Notes
Article history
The research reported in this issue of the journal was commissioned by the HTA programme as project number 02/35/02. The contractual start date was in November 2004. The draft report began editorial review in October 2009 and was accepted for publication in May 2010. As the funder, by devising a commissioning brief, the HTA programme specified the research question and study design. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the referees for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2012. This work was produced by Lamb et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to NETSCC. This journal is a member of and subscribes to the principles of the Committee on Publication Ethics (COPE) (http://www.publicationethics.org/). This journal may be freely reproduced for the purposes of private research and study and may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NETSCC, Health Technology Assessment, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
2012 Queen’s Printer and Controller of HMSO
Chapter 1 Introduction
Background
Whiplash injuries (acceleration–deceleration injuries to the neck) are a common type of injury and the sequelae make up a significant proportion of the workload of emergency departments (EDs) as well as having significant implications for orthopaedic services, physiotherapy and primary care. Most often the injury results from rear-end or side-impact motor vehicle collisions, but it may also occur during other activities such as diving. Although whiplash injuries are usually not serious, they may cause substantial long-term morbidity, and because they are so common they are a major health and economic problem around the world. In the UK, the annual cost to the economy was about £2553M in 1990, representing about 18% of the total costs of all road traffic collisions and 0.4% of the gross domestic product. 1 More recent estimates suggest the costs maybe circa £3.1B per annum. 2 The costs are caused mainly by lost productivity owing to absence from work and considerable health service costs involved in the treatment of patients who develop chronic symptoms.
The incidence of whiplash injuries varies around the world, being largely dependent on traffic volumes and road conditions. Not surprisingly, high rates are found in developed countries with high population density and high car ownership. Different studies have estimated incidences of 380 per 100,0003 or 106 per 100,0004 in Australia, 266 to 387 per 100,000 in the USA,5 70 per 100,000 in Quebec,6 and 188 to 325 per 100,000 in the Netherlands. 7 In the UK, there appears to have been a substantial increase in the incidence of whiplash injuries during the 1980s and 1990s and there were around 250,000 new cases in 2003. 1 Similar increases have been reported in Germany8 and the Netherlands. 7 The reasons for the increasing incidence are not completely clear, but there are probably several contributory factors, including increase in traffic volume and, possibly, increased litigation leading to an increase in the reporting of symptoms after road accidents.
Classification of whiplash injuries
Early studies of whiplash used terms such as ‘whiplash’ to mean a variety of different things. Terminology was standardised by the Quebec Task Force (QTF), an international expert group, in 1995. 6 These definitions are now internationally accepted and are used throughout this study. According to the QTF definitions, ‘whiplash’ is the mechanism of injury (acceleration–deceleration injuries usually in the frontal plane), ‘whiplash injuries’ are the soft tissue injuries that result and ‘whiplash-associated disorder (WAD)’ describes the pattern of signs and symptoms that arise. There are five grades of WAD, from grade 0 (no neck complaints or signs) to grade IV (fracture or dislocation) see Table 1. 3
| Term | Definition |
|---|---|
| WAD grade 0 | No neck complaints or signs |
| WAD grade I | Complaint of pain, stiffness or tenderness, but no physical signs |
| WAD grade II | Complaint of pain, stiffness or tenderness, and musculo-skeletal signs (decreased range of motion, point tenderness, etc.) |
| WAD grade III | Complaint of pain, stiffness or tenderness and neurological signs (decreased or absent deep tendon reflexes, weakness and sensory deficits). Could also have musculo-skeletal signs |
| WAD grade IV | Fracture or dislocation |
The term ‘late whiplash syndrome (LWS)’ is used throughout the study to describe the chronic complications of whiplash, and defined as: ‘Presence of pain, restriction of motion or other symptoms at 6 months or more after the injury, sufficient to hinder return to normal activities such as driving, usual occupation and leisure’.
Prognostic factors for late whiplash syndrome
The most common symptoms after acute whiplash injury are neck pain and headache, with other symptoms such as neck stiffness, shoulder pain, arm pain or numbness (or both), paraesthesia, weakness, dysphagia, visual and auditory symptoms, dizziness and concentration difficulties occurring in smaller numbers of patients. In most cases, symptoms are short lived, but a substantial minority go on to develop LWS, i.e. persistence of significant symptoms beyond 6 months after injury. Different studies have estimated variable proportions of patients to have persistent symptoms, and the incidence of LWS is not known precisely. In part the differences in reported incidence between studies are due to differences in the definitions of chronic symptoms and differences in the populations studied. However, it is generally accepted that between 20% and 50% of patients will report symptoms persisting for more than 6 months. 9 These patients generate the majority of costs associated with WAD in terms of lost productivity and costs to the health service of providing treatment. 1 Therefore, an important aim in the management of acute WAD injuries is to prevent the development of LWS.
A wide range of factors have been reported to be associated with the development of LWS, including physical factors such as pain intensity and psychological factors such as previous psychological problems, stress and acute psychological response to injury. The existing literature is generally of poor methodological quality and does not provide strong evidence for the association of any risk factor with LWS, but initial pain intensity and neck pain-related disability appear to have the most consistent associations. 10–12 The literature is not of sufficient quality to allow any quantitative assessment of the relative importance of the different risk factors. There is limited evidence for the importance of other risk factors such as post-traumatic stress, self-efficacy and previous chronic pain in development of LWS. 13 Despite considerable research effort, the factors associated with LWS and their relative importance are not well known. Several risk factors identified by various studies are potentially modifiable in the early stages of recovery after whiplash injury, so effective treatment may be able to reduce the proportion of patients who subsequently develop LWS.
Management of whiplash-associated disorders
There are few good-quality randomised trials upon which to base recommendations for practice and the optimum treatment for acute whiplash injury is unknown. In the mid-1990s the QTF review found insufficient evidence supporting the treatments in use at that time. It concluded that promoting activity in the early stages of recovery was probably the most effective strategy, soft collars were not helpful, and physiotherapy, a very common treatment, required rigorous evaluation because of its high costs. The Cochrane review Conservative Treatments for Whiplash14 included 17 studies of treatments for acute whiplash. These evaluated a wide range of treatments, but most were of low methodological quality and differences between them precluded any meta-analyses. Although some individual trials appeared to show superiority of one treatment, results were inconsistent and no clear conclusions could be drawn about the most effective therapy. The authors concluded that large, high-quality trials are needed.
The QTF proposed a ‘stepped care’ clinical pathway in which patients are given advice and education at the initial contact, and then reviewed at 3 weeks. Patients with persisting symptoms would then be provided with more intensive treatment aimed at amelioration of modifiable risk factors for LWS to prevent development of chronic symptoms. Such a strategy is likely to yield the most cost-effective method of providing care for acute whiplash injuries, as it should target intensive (and expensive) treatment to those patients who are most likely to benefit. However, the QTF did not make any recommendations about the specific treatments that should be used.
Another review15 suggested that psychological risk factors predominate as risk factors for poor outcome after whiplash injury, and argue that advice to resume normal activity, using a cognitive behavioural approach, should be the treatment of choice for early management of whiplash. The review was used to develop The Whiplash Book,16 which is a booklet that uses a psychoeducational approach to deliver positive messages about prognosis, pain, returning to normal activities, exercise and self-management of symptoms. The Whiplash Book was developed by an internationally recognised multidisciplinary group. 16 Using recommendations for developing patient information and experience of developing similar material for low back pain,17,18 a draft booklet was peer reviewed by independent multidisciplinary experts. The booklet was formatted by design experts, and tested for proof of concept. 19 The results were promising in so far as patient’s beliefs about pain and poor recovery were modified, and the potential for modifying behaviours on the causal pathway to disability suggested. 19 Disability outcomes were not investigated. Experience gained in back pain research emphasised the importance of practitioner training in using The Whiplash Book to ensure that verbal consultations and written material were consistent. The overall approach is called ‘active management’.
Whether or not The Whiplash Book and active management approach is effective is not yet known. Other systematic reviews have suggested that physical as well as psychological factors may also carry significant amounts of risk for poor outcome,12,20 and some of the evidence used to support the strategy of The Whiplash Book was from the field of low back pain or other chronic conditions, and may not be directly transferable to management of WAD. There are notable differences between WAD and low back pain in terms of the mechanism of injury and psychological consequences. For example, phobic travel anxiety and other psychological manifestations of shock may occur in 50% of people after whiplash injury21,22 but are rarely, if ever, reported in low back pain.
Current UK practice for acute whiplash-associated disorder
The most common treatment for WADs in EDs is advice, but the content and quality of the advice varies. 23 Over 90% of departments suggest using analgesics and gradually increasing movement of the neck. Some departments use soft collars as well, suggesting that they should be removed and the neck exercised on a regular basis. Referral to radiological investigations and physiotherapy occurs in 50% of departments for those patients with more severe symptoms. Physiotherapy is a common treatment for WAD but there are no published data on the types of physiotherapy currently delivered in the UK. The most recent UK guidelines for the physiotherapy management of WAD advocates the use of joint manipulation and mobilisation, soft tissue mobilisations, exercises, education and advice, transcutaneous electrical nerve stimulation (TENS) and multimodal packages. 24
Rationale for Managing Injuries of the Neck Trial
Current treatments for acute WAD are variable and are not supported by good-quality evidence. A stepped care approach to treating whiplash injuries, as proposed by the QTF, is potentially the most cost-effective solution but it requires evaluation and identification of the optimal components of treatment. In this approach, EDs would provide advice on management of WAD. Currently, advice given by EDs in the UK is variable and often contains outdated recommendations. The advice contained in The Whiplash Book may potentially be superior to current standard care, and could become a standard treatment across the NHS. Evaluation is needed to determine whether or not it is beneficial.
The second component of the stepped care pathway is physiotherapy treatment, for patients with persistent symptoms. In the Managing Injuries of the Neck Trial (MINT) we evaluate a package of physiotherapy treatments that are, as far as possible, evidence based and acceptable to physiotherapists and could be implemented throughout the NHS if shown to be effective.
Research objectives
-
To estimate the clinical effectiveness of a stepped care approach over a 12-month period after an acute whiplash injury.
-
Step 1: The Whiplash Book versus usual care advice (UCA) in EDs.
-
Step 2: In patients with symptoms persisting at 3 weeks (WAD grades I–III), supplementary treatment comprising either a package of physiotherapy treatments and reinforcement of advice versus reinforcement by a physiotherapist of advice provided at the initial ED contact.
And: the combined effect of the treatments.
-
-
To estimate the clinical effectiveness in pre-specified subgroups of patients: those with prior neck problems, psychological or physical risk factors for poor outcome, and those seeking compensation.
-
To estimate the costs of each strategy including treatment and subsequent health-care costs over a period of 12 months and to estimate cost-effectiveness.
-
To gain a participant’s perspective on experiencing a whiplash injury, NHS treatment and recovery within the context of MINT.
Chapter 2 Methods
Introduction
MINT used a design consisting of two linked randomised controlled trials (RCTs). The first step was a cluster randomised trial in which NHS trusts were randomised to one or other of the ED advice interventions to be compared (The Whiplash Book or UCA), for all patients presenting with acute problems following a whiplash injury. The second step was an individually randomised trial, for patients still experiencing symptoms 3 weeks after their injury, comparing physiotherapy with a single advice session reinforcing the advice given in the ED. The two parts of the trial used a common system of follow-up at 4, 8 and 12 months.
The trial was run in hospitals of 12 NHS acute trusts in the UK: Heart of England NHS Foundation Trust (Heartlands and Solihull Hospitals), North Bristol NHS Trust (Frenchay Hospital), Oxford Radcliffe Hospitals NHS Trust (John Radcliffe Hospital), University Hospitals Coventry and Warwickshire NHS Trust [University Hospital (Walsgrave Site) and Hospital of St Cross, Rugby], Gloucestershire Hospitals NHS Trust (Cheltenham General and Gloucester Royal Hospitals), South Warwickshire General Hospitals NHS Trust (Warwick Hospital), Worcestershire Acute Hospitals NHS Trust (Alexandra Hospital, Redditch and Princess of Wales Community Hospital), University Hospitals Birmingham NHS Foundation Trust (Selly Oak Hospital), Kettering General Hospital NHS Foundation Trust (Kettering General Hospital), Buckinghamshire Hospitals NHS Trust (Stoke Mandeville Hospital), Countess of Chester Hospital NHS Foundation Trust (Countess of Chester Hospital), and Gwent Healthcare NHS Trust (Royal Gwent Hospital, Newport). Some trusts comprised several hospitals and hence some clusters contained more than one ED.
Ethics committee approval
MINT was approved by the Trent Multicentre Research Ethics Committee (MREC, reference MREC/04/4/003), the Local Research Ethics Committee and the Research and Development Committee of each participating centre.
Step 1: Cluster randomised trial of The Whiplash Book versus usual advice
Inclusion and exclusion criteria
All people who attended ED with a history of whiplash injury of less than 6 weeks’ duration were eligible for the trial, except those with any of the following exclusion criteria:
-
age < 18 years
-
fractures or dislocations of the spine or other bones
-
head injuries with more than a transient loss of consciousness or with a Glasgow Coma Score of ≤ 12 at any stage of their assessment in hospital
-
admission to inpatient services
-
severe psychiatric illness.
Identifying participants and consent
Because the first part of the trial was cluster randomised, individual consent for participation was not sought. This is an accepted procedure for cluster randomised trials where individuals do not have a choice of whether or not to receive the trial intervention. 25
Clinicians in each participating ED were responsible for identifying eligible participants. Posters were displayed in the ED to inform patients that the trial was taking place and also versions with the study inclusion/exclusion criteria to remind clinicians about the trial. In addition, resources such as credit card-sized laminated card reminders of WAD grades and inclusion/exclusion criteria were also distributed. Details of patients with WADs were recorded on a trial proforma, a short carbonised form developed specifically for MINT. It allowed collection of a routine core clinical data set, including injury severity, pain intensity and WAD grade diagnosis. It contained tick boxes to ensure that clinicians provided potential participants with the trial information sheet, discussed the study with them, and also recorded if the patient would prefer not to receive the study questionnaires. A copy of the proforma was filed in the medical notes as a treatment record and the second copy was passed to the research team to notify them that a patient had been asked to participate. Completed proformas were collected twice a week by the research therapists/nurses and returned to the study co-ordinating centre (Warwick Clinical Trials Unit) either by post or in person, depending on the centre.
Patients were informed about the possibility that they may be eligible for Step 2 of the study but did not receive detailed information at this stage, because the majority of patients who participated in Step 1 were not expected to have persistent symptoms at 3 weeks and hence were not eligible for Step 2. Patients were also asked for their contact details (address, telephone number, mobile telephone number and e-mail address), to assist with sending out and following up questionnaires.
Randomisation
The unit of randomisation was the NHS trust. Participating trusts were randomised by the project statisticians before the start of recruitment to UCA or The Whiplash Book advice (WBA). We randomised by trust rather than by ED to avoid contamination; this could arise if different EDs within a trust were allocated to different interventions, because staff frequently worked in more than one ED. Randomisation used a table of random numbers, starting at a random place to ensure that the allocations were not known before randomisation. The allocation depended on whether or not the next digit was odd or even. Clusters were pair matched by size (number of ED attendances per year) prior to randomisation; one of each pair of trusts was randomised to The Whiplash Book arm and the other to the UCA arm.
Interventions
The interventions, their delivery and training of ED staff are described fully in Chapter 3.
Eligible patients were given a trial information pack containing a letter of introduction about the study, signed by their local ED consultant, and the appropriate advice leaflet. The pack was identical for both arms of the trial apart from the advice materials. ED clinicians discussed the study with patients. If patients were willing to participate, they were told that they would receive a questionnaire in a few days time. They were asked to return this and to contact the MINT study team if they continued to have problems after approximately 2 weeks. The introduction letter did not mention randomisation of hospitals to The Whiplash Book or UCA, but simply stated that the hospital was taking part in a study of advice given to patients with whiplash injuries. ED clinicians provided each patient with either a copy of the ED’s usual advice leaflet or The Whiplash Book, and verbal guidance on management of WAD. A patient user group was consulted when developing the trial materials provided to patients explaining the study.
Some of the EDs involved in the trial serve large populations from minority ethnic groups. With permission from the publishers, The Whiplash Book was translated into five south Asian languages (Bengali, Gujarati, Hindi, Punjabi and Urdu).
Monitoring the intervention delivery
Research staff visited the centres regularly throughout the recruitment period to provide recruitment and educational support. Where possible, hospital records were audited to monitor ED attendance rates and referral rates. To assist in monitoring the delivery of the intervention additional audits were carried out to see if the number of proformas completed matched the number of MINT patient information packs (containing the advice leaflet and trial information) being used.
Patient inclusion, outcome measures and data collection
All patients attending for treatment of a whiplash injury that did not ask to be excluded were sent the 2-week and 4-month follow-up questionnaires, and were included in the trial if either of these was returned. The 2-week questionnaire was sent within a week of their ED attendance. It included demographic information and administration of some of the outcome measures [Short Form questionnaire-12 items (SF-12) version 1, European Quality of Life-5 Dimensions (EQ-5D) and ED treatment satisfaction]. If the questionnaire was not returned within a week, a second copy of the questionnaire was dispatched.
Step 2: Individually randomised trial of physiotherapy versus reinforcement of advice given in emergency departments
Inclusion and exclusion criteria
Participants were eligible for randomisation into the second step of the trial if they:
-
reported symptoms in the 24 hours before attendance at the physiotherapy research clinic approximately 3 weeks after attendance at ED
-
were WAD grades I–III at this time
-
did not have any contraindications to physiotherapy treatment – these include central cord compression or upper motor neuron lesion, complete nerve root compression or lower motor neuron lesion, suspected vascular injury or haemorrhagic event.
Identifying participants and consent
Patients who attended participating EDs and received either of the advice interventions were asked to contact the study co-ordinating centre if they continued to have symptoms 3 weeks after their ED attendance. All participating patients who reported ongoing symptoms at this time were contacted by telephone by a research therapist to ensure they were potentially eligible and, if so, an appointment was then made for the patient with a research physiotherapist based at their local hospital. At this appointment, their eligibility for Step 2 of the trial was assessed. If eligible, trial participation was discussed and the patient was asked to sign a study consent form prior to randomisation. Information about Step 2 of MINT was sent to patients several days before their research clinic appointment, ensuring that they had sufficient time to consider participation.
Randomisation
Randomisation to physiotherapy or reinforcement of advice was via a central telephone randomisation service, based at the Cancer Research Clinical Trials Unit, University of Birmingham, Birmingham, UK. Randomisation was stratified by centre to ensure balance between the different ED interventions used in Step 2, and members of the same household were assigned to the same intervention to reduce the chance of contamination. This was taken into account in the trial analysis. If eligible patients declined participation, their reasons for doing so were recorded.
Interventions
Full details of the interventions are given in Chapter 3, but are described briefly here.
The physiotherapy package consisted of up to six sessions of therapy, over an 8-week period. The components of the intervention were described in a training and reference manual. The choice of physiotherapy treatments was made using two principles. Firstly, if there was evidence that the treatments were potentially effective in a WAD population or, where this was lacking, evidence of treatments that were effective for chronic neck dysfunction and likely to be effective for WAD, based on expert opinion or limited trial evidence. Secondly, if the treatments targeted established and potentially modifiable risk factors for developing LWS, including reduced cervical range of motion, high pain intensity, and adverse psychological reactions to the injury.
Participants randomised to reinforcement of advice received a single 40-minute session of advice with a physiotherapist, in which the therapist restated the advice that the patient was given at the time of their ED attendance (either The Whiplash Book or the hospital’s usual advice leaflet), discussed any queries that the patient had, and if applicable, checked the exercises that the patient was given in the ED. The physiotherapist could only give advice regarding progression of exercises or activities specified in The Whiplash Book or usual advice leaflet, and could not prescribe new exercises or use any ‘hands-on’ treatment. No review appointments were offered to these patients. They were advised to see their general practitioner (GP) if they had ongoing problems.
Physiotherapists who were independent of the recruitment and randomisation procedures, and had attended a 1.5-day training session from the trial team, delivered all interventions. The same therapists delivered both the physiotherapy and the control interventions, and each treatment session was recorded in a treatment log. All treatments were intended to be completed within 4 months of the patient’s first attendance at the ED. Participants were able to seek additional treatment outside the trial, and use of any such treatment was recorded in the follow-up questionnaires.
Monitoring the intervention delivery
The primary method of monitoring attendance rates and the treatments delivered was treatment logs. Treatment logs were completed for all patients by the trial physiotherapists and returned to the study co-ordinating centre. We liaised closely with the physiotherapy departments to ensure that all treatment logs were returned, and to address any problems identified via the treatment logs. From these treatment logs the patients were classified into four categories of attendance: did not attend any sessions; attended assessment only; partial completion; and completed treatment. In the physiotherapy arm, patients were classified as partial completers if they attended for the assessment and at least one treatment session. Treatment was terminated when the patient failed to attend for subsequent treatment. Physiotherapy package patients were classified as having completed treatment if the treatment was completed as intended and discharge was by mutual agreement between the physiotherapist and patient. Those allocated to the advice session were deemed to have completed treatment if they attended the advice session.
In addition, some centres were visited in the early stages of the trial to ensure the smooth implementation of the intervention. This involved auditing a selection of patient notes who were receiving the physiotherapy package and the observation of an advice session.
Outcome measures and data collection
A common follow-up procedure was used for all participants. Follow-up data collection was by postal questionnaires, completed at 4, 8 and 12 months after ED attendance. The primary outcome was the Neck Disability Index (NDI). The NDI is a self-completed questionnaire that has been used successfully in a postal format in trials of neck treatments. 26,27 It assesses pain-related activity restrictions in 10 areas including personal care, lifting, sleeping, driving, concentration, reading and work, each of which is scored from 0 to 5 (0 = no disability, 5 = total disability).
The SF-12 and EQ-5D were included to assess generic health-related quality of life (HRQoL), and to enable a single utility score for economic evaluation to be derived from the EQ-5D. We used the acute (1 week) recall version of the SF-12 in order to obtain more accurate change in health status. Participants also rated whether or not they had improved, remained the same, or worsened. Resource use was assessed by a short questionnaire that asked about additional NHS or private hospital treatment for the whiplash injury, any GP consultations, manipulation, massage or other treatment. Participants were asked to distinguish between prescription and out-of-pocket expenses.
Follow-up questionnaires were mailed to participants 4, 8 and 12 months after their ED attendance. If questionnaires were not returned within a week, a standardised series of reminders were used:
-
questionnaire sent to participant
-
questionnaire not returned after 1 week: first telephone prompt
-
second copy of questionnaire dispatched if necessary
-
questionnaire not returned after a further week: second telephone prompt
-
questionnaire not returned: contact participant to collect core outcome data by telephone
-
unable to contact participant by telephone: class as ‘non-responder’ and close case.
Follow-ups were classed as ‘closed cases’ when a questionnaire was received from the patient, data were collected by telephone, or the procedure was followed to the end and the patient was classed as a ‘non-responder’.
Participants were asked only at the 12-month follow-up whether or not they had pursued and settled a compensation claim related to their whiplash injury. This was not asked at 4- or 8-month follow-up to avoid stimulation of claims among the trial population.
A research assistant not involved in the recruitment or randomisation processes was responsible for mailing follow-up questionnaires, and for entering responses onto the study database. Blinding of the study team was maintained until final analysis of the data was completed.
Database and data processing
The database was designed and developed in house (Wolfson Institute) using Microsoft Access 2002 (Microsoft Corporation, Redmond, WA, USA). All data were kept and backed up using a LaCie Biometric Safe Drive (London, UK) that was only accessible by authorised staff. For an added security to personal data, the database was encrypted using the encryption software Cryptainer, and Groove Virtual Office software was used to transfer files between secured PCs in the study co-ordinating centre (Warwick Clinical Trials Unit) and the statistical team (Wolfson Institute).
The database imposed rules for data entry which include valid range for responses, linked dates and patient identity among data tables, auto-generated patient identity with check digits, auto-generated dates for despatch records and pop-up warnings for ambiguous entries, which eliminated implausible errors on data entry. Queries were set up to automate checks between linked tables.
Data were single entered into the database by study personnel. The data sets were automatically cleaned on a weekly basis using a computer program to standardise missing and ambiguous responses on follow-up questionnaires according to coding rules developed during the study.
For data quality assessment, 10% of baseline, 5% of 4-month follow-up, 5% of 8-month follow-up, and 10% of 12-month follow-up questionnaires were randomly selected for double entry. We found that the clinical sections of the questionnaires have very low item-level percentage of error and very low overall error rates throughout, less than 5%. The health economics sections suffered some higher percentages of item-level discordance, but most of the discordances were attributed to coding of missing values. Small denominators were also responsible for the higher percentages of item-level discordance. All disagreements found between the two databases during the check were corrected and we also corrected any systematic faults that were detected. We concluded that data quality was good and full double entry was not necessary. In addition, we checked manually for data inconsistencies every 3–4 months using the queries mentioned above, and compared any anomalies found with the paper questionnaires. Amendments were made to the data (both paper and electronic) if necessary.
Statistical analysis
Outcome data
For the NDI, an overall score was calculated for each participant by summing the score for individual components (a score out of five for each of the 10 components) and was expressed as a percentage (i.e. double the sum of the components). In addition, we summarised poor recovery at two time points as acute whiplash injury and LWS as below.
Acute whiplash injury
‘Whiplash is an acceleration–deceleration mechanism of energy transfer to the neck. It may result from rear end or side-impact motor vehicle collisions, but can also occur during diving or other mishaps. The impact may result in bony or soft tissue injuries (whiplash injury), which in turn may lead to a variety of clinical manifestations’ [Whiplash Association Disorders (WAD)]. 6
Operationally, this is defined as ‘if participant scores either ≥ two on Question two (personal care) OR Question seven (work) OR Question 10 (recreation) of the Neck Disability Index on their 4 month follow-up questionnaire they will be deemed to have Acute Whiplash Injury’.
Late whiplash syndrome
Late whiplash syndrome is the presence of pain, restriction of motion or other symptoms at 6 months or more after the injury, sufficient to hinder return to normal activities such as driving, usual occupation and leisure.
Operationally this is defined as ‘if participant scores either ≥ two on Question two (personal care) OR Question seven (work) OR Question 10 (recreation) of the Neck Disability Index on the 12 month follow-up questionnaire they will be deemed to have LWS’.
We found no published literature available on the strategy for handling missing data on the NDI items. For the purpose of calculating the overall score, no imputation was made for the question on driving (question 7). If this item was missing, the NDI was scored based on the other nine items, as the question is not relevant to any participants who do not drive. Other missing item scores were imputed using multiple imputation by chained equations (MICE) technique. 28 This is implemented by the ‘ice’ package commands in Stata (StataCorp LP, College Station, TX, USA).
Work days lost was determined by the number of days off sick in the last 4 months. We assumed the maximum days and hours of work possible within the period in question. A high proportion of missing data for these items was expected and was dealt with by multiple imputation in the Poisson regressions as for NDI.
The SF-12 was scored according to standard methods (SF-12v1). 29 We analysed mean scores for the mental component score (MCS) and physical components score (PCS). We used US norms because there is little difference in using country-specific norms to calculate SF-12 summary measures and so that data can be compared and interpreted across countries in relation to the US standard benchmark. 30 Missing responses were dealt with by multiple imputation, as with the NDI.
The EQ-5D was used mainly for economic evaluation. A standard scoring algorithm was used to calculate the health-utility score. 31 Missing responses were again addressed using multiple imputation.
Analytical strategy
All participants were analysed in the groups to which they were randomised, regardless of the treatment that they may have eventually received (intention to treat analysis). The analysis was conducted in three separate parts:
-
cluster randomised (Step 1)
-
individually randomised (Step 2)
-
interaction between cluster randomised and individually randomised.
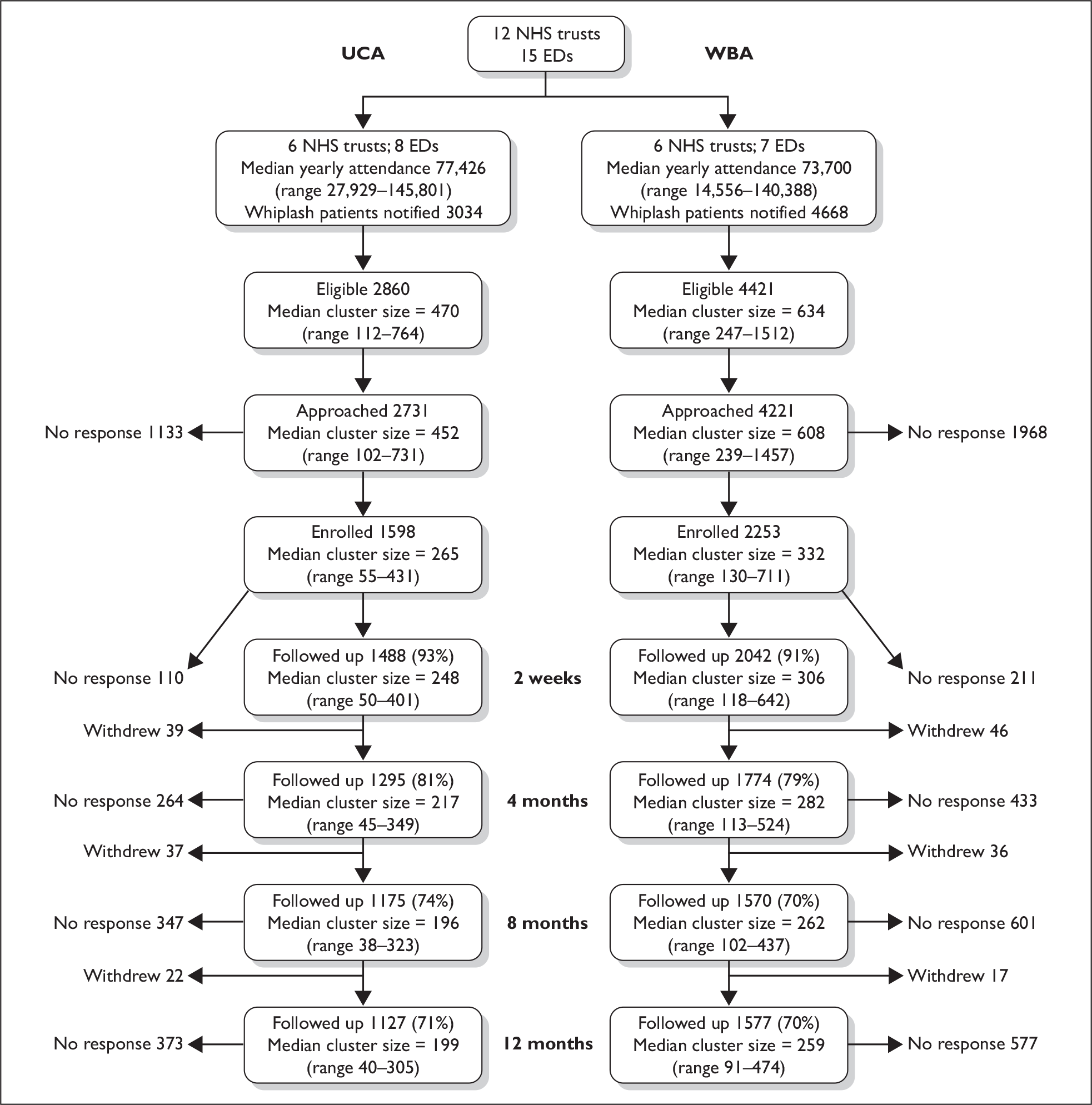
Descriptive statistics for demographics of participants at baseline were analysed separately for each component, and a Consolidated Standards of Reporting Trials (CONSORT) diagram was produced for both stages of the trial (see Figures 2 and 14).
Step 1
We included all participants in Step 1 in the comparison of WBA versus UCA, irrespective of whether or not they took part in Step 2 of the trial. Cluster characteristics were tabulated, and intracluster correlation coefficient (ICC) estimates for NHS trusts were calculated (see Appendix 3). We used hierarchical regression modelling to incorporate the effects of clustering owing to randomisation of NHS trusts. Random effects multiple linear regressions were used for all primary and secondary outcome measures on continuous scales, and random effects multiple logistic regressions on the binary outcomes acute whiplash injury and LWS. Work days lost was analysed using Poisson regression. Models were adjusted for clustering of NHS trusts and WAD grades at ED attendance at each time point on observed data and multiply imputed data.
Step 2
We performed random effects multiple regressions, as in Step 1, to compare the physiotherapy arm with reinforcement of advice, but with adjustment for advice intervention in Step 1, clustering of NHS trusts, clustering of therapists within NHS trusts, and NDI score at research clinic.
Statistical analyses were carried out in Stata 10 and MLwiN 2.1 (MLwiN, Centre for Multilevel Modelling, Bristol, UK). 32
Interaction between cluster and individually randomised analysis
We investigated whether or not there were any effects of interactions between interventions given in Step 1 and Step 2. We performed random effects multiple regressions as in Step 2, with additional adjustment for interaction term between The Whiplash Book intervention and physiotherapy intervention.
Adverse events
Adverse events are reported qualitatively in Chapter 5. We tabulated reasons for withdrawal for participants in Step 1 and Step 2 separately.
Subgroup analyses
Four pre-specified subgroup analyses were undertaken in both Step 1 and Step 2:33
-
severe physical symptoms at trial entry (WAD grade I vs WAD grades II or III)
-
adverse psychological reactions at trial entry (measured by EQ-5D question 5 in Step 1 and the Impact of Events Scale in Step 2)
-
pre-existing neck pain versus no pre-existing neck pain
-
compensation – claim being pursued versus not being pursued (as identified by the 12-month follow-up questionnaire).
Statistical tests of interaction were used to perform subgroup analyses. 34
Sensitivity analysis
Sensitivity analysis were planned to explore the effects on the results of adjustment for imbalance in baseline characteristics. Exploratory analyses of adjustment for the effects of ethnicity were performed because of an observed imbalance in the ethnic mix of participants in Step 1.
Sample size
For the primary outcome (NDI), there is consensus that a minimal clinically important difference lies in the range of three to five absolute points, with a standard deviation (SD) of about 8%. 35 We therefore aimed to be able to detect a difference between the groups of three absolute points (i.e. 0.375 SDs), both for the comparison of The Whiplash Book and UCA, and for physiotherapy versus reinforcement of advice. For the individually randomised comparison (physiotherapy vs reinforcement of advice), 211 per group were required, based on 90% power and 1% significance level. Assuming a worst-case scenario of 30% loss to follow-up gives a total sample size of 300 per group (600 in total). 36 The comparison of ED advice interventions was cluster randomised, so larger numbers were needed. Originally it was planned that eight centres would participate, recruiting 4800 participants. This was revised with the inclusion of four additional centres, which allowed reduction of the overall sample size required to achieve the same power. Assuming a ICC of 0.02, an average of 120 patients per centre gives an inflation factor of 5.94,37 leading to a sample size of 713 in each group. Allowing for 30% loss to follow-up, 1020 participants per group were needed (2040 in total). To allow for a reduction in power caused by unequal sample sizes among clusters, the target sample size was set to 3000 (an average of 250 per cluster). The change to the sample size was agreed by the Data Monitoring and Ethics Committee (DMEC), who monitored parameters that affect power throughout recruitment.
Monitoring
Trial Steering Committee
A Trial Steering Committee (TSC) was responsible for monitoring and supervising the progress of MINT towards its interim and overall objectives. Membership of the TSC is given in Appendix 1.
Data Monitoring and Ethics Committee
The DMEC was independent of the trial and monitored the ethical, safety and data integrity aspects of the trial. The DMEC determined what analyses were required at each of the meetings and the trial statistician supplied these. Membership of the DMEC is given in Appendix 2.
Chapter 3 Intervention description and rationale
Introduction
The commissioning brief requested a trial of non-surgical, non-pharmacological treatments for acute WAD, applied within the first 6 weeks of injury.
Treatments provided in the early phase of recovery after whiplash injury are targeted to the rapid alleviation of acute symptoms and prevention of LWS. The ranges of treatment possibilities include watchful waiting, advice to promote return of normal activity, psychosocial educational materials, physiotherapy, complementary therapies (not widely available in the NHS), or psychological counselling. More intensive multimodal rehabilitation interventions are applied only when chronic symptoms are established.
The QTF provided useful guidance for determining the treatments to be compared in the trial,6 and suggested that promoting activity in the early stages of the injury was probably the most effective way forward, and that soft collars are not helpful.
The QTF proposed a stepped care clinical pathway in which patients are given advice and education at the initial contact, and then reviewed at 3 weeks and considered for further treatment. The QTF suggest that patients with persisting symptoms should be provided with more intensive treatments by health professionals experienced in the management of WAD. This was the broad schema that we adopted for testing within the trial. At the outset of the trial, we believed that the stepped care model was most likely to yield a cost-effective strategy for management of WAD. However, the QTF did not make precise recommendation about which treatments should be used for people who have persisting symptoms. Physiotherapy is the most widely available treatment for WAD in the UK NHS, and the QTF highlighted the lack of evidence and need for rigorous evaluation of physiotherapy because of the potential high cost. The Cochrane review Conservative Treatments for Whiplash drew similar conclusions. 38
Therefore, we decided to draw the following comparisons:
-
For all participants, either UCA versus an active management advice strategy supplemented by The Whiplash Book at ED attendance.
-
For those participants who had persisting symptoms, a single advice session of physiotherapy versus an intensive physiotherapy programme consistent with dose and method of delivery for the UK NHS.
Advice and usual care interventions tested in Step 1
Advice is considered to be the cornerstone of clinical management for acute WAD. In 1995 the QTF proposed that initial treatment should be advice and reassurance about the favourable prognosis following a whiplash injury. Suggested key messages were that pain is usually short-lived and is controllable, that early return to usual activities with the help of exercises produces a favourable outcome and that the use of soft collars may prolong recovery times.
Subsequent research has suggested that psychological risk factors are important as risk factors for poor outcome, and psychoeducational advice materials [based on cognitive behavioural (CB) model] may prove efficacious in the management of acute WAD outcome. 13,39–41 Prior to and independently of the MINT trial, an expert group developed a psychoeducational booklet for use in acute WAD which has been advocated widely in the UK16 and efficacy trials provided proof of concept evidence that the book challenged and modified people’s thinking about the injury. Experienced gained in back pain research emphasised the importance of practitioner training in using The Whiplash Book to ensure the verbal consultation and written material were consistent. The overall approach is called ‘active management’.
Hence we selected to make two treatment comparisons at the point participants presented to the ED:
-
usual care advice
-
an active management strategy which emphasised the importance of resuming normal activity, the short-lived nature of pain, and positive prognosis after a whiplash injury, using both the consultation with the participants to deliver this message and The Whiplash Book as reinforcement.
This presented a number of challenges. Firstly to determine what usual care is, and secondly, to develop a training package using the active management strategy and The Whiplash Book which promoted routine use within EDs.
Defining usual care
Before starting the trial we undertook a national survey of ED consultants across the UK to estimate the usual care in UK EDs, and a content analysis of advice sheets used. 23
A postal questionnaire was sent to 316 lead consultants from all UK EDs with annual new attendances of > 50,000 people. Consultant leads were asked to indicate the use of a range of treatments and the frequency with which these treatments were used. Samples of written advice were requested and content analysis was conducted and compared with survey responses.
The response rate was 79% (251 of 316). The intervention most frequently used was verbal advice to exercise, reported by 84% of respondents for most or all cases, and advice against the use of a collar (83%). Other treatments reported as being used frequently were written advice and anti-inflammatory medication. One hundred and six consultants (42%) provided a sample of written materials. Reference to expected recovery and encouragement for early return to activities (including work) were included in less than 6% of the written advice leaflets. There were important differences between reported verbal behaviours and written advice. Nearly 50% of written materials suggested the use of a soft collar and contained information on how to use a soft collar, and 61% contained information on solicitors and pursuing a personal injury claim.
Radiological investigations, physiotherapy and analgesics other than non-steroidal anti-inflammatory drugs (NSAIDs) were used only in selected cases, and in only 50% of departments. Case selection criteria were greater pain and more severe symptoms at initial presentation, and those who did not improve.
Of the departments providing written advice to patients, the most common format was material developed by the department [supplied by 176 of 251 (70%) departments to most or all cases]. Only 10 out of the 251 departments (4%) used The Whiplash Book for most or all cases, and the remainder used other formats. The majority of departments who gave advice to exercise did not provide information on exercise in their written information.
Content analysis of the UCA leaflets, demonstrated they did not include information about longer-term recovery, the benefits of early return to activity or the appropriate use of collars.
We concluded that verbal advice is the primary method for managing WAD in EDs and is usually supplemented by written advice. Within individual hospitals there is a lack of consistency between verbal and written advice.
Logan and Holt42 also reported a survey of ED practice for the management of WAD in Wales. They found that most departments (19 of 20) used patient advice sheets, but there was a large disparity in the verbal advice given both within and between departments.
Active management strategy for acute whiplash-associated disorder
We designed a programme to train ED clinicians (medical and other) in the active management strategy. We utilised similar approaches to those found successful in implementing The Back Book and active management strategy for low back pain in primary care. 43,44 We implemented a systematic approach to assessment, and provided regular training to ensure delivery of the active management strategy.
ED staff were asked to emphasise key messages during the consultation as well as give a copy of The Whiplash Book. The messages were:
-
reassurance that prognosis following a whiplash injury is good
-
encouragement to return to normal activities as soon as possible using exercises to facilitate recovery
-
reassurance that pain is normal following a whiplash injury and patients should use analgesia consistently to control this
-
advice against using a collar.
The training programme used behavioural learning theories. 45 We used existing training slots (ED rotational induction or in-service training programmes), using the usual session lengths for each hospital. At most departments training occurred once every 4 months in tandem with junior medical staff rotations. Nursing and allied health professionals working in ED were trained through existing programmes within the department.
The training consisted of a 30- to 40-minute session. Clear objectives were set for clinicians to understand WAD and the need to provide clear, well-articulated messages of the active management strategy alongside The Whiplash Book. Clinicians were asked to use this approach for all patients with WAD grades I–III. 6 The training was delivered by the research team (physiotherapists). If ED staff were unable to take part in training programmes, the research team spoke with clinicians individually and provided summary training sheets.
Training sessions for usual care
We developed a training session for the usual care departments that comprised a session of similar length to the active management session. The content was an educational package about WAD, but included no instructions on the management of WAD. Emphasis was placed on continuing with usual advice for all patients with WAD grades I–III6 and providing participants with information on the trial. The package was delivered in the same way in both arms of the trial.
Comparison of active management and usual care interventions
Advice leaflets from all of the departments who agreed to be randomised into the trial were collected and reviewed prior to randomisation. In comparison to the national survey of ED practice, the leaflets were consistent with the most frequently occurring pattern of advice in the UK (Table 2). The advice sheets were brief; with all being limited to one sheet of A4 or A5 sized paper.
| Theme | Present in advice leaflet, n (%) | |
|---|---|---|
| Departments in UK ED survey (n = 106) | All departments involved in MINT (n = 16) | |
| Reassurance that serious injury is rare | 6 (6) | 2 (13) |
| Reassurance about early recovery | 40 (38) | 2 (13) |
| Advice about early return to activity and work | 5 (5) | 2 (13) |
| Advice on pain control and medication | 84 (79) | 15 (94) |
| Advice on exercises | 83 (78) | 12 (75) |
| Advice that a collar should not be used | 17 (16) | 1 (6) |
| Reassurance to minimise psychological symptoms | 5 (5) | 1 (6) |
| Advice on posture | 39 (37) | 4 (25) |
| Advice on sleeping | 89 (84) | 15 (94) |
| Solicitors advert included | 65 (61) | 9 (56) |
Content analysis of The Whiplash Book demonstrated it to be substantially different to the materials used for usual care, not only in length and detail, but also:
-
– in delivering positive messages about prognosis, promoting the message that pain is nothing to worry about
-
– in promoting early return to normal activities and work. Making recommendations about physical activity, exercise and self-management of symptoms.
A notable exclusion from The Whiplash Book compared with the ED advice leaflets was information on pursuing claims or sponsorship from solicitors.
The Whiplash Book consists of 26 pages of A5 and contains approximately 5000 words and illustrations on every page. 16
The trial team were satisfied that all departments potentially randomised to the usual care arm of the trial would provide what constituted UCA in the UK if they continued to issue patients with the advice leaflet that was normally in use at their department (see Table 2). Departments were monitored for any changes in materials throughout the trial. No changes were detected.
Pilot study (Step 1)
We piloted the active management strategy at one ED from April to August 2005. A video recording of the pilot training session was reviewed by a medical educational specialist and feedback supplied. Communication, structure, content and interaction were evaluated. The overall impression was of a ‘very competent’ teaching session.
Feedback on the training was also sought from the clinicians (mixture of grades) immediately after the training session. All clinicians who were surveyed rated the delivery, content and materials as either good or very good. Minor changes were made to presentation slides and handouts following these evaluations.
Details of the final ED intervention and associated materials are in Appendix 8.
Physiotherapy interventions tested in Step 2
Development of the physiotherapy intervention
We used a number of principles to develop the physiotherapy package:
-
To design an intervention that was reflective of best practice in the UK NHS and was consistent with high-quality, evidence-based clinical guidelines.
-
To ensure the evidence base informed the intervention and discouraged the use of treatments for which there is evidence of no effect. Evidence considered comprised both RCTs, and observational studies of risk factors for poor recovery.
-
To ensure the intervention could be delivered within the context of the UK NHS in terms of staffing and time, and respected physiotherapist’s autonomy in clinical decision-making.
-
To ensure the intervention was documented to a standard that promoted consistency in delivery, and would enable replication.
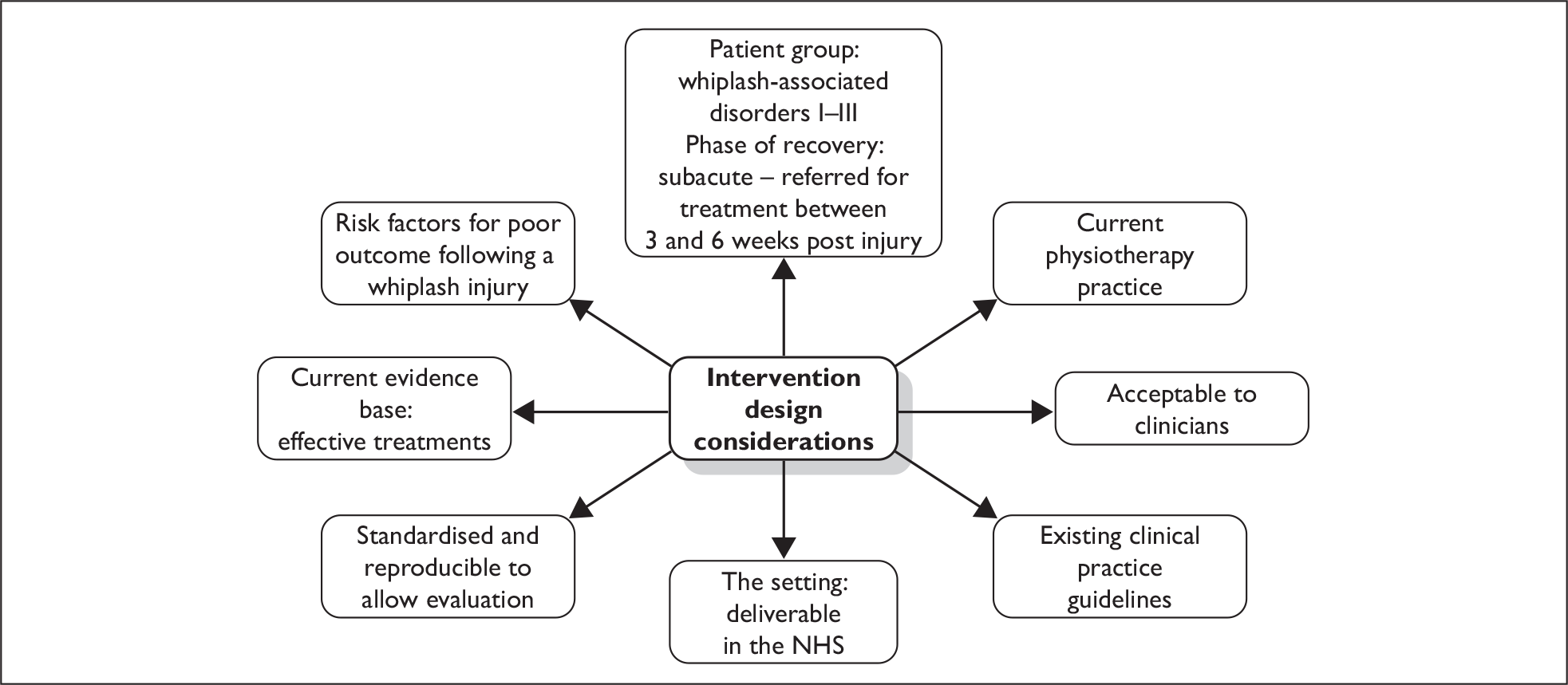
This was achieved by a triangulation of methods (Figure 1) – including systematic reviews of the RCTs and observational studies, a review of clinical guidelines, expert peer review and piloting to test the feasibility and acceptability of the intervention.
FIGURE 1.
Intervention design considerations.
