Notes
Article history paragraph text
The research reported in this issue of the journal was commissioned and funded by the HTA programme on behalf of NICE as project number 11/57/01. The protocol was agreed in November 2011. The assessment report began editorial review in April 2012 and was accepted for publication in September 2012. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors' report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
The present monograph presents as full a version of the report as is possible while retaining readability, but some sections, sentences, tables and figures have been removed. Readers should bear in mind that the discussion, conclusions and implications for practice and research are based on all the data considered in the original full NICE report.
Note
This monograph is based on the Diagnostic Assessment Report produced for NICE. The full report contained a considerable number of data that were deemed commercial-in-confidence. The full report was used by the Appraisal Committee at NICE in their deliberations. The full report with each piece of commercial-in-confidence data removed and replaced by the statement ‘commercial-in-confidence data removed’ is available on the NICE website: www.nice.org.uk.
The present monograph presents as full a version of the report as is possible while retaining readability, but some sections, sentences, tables and figures have been removed. Readers should bear in mind that the discussion, conclusions and implications for practice and research are based on all the data considered in the original full NICE report.
Permissions
Copyright statement
© Queen's Printer and Controller of HMSO 2013. This work was produced by Shepherd et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Scientific summary
Background
It is important that the level of general anaesthesia (GA) is appropriate for the individual patient undergoing surgery. If anaesthesia is deeper than required to keep a patient unconscious, there might be increased risk of anaesthetic-related morbidity, such as postoperative nausea, vomiting and cognitive dysfunction. If anaesthesia is too light, patients may not be fully unconscious and could be at risk of intraoperative awareness. Intraoperative awareness is a relatively rare event with an incidence typically of around one to two patients per 1000. However, over time, awareness may cause depression, anxiety and post-traumatic stress disorder (PTSD).
During GA, patients are routinely monitored for signs of potential intraoperative awareness, including tachycardia (rapid heart rate), hypertension, sweating, lacrimation (tear production), movement/grimacing and tachypnoea (rapid breathing). In patients receiving inhaled GA, end-tidal (exhaled) anaesthetic gas concentrations may be assessed to gauge depth of anaesthesia. However, clinical observation alone may not be a reliable surrogate marker of depth of anaesthesia. Technologies have been developed using electroencephalography (EEG) to measure and interpret electrical activity in the brain to provide a measure of unconsciousness. Most devices comprise a module that collects raw EEG data via sensors placed on the patient's forehead and then processes and analyses these using a mathematical algorithm. The output is then displayed numerically on a monitor for use by the anaesthetist to judge depth of unconsciousness, and to alter anaesthetic dose accordingly. Three such devices prioritised for this report are Bispectral Index (BIS), E-Entropy and Narcotrend.
Objectives
The objective of this report is to assess the clinical effectiveness and cost-effectiveness of BIS, E-Entropy and Narcotrend technologies to monitor the depth of anaesthesia in surgical patients undergoing GA.
Methods
Systematic review of patient outcomes
A systematic review of patient outcomes associated with depth of anaesthesia monitoring was conducted. A search strategy was developed and run on eight bibliographic electronic databases. Reference lists supplied by the device manufacturers were checked to identify potentially relevant studies. Eligibility criteria were applied to titles and abstracts and to full papers by two reviewers independently. Because of the relatively large volume of evidence for BIS, we included only trials that were supplemental to a recent Cochrane systematic review of BIS. Included studies were data extracted using a standard template. Risk of bias and markers of quality were assessed. The studies were synthesised narratively, with meta-analyses from the Cochrane review of BIS updated with supplemental studies where feasible and appropriate.
Systematic review of cost-effectiveness
A systematic review of the literature on the cost-effectiveness of depth of anaesthesia monitoring compared with standard clinical monitoring was undertaken. Included studies were evaluated for their quality and for generalisability to the UK. Eligibility criteria were applied to titles and abstracts and to full papers by two reviewers independently, and the studies were synthesised narratively.
Economic evaluation
A decision-analytic model was developed to assess the cost-effectiveness of depth of anaesthesia monitoring compared with standard clinical observation. A simple decision tree was developed, which accounted for patients' risk of experiencing short-term anaesthetic-related complications in addition to a risk of experiencing intraoperative awareness.
It was assumed that a proportion of patients who experience awareness will suffer psychological symptoms and that a proportion of those will develop PTSD and may seek treatment. A systematic review of health-related quality of life (HRQoL) in PTSD was undertaken in order to estimate the quality-of-life decrement to be applied as the result of any psychological symptoms arising from an awareness episode. The costs of depth of anaesthesia monitoring consist of the capital costs associated with acquisition of the monitor and recurring costs associated with sensors that are attached to the patient. Equivalent annual costs for each monitor were calculated for an effective equipment life of 5 years. Unit costs of anaesthetic drugs were derived from the British National Formulary (BNF) and supplied from an NHS Trust. The baseline incidence of awareness in high-risk patients was calculated from the control arms of randomised controlled trials (RCTs) in this group of patients. The summary values of the effectiveness of depth of anaesthesia monitoring were taken from our systematic review of patient outcomes.
The model evaluates costs [UK sterling (pounds) using a 2011 price base] from the perspective of the NHS and Personal Social Services. Outcomes in the model are expressed as quality-adjusted life-years (QALYs). Both costs and outcomes are discounted using a 3.5% annual discount rate, in line with current guidance.
Results
Systematic review of patient outcomes
From a total of 776 bibliographic records, 22 RCTs comparing BIS, E-Entropy and Narcotrend with standard clinical monitoring were included in the systematic review of patient outcomes. Fifteen trials of BIS, seven trials of E-Entropy and four trials of Narcotrend all compared with standard clinical monitoring. (Note that some trials compared more than one of the three devices to standard clinical monitoring.) Some of the trials reported that in the EEG arm anaesthesia doses were titrated according to device values in conjunction with clinical signs. In other trials the use of clinical signs alongside EEG monitoring was not explicit. The Cochrane review of BIS included 31 RCTs. The trials included in both reviews span the period between 1997 and 2011 in terms of publication date.
In many cases, the risk of bias in the trials was unclear because of limitations in reporting of methodological details. The trials varied in terms of their sample sizes, from as low as 20 to over 6000 patients, but, in general, sample sizes were relatively small (e.g. fewer than 200). Fifteen of the trials in this systematic review and all of the trials in the Cochrane BIS review were conducted in adult patients, of varying mean ages. Seven of the trials in this review were conducted with children. The trials were generally single-centre studies conducted in a range of locations including Europe, North America and Asia.
Six trials were conducted with patients classified as having one or more risk factors for intraoperative awareness (e.g. planned cardiac surgery, pulmonary hypertension, end-stage lung disease), all of which evaluated BIS monitoring. The trials tended to exclude patients with significant ill health or factors that may interfere with EEG recordings.
Explicit intraoperative awareness was assessed in 16 of the trials, but in most of these no episodes were recorded. However, awareness is a relatively rare event and the trials were not statistically powered to detect it. The six trials of patients classified with risk factors for intraoperative awareness, all of which evaluated BIS, were combined in a fixed-effect meta-analysis. The overall pooled Peto's odds ratio (OR) was 0.45 [95% confidence interval (CI) 0.25 to 0.81] in favour of BIS.
Caution is advised in the interpretation of this result as, overall, there was statistically significant heterogeneity (p = 0.009; I2 = 79%). Both the subgroup of trials, which included a trial of mixed inhaled and intravenous anaesthesia, and the subgroup, which included trials of total intravenous anaesthesia (TIVA), statistically favoured BIS monitoring. However, in the subgroup of trials that used only inhaled anaesthesia, the Peto's OR was 1.79 (95% CI 0.63 to 5.11), favouring standard clinical monitoring, although not statistically significant.
Systematic review of cost-effectiveness
A total of 134 potentially relevant references were identified by the cost-effectiveness searches. Of these, one study comparing BIS with standard clinical monitoring met all of the inclusion criteria. The study reported cost per avoided intraoperative recall, with the incidence of recall with BIS reported as 0.04% compared with 0.18% for standard monitoring, resulting in a cost per avoided recall of US$4410. The authors of the study concluded that BIS monitoring did not appear cost-effective. However, the results and conclusions should be viewed with caution because of poor methodological and reporting quality.
Economic evaluation
For each technology we presented a base-case analysis for two modes of anaesthetic administration {TIVA and mixed anaesthesia [induction with intravenous (i.v.) anaesthesia and maintenance with inhaled anaesthesia or a combination of inhaled and i.v. anaesthetic]} and for two patient populations (those considered at high risk of intraoperative awareness and a general surgical population, at average risk of intraoperative awareness).
Bispectral Index compared with standard clinical monitoring
In cohorts of 10,000 patients at high risk of intraoperative awareness undergoing GA with TIVA, the incremental cost-effectiveness ratio (ICER) for BIS compared with standard clinical monitoring in this population was £22,339.
For the population of general surgical patients undergoing GA with TIVA, BIS monitoring was modelled as being associated with 3.8 cases (per 10,000 patients) of awareness, compared with 16 in patients receiving standard clinical monitoring. Given the lower baseline risk of awareness in this population, the QALY gain with BIS monitoring was lower (0.0003) than for high-risk patients. This resulted in a higher ICER (£34,565).
Deterministic sensitivity analyses indicated that the ICER was sensitive to the same input parameters as for the population at high risk of awareness.
The baseline estimates of awareness, late psychological symptoms (LPS) and PTSD for high-risk patients undergoing mixed GA were the same as for high-risk patients undergoing TIVA. However, given that the OR of awareness with BIS monitoring was higher in this analysis, the estimated reduction in LPS and PTSD was lower. The ICER for BIS compared with standard clinical monitoring in this population was £29,634.
The baseline estimates of awareness, LPS and PTSD in the population of general surgical patients undergoing mixed GA were the same as for TIVA. Although a proportion of the higher cost associated with BIS monitoring was offset by reduction in anaesthetic consumption, the cost-saving for inhaled anaesthesia was lower than for TIVA. As a result the incremental cost was greater. Given the lower baseline risk of awareness in this population, the QALY gain with BIS monitoring was lower (0.0003) than for high-risk patients, resulting in a higher ICER (£49,198).
Deterministic sensitivity analyses indicated that the ICER was sensitive to a number of parameters, including the baseline incidence of awareness and the effectiveness of BIS in reducing awareness.
E-Entropy compared with standard clinical monitoring
In patients at high risk of awareness undergoing GA with TIVA, the modelled cost per patient with E-Entropy monitoring was higher than with standard clinical monitoring, although some of the additional cost was offset by reduced cost associated with psychological sequelae of awareness. The ICER for E-Entropy compared with standard clinical monitoring in this population was £14,421.
In the population of general surgical patients undergoing GA with TIVA, E-Entropy monitoring had a higher cost per patient than standard clinical monitoring. There was no reduction in anaesthetic drug costs to offset the additional costs of E-Entropy monitoring. Given the lower baseline risk of awareness in this population, the QALY gain was lower than for high-risk patients, which resulted in a higher ICER (£31,131–31,430).
In patients considered at high risk of awareness undergoing mixed GA, E-Entropy monitoring had higher costs and improved outcomes compared with standard clinical monitoring. However, the QALY gain was lower than for patients undergoing TIVA. The ICER for E-Entropy compared with standard clinical monitoring in this population was £19,367.
In the population of general surgical patients undergoing mixed GA, E-Entropy monitoring had higher costs than standard clinical monitoring. In contrast with the analysis for TIVA, the clinical trial used to estimate inhaled anaesthetic drug consumption reported a substantial decrease (29%), which resulted in approximately half of the additional cost of E-Entropy monitoring being offset by a reduction in anaesthetic drug costs. Despite the lower baseline risk of awareness, which resulted in a lower QALY gain with E-Entropy monitoring than for high-risk patients, the lower incremental cost resulted in an equivalent ICER (£19,000).
Deterministic sensitivity analyses indicated that the ICER was sensitive to a number of parameters, including the baseline incidence of awareness and the effectiveness of E-Entropy in reducing awareness.
Narcotrend compared with standard clinical monitoring
In patients at high risk of awareness undergoing GA with TIVA, the modelled cost per patient with Narcotrend monitoring was higher than with standard clinical monitoring, although some of the additional cost was offset by reduced cost associated with psychological sequelae of awareness. The ICER for Narcotrend compared with standard clinical monitoring in this population was £5681. Deterministic sensitivity analyses indicated that the ICER was sensitive to a number of parameters, including the baseline incidence of awareness and the effectiveness in reducing awareness.
In the general surgical population undergoing GA with TIVA, and also undergoing mixed GA, Narcotrend monitoring had a lower cost per patient than standard clinical monitoring. The additional cost of monitoring was more than offset by reduction in anaesthetic drug consumption. Given the lower baseline risk of awareness in this population, the QALY gain was lower than for high-risk patients. Narcotrend dominated standard clinical monitoring. Narcotrend remained dominant in the majority of deterministic sensitivity analyses.
In patients at high risk of awareness undergoing mixed GA, Narcotrend monitoring had higher costs and improved outcomes than standard clinical monitoring, although the QALY gain (0.0005) was lower than for patients undergoing TIVA. The ICER for Narcotrend compared with standard clinical monitoring in this population was £8033. Deterministic sensitivity analyses indicated that the ICER was sensitive to the same parameters as for high-risk patients undergoing TIVA.
Conclusion
In general, BIS, E-Entropy and Narcotrend technologies for monitoring the depth of anaesthesia are associated with reductions in general anaesthetic consumption, and decreased anaesthetic recovery times, compared with monitoring of clinical signs alone. However, these reductions may be considered clinically modest. The available evidence on the impact of the technologies on reducing the likelihood of intraoperative awareness is limited. Overall, BIS was associated with a statistically significant reduction in intraoperative awareness in patients classified as at higher risk, although there is uncertainty in effect estimates because of significant heterogeneity. Caution is advised because of uncertainties about the risk of bias of many of the included trials, and because many outcome measures were not statistically powered.
The cost-effectiveness of depth of anaesthesia monitoring appears to be highly dependent on the incidence of awareness, the HRQoL impact of psychological sequelae of awareness and the probability of developing psychological illness following awareness, as well as the effectiveness of depth of anaesthesia monitoring in reducing awareness. Cost-savings resulting from reduced use of anaesthetic drugs may offset some of the additional cost of depth of anaesthesia monitoring. The cost of sensors attached to the patient appears to be a key factor in the additional cost of depth of anaesthesia monitoring.
This report makes the following research recommendations (in priority order):
-
RCTs of E-Entropy- and Narcotrend-guided anaesthesia monitoring are needed, in high-risk patients, with adequate statistical power to detect explicit intraoperative awareness, and of sufficient length of follow-up to detect delayed cases of awareness.
-
RCTs of all three technologies should also evaluate the effects of anaesthesia overdosing, including short-term effects, such as nausea and vomiting, as well as longer-term impact on cognitive function.
-
RCTs of E-Entropy- and Narcotrend-guided anaesthesia monitoring are also needed in children.
Study registration
This study is registered as PROSPERO CR042011001834.
Funding
Funding for this study was provided by the Health Technology Assessment programme of the National Institute for Health Research.
Chapter 1 Background and definition of the decision problem
Condition and aetiology
Background
When patients sundergo surgical procedures under general anaesthesia (GA) it is important that the depth of anaesthesia provided by the anaesthetist is neither too light nor too deep. If the depth is too light, patients may not be fully unconscious and may be at risk of intraoperative awareness, which may lead to longer-term postoperative sequelae such as post-traumatic stress disorder (PTSD). If the depth of anaesthesia is deeper than the minimum needed to keep a patient unconscious, the patient may be at risk of anaesthetic-related morbidity, which can include postoperative nausea, vomiting and varying degrees of cognitive dysfunction. Provision of lighter anaesthesia is more likely to facilitate prompt recovery, and therefore potential health-care savings, but has to be balanced against the risks of inadequate analgesia and intraoperative awareness. A challenge facing the anaesthetist is to avoid under- or overdosing the anaesthetic, as the response to anaesthetic agents varies among individuals.
A primary concern with inadequate depth of anaesthesia is that a patient may experience intraoperative awareness, which the patient may recall postoperatively (explicit awareness) or may not subsequently recall (implicit awareness). 1 Although implicit awareness can exist without conscious recall, it may (or may not) influence patients' experience and behaviours after anaesthesia. Conscious recall may underestimate instances of awareness, as people are generally aware of more things intraoperatively than they remember. 2,3 Some authors have used ‘wakefulness’ as a term to describe the ability of a patient to respond to a command during GA without recollection of this in the postoperative period. 4 Examples of intraoperative events that have been classed as awareness by researchers but which were not recalled by patients when questioned after their surgery, include eye opening and gross motor responses during anaesthesia. 2,3
Awareness symptoms and sequelae
Intraoperative awareness is commonly reported by patients as hearing noises or voices, a sensation of paralysis, anxiety, helplessness, panic and/or pain during their operation. 5,6 Some patients may report intraoperative awareness when interviewed in the recovery room, but many patients do not recall intraoperative awareness until several weeks after surgery. 7,8 Patients who experience intraoperative awareness may go on to experience problems including sleep disturbances, nightmares, flashbacks, anxiety during the day and/or fear about future anaesthetics,5,7,9 and may be diagnosed with PTSD. 5,6,8,10 Some patients who have experienced symptoms following awareness will not seek treatment because the episode was so traumatic that they do not wish to discuss it, particularly if they have subsequently developed a phobia of medical personnel.
Studies that have followed up patients with intraoperative awareness for 2 years11 or 5 years8 estimated that around half of the patients with intraoperative awareness experienced PTSD. In these patients, the PTSD was not detectable immediately after surgery, but commenced several weeks afterwards, and then persisted throughout the follow-up period. The findings from these studies highlight the importance of conducting long-term follow-up of patients who might be at risk of intraoperative awareness, and emphasise that interviews to detect intraoperative awareness within the first few days of surgery may not detect either intraoperative awareness or sequelae including PTSD.
Incidence of intraoperative awareness
Intraoperative awareness is a rare event, so large studies are needed in order to accurately estimate the incidence. Large studies (with sample size of at least 10,000 patients) have not been conducted in the UK. Large studies in other countries, which have all been based on adult populations, suggest that the incidence rate for intraoperative awareness and recall is typically one to two patients per 1000, although a considerably lower incidence of 0.07 per 1000 patients was found in the largest study14 which included over 87,000 patients, whereas a higher incidence of 4.1 per 1000 patients was found in a Chinese study15 (Table 1).
| Study | Country | Sample size (number of patients) | Awareness assessment method | Estimated incidence of intraoperative awareness per 1000 patients |
|---|---|---|---|---|
| Myles et al. (2000)12 | Australia | 10,811 | NR | 1.1 |
| Sandin et al. (2000)9 | Sweden | 11,785 | Modified Brice interview | 1.0 without neuromuscular block, 1.8 with neuromuscular block |
| Sebel et al. (2004)13 | USA | 19,575 | Modified Brice interview | 1.3 overall (one or two per site) |
| Pollard et al. (2007)14 | USA | 87,361 | Modified Brice interview | 0.07 |
| Xu et al. (2009)15 | China | 11,101 | Modified Brice interview | 4.1 (all patients had neuromuscular block) |
Differences in incidence estimates between these studies might be explained by variations in data collection methods, the frequency and timing of interviews, or the characteristics of the patient populations and surgical procedures included. 14 The notably high incidence of intraoperative awareness in the Chinese study was considered by the authors to be possibly attributable to differences between Chinese and Western medical practices, including inappropriately light anaesthesia in the Chinese population. 15
Risk factors for intraoperative awareness
Some groups of patients undergoing GA are at increased risk of intraoperative awareness because they cannot tolerate adequate doses of anaesthetic or because signs of inadequate anaesthesia are masked or because, owing to the nature of the patient's condition and the surgery, higher doses of anaesthetic were considered to be risky. 7,16 For example, patients undergoing procedures such as caesarean section were often given lower anaesthetic doses because of concerns over adverse fetal effects. However, most caesarean sections are now performed under regional anaesthesia (epidural or spinal) rather than under GA. Similarly, patients undergoing cardiac surgery were given lower doses because of concerns over adverse effects on their circulation. However, modern anaesthetic agents and improved treatment of haemodynamic effects have lessened the risks. 17
Use of muscle relaxant drugs (e.g. to facilitate tracheal extubation) is an important risk factor for intraoperative awareness because it permits the use of less anaesthetic while at the same time preventing patients' movement responses that could signal inadequacy of anaesthesia to the anaesthetist, potentially allowing anaesthetic insufficiency to remain uncorrected. Some patients who have received muscle relaxants (and are therefore paralysed) have reported feelings of impending doom and death while experiencing intraoperative awareness, and have suffered long-term psychological ill health. Around half of all operations under GA involve the use of muscle relaxants.
Other risk factors for intraoperative awareness that have been identified include a high American Society of Anesthesiologists (ASA) physical status classification (indicating worse illness);13,14 use of total intravenous anaesthesia (TIVA);18 history of depression;6 lack of benzodiazepine premedication;18 and emergency surgery performed at night. 18
Impact of intraoperative awareness
Patients who experienced severe long-term psychological or psychiatric symptoms following intraoperative awareness have reported that the symptoms caused a definite impairment of their lives. 11 For example, it may limit their ability to work, and have an adverse effect on relationships with family and friends. Patients with less severe symptoms of intraoperative awareness frequently experience a sense of dissatisfaction with their anaesthetic experience. 12 Such patients may be at risk of avoiding certain health-care procedures if they feel anxious or if they mistrust health professionals as a result of their previous experience.
Aside from the cost of managing the sequelae of intraoperative awareness, the NHS could be at risk of professional liability claims from those who have experienced intraoperative awareness. 19 However, the psychological trauma experienced by some people may be so great that they may be discouraged from reporting intraoperative awareness because they do not want to discuss it. The incidence of explicit awareness may therefore be underestimated. High-profile cases of intraoperative awareness in the media may influence public perceptions of the safety of anaesthetic procedures, which could influence how patients perceive information and services provided to them by the NHS. Some patients who have experienced intraoperative awareness have developed a fear of anaesthesia, which, in the event that further anaesthesia is required, could have implications for their acceptance or tolerance of subsequent care.
Measurement of intraoperative awareness
Basic signs of intraoperative awareness during anaesthesia include tachycardia (rapid heart rate), hypertension, sweating, lacrimation (tear production), movement/grimacing and tachypnoea (rapid breathing). Intermittent checking of these clinical signs has low sensitivity and specificity for detecting awareness. 20,21 Cases of intraoperative awareness do not always involve changes in haemodynamic parameters. 22
Tests of intraoperative awareness may seek to identify awareness in situ, often using verbal, tactile or noxious stimulation,1,2 and/or by interviewing the patient after surgery to establish whether or not they recall having been aware during the period of anaesthesia. During surgery the isolated forearm technique is one of the methods of detecting possible awareness in patients who have received neuromuscular blockade. A tourniquet is applied to the patient's upper arm, and inflated above systolic blood pressure to isolate the patient's forearm from the effects of the block. Movement of the arm, either spontaneously or to command, indicates wakefulness, although not necessarily explicit awareness. The isolated forearm technique has not been widely used in practice, though it has been used as a research tool in a number of studies. 21,23
The most popular approach for postoperative assessment of awareness (as illustrated in Table 1) is to question patients using a version of the Brice interview. 24 The Brice interview poses five questions: (1) What was the last thing you remembered happening before you went to sleep? (2) What was the first thing you remember happening on waking? (3) Did you dream or have any other experiences while you were asleep? (4) What was the worst thing about your operation? (5) What was the next worst? In addition to an interview to detect intraoperative awareness, some studies have used a second interview (sometimes referred to as a follow-up questionnaire) to characterise the awareness episodes in more detail. 25,26 In some studies, independent expert verification of interview responses has been used to determine definite cases of awareness. 27
Studies that report using modified versions of the Brice interview have to be interpreted with caution, as there may be considerable variation in the number of questions, their content and extent of overlap with the original Brice interview. None of the studies has looked into the psychometric properties of the interview questionnaires that it used, so their reliability and validity could be questionable. As noted above, not all cases of awareness would be detected if interviews are conducted immediately after surgery with a single interview,9 as recall of intraoperative awareness has been reported up to 19 years after the event. 5 Other issues to consider when interpreting postoperative interviews are: repeated questioning may induce false memories,3,27 and three of the five Brice questions are about pre or post surgery or dreaming, which would not specifically reveal remembrance of an intraoperative awareness event. 28 The interview approach to assessing awareness with recall has also been criticised because it cannot assess awareness without recall, even though this may include implicit memory (i.e. still impact on postoperative patient experience or behaviour).
As noted above, awareness without explicit recall can be assessed using specialist interview approaches,29 but these appear to be rarely used and have been restricted to experimental research settings. It is not known whether or not changes in behaviour as a result of implicit awareness are associated with longer-term morbidity.
Consequences of anaesthesia overdose
It is suggested that anaesthetists tend to provide higher doses of anaesthetic than may be necessary, in order to reduce the risk of intraoperative awareness. 23 Potential consequences of anaesthesia overdose include prolonged recovery time (which in severe cases may lead to potentially life-threatening cardiovascular and respiratory collapse), vomiting, headaches, dizziness and, less commonly, short- or long-term cognitive dysfunction, particularly in elderly patients. 30
Outcomes relevant to assessing the consequences of anaesthesia overdose include postoperative nausea and vomiting (PONV) assessed using patient questionnaires or rating scales; assessments of time to recovery from anaesthesia using various measures (e.g. the time to extubation, eye opening, purposeful movement, discharge from the operating theatre or the recovery room or time to attain a specified recovery score); consumption of general anaesthetic or other drugs (such as analgesics and antinausea agents); and assessment of cognitive or neurological function.
Description of technologies under assessment
The depth of anaesthesia and likelihood of awareness may be monitored using a number of different approaches. As mentioned, potential awareness may be identified by monitoring of basic clinical signs such as blood pressure and heart rate (for more information see Comparators). Other techniques which have been used, but are considered historical, include spontaneous and provoked lower oesophageal sphincter contractility, forehead galvanometry and saccadic eye movements.
Electroencephalography (EEG) is the study of patient electrical brain activity to assess unconsciousness. During the last 15–20 years a number of EEG-based technologies have become commercially available for measuring depth of anaesthesia and for use in guiding anaesthetic management during surgery. Most comprise a module that collects raw EEG data via sensors placed on the patient's forehead and then processes and analyses these using a mathematical algorithm. Raw EEG signals can be difficult to interpret; therefore, many modules convert the signal to a number displayed on a monitor to indicate to the anaesthetist the depth of unconsciousness (e.g. from 0 to 99). EEG can be distinguished as spontaneous or derived from middle latency evoked potentials (auditory and visual). Evoked potentials measure the EEG responses to repetitive auditory or visual stimuli, and measure the integrity of the neural pathways that bring information from the periphery to the cortex. 21 A number of EEG-derived indexes have been devised based on different algorithms,23 including the Bispectral Index (BIS), E-Entropy, Narcotrend, Cerebral State Index, the Patient State Index and NeuroSENSE.
In practice, EEG devices can be used in conjunction with observation of clinical signs to titrate anaesthetic dose (see the section Comparators). Expert opinion suggests that anaesthetists primarily use clinical signs with EEG values as an additional source of information. If there is a difference between them then the anaesthetist will usually favour the clinical signs and their judgement.
After consultation by the National Institute for Health and Care Excellence (NICE) with relevant stakeholders, three of the technologies currently available were prioritised for the current assessment: the BIS, E-Entropy and Narcotrend.
Bispectral Index (Covidien, Mansfield, MA, USA)
The BIS system, introduced in 1994, uses a sensor on the patient's forehead to measure electrical activity in the brain before using proprietary algorithmic analysis to process the EEG data and calculate a number between 0 (absence of brain electrical activity) and 100 (wide awake). This provides a measure of cerebral electrical response to increasing doses of anaesthetic drugs. The target range of BIS values during GA is 40–60, which indicates a low probability of consciousness.
Bispectral Index technology is compatible with a wide range of patient monitoring platforms through an interface for ‘BIS Ready’ systems [such as those manufactured by Mennen Medical Corporation, Feasterville-Trejose, PA, USA (e.g. VitaLogik series monitors); Philips Healthcare, Da Best, the Netherlands (e.g. IntelliVue series monitors); and Dräger Medical Inc., Telford, PA, USA (e.g. Infinity series monitors). This works via the BISx or BISx4 plug-in connector, which allows integration with existing anaesthesia systems.
E-Entropy module (GE Healthcare, Medical Diagnostics, Amersham, UK)
Entropy monitoring in anaesthesia has been studied over the last 10 years. E-Entropy (previously known as M-Entropy) is designed to aid the management of GA in patients by measuring the level of order or disorder in spontaneous brain and frontalis muscular activity. It uses a proprietary algorithm to process EEG and frontal electromyography data to produce two values that indicate the depth of anaesthesia. The first value, response entropy, is based on both EEG and frontal electromyography signals and provides an indication of the patient's responses to external stimuli and may signal early awakening. The second value, state entropy, is a stable parameter based on EEG and may be used to assess the hypnotic effect of anaesthetic agents on the brain. Response entropy is always higher than or equal to the state entropy value. The response entropy–state entropy difference may be used as a secondary target value when monitoring depth of anaesthesia.
More ordered signals, with less variation in the wavelength and amplitude, over time, produce high values of entropy and may indicate that the patient is awake. Regular signals, with a constant wavelength and amplitude over time, produce low or zero entropy values, indicating a low probability of recall and suppression of brain electrical activity. The response entropy scale ranges from 0 (no brain activity) to 100 (fully awake) and the state entropy scale ranges from 0 (no brain activity) to 91 (fully awake). The clinically relevant target range for entropy values is 40–60. Response entropy and state entropy values near 40 indicate a low probability of consciousness.
E-Entropy is a plug-in module that is compatible with the Ohmeda S/5 Anaesthesia monitor and S/5 Compact Anaesthesia monitor using software L-ANE03(A) and L-CANE03(A), and all subsequent software releases since 2003. The module will not work with software levels that are older than indicated. It is also compatible with GE Healthcare's latest monitoring product range (CARESCAPE Monitors B850 and B650), but is incompatible with monitors made by other manufacturers.
Narcotrend monitor (MonitorTechnik, Bad Bramstedt, Germany)
The Narcotrend monitor automatically analyses the raw EEG using spectral analysis to produce a number of parameters. Multivariate statistical methods using proprietary pattern recognition algorithms are then applied to these parameters to provide an automatically classified EEG. The basis for the development of the automatic classification functions were visually classified EEG. The EEG visual classification scale is from stage A (awake) to stage F (very deep hypnosis), with stage E indicating the appropriate depth of anaesthesia for surgery. As a refinement to the A–F scale, an EEG index (100 = awake, 0 = very deep hypnosis) is also calculated.
The Narcotrend-Compact M is a stand-alone monitor that stores recorded EEG data on its hard disk and can send raw and processed EEG data in real time to other anaesthesia monitors. Data can also be saved to a USB flash drive for processing and evaluation of Narcotrend EEG recordings on a remote PC using the software NarcoWin. The Narcotrend algorithms are revised continually.
Subgroups of patients
Unsuitable patient populations include those undergoing specific surgical procedures in which the sensors would impede access to the surgical site, and therefore certain ENT, ophthalmic and neurosurgical procedures may be unsuitable for EEG monitoring. In neonates the immature EEG has resulted in inconsistent linkages between anaesthetic dosing and displayed BIS values, and an inability to demonstrate a titration potential for BIS-guided anaesthesia care. The manufacturer of BIS recommends that BIS values should be interpreted cautiously in patients with known neurological disorders and patients taking psychoactive medications. E-Entropy is validated only for patients over the age of 2 years; it is not for patients undergoing procedural or conscious sedation, and seizure activity may cause interference. In addition, E-Entropy readings may be inconsistent when monitoring patients with neurological disorders or patients on psychoactive medication. Limited information is available for subgroups of patients for whom Narcotrend may not be suitable, although Narcotrend values should be interpreted cautiously in patients with a history of central nervous system diseases.
Artefacts
All EEG monitoring is subject to contamination by artefacts generated either by the patient (e.g. by eye movements, muscle activity) or from external sources (poor skin contact, mains or power line interference, electrocautery). With the BIS system most artefacts present as elevated BIS values and the recommended strategy from the manufacturer for an unexpected elevated BIS value is prompt patient assessment, confirmation of anaesthetic dosing and delivery, and consideration of artefacts. Narcotrend is equipped with artefact detection algorithms to exclude segments contaminated with artefact from further analysis. If too many artefacts are detected, no classification result will be output and only raw EEG will be visible onscreen.
Current usage in the UK
Expert opinion suggests that there is low use of EEG in practice to monitor depth of anaesthesia. Current penetration of BIS technology in UK operating theatres is still relatively low but, as most anaesthetic monitors used in the UK could be compatible with the BIS module, BIS technology could be available in the majority of UK operating theatres. The manufacturers of E-Entropy in their submission to NICE estimate that nearly 45% of UK theatres would be ready and compatible with E-Entropy and ‘believe our theatre installed base to be around 60 to 65% of UK theatres’. No data are available on the provision or diffusion of Narcotrend in the UK. (Commercial-in-confidence information removed.)
Training
It appears that little additional training in the use of these technologies is needed. The manufacturer states that no specific additional training is required to use the BIS monitoring system (although expert clinical opinion disputes this). Instructions for use are provided with both the BIS device (stand-alone or module) as well as the BIS sensors and are regarded as sufficient guidance by the manufacturer for safe and effective use. Additional educational resources are provided by the manufacturer if necessary, such as simulation devices and online multimedia courses. For E-Entropy, 30 minutes of introductory training is suggested for health-care staff before use, with particular attention being paid to sensor application. A 1-day visit from staff to give a lecture and to demonstrate the use of Narcotrend in the operating theatre is judged sufficient training by the manufacturer for the majority of Narcotrend users.
Comparators
A number of clinical signs that are routinely monitored during anaesthesia can be used to assess potential awareness. Prior to induction of anaesthesia a variety of monitoring devices may be attached to the patient, including a pulse oximeter (to measure oxygen levels); a non-invasive blood pressure monitor; an electrocardiograph (to measure heart rate); and a capnograph (to measure inhaled and exhaled carbon dioxide concentration). Devices are also used to measure airway pressure and the patient's temperature. Other markers of awareness that are monitored include movement, lacrimation and sweating.
End-tidal anaesthetic gas concentrations (ETACs) may be used to assess the concentration of volatile (inhaled) anaesthetic in a patient, expressed as a percentage. ETAC can be used to calculate the minimum alveolar concentration (MAC), which is the minimum concentration of anaesthetic agent in the lungs at one atmosphere pressure that is required to prevent movement in 50% of individuals when exposed to a standard painful stimulus. MAC provides a measure of the potency for comparison between different inhaled general anaesthetics (see Care pathways), and anaesthesia can be titrated to keep within a certain MAC range.
Of all the signs and variables, the key things to observe are ETAC (where inhaled anaesthetics have been used), blood pressure and heart rate. However, in practice, the combination of signs that are used is likely to vary. 31
Care pathways
In UK health-care settings, GA is usually administered in an anaesthetic room32 (sometimes referred to as the induction room), following which the patient is transferred to the operating theatre. Monitoring of clinical signs always commences prior to administration of GA, and continues until surgery is complete and the patient is moved from the theatre to the recovery room (also referred to as the postanaesthesia care unit, PACU), or to intensive care or a high-dependency unit if applicable. Supplementary monitoring devices such as EEG-based technologies may also be attached during anaesthesia induction and continued until surgery is complete, anaesthesia has ceased and the patient has entered the recovery phase.
General anaesthetics are generally classified as intravenous (i.v.) or inhalational. Propofol is a commonly used i.v. anaesthetic and can be used for induction and/or maintenance of anaesthesia. Use of an i.v. anaesthetic for induction and maintenance is sometimes referred to as TIVA. Ketamine is also available for induction and maintenance of anaesthesia, but is rarely used. Inhaled anaesthetics are classified as volatile agents or nitrous oxide. The latter is used for maintenance of anaesthesia in combination with i.v. or volatile agents, in a concentration of 50–66% in oxygen33 (it can also be used for analgesia). Volatile anaesthetics can be used for induction and maintenance of anaesthesia, and also following induction with an i.v. anaesthetic. Volatile agents include isoflurane, desflurane and sevoflurane. Isoflurane is the preferred inhalational anaesthetic for use in obstetrics. 33 Desflurane is rapid acting and has about one-fifth of the potency of isoflurane. It is not recommended for induction of GA. Sevoflurane is also rapid acting, is more potent than desflurane and can be used for induction of anaesthesia. The MACs of desflurane, sevoflurane and isoflurane are 6.0, 1.8 and 1.2 for people of ages 30–60 years, and 5.2, 1.5 and 1.0 for people older than 65 years respectively. 34 MAC would be higher in children and young adults.
Summary of the decision problem
As has been described, the purpose of anaesthesia monitoring is to ensure adequate sedation of the patient under GA. If anaesthesia is too deep the patient may be at risk of adverse effects, such as a prolonged recovery time. However, if anaesthesia is not deep enough patients may be more likely to experience awareness of their surroundings, and this may have short- and long-term psychological effects, including depression and anxiety. Optimum anaesthetic dosing may also potentially lead to drug cost-savings.
Currently, anaesthetists generally use clinical observation of vital signs and other markers to assess unconsciousness and the possibility of awareness. However, clinical observation alone may not be a reliable surrogate marker of anaesthetic depth. As an alternative, technologies have been developed using EEG to measure and interpret patient electrical brain activity to provide a measure of unconsciousness. Three such technologies, prioritised for assessment, are BIS, E-Entropy and Narcotrend.
The aim of this report, therefore, is to assess the clinical effectiveness and cost-effectiveness of BIS, E-Entropy and Narcotrend to monitor the depth of anaesthesia in surgical patients undergoing GA.
Chapter 2 Assessment methods
Systematic review of patient outcomes
The purpose of this section is to describe the methods used in the systematic review of patient outcomes associated with depth of anaesthesia monitoring. These methods were stated a priori in the published research protocol. An extract of the protocol outlining the methods is given in Appendix 1.
Identification of studies
A search strategy was developed for MEDLINE and pilot tested by an experienced information scientist. The MEDLINE strategy (see Appendix 2) was adapted where necessary to the specific vocabulary and rules of other electronic bibliographic databases. Searches were run in the following databases: Ovid MEDLINE; Ovid EMBASE; Centre for Reviews and Dissemination (CRD); The Cochrane Library (Cochrane Database of Systematic Reviews (CDSR); Cochrane Central Register of Controlled Trials (CENTRAL); Database of Abstracts of Reviews of Effects (DARE); and Health Technology Assessment (HTA) database. For E-Entropy and Narcotrend the electronic searches were conducted from 1995 (around the time of the introduction of EEG technologies) to November 2011 (with an update search performed in February 2012).
Scoping searches indicated that the volume of evidence for BIS was relatively larger than for Narcotrend and E-Entropy and it would be beyond the resources available to include all of the BIS studies in the systematic review. During preliminary scoping searches we identified a recent Cochrane systematic review of BIS34 that had similar study eligibility criteria to our review (with the exception that it did not include studies of children). We therefore based our review of BIS on a Cochrane systematic review,34 which contained 31 randomised controlled trials (RCTs) of BIS. The most recent date of literature searching in the Cochrane review was May 2009. We therefore searched from the beginning of 2009 to November 2011 for studies of BIS (and then updated in February 2012) (see Method of data synthesis for further information about how results from the Cochrane review are integrated into the current review).
In addition to the searches of electronic bibliographic databases, the following sources were searched to identify potentially relevant studies:
-
contact with experts in the field (identified by NICE as part of the consultation process)
-
bibliographic lists of potentially relevant studies on BIS, E-Entropy and Narcotrend as supplied by the device manufacturers (via NICE)
-
reference lists of included studies
-
databases of research in progress, searched on 7 December 2011: UK Clinical Research Network (UKCRN); controlled-trials.com; ClinicalTrials.gov; NIHR-Clinical Research Network Portfolio; WHO ICTRP (International Clinical Trials Registry Platform).
The titles and abstracts of studies identified from these searches were imported into a Reference Manager bibliographic database. All titles and abstracts in this database were assessed against the inclusion/exclusion criteria (see Inclusion/exclusion criteria). Bibliographic records that clearly did not meet any of the inclusion criteria, or met at least one of the exclusion criteria, were excluded from further consideration. For each bibliographic record that met all of the inclusion criteria, or was of unclear relevance, a full-text version was obtained and assessed against the inclusion/exclusion criteria. Full-text records that clearly did not meet all of the inclusion criteria were excluded from further consideration, and the reasons for their exclusion were noted.
Both the title and abstract selection step and the full-text selection step were conducted independently by two reviewers. After screening the bibliographic records, the reviewers compared their selection results. All initial differences in opinion were resolved through discussion, without needing to involve a third reviewer.
Inclusion/exclusion criteria
The inclusion/exclusion criteria for this report were based on the scope of the appraisal set by NICE. Only articles published in the English language were included. Abstracts that had no corresponding full-text record (e.g. conference abstracts) were excluded unless they met two criteria: they were published in 2010 or later; and they provided sufficient details to allow appraisal of the methodology and the assessment of results to be undertaken.
The inclusion/exclusion criteria were provided to each reviewer as a standard list against which each title/abstract or full-text record could be readily assessed (see Appendix 3). In addition to the language and publication type restrictions, the following selection criteria were applied:
Population
Studies were included if they included patients who received GA for surgery, including adults and children (over the age of 2 years) in whom the technology is licensed. Studies involving patients receiving sedation in intensive care or high-dependency units, studies carried out in healthy volunteers and studies of non-surgical anaesthesia were excluded.
Diagnostic technologies
The diagnostic technologies included were E-Entropy, BIS and Narcotrend.
Comparators
Comparators included standard clinical monitoring for monitoring delivery of anaesthesia, including one or more of the following clinical markers: end-tidal anaesthetic gas concentrations (for inhaled anaesthesia); pulse measurement; heart rhythm; blood pressure; lacrimation; and sweating.
Outcomes
Studies were included if at least one of the following outcomes was reported:
-
probability of intraoperative awareness
-
patient distress and other sequelae resulting from intraoperative awareness
-
recovery status (e.g. Aldrete scoring system)
-
time to emergence from anaesthesia
-
time to extubation
-
time to discharge from the recovery room
-
consumption of anaesthetic agents
-
morbidity and mortality including postoperative cognitive dysfunction (POCD) from anaesthetic agents, pain-relieving drugs, antibiotics, antisickness drugs and muscle relaxants.
Study design
The review was limited to prospective controlled trials (once studies had been included in the systematic review, priority was given to RCTs unless no RCT evidence for relevant parameters was available in which case non-RCT data would be considered). Systematic reviews that met the inclusion criteria were retrieved in order to check their reference lists for potentially relevant studies but were not themselves evaluated (except for the Cochrane systematic review of BIS technologies,34 which was considered in more detail when conducting data synthesis: see Data extraction and critical appraisal methods).
Data extraction and critical appraisal methods
A standardised data extraction and quality appraisal template (see Appendix 5) was used to extract information on the relevant study characteristics for assessing the impact of the interventions on the outcomes listed above (see Inclusion/exclusion criteria) and for assessing study quality. Study quality assessment criteria included: Cochrane Collaboration Risk of Bias criteria,35 as specified in the review protocol; methods of data analysis, including the statistical tests used and whether or not studies were powered statistically to detect differences in outcomes between intervention and comparator groups; participant attrition; generalisability of the studies; and conflict of interests. Criteria for the critical appraisal of non-randomised and observational studies were specified in the protocol but were not required, as all the included studies were RCTs (see Results of systematic review of patient outcomes).
The data extraction and critical appraisal template was completed for each study included in the systematic review by one reviewer and was checked by a second reviewer. All initial discrepancies between the reviewers were resolved by discussion, without needing to involve a third reviewer.
Method of data synthesis
Analyses of the three monitoring devices are presented in respective separate subsections of this report (see Results of systematic review of patient outcomes). For each device a narrative synthesis was conducted, with characteristics of the included trials, and their outcomes, described in the text and tabulated.
As stated, the analysis of BIS was based on trials included in an existing Cochrane review of BIS,34 and supplemented by trials identified and included in the current systematic review. For each BIS outcome measure we present a narrative synthesis of the studies identified in the current systematic review, in addition to the pooled meta-analysis estimates from the Cochrane review. Where possible, we have updated the Cochrane meta-analyses for BIS with trials identified in the current review. However, the Cochrane BIS review included only trials of adults, and it was not considered appropriate to combine trials of children identified in our searches with the existing adult trials. We used Cochrane Review Manager 5.1.6 (The Cochrane Collaboration, The Nordic Cochrane Centre, Copenhagen, Denmark) to conduct the meta-analyses.
Systematic review of cost-effectiveness
Identification of studies
A comprehensive search strategy was developed, tested and refined by an experienced information scientist to identify studies of the cost-effectiveness of depth of anaesthesia monitoring. The MEDLINE search strategy is provided in Appendix 2.
A total of six electronic resources were searched. Searches were from database inception to November 2011 (an update search was done in February 2012). The following electronic databases were searched: MEDLINE (Ovid); MEDLINE In-Process & Other Non-Indexed Citations (MEIP); EMBASE; The Cochrane Library including CENTRAL and CDSR; CRD including HTA database, DARE and National Health Service Economic Evaluation Database (NHS EED); and EconLit. Bibliographies of retrieved articles were checked for any additional references, and the expert advisory group was contacted to identify additional published and unpublished studies.
Inclusion/exclusion criteria
Studies were selected for inclusion in the systematic review of cost-effectiveness through a two-stage process using predefined and explicit criteria. The full literature search results were independently screened by two reviewers to identify all citations that possibly met the inclusion criteria (Table 2).
| Criterion | Eligibility |
|---|---|
| Population | Patients receiving general anaesthetic for surgery, including adults and children in whom the technology is licensed |
| Interventions | Any depth of anaesthesia monitoring device |
| Design | Economic evaluation (cost-consequence analysis, cost-effectiveness analysis, cost–utility analysis, cost–benefit analysis) |
| Outcomes | Cost per patient, cost per episode of intraoperative awareness or cost per QALY |
| Other | Exclude non-English language |
| Exclude conference abstracts |
Full papers of relevant studies were retrieved and assessed independently by two reviewers using a standardised eligibility form, using the same inclusion/exclusion criteria, except that only studies with standard treatment specified as ‘no depth of anaesthesia monitor’ were included. Studies reporting other outcomes (one or more of probability of intraoperative awareness, consumption of anaesthetic agents, postoperative morbidity or mortality, HRQoL) were not included in the review, but were retained to inform the development and population of the decision-analytic model.
Data extraction and critical appraisal methods
Data were extracted by one reviewer using a standard data extraction form (see Appendix 6) and checked by a second reviewer. At each stage, any disagreements between reviewers were resolved by consensus.
The quality of the included economic evaluations was assessed using a critical appraisal checklist based on that proposed by Drummond and colleagues36 and Philips and colleagues37 (see Appendix 6).
Method of data synthesis
Studies of cost-effectiveness were synthesised through a narrative review with tabulation of results of included studies, where appropriate.
Economic evaluation
We developed a decision-analytic model to assess the cost-effectiveness of depth of anaesthesia monitoring, compared with standard clinical monitoring, adopting the perspective of the UK NHS. Separate analyses are presented for each of the included technologies, compared with standard clinical monitoring – the included technologies are not compared with each other.
The scope issued by NICE identified a number of health outcomes, including morbidity and mortality from anaesthetic agents, pain-relieving drugs, antibiotics, antisickness drugs and muscle relaxants, as well as patient discomfort and sequelae resulting from intraoperative awareness. The model was developed to allow for the inclusion of these outcomes, if suitable data on baseline values and the effect of depth of anaesthesia monitoring on these outcomes was identified in our systematic review of patient outcomes. Outcomes in the model are expressed as quality-adjusted life-years (QALYs). The model evaluates costs from the perspective of the NHS and Personal Social Services. Costs are expressed in UK sterling (pounds, £) at a 2011 price base. Both costs and outcomes are discounted using a 3.5% annual discount rate, in line with current guidance. 38,39
Analytical methods
Base case
A base-case analysis is presented for a general surgical population (at average risk of intraoperative awareness) and for a population assumed to be at high risk of intraoperative awareness. In the general surgical population, additional potential benefits (in terms of reductions in anaesthetic dose and reduction in anaesthetic-related complications) that may be associated with depth of anaesthesia monitoring are included in the base-case analysis, based on data from our systematic review of patient outcomes. Where data from the systematic review of patient outcomes were insufficiently robust, or where no evidence specific to the technology being considered was identified, data derived for other included technologies were used to populate the model.
Deterministic sensitivity analysis
Uncertainties around the probability, resource use and cost estimates, as well as effect parameters derived in the systematic review of patient outcomes, were investigated by applying ranges around the point estimates used in the base-case analysis. Where possible the ranges used in the deterministic sensitivity analyses were based on 95% confidence intervals (CIs) estimated for each input parameter. The method adopted was univariate sensitivity analysis – that is, varying one parameter at a time, leaving all other variables unchanged. This is to highlight the impact, if any, of each selected parameter alone on the cost-effectiveness results.
Scenario analysis
Scenario analysis was used to address uncertainty associated with the choice of data source adopted for parameter values in the base case and for variables omitted from the model.
Commercial-in-confidence information
This report contains reference to confidential information provided as part of the NICE appraisal process. This information has been removed from the report, and the results, discussions and conclusions of the report do not include the confidential information. These sections are clearly marked in the report.
Chapter 3 Assessment results
Results of systematic review of patient outcomes
Quantity and quality of research available
In total, 776 bibliographic records were identified from electronic bibliographic databases and reference lists provided by the manufacturers of the BIS, E-Entropy and Narcotrend monitors (Figure 1).
FIGURE 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta Analyses) flow chart showing the study selection process for bibliographic records (excluding those already identified in a Cochrane systematic review of BIS studies).
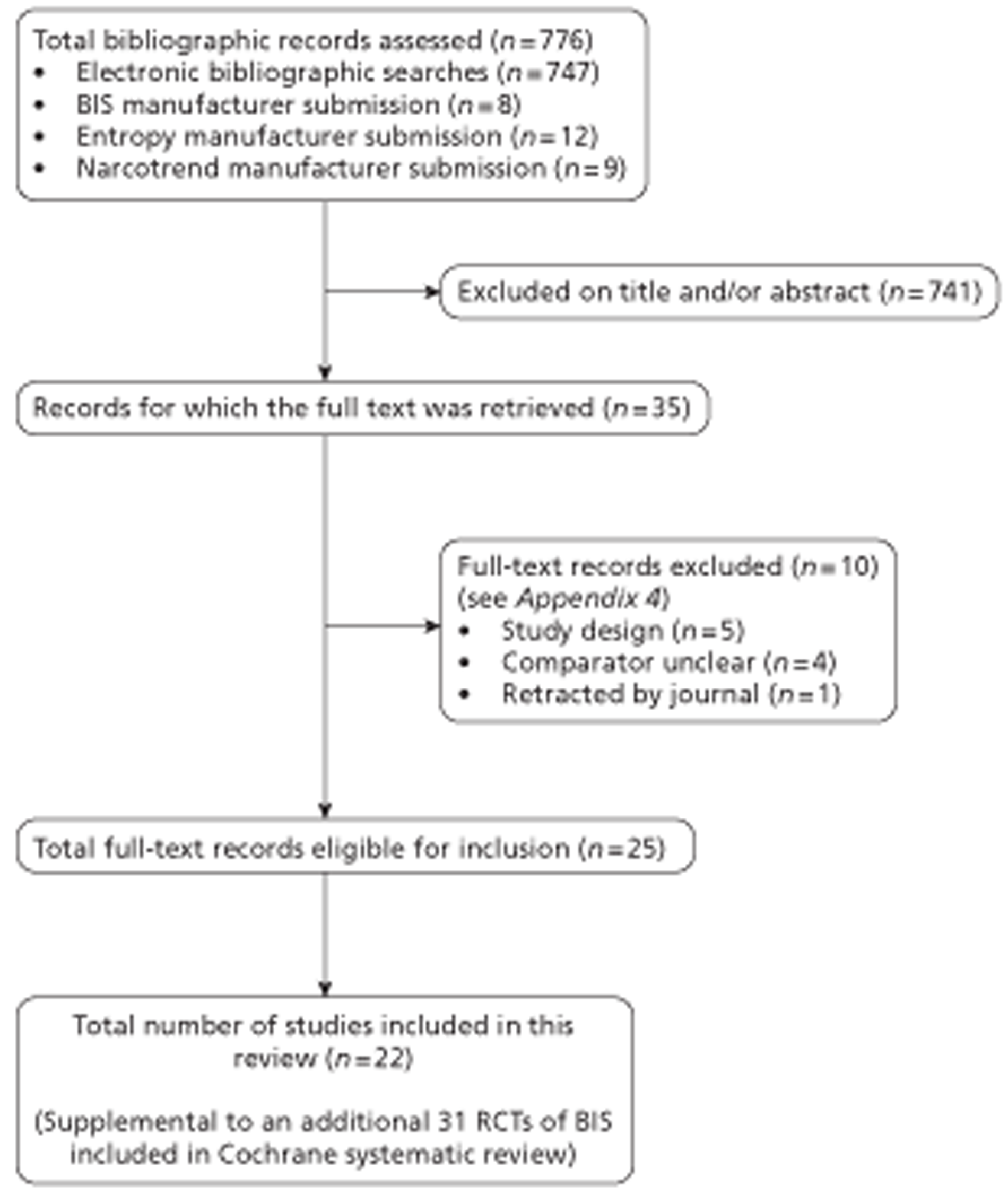
Of these 776 records, 741 were excluded, based on information provided in the title and/or abstract. Full-text publications were obtained and assessed for the remaining 35 records, of which 10 were found on further scrutiny to not meet the inclusion criteria. Reasons for excluding the 10 full-text records were that they were not RCTs (five publications), they included an inappropriate or unclear comparator group (four publications) and, in one case, the publication was retracted by the journal (see Appendix 4).
The remaining 25 full-text publications reported 25 studies, which were eligible for inclusion in the systematic review. Four of the 25 RCTs were identified by our update searches in February 2012, all evaluating BIS. Because of finite time and resources we prioritised the largest of these for inclusion in the review (a trial of around 5000 patients, specifically designed to assess intraoperative awareness40). The other three were smaller trials (80 patients,41 40 patients,42 and 20 patients43 respectively) and their inclusion in the review was unlikely to change the findings. In summary, a total of 22 RCTs were included in this systematic review.
The 22 included studies were all RCTs that included study arms for at least one relevant technology (BIS, E-Entropy or Narcotrend) and a comparator that reflected standard clinical monitoring.
The 22 included studies were two- or three-arm RCTs that compared the following technologies against standard clinical monitoring:
These 22 studies provide 15 comparisons of BIS against standard clinical monitoring, seven comparisons of E-Entropy against standard monitoring and four comparisons of Narcotrend against standard monitoring (Table 3).
| Author | BIS | Entropy | Narcotrend |
|---|---|---|---|
| Aime et al.61 | ✓ | ✓ | |
| Avidan et al.44 | ✓ | ||
| Bannister et al.45 | ✓ | ||
| Bhardwaj and Yaddanapudi46 | ✓ | ||
| Chan et al.47 | ✓ | ||
| Choi et al.54 | ✓ | ||
| Ellerkmann et al.62 | ✓ | ✓ | |
| Gruenewald et al.55 | ✓ | ||
| Kamal et al.48 | ✓ | ||
| Kerssens et al.49 | ✓ | ||
| Kreuer et al.63 | ✓ | ✓ | |
| Kreuer et al.64 | ✓ | ✓ | |
| Lai et al.59 | ✓ | ||
| Leslie et al.50 | ✓ | ||
| Liao et al.51 | ✓ | ||
| Messieha et al.52 | ✓ | ||
| Messieha et al.53 | ✓ | ||
| Rundshagen et al.60 | ✓ | ||
| Talawar et al.56 | ✓ | ||
| Vakkuri et al.57 | ✓ | ||
| Wu et al.58 | ✓ | ||
| Zhang et al.40 | ✓ |
The 15 comparisons of BIS against standard monitoring supplement the Cochrane review,34 which included 31 RCTs of BIS against standard clinical practice. 27,61,63–91
Note that only 11 of the 15 BIS studies in the current review are presented in the following BIS subsections for the following reasons:
-
One of the trials of BIS and E-Entropy compared with standard clinical monitoring was included in the Cochrane BIS review,61 and therefore is described only within the E-Entropy subsections of this report (i.e. for the comparison of E-Entropy with standard clinical monitoring).
