Notes
Article history paragraph text
The research reported in this issue of the journal was funded by the HTA programme as project number 06/02/01. The contractual start date was in February 2008. The draft report began editorial review in January 2012 and was accepted for publication in July 2012. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors' report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Permissions
Copyright statement
© Queen's Printer and Controller of HMSO 2013. This work was produced by Underwood et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Care homes
The population of Britain, like that of other countries, is ageing. The biggest change for health and social care systems is the expansion in the number of the oldest old (aged ≥ 85 years). In mid-2010, there were 1,410,700 people aged ≥ 85 years in the UK1 – an increase from 600,000 in 1981. Increasing age is associated with increasing disability. This large burden of illness and disability inevitably places huge demands on health and social care services. One consequence of this is an increase in demand for long-term care for the oldest old, which, despite the increased emphasis on community care,2 will remain a necessary component of health and social care provision. 3,4
Even the most optimistic projections for increasing quantity and quality of care in the community leave society facing the prospect of greatly increased numbers of older people in care homes. 4 There are 18,000–19,000 care homes in England with a capacity of 450,000–469,000 places; the majority of places are residential, not involving specialist nursing care. 5,6 Nearly 90% of residents in care homes require care because of disability from long-term conditions, 72% have mobility problems, and 62% are described as confused. 7 Concerns exist about the standards of care received by care home residents. 6,8 Care standards introduced by the Care Quality Commission9 for all care homes in England and Wales in 2011 defined minimum standards of care. These include overriding principles including that residents will be told what is happening to them; that they will receive care and support to meet their needs; that they can expect to be safe; that they will be cared for by qualified staff; and that their care will be constantly checked. The care home business has some inherent instabilities. The Care Quality Commission's 2011 report6 on the state of health care and adult social care in England identified substantial potential for improving the quality of care homes. Even quite modest improvements in mental and physical health are likely to produce large relative increases in the number of quality-adjusted life-years available to this group, which has an extremely poor baseline level of health and life expectancy.
As much of this long-term care provision is in the private sector, and privately funded, one might question the National Health Service's interest in this area. The financial collapse of the Southern Cross Group in 2011, however, emphasises the over-riding role of the state in sponsoring an ostensibly private sector of the economy; what happens in care homes is everybody's business. 10 Large chains of care homes report that between 40% and 75% of their residents are state funded. 11
There is a clear need for more high-quality research to identify effective and cost-effective approaches that can improve the quality of life of care home residents. Because of the very large numbers of National Health Service patients in this sector, and their major health problems, it is an appropriate area for health services research.
Care home terminology
At the time this study was designed the terms residential home and nursing home were used to distinguish between residential facilities that did, or did not, provide nursing care. Since then, the terminology has changed to care homes with, or without, nursing. All of our study materials and our protocol papers used the old terminology. 12,13 The results of this study will be interpreted within the current terminology. Henceforth, we will use the terms care homes with, or without nursing, in preference to the terms residential home and nursing home except when the older terms are critical in understanding the work or when we are reporting work by others and use their original terminology.
Depression in care home residents
Untreated depression is a major cause of morbidity in older people, particularly in those who live in care homes. Up to 40% of care home residents meet criteria for significant depression on validated depression symptom scales. 14,15 Incidence rates for depression in care home residents are typically 6–12% per year for major depression,16–18 with persistence of depression among people already depressed also a major contributor to the burden of morbidity. 19
Multiple physical morbidities are expected in care home residents20 and there is often a lack of social interaction among those living in nursing homes. 21 There is good evidence that both functional impairment and loneliness are risk factors for depression in care home residents. 22
In many cases depression is not recognised by the care home staff or by the resident's general practitioner23–25 and, even if recognised, it is often not treated. 26 Using various depression identification methods, only between 15% and 27% of depressed residents were identified by staff in 30 UK care homes. 27 Evidence from the USA, in contrast, suggests substantial increases in the diagnosis of depression among nursing home residents28 and in the rates of prescription of antidepressants among nursing home residents. 28,29 This matters because depression is an important, independent predictor of adverse outcomes in older people. Among older people living in the community, depression is an independent predictor of both admission to care homes and death. 30–33 Furthermore, in care home residents, it is an independent predictor of more rapid cognitive decline,34 increased medical service use35 and death. 18,27 For people with dementia living in care homes, depressive symptoms are the most important single influence on their quality of life. 36 In care homes, the likelihood of persistence of depression has been shown to be between 45%18 and 63%. 35 Depression is therefore an important target for interventions within care homes.
Approaches to managing depression among care home residents include staff training in detection,25 multifaceted interventions involving highly qualified specialists,15 adaptations of cognitive behavioural therapy for care home populations,37 antidepressant medication and exercise. The evidence that exercise has a beneficial effect on depression in older people with dementia is limited. 38 Antidepressant medication has attractions and there is some evidence of increased use in care homes, especially in the USA. 28,29 Evidence for the efficacy of antidepressants remains modest in this patient group, whereas they have major potential for adverse events due to comorbidity20 and direct toxicity; for example, there is a twofold increase in falls in those taking tricyclic or selective serotonin re-uptake inhibitor (SSRI) antidepressants. 39 Reducing the burden of depression in care home residents, by using a conventional medical model of diagnosis and drug treatment, is likely to fail, at least in the UK, because of poor recognition, low intervention rates and the toxicity of medications. More generally there is a move away from drug treatment for mild/moderate depression. The National Institute for Health and Care Excellence (NICE) guidelines do not recommend drug treatment for mild depression; they suggest that drugs should be used only as part of a more holistic package of care for those with moderate depression. 40 Specifically for the elderly, the guidelines recommend that their poor physical state and social isolation should be addressed. 40 Interventions that may address these multiple requirements are therefore needed. Exercise shows promise as a non-drug intervention that may be helpful for depression.
Exercise/activity as treatment for depression
Evidence for the use of the structured exercise programme
Physical activity is ‘any bodily movement produced by skeletal muscles that results in caloric expenditure’. 41 Exercise is a subcategory of physical activity; it is planned, structured, repetitive and results in improvement or maintenance of one or more facets of physical fitness. There are several types of exercise, including aerobic exercise (submaximal, rhythmic, repetitive exercise of large muscle groups, during which the needed energy is supplied by inspired oxygen) and resistance exercise (any form of active exercise in which a dynamic or static muscular contraction is resisted by an outside force). 42
The endorphin hypothesis suggests that physical activity and exercise cause an increase in the release of ß-endorphins, believed to be related to a positive mood and an enhanced sense of well-being. 43 Although it was originally thought that these ß-endorphins could not cross the blood–brain barrier,44 the endogenous release of central opioids with strenuous exercise may directly account for the sensations of euphoria associated with this type of exercise. 45 Some of the endorphin-related effects may be elicited during aerobic physical activity via an increased discharge from the mechanosensitive nerve fibres within contracting skeletal muscles. 46,47 The level of these increases in endorphins also appears to be directly related to the use of more intense resistance exercise. 48
The monoamine hypothesis suggests that exercise leads to an increase in the availability of brain neurotransmitters (such as serotonin, dopamine and noradrenaline) that are often decreased in depression. 43,47 Exercise also appears to cause increases in levels of monoamines in the blood and urine, and may do so centrally. This theory is based on animal work, and the connection to central increases in monoamines following exercise in humans is as yet unproven. 43
Neurotrophins, especially brain-derived neurotrophic factor, can counteract the hippocampal atrophy that appears to be associated with the high plasma cortisol levels seen in stress and depression,49 and may make the brain more resistant to stress. Neurotrophins are a family of closely related proteins that control many aspects of survival, development and function of neurons in both the peripheral and central nervous system. 50 Exercise appears to activate cellular cascades, such as increases in brain-derived neurotrophic factor expression, which may be both time and intensity dependent. 51,52 Moderate intensity aerobic exercise for a period of 12 months may have the capacity to significantly increase hippocampal size in healthy older adults53 and there appear to be links between resistance exercise and mood changes via the brain-derived neurotrophic factor system,54 although the evidence for the direct effects of resistance exercise on brain-derived neurotrophic factor levels have so far been inconsistent. 55
Engaging in exercise may have the capacity to counteract common symptoms of depression, such as negative thought patterns, low self-esteem and anhedonia (the inability to gain pleasure from enjoyable experiences)56 through distraction, mastery experience,43,57 improvements in self-evaluation58,59 and a sense of achievement. 60 A further theoretical underpinning comes from the theories of positive psychology, considering the potential of exercise interventions to build on ‘virtues’ and ‘character strengths’, such as love of learning (mastery of new skills), bravery (not shrinking from challenge or difficulty) and hope (expecting the best and working to achieve it). 61
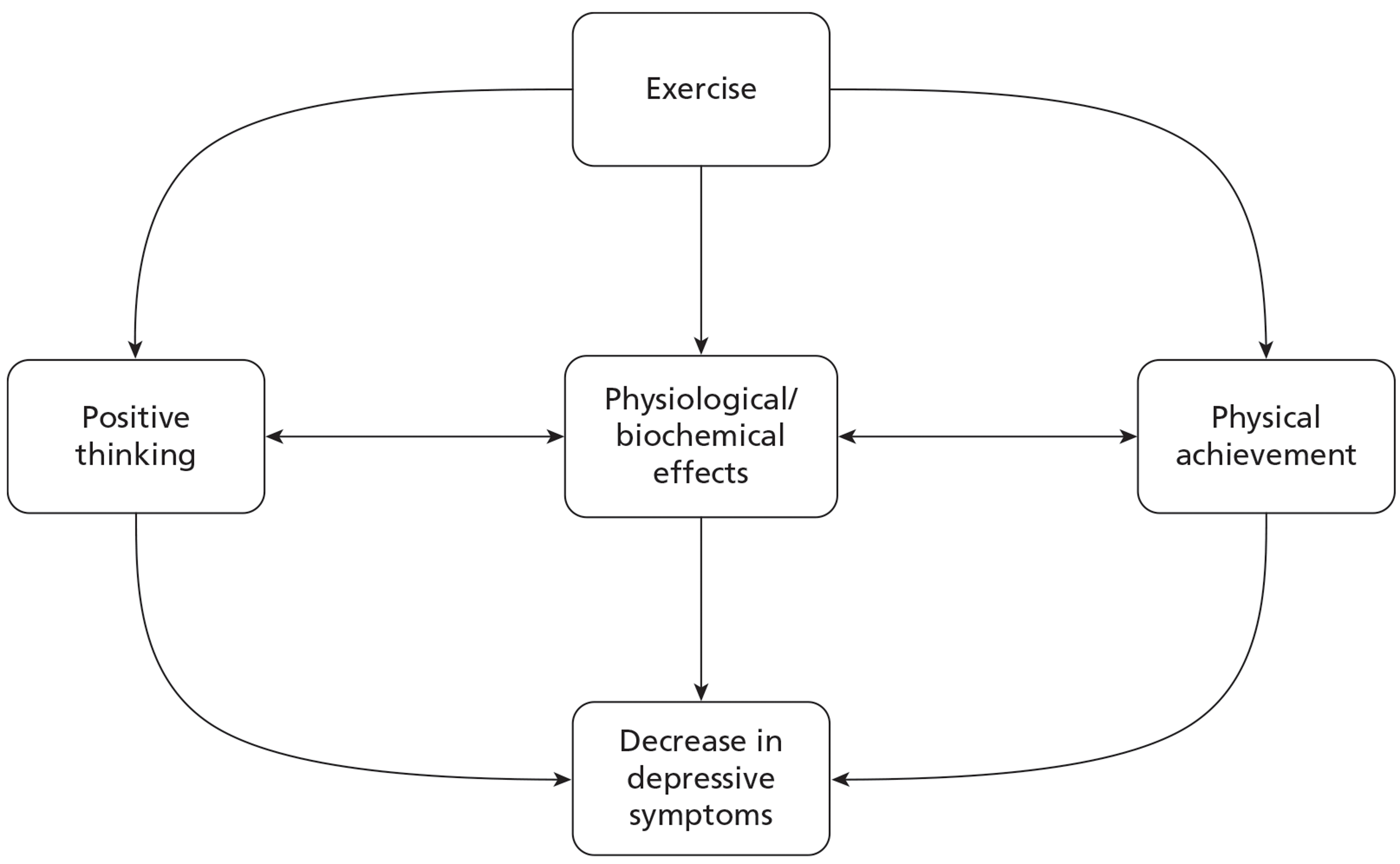
Based on our literature review we developed a theoretical model for how exercise might reduce depressive symptoms (Figure 1).
FIGURE 1.
Theoretical model of effect of exercise on depressive symptoms.
A systematic review of the evidence for the effects of exercise and physical activity on depression in older people concluded that aerobic and resistance exercise are likely to be the most effective forms of exercise for decreasing depressive symptoms in this group. The review also found that interventions using moderate or high intensities of training appeared to be the most effective, signifying that there may be a dose–response effect. 62 A second review examined the evidence for the effect of physical activity and exercise interventions in older people with dementia and depression. It concluded that although there is no clear indication of effect on depressive symptoms or quality of life, there appears to be good potential for people with dementia to participate in physical activity and group exercise programmes, including the use of strength training and higher exercise intensities. 38
Exercise participation for older people with dementia
Kitwood's principles of ‘positive person work’ emphasises the need to understand people with dementia as individuals with very different experiences of life, and different needs, feelings, likes and dislikes63 (Box 1). The features of a person-centred dementia care approach are most likely to support well-being and enable any intervention to create the best possible effects.
Recognition To be acknowledged as a person, known by name, unique
Negotiation To be consulted about preferences, desires and needs, skills needed to take into account anxieties and insecurities
Collaboration Align on a shared task, person's own initiative and abilities are involved
Play To encourage development of spontaneity and self-expression
Timalation The use of interactions of which the prime modality is sensory, without the use of complex cognitive strategies, so that it provides contact, reassurance and pleasure while making few demands
Celebration To enable life to be experienced as intrinsically joyful
Relaxation To enable a person to relax in solitude or with others near them (considering that some people with dementia have strong social needs)
Validation To accept someone's subjective truth, and acknowledge that person's emotions and feelings
Holding To provide a safe psychological space, to help ‘hold’ someone psychologically or physically. This can help the person feel that there is hope that things will get better, and that there is someone who will stay with them however bad things (or they) get
Facilitation Where enabling merges into collaboration, to enable an interaction to get started and to amplify it. This requires great sensitivity to the possible meaning in a person's movements
Neurophysiology of dementia and motor control theory
Motor learning principles can further support maximum participation, success and adherence within both a physical activation programme and exercise groups. A person with dementia can face many challenges in processing visual, auditory, proprioceptive and somatosensory information, indicating the need to provide adequate time to achieve this processing, along with other props that might support their responses, such as the use of rhythm, familiar actions and tasks. 64,65
Because of the pattern of initial change in declarative or explicit memory and learning (for names and facts) among most people with dementia, the use of procedural or implicit memory stimulation and learning strategies (for processes and routines) can be very useful66,67 via the use of:
-
Preserved functions:
-
Repetition:
-
Procedural learning accumulates slowly through much repetition in varying circumstances, where the person (possibly unconsciously) begins to form rules associated with the task. 70
-
-
Feedback and demonstration:
-
The use of targeted feedback and demonstration is linked to classical conditioning and the formation of a predictive relationship between stimuli,68 which can further support the development of automatic responses to those stimuli.
-
Associated with these procedural learning strategies are specific training techniques:
-
Errorless learning:
-
Where multiple cues are provided to prevent errors and so enable success at every stage of a task. This is particularly useful in training people with memory losses, as it avoids the learning of the ‘error’ that might be encountered in ‘trial and error’ techniques, and is effective in promoting the mastery experiences mentioned previously. 71
-
-
Backward chaining:
-
Where a task is broken down into small, achievable parts, with assistance provided until the end of the task (e.g. guide each stage of ‘turn to sit’, but allow person to descend to sitting independently). This is also useful for people with cognitive impairment as it is more likely to promote success and mastery. 72–74
-
-
Functional approach:
-
Owing to the frequent involvement of the parietal cortex and the resultant presence of dyspraxia as a symptom of dementia, the functional approach can be a valuable tool. This employs the use of visual, verbal and physical prompting to support and enhance either the learning of new compensatory strategies or the regaining of previously learned skills. 75
-
Music can be used to increase the efficiency of exercise efforts with evidence indicating improved respiratory efficiency associated with the use of synchronous music, and improved running speeds associated with the use of motivational synchronous music. 76 Music may act as a cue to improve performance, especially in neurological conditions,77 as well as to support memory via the use of classical conditioning. 68 Music may also positively influence adherence via its influences on cerebral areas associated with arousal, emotions and reward,78,79 as well as the attainment of flow (a state of focused motivation/concentration). 76
A group format for structured exercise may offer the protective and positive effects associated with social activities on well-being and mental health. 80,81 Delivering exercise in groups is also likely to enhance adherence and may improve the cost-effectiveness of an intervention. 82,83
Theoretical concepts supporting the use of a whole-home approach
Older adults are more likely than any other age group to lead a sedentary lifestyle despite an awareness of the benefits of being physically active. They cite deterrent factors such as lack of interest, shortness of breath, joint pain, perceived lack of fitness and lack of energy. 84 Frail older adults with multiple comorbidities and high disability levels residing in care homes are even more likely to have very limited physical activity levels. 85,86 To influence the physical activity behaviour of as many residents as possible, and maximise exposure to the exercise sessions, any activity/exercise intervention should offer a variety of physical activity opportunities without placing unreasonable demands on care home staff.
A large number of factors create barriers to physical activity within care homes: resource limitations, perceived role boundaries, limited staff training opportunities and restricted access to appropriate health-care providers. 86–92 Hence, any intervention to increase exercise participation should include approaches to create the culture change needed to effectively address these barriers. 92,93
A whole-home intervention, using an organisational approach to encourage all residents and staff in efforts to increase the residents' level of physical activity, is more likely to achieve the positive effects sought than simply providing group exercise sessions. Such whole-home interventions need to consider the full range of physical, organisational and attitudinal barriers that may be encountered.
Cluster randomised trials in care homes
A systematic review identified 73 cluster randomised trials in residential facilities for the aged, of which 70 were conducted in care homes (Table 1). 94 The earliest trial identified was published in 1992. The trials randomised between 3 and 230 homes, and recruited between 49 and 10,558 participants. The review identified variable quality among the trials, with particularly low proportions accounting for clustering in the sample size calculations and reporting the intracluster correlation coefficients for the homes.
| Characteristics | Median | Minimum | Maximum |
|---|---|---|---|
| Year of publication | 2006 | 1992 | 2010 |
| No. of clusters randomised | 15 | 3 | 230 |
| Mean cluster size (participants per cluster) | 28 | 2 | 217 |
| No. of participants recruited | 352 | 49 | 10,558 |
| Country | No. | ||
| USA | 16 | ||
| UK | 16 | ||
| Netherlands | 9 | ||
| Canada | 6 | ||
| Sweden | 5 | ||
| Others | 18 | ||
| Type of outcome | |||
| Falls | 15 | ||
| Medication prescription | 13 | ||
| Quality of life | 9 | ||
| Mobility | 6 | ||
| Fractures | 5 | ||
| Others | 22 | ||
Most commonly, the trials focused on falls, use of medications, use of physical restraints or quality of life. Two trials focused on depression. There were 13 trials for which physical exercise formed part of the experimental intervention. Overall, the quality of these trials was varied (based on their potential for recruitment/identification bias of participants, and accounting for clustering in design and analyses). The nature of the exercise interventions was also very varied, ranging from gentle exercises based on activities of daily living (six trials) to balance and resistance exercises (seven trials). The frequency of the exercises ranged from once to thrice weekly (except for one trial on hand motor activity for 30 minutes, 5 days a week, during 6 weeks).
The outcomes of these exercise interventions included physical function, falls, quality of life and depressive symptoms. One trial95 tested the effect of a moderate-intensity functional exercise programme, of 3 months' duration. There was no evidence of effect of the intervention on depression. This trial,95 published after OPERA had completed recruitment, was too small, however, to exclude a positive effect from the intervention, particularly in those with depressive symptoms. 95
Ethical issues
Cluster randomised trials have become increasingly common in health service research for a range of pragmatic and methodological reasons. However, the nature of cluster randomised trials, where randomisation, and often also the intervention, is at the level of the cluster rather than the individual, means that the standard ethical requirement of informed consent from all research participants prior to participation cannot be achieved.
The diverse range of models for cluster randomised trials means that how researchers need to secure appropriate consent, while respecting the rights of research participants, is complex. 96–98 MacRae et al. 99 draw on the moral foundations of informed consent and international regulatory guidelines to offer a framework for consent in cluster randomised trials. 99 This includes justificatory reasons for waiver of consent, when consent to randomisation may not be necessary, and the level of information required to be provided following randomisation. When the unit of randomisation in a cluster randomised trial is a care home, the ‘cluster guardian’, who provides consent for participation in the study, will usually be the care home manager. The manager also acts as a gate keeper, controlling access to individual residents for recruitment. The importance of care home managers and staff in the recruitment of participants to research in care home settings has been noted previously. 100 Reasons for excluding access include the views of care home staff on the resident's capacity to consent, the resident's or their next of kin's (NOK's) physical frailty, and the value they place on their privacy. There is a difficult ethical balance to be struck by care home managers in protecting their residents' interests while not denying them the opportunity to participate in research if they wish.
A further difficulty in conducting research in care homes is the substantial number of residents who have a degree of cognitive impairment and who therefore may lack capacity to consent. Cognitive impairment, per se, is not determinative of whether or not a person has capacity to make a specific decision such as consenting or refusing to participate in a research project. There is no direct correlation between Mini Mental State Examination scores and capacity to consent,101 and there is considerable variability in judgements of the capacity of people with Alzheimer's disease to consent to research, even among experienced psychiatrists. 102 A key message from these studies would appear to be that researchers must take responsibility for assessing capacity of participants for their specific study, and recording the process and reasoning for their assessment. It is not clear from the literature that this is currently regarded as standard research practice. A systematic review of cluster randomised trials in care homes found that of the 46 papers that reported consent processes, three trials relied on the opinion of care home staff to assess capacity and seven assumed lack of capacity in all participants by virtue of being resident in a dementia specialist home. 94
Some potential research participants in care homes will clearly lack capacity to consent to take part in research. International research ethics guidelines permit research involving participants who lack capacity if specific criteria are met, for example that the risk of harm to the participant should be no more than slightly greater than that of ordinary medical care103 or that consent is given by a legal representative. 104
The Mental Capacity Act 2005105 requires researchers to consult with either a personal or nominated consultee to seek advice on whether or not the person who lacks capacity would have objected to taking part in the research if they were able to consent. Confusion among research ethics committees and researchers regarding this consultation process has been identified. 106,107 There are also concerns about the impact of this requirement on recruitment of participants who lack capacity to consent. Two UK studies that specified recruitment rates for care home residents through proxies or consultees reported levels of 61% and 41%, respectively. 100,108
In developing this study we identified several ethical issues:
-
the ethics of cluster randomisation and the role of care home managers as cluster guardians providing consent for participation in the study
-
recruitment and consent of individuals for assessments and data gathering in an institutional setting, including the role of home staff as gatekeepers
-
obtaining valid consent for individual participation in a population that will include a high number of cognitively impaired participants, including assessment of capacity to consent
-
the involvement of personal and nominated consultees in decisions about recruitment of residents who lacked capacity to consent
-
the challenges of fluctuating mental capacity throughout the study.
Process evaluations of complex interventions
The effectiveness of any intervention is only partly determined by the content of the intervention. The context in which it is delivered, including the process of delivery and the physical and social environment, has a major influence and should be considered. 109 Process evaluation involves an examination of the processes by which a programme or intervention is implemented. A number of authors have described the use of process evaluation in complex intervention trials, pointing out the value of being able to place findings into context, understanding both how the intervention was delivered and how the social, political and physical context impacted on its effectiveness. 109–111
Aims and objectives of OPERA
The overall aim of the OPERA study was to evaluate the impact of a whole-home intervention, consisting of training for residential and nursing home staff backed up with a twice-weekly, physiotherapist-led exercise class on depressive symptoms in care home residents. Specifically, we sought to test the effect of the OPERA intervention on:
-
the prevalence of depression in those able to complete assessments 12 months after their homes were randomised (cross-sectional analysis)
-
the change in number of depressive symptoms 6 months after randomisation in those who were depressed at baseline (cohort analysis)
-
the change in the number of depressive symptoms in all residents 12 months after randomisation (cohort analysis).
In parallel with this effectiveness analysis, there was a cost-effectiveness analysis, a process evaluation of the study, an ethics substudy and a post-study evaluation.
Chapter 2 Methods
Trial design considerations
The focus of OPERA was on testing an intervention that could be implemented as part of routine health/social care. The original brief from the National Institute for Health Research Health Technology Assessment programme called for a cluster randomised trial of the effect of a programme of group exercise on the remission of depression in care home residents. An exercise intervention would be difficult to introduce into normal practice if it is to be available only to those who have been diagnosed with depression. This is because of the need to pre-screen residents for depression. It also may be less likely to be effective if only those who are depressed attend, as positive social interactions and peer modelling of maximal effort may contribute to effectiveness. If a positive approach to increasing exercise in the residents is built into the values of care home staff, the likelihood of a group exercise intervention having a positive effect will be maximised. We, therefore, chose to test a whole-home intervention, consisting of a training programme for care home staff backed up by a twice-weekly, physiotherapist-led exercise class. As all residents were exposed to the OPERA intervention, its effects, positive or negative, on mental and physical health, may affect both those who are depressed and those who are not depressed. Furthermore, there is a high turnover of care home residents, with many new residents also being exposed to the intervention. For these reasons measurement of outcomes on all residents is important. The potential for harm from the intervention meant that it was very important to collect data on all residents, not just those with depression. With an ongoing intervention any effects, positive and negative, will continue to accrue in the long term. Indeed, only if long-term beneficial effects can be demonstrated would it be appropriate to build such a programme into the work of care homes. The outcome of interest then becomes the prevalence of depression in all of those residents in the care home at the end of the study. This includes any new residents who joined the study after randomisation. Thus, our pragmatic primary outcome of interest was the proportion of care home residents who were depressed 12 months after their care home was randomised. Henceforth, we will refer to this as the cross-sectional analysis, recognising that this population includes participants who had been in the study for variable lengths of time. The term cohort analysis will be used when referring to our more explanatory primary outcomes of change in depressive symptoms, involving those residents who were present in the home, and who had provided data, prior to randomisation. Where appropriate, we refer specifically to the depressed cohort of residents, who were classified as depressed on the Geriatric Depression Scale-15. 112 Likewise, the results of secondary analyses are similarly reported as cross-sectional analysis and depressed cohort analysis.
We collected data from several sources:
-
Directly from the participants, henceforth assessment data.
-
Indirectly from the care homes and the National Health Service, henceforth care home data. This includes data collected from routine care home records, henceforth record data, and assessments by care home staff of participant's health state and social interaction, henceforth proxy data, and data from the Secondary Uses Services databases held by participating primary care trusts, and the National Health Service Medical Record Information Service, henceforth National Health Service data.
A participant in the OPERA study is anyone for whom we have consent/agreement to provide data; a resident is anyone living an OPERA home. Some participating residents might not have been present in the home at the time assessments were carried out, for example because they were in hospital. On occasion when referring to the group exercise sessions we refer to exercise group participation which is distinct from study participation.
Some participants did not complete face-to-face assessments, and thus did not provide assessment data, but they did provide care home data. The reasons for this were either that the relevant permissions (consent/assent) were not obtained to allow face-to face assessments, the participant was not present at the time assessments were done, or that when approached the residents were unable, or unwilling, to engage with the assessment process because they were cognitively impaired. A small number of participants agreed to provide assessment data but not to allow access to care home data.
In addition to those included in the cross-sectional analyses and the cohort analyses there are two further groups of residents who have contributed data to the study. Firstly, there are those who provided individual baseline data after their home was randomised but who did not provide data for the cross-sectional analysis; typically these were people who were only resident in the home for part of the year. This group contribute to the specific data on fracture rates. Secondly, as any harms from the intervention might also affect non-participants we collected some safety data from all residents.
Although the core of this study was a very simple trial to find out if exercise helps depression, there are a number of different populations contributing to the different analyses. Only by including these different populations are we able to give the full picture of how the intervention might affect care home residents. This added overall value to the study.
Pilot study
In the pilot study we tested the recruitment processes and refined the study interventions and process evaluation design prior to the main study.
We recruited three local care homes in Coventry in June/July 2008: two residential care homes and one dementia specialist care home. The residential homes were selected to represent care homes in the locality, and the dementia specialist home to test the assessment procedures and exercise intervention with more cognitively impaired residents. We assessed recruitment flow for the three care homes to allow comparison of recruitment rates between the two residential homes and the dementia specialist home (Figure 2).
FIGURE 2.
Recruitment in pilot homes. CH, care home; DSCH, dementia specialist care home.
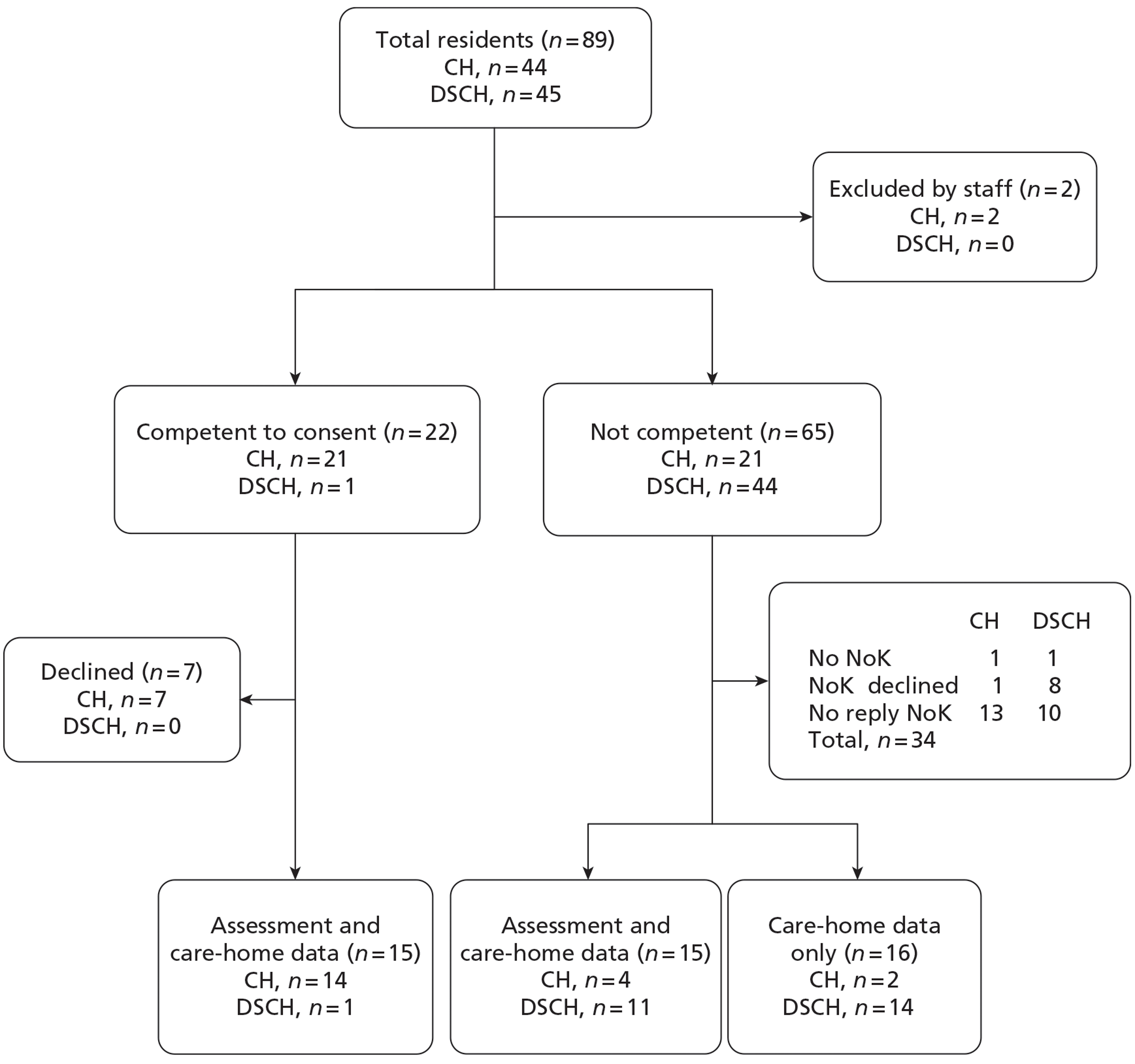
There were 89 residents in the three care homes at the time of recruitment; staff excluded two residents because they were considered too ill to take part in the study. Half of residents in the two residential care homes were judged to have capacity to consent and one resident in the dementia specialist home. Fifteen residents gave consent to take part in the study assessments and permission for staff to collect data from their home records.
Twenty-three (37%) NOK did not respond to written request for assent and nine NOK did not want their relatives to take part in the study. Assent/agreement was obtained for 31 residents to take part in the study; however, 16 of these, when approached by the recruitment team, were unable to complete study assessments and provided access to care home data only. That 14 of these participants were resident in the dementia specialist home identified initial challenges in collecting assessment data from more cognitively impaired residents.
Following the recruitment phase of the pilot study a number of processes were revised:
-
Permission was approved by the ethics committee to contact NOK by telephone if no reply for assent/agreement had been received 2 weeks after the written request in an attempt to improve response rates.
-
Owing to difficulties experienced in recruiting residents from, and collecting the primary outcomes in, the dementia specialist home, the management team proposed re-evaluating the inclusion of dementia specialist homes in the main study.
Once potential participants were recruited to the pilot, we randomised the two residential care homes: one to the control intervention and one the exercise intervention. The dementia specialist care home was allocated the exercise intervention so that we could evaluate the feasibility of running the exercise groups for residents with moderate to severe cognitive impairment.
The exercise groups were well attended in the residential homes and dementia specialist home, and proved to be appropriate for residents with and without cognitive impairment. Following observation by a member of the process evaluation team and staff delivering the exercise groups, small changes were made to the physiotherapist assessments of residents and the format of the exercise groups.
The pilot study demonstrated that the depression awareness training (a component of both the control and active intervention, which is outlined in detail later) was well received by care home staff, and the format required very little change prior to the start of the main study.
Observation visits to the three care homes helped inform the development of the process evaluation protocol for the main study. The wide range of cognitive and physical abilities observed in the residents in the care homes identified the importance of developing an inclusive approach to recruitment to ensure that findings reflected the experiences of all residents. As a consequence of our observations in the pilot homes we felt that none of the planned outcome measures captured levels of activity or social engagement in the homes. We therefore decided to add the Social Engagement Scale as a secondary outcome measure. 113
Developing the process evaluation
The process evaluation pilot had two main aims: to inform (1) the development and implementation of both the whole-home intervention and the control intervention for the main study, and (2) the design of the process evaluation of the main study. We used a formative approach in the pilot phase to ensure that any problems were identified and addressed in the main study protocols and procedures. As part of the process evaluation of the pilot study, one researcher (DE) spent time in the three pilot study homes observing the research staff activity and talking to staff and residents. Although we aimed to conduct non-participant observation, it proved impossible to maintain non-participant observer status in this setting. The researcher was inevitably drawn into the activities in the home; residents became familiar with him and expected him to interact with them socially. We used both non-participant and participant observation in the main study process evaluation as these approaches are complementary. 114
Other challenges were identified in the pilot process evaluation13 and influenced our development of the process evaluation protocol including:
-
We were working with a vulnerable population with varying degrees of cognitive and physical abilities. We had to take care to be inclusive in our approach to ensure that our findings reflected the experiences of the whole population of the care homes.
-
In many homes space to carry out interviews in private was limited. We needed to establish standard operating procedures that as far as possible respected residents' right to privacy.
-
A normal day in a care home is structured with set times for meals, breaks, activities and drug rounds, which can leave little time for a researcher to engage with residents. During the pilot study, we found that there was often a narrow window of opportunity to engage in individual interviews. Residents tended to be more receptive in the mornings (a common finding in populations with a high prevalence of dementia), with many homes running activities at these times for this very reason. This coupled with prearranged interviews being cancelled when the resident was found to be asleep further narrowed the opportunities for carrying out interviews.
-
Observations and feedback from team members revealed that the process of recruiting participants and, in particular, gaining informed consent, took considerably longer than originally envisaged. During the pilot phase, a number of problems with the process of gaining consent were noted, including the content of the consent forms and the difficulties of ensuring that participants had given informed consent.
In a focus group with the recruiting team, to discuss issues in the process of gaining consent, the team reported finding the process challenging, and thought the consent form was too complex for residents. It took up to 20 minutes to complete the process for each individual resident, and some of the residents found the information difficult to understand and to retain. Those study recruitment staff who had carried out the assent/agreement process (with relatives of residents deemed unable to give informed consent) found it easier, with fewer tick boxes, making it simpler to complete. This led to the consent form being shortened to make it easier for residents to complete.
A number of other changes to the conduct of the main study were implemented as a result of the pilot study process evaluation, including changes to data collection forms. Other recommendations arising from the pilot process evaluation are described in Box 2.
Ensuring that the intervention homes were aware of what the exercise intervention entailed and the need for support from the staff
A review of the physiotherapist assessment of residents to reduce burden on physiotherapist
A review of the exercise sessions and the use of leg weights in the classes
A review of whether or not dementia specialist homes should be included, given the low numbers or residents who were able to complete the primary outcome measure, the Geriatric Depression Scale-15
As a result of the recommendations from the pilot study, amendments were made to the process evaluation protocol: nursing homes were included as a separate category in the sampling frame for case study homes and two focus groups (one for the recruiting team and one for the physiotherapists) were planned instead of individual interviews
Recruitment
Homes
We recruited homes from two geographical locations: Coventry and Warwickshire (C&W) and north-east London (NEL). The practicalities of delivering the intervention meant that all care homes needed to be within reasonable travelling distance for the physiotherapists delivering the intervention: either Warwick Clinical Trials Unit for C&W or Barking & Dagenham Primary Care Trust's physiotherapy department for NEL. Together, these two locations provided a wide range of populations broadly representative of the social mix within the UK, ranging from prosperous rural South Warwickshire through to deprived multicultural urban communities in Coventry and NEL.
We identified all care homes within the relevant primary care trust areas (Barking & Dagenham, Coventry, Havering, Redbridge, Waltham Forest, Warwickshire and West Essex). Following primary care trust approval we approached all care homes with between 16 and 60 beds, but from 11 February 2009 increased the maximum number of beds to 70. Also, from this date we specified that a minimum of six residents needed to have been assessed to be included in the study; our lower limit for home size was based on being able to recruit a minimum of six participants from each home. We excluded smaller homes to ensure that we could collect, from each home, follow-up data from at least one resident with five or more depressive symptoms at baseline. We excluded larger homes because the reduced statistical power from larger clusters meant the additional time taken in recruitment and delivering the intervention was an inefficient use of available resources. With the agreement of the Trial Steering Committee we decided to exclude homes in which more than half of the beds were registered as dementia specialist beds. We took this decision because recruiting in the first dementia specialist home for the main study confirmed our observation from the pilot study, that too few residents in dementia specialist homes were able to provide data on the primary outcome measure. With the agreement of the Trial Steering Committee we changed our protocol to exclude these homes after the first of them had been randomised.
We approached, by post, all apparently eligible homes, apart from three in C&W included in our pilot study. Interested homes were then visited by a member of the recruitment team to assess their suitability. At this time homes were excluded if fewer than six residents were likely to be able to take part in the study; more than half of the residents had severe cognitive impairment; the majority of residents were non-English speaking; or, after discussion with the study team, the home felt they were too busy to participate. Towards the end of the study some interested homes were unable to participate because we had reached our target for home recruitment.
Inclusion and exclusion criteria
Inclusion criteria:
-
permanent resident in the care home
-
aged ≥ 65 years
-
English speaker (for assessments).
Exclusion criteria:
-
terminal illness or too ill to be seen at the time of assessment
-
severe problems communicating (for assessments).
Many care home residents had multiple comorbidities, which meant that they would not be able to provide data for some, or all, of our assessments. The whole-home nature of our intervention meant, however, that all home residents would be exposed to the intervention regardless of their ability to provide data for our primary outcome or to participate in the exercise groups. For this reason we asked residents to give consent, or their NOK to give agreement, for us to collect assessment data directly from participants, and also to collect indirect care home data. Furthermore, any harms relating to the intervention would affect both participants and non-participants. For this reason we collected safety data (fractures and deaths) on all residents.
In some instances NOK had provided assent/agreement for us to assess a resident but upon approaching them the assessment was abandoned due to the resident being uncooperative or too cognitively impaired.
Ethical considerations
Obtaining appropriate valid consent from participants is essential to any research study and there are specific ethical concerns regarding consent in both cluster randomised trials and research conducted in care homes (see Chapter 1, Ethical issues). Many residents were likely to have substantial cognitive impairment and therefore may have lacked capacity to consent to taking part in a research study, which involves completing a series of assessments and allowing access to their records.
In the OPERA study the clusters were the care homes where the home managers not only acted as gatekeepers to individual residents, or their NOK, for the purposes of consent to the assessments, but were also the cluster guardians for the home giving consent for the home to participate, and actively participated in the whole-home intervention. 96
To ensure that participants had given valid consent particular attention needed to be paid to assessment of capacity during the information-giving process. We therefore developed a two-stage approach to gaining consent; first assessing capacity and at a second visit obtaining consent (see Obtaining consent, below). All of the research nurses and physiotherapists who were part of the recruitment team received specific training in assessment of capacity and taking consent by the study ethicist.
Enrolling participants who are unable to consent into a study is ethically problematic, as it can be difficult to argue that participation is necessarily in their best interests. For those residents who were unable to consent to take part in the assessment component of the study we followed the requirements of The Mental Capacity Act 2005,105 which provides the legal framework for involving people who lack capacity in medical research. Initially, the NOK was approached as the personal consultee, as defined in the Act, and if no personal consultee could be identified then a nominated consultee, as defined in the Act, was sought.
If the consultee agreed that the resident should take part in the study then the resident was enrolled as a participant. The process of setting up the study and obtaining ethics approval took place very soon after enactment of The Mental Capacity Act 2005, when researchers were still familiarising themselves with the practical implications of its requirements for research. As a result, our documentation referred to assent/agreement of the consultee to the resident taking part in the research. We are aware that there has been discussion in the literature about the initial failure of researchers and research ethics committees to fully understand the precise intention of the Act in this regard. 106
There has been a subsequent movement towards seeking a consultee's views about the likely wishes of the individual (the resident) about participating in the research, rather than their agreement on their behalf. Our own research practice has mirrored this development in thinking. However, as our study documentation, which had been subjected to ethical review, included the terms assent and agreement, we will continue to use these throughout this report to describe this research process.
Residents who lacked capacity to consent to take part in the research may still have been able to give consent, or refuse, to take part in an individual assessment. Therefore, at each assessment their consent or agreement was sought for that particular assessment. If at any time during the assessment a participant indicated that they did not want to take part their wishes were respected, whether or not they had formally consented or agreement had been provided by NOK.
Ethical review for the study was provided by the Joint University College London/University College London Hospital Committees on the Ethics of Human Research (Committee A), now known as Central London REC 4. The REC reference for the study is 07/Q0505/56. The Committee also approved 10 Substantial Amendments for the study.
Obtaining consent
At the first visit to the care home the care home manager, or delegated staff member, was asked to exclude any residents whom they felt it would be inappropriate to approach to take part in the study, for example those with a terminal illness. A specially trained research nurse or physiotherapist approached the remaining residents to tell them about the study and assess their capacity to give consent (stage 1). Those who, in the opinion of the recruitment team, lacked capacity to give consent to participate were not approached further; we did, however, approach their NOK. Residents not interested in taking part in the study were excluded.
Information sheets were given to residents who were considered competent to consent, and left in a prominent place so that they could discuss it with their relatives or friends. Large print or audio versions were available for those with visual impairment. Mutually agreed appointments were made for study assessments within about 1 week of the initial approach, giving residents time to consider taking part in the study.
Residents had the option to consent, or NOK had the option to give assent, either to the assessments, the use of care home data or to both. Residents (or NOK) could also consent (or assent) to the results of assessments being shared with the care home manager and their NOK, and/or their general practitioners being informed of their participation in the study. The research nurse/physiotherapist conducting the recruitment assessment checked that the resident had read, or otherwise availed themselves of, the information sheet and understood the broad nature of the study, and answered any questions that the resident had. In practice, family members were sometimes present for these discussions. Each statement on the consent form was discussed and initialled by the resident; if they were in agreement then the consent form was signed by the resident and witnessed by the research nurse. For those residents with sight impairment a member of the care home staff witnessed the consent process. The process of going through the information sheet and consent form and checking understanding provided a further check on the resident's capacity to consent (stage 2). If at this stage it was clear that the resident lacked capacity then the process was stopped and a personal consultee was approached.
Care homes wrote to the NOK of residents who lacked capacity to consent, enclosing information about the study and an expression-of-interest slip. Residents who were unable to communicate were identified by the care home manager at the initial meeting, and agreement was requested for access to care home data only. NOK who expressed an interest in their relative/friend taking part in the study were contacted by telephone to answer any queries and arrange for an assent form to be sent to them by post or to be completed with the research nurse at the care home.
If after 2 weeks there had been no response to the request from the initial letter the relatives were contacted by telephone. It had been anticipated that if a resident had no known NOK then an appropriate nominated person could be contacted as permitted by The Mental Capacity Act 2005. 105
We consulted with local social services departments and the Independent Mental Capacity Advocacy (IMCA); neither organisation felt able to provide this service. In view of the relatively small numbers of residents involved we decided not to explore other possibilities for a nominated consultee and therefore residents who were unable to give consent and who had no contactable NOK were not recruited.
Baseline data collection
Assessments were carried out in the resident's own room or an alternative quiet location in the care home in which the resident felt most comfortable. Assessment lasted between 30 and 60 minutes and the research nurse/physiotherapist administered the questionnaire instruments; Geriatric Depression Scale-15,112 Mini Mental State Examination,115 European Quality of Life-5 Dimensions (EQ-5D),116 fear of falling and current pain. They also did a brief physical assessment: the Short Physical Performance Battery. 117,118 The results were recorded on paper whilst with the resident, and entered directly on to a laptop computer after the assessment had finished. Assessments were terminated if the resident expressed any distress or desire to withdraw.
Wherever possible all baseline assessments were collected prior to randomisation. For a small number of residents the recruitment process was started prior to randomisation but consent/assent was not obtained until after randomisation. Data collection for these participants was then carried out as soon as possible after randomisation. These participants' data were not included in the cohort analysis but were included in safety analyses, and if present at the end of the study they were included in the cross-sectional analyses.
Where consent/agreement had been given we provided the care home manager with the resident's Geriatric Depression Scale-15 scores and a brief interpretation/suggested action. Residents with Geriatric Depression Scale-15 scores of 0–4 were considered to have no depression. It was suggested that residents with Geriatric Depression Scale-15 scores of between 5 and 10 (moderate depression) were encouraged to take part in activities and be monitored by care home staff. Care home staff were encouraged to refer residents with Geriatric Depression Scale-15 scores of between 11 and 15 (severe depressive symptoms) to their general practitioner or Community Mental Health Team. For those residents who were unable to complete all 15 questions (but did complete ≥ 10) we used an algorithm to calculate and report the score, based on proportion of positive replies from questions answered (see Appendix 1).
Residents recruited after randomisation
At the 3- and 6-month visits the care home manager was asked to identify any new permanent residents (see Follow-up, below). We did not do this at 9 months to ensure that all those contributing to the cross-sectional analyses had been exposed to the environment within the care home long enough to be exposed to at least 4 months of the environment of that home. If the resident was eligible and interested in taking part in the study, the research nurse/physiotherapist explained the study and assessed their capacity to give informed consent, allowing the resident at least 24 hours to consider taking part in the study. NOK of residents unable to give informed consent were contacted in the same manner as those approached prior to randomisation. All processes for data collection were the same as for participants recruited prior to randomisation (see Obtaining consent, above).
Care home data
We collected demographic data (age, sex, ethnicity, social class, age at leaving full-time education), comorbidities (cancer, stroke, dementia, depression, anxiety, osteoporosis, chronic lung disease, urinary incontinence) and data on length of residence from the care home records. Data on current medication use were obtained directly from residents' Medication Administration Record Sheets. The resident's key carer, or carer looking after them on the day of data collection, was asked to complete a proxy EQ-5D, Barthel Index and Social Engagement Scale (Table 2). 113,116,119
| Data collection | Time recruited | |||
|---|---|---|---|---|
| Baseline | 3 months | 6 months | 9 months | |
| Before randomisation and immediately post randomisation | Sociodemographic data, comorbidities, GDS-15, MMSE, EQ-5D, SPPB, fear of falling, pain, Barthel Index, proxy EQ-5D, SES, medications | |||
| 3 months | Proxy EQ-5D, SES, medications, fractures, deaths | Sociodemographic data, comorbidities, GDS-15, MMSE, EQ-5D, SPPB, fear of falling, pain, Barthel Index, proxy EQ-5D, SES, medications | ||
| 6 months | GDS-15, MMSE, EQ-5D, fear of falling, pain, proxy EQ-5D, SES, medications, fractures, deaths | Proxy EQ-5D, SES, medications, fractures, deaths | Sociodemographic data, comorbidities, Barthel Index, GDS-15, MMSE, EQ-5D, SPPB, fear of falling, pain, Barthel Index, proxy EQ-5D, SES, medications | |
| 9 months | Proxy EQ-5D, SES, medications, fractures, deaths | GDS-15, MMSE, EQ-5D, fear of falling, pain, proxy EQ-5D, SES, medications, fractures, deaths | Proxy EQ-5D, SES, medications, fractures, deaths | Sociodemographic data, comorbidities, Barthel Index, GDS-15, MMSE, EQ-5D, SPPB, fear of falling, pain, Barthel Index, proxy EQ-5D, SES, medications |
| 12 months, end of study | GDS-15, MMSE, EQ-5D, SPPB, fear of falling, pain, proxy EQ-5D, SES, medications, fractures, deaths | |||
Follow-up
We did four cycles of follow-up in each home. Follow-up data were collected over several visits, at around 3, 6, 9 and 12 months after the home was randomised.
Follow-up data collection
At 6 and 12 months we sought to complete follow-up assessments on all residents from whom we had consent or agreement to take part in study assessments. The research nurse/physiotherapist confirmed with the care home manager that it was an appropriate time to approach the resident. Residents who agreed to take part in follow-up assessment completed the same questionnaire instruments as baseline apart from the physical assessment Short Physical Performance Battery, which was not administered at 6 months.
Residents who were known to have died or had moved from the home were reported to the study team by the care home manager at each visit. At 6 and 12 months residents who were in hospital, or too unwell at the time of assessment, were contacted within 1 month to see if they were now well enough to be assessed. Participants who had moved to another participating care home were contacted and assessed, at the time that assessments were being done in their original home. We were unable to follow-up participants who had moved to a non-participating home.
Care home data were collected for those for whom we had consent/agreement and who were present in the care home at 3, 6, 9 and 12 months. Medication use, visits by health-care professionals, outpatient appointments, accident and emergency (A&E) attendances, and hospital admissions were recorded. The resident's key carer, or carer looking after them on the day of data collection, was asked to complete a proxy EQ-5D and the Social Engagement Scale at the 3-, 6-, 9- and 12-month follow-up visits.
Residents recruited after randomisation
Follow-up assessments were completed in the same manner as those recruited prior to randomisation with an assessment 6 months after they had joined the study. All participating new residents had an end of study assessment when their home came to the end of its 12-month study period. The majority of new residents were identified and recruited at 3- and 6-month follow-up visits to the care homes; a small number requiring assent from NOK were recruited at between 6 and 9 months post randomisation.
Evaluation of recruitment processes
As part of the process evaluation, recruitment processes, including home recruitment and recruitment of individual participants, were evaluated (see Process evaluation, below).
Independent observations of the process of consenting participants were carried out by the process evaluation research fellow. This involved shadowing the recruiting staff on a number of occasions and observing the consent and assessment process in different homes. Results of these observations are reported in the quality control section and are mentioned in the consent substudy section (see Ethics substudy, below).
Assessment
In light of the poor state of health of many of our study participants we used a parsimonious set of outcome assessments. For the cohort analyses we collected follow-up data, directly from participants, at 6 and 12 months after randomisation. A drug trial for the treatment of depression would expect maximal effect to be seen by 4 months. 40 If exercise were an effective treatment for depression we might expect a response in a similar time. However, there is a time lag between randomisation and participants gaining any benefits from the exercise programme because of the time taken to start changing the attitudes of the care home staff and to establish exercise groups as a regular routine in the care home. Anticipating that the intervention would be fully functional 2 months after randomisation, we did our first assessment 6 months after the home was randomised.
We originally intended to collect 6-month follow-up data just from those with five or more depressive symptoms (or equivalent) at baseline. Early in the study it became clear that the average cluster size was smaller than anticipated. In view of concerns about obtaining sufficient data for any 6-month analysis, and with the agreement of the Trial Steering Committee, we changed to collecting 6-month assessment data from all participants. We did not, however, have sufficient research nurse/physiotherapist capacity to also collect the Short Physical Performance Battery on all participants at 6 months and therefore did not include the 6-month physical assessment. For the cross-sectional analyses we included residents who had been in an OPERA care home for at least 3 months prior to the end-of-study (12-month) data collection.
At each assessment we started by collecting our primary outcome measure, the Geriatric Depression Scale-15, to maximise response rates in those who might not be able to complete the full assessment. 112 We had originally set an exclusion criterion of a Mini Mental State Examination score of < 10 for severe cognitive impairment, as we thought that those with lower scores would be unable to complete the Geriatric Depression Scale-15. 115 Experience in the pilot study was that we were collecting satisfactory Geriatric Depression Scale-15 scores prior to attempted completion of the Mini Mental State Examination. We therefore removed this exclusion criterion from the main study. This concurs with reports of successful completion of the Geriatric Depression Scale-15 in people with severe cognitive impairment. 120
Primary outcome measure
Our primary outcome measure was the Geriatric Depression Scale-15. 112 This brief instrument consists of 15 yes/no questions and has been well validated in care home populations. It avoids using potentially somatic features of depression that may be misleading in this age group, focusing more on mood and functional symptoms of depression. 121 It is one of the most widely used measures in this field. It is simple to complete, with 97% of cognitively intact nursing home residents producing analysable data, and showed high internal consistency in a large sample of US nursing home residents. 122 The Geriatric Depression Scale-15 can be interpreted as an indication of the presence/absence of depressive mood. A score of ≥ 5 appears to give the best sensitivity and specificity for presence/absence of depressive mood. 120,123 Nevertheless, the Geriatric Depression Scale-15 is not a substitute for a clinical diagnosis of depression. However, in this report we will refer henceforth to the presence of five or more depressive symptoms, or its equivalent, on the Geriatric Depression Scale-15 as depression (Table ). Some individuals completed fewer than 15 items on the Geriatric Depression Scale. The recommended score indicating depression is ‘5’ when 13 or more items are completed, ‘4’ when 12 or 11 items are completed and ‘3’ when 10 items are completed (see Table 3). When nine items or fewer were completed the Geriatric Depression Scale-15 score was set to missing. Henceforth the presence of the appropriate number of positive items is referred to as depression. The Geriatric Depression Scale-15 has been used as a continuous measure in other randomised controlled trials based in care homes. 95,124 We also use the Geriatric Depression Scale-15 as a continuous measure in some of our analyses.
| Responses to GDS | Score indicating depression |
|---|---|
| 15 | ≥ 5 |
| 14 | ≥ 5 |
| 13 | ≥ 5 |
| 12 | ≥ 4 |
| 11 | ≥ 4 |
| 10 | ≥ 3 |
Data collection
For the cohort study we collected Geriatric Depression Scale-15 and the other participant reported outcomes prior to randomisation and then at 6- and 12-month follow-up. For those joining the study after randomisation we collected these data at study entry, 6 months after study entry and/or at the end of the study.
Other participant reported outcomes
Health-related quality of life
The EQ-5D is a widely-used brief measure of health utility. 125–127 [The EQ-5D and proxy EQ-5D were used with the permission of the EuroQol Executive Office. All copyrights in the EQ-5D, its (digital) representations, and its translations exclusively in the EuroQol Group. The EQ-5D™ is a trade mark of the EuroQol Group.] It measures quality of life using questions in five domains, the EQ-5D, plus the EuroQol Visual Analogue Scale (thermometer). To reduce questionnaire load we used the EQ-5D as our overall measure of health-related quality of life and for our health economic analyses. It has been used satisfactorily in previous studies of nursing home residents. 127
Cognitive function
We measured cognitive function using the Mini Mental State Examination115 (The Mini Mental State Examination was used with permission of Psychological Assessment Resources Inc., which retains the copyright). The Mini Mental State Examination is the most widely used measure of cognitive impairment worldwide. 128 It is quick, validated in relevant populations, sensitive to change and allows comparisons to be made with other studies. There is a suggestion that exercise may have a direct effect on preventing cognitive decline. 129 This is therefore an important secondary outcome.
Fear of falling
Although there are grounds for optimism that exercise intervention of the type used in OPERA may reduce both falls and falls injury, there is a justifiable concern that, by encouraging residents to be more active, it might lead to an increase in falls. 130,131 Recording of falls within care homes is likely to be unreliable and within a cluster randomised trial of this nature it is prone to reporting bias. In community studies fear of falling has been shown to be an independent predictor of falls risk. 132 For this study we used a simple yes/ no question of fear of falling to make completion easier. Others have found, in similar populations, that many residents are unable to complete a scale for fear of falling. 133
Pain
The association between pain and depression in older people is well recognised. 134,135 Exercise may have a beneficial effect on pain in this population, independent of the beneficial effects it may have on depression. 33 We ascertained presence or absence of pain from the EQ-5D pain question. For those with pain we then assessed their current level of pain on a five-point ordinal scale, i.e. pain now: no pain, mild pain, moderate pain, severe pain, and pain as bad as it could be. For analysis we collapsed this into three groups: no pain, mild/moderate pain, and pain as severe or as bad as can be.