Current practice
Physiotherapy is a common treatment for WAD but there is no published information that outlines the treatments most commonly used by physiotherapists or the amount and frequency of physiotherapy treatment provided in the UK. Spitzer et al. 6 suggest the following treatments are used in the treatment of whiplash injuries: manipulation, mobilisation, exercises, postural advice, relaxation, traction, heat, ice, massage, acupuncture and electrotherapy. These are the types of treatments available to physiotherapists who practise in the UK and reflect the types of treatments upon which recommendations have been made in published clinical guidelines. 24
Evidence base
Randomised controlled trials
Over 10 years ago, the QTF identified a lack of good-quality trial evidence to inform recommendations for physiotherapy practice in WAD management. 6 In 2007 the field had not moved much further forward – the Cochrane review Conservative Treatments for Whiplash14 concluded that there was no clear evidence to recommend the best treatment for WAD. However, there was a trend that active interventions were more effective than passive interventions. Two studies supported exercise to reduce pain intensity27,46 although there is no direct comparative evidence to inform the exact choice of exercise type. Studies have reported favourable outcomes for manual therapy,47,48 but are methodologically weak, with only short-term follow-up and no patient-rated outcomes. Provinciali et al. 49 describe an intervention of relaxation and postural training, psychological support, eye fixation exercises and manual treatment, which resulted in quicker return to work. The intervention was not described sufficiently to allow detailed scrutiny of the components.
Although weak, the evidence suggests that interventions that comprise exercise, manual therapy and psychological approaches are most likely to be successful. Similar observations have been made in chronic neck pain treatments,50 with the strongest evidence being for the combination of mobilisation and exercises. No evidence was found in RCTs evaluating the use of electrotherapy, acupuncture, massage, traction, heat and cold to support their inclusion in the intervention.
Observational studies
There is an extensive literature of observational studies related to WAD and these were explored to assist in the identification of potentially modifiable risk factors for poor outcome (treatment targets). We carried out two systematic reviews investigating risk factors for the development of chronic whiplash symptoms. The first review focused on physical risk factors12 and highlighted initial pain intensity and functional impairment as risk factors. While the evidence was less extensive, range of movement (ROM) has been shown to be predictive of chronicity. People with persisting symptoms demonstrate at least 25% reduction in ROM when compared with normal subjects. 51 Deficits in cervical joint position sense52 and muscle function53,54 have also been identified in both acute and chronic subjects with WAD, suggesting that exercises that address these factors may be beneficial.
The second review focused on psychological risk factors13 and identified low levels of self-efficacy and an elevated post-traumatic stress response (measured on the Impact of Event Scale55) as risk factors for poor outcome. Fear avoidance, catastrophising, coping and distress management were also identified as potential treatment targets (evidence summarised in Williamson et al. ). 13
Clinical guidelines and expert opinion
The physiotherapy intervention was developed in 2005 and, at that time, the only published guidelines available were those by Scholten-Peeters et al. 56 These guidelines emphasised the importance of ROM exercises, muscle retraining, postural retraining and encouragement of an incremental increase in activities. There was also endorsement of the need to address the psychological risk factors. Since then, the Chartered Society of Physiotherapy (CSP) has also produced clinical guidelines for the management of WAD which include endorsement for manual therapy techniques (both articular and soft tissue techniques). 24 The intervention we developed and implemented is consistent with both of these guidelines. The targeting of the psychological factors was also supported by a Delphi survey published in 2008. 57
In the second step of MINT we compared two treatments, in people who considered themselves as not recovering well:
-
reinforcement of the advice in an appointment with a physiotherapist (either usual care or The Whiplash Book depending on the centre)
-
a more intensive physiotherapy intervention allowing for up to six sessions of one-to-one therapist contact in an 8-week time period (representative of the usual numbers of sessions available within the NHS).
Intensive physiotherapy intervention
Having identified potential risk factors for poor recovery after the injury, as well as potentially effective treatments, we utilised a framework common in physiotherapy; assessment of a range of risk factors (history, physical examination, psychological factors) to identify treatment targets and matched treatments to the risk factor profile (detailed in Table 3). The intervention consisted of an assessment session and up to six sessions of treatment over an 8-week period. If further treatment was deemed essential, this was permitted.
| Risk factor | Treatment aim | Method of assessment | Interventions to modify risk factors |
|---|---|---|---|
| Physical risk factors | |||
| Restricted range of movement | Restore range of movement |
Subjective report from the patient Objective measurement of active cervical, thoracic and shoulder range of movement Assessment of passive joint movements including physiological and accessory movements |
Manual therapy Range of movement exercises Paced return to functional activities Education regarding: active involvement of the patient in their recovery; setting baseline and pacing |
| High pain intensity | Reduce pain |
Subjective report by patient regarding sleep, ability to control pain, ability to function Visual analogue scale |
Education regarding: pain mechanisms; activity modification and pacing; relaxation; symptom control, e.g. use of heat/cold, medication; and posture Reassurance Manual therapy |
| Psychological risk factors | |||
| Self-efficacy | Increase self-efficacy through equipping the patient with effective coping skills |
Questioning about their ability to cope with the injury/pain or concerns about their condition SOPA |
Reassurance and encouragement Achievement of goals through realistic goal setting and effective pacing Educate/discuss ways of coping, e.g. heat/cold, positioning, relaxation techniques, exercises and pacing |
| Beliefs about pain and injury | Modify/address unhelpful beliefs |
Questioning of patient about their expectations of treatment, ways they cope, the meaning of pain, reasons for not returning to activities, concerns about their condition expectations for recovery SOPA General observation, e.g. looking for reluctance to move which may mean they are fear avoidant |
Address unhelpful beliefs about pain/injury: education about pain mechanisms/meaning of pain, role of physiotherapy in their recovery and ways to control pain Address fear avoidance: education regarding fear avoidance cycle, exercises and manual therapy Reassurance Teach pacing and goal setting |
| Anxiety and stress |
Reduce psychological distress related to symptoms Facilitate reduction of post-traumatic stress through referral to appropriate agencies |
Questioning of patient, e.g. sleep patterns, ability to drive General observation for signs of anxiety, e.g. patient is agitated or on edge |
Distress related to symptoms: education and advice regarding symptom management; reassurance; and relaxation Post-traumatic stress: refer to GP or psychologist for appropriate management |
Patients were to be offered an appointment within 14 days of referral from the research clinic if possible.
A standardised assessment form was used to record risk factors and treatment targets. This included several questions to elicit health beliefs and the short version of the Survey of Pain Attitudes (SOPA) questionnaire. 58 A treatment planner was devised to encourage consistency in clinical decision making by facilitating physiotherapists toward identifying risk factors/treatment targets. The treatment planner encouraged an integrated approach to the management of both physical and psychological factors utilising three main components:
-
manual therapy
-
exercise
-
psychological strategies and self-management advice.
Manual therapy
The Maitland approach59 was used because it is widely practised in the UK and is taught in all undergraduate courses. A small number of other related techniques [natural apophyseal glides (NAGS) and sustained natural apophyseal glides (SNAGS)]60 and soft tissue techniques were also included as they are frequently used by physiotherapists in the UK. Treatments were aimed at the cervical, upper thoracic and shoulder region. Treatment of the upper thoracic spine was included because 15–20% of people experience thoracic spine pain after whiplash. 22 The following techniques were permitted:
-
cervical spine mobilisations, i.e. Maitland techniques grades I–IV
-
thoracic spine mobilisations, i.e. Maitland techniques grades I–IV
-
thoracic spine manipulation, i.e. Maitland techniques grade V
-
shoulder-complex mobilisations.
Cervical spine grade V manipulations were not included. Although the risk of adverse event are relatively small, vertebral artery dissection is a potential complication of manipulation61 and it has been recognised that pre-manipulative testing may fail to identify those at risk. 62 There are reports of vertebral artery damage in patients with minor whiplash injuries making this patient group higher risk for an adverse reaction to manipulation. 63–65 While we recognise that the safety of manipulation is contested from both sides, we decided that the potential benefit did not outweigh the risk that maybe involved.
Exercise therapy
The majority of exercises included in the intervention were exercises for the cervical, thoracic and shoulder regions aimed at the restoration of movement. Two exercises were also included to improve postural muscle control in standing (upper cervical flexion exercises and scapular setting) as well as a simple proprioception-enhancing exercise.
Exercises were prescribed according to a participant’s risk profile, and exercises were reviewed regularly and progressed to facilitate return to activities and work. A graded approach was used to minimise flare-ups. Skills such as goal setting and pacing were taught to assist in this process. 66,67 Exercise sheets were provided to help standardise the exercises used.
Psychological strategies and self-management advice
The third aspect of the physiotherapy intervention involved psychological strategies and self-management advice. Simple strategies for dealing with psychological factors were to be delivered alongside the other elements of the intervention. Although this was not a CB intervention, a CB therapist was consulted to develop these strategies which included the use of specific questioning techniques to identify treatment targets and included questioning about beliefs about pain, injury and recovery, and coping strategies used. Specific approaches for the management of identified treatment targets included goal setting and pacing, education about pain and recovery, facilitation of effective coping strategies and reassurance. Physiotherapists also provided self-management advice covering aspects such as posture and positioning.
A clinical psychologist was consulted to develop guidelines for managing patients who may be suffering from a stress reaction. This included how to identify these patients and the action to be taken (i.e. where to refer patients). It was emphasised that it was important that their physiotherapy management continued where possible. Guidelines were also developed for advice on managing mild travel anxiety with an emphasis on when it was appropriate to refer these patients on for management.
More information (including the assessment form and treatment planner) is available at: www.warwick.ac.uk/go/whiplash.
Comparator treatment: reinforcement of advice
The control intervention was a single advice session that aimed to re-enforce the advice provided in the ED. The advice was given by a physiotherapist, and included a brief assessment of symptoms and movements to allow individual tailoring of advice. For example, the physiotherapist could highlight a particular exercise on the advice sheet and advise the patient about performing it, but they could not prescribe a new exercise.
Pilot study
The acceptability and feasibility of the intervention was tested in a pilot study that ran from May to September 2005 and involved three senior outpatient physiotherapists. The physiotherapists attended a half-day training session and each received a comprehensive manual describing the intervention. The physiotherapy package was then delivered to seven patients who fulfilled the criteria for the trial. The treating physiotherapists provided feedback on the training and the intervention. The main feedback from the physiotherapists was that they lacked confidence in the use of the psychological strategies. More time was allocated to this in subsequent training sessions.
Peer review
Following the pilot study minor modifications were made to the intervention manual and reviewed by two experienced researchers (Christopher McCarthy and Michele Sterling, one of whom was involved in research into WAD) and an experienced senior physiotherapist (Heidi Williams). Minor changes were made in response to their feedback.
Physiotherapist training
All physiotherapists received training in the package. Training was held over 1 or 1.5 days depending on the number of physiotherapists attending. The research team physiotherapists provided the training. Participating physiotherapists were provided with a training manual that contained details about the trial, physiotherapy assessment, treatment planning and treatments.
We also provided training on the advice session, including role-play. Guidelines for the delivery of the advice session were provided in the training manual.
Physiotherapist support
The MINT team were in contact with the treating physiotherapists throughout the duration of the trial. An update evening was held in November 2006 to provide a forum for physiotherapists to discuss any problems that had arisen. These were held at 2 centres (Frenchay Hospital and the University of Warwick) and were attended by 23 physiotherapists from 9 out of 11 trusts that were recruiting (Stoke Mandeville had yet to start recruitment). The physiotherapists from the two trusts that were unable to attend were visited to provide an update on the trial.
Chapter 4 Results
Introduction
The results section is structured to present the results of the cluster randomised trial of ED advice interventions (Step 1) first, followed by the results of the individually randomised comparison of physiotherapy versus no physiotherapy (Step 2).
Step 1
Participating departments and staff
Fifteen EDs managed by 12 NHS trusts participated in the study. Six trusts (managing seven EDs) were randomised to deliver WBA and six trusts (managing eight EDs) were randomised to deliver their UCA. Recruitment to the trial took place between December 2005 and November 2007, and departments were enrolled in the trial for between 12 and 23 months. Over 500 clinicians were trained in the trial procedures across all sites during this period.
Management of whiplash patients in participating emergency departments
Table 4 shows the management strategies used by EDs by trial arm for patients who were included in the trial. There were no significant differences between the trial arms in the management strategies used, other than the use of The Whiplash Book. There was no indication of any difference in the management of patients who participated in the trial and those who did not.
| Management strategy used | UCA n = 1598 (%) |
WBA n = 2253 (%) |
|---|---|---|
| Education | 1043 (65) | 1342 (60) |
| Analgesia | 1257 (79) | 1725 (77) |
| Provision of advice leaflet appropriate to trial arm | 1173 (73) | 1716 (76) |
| X-ray | 347 (42) | 484 (58) |
| Exercise | 777 (49) | 1106 (49) |
| Other | 68 (4) | 85 (4) |
Recruitment to Step 1
During the recruitment period ED staff completed trial proformas for 7702 patients; 3034 from UCA departments and 4668 from WBA departments (Figure 2).
FIGURE 2.
CONSORT flow diagram for Step 1.
The results of audits conducted to monitor the proportion of patients referred to the trial (see Table 6) are summarised in Table 5. It was not possible to conduct audits in three departments. The average period of audit over the course of recruitment was 10 weeks per hospital. Just under half of all eligible patients attending a participating ED were reported to the trial through completion of a trial proforma. The proportion was slightly higher in the UCA centres compared with the WBA centres, but this was offset by the slightly higher numbers of eligible patients seen per day in the WBA centres (2.7 vs 2.3). There were no major differences between the trial arms in the proportion of eligible patients referred to the trial. Audit of the number of proformas completed and the number of advice leaflet packs given out showed that in all centres (where audits were possible), except one, the number of information packs given out exceeded the number of patients referred to the trial (Table 6). This suggests that virtually all patients for whom a proforma was completed also received the information pack, but also that some patients who were not referred to the trial also received an information pack (340 proformas were completed and 372 advice leaflet packs were used).
| Centre | Average daily attendances (eligible patients per day) | % patients with proforma completed |
|---|---|---|
| WBA centres | ||
| University Hospitals Birmingham NHS Foundation Trustb | 2.9 | 38 |
| University Hospitals Birmingham NHS Foundation Trustb | 2.2 | 36 |
| Oxford Radcliffe Hospitals NHS Trust | 2 | 49 |
| Gwent Healthcare NHS Trust | 1.8 | 48 |
| University Hospitals Birmingham NHS Foundation Trust | 2.8 | 54 |
| South Warwickshire General Hospitals NHS Trust | 1.8 | 51 |
| Average daily attendance per cluster | 2.7 | 46 |
| UCA centres | ||
| University Hospitals Coventry and Warwickshire NHS Trustb | 3.2 | 37 |
| University Hospitals Coventry and Warwickshire NHS Trustb | 1.3 | 54 |
| Gloucestershire Hospitals NHS Trustb | 1.5 | 56 |
| Gloucestershire Hospitals NHS Trustb | 0.6 | 61 |
| Kettering General Hospital NHS Foundation Trust | 1.5 | 46 |
| North Bristol NHS Trust | 1.9 | 28 |
| Worcestershire Acute Hospitals NHS Trust | 1.7 | 61 |
| Average daily attendance per cluster | 2.3 | 49 |
| Centre | No. of days audited | No. of proformas received | No. of information packs given out |
|---|---|---|---|
| WBA centres | |||
| University Hospitals Birmingham NHS Foundation Trusta | 24 | 42 | 44 |
| University Hospitals Birmingham NHS Foundation Trusta | 12 | 15 | 21 |
| Oxford Radcliffe Hospitals NHS Trust | 70 | 46 | 58 |
| Gwent Healthcare NHS Trust | 14 | 11 | 11 |
| University Hospitals Birmingham NHS Foundation Trust | 13 | 31 | 31 |
| South Warwickshire General Hospitals NHS Trust | 40 | 31 | 35 |
| UCA centres | |||
| North Bristol NHS Trust | 161 | 84 | 92 |
| Worcestershire Acute Hospitals NHS Trust | 13 | 11 | 12 |
| University Hospitals Coventry and Warwickshire NHS Trusta | 36 | 60 | 58 |
| University Hospitals Coventry and Warwickshire NHS Trusta | 32 | 9 | 10 |
Of the 7702 patients referred to the trial, 6952 were eligible and were approached to be included in the trial by sending the trial 2-week questionnaire. A total of 3851 (55%) patients agreed to participate by returning the questionnaire: 2253 from WBA centres and 1598 from UCA centres. The number of patients recruited by each centre is given in Table 7. More patients were recruited to centres in the WBA arm than to centres in the UCA arm (Figure 3), which was a result of a higher recruitment rate (per 10,000 attendances) in the WBA arm (Figure 4).
| Cluster number | Trust | Start date | Months of recruitment | Size (attendances/year) | Numbers recruited (recruits per 10,000 attendances) |
|---|---|---|---|---|---|
| UCA | |||||
| 1 | University Hospitals Coventry and Warwickshire NHS Trust | 17 January 2006 | 22 | 145,801 | 370 (25) |
| 2 | North Bristol NHS Trust | 9 December 2005 | 23 | 89,829 | 228 (25) |
| 3 | Gloucestershire Hospitals NHS Trust | 9 February 2006 | 21 | 127,461 | 431 (34) |
| 4 | Worcestershire Acute Hospitals NHS Trust | 11 April 2006 | 19 | 49,524 | 302 (61) |
| 5 | Kettering General Hospital NHS Foundation Trust | 22 May 2006 | 17 | 65,022 | 212 (33) |
| 6 | Buckinghamshire Hospitals NHS Trust | 6 December 2006 | 12 | 27,929 | 55 (20) |
| WBA | |||||
| 7 | Heart of England NHS Foundation Trust | 6 December 2005 | 23 | 140,388 | 711 (51) |
| 8 | University Hospitals Birmingham NHS Foundation Trust | 5 December 2005 | 23 | 76,845 | 524 (68) |
| 9 | Oxford Radcliffe Hospitals NHS Trust | 8 February 2006 | 21 | 117,073 | 224 (19) |
| 10 | South Warwickshire General Hospitals NHS Trust | 24 April 2006 | 19 | 53,008 | 252 (48) |
| 11 | Gwent Healthcare NHS Trust | 21 September 2006 | 13 | 70,554 | 130 (18) |
| 12 | Countess of Chester Hospital NHS Foundation Trust | 31 July 2006 | 15 | 56,240 | 412 (73) |
FIGURE 3.
Observed versus expected cumulative patient recruitment by trial arm. The expected number of recruits was reset to the actual observed number at the time of the extension to recruitment, hence the discontinuity in the ‘expected’ line.
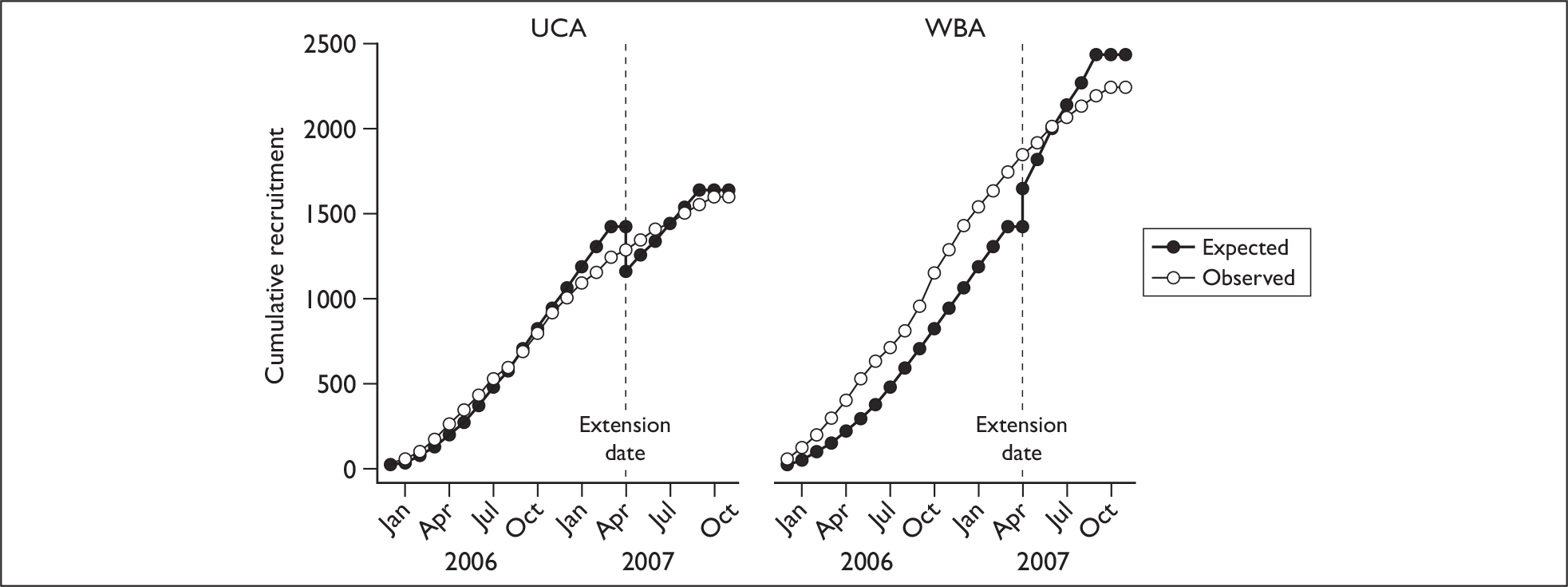
FIGURE 4.
Average monthly recruitment rates by trial arm.
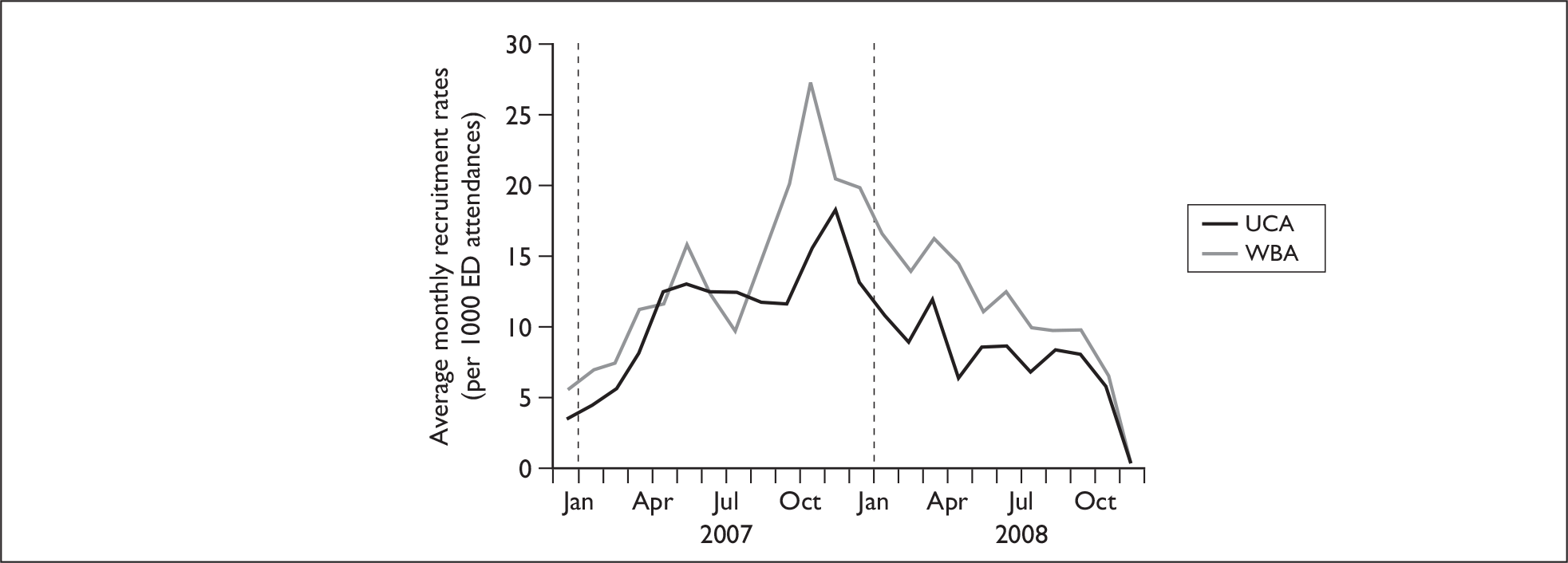
The characteristics of patients recruited to the trial are summarised in Table 8. The WBA and UCA arms were well matched but there were small differences between them in ethnicity; there were slightly more people of Pakistani origin in the WBA group than in the UCA group (8% vs 2%), and fewer people of white ethnic origin (70% vs 84%). This difference reflects differences in the populations served by the hospitals in the two arms. The majority of the participants were of working age (mean age 37 years, SD 13), and were employed. There was a small difference between the arms in the proportion that were working (UCA 75%, WBA 69%). The age distributions of the participants were similar in the two arms (Figure 5), with a peak between 20 and 30 years. Road traffic accidents were by far the most common mechanism of injury, with other causes accounting for only 5% of the participants (200 of 3851). WAD grade III injuries (involving neurological signs as well as pain and musculoskeletal signs) were rare (104 of 3851, 2.7% of participants).
| UCA | Missing | WBA | Missing | |
|---|---|---|---|---|
| Number enrolled | 1598 | 2253 | ||
| Gender – male | 666 (42%) | 18 | 995 (44%) | 39 |
| Age in years, mean [SD] | 37 [13] | 0 | 37 [13] | 0 |
| Ethnic group | 118 | 224 | ||
| White | 1336 (84%) | 1586 (70%) | ||
| Mixed | 19 (1%) | 42 (2%) | ||
| Indian | 49 (3%) | 95 (4%) | ||
| Pakistani | 24 (2%) | 179 (8%) | ||
| Bangladeshi | 9 (1%) | 21 (1%) | ||
| Black or Black British | 31 (2%) | 69 (3%) | ||
| Chinese or other | 12 (1%) | 37 (2%) | ||
| Mechanism of injury | 15 | 14 | ||
| Road traffic accident | 1495 (94%) | 2127 (94%) | ||
| Other | 88 (6%) | 112 (5%) | ||
| Location of pain | 37 | 73 | ||
| C-spine only | 1046 (65%) | 1365 (61%) | ||
| C-spine and other spinal area | 275 (17%) | 400 (18%) | ||
| Other spinal area only | 31 (2%) | 65 (3%) | ||
| Spinal and other area | 141 (9%) | 190 (8%) | ||
| Other area only | 23 (1%) | 56 (2%) | ||
| No pain | 45 (3%) | 104 (5%) | ||
| Pain intensity (/10), mean [SD] | 4.9 [1.9] | 349 | 5.3 [1.9] | 574 |
| History | ||||
| Previous neck problems | 190 (12%) | 58 | 218 (10%) | 94 |
| Previous back problems | 199 (12%) | 308 | 285 (13%) | 396 |
| Neurological symptoms | 98 (6%) | 57 | 121 (5%) | 86 |
| WAD grades | 0 | 0 | ||
| I: Complaint of pain, stiffness or tenderness, no physical signs | 883 (55%) | 1205 (53%) | ||
| II: Complaint of pain, stiffness or tenderness, musculoskeletal signs | 662 (41%) | 997 (44%) | ||
| III: Complaint of pain, stiffness or tenderness, neurological signs | 53 (3.3%) | 51 (2.3%) | ||
| Employment | 155 | 272 | ||
| Working/earninga | 1185 (74%) | 1549 (69%) | ||
| Unpaid work | 4 (0.25%) | 7 (0.31%) | ||
| Not workingb | 254 (16%) | 425 (19%) |
FIGURE 5.
Age at ED attendance.
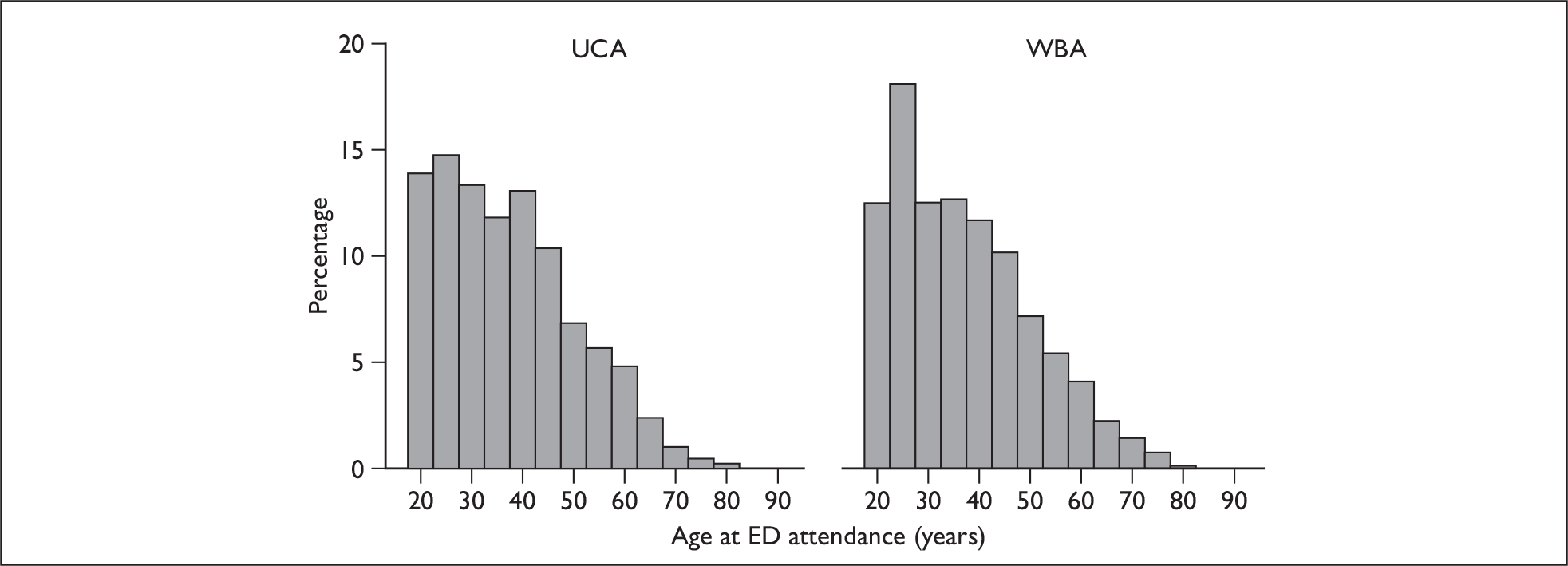
Follow-up questionnaires
The chronology of trial questionnaires for a participant in Step 1 is summarised in Figure 6.
FIGURE 6.
Step 1: chronology of trial questionnaires.
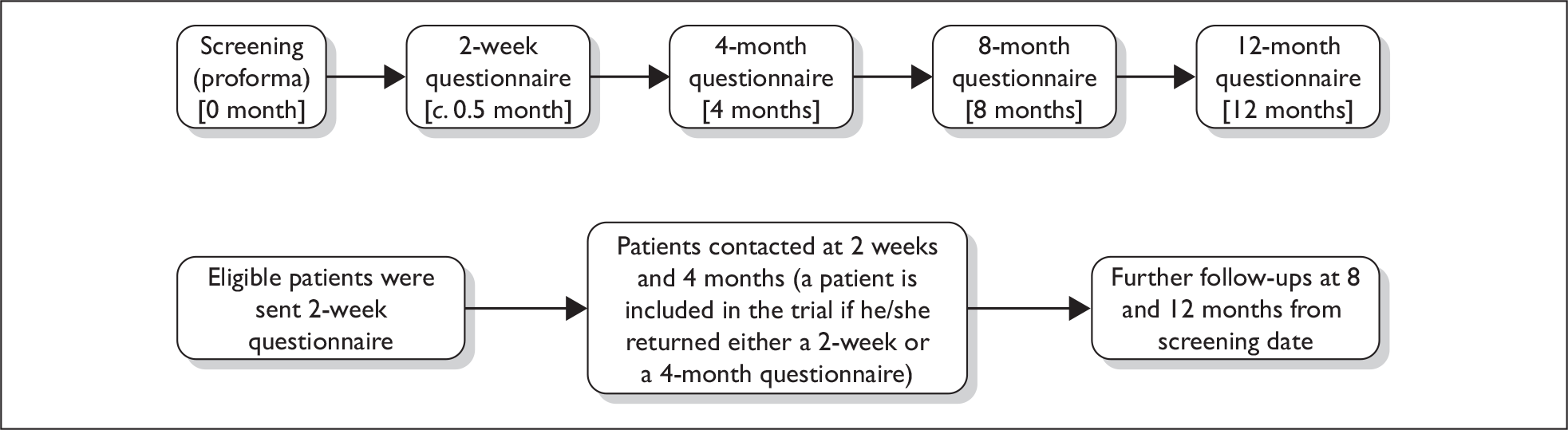
Because many participants did not return their follow-up questionnaires immediately the actual times until questionnaire return were slightly longer than the specified follow-up periods (Table 9).
| UCA Median (IQR) |
WBA Median (IQR) |
|
|---|---|---|
| Time to 2-week follow-up | 0.5 (0.4–0.8) | 0.5 (0.3–0.8) |
| Time to 4-month follow-up | 4.3 (4.1–4.9) | 4.3 (4.1–5.0) |
| Time to 8-month follow-up | 8.4 (8.1–9.0) | 8.4 (8.1–9.0) |
| Time to 12-month follow-up | 12.4 (12.2–13.1) | 12.5 (12.2–13.2) |
In total 197 participants withdrew from the trial during follow-up, and were not sent any further follow-up questionnaires after their withdrawal. Withdrawals were well balanced between the trial arms: 39 UCA (2.4%) and 46 WBA (2.0%) participants withdrew after returning the 2-week questionnaire, 37 UCA (2.3%) and 36 WBA (1.6%) participants withdrew after the 4-month questionnaire, and 22 UCA (1.4%) and 17 WBA (0.1%) participants withdrew after the 8-month questionnaire. A reason for withdrawal was given by the majority of participants who withdrew (Table 10). There were no serious adverse events reported in Step 1 of the trial.
| Reasons for withdrawal | UCA | WBA | Total |
|---|---|---|---|
| Illness of family member | 0 | 1 | 1 |
| Inconvenient to attend treatment | 0 | 1 | 1 |
| Language barrier | 0 | 1 | 1 |
| Moved away | 4 | 11 | 15 |
| No longer interested | 60 | 52 | 112 |
| No reasons given | 3 | 2 | 5 |
| Patient died – unrelated to trial | 0 | 4 | 4 |
| Post inclusion ineligibility | 2 | 2 | 4 |
| Recovered and no longer interested | 11 | 11 | 22 |
| Self-reported ineligibility | 9 | 6 | 15 |
| Unhappy with NHS service | 1 | 2 | 3 |
| Unhappy with trial | 8 | 6 | 14 |
| Total | 98 | 99 | 197 |
The proportion of participants providing outcome data was 80% at 4 months, 71% at 8 months and 70% at 12 months (Figure 2). Non-response was the major cause of missing outcome data. There was no evidence of major differences in age, sex or injury severity between participants retained by the trial at 12 months and those lost to follow-up (Table 11), though there was a slightly higher proportion of male participants among those lost.
| Patients retained at 12 months | Patients lost to follow-up | |
|---|---|---|
| UCA | n = 1127 | n = 471 |
| Age, mean (SD) | 39 (14) | 34 (13) |
| Male, n (%) | 438 (39) | 228 (48) |
| WAD I, n (%) | 631 (56) | 252 (54) |
| WAD II, n (%) | 459 (41) | 203 (43) |
| WAD III, n (%) | 37 (3) | 16 (3) |
| WBA | n = 1577 | n = 676 |
| Age, mean (SD) | 38 (14) | 34 (13) |
| Male, n (%) | 681 (43) | 314 (47) |
| WAD I, n (%) | 862 (55) | 343 (51) |
| WAD II, n (%) | 684 (43) | 313 (46) |
| WAD III, n (%) | 31 (2) | 20 (3) |
Comparison of The Whiplash Book advice and usual care advice arms
The tables in this section present the results of the analyses described in Chapter 2, Statistical analysis. Each table includes two analyses: the complete case analysis (i.e. using all participants who provided outcome data) and the multiply imputed analyses, which allows for the estimated effects of missing data. All analyses were adjusted for WAD grade at ED clustering of NHS trusts. Estimates of the ICC for each outcome are presented in Appendix 3. The ICC estimate for the primary outcome (NDI) was 0.0136 at 4 months and substantially lower at 8 and 12 months (0.0075 and 0.0033, respectively).
Primary outcomes: Neck Disability Index
There was no evidence of a difference in NDI score between the two ED advice intervention arms (Table 12 and Figure 7). Because of the imbalance in ethnicity between the advice interventions, we reran the analysis on complete cases with additional adjustment for ethnicity, as a sensitivity analysis. There was no material difference in the treatment effect estimates (Table 13). A further sensitivity analysis restricted to white participants only, produced very similar results.
| 4 months | 8 months | 12 months | |
|---|---|---|---|
| UCA | |||
| Mean (SD) | 20.4 (17.2) | 16.0 (16.4) | 14.4 (16.0) |
| n (missing/total) (%) | 42/1,295 (3%) | 36/1175 (3%) | 25/1127 (2%) |
| WBA | |||
| Mean (SD) | 21.5 (17.6) | 16.6 (16.5) | 14.4 (15.9) |
| n (missing/total) (%) | 64/1774 (4%) | 35/1570 (2%) | 41/1577 (3%) |
| Treatment estimatea | |||
| ∆ (95% CI) | 0.5 (–1.8 to 2.8) | 0.3 (–1.6 to 2.2) | –0.1 (–1.6 to 1.4) |
| Treatment estimateb | |||
| ∆ (95% CI) | 0.5 (–2.1 to 3.0) | 0.8 (–1.6 to 3.1) | 0.5 (–1.5 to 2.5) |
FIGURE 7.
Observed NDI scores (%) (mean and 95% CIs) by advice intervention. Higher score indicates greater disability.
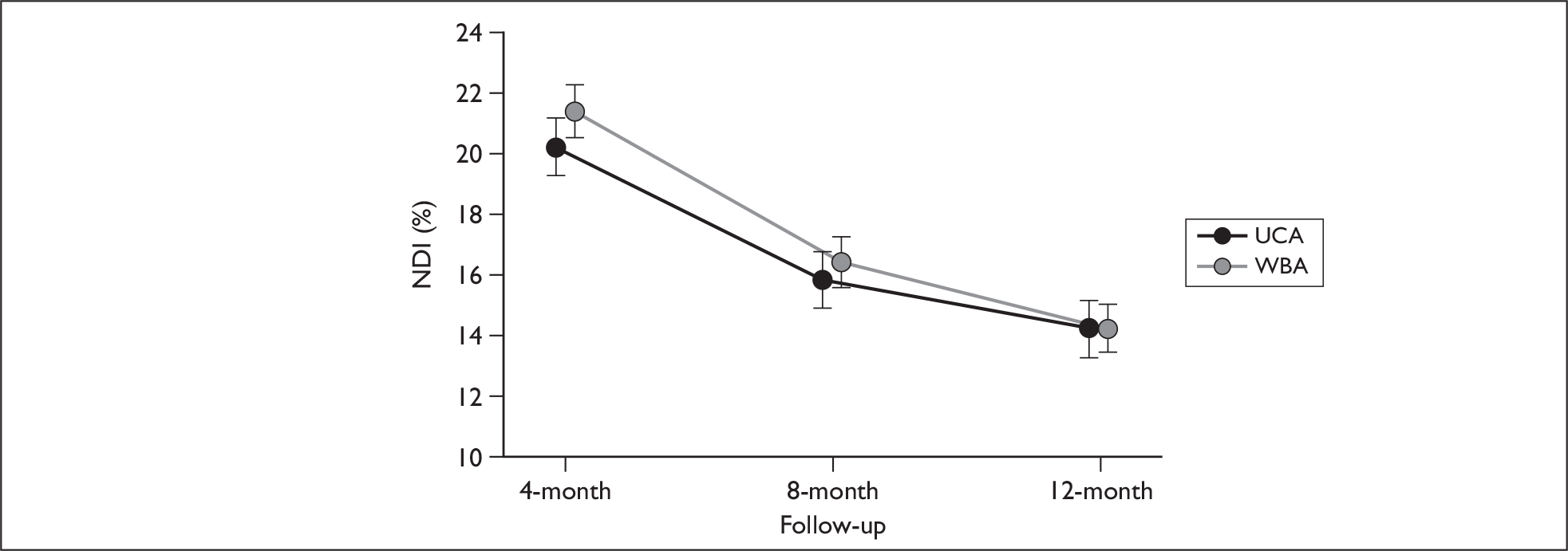
| 4 months | 8 months | 12 months | |
|---|---|---|---|
| Treatment estimatea | |||
| ∆ (95% CI) | –0.4 (–1.7 to 0.9) | –0.5 (–2.5 to 1.5) | –0.6 (–2.9 to 1.6) |
Secondary outcomes
There were no statistically or clinically significant differences between the UCA and WBA groups for the physical or mental health components of the SF-12 (Tables 14 and 15, Figures 8 and 9). We also reran these analyses by further adjusting the regressions for the effect of ethnicity, because of the observed imbalance. This did not alter the results for either the mental or physical components of the SF-12 (see Appendix 4).
| MCS | 2 weeks | 4 months | 8 months | 12 months |
|---|---|---|---|---|
| UCA | ||||
| Mean (SD) | 40.9 (13.0) | 48.0 (11.6) | 49.4 (11.3) | 49.6 (10.9) |
| n (missing/total) (%) | 183/1488 | 256/1295 | 266/1175 | 277/1127 |
| WBA | ||||
| Mean (SD) | 40.7 (12.7) | 47.1 (12.1) | 48.7 (11.5) | 49.3 (10.9) |
| n (missing/total) (%) | 271/2042 | 406/1774 | 359/1570 | 487/1577 |
| Treatment estimatea | ||||
| ∆ (95% CI) | –0.1 (–1.8 to 1.5) | –0.9 (–1.9 to 0.0) | –0.8 (–1.8 to 0.2) | –0.3 (–1.3 to 0.7) |
| Treatment estimateb | ||||
| ∆ (95% CI) | –0.4 (–1.9 to 1.2) | –0.3 (–1.6 to 1.0) | –0.5 (–1.7 to 0.7) | –0.3 (–1.4 to 0.9) |
| PCS | 2 weeks | 4 months | 8 months | 12 months |
|---|---|---|---|---|
| UCA | ||||
| Mean (SD) | 40.3 (9.0) | 46.5 (9.7) | 48.9 (9.2) | 49.9 (9.0) |
| n (missing/total) (%) | 183/1488 | 256/1295 | 266/1175 | 277/1127 |
| WBA | ||||
| Mean (SD) | 40.2 (8.9) | 46.0 (9.8) | 48.5 (9.2) | 49.8 (9.1) |
| n (missing/total) (%) | 271/2042 | 406/1774 | 359/1570 | 487/1577 |
| Treatment estimatea | ||||
| ∆ (95% CI) | –0.3 (–2.3 to 1.7) | –0.4 (–1.9 to 1.2) | –0.4 (–1.2 to 0.4) | –0.2 (–1.6 to 1.2) |
| Treatment estimateb | ||||
| ∆ (95% CI) | –0.3 (–2.2 to 1.5) | –0.5 (–2.0 to 1.1) | –0.0 (–1.1 to 1.0) | 0.0 (–1.5 to 1.5) |
FIGURE 8.
Observed mental component scores of SF-12v1 (mean and 95% CI) by advice intervention. Higher scores indicate better mental health-related quality of life.
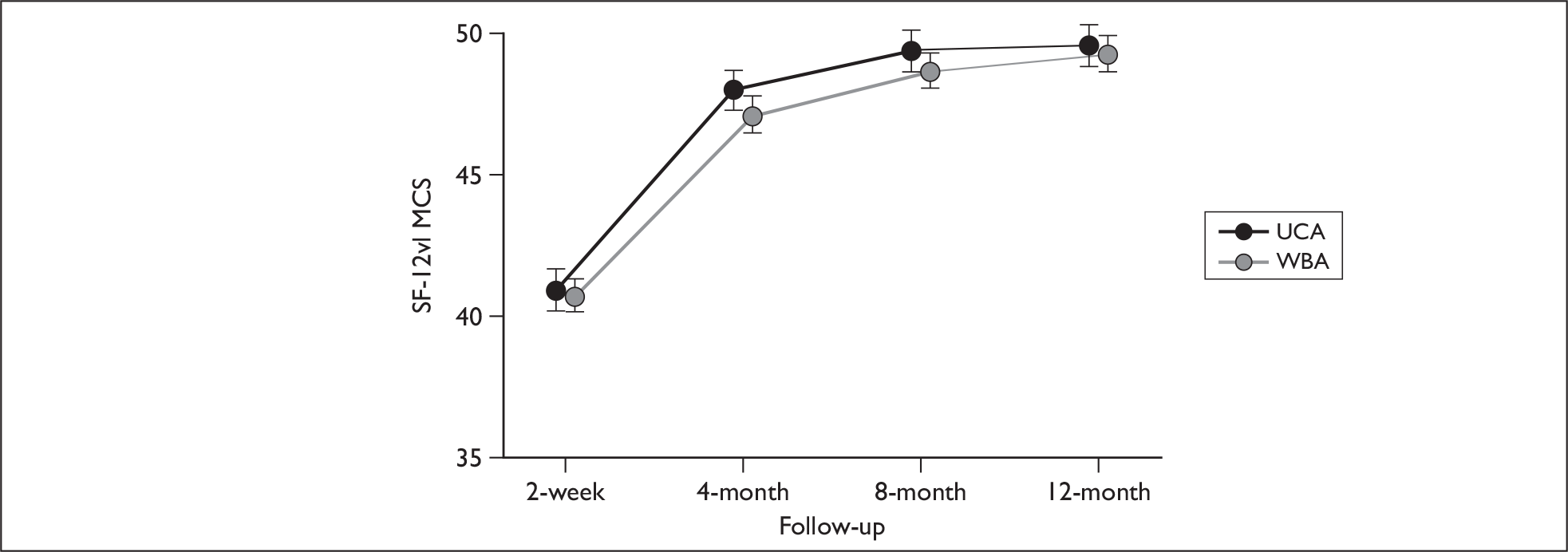
FIGURE 9.
Observed physical component scores of SF-12v1 (mean and 95% CI) by advice intervention. Higher scores indicate better physical health-related quality of life.
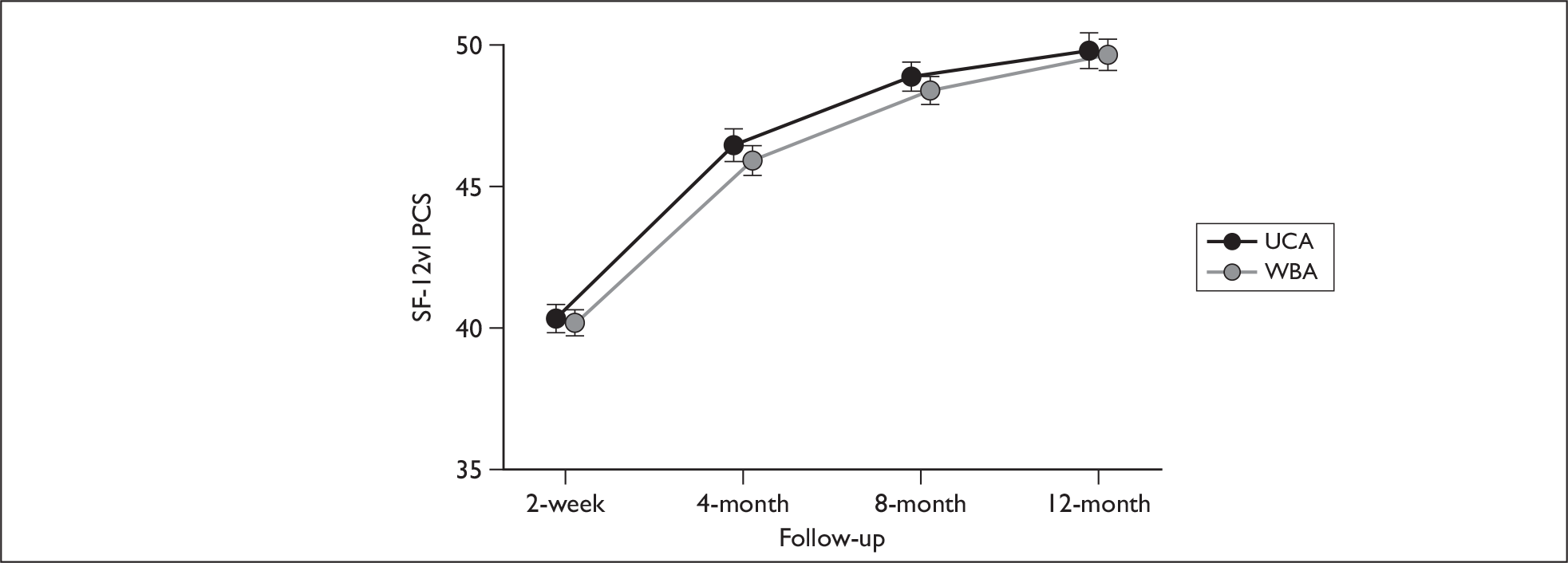
There were no statistically significant differences between the UCA and WBA groups for acute whiplash injury and LWS (Tables 16 and 17).
| n (%) or odds ratio (OR) (95% CI) | |
|---|---|
| UCA | |
| Present | 492 (31%) |
| Absent | 796 (50%) |
| n (missing/total) (%) | 310/1598 (19%) |
| WBA | |
| Present | 704 (31%) |
| Absent | 1061 (47%) |
| n (missing/total) (%) | 488/2253 (22%) |
| Treatment estimatea | |
| ∆ (OR 95% CI) | 1.00 (0.76 to 1.33) |
| Treatment estimateb | |
| ∆ (OR 95% CI) | 1.01 (0.77 to 1.33) |
| n (%) or odds ratio (OR) (95% CI) | |
|---|---|
| UCA | |
| Present | 286 (18%) |
| Absent | 839 (53%) |
| n (missing/total) (%) | 473/1598 (30%) |
| WBA | |
| Present | 397 (18%) |
| Absent | 1176 (52%) |
| n (missing/total) (%) | 680/2253 (30%) |
| Treatment estimatea | |
| ∆ (OR 95% CI) | 0.95 (0.73 to 1.25) |
| Treatment estimateb | |
| ∆ (OR 95% CI) | 1.05 (0.86 to 1.29) |
There were no statistically significant differences between the UCA and WBA groups for work days lost (Tables 18–20).
| 4 months | 8 months | 12 months | |
|---|---|---|---|
| UCA | |||
| Mean (SD) | 4.4 (13.1) | 5.1 (14.5) | 5.6 (15.8) |
| Missing/total | 9/1295 (1%) | 0/1175 (0%) | 2/1127 (0%) |
| WBA | |||
| Mean (SD) | 4.4 (13.5) | 5.4 (15.9) | 5.8 (17.4) |
| Missing/TOTAL | 8/1774 (0%) | 4/1570 (0%) | 3/1577 (0%) |
| Treatment effect | |||
| Δ (95% CI)a | –7.5 (–26.8 to 17.0) | –24.4 (–62.8 to 53.4) | –21.3 (–42.3 to 7.3) |
| Δ (95% CI)b | –7.0 (–26.0 to 17.0) | –24.3 (–62.6 to 53.2) | –18.4 (–39.7 to 10.4) |
| 4 months | 6 months | 12 months | |
|---|---|---|---|
| Δ (95% CI)a | –15.2 (–33.9 to 8.7) | –24.5 (–63.8 to 57.5) | –23.7 (–45.4 to 6.5) |
| Δ (95% CI)b | –14.4 (–32.8 to 9.2) | –24.1 (–63.5 to 57.9) | –20.3 (–42.4 to 10.2) |
| 4 months | 8 months | 12 months | |
|---|---|---|---|
| UCA | |||
| Mean (SD) | 5.3 (14.3) | 6.2 (15.9) | 6.7 (17.5) |
| Missing/total | 5/950 (1%) | 0/901 (0%) | 0/863 (0%) |
| WBA | |||
| Mean (SD) | 4.7 (13.1) | 5.8 (16.0) | 6.3 (17.8) |
| Missing/total | 1/1194 (0%) | 1/1131 (0%) | 2/1134 (0%) |
| Treatment effect | |||
| Δ (95% CI)a | –17.4 (–35.3 to 5.5) | –26.4 (–64.5 to 52.3) | –26.8 (–47.3 to 1.7) |
| Δ (95% CI)b | –16.3 (–34.3 to 6.5) | –25.8 (–64.2 to 53.5) | –23.6 (–44.6 to 5.5) |
Subgroup analyses
Three subgroup analysis of the primary outcome are presented, stratifying by injury severity (WAD grade at ED presentation), previous neck pain, and early psychological response to whiplash injury. The analysis of injury severity was not adjusted for WAD grade, as this was the factor used to classify the subgroups. Otherwise adjustments were consistent with previous analyses and are detailed in footnotes of each table.
