Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 06/37/04. The contractual start date was in September 2008. The draft report began editorial review in July 2012 and was accepted for publication in November 2012. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors' report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Paul Stallard holds other grants paid to his institution from the National Institute of Health Research (NIHR) and has received funding to speak at the Excellence in Paediatrics Conference in Istanbul in December 2012. Glyn Lewis has grants/grants pending to his institution from the NIHR, Medical Research Council, Wellcome Trust, and US National Institute on Alcohol Abuse and Alcoholism that are relevant to this work and has received funding to speak at the Austrian Society of General Practice and Family Medicine conference, Vienna, in 2012. Abigail Millings is currently employed by Ultrasis UK Ltd and has stock options with her employer. All other authors declare (1) no financial support for the submitted work from anyone other than their employer; (2) no financial relationships with commercial entities that might have an interest in the submitted work; (3) no spouses, partners or children with relationships with commercial entities that might have an interest in the submitted work; and (4) no non-financial interests that may be relevant to the submitted work.
Permissions
Copyright statement
© Queen's Printer and Controller of HMSO 2013. This work was produced by Stallard et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Background
Depression is common in adolescents, with cumulative rates indicating that up to 20% of young people will suffer at least one clinically depressive episode by the age of 18 years. 1 Adolescent depression causes significant impairment, impacts on developmental trajectories, interferes with educational attainment and increases the risk of attempted and completed suicide as well as major depressive disorder in adulthood,2–5 yet it often remains unrecognised and untreated. 6,7 Depression in adolescence is an important public health issue and there has been growing interest in the development of preventative and early interventions. Systematic reviews of programmes designed to reduce symptoms of depression in adolescents have noted considerable variability in results but remain supportive of prevention and early intervention approaches delivered in schools. 8,9 However, significant methodological shortfalls, limited follow-up and absence of attention control or placebo comparisons have been noted as important omissions in previous studies10 and the cost-effectiveness of school-based depression prevention programmes has not yet been established.
Several evaluations have been carried out of depression prevention programmes based on cognitive–behavioural therapy (CBT) principles, including the Penn Resiliency Programme,11,12 Coping with Stress,13 Problem Solving for Life,14 FRIENDS,15 Resourceful Adolescent Programme (RAP)16 and other CBT programmes. 17 Although a number of studies have demonstrated short-term reduction in symptoms of depression, there is often an absence of long-term follow-up and where this is present effects typically diminish after 6 months. 1,10,18–20 Given the limited evidence of long-term gains for depression preventative interventions, it is possible that additional booster sessions could be useful in maintaining short-term benefits. Furthermore, active interventions need to be compared with appropriate controls, including placebo conditions, to account for non-specific treatment effects and spontaneous recovery. 1,8,9,18
Cognitive–behavioural therapy-based depression prevention programmes have been delivered as indicated (selective or targeted) interventions to adolescents with elevated symptoms of depression21,22 or as universal interventions to whole populations. 16,23 A meta-analytic review of school-based depression prevention programmes revealed that indicated programmes typically have larger effects than universal approaches. 9 However, indicated preventative interventions do not provide any input to low-risk children that would prevent symptoms developing and they encounter significant recruitment problems that severely limit their reach and potential impact. 11,21,24 Universal prevention programmes provide an alternative pragmatic approach, increasing reach (recruitment rates of 67–88% reported), reducing possible negative effects of stigma and labelling and resulting in lower rates of dropout. 13,14,16,25 Thus, although universal approaches might have a marginally smaller effect on symptoms of depression for individuals, they can potentially reduce far more disorders in the population as a whole. 26 The question of who delivers school-based interventions also needs to be considered, as depression prevention programmes that are led by trained facilitators typically have larger effects than those led by teachers. 9
Of the evaluated universal depression prevention programmes, the RAP appears particularly promising. Three studies have demonstrated a reduction in symptoms of depression relative to a control group post intervention, and all have demonstrated good reach (> 70% of the eligible population) and low attrition (< 10%),16,24,25 although sustained effects at long-term follow-up (12 months) were not assessed in two of these studies. 24,25 The largest of these studies was a multisite randomised controlled effectiveness trial in Australia of RAP involving 2664 students from 12 schools. 24 Of the ‘at-risk’ students, 49.1% in the RAP condition moved into the healthy category post intervention compared with 35.3% in the control group. This difference was maintained at 12-month follow-up and qualitative feedback indicated a high level of skills usage in the RAP group. 24
The current project aimed to undertake a pragmatic trial to evaluate the clinical effectiveness of a universally delivered classroom-based CBT depression prevention programme implemented under everyday conditions in the UK school context. To maximise the potential for effectiveness, an efficacious programme was selected (RAP), booster sessions were offered, and the programme was delivered by trained professionals external to the school. To overcome the methodological limitations of previous studies, classroom-based CBT was compared with usual Personal, Social and Health Education (PSHE) curriculum and attention control PSHE groups, and a long-term follow-up (12 months) was included.
Objectives
-
Examine the effectiveness of classroom-based CBT in reducing symptoms of depression in high-risk adolescents (aged 12–16 years) 12 months from baseline compared with the usual school curriculum and an attention control group.
-
Examine the effectiveness of classroom-based CBT compared with the control groups on the secondary outcomes on symptoms of depression, negative thoughts, self-esteem and anxiety (6 and 12 months from baseline).
-
Undertake secondary subgroup analysis to investigate effect modification on symptoms of depression (6 and 12 months from baseline) according to sex, age and baseline report of school connectedness, bullying, self-harm, and alcohol and drug use.
-
Assess the cost-effectiveness of the intervention in terms of reduction in symptoms of depression, health-related quality of life and cost–utility (6 and 12 months from baseline).
-
Undertake a process evaluation to assess factors associated with adherence, acceptability and sustainability of the intervention (post intervention).
Chapter 2 Methods
Design
The study was a pragmatic cluster randomised controlled trial comparing three arms: classroom-based CBT, attention control PSHE and usual PSHE (Table 1). The programmes were delivered universally to whole classes of young people during lessons when they would usually be following the school PSHE curriculum. However, the focus of the evaluation was on assessing the effect upon students who had consistent elevated levels of depressive symptoms (‘high risk’) at screening and baseline assessments.
| Trial arm | Content | Delivery |
|---|---|---|
| Classroom-based CBT | The RAP, a focused CBT programme | Two facilitators (leading sessions) |
| Attention control PSHE | Usual school PSHE curriculum | One member of school staff (leading sessions) plus two facilitators |
| Usual PSHE | Usual school PSHE curriculum | One member of school staff |
A pilot phase was carried in one school in the South West region during the 2008–9 academic year. A further eight schools took part in the main trial, with interventions delivered during the 2009–10 academic year.
Ethical approval and consent
The study was approved by the University of Bath School for Health Research Ethics Approval Panel (14 November 2007). Consent/assent involved three stages: interested schools were required to opt in to the study; parents/carers of all eligible students were sent information and invited to opt out if they did not wish their child to complete the project assessments; and, finally, young people were required to opt in and provide written consent if they were willing to complete the assessments.
Participants and procedure
Sample size
The study was powered to detect a difference of two points in mean Short Mood and Feelings Questionnaire (SMFQ) scores at 12-month follow-up between classroom-based CBT and each of the control arms. The pilot study provided estimates of intraclass correlation coefficients (ICCs; 0.025), mean year group size (n = 203), consent rate (84%) and SMFQ standard deviation (SD; 4.9) in the target population. Based on 80% consent, 80% retention and 20% of children being classified as high risk, a mean cluster size for analysis of 26 high-risk participants per year group was anticipated, requiring a minimum of 22 year groups to detect a difference of two points with 80% power and 2.7% Dunnett-correction two sided alpha.