-
Two of the trials of BIS and Narcotrend compared with standard clinical monitoring were included in the Cochrane BIS review,63,64 and are therefore described only within the Narcotrend subsections of this report (i.e. for the comparison of Narcotrend with standard clinical monitoring).
-
One of the BIS publications identified in the current systematic review (Leslie and colleagues50) is a long-term follow-up publication of one of the trials (the B-Aware trial by Myles and colleagues79) included in the Cochrane review. 73 We report the long-term results of this trial in this report (see Assessment of outcomes: Bispectral Index) but details of the characteristics of the trial (including the risk of bias judgement) can be found in the Cochrane review itself.
Risk of bias in Bispectral Index trials
Table 4 reports a summary of the risk of bias judgements for the trials of BIS included in this systematic review (NB. The risk of bias judgements for the 31 RCTs in the Cochrane BIS review are not tabulated in this report, but are summarised in the text below).
| Study | Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting |
|---|---|---|---|---|---|---|
| Avidan et al.44 | Low | Low | Unclear | Low | Low | Low |
| Bannister et al.45 | Unclear | Unclear | Unclear | Unclear | Unclear | Low |
| Bhardwaj and Yaddanapudi46 | Low | Unclear | Unclear | Unclear | Low | Low |
| Chan et al.47 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Ellerkmann et al.62 | Low | Unclear | Unclear | Unclear | High | Low |
| Kamal et al.48 | Unclear | Unclear | Unclear | Unclear | Low | Low |
| Kerssens et al.49 | Low | Unclear | Unclear | Low | Unclear | Unclear |
| Liao et al.51 | Unclear | Unclear | Unclear | Unclear | Low | Low |
| Messieha et al.52 | Unclear | Unclear | Unclear | Unclear | Unclear | Low |
| Messieha et al.53 | Unclear | Unclear | Unclear | Unclear | Unclear | Low |
| Zhang et al.40 | Low | Unclear | Low | Low | Unclear | Low |
In many cases the risk of bias in the trials was unclear because of limitations in reporting of methodological details. Uncertainty was greatest in relation to concealment of the random allocation process, where details were unclear in all but two trials. In the Cochrane systematic review of BIS, 12 of the 31 (39%) trials were considered to have adequately concealed random allocation, with most of the remainder judged as unclear.
Details of blinding of participants and trial personnel to trial arm were also generally unclear, as was the case of blinding of outcome assessors. In the Cochrane BIS review34 just over half of the studies were judged to be of a low risk of bias because of blinding of outcome assessors (17/31; 55%).
Random sequence generation was one of the domains where risk of bias was lowest. However, although all studies were reported to be randomised trials, in six trials (46%) the method of randomisation was not given. In the Cochrane systematic review of BIS34 just under half of the included studies (15/31; 48%) were judged to be of a low risk of bias because of adequate random sequence generation. Most of the remainder were unclear because of lack of details given in trial publications.
In general, there appeared to be low risk of bias in terms of selective reporting of outcomes, as could be judged from the details reported in the trial publications. This was also the case in the Cochrane BIS review. 34 Bias associated with incomplete outcome data was judged low in around half of the trials (and in just under half in the Cochrane BIS review,34 15/31; 48%). In the remainder it was unclear, and in one trial it was judged to be high because of an imbalance in the percentage of patients excluded from the analysis between trial arms. 62 In general, it was not considered that risk of other forms of bias were present. However, in one trial the risk was considered high because of the study being funded in part by the BIS module manufacturer. 45
The trials varied in terms of their sample sizes, from as low as 20 patients to over 6000. There were seven (46%)45,46,48,52,53,59,62 that included fewer than 100 patients and five (33%)48,51,61,63,64 that had between 101 and 200 patients. One trial included 921 patients,47 another included 530940 and another, the largest, included 6041 patients. 44 In the Cochrane BIS review34 the majority of trials included fewer than 100 patients (21/31; 68%). Seven trials (23%) included between 101 and 200 patients. Another study – the B-Unaware trial by Avidan and colleagues 2008 – included 1941 patients,27 and the largest included 2463 patients. 79 (NB. The Cochrane BIS review appears to count two publications relating to this single trial as two separate studies. One publication reports the main trial results,79 and a second publication focuses on recovery outcomes from the trial. 74)
Six (55%)40,44,46,49,51,62 of the 11 BIS trials reported a statistical sample size calculation based on a nominated primary outcome, although one of these trials reported that the number of patients chosen was arbitrary rather than being based on a statistical calculation. 49 The Cochrane BIS review34 did not comment on sample size power calculations in the studies included.
Six (55%)40,44,46,48,49,62 of the 11 BIS trials reported patient attrition. The attrition rate varied from 1.5%40 to 15% 49 of the total number of patients enrolled. Most of the studies reported the reasons for attrition, generally comprising exclusions from the analyses as a result of deviations from the study protocol. Given the nature of the procedure and the relatively short follow-up duration, loss to follow-up was rarely reported. In five (45%) studies it was reported by the authors that there was no attrition, or there did not appear to be any attrition. 45,47,51–53 Whether or not an intention-to-treat (ITT) analysis had been employed was rarely mentioned in the trial reports. Only two trials mentioned that patients had been analysed according to the procedure to which they had been randomised. 44,46
Five of the BIS trials disclosed information about funding. 40,44,45,49,51 Funding for two of these trials was provided by medical research funding organisations and/or hospital departmental grants. 44,51 The other three trials reported varying financial associations with BIS manufacturers. 40,44,49 The trial by Bannister and colleagues45 stated that Aspect Medical Systems supplied the BIS monitor, and that one author was employed by Aspect Medical Systems and another author was a paid consultant to Aspect Medical Systems. This funding therefore represents a conflict of interest. The trial by Kerssens and colleagues49 reported that Aspect Medical Systems did not financially support the study, but that the lead author had received an educational grant in support of her salary from Aspect Medical Systems, and one co-author was a paid consultant to Aspect Medical Systems. In the trial by Zhang and colleagues,40 Aspect Medical Systems provided BIS electrodes, but no further detail on funding was given. None of the other BIS trials stated or appeared to have any major conflicts of interest. The Cochrane BIS review34 did not report funding details of the included trials, or whether or not any of the trials had conflicts of interests.
Risk of bias in E-Entropy trials
Table 5 reports a summary of the risk of bias judgements for the trials of E-Entropy included in this systematic review.
| Study | Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting |
|---|---|---|---|---|---|---|
| Aime et al.61 | Low | Unclear | Unclear | Unclear | Low | Low |
| Choi et al.54 | Unclear | Unclear | Unclear | Unclear | Low | Low |
| Ellerkmann et al.62 | Low | Unclear | Unclear | Unclear | High | Low |
| Gruenewald et al.55 | Unclear | Unclear | Unclear | Unclear | Unclear | Low |
| Talawar et al.56 | Low | Unclear | Unclear | Low | Low | Low |
| Vakkuri et al.57 | Low | Unclear | Unclear | Unclear | Unclear | Unclear |
| Wu et al.58 | Unclear | Unclear | Unclear | Unclear | Unclear | Low |
The risk of bias in the E-Entropy trials was unclear in many cases because of limitations in the reporting of methodological details. Uncertainty was greatest concerning allocation concealment and the blinding of participants and personnel, which were not adequately reported in any of the seven E-Entropy trials.
Risk of bias because of random sequence generation was considered low in four of the trials, in which sequences were generated either by computer56,57,61 or by drawing lots. 62 Risk of bias because of random sequence generation was deemed unclear in the remaining three trials, which provided no information on the method of sequence generation.
The method of allocation concealment was considered to pose unclear risk of bias in all seven of the trials, either because no relevant information was reported58,61,62 or sealed envelopes were used for allocation codes, but it was not stated whether or not the envelopes were opaque. 54–57
Anaesthetists who administered anaesthesia according to standard clinical monitoring were blinded to E-Entropy values. However, none of the studies unequivocally reported that study participants and personnel were blinded to the study groups. The risk of bias because of inadequate blinding in each of the E-Entropy studies was therefore judged to be unclear.
In three of the seven E-Entropy trials, the risk of attrition bias because of analysis of incomplete outcome data was considered low, as exclusions were a minor proportion of the sample size,54 or were generally balanced between groups with generally similar reasons given,61 or the analysis was conducted by ITT with no discernible attrition. 56 Two trials were considered at high risk of attrition bias because the rate of attrition was ≥ 10% in at least one of the study arms, and not balanced across the arms. 58,62 The remaining two trials were judged to have unclear risk of attrition bias because of incomplete outcome data, either because attrition was not reported at all55 or it was not reported separately by study arm. 57
The risk of bias because of selective reporting of outcomes was judged to be low for six of the seven E-Entropy trials, as there was no indication within the primary publications that more outcomes had been measured than were subsequently reported (in general, there was concordance between the outcomes specified in the methods and results sections of the publications). In the remaining trial,57 risk of bias from selective reporting was considered unclear as several outcomes were reported narratively without any supporting quantitative data that could be checked by the reviewers.
One of the E-Entropy trials56 reported that no external funding was used, and one trial62 did not report whether or how the work was funded. Two trials were funded by non-commercial sponsors, which were a university54 and a national science organisation. 58 The remaining three E-Entropy trials were supported by the E-Entropy device manufacturer (GE Healthcare; formerly Datex-Ohmeda), either through provision of equipment alone55,61 or through provision of equipment, funding and also technical support. 57 The authors of this latter trial57 included a research engineer, research scientist and chief scientist of the device manufacturer and two medical advisors to the device manufacturer. These three trials that involved support from the device manufacturer could be at risk of bias because of conflict of interests. The study that involved the most extensive links with the manufacturer57 was deemed by the reviewers to be at high risk of bias because of a high likelihood of conflicting interests. In the four E-Entropy trials that were not supported by the E-Entropy device manufacturer, three did not refer to conflict of interests54,58,62 and one stated that no conflicts were disclosed. 56
The seven E-Entropy studies were published during 2005 to 2010 and ranged in their total sample size from 50 to 335 patients. 54–58,61,62 Five of the trials involved a two-arm comparison of E-Entropy against standard clinical monitoring. 54–58 One trial involved a three-arm comparison of BIS, E-Entropy and standard clinical monitoring. 61 The remaining trial was a three-arm comparison of E-Entropy, E-Entropy and BIS, and standard practice. 62 The number of patients randomised per arm ranged from 25 to 40 in six trials. 54–56,58,61,62 In the seventh (largest) trial, only the number per arm after attrition (160 patients) was reported. 57
Only one of the E-Entropy trials did not report a sample size calculation. 58 Three trials calculated the sample size needed to detect a specified percentage difference in anaesthetic consumption for sevoflurane54,61 or propofol. 62 The remaining three trials calculated the sample size needed to detect differences in patient recovery from anaesthesia, namely the time to eye opening,55 time to awakening (not defined)56 or the time to response to a verbal command. 57
Overall, the range of attrition in the trials was 0–11% of the total population per trial, or 0–17% of the population per study arm. Attrition appeared to be zero in one trial,56 and was not reported in one trial. 55 Among the remaining five trials, reasons for attrition were clearly reported separately by study group in two trials;54,61 were reported only for aggregated data across study groups in one trial;57 were vaguely specified as resulting from ‘technical problems’ in one trial;54 and were not specified in the remaining trial. 58
An analysis by ITT was explicitly reported in one trial and appears valid as no attrition was discernible in the study report. 56 Another trial55 did not explicitly mention ITT analysis but appeared to have used an ITT approach, as it was stated that all patients were included in the final analysis, although attrition was not reported. A third trial54 analysed nearly all the randomised patients [only 1/40 per group (2.5%) were excluded], which may be considered close to an ITT approach. The remaining four trials57,58,61,62 did not follow the ITT principle as their analyses excluded from 4% to 17% of the randomised patients per study arm.
Risk of bias in Narcotrend trials
Table 6 reports a summary of the risk of bias judgements for the trials of Narcotrend included in this systematic review.
| Study | Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting |
|---|---|---|---|---|---|---|
| Kreuer et al.63 | Low | Unclear | Unclear | Low | Low | Low |
| Kreuer et al.64 | Low | Unclear | Unclear | Low | Low | Low |
| Lai et al.59 | Unclear | Unclear | Unclear | Unclear | Low | Low |
| Rundshagen et al.60 | Unclear | Unclear | Unclear | Unclear | Unclear | Low |
In many cases the risk of bias in the trials was unclear because of limitations in reporting of methodological details. Uncertainty was greatest in relation to concealment of the random allocation process and blinding of participants and personnel, where details were unclear in all four trials. 59,60,63,64
Both the method of random sequence generation and blinding of outcome assessment were unclear in two trials,59,60 with low risk of bias for these domains in the other two trials. 63,64 Risk of bias because of incomplete outcome data was low in all but one trial in which details were unclear. 60
In general, there appeared to be low risk of bias in terms of selective reporting of outcomes, as could be judged from the details reported in the trial publications. Other sources of bias were reported for only one study where the paper was translated from Chinese to English prior to publication and it is unclear whether or not any checks were made to ensure fidelity of the published version to the original work. 59
The trials were conducted between 2003 and 2010 and trial sizes ranged from 120 patients63,64 to 48 patients60 and 40 patients. 59 All but the smallest study reported the use of a sample size calculation. No attrition was reported for three trials59,63,64 and these studies conducted ITT analyses. The fourth trial60 reported attrition although not by study group, and analyses did not include all patients who started but it is unclear whether or not attrition happened pre or post randomisation. All four trials59,60,63,64 did not report any conflict of interest. Two studies63,64 stated that the study was solely supported by departmental funding, one59 did not report any details of the sponsor and the fourth60 reported that the study was supported by a pharmaceutical company and a university institutional research grant.
Characteristics of included studies: Bispectral Index
The following subsections describe the key characteristics of the BIS trials included in this systematic review. The characteristics of the 31 trials included in the Cochrane BIS review are summarised alongside.
Study populations
Five of the 11 BIS trials were conducted in children, with mean ages of between 4 and 6 years, and age ranges from 2 to 18 years. 45,46,51–53 The remaining six studies were conducted in adults,40,44,47–49,62 with mean ages ranging across the studies from 43 to 64 years. One study was conducted to investigate POCD in an elderly population, defined as > 60 years (no further age information given) (conference abstract). 47 All of the trials included in the Cochrane BIS review34 studied adult patients (the review's inclusion criteria specified adults over the age of 18 years).
All of the trials included mixed-sex populations. Generally, there was an even mix of males and females in the trials, though there was a higher percentage of males (i.e. > 60%) in three studies. 46,48,51 One study did not report the sex of the included patients. 47
All but one of the studies reported patients' weight. 47 The majority of studies reported weight in kilograms, ranging from a mean of 68–91 kg in the adult studies, and of 17–28 kg in the children studies. In addition to reporting weight in kilograms, one trial also reported body mass index (BMI), which was between 28 and 30 kg/m2. 49 Another trial reported weight only in terms of BMI, with a mean of 30 kg/m2, indicating an overweight/obese population. 44 The Cochrane BIS review34 included one study of obese patients.
Racial origin was reported in only one trial, in which the population was predominantly (> 80%) classified as white. 44 The countries in which the trials were conducted included the USA,45,49,52,53 USA/Canada,44 China,40,47,51 Germany,62 Egypt48 and India. 46 In the Cochrane BIS review34 the majority of studies were conducted in Europe or the USA. Seven of the trials were conducted in single centres,45,46,48,51–53,62 with one trial taking place in two centres,47 another taking place in three centres,44 one trial taking place in 13 centres40 and a trial not reporting the number of centres. 49
The type of surgery reported in the adult trials varied: open heart,44 major non-cardiac,47 major orthopaedic,49 orthopaedic,62 and elective moderate abdominal surgery. 48 The surgical procedures in the trials of children included tonsillectomy and/or adenoidectomy,45 urogenital/urological surgery46,51 and dental rehabilitation. 52,53
Only two of the trials reported patient risk factors for awareness. 40,44 To be included in the trial by Avidan and colleagues44 patients had to be at high risk for intraoperative awareness, demonstrating one or more of the following risk factors: planned open heart surgery; aortic stenosis; pulmonary hypertension; use of opiates; use of benzodiazepines; use of anticonvulsant drugs; daily alcohol consumption; ASA status 4; end-stage lung disease; history of intraoperative awareness; history of, or anticipated, difficult intubation; cardiac ejection fraction of < 40%; and marginal exercise tolerance. The trial by Zhang and colleagues40 included patients receiving TIVA, which they cited as a risk factor for intraoperative awareness. The Cochrane BIS review34 included four trials that were classified as including patients at high risk of intraoperative awareness. 27,78,79,82
The eligibility criteria employed by the trials generally excluded patients with significant comorbidities, or factors that may interfere with EEG readings, including epilepsy, cerebrovascular disease, dementia, treatment with opioids and antipsychotic medication, and illicit drug use. Two of the studies permitted inclusion of children with mild cerebral palsy without significant neurological deficit. 52,53 The trials included in the Cochrane BIS review34 also generally excluded patients with the above factors. Some of these trials also excluded patients considered obese, or patients with diabetes or impaired renal or hepatic function.
The ASA physical status classification of the patients in the trials was generally between I and II, indicating that they were generally healthy, with only mild disease. In three of the trials the ASA status was not reported45,47,48 (although in one of these trials the inclusion criteria specified patients had to be within I–III48). In one trial the proportion of patients with ASA status I–II was 50%, and the remainder of patients were classified as III (severe systemic disease). 49 There was one trial in which patients were predominantly classified as III–IV (IV being classified as a patient with severe systemic disease that is a constant threat to life). 44
Technologies
The trials varied in the level of detail given on the BIS module and monitors used. Two studies did not provide any information other than that a BIS module was used. 44,47 Most commonly reported was the BIS Monitor Model A-2000 as mentioned in four trials. 40,45,48,62 In one this was described as: ‘IP X 2’46 in another ‘version XP, software version 4.0’62 and in the third trial using Aspect Medical Systems ‘Software program Datex-Ohmeda S/5 Collect (v4.0)’ (Aspect Medical Systems Inc., Norwood, MA, USA). 48 One trial used BIS (version 3.3, Aspect Medical Systems) using an A-1050 EEG monitor,45 while another used BIS monitor (XP, algorithm 3.4; Aspect Medical Systems). 49 A further two trials reported using BIS (Aspect Medical Systems), but gave no further information on the software version or the monitor used. 52,53 Although most studies reported using Aspect Medical Systems BIS, one trial reported using the BIS monitor as manufactured by Phillips but using ‘Aspect Medical Systems' XP platform technology’. 51 Given the variability in reporting it is not clear how comparable the trials are in terms of the software and BIS algorithms used, which may have implications for the interpretation of the results of the trials.
All of the trials reported the target BIS values to be achieved during anaesthesia. In five trials the target was 40–60. 40,44,45,47,51 In one of these trials the target was increased to 60–70 during last 15 minutes of surgery. 45 In the remaining trials the target values were higher: 45–60;46 50 during maintenance (target value of 60 to facilitate rapid emergence from anaesthesia 15 minutes before expected end of surgery);62 50–60;48,49 55–65;53 and 60–70. 52
Although all of the trials compared BIS against standard clinical monitoring, the monitored parameters varied. Only one trial measured ETAC in order to detect possible intraoperative awareness. 44 Audible alarms sounded if the age-adjusted MAC fell outside of 0.7 to 1.3. The remaining nine trials used clinical signs to guide anaesthetic use. In general, a combination of signs were monitored in each trial, most commonly: blood pressure;46,48,49,52,62,94 heart rate;48,49,52,53,62 surgical stimulation;52,53 sweating;62 tear production;62 and movement. 62
Two trials did not explicitly define which signs were monitored other than that they were clinical signs and haemodynamic changes. 45,47 A further trial mentioned that the aim of standard clinical monitoring was to maintain haemodynamic stability while avoiding patient movement and achieving a rapid recovery. 51
Some of the trials reported that clinical signs were also monitored in the BIS arm, suggesting that adjustment of anaesthesia was based on signs of inadequate anaesthesia as well as BIS values. 48,52,53,62 For example, in one trial48 changes in anaesthesia were guided by the presence of clinical signs in relation to the BIS value. If the patient exhibited hypertension or tachycardia and the BIS was > 60 then sevoflurane was increased. If BIS was in the target range of 50–60, then fentanyl was given. If BIS was < 50 then sevoflurane was decreased and the patient checked for lack of analgesia. In the one trial that used ETAC as the comparator to BIS,44 it was stated that both forms of monitoring were used as part of structured protocols. It was not intended that these protocols would prescribe or restrict the use of anaesthetic agents. Practitioners were able to increase or decrease anaesthetic administration at their discretion if a patient's condition was haemodynamically unstable. The protocols were designed to increase vigilance and to provide warnings that patients might be experiencing awareness. Some trials did not explicitly report whether or not clinical signs were monitored in the BIS arm, and it is possible that in these studies anaesthesia was adjusted based on BIS monitoring in conjunction with changes in clinical signs.
All trials reported that a BIS monitor was used in the standard clinical monitoring arm, but that the values were hidden from the anaesthetist, for example by placing it out of their line of sight, or using a curtain or cover, and also switching off any audible alarms.
The majority of trials did not explicitly report where or when monitoring commenced and ceased. Where details were provided, monitoring started prior to anaesthesia induction45,46 and in the operating theatre. 46,51,62 Three studies reported cessation of monitoring: until patients achieved discharge criteria from the recovery room (Steward score of 6)46 and until discharge from the PACU. 52,53
The training and experience of the anaesthetist in using BIS was rarely mentioned in the trials. The trial by Avidan and colleagues44 reported that summaries of BIS and ETAC protocols were given to the practitioners to provide education and to increase adherence. Furthermore, signs were affixed to anaesthesia machines to remind practitioners to check BIS/ETAC and consider patient awareness. One of the trials mentioned that the anaesthetist was experienced, but provided no further information. 62
Anaesthetic agents and protocols
Five of the trials reported that an inhaled general anaesthetic was used for both induction and maintenance. 44,45,51–53 In all but one of these trials sevoflurane was the inhaled anaesthetic used. 53 Two of these trials also gave nitrous oxide in oxygen. 45,51 In the fifth trial patients either received isoflurane, sevoflurane or desflurane. 44 Three trials reported that both i.v. and inhalational general anaesthetic were used. 47–49 In two of these propofol was used for induction of anaesthesia and sevoflurane was given for maintenance. 48,49 The third trial implied that both propofol and an inhalational anaesthetic were given, but did not provide any further detail. 47 Three trials reported that propofol was given for both induction and maintenance of general anaesthesisa. 40,46,62 One of these also used nitrous oxide in oxygen during the maintenance period. 46
Only one trial stated that regional anaesthesia was used, although no information was provided on which agent was used. 62 One trial mentioned that regional anaesthesia was used for postoperative pain management. 49 In the remaining nine trials44–48,51–53,62 it was either reported that regional anaesthesia was not used or the use of regional anaesthesia was not stated.
Use of analgesia at various points during surgery was reported by seven of the trials, including fentanyl,49,51–53 fentanyl or morphine45,46 or remifentanil (during induction). 62 One trial reported that analgesia was used at the discretion of the anaesthetist. 40 In three trials the use of analgesia was not stated. 44,47,48 Premedication with midazolam was used in seven trials. 40,44–46,52,53,62 In two of these trials ketamine was also used as premedication. 52,53
Muscle relaxants were used in seven of the trials, including atracurium,46,48 cisatracurium,63 vecuronium bromide49 and rocuronium bromide. 52,53 One trial did not specify which agent was used. 40
Duration of anaesthesia was reported by five of the BIS trials46,48,49,51,62 and ranged from a mean of 40 minutes (paediatric urological surgery)51 to 126 minutes (major orthopaedic surgery in adults). 49 In the trials featuring adults, duration of anaesthesia was, in general, between 100 and 120 minutes. Duration of surgery was reported by seven of the BIS trials,40,45,46,48,51–53 and ranged from around 30 minutes (in children undergoing tonsillectomy and/or adenoidectomy)45 to 160 minutes (children undergoing dental surgery). 52 Not all trials reported both duration of anaesthesia and duration of surgery.
Outcomes
Table 7 illustrates the distribution of outcomes reported by the trials included in this systematic review. The table also shows the frequency of the outcomes in this review, the Cochrane BIS review34 and the grand total for both reviews.
| Study | Avidan44 | aBannister45 | aBhardwaj46 | Chan47 | Ellerkmann62 | Leslie50 | Kamal48 | Kerssens49 | aLiao51 | aMessieha52 | aMessieha53 | aZhang40 | Total this review | Total Cochrane BIS review34 | Grand Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcomes | |||||||||||||||
| Anaesthetic consumption | ✗ | P | ✗ | P | ✗ | ✗ | 6 | 24 | 30 | ||||||
| Intraoperative awareness | P | ✗ | ✗ | P | ✗ | P | 6 | 4 | 10 | ||||||
| Distressing experience of awareness | ✗ | 1 | 0 | 1 | |||||||||||
| Analgesic consumption | ✗ | ✗ | ✗ | ✗ | ✗ | 5 | 6 | 11 | |||||||
| Muscle relaxant requirement | 0 | 2 | 2 | ||||||||||||
| Time to response to commands | ✗ | 1 | 12 | 13 | |||||||||||
| Time to eye opening | ✗ | ✗ | ✗ | 3 | 19 | 22 | |||||||||
| Time to extubation | ✗ | ✗ | ✗ | ✗ | ✗ | 5 | 21 | 26 | |||||||
| Time to laryngeal mask airway removal | ✗ | 1 | 0 | 1 | |||||||||||
| Time to first movement response | ✗ | P | 1 | 0 | 1 | ||||||||||
| Time to recovery of orientation | ✗ | 1 | 7 | 8 | |||||||||||
| Time to phonation | ✗ | 1 | 0 | 1 | |||||||||||
| PACU stay | ✗ | ✗ | ✗ | ✗ | 4 | 12 | 16 | ||||||||
| Time to home readiness | 0 | 7 | 7 | ||||||||||||
| Monitoring device values | ✗ | ✗ | ✗ | 3 | 0 | 3 | |||||||||
| Postoperative nausea and vomiting | ✗ | 1 | 2 | 3 | |||||||||||
| Emergence delirium | ✗ | 1 | 0 | 1 | |||||||||||
| POCD | ✗ | 1 | 1 | 2 | |||||||||||
| Parental satisfaction | ✗ | 1 | 0 | 1 | |||||||||||
| Treatment of haemodynamic events | 0 | 0 | 0 | ||||||||||||
| Haemodynamic profiles | ✗ | ✗ | ✗ | 3 | 3 | 6 | |||||||||
| Stroke | ✗ | 1 | 0 | 1 | |||||||||||
| Myocardial infarction | ✗ | 1 | 0 | 1 | |||||||||||
| Mortality | ✗ | 1 | 0 | 1 | |||||||||||
The most commonly reported outcome was anaesthetic consumption (n = 30 trials), followed by recovery outcomes such as time to extubation (n = 26 trials); time to eye opening (either spontaneously or in response to command) (n = 22 trials); and time to discharge from the PACU. Intraoperative analgesic consumption was reported in 11 trials.
Adverse outcomes were less commonly reported, such as PONV (n = 3 trials); and emergence delirium (n = 1 trial59). One trial, by Leslie and colleagues,50 reported stroke, myocardial infarction, mortality for all surviving and available patients 30 days post operation. This is a long-term follow-up (median = 4.1 years) publication of the B-Aware trial [NB. A publication of the short-term results of this trial by Myles and colleagues 200479 (primary outcome: intraoperative awareness) was included in the Cochrane BIS review34].
Six of the 11 BIS trials40,44,46,49,59,62 included in this systematic review specified a primary outcome measure. In two trials the primary outcome measure was anaesthetic consumption,46,62 and in another trial the primary outcome measure was time to first movement response. 59 In the other three trials the primary outcome measure was intraoperative awareness. 40,44,49
In the trial by Avidan and colleagues44 – which recruited patients classified as at high risk of intraoperative awareness – the incidence of definite intraoperative awareness was the primary outcome measure. The incidence of definite or possible awareness was a secondary outcome. Awareness was assessed by a modified Brice questionnaire (references cited), and assessments were made 72 hours after surgery and 30 days after extubation. Patients who reported memories of the period between ‘going to sleep’ and ‘waking up’ were contacted by a different evaluator, who asked additional structured questions. Responses to the questionnaire from patients who had reported memories were reviewed by three independent experts, who determined whether the reported event involved definite awareness, possible awareness or no awareness. Where there was a difference in judgement over an awareness episode a fourth expert made the final determination. This study was designed specifically to evaluate the effects of BIS on intraoperative awareness, and to overcome methodological limitations of a previous single-centre trial by the same investigators (the B-Unaware trial27 – included in the Cochrane BIS review34) by including a study sample sufficiently large enough to detect a relatively rare outcome such as awareness.
The trial by Zhang and colleagues40 also reported incidence of confirmed awareness, or possible awareness, using a Brice questionnaire. Assessments were made on the first and fourth day following surgery. An independent evaluating committee was used to verify cases of awareness. The patients in this trial were noted to be at increased risk of intraoperative awareness after receiving TIVA.
The trial by Kerssens and colleagues49 measured explicit awareness, via a patient interview, as well as implicit awareness, via a word recognition test. This is the only trial identified by the current systematic review that measured implicit awareness. The underlying hypothesis was that intraoperative memory could occur either because of insufficient anaesthetic or stress-induced learning mechanisms during unconsciousness (i.e. intraoperative memory could be dependent on and/or independent of depth of anaesthesia). Six hours after surgery, patients were interviewed using questions similar to the Brice interview, consisting of five questions, with additional questions asked as necessary. Following the interview a recognition memory test was performed. During anaesthesia, sequences of pre-determined neutral words were played to patients through headphones. The postoperative memory test involved playing pre-determined combinations of words that had been used during anaesthesia, and distractor words, to patients though headphones. Patients were instructed to listen to each test sequence and select the word played during surgery, or to guess if necessary. The main analysis of this study was the effect of study group assignment on recognition memory test performance, but given the low incidence of explicit recall (awareness) the study was not powered to detect differences in explicit recall. An arbitrary sample size of 100 patients was chosen to assess recognition memory.
Intraoperative awareness was also reported as a non-primary outcome by three other BIS trials included in this systematic review. 48,51,62 In these trials, awareness was one of a number of outcomes measured, and patients were not identified as being at particular risk. Awareness was assessed by a patient interview administered at various times up to 3 days post operation. In the trial by Ellerkmann and colleagues62 interviews took place on the first and third postoperative days, in the trial by Kamal and colleagues48 interviews took place on the first, second and third days postoperatively, and in the trial by Liao and colleagues51 the timing was not specified. Little detail of the interviews was given other than that ‘patients were questioned for recall of events, hearing vague sounds, feeling surgical instruments or dressing application, or dreaming’48 or patients were asked ‘whether they could recall any event or dreaming during the intraoperative period’51 or that a ‘standardised interview’ was used (reference cited). 62
The Cochrane BIS review conducted a meta-analysis of explicit intraoperative awareness, which included four RCTs. 27,78,79,82 The Cochrane review also included a further eight trials61,63,66,83,84,87–89 that reported explicit intraoperative awareness, but the review did not classify these as featuring patients at higher risk. They were not included in any meta-analysis and the impact on awareness was not commented on by the Cochrane review. The Cochrane BIS review did not report whether any of the included trials measured implicit awareness or assessed awareness during surgery using techniques such as the isolated forearm technique.
Assessment of outcomes: Bispectral Index
The following sections report the results of the BIS trials included in this systematic review. Tabulated data are from the studies identified by this review (i.e. supplemental to the trials in the Cochrane BIS review). Where appropriate we have updated the meta-analyses of the Cochrane BIS review with studies from the current review, presented graphically in forest plots. Where it was not appropriate to update the Cochrane BIS meta-analysis we have presented the results of the meta-analysis narratively.
Intraoperative awareness
Table 8 gives the results of the six trials included in this systematic review which measured the impact of BIS monitoring on explicit intraoperative awareness, as assessed by patient interview.
| Study | BIS | Standard clinical monitoring | Mean difference (95% CI), p-value |
|---|---|---|---|
| Avidan et al.,44 n/N (%) | |||
| Definite awareness | 7/2861 (0.24) | 2/2852 (0.07) | 0.17 (−0.03 to 0.38), p = 0.98 |
| Definite or possible awareness | 19/2861 (0.66) | 8/2852 (0.28) | 0.38 (0.03 to 0.74), p = 0.99 |
| Patient distress and sequelae resulting from intraoperative awareness | 8/2861 (0.28) | 1/2852 (0.04) | 0.24 (0.04 to 0.45), p = 0.99 |
| Ellerkmann et al.,62 n/N | 0/27 | 0/27 | – |
| Kamal et al.,48 n/N | 0/28 | 0/29 | – |
| Kerssens et al.,49 n/N (%) | 2/67 (3) | 1/61 (2) | NR |
| aLiao et al.,51 n/N | 0/52 | 0/54 | – |
| Zhang et al.,40 n/N (%) | |||
| Confirmed awareness | 4/2919 (0.14) | 15/2309 (0.65) | OR 0.21 (0.07 to 0.63), p = 0.002 |
| Possible awareness | 4/2919 (0.14) | 6/2309 (0.26) | p = 0.485 |
| Confirmed or possible awareness | 8/2919 (0.27) | 21/2309 (0.9) | p = 0.01 |
No cases of awareness were reported at all in three trials,48,51,62 and a very low number of cases were reported in a fourth trial. 49 As stated earlier, these trials were not specifically designed to detect the effect of depth of anaesthesia monitoring on awareness, and therefore are unlikely to have sufficiently large enough sample sizes for relatively rare awareness events. In the trial by Avidan and colleagues,44 which included patients classified at higher risk for intraoperative awareness and was statistically powered for this outcome, there was a higher percentage of both definite awareness, and of definite or possible awareness cases, in the group who received BIS monitoring than the group who had standard clinical monitoring. However, these differences were not statistically significant. Avidan and colleagues44 also reported patient distress and sequelae resulting from intraoperative awareness, as a post hoc secondary outcome. Distress was measured using the Michigan Awareness Classification tool (reference supplied) and was characterised by reports of fear, anxiety, suffocation, sense of doom or sense of impending death. There was a higher percentage of distress reported in the BIS-monitored group, but no statistically significant difference between groups.
In contrast to Avidan and colleagues,44 Zhang and colleagues40 reported a significantly lower incidence of confirmed intraoperative awareness in patients monitored by BIS than in those who received standard clinical monitoring. Incidence of possible awareness was also lower for BIS-monitored patients, although not statistically significant. The incidence of confirmed or possible awareness was significantly lower for BIS-monitored patients.
Intraoperative awareness was the primary outcome measure in the Cochrane BIS review. 34 However, as stated earlier, the review reported awareness outcomes only for trials in its set which were conducted with patients considered to be at higher risk of awareness (n = 4). 27,78,79,82 The Cochrane review combined these four trials in a fixed-effect meta-analysis, and we have updated this meta-analysis to include the two trials from our study set that featured higher risk patients. 40,44Figure 2 reports the results of this meta-analysis.
FIGURE 2.
Meta-analysis of intraoperative awareness during BIS monitoring (patients classified at higher risk of awareness)
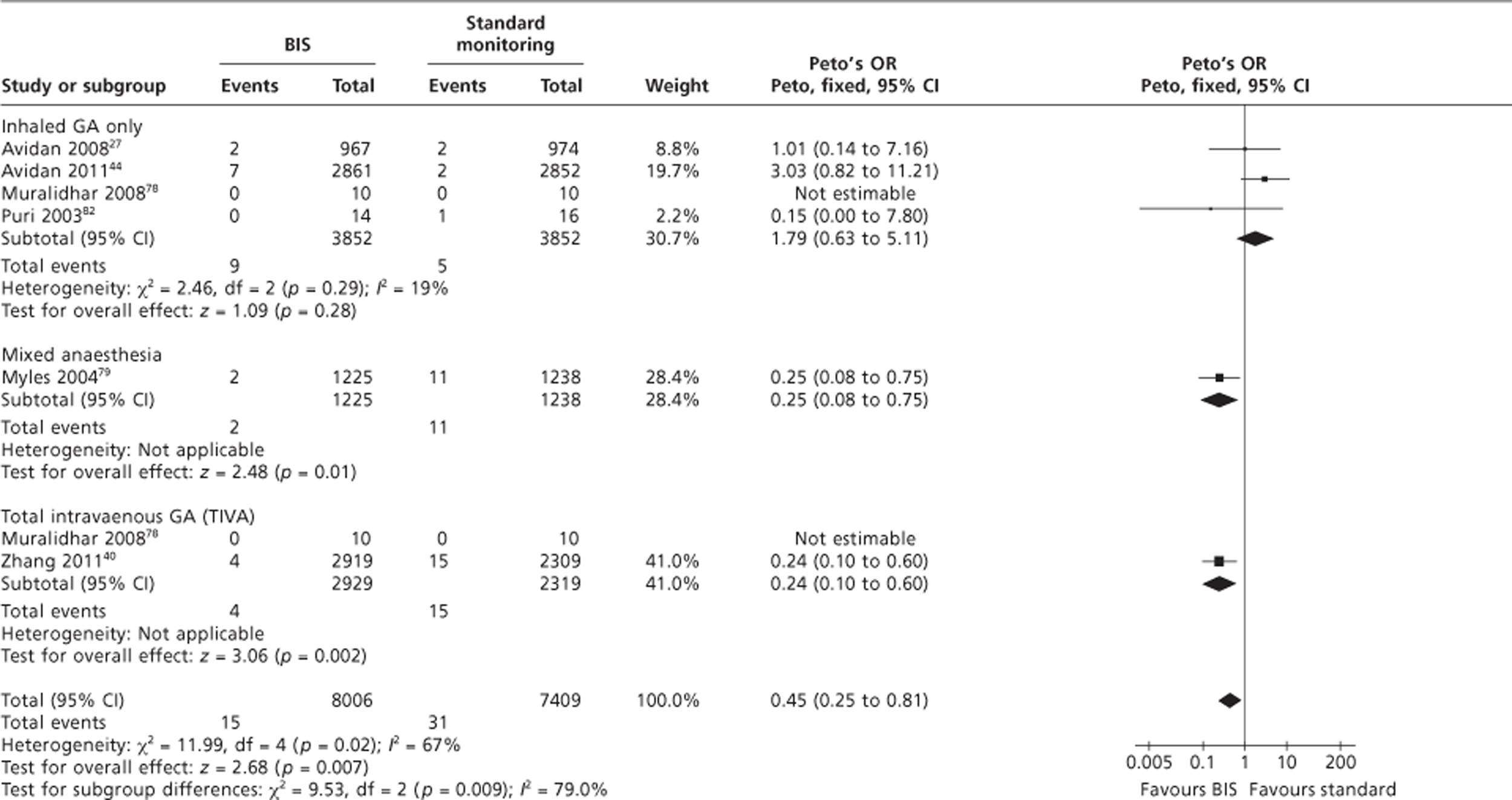
The meta-analysis included three subgroup analyses: trials that used inhaled GA only; trials that used a mixture of inhaled and i.v. anaesthesia; and trials that used TIVA. The original overall pooled Peto's odds ratio (OR) from the Cochrane review was 0.33 [95% confidence interval (CI) 0.13 to 0.84], indicating a statistically significant difference between groups favouring BIS. The addition of the trials by Avidan and colleagues44 and Zhang and colleagues40 increased the OR to 0.45 (95% CI 0.25 to 0.81). Caution is advised in the interpretation of this result as, overall, there was statistically significant heterogeneity (p = 0.009; I2 = 79%). In the subgroup of trials that used only inhaled anaesthesia the Peto's OR was 1.79 (95% CI 0.63 to 5.11) in favour of standard clinical monitoring. This is in contrast with the other two subgroups, which favoured BIS monitoring.
Explicit intraoperative awareness was an outcome measured in a further eight trials included in the Cochrane BIS review. However, as stated earlier, the review did not report the results of these trials for this outcome. We examined these studies (data not formally extracted) and note that no patients in any of these eight trials reported experiencing intraoperative awareness. It is unlikely that these studies were adequately statistically powered to detect awareness.
The trial by Kersens and colleagues49 was the only study to report implicit awareness, that is awareness that the patient does not necessarily recall experiencing. The probability of postoperatively selecting a word presented during anaesthesia (target) was higher in the BIS monitoring group (mean 0.371 ± 0.132) than in the standard clinical monitoring group (mean 0.323 ± 0.132). The probability of postoperatively selecting a word not presented during anaesthesia (distractor) was lower in the BIS monitoring group (mean 0.315 ± 0.117) than in the standard clinical monitoring group (mean 0.338 ± 0.119). It was not reported whether or not differences between study groups were statistically significant. Intragroup and overall differences between postoperative target and distractor word recall suggest that BIS-monitored patients were more likely to select words presented during anaesthesia than words not presented during anaesthesia, but standard clinical monitoring patients performed no better than chance in word selection (within-group difference in probability of selecting target word or distraction word: BIS: p = 0.001; standard clinical monitoring: p≥ 0.05).
Anaesthetic consumption
Table 9 reports the impact of BIS monitoring on intraoperative general anaesthetic requirement.
| Study | BIS | Standard clinical monitoring | Mean difference (95% CI), p-value |
|---|---|---|---|
| Volatile anaesthetic (sevoflurane), mean ± SD end-tidal sevoflurane concentration (%) | |||
| aBannister et al.45 | |||
| Maintenance of GA | 1.8 ± 0.4 | 2.4 ± 0.6 | p < 0.05 |
| Last 15 minutes of GA | 1.6 ± 0.6 | 2.1 ± 0.7 | p < 0.05 |
| End of procedure | 1.1 ± 0.6 | 1.5 ± 0.7 | NS |
| Kerssens et al.49 | |||
| Maintenance phase | 1.31 ± 0.29 | 1.56 ± 0.29 | p < 0.001 |
| aLiao et al.51 | |||
| Maintenance | 2.5 ± 0.4 | 2.9 ± 0.5 | 0.001;b p < 0.01c |
| Propofol consumption | |||
| aBhardwaj et al.46 | |||
| Maintenance phase μg/kg/minute, mean (SD) | 108.6 (37.8) | 106.6 (38.9) | Mean difference 1.9 (−19.9 to 23.7), p-value NR |
| Chan et al.47 | 25.3% reduction vs standard clinical monitoringd | ||
| Ellerkmann et al.62 | |||
| Maintenance phase μg/kg/minute, mean (SD) | 104 (20) | 101 (22) | Entropy/BIS vs standard clinical monitoring, p = 0.27 |
Six of the 11 BIS trials included in this systematic review reported this outcome measure,45–47,49,51,62 two of which reported it to be the primary outcome. 46,62 Three of the trials reported volatile anaesthetic consumption, all of which were for sevoflurane. Two of these three trials were conducted in children. 45,51 The mean end-tidal sevoflurane concentration (%) during maintenance of GA in each of these three trials was statistically significantly lower in the BIS-monitored group than in the standard clinical monitoring group. The other three trials46,47,62 reported i.v. anaesthetic consumption, all of which used propofol. One of these trials was conducted with children. 46 In two of the three trials the maintenance dose was higher in BIS-monitored patients than standard clinical monitoring, but with no statistically significant differences between groups. 46,62 The third trial was reported in a conference abstract, and limited results are given, except that there was a 25.3% reduction in propofol consumption compared with standard clinical monitoring. 47
The Cochrane BIS review34 conducted random-effects meta-analyses for anaesthetic consumption, producing separate meta-analyses for volatile anaesthetic consumption and for propofol consumption. We have updated these meta-analyses with studies included in our systematic review. Figure 3 shows the results of the meta-analysis of volatile anaesthetic consumption (sevoflurane).
FIGURE 3.
Meta-analysis of volatile anaesthetic consumption (sevoflurane) during BIS monitoring, MAC equivalents. IV, inverse variance, SD, standard deviation.
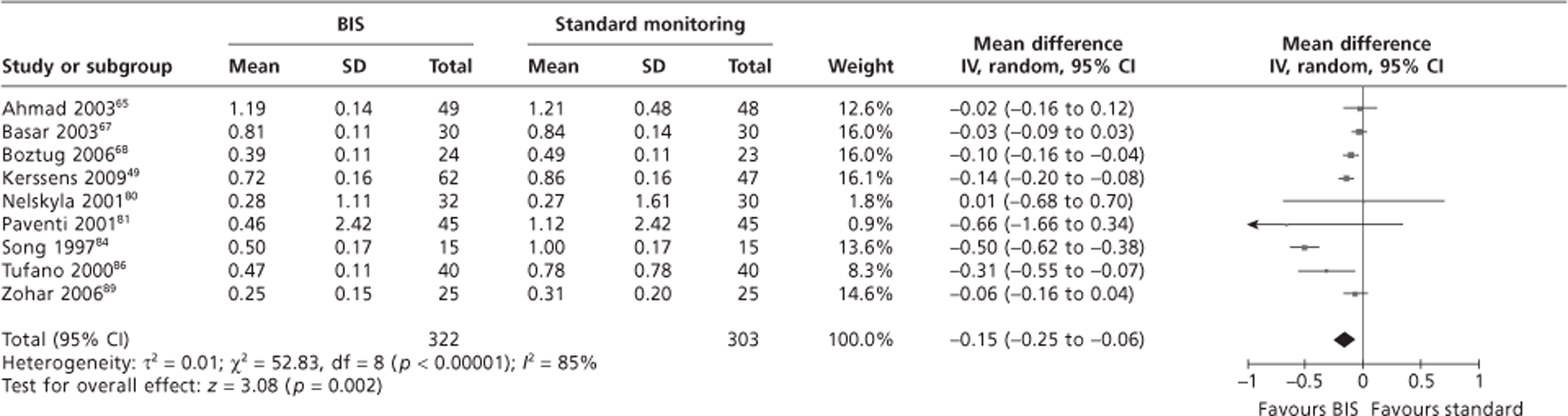
As stated, two of the three studies measuring sevoflurane consumption in our systematic review were conducted in children. The Cochrane BIS review34 only included studies of adults, therefore we have only updated their meta-analysis with the one study of adults from our set (Kerssens and colleagues49). The original mean difference in MAC equivalents from the Cochrane review for sevoflurane consumption was −0.16 (−0.29 to −0.04), indicating a statistically significant difference in favour of BIS. Updating the meta-analysis with the trial by Kerssens and colleagues49 reduced the mean difference slightly to −0.15 (95% CI −0.25 to −0.06), but remained statistically significant. However, caution is advised because of a high degree of unexplained statistical heterogeneity (p < 0.00001; I2 = 85%).
Figure 4 shows the results of the meta-analysis of propofol consumption.
FIGURE 4.
Meta-analysis of propofol consumption during BIS monitoring, mg/kg/minute. IV, inverse variance; SD, standard deviation.
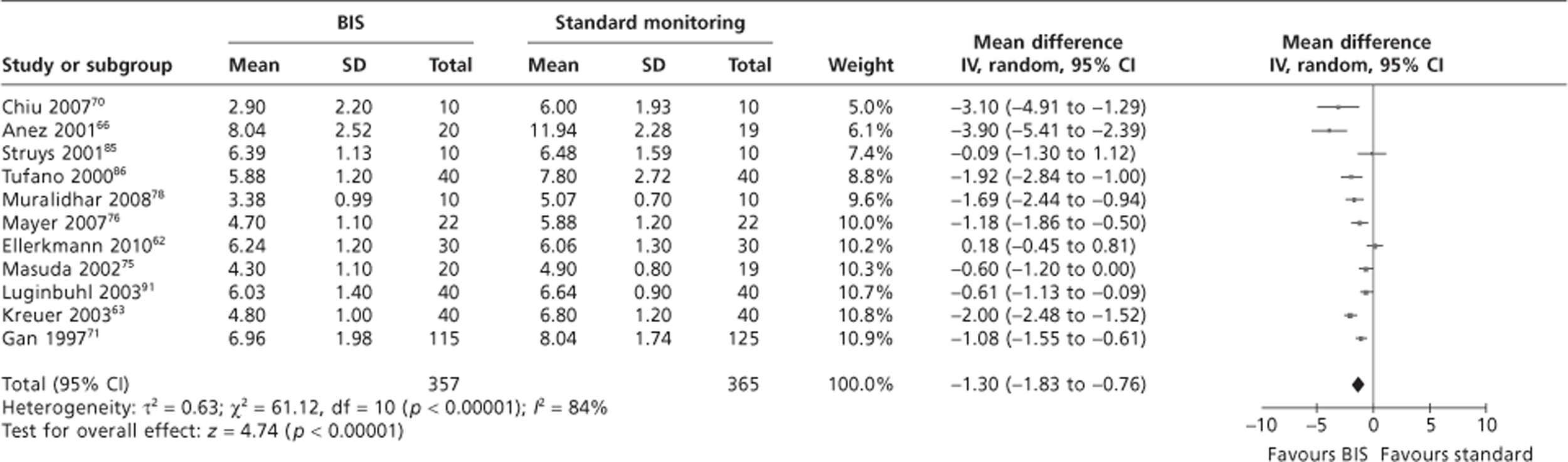
As stated, one of the three studies measuring propofol consumption in our systematic review was conducted in children. 46 As the Cochrane BIS review34 only included studies of adults, therefore we have updated their meta-analysis with one of the two studies of adults from our set. 62 (NB. The other adult study47 was only reported in a conference abstract and the results were not reported in a format amenable to meta-analysis.) The original mean difference propofol consumption (mg/kg/minute) in the Cochrane review was −1.44 (−1.95 to −0.93), indicating a statistically significant difference in favour of BIS. Updating the meta-analysis with the trial by Ellerkmann and colleagues62 reduced the mean difference slightly to −1.30 (95% CI −1.83 to −0.76), but remained statistically significant. Again, caution is required because of highly significant unexplained statistical heterogeneity (p < 0.00001; I2 = 80%).
Outcomes related to postanaesthesia care unit stay
Five of the 11 BIS trials45,46,48,52,53 in our systematic review reported this outcome, of which four were conducted with children. 45,46,52,53 In none of the trials was use of PACU a primary outcome. All of the studies appear to have reported the time to discharge from the PACU. However, it was not always clear exactly when the time to discharge began (e.g. from the end of skin closure, termination of anaesthetic or from admittance to the PACU). Bannister and colleagues45 reported time from end of surgery to PACU discharge, whereas Kamal and colleagues48 and both the trials by Messieha and colleagues52,53 stated measuring the end of general anaesthetic to PACU discharge (although in one of these trials48 data do not appear to be reported for that outcome). Bhardwaj and colleagues46 did not provide any detail on timing. Detail of discharge criteria varied between the trials. Bannister and colleagues45 and Kamal and colleagues48 both used the Aldrete scoring system (score of > 9), whereas Bhardwaj and colleagues46 used the Steward recovery scoring system (eligibility = score of 6). Messieha and colleagues52,53 did not report use of discharge criteria.
Table 10 shows the results of the trials relating to stay in the PACU.
| Study | BIS | Standard clinical monitoring | Mean difference (95% CI), p-value |
|---|---|---|---|
| aBannister et al.45 | |||
| Time to discharge from the PACU minutes mean (SD) | 20.0 (± 7.9) | 26.7 (± 11.2) | p < 0.05 |
| aBhardwaj et al.46 | Time to achieve a Steward recovery score of 6 (for discharge from the recovery room) reported to be comparable in the two groups | ||
| Kamal et al.48 | |||
| Arrival at PACU (minutes), mean (SD) | 9.4 (± 1.9) | 14.1 (± 2.8) | p < 0.01 |
| PACU discharge (minutes), mean (SD) | 53.9 (± 14.7) | 78.6 (± 21.5) | p < 0.01 |
| aMessieha et al.52 | |||
| Time to PACU discharge (minutes), mean (SD) | 60 (± 13) | 90 (± 11) | p < 0.001 |
| Duration of PACU stay (minutes), mean (SD) | 45 (± 8) | 71 (± 9) | p < 0.001 |
| aMessieha et al.53 | |||
| Duration of PACU stay (minutes), mean (SD) | 47 (± 17) | 63 (± 17) | p = 0.02 |
In all trials, time to discharge from the PACU was statistically significantly greater in the standard clinical monitoring group than in the BIS monitoring group, with mean differences in the range of 6.7–30 minutes. One trial did not report data for this outcome, mentioning that time to discharge was comparable between groups. There was also a statistically significant difference in the one trial that measured time to arrival at the PACU, with reduction of 4.7 minutes for BIS monitoring. 48 The two trials that reported duration of stay in the PACU both reported statistically significant differences in favour of BIS. 52,53
Eligibility for discharge from the PACU unit was one of the secondary outcomes from the Cochrane BIS review. 34 The review meta-analysed the outcome ‘PACU’ stay, including data from 12 trials. Examination of characteristics of the trials included in this meta-analysis, as summarised in the Cochrane review, show that some of the trials reported time to arrival in the PACU, time to discharge from the PACU and length of stay in the PACU. These all appear to have been included in the same meta-analysis, and there is no discussion about how timings may differ according to these different outcomes. Given this lack of clarity, and the fact that the Cochrane review included only trials of adults, we decided not to update this meta-analysis with data from trials identified in the current review. The pooled random-effects mean difference reported in the Cochrane review was −7.63 minutes (95% CI −12.50 to −2.76 minutes) in favour of BIS. However, caution is advised for the reasons given above, as well as a high degree of statistical heterogeneity (p < 0.00001; I2 = 82%). The results of the meta-analysis are similar to the results of the trials included in the current review (i.e. showing a benefit for BIS monitoring).
Time to recovery from anaesthesia
The trials included in the current systematic review reported a variety of outcomes relating to recovery from anaesthesia, including time to tracheal extubation, time to eye opening and movement responses.
Table 11 reports the time to tracheal extubation following surgery.
| Study | BIS | Standard clinical monitoring | Mean difference (95% CI), p-value |
|---|---|---|---|
| Mean (SD) time to extubation (minutes) | |||
| aBannister et al.45 | 7.1 (3.7) | 11.3 (5.9) | p < 0.05 |
| aBhardwaj et al.46 | Time to extubation reported to be comparable in the two groups | ||
| Kamal et al.48 | 4.3 (2.1) | 4.8 (2.3) | p > 0.05 |
| aMessieha et al.52 | 9 (5) | 13 (5) | p = 0.07 |
| aMessieha et al.53 | 5 (2) | 10 (7) | p = 0.04 |
Five of the 11 BIS trials included in the current systematic review measured time to extubation, of which four were conducted with children. 45,46,52,53 None of these studies considered this to be a statistically powered primary outcome measure. Timing was reported to have begun from end of surgery in three studies,45,52,53 and from termination of anaesthetic in two studies. 46,48 Extubation times were shorter for BIS-monitored patients than for those receiving standard clinical monitoring by as much as 5 minutes or as little as 0.5 minutes. Differences between groups were reported to be statistically significant in two trials,45,53 but not in two other trials. 48,52 One trial did not report numerical data, stating that times were comparable between groups. 46
A sixth study, conducted with children, reported time to laryngeal mask airway removal following surgery as an outcome. 51 The mean time [standard deviation (SD)] in minutes was 1.8 (1.6) in the BIS-monitored group, and 2.1 (2.4) in the standard clinical monitoring group (p = 0.93), indicating no statistically significant differences between groups.
Time to extubation was one of the secondary outcomes from the Cochrane BIS review. 34 The review meta-analysed data from 21 trials. Given that four of the five trials45,46,52,53 in the current systematic review were conducted in children and the Cochrane review was restricted to trials of adults, we have not updated their meta-analysis. The overall random-effects mean difference in time to extubation was −2.87 minutes (95% CI −3.74 to −1.99 minutes), indicating a statistically significant difference in favour of BIS. Caution is advised as there was a high degree of statistical heterogeneity (p < 0.00001; I2 = 79%).
Table 12 reports time to eye opening following surgery.
| Study | BIS | Standard clinical monitoring | Mean difference (95% CI), p-value |
|---|---|---|---|
| Mean (SD) time to eye opening (minutes) | |||
| aBhardwaj et al.46 | Time to eye opening reported to be comparable in the two groups | ||
| Kamal et al.48 | 4.1 (1.6) | 4.4 (1.9) | p > 0.05 |
| aLiao et al.51 | 15.0 (16.4) | 16.1 (11.3) | p = 0.17b |
Three trials included in the current systematic review reported time to eye opening, two of which were conducted with children. 46,51 Timing was reported to have begun immediately after the last surgical stitch in two studies48,51 and from the end of surgery in one trial. 46 Times were shorter in BIS-monitored patients, although by modest duration (up to 1 minute) and there were no statistically significant differences between groups. One trial provided only narrative results, reporting comparable times between groups.