Physical assessment
Mobility
To assess the effect of the programme on mobility we used the Short Physical Performance Battery, which incorporates three essential aspects of physical function that should be improved by the exercise programme: static balance, lower limb strength and dynamic balance. 117 Because of the central importance of physical function to the ability to thrive, the Short Physical Performance Battery has been used extensively in trials and observational studies of older people. It has well-established and surprisingly strong relationships with a range of important public health outcomes, including onset and progression of disability, mortality and nursing home admission. 136 Testing procedures are standardised and timed. 117,118 A change in the Short Physical Performance Battery would indicate if the OPERA intervention has had an effect on its primary target of improving physical activity.
Data collection
For the cohort study we collected Short Physical Performance Battery prior to randomisation and at the end-of-study assessment. For those joining the study after randomisation, we collected these data at study entry and at the end of the study. In the original protocol we were planning to collect only 6-month outcome data on those who were depressed at baseline. As a sustained effect on mobility was the outcome of interest this was measured at study entry and end-of-study assessments only.
Proxy measures
We collected proxy data on all of those for whom we had permission to collect care home data. Thus, more proxy data are available on participants than data from the participant-completed measures.
Activities of daily living
At baseline only we collected data on activities of daily living in order to provide data on the severity of physical disability in our population. We used the Barthel Index, a widely used measure of activities of daily living. 119
Health-related quality of life
The use of proxy measures of the EQ-5D, where the proxy is asked to report on how they think the subject feels, is well established. 137 Many of our participants would be unable to satisfactorily complete the EQ-5D. In particular, the use of the EQ-5D Visual Analogue Scale (thermometer) is difficult for those with substantial cognitive impairment or visual impairment. The level of agreement between self-completed and proxy scores varies according to subjects' underlying illnesses and who the proxy is (family member or health-care professional). Agreement is better for the EQ-5D index score than the Visual Analogue Scale but varies across EQ-5D domains. Agreement is reasonable for people living with stroke and better for Parkinson's disease. 138,139 One study in dementia found an intracluster correlation coefficient of 0.42 for the index score between health-care professionals and patients for EQ-5D index score in people suffering from dementia. 140 Whatever the absolute level of agreement between proxy and self-completed EQ-5D might be in individual cases, the proxy values should reliably identify changes in health state.
The calculation of quality-adjusted life-years requires multiple measures at different time points. It is likely that the health of a substantial proportion of participants will deteriorate over 12 months, reducing the proportion who can contribute to the health economic analysis. For this reason we collected proxy EQ-5D at each time point on all participants, even if they had satisfactorily completed an EQ-5D themselves. We asked carers to rate how he/she (the proxy) thought the resident would rate his/her own health-related quality of life if he/she (the resident) was able to communicate it (EQ-5D, proxy version 2). 137
Social engagement
Improving level of social engagement in care home residents through group activity and increased mobility is an alternate pathway through which the OPERA intervention might affect mood. Collecting data by direct observation across 78 homes would be impractical. For this reason we used the Social Engagement Scale, which is completed by carers to give an indication of the involvement of a resident in activities within a nursing or residential home. (The Social Engagement Scale is part of assessment instruments owned by interRAI, a non-profit corporation with central offices in the USA. However, use of these instruments in the UK is handled by an English affiliate led by Dr Iain Carpenter, University of Kent. Dr Carpenter kindly gave us permission to use this item.) The Social Engagement Scale uses six Minimum Data Set Resident Assessment Instrument items. 141 As part of the Minimum Data Set Resident Assessment Instrument the Social Engagement Scale is normally administered by direct observation of the resident by the researcher as well as asking the residents and care home staff. This was impractical in our study and the Social Engagement Scale was added to proxy measures completed by care staff. The items are scored with yes (1) or no (0) responses indicating the presence or absence of the behaviour in question. 113,142 Scores range from 0 to 6, with a higher score indicating higher levels of social engagement. For the purposes of reporting, individual scores were calculated and then grouped into low (scores of 0 or 1), medium (scores 2–4), and high social engagement (scores of 5 or 6).
Data collection
For the cohort analyses we collected proxy EQ-5D and proxy Social Engagement Scale prior to randomisation and then at 3-, 6-, 9- and 12-month follow-up. For those joining the study after randomisation we collected these data at study entry, and 3 and 6 months after study entry and/or at the end of the study.
Care home data
Participant characteristics.
We collected demographic data (age, sex, ethnicity, social class and age at leaving full-time education), comorbidities (cancer, stroke, dementia, depression, anxiety, osteoporosis, chronic lung disease, urinary incontinence) and data on length of residence and current medication from the care home records.
Medication
We collected data on all medications used over a 1-week period from the home records. We extracted the exact drug name (as written in care home records), preparation and dose used, plus the number of times any medication was actually administered over a 1-week period. We then used the prescription cost analysis database to attach a code to each unique preparation used. 143 In this way we were able to attach a cost to each individual preparation used, and to estimate total amount used of each individual drug listed in the British National Formulary. 144 Using the World Health Organization (WHO)-defined daily dose for each drug we were able to generate number of days of medication used by British National Formulary chapter and subchapter. 145
For some products estimating total usage from care home records was not possible. For example, the amount of topical preparation used at each administration is not recorded, and the degree of variability in recording of appliances and dressing between care homes meant that these data were not reliable.
We collected these care home record data on all of those for whom we had permission to access records. We collected data on medication use prior to randomisation and then at 3-, 6-, 9 and 12-month follow-up. For those joining the study after randomisation we collected these data at study entry, and at 3 and 6 months after study entry and/or at the end of the study. We restricted our collection of medication use to no more than 5 weeks over the study period to ensure the task remained manageable within the available resources.
Safety data
Care home record data
Everyone in the home is exposed to the intervention, including those who are not study participants. Safety monitoring, therefore, needs to include all residents. To get an overall picture for each home we used the routinely collected data that care homes are required to keep on deaths and fractures. Care homes are specifically required to record and report deaths and serious injury, including falls and fractures, under Regulation 37, Part V11 of The Care Home Regulations (2001). 146 These regulations were made under the Care Standards Act (2000). 147
We extracted pooled anonymous data unlinked to identity for the preceding 3 months from each home for all residents (participants and non-participants) at 3, 6, 9 and 12 months after randomisation (see Directly attributable diverse events, below).
National Health Service data fractures
At the end of the study, Hospital Episodes Statistics Secondary Uses Service data were collected from each primary care trust in which the study had been run. 148 Permission to access these data was obtained from the primary care trusts' respective Caldicott Guardians. Once the relevant permissions had been obtained, the primary care trusts' information analysts provided us with data for each of our participants for whom we had permission to access National Health Service data (a small number of participants who were assessed did not wish their care home data to be used) (see Economic valuation, below). This included data for A&E department attendances, hospital admissions, outpatient attendances and use of community services.
Fractures of interest were prespecified as peripheral fractures, defined as fractures not involving the spine. All spinal fractures were excluded, as these are not strongly related to fall injury. We identified all fracture codes in The International Statistical Classification of Diseases and Related Health Problems, Tenth revision (ICD-10)149 and then searched diagnostic descriptions from the inpatient, outpatient and A&E departments for fracture diagnoses.
One fracture event may lead to multiple heath service encounters, for example an A&E department attendance followed by an admission and a subsequent outpatient appointment. We therefore cross-referred between data sets to identify linked episodes that represented a single fracture event. The quality of coding in A&E data was poor; typically, these reported an attendance accompanied by a broad, non-specific diagnostic description of ‘dislocation/fracture/joint injury/amputation’. Outpatient data typically reported the clinic attended but not the diagnosis. We were not able to link these to care home records' data on fractures, as these had been provided to us as pooled anonymous data. When a participant had multiple peripheral fractures for one episode of care, this was treated as a single fracture event. We then allocated events to different levels of certainty that there had been a fracture:
-
confirmed fracture definite fracture code identified, typically an inpatient admission
-
probable fracture an A&E attendance followed by an orthopaedic outpatient appointment
-
potential fracture an A&E attendance for an injury in which the term fracture appeared (among other diagnostic terms) in the diagnostic description with no further data provided.
National Health Service data deaths
At the end of the study we collected data on date and cause of death for all of the participants for whom we had permission to access medical record data from the Medical Record Information Service. 150
Health service activity
Care home data
We collected data on all general practitioner and practice nurse consultations from the care home records.
For the cohort study we collected follow-up data on medication use at 3-, 6-, 9- and 12-month follow-up. For those joining the study after randomisation we collected these data at study entry, 3, 6 and 9 months after study entry and/or at the end of the study. We collected these care home data on all of those for whom we had permission to access records.
National Health Service data
As described above, we used routine primary care trust Secondary User Services data on visits by community services, A&E attendances, outpatient appointments and hospital admissions. In addition to the episode statistics, these data included the price of each encounter with secondary care services. We were not able to collect general practitioner consultation data from these records. We collected these data at the end of the study on all those for whom we had permission to access records.
Interventions
In line with the Medical Research Council's framework151 we used an active control intervention in all participating care homes to ensure that they are aware of current best care for the identification and management of depression in this population.
-
By using current best care as our control, we could ensure that any benefits identified were due specifically to our intervention package rather than to raising awareness of depression within the intervention homes.
-
We reduced the risk of ‘resentful demoralisation’ in the control homes affecting recruitment of new residents after randomisation or even leading to the care home withdrawing from the study. 152
Control intervention
Our control intervention mirrored as closely as possible a realistic depression intervention which the National Health Service might introduce in care homes that would constitute a best usual care implementable by the National Health Service. The depression awareness training was designed to be short, inexpensive, deliverable by a non-expert clinician, and to address relevant learning objectives for staff in the care home sector. We used a scripted interview that was filmed using a trained simulator (actor) playing a 67-year-old care home resident with clinical depression being visited by a community psychiatric nurse. This video lasted six minutes and was used in the middle part of the depression awareness training session to illustrate key clues to diagnosing depression and possible ways to treat depression.
Each clinician delivering the depression awareness training intervention session in the care homes attended a 120- to 150-minute training session. The session reviewed the definition and epidemiology of depression, the place of depression awareness training in the OPERA study, the care home sector and its staff in the UK, and exercises including role play in delivering the session. Clinicians were able to deliver the depression awareness training only if, after a training session, in the opinion of an experienced training clinician, they had achieved the expertise to deal with this. The implementation of the depression awareness training intervention was studied as part of the process evaluation.
The depression awareness training was delivered to staff in every care home in OPERA. Each session was delivered by a clinically qualified member of the research team (e.g. nurse/physiotherapist/general practitioner) and lasted approximately 30–40 minutes. Staff members at care homes were asked to attend on one occasion. Sessions were designed for 3 to 10 staff. Requirements for the session were a room which could hold the staff group and was quiet, and a session time suitable for the care home staff; this depended on care home arrangements but was typically during the middle part of the day, around staff handovers. A method of delivering a video to staff was needed; either a DVD player and television, or a laptop computer with loudspeakers. In many care homes, more than one session was required to allow as many staff as possible to attend.
The stated aims of the session for staff attending were to be able to:
-
say what depression is
-
distinguish depression from normal sadness
-
name two things that can be done to help people with depression in a care home.
The session was structured as shown below:
-
introduction (3–4 minutes)
-
talk/discussion on what is depression, supported by written materials (6–8 minutes)
-
video of simulated resident/nurse encounter (6–7 minutes)
-
case discussion (15–18 minutes).
At the end of each session care home staff completed feedback forms that recorded attendance, satisfaction with the sessions, and suggestions for development.
Active intervention
The OPERA intervention was designed to test the effects of exercise and increased physical activity on depression and other important outcomes (Figure 3). Our plan was to deliver a whole-home exercise intervention, consisting of training for care home staff backed up with a twice-weekly physiotherapist-led exercise groups.
FIGURE 3.
Design considerations for OPERA intervention.
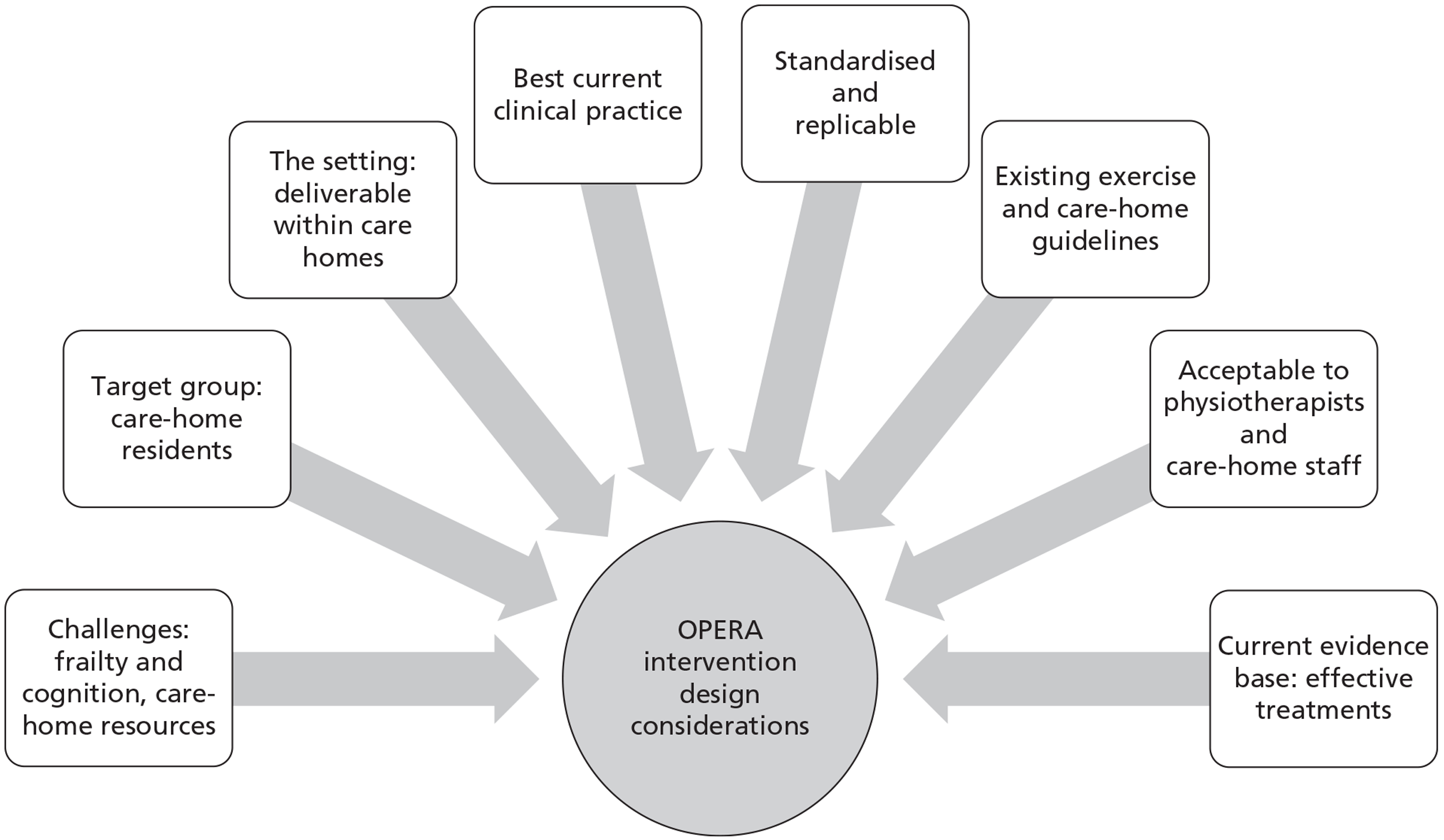
Whole-home intervention
The aims of the whole-home intervention were to:
-
increase the physical activity levels of care home residents over the length of the study in each home (12 months) using simple approaches
-
engage residents' participation in twice-weekly exercise groups delivered by the OPERA physiotherapists.
To promote the effectiveness and sustainability of the OPERA intervention it was envisaged as a whole-home, ‘ecological’ intervention153 directed at changing the whole-home environment and the culture within care homes. To this end the intervention adopted the WHO ‘settings approach’,154 aiming to strengthen the resources for health in a ‘setting of everyday life’. Such systemic interventions have been shown to be effective in significantly changing behaviour within cluster randomised trials in other settings. 155
The intervention was limited to specific pathways and treatments thought to affect depression. It was not intended to provide physiotherapy more broadly. The approach to safety and risk management was grounded in available evidence, supplemented by pragmatic opinion of professional bodies and internationally respected opinion leaders. The aim was to include and address the problems of as many residents of care homes as possible, including those with dementia.
The whole-home intervention consisted of training for residential and nursing home staff backed up with a twice-weekly physiotherapist-led exercise class. This approach, with the regular exercise groups at its core, was used to ensure that residents had maximum opportunity to engage in the exercise groups and to maintain physical activity outside the formal exercise session.
The development of the whole-home intervention drew on components of both Greenhalgh's ‘diffusion of innovations’ model156 and Cialdini's ‘model of persuasion and influence’. 157 A dementia/person-centred care approach was robustly promoted within the OPERA intervention along with the use of an ‘unconditional positive regard’. 63
Diffusion of innovations model
The interaction between an innovation, its adopters and the context of the innovation will determine its adoption in service organisations. 156 Greenhalgh et al. 156 presented a conceptual model ‘intended mainly as a memory aide for considering the different aspects of a complex situation and their many interactions’.
We took into account the full range of components in this model when considering the design of the whole-home OPERA intervention, for example ‘key interactions to help innovations be adopted’ listed below:
-
Compatibility – needing to ensure that the innovation is compatible with the adopter's values, norms and perceived needs Before setting any training, mobility recommendations or exercise groups into action, the physiotherapists ensured that they became familiar with each care home's daily routines and the full range of constraints and opportunities faced by both the management and the care home staff, as well as those faced by the residents, in terms of time, equipment, environment, training and available health-care support.
-
Reinvention – the innovation can be adapted, refined or modified The care home staff were encouraged to raise their concerns and make suggestions about the timing, location of and arrangements for the exercise groups on an ongoing basis; the physiotherapists were encouraged to be open and responsive and to these ideas. The physiotherapists also paid attention to the care home staff's and residents' feedback on the outcome of physical activity recommendations, and disseminated relevant findings to the rest of the physiotherapy team via e-mail networks throughout the study period.
-
Risk – a lower degree of uncertainty of outcome for personal risk It was essential that the physical activity recommendations for any resident accounted for carers' and home management's safety concerns, while promoting an alternative ethos of positive risk-taking within the home.
-
Task issues – tasks need to be relevant to the performance of users' work and improve task performance The individualised physical activity recommendations, created through co-operation and discussion with the care home staff, had the potential to increase the efficiency of the carers' working routines when they were able to identify approaches which enabled residents to increase their independent mobility and then take on more of their own care tasks over time.
-
Augmentation/support – innovation supplied as an ‘augmented product’ with customisation and training The carer training programme provided care home staff with free on-site health-related training and used simple visual materials designed to be accessible and acceptable to a wide range of care staff in terms of previous training and experience, education and language. The physiotherapists could support this further by providing frequent opportunities for discussion and hands-on training sessions throughout the intervention period.
Persuasion and influence model
Theories relating to the psychology of persuasion and influence can also inform actions aimed at changing both residents' and care home staff's attitudes and behaviours. 157 We used Cialdini's framework of behavioural principles of social influence to develop the OPERA intervention. 158
We used the following components of this model:
-
Reciprocation Frequent verbal recognition of, and praise for, care home staff efforts to get residents more active and involved in groups, or rewards for staff, for example evidence for National Vocational Qualification, built up from attending groups or finding ways to increase individual resident's physical activity.
-
Consistency Aiming to facilitate ‘commitment replies’ via questions like: ‘What do you think would help Mrs X come to the group next time?’ or ‘Which of the residents do you think might come to the next session?’
-
Concessions Regular informal discussions took place during care home staff handover periods and more formal (recorded) sessions at least 2-monthly intervals or as/when the need arose. These discussions focused on the constraints that both the physiotherapist and the care home staff faced when encouraging residents to increase their levels of physical activity, with the aim of developing acceptable and appropriate solutions to these constraints, as well as providing opportunities to create increased rapport and feelings of mutual interest.
-
Liking Developing personal relationships with care home staff though shared ‘social’ time, demonstrating awareness of their personal strengths and qualities, as well as their particular constraints and obstacles.
-
Authority Linking the OPERA programme to the importance of activities for Care Quality Commission requirements.
-
Scarcity Promoting the fact that this might be a chance to have some expert guidance on mobility needs from an ‘in-house’ physiotherapist, to have a hands-on opportunity to learn how to promote physical activity and develop exercise groups in care homes with the ongoing close support of a health professional, and to be involved in a national level research programme that might influence policy.
The actual intervention design was also based on a number of other principles and considerations (see Figure 3). This included the biological rationale for the proposed therapeutic effect and two systematic reviews of randomised trials. 38,62 It was also informed by physical activity guidelines for older adults159,160 and exercise prescription guidelines,161–163 with adaptations to account for the high levels of frailty and multiple comorbidities seen in this population. 164 The design followed the principles of person-centred dementia care approaches advocated for use in UK care homes,165,166 was consistent with the guidelines affecting care home staff such as those specified by the Care Quality Commission, and accounted for the context of UK residential and nursing homes in terms of staffing, time, environment and equipment. Additional expert opinion was gathered in discussion with clinical and exercise specialists in older people's physical and mental health care. We considered the deliverability within care home settings, the frailty of the target group, and the acceptability to physiotherapists and care home staff who would be delivering the intervention. Finally, the design included documentation and training to promote consistency in delivery.
The OPERA intervention
The OPERA study was located in UK care homes in which up to 70% of residents are likely to be living with dementia. 167 A dementia/person-centred care approach was robustly promoted within the OPERA intervention and team members, along with the use of an ‘unconditional positive regard’. The intervention was delivered by a physiotherapist who was assigned to work with an individual home for 12 months.
The physiotherapists were allocated two half-days per week to each care home – more in some larger homes in which we ran more exercise groups. There were seven components to the intervention (Figure 4).
FIGURE 4.
OPERA intervention flow chart.
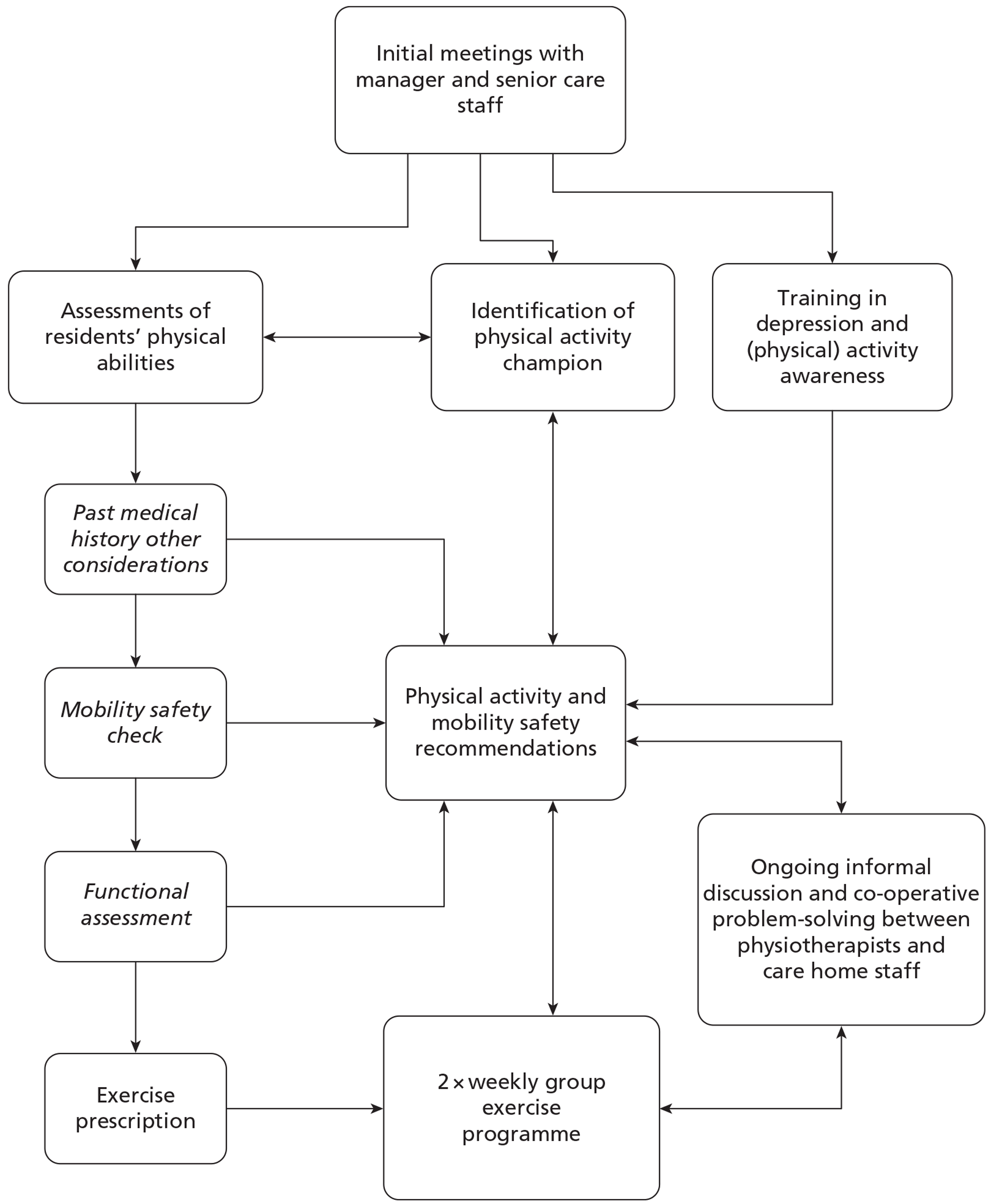
Initiation and assessment period:
-
Initial meetings with the care home manager and senior care home staff.
-
The identification of a physical activity champion from within the care home staff.
-
Carer training in depression and activity awareness.
-
Physical activity assessments.
Ongoing physical activity and exercise programme:
-
5. Physical activity (and mobility safety) recommendations for care home staff.
-
6. A twice-weekly group exercise programme. The exercise groups were the most resource intensive and most tangible component of the intervention.
-
7. Ongoing informal discussion and co-operative problem-solving between physiotherapists and care home staff.
Initial meetings with care home manager
The physiotherapist set up an initiation meeting with the care home manager and senior carers aimed at establishing rapport with the care home staff, understanding and agreeing roles within the intervention, and to sort out logistical details such as locations for the exercise groups.
Physical activity champion
A ‘champion’ (a key individual in an organisation) may assist in the assimilation of an innovation, so we sought to identify a physical activity champion in collaboration with the care home manager and senior care staff to act as a key link within the home. Their role was to assist with planning the exercise groups, and to attend the groups whenever possible, to act as a link between the physiotherapist and home, and to facilitate the implementation of the physical activity recommendations for each resident.
Care home staff depression awareness and activity training
The aims of the care home staff depression awareness and activity training, in addition to the aims of the depression awareness training programme described above, were to:
-
highlight the importance of promoting and increasing physical activity to aid the physical and mental health of residents
-
establish a collaborative approach towards increasing physical activity within the home
-
describe the specific elements of the OPERA intervention and how the staff would be involved.
The session was based on the best current adult pedagogical practice and previous experience of what works in training in care homes. To this end it involved short sessions, used a variety of teaching methods including the depression awareness DVD, and included discussion of cases.
Staff training sessions took about 60 minutes to complete and were repeated when new staff needed to be trained. The training materials used were the same as in the control arm depression awareness training sessions, with the addition of posters illustrating the physical and mental health benefits of physical activity and cycles of activity avoidance related to falls and pain. The training booklets for care home staff had additional pages for copies of these posters plus a mobility safety advice section outlining important enabling techniques and considerations for the care home staff.
Physical activity assessment and recommendations
In consultation with the care home manager all eligible residents were invited to undergo a mobility and physical activity assessment, and received a tailored physical activity recommendation to promote day-to-day activity alongside an invitation to attend the exercise classes. The assessment took place in the resident's room or other locations according to the resident's preference or abilities. The physiotherapist assessed functional capacity, medical history, pain, fear, anxiety, sensory and communication abilities.
On the basis of the assessment the physiotherapist determined a plan of action for the intervention programme elements. The first was a bespoke physical activity programme tailored to each resident and aimed at increasing the level of habitual physical activity, developed in co-operation with the physical activity champion/senior carers. This included the provision of mobility aids, advice on footwear, and manual handling tips to enable mobility. The second was to determine the appropriate level of exercise activities for the group exercise programme.
Group exercise programme
The aim was to provide a structured, standardised and replicable programme of exercise targeted at the physiological, biochemical and psychological mechanisms considered responsible for depressive symptoms in older people, which also accounted for the frailty of residents. This consisted of:
-
An initial adaptive 4-week period utilising shorter exercise times, lower exercise intensity levels, lower numbers of weight lift sets and repetitions, longer repetition durations, and low starting weights set according to functional ability levels.
-
Twice-weekly exercise sessions in a group format, lasting approximately 1 hour each, with at least 45 minutes of expected exercise time per session.
-
Each session included:
-
a 15-minute section of moderate intensity aerobic exercise
-
an approximately 15-minute section of moderate intensity progressive resistance exercise aiming for two sets of 15 repetitions for each muscle group targeted
-
warm-up and cool-down sections of 5–10 minutes each.
An important concept in exercise therapy is to ensure that the training stimulus is sufficient for each participant to ensure a biological response. Residents' functional status, including their postural stability, was categorised on a three-point scale and the exercise activities used during the class were matched to this. In the first instance the exercise level of the class was set at the level of the least functionally able resident and then progressed on an individual basis in each class.
Screening for exercise safety
All residents were assessed to identify the aspects of their medical history, psychological and physical abilities that would need to be considered in the delivery of moderately intense group exercise activities and screened for absolute contraindications to exercise such as recent operations and severe breathlessness at rest according to New York Heart Association Class IV. 168 This information was drawn from observations, resident's report, care home records or care home staff. Residents who were unable to maintain a seated position while moving their limbs were excluded, and the levels of exercise activities matched to both aerobic/strength capacity and postural stability. Review of resident's health and ability to participate in the exercise and physical activity programme were undertaken by the physiotherapist and care home staff on an ongoing basis in order to ensure safety and progression where changes in functional status were occurring.
The OPERA exercise prescription
We developed three levels of exercise to match the expected levels of functional ability (Table 4). These levels were developed to enable the physiotherapists to develop a ‘profile’ of the likely group participants, both for setting the exercise level for group sessions and as a reminder to increase the exercise challenges for the more physically able residents over time, as well as for ease of communication to physiotherapists providing cover.
| Level | Functional ability |
|---|---|
| 1 | Person able to exercise safely when seated, with lower intensity aerobic and strength challenges |
| 2 | Person able to exercise safely when seated and in supported standing, and to work at a moderate level of intensity |
| 3 | Person able to exercise more dynamically in sitting and standing with some walking-/dancing-based activities and to work at a sustained moderate to high-intensity aerobic and strength training level |
After an initial low to moderate intensity start-up phase of several sessions (which varied according to the frailty levels of the residents) group members were encouraged to exercise for up to 45 minutes at moderate intensity. The sessions comprised the following three components.
Progressive resistance exercise
In order to achieve an increase in muscle strength or aerobic conditioning, the demands placed on the musculoskeletal and cardiopulmonary systems must progressively increase over time and stress them beyond their accustomed loads. 169,170 Informed by American College of Sports Medicine161 and by several existing evidence-based exercise programmes for older people, we aimed to increase general muscle work and strength.
We decided not to use the one repetition maximum to calculate starting weights or progressions, because many of the residents in the pilot study were not able to be accurately tested with free weights or a dynamometer. Instead, our starting weights (Table 5) were set according to functional ability level, which could be adapted according to individual preference for acceptability and promotion of adherence.
| Level | Soft hand weights | Ankle weights |
|---|---|---|
| 1 | Juggling ball (∼200 g) | 0.5 kg |
| 2 | 0.5 kg | 1.0 kg |
| 3 | 1.0 kg | 1.5 kg |
For the OPERA study we chose to use an observed form of the Borg Scale of Perceived Exertion for resistance exercise. 171–173 It is unlikely that many residents would be able to subjectively report their rate of perceived exertion owing to the high levels of observed cognitive decline observed in residents in the pilot study, and the high prevalence of dementia in the study population as mentioned earlier. We are not aware of any studies that have examined the use of such observed measures in older adults.
Owing to the high levels of frailty common in UK care home residents, it would be likely that few residents could attain or tolerate the higher level of Progressive Resistance Exercise intensity used in previous studies, which demonstrated positive effects on the symptoms of depression. 174–176
Aerobic exercises
Aerobic exercises are activities that are most likely to increase cardiorespiratory demand, and need to be sustained for 15–20 minutes. Aerobic intensity was monitored by rating perceived exertion using the adapted 10-point Borg rate of perceived exertion scale. 173,177
Given the frailty of this population, and the setting, the aim was to achieve (the higher end of) a moderate level of intensity, built up over time, using the ‘start low, go slow’ maxim. 178,179
Warm-up and cool-down sections
These sections included activities designed to gradually increase or decrease heart/respiratory/circulatory rates as recommended by American College of Sports Medicine. 161
In order to ensure and maintain a training effect over time, each resident was progressed within the exercise activities at their starting level or up to next level (Figures 5 and 6). Residents could progress between levels on an individual basis by changing their position, for example by standing up in some parts of the aerobic section (level 2). The group could also progress as a whole through the use of changes in music tempo and routines. The exercise progression models were, again, set according to the American College of Sports Medicine Guidelines,161,162 and informed by several existing evidence-based exercise programmes for older people (see Figures 5 and 6). 174,180–182
FIGURE 5.
Flow chart for the progressive resistance exercise progressions. RPE, rate of perceived exertion.
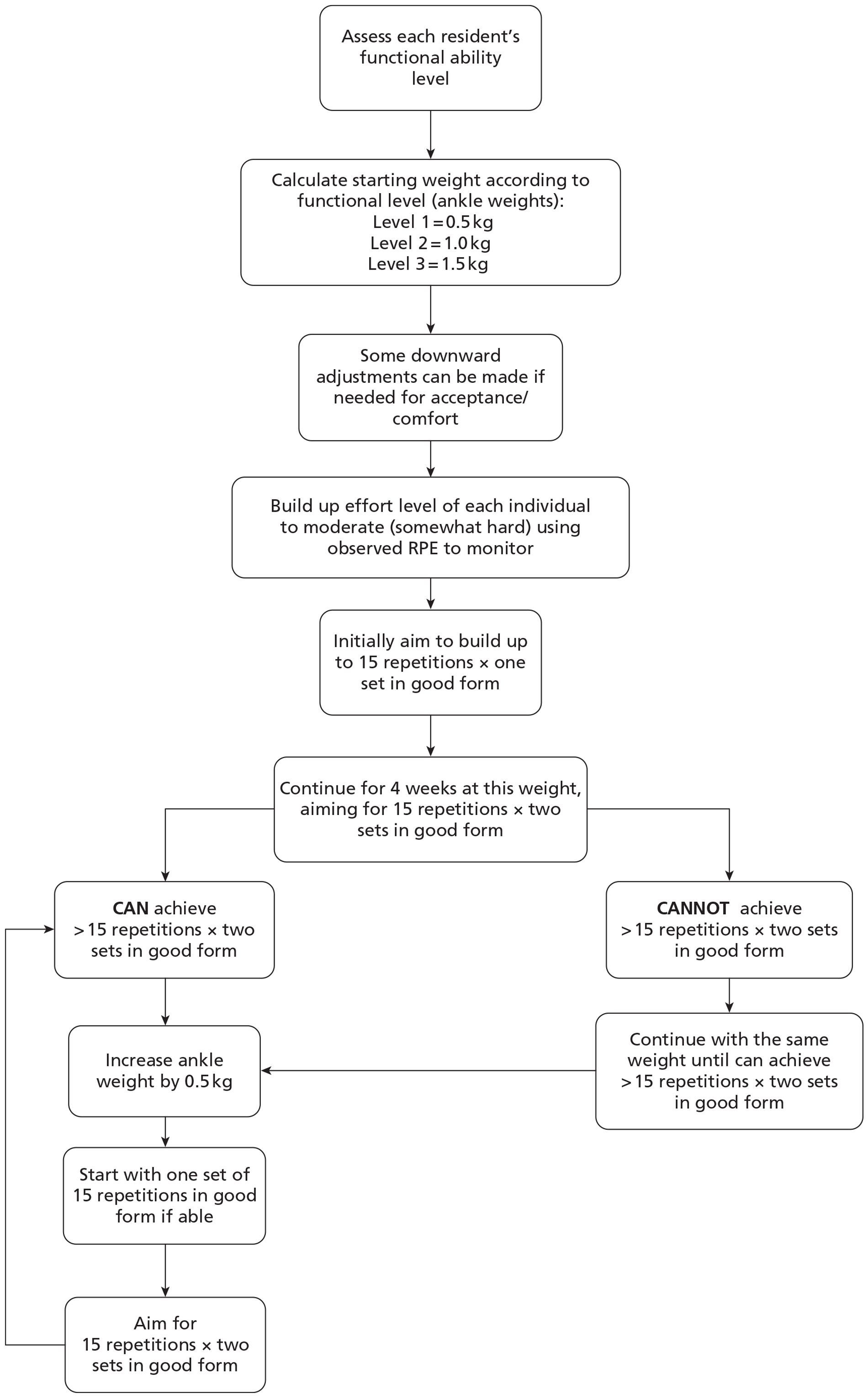
FIGURE 6.
Flow chart for progression of aerobic exercise. RPE, rate of perceived exertion.
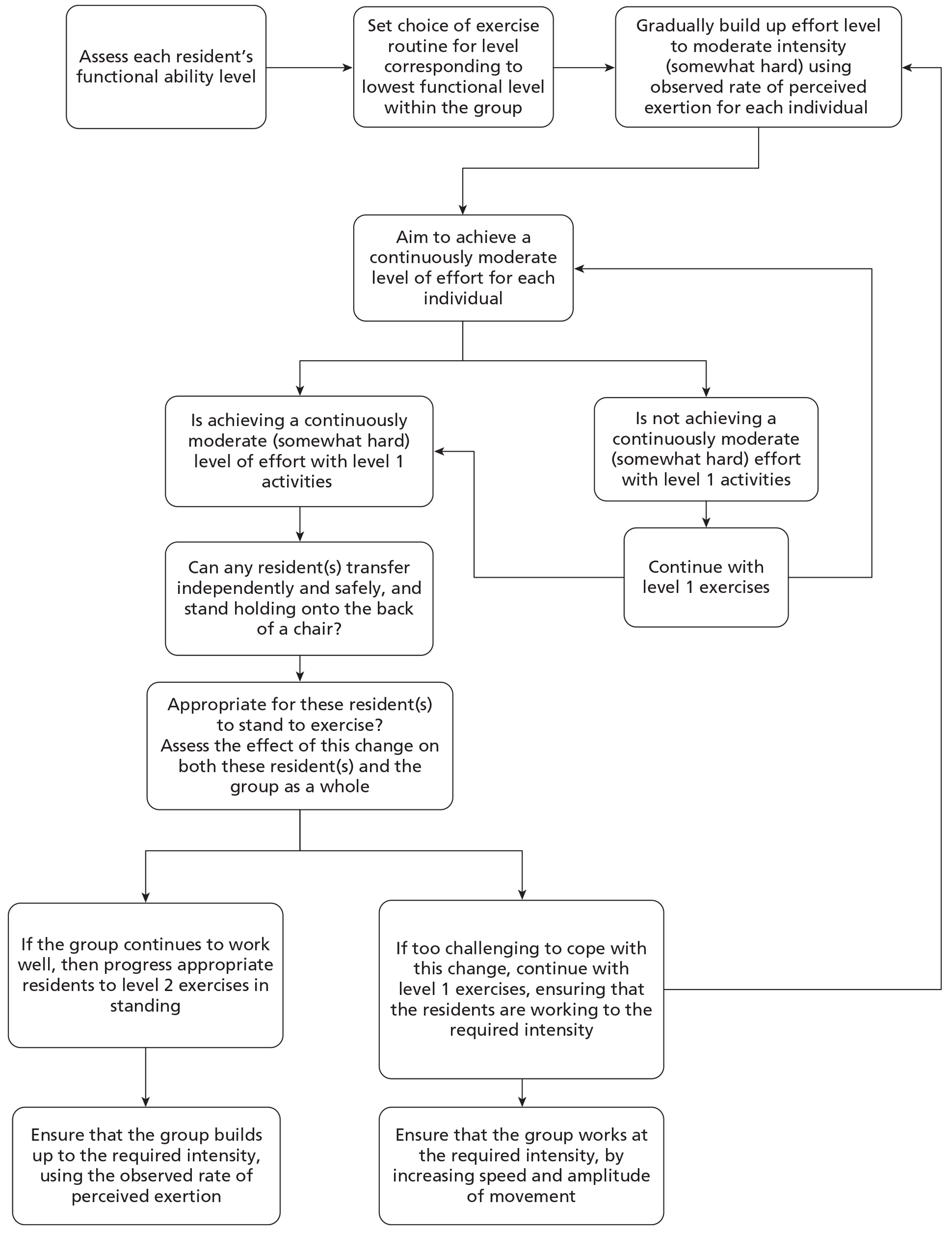
OPERA music and equipment
The exercise activities were set within a structured routine, with the target timings matched to selected music tracks for each ability level. The music tracks were carefully selected and arranged to exploit their tempo, themes and psychological appeal. 76,78,183 The choice of music tracks was also based on the likely preferences of older people living in care homes, developed out of experience and expert opinions, and not limited to any musical era in recognition of the potential breadth of musical tastes of this population group. These were provided on a CD [we obtained an annual Limited Manufacture Licence from Mechanical Copyright Protection Society (MCPS) to allow us to disseminate copies of these CDs to all the OPERA physiotherapists] for levels 1, 2 and 3 to each physiotherapist for easy reference before, and during, the group sessions (see Appendix 2).
The exercise equipment comprised small and large soft foam/inflatable footballs (principally for the warm-up period), soft weighted hand balls and ankle weights, plus a 10-metre stretchy velvet band for the aerobic section. This equipment had been chosen for safety reasons (no hard metals or sharp edges), for practicability within UK care home facilities (no space for resistance exercise machines), and for their potential to enable participation, enjoyment, success and so maximise possible adherence for all residents, however frail or cognitively impaired.
Group size and levels of supervision
Although it had initially been planned that group size would be limited to eight residents, because of the numbers of residents in some homes, pragmatically the group size was instead based on the numbers of residents willing and able to attend the exercise sessions. In addition, in many homes the group sessions were run in the main lounge, where residents who expressed a wish not to take part usually sat during the day. These residents remained in their chairs during the sessions, sometimes joining in over time or in a limited manner according to their preference or abilities. Each intervention home was asked to provide a member of the care home staff to help the physiotherapist with running the exercise group sessions.
Logistics of delivering the OPERA intervention
Physiotherapist recruitment and training
The intervention was delivered by chartered physiotherapists registered with the Health Professions Council.
We developed a 2-day training programme to train the physiotherapists, reflecting the typical length of informal training programmes for qualified staff currently available in the UK. The training included a background of the neurophysiology of exercise and depression, exercise prescription guidelines, person-centred dementia care and neurofacilitation techniques relevant to people living with dementia. Physiotherapists were trained in how to deliver the exercise prescription and programme, including practice sessions. The training also covered the assessment of residents, physical activity programme, whole-home approach, carer training package and the logistics of preparing and completing the data collection and clinical record forms. The training was delivered by a physiotherapist with specialist expertise in the management of dementia and mental health, and documented in an extensive training manual (NA).
Physiotherapist support
In addition each physiotherapist received a carer training pack (with cue cards, posters and DVD) and a set of the specially produced OPERA CDs to accompany the exercise routines. Ongoing support was provided to each physiotherapist via e-mail communications and a study day half-way through the 2-year recruitment and delivery period. Clinical supervision and support was provided by local team leaders and supplemented by regular visits from the research team. The frequency of supervisory support visits was between 2- and 6-monthly, depending on the experience and confidence levels of the physiotherapists.
Physiotherapy team
There were two distinct models of physiotherapy delivery in OPERA. These were planned from the outset with oversight of the whole of the intervention delivery being provided by the lead physiotherapist in C&W. In C&W the physiotherapists were employed by the University of Warwick and their main role was OPERA intervention delivery (some on casual or part-time contracts). In NEL the physiotherapists were seconded from Barking & Dagenham Primary Care Trust and generally had a clinical caseload as well as OPERA commitments. At times of peak demand some sessions were delivered by a private physiotherapy service. One primary care trust physiotherapist in NEL acted as the main contact with the primary care trust physiotherapists. Training for physiotherapists at both sites was provided by the lead physiotherapist in C&W.
Consent to exercise
As this was a cluster randomised trial, all residents were exposed to the intervention that included the opportunity to take part in the exercise classes. Formal written consent was not taken for participation in the classes. A more informal approach was taken that reflected best clinical practice. Residents were encouraged to take part in a home activity, which was briefly described during the assessment, with visual/aural clues acting as non-verbal descriptors and reminders during the classes themselves (setting out the equipment, playing the music, demonstrating the exercises). Residents then expressed their implied consent or refusal, by either participating, leaving the room or requesting to leave the room (could be expressed non-verbally), or by not doing the exercises.
Directly attributable adverse events
We defined a directly attributable adverse event as an event needing external medical attention as a consequence of participation in OPERA. This included events occurring during an intervention exercise group, or when participants in the groups were getting to and from the session. Events to be included (but not restricted to) were injurious falls, myocardial infarction, angina, stroke, respiratory distress, musculoskeletal injuries, severe psychological distress or death. For any such events, which were suspected to be a directly attributable adverse event, the treating physiotherapist completed a notification form and notified the study manager. Clinical members of the team then assessed if this event was a directly attributable adverse event. In the event that the home manager became aware of such an event after the physiotherapist had left the home they completed a suspected serious adverse event form and notified the study manager. We used the same system for assessing any suspected adverse events that occurred during study assessments.
Summary
We designed a structured exercise and physical activation programme, within a whole-home approach, to affect the physiological and psychological processes most likely to be able to decrease or prevent depressive symptoms in older people residing in care homes in the UK. The intervention adhered to the principles of exercise prescription, person-centred care and innovation adoption, and was structured with sufficient flexibility to be delivered within a range of different care home settings, to a variety of resident profiles. The training and support package was practical to allow for roll out within the National Health Service if the intervention proved effective.
Methodological considerations
Objectives
Our primary objective was to compare depression levels between intervention and control care homes, addressed via three primary analyses that represent different ways of expressing depression levels:
-
the prevalence of depression (defined as proportion of participants with five or more positive responses to the Geriatric Depression Scale-15 or equivalent) in intervention homes with that in control homes in all residents contributing data 12 months after homes were randomised (cross-sectional analyses)
-
the number of depressive symptoms at 6 months between intervention and control homes in residents who were depressed at pre-randomisation baseline assessment (depressed cohort analyses)
-
the number of depressive symptoms at 12 months between intervention and control homes in all residents who were assessed prior to randomisation (cohort analyses).
In our original proposal we planned to include, as part of our primary analyses, comparisons of the rates of remission from depression at 6 months and the number of depressive symptoms at 12 months in those who were depressed at pre-randomisation baseline. Early in the study it became clear that the average cluster size and follow-up rates would be smaller than originally anticipated and that we would be unlikely to obtain sufficient data to produce robust comparisons. We therefore changed our primary analyses with the agreement of the independent Trial Steering Committee, Data Monitoring and Ethics Committee (DMEC) and the funder (see below). Remission of depression became a secondary outcome.
Our secondary objectives were:
-
to compare, between intervention and control arms:
-
remission of depression
-
cognitive function
-
health-related quality of life
-
mobility and exercise tolerance
-
pain
-
fear of falling
-
social engagement
-
-
to report descriptive statistics on:
-
the prescribing of antidepressants, hospital admissions
-
-
to report the following safety outcomes:
-
injurious falls as indicated by peripheral fractures, mortality rates.
-
For the depressed cohort we just report a 6-month analysis. For remaining analyses we report on each time point at which we collected data.
Sample size
Unusually, three linked primary analyses were specified for this study. The funder's brief specified a cluster randomised trial with the outcome of interest to be remission of depression. In designing the study, the research team developed a whole-home intervention that would have a long-term impact on all residents. Thus, the outcome of greatest interest to the research team was the difference in the prevalence of depression (as indicated by five or more depressive symptoms or equivalent) at 12 months. (If 15–13 items on the Geriatric Depression Scale-15 have been completed a score of ≥ 5 is indicative of depression; if 12–11 items on the Geriatric Depression Scale-15 have been completed a score of ≥ 4 is indicative of depression; if 10 items on the Geriatric Depression Scale-15 have been completed a score of ≥ 3 is indicative of depression.) For completeness we also considered the long-term effect the intervention may have on the mean level of depressive symptoms at 12 months for all study participants with baseline assessments prior to randomisation.
The remission of depression question originally specified by the funders required the largest number of participating homes; it was therefore this comparison we used to set our original sample size of 77 homes. To reduce treatment costs we planned an unbalanced randomisation of 1 : 1.5 in favour of control.
Original sample size
To show an increase in the remission rate after 6 months from 25% to 40% in those depressed at baseline, with 80% power at the 5% significance level, with this unbalanced randomisation using a simple sample size calculation requires data on 343 subjects. Assuming an average home size of 32 and a 50% recruitment rate to the study the average cluster size at randomisation would be 16. Assuming that 40% of the residents recruited had five or more depressive symptoms and a 15% loss to follow-up at 6 months, the average cluster size for the analysis would be 5.44. Few previous studies were available to allow us to estimate the range of likely values for the intracluster correlation coefficient needed to estimate the inflation factor required for a cluster randomised trial in care homes. We therefore used a conservative value of 0.05 for the intracluster correlation coefficient; towards the upper end of the range seen in previous primary care studies. We inflated our sample size by a factor of 1.22, meaning that we required data on 418 subjects at follow-up for this analysis. This in turn means we needed to recruit 77 homes to achieve this target (Table 6).
| ICC = 0.05 | A. To show a reduction in the proportion of participating residents depressed (GDS-15 score < 5) at the end of the study from 40% to 25% | B. To show an increase in the remission rate after 6 months from 25% to 40% in those depressed at baseline | C. To show a mean reduction in GDS-15 score of 1.2 after 12 months in those depressed at baseline |
|---|---|---|---|
| Power | 80% | 80% | 80% |
| Significance | 5% | 5% | 5% |
| Simple sample size | 343 | 343 | 280 |
| Mean cluster size at follow-up | 15.0 | 5.4 | 4.5 |
| Inflation factor | 1.7 | 1.22 | 1.175 |
| Total no. required at follow-up | With complete assessments: 583 | With depression at baseline and complete assessments: 418 | With depression at baseline and complete assessments: 330 |
| Care homes required | 39 | 77 | 74 |
The mean change in the Geriatric Depression Scale-15 score in a community sample of people aged > 85 years after a major negative life event (e.g. death of partner) is 1.2. 121 This is indicative of a clinically important mean difference in Geriatric Depression Scale-15. In previous studies the standard deviation (SD) of the Geriatric Depression Scale-15 in care home residents was in the range of 3.2–3.6;120,122,124 for depressed care home residents it was 3.5. 26 We therefore used a minimally important difference of 1.2 and a SD of 3.5 in the sample size calculation for the comparison of depressive symptoms.
Revised sample size
We revisited this sample size, using baseline data, part-way during recruitment because the average cluster size was smaller than anticipated. After we had randomised 47 care homes the mean cluster size at baseline was 10.7, intracluster correlation coefficient = 0.053, 6-month follow-up rate 70%, 46% of our participants had a baseline Geriatric Depression Scale-15 score of ≥ 5, and the SD of the Geriatric Depression Scale-15 was 2.2 and 3.1 for depressed and all residents, respectively. Reworking our sample size in light of these data showed that we were unlikely to have sufficient statistical power to show our prespecified increase in rate of remission from depression – comparison B (Table 7).
| ICC = 0.053 | A. To show a reduction in the proportion depressed (GDS-15 score < 5) at 12 months from 46.1% to 28.8%a | B. To show an increase in the remission rate after 6 months from 25% to 40% in those depressed at baselineb | C. To show a mean reduction in GDS-15 score of 1.2 after 6 months in those depressed at baseline: from 7.27 to 6.07 (SD = 2.21) | D. To show a mean reduction in GDS-15 score of 1.2 after 12 months: from 4.5 to 3.3 (SD = 3.12) |
|---|---|---|---|---|
| Power | 80% | 80% | 80% | 80% |
| Significance | 5% | 5% | 5% | 5% |
| Simple sample size | 281a | 343 | 112 | 224a |
| Mean cluster size at follow-up | 9.6 | 3.9 | 3.9 | 7.5 |
| Inflation factor | 1.46 | 1.16 | 1.16 | 1.34 |
| Total no. required at follow-up | With complete assessments: 409 | With depression at baseline and complete assessments: 396 | With depression at baseline and complete assessments: 130 | With complete assessments: 301 |
| Care homes required | 43 | 101 | 33 | 41 |
With the agreement of the Trial Steering Committee, DMEC and funder we therefore dropped comparison B as one of our primary analyses, replacing this with new comparison C (see Table 7), seeking to show a mean difference of 1.2 points in the Geriatric Depression Scale-15 for those depressed at baseline. Consequential upon this change, to avoid making multiple comparisons on the same group, i.e. those depressed at baseline, we changed our third primary analysis to comparing change in depressive symptoms at 12 months in all of those present at baseline – new comparison D (see Table 7). In this way we ensured that we had adequate statistical power to test the effect of our intervention on all three overlapping populations of interest: those resident in the homes at the end of 12 months, those who were depressed at baseline and able to provide 6-month data, and all residents present at baseline who were still able to give data at 12 months. To allow for unforeseen events we continued to recruit to our original target of 77 care homes.
Randomisation
This was a cluster randomised trial with care homes as the unit of randomisation. Care homes were first stratified by location (NEL or C&W) and then minimised into intervention and control arms using the MINIM programme (www-users.york.ac.uk/∼mb55/guide/minim.htm). This programme uses minimisation with a random element, allocating care homes to the arm of the study that gives the better balance with a probability of 70%. The minimisation factors were type of home (local authority, voluntary, private and care home, private and nursing home), and size of home (32 beds or fewer, > 32 beds). Initially, we had intended to use a third randomisation factor, dementia home or not, but only one dementia home was recruited (see Homes, above).
Allocation concealment and identification/recruitment bias
Allocation concealment was ensured by using a statistician who was independent of the study, based at the Pragmatic Clinical Trials Unit, Barts and The London School of Medicine and Dentistry, to carry out the minimisation. Researchers recruiting homes provided details of a recruited home by e-mail directly to the independent statistician. They were always notified, by telephone, of allocation within a week but usually within a few days.
Bias can occur in cluster randomised trials when identifying and recruiting participants is carried out after randomisation. The issues that arise are similar to those arising when allocation is not concealed. This identification/recruitment bias has the potential to be a serious source of bias in these studies. 184–186 This bias is avoided if those identifying and/or recruiting participants do so before randomisation. In OPERA the majority of participants were recruited prior to the care homes being randomised. In addition, the majority of these individuals provided baseline data prior to randomisation thus avoiding the chance of participant responses to the baseline questionnaires being influenced by their knowledge of the intervention they would be receiving. Some baseline data were collected from participants after randomisation, either from participants who had been approached before randomisation, for whom assent was only obtained after randomisation, or from participants who had been unable to provide a complete data set prior to randomisation, for example if records data were available but the resident was not available for assessment. Data from these participants collected after randomisation were not used in the cohort analyses.
Some participants joined the study because they moved into participating homes after the homes had been randomised. We could not avoid the possibility of identification and/or recruitment bias for those participants; both their likelihood of identification as a potential study participant and their likelihood of participation might have been affected by their knowledge, and knowledge of care home staff, of the intervention in their home.
Baseline comparisons
We compared baseline characteristics of homes and characteristics of participants in the intervention and control arms. We compared the baseline characteristics between intervention and control groups for the cohort and the depressed cohort (these individuals are included in our cohort comparisons). We also compared these characteristics for those participants who joined the study after randomisation.
Analysis
Our full analysis plan is included in Appendix 3. In this overview we describe the general principles for our primary and secondary analyses. Safety analyses are described later in this chapter (see Safety analyses, below).
We conducted available case analyses using intention-to-treat principles. This meant that, for the cohort analyses, when we were able to obtain data for an individual at a specified outcome point (6 or 12 months), we analysed them in the care home they were recruited to regardless of whether they were still in this care home, had moved to another OPERA care home, or had moved to a home outside OPERA or elsewhere. For the cross-sectional comparisons we analysed data according to which care home they were in at the time data were collected. We did not impute missing values in our clinical analyses.
To account for cluster randomisation, we used mixed-effect models with care home as a random effect, and intervention and minimisation factors as fixed effects. Baseline values of outcome and other covariates were also used as summarised in Table 8. All covariates were selected prior to any analyses, as specified in the analysis plan, and all were retained in the analysis, unless there was evidence of multicollinearity. To assess any potential multicollinearity we examined correlations between covariates. If severe multicollinearity was present we dropped one of the collinear covariates, retaining the covariate providing the best fit.
| Outcome | Covariates at home level | Covariates at individual level |
|---|---|---|
| All outcomes | Location (C&W or NEL) | Sex |
| Home size | Whether or not individual on antidepressants when recruited | |
| Home type (voluntary and local authority; private and care home; private and nursing home) | SPPB when recruited | |
| Proportion of residents in home with MMSE score of < 20 | ||
| Cross-sectional outcomes only | Mean outcome measure in home at baseline (except for MMSE) | Age at study end |
| Cohort outcomes only | Baseline value of outcome | |
| Baseline value of GDS-15 | ||
| Age at baseline |
An appropriate link function was used in the analyses depending on the type of outcome:
-
continuous outcomes an identity link function
-
binary outcomes a logit link function
-
count outcomes a Poisson link function
-
ordinal outcomes cumulative logit link function.
We used model diagnostics to check distributions of residuals and homoscedasticity as appropriate.
Populations of interest
The nature of OPERA study design is that there are several populations of interest, each being relevant to different comparisons. On each occasion our analyses refer to the individuals in that population of interest.
-
Cohort analyses, assessment data All of those who provided one or more outcome at an assessment prior to randomisation and who were alive the day before their care home was randomised.
-
Cohort analyses, care home data All those for whom we had consent/assent to collect data prior to randomisation and who were alive the day before their care home was randomised.