Tables 21–23 provide the estimates for the NDI in each subgroup and the statistical significance of interaction terms at each time point of follow-up. There were no statistically significant differences between the subgroups in the effects of the intervention. Estimates [mean and 95% confidence interval (CI)] of all terms tested in the NDI subgroup analyses are given in Appendix 5.
| 4 months Mean (SD) [n] |
8 months Mean (SD) [n] |
12 months Mean (SD) [n] |
|
|---|---|---|---|
| Severe symptoms | |||
| UCA | 22.5 (17.9) [540] | 18.5 (17.6) [498] | 16.1 (16.9) [479] |
| WBA | 23.5 (18.1) [793] | 18.1 (17.1) [714] | 16.0 (16.8) [695] |
| Milder symptoms | |||
| UCA | 18.8 (16.4) [713] | 14.0 (15.2) [641] | 13.1 (15.1) [623] |
| WBA | 19.8 (17.1) [917] | 15.2 (15.9) [821] | 13.2 (14.9) [842] |
| p-value for interactiona | 0.96 | 0.22 | 0.88 |
| p-value for interactionb | 0.94 | 0.90 | 0.66 |
| 4 months Mean (SD) [n] |
8 months Mean (SD) [n] |
12 months Mean (SD) [n] |
|
|---|---|---|---|
| Early psychological response present | |||
| UCA | 25.6 (17.8) [644] | 20.8 (18.0) [606] | 18.5 (17.6) [563] |
| WBA | 26.4 (17.7) [867] | 20.9 (17.4) [808] | 18.3 (16.9) [787] |
| Early psychological response absent | |||
| UCA | 14.0 (14.2) [492] | 10.2 (12.0) [475] | 9.7 (12.3) [460] |
| WBA | 14.0 (13.7) [634] | 10.5 (12.1) [617] | 9.3 (12.1) [622] |
| p-value for interactiona | 0.56 | 0.91 | 0.82 |
| p-value for interactionb | 0.73 | 0.79 | 0.81 |
| 4 months Mean (SD) [n] |
8 months Mean (SD) [n] |
12 months Mean (SD) [n] |
|
|---|---|---|---|
| Had previous neck pain | |||
| UCA | 27.1 (18.2) [62] | 23.4 (17.7) [61] | 21.6 (17.9) [64] |
| WBA | 31.7 (18.1) [93] | 25.5 (17.3) [89] | 21.6 (18.2) [84] |
| No previous neck pain | |||
| UCA | 20.1 (17.0) [1077] | 15.7 (16.2) [1022] | 14.0 (15.7) [961] |
| WBA | 20.5 (17.1) [1407] | 15.7 (15.8) [1336] | 13.9 (15.5) [1314] |
| p-value for interactiona | 0.18 | 0.49 | 0.93 |
| p-value for interactionb | 0.24 | 0.61 | 0.87 |
p-value for interaction is the interaction between WBA and injury severity. No adjustment for WAD grade at ED attendance was made here because of collinearity (injury severity was determined from WAD grade at ED attendance).
Additional subgroup analyses were performed for the SF-12, LWS and acute whiplash indicator. There were no statistically significant differences between the subgroups in the effects of the interventions, for any of these other outcomes. A few of the interaction tests had p-values between 0.05 and 0.10, but given the large number of tests performed these are likely to have been due to chance.
Compensation pursued
We also performed a subgroup analysis stratifying patients by whether or not they were pursuing or had pursued a claim for compensation in relation to their whiplash injury. This information was collected only at the 12-month follow-up to avoid stimulating compensation claims among the trial population. Hence this is not a true subgroup analysis, as it does not classify participants by a baseline characteristic; the compensation claim would certainly have been initiated after injury, and may also have been after enrolment in the trial.
Table 24 presents the characteristics of participants who did and did not pursue a compensation claim (as reported at 12 months). There were few participants who did not pursue a compensation claim in either trial arm, hence there is limited power to detect any differences between those who did and did not pursue a claim. There was no evidence that the ED advice intervention had any effect on the number of participants pursuing a claim (Table 25), nor that its effects differed between those who pursued a compensation claim and those who did not (Table 26).
| UCA | Missing, n | WBA | Missing, n | |
|---|---|---|---|---|
| Pursued compensation | 1037 | 1441 | ||
| Male, n (%) | 401 (39%) | 12 | 626 (43%) | 16 |
| Age in years, mean (SD) | 39 (13) | 0 | 38 (13) | 0 |
| Injury severity, n (%) | 0 | 0 | ||
| WAD I | 584 (56%) | 787 (55%) | ||
| WAD II | 418 (40%) | 626 (43%) | ||
| WAD III | 35 (3%) | 28 (2%) | ||
| Medium used to claim | 643 (62%) | 394 | 936 (65%) | 505 |
| Through solicitor | 424 (41%) | 582 (40%) | ||
| Directly from insurer | 205 (20%) | 328 (23%) | ||
| Other medium | 14 (1%) | 26 (2%) | ||
| Claim has been resolved | 375 (36%) | 3 | 560 (39%) | 4 |
| Did not pursue compensation | 63 | 93 | ||
| Male, n (%) | 23 (37%) | 2 | 36 (39%) | 2 |
| Age in years, mean (SD) | 37 (15) | 0 | 33 (12) | 0 |
| Injury severity, n (%) | 63 (100%) | 0 | 93 (100%) | 0 |
| WAD I | 33 (52%) | 51 (55%) | ||
| WAD II | 28 (44%) | 40 (43%) | ||
| WAD III | 2 (3%) | 2 (2%) | ||
| Missing compensation status | 498 | 719 |
| n (%) or odds ratio (95% CI) | |
|---|---|
| UCA | |
| Pursued | 1037 (65%) |
| Did not pursue | 63 (4%) |
| n (missing/total) (%) | 498/1598 (31%) |
| WBA | |
| Pursued | 1441 (64%) |
| Did not pursue | 94 (4%) |
| n (missing/total) (%) | 718/2253 (32%) |
| Treatment estimatea | |
| ∆ (95% CI) | 1.21 (0.31 to 4.81) |
| Treatment estimateb | |
| ∆ (95% CI) | 1.21 (0.31 to 4.81) |
| 4 months Mean (SD) [n] |
8 months Mean (SD) [n] |
12 months Mean (SD) [n] |
|
|---|---|---|---|
| Pursued compensation | |||
| UCA | 20.2 (17.1) [925] | 16.3 (16.4) [900] | 14.9 (16.1) [1017] |
| WBA | 20.5 (17.2) [1249] | 16.1 (15.9) [1216] | 14.7 (16.1) [1412] |
| Did not pursue compensation | |||
| UCA | 11.6 (15.9) [42] | 10.2 (13.7) [47] | 7.2 (10.3) [62] |
| WBA | 14.4 (15.6) [67] | 9.8 (12.9) [71] | 8.7 (10.8) [93] |
| p-value for interactiona | 0.56 | 0.90 | 0.62 |
| p-value for interactionb | 0.83 | 0.89 | 0.48 |
Step 2
Recruitment to Step 2
Recruitment to Step 2 took place concurrently with recruitment to Step 1, from December 2005 to November 2007. Although we expected that all participants in Step 2 would already be taking part in Step 1, in fact 25 patients were randomised into Step 2 before returning their 2-week questionnaire, and subsequently failed to return either this or the 4-month questionnaire. Hence these 25 patients were randomised into Step 2 and are included in the results, but were not included in the earlier follow-up stages of Step 1.
A total of 949 patients reported on-going problems to the trial office, and were considered for the second stage of the trial. Of these, 693 were assessed as potentially eligible and were invited to a research clinic appointment. Seventy-seven did not attend or cancelled, and 616 patients were assessed for eligibility, of whom 2 were ineligible, 15 declined participation and 599 were randomised. No patients were excluded because of contraindications to physiotherapy.
Table 27 summarises the characteristics of the participants randomised to Step 2 and those who were not randomised. The differences were not large, but the population randomised to Step 2 included a slightly lower proportion of males, a higher proportion of people with more serious injuries (WAD grade II or III) at ED attendance, and lower SF-12 scores.
| Randomised | Missing | Not randomised | Missing | |
|---|---|---|---|---|
| Number of patients | 599 | 0 | 3277 | 0 |
| Sex – male | 221 (37%) | 0 | 1456 (44%) | 50 |
| Age in years, mean [SD] | 40 [13] | 0 | 36 [13] | 0 |
| Had previous neck pain | 77 (13%) | 40 | 334 (10%) | 115 |
| WAD grades | 0 | 0 | ||
| 0: No neck complaints or signsa | 0 (0%) | 0 (0%) | ||
| I: Complaints of pain, stiffness or tenderness, no physical signs | 275 (46%) | 1823 (56%) | ||
| II: Complaint of pain, stiffness or tenderness, musculoskeletal signs | 299 (50%) | 1375 (42%) | ||
| III: Complaint of pain, stiffness or tenderness, neurological signs | 25 (4%) | 79 (2%) | ||
| IV: Fracture/dislocationa | 0 (0%) | 0 (0%) | ||
| SF-12v1 scores, mean [SD] | ||||
| Mental component score | 36 [12] | 108 | 42 [13] | 692 |
| Physical component score | 36 [7] | 108 | 41 [9] | 692 |
| Received public fund | 192 (33%) | 37 | 748 (23%) | 332 |
Previous neck pain and WAD grades were collected at ED attendance. Gender, age, MCS, and PCS were collected via the 2-week follow-up questionnaire.
Participants were recruited from the two Step 1 arms of the trial in approximately the proportions that were expected given the difference in numbers recruited to the WBA and UCA arms. Randomisation was stratified by site, and there was equal balance of participants in each of the Step 2 arms who had received usual care and active management advice. The proportion of participants being randomised to Step 2 was similar across all recruiting sites (Table 28). Cumulative target and actual recruitment is shown in Figure 10.
| Cluster number | Advice n (% of Step 1) |
Physiotherapy n (% of Step 1) |
Not randomised n (% of Step 1) |
|
|---|---|---|---|---|
| UCA | ||||
| 1 | University Hospitals Coventry and Warwickshire NHS Trust | 33 (9%) | 32 (9%) | 309 (84%) |
| 2 | North Bristol NHS Trust | 19 (8%) | 17 (7%) | 194 (85%) |
| 3 | Gloucestershire Hospitals NHS Trust | 41 (10%) | 42 (10%) | 352 (82%) |
| 4 | Worcestershire Acute Hospitals NHS Trust | 24 (8%) | 26 (9%) | 253 (84%) |
| 5 | Kettering General Hospital NHS FoundationTrust | 16 (8%) | 14 (7%) | 183 (86%) |
| 6 | Buckinghamshire Hospitals NHS Trust | 3 (5%) | 5 (9%) | 47 (85%) |
| WBA | ||||
| 7 | Heart of England NHS Foundation Trust | 51 (7%) | 50 (7%) | 616 (87%) |
| 8 | University Hospitals Birmingham NHS Foundation Trust | 29 (6%) | 31 (6%) | 468 (89%) |
| 9 | Oxford Radcliffe Hospitals NHS Trust | 23 (10%) | 24 (11%) | 180 (80%) |
| 10 | South Warwickshire General Hospitals NHS Trust | 25 (10%) | 25 (10%) | 202 (80%) |
| 11 | Gwent Healthcare NHS Trust | 14 (11%) | 15 (12%) | 101 (78%) |
| 12 | Countess of Chester Hospital NHS Foundation Trust | 21 (5%) | 19 (5%) | 372 (90%) |
FIGURE 10.
Step 2 recruitment versus target graph by advice intervention.
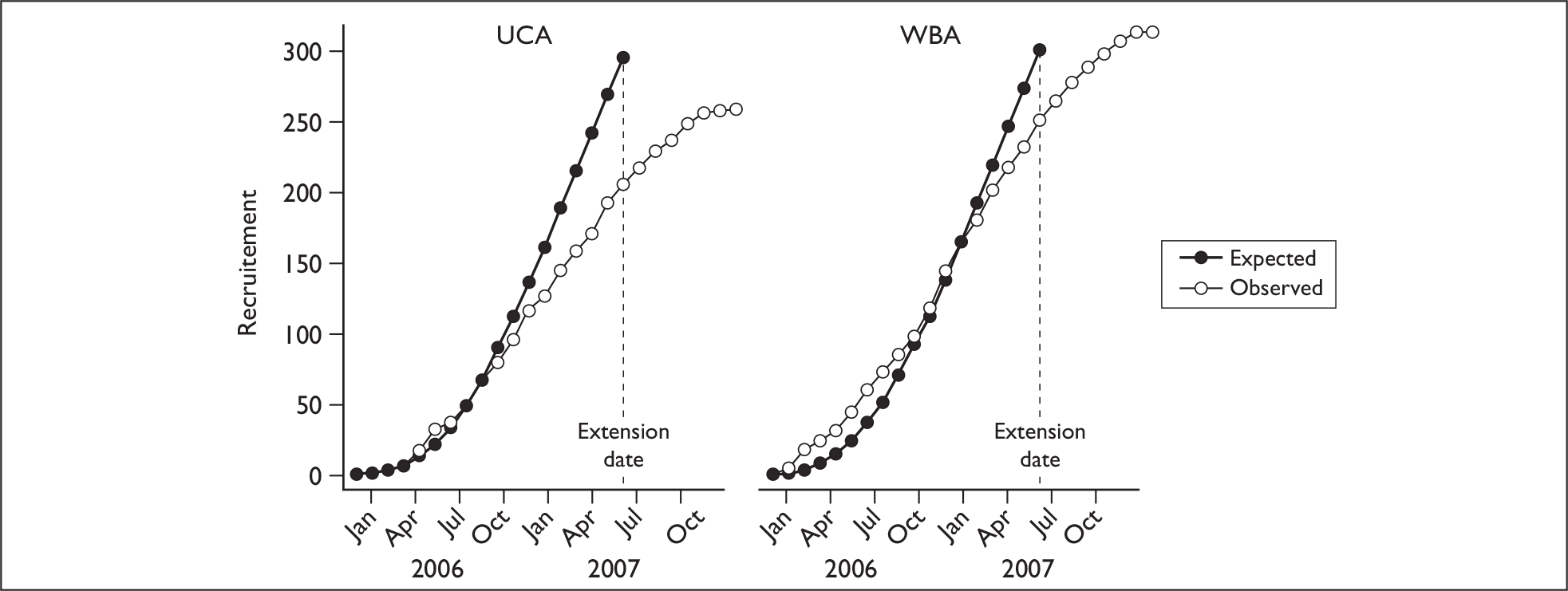
Characteristics of the population at randomisation are summarised in Table 29. The groups were well matched, with no baseline imbalances apart from a five-point difference in mean NDI scores between the groups [physiotherapy 44 (SD 16), advice 39 (SD 16)], indicating that participants randomised to physiotherapy had slightly greater neck disability. Analyses were therefore adjusted for this baseline imbalance.
| Advice | Missing | Physiotherapy | Missing | |
|---|---|---|---|---|
| Number randomised | 299 | 300 | ||
| Sex – male | 115 (38%) | 0 | 106 (35%) | 0 |
| Age in years, mean [SD] | 40 [13] | 0 | 40 [13] | 0 |
| Ethnic Group | 16 | 20 | ||
| White | 229 (77%) | 226 (75%) | ||
| Mixed | 2 (67%) | 3 (1%) | ||
| Indian | 18 (6%) | 19 (6.3%) | ||
| Pakistani | 19 (6.4%) | 19 (6.3%) | ||
| Bangladeshi | 2 (67%) | 1 (33%) | ||
| Black or Black British | 10 (3.3%) | 7 (2.3%) | ||
| Chinese or other | 3 (1%) | 5 (1.7%) | ||
| Mechanism of injury | 2 | 1 | ||
| Road traffic accident | 284 (95%) | 286 (95%) | ||
| Other | 13 (4.3%) | 13 (4.3%) | ||
| Location of pain | 8 | 12 | ||
| C-spine only | 178 (60%) | 178 (59%) | ||
| C-spine and other spinal area | 60 (20%) | 62 (21%) | ||
| Other spinal area only | 10 (3%) | 3 (1%) | ||
| Spinal + other area | 27 (9%) | 27 (9%) | ||
| Other area only | 3 (1%) | 6 (2%) | ||
| No pain | 13 (4%) | 12 (4%) | ||
| Pain intensity (/10), mean [SD] | 5.4 [1.9] | 69 | 5.6 [1.9] | 91 |
| History | ||||
| Previous neck problems | 36 (12%) | 21 | 41 (14%) | 19 |
| Previous back problems | 40 (13%) | 56 | 43 (14%) | 65 |
| Neurological symptoms | 26 (9%) | 19 | 29 (10%) | 15 |
| WAD gradesa | 0 | 0 | ||
| 0: No neck complaints or signsb | 0 (0%) | 0 (0%) | ||
| I: Complaints of pain, stiffness or tenderness, no physical signs | 39 (13%) | 45 (15%) | ||
| II: Complaint of pain, stiffness or tenderness, musculoskeletal signs | 222 (74%) | 220 (73%) | ||
| III: Complaint of pain, stiffness or tenderness, neurological signs | 38 (13%) | 35 (12%) | ||
| IV: Fracture/dislocationb | 0 (0%) | 0 (0%) | ||
| SF-12v1 scores, mean [SD] | ||||
| Norm-based MCS | 37 [12] | 53 | 35 [12] | 55 |
| Norm-based PCS | 36 [7] | 53 | 36 [6.9] | 55 |
| Received any public funds | 91 (30%) | 17 | 101 (34%) | 20 |
| NDI (%), mean [SD]a | 39 [16] | 3 | 44 [16] | 7 |
| Employment | 22 | 29 | ||
| Working/earningc | 225 (75%) | 210 (70%) | ||
| Unpaid work | 0 (0%) | 2 (1%) | ||
| Not workingd | 52 (17%) | 59 (20%) |
The flow of participants through the trial is summarised in Figure 11. There were 17 notifications of withdrawal from the trial (12 in the advice group and 5 in the physiotherapy group), and these participants were not followed-up at time points after their withdrawal (Table 30). Outcome data were available for 92% of participants at 4 months, 87% at 8 months and 80% at 12 months. There were no serious adverse events in Step 2.
FIGURE 11.
Step 2 CONSORT flowchart. (a) Two symptoms not appropriate, 15 not willing to participate; (b) 55 failed to attend, and 22 cancelled.
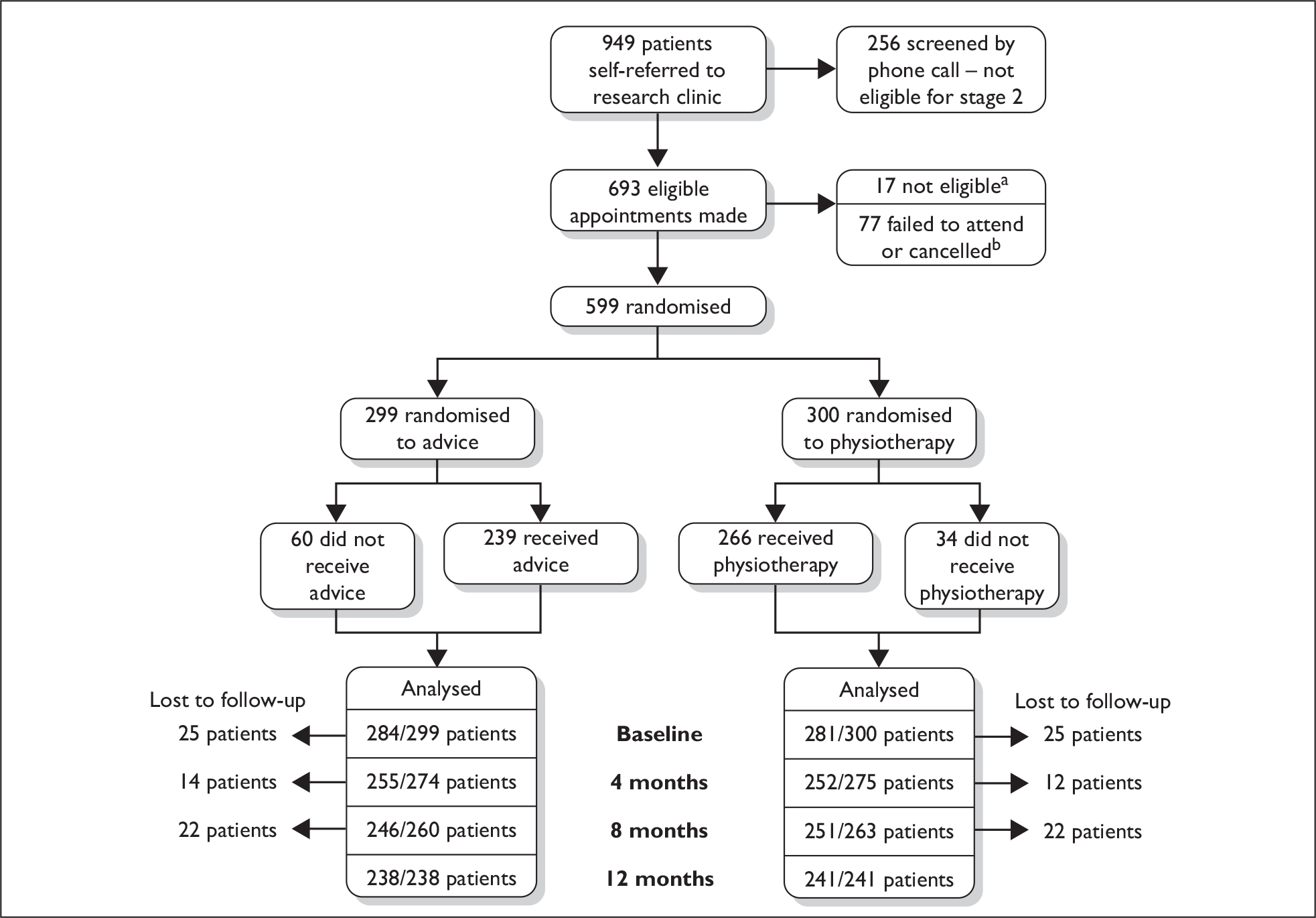
| Reasons | Advice | Physiotherapy | Total |
|---|---|---|---|
| Moved away | 2 | 1 | 3 |
| No longer interested | 4 | 0 | 4 |
| No reasons given | 1 | 0 | 1 |
| Recovered and no longer interested | 1 | 0 | 1 |
| Unhappy with trial | 4 | 4 | 8 |
| Total | 12 | 5 | 17 |
Participating physiotherapists
Fifty-five physiotherapists from 12 NHS trusts (16 physiotherapy departments, 4 trusts, had 2 departments) participated. All of the physiotherapists were senior clinicians, with the majority being a Senior II (24 of 55, 44%) or Senior I (25 of 55, 45%). They had been qualified for between 2 and 33 years [median 6.5 years, interquartile range (IQR) 4.5–18] with a median of 4 years of experience working in musculoskeletal (range 1–28 years, IQR 3.0–11.25).
Of the 55 physiotherapists, 45 provided feedback on the Step 2 intervention training (82%). All respondents rated the overall quality of the training as ‘good’ or ‘very good’. In the aspects of the protocol that were taught in addition to usual physiotherapy practice, all the physiotherapists rated themselves as ‘very confident’ or ‘fairly confident’ in using the assessment form. The majority of therapists reported being ‘very confident’ or ‘fairly confident’ in using the pain beliefs protocol (44 of 45, 98%), pacing protocols (43 of 45, 96%), and goal setting protocols (43 of 45, 96%). All the physiotherapists rated the trial materials (training manual, assessment form and patient education materials) as ‘good’ or ‘very good’ except for one (2%) respondent who rated the manual as ‘average’ and three (7%) participants who rated the patient education material as ‘average’.
Study treatments
Treatment attendance rates
Treatment attendance rates are shown in Table 31 (see Chapter 2, Monitoring the intervention delivery).
| Physiotherapy package (n = 300) |
Advice session (n = 299) |
|
|---|---|---|
| Failed to attend any appointments | 34 (11%) | 60 (20%) |
| Attended for assessment onlya | 26 (9%) | N/A |
| Partial completion of treatment | 45 (15%) | N/A |
| Completed treatmenta | 201 (67%) | 239 (80%) |
We investigated factors associated with attendance. The baseline characteristics (age, gender, NDI and WAD grade) of those who attended and those who did not were compared for both the physiotherapy package and the advice session. No statistically significant difference was observed between the different categories of attendance.
The amount of treatment
The number of treatment sessions delivered in the physiotherapy package (excluding the assessment) ranged from 0 to 23 (median = 3.0, IQR = 1.0–5.0) with 14 (4.7%) patients receiving greater than the recommended six treatment sessions. Assessment sessions were between 40 and 60 minutes long, and treatment sessions were between 20 and 30 minutes. All participants in the control intervention who attended for treatment received one session of advice, 30–60 minutes in duration.
Timing of treatment
The timing of delivery of the interventions is presented in Table 32. Sixty-three per cent of patients attending for the physiotherapy intervention were seen within 14 days of randomisation, and 91% were seen within 28 days. Sixty-two per cent of patients completed their treatment in the recommended 8 weeks (56 days) and 87% of patients completed within 12 weeks (84 days). Fifty-three per cent of those receiving the advice session were seen within 14 days. Eighty-six per cent of those attending for the control intervention were seen within 28 days.
| Physiotherapy package | Advice session | |
|---|---|---|
| Days post injury when referred for treatment |
Median = 31 IQR = 24–39 Range = 7–74 |
Median = 30 IQR = 23–40 Range = 10–65 |
| Physiotherapy waiting times – days from date of referral to first appointmenta |
Median = 12 IQR = 7–19 Range = 0–129 (missing data n = 14a) |
Median = 14 IQR = 8–21 Range 1–116 (missing data n = 10a) |
| Days post injury until first appointment |
Median = 45 IQR = 35–55 Range = 15–177 (missing data n = 14a) |
Median = 47 IQR = 36–60 Range = 17–143 (missing data n = 10a) |
| Time from initial to final physiotherapy package appointment (days) (n = 246)b |
Median = 45 IQR = 28–71 Range = 0–428 |
N/A |
| Time from ED attendance to final physiotherapy package appointment (days) (n = 246)b |
Median = 86 IQR = 66–115 Range = 25–461 |
N/A |
Content of treatment
Information about the content of the treatments delivered was available for 259 of the 266 patients who attended at least one appointment (Table 33). Seven of the 26 patients who attended the assessment session were assessed but did not receive any treatment. Psychological strategies and self-management advice were used with the majority of patients (246 of 259, 95%), and almost all received guidance on some form of exercises (246 of 259, 95%). The most common form of exercises was cervical ROM exercises. Manual therapy was used to a somewhat lesser degree (211 of 259, 81%), with soft tissue techniques and Maitland cervical mobilisations being used most frequently. The majority of patients (73%) received a combination of manual therapy, exercises and psychological strategies. Two protocol violations were reported which involved the use of electrotherapy. Both of the patients received the treatment only once.
| Type of treatment delivered | No. of patients receiving the treatment (%) |
|---|---|
| Combinations of treatments | n = 259 |
| Manual therapy, exercises and psychological strategies | 190 (73) |
| Exercises and psychological strategies | 45 (17) |
| Manual therapy and psychological strategies | 10 (4) |
| Manual therapy and exercises | 9 (3) |
| Manual therapy only | 2 (1) |
| Exercises only | 2 (1) |
| Psychological strategies only | 1 (0) |
| Manual therapy techniques | n = 211 |
| Soft tissue techniques | 123 (58) |
| Maitland cervical mobilisations | 123 (58) |
| NAGS and SNAGS (cervical or thoracic) | 86 (41) |
| Maitland thoracic mobilisations | 71 (34) |
| Other manual therapy | 42 (20) |
| Shoulder mobilisations | 15 (7) |
| Thoracic manipulation | 5 (2) |
| Exercises | n = 246 |
| Cervical ROM exercises | 244 (99) |
| Cervical or scapular stability exercises | 118 (48) |
| Thoracic ROM exercises | 106 (43) |
| Shoulder ROM exercises | 88 (36) |
| Other exercises | 69 (28) |
| Proprioception exercises | 28 (11) |
| Psychological strategies and self-management advice | n = 246 |
| Advice regarding posture and positioning | 194 (79) |
| Reassurance | 194 (79) |
| Pain education | 144 (59) |
| Advice regarding return to work or activities | 145 (59) |
| Goal setting or pacing | 119 (48) |
| Advice regarding medication and symptomatic control | 87 (35) |
| Relaxation | 56 (23) |
| Advice regarding travel anxiety | 27 (11) |
| Referral to GP/psychologist for stress reaction | 10 (4) |
In the advice arm (Table 34), 163 patients received advice based on The Whiplash Book and 136 received advice based on the usual leaflet issued at the ED they attended. The physiotherapist referred two patients on after they were assessed as having developed potentially serious complications between the randomisation assessment and commencing treatment. This included one patient who presented with swallowing problems and one who presented with dizziness, dysarthria, dysphagia and gait disturbance.
| Advice | No. of patients receiving the advice, n = 239 (%) |
|---|---|
| Assessed ROM | 232 (97) |
| Neurological examination | 87 (36.5) |
| Referred on owing to serious complication | 2 (0.8) |
| Reviewed exercises given in the ED | 228 (95) |
| Progressed exercises within the guidelines of The Whiplash Booka | 108 (45) |
| Postural or positioning advice | 200 (83.5) |
| Advice regarding collar | 56 (22) |
| Advice regarding pain control or medication use | 185 (77.5) |
| Advice regarding graded return to activities, return to work or staying activea | 119 (50) |
| Relaxation techniquesa | 82 (34.5) |
| Reassurancea | 119 (50) |
| Reinforced the ‘hurt does not equal harm’ messagea | 121 (50.5) |
| Advised to see their GP if they had ongoing problems | 220 (92) |
| Other advice | 25 (8.4) |
In addition to the physiotherapists’ records of treatments, the trial team conducted formal quality control assessments of the delivery of the physiotherapy intervention at seven of the participating departments. All were satisfactory. Overall, there was no evidence of any departure from the intervention protocol, and the physiotherapy and advice interventions were delivered as intended.
Comparison of physiotherapy versus advice
For all outcomes, two series of analyses were performed; first, a complete case analysis, using all participants with data at each time point; and, second, a multiply imputed analysis to allow for the effects of missing data. Both analyses were adjusted for the effects of clustering in Step 1, NDI score at randomisation, and therapist. Estimates of the ICC for therapist effects are provided in Appendix 6. The ICC for therapists was consistent with only small proportions of variance (< 2%) being explained by therapists, and made minimal difference to the statistical models.
Primary outcome
The NDI scores for the physiotherapy group were on average 3.2 (95% CI –5.8 to 0.7) percentage points lower than those of the advice group at 4-month follow-up, but there was no evidence of a difference at 8 and 12 months. Physiotherapy therefore has a modest beneficial effect in the short term (see Table 35, Figures 12–14).
| 4 months | 8 months | 12 months | |
|---|---|---|---|
| Advice | |||
| Mean (SD) | 27.8 (17.4) | 21.5 (16.7) | 19.5 (17.0) |
| n (missing/total) (%) | 5/255 (2%) | 11/246 (4%) | 3/238 (1%) |
| Physiotherapy | |||
| Mean (SD) | 28.0 (17.9) | 24.1 (18.4) | 21.7 (18.4) |
| n (missing/total) (%) | 11/252 (4%) | 7/251 (3%) | 6/241 (2%) |
| Treatment estimatea | |||
| ∆ (95% CI) | –3.2 (–5.8 to –0.7) | –0.2 (–2.9 to 2.4) | –1.2 (–4.0 to 1.5) |
| Treatment estimateb | |||
| ∆ (95% CI) | –3.7 (–6.1 to –1.3) | –1.0 (–3.6 to 1.6) | –2.0 (–4.6 to 0.6) |
FIGURE 12.
Observed NDI scores (%) and 95% CIs by physical intervention.
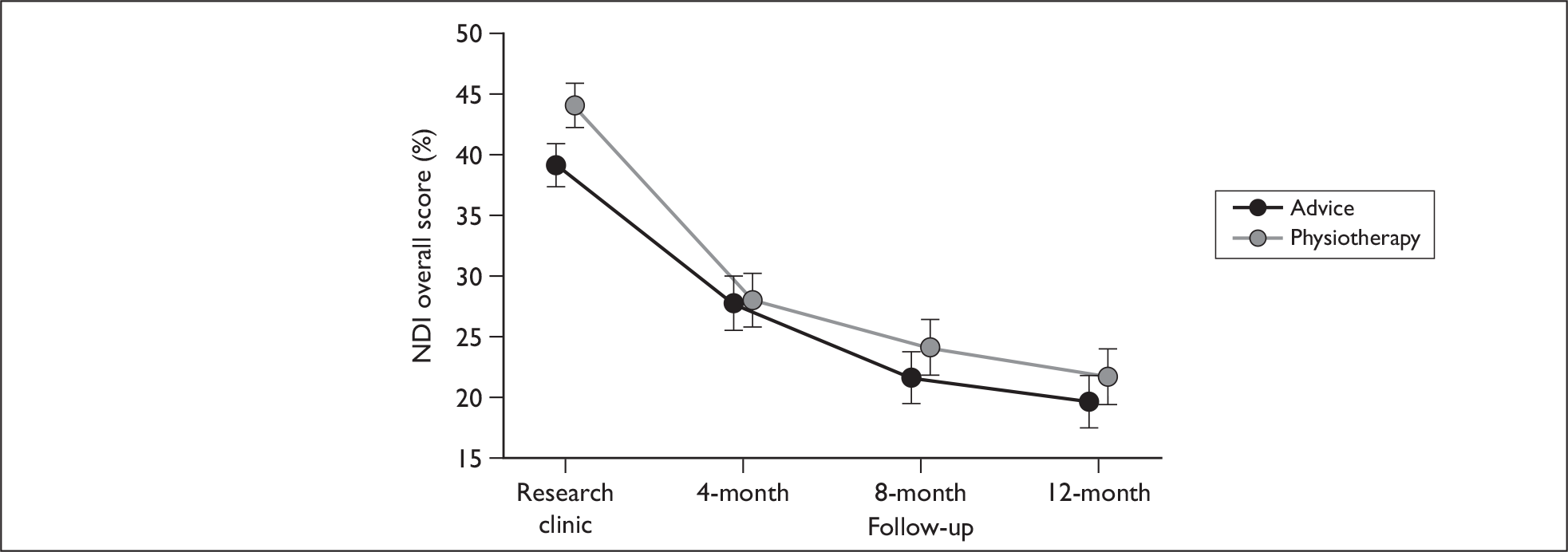
FIGURE 13.
Unadjusted change in NDI from baseline research clinic for patients in Step 2 by individually-randomised treatment groups and month of follow-up.
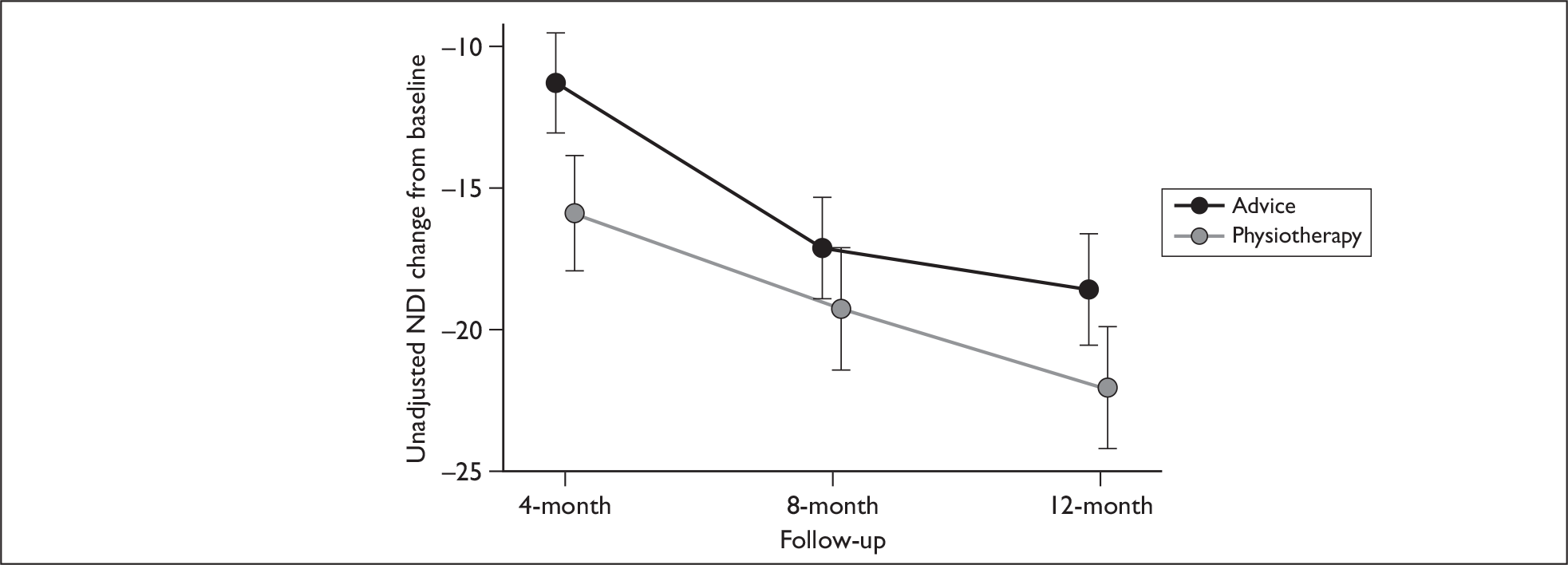
FIGURE 14.
Multiply imputed estimate of physiotherapy effects on NDI by month of follow-up for patients in Step 2.
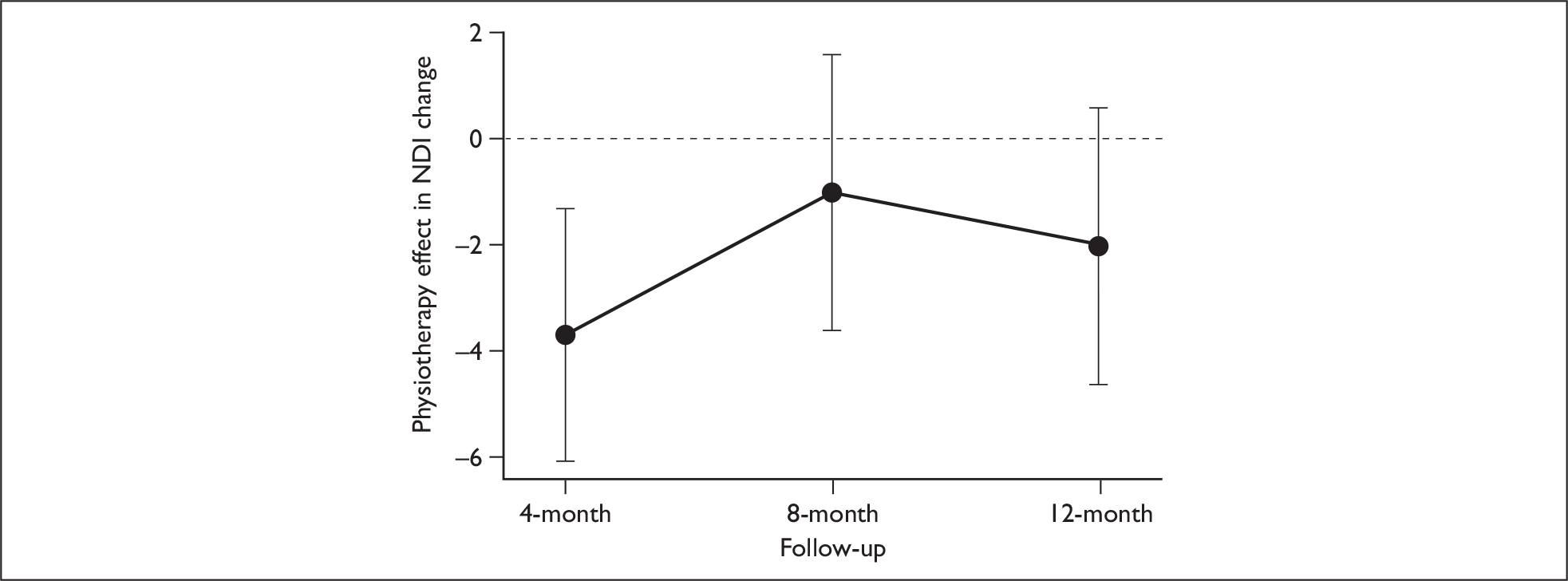
Secondary outcomes
There were no statistically or clinically significant differences in the treatment outcomes for the physical or mental health components of the SF-12v1, nor for acute whiplash injury and LWS (Tables 36–39).
| 4 months | 8 months | 12 months | |
|---|---|---|---|
| Advice | |||
| Mean (SD) | 45.9 (12.5) | 47.1 (11.4) | 48.8 (10.6) |
| n (missing/total) (%) | 54/255 (21%) | 54/246 (22%) | 69/238 (29%) |
| Physiotherapy | |||
| Mean (SD) | 46.3 (12.1) | 46.2 (12.7) | 47.5 (11.8) |
| n (missing/total) (%) | 65/252 (26%) | 60/251 (24%) | 81/241 (34%) |
| Treatment estimatea | |||
| ∆ (95% CI) | 1.4 (–0.9 to 3.7) | –0.1 (–2.5 to 2.2) | 0.1 (–2.3 to 2.4) |
| Treatment estimateb | |||
| ∆ (95% CI) | 1.3 (–0.9 to 3.5) | –0.3 (–2.6 to 2.0) | –0.0 (–2.2 to 2.1) |
| 4 months | 8 months | 12 months | |
|---|---|---|---|
| Advice | |||
| Mean (SD) | 43.5 (9.7) | 45.8 (9.5) | 47.1 (9.9) |
| n (missing/total) (%) | 54/255 (21%) | 54/246 (22%) | 69/238 (29%) |
| Physiotherapy | |||
| Mean (SD) | 42.3 (9.2) | 45.3 (9.8) | 46.5 (10.2) |
| n (missing/total) (%) | 65/252 (26%) | 60/251 (24%) | 81/241 (34%) |
| Treatment estimatea | |||
| ∆ (95% CI) | –0.1 (–1.8 to 1.6) | 0.5 (–1.3 to 2.3) | 1.0 (–1.0 to 3.0) |
| Treatment estimateb | |||
| ∆ (95% CI) | 0.2 (–1.4 to 1.8) | 0.2 (–1.5 to 2.0) | 1.1 (–0.7 to 2.9) |
| n (%) or odds ratio (95% CI) | |
|---|---|
| Advice | |
| Present | 135 (47%) |
| Absent | 120 (42%) |
| n (missing/total) (%) | 32/287 (11%) |
| Physiotherapy | |
| Present | 135 (47%) |
| Absent | 114 (40%) |
| n (missing/total) (%) | 38/287 (13%) |
| Treatment estimatea | |
| ∆ (OR 95% CI) | 0.81 (0.55 to 1.20) |
| Treatment estimateb | |
| ∆ (OR 95% CI) | 0.76 (0.51 to 1.12) |
| n (%) or odds ratio (95% CI) | |
|---|---|
| Advice | |
| Present | 86 (30%) |
| Absent | 152 (53%) |
| n (missing/total) (%) | 49/287 (17%) |
| Physiotherapy | |
| Present | 100 (49%) |
| Absent | 141 (49%) |
| n (missing/total) (%) | 46/287 (16%) |
| Treatment estimatea | |
| ∆ (OR 95% CI) | 0.91 (0.59 to 1.39) |
| Treatment estimateb | |
| ∆ (OR 95% CI) | 0.84 (0.56 to 1.28) |
Physiotherapy had a beneficial effect on absences from work; participants randomised to physiotherapy treatment had on average a 41.4% reduction in work days lost over the first 4 months since their injury (95% CI –45.4% to –37.0%). This effect persisted to 8 and 12 months (Tables 40–42). We also performed an analysis of log-transformed data (using a bootstrap procedure to calculate CIs), to obtain an estimate of the absolute difference in work days lost (adjusted for clustering, advice intervention, NDI score at baseline and therapist). The results of this analysis were consistent with the Poisson regression. The estimated reduction in work days lost was 4.2 days (95% CI 1.1 to 7.9 days) (see Appendix 10).
| 4 months | 8 months | 12 months | |
|---|---|---|---|
| Advice | |||
| Mean (SD) | 8.9 (22.9) | 9.9 (25.3) | 10.7 (26.2) |
| Missing/total | 1/255 (0%) | 0/246 (0%) | 0/238 (0%) |
| Physiotherapy | |||
| Mean (SD) | 6.3 (14.8) | 8.2 (17.7) | 9.2 (18.9) |
| Missing/total | 0/252 (0%) | 1/251 (0%) | 1/241 (0%) |
| Treatment effect | |||
| Δ (95% CI)a | –41.4 (–45.4 –37.0) | –33.3 (–37.5 to –28.9) | –17.5 (–22.5 to –12.0) |
| Δ (95% CI)b | –43.5 (–50.0 to –36.1) | –31.2 (–41.3 to –19.5) | –15.13 (–27.0 to –1.4) |
| 4 months | 8 months | 12 months | |
|---|---|---|---|
| Δ (95% CI)a | –39.3 (–43.6 to –34.5) | –33.6 (–37.9 to –29.0) | –8.3 (–14.1 to –2.1) |
| Δ (95% CI)b | –37.0 (–44.4 to –28.6) | –26.7 (–37.1 to –14.6) | –8.21 (–21.1 to 6.8) |
| 4 months | 8 months | 12 months | |
|---|---|---|---|
| Advice | |||
| Mean (SD) | 11.1 (25.4) | 12.3 (28.1) | 13.3 (29.1) |
| Missing/total | 0/202 (0%) | 0/192 (0%) | 0/184 (0%) |
| Physiotherapy | |||
| Mean (SD) | 7.4 (15.2) | 9.4 (18.3) | 10.6 (19.7) |
| Missing/total | 0/189 (0%) | 1/185 (1%) | 1/180 (1%) |
| Treatment effect | |||
| Δ (95% CI)a | –42.6 (–46.8 to –38.0) | –36.6 (–40.9 to –32.1) | –13.5 (–19.2 to –7.5) |
| Δ (95% CI)b | –41.0 (–49.6 to –30.8) | –31.6 (–42.7 to –18.3) | –13.4 (–26.9 to 2.4) |
Subgroup analyses: injury severity, previous neck pain and early psychological response
There were no statistically significant interactions between the NDI and severity of initial injury, psychological reaction to the injury or previous neck pain (Tables 43–45). Estimates (mean and 95% CIs) of all terms tested in the NDI subgroup analyses are given in Appendix 7.
| 4 months Mean (SD) [n] |
8 months Mean (SD) [n] |
12 months Mean (SD) [n] |
|
|---|---|---|---|
| Severe symptoms | |||
| Advice | 28.7 (17.5) [216] | 22.5 (16.7) [203] | 20.3 (17.2) [204] |
| Physiotherapy | 29.5 (18.1) [202] | 25.2 (19.1) [205] | 23.0 (19.0) [197] |
| Milder symptoms | |||
| Advice | 21.9 (16.0) [34] | 15.5 (15.3) [32] | 14.2 (14.6) [31] |
| Physiotherapy | 20.0 (14.6) [39] | 18.4 (13.3) [39] | 15.1 (13.0) [38] |
| p-value for interactiona | 0.23 | 0.96 | 0.35 |
| p-value for interactionb | 0.24 | 0.62 | 0.42 |
| 4 months Mean (SD) [n] |
8 months Mean (SD) [n] |
12 months Mean (SD) [n] |
|
|---|---|---|---|
| Early psychological response present | |||
| Advice | 29.6 (17.8) [178] | 23.1 (17.3) [166] | 21.1 (17.8) [160] |
| Physiotherapy | 30.6 (18.9) [176] | 26.7 (19.7) [177] | 24.1 (19.4) [173] |
| Early psychological response absent | |||
| Advice | 22.5 (13.9) [68] | 17.0 (13.4) [66] | 15.7 (14.2) [71] |
| Physiotherapy | 20.5 (12.0) [55] | 17.6 (11.4) [57] | 15.1 (13.0) [55] |
| p-value for interactiona | 0.64 | 0.70 | 0.72 |
| p-value for interactionb | 0.66 | 0.86 | 0.45 |
| 4 months Mean (SD) [n] |
8 months Mean (SD) [n] |
12 months Mean (SD) [n] |
|
|---|---|---|---|
| Had previous neck pain | |||
| Advice | 31.0 (19.8) [21] | 26.7 (16.6) [23] | 26.5 (17.0) [24] |
| Physiotherapy | 34.4 (19.8) [19] | 32.8 (19.1) [18] | 28.3 (20.8) [14] |
| No previous neck pain | |||
| Advice | 27.3 (17.1) [223] | 21.0 (16.7) [207] | 18.6 (16.8) [205] |
| Physiotherapy | 27.3 (17.7) [215] | 23.6 (18.2) [219] | 21.5 (18.4) [214] |
| p-value for interactiona | 0.96 | 0.72 | 0.41 |
| p-value for interactionb | 0.84 | 0.81 | 0.61 |
Compensation pursued
As in Step 1, we performed an exploratory analysis comparing the outcomes of those who pursued a compensation claim versus those who did not. This was limited in power by the fact that only 13 participants reported at 12 months that they had not pursued a claim for compensation.