Recruitment of schools
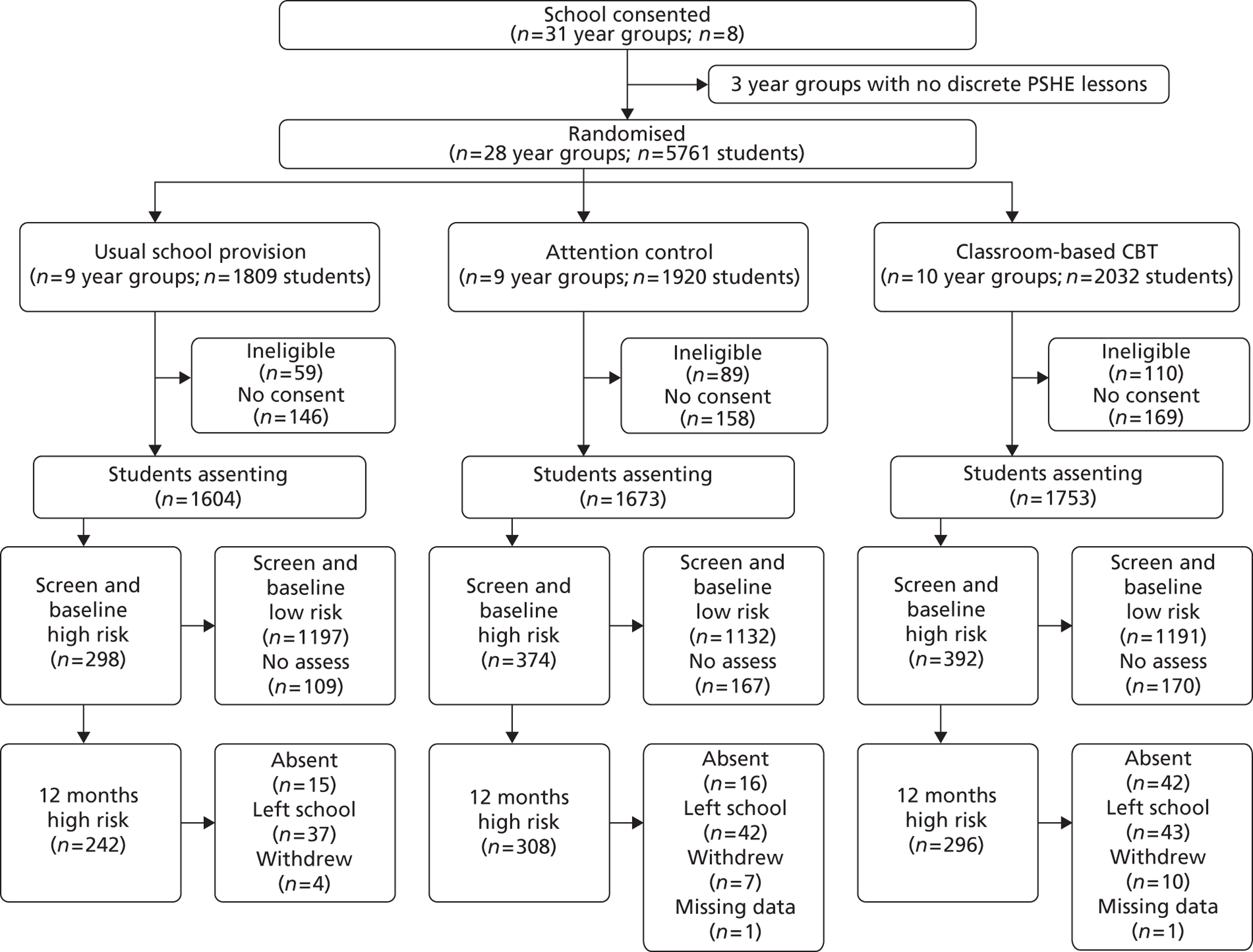
Information about the project was sent to 66 non-denominational comprehensive secondary schools in Bath and North East Somerset, Bristol, Wiltshire, Nottingham City and Nottinghamshire County. Schools that expressed an interest were contacted by the research team and a face-to-face meeting was arranged to discuss the project. Nine schools were recruited: one for the pilot study and eight for the main trial. In the participating schools, three year groups could not be included as they did not have discrete PSHE lessons. Therefore, 28 year groups were included in the randomisation process for the main trial. Details of participant flow are provided in Figure 1 (pilot study) and Figure 2 (main trial).
FIGURE 1.
Consolidated Standards of Reporting Trials diagram: pilot trial participant flow.
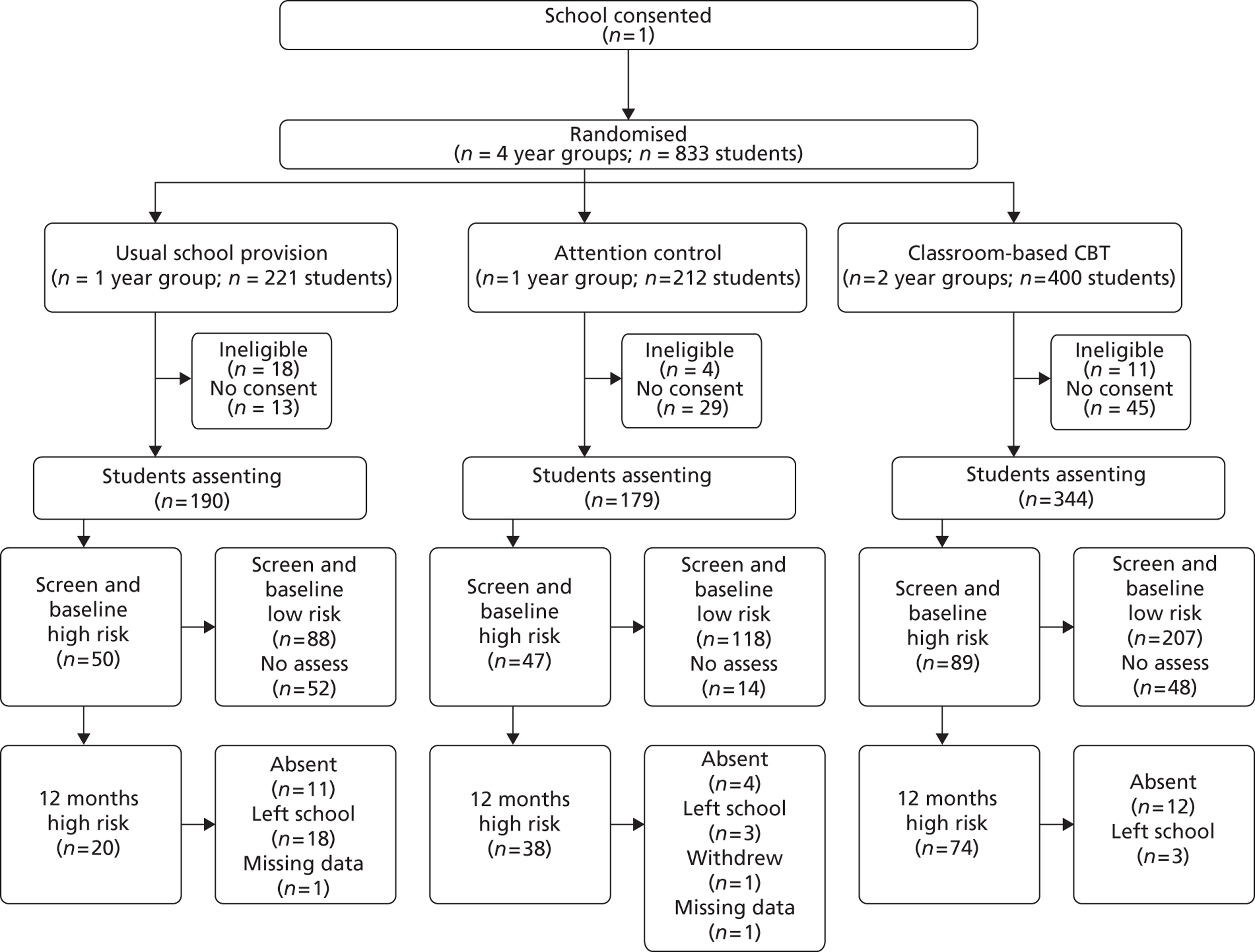
FIGURE 2.
Consolidated Standards of Reporting Trials diagram: main trial participant flow.
Inclusion/exclusion criteria
Interventions were provided during the school day as part of the school PSHE curriculum. All children were eligible unless they did not attend PSHE lessons (e.g. if they were away from school on long-term sickness absence, were withdrawn from PSHE for religious reasons or were educated elsewhere). Young people and their carers were contacted if they were identified as possibly clinically depressed during assessments (i.e. in the highest 2–3% of SMFQ scores). They were provided with information on how to seek further help should they require it, but these young people continued to participate in the programmes running in the school as usual.