Time to eye opening was one of the secondary outcomes from the Cochrane BIS review. 34 The review meta-analysed data from 19 trials. Given that two of the three trials in the current systematic review were conducted in children and the Cochrane review was restricted to trials of adults, we have not updated their meta-analysis. The overall random-effects mean difference in time to extubation was −2.14 minutes (95% CI −2.99 to −1.29 minutes), indicating a statistically significant difference in favour of BIS. Caution is advised as there was a high degree of statistical heterogeneity (p < 0.00001; I2 = 83%). The results of the meta-analysis are more conclusive than those of the relatively smaller number of trials included in the current review.
Table 13 reports the results of three trials that reported other recovery outcomes.
| Study | BIS | Standard clinical monitoring | Mean difference (95% CI), p-value |
|---|---|---|---|
| aBannister et al.45 | |||
| Mean ± SD time to first movement response (minutes) | 4.2 ± 3.7 | 7.0 ± 3.9 | p < 0.05 |
| aBhardwaj et al.46 | |||
| Time to response commands | Time to response to commands reported to be comparable in the two groups | ||
| aLiao et al.,51 mean ± SD time to emergence from anaesthesia (minutes) | |||
| Spontaneous movement | 3.6 ± 2.7 | 6.1 ± 5.7 | 0.02b; p < 0.05c |
| Phonation | 8.4 ± 5.2 | 12.9 ± 9.0 | 0.11b |
All three of the trials45,46,51 reporting other recovery outcomes were conducted with children. Bannister and colleagues45 reported mean time to first movement, with a statistically significant reduction for BIS-monitored patients of 2.8 minutes. Similarly, Liao and colleagues51 reported a statistically significant reduction in time to first spontaneous movement of 2.5 minutes. This trial51 also reported a shorter time to phonation (making a vocal sound) of 4.5 minutes, but this was not statistically significant. Bhardwaj and colleagues46 reported time to response to commands, commenting that this was comparable in the two groups but not reporting any numerical data.
Postoperative nausea and vomiting
Postoperative nausea and vomiting was reported by only one of the trials included in the current systematic review, the trial by Liao and colleagues. 51 There was no difference between patients in the BIS and standard clinical monitoring groups in terms of nausea [n = 5 (10%); n = 6 (11%), respectively, p = 0.95] or vomiting [n = 2 (4%); n = 3 (6%), respectively, p = 0.88]. Postoperative nausea and vomiting was not reported by the Cochrane BIS review. 34
Emergence delirium
Liao and colleagues51 also reported the incidence of emergence delirium, as measured by the Paediatric Anaesthetic Emergence Delirium (PAED) instrument (noted to be valid and reliable by the authors, reference cited). Assessment took place by a trained observer in the PACU every 5 minutes after awakening for 30 minutes. The highest score during this period was used in the final PAED score. (NB. A description of the instrument and what the scores mean is not given.) There was no statistically significant difference between BIS and standard clinical practice monitored patients [median (interquartile range) score 18 (14–16); 15 (13–15), respectively, p = 0.94].
Postoperative cognitive dysfunction
The only trial to report postoperative cognitive dysfunction was that of Chan and colleagues, who studied an elderly patient population. 47 Cognitive dysfunction was assessed by a battery of eight neuropsychology tests before and at 1 and 3 weeks after surgery (no information on the tests reported). POCD was confirmed when two or more test parameters or the combined z-value > 1.96 (no further information given). There was no statistically significant difference between BIS and standard clinical monitoring in rates of dysfunction at 1 week post surgery [146 (32.5%); 177 (39.1%), respectively, p = 0.07]. However, the difference between groups become significant at 3 months post surgery [36 (8.1%); 54 (12%), respectively, p = 0.03; OR 1.6 (95% CI 1.0 to 2.4)]. Caution is advised as this trial47 was reported in a conference abstract therefore detail of its characteristics are lacking, prohibiting a thorough appraisal of its methodological quality. As the abstract was published in 2010 a full publication potentially may be available in the near future.
Mortality, myocardial infarction and stroke
One trial, by Leslie and colleagues,50 reported stroke, myocardial infarction and mortality for all surviving and available patients 30 days post operation (Table 14). This is a long-term follow-up (median = 4.1 years) publication of the B-Aware trial79 in patients classified at higher risk of intraoperative awareness because of factors such as type of surgery (e.g. high-risk cardiac surgery), health status (e.g. cardiovascular impairment) and lifestyle (e.g. heavy alcohol intake). [NB. A publication of the short-term results of this trial by Myles and colleagues79 (primary outcome: intraoperative awareness) was included in the Cochrane BIS review. 34 Results of this trial are presented earlier in this report.]
| Outcome | Group 1 BIS | Group 2 Routine care | OR or HR (95% CI), p-value |
|---|---|---|---|
| Mortality rate per 1000 patient-years (95% CI) | 67 (60 to 76) | 70 (62 to 79) | HR 0.86 (0.72 to 1.01), p = 0.07 |
| Myocardial infarction, n (%) | 105 (9) | 111 (9) | OR 0.85 (0.64 to 1.14), p = 0.28 |
| Stroke, n (%) | 53 (4) | 62 (5) | OR 0.79 (0.54 to 1.16), p = 0.22 |
There was no statistically significant difference between BIS-monitored patients and patients who received routine care in mortality, myocardial infarction or stroke.
Summary of Bispectral Index assessment
-
Six trials included in this systematic review measured the impact of BIS monitoring on explicit intraoperative awareness. Four of these trials reported few or no cases of awareness; however, they were not statistically powered to detect this outcome. The other two trials were powered to detect awareness and we added them to the meta-analysis from the Cochrane BIS review (restricted to patients considered to be at higher risk of awareness). The pooled Peto's OR was 0.45 (95% CI 0.25 to 0.81), in favour of BIS. However, there was statistically significant heterogeneity and a non-significant difference in the subgroup of trials in which only inhaled GA was used.
-
Three trials included in this systematic review reported changes in sevoflurane consumption, all of which were statistically significantly lower with BIS monitoring. We updated the Cochrane meta-analysis with one of these trials, producing a pooled mean difference of −0.15 (95% CI −0.25 to −0.06) MAC equivalents in favour of BIS (with unexplained statistically significant heterogeneity).
-
Three trials included in this systematic review reported changes in propofol consumption. In two of these the maintenance dose was higher in BIS-monitored patients than standard clinical monitoring, but not statistically significant. In the third trial propofol consumption was lower for BIS. We updated the Cochrane meta-analysis with one of these trials, producing a pooled mean difference of −1.33 mg/kg/minute (95% CI −1.82 to −0.84 mg/kg/minute), in favour of BIS (with unexplained statistically significant heterogeneity).
-
Five trials included in this systematic review reported time to discharge from the PACU, all of which appeared to be secondary outcomes. In all trials time to discharge was statistically significantly shorter in BIS-monitored patients, with mean differences in the range of 6.7–30 minutes. The Cochrane BIS review did a meta-analysis of the outcome ‘PACU stay’ (including time to arrival in the PACU, time to discharge from the PACU, and length of stay in the PACU). The pooled mean difference was −7.63 minutes (95% CI −12.50 to −2.76 minutes) in favour of BIS (with unexplained statistically significant heterogeneity).
-
Five trials included in this systematic review measured time to tracheal extubation, as a secondary outcome. Extubation times were shorter for BIS-monitored patients compared with standard clinical monitoring by as much as 5 minutes, and as little as 0.5 minutes, but not always statistically significant. The pooled mean difference in the Cochrane review for this outcome was −2.87 minutes (95% CI −3.74 to −1.99 minutes) in favour of BIS (with unexplained statistically significant heterogeneity).
-
Three trials included in the current systematic review reported time to eye opening as a secondary outcome. Times were shorter in BIS-monitored patients, although by modest duration (up to 1 minute), and there were no statistically significant differences between groups. The pooled mean difference in the Cochrane review for this outcome was −2.14 minutes (95% CI −2.99 to −1.29 minutes), indicating a statistically significant difference in favour of BIS (with unexplained statistically significant heterogeneity).
-
Postoperative nausea and vomiting was reported by only one trial. Incidence of nausea and vomiting was low (around 10% or less) and there was no statistically significant difference between groups.
-
Only one trial reported the incidence of postoperative cognitive dysfunction. There was no statistically significant difference between groups in rates of dysfunction at 1 week post surgery. By 3 months post surgery, incidence had fallen to around 8–12%, with a significant difference in favour of BIS. This study was reported only as a conference abstract and it is not clear whether or not this outcome was adequately statistically powered.
-
Longer-term postoperative outcomes of stroke, myocardial infarction and mortality were reported by only one trial (median of 4.1 years post operation), as secondary outcomes. Mortality was lower in BIS-monitored patients, although not statistically significant. Incidence of stroke and myocardial infarction was similar between groups.
-
In summary, BIS monitoring was associated with overall lower rates of explicit intraoperative awareness (limited to patients classified at higher risk of awareness, and non-significant effects in the subgroup of patients receiving only inhaled anaesthesia), lower general anaesthetic consumption and shorter recovery times (e.g. PACU discharge, time to extubation, time to eye opening). Generally, there was little difference between BIS and standard clinical monitoring in complications arising from excessive anaesthetic dose (e.g. nausea, vomiting and cognitive dysfunction). Caution is advised in the interpretation of the results as not all outcomes appeared to be adequately statistically powered, and there was significant heterogeneity. There was much variation between the trials in terms of patient characteristics and surgical procedures.
Characteristics of included studies: E-Entropy
Study populations
Two of the seven E-entropy trials were conducted with children, with median age 4–6 years (range 3–12 years). 54,56 The remaining five trials were in adults, with the mean age of patients ranging from 33 years55 to 69 years. 58 The trials varied in their sex composition. One trial was entirely on adult women,55 whereas another trial was almost entirely on young boys (the trial included 12% girls in one study arm only). 56 One trial included more elderly men than women (men–women ratio approximately 4:1),58 whereas another trial included more middle-aged women than men (male–female ratio approximately 1:3). The remaining three E-Entropy trials included a more even balance of males and females. 54,61,62 In all seven trials the mean body weight of patients appeared to be within the normal range, with mean weights ranging from 16 kg to 22 kg in the child studies and from 65 kg to 82 kg in the adult studies. One trial was conducted at six centres in three countries (Finland, Sweden and Norway). 57 The remaining trials appeared to be single-centre studies (not explicitly stated in two trials) that were each carried out in one country: Germany,55,62 France,61 India,56 South Korea54 and Taiwan. 58 None of the E-Entropy trials reported the ethnicity of their participants.
Four of the E-Entropy trials were in patients undergoing a mix of abdominal, urological, gynaecological and/or orthopaedic surgical procedures,56,61,62 which also included breast and thyroid surgery in one trial. 57 One trial specifically involved children undergoing tonsillectomy or adenoidectomy. 54 Another trial was carried out specifically in women undergoing laparoscopic gynaecological procedures. 55 The remaining trial focused on total knee replacement surgery. 58 Only one of the E-Entropy trials was clearly limited to day surgery patients. 56 None of the seven trials identified any specific risk factors for intraoperative awareness among their populations and none reported whether or not patients had any comorbidities that affect EEG monitoring. However, all the E-Entropy trials stated that they excluded patients with any history of cerebrovascular and/or neurological disorders. The ASA grade of patients was I–II in four of the trials,54–56,58 and I-III in the remaining three trials. 57,61,62 The proportion of grade III patients varied by study groups within these three trials, ranging 1–3%,57 11–15%61 and 3–26%. 62
Technologies
Four of the seven E-Entropy trials reported that they used the E-Entropy module manufactured by GE Healthcare,55,57,61,62 and six of the trials reported that they used the S/5TM monitor (Datex-Ohmeda). 54–58,61 Very little other information about the modules and monitors was provided: only one trial mentioned the version of the S/5 monitor used (Avance),56 and none of the studies stated the version of the E-Entropy algorithm software used.
The target E-Entropy values during anaesthesia maintenance were mostly in the range 40–65. Four trials specified target ranges for state entropy, which were either 40–6054,55 or 45–65. 56,57 A further trial specified a specific state entropy target of 50. 62 The remaining two trials specified target ranges for both state entropy and response entropy, which were 35–4558 and 40–60. 61 Four of the trials that specified target values for state entropy permitted an increase in the state entropy value during the last 15 minutes of surgery. During this period, the target values were specified as 60,62 65–70,56 ‘ideally 65, but not > 70’57 and ‘> 60 acceptable’. 55 In addition to the target values of state and response entropy, three trials also specified target values of the difference between response entropy and state entropy: these were < 10 in two trials55,57 and 5–10 in the remaining trial. 58
Two of the seven E-Entropy trials reported that E-Entropy monitoring for anaesthesia delivery was done in conjunction with monitoring haemodynamic changes. One of these trials specified that heart rate and blood pressure were to be kept within ± 20% of their baseline (preoperative visit) values. 57 The second trial stated that E-Entropy was used to guide anaesthesia unless (unspecified) haemodynamic changes of 30% persisted for > 5 minutes.
In addition to titrating anaesthesia to maintain the specified target entropy values, two trials specified corrective action if target values were exceeded. One trial specified intermittent provision of a sufentanil bolus if the response entropy–state entropy difference exceeded 10 for > 2 minutes. 61 The other trial specified administration of a propofol bolus if the state entropy value increased suddenly above 65.
In all seven of the E-Entropy trials, the E-Entropy monitoring was initiated in the operating theatre. Two trials stated57 or implied58 that E-Entropy monitoring was started before anaesthesia induction, and two trials stated that E-Entropy monitoring began after anaesthesia induction. 55,56 The remaining three trials did not report whether E-Entropy monitoring commenced before or after anaesthesia induction.
Comparators
Standard clinical monitoring was based on blood pressure and heart rate in three trials. 54,57,61 As well as blood pressure and heart rate, a further two trials also monitored sweating, lacrimation or movement,62 or coughing, chewing, grimacing or purposeful movement. 55 The remaining trials monitored heart rate, mean arterial pressure and lacrimation, and either movement in response to surgical stimulation,56 or sweating, flushing or wrinkling of frontal facial muscles, together with monitoring the end-tidal anaesthetic concentration. 58 Quantitative thresholds for the clinical parameters that were used to guide anaesthesia titration were specified in five of the seven E-Entropy trials. 54–58
In addition to titrating anaesthesia according to the clinical parameters, in one trial58 the ETAC was adjusted to maintain mean arterial pressure and heart rate fluctuations to within ± 30% of the baseline values. In another trial, i.v. fentanyl was given if clinical parameters were not stabilised after increasing the anaesthetic concentration to 1.3 MAC. 56
Anaesthetic agents and protocols
Three of the seven trials used i.v. propofol for anaesthesia induction. 55,61,62 One trial used i.v. propofol with alfentanil analgesic for induction. 57 A further trial employed propofol if patients had an i.v. line, but otherwise used inhaled sevoflurane for induction. 56 The remaining two trials both used inhaled sevoflurane for induction in all their patients. 54,58
For maintenance of anaesthesia, three trials used inhaled sevoflurane,54,58,61 and one trial used inhaled isoflurane. 56 The remaining trials used i.v. delivery of propofol,62 propofol and remifentanil,55 or propofol and alfentanil analgesic. 57
Overall, two trials used the same inhaled agent (sevoflurane) for both induction and maintenance;54,58 three trials used i.v. agents (all included propofol) for both induction and maintenance;55,57,62 and two trials used an i.v. anaesthetic for induction followed by an inhaled anaesthetic for maintenance. 56,61
Regional anaesthesia was only clearly reported in one of the E-Entropy trials, in which a caudal block was placed with bupivacaine. 56 Two trials stated that regional anaesthesia was not used. 58,61 One trial referred to regional anaesthesia in the publication abstract but did not provide details. 62 The remaining three trials did not refer to regional anaesthesia.
One of the E-Entropy trials stated that analgesics were not used during induction or maintenance of anaesthesia, although ketorolac was used after anaesthetic cessation. 54 One trial used i.v. sufentanil during induction and maintenance, with morphine during the last 15 minutes of surgery, followed by paracetamol, nefopam or non-steroidal anti-inflammatory drugs postoperatively. 61 Two trials used fentanyl during anaesthesia maintenance. Of these, one also used fentanyl and lidocaine during induction,58 whereas the other used fentanyl postoperatively, according to the patient's pain score. 56 One trial used piritramide during the last 15 minutes of surgery only. 55 The remaining two trials did not refer to analgesia either during induction, maintenance or post surgery. 57,62
Premedication was reported in five of the E-Entropy trials. The agents used were oral hydroxyzine,61 oral midazolam alone,62 oral midazolam with a benzodiazepine,55 i.v. midazolam54 and oral diazepam (in five of six study centres). 57 The remaining two trials did not specify whether or not premedication was used.
All of the E-Entropy studies except one56 used muscle relaxants. The muscle relaxants were atracurium,58,61,62 rocuronium54,55 or were not specified a priori but were chosen at the anaesthetist's discretion when needed. 57
In five trials anaesthesia was administered in the operating theatre. 56–58,61,62 The two remaining trials did not report where anaesthetics were administered.
The mean duration of anaesthesia was reported in six studies and ranged from 64.3 minutes for tonsillectomy or adenoidectomy procedures in children54 to 190.8 minutes for general surgical procedures in adults. 61 The remaining study reported median duration of anaesthesia which was 68–72 minutes (range 32–180 minutes) for lower abdominal or urological surgical procedures in children. 56
Duration of the surgery itself was reported less precisely than the duration of anaesthesia. Surgical duration was described as a minimum of 1 hour,55,61 approximately 1.5 hours,58 a mean of 41.4–48.1 minutes,54 or a median of 29–30 minutes (range 15–95 minutes)56 or was not reported. 57,62
The training and experience of the anaesthetists in E-Entropy module use was reported in four of the seven E-Entropy trials. 55,57,61,62 One trial stated that anaesthetists were allowed to accustom themselves to the use of E-Entropy monitoring for 3 weeks, and all participants had substantial previous experience with EEG-based depth of anaesthesia monitors. 57 In the remaining three trials the descriptions provided for training or experience were only superficial: ‘more than 3 months of routine use’61 ‘experienced anaesthesiologist’;62 and ‘anaesthesia was supervised by an experienced staff anaesthetist’. 55
Outcomes
Anaesthetic consumption was the primary outcome in four of the seven E-Entropy studies (Table 15). 54,58,61,62 The method of assessing anaesthetic consumption was by weighing the vaporiser,61 measuring the end-tidal concentration,54 using data from the S/5 anaesthetic delivery system58 or was not reported. 62 In the remaining three trials the primary outcomes were time to eye opening55,56 and time to response to a verbal command,57 after cessation of anaesthesia.
| Outcome | Study | ||||||
|---|---|---|---|---|---|---|---|
| Aime et al.61 | aChoi et al.54 | Ellerkmann et al.62 | Gruenewald et al.55 | aTalawar et al.56 | Vakkuri et al.57 | Wu et al.58 | |
| Anaesthetic consumption | P | P | P | ✗ | ✗ | ✗ | P |
| Intraoperative awareness | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| Analgesic consumption | ✗ | ||||||
| Time to response to commands | P | ||||||
| Time to eye opening | ✗ | ✗ | ✗ | P | P | ✗ | |
| Time to extubation | ✗ | ✗ | ✗ | ||||
| Time to recovery of orientation | ✗ | ✗ | |||||
| Time to PACU admission or discharge | ✗ | ✗ | |||||
| Monitoring device values | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ |
| Postoperative nausea and vomiting | ✗ | ||||||
| Parental satisfaction | ✗ | ||||||
| Treatment of haemodynamic events | ✗ | ||||||
| Haemodynamic profiles | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| % time with adverse haemodynamic profiles | ✗ | ||||||
| Time to complete recovery (Aldrete score of at least 9) | ✗ | ||||||
| Recovery score (modified Steward recovery score) | ✗ | ||||||
| Postoperative pain | ✗ | ✗ | |||||
| Patient satisfaction | ✗ | ||||||
The most frequently reported outcomes overall for which quantitative results were reported were: anaesthetic consumption (a primary outcome in four trials54,58,61,62 and a secondary outcome in three trials55–57); entropy values (a secondary outcome in all seven trials); time to eye opening (a primary outcome in two trials55,56 and a secondary outcome in four trials54,57,61,62); intraoperative awareness (a secondary outcome in all except one trial56); haemodynamic profiles (a secondary outcome in all except one trial62); time to extubation (a secondary outcome in three trials54,57,61); and postoperative pain (a secondary outcome in two trials55,56). Other outcomes that were reported quantitatively in one trial each were postoperative pain, analgesia consumption, PONV, time to recovery based on Aldrete or Steward scores, time spent with adverse haemodynamic profiles, probability of emergence and (in a study with children) parental satisfaction. Some of the trials provided only a narrative report of outcomes. These outcomes were not extracted from the primary trials as no estimates of effect or variance could be determined. For example, two trials57,58 stated narratively that pain scores, analgesic use and incidence of PONV did not differ between E-Entropy and clinical practice groups but no quantitative results were reported for these outcomes and so these are not included in Table 15.
Three of the six trials that measured intraoperative awareness employed versions of standard patient questionnaires published by Brice and colleagues24 (two studies57,61) or Nordström and colleagues96 (one study62). The three remaining trials stated only that intraoperative recall was assessed by independent nurses;54 patients were questioned about memory and awareness;55 or the level of awareness was assessed. 58 Four trials reported the timing of the intraoperative awareness assessments, which were 24 hours after surgery,55 on the first postoperative day,62 in the PACU and on the first day post surgery,57 or on the first and third days post surgery. 61 The remaining two trials did not specify the timing of the awareness outcome assessments. No further details of the methods for assessing intraoperative awareness were reported.
Length of follow-up was relatively short in all the trials, being 1 day post surgery (for intraoperative awareness) in three trials,54,55,57 3 days post surgery (for intraoperative awareness) in three trials,58,61,62 and only 2 hours post surgery (for pain assessment) in the remaining trial. 56 The duration of follow-up would not have been adequate for detecting delayed onset of awareness recall, which may occur more than 1 week post surgery.
Assessment of outcomes: E-Entropy
Intraoperative awareness
Only one case of intraoperative awareness was reported in the six trials that measured this outcome (Table 16). This was experienced by an adult woman in the standard clinical practice group of the trial by Gruenewald and colleagues. 55 It should be noted that the sample sizes of these studies may have been too small to detect rare events such as intraoperative awareness.
| Study | Entropy | Standard clinical monitoring | Mean difference (95% CI), p-value |
|---|---|---|---|
| Aime et al.,61 n/N (%) | 0/40 (0) | 0/60 (0) | NR |
| aChoi et al.,54 n/N (%) | 0/39 (0) | 0/39 (0) | NR |
| Ellerkmann et al.,62 n/N (%) | 0/30 (0) | 0/30 (0) | NR |
| Gruenewald et al.,55 n/N (%) | 0/37 (0) | 1/35 (2.8) | NR |
| bVakkuri et al.,57 n/N (%) | 0/160 (0) | 0/160 (0) | NR |
| Wu et al.,58 n/N (%) | 0/34 (0) | 0/31 (0) | NR |
Anaesthetic consumption
Four trials that assessed volatile anaesthetic consumption either as the primary outcome for sevoflurane54,58,61 or a secondary outcome for isoflurane,56 all demonstrated statistically significant reductions in the E-Entropy-guided anaesthesia group compared with the standard clinical monitoring group (Table 17). In the trial by Aime and colleagues,61 the rates of sevoflurane consumption, but not the total amount consumed, were significantly lower in the E-Entropy group. In this trial61 the difference in sevoflurane consumption rates between groups was more pronounced when the consumption rate was normalised to patients' body weight.
| Study | Entropy | Standard clinical monitoring | Mean difference (95% CI), p-value |
|---|---|---|---|
| Volatile anaesthetic consumption (sevoflurane), mean ± SD vaporiser weight change | |||
| Aime et al.61 | |||
| Total (g) | 22.8 ± 14.4 | 25.6 ± 17.2 | p = 0.49 |
| Rate (g/hour) | 7.8 ± 3.4 | 9.4 ± 5.6 | p = 0.07 |
| aRate normalised (g/kg/hour) | 0.10 ± 0.05 | 0.14 ± 0.09 | p = 0.003 |
| Volatile anaesthetic consumption (sevoflurane), mean ± SD end-tidal sevoflurane concentration (%) | |||
| bChoi et al.54 | 2.2 ± 0.3 | 2.6 ± 0.4 | p < 0.05 |
| Volatile anaesthetic consumption (sevoflurane), mean ± SD total sevoflurane consumption recorded by S/5 monitor | |||
| Wu et al.58 | |||
| Total consumption (ml) | 27.79 ± 7.4 | 31.42 ± 6.9 | p = 0.023 |
| Volatile anaesthetic consumption (isoflurane), mean end-tidal isoflurane concentration (%) | |||
| bTalawar et al.56 | |||
| Immediately before LMAI | 0.81 | 1.24 | p < 0.05 |
| 15 seconds after LMAI | 0.78 | 1.24 | p < 0.05 |
| 15 seconds after caudal analgesia | 0.69 | 0.84 | p < 0.05 |
| 15 seconds after skin incision | 0.68 | 0.78 | p < 0.05 |
| 5 minutes after skin incision | 0.68 | 0.79 | p < 0.05 |
| Immediately before LMAR | 0.35 | 0.38 | p≥ 0.05 |
| Intravenous anaesthetic consumption (propofol and remifentanil), mean ± SD consumption rate and number (%) requiring propofol bolus based on E-Entropy | |||
| Ellerkmann et al.62 | |||
| Propofol (μg/kg/minute) | 106 ± 24 | 101 ± 22 | p = 0.27 |
| Remifentanil (μg/kg/minute) | 0.08 ± 0.02 | 0.09 ± 0.02 | p = 0.56 |
| Requiring bolus, n/N (%) | 12/30 (40) | 10/30 (33) | NR |
| Gruenewald55 | |||
| Propofol (μg/kg/minute) | 81 ± 22 | 95 ± 14 | p < 0.01 |
| Remifentanil (μg/kg/minute) | 0.46 ± 0.08 | 0.39 ± 0.08 | p < 0.001 |
| Intravenous anaesthetic consumption (propofol and alfentanil), median (range) consumption rate | |||
| cVakkuri57 | |||
| Propofol (mg/kg/minute) | 0.10 (0.04–0.23) | 0.11 (0.03–0.21) | p < 0.001 |
| Alfentanil (μg/kg/minute) | 0.60 (0.12–2.2) | 0.57 (0.16–1.6) | p = 0.54 |
Three trials that assessed consumption of i.v. anaesthetics55,57,62 showed mixed results (Table 17). Propofol consumption in the E-Entropy group was statistically significantly lower than in the standard clinical practice group in two trials that assessed anaesthetic consumption as secondary outcomes,55,57 but not in a trial that assessed anaesthetic consumption as the primary outcome. 62 Remifentanil consumption was significantly higher in the E-Entropy group in one trial that assessed this as a secondary outcome,55 but did not differ between groups in the trial that assessed this as the primary outcome. 62 Alfentanil consumption, assessed as a secondary outcome in one trial, did not differ significantly between the study groups. 57
The trials that assessed anaesthetic consumption measured outcomes in different ways, expressed their outcomes in different units (total consumption or rates) and, as noted above, differed in the patient populations that they included. These differences would preclude the meaningful pooling of the anaesthetic consumption outcomes that were reported (Table 17).
Time to recovery from anaesthesia
Results are summarised in Table 18 for the trials that reported time to eye opening;54–57,61,62 extubation;54,57,61 spontaneous breathing;57 recovery of orientation;54,57 response to commands;57 recovery defined by Aldrete score;54 and recovery defined by modified Steward score. 56
| Study | Entropy | Standard clinical monitoring | Mean difference (95% CI), p-value |
|---|---|---|---|
| Time (minutes) to eye opening, mean ± SD or median (range) [interquartile range] time since cessation of anaesthetic (or time from last suture62) | |||
| Aime et al.61 | 7.6 ± 4.1 | 7.2 ± 4.7 | NR |
| aChoi et al.54 | 14.3 ± 3.6 | 18.0 ± 3.3 | Stated not significant |
| Ellerkmann et al.62 | 9.2 ± 3.9 | 7.3 ± 2.9 | Not reported |
| bGruenewald et al.55 | 3 (0–9) [1–5] | 4 (0–14) [3–6] | Stated not significant |
| a,bTalawar et al.56 | 8.2 ± 4.49, 7 (3–18) | 10.96 ± 3.86, 10 (5–21) | 2.72 (0.34–5.1), p = 0.017 |
| Vakkuri et al.57 | 6.08 (0.15–37.5) | 10.8 (2.23–43.2) | p < 0.001 |
| Time (minutes) to extubation, mean ± SD or median (range) time since cessation of anaesthetic (or start time not reported57) | |||
| Aime et al.61 | 11.5 ± 5.8 | 14.2 ± 9.0 | NR |
| aChoi et al.54 | 8.3 ± 1.4 | 11.9 ± 2.5 | p < 0.05 |
| Vakkuri et al.57 | 5.80 (3.00–27.3) | 9.16 (1.67–32.3) | p < 0.001 |
| Time (minutes) to spontaneous breathing, median (range) (start time not reported) | |||
| Vakkuri et al.57 | 4.74 (0.00–18.0) | 7.07 (−1.00–28.5) | p < 0.001 |
| Time (minutes) to recovery of orientation, mean ± SD or median (range) time since cessation of anaesthetic (or start time not reported57) | |||
| aChoi et al.54 | 18.2 ± 4.0 | 23.3 ± 5.0 | p < 0.05 |
| Vakkuri et al.57 | 10.3 (1.17–48.7) | 15.1 (4.08–113) | p < 0.001 |
| Time (minutes) to response to commands, median (range) time to hand squeezing (start time not reported) | |||
| Vakkuri et al.57 | 8.60 (1.17–47.4) | 12.7 (2.43–48.1) | p < 0.001 |
| Time (minutes) to complete recovery (Aldrete score ≥ 9), mean ± SD time since cessation of anaesthetic | |||
| aChoi et al.54 | 24.3 ± 7.3 | 28.8 ± 5.7 | p < 0.05 |
| Time (minutes) to recovery (Steward score of 6), mean ± SD time since cessation of anaesthetic | |||
| aTalawar et al.56 | 7.08 ± 3.78, 6 (1–15) | 8.36 ± 4.8, 8 (2–24) | 1.3 (−1.2–3.7), p = 0.464 |
Time to eye opening was significantly shorter, by approximately 2–4 minutes, in the E-Entropy group than in the standard clinical practice group in two of six trials. 56,57 One of these assessed this as a primary outcome in children56 and the other assessed it as a secondary outcome in adults. 57 In the remaining four trials54,55,61,62 (one of which specified this as a primary outcome55) the time to eye opening did not differ between the study groups (Table 18).
Time to extubation (a secondary outcome) was shorter, by approximately 3–4 minutes, in the E-Entropy group than in the standard clinical monitoring group in all three trials that assessed this outcome. 54,57,61 The differences were stated as statistically significant in two of the trials54,57 but statistical significance was not reported in the remaining trial61 (see Table 18).
The times to spontaneous breathing (a secondary outcome);57 recovery of orientation (a secondary outcome);54,57 response to commands (a primary outcome);57 and recovery defined by an Aldrete score of at least 9 (a secondary outcome)54 were each significantly shorter in the E-Entropy group than the standard clinical practice group in the two trials54,57 that reported these outcomes (see Table 18). However, the time to recovery as defined by reaching a Steward score of 6 (a secondary outcome) did not differ between the study groups in one trial that assessed this outcome. 56
Outcomes related to postanaesthesia care unit stay
The time from discharge from the operating room to the PACU was shorter by approximately 3–4 minutes in the E-Entropy group than the standard clinical practice group in the two trials that monitored these outcomes56,57 (Table 19). The differences in both trials were statistically significant, although only marginally so in one of the trials. 56
| Study | Entropy | Standard clinical monitoring | Mean difference (95% CI); p-value |
|---|---|---|---|
| Time (minutes) from discharge from operating room to PACU admission, mean ± SD or median (range) time since cessation of anaesthetic56 or since discharge from operating room57 | |||
| aTalawar et al.56 | 15.32 ± 6.6, 15 (5–31) | 19.32 ± 7.12, 19 (10–40) | 4.0 (0.07–7.9), p = 0.045 |
| Vakkuri et al.57 | 10.3 (3.83–42.4) | 13.0 (5.00–49.8) | p < 0.001 |
| Time (minutes) to discharge from PACU, median (range) – not stated whether time since discharge from operating room or since admission to PACU | |||
| Vakkuri et al.57 | 134 (50–1293) | 150 (7–1020) | p = 0.21 |
The time to discharge from the PACU was shorter in the E-Entropy group than the standard clinical monitoring in the only trial that assessed this outcome,57 although the difference was not statistically significant. The time from which discharge from the PACU was measured was not reported, however, which makes interpretation of this outcome unclear57 (see Table 19).
Postoperative pain
Two trials reported postoperative pain, using different rating scales (Table 20). Pain was assessed as a score on a 0–10 scale55 or using the Children's Hospital of Eastern Ontario Pain Score (CHEOPS). 56 Pain scores were significantly lower in the E-Entropy group than standard clinical practice for the adult population. 55 In the paediatric population, the CHEOPS scores were significantly lower in the E-Entropy group at 60, 90 and 120 minutes after arrival in the PACU but not at 30 minutes after arrival. 56
| Study | Entropy | Standard clinical monitoring | Mean difference (95% CI), p-value |
|---|---|---|---|
| Pain intensity score on arrival in recovery room (0–10 scale; no other details), median (range) [interquartile range] | |||
| Gruenewald et al.55 | 6 (2–10) [4–7] | 4 (1–10) [3–5] | p = 0.03 |
| Pain intensity score based on CHEOPS scale, mean (standard error) | |||
| a,bTalawar et al.56 | |||
| After 30 minutes in PACU | 4.88 (0.319) | 4.76 (0.09) | 0.12 (−0.53 to 0.77), p = 0.71 |
| After 60 minutes in PACU | 4.48 (0.10) | 4.76 (0.08) | −0.28 (4.59 to 4.92), p = 0.01 |
| After 90 minutes in PACU | 4.56 (0.10) | 4.76 (0.08) | −0.2 (4.59 to 4.92), p = 0.01 |
| After 120 minutes in PACU | 4.88 (0.21) | 5.44 (0.33) | −0.56 (4.77 to 6.09), p = 0.01 |
Analgesic consumption
Only one E-Entropy trial assessed analgesic consumption. 61 Consumption of sufentanil was slightly lower in the E-Entropy group than the standard clinical monitoring group during both induction and maintenance of anaesthesia, but the differences were not statistically significant (Table 21).
| Study | Entropy | Standard clinical monitoring | Mean difference (95% CI), p-value |
|---|---|---|---|
| Sufentanil consumption per patient, mean ± SD | |||
| Aime et al.61 | |||
| Induction dose (μg/kg) | 0.21 ± 0.05 | 0.23 ± 0.06 | p = 0.18 |
| Maintenance consumption (μg/hour) | 13.6 ± 6.1 | 14.9 ± 8.3 | p = 0.66 |
| Maintenance consumption (μg/kg/hour) | 0.18 ± 0.09 | 0.22 ± 12 | p = 0.26 |
Postoperative nausea and vomiting
One trial that assessed PONV after arrival in the recovery room55 reported similar frequencies in the E-Entropy and standard clinical monitoring that did not differ significantly (Table 22).
| Study | Entropy | Standard clinical monitoring | Mean difference (95% CI), p-value |
|---|---|---|---|
| Nausea and vomiting on arrival in recovery room, n/N (%) | |||
| Gruenewald et al.55 | 15/37 (41) | 13/35 (37) | Stated not significant |
In addition to the outcomes reported above, the E-Entropy trials reported that the following outcomes did not differ between E-Entropy and standard clinical practice groups (data not extracted): patient satisfaction scores;55 parent satisfaction scores for children at 24 hours post surgery;55 time spent by patients with adverse haemodynamic profiles;61 and treatment for haemodynamic events. 61
Summary of E-Entropy assessment
-
Six trials monitored intraoperative awareness in adults and children receiving different volatile and i.v. anaesthetics. Only one case of awareness occurred, in the standard clinical practice group of one trial. However, sample sizes were relatively small in these trials.
-
Four trials monitored consumption of volatile anaesthetic (three monitored sevoflurane as a primary outcome, one monitored isoflurane as a secondary outcome). Consumption was significantly lower in the E-Entropy monitoring than standard clinical practice groups of all trials, with the proviso that in one of these trials the difference in sevoflurane consumption was statistically significant for rates of consumption but not for total anaesthetic dose.
-
Three trials that monitored consumption of i.v. anaesthetic yielded mixed results. Trials that monitored consumption of propofol, remifentanil and alfentanil as primary outcomes found no statistically significant differences between the study groups. However, significantly lower consumption of propofol and remifentanil in the E-Entropy group was reported in trials that assessed these as secondary outcomes.
-
Time to eye opening was significantly shorter in the E-Entropy group than the standard clinical practice group in two of six trials, one of which assessed this as a primary outcome, but did not differ in the remaining four trials.
-
Time to extubation (a secondary outcome) was shorter in the E-Entropy group than the standard practice group in all three trials that assessed this outcome. The differences were stated as statistically significant in two of the trials but statistical significance was not reported in the remaining trial.
-
The times to spontaneous breathing (a secondary outcome), recovery of orientation (a secondary outcome), response to commands (a primary outcome) and recovery defined by an Aldrete score of at least 9 (a secondary outcome) were each significantly shorter in the E-Entropy group than in the standard clinical practice group. Except for time to orientation (two trials), these outcomes were reported by only one trial each. The time to recovery as defined by reaching a Steward score of 6 (a secondary outcome) did not differ between the study groups in one trial that assessed this outcome.
-
The limited evidence available (from two trials which assessed secondary outcomes only) suggests that E-Entropy monitoring favours shorter time to discharge to and from the PACU, but it is unclear whether or not the time gains are clinically important.
-
No firm conclusions can be drawn about effects of E-Entropy monitoring on postoperative pain because the only two trials that assessed this used different rating scales, and the effect of E-Entropy monitoring on pain scores was temporally variable in one of the trials. Analgesic consumption and frequency of PONV were assessed in one trial each and did not differ between the E-Entropy and standard clinical practice groups. Postoperative pain, nausea and vomiting, and analgesic consumption were assessed only as secondary outcomes in these trials.
-
In summary, compared with standard clinical monitoring, E-Entropy monitoring favoured: lower consumption of volatile anaesthetics and some, but not all, i.v. anaesthetics; and shorter times to recovery and discharge to and from the PACU, assessed by various measures. E-Entropy monitoring had no consistent impact on other outcomes that were monitored, including intraoperative awareness, but the small sample sizes in the trials may not have provided adequate statistical power to detect meaningful differences in rare events. Pooled effect estimates would not be estimable reliably for these outcomes, because of the uniqueness of the individual studies (which included different populations in terms of age, sex and ethnicity, undergoing different surgical procedures) and differences between the trials in the way that outcomes were assessed and reported. Also, the majority of the outcomes were secondary and may not have been adequately powered statistically to detect clinically relevant differences between the E-Entropy and standard clinical practice groups.
Characteristics of included studies: Narcotrend
Study populations
In all trials of Narcotrend, the study population was adults (mean age 40–50 years) and 33–50% of participants were males for the three studies reporting sex. Mean weight ranged from 60 kg to about 84 kg. All studies appeared to be single-centred studies with three conducted in Germany and one in China. 59 Ethnicity of participants was not reported in any study.
The type of surgery was minor orthopaedic surgery,63,64 microwave coagulation for liver cancer,59 and all kinds of elective surgery, including surgery for ‘malignoma’ and peripheral vascular surgery. 60 No trial reported risk factors for awareness. Comorbidities were reported in two trials:59,60 hypertension was reported in both of these and one trial60 also reported cardiac arrhythmia, diabetes type II, asthma and miscellaneous comorbidities. Three trials included the number of participants with ASA grade I, II or III, with most grade II and fewest grade III; the fourth trial59 reported only that participants were ASA grade II or III.
Technologies
The Narcotrend monitor with software version 2.0 AF was used in three trials,60,63,64 whereas in the fourth trial59 no details of the software version are reported. Two trials report using the MonitorTechnik (Germany) with Blue Sensor (Denmark). 59,60
The Narcotrend target value during maintenance anaesthesia was D0 and then adjusted to C1 15 minutes before the expected end of surgery in two studies,63,64 and D2–E0 during maintenance adjusted to D0–D1 10 minutes before the end of surgery in one study. 59 In the fourth study60 the Narcotrend target value was D2–E0 with no further details given. The two studies59,60 using Narcotrend target values of D2–E0 therefore used deeper levels of anaesthesia and hypnosis than the other two studies. Monitoring started in the operating theatre in two studies,63,64 in the computed tomography department where surgery took place in one study59 and was not reported in the fourth study. 60
Only one trial59 explicitly stated that observational indices of electrocardiography (ECG), heart rate and mean arterial blood pressure were continuously monitored alongside Narcotrend scores. The other three studies did not explicitly state whether or not standard clinical monitoring took place in addition to Narcotrend. However, as signs of inadequate anaesthesia were based on vital signs and clinical parameters it can be assumed that it did. For example, signs of inadequate anaesthesia were hypertension, tachycardia or patient movement, eye opening, swallowing, grimacing, lacrimation and sweating. 63,64 Vital clinical parameters of heart rate, pulse oximetry readings, rectal temperature and end-expiratory carbon dioxide were continuously measured in the fourth study. 60
Comparators
Standard clinical continuous monitoring included heart rate, systemic arterial blood pressure, respiratory rate, oxygen saturation and end-tidal concentrations of carbon dioxide63,64 plus end-tidal desflurane64 and heart rate, pulse oximetry readings, rectal temperature and end-expiratory carbon dioxide. 60 In one study59 heart rate, blood pressure and body movement were used for monitoring.
Anaesthetic agents and protocols
Three studies used total i.v. anaesthesia: two60,63 used propofol–remifentanil for induction and maintenance anaesthesia; one used propofol–fentanyl induction and propofol anaesthesia maintenance. 59 The fourth study used desflurane–remifentanil anaesthesia. 64 Regional anaesthesia was not reported in any of the studies. Premedication was used in three studies in the form of midazolam60,64 and diazepam. 63 Analgesia included metamizol with sodium chloride,63,64 fentanyl59 and novaminsulfone, piritramide or morphine. 60 Muscle relaxants used included atracurium,64 cisatracurium63 and rocuronium. 60
Mean duration of anaesthesia ranged from 113 to 125 minutes,64 from 108 to 127 minutes,63 from 88 to 91 minutes59 and from 105 to 111 minutes60 in the four trials, with no significant differences between groups within each study. Duration of surgery was not reported in any study. Three studies60,63,64 reported that all patients were anaesthetised by the same experienced anaesthesiologist, one of which mentions specific experience in Narcotrend. 63 No details are given for the length of experience/training of the anaesthetist in the fourth study. 59
Outcomes
The primary outcome (statistically powered) specified in three trials was time to eye opening63,64 and time to extubation60 (Table 23). Time to tracheal extubation was also an outcome in two other studies. 63,64 All four studies59,60,63,64 report anaesthetic consumption and intraoperative awareness. Other reported outcomes include time to arousal time59 (defined as the time between cessation of drugs and the patient being able to open their eyes on command) and time to recovery of orientation (defined as the time between a patient opening their eyes on command and the restoration of orientation). 59 Two studies63,64 report time to discharge to the PACU and two report PONV. 59,60
| Outcomes | Study | |||
|---|---|---|---|---|
| Kreuer et al.64 | Kreuer et al.63 | Lai et al.59 | Rundshagen et al.60 | |
| Anaesthetic consumption | ✗ | ✗ | ✗ | ✗ |
| Intraoperative awareness | ✗ | ✗ | ✗ | ✗ |
| Analgesic consumption | ✗ | ✗ | ||
| Time to response to commands | ✗ | |||
| Time to eye opening | P | P | ||
| Time to extubation | ✗ | ✗ | P | |
| Time to recovery of orientation | ✗ | |||
| Time to arrival at PACU | ✗ | ✗ | ||
| PONV | ✗ | ✗ | ||
Assessment of outcomes: Narcotrend
Intraoperative awareness
No patients in any of the trials of Narcotrend reported intraoperative awareness as explicit memory during anaesthesia, although two patients (8%) receiving Narcotrend anaesthetic monitoring recalled dreaming during anaesthesia. 60
Anaesthetic consumption
Three studies report consumption of propofol; two59,63 found a statistically significant reduction in the group receiving Narcotrend monitoring compared with standard clinical monitoring, whereas the third60 found no difference in consumption between groups (Table 24).
| Study | Narcotrend | Standard clinical monitoring | p-value |
|---|---|---|---|
| Propofol consumption per patient | |||
| Kreuer et al.63 | |||
| Mean ± SD (mg) | 721.3 ± 401.2 | 970.5 ± 384.4 | p < 0.05 |
| Mean ± SD (mg/kg/hour) | 4.5 ± 1.1 | 6.8 ± 1.2 | p < 0.001 |
| Lai et al.59 | |||
| Mean ± SD (mg) | 380 ± 35 | 460 ± 30 | p < 0.01 |
| Rundshagen et al.60 | |||
| Mean ± SD (μg/kg/minute) | 0.093 ± 0.042 | 0.114 ± 0.035 | p = 0.089 |
| Remifentanil consumption per patient | |||
| Kreuer et al.64 | |||
| Mean ± SD normalised remifentanil infusion rate (μg/kg/minute) | 0.22 ± 0.06 | 0.23 ± 0.07 | NS |
| Kreuer et al.63 | |||
| Mean ± SD normalised remifentanil infusion rate (μg/kg/minute) | 0.21 ± 0.07 | 0.20 ± 0.07 | NS |
| Rundshagen et al.60 | |||
| Mean ± SD remifentanil dose (μg/kg/minute) | 0.31 ± 0.10 | 0.34 ± 0.11 | NS |
| Desflurane consumption per patient | |||
| Kreuer et al.64 | |||
| Mean ± SD (mg) | 4655.9 ± 2891.7 | 5547.3 ± 2396.4 | NS |
| Mean ± SD (mg/minute) | 374.6 ± 124.2 | 443.6 ± 71.2 | p < 0.05 |
Three studies reported remifentanil consumption and all found no statistically significant difference between Narcotrend and standard clinical monitoring. 60,63,64
Desflurane consumption per patient was not different between the Narcotrend monitoring group and standard anaesthetic practice, although desflurane consumption per patient per minute was statistically significantly lower in the Narcotrend group. 64
Time to arrival at postanaesthetia care unit
Two studies reported time to arrival at PACU and found statistically significantly shorter times in the Narcotrend monitoring group compared with the standard care monitoring group63,64 (Table 25).
Time to eye opening
Time to eye opening was the primary outcome in two trials and results between the studies differ (Table 26). One trial64 reported no statistically significant difference between Narcotrend monitoring and standard clinical monitoring, whereas the other trial63 reported a statistically significant reduction in time to eye opening of 5.9 minutes in the Narcotrend group compared with standard care.
Time to extubation
Time to tracheal extubation was the primary outcome in one study60 and no difference was found between monitoring of anaesthesia by Narcotrend and standard clinical monitoring (Table 27). In contrast, two other studies that reported time to extubation found statistically significant reductions in time to extubation of between 1.4 to 6 minutes with Narcotrend monitoring compared with standard clinical monitoring. 63,64
Other measures of time to emergence from anaesthesia
Time to arousal (defined as the time between cessation of drugs and the patient being able to open their eyes on command) was statistically significantly shorter in the group receiving Narcotrend monitoring than the group receiving standard clinical monitoring. 59 Duration of orientation recovery was also shorter with Narcotrend monitoring (Table 28). 59
| Study | Time to emergence from anaesthesia (minutes) | p-value | |
|---|---|---|---|
| Narcotrend | Standard clinical monitoring | ||
| Lai et al.59 | |||
| Mean ± SD time to arousal | 4.9 ± 2.2 | 9.5 ± 2.9 | p < 0.01 |
| Mean ± SD orientation recovery | 6.6 ± 3.2 | 12.2 ± 3.5 | p < 0.01 |
Postoperative nausea and vomiting
One study found that no nausea or vomiting was reported after surgery in either group. 59 Another study60 reported that nausea scores were statistically significantly higher in the group receiving anaesthesia monitoring by standard clinical practice than by Narcotrend at 10 minutes after extubation (mean ± SD, 24.06 ± 34.04 vs 6.88 ± 15.2, respectively, p = 0.005); however, there were no significant differences at other time points.
Analgesic consumption
Two studies59,60 reported consumption of pain-relieving drugs and found no statistically significant differences between Narcotrend and standard care monitoring groups.
Summary of Narcotrend assessment
-
Four trials59,60,63,64 monitored intraoperative awareness in adults receiving different volatile and i.v. anaesthetics; no patients reported explicit memory during anaesthesia although two patients receiving Narcotrend monitoring recalled dreaming during anaesthesia.
-
Three studies59,60,63 that measured consumption of propofol reported different results; significantly lower consumption was found in the Narcotrend group in two studies, whereas no difference was reported between groups in the third study.
-
Three studies60,63,64 found no significant difference between groups in remifentanil or desflurane consumption.
-
Two studies63,64 reported time to arrival at PACU and found statistically significantly shorter times in the Narcotrend group compared with standard care.
-
Time to eye opening was the primary outcome in two studies63,64 which yielded conflicting results; one reported a significantly lower time in the Narcotrend group than with standard care and the other reported no difference between groups.
-
Time to extubation was the primary outcome in one study60 which found no difference between groups; two other studies63,64 that reported this measure as a secondary outcome found significantly shorter time to extubation with Narcotrend monitoring than with standard care.
-
Time to arousal and duration of orientation recovery were reported to be shorter with Narcotrend monitoring compared with standard care in the one study59 reporting these outcomes.
-
Results suggest that there are no differences between groups in PONV after surgery or analgesic consumption from the two studies that report these outcomes.
-
In summary, Narcotrend monitoring compared with standard practice during minor orthopaedic surgery resulted in shorter recovery times (eye opening, arrival at PACU and time to extubation) and reduced propofol consumption. It was also associated with lower doses of propofol and shorter recovery during TIVA with propofol and fentanyl in liver cancer microwave coagulation. Narcotrend-assisted propofol–remifentanil anaesthesia did not reduce propofol or remifentanil consumption or time to extubation compared with standard clinical assessment in patients undergoing a range of elective surgery. The majority of the outcomes reported in the studies of Narcotrend were secondary and may not have been adequately powered statistically to detect clinically relevant differences. Also, the trial results are applicable to the specific patient groups included in the studies for the type of anaesthesia used and are not generalisable beyond this.
Results of systematic review of cost-effectiveness
The aim of this section is to assess the current state of evidence on the cost-effectiveness of depth of anaesthesia monitoring compared with standard clinical monitoring through a systematic review of the literature. The methods used for the search strategy are described in Identification of studies, and inclusion criteria are shown in Inclusion/exclusion criteria. Included studies were evaluated for their quality and for generalisability to the UK. This section concludes a statement on the current state of evidence on the cost-effectiveness of depth of anaesthesia monitoring and a discussion of key issues arising from included studies. The full data extraction forms for included studies are shown in Appendix 6.
Quantity and quality of research available
A total of 134 potentially relevant references were identified in the cost-effectiveness searches. Of these, the full text of 14 papers was retrieved and one study97 met all of the a priori inclusion criteria. A summary of the selection process and the reasons for exclusion are presented in Figure 5 – a list of excluded studies can be found in Appendix 7.
FIGURE 5.
Flow chart of identification of studies for inclusion in the review of cost-effectiveness.
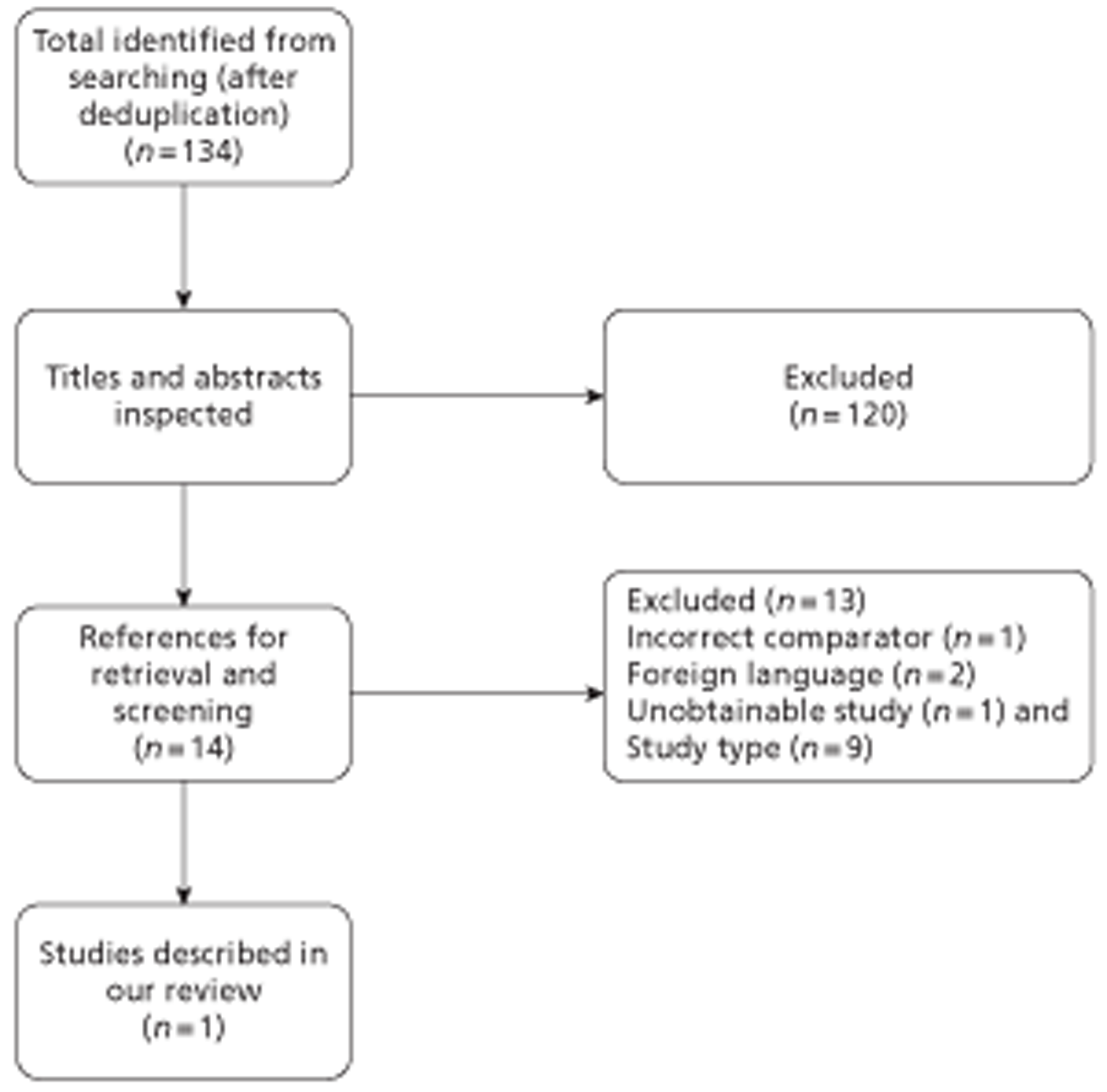
The excluded studies were predominantly cost analyses, completed as part of BIS trials, which reported the difference in drug cost between the BIS and control arms. An update search, conducted in February 2012, identified six possible studies. These were all excluded on the basis of title and abstract as either not being full economic evaluations or did not include the specified interventions and comparators. The included study was simple calculation models of BIS monitoring compared with standard treatment. The completed checklist for quality assessment of the included study is shown in Table 29.
| Item | Abenstein97 | |
|---|---|---|
| 1 | Is there a clear statement of the decision problem? | Y |
| 2 | Is the comparator routinely used in the UK NHS? | Y |
| 3 | Is the patient group in the study similar to those of interest in the UK NHS? | Y |
| 4 | Is the health-care system comparable to the UK? | N |
| 5 | Is the setting comparable to the UK? | Y |
| 6 | Is the perspective of the model clearly stated? | N |
| 7 | Is the study type appropriate? | Y |
| 8 | Is the modelling methodology appropriate? | Y |
| 9 | Is the model structure described and does it reflect the disease process? | Y |
| 10 | Are assumptions about model structure listed and justified? | N |
| 11 | Are the data inputs for the model described and justified? | ? |
| 12 | Is the effectiveness of the intervention established based on a systematic review? | N |
| 13 | Are health benefits measured in QALY? | N |
| 14 | Are health benefits measured using a standardised and validated generic instrument? | N |
| 15 | Are the resource costs described and justified? | ? |
| 16 | Have the costs and outcomes been discounted? | N |
| 17 | Has uncertainty been assessed? | N |
| 18 | Has the model been validated? | N |
Characteristics and results of included studies
The included study was a simple calculation model of BIS monitoring compared with standard treatment. Characteristics of the study are shown in Table 30 and a full data extraction form can be found in Appendix 6.
| Author | Abenstein97 |
|---|---|
| Publication year | 2009 |
| Country | USA |
| Study type | Cost-effectiveness analysis |
| Intervention(s) | BIS |
| Model type | Simple calculation |
| Intervention effect | Reduction in awareness for all patients from 0.18% to 0.04% |
| Base-case results | Cost of preventing each episode of awareness is US$11,294 for all patients |
The included study employed a relevant comparator and similar patient group to the UK NHS. However, the study was of poor quality, with limited information reported on the methods, and sources used for the model parameters. Assumptions were not justified. The study did not include health-related quality of life (HRQoL) or investigate uncertainty through sensitivity analyses.