Among participants who pursued compensation, those randomised to physiotherapy tended to have slightly higher NDI scores at all time points. However, among those who did not pursue compensation, participants randomised to physiotherapy had considerably lower NDI scores, indicating less neck injury-related disability (Table 46). The interaction between physiotherapy treatment and compensation approached statistical significance (p = 0.06) at 12-month follow-up for complete cases and multiply imputed models.
| 4 months Mean (SD) [n] |
8 months Mean (SD) [n] |
12 months Mean (SD) [n] |
|
|---|---|---|---|
| Pursued compensation | |||
| Advice | 26.7 (17.6) [210] | 20.3 (16.0) [206] | 19.3 (17.2) [227] |
| Physiotherapy | 27.7 (17.5) [203] | 24.1 (18.2) [208] | 22.0 (18.4) [221] |
| Did not pursue compensation | |||
| Advice | 34.0 (17.0) [2] | 25.2 (10.0) [5] | 28.8 (7.3) [5] |
| Physiotherapy | 12.7 (13.3) [6] | 20.0 (21.1) [8] | 11.0 (14.7) [8] |
| p-value for interactiona | 0.27 | 0.77 | 0.06 |
| p-value for interactionb | 0.53 | 0.68 | 0.06 |
The interaction term between SF-12v1 physical component score and compensation was also significant at 12-month follow-up for complete cases model, but was no longer significant in the multiply imputed model. Given the small number of participants who did not pursue compensation, it is difficult to assess the possible significance of these results.
There were no other suggestions of any interaction between any the treatment group and compensation for any outcome.
Additional analyses: the effectiveness of physiotherapy interventions in combination with different advice interventions
We investigated the potential interactions between the two physiotherapy interventions provided in Step 2 and the two advice interventions provided in Step 1, in those participants randomised to Step 2. The randomisation procedure resulted in an even distribution of characteristics within each of the four possible treatment combinations (UCA/physiotherapy advice session; UCA/physiotherapy package; active management advice/ physiotherapy advice session; active management advice/physiotherapy package; shown in Table 47).
| UCA | WBA | |||
|---|---|---|---|---|
| Advice | Physiotherapy | Advice | Physiotherapy | |
| Number randomised | 136 | 136 | 163 | 164 |
| Sex – male | 54 (40%) | 40 (29%) | 61 (37%) | 66 (40%) |
| Age in years, mean (SD)a | 40 (13) | 41 (14) | 39 (13) | 39 (13) |
| Ethnic group | ||||
| White | 116 (85%) | 113 (83%) | 113 (69%) | 113 (69%) |
| Mixed | 0 (0%) | 1 (1%) | 2 (1%) | 2 (1%) |
| Indian | 5 (4%) | 9 (7%) | 13 (8%) | 10 (6%) |
| Pakistani | 2 (2%) | 3 (2%) | 17 (10%) | 16 (10%) |
| Bangladeshi | 1 (1%) | 1 (1%) | 1 (1%) | 0 (0%) |
| Black or Black British | 4 (3%) | 1 (1%) | 6 (4%) | 6 (4%) |
| Chinese or other | 1 (1%) | 1 (1%) | 2 (1%) | 4 (2%) |
| Mechanism of injury | ||||
| Road traffic accident | 130 (96%) | 127 (93%) | 154 (94%) | 159 (97%) |
| Other | 4 (3%) | 8 (6%) | 9 (6%) | 5 (3%) |
| Location of pain | ||||
| C-spine only | 87 (64%) | 85 (63%) | 91 (56%) | 93 (57%) |
| C-spine and other spinal area | 21 (15%) | 28 (21%) | 39 (24%) | 34 (21%) |
| Other spinal area only | 4 (3%) | 0 (0%) | 6 (4%) | 3 (2%) |
| Spinal + other area | 10 (7%) | 13 (10%) | 17 (10%) | 14 (9%) |
| Other area only | 1 (1%) | 2 (1%) | 2 (1%) | 4 (2%) |
| No pain | 8 (6%) | 4 (3%) | 5 (3%) | 8 (5%) |
| Pain intensity (/10), mean (SD) | 4.9 (1.9) | 5.5 (1.9) | 5.8 (1.9) | 5.7 (1.9) |
| History | ||||
| Previous neck problems | 20 (15%) | 24 (18%) | 16 (9.8%) | 17 (10%) |
| Previous back problems | 21 (15%) | 18 (13%) | 19 (12%) | 25 (15%) |
| Neurological symptoms | 15 (11%) | 12 (8.8%) | 11 (6.7%) | 17 (10%) |
| WAD gradesb | ||||
| 0: No neck complaints or signsc | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| I: Complaint of pain, stiffness or tenderness, no physical signs | 10 (7%) | 12 (9%) | 29 (18%) | 33 (20%) |
| II: Complaint of pain, stiffness or tenderness, musculoskeletal signs | 104 (76%) | 109 (80%) | 118 (72%) | 111 (68%) |
| III: Complaint of pain, stiffness or tenderness, neurological signs | 22 (16%) | 15 (11%) | 16 (10%) | 20 (12%) |
| IV: Fracture/dislocationc | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| SF-12v1 scores, mean (SD) | ||||
| Norm-based MCS | 37 (12) | 36 (13) | 36 (12) | 34 (11) |
| Norm-based PCS | 37 (6.9) | 36 (6.9) | 36 (7.1) | 36 (6.9) |
| Received any public funds | 43 (32%) | 48 (35%) | 48 (29%) | 53 (32%) |
| NDI (%), mean (SD)b | 39 (15) | 43 (17) | 40 (17) | 45 (16) |
Mechanism of injury, location of pain, pain intensity, and medical history were collected at ED attendance. Gender, age, and ethnic group were collected via the 2-week follow-up questionnaire in Step 1.
Tables 48–55 give the estimate of treatment effectiveness for physiotherapy and The Whiplash Book elements separately for the NDI and other outcomes, and the interaction between them. There was no suggestion of an interaction between the treatments provided in Step 1 and those provided in Step 2.
| 4 months | 8 months | 12 months | |
|---|---|---|---|
| UCA | |||
| Advice | |||
| Mean (SD) | 27.2 (17.1) | 21.9 (16.4) | 20.1 (17.5) |
| n (missing/total) (%) | 4/117 (3%) | 7/116 (6%) | 1/110 (1%) |
| Physiotherapy | |||
| Mean (SD) | 28.1 (17.2) | 23.7 (18.3) | 21.1 (17.9) |
| n (missing/total) (%) | 5/118 (4%) | 3/117 (3%) | 1/109 (1%) |
| WBA | |||
| Advice | |||
| Mean (SD) | 28.3 (17.7) | 21.2 (17.0) | 19.0 (16.7) |
| n (missing/total) (%) | 1/138 (3%) | 4/130 (6%) | 2/128 (1%) |
| Physiotherapy | |||
| Mean (SD) | 27.9 (18.5) | 24.5 (18.6) | 22.2 (18.8) |
| n (missing/total) (%) | 6/134 (4%) | 4/134 (3%) | 5/132 (1%) |
| Combined treatment estimatesa | |||
| ∆interaction (95% CI) | –0.2 (–5.2 to 4.9) | 0.0 (–5.2, 5.3) | 0.9 (–4.6, 6.3) |
| ∆physiotherapy (95% CI) | –3.1 (–6.9 to 0.7) | –0.2 (–4.1, 3.6) | –1.7 (–5.7, 2.3) |
| ∆WBA (95% CI) | 0.3 (–3.8 to 4.4) | –1.2 (–5.0, 2.7) | –1.2 (–5.3, 3.0) |
| Combined treatment estimatesb | |||
| ∆interaction (95% CI) | 1.1 (–3.8 to 5.9) | 1.3 (–3.9 to 6.4) | 1.4 (–3.7 to 6.5) |
| ∆physiotherapy (95% CI) | –4.3 (–7.9 to –0.7) | –1.7 (–5.5 to 2.1) | –2.8 (–6.6 to 1.0) |
| ∆WBA (95% CI) | –0.2 (–4.2 to 3.9) | –0.5 (–5.2 to 4.1) | –0.9 (–4.9 to 3.0) |
| 4 months | 8 months | 12 months | |
|---|---|---|---|
| UCA | |||
| Advice | |||
| Mean (SD) | 46.2 (12.8) | 48.1 (11.0) | 49.0 (10.3) |
| n (missing/total) (%) | 24/117 (21%) | 25/116 (22%) | 32/110 (29%) |
| Physiotherapy | |||
| Mean (SD) | 46.7 (12.2) | 47.0 (13.2) | 48.0 (11.8) |
| n (missing/total) (%) | 31/118 (26%) | 31/117 (26%) | 34/109 (31%) |
| WBA | |||
| Advice | |||
| Mean (SD) | 45.7 (12.2) | 46.2 (11.7) | 48.7 (10.9) |
| n (missing/total) (%) | 30/138 (21%) | 29/130 (22%) | 37/128 (29%) |
| Physiotherapy | |||
| Mean (SD) | 45.9 (12.1) | 45.5 (12.3) | 47.0 (11.8) |
| n (missing/total) (%) | 34/134 (26%) | 29/134 (26%) | 47/132 (31%) |
| Combined treatment estimatesa | |||
| ∆interaction (95% CI) | –0.4 (–5.1 to 4.2) | 0.9 (–3.8 to 5.6) | –0.6 (–5.3 to 4.1) |
| ∆physiotherapy (95% CI) | 1.6 (–1.8 to 5.1) | –0.6 (–4.1 to 2.9) | 0.4 (–3.1 to 3.9) |
| ∆WBA (95% CI) | –0.2 (–3.5 to 3.1) | –1.8 (–5.2 to 1.6) | 0.1 (–3.3 to 3.4) |
| Combined treatment estimatesb | |||
| ∆interaction (95% CI) | 0.1 (–4.0 to 4.2) | 0.2 (–4.1 to 4.6) | –0.2 (–4.2 to 3.9) |
| ∆physiotherapy (95% CI) | 1.3 (–1.9 to 4.4) | –0.4 (–3.6 to 2.9) | 0.1 (–3.0 to 3.1) |
| ∆WBA (95% CI) | –0.5 (–5.5 to 4.5) | –0.9 (–5.9 to 4.0) | –0.4 (–4.8 to 3.9) |
| 4 months | 8 months | 12 months | |
|---|---|---|---|
| UCA | |||
| Advice | |||
| Mean (SD) | 43.5 (8.8) | 46.4 (9.1) | 46.7 (10.7) |
| n (missing/total) (%) | 24/117 (21%) | 25/116 (22%) | 32/110 (29%) |
| Physiotherapy | |||
| Mean (SD) | 41.9 (8.5) | 45.8 (10.0) | 46.6 (10.1) |
| n (missing/total) (%) | 31/118 (26%) | 31/117 (26%) | 34/109 (31%) |
| WBA | |||
| Advice | |||
| Mean (SD) | 43.6 (10.4) | 45.4 (9.9) | 47.5 (9.1) |
| n (missing/total) (%) | 30/138 (21%) | 29/130 (22%) | 37/128 (29%) |
| Physiotherapy | |||
| Mean (SD) | 42.7 (9.9) | 44.8 (9.6) | 46.4 (10.4) |
| n (missing/total) (%) | 34/134 (26%) | 29/134 (26%) | 47/132 (31%) |
| Combined treatment estimatesa | |||
| ∆interaction (95% CI) | 0.4 (–3.0 to 3.8) | 1.1 (–2.5 to 4.6) | –0.8 (–4.8 to 3.2) |
| ∆physiotherapy (95% CI) | –0.3 (–2.9 to 2.2) | –0.1 (–2.7 to 2.5) | 1.4 (–1.5 to 4.4) |
| ∆WBA (95% CI) | 0.4 (–2.1 to 2.9) | –0.8 (–3.3 to 1.7) | 1.2 (–1.6 to 4.1) |
| Combined treatment estimatesb | |||
| ∆interaction (95% CI) | –0.3 (–3.4 to 2.9) | –0.2 (–3.5 to 3.1) | –0.2 (–3.7 to 3.2) |
| ∆physiotherapy (95% CI) | 0.4 (–1.9 to 2.6) | 0.3 (–2.1 to 2.8) | 1.3 (–1.2 to 3.8) |
| ∆WBA (95% CI) | 0.1 (–2.3 to 2.6) | –0.1 (–4.0 to 3.8) | 0.3 (–3.2 to 3.8) |
| 4 months | 8 months | 12 months | |
|---|---|---|---|
| UCA | |||
| Advice | |||
| Mean (SD) | 10.1 (24.7) | 10.4 (24.8) | 11.6 (26.8) |
| Missing/total | 0/117 (0%) | 0/116 (0%) | 0/110 (0%) |
| Physiotherapy | |||
| Mean (SD) | 4.6 (10.6) | 5.4 (11.3) | 6.4 (13.3) |
| Missing/Total | 0/118 (0%) | 0/117 (0%) | 0/109 (0%) |
| WBA | |||
| Advice | |||
| Mean (SD) | 7.8 (21.3) | 9.5 (25.8) | 9.9 (25.8) |
| Missing/total | 1/138 (0%) | 0/130 (0%) | 0/128 (0%) |
| Physiotherapy | |||
| Mean (SD) | 7.8 (17.6) | 10.6 (21.5) | 11.6 (22.4) |
| Missing/total | 0/134 (0%) | 1/134 (0%) | 1/132 (0%) |
| Treatment estimatea | |||
| ∆interaction (95% CI) | 147.2 (113.6 to 186.1) | 98.0 (72.9 to 126.6) | 111.6 (85.4 to 141.5) |
| ∆physiotherapy (95% CI) | –66.8 (–70.4 to –62.6) | –57.0 (–61.4 to –52.0) | –48.0 (–53.2 to –42.3) |
| ∆WBA (95% CI) | –44.4 (–69.0 to –0.3) | –34.9 (–65.1 to 21.6) | –35.7 (–64.6 to 17.0) |
| Treatment estimateb | |||
| ∆interaction (95% CI) | 187.0 (138.0 to 246.0) | 106.3 (48.8 to 186.1) | 105.9 (42.9 to 196.6) |
| ∆physiotherapy (95% CI) | –70.5 (–74.8 to –65.6) | –56.4 (–67.7 to –41.1) | –46.0 (–59.6 to –27.7) |
| ∆WBA (95% CI) | –37.2 (–65.1 to 12.9) | –25.0 (–61.2 to 45.0) | –28.7 (–62.7 to 36.3) |
| 4 months | 8 months | 12 months | |
|---|---|---|---|
| Treatment estimatea | |||
| ∆interaction (95% CI) | 99.6 (71.4 to 132.4) | 70.8 (48.5 to 96.3) | 97.6 (72.4 to 126.4) |
| ∆physiotherapy (95% CI) | –60.4 (–65.0 to –55.3) | –53.0 (–58.0 to –47.4) | –40.2 (–46.4 to –33.3) |
| ∆WBA (95% CI) | –39.8 (–66.1 to 6.7) | –29.6 (–61.6 to 29.2) | –37.2 (–64.4 to 10.7) |
| Treatment estimateb | |||
| ∆interaction (95% CI) | 176.5 (128.5 to 234.6) | 97.3 (41.3 to 175.6) | 96.3 (35.9 to 183.5) |
| ∆physiotherapy (95% CI) | –66.6 (–71.8 to –60.4) | –52.5 (–65.1 to –35.3) | –39.9 (–55.7 to –18.6) |
| ∆WBA (95% CI) | –34.2 (–62.5 to 15.2) | –20.7 (–57.9 to 49.2) | –27.8 (–61.0 to 33.6) |
| 4 months | 8 months | 12 months | |
|---|---|---|---|
| UCA | |||
| Advice | |||
| Mean (SD) | 12.2 (26.8) | 12.5 (26.9) | 13.9 (29.1) |
| Missing/total | 0/97 (0%) | 0/95 (0%) | 0/88 (0%) |
| Physiotherapy | |||
| Mean (SD) | 5.9 (11.8) | 6.9 (12.3) | 8.1 (14.5) |
| Missing/total | 0/89 (0%) | 0/86 (0%) | 0/80 (0%) |
| WBA | |||
| Advice | |||
| Mean (SD) | 10.1 (24.1) | 12.2 (29.3) | 12.7 (29.3) |
| Missing/total | 0/105 (0%) | 0/97 (0%) | 0/96 (0%) |
| Physiotherapy | |||
| Mean (SD) | 8.7 (17.7) | 11.6 (22.1) | 12.9 (23.2) |
| Missing/total | 0/100 (0%) | 1/99 (0%) | 1/100 (0%) |
| Treatment estimatea | |||
| ∆interaction (95% CI) | 78.8 (53.1 to 108.8) | 53.1 (32.8 to 76.5) | 68.8 (46.9 to 94.0) |
| ∆physiotherapy (95% CI) | –59.6 (–64.3 to –54.4) | –51.6 (–56.9 to –45.8) | –37.4 (–43.9 to –30.1) |
| ∆WBA (95% CI) | –36.9 (–64.6 to 12.5) | –26.3 (–60.2 to 36.5) | –33.4 (–62.5 to 18.2) |
| Treatment estimateb | |||
| ∆interaction (95% CI) | 160.3 (103.9 to 232.3) | 90.0 (34.5 to 168.5) | 79.3 (26.0 to 155.1) |
| ∆physiotherapy (95% CI) | –67.2 (–72.6 to –60.6) | –54.2 (–66.5 to –37.4) | –39.5 (–55.2 to –18.4) |
| ∆WBA (95% CI) | –31.6 (–61.2 to 20.3) | –16.9 (–55.7 to 56.1) | –25.7 (–59.6 to 36.4) |
| n (%) or odds ratio (95% CI) | |
|---|---|
| UCA | |
| Advice | |
| Present | 68 (52%) |
| Absent | 49 (38%) |
| n (missing/total) (%) | 13/130 (10%) |
| Physiotherapy | |
| Present | 67 (52%) |
| Absent | 50 (38%) |
| n (missing/total) (%) | 13/130 (10%) |
| WBA | |
| Advice | |
| Present | 67 (43%) |
| Absent | 71 (45%) |
| n (missing/total) (%) | 19/157 (12%) |
| Physiotherapy | |
| Present | 68 (43%) |
| Absent | 64 (41%) |
| n (missing/total) (%) | 25/157 (16%) |
| Combined treatment estimatesa | |
| ∆interaction (95% CI) | 1.32 (0.60 to 2.89) |
| ∆physiotherapy (95% CI) | 0.70 (0.39 to 1.25) |
| ∆WBA (95% CI) | 0.60 (0.33 to 1.10) |
| Combined treatment estimatesb | |
| ∆interaction (95% CI) | 1.35 (0.63 to 2.89) |
| ∆physiotherapy (95% CI) | 0.64 (0.36 to 1.15) |
| ∆WBA (95% CI) | 0.61 (0.34 to 1.11) |
| n (%) or odds ratio (95% CI) | |
|---|---|
| UCA | |
| Advice | |
| Present | 45 (35%) |
| Absent | 65 (50%) |
| n (missing/total) (%) | 20/130 (15%) |
| Physiotherapy | |
| Present | 44 (34%) |
| Absent | 65 (50%) |
| n (missing/total) (%) | 21/130 (16%) |
| WBA | |
| Advice | |
| Present | 41 (26%) |
| Absent | 87 (55%) |
| n (missing/total) (%) | 29/157 (18%) |
| Physiotherapy | |
| Present | 56 (36%) |
| Absent | 76 (48%) |
| n (missing/total) (%) | 25/157 (16%) |
| Combined treatment estimatesa | |
| ∆interaction (95% CI) | 1.57 (0.67 to 3.68) |
| ∆physiotherapy (95% CI) | 0.71 (0.38 to 1.33) |
| ∆WBA (95% CI) | 0.58 (0.30 to 1.12) |
| Combined treatment estimatesb | |
| ∆interaction (95% CI) | 1.74 (0.77 to 3.91) |
| ∆physiotherapy (95% CI) | 0.63 (0.34 to 1.15) |
| ∆WBA (95% CI) | 0.62 (0.34 to 1.14) |
Additional analyses: recovery in participants not randomised to Step 2
We examined recovery in the people who participated in Step 1 but were not randomised to Step 2 (Table 56). Figure 15 demonstrates that overall symptoms were milder than those within Step 2, but that recovery was not complete at 12 months.
| 4 months | 8 months | 12 months | |
|---|---|---|---|
| UCA | |||
| Mean (SD) | 18.8 (16.8) | 14.3 (15.7) | 12.9 (15.1) |
| n (missing/total) (%) | 33/1060 (3%) | 26/942 (3%) | 23/908 (3%) |
| WBA | |||
| Mean (SD) | 20.3 (17.3) | 15.3 (15.9) | 13.2 (15.2) |
| n (missing/total) (%) | 57/1502 (4%) | 27/1306 (2%) | 34/1317 (3%) |
| Treatment estimatea | |||
| ∆ (95% CI) | 0.9 (–1.8 to 3.5) | 0.7 (–1.4 to 2.7) | 0.2 (–1.5 to 1.9) |
| Treatment estimateb | |||
| ∆ (95% CI) | 0.9 (–2.0 to 3.7) | 1.1 (–1.4 to 3.7) | 0.8 (–1.2 to 2.8) |
FIGURE 15.
Neck Disability Index (%) for those who did not enter Step 2 by advice intervention.
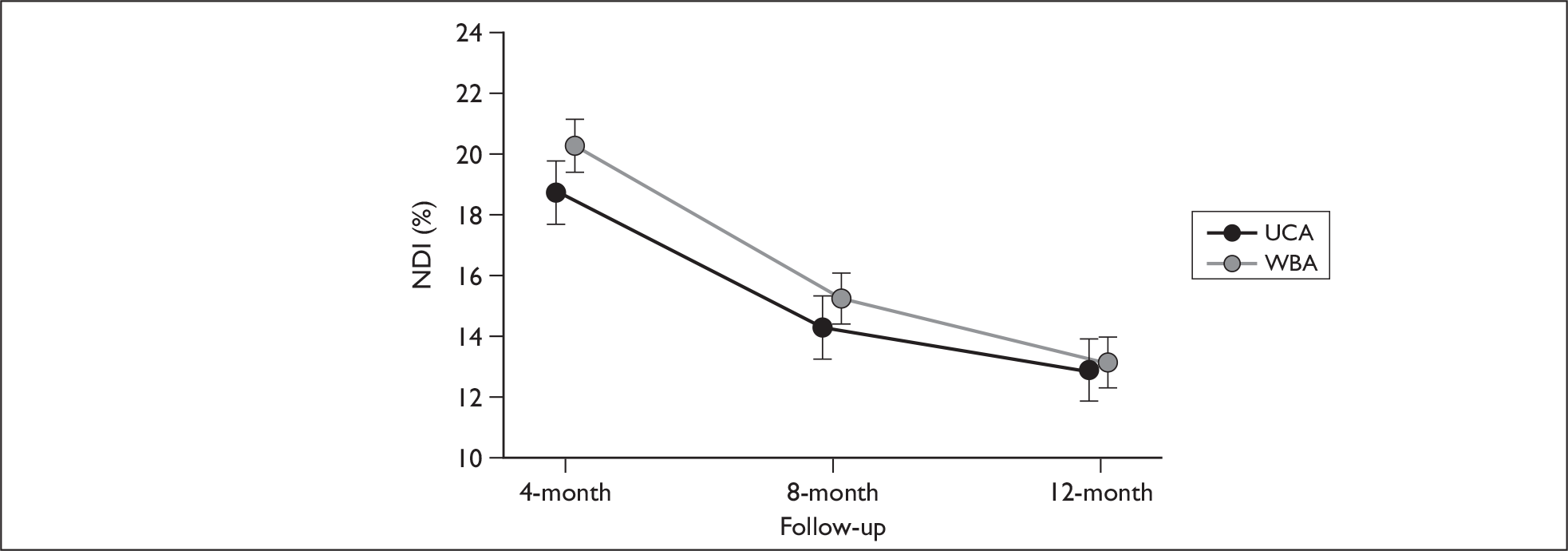
Chapter 5 Qualitative study
Introduction
The aim of the qualitative study was to gain the participant’s perspective on the experience of having a whiplash injury, and the experience of treatment and recovery within the context of MINT. Despite the recognised importance of qualitative data to understanding patient experiences, there are very few qualitative studies in the field of WADs. 68
Method
Semi-structured interviews were conducted with 20 participants after they had received their allocated treatments. All people interviewed were participants in Step 1 and 2 of the trial.
Sample
Participants were sampled purposively from trial clinics in four NHS trusts in the West Midlands (University Hospital Birmingham, University Hospitals Coventry and Warwickshire, Heart of England, Worcestershire Acute Hospitals) aiming for equal numbers of people from the four possible treatment combinations.
Participant recruitment
While attending the clinic for entry to Step 2 of the trial, 25 people were invited to participate, given an information sheet detailing the purpose and content of the interviews, and advised that a researcher (EMW) would contact them on completion of their treatment. Of these, 20 were contacted and completed the interview and one was contacted and arranged an interview but failed to attend (Figure 16).
FIGURE 16.
Participant recruitment to the interview study.
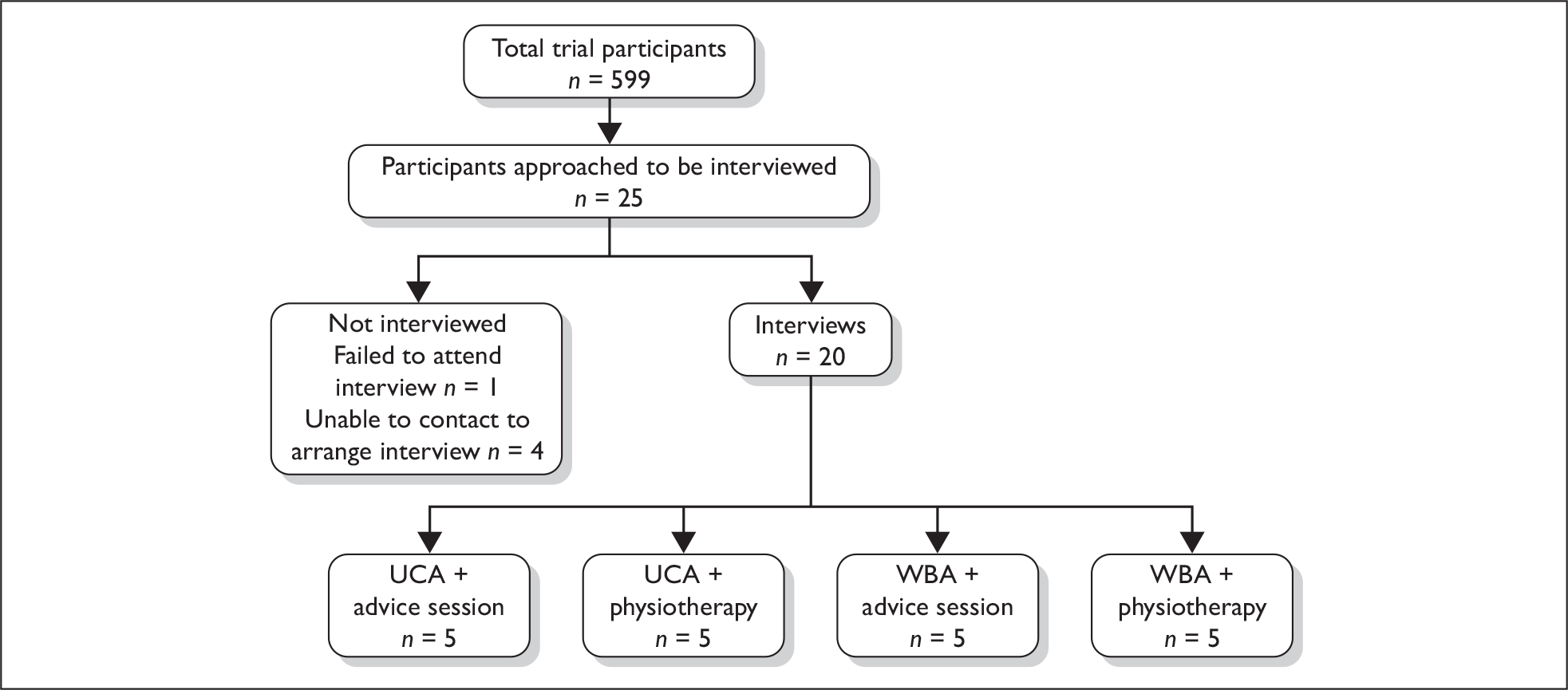
The interview
Interviews were carried out between 54 and 167 days after ED attendance following whiplash injury (mean = 102). The venues for the interview, chosen by participants, were: own home (n = 8); physiotherapy department (n = 9); ED (n = 2); and workplace (n = 1). The intention was to interview participants on completion of treatment, but owing to time constraints three participants receiving the physiotherapy package were interviewed towards the end of their treatment programme.
We used semi-structured interviews. The research team developed the interview schedule. Participants were encouraged to talk about their personal experience of having a whiplash injury and the treatment and recovery phase through the use of open questions and prompts. 69 Participants provided signed consent prior to the start of the interview. Interviews lasted up to 1 hour and were audio recorded. The interview schedule is given at www2.warwick.ac.uk/fac/med/research/hsri/emergencycare/research/whiplash/webresource.
Analysis
For this descriptive analysis we used thematic analysis, identifying themes that participants had in common and where they differed. 69 The research team discussed and agreed coding themes based on the interview transcripts. This was then developed and discussed further as new themes emerged during analysis. The data were coded, and we compared participants in each of the four treatment pathways, to identify both consistency and disparity in their experiences.
For reporting results, the coded data was summarised for each theme and illustrative quotes identified. To give an indication of whether a theme was commonly mentioned or not we report the number of participants mentioning a theme. The analysis describes and summarises participants’ experiences of attending the ED after whiplash injury and their treatment within the trial, and compares the accounts from participants following different treatment pathways.
Data management and quality checks
Interviews were transcribed and anonymised. The transcriptions were checked by the interviewer and then coded. The software nvivo, version 7 (QSR International Pty Ltd, Doncaster, VIC, Australia), was used to assist with the analysis. EW coded all the interviews. A second researcher independently coded 20% of interviews and the coding was compared. There was little disagreement in the allocation of codes. Where they occurred, disagreements were resolved by discussion. Coding and analysis was completed prior to completion of the trial.
Results
Participant characteristics including treatment attendance
The profile of the interview participants was similar to that of the average participant in Step 2 of the trial (Table 57).
| Interview participants (N = 20) | Step 2 participants (N = 599) | ||
|---|---|---|---|
| Gender |
Male Female |
n = 8 (40%) n = 12 (60%) |
n = 220 (37%) n = 379 (64%) |
| Age (years) | Mean (SD) | 41 (10.8) | 39(13.1) |
| NDI scores at research clinic | Mean (SD) | 21 (8.7) | 21 (8.1) |
| Disability severity (based on NDI scores) at research clinica |
No disability Mild disability Moderate disability Severe disability Complete disability |
n = 0 (0%) n = 5 (25%) n = 7 (35%) n = 7 (35%) n = 1 (5%) |
n = 3 (1%) n = 127 (21%) n = 266 (45%) n = 155 (26%) n = 48 (8%) |
| WAD grading at research clinic |
WAD I WAD II WAD III |
n = 2 (10%) n = 17 (85%) n = 1 (5%) |
n = 84 (14%) n = 442 (74%) n = 73 (12%) |
Treatment attendance in Step 2
All participants who were randomised to the physiotherapy advice session attended with a mean wait of 18 days (SD = 11) between the research clinic and the physiotherapy advice session. Waiting times were similar to the main trial (mean = 18 days, SD = 13.8). Mean time between injury and attending the physiotherapy advice session was 50 days (SD = 13.6), similar to the main trial (mean = 49.7 days, SD = 17.47). Mean time between injury and interview was 84 days (SD = 18).
For the group randomised to the physiotherapy package, seven of the 10 participants (70%) interviewed completed their full course of treatment, two participants (20%) partially completed treatment and one (10%) attended the initial assessment only. This attendance pattern was similar to that of the main trial where 67% completed treatment, 15% partially completed treatment and 9% only attended the assessment session. The mean number of treatments attended in addition to the assessment session was five (SD = 3.7), somewhat larger than in the trial overall (mean = 3, SD = 2.7) (Table 58). Mean wait from referral to first physiotherapy appointment was 13 days (SD = 12.2), similar to the main trial (mean = 15 days, SD = 13.4). Mean time between injury and interview was 120 days (SD = 28).
The experience of the emergency department
Almost all participants made positive and negative comments about their experience of attending the ED. They commented on waiting times, attentiveness of staff, their expectations of treatment and treatments delivered. These data were similar to findings from previous studies of ED attendance in other conditions. 71 We focused on participants’ comments about MINT treatments.
Verbal advice received in the emergency department
Regardless of the trial arm that they were randomised to, all participants reported being given advice about or a prescription for pain relief in the ED. Other verbal information/advice reported was: information about their injury (n = 11), reassurance their injury was not serious (e.g. no fracture or dislocation) (n = 9), reassurance to exercise and/or stay active (n = 8), advice about who to see if they had ongoing or worsening problems (n = 6), information on prognosis (n = 5), and information about what symptoms to expect (n = 3). Some participants were given advice to rest – this was an observation in both treatment arms.
The influence of advice was evident through the narratives, for example
He just said ‘you’ve just pulled all your muscles and you’ve damaged your neck’, but he said ‘it will get better’ so … and that was enough for me.
Participant T, usual care, ED
Seven participants mentioned they were not given any verbal advice about exercise or staying active with three participants recalled being told specifically to rest.
… he just said ‘you need rest and a big dose of painkillers’.
Participant H, The Whiplash Book, ED
In the sample interviewed, there was no evidence of a systematic difference in the verbal advice given by clinical staff in the ED.
Engagement with written advice
All but one participant recalled receiving an advice leaflet in the ED. Almost all participants mentioned reading at least part of the leaflet they received. Those receiving The Whiplash Book were more likely to recall its content than those receiving the leaflet for usual care.
Of the 10 participants who received The Whiplash Book, six said they had read it all the way through, three had read some of it and one said he had not read it because he felt he knew enough about managing his injury himself. Of the nine participants who received the usual care leaflet, all but one participant indicated that they had read it at least once. This participant had already attended another hospital and read their information sheet.
Most participants receiving The Whiplash Book were able to recall something about its content.
It really made me think because there is a chapter in the book that says what you want to do now. ‘You want to sit down and do nothing’ or ‘you want to get better and keep moving’, so … you know … that really … So ‘hold on a minute. No, I want to be in the next one. I want to keep moving and get my life back’ because I was like really upset.
Participant H, The Whiplash Book, ED
Many participants receiving the usual care leaflet could not recall anything about its content and the four that did, commented mainly on how it could be improved.
Messages recalled by participants from the written advice
Most participants recalled information about exercises from written advice, particularly those receiving The Whiplash Book. By the time they were interviewed, only four participants recalled information about other non-exercise components in the written advice. Three out of the four participants able to recall this additional information had received The Whiplash Book.
When asked, eight of the 10 participants receiving The Whiplash Book recalled the exercises or advice to stay active.
I mainly went straight to the exercises. To me that was … First things first; ‘that’s the one for literature and that’s what is going to get me better … I just went to the diagrams to get myself better.
Participant I, The Whiplash Book, ED
Five of The Whiplash Book participants appeared to concentrate solely on the exercises and to pay little or no attention to the rest of the content of The Whiplash Book considering the exercises as the most likely thing that would help their recovery.
The exercises were enough if you are with me. I knew that it was doing something because I was getting a feeling from it.
Participant D, The Whiplash Book, ED
Three participants recalled other advice in The Whiplash Book of which two had read it thoroughly and recalled detailed information.
I think when I read the booklet it did say very rarely is it a long-term problem that you can’t solve so I think I was reassured by that that it would be … get better.
Participant C, The Whiplash Book, ED
Of the four participants receiving the usual care leaflet who could recall any content, all mentioned exercises and one mentioned information about pain relief and possible symptoms.
I can remember they gave me a whole pack and it was about pain relief. Everyday I was getting a headache and it was on the leaflet to expect to have headache.
Participant L, usual care, ED
Use of the written advice to exercise
Only half the participants had started exercising based on written advice alone. For the others, starting to exercise was not straightforward. They talked about the importance of encouragement from other people in getting them started, fear of doing more damage through exercise or concern about not getting the exercises right. A larger proportion of participants receiving The Whiplash Book mentioned they had started the exercises before their advice/physiotherapy sessions than those receiving the usual care leaflet.
Participants were not asked directly whether or not they had used the written advice they received. Analysis focused on accounts of their experience following attendance at the ED. This may result in under-reporting of use of the written advice but aimed to reduce eliciting what participants might consider an acceptable answer if asked directly.
Six of the 10 patients who received The Whiplash Book talked about carrying out exercises before attending for the treatments provided in Step 2 of the trial, including one who did his own exercises rather than those in the book. Two participants did not start any exercises until they attended for Step 2 treatments, one started the exercises but stopped them because they were too painful and it was not clear when the remaining participant started exercises.
Of the patients receiving the usual care leaflet, four participants talked about doing exercises prior to attending for Step 2 treatments. One had followed the advice in the usual care leaflet, one continued with an exercise regime they had been doing prior to their injury, not those on the leaflet, one had started exercising on encouragement from a friend who was an occupational therapist and one started the exercises, stopped them as they were too painful then restarted after advice from her GP on how to exercise.
Within their interview accounts, participants spoke of not feeling confident to start doing the exercises without reassurance or guidance from someone else.
You need someone to reassure you and I’m a person that won’t just believe a book.
Participant H, The Whiplash Book, ED
My neck was still … it seemed to have got worse. I thought … I did try and avoid hospital so I went to the GP and the GP said get movement back in my neck by holding on either side of your head and manipulating … not manipulating but gently move my head up and down, side to side so I could exercise the muscles.
Participant L, usual care, ED
Fear of doing further damage or concern about doing the right thing was mentioned by some participants.
I find that quite difficult because its … you can have something visually in front of you telling you what to do but its so different actually doing it that I was scared of doing more damage than getting it right because of how much it hurt when I move in certain positions.
Participant N, usual care, ED
The Whiplash Book showed a fair bit of, sort of, information in it, and there were various exercises in it. Now, um, I was not too sure, if I should go on the basic neck exercises or the extreme exercises. I mean I could do something more extreme but that could have done more damage to my neck as such.
Participant B, The Whiplash Book, ED
I didn’t know whether I’d be doing the right thing or the wrong thing and I thought I’d give it time to settle before I tried it.
Participant G, The Whiplash Book, ED
These narratives suggest that fear of movement and reinjury has not been allayed by The Whiplash Book sufficiently to modify behaviour.
Step 2 interventions
The experience of the physiotherapy advice session
Most participants found the physiotherapy advice session helpful for managing their injury especially when access was relatively quick. Nearly half of the participants felt that one session was sufficient for their injury.
Six participants talked about how the guidance from a physiotherapist had helped them.
… because I was doing exercises from the book, but she was able to specifically say ‘ok this is how you have hurt your neck and this is how much you need to do’ and I felt more comfortable having it from her telling me exactly what was right.
Participant C
Even having just that one and speaking to somebody that that knew, somebody who could show me things, that meant a lot. That was a lot more helpful than just going to the doctors and the doctors saying just take your painkillers and do your exercises. You know, it was nice for somebody to be there and be able to speak to somebody and for them to show you. You know the best things to do. Just do some with you and that.
Participant A
Three participants felt timely access to the advice had helped, compared with what they perceived to be normal access to physiotherapy.
I must admit that I think the trial is really good. I wouldn’t have got that physio session. That would have took me ages to get that through the doctor. By the time I would have gotten it through the doctor it wouldn’t have been worth it. Even having just that one and speaking to somebody that that knew, somebody who could show me things, that meant a lot.
Participant A
One participant mentioned the holistic approach taken by the physiotherapist.
Not only did she look at my past but the immediate problem I had she also looked at. She looked at me holistically. It wasn’t just one problem she was interested. She was interested in all.
Participant E
Two participants mentioned a temporary increase in neck pain in the days following the advice session.
She was really nice but I found afterwards my neck was actually sore for about 5 days after the actual session so I don’t know if it was from the exercises I did. I think it was a bit of a shock to my neck but I still do the exercises and it has helped a lot.
Participant L
Three participants said the information received during the advice session was not new to them. This is not unexpected as the advice session was based on the written advice. However, these participants said the advice session was still useful.
No really its stuff that I knew already but she just kind of went over it and I thought ‘oh yes I forgot about that’ so it was useful.
Participant L
Four of the participants receiving the physiotherapy advice session felt that it was sufficient for their injury.
I thought that, it was explained to me, that I would be checked and if my neck injury was a lot more worse then, obviously I would have a few more sessions as such but I felt at the time that one session was probably right for me. After the initial painkillers and doing the actual neck exercises, I mean my neck weren’t too bad. It is still fairly stiff but it is a lot better than probably a few weeks back. The time given to me just to explain that if you kept doing these exercises I thought that was enough treatment for my neck injury.
Participant B
One of the four participants who felt the physiotherapy advice session was sufficient did suggest that a follow-up session may have been useful but also acknowledged it was up to them to do the exercises.
Just the one session. Yes well I know you could … there was … thinking either one session or a few sessions but actually I thought one session was quite adequate because I needed the exercises and its only me that can do them, so for me that worked fine. I mean the only … I mean maybe one follow up session a while later, but not sort of straight afterwards because I couldn’t be seen if that was a … now I might say ‘well it’s still not better but perhaps that’s because I’ve been a bit lax with my exercises’ so actually just one is fine.
Participant C
Although appreciative of the physiotherapy advice session, four participants would have liked more contact with the physiotherapist.
If it was improving, which it did, whether I could be like doing more of the exercises or if there were different ones to do to progress, yes – just to monitor it really yes.
Participant M
Two participants were unhappy with the physiotherapy advice session. One had a strong preference for physiotherapy treatment and felt attending the physiotherapy advice session had delayed her receiving this. The other said he attended to be helpful rather than expecting the session to help him, and that he was not told anything he did not know already.
The participants’ accounts were also examined to determine if the physiotherapy advice sessions were delivered in line with the trial protocol. This was generally the case and there was evidence that the advice was tailored to the individual participants as intended. Two deviations from the protocol were noted. One participant reported that they were told they would definitely need physiotherapy and to see their GP to arrange this. The other participant was referred by the trial physiotherapist for another physiotherapy assessment for his lower back pain (LBP). Both participants should have been advised to see their GP after trying the advice given if their symptoms did not settle.
The experience of the physiotherapy package
Participants receiving the physiotherapy package were pleased with the treatment and mentioned, in particular, how helpful the guidance and reassurance specifically in relation to undertaking exercises and the manual therapy was. A minority of those receiving the physiotherapy package felt they needed more treatment.
When asked what was most helpful about the physiotherapy sessions, six participants mentioned reassurance and guidance.
I wouldn’t have done the exercises at home without [Name] helping me – I mean without her saying ‘that’s the right thing to do and this is the right thing. This way is going to hurt you less’ or ‘this way is going to hurt you more’ and the positions and the postures. I think that helps.
Participant H
I do think that you do your best following charts and written instructions but I do think you need an expert to say whether you are doing it quite right.
Participant P
Six participants indicated that the exercises were helpful.
I did a lot of exercises to try to loosen the muscles and, you know, try to reduce the stiffness and that was really useful.
Participant F
Five participants indicated that the manual therapy was helpful.
… when she was manipulating and helping cause it was such a nice feeling and when I actually walked out I felt that I was walking better, more upright and just felt better and different. More aligned I presumed.
Participant P
When asked about the impact of the physiotherapy package, six participants felt the package had contributed to improving their movement, five that it had helped with pain relief, at least temporarily, and two attributed their increase in function to the physiotherapy.
Yes she told me to go swimming and then she told me that I could probably do my Tai Chi. She said ‘don’t stop going, just do the movements that you can do’ and as I say I did go swimming.
Participant J
Well, because I have achieved a lot and I am sure if I didn’t have the physiotherapy session I wouldn’t have achieved what I have achieved. I would not be able to move and you know, um, and do the exercises I am doing now. Maybe I would not be back to work.
Participant F
Three participants reported minor and temporary side effects following treatment that included a reaction to the tape used to improve posture, post-treatment soreness and feeling dizzy.
Six of the nine participants attending physiotherapy package indicated that they were happy with the amount of treatment they received and three felt they would have benefited from more. Of these three, one suggested a follow-up session a few months later.
Maybe another session in 3 months and gradually sort of ease it off and then one after 6 months just to check up.
Participant G
Some participants spoke about the difficulty in attending all of the sessions. One participant attended only the initial assessment session. He had missed his first appointment and subsequently had been unable to arrange a further appointment at an appropriate time. However, he said if he had not been coping well he would have made more of an effort to sort out the appointments.
I just … but anyway, what happened from that is I missed that appointment and I said ‘well, can I make an appointment for next week then please? Next Friday would be perfect.’ ‘[Physiotherapist] doesn’t do Fridays.’ ‘OK, then. I’ve got work commitments here and I have to take time off; ‘can I … ?’ ‘He’s off.’ ‘Oh what about the week after?’ ‘Oh no, he’s off for 2 weeks. He can do 3 weeks’ time.’ So obviously I’ve just missed 1 week. Another 3 weeks – that’s a month and I said ‘well, it’s a waste of time. I might as well continue doing my own exercises.
Participant I
Two other participants also found it difficult to attend for the six sessions offered owing to work or family commitments.
Well I originally should have had six I think but I ended up having four because one of the appointments, on the fifth one I got really busy. Work got busy half an hour before the appointment and I phoned to get it moved but it couldn’t and I was waiting for another appointment.
Participant R
One participant commented how pleased they were with how quickly they received treatment and another commented it would have been better to have the treatment sooner.
The transcripts were also examined to determine if the treatments had been delivered in line with the trial protocol. The participants’ accounts of their physiotherapy treatment were consistent with the physiotherapy package protocol.
Participants’ sources of treatment or advice beyond the clinical trial
In total, 15 participants (eight participants attending The Whiplash Book centres and seven participants attending usual care centres) mentioned seeking treatment or advice from other sources, nine of those who received the physiotherapy package and six of those receiving the physiotherapy advice session.
All 15 participants consulted their GP following their injury. Reasons for consulting were pain relief (n = 8), obtaining or enquiring about a sick note (n = 3), low back pain (n = 2), headaches (n = 2), sleeping problems (n = 1), and asking for a physiotherapy referral (n = 1). Three participants said they consulted a physiotherapist other than the MINT physiotherapist: one received some physiotherapy through her GP, one had an assessment with a physiotherapist before deciding to take part in MINT and one was referred for a physiotherapy assessment for their back pain by their MINT physiotherapist. Other sources of treatment or advice were a masseuse, work-place occupational health service, counsellor for anxiety related to driving, fitness instructor, occupational therapist who was also a friend, and NHS Direct contacted prior to attending the ED.
Conclusion
This study has explored the experience of treatment following a whiplash injury, particularly how the different components of the treatment were perceived and used by participants and how they impacted on recovery.