Classification of the high-risk group
The target group for the effectiveness analysis were those who were at high risk of depression, that is those who had elevated and persistent symptoms of depression assessed using the SMFQ. 27 Those with scores of ≥ 5 at both screening and baseline assessments were classified as high risk.
Procedure for individual assessments with young people
Assessments were carried out at four time points: screening (SMFQ only), baseline, and 6 and 12 months from baseline. Some variation in assessment intervals occurred to fit around school holidays, examinations and other events. Mean times between assessments were baseline to 6 months = 176 days (SD 34.2); 6 months to 12 months = 181 days (SD 35.8); and baseline to 12 months = 359 days (SD 20.4). There was no difference between trial arms for the interval between time points for primary analysis (baseline to 12 months).
Assessments with young people were self-completed in schools during lesson time in sessions that were led by the research team. Following the pilot study, we anticipated that there would be differential dropout for the year 11 students who had left school by the time of their 12-month follow-up. To maximise response rates in this group in the main trial, any year 11 students who had stayed on for year 12 were assessed in school after 12 months. Those who had left school were contacted by post and/or e-mail (contact details and permission were obtained at 6-month assessment) and offered an option of filling in the questionnaire online and an incentive of entry to a prize draw (the prize was a gift voucher: 10 of £10 and 20 of £5 were available).
Randomisation
Year groups were randomly allocated on a 1 : 1 : 1 basis once all schools had been recruited. Balance between trial arms with respect to number of classes, number of students, PSHE frequency and scheduling of PSHE lessons within the school was achieved by calculating an imbalance statistic28 of all possible allocation sequences, restricted to those in which every school had at least one year group allocated to classroom-based CBT. Using a computer random numbers generator, a statistician with no other involvement in the study randomly selected one sequence from a subset of 100 with the most desirable balance properties.
Interventions
Classroom-based cognitive–behavioural therapy: the Resourceful Adolescent Programme UK
The RAP is a manualised depression prevention programme designed for use with groups of young people aged 12–15 years. It is based on a CBT model and interpersonal therapy principles. CBT recognises the importance of negative thoughts and low self-worth/image in the onset and maintenance of depression. These are actively targeted with core treatment components including psycho-education, identifying and challenging negative/dysfunctional thoughts, identifying personal strengths (thereby enhancing self-esteem/image), managing social problems, and learning to problem solve. Students complete their own workbook and group leaders have a detailed manual specifying key learning points and objectives.
For this study, the RAP was modified for use in the UK (RAP-UK). The content, key messages and goals were consistent with the original RAP, but the structure and method of delivery were revised to fit in with the UK education system. The key elements of RAP-UK – personal strengths, helpful thinking, keeping calm, problem solving, support networks and keeping the peace – are organised into nine sessions, each approximately 50–60 minutes long. RAP-UK was designed with a flexible method of delivery in mind to ensure that it could fit into a busy school timetable while retaining the key elements of the programme. Two additional booster sessions were offered to schools approximately 6 months after the initial programme had been completed. These provided an opportunity to review RAP-UK skills and to practise applying them to current difficulties. RAP-UK was delivered by two trained facilitators external to the school.
Attention control Personal, Social and Health Education
The attention control PSHE intervention involved similar time and contact with external providers to classroom-based CBT, but did not include the active components of the CBT intervention. The school delivered its usual PSHE curriculum, but the class teacher was joined by two facilitators from outside the school who assisted with delivering the lessons and engaging with young people. This controlled for the non-specific effects of interventions that are considered important in studies of depression. 29 As with classroom-based CBT, delivery of attention control PSHE was designed around nine 50- to 60-minute sessions, with flexibility to fit in with existing school PSHE programmes.
Usual Personal, Social and Health Education
‘Usual PSHE’ was the usual school PSHE curriculum provided by the school staff and did not involve any external input from the research team.
Programme facilitators
Facilitators had completed at least an undergraduate degree and had experience of working with young people and/or in a health-care setting. They were employed on a sessional basis. Different facilitators delivered the classroom-based CBT and attention control PSHE interventions to minimise therapist contamination. Facilitators received initial training, which covered the identification and management of mental health concerns, group management techniques and training in delivering their specific intervention. This was usually carried out with groups of new staff over 2 or 3 days, with condensed one-to-one training provided for staff joining at different points in the year as required. During the course of delivery, regular separate supervision groups were provided for classroom-based CBT and attention control PSHE facilitators. Teachers were present in all PSHE sessions and remained responsible for managing class behaviour.
Outcome measures: individual assessments with young people
Assessments completed by young people focused on the following areas: psychological functioning, social relationships, risk behaviours, health-care resource usage and sociodemographics. A copy of the questionnaire is provided in Appendix 1 and additional details on these measures are included in the trial protocol (see Appendix 2).
Primary outcome
The SMFQ27 is a 13-item scale derived from the 33-item Mood and Feelings Questionnaire. 30 Each item consists of a simple statement (e.g. ‘I didn't enjoy anything at all’), which is rated as being ‘true’ (scores 2), ‘sometimes true’ (scores 1) or ‘not true’ (scores 0). The SMFQ correlates well with other measures of depression and has good test–retest reliability, and higher scores are associated with fulfilling diagnostic criteria for clinical depression. 31–33
Secondary outcomes
Secondary outcomes were the personal failure subscale of the Children's Automatic Thoughts Scale (CATS),34 Rosenberg Self-Esteem Inventory,35 Revised Child Anxiety and Depression Scale (RCADS),36 School Connectedness Scale,37 Attachment Questionnaire for Children38 and items relating to bullying (Olweus Bully/Victim Questionnaire39), self-harm, cannabis use, use of other ‘street drugs’ (e.g. amphetamines, LSD, ecstasy, cocaine, ketamine, crack, heroin), and alcohol use over the last 6 months.
Resource and service use
As part of their standard assessments, all participants were asked to complete the European Quality of Life-5 Dimensions40 (EQ-5D: a standardised measure of quality of life/health outcome) and a modified self-report version of the Client Service Receipt Inventory (CSRI). 41 The CSRI is widely used and has been adapted across the child and adult age range and for different services. 41 The wording and presentation of the questions were simplified and pilot tested for clarity and ease of completion by the younger age group during the pilot phase of this trial. The modified CSRI (see Appendix 2) retrospectively assessed time off school; receipt of mental health or other health services; educational support; antipsychotropic medication (i.e. antidepressants or others); and social work/care services over a 6-month period. The specific service use information recorded in the assessment for each type of service use is summarised in Table 2.
| Types of service use | Details recorded | Notes or limits |
|---|---|---|
| Overnight hospital stays | Reason for stay and number of days in hospital | For up to three stays |
| A&E visits | Number of visits, reasons for visits | Up to three reasons |
| Hospital outpatient appointments | Number of visits, reasons for visits | Up to three reasons |
| Visits to the GP | Number of visits, number of visits for worry anxiety or unhappiness | |
| ‘Seen anyone else for psychological problems (such as worry, anxiety or unhappiness)’ | Number of times seen (for each of nurse at GP's practice, school nurse, counsellor, child mental health service, child psychologist, social worker or ‘someone else, please say who’) | |
| Taking medication (for anxiety or depression) | Name of medicine, how long taken | Up to two medicines |
Sociodemographic data
Basic demographic data were collected (sex, age, who you usually live with, ethnicity). The Family Affluence Scale42 was used as an indicator of socioeconomic status.
Process evaluation
The process evaluation followed the RE-AIM (Reach, Efficacy/effectiveness, Adoption, Implementation and Maintenance) framework. 43 Data were collected on attendance and attrition for classroom-based CBT and attention control PSHE by programme facilitators. An independent observer attended 5% of classroom-based CBT sessions to assess treatment fidelity. Feedback was gathered from teachers, young people and facilitators using questionnaires and qualitative interviews.