-
Depressed cohort analyses Assessment data and care home data; all of those with a Geriatric Depression Scale-15 score of ≥ 5 (or its equivalent) completed prior to randomisation and who were alive the day before their care home was randomised.
-
Cross-sectional analysis, assessment data All those for whom we had consent/agreement to collect assessment data and who were present in an OPERA home at the time of the end-of study assessment for that care home.
-
Cross-sectional analysis, care home data All of those for whom we had consent/agreement to collect care home data and who were present in an OPERA home at the time of the end-of study assessment for that care home.
-
Safety analysis All residents in OPERA homes at any time during the study period for that care home.
Cross-sectional analyses were performed for outcomes only at 12 months. In these analyses we included all residents who had been resident in the home for at least 3 months. This included all of those who had been resident prior to randomisation regardless of whether they had provided baseline data before or after randomisation, plus residents who were recruited to the study after randomisation. In our reporting we assumed that those assessed within 6 weeks of randomisation were present at randomisation; those assessed between 6 weeks and 4.5 months post recruitment moved into homes within 3 months of randomisation and were recruited at a 3-month follow-up visit; those assessed between 4.5 and 7.5 months were recruited at a 6-month follow-up visit; and those assessed between 7.5 and 9 months were recruited at a 9-month visit.
Cohort analyses were conducted for outcomes at both 6 and 12 months. In these analyses, we included only those who had provided the outcome of interest prior to randomisation and who also provided the same outcome at the specified outcome point. Thus, our cohort comparisons were always smaller than our equivalent cross-sectional comparisons.
All analyses were undertaken in Stata release 11 (StataCorp LP, College Station, TX, USA), using xtmixed and xtmelogit commands, with the exception of ordinal outcomes, for which SAS 9.2 (SAS Institute Inc., Cary, NC, USA) proc glimmix was used. We report intracluster correlation coefficients for all outcomes. For linear and Poisson models, intracluster correlation coefficients were produced directly from the models. For logistic models, intracluster correlation coefficients were produced on the logistic scale. These were converted on to the linear scale using a method. 187 For the glimmix routines in SAS we used the ordinal scales for pain and social engagement. Intracluster correlation coefficients were obtained using intracluster correlation coefficient = σu/(σu + π2)/3 and are on the logistic scale. There is currently no straightforward way of converting these on to a linear scale for ordered logistic regression but the intracluster correlation coefficients are likely to be slightly smaller on the linear scale.
Primary analyses
-
To compare the prevalence of depression in intervention homes with that in control homes (cross-sectional comparison) we used a mixed model with a logit link. We included those who had been in the study for > 3 months at the 12-month outcome point. To assess the effect of recruitment post randomisation when there was a chance of identification/recruitment bias, we conducted a sensitivity analysis that excluded those whose baseline assessments occurred after randomisation of the home into which they were originally recruited.
-
To compare (1) the number of depressive symptoms at 6 months between intervention and control homes in participants who were depressed when assessed prior to randomisation and (2) the number of depressive symptoms at 12 months in all participants assessed prior to randomisation (cohort comparisons), we used mixed models with an identity link and with the number of depressive symptoms at baseline as a covariate. Those recruited post randomisation were not included in the primary analyses because the effects on these individuals was likely to be less given that they had been resident in the homes for a shorter period and there was potential for identification/recruitment bias among these individuals.
Note that we hypothesised a reduction in depression score and prevalence of depression as a result of our intervention, thus negative mean difference or an odds ratio (OR) of < 1 favours the intervention.
Secondary analyses
Secondary analyses used the same principles as the analyses of primary outcomes. Note that we hypothesised that our intervention would increase the score or prevalence for most outcomes, thus in general positive mean differences and ORs of > 1 favour the intervention. The only exceptions are the outcomes levels of depression, pain and fear of falling, all of which were hypothesised to reduce as a result of our intervention.
Safety analyses
Two of our safety analyses (on fracture and death rates) were based on data relating to study participants and conducted in a similar fashion to our primary (Table 9) and secondary analyses (Table 10), using mixed-effects logistic models. The third analysis (Table 11) was of fractures among all care home residents (aggregated fracture level). These fractures could not be attributed to individuals so we used a Poisson model at the care home level, adjusting for clustering with a random effect, and home location, home size, home type, mean age of home participants at pre-randomisation baseline, proportion female, percentage on antidepressants at pre-randomisation baseline, proportion of residents with moderate or severe cognitive impairment at pre-randomisation baseline assessment.
| Outcome | Measurementa | Population of interestb | Source of datab | Model, programme and command | Effect and interpretation |
|---|---|---|---|---|---|
| Prevalence of depression | Proportion of those depressed as measured by GDS-15 | Cross-sectional at 12 months | Assessment | Mixed model, logit link | OR <1 favours intervention |
| Stata | |||||
| xtmelogit | |||||
| Level of depression | No. of depressive symptoms as measured by GDS-15 | Cohort at 12 months | Assessment | Mixed model, identity link | Negative mean difference favours intervention |
| Depressed cohort at 6 months | Stata | ||||
| xtmixed |
| Outcome | Measurement | Populations of interesta | Source of dataa | Model, programme and command | Effect and interpretation |
|---|---|---|---|---|---|
| Secondary analyses of GDS-15 | |||||
| Remission of depression | Proportion not depressed as measured by GDS-15 | Depressed cohort at 6 months | Assessment | Logistic-mixed model, logit link | OR > 1 favours intervention |
| Stata | |||||
| xtmelogit | |||||
| Level of depression | No. of depressive symptoms as measured by GDS-15 | Cross-sectional at 12 months | Assessment | Linear-mixed model, identity link | Negative mean difference favours intervention |
| Stata | |||||
| xtmixed | |||||
| Other outcome measures | |||||
| Health-related quality of life | Self-assessed EQ-5D score | Cohort at 6 months | Assessment | Linear-mixed model, identity link | Positive mean difference favours intervention |
| Cohort at 12 months | Stata | ||||
| Cross-sectional at 12 months | xtmixed | ||||
| Cognitive function | MMSE score | Cohort at 6 months | Assessment | Linear-mixed model, identity link | Positive mean difference favours intervention |
| Cohort at 12 months | |||||
| Stata | |||||
| Cross-sectional at 12 months | xtmixed | ||||
| Fear of falling | Yes/no question | Cohort at 6 months | Assessment | Logistic-mixed model, logit link | OR < 1 favours intervention |
| Cohort at 12 months | Stata | ||||
| Cross-sectional at 12 months | xtmixed | ||||
| Pain | Ordinal five-point scale reduced to three points for analysis | Cohort at 6 months | Assessment | Ordinal logistic-mixed model, cumulative logit link | Proportional OR < 1 favours intervention |
| Cohort at 12 months | |||||
| Cross-sectional at 12 months | SAS | ||||
| glimmix | |||||
| Mobility | SPPB | Cohort at 12 months | Physical assessment | Linear-mixed model, identity link | Positive mean difference favours intervention |
| Cross-sectional at 12 months | Stata | ||||
| xtmixed | |||||
| Health-related quality of life | Proxy EQ-5D | Cohort at 6 months | Care home, proxy | Linear-mixed model, identity link | Positive mean difference favours intervention |
| Cohort at 12 months | Stata | ||||
| Cross-sectional at 12 months | xtmixed | ||||
| Social engagement | SES, six binary items reduced to three-point scale for analysis | Cohort at 6 months | Care home, proxy | Ordinal logistic-mixed model, cumulative logit link | Proportional OR > 1 favours intervention |
| Cohort at 12 months | SAS | ||||
| Cross-sectional at 12 months | glimmix | ||||
| Outcome | Measurement | Populations of interesta | Source of datab | Model, programme and command | Effect and interpretation |
|---|---|---|---|---|---|
| Aggregated fracture rate | No. of fractures at home level | All residents of the home over the year following randomisation, regardless of whether or not they were participants in the study | Care home records | Poisson mixed model in SASc | OR < 1 favours intervention |
| Stata | |||||
| xtmepoisson | |||||
| Fracture rate | Fracture or not | Study participants over the year following randomisation | NHS data | Logistic-mixed effects model, logit link | OR < 1 favours intervention |
| Stata | |||||
| melogit | |||||
| Mortality | Death | Study participants over the year following randomisation | NHS data | Logistic-mixed effects model, logit link | OR < 1 favours intervention |
| Stata | |||||
| melogit |
Descriptive analyses
We collected data on medication use. We present descriptive data on use of medications most relevant to our study hypotheses: hypnotics and anxiolytics, antipsychotics, antidepressants, tricyclic antidepressants, SSRIs, analgesics and non-steroidal anti-inflammatory drugs (NSAIDs).
Blinding
As described above (see Allocation concealment and identification/recruitment bias), new residents joining the study after randomisation could not be blinded to their care home's allocation status prior to recruitment. Identification/recruitment bias was possible for these participants because all care home staff and study staff visiting the care homes were aware of the care home's allocation. Indeed, one marker of success for the programme would be achieving this obvious level of awareness. Additionally, recruitment and treatment visits might coincide.
We protected against this by asking care homes to notify us of all new residents and monitored reasons for exclusion from the study and considered basing our analysis of the proportion of residents depressed at the end of the study only on those residents who joined the study before randomisation and who were present at the end of the study if there were baseline differences between intervention and control homes in characteristics of those who joined the study after randomisation.
Members of the research team collecting follow-up data were aware of the care homes' randomisation status leading to possible bias in data collection. We would anticipate more potential for bias in the physical function assessment – the Short Physical Performance Battery – than for patient-completed outcomes. As part of staff training we emphasised the importance of consistency of approach in the two arms of the study. Results from proxy outcomes, collected from care home staff, might be more likely to be prone to bias than those collected by the research team.
The routine data collected were less prone to bias. Drug-use data were extracted from routine care home records; data on fractures and deaths collected under Regulation 37, Part V11188 are unlikely to be biased because this recording by care homes is a statutory obligation. Routine National Health Service data used for deaths, fractures in study participants and other health service activity (except general practitioner consultations) would not be prone to bias. Where coding of these data was required (fracture-related deaths), this was undertaken by a study team member blind to allocation. Our overall mortality data are not prone to bias.
Economic evaluation
The whole-home aspect of the intervention means that those residents who did not wish to participate in the study were also exposed to the intervention. This was a result of the training given to the care home staff who looked after them and, in the intervention homes, due to the ability of residents who were not participating in the evaluation to participate in the exercise groups. The economic evaluation was designed to capture the costs associated with these changes. Our aim was to examine the cost–utility of the whole-home exercise intervention to alleviate depression among care home residents aged ≥ 65 years, as compared with current best practice for the identification and management of depression in this population from the National Health Service provider perspective.
Data collection
Data for the economic evaluation covered a 12-month time period from when the home was randomised. We collected data needed to calculate costs at the individual-level through the care home records at 3, 6, 9 and 12 months and from routine primary care trust data provided after the study was finished (Table 12).
| Item | Unit | Unit cost (£) | Source of resource use collection |
|---|---|---|---|
| A&E | Investigation | Variable | PCT data extract |
| Community visits | Visit | 47 | PCT data extract |
| GP home visit | Visit | 120 | Care home records |
| GP surgery visit | Visit | 36 | Care home records |
| Inpatient service | Dominant episode | Variable | PCT data extract |
| Medications | |||
| Tablets | Tablet | Variable | Care home records |
| Liquid medicines | ml | Variable | Care home records |
| Patches | Patch | Variable | Care home records |
| Suppositories | Suppository | Variable | Care home records |
| Metered-dose inhalers | Dose | Variable | Care home records |
| Mental health team | Visit | 108 | Care home records |
| Outpatient service | Visit | Variable | PCT data extract |
| Practice nurse | Visit | 12 | Care home records |
| Transport to A&E via ambulance | Trip | 246 | PCT data extract |
We used the EQ-5D to measure gains in quality-adjusted life-years. The research team collected proxy EQ-5D data on all participants at baseline, and 3, 6, 9 and 12 months after randomisation. Additionally, we collected self-completed EQ-5D scores at baseline and 6- and 12-month assessments on participants able to complete these. They are not reported here but will be used to look at a secondary analysis of the relationship between EQ-5D and proxy EQ-5D.
For residents joining the study after their care home was randomised, we collected data in the same way but participation in the study is deemed to start from the time they were first assessed, i.e. 3, 6 or 9 months after randomisation (see Table 12). These participants were included only in our secondary analysis.
Costs
Individual-level resource use was combined with unit costs to calculate the total health-care cost for each resident. The data received from the primary care trusts on inpatient services, outpatient services and A&E visits included diagnostic related groups and associated tariffs. These costs included staff costs, consumables and procedure costs. For those A&E attendances that recorded arrival ‘via ambulance or air ambulance’, the primary care trusts confirmed that most, or indeed all, arrivals were via road and the cost for a road ambulance journey188 was added to the tariff for the visit. For resource use coming from care home records and community data provided by primary care trusts, we obtained unit costs for the UK from published sources. 189,190 Unit costs are inclusive of ancillary staff costs, overheads and training costs. We used unit costs for the year 2010, actualising unit costs for inflation using the Healthcare Price Index when necessary. 189 Table 12 shows all unit costs derived from published sources. We were unable to procure data on diagnostic tests.
Unit costs for medications were obtained from the Prescription Cost Analysis database for 2010. 190 We included all medication costs where reliable data could be collected, as there were unlikely to be many health costs that could not plausibly be related to the intervention. We obtained details for medications that were being taken by study participants over the 1-week time period that preceded the data collection visit (see Health service activity, above). We calculated the total medication costs using the average cost per dose for each product obtained from the database, and the mean quantity taken per day of each product during the 7 days prior to data collection. These costs were extrapolated for the 91 days prior to the follow-up visits at 3, 6, 9 and 12 months. If the daily drug cost was missing for a time point then we used the midpoint of the adjacent time points.
Where a dose range is cited as ‘as required’, we coded it as the midpoint of that range. For common analgesics such as paracetamol and co-codamol, the dose was considered to be two tablets unless another dose was clearly specified. If the dose of the drug had not been recorded, the standard dose for that drug was assumed. If the quantity was not recorded, the standard quantity for that drug was assumed. Good data were available for tablets, liquid medicines, patches, suppositories and metered-dose inhalers. Owing to inconsistencies in the way dosing was recorded within care homes, the following items were excluded from our analyses: all wound dressings (including bandages), creams and lotions, sprays, eye drops, ear drops, injections (including insulin), glucose strips and lancets, catheters and catheter solutions and appliances.
Active control and intervention costs
Control home costs included the cost of training a nurse to deliver the depression awareness intervention, the costs of the nurse's time and travel to deliver the intervention at the care homes, and the materials for the training sessions. In the control homes, the total cost of implementing ‘best practice’ for diagnosis of depression was divided by all residents in the home to arrive at the unit cost.
Intervention care home costs included the training of physiotherapy staff, the delivery of the depression awareness training, the implementation of the exercise regime, physiotherapists' time and travel expenses for organising and running the exercise class, and equipment used both for the exercise programme and to aid resident mobility. Data on the National Health Service costs of providing equipment resulting from mobility assessments with the physiotherapists were not easily available. The likely differences between the market purchase price and National Health Service costs, including a discount, would be small for most items, as items were of relatively low cost. These items were estimated by study staff at the aggregate level for residents in the intervention homes and this cost was attributed to the total cost of the intervention.
Deciding how to attribute the cost of intervention delivery to study participants, and hence arrive at unit cost for the intervention was not straightforward. This was because non-study participants are also exposed to the intervention and a proportion of the cost could also be attributable them.
We considered four different ways of attributing costs to study participants:
-
Cost per study participant The fixed cost is divided by number of study participants to develop a cost of delivery of the intervention package to each study participant; however, this may overestimate the costs to study participants, as many non-study participants were exposed. Furthermore, some study participants did not attend any exercise groups.
-
Cost per session attendance The fixed cost (TC) is divided by the number of attendances at the exercise intervention sessions, regardless of whether or not the attendee was a study participant, to estimate a cost per session attendance, i.e. TC/(ap + anp) (where ap equals the number of attendances to exercise classes by study participants and anp equals the number of attendances to exercise classes by non-study participants). This cost per session attendance can then be applied at an individual study participant based on the number of sessions attended by each study participant. This method ignores the whole-home aspect of the intervention as residents who did not attend any sessions could still benefit from the intervention through the mobility assessments and general changes to the atmosphere of the care home.
-
Cost per resident The fixed cost is divided by the number of residents to develop a cost of delivery of the intervention package to each resident. This may underestimate the cost to participants as some non-participants, for example those with severe disability or cognitive impairment, will not have had substantial exposure to the intervention.
-
Weighted cost per resident The fixed cost is divided by the overall percentage of residents assessed for eligibility to participate in the exercise sessions. This method has the advantage of reflecting the whole-home aspect of the intervention while removing the cost burden from those residents who were unlikely to receive much benefit from the programme due to communication difficulties or serious illness.
We chose to use option 4, the weighted cost per resident, to attribute costs to study participants. In addition, for those leaving the care homes or dying, the costs were truncated at the point of leaving or death.
Quality-adjusted life years
The proxy EQ-5D is a well-accepted measure that has been used for stroke patients. 138,191 Responses from proxy EQ-5D questionnaires were transformed into quality of life weights (utility) derived from at UK general population sample using an algorithm developed by Dolan et al. 192 We specified a priori that we would use proxy EQ-5D data rather than self-completed EQ-5D. This was because of an anticipated poor completion rate and to avoid problems with participants whose health deteriorated making them unable to complete the EQ-5D at follow-up time points. In practice, the proxy EQ-5D was completed for a larger proportion of participants than the self-reported EQ-5D.
In order to ensure that quality-adjusted life-year calculations were as accurate as possible, we chose to use multiple imputation to guard against any bias that may result from missing proxy EQ-5D scores. As the study was cluster randomised rather than individual randomised, the data were multilevel. To adjust for this characteristic of the data, a multiple imputation model that accounted for clustering (by means of a random cluster effect) by care home was used to generate the missing proxy EQ-5D scores at each of the five time points (baseline and 3, 6, 9 and 12 months). The imputation model was multivariate for the five EQ-5D scores at each time point, and used the auxiliary variables home size, baseline age of resident and proxy EQ-5D scores at all five time points. Five imputed data sets were created in this way.
The EQ-5D scores, including those scores that were generated by the multiple imputation, were then used to calculate five quality-adjusted life-years, one for each imputed data set. We calculated the total utility for each participant from point estimates at baseline, 3, 6, 9 and 12 months, using the ‘area under the curve’. To estimate the total utility, we assumed that utility for each person followed a linear trend line between these point estimates. 193 We then added up these utility estimates. As many study participants died over the course of the study, we assumed a linear relationship from last proxy EQ-5D measurement to death.
Analyses
Our primary analysis was a cost–utility analysis over 12 months examining the cost per quality-adjusted life-year gained for all participants, who were assessed for proxy EQ-5D prior to randomisation and had primary care trust data extracts. Importantly, the health economics criteria for inclusion were slightly more restrictive than those for the statistical analysis. The clinical effectiveness analysis included residents with and without primary care trust data extracts, whereas the health economic analysis included only those residents with primary care trust data extracts. This should not be confused with the notion of complete or missing data, as all participants with a primary care trust data extract were included irrespective of the completeness of their records. This analysis included those who were not depressed as well as those who were depressed. This was a more meaningful analysis than the alternative of only examining those who were depressed at baseline, as the costs and any potential benefits were related to all of those exposed to the intervention. In order to be aligned with the clinical effectiveness analysis, we included only those who provided the primary outcome, in this case proxy EQ-5D, prior to the home being randomised. Unlike the clinical effectiveness analysis, we included those residents with partially incomplete proxy EQ-5D scores, as these scores could be imputed for our analyses. In line with an intention-to-treat principle, any participants who moved between care homes during the study were analysed as if they had remained in their original care home.
For each cost category, we multiplied the number of items, or contacts with each type of health-care service, by their unit cost. We calculated the mean total costs per participant from an National Health Service provider perspective adding the cost of consultations, admissions, equipment, rehabilitation and physiotherapy services, prescriptions and applicable intervention costs.
As the outpatient data had a large proportion of missing costs, and these missing data were more frequent with some primary care trusts than with others, we imputed these data using the same methodology as we did for the missing EQ-5D scores before calculating the total outpatient cost. We log-transformed costs before imputing, to make the assumption of normality more plausible. The imputation model also accounted for clustering using random home effects and used the auxiliary variables home size, baseline age of resident and the specialty code provided by the primary care trust. Five data sets with imputed data were created. From these sets, the total outpatient cost per resident was calculated and added to the total cost from the other cost categories to produce five total cost data sets, which were used in the baseline analysis.
To compare differences in mean resource use and mean costs between participants in the intervention and control arms of the study, a univariate linear-mixed model was used. To aid in the comparison of costs between the two groups for the outpatient data and total costs, the univariate linear-mixed model was applied to one of the data sets generated by multiple imputation.
Base-case analysis
The correlation between individual costs and outcomes needs to be considered in the cost-effectiveness analysis. In order to acknowledge this correlation when estimating mean incremental costs and mean incremental quality-adjusted life-years, we used bivariate normal mixed models with cluster random effect to obtain maximum likelihood estimates. 194 Originally, we planned to use seemingly unrelated regression, but this method does not strictly recognise the hierarchical nature of our data and so multilevel models have been reported instead. 194 The hierarchical multiple imputation of EQ-5D and outpatient data resulted in five sets of total costs and five sets of EQ-5D scores from which we calculated total costs and total quality-adjusted life-years. Rubin's rules were used to combine these estimates of incremental costs and incremental quality-adjusted life-years with multiple imputation standard errors. 195 Intracluster correlation coefficients were calculated using a mixed model without adjusting for any covariates.
We plotted the spread of incremental cost-effectiveness ratio across the four quadrants of cost-effectiveness, but calculated a mean incremental cost-effectiveness ratio only if it would be informative. For example, with data that show an insignificant quality-adjusted life-year gain, it was more informative to report disaggregated data on costs and effects than report a mean incremental cost-effectiveness ratio. As a definite threshold has proven difficult to set empirically, we planned to assess the cost–utility of the intervention using willingness-to-pay thresholds ranging between £0 and £40,000. 196 The probability that the intervention was cost-effective at willingness-to-pay thresholds was calculated based on the incremental net benefit, which was assumed to be normally distributed, with both mean and SD equal to their multiple imputation estimates.
Sensitivity analyses
To assess the robustness of the analysis to changes of key input values and assumptions, we conducted the cost-effectiveness analysis using alternative scenarios for some cost items. The following were considered:
-
Excluding high cost individuals This analysis excluded those individuals who were above the 95th percentile of total cost of care including intervention costs at 12 months.
-
Including costs from the societal perspective This perspective includes the cost of care home staff time lost to training and gained by having the residents in the physiotherapy sessions. For the societal perspective, we included the costs of the exercise programme to care homes in terms of time taken to set up and monitor the exercise routines, or to implement the control intervention, as estimated by study staff.
Secondary analysis
A secondary analysis was conducted to include the costs and quality-adjusted life-years for all those participants who joined after the homes were randomised. These individuals provide cost and proxy EQ-5D for the period following their first EQ-5D at a home follow-up visit until the end of the study for the home in which they were recruited.
Process evaluation
Alongside the main study we carried out a process evaluation, using both qualitative and quantitative methodologies, to explore the process of implementing the study in a care home setting, to develop a set of transferable principles, regarding both the OPERA depression awareness training and the OPERA whole-home exercise intervention, and to inform its implementation on a wider scale.
No data from the process evaluation of the main study were provided to the research team until after the intervention phase was complete. A full process evaluation report was completed and submitted to the chief investigator before any analyses of outcome data were performed (September 2011). This ensured that this assessment was conducted blind to the outcomes of the study.
We used the Theory of Change197 to identify the important processes to consider in the process evaluation. 109 The Theory of Change identifies the causal processes through which change comes about as a result of a programme's strategies and action. 197 It relates to how practitioners believe individual, intergroup, and social/systemic change happens and how, specifically, their actions will produce positive results.
Figure 7 is a representation of the Theory of Change in relation to the active whole-home intervention in the OPERA study. In this model the primary outcomes (on the right) are brought about by a series of ‘changes’ as a result of introducing the intervention into the care.
FIGURE 7.
Theory of change model for how the OPERA ‘active intervention’ might work. The bold arrows depict the main direction in which we believe OPERA will have an impact.
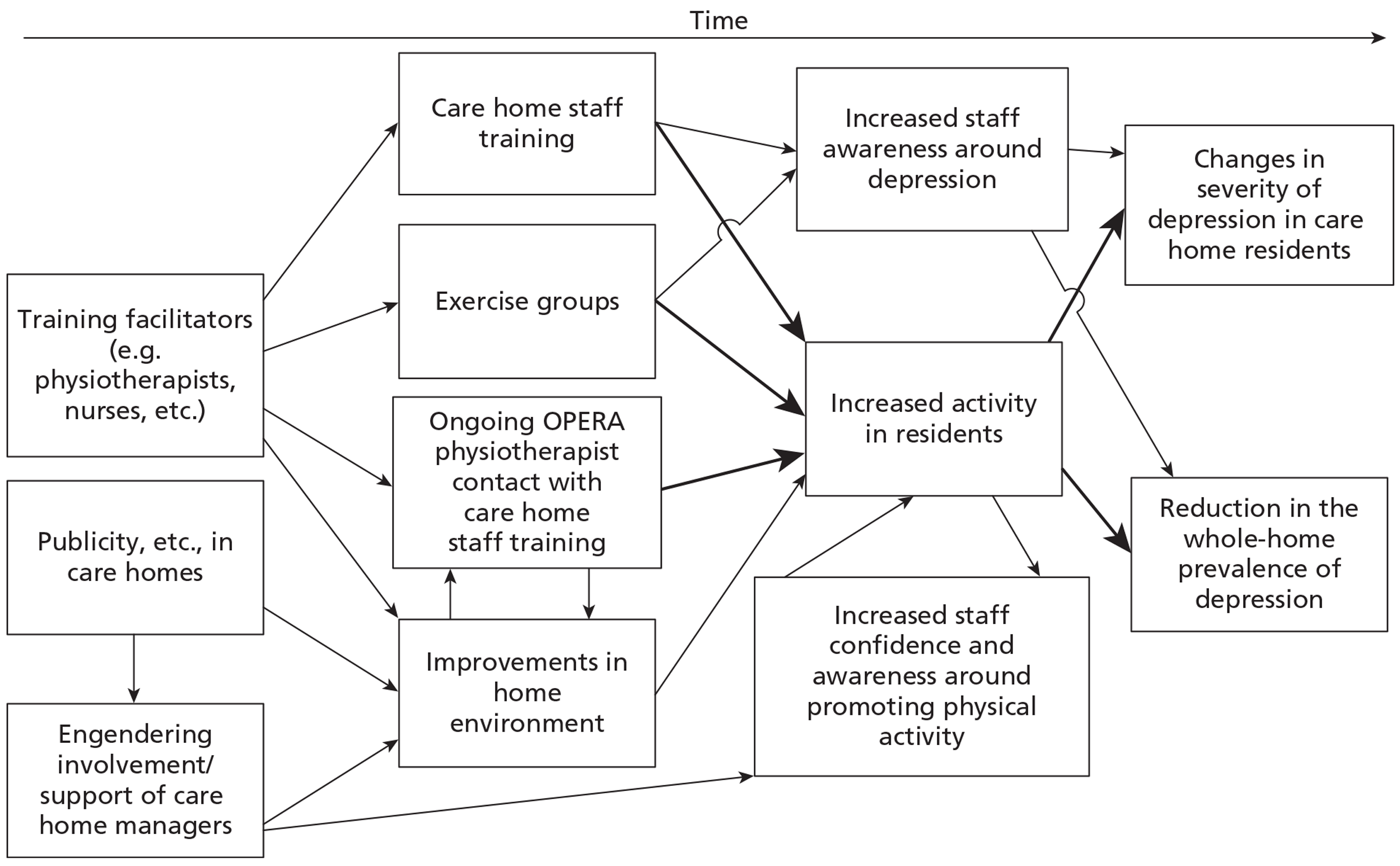
The process evaluation followed the key components of process evaluation proposed by Steckler and Linnan:198 context, reach, dose delivered, dose received, fidelity and recruitment (Box 3). We omitted implementation (‘a composite score that indicates the extent to which an intervention has been implemented as planned’). Additionally, we sought the views of participants, including residents, care workers and members of the research team. Their experiences, their attitudes to the intervention and their suggestions for improving the intervention have a significant role in interpreting the study outcomes and informing policy development.
| Component | Definition |
|---|---|
| Context | Aspects of the larger social political and economic environment that may influence implementation |
| Reach | The proportion of the intended target audience that participates in the intervention |
| Dose delivered | The number or amount of intended units of each intervention or each component delivered or provided |
| Dose received | The extent to which participants actively engage, and interact, with the recommended resources |
| Fidelity | The extent to which the intervention was delivered as planned |
| Recruitment | Procedures used to approach and attract participants |
We used a mixed-methods approach, combining quantitative and qualitative data199,200 to facilitate exploration of apparent discrepancies between findings. 109,201 Integrating quantitative and qualitative methodologies into a single study requires careful planning. 202 Considerations include the priority given to a particular methodological approach and how other methods will complement this. In this process evaluation the principal data collection method was quantitative, while the qualitative data, which complemented and illuminated the quantitative data, were collected from only a small sample of care homes.
Aims and objectives
The aims of the process evaluation were to
-
assist in the interpretation of the results of the main effectiveness study
-
develop a set of transferable principles regarding the whole-home intervention to inform its implementation on a wider scale.
The objectives were to
-
collect quantitative data on the delivery of the intervention in both intervention and control care homes
-
observe the exercise programme delivery and the depression awareness training (see Interventions, above)
-
document the care home environment in case study care homes and document any changes observed
-
carry out in-depth interviews with care home managers, care home staff, patients and carers in a purposive sample of the care homes
-
collate and interpret the resulting data.
Methods
All of the OPERA care homes contributed quantitative data to the process evaluation; eight purposively sampled care homes (six intervention and two control) were selected as case study care homes where additional quantitative and qualitative data collection took place.
Data were collected from all care homes using specially designed case report forms and from other sources, including the Commission for Social Care Inspection reports for the care homes (i.e. data from the last published report prior to randomisation), and the records of exercise classes kept by the physiotherapists. Box 4 shows the data that were collected from each participating care home and from the residents and staff within each care home.
No. of homes overall
Size of home (including number beds and actual occupancy)
Type of home (i.e. registered as a dementia specialist home or not)
Type of home in terms of funding (i.e. independent, charity, group or local authority/run)
Pre-existing reported level of opportunity for physical activity already within home (e.g. groups, trips out)
Facilities available within the home, such as an accessible garden
ResidentsNos. approached
Type of consent [personal or third party (assent)]
Nos. agreeing to take part
Dropouts, adverse events or other attrition
Attendance at the exercise groups
Care staffNo. of staff (day and night), grade, vacancies, qualifications and number and type of ancillary staff
No. of OPERA control or active intervention care home staff training sessions conducted
No. of care staff trained
Satisfaction with the training programmes
All staff in the care homes (control and intervention) were invited to participate in a brief training session on depression awareness. Staff in the intervention homes received additional information about promoting and increasing physical activity amongst residents. Key elements included staff response to these sessions, how confident the presenter was in engaging/adapting to residents' needs, the environment used for the training, timing, and the level of interest of participants.
In addition to observing some sessions, feedback on the value and quality of the training package was sought from attendees using an evaluation form distributed immediately after the session. A follow-up questionnaire with a return envelope was mailed to care home staff 4 weeks later exploring how useful the training had been and if it had been put into practice.
Case study homes
Recruitment of case study homes took place after randomisation, and was staggered through the first 6 months of randomisation of homes into the study. All care homes at the point of recruitment were informed about the process evaluation and the possibility that they may be asked to take part. No more than two homes and no more than one intervention home were recruited in any 4-week period. The main sampling criterion was ownership of the care homes and a secondary criterion in the intervention homes was which physiotherapist would be leading intervention delivery. Research carried out in the case study homes was predominantly ethnographic and consisted of semistructured interviews and repeated observation with field notes. 203
In each case study home we invited for interview the care home managers, care home staff, care home residents, residents' relatives/NOK, and the physiotherapists who were involved in the delivery of the intervention in that home.
The inclusion criteria for residents were:
-
ability to understand and communicate in spoken English
-
provision of consent to participate in OPERA.
We did baseline interviews after randomisation and before the OPERA interventions were implemented. Semistructured, face-to-face interviews were conducted at a time and place to suit participants, were digitally recorded, transcribed verbatim and anonymised. Baseline interviews explored life in the home and the current levels of activity, staff/resident interactions and the process of consent to the OPERA study. We did follow-up interviews with a few of the key informants, where possible, at 6 months and again at the end of the study. Potential interviewees were invited to give written informed consent to participate in the interview.
These interviews explored in more depth perceptions about the care home and its levels of activity and in intervention homes, perceptions of the activity programme and its impact. Follow-up interviews also explored feelings about the withdrawal of OPERA involvement in the home at the end of the study. Topic guides for interviews are shown in Appendix 5.
Additional information was sought from the care home managers about their reasons for taking part in OPERA, their feelings about the whole-home intervention and their beliefs about potential long-term changes in the care home as a result of the intervention.
Field observation
Observation of the case study homes was carried out by DE. He spent at least 4 days in each home at baseline and at least 3 days at each follow-up. Observation spells were typically spread over a period of 2 weeks and involved observation of the home environment, the delivery of the depression awareness training in control homes, the depression awareness/activity training in intervention homes and delivery of the exercise groups. At each visit, DE wrote field notes, noting time of day, what residents were doing, any home activity sessions and staff resident interactions.
To quantify the kind of activity that was taking place in the care homes, we did a series of observational sweeps of all the public spaces at baseline and follow-ups. We adapted the observational instrument of activity and well-being Behaviour Category Codes. 204,205 This involved the researcher completing a checklist of where residents were and what they were doing (including interactions with staff and others) at regular intervals in the day (Box 5). Observational data sweeps occurred every 15 minutes for a 90-minute period (i.e. six sweeps in 90 minutes). The sweeps recorded the number of residents within each public area exhibiting a particular behaviour. Observations were carried out starting at different times but covering a whole day over a number of visits. The recommended time periods were 1000–1130, 1200–1330, 1400– 1530, 1600–1730 and 1800–1930 but we stopped doing observations for the period 1800–1930 as most residents had retired to their bedrooms by then. We collected data at baseline and at follow-up near to the end of the study (12 months). To preserve the privacy and rights of non-participants in the OPERA study no individuals were identified in written records and no researcher entered a resident's bedroom (unless invited by the resident).
The seven categories used are based on the Behavioural Category Code observational instrument of activity and well-being Behaviour Category Codes,204,205 which has 10 categories. [Four categories were not used: communicating with no response, other, receiving care (as this mostly took place away from observation) and unavailable for observation (not relevant as we were not mapping individuals)]
| Active social interaction | Interacting with others verbally or otherwise |
| Eating/drinking | Meals, snacks or drinks |
| Recreational activity (not exercise) | Participating in a game, craft activities, using intellectual abilities, performing work or pseudo-work, engaging with media (e.g. ‘actively watching TV or listening to radio’) or participating in religious activity |
| Sport or exercise | Exercise (this was separated from the recreational activity category, as we were specifically interested in knowing if exercise took place) |
| Passive social interaction | Being socially involved but passively, for example sits quietly but aware of what is going on and contributes if needed |
| Socially inactive | Being socially uninvolved, withdrawn, sleeping, dozing |
| Walking/wandering |
When coding, the observer, where possible, noted specific interactions with others. For example, if a resident was talking to another resident then this was marked as ‘active social interaction’ [with S T, RE or OT to indicate whether the interaction was primarily with a STaff member or REsident, or OTher (e.g. relative)]. This was repeated for all categories in which an interaction could be taking place. The results of these individual interactions are not reported here. For the purposes of the results these different interactions were collapsed into the overall category.
Observations included how the exercise classes fitted into the day; how the residents reacted; how the physiotherapist interacted with the residents; the involvement of the staff/home; and what happened at the end of the exercise group.
Quantitative data analyses
Quantitative data were analysed using the statistical package SPSS version 18 (SPSS Inc., Chicago, IL, USA) and reported in descriptive tables. Charts, presenting average monthly attendances at exercise groups, were based on the month the first group was delivered. For each calendar month all attendance register data (see Box 4) were pooled and an average attendance calculated. Although this was a 12-month intervention, several homes did, using this method, cover 13 months due to them starting late in the first calendar month.
Data from the activity sweeps described above were summarised in a 100% stacked bar chart, each bar within the chart representing a home displaying the means of 12–14 individual activity sweeps. Activities were grouped into one of seven categorises, elaborated in Box 5.
Data collected from OPERA staff
We ran focus groups to explore the experiences of both the recruiting team and the physiotherapists. These were carried out as the study was drawing to a close. Both of these groups were day-long events and involved a facilitator (DE) and a scribe.
The recruitment team focus group discussions included asking about experiences and thoughts on OPERA in respect to
-
recruitment of homes
-
recruitment of participants including consent/assent process
-
assessments
-
follow-ups
-
general points about involvement and experiences (e.g. questions on questionnaires, working with care homes and care home staff, interactions with OPERA office).
The physiotherapy team focus group discussions included exploration of the following topics:
-
initial meetings with care homes
-
assessment of residents
-
training of care home staff
-
the exercise intervention
-
delivery of the sessions
-
paperwork
-
‘whole–home’ interactions
-
interactions with care home staff/management
-
closing of care homes.
In these sessions topics were discussed and then main points were brought together and agreed by the group and the scribe produced a summary result on each topic. The results of these groups are interlaced in the process evaluation results and the results presented in the ethics substudy section (see Chapter 3, Ethics).
Qualitative data analyses
The analysis was thematic and we adopted the framework method described by Ritchie and Spencer206 and Pope et al. ,207 which involved the following:
-
Data familiarisation Repeated reading of interview transcripts and field notes and listening to original audio-recordings.
-
Identifying a thematic framework Key issues, concepts and themes were identified and an index of codes developed.
-
Indexing The index generated through identification of the thematic framework was applied to all data.
-
Charting A summary of each passage of text was transferred into a table to allow more overall and abstract consideration of index codes across the data set.
-
Mapping and interpretation Understanding the meaning of key themes, dimensions and broad overall picture of the data, and identifying and understanding the typical associations between themes and dimensions.
Researcher bias was minimised through regular cross-checking of data and findings by the members of research team. In addition, transcripts were returned to participants (where appropriate) providing them with the opportunity to check the transcripts for accuracy and authenticity, and to offer any subsequent reflections. Quotes are used as exemplars of key themes.
Ethics substudy
In order to explore some of the ethical issues around recruitment and consent for research involving people who are vulnerable because of either their situation (in this case residents in care homes) or a degree of cognitive impairment, we nested an ethics substudy within the OPERA study.
The aims of the ethics substudy were to
-
describe the process of obtaining consent to participate in a complex intervention research study involving people who lack capacity
-
consider this in relation to current legislation and international ethical guidelines for the conduct of medical research
-
explore the views of older people and key stakeholders on consent to research involving older people who lack capacity.
The study used a combination of the following research methods:
-
Observation of the recruitment and consent process (part of the process evaluation study reported in Quality control, below).
-
Interviews with care home staff, residents and NOK of participants in the study (see Case study homes, above).
-
Focus group with recruitment staff (see Data collected from OPERA staff, above).
-
Focus groups with older people not currently in a care home to elicit their views on research in general and research with people who are unable to consent in particular.
-
Interviews with key professional informants, including researchers, ethicists, academics, health professionals, representative of a national care provider, and representatives of elderly care-related voluntary organisations.
Data collection
Data collection methods for items 1–3 are described in the above sections Case study homes and Data collected from OPERA staff, respectively.
We conducted three focus groups with elderly people who were not currently living in a care home. Initial attempts at recruitment using advertising through local contact with two national, elderly care-related voluntary organisations were unsuccessful. Final recruitment was through local support groups providing day care or activities for the elderly. The managers of centres within C&W were contacted by the research team via telephone and asked if they would be interested in participating. The first two centres contacted expressed an interest and were sent information and posters about the study. Centre managers spoke with different groups within their centres, using posters and participant information sheets provided by the study team. Three groups from two centres agreed to participate and members of these groups were given copies of the participant information sheet and a consent form. Focus groups were organised on days and times specified by the centre managers to coincide with regular timetabled group meetings and were carried out by two researchers: a lead and a scribe (note taker). All participants provided written informed consent on the day of the meeting. As an introduction to the focus group topic the researcher opened the group discussion with a question about the process of consent that the participants had just experienced. A schedule of open questions followed by prompts where necessary guided the main discussion. Questions focused on experiences, perceptions or feelings about the involvement of elderly people in research, particularly about how decisions to take part in research are made (a copy of the schedule can be found in Appendix 6). All focus groups were audio-recorded and field notes were taken. Key points were identified on a flip chart and fed back to participants to check that we had accurately captured their views.
We conducted interviews with key informants, who were purposively selected to provide a range of points of view from different stakeholder and professional groups. We initially contacted 40 potential participants by e-mail with an invitation to participate in the study. Following an expression of interest we sent an information sheet and consent form to complete and return to us. Interviews took place either face to face or by telephone, according to the participant's preference. All interviews were audio-recorded and transcribed.
Interviews were structured around a topic guide that focused on their views about health research in elderly or care home populations. Specific prompts were given, where necessary, regarding potential difficulties in conducting research in these populations and on the question of consent. Finally, participants were asked whether or not they would be prepared to be involved in a consent process for research involving a relative who lacked capacity to consent, and who if anyone would they wish to be involved in such a process for them. Personal involvement in this kind of research, for example as a researcher, was explored. (A copy of the interview schedule can be found in Appendix 7.)
Analysis
All interviews were recorded, transcribed and analysed using NVivo 7 software (QSR International, Southport, UK). Focus group field notes and flip chart records were used as the basis of analysis with reference to the recordings for clarification of points and illustrative quotes. We used a thematic content analysis based on the framework approach and matching that we used in the process evaluation (see Process and evaluation, above). We analysed the process evaluation interview data separately looking for any factors or themes relating to the process of recruitment and consent. We then compared themes emerging from all sources of data (key informant interviews, focus groups, process evaluation interviews and observations) to look for congruence and areas of divergence. In identifying and mapping themes across the data we framed our analysis within the theoretical foundation of informed consent to research and current policy and regulatory frameworks on research ethics. Using a process of reflective equilibrium between empirical data and ethical theory as described by Ives and Draper,208 we were able to achieve a contextual understanding of the ethical requirement of informed consent to research in older people in care homes.
OPERA end-of-study feedback
At the end of the study, all care homes were sent an end-of-study questionnaire. Two versions were developed: one for intervention homes and one for the control (copies of these can be found in Appendices 8 and 9). Both versions included questions about the recruitment process, raising awareness of depression in the home, staff training (i.e. OPERA Depression Awareness or Depression Awareness and Activity Training), interactions with the research team and any contacts made with the OPERA office staff. The intervention version also included questions about interactions with the physiotherapists and the exercise groups. Most of the questions were statements that required a box to be ticked on a four-point scale (‘totally agree’, ‘agree’, ‘disagree’ or ‘totally disagree’); some questions required a ‘yes’ or ‘no’ answer. Space was provided for free-text comments.
Responses from the questionnaires were collated on a study database and summary statistics generated (i.e. number of particular responses to each question).
Quality control
Recruitment (consent and assessments) and data security (in homes)
As part of the process evaluation a researcher (DE) included quality control assessments as part of the work within the eight case study homes (five in NEL and three in C&W). The researcher observed the consenting of residents; the initial Short Physical Performance Battery; and the completion of baseline outcome measures (e.g. Mini Mental State Examination and Geriatric Depression Scale-15). A formal check was also made that OPERA data/files were being maintained and stored correctly within the care home.
Depression awareness training (control intervention)
Observations were carried out during training sessions. Checklists were completed to ensure training was delivered as per protocol. Interactions with the care home staff during the training were also noted.
Intervention delivery
Although the lead physiotherapist assessed the fidelity of the delivery of the exercise intervention in terms of the individuals (physiotherapists) delivering it [see Intervention fidelity (physiotherapist), below], independent observations were also carried out by the process evaluation research fellow. Observation at these times included how the session fitted into the day, how the residents were reacting, how the physiotherapist was interacting with the residents, staff/home involvement and what happened when it ended.
Data security and data collection accuracy at base
All of the electronic OPERA data are stored on the OPERA web application. The OPERA web application is a secure, password-protected, ASP.net web application developed by the Warwick Clinical Trials Unit programming team. The OPERA web application is hosted on the Warwick University Clinical Trials Unit SQL Server 2005 Enterprise edition database. Full back-ups of the OPERA database are completed once every 24 hours.
Baseline and follow-up data were collected on laptops or on paper case report forms. Data entered on to laptops were directly uploaded on to the OPERA web application. Paper case report forms were returned to the study office. Case report forms received, which had not been inputted on to the online database by the recruitment team, were then inputted directly by a data entry clerk, after having been checked by the study manager. The OPERA web application was equipped with computerised validation criteria to minimise data entry errors. These validations placed limitations and checks on data fields to ensure that only the expected responses could be inputted. The database would flag up unexpected responses, prompting the data entry clerk to investigate the query and to correct it. The programmer produced a regular report to identify any possible anomalies on the database in order that they may be investigated in a timely fashion. After data entry had been completed, a 100% data check was conducted on the primary outcome measure (Geriatric Depression Scale-15). This involved checking all of the data points on all of the Geriatric Depression Scale-15 case report forms. For all other outcomes a random 10% check was carried out. This involved checking all of the data points on a randomly selected 10% of the case report forms that contained secondary outcome data. The data checks revealed an error rate lower than the pre-set maximum error rate of one error in 1000 data points. All data management and quality control checks were in line with the standard operating procedures of the Warwick Clinical Trials Unit.
Intervention fidelity (physiotherapist)
The quality and fidelity of the intervention delivery was checked via a site visit to each physiotherapist at one of their assigned care homes on at least two occasions – at least at 6 weeks and at 6 months after the intervention started in that home. These visits were made by the lead (C&W) physiotherapist, or during annual leave an assigned deputy. The delivery of the exercise group and use of the whole-home approach was assessed by observation, and sample of the intervention case report forms and registers were checked. If any major issues were identified, in which case all were checked, that physiotherapist was then visited again within the next few weeks.
In-depth discussions with individual physiotherapists around strategies to maintain and improve treatment fidelity were held on each visit whenever possible, but particularly whenever an area of concern was observed, especially if that difficulty persisted on later visits. The intervention session content and skills demonstrated by their physiotherapist were assessed using a checklist that included items on administration, group locations, resources, self-assessment, progress of participants, working with the care home and mobility safety.
Long-term follow-up
Culture within an organisation is constructed from commonly held and relatively stable beliefs and attitudes, and is realised through behaviours and working practices. In OPERA we provided the opportunity for care homes to adopt practices (i.e. increasing activity and safe mobility of residents) that it was hoped would become embedded in the culture of the care home and be sustained over time.
The experience of research team and interim data from the process evaluation indicated that the OPERA intervention was popular in the care homes and that we were producing the desired culture change. Any longer term effects that OPERA had on the culture of homes is a further facet of understanding the effects of the study. We were provided with additional funding by the Health Technology Assessment in the latter part of 2010 to explore this issue further.
Research questions
Primary question:
-
Do any beneficial changes brought about by having participated in the OPERA intervention appear to be persistent?
Secondary questions:
-
What factors appear to support sustained beneficial changes?
-
Are there any sustained effects from having participated in the research in control homes?
Methods
We planned to recruit all 35 of the OPERA intervention homes and a sample of 18 of the control homes. Within this sample we planned to invite all eight case study homes from the process evaluation (six intervention and two control) to take part in both the interview and the observational parts of this follow-up.
This follow-up study followed homes as they reached approximately 6 months after the end of their participation in OPERA. However, as a few of the homes would not reach this 6-month milestone until October 2011, some were approached at about 4 months to ensure their inclusion.
Interviews with care home managers or their delegates were carried out either face to face (in case study homes or some local homes in C&W) or via telephone. Questions explored reflections on the care homes' experiences of OPERA (e.g. interaction with OPERA team, depression awareness training, exercise groups, what went well and what we could have done differently/better), the impact of OPERA interventions on the home during the period of the study and since its end (e.g. awareness of depression, continued use of information, continuation of OPERA-type exercise interventions or other activities), and the impact of the withdrawal of the physiotherapist and the exercise intervention (intervention homes only) (see Appendix 10). Analysis was grounded on contemporaneous notes taken during interviews, with transcripts and original recordings available, when needed, for clarification.
We repeated the ethnographic observations that we carried out in process evaluation case study homes during the OPERA intervention period. The method for the activity sweeps carried out during these observations is explained fully in the process evaluation section above (see Methods).
Chapter 3 Results
Recruitment
Recruitment of homes
There were 323 care homes across the two localities. Of these, 180 met our inclusion criteria and were sent letters inviting them to take part in the study (Figure 8). Around half of these (98, 54%) expressed an interest in participating; 17 of these were excluded after a visit by the study team because they had too few residents at the time of recruitment, were too busy, had too many residents with severe cognitive impairment, had too few residents aged ≥ 65 years or the residents were too frail/disabled. After having completed service-level agreements and consent processes, we recruited 78 of the 81 eligible homes to the study between January 2009 and March 2010; follow-up was completed 1 year later (see Figure 8).
FIGURE 8.
Recruitment of homes. a, Did not want to take part.
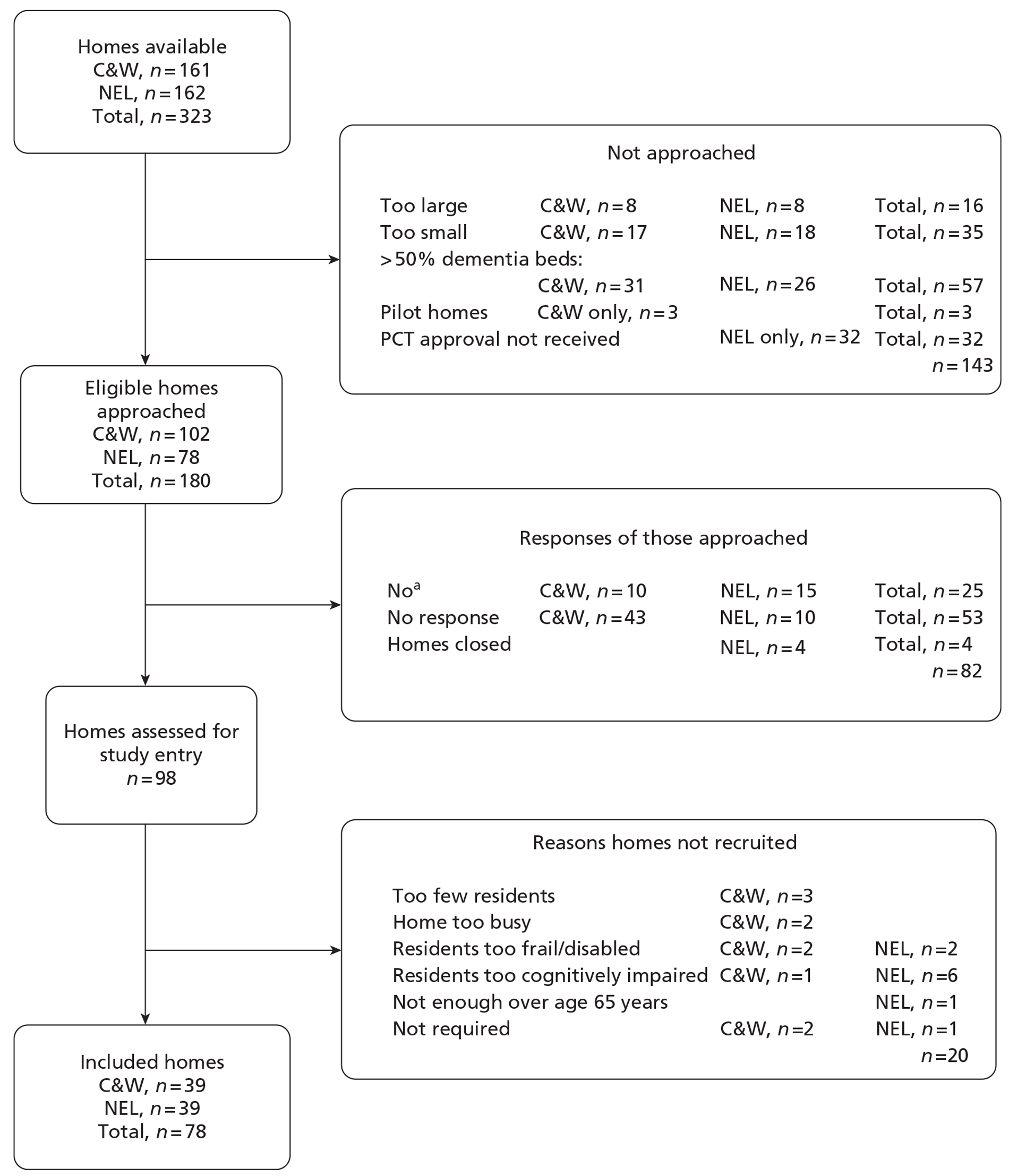
Home characteristics
We recruited equal numbers of care homes from C&W and NEL, and 18 (23%) were care homes with nursing. One residential home was a dementia specialist home, 61 (78%) were privately owned (Table 13), 16 (21%) were voluntary or charity owned and one (1%) was owned by the local authority. Fifty-one of the privately run homes were in independent (small company) ownership. Most homes had a large number of residents with cognitive impairment; 22 were registered for dementia care. 209 Most of the participating care homes were rated as good (54/78, 69%) or excellent (11/78, 14%) in the last reported Commission for Social Care Inspection data (Table 14). 209
| Characteristic | All care homes | OPERA care homes |
|---|---|---|
| No. of homes | 323 | 78 |
| Type of home (n, %) | ||
| Nursing | 81 (25) | 18 (23) |
| Residential | 242 (75) | 60 (77) |
| Ownership (n, %) | ||
| Private | 262 (81) | 61 (78) |
| Voluntary/charity | 36 (11) | 16 (21) |
| Local authority | 25 (8) | 1 (1) |
| No. of beds | ||
| Average | 36 | 32 |
| Range | 3–121 | 17–65 |
| Location | ||
| C&W | 161 | 39 |
| NEL | 162 | 39 |
| Rating | Intervention | Control | Total (no. of homes) |
|---|---|---|---|
| Poor (no stars) | 2 | 0 | 2 |
| Adequate (one star) | 6 | 5 | 11 |
| Good (two stars) | 23 | 31 | 54 |
| Excellent (three stars) | 4 | 7 | 11 |
| Total | 35 | 43 | 78 |
Care homes ranged in size from 17 to 65 beds across the study; 2140 of the 2450 (87%) of beds were occupied when recruitment started (Table 15). Three-quarters of participating homes (60/78) were classed as residential, 15 were classified as nursing and a further three homes were mixed nursing/residential homes (see Table 13). Most of the care homes (67/78, 86%) also offered (temporary) respite care.
| Characteristics | Intervention | Control | Combined | ||||||
|---|---|---|---|---|---|---|---|---|---|
| C&W | NEL | Total | C&W | NEL | Total | ||||
| No. of beds | Median | 26 | 33 | 28 | 32 | 26 | 31 | 30 | |
| Range | 17–47 | 18–62 | 17–62 | 19–65 | 17–61 | 17–65 | 17–65 | ||
| Total | 479 | 625 | 1104 | 737 | 609 | 1346 | 2450 | ||
| Reported occupancy | n | 408 | 565 | 973 | 617 | 550 | 1167 | 2140 | |
| % occupancy at baseline | Mean | 85 | 90 | 88 | 84 | 90 | 87 | 87 | |
| Respite services available | No. of homes | 13 | 17 | 30 | 21 | 16 | 37 | 67 | |
| Reported staff– resident ratioa | Morning | Mean (SD) | 0.24 (0.22) | 0.29 (0.23) | 0.26 (0.11) | 0.28 (0.26) | 0.23 (0.21) | 0.25 (0.10) | 0.26 (0.10) |
| Afternoon | Mean (SD) | 0.19 (0.05) | 0.21 (0.07) | 0.20 (0.06) | 0.21 (0.09) | 0.18 (0.05) | 0.20 (0.07) | 0.20 (0.03) | |
| Night | Mean (SD) | 0.10 (0.03) | 0.10 (0.02) | 0.10 (0.02) | 0.10 (0.04) | 0.11 (0.03) | 0.11 (0.04) | 0.11 (0.03) | |
| Homes with qualified nurse | One nurse employed | n | 2 | 2 | 4 | 2 | 1 | 3 | 7 |
| Two or more nurses employed | n | 1 | 2 | 3 | 2 | 3 | 5 | 8 | |
These results suggest that the care homes in OPERA were broadly representative of care homes in England, with respect to home ownership, and Commission for Social Care Inspection rating. Local authority-run homes were, however, under-represented in our sample, with only one home included (local authority homes represented 10% of care homes in England in 2010),209 and no very large homes were included. The allocation to intervention and control homes was appropriately balanced in terms of size and location (see Tables 13–15).
On average there was one member of staff for every four home residents during the morning and one for every five in the afternoon. At night there was on average of one member of staff for every 10 residents. Few nurses were employed by homes. We are unable to report the different staff types within the homes, as the self-reported data from the homes did not differentiate type of staff and reported numbers may include ancillary staff, thus staff–resident ratios are likely to be overestimates.