In the narratives recorded in this small group of participants, the recall of the content of verbal advice given in the EDs was similar regardless of the arm of the trial. Although generally of high quality, the advice given was not always consistent with the concept of active management as a few participants reported being told to rest. The interviews were conducted after all treatments had been completed, and it is probable that the recall of specific details of treatments given is limited by recall bias. However, given the long recall period it is perhaps surprising that people do remember at least some of the content of the ED consultation. Messages regarding physical activity and rest appear to be retained over time. Although it would be important to understand the context in which instructions to rest had been made, the indication is that the educational packages given to clinicians in EDs may have been insufficient to ensure that all clinicians had embraced the core components of the active management strategy.
The interviews suggest that The Whiplash Book is well received by patients. Participants receiving The Whiplash Book and active management advice described greater engagement with the written advice, than those receiving the usual care leaflet. A higher proportion of participants receiving The Whiplash Book initiated the recommended exercises promptly. The narratives suggest that The Whiplash Book gives added value over the usual care leaflet. However, we need to be cautious in drawing conclusions. All participants in the interview study were participants in the second stage of the trial, and, as such, the advice encapsulated in the original ED consultation was reinforced during the follow-up treatment. The added value of The Whiplash Book may be, at least in part, that it provides an adequate basis for consistent reinforcement by health professionals who may see people later in the course of their recovery. However, on its own The Whiplash Book seems to have enabled more people to start on exercises for their neck than the usual care leaflets.
Despite receiving written advice, some participants expressed hesitation about doing exercises without further guidance or reassurance. This hesitation was in part because participants wanted reassurance that they were doing the exercises in the right way, but some participants expressed a fear of making themselves worse. The hesitant behaviour was found among participants in the usual care and active management advice arms. Fear of damage is known to lead to activity restriction in other musculoskeletal problems, and is hypothesised to be an important mediator on the path to chronic symptoms. 72 For individuals where fear avoidance plays an important role in their reaction to injury and recovery, The Whiplash Book alone does not seem to be sufficient to allay their fear. Participants reported using The Whiplash Book selectively, often only using the exercise component. Improving the accessibility and format of the other sections of the booklet may improve effectiveness. Providing advice about what to do if you cannot get started on activity and movement may prove a useful addition to the text.
All participants reported that a follow-on session or sessions with a physiotherapist were important in allaying their hesitation to exercise, and enabling them to start exercise.
The single physiotherapy advice session appeared sufficient to many participants. Great value was placed on rapid access to the service. Some participants felt they would have benefited from a follow-up session, or at least have this as an option. For participants it was important that the physiotherapist assessed them as individuals and helped them understand how to undertake the exercises, including demonstrating the exercises.
Those attending the physiotherapy package also highlighted guidance, reassurance, and continuing exercises as helpful. Some participants appreciated manual therapy. For most participants, the physiotherapy package was considered sufficient. More flexible appointment times may have made it easier for some participants to attend, and allows people to be able to continue with important commitments such as work. Although it is common practice for a package of physiotherapy to be delivered by the same physiotherapist, future research should examine whether or not this continuity in delivery is essential.
Some participants sought advice or treatment for their whiplash beyond the trial.
There are a number of limitations and caveats to note. Qualitative research usually involves in depth analysis of small samples, and it is not possible (nor an intended aim of the method) to generalise the findings to a wider population. We undertook purposive sampling to try to maximise the representativeness of the sample in terms of injury severity and gender, and of the overall clinical trial sample. We interviewed 20 participants, with data saturation sufficient to develop a meaningful and internally consistent thematic framework.
There are some limitations specific to this study. The length of time between attending the ED and having the qualitative interview may have affected recall, particularly of treatments delivered in the first step of the trial. Also we need to highlight that remembering advice does not equate to changing exercise, illness and pain behaviours. Some of the participants had been registered in to the second step of the trial by the same researcher who conducted the interviews, and hence may have been reluctant to provide criticism of the treatments provided.
In conclusion, these interviews suggest – that The Whiplash Book can give added value over the usual care provided in the ED. However, as intentions do not necessarily translate into trying exercises, and the non-exercise components of the book are overlooked, The Whiplash Book may not affect clinically important end points. Both the physiotherapy advice session and the physiotherapy package were beneficial to participants. Consistent reinforcement of the same messages about how to manage a whiplash injury was helpful for many participants particularly when a therapist engaged with the individual and tailored the messages to each individual.
Chapter 6 Economic analysis
Introduction
This section reports the cost-effectiveness analysis of the stepped care approach to managing neck injuries including education and advice based on The Whiplash Book at the initial contact, compared with usual care in EDs, and, in patients with persisting symptoms, the supplementation of reinforcement of advice with physiotherapy treatment, compared with reinforcement of advice only.
We assessed the cost–utility of advice based on The Whiplash Book and of physiotherapy. The cost–utility analysis compared The Whiplash Book with usual care and separately, physiotherapy with reinforcement of advice, reflecting the study design. The primary analysis was a within-trial cost–utility, expressed as the cost–utility ratio, the cost of gaining one additional quality-adjusted life-year (QALY) with each of the two interventions considered.
The cost–utility was assessed over a time frame of 12 months. Costs were expressed in UK pounds (£) actualised to current prices using the Office for National Statistics Retail Price Index. 73 2009 was the base year of the analysis. Costs and QALYs were not discounted as the time horizon of the analysis was 1 year.
We calculated the cost–utility from both the UK NHS perspective and a general health-care perspective including all private health care and related costs supported by participants.
Data
Outcome data
The cost–utility analysis used health outcome data estimated from the trial and expressed as QALYs. Utility weights were estimated using EQ-5D questionnaires administered at baseline and 4, 8 and 12 months. The EQ-5D is a well-known generic measure of health status that includes five dimensions: mobility, self-care, usual activities, pain or discomfort and depression or anxiety. The respondent rates their current health status choosing from three levels: ‘no problem’, ‘some problems’ and ‘unable to perform’. The EQ-5D spans 243 states that range from worst possible to best possible health.
Resource-use data
The use of health-care resources was collected during the trial at the 4-, 8- and 12-month follow-up using self-recorded patient utilisation. Resources included any type and quantity of each health-care service or good used during treatment or in the course of follow-up. Resource uses were number and type of GP or outpatient consultations, or contacts with nurses, physiotherapists, psychologists, surgeons or medical specialists, consulted within the NHS or on a private basis. Other NHS resources included were diagnostic tests [including X-ray, magnetic resonance imaging (MRI) scan, computerised tomography (CT) scan and blood tests], accident and emergency attendances, hospital admissions and drugs (including painkillers, anti-inflammatory drugs, sleeping tablets, antidepressants, topical medications, gels and creams and other drugs indicated by patients as being related to neck injury).
We collected data on out-of-pocket expenses and health care provided by the non-NHS sector. Items included were the resource use and costs for services accessed to treat neck injury, such as private physiotherapy, chiropractic, counselling, massage, osteopathy, orthopaedics and other consultations, diagnostic tests and admissions. Other resources were drugs paid for out-of-pocket and equipment, housing adaptations and aids. Participants were asked to indicate both the type and quantity of the goods and services purchased privately and the total amount paid either directly out-of-pocket or reimbursed by private medical insurance.
Unit costs
NHS costs
Total health-care costs were obtained multiplying resource use by their unit costs. Unit costs were those of physiotherapy or The Whiplash Book, primary care and outpatient consultations, ED and hospital admissions, the cost of drugs, diagnostic and other community care services, and finally the costs of privately purchased equipment, aids and adaptations (Table 59).
| Item | Unit cost (£) | Source |
|---|---|---|
| GP visit (surgery) | 36.00 | Curtis 200874 |
| Nurse visit (surgery) | 11.00 | Curtis 200874 |
| Physiotherapy visit | 33.90 | Curtis 200874 |
| Physiotherapy cycle | 218.00 | Curtis 200874 |
| Outpatient consultation | 116.50 | NHS reference costs 75 |
| Orthopaedic consultation | 119.00 | NHS reference costs 75 |
| Psychologist consultation | 72.00 | Curtis 200874 |
| Accident and emergency admission | 148.00 | NHS reference costs 75 |
| Occupational health consultation | 84.80 | NHS reference costs 75 |
| Ambulance | 263.00 | NHS reference costs 75 |
| NHS Direct telephone consultation | 16.40 | NHS reference costs 75 |
| Pain management clinic | 127.00 | NHS reference costs 75 |
| Diagnostics: X-rays | 30.95 | NHS reference costs 75 |
| Diagnostics: CT scan | 130.50 | NHS reference costs 75 |
| Diagnostics: MRI scan | 225.50 | NHS reference costs 75 |
| Diagnostics: blood tests | 3.39 | NHS reference costs 75 |
| Painkillers | 4.57 | PCA database76 |
| Anti-inflammatory drugs | 8.22 | PCA database76 |
| Gels, creams and ointments | 5.75 | PCA database76 |
| Sleeping pills | 3.66 | PCA database76 |
| Antidepressants | 5.86 | PCA database76 |
Unit costs used in the cost-effectiveness analysis were obtained from published UK sources and updated to 2009 prices using the UK National Statistics Healthcare Price Inflation Index.
Drug unit costs were calculated based on the typical drugs commonly prescribed for back pain, based on a consensus exercise among six academic GPs conducted alongside a trial of CB therapy in LBP. 77 The average cost of the prescriptions was then computed based on the bundle of typical drugs and drugs unit costs taken from the Prescription Cost Analysis database. 78
The cost of drugs other than the five typical groups above was included based on the costs declared by participants.
The costs of diagnostic tests, hospital and ED admissions were obtained from the NHS Reference Costs database. The cost of blood tests was the average of the cost of blood tests (speciality codes DAP823 and DAP839). The cost of ED was the cost of a ED consultation without a subsequent admission. Unit costs were obtained from the most recent NHS Reference Costs Database (2007)75 and updated to 2009 prices.
Private health-care unit costs
Private health-care costs were estimated using the costs paid for privately purchased health care (Table 60). This included physiotherapy, consultations with a variety of health-care professionals (osteopath, chiropractor, psychologist and outpatient consultations) as well as diagnostic tests, drugs, equipment and admissions. Resource consumption for each type of visit was collated from data declared by patients.
| Item | Unit cost (£) | Source |
|---|---|---|
| Outpatient consultation with NHS consultant | 182.50 | Telephone survey of six consultants’ private consultation fees for patients with LBP, at BMI Alexandra Hospital (Cheadle); BMI Meriden Hospital (Coventry); BMI Sarum Road Hospital (Winchester); Spire Bristol; Spire Gatwick Park; and Spire Leicester. Conducted in February 2008. Estimates are the average cost |
| X-ray | 86.20 | |
| CT scan | 551.60 | |
| MRI scan | 597.90 | |
| Blood tests | 109.80 | |
| Physiotherapy | 38.20 | Telephone survey of six specialists’ private consultation fees for patients with LBP, at Coventry Essex, Liverpool, London, Manchester and Newcastle. Conducted between 1 and 5 February 2008. Estimates are the average cost77 |
| Osteopath | 44.30 | |
| Chiropractor | 35.30 | |
| Psychologist | 70.40 | |
| Counsellor | 50.00 | |
| Massage therapist | 24.80 | |
| Acupuncture | 34.50 |
Privately purchased drugs were costed using the NHS costs for each group of drugs as reported in the previous section.
Hospital admissions were costed based on the total cost declared by patients, including both the cost directly paid by the patient and the medical insurance reimbursement. The costs of equipment and housing adaptations were included based on the costs declared by participants only.
Analysis
The base-case analysis included the sample of all participants who returned at least one resource use questionnaire at 4 months. Missing data were imputed only in a limited number of cases. For individuals who had missing NHS costs, data were imputed if the respondent had indicated the use of a resource but not the quantity. Data were not imputed for self-funded items as the patients declared the total amount disbursed; therefore, the cost of each type of private service consumed was not available.
The cost–utility analysis was conducted using data from cases that had completed at least one follow-up questionnaire. For patients who failed to return at least one questionnaire, data were not imputed, as the inverse-weighted analysis (illustrated below) allows adjusting for the total time of follow-up for each patient. Furthermore, the number of missing resource-use and cost data was low.
We also conducted a descriptive analysis of cost and resource-use data to provide cost data in reusable form. To ensure that the resource use and costs were based on a homogeneous time period, the descriptive analysis was conducted on complete cases only, including cases that had returned resource consumption data over a 12-month period.
Quality-adjusted life-years
The EQ-5D data obtained from participants questionnaires were converted into utility weights using an econometric model developed from a survey of time trade-off valuations of health states from members of the British general public. 31 Utility weights are a measure of the relative value of a health state compared with perfect health and are between 0 and 1. These extremes indicate the utility associated with death and perfect health, respectively.
Quality-adjusted life-years were then calculated for each participant using the area under the curve, which is the weighted sum of the utility at baseline and at 4, 8 and 12 months, and the time spent in each period expressed in years.
The trial did not collect utility data at baseline, because participants were enrolled at EDs with minimal data collection. Utility data were collected in the 2-week, 4-month, 8-month and 12-month follow-up questionnaires. Therefore, we imputed utility values at baseline using utility data from the general population derived from the Health Survey for England,79 matching values by age. This is justified as the population in this trial is made up by individuals from the general population who had an accident, but were otherwise no different from the general public. Baseline utility values were applied from the day of randomisation to 2 weeks, whereas data on utility collected in the trial were used thereafter.
Descriptive summaries for utility weights were calculated and the difference in weights between interventions and controls was tested using t-tests for differences in mean.
We explored the determinants of QALYs using a regression-based approach, including clinical and behavioural prognostic factors, such as a range of clinical indicators of severity of neck injury and neck pain, age, gender, psychological problems, utility at baseline and whether or not the participant sought compensation for neck injury.
Cost of care
Total cost of care was computed for each participant, multiplying the number and type of resources used by their unit costs.
The total cost of care was computed from the NHS and from the general health-care perspectives, including the cost components indicated previously (see Chapter 6, Data). The broad classes of costs included in the NHS perspective were the cost of consultations, admissions, physical and other therapies, drugs and diagnostic tests. The health-care perspective included, in addition to NHS costs, the costs of consultations, admissions, therapies, drugs, diagnostics and equipment privately purchased.
We conducted a descriptive analysis of mean costs using a complete case analysis at 4, 8 and 12 months. This includes patients who returned all questionnaires and patients whose data were collected on follow-up telephone calls if non-respondent and were asked to provide NHS and private resource consumption data.
Mean resources and costs were tabulated for each type of health-care resource separately for Step 1 and Step 2 of the study. Mean differences in costs by groups were tested for both steps of the study, using a t-test of difference in means.
As the cost of care is not symmetrically distributed, standard errors were also constructed using bootstrap procedures, sampling 5000 random samples from the original study data and calculating the mean at each sample. The 95% confidence bounds were computed from the empirical distribution of the means obtained from the bootstrap procedure.
We explored the determinants of costs using the same prognostic factors used in the analysis of QALYs, indicators of severity of neck injury and neck pain, age, gender, psychological problems, utility at baseline and whether or not the participant sought compensation for neck injury. This analysis aimed to establish the significant prognostic factors included in the incremental cost-effectiveness analysis. We analysed the significance of prognostic factors using ANOVA.
Incremental analysis
The incremental cost–utility ratio (ICUR) was calculated as the ratio between the difference in the mean cost of care and the difference in mean QALYs. The incremental cost–utility was calculated separately for the Step 1 and Step 2 comparisons, The Whiplash Book compared with standard care and physiotherapy compared with reinforcement of advice.
Incremental QALYs and costs were calculated using a regression approach. Mean costs and mean QALYs were estimated in a regression including a term for treatment, and controlling for length of follow-up and baseline utility as continuous factors, as these factors are correlated with total QALYs and total costs. The regression was also controlled for prognostic factors that emerged from the descriptive analysis of costs and QALYs.
The difference in mean costs and mean QALY was the coefficient of the treatment term in the regression. A positive coefficient indicated that treatment was an independent predictor of increased costs and of health gain, (expressed in QALYs); therefore, the ICUR was computed as the ratio of the coefficient of costs and QALYs obtained from the regressions.
Mean QALYs were estimated as the inverse probability weighted mean of the total quality-adjusted survival for each participant in the four groups. The use of inverse probability weighting is justified to account for censoring of participants data owing to loss of follow-up and as the accrual of costs and QALYs are believed to be correlated with the duration of participation into the study. Therefore, the accrual of QALYs may differ between patients who were followed up for the entire duration of the trial and those that were lost to follow-up at earlier dates. In this analysis we applied the inverse-weight adjustment to the estimation of QALYs only.
Furthermore, we used the regression approach to control for factors that may be important in the prediction of costs and quality of life (QoL). The estimation of mean costs and QALYs should be adjusted a priori by utility at baseline. This is because the value of utility at baseline correlates with the total QALY as it enters its calculation directly. Any randomised comparison between treatments is likely to show a difference in utility by group at baseline. Any imbalance in the utility at baseline, regardless of statistical significance, should always be regarded as a source of bias in the computation of the total QALY difference between the two groups. In addition, such analysis allows for the incorporation of adjustments for control factors depending on the results of the cost and QALY analysis, which may reveal additional significant predictors of costs and QALYs.
To explore the uncertainty in the cost–utility analysis, we used a non-parametric bootstrap approach, sampling 5000 random samples for costs and QALYs from the original study. A group of equal number of cases than the original study groups was sampled for each bootstrap iteration and the incremental costs and QALYs were calculated using a regression.
Incremental costs and QALYs were plotted on the cost-effectiveness plane, which shows the joint distribution of the difference in costs and the difference in QALYs generated by the bootstrap procedure. The cost-effectiveness plane is divided in four quadrants, each of them representing a potential combination of incremental costs and QALYs:
-
The active intervention (The Whiplash Book or physiotherapy) is more effective than the comparator (usual care or reinforcement of advice) but also more expensive. This combination identifies points on quadrant I of the cost-effectiveness plane. In this case, the intervention is deemed cost-effective if the incremental cost–utility ratio falls below the societal decision maker’s willingness to pay (WTP) the monetary value that the decision maker is willing to pay for one additional QALY. The societal decision maker’s WTP has proven empirically difficult to set, although it has been suggested that, for the UK, the societal cost-effectiveness threshold could be at around £30,000. Therefore, the cost–utility was presented over the range £0–50,000. The decision-maker’s cost-effectiveness threshold is also known with the symbol λ.
-
The active intervention is both less costly and less effective than the comparator (points on quadrant III). This combination indicates that the usual care or reinforcement of advice is cost-effective and therefore the comparator should be chosen if the ICUR is lower than the decision maker’s cost-effectiveness threshold.
-
The Whiplash Book or physiotherapy is less expensive, yet more effective than usual care or reinforcement of advice (quadrant IV). Then the interventions are ‘dominant’ therefore should be always chosen.
-
The Whiplash Book or physiotherapy is more expensive and less effective (quadrant II). Therefore, the interventions are ‘dominated’ as there is no cost-effectiveness threshold at which the decision maker would be willing to pay.
The cost-effectiveness plane provides a visual illustration of the extent of cost-effectiveness or dominance combinations and the extent of cost–effective combinations for The Whiplash Book or physiotherapy.
Because of the presence of dominance combinations, the variability of the incremental cost–utility ratio cannot be represented with confidence intervals. Therefore, we investigated the uncertainty around the ICUR calculating the net benefit (NB) statistic,
which is a summary statistic for the net value of The Whiplash Book or of physiotherapy expressed as the monetary value of the incremental gain, weighted by the WTP of the decision maker, and net of the cost of the intervention. Therefore, an intervention is cost-effective when the total monetary value of health gain is higher than its costs, hence when the net benefit is positive.
From the incremental costs and QALYs obtained from the bootstrap sample, the net benefit was calculated for a range of cost-effectiveness threshold values. The empirical proportion of positive net benefit was estimated and plotted on a graph, the cost-effectiveness acceptability curves (CEACs), a representation of the probability that each intervention is cost-effective given the range of WTP of the decision-maker. CEACs were presented for both The Whiplash Book and physiotherapy.
The cost–utility analysis was reported presenting the results of the regression models used to estimate the incremental QALYs and the incremental costs. To explore the impact of methodological assumptions, we report the results of the cost–utility analysis with and without the inverse probability weight adjustment applied in the regression models used to estimate incremental costs and QALYs. Furthermore, to assess the performance of the bootstrap procedure, we also report the results of the regressions estimated using the bootstrap procedure and compare them with the results of the exact regression models.
For each comparison, The Whiplash Book versus usual care and physiotherapy versus reinforcement of advice, we then report the CEACs illustrating the probability of cost-effectiveness over a range of decision makers’ WTP between £0 and £50,000.
Results
Cases included in the economic evaluation
The descriptive analysis of costs was conducted on a sample of 2706 cases. The number of valid cost questionnaires at each follow-up is reported in Table 61.
| Period of collection | No. of valid questionnaires | % of total participants |
|---|---|---|
| Baseline | 3851 | 100 |
| 2 weeks | 3851 | 100 |
| 4 months | 3088 | 80 |
| 8 months | 2745 | 71 |
| 12 months | 2706 | 70 |
The regression models for QoL and costs use all data from patients with QoL scores and valid cost data. However, information on prognostic factors was not available for all cases. Therefore, the regression sample was of 2386 cases and the cost regression sample was of 2104 for the Step 1 analysis and 413 for the Step 2 analysis (Table 62).
| No. of complete cases | |
|---|---|
| NDI score | 2963 |
| Claimants | 2617 |
| Severity of neck injury | 3851 |
| Psychological problems | 3483 |
| Neck pain | 3480 |
Utility scores
Raw utility scores collected from participants did not differ by group over the course of the study. Table 63 illustrates the average EQ-5D scores at baseline and 2 weeks, 4, 8 and 12 months, by treatment groups. These are the crude scores, and are intended to provide a description of the data used in the cost-effectiveness analysis.
| Baseline | 2 weeks | 4 months | 8 months | 12 months | |
|---|---|---|---|---|---|
| Step 1 (n = 3851) | |||||
| The Whiplash Book | 0.900 | 0.577 | 0.723 | 0.771 | 0.804 |
| Usual care | 0.899 | 0.593 | 0.747 | 0.791 | 0.807 |
| Difference | –0.001 | –0.016 | –0.024a | –0.020b | –0.003 |
| Step 2 (n = 584) | |||||
| Physiotherapy | 0.891 | 0.455 | 0.673 | 0.693 | 0.721 |
| Reinforcement of advice | 0.890 | 0.470 | 0.664 | 0.726 | 0.765 |
| Difference | –0.001 | –0.015 | 0.008 | –0.033 | –0.044c |
Incremental quality-adjusted life-years
From the raw scores collected at study follow-up, we estimated the mean QALY per group using a regression model including a treatment term. The results of the regression models are reported in the sections below, presented by model and by whether or not inverse-weight adjustments were used.
Model 1: non-inverse-weighted incremental quality-adjusted life-years
Table 64 reports the coefficients of the regression model used to estimate QALYs. This is a deterministic regression in that it is run on the data set and is not inverse-probability weighted.
| Coefficient | Standard error | p-value | 95% CI | |
|---|---|---|---|---|
| Step 1 | ||||
| Constant | 0.2460 | 0.1514 | 0.104 | –0.0509 to 0.5429 |
| Treatment (The Whiplash Book) | –0.0022 | 0.0052 | 0.67 | –0.0124 to 0.008 |
| NDI score at baseline | –0.0076 | 0.0002 | 0 | –0.008 to –0.0073 |
| Utility at baseline | –0.0765 | 0.1456 | 0.60 | –0.3621 to 0.2091 |
| Age | –0.0013 | 0.0005 | 0.01 | –0.0023 to –0.0004 |
| Gender | 0.0041 | 0.0054 | 0.44 | –0.0064 to 0.0146 |
| Claimed compensation | 0.0040 | 0.0058 | 0.50 | –0.0074 to 0.0153 |
| Severe | –0.0013 | 0.0052 | 0.80 | –0.0116 to 0.0089 |
| Psychological problems | –0.0517 | 0.0055 | 0 | –0.0625 to –0.0409 |
| Previous neck problems | –0.0044 | 0.0109 | 0.68 | –0.0257 to 0.0169 |
| Length follow-up | 0.0021 | 0.0001 | 0 | 0.002 to 0.0023 |
| Model fit: probability > F(10,2043) = 0.000, r2 = 0.6392 | ||||
| Step 2 | ||||
| Constant | 0.7931 | 0.3965 | 0.05 | 0.0135 to 1.573 |
| Treatment (physiotherapy) | –0.0102 | 0.0129 | 0.43 | 0.0356 to 0.0152 |
| NDI score at baseline | –0.0075 | 0.0004 | 0.00 | –0.0084 to –0.0068 |
| Utility at baseline | –0.5642 | 0.3751 | 0.13 | –1.3017 to 0.1733 |
| Age | –0.0032 | 0.0014 | 0.02 | –0.0059 to –0.0006 |
| Gender | 0.0015 | 0.0139 | 0.91 | –0.0258 to 0.0289 |
| Claimed compensation | 0.0172 | 0.0167 | 0.30 | –0.0157 to 0.0501 |
| Severe | –0.0223 | 0.0182 | 0.22 | –0.0134 to 0.0580 |
| Psychological problems | –0.0464 | 0.0148 | 0.00 | –0.0755 to –0.0174 |
| Previous neck problems | –0.0479 | 0.0241 | 0.05 | –0.0952 to 0.0006 |
| Length follow-up | 0.0020 | 0.0003 | 0.00 | 0.0013 to 0.0026 |
| Model fit: probability > F(10,392) = 0.000, r2 = 0.562 | ||||
This regression is estimated using all cases with valid or imputed EQ-5D; therefore, all patients are potentially included in the regression, however, there are a large number of participants with missing values for predictors.
Overall the model seems to fit reasonably well. Using this model, the (deterministic) base-case incremental QALY are calculated for both Step 1 and Step 2. The Whiplash Book achieves 0.7547 QALYs and usual care achieves 0.7577, with a negative incremental QALY of –0.003. At Step 2, physiotherapy achieves 0.6908 QALYs and reinforcement of advice 0.7019, with a negative incremental QALY of –0.011.
The negative incremental QALY for Step 2 indicates that physiotherapy does not improve QoL. The Whiplash Book has a very small yet negative incremental QALY in the deterministic analysis.
To estimate the variation around the incremental cost-effectiveness ratio (ICER) a bootstrap procedure is used to estimate the incremental QALYs using 5000 replications. The expected incremental QALYs are reported in Table 65 below.
| Non-inverse weight-adjusted (deterministic results) | Non-inverse weight-adjusted (probabilistic bootstrap estimation) | |
|---|---|---|
| Step 1 | ||
| The Whiplash Book | 0.7547 | 0.7546 |
| Usual care | 0.7577 | 0.7576 |
| Incremental QALY | –0.00298 | –0.0031 |
| Step 2 | ||
| Physiotherapy | 0.6908 | 0.6855 |
| Reinforcement of advice | 0.7019 | 0.6967 |
| Incremental QALY | –0.0111 | –0.0112 |
Model 2: inverse-weighted incremental quality-adjusted life-years
The inverse-weights adjusted analysis shows similar results compared with the standard regression approach (Table 66). Overall, The Whiplash Book achieves 0.7912 QALYs and reports a negative QALY gain when compared with usual care, –0.0046 incremental QALYs. Likewise, physiotherapy achieves 0.718 QALYs with a decrement of –0.0115 QALYs when compared with reinforcement of advice.
| Inverse-weighted, deterministic | Inverse-weighted (probabilistic, bootstrapped) | |
|---|---|---|
| Step 1 | ||
| The Whiplash Book | 0.7912 | 0.7918 |
| Usual care | 0.7958 | 0.7959 |
| Incremental QALY | –0.0046 | –0.0041 |
| Step 2 | ||
| Physiotherapy | 0.7183 | 0.7186 |
| Reinforcement of advice | 0.7298 | 0.7297 |
| Incremental QALY | –0.0115 | –0.0111 |
These results are similar when the analysis is conducted using bootstrap, with The Whiplash Book reporting an incremental QALY of –0.0041 and physiotherapy a decrement in total QALY of –0.0111 (Table 66). Overall the interventions do not improve QoL and although the differences are small, the incremental QALYs remain negative regardless of methodological approach.
Resource use
This section describes the patterns of health care used by individuals in the trial. Tables 67 and 68 report a breakdown of resource consumption for each stage, for NHS resources and for resources privately purchased, respectively. Overall, there are no reported differences in the use of health-care resources between individuals who are given The Whiplash Book and those who receive usual care in Step 1.
| Type of care | Step 1 | Step 2 | ||
|---|---|---|---|---|
| The Whiplash Book | Usual care | Physiotherapy | Reinforcement of advice | |
| Consultations | ||||
| GP consultations | 2.03 | 1.93 | 2.97 | 2.18a |
| Nurse consultations | 0.11 | 0.12 | 0.26 | 0.11 |
| Physiotherapy sessions | 2.15 | 2.24 | 4.15 | 2.79b |
| ED | 0.33 | 0.30 | 0.44 | 0.28b |
| Outpatient consultations | 0.19 | 0.21 | 0.22 | 0.26 |
| Psychologist | 0.21 | 0.09 | 0.19 | 0.10 |
| Orthopaedician | 0.10 | 0.13 | 0.11 | 0.14 |
| Other | 0.08 | 0.1 | 0.16 | 0.09 |
| Diagnostics | ||||
| X-ray test | 0.19 | 0.19 | 0.25 | 0.19 |
| CT scan | 0.02 | 0.01 | 0.03 | 0.03 |
| MRI scan | 0.05 | 0.04 | 0.07 | 0.04 |
| Blood tests | 0.10 | 0.14 | 0.18 | 0.09 |
| Other | 0.33 | 0.53 | 0.01 | 0.41 |
| Drugs (prescriptions) | ||||
| Painkillers | 1.53 | 1.39 | 2.57 | 1.76a |
| Anti-inflammatory | 0.85 | 0.91 | 1.42 | 0.84b |
| Gels and creams | 0.18 | 0.19 | 0.34 | 0.15 a |
| Sleeping drugs | 0.19 | 0.12 | 0.42 | 0.10 a |
| Antidepressants | 0.27 | 0.326 | 0.67 | 0.29 |
| Admissions (number) | ||||
| Admissions, total | 0.01 | 0.01 | 0.01 | 0.02 |
| Type of care | Step 1 | Step 2 | ||
|---|---|---|---|---|
| The Whiplash Book | Usual care | Physiotherapy | Reinforcement of advice | |
| Consultations | ||||
| Physiotherapy | 1.42 | 1.81a | 1.09 | 1.60 |
| Outpatient | 0.11 | 0.08 | 0.12 | 0.09 |
| Osteopath | 0.18 | 0.39b | 0.33 | 0.45 |
| Chiropractor | 0.48 | 0.44 | 0.67 | 0.29 |
| Psychologist | 0.09 | 0.04 | 0.20 | 0.05 |
| Other consultations | 0.28 | 0.27 | 0.31 | 0.45 |
| Diagnostics | ||||
| X-ray | 0.03 | 0.02 | 0.02 | 0.02 |
| CT scan | 0 | 0 | 0 | 0 |
| MRI scan | 0.01 | 0.01 | 0.01 | 0.02 |
| Blood tests | 0.03 | 0.01 | 0.02 | 0.03 |
| Other diagnostics | 0.01 | 0.01 | 0.02 | 0.01 |
| Drugs | ||||
| Painkillers | 3.95 | 4.08 | 6.52 | 6.28 |
| Anti-inflammatory | 2.22 | 2.63 | 3.48 | 3.06 |
| Gels and creams | 0.58 | 0.68 | 0.80 | 0.85 |
| Sleeping pills | 0.12 | 0.11 | 0.13 | 0.03a |
| Antidepressants | 0.05 | 0.08 | 0.05 | 0.01 |
In Step 2, individuals treated with physiotherapy report a more intensive use of GP consultations and accident and emergency services. Unsurprisingly, those allocated to physiotherapy report higher use of this service, although the group allocated to reinforcement of advice makes more intensive use of physical therapy compared with individuals who participate in Step 1 only.
Health-care costs
In this section we present the descriptive analysis of total health-care costs of services provided by the NHS or, separately, of costs for health-care services privately paid for by participants.
The costs reported in this section are simple means of costs per quarter for people who returned the questionnaire or had core questionnaires filled-in over the telephone. The overall cost at 1 year includes the total costs for all patients who had completed follow-up at 12 months; therefore, it excludes the costs of participants who neither returned further questionnaires nor were interviewed on the phone for questionnaires at month 8 or 12. The final difference over 1 year is reported here for descriptive purposes, but will differ from the incremental cost in the regression. This section simply aims to describe the nature of the cost data.
NHS costs
Tables 69 and 70 illustrate the costs supported for health care provided by the NHS. There were few differences in costs of NHS care between The Whiplash Book group and the usual care group. The total cost of NHS care was £311 with The Whiplash Book and £283 with usual care. The difference was not statistically significant and was mostly made up of the difference in costs for admissions, which were very few in number.
| Type of care | Step 1 | Step 2 | ||
|---|---|---|---|---|
| The Whiplash Book (£) | Usual care (£) | Physiotherapy (£) | Reinforcement of advice (£) | |
| (a) Consultations, total | 247.42 | 237.87 | 370.06 | 272.47a |
| GP consultations | 73.15 | 69.58 | 106.99 | 78.48a |
| Nurse consultations | 1.22 | 1.30 | 2.88 | 1.20 |
| Physiotherapy sessions | 73.03 | 75.93 | 140.51 | 94.63b |
| Accident and emergency | 48.93 | 43.98 | 65.70 | 41.38b |
| Outpatient consultations | 22.17 | 24.01 | 26.13 | 30.37 |
| Psychologist | 15.18 | 6.33 | 13.79 | 7.17 |
| Orthopaedist | 12.40 | 15.10 | 13.35 | 16.92 |
| Other | 1.35 | 1.65 | 0.71 | 2.32 |
| (b) Diagnostics, total | 19.71 | 16.55 | 26.68 | 19.77 |
| X-ray | 5.97 | 5.77 | 7.67 | 5.72 |
| CT scan | 2.89 | 1.70 | 3.66 | 3.71 |
| MRI scan | 10.17 | 8.07 | 14.75 | 9.62 |
| Blood tests | 0.35 | 0.47 | 0.60 | 0.31 |
| Other | 0.33 | 0.53 | 0.00 | 0.41 |
| (c) Drugs, total | 17.24 | 17.22 | 30.74 | 17.93c |
| Painkillers | 6.99 | 6.33 | 11.72 | 8.06a |
| Anti-inflammatory | 6.95 | 7.44 | 11.64 | 6.93b |
| Gels and creams | 1.03 | 1.10 | 1.93 | 0.87a |
| Sleeping drugs | 0.70 | 0.44 | 1.52 | 0.35a |
| Antidepressants | 1.56 | 1.91 | 3.92 | 1.72 |
| (d) Admissions, total | 26.84 | 11.83 | 12.74 | 25.85 |
| Total costs (a + b + c + d) | 311.22 | 283.47 | 440.22 | 336.02a |
| Groups | 4 months (£) | 8 months (£) | 12 months (£) | Overall costs 1 year (£) |
|---|---|---|---|---|
| Step 1 | ||||
| The Whiplash Book (n = 1219) | 167.85 | 80.24 | 63.14 | 311.22 |
| Usual care (n = 922) | 162.44 | 69.71 | 51.32 | 283.47 |
| Difference | + 5.41 | + 10.53 | + 11.82 | + 27.76 |
| Step 2 | ||||
| Physiotherapy (n = 214) | 254.75 | 112.46 | 73.01 | 440.22 |
| Reinforcement of advice (n = 211) | 179.93 | 84.42 | 71.68 | 336.02 |
| Difference | + 74.83b | + 28.04 | + 1.32 | + 104.19a |
The difference in costs between the physiotherapy and the reinforcement of advice groups were on the contrary statistically significant. Physiotherapy cost approximately £105 more than reinforcement of advice. The higher costs were due to consultations, physiotherapy sessions and emergency admissions. Overall, this group also had a higher expenditure on drugs. However, most cost differences were accrued at the start of the study indicating that the initial costs of physiotherapy were probably the main determinant of cost differences. Physiotherapy did not seem to reduce later health-care and treatment costs.
Non-NHS health-care costs and cost of privately purchased services
The cost of privately purchased health care is reported in Tables 71 and 72. Overall there is no difference in the cost of privately purchased care between The Whiplash Book and usual care and between the physiotherapy and reinforcement of advice groups. Nevertheless, in Step 2, the reinforcement of advice group spent more in privately paid physiotherapy compared with the physiotherapy group.
| Type of care | Step 1 | Step 2 | ||
|---|---|---|---|---|
| The Whiplash Book (£) | Usual care (£) | Physiotherapy (£) | Reinforcement of advice (£) | |
| Consultations | ||||
| Physiotherapy | 38.53 | 35.34 | 24.16 | 42.95 |
| Outpatient | 22.05 | 14.03 | 15.39 | 20.97 |
| Osteopath | 8.09 | 10.27 | 10.24 | 12.58 |
| Chiropractor | 13.45 | 12.07 | 25.82 | 11.94 |
| Psychologist | 8.11 | 1.36 | 5.69 | 3.86 |
| Other consultations | 6.26 | 16.01 | 11.12 | 12.98 |
| Diagnostics | ||||
| All diagnostics | 17.70 | 15.25 | 24.87 | 17.94 |
| Drugs | ||||
| Painkillers | 8.56 | 8.17 | 12.39 | 12.36 |
| Anti-inflammatory | 4.65 | 8.65 | 7.65 | 6.66 |
| Gels and creams | 2.85 | 2.81 | 3.74 | 4.89 |
| Sleeping pills | 0.58 | 0.45 | 0.71 | 0.28a |
| Antidepressants | 0.30 | 0.46 | 0.61 | 0.05a |
| Other | 0.65 | 8.25 | 1.37 | 0.70 |
| Admissions | 14.60 | 0.00 | 1.37 | 0.00 |
| Equipment | 8.28 | 9.30 | 14.37 | 15.14 |
| Total | 154.66 | 142.42 | 159.50 | 163.28 |
| Groups | 4 months (£) | 8 months (£) | 12 months (£) | Overall costs 1 year (£) |
|---|---|---|---|---|
| Step 1 | ||||
| The Whiplash Book (n = 1219) | 61.76 | 35.36 | 57.54 | 154.66 |
| Usual care (n = 922) | 62.31 | 41.36 | 38.75 | 142.42 |
| Difference | –0.55 | –6.00 | 18.79 | 12.24 |
| Step 2 | ||||
| Physiotherapy (n = 214) | 63.40 | 49.26 | 46.84 | 159.50 |
| Reinforcement of advice (n = 211) | 63.64 | 51.62 | 48.02 | 163.28 |
| Difference | –0.24 | –2.36 | –1.18 | –3.78 |
Private health-care expenditure did not show any significant reduction in time (Table 72) with similar costs of care in each group at the start of the study and during follow-up.
Incremental costs: NHS perspective
We estimated incremental costs of The Whiplash Book compared with usual care and of physiotherapy compared with reinforcement of advice using a set of regression models.
The regression models were run on all patients who had at least one economics questionnaire for the follow-up at 4 months. Participants excluded from the cost-effectiveness analysis were those with no follow-up data at all.
We used two models for the regression, with and without inverse-weight adjustments. In the non-inverse weight-adjusted model, the regressions were run using the same predictors used for utility, with the exception of age (as continuous variable) and gender as these predictors were not significant. The differences in results between the two methods were very small and only the non-inverse-weighted results are presented.
Table 73 shows the results of the regression model for both Step 1 and Step 2. The Whiplash Book resulted in higher costs compared with usual care, with a difference of approximately £28. The difference in cost by treatment was not statistically significant.
| Coefficient (£) | Standard error (£) | p-value | CI (£) | |
|---|---|---|---|---|
| Step 1 | ||||
| Constant | 110.87 | 52.75 | 0.04 | 7.41 to 214.32 |
| Treatment (The Whiplash Book) | 27.95 | 21.93 | 0.20 | –15.06 to 70.96 |
| NDI score at baseline | 11.14 | 0.79 | 0.00 | 9.59 to 12.68 |
| Utility at baseline | –189.87 | 49.87 | 0.00 | –287.67 to –92.08 |
| Claimed compensation | 44.29 | 24.57 | 0.07 | –3.89 to 92.47 |
| Severe neck injury | 33.58 | 22.06 | 0.13 | –9.69 to 76.84 |
| Psychological problems | 20.87 | 25.57 | 0.42 | –29.28 to 71.01 |
| Previous neck problems | –39.17 | 45.49 | 0.39 | –128.39 to 50.05 |
| Model fit: probability > F(7, 2047) = 0.000, r2 = 0.1888 | ||||
| Step 2 | ||||
| Constant | 3.09 | 116.71 | 0.98 | –226.37 to 232.55 |
| Treatment (physiotherapy) | 58.36 | 46.59 | 0.21 | –33.25 to 149.96 |
| NDI score at baseline | 9.75 | 1.52 | 0.00 | 6.78 to 12.74 |
| Utility at baseline | –144.97 | 89.74 | 0.11 | –321.40 to 31.46 |
| Claimed compensation | 114.26 | 60.28 | 0.06 | –4.26 to 232.77 |
| Severe neck injury | 35.59 | 65.57 | 0.59 | –93.32 to 164.50 |
| Psychological problems | 74.04 | 57.12 | 0.120 | –38.24 to 186.33 |
| Previous neck problems | –199.63 | 85.36 | 0.02 | –367.46 to –31.81 |
| Model fit: probability > F(7, 395) = 0.000, r2 = 0.1880 | ||||
Independent cost drivers for Step 1 were baseline utility, with individuals starting the study with better QoL reporting fewer costs. NDI scores at study entry were also associated with a statistically significant increase in the cost of care, although the absolute value of this difference was not large. Finally individuals that claimed compensation were somehow more likely to report higher health-care costs with borderline statistical significance.
Reporting previous neck problems, psychological problems or severe neck injury were overall associated with higher costs of care, but the coefficients for these factors did not reach statistical significance.
For Step 2, the incremental cost of physiotherapy compared with reinforcement of advice was £58, although again the difference in costs was not statistically significant. Patients assigned to the physiotherapy group were more likely to report higher costs as a function of NDI score at baseline and whether or not they reported previous neck problems. These higher costs were statistically significant. Total incremental costs from the NHS perspective are summarised in Table 74.
| Non-inverse weight-adjusted (deterministic regression) (£) | Non-inverse weight-adjusted (probabilistic, bootstrapped) (£) | |
|---|---|---|
| Step 1 | ||
| The Whiplash Book | 305.37 | 299.12 |
| Usual care | 277.42 | 271.58 |
| Incremental cost | 27.95 | 27.54 |
| Step 2 | ||
| Physiotherapy | 414.73 | 412.92 |
| Reinforcement of advice | 356.37 | 353.64 |
| Incremental cost | 58.36 | 59.27 |
Incremental costs: general health-care perspective
Costs from the general health-care perspective were the sum of those supported by the NHS and the costs disbursed for privately purchased health care. Regression models were run for total health-care costs, reflecting the analysis conducted for the NHS costs only.
Table 75 illustrates the coefficients resulting from the estimation of costs based on treatment and predictors. The incremental costs with The Whiplash Book from the total health-care perspective was –£22, indicating that, when controlling for predictors of costs, The Whiplash Book cost less than usual care. This difference was not statistically significant.
| Coefficient (£) | Standard error (£) | p-value | CI (£) | |
|---|---|---|---|---|
| Step 1 | ||||
| Constant | 160.44 | 74.97 | 0.032 | 13.41 to 307.46 |
| Treatment (The Whiplash Book) | –21.93 | 31.17 | 0.48 | –83.05 to 39.19 |
| NDI score at baseline | 15.84 | 1.12 | 0.00 | 13.64 to 18.03 |
| Utility at baseline | –183.23 | 70.87 | 0.01 | –322.20 to –44.25 |
| Claimed compensation | 78.99 | 34.91 | 0.02 | 10.52 to 147.46 |
| Severe neck injury | 16.57 | 31.35 | 0.60 | –44.91 to 78.05 |
| Psychological problems | 32.71 | 36.34 | 0.37 | –38.55 to 103.97 |
| Previous neck problems | –23.60 | 64.65 | 0.72 | –150.39 to 103.19 |
| Model fit: probability > F(7, 2047) = 0.000, r2 = 0.1741 | ||||
| Step 2 | ||||
| Constant | –11.12 | 159.13 | 0.94 | –323.96 to 301.73 |
| Treatment (physiotherapy) | 48.29 | 63.53 | 0.45 | –76.61 to 173.18 |
| NDI score at baseline | 14.04 | 2.07 | 0.00 | 9.97 to 18.10 |
| Utility at baseline | –168.58 | 122.35 | 0.17 | –409.12 to 71.96 |
| Claimed compensation | 195.47 | 82.19 | 0.02 | 33.88 to 357.05 |
| Severe neck injury | 33.02 | 89.40 | 0.71 | –142.73 to 208.78 |
| Psychological problems | 99.07 | 77.87 | 0.20 | –54.02 to 252.17 |
| Previous neck problems | –191.48 | 116.39 | 0.10 | –420.29 to 37.34 |
Predictors of total health-care costs were NDI score at baseline (+ £16), utility at baseline (–£183) and whether or not the participant claimed compensation (+ £79).
For Step 2, physiotherapy carried an incremental cost of £48 that was not statistically significant. Similarly to Step 1, the predictors of costs were NDI scores at baseline and whether or not the participant claimed compensation. Baseline utility had a large effect on costs (–£169); however, this effect failed to reach statistical significance.
Table 76 summarises the incremental costs for The Whiplash Book and physiotherapy obtained from the regression models. These costs are the inputs to the cost-effectiveness analysis in the following section.
| Non-inverse weight-adjusted (deterministic regression) (£) | Non-inverse weight-adjusted (probabilistic, bootstrapped) (£) | |
|---|---|---|
| Step 1 | ||
| The Whiplash Book | 420.89 | 304.43 |
| Usual care | 442.82 | 283.81 |
| Incremental cost | –21.93 | –20.62 |
| Step 2 | ||
| Physiotherapy | 576.80 | 522.23 |
| Reinforcement of advice | 528.51 | 575.77 |
| Incremental cost | + 48.29 | + 53.54 |
Incremental cost-effectiveness
Incremental cost-effectiveness: NHS
The ICER was obtained from the regressions of costs and QALYs for the two steps of the study.
The Whiplash Book was associated with higher costs and lower QALYs and therefore was dominated by usual care. Similarly, physiotherapy was both more expensive and less effective than reinforcement of advice (Table 77).
| Incremental costs (£) | Incremental QALYs | ICER | |
|---|---|---|---|
| Non-inverse weight-adjusted (deterministic results) | |||
| Step 1 | |||
| The Whiplash Book vs usual care | 27.95 | –0.00298 | Dominated |
| Step 2 | |||
| Physiotherapy vs reinforcement of advice | 58.36 | –0.0111 | Dominated |
| Non-inverse weight-adjusted (probabilistic, bootstrapped expectation) | |||
| Step 1 | |||
| The Whiplash Book vs usual care | 27.54 | –0.0031 | Dominated |
| Step 2 | |||
| Physiotherapy vs reinforcement of advice | 59.27 | –0.0112 | Dominated |
These results were invariant with respect to the methods used to estimate costs and QALYs. In the bootstrap analysis, both The Whiplash Book in Step 1 and physiotherapy in Step 2 are dominated at any level of WTP. The inverse weighting also did not have an impact on the results (Tables 77 and 78).
| Incremental costs (£) | Incremental QALYs | ICER | |
|---|---|---|---|
| Inverse weight-adjusted (deterministic results) | |||
| Step 1 | |||
| The Whiplash Book vs usual care | 27.95 | –0.0046 | Dominated |
| Step 2 | |||
| Physiotherapy vs reinforcement of advice | 58.36 | –0.0115 | Dominated |
| Inverse weight-adjusted (probabilistic, bootstrapped expectation) | |||
| Step 1 | |||
| The Whiplash Book vs usual care | 27.54 | –0.0041 | Dominated |
| Step 2 | |||
| Physiotherapy vs reinforcement of advice | 59.27 | –0.0111 | Dominated |
The CEACs (Figure 17) for Step 1 and Step 2 show that both interventions at Step 1 (The Whiplash Book) and Step 2 (physiotherapy) are dominated by the comparators at any threshold of cost-effectiveness used by decision makers.
FIGURE 17.
Cost-effectiveness acceptability curves for Step 1 and Step 2: NHS perspective (inverse probability weighted model).