Feedback questionnaires
Twenty per cent of classes were asked to complete evaluation questionnaires post intervention. This included a series of 11-point Likert scales (0–10), asking students about engagement and usefulness of the PSHE programmes. All teachers involved with classroom-based CBT were invited to complete evaluation questionnaires, where they rated on the following five-point Likert scales (0–4): quality of organisation of the programme; relevance to young people; age appropriateness; extent to which they thought the programme would help young people with their mood and dealing with challenges in day-to-day life; whether or not the number of sessions was appropriate; and how likely they would be to continue with the programme in the future. Facilitators were asked to rate on the following five-point scales (0–4): the adequacy of training and supervision; how much they enjoyed delivering the programme; how challenging they had found it; how much they thought it would make a difference to young people's mental health; and student engagement.
Qualitative evaluation
Purposive sampling was used for the focus groups with young people to ensure that a range of views was captured across schools, year groups and sexes. There was a combination of same- and mixed-sex groups to allow for variations in discussion influenced by group composition. In total, 42 young people (19 male and 23 female) participated across seven focus groups, with all year groups being represented at least once.
The school link person (either the PSHE coordinator or a member of the senior management team) and any other teachers involved in the trial at each school were invited to provide feedback via either interviews or focus groups. Members of school staff (four male and eight female) participated across seven interviews or focus groups. For focus groups with facilitators, 39 individuals (6 male and 33 female) participated across six groups (separate groups for classroom-based CBT and attention control PSHE facilitators).
Semi-structured topic guides were used to gather the qualitative feedback, focusing on overall views of RAP, individual sessions (what worked and what did not), delivery, pupils' perceptions and maintenance of RAP (including likelihood of continuing the programme, giving consideration to cost and resources). Summary cards of RAP sessions and RAP manuals were provided to facilitate discussion. Interviews also captured general feedback on the trial, attention control PSHE, views on how PSHE is delivered in schools in general and any other comments. Focus groups were facilitated by a researcher and a co-facilitator/note-taker.
Analysis: pilot study
The aims of the pilot study were to establish whether or not the trial protocol was feasible in terms of reach and acceptability, gather data to check the sample size calculation for the main trial and trial the programmes and assessment procedure. The analysis focused on participant flow (recruitment and retention), descriptive analysis of change in symptoms over the course of the study, success in delivering sessions as intended and adherence/attrition and brief thematic analysis of feedback from students and teachers on acceptability.
Analysis: main trial
Statistical analysis
Statistical analyses were conducted using Stata 11 (StataCorp LP, College Station, TX, USA). Descriptive statistics were used to assess the balance between the trial arms at baseline. Effects on the primary outcome (SMFQ at 12-month follow-up) were assessed by intention to treat without imputation. In order to take appropriate account of the hierarchical nature of the data, multivariable mixed-effects regression was used to compare mean SMFQ at 12 months for classroom-based CBT with attention control PSHE and usual PSHE, with adjustment for baseline SMFQ and randomisation variables. In a secondary analysis, further adjustment was made for variables that were imbalanced between the trial arms at baseline. These analyses were repeated for secondary outcomes.
For SMFQ, repeated-measures mixed-effects regression models were used to investigate convergence/divergence between trial arms over time. Preplanned subgroup analyses44 were carried out using interaction terms in the regression models between the randomised arm and the following baseline variables: symptom severity (SMFQ score 5–10, ≥11); self-harm (no/yes); alcohol and/or drug misuse (no/yes); year group (8–11); and family affluence.
Sensitivity analyses were conducted to assess the potential effect of missing data using multiple imputation chained equation methods,45 with the imputation model including all variables associated with absence of primary outcome at 12 months. Variance at class and school level was investigated by including these in the multilevel models. Neither of these sensitivity analyses made any material difference to the primary results and therefore the data presented are those from two-level (individual and year group) models based on observed data only.
Finally, the effect of actual attendance at allocated lessons was examined by estimating the compiler-average causal effect (CACE) using instrumental variable regression,46 weighted using inverse probability weights constructed using baseline SMFQ scores, randomised group and ‘adherence’ (defined as attendance at ≥ 60% of sessions).
Qualitative analysis
Interviews and focus groups were digitally audio recorded and transcribed verbatim. The transcripts were thematically analysed, broadly following the guidelines of Braun and Clarke. 47 Transcripts were coded using NVivo 9 (QSR International, Southport, UK) software. A predefined, broad and descriptive coding framework was developed to enable the generation of initial codes. Each coding unit was coded exclusively into just one category as this allows very clearly defined coding categories to be developed. 48 Three members of the research team independently coded three randomly selected transcripts. Inter-rater reliabilities calculated using NVivo 9 revealed coding agreement ranging from 78% to 100%, indicating satisfactory consistency of interpretation. Any coding inconsistencies were resolved by discussion and consensus. The remaining 14 transcripts were then divided between the researchers and coded using the same framework. Data were then reviewed by the researchers and the themes were redefined as required. The emergent inductively coded themes were examined for consensus and conflict across the different participant groups.
Economic analysis
The service and resource use and cost-effectiveness analysis was carried out according to current best practice methods for conducting economic evaluation alongside trials,49 and specifically alongside cluster randomised controlled trials. 50
The unit costs applied to different types of health service use and for visits to different types of professionals or services because of anxiety or depression are provided in Table 3. The two main sources for the unit costs were the Department of Health's National Schedule of Reference Costs51 [for primary care trusts (PCTs) and NHS trusts combined] and the Personal Social Services Research's Unit Costs of Health and Social Care52 (hourly costs of patient or client contact for various types of health or social care professional).
The service/resource use data were checked and cleaned manually where required. Reported reason(s) for inpatient stays were assessed as being either elective or non-elective and relevant unit costs were applied (see Table 3). For a small minority (< 1%) of participants who reported taking medication for anxiety or depression, the information provided on medication names and on how long they had been taken was too unreliable to use as a basis for estimating these costs (e.g. where young people simply recorded ‘dunno’ or ‘can't remember’, or stated that they used ‘paracetamol’, other over-the-counter medications or herbal remedies, which would have no cost implications for the NHS) and was therefore excluded from further analysis.
The classroom-based CBT and attention control PSHE programmes were costed using detailed project records of resource use. This included the paid time of facilitators delivering the programme, the cost of their training, travel costs, printing costs of course booklets, and an apportionment of the cost of recruiting schools. All costs were calculated as either the amount of resource used multiplied by a unit cost or the total amount incurred over the trial period divided by the number of pupils in participating classes, number of sessions delivered or number of schools, depending on the level at which the cost was incurred.
Cleaning and correction of resource use and EQ-5D data and calculation of service use costs were conducted using PASW Statistics 18 (SPSS Inc., Chicago, IL, USA). Models for analysing incremental cost-effectiveness were fitted using Stata 12.0 software. Two cost-effectiveness analyses were conducted, the first using the SMFQ score and the second using quality-adjusted life-years (QALYs) based on responses to the EQ-5D questionnaire. Derivation of the per-person QALYs from baseline to 12 months involved calculating the social preference weight (or utility) for all those who completed the EQ-5D at each of the three time points, estimating the ‘area under the curve’ between baseline and 6 months and between 6 months and 12 months and summing them. QALYs were therefore calculated only for students who had complete EQ-5D data at all three time points. The social preference weights for the EQ-5D were from a representative sample survey of the UK general population in 1993. 53
| Question numbers | Resource type and unit | Unit cost (£) | Source |
|---|---|---|---|
| 6–11 | Inpatient stays – elective | 781 per day | NSRC2009–10c |
| 6–11 | Inpatient stays – non-elective short stay (1 day/night) | 520 per day | NSRC2009–10c |
| 6–11 | Inpatient stays – non-elective long stay (> 1 day/night) | 386 per day | NSRC2009–10c |
| 13–16 | A&E attendances | 103 | NSRC2009–10 A&E services not leading to admitted (sheet: TPCTA and EMSNA) |
| 18–21 | Hospital outpatient clinics | 99 | NSRC2009–10 face-to-face outpatient appointments (weighted average, consultant and non-consultant led, first attendance and follow-ups) |
| 23 and 24 | Visit to GP | 32 | UC2010 Section 2.8 (11.7-minute consultation)a |
| 25a | GP practice nurse consultation | 10 | UC2010 Section 10.6 (nurse GP practice, per consultation)a |
| 25b | School nurse time (per hour) | 64 | UC2010 (community nurse, per hour with patient, £16 per 15-minute appointment)a |
| 25c | Counsellor (per hour)b | 44 | UC2010 Section 2.14 (counselling services in primary medical care, per hour with patient or per contact hour)a |
| 25d | Child mental health service (per hour)b | 48 | UC2010 (mental health nurse, per hour with patient)a |
| 25e | Child psychologist (per hour)b | 81 | UC2010 Section 9.5 (clinical psychologist, per hour with patient)a |
| 25f | Social worker (per hour)b | 53 | UC2010 Section 11.3 [social worker (children), per hour with client]a |
Incremental costs, incremental effects and, where relevant, incremental cost-effectiveness ratios (ICERs) were estimated, comparing each of the classroom-based CBT and attention control PSHE trial arms with usual PSHE. The incremental cost per unit decrease in the SMFQ score (as lower scores on the SMFQ indicate better outcome) and the incremental cost per unit QALY increase were estimated. Both unadjusted and adjusted analyses (adjusting for site, mode of delivery, number of students and number of classes) were carried out. The incremental cost per unit decrease in SMFQ was additionally adjusted for SMFQ score at baseline.