Exercise groups at baseline
Nearly all of the care homes reported that they offered established exercise classes, with two-thirds reporting running a class at least once per week (Table 16). About half of the classes were reported as being run by members of the care home staff and around half by external fitness instructors but only two care homes reported external physiotherapist-led exercise classes. Reported attendance at these groups ranged from 3 to 25, with a median of 10, but many care home managers (22) failed to give an estimated attendance. However, observations carried out in the case study care homes (see below) and anecdotal reports by the field staff suggest that exercise groups outside the OPERA intervention were, in fact, uncommon. Observations showed that care homes commonly advertised activities on weekly calendars but that these did not always take place.
| Item | Intervention | Control | Total |
|---|---|---|---|
| Activities co-ordinator employed by home? | 24/35 | 29/43 | 53/78 |
| No. of homes reporting exercise classes being delivered | 31 | 42 | 73 |
| Frequency of exercise classes | |||
| Less than once per week | 9 | 16 | 25 |
| Once per week | 10 | 12 | 22 |
| Twice per week | 9 | 7 | 16 |
| Three times per week | 2 | 3 | 5 |
| More than three times per week | 1 | 4 | 5 |
| Who runs these classes? | |||
| Home staff | 16 | 21 | 37 |
| External fitness instructor | 13 | 19 | 32 |
| External physiotherapist | 2 | 0 | 2 |
| Not reported | 0 | 2 | 2 |
| How long have these exercise classes been running? | |||
| 0–6 months | 3 | 4 | 7 |
| 7–11 months | 3 | 4 | 7 |
| 12–24 months | 5 | 13 | 18 |
| > 24 months | 20 | 19 | 39 |
| Not reported | 0 | 2 | 2 |
| Homes providing average attendance figures | 23 | 33 | 56 |
| Reported average attendance to exercise groups: median (range) | 10 (5–25) | 12 (3–23) | 22 (3–25) |
Individual recruitment
When we started individual recruitment in the care homes we identified 2133 residents. This is slightly different to the number of residents who were present at the time homes were recruited (2140) because of resident turnover. Fifty-five residents (3%) were not eligible as there were aged < 65 years or were not permanent residents. We screened the remaining 2078 for study entry. Some residents were excluded because the care home manager felt it was inappropriate to approach them or they were too ill (245 and 279, respectively) (Figure 9). We obtained consent from 607 residents and assent from the NOK of 300 (Table 17). Ninety-four per cent (853) agreed to both assessment and use of care home data, 50 to use of care home data only and four to assessments only. Of the 907 residents screened and providing consent or assent before randomisation, six died prior to randomisation (five of whom had provided some assessment or proxy/care home data), baseline data collection was completed on a further six within 6 weeks of randomisation, one did not complete assessments until 3 months and one completed assessments around 6 months. A further two residents did not provide outcome assessment or proxy/care home data at any point. In total, 897/2078 (43%) of residents screened provided some baseline outcome data prior to randomisation. After excluding the six who died before randomisation, it is the remaining 891 who form our population of interest for the cohort analyses. For a few care homes the number of residents providing a baseline Geriatric Depression Scale-15 prior to randomisation was five rather than six. This was because the lower cluster size criterion for study entry applied to the number of assessments completed rather than the number of baseline Geriatric Depression Scale-15 scores obtained (see Table 17). Proportionally more participants in C&W had given assent than in NEL. This was because care homes in NEL had proportionally fewer cognitively impaired residents and some time constraints for the NEL research team limiting time to obtain assent.
FIGURE 9.
Reasons for being unable to gain consent/assent prior to randomisation. a, Eligible.
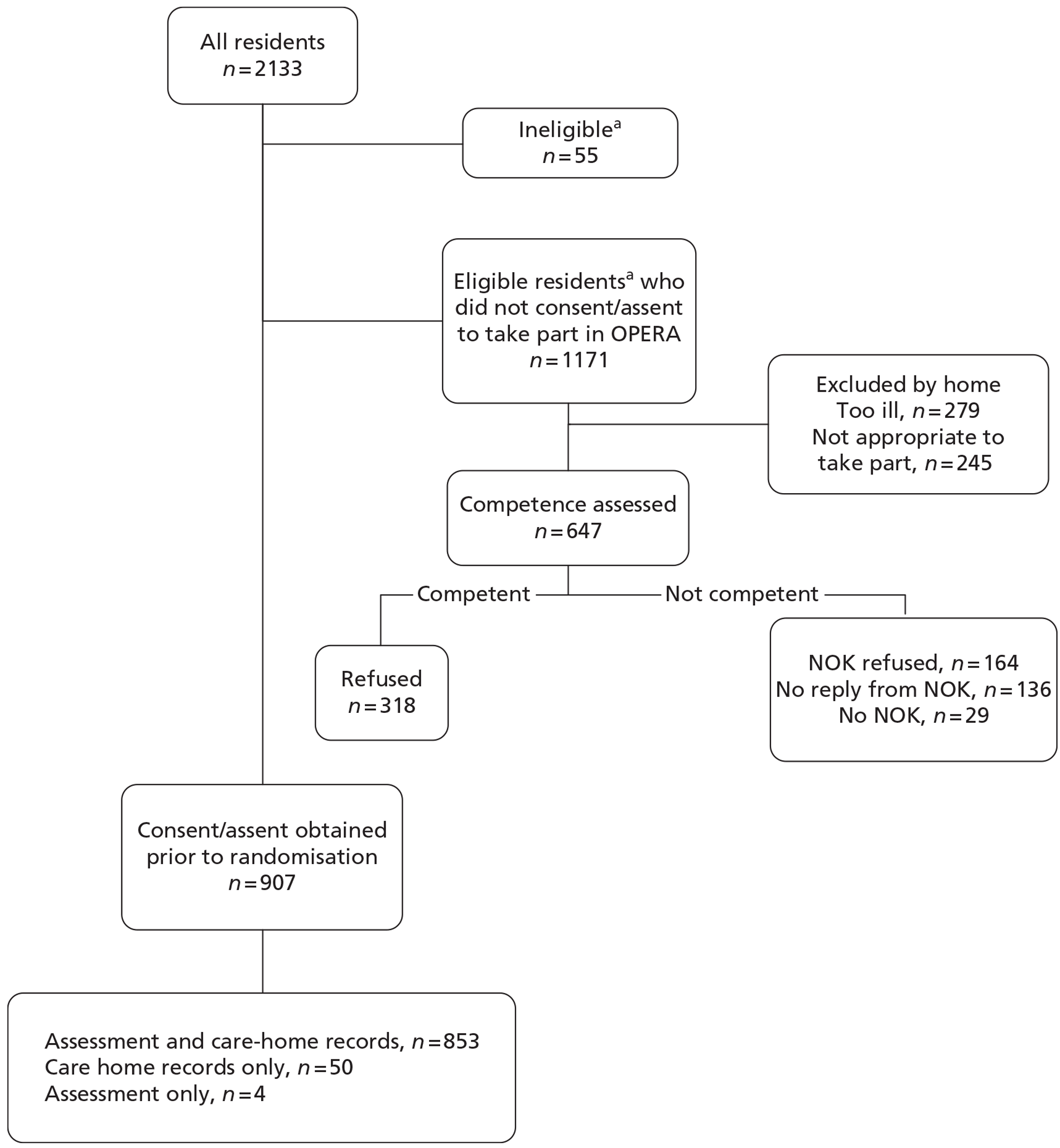
| Site | Recruited | |||
|---|---|---|---|---|
| Assessment and care home data | Care home data only | Assessment only | Total | |
| C&W | ||||
| Consented | 284 | 1 | 1 | 286 |
| Assented | 174 | 31 | 2 | 207 |
| NEL | ||||
| Consented | 319 | 1 | 1 | 321 |
| Assented | 76 | 17 | 0 | 93 |
| Total | 853 | 50 | 4 | 907 |
| Includes those who died prior to randomisation. | ||||
Individual characteristics
We had consent/agreement to directly assess 857/907 of the residents who consented or assented to join the study prior to randomisation (see Table 17). We assessed 783 (91%) of these. Two died between assessment and the day the home was randomised. (We do not have data on time of death. Some deaths may have occurred on the day of randomisation and prior to the time randomisation was performed.) It is the remaining 781 residents who constitute our population of interest for participant-reported outcomes. We obtained a Geriatric Depression Scale-15 score from 765 (98%) of this population at baseline. Overall we recruited an elderly (age range 65–107 years), predominantly (76%) female sample. Of the 781 individuals included in the analyses for patient-reported outcomes, 94–98% responded to each item of measurement at baseline except for self-assessed EQ-5D for which the response rate was only 81%. We anticipated this low response rate prior to the study and consequently also collected proxy EQ-5D. The majority of residents were not in pain, but almost half were afraid of falling and almost one-third were on antidepressants. Baseline characteristics of those who provided data prior to randomisation were similar in the intervention and control groups (Tables 18–21).
| Characteristics | Group | |
|---|---|---|
| Intervention (n = 398) | Control (n = 493) | |
| Female | 294/398, 74% | 383/493, 78% |
| White | 385/393, 98% | 480/488, 98% |
| Age, mean (SD) | 86.7 (7.2) | 86.3 (7.5) |
| Age left full-time education: mean (SD) | 15.0 (1.8) | 14.9 (1.9) |
| ≤ 14 years of age | 178/304, 59% | 207/348, 59% |
| 14–16 years of age | 89/304, 29% | 90/348, 26% |
| > 16 years of age | 37/304, 12% | 51/348, 15% |
| Length of stay in home | 392 | 488 |
| Years, mean (SD) | 2.4 (2.6) | 2.5 (2.6) |
| Interquartile range | 0.7–3.3 | 0.8–3.4 |
| On antidepressants | 110/397, 28% | 156/490, 32% |
| This table includes 696 individuals who had direct assessment, proxy and drugs data prior to randomisation, 84 who had proxy and drugs data, 66 who had direct assessment and drugs data, 23 who had drugs data only, 15 who had direct assessment and proxy data, four who had assessment data only and three who had proxy data only. | ||
| Comorbidities | Group | |||
|---|---|---|---|---|
| Intervention (n = 397) | Control (n = 490) | |||
| n | % | n | % | |
| Cancer | 28/389 | 7 | 40/485 | 8 |
| Stroke | 97/392 | 25 | 109/488 | 22 |
| Dementia | 113/393 | 29 | 134/488 | 27 |
| Depression | 84/392 | 21 | 96/486 | 20 |
| Anxiety | 67/391 | 17 | 84/485 | 17 |
| Osteoporosis | 45/392 | 11 | 50/486 | 10 |
| Chronic lung disease | 47/391 | 12 | 56/489 | 11 |
| Urinary incontinence | 214/393 | 54 | 286/489 | 58 |
| Characteristics | Group | |||||
|---|---|---|---|---|---|---|
| Intervention (n = 355) | Control (n = 426) | |||||
| n | Mean | SD | n | Mean | SD | |
| GDS-15 (0–15, 0 being the best score) | 345 | 4.8 | 3.3 | 420 | 4.8 | 3.3 |
| MMSE (0–30, 30 being the best score) | 346 | 18.7 | 6.9 | 404 | 18.1 | 6.6 |
| SPPB (0–12, 12 being the best score) | 348 | 1.9 | 2.2 | 413 | 1.8 | 2.0 |
| EQ-5D (–0.594 to 1, 1 being the best score) | 297 | 0.54 | 0.39 | 335 | 0.59 | 0.37 |
| ‘Pain now’ rating | n = 335 | % | n = 397 | % | ||
| No pain | 221 | 66 | 264 | 66 | ||
| Mild/moderate pain | 107 | 32 | 116 | 30 | ||
| Severe | 7 | 2 | 17 | 4 | ||
| Fear of falling | n = 341 | % | n = 405 | % | ||
| Yes | 141 | 41 | 189 | 47 | ||
| No | 200 | 59 | 216 | 53 | ||
| Characteristics | Group | ||||||
|---|---|---|---|---|---|---|---|
| Intervention (n = 352) | Control (n = 446) | ||||||
| n | Mean | SD | n | Mean | SD | ||
| Barthel Index (0–100, 100 being the best score) | 337 | 54.5 | 29.4 | 417 | 54.0 | 27.8 | |
| Proxy EQ-5D (−0.594 to 1, 1 being the best score) | 345 | 0.44 | 0.35 | 431 | 0.46 | 0.34 | |
| n = 342 | % | n = 435 | % | ||||
| Social engagement | Low | 34 | 10 | 43 | 10 | ||
| Medium | 97 | 28 | 133 | 31 | |||
| High | 211 | 62 | 259 | 60 | |||
Prior to randomisation, we had consent/agreement to obtain care home data on 903/907 residents. Six of these died between consent/agreement being obtained and the day the care home was randomised, and a further 16 had no care home data collected prior to randomisation. It is the remaining 887 participants who constitute our population of interest for care home data. We obtained proxy EQ-5D and Social Engagement Scale data on 88% of these participants.
The prevalence of comorbidities was high and similar in the intervention and control groups (see Table 19).
Depressed cohort baseline characteristics
Forty-nine per cent (374/765) of those who provided GDS-15 data at baseline were classified as depressed (GDS-15 score of ≥ 5 or equivalent) (Table 22). It is these participants who are our population of interest for all the depressed cohort analyses. For participants in the depressed cohort, GDS-15 scores were inevitably higher (mean = 7.5), but other baseline characteristics, including the proportion on antidepressants, were broadly similar to those in the overall cohort (Tables 23–25). Baseline characteristics of the depressed cohort were also similar in the intervention and control groups. Of those in the depressed cohort, 25% (92/365) had been diagnosed with depression according to care home records and 30% (112/371) were taking antidepressants (see Table 22).
| Status | GDS-15 score ≥ 5, N = 374: n (%) | GDS-15 score < 5, N = 391: n (%) |
|---|---|---|
| On antidepressants | 112 (30) | 102 (26) |
| Not on antidepressants | 259 (70) | 288 (74) |
| Diagnosed depression | 92 (25) | 60 (16) |
| Not diagnosed depression | 273 (75) | 327 (84) |
| Characteristics | Intervention group (n = 174) | Control group (n = 200) | ||
|---|---|---|---|---|
| Female: n (%) | 130/174 | 75 | 148/200 | 74 |
| White | 167/169 | 99 | 192/197 | 98 |
| Age, years (SD) | 86.6 | (7.4) | 86.7 | (7.8) |
| Age left full-time education, years: mean (SD) | 14.8 | (1.6) | 15.0 | (2.1) |
| ≤ 14 years of age | 101/156 | 65 | 100/166 | 60 |
| 14–16 years of age | 40/156 | 26 | 42/166 | 25 |
| > 16 years of age | 15/156 | 10 | 24/166 | 14 |
| Length of stay in home (n) | 169 | 197 | ||
| Years: mean (SD) | 2.4 | (2.7) | 2.2 | (2.7) |
| On antidepressants | 49/173 | 28 | 63/198 | 32 |
| Characteristics | Group | |||||||
|---|---|---|---|---|---|---|---|---|
| Intervention (n = 174) | Control (n = 200) | |||||||
| n | Mean | SD | n | Mean | SD | |||
| GDS-15 (0–15, 0 being the best score) | 174 | 7.4 | 2.4 | 200 | 7.6 | 2.4 | ||
| MMSE (0–30, 30 being the best score) | 170 | 19.4 | 6.7 | 186 | 18.5 | 6.4 | ||
| SPPB (0–12, 12 being the best score) | 171 | 1.6 | 2.2 | 190 | 1.3 | 1.7 | ||
| EQ-5D (–0.594 to 1, 1 being the best score) | 143 | 0.38 | 0.40 | 148 | 0.43 | 0.36 | ||
| ‘Pain now’ rating | % | % | ||||||
| No pain | 84 | 51 | 109 | 59 | ||||
| Mild/moderate pain | 73 | 45 | 65 | 36 | ||||
| Severe | 7 | 4 | 10 | 5 | ||||
| Fear of falling | % | % | ||||||
| Yes | 97 | 57 | 104 | 56 | ||||
| No | 72 | 43 | 83 | 44 | ||||
| Characteristics | Intervention (n = 174) | Control (n = 200) | ||||
|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | |
| Barthel Index (0–100, 100 being the best score) | 164 | 56.0 | 27.7 | 180 | 53.5 | 25.9 |
| Proxy EQ-5D (−0.594 to 1, 1 being the best score) | 168 | 0.42 | 0.34 | 190 | 0.44 | 0.32 |
| Social engagement | % | % | ||||
| Low | 16 | 10 | 16 | 8 | ||
| Medium | 42 | 25 | 63 | 33 | ||
| High | 107 | 65 | 111 | 58 | ||
The prevalence of comorbidities was high and similar in the intervention and control groups. Prevalence of comorbidities was similar to that observed in the overall cohort (Table 26).
| Comorbities | Group | |||
|---|---|---|---|---|
| Intervention (n = 174) | Control (n = 200) | |||
| n | % | n | % | |
| Cancer | 7/169 | 4 | 20/195 | 10 |
| Stroke | 43/169 | 25 | 50/197 | 25 |
| Dementia | 37/169 | 22 | 42/197 | 21 |
| Depression | 45/169 | 27 | 47/196 | 24 |
| Anxiety | 34/169 | 20 | 39/195 | 20 |
| Osteoporosis | 14/169 | 8 | 18/195 | 9 |
| Chronic lung disease | 22/168 | 13 | 19/197 | 10 |
| Urinary incontinence | 99/169 | 59 | 111/197 | 56 |
Participants joining study after randomisation
A further 163 residents provided baseline data after randomisation; of these 150 provided assessment data and care home data, and 13 provided just care home data. Ten were screened for eligibility prior to randomisation but the recruitment and/or baseline data collection processes were completed only after randomisation (six by 6 weeks, one around 3 months and one around 6 months). Fifty-seven were residents who were already living in the homes (26 recruited around 3 months, 19 around 6 months and 4 around 9 months), 45 were new residents recruited at the 3-month data collection visits, 59 were recruited at the 6-month visits; the remaining two were recruited at the 9-month visits (Table 27). In total, 127 of the 163 were present at the end of the study. Of these, 107 contributed direct assessment data and 126 contributed proxy data to the cross-sectional analyses.
The baseline characteristics of participants included in the cross-sectional analyses who were first assessed after randomisation were similar to those recruited before randomisation. Characteristics of intervention and control groups were similar, although larger numbers were recruited in the intervention than in the control arm (Tables 28–30).
| Type | Time of baseline data collection | No assessed datae | n | ||||
|---|---|---|---|---|---|---|---|
| 0a | By 6 weeksb | Around 3 monthsc | Around 6 monthsd | Around 9 months | |||
| Consent | |||||||
| Assessment and care home data | 599f | 0 | 51 | 51 | 1 | 1f | 703 |
| Assessment only | 2f | 0 | 0 | 0 | 0 | 0 | 2 |
| Care home data only | 2 | 0 | 0 | 0 | 0 | 0 | 2 |
| Assent | |||||||
| Assessment and care home data | 242f | 4f | 17 | 22 | 2 | 1f | 288 |
| Assessment only | 2f | 0 | 0 | 0 | 0 | 0 | 2 |
| Care home data only | 44 | 2 | 3 | 5 | 3 | 0 | 57 |
| Total | 891 | 6 | 71 | 78 | 6 | 2 | 1054 |
| Characteristic | Intervention (n = 76) | Control (n = 51) | ||||
|---|---|---|---|---|---|---|
| n | Mean/% | SD | n | Mean/% | SD | |
| Age (years) | 76 | 86.9 | 8.0 | 51 | 86.9 | 7.2 |
| Females | 59/76 | 78% | 41/51 | 80% | ||
| White | 74/76 | 97% | 50/51 | 98% | ||
| Age when left full-time education (years) | 63 | 14.7 | 2.0 | 39 | 15.4 | 2.0 |
| ≤ 14 years of age | 39 | 62% | 19 | 49% | ||
| 14–16 years of age | 18 | 29% | 13 | 33% | ||
| > 16 years of age | 6 | 9% | 7 | 18% | ||
| On antidepressants | 18/76 (24%) | 13/51 (25%) | ||||
| Characteristic | Intervention (n = 73) | Control (n = 49) | ||||
|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | |
| GDS-15 (0–15, 0 being the best score) | 71 | 5.4 | 3.2 | 44 | 5.4 | 3.2 |
| MMSE (0–30, 30 being the best score) | 69 | 19.1 | 6.4 | 42 | 18.3 | 7.0 |
| SPPB (0–12, 12 being the best score) | 69 | 1.9 | 2.2 | 43 | 1.9 | 2.3 |
| EQ-5D (self) (–0.594 to 1, 1 being the best score) | 58 | 0.51 | 0.37 | 36 | 0.49 | 0.40 |
| Intervention total: n (%) | Control total: n (%) | |||||
| ‘Pain now’ rating | ||||||
| No pain | Mild/moderate | Severe | No pain | Mild/moderate | Severe pain | |
| 50 (72) | 16 (23) | 3 (4) | 27 (64) | 14 (33) | 1 (2) | |
| Fear of falling | ||||||
| Yes | No | Yes | No | |||
| 33 (48) | 36 (52) | 15 (35) | 28 (65) | |||
| Characteristic | Intervention (n = 76) | Control (n = 51) | ||||
|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | |
| EQ-5D (proxy) (−0.594 to 1, 1 being the best score) | 72 | 0.55 | 0.32 | 48 | 0.50 | 0.35 |
| Intervention total: n (%) | Control total: n (%) | |||||
| Social engagementa | Low | Medium | High | Low | Medium | High |
| 8 (11) | 15 (21) | 49 (68) | 1 (2) | 11 (23) | 35 (75) | |
Follow-up
Two different types of analyses were conducted in this study: (1) cohort analyses, in which study participants were included only if they had baseline assessments conducted prior to randomisation, and (2) cross-sectional analyses, in which study participants were included if they were present in the care home 12 months after randomisation (end-of-study assessment) regardless of when they were recruited and assessed.
In addition, data were collected either from direct assessment of participants or using care home data collected either from home staff or from records. We therefore present three different Consolidated Standards of Reporting Trials (CONSORT) charts. A CONSORT checklist is included as Appendix 11.
-
cohort, assessment data (Figure 10)
-
cohort, care home data (Figure 11)
-
depressed cohort, assessment data (Figure 12).
FIGURE 10.
Consolidated Standards of Reporting Trials diagram: cohort assessment. GDS, Geriatric Depression Scale; MMSE, Mini Mental State Examination; SPPB, Short Physical Performance Battery.
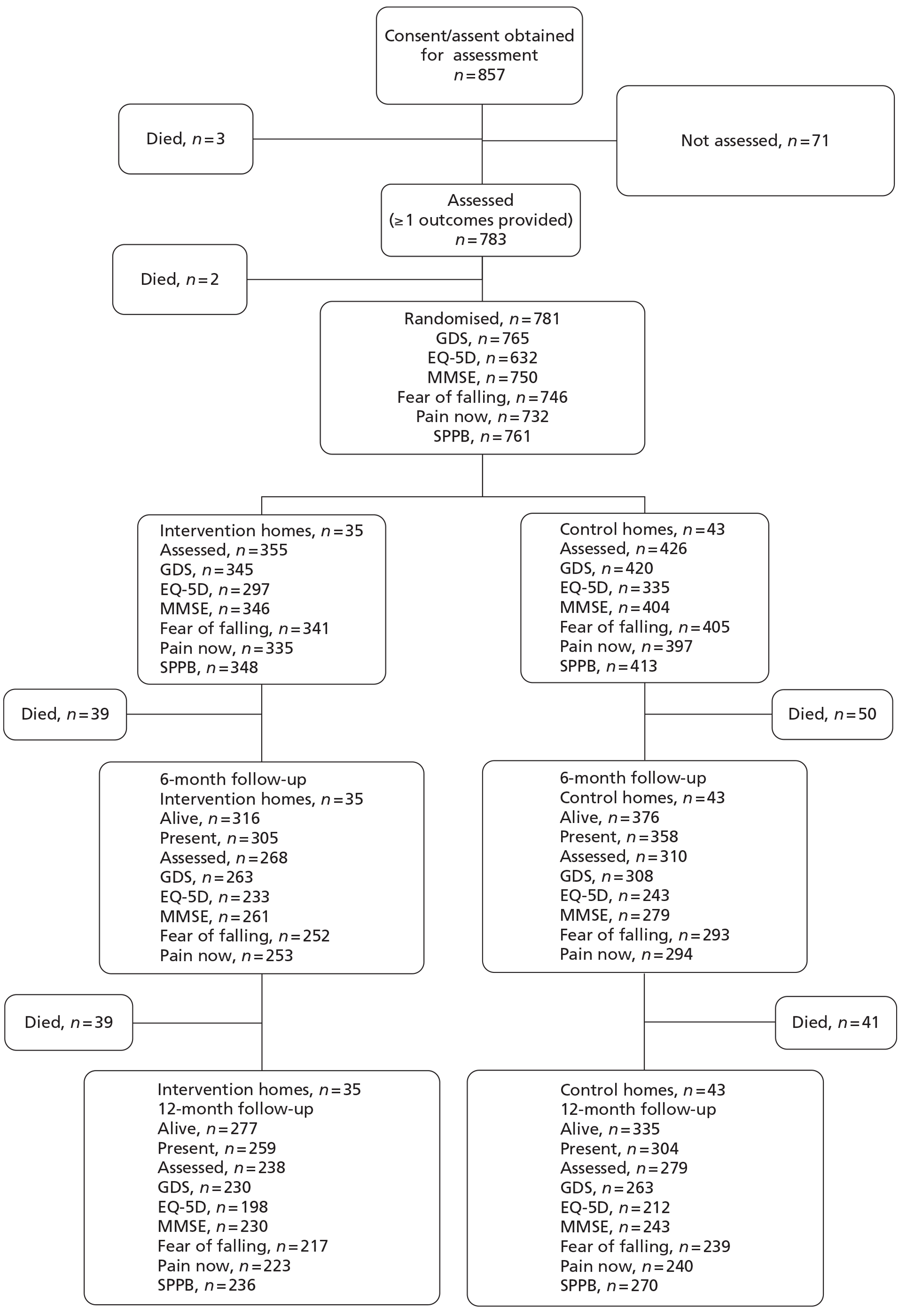
FIGURE 11.
Consolidated Standards of Reporting Trials diagram; cohort, care home data. a, One home did not provide proxy EQ-5D or SES data during follow-up. SES, Social Engagement Scale.
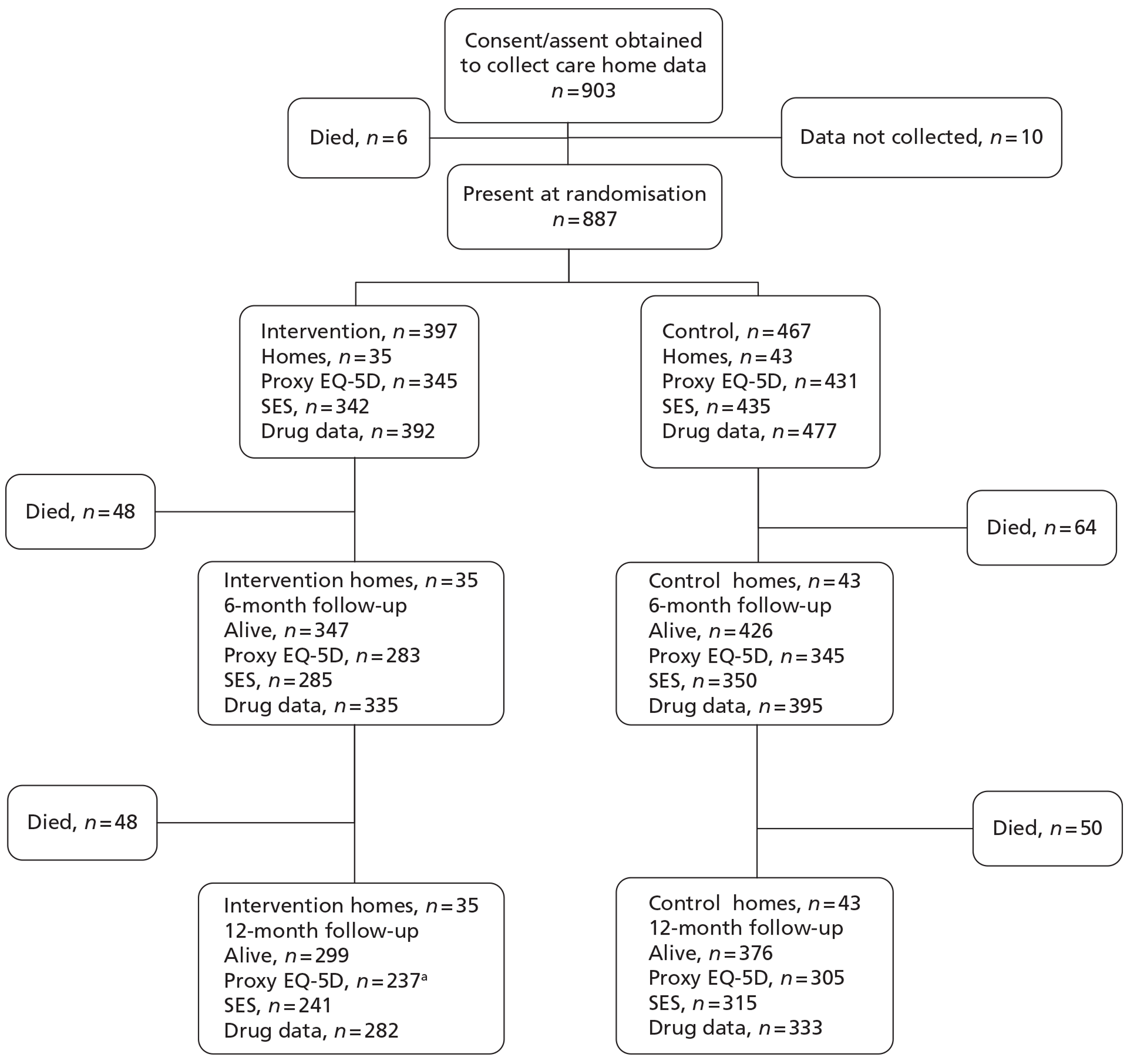
FIGURE 12.
Consolidated Standards of Reporting Trials diagram; depressed cohort. GDS, Geriatric Depression Scale.
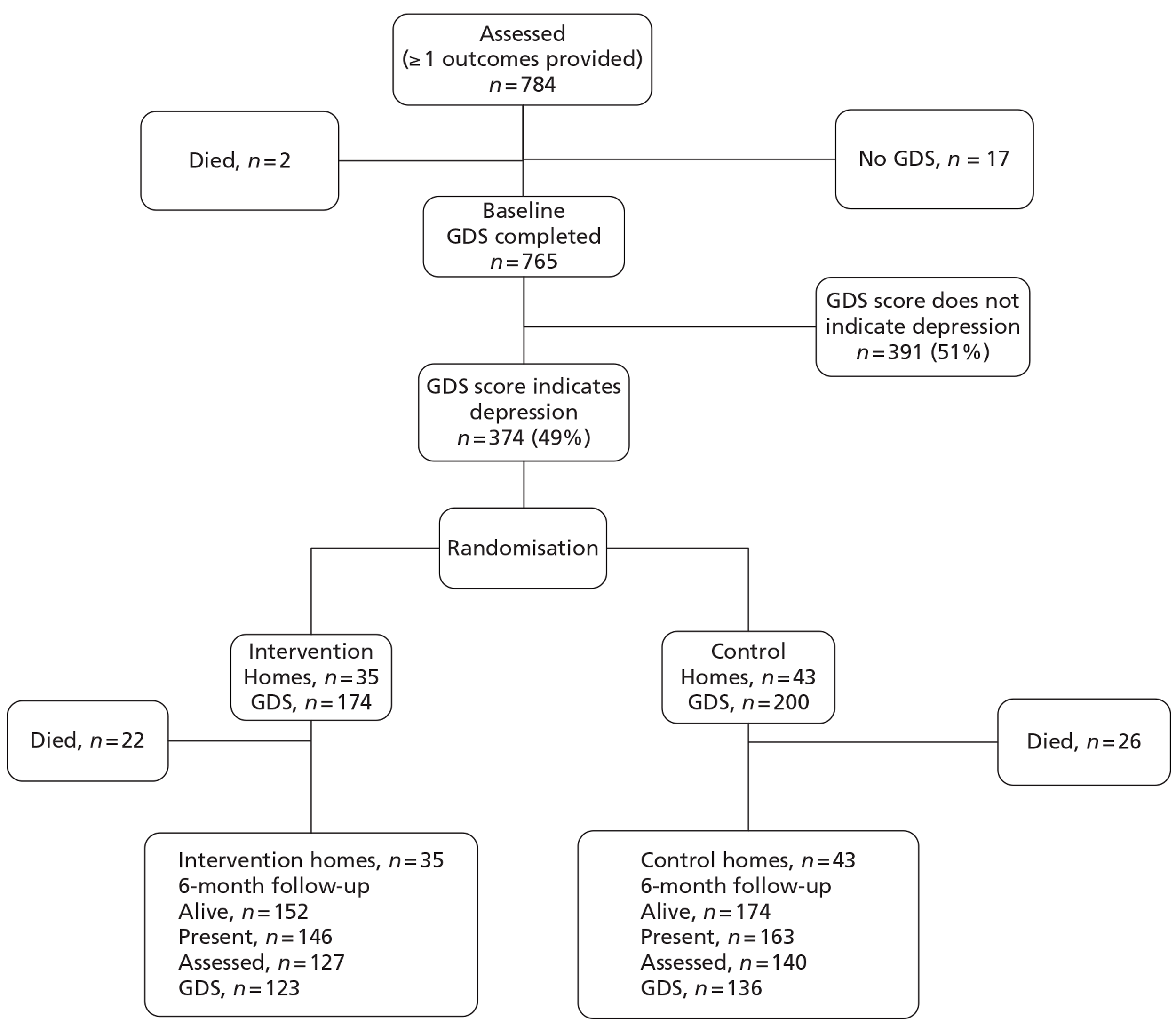
No care homes dropped out of the OPERA study and so no clusters were lost to follow-up. One home, in the intervention arm, was unable to provide proxy data at the follow-up assessments. All other data were collected as normal in this care home. The therapy team found in one care home, randomised to the intervention arm, that the residents were too disabled to participate in the exercise groups and no intervention was delivered. We collected follow-up data in this care home and their data are included in the relevant analyses.
At each time point we were unable to collect assessment data on some participants. There was a small but consistent trend, to collect more outcomes within each assessment in the intervention care homes than the control homes (Tables 31 and 32).
| Analysis | Outcome | |||||
|---|---|---|---|---|---|---|
| Cohort, 6 months | Cohort, 12 months | Depressed cohort, 6 months | ||||
| Intervention | Control | Intervention | Control | Intervention | Control | |
| No. of homes | 35 | 43 | 35 | 43 | 35 | 43 |
| Present at randomisation | 387 | 465 | 387 | 465 | 174 | 200 |
| Assessed at baseline | 355 | 426 | 355 | 426 | 174 | 200 |
| GDS-15 at randomisation | 345 | 420 | 345 | 420 | ||
| EQ-5D at randomisation | 297 | 335 | 297 | 335 | ||
| MMSE at randomisation | 346 | 404 | 346 | 404 | ||
| Fear of falling at randomisation | 341 | 405 | 341 | 405 | ||
| Pain now at randomisation | 335 | 397 | 335 | 397 | ||
| SPPB at randomisation | 348 | 413 | ||||
| Died randomisation date | 39 | 50 | 78 | 91 | 22 | 26 |
| Alive at end point n (% of all) | 316 (89) | 376 (88) | 277 (78) | 335 (79) | 152 (87) | 174 (86) |
| Present at end point | 305 | 358 | 259 | 304 | 146 | 163 |
| Assessed at end point (% of all, % of alive, % of present) | 268 (75, 85, 88) | 310 (73, 82, 87) | 238 (67, 86, 92) | 279 (65, 83, 92) | 127 (73, 84, 87) | 140 (70, 80, 86) |
| GDS-15 at end point (% of all, % of alive) | 263 (74, 83) | 310 (73, 82) | 230 (65, 83) | 263 (62, 79) | 123 (71, 81) | 136 (68, 78) |
| EQ-5D at end point (% of all, % of alive) | 233 (66, 74) | 243 (57, 65) | 198 (56, 71) | 212 (50, 63) | ||
| MMSE at end point (% of all, % of alive) | 261 (74, 83) | 279 (65, 74) | 230 (65, 83) | 243 (57,73) | ||
| Fear of falling at end point (% of all, % of alive) | 252 (71, 80) | 293 (69, 78) | 217 (61, 78) | 239 (56, 71) | ||
| Pain now at end point (% of all, % of alive) | 253 (71, 80) | 293 (69, 78) | 223 (64, 81) | 240 (56, 72) | ||
| SPPB at end point (% of all, % of alive) | 236 (66, 85) | 270 (63, 81) | ||||
| Analysis | Outcome | |
|---|---|---|
| Intervention (n = 397) | Control (n = 490) | |
| No. of homes | 35a | 43 |
| Proxy EQ-5D at randomisation | 345 | 431 |
| SES at randomisation | 342 | 435 |
| Drug data at randomisation | 392 | 477 |
| Alive at 6 months (%) | 347 (87) | 426 (87) |
| Proxy EQ-5D at 6 months (% of all, % of alive) | 283 (71, 82) | 345 (70, 81) |
| SES at 6 months (% of all, % of alive) | 285 (72, 82) | 350 (71, 82) |
| Drug data at 6 months (% of all, % of alive) | 335 (84, 97) | 395 (81, 93) |
| Alive at 12 months (%) | 299 (75) | 376 (77) |
| Proxy EQ-5D at 12 months (% of all, % of alive) | 237 (60, 68) | 305 (62, 72) |
| SES at 12 months (% of all, % of alive) | 241 (61, 81) | 315 (64, 84) |
| Drug data at 12 months (% of all, % of alive) | 282 (71, 94) | 333 (68, 89) |
Overall, however, considering the poor state of health of our participants, we achieved good follow-up rates for our primary outcomes. We obtained Geriatric Depression Scale-15 data from 81% of survivors in the cohort analysis at 12 months and 79% of survivors in the depressed cohort analysis at 6 months.
We collected drug use data prior to randomisation on 869/887 (98%) of the proxy/care home data cohort participants who had agreed to provide care home data. At 3, 6, 9 and 12 months we collected data on 786/804 (98%), 730/758, (96%), 670/704 (95%) and 615/660 (93%), respectively, of those alive at each time point.
For the cross-sectional analyses of assessment data, 722 participants were present in OPERA homes at the time that end-of-study assessments were made, which constitute our population of interest for these analyses. For the cross-sectional analyses of care home data there were 749 participants resident in OPERA homes at the time that end-of-study assessments were made, which constitute our population of interest for these analyses. For our cross-sectional analysis of Geriatric Depression Scale, we obtained responses from 595/722 (82%) of these participants (Tables 33 and 34).
| Analysis | Outcome | |
|---|---|---|
| Intervention | Control | |
| No. of homes | 35 | 43 |
| Recruited before randomisation | 258 | 305 |
| Recruited after randomisation | 97 | 70 |
| Total present at end of study | 355 | 375 |
| Assessed at end of study | 303 | 328 |
| GDS-15, n (% of present) | 288 (82) | 307 (80) |
| MMSE, n (% of present) | 284 (81) | 285 (74) |
| EQ-5D, n (% of present) | 251 (71) | 245 (64) |
| Pain now, n (% of present) | 278 (79) | 281 (73) |
| Fear of falling, n (% of present) | 273(78) | 280 (73) |
| SPPB, n (% of present) | 296 (84) | 315 (82) |
| Analysis | Outcome | |
|---|---|---|
| Intervention | Control | |
| No. of homes | 35 | 43 |
| Recruited before randomisation | 243 | 321 |
| Recruited after randomisation | 112 | 73 |
| Total resident at end of study | 355 | 394 |
| EQ-5D at end point,an (% of participating residents) | 346 (95) | 378 (92) |
| SES at end point,an (% of participating residents) | 349 (96) | 386 (94) |
Primary outcomes: Geriatric Depression Scale-15
In this section we present results for our three co-primary outcomes: (1) prevalence of depression at 12 months; (2) number of depressive symptoms at 6 months in those depressed prior to randomisation; and (3) number of depressive symptoms at 12 months of all those with Geriatric Depression Scale data prior to randomisation.
In the 12-month cross-sectional analysis, 595 participants provided Geriatric Depression Scale-15 data. Forty-eight per cent in the control group and 43% in the intervention group were depressed (Geriatric Depression Scale score of ≥ 5 or equivalent) (Table 35). In a mixed effects logistic regression model adjusting for clustering (with a random effect) and for site (C&W/NEL), home type, number of beds, mean Geriatric Depression Scale-15 score and proportion moderately to severely cognitively impaired in the care home prior to randomisation, whether or not on antidepressants and Short Physical Performance Battery at participant baseline assessment (whether before or after randomisation), age and sex, the odds for being depressed were 0.76 [95% confidence interval (CI) 0.53 to 1.09] lower in the intervention group (see Table 35); this effect was not statistically significant (p = 0.130). The model included 576 participants who had complete data on all covariates. Our pre-planned sensitivity analysis excluding those who provided baseline data after randomisation did not materially alter our results.
| Outcome | Population | Intervention | Control | Effect estimate | 95% CI | ICC | ||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) or n (%) | n | Mean (SD) or n (%) | n | |||||
| Prevalence of depression at 12 monthsa | All with GDS at 12 months | ≥ 5: 124 (43%) | 288 | ≥ 5: 149 (49%) | 307 | 0.76b (OR for presence of depression) | 0.53 to 1.09 | 0 |
| < 5: 164 (57%) | < 5: 158 (51%) | |||||||
| GDS-15 score at 12 months | GDS at 0 and 12 months | At 0 months: 4.5 (3.2) | 224 | At 0 months: 4.7 (3.2) | 260 | 0.13c (mean difference) | −0.33 to 0.60 | 0 |
| At 12 months: 4.6 (3.3) | At 12 months: 4.6 (3.3) | |||||||
| GDS-15 score at 6 months (depressed cohort) | Depressed at 0 months, with GDS at 6 months | At 0 months: 7.3 (2.2) | 123 | At 0 months: 7.4 (2.4) | 136 | 0.22d (mean difference) | −0.52 to 0.95 | 0.03 |
| At 6 months: 6.3 (3.1) | At 6 months: 6.5 (3.0) | |||||||
We included 484 participants with baseline and follow-up Geriatric Depression Scale-15 in the 12-month cohort analysis. There was a mean increase in the number of depressive symptoms of 0.05 in the intervention group and a decrease of 0.03 in the control group between baseline and 12 months. In a mixed-effects linear regression model adjusting for clustering (with a random effect) for site (C&W/NEL), home type, number of beds, proportion moderately to severely cognitively impaired in the home prior to randomisation, whether or not a participant was on antidepressants and Short Physical Performance Battery and Geriatric Depression Scale-15 scores at baseline, age and sex, the mean Geriatric Depression Scale-15 was 0.13 points higher in the intervention group (95% CI −0.33 to 0.60); this effect was not statistically significant (p = 0.576). The model included 475 participants who had complete data on all covariates.
Of the 374 individuals who were depressed prior to randomisation, 259 had Geriatric Depression Scale measurements at 6 months and were included in the depressed cohort analysis. For these individuals, Geriatric Depression Scale-15 scores decreased slightly at 6 months in both groups. In a mixed-effects model similar to that used for number of depressive symptoms, the estimated decrease in Geriatric Depression Scale was 0.22 points greater in the intervention group (95% CI −0.52 to 0.95); this effect was not statistically significant (p = 0.566). The model included 253 participants who had complete data on all covariates.
Secondary outcomes: cohort analyses
We present results for our secondary outcomes in two sections. In this section we present results from analyses conducted on those individuals who provided data on the relevant outcomes prior to randomisation, as well as at the appropriate follow-up time (cohort analyses); thus in these analyses those who were recruited post randomisation are excluded. In the following section we present results from analyses conducted on all individuals who provided outcome data at the end of study in each home, irrespective of when they were recruited.
Among those who were depressed prior to randomisation and had Geriatric Depression Scale-15 scores at 6 months (n = 259), 29% were no longer depressed at 6 months. In a mixed-effects logistic regression adjusting for covariates (remission of depression at 6 months for those depressed prior to randomisation) and for clustering, there were very slightly greater odds of those in the intervention group having remission from depression at this stage (30% vs 27%), but the difference between groups was not statistically significant (p = 0.820) (Table 36).
| Outcome | Intervention (6 months) | Control (6 months) | ORa (for remission of depression) | 95% CI | ICC |
|---|---|---|---|---|---|
| GDS < 5 (not depressed) | 37 | 37 | 1.07b | 0.59 to 1.95 | 0 |
| GDS ≥ 5 (depressed) | 86 | 99 |
For those with data prior to randomisation for the relevant outcome, there was little change in mean proxy and self-assessed EQ-5D, Mini Mental State Examination and mean Short Physical Performance Battery scores over the study period or in the odds of being fearful of falling (Tables 37–40), although we were not able to collect data on all of those for proxy EQ-5D at each time point. For those who provided data on the relevant outcome at baseline and 6 months there was no evidence of differential change between the intervention and control groups, and this was also true for the change from baseline to 12 months.
| Outcome | Time point (months) | Total | Intervention at baseline | Control at baseline | Intervention at end point | Control at end point | Effect estimate | 95% CI | ICC |
|---|---|---|---|---|---|---|---|---|---|
| Self-assessed EQ-5D | 6 | n | 214 | 201 | 214 | 201 | 0.03a | −0.02 to 0.08 | 0 |
| Mean | 0.58 (0.38) | 0.60 (0.36) | 0.59 (0.36) | 0.57 (0.37) | |||||
| 12 | n | 184 | 182 | 184 | 182 | 0.01b | −0.05 to 0.06 | 0.02 | |
| Mean | 0.56 (0.39) | 0.60 (0.36) | 0.56 (0.40) | 0.58 (0.38) |
| Outcome | Time point (months) | Total | Intervention at baseline | Control at baseline | Intervention at end point | Control at end point | Effect estimate | 95% CI | ICC |
|---|---|---|---|---|---|---|---|---|---|
| Proxy EQ-5D | 6 | n | 278 | 336 | 278 | 336 | 0.05a | −0.01 to 0.11 | 0.10 |
| Mean | 0.44 (0.34) | 0.47 (0.33) | 0.45 (0.35) | 0.44 (0.35) | |||||
| 12 | n | 232 | 294 | 232 | 294 | 0.01b | −0.06 to 0.08 | 0.17 | |
| Mean | 0.46 (0.35) | 0.49 (0.33) | 0.43 (0.36) | 0.45 (0.35) |
| Outcome | Time point (months) | Intervention | Control | Effect estimate | 95% CI | ICC | |
|---|---|---|---|---|---|---|---|
| MMSE | 6 | n | 257 | 269 | −0.53a | −0.16 to 1.22 | 0.02 |
| Mean at baseline | 19.5 (6.4) | 19.1 (6.1) | |||||
| Mean at 6 months | 18.8 (7.0) | 17.8 (6.6) | |||||
| 12 | n | 227 | 234 | 0.02b | −0.78 to 0.83 | 0.03 | |
| Mean at baseline | 19.6 (6.4) | 19.0 (6.3) | |||||
| Mean at 12 months | 18.2 (7.5) | 17.3 (6.9) |
| Time point (months) | Fear of falling | Total | Intervention | Control | OR (intervention/control)a | 95% CI | ICCb |
|---|---|---|---|---|---|---|---|
| 6 | Yes | 229 | 93 | 136 | 0.76c | 0.51 to 1.15 | 0 |
| No | 298 | 153 | 145 | ||||
| 12 | Yes | 171 | 76 | 95 | 1.07d | 0.68 to 1.67 | 0 |
| No | 268 | 135 | 133 |
Prior to randomisation, 330/746 (44%) of participants were afraid of falling; 527 (71%) provided data on this outcome at 6 months and 439 (59%) at 12 months. The proportions afraid of falling were 43% at 6 months and 39% at 12 months. There was no evidence of a difference in the proportions fearing falling in the two intervention groups at either 6 or 12 months (see Table 40).
Mean Short Physical Performance Battery scores at baseline were low (2.2 ± 2.4 intervention and 2.0 ± 2.1 control) indicating poor levels of lower limb function. These had slightly worsened by the end of the study (1.9 ± 2.4 intervention and 1.6 ± 2.1 control). No significant difference is found (Table 41).
| Outcome | Time point | Total | Intervention at baseline | Control at baseline | Intervention at end point | Control at end point | Effect estimate | 95% CI | ICC |
|---|---|---|---|---|---|---|---|---|---|
| SPPB | 12 months | n | 231 | 261 | 231 | 261 | 0.30a | −0.05 to 0.64 | 0.09 |
| Mean | 2.2 (2.4) | 2.0 (2.1) | 1.9 (2.4) | 1.6 (1.9) |
Sixty per cent (470/777) of participants had high social engagement prior to randomisation. This outcome measure was completed for 616 (79%) of individuals at 6 months and 541 (70%) at 12 months. The proportions with high social engagement at 6 and 12 months were 56% and 54%, respectively. Among those who had values for social engagement at all three time points, the proportions with high social engagement were 64% at baseline, 59% at 6 months and 54% at 12 months. Thus social engagement appears to have diminished over time among these participants. There was no evidence of a difference between intervention and control groups in terms of their social engagement (Table 42).
| Time point (months) | Social engagement | Total | Intervention | Control | ORa | 95% CI | ICCb |
|---|---|---|---|---|---|---|---|
| 6 | Low | 90 | 43 | 47 | 1.11 | (0.73 to 1.69) | 0.06 |
| Moderate | 184 | 72 | 112 | ||||
| High | 343 | 161 | 182 | ||||
| 12 | Low | 73 | 27 | 46 | 1.08 | (0.64 to 1.83) | 0.14 |
| Moderate | 177 | 80 | 97 | ||||
| High | 291 | 128 | 163 |
Of those providing data on their experiences of pain prior to randomisation, 485/732 (66%) experienced no pain. 523 (71%) provided data on their experience of pain at 6 months and 443 (61%) at 12 months. The proportions experiencing no pain rose from 66% prior to randomisation to 70% at 6 months and 73% at 12 months. Nevertheless, the absolute numbers experiencing no pain fell. Thus the rise in proportion experiencing no pain may reflect a greater loss to follow-up among those with moderate and severe pain prior to randomisation rather than a general decrease in pain felt by residents over the study period. There was no evidence of a difference in the experience of pain between intervention and control groups at either 6 or 12 months (Table 43).
| Time point (months) | Pain now? | Total | Intervention | Control | ORa | 95% CI | ICCb |
|---|---|---|---|---|---|---|---|
| 6 | No pain | 364 | 168 | 196 | 1.08 | 0.70 to 1.66 | 0.03 |
| Moderate pain | 141 | 69 | 72 | ||||
| Severe pain | 18 | 8 | 10 | ||||
| 12 | No pain | 322 | 155 | 167 | 1.07 | 0.67 to 1.72 | < 0.0001 |
| Moderate pain | 105 | 51 | 54 | ||||
| Severe pain | 16 | 10 | 6 |
We calculated intracluster correlation coefficients for all outcomes. These were near zero for outcomes reflecting mental and emotional well-being and quality of life, and considerably higher for outcomes reflecting physical functioning, pain and social engagement (these factors may vary more between care homes because of the type of care provided by the home and the type of residents that homes look after).
Cross-sectional analyses
Secondary outcomes: cross-sectional analyses
As for the cohort analyses (see Follow-up and Primary outcomes: Geriatric Depression Scale-15, above), cross-sectional analyses including all those resident in the home at 12 months do not provide any evidence of an effect of the intervention on any secondary outcomes (Tables 44 and 45).
| Outcome | Intervention | Control | Effect estimate | 95% CI | ICC |
|---|---|---|---|---|---|
| GDS-15 | |||||
| n = 595 | 288 | 307 | 0.03a (mean difference) | −0.54 to 0.61 | 0 |
| Mean age (years) | 87.3 | 87.1 | (positive change favours control) | ||
| % female | 75 | 78 | |||
| Mean (SD) | 4.67 (3.39) | 4.74 (3.29) | |||
| EQ-5D self-completed | |||||
| n = 496 | 251 | 245 | 0.00b (mean difference) | −0.06 to 0.06 | 0 |
| Mean age (years) | 87.0 | 86.9 | |||
| % female | 73 | 77 | (positive change favours intervention) | ||
| Mean (SD) | 0.55 (0.39) | 0.57 (0.38) | |||
| MMSE | |||||
| n = 569 | 284 | 285 | 0.68c (mean difference) | −0.46 to 1.82 | 0 |
| Mean age (years) | 87.2 | 87.0 | (positive change favours intervention) | ||
| % female | 74 | 77 | |||
| Mean (SD) | 18.6 (7.3) | 17.7 (6.9) | |||
| SPPB | |||||
| n = 611 | 296 | 315 | 0.20d (mean difference) | −0.14 to 0.53 | 0 |
| Mean age (years) | 87.3 | 86.9 | (positive change favours intervention) | ||
| % female | 74 | 78 | |||
| Mean (SD) | 1.9 (2.4) | 1.5 (1.9) | |||
| Proxy EQ-5D | |||||
| n = 724 | 346 | 378 | 0.02e (mean difference) | −0.05 to 0.08 | 0.09 |
| Mean age (years) | 87.6 | 87.1 | (positive change favours intervention) | ||
| % female | 75 | 79 | |||
| Mean (SD) | 0.45 (0.37) | 0.44 (0.36) |
| Outcome | Intervention | Control | Effect estimate | 95% CI | ICC | |
|---|---|---|---|---|---|---|
| Fear of falling | ||||||
| No | n = 340 | 170 | 170 | 1.16a (OR) | 0.79 to 1.71 | 0 |
| Mean age | 86.9 | 87.2 | (positive change favours control) | |||
| % female | 71 | 75 | ||||
| Yes | n = 213 | 103 | 110 | |||
| Mean age | 87.9 | 86.6 | ||||
| % female | 82 | 88 | ||||
| Pain now | ||||||
| No pain | n = 411 | 198 | 213 | 1.39b | 0.92 to 2.08 | 0 |
| Mean age | 87.4 | 87.5 | (OR < 1 favours intervention) | |||
| % female | 73 | 78 | ||||
| Moderate | n = 131 | 70 | 61 | |||
| Mean age | 87.0 | 85.9 | ||||
| % female | 76 | 69 | ||||
| Severe | n = 17 | 10 | 7 | |||
| Mean age | 84.4 | 81.2 | ||||
| % female | 70 | 100 | ||||
| Social engagement | ||||||
| Low | n = 100 | 49 | 51 | 0.89c | 0.57 to 1.38 | 0.12 |
| Mean age | 87.6 | 87.1 | (OR < 1 favours control) | |||
| % female | 80 | 82 | ||||
| Moderate | n = 233 | 108 | 125 | |||
| Mean age | 87.7 | 86.8 | ||||
| % female | 69 | 78 | ||||
| High | n = 402 | 192 | 210 | |||
| Mean age | 87.3 | 87.0 | ||||
| % female | 77 | 80 | ||||
Medication use
We obtained baseline drug use data on 869/887 (98%) of participants in the care home data cohort. We obtained data on progressively fewer residents at each time point falling to 615 at 12 months. We obtained data on 91% of those who were alive at 12 months. A large proportion of these were taking psychoactive drugs; with one in six taking hypnotics or anxiolytics, one in three taking antidepressants, and one in nine taking antipsychotic drugs. There were no differences in the number of participants using these drugs, over time or between the intervention and control (Tables 46–48).
| BNF chapter | Time point | n/total (%) | Intervention n/N (%) | Control n/N (%) |
|---|---|---|---|---|
| 4.1 Hypnotics and anxiolytics | Baseline | 139/869 (16) | 53/392 (14) | 86/477 (18) |
| 3 months | 126/786 (16) | 45/359 (13) | 81/427 (19) | |
| 6 months | 112/730 (15) | 42/335 (13) | 70/395 (18) | |
| 9 months | 107/670 (16) | 43/306 (14) | 64/364 (18) | |
| 12 months | 98/615 (16) | 40/282 (14) | 58/333 (17) | |
| 4.2 Antipsychotics | Baseline | 100/869 (12) | 40/392 (10) | 60/477 (13) |
| 3 months | 88/786 (11) | 38/359 (11) | 50/427 (12) | |
| 6 months | 80/730 (11) | 35/335 (10) | 45/395 (11) | |
| 9 months | 81/670 (12) | 35/306 (11) | 46/364 (13) | |
| 12 months | 74/615 (12) | 32/382 (11) | 42/333 (13) | |
| 4.3 Any antidepressants | Baseline | 260/869 (30) | 110/392 (28) | 150/477 (31) |
| 3 months | 231/786 (29) | 100/359 (28) | 131/427 (31) | |
| 6 months | 221/730 (30) | 97/335 (29) | 124/395 (31) | |
| 9 months | 193/670 (29) | 88/306 (29) | 105/364 (29) | |
| 12 months | 186/615 (30) | 83/282 (29) | 103/333 (31) | |
| 4.3.1 Tricyclic antidepressants | Baseline | 54/869 (6) | 18/392 (5) | 36/477 (8) |
| 3 months | 46/786 (6) | 16/359 (4) | 30/427 (7) | |
| 6 months | 48/730 (6) | 15/335 (4) | 28/395 (7) | |
| 9 months | 40/670 (6) | 13/306 (4) | 27/364 (7) | |
| 12 months | 36/615 (6) | 13/282 (5) | 23/333 (7) | |
| 4.3.3 Selective serotonin re-uptake inhibitors | Baseline | 189/869 (22) | 86/392 (22) | 103/477 (22) |
| 3 months | 177/786 (23) | 82/359 (23) | 95/427 (22) | |
| 6 months | 171/730 (23) | 79/335 (24) | 93/395 (23) | |
| 9 months | 147/670 (22) | 70/306 (23) | 77/364 (21) | |
| 12 months | 144/615 (23) | 65/282 (23) | 79/333 (24) | |
| 4.3.4 Other antidepressants | Baseline | 46/869 (5) | 17/392 (4) | 29/477 (6) |
| 3 months | 39/786 (5) | 14/359 (4) | 25/427 (5) | |
| 6 months | 32/730 (4) | 12/335 (4) | 20/395 (5) | |
| 9 months | 29/670 (4) | 12/306 (4) | 17/364 (5) | |
| 12 months | 27/615 (4) | 12/282 (4) | 15/333 (5) | |
| 4.7 Analgesics | Baseline | 420/869 (48) | 166/392 (42) | 254/477 (53) |
| 3 months | 344/786 (44) | 141/359 (39) | 203/427 (48) | |
| 6 months | 345/730 (47) | 137/335 (41) | 208/395 (53) | |
| 9 months | 316/670 (47) | 132/306 (43) | 184/364 (51) | |
| 12 months | 289/615 (47) | 117/282 (41) | 172/333 (52) | |
| 10.1.1 Non-steroidal anti-inflammatory drugs | Baseline | 31/869 (3) | 12/392 (3) | 19/477 (4) |
| 3 months | 29/786 (4) | 14/359 (4) | 15/427 (4) | |
| 6 months | 26/730 (4) | 9/335 (3) | 17/395 (4) | |
| 9 months | 22/670 (3) | 9/306 (3) | 13/364 (4) | |
| 12 months | 19/615 (3) | 9/282 (3) | 10/333 (3) |
| BNF chapter | Intervention | Control | ||
|---|---|---|---|---|
| n | % | n | % | |
| Total | 282 | 333 | ||
| 4.1 Hypnotics and anxiolytics | ||||
| On drug beginning and end | 29 | 10 | 47 | 14 |
| On drug only at end | 11 | 4 | 11 | 3 |
| On drug only at beginning | 5 | 2 | 9 | 3 |
| Never on drug | 237 | 84 | 266 | 80 |
| 4.2 Antipsychotics | ||||
| On drug beginning and end | 24 | 9 | 37 | 11 |
| On drug only at end | 8 | 3 | 5 | 2 |
| On drug only at beginning | 7 | 2 | 5 | 2 |
| Never on drug | 245 | 87 | 284 | 85 |
| 4.3 Antidepressants | ||||
| On drug beginning and end | 73 | 26 | 84 | 25 |
| On drug only at end | 10 | 4 | 19 | 6 |
| On drug only at beginning | 10 | 4 | 11 | 3 |
| Never on drug | 189 | 67 | 219 | 66 |
| BNF chapter | Mean total number of DDDs over whole resident follow-up in cohort | |||
|---|---|---|---|---|
| N = 869 | Intervention (n = 392) | Control (n = 477) | Mann–Whitney U-test: p-value | |
| Mean total (SD), 90th centile | Mean total (SD), 90th centile | Mean total (SD), 90th centile | ||
| 4.1 Hypnotics and anxiolytics | 23 (69), 111 | 17 (52), 56 | 29 (80), 139 | 0.131 |
| 4.2 Antipsychotics | 6 (39), 5 | 7 (48), 2 | 6 (29), 5 | 0.630 |
| 4.3 Antidepressants | 68 (151), 277 | 59 (123), 242 | 76 (171), 282 | 0.168 |
There was no evidence of a change in participants' use of psychoactive drugs during the lifetime of the study. Few residents either started or stopped these medications, and there was no suggestion of a difference in the pattern of change between intervention and control homes (see Table 47).