Abenstein97 used a simple calculation model to compare GA with BIS monitoring to GA for high- and general-risk patients. The cost per avoided intraoperative recall is:
The cost per patient of BIS monitoring consisted of the cost of the sensors (US$17 each) and the cost of the monitor. The monitor was assumed to cost US$9000 and have a lifespan of 7 years, and be used by four patients per day for 300 days per year (US$1.07 per patient). The incidence of intraoperative recall for patients of general risk was taken from a prospective study by Ekman and colleagues98 who reported a recall rate of 0.04% (GA with BIS) compared with 0.18% (GA). The cost per avoided intraoperative recall was US$11,294. Abenstein97 estimated the cost per avoided intraoperative recall for high-risk patients to be US$4410 per avoided intraoperative recall. They used estimates of the incidence of intraoperative recall by averaging the difference between the studies by Myles and colleagues79 and Avidan and colleagues,27 which gave a reduction in incidence of intraoperative recall from 0.59% to 0.18%. The authors concluded that the general use of BIS monitoring does not seem warranted and appears not to be cost-effective.
Summary
One cost-effectiveness analysis97 was included in this systematic review, which compared BIS with standard clinical monitoring, using a simple calculation model. The study concluded that addition of BIS to GA was not cost-effective. However, the results and conclusions should be viewed with caution because of the poor methodological and reporting quality.
Model structure, model parameterisation and results of economic evaluation
Description of decision-analytic model
Overview
A decision-analytic model was developed to assess the cost-effectiveness of depth of anaesthesia monitoring, compared with standard clinical monitoring, in accordance with the scope of the appraisal issued by NICE. Separate analyses are presented for each of the three included technologies (the included technologies are not compared with each other).
The model was structured to include outcomes identified in the scope issued by NICE for this appraisal, where suitable data on the relative effectiveness of included technologies was identified in our systematic review of patient outcomes (see Results of systematic review of patient outcomes). The model evaluates costs (UK pounds using a 2011 price base) from the perspective of the NHS and Personal Social Services. Outcomes in the model are expressed as QALY. Both costs and outcomes are discounted using a 3.5% annual discount rate, in line with current guidance. 38,39
Modelling approach and model structure
The model developed for this assessment was a simple decision tree, which accounted for patients' risk of experiencing short-term anaesthetic-related complications (such as PONV) and more serious complications that may be associated with risk of morbidity or mortality. These were included, in addition to a risk of experiencing intraoperative awareness, see Figure 6.
FIGURE 6.
Decision tree evaluating cost-effectiveness of depth of anaesthesia monitoring compared with standard clinical monitoring.
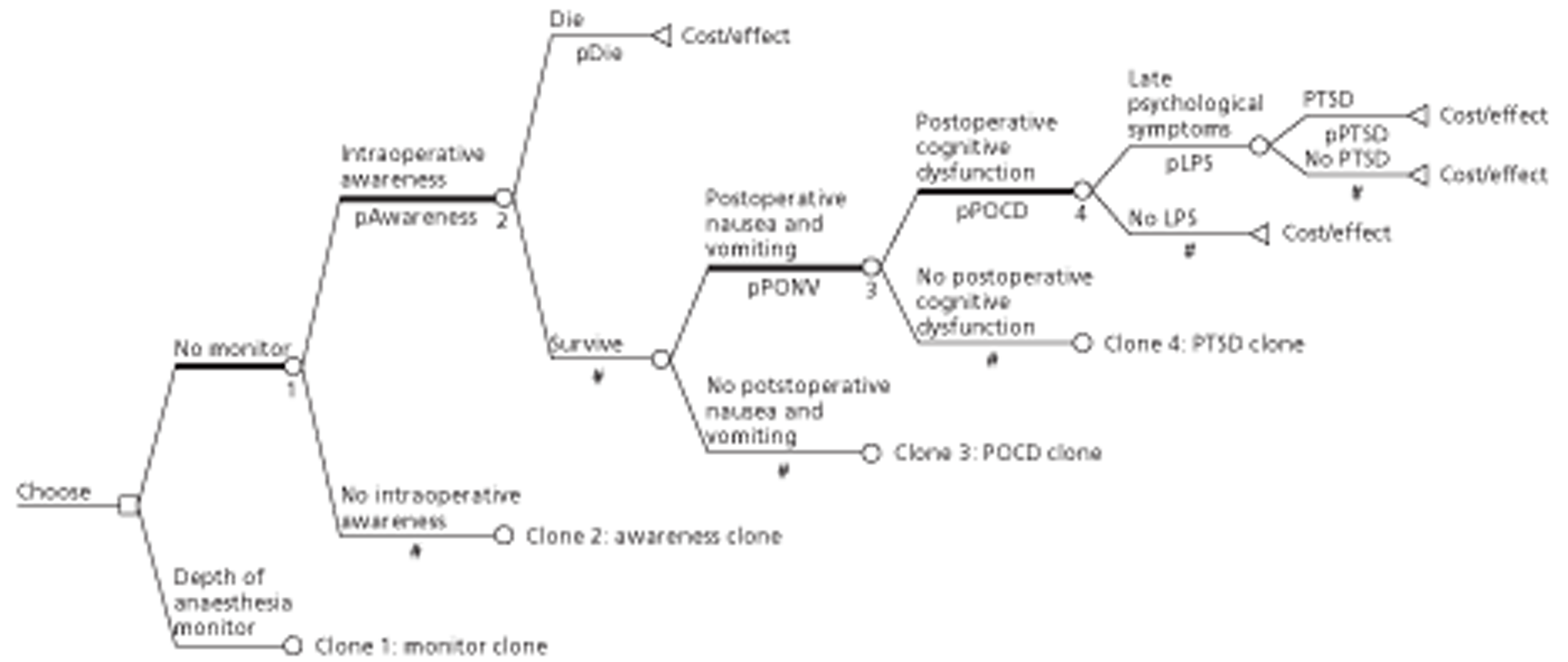
Each of the short-term anaesthetic-related complications could be associated with additional treatment costs (such as antiemetic medication for patients experiencing PONV, whereas for patients experiencing POCD there may be in-hospital costs of managing the condition, additional days of hospital stay and, for longer-term cases, additional costs of managing the condition following discharge). No direct cost-consequences for intraoperative awareness are included in the model. However, it is assumed that a proportion of patients who experience awareness will suffer psychological symptoms arising from the awareness episode and that a proportion of those will develop PTSD and may seek treatment.
We assumed that monitoring of basic clinical signs, including blood pressure and heart rate (mandatory worldwide), would be common components to standard clinical monitoring and to depth of anaesthesia monitoring using EEG devices (as discussed in Description of technologies under assessment) and, therefore, these have not been costed in the model. The key cost components identified for the standard clinical monitoring branch of the model are the costs of anaesthesia, costs of anaesthesia-related complications and costs of managing long-term sequelae of intraoperative awareness, with baseline levels (unit costs, estimated baseline consumption of anaesthetics and estimated baseline incidence of anaesthesia-related complications/intraoperative awareness) defined at the root node of the tree. The effects of EEG-based depth of anaesthesia monitoring (using the included technologies) compared with standard clinical monitoring, which have been identified and assessed in the systematic review of patient outcomes, are applied to the baseline estimates, at the depth of anaesthesia monitoring node. These are applied as proportionate changes or OR/relative risks.
No quality-of-life (QoL) impact (utility loss) is included in the model for short-term anaesthesia-related complications (such as PONV) as these are expected to be of limited duration. Similarly, the model does not include an estimate of the QoL impact (utility loss) for an intraoperative awareness episode. The most significant quality-of-life QoL impact of any intraoperative awareness experience is assumed to be captured by estimating the incidence of psychological symptoms arising as a result of the awareness episode (including cases of PTSD).
As indicated, data population of the model required the estimation of baseline risks for a number of parameters in addition to the effectiveness estimates drawn from the systematic review of patient outcomes. The following section identifies the model parameters and the data sources used in the model.
Model parameters
Cost of depth of anaesthesia monitoring
The costs of depth of anaesthesia monitoring consist of the capital costs associated with acquisition of the module and recurring costs associated with sensors which are attached to the patient. Table 31 summarises the costs supplied by manufacturers for each of the modules included in the assessment.
| Depth of anaesthesia model | Manufacturer | Cost of depth of anaesthesia monitor (£) | Sensor cost, per patient (£) |
|---|---|---|---|
| E-Entropy module | GE Healthcare | 5352 | 8.68a |
| Vista module (BIS) | Covidien | 4350b | 14.50c |
| Compact M monitor | Narcotrend | 8572–11,998d | 0.56e |
Equivalent annual costs for each module (assuming a 5-year useful life for the equipment and a discount rate of 3.5%) are presented in Table 32.
| Depth of anaesthesia module | Equivalent annual cost (£) |
|---|---|
| E-Entropy module | 1185 |
| BIS module | 963 |
| Narcotrend monitora | 2278 |
The annual throughput of patients for each module is assumed to be 1000 patients per year (equivalent to four patients per day for a working year of 250 days) if used for patients at average risk of intraoperative awareness, based on discussion with clinical experts. We assumed that throughput would be halved if depth of anaesthesia monitoring was limited only to patients at high risk of intraoperative awareness (equivalent to two patients per day for a working year of 250 days) – the impact of assumptions regarding patient throughput on the unit costs for DoA modules is tested in scenario analyses.
Additional costs
The manufacturers' submissions to NICE indicate minimal additional power consumption associated with the modules. Therefore no additional costs were added to account for this.
The need for additional training for staff to operate the monitor appears to vary by model, according to the industry submissions. Narcotrend models require a day for the delivery of a lecture and training in the operating theatre or intensive care unit (ICU). The technical part of the training (handling the Narcotrend device, electrode placing) requires < 1 hour. The manufacturer of the E-Entropy model states that a 30-minute introductory training session is required in placement of the sensors, whereas no additional training is required for the use of a BIS monitor. This is not currently accounted for in the model.
The Narcotrend device included in this assessment is a stand-alone monitor [although the manufacturer's submission states that it can also send data in real time to other anaesthesia monitors (makes and coverage not specified)], whereas BIS and E-Entropy are modules designed to operate with other anaesthesia monitors. BIS is compatible with a range of monitoring platforms.
(Commercial-in-confidence information has been removed.) E-Entropy is compatible with GE Healthcare's most recent monitor range (CARESCAPE Monitors B850 and B650), but not older software levels (in GE Healthcare monitors) or with monitors produced by other manufacturers. The manufacturer's submission estimates that 45% of all UK operating theatres would be compatible with E-Entropy – for the remaining 55% significant investment in new monitoring equipment may be required for compatibility. Costs based on Table 31 would not be representative for facilities requiring such investment in new monitoring equipment.
The manufacturers did not supply any information on maintenance costs or costs of maintenance contracts for any of the depth of anaesthesia modules. As a result, the base case excludes any costs for recurrent maintenance. The potential impact of maintenance costs are examined in scenario analyses using assumptions regarding maintenance costs (annual maintenance costs estimated at 10% and 20% of the module acquisition cost).
Summary of unit costs for depth of anaesthesia modules
Unit costs for DoA modules include acquisition costs for the module (annualised, assuming a 5-year effective life, and converted to an average cost per patient using assumptions on patient throughput) and recurring costs arising from the single-use sensors attached to the patient.
Unit costs included in the base case do not include estimates of the cost of formal training or familiarisation with equipment or maintenance costs.
Anaesthetic dose
Baseline value
We undertook targeted searches for studies reporting costs of anaesthetics or estimates of anaesthetic consumption against duration of anaesthesia. Elliott and colleagues99 reported a national survey of anaesthetic practice for paediatric and adult day surgery in UK and undertook a prospective RCT comparing the cost-effectiveness of anaesthetic regimens in adults (general, orthopaedic and gynaecology patients) and paediatric cases (general plus ear, nose and throat patients). They reported total costs (broken down by variable, semi-fixed and fixed components) for four anaesthetic regimens. The included regimens were TIVA (propofol induction, propofol maintenance), i.v./inhalational anaesthesia (propofol induction, isoflurane/N2O maintenance or propofol induction, sevoflurane/N2O maintenance) and total inhalational anaesthesia (sevoflurane induction, sevoflurane/N2O maintenance).
A total of 1063 adult patients remained in the study until hospital discharge (265 propofol/propofol, 267 propofol/isoflurane, 280 propofol/sevoflurane, 251 sevoflurane/sevoflurane). The mean total and variable costs reported for the RCTs are shown in Table 33.
| Cost | Propofol/propofol | Propofol/isoflurane | Propofol/sevoflurane | Sevoflurane/sevoflurane | Total |
|---|---|---|---|---|---|
| Mean total cost (£) | 131.70 | 118.70 | 123.40 | 131.30 | 126.10 |
| Mean variable cost (£) | 21.10 | 7.10 | 13.80 | 15.30 | 14.40 |
Variable costs included for each anaesthetic regimen in the trial were reported as being primarily drug costs (including anaesthetic agent use), but also included other items such as disposable equipment and therefore may not be the best basis for estimating savings that may be realised by reducing anaesthetic use associated with DoA monitoring.
Baseline consumption of inhaled anaesthetic agents in the economic model was estimated using an equation reported by Chernin,100 based on a formula originally presented by Dion. 101
where concentration is the concentration (%) of gas delivered, FGF is the fresh gas flow rate in litres/minute, duration is duration of inhaled anaesthetic delivery in minutes, MW is molecular weight in grams, D is density in grams/ml and 2412 is a factor to account for the molar volume of a gas at 21 °C. If duration is set to 60 minutes, the above formula would estimate the cost per MAC hour for a given inhaled anaesthetic agent. Table 34 presents the required values for calculating the cost per MAC hour of isoflurane, desflurane and sevoflurane at fresh gas flow rates of 2 l/minute for maintenance of anaesthesia.
| Input | Units | Sevoflurane | Isoflurane | Desflurane |
|---|---|---|---|---|
| Anaesthetic concentration | % | 1.80 | 1.15 | 6.60 |
| Fresh gas flow | l/minute | 2 | 2 | 2 |
| Duration | Minutes | 60 | 60 | 60 |
| Molecular weight of anaesthetic | g | 200.00 | 184.50 | 168.00 |
| Density | g/ml | 1.52 | 1.50 | 1.45 |
| Cost | £/ml | 0.5920 | 0.2280 | 0.3040 |
| ml per MAC hour | ml | 11.78 | 7.04 | 38.04 |
| Cost per MAC hour | £ | 6.98 | 1.60 | 11.57 |
Consumption of i.v. anaesthetic (e.g. propofol) will be based on reported total consumption in included trials. Where this is not reported consumption will be estimated based on normalised rates (mg/kg/hour or mg/kg/hour where appropriate), average patient weight and duration of anaesthesia.
Change in anaesthetic consumption associated with depth of anaesthesia monitoring
The summary values reproduced in Table 35 below are taken from the systematic review of patient outcomes reported earlier in Results of systematic review of patient outcomes.
| Technology | Anaesthetic agent | Population | Number of trials | Mean difference (95% CI) | Proportionate change (95% CI) |
|---|---|---|---|---|---|
| BIS vs standard clinical monitoring | Sevoflurane | General surgical | 949,65,67,68,80,81,84,86,89 | −0.15 (−0.25 to −0.06) | −0.202a (−0.330 to −0.074) |
| Propofol | General surgical | 1162,63,66,70,71,75,76,78,85,86,91 | −1.30 (−1.83 to −0.76) | −0.193b (−0.272 to −0.113) | |
| E-Entropy vs standard clinical monitoring | Sevoflurane | General surgical | 161 | −0.04c (−0.07 to −0.01) | −0.286 (−0.492 to −0.079) |
| Propofol | Orthopaedic surgery | 162 | 5d (−7.54 to 17.54) | 0.050 (−0.075 to 0.174) | |
| Remifentanil | −0.01e (−0.02 to 0.00) | −0.111 (−0.232 to 0.010) | |||
| Propofol | Elective gynaecological laparoscopy | 155 | −14f (−22.47 to −5.53) | −0.147 (−0.237 to −0.058) | |
| Remifentanil | 0.07g (0.03 to 0.11) | 0.179 (0.085 to 0.274) | |||
| Narcotrend vs standard clinical monitoring | Desflurane | Orthopaedic surgery | 164 | −69h (−113.37 to −24.63) | −0.156 (−0.256 to −0.056) |
| Remifentanil | −0.01i (−0.04 to 0.02) | −0.043 (−0.168 to 0.081) | |||
| Propofol | Minor orthopaedic surgery | 260,63 | −1.99j (−2.922 to −1.06) | −0.292 (−0.429 to −0.155) | |
| Remifentanil | −0.01k (−0.04 to 0.01) | −0.054 (−0.158 to 0.050) |
Consumption of anaesthetic drugs used in TIVA, for the comparison of E-Entropy and standard clinical monitoring, is based on data reported in two clinical trials55,62 that were modelled separately, as we considered them unsuitable for pooling, given substantial differences in the patient populations.
Unit cost of anaesthetic agents
Unit costs for propofol are taken from the British National Formulary (BNF33). Unit costs for volatile inhaled anaesthetic gases are not available in the BNF. As a result, these costs have been provided by University Hospital Southampton NHS Foundation Trust. The unit costs reported for inhaled anaesthetic gases are based on currently quoted wholesale prices and do not reflect any discounts that may be available to NHS purchasers (Table 36).
Estimated baseline (standard clinical monitoring) cost of anaesthetic agents adopted in the model
Table 37 presents a summary of estimated baseline costs, change in anaesthetic consumption and cost of anaesthetic associated with use of DoA monitoring, based on assumptions presented in Tables 34 and Table 36.
| Comparison | Source | Agent | Cost (£) | Proportionate change | Estimated cost with depth monitoring (£) |
|---|---|---|---|---|---|
| BIS vs standard clinical monitoring | Meta-analysis | Sevoflurane | 11.04a | −0.202 | 8.81 |
| Propofol | 20.92 | −0.193 | 16.90 | ||
| Entropy vs standard clinical monitoring | Aime et al.61 | Sevoflurane | 15.93c | −0.286 | 11.38 |
| Ellerkmann et al.62 | Propofol | 18.85d | 0.050 | 19.78 | |
| Remifentanil | 4.26e | −0.111 | 3.78 | ||
| Gruenewald et al.55 | Propofol | 14.35f | −0.147 | 12.24 | |
| Remifentanil | 14.94g | 0.179 | 17.62 | ||
| Narcotrend vs standard clinical monitoring | Kreuer et al.64 | Desflurane | 24.09h | −0.156 | 20.35 |
| Remifentanil | 11.63i | −0.043 | 11.12 | ||
| Kreuer et al.63 and Rundshagen et al.60 | Propofol | 19.39j | −0.292 | 13.72 | |
| Remifentanil | 10.79k | −0.054 | 10.20 |
Postoperative nausea and vomiting
Our systematic review of patient outcomes identified limited evidence of the impact of DoA monitoring on the risk of PONV. A baseline risk of PONV (30%)102–104 for standard clinical monitoring and DoA monitoring has been included in the model. The sensitivity of the results to the potential impact of depth of anaesthesia monitoring on the risk of PONV is explored in a scenario analysis using data from a meta-analysis on the effectiveness of BIS on a range of outcomes including PONV by Liu. 105 We assumed that all treatments (such as prophylaxis against PONV) were the same for each monitoring group, and that all patients experiencing PONV were treated using 4 mg ondansetron by intramuscular or slow i.v. injection (unit cost = £5.39; BNF33).
Postoperative cognitive dysfunction
Baseline value
Our systematic review of patient outcomes identified limited evidence of the impact of depth of anaesthesia monitoring on the risk of POCD. One study, conducted in an elderly population (> 60 years old) available as an abstract, reported a reduction in POCD for BIS-monitored patients at 7 days and 3 months, although the difference at 7 days was reported to not be statistically significant. There is disagreement over the true incidence of POCD, with some authors arguing that this may be underestimated because of loss to follow-up for the most severe cases,106 whereas others argue that it may be overestimated by identifying as POCD what was a pre-existing cognitive decline. Duration of POCD was estimated using data reported for the International Study of Post-Operative Cognitive Dysfunction (ISPOCD). 107 This study recruited people over the age of 60 years who were presenting for major abdominal, non-cardiac thoracic or orthopaedic surgery under GA. Subjects with Mini Mental State Examination (MMSE) score of < 23 at baseline were excluded. Incidence of POCD at 1 week after surgery was 25.8% and was present in 9.9% of subjects at 3 months. This compared with 3.4% at 1 week and 2.8% at 3 months in non-surgical controls. Longer-term follow-up of subjects in the ISPOCD study,108 between 1 and 2 years, reported cognitive dysfunction in 10.4% of patients and 10.6% of controls, although there was considerable attrition of the cohort (336 of the original 1218 subjects followed up between 1 and 2 years). For this assessment we have assumed that the excess (22.4% at 1 week and 7.1% at 3 months) represents cognitive dysfunction attributable to undergoing GA, which will then gradually reduce to zero (at 18 months). Using these proportions (22.4% at 1 week, 7.1% at 3 months and zero at 18 months), we used the area under the curve to estimate the mean duration of POCD at 29.65 days for patients over the age of 60 years. We estimated the proportion of surgical patients experiencing POCD using data on the proportion of patients undergoing any procedure available from Health Episode Statistics (HES) online,109 which reported that 45% of patients were age 60 years and above.
Change in postoperative cognitive dysfunction associated with depth of anaesthesia monitoring
Odds ratios for POCD at 7 days and at 3 months were estimated using data tabulated in the abstract by Chan and colleagues47 (Table 38).
| Time | Routine care (n = 452) | BIS-guided anaesthesia (n = 449) | Estimated OR |
|---|---|---|---|
| 1 week | 39.1% | 32.5% | 0.750 |
| 3 months | 12.0% | 8.1% | 0.646 |
The ORs were applied to the baseline proportions with cognitive dysfunction at 7 days and 3 months, and mean duration of POCD associated with BIS monitoring was estimated at 21.10 days.
Quality of life impact of postoperative cognitive dysfunction associated with depth of anaesthesia monitoring
The QoL impact of POCD was based on the utility decrement reported by Jonsson and colleagues110 for the difference between a MMSE evaluation score of > (no dysfunction), which had a utility of 0.69, and a MMSE evaluation score of between 21 and 25 (indicating mild cognitive impairment), which had a utility of 0.64.
Intraoperative awareness
Baseline value
Awareness (defined as postoperative recollection of events occurring during GA) has generally been described as a rare occurrence, with an incidence of 0.1–0.2% in the general surgical population. Although still rare, the risk of awareness has historically been greater (up to 1%) in particular types of surgery (cardiac surgery, caesarean section and trauma surgery). 79,111,112
We conducted targeted searches for studies reporting incidence of intraoperative awareness in general surgical populations and in those populations identified as being at greater risk of awareness. Table 39 reports the studies identified by the searches, the study populations as well as the methods used to assess and measure awareness. The majority of studies reported using the Brice interview24 or modified versions of the Brice interview administered on at least two occasions (with the first interview in the PACU). Three comparatively large studies (sample sizes between 10,000 and 20,000 patients) in general surgical populations estimated similar incidences and are commonly cited in support of the previously quoted incidence of 0.1–0.2%. However, two more recent studies have suggested wildly divergent incidence in the general surgical population (from 0.007% up to 0.99%). Although the authors of the study18 indicating the highest incidence in a general surgical population reported lower values when excluding high-risk cases (emergency surgery, intraoperative hypotension-shock and caesarean section) and those patients who (in subsequent interviews) denied experiencing awareness, the reported incidence remained substantially in excess of the assumed risk for the general surgical population and closer to that assumed for high-risk patients.
| Study | Study design (dates) | Population description | Sample size | Measure of awareness | Timing and frequency of measure | Incidence of awareness, n (%) |
|---|---|---|---|---|---|---|
| Liu et al.113 | One centre, prospective (2/1990–4/1990) | Patients aged 16 years or older undergoing GAa | 1000 | Brice interview | Single interview between 20 and 36 hours after surgery | 2 (0.2) |
| Ranta et al.6 | One centre prospective (8/1994–8/1995) | Patients aged 12 years or older undergoing GA | 2612b | Brice interview | Twice: in PACU; re-interviewed the same day or day after | 10 (0.38)c |
| Sandin et al.79 | Two centre prospective (1998–1998) | Patients undergoing GA | 11,785 | Modified Brice interview | Three times: in PACU; 1–3 days and 7–14 days later | 18 (0.15) |
| Myles et al.12 | QA programme, single centre (not stated) | 10,811 | Not stated | Once: ‘first day after operation’ | 12 (0.11) | |
| Sebel et al.13 | Multicentre, cohort (4/2001 – 12/2002) | Patients undergoing GA | 19,575 | Modified Brice interview | Twice: in PACU; and then ≥ 1 week later | 25 (0.13; includes 13 BIS-monitored cases) |
| Pollard et al.14 | Quality assurance programme, eight centres (2002–4) | Patients aged 18 years or older undergoing GA | 87,361d | Modified Brice interview | Twice: in PACU; and within 1–2 days of anaesthesia | 6 (0.0068) |
| Errando et al.18 | One centre, prospective (4/1995–11/2001)e | Patients undergoing GA | 4001 | Structured interview – does not appear to include Brice questions | Three times: in PACU; 7 days and 30 days later | 39 (0.99)f |
| Lyons et al.111 | (1982–9) | Patients undergoing GA for caesarean section | 3000 | Unclear | Unclear | 8 (0.93) |
| Ranta et al.112 | Cardiac surgery patients | 204 | Unclear | Unclear | 3 (1.5) | |
| gPuri et al.82 | Multicentre RCT | High-risk patients | 16h | NR | NR | 1 (6.25) |
| Myles et al.79 | Multicentre RCT | High-risk patients | 1238i | Structured questionnaire, not defined | Three times: 2–6 hours, 24–36 hours and 30 days after surgery | 11 (0.89) |
| Avidan et al.27 | RCT | High risk – at least one major criterion | 974j | Brice questionnaire | Three times: within 24 hours, between 24 and 72 hours and at 30 days after extubation | 2 (0.20) |
| gMuralidhar et al.78 | High risk | 20k | NR | NR | 0 (0.00) | |
| Avidan et al.44 | Multicentre RCT | High-risk patients – at least one risk factor | 2852l | Modified Brice interview. Michigan awareness classification for assigning to possible or definite awareness | Twice: 72 hours and 30 days after extubation | 2 (0.07)m |
A pooled estimate from all these studies gives a cumulative incidence of awareness of 0.21% (95% CI 0.06% to 0.45%) assuming random effects [Cochran's Q = 212.55 (df = 5); p < 0.0001; I2 = 97.6% for fixed-effect model; see Appendix 9 for details]. Excluding the two outlying studies (Pollard and colleagues14 and Errando and colleagues18) yields a slightly lower estimate, with narrower CI (0.16%; 95% CI 0.10% to 0.23%) assuming random effects [Cochran's Q = 7.85 (df = 3); p = 0.0493; I2 = 61.8% for fixed-effect model].
The incidence of awareness in high-risk patients has been calculated from the standard clinical monitoring arms of RCTs in this group of patients from our systematic review of patient outcomes (Results of systematic review of patient outcomes). Pooling these estimates gives a cumulative incidence of awareness of 0.45% (95% CI 0.06% to 1.19%) assuming random effects [Cochran's Q = 19.97 (df = 4); p = 0.0005; I2 = 80.0% for fixed-effect model; see Appendix 9 for details].
In the model we apply the pooled estimates of 0.16% (95% CI 0.10% to 0.23%) for risk of awareness in the base case for general surgical patients and 0.45% (95% CI 0.06% to 1.19%) for high-risk patients. The lowest incidence (0.007%), reported by Pollard and colleagues,14 and highest incidence (0.99%), reported by Errando and colleagues,18 are used in scenario analyses for general surgical patients. A high value of 1% is used in scenario analyses for high-risk patients.
Change in incidence of intraoperative awareness associated with depth of anaesthesia monitoring
The summary values reproduced in Table 40 are taken from the systematic review of patient outcomes reported earlier in Results of systematic review of patient outcomes. There are no entries for E-Entropy and Narcotrend in this table as insufficient data were identified in the systematic review of patient outcomes to derive robust results. As a result the relevant OR derived for BIS were used in the model to estimate the impact on intraoperative awareness of depth of anaesthesia monitoring with E-Entropy and Narcotrend.
| Model of general anaesthetic | Population | Number of trials | Peto's OR | 95% CI |
|---|---|---|---|---|
| Mixed anaesthesia (includes both patients undergoing TIVA and patients undergoing inhaled GA)a | High risk | 1 | 0.25 | 0.08 to 0.75 |
| Inhaled GA only | High risk | 4 | 1.79 | 0.63 to 5.11 |
| TIVA | High risk | 2 | 0.24 | 0.10 to 0.60 |
| Pooled effect | High risk | 7 | 0.45 | 0.25 to 0.81 |
In addition, the systematic review did not identify any robust data on the effect of depth of anaesthesia monitoring on the incidence of intraoperative awareness in patients considered at average risk of awareness. Consequently, the relevant OR derived for high-risk patients were used in the model to estimate the impact on intraoperative awareness of depth of anaesthesia monitoring for general surgical patients considered at average risk of awareness.
Sequelae of intraoperative awareness
A targeted search for studies reporting symptoms of patients who had reported awareness during surgery was undertaken in order to understand the health-related consequences of intraoperative awareness.
Eight studies were identified5,7,8,10,11,19,114,115 (Table 41). These suggested that the patients who had experienced intraoperative awareness fall into three groups: those who do not experience any sequelae, those who experience ‘late psychological symptoms’ and those who go on to suffer from PTSD. Late psychological symptoms (LPS) comprise anxiety, chronic fear, nightmares, flashbacks, indifference, loneliness and a lack of confidence in future life. Anxiety, nightmares and flashbacks appeared to be the predominant symptoms in the study by Samuelsson and colleagues115 in patients with an LPS duration of < 2 months; those experiencing symptoms for a longer duration reported nightmares and flashbacks alone. A diagnosis of PTSD is made if all six criteria of the clinician-administered PTSD scale (CAPS) are positive. These include symptoms of re-experiencing trauma, avoidance, hyper-arousal, significant distress and the duration of symptoms lasting longer than 1 month. 8
| Study | Date | Method of recruitment | Identification/classification of LPS and PTSD | Aware | LPS | PTSD | ||
|---|---|---|---|---|---|---|---|---|
| n | n | % | n | % | ||||
| Evans116 | 1987 | Advertisement in four British newspapers | 27 | |||||
| Moerman et al.5 | 1993 | Referral from university hospital anaesthesiology department | Response to (open-ended) interview question – ‘have there been any consequences?’ (of the identified awareness episode). Patients reported sleep disturbance, dreams and nightmares, flashbacks and anxiety during the day | 26 | 18 | 69 | NR | |
| Schwender et al.114 | 1998 | Advertisements in four German papers and on internet (n = 21) or referral from three hospital anaesthesia departments (n = 24) | Response to questionnaire items on after effects (including anxiety and nightmares). No definition for PTSD reported (simply states ‘whether … PTSD syndrome developed’) | 45 | 22 | 49 | 3 | 7 |
| Domino et al.19 | 1999 | Retrospective analysis of American Society of Anaesthetists Closed Claims Project (malpractice claims) – data from 1961 to 1995a | No definitions – reports states ‘% (n) sustained temporary emotional distress, whereas in % (n) post-traumatic stress disorder developed’ | 61 | 51 | 84 | 6 | 10 |
| Osterman et al.10 | 2001 | Advertisement in newspapers, fliers in hospitals, self-referral following print and TV news stories or referral by anaesthetist | PTSD defined using CAPS | 16 | NR | 9 | 56 | |
| Lennmarken et al.11 | 2002 | 18 patients identified as experiencing awareness during GA in two hospitals (reported by Sandin and colleagues9) were followed up for interview regarding psychological symptomsb | PTSD defined using diagnostic criteria A1-F in the DSM-IV, American Psychiatry Association117 | 9 | 7 | 78 | 4 | 44 |
| Samuelsson et al.115 | 2007 | Consecutive patients who had undergone GA were interviewed regarding awareness during previous GA | LPS were any one of: anxiety, chronic fear, nightmares, flashbacks, indifference, loneliness and lack of confidence in future life (each rated on a scale from zero to two). PTSD appears to be defined on basis of existing clinical diagnosis (not specifically identified or classified in study) | 46 | 15c | 33 | 1 | 2 |
| Ghoneim et al.7 | 2009 | Data extracted from published case reports on ‘awareness’ and ‘anaesthesia’ – from PubMed between 1950 and August 2005 | No definition of LPS | 271 | NR | 22 | NR | |
| Leslie et al.8 | 2010 | 13 patients identified as experiencing awareness in the B-Aware trial (reported by Myles and colleagues79) were followed up for interview regarding psychological symptomsd | PTSD defined using CAPS | 7 | NR | 5 | 71 | |
Just two of the studies had a prospective design. 8,115 The study by Samuelsson and colleagues115 reported 46 awareness cases in a cohort of 2681 interviewed after surgery. This is therefore the strongest evidence for development of PTSD and LPS that was identified in the targeted search. Leslie and colleagues,8 although reporting a small cohort, were the only authors among those identified to report time to onset and duration of symptoms. However, some cases of PTSD reported were ongoing, and it is unclear how this may impact on the duration results. The two prospective studies were used to inform the baseline data inputs, for the states of LPS and PTSD, into the model, as presented in Table 42 below. The six remaining studies were small, with limited usefulness for understanding the prevalence of psychological symptoms associated with awareness, because of retrospective design, participant recruitment methods or low recruitment levels. 5,7,10,11,19,114
| Sequelae | Value (95% CI) | Method | Source |
|---|---|---|---|
| LPS | |||
| Probability, given awareness | 0.326 (0.195 to 0.480) | 15/46 patients with awareness | Samuelsson et al.115 |
| PTSD | |||
| Probability, given awareness | 0.177 (0.113 to 0.230) | Pooled proportion of subjects with LPS having PTSD or severe symptoms, from (two) studies reporting this proportion, applied to probability of LPS | Samuelsson et al.115 and Lennmarken et al.11 |
| Pooled estimate based on 0.57111 (4/7) and 0.0533115 (8/15) = 0.542 (95% CI 0.345 to 0.733) | |||
| Probability PTSD = (15/46) × 0.542 | |||
Leslie and colleagues8 reported a median duration of 4.7 years (range 4.4 to 5.6 years) for patients experiencing symptoms of PTSD. No further information on the distribution is provided so it unclear how well the median approximates to the mean duration of symptoms, as these cases of PTSD reported were ongoing, and it is unclear how this may impact on the duration results. Targeted searches did not identify any other studies reporting duration of PTSD symptoms associated with intraoperative awareness. One study was identified which reported duration of PTSD (median duration and survival curves) in a non-institutionalised, civilian population aged 15–54 years, conducted in the USA. 118 These data were from the National Comorbidity Survey (a survey designed to study the distribution, correlates and consequences of psychiatric disorder in the USA) and included 5877 respondents from 48 states. Response rates to part 2 of the survey, which included components related to PTSD, were between 98.1% (for those screening positive for any lifetime diagnosis in part 1 of the survey) and 99% (for a random subsample of those not screening positive in part 1 of the survey). The median duration of symptoms for respondents who had ever sought professional treatment (n = 266) was 36 months and for those who had not sought professional treatment (n = 193) was 64 months. We estimated the mean duration of PTSD symptoms for the population who had not sought professional treatment, by fitting a regression (assuming a Weibull distribution for the survival function; see Appendix 10 for details) to the reported survival curves. The mean duration of PTSD symptoms derived in this analysis was 152 months (12.7 years) (Figure 7).
FIGURE 7.
Survival curve based on duration of symptoms for respondents who did not seek treatment for PTSD, reported by Kessler and colleagues,118 and fitted Weibull model.
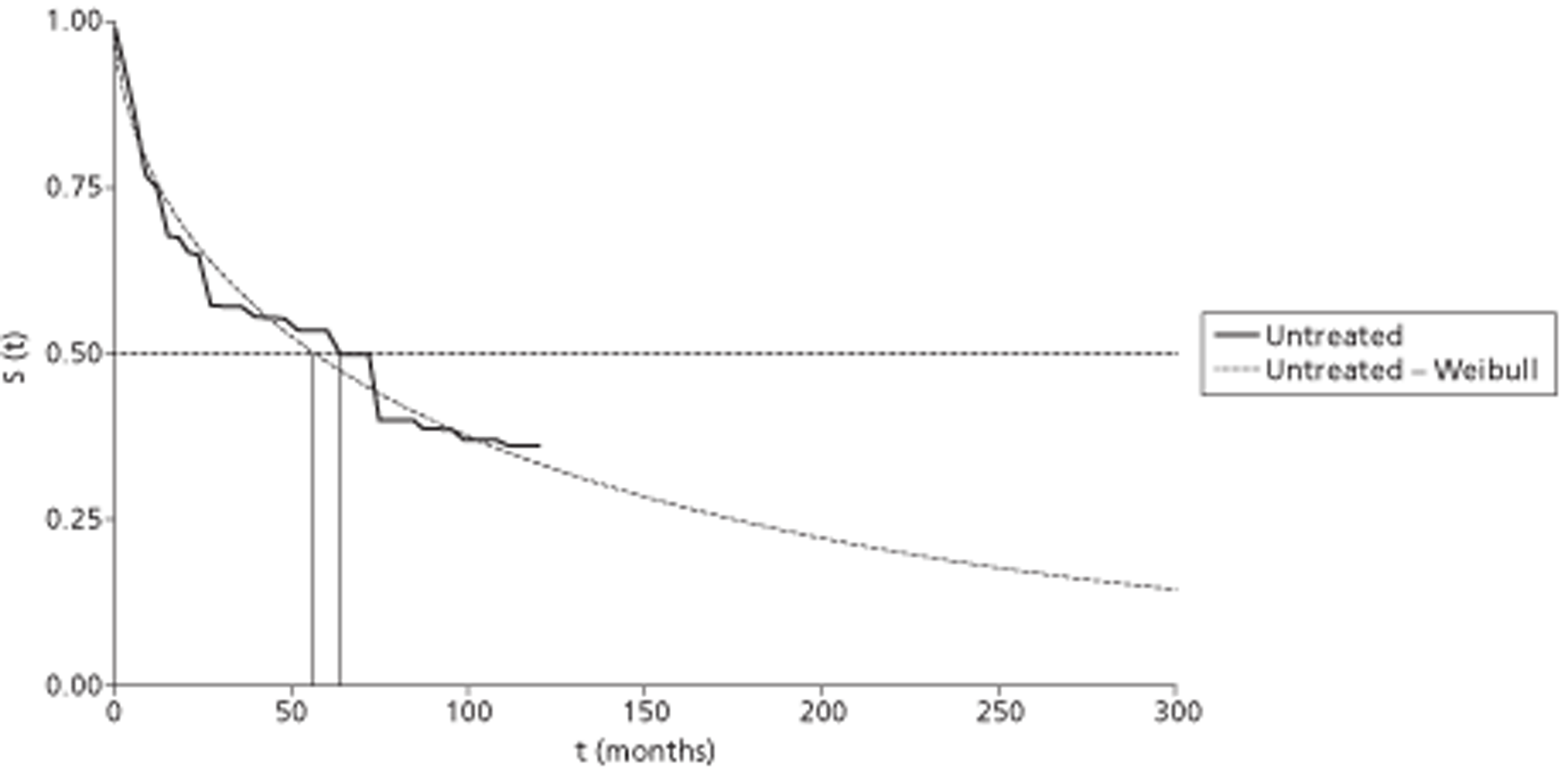
A review of the HRQoL of patients with PTSD was undertaken in order to explore the differences in scores between PTSD patients and those who had also experienced trauma, but had not gone on to develop PTSD. These scores were used to inform those in the model for patients experiencing awareness and developing psychological symptoms.
Methods
A systematic search was undertaken in order to identify studies reporting utility values associated with PTSD. The details of the search strategy are documented in Appendix 11. A total of 334 studies were initially identified by the search. The abstracts were screened by two independent reviewers and 21 full papers were retrieved (Figure 8). These were assessed against the inclusion criteria detailed in Table 43.
FIGURE 8.
Flow chart of identification of QoL studies for inclusion in the review.
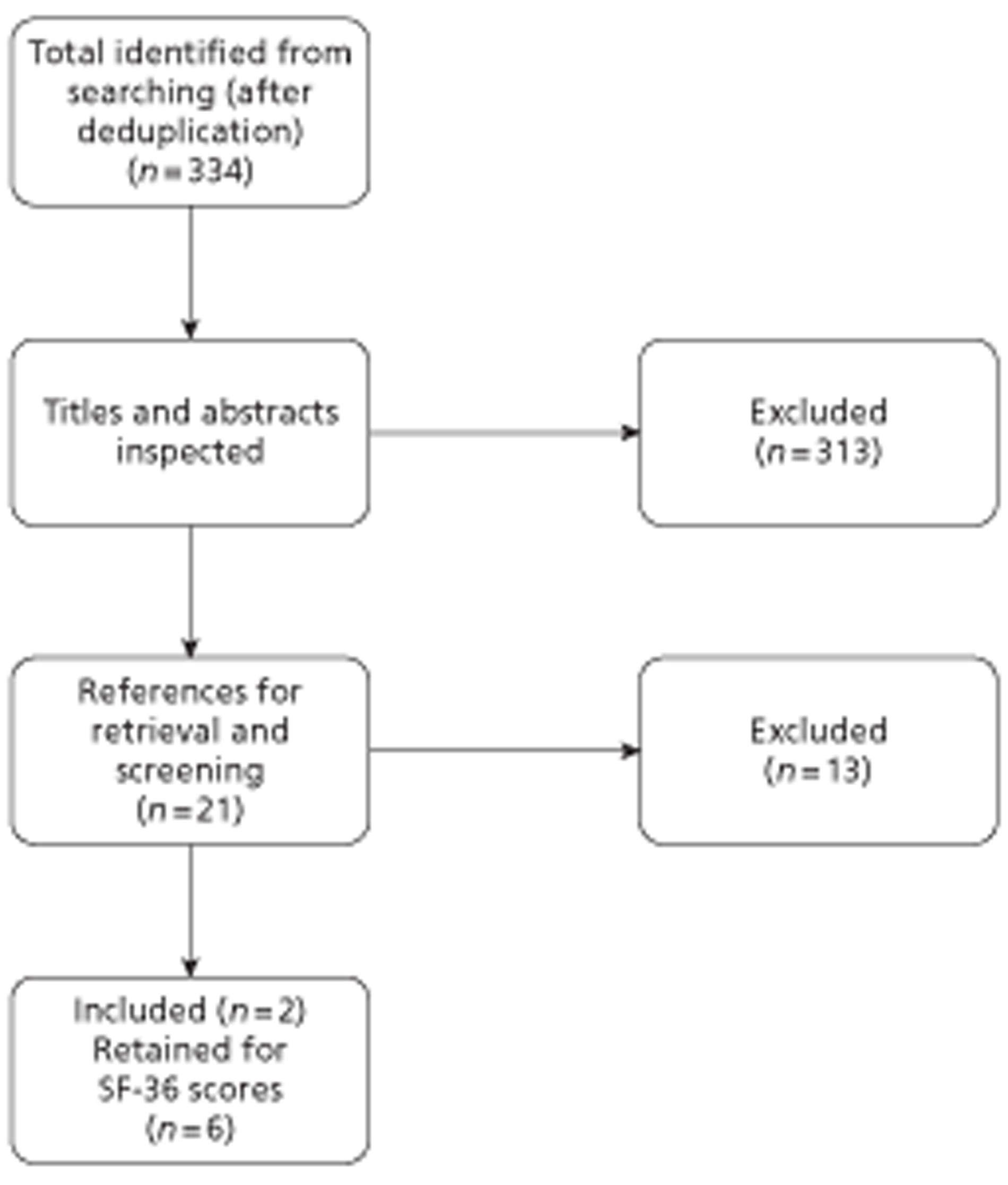
| Criteria | Include | Exclude |
|---|---|---|
| Participants | Adults with PTSD | Studies related to or concerning specific morbidities, with the exception of psychiatric (or related) illness |
| Design | Studies that report a utility value, based on generic preference based measures for QoL, such as EQ-5D, SF-6D, or other standard valuation technique such as standard gamble or TTO | |
| Interventions | Any | |
| Other | Articles published in English | Articles in languages other than English |
| Conference abstracts |
Characteristics of the included studies
Two papers119,120 met the inclusion criteria for the review. The study design and population baseline characteristics are shown in Table 44.
| Criteria | Doctor et al.119 | Freed et al.120 |
|---|---|---|
| Patient group | Patients with PTSD | Veterans with PTSD |
| Country and setting | US, multicentre trial, setting not reported | US study, British sample, primary care clinics |
| Sample size | 184 | 840 |
| Duration of symptoms | Patients were a minimum of 12 weeks from the traumatic event | NR |
| Age, mean ± SD (years) | 37.31 ± 11.33 | 60 ± 12 |
| Sex (F) | 141 (76%) | 176 (21%) |
| QoL instrument | SG/TTO/VAS | SF-36a |
The two included studies119,120 were both undertaken in patients with PTSD. This population is diverse and there are a range of types of trauma that can trigger the disorder, such as domestic abuse, natural disaster or serious illness. 122–124 Freed and colleagues interviewed veterans with PTSD,120 whereas Doctor and colleagues125 interviewed a sample of patients taking part in a trial of treatments for chronic PTSD at baseline.
The two studies119,120 were considerably different in size, with the Freed study120 having approximately four times as many respondents. The two studies reported differing populations in respect to both age and sex, which may have contributed to the differing results. In the study by Freed and colleagues,120 female patients constituted 21% of the sample, and the average age was 60 years. In the Doctor and colleagues study125 the sample was on average younger, with a mean age of 37, and 76% of the respondents were female.
In addition, the two studies generated the results using different valuation tools and methods. Neither of the included studies was based on the European Quality of Life-5 Dimensions (EQ-5D) questionnaire, as prescribed by the NICE reference case. 38 Doctor and colleagues119 asked respondents to respond using standard gamble (SG), visual analogue scale (VAS), and time trade-off (TTO) techniques, the last of which is recommended as an alternative. 38 Freed and colleagues126 used the Short Form questionnaire-36 items (SF-36) responses from a previous study127 and converted these to preference weighted health scores (PWHSs) using the formula developed by Brazier and colleagues. 121
Both studies included the results of statistical models generated in order to identify predictors for worsening or improvement of utility scores. 119,120
Doctor and colleagues119 clearly reported inclusion and exclusion criteria for patients entering the trial, which appeared appropriate. The methods employed to elicit utility scores were clearly described, although the description of TTO does not appear to be correct, which could undermine the results. Freed and colleagues120 have based their analysis on the results of a previous study, the sources for the analysis are clearly stated, and the interview methods and scales employed are adequately described. The sample is of British veterans, which is relevant to the UK, but the generalisability of the HRQoL of veterans to different patient populations is unclear. Freed and colleagues120 have also carried out ordinary least squares regressions (OLS) in order to allow researchers to adjust the estimates of patients' PWHS. The methods for these were adequately described, but contradictory results are reported: the PWHS is reported to increase if a patient has both a PTSD diagnosis and increasing severity of symptoms on the PTSD checklist (PCL). These contradictions are not fully considered or explained, and therefore limit the usefulness of the regression results in estimating HRQoL in patients with PTSD.
Results
The mean utility scores reported in each of the included studies are presented in Table 45.
| Patient group | Doctor et al.119 | Freed et al.120 | ||
|---|---|---|---|---|
| SG | TTO | VAS | ||
| HRQoL score in patients with PTSD (mean ± SD) | 0.87 ± 0.25 | 0.66 ± 0.28 | 0.64 ± 0.2 | 0.535a |
| HRQoL score in patients without PTSD (mean ± SD) | NR | NR | NR | 0.652a |
The scores for veterans in the Freed study120 with PTSD is lower than that of veterans without PTSD, with a difference of 0.11, suggesting that PTSD does negatively impact on HRQoL.
Doctor and colleagues119 report three separate scores according to the valuation method. The scores for TTO and VAS are similar (0.66 and 0.64 respectively), whereas the score for SG appears high at 0.87. The authors argue that the mixed-effect model employed has accounted for possible bias in SG methods (SG requires the participants to state the probability that they would accept a treatment that has a certain probability of conferring full health, with the concomitant probability of immediate death). However, they also state that the TTO method has a lower risk of bias, although justification for this is not reported. 119 TTO is also recommended by NICE where EQ-5D scores are unavailable. 38 The study does not provide a raw comparable score for a group without PTSD using these methods, and therefore it is not possible to draw conclusions as to the decrement in utility resulting from developing PTSD from this paper.
Studies reporting Short Form questionnaire-36 items scores
A further six studies122–124,129–131 that did not meet our inclusion criteria, but which reported the eight subscales of the SF-36, were identified. A preference-based utility score can be estimated from studies that report scores for the eight subscales of the SF-36. 128 Preference-based health-related utilities from these results have been estimated by SHTAC in order to assess the robustness of the estimates in the study by Freed and colleagues. 120 These were converted using the algorithm published by Ara and Brazier,128 and are reported in Table 46.
| Study | Patient group | Utility | ||
|---|---|---|---|---|
| PTSD | No PTSD | Difference | ||
| Laffaye et al.122 | Women experiencing domestic abuse | 0.634 | 0.748 | 0.114 |
| Meeske et al.124 | Young adult survivors of childhood cancer | 0.666 | 0.799 | 0.132 |
| Berger et al.129 | Male ambulance workers | 0.705 | 0.790 | 0.085 |
| Shiner et al.130 | Veterans | 0.508 | – | – |
| Tsai et al.123 | Earthquake survivors (0.5 years post)a | 0.649 | 0.783 | 0.134 |
| Evren et al.131 | Alcohol-dependent men with history of emotional abuse | 0.592 | 0.659 | 0.068 |
Scores derived using the SF-36 do not meet the NICE reference case,38 which recommends the EQ-5D, and that values generated from the Short Form questionnaire-6 Dimensions (SF-6D) 132 be employed in the sensitivity analysis. The studies reporting the SF-36 scores were carried out in diverse groups, with differing traumatic triggers for PTSD. Furthermore, caution should be exercised in the interpretation of this table as these studies have not been fully data extracted or quality assessed. However, the scores consistently indicate similar differences in HRQoL between groups of patients who have similar experiences who go on to develop PTSD, and those who do not, and the differences are consistent with those reported by Freed and colleagues. 120 On average across these papers the difference is 0.10. These results lend weight to the estimates of decrement in utility as a result of PTSD, and may also be useful for sensitivity analysis. However, the results for the utility scores in patients with and without PTSD are generally higher than those reported by Freed and colleagues,120 with the exception of those reported by Shiner and colleagues130 also elicited from veterans.
Summary
-
Two papers met the inclusion criteria for this review of utility scores in PTSD. Six other papers reporting SF-36 scores for people with PTSD were also retained.
-
Neither of the studies meeting the inclusion criteria (reporting a utility value based on a generic, preference-based measure) was based on the EQ-5D.
-
One study reported a utility score for patients with PTSD based on TTO. 119 However, no score for patients without PTSD was reported, and therefore no difference in these can be derived.
-
The second study reported scores for patients both with and without PTSD, but these were based on the SF-36 and converted to a utility score. 120
-
Therefore the evidence base for HRQoL in patients with PTSD is limited.
-
Six further studies provide SF-36 scores, which have been transformed into utility values. These can provide context and values for sensitivity analysis.
The costs of treating PTSD have been estimated based on assumptions contained in the national cost impact report133 associated with NICE Clinical Guideline no. 26133 on the management of PTSD in adults and children in primary and secondary care. 134 The costing report acknowledged that there has been little systematic collection of information about PTSD, on services provided to people with PTSD or on uptake of these services. This limited the feasibility of developing a comprehensive bottom-up costing model and resulted in the costing being based on a series of assumptions – developed and validated through discussion with members of the Guideline Development Group (GDG) and key clinical practitioners in the NHS. These assumptions, in terms of uptake and services available, are summarised in Figure 9 and are discussed below.
FIGURE 9.
Care pathways and costing assumptions developed for NICE.
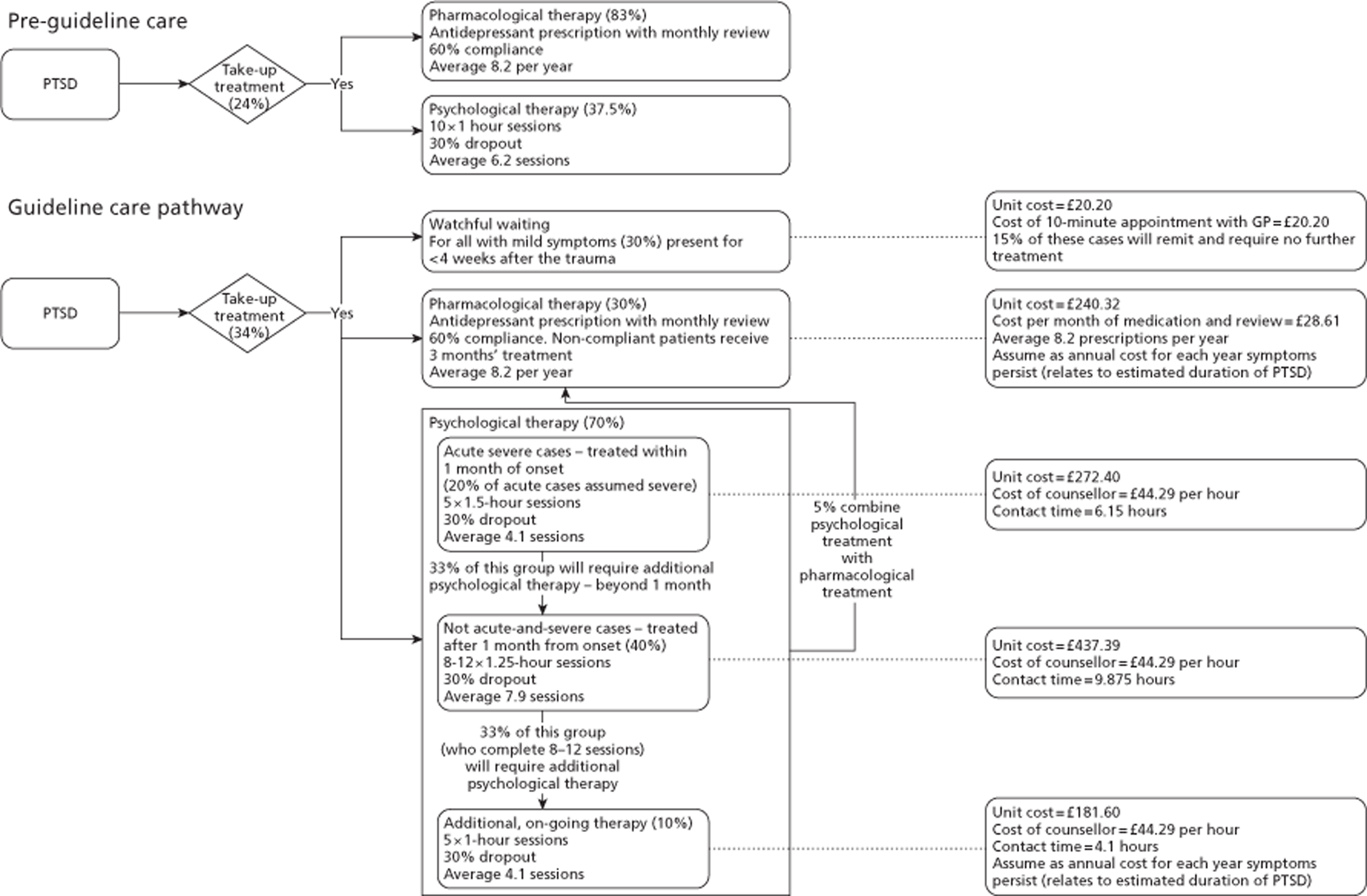
Data from the adult psychiatric morbidity survey,135 which reported that 24% respondents assessed as having a neurotic disorder were receiving treatment of some kind at the time of interview, were used as the basis for estimating the current proportion of people with PTSD who seek treatment. On the basis of additional data from the same survey, 62.5% of these were assumed to be receiving pharmacological therapy alone, 16.7% were receiving counselling or therapy alone and 20.8% were receiving both. It was assumed that, following implementation of the guideline, the proportion receiving treatment would increase by 10%, to 34%. Moreover, the guideline proposed a substantially different care pathway with significantly fewer patients expected to receive medication (with a recommendation that drug treatments not be offered routinely as first line, but to provide trauma-focused psychological treatment to more patients with PTSD symptoms). We estimated an average cost for management of PTSD using the assumptions regarding take-up of treatment options (70% of patients accept psychological treatment, and 30% initially accept pharmacological treatment) and severity (30% patients have mild symptoms and are initially managed through watchful waiting, and 20% have severe symptoms and are offered trauma-focused psychological treatment within the first month after the traumatic event). Table 47 summarises the unit costs, assumptions regarding the proportion of patients receiving each treatment and the overall cost estimated for PTSD.
| Treatment | Unit cost (£) | Proportion (%) | Cost (£) |
|---|---|---|---|
| Watchful waiting | 20.20 | 16.50 | 3.33 |
| Pharmacological therapy | 240.32 | 30.00 | 915.62 |
| Combined pharmacological and psychological therapy | 240.32 | 5.00 | 152.60 |
| Psychological therapy (severe acute cases < 1 month) | 272.40 | 14.00 | 38.14 |
| Psychological therapy (> 1 month after traumatic event) | 437.39 | 38.53 | 168.50 |
| Psychological therapy (severe acute cases > 1 month) | 437.39 | 4.62 | 20.21 |
| Additional, ongoing psychological therapy | 181.60 | 9.97 | 229.86 |
| Total | 1528.26 |
The NICE guideline133 does not include any estimates for inpatient care for people with PTSD. Targeted searches did not identify any UK studies of health service use, in particular use of secondary services and inpatient care for people with PTSD. One US study identified by the searches reported health-care utilisation, derived from electronic medical records, for civilian primary care patients, including a proportion who had current PTSD. 136 This study reported an incidence rate ratio of 2.22 (adjusted for age, sex, income, substance dependence, depression and comorbidity) for hospitalisation in subjects with PTSD compared with those without PTSD. Unadjusted mean number of hospitalisations among the PTSD group was 0.43 compared with 0.18 in those without PTSD. No further details are reported on the reason for hospitalisation or length of stay. In the absence of data specific to the UK for people with PTSD, we have assumed, based on the mean values reported in this study, an excess hospitalisation probability of 0.25 per year among people with PTSD. We derived a crude estimate of the average cost of hospitalisation (£2590), based on 2010–11 NHS Reference Costs,137 by summing the total costs reported for elective and non-elective inpatient HRG data and dividing by the total activity under these headings. On this basis we estimated an additional £7576 for hospitalisations among people with PTSD over the average duration of symptoms of 12.7 years.