Random effects bivariate linear regression models54 were fitted to model cost and effectiveness (SMFQ or QALY) simultaneously, allowing for correlation within clusters and correlation between cost and effectiveness score within participants. Estimates of the mean difference in costs and corresponding standard error, the mean difference in effect and corresponding standard error and (indirectly via the variance–covariance matrix of the regression coefficients) the correlation between the mean cost difference were obtained from these models. Where the ICER was in the north-east quadrant of the cost-effectiveness plane (i.e. intervention has both higher costs and greater effectiveness than control), Fieller's method was applied to obtain a parametric estimate of the 95% confidence interval (CI) for the ICER and construct the cost-effectiveness acceptability curve (CEAC). 49 The degrees of freedom (df) for these calculations (implemented in Stata using the ‘fielleri’ and ‘accepti’ commands) were based on the number of clusters.
For all adjusted analyses, the joint distribution of the difference in costs and effects was displayed using a scatterplot with 2000 cost–effect data pairs generated parametrically (using simulation) from a bivariate normal distribution based on the estimates from the random effects bivariate regression model used to model the cost and effect outcomes. The parametric scatterplots were similar to those generated using a non-parametric bootstrap approach and so, for consistency, we present only the former. Note that because the cost of the intervention must be apportioned across all participants in a given trial arm, both the SMFQ- and QALY-based cost-effectiveness results are based on the whole sample with valid cost and outcome data (i.e. not just those assessed as high risk as in the primary effectiveness analysis). Given the short time horizon, neither costs nor outcomes were discounted to present values.
Chapter 3 Results: pilot study
Altogether, 326 and 387 girls agreed to participate in the pilot study (89.1% of the eligible population). Ninety-two per cent of those who completed the baseline assessment were retained at 6 months and 80.2% were retained at 12 months. Details of participant flow by trial arm are provided in Figure 1.
Symptom change
A decrease in SMFQ scores was observed across all trial arms in the high-risk group from the baseline assessment to the 12-month follow up (F = 7.55, df 1; p < 0.01). However, the pilot study was not powered to assess between group differences on the primary outcome measure (SMFQ).
Feasibility of intervention delivery
Classroom-based CBT was provided to students in school years 8 and 10. All nine RAP-UK sessions were delivered to 15 classes, with the remaining class receiving eight sessions. A total of 137 (95.2%) RAP-UK sessions were delivered as intended by two facilitators, with the other seven sessions being led by one facilitator. A total of seven sessions were unexpectedly cancelled owing to adverse weather (n = 2), early school closure (n = 1), bank holidays (n = 1), examinations (n = 1), a school project day (n = 1) and PSHE itself being cancelled (n = 1). Of the 409 eligible children in years 8 and 10, only nine (2.2%) failed to attend any RAP-UK sessions. Of these, five had either been excluded from or moved school before the sessions started. Approximately half (n = 188; 46.0%) attended all nine sessions, with 357 (87.3%) attending seven or more sessions.
Classroom-based CBT facilitators rated the coverage of self-esteem, emotional awareness and positive thinking over the course of the programme significantly higher (p < 0.05) than the attention control PSHE facilitators, who gave the highest ratings to the coverage of topics traditionally covered in PSHE (i.e. bullying, smoking, drugs, alcohol, sex education, ethical issues, diversity, religion and citizenship). There was no significant difference between the groups in the specific focus on depression, although classroom-based CBT facilitators rated the direct focus on mental health more highly.
Acceptability of the classroom-based cognitive–behavioural therapy programme (Resourceful Adolescent Programme UK)
Semi-structured interviews were undertaken with 19 students (nine from year 8 and 10 from year 10) who took part in the classroom-based CBT (RAP-UK). Overall, feedback was positive. Students liked the content, the positive focus and the way in which the individual sessions built upon each other. The accompanying workbook was liked by most of the younger students, but some of the older students thought that it was pitched at too young a level. Some students expressed a preference for more ‘hands-on’ activities, role plays and discussions. A number of students also felt that the video clips were outdated or unclear. The sessions that students found most helpful were those focusing on problem solving, emotional recognition, the connection between thoughts and feelings, thought checking and relaxation. Those that focused on identifying and changing unhelpful thoughts were seen as repetitive and the support network session was considered by some to be too long.
A focus group was undertaken with the eight teachers whose classes received the classroom-based CBT. Initially, teachers were concerned about addressing mental health in a group, but they felt reassured by the end of the programme. Teachers were generally positive about the programme facilitators and the way in which assessments were conducted. They felt that some of the concepts in RAP-UK were memorable for themselves as well as for the students, such as negative thinking traps and ‘snowballing’. It was felt that the benefits of the programme might not be obvious immediately, but that the skills students acquired could be useful when they encountered problems later in their lives. Teachers liked the content of the programme, but at times felt it was pitched more towards the younger students (year 8) and may not have stretched the most able students. Teachers also raised concerns about the ability of less able students to engage with the classroom-based CBT.
Disruptive student behaviour in classes was a major issue, particularly if students became disengaged. The ability of facilitators to manage student behaviour came to light, with additional support from other members of staff in the classroom being viewed as essential, particularly when working with large classes and managing small group activities. Teachers felt that the sessions were sometimes repetitive and had many ideas about how sessions could be more interactive and engaging, such as making the graphics in the workbooks more age appropriate, updating some of the materials (particularly the video clips) and using more practical tasks in addition to the discussions.
The feedback from teachers and young people was used to revise RAP-UK by condensing some of the sessions, adding more interactive tasks, modifying the workbook so that it was more age appropriate (e.g. using photos instead of cartoons, changing the colour scheme and font) and updating multimedia materials.
Chapter 4 Results: main trial
Reach and attrition
Participant flow for the main trial is shown in Figure 2.
A summary of the demographic profile of the eight participating schools compared with national averages is presented in Table 4.
| School | Pupils in trial (n) | White (%)55 | Special needs without statements (%)55 | Overall absence (%)56 | Persistent absence (%)56 | Achieving five A*–C GCSE passes including level 2 English and maths (%)57 | Eligible for free school meals (%)55 |
|---|---|---|---|---|---|---|---|
| 1 | 710 | 63.8 | 20.2 | 5.4 | 2.7 | 69 | 11.9 |
| 2 | 623 | 89.7 | 8.1 | 8.3 | 7.7 | 61 | 7.0 |
| 3 | 835 | 93.2 | 17.9 | 6.5 | 5.1 | 55 | 9.5 |
| 4 | 783 | 95.3 | 6.9 | 6.1 | 2.8 | 75 | 2.5 |
| 5 | 848 | 77.6 | 36.0 | 11.1 | 13.8 | 36 | 31.2 |
| 6 | 530 | 83.5 | 10.5 | 4.7 | 1.7 | No year 11 | 3.3 |
| 7 | 534 | 92.8 | 10.1 | 7.7 | 6.2 | 47 | 7.6 |
| 8 | 167 | 98.7 | 19.7 | 7.9 | 7.4 | 48 | 9.2 |
| Total trial | 5030 | 85.5 | 16.8 | 7.3 | 6.0 | 56.7 | 11.2 |
| UK national average | NA | 81.2 | 19.7 | 6.9 | 4.4 | 50 | 15.4 |
The study cohort had a greater percentage of white students, were more academically able and had fewer students eligible for free school meals than the national average.