Only a minority of residents used any medication from each of the three selected groups of psychoactive drugs. The mean number of defined daily doses taken was small for antipsychotics, larger for hypnotics and anxiolytics and largest for antidepressants. There was no evidence of a difference in amount of these drugs used between intervention and control homes (see Table 48).
Adverse events
Indirectly attributable adverse events
There was a total of 90 fractures identified from home records over the study period; these occurred in both study participants and in non-participants. There was no evidence of a differential fracture rate between intervention and control homes (Table 49).
| Outcome | Total no. of fractures | No. of fractures | |||||
|---|---|---|---|---|---|---|---|
| Intervention | Control | Estimatea | 95% CI | ICC | |||
| Peripheral fractures | Aggregated | 90 | 48 | 42 | RR = 1.14 | 0.80 to 1.63 | 0.03 |
Among those who had provided consent or assent to have their data examined, there were 56 definite fractures, eight probable fractures and nine possible fractures. Again, there was no evidence of a difference in fracture rate between the intervention and control homes (Table 50). Of the definite fractures, i.e. those requiring hospital admission, 39/56 (70%) were fractures of the femur.
There were 241 deaths among the 1054 study participants: 119 in the intervention group and 122 in the control group. There was no evidence of differential death rates between intervention and control groups (Table 51).
| Type | Total no. of fractures | No. of fractures | |
|---|---|---|---|
| Intervention | Control | ||
| Definite | 56 | 29 | 27 |
| Probable | 8 | 1 | 7 |
| Possible | 9 | 5 | 4 |
| Total | 75 | 35 | 38 |
| Deaths | Total | Intervention | Control |
|---|---|---|---|
| All-cause mortality | 241/1054a (23%) | 119/501 (24%) | 122/553 (22%) |
Directly attributable adverse events
Five residents in intervention homes, including one resident who was not a study participant, experienced adverse events during the exercise groups or when preparing for the groups; none was serious (Table 52). Although two residents fell in the lounge of their care home this was before the group started and no injuries were sustained. Two residents had other health problems that became apparent during the groups and one suffered a minor injury, not requiring treatment. Thus incidence of directly attributable serious adverse events was < 1 : 30,000 attendances.
| Resident | Study participant? | Nature of event | Consequences | Serious adverse event? |
|---|---|---|---|---|
| 1 | Yes | Fall in lounge before exercise group session | No injury, no medical intervention needed | No |
| 2 | Yes | Fresh graze on lower leg noted after removal of soft ankle weight | Seen by community nurse, no medical intervention needed | No |
| 3 | Yes | Unwell during exercise, low haemoglobin level, started on treatment for Parkinson's disease | Returned to care home after overnight admission | No |
| 4 | Yes | Increased hip and knee pain after joining exercise group sessions, radiograph showed acetabular erosion associated with hemiarthroplasty, change since previous film 4 years earlier | Referred to orthopaedics | No |
| 5 | No | Fall in lounge before exercise group session | No injury, no medical intervention needed | No |
Economic evaluation
Resource use and quality-adjusted life-year data were available for 798 participants recruited prior to randomisation. The economic analysis includes those participants who consented or assented to us collecting data from their medical records and the collection of proxy EQ-5D scores. As self-completed questionnaire data were not required for this analysis, the economic evaluation includes two participants who were not included in the analysis of primary outcomes. As the economic analysis required a National Health Service number to get primary care trust data extracts, the economic evaluation excluded two participants who were included in the cohort analysis of effectiveness.
Costs
Resource use was broadly comparable between the control and intervention homes (Table 53). Participants were frequent users of community services and general practitioner home visits. Use of general practitioner surgery visits, mental health team visits and practice nurse visits was infrequent. Using the univariate linear-mixed model, no significant differences were seen between the two arms of the study. All event types were more frequent in the intervention arm.
| Contact type | Unit | Intervention mean | Control mean | Mean difference | 95% CI of the difference |
|---|---|---|---|---|---|
| A&E attendances | Investigations | 0.94 | 0.91 | 0.03 | −0.23 to 0.30 |
| Community visit | Visit | 7.03 | 5.25 | 1.77 | −1.43 to 11.92 |
| GP home visit | Visit | 5.23 | 4.97 | 0.26 | −1.42 to 1.94 |
| GP surgery visit | Visit | 0.31 | 0.29 | 0.02 | −0.23 to 0.27 |
| Inpatient service | Dominant episode | 0.87 | 0.74 | 0.13 | −0.09 to 0.35 |
| Mental health team visit | Visit | 0.17 | 0.15 | 0.02 | −0.10 to 0.14 |
| Outpatient service | Visit | 1.56 | 1.27 | 0.29 | −0.16 to 0.73 |
| Practice nurse visit | Visit | 0.14 | 0.10 | 0.03 | −0.05 to 0.12 |
The inpatient and A&E cost data collected from the primary care trusts had some missing data. For the outpatient attendance cost data, 36% of attendances had missing cost values, and 96% of these missing values came from two of the primary care trust data sets. Consequently, the outpatient costs were calculated using data for missing values that had been generated by multiple imputation. Outpatient attendances, however, constitute only a small proportion of the total costs.
The distribution of costs was skewed, as is typical for health-care costs (Figure 13).
FIGURE 13.
Distribution of participants' costs at 12 months, across all homes. (The outpatient costs used in this figure were derived by taking the mean cost of the five data sets generated by multiple imputation.)
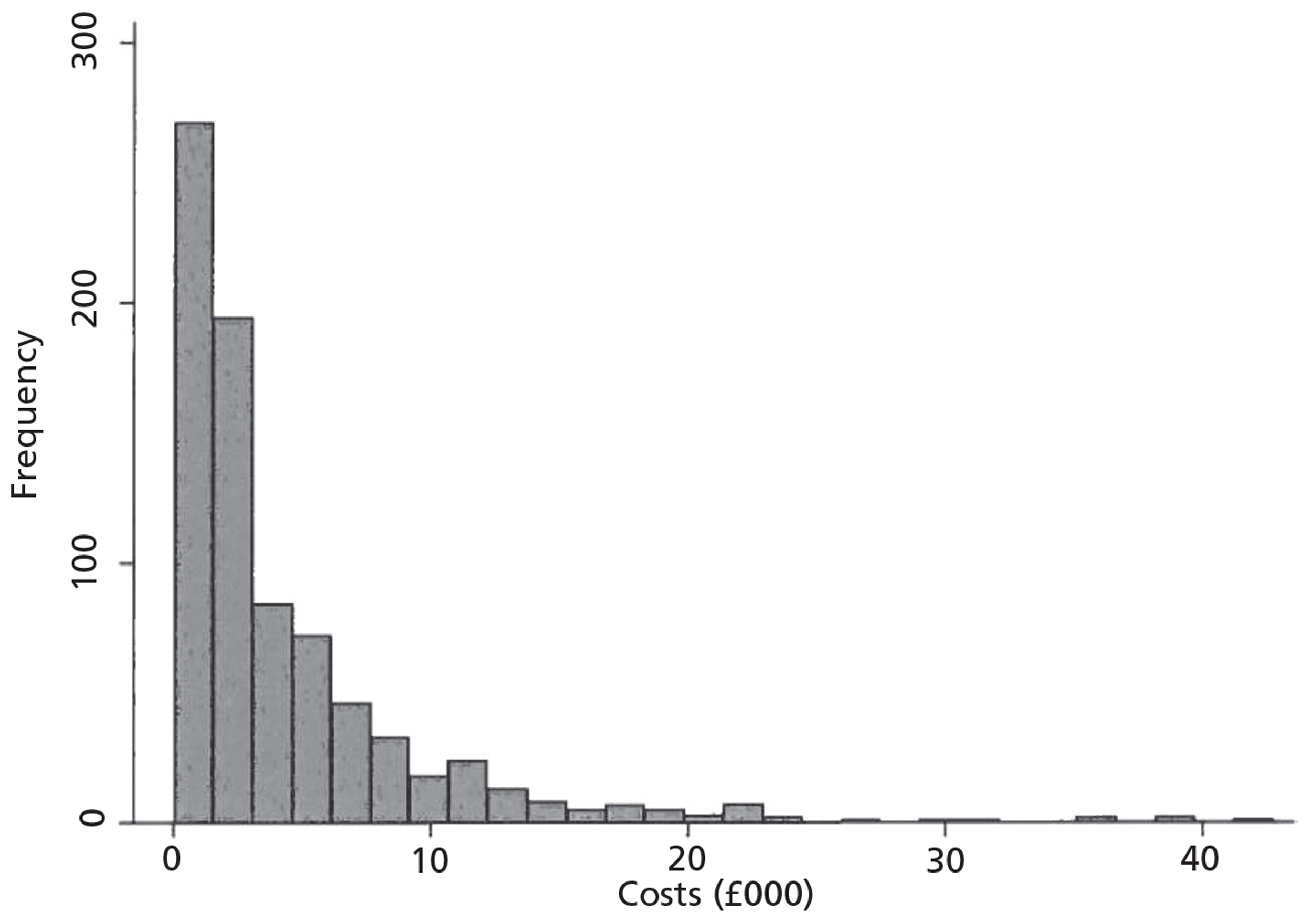
As with the resource use, no significant differences were found (Table 54). For the costs associated with medications, the intervention arm had lower costs. For all other categories, the mean cost of the control arm was lower. The mean National Health Service cost per individual in the intervention arm over 12 months was £4639, whereas the cost per participant in the active control arm was £4251 (mean difference = £388, 95% CI −£604 to £1380).
| Cost category | Intervention mean | Control mean | Mean difference | 95% CI of the difference |
|---|---|---|---|---|
| A&E attendances | 319 | 306 | 13 | −79 to 105 |
| Community visit | 330 | 247 | 83 | −393 to 560 |
| GP home visit | 628 | 597 | 31 | −170 to 232 |
| GP surgery visit | 11.2 | 10.5 | 0.7 | −8.2 to 9.6 |
| Inpatient services | 2319 | 2264 | 55 | −688 to 797 |
| Medications | 525 | 626 | −101 | −268 to 67 |
| Mental health team contacts | 19 | 17 | 2 | −11 to 15 |
| Outpatient visitsa | 450 | 379 | 71 | −24 to 166 |
| Practice nurse contacts | 1.6 | 1.2 | 0.4 | −0.6 to 1.4 |
| Total costsa | 4639 | 4251 | 388 | −604 to 1380 |
Active control and intervention costs
The time and materials needed to deliver both the depression awareness training and the intervention programme were collected alongside the study. Unless otherwise noted, all costs associated with delivering the active control and intervention programmes were taken from the study records (Tables 55 and 56). In the control arm the cost of depression awareness training sessions was the highest cost, followed by the materials. For the intervention arm, the cost of the exercise sessions was the highest cost, followed by the mobility assessments.
| Item | NHS cost | Societal cost | Notes |
|---|---|---|---|
| Depression awareness training sessions | 5111 | 5111 | Nursing/physiotherapy staff time to deliver the intervention, including travel |
| Materials for depression awareness training sessions | 1294 | 1294 | Included pack for trainers and booklets for home staff |
| Nurse/physiotherapist training | 166 | 166 | Nursing/physiotherapy staff time being trained to deliver the sessions, including travel |
| Trainer costs | 508 | 508 | Based on £127 per hour for a psychiatric consultant189 |
| Home staff carers' time in training | 2147 | Based on £6 per hour for a care worker188 | |
| Home staff nurses' time in training | 302 | Based on £22 per hour for Agenda for Change Band 6189 | |
| Home staff managers' time in training | 405 | Based on £17 per hour for a registered manager188 | |
| Total | 7078 | 9932 | |
| Cost per home | 165 | 231 | |
| Cost per participant | 5 | 7 | Weighted cost per participant: assumes that 87% of residents in homes are eligible to participate (see Table 64) |
| Item | NHS cost | Societal cost | Notes |
|---|---|---|---|
| Training of physiotherapists | 13,014 | 13,014 | Includes physiotherapists' time spent being trained to deliver the intervention, travel, materials and lunches. Excludes room hire. Based on £25 per hour for a community physiotherapist189 |
| Training of care home staff | 3842 | 3842 | Physiotherapists' time to deliver the training to care home staff and associated travel costs. Based on £25 per hour for a community physiotherapist189 |
| Mobility assessments | 32,425 | 32,425 | Physiotherapists' time to conduct mobility assessments for participants and associated travel costs. Based on £25 per hour for a community physiotherapist189 |
| Exercise sessions | 287,403 | 287,403 | Physiotherapists' time to deliver the exercise sessions and travel costs. Based on £25 per hour for a community physiotherapist189 |
| Equipment for exercise sessions | 12,511 | 12,511 | Includes items such as, leg weights and balls |
| Materials for home staff training | 1747 | 1747 | Includes pack for trainers and booklets for home staff |
| Mobility equipment | 1566 | 1566 | Items requested by physiotherapist to aid mobility |
| Trainer costs | 7771 | 7771 | Trainer time spent with physiotherapists, travel and accommodation. Based on £127 per hour for a psychiatric consultant and £21 per hour for a Band 6 physiotherapist189 |
| Home staff carers' time in training | 2292 | Based on £6 per hour for a care worker210 | |
| Home staff nurses' time in training | 381 | Based on £22 per hour for Agenda for Change Band 6189 | |
| Home staff managers' time in training | 539 | Based on £17 per hour for a registered manager210 | |
| Carer time assisting with mobility assessments | 1185 | Based on £6 per hour mean cost assuming a ratio of 9 : 1 carers to senior carers210 | |
| Carer time in informal 1 : 1 training with physiotherapists | 3634 | Based on £7 per hour mean cost assuming a ratio of 7 : 13 ratio of carers to senior carers210 | |
| Carer time saved by physiotherapists transporting participants | −17,111 | Based on £6 per hour mean cost assuming a ratio of 9 : 1 carers to senior carers.210 Gain of 5 minutes per participant attendance at exercise session | |
| Total | 360,278 | 351,199 | |
| Cost per home | 10,294 | 10,034 | |
| Cost per participant | 322 | 314 | Weighted cost per participant: assumes that 87% of participants in homes are eligible to participant (see Table 64) |
The weighted cost per participant in the intervention homes was £322. For participants in the active control homes, it was £5. The societal cost per participant in the intervention home was £314 and for the participants in the control home it was £7. The lower societal cost in the intervention care homes was due to home staff time saved by the assistance and occupation of the physiotherapists while in the home, which outweighed the care home staff time spent training. The higher societal cost in the control care homes was due to the staff time spent in depression awareness training.
Quality-adjusted life-years
The level of missing data ranged from 4% to 16% per time point for the proxy EQ-5D scores; consequently, the quality-adjusted life-years for the primary analyses were calculated from the five data sets (one for each time point) with missing values replaced by values generated by multiple imputation.
Analyses
All reported incremental costs and quality-adjusted life-years are from multilevel models to recognise clustering.
Base-case analysis
In the control arm the multiple imputation averaged correlation between total cost and quality-adjusted life-year is −0.13, whereas in the intervention this correlation is −0.05.
Each of the five sets of total costs and quality-adjusted life-years were analysed using multilevel models to account for clustering. These produced an incremental cost of £374 (SE = £525, 95% CI −£655 to £1404). The incremental quality-adjusted life-year gain was −0.0014 (SE = 0.036, 95%CI −0.0727 to 0.0699). The intracluster correlation coefficient for the total costs was 0.07, and the intracluster correlation coefficient for the quality-adjusted life-years was 0.14.
To obtain a graphical representation of the uncertainty of the cost-effectiveness estimates, we used bootstrapping. We sampled at random with replacement each of our five cost-effectiveness sets including the imputed data, producing 2000 incremental cost and incremental quality-adjusted life-years estimates for each data set. These estimates were plotted in a cost-effectiveness plane. Figure 14 shows one of these graphs. The graph of bootstrapped estimates provides a graphical description of the distribution of the incremental costs and quality-adjusted life-years and the uncertainty surrounding these values. From Figure 14, it is apparent that more points lie above the x-axis, indicating that the intervention is more costly, and that more points are to the left of the y-axis, indicating that the intervention produces fewer quality-adjusted life-years. This also displays how other combinations of costs and quality-adjusted life-years that were consistent with the data produced sample means in all four quadrants.
FIGURE 14.
Cost-effectiveness plane generated from bootstrapped mean cost and quality-adjusted life-year differences for residents over 12 months (positive values indicate that the intervention was more costly or more effective).
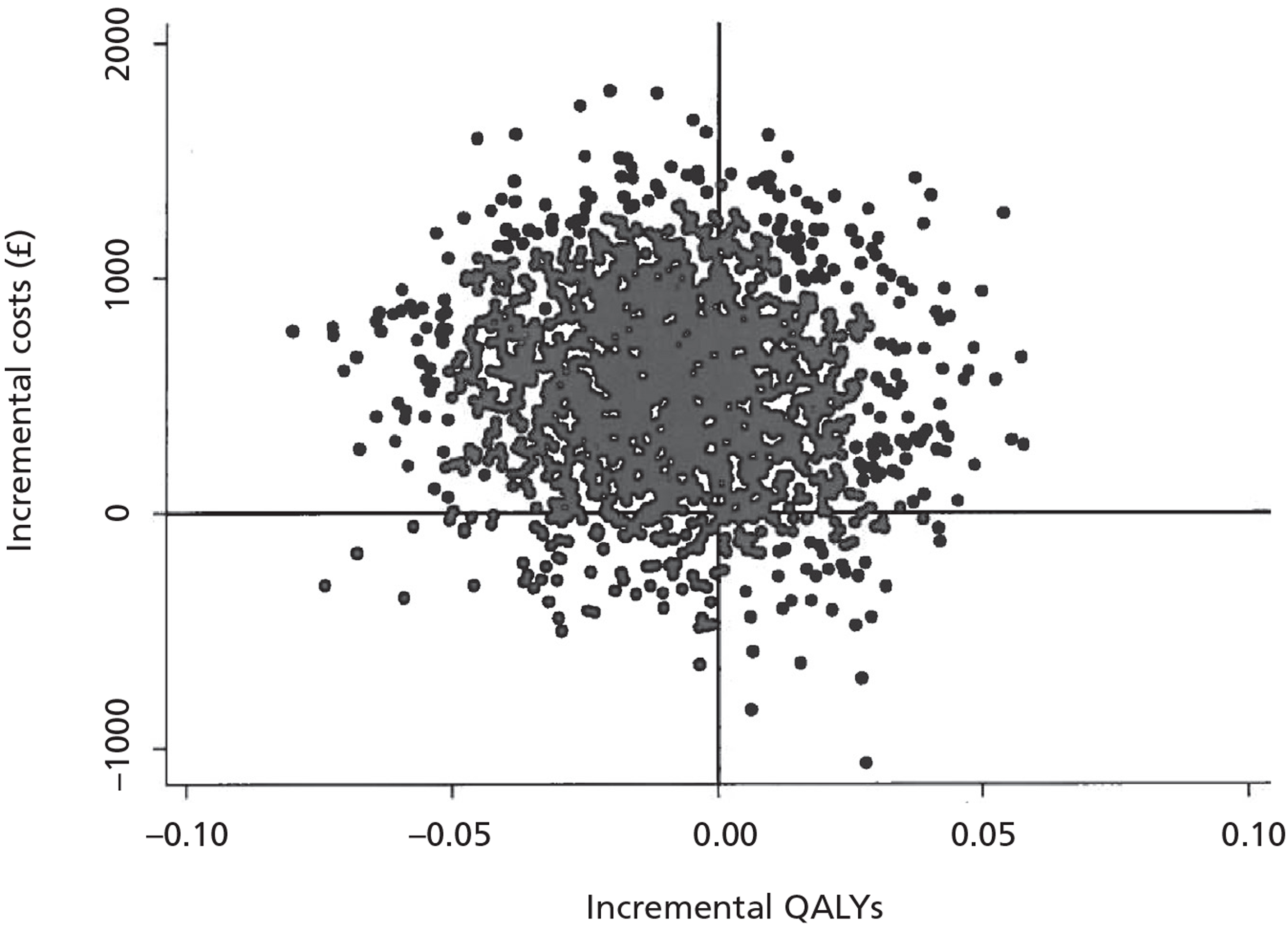
The incremental cost-effectiveness ratio was not calculated as the intervention was more expensive with a net reduction in quality-adjusted life-years. Under these circumstances, disaggregated data on costs and effects are considered to be more informative. The probability of the intervention being cost-effective at a willingness-to-pay threshold of £20,000 per quality-adjusted life-year was 33% and at a threshold of £30,000 was 37%.
Sensitivity analyses
For the sensitivity analysis excluding participants with high costs, the 39 participants with the top 5% of costs were dropped. This resulted in an incremental cost of £402 (SE = £319, 95% CI −£224 to £1028). The incremental gains in quality-adjusted life-years remained negative and very small at −0.0023 (SE = 0.0380, 95% CI −0.076 to 0.072).
The second sensitivity analysis expanded our analysis to the societal perspective. This analysis accounted for the training time of home staff, the time saved by carers in the intervention homes owing to the physiotherapists assisting with participant transport and the time lost by carers owing to mobility assessments and informal training. The incremental societal cost was £366 (SE = £525, 95% CI −£664 to £1396). The quality-adjusted life-year gain was unaltered from the base-case analysis.
For both sensitivity analyses, the mean cost per participant in the intervention arm was higher, and the mean difference in quality-adjusted life-year value was very small and favoured the control arm (Table 57).
| Analysis | Mean difference | 95% CI |
|---|---|---|
| Base-case analysis | ||
| Total costs, £ | 374 | −655 to 1404 |
| QALY | −0.0014 | −0.0728 to 0.0699 |
| Excluding high-cost participants | ||
| Total costs, £ | 402 | −224 to 1028 |
| QALY | −0.0023 | −0.076 to 0.072 |
| Societal perspective | ||
| Total costs, £ | 366 | −664 to 1396 |
| QALY | −0.0014 | −0.0728 to 0.0699 |
| Secondary analysis | ||
| Total costs, £ | −176 | −450 to 802 |
| QALY | −0.0340 | −0.0717 to 0.0037 |
Secondary analysis
For the secondary analysis including participants recruited after the randomisation of the homes, the analysis included 1025 residents. Of these, 798 were from the baseline cohort and 291 had been recruited at 3, 6 or 9 months. This resulted in an incremental cost of −£176 (SE = £319, 95% CI −£450 to £802). The incremental quality-adjusted life-years were −0.0340 (SE = 0.0193, 95% CI −0.0717 to 0.0037). In this analysis the mean cost per participant in the intervention arm was lower and the mean difference in quality-adjusted life-year was small (see Table 57). The CIs for the incremental costs remained very large and overlapped zero, indicating that this finding is not significant. Care is needed in interpreting these results as there is some evidence of differential recruitment in those who joined the study after randomisation and we may not have been able to fully control for differences in length of follow-up between the treatment and control groups.
Process evaluation results
The case study care homes
We recruited four homes each from NEL and C&W. In each area one home was a control home and three intervention homes. The three intervention homes were selected so that one was an independent home (where the owner owned fewer than 10 homes), one was part of a larger chain, and one was designated as a nursing home (Table 58). All of the case study care homes were located in residential areas – several with local shops and amenities within a short walking distance, and several had access to nearby parkland. They all had gardens, usually well maintained, although one was poorly tended with very limited access. Smokers (staff and residents) were the main users of the outside space.
| Home | Intervention/control | Area | Ownership | No. beds | CSCI rating |
|---|---|---|---|---|---|
| 1 | Control | NEL | Independent < 10a | 39 | 3 star |
| 2 | Intervention | NEL | Independent, nursing | 28 | 2 star |
| 3 | Intervention | NEL | Independent, part of chain | 40 | 3 star |
| 4 | Intervention | NEL | Independent < 10a | 24 | 2 star |
| 5 | Control | C&W | Voluntary | 28 | 2 star |
| 6 | Intervention | C&W | Voluntary | 45 | 2 star |
| 7 | Intervention | C&W | Independent < 10a | 21 | 2 star |
| 8 | Intervention | C&W | Private/nursing | 30 | 2 star |
Of the four homes in NEL, one was a purpose-built home (which in the past was in local authority control) and had two floors. Two were converted houses, while the remaining home was a converted block of flats. With one exception, public areas (e.g. lounges and dining rooms) were all on the ground floor. The purpose-built home had an additional little-used small lounge on the first floor (used as a store room). All care homes had ground floor bedrooms and had lifts to the upper floors. Two of the homes had separate dining rooms next to the kitchen, while in the other two food was served either in the main lounge or an area used during the day as a ‘quiet’ room for reading or craft activities. Three of the homes had multiple areas for residents to sit and/or become involved in activities, while the other had a large multiuse room.
In C&W, there was one purpose-built home, one converted hospital building and two converted houses. Two of these homes had public areas on each of the floors. There were residents' rooms on all floors and all of the homes had lifts to all floors. In the purpose-built home there were also small kitchen/dining rooms in each of the three wings. One of the converted houses had one large central space divided into three areas: a dining area, a lounge for activities and a TV lounge, with no physical dividers between the areas.
Interviews undertaken
The process evaluation fellow (DE) carried out 48 interviews with 35 people; 21 were from NEL and 14 were from C&W (eight care home managers, six carers, three senior carers, four activities co-ordinators, eleven residents and three NOK). Where direct quotations are used to illustrate themes, an assigned code identifies the respondent and time point within the study. A full table of the interviewees and their corresponding codes is given in Appendix 12.
We could not complete as many interviews as we had planned. Care home managers and staff were very busy and often had to cancel interviews. We could interview residents only if they had, themselves, consented to the OPERA study, which restricted the number of potential interviewees. These numbers reduced further as people left the home, were in hospital or died. We also found that participants were reluctant to be formally interviewed. It was particularly difficult to arrange interviews with NOK as we had no access to their contact details.
Evaluation of recruitment processes
Home recruitment
A focus group with the research staff involved in recruiting the homes revealed that the main reasons given by care home managers for not wanting to take part in the study were that the care home already had exercise classes or provided some sort of depression training or dementia training, or the timing of the study was inconvenient. The recruiting team found if the care home manager agreed to a meeting they generally agreed to the home taking part. Early challenges included clarifying the inclusion criteria for homes. Recruiting staff adopted a policy of checking the inclusion criteria by phone before visiting the care homes. The team all noted that information about the care homes obtained from the Commission for Social Care Inspection (now Care Quality Commission) reports was not always accurate.
At baseline interview some care home managers expressed a preference for which arm of the study they might be randomised to. Many managers were interested in the opportunity for regular exercise groups but some preferred the control intervention. Care home staff training in depression was limited and care home managers felt that such training would be an advantage.
At first we were really ‘Oh I hope we get the [exercise] sessions’, but then as we were looking at it and we've got more and more to learn more about it, we were like we actually want the training.
5 manager
If we'd have got the staff trained then fine, but I made it perfectly clear what really would have been the massive carrot for me and luckily, we got it (the intervention).
16 manager
I could not influence anything. Of course I could not, but I was really hoping it was going to be a physiotherapist, rather than the training.
19 manager
Recruiting individual participants
We include here data gathered from observations, interviews and a reflective focus group held with the recruiting staff at the end of the study recruitment period.
Care home managers were asked to help identify any residents who were too ill or not eligible for the study for other reasons. The recruitment team found that some care home managers were also excluding people they felt would not want to take part in the study, and the recruiting team made strenuous efforts to ensure that this did not happen.
The recruitment team felt it would have been useful to be able to present the study to the care home staff and residents prior to recruitment but the tight recruitment schedule prevented this. Managers were asked to inform the staff and residents about the study before recruitment started, but this did not always happen. When it did, residents were more interested. Some managers put up notices they had designed themselves to inform staff and relatives about the study.
Assessing capacity to consent in all residents in the care home could mean assessing up to 50 residents; this was time consuming and challenging despite help from care home managers in identifying residents who would definitely not have capacity to consent. Time pressure on the recruiting staff, especially at the peak of recruitment, meant they may have missed a few eligible participants. In some cases the family of a resident who had consented would also ask for information about the study, and some residents with capacity to consent wanted one of their relatives to sign the consent form on their behalf. One resident went to great lengths to report her experience of the physical assessment carried out by the research team after she gave consent to participate.
Well, when she came I amazed myself because I think it was about an hour and a half. It was a mental test ... And doing it without being warned I was going to do it, I would not have thought I could but I did ... And she was surprised herself! I mean I still do not know how I did it, she was surprised and when it came to walking she had a white line over there ... She asked me to walk over there and stand upright and leave that, so my standing is not quite good but she was there. She said ‘You will not fall.’ ... She timed me on how long I could stand without holding that.
11 resident
Care home managers who were interviewed were positive about the process of resident recruitment:
No, no problems at all. No, none whatsoever. I mean he's been here – [Name] on ... I think he's been here about four times in total, four or so times, and he's been good ... It was very good, yes. Nobody was put under any pressure to participate.
37 manager
Additional data on the use and administration of the outcome measures are summarised in Appendix 13.
Impact of recruitment on the care homes
In addition to being asked about their interactions with the physiotherapists, care home managers and carers were also asked about interactions with the OPERA team (including the recruitment/assessment staff, research fellows and contact with the study office). All managers and a number of the care staff commented that the visiting OPERA team, although sometimes viewed warily at the start, became welcome in the home. Care home managers noted that appointments were made for visits and the team were no burden on the homes' residents or staff. Several reported good outcomes from problems that were raised.
I think it was excellent. There wasn't any problem at all. I mean the residents, they [the OPERA team] did not impose. They knew which residents were not able to make the decision and so they contacted relatives. I think it was done very well – no problem.
19 manager
And it was a pleasure having [Names] here. I mean all of you ... I've never had any problems. You've actually fitted in and people have accepted you.
20 manager
Even when you did the interviews here, we did not have any problems. Everybody was just so respectful and kind and just nice people – just a nice bunch of people.
32 senior carer
Delivery of care home staff training
We delivered at least 142 depression awareness training sessions to at least 902 care home staff; eight of these training sessions were observed (five intervention and three control) (Table 59). Registers are missing from one home where at least one training session was delivered. One home had six sessions delivered covering most of the staff. Overall less than half of the care homes' staff were exposed to the training. OPERA research staff in both arms of the study reported difficulties at times in organising the training sessions. On at least 15 occasions no care home staff attended a booked training session. It proved to be particularly difficult to deliver training in some care homes, and after several failed attempts training was abandoned in one home in the control arm.
| Item | Intervention: depression awareness and activity training | Control: depression awareness training | Total |
|---|---|---|---|
| No. homes (n) | 35 | 43 | 78 |
| No. of staff | 884 | 1126 | 2010 |
| Training sessions delivered (n) | 69 | 73 | 142 |
| Total attendance | 406 | 496 | 902 |
| Mean attendance | 5.9 | 6.8 | 6.4 |
| Percentage of staff trained | 46% | 44% | 45% |
| No training delivered | 0 | 1 | 1 |
| One session delivered (n homes) | 8 | 21 | 29 |
| Two sessions delivered (n homes) | 18 | 15 | 33 |
| Three or more sessions delivered (n homes) | 8 | 6 | 14 |
| Missing data (n homes) | 1 | 0 | 1 |
We received 916 completed feedback forms at the end of the training sessions (this included 14 forms from the care home with a missing register); 174 (19%) participants had worked in a care home setting for < 1 year, while 421 (46%) had worked in such a setting for > 5 years. Ethnographic observations in the case study care homes and interviews suggested that a majority of care staff have been working in the sector for many years. We observed cases of a changing staff population but there was a large core of staff with long-term experience.
Specific observations of the delivery of the training revealed some of the challenges faced by the research team delivering the session. Quiet space within homes for staff to attend training was not always available and the attendance varied. Some of the care home managements did not pay staff for time spent in training with the result that there was little incentive to attend, especially if staff had a day off or if training took place outside their shift hours. A number of staff attended the training during their normal shift but in some cases this resulted in them being called away from the training to carry out a caring task. Some home managers actively encouraged all staff to attend (including ancillary staff and night staff) but this was not universal.
Observations during the training sessions generally supported the results of the feedback questionnaire described below (Table 60). Care home staff appeared to enjoy the DVD and it generated discussion. The levels of engagement with the training were variable – some got involved and asked questions or made comments, while others said very little.
| Statement | n | Strongly disagree | Disagree | Neither agree or disagree | Agree | Strongly agree |
|---|---|---|---|---|---|---|
| The session was relevant to my job | 888 | 16 (2%) | 6 (1%) | 25 (3%) | 296 (33%) | 545 (61%) |
| I learned something new from this session | 891 | 19 (2%) | 17 (2%) | 48 (5%) | 421 (47%) | 386 (43%) |
| I am glad I attended this session | 889 | 14 (2%) | 7 (1%) | 24 (3%) | 371 (42%) | 473 (53%) |
| The session was just the right length | 881 | 19 (2%) | 34 (4%) | 36 (4%) | 397 (45%) | 395 (45%) |
The immediate participant feedback questionnaires suggested that the training was felt to be relevant and provided new information. However, the response rate to the mailed, 3-month questionnaire was very poor (15%). Investigation suggests that there was no monitoring of returns and no reminders were sent. Those who did respond provided interesting feedback, more detail of which is provided in Appendices 14 and 15; in summary it suggested that:
-
the training was well liked
-
the materials were useful
-
the training sensitised people to be aware of low mood and depression
-
the training changed people's perceptions of what to look for in a resident.
However, there was not much evidence in the feedback that the training changed the way people did their jobs. Most respondents said they would have liked more training.
Interviews with care home staff and home managers support the findings of the training feedback. Most of the managers had attended the training themselves and several had received positive feedback from their staff. Although the training was seen as a good thing there were comments about the level of the training.
... to be honest, most of it I felt like I already knew really
28 activity co-ordinator
I thought it was very basic and I would have liked something more sophisticated because I think basically what she said, we already knew and we really needed the next level up.
23 manager
Equally, there were positive comments such as:
I think it was an eye-opener. There was the DVD she brought with her as well. I think it did get people questioning and there was a lot of interacting going on in that session.
20 manager
Yes, I mean the whole thing that [Name] and [Name] did was good. It wasn't too technical and it wasn't talking down to people. It wasn't talking under people. It wasn't too complex, too simple, too fussy, too thin or whatever.
25 manager
Many of the research staff who delivered the care home staff training reported that managers and staff would have liked more than just a one-off depression awareness session, and some care homes would have liked the training to be in more depth, supporting the findings from the interviews. One care home requested additional depression training for staff after follow-up was completed (post OPERA). Several physiotherapists were aware that the training helped the home fulfil its requirements for the Care Quality Commission supported by the certificates provided to attendees.
Set-up of the exercise groups
Thirty-five homes were randomised to the ‘whole-home’ intervention: 18 in NEL and 17 in C&W. After randomisation to the active arm of the study, one care home in NEL was found to be unsuitable for the intervention during the physiotherapist assessments of residents and no exercise groups were delivered in this home. Thus the following data, for the delivery of exercise classes, are from 17 homes in each area. Data presented in this section include all residents within the care homes and are split by those who are study participants and those who are not. There was considerable variation in the time taken getting the intervention started (between 3 and 14 weeks) (Table 61). There was a shorter average set-up time in C&W and hence a longer period of actual intervention delivery.
| Time Frame | Time (weeks) | ||
|---|---|---|---|
| C&W: median (range) | NEL: median (range) | Overall: median (range) | |
| Period from randomisation to first exercise group | 5 (3–10) | 6 (3–14) | 6 (3–14) |
| Intervention delivery period | 48 (39–51) | 45 (37–50) | 48 (37–51) |
| Period from randomisation to last exercise group | 54 (49–56) | 52 (47–55) | 53 (47–56) |
Before the exercise intervention started, there were some anxieties among staff of the homes. Both care home managers and carers anticipated a number of potential barriers, including difficulties in fitting into the care homes‘ routines and sustaining the participation of residents.
Well, one thing that could stop you from doing it is if none of the residents joined in, obviously ... but other than that, I do not really think there is anything that would stop you from doing it.
1 manager
It's a bit of hard question because they might say ‘yes’ and when it comes to it, they'll probably change their minds – the residents, because they like doing that to us. I mean one or two might do it.
12 carer
Well, I think some barriers have probably already come across and that is ... and I said this from the start, that some residents ... You know, they're having it twice a week – the exercises and some residents, they may want to be totally committed one week but then the next week they cannot be bothered, and this happens.
19 manager
There were also some reported problems arising from differences in expectations, although these were all resolved relatively quickly.
With regards to myself and the staff, I think she's just a little bit overpowering and I do not think they understood that she would have such an active part that it would be twice a week and it would be so intense, and she would want so much from the other staff. We did not expect that, so I think that's been a bit of a learning curve really.
44 manager
Well, I think it's a bit over the top with [Name] occasionally. You know ... all I can do as a manager is just put it to the company and it's not my decision. It's the company's decision whether we change things.
19 manager
The residents interviewed at baseline could see no barriers to the research team delivering OPERA into the home and in general thought it was a good idea although two residents doubted that people would participate:
But people will not join in, will they?
11 resident
Yes, that would be good [the exercise groups]. They do not always join in anything here.
34 resident
Dose delivered
In one of the 35 intervention homes the dose delivered was zero because residents were too disabled to participate. We report here on activity in the remaining 34 homes. Delivery of two exercise groups per week over 12 months (allowing for set-up time and key public holidays) gives a potential 100% dose delivered of 92 groups in a home (Table 62). The study achieved a 90% dose delivered: 90% in C&W and 89% in NEL. Four homes were so big, or laid out in such a way, that they required more than one pair of exercise classes per week. Some planned exercise classes failed to happen. The physiotherapist team reported a number of reasons for this including infection control issues (e.g. outbreaks of diarrhoea and vomiting, norovirus and the influenza H1N1 epidemic), and adverse weather conditions (e.g. snow and ice, or days that were too hot for residents to exercise).
| Area | n homes | Sets deliverda | Median n of sessions delivered | Percentiles | Dose delivered: median, % (range)b | ||
|---|---|---|---|---|---|---|---|
| 25 | 50 | 75 | |||||
| C&W | 17 | 19 | 83 | 80 | 83 | 91 | 90% (76–118) |
| NEL | 17 | 19 | 82 | 72 | 82 | 88 | 89% (73–116) |
| Totals | 34 | 38 | 82 | 76 | 83 | 89 | 90% (73–118) |
The 34 intervention homes had a total resident population of 1439 (based on study registers during the period of the intervention delivery); of these, 494 (34%) were study participants. Not all residents were judged by the physiotherapists to be fit enough to participate in the exercise groups. There were around 1256 (87%) residents who were eligible to attend groups of whom 478 (38%) were study participants.
During the study physiotherapists delivered 3191 exercise groups in 34 homes. In total 65,196 person sessions were made available, calculated by summing the number of groups each of the 1256 eligible residents would be able to attend (i.e. excluding sessions for which they were ineligible or when they were not at that point a resident in the home). On average residents attended about half of the available sessions (31,705). An average group size of 10 (5.3 study participants and 4.6 non-study participants) was calculated by dividing the total number of person attendances (31,705) by the total number of groups delivered (3191) (Table 63). Figure 15 groups study participants into the number of groups they attended. The reasons for not attending the available sessions are discussed in more detail below.
| Item | n or % | Study participant | Non-study participant | Total |
|---|---|---|---|---|
| Residents (all) | n | 494 | 945 | 1439 |
| Residents eligible to attend groupsa | n | 478 | 778 | 1256 |
| No. of groups deliveredb | n | 3191 | ||
| No. of eligible groups availablec | n | 31,330 | 33,866 | 65,196 |
| Total attendancesd | n | 16,986 | 14,719 | 31,705 |
| Percentage of maximum possible | % | 54 | 43 | 49 |
| Average attendancee | n | 5.32 | 4.61 | 9.94 |
| Reasons for non-attendance | ||||
| Out | n | 382 | 1067 | 1449 |
| % | 1 | 3 | 2 | |
| In hospital | n | 719 | 937 | 1656 |
| % | 2 | 3 | 3 | |
| Unwell | n | 1670 | 1497 | 3167 |
| % | 5 | 4 | 5 | |
| Visitors | n | 369 | 396 | 765 |
| % | 1 | 1 | 1 | |
| Unwilling | n | 8339 | 11,930 | 20,269 |
| % | 27 | 35 | 31 | |
| Other | n | 2865 | 3320 | 6185 |
| % | 9 | 10 | 9 | |
FIGURE 15.
Study participants: number of groups attended.
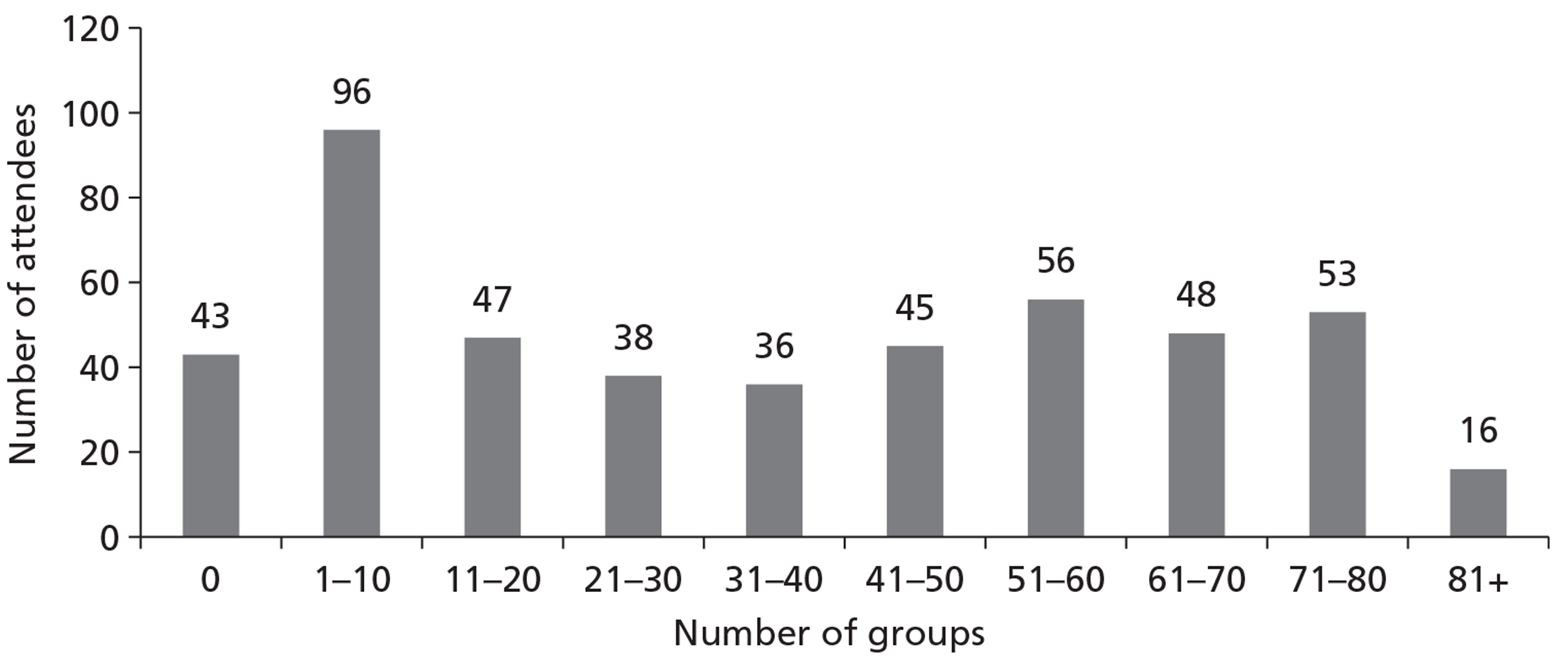
The most cited reason for non-attendance was the unwillingness of participants. Unwillingness to attend appears to be consistently higher in the NEL homes at 31% compared with 21% in C&W. We observed 21 exercise groups in case study care homes; seven in the early stages of their introduction (five homes once and one home twice), six at about the midpoint (once in each of six homes) and eight at the end of the 12-months (four homes once and two homes twice).
During the interviews little was said about why residents attended or did not attend. However, a care home manager and an activities co-ordinator noted that the time of day could have an impact on attendance.
The only thing we actually found was that someone could not come in the morning, but wanted to come in the afternoon and they were not having none of it (the residents) ... They know their own mind ... And no, they're all tired and they've had lunch and no, and it's really funny but that day none of them wanted to do it.
31 manager
... what I've found is the best time for me to do it, like you've seen I come in the mornings and I do it straight off in the morning, because the best time is to get them in the morning because they do it before their lunch, they're sitting there, they're tired, they do not ... if you allow them to, they'll sit and they'll smoke away in the chairs and be relaxed and just listen to the television or watch the television. Get them up and moving, and then it's easier to get them more involved in other activities later on in the day, where if I do other activities and then just put the exercise at the end of the day, they're normally you've got less of a chance to get them to participate in the afternoon, as you would in the morning.
50 activity co-ordinator
Home observation suggested that some residents preferred groups in the morning and some in the afternoon.
A priori we set the threshold for the minimum effective dose as attending 51 sessions, an average of one per week; 36% of our participants achieved this. Nine per cent of our study participants attended no groups, 20% attended 10 groups or fewer (Table 64).
| Area | n or % | Total residents | Total eligible residentsa | No. of groups | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1–10 | 11–20 | 21–30 | 31–40 | 41–50 | 51–60 | 61–70 | 71–80 | 81+ | ||||
| Total study | n | 494 | 478 | 43 | 96 | 47 | 38 | 36 | 45 | 56 | 48 | 53 | 16 |
| participants | % | 97 | 9 | 20 | 10 | 8 | 8 | 9 | 12 | 10 | 11 | 3 | |
| Total overallb | n | 1439 | 1256 | 187 | 384 | 132 | 103 | 83 | 85 | 96 | 80 | 81 | 25 |
| % | 87 | 15 | 31 | 11 | 8 | 7 | 7 | 8 | 6 | 6 | 2 | ||
Overall, there was little attrition in the attendance at groups over the year (Figures 16–18 and Table 65).
| Month | NEL | C&W | Overall | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n (homes) | Mean | SD | n (homes) | Mean | SD | n (homes) | Mean | SD | |
| 1 | 17 | 11 | 4 | 17 | 13 | 5 | 34 | 12 | 4 |
| 2 | 17 | 11 | 4 | 17 | 11 | 4 | 34 | 11 | 4 |
| 3 | 17 | 11 | 4 | 17 | 11 | 4 | 34 | 11 | 3 |
| 4 | 17 | 11 | 4 | 17 | 11 | 4 | 34 | 11 | 4 |
| 5 | 17 | 10 | 4 | 17 | 11 | 4 | 34 | 11 | 4 |
| 6 | 17 | 11 | 4 | 17 | 11 | 4 | 34 | 11 | 4 |
| 7 | 17 | 10 | 3 | 17 | 11 | 4 | 34 | 11 | 4 |
| 8 | 17 | 9 | 3 | 17 | 11 | 4 | 34 | 10 | 3 |
| 9 | 17 | 9 | 3 | 17 | 11 | 4 | 34 | 10 | 3 |
| 10 | 17 | 9 | 3 | 17 | 11 | 4 | 34 | 10 | 4 |
| 11 | 12 | 9 | 3 | 16 | 11 | 4 | 28 | 10 | 4 |
| 12 | 6 | 7 | 5 | 15 | 11 | 4 | 21 | 10 | 4 |
| 13 | 1 | 6 | NA | 4 | 10 | 5 | 5 | 9 | 4 |
FIGURE 16.
Average monthly attendance to exercise groups: all homes (± SD).
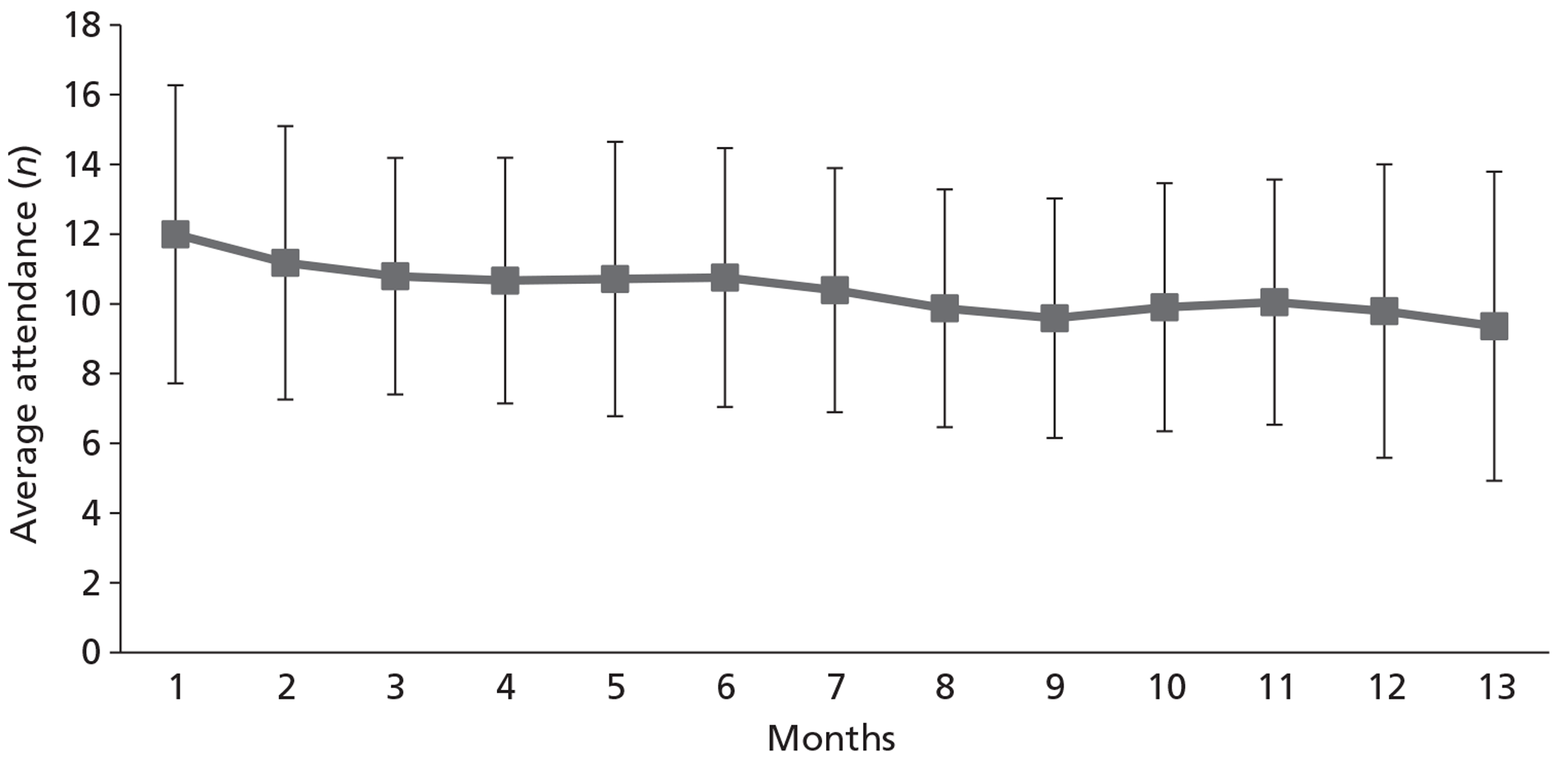
FIGURE 17.
Average monthly attendance to exercise groups: NEL homes (± SD).
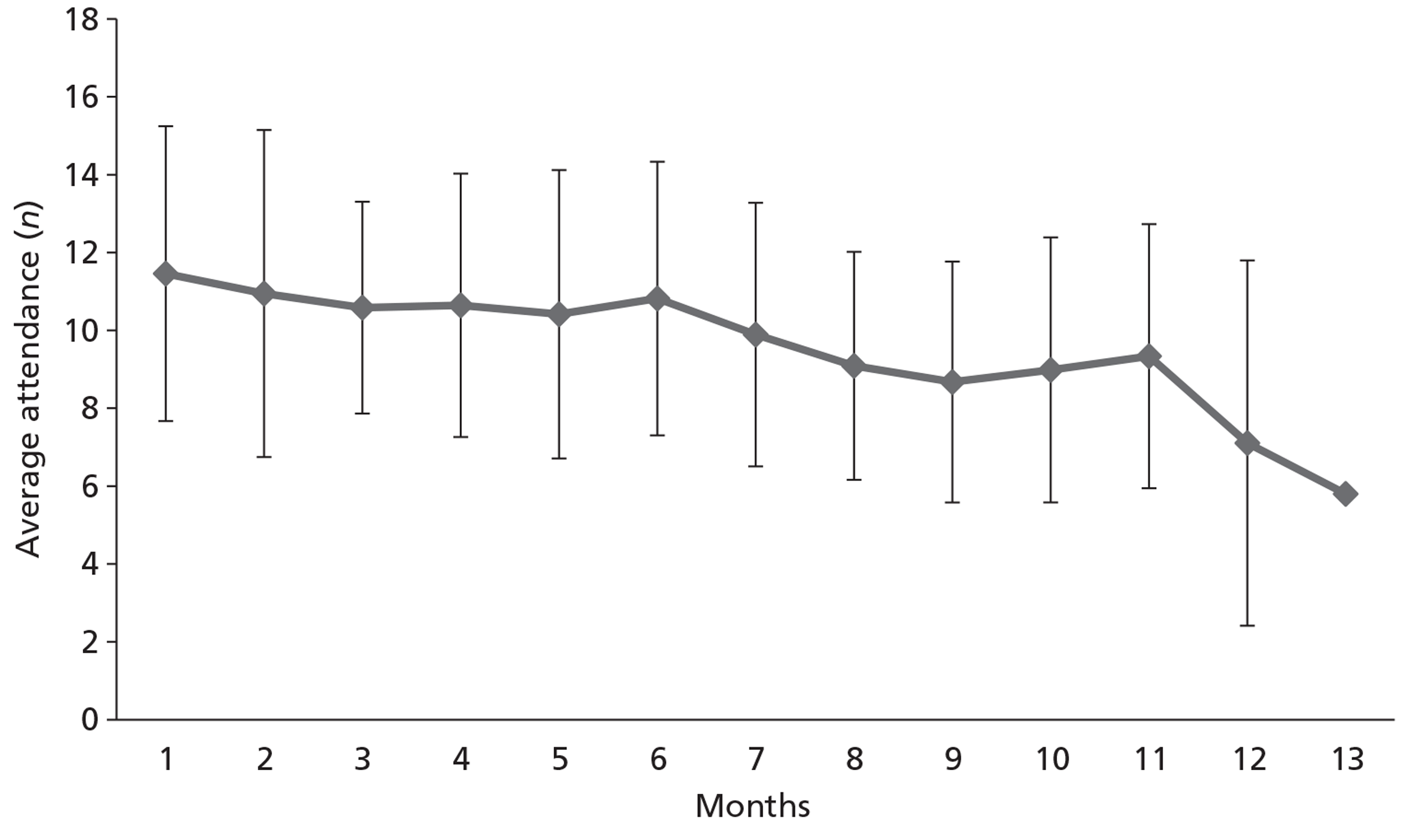
FIGURE 18.
Average monthly attendance to exercise groups: C&W homes (± SD).