The total cost associated with PTSD was £9104 (undiscounted) or £6128 (discounted at 3.5%).
The following tables contain a summary of the input parameters in the model, the base-case value and a brief overview of how the data were derived including a source, where relevant. Table 48 provides a summary of the cost per patient of each depth of anaesthesia technology, including an estimated cost per patient of the depth-monitoring device as well as the cost of consumables (single-use sensors attached to the patient). Table 49 provides a summary of the baseline cost of anaesthetic drug calculated for standard clinical monitoring in each comparison and the proportionate reduction in consumption associated with depth of anaesthesia monitoring. We have assumed that the reduction in consumption of anaesthetic will be realised only for the general surgical population and not in the population at high risk of awareness, as the raised risk of awareness may be an indication that this group of patients are already at a risk of being underdosed.
| Parameter | Value (£) | Source |
|---|---|---|
| BIS | ||
| Cost per patient of depth monitoring device | 0.96 | Equivalent annual cost for depth monitor (acquisition cost £4350) assuming an effective life of 5 years and using a discount rate of 3.5%. Patient throughput assumed at 1000 per year |
| Cost per patient of depth monitor sensors | 14.50 | Manufacturer's price of £362.50 for a box of 25 sensors (for Vista monitor) |
| E-Entropy | ||
| Cost per patient of depth monitoring device | 1.19 | Equivalent annual cost for depth monitor (acquisition cost £5352) assuming an effective life of 5 years and using a discount rate of 3.5%. Patient throughput assumed at 1000 per year |
| Cost per patient of depth monitor sensors | 8.68 | Manufacturer's price of £217 for a box of 25 sensors |
| Narcotrend | ||
| Cost per patient of depth monitoring device | 2.28 | Equivalent annual cost for depth monitor (acquisition cost £10,285, mid-point of range quoted by manufacturer) assuming an effective life of 5 years and using a discount rate of 3.5%. Patient throughput assumed at 1000 per year |
| Cost per patient of depth monitor sensors | 0.56 | Average across manufacturer's price of £0.14 per sensor, using three for one-channel recording and five for two-channel recording |
| Parameter | Value (95% CI) | Source |
|---|---|---|
| BIS | ||
| Baseline inhaled anaesthetic cost | £11.04 | Cost for 1.6 MAC hours (95 minutes) of sevoflurane (concentration of 1.8% and fresh gas flow rate of 4 l/minute). Unit cost of £0.59 per ml, based on price of £148 per 250 ml |
| Reduction in consumption of inhaled anaesthetic using depth monitor (proportionate reduction compared with standard clinical care) | −0.202 (−0.330 to −0.074) | Mean difference of −0.15 from a (weighted) mean consumption of 0.765 MAC equivalents |
| Baseline i.v. anaesthetic cost | £20.92 | Cost for 2 hours of propofol [at 6.77 mg/kg/hour (from control arms of RCT in meta-analysis) and patient average weight of 77 kg]. Unit cost of £0.0202 per mg |
| Reduction in consumption of i.v. anaesthetic using depth monitor | −0.193 (−0.272 to −0.113) | Mean difference of −0.130 from a (weighted) mean consumption of 6.73 mg/kg/hour |
| E-Entropy | ||
| Baseline inhaled anaesthetic cost | £15.93 | Cost for 2.3 MAC hours (137 minutes) of sevoflurane (concentration of 1.8% and fresh gas flow rate of 4 l/minute). Unit cost of £0.59 per ml, based on price of £148 per 250 ml |
| Reduction in consumption of inhaled anaesthetic using depth monitor | −0.286 (−0.492 to 0.079) | Mean difference of −0.04 from patient normalised consumption of 0.14 g/kg/hour (in standard care arm, Aime et al.61) |
| Baseline i.v. anaesthetic cost | Propofol = £18.85 | Ellerkmann et al.62 |
| Remifentanil = £4.26 | ||
| Propofol = £14.35 | Gruenewald et al.55 | |
| Remifentanil = £14.94 | ||
| Reduction in consumption of i.v. anaesthetic using depth monitor | 0.050 (−0.075 to 0.174) | Propofol mean difference of 5 from baseline rate of 101 mg/kg/hour (Ellerkmann et al.62) |
| −0.111 (−0.232 to 0.010) | Remifentanil mean difference of −0.01 from baseline rate of 0.09 mg/kg/hour (Ellerkmann et al.62) | |
| −0.147 (−0.237 to −0.058) | Propofol mean difference of −14 from baseline rate of 95 mg/kg/hour (Gruenewald et al.55) | |
| 0.179 (0.085 to 0.274) | Remifentanil mean difference of 0.07 from baseline rate of 0.39 mg/kg/hour (Gruenewald et al.55) | |
| Narcotrend | ||
| Baseline inhaled anaesthetic cost | £24.09 | Cost for 2.1 MAC hours (125 minutes) of desflurane (concentration of 6.6% and fresh gas flow rate of 4 l/minute). Unit cost of £0.30 per ml, based on price of £76 per 250 ml |
| Reduction in consumption of inhaled anaesthetic using depth monitor | −0.156 | Mean difference of −69 mg/minute from 443.6 mg/minute (in standard care arm, Kreuer et al.64) |
| Baseline i.v. anaesthetic cost | Propofol = £19.39 | Cost for 108 minutes of propofol [at 6.81 mg/kg/hour (from control arms of RCT) and patient average weight of 80 kg]. Unit cost of £0.0202 per mg |
| Remifentanil = £10.79 | Cost for 108 minutes of remifentanil [at 0.120 mg/kg/hour (from control arms of RCT) and patient average weight of 80 kg]. Unit cost of £5.12 per mg | |
| Reduction in consumption of i.v. anaesthetic using depth monitor | −0.292 (−0.429 to −0.155) | Propofol mean difference of −1.99 from baseline rate of 6.8 mg/kg/hour60,63 |
| −0.054 (−0.158 to 0.050) | Remifentanil mean difference of −0.01 from baseline rate of 0.25 mg/kg/hour60,63 | |
Table 50 provides a summary of model inputs related to awareness including the baseline risks for patients considered at high risk of awareness and a general surgical population, the risk reduction associated with depth of anaesthesia monitoring and a list of assumptions underlying the estimation of the cost and outcomes associated with the psychological sequelae of intraoperative awareness.
| Parameter | Value (95% CI) | Source |
|---|---|---|
| Intraoperative awareness | ||
| Baseline awareness in surgical population at high risk of awareness | 0.45% (0.06% to 1.19%) | Pooled estimate from control arms of RCT in high-risk patients |
| Reduction in awareness using depth monitor | Meta-analysis of RCT in high-risk patients, undertaken as part of this review (see Assessment of outcomes: Bispectral Index) | |
| High-risk patients undergoing TIVA (Peto's OR) | 0.24 (0.10 to 0.60) | |
| High-risk patients undergoing anaesthetic induction with i.v. and maintenance with inhaled anaesthetic (Peto's OR) | 0.45 (0.25 to 0.81) | |
| Baseline awareness in general surgical population | 0.16% (0.10% to 0.23%) | Pooled estimate from studies reporting incidence of awareness, not specified to be high risk |
| Reduction in awareness using depth monitor | ||
| General surgical population undergoing TIVA (Peto's OR) | 0.24 (0.10 to 0.60) | Meta-analysis of RCT in high-risk patients, undertaken as part of this review (see Assessment of outcomes: Bispectral Index). |
| General surgical population undergoing anaesthetic induction with i.v. and maintenance with inhaled anaesthetic (Peto's OR) | 0.45 (0.25 to 0.81) | Effect assumed to be the same as for high-risk patients |
| Psychological sequelae of intraoperative awareness | ||
| Probability of LPS, given awareness | 0.326 (0.195 to 0.480) | Samuelsson et al.115 |
| Duration of LPS | 6 months | Assumption |
| Unit cost of LPS | 0 | Assumption |
| Utility reduction due to LPS | Same as PTSD | Assumption |
| Probability of PTSD, given awareness | 0.177 (0.113 to 0.230) | Samuelsson et al.115 and Lennmarken et al.11 |
| Duration of PTSD | 12.7 years | Kessler et al.118 |
| 7.32 years, discounted at 3.5% (8.2 to 21.6 years, 5.6 to 9.6 discounted at 3.5%) | ||
| Unit cost of PTSD | £9104 | NICE [consists of £915.62 (60%) pharmacological therapy, £456.71 (30%) psychological therapy and £152.60 (10%) combined pharmacological and psychological therapy]. Excess risk of hospitalisation 25% annually.136 Average cost of inpatient stay. NHS Reference Costs 2010–2011137 |
| Utility reduction due to PTSD | 0.12 | Various |
Table 51 provides a summary of model inputs relating to anaesthetic complications (PONV and POCD in the model), including the baseline risks and the risk reduction associated with depth of anaesthesia monitoring for POCD.
| Parameter | Value | Source |
|---|---|---|
| PONV | ||
| Baseline PONV | 30% | Cohen MM, Duncan PG, DeBoer DP, Tweed WA. The postoperative interview: assessing risk factors for nausea and vomiting. Anaesth Analg 1994;78:7–16 |
| Reduction in PONV using depth monitor | Not included in base case | Included as a scenario analysis |
| Unit cost of PONV | £5.39 | £5.39 (4 mg of ondansetron) |
| Utility reduction due to PONV | 0 | |
| POCD | ||
| Baseline POCD | Average duration of 29.65 days | ISPOCD study reported POCD in 25.8% (95% CI 23.1% to 28.5%) of patients at 1 week and in 9.9% (95% CI 8.1% to 12.0%) of patients at 3 months after surgery: compared with 3.4% and 2.8%, respectively, in UK controls. At median follow-up of 532 days, 10.4% patients had cognitive dysfunction compared with 10.6% controls (47 non-hospitalised volunteers of similar age). Assume excess of 22.4% at 7 days, reducing to excess of 7.10% at 3 months and excess of 0% at 1.5 years (532/365.25 years) – area under curve = 29.65 days |
| Reduction in POCD using depth monitor | Average duration of 21.10 days | Chan and colleagues'47 abstract reported 32.5% (BIS) vs 39.1% (standard clinical monitoring) at 7 days and 8.1% (BIS) vs 12% (standard clinical monitoring) at 3 months |
| OR estimated as 0.75 (at 7 days) and 0.646 (at 3 months) – applied to excess proportions above. Assume average duration of 21.10 days | ||
| Unit cost of POCD | 0 | |
| Utility reduction due to POCD | 0.05 | Jonsson et al.:110 difference in utility between an MMSE score > 25 (0.69) and an MMSE score between 21 and 25 (0.64). Normal to mild cognitive dysfunction |
Model results
The model results are presented in separate subsections for BIS, E-Entropy and Narcotrend respectively. Analyses are presented by mode of administration [TIVA and mixed anaesthesia (induction with i.v. anaesthetic and maintenance with inhaled anaesthetic)], with separate analyses reported for patients considered at high risk of awareness and for a general surgical population. No analysis is presented for inhaled GA only. Although trials using this mode of anaesthesia delivery were included in the systematic review of patient outcomes, these did not report any information on anaesthetic drug consumption on which to base a reliable costing.
Bispectral Index compared with standard clinical monitoring
Base case
The costs, QALY and ICER modelled for patients considered at high risk of intraoperative awareness undergoing GA with TIVA, comparing standard clinical monitoring with BIS are presented in Table 52.
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Standard clinical monitoring | 24.19 | −0.0011 | 22,339 | ||
| BIS | 39.36 | 15.17 | −0.0005 | 0.0007 |
Bispectral Index monitoring was modelled as being associated with 10.8 cases of awareness, compared with 45 cases for patients receiving standard clinical monitoring, in cohorts of 10,000 patients. This resulted in a reduction of 11.1 cases of LPS (from 14.7 to 3.5), which included a reduction of six cases of PTSD (from 8.0 to 1.9).
The cost of standard clinical monitoring during anaesthesia in high-risk patients was lower than for BIS, with a cost difference of £15.17. The increased cost for BIS monitoring is primarily the result of the sensors attached to the patient (88% of the cost per patient cost) rather than the module. There is no reduction in anaesthetic costs associated with depth of anaesthesia monitoring in this group of patients, although a small amount of the additional cost of depth of anaesthesia monitoring is offset by reduced costs associated with psychological sequelae of awareness (Table 53).
| Cost | Standard clinical monitoring (£) | BIS (£) |
|---|---|---|
| Depth of anaesthesia monitoring | 0.00 | 16.43 |
| Anaesthetic drugs | 20.92 | 20.92 |
| PONV | 1.62 | 1.62 |
| POCD | 0.00 | 0.00 |
| PTSD | 1.66 | 0.40 |
The comparatively high cost of sensors for use with BIS suggests that it is unlikely to generate sufficient savings to offset fully the additional costs of depth of anaesthesia monitoring. This analysis suggests that the cost-effectiveness of BIS is likely to be highly dependent on the extent to which it delivers improved patient outcomes (such as reduction in episodes of awareness (and the psychological sequelae) or POCD). A threshold analysis showed that, for patients considered at high risk of intraoperative awareness undergoing GA with TIVA, BIS monitoring would be cost-effective (at a threshold of £30,000 per QALY gained) where the OR for awareness (BIS vs standard clinical monitoring) was < 0.458.
The costs, QALY and ICER modelled for a general surgical population undergoing GA with TIVA, comparing standard clinical monitoring with monitoring by BIS are presented in Table 54.
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Standard clinical monitoring | 23.13 | −0.0007 | |||
| BIS | 34.10 | 10.98 | −0.0004 | 0.0003 | 34,565 |
Although the cost of standard clinical monitoring in this group of patients was slightly lower than for the subgroup of patients at high risk of intraoperative awareness, the incremental cost of BIS monitoring is lower. This is attributable to the potential to offset a reduction in consumption of anaesthetic against the additional costs of depth of anaesthesia monitoring (Table 55). Propofol consumption for maintenance of anaesthesia was estimated as being 19.3% lower in the BIS-monitored group, compared with standard clinical monitoring. Given the lower probability of intraoperative awareness in this group of patients, the QALY losses for standard clinical monitoring and BIS monitoring [resulting from psychological sequelae of awareness (LPS and PTSD)] are lower than for the high-risk group. The QALY gain of 0.0003 was lower than in the high-risk group and results in an increased ICER of £34,565 per QALY gained.
| Cost | Standard clinical monitoring (£) | BIS (£) |
|---|---|---|
| Depth of anaesthesia monitoring | 0.00 | 15.46 |
| Anaesthetic drugs | 20.92 | 16.88 |
| PONV | 1.62 | 1.62 |
| POCD | 0.00 | 0.00 |
| PTSD | 0.59 | 0.14 |
The costs, QALY and ICER modelled for patients considered at high risk of intraoperative awareness undergoing GA, comparing standard clinical monitoring with monitoring by BIS, are presented in Table 56.
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Standard clinical monitoring | 14.31 | −0.0011 | |||
| BIS | 29.83 | 15.52 | −0.0006 | 0.0005 | 29,634 |
Bispectral Index monitoring was modelled as being associated with 20.3 cases of awareness, compared with 45 cases among patients receiving standard clinical monitoring, in cohorts of 10,000 patients. This resulted in a reduction of 8.1 cases of LPS (from 14.7 to 6.6), which included a reduction of 4.4 cases of PTSD (from 8.0 to 3.6).
The cost of BSI during anaesthesia in high-risk patients was higher than for standard clinical monitoring, with an incremental cost of £15.52. As discussed previously, the majority of the cost increase with BIS monitoring is attributable to the sensors attached to the patient rather than the depth-monitoring module. As with TIVA in high-risk patients, there is no reduction in anaesthetic costs associated with depth of anaesthesia monitoring and limited scope to offset the additional cost of depth of anaesthesia monitoring by reduction in costs associated with psychological sequelae of awareness (Table 57).
| Cost | Standard clinical monitoring (£) | BIS (£) |
|---|---|---|
| Depth of anaesthesia monitoring | 0.00 | 16.43 |
| Anaesthetic drugs | 11.04 | 11.04 |
| PONV | 1.62 | 1.62 |
| POCD | 0.00 | 0.00 |
| PTSD | 1.66 | 0.75 |
Bispectral Index monitoring in a general surgical population undergoing mixed anaesthesia was modelled as being associated with 7.2 cases of awareness, compared with 16 cases among patients receiving standard clinical monitoring. This resulted in a reduction of three cases of LPS (from 5.2 to 2.33), which included a reduction of 1.5 cases of PTSD (from 2.8 to 1.3). The costs, QALY and ICER modelled for this population undergoing mixed GA, comparing standard clinical monitoring with monitoring by BIS, are presented in Table 58.
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Standard clinical monitoring | 13.25 | −0.0007 | |||
| BIS | 26.16 | 12.91 | −0.0004 | 0.0003 | 49,198 |
Costs of standard clinical monitoring and BIS monitoring in this group of patients are both lower than for the subgroup of patients at high risk of intraoperative awareness. The cost difference is lower, because of the potential to offset a reduction in consumption of anaesthetic against the additional costs of depth of anaesthesia monitoring (Table 59). Sevoflurane consumption for maintenance of anaesthesia was estimated as being 20.2% lower in the BIS-monitored group, compared with standard clinical monitoring. Given the lower probability of intraoperative awareness in this group of patients, the QALY losses for standard clinical monitoring and BIS monitoring are lower than for the high-risk group. The effectiveness of BIS monitoring at reducing intraoperative awareness was also assumed to be lower with inhaled anaesthesia (Peto's OR 0.45) compared with TIVA (Peto's OR 0.24). The QALY gain of 0.0003 was lower than in the high-risk group and results in an increased ICER of £49,198 per QALY gained.
| Cost | Standard clinical monitoring (£) | BIS (£) |
|---|---|---|
| Depth of anaesthesia monitoring | 0.00 | 15.46 |
| Anaesthetic drugs | 11.04 | 8.81 |
| PONV | 1.62 | 1.62 |
| POCD | 0.00 | 0.00 |
| PTSD | 0.59 | 0.27 |
Deterministic sensitivity analysis
One-way sensitivity analyses of key parameters were undertaken in both the general surgical population, and the high-risk surgical population undergoing GA with TIVA. The results are shown in Tables 60 and 61.
| Parameter | Input value | Standard clinical monitoring | BIS | Incremental | ICER (£/QALY gained) | |||
|---|---|---|---|---|---|---|---|---|
| Cost (£) | QALY | Cost (£) | QALY | Cost | QALY | |||
| Probability awareness | 0.0006 | 22.76 | −0.0005 | 39.02 | −0.0003 | 16.26 | 0.0002 | 84,305 |
| 0.0119 | 26.92 | −0.0024 | 40.03 | −0.0008 | 13.11 | 0.0016 | 8196 | |
| Operating room awareness with depth of anaesthesia monitor | 0.1 | 24.19 | −0.0011 | 39.13 | −0.0004 | 14.94 | 0.0008 | 19,080 |
| 0.6 | 24.19 | −0.0011 | 39.96 | −0.0007 | 15.77 | 0.0004 | 38,193 | |
| Duration of LPS (years) | 0.25 | 24.19 | −0.0011 | 39.36 | −0.0005 | 15.17 | 0.0007 | 22,854 |
| 1 | 24.19 | −0.0012 | 39.36 | −0.0005 | 15.17 | 0.0007 | 21,375 | |
| Probability of LPSa | 0.195 | 23.53 | −0.0125 | 39.20 | −0.0121 | 15.67 | 0.0004 | 37,905 |
| 0.48 | 24.98 | −0.0302 | 39.55 | −0.0293 | 14.58 | 0.0008 | 17,239 | |
| Duration of PTSD (years) | 5.6 | 24.19 | −0.0010 | 39.36 | −0.0004 | 15.17 | 0.0006 | 27,364 |
| 9.6 | 24.19 | −0.0014 | 39.36 | −0.0005 | 15.17 | 0.0008 | 17,969 | |
| Proportion PTSDb | 0.345 | 23.59 | −0.0009 | 39.22 | −0.0004 | 15.63 | 0.0005 | 31,289 |
| 0.733 | 24.78 | −0.0014 | 39.50 | −0.0005 | 14.73 | 0.0009 | 17,259 | |
| LPS QoL decrement | −0.075 | 24.19 | −0.0011 | 39.36 | −0.0005 | 15.17 | 0.0007 | 22,723 |
| −0.05 | 24.19 | −0.0011 | 39.36 | −0.0005 | 15.17 | 0.0007 | 22,942 | |
| PTSD QoL decrement | −0.134 | 24.19 | −0.0012 | 39.36 | −0.0005 | 15.17 | 0.0007 | 20,473 |
| −0.068 | 24.19 | −0.0008 | 39.36 | −0.0004 | 15.17 | 0.0004 | 33,770 | |
| Probability people with PTSD seek treatment | 0 | 22.54 | −0.0011 | 38.96 | −0.0005 | 16.43 | 0.0007 | 24,191 |
| 1 | 27.41 | −0.0011 | 40.14 | −0.0005 | 12.73 | 0.0007 | 18,742 | |
| Cost of sensors (£) | 10.875 | 24.19 | −0.0011 | 35.74 | −0.0005 | 11.54 | 0.0007 | 17,000 |
| 18.125 | 24.19 | −0.0011 | 42.99 | −0.0005 | 18.79 | 0.0007 | 27,677 | |
| Parameter | Input value | Standard clinical monitoring | BIS | Incremental | ICER (£/QALY gained) | |||
|---|---|---|---|---|---|---|---|---|
| Cost (£) | QALY | Cost (£) | QALY | Cost (£) | QALY | |||
| Proportional change in propofol use | −0.272 | 23.13 | −0.0007 | 32.45 | −0.0004 | 9.33 | 0.0003 | 29,362 |
| −0.113 | 23.13 | −0.0007 | 35.78 | −0.0004 | 12.65 | 0.0003 | 39,835 | |
| Probability awareness | 0.001 | 22.91 | −0.0006 | 34.05 | −0.0003 | 11.15 | 0.0002 | 45,913 |
| 0.0023 | 23.38 | −0.0008 | 34.17 | −0.0004 | 10.78 | 0.0004 | 26,630 | |
| Operating room awareness with depth of anaesthesia monitor | 0.1 | 23.13 | −0.0007 | 34.02 | −0.0003 | 10.90 | 0.0004 | 30,741 |
| 0.6 | 23.13 | −0.0007 | 34.32 | −0.0004 | 11.19 | 0.0002 | 50,184 | |
| Duration of LPS (years) | 0.25 | 23.13 | −0.0007 | 34.10 | −0.0004 | 10.98 | 0.0003 | 35,168 |
| 1 | 23.13 | −0.0007 | 34.10 | −0.0004 | 10.98 | 0.0003 | 33,419 | |
| Probability of LPSa | 0.195 | 22.89 | −0.0122 | 34.05 | −0.0120 | 11.16 | 0.0002 | 50,006 |
| 0.48 | 23.40 | −0.0295 | 34.17 | −0.0292 | 10.77 | 0.0004 | 28,573 | |
| Duration of PTSD (years) | 5.6 | 23.13 | −0.0006 | 34.10 | −0.0003 | 10.98 | 0.0003 | 40,178 |
| 9.6 | 23.13 | −0.0007 | 34.10 | −0.0004 | 10.98 | 0.0004 | 29,170 | |
| Proportion PTSDb | 0.345 | 22.91 | −0.0006 | 34.05 | −0.0003 | 11.14 | 0.0003 | 43,915 |
| 0.733 | 23.33 | −0.0008 | 34.15 | −0.0004 | 10.82 | 0.0004 | 28,507 | |
| LPS QoL decrement | −0.075 | 23.13 | −0.0007 | 34.10 | −0.0004 | 10.98 | 0.0003 | 35,016 |
| −0.05 | 23.13 | −0.0007 | 34.10 | −0.0004 | 10.98 | 0.0003 | 35,271 | |
| PTSD QoL decrement | −0.134 | 23.13 | −0.0007 | 34.10 | −0.0004 | 10.98 | 0.0003 | 32,324 |
| −0.068 | 23.13 | −0.0006 | 34.10 | −0.0003 | 10.98 | 0.0002 | 46,553 | |
| Probability people with PTSD seek treatment | 0 | 22.54 | −0.0007 | 33.96 | −0.0004 | 11.43 | 0.0003 | 35,975 |
| 1 | 24.27 | −0.0007 | 34.38 | −0.0004 | 10.11 | 0.0003 | 31,830 | |
| Cost of sensors (£) | 10.875 | 23.13 | −0.0007 | 30.48 | −0.0004 | 7.35 | 0.0003 | 23,152 |
| 18.125 | 23.13 | −0.0007 | 37.73 | −0.0004 | 14.60 | 0.0003 | 45,979 | |
The changes in the probability of awareness in the patients at high risk of intraoperative awareness receiving TIVA resulted in a substantially altered ICER from the base case: £8196 per QALY gained and £84,305 per QALY gained respectively. The ICER was also sensitive to decreased effectiveness of the BIS module, changes in the probability of LPS, the duration of PTSD at 9.6 years, changes in the probability of PTSD, the lower PTSD decrement and the lower unit cost of sensors. Changes in the duration of LPS, or the LPS QoL decrement, had little impact on the ICER.
These results suggest that the ICER for the general surgical population is relatively robust to changes in the duration of LPS, changes in the QoL decrement applied to LPS, and to the probability of patients seeking treatment for PTSD and the duration of PTSD symptoms.
The ICER appears sensitive to the lower probability of awareness, the relative risk of awareness with BIS modules, the decrease in probability of developing LPS, the decreased probability of developing PTSD and changes in the QoL decrement applied to PTSD.
One-way sensitivity analyses of key parameters were undertaken in both the general surgical population and the high-risk surgical population undergoing mixed GA. The results are shown in Tables 62 and 63.
| Parameter | Input value | Standard clinical monitoring | BIS | Incremental | ICER (£/QALY gained) | |||
|---|---|---|---|---|---|---|---|---|
| Cost (£) | QALY | Cost (£) | QALY | Cost (£) | QALY | |||
| Probability awareness | 0.0006 | 12.88 | −0.0005 | 29.18 | −0.0003 | 16.31 | 0.0002 | 94,710 |
| 0.0119 | 17.04 | −0.0024 | 31.07 | −0.0012 | 14.03 | 0.0012 | 11,819 | |
| Operating room awareness with depth of anaesthesia monitor | 0.25 | 14.31 | −0.0011 | 29.50 | −0.0005 | 15.19 | 0.0007 | 22,610 |
| 0.81 | 14.31 | −0.0011 | 30.43 | −0.0009 | 16.11 | 0.0003 | 62,482 | |
| Duration of LPS (years) | 0.25 | 14.31 | −0.0011 | 29.83 | −0.0006 | 15.52 | 0.0005 | 30,274 |
| 1 | 14.31 | −0.0012 | 29.83 | −0.0006 | 15.52 | 0.0005 | 28,432 | |
| Probability of LPSa | 0.195 | 13.65 | −0.0125 | 29.53 | −0.0122 | 15.88 | 0.0003 | 47,890 |
| 0.48 | 15.10 | −0.0302 | 30.18 | −0.0295 | 15.09 | 0.0006 | 23,430 | |
| Duration of PTSD (years) | 5.6 | 14.31 | −0.0010 | 29.83 | −0.0006 | 15.52 | 0.0004 | 35,798 |
| 9.6 | 14.31 | −0.0014 | 29.83 | −0.0007 | 15.52 | 0.0006 | 24,132 | |
| Proportion PTSDb | 0.345 | 13.71 | −0.0009 | 29.56 | −0.0005 | 15.85 | 0.0004 | 40,248 |
| 0.733 | 14.90 | −0.0014 | 30.09 | −0.0007 | 15.20 | 0.0006 | 23,396 | |
| LPS QoL decrement | −0.075 | 14.31 | −0.0011 | 29.83 | −0.0006 | 15.52 | 0.0005 | 30,112 |
| −0.05 | 14.31 | −0.0011 | 29.83 | −0.0006 | 15.52 | 0.0005 | 30,383 | |
| PTSD QoL decrement | −0.134 | 14.31 | −0.0012 | 29.83 | −0.0007 | 15.52 | 0.0006 | 27,301 |
| −0.068 | 14.31 | −0.0008 | 29.83 | −0.0005 | 15.52 | 0.0004 | 43,413 | |
| Probability people with PTSD seek treatment | 0 | 12.66 | −0.0011 | 29.08 | −0.0006 | 16.43 | 0.0005 | 31,371 |
| 1 | 17.53 | −0.0011 | 31.28 | −0.0006 | 13.75 | 0.0005 | 26,262 | |
| Cost of sensors (£) | 10.875 | 14.31 | −0.0011 | 26.21 | −0.0006 | 11.89 | 0.0005 | 22,711 |
| 18.125 | 14.31 | −0.0011 | 33.46 | −0.0006 | 19.14 | 0.0005 | 36,557 | |
| Parameter | Input value | Standard clinical care | BIS | Incremental | ICER (£/QALY gained) | |||
|---|---|---|---|---|---|---|---|---|
| Cost (£) | QALY | Cost (£) | QALY | Cost (£) | QALY | |||
| Proportional change in sevoflurane use | −0.330 | 13.25 | −0.0007 | 24.74 | −0.0004 | 11.50 | 0.0003 | 43,813 |
| −0.074 | 13.25 | −0.0007 | 27.57 | −0.0004 | 14.32 | 0.0003 | 54,583 | |
| Probability awareness | 0.001 | 13.03 | −0.0006 | 26.06 | −0.0004 | 13.03 | 0.0002 | 62,569 |
| 0.0023 | 13.50 | −0.0008 | 26.27 | −0.0005 | 12.77 | 0.0003 | 39,224 | |
| Operating room awareness with depth of anaesthesia monitor | 0.25 | 13.25 | −0.0007 | 26.04 | −0.0004 | 12.79 | 0.0003 | 40,611 |
| 0.81 | 13.25 | −0.0007 | 26.37 | −0.0005 | 13.12 | 0.0002 | 78,178 | |
| Duration of LPS (years) | 0.25 | 13.25 | −0.0007 | 26.16 | −0.0004 | 12.91 | 0.0003 | 49,948 |
| 1 | 13.25 | −0.0007 | 26.16 | −0.0004 | 12.91 | 0.0003 | 47,764 | |
| Probability of LPSa | 0.195 | 13.01 | −0.0122 | 26.05 | −0.0121 | 13.04 | 0.0002 | 67,196 |
| 0.48 | 13.52 | −0.0295 | 26.28 | −0.0292 | 12.76 | 0.0003 | 41,792 | |
| Duration of PTSD (years) | 5.6 | 13.25 | −0.0006 | 26.16 | −0.0004 | 12.91 | 0.0002 | 56,055 |
| 9.6 | 13.25 | −0.0007 | 26.16 | −0.0004 | 12.91 | 0.0003 | 42,340 | |
| Proportion PTSDb | 0.345 | 13.03 | −0.0006 | 26.06 | −0.0004 | 13.03 | 0.0002 | 60,266 |
| 0.733 | 13.45 | −0.0008 | 26.25 | −0.0004 | 12.80 | 0.0003 | 41,648 | |
| LPS QoL decrement | −0.075 | 13.25 | −0.0007 | 26.16 | −0.0004 | 12.91 | 0.0003 | 49,758 |
| −0.05 | 13.25 | −0.0007 | 26.16 | −0.0004 | 12.91 | 0.0003 | 50,075 | |
| PTSD QoL decrement | −0.134 | 13.25 | −0.0007 | 26.16 | −0.0004 | 12.91 | 0.0003 | 46,382 |
| −0.068 | 13.25 | −0.0006 | 26.16 | −0.0004 | 12.91 | 0.0002 | 63,521 | |
| Probability people with PTSD seek treatment | 0 | 12.66 | −0.0007 | 25.89 | −0.0004 | 13.23 | 0.0003 | 50,432 |
| 1 | 14.39 | −0.0007 | 26.67 | −0.0004 | 12.28 | 0.0003 | 46,803 | |
| Unit cost of sensors (£) | 10.875 | 13.25 | −0.0007 | 22.53 | −0.0004 | 9.28 | 0.0003 | 35,383 |
| 18.125 | 13.25 | −0.0007 | 29.78 | −0.0004 | 16.53 | 0.0003 | 63,013 | |
The ICER was sensitive to several key parameters in high-risk patients undergoing mixed anaesthesia. The largest variation is seen where the probability of awareness is decreased to 0.0006 and 0.0119, resulting in an ICER of £11,819 and £94,710 per QALY gained respectively. Changes in the relative risk of awareness with the BIS module, probability of developing LPS or PTSD, the duration of PTSD and a decreased PTSD QoL decrement all lead to large variations in the ICER, ranging from £22,610 to £62,482 per QALY gained.
The ICER is again sensitive to several key parameters in a general surgical population undergoing mixed anaesthesia. In this group, an increase in the probability of LPS resulted in the largest variation, to £67,196 per QALY gained. The ICER was again driven by probability of awareness, the relative risk of awareness with the BIS module (increase and decrease), duration and probability of PTSD, and the unit costs of the sensors.
Scenario analysis
The systematic review of patient outcomes did not identify any robust data which reported an estimate of the effect of BIS monitoring on risk of PONV. We developed a scenario analysis using data from the meta-analysis by Liu105 to investigate the potential impact of including this outcome on the cost-effectiveness results.
For this scenario analysis we used the baseline (control group) risk of PONV as the estimated risk for standard clinical monitoring and applied the OR derived in the meta-analysis (0.77, 95% CI 0.56 to 0.99) and the lower limit of the 95% CI to estimate risk for BIS-monitored patients. We assumed that all treatments (such as prophylaxis against PONV) were the same for each treatment group, and that all patients experiencing PONV were treated using 4 mg ondansetron by intramuscular or slow i.v. injection (unit cost = £5.39; BNF33).
Tables 64 and 65 report the results of the scenario analysis for patients at high risk of intraoperative awareness and a general surgical population, respectively, undergoing GA with TIVA. The incremental costs for BIS monitoring are reduced, from the value reported for the base-case analyses (Tables 52 and 54), by including an estimate of PONV. However, the change in costs is slight and leaves the ICER largely unchanged.
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| OR = 0.77: baseline risk = 0.3, risk with BIS monitoring = 0.248 | |||||
| Standard clinical monitoring | 24.19 | −0.0011 | |||
| BIS | 39.08 | 14.89 | −0.0005 | 0.0007 | 21,927 |
| OR = 0.56a: baseline risk = 0.3, risk with BIS monitoring = 0.194 | |||||
| Standard clinical monitoring | 24.19 | −0.0011 | |||
| BIS | 38.79 | 14.60 | −0.0005 | 0.0007 | 21,494 |
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| OR = 0.77: baseline risk = 0.375, risk with BIS monitoring = 0.248 | |||||
| Standard clinical monitoring | 23.13 | −0.0007 | |||
| BIS | 33.82 | 10.70 | −0.0004 | 0.0003 | 33,685 |
| OR = 0.56:a baseline risk = 0.375, risk with BIS monitoring = 0.194 | |||||
| Standard clinical monitoring | 23.13 | −0.0007 | |||
| BIS | 33.53 | 10.40 | −0.0004 | 0.0003 | 32,759 |
Tables 66 and 67 report the results of the scenario analysis for patients at high risk of intraoperative awareness and a general surgical population, respectively, undergoing mixed GA. As before, the incremental costs for BIS monitoring are reduced. However, the change in costs is slight and leaves the ICER largely unchanged.
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| OR = 0.77: baseline risk = 0.3, risk with BIS monitoring = 0.248 | |||||
| Standard clinical monitoring | 14.31 | −0.0011 | |||
| BIS | 29.55 | 15.24 | −0.0006 | 0.0005 | 29,100 |
| OR = 0.56:a baseline risk = 0.3, risk with BIS monitoring = 0.194 | |||||
| Standard clinical monitoring | 14.31 | −0.0011 | |||
| BIS | 29.26 | 14.94 | −0.0006 | 0.0005 | 28,538 |
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| OR = 0.77: baseline risk = 0.3, risk with BIS monitoring = 0.248 | |||||
| Standard clinical monitoring | 13.25 | −0.0007 | |||
| BIS | 25.88 | 12.63 | −0.0004 | 0.0003 | 48,132 |
| OR = 0.56:a baseline risk = 0.3, risk with BIS monitoring = 0.194 | |||||
| Standard clinical monitoring | 13.25 | −0.0007 | |||
| BIS | 25.58 | 12.34 | −0.0004 | 0.0003 | 47,011 |
Inclusion of the impact of PONV with BIS monitoring into the base-case analysis is unlikely to substantially affect decisions based on cost-effectiveness criteria.
Our review of published studies of the incidence of intraoperative awareness identified substantial uncertainty over the estimated values. We used pooled values across identified studies in the base-case analysis. However, the value adopted for ‘high risk’ is lower than that commonly quoted as indicating high risk, and the pooled estimate adopted for a general surgical population excluded two outlying studies (one high and one low extreme value).
For this scenario analysis we replace the base-case estimate for probability of awareness in the high-risk population (0.45%) with a value of 1.0% reported for certain types of surgery (cardiac surgery, caesarean section and trauma surgery). 79,111,112 The effect of this is to approximately double the QALY loss for each group, resulting in a doubling of the QALY gain associated with BIS monitoring, while incremental costs are largely unchanged. The effect of this is to reduce the ICER by about half (Table 68).
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| TIVA | |||||
| Standard clinical monitoring | 26.22 | −0.0021 | |||
| BIS | 39.85 | 13.64 | −0.0007 | 0.0014 | 10,003 |
| Mixed anaesthesia | |||||
| Standard clinical monitoring | 16.34 | −0.0021 | |||
| BIS | 30.75 | 14.41 | −0.0010 | 0.0010 | 14,168 |
In the general surgical population, we replaced the base-case estimate for probability of awareness (0.16%) with the incidences reported in the two outlying studies (Tables 69 and 70). The results from these two scenarios contrast sharply. At the highest reported incidence of awareness – equivalent to that frequently cited for ‘high-risk’ populations – the QALY loss for each group increases approximately 2.5-fold, resulting in a three- to fourfold increase in the QALY gain associated with BIS monitoring. The incremental costs are slightly reduced, compared with the base case, and the resulting ICERs are substantially reduced. In the case of the lowest reported probability of awareness, the QALY gain from BIS monitoring is negligible resulting in high-value ICER.
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Baseline probability of awareness = 0.99% | |||||
| Standard clinical monitoring | 26.18 | −0.0020 | |||
| BIS | 34.84 | 8.66 | −0.0007 | 0.0014 | 6413 |
| Baseline probability of awareness = 0.007% | |||||
| Standard clinical monitoring | 22.56 | −0.0004 | |||
| BIS | 33.97 | 11.41 | −0.0003 | 0.0001 | 90,014 |
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Baseline probability of awareness = 0.99% | |||||
| Standard clinical monitoring | 16.30 | −0.0020 | |||
| BIS | 27.54 | 11.24 | −0.0010 | 0.0010 | 11,146 |
| Baseline probability of awareness = 0.007% | |||||
| Standard clinical monitoring | 12.68 | −0.0004 | |||
| BIS | 25.90 | 13.22 | −0.0003 | 0.0001 | 106,347 |
In order to apportion the capital cost of the depth of anaesthesia monitoring modules, we required an estimate of the number of patients in whom the monitor module was used in each year (patients per device-year), throughout its assumed 5-year effective life. The estimate used for the general surgical population was 1000 patients per year (equivalent to four patients per day over 250 working days per year) was based on discussion with clinical experts. This scenario analysis investigates the impact of this assumption on the estimated incremental cost associated with BIS monitoring, compared with standard clinical monitoring, and the resulting effect on the ICER. Tables 71 and 72 report the incremental cost and ICER for BIS, compared with standard clinical monitoring, at four selected values for the number of patients per device-year: the base-case value of 100 and also for a low value of 10 and a high value of 1500 (six patients per day over 250 working days per year). This suggests that the assumed number of patients per device-year only has a substantial impact on incremental cost (hence on the ICER) at comparatively low volumes.
| Patients per device-year | High-risk patients undergoing TIVA | General surgical population undergoing TIVA | ||
|---|---|---|---|---|
| Incremental cost (£) | ICER (£/QALY gained) | Incremental cost (£) | ICER (£/QALY gained) | |
| 100 | 22.88 | 33,689 | 19.65 | 61,866 |
| 500 | 15.17 | 22,339 | 11.94 | 37,599 |
| 1000 | 14.21 | 20,920 | 10.98 | 34,565 |
| 1500 | 13.88 | 20,447 | 10.66 | 33,554 |
| Patients per device-year | High-risk patients undergoing mixed anaesthesia | General surgical population undergoing mixed anaesthesia | ||
|---|---|---|---|---|
| Incremental cost (£) | ICER (£/QALY gained) | Incremental cost (£) | ICER (£/QALY gained) | |
| 100 | 23.22 | 44,354 | 21.58 | 82,243 |
| 500 | 15.52 | 29,634 | 13.87 | 52,870 |
| 1000 | 14.55 | 27,794 | 12.91 | 49,198 |
| 1500 | 14.23 | 27,181 | 12.59 | 47,974 |
The QoL decrement applied in the base-case analysis was based on Freed and colleagues'120 paper on veterans with PTSD. In order to investigate the impact of a sparse evidence base on HRQoL in a group of patients with PTSD, a scenario analysis was undertaken. The utility decrement was adjusted to 0.50 and 0.75 in high-risk and general surgical groups receiving either TIVA or mixed anaesthesia (Table 73).
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| TIVA | |||||
| Utility decrement for PTSD = −0.5 | |||||
| Standard clinical monitoring | 24.19 | −0.0034 | |||
| BIS | 39.36 | 15.17 | −0.0010 | 0.0024 | 6431 |
| Utility decrement for PTSD = −0.75 | |||||
| Standard clinical monitoring | 24.19 | −0.0048 | |||
| BIS | 39.36 | 15.17 | −0.0014 | 0.0035 | 4379 |
| Mixed anaesthesia | |||||
| Utility decrement for PTSD = −0.5 | |||||
| Standard clinical monitoring | 14.31 | −0.0034 | |||
| BIS | 29.83 | 15.52 | −0.0016 | 0.0017 | 8928 |
| Utility decrement for PTSD = −0.75 | |||||
| Standard clinical monitoring | 14.31 | −0.0048 | |||
| BIS | 29.83 | 15.52 | −0.0023 | 0.0025 | 6116 |
The ICER was sensitive to these alternative scenarios in high-risk patients, both receiving TIVA and mixed anaesthesia. Where the PTSD decrement was increased to −0.5 in TIVA and mixed anaesthesia the ICER reduced to £6431 per QALY gained and £8928 per QALY gained respectively. Where the PTSD decrement was increased further, the ICER decreased again to £4379 and £6116 per QALY gained in the TIVA and mixed anaesthesia groups respectively.
The scenario analyses using alternative PTSD decrements in the general surgical population reflect the results in the high-risk population: there is a substantial reduction in the ICER where these are increased (Table 74).
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| TIVA | |||||
| Utility decrement for PTSD = −0.5 | |||||
| Standard clinical monitoring | 23.13 | −0.0015 | |||
| BIS | 10 | 10.98 | −0.0005 | 0.0009 | 11,994 |
| Utility decrement for PTSD = −0.75 | |||||
| Standard clinical monitoring | 23.13 | −0.0020 | |||
| BIS | 34.10 | 10.98 | −0.0007 | 0.0013 | 8390 |
| Mixed anaesthesia | |||||
| Utility decrement for PTSD = −0.5 | |||||
| Standard clinical monitoring | 13.25 | −0.0015 | |||
| BIS | 26.16 | 12.91 | −0.0008 | 0.0007 | 18,581 |
| Utility decrement for PTSD = −0.75 | |||||
| Standard clinical monitoring | 13.25 | −0.0020 | |||
| BIS | 26.16 | 12.91 | −0.0010 | 0.0010 | 13,183 |
E-Entropy compared with standard clinical monitoring
Base case
The costs, QALY and ICER modelled for patients considered at high risk of intraoperative awareness undergoing GA with TIVA, comparing standard clinical monitoring with monitoring by E-Entropy, are presented in Table 75.
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Standard clinical monitoring | 26.38 | −0.0011 | |||
| E-Entropy | 36.18 | 9.79 | −0.0005 | 0.0007 | 14,421 |
E-Entropy monitoring was modelled as being associated with 10.8 cases of awareness, compared with 45 cases in patients receiving standard clinical monitoring, in cohorts of 10,000 patients. This resulted in a reduction of 11.1 cases of LPS (from 14.7 to 3.5), which included a reduction of six cases of PTSD (from 8.0 to 1.9).
The cost of standard clinical monitoring during anaesthesia in high-risk patients was lower than for E-Entropy monitoring, with the incremental cost being £9.79. The breakdown of total cost for standard clinical monitoring and E-Entropy is reported in Table 76; the costs of anaesthetic drug use outlined in this table apply to the Ellerkmann and colleagues study only. 62 As no reduction in drug costs is expected in the population at high risk of awareness, the cost assumption (for anaesthetic drugs) has no impact on the ICER. The increased cost for E-Entropy monitoring is partially offset by the reduction in costs of patients with PTSD.
| Cost | Standard clinical monitoring (£) | E-Entropy (£) |
|---|---|---|
| Depth of anaesthesia monitoring | 0.00 | 11.05 |
| Anaesthetic drugs | 23.11 | 23.11 |
| PONV | 1.62 | 1.62 |
| POCD | 0.00 | 0.00 |
| PTSD | 1.66 | 0.40 |
As a result of the psychological sequelae of awareness, including LPS, PTSD and POCD, patients in both groups incurred a slight QALY loss. This was lower in the E-Entropy-monitored patients, with a difference of 0.0007 QALY, resulting in an ICER of £14,421 per QALY gained.
In a general surgical population (not just those at high risk of intraoperative awareness) undergoing GA with TIVA, E-Entropy monitoring was modelled as being associated with 3.8 cases of awareness, compared with 16 cases for patients receiving standard clinical monitoring, in cohorts of 10,000 patients. This resulted in a reduction of four cases of LPS (from 5.2 to 1.3), which included a reduction of 2.1 cases of PTSD (from 2.8 to 0.7). The costs, QALY and ICER modelled for this population, comparing standard clinical monitoring with monitoring by E-Entropy are presented in Table 77 (based on anaesthetic drug consumption from the RCT by Ellerkmann and colleagues62) and in Table 78 (based on anaesthetic drug consumption from the RCT by Gruenewald and colleagues55).
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Standard clinical monitoring | 25.32 | −0.0007 | |||
| E-Entropy | 35.20 | 9.89 | −0.0004 | 0.0003 | 31,131 |
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Standard clinical monitoring | 31.50 | −0.0007 | |||
| E-Entropy | 41.48 | 9.98 | −0.0004 | 0.0003 | 31,430 |
Applying the costs of anaesthetic drugs from both the Ellerkmann and colleagues62 and Gruenewald and colleagues55 RCTs results in increased costs with E-Entropy. Both RCTs reported slightly lower costs for anaesthetic drug use in the standard clinical monitoring group than with the E-Entropy group. Again, costs for PTSD were slightly lower in the E-Entropy group as a result of lower incidence of awareness (Table 79).
| Cost | Standard clinical monitoring (£) | E-Entropy (£) |
|---|---|---|
| Depth of anaesthesia monitoring | 0.00 | 9.87 |
| Anaesthetic drugs | ||
| Gruenewald et al.55 | 29.29 | 29.85 |
| Ellerkmann et al.62 | 23.11 | 23.58 |
| PONV | 1.62 | 1.62 |
| POCD | 0.00 | 0.00 |
| PTSD | 0.59 | 0.14 |
The QALY loss incurred by patients undergoing E-Entropy monitoring was slightly less than that of patients in the standard clinical monitoring group, giving an incremental QALY gain of 0.0003. This resulted in an ICER of £31,131 per QALY gained where the anaesthetic consumption from the Ellerkmann and colleagues RCT62 were applied, and £31,430 where anaesthetic consumption from Gruenewald and colleagues55 were applied.
The costs, QALY and ICER modelled for patients considered at high risk of intraoperative awareness undergoing mixed anaesthesia, comparing standard clinical monitoring with monitoring by E-Entropy are presented in Table 80.
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Standard clinical monitoring | 19.20 | −0.0011 | |||
| E-Entropy | 29.35 | 10.14 | −0.0006 | 0.0005 | 19,367 |
E-Entropy monitoring was modelled as being associated with 20.3 cases of awareness, compared with 45 cases among patients receiving standard clinical monitoring, in cohorts of 10,000 patients. This resulted in a reduction of 8.1 cases of LPS (from 14.7 to 6.6), which included a reduction of 4.4 cases of PTSD (from 8.0 to 3.6).
The costs of anaesthetic drugs in each group were the same, as shown in the breakdown of total cost in Table 81. Sufentanil costs are not included as it is not available in the UK and therefore the costs are not available in the BNF. Given the reduced incidence of awareness, and consequent reduction in cases of PTSD, costs for PTSD were lower in the group undergoing E-Entropy monitoring. The incremental cost of E-Entropy monitoring was £10.14.
| Cost | Standard clinical monitoring (£) | E-Entropy (£) |
|---|---|---|
| Depth of anaesthesia monitoring | 0.00 | 11.05 |
| Anaesthetic drugs | 15.93 | 15.93 |
| PONV | 1.62 | 1.62 |
| POCD | 0.00 | 0.00 |
| PTSD | 1.66 | 0.75 |
Again, each group incurred a QALY loss as a result of psychological sequelae such as LPS and PTSD, which resulted in an incremental QALY gain for E-Entropy patients of 0.0005. This yielded an ICER of £19,367 per QALY gained.
In a general surgical population E-Entropy monitoring was modelled as being associated with 7.2 cases of awareness, compared with 16 cases in patients receiving standard clinical monitoring, in cohorts of 10,000 patients. This resulted in a reduction of three cases of LPS (from 5.2 to 2.3), which included a reduction of 1.5 cases of PTSD (from 2.8 to 1.3). The costs, QALYs and ICER modelled for this population undergoing GA with both i.v. and inhaled anaesthetic, comparing standard clinical monitoring with monitoring by E-Entropy, are presented in Table 82.
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Standard clinical monitoring | 18.14 | −0.0007 | |||
| E-Entropy | 23.12 | 4.99 | −0.0004 | 0.0003 | 19,000 |
In a general surgical population undergoing mixed anaesthesia with sufentanil and sevoflurane, the costs of E-Entropy monitoring were higher, with an incremental cost of £4.99 (Table 83). Costs of anaesthetic drugs were lower in the E-Entropy arm, as were costs associated with PTSD, offsetting a proportion of the additional costs associated with depth of anaesthesia monitoring.
| Cost | Standard clinical monitoring (£) | E-Entropy (£) |
|---|---|---|
| Depth of anaesthesia monitoring | 0.00 | 9.87 |
| Anaesthetic drugs | 15.93 | 11.37 |
| PONV | 1.62 | 1.62 |
| POCD | 0.00 | 0.00 |
| PTSD | 0.59 | 0.27 |
The general surgical population accrued a slightly lower incremental QALY gain of 0.0003, which resulted in an ICER of £19,000 per QALY gained.
Deterministic sensitivity analysis
One-way sensitivity analyses of key parameters were undertaken in both the general surgical population and the high-risk surgical population undergoing general anaesthetic using TIVA. The results for the high-risk surgical population are shown in Table 84. Here the anaesthetic drug costs are based on Ellerkmann and colleagues' study. 62 As there is no expected reduction in drug use in this high-risk population, this assumption has no overall impact: anaesthetic drug costs are the same for both standard clinical monitoring and E-Entropy and therefore cancel out in the calculation of incremental cost and in the ICER.
| Parameter | Input value | Standard clinical monitoring | E-Entropy | Incremental | ICER (£/QALY gained) | |||
|---|---|---|---|---|---|---|---|---|
| Cost (£) | QALY | Cost (£) | QALY | Cost (£) | QALY | |||
| Probability awareness | 0.0006 | 24.95 | −0.0005 | 35.83 | −0.0003 | 10.88 | 0.0002 | 56,429 |
| 0.0119 | 29.11 | −0.0024 | 36.84 | −0.0008 | 7.73 | 0.0016 | 4834 | |
| Operating room awareness with depth of anaesthesia monitor | 0.1 | 26.38 | −0.0011 | 35.94 | −0.0004 | 9.56 | 0.0008 | 12,212 |
| 0.6 | 26.38 | −0.0011 | 36.77 | −0.0007 | 10.39 | 0.0004 | 25,169 | |
| Duration of LPS (years) | 0.25 | 26.38 | −0.0011 | 36.18 | −0.0005 | 9.79 | 0.0007 | 14,754 |
| 1 | 26.38 | −0.0012 | 36.18 | −0.0005 | 9.79 | 0.0007 | 13,799 | |
| Probability of LPSa | 0.195 | 25.72 | −0.0125 | 36.02 | −0.0121 | 10.30 | 0.0004 | 24,904 |
| 0.48 | 27.17 | −0.0302 | 36.37 | −0.0293 | 9.20 | 0.0008 | 10,880 | |
| Duration of PTSD (years) | 5.6 | 26.38 | −0.0010 | 36.18 | −0.0004 | 9.79 | 0.0006 | 17,666 |
| 9.6 | 26.38 | −0.0014 | 36.18 | −0.0005 | 9.79 | 0.0008 | 11,601 | |
| Proportion PTSDb | 0.345 | 25.78 | −0.0009 | 36.03 | −0.0004 | 10.25 | 0.0005 | 20,524 |
| 0.733 | 26.97 | −0.0014 | 36.32 | −0.0005 | 9.35 | 0.0009 | 10,958 | |
| LPS QoL decrement | −0.075 | 26.38 | −0.0011 | 36.18 | −0.0005 | 9.79 | 0.0007 | 14,669 |
| −0.05 | 26.38 | −0.0011 | 36.18 | −0.0005 | 9.79 | 0.0007 | 14,811 | |
| PTSD QoL decrement | −0.134 | 26.38 | −0.0012 | 36.18 | −0.0005 | 9.79 | 0.0007 | 13,217 |
| −0.068 | 26.38 | −0.0008 | 36.18 | −0.0004 | 9.79 | 0.0004 | 21,801 | |
| Probability people with PTSD seek treatment | 0 | 24.73 | −0.0011 | 35.78 | −0.0005 | 11.05 | 0.0007 | 16,274 |
| 1 | 29.60 | −0.0011 | 36.95 | −0.0005 | 7.35 | 0.0007 | 10,825 | |
| Unit cost of sensors (£) | 6.51 | 26.38 | −0.0011 | 34.01 | −0.0005 | 7.62 | 0.0007 | 11,226 |
| 10.85 | 26.38 | −0.0011 | 38.35 | −0.0005 | 11.96 | 0.0007 | 17,617 | |
The ICER resulting from the one-way sensitivity analysis in a high-risk population receiving TIVA ranged from £4834 to £56,429 per QALY gained. The ICER was insensitive to decreases in the LPS QoL decrement, and to the unit costs of sensors, but a decrease in the PTSD decrement pushed the ICER up to £21,801 per QALY gained from the base case of £14,421. The ICER appears driven by changes in the effectiveness of the E-Entropy module: where the relative risk of awareness is increased to 0.6, the ICER increases to £25,169 per QALY gained. Similarly, the ICER was very sensitive to changes in the probability of awareness. A decrease in this probability to 0.0006 increases the ICER substantially to £56,429 per QALY gained. Conversely, an increase in this probability to 0.0119 decreased the ICER to £4834 per QALY gained.