Altogether, 2563 boys and 2467 girls agreed to participate (91.4% of the eligible population). Of the 5030 participants, 1064 (21.2%) were classified as high risk. These had been allocated to usual PSHE (n = 298), attention control PSHE (n = 374) or classroom-based CBT (n = 392). Valid primary outcome data at 12 months were available for usual PSHE (n = 242; 81%), attention control PSHE (n = 308; 82%) and classroom-based CBT (n = 296; 76%).
For all participants, the median percentage of sessions attended was 89% (quartiles 67–100) in the classroom-based CBT group and 100% (quartiles 88–100) in the attention control PSHE group, with 80% of those in the classroom-based CBT group and 95% of the attention control PSHE groups attending at least 60% of sessions. One year group (n = 199) was withdrawn from classroom-based CBT after four sessions because of school closures in adverse weather. When this year group was removed from analysis, the median percentage of classroom-based CBT sessions attended was 89% (quartiles 78–100), with 92.2% attending at least 60% of sessions. For the high-risk participants, the median percentage of sessions attended was 88% (quartiles 67–100) in the classroom-based CBT arm and 89% (quartiles 78–100) in the attention control PSHE arm. The percentage of participants attending more than 60% of sessions was 80% and 93% in the classroom-based CBT and attention control PSHE groups, respectively. Details were not collected on PSHE attendance in the usual PSHE arm.
Balance between trial arms
Characteristics of high-risk individuals at baseline were well balanced between trial arms, apart from alcohol, street drug and cannabis use and bullying others, which were reported by fewer participants in the usual PSHE group (Table 5).
The proportion of high-risk participants within the arms was also slightly higher in the classroom-based CBT and attention control PSHE arms than in the usual PSHE arm (22.4%, 22.4% and 18.6%, respectively) (Table 6).
| Variable | Level | High-risk group (N = 1064) | All participants (N = 5030) | ||||
|---|---|---|---|---|---|---|---|
| Usual PSHE (n = 298) | Classroom-based CBT (n = 392) | Attention control PSHE (n = 374) | Usual PSHE (n =1604) | Classroom-based CBT (n = 1753) | Attention control PSHE (n = 1673) | ||
| Sex | Male | 101 (33.9) | 132 (33.7) | 135 (36.1) | 834 (52.0) | 880 (50.2) | 849 (50.7) |
| Female | 197 (66.1) | 260 (66.3) | 239 (63.9) | 770 (48.0) | 873 (49.8) | 824 (49.3) | |
| Ethnicity | White | 246 (86.6) | 314 (87.7) | 286 (81.7) | 1275 (86.1) | 1372 (86.7) | 1271 (83.6) |
| Non-white | 38 (13.4) | 44 (12.3) | 64 (18.3) | 205 (13.9) | 210 (13.3) | 250 (16.4) | |
| Living situation | Mother and father | 149 (53.4) | 186 (52.0) | 189 (53.7) | 981 (66.9) | 972 (62.2) | 1019 (67.1) |
| Parent and partner | 46 (16.5) | 64 (17.9) | 69 (19.6) | 193 (13.2) | 224 (14.3) | 189 (12.4) | |
| Single parent | 73 (26.2) | 96 (26.8) | 87 (24.7) | 262 (17.9) | 343 (22.0) | 283 (18.6) | |
| Other | 11 (3.9) | 12 (3.4) | 7 (2.0) | 30 (2.0) | 23 (1.5) | 29 (1.9) | |
| Year group | 8 | 112 (37.6) | 66 (16.8) | 79 (21.1) | 569 (35.5) | 470 (26.8) | 374 (22.4) |
| 9 | 89 (29.9) | 81 (20.7) | 102 (27.3) | 469 (29.2) | 384 (21.9) | 541 (32.3) | |
| 10 | 17 (5.7) | 153 (39.0) | 144 (38.5) | 179 (11.2) | 583 (33.3) | 562 (33.6) | |
| 11 | 80 (26.8) | 92 (23.5) | 49 (13.1) | 387 (24.1) | 316 (18.0) | 196 (11.7) | |
| Age, mean (SD) | Years | 13.9 (1.2) | 14.4 (1.0) | 14.1 (1.0) | 13.9 (1.2) | 14.1 (1.1) | 14.0 (1.0) |
| Trial arm | 6 months | 12 months | ||
|---|---|---|---|---|
| Low risk | High risk | Low risk | High risk | |
| Usual PSHE (n = 1495) | ||||
| Risk status | ||||
| Low (n = 1197) | 929/1110 (83.7%) | 181/1110 (16.3%) | 890/1040 (85.6%) | 150/1040 (14.4%) |
| High (n = 298) | 77/264 (29.2%) | 187/264 (70.8%) | 104/242 (43.0%) | 138/242 (57.0%) |
| Classroom-based CBT (n = 1583) | ||||
| Risk status | ||||
| Low (n = 1191) | 886/1090 (81.3%) | 204/1090 (18.7%) | 821/994 (82.6%) | 173/994 (17.4%) |
| High (n = 392) | 83/330 (25.2%) | 247/330 (74.8%) | 106/296 (35.8%) | 190/296 (64.2%) |
| Attention control (n = 1506) | ||||
| Risk status | ||||
| Low (n = 1132) | 839/1022 (82.1%) | 183/1022 (17.9%) | 789/954 (82.7%) | 165/954 (17.3%) |
| High (n = 374) | 78/341 (22.9%) | 263/341 (77.1%) | 90/308 (29.2%) | 218/308 (70.8%) |
Implementation
Classroom-based cognitive–behavioural therapy delivery
The classroom-based CBT arm included 79 classes. Intervention delivery was adapted to fit in with the existing structure of PSHE delivery within schools, with all programmes covering the core content and key tasks. The RAP-UK programme used was delivered in weekly lessons to 41 classes, while 22 classes had fortnightly lessons and 16 classes had other formats (project days or condensed programme over 3 weeks). All nine sessions were delivered to 71 classes, while four classes had a condensed eight-session programme and four classes had a seven-session programme. The RAP-UK programme was terminated after the fourth session for a whole year group (eight classes) in one school. This was due to disruption caused by adverse weather, which led to several days of school closure. Owing to competing priorities (i.e. making up time for examined subjects), the school was unable to complete the programme.
The additional RAP-UK booster sessions offered were completed by 40 of the classroom-based CBT classes. Of those classes that did not complete the boosters, eight were those that had terminated the programme at session 4, 16 classes were originally in year 11 so either had left school or were not doing PSHE the following academic year, eight classes had moved from year 10 to year 11 and no longer did PSHE, and one year group opted not to complete the booster sessions. Therefore, a total of 832 young people in the classroom-based CBT group (47.8%) attended at least one RAP-UK booster session to refresh and consolidate their skills approximately 6 months after completing the core programme.
Facilitators
Classroom-based CBT was delivered by 39 facilitators, while 35 people facilitated the attention control PSHE sessions. Classroom-based CBT was led by two facilitators, as intended, in 94.3% of sessions, with 5.7% being led by a single facilitator. There were two facilitators present at 83.1% of attention control PSHE sessions with 16.9% being attended by a single facilitator. To fit in with school timetables, a large number of facilitators were required as whole year groups or even whole schools received PSHE at the same time in some cases. This meant recruiting, training and managing a much larger team of facilitators than was originally anticipated. This had an impact on cost as well as causing operational difficulties with cover for staff absences/sickness and ensuring that the facilitators had sufficient regular working hours to make the posts viable.
Treatment fidelity
Of the 36 classroom-based CBT sessions observed to assess intervention fidelity, 31 covered all the core tasks, with at least 75% of core tasks being covered in the remaining five sessions. Differences in facilitator ratings of lesson content for classroom-based CBT versus attention control PSHE were examined using one-way analysis of variance and indicated that the classroom-based CBT focused more on self-esteem, emotional awareness and positive thinking, and less on topics traditionally covered in PSHE, i.e. sex education, ethical issues, diversity, religion and citizenship (all p < 0.05). There was no difference between classroom-based CBT and attention control PSHE in facilitators' views of student engagement with lessons.