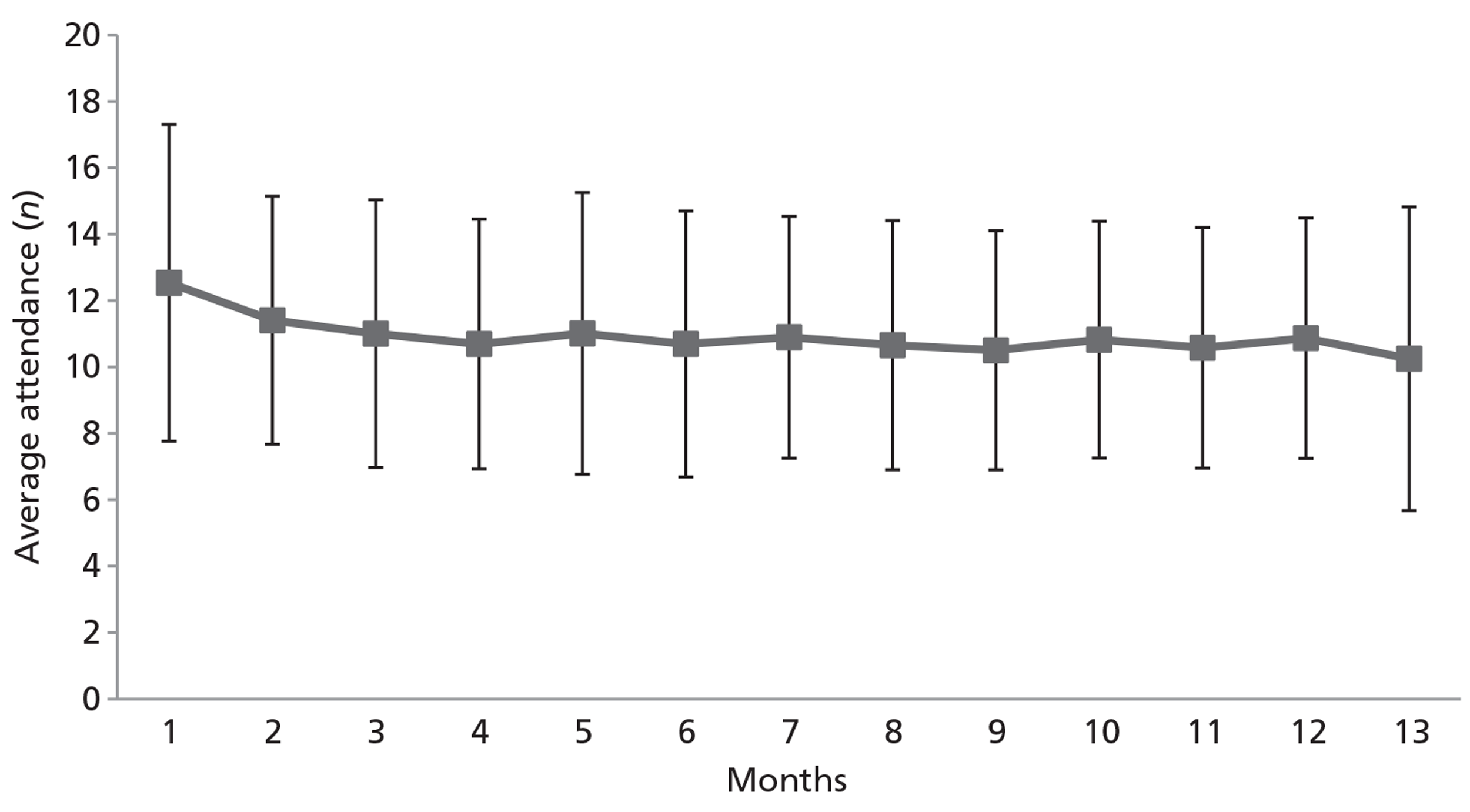
Dose received by those providing primary outcome
In a post hoc analysis we examined the attendance at the exercise groups by just those participants who provided the primary outcome for our two cohort analyses (Table 66). This shows that over half of our participants contributing to these analyses had attended over half of the group exercise sessions, with around three-quarters attending at least one-quarter of the sessions over a 12-month period. This indicates that an adequate dose was received by a larger proportion of those contributing to our primary analyses.
| Cohort | n | Attendance at exercise groups | > 50% dose receiveda | ||
|---|---|---|---|---|---|
| Median (range) | Interquartile range | n | % | ||
| Depressed cohortb (6 months) | 123 | 37 (0 to 82) | 7 to 62 | 66 | 54 |
| Cohort (12 months)a,c | 224 | 55 (0 to 91) | 23 to 72 | 124 | 51 |
Perceptions of exercise groups
Interviews at the end of the study illustrate the impact that the groups had on the residents and care home staff. Most were positive about the planning and execution of the groups, noting that the regular and consistent time slots were appreciated and that the physiotherapist liaised well with the care home managers. Care home staff also appreciated having a professional in charge of the exercise class.
I mean it's very good because it's always Monday and Wednesday ...
29 manager
... and [Name] was very good. You know they would come in and tell us what they were doing and how they were going to do it and what was going to happen so the communication even from them to us was very very good.
51 manager
You know, at first even when I used to do my little five minutes and workouts or we'd do a daily dance, it could be quite worrying; ‘Oh my legs hurt so I'm not going to do anything’, whereas because they've got a professional guiding them, using the weights and even telling her what weights to use ... You know, there's a sudden interest in their own well-being.
27 activities co-ordinator
The physiotherapists reported that residents, care home staff and visiting relatives enjoyed the exercise groups. Physiotherapists felt that they gained increased confidence in running a group, job satisfaction, and liked being involved in research. The practicalities of running a group raised issues relating to variation in the amount of care home staff input. Examples were given where there was no-one to help get people to the group or help with running it. This was therefore more time-consuming especially if there was little flexibility in time allocated to OPERA. For the physiotherapists, having an activity co-ordinator or member of staff designated to assist was a great help, and they felt that continuity in the staffing was important, and that the bond and understanding of the residents' idiosyncrasies made it easier to gauge the group. However, some of the care home staff felt that the group was a time during which they could ‘do other things’ (sometimes a highly appreciated aspect of the intervention).
Interviews with physiotherapists, care home managers, care home staff and residents revealed that the delivery of the group worked well and was easy to follow. Equipment was considered appropriate and the music an important part. Some explanations for the positive impact of music were that it helped to establish a routine, increased enjoyment, promoted activity, encouraged singing, which helped lung function, and promoted discussion about the music and artist.
The positive impact of the exercise groups was mentioned by many interviewees, talking about changes in residents' mood and physical ability and about the changes they have seen in residents' attitude towards exercise:
They have become happier in their mood and I think it has achieved what it set out to do. Certainly towards the end of the programme once everyone got into the swing of it, it really picked up.
48 manager
I'd often walk by and see them and they were always smiling. There was always ... a good rapport in there. There was always laughter in there. The music would be going and you would see them all doing this [gesture] and I never saw anybody sitting there sort of looking glum.
32 senior carer
You know it has been wonderful, it has been good for our residents, it has been excellent in their development; you know they are happier
51 manager
I just feel a lot better. I mean I can ... (shows me he can stand) I can (So is that better than it was?) Oh yes (note: was very reliant on wheelchair at start of study).
39 resident
During observation of the exercise groups the challenges faced by the team and the general enjoyment of the residents were noted. As a relationship developed between the physiotherapists and the residents the groups appeared easier but there were still some residents who were reluctant to be involved and others with challenging behaviour. During the groups there was laughter and smiles, and at times the groups became competitive. The music was well liked and residents often sang along, and indeed knew which exercise they should be doing with a particular tune. It was clear in the homes that there were a number of residents who looked forward to the groups.
The physiotherapists running the groups noted that the exercise involving a velvet rope promoted inclusion and involvement, and gave a tactile experience. They also noted that the use of equipment (e.g. balls and weights) promoted activity, especially in the cognitively impaired, but could be problematic. Some of the physiotherapists found the weights hard work and some residents were initially resistant and said that the weights, for example, ‘looked like manacles’. In some cases, weights and the weighted balls created some competition between residents, with banter about how much they had done that day in the session.
There were some issues around safety, for example, when throwing and kicking balls, or the potential to wrap the rope around one's neck. Space, temperature, arguments over seats or routines, and group disruptions were also challenges that had to be faced.
The whole-home intervention and role of the physiotherapist
The aim of the intervention was to achieve a change in the whole culture of the home, so that the importance of helping residents to be active was embedded permanently. Home champions were intended to be part of this intervention and it was planned that these would be identified early on. However, this did not happen in all homes. Some of the activity co-ordinators in homes became involved but not all felt it was in their remit. Again, some carers were identified as ‘champions’ but problems with shifts, time or enthusiasm limited their effectiveness. It seems that the role of home champion was unrealistically demanding for most staff in most homes.
The physiotherapists felt that it was sometimes difficult to explain their remit to care home staff and that some staff were very wary of them. Nevertheless, the physiotherapists reported that clinical assessments of the residents gave opportunities to meet residents and staff, to build a rapport and increase the understanding of the importance of physical activity and lay good foundations within the home. Several care home staff commented on how staff were encouraging residents to walk more.
She said ‘Wheelchair’ and I said ‘No, you can walk.’ She said ‘Oh I don't know whether I could’ and I said ‘But you can because you used to walk all the way up there.’ She said ‘Oh yes, I did’ and she walked down there fine. She was slow but she walked there fine because everybody keeps sticking her in the wheelchair to take her to bed, but she can actually walk and I think if she can walk then for G**'s sake, let her walk.
1 Carer
But generally, sort of one of the ladies downstairs, she was having the wheelchair quite a lot and then they said ‘Well, maybe if we encourage her to walk little bits at a time and then a bit more and a bit more’ and it's worked really well and she's walking everywhere now.
2 Senior carer
Physiotherapists reported seeing their suggestions being acted upon, as for example, where residents were seen to be walking instead of using a wheelchair. The physiotherapists also felt that they had reinforced good principles of manual handling and promoting activity, and had broken down barriers to mobility. Physiotherapists encouraged exercise progression by setting individual goals and helping care home staff to recognise and reinforce these.
Care home managers were generally happy to have a physiotherapist working in the home, and communication and understanding increased as the intervention progressed, although not all staff were receptive to the physiotherapists' advice.
The staff definitely do not feel that (the physiotherapist is an imposition) and as time has gone on with [Name], they've really got to know [Name] and she sits and has her lunch with them – not for long, but she does and they look forward to her coming in, to be honest
19 manager
Yes, because I think that gave us a sort of opening as well to actually think, ‘Well, I'll do ... this person can actually do more than what they're actually saying that they can actually do’, so they brought a sort of ... they brought a lot of that out
31 manager
The hardest part I think for me was trying to get the staff on board to realise what this was about, who it was for and how people would benefit.
32 senior carer
One manager noted the challenge she faced in trying to increase mobility.
It is a collective protective culture and that's why they come into care. They think people should be protected, but I think in this situation because we deal with people who have very high dependency needs that it sometimes is that we de-skill them, rather than enhance them because it's a protective mechanism.
44 manager
And another talked about the challenge in bringing about changes to thinking:
Yes, that's what I say to the staff because I mean when people talk about activities I think it's still there – the old belief that it is about doing the art work, doing bingo and you need to get away from that because that's not what it's about.
20 manager
Two interviewees reported that OPERA has had a positive impact on external views of the home. One home found the study mentioned approvingly in a Care Quality Commission report and in another home a social workers' report highlighted the positive effect of OPERA.
Yes, she'd actually heard of it (Care Quality Commission inspector). She must have gone to another home before she came in here and we actually saw the file and she said it was a very good study and she actually had feedback from another home.
32 senior carer
Social Services, they have to have regular reviews and one of the residents who's involved in this study, she had her review and they ... The reviewing officer always sends me a copy of the review ... and I read it yesterday and I was so proud of, you know ... Her and her family could not thank the home enough but also, OPERA was mentioned in that review ... and about how she's enjoying it and that's recorded.
19 manager
By 6 months and at the end of the study interviewees were positive about the intervention. Most commented on how the relationship developed between the care home (the manager, residents, staff and sometimes relatives) and the physiotherapist and in all cases the physiotherapist became seen as ‘members of staff’, ‘members of the team’ or ‘one of us’.
Brilliant and that's never petered off. In fact, it's just got more positive. They're brilliant with her. They trust her with everything and that in itself is a feat.
40 manager
I think the staff ... well, certainly we will miss her and they really will. The residents ... my G** they'll miss her
43 manager
One senior carer felt that the number of falls had reduced and attributed some of this to OPERA physiotherapist input.
There was one resident here with a walking stick, ‘Where's his stick?’ and he kept falling. We had a terrible history of falling with him. With a lot of perseverance, [Name] got the frame and now he actually walks with a frame very well. He's reduced his risk of falls. We've had hardly any falls with this man and he doesn't mention his stick any more ... Yes, so we have seen some good results ... (falls). They have been reduced, I'd say definitely ... And I think if you've got the right aids – and a lot of them didn't have, it has minimised the falls. They now use the proper things they should be using.
32 senior carer
The professional conduct of the physiotherapist was seen as very important, as was having the same physiotherapist over time.
Well that's very important, yes because the residents get used to that person coming in and they build up ... They kind of bond with them don't they?
28 activities co-ordinator
... yes and I think it definitely makes a difference what physio you use because I think it depends on the person they send down as well. I mean [Name] is very ... She's sort of a bubbly character. She's not afraid to motivate them to join in.
29 manager
It doesn't matter what sector you come from, whether it's general practitioner, physio or district nurse, (continuity) is really important because each time a new person comes in you're starting from the beginning again.
40 manager
However, despite the intervention lasting for a 12-month period physiotherapists felt there was little time to facilitate a change in staff behaviour around encouraging residents' mobility. The barriers to facilitating change included staff turnover, staff attitudes towards manual handling, staff morale and time constraints.
The key facilitators were the physiotherapists and several care home managers saw this as an important benefit for the residents. Physiotherapists were seen as supplying both practical advice on mobility aids and more general advice on navigating the services available.
That time when we'd got a problem with ... oh that lady who passed away eventually. We were really struggling with the doctors and the mental health team. It was evident that she needed something and [Name] just came and said, ‘You can refer her online to the mental health team’ and we didn't even know that did we, and because she's a professional, we got somebody here the same day.
43 manager
Yes, that was another asset I think that [Name] and the team brought in, which was yes, we have people walking with the walking aids and the frames and the walking sticks, but the good thing is that for me to get everybody checked here ... It would be crazy of us. [Name] came in and [Name] and they assessed each person ...
20 manager
[Name] was excellent there. We were using the wrong aids and we still had walking sticks on the premises we shouldn't have had. [Name] was brilliant that way and that saved us a lot of time I think, referring them from the general practitioner to a physio, for them to come in and then now, the (National Health Service) physios don't actually come on the premises.
32 senior carer
The importance that care home managers placed on having access to a physiotherapist was no doubt influenced by the difficulties they reported in accessing routinely available physiotherapy services and mobility aids.
There are the initial referrals – especially via the general practitioner. Sometimes you get some of the district nurses that um and aah and all the rest of it and then eventually do and I said to [S] last week, I'm finding it quite hard to understand why she's put in her referrals and the equipment had come within a couple of days. If you go via the other channels we've waited an age.
16 manager
Activity in case study care homes
A total of 109 activity sweeps were carried out: 53 at baseline and 56 at follow-up, with 12 to 14 observations in each home at each time point. Across the case study care homes a substantial amount of residents' time was spent in activities associated with eating and drinking with active social interaction only amounting to between 5% and 15% of daily activity. The proportion of time spent in recreational activity, passive social interaction and being socially inactive appeared to vary across the homes. With only one exception (home 4), no exercise groups or ‘exercise’ activities were observed (Figure 19).
FIGURE 19.
Summary of day-time activity in homes, baseline vs follow-up. BL, baseline; FU, follow-up.
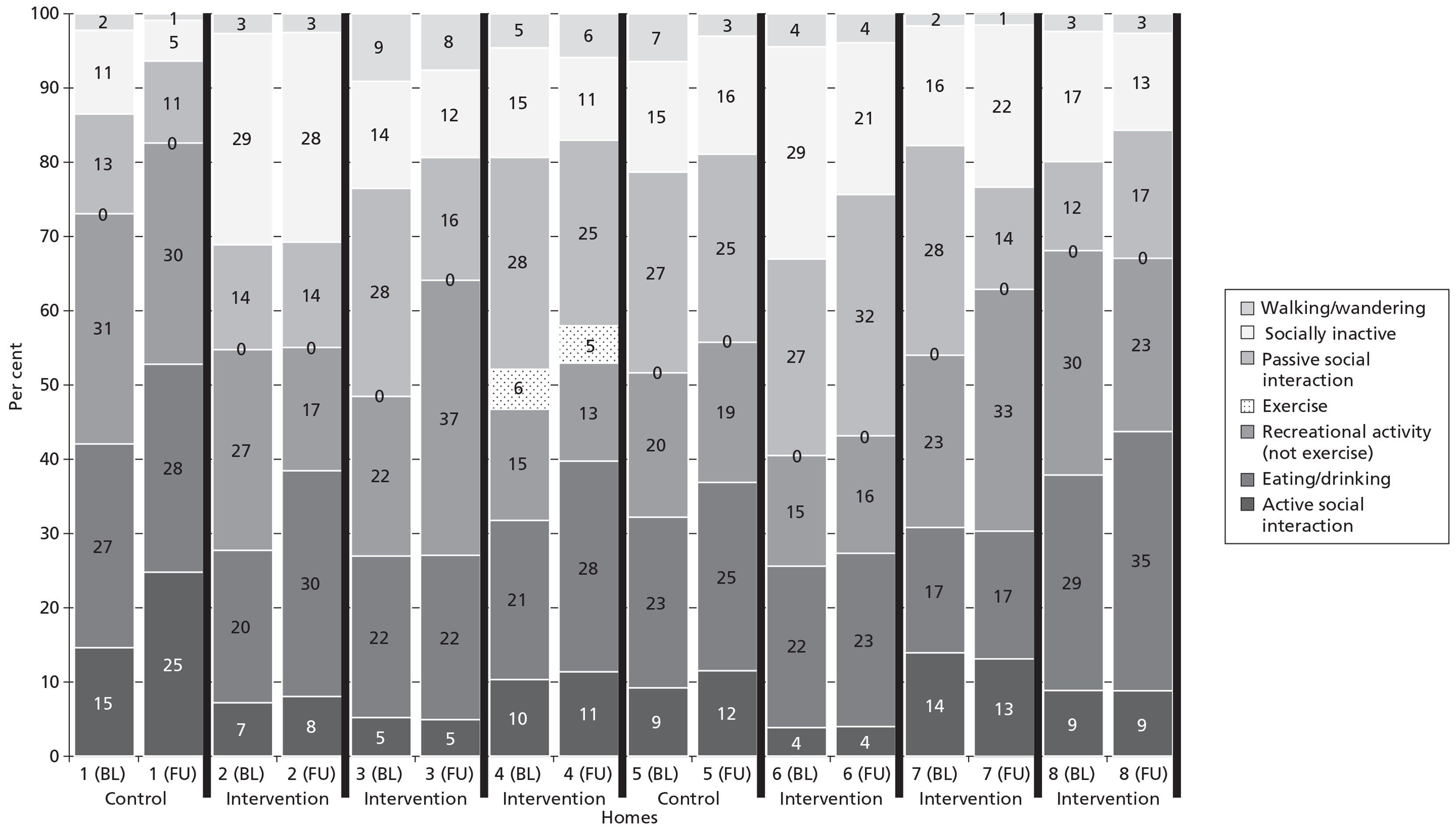
In contrast with the different patterns of activity and inactivity seen between the homes, within homes the patterns of activity were remarkably consistent between baseline and follow-up. None of these data was analysed until all data were collected, so it is unlikely that the researcher was influenced at follow-up by the findings at baseline (see Figure 19).
The observation sweeps do not show any major changes in activity within the homes; two homes had some increase in recreational activity and one a decrease, and in one social interaction increased. These may be chance differences because of the large number of comparisons made. General observation in the homes supported the conclusion that there was little change in overall activity levels within the homes.
Ending the intervention
When the intervention was coming to an end, staff in the homes expressed some concern about what would happen when the study was finished. Without exception all interviewees expressed a feeling of sadness, and in some cases concern, about the withdrawal of the exercise groups and the physiotherapist.
Oh yes they will miss it as well. They used to come to the exercise class as well so. Yes they will miss it. And I think it is a shame that it has come to an end but everything has to come to an end, and hopefully when all the powers that be have done their research and they have got all of their figures and everything together maybe ...
48 manager
No, I'm just hoping that something can be done for them when this course is over and done with. I just don't like to see them be let down. I've seen it too often and it can actually damage them – and I have seen it, so ... and if you can do anything for the staff that would be fantastic. We need to be de-stressed.
17 carer
Yes, they love it. They really love it and it's actually a shame if it actually stops, because it's something that they've got there that they have every week. You know, it is a shame ...
31 manager
Many of the care homes brought gifts for the physiotherapists and had celebrations at the end of OPERA and there were tears and sadness on both sides. Several of the physiotherapists have stayed in contact with some of the homes and residents. Some physiotherapists felt unprepared, as the closing process was not in original paperwork. Some homes have kept exercises classes going in a modified form, some have purchased some physiotherapist input, and other homes have no funds to continue.
Ethics
The ethics substudy focused on issues relating to recruitment and consent to research of older, vulnerable adults. Data were drawn from the OPERA process evaluation study and a separate qualitative study of key informants‘ interviews and three focus groups of older people. Key informants included four senior researchers working in elderly care research, three research commissioners/funders of elderly care research including age-related charities, a director of services for an age-related charity, a director of public health, an acute National Health Service Trust chief executive, and a professor of medical ethics. The focus groups were based on groups attending a range of day care or activity-related services for older people. The number of participants ranged from seven to nine in each group and the majority were female (only three males).
Analysis of the observation and interview data from the process evaluation study relating to recruitment and consent identified three broad themes that framed the experience for those involved (participants, care home managers and research staff).
Experience within the OPERA study
The care home manager as gatekeeper and facilitator
Care home managers who were interviewed expressed no concerns about their role as consent giver for the home to take part in the study. They perceived themselves as decision-makers for the home, with a responsibility for improving resident well-being and staff training, and therefore a decision to participate in OPERA was not qualitatively different from other decisions about home activities and processes.
The possibility from a selfish point of view for the home; that we could potentially get something out of it and I made it clear right from the very beginning what my interest would be, more for the service users ... and it was for them more so than the staffing and the home. If we'd have got the staff trained then fine, but I made it perfectly clear what really would have been the massive carrot for me and luckily, we got it.
16 manager
One or two managers commented on the importance of doing research on these issues but this was not the main consideration in deciding to participate.
Managers, and recruiting staff, also identified a gatekeeper role in allowing access to individual residents for participation in the assessment processes, a role recognised and utilised by the recruiting staff. Access to residents for recruitment was negotiated with managers who identified residents whom they considered too ill or frail to be approached, as well as residents who were unable to communicate, thus protecting residents from unnecessary intrusion or distress. Managers also identified residents who, in the manager's opinion, would not want to take part or who might not understand sufficiently to give consent. In line with the legal and ethical requirement that adults with capacity should make their own decisions, and that capacity is decision specific, the study protocol stipulated that trained recruiting staff should assess all residents for capacity to consent following exclusion of those too ill or frail to participate. Thus there was a potential tension between recruiting staff's aims and managers' perceived gate-keeping role. In practice, recruiting staff learned through dialogue with managers to develop a shared understanding of a threshold level at which managers would predict a resident's lack of capacity to make a decision regarding participation, triggering an approach to a personal consultee, which facilitated the effective running of the recruitment process while minimising the risk of a resident being excluded from a decision that they had capacity to make.
The negotiated process between recruiters and care home managers demonstrates a further facet of the manager's role, that of facilitator of the research. In identifying residents who clearly could not consent they assisted in the efficient roll-out of the study, as well as protecting residents from unnecessary intrusion. Some managers also adopted a facilitation role in individual resident recruitment by being present during the interview, and so acting as a reassuring presence and guarantor of the legitimacy of the study for residents who might feel concerned at a stranger coming to talk to them.
... and I think we find that the residents are quite wary of new people and I think it's one of the things that sometimes means they say no ... I sat in on it, you know... to let them know we know what's going on. We're not trying to trick them and there's nothing strange about it.
16 manager
The challenge of assessing capacity and validity of consent
Assessing capacity to consent was seen as the most difficult and challenging part of the recruitment process by recruitment staff. Two particular difficulties that were identified related to the understanding and retention requirements for capacity set out in The Mental Capacity Act 2005. 105 Recruiting staff felt that the information sheet and consent form were too lengthy and difficult for participants to understand. However, despite recruiting staff's concerns in this regard, observation of the consent process confirmed that with careful explanation of each section of the information sheet and consent form by the recruiting staff the participants were able to understand what was required of them and provided valid consent. This highlights the particular importance of the recruiting staff's role in promoting participants' capacity.
The question of how long someone must retain relevant information in order to have capacity to make a decision based on that information is particularly pertinent for consent to research where the usual requirement is for at least 24 hours between provision of information and taking of consent. In OPERA none of the residents whose consent process was observed, and who had been assessed as having capacity to consent to participate the previous day, remembered what the study was about. This problem with retention was confirmed in the interviews with residents, most of whom could not recall that they had given consent although they remembered meeting the recruiting staff member. The Mental Capacity Act 2005 does not specify a required time for fulfilment of this element of the capacity assessment although section 3(3) states that ‘the fact that a person is able to retain the information relevant to a decision for a short period only does not prevent him from being regarded as able to make the decision’.
Goodman has used the concept of capacity to consent ‘in the moment’ with retention only necessary for the period of the conversation with the researcher. 100 In effect this was the standard used by recruiting staff in OPERA as failure to remember information given to them 24 hours previously was not seen as a bar to consenting if the resident was able to understand the information and retain it during the discussion prior to signing the consent form.
Some recruiting staff suggested that the efficiency of recruitment would be increased if the initial step of assessing capacity by talking through the study with potential participants could be dropped, and capacity assessment combined with consent using an ‘in the moment’ test for retention of information. However, two reasons for retaining this step emerged. First, although the residents did not recall the specific information about the study they had been given previously, some did have vague recollections of discussing it beforehand with the researcher, and repeating the information during the consent process may have acted as a reminder helping to consolidate understanding and reduce concern. Recruiting staff in OPERA also identified the 24-hour period between providing information and consent as an opportunity for staff, or the resident's family, to discuss the study with them. In addition to the importance of beginning the process of consolidating information, the initial visit by the recruiting team member marked the development of a relationship between the recruiter and the resident, the first step in a process of information giving, consent checking and engagement that was to continue throughout the study. Observations of the consent process noted that despite having no recollection of the patient information sheet or the details of the study, residents remembered the researcher and were pleased to see them, appearing relaxed in their presence and happy to discuss the study. Given that care home managers had expressed concern that some residents might be unwilling to speak to a stranger, the building of a positive relationship between recruiter and resident could be seen as an important factor in facilitating recruitment in this kind of study.
The creation of a relationship between recruiter and resident, however transitory, does, however, raise potential concerns regarding the voluntariness of the resident's consent to participate in the study. Making these fine judgements about capacity, and validity of consent, in the context of the knowledge that there was a need to recruit posed ongoing challenges for all recruiting staff.
We also had the added pressure of needing to recruit numbers, we all felt obliged to make the recruitment work so all tended to give resident's the ‘benefit of the doubt’ when capacity seemed difficult to assess.
Focus Group, recruiting staff
The importance of relationships
The relationship between recruiter and participant is one of a number of relationships impacting on the process of recruitment and consent identified in the qualitative data from the process evaluation study. The relationship between care home staff and resident has already been noted in the role of the care home manager as gatekeeper and facilitator. Recruiting staff also identified the importance of their relationship with the care home manager for gaining access to residents and, where necessary, their NOK, and also facilitating the consent process. The other key set of relationships involved the families of the residents. The importance of recognising the nature of the relationship between a resident and his or her family was identified by both recruiting staff and care home managers. Some families were heavily involved in their relative's care and expected to be involved in any decision-making process, even if their relative was competent to make their own decisions about care or, in this case, research participation. Recruiting staff noted that this was an unanticipated step in the recruitment process. The notification of families of residents who had capacity to consent seems at odds with the concept of respecting individual autonomy and is contrary to practice in other research contexts. However, involvement of the family in this way was endorsed by at least some residents in the study who, although being assessed as having capacity to consent for themselves, expressed a wish that a relative sign the consent form on their behalf. Care home managers also placed importance on their own relationship with residents' families, emphasising the need to maintain families' trust that the care home would act in their relative's best interests and respect their privacy.
... you know, I was happier personally signing them myself because then I could honestly say to any relative who said anything that no details had been given, ‘No one has been given your address and I've done it’ ...
25 manager
Data external to OPERA
The ethical challenges of recruitment and consent to participation in research studies involving adults who may lack capacity were further explored through analysis of data from the focus groups and key informant interviews. There was a consensus that conducting research with elderly participants was important and focus group participants were prepared to consider participation in a wide range of research studies. Key informants considered that excluding people because of frailty, comorbidities or cognitive impairment was discriminatory. They identified a number of practical and ethical difficulties in organising and conducting research in this population, including protectiveness of research ethics committees or research governance processes stopping research proceeding, the need to minimise the burden on frail and/or ill people in the research design, the demands placed on care home staff in facilitating research, and the difficulty of assessing capacity and obtaining valid consent. Two key themes emerged from the analysis, identified by both focus group participants and key informants from their different perspectives. These were (a) difficulties with the standard consent process, and (b) the importance of trust.
Difficulties with the standard consent process
Focus group participants considered study information sheets too long winded and complicated and were particularly likely to ignore information sheets sent in the post. One participant had withdrawn from a previous research study because of ‘too much paperwork’. Generally the participants considered the study paperwork as protection for the researchers rather than protection for them as participants. Verbal communication was valued over written and this was linked to the importance given to a trusted person providing the information and obtaining consent. Several participants expressed a reluctance to sign a consent form for a research study (two participants refused to sign a consent form for the focus group but were happy to give verbal consent). The idea of a son or daughter signing on their behalf, or advising on whether or not to sign, was raised by some participants. One commented that she never signed anything without her daughter. A reluctance of older people to sign consent forms was also noted by researcher key informants.
So my feeling would be if there was some way of making the consent process less scary. I mean especially people in care homes they sometimes feel they're signing away their house or something.
31 key informant
One researcher described a study where verbal consent was used specifically to overcome this reluctance to sign a formal document for a stranger.
I think when you're working with the older population that you may need to have that sort of flexibility.
32 key informant
The importance of trust
Both focus group participants and key informants identified trust as an essential feature of the process of gaining consent and of making a decision for someone who cannot give consent. Although focus group participants wanted clear and simple information sheets, the determinative factor in whether or not they would agree to take part in a study was whether or not they trusted the person who provided the information. So approaches from someone who knew them, such as their general practitioner or hospital consultant, were likely to be considered, whereas cold call approaches from research groups were likely to be ignored or ‘binned’. Similarly, the person providing the information and taking consent was crucial. Given participants' concerns about their own ability to understand the written information, a verbal explanation by someone they trusted as having their interests at heart was seen as providing reassurance and confidence in the study. The importance of trust was also identified by key informants.
... so when we're trying to reach out to people in their homes where there isn't the level of contact with services – the older person might not have a trusting relationship with a health worker – we're going through the voluntary sector because they have – and we're going through peer systems to help them trust what we are doing.
39 key informant
A trustworthy individual was also required for making decisions for a person who was unable to consent. Most focus group participants and key informants considered that if they lacked capacity to consent then close family members would be most appropriate either as proxy decision-makers or as providing advice on what the person would have wished, although it was noted that some families are estranged or may have different views from the person who lacks capacity. Important criteria for family members, and other proxies/advisors, were knowledge of the person's views about research, ability to assess the value of the research, and an understanding of the risks of the research for the participant. Although participants in general were prepared to trust the relevant individual to make decisions about their participation in a range of research, when asked to imagine taking on this role for a family member who lacked capacity participants expressed some concern about the burden of this responsibility and were more reluctant to agree to drug trials compared with other less risky interventions. Research advance directives were seen as potentially helpful in this regard.
Yeah, I'm sure I would give an indication to my family, I mean especially with how we're thinking now with The Mental Capacity Act, so I would probably indicate that I would be wanting to be involved in research ... But again I'd probably want somebody with an understanding of research to at least look at the protocols and to have an idea of the sort of quality of the research.
32 key informant
The difficulties with the formal consent process and the importance of trust in the researcher were strong themes in the observational and interview data in the OPERA process evaluation. The importance of relationships, particularly family relationships, for older people participating in research was also experienced in OPERA. Our data suggest that older people participating in research may think and act in ways that are not necessarily congruent with the accepted model of individual autonomy underpinning the standard informed consent framework of provision of full information and explicit written consent uninfluenced by others.
OPERA end-of study feedback
We obtained responses from 56 of our 78 homes (72%). Without exception, across all of the responses, answers to the statements that had the four anchor points (‘totally agree’, ‘agree’, ‘disagree’ or ‘totally disagree’) were either ‘agree’ or ‘totally agree’.
Eighty-nine per cent of respondents found the information about a resident's baseline Geriatric Depression Scale-15 score useful (Table 67). Control homes seem to have appreciated this information more than intervention homes. When asked how they had used this information the most popular responses were to encourage the residents (80%) and to monitor the residents (75%). Over half had contacted a general practitioner and about one-third had contacted the mental health team; other health professionals who were contacted in relation to this included community occupational therapy and district nurses. Some respondents reported that they had discussed the information with families and encouraged their involvement.
| Item | Intervention | Control | Total | ||||
|---|---|---|---|---|---|---|---|
| Returns (from 78 homes mailed) | 22 (63%) | 34 (79%) | 56 (72%) | ||||
| Paraphrased questions from end-of-study questionnaire a | |||||||
| Recruitment processes | |||||||
| n | % | n | % | n | % | ||
| Study was fully explained | Agree | 3 | 14 | 7 | 21 | 10 | 18 |
| Totally agree | 19 | 86 | 27 | 79 | 46 | 82 | |
| Mutually agreeable times (for assessments, etc.) | Agree | 3 | 14 | 8 | 23 | 11 | 20 |
| Totally agree | 19 | 86 | 26 | 77 | 45 | 80 | |
| Easily able to provide | Agree | 3 | 14 | 5 | 15 | 8 | 14 |
| Totally agree | 19 | 86 | 29 | 85 | 48 | 86 | |
| Identifying eligible residents (not burdensome) | Agree | 4 | 18 | 10 | 30 | 14 | 25 |
| Totally agree | 18 | 82 | 24 | 70 | 42 | 75 | |
| Raising awareness of depression | |||||||
| Depression score useful? (smiley faces) | Yes | 22 | 100 | 50 | 84 | 72 | 89 |
| How the depression information/score was used | |||||||
| Monitor resident | 18 | 82 | 24 | 71 | 42 | 75 | |
| Encourage resident | 19 | 86 | 26 | 79 | 45 | 80 | |
| Contact GP | 14 | 64 | 17 | 50 | 31 | 55 | |
| Contacted mental health team | 6 | 27 | 12 | 35 | 18 | 32 | |
| Contacted other health professional | 4 | 18 | 6 | 18 | 10 | 18 | |
| Other | 5 | 23 | 4 | 12 | 9 | 16 | |
Responses to questions related to training provided to the care staff in depression awareness and questions about any potential burden placed on the home by the OPERA research team when carrying out follow-up visits were again universally 100% positive (Table 68). Twenty-three respondents reported they had needed to contact the OPERA office for one reason or another. Twenty-two of these reported a very positive experience and outcome; the one negative comment relates to changes in study staff and issues not being passed on.
| Item | Intervention | Control | Total | ||||
|---|---|---|---|---|---|---|---|
| Returns (from 78 homes mailed) | 22 (63%) | 34 (79%) | 56 (72%) | ||||
| Paraphrased questions from end-of-study questionnaire a | |||||||
| Staff training | |||||||
| n | % | n | % | n | % | ||
| (Staff training) times mutually agreed? | Agree | 6 | 27 | 12 | 35 | 18 | 32 |
| Totally agree | 16 | 73 | 22 | 65 | 38 | 68 | |
| Staff responded well (to training)? | Agree | 7 | 32 | 13 | 38 | 20 | 36 |
| Totally agree | 15 | 68 | 21 | 62 | 36 | 64 | |
| Staff found training useful? | Agree | 7 | 32 | 10 | 29 | 17 | 30 |
| Totally agree | 15 | 68 | 24 | 71 | 39 | 70 | |
| Follow-up visits (3, 6, 9 and 12 months) | |||||||
| Follow-up visits not burdensome on the home? | Agree | 8 | 36 | 8 | 24 | 16 | 29 |
| Totally agree | 14 | 64 | 26 | 76 | 40 | 71 | |
| Follow-up visits not burdensome on the residents? | Agree | 8 | 36 | 9 | 26 | 17 | 30 |
| Totally agree | 14 | 64 | 25 | 74 | 39 | 70 | |
| Records easily available for review (at follow up)? | Agree | 5 | 23 | 9 | 26 | 14 | 25 |
| Totally agree | 17 | 77 | 25 | 74 | 42 | 75 | |
| Contact with OPERA office/team | |||||||
| Did you need to contact the OPERA office? | Yes (n = ) | 10 | 13 | 23 | |||
| Were concerns dealt with satisfactorily? | Yes | 9/10 | 13/13 | 22/23 | |||
We also obtained 100% positive feedback on the interactions with physiotherapists (Table 69) with respondents reporting that the physiotherapists worked well with the care homes and provided useful advice and information. Exercise groups too fitted well into the homes, were run as expected, the residents liked them and the home enjoyed having them twice a week.
| Item | Total | |
|---|---|---|
| Returns (35 intervention homes mailed) | 22 (63%) | |
| Paraphrased questions from end-of-study questionnaire a | ||
| % | ||
| Physiotherapist assessments (of residents) | ||
| Mutually agreeable times arranged? | Agree | 18 |
| Totally agree | 82 | |
| Usefulness of the physiotherapist (to the home) | ||
| Helping in solving mobility issues? | Agree | 18 |
| Totally agree | 82 | |
| Advice increasing physical activity? | Agree | 23 |
| Totally agree | 77 | |
| Exercise groups | ||
| Fitted well into the home? | Agree | 5 |
| Totally agree | 95 | |
| Ran as regularly as expected? | Agree | 5 |
| Totally agree | 95 | |
| Residents liked going? | Agree | 18 |
| Totally agree | 82 | |
| We enjoyed twice-weekly groups? | Agree | 5 |
| Totally agree | 95 | |
Thirty-nine of the follow-up respondents included comments about OPERA. A small selection of these are presented below:
-
We are grateful for having had the opportunity to participate in this study. The training that you supplied was helpful and the time that your trained nurse spent with the chosen residents was appreciated. I think that this study will be of value in the future.
-
Thank you all very much for allowing my home to participate in this study. We will now continue to maintain exercise groups with our residents because of the positive impact it has had.
-
Smiley faces and sad faces were extremely helpful. Doctor professional of medical issues were brought in and medication change, some up, some came off medication all together, now they all have smiley faces.
-
The staff and residents appreciated the visits by professionals.
-
OPERA took into account the need and well-being of our residents. A friendship was built up between residents, members of staff and management with all who came to our home involved with OPERA. Our residents will be carrying on with the exercise plan.
Quality control
The recruitment process and baseline assessments of participants were observed on a 13 occasions; this included observing the process of consent when this is being given by a third party owing to the cognitive impairment of the participant (one occasion).
The recruiting staff who were observed were all seen to adhere to the study procedures and there were no significant deviations from protocol (Table 70).
| Item | C&W | NEL |
|---|---|---|
| No. of recruitment staff | 3 | 2 |
| No. of recruitment staff assessed | 3 | 2 |
| No. of observations | 5 | 8 |
| Percentage of QC assessments where no significant action needed to assure adherence to procedures | 100 | 100 |
| Percentage of QC assessments where minor action needed to assure adherence to procedures | 0 | 0 |
| Maintenance/updating of OPERA files (in homes): percentage of QC assessments where no significant action needed to assure adherence to procedures | 100 | 100 |
| OPERA files security (in homes): percentage of QC assessments where no significant action needed to assure adherence to procedures | 100 | 100 |
During these observations, the challenges that recruiting staff face with this population in this setting have been noted. For example, these include:
-
the higher levels of cognitive impairment and frailty of the population
-
fitting in to a home's timetable (limited window of opportunity to carry out recruitment activities)
-
space to carry out assessment (often limited space and not very private).
On visits to the care homes above to carry out the recruitment checks and also on the numerous visits to the eight case study care homes the OPERA sites files were checked. It was found that data were being updated within care home files (e.g. new residents added or deaths/movements recorded) and storage of these files was generally secure within home managers' offices and were easily accessible to OPERA research staff if needed.
Depression awareness training (control intervention)
Research staff who were delivering the control intervention were observed on several occasions. These observations have shown that staff were delivering the intervention as the protocol stated and there were no significant problems. However, it has been noted that these research staff faced a number of challenges when carrying out this work. For example:
-
difficulties with some care homes making appointments for training
-
trainer turning up and care home staff not being there or aware
-
presentation equipment being a little small for large groups (laptops and speakers).
Intervention delivery
Although the lead physiotherapist measured the fidelity of the delivery of the exercise intervention, in terms of the individuals (physiotherapists) delivering it (see below), independent observations were also carried out by the process evaluation research fellow. Twenty-one of the exercise classes in the case study care homes were observed; seven in the early stages of their introduction (five homes once and one home twice), six at about the mid-point (once in each home) and eight at the end of the 12 months (four homes once and two homes twice). Observation at these times included how the session fitted into the day, how the residents were reacting, how the physiotherapist was interacting with the residents, care staff/ home involvement and what happened when it ended. These observations proved to be very positive, with groups being delivered as per protocol. Comments from interviews and notes from these field observations can be found within the process evaluation results section (see Chapter 2, Process evaluation).
Data security and data collection accuracy at base
All data were stored as per protocol and were secure. Although laptops proved to be difficult to use with this population for direct entry of data, there were no problems with the security of downloading of information from remote sites. All participant data were accounted for and entered. Problems were encountered because of the complexity of the study. These related to linking tables for participants who might have very different trajectories in the study and also related to the large amount of data on the intervention delivery. Following internal audits these were resolved by the study team.
Intervention physiotherapists
The lead physiotherapist trained a total of 26 physiotherapists to deliver the OPERA intervention, 24 of whom went on to deliver the intervention on a regular basis (owing to changes in personal circumstances two left before delivering any groups). The 24 physiotherapists who delivered the intervention had an average of 10 years' post-qualification experience (range 0–42 years) and their banding levels ranged between 5 and 7, with 67% of the physiotherapists having previously run therapeutic exercise groups and/ or worked in a care home setting (Table 71).
| Characteristics | C&W | NEL | Total |
|---|---|---|---|
| No. of physiotherapists | 8 | 16 | 24 |
| Employer (n) | |||
| University of Warwick | 8 | 2 | 10 |
| NHS | 0 | 12 | 12 |
| Private | 0 | 2 | 2 |
| Band on entrya (n) | |||
| Band 7 | 6 | 3 | 9 |
| Band 6 | 1 | 0 | 1 |
| Band 5 | 2 | 12 | 14 |
| Years qualified on entry: median (range) | 18 (1–32) | 7 (0–42) | 10 (0–42)b |
| No. of months working in OPERA homes: median (range) | 16.5 (4–27) | 6 (0–18) | 9 (0–27) |
| No. of homes assigned: median (range) | 3 (1–5) | 2 (0–5) | 2 (0–5) |
Satisfaction with training
All physiotherapists were asked to provide anonymous feedback in a questionnaire completed after the initial training days; 55% of the physiotherapists who completed the evaluation forms rated the training as ‘very good’, with the remaining 45% rating it as ‘good’ or ‘average’. The physiotherapists rated themselves as ‘very confident’ or ‘fairly confident’ to deliver 87% of the intervention elements and ‘a little confident’ to deliver 13% of the intervention elements. None of the physiotherapists rated themselves as not at all confident to deliver any of the intervention elements.
Intervention fidelity (physiotherapist)
The quality and fidelity of the intervention delivery was checked via a site visit made to each physiotherapist at one of their assigned care homes on at least two occasions: at 6 weeks and at 6 months after the intervention started in that home. The delivery of the exercise group and use of the whole-home approach were assessed by observation, and a sample of each of the intervention data collection and clinical record forms and registers was checked (unless any major issues were identified, in which case all were checked). The results of these quality assurance visits were documented, with the results shown in Table 72.
| Item | Not achieved: n (% of total) | Partially achieved: n (% of total) | Satisfactorily achieved: n (% of total) |
|---|---|---|---|
| Administration/record-keeping (completion of all forms/registers) | 3 (7) | 8 (20) | 30 (73) |
| Preparation for group (room, residents, resources, staffing) | 0 (0) | 0 (0) | 41 (100) |
| Storage and organisation of equipment | 0 (0) | 1 (3) | 40 (97) |
| Personal performance in running group (use of communication, music, facilitation) | 0 (0) | 6 (15) | 35 (85) |
| Content of group exercise session (intensity, progression, equipment use) | 0 (0) | 8 (20) | 33 (80) |
| Whole-home approach activities/communication/cooperation/support to care staff, mobility recommendations, equipment procurement | 0 (0) | 18 (44) | 23 (56) |
Long-term follow-up
Sample
We invited all 78 care homes to participate in the follow-up study (postal invitation with telephone follow-up). Thirty declined, a high proportion of which were control homes (n = 26). Thirty of the 35 intervention homes completed interviews (including five of the six case study care homes), one care home had closed down and four others declined. Seventeen interviews were completed with control homes (including one of the two case study care homes; the other home declined) (Table 73). Observations were undertaken in the six case study care homes that consented.
| Item | Intervention total | Control total | Total |
|---|---|---|---|
| All OPERA homes | 35 | 43 | 78 |
| Sample required (for follow-up) | 35 | 18 | 53 |
| Homes approached | 35 | 43 | 78 |
| Refused | 4 | 26 | 30 |
| Closed down | 1 | 0 | 1 |
| Total included | 30 | 17 | 47 |
| % of required sample recruited | 86 | 94 | 89 |
Quotations used in this section are illustrative of the themes within the heading. These quotes will include reference to their source, including the role of the interviewee and a number to indicate a home/origin (homes numbers 1–30 are intervention homes and numbers 31–47 are control homes).
Table 73 shows that 86% of the intervention homes took part in the follow-up substudy and for control homes 94% of the planned sample participated.
Activities co-ordinators and exercise groups
We asked specific questions about the homes having activities co-ordinators and the running of regular exercise groups (Table 74). With the exception of three cases, the role of activities co-ordinator was to promote ‘activity’ in the care homes. The three exceptions were that two were also the manager of the home and one was also a care assistant. When asked if the role had changed over the last 2 years most gave a positive answer. Some talked about how it had developed.
| Question/response | Intervention total | Control total | Total | |
|---|---|---|---|---|
| Someone responsible for ‘activity’? | Yes | 21 | 10 | 31 |
| No | 9 | 7 | 16 | |
| Activity co-ordinator working hours? | Full-time | 12 | 4 | 16 |
| Part-time | 9 | 7 | 16 | |
| Has role changed over the last 2 years? | Yes | 18 | 9 | 27 |
| No | 3 | 9 | 12 | |
| Does the home run regular exercise classes? | No | 7 | 4 | 11 |
| Yes | ||||
| External or staff run | 6 | 13 | 19 | |
| OPERA type | 17 | N/A | 17 | |
| How often are exercise classes run? | Daily | 1 | 0 | 1 |
| Once a week | 8 | 5 | 13 | |
| Twice a week | 8 | 4 | 12 | |
| Once a fortnight | 5 | 4 | 9 | |
It has developed. Before started no activities co-ordinator and it has grown over time.
Home 7, activities co-ordinator
We have become more proactive at getting them active.
Home 12, manager
Yes, adapted to changing needs of residents.
Home 47, manager
Interviewees also commented on how OPERA had influenced their decisions to employ an activities co-ordinator:
We didn't have an activities co-ordinator when OPERA started but OPERA showed us what could be done. We employed someone who was very good. And as OPERA ended she was able to continue with the groups. Sadly she had to leave us and we are currently looking for a replacement. It is OPERA that have given us this will to have someone.
Home 18, manager
Yes, when OPERA started we did have an activities co-ordinator but he was ineffective and after a short time left. Did not employ anyone during OPERA as OPERA were in twice a week; employed new person post OPERA.
Home 1, manager
Yes, got activities co-ordinator after OPERA as realised that resident well-being improved (made them happier).
Home 27, manager
Three homes reported having vacancies for activities co-ordinators, which they hoped would be filled soon.
Thirty-six of the 47 homes interviewed reported that they ran regular exercise groups. When asked when the last of these groups took place, most indicated that they had held exercise groups within the last week. Seventeen of the intervention care homes (around 50% of the total intervention care homes) had adopted versions of the OPERA exercise groups. Most of these were delivered by the care home staff (usually the activities co-ordinator); some took place twice a week, others just once. Several care homes had negotiated privately with the physiotherapist who either went in to deliver groups or went in to support the activities co-ordinator by doing regular assessments of the residents and providing advice and support. Two other intervention care homes were using OPERA-type groups but they have had to stop due to staffing problems in the homes and organisational changes (a number of our homes were part of the ‘Southern Cross’ chain, which went into receivership post OPERA). Another home was going to be starting OPERA-type groups again after residents at a residents meeting had asked for them to be reinstated.
Motivation went a bit and we stopped (after a number of deaths in the home). However, at a residents meeting a month ago a resident raised the issue and as a result we are reinstating it (OPERA groups); not yet started.
Home 22, manager
Awareness of depression and activity in the home
We asked specific questions about depression awareness and levels of activity within the homes. From those who responded to the question asking if they are ‘more aware of depression’, many linked this to the care home staff training we provided early in the project (Table 75). Many stated that they already knew about depression and were acting upon it. Others felt that they were more aware since OPERA, and several felt that they were seeing less depression.
| Question/response | Intervention total | Control total | Total | |
|---|---|---|---|---|
| Do you think you are more aware of depression/low mood in residents since OPERA? | Knew already | 7 | 4 | 11 |
| It was a good reminder | 2 | 0 | 2 | |
| Noticed less depression | 3 | 0 | 3 | |
| More aware | 9 | 8 | 17 | |
| No | 1 | 3 | 4 | |
| Has your approach to encouraging residents to be active changed? | No | 5 | 12 | 17 |
| Yes | ||||
| Activities co-ordinator now | 3 | 0 | 3 | |
| Run OPERA groups | 9 | 0 | 9 | |
| Do more activities | 12 | 4 | 16 | |
| Would you recommend changing the depression awareness training in any way? | No | 11 | 13 | 24 |
| More sessions or a follow-up | 19 | 4 | 23 | |
Saw a big change in staff; more aware of problems now and will report/refer.
Home 5, manager
Yes it has changed their mood they were much happier and more social.
Home 27, manager
Definitely noticed less depression.
Home 12, manager
We asked if their approach to encouraging residents to be active had changed; 17 of the interviewees said no. Within intervention homes the most reported change was the introduction of OPERA-type groups. There were also reports of more activities in general taking place in some care homes and the introduction of activity co-ordinators in others.
Yes, getting the residents going, lots organised including gardening.
Home 21, manager
Yes, we run regular OPERA-type groups now.
Home 2, activities co-ordinator
OPERA has changed us and we are now getting an activity co-ordinator.
Home 18, manager
Yes I have seen what the OPERA intervention can do for residents.
Home 30, manager
We do more with them now. Cooking, games puzzles arts and crafts floor games.
Home 10, manager
When asked about the staff training (depression awareness training in control homes and depression awareness and activity training in intervention homes), just under half of the interviewees reported that they would have liked the training to be either longer (with more sessions or a follow-up) or more in-depth (noted by some as too basic).
We asked two specific questions. The first was about the involvement of physiotherapists in the care home (and was asked only in intervention homes). The second asked about observed changes in the care home during OPERA (which was asked in both intervention and control homes) (Table 76). Control homes reported no OPERA-related changes in the home during the study. Without exception, all of the intervention homes placed high value on having access to a physiotherapist for 12 months and noted that this was not just owing to having them deliver the exercise groups; there were other benefits also. The most cited of these was the help, advice and support provided.
| Intervention homes | Total |
|---|---|
| What else did you get from having a physiotherapist on site twice a week? | |
| Help/advice/support | 29 |
| Equipment and aids | 10 |
| Freed up staff time | 4 |
| Increased resident social circle | 1 |
| Did you see changes in the home during OPERA? | |
| Residents | |
| More awake | 3 |
| Mobilise easier/more mobile | 16 |
| Increased mental alertness | 4 |
| Improved mood | 9 |
| Happier | 9 |
| Physically improved | 7 |
Advice and support ... Staff, families and residents asked for advice from physio ... Physio services very difficult to get in care home.
Home 30, manager
This theme was expanded to include the support and help given about equipment and aids which many homes found invaluable.
Physio really nice with residents, helped with equipment and advice.
Home 21, manager
Source of encouragement and information. Helpful to needs of residents. Aids, grab rails. Residents trusted her.
Home 24, manager
Noticed things, gave advice, aids (Zimmers, height of) helped staff.
Home 19, manager
Two care home managers commented that having the physiotherapist in the home twice a week freed up time for staff to do other things. One manager noted that the physiotherapist, and indeed the whole OPERA team, provided added social interaction for the residents, as we were someone different for them to talk to.
The most reported change observed in the intervention homes was that residents seemed more mobile. Some noted improvements in alertness and mood with some describing their residents as ‘happier’.
Yes, moods were better. One resident much more mobile. Physio spent time helping residents.
Home 11, activities co-ordinator
A lot of enjoyment in residents and staff ... mobility improved. Mood (of residents) got better.
Home 12, manager
Yes definitely some physical and mental changes improvements. They were happier
Home 6, manager
Residents were more awake some changes physically (able to mobilise easier) and mentally more alert.
Home 1, manager
More mobility and happiness.
Home 23, manager and carer
When asked if they would change the exercise groups in any way most said ‘no’; however, several did make some suggestions. These included sessions being a little longer, changes to the music (‘more jolly’), need to consider the residents with dementia, and, finally, perhaps breaking the sessions up with other activities.
Hard to get services some rehabilitation services but not a lot.
Home 16, manager
Difficult to get physio services in the home.
Home 28, manager
Many felt that if they were to pay for an OPERA-type service it would have to be reduced to perhaps once a week again due to cost. All stated that if the service were provided free of charge they would welcome it with open arms.
Over the moon.
Home 20, manager
Bring it ON.
Home 1, manager
Would grab with both hands.
Home 26, manager
Yes with open arms, such a good thing.
Home 15, manager
Asked if they would pay for an OPERA-type service for the care home all agreed that it would be nice if it were available. However, cost would be a huge issue as homes have limited or no budgets for these things. Some fund external activities via fundraising (e.g. raffles, garden parties) while other homes have small ‘activities’ budgets that have to be prioritised (e.g. how can the money be used to benefit the most residents).
Cost an issue may be able to pay about £50 but would have to come out of fundraising and residents fund.
Home 7, activities co-ordinator
Cost an issue have no funding for it. We pay up to £70 (for an entertainer) but this would not be every week.
Home 16, manager
£50/h (price they put on it) not feasible twice a week.
Home 11, manager
All felt that OPERA provided a valuable service to the care homes, a service that most found very hard to get. With a few exceptions, care home managers reported that access to physiotherapy services was very difficult. Most were required to ‘refer’ via the general practitioner and services could take weeks or months to appear and in some cases never appeared.
Asked about the overall experience of having OPERA in the home, all interviewees, from both control and intervention homes, reported this was a very positive experience. Intervention homes again referred back to the exercise groups and the role of the physiotherapist within the home and interviewees from control homes and intervention homes were very positive about day-to-day interactions with the OPERA team, stating that the team were always polite, made mutually agreeable appointments and were never a burden on the home, its residents and staff.
Really nice people, forms easy to complete not a burden, appointments always made.
Home 39, manager
Very motivating really enjoyed the experience.
Home 21, manager
Blended in ... part of Team ... all fitted into home really well
Home 23, manager and carer
Very positive, everyone was very professional and not a burden on the home staff or its residents. You placed no pressure on us.
Home 36, manager
Residents liked seeing the kind OPERA staff. It was easy for us and not a burden.
Home 38, manager
Asked at the end of the interviews if they had any more comments about OPERA, the most persistent comments were from interviews with intervention homes who expressed their sadness at OPERA ending and wishing it could continue.
Fantastic, sorry it has gone.
Home 10, activities co-ordinator
Drawback was it was only 12 months.
Home 2, activities co-ordinator
It was wonderful and we all miss it greatly it has left a big hole.
Home 6, manager
Observations and activity sweeps (case study care homes)
Six of the eight case study care homes (from the process evaluation) agreed to participate in this follow-up. Of the two which did not, one of the control homes had major staff changes and current staff could not comment on OPERA while the other (intervention home) had gone through ownership and managerial changes; thus both declined to take part.
Figure 20 represents an average of activity sweeps in each of the homes (at least eight sweeps of 90 minutes in each home over several days). These were compared with those undertaken at the end of the study (Table 77). Observation visits and these activity sweeps revealed that generally little had changed within the care homes since OPERA finished. In the five intervention homes, three carried on the OPERA groups at least once a week using their staff, one stated that they were unable to afford to run groups and the other did not as they had staffing problems. Comparison of the activity (see Table 77) shows that home 4 maintained a fairly good level of activity despite the fact that they recently lost their activities co-ordinator. Home 3 showed a reduction in recreational activities and this too was observed during visits. The care home manager reported she was struggling to motivate staff at present and this was clearly having an impact.
FIGURE 20.
Summary of daytime activity in six of the case study homes at post-OPERA follow-up.