The results for the one-way sensitivity analyses in the general surgical population are shown in Table 85 (anaesthetic drug costs based on usage reported by Ellerkmann and colleagues62) and Table 86 (anaesthetic drug costs based on usage reported by Gruenewald and colleagues55).
| Parameter | Input value | Standard clinical monitoring | E-Entropy | Incremental | ICER (£/QALY gained) | |||
|---|---|---|---|---|---|---|---|---|
| Cost (£) | QALY | Cost (£) | QALY | Cost (£) | QALY | |||
| Proportional change in propofol use | −0.075 | 25.32 | −0.0007 | 32.85 | −0.0004 | 7.53 | 0.0003 | 23,712 |
| 0.174 | 25.32 | −0.0007 | 37.54 | −0.0004 | 12.22 | 0.0003 | 38,490 | |
| Proportional change in remifentanil | −0.232 | 25.32 | −0.0007 | 34.69 | −0.0004 | 9.37 | 0.0003 | 29,508 |
| 0.010 | 25.32 | −0.0007 | 35.72 | −0.0004 | 10.40 | 0.0003 | 32,754 | |
| Probability awareness | 0.0010 | 25.10 | −0.0006 | 35.15 | −0.0003 | 10.06 | 0.0002 | 41,419 |
| 0.0023 | 25.57 | −0.0008 | 35.27 | −0.0004 | 9.69 | 0.0004 | 23,936 | |
| Operating room awareness with depth of anaesthesia monitor | 0.1 | 25.32 | −0.0007 | 35.12 | −0.0003 | 9.80 | 0.0004 | 27,663 |
| 0.6 | 25.32 | −0.0007 | 35.42 | −0.0004 | 10.10 | 0.0002 | 45,292 | |
| Duration of LPS (years) | 0.25 | 25.32 | −0.0007 | 35.20 | −0.0004 | 9.89 | 0.0003 | 31,674 |
| 1 | 25.32 | −0.0007 | 35.20 | −0.0004 | 9.89 | 0.0003 | 30,099 | |
| Probability of LPSa | 0.195 | 25.08 | −0.0122 | 35.15 | −0.0120 | 10.07 | 0.0002 | 45,117 |
| 0.48 | 25.59 | −0.0295 | 35.27 | −0.0292 | 9.68 | 0.0004 | 25,678 | |
| Duration of PTSD (years) | 5.6 | 25.32 | −0.0006 | 35.20 | −0.0003 | 9.89 | 0.0003 | 36,186 |
| 9.6 | 25.32 | −0.0007 | 35.20 | −0.0004 | 9.89 | 0.0004 | 26,271 | |
| Proportion PTSDb | 0.345 | 25.10 | −0.0006 | 35.15 | −0.0003 | 10.05 | 0.0003 | 39,615 |
| 0.733 | 25.52 | −0.0008 | 35.25 | −0.0004 | 9.73 | 0.0004 | 25,633 | |
| LPS QoL decrement | −0.075 | 25.32 | −0.0007 | 35.20 | −0.0004 | 9.89 | 0.0003 | 31,536 |
| −0.05 | 25.32 | −0.0007 | 35.20 | −0.0004 | 9.89 | 0.0003 | 31,766 | |
| PTSD QoL decrement | −0.134 | 25.32 | −0.0007 | 35.20 | −0.0004 | 9.89 | 0.0003 | 29,112 |
| −0.068 | 25.32 | −0.0006 | 35.20 | −0.0003 | 9.89 | 0.0002 | 41,927 | |
| Probability people with PTSD seek treatment | 0 | 24.73 | −0.0007 | 35.06 | −0.0004 | 10.34 | 0.0003 | 32,540 |
| 1 | 26.46 | −0.0007 | 35.48 | −0.0004 | 9.02 | 0.0003 | 28,395 | |
| Unit cost of sensors (£) | 6.51 | 25.32 | −0.0007 | 33.03 | −0.0004 | 7.72 | 0.0003 | 24,298 |
| 10.85 | 25.32 | −0.0007 | 37.37 | −0.0004 | 12.06 | 0.0003 | 37,963 | |
| Parameter | Input value | Standard clinical monitoring | Entropy | Incremental | ICER (£/QALY gained) | |||
|---|---|---|---|---|---|---|---|---|
| Cost (£) | QALY | Cost (£) | QALY | Cost (£) | QALY | |||
| Proportional change in propofol use | −0.237 | 31.50 | −0.0007 | 40.19 | −0.0004 | 8.69 | 0.0003 | 27,364 |
| −0.058 | 31.50 | −0.0007 | 42.76 | −0.0004 | 11.26 | 0.0003 | 35,452 | |
| Proportional change in remifentanil | 0.085 | 31.50 | −0.0007 | 40.07 | −0.0004 | 8.58 | 0.0003 | 27,009 |
| 0.274 | 31.50 | −0.0007 | 42.90 | −0.0004 | 11.40 | 0.0003 | 35,899 | |
| Probability awareness | 0.001 | 31.28 | −0.0006 | 41.43 | −0.0003 | 10.15 | 0.0002 | 41,811 |
| 0.0023 | 31.75 | −0.0008 | 41.54 | −0.0004 | 9.79 | 0.0004 | 24,171 | |
| Operating room awareness with depth of anaesthesia monitor | 0.1 | 31.50 | −0.0007 | 41.40 | −0.0003 | 9.90 | 0.0004 | 27,932 |
| 0.6 | 31.50 | −0.0007 | 41.69 | −0.0004 | 10.19 | 0.0002 | 45,719 | |
| Duration of LPS (years) | 0.25 | 31.50 | −0.0007 | 41.48 | −0.0004 | 9.98 | 0.0003 | 31,979 |
| 1 | 31.50 | −0.0007 | 41.48 | −0.0004 | 9.98 | 0.0003 | 30,388 | |
| Probability of LPSa | 0.195 | 31.26 | −0.0122 | 41.42 | −0.0120 | 10.16 | 0.0002 | 45,544 |
| 0.48 | 31.77 | −0.0295 | 41.55 | −0.0292 | 9.77 | 0.0004 | 25,931 | |
| Duration of PTSD (years) | 5.6 | 31.50 | −0.0006 | 41.48 | −0.0003 | 9.98 | 0.0003 | 36,534 |
| 9.6 | 31.50 | −0.0007 | 41.48 | −0.0004 | 9.98 | 0.0004 | 26,524 | |
| Proportion PTSDb | 0.345 | 31.28 | −0.0006 | 41.43 | −0.0003 | 10.15 | 0.0003 | 39,990 |
| 0.733 | 31.70 | −0.0008 | 41.53 | −0.0004 | 9.82 | 0.0004 | 25,884 | |
| LPS QoL decrement | −0.075 | 31.50 | −0.0007 | 41.48 | −0.0004 | 9.98 | 0.0003 | 31,840 |
| −0.05 | 31.50 | −0.0007 | 41.48 | −0.0004 | 9.98 | 0.0003 | 32,072 | |
| PTSD QoL decrement | −0.134 | 31.50 | −0.0007 | 41.48 | −0.0004 | 9.98 | 0.0003 | 29,393 |
| −0.068 | 31.50 | −0.0006 | 41.48 | −0.0003 | 9.98 | 0.0002 | 42,331 | |
| Probability people with PTSD seek treatment | 0 | 30.91 | −0.0007 | 41.34 | −0.0004 | 10.43 | 0.0003 | 32,840 |
| 1 | 32.64 | −0.0007 | 41.75 | −0.0004 | 9.11 | 0.0003 | 28,695 | |
| Unit cost of sensors (£) | 6.51 | 31.50 | −0.0007 | 39.31 | −0.0004 | 7.81 | 0.0003 | 24,598 |
| 10.85 | 31.50 | −0.0007 | 43.65 | −0.0004 | 12.15 | 0.0003 | 38,263 | |
The one-way sensitivity analysis results in the general surgical population undergoing TIVA, and using costs applied from Ellerkmann and colleagues62 (Table 85) reflects those in the high-risk population. Again, the results are generally insensitive to changes in the duration of LPS, and the LPS QoL decrement. The greatest changes in ICERs were again generated as a result of changes in the probability of awareness (£23,936 per QALY gained, and £41,419 per QALY gained), a reduction in effectiveness of the E-Entropy module (£45,292 per QALY gained,) and the probability of LPS and a reduction in the PTSD QoL decrement.
Again, the one-way sensitivity analysis in the general surgical population receiving TIVA and applying costs from Gruenewald and colleagues55 (Table 86) reflect the results in the high-risk group. Whereas the ICER appears relatively insensitive to the changes in LPS QoL and LPS duration, the key parameters driving the results are a reduction in the probability of awareness, an increase in the relative risk of awareness with the E-Entropy module, a reduction in the probability of LPS and a reduction in the PTSD decrement applied.
One-way sensitivity analyses of key parameters were undertaken in both the general surgical population and the high-risk surgical population undergoing general anaesthetic using mixed anaesthesia [induction with i.v. anaesthetic (remifentanil) and maintenance with i.v. and inhaled anaesthetic (remifentanil and sevoflurane)]. The results are shown in Tables 87 and 88.
| Parameter | Input value | Standard clinical monitoring | E-Entropy | Incremental | ICER (£/QALY gained) | |||
|---|---|---|---|---|---|---|---|---|
| Cost (£) | QALY | Cost (£) | QALY | Cost (£) | QALY | |||
| Probability awareness | 0.0006 | 17.77 | −0.0005 | 28.70 | −0.0003 | 10.93 | 0.0002 | 63,483 |
| 0.0119 | 21.93 | −0.0024 | 30.58 | −0.0012 | 8.65 | 0.0012 | 7290 | |
| Operating room awareness with depth of anaesthesia monitor | 0.25 | 19.20 | −0.0011 | 29.01 | −0.0005 | 9.81 | 0.0007 | 14,605 |
| 0.81 | 19.20 | −0.0011 | 29.94 | −0.0009 | 10.74 | 0.0003 | 41,635 | |
| Duration of LPS (years) | 0.25 | 19.20 | −0.0011 | 29.35 | −0.0006 | 10.14 | 0.0005 | 19,785 |
| 1 | 19.20 | −0.0012 | 29.35 | −0.0006 | 10.14 | 0.0005 | 18,582 | |
| Probability of LPSa | 0.195 | 18.54 | −0.0125 | 29.04 | −0.0122 | 10.51 | 0.0003 | 31,680 |
| 0.48 | 19.99 | −0.0302 | 29.70 | −0.0295 | 9.71 | 0.0006 | 15,082 | |
| Duration of PTSD (years) | 5.6 | 19.20 | −0.0010 | 29.35 | −0.0006 | 10.14 | 0.0004 | 23,395 |
| 9.6 | 19.20 | −0.0014 | 29.35 | −0.0007 | 10.14 | 0.0006 | 15,771 | |
| Proportion PTSD | 0.345 | 18.60 | −0.0009 | 29.07 | −0.0005 | 10.47 | 0.0004 | 26,595 |
| 0.733 | 19.79 | −0.0014 | 29.61 | −0.0007 | 9.82 | 0.0006 | 15,119 | |
| LPS QoL decrement | −0.075 | 19.20 | −0.0011 | 29.35 | −0.0006 | 10.14 | 0.0005 | 19,679 |
| −0.05 | 19.20 | −0.0011 | 29.35 | −0.0006 | 10.14 | 0.0005 | 19,857 | |
| PTSD QoL decrement | −0.134 | 19.20 | −0.0012 | 29.35 | −0.0007 | 10.14 | 0.0006 | 17,843 |
| −0.068 | 19.20 | −0.0008 | 29.35 | −0.0005 | 10.14 | 0.0004 | 28,372 | |
| Probability people with PTSD seek treatment | 0 | 17.55 | −0.0011 | 28.60 | −0.0006 | 11.05 | 0.0005 | 21,104 |
| 1 | 22.42 | −0.0011 | 30.80 | −0.0006 | 8.38 | 0.0005 | 15,995 | |
| Unit cost of sensors (£) | 6.51 | 19.20 | −0.0011 | 27.18 | −0.0006 | 7.97 | 0.0005 | 15,223 |
| 10.85 | 19.20 | −0.0011 | 31.52 | −0.0006 | 12.31 | 0.0005 | 23,511 | |
| Parameter | Input value | Standard clinical monitoring | Entropy | Incremental | ICER (£/QALY gained) | |||
|---|---|---|---|---|---|---|---|---|
| Cost (£) | QALYs | Cost (£) | QALYs | Cost (£) | QALYs | |||
| Proportional change in sevoflurane | −0.492 | 18.14 | −0.0007 | 19.84 | −0.0004 | 1.70 | 0.0003 | 6494 |
| −0.079 | 18.14 | −0.0007 | 26.42 | −0.0004 | 8.28 | 0.0003 | 31,567 | |
| Probability awareness | 0.001 | 17.92 | −0.0006 | 23.02 | −0.0004 | 5.11 | 0.0002 | 24,521 |
| 0.0023 | 18.39 | −0.0008 | 23.24 | −0.0005 | 4.84 | 0.0003 | 14,881 | |
| Operating room awareness with depth of anaesthesia monitor | 0.25 | 18.14 | −0.0007 | 23.00 | −0.0004 | 4.87 | 0.0003 | 15,454 |
| 0.81 | 18.14 | −0.0007 | 23.33 | −0.0005 | 5.20 | 0.0002 | 30,967 | |
| Duration of LPS (years) | 0.25 | 18.14 | −0.0007 | 23.12 | −0.0004 | 4.99 | 0.0003 | 19,290 |
| 1 | 18.14 | −0.0007 | 23.12 | −0.0004 | 4.99 | 0.0003 | 18,446 | |
| Probability of LPSa | 0.195 | 17.90 | −0.0122 | 23.02 | −0.0121 | 5.12 | 0.0002 | 26,362 |
| 0.48 | 18.41 | −0.0295 | 23.25 | −0.0292 | 4.83 | 0.0003 | 15,833 | |
| Duration of PTSD (years) | 5.6 | 18.14 | −0.0006 | 23.12 | −0.0004 | 4.99 | 0.0002 | 21,648 |
| 9.6 | 18.14 | −0.0007 | 23.12 | −0.0004 | 4.99 | 0.0003 | 16,351 | |
| Proportion PTSDb | 0.345 | 17.92 | −0.0006 | 23.03 | −0.0004 | 5.10 | 0.0002 | 23,609 |
| 0.733 | 18.34 | −0.0008 | 23.22 | −0.0004 | 4.87 | 0.0003 | 15,856 | |
| LPS QoL decrement | −0.075 | 18.14 | −0.0007 | 23.12 | −0.0004 | 4.99 | 0.0003 | 19,216 |
| −0.05 | 18.14 | −0.0007 | 23.12 | −0.0004 | 4.99 | 0.0003 | 19,339 | |
| PTSD QoL decrement | −0.134 | 18.14 | −0.0007 | 23.12 | −0.0004 | 4.99 | 0.0003 | 17,912 |
| −0.068 | 18.14 | −0.0006 | 23.12 | −0.0004 | 4.99 | 0.0002 | 24,531 | |
| Probability people with PTSD seek treatment | 0 | 17.55 | −0.0007 | 22.86 | −0.0004 | 5.31 | 0.0003 | 20,234 |
| 1 | 19.28 | −0.0007 | 23.64 | −0.0004 | 4.36 | 0.0003 | 16,604 | |
| Unit cost of sensors (£) | 6.51 | 18.14 | −0.0007 | 20.95 | −0.0004 | 2.82 | 0.0003 | 10,730 |
| 10.85 | 18.14 | −0.0007 | 25.29 | −0.0004 | 7.16 | 0.0003 | 27,270 | |
The results of the one-way sensitivity analysis in high-risk patients receiving mixed anaesthesia reflect those in patients receiving TIVA. The ICER in a high-risk surgical group receiving mixed anaesthesia is very sensitive to both increase and decrease in the probability of awareness (Table 87), resulting in ICER of £7290 per QALY gained and £63,483 per QALY gained respectively. The ICER was also sensitive to increase in the relative risk of awareness with the E-Entropy module, giving £41,635 per QALY gained. Again, the ICER was sensitive to changes in the probability of LPS, a decrease in the probability of PTSD, and a decrease in the PTSD QoL decrement, while being insensitive to the LPS decrement and duration.
In the general surgical population the largest variation in the ICER from the base case of £19,000 per QALY gained was driven by proportional decreases in sevoflurane, resulting in ICER of £6494 per QALY gained and £31,567 per QALY gained. The remaining results reflect the sensitivity in other patient groups undergoing TIVA and mixed anaesthesia, but to a lesser extent. The decrease and increase in probability of awareness yielded ICERs of £14,881 per QALY gained and £24,521 per QALY gained respectively. Again, the ICER is sensitive to a decrease in the effectiveness of the E-Entropy module, which results in an ICER of £30,967 per QALY gained. Changes in the probability of LPS, of PTSD, a reduction in the QoL decrement for PTSD and the changes in the unit costs of sensors appear to drive the results in this group of patients.
Scenario analysis
The systematic review of patient outcomes did not identify any robust data that reported an estimate of the effect of E-Entropy monitoring on risk of PONV. We developed a scenario analysis using data from a meta-analysis by Liu,105 on the effectiveness of BIS on a range of outcomes including PONV, to investigate the potential impact of including this outcome on the cost-effectiveness results.
For this scenario analysis we assumed a baseline PONV risk of 30%,102–104 for standard clinical monitoring and applied the OR derived in the meta-analysis (0.77, 95% CI 0.56 to 0.99) to estimate risk for E-Entropy monitored patients. We assumed that all treatments (such as prophylaxis against PONV) were the same for each treatment group, and that all patients experiencing PONV were treated using 4 mg ondansetron by intramuscular or slow i.v. injection (unit cost = £5.39, BNF33).
Tables 89 and 90 report the results of this scenario analysis for high-risk patients and general surgical patients, respectively, undergoing GA with TIVA.
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| OR = 0.77: baseline risk = 0.3, risk with E-Entropy monitoring = 0.248 | |||||
| Standard clinical monitoring | 26.38 | −0.0011 | |||
| E-Entropy | 35.60 | 9.51 | −0.0005 | 0.0007 | 14,010 |
| OR = 0.56:a baseline risk = 0.3, risk with E-Entropy monitoring = 0.194 | |||||
| Standard clinical monitoring | 26.38 | −0.0011 | |||
| E-Entropy | 35.60 | 9.22 | −0.0005 | 0.0007 | 13,576 |
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Anaesthetic drug consumption based on Ellerkmann et al.62 | |||||
| OR = 0.77: baseline risk = 0.3, risk with E-Entropy monitoring = 0.248 | |||||
| Standard clinical monitoring | 25.32 | −0.0007 | |||
| E-Entropy | 34.92 | 9.61 | −0.0004 | 0.0003 | 30,250 |
| OR = 0.56: baseline risk = 0.3, risk with E-Entropy monitoring = 0.194 | |||||
| Standard clinical monitoring | 25.32 | −0.0007 | |||
| E-Entropy | 34.63 | 9.31 | −0.0004 | 0.0003 | 29,324 |
| Anaesthetic drug consumption based on Gruenewald et al.55 | |||||
| OR = 0.77: baseline risk = 0.3, risk with E-Entropy monitoring = 0.248 | |||||
| Standard clinical monitoring | 31.50 | −0.0007 | |||
| E-Entropy | 41.20 | 9.70 | −0.0004 | 0.0003 | 30,550 |
| OR = 0.56: baseline risk = 0.3, risk with E-Entropy monitoring = 0.194 | |||||
| Standard clinical monitoring | 31.50 | −0.0007 | |||
| E-Entropy | 40.90 | 9.41 | −0.0004 | 0.0003 | 29,624 |
The base-case ICER of £14,421 per QALY gained was insensitive to both changes in OR of PONV with E-Entropy monitoring. An OR of 0.77 applied to the baseline risk resulted in an ICER of £14,010 per QALY gained, whereas an OR of 0.56 resulted in an ICER of £13,576 per QALY gained.
Again, changes in the OR of PONV as a result of E-Entropy monitoring make little difference to the ICER in a general surgical population undergoing TIVA. The base-case ICER of £31,131 applying Ellerkmann and colleagues' anaesthetic consumption estimates, became £29,324 and £30,250 per QALY gained with ORs applied to the baseline risk of 0.56 and 0.77 respectively. Applying Gruenewald and colleagues' anaesthetic consumption estimates resulted in ICERs of £30,550 per QALY gained (OR 0.77) and £29,624 per QALY gained (OR 0.56).
Tables 91 and 92 report the results of this scenario analysis for patients at high risk and for patients at average risk of intraoperative awareness, respectively, undergoing GA with mixed anaesthesia (induction with i.v. anaesthetic and maintenance with i.v. and inhaled anaesthetic).
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| OR = 0.77: baseline risk = 0.3, risk with E-Entropy monitoring = 0.248 | |||||
| Standard clinical monitoring | 19.20 | −0.0011 | |||
| E-Entropy | 29.07 | 9.86 | −0.0006 | 0.0005 | 18,833 |
| OR = 0.56: baseline risk = 0.3, risk with E-Entropy monitoring = 0.194 | |||||
| Standard clinical monitoring | 19.20 | −0.0011 | |||
| E-Entropy | 28.77 | 9.57 | −0.0006 | 0.0005 | 18,271 |
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALYs | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| OR = 0.77: baseline risk = 0.3, risk with E-Entropy monitoring = 0.248 | |||||
| Standard clinical monitoring | 18.14 | −0.0007 | |||
| E-Entropy | 22.84 | 4.71 | −0.0004 | 0.0003 | 17,934 |
| OR = 0.56: baseline risk = 0.3, risk with E-Entropy monitoring = 0.194 | |||||
| Standard clinical monitoring | 18.14 | −0.0007 | |||
| E-Entropy | 22.55 | 4.41 | −0.0004 | 0.0003 | 16,813 |
Where the OR for PONV was changed to 0.77 and 0.56 in a high-risk population receiving mixed anaesthesia, the ICER reduced slightly, but was generally insensitive to the changes, which resulted in ICER of £18,833 and £18,271 per QALY gained respectively.
The changes in OR for PONV to 0.77 and 0.56 again resulted in a slightly larger reduction in the ICER in this scenario (in a general surgical population receiving mixed anaesthesia), to £17,934 per QALY gained and £16,813 per QALY gained respectively.
Our review of published studies of the incidence of intraoperative awareness identified substantial uncertainty over the estimated values. We used pooled values across identified studies in the base-case analysis. However, the value adopted for ‘high risk’ is lower than the 1% incidence cited in the publication reporting one of the included trials44 (based on incidences reported by Phillips and colleagues,138 Ranta and colleagues112 and Myles and colleagues79), and the pooled estimate adopted for a general surgical population excluded two outlying studies (one high and one low extreme value).
For this scenario analysis we replace the base-case estimate for probability of awareness in high-risk population (0.45%) with the higher value of 1% (Table 93). The effect of this is to reduce the ICER to £6059 per QALY gained for TIVA and to £8882 for mixed anaesthesia.
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| TIVA | |||||
| Standard clinical monitoring | 28.41 | −0.0021 | |||
| E-Entropy | 36.67 | 8.26 | −0.0007 | 0.0014 | 6059 |
| Mixed anaesthesia | |||||
| Standard clinical monitoring | 21.23 | −0.0021 | |||
| E-Entropy | 30.26 | 9.03 | −0.0010 | 0.0010 | 8882 |
For the general surgical population, we replaced the base-case estimate for probability of awareness (0.16%) with the extreme high and low values reported in the literature (0.99% and 0.007%, Tables 94 and 95).
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Anaesthetic drug consumption based on Ellerkmann et al.62 | |||||
| Baseline probability of awareness = 0.99% | |||||
| Standard clinical monitoring | 28.37 | −0.0020 | |||
| E-Entropy | 35.94 | 7.57 | −0.0007 | 0.0014 | 5605 |
| Baseline probability of awareness = 0.007% | |||||
| Standard clinical monitoring | 24.75 | −0.0004 | |||
| E-Entropy | 35.07 | 10.32 | −0.0003 | 0.0001 | 81,406 |
| Anaesthetic drug consumption based on Gruenewald et al.55 | |||||
| Baseline probability of awareness = 0.99% | |||||
| Standard clinical monitoring | 34.55 | −0.0020 | |||
| E-Entropy | 42.22 | 7.67 | −0.0007 | 0.0014 | 5676 |
| Baseline probability of awareness = 0.007% | |||||
| Standard clinical monitoring | 30.93 | −0.0004 | |||
| E-Entropy | 41.34 | 10.41 | −0.0003 | 0.0001 | 82,157 |
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Baseline probability of awareness = 0.99% | |||||
| Standard clinical monitoring | 21.19 | −0.0020 | |||
| E-Entropy | 24.51 | 3.31 | −0.0010 | 0.0010 | 3286 |
| Baseline probability of awareness = 0.007% | |||||
| Standard clinical monitoring | 17.57 | −0.0004 | |||
| E-Entropy | 22.87 | 5.30 | −0.0003 | 0.0001 | 42,599 |
The ICER was sensitive to changes in the probability of awareness, where the outlying values were adopted. In each case (where anaesthetic consumption estimates were applied from either Ellerkmann and colleagues62 or Gruenewald and colleagues55), these range from approximately £5600 per QALY gained to approximately £80,000 per QALY gained respectively.
In threshold analyses we found that depth of anaesthesia monitoring with E-Entropy for patients undergoing GA with TIVA was cost-effective if the probability of awareness was > 0.192–0.194%, at a willingness-to-pay threshold of £30,000 per QALY gained. Depth of anaesthesia monitoring with E-Entropy was cost-effective if the probability of awareness was > 0.315–0.318%, at a willingness-to-pay threshold of £20,000 per QALY gained. We report a range of values for the probability of awareness, as the exact values depend on which study the anaesthetic drug consumption is based (Ellerkmann and colleagues62 or Gruenewald and colleagues55).
The ICER is sensitive to a scenario where the outlying probabilities of awareness are applied in a general population undergoing mixed anaesthesia. Where the lower probability of 0.007 is applied, the ICER increases to £42,599 per QALY gained. Where the probability is set at 0.99%, the ICER decreases considerably to £3286.
In threshold analyses we found that depth of anaesthesia monitoring with E-Entropy for patients undergoing mixed GA was cost-effective if the probability of awareness was > 0.098%, at a willingness-to-pay threshold of £30,000 per QALY gained. The required probability, at a willingness-to-pay threshold of £20,000 per QALY gained, is 0.196%.
In order to apportion the capital cost of the depth of anaesthesia monitoring modules we required an estimate of the number of patients/cases in which the monitor module was used in each year (patients per device-year), throughout its assumed 5-year effective life. The estimate used for the general surgical population was 1000 patients per year (equivalent to four patients per day over 250 working days per year), based on discussion with clinical experts. This scenario analysis investigates the impact of this assumption on the estimated incremental cost associated with E-Entropy monitoring, compared with standard clinical monitoring, and the resulting effect on the ICER. Table 96 reports the incremental cost and ICER for E-Entropy compared with standard clinical monitoring at four selected values for the number of patients per device-year: the base-case value of 500 and also for a low value of 10 and high values of 1000 (four patients per day over 250 working days per year) and 1500 (six patients per day over 250 working days per year). This suggests that the assumed number of patients per device-year only has a substantial impact on incremental cost (hence on the ICER) at very low volumes.
| Patients per device-year | Standard clinical monitoring (£) | E-Entropy (£) | Incremental cost (£) | ICER (£/QALY gained |
|---|---|---|---|---|
| TIVA | ||||
| 100 | 25.32 | 45.87 | 20.56 | 64,720 |
| 500 | 25.32 | 36.39 | 11.07 | 34,863 |
| 1000 | 25.32 | 35.20 | 9.89 | 31,131 |
| 1500 | 25.32 | 34.81 | 9.49 | 29,887 |
| Mixed anaesthesia | ||||
| 100 | 18.14 | 33.79 | 15.65 | 59,657 |
| 500 | 18.14 | 24.31 | 6.17 | 23,517 |
| 1000 | 18.14 | 23.12 | 4.99 | 19,000 |
| 1500 | 18.14 | 22.73 | 4.59 | 17,494 |
The QoL decrement applied in the base case was based on Freed and colleagues'120 paper on veterans with PTSD. In order to investigate the impact of a sparse evidence base on HRQoL in a group of patients with PTSD, a scenario analyses was undertaken. The utility decrement was adjusted to 0.50 and 0.75 in high-risk and general surgical groups receiving either TIVA or mixed anaesthesia (Tables 97 and 98).
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| TIVA | |||||
| Utility decrement for PTSD = 0.50 | |||||
| Standard clinical monitoring | 26.38 | −0.0034 | |||
| E-Entropy | 36.18 | 9.79 | −0.0010 | 0.0024 | 4152 |
| Utility decrement for PTSD = 0.75 | |||||
| Standard clinical monitoring | 26.38 | −0.0048 | |||
| E-Entropy | 36.18 | 9.79 | −0.0014 | 0.0035 | 2827 |
| Mixed anaesthesia | |||||
| Utility decrement for PTSD = 0.50 | |||||
| Standard clinical monitoring | 19.20 | −0.0034 | |||
| E-Entropy | 29.35 | 10.14 | −0.0016 | 0.0017 | 5835 |
| Utility decrement for PTSD = 0.75 | |||||
| Standard clinical monitoring | 19.20 | −0.0048 | |||
| E-Entropy | 29.35 | 10.14 | −0.0023 | 0.0025 | 3997 |
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| TIVA | |||||
| Utility decrement for PTSD = 0.50 | |||||
| Standard clinical monitoring | 25.32 | −0.0015 | |||
| E-Entropy | 35.20 | 9.98 | −0.0005 | 0.0009 | 10,803 |
| Utility decrement for PTSD = 0.75 | |||||
| Standard clinical monitoring | 25.32 | −0.0020 | |||
| E-Entropy | 35.20 | 9.89 | −0.0007 | 0.00013 | 7556 |
| Mixed anaesthesia | |||||
| Utility decrement for PTSD = 0.50 | |||||
| Standard clinical monitoring | 18.14 | −0.0015 | |||
| E-Entropy | 23.12 | 4.99 | −0.0008 | 0.0007 | 7176 |
| Utility decrement for PTSD = 0.75 | |||||
| Standard clinical monitoring | 18.14 | −0.0020 | |||
| E-Entropy | 23.12 | 4.99 | −0.0010 | 0.0010 | 5091 |
The ICER was sensitive to these alternative scenarios in high-risk patients, both receiving TIVA and mixed anaesthesia. Where the PTSD decrement was increased to 0.5 in TIVA and mixed anaesthesia, the ICER reduced to £4152 per QALY gained and £5835 per QALY gained respectively. Where the PTSD decrement was increased further, the ICER decreased again to £2827 and £3997 per QALY gained in the TIVA and mixed anaesthesia groups respectively.
The scenario analyses using alternative PTSD decrements in the general population reflect the results in the high-risk population: there is a substantial reduction in the ICER where these are decreased.
Narcotrend compared with standard clinical monitoring
Base case
The costs, QALY and ICER modelled for patients considered at high risk of intraoperative awareness undergoing GA with TIVA, comparing standard clinical monitoring with depth of anaesthesia monitoring by Narcotrend are presented in Table 99.
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Standard clinical monitoring | 33.45 | −0.0011 | |||
| Narcotrend | 37.31 | 3.86 | −0.0005 | 0.0007 | 5681 |
Narcotrend monitoring was modelled as being associated with 10.8 cases of awareness, compared with 45 cases among patients receiving standard clinical monitoring, in a cohort of 10,000 patients. This results in a reduction of 11.1 cases of LPS (from 14.7 to 3.5), which includes a reduction of six cases of PTSD (from 8.0 to 1.9).
The cost of standard clinical monitoring during anaesthesia in high-risk patients was lower than for Narcotrend depth of anaesthesia monitoring, with the incremental cost being £3.86. The increased cost for Narcotrend monitoring is largely the result of the additional costs of the depth monitor (80% of the per patient cost) rather than the sensors attached to the patients (20% of the per patient cost). There is no reduction in anaesthetic costs associated with depth of anaesthesia monitoring, for this group of patients, although some of the additional cost of depth of anaesthesia monitoring is offset by reduced costs associated with psychological sequelae of awareness (Table 100).
| Cost | Standard clinical monitoring (£) | Narcotrend (£) |
|---|---|---|
| Depth of anaesthesia monitoring | 0.00 | 5.12 |
| Anaesthetic drugs | 30.18 | 30.18 |
| PONV | 1.62 | 1.62 |
| POCD | 0.00 | 0.00 |
| PTSD | 1.66 | 0.40 |
Patients in both groups incurred a slight QALY loss, resulting from psychological sequelae of awareness (LPS and PTSD) and from POCD in older patients. This was lower in the Narcotrend-monitored patients, with a difference of 0.0007 QALY, resulting in an ICER of £5681 per QALY gained.
The costs, QALY and ICER modelled for a general surgical population (not just those at high risk of intraoperative awareness) undergoing GA with TIVA, comparing standard clinical monitoring with depth of anaesthesia monitoring by Narcotrend are presented in Table 101.
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Standard clinical monitoring | 32.39 | −0.0007 | |||
| Narcotrend | 28.53 | −3.85 | −0.0004 | 0.0003 | Narcotrend dominates |
In the general surgical population, Narcotrend monitoring was modelled as being associated with 3.8 cases of awareness, compared with 16 cases in patients receiving standard clinical monitoring, in cohorts of 10,000 patients. This results in a reduction of four cases of LPS (from 5.2 to 1.3), which includes a reduction of 2.1 cases of PTSD (from 2.8 to 0.7).
In this patient population, depth of anaesthesia monitoring with Narcotrend is associated with lower costs than for standard clinical monitoring (see Table 101). This results from reduction in the use of anaesthetic drugs (and to a lesser extent with lower PTSD-related costs, because of the lower incidence of awareness), which offset the additional costs associated with depth of anaesthesia monitoring (Table 102).
| Cost | Standard clinical monitoring (£) | Narcotrend (£) |
|---|---|---|
| Depth of anaesthesia monitoring | 0.00 | 2.84 |
| Anaesthetic drugs | 30.18 | 23.94 |
| PONV | 1.62 | 1.62 |
| POCD | 0.00 | 0.00 |
| PTSD | 0.59 | 0.14 |
Given the lower probability of intraoperative awareness in this group of patients, the QALY losses for both standard clinical monitoring and Narcotrend monitoring, resulting from psychological sequelae of awareness (LPS and PTSD), are lower than for the high-risk group. The QALY loss arising from the LPS and PTSD following awareness and from POCD are lower for patients monitored with Narcotrend compared with those receiving standard clinical monitoring. As better outcomes are modelled as being achieved at lower costs, Narcotrend dominates standard clinical monitoring for this population.
The costs, QALY and ICER modelled for patients considered at high risk of intraoperative awareness undergoing mixed anaesthesia, comparing standard clinical monitoring with depth of anaesthesia monitoring by Narcotrend are presented in Table 103.
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALYs | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Standard clinical monitoring | 38.99 | −0.0011 | |||
| Narcotrend | 43.20 | 4.21 | −0.0006 | 0.0005 | 8033 |
Narcotrend monitoring is modelled as being associated with 20.3 cases of awareness, compared with 45 cases among patients receiving standard clinical monitoring, in cohorts of 10,000 patients. This results in a reduction of 8.1 cases of LPS (from 14.7 to 6.6), which includes a reduction of 4.4 cases of PTSD (from 8.0 to 3.6).
In a high-risk population receiving mixed anaesthesia, Narcotrend monitoring resulted in an incremental cost of £4.21. The increased costs in the Narcotrend group are associated with the depth of anaesthesia monitoring costs. Anaesthetic drug costs are the same in each group, but again the monitoring costs incurred by the Narcotrend group are, to an extent, offset by reduced costs associated with PTSD (see Table 104).
| Cost | Standard clinical monitoring (£) | Narcotrend (£) |
|---|---|---|
| Depth of anaesthesia monitoring | 0.00 | 5.12 |
| Anaesthetic drugs | 35.72 | 35.72 |
| PONV | 1.62 | 1.62 |
| POCD | 0.00 | 0.00 |
| PTSD | 1.66 | 0.75 |
The reduced QALY loss in high-risk patients undergoing monitoring with Narcotrend compared with patients undergoing standard monitoring occurred as a result of the lower probability of awareness in this group, with a difference of 0.0005 QALY. This resulted in an ICER of £8033 per QALY gained.
The costs, QALY and ICER modelled for a general surgical population (not just those at high risk of intraoperative awareness) undergoing mixed GA, comparing standard clinical monitoring with depth of anaesthesia monitoring by Narcotrend are presented in Table 105.
| Intervention | Cost | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Standard clinical monitoring | 37.93 | −0.0007 | |||
| Narcotrend | 36.18 | −1.74 | −0.0004 | 0.0003 | Narcotrend dominates |
Narcotrend monitoring was modelled as being associated with 7.2 cases of awareness, compared with 16 cases among patients receiving standard clinical monitoring, in cohorts of 10,000 patients. This results in a reduction of three cases of LPS (from 5.2 to 2.3), which includes a reduction of 1.5 cases of PTSD (from 2.8 to 1.3).
Narcotrend monitoring is associated with lower costs than for standard clinical monitoring in this patient population (Table 106). This arises from the relatively small additional cost of depth of anaesthesia monitoring with Narcotrend (the sensors are available at a low cost, whereas the capital cost of the monitor is spread across a relatively large patient throughput) and from savings because of a reduction in the use of anaesthetic drugs (and to a lesser extent with lower PTSD-related costs, because of the lower incidence of awareness).
| Cost | Standard clinical monitoring (£) | Narcotrend |
|---|---|---|
| Depth of anaesthesia monitoring | 0.00 | 2.84 |
| Anaesthetic drugs | 35.72 | 31.46 |
| PONV | 1.62 | 1.62 |
| POCD | 0.00 | 0.00 |
| PTSD | 0.59 | 0.27 |
As better outcomes are modelled as being achieved at lower costs, Narcotrend dominates standard clinical monitoring for this population.
Deterministic sensitivity analysis
One-way sensitivity analyses of key parameters were undertaken in both the general surgical population and the high-risk surgical population undergoing general anaesthetic using TIVA. The results are shown in Tables 107 and 108.
| Parameter | Input value | Standard clinical monitoring | Narcotrend | Incremental | ICER (£/QALY gained) | |||
|---|---|---|---|---|---|---|---|---|
| Cost (£) | QALY | Cost (£) | QALY | Cost (£) | QALY | |||
| Probability awareness | 0.0006 | 32.02 | −0.0005 | 36.97 | −0.0003 | 4.95 | 0.0002 | 25,656 |
| 0.0119 | 36.18 | −0.0024 | 37.97 | −0.0008 | 1.80 | 0.0016 | 1123 | |
| Operating room awareness with depth of anaesthesia monitor | 0.1 | 33.45 | −0.0011 | 37.08 | −0.0004 | 3.63 | 0.0008 | 4631 |
| 0.6 | 33.45 | −0.0011 | 37.91 | −0.0007 | 4.45 | 0.0004 | 10,792 | |
| Duration of LPS (years) | 0.25 | 33.45 | −0.0011 | 37.31 | −0.0005 | 3.86 | 0.0007 | 5812 |
| 1 | 33.45 | −0.0012 | 37.31 | −0.0005 | 3.86 | 0.0007 | 5436 | |
| Probability of LPSa | 0.195 | 32.79 | −0.0125 | 37.15 | −0.0121 | 4.36 | 0.0004 | 10,552 |
| 0.48 | 34.24 | −0.0302 | 37.50 | −0.0293 | 3.26 | 0.0008 | 3861 | |
| Duration of PTSD (years) | 5.6 | 33.45 | −0.0010 | 37.31 | −0.0004 | 3.86 | 0.0006 | 6959 |
| 9.6 | 33.45 | −0.0014 | 37.31 | −0.0005 | 3.86 | 0.0008 | 4570 | |
| Proportion PTSDb | 0.345 | 32.85 | −0.0009 | 37.17 | −0.0004 | 4.32 | 0.0005 | 8640 |
| 0.733 | 34.04 | −0.0014 | 37.45 | −0.0005 | 3.41 | 0.0009 | 4002 | |
| LPS QoL decrement | −0.075 | 33.45 | −0.0011 | 37.31 | −0.0005 | 3.86 | 0.0007 | 5779 |
| −0.05 | 33.45 | −0.0011 | 37.31 | −0.0005 | 3.86 | 0.0007 | 5835 | |
| PTSD QoL decrement | −0.134 | 33.45 | −0.0012 | 37.31 | −0.0005 | 3.86 | 0.0007 | 5207 |
| −0.068 | 33.45 | −0.0008 | 37.31 | −0.0004 | 3.86 | 0.0004 | 8589 | |
| Probability people with PTSD seek treatment | 0 | 31.80 | −0.0011 | 36.91 | −0.0005 | 5.12 | 0.0007 | 7534 |
| 1 | 36.67 | −0.0011 | 38.09 | −0.0005 | 1.42 | 0.0007 | 2085 | |
| Unit cost of sensors (£) | 0.42 | 33.45 | −0.0011 | 37.17 | −0.0005 | 3.72 | 0.0007 | 5475 |
| 0.70 | 33.45 | −0.0011 | 37.45 | −0.0005 | 4.00 | 0.0007 | 5887 | |
| Parameter | Input value | Standard clinical monitoring | Narcotrend | Incremental | ICER (£/QALY gained) | |||
|---|---|---|---|---|---|---|---|---|
| Cost (£) | QALY | Cost (£) | QALY | Cost (£) | QALY | |||
| Proportional change in propofol use | −0.429 | 32.39 | −0.0007 | 24.65 | −0.0004 | −7.73 | 0.0003 | Narcotrend dominates |
| −0.0155 | 32.39 | −0.0007 | 31.19 | −0.0004 | −1.20 | 0.0003 | ||
| Proportional change in remifentanil | −0.158 | 32.39 | −0.0007 | 27.41 | −0.0004 | −4.98 | 0.0003 | |
| 0.050 | 32.39 | −0.0007 | 29.65 | −0.0004 | −2.73 | 0.0003 | ||
| Probability awareness | 0.001 | 32.17 | −0.0006 | 28.48 | −0.0003 | −3.69 | 0.0002 | |
| 0.0023 | 32.64 | −0.0008 | 28.59 | −0.0004 | −4.05 | 0.0004 | ||
| Operating room awareness with depth of anaesthesia monitor | 0.1 | 32.39 | −0.0007 | 28.45 | −0.0003 | −3.94 | 0.0004 | |
| 0.6 | 32.39 | −0.0007 | 28.74 | −0.0004 | −3.64 | 0.0002 | ||
| Duration of LPS (years) | 0.25 | 32.39 | −0.0007 | 28.53 | −0.0004 | −3.85 | 0.0003 | |
| 1 | 32.39 | −0.0007 | 28.53 | −0.0004 | −3.85 | 0.0003 | ||
| Probability of LPSa | 0.195 | 32.15 | −0.0122 | 28.48 | −0.0120 | −3.67 | 0.0002 | |
| 0.48 | 32.66 | −0.0295 | 28.60 | −0.0292 | −4.07 | 0.0004 | ||
| Duration of PTSD (years) | 5.6 | 32.39 | −0.0006 | 28.53 | −0.0003 | −3.85 | 0.0003 | |
| 9.6 | 32.39 | −0.0007 | 28.53 | −0.0004 | −3.85 | 0.0004 | ||
| Proportion PTSDb | 0.345 | 32.17 | −0.0006 | 28.48 | −0.0003 | −3.69 | 0.0003 | |
| 0.733 | 32.59 | −0.0008 | 28.58 | −0.0004 | −4.01 | 0.0004 | ||
| LPS QoL decrement | −0.075 | 32.39 | −0.0007 | 28.53 | −0.0004 | −3.85 | 0.0003 | |
| −0.05 | 32.39 | −0.0007 | 28.53 | −0.0004 | −3.85 | 0.0003 | ||
| PTSD QoL decrement | −0.134 | 32.39 | −0.0007 | 28.53 | −0.0004 | −3.85 | 0.0003 | |
| −0.068 | 32.39 | −0.0006 | 28.53 | −0.0003 | −3.85 | 0.0002 | ||
| Probability people with PTSD seek treatment | 0 | 31.80 | −0.0007 | 28.39 | −0.0004 | −3.41 | 0.0003 | |
| 1 | 33.53 | −0.0007 | 28.81 | −0.0004 | −4.72 | 0.0003 | ||
| Unit cost of sensors (£) | 0.42 | 32.39 | −0.0007 | 28.39 | −0.0004 | −3.99 | 0.0003 | |
| 0.70 | 32.39 | −0.0007 | 28.67 | −0.0004 | −3.71 | 0.0003 | ||
The one-way sensitivity analysis of key parameters in the high-risk surgical group receiving TIVA resulted in ICER ranging from £1123 to £25,656 per QALY gained. However, the ICER appears robust to the majority of changes in parameters in this group. The ICER also increases where the probability of awareness, of LPS, and the PTSD decrements are reduced, and the relative risk of awareness increases.
The one-way sensitivity analysis of key parameters demonstrated that the ICER in the general surgical population is robust where these parameters are varied. In each case Narcotrend dominates standard clinical monitoring in the general surgical population receiving TIVA, by generating improved outcome at reduced cost.
One-way sensitivity analyses of key parameters were undertaken in both the general surgical population and the high-risk surgical population undergoing general anaesthetic using mixed anaesthesia [induction with i.v. anaesthetic (remifentanil) and maintenance with i.v. and inhaled anaesthetic (remifentanil and desflurane)]. The results are shown in Tables 109 and 110.
| Parameter | Input value | Standard clinical monitoring | Narcotrend | Incremental | ICER (£/QALY gained) | |||
|---|---|---|---|---|---|---|---|---|
| Cost (£) | QALY | Cost (£) | QALY | Cost (£) | QALY | |||
| Probability awareness | 0.0006 | 37.56 | −0.0005 | 42.55 | −0.0003 | 4.99 | 0.0002 | 29,010 |
| 0.0119 | 41.72 | −0.0024 | 44.44 | −0.0012 | 2.72 | 0.0012 | 2290 | |
| Operating room awareness with depth of anaesthesia monitor | 0.25 | 38.99 | −0.0011 | 42.87 | −0.0005 | 3.87 | 0.0007 | 5769 |
| 0.81 | 38.99 | −0.0011 | 43.80 | −0.0009 | 4.80 | 0.0003 | 18,621 | |
| Duration of LPS (years) | 0.25 | 38.99 | −0.0011 | 43.20 | −0.0006 | 4.21 | 0.0005 | 8206 |
| 1 | 38.99 | −0.0012 | 43.20 | −0.0006 | 4.21 | 0.0005 | 7707 | |
| Probability of LPSa | 0.195 | 38.33 | −0.0125 | 42.90 | −0.0122 | 4.57 | 0.0003 | 13,785 |
| 0.48 | 39.78 | −0.0302 | 43.55 | −0.0295 | 3.78 | 0.0006 | 5865 | |
| Duration of PTSD (years) | 5.6 | 38.99 | −0.0010 | 43.20 | −0.0006 | 4.21 | 0.0004 | 9704 |
| 9.6 | 38.99 | −0.0014 | 43.20 | −0.0007 | 4.21 | 0.0006 | 6542 | |
| Proportion PTSDb | 0.345 | 38.39 | −0.0009 | 42.93 | −0.0005 | 4.54 | 0.0004 | 11,522 |
| 0.733 | 39.58 | −0.0014 | 43.46 | −0.0007 | 3.89 | 0.0006 | 5982 | |
| LPS QoL decrement | −0.075 | 38.99 | −0.0011 | 43.20 | −0.0006 | 4.21 | 0.0005 | 8162 |
| −0.05 | 38.99 | −0.0011 | 43.20 | −0.0006 | 4.21 | 0.0005 | 8236 | |
| PTSD QoL decrement | −0.134 | 38.99 | −0.0012 | 43.20 | −0.0007 | 4.21 | 0.0006 | 7401 |
| −0.068 | 38.99 | −0.0008 | 43.20 | −0.0005 | 4.21 | 0.0004 | 11,768 | |
| Probability people with PTSD seek treatment | 0 | 37.34 | −0.0011 | 42.45 | −0.0006 | 5.12 | 0.0005 | 9770 |
| 1 | 42.21 | −0.0011 | 44.65 | −0.0006 | 2.44 | 0.0005 | 4661 | |
| Unit cost of sensors (£) | 0.42 | 38.99 | −0.0011 | 43.06 | −0.0006 | 4.07 | 0.0005 | 7766 |
| 0.70 | 38.99 | −0.0011 | 43.34 | −0.0006 | 4.35 | 0.0005 | 8300 | |
| Parameter | Input value | Standard clinical monitoring | Narcotrend | Incremental | ICER (£/QALY gained) | |||
|---|---|---|---|---|---|---|---|---|
| Cost (£) | QALY | Cost (£) | QALY | Cost | QALY | |||
| Proportional change in desflurane | −0.256 | 37.93 | −0.0007 | 33.77 | −0.0004 | −4.15 | 0.0003 | Narcotrend dominates |
| −0.056 | 37.93 | −0.0007 | 38.59 | −0.0004 | 0.66 | 0.0003 | 2534 | |
| Proportional change in remifentanil | −0.168 | 37.93 | −0.0007 | 34.73 | −0.0004 | −3.20 | 0.0003 | Narcotrend dominates |
| 0.081 | 37.93 | −0.0007 | 37.62 | −0.0004 | −0.30 | 0.0003 | ||
| Probability awareness | 0.001 | 37.71 | −0.0006 | 36.08 | −0.0004 | −1.62 | 0.0002 | |
| 0.0023 | 38.18 | −0.0008 | 36.30 | −0.0005 | −1.89 | 0.0003 | ||
| Operating room awareness with depth of anaesthesia monitor | 0.25 | 37.93 | −0.0007 | 36.06 | −0.0004 | −1.86 | 0.0003 | |
| 0.81 | 37.93 | −0.0007 | 36.39 | −0.0005 | −1.53 | 0.0002 | ||
| Duration of LPS (years) | 0.25 | 37.93 | −0.0007 | 36.18 | −0.0004 | −1.74 | 0.0003 | |
| 1 | 37.93 | −0.0007 | 36.18 | −0.0004 | −1.74 | 0.0003 | ||
| Probability of LPSa | 0.195 | 37.69 | −0.0122 | 36.08 | −0.0121 | −1.61 | 0.0002 | |
| 0.48 | 38.20 | −0.0295 | 36.31 | −0.0292 | −1.90 | 0.0003 | ||
| Duration of PTSD (years) | 5.6 | 37.93 | −0.0006 | 36.18 | −0.0004 | −1.74 | 0.0002 | |
| 9.6 | 37.93 | −0.0007 | 36.18 | −0.0004 | −1.74 | 0.0003 | ||
| Proportion PTSDb | 0.345 | 37.71 | −0.0006 | 36.09 | −0.0004 | −1.63 | 0.0002 | |
| 0.733 | 38.13 | −0.0008 | 36.28 | −0.0004 | −1.86 | 0.0003 | ||
| LPS QoL decrement | −0.075 | 37.93 | −0.0007 | 36.18 | −0.0004 | −1.74 | 0.0003 | |
| −0.05 | 37.93 | −0.0007 | 36.18 | −0.0004 | −1.74 | 0.0003 | ||
| PTSD QoL decrement | −0.134 | 37.93 | −0.0007 | 36.18 | −0.0004 | −1.74 | 0.0003 | |
| −0.068 | 37.93 | −0.0006 | 36.18 | −0.0004 | −1.74 | 0.0002 | ||
| Probability people with PTSD seek treatment | 0 | 37.34 | −0.0007 | 35.92 | −0.0004 | −1.42 | 0.0003 | |
| 1 | 39.07 | −0.0007 | 36.70 | −0.0004 | −2.37 | 0.0003 | ||
| Unit cost of sensors (£) | 0 | 37.93 | −0.0007 | 36.04 | −0.0004 | −1.88 | 0.0003 | |
| 1 | 37.93 | −0.0007 | 36.32 | −0.0004 | −1.60 | 0.0003 | ||
The results of the one way-sensitivity analysis in high-risk patients undergoing mixed anaesthesia range from £2290 to £29,010 per QALY gained. The ICER appears least sensitive to changes in the LPS decrement and most affected by the changes in probability of awareness to 0.0119 and 0.006, resulting in the lowest and highest ICERs of £2290 and £29,010 per QALY gained respectively. The results are also sensitive to the estimated effect of monitoring on the incidence of awareness, the proportion of patients with LPS who develop PTSD and to the size of utility decrement for PTSD.
The one-way sensitivity analysis suggests that the results in the general surgical population are generally robust to variation in key input parameters. The exception is the proportional change in use of desflurane. The upper limit of the 95% CI is close to zero, indicating only limited savings in cost of anaesthetic gas to offset against the cost of Narcotrend monitoring, resulting in a positive incremental cost.
Scenario analysis
The systematic review of patient outcomes did not identify any robust data that reported an estimate of the effect of Narcotrend monitoring on risk of PONV. We developed a scenario analysis using data from a meta-analysis by Liu,105 on the effectiveness of BIS on a range of outcomes including PONV, to investigate the potential impact of including this outcome on the cost-effectiveness results.
For this scenario analysis we assumed a baseline PONV risk of 30%,102–104 for standard clinical monitoring and applied the OR derived in the meta-analysis (0.77, 95% CI 0.56 to 0.99) to estimate risk for Narcotrend-monitored patients. We assumed that all treatments (such as prophylaxis against PONV) were the same for each treatment group, and that all patients experiencing PONV were treated using 4 mg ondansetron by intramuscular or slow i.v. injection (unit cost = £5.39; BNF33).
Tables 111 and 112 report the results of this scenario analysis for high-risk patients and general surgical patients, respectively, undergoing GA with TIVA.
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| OR = 0.77: baseline risk = 0.3, risk with Narcotrend monitoring = 0.248 | |||||
| Standard clinical care | 33.45 | −0.0011 | |||
| Narcotrend | 37.03 | 3.58 | −0.0005 | 0.0007 | 5270 |
| OR = 0.56: baseline risk = 0.3, risk with Narcotrend monitoring = 0.194 | |||||
| Standard clinical care | 33.45 | −0.0011 | |||
| Narcotrend | 36.74 | 3.28 | −0.0005 | 0.0007 | 4836 |
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| OR = 0.77: baseline risk = 0.3, risk with Narcotrend monitoring = 0.248 | |||||
| Standard clinical care | 32.39 | −0.0007 | |||
| Narcotrend | 28.25 | −4.13 | −0.0004 | 0.0003 | Narcotrend dominates |
| OR = 0.56: baseline risk = 0.3, risk with Narcotrend monitoring = 0.194 | |||||
| Standard clinical care | 32.39 | −0.0007 | |||
| Narcotrend | 27.96 | −4.13 | −0.0004 | 0.0003 | Narcotrend dominates |
Variation in the OR of PONV applied in the model does not have an impact on the ICER, either in the case of the high-risk population (Table 111) or in the general surgical population (Table 112) undergoing TIVA.
Tables 113 and 114 report the results of this scenario analysis for patients at high risk and for patients at average risk of intraoperative awareness, respectively, undergoing GA with mixed anaesthesia (induction with i.v. anaesthetic and maintenance with i.v. and inhaled anaesthetic).