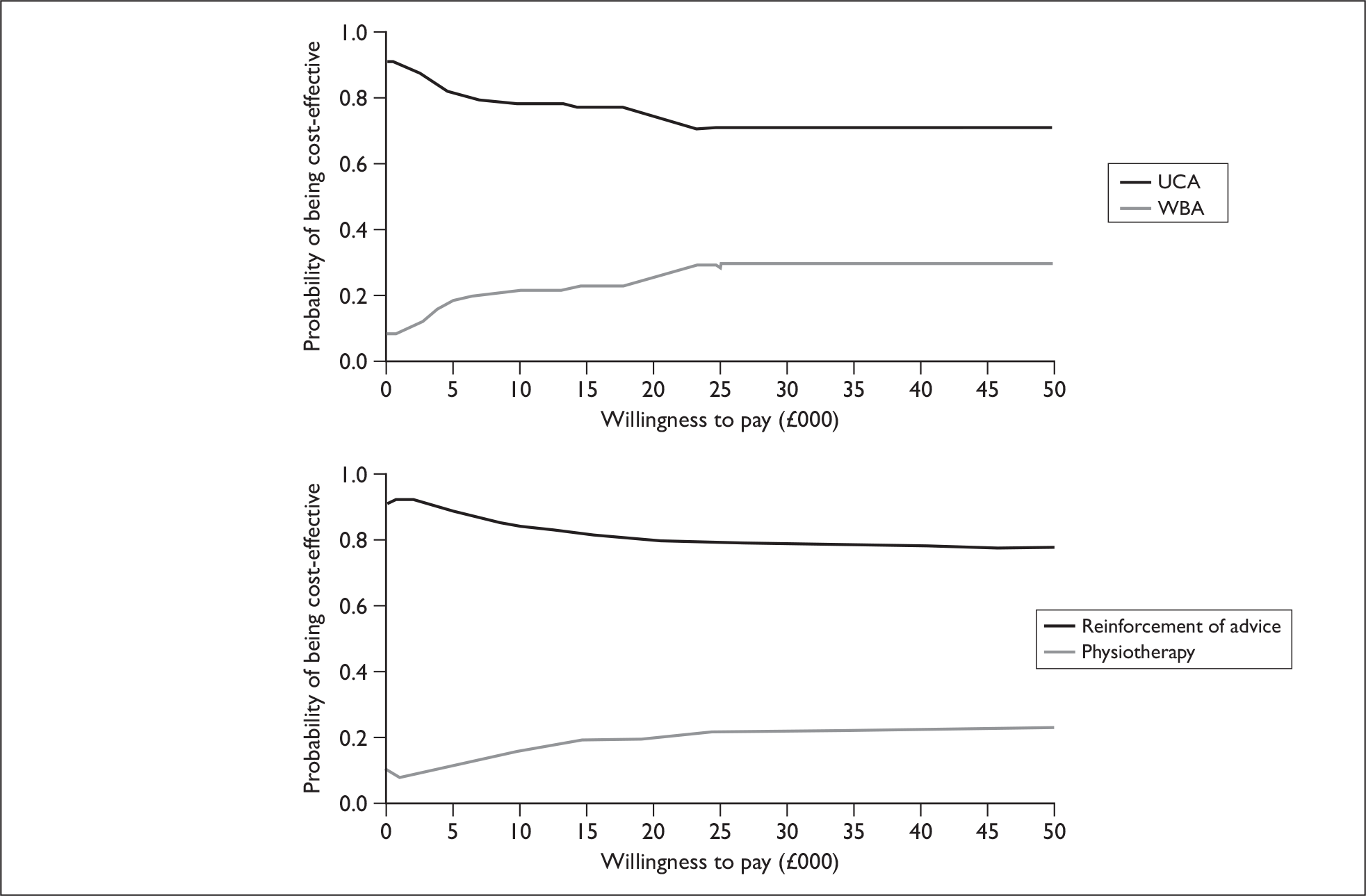
Incremental cost-effectiveness: general health-care perspective
The results of the incremental cost-effectiveness analysis from the viewpoint of the general health-care sector are similar to those of the NHS. The Whiplash Book is not cost-effective compared with usual care (Table 79). The intervention reduces the total QALYs slightly; however, the reduction in costs is not sufficient to compensate for the loss of health outcomes and therefore usual care remains cost-effective at a ICER of approximately £7000. Physiotherapy remains dominated as it remains associated with an increase in costs and a decrease in health outcomes. Again these results are robust to the analytical methods adopted in the cost-effectiveness (Tables 79 and 80).
| Incremental costs (£) | Incremental QALYs | ICER | |
|---|---|---|---|
| Non-inverse weight-adjusted (deterministic results) | |||
| Step 1 | |||
| The Whiplash Book vs usual care | –21.93 | –0.0030 |
£7359 Usual care is cost-effective |
| Step 2 | |||
| Physiotherapy vs reinforcement of advice | 48.29 | –0.0111 | Dominated |
| Non-inverse weight-adjusted (probabilistic, bootstrapped expectation) | |||
| Step 1 | |||
| The Whiplash Book vs usual care | –20.62 | –0.0031 |
£6652 Usual care is cost-effective |
| Step 2 | |||
| Physiotherapy vs reinforcement of advice | 53.54 | –0.0112 | Dominated |
| Incremental costs (£) | Incremental QALYs | ICER | |
|---|---|---|---|
| Inverse weight-adjusted (deterministic results) | |||
| Step 1 | |||
| The Whiplash Book vs usual care | –21.93 | –0.0046 |
£4767 Usual care is cost-effective |
| Step 2 | |||
| Physiotherapy vs reinforcement of advice | 48.29 | –0.0115 | Dominated |
| Inverse weight-adjusted (probabilistic, bootstrapped expectation) | |||
| Step 1 | |||
| The Whiplash Book vs usual care | –20.62 | –0.0041 |
£5029 Usual care is cost-effective |
| Step 2 | |||
| Physiotherapy vs reinforcement of advice | 53.54 | –0.0111 | Dominated |
In the bootstrap analysis from the general health-care perspective, usual care is cost-effective at generally accepted cost-effectiveness thresholds. Physiotherapy remains dominated at any level of WTP. This is reflected in the CEACs for Step 1 and Step 2 (see Figure 18).
FIGURE 18.
Cost-effectiveness acceptability curves for Step 1 and Step 2: general health-care perspective (inverse probability weighted model).
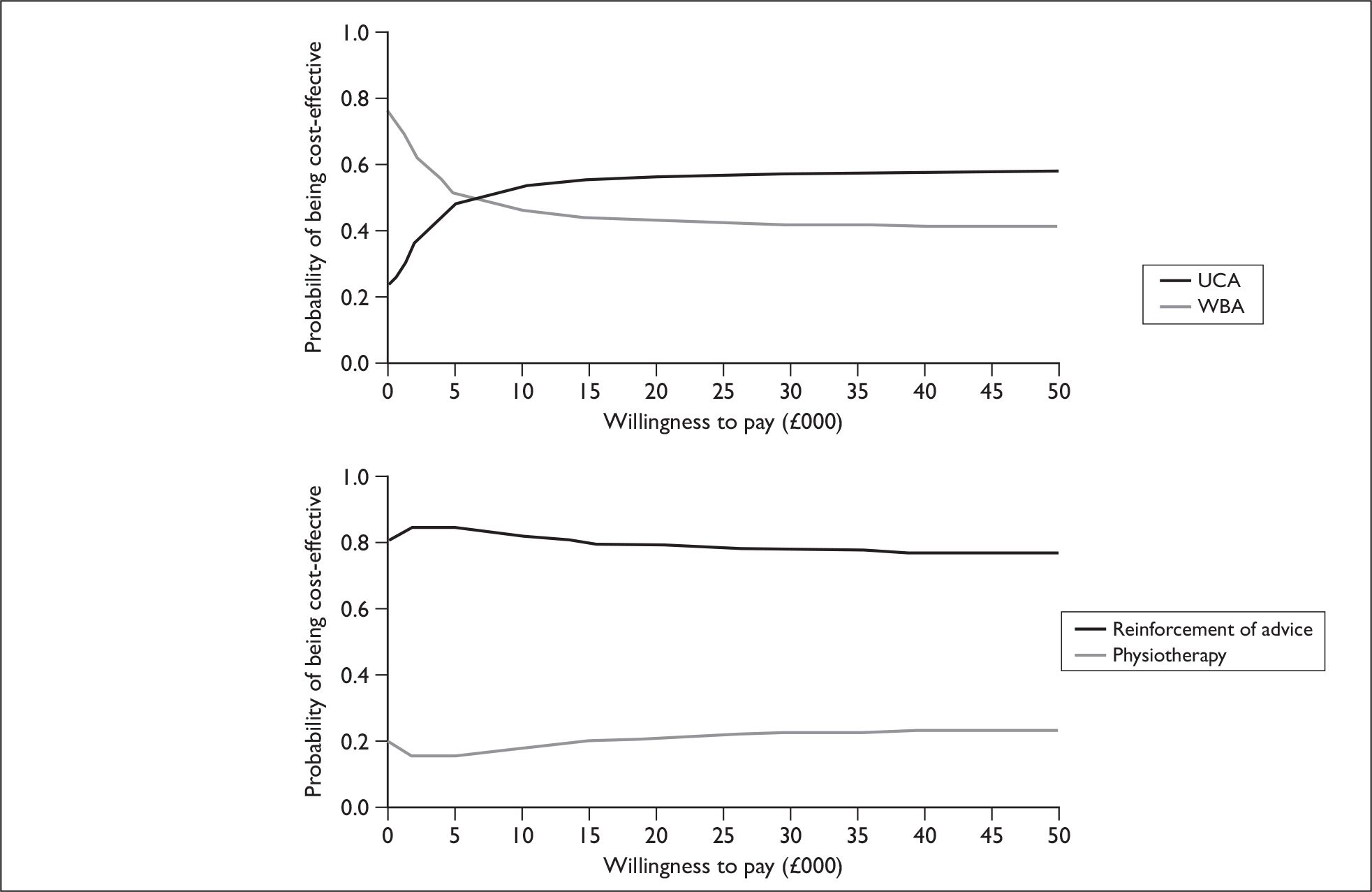
Chapter 7 Discussion
Aims and overview of the trial findings
In 1995, the QTF on whiplash injuries and disorders recognised the need for a definitive trial of treatments commonly used in whiplash injury, and, in particular, for a trial of physiotherapy. This need was reiterated by the British Bone and Joint Decade Task Force on whiplash injury in 2008, which, on reviewing the accumulating evidence base, concluded that progress in terms of large, definitive trials had been poor, and fundamental questions about the clinical management of whiplash remained. 80
MINT is the largest trial of treatments for acute whiplash injury completed to date. It was designed to provide a definitive answer to several questions about the clinical management of acute WAD. The sample size was large, to enable detection of small but potentially worthwhile clinical benefits and to allow a robust economic evaluation alongside the trial. The trial was also designed to track and evaluate a two-step process of delivering treatment which is observed frequently in clinical practice, that being the provision of a ‘light touch’ treatment of advice in the first instance, followed by a more resource-intensive second step of treatment to those who are struggling to recover. 81
The first step of the trial examined whether or not an enhanced advice and active management strategy, supplemented by a relatively inexpensive and bespoke advice booklet, was more effective than usual care. Overall, it was not. The second step of the trial examined two approaches to providing additional physiotherapy: a single session of advice or a typical package of physiotherapy allowing for up to six sessions of physiotherapy treatment. Although there was some small benefit of the additional physiotherapy package at 4 months after the injury, in the longer term this made no difference to the clinical outcome, and importantly, from a health-care perspective, the small clinical gain was not worth the additional cost at current accepted levels of WTP. We conclude, overall, that for those individuals who perceive they are struggling with recovery, a single session of advice from a physiotherapist is sufficient. Our design does not allow us to draw a direct comparison of no follow-up treatment. However, the qualitative data collected suggest strongly that the advice session provides much needed reinforcement and encouragement to engage with doing exercises and taking a positive approach to recovery. Overall, the best combination of treatment was UCA followed by a single physiotherapy advice session for those struggling. The pattern of clinical response was consistent across similar outcomes.
Internal validity and methodological limitations
The trial was powered to detect a moderate effect size (0.375), assuming a pooled SD of eight absolute points (16 percentage points). Overall, the assumptions underlying the sample estimate appear correct. For Step 1 of the trial, the pooled SD at each of the follow-up points was within our anticipated range. For Step 2 of the trial, the pooled SD at baseline was within the anticipated range, although it increased slightly over the follow-up time points. We estimated an ICC coefficient of 0.02 and an average of 350 patients per centre, giving an inflation factor of 7.98.
In the early phases of the study, we recognised that we would not achieve the desired sample size, and increased the number of clusters recruiting into the trial. This had the overall effect of reducing the sample size. At the close of the trial, the point estimate for the ICC suggested a much smaller clustering. This, combined with a smaller loss to follow-up than anticipated, means that MINT had good power to detect the differences we originally specified.
Acute injury trials present a particular difficulty in being able to estimate accurately the pre-injury status. A number of options exist – to collect the data retrospectively (which is subject to recall bias) or to accept the premise that randomisation will result in well-matched groups. Within the constraints of a large pragmatic trial in which treatments and trial procedures are being implemented alongside the day-to-day operations of EDs, we did not have the option to collect an extensive data set. Pre-treatment WAD grades were collected and a four-point indicator of HRQoL.
Randomisation resulted in two groups that were well matched in the first step of the trial. Although the ethnic mix of the sample was representative of the UK population, there were slightly more participants of Pakistani origin in one arm of the trial than in the other. Sensitivity analyses concluded that this small imbalance made no qualitative or quantitative difference to the overall estimates of treatment effect. In the second step of the trial, there was a difference in the NDI scores collected at the research clinic. We have examined our procedures carefully. The risk of allocation subversion is small, as we used a quality-assured telephone randomisation system. We stratified by site, but did not use blocking, thus minimising the chance that recruitment staff could anticipate and hold patients for favourable allocations. Allocation lists have been checked for date and sequence, and all found to be normal. The most likely explanation is that these differences have arisen by chance. Overall, the difference will not have affected our overall estimate of treatment effect; the difference was accounted for in the analysis.
Although we did not account for clustering attributable to therapist effects in the original sample size estimation, the final models of treatment effect were adjusted for these effects. The ICC for therapist effects was of the order of 0.02 for the primary outcome, indicating a minimal amount of intertherapist variability in the intervention effectiveness. In comparison with other studies, the therapist effects are small, and carry most influence at the time points nearest to the delivery of treatment.
Loss to follow-up was lower than expected for a trial of an acute injury. Previous pragmatic studies of acute injury management in EDs have reported loss to follow-up of ≥ 30% at 9 months. 82 We used a system of repeat questionnaires, supplemented by a telephone interview, to collect the core primary outcomes where postal response could not be elicited. Telephone data collection worked well, although we were unable to collect as much information and the process required substantial dedication from the trial team, including out-of-hours working. Although there was a tendency for younger men to respond less often, our estimates of the treatment effectiveness appear insensitive to missing data.
Analytically the greatest challenge posed by the trial was the lack of EQ-5D estimate prior to initiation of treatment in the ED, and prior to the injury in the first step of the trial. We addressed this by imputing a value based on the age and gender expected norms for each individual. This inevitably introduces some underestimation of variance in the EQ-5D, and an assumption that the population we recruited from is broadly reflective of the age- and gender-matched population. Overall, however, these assumptions and shortfalls are small, and we are confident in the conclusions of the economic analysis for Step 1 of the trial. Baseline values were available for Step 2 of the trial.
External validity and generalisability of the findings
Overall we believe the generalisability of the trial to be good, with good representation of the injury grades usually encountered in clinical practice, a wide range of hospitals and substantial numbers of participants. We recruited 15 EDs, comprising large teaching hospitals, foundation hospitals and district general hospitals. The EDs served a mix of urban and semi-rural catchment areas. The services available in these hospitals reflected the normal services in UK hospitals, with none having specific specialist services applicable to whiplash injuries. The level of training provided in WAD management was consistent with the best that could be achieved under the constraints of routine clinical practice. The population recruited was reflective of the expected incidence of different injury severity within the UK, and was similar in terms of age and gender to previous UK series. The recovery trajectory was consistent with published rates of recovery from smaller studies based on the UK population where reports of persistent symptoms at least 1 year post injury ranged from 16% to 48% of participants. 21,22,83–85 In MINT, approximately 18% of participants in Step 1 and 32% in Step 2 had persistent symptoms at 12 months (LWS). Forty-eight per cent of people had recovered at 4 months in Step 1 and 41% in Step 2.
The wide, pragmatic inclusion criteria have allowed us to investigate the effects in pre-specified subgroups of patients. Subgroup effects should be analysed through formal tests of statistical interaction and be pre-specified to avoid potentially spurious results. 34 We adopted both these approaches. The sample size allowed for detection of large subgroup effects (approximately double the size of the main effect), provided imbalance between the subgroups was no greater than 70 : 30. We investigated three potential subgroup effects: (1) severity of the index injury; (2) adverse psychological reactions to the injury; and (3) neck pain prior to the injury. We cannot draw any conclusions relating to neck pain prior to the injury because the subsample of people with prior neck pain is too small (< 7%). The distribution of other pre-specified subgroups was within the acceptable range within the first step of the trial. We can conclude that there were no substantial interactions between the psychological factors or injury severity and the provision of advice. In the second step of the trial there was a statistically significant interaction between symptom severity and treatment allocation, suggesting that the physiotherapy package is more effective in people with severe symptoms. However, this should be interpreted with caution as there were relatively few cases with mild symptoms in the second step of the trial.
Interpretation and implications for clinical practice and policy
Overall, there was no benefit to training EDs in an active management strategy and supplementing this advice with The Whiplash Book. The most probable explanation is that active management (as promoted by The Whiplash Book) is no more effective (or ineffective) in encouraging people to return to normal activities or to initiate exercise, and hence influence clinical outcome.
Although the extended physiotherapy package resulted in some short-term symptomatic relief in neck disability (or more rapid restoration of function), this additional treatment had no impact on generic HRQoL. This is perhaps surprising, and there are several potential explanations. First is that injury has minimal impact on HRQoL. We used two measures of generic HRQoL in this trial, the EQ-5D and the SF-12. The injury is isolated in its nature, and is unlikely to substantially impact on the locomotor system, which is an important component of measures of generic HRQoL. The injury is painful, and our data suggest that it affects fatigue, sleep, driving and reading predominantly – these domains do not feature strongly in either the SF-12 or EQ-5D. The conclusion of the health economic analysis, which is based on currently accepted methods of using the EQ-5D to facilitate comparison of the benefits across conditions, is that the cost of the additional treatment dominates the benefits. Hence, despite some short-term symptomatic relief, we do not recommend an extended physiotherapy package as a cost-effective treatment for routine clinical practice. The single supplementary advice session with the physiotherapist does appear beneficial in encouraging people to exercise and undertake self-management activities, but this conclusion is based on the qualitative component of the study, not any quantitative comparison.
There are a number of other potential reasons why the extended package is less effective than anticipated. This was a pragmatic trial, and the treatment effect may have been diluted by participants seeking physiotherapy or similar treatment elsewhere. Self-reported resource use suggests that, overall, people randomised to the additional physiotherapy package did receive extra treatment, and examination of the treatment records suggests that the therapists were broadly compliant with the treatment protocol.
As with all trials of complex interventions, it was necessary to select the components of the intervention to be evaluated from a range of possible treatments. We selected the treatments that are most commonly applied in contemporary clinical practice, and have some evidence supporting their effectiveness. The treatment package contained exercise, manual therapy, advice and reassurance, all of which have been reported to be efficacious in small trials,27,46–49 and it was consistent with the CSP guidelines for the management of WAD. However, the evidence base supporting these treatments is not high quality, and it is possible that there may be other techniques, for example CB therapy, that would be more effective. These require evaluation in future trials.
It is reassuring that the great majority of people we studied eventually recovered from their injury. We found that injury severity had some impact on treatment effectiveness, with the more serious injuries benefiting more from additional treatment. Serious adverse events were rare, and all of the treatments applied had an acceptable safety profile. Although there is some evidence of ceiling effects in the NDI score, we do not believe these to have had a substantial effect on our being able to detect clinically important differences.
There has been a long-standing interest surrounding the possible negative effect compensation has on outcome of whiplash injuries. 21,85–92 We investigated this from two perspectives. The number of people who pursued compensation was high, > 90% of participants who responded in both the Step 1 and Step 2 cohorts. Neither of the advice treatments affected the proportion of people pursing compensation. There was a suggestion in the analysis of Step 2 that physiotherapy treatment appeared more effective in those not pursuing a claim for compensation, but given the very small number of participants in this subgroup, this is uncertain.
Chapter 8 Conclusions
The active management strategy supplemented by The Whiplash Book is not more effective in promoting recovery from whiplash than UCA.
The active management strategy supplemented by The Whiplash Book costs more than UCA. The evidence generated in this trial suggests that the active management approach is not cost-effective in comparison with usual care.
For those people who are struggling with recovery, a physiotherapy package of up to six treatments produces some symptomatic improvements, but no difference in long-term outcomes. It has minimal impact on HRQoL and is not a cost-effective intervention from a health-care perspective. However, the number of work days lost is reduced.
The single session of advice from a physiotherapist appears useful in reinforcing the need to exercise and providing reassurance. It should be considered in preference to a more intensive physiotherapy package.
Future research questions
Further research is needed to better understand the importance of whiplash injuries in the spectrum of injury that are managed by the NHS. Although not part of the remit of the commissioned trial, the MINT data will be important in determining costs of whiplash injury by different grades of severity, and to determine whether or not poor recovery can be predicted with reasonable accuracy at different time points in the recovery trajectory. A better understanding of the basic epidemiology of disability after whiplash injury will also serve to develop new treatments. We would recommend further research to develop group-based CB programmes, which have been successful in the management of subacute and chronic lower back pain, for the management of WAD. Understanding the optimal time point to administer these programmes will be an important element of future research. Improved educational strategies in the ED, particularly those that can be given to a patient and result in a behavioural change, seem suitable candidates for further testing and development. Improving the content and relevance of The Whiplash Book, for example by addressing problems related to travel anxiety and other psychological manifestations related to stress, may improve effectiveness of the educational materials.
Acknowledgements
Contribution of authors
Sallie Lamb: chief investigator, study conception and design, development of interventions, supervision, writing and reviewing report.
Mark Williams: study management, development of interventions, writing and reviewing report.
Esther Williamson: development of interventions, study management, writing and reviewing report.
Simon Gates: study supervision, writing and reviewing report.
Emma Withers: study management, writing and reviewing report.
Shahrul Mt-Isa: designing and conducting statistical analysis, writing and reviewing report.
Deborah Ashby: study conception and design, study supervision, designing and conducting statistical analysis, writing and reviewing report.
Emanuela Castelnuovo: designing and conducting economic analysis, writing and reviewing report.
Martin Underwood: study conception and design, study supervision, writing and reviewing report.
Matthew Cooke: study conception and design, study supervision, writing and reviewing report.
Trial team
Trial management group
Professor Sallie Lamb, chief investigator
Professor Martin Underwood, co-applicant
Mr Mark Williams, clinical research fellow
Mrs Esther Williamson, clinical research fellow
Dr Simon Gates, principal research fellow
Professor Matthew Cooke, co-applicant
Mrs Emma Withers, study co-ordinator
Professor Deborah Ashby, co-applicant – statistician
Mr Shahrul Mt-Isa, statistician
Trial applicants
Professor Sallie Lamb, chief investigator
Professor Martin Underwood, co-applicant
Professor Matthew Cooke, co-applicant
Professor Ala Szczepura, co-applicant
Professor Deborah Ashby, co-applicant
Dr Richard Mayou, co-applicant
Dr Stephen Joseph, co-applicant
Dr Frances Griffiths, co-applicant
Trial Steering Committee
Mr Peter Driscoll, chairperson
Professor Deborah Ashby, statistician
Professor Matthew Cooke, co-applicant
Professor Sandra Eldridge, independent member
Professor Jennifer Klaber-Moffatt, independent member
Professor Sallie Lamb, chief investigator
Professor Ala Szczepura, health economist
Professor Martin Underwood, co-applicant
Mrs Anne Carson, lay member
Mr Mike Wakeman, lay member
Data Monitoring and Ethics Committee
Professor Tim Peters, chairperson
Dr Karen Barker, independent member
Professor Timothy Coats, independent member
Data management group
Mrs Emma Withers
Miss Lisa Craven
Mr Chris Rubery
Statistician
Professor Deborah Ashby
Mr Shahrul Mt-Isa
Health economist
Ms Emanuela Castelnuovo
Professor Ala Szczepura
Mr Anil Gumber
Research team (ED clinicians, nurses, physiotherapists, etc.)
Gemma Artz, physiotherapist
Nick Ashton, physiotherapist
Liz Ball, Research, clinician
Lucy Bardell, physiotherapist
Mitam Barooah, principal investigator
Alison Bartlett, physiotherapist
Nick Barton, physiotherapist
Kate Baskill, physiotherapist
Anna Beardshaw, physiotherapist
Charlotte Biggin, physiotherapist
Debbie Blassberg, physiotherapist
Louise Brooks, physiotherapist
Jane Callaway, physiotherapist
Joseph Chimera, physiotherapist
Prue Churchley, physiotherapist
Chris Cowley, physiotherapist
Liz Creak, physiotherapist
Sue Crew-Smith, physiotherapist
Linda Davies, physiotherapist
Frances Deery, physiotherapist
Alison Douglas, physiotherapist
Peter Doyle, principal investigator
Lesley Dransfield, physiotherapist
Matthew Dunn, principal investigator
Dr Kym Fraser, training advisor
Katie Glover, physiotherapist
Bridget Gray, research clinician
Joanne Hack, physiotherapist
Helen Harrison, research clinician
Yasmeen Hasnain, principal investigator
Alison Heap, physiotherapist
Amanda Hicks, physiotherapist
Katie Holt, physiotherapist
Phil Hormbrey, principal investigator
Claire Hunt, research clinician
Virginia Kay, physiotherapist
Susan Kempson, research clinician
Jason Kendall, principal investigator
Janet King, physiotherapist
Mary Kinsey, physiotherapist
Steven Lodge, research clinician
Janet Lowe, research clinician
Rebecca Mallin-Jones, physiotherapist
Dave Mason, physiotherapist
Steve McCabe, principal investigator
Chris McCarthy, expert review of intervention
Cathy McDonald, physiotherapist
Stewart McMorran, principal investigator
Melissa Minshull, research clinician
Cath Morgan, physiotherapist
Richard Morrell, principal investigator
Anne Nooney, physiotherapist
Elizabeth Oastler, research clinician
Andrea Powell, physiotherapist
Gill Pratt, physiotherapist
Dominic Price, physiotherapist
Lynne Reddyhough, physiotherapist
Kate Rees, research clinician
Francis Richardson, principal investigator
Cheryl Ritchie, research clinician
Nicola Rose, research clinician
Magdy Sakr, principal investigator
Jeanette Saunders, physiotherapist
Heather Shilliday, research clinician
John Sloan, principal investigator
Michele Sterling, expert review
Hilary Stock, physiotherapist
Lucie Stringer, physiotherapist
Andy Szykuta, physiotherapist
Tammy Tang, physiotherapist
Rachel Tidbull, physiotherapist
Esme Trevelyan, physiotherapist
Rachel Trickey, research clinician
Lauren Tromans, physiotherapist
Sue Tura, physiotherapist
Nicola Vaux, physiotherapist
Anna Vines, physiotherapist
Antonia Wadley, physiotherapist
Nicky Walker, physiotherapist
Heidi Williams, expert review of intervention
Esther Williamson, research physiotherapist
Elaine Willmore, research clinician
Troy Wilson, physiotherapist
Chloe Wilson, physiotherapist
Jackie Young, physiotherapist
Publication
Lamb SE, Gates S, Underwood MR, Cooke MW, Ashby D, Szczepura A, et al. Managing Injuries of the Neck Trial (MINT): design of a randomised controlled trial of treatments for whiplash associated disorders. BMC Musculoskelet Disord 2007;8:7.
Lamb SE, Gates S, Williams MA, Williamson EM, Mt-Isa S, Withers EJ, et al. Emergency department treatments and physiotherapy for acute whiplash: a pragmatic, two-step, randomised controlled trial. Lancet 2012;in press. DOI: 10.1016/S0140-6736(12)61304-X.
Disclaimers
The views expressed in this publication are those of the authors and not necessarily those of the HTA programme or the Department of Health.
References
- Galasko CSB, Gunzberg R, Szpalski M. Whiplash injuries: current concepts in prevention, diagnosis, and treatment of the cervical chiplash syndrome. Philadelphia, PA: Lippincott-Raven; 1998.
- Galasko G, Murray P, Stephenson W. Incidence of whiplash-associated disorder. BCMJ 2002;44:237-40.
- Barnsley L, Lord S, Bogduk N. Whiplash injury. Pain 1994;58:283-307.
- Miles K, Maimaris C, Finlay D, Barnes M. The incidence and prognostic significance of radiological abnormalities in soft tissue injuries to the cervical spine. Skeletal Radiol 1988;17:493-6.
- Quinlan K, Annest J, Myers B, Ryan G, Hill H. Neck strains and sprains among motor vehicle occupants-United States, 2000. Accid Anal Prev 2004;36:21-7.
- Spitzer W, Skovron M, Salmi L, Cassidy J, Duranceau J, Suissa S, et al. Scientific monograph of the Quebec Task Force on whiplash-associated disorders: redefining ‘whiplash’ and its management. Spine 1995;20:1S-73S.
- Versteegen G, Kingma J, Meijler W, ten Duis H. Neck sprain after motor vehicle accidents in drivers and passengers. Eur Spine J 2000;9:547-52.
- Richter M, Otte D, Pohlemann T, Krettek C, Blauth M. Whiplash-type neck distortion in restrained car drivers: frequency, causes and long-term results. Eur Spine J 2000;9:109-17.
- Carroll L, Holm L, Hogg-Johnson S, Côté P, Cassidy J, Haldeman S, et al. Course and prognostic factors for neck pain in whiplash-associated disorders (WAD): results of the bone and joint decade 2000–2010 task force on neck pain and its associated disorders. Spine 2008;33:S83-92.
- Cote P, Cassidy JD, Carroll L, Frank JW, Bombardier C. A systematic review of the prognosis of acute whiplash and a new conceptual framework to synthesize the literature. Spine 2001;26:E445-58.
- Scholten-Peeters G, Verhagen A, Bekkering G, van der Windt D, Barnsley L, Oostendorp R, et al. Prognostic factors of whiplash-associated disorders: a systematic review of prospective cohort studies. Pain 2003;104:303-22.
- Williams MA, Williamson EM, Gates S, Lamb SE, Cooke M. A systematic literature review of physical factors and the development of late whiplash syndrome. Spine 2007;32:E764-80.
- Williamson E, Williams M, Gates S, Lamb S. A systematic literature review of psychological factors and the development of late whiplash syndrome. Pain 2008;135:20-3.
- Verhagen A, Scholten-Peeters G, van Wijngaarden S, de Bie R, Bierma-Zeinstra S. Conservative treatments for whiplash. Cochrane Database Syst Rev 2007;2.
- McClune T, Burton AK, Waddell G. Whiplash associated disorders: a review of the literature to guide patient information and advice. Emerg Med J 2002;19:499-506.
- Burton K, Tim M, Gordon W. The Whiplash Book. London: TSO; 2005.
- Coulter A. Evidence based patient information. is important, so there needs to be a national strategy to ensure it. BMJ 1998;317:225-6.
- Burton A, Waddell G, Tillotson K, Summerton N. Information and advice to patients with back pain can have a positive effect. A randomized controlled trial of a novel educational booklet in primary care. Spine 1999;24:2484-91.
- McClune T, Burton AK, Waddell G. Evaluation of an evidence based patient educational booklet for management of whiplash associated disorders. Emerg Med J 2003;20:514-17.
- Pietrobon R, Coeytaux RR, Carey TS, Richardson WJ, DeVellis RF. Standard scales for measurement of functional outcome for cervical pain or dysfunction: a systematic review. Spine 2002;27:515-22.
- Mayou R, Bryant B. Outcome of ‘whiplash’ neck injury. Injury 1996;27:617-23.
- Mayou R, Bryant B. Psychiatry of whiplash neck injury. Br J Psychiatry 2002;180:441-8.
- Lamb S, Williams M, Withers E, Perry J, Gates S, Williamson E, et al. A national survey of clinical practice for the management of whiplash-associated disorders in UK emergency departments. Emerg Med J 2009;26:644-7.
- Moore A, Jackson A, Jordan J, Hammersley S, Hill J, Mercer C, et al. Clinical guidelines for the physiotherapy management of whiplash associated disorder. London: Chartered Society of Physiotherapy; 2005.
- Eldridge S, Ashby D, Feder G. Informed patient consent to participation in cluster randomized trials: an empirical exploration of trials in primary care. Clin Trials 2005;2:91-8.
- Hoving JL, Koes BW, de Vet HC, van der Windt DA, Assendelft WJ, van Mameren H, et al. Manual therapy, physical therapy, or continued care by a general practitioner for patients with neck pain. A randomized, controlled trial. Ann Intern Med 2002;136:713-22.
- Rosenfeld M, Gunnarsson R, Borenstein P. Early intervention in whiplash-associated disorders: a comparison of two treatment protocols. Spine 2000;25:1782-7.
- van Buuren S, Boshuizen H, Knook D. Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med 1999;18:681-94.
- Ware J, Kosinski M, Keller S. SF-12: how to score the SF-12 physical and mental health summary scales. Lincoln, RI: QualityMetric Incorporated; 1998.
- Gandek B, Ware J, Aaronson N, Apolone G, Bjorner J, Brazier J, et al. Cross-validation of item selection and scoring for the SF-12 health survey in nine countries: results from the IQOLA project. International quality of life assessment. J Clin Epidemiol 1998;51:1171-8.
- Dolan P, Gudex C, Kind P, Williams A. A social tarrif for EuroQol: results from a UK general population survey. University of York: Centre for Health Economics; 1995.
- Rasbash J, Charlton C, Browne WJ, Healy M, Cameron B. MLwiN version 2.1. Bristol: Centre for multilevel modelling, University of Bristol; 2009.
- Lamb S, Gates S, Underwood M, Cooke M, Ashby D, Szczepura A, et al. Managing Injuries of the Neck Trial (MINT): design of a randomised controlled trial of treatments for whiplash associated disorders. BMC Musculoskelet Disord 2007;8.
- Brookes S, Whitley E, Peters T, Mulheran P, Egger M, Davey Smith G. Subgroup analyses in randomised controlled trials: quantifying the risks of false-positives and false-negatives. Health Technol Assess 2001;5.
- Stratford PW, Riddle DL, Binkley JM, Spadoni G, Westaway MD, Padfield B. Using the Neck Disability Index to make decisions concerning individual patients. Physiother Can 1999;51:107-19.
- Pocock S. Clinical trials: a practical approach. Chichester: Wiley; 1983.
- Eldridge S, Ashby D. Statistical concepts. London: Royal College of General Practitioners; 2000.
- Verhagen AP, Peeters GG, de Bie RA, Oostendorp RA. Conservative treatment for whiplash. Cochrane Database Syst Rev 2001;4.
- Cote P, Cassidy JD, Carroll L, Frank JW, Bombardier C. A systematic review of the prognosis of acute whiplash and a new conceptual framework to synthesize the literature. Spine 2001;26:E445-58.
- Scholten-Peeters GG, Verhagen AP, Bekkering GE, van der Windt DA, Barnsley L, Oostendorp RA, et al. Prognostic factors of whiplash-associated disorders: a systematic review of prospective cohort studies. Pain 2003;104:303-22.
- Williams M, Williamson E, Gates S, Lamb S, Cooke M. A systematic literature review of physical prognostic factors for the development of late whiplash syndrome. Spine 2007;32:E764-80.
- Logan AJ, Holt MD. Management of whiplash injuries presenting to accident and emergency departments in Wales. Emerg Med J 2003;20:354-5.
- Grimshaw J, Russell I. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet 1993;342:1317-22.
- Underwood M, O’Meara S, Harvey E. The acceptability to primary care staff of a multidisciplinary training package on acute back pain guidelines. Fam Pract 2002;19:511-15.
- Rogers A. Teaching adults. Philadelphia, PA: Open University Press; 2002.
- Schnabel M, Ferrari R, Vassiliou T, Kaluza G. Randomised, controlled outcome study of active mobilisation compared with collar therapy for whiplash injury. Emerg Med J 2004;21:306-10.
- Mealy K, Brennan H, Fenelon G. Early mobilization of acute whiplash injuries. Br Med J 1986;292:656-7.
- McKinney L, Dornan J, Ryan M. The role of physiotherapy in the management of acute neck sprains following road-traffic accidents. Arch Emerg Med 1989;6:27-33.
- Provinciali L, Baroni M, Illuminati L, Ceravolo M. Multimodal treatment to prevent the late whiplash syndrome. Scand J Rehabil Med 1996;28:105-11.
- Gross AR, Kay T, Hondras M, Goldsmith C, Haines T, Peloso P, et al. Manual therapy for mechanical neck disorders: a systematic review. Man Ther 2002;7:131-49.
- Dall’Alba P, Sterling M, Treleaven J, Edwards S, Jull G. Cervical range of motion discriminates between asymptomatic persons and those with whiplash. Spine 2001;26:2090-4.
- Treleaven J, Jull G, Sterling M. Dizziness and unsteadiness following whiplash injury: characteristic features and relationship with cervical joint position error. J Rehabil Med 2003;35:36-43.
- Sterling M, Jull G, Vicenzino B, Kenardy J, Darnell R. Development of motor system dysfunction following whiplash injury. Pain 2003;103:65-73.
- Jull G, Kristjansson E, Dall’Alba P. Impairment in the cervical flexors: a comparison of whiplash and insidious onset neck pain patients. Man Ther 2004;9:89-94.
- Horowitz M, Wilner N, Alvarez W. Impact of event scale: a measure of subjective stress. Psychosom Med 1979;41:209-18.
- Scholten-Peeters G, Bekkering G, Verhagen A, van Der Windt D, Lanser K, Hendriks E, et al. Clinical practice guideline for the physiotherapy of patients with whiplash-associated disorders. Spine 2002;27:412-22.
- Miró J, Nieto R, Huguet A. Predictive factors of chronic pain and disability in whiplash: a Delphi poll. Eur J Pain 2008;12:30-47.
- Jensen M, Keefe F, Lefebvre J, Romano J, Turner J. One- and two-item measures of pain beliefs and coping strategies. Pain 2003;104:453-69.
- Maitland G, Hengeveld E, Banks L, English K. Maitland’s vertebral manipulation. Oxford: Butterworths Heinemann; 2001.
- Mulligan B. Manual therapy: NAGS, SNAGS, MWMS etc. Wellington: Plane View Science Ltd; 1995.
- Di Fabio R. Manipulation of the cervical spine: risks and benefits. Phys Ther 1999;79:50-65.
- Refshauge K, Parry S, Shirley D, Larsen D, Rivett D, Boland R. Professional responsibility in relation to cervical spine manipulation. Aust J Physiother 2002;48:171-85.
- Norris JW, Beletsky V, Nadareishvili ZG. Sudden neck movement and cervical artery dissection. The Canadian stroke consortium. CMAJ 2000;163:38-40.
- De Decker K, Van Havenbergh T, D’Archambeau O, Jorens P. Basilar artery thrombosis in a trauma patient. Case report and review of the literature. Resuscitation 2003;59:147-54.
- Friedman D, Flanders A, Thomas C, Millar W. Vertebral artery injury after acute cervical spine trauma: rate of occurrence as detected by MR angiography and assessment of clinical consequences. AJR Am J Roentgenol 1995;164:443-9.
- Harding V, Gifford L. Topical issues in pain physiotherapy pain association year book. Cornwall: NOI Press; 1998.
- Moseley L, Butler D. Explain pain. Adelaide, SA: NOI Australasia Pty Ltd; 2003.
- Russell G, Nicol P. ‘I’ve broken my neck or something!’ The general practice experience of whiplash. Fam Pract 2009;26:115-20.
- Green J, Thorogood N. Qualitative methods for health research. London: Sage; 2004.
- Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther 1991;14:409-15.
- Taylor C, Benger J. Patient satisfaction in emergency medicine. Emerg Med J 2004;21:528-32.
- Vlaeyen J, Kole-Snijders A, Boeren R, van Eek H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain 1995;62:363-72.
- Office of National Statistics . Retail Price Index Monthly Percentage Changes, 1988 to 2009 2009. www.statistics.gov.uk/statbase/TSDSelection1.asp (accessed 13 October 2010).
- Curtis L. Unit costs of health and social care 2008. University of Kent, Canterbury: Personal Social Services Research Unit; 2008.
- Department of Health . Reference Costs, 2006–07 2008. www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_082571 (accessed 10 January 2011).
- Prescribing Support Unit . Prescription Cost Analysis 2007 2008. www.ic.nhs.uk/statistics-and-data-collections/primary-care/prescriptions/prescription-cost-analysis-2007 (accessed 10 January 2011).
- Lamb S, Lall R, Hansen Z, Castelnuovo E, Withers E, Nichols V, et al. A multicentred randomised controlled trial of a primary care-based cognitive behavioural programme for low back pain. The Back Skills Training (BeST) trial. Health Technol Assess 2010;14.
- NHS Information Centre PSU . Prescribing Analysis and CosT (PACT) 2008. www.ic.nhs.uk/statistics-and-data-collections/primary-care/prescriptions/prescription-cost-analysis-2007 (accessed 13 October 2010).
- National Centre for Social Research and University of College London . Department of Epidemiology and Public Health HSfE. Health Survey for England 2006 n.d.:1991-2007.
- Hurwitz E, Carragee E, van der Velde G, Carroll L, Nordin M, Guzman J, et al. Treatment of neck pain: noninvasive interventions: results of the bone and joint decade 2000–2010 task force on neck pain and its associated disorders. Spine 2008;33:S123-52.
- Von Korff M, Moore J. Stepped care for back pain: activating approaches for primary care. Ann Intern Med 2001;134:911-17.
- Lamb S, Marsh J, Hutton J, Nakash R, Cooke M. Mechanical supports for acute, severe ankle sprain: a pragmatic, multicentre, randomised controlled trial. Lancet 2009;373:575-81.
- Gargan MF, Bannister GC. The rate of recovery following whiplash injury. Eur Spine J 1994;3:162-4.
- Gargan M, Bannister G, Main C, Hollis S. The behavioural response to whiplash injury. J Bone Joint Surg Br 1997;79:523-6.
- Pennie B, Agambar L. Patterns of injury and recovery in whiplash. Injury 1991;22:57-9.
- Kasch H, Bach FW, Jensen TS. Handicap after acute whiplash injury: a 1-year prospective study of risk factors. Neurology 2001;56:1637-43.
- Brison L, Hartling, Pickett W. Prospective study of neck injuries following rear-end motor vehicle collisions. J Musculoskelet Pain 2000;8:97-113.
- Cassidy JD, Carroll LJ, Cote P, Lemstra M, Berglund A, Nygren A. Effect of eliminating compensation for pain and suffering on the outcome of insurance claims for whiplash injury. N Engl J Med 2000;342:1179-86.
- Cote P, Hogg-Johnson S, Cassidy JD, Carroll L, Frank JW. The association between neck pain intensity, physical functioning, depressive symptomatology and time-to-claim-closure after whiplash. J Clin Epidemiol 2001;54:275-86.
- Hohl M. Soft-tissue injuries of the neck in automobile accidents. J Bone Joint Surg Am 1974;56:1675-82.
- Hodgson S, Grundy M. Whiplash injuries: their long prognosis and its relationship to compensation. Neuro-orthopedics 1998;7:88-91.
- Norris S, Watt I. The prognosis of neck injuries resulting from rear-end vehicle collisions. J Bone Joint Surg Br 1983;65:608-11.