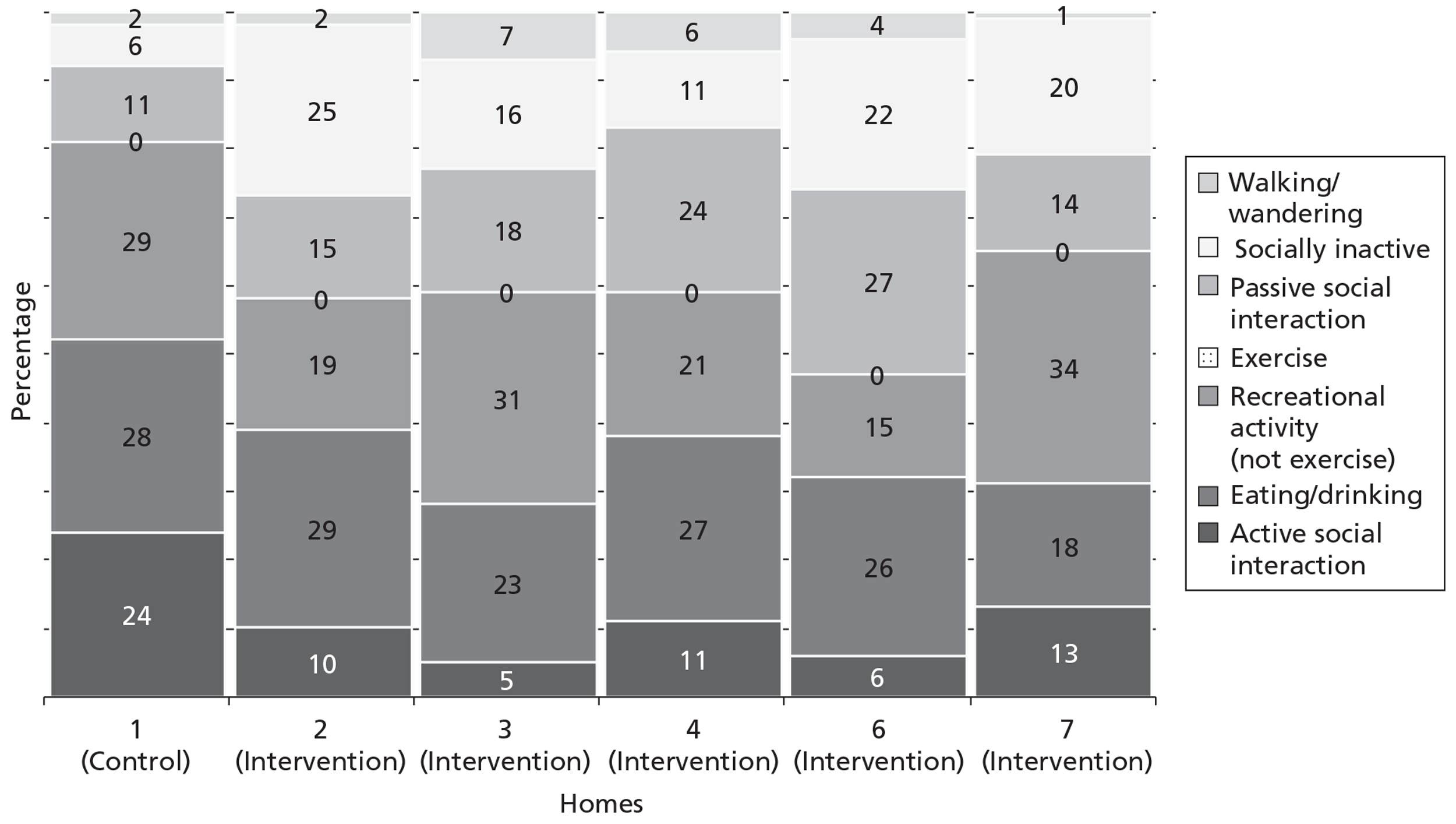
| Home | Time points/change | Activity codesb | ||||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
| Home 1 | a. Trial end | 25 | 28 | 30 | 0 | 11 | 5 | 1 |
| b. Follow-up | 24 | 28 | 29 | 0 | 11 | 6 | 2 | |
| c. Change (b–a) | −1 | 0 | −1 | 0 | 0 | 1 | 1 | |
| Home 2 | a. Trial end | 8 | 30 | 17 | 0 | 14 | 28 | 3 |
| b. Follow-up | 10 | 29 | 19 | 0 | 15 | 25 | 2 | |
| c. Change (b–a) | 2 | −1 | 2 | 0 | 1 | −3 | −1 | |
| Home 3 | a. Trial end | 5 | 22 | 37 | 0 | 16 | 12 | 8 |
| b. Follow-up | 5 | 23 | 31 | 0 | 18 | 16 | 7 | |
| c. Change (b–a) | 0 | 1 | −6 | 0 | −2 | 4 | −1 | |
| Home 4 | a. Trial end | 12 | 28 | 13 | 5 | 25 | 11 | 6 |
| b. Follow-up | 11 | 27 | 21 | 0 | 24 | 11 | 6 | |
| c. Change (b–a) | −1 | −1 | 8 | −5 | −1 | 0 | 0 | |
| Home 6 | a. Trial end | 4 | 23 | 16 | 0 | 32 | 21 | 4 |
| b. Follow-up | 6 | 26 | 15 | 0 | 27 | 22 | 4 | |
| c. Change (b–a) | 2 | 3 | −1 | 0 | −5 | 1 | 0 | |
| Home 7 | a. Trial end | 13 | 17 | 33 | 0 | 14 | 22 | 1 |
| b. Follow-up | 13 | 18 | 34 | 0 | 14 | 20 | 1 | |
| c. Change (b–a) | 0 | 1 | 1 | 0 | 0 | −2 | 0 | |
Chapter 4 Discussion
Overview
OPERA was a complex multifaceted study. The nature of both the intervention being studied and the population studied means that a simpler study design would not capture all of the active intervention's possible effects (positive or negative) on care home residents. In addition to obtaining data on the effects of the intervention we have also been able to investigate, in detail, both the process of running the study and of implementing a complex intervention within care homes. This has generated high-quality data on how to do research and on change implementation in this environment.
At the time we started OPERA we had serious concerns regarding whether or not the study was feasible. In particular there were concerns that care homes, which are often unfamiliar with research, might be reluctant to participate. Contrary to expectations, over half of the care homes we approached were interested in participating. Furthermore, no homes dropped out of the study after randomisation, meaning that we were able to collect ample follow-up data for our cohort analyses and for our end-of-study cross-sectional analysis we had a full complement of homes. Care homes and residents maintained their commitment to the study through what, for some, were difficult times or after many care home staff changes. For example, one care home needed to close during the study because of safety issues and residents were moved to other homes. We were able to follow up most of these residents in their temporary care homes, and after building work was completed, the home re-opened and residents returned, and we were able to complete our 12-month study assessments as planned.
The number of participants per care home was fewer than anticipated at the study design stage. This was partly because of the surprisingly high number of vacant beds in our homes and also the high proportion of residents who were too ill or too cognitively impaired to complete study assessments. For this reason, during the study we changed one of our primary outcomes to ensure that we had adequate statistical power, while still recruiting the originally planned number of homes. Our original sample size estimates were inflated to allow for clustering effects. One of the striking findings was that the intracluster correlation coefficients for participant assessments were very small or zero. These factors meant that although we recruited substantially fewer participants than originally planned (765 vs 1231, with a Geriatric Depression Scale-15 prior to randomisation) the effective number of participants contributing to our three primary analyses is substantially greater than specified in our revised sample size calculation. This means that all of our main effect estimates are much more precise than planned, giving reassurance that our findings are robust.
The overall findings of the study are clear and conclusive. We developed a high-quality intervention that was received extremely well both by staff and residents within the care homes. Uptake of the intervention was very good and was maintained throughout the 12-month intervention period. We have some evidence that homes welcomed, and were supportive of, the intervention package. There was not, however, any benefit on any of our primary or secondary outcome measures. The OR for residents being depressed at the end of the study was 0.75 (95% CI 0.52 to 1.08), the mean difference in Geriatric Depression Scale-15 in the cohort analysis at 12 months was 0.14 (95% CI −0.33 to 0.60) and for the depressed cohort at 6 months this was 0.23 (95% CI −0.50 to 0.96) (Table 35). The limits of the 95% CIs for the mean differences are less than the minimally clinically important difference specified for the study (1.2 points in the Geriatric Depression Scale-15), effectively excluding the possibility that the OPERA intervention has a meaningful effect on depressive symptoms as measured by the Geriatric Depression Scale-15. Furthermore, in our health economic evaluation the OPERA intervention was both more costly and less effective than the control intervention. We conclude that the OPERA intervention cannot be recommended as a means of reducing the burden of depression in care home residents.
OPERA care homes
The OPERA care homes were broadly representative of care homes in the two localities, except that we excluded larger homes and we recruited only one local authority-run home. Local authority homes have also been under-represented in previous studies.86 It is unlikely that the process of implementing the intervention in large or local authority-run homes would be so different from that in our included homes that the intervention would be substantially more effective. Our findings are generalisable to residents in these homes.
We included only one dementia specialist home. This was because of practical difficulties in obtaining our primary outcome data from residents in these homes. We observed substantial differences in approach to activity between dementia specialist units within OPERA care homes and the rest of the homes; these units were generally more proactive in encouraging activity. This is a difference we would expect to be seen also in dementia specialist homes. It is possible that within a dementia specialist home improved adherence to the exercise regimen might produce beneficial outcomes. Thus, although a large proportion of our participants had substantial cognitive impairment our findings are not necessarily applicable to dementia specialist homes.
OPERA participants
Recruitment
The number of participating residents per care home was fewer than originally planned; the number of eligible residents per home was 28 rather than the anticipated 32. Only 37% of eligible residents provided a baseline Geriatric Depression Scale-15 score and only 43% agreed to provide care home data. This is similar to the proportion of residents recruited to another recent UK care home study of a physiotherapy intervention, targeted just at those with mobility limitations. 86
Substantial numbers of residents were excluded (524/2078, 25%) (either because their health was too poor or because the care home manager felt that it was inappropriate to approach that individual for another reason). Those residents with poor health would have been unlikely to be able to participate in the exercise groups and would be unlikely to benefit from the intervention.
The baseline characteristics of those recruited prior to randomisation were broadly similar to population values. The baseline Geriatric Depression Scale-15 scores for our population (mean Geriatric Depression Scale-15 score 4.8, SD 3.3) (Table 19) are very close to those reported for care home populations in the UK (mean Geriatric Depression Scale-15 score 5.4, SD 3.2)120 and in the USA (mean Geriatric Depression Scale-15 score 4.8, SD 3.5). 122 This mean Geriatric Depression Scale-15 score also supports reports that a cut-off of 4/5 on Geriatric Depression Scale-15 has good sensitivity and specificity for detecting clinically significant depression among older people, with an expected prevalence of significant depression of 40% in a care home population.
Around half of our participants were depressed, with a mean Geriatric Depression Scale score of 4.8 (SD 3.3). Of the 374 participants depressed at baseline, only 92 (25%) had a recorded diagnosis of depression and only 126 (34%) were taking antidepressants (Table 22). This is indicative of substantial under-recognition and undertreatment of depression in care homes and concurs with findings in previous studies. 24,26
The mean Mini Mental State Examination score of 18.4 indicates that our participants had substantial levels of cognitive impairment and that our findings are applicable to the many care home residents with cognitive impairment. The mean EQ-5D scores of 0.57 (self-report) and 0.45 (proxy) attest to the overall poor quality of life of our participants. UK norms for people in the community aged ≥ 75 years were 0.73 (SD 0.27). 211 This is consistent with findings from previous studies. Of participants recruited in intervention homes, 16 (3%) were considered ineligible for the group sessions by the study physiotherapists. Our participants overall state of health was, as anticipated, very poor and representative of our target population of care home residents able to participate in exercise sessions.
The mean baseline Short Physical Performance Battery scores indicate poor levels of lower limb function. To our knowledge we are the first study to administer the Short Physical Performance Battery among a care home-dwelling population in the UK. Some studies in the USA have used the Short Physical Performance Battery in assisted living populations;212–214 however, it is not apparent that assisted living facilities in the USA are comparable with care homes within the UK. The floor effect, demonstrated in the baseline Short Physical Performance Battery scores, limits the ability of the Short Physical Performance Battery to detect deterioration in scores at the follow-up time points. Furthermore, as the Short Physical Performance Battery was designed for community-dwelling older adults, it may not be sufficiently sensitive to detect changes in lower limb function of the OPERA participants who are considerably more frail than older people living in the community.
Baseline social engagement shows a high percentage of residents reported as being highly socially engaged (i.e. interacting with others, very involved in activities, not withdrawn) in both the intervention and control groups (62% and 60%, respectively). In contrast, an international study of nursing home residents in five countries (Denmark, Iceland, Italy, Japan and USA) reported at most 30% of residents reporting high scores. In a large sample in the USA with high social engagement, residents also had high levels of cognitive function and high levels of activity of daily living. 142 This difference in apparent social activity may be related to how we used the measure. As originally designed, it was based on direct observation. For this study we used carer report, which might be subject to bias in measurement of absolute score. We would, however, expect it still to be sensitive to change.
Unusually in the OPERA study we also recruited participants after care homes were randomised to ensure that for our end-of-study cross-sectional analyses we were studying a representative population rather than just relatively healthy survivors. This analysis tells us the likely long-term effect of implementing the OPERA intervention on overall prevalence of depressive symptoms in care home residents. Again this population was broadly representative of the population of care home residents overall, ensuring that our findings are generalisable.
Follow-up
Overall we obtained good follow-up rates. As expected there was a lot of attrition due to death but loss to follow-up arising from residents moving out of an OPERA home was higher than expected. Thus although we were able to obtain a Geriatric Depression Scale-15 on around 90% of participants present in an OPERA home at each end point this represents only 61% of our population of interest for individual assessment data in the cohort analysis at 12 months in the control homes. Nevertheless, our follow-up rate was always in excess of three-quarters of those who were alive for the primary outcome – ensuring that our conclusions in the cohort analysis are robust. There was a consistent trend for more follow-up data to be collected in the intervention homes than in the control homes. Our findings did not, however, change materially in a sensitivity analysis in which missing data were imputed or when an extreme scenario sensitivity analysis was conducted (data not presented). As the study had a much more visible presence in the intervention homes it is not surprising that there was some differential follow-up. The process evaluation has identified how warmly the intervention was received in the homes. It is likely that this was translated into an extra willingness on the part of the care home staff to help follow-up assessments and, of course, an increased interest in assisting in data collection from residents and providing data on residents. The difference is small, however, and any bias introduced by this differential follow-up would be very unlikely to change our conclusions.
In this study we have made use of Secondary Uses Service data from primary care trusts to collect most health service activity. We are extremely grateful to the primary care trusts who kindly collated these data for us during a difficult time of organisational change within the National Health Service. These data became available just 12 weeks after the end of the study period. Although these data may not be as clean as a final Hospital Episodes Statistics data set, available 6 months after the end of the financial year in which the activity accrued, this has provided a very timely resource for monitoring health service costs in a standardised manner. This data set does, however, have some limitations for collecting causes of A&E attendances and outpatient appointments. Although we cannot be certain that any attendance for injury at an A&E department or at a fracture clinic is the result of a fracture, these are likely to be indicative of a significant injury and are a good marker for the safety of the OPERA intervention.
Clinical effectiveness
This is one of the larger intervention studies run in a care home environment. Surprisingly, for many of the participant-reported outcomes the intracluster correlation coefficient was zero, or close to zero. This is in contrast with findings in some other UK-based cluster randomised care home studies, which have found intracluster correlation coefficients in the range 0.37 to 0.49 for some outcome measures. 86,215 These intracluster correlation coefficients were, however, for measures such as the Barthel Index and the Rivermead Mobility Index, which were collected by independent assessors rather than directly from residents. Our largest intracluster correlation coefficient for assessment data, collected directly from residents, was 0.09 for the Short Physical Performance Battery; a larger intracluster correlation coefficient for measuring an outcome that is dependent on environmental and, possibly, assessor factors is not surprising.
We collected our proxy data from care home staff. Although the intracluster correlation coefficients were large enough to affect our statistical power (0.17 for proxy EQ-5D and 0.16 for Social Engagement Scale at 12 months) they were, surprisingly, much smaller than those found by others.
As a consequence of these small intracluster correlation coefficients we have sufficient data to make quite precise estimates for most of our primary and secondary analyses for between-group differences. Although we have conducted a large number of primary and secondary analyses we have failed to show any statistically significant differences in any of our outcome measures. The large numbers of participants means that we can be confident that these are true-negative effects.
Geriatric Depression Scale-15
Surprisingly, the point estimates for benefit from the OPERA intervention on the Geriatric Depression Scale-15 in both the cohort analysis (0.14, 95% CI −0.33 to 0.60) and depressed cohort (0.23, 95% CI −0.50 to 0.96) favour the control intervention (Table 35). We originally set the clinically important difference on the Geriatric Depression Scale-15 score as 1.2. It could be argued that this was based upon a minimally clinically important change for an individual, equivalent to the effect of loss of a spouse, rather than a minimally important change for a population and that we should have chosen a smaller mean difference as clinically important. 216 The limit of the 95% confidence for possible benefit from the OPERA intervention is around one-quarter of the minimally clinically important change for an individual and equates to a standardised mean difference of 0.1 (lower limit 95% CI 0.33, SD at baseline = 3.3), effectively excluding any possibility of a beneficial effect on depressive symptoms, as measured on the Geriatric Depression Scale-15, from the OPERA intervention. For the original research question set by the funders, the proportion of residents with depressive symptoms at baseline who experienced remission of depression (at 6 months), we had data on 259 participants. This is fewer than the 343 participants specified in the simple sample size from our original application, justifying our a priori decision not to consider this as a primary analysis. In this case the direction of change was in favour of the OPERA intervention. This might suggest a possibility that we are overlooking a true effect. However, this would seem unlikely, given that the direction of change for mean scores in the cohort analysis favours the control intervention.
That there was no difference in the prevalence of depressive symptoms between baseline and follow-up in the control group (mean Geriatric Depression Scale-15 at baseline and follow-up 4.7 and 4.6, respectively) (Table 35) suggests the control intervention was also ineffective and it is not the success of depression awareness training that means we failed to find a beneficial effect from the OPERA intervention. There was not a significant difference in the rates of antidepressant use between the intervention and control homes at any time point (Tables 46 and 47). Neither was there any suggestion of a difference in how many participants started or stopped antidepressants. It is therefore unlikely that changes in medication use, for example increased use of antidepressants in the control arm, masked a beneficial effect from the OPERA intervention.
We are aware of one other cluster randomised trial that has reported the effect of a reasonably similar exercise programme on Geriatric Depression Scale-15 scores delivered to a reasonably similar population in residential accommodation. Conradsson et al. 95 tested a moderate intensity functional exercise, delivered 29 times over 3 months, which did not include a whole-home approach. They found no benefit on the Geriatric Depression Scale-15 score at either 3 months (mean difference 0.09, 95% CI −0.55 to 0.74) or 6 months (n = 191)95 for all participants, or for those with a Geriatric Depression Scale-15 score of > 4 at baseline (mean difference −0.59, 95% CI −1.66 to 0.48 at 3 months; mean difference, 0.12 95% CI −1.12 to 1.37 at 6 months). Meta-analysis of these data and the OPERA data, for the main cohort and the depressed cohort, provide further support for the notion that such exercise interventions are unlikely to be effective in this population (Figures 21 and 22). For these analyses we have used Conradsson's 3-month data, which was at the end of the intervention period rather than 6-month follow-up, as it is at this time that any positive effect was most likely to be evident (the direction of change does favour the intervention in one of Conradsson's analyses), and pooled this with data from our primary analyses for these two populations.
FIGURE 21.
Meta-analysis of mean difference on Geriatric Depression Scale-15 in those with depressive symptoms at baseline.
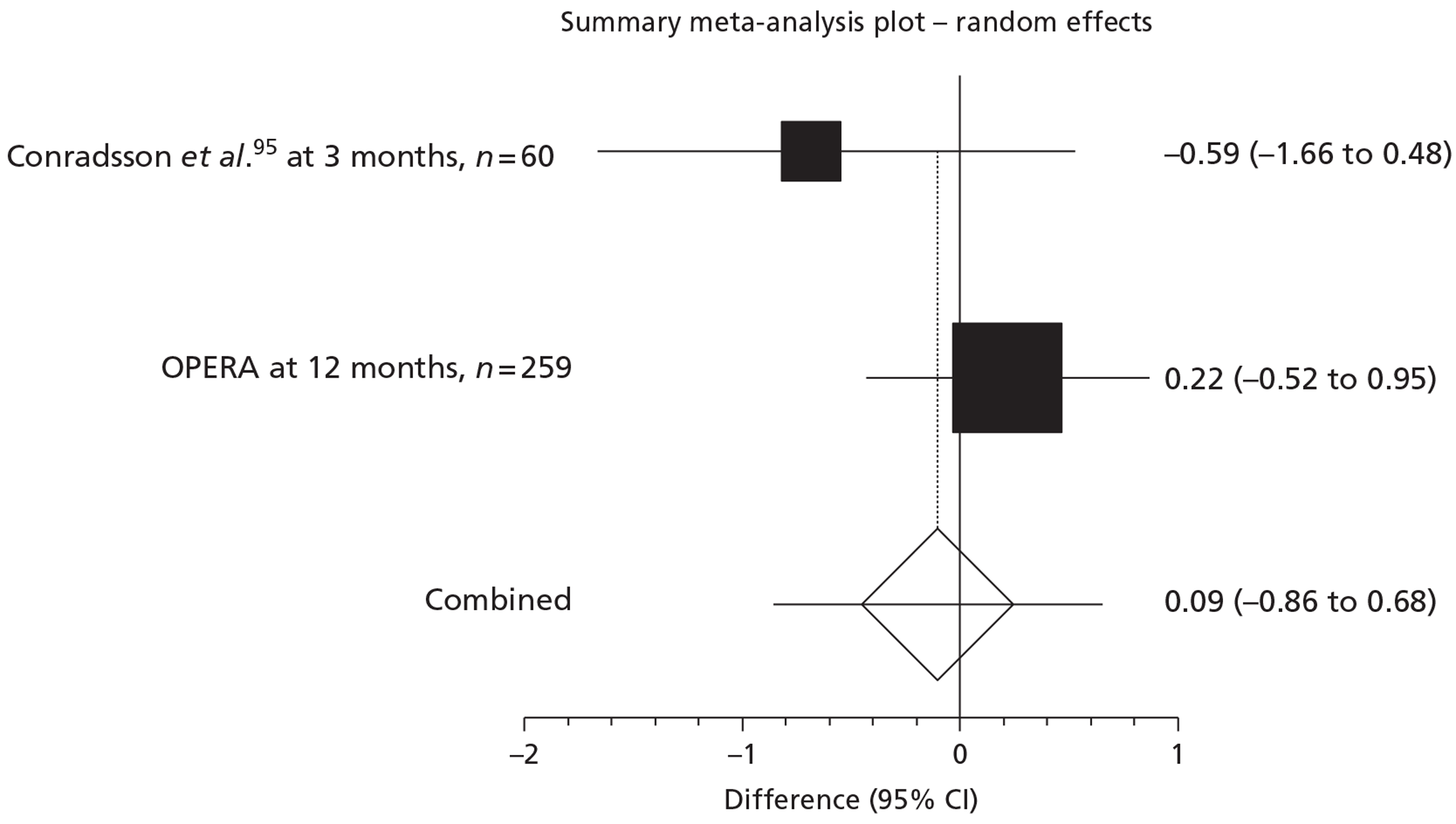
FIGURE 22.
Meta-analysis of mean difference on Geriatric Depression Scale-15 in all participants.
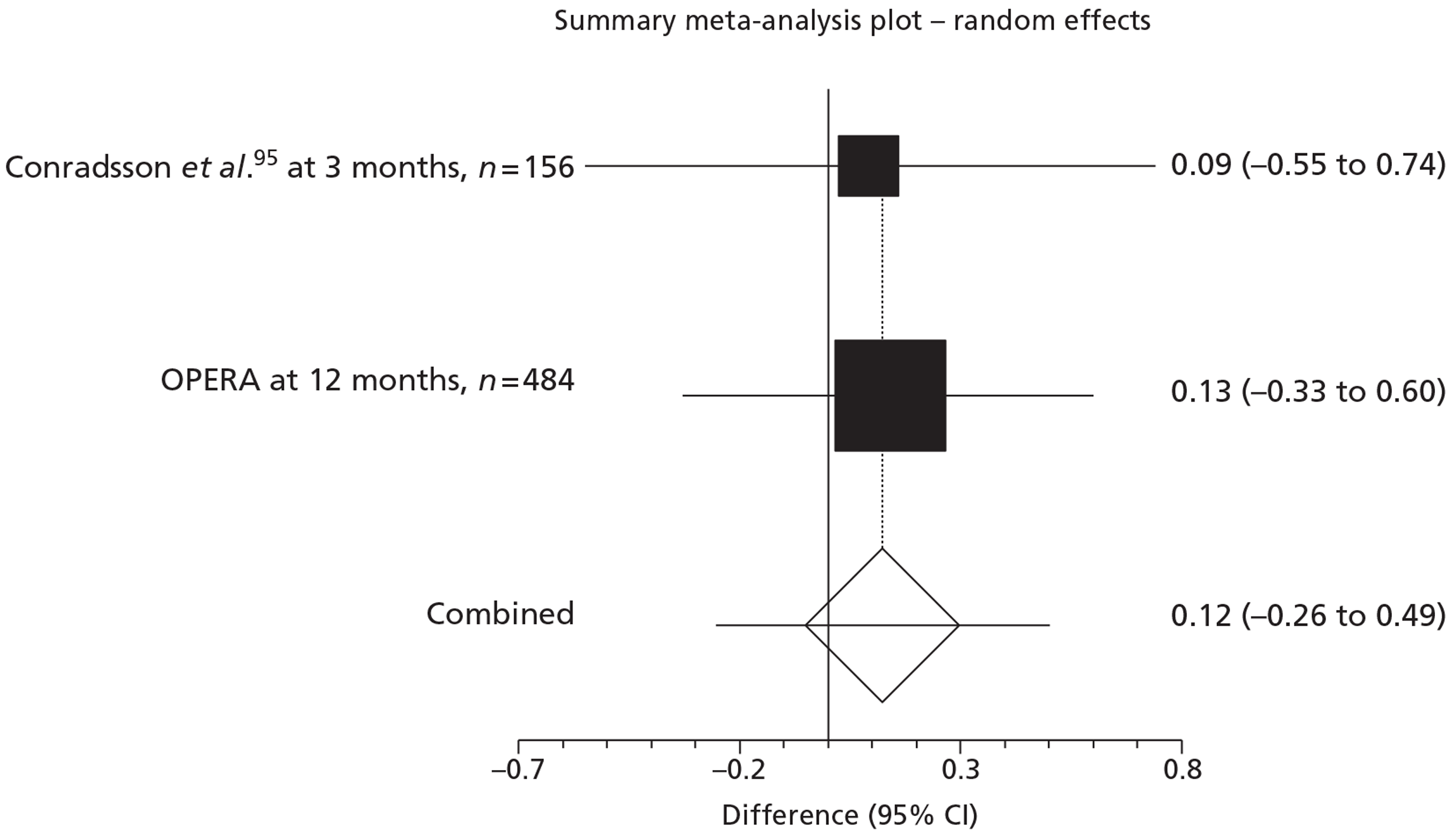
Other outcomes
The absence of any statistically significant difference in any of our other outcomes is notable. Only for the Short Physical Performance Battery does the difference approach statistical significance; this is the case on both the cohort analysis (0.30, 95% −0.05 to 0.64) (Table 41) and the cross-sectional analysis (0.24, 95% CI −0.1 to 0.57) (Tables 44 and 45). A change of 0.5 points on the Short Physical Performance Battery is considered a small but meaningful change, and 1.0 points a substantial change. 217,218 We have effectively excluded the possibility that the OPERA intervention will have a substantial effect on mobility and lower limb function. We have not excluded the possibility that the OPERA intervention might have a small but meaningful effect on mobility and lower limb function.
Failing to show a positive effect on the Short Physical Performance Battery may not be a surprising result given that the structured exercise activities needed to be performed largely seated due to the poor physical health and abilities of the exercise group participants, and so were less likely to positively affect the abilities measured by the Short Physical Performance Battery. Although the whole-home intervention included efforts to increase the amount of safe walking for all residents, it appears that the main effect of this approach was improved attendance and adherence to the structured exercise programme offered by participation in the exercise groups.
There is also an emerging literature suggesting that many very frail elderly people, such as those included in OPERA, may be unable to exercise at levels sufficient to fully participate in exercise activities and exercise intensities that might activate the physiological processes hypothesised to ameliorate depressive symptoms. 178,219–221
Our overall measure of health-related quality of life was the EQ-5D, self-reported and proxy. A priori we decided to use the proxy values, as we were anticipating a large amount of missing data, in particular for completion of the EuroQol thermometer. Although this was the case, fewer participants satisfactorily completed this at baseline and follow-up and the difference in intracluster correlation coefficients between the self-assessed EQ-5D (0.02) (Table 37) and the proxy EQ-5D (0.17) (Table 38) mean that the precision for the estimate is similar for both proxy and self-completed EQ-5D. Neither shows any significant benefit from the intervention in any of our analyses, with point estimates at, or very close to, zero; effectively ruling out any meaningful benefit on overall health-related quality of life from the OPERA intervention.
Safety
At the time we started OPERA there were significant concerns that we might have been exposing residents to some risk of harm. This was both around the time of the group exercise sessions and at other times when mobility was being encouraged. No directly attributable serious adverse events occurred during over 30,000 individual attendances at the exercise sessions by a very frail elderly population, which is a tribute to the professionalism of the physiotherapy team. Ascertainment of fractures in the population exposed to the intervention is important. We were able to collect medical record data only on study participants and so we needed to rely on pooled data from the care homes to ascertain overall fracture rates among all residents. Because there is a statutory duty to record these they should be a complete record but they do not give us data on person-years of exposure or identify those with multiple fractures at different times. There was, however, no suggestion of a difference here. The use of routine National Health Service statistics to identify fractures has the potential to provide confirmatory information on fracture rates, based on years of exposure. For inpatient events the data are of high quality but the quality of reporting in routine data sets of events in A&E departments and fracture clinics does not allow for definite diagnosis of fractures. Notwithstanding this problem the data clearly do not show any increased risk of injury fracture in the intervention group. Thus the OPERA intervention is very safe to deliver.
Cost-effectiveness
The results show that the exercise intervention made no significant difference in the number of quality-adjusted life-years accrued by residents while increasing overall costs due to the cost of delivery of the intervention. A high cost of implementation (£322 per resident) was expected for such an intensive intervention. This cost was not offset through decreases in health services use during the 12 months of the study. The intervention did not contribute to an increase in health service use. The findings of no significant difference in mean costs between residents in the intervention and control arms were consistent across all types of health-care visits. Consequently, the incremental cost of the intervention from an National Health Service perspective was £374 (95% CI −£655 to £1404) and £366 (95% CI −£664 to £1396) from a societal perspective.
The base-case analysis found the incremental quality-adjusted life-year figure to favour the control arm of the study; the difference was negligible (0.0014) with a wide CI (−0.0728 to 0.0699). The wide CI means that we cannot formally conclude equivalence in quality-adjusted life-years, as the limits of the 95% CI include values where we might have concluded that the intervention was cost-effective. The sensitivity and secondary analyses showed similar results. In light of the small negative effect from the intervention in all analyses, the economic evaluation does not support the use of the OPERA intervention. The low probability of the OPERA intervention being cost-effective at a willingness-to-pay of £20,000 and £30,000 demonstrates fairly conclusively that this is not a cost-effective intervention.
In such an elderly and frail population, it can be difficult to influence EQ-5D scores because there may be limited potential to achieve the relatively large changes in states within a domain (e.g. from confined to bed to some problems walking about). Often interventions in these populations are only able to slow the deterioration in quality of life rather than improve it. Furthermore, quality-adjusted life-years using the EQ-5D may not be an appropriate outcome for those receiving palliative care. 222 Twenty-three per cent of the residents included in the economic evaluation died during the 12-month follow-up period, indicating that many residents were effectively receiving palliative care at some point during the study. No better method currently exists to measure health utility for those at the end of life.
If there was a measure of health utility that was more suitable for use in this population, and that was more sensitive to change than the EQ-5D, then it might be easier to demonstrate cost-effectiveness of interventions in care homes. As the incremental cost of delivering the OPERA intervention is £374 per resident per year it would still need to show a net quality-adjusted life-year gain of at least 0.012 to be considered as cost-effective at a willingness to pay of £30,000 per quality-adjusted life-year.
Proxy EQ-5D data was chosen a priori for this analysis as it was more complete and collected more frequently, allowing for more residents to be included in our analysis. Over 25% of the self-reported EQ-5D data were missing at each time point. Some residents were unable to fill out the self-completed surveys because they were too unwell or cognitively impaired. Proxy data, however, has some shortcomings, as demonstrated by studies that compare self-completed quality-of-life surveys with those completed by a proxy. 138–140 In some homes, these surveys were completed by the care home manager due to language or literacy barriers or time constraints among the care workers working with the residents on a day-to-day basis. Although these care workers may have found it more difficult to complete the survey, they may have had a more comprehensive understanding of what life entailed for the residents. The care home managers, paradoxically, may have had a better understanding of the survey but may have had less interaction with the residents, which might have affected their interpretation of the residents' quality of life, although, particularly in smaller homes, the managers had a great deal of contact with their residents.
Process evaluation of the study
The process evaluation had some limitations. The number and spread of interviews carried out was smaller than planned, particularly with residents in the care homes. Relatives were also difficult to approach as we had no access to their contact information. Here we consider our finding under the different components of our process evaluation.
Context: aspects of the larger social political and economic environment that may influence implementation198
Our quantitative and qualitative data clearly illustrate the frailty of care home residents. A 2011 report from the British Geriatric Society concluded:223
Care homes and the residents they support have changed. They are no longer housing options for frail and financially insecure older people, as might be inferred from reading the National Assistance Act (1948) which set out in Part III the duty of local authorities to provide accommodation. They are now a major component of the welfare system's provision of care for vulnerable and clinically unstable older people. Many are now providing highly specialised services, for instance for older people with dementia.
The frailty of the residents and the high prevalence of cognitive impairment seen (see Chapter 3, Individual characteristics) led some care home managers to be pessimistic about the prospects of residents' participation at the start of the study, and doubtless impacted on the implementation of the OPERA intervention. Nevertheless, the principal message from our process evaluation is that, even in this challenging population, it was possible to recruit participants and to implement a complex, multicomponent intervention which made considerable demands on care home staff and residents.
Providing seamless health-care provision for residents in care homes within the independent sector has been identified as an important problem. For example, the OPERA physiotherapists succeeded in obtaining simple, relatively low-cost mobility aids that care homes had been either unaware of or unable to access.
The OPERA study took place across a period of increasing economic uncertainty and, latterly, in an evolving economic recession. The majority of UK care homes are part of the independent sector and one of the largest groups in the UK, Southern Cross, announced it was closing down just after the end of the study;224 four care homes from the chain took part in OPERA. Even at baseline the mean occupancy was 87% and the recruitment team reported that the number of vacant beds increased during the study. Observation and interviews in the care homes suggested that care home staff often have to work very hard and some resource-stretched care homes may have little spare capacity to engage in cultural shifts that might consume more carer time, such as promoting physical activity among frail elderly residents. Overall in England in 2009 about one-third of adult social care workers had been in their post for < 3 years, and one-third for 3–7 years (see State of the Adult Social Care Workforce 2010, Skills for Care, p. 11210).
One interesting finding from this evaluation is the difference between care homes within the OPERA study. The activity sweeps show patterns of activity that appear to be relatively consistent across time within the homes, but very different between homes, suggesting that there are huge differences across the care home sector. We do not fully understand why the culture around physical activity appears to differ so much between care homes and it seems unlikely that these differences could be completely explained by a difference in the mix of residents. The process evaluation identified some of the very different physical environments provided by different care homes but it is not fully understood how these environmental differences may impact on residents and care staff. The stability of patterns of activity across 12 months within the case study care homes suggests that changing the culture of homes, at least with regard to patterns of activity among residents, might be difficult.
Reach: the proportion of the intended target audience that participates in the intervention198
The OPERA study succeeded in recruiting a representative sample of care homes and the process evaluation suggests that care home managers and staff were enthusiastic about the intervention (even if they did initially express doubts about attendance). The evaluation suggests that it would be possible to introduce the intervention across the care home sector and it would prove popular with most homes.
The cluster randomised design meant that residents within participating homes were exposed to the intervention whether or not they participated in the evaluation of OPERA. Some residents who had neither consented nor been assented into the OPERA evaluation choose to participate in the exercise classes. Unfortunately, because we cannot collect outcome data on these residents we will not be able to measure any potential benefits or disbenefits and in this regard the true magnitude of the effect of the OPERA intervention remains partly unknown.
Dose delivered: the number or amount of intended units of each intervention or each component delivered or provided198
All 35 intervention homes and 42 out of 43 control homes received the depression awareness training session, although it was very difficult to arrange, and required considerable persistence, in a few homes. In one intervention home we were unable to deliver the intervention because the residents were too disabled to participate in the exercise group. The physiotherapists assessed all residents for eligibility and safety before they attended the exercise classes and fed this information back to the care home staff. Assessments also provided the opportunity to consider the aids a resident was using, and where necessary to make adjustments or indeed obtain suitable mobility aids/equipment. Across the intervention homes the physiotherapists delivered on average 90% of the maximum dose of exercise classes (Table 61).
We are not able to quantify the dose delivered of one aspect of this whole-home intervention, ongoing support and advice from the visiting physiotherapist to the care home staff, but it seems likely from the process evaluation that this aspect of the intervention may have differed between the two geographical locations of the study because of the different ways the physiotherapists delivering the OPERA intervention were employed at the two sites. If the intervention were to be rolled out across the care sector it is more likely that the model seen in NEL, where physiotherapists were seconded from the National Health Service to provide the intervention, would be followed. Our evaluation suggests that this model makes this aspect of the intervention more difficult to deliver.
Dose received: the extent to which participants actively engage with and interact with the recommended resources198
Just over one-third of participants attended 51 classes, our predefined estimate of an effective dose, with nearly 10% attending 41–50 classes (Table 63). In particular, attendance was good in those who contributed to our primary analyses. Attendance at the class does not, of course, mean that residents exercised to their set target level. There was little evidence of fall off in the numbers attending exercise groups across time, suggesting that ongoing group-based exercise in care home settings is viable. Only 9% of participating individuals attended no classes. This slightly disappointing attendance rate should be seen in the context of the very frail, sedentary, elderly population in the care homes and attendance rates at other exercise or other self-management interventions in community settings, which commonly have low attendance rates.
Vectors for change
Alongside the components of a process evaluation198 this evaluation was underpinned by the theory of change197 which we outlined in Chapter 2 (see Process evaluation). We identified four vectors through which activity among residents in the homes might be increased: care home staff training, exercise groups, physiotherapist contact with care home staff and improvements in the home environment.
Care home staff training took place and was positively received by those who participated. However, only around 39% of staff in intervention homes in C&W and 54% of staff in intervention homes in NEL actually attended the training. Initial feedback from both the intervention and control training suggests that there was some increase in care home staff's awareness of depression and how to deal with it, and there was some indication that intervention home staff were, with the help of the physiotherapist, more confident in promoting physical activity. However, in the very small proportion who returned a 3-month follow-up evaluation questionnaire, there was little evidence that attendance at the training had changed their practice. In contrast, interview and focus group data strongly suggested that, at least in some cases, the training of care home staff made a real difference to their awareness, ability and practice around promoting increased physical activity in residents. There was less evidence from qualitative sources that the training had influenced the awareness and recognition of depression in practice among care home staff.
The exercise groups were delivered as planned and information from the focus groups and interviews identified many positive effects of the groups and almost universal enthusiasm from the care home staff and residents for the groups, which only appeared to increase across the duration of the study.
Measuring the effect of the physiotherapists' contact with care home staff proved more difficult, and we have relied mainly on data from the observations, interviews and focus groups. Most of the comments about the physiotherapists, especially later in the study, were very positive, making it clear that they had come to be regarded as one of the team and would be sorely missed. However, it was clear that continuity was important. In cases where there were changes of physiotherapist, there were comments about the difficulties this raised. Care home managers and carers also valued the access to professional advice from the physiotherapists about their residents, which they seemed otherwise to find almost impossible to access. A further unexpected benefit of the visits of the physiotherapists was their role as an advisor or guide for care home staff negotiating access to other National Health Service services, including particularly the provision of appropriate mobility aids, but also, for example, providing advice on accessing mental health services.
Measuring changes in the home environment also proved challenging. The activity sweeps that we carried out in the case study care homes provided some insight into the variation between homes in patterns of activity (or inactivity), but failed to provide any evidence of change in activity over the duration of the intervention. Several care homes reported having regular exercise sessions at baseline but there was little evidence of such sessions in either control or intervention homes during the study. Indeed, some homes were seen to struggle to maintain a full activity programme, most commonly due to shortage of staff. Some care homes had activities co-ordinators appointed, but their effectiveness varied. Some were successful in promoting social interaction and activity, but others had many competing demands on their time (e.g. being a carer, errands) and were less effective as activities co-ordinators. Reported staff–resident ratio seems low across the day and in some cases it does seem that there were staff shortages.
There were two models of physiotherapist delivery: one used by the team in C&W and one used by the team in NEL. In C&W, the physiotherapists were employed directly by the University of Warwick to carry out the groups and usually had no other clinical commitments. This resulted in more continuity in provision and may also have meant that physiotherapists were less rushed and more likely to spend time talking to the staff in the care homes. In NEL, there was a contract with the local National Health Service physiotherapy service to deliver the groups; this resulted in less continuity and, because the physiotherapists had many other clinical commitments, may have meant that they were less able to linger to talk to staff in the care homes.
Hypotheses derived from the process evaluation
One very striking finding from all the observational work was the very large variation between homes in culture, daily activity and staffing level (Tables 15 and 16). At the time the process evaluation was being completed and before seeing the final results of the study, we hypothesised that the magnitude of any effect from the OPERA intervention is likely to vary considerably between care homes and this variability will lessen any overall effect size. This is because there is enormous variation between the care homes in the level of engagement of care home staff with the residents, and in the opportunities for activity within the care homes (including the opportunity for trips and activities outside the homes). We also hypothesised that there would be a dose effect, such that the intervention will have a greater effect on those attending a greater number of group exercise sessions. A caveat is that such a dose effect may be hard to detect if it should be found that the absence of depression is a key determinant of whether or not residents were frequent attendees at exercise classes.
Long-term follow-up
The aim of this follow-up was to explore if any beneficial changes in culture within homes brought about by having participated in the OPERA intervention appear to be persistent. It is clear that OPERA was well liked by the care homes and it also seems that it has had a lasting impact. Some care homes have adopted versions of the OPERA intervention and in some cases are still getting input from OPERA-trained physiotherapists (privately). It seems that OPERA has impacted on outcomes far beyond those measured, with reports of ‘happier’ residents and services beyond those normally available in care homes. There is some evidence that staff have benefited from the training and interactions with the OPERA team but little evidence that OPERA has changed practice other than promoting some homes to employ an activities co-ordinator and inspiring some activities co-ordinators to do more.
In terms of the factors that support beneficial change it is hard to be conclusive. Care homes that have adopted OPERA have probably increased ‘activity’ and social interaction in their homes, which should benefit the residents. Staffing and funding are barriers to sustainability of programmes such as this, as homes have to prioritise limited budgets. In light of the ineffectiveness of the OPERA intervention on depressive symptoms, it is unlikely to be prioritised by care homes for funding.
Little change was seen in control homes. Staff who were interviewed were complimentary about the training and interactions with the OPERA team. As with the intervention homes, there were control homes with lots of activities for residents and some with very few.
Ethics
Cluster randomised trials and care home managers as gatekeepers for research in care homes
Cluster randomised trials raise particular ethical considerations due to lack of individual consent from all participants in the clusters for at least some aspects of the study. National and international ethics guidelines allow for waiver of consent in specific circumstances and cluster randomised trials are recognised as one potential justification for not obtaining explicit individual consent from all research participants. 225 However, the ethical justification for this must include strong scientific, practical or economic reasons as to why a cluster randomised design is necessary for the research question to be answered. This should include an explanation of the importance of the benefit of the research to the community in which the research takes place (and the individuals in that community), and that the potential harm to individuals within the cluster as a result of the research will be minimal. In addition, researchers should endeavour to seek individual consent whenever possible within the research project, and take steps to ensure appropriate cluster representation mechanisms to protect the interests of the cluster. 225 The OPERA intervention was a whole-home intervention and therefore individual consent for the intervention was not possible. Individual consent (or use of a personal consultee) was obtained for data collection at the individual level, although some pooled anonymous data on fracture rates were also collected at a home level without consent. The whole-home intervention, however, included a physiotherapist-led group exercise class that was offered to individual residents. All residents, whether or not they had consented to participate in data collection, were encouraged to attend the exercise classes but a refusal to attend, or a resident's request to leave during the class, was respected in line with normal clinical or home practice for group activities. Thus agreement to participate was obtained but there was no formal research consent process for participation in the intervention. Clinical records were kept for residents attending the exercise classes in line with Good Clinical Practice but these were kept separate from the research data for residents who had not consented to data collection. The complexity of the different levels of consent and arrangements for data confidentiality in OPERA reflects the endeavours of the research team to comply with guidance on cluster randomised trials and illustrates the need for researchers to consider the ethical and practical issues of consent carefully in relation to the specifics of the particular cluster randomised trial being conducted, as recommended by Eldridge et al. 98
The care home managers in OPERA had a key role as both cluster guardians, providing consent for randomisation and implementation of the interventions, and gatekeepers to individual residents for recruitment for the assessments. The literature on cluster randomised trials emphasises the role of cluster guardians in protecting the interests of cluster members. Our interview data from care home managers suggest that they took this role very seriously, choosing to participate in OPERA because they considered that the intervention was likely to benefit their residents but also monitoring the researchers and controlling access to residents and relatives. The importance of care home managers and staff in the recruitment of participants to research in care home settings has been noted previously. 100 Reasons for excluding access varied and included the care home staff's views on a resident's capacity to consent, a resident's or their NOK's physical frailty, and the value they placed on their privacy. We found similar reasons in OPERA. There is a difficult ethical balance to be struck by care home managers in protecting their residents' interests while not denying them the opportunity to participate in research if they wish. Some home managers in OPERA were surprised when residents made decisions that were different to those they had predicted. On the other hand enthusiasm and a sense of ownership of the study could lead to care home staff putting implicit pressure on residents to take part, either in the intervention or the assessments. The care home staff we interviewed were aware of their position as trusted intermediary between residents and their families, and the research team, reassuring residents about the study but respecting their right to say no.
Assessment of capacity and the process of consent
A major challenge identified by the recruitment team in OPERA was the process of assessing capacity and gaining consent from individual residents for the assessments and access to medical records. The difficulty of obtaining valid consent when a substantial number of the relevant population have cognitive impairment was also identified by key informants in the ethics substudy. Notwithstanding that many OPERA participants had substantial cognitive impairment, 67% of participants were assessed as having capacity and gave consent. A similar mismatch between Mini Mental State Examination scores and capacity to consent was found by Warner et al. 101 Cognitive impairment, per se, is clearly not determinative of whether or not a person has capacity to make a specific decision such as consenting or refusing to participate in a research project. This poses serious challenges for recruitment staff, placing on them the burden of assessing capacity, ensuring that potential participants have the opportunity to exercise their autonomous wishes but not accepting agreement where there is no understanding. Assessing capacity in people with cognitive impairment is not straightforward, even when using standardised capacity assessment tools. Kim et al. 102 found marked variability in judgements of capacity of people with Alzheimer's disease to consent to research or to appoint a research proxy by experienced psychiatrists, including both between expert and within expert variability. An added difficulty is that capacity may fluctuate, not only over the course of a longitudinal study, which is well recognised, but also from day to day, for example between assessment of capacity and taking of consent. Given the above difficulties it may need to be accepted that judgement of capacity to consent to research in this population may have to be different to those judgements in other populations.
The Mental Capacity Act 2005 specifies retention of relevant information as a component of the capacity test but does not require indefinite retention. 105 Usual practice for the research consent process is to provide participants with at least 24 hours between provision of information and obtaining consent to allow the person to consider the information at greater length and to minimise any likelihood of implicit coercion. This raises the question of whether or not the participant must retain the information over this period for them to be assessed as having capacity. There is no consensus on this issue among researchers or the research ethics community. Goodman et al. 100 have described conflicting views on retention by care home managers directly affecting their recruitment of residents with dementia into a research study. The experience in OPERA was that retention for 24 hours was often not achieved but that provision of information some time before the consent process was useful as a first step in the process of information consolidation and in the establishment of a relationship between the researcher and resident.
The importance of a relationship of trust between researcher and participant for the success of the consent process was a key finding of the ethics substudy. Older people are more likely to consent to take part in research if they know and trust the person giving them the information about the study. This will be particularly true for residents of care homes who have less independence and may have cognitive impairment, contributing to feelings of vulnerability. The presence of care home staff or relatives to support, reassure and advise residents can be seen as facilitating autonomous decision making, although the risk of implicit coercion must be borne in mind. However, the idea that the trustworthiness and familiarity of the researcher encourages consent, perhaps even when understanding of the research by the participant is limited, requires further exploration. Difficulties with the formality and complexity of research paperwork and a reluctance of older people to sign documents, or preferring a relative to sign on their behalf, raise further issues for researchers in developing an appropriate consent process that respects older people's preferences and experience.
Recruiting participants who lack capacity
Many research participants in care homes lack capacity to consent to take part in the research (33% of participants in OPERA). Prior to the implementation of The Mental Capacity Act 2005,105 the legal position regarding research with adults who lacked capacity to consent was unclear for studies not covered by the Medicines for Human Use (Clinical Trials) Regulations (2004). 226 The Mental Capacity Act 2005105 sets out the criteria under which such research may be lawful, which includes a requirement that researchers consult with either a personal or nominated consultee to seek advice on whether or not the person who lacks capacity would have objected to taking part in the research if they were able to consent. OPERA commenced in 2007, shortly after implementation of The Mental Capacity Act 2005,105 when there was still some confusion among researchers and research ethics committees regarding the process of involving personal and nominated consultees for people who lacked capacity to consent to research. 106,107 Our recruiting staff found the process of identifying and approaching personal consultees straightforward but very time-consuming, an experience shared by other researchers. The recruitment rate through personal consultees was disappointing (48%), with 23% not responding to letters of invitation. In addition, we were unable to identify anyone willing to be a nominated consultee when no personal consultee was identified. The difficulty in engaging both personal and nominated consultees for conducting research will pose a challenge for future research. A substantial proportion of the relevant population could be excluded from participation in research studies. This could potentially affect generalisability of results, although the nature of the OPERA results is such that this would be unlikely in this case.
The difficulties of identifying appropriate proxy decision-makers for consent to research in the emergency setting has led to the recognition of waiver of consent for this type of research in some research ethics guidelines. 103 However, in non-emergency settings the argument of urgency does not hold and the requirements of the relevant legislation (clinical trials regulations or The Mental Capacity Act 2005105) must be fulfilled. In many settings identification of a personal consultee will be straightforward as they are likely to be living with the person or in close contact. Care home residents, however, may not have a readily identifiable person to consult, for example if they have no close family or friends and their designated NOK is not in regular contact. Two UK studies that specified recruitment rates for care home residents through proxies or consultees reported levels of 61% and 41%, respectively. 100,108 Recruitment of research participants who lack capacity by using consultees or proxy decision-makers raises a range of legal, ethical and practical issues that may be context dependent and that require further exploration.
The OPERA study met the criteria for waiver of consent in that (1) it had appropriate approval from a multicentre research ethics committee; (2) the intervention was a whole-home intervention, with the exercise classes including people who had cognitive impairment that may have affected their capacity; (3) it was not possible to provide the intervention selectively to residents with capacity and all residents had the potential to benefit without a disproportionate burden of taking part; (4) residents in the control homes, and those taking part in the assessments, were at negligible risk of harm; and (5) the research provided knowledge of the effect of the intervention on depression in residents of care homes, a condition that either affected or had the potential to affect all participants.
Strengths and weaknesses
Particular strengths of this study are that we have recruited a large sample of residents from a representative sample of care homes. This indicates that these findings are generalisable to UK care homes. Although we recruited a smaller proportion of residents than planned (38% vs 50%), the results will be applicable to the overall care home population; as the intervention was ineffective in the more capable and motivated residents who joined the study it is unlikely that it would have any positive effect on those who were too ill to participate. We achieved good follow-up rates. Within the limitations of the outcome measures used we have achieved very precise estimates of the possible effect of the OPERA intervention. However, the study is limited by the sensitivity of the measures used and it might be that other, more sensitive, outcome measures might have shown a benefit, particularly on health-related quality of life.
Any outcome measure measuring depression in a trial focusing on depression in a frail population such as ours should ideally be short, sensitive to change, have face validity, have a relative lack of directly or indirectly somatic items that are likely to be affected by physical health problems, and should have concurrent validity against a gold standard measure (expert clinician judgement). The Geriatric Depression Scale-15 has been shown to be sensitive to change. 121 The full Geriatric Depression Scale–30, from which the shorter 15-item version is drawn, has been shown to demonstrate significant change in intervention among a very similar population of Australian care home residents. 15 It has been used as a primary outcome measure in trials of interventions for depression among older people. 95,124,227–229 In Conradsson et al. 95 the Geriatric Depression Scale-15 was used as the primary outcome measure in a trial of a reasonably similar intervention (exercise) and setting (residential care homes) and range of cognitive impairment. At the core of depressive disorders are low mood, reduced energy and reduced enjoyment; the Geriatric Depression Scale–15 items have demonstrated ability to distinguish older people with depressive disorder from those without and despite the atypical situation of care home residents, we believe that any intervention with antidepressant effect should be able to show a reduction on Geriatric Depression Scale-15 symptoms.
Potential alternative outcome measures for trials among people with depression include The Montgomery–Åsberg Depression Rating Scale (MADRS),230 the Hamilton Depression Rating Scale (HDRS),231 Center for Epidemiologic Studies Depression Scale (CES-D)232 and the Cornell Scale. 233 Importantly, very similar outcomes have been found for the Geriatric Depression Scale-15 against alternative established measures of depression, including MADRS and CES-D,229 and against clinician ICD-10 diagnosis149 of depressive disorder. 227
Against other potential measures the Geriatric Depression Scale-15 is significantly shorter than the MADRS,230 the HDRS,231 CES-D232 and the Cornell Scale. 149 Of these scales, the Cornell Scale149 includes 3/19 items that are indirectly affected by physical disorder (appetite loss, weight loss and lack of energy), the MADRS230 includes items on lack of sleep and reduced appetite, the HDRS includes – within its 17 symptom areas – three directly somatic items including gastrointestinal, genitourinary and general somatic symptoms, while the CES-D232 includes one item on lack of appetite.
What was perhaps surprising in the OPERA study was the degree of frailty and cognitive impairment among potential participants, which limited the pool of potential participants who were able to complete the primary outcome measure. Nevertheless, with the substantial numbers in the analyses with full data on Geriatric Depression Scale-15, the choice of instrument was appropriate for this population and the findings are robust.
The primary hypothesis for this study was that promoting physical activity might reduce depressive symptoms. Depression rating scales are, however, only one way of measuring low mood. Since we designed this study there has been a developing interest in well-being as a health outcome. The observational work in our process evaluation suggests that although we did not change any of our objective outcomes, the OPERA intervention did effect some changes within the care homes and we had good participation in the group exercise sessions. It may be that if we had measured well-being instead of either depression or health-related quality of life we might have had a positive impact. Although measures are becoming established for the measurement of well-being in the general population, for example the Warwick–Edinburgh Mental Well-being Scale (WEMWBS),234 these are not yet well established in care home residents. The social well-being of nursing home residents (SWON-scale) is a candidate that was developed during the lifetime of the OPERA study and might be a suitable measure. 235 Furthermore, we have not measured the effect that our intervention may have had on the care home staff. It was clear from our observations in the homes that the level of interest in the work and training of care home staff was greater than that which they normally experienced. The staff also particularly valued the contact with the OPERA physiotherapists. We have not been able to measure, and account for, these effects in our analyses.
We were unable to collect Short Physical Performance Battery data at the 6-month follow-up data when we changed to collecting 6-month outcomes on all participants rather than just those with depression. This was because much of this was a particularly time-consuming test taking around 15 minutes per participant; this was substantially greater than anticipated at the time we designed the study. With the help of research nurses from the primary care and mental health research networks we were able to collect these data at baseline and 12 months but adding in 6-month data would have increased the workload above capacity at a time when we were at our maximal home recruitment rate. This does mean, however, that we are not able to examine if changes in Short Physical Performance Battery at 6 months mediate any possible changes in depressive symptoms at 12 months.
We have developed a high-quality, theoretically informed intervention that was popular with care homes. We were able to deliver this satisfactorily within homes without any related serious adverse events.
Overall we believe this is a very robust study that has obtained a clear answer to the research question set and has helped to develop our understanding both of how to undertake research in a care home environment and how care is delivered in this environment.
Conclusions
Implications for health care
There is a high prevalence of depressive symptoms in those living in care homes; much of this is unrecognised. There is a clear need for research to reduce the burden of depression in this group, many of whom are extremely frail and have a very limited life expectancy. It is possible to recruit care home residents with substantial cognitive impairment to studies; however, there remain some structural problems for obtaining agreement from those whose NOK cannot be contacted to take part in research. The OPERA intervention, targeted at improving physical fitness and social interaction, could be delivered safely and to a high standard over a prolonged period. Both residents and care home staff valued participation in the study, and also the activities of the physiotherapists in promoting physical activity within the homes. There was less evidence of achieving a cultural shift in the attitude towards physical activity in care homes. In some homes, however, we were able to achieve some sustained changes that were maintained after the end of the study. The OPERA intervention had no positive effect on any of our primary or secondary outcome measures and it was dominated by the control intervention in the health economic analysis. This evidence does not support the use of moderate-intensity functional exercise programmes, such as the OPERA intervention, to reduce depression in care home residents.
Recommendations for future research
-
A cluster randomised trial of care home staff training in basic psychological/behavioural techniques may include cognitive approaches (positive thinking/installing hope) and behavioural approaches (suggesting positive activities). This could also include case finding followed by referral for advice on optimisation of drug regimen.
-
Development and evaluation of measures of wellness and health utility that are specific for care home populations, suitable for completion either by residents or by proxies on their behalf.
-
Observational studies to identify modifiable factors that impact on the wellness of care home residents.
-
Work to further develop the evidence base of best practice for recruitment of those who lack capacity, in a variety of clinical situations, to take part in clinical trials, informed both by ethical and legal analysis and empirical data from key stakeholders including trial participants or their NOK.