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| OR = 0.77: baseline risk = 0.3, risk with Narcotrend monitoring = 0.248 | |||||
| Standard clinical care | 38.99 | −0.0011 | |||
| Narcotrend | 42.92 | 3.93 | −0.0006 | 0.0005 | 7499 |
| OR = 0.56: baseline risk = 0.3, risk with Narcotrend monitoring = 0.194 | |||||
| Standard clinical care | 38.99 | −0.0011 | |||
| Narcotrend | 42.63 | 3.63 | −0.0006 | 0.0005 | 6937 |
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| OR = 0.77: baseline risk = 0.3, risk with Narcotrend monitoring = 0.248 | |||||
| Standard clinical care | 37.93 | −2.02 | −0.0007 | 0.0003 | Narcotrend dominates |
| Narcotrend | 35.90 | −0.0004 | |||
| OR = 0.56: baseline risk = 0.3, risk with Narcotrend monitoring = 0.194 | |||||
| Standard clinical care | 37.93 | −2.32 | −0.0007 | 0.0003 | Narcotrend dominates |
| Narcotrend | 35.61 | −0.0004 | |||
Where the variations in the OR of PONV are applied to the high-risk patients undergoing mixed anaesthesia there is a slight reduction in the ICER. An OR of 0.77 results in an ICER of £7499 per QALY gained and an OR of 0.56 yields an ICER of £6937 per QALY gained in this group.
In the case of the general risk group receiving mixed anaesthesia, the ICER is robust to the variation in risk of PONV, and Narcotrend continues to dominate.
Our review of published studies of the incidence of intraoperative awareness identified substantial uncertainty over the estimated values. We used pooled values across identified studies in the base-case analysis. However, the value adopted for ‘high risk’ is lower than the 1% incidence cited in the publication reporting one of the included trials44 (based on incidences reported by Phillips and colleagues,138 Ranta and colleagues112 and Myles and colleagues79), and the pooled estimate adopted for a general surgical population excluded two outlying studies (one high and one low extreme value).
For this scenario analysis we replace the base-case estimate for probability of awareness in high-risk population (0.45%) with the higher value of 1% (Table 115).
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| TIVA | |||||
| Standard clinical care | 35.48 | −0.0021 | |||
| Narcotrend | 37.80 | 2.32 | −0.0007 | 0.0014 | 1705 |
| Mixed anaesthesia | |||||
| Standard clinical care | 41.02 | −0.0021 | |||
| Narcotrend | 44.12 | 3.10 | −0.0010 | 0.0010 | 3047 |
The ICERs decrease substantially in the high-risk population receiving either TIVA or mixed anaesthesia, where the probability of awareness is set to 1%, from £8033 to £3047 per QALY gained in the group receiving mixed, and from £5681 to £1705 in the group receiving TIVA.
In the general surgical population, we replace the base-case estimate for probability of awareness (0.16%) with the extreme high and low values reported in the literature (0.99% and 0.007%, Tables 116 and 117).
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Baseline probability of awareness = 0.99% | |||||
| Standard clinical care | 35.44 | −0.0020 | Narcotrend dominates | ||
| Narcotrend | 29.27 | −6.17 | −0.0007 | −0.0014 | |
| Baseline probability of awareness = 0.007% | |||||
| Standard clinical care | 31.82 | −0.0004 | Narcotrend dominates | ||
| Narcotrend | 28.40 | −3.43 | −0.0003 | 0.0001 | |
| Intervention | Cost per patient (£) | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| Baseline probability of awareness = 0.99% | |||||
| Standard clinical care | 40.98 | −0.0020 | |||
| Narcotrend | 37.57 | −3.42 | −0.0010 | 0.0010 | Narcotrend dominates |
| Baseline probability of awareness = 0.007% | |||||
| Standard clinical care | 37.36 | −0.0004 | |||
| Narcotrend | 35.93 | −1.43 | −0.0003 | 0.0001 | Narcotrend dominates |
Where the outlying probabilities are applied the ICER is robust and Narcotrend continues to dominate in TIVA and mixed anaesthesia patients.
In order to apportion the capital cost of the depth of anaesthesia monitoring modules, we required an estimate of the number of patients/cases in which the monitor module was used in each year (patients per device-year), throughout its assumed 5-year effective life. The estimate used for the general surgical population was 1000 patients per year (equivalent to four patients per day over 250 working days per year), which was based on discussion with clinical experts. This scenario analysis investigates the impact of this assumption on the estimated incremental cost associated with Narcotrend monitoring, compared with standard clinical monitoring, and the resulting effect on the ICER. Table 118 reports the incremental cost and ICER for Narcotrend compared with standard clinical monitoring, at four selected values for the number of patients per device-year: the basecase value of 1000 and also for a low value of 10, intermediate value of 500 and a high value of 1500 (six patients per day over 250 working days per year). This suggests that the assumed number of patients per device-year only has a substantial impact on incremental cost (hence on the ICER) at very low throughput.
| Patients per device-year | Standard clinical monitoring (£) | Narcotrend (£) | Incremental cost (£) | ICER (£/QALY gained |
|---|---|---|---|---|
| TIVA | ||||
| 100 | 32.39 | 49.03 | 16.65 | 52,414 |
| 500 | 32.39 | 30.81 | −1.58 | Narcotrend dominates |
| 1000 | 32.39 | 28.53 | −3.85 | Narcotrend dominates |
| 1500 | 32.39 | 27.7 | −4.61 | Narcotrend dominates |
| Mixed anaesthesia | ||||
| 100 | 37.93 | 26.68 | 18.76 | 71,484 |
| 500 | 37.93 | 38.46 | 0.53 | 2035 |
| 1000 | 37.93 | 36.18 | −1.74 | Narcotrend dominates |
| 1500 | 37.93 | 35.42 | −2.50 | Narcotrend dominates |
The QoL decrement applied in the base case was based on Freed and colleagues'120 paper on veterans with PTSD. In order to investigate the impact of a sparse evidence base on HRQoL in a group of patients with PTSD, a scenario analysis was undertaken. The utility decrement was adjusted to 0.50 and 0.75 in high-risk and general surgical groups receiving either TIVA (Table 119) or mixed anaesthesia (Table 120).
| Intervention | Cost | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| TIVA | |||||
| Utility decrement for PTSD = 0.50 | |||||
| Standard clinical care | 33.45 | −0.0034 | |||
| Narcotrend | 37.31 | 3.86 | −0.0010 | 0.0024 | 1636 |
| Utility decrement for PTSD = 0.75 | |||||
| Standard clinical care | 33.45 | −0.0048 | |||
| Narcotrend | 37.31 | 3.86 | −0.0014 | 0.0035 | 1114 |
| Mixed anaesthesia | |||||
| Utility decrement for PTSD = 0.50 | |||||
| Standard clinical care | 38.99 | −0.0034 | |||
| Narcotrend | 43.20 | 4.21 | −0.0016 | 0.0017 | 2420 |
| Utility decrement for PTSD = 0.75 | |||||
| Standard clinical care | 38.99 | −0.0048 | |||
| Narcotrend | 43.20 | 4.21 | −0.0023 | 0.0025 | 1658 |
| Intervention | Cost | Incremental cost (£) | QALY | Incremental QALY | ICER (£/QALY gained) |
|---|---|---|---|---|---|
| TIVA | |||||
| Utility decrement for PTSD = 0.50 | |||||
| Standard clinical care | 32.39 | −0.0015 | Narcotrend dominates | ||
| Narcotrend | 28.53 | −3.85 | −0.0005 | 0.0009 | |
| Utility decrement for PTSD = 0.75 | |||||
| Standard clinical care | 32.39 | −0.0020 | Narcotrend dominates | ||
| Narcotrend | 28.53 | −3.85 | −0.0007 | 0.0013 | |
| Mixed anaesthesia | |||||
| Utility decrement for PTSD = 0.50 | |||||
| Standard clinical care | 37.93 | −0.0015 | Narcotrend dominates | ||
| Narcotrend | 36.18 | −1.74 | −0.0008 | 0.0007 | |
| Utility decrement for PTSD = 0.75 | |||||
| Standard clinical care | 37.93 | −0.0020 | Narcotrend dominates | ||
| Narcotrend | 36.18 | −1.74 | −0.0010 | 0.0010 | |
The ICER is substantially reduced in the high-risk surgical population where higher decrements for PTSD QoL are applied (see Table 119). These are reduced to £1636 and £1114 per QALY gained for a 0.5 and 0.75 decrement, respectively, in the group undergoing TIVA. The ICER is reduced to £2420 and £1658 for a 0.5 and 0.75 decrement in the group undergoing mixed anaesthesia.
Where the alternative values for PTSD decrement are applied for the general surgical population in both the TIVA and mixed anaesthesia groups, Narcotrend continues to dominate (see Table 120).
Cost-effectiveness summary
We have presented modelled cost-effectiveness analyses for BIS, E-Entropy and Narcotrend compared with standard clinical monitoring, for two modes of anaesthetic administration. There is substantial uncertainty associated with the analysis, given the weakness of the evidence base for the majority of outcomes included in the model. No robust evidence was identified on the effectiveness of E-Entropy or Narcotrend in avoiding intraoperative awareness or POCD and, in the absence of such evidence, we have assumed that the effect estimates derived for BIS can be applied. However, even in the case of BIS the evidence base is currently severely lacking. There is also limited evidence on the baseline incidence of anaesthetic complications included in the model. There is more evidence on the benefit in terms of reduced anaesthetic drug consumption, although for some technologies the evidence is inconclusive.
Overall the economic evaluation indicates that, for general surgical patients, some of the additional costs of depth of anaesthesia monitoring may be offset by reduction in consumption of anaesthetic drugs. However, the size of these savings may not fully offset the additional cost. Given the comparative rarity of awareness, cost-savings through the avoidance of PTSD are unlikely to offset the additional costs. However, avoidance of the psychological sequelae of awareness yields gains in outcome that, depending on the utility losses associated with these conditions, may be acceptable in cost-effectiveness terms. The economic analysis suggests that, other than at comparatively low patient volumes, the acquisition cost of the DoA modules may be less significant in determining cost-effectiveness than the cost of consumables – in particular the sensors attached to the patient. Other key determinants of the cost-effectiveness of depth of anaesthesia monitoring appear to be the baseline risk of awareness and, unsurprisingly, the effect size in terms of avoiding awareness.
Chapter 4 Assessment of factors relevant to the NHS and other parties
Few of the trials included in this report reported whether or not anaesthetists had received training in use of the EEG devices. In their evidence submissions to NICE, the manufacturers of the three EEG devices assessed suggested varying lengths of training necessary, from 30 minutes' instruction in placing of the sensors for the E-Entropy module, to a whole day of lecture and training for Narcotrend in the operating theatre. The manufacturer of BIS suggests no additional training is necessary, but that a modest amount of additional training further enhances safe and effective use. Expert clinical opinion suggests that it is relatively straightforward to learn how to attach sensors and interpret the device values, but also that some training may be of benefit. In terms of cost implications, training would be provided for free by the manufacturer in the operating theatre, and/or anaesthetists would be able to access education materials including online multimedia courses. The main cost would therefore be for the operating theatre and the anaesthetist's time. Once a device has been installed and any initial training given, anaesthetists would need a period of time to become accustomed to using the device in practice.
The long-term impact of intraoperative awareness can have a profound impact on the health and well-being of patients. Psychological symptoms7 such as disturbed sleep, phobias, depression, anxiety and PTSD may limit daily activities including their ability to work, resulting in periods of sickness absence and with consequent financial implications for employers. In extreme cases patients may have to cease working altogether and therefore their financial livelihood will be significantly impaired, and they may become reliant on welfare services. There may also be knock-on effects on patients' families and friends, for example, to provide social, emotional and practical support. Strain may be placed on marriages and partnerships, leading to separation in more severe cases. Patients may seek treatment for their symptoms which will involve primary and community care services (e.g. to provide counselling and/or medication) and in some cases secondary care (e.g. psychiatric supervision).
Chapter 5 Discussion
Statement of principal findings
Systematic review of patient outcomes
The eligible evidence base for BIS-guided anaesthesia (11 RCTs, plus 31 RCTs included in the Cochrane BIS review34) is larger than that for entropy-guided or Narcotrend-guided anaesthesia (seven and four RCTs respectively). A notable feature of the primary studies within each of the BIS, E-Entropy and Narcotrend technologies is that very few RCTs were methodologically similar to one another, which in most cases precluded the pooling of outcomes across studies.
Explicit intraoperative awareness
The effect estimate for intraoperative awareness in the Cochrane BIS review34 was updated using data from two recent large RCTs. One of these was the BAG-RECALL RCT by Avidan and colleagues,44 which compared BIS monitoring with monitoring of end-tidal anaesthetic agent concentration. The trial, which took place across three centres in the USA and Canada, randomised at least 3020 patients per study group, and patients received only inhaled GA. The RCT by Zhang and colleagues40 also recruited large numbers of patients (around 5000) but was conducted in China across 13 centres, and patients received TIVA, rather than inhaled anaesthesia. BIS-guided TIVA was compared against routine TIVA (no further details given). Both trials were statistically powered to detect explicit intraoperative awareness in patients considered to be at higher risk. The trials reported contrasting findings, with Avidan and colleagues44 noting a higher but non-statistically significant incidence of definite awareness in BIS-monitored patients, and Zhang and colleagues40 finding a statistically significantly lower incidence of confirmed awareness in patients monitored with BIS.
When both of these trials were added to the Cochrane meta-analysis the pooled Peto's OR remained statistically significant 0.45 (95% CI 0.25 to 0.81), favouring BIS, though with significant heterogeneity. We classified the trials into subgroups based on the type of GA used (inhaled only; mixed inhaled and i.v.; total i.v.). The pooled Peto's OR for the subgroups of mixed inhaled and i.v. GA, and TIVA were both consistent with the overall pooled OR (i.e. statistically significant in favour of BIS). In contrast, the pooled estimate for the trials of inhaled GA, including the BAG-RECALL RCT44 and another large RCT (the B-Unaware trial27), favoured standard clinical monitoring although the confidence intervals overlapped with 1 indicating potential advantage to both BIS and to standard clinical monitoring. Importantly the BAG-RECALL RCT44 was designed to overcome some of the methodological limitations of the B-Unaware trial,27 such as use of a larger sample of patients, more than one centre, and use of only major risk factors for awareness. It is not fully clear why the results of this trial were contrary to expectation. Notably these trials compared a structured BIS protocol with a structured ETAC protocol, comprising target anaesthetic concentration-linked audible alarms, staff education and checklists. The comparators reported in the other trials in the meta-analysis did not report use of structured protocols.
The remaining trials that reported intraoperative awareness either assessed this as a main outcome (one RCT on BIS49) or as a secondary outcome (three RCTs on BIS,48,51,62 six of the seven RCTs on entropy,54,55,57,58,61,62 and all four of the RCTs on Narcotrend59,60,63,64). Although the RCT by Kerssens and colleagues49 specified that intraoperative awareness was the main outcome, the authors reported that the study was not powered statistically for this outcome. None of the remaining studies reported whether or not it was powered statistically for detecting a clinically meaningful difference in intraoperative awareness. In these RCTs the sample sizes ranged from 10 to 160 patients per study group, which most likely would be insufficient for detecting clinically meaningful differences in intraoperative awareness, given the low incidence of this event (see Table 1 in Incidence of intraoperative awareness). Only two of these RCTs reported cases of intraoperative awareness, both in adult populations, but did not test differences between the study groups statistically. Kerssens and colleagues49 reported that incidence rates in BIS-guided and standard clinical monitoring groups were 2.9% (2/67) and 1.6% (1/61) respectively. Gruenewald and colleagues55 reported that incidence rates of intraoperative awareness in entropy-guided and standard clinical practice groups were 0% (0/37) and 2.9% (1/35) respectively. These incidence rates are relatively high compared with those estimated from much larger studies (see Table 1), although in the Gruenewald study awareness was experienced by only one patient. 55
The case of awareness reported by Gruenewald and colleagues55 might have happened outside of the period of GA, as patients were asked if they had any memory or awareness during different stages of their procedure, including in the ward, induction room, during surgery or extubation, or in the recovery room. 55 The reason for the relatively high incidence of awareness observed in the Kerssens study49 is not clear. Although Kerssens and colleagues49 did not specify that their patients were at risk of awareness, the patients did appear to be relatively old (early 60s), possibly overweight or obese, and half of them had notable illness (ASA physical score grade III). The awareness assessment conducted by Kerssens and colleagues49 involved asking patients five questions that were very similar to those of the Brice interview. Both of these RCTs49,55 stated that their outcome assessors were blinded to the study group. Assessment of awareness in these RCTs took place 6 hours49 or 24 hours55 after surgery, without any longer-term follow-up. In fact, only the large trial by Avidan and colleagues44 conducted follow-up assessments longer than 3 days after surgery (30 days after extubation); all other trials that assessed intraoperative awareness conducted follow-up assessments only 1 day or less post surgery,54,57,59,60 3 days post surgery48,58,61–64 or did not state when follow-up occurred. 51 As occurrences of intraoperative awareness may take time to develop (see Incidence of intraoperative awareness), these follow-up periods may have been too short for detecting all cases of awareness.
Weighing up the strengths and limitations of the studies, an appropriate conclusion would be that, in patients considered to be at increased risk of awareness, BIS monitoring is associated with a reduced likelihood of explicit intraoperative awareness. However, this may not be applicable where inhaled GA is solely used. There is no evidence that EEG device-titrated anaesthesia significantly affects incidence of explicit intraoperative awareness in surgical patients not considered to be at increased risk, primarily as trials large enough to detect awareness have not been conducted.
Implicit intraoperative awareness
Implicit awareness (i.e. awareness that the patient does not necessarily recall experiencing) was reported only in one BIS trial, as a secondary outcome. 49 The assessment involved presenting patients audibly with words during anaesthesia then conducting specialist word recall tests after recovery from anaesthesia. The results showed that only patients in the BIS group selected target words more often than distractor words, and that patients in the BIS group selected target words more often than in the standard clinical monitoring group. Although appearing to indicate implicit intraoperative awareness, these findings would only have clinical relevance if the patients were followed up and found to have related clinical sequelae. Such follow-up has not been done and, in general, the possible longer-term implications for patients of implicit intraoperative awareness are not well understood.
Sequelae and long-term consequences of intraoperative awareness
None of the trials reported longer-term detrimental impacts of awareness such as PTSD. The BAG RECALL trial by Avidan and colleagues44 reported patient distress and sequelae associated with awareness as a post hoc secondary outcome, based on the Michigan Awareness Classification Instrument, in which distress related to intraoperative awareness includes reports of fear, anxiety, suffocation, a sense of doom or a sense of impending death. Avidan and colleagues44 found a higher percentage of distress in the BIS-monitored group (0.28% compared with 0.04%), but no statistically significant difference between the groups. No other trials included in the systematic review assessed patients' distress, anxiety or depression.
Anaesthetic consumption
The RCTs that reported anaesthesia consumption as an outcome can be summarised in various ways, as they differed in their populations (adults or children) anaesthesia (volatile or i.v.), sample sizes, and the methods used to measure anaesthetic consumption. The specific details of the outcomes summarised in the table can be obtained from Table 9 (BIS), Table 17 (E-Entropy) and Table 24 (Narcotrend) in Results of systematic review of patient outcomes of this report.
Anaesthetic consumption was a statistically powered outcome in four RCTs: for sevoflurane in adults,61 propofol in adults,62 sevoflurane in children54 and propofol in children. 46 The outcomes were powered to detect either a 20% reduction in anaesthetic consumption46,54,62 or a 50% reduction. 61 A further RCT on adults specified sevoflurane as the main outcome but the outcome was not powered statistically. 58 The statistically powered RCT reported significant reductions of sevoflurane consumption under entropy-guided anaesthesia relative to standard clinical monitoring (i.e. favouring the E-Entropy group) in both adults61 and children,54 but no difference in propofol consumption between BIS, E-Entropy and standard clinical monitoring groups in adults. 62 However, the last trial62 has high risk of bias because of an imbalance in the patient attrition between the study groups (see Quantity and quality of research available). The one trial that was powered to detect clinically relevant differences in propofol consumption in children46 did not report a statistical comparison between the study groups, but in this trial, by Bhardwaj and colleagues,46 the propofol consumption rate was higher in the BIS-guided than the standard clinical monitoring group (see Table 9). Overall, the findings from the statistically powered RCT indicate that E-Entropy-guided and BIS-guided anaesthesia reduce the consumption of sevoflurane but not propofol in both adults and children, although it should be noted that the methods used to assess anaesthesia consumption differed between the studies. None of the trials of Narcotrend were statistically powered to detect differences in anaesthetic consumption.
The remaining trials were not specifically powered to detect differences in anaesthetic consumption but their findings for sevoflurane consumption are similar to those of the powered trials. Three RCTs that assessed sevoflurane consumption in adults found that consumption was significantly lower in the BIS-guided group45,49 or E-Entropy-guided group58 than under standard clinical monitoring. Two RCTs that assessed sevoflurane in children also found consumption to be lower in the BIS group51 or E-Entropy group. 54 In contrast with the statistically powered trials, most of the trials that assessed consumption of propofol as a secondary outcome, which were all on adult populations, reported significant differences in consumption in favour of the EEG-guided anaesthesia group. These differences were reported for E-Entropy-guided anaesthesia55,139 and Narcotrend-guided anaesthesia,59,60,63 whereas one RCT on BIS-guided anaesthesia reported a reduced propofol consumption in the BIS group but without an indication of statistical significance. 47
Two RCTs assessed the consumption of other anaesthetics as secondary outcomes. These were desflurane consumption in adults64 and isoflurane consumption in children. 56 These trials found that EEG-guided anaesthesia significantly reduced consumption, either using Narcotrend monitoring in adults64 or E-Entropy monitoring in children. 56
It was possible to update effect estimates for anaesthetic consumption in the Cochrane review34 for volatile anaesthesia (sevoflurane) using data from a RCT by Kerssens and colleagues,49 and for TIVA (propofol) using data from a RCT by Ellerkmann and colleagues. 62 For both types of anaesthesia, the updated effect estimate (mean difference) remained statistically significantly different from zero and in favour of the BIS group. However, heterogeneity was statistically significant even when using a random-effects model.
Time to recovery from anaesthesia
Recovery from anaesthesia was assessed in several different ways. The most frequent measurements reported were time to eye opening (11 RCTs) and time to extubation (11 RCTs).
Other recovery outcomes that were assessed included time to arrival in the PACU (five RCTs); duration of stay in the PACU (two RCTs); time to discharge from the PACU (five RCTs); time to response to commands (three RCTs) time to recovery of orientation (three RCTs); time to first movement response (two RCTs); time to recovery based on recovery scores (two RCTs); time to spontaneous breathing (one RCT); time to laryngeal mask airway removal (one RCT); and time to phonation (one RCT). ‘PACU stay’ was an outcome in the Cochrane review34 but does not appear to distinguish between PACU admissions, stay and discharge times. For this reason the Cochrane review meta-analysis was not updated with data from the RCTs identified in the current review.
Time to eye opening
Four of the 11 RCTs that assessed this outcome were powered statistically to detect a difference between the study groups of 1.5 minutes,64 3 minutes55,63 or 5 minutes. 56 Two of these powered trials detected a statistically significant difference in time to eye opening56,63 and two did not. 55,64 Among the remaining seven RCTs46,48,51,54,57,61,62 that were not specifically powered for this outcome, one57 detected a significant difference between the study groups in time to eye opening and six46,48,51,54,61,62 did not. In the three RCTs56,57,63 that reported significant effects, the time to eye opening was consistently shorter in the EEG group than the standard clinical monitoring group. The significant reductions did not show any clear pattern with regard to whether the population (adults/children), EEG device used (BIS, E-Entropy, Narcotrend) or type of anaesthesia (volatile, total i.v. or mixed) could be explanatory variables. It is unclear whether or not these differences would impact on the comparability of the findings (and they do not appear to have been considered in the Cochrane review34). The statistically significant reductions in time to eye opening ranged from 2.72 to 5.9 minutes. It is not possible to draw any firm conclusions about the clinical significance of these reductions (e.g. their implications for health services) because the majority of the RCTs did not detect significant reductions in time to eye opening; one of the four trials that did report a significant effect is at high risk of bias because of the authors' conflict of interests57 (see Quantity and quality of research available); and the pooled effect estimate from the Cochrane review,34 although statistically significant, has high heterogeneity in the random-effects model used.
Time to extubation
One of the 11 RCTs that assessed this outcome was powered statistically to detect a specific difference (of 3 minutes) between the study groups, but did not detect a significant effect of Narcotrend monitoring on time to extubation. 60 Among the remaining 10 RCTs, six reported a significant reduction in the time to extubation, which, in all cases, favoured the EEG group relative to standard clinical monitoring. The reductions in time to extubation in these six trials ranged from 1.4 minutes to 6 minutes, with the largest reductions being for Narcotrend-guided total i.v. anaesthesia in adults (6 minutes),63 BIS-guided volatile anaesthesia in children (5 minutes)53 and BIS-guided volatile anaesthesia in adults (4.2 minutes). 45
In general, the same cautions in interpreting these results apply as noted above for the time to eye opening. Taking these limitations into consideration, there appears to be an overall favourable effect of EEG-guided anaesthetic monitoring on time to extubation but no clear pattern that would identify possible explanatory variables (such as the importance of population, EEG monitor or type of anaesthesia). It is unlikely that a saving of 6 minutes (the best achieved) in the time to extubation would have importance for patients or for service provision, given that it represents < 10% of the total time patients were undergoing surgical procedures.
Outcomes related to postanaesthesia care unit stay
None of the RCTs that assessed outcomes related to PACU stay was specifically powered statistically to detect differences in these outcomes.
All five RCTs that reported the time to arrival at the PACU found that the arrival time was significantly shorter under EEG-guided anaesthesia than following standard clinical monitoring. 48,56,57,63,64 Together, these RCTs represented both adults and children, different types of anaesthesia, and different EEG monitoring devices. The time savings ranged from 1.4 minutes to 5.8 minutes, with the largest differences being for Narcotrend-guided TIVA in adults (5.8 minutes),63 BIS-guided mixed anaesthesia in adults (4.7 minutes)48 and E-Entropy-guided mixed anaesthesia in children (4.0 minutes). 56 A difficulty in comparing these studies is that the starting point for measuring the time of arrival at the PACU was variable and sometimes unclear.
The two RCTs that reported the duration of stay in the PACU both examined BIS-guided volatile anaesthesia in children and both reported significant reductions in the duration of stay in the BIS-guided anaesthesia group compared with standard clinical monitoring. 52,53 In these RCTs the time savings in PACU stay ranged from 16 minutes53 to 26 minutes. 52 These RCTs, which were both by Messieha and colleagues,52,53 were similar and studied children undergoing complete dental rehabilitation. A notable difference is that in one RCT the target BIS value was 55–65,53 whereas in the other RCT the target BIS value was 65–70. 52 Although the higher BIS values in the latter trial would represent lighter depth of anaesthesia, both of these trials supplemented their BIS-guided anaesthesia with monitoring of clinical signs, which makes it difficult to determine whether or not the differences between the trials in PACU stay relate directly to the use of different target BIS values.
Three of the five RCTs that reported time to PACU discharge found significant differences between EEG-guided anaesthesia and standard clinical monitoring. 45,48,52 These trials were all on BIS-guided anaesthesia, and included volatile anaesthesia in adults,45 mixed anaesthesia in adults48 or volatile anaesthesia in children. 52 In all cases the time to discharge was shorter in the BIS-guided group, with the time saved ranging from 6.7 minutes to 30 minutes. The trials that reported the longest time savings, of 30 minutes52 and 24.7 minutes,48 both measured time to discharge from the end of GA. These reductions in discharge times are relatively large compared with the total durations of surgery in these trials, which were approximately 91 minutes (adults)48 and 139 minutes (children),52 suggesting possible benefits for patient throughput or PACU bed occupancy, as well as indicating improved clinical recovery of patients.
As noted above, the ‘PACU stay’ outcome in the Cochrane review34 seems to combine different aspects of time to PACU arrival, stay and/or discharge so may be difficult to interpret precisely. The outcome is consistent with the overall results of the individual RCTs included in the current systematic review, which indicate that EEG-guided anaesthesia reduces time to PACU admission, stay and discharge. However, although the pooled effect estimate in the Cochrane review is statistically significant, it has high statistical heterogeneity in the random-effects model used.
Time to response to commands
One RCT was powered statistically to detect a 20% difference in the time to response to verbal commands. 57 This trial and a further RCT59 reported statistically significant reductions in time to response in E-Entropy-guided anaesthesia57 and Narcotrend-guided anaesthesia59 compared with standard clinical practice. Both these trials were on adults receiving TIVA. The third RCT, on children receiving TIVA, did not provide quantitative data but stated that the study groups were comparable. 46 The reductions in time to response to commands were 4.1 minutes (median) for time to hand squeezing on command (start time not reported)57 and 4.6 minutes (mean) for time from end of anaesthetic to eye opening on command (also referred to as ‘arousal time’). 59
Time to recovery of orientation
The three RCTs measuring this outcome all reported statistically significant reductions in time to orientation in E-Entropy-guided54,57 or Narcotrend-guided59 anaesthesia compared with standard clinical practice. The reported time savings were 4.8 minutes (median) in E-Entropy-guided TIVA in adults,57 5.1 minutes (mean) in E-Entropy-guided volatile anaesthesia in children54 and 5.6 minutes (mean) in Narcotrend-guided TIVA in adults. 59 However, these RCTs were not specifically powered for this outcome; none of them defined orientation, and only one defined the time period to orientation [stated as the time between opening eyes on command and (undefined) orientation59].
Time to first movement response
Both of the RCTs measuring this outcome examined BIS-guided volatile anaesthesia, in adults45 or children. 51 The latter RCT was powered statistically to detect a 30% reduction in the time to first movement response. Both the trials reported statistically significant reductions in time to first movement in the BIS-guided anaesthesia group compared with standard clinical monitoring. The mean time savings were 2.8 minutes45 and 2.5 minutes. 51
Time to achieve specified recovery scores
Both of the RCTs measuring this outcome evaluated E-Entropy-guided anaesthesia in children who received either volatile anaesthetic (sevoflurane)54 or mixed anaesthetic (comprising propofol or sevoflurane for induction and isoflurane for maintenance). 56 One trial defined time to complete recovery as the time to reach a score of ≥ 9 on a modified Aldrete scale. 54 In the other trial time to recovery was defined as the time to reach a score of 6 on a modified Steward scale. 56 Time to recovery was significantly shorter, by a mean of 4.5 minutes, in the E-Entropy-guided than the standard clinical practice group in one trial (Aldrete score),54 but did not differ significantly in the other trial. 56
Time to spontaneous breathing
This RCT57 evaluated BIS-guided TIVA in adults and found a significantly shorter time to spontaneous breathing in the E-Entropy-guided than the standard clinical practice group. The median time difference was 2.33 minutes. Limitations to interpretation are: the RCT was not powered specifically for this outcome; the time to spontaneous breathing was not formally defined.
Time to laryngeal mask airway removal and time to phonation
This RCT51 evaluated BIS-guided volatile anaesthesia in children. The times from the last surgical suture to removal of the laryngeal mask airway and to phonation did not differ significantly between the BIS and standard clinical practice groups. A potential limitation to interpretation is that this trial was not specifically powered to detect differences in these outcomes.
Adverse effects of anaesthesia
Few of the trials reported anaesthesia-related adverse effects outcomes. The most frequently reported adverse outcomes were PONV (four RCTs), postoperative pain (two RCTs), POCD in elderly patients (one RCT) and emergence delirium in children (one RCT). These adverse effects are particularly relevant to situations in which overdosing of anaesthesia occurs. They were all reported as secondary outcomes (i.e. they were not specifically powered statistically) in the RCTs.
Postoperative nausea and vomiting
The four RCTs reporting this outcome evaluated BIS-guided volatile anaesthesia in children,51 entropy-guided TIVA in adults55 and Narcotrend-guided TIVA in adults. 59,60 In two trials PONV occurred but did not differ significantly in frequency between standard clinical monitoring and the BIS group51 or E-Entropy group. 55 In the third trial no cases of PONV occurred in either the Narcotrend or standard monitoring practice groups. 59 The remaining RCT reported PONV scores based on a VAS (no details provided) rather than frequency of occurrence, and found significantly higher (better) scores (indicating less frequent PONV) in the Narcotrend group compared with standard clinical practice. 60 However, this difference was significant only 10 minutes after the end of surgery and not at 30 or 90 minutes post surgery.
Postoperative pain
The two RCTs that assessed postoperative pain evaluated E-Entropy-guided anaesthesia, either in adults under TIVA55 or in children under mixed anaesthesia. 56 Pain was assessed as a score on a 0–10 scale55 or using the CHEOPS. 56 Pain scores were significantly lower in the E-Entropy group than standard clinical monitoring for the adult population. 55 In the paediatric population, the CHEOPS scores were significantly lower in the E-Entropy group at 60, 90 and 120 minutes after arrival in the PACU but not at 30 minutes after arrival. 56
Postoperative cognitive dysfunction
The RCT that assessed this outcome evaluated BIS-guided i.v. anaesthesia in elderly patients. 47 At 1 week post surgery, the incidence of POCD was 32.5% in the E-Entropy group and 39.1% in the standard clinical monitoring group. At 3 months post surgery the incidences were 8.1% and 12.0% respectively. Only the 3-month results were statistically significant. Interpretation is limited because the RCT is reported only in a conference abstract, which provides very limited information about the study.
Emergence delirium
The RCT that assessed this outcome was a study of BIS-guided volatile anaesthesia in children. 51 In this trial, emergence delirium was assessed using the PAED Instrument. The highest PAED scores recorded during the first 30 minutes after awakening were compared between the study groups and did not differ significantly.
Economic evaluation
Systematic review of published economic evaluations
Systematic searches identified 134 potentially relevant references. Studies were eligible for inclusion if they were full economic evaluations, including an assessment of any depth of anaesthesia monitoring device, conducted in patients receiving general anaesthetic for surgery. One study met all of the a priori inclusion criteria. This was a cost-effectiveness study reporting outcomes as cost of preventing an episode of awareness in all patients97 using data drawn from a prospective study by Ekman and colleagues98 and from the RCT reported by Myles and colleagues79 and Avidan and colleagues. 27 The analysis was limited only to the cost of the BIS and sensors to be attached to the patient, whereas outcomes were limited to cases of awareness. Based on an estimated incidence of awareness of 0.04% with BIS and 0.18% with standard clinical monitoring the cost-effectiveness of depth of anaesthesia monitoring was estimated as US$4410 per case avoided. The authors of the study concluded that the use of BIS monitoring was unlikely to be cost-effective. However, the results and conclusions should be viewed with caution because of weaknesses in methodology and poor reporting quality.
De novo economic evaluation
We developed a decision-analytic model to assess the cost-effectiveness of depth of anaesthesia monitoring compared with standard clinical monitoring. The model incorporated evidence on outcomes from the systematic review of patient outcomes (change in anaesthetic drug consumption, change in incidence of awareness and POCD) combined with data identified through targeted searches (incidence of long-term psychological sequelae of awareness, duration and cost of PTSD, QOL impact of LPS and PTSD, duration of POCD). Outcomes in the model are expressed as QALY. The model evaluates costs from the perspective of the NHS and Personal Social Services. Costs are expressed in UK sterling (pounds, £) at a 2011 price base. Cost-effectiveness was assessed using ICER for each technology, compared with standard clinical monitoring. Separate analyses are presented for each of the included technologies, compared with standard clinical monitoring – the included technologies are not compared with each other as this was not within the scope of the appraisal issued by NICE.
Bispectral Index compared with standard clinical monitoring
We presented a base-case analysis for two modes of anaesthetic administration [TIVA and mixed anaesthesia (induction with i.v. anaesthesia and maintenance with inhaled anaesthesia or a combination of inhaled and i.v. anaesthetic)] and for two patient populations (those considered at high risk of intraoperative awareness and a general surgical population, at average risk of intraoperative awareness).
For patients undergoing GA with TIVA, we used the OR of awareness with BIS monitoring (0.24), compared with standard clinical monitoring, reported in the meta-analysis in our systematic review of patient outcomes (see Results of systematic review of patient outcomes) and baseline awareness risks identified and pooled in this assessment (0.45% in patients at high risk of intraoperative awareness and 0.16% for a general surgical population, at average risk of intraoperative awareness) to estimate the risk reduction for awareness and its psychological sequelae associated with BIS monitoring. All of the trials included in the meta-analysis were conducted in patients at high risk of awareness. In the absence of any evidence on the effectiveness of BIS on the incidence of awareness in the general surgical population, we applied the same OR reported in the meta-analysis to both groups of patients.
Anaesthetic drug costs were based on reported consumption in trials included in the meta-analysis reported in the systematic review of patient outcomes (see Results of systematic review of patient outcomes). None of the trials included in the meta-analysis of drug consumption were conducted in patients at high risk of awareness, as these did not report anaesthetic drug consumption. In the model we assumed that the clinical characteristics of high-risk patients mean that anaesthetists will be particularly cautious regarding the dose of anaesthetic drugs and that the higher risk of awareness is associated with a tendency to underdose patients. As a result, we assumed that the potential reduction in anaesthetic dose, through the use of depth of anaesthesia monitoring, would not apply in this group of patients.
In cohorts of 10,000 patients, at high risk of intraoperative awarenes GA with TIVA, BIS monitoring was modelled as being associated with 10.8 cases of awareness, compared with 45 in patients receiving standard clinical monitoring. This resulted in a reduction of 11 cases of LPS (from 14.7 to 3.5), which included a reduction of six cases of PTSD (from 8.0 to 1.9). The modelled cost per patient was higher with BIS monitoring than for standard clinical monitoring, although some of the additional cost was offset by reduced costs associated with psychological sequelae of awareness. The majority of the additional cost of BIS monitoring was attributable to the sensors attached to the patient (88% of additional cost, per patient). By reducing the incidence of awareness and longer-term effects of POCD, BIS monitoring was associated with improved outcomes. The ICER, for BIS compared with standard clinical monitoring in this population was £22,339. Deterministic sensitivity analyses indicated that the ICER was sensitive to the baseline incidence of awareness, effectiveness of BIS in reducing awareness, probability of LPS, QoL decrement for PTSD, the proportion of people with LPS who have PTSD and the cost of sensors. Scenario analyses were undertaken to address the question of variables omitted from the base case and to explore the impact of key baseline assumptions. These indicate that the cost-effectiveness results were largely insensitive to including an effect of BIS on PONV and to assumptions regarding patient throughput (except at comparatively low volumes, below 500 cases per year per module), whereas they were highly sensitive to assumptions regarding the baseline risk of awareness and the QoL decrement for PTSD.
For the population of general surgical patients undergoing GA with TIVA, BIS monitoring was modelled as being associated with 3.8 cases (per 10,000 patients) of awareness, compared with 16 in patients receiving standard clinical monitoring. This resulted in a reduction of four cases of LPS (from 5.2 to 1.3), which included a reduction of two cases of PTSD (from 2.8 to 0.7). Although the modelled cost per patient was higher with BIS than with standard clinical monitoring, a larger proportion was offset by reductions in other costs (primarily anaesthetic drug costs) than was the case for patients at high risk of intraoperative awareness (where no saving in anaesthetic drug costs was included). As with the analysis for high-risk patients, the majority of the additional cost of BIS monitoring was attributable to the sensors attached to the patient, rather than the monitor module itself. Given the lower baseline risk of awareness in this population, the QALY gain with BIS monitoring was lower (0.0003) than for high-risk patients. This resulted in a higher ICER (£34,565) despite the lower incremental cost estimated for this population, arising from reduced anaesthetic consumption. Deterministic sensitivity analyses indicated that the ICER was sensitive to the same input parameters as for the population at high risk of awareness. In the majority of cases the ICER remained above £30,000 per QALY gained – the most favourable ICER was associated with a reduction in the cost of sensors. Conclusions from the scenario analyses were similar to those undertaken for high-risk patients. In particular, more favourable ICERs were associated with a higher baseline incidence of awareness and with a higher utility decrement for PTSD.
For patients undergoing mixed GA (induction with i.v. and maintenance including inhaled anaesthetic), we used the pooled OR of awareness with BIS monitoring, compared with standard clinical monitoring, calculated in the meta-analysis reported in the systematic review of patient outcomes (0.45) and baseline awareness risks identified and pooled in this review to estimate the risk reduction for awareness and its psychological sequelae associated with BIS monitoring.
The baseline estimates of awareness, LPS and PTSD were the same as for high-risk patients undergoing TIVA (45, 14.7 and 8 per 10,000 patients respectively). However, given that the OR of awareness with BIS monitoring was higher in this analysis, the estimated reduction in LPS and PTSD was lower. In this patient population BIS monitoring was associated with 20.3 cases of awareness, 6.6 cases of LPS, including 3.6 cases of PTSD. BIS monitoring had higher costs and improved outcomes compared with standard clinical monitoring. However, the QALY gain (0.0005) was lower than for patients undergoing TIVA. The ICER, for BIS compared with standard clinical monitoring in this population was £29,634. Deterministic sensitivity analyses indicated that the ICER was sensitive to the baseline incidence of awareness, effectiveness of BIS in reducing awareness, probability of LPS, QoL decrement for PTSD, the proportion of people with LPS who have PTSD and the cost of sensors. The highest incidence of awareness (1.19%), largest effect size (0.25, lower 95% confidence limit for OR of awareness with BIS vs standard clinical care), longest duration of LPS (1 year), highest probability of LPS (0.48), longest duration of PTSD (21.6 years), highest probability of PTSD (0.239), greatest utility reduction associated with PTSD (−0.134), largest proportion of PTSD patients being treated (100%) and lowest cost of sensors (£10.875, 75% of base-case value) tested in the sensitivity analysis resulted in ICERs below £30,000 per QALY gained, although the majority remained above £20,000 per QALY gained. Conclusions from the scenario analyses were similar to those for high-risk patients undergoing TIVA.
The baseline estimates of awareness, LPS and PTSD in the population of general surgical patients undergoing mixed GA were the same as for TIVA (16, 5.2 and 2.8 per 10,000 patients respectively), whereas BIS monitoring in this patient population was modelled as being associated with 7.2, 2.3 and 1.3 cases respectively. Although a proportion of the higher cost associated with BIS monitoring was offset by reduction in anaesthetic consumption, the cost-saving for inhaled anaesthesia was lower than for TIVA. As a result the incremental cost was greater (£12.91 compared with £10.98). Given the lower baseline risk of awareness in this population, the QALY gain with BIS monitoring was lower (0.0003) than for high-risk patients, resulting in a higher ICER (£49,198). Deterministic sensitivity analyses indicated that the ICER was sensitive to the same input parameters as for the population at high risk of awareness. However, in all cases the ICER remained above conventional thresholds – the most favourable ICER was associated with a reduction in the cost of sensors. Conclusions from the scenario analyses were also similar to those undertaken for high-risk patients.
E-Entropy compared with standard clinical monitoring
A base-case analysis was presented for two modes of anaesthetic administration [TIVA and mixed anaesthesia (induction with i.v. anaesthesia and maintenance with inhaled anaesthesia or a combination of inhaled and i.v. anaesthetic)] and for two patient populations (those considered at high risk of intraoperative awareness and a general surgical population, at average risk of intraoperative awareness).
Insufficient evidence was identified to estimate the effectiveness of depth of anaesthesia monitoring with E-Entropy on the incidence of intraoperative awareness or on POCD. In the absence of evidence specific to E-Entropy we have applied the effectiveness estimates derived for BIS, described above. This meant that the modelled clinical effectiveness of E-Entropy was identical to that reported for BIS – this is an untested assumption and must be considered a weakness in the evidence base for E-Entropy. Anaesthetic drug costs were based on consumption reported in the included trials, and were valued using current unit costs.
In patients considered at high risk of awareness undergoing GA with TIVA, the modelled cost per patient with E-Entropy monitoring was higher than with standard clinical monitoring, although some of the additional cost was offset by reduced cost associated with psychological sequelae of awareness. The additional cost of E-Entropy monitoring was approximately two-thirds that of BIS monitoring, with the majority being attributable to the sensors attached to the patient (80% of additional cost per patient). E-Entropy monitoring was associated with improved outcomes, based on applying clinical effectiveness evidence reported for BIS. The ICER for E-Entropy compared with standard clinical monitoring in this population was £14,421. Deterministic sensitivity analyses indicated that the ICER was sensitive to the baseline incidence of awareness, effectiveness of E-Entropy in reducing awareness, probability of LPS, QoL decrement for PTSD, the proportion of people with LPS who have PTSD and the cost of sensors. The least favourable ICERs were for low baseline incidence of awareness, lower effectiveness on incidence of awareness and a lower probability of patients with awareness developing LPS. Scenario analyses, undertaken to consider variables omitted from the base case and to explore the impact of key baseline assumptions, indicated that the cost-effectiveness results were highly sensitive to assumptions regarding the baseline risk of awareness and the QoL decrement for PTSD, whereas they were largely insensitive to including an effect of E-Entropy on PONV and to assumptions regarding patient throughput (except at comparatively low volumes, < 500 cases per year per module).
In the population of general surgical patients undergoing GA with TIVA, E-Entropy monitoring had a higher cost per patient than standard clinical monitoring. Anaesthetic drug costs derived from two clinical trials were modelled separately, as we considered them unsuitable for pooling, given substantial differences in the patient populations (one trial in orthopaedic surgery and the other in elective gynaecological laparoscopy). Neither of the trials showed an overall reduction in anaesthetic drug consumption and as a result there was no reduction in anaesthetic drug costs to offset the additional costs of E-Entropy monitoring. As with the analysis for high-risk patients, the majority of the additional cost of monitoring was attributable to the sensors attached to the patient. Given the lower baseline risk of awareness in this population, the QALY gain was lower than for high-risk patients, which resulted in a higher ICER (£31,131–31,430). Deterministic sensitivity analyses indicated that the ICER was sensitive to the baseline incidence of awareness, effectiveness in reducing awareness, probability of LPS, QoL decrement for PTSD, the proportion of people with LPS who have PTSD and the cost of sensors. The lower limit of anaesthetic drug consumption, the highest incidence of awareness, largest effect size, greatest probability of LPS, longest duration of PTSD, greatest probability of PTSD and lowest cost of sensors tested in the sensitivity analysis resulted in an ICER of < £30,000 per QALY gained, although they remained above £20,000 per QALY gained. Conclusions from the scenario analyses were similar to those undertaken for high-risk patients.
As noted above, in the absence of evidence specific to E-Entropy, we have applied the effectiveness estimates derived for BIS in this analysis. For patients undergoing mixed GA (induction with i.v. and maintenance including inhaled anaesthetic), the pooled OR of awareness with BIS monitoring, compared with standard clinical monitoring, (0.45) was higher than for TIVA, resulting in a smaller reduction in cases of awareness, LPS and PTSD.
In patients considered at high risk of awareness undergoing mixed GA, E-Entropy monitoring had higher costs and improved outcomes compared with standard clinical monitoring. However, the QALY gain (0.0005) was lower than for patients undergoing TIVA. The ICER for E-Entropy compared with standard clinical monitoring in this population was £19,367. Deterministic sensitivity analyses indicated that the ICER was sensitive to the baseline incidence of awareness, effectiveness in reducing awareness, probability of LPS, QoL decrement for PTSD, the proportion of people with LPS who have PTSD and the cost of sensors. The least favourable ICERs were found with a low incidence of awareness (lower limit of 95% CI), lesser effect size (upper limit of 95% CI for OR of awareness with monitoring vs standard clinical care) and greater probability of LPS (0.48). The majority of the ICERs remained at < £20,000 per QALY gained. Conclusions from the scenario analyses were similar to those undertaken for high-risk patients undergoing TIVA.
In the population of general surgical patients undergoing mixed GA, E-Entropy monitoring had higher costs than standard clinical monitoring. In contrast with the analysis for TIVA, the clinical trial used to estimate inhaled anaesthetic drug consumption reported a substantial decrease (29%), which resulted in approximately half of the additional cost of E-Entropy monitoring being offset by a reduction in anaesthetic drug costs. Despite the lower baseline risk of awareness, which resulted in a lower QALY gain with E-Entropy monitoring than for high-risk patients, the lower incremental cost resulted in an equivalent ICER (£19,000). Deterministic sensitivity analyses indicated that the ICER was sensitive to the same input parameters as for the population at high risk of awareness. The least favourable ICERs were found with a low reduction in anaesthetic drug consumption (lower limit of 95% CI) and lesser effect size (upper limit of 95% CI for OR of awareness with monitoring vs standard clinical care). The majority of the ICERs remained below £20,000 per QALY gained. Conclusions from the scenario analyses were also similar to those undertaken for high-risk patients.
Narcotrend compared with standard clinical monitoring
We presented a base-case analysis for two modes of anaesthetic administration [TIVA and mixed anaesthesia (induction with i.v. anaesthesia and maintenance with inhaled anaesthesia or a combination of inhaled and i.v. anaesthetic)] and for two patient populations (those considered at high risk of intraoperative awareness and a general surgical population, at average risk of intraoperative awareness).
Anaesthetic drug costs were based on consumption reported in the included trials, and were valued using current unit costs. Insufficient evidence was identified to estimate the effectiveness of depth of anaesthesia monitoring with Narcotrend on the incidence of intraoperative awareness or on POCD. In the absence of evidence specific to Narcotrend, we have applied the effectiveness estimates derived for BIS, described above. This means that the modelled clinical effectiveness of Narcotrend is identical to that reported for BIS – this is an untested assumption and must be considered a weakness in the evidence base for Narcotrend.
In patients considered at high risk of awareness undergoing GA with TIVA, the modelled cost per patient with Narcotrend monitoring was higher than with standard clinical monitoring, although some of the additional cost was offset by reduced cost associated with psychological sequelae of awareness. The additional cost of Narcotrend monitoring was approximately half that of E-Entropy monitoring, and approximately one-quarter that of BIS – primarily because of differences in the cost of the sensors attached to the patient. In contrast with BIS and E-Entropy, the majority of the additional cost of Narcotrend monitoring was attributable to the monitor (90% of additional cost per patient) rather than the sensors. Narcotrend monitoring was associated with improved outcomes, based on applying clinical effectiveness evidence reported for BIS. The ICER for Narcotrend compared with standard clinical monitoring in this population was £5681. Deterministic sensitivity analyses indicated that the ICER was sensitive to the baseline incidence of awareness, effectiveness in reducing awareness, probability of LPS, QoL decrement for PTSD, the proportion of people with LPS who have PTSD and the cost of sensors. The least favourable ICER was for low baseline incidence of awareness. Scenario analyses, undertaken to consider variables omitted from the base case and to explore the impact of key baseline assumptions, indicated that the cost-effectiveness results were highly sensitive to assumptions regarding the baseline risk of awareness and the QoL decrement for PTSD, whereas they were largely insensitive to including an effect of E-Entropy on PONV.
In the general surgical population undergoing GA with TIVA Narcotrend monitoring had a lower cost per patient than standard clinical monitoring. The additional cost of monitoring was reduced to £2.84 per patient (£2.28 per patient for the monitor and £0.56 for the sensors attached to the patient). This was more than offset by reduction in anaesthetic drug consumption. Given the lower baseline risk of awareness in this population, the QALY gain was lower than for high-risk patients. However, given that Narcotrend was associated with improved outcomes and reduced costs it dominated standard clinical monitoring. Narcotrend remained dominant in all the deterministic sensitivity analyses. Conclusions from the scenario analyses were similar to those undertaken for high-risk patients.
As noted above, in the absence of evidence specific to Narcotrend, we have applied the effectiveness estimates derived for BIS in this analysis. For patients undergoing mixed GA (induction with i.v. and maintenance including inhaled anaesthetic), the pooled OR of awareness with BIS monitoring compared with standard clinical monitoring (0.45) is higher than for TIVA, resulting in a smaller reduction in cases of awareness, LPS and PTSD.
In patients considered at high risk of awareness undergoing mixed GA, Narcotrend monitoring had higher costs and improved outcomes compared with standard clinical monitoring, although the QALY gain (0.0005) was lower than for patients undergoing TIVA. The ICER for Narcotrend compared with standard clinical monitoring in this population was £8033. Deterministic sensitivity analyses indicated that the ICER was sensitive to the baseline incidence of awareness, effectiveness in reducing awareness, probability of LPS, QoL decrement for PTSD, the proportion of people with LPS who have PTSD and the cost of sensors. The least favourable ICERs were found with a low incidence of awareness (lower limit of 95% CI) and lesser effect size (upper limit of 95% CI for OR of awareness with monitoring vs standard clinical care). Conclusions from the scenario analyses were similar to those undertaken for high-risk patients undergoing TIVA.
In the population of general surgical patients undergoing mixed GA, Narcotrend monitoring had higher costs than standard clinical monitoring. Although the proportionate reduction in consumption of inhaled anaesthetic (desflurane) was lower than the reduction in i.v. anaesthetic (propofol) for TIVA, the reduction in cost of anaesthetic (£4.26) was sufficient to offset the additional cost of Narcotrend monitoring (£2.84). Given the lower baseline risk of awareness in this population, the QALY gain was lower than for high-risk patients. However, as Narcotrend was associated with improved outcomes and reduced costs, it dominated standard clinical monitoring. Narcotrend remained dominant in the majority of deterministic sensitivity analyses. At the upper limit of the 95% CI for proportional change in desflurane use, the reduction in cost of anaesthetic was insufficient to offset the additional cost of Narcotrend monitoring and the resulting ICER was £2534. Conclusions from the scenario analyses were similar to those undertaken for high-risk patients.
Strengths and limitations of the assessment
The current evidence synthesis followed an accepted standard procedure for conducting a systematic review of the evidence, based on a published protocol, so as to minimise bias and, where possible, provide the most precise estimates of effects for relevant outcomes. The work was carried out by a team experienced in health technology appraisal, independent of any vested interest.
We know of only two other relevant systematic reviews in this topic area, both of which focused on the effects of BIS-guided depth of anaesthetic monitoring. A systematic review and meta-analysis reported by Liu (2004)105 investigated the use of BIS-guided anaesthetic delivery in ambulatory anaesthesia. Eleven RCTs were included and BIS-guided anaesthesia was found to significantly reduce anaesthetic consumption, PONV and time spent in the recovery room (PACU). However, the benefits did not reduce the time spent in the ambulatory surgery unit overall. More recently, a more comprehensive Cochrane systematic review and meta-analysis of the use of BIS monitoring to improve anaesthetic delivery and postoperative recovery, not limited to ambulatory anaesthesia, was conducted by Punjasawadwong and colleagues. 34 As noted above, our current systematic review complements this Cochrane review for BIS studies and, where possible, we have updated meta-analyses in the Cochrane review using data from new RCTs that we have identified. For pragmatic reasons (to keep the work manageable with the available resources), we did not duplicate the searches of the Cochrane review or re-extract data for those RCTs already included in it, but instead systematically sought and appraised new RCTs about BIS-guided anaesthesia that have been published since the search dates of the Cochrane review. The Cochrane review was limited to RCTs on adults but, as specified in the protocol, we have included in our systematic review RCTs on children as well as adults. In practice, we found new evidence to update the Cochrane review meta-analysis for three outcomes (intraoperative awareness, consumption of volatile anaesthetic and consumption of i.v. anaesthetic), although for anaesthetic consumption the precision of the existing effect estimates was not necessarily improved because of significant statistical heterogeneity. A disadvantage of our pragmatic approach is that we have not presented full details of those BIS trials included in the Cochrane review, although these can be ascertained from the Cochrane review itself. Although Cochrane reviews are generally conducted to high standards, there appear to be some limitations in the publication by Punjasawadwong and colleagues,34 which we have noted above when interpreting specific outcomes. For instance, a meta-analysis relating to ‘PACU stay’ appears to have combined several outcomes concerning the time to PACU arrival, stay and discharge, which would be more informative if analysed separately.
As no systematic reviews of E-Entropy-guided anaesthesia or Narcotrend-guided anaesthesia appear to have been published, for these technologies we conducted more extensive searches to locate all relevant RCTs, on both adults and children, which were then screened for relevance and, where they met the inclusion criteria, were subjected to full systematic review. The current work represents the most comprehensive systematic review of BIS-, E-Entropy- and Narcotrend-guided anaesthesia that has been conducted to date.
A notable limitation to our assessment of patient outcomes is that the quality of reporting in the primary studies was often limited, which gives rise to numerous uncertainties in the interpretation of the primary evidence (see Uncertainties). As discussed above, the studies were diverse in their methodological characteristics, which limited opportunities to pool their data in meta-analyses. The primary studies also predominantly reported secondary outcomes, which were often based on relatively small sample sizes, with unknown statistical validity.