Appendix 1 Membership of the Trial Steering Committee
Mr Peter Driscoll – Chairperson
Professor Deborah Ashby
Professor Matthew Cooke
Professor Sandra Eldridge
Professor Jennifer Klaber-Moffatt
Professor Sallie Lamb
Professor Ala Szczepura
Professor Martin Underwood
Mrs Anne Carson
Mr Mike Wakeman
Appendix 2 Membership of the Data Monitoring and Ethics Committee
Professor Tim Peters – Chairperson
Dr Karen Barker
Professor Timothy Coats
Appendix 3 Observed intracluster correlation coefficients at Step 1
Intracluster correlation coefficients for Step 1 are based on full model adjusted for clustering, advice intervention and WAD grade at ED attendance. We present observed ICC estimates at 4-, 8- and 12-month time points. The full models were replicated in MLwiN 2.1128 using iterative generalised least squares (IGLS) procedure, and ICC estimates were subsequently calculated. We also present ICC estimates under null model by intervention and overall.
| Null model | yij = β0 + u0j = eij |
| Adjusted (full) model |
yij = β0 + β1WBAij + β2kWADijk + u0j + eij Where u0j ∼ N(0, σu2) is the random effect ED of clustering, eij ∼ N(0, σE2) is the individual random error, and WADijk is the identifier for WAD grade k at ED attendance |
| ICC between ED clusters | σu2σu2+σE2 |
| ICC at 4 months | ICC at 8 months | ICC at 12 months | ||||
|---|---|---|---|---|---|---|
| Stata | MLwiN | Stata | MLwiN | Stata | MLwiN | |
| UCAa | –0.0010 | –0.0005 | –0.0017 | |||
| WBAa | 0.0213 | 0.0120 | 0.0056 | |||
| Overalla | 0.0151 | 0.0080 | 0.0029 | |||
| Overallb | 0.0136 | 0.0095 | 0.0075 | 0.0060 | 0.0033 | 0.0026 |
| ICC at 4 months | ICC at 8 months | ICC at 12 months | ||||
|---|---|---|---|---|---|---|
| Stata | MLwiN | Stata | MLwiN | Stata | MLwiN | |
| UCAa | –0.0036 | –0.0031 | –0.0044 | |||
| WBAa | 0.0051 | 0.0044 | –0.0019 | |||
| Overalla | 0.0040 | 0.0032 | –0.0026 | |||
| Overallb | 0.0012 | 0.0008 | 0.0017 | 0.0013 | –0.0030 | –0.0028 |
| ICC at 4 months | ICC at 8 months | ICC at 12 months | ||||
|---|---|---|---|---|---|---|
| Stata | MLwiN | Stata | MLwiN | Stata | MLwiN | |
| UCAa | 0.0090 | –0.0028 | 0.0016 | |||
| WBAa | 0.0117 | 0.0042 | 0.0121 | |||
| Overalla | 0.0121 | 0.0024 | 0.0085 | |||
| Overallb | 0.0112 | 0.0101 | 0.0018 | 0.0015 | 0.0088 | 0.0089 |
| ICC at 4 months | ICC at 8 months | ICC at 12 months | ||||
|---|---|---|---|---|---|---|
| Stata | MLwiN | Stata | MLwiN | Stata | MLwiN | |
| UCAa | –0.0005 | 0.0012 | –0.0017 | |||
| WBAa | 0.0142 | 0.0055 | –0.0001 | |||
| Overalla | 0.0134 | 0.0058 | –0.0007 | |||
| Overallb | 0.0094 | 0.0078 | 0.0040 | 0.0036 | –0.0005 | –0.0005 |
Appendix 4 Effect of ethnicity on SF-12v1 mental and physical component scores
| 2 weeks | 4 months | 8 months | 12 months | |
|---|---|---|---|---|
| UCA | ||||
| Mean (SD) | 40.9 (13.0) | 48.0 (11.6) | 49.4 (11.3) | 49.6 (10.9) |
| n (missing/total) (%) | 183/1488 (12%) | 256/1295 (20%) | 266/1175 (23%) | 277/1127 (25%) |
| WBA | ||||
| Mean (SD) | 40.7 (12.7) | 47.1 (12.1) | 48.7 (11.5) | 49.3 (10.9) |
| n (missing/total) (%) | 271/2042 (13%) | 406/1774 (23%) | 359/1570 (23%) | 487/1577 (31%) |
| Treatment estimatea | ||||
| ∆ (95% CI) | 0.3 (–0.7 to 1.2) | –0.4 (–1.7 to 1.0) | –0.3 (–1.3 to 0.7) | 0.1 (–0.9 to 1.1) |
| Treatment estimateb | ||||
| ∆ (95% CI) | 0.2 (–1.0 to 1.4) | –0.0 (–0.9 to 0.9) | –0.2 (–1.1 to 0.7) | 0.1 (–1.0 to 1.1) |
| 2 weeks | 4 months | 8 months | 12 months | |
|---|---|---|---|---|
| UCA | ||||
| Mean (SD) | 40.3 (9.0) | 46.5 (9.7) | 48.9 (9.2) | 49.9 (9.0) |
| n (missing/total) (%) | 183/1488 (12%) | 256/1295 (20%) | 266/1175 (23%) | 277/1127 (25%) |
| WBA | ||||
| Mean (SD) | 40.2 (8.9) | 46.0 (9.8) | 48.5 (9.2) | 49.8 (9.1) |
| n (missing/total) (%) | 271/2042 (13%) | 406/1774 (23%) | 359/1570 (23%) | 487/1577 (31%) |
| Treatment estimatea | ||||
| ∆ (95% CI) | 0.0 (–1.4 to 1.4) | 0.2 (–0.7 to 1.0) | 0.0 (–0.8 to 0.8) | 0.2 (–0.6 to 1.1) |
| Treatment estimateb | ||||
| ∆ (95% CI) | –0.1 (–1.5 to 1.4) | 0.0 (–0.8 to 0.8) | 0.4 (–0.3 to 1.1) | 0.4 (–1.0 to 1.7) |
Appendix 5 Subgroup analyses
| 4-month follow-up (95% CI) | 8-month follow-up (95% CI) | 12-month follow-up (95% CI) | |
|---|---|---|---|
| Injury severity | |||
| WBA | 0.4 (–2.2 to 3.1) | 0.9 (–1.7 to 3.5) | –0.1 (–2.0 to 1.8) |
| Severe | 3.8 (1.9 to 5.7) | 4.4 (2.5 to 6.4) | 3.0 (1.1 to 4.9) |
| WBA × severe | –0.1 (–2.6 to 2.5) | –1.6 (–4.1 to 0.9) | –0.2 (–2.7 to 2.3) |
| Early psychological response (psych) | |||
| WBA | –0.1 (–2.0 to 1.8) | 0.2 (–1.6 to 2.1) | –0.5 (–2.5 to 1.5) |
| Psych | 11.5 (9.6 to 13.4) | 10.4 (8.6 to 12.3) | 8.6 (6.7 to 10.4) |
| WBA × psych | 0.7 (–1.8 to 3.3) | –0.1 (–2.6 to 2.3) | 0.3 (–2.2 to 2.7) |
| Previous neck pain | |||
| WBA | –0.1 (–2.5 to 2.2) | –0.2 (–2.4 to 2.0) | –0.1 (–1.7 to 1.5) |
| Neck pain | 7.0 (2.7 to 11.4) | 7.7 (3.6 to 11.8) | 7.6 (3.6 to 11.5) |
| WBA × neck pain | 3.9 (–1.7 to 9.5) | 1.9 (–3.5 to 7.2) | –0.2 (–5.5 to 5.0) |
| Pursued compensation | |||
| WBA | 2.0 (–4.7 to 8.7) | –0.7 (–6.6 to 5.2) | 1.1 (–4.1 to 6.3) |
| Compensation | 8.5 (3.2 to 13.7) | 6.1 (1.5 to 10.7) | 7.7 (3.6 to 11.7) |
| WBA × compensation | –2.0 (–8.7 to 4.7) | 0.4 (–5.6 to 6.4) | –1.3 (–6.6 to 3.9) |
| 4-month follow-up (95% CI) | 8-month follow-up (95% CI) | 12-month follow-up (95% CI) | |
|---|---|---|---|
| Injury severity | |||
| WBA | 0.4 (–2.5 to 3.3) | 0.8 (–1.9 to 3.5) | 0.3 (–2.1 to 2.7) |
| Severe | 4.2 (2.3 to 6.1) | 3.7 (1.9 to 5.5) | 2.3 (0.5 to 4.1) |
| WBA × severe | 0.1 (–2.3 to 2.5) | –0.2 (–2.5 to 2.2) | 0.5 (–1.8 to 2.8) |
| Early psychological response (psych) | |||
| WBA | 0.4 (–1.6 to 2.4) | 0.6 (–1.3 to 2.5) | 0.1 (–1.7 to 1.9) |
| Psych | 10.4 (8.6 to 12.3) | 9.1 (7.3 to 10.9) | 8.3 (6.6 to 10.1) |
| WBA × psych | 0.4 (–1.9 to 2.7) | 0.3 (–2.0 to 2.6) | 0.3 (–2.0 to 2.5) |
| Previous neck pain | |||
| WBA | –0.0 (–2.5 to 2.4) | 0.3 (–2.2 to 2.8) | 0.2 (–1.8 to 2.2) |
| Neck pain | 5.8 (1.5 to 10.0) | 7.1 (3.1 to 11.1) | 7.1 (3.1 to 11.1) |
| WBA × neck pain | 3.2 (–2.1 to 8.5) | 1.3 (–3.8 to 6.5) | 0.4 (–4.6 to 5.4) |
| Pursued compensation | |||
| WBA | 0.6 (–5.4 to 6.6) | –0.4 (–6.0 to 5.2) | 1.6 (–3.6 to 6.8) |
| Compensation | 7.4 (2.9 to 11.9) | 6.0 (1.8 to 10.2) | 7.9 (3.8 to 11.9) |
| WBA × compensation | –0.7 (–6.5 to 5.2) | 0.4 (–5.1 to 5.9) | –1.9 (–7.1 to 3.4) |
Appendix 6 Observed intracluster correlation coefficients at Step 2
Intracluster correlation coefficients for Step 2 are based on model adjusted for NHS trusts and therapists within NHS trusts clustering, advice intervention, physical intervention, and NDI score measured at research clinic. We present observed ICC estimates at 4-, 8- and 12-month time points. The ICC estimates were subsequently calculated. We also present ICC estimates under null model by physical intervention and overall.
| Null model | yijk = β0 + u0k + v0jk + eijk |
| Adjusted model |
yijk = β0 + β1WBAijk + β2Physiotherapyijk + β3NDIijk + u0k + v0jk + eijk Where u0k ∼ N(0, σu2) is the random effect of NHS trusts clustering, v0jk ∼ N(0, σv2) is the random effect of therapists, eijk ∼ N(0, σE2) is the individual random error, and NDIijk is the NDI score measured at research clinic assessment |
| ICC between NHS trusts clusters | ICCNHS trusts=σu2σu2+σv2+σE2 |
| ICC between therapists within NHS trusts | ICCTherapists=σv2σv2+σE2 |
NHS trusts clustering
Model adjusted for NHS trusts and therapists within NHS trusts clustering, advice intervention, physical intervention and NDI score at research clinic.
| ICC at 4 months | ICC at 8 months | ICC at 12 months | ||||
|---|---|---|---|---|---|---|
| Stata | MLwiN | Stata | MLwiN | Stata | MLwiN | |
| Advicea | 0.0000 | 0.0009 | 0.0004 | |||
| Physiotherapya | 0.0001 | 0.0003 | 0.0003 | |||
| Overalla | 0.0044 | 0.0007 | 0.0002 | |||
| Adjustedb | 0.0039 | 0.0111 | 0.0002 | –0.0093 | 0.0001 | –0.0158 |
| ICC at 4 months | ICC at 8 months | ICC at 12 months | ||||
|---|---|---|---|---|---|---|
| Stata | MLwiN | Stata | MLwiN | Stata | MLwiN | |
| Advicea | 0.0138 | 0.0319 | 0.0003 | |||
| Physiotherapya | 0.0002 | 0.0001 | 0.0002 | |||
| Overalla | 0.0008 | 0.0002 | 0.0003 | |||
| Adjustedb | 0.0090 | –0.0016 | 0.0002 | –0.0057 | 0.0001 | –0.0053 |
| ICC at 4 months | ICC at 8 months | ICC at 12 months | ||||
|---|---|---|---|---|---|---|
| Stata | MLwiN | Stata | MLwiN | Stata | MLwiN | |
| Advicea | 0.0000 | 0.0336 | 0.0004 | |||
| Physiotherapya | 0.0006 | 0.0003 | 0.0002 | |||
| Overalla | 0.0073 | 0.0113 | 0.0001 | |||
| Adjustedb | 0.0001 | –0.0195 | 0.0003 | –0.0096 | 0.0001 | 0.0022 |
| ICC at 4 months | ICC at 8 months | ICC at 12 months | ||||
|---|---|---|---|---|---|---|
| Stata | MLwiN | Stata | MLwiN | Stata | MLwiN | |
| Advicea | 0.0002 | 0.0000 | 0.0000 | |||
| Physiotherapya | 0.0004 | 0.0144 | 0.0002 | |||
| Overalla | 0.0000 | 0.0000 | 0.0001 | |||
| Adjustedb | 0.0000 | –0.0054 | 0.0000 | –0.0182 | 0.0000 | –0.0173 |
| Outcome | ICC at 4 months | ICC at 8 months | ICC at 12 months | |||
|---|---|---|---|---|---|---|
| Stata | MLwiN | Stata | MLwiN | Stata | MLwiN | |
| NDI | 0.0544 | 0.0772 | 0.0009 | 0.0789 | 0.0303 | 0.0672 |
| MCS | 0.0008 | 0.0019 | 0.0007 | 0.0908 | 0.0008 | 0.0530 |
| PCS | 0.0318 | 0.1238 | 0.0016 | 0.0213 | 0.0007 | 0.0263 |
| EQ-5D | 0.0144 | 0.0802 | 0.0003 | 0.0134 | 0.0062 | –0.0411 |
Appendix 7 Subgroup analyses
Complete cases analyses
| 4-month follow-up (95% CI) | 8-month follow-up (95% CI) | 12-month follow-up (95% CI) | |
|---|---|---|---|
| Injury severity | |||
| Physiotherapy | –6.8 (–13.3 to –0.3) | –1.2 (–7.9 to 5.5) | –4.3 (–11.4 to 2.8) |
| Severe | –1.2 (–6.4 to 4.1) | –0.4 (–6.0 to 5.2) | –1.0 (–6.8 to 4.8) |
| Physiotherapy × severe | 4.2 (–2.8 to 11.3) | 0.2 (–7.1 to 7.5) | 3.7 (–4.0 to 11.3) |
| Early psychological response (psych) | |||
| Physiotherapy | –3.7 (–7.3 to 0.0) | –1.1 (–4.9 to 2.8) | –0.3 (–4.2 to 3.6) |
| Psych | 3.0 (–0.6 to 6.6) | 2.0 (–1.9 to 5.9) | 2.2 (–1.8 to 6.1) |
| Physiotherapy × psych | 1.2 (–3.9 to 6.3) | 1.1 (–4.2 to 6.3) | –1.0 (–6.5 to 4.5) |
| Previous neck pain | |||
| Physiotherapy | –3.1 (–5.8 to –0.4) | –0.6 (–3.4 to 2.2) | –0.4 (–3.2 to 2.5) |
| Neck pain | 3.1 (–3.2 to 9.4) | 5.1 (–1.0 to 11.3) | 7.4 (1.2 to 13.6) |
| Physiotherapy × neck pain | 0.2 (–9.0 to 9.4) | 1.7 (–7.6 to 11.0) | –4.3 (–14.4 to 5.9) |
| Pursued compensation | |||
| Physiotherapy | –15.7 (–38.8 to 7.3) | 2.1 (–13.9 to 18.0) | –16.8 (–33.4 to –0.2) |
| Compensation | –5.5 (–25.6 to 14.5) | –1.8 (–14.3 to 10.8) | –10.4 (–23.6 to 2.9) |
| Physiotherapy × compensation | 13.2 (–10.0 to 36.4) | –2.4 (–18.6 to 13.8) | 16.2 (–0.7 to 33.0) |
Multiple imputation analyses
| 4-month follow-up (95% CI) | 8-month follow-up (95% CI) | 12-month follow-up (95% CI) | |
|---|---|---|---|
| Injury severity | |||
| Physiotherapy | –7.2 (–13.6 to –0.8) | –2.6 (–9.3 to 4.2) | –4.6 (–11.3 to 2.1) |
| Severe | –1.7 (–6.9 to 3.5) | –1.4 (–6.9 to 4.1) | –1.5 (–7.0 to 4.0) |
| Physiotherapy × severe | 4.1 (–2.8 to 11.1) | 1.8 (–5.4 to 9.1) | 3.0 (–4.3 to 10.3) |
| Early psychological response (psych) | |||
| Physiotherapy | –4.3 (–8.3 to –0.3) | –0.5 (–4.9 to 3.8) | –0.7 (–4.9 to 3.6) |
| Psych | 2.4 (–1.1 to 6.0) | 3.1 (–0.8 to 7.0) | 2.2 (–1.6 to 6.0) |
| Physiotherapy × psych | 1.1 (–3.9 to 6.2) | –0.5 (–6.0 to 5.0) | –2.0 (–7.3 to 3.2) |
| Previous neck pain | |||
| Physiotherapy | –3.5 (–6.1 to –0.9) | –0.6 (–3.4 to 2.1) | –1.6 (–4.4 to 1.2) |
| Neck pain | 2.1 (–3.9 to 8.1) | 5.2 (–1.1 to 11.5) | 5.7 (–0.5 to 11.9) |
| Physiotherapy × neck pain | 0.9 (–8.1 to 10.0) | –1.2 (–10.7 to 8.3) | –2.5 (–12.2 to 7.1) |
| Pursued compensation | |||
| Physiotherapy | –8.3 (–25.1 to 8.4) | –3.4 (–20.1 to 13.2) | –16.8 (–33.4 to –0.1) |
| Compensation | 0.4 (–13.1 to 13.9) | –4.5 (–17.7 to 8.7) | –10.5 (–23.7 to 2.8) |
| Physiotherapy × compensation | 5.4 (–11.7 to 22.5) | 3.5 (–13.4 to 20.4) | 16.4 (–0.5 to 33.3) |
Appendix 8 Emergency department intervention and materials
Emergency department proforma.
Assessment form and treatment planner.
Survey of Pain Attitudes questionnaire.
Exercises handout.
Proprioception handout.
Postural advice handout.
Relaxation advice handout.
Discharge advice handout.
Manual therapy manual.
Exercise therapy manual.
Psychological strategies manual.
Fear avoidance cycle.
Overactivity, underactivity cycle 1.
Overactivity, underactivity cycle 2.
The above documents can all be found at: www2.warwick.ac.uk/fac/med/research/hsri/emergencycare/research/whiplash/webresource
Appendix 9 Emergency department survey paper
This document can be found at: www2.warwick.ac.uk/fac/med/research/hsri/emergencycare/research/whiplash/webresource
Appendix 10 Analysis of work days lost using random-effects multiple linear regression model with bootstrapping
| 4 months | 8 months | 12 months | |
|---|---|---|---|
| Advice | |||
| Mean (SD) | 8.9 (22.9) | 9.9 (25.3) | 10.7 (26.2) |
| Missing/total | 1/255 (0%) | 0/246 (0%) | 0/238 (0%) |
| Physiotherapy | |||
| Mean (SD) | 6.3 (14.8) | 8.2 (17.7) | 9.2 (18.9) |
| Missing/total | 0/252 (0%) | 1/251 (0%) | 1/241 (0%) |
| Treatment effect | |||
| Δ (95% CI)a | –4.2 (–7.9 to –1.1) | –4.0 (–7.7 to –0.5) | –3.6 (–7.5 to –0.02) |
| 4 months | 8 months | 12 months | |
|---|---|---|---|
| Treatment effect | |||
| Δ (95% CI)a | –4.3 (–7.3 to –1.3) | –4.0 (–7.4 to –0.5) | –3.9 (–7.7 to –0.6) |
| Month 4 | Month 8 | Month 12 | |
|---|---|---|---|
| Advice | |||
| Mean (SD) | 11.1 (25.4) | 12.3 (28.1) | 13.3 (29.1) |
| Missing/total | 0/202 (0%) | 0/192 (0%) | 0/184 (0%) |
| Physiotherapy | |||
| Mean (SD) | 7.4 (15.2) | 9.4 (18.3) | 10.6 (19.7) |
| Missing/total | 0/189 (0%) | 1/185 (1%) | 1/180 (1%) |
| Treatment effect | |||
| Δ (95% CI)a | –5.1 (–9.4 to –1.4) | –4.9 (–9.7 to –0.7) | –4.9 (–10.2 to –0.9) |
Appendix 11 Final trial proposal
Protocol version 2 – 6 April 2004 MREC changes incorporated
Project Title: Managing Injuries of the Neck Trial (MINT): a multi-centred randomised controlled trial of education and advice versus a targeted intervention to prevent late whiplash syndromes.
1. How the project has changed since the outline proposal was submitted
The study team has met on several occasions. We have: (1) addressed the issues raised by the board at the outline stage; (2) undertaken extensive searching for reviews and trials and of the National Research and other registers to investigate if any new trials are underway. We have considered the findings of the Cochrane Review of methods to promote postal follow up; (3) gained formal agreements from A&E consultants, physiotherapists and R&D managers in over 15 hospitals who would take part in the trial; (4) conducted a national survey of current practice for whiplash injuries in over 350 UK A&E departments to guide our decision-making and audited information leaflets on whiplash provided by over 60 departments; (5) estimated the numbers of whiplash injuries at clinical sites to specify recruitment targets; and (6) Drs Joseph and Griffiths have joined the team.
1.1 Definition of terms used in the brief
The term whiplash-associated disorders (WAD) is used variously in the literature. The Quebec Task Force definition is internationally recognised and the most widely used definition, and the one we will use for this trial (Spitzer, 1995). Whiplash is the mechanism of injury (acceleration–deceleration injuries usually in the frontal plane), whiplash injuries are the soft tissue injuries that result and WAD describes the pattern of symptoms that arise (see Table 1). A further term, late whiplash syndrome, is used to describe the chronic complications of whiplash that occur in the minority of patients.
|
WAD Grade 0: No neck complaints or signs WAD Grade I: Complaint of pain, stiffness or tenderness, but no physical signs WAD Grade II: Complaint of pain, stiffness or tenderness, and musculo-skeletal signs (decreased range of motion, point tenderness, etc.) WAD Grade III: Compliant of pain, stiffness or tenderness and neurological signs (decreased or absent deep tendon reflexes, weakness and sensory deficits). Could also have musculo-skeletal signs WAD Grade IV: Fracture or dislocation Late whiplash syndrome: presence of pain, restriction of motion or other symptoms at six months or more after the injury, sufficient to hinder return to normal activities such as driving, usual occupation and leisure |
The brief requests a trial of non-surgical, non-pharmacological treatments of WAD, applied within the first 6 weeks of the injury. Treatment should be targeted at rapid alleviation of acute symptoms, and importantly, prevention of late whiplash syndrome. The alternative would be a ‘wait and see approach’, targeting late whiplash syndrome once it was established and leaving acute symptoms to resolve naturally. Research from the chronic pain and whiplash literature strongly supports a preventive approach (Waddellet al. 1996). The term active treatment covers a wide range of treatment options, from advice to promote return of normal activity (as for example in the recently published The Whiplash Book) to interventions such as physiotherapy, psychological counselling or multi-modal rehabilitation.
2. Existing research
Background
The annual cost of whiplash injuries to the UK economy was £2,553 million (1990 prices), representing about 18% of the total costs of all road traffic accidents and 0.4% of the Gross Domestic Product (Galasko, 1998). The average time off work for WAD was 81 days. Health services costs are considerable, with physiotherapy costs representing a substantial component of health care expenditure (Spitzer 1995). Late whiplash syndrome is estimated to occur in 30% of patients (Mayouet al. 2002) and it is generally accepted, although a minority, the patients who progress to having chronic symptoms generate the majority of costs (Galasko 1998). From a societal perspective, prevention of chronic symptoms is a priority in terms of return to full work and pre-injury quality of life. Rapid, symptomatic relief is likely to be a high priority for NHS users.
The Quebec Task Force recommendations, systematic reviews and trial evidence
Despite whiplash being a common injury, there are virtually no good quality trials upon which to base recommendations for practice. Expert opinion dominates. In 1995 the Quebec Task Force (QTF) undertook an extensive review and expert consensus exercise. The conclusions were: (1) there was insufficient evidence to support the use of treatments currently used for WAD; (2) promoting activity in the early stages was probably the most effective way forward; (3) soft collars are not helpful; (4) physiotherapy was a very common treatment, but required rigorous evaluation because of the high costs. The Cochrane Review of Conservative Treatments for Whiplash drew similar conclusions (Vergangenet al. 2002). The QTF proposed a clinical pathway in which patients are given advice and education at the initial contact, and then reviewed at 3 weeks. At this point, patients with persisting symptoms would be provided with more intensive treatment by health professionals experienced in the management of whiplash. We believe that the stepped care clinical pathway proposed by the QTF is the model most likely to yield a cost-effective strategy for WAD and is the clinical approach we have chosen for this trial. The QTF did not make recommendations about the treatments that should be used.
A subsequent review has reported little progress in the literature in terms of trials (McCluneet al. 2002). The authors suggested that psychological risk factors predominate as risk factors for poor outcome, and argue that advice to resume normal activity, using a cognitive-behavioural approach, is the treatment of choice for early management of whiplash. The review was used to develop The Whiplash Book (HMSO 2001). The review can be criticised because it has been selective in it’s use of evidence. Subsequent systematic reviews of risk factors for poor outcome have shown that physical and psychological factors carry equivalent amounts of risk for poor outcome (Pietrobonet al. 2002). Also 11 out of 12 references used to support early activity and key health promotion messages were from the field of low back pain or other chronic conditions. Implementation without research would require a leap of faith to be confident that lessons learnt in the field of sub-acute and chronic LBP, and on which The Whiplash Book is based, are transferable to acute whiplash injuries. There are notable differences between the conditions in terms of the mechanism of injury and psychological consequences, and between the advice delivered in the booklet and that given by most A&E departments. For example, phobic travel anxiety and other psychological manifestations of shock occur in about 50% of people after whiplash (Mayou 1996, 2002), but are rarely, if ever, reported in the low back pain.
Physiotherapy includes hot and cold therapy, electrotherapies, mobilisation, manipulation, exercise (of many different kinds), and traction. If a causal pathway between pain and zygoapophyseal joint dysfunction, limited range of motion and long-term disability is assumed (and as is suggested by the epidemiologic literature, Bodguk 1999), spinal mobilisation and exercises to improve range of motion should be effective treatments. There is good quality trial evidence to support the effectiveness of mobilisation and exercise in the management of chronic neck pain (e.g. Hovinget al. 2002; Evanset al. 2002; Kjellmanet al. 2002). A review of the evidence for whiplash outcomes concluded that there was moderate quality evidence for exercises and mobilisations commonly used by physiotherapists (Sagit-Barat 2003). However, this review has to be interpreted with caution. The conclusions are based on three trials, all of which reported short term outcome, had sample sizes of less then 60 patients, did not undertake an intention to treat analysis, and failed to ensure blinding of investigators involved in the collection of outcome data. Our proposal for a well-designed trial, if funded, that will make a significant contribution to improving knowledge of effective treatments for whiplash.
Risk factors for developing chronic whiplash syndrome and information for the choice of sub-groups
The brief requests a sub-group analysis, which requires an understanding of prognostic factors. In the UK about 30% of people with whiplash develop chronic symptoms (Mayou 1996, 2002). Estimates vary by the origin of the study and the outcomes studied. Age, gender, and severity of physical symptoms in the early post injury stage predict outcome at 6–12 months. People with severe physical and psychological signs are twice as likely to experience a poor outcome; for chronic neck pain this rises to seven times more likely (reviewed by Pietrobonet al. 2002). More recent studies have focused on the psychological factors, identifying anger, blame and pre-existing life stresses to be important (Sullivanet al. 2002). Few studies have examined the effect of physical and psychological factors in the same cohort, but it is likely that the resolution of pain is critical to alleviation of psychological symptoms (Walliset al. 1997). There have been no studies of the interaction between prognostic factors and treatment outcomes in a randomised trial.
Compensation
Indications that WAD and late whiplash syndromes are influenced by litigation arise from a variety of sources. A change from tort to no-fault insurance in Saskatchewan resulted in a significant reduction in late whiplash syndrome (Spitzer 1995). Schraderet al. (1996) suggested the low incidence of late whiplash syndrome in Lithuania was due to a lack of financial incentive. More recent research has suggested that expectations of the outcome of whiplash vary across cultures because of differences in litigation systems (Ferrariet al. 2002). These suggestions have been heavily rebuffed on the basis of poor study methods, persuasive evidence for a biomechanical mechanism of injury that can result in chronic pain (Bodguk, 1999), and studies that show pain does not resolve once litigation is resolved (e.g. Pennie and Agambar 1991). The issue is unresolved.
4. Research objectives
-
To estimate the clinical effectiveness of a stepped care approach over a 12 month period after an acute injury.
-
1.1 Step One: The Whiplash Book versus usual care advice in Accident & Emergency.
-
1.2 Step Two: In patients with symptoms persisting at 3 weeks (WAD Grades I-III), supplementary treatment comprising either a package of physiotherapy treatments and reinforcement of advice versus reinforcement of advice provided at the initial A&E contact only.
-
1.3 The combined effect of the various treatments using a 2 by 2 factorial design.
-
-
To estimate the clinical effectiveness in pre-specified sub-groups of patients – those with prior neck problems, psychological or physical risk factors for poor outcome, and those seeking compensation.
-
To estimate the costs of each strategy including treatment and subsequent health care costs over a period of 12 months and to estimate cost-effectiveness.
5. Research methods
Summary: A 2 × 2 factorial randomised controlled trial to enable the estimation of a stepped care approach to the alleviation of acute symptoms of WAD, and prevention of late whiplash syndrome. We will compare two advice interventions; usual care advice and The Whiplash Book, provided at the first A&E contact. Patients will be reviewed three weeks later, and those with unresolved symptoms (WAD Grade I-III) will be asked to continue their treatment in the framework of an individually randomised controlled trial of a physiotherapy package versus reinforcement of the advice originally provided. The physiotherapy package will include pre-specified treatments for pain, motion and psychological risk factors for poor outcome. We will include a sub-group analysis to determine if the treatments are more effective and cost-effective in people with one or more symptoms associated with poor outcome. The sub-groups will be [1] physical risk factors for poor outcome (WAD Grade III injuries) [2] psychological risk factors e.g. anger or phobic travel anxiety and/or [3] neck pain in the six months prior to the injury. We will also examine the role of compensation as a predictor of poor outcome. Sample size requirements have been estimated with care to reflect the power needed to account for clustering, main and interaction effects, and sub-group analyses, and the proposal includes a cost and cost-effectiveness analysis. We will require a minimum of 8 departments, 4 of which have been cluster randomised to usual care advice, and the remainder of which have been cluster randomised to The Whiplash Book advice intervention. We have an extensive and established network of A&E departments across the UK (> 15) willing to participate in research. We have already gained formal agreements from sufficient A&E, physiotherapy and R&D departments to ensure that we can achieve our recruitment targets, with the capacity to increase the number of departments if needs be. All treatments will be delivered to a defined standard. The trial team will provide a training programme to A&E departments and to the physiotherapy departments. Outcomes will be measured over a 12-month period using postal questionnaires. An economic evaluation will run prospectively alongside the trial.
6. Study design, approach and randomisation
Design: A multi-centred randomised controlled trial with blinded assessment of outcomes. We will compare:
-
The Whiplash Book versus usual care and advice in A&E using a cluster randomised trial
-
If symptoms persist at 3 weeks, the effectiveness a package of physiotherapy treatments versus reinforcement of the advice as supplementary treatments using an individually randomised trial.
-
The combination of different approaches to advice and follow-up treatments using the principles of factorial design.
Setting: Treatment and recruitment will occur in NHS hospitals. A summary of the departments who have indicated they are willing to participate is given in Appendix 1. The trial simulates the most likely service delivery model if the treatments were found to be effective. The A&E departments have been selected because: (1) they are committed to participating in research and have a nominated a lead clinician who is prepared to take an active role in implementing the study at their site; (2) the volume of patients attending with whiplash injuries is more than adequate to ensure that we can achieve our recruitment targets; and (3) there is a lead physiotherapist who is prepared to take an active role in implementing the study at the site. The departments are in the North West, South West and West Midlands.
Inclusion criteria: All people who attend A&E with a whiplash injury of less than 6 weeks duration (as specified in the brief) will be invited to participate in the trial. Patients must be considered able to give informed consent to participate in the trial.
Exclusion criteria: Age less than 18 years. Fractures or dislocations of the spine or other bones. Head injuries (Glasgow Coma Score 12 at the time of the accident). Admission to in-patient services as a result of the accident. Severe psychiatric illness.
Identifying potential participants: Clinicians working in A&E will provide all people presenting with acute whiplash (of less than 6 weeks duration) with information about the trial as well as education and advice, at their first attendance. A standard approach will be instituted across all A&E departments based on our experience of running previous trials. We will develop a short pro-forma that serves two purposes (1) collection of routine core clinical data set in a tick box format (2) A tick box to ensure that clinicians have provided potential participants with the trial information pack and a brief explanation of the trial. One copy of the form will be filed to the medical notes as a treatment record and a second copy is passed to the research team (with the patients consent) to notify them that a patient has been asked to participate in the trial. Provided that the clinical centres are involved in the development of the pro-forma, we have found this system to work well and once embedded in the system, to act as a reminder to invite patients into the trial. We are also able to check against routine attendance data to ensure that all people with whiplash injuries have been approached. An appointment will be made for patients to attend a review clinic at 3 weeks after the injury, using the normal A&E scheduling for follow up. The clinic will be run by a research physiotherapist, who will assess the patient’s progress, confirm that they are eligible for the supplementary treatments and wish to participate in the trial. If so, the physiotherapist will gain informed consent, re-affirm the site-specific advice provided to all participants in A&E, arrange for randomisation and any other trial treatments and complete the on-study forms. We will telephone to confirm the time of attendance at the follow up clinic a couple of days prior to the clinic. If participants have no on-going symptoms they need not attend. Patients who indicate that they do not wish to participate in the study at the initial contact will be scheduled for follow up in accordance with local policy. Reasons for declining to participate in the trial will be recorded, along with age, sex, ethnicity, and severity of whiplash associated disorders (using the QTF classification) of all people approached to allow an assessment of the generalisability of the study results.
FIGURE 1.
Study design.
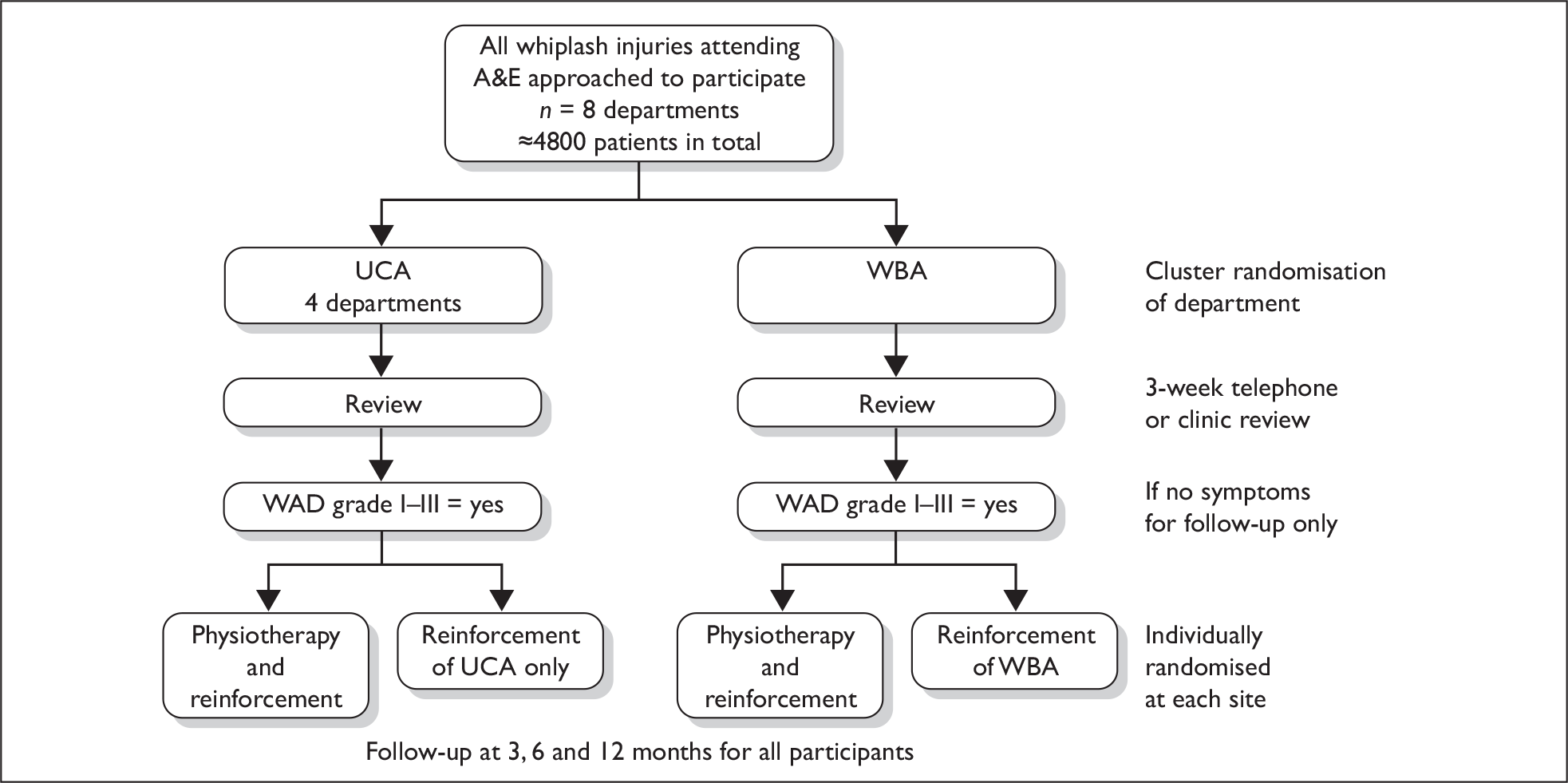
Consent and ethical committee approval: Patients will receive usual care advice or The Whiplash Book advice without giving consent. This is the standard and accepted method for cluster randomised trials (Edwards SJet al. 1999). All patients will receive an information letter and pack explaining the trial at their first A&E attendance and requesting their consent to postal questionnaire follow up over the next 12 months. They will be informed of the second phase of the trial (giving at least two weeks before they would be approached for participation). As the majority of A&E departments in the UK currently follow up patients in one form or another (sometimes in primary care), patients will be scheduled an appointment to attend a review clinic to have their symptoms re-assessed. The second phase of the trial will be re-iterated at the review clinic. All participants will be asked to give informed consent to enter the trial, and for access to their medical records. MREC approval will be sought from the West Midlands region, the next meeting being in September 2002.
Randomisation method: A&E departments will be randomised to usual advice or The Whiplash Book using a pre-prepared, computer generated randomisation list and procedures to ensure allocation concealment. For the randomisation to physiotherapy or reinforcement of advice we will use a telephone registration and randomisation, stratified by site. Allocation concealment, which shields people who enter patients into a trial from knowing future allocations, will be ensured by using a remote computer generated randomisation system that is independently administered and quality controlled. In the situation where family members or close relatives are eligible for the second stage of the study, these ‘units’ will be randomised to one arm of the trial, and this will be accounted for in the analysis.
7. Intervention protocols
Educational package: Usual care advice (reference group) or The Whiplash Book: We have undertaken a survey to determine current practice in A&E departments. The most popular form of treatment is advice, but the content and quality of the advice varies. The most common form of advice is to take analgesics and gradually increase movement of the neck (over 90% of departments use this approach). Some departments use soft collars as well, suggesting that they should be removed and neck exercised on a regular basis (also reported by Holt and Logan 2003). Most advice sheets are explicit in encouraging patients to pursue a claim, the incentive being that A&E departments can claim back costs through the Department of Health Compensation Recovery Unit and generate income through sponsorship from local Law firms. None contain information on the range of symptoms to be expected or the prognosis of whiplash. The Whiplash Book is quite different. It uses a psycho-educational approach to [1] deliver positive, although not necessarily accurate messages about prognosis, promoting the message that pain (including radicular pain) is nothing to worry about. [2] Promotion and guidance on getting back to work and normal activities early [3] Excludes information on pursing claims or sponsorship from Solicitors [4] Recommendations about physical activity, exercise and self-management of symptoms.
In all other respects, the advice interventions will be same and will be implemented using an organisational approach. All A&E clinicians and support workers will be trained in the advice approach to ensure consistency. The general practitioner is an important link in the system, and will receive a faxed communication outlining the advice. The organisational approach has been the most successful method of introducing clinical guidelines (Grimshawet al. 1993). This approach was used to introduce The Back Book (on which The Whiplash Book is based) in to primary care as part of the UK – Back Exercise and Manipulation Trial (Underwood et al. in press). All patients will be offered a review of their symptoms at 3 weeks. Expert opinion and epidemiologic evidence suggests that this is the optimal time point for review (Spitzer 1995). If there are persistent physical symptoms (WAD I–III), and/or psychological symptoms (anger, phobia, depression or anxiety) participants will be eligible for supplementary treatment and the second phase of the trial.
Supplementary treatment – the physiotherapy package: In addition to the reinforcement of advice, participants who are randomised to the physiotherapy package will have up to six sessions of therapy, over a 6-week time period. The physiotherapy package will be delivered by a therapist who is independent of the recruitment and randomisation procedures. Physiotherapy is a multi-component intervention, and we will therefore follow the guidance of the MRC for the design of trials of complex interventions (MRC, 2000) in ensuring that adequate documentation is assured. In particular, the components of the intervention will be described in a training and reference manual. We will adopt a standard and pre-specified approach across sites and monitor treatment quality by observing a random sub-sample of the treatment sessions. The choice of physiotherapy treatments has been made using two principles: (1) there is evidence that the treatments are effective for chronic neck dysfunction and are likely to be effective for whiplash injuries, based on expert opinion or limited trial evidence (see section 4); and (2) The treatments target established and potentially modifiable risk factors for developing late whiplash syndrome, including restrictions of motion, persisting or radicular pain, and adverse psychological reactions to the injury.
The treatments will be:
-
Mobilisation (gentle manipulation) of the cervical spine according to Maitland (1984).
-
Stretching exercises to increase range of motion of the cervical spine according to Kisneret al. 2002.
-
A cognitive behavioural approach to treatment delivery, as this has been found to be highly effective in physiotherapy for other painful conditions (e.g. Klaber Moffetet al. 1999). The approach will promote self-management using: (1) patient education to counter negative beliefs about whiplash, highlight inactivity and over activity cycles; (2) use of cognitive re-structuring techniques to improve pain management, coping and pacing skills; and (3) graded physical activity programme and exposure to activities (such as driving). Physiotherapists will be trained to recognise and deal with phonic travel anxiety and anger. We will train physiotherapists in the trial treatment package, and this will take no longer than one day.
Co-interventions: It is possible that participants or GPs will seek other forms of treatment during the follow up period. If the early provision of physiotherapy and/or advice is effective, this should be evident in a reduction in additional treatments. It would not be ethically acceptable to constrain the use of other treatments. Therefore, their use including changes in the amount or types of analgesia used, use of physical treatments (osteopathy, chiropractic or physiotherapy), alternative therapies, or referral to secondary care services will be monitored as a treatment outcome and considered in the final analysis.
Contamination: The advice trial has been designed as a clustered randomised trial to minimise the problem of contamination. The Department of Health is currently promoting The Whiplash Book, and we will co-ordinate with their team to minimise contamination. We do not anticipate that this will be a problem; only 1% of departments are using the booklet. Many departments report difficulties in funding the provision of a booklet to each patient. We are confident the physiotherapy package we are proposing is not currently used in acute whiplash. Therapists who administer the physiotherapy package will be asked to restrict their clinical contact with whiplash cases to those recruited via randomisation to the physiotherapy arm at the second stage. All departments have the capacity to ensure that non-trial participants or those randomised to other arms are allocated to therapists who have not been on the training programme. Services will be monitored in each locality to monitor for and overcome any potential problems with contamination. The selection of effect size for the trial accounts for the possibility that a minority of patients may seek additional physical treatments such as chiropractic. This is usual for pragmatic trials in this field. Any treatment provided for whiplash in addition to the defined trial treatments will be identified, and accounted for as outcome in the analysis.
8. Baseline assessment and explanatory variables
A minimum data set will be collected from all patients using the clinical proforma described. We will seek consent to take a minimum data set at initial contact when the patients are informed of the trial. The minimum data set will include patient’s age, sex, and injury severity [as determined by the Quebec Task Force guidelines (Spitzer 1995)], a simple psychological screen, and history of previous neck problems. We are confident that will be able to reach agreement with the Multicentre Research Ethics Committee for this activity, as this would be in accordance with normal practice for cluster randomised trials (Edwards SJet al. 1999). These data will be provided in an anonymised format by the A&E departments. This system has worked successfully in previous trials.
9. Outcome measures
Outcome measures will be timed from the initial contact in A&E. We will request that all trial treatments should have been given within the first three months of the first A&E attendance. Our clinical collaborators in physiotherapy do not anticipate this to be a problem; they have reserved slots exist for acute injury management and some of the centres provide an acute injury management service within A&E. The outcomes for the trial are detailed in Table 2. The total outcome measurement package that trial participants will have to complete includes 1 × 10 item scale (items answered on a yes/no basis), 1 × 36 item, 2 × 3 item scale 1 × 5 item scale, 5 single item questions and should take between 15 and 25 minutes to complete.
| Domain | Measures | Details | Time points (months) | |
|---|---|---|---|---|
| Function | Primary |
Neck Disability Index Time to return to work and normal activities (including driving |
Self-completed questionnaire, postal Self-report questionnaire supplemented by calendar |
3, 6, 12 3, 6, 12 |
| Symptoms | Secondary | Cervical Spine Outcomes Questionnaire | Self-completed questionnaire, postal | 3, 6, 12 |
| HR-QoL | Secondary | SF36 | Self-completed questionnaire, postal | 3, 6, 12 |
| Satisfaction | Secondary | Single item rating | Self-completed, postal | 3, 6, 12 |
| Economics |
Resource use questionnaire EQ-5D (health utility) |
Self-completed questionnaire, postal Self-completed questionnaire, postal |
3, 6, 12 3, 6, 12 |
Primary outcome: Return to normal function after the whiplash injury. We will measure this in two ways. Firstly, using the Neck Disability Index (NDI). The NDI is a self-completed questionnaire that has been used successfully in a postal format in trials of neck treatments (e.g. Hovinget al. 2002; Rosenfeldet al. 2000). It assesses pain-related activity restrictions in 10 areas including personal care, lifting, sleeping, driving, concentration, reading and work. In a recent systematic review of outcome measures for neck conditions (Coteet al. 2001), the NDI was considered to be the industry standard for trials – having been validated across a range of studies and broad spectrum of neck conditions. It has good reliability and is responsive to change in clinical status (Coteet al. 2001). Importantly there is consensus that a minimal clinically importance difference lies in the range of 3–5 percentage score points, with a standard deviation of about 8% (e.g. Coteet al. 2001; Riddleet al. 1997). In studies of chronic neck problems, the item on driving is often missed because many patients are not regular drivers. We do not anticipate this being a problem in this trial since most injuries will have been sustained through a vehicular accident. We will also ask participants to estimate the time to recovery of key milestones including return to usual pre-injury occupation, driving and leisure activities. We have developed a system of bespoke calendars to remind participants to record the dates of key milestones in the recovery process and are currently investigating their effectiveness. Our data so far suggests that it is helpful. We will also ask participants to report at each assessment interval the degree to which they have been able to return to their normal activities, recognising that many individuals return to sport, light work or driving but at a reduced level (according to Kaschet al. 2001).
Secondary outcomes: We have been guided in our selection of measures by the HTA monograph authored by Fitzpatrick et al. 1999. We have included additional measures to assess generic health related quality of life, and to address any potential inadequacies in the primary outcome measures. The NDI is very similar in construct to measures used in low back pain research, where it has been found on occasion, that focusing assessment only on pain-related activity limitation can be restrictive (Hovinet al. 2003). For instance, many patients experience significant levels of pain, with no activity restriction. Likewise, some patients perceive stiffness and difficulty to move as opposed to pain.
Cervical Spine Outcomes Questionnaire (BenDebba 2000): Is designed to capture changes in symptoms resulting from treatment. The items include stiffness, dizziness, memory, feelings, self-confidence, jaw pain, vision and soreness. These items are rated on separate scales, summed to provide an overall score. Although a relatively new measure, we recommend that it should be included to ensure the range of possible disease specific outcomes can be captured. We will undertake a formal and comparative assessment of the various measures at the end of the trial to contribute to the design of efficient trials in the future.
SF36: A 36-item measure of health-related quality of life (HR-QoL) (Jenkinsonet al. 1999). We will use the physical role sub-scales to further quantify changes in normal occupation, as well as the total score to reflect the broader impact that the treatments might have on HR-QoL. The SF36 has performed well in trials of spinal pain and is more sensitive than the SF-12 (Bombardieret al. 2001).
Patient rated response to treatment, satisfaction and need for further treatment: Patients will be asked to rate whether they have improved, declined or remained the same as a result of treatment. They will be asked ‘How satisfied are you with your overall care for your neck?’ (Evaluated using a five point scale ranging from extremely satisfied, to extremely dissatisfied), and to provide an indication of whether they consider they need further treatment (Kaschet al. 1999).
EQ-5D: In order to conduct an economic evaluation, it will also be necessary to have a single index measure of health status differences. The EQ-5D is currently the best available measure (Williams, 1995). It measures health on five dimensions and a tariff is available for deriving a single utility score.
Resource use: Will be monitored for the economic analysis. A short questionnaire will be administered at pre-defined assessment intervals. It will ascertain whether participants have had additional hospital treatment for their whiplash injury in the intervening period, specifying whether this was NHS or private treatment paid for by the individual or insurance provider; any GP consultations; and any manipulation, massage etc. which they have received during this period. Participants will also be asked about the number and types of any medications and treatments during the previous 4 weeks, including pain-relieving medications. Participants will be asked to distinguish between prescription and out-of-pocket expenses. We will use a structured closed questionnaire to ascertain these data, based on a questionnaire that has been modified from trials of low back pain treatments (Oxfordshire Low Back Pain Trial and UK-BEAM). Patient self-reported information on service use has been shown to be accurate in terms of intensity of use of different services (Van de Brink Met al. 2000).
The assessment intervals (detailed in Table 2) have been selected to balance between the possibility of questionnaire fatigue and recall bias. We will only ask whether participants have pursued and settled on a compensation claim at 12 months to avoid contamination.
10. Blinding to allocation and outcome measures
An independent research assistant will be responsible for mailing follow up questionnaires, and for entering responses onto a computer. S/he will not have been involved in the recruitment or randomisation processes. Blinding of the intervention will be maintained until final analysis of the data has been completed. The only exception to this rule will be if the data monitoring committee require unblinded data, and in this circumstance, only the independent Chairperson will be aware of assignments.
11. Missing data
There are three levels at which data might not be forthcoming: patient’s withdrawal, loss of patients to follow-up and incomplete responses from individual questionnaires.
Handling withdrawals: Participants will be free to withdraw from the trial at any time. Where possible reasons for withdrawal will be ascertained, including dissatisfaction with the treatment provided.
Potential problems with loss to follow up: Estimates from 2 recent trials of spinal treatments in community dwelling samples suggest that loss to follow up will be approximately 20–25% at 12 months (UK-BEAM and the Oxfordshire Low Back Pain Trial). We will use postal questionnaires at 1 month to ‘imprint’ and minimise loss to follow up, and institute a system of reminder letters and telephone calls to contact people who do not reply. We have studied the Cochrane review of methods to promote postal follow up carefully (ref). We have noted a number of strategies to promote follow up, including using recorded mail delivery for reminder questionnaires. We will adopt a strategy of two questionnaires being sent 1st class in standard mail, with a personalised letter and including a stamped addressed reply envelope (not pre-paid). The third reminder will be sent by recorded delivery, and finally if needed a telephone call from the research office to ascertain a core set of data over the telephone.
Questionnaires: Questionnaires will be designed to minimise this possibility of systematic missing responses (e.g. avoidance of double sided photocopying). The SF36 includes guidance on imputing missing values. For other measures we will use appropriate statistical methods (Schafar 1997). In the pilot phase of the study we will assess patterns of missing data, and rectify any problems with individual item response to questionnaires. For data relating to resource use and complications, we will gain consent at the beginning of the study to access patient records. These can provide additional information where participants are lost to follow up and will be used to assess whether data are missing at random, and to develop test assumptions about the patterns of missing data.
12. Sample size estimates
Choice of treatment effect size: Increasingly it is recognised that advances in modern health care are most likely to yield moderate improvements, but in the context of highly prevalent conditions such as whiplash, these are worthwhile (Peto & Baigent 1998). For the primary end-point of NDI, the estimated standard deviation is 8 and we wish to detect a difference of 3 points between groups would be considered clinically important. This translates into an effect size of 0.375 (moderate size). This is the difference we wish to detect both for the comparison of advice interventions, and for the physiotherapy versus reinforcement of advice. For subgroup analysis, we are only interested in large differences, and are interested in detecting differences between the treatment effects in the subgroups of twice this magnitude. We have enough power for secondary endpoints at comparable effect sizes.
Power: We have selected a power of 90% recognising that economic analyses can require greater power. Based on the experience of previous trials, the number of participants we intend to recruit should be adequate for the purposes of the economic analysis (Torgerson & Campbell 2000).
Alpha: We have selected p = 0.01 because of the need for a definitive trial.
Loss to follow up: We are assuming a worst case scenario of loss to follow up of 30%.
Sample size calculation
Main effects: For the individually randomised component of the trial (i.e. physiotherapy versus reinforcement of advice), we wish to detect a difference of 3 points on the NDI scale, with a standard deviation of 8, at alpha = 1%, and power of 90%. This will require 211 in each group (Pocock, 1983). The comparison of advice interventions is cluster randomised, so the numbers need to be larger. Assuming an intra-cluster correlation co-efficient of 0.02, and an average of 350 patients per centre gives an inflation factor of 7.98 (Eldridge and Ashby, 2000), leading to a sample size of 1683 in each group, or 4 clusters randomised to each group. To allow for loss to follow up of 30%, the initial recruitment needs to be inflated by 1/0.7 = 1.43, giving 2407 per group (from 4 centres) for the advice comparison, and 300 per group for the comparison of physiotherapy versus reinforcement of advice. It is logistically easier and more efficient to deal with a smaller number of larger clusters, we have the luxury of being able to add in more clusters in the event that recruitment rates fall below the expected. For example, if each centre were to recruit 100 patients, the inflation factor would be 2.98, giving a total sample size of 628 per group (900 with loss to follow up). Although this would cost less in terms of patient follow up, the set up and cluster maintenance costs would be greater.
Subgroup analysis: To test for the existence of modest interactions between subgroups increases the required sample size. A recent HTA report (Brookeset al. , 2001) gives details and shows that to detect interactions twice of the main effect requires no increase in sample size, provided the subgroups are of equal size. However, to detect an interaction equal to that of the main effect would necessitate quadrupling sample sizes, which seems infeasible. Although the main effects are powered at a significance level of 1%, a significance level of 5% is adequate for subgroups, which at 90% power requires 1189 per group for trial 1 and 149 per group for trial 2. Because our subgroups of interest are determined from observational factors, equal size subgroups will not, in general, be the case. A conservative inflation is to use 0.5/s, where s is the proportion in the smaller of the subgroups. The most extreme distribution of the subgroups proposed in 70%/30% (for example, for claimants and those with previous neck pain), leading to an inflation factor of 0.5/0.3 = 1.7. Thus the sample sizes planned for the main effects will more than suffice for the subgroup analyses proposed.
Pragmatic approach: We have used conservative estimates in calculating the sample size, both in terms of the treatment effect, power and statistical significance and have based our plans on recruiting up to 4800 attendees to the advice comparison, and 600 participants to the second phase. The assumptions underlying the power calculation will be monitored by the DMEC at pre-defined time-points throughout the trial, and the sample size adjusted accordingly. Changes to the sample size are unlikely, but will be made only with HTA approval.