High-risk participants: primary outcome (Short Mood and Feelings Questionnaire)
There was a decrease in symptoms of depression between baseline and 12 months for the high-risk group overall (F = 158.8, df 1, p < 0.001). However, there was no evidence of an effect of classroom-based CBT on SMFQ at 12 months relative to attention control PSHE or usual PSHE (see Table 5). The 95% CIs for the adjusted treatment difference excluded the predefined clinically important difference of two points. Likewise, there was no evidence of an effect of classroom-based CBT when compared with usual PSHE on continuous SMFQ score at 6 months (Table 7).
| Time point | Usual PSHE, mean (SD) | Classroom-based CBT vs. usual PSHE adjusted difference from baseline (95% CI) | Classroom-based CBT, mean (SD) | Classroom-based CBT vs. attention control adjusted difference from baseline (95% CI) | Attention control PSHE, mean (SD) |
|---|---|---|---|---|---|
| Baseline | 10.56 (4.93) | NA | 10.64 (4.91) | NA | 10.60 (4.67) |
| 12 months | 6.81 (5.70) (n = 242) | 0.97 (−0.34 to 2.28); p = 0.067 | 8.22 (6.45) (n = 296) | −0.63 (−1.99 to 0.73); p = 0.249 | 8.50 (5.88) (n = 308) |
| 6 months | 8.61 (6.01) (n = 264) | 0.56 (−0.41 to 1.53); p = 0.259 | 9.22 (6.39) (n = 330) | −0.35 (−1.38 to 0.68); p = 0.505 | 9.44 (5.84) (n = 341) |
Further adjustment for variables that were imbalanced at baseline indicated that classroom-based CBT may have had a small but potentially harmful effect compared with usual PSHE (1.21, 95% CI 0.11 to 2.30, p = 0.031).
There was some evidence of a beneficial effect of classroom-based CBT when compared with attention control PSHE at 12 months for SMFQ as a binary outcome (which indicates the odds of being reclassified as ‘low risk’ at follow-up) (Table 8).
| Usual PSHE: 12 months, n (%) | Classroom-based CBT vs. usual PSHE, adjusted OR (95% CI) | Classroom-based CBT: 12 months, n (%) | Classroom-based CBT vs. attention control PSHE, adjusted OR (95% CI) | Attention control PSHE: 12 months, n (%) |
|---|---|---|---|---|
| 104/242 (43.0) | 0.85 (0.58 to 1.26); p = 0.429 | 106/296 (35.8) | 1.64 (1.08 to 2.51); p = 0.021 | 90/308 (29.2) |
Repeated-measures mixed-effects analyses showed no effect of classroom-based CBT over time for SMFQ score (classroom-based CBT vs. attention control PSHE interaction coefficient −0.17, 95% CI −1.40 to 1.06, p = 0.785; classroom-based CBT vs. usual PSHE interaction coefficient 0.72, 95% CI −0.59 to 2.03, p = 0.282). The effect of classroom-based CBT in high-risk participants was not modified by any of the predefined subgroups we examined (Table 9). A post hoc interaction analysis showed no modification of effect by sex.
| Variable | Level | Classroom-based CBT vs. usual PSHE | Classroom-based CBT vs. attention control PSHE | ||
|---|---|---|---|---|---|
| Interaction (95% CI) | p-value | Interaction (95% CI) | p-value | ||
| SMFQ | 5–10 | Reference | 0.583 | Reference | 0.778 |
| 11+ | 0.56 (−1.44 to 2.55) | −0.27 (−2.14 to 1.60) | |||
| Self-harm thoughts | Yes | 0.52 (−1.48 to 2.53) | 0.607 | 0.15 (−1.73 to 2.03) | 0.880 |
| Self-harm behaviour | Yes | 0.52 (−1.69 to 2.73) | 0.644 | −1.35 (−3.38 to 0.68) | 0.192 |
| Alcohol use | Yes | −0.75 (−3.05 to 1.55) | 0.522 | −1.10 (−3.22 to 1.02) | 0.308 |
| Street drug use | Yes | −4.37 (−11.38 to 2.65) | 0.222 | −2.71 (−6.78 to 1.37) | 0.193 |
| Cannabis use | Yes | −1.95 (−5.37 to 1.46) | 0.263 | −2.30 (−5.08 to 0.48) | 0.105 |
| Year group | 8 | Reference | 0.832 | Reference | 0.212 |
| 9 | −1.64 (−6.44 to 3.16) | −1.95 (−6.41 to 2.50) | |||
| 10 | −2.44 (−7.83 to 2.95) | −1.83 (−5.32 to 1.66) | |||
| 11 | −1.59 (−6.64 to 3.47) | −5.33 (−10.55 to −0.11) | |||
| Sex | Female | −0.02 (−2.03 to 1.99) | 0.981 | 0.87 (−1.02 to 2.76) | 0.365 |
| Age | −0.32 (−1.39 to 0.75) | 0.559 | −0.81 (−1.90 to 0.28) | 0.144 | |
| Family Affluence Scale | −0.45 (−1.11 to 0.21) | 0.183 | −0.02 (−0.68 to 0.64) | 0.945 | |
High-risk participants: secondary outcomes
In the high-risk group, there was some evidence of a potentially harmful effect of classroom-based CBT relative to usual PSHE for CATS personal failure scores at 12 months (adjusted difference 1.95, 95% CI 0.25 to 3.66). However, there was also evidence of a potentially beneficial effect of classroom-based CBT on RCADS depression at 12 months compared with usual PSHE (adjusted difference 0.64, 95% CI 0.06 to 1.21) and on self-harm thoughts at 6 months compared with attention control PSHE [odds ratio (OR) 0.58, 95% CI 0.35 to 0.97]. Details of adjusted differences, adjusted ORs and CIs for analysis of the secondary outcomes are provided in Tables 10 and 11.
In repeated-measures regression analysis, no effect of classroom-based CBT over time was observed for any of the secondary outcomes in either high-risk participants or all participants.
| Variable | Usual PSHE | Adjusted OR (95% CI):a 6 months, 12 months | Classroom-based CBT | Adjusted OR (95% CI):a 6 months, 12 months | Attention control PSHE | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline, n (%) | 6 months, n (%) | 12 months, n (%), | Baseline, n (%) | 6 months, n (%) | 12 months, n (%) | Baseline, n (%) | 6 months, n (%) | 12 months, n (%) | |||
| Bullying others | 80 (28.88) | 77 (30.08) | 41 (18.06) | 0.66 (0.42 to 1.05), 1.29 (0.75 to 2.23) | 96 (26.82) | 73 (23.25) | 55 (20.83) | 0.79 (0.47 to 1.32), 0.96 (0.55 to 1.69) | 118 (33.71) | 88 (26.51) | 57 (20.50) |
| Self-harming thoughts | 147 (53.07) | 111 (43.53) | 90 (38.96) | 0.92 (0.58 to 1.45), 1.06 (0.69 to 1.63) | 197 (55.18) | 142 (45.08) | 123 (46.42) | 0.58 (0.35 to 0.97), 0.93 (0.59 to 1.46) | 189 (54.15) | 167 (50.76) | 126 (45.00) |
| Self-harming behaviour | 77 (27.70) | 69 (27.17) | 51 (22.17) | 0.92 (0.56 to 1.51), 1.18 (0.71 to 1.99) | 106 (29.86) | 95 (30.16) | 77 (29.39) | 0.93 (0.55 to 1.58), 1.00 (0.56 to 1.74) | 109 (31.23) | 105 (32.31) | 71 (25.54) |