Acknowledgements
OPERA care homes
We are grateful to the staff and residents of the following care homes: Abbcross Nursing Home, Essex; Abbeyfield Residential Home, Essex; Abbotsford Nursing Home, Essex; Albany Nursing Home, London; Albion Park House, Essex; Alton House, Essex; Alveston Leys, Stratford-upon-Avon; Angel Lodge, Ilford, Essex; Apple Garth Residential Care Home, Coventry; Arden House, Leamington Spa; Arden Park Care Home, Coventry; Arran Manor, Essex; Attleborough Grange Residential Home, Nuneaton; Avondale Nursing Home, Essex; Bentley Home Care Centre, Warwick; Bethany Residential Home, Leamington Spa; Birchwood Residential Home, Essex; Cambridge Nursing and Residential Care Home, London; Charnwood Residential Home, Coventry; Clarendon House, Coventry; Clarendon Manor, Leamington Spa; Collyhurst Residential Care Home, Bedworth; Compton Manor Care Home, Coventry; Cranvale RCH, Essex; Dewar Close Residential Home, Rugby; Drayton Court, Nuneaton; Dury Falls Residential Care House, Essex; Eastwood Lodge, Essex; Ebury Court, Essex; Eric Williams House, Coventry; Eversleigh Nursing Home, Leamington Spa; Fairfield, Coventry; Forest View Residential Home, London; Forest Dene, London; Fountain Lodge, Coventry; Fountains Care Centre, Essex; Four Ways, Leamington Spa; Grove House, Coventry; Hall Green Residential Home, Coventry; Hanbury Court, Essex; Haven House, Kineton; Havering Court Nursing Home, Essex; Hillside Nursing Home, Essex; Homesdale, London; Homewood, Leamington Spa; James Hirons Care Home, Leamington Spa; Kenilworth Manor Nursing Home, Kenilworth; Ladyville Lodge, Upminster; Lammas House, Coventry; Lisnaveane House, London; Longlea, Nuneaton; Malvern House, Essex; Manor Court, Nuneaton; Minster Residential Care Home, Coventry; Newstead Lodge Nursing Home, Southam; Palm Nursing Home, Essex; Parkside, Essex; Pinewood, Essex; Romford Grange, Essex; Rosewood Lodge, Essex; Rowallan House, Essex; Selborne Court, Coventry; Spencer Newham House, Coventry; St Andrews House, Coventry; St Catherine's, Leytonstone; St Ives Lodge, Chingford; St Joseph's Rest Home, Essex; St Martin's Rest Home, London; Stratford Bentley Nursing Home, Stratford-upon-Avon; Sycamores, Leamington Spa; The Knowles Care Home Ltd, Coventry; The Oak's Residential Care Home, Essex; The Spinney Residential Home, Coventry; The Willows, Coventry; Three Willows, London; Victoria Gardens, Coventry; Victoria Lodge, Essex; Victoria Park Residential Home, Coventry; Weavers Care Home, Coventry; West Lodge Residential Care Home, Essex; and Woodside Residential Home, Warwick, for their co-operation and enthusiastic participation in the OPERA trial.
We are grateful for the support of the following research networks and individuals:
Jo Burns (Manager, Greater London PCRN and Network), Primary Care Research Network – West Midlands South, Heart of England Hub Mental Health Research Network, Sandra O'Sullivan (Manager, North London Hub of the Mental Health Research Network and Hub), Central and East London Comprehensive Clinical Research Network.
We are grateful to the following primary care trusts and individuals:
Fay Baillie (Caldicott Guardian, Coventry Primary Care Trust), Simon Burton (Information Analyst, West Essex Primary Care Trust), Mark Chapman (Intelligence Consultant Community & Mental Health, Warwickshire Primary Care Trust), Lisa De Bruin (Business and Performance, North East London Foundation Trust), Mark Elverstone (Business and Performance, North East London Foundation Trust), Julia Hardcastle (Personal Assistant, Havering Primary Care Trust), Jacky Hayter (Head of Information and Performance, Havering Primary Care Trust), Kevin Hough (Head of Information, North East London Foundation Trust), Steve Johns (Information Analyst, Coventry Primary Care Trust), Jane Marley (Information Governance Manager, West Essex Primary Care Trust), Marie Matthews (Information Governance Manager, Coventry Primary Care Trust), Jenny Minihane (Director of Nursing and Quality, West Essex Primary Care Trust), Marie Price (Director of Corporate Affairs, Redbridge Primary Care Trust), Pat Ryan (CLRN Information Manager, West Midlands South), Jacqueline Sinclair (Information Governance Manager, Barking & Dagenham Primary Care Trust), Andy Wan (Senior Information Analyst, Barking & Dagenham Primary Care Trust), Carl Wilson (Information Analyst, West Essex Primary Care Trust) and Tim Woodman (Medical Director, Outer North East London Community Services), for their assistance in collecting Secondary Uses Service data.
This project benefited from facilities funded through the Birmingham Science City Translational Medicine, Clinical Research and Infrastructure Trials Platform, with support from Advantage West Midlands (AWM).
Contribution of authors
Martin Underwood (Professor of Primary Care Research, University of Warwick) was the lead applicant and chief investigator for the OPERA trial. Substantial contributions were made to the overall design of the study, the statistical analysis plan, and the writing of the background, methods, results and discussion sections of the report.
Sallie E Lamb (Professor of Rehabilitation and Director of CTU, University of Warwick) was a co-applicant, led the design of the OPERA exercise intervention and contributed to the writing of the background and methods sections of the report.
Sandra Eldridge (Professor of Biostatistics, Queen Mary, University of London) was a co-applicant, lead trial statistician, contributed to the statistical analysis plan and writing of the results section of the report.
Bart Sheehan (Associate Clinical Professor of Old Age Psychiatry, University of Warwick) was a co-applicant, designed the depression awareness component of the OPERA trial intervention and contributed to the writing of the background, methods and discussion sections of the report.
Anne Slowther (Associate Professor of Clinical Ethics, University of Warwick) was a co-applicant, designed the ethics substudy and contributed to the writing of the methods and discussion sections of the report.
Anne Spencer (Co-applicant, Queen Mary, University of London) was a co-applicant and health economics lead. She contributed to the health economic analysis plan and commented on final draft of the report.
Margaret Thorogood (Professor of Epidemiology, University of Warwick) was a co-applicant and a joint process evaluation lead, and contributed the writing of the background, methods, results and discussion section of the report.
Nicky Atherton (Clinical Research Fellow, University of Warwick) designed, led and delivered the OPERA exercise intervention, and contributed to the writing of the background, methods and results section.
Stephen A Bremner (Lecturer in Medical Statistics, Queen Mary, University of London) made a major contribution to the statistical analysis plan, undertook the analysis of the trial data and the writing of the results section of the report.
Angela Devine (Health Economist, Queen Mary, University of London) produced the health economics analysis plan, undertook the health economics analysis and wrote the health economics section of the report.
Karla Diaz-Ordaz (Research Fellow, Medical Statistics, Queen Mary, University of London) contributed to the statistical analysis plan and the health economic analysis plans, and assisted in the analysis of the trial and health economic data and the writing of the results section of the report.
David R Ellard (Senior Research Fellow, University of Warwick) contributed to the design of the process evaluation, collected the process evaluation data, undertook the qualitative and quantitative analyses of the process evaluation, and contributed to the writing of the background, methods, results and discussion sections of the report.
Rachel Potter (Research Nurse, University of Warwick) led the recruitment of care homes and participants for the trial and contributed to the writing of the methods and results sections of the report.
Katie Spanjers (Research Associate, University of Warwick) assisted in the delivery of the OPERA intervention, made a minor contribution to the statistics analysis plan, arranged the collection and undertook the analyses of the Secondary Uses Services data and contributed to the writing of the methods, results and discussion section.
Stephanie JC Taylor (Professor of Public Health and Primary Care, Queen Mary, University of London) was a co-applicant and Principal Investigator for London, designed the whole-home approach of the OPERA trial, was joint lead for process evaluation and contributed to the writing of the background, methods, results and discussion sections of the report.
Other members of the trial team
Amy Campbell (Trainee Clinical Trial Manager, University of Warwick) provided administrative support to the OPERA team, and was responsible for the collation and formatting of the report. Sarah Duggan (Warwick Clinical Trials Unit Manager, University of Warwick) co-ordinated the provision of administrative support for the OPERA team members based at the Warwick Clinical Trial Unit, and proofread the report. Suzanne Parsons (Research Fellow, Queen Mary, University of London) was a co-applicant and contributed to early design of the process evaluation. Emma Withers (Clinical Trial Manager, University of Warwick), Maryam Zare (Clinical Trial Manager, University of Warwick), Jenny Exton (Trainee Clinical Trial Manager, University of Warwick) and Nilu Ahmed (Research Fellow, Queen Mary, University of London) undertook the initial set-up of the trial.
Other contributors
Scott Weich (co-applicant, Professor of Psychiatry, University of Warwick).
OPERA intervention team
We would like to thank all of the OPERA intervention physiotherapists who delivered the OPERA exercise groups led by Morag Barber (Research Physiotherapist, Local Intervention Lead for North East London Primary Care Trust) Fiona Stock (Acting Head of Adult Therapies, Barking & Dagenham Primary Care Trust) , Debbie Feltham (Intermediate Care Therapies Lead, Barking & Dagenham Primary Care Trust) and Caroline O'donnell (Associate Director for Adult Services, Barking & Dagenham Primary Care Trust ) in London, and supported by Simon Cannon (Research Physiotherapist, Barking & Dagenham Primary Care Trust), Marie Clarke (Research Physiotherapist, Barking & Dagenham Primary Care Trust), Peta Cook (Research Physiotherapist, E Physio Associates), Coral Gladwell (Research Physiotherapist, E Physio Associates), Steven Jay (Research Physiotherapist, Barking & Dagenham Primary Care Trust), Sarah Lazenby (Research Physiotherapist, Barking & Dagenham Primary Care Trust), Cheryl Lewis (Research Physiotherapist, Barking & Dagenham Primary Care Trust), Nadia Masri (Research Physiotherapist, Barking & Dagenham Primary Care Trust), Judith Moss (Research Physiotherapist, Barking & Dagenham Primary Care Trust), Hannah Pickford (Research Physiotherapist, Barking & Dagenham Primary Care Trust), Maduri Ratnayake (Research Physiotherapist, Barking & Dagenham Primary Care Trust), Ellie Rowling (Research Physiotherapist, Barking & Dagenham Primary Care Trust), Peh Yan Soo (Research Physiotherapist, Barking & Dagenham Primary Care Trust), and in C&W: Elizabeth Ball (Research Physiotherapist, University of Warwick), Sarah Bridgewater (Research Physiotherapist, University of Warwick), Sue Davies (Research Physiotherapist, University of Warwick), Susanne Finnegan (Research Physiotherapist, University of Warwick), Janet Lowe (Research Physiotherapist, University of Warwick), Sherine Mathews (Research Physiotherapist, University of Warwick), Namonga Mtonga (Research Physiotherapist, University of Warwick) and Jill Nussbaum (Research Physiotherapist, University of Warwick).
Field research team
We would like to thank all of the OPERA recruitment team led by Sobhash Jhuree (Research Nurse, Queen Mary, University of London) and Denise Tedder (Research Nurse, Queen Mary, University of London) in London, and supported by Jamil Ahmad (Research Officer, Primary Care Research Network, Greater London), Helen Blake (Research Officer, London Hub Mental Health Research Network), Rachel Evered (Research Officer, London Hub Mental Health Research Network), Shreena Ghelani (Research Officer, London Hub Mental Health Research Network), Deborah Haworth (Research Officer, Primary Care Research Network, Greater London), Kofi Kramo (Research Officer, London Hub Mental Health Research Network), Amy Murphy (Research Officer, London Hub Mental Health Research Network), Anna Piasecka (Research Officer, London Hub Mental Health Research Network), Stephanie Pohlmann (Research Officer, Primary Care Research Network, Greater London), Pat Sturdy (Research Assistant, Queen Mary, University of London), Charlotte Watson (Research Officer, London Hub Mental Health Research Network).
Vivien Nichols (Research Physiotherapist, University of Warwick) and Cheryl Ritchie (Research Physiotherapist, University of Warwick) headed recruitment in C&W supported by Shabana Bashir (Research Officer, Heart of England Hub Mental Health Research Network), Pauline Darbyshire (Research Nurse, Primary Care Research Network, West Midlands South), Victoria Gordon (Research Nurse, Primary Care Research Network, West Midlands South), Nicola McHugh (Research Nurse, University of Warwick), Ruman Sandhu (Research Officer, Heart of England Hub Mental Health Research Network), Sandra Ward (Research Facilitator, Primary Care Research Network, West Midlands South) and Sue Webb (Research Nurse, University of Warwick).
Independent members of the Data Monitoring and Ethics Committee
Kerenza Hood (DMEC chairperson, Cardiff University), Michael Parker (University of Oxford), Adrian Renton (University of East London) and Andrew Stevens (The University of Birmingham).
Independent members of the Trial Steering Committee
Sube Banerjee (Trial Steering Committe chairperson, King's College London), Julia Burton-Jones (Trial Steering Committee Lay Member), Sally Kerry (St George's University of London), Dawn Skelton (Glasgow Caledonian University) and Andre Tylee (King's College London).
Administrative team
Cheryl Billingham (Data Entry Clerk, University of Warwick), Paula Broome (PA to Professor Taylor, Queen Mary, University of London), Naheedah Choudhury (Assistant Trial Administrator, Queen Mary, University of London), Claire Daffern (Quality Assurance Manager, University of Warwick), Sarah Lowe (Data Entry Clerk, University of Warwick), Muriel McAughtrie (Centre Manager, Queen Mary, University of London), Anne Ngunjiri (Trial Administrator, University of Warwick), John Owen (Research Grant Administrator, Queen Mary, University of London), Claire Rutherford (Randomisation Officer, Queen Mary, University of London) and Nancy Schumann (Trial Administrator, Queen Mary, University of London).
Programming team
Henry Adjei (Programmer, University of Warwick), Chockalingam Muthiah (Programmer, University of Warwick) and Adrian Willis (Senior Programmer, University of Warwick).
Publications
1. Atherton N. Could exercise combat depression in nursing and residential homes? J Dement Care 2008;39.
2. Potter R, Ellard D, Karen R, Thorogood M. A systematic review of the effects of physical activity on physical functioning, quality of life and depression in older people with dementia. Int J Geriatr Psychiatry 2011;26:1000–11.
3. Ellard D, Taylor S, Parsons S, Thorogood M. The OPERA trial: a protocol for the process evaluation of a randomised trial of an exercise intervention for older people in residential and nursing accommodation. Trials 2011;12:28.
4. Bridle C, Spanjers K, Patel S, Atherton NM, Lamb SE. Effect of exercise on depression severity in older people: systematic review and meta-analysis of randomised controlled trials. Br J Psychiatry 2012;201:180–5.
5. Underwood M, Eldridge S, Lamb S, Potter R, Sheehan B, Slowther AM, et al. The OPERA trial: protocol for a randomised trial of an exercise intervention for older people in residential and nursing accommodation. Trials 2011;12:27.
6. Underwood M, Lamb SE, Eldridge S, Sheehan B, Slowther A, Spencer A, et al. Exercise for depression in older care home residents. A cluster randomised controlled trial. Lancet 2013: in press. Published online on 2 May 2013. URL: http:dx.doi.org/S0140-6736(13)60649-2.
Disclaimer
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Office for National Statistics (ONS) . Population Estimates for UK, England and Wales, Scotland and Northern Ireland, Mid 2010 Population Estimates 2010. www.ons.gov.uk/ons/publications/re-reference-tables.html?edition=tcm%3A77–231847 (accessed 7 December 2011).
- Our health, our care, our say: a new direction for community services. London: DoH; 2006.
- Harwood R. Do we still need care homes?. Age Ageing 2004;33:529-30.
- Macdonald A, Cooper B. Long-term care and dementia services: an impending crisis. Age Ageing 2007;36:16-22.
- Care homes for older people in the UK: a market study. London: OFT; 2005.
- The state of health care and adult social care in England: an overview of key themes in care in 2010/11. London: The Stationery Office; 2011.
- CCC . Care at the Cross-Road: CCC Care Census Survey Points the Way Forward 2006. www.ccc-ltc.org.uk/pr/2006–07–03.pdf (accessed 3 January 2012).
- Fahey T, Montgomery AA, Barnes J, Protheroe J. Quality of care for elderly residents in nursing homes and elderly people living at home: controlled observational study. BMJ 2003;326.
- What standards to expect from the regulation of your care home: an introduction to important changes to how adult social care services are regulated. London: The Stationery Office; 2011.
- Coward R. Southern Cross wakes us up to the business of caring: We can't leave our elderly to the market's mercies – yet this government will not commit to averting a funding catastrophe. Guardian News and Media Ltd.; 2011.
- Samuel M. Fall in Council Income Puts Many Care Homes in Financial Peril 2011. www.communitycare.co.uk/Articles/22/03/2011/116515/fall-in-council-income-puts-many-care-homes-in-financial-peril.htm (accessed 14 November 2011).
- Underwood M, Eldridge S, Lamb S, Potter R, Sheehan B, Slowther AM, et al. The OPERA trial: protocol for a randomised trial of an exercise intervention for older people in residential and nursing accommodation. Trials 2011;12.
- Ellard DR, Taylor SJ, Parsons S, Thorogood M. The OPERA trial: a protocol for the process evaluation of a randomised trial of an exercise intervention for older people in residential and nursing accommodation. Trials 2011;12.
- Mann AH, Graham N, Ashby D. Psychiatric illness in residential homes for the elderly: a survey in one London borough. Age Ageing 1984;13:257-65.
- Llewellyn-Jones R, Baikie K, Smithers H, Cohen J, Snowdon J, Tennant C. Multifaceted shared care intervention for late life depression in residential care: randomised controlled trial. BMJ 1999;319:676-82.
- Parmelee PA, Katz IR, Lawton MP, Parmelee PA, Katz IR, Lawton MP. Incidence of depression in long-term care settings. J Gerontol 1992;47:M189-96.
- Hoover DR, Siegel M, Lucas J, Kalay E, Gaboda D, Devanand DP, et al. Depression in the first year of stay for elderly long-term nursing home residents in the USA. Int Psychogeriatr 2010;22:1161-71.
- Barca ML, Engedal K, Laks J, Selbaek G. A 12 months follow-up study of depression among nursing-home patients in Norway. J Affect Disord 2010;120:141-8.
- Smalbrugge M, Jongenelis L, Pot AM, Eefsting JA, Ribbe MW, Beekman AT. Incidence and outcome of depressive symptoms in nursing home patients in the Netherlands. Am J Geriatr Psychiatry 2006;14:1069-76.
- van Dijk PT, Mehr DR, Ooms ME, Madsen R, Petroski G, Frijters DH, et al. Comorbidity and 1-year mortality risks in nursing home residents. J Am Geriatr Soc 2005;53:660-5.
- Schreiner AS, Yamamoto E, Shiotani H. Positive affect among nursing home residents with Alzheimer's dementia: the effect of recreational activity. Aging Ment Health 2005;9:129-34.
- Eisses AM, Kluiter H, Jongenelis K, Pot AM, Beekman AT, Ormel J. Risk indicators of depression in residential homes. Int J Geriatr Psychiatry 2004;19:634-40.
- Bagley H, Cordingley L, Burns A, Mozley CG, Sutcliffe C, Challis D, et al. Recognition of depression by staff in nursing and residential homes. J Clin Nurs 2000;9:445-50.
- Llewellyn-Jones RH, Baikie KA, Castell S, Andrews CL, Baikie A, Pond CD, et al. How to help depressed older people living in residential care: a multifaceted shared-care intervention for late-life depression. Int Psychogeriatr 2001;13:477-92.
- Eisses AM, Kluiter H, Jongenelis K, Pot AM, Beekman AT, Ormel J, et al. Care staff training in detection of depression in residential homes for the elderly: randomised trial. Br J Psychiatry 2005;186:404-9.
- McCabe M, Davison T, Mellor D, George K, Moore K, Ski C. Depression among older people with cognitive impairment: prevalence and detection. Int J Geriatr Psychiatry 2006;21:633-44.
- Sutcliffe C, Burns A, Challis D, Mozley CG, Cordingley L, Bagley H, et al. Depressed mood, cognitive impairment, and survival in older people admitted to care homes in England. Am J Geriatr Psychiatry 2007;15:708-15.
- Gaboda D, Lucas J, Siegel M, Kalay E, Crystal S. No longer untreated? Depression diagnosis and antidepressant therapy in elderly long-stay nursing home residents, 1999 to 2007. J Am Geriatr Soc 2011;59:673-80.
- Hanlon JT, Handler SM, Castle NG. Antidepressant prescribing in US nursing homes between 1996 and 2006 and its relationship to staffing patterns and use of other psychotropic medications. J Am Med Dir Assoc 2010;11:320-4.
- Luppa M, Luck T, Matschinger H, König H-H, G Riedel-Heller S. Predictors of nursing home admission of individuals without a dementia diagnosis before admission – results from the Leipzig Longitudinal Study of the Aged (LEILA 75+). BMC Health Serv Res 2010;10.
- Luppa M, Luck T, Weyerer S, Konig HH, Brahler E, Riedel-Heller SG. Prediction of institutionalization in the elderly. A systematic review. Age Ageing 2010;39:31-8.
- Onder G, Liperoti R, Soldato M, Cipriani MC, Bernabei R, Landi F. Depression and risk of nursing home admission among older adults in home care in Europe: results from the Aged in Home Care (AdHOC) study. J Clin Psychiatry 2007;68:1392-8.
- Penninx BW, Geerlings SW, Deeg DJ, van Eijk JT, van Tilburg W, Beekman AT. Minor and major depression and the risk of death in older persons. Arch Gen Psychiatry 1999;56:889-95.
- Rapp M, Schnaider-Beeri M, Wysocki M, Guerrero-Berroa E, Grossman H, Heinz A, et al. Cognitive decline in patients as a function of depression. Am J Geriatr Psychiatry 2011;19:357-63.
- Smalbrugge M, Pot A, Jongenelis L, Gundy C, Beekman A, Eefsting J. The impact of depression and anxiety on well being, disability and use of health care services in nursing home patients. Int J Geriatr Psychiatry 2006;21:325-32.
- Hoe J, Hancock G, Livingston G, Orrell M. Quality of life of people with dementia in residential care homes. Br J Psychiatry 2006;188:460-4.
- Konnert C, Dobson K, Stelmach L. The prevention of depression in nursing home residents: a randomized clinical trial of cognitive–behavioral therapy. Aging Ment Health 2009;13:288-99.
- Potter R, Ellard D, Rees K, Thorogood M. A systematic review of the effects of physical activity on physical functioning, quality of life and depression in older people with dementia. Int J Geriatr Psychiatry 2011;26:1000-11.
- Thapa PB, Gideon P, Cost TW, Milam AB, Ray WA, Thapa PB, et al. Antidepressants and the risk of falls among nursing home residents. N Engl J Med 1998;339:875-82.
- Clinical Guidelines 90. London: NICE; 2009.
- Casperson C, Powell K, Christenson G. Physical activity, exercise, and physical fitness: definitions and distinctions of health-related research. Publ Health Rep 1985;100:126-31.
- Kisner C, Colby LA. Therapeutic exercise. Philadelphia, PA: FA Davis; 2007.
- Craft L, Perna F. The benefits of exercise for the clinically depressed. Prim Care Companion J Clin Psychiatry 2004;6:104-10.
- Frederickson RCA, Geary LE. Endogenous opioid peptides: review of physiological, pharmacological and clinical aspects. Prog Neurobiol 1982;19:19-6.
- Boecker H, Sprenger T, Spilker ME, Henriksen G, Koppenhoefer M, Wagner KJ, et al. The runner's high: opioidergic mechanisms in the human brain. Cereb Cortex 2008;18:2523-31.
- Morgan W. Physical activity and mental health. Washington, DC: Taylor & Francis; 1997.
- Manji HK, Drevets WC, Charney DS. The cellular neurobiology of depression. Nat Med 2001;7:541-7.
- Thoren P, Floras J, Hoffmann P, Seals D. Endorphins and exercise: physiological mechanisms and clinical implications. Med Sci Sports Exerc 1990;22:417-28.
- Duman RS, Monteggia LM. A neurotrophic model for stress-related mood disorders. Biol Psychiatry 2006;59:1116-27.
- Reichardt LF. Neurotrophin-regulated signalling pathways. Phil Trans Roy Soc Lond B Biol Sci 2006;361:1545-64.
- Adlard PA, Perreau VM, Engesser-Cesar C, Cotman CW. The timecourse of induction of brain-derived neurotrophic factor mRNA and protein in the rat hippocampus following voluntary exercise. Neurosci Lett 2004;363:43-8.
- Ferris LT, Williams J, Shen C-L. The effect of acute exercise on serum brain-derived neurotrophic factor levels and cognitive function. Med Sci Sports Exerc 2007;39:728-34.
- Erickson KI, Voss MW, Prakash RS, Basak C, Szabo A, Chaddock L, et al. Exercise training increases size of hippocampus and improves memory. Proc Natl Acad Sci USA 2011;108:3017-22.
- Deslandes A, Moraes H, Ferreira C, Veiga H, Silveira H, Mouta R, et al. Exercise and mental health: many reasons to move. Neuropsychobiology 2009;59:191-8.
- Zoladz J, Pilc A. The effect of physical activity on the brain derived neurotrophic factor: from animal to human studies. J Physiol Pharmacol 2010;61:533-41.
- Manthorpe J, Iliffe S. Depression in later life. London: Jessica Kingsley Publishers; 2005.
- Bandura A, Ramachaudran VS. Encyclopedia of human behavior. New York, NY: Academic Press; 1994.
- Barbour KA, Blumenthal JA. Exercise training and depression in older adults. Neurobiol Aging 2005;26:119-23.
- Fox K, Stathi A, McKenna J, Davis M. Physical activity and mental well-being in older people participating in the Better Ageing Project. Eur J Appl Physiol 2007;100:591-602.
- Blumenthal J, Williams R, Needels T, Wallace A. Psychological changes accompany aerobic exercise in healthy middle-aged adults. Psychosom Med 1982;44:529-36.
- Seligman M, Steen T, Park N, Peterson C. Positive psychology progress: empirical validation of interventions. Am Psychol 2005;60:410-21.
- Bridle C, Spanjers K, Patel S, Atherton N, Lamb S. Effect of exercise on depression severity among older people with clinically significant symptoms of depression: Systematic review and meta-analysis of randomised controlled trials. Br J Psychiatry 2012;201:180-5.
- Kitwood T. The dialectics of dementia: with particular reference to Alzheimer's disease. Ageing Soc 1990;10:177-96.
- Oddy R. Promoting mobility in patients with dementia: some suggested strategies for physiotherapists. Physiother Pract 1987;3:18-27.
- Oddy R. Promoting mobility for people with dementia: a problem-solving approach. London: Age Concern; 2003.
- Willingham D, Peterson E, Manning C, Brashear R. Patients with Alzheimer's disease who cannot perform some motor skills show normal learning of other skills. Neuropsychology 1997;2:261-71.
- Zanetti O, Binetti G, Magni E, Rozzini L, Bianchetti A, Trabucchi M. Procedural memory stimulation in Alzheimer's disease: impact of a training programme. Acta Neurol Scand 1997;95:152-7.
- Shumway-Cook A, Woolacott M. Motor control: theory and practical applications. London: Lippincott Williams & Wilkins; 2001.
- Willingham DB. A neuropsychological theory of motor skill learning. Psychol Rev 1998;105:558-84.
- Kandel E, Jessel T, Schwartz J. Essentials of neural science and behaviour. London: Prentice Hall; 1995.
- Clare L, Jones R. Errorless learning in the rehabilitation of memory impairment: a critical review. Neuropsychol Rev 2008;18:1-23.
- Hellen C. Enabling success: hands-on care strategies and behavioural refocusing interventions. Alzheim Care Q 2004;5:178-82.
- McEvoy CL, Patterson RL. Behavioral treatment of deficit skills in dementia patients. Gerontologist 1986;26:475-8.
- McGilton KS, Rivera TM, Dawson P. Can we help persons with dementia find their way in a new environment?. Aging Ment Health 2003;7:363-71.
- Zoltan B. Vision, perception, and cognition. A manual for the evaluation and treatment of the neurologically impaired adult. Thorofare: N Slack Inc.; 1996.
- Karageorghis C, Priest D-L. Music in sport and exercise: an update on research and application. Sport J 2008;11.
- Nieuwboer A, Kwakkel G, Rochester L, Jones D, van Wegen E, Willems AM, et al. Cueing training in the home improves gait-related mobility in Parkinson's disease: the RESCUE trial. J Neurol Neurosurg Psychiatry 2007;78:134-40.
- Popescu M, Otsuka A, Ioannides AA. Dynamics of brain activity in motor and frontal cortical areas during music listening: a magnetoencephalographic study. NeuroImage 2004;21:1622-38.
- Blood AJ, Zatorre RJ. Intensely pleasurable responses to music correlate with activity in brain regions implicated in reward and emotion. Proc Natl Acad Sci USA 2001;98:11818-23.
- Everard KM, Lach HW, Fisher EB, Baum MC. Relationship of activity and social support to the functional health of older adults. J Gerontol B Psychol Sci Soc Sci 2000;55.
- Glass TA, De Leon CFM, Bassuk SS, Berkman LF. Social Engagement and Depressive Symptoms in Late Life. J Aging Health 2006;18:604-28.
- Woodard CM, Berry MJ. Enhancing adherence to prescribed exercise: structured behavioral interventions in clinical exercise programs. J Cardpulm Rehabil Prev 2001;21.
- Lowensteyn I, Coupal L, Zowall H, Grover SA. The cost-effectiveness of exercise training for the primary and secondary prevention of cardiovascular disease. J Cardpulm Rehabil Prev 2000;20.
- Crombie IK, Irvine L, Williams B, McGinnis AR, Slane PW, Alder EM, et al. Why older people do not participate in leisure time physical activity: a survey of activity levels, beliefs and deterrents. Age Ageing 2004;33:287-92.
- Resnick B, Gruber-Baldini AL, Zimmerman S, Galik E, Pretzer-Aboff I, Russ K, et al. Nursing Home resident outcomes from the Res-Care Intervention. J Am Geriatr Soc 2009;57:1156-65.
- Sackley CM, van den Berg ME, Lett K, Patel S, Hollands K, Wright CC, et al. Effects of a physiotherapy and occupational therapy intervention on mobility and activity in care home residents: a cluster randomised controlled trial. BMJ 2009;339.
- Resnick B, Fleishell A. Developing a restorative care program. Am J Nurs 2002;102.
- Engelman KK, Altus DE, Mosier MC, Mathews RM. Brief training to promote the use of less intrusive prompts by nursing assistants in a dementia care unit. J Appl Behav Anal 2003;36:129-32.
- Davies S, Ellis L, Laker S. Promoting autonomy and independence for older people within nursing practice: an observational study. J Clin Nurs 2000;9:127-36.
- Lekan-Rutledge D, Palmer MH, Belyea M. In their own words: nursing assistants' perceptions of barriers to implementation of prompted voiding in long-term care. Gerontologist 1998;38:370-8.
- Jirovec MM. The impact of daily exercise on the mobility, balance and urine control of cognitively impaired nursing home residents. Int J Nurs Stud 1991;28:145-51.
- Szczepura A, Clay D, Nelson S, Wild D, Spilsbury K. Improving care in residential homes: a literature review. York: Joseph Rowntree Foundation; 2008.
- Resnick B. Restorative care nursing for older adults: a guide for all care settings. New York, NY: Springer; 2004.
- Diaz-Ordaz K. Queen Mary, University of London; 2012.
- Conradsson M, Littbrand H, Lindelof N, Gustafson Y, Rosendahl E. Effects of a high-intensity functional exercise programme on depressive symptoms and psychological well-being among older people living in residential care facilities: a cluster-randomized controlled trial. Aging Ment Health 2010;14:565-76.
- Edwards SJ, Braunholtz DA, Lilford RJ, Stevens AJ. Ethical issues in the design and conduct of cluster randomised controlled trials. BMJ 1999;318:1407-9.
- Hutton JL. Are distinctive ethical principles required for cluster randomized controlled trials?. Stat Med 2001;20:473-88.
- Eldridge SM, Ashby D, Feder GS. Informed patient consent to participation in cluster randomized trials: an empirical exploration of trials in primary care. Clin Trials 2005;2:91-8.
- McRae AD, Weijer C, Binik A, Grimshaw JM, Boruch R, Brehaut JC, et al. When is informed consent required in cluster randomized trials in health research?. Trials 2011;12.
- Goodman C, Baron NL, Machen I, Stevenson E, Evans C, Davies SL, et al. Culture, consent, costs and care homes: enabling older people with dementia to participate in research. Aging Ment Health 2011;15:475-81.
- Warner J, McCarney R, Griffin M, Hill K, Fisher P. Participation in dementia research: rates and correlates of capacity to give informed consent. J Med Ethics 2008;34:167-70.
- Kim SY, Appelbaum PS, Kim HM, Wall IF, Bourgeois JA, Frankel B, et al. Variability of judgments of capacity: experience of capacity evaluators in a study of research consent capacity. Psychosomatics 2011;52:346-53.
- International ethical guidelines for biomedical research involving human subjects. Geneva: CIOMS; 2002.
- ICH Topic E 6 (R1) Guideline for Good Clinical Practice. London: EMA; 2002.
- The Mental Capacity Act 2005. London: The Stationery Office; 2005.
- Dixon-Woods M, Angell EL. Research involving adults who lack capacity: how have research ethics committees interpreted the requirements?. J Med Ethics 2009;35:377-81.
- Dobson C. Audit of research studies including participants not having the capacity to consent to their involvement. Preston: Lancashire Care NHS Foundation Trust; 2011.
- Zermansky AG, Alldred DP, Petty DR, Raynor DK. Striving to recruit: the difficulties of conducting clinical research on elderly care home residents. J R Soc Med 2007;100:258-61.
- Oakley A, Strange V, Bonell C, Allen E, Stephenson J, Team RS. Process evaluation in randomised controlled trials of complex interventions. BMJ 2006;332:413-16.
- Dignan MB, Carr PA. Program planning for health education and promotion. Philadelphia, PA: Lea & Febiger; 1987.
- Geraets JJ, Goossens ME, van Haastregt JC, de Groot IJ, de Bruijn CP, de Bie RA, et al. Implications of process evaluation for clinical effectiveness and clinical practice in a trial on chronic shoulder complaints. Patient Educ Couns 2006;61:117-25.
- Sheikh J, Yesavage J. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontol 1986;5:165-73.
- Morris JN, Hawes C, Fries BE, Phillips CD, Mor V, Katz S, et al. Designing the national resident assessment instrument for nursing homes. Gerontologist 1990;30:293-307.
- Cohen D, Crabtree B. Qualitative Research Guidelines Project 2006. www.qualres.org/HomeObse-3594.html (accessed 12 January 2012).
- Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189-98.
- EuroQol Group . EuroQol: a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208.
- Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 1994;49:M85-94.
- Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci 2000;55:M221-31.
- Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md Med J 1965;14:61-5.
- Sutcliffe C, Cordingley L, Burns A, Mozley CG, Bagley H, Huxley P, et al. A new version of the geriatric depression scale for nursing and residential home populations: the geriatric depression scale (residential) (GDS-12R). Int Psychogeriatr 2000;12:173-81.
- Vinkers DJ, Gussekloo J, Stek ML, Westendorp RG, Van Der Mast RC, Vinkers DJ, et al. The 15-item Geriatric Depression Scale (GDS-15) detects changes in depressive symptoms after a major negative life event. The Leiden 85-plus Study. Int J Geriatr Psychiatry 2004;19:80-4.
- Koehler M, Rabinowitz T, Hirdes J, Stones M, Carpenter GI, Fries BE, et al. Measuring depression in nursing home residents with the MDS and GDS: an observational psychometric study. BMC Geriatrics 2005;5.
- Jongenelis K, Pot AM, Eisses AM, Gerritsen DL, Derksen M, Beekman AT, et al. Diagnostic accuracy of the original 30-item and shortened versions of the Geriatric Depression Scale in nursing home patients. Int J Geriatr Psychiatry 2005;20:1067-74.
- Kotynia-English R, McGowan H, Almeida OP. A randomized trial of early psychiatric intervention in residential care: impact on health outcomes. Int Psychogeriatr 2005;17:475-85.
- EuroQol Group . A new facility for the measurement of health-related quality of life. Health Pol 1990;16:199-208.
- Brooks R. EuroQol: the current state of play. Health Pol 1996;37:53-72.
- Borowiak E, Kostka T, Borowiak E, Kostka T. Predictors of quality of life in older people living at home and in institutions. Aging Clin Exp Res 2004;16:212-20.
- O’Bryant SE, Humphreys JD, Smith GE, Ivnik RJ, Graff-Radford NR, Petersen RC, et al. Detecting dementia with the mini-mental state examination in highly educated individuals. Arch Neurol 2008;65:963-7.
- Larson EB, Wang L, Bowen JD, McCormick WC, Teri L, Crane P, et al. Exercise is associated with reduced risk for incident dementia among persons 65 years of age and older. Ann Int Med 2006;144:73-81.
- Mulrow CD, Gerety MB, Kanten D, Cornell JE, DeNino LA, Chiodo L, et al. A randomized trial of physical rehabilitation for very frail nursing home residents. JAMA 1994;271:519-24.
- Skelton D. EU Working Party on Effective Falls Prevention. Brussels; 2003.
- Friedman SM, Munoz B, West SK, Rubin GS, Fried LP, Friedman SM, et al. Falls and fear of falling: which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatr Soc 2002;50:1329-35.
- Kerse N, Peri K, Robinson E, Wilkinson T, von Randow M, Kiata L, et al. Does a functional activity programme improve function, quality of life, and falls for residents in long term care? Cluster randomised controlled trial. BMJ 2008;337.
- Gallagher RM, Verma S, Mossey J. Chronic pain. Sources of late-life pain and risk factors for disability. Geriatrics 2000;55:40-4.
- Sheehan B, Bass C, Briggs R, Jacoby R, Sheehan B, Bass C, et al. Somatic symptoms among older depressed primary care patients. Int J Geriatr Psychiatry 2003;18:547-8.
- Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med 1995;332:556-61.
- EuroQol Group . EQ-5D. A Standardised Instrument for Use As a Measure of Health Outcome n.d. www.euroqol.org/ (accessed 8 December 2011).
- Dorman PJ, Waddell F, Slattery J, Dennis M, Sandercock P. Are proxy assessments of health status after stroke with the EuroQol questionnaire feasible, accurate, and unbiased?. Stroke 1997;28:1883-7.
- Martinez-Martin P, Benito-Leon J, Alonso F, Catalan MJ, Pondal M, Zamarbide I. Health-related quality of life evaluation by proxy in Parkinson's disease: approach using PDQ-8 and EuroQoL-5D. Mov Disord 2004;19:312-18.
- Ankri J, Beaufils B, Novella JL, Morrone I, Guillemin F, Jolly D, et al. Use of the EQ-5D among patients suffering from dementia. J Clin Epidemiol 2003;56:1055-63.
- Mor V, Branco K, Fleishman J, Hawes C, Phillips C, Morris J, et al. The structure of social engagement among nursing home residents. J Gerontol B Psychol Sci Soc Sci 1995;50:P1-8.
- Schroll M, Jonsson PV, Mor V, Berg K, Sherwood S. An international study of social engagement among nursing home residents. Age Ageing 1997;26:55-9.
- Prescription cost analysis England 2010–2011. London: PSU; 2011.
- British National Formulary (BNF) 2011. http://bnf.org/bnf/index.htm (accessed 12 January 2012).
- World Health Organization (WHO) . ATC/DDD/Index/2011 2010. www.whocc.no/atc_ddd_index/ (accessed 12 January 2012).
- Social Care England Children and Young Persons England The Care Homes Regulations. 2001. United Kingdom: HMSO; 2001.
- Care Standards Act 2000. London: HMSO; 2000.
- NHS . Using the Secondary Users Service. The Health and Social Care Information Centre 2011. www.ic.nhs.uk/services/secondary-uses-service-sus/using-the-sus-service (accessed 12 January 2012).
- World Health Organization (WHO) . ICD-10 Version: 2010 2010. http://apps.who.int/classifications/icd10/browse/2010/en (accessed 12 January 2012).
- NHS . Medical Research Information Service 2011. www.ic.nhs.uk/services/data-linkage-service (accessed 12 January 2012).
- A framework for development and evaluation of RCTs for complex interventions to improve health. London: MRC; 2000.
- Cook T, Campbell D. Quasi-experimentation: design and analysis issues for field settings. Boston, MA: Houghton Miffline; 1979.
- Egger G, Swinburn B. An ‘ecological’ approach to the obesity pandemic. BMJ 1997;315:477-80.
- Kickbusch I. The contribution of the World Health Organization to a new public health and health promotion. Am J Public Health 2003;93:383-8.
- Bond L, Patton G, Glover S, Carlin JB, Butler H, Thomas L, et al. The Gatehouse Project: can a multilevel school intervention affect emotional wellbeing and health risk behaviours?. J Epidemiol Community Health 2004;58:997-1003.
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004;82:581-629.
- Cialdini RB. The science of persuasion. Sci Am Spec Edn 2004;14:70-7.
- Redelmeier DA, Cialdini RB. Problems for clinical judgement: 5. Principles of influence in medical practice. CMAJ 2002;166:1680-4.
- Nelson M, Rejeski J, Blair S, Duncan P, Judge J, King A, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc 2007;39:1435-45.
- A report from the Chief Medical Officer. London: DoH; 2004.
- ACSM's Guidelines for Exercise Testing and Prescription. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.
- ACSM's Resource Manual for Guidelines for Exercise Testing and Prescription. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.
- Ratamess N, Alvar B, Evetoch T, Housh T, Kibler W, Kraemer W. Progression models in resistance training for healthy adults [ACSM position stand]. Med Sci Sports Exerc 2009;41:687-708.
- Armstrong JJ, Stolee P, Hirdes JP, Poss JW. Examining three frailty conceptualizations in their ability to predict negative outcomes for home-care clients. Age Ageing 2010;39:755-8.
- Home from home: a report highlighting opportunities for improving standards of dementia care in care homes. London: Alzheimer's Society; 2008.
- Stokes G, Goudie F. The essential dementia care handbook. Bicester, UK: Speechmark Publishing; 2002.
- Matthews FE, Dening T. Prevalence of dementia in institutional care. Lancet 2002;360:225-6.
- Heart Failure Society of America (HFSA) . The Stages of Heart Failure – NYHA Classification 2002. www.abouthf.org/questions_stages.htm (accessed 25 July 2011).
- Kramer W, French D, Jones CJ RD. Physical activity instruction of older adults. Champaign, IL: Human Kinetics; 2005.
- Dinan S, Skelton D, Malbut K, Jones CJ RD. Physical activity instruction of older adults. Champaign, IL: Human Kinetics; 2005.
- Lagally K, Amorose A. The validity of using prior ratings of perceived exertion to regulate resistance exercise intensity. Percept Mot Skills 2007;104:534-42.
- Lagally K, Robertson R. Construct validity of the OMNI resistance exercise scale. J Strength Cond Res 2006;20:252-6.
- Borg G. Borg's perceived exertion and pain scales. Champaign, IL: Human Kinetics; 1998.
- Littbrand H, Rosendahl E, Lindelof N, Lundin-Olsson L, Gustafson Y, Nyberg L. A high-intensity functional weight-bearing exercise program for older people dependent in activities of daily living and living in residential care facilities: evaluation of the applicability with focus on cognitive function. Phys Ther 2006;86:489-98.
- Singh N, Stavrinos T, Scarbek Y, Galambos G, Liber C, Fiatarone Singh M. A randomized controlled trial of high versus low intensity weight training versus general practitioner care for clinical depression in older adults. J Gerontol A Biol Sci Med Sci 2005;60:768-76.
- Singh N, Clements K, Singh M. The efficacy of exercise as a long-term antidepressant in elderly subjects: a randomized, controlled trial. J Gerontol A Biol Sci Med Sci 2001;56:M497-504.
- Borg G. The Borg CR 10 Scale Folder. A method for measuring intensity of experience. Hasselby, Sweden: Borg Perception; 2004.
- Gill TM, DiPietro L, Krumholz HM. Role of exercise stress testing and safety monitoring for older persons starting an exercise program. JAMA 2000;284:342-9.
- Morey MC, Sullivan RJ. Medical assessment for health advocacy and practical strategies for exercise initiation. Am J Prev Med 2003;25:204-8.
- Gardner MM, Buchner DM, Robertson MC, Campbell AJ. Practical implementation of an exercise-based falls prevention programme. Age Ageing 2001;30:77-83.
- Skelton D. Appendix 3, Exercises (FaME). London: Later life Training; 2008.
- Skelton D, Dinan S, Campbell M, Rutherford O. Tailored group exercise (Falls Management Exercise – FaME) reduces falls in community-dwelling older frequent fallers (an RCT). Age Ageing 2005;34:636-9.
- Levitin DJ. The Neural Correlates of Temporal Structure in Music. Music Med 2009;1:9-13.
- Farrin A, Russell I, Torgerson D, Underwood M. Differential recruitment in a cluster randomized trial in primary care: the experience of the UK back pain, exercise, active management and manipulation (UK BEAM) feasibility study. Clin Trials 2005;2:119-24.
- Puffer S, Torgerson D, Watson J. Evidence for risk of bias in cluster randomised trials: review of recent trials published in three general medical journals. BMJ 2003;327:785-9.
- Eldridge S, Ashby D, Bennett C, Wakelin M, Feder G. Internal and external validity of cluster randomised trials: systematic review of recent trials. BMJ 2008;336:876-80.
- Eldridge S, Ukoumunne O, Carlin J. The Intra-Cluster Correlation Coefficient in Cluster Randomized Trials: A Review of Definitions. International Statistical Review 2009;77:378-94.
- NHS reference costs 2009–2010. London: DoH; 2011.
- Curtis L. Unit costs of health and social care. Canterbury: PSSRU: University of Kent; 2010.
- Prescription Cost Analysis, England – 2010. Leeds: NHS; 2011.
- Pickard AS, Johnson JA, Feeny DH, Shuaib A, Carriere KC, Nasser AM. Agreement between patient and proxy assessments of health-related quality of life after stroke using the EQ-5D and Health Utilities Index. Stroke 2004;35:607-12.
- Dolan P, Gudex C, Kind P, Williams A. A social tariff for Euroqol: results from a UK general population survey. York: University of York; 1995.
- Richardson G, Manca A. Calculation of quality adjusted life years in the published literature: a review of methodology and transparency. Health Econ 2004;13:1203-10.
- Gomes M, Ng ES-W, Grieve R, Nixon R, Carpenter J, Thompson SG. Developing appropriate methods for cost-effectiveness analysis of cluster randomized trials. Med Decis Making 2012;32:350-61.
- Rubin D. Multiple imputation for nonresponse in surveys. New York, NY: John Wiley & Sons; 1987.
- Towse A. Should NICE's threshold range for cost per QALY be raised? Yes. BMJ 2009;338.
- Weiss CH. Evaluation research. Englewood Cliffs, NJ: Prentice Hall; 1972.
- Steckler A, Linnan L. Process evaluation for public health interventions and research. San Francisco, CA: Jossey-Bass; 2002.
- Bryman A. Integrating quantitative and qualitative research: how is it done?. Qual Res 2006;6:97-113.
- Pope C, Mays N. Qualitative research: reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ 1995;311:42-5.
- Oakley A, Strange V, Stephenson J, Forrest S, Monteiro H. Evaluating processes: a case study of a randomized controlled trial of sex education. Evaluation 2004;10:440-62.
- Morgan DL. Practical strategies for combining qualitative and quantitative methods: applications to health research. Qual Health Res 1998;8:362-76.
- Taylor S. Ethnographic research: a reader. London: Sage Publications; 2002.
- McKee KJ, Houston DM, Barnes S. Methods for assessing quality of life and well-being in frail older people. Psychol Health 2002;17:737-51.
- Parker C, Barnes S, McKee K, Morgan K, Torrington J, Tregenza P. Quality of life and building design in residential and nursing homes for older people. Ageing Soc 2004;24:941-62.
- Ritchie J, Spencer L, Bryman A, Burgess R. Analysing qualitative data. London: Routledge; 1994.
- Pope C, Ziebland S, Mays N. Qualitative research in health care: analysing qualitative data. BMJ 2000;320:114-16.
- Ives J, Draper H. Appropriate methodologies for empirical bioethics: it's all relative. Bioethics 2009;23:249-58.
- Care Quality Commission (CQC) . Our job is to check whether hospitals, care homes and care services are meeting government standards. Care Quality Commission 2011. www.cqc.org.uk/ (accessed 12 January 2012).
- Eborall C, Fenton W, Woodrow S. State of the Adult Social Care Workforce in England 2010 n.d. www.skillsforcare.org.uk/research/research_reports/state_of_the_adult_social_care_workforce_reports.aspx (accessed 7 December 2011).
- Kind P, Hardman G, Macran S. Centre for Health Economics discussion paper 172. York: Centre for Health Economics, University of York; 1999.
- Mihalko SL, Wickley KL, Sharpe BL. Promoting physical activity in independent living communities. Med Sci Sports Exerc 2006;38:112-15.
- Gnjidic D, Le Couteur DG, Abernethy DR, Hilmer SN. Drug Burden Index and Beers Criteria: impact on functional outcomes in older people living in self-care retirement villages. J Clin Pharmacol 2012;52:258-65.
- Hall KS, McAuley E. Examining indirect associations between physical activity, function, and disability in independent- and assisted-living residents. J Phys Activ Health 2011;8:716-23.
- Sackley CM, Rodriguez NA, van den Berg M, Badger F, Wright C, Besemer J, et al. A phase II exploratory cluster randomized controlled trial of a group mobility training and staff education intervention to promote urinary continence in UK care homes. Clin Rehabil 2008;22:714-21.
- Froud R, Eldridge S, Lall R, Underwood M. Estimating the number needed to treat from continuous outcomes in randomised controlled trials: methodological challenges and worked example using data from the UK Back Pain Exercise and Manipulation (BEAM) trial. BMC Med Res Methodol 2009;9.
- Perera S, Mody SH, Woodman RC, Studenski SA, Perera S, Mody SH, et al. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc 2006;54:743-9.
- Kwon S, Perera S, Pahor M, Katula JA, King AC, Groessl EJ, et al. What is a meaningful change in physical performance? Findings from a clinical trial in older adults (the LIFE-P study). J Nutr Health Aging 2009;13:538-44.
- Wedzicha JA, Bestall JC, Garrod R, Garnham R, Paul EA, Jones PW. Randomized controlled trial of pulmonary rehabilitation in severe chronic obstructive pulmonary disease patients, stratified with the MRC dyspnoea scale. Eur Respir J 1998;12:363-9.
- Billinger SA, Vidoni ED, Honea RA, Burns JM. Cardiorespiratory Response to Exercise Testing in Individuals With Alzheimer's Disease. Arch Phys Med Rehabil 2011;92:2000-5.
- Theou O, Stathokostas L, Roland KP, Jakobi JM, Patterson C, Vandervoort AA, et al. The effectiveness of exercise interventions for the management of frailty: a systematic review. J Aging Res 2011.
- Normand C. Measuring outcomes in palliative care: limitations of QALYs and the road to PalYs. J Pain Symptom Manag 2009;38:27-31.
- British Geriatrics Society . for Older People in Care Homes: A Call for Leadership, Partnership and 2011. www.bgs.org.uk/campaigns/carehomes/quest_quality_care_homes.pdf (accessed 12 January 2012).
- BBC . Southern Cross Set to Shut down and Stop Running Homes 2011. www.bbc.co.uk/news/business-14102750 (accessed 11 October 2011).
- Cluster randomised trials: methodological and ethical considerations. London: MRC; 2002.
- The Medicines for Human Use (Clinical Trials) Regulations 2004 n.d.
- Cullum S, Tucker S, Todd C, Brayne C. Effectiveness of liaison psychiatric nursing in older medical inpatients with depression: a randomised controlled trial. Age Ageing 2007;36:436-42.
- Tajalizadekhoob Y, Sharifi F, Fakhrzadeh H, Mirarefin M, Ghaderpanahi M, Badamchizade Z, et al. The effect of low-dose omega 3 fatty acids on the treatment of mild to moderate depression in the elderly: a double-blind, randomized, placebo-controlled study. Eur Arch Psychiatry Clin Neurosci 2011;261:539-49.
- van de Rest O, Geleijnse JM, Kok FJ, van Staveren WA, Hoefnagels WH, Beekman AT, et al. Effect of fish-oil supplementation on mental well-being in older subjects: a randomized, double-blind, placebo-controlled trial. Am J Clin Nutr 2008;88:706-13.
- Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry 1979;134:382-9.
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry 1960;23:56-62.
- Radloff SL, Teri L. Use of the Center for Epidemiological Studies-Depression Scale with Older Adults. Clin Gerontologist 1986;5:119-36.
- Alexopoulos GS, Abrams RC, Young RC, Shamoian CA. Cornell Scale for Depression in Dementia. Biol Psychiatry 1988;23:271-84.
- Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. BioMed Central 2007;5.
- Gerritsen DL, Steverink N, Frijters DH, Ooms ME, Ribbe MW. Social well-being and its measurement in the nursing home, the SWON-scale. J Clin Nurs 2010;19:1243-51.
Appendix 1 Scoring and algorithm for Geriatric Depression Scale-15
Scoring and algorithm for Geriatric Depression Scale-15 (PDF download)
Appendix 2 Level 1 OPERA exercise routine with links to music
Level 1 OPERA exercise routine with links to music (PDF download)
Appendix 3 Statistical analysis plan
Appendix 4 Notes on statistical analysis plan v1.1 for OPERA
Notes on statistical analysis plan v1.1 for OPERA (PDF download)
Appendix 5 Process evaluation interview topic guides
Appendix 6 Ethics substudy: focus group guide
Appendix 7 OPERA ethics substudy: key informant topic guide
OPERA ethics substudy: key informant topic guide (PDF download)
Appendix 8 End-of-study questionnaire: intervention
Appendix 9 End-of-study questionnaire: control
Appendix 10 Six-month post-OPERA follow-up interview schedule
Six-month post-OPERA follow-up interview schedule (PDF download)
Appendix 11 Consolidated Standards of Reporting Trials checklist
Consolidated Standards of Reporting Trials checklist (PDF download)
Appendix 12 Process evaluation interviewees: basic characteristics and data source codes
Process evaluation interviewees: basic characteristics and data source codes (PDF download)
Appendix 13 Feedback notes on recruitment and assessments (from recruiting team)
Feedback notes on recruitment and assessments (from recruiting team) (PDF download)
Appendix 14 Example responses from training feedback
Appendix 15 Training follow-up: exemplars of themes
Appendix 16 OPERA protocol v3
Glossary
- Assessment data
- Study data collected directly from participants.
- Caldicott Guardian
- A Caldicott Guardian is a senior person in each National Health Service organisation, who is responsible for the protection and confidentiality of patient and service-user information.
- Care homes (with or without nursing)
- Care homes are residential settings where a number of older people live together and have staff available 24-hours to provide personal care. Care homes with nursing must have a qualified nurse on duty 24-hours to provide additional nursing care for more dependent residents.
- Care home data
- Data collected indirectly from care home records and National Health Service records. This includes data collected from routine care home records (see Record data), from staff (see Proxy data), and the National Health Service (see National Health Service data).
- Care Quality Commission
- The Care Quality Commission (formally Commission for Social Care Inspection) is the independent regulator of health and social care in England. It promotes the rights and interests of people who use services and it has a wide range of enforcement powers to take action on their behalf if services are unacceptably poor.
- Case report form
- A paper or electronic form used to collect research data from each participant or participating site.
- Clinical record form
- A paper form used by the physiotherapists to record each resident's physical performance during each exercise group that they attended.
- Cohort population
- Study participants who were present and provided baseline assessment data prior to randomisation.
- Cross-sectional population
- All study participants irrespective of the time point at which they entered the study who provided data for end of study assessments.
- Data Monitoring and Ethics Committee
- The Data Monitoring and Ethics Committee is an independent committee, the role of which is to safeguard the interests of the study participants, assess the safety and efficacy of the study interview, and monitor the overall conduct of the study.
- Dementia specialist homes
- Care homes where residents must have a diagnosis of dementia to be considered for admission to the home.
- Depressed cohort
- Study participants who provided baseline assessment data prior to randomisation and whose Geriatric Depression Scale-15 scores indicated that they were depressed at baseline.
- Group exercise programme
- Exercise activities that are provided in a group format (and do not include teaching of skills, such as might be taught in an exercise class).
- Independent Mental Capacity Advocacy
- Independent Mental Capacity Advocacy provides an independent advocacy service for people who lack capacity in facing decisions made by the National Health Service or local authorities on serious medical treatment, change of residence, a care review or adult protection issue.
- Mental Capacity Act
- The Mental Capacity Act (2005) for England and Wales is designed to support and protect people who cannot make decisions for themselves or lack the mental capacity to do so.
- National Health Service data
- Data from the Secondary Uses Services databases held by participating primary care trusts, and the National Health Service Medical Record Information Service.
- Nominated consultee
- If a person who lacks capacity has no personal consultee (see below), a nominated consultee can be proposed. This could be someone from an organisation (church, charity) or a professional (general practitioner, social worker), providing that they have no connection with the research study.
- Personal consultee
- Someone trusted by the person who lacks capacity, such as a family member or friend who is not acting in a professional or paid capacity.
- Physical activity assessment
- Assessment of physical abilities and mobility factors, along with other considerations relating to participation in a moderate-intensity exercise programme.
- Primary care trust
- Primary care trusts receive budgets from the Department of Health to commission and provide primary care and community services across the local area and to commission hospital services for patients.
- Process evaluation
- A process evaluation can assess to what degree a programme was implemented, including what activities were carried out, the degree to which the priority population was reached, and what the barriers were to adoption and implementation of the intervention.
- Proxy data
- Assessments by care home staff of participant's health state and social interaction.
- Record data
- Data collected directly from routine care home records.
- Trial Steering Committee
- The Trial Steering Committee is a committee responsible for the overall supervision and progress of a study ensuring it is conducted in accordance with the principles of Good Clinical Practice and the relevant regulatory requirements.
- Whole-home intervention
- A whole-home, ‘ecological’ intervention directed at changing the whole-home environment and culture within care homes.
List of abbreviations
- A&E
- accident and emergency
- C&W
- Coventry and Warwickshire
- CES-D
- Center for Epidemiologic Studies Depression Scale
- CI
- confidence interval
- CONSORT
- Consolidated Standards of Reporting Trials
- DMEC
- Data Monitoring and Ethics Committee
- EQ-5D
- European Quality of Life-5 Dimensions
- HDRS
- Hamilton Depression Rating Scale
- ICD-10
- International Statistical Classification of Diseases and Related Health Problems, Tenth revision
- MADRS
- Montgomery-Åsberg Depression Rating Scale
- NA
- not available
- NEL
- north-east London
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NOK
- next of kin
- NSAID
- non-steroidal anti-inflammatory drugs
- OR
- odds ratio
- SD
- standard deviation
- SSRI
- selective serotonin re-uptake inhibitor
- WHO
- World Health Organization