13. Statistical methods and planned analyses
The analysis will be conducted as intention to treat. All patients will be analysed in the groups to which they were randomised, regardless of the treatment that they may have eventually received. An analysis of all people who completed the trial will be undertaken, and in addition, a sensitivity analysis will be undertaken to assess the range of potential biases that could result from loss to follow up or withdrawal. Numerical and graphical summaries of all the data will be compiled, including a detailed description of missing data at the questionnaire and individual level. Estimates of treatment effect will reported with 95% confidence intervals, and the numbers needed to treat.
We will make the following comparison:
-
The Whiplash Book versus standard advice
-
physiotherapy package versus reinforcement of the advice
-
whether there is an interaction between The Whiplash Book and physiotherapy
-
whether there are interactions with predefined subgroups (compensation, severe physical symptoms (yes/no), adverse psychological reactions (yes/no) and pre-existing neck pain).
For (1) we will compare all individuals within clusters with The Whiplash Book versus all individuals within clusters with standard advice, IRRESPECTIVE of whether or not they were subsequently randomised to physiotherapy package/ not, or to what they were randomised. For analysis we will use linear or logistic regression models or survival analysis (depending on the outcome).
For (2) We will compare all individuals randomised to physiotherapy package versus all those randomised to control IRRESPECTIVE of book/ advice cluster. For analysis we will use linear or logistic regression model or survival analysis (depending on the outcome), stratified by cluster, with random effects for therapist.
For (3) and (4) we will use the same individuals as for (2) and build on that hierarchical analysis by incorporating a booklet/physio interaction term.
Area under the curve will be used to summarise NDI outcomes over the 1-year period, using last value carried forward for those lost to follow up.
14. Economic analyses
Estimates of cost consequences: Whiplash-associated disorders will have a range of direct healthcare cost consequences, in both the primary and secondary care sectors, as well as indirect cost consequences depending on whether or not hospitals can claim for the cost of care through the Hospital Compensations Mechanism (i.e. when patients make a compensation claim). There are also consequences for patients and society, in terms of personal expenditure and return to work. The costing study will therefore take a broad societal perspective and seek to estimate any differences in these various costs incurred by different trial groups. This will enable costs and consequences to be compared from various perspectives, including a societal one and a health care perspective. The latter is likely to be of more interest to NHS decision-makers.
The cost of different interventions (educational/ treatment) will be determined to include staff time, capital costs, consumables, overheads etc. NHS service use associated with each patient management pathway will be collected across study sites. Where participants are lost to follow up, patient records will be used to assess whether data are missing at random, and to develop assumptions about missing service use data. The use of primary care and hospital services will be costed from a variety of sources, including the finance departments of the hospitals, PCTs concerned and national sources (Netten Aet al. 1996).
The consequences for patients in terms of travel expenses, time off work, and personal expenditure on self-medication or private practitioner input will be obtained from resource use questions added to the follow-up outcome questionnaires as described above (section 9). In addition, because a significant number of patients will pursue a compensation claim, information will be collected on the level and outcome of these claims at the end of the 12 month follow-up period. Since final compensation figures may not yet be agreed, data from bodies such as the British Insurers Association will be used to provide further estimates. Additional healthcare costs incurred due to the compensation claim (e.g. extra imaging) will also be recorded.
Sensitivity analysis: There will be uncertainties in many of the resource use estimates (e.g. number of GP visits) and certain assumptions (e.g. the average cost per visit). A careful analysis of the sensitivity of any observed cost differences between groups will be undertaken, based on the confidence intervals around the statistical estimates and alternative assumptions; estimates of critical values of key variables that can reverse the result will be calculated.
Comparison of costs and consequences: A full economic evaluation will be performed based on a comparative assessment of the marginal costs and outcomes of the intervention regimes assessed. This will be performed from a societal perspective and from a health care perspective. The appropriate technique of economic evaluation will depend on the results of the study, and it is recognised that a well-designed economic study should allow for different eventualities (Drummond MFet al. 1990). The simplest eventuality would be where the least expensive intervention is found to be better on at least one outcome measure and no worse on any other, i.e. dominant. Another is where two interventions have the same outcomes (e.g. no differences in disability) in which case the economic evaluation required is a cost-minimisation analysis. However, where the better intervention in terms of outcome is also more costly, two different approaches will be used in the economic analysis.
-
Cost-effectiveness analysis: One approach will be to compare the different interventions in terms of their cost-effectiveness. This requires a single outcome measure common to all interventions. Occupational function (i.e. number of work days lost) will be the primary outcome measure used, and the marginal cost per additional work day will be used to provide an estimate of relative cost-effectiveness.
-
Cost–utility analysis: Where interventions vary in terms of their impact on health related quality of life over time, another approach is to compare them in terms of cost–utility. In the present study, the EQ-5D instrument will be used to generate utility scores and a cost–utility analysis will be undertaken to provide an estimate of the incremental cost of any benefit gained in terms of improved health status. This analysis will be undertaken both in summary form in terms of incremental cost per QALY, and also using a ‘disaggregated’ approach where the extra costs are presented alongside the outcome gains in terms of improvements in pain, physical activity, mental well-being etc. In all these analyses, the uncertainties in the cost and outcomes data will be incorporated into a sensitivity analysis.
Decision-modeling analysis: Finally, decision-modeling analysis will be used to model the costs and benefits of the different patient management routes (treatment and/or education). Resource implications will be combined with estimates of effectiveness derived for the various components of the study. Decision analysis will then be used to determine the optimal course of action among competing alternatives. The principal analysis of the data will be based on the 12-month costs and outcomes associated with different intervention strategies. The analysis will be run from a number of different perspectives, including minimum NHS costs, minimum societal costs, maximum outcome, and net expected cost savings (positive or negative). The impact of compensation claims and their outcome will be included in the model. Estimates of uncertainty will be quantified by multi-way sensitivity analyses (Huninket al. 1998).
15. Recruitment rates and targets
We have set a recruitment target of 40 patients per month per site to advice component of the trial, for a 15-month time period. This translates to 600 patients. Each site will be set a randomisation target of 5 patients per month for 15 months for individually randomised component of the study, translating to a target of 75 patients. In 2002 the average number of potential participants seen in each of two participating A&E departments (Countess of Chester and Universities of Coventry and Warwick NHS Trust) was 1240, more or less evenly spread across the year (there is slight dip in August). Similar annual attendance is reported by the other centres. The recruitment target is realistic and feasible. It contains a generous allowance for quantitative and qualitative differences in case mix between departments, departments withdrawing or failing to recruit, for variations in the proportion of people who attend for review clinic and agree to participate in the trial and who are lost to follow up. One factor, which can be over-looked in trials, is the capacity of the NHS to provide the trial treatments. We have considered this as a possibility particularly in the delivery of the physiotherapy intervention. A target of 5 patients per month should be achievable without placing excessive strain on current service provision.
16. Pilot work already undertaken
National survey of current management of whiplash injuries, structured audit of information provided by over 60 A&E departments. We have contacted all hospitals in our Emergency Medicine Research Network, physiotherapy and R&D departments to obtain agreements to participate in the trial. We have piloted a similar cognitive behavioural intervention for physiotherapists treating low back pain.
17. Pilot study
The commissioning board has asked us to consider piloting the interventions first. We suggest that the pilot should also include an appraisal of the package of trial materials (outcome measures, intervention materials) with NHS users and a dummy run of the trial procedures (including data capture systems). The pilot phase of the trial will run for the first 9 months, allowing sufficient time to appoint staff, finalise the interventions, gain LREC approval, honorary contracts for research staff, and enable hospitals sufficient notice to purchase treatment materials before starting. Our experience is that even when MREC approval and local R&D approvals have been obtained, the preparation for a trial and setting up pilot sites is time consuming. The pilot study will monitor the attendance and potential uptake of the trial at all centres. A pilot evaluation of the interventions will be run at centre in the West Midlands. The pilot study will not have sufficient power to detect whether the intervention is effective, but we will be able to monitor adverse event rates and gain a general impression of acceptability and satisfaction with the interventions from the participants. We will undertake some qualitative interviewing to gain the user perspective on the acceptability of the treatments, their concerns about whiplash, and of the study outcomes.
We will monitor attendance for whiplash in selected primary care sites to estimate potential recruitment bias and to determine if it is possible to use a combined primary care/A&E recruitment strategy. In the first instance we will undertake a computerised record search of 6 general practices that comprise the Coventry Research Framework (the pilot study will be centred around Coventry). The aim will be to determine the number of whiplash injuries that are presenting to primary care in comparison to A&E departments in a one-month period. This record search will be undertaken by a practice nurse employed by the practice, (practices will be re-imbursed) or by a PCT employed research nurse working within the Framework. The time that has elapsed between injury and first appointment with the GP will be abstracted from the records where possible. The data will be provided to the research team in an anonymised format. The TSC and DMEC will consider these data and decide whether a primary care recruitment strategy is required. If so, the MREC will be informed and all relevant documentation will be submitted as an amendment to the protocol.
| Jan | Feb | Mar | April | May | June | July | Aug | Sept | Oct | Nov | Dec | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Attendance (n) | 99 | 111 | 117 | 110 | 110 | 91 | 107 | 75 | 90 | 122 | 105 | 103 | 1240 |
We are confident that this trial will run and recruit well. Our group has been funded to undertake a trial of mechanical support for ankle sprains for the NCC-HTA. We have problem-solved effectively and efficiently on this trial, and are delivering on our recruitment targets and timetable.
18. Other analyses
We have pre-specified sub-group analyses in the section on statistical analysis. We will contribute additional work on outcomes and trial methodology in accident and emergency settings.
19. Ethical considerations
Risks and benefits: The risks to patients are small. The potential benefits are minimisation of neck symptoms and prevention of chronic problems.
Potential side effects and monitoring: There are unlikely to be any serious side effects from the treatments. Potential side effects may be worsening of symptoms if other more effective treatments are withheld. We have taken steps within the protocol to ensure that this is not the case. All adverse events will be reported to the DMEC. A serious adverse event will be defined as one that requires hospitalisation as a result of the intervention, or that causes unwarranted distress to a participant.
Participant confidentiality: All approaches to potential participants will be made through their treating departments. The research team will only know the identity of those who have agreed to participate. All study paper work will identify participants by study number only. We will display posters in all participating departments informing potential participants about the study so that those who do not want to be approached can be excluded.
20. Inclusion of people from ethnic minorities
Some of the localities we will be using include a large proportion of people of South Asian origin. We consider that it is feasible in some of the localities (based on the availability of interpretation services) to recruit non-English speaking Asians into the study. Dr Anil Gumbar at the ESRC Centre for Evidence in Ethnicity, Health and diversity at Warwick University will assist us in translating the Neck Disability Index into appropriate languages. We will report the translated versions of these questionnaires. In the pilot study will examine the performance of the translated versions of the outcomes, to verify that we can use them in the main trial.
21. Patient perspectives
Patient perspectives will be collected as part of the treatment credibility/acceptance study, and user input will be provided at key points in the trial by the newly constituted Users panel for the Warwick Emergency Care Group (chaired by the Bishop of Warwick).
22. Expertise
A strength of this application is the expertise pulled together from a number of University Institutions and an established network of clinical collaborators, many of whom have worked together and with us before. A trial of this nature is large and complex. It will require excellent organisation and an efficient network of A&E departments that are willing and able to recruit sufficient numbers of patients. The study will also require people experienced in the design and management of health services research, including economics, statistics and sociological research (Lamb, Underwood, Cooke, Ashby, Szczepura, Griffiths). It will require people experienced in the clinical management of whiplash, psychological aspects of trauma and physiotherapy in the UK (Lamb, Cooke, Underwood, Joseph and Mayou). The Emergency Medicine Research Group, based at Warwick University has a good track record in designing and running large trials in A&E, having just successfully launched the HTA funded trial of mechanical support for severe ankle sprains. Dr Cooke is Department of Health advisor on A&E, and is well networked with departments across the country. Professor Szczpura has an excellent track record in health services research, particularly economics. She is Director of the Centre for Health Service Studies and Co-Director of the ESRC Centre for Ethnicity, Health and Diversity. Professor Underwood holds a NHS Career Scientist Fellowship to develop a portfolio of work in chronic musculo-skeletal conditions in primary care and is principal investigator of a study of psychological factors associated with musculo-skeletal diseases (principal investigator on BEXS). He has excellent experience of designing and running large trials, and providing a general practice perspective. Professor Lamb also has experience of the design and management of trials of complex interventions, including physiotherapy, physical activity interventions and rehabilitation. Dr Stephen Joseph, a health psychologist, has published and researched widely in post-traumatic stress disorders after accidents. Dr Frances Griffiths will provide input into the qualitative aspects of the trial. Professor Ashby is an experienced statistician with relevant experience of the analysis of complex interventions.
23. Trial management
The framework for the collaboration for this study is well established. Professor Lamb will assume overall responsibility for the trial. The trial will be managed on a day to day basis by a Senior Clinical Trial Co-ordinator, supported by a half time administrative assistant. A senior physiotherapist who is experienced in whiplash will be appointed to undertake the training of, and interface with clinicians at each of the sites and be responsible for recruiting patients. We will employ clinical staff on temporary contracts at remote sites to undertake recruitment and act as local co-ordinators. Trial meetings will be held at monthly intervals with the principal investigators to monitor progress and provide support. The responsibilities of each of the applicants are specified in the application form. The trial statistician and economist will be closely involved in setting up data capture systems, design of data bases, protocols for data entry and cleaning, trial steering committee meetings, preparation of DMEC reports, and analysis.
24. Project timetable and milestones
A cross indicates active phases for each task with dated milestones. Each milestone has a measurable output. Recruitment rates for the RCT have been calculated carefully to ensure that all departments will be able to recruit the desired number of participants. Data monitoring reports will include numbers of subjects approached, consenting, being randomised, dropping out and any adverse events. We are requesting funding over a 4-year period.
25. Trial steering committee
The remit will be to (1) monitor and supervise the progress of the trial towards its interim and overall objectives (2) review at regular intervals relevant information from other sources (3) consider the recommendations of the DMEC (4) inform the HTA on the progress of the trial. The membership will include an independent chairperson (to be confirmed), two additional independent members; investigators: Lamb, Underwood, Ashby, Cooke, Szcepura.
26. Data monitoring and ethics committee (DMEC)
The terms of reference will be to: (1) Review the assumptions underlying the sample size and determine if interim analyses of trial data should be undertaken; (2) Consider data from interim analyses, unblinded if considered appropriate, plus any additional safety issues for the trial and relevant information from elsewhere; (3) Ensure that ethical considerations are of prime importance; (4) Consider any requests for the release of interim trial data and to recommend the TSC on the advisability of this; and (5) Advise on funding issues. The DMEC will comprise three independent members, including a senior statistician, an A&E consultant and physiotherapist.
27. Study outcomes and dissemination strategy
The study will provide important data to guide decision making in allocation of resources and of treatment choices to patients and clinicians. In addition to producing a report for the HTA, we plan publications for a wide audience, including practice and academic journals. Important methodological work will be undertaken as part of the study, and will advance the field in terms of outcome measures and trial design. These end-points will also be reported in academic journals. Dissemination will be aimed at A&E staff, general practice, psychologists, orthopaedic, nursing, physiotherapy, chiropractors, osteopaths and other professionals involved in WAD. If effective, we will also run practical courses on implementing the clinical methods used and publish a paper based version of the intervention manual (at cost only). In addition, we would like to prepare a web-based manual and learning kit for dissemination (subject to securing funding).
| Task (to be completed by the end of month … ) | 0 | 3 | 6 | 9 | 12 | 15 | 18 | 21 | 24 | 27 | 30 | 36 | 39 | 42 | 48 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Recruit study personnel | ✗ | ||||||||||||||
| 2. Prepare and refine materials | ✗ | ✗ | |||||||||||||
| 3. Pilot study launched by month 6 | ✗ | ✗ | |||||||||||||
| 4. Presentation of results to steering committee | ✗ | ||||||||||||||
| 5. Set up remaining sites (staggered) | ✗ | ✗ | ✗ | ✗ | |||||||||||
| 6. Recruitment and randomisation | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||||||
| 7. Data monitoring report | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| 8. Finish all data collection | ✗ | ||||||||||||||
| 9. Finish all economic collection data | ✗ | ||||||||||||||
| 10. Statistical and economic input/analyses | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||
|
11. Data monitoring committee Trial steering committee |
✗ ✗ |
✗ | ✗ | ✗ |
✗ ✗ |
✗ ✗ |
✗ ✗ |
||||||||
| 12. Preparation HTA report/ publications | ✗ | ✗ | |||||||||||||
| 13. Preparation of other dissemination | ✗ |
28. Justification of the support required
Research costs: The study requires a full-time experienced research co-ordinator, to manage the day-to-day running of the trial. The post has been re-numerated at a level that reflects the responsibilities of a senior position. We are asking for a 0.5 FTE research assistant to support the co-ordinator, in duties such as arranging meetings and office duties, but we will use this money flexibly across the study period. We have also sought additional monies for hourly paid or temporary staff to assist with data entry, recruitment and patient interviewing. We have a bank of dedicated temporary staff that undertakes these duties diligently. We intend to run the study in two regions: most likely the Northwest and Midlands region, although we have a cluster of departments in the South West as well. A clinical research fellow will be appointed to the remote cluster to recruit, consent, randomise, and undertake baseline assessments at each of the sites. One fellow will be based at Warwick University (lead fellow) and will co-ordinate the activities of clinical fellows at remote sites. There are also costs for quality control checks, and to cover the eventuality that a small number of participants will be telephoned during follow up. We have requested a 25% junior statistician and economist for each of the four years of the study to be used flexibly across the grant. The health economist will be involved in the refinement of data collection tools prior to the start of the study, conduct of the pilot study, and take responsibility for the costing study, cost analyses and economic modelling as well as contributing to the final report. A consultancy fee is included for Professor Szczpura (15 days at £700.00 per day). Expenses for travel and subsistence include travel to training days, steering group meetings, travel between the clinical sites and have been estimated at either 2nd class rail rates, or at mileage rate of 35p per mile. Phone and stationary are costed at cheapest rates. We will require 3 desktop computers, 2 laser printers and a fax machine for the study. A fee of £10,000 has been included for telephone randomisation, and £3,000 for software licences. We have included monies for recruitment, staff training (such as attendance on a clinical trials course) and conference attendance.
Service support costs: The NHS R&D costs have been estimated by the lead centre (Universities of Coventry and Warwick Hospitals) and agreed in principle by the R&D departments of the collaborating hospitals. Whiplash Books and a contribution toward the costs of physiotherapy are sought through the excess treatment costs. Physiotherapy is provided to selected patients at the moment, but we anticipate that the study will result in a doubling of demand on physiotherapy services in the collaborating centres.
29. Concluding remarks
The board raised a number of points at the outline stage. We have provided justification of why we consider the interventions will be effective and should be tested. The trial could be simplified by a straight comparison between the Whiplash Book and a physiotherapy intervention. However, we believe that the Whiplash Book requires rigorous evaluation before it is recommended for practice because the evidence on which it is based is weak. Advice interventions may appear benign, but can harm patients, particularly where they minimise the importance of ‘red flags’ as The Whiplash Book does (Grosset al. 1997). There is a significant danger that if The Whiplash Book is used as the comparison the clinical community may not accept the result. The criticism will be that we should have a control that reflected ‘usual practice’. If ‘usual practice’ advice is used, then the question of whether physiotherapy is better than The Whiplash Book or not will remains.
Whiplash incurs significant costs and the cost of the trial would soon be recouped if the treatments were shown to be effective at preventing late whiplash syndrome. A finding that suggests additional intensive therapy is not effective, would guide commissioners in the appropriate direction when purchasing services for whiplash. Physiotherapists are well placed to make a significant contribution to the management of whiplash injuries. They would require a small amount of additional training to deliver the psychological component of the intervention, but otherwise all of the skills (musculo-skeletal assessment, soft tissue injury management, exercise prescription and mobilisation) are gained in under-graduate training. However, it is essential that the effectiveness and cost-effectiveness of Physiotherapy treatments are established in large-scale trials. We have proposed a 2 × 2 factorial trial. The two trials could stand independently, and a cost saving would be achieved by dropping either trial from the commissioning process.
The comments from the board ask how patients with WAD are going to be included in the trial. We expect that nearly all patients consulting at A&E will have WAD (using QTR definitions, Table 1), of varying severity. Only patients with WAD grades I to III will be eligible for the second phase of the trial. Inclusion of patients with late whiplash syndrome at baseline would require the brief to be changed. We believe the brief is correct to focus on early, preventive treatments. The QTF have identified that trials are needed in A&E, but we will explore the possibility of a combined recruitment strategy between primary care and A&E at each of the sites.
Our application will look at the issue of compensation from two perspectives. We will record whether or not people have pursued a claim (yes/no), and whether this has been successfully resolved at one year (yes/no), and investigate whether compensation determines success of treatment at one year. Data concerning claims will be ascertained at the last follow up (12 months) only. The Whiplash Book has no reference to compensation. We will be able to determine whether or not this has any effect on pursing a claim.
The randomisation targets will be 40 patients per centre randomised per month for 15 months with 5 patients per month being randomised into the physiotherapy trial. We expect a response rate of 70% in the worst case scenario.
30. References
- Logan AJ, Holt MD. Management of whiplash injuries presenting to accident and emergency departments in Wales. Emerg Med J 2003;20:354-5.
- BenDebba M, . Cervical spine outcomes questionnaire. Spine 2002;27:2116-124.
- Berry H. Chronic whiplash as a functional disorder. Arch Neurolo 2000;57:592-3.
- Bodguk Teasall R. Whiplash: the evidence for an organic aetiology. Arch Neurology n.d.;57:590-1.
- Bombardier C. (2000) Outcome assessments in the evaluation of treatment of spinal disorders: summary and general recommendations. Spine n.d.;25:3100-3.
- Brookes ST, Whitley E, Peters TJ, . Sub-group analyses in randomised controlled trial: quantifying the risks of false-positives and false-negatives. Health Technol Assess 2001;5.
- Cote P, . A systematic review of the prognosis of acute whiplash and a new conceptual framework to synthesize the literature. Spine 2001;26:E445-58.
- Donner OA, . Randomization by cluster. Sample size requirements and analysis. Am J Epidemiol 1981;114:906-14.
- Drummond MF, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Oxford University Press; 1990.
- Edwards P, . Methods to influence response to postal questionnaires. Oxford: Update Software; 2003.
- Edwards SJ, Braunholtz DA, Lilford RJ, Stevens AJ. Ethical issues in the design and conduct of cluster randomised controlled trials. BMJ 1999;318:1407-9.
- Eldridge SM, Ashby D. Statistical Concepts. Royal College of General Practitioners; 2000.
- Evans R, . Two-year follow-up of a randomized clinical trial of spinal manipulation and two types of exercise for patients with chronic neck pain. Spine 2002;27:2383-9.
- Ferrari R, . Layperson’s expectation of the seqeale of whiplash injury. A cross cultural comparative study between Canada and Lithuania. Med Sci Monit 2002;8:CR728-34.
- Galasko SB, Gunzburg R, Szpalski M. Whiplash Injuries: current concepts in prevention diagnosis, and treatment of the cervical whiplash syndrome. Philadelphia, Lippincott-Raven; 1998.
- Giroux M, , Gunzburg R, Szpalski M. Whiplash injuries: current concepts in prevention, diagnosis and treatment of the cervical whiplash syndrome. Philadelphia, Lippincott-Raven; 1998.
- Grimshaw JM, Russell IT. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet 1993;342:1317-22.
- Gross A, . Patient education for mechanical neck disorders (Cochrane Review). The Cochrane Library; 2002.
- Group E. EuroQol: a new facility for the measurement of health related quality of life. Health Policy 1991;16:199-208.
- Hollis S, Campbell F. What is meant by intention to treat analysis?. BMJ 1999;319:670-74.
- Hoving JL, . Manual therapy, physical therapy, or continued care by a general practitioner for patients with neck pain. A randomized, controlled trial. Ann Intern Med 2002;136:713-22.
- Hunink MGM, Bult JR, deVries J, Weinstein MC. Uncertainty in decision models analysing cost-effectiveness: the joint distribution of incremental costs and effectiveness evaluated with a nonparametric bootstrap method. Medical Decision Making 1998;18:337-46.
- Jenkinson C, Stewart-Brown S, . Assessment of the SF-36 version 2 in the United Kingdom. J Epidemiol Community Health 1999;53:46-50.
- Johnston K, . Assessing the costs of healthcare technologies in clinical trials. Health Technol Assess 1999;3.
- Kasch H, . Handicap after acute whiplash injury: a 1-year prospective study of risk factors. Neurology 2001;56:1637-43.
- Kjellman G, . A randomized clinical trial comparing general exercise, McKenzie treatment and a control group in patients with neck pain. J Rehabil Med 2002;34:183-90.
- Kisner C, . Therapeutic exercise goundations and techniques. F.A. Davis Company; n.d.
- Maitland GD. Peripheral Manipulation. Butterworth-Heinemann; n.d.
- Mayou R, . Outcome of ‘whiplash’ neck injury. Injury 1996;27:617-23.
- Mayou R, . Psychiatry of whiplash neck injury. Br J Psychiatry 2002;180:441-8.
- McClune T, . Whiplash associated disorders: a review of the literature to guide patient information and advice. Emerg Med J 2002;19:499-506.
- Medical Research Council London . A Framework for Development and Evaluation of RCTs for Complex Interventions to Improve Health 2000.
- Moffett JK, . Randomised controlled trial of exercise for low back pain: clinical outcomes, costs, and preferences. BMJ 1999;319:279-83.
- Netten A, Dennett J. Unit costs of health and social care. PSSRU, University of Kent at Canterbury; 1996.
- Peto R, Baigent C. Large scale randomised evidence of moderate benefits. BMJ 1998;317:1170-1.
- Pietrobon R, . (2002). Standard scales for measurement of functional outcome for cervical pain or dysfunction: a systematic review. Spine 2002;27:515-22.
- Pocock SJ. Clinical trials: a practical approach. Chichester: Wiley; 1983.
- Polit DF, Hungler BP. Essentials of nursing research; methods, appraisal and utilization. Philadelphia, Lippincott; 1997.
- Riddle DL, . Use of generic versus region-specific functional status measures on patients with cervical spine disorders. Physical Therapy 1998;78:951-63.
- Roland MG, Waddell JA, . The Back Book. Norwich: The Stationery Office; 1997.
- Rosenfeld M, . Early intervention in whiplashassociated disorders: a comparison of two treatment protocols. Spine 2000;25:1782-7.
- Sarig-Bahat H. Evidence for exercise therapy in mechanical neck disorders. Man Ther 2003;8:10-2.
- Schafer JL. Analysis of incomplete multivariate data. London: Chapman & Hall; 1997.
- Scholten-Peeters GG, . Clinical practice guideline for the physiotherapy of patients with whiplashassociated disorders. Spine 2002;27:412-22.
- Schrader . Natural evolution of late whiplash syndrome outside the medicolegal context. Lancet 1996;347:1201-11.
- Spitzer WO, . Scientific monograph of the Quebec Task Force on whiplash-associated disorders: redefining “whiplash” and its management. Spine 1995;20:1S-73S.
- Stratford PW, . Using the Neck Disability Index to make decisions concerning individual patients. Physiotherapy Canada 1999:107-19.
- Sullivan MJ, . Perceived cognitive deficits, emotional distress and disability following whiplash injury. Pain Research &Amp; Management 2002;7:120-6.
- Torgerson DJ, Campbell MK. Cost-effectiveness calculations and sample size. BMJ 2000;321.
- Underwood MR, O’Meara S, Harvey E. (2002b) on behalf UK BEAM . The active management of low back pain: the acceptability of a training package for primary care staff. Family Practice n.d.
- Van de Brink M, Van de Hout WB, . Self Reports of Health Care Utilisation; Can a Questionnaire Replace a Diary n.d.
- Vergagen AP, . Conservative treatment for whiplash (Cochrane Review). The Cochrane Library; 2003.
- Waddell G, Feder G, McIntosh A, Lewis M, Hutchinson A. Low back pain: clinical guidelines and evidence review. London: Royal College of General Practitioners; 1996.
- Wallis BJ, . Resolution of psychological distress of whiplash patients following treatment by radio frequency neurotmoy a randomised double blind placebo controlled trial. Pain 1997;73:15-22.
- Williams A. Measurement and valuation of health: a chronicle. University of York; 1995.
List of abbreviations
- CB
- cognitive behavioural
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- CSP
- Chartered Society of Physiotherapy
- CT
- computerised tomography
- DMEC
- Data Monitoring and Ethics Committee
- ED
- emergency department
- EQ-5D
- European Quality of Life-5 Dimensions
- GP
- general practitioner
- HRQoL
- health-related quality of life
- ICC
- intracluster correlation coefficient
- ICER
- incremental cost-effectiveness ratio
- ICUR
- incremental cost–utility ratio
- IGLS
- iterative generalised least squares
- IQR
- interquartile range
- LBP
- lower back pain
- LWS
- late whiplash syndrome
- MCS
- mental component score
- MICE
- multiple imputation by chained equations
- MINT
- Managing Injuries of the Neck Trial
- MREC
- Multicentre Research Ethics Committee
- MRI
- magnetic resonance imaging
- NAGS
- natural apophyseal glides
- NDI
- Neck Disability Index
- NSAIDs
- non-steroidal anti-inflammatory drugs
- OR
- odds ratio
- PCS
- physical components score
- QALY
- quality-adjusted life-year
- QoL
- quality of life
- QTF
- Quebec Task Force
- RCT
- randomised controlled trial
- ROM
- range of movement
- SD
- standard deviation
- SF-12
- Short Form questionnaire-12 items
- SNAGS
- sustained natural apophyseal glides
- SOPA
- Survey of Pain Attitudes
- TSC
- Trial Steering Committee
- UCA
- usual care advice
- WAD
- whiplash-associated disorder
- WBA
- The Whiplash Book advice
- WTP
- willingness to pay
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.
Notes
Health Technology Assessment programme
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, Department of Pharmacology and Therapeutics, University of Liverpool
-
Professor of Dermato-Epidemiology, Centre of Evidence-Based Dermatology, University of Nottingham
Prioritisation Group
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, Department of Pharmacology and Therapeutics, University of Liverpool
-
Professor Imti Choonara, Professor in Child Health, Academic Division of Child Health, University of Nottingham
Chair – Pharmaceuticals Panel
-
Dr Bob Coates, Consultant Advisor – Disease Prevention Panel
-
Dr Andrew Cook, Consultant Advisor – Intervention Procedures Panel
-
Dr Peter Davidson, Director of NETSCC, Health Technology Assessment
-
Dr Nick Hicks, Consultant Adviser – Diagnostic Technologies and Screening Panel, Consultant Advisor–Psychological and Community Therapies Panel
-
Ms Susan Hird, Consultant Advisor, External Devices and Physical Therapies Panel
-
Professor Sallie Lamb, Director, Warwick Clinical Trials Unit, Warwick Medical School, University of Warwick
Chair – HTA Clinical Evaluation and Trials Board
-
Professor Jonathan Michaels, Professor of Vascular Surgery, Sheffield Vascular Institute, University of Sheffield
Chair – Interventional Procedures Panel
-
Professor Ruairidh Milne, Director – External Relations
-
Dr John Pounsford, Consultant Physician, Directorate of Medical Services, North Bristol NHS Trust
Chair – External Devices and Physical Therapies Panel
-
Dr Vaughan Thomas, Consultant Advisor – Pharmaceuticals Panel, Clinical
Lead – Clinical Evaluation Trials Prioritisation Group
-
Professor Margaret Thorogood, Professor of Epidemiology, Health Sciences Research Institute, University of Warwick
Chair – Disease Prevention Panel
-
Professor Lindsay Turnbull, Professor of Radiology, Centre for the MR Investigations, University of Hull
Chair – Diagnostic Technologies and Screening Panel
-
Professor Scott Weich, Professor of Psychiatry, Health Sciences Research Institute, University of Warwick
Chair – Psychological and Community Therapies Panel
-
Professor Hywel Williams, Director of Nottingham Clinical Trials Unit, Centre of Evidence-Based Dermatology, University of Nottingham
Chair – HTA Commissioning Board
Deputy HTA Programme Director
HTA Commissioning Board
-
Professor of Dermato-Epidemiology, Centre of Evidence-Based Dermatology, University of Nottingham
-
Professor of Bio-Statistics, Department of Public Health and Epidemiology, University of Birmingham
-
Professor of Clinical Pharmacology, Director, NIHR HTA programme, Department of Pharmacology and Therapeutics, University of Liverpool
-
Professor Zarko Alfirevic, Head of Department for Women’s and Children’s Health, Institute of Translational Medicine, University of Liverpool
-
Professor Judith Bliss, Director of ICR-Clinical Trials and Statistics Unit, The Institute of Cancer Research
-
Professor David Fitzmaurice, Professor of Primary Care Research, Department of Primary Care Clinical Sciences, University of Birmingham
-
Professor John W Gregory, Professor in Paediatric Endocrinology, Department of Child Health, Wales School of Medicine, Cardiff University
-
Professor Steve Halligan, Professor of Gastrointestinal Radiology, Department of Specialist Radiology, University College Hospital, London
-
Professor Angela Harden, Professor of Community and Family Health, Institute for Health and Human Development, University of East London
-
Dr Joanne Lord, Reader, Health Economics Research Group, Brunel University
-
Professor Stephen Morris, Professor of Health Economics, University College London, Research Department of Epidemiology and Public Health, University College London
-
Professor Dion Morton, Professor of Surgery, Academic Department of Surgery, University of Birmingham
-
Professor Gail Mountain, Professor of Health Services Research, Rehabilitation and Assistive Technologies Group, University of Sheffield
-
Professor Irwin Nazareth, Professor of Primary Care and Head of Department, Department of Primary Care and Population Sciences, University College London
-
Professor E Andrea Nelson, Professor of Wound Healing and Director of Research, School of Healthcare, University of Leeds
-
Professor John David Norrie, Director, Centre for Healthcare Randomised Trials, Health Services Research Unit, University of Aberdeen
-
Professor Barney Reeves, Professorial Research Fellow in Health Services Research, Department of Clinical Science, University of Bristol
-
Professor Peter Tyrer, Professor of Community Psychiatry, Centre for Mental Health, Imperial College London
-
Professor Martin Underwood, Professor of Primary Care Research, Warwick Medical School, University of Warwick
-
Professor Caroline Watkins, Professor of Stroke and Older People’s Care, Chair of UK Forum for Stroke Training, Stroke Practice Research Unit, University of Central Lancashire
-
Dr Duncan Young, Senior Clinical Lecturer and Consultant, Nuffield Department of Anaesthetics, University of Oxford
-
Dr Tom Foulks, Medical Research Council
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
HTA Clinical Evaluation and Trials Board
-
Director, Warwick Clinical Trials Unit, Warwick Medical School, University of Warwick and Professor of Rehabilitation, Nuffield Department of Orthopaedic, Rheumatology and Musculoskeletal Sciences, University of Oxford
-
Professor of the Psychology of Health Care, Leeds Institute of Health Sciences, University of Leeds
-
Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Professor Keith Abrams, Professor of Medical Statistics, Department of Health Sciences, University of Leicester
-
Professor Martin Bland, Professor of Health Statistics, Department of Health Sciences, University of York
-
Professor Jane Blazeby, Professor of Surgery and Consultant Upper GI Surgeon, Department of Social Medicine, University of Bristol
-
Professor Julia M Brown, Director, Clinical Trials Research Unit, University of Leeds
-
Professor Alistair Burns, Professor of Old Age Psychiatry, Psychiatry Research Group, School of Community-Based Medicine, The University of Manchester & National Clinical Director for Dementia, Department of Health
-
Dr Jennifer Burr, Director, Centre for Healthcare Randomised trials (CHART), University of Aberdeen
-
Professor Linda Davies, Professor of Health Economics, Health Sciences Research Group, University of Manchester
-
Professor Simon Gilbody, Prof of Psych Medicine and Health Services Research, Department of Health Sciences, University of York
-
Professor Steven Goodacre, Professor and Consultant in Emergency Medicine, School of Health and Related Research, University of Sheffield
-
Professor Dyfrig Hughes, Professor of Pharmacoeconomics, Centre for Economics and Policy in Health, Institute of Medical and Social Care Research, Bangor University
-
Professor Paul Jones, Professor of Respiratory Medicine, Department of Cardiac and Vascular Science, St George‘s Hospital Medical School, University of London
-
Professor Khalid Khan, Professor of Women’s Health and Clinical Epidemiology, Barts and the London School of Medicine, Queen Mary, University of London
-
Professor Richard J McManus, Professor of Primary Care Cardiovascular Research, Primary Care Clinical Sciences Building, University of Birmingham
-
Professor Helen Rodgers, Professor of Stroke Care, Institute for Ageing and Health, Newcastle University
-
Professor Ken Stein, Professor of Public Health, Peninsula Technology Assessment Group, Peninsula College of Medicine and Dentistry, Universities of Exeter and Plymouth
-
Professor Jonathan Sterne, Professor of Medical Statistics and Epidemiology, Department of Social Medicine, University of Bristol
-
Mr Andy Vail, Senior Lecturer, Health Sciences Research Group, University of Manchester
-
Professor Clare Wilkinson, Professor of General Practice and Director of Research North Wales Clinical School, Department of Primary Care and Public Health, Cardiff University
-
Dr Ian B Wilkinson, Senior Lecturer and Honorary Consultant, Clinical Pharmacology Unit, Department of Medicine, University of Cambridge
-
Ms Kate Law, Director of Clinical Trials, Cancer Research UK
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
Diagnostic Technologies and Screening Panel
-
Scientific Director of the Centre for Magnetic Resonance Investigations and YCR Professor of Radiology, Hull Royal Infirmary
-
Professor Judith E Adams, Consultant Radiologist, Manchester Royal Infirmary, Central Manchester & Manchester Children’s University Hospitals NHS Trust, and Professor of Diagnostic Radiology, University of Manchester
-
Mr Angus S Arunkalaivanan, Honorary Senior Lecturer, University of Birmingham and Consultant Urogynaecologist and Obstetrician, City Hospital, Birmingham
-
Dr Diana Baralle, Consultant and Senior Lecturer in Clinical Genetics, University of Southampton
-
Dr Stephanie Dancer, Consultant Microbiologist, Hairmyres Hospital, East Kilbride
-
Dr Diane Eccles, Professor of Cancer Genetics, Wessex Clinical Genetics Service, Princess Anne Hospital
-
Dr Trevor Friedman, Consultant Liason Psychiatrist, Brandon Unit, Leicester General Hospital
-
Dr Ron Gray, Consultant, National Perinatal Epidemiology Unit, Institute of Health Sciences, University of Oxford
-
Professor Paul D Griffiths, Professor of Radiology, Academic Unit of Radiology, University of Sheffield
-
Mr Martin Hooper, Public contributor
-
Professor Anthony Robert Kendrick, Associate Dean for Clinical Research and Professor of Primary Medical Care, University of Southampton
-
Dr Nicola Lennard, Senior Medical Officer, MHRA
-
Dr Anne Mackie, Director of Programmes, UK National Screening Committee, London
-
Mr David Mathew, Public contributor
-
Dr Michael Millar, Consultant Senior Lecturer in Microbiology, Department of Pathology & Microbiology, Barts and The London NHS Trust, Royal London Hospital
-
Mrs Una Rennard, Public contributor
-
Dr Stuart Smellie, Consultant in Clinical Pathology, Bishop Auckland General Hospital
-
Ms Jane Smith, Consultant Ultrasound Practitioner, Leeds Teaching Hospital NHS Trust, Leeds
-
Dr Allison Streetly, Programme Director, NHS Sickle Cell and Thalassaemia Screening Programme, King’s College School of Medicine
-
Dr Matthew Thompson, Senior Clinical Scientist and GP, Department of Primary Health Care, University of Oxford
-
Dr Alan J Williams, Consultant Physician, General and Respiratory Medicine, The Royal Bournemouth Hospital
-
Dr Tim Elliott, Team Leader, Cancer Screening, Department of Health
-
Dr Joanna Jenkinson, Board Secretary, Neurosciences and Mental Health Board (NMHB), Medical Research Council
-
Professor Julietta Patrick, Director, NHS Cancer Screening Programme, Sheffield
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Disease Prevention Panel
-
Professor of Epidemiology, University of Warwick Medical School, Coventry
-
Dr Robert Cook, Clinical Programmes Director, Bazian Ltd, London
-
Dr Colin Greaves, Senior Research Fellow, Peninsula Medical School (Primary Care)
-
Mr Michael Head, Public contributor
-
Professor Cathy Jackson, Professor of Primary Care Medicine, Bute Medical School, University of St Andrews
-
Dr Russell Jago, Senior Lecturer in Exercise, Nutrition and Health, Centre for Sport, Exercise and Health, University of Bristol
-
Dr Julie Mytton, Consultant in Child Public Health, NHS Bristol
-
Professor Irwin Nazareth, Professor of Primary Care and Director, Department of Primary Care and Population Sciences, University College London
-
Dr Richard Richards, Assistant Director of Public Health, Derbyshire County Primary Care Trust
-
Professor Ian Roberts, Professor of Epidemiology and Public Health, London School of Hygiene & Tropical Medicine
-
Dr Kenneth Robertson, Consultant Paediatrician, Royal Hospital for Sick Children, Glasgow
-
Dr Catherine Swann, Associate Director, Centre for Public Health Excellence, NICE
-
Mrs Jean Thurston, Public contributor
-
Professor David Weller, Head, School of Clinical Science and Community Health, University of Edinburgh
-
Ms Christine McGuire, Research & Development, Department of Health
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
External Devices and Physical Therapies Panel
-
Consultant Physician North Bristol NHS Trust
-
Reader in Wound Healing and Director of Research, University of Leeds
-
Professor Bipin Bhakta, Charterhouse Professor in Rehabilitation Medicine, University of Leeds
-
Mrs Penny Calder, Public contributor
-
Dr Dawn Carnes, Senior Research Fellow, Barts and the London School of Medicine and Dentistry
-
Dr Emma Clark, Clinician Scientist Fellow & Cons. Rheumatologist, University of Bristol
-
Mrs Anthea De Barton-Watson, Public contributor
-
Professor Nadine Foster, Professor of Musculoskeletal Health in Primary Care Arthritis Research, Keele University
-
Dr Shaheen Hamdy, Clinical Senior Lecturer and Consultant Physician, University of Manchester
-
Professor Christine Norton, Professor of Clinical Nursing Innovation, Bucks New University and Imperial College Healthcare NHS Trust
-
Dr Lorraine Pinnigton, Associate Professor in Rehabilitation, University of Nottingham
-
Dr Kate Radford, Senior Lecturer (Research), University of Central Lancashire
-
Mr Jim Reece, Public contributor
-
Professor Maria Stokes, Professor of Neuromusculoskeletal Rehabilitation, University of Southampton
-
Dr Pippa Tyrrell, Senior Lecturer/Consultant, Salford Royal Foundation Hospitals’ Trust and University of Manchester
-
Dr Nefyn Williams, Clinical Senior Lecturer, Cardiff University
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Interventional Procedures Panel
-
Professor of Vascular Surgery, University of Sheffield
-
Consultant Colorectal Surgeon, Bristol Royal Infirmary
-
Mrs Isabel Boyer, Public contributor
-
Mr Sankaran Chandra Sekharan, Consultant Surgeon, Breast Surgery, Colchester Hospital University NHS Foundation Trust
-
Professor Nicholas Clarke, Consultant Orthopaedic Surgeon, Southampton University Hospitals NHS Trust
-
Ms Leonie Cooke, Public contributor
-
Mr Seumas Eckford, Consultant in Obstetrics & Gynaecology, North Devon District Hospital
-
Professor Sam Eljamel, Consultant Neurosurgeon, Ninewells Hospital and Medical School, Dundee
-
Dr Adele Fielding, Senior Lecturer and Honorary Consultant in Haematology, University College London Medical School
-
Dr Matthew Hatton, Consultant in Clinical Oncology, Sheffield Teaching Hospital Foundation Trust
-
Dr John Holden, General Practitioner, Garswood Surgery, Wigan
-
Dr Fiona Lecky, Senior Lecturer/Honorary Consultant in Emergency Medicine, University of Manchester/Salford Royal Hospitals NHS Foundation Trust
-
Dr Nadim Malik, Consultant Cardiologist/Honorary Lecturer, University of Manchester
-
Mr Hisham Mehanna, Consultant & Honorary Associate Professor, University Hospitals Coventry & Warwickshire NHS Trust
-
Dr Jane Montgomery, Consultant in Anaesthetics and Critical Care, South Devon Healthcare NHS Foundation Trust
-
Professor Jon Moss, Consultant Interventional Radiologist, North Glasgow Hospitals University NHS Trust
-
Dr Simon Padley, Consultant Radiologist, Chelsea & Westminster Hospital
-
Dr Ashish Paul, Medical Director, Bedfordshire PCT
-
Dr Sarah Purdy, Consultant Senior Lecturer, University of Bristol
-
Dr Matthew Wilson, Consultant Anaesthetist, Sheffield Teaching Hospitals NHS Foundation Trust
-
Professor Yit Chiun Yang, Consultant Ophthalmologist, Royal Wolverhampton Hospitals NHS Trust
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Pharmaceuticals Panel
-
Professor in Child Health, University of Nottingham
-
Senior Lecturer in Clinical Pharmacology, University of East Anglia
-
Dr Martin Ashton-Key, Medical Advisor, National Commissioning Group, NHS London
-
Dr Peter Elton, Director of Public Health, Bury Primary Care Trust
-
Dr Ben Goldacre, Research Fellow, Division of Psychological Medicine and Psychiatry, King’s College London
-
Dr James Gray, Consultant Microbiologist, Department of Microbiology, Birmingham Children’s Hospital NHS Foundation Trust
-
Dr Jurjees Hasan, Consultant in Medical Oncology, The Christie, Manchester
-
Dr Carl Heneghan, Deputy Director Centre for Evidence-Based Medicine and Clinical Lecturer, Department of Primary Health Care, University of Oxford
-
Dr Dyfrig Hughes, Reader in Pharmacoeconomics and Deputy Director, Centre for Economics and Policy in Health, IMSCaR, Bangor University
-
Dr Maria Kouimtzi, Pharmacy and Informatics Director, Global Clinical Solutions, Wiley-Blackwell
-
Professor Femi Oyebode, Consultant Psychiatrist and Head of Department, University of Birmingham
-
Dr Andrew Prentice, Senior Lecturer and Consultant Obstetrician and Gynaecologist, The Rosie Hospital, University of Cambridge
-
Ms Amanda Roberts, Public contributor
-
Dr Gillian Shepherd, Director, Health and Clinical Excellence, Merck Serono Ltd
-
Mrs Katrina Simister, Assistant Director New Medicines, National Prescribing Centre, Liverpool
-
Professor Donald Singer, Professor of Clinical Pharmacology and Therapeutics, Clinical Sciences Research Institute, CSB, University of Warwick Medical School
-
Mr David Symes, Public contributor
-
Dr Arnold Zermansky, General Practitioner, Senior Research Fellow, Pharmacy Practice and Medicines Management Group, Leeds University
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Mr Simon Reeve, Head of Clinical and Cost-Effectiveness, Medicines, Pharmacy and Industry Group, Department of Health
-
Dr Heike Weber, Programme Manager, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health
Psychological and Community Therapies Panel
-
Professor of Psychiatry, University of Warwick, Coventry
-
Consultant & University Lecturer in Psychiatry, University of Cambridge
-
Professor Jane Barlow, Professor of Public Health in the Early Years, Health Sciences Research Institute, Warwick Medical School
-
Dr Sabyasachi Bhaumik, Consultant Psychiatrist, Leicestershire Partnership NHS Trust
-
Mrs Val Carlill, Public contributor
-
Dr Steve Cunningham, Consultant Respiratory Paediatrician, Lothian Health Board
-
Dr Anne Hesketh, Senior Clinical Lecturer in Speech and Language Therapy, University of Manchester
-
Dr Peter Langdon, Senior Clinical Lecturer, School of Medicine, Health Policy and Practice, University of East Anglia
-
Dr Yann Lefeuvre, GP Partner, Burrage Road Surgery, London
-
Dr Jeremy J Murphy, Consultant Physician and Cardiologist, County Durham and Darlington Foundation Trust
-
Dr Richard Neal, Clinical Senior Lecturer in General Practice, Cardiff University
-
Mr John Needham, Public contributor
-
Ms Mary Nettle, Mental Health User Consultant
-
Professor John Potter, Professor of Ageing and Stroke Medicine, University of East Anglia
-
Dr Greta Rait, Senior Clinical Lecturer and General Practitioner, University College London
-
Dr Paul Ramchandani, Senior Research Fellow/Cons. Child Psychiatrist, University of Oxford
-
Dr Karen Roberts, Nurse/Consultant, Dunston Hill Hospital, Tyne and Wear
-
Dr Karim Saad, Consultant in Old Age Psychiatry, Coventry and Warwickshire Partnership Trust
-
Dr Lesley Stockton, Lecturer, School of Health Sciences, University of Liverpool
-
Dr Simon Wright, GP Partner, Walkden Medical Centre, Manchester
-
Dr Kay Pattison, Senior NIHR Programme Manager, Department of Health
-
Dr Morven Roberts, Clinical Trials Manager, Health Services and Public Health Services Board, Medical Research Council
-
Professor Tom Walley, CBE, Director, NIHR HTA programme, Professor of Clinical Pharmacology, University of Liverpool
-
Dr Ursula Wells, Principal Research Officer, Policy Research Programme, Department of Health