We undertook a comprehensive search for studies that would be potentially relevant to the assessment of cost-effectiveness, by identifying full economic evaluations of any depth of anaesthesia monitoring device compared with standard clinical monitoring. One published study was identified, which reported ICER as the incremental cost of BIS monitoring per case of intraoperative recall avoided. We did not identify any published economic evaluations that reported outcomes in terms of QALY or similar units, nor did we identify any studies that explicitly compared the additional costs of depth of anaesthesia monitoring with potential savings in anaesthetic drug use. We developed a de novo decision-analytic model to provide an assessment of the cost-effectiveness of depth of anaesthesia monitoring, compared with standard clinical monitoring, incorporating patient outcomes (in terms of avoided cases of PTSD and POCD) as QALY and anaesthetic drug use. The model provided a means to synthesise data from the systematic review of patient outcomes (in terms of the effectiveness of depth of anaesthesia monitoring on intraoperative awareness, POCD and anaesthetic drug use). This was supplemented by information identified using targeted searches (on the baseline incidence of intraoperative awareness in high-risk and general surgical populations, proportion of patients who experience POCD, the proportion of patients experiencing intraoperative awareness who develop long-term psychological illness, the duration, cost and the QoL impact of those conditions).
In the model, GA exposes patients to a risk of intraoperative awareness that is defined either as high or average (the latter corresponding to the risk of awareness in the general surgical population), and to POCD, which have consequences for QoL. In patients experiencing long-term psychological illness as a consequence of an awareness episode, there are also associated health-care costs. Other costs considered in the model are costs of anaesthetic drugs, as well as the cost of the depth of anaesthesia monitors. Cost-effectiveness was assessed by estimating ICER for each mode of anaesthesia and each technology. We undertook a range of sensitivity analyses and scenario analysis to identify the key determinants of the cost-effectiveness results as well as the impact of key assumptions and of variables missing from the analysis.
Evidence to populate the model was limited. In particular no evidence on the effectiveness of E-Entropy and Narcotrend on the incidence of intraoperative awareness was identified. In the case of BIS, where such evidence was identified it was limited to patients considered at high risk of awareness. We have assumed in the model that the effectiveness evidence in high-risk patients can be applied to the general surgical population (at average risk of awareness) and that the effectiveness evidence for BIS can be applied to both E-Entropy and Narcotrend. These are untested assumptions and must be considered a weakness in the cost-effectiveness evidence base. Whereas more evidence is available on the baseline risk of awareness, there was considerable inconsistency in the estimated incidence in studies identified in our targeted searches. As a result we used pooled values (excluding outliers) in the base-case analyses, with the outlying values adopted in scenario analyses.
Evidence on the effectiveness of any depth of anaesthesia monitoring on POCD is also limited to BIS, with the only published study being available only in abstract form. As with the evidence on effectiveness with respect to awareness, we have assumed that evidence for BIS can also be applied to E-Entropy and Narcotrend – again this is an untested assumption. Evidence on the incidence of POCD was also limited and is subject to considerable uncertainty (primarily concerning the extent to which pre-existing, but unrecognised, cognitive dysfunction may be incorrectly identified as a postoperative complication). The best evidence we could identify that reported POCD in patients who had been assessed preoperatively compared with a matched group of non-surgical controls is over 10 years old, and it is not clear whether or not this will reflect incidence of POCD in current practice.
Although we were able to identify some evidence on the incidence of PTSD in patients who experienced awareness during GA, we did not identify any studies reporting overall QoL impact, health state utilities or mean duration of symptoms in PTSD sufferers with awareness as the trigger. The evidence base for people with PTSD relates to a range of trauma exposures (including military service and other wartime exposures, natural disaster, domestic abuse), and it is not clear whether or not this can be applied directly to people who have developed psychological illness following intraoperative awareness.
We adopted a modelling approach that did not explicitly identify patients exposed to overdose or underdose of anaesthetics, although this may allow a clearer assessment of the potential benefits of depth of anaesthesia monitoring. Intraoperative awareness may be identified as being particularly closely associated with anaesthetic underdose, whereas POCD and PONV may be more closely associated with overdose. The potential for savings in terms of anaesthetic drug use may also primarily arise in this latter group. Although it may have been preferable to adopt this more explicit structure, we did not identify data to support this approach. We have therefore adopted a more simple model structure, although we have implicitly incorporated some of these assumptions into our model.
The scope of the appraisal issued by NICE required the three depth of anaesthesia monitoring devices to be compared with standard clinical monitoring, rather than with each other. A direct comparison of the cost-effectiveness of the three technologies was therefore not conducted. However, such a comparison would not be feasible as there is limited direct trial evidence comparing the technologies with each other, and an indirect comparison would not be possible because of the lack of outcome data on intraoperative awareness for E-Entropy and Narcotrend. Indeed, because of the lack of awareness data, one of the assumptions we have had to make is that all three technologies would be similar in terms of preventing awareness, based on the data available for BIS.
Uncertainties
One of the biggest uncertainties in the evidence base assessed in this report is the impact of EEG monitoring on intraoperative awareness, and other significant adverse effects such as POCD. The lack of outcome data from RCTs on awareness was particularly the case for E-Entropy and Narcotrend. Likewise, the only RCT data available for POCD was for BIS and was available only in a conference abstract. In situations where evidence for specific outcomes from RCTs is lacking, it is pragmatic to use data from other types of study design, including non-experimental studies (e.g. cohort studies). However, we did not identify any such studies of BIS, E-Entropy and Narcotrend in our literature searches that reported on intraoperative awareness or POCD.
The nature of standard clinical monitoring varied across the included trials, with some trials giving more information than others. For example, in one study59 it is reported that ‘in the clinical group, the depth of anaesthesia was primarily evaluated by clinical indices including heart rate, blood pressure and body movement’ (our emphasis) so it is not known what other methods may have been used. Also patients in the EEG arm of some of the trials were potentially assessed on the basis of standard clinical monitoring with the EEG reading used as an adjunct to other physiological parameters in assessing the effects of anaesthetic agents; however, this was not always explicitly stated in the trials. The BAG-RECALL trial by Avidan and colleagues44 used ‘structured protocols’ to remind anaesthesiologists that patients may be aware, but not necessarily to prescribe changes in anaesthetic. As patients can have their anaesthesia adjusted on the basis of standard clinical monitoring or EEG monitoring or both, the effect is not solely as a result of the technology being considered (BIS, E-Entropy and Narcotrend) in the intervention arm of most of the studies.
Details of the technologies used in the trials are also often limited and confusing. It is not always clear or specified as to which monitor has been used or which version of the software has been used. There also seems to be some confusion between monitor version and software version in the reporting of the trials, and also between the terms ‘monitor’ and ‘module’. For example, the trials of Narcotrend report Narcotrend Monitor version 2.0 AF,60 Narcotrend monitor (software version 2.0 AF)63,64 and Narcotrend monitor (MonitorTechnik, Germany). 59 This also happens in the studies reported in Cochrane review of BIS. 34 Anaesthesia monitors assess a range of parameters such as EEG, ECG, respiration, temperature, anaesthetic gases, and can be used for viewing and processing information (e.g. Datex-Ohmeda S/5 monitor); an EEG monitor with BIS, monitors the state of the brain by data acquisition of EEG and BIS is the processed EEG variable. However, device manufacturers also use the terms monitor and module interchangeably. This is probably because some monitors incorporate processing modules. For example, the A-2000 EEG monitor with BIS was upgraded to the A-3000 EEG monitor, which incorporated a BIS module and is known as a BIS monitor.
It therefore appears that the technologies considered are continually evolving, and different versions of the software have been used to interpret EEG readings in the different trials. It is not clear exactly what alterations have been made to the algorithms and how these influence the trial results as the algorithms are proprietary and not completely published. However, it is suggested by the manufacturer of BIS that update versions of the module have focused on artefact detection and removal, rather than fundamental changes to the algorithm. In the Narcotrend industry submission to NICE, one trial showed that Narcotrend does not differentiate reliably between conscious and unconscious patients. The reason given to explain these results is that both these studies were carried out using older versions of the algorithm and that the studies had methodological flaws. Whatever the reasons are for these results, this does emphasise the potential lack of consistency between the different versions and need for care when interpreting results from studies using different software versions.
There is also inconsistency in EEG values used in the trials, both overall and at different time points during surgery, making comparison across trials difficult. In the BIS trials there was notable variation in target values from 40 to 70. E-Entropy values during the maintenance phase of anaesthesia ranged from 35 to 60 for response entropy and 40–65 for state entropy, but in some trials higher values were permitted near the end of surgery, and the response entropy–state entropy difference was also used as a target value in some trials. Narcotrend values ranged from D0 to C1, D2 to E0 adjusted to D0 to D1 and D2 to E0, which means that the level of anaesthesia varied across trials within the same technology.
Outcomes were also defined differently in the different studies, which may affect results. For example, the starting point for the recovery process can be the last stitch performed during surgery or the end of application of dressings.
Other issues to consider when interpreting results are investigator bias (subtle unconscious or conscious influence of investigator on results which can overestimate results) and ‘learning contamination bias’ (the unintended improvement of standard clinical monitoring occurring with the introduction of a new monitoring device which can reduce the difference in results). Not many of the included studies discussed these aspects or reported experience of the anaesthetist. Ellerkmann and colleagues62 used experienced anaesthesiologists and suggest that results may have been different had they used less experienced staff. Kreuer and colleagues63 discount learning contamination bias in the standard clinical monitoring group of their trials as the anaesthesiologist was also experienced in use of Narcotrend/BIS.
Additional factors for consideration include inter-individual variability and sex differences in response to anaesthesia which complicate interpretation of results. For example in one trial, with comparable amounts of propofol, women in the standard clinical monitoring group had significantly shorter recovery times than men; in EEG-monitored groups (BIS and Narcotrend) propofol consumption was lower for men. 63 Also effects differ between i.v. anaesthesia and volatile anaesthetics and also depend on the specific drug used. For example, more rapid recovery can be expected with desflurane/remifentanil (which is washed out quicker) compared with propofol, so comparisons across trials using different anaesthetic agents are not valid. In addition, as anaesthesia is the interaction between hypnosis and sedation, the relative proportion of the drugs used to achieve these elements of anaesthesia may have an impact on EEG monitoring. Also, different approaches were used in the trials to manage inadequate anaesthesia, such as narcotics (fentanyl, sufentanil, alfentanil), which could impact on results.
Taking into account the above issues such as the methodology of the trials, the lack of clarity of reporting, the differences in patient characteristics and differences in technologies and anaesthesia used, brings into question the overall generalisability of the results and makes interpretation of results problematic, especially as some of the observed differences are minimal and may not be judged as clinically significant.
Chapter 6 Conclusions
In general, BIS, E-Entropy and Narcotrend technologies for monitoring the depth of anaesthesia are associated with reductions in general anaesthetic consumption and decreased anaesthetic recovery times, compared with monitoring of clinical signs alone. However, these reductions may be considered clinically modest. The available evidence on the impact of the technologies on reducing the likelihood of intraoperative awareness is limited. Overall, BIS was associated with a statistically significant reduction in intraoperative awareness in patients classified as at higher risk, although there is uncertainty in effect estimates because of significant heterogeneity. Caution is advised because of uncertainties about the risk of bias of many of the included trials, and because many outcome measures were not statistically powered.
The cost-effectiveness of depth of anaesthesia monitoring appears to be highly dependent on the incidence of awareness, the HRQoL impact of psychological sequelae of awareness, the probability of developing psychological illness following awareness as well as the effectiveness of depth of anaesthesia monitoring in reducing awareness. Cost-savings, resulting from reduced use of anaesthetic drugs may offset some of the additional cost of depth of anaesthesia monitoring. The cost of sensors attached to the patient appears to be a key factor in the additional cost of depth of anaesthesia monitoring.
Implications for service provision
The main implications for service provision will be the installation of the EEG module, any training required, and follow-up module maintenance. Module installation is unlikely to be particularly disruptive, although a separate compatible monitor may also be required, depending on which module is being introduced. As discussed earlier, training in use of the modules is not likely to be extensive.
Suggested research priorities
The following research recommendations are listed in order of perceived priority.
-
There is a lack of RCTs of E-Entropy-guided and Narcotrend-guided anaesthesia monitoring to detect explicit intraoperative awareness, specifically in high-risk patients. Given that incidence of awareness will be higher in this group, it may be more feasible to mount a trial than in the general surgical population, notwithstanding an adequate a priori statistical power calculation (although see below). Future trials should incorporate adequate length of follow-up to detect delayed cases of awareness. Cases of awareness may emerge after the first postoperative week, but in nearly all of the currently available RCTs of BIS, E-Entropy and Narcotrend, intraoperative awareness was assessed only within 1–3 days post surgery. It should be noted that in the RCTs we reviewed, the timing of follow-up was not always clearly specified and/or it was not clear to which outcomes the specified follow-up periods applied. Clear reporting of these crucial aspects of the RCT should be strongly encouraged. Future RCTs should also evaluate the effects of anaesthesia overdosing, including short-term effects such as nausea and vomiting, as well as longer-term impact on cognitive function.
-
There were no trials of the use of Narcotrend in children, and only two paediatric studies of E-Entropy in our systematic review. Future evaluation of these technologies would be warranted in these groups.
-
Further evidence on the incidence of intraoperative awareness is needed. The Royal College of Anaesthetists ran the National Audit Project (NAP) 5 to estimate the incidence of awareness in all UK hospitals (1 June 2012 until 31 May 2013). This may provide useful data for future economic modelling of depth of anaesthesia technologies in the UK.
-
Our literature searches identified three ongoing RCTs that would meet the inclusion criteria of our systematic review (see Appendix 12), all of which are investigating anaesthesia depth titrated according to BIS values. A further recent RCT (accepted for publication), which is similar to our inclusion criteria, is the Michigan Awareness Control Study, comparing BIS-guided and MAC-guided electronic alerts for the prevention of awareness under GA. 140 The target sample size was 15,000 patients in each group (aged > 18 years) at both low and high risk for awareness, and a total of 21,601 patients were enrolled at the time of interim analysis. The primary outcome measure was intraoperative awareness, with explicit recall measured at 28–30 days post anaesthesia. Modified ITT interim analysis found no statistically significant difference between BIS- and MAC-guided alerts in incidence of definite awareness, and the trial was therefore terminated because of futility. Post hoc power analysis showed that around 30,000 patients in each group would be required to detect a difference between the two interventions. 141 This calls into question the feasibility of future RCTs of depth of anaesthesia monitoring, particularly in the general surgical population.
Acknowledgements
We would like to thank members of our advisory group panel who provided expert advice and comments on the protocol and a draft of this report:
Professor Brian Pollard, Professor of Anaesthesia, Manchester Royal Infirmary, UK. (Professor Pollard has in the past received funding from Aspect Medical, the manufacturers of the BIS monitor, to undertake some research using the BIS monitor.)
Marta Soares, Research Fellow, Centre for Health Economics, University of York, UK.
Dr Gerlinde Mandersloot, Consultant in Intensive Care and Anaesthesia, The Royal London Hospital Whitechapel, UK (Representing ICU Steps The Intensive Care Patient Support Charity).
We are also grateful to Karen Welch, Information Scientist, SHTAC, University of Southampton, for generating and running the literature searches, and Andy Clegg, Professor of Health Services Research, SHTAC, University of Southampton, for reviewing a draft of this report.
Contribution of authors
J Shepherd (Principal Research Fellow) developed the research protocol, assisted in the development of the search strategy, assessed studies for inclusion, extracted data from, and quality assessed, included studies, synthesised evidence, drafted and edited the final report, and project managed the study.
J Jones (Principal Research Fellow) developed the research protocol, assessed studies for inclusion, extracted data from, and quality assessed, included studies, synthesised evidence, developed the economic evaluation, and drafted the final report.
GK Frampton (Research Fellow) assessed studies for inclusion, extracted data from, and quality assessed, included studies, synthesised evidence, and drafted the final report.
L Baxter (Research Fellow) assessed studies for inclusion, extracted data from, and quality assessed, included studies, synthesised evidence, assisted in developing the economic evaluation and drafted the final report.
J Bryant (Principal Research Fellow) developed the research protocol, contributed to the background section, extracted data from, and quality assessed, included studies, synthesised evidence, drafted and edited the final report.
K Cooper (Senior Research Fellow) assessed studies for inclusion, extracted data from, and quality assessed, included studies, synthesised evidence, and developed the economic evaluation.
Disclaimer
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Jones JG, Konieczko K. Hearing and memory in anaesthetised patients. Br Med J 1986;292. http://dx.doi.org/10.1136/bmj.292.6531.1291.
- Kerssens C, Klein J, Bonke B. Awareness: Monitoring versus remembering what happened. Anesthesiology 2003;99:570-5. http://dx.doi.org/10.1097/00000542-200309000-00011.
- Enlund M, Hassan HG. Intraoperative awareness: detected by the structured Brice interview?. Acta Anaesthesiol Scand 2002;46:345-9. http://dx.doi.org/10.1034/j.1399-6576.2002.460402.x.
- Russell IF. Comparison of wakefulness with two anaesthetic regimens. Br J Anaesth 1986;58:965-8. http://dx.doi.org/10.1093/bja/58.9.965.
- Moerman N, Bonke B, Oosting J. Awareness and recall during general anaesthesia. Anesthesiology 1993;79:454-64. http://dx.doi.org/10.1097/00000542-199309000-00007.
- Ranta S, Laurila R, Saario J, Ali-Melkkila T, Hynynen M. Awareness with recall during general anaesthetia: incidence and risk factors. Anesth Analg 1998;86:1084-9.
- Ghoneim MM, Block RI, Haffarnan M, Mathews MJ. Awareness during anaesthesia: risk factors, causes and sequelae: A review of reported cases in the literature. Anesth Analg 2009;108:527-35. http://dx.doi.org/10.1213/ane.0b013e318193c634.
- Leslie K, Chan MTV, Myles PS, Forbes A, McCulloch TJ. Posttraumatic stress disorder in aware patients from the B-Aware trial. Anesth Analg 2010;110:823-8. http://dx.doi.org/10.1213/ANE.0b013e3181b8b6ca.
- Sandin RH, Enlund G, Samuelsson P, Lennmarken C. Awareness during anaesthesia: a propsective case study. Lancet 2000;355:707-11. http://dx.doi.org/10.1016/S0140-6736(99)11010-9.
- Osterman JE, Hopper J, Heran WJ, Keane TM, van der Volk BA. Awareness under anaesthesia and the development of posttraumatic stress disorder. Gen Hosp Psychiatry 2001;23:198-204. http://dx.doi.org/10.1016/S0163-8343(01)00142-6.
- Lennmarken C, Bildfors K, Enlund G, Samuelsson P, Sandin R. Victims of awareness. Acta Anaesthesiol Scand 2002;46:229-31. http://dx.doi.org/10.1034/j.1399-6576.2002.t01-1-460301.x.
- Myles PS, Williams DL, Hendrata M, Anderson H, Weeks AM. Patient satisfaction after anaesthesia and surgery: results of a prospective survey of 10,811 patients. Br J Anaesth 2000;84:6-10. http://dx.doi.org/10.1093/oxfordjournals.bja.a013383.
- Sebel PS, Bowdle TA, Ghoneim MM, Rampil IJ, Padilla RE, Gan TJ, et al. The incidence of awareness during anaesthesia: a multicenter United States study. Anesth Analg 2004;99:833-9. http://dx.doi.org/10.1213/01.ANE.0000130261.90896.6C.
- Pollard RJ, Coyle JP, Gilbert RL, Beck JR. Intraoperative awarenes in a regional medical system. A review of 3 years' data. Anesthesiology 2007;106:269-74. http://dx.doi.org/10.1097/00000542-200702000-00014.
- Xu L, Wu A-S, Yue Y. The incidence of intra-operative awareness during general anaesthesia in China: a multi-center observational study. Acta Anaesthesiol Scand 2009;53:873-82. http://dx.doi.org/10.1111/j.1399-6576.2009.02016.x.
- Leslie K, Davidson AJ. Awareness during anesthesia: a problem without solutions?. Minerva Anestesiol 2010;76:624-8.
- Ronald A, Abdul Aziz KA, George Day T, Scott M. In patients undergoing cardiac surgery, thoracic epidural analgesia combined with general anaesthesia results in faster recovery and fewer complications but does not affect length of hospital stay. Interact Cardiovasc Thorac Surg 2006;5:207-16. http://dx.doi.org/10.1510/icvts.2005.125054.
- Errando CL, Sigl JC, Robles M, Calabuig E, Garcia J, Arocas F, et al. Awareness with recall during general anaesthesia: a propsective observational evaluation of 4001 patients. Br J Anaesth 2008;101:178-85. http://dx.doi.org/10.1093/bja/aen144.
- Domino KB, Posner KL, Caplan RA, Cheney FW. Awareness during anaesthesia. A closed claims analysis. Anesthesiology 1999;90:1053-61. http://dx.doi.org/10.1097/00000542-199904000-00019.
- Hardman JG, Aitkenhead AR. Awareness during anesthesia. Contin Educ Anaesth Crit Care Pain 2005;5:183-6. http://dx.doi.org/10.1093/bjaceaccp/mki049.
- Thomas G, Morgan M. Monitoring neuromuscular blockade and depth of anaesthesia. Anaesth Intensive Care Med 2011;12:271-4. http://dx.doi.org/10.1016/j.mpaic.2011.03.008.
- Orser BA, Mazer D, Baker AJ. Awareness during anesthesia. Can Med Assoc J 2008;178:185-8. http://dx.doi.org/10.1503/cmaj.071761.
- Bruhn J, Myles PS, Sneyd R, Struys MMRF. Depth of anaesthesia monitoring: What's available, what's validated and what's next?. Br J Anaesth 2006;97:85-94. http://dx.doi.org/10.1093/bja/ael120.
- Brice DD, Hetherington RR, Utting JE. A simple study of awareness and dreaming during anaesthesia. Br J Anaesth 1970;42:535-41. http://dx.doi.org/10.1093/bja/42.6.535.
- Wennervita J, Ranta SO, Hynynen M. Awareness and recall in outpatient anesthesia. Anesth Analg 2002;95:72-7. http://dx.doi.org/10.1097/00000539-200207000-00013.
- Avidan MS, Palanca BJ, Glick D, Jacobsohn E, Villafranca A, O’Connor M, et al. Protocol for the BAG-RECALL clinical trial: a prospective, multi-center, randomized, controlled trial to determine whether a bispectral index-guided protocol is superior to an anesthesia gas-guided protocol in reducing intraoperative awareness with explicit recall in high risk surgical patients. BMC Anesthesiol 2009;9.
- Avidan MS, Zhang L, Burnside BA, Finkel KJ, Searleman AC, Selvidge JA, et al. Anesthesia awareness and the bispectral index. N Engl J Med 2008;358:1097-108. http://dx.doi.org/10.1056/NEJMoa0707361.
- Eger EI, Sonner JM. Response to Enlund M: TIVA, awareness and the Brice interview. Anesth Analg 2006;102. http://dx.doi.org/10.1213/01.ANE.0000190857.67309.1E.
- Lubke GH, Kerssens C, Gershon RY, Sebel PS. Memory formation during general anesthesia for emergency cesarean sections. Anesthesiology 2000;92:1029-34. http://dx.doi.org/10.1097/00000542-200004000-00020.
- Hudson AE, Hemmings HC. Are anaesthetics toxic to the brain?. Br J Anaesth 2011;107:30-7. http://dx.doi.org/10.1093/bja/aer122.
- Recommendations for standards of monitoring during anaesthesia and recovery. London: The Association of Anaesthetists of Great Britain and Ireland; 2007.
- Bromhead HJ, Jones NA. The use of anaesthetic rooms for induction of anaesthesia: a postal survey of current practice and attitudes in Great Britain and Northern Ireland. Anaesthesia 2002;57:850-4. http://dx.doi.org/10.1046/j.1365-2044.2002.02779.x.
- British national formulary No. 62. London: BMA and RPS; 2011.
- Punjasawadwong Y, Phongchiewboon A, Bunchungmongkol N. Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database Syst Rev 2007;4.
- Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343. http://dx.doi.org/10.1136/bmj.d5928.
- Drummond M, Sculpher M, Torrance G, O’Brien B, Stoddart G. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2005.
- Philips Z, Bojke L, Sculpher M, Claxton K, Golder S. Good practice guidelines for decision-analytic modelling in health technology assessment: A review and consolidation of quality assessment. Pharmacoeconomics 2006;24:355-71. http://dx.doi.org/10.2165/00019053-200624040-00006.
- Guide to the methods of technology appraisal. 2008.
- Treasury HM. The Green Book. Appraisal and Evaluation in Central Government. 2010. www.hm-treasury.gov.uk/data_greenbook_index.htm.
- Zhang C, Xu L, Ma Y-Q, Sun Y-X, Li Y-H, Zhang L, et al. Bispectral index monitoring prevent awareness during total intravenous anesthesia: A prospective, randomized, double-blinded, multi-center controlled trial. Chin Med J 2011;124:3664-9.
- Sahni N, Anand LK, Gombar KK, Gombar S. Effect of intraoperative depth of anesthesia on postoperative pain and analgesic requirement: A randomized prospective observer blinded study. J Anaesthesiol Clin Pharmacol 2011;27:500-5. http://dx.doi.org/10.4103/0970-9185.86595.
- Sakaguchi M, Higuchi H, Maeda S, Miyawaki T. Dental sedation for patients with intellectual disability: A prospective study of manual control versus Bispectral Index-guided target-controlled infusion of propofol. J Clin Anesth 2011;23:636-42. http://dx.doi.org/10.1016/j.jclinane.2011.04.008.
- Hampshire P, Guha A, Welters I, Murphy J, Poole L. Bispectral index monitoring reduces sedative and vasopressor requirements during percutaneous tracheostomy. Crit Care 2011;15:S123-4. http://dx.doi.org/10.1186/cc9768.
- Avidan MS, Jacobsohn E, Glick D, Burnside BA, Zhang L, Villafranca A, et al. Prevention of intraoperative awareness in a high-risk surgical population. New Engl J Med 2011;365:591-600. http://dx.doi.org/10.1056/NEJMoa1100403.
- Bannister CF, Brosius KK, Sigl JC, Meyer BJ, Sebel PS. The effect of bispectral index monitoring on anesthetic use and recovery in children anesthetized with sevoflurane in nitrous oxide. Anesth Analg 2001;92:877-81. http://dx.doi.org/10.1097/00000539-200104000-00015.
- Bhardwaj N, Yaddanapudi S. A randomized trial of propofol consumption and recovery profile with BIS-guided anesthesia compared to standard practice in children. Paediatr Anaesth 2010;20:160-7. http://dx.doi.org/10.1111/j.1460-9592.2009.03240.x.
- Chan MTV, Cheng B, Gin T, Lee T, Koo E. Cognitive dysfunction after anesthesia: a randomized controlled trial. J Neurosurg Anesthesiol 2010;22:408-9.
- Kamal NM, Omar SH, Radwan KG, Youssef A. Bispectral index monitoring tailors clinical anesthetic delivery and reduces anesthetic drug consumption. J Med Sci 2009;9:10-6. http://dx.doi.org/10.3923/jms.2009.10.16.
- Kerssens C, Gaither JR, Sebel PS. Preserved memory function during bispectral index-guided anesthesia with sevoflurane for major orthopedic surgery. Anesthesiology 2009;111:518-24. http://dx.doi.org/10.1097/ALN.0b013e3181b05f0b.
- Leslie K, Myles PS, Forbes A, Chan MT. The effect of bispectral index monitoring on long-term survival in the B-aware trial. Anesth Analg 2010;110:816-22. http://dx.doi.org/10.1213/ANE.0b013e3181c3bfb2.
- Liao WW, Wang JJ, Wu GJ, Kuo CD. The effect of cerebral monitoring on recovery after sevoflurane anesthesia in ambulatory setting in children: a comparison among bispectral index, A-line autoregressive index, and standard practice. J Chin Med Assoc 2011;74:28-36. http://dx.doi.org/10.1016/j.jcma.2011.01.004.
- Messieha ZS, Ananda RC, Hoffman WE, Punwani IC, Koenig HM. Bispectral Index System (BIS) monitoring reduces time to discharge in children requiring intramuscular sedation and general anesthesia for outpatient dental rehabilitation. Pediatr Dent 2004;26:256-60.
- Messieha ZS, Ananda RC, Hoffman WE, Punwani IC, Koenig HM. Bispectral index system (BIS) monitoring reduces time to extubation and discharge in children requiring oral presedation and general anesthesia for outpatient dental rehabilitation. Pediatric Dent 2005;27:500-4.
- Choi SR, Lim YH, Lee SC, Lee JH, Chung CJ. Spectral entropy monitoring allowed lower sevoflurane concentration and faster recovery in children. Acta Anaesthesiol Scand 2010;54:859-62. http://dx.doi.org/10.1111/j.1399-6576.2010.02212.x.
- Gruenewald M, Zhou J, Schloemerkemper N, Meybohm P, Weiler N, Tonner PH, et al. M-Entropy guidance vs standard practice during propofol–remifentanil anaesthesia: a randomised controlled trial. Anaesthesia 2007;62:1224-9. http://dx.doi.org/10.1111/j.1365-2044.2007.05252.x.
- Talawar P, Chhabra A, Trikha A, Arora MK, Chandralekha. Entropy monitoring decreases isoflurane concentration and recovery time in pediatric day care surgery: a randomized controlled trial. Paediatr Anaesth 2010;20:1105-10. http://dx.doi.org/10.1111/j.1460-9592.2010.03441.x.
- Vakkuri A, Yli-Hankala A, Sandin R, Mustola S, Hoymork S, Nyblom S, et al. Spectral entropy monitoring is associated with reduced propofol use and faster emergence in propofol-nitrous oxide-alfentanil anesthesia. Anesthesiology 2005;103:274-9. http://dx.doi.org/10.1097/00000542-200508000-00010.
- Wu SC, Wang PC, Liao WT, Shih TH, Chang KA, Lin KC, et al. Use of spectral entropy monitoring in reducing the quantity of sevoflurane as sole inhalational anesthetic and in decreasing the need for antihypertensive drugs in total knee replacement surgery. Acta Anaesthesiol Taiwan 2008;46:106-11. http://dx.doi.org/10.1016/S1875-4597(08)60003-X.
- Lai R-C, Lu Y-L, Huang W, Xu M-X, Lai J-L, Xie J-D, et al. Application of a narcotrend-assisted monitor for depth of anesthesia on microwave coagulation for the patients with liver cancer during total intravenous anesthesia with propofol and fentanyl. Chin J Cancer 2010;29:110-13. http://dx.doi.org/10.5732/cjc.009.10244.
- Rundshagen I, Hardt T, Cortina K, Pragst F, Fritzsche T, Spies C. Narcotrend-assisted propofol/remifentanil anaesthesia vs clinical practice: does it make a difference?. Br J Anaesth 2007;99:686-93. http://dx.doi.org/10.1093/bja/aem231.
- Aime I, Verroust N, Masson-Lefoll C, Taylor G, Laloe PA, Liu N, et al. Does monitoring bispectral index or spectral entropy reduce sevoflurane use?. Anesth Analg 2006;103:1469-77. http://dx.doi.org/10.1213/01.ane.0000246838.93153.23.
- Ellerkmann RK, Soehle M, Riese G, Zinserling J, Wirz S, Hoeft A, et al. The Entropy Module and Bispectral Index as guidance for propofol-remifentanil anaesthesia in combination with regional anaesthesia compared with a standard clinical practice group. Anaesth Intensive Care 2010;38:159-66.
- Kreuer S, Biedler A, Larsen R, Altmann S, Wilhelm W. Narcotrend monitoring allows faster emergence and a reduction of drug consumption in propofol-remifentanil anesthesia. Anesthesiology 2003;99:34-41. http://dx.doi.org/10.1097/00000542-200307000-00009.
- Kreuer S, Bruhn J, Stracke C, Aniset L, Silomon M, Larsen R, et al. Narcotrend or bispectral index monitoring during desflurane-remifentanil anesthesia: a comparison with a standard practice protocol. Anesth Analg 2005;101:427-44. http://dx.doi.org/10.1213/01.ANE.0000157565.00359.E2.
- Ahmad S, Yilmaz M, Marcus RJ, Glisson S, Kinsella A. Impact of bispectral index monitoring on fast tracking of gynecologic patients undergoing laparoscopic surgery. Anesthesiology 2003;98:849-52. http://dx.doi.org/10.1097/00000542-200304000-00010.
- Anez C, Papaceit J, Sala JM, Fuentes A, Rull M. The effect of encephalogram bispectral index monitoring during total intravenous anesthesia with propofol in outpatient surgery. Rev Esp Anestesiol Reanim 2001;48:264-9.
- Basar H, Ozcan S, Buyukkocak U, Akpinar S, Apan A. Effect of bispectral index monitoring on sevoflurane consumption. Eur J Anaesthesiol 2003;20:396-400. http://dx.doi.org/10.1097/00003643-200305000-00008.
- Boztug N, Bigat Z, Akyuz M, Demir S, Ertok E. Does using the bispectral index (BIS) during craniotomy affect the quality of recovery?. J Neurosurg Anesthesiol 2006;18:1-4. http://dx.doi.org/10.1097/01.ana.0000188028.80960.dd.
- Bruhn J, Kreuer S, Bischoff P, Kessler P, Schmidt GN, Grzesiak A, et al. Bispectral index and A-line AAI index as guidance for desflurane-remifentanil anaesthesia compared with a standard practice group: a multicentre study. Br J Anaesth 2005;94:63-9. http://dx.doi.org/10.1093/bja/aei013.
- Chiu CL, Ong G, Majid AA. Impact of bispectral index monitoring on propofol administration in patients undergoing cardiopulmonary bypass. Anaesth Intensive Care 2007;35:342-7.
- Gan TJ, Glass PS, Windsor A, Payne F, Rosow C, Sebel P, et al. Bispectral index monitoring allows faster emergence and improved recovery from propofol, alfentanil, and nitrous oxide anesthesia. BIS Utility Study Group. Anesthesiology 1997;87:808-15. http://dx.doi.org/10.1097/00000542-199710000-00014.
- Hachero A, Alamo F, Caba F, Echevarria M, Merino S, Gomez P, et al. Influence of bispectral index monitoring on fentanyl requirements during total intravenous anesthesia for major gynecological surgery. Rev Esp Anestesiol Reanim 2001;48:364-9.
- Ibraheim O, Alshaer A, Mazen K, El-Dawlaty A, Turkistani A, Alkathery K, et al. Effect of bispectral index (BIS) monitoring on postoperative recovery and sevoflurane consumption among morbidly obese patients undergoing laparoscopic gastric banding. Middle East J Anesthesiol 2008;19:819-30.
- Leslie K, Myles PS, Forbes A, Chan MT, Short TG, Swallow SK. Recovery from bispectral index-guided anaesthesia in a large randomized controlled trial of patients at high risk of awareness. Anaesth Intensive Care 2005;33:443-51.
- Masuda T, Yamada H, Takada K, Sagata Y, Yamaguchi M, Tomiyama Y, et al. Bispectral index monitoring is useful to reduce total amount of propofol and to obtain immediate recovery after propofol anesthesia. Masui 2002;51:394-9.
- Mayer J, Boldt J, Schellhaass A, Hiller B, Suttner SW. Bispectral index-guided general anesthesia in combination with thoracic epidural analgesia reduces recovery time in fast-track colon surgery. Technol Comput Simulation 2007;104:1145-9.
- Morimoto Y, Oka S, Mii M, Shinjo Y, Yamashita A, Gohara T, et al. Efficacy of bispectral index monitoring in improving anesthetic management, economics, and use of the operating theater. Masui 2002;51:862-68.
- Muralidhar K, Banakal S, Murthy K, Garg R, Rani GR, Dinesh R. Bispectral index-guided anaesthesia for off-pump coronary artery bypass grafting. Ann Card Anaesth 2008;11:105-10. http://dx.doi.org/10.4103/0971-9784.41578.
- Myles PS, Leslie K, McNeil J, Forbes A, Chan MT. Bispectral index monitoring to prevent awareness during anaesthesia: the B-Aware randomised controlled trial. Lancet 2004;363:1757-63. http://dx.doi.org/10.1016/S0140-6736(04)16300-9.
- Nelskyla KA, Yli-Hankala AM, Puro PH, Korttila KT. Sevoflurane titration using bispectral index decreases postoperative vomiting in phase II recovery after ambulatory surgery. Anesth Analg 2001;93:1165-9. http://dx.doi.org/10.1097/00000539-200111000-00021.
- Paventi S, Santevecchi A, Metta E, Annetta MG, Perilli V, Sollazzi L, et al. Bispectral index monitoring in sevoflurane and remifentanil anesthesia. Analysis of drugs management and immediate recovery. Minerva Anestesiol 2001;67:435-9.
- Puri GD, Murthy SS. Bispectral index monitoring in patients undergoing cardiac surgery under cardiopulmonary bypass. Eur J Anaesthesiol 2003;20:451-6. http://dx.doi.org/10.1097/00003643-200306000-00004.
- Recart A, Gasanova I, White PF, Thomas T, Ogunnaike B, Hamza M, et al. The effect of cerebral monitoring on recovery after general anesthesia: a comparison of the auditory evoked potential and bispectral index devices with standard clinical practice. Anesth Analg 2003;97:1667-74. http://dx.doi.org/10.1213/01.ANE.0000087041.63034.8C.
- Song D, Joshi GP, White PF. Titration of volatile anesthetics using bispectral index facilitates recovery after ambulatory anesthesia. Anesthesiology 1997;87:842-8. http://dx.doi.org/10.1097/00000542-199710000-00018.
- Struys MM, De ST, Versichelen LF, Van DV, Van den Broecke R, Mortier EP. Comparison of closed-loop controlled administration of propofol using Bispectral Index as the controlled variable versus ‘standard practice’ controlled administration. Anesthesiology 2001;95:6-17. http://dx.doi.org/10.1097/00000542-200107000-00007.
- Tufano R, Palomba R, Lambiase G, Giurleo LG. The utility of bispectral index monitoring in general anesthesia. Minerva Anestesiol 2000;66:389-93.
- White PF, Ma H, Tang J, Wender RH, Sloninsky A, Kariger R. Does the use of electroencephalographic bispectral index or auditory evoked potential index monitoring facilitate recovery after desflurane anesthesia in the ambulatory setting?. Anesthesiology 2004;100:811-17. http://dx.doi.org/10.1097/00000542-200404000-00010.
- Wong J, Song D, Blanshard H, Grady D, Chung F. Titration of isoflurane using BIS index improves early recovery of elderly patients undergoing orthopedic surgeries. Can J Anaesth 2002;49:13-8. http://dx.doi.org/10.1007/BF03020413.
- Zohar E, Luban I, White PF, Ramati E, Shabat S, Fredman B. Bispectral index monitoring does not improve early recovery of geriatric outpatients undergoing brief surgical procedures. Can J Anaesth 2006;53:20-5. http://dx.doi.org/10.1007/BF03021523.
- Assare H, Anderson RE, Jakobsson J. Sevoflurane requirements during ambulatory surgery: a clinical study of bispectral index and auditory evoked potential guided anaesthesia. Ambul Surg 2002;9:207-11. http://dx.doi.org/10.1016/S0966-6532(02)00004-5.
- Luginbuhl M, Wuthrich S, Petersen-Felix S, Zbinden AM, Schnider TW. Different benefit of bispectral index (BIS) in desflurane and propofol anesthesia. Acta Anaesthesiol Scand 2003;47:165-73. http://dx.doi.org/10.1034/j.1399-6576.2003.00041.x.
- McCormack J, Mehta D, Peiris K, Dumont G, Fung P, Lim J, et al. The effect of a target controlled infusion of propofol on predictability of recovery from anesthesia in children. Paediatr Anaesth 2010;20:56-62. http://dx.doi.org/10.1111/j.1460-9592.2009.03196.x.
- Wennervirta J, Hynynen M, Koivusalo AM, Uutela K, Huiku M, Vakkuri A. Surgical stress index as a measure of nociception/antinociception balance during general anesthesia. Acta Anaesthesiol Scand 2008;52:1038-45. http://dx.doi.org/10.1111/j.1399-6576.2008.01687.x.
- Medical Advisory Secretariat. Bispectral index monitor. 2004.
- Choi BM, Shin DH, Noh MH, Kim YH, Jeong YB, Lee SH, et al. Temporal linear mode complexity as a surrogate measure of the effect of remifentanil on the central nervous system in healthy volunteers. Br J Clin Pharmacol 2011;71:871-85. http://dx.doi.org/10.1111/j.1365-2125.2011.03904.x.
- Nordström O, Engström AM, Persson S, Sandin R. Incidence of awareness in total i.v. anaesthesia based on propofol, alfentanil and neuromuscular blockade. Acta Anaesthesiol Scand 1997;41:978-84. http://dx.doi.org/10.1111/j.1399-6576.1997.tb04823.x.
- Abenstein JP. Is BIS monitoring cost-effective?. Conference Proceedings: Annual International Conference of the IEEE Engineering in Medicine &Amp; Biology Society 2009 n.d.:7041-4.
- Ekman A, Lindholm ML, Lennmarken C, Sandin R. Reduction in the incidence of awareness using BIS monitoring. Acta Anaesthesiol Scand 2004;48:20-6. http://dx.doi.org/10.1111/j.1399-6576.2004.00260.x.
- Elliott RA, Payne K, Moore JK, Davies LM, Harper NJN, St Leger AS, et al. Which anaesthetic agents are cost-effective in day surgery? Literature review, national survey of practice and randomised controlled trial. Health Technol Assess 2002;6.
- Chernin EL. Pharmacoeconomics of Inhaled Anesthetic Agents: Considerations for the Pharmacist. Am J Health Syst Pharm 2004;61:18-22.
- Dion P. The cost of anaesthetic vapours. Can J Anaesth 1992;39. http://dx.doi.org/10.1007/BF03008331.
- Chatterjee S, Rudra A, Sengupta S. Current concepts in the management of postoperative nausea and vomiting. Anesthesiol Res Pract 2011;2011.
- Ku CM, Ong BC. Postoperative nausea and vomiting: a review of current literature. Singapore Med J 2003;44:366-74.
- Gan TJ. Postoperative nausea and vomiting – Can it be eliminated?. J Am Med Assoc 2002;287:1233-6. http://dx.doi.org/10.1001/jama.287.10.1233.
- Liu SS. Effects of Bispectral Index Monitoring on Ambulatory Anesthesia. Anesthesiology 2004;101:311-15. http://dx.doi.org/10.1097/00000542-200408000-00010.
- Deiiner S, Silverstein JH. Postoperative delirium and cognitive function. Br J Anaesth 2009;103.
- Moller JT, Cluitmans P, Rasmussen LS, Canet J, Rabbitt P, Jolles J, et al. Long term postoperative cognitive dysfunction in the elderly: ISPOCD1 study. Lancet 2012;351:857-61. http://dx.doi.org/10.1016/S0140-6736(97)07382-0.
- Abildstrom H, Rasmussen LS, Rentowl P, Rasmussen H, Kristensen PA, Moller JT. Cognitive dysfunction 1–2 years afternon-cardiac surgery in the elderly. Acta Anaesthesiol Scand 2000;44:1246-51. http://dx.doi.org/10.1034/j.1399-6576.2000.441010.x.
- The Information Centre for Health and Social Care . HES Online – Main Procedures and Intervention Tables 2012. www.hesonline.nhs.uk.
- Jonsson L, Andreasen N, Kilander L, Soininen H, Waldemar G, Nygaard H, et al. Patient and proxy-reported utility in Alzheimer Disease using the EuroQol. Alzheimer Dis Assoc Disord 2006;20:49-55. http://dx.doi.org/10.1097/01.wad.0000201851.52707.c9.
- Lyons G, Macdonald R. Awareness during Caesarean section. Anaesthesia 1991;46:62-4. http://dx.doi.org/10.1111/j.1365-2044.1991.tb09321.x.
- Ranta S, Jussila J, Hynynen M. Recall of awareness during cardiac anaesthesia: influence of feedback information to the anaesthesiologist. Acta Anaesthesiol Scand 1996;40:554-60. http://dx.doi.org/10.1111/j.1399-6576.1996.tb04487.x.
- Liu WHD, Thorp TAS, Graham SG, Aitkenhead AR. Incidence of awareness with recall during general anaesthesia. Anaesthesia 1991;46:435-7. http://dx.doi.org/10.1111/j.1365-2044.1991.tb11677.x.
- Schwender D, Kunze-Kronawitter H, Dietrich P, Klasing S, Forst H, Madler C. Conscious awareness during general anaesthesia: patients' perceptions, emotions, cognition and reactions. Br J Anaesth 1998;80:133-9. http://dx.doi.org/10.1093/bja/80.2.133.
- Samuelsson P, Brudin L, Sandin RH. Late psychological symptoms after awareness among consecutively included surgical patients. Anesthesiology 2007;106:26-32. http://dx.doi.org/10.1097/00000542-200701000-00009.
- Evans JM, Rosen M, Lunn JN. Consciousness, awareness and pain in general anesthesia. London: Butterworth; 1987.
- Diagnostic and statistical manual of mental disorders. Washington, DC: American Psychiatric Association; 1994.
- Kessler RC, Sonnega A, Bromet E, Hughes M, Neslon CB. Posttraumatic stress disorder in the national comorbidity survey. Arch Gen Psychiatry 1995;52:1048-60. http://dx.doi.org/10.1001/archpsyc.1995.03950240066012.
- Doctor JN, Zoellner LA, Feeny NC. Predictors of health-related quality-of-life utilities among persons with posttraumatic stress disorder. Psychiatr Serv 2011;62:272-7. http://dx.doi.org/10.1176/appi.ps.62.3.272.
- Freed MC, Yeager DE, Liu X, Gore KL, Engel CC, Magruder KM. Preference-weighted health status of PTSD among veterans: an outcome for cost-effectiveness analysis using clinical data. Psychiatr Serv 2009;60:1230-8. http://dx.doi.org/10.1176/appi.ps.60.9.1230.
- Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ 2002;21:271-92. http://dx.doi.org/10.1016/S0167-6296(01)00130-8.
- Laffaye C, Kennedy C, Stein MB. Post-traumatic stress disorder and health-related quality of life in female victims of intimate partner violence. Violence Vict 2003;18:227-38. http://dx.doi.org/10.1891/vivi.2003.18.2.227.
- Tsai KY, Chou P, Chou FH, Su TT, Lin SC, Lu MK, et al. Three-year follow-up study of the relationship between posttraumatic stress symptoms and quality of life among earthquake survivors in Yu-Chi, Taiwan. J Psychiatr Res 2007;41:90-9. http://dx.doi.org/10.1016/j.jpsychires.2005.10.004.
- Meeske KA, Ruccione K, Globe DR, Stuber ML. Posttraumatic stress, quality of life, and psychological distress in young adult survivors of childhood cancer. Oncol Nurs Forum 2001;28:481-9.
- Hernandez-Gancedo C, Pestana D, Perez-Chrzanowska H, Martinez-Casanova E, Criado A. Comparing Entropy and the Bispectral index with the Ramsay score in sedated ICU patients. J Clin Monit Comput 2007;21:295-302. http://dx.doi.org/10.1007/s10877-007-9087-7.
- Weil G, Passot S, Servin F, Billard V. Does spectral entropy reflect the response to intubation or incision during propofol-remifentanil anesthesia?. Anesth Analg 2008;106:152-9. http://dx.doi.org/10.1213/01.ane.0000296454.00236.fc.
- Magruder KM, Frueh B, Knapp R, . Prevalence of posttraumatic stress disorder in Veteran's Affairs primary care clinics. Gen Hosp Psychiatry 2005;27:169-79. http://dx.doi.org/10.1016/j.genhosppsych.2004.11.001.
- Ara R, Brazier J. Predicting the short form-6D preference-based index using the eight mean short form-36 health dimension scores:estimating preference-based health-related utilities when patient level data are not available. Value Health 2009;12:346-53. http://dx.doi.org/10.1111/j.1524-4733.2008.00428.x.
- Berger W, Figueira I, Maurat AM, Bucassio EP, Vieira I, Jardim SR, et al. Partial and full PTSD in Brazilian ambulance workers: prevalence and impact on health and on quality of life. J Trauma Stress 2007;20:637-42. http://dx.doi.org/10.1002/jts.20242.
- Shiner B, Watts BV, Pomerantz A, Young-Xu Y, Schnurr PP. Sensitivity of the SF-36 to PTSD symptom change in veterans. J Trauma Stress 2011;24:111-15. http://dx.doi.org/10.1002/jts.20613.
- Evren C, Sar V, Dalbudak E, Cetin R, Durkaya M, Evren B, et al. Lifetime PTSD and quality of life among alcohol-dependent men: impact of childhood emotional abuse and dissociation. Psychiatry Res 2011;186:85-90. http://dx.doi.org/10.1016/j.psychres.2010.07.004.
- SCHARR . SF-6D 2012. www.shef.ac.uk/scharr/sections/heds/mvh/sf-6d.
- Post-traumatic stress disorder (PTSD). The management of PTSD in adults and children in primary and secondary care. National costing report. 2005.
- Post-traumatic stress disorder (PTSD). The management of PTSD in adults and children in primary and secondary care. Clinical Guideline 26. 2005.
- Singleton N, Bumpstead R, O’Brien M, Lee A, Meltzer H. Psychiatric morbidity among adults living in private households, 2000. London: HMSO; 2001.
- Kartha A, Brower V, Saitz R, Samet JH, Keane TM, Liebschutz J. The impact of trauma exposure and post-traumatic stress disorder on health care utilization among primary care patients. Med Care 2008;46:388-93. http://dx.doi.org/10.1097/MLR.0b013e31815dc5d2.
- Department of Health . NHS Reference Costs 2010–2011 2012. www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_131140 (accessed 17 May 2013).
- Phillips AA, McLean RF, Devitt JH, Harrington EM. Recall of intraoperative events after general anaesthesia and cardiopulmonary bypass. Can J Anaesth 1993;40:922-6. http://dx.doi.org/10.1007/BF03010093.
- Russell IF. The Narcotrend ‘depth of anaesthesia’ monitor cannot reliably detect consciousness during general anaesthesia: an investigation using the isolated forearm technique. Br J Anaesth 2006;96:346-52. http://dx.doi.org/10.1093/bja/ael017.
- Mashour GA, Tremper KK, Avidan MS. Protocol for the ‘Michigan Awareness Control Study’: A prospective, randomized, controlled trial comparing electronic alerts based on bispectral index monitoring or minimum alveolar concentration for the prevention of intraoperative awareness. BMC Anesthesiol 2009;9. http://dx.doi.org/10.1186/1471-2253-9-7.
- Mashour GA, Shanks A, Tremper K, Kheterpal S, Turner C, Ramachandran S, et al. Prevention of intraoperative awareness with explicit recall in an unselected surgical population: a randomized comparative effectiveness trial. Anesthesiology 2012;117:717-25.
- Medical Advisory Secretariat Bispectral index monitor: an evidence-based analysis. ONT Health Technol Assess Ser 2004;4:1-72.
- El Menesy TM, Hamden GA, Amin SM, Zakaria D. Continuous intraoperative high state and response entropies reduced desflurane emergence agitation in pediatric laparoscopic surgery. Egypt J Anaesth 2008;24:85-93.
- Pelletier N, Passot S, Zufferey P, Molliex S. Benefit of EEG guided anaesthesia: a meta-analysis. Anesthesiology 2011.
- Smajic J, Praso M, Hodzic M, Hodzic S, Srabovic-Okanovic A, Smajic N, et al. Assessment of depth of anesthesia: PRST score versus bispectral index. Medicinski Arhiv 2011;65:216-20. http://dx.doi.org/10.5455/medarh.2011.65.216-220.
- Bauer M, Wilhelm W, Kraemer T, Kreuer S, Brandt A, Adams HA, et al. Impact of bispectral index monitoring on stress response and propofol consumption in patients undergoing coronary artery bypass surgery. Anesthesiology 2004;101:1096-104. http://dx.doi.org/10.1097/00000542-200411000-00008.
- Riad W, Schreiber M, Saeed AB. Monitoring with EEG entropy decreases propofol requirement and maintains cardiovascular stability during induction of anaesthesia in elderly patients. Eur J Anaesthesiol 2007;24:684-8. http://dx.doi.org/10.1017/S026502150700018X.
- Singh M, Kulkarni D, Gopinath R. Bispectral index monitoring may not enhance performance of the ‘wake-up’ test during scoliosis surgery. J Anaesthesiol Clin Pharmacol 2009;25:179-82.
- Weber F, Pohl F, Hollnberger H, Taeger K. Impact of the Narcotrend Index on propofol consumption and emergence times during total intravenous anaesthesia with propofol and remifentanil in children: a clinical utility study. Eur J Anaesthesiol 2005;22:741-7. http://dx.doi.org/10.1017/S0265021505001237.
- Tappenden P, Jones R, Paisley S, Carroll C. Systematic review and economic evaluation of bevacizumab and cetuximab for the treatment of metastatic colorectal cancer. Health Technol Assess 2007;11.
Appendix 1 Report methods for synthesis of evidence of clinical effectiveness and cost-effectiveness as described in the research protocol
Report methods for synthesis of evidence of clinical effectiveness and cost-effectiveness as described in the research protocol (PDF download)
Appendix 2 Literature search strategies
Appendix 3 Inclusion/exclusion worksheet used in systematic review of patient outcomes
Inclusion/exclusion worksheet used in systematic review of patient outcomes (PDF download)
Appendix 4 Reasons for the exclusion of full-text publications from systematic review of patient outcomes
Reasons for the exclusion of full-text publications from systematic review of patient outcomes (PDF download)
Appendix 5 Data extraction and critical appraisal forms used in the systematic review of patient outcomes
Data extraction and critical appraisal forms used in the systematic review of patient outcomes (PDF download)
Appendix 6 Data extraction and critical appraisal forms used in the systematic review of cost-effectiveness
Data extraction and critical appraisal forms used in the systematic review of cost-effectiveness (PDF download)
Appendix 7 Studies excluded from the review of economic evaluations
Studies excluded from the review of economic evaluations (PDF download)
Appendix 8 Pooled intravenous anaesthetic consumption for Narcotrend randomised controlled trials
Pooled intravenous anaesthetic consumption for Narcotrend randomised controlled trials (PDF download)
Appendix 9 Derivation of the pooled estimates of cumulative incidence of awareness used in the model
Derivation of the pooled estimates of cumulative incidence of awareness used in the model (PDF download)
Appendix 10 Survival modelling methodology
Appendix 11 Search strategy to identify utility values for post-traumatic stress disorder
Search strategy to identify utility values for post-traumatic stress disorder (PDF download)
Appendix 12 Ongoing trials identified
List of abbreviations
Technical terms and abbreviations are used throughout this report. The meaning is usually clear from the context, but a glossary is provided for the non-specialist reader.
- ASA
- American Society of Anesthesiologists
- BAG-RECALL
- BIS or Anaesthetic Gas to Reduce Explicit Recall
- BIS
- Bispectral Index
- BMI
- body mass index
- BNF
- British National Formulary
- CHEOPS
- Children's Hospital of Eastern Ontario Pain Score
- CI
- confidence interval
- ECG
- electrocardiography
- EEG
- electroencephalography
- EQ-5D
- European Quality of Life-5 Dimensions
- ETAC
- end-tidal anaesthetic concentration
- FGF
- fresh gas flow
- GA
- general anaesthesia
- HRQoL
- health-related quality of life
- HTA
- health technology assessment
- ICER
- incremental cost-effectiveness ratio
- ITT
- intention to treat
- i.v.
- intravenous
- IV
- inverse variance
- LPS
- late psychological symptoms
- MAC
- minimum alveolar concentration
- MMSE
- Mini Mental State Examination
- NICE
- National Institute for Health and Care Excellence
- PACU
- postanaesthesia care unit
- PAED
- Paediatric Anaesthetic Emergence Delirium
- POCD
- postoperative cognitive dysfunction
- PONV
- postoperative nausea and vomiting
- PTSD
- post-traumatic stress disorder
- PWHS
- preference weighted health score
- QALY
- quality-adjusted life-year
- QoL
- quality of life
- RCT
- randomised controlled trial
- SD
- standard deviation
- SF-36
- Short Form questionnaire-36 items
- SF-6D
- Short Form questionnaire-6 Dimensions
- SG
- standard gamble
- STAI
- StateTrait Anxiety Inventory
- TIVA
- total intravenous anaesthesia
- TTO
- time trade-off
- VAS
- visual analogue scale
All abbreviations that have been used in this report are listed here unless the abbreviation is well known (e.g. NHS), or it has been used only once, or it is a non-standard abbreviation used only in figures/tables/appendices, in which case the abbreviation is defined in the figure legend or in the notes at the end of the table.