| Alcohol misuse | 77 (28.00) | 81 (31.89) | 70 (30.57) | 0.89 (0.54 to 1.46), 1.44 (0.84 to 2.47) | 112 (31.28) | 108 (34.73) | 105 (39.33) | 1.00 (0.60 to 1.68), 1.26 (0.72 to 2.20) | 97 (27.95) | 109 (33.33) | 99 (35.61) |
| Street drug misuse | 7 (2.55) | 10 (3.94) | 13 (5.70) | 0.93 (0.26 to 3.38), 1.22 (0.43 to 3.44) | 25 (7.00) | 18 (5.79) | 20 (7.55) | 1.47 (0.47 to 4.68), 2.93 (1.00 to 8.61) | 16 (4.58) | 15 (4.55) | 12 (4.30) |
| Cannabis misuse | 30 (10.87) | 31 (12.35) | 44 (19.30) | 1.18 (0.58 to 2.42), 0.67 (0.36 to 1.27) | 53 (14.85) | 57 (18.15) | 65 (24.34) | 0.94 (0.45 to 1.97), 1.30 (0.70 to 2.42) | 63 (17.95) | 66 (20.06) | 55 (19.57) |
| Variable | Usual PSHE | Adjusted difference (95% CI):a 6 months, 12 months | Classroom-based CBT | Adjusted difference (95% CI):a 6 months, 12 months | Attention control PSHE | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline, mean (SD) | 6 months, mean (SD) | 12 months, mean (SD) | Baseline, mean (SD) | 6 months, mean (SD) | 12 months, mean (SD) | Baseline, mean (SD) | 6 months, mean (SD) | 12 months, mean (SD) | |||
| CATS | 12.20 (9.28) | 10.16 (9.52) | 8.18 (8.68) | 1.20 (−0.39 to 2.78), 1.95 (0.25 to 3.66) | 12.40 (9.21) | 11.51 (10.53) | 10.48 (10.00) | 0.71 (−1.03 to 2.45), 0.29 (−1.48 to 2.07) | 13.35 (8.99) | 11.64 (9.87) | 10.63 (9.94) |
| Self-esteem | 15.88 (4.80) | 16.58 (5.22) | 17.39 (5.34) | 0.02 (−0.81 to 0.85), 0.12 (−0.81 to 1.05) | 15.54 (4.70) | 16.33 (5.39) | 16.93 (5.65) | 0.13 (−0.76 to 1.02), −0.13 (−1.12 to 0.87) | 15.36 (4.38) | 16.02 (4.38) | 16.68 (5.25) |
| General anxiety | 5.74 (2.87) | 5.55 (2.96) | 4.67 (3.05) | 0.16 (−0.34 to 0.66), 0.41 (−0.15 to 0.97) | 5.92 (2.84) | 5.63 (2.96) | 5.18 (3.12) | −0.00 (−0.54 to 0.53), −0.24 (−0.82 to 0.35) | 5.77 (2.86) | 5.76 (3.08) | 5.40 (2.91) |
| Separation anxiety | 2.26 (2.19) | 1.94 (2.36) | 1.65 (2.17) | 0.15 (−0.25 to 0.54), 0.04 (−0.37 to 0.44) | 2.27 (2.26) | 2.07 (2.50) | 1.98 (2.34) | 0.11 (−0.31 to 0.53), −0.18 (−0.60 to 0.25) | 2.35 (2.31) | 2.12 (2.56) | 2.09 (2.45) |
| Social phobia | 6.64 (3.24) | 6.11 (3.17) | 5.72 (3.31) | 0.24 (−0.27 to 0.76), 0.34 (−0.26 to 0.93) | 6.87 (3.33) | 6.39 (3.43) | 6.26 (3.57) | 0.27 (−0.27 to 0.82) 0.02 (−0.60 to 0.64) | 6.58 (3.22) | 6.34 (3.52) | 6.34 (3.48) |
| Panic | 4.15 (3.19) | 3.85 (3.48) | 3.17 (3.23) | 0.25 (−0.28 to 0.77), 0.25 (−0.31 to 0.81) | 4.35 (3.17) | 4.25 (3.48) | 3.79 (3.49) | 0.11 (−0.44 to 0.66), −0.25 (−0.84 to 0.34) | 4.14 (3.16) | 4.05 (3.34) | 3.59 (3.18) |
| Depression | 5.27 (2.83) | 4.69 (3.19) | 4.06 (3.26) | 0.24 (−0.28 to 0.75), 0.64 (0.06 to 1.21) | 5.64 (2.88) | 5.20 (3.39) | 4.94 (3.32) | −0.10 (−0.65 to 0.46), −0.02 (−0.65 to 0.60) | 5.47 (3.10) | 5.10 (3.25) | 4.83 (3.19) |
| RCADS | 24.07 (10.69) | 22.11 (11.59) | 19.27 (11.64) | 1.07 (−0.81 to 2.95), 1.48 (−0.64 to 3.59) | 25.04 (10.80) | 23.42 (12.22) | 22.16 (12.38) | 0.23 (−1.76 to 2.23), −0.60 (−2.88 to 1.67) | 24.29 (11.01) | 23.39 (12.23) | 22.27 (11.74) |
| School connectedness | 26.22 (6.19) | 25.82 (6.76) | 26.84 (6.94) | 0.11 (−0.86 to 1.08), 0.42 (−0.70 to 1.55) | 25.36 (6.20) | 25.85 (6.85) | 26.18 (6.80) | 0.25 (−0.78 to 1.29), 0.57 (−0.65 to 1.80) | 25.17 (6.04) | 25.29 (6.36) | 25.94 (6.64) |
All participants: primary outcome (Short Mood and Feelings Questionnaire)
Including all participants in the analysis, there was no evidence of an effect of classroom-based CBT on SMFQ score at 12 months (classroom-based CBT vs. usual PSHE 0.27, 95% CI −0.08 to 0.62; classroom-based CBT vs. attention control PSHE −0.01, 95% CI −0.42 to 0.39) or an effect of classroom-based CBT on SMFQ score over time (classroom-based CBT vs. attention control PSHE interaction coefficient −0.04, 95% CI −0.47 to 0.40, p = 0.869; classroom-based CBT vs. usual PSHE 0.04, 95% CI −0.39 to 0.48, p = 0.848).
In the subgroup analysis (Table 12), there was some suggestion of a beneficial effect of classroom-based CBT compared with both control groups in those who used ‘street drugs’ (classroom-based CBT vs. usual PSHE interaction coefficient −4.62, 95% CI −8.14 to −1.11; classroom-based CBT vs. attention control PSHE interaction coefficient −3.41, 95% CI −5.82 to −0.99), but of a possible harmful effect compared with usual PSHE among those who reported self-harm behaviour (interaction coefficient 1.57, 95% CI 0.37 to 2.78).
| Variable | Level | Classroom-based CBT vs. usual PSHE | Classroom-based CBT vs. attention control PSHE | ||
|---|---|---|---|---|---|
| Interactiona | p-value | Interactiona | p-value | ||
| SMFQ | < 5 | Reference | 0.069 | Reference | 0.117 |
| 5–10 | −0.01 (−0.88 to 0.85) | −0.81 (−1.65 to 0.02) | |||
| 11+ | 1.35 (0.19 to 2.51) | −0.64 (−1.76 to 0.47) | |||
| Self-harm thoughts | Yes | 0.86 (−0.00 to 1.71) | 0.051 | −0.31 (−1.12 to 0.50) | 0.457 |
| Self-harm behaviour | Yes | 1.57 (0.37 to 2.78) | 0.010 | −0.47 (−1.56 to 0.60) | 0.393 |
| Alcohol use | Yes | −0.39 (−1.28 to 0.51) | 0.400 | −0.57 (−1.49 to 0.35) | 0.225 |
| Street drug misuse | Yes | −4.62 (−8.14 to −1.11) | 0.010 | −3.41 (−5.82 to −0.99) | 0.006 |
| Cannabis misuse | Yes | −0.18 (−1.61 to 1.25) | 0.800 | −1.33 (−2.64 to −0.02) | 0.047 |
| Year group | 8 | Reference | 0.892 | Reference | 0.994 |
| 9 | 0.23 (−1.36 to 1.82) | 0.03 (−1.44 to 1.50) | |||
| 10 | 0.48 (−1.06 to 2.03) | −0.11 (−1.28 to 1.06) | |||
| 11 | 0.56 (−1.21 to 2.33) | −0.12 (−2.14 to 1.89) | |||
| Sex | Female | −0.09 (−0.73 to 0.55) | 0.780 | −0.26 (−0.90 to 0.38) | 0.428 |
| Age | 0.20 (−0.17 to 0.56) | 0.294 | −0.00 (−0.41 to 0.41) | 0.998 | |
| Family Affluence Scale | −0.21 (−0.45 to 0.04) | 0.100 | 0.07 (−0.19 to 0.32) | 0.619 | |
All participants: secondary outcomes
Among all participants, there was some evidence of a beneficial effect of classroom-based CBT on bullying status at 12 months when compared with attention control PSHE (OR 0.69, 95% CI 0.51 to 0.94) and on cannabis use at 6 months (OR 0.56, 95% CI 0.38 to 0.82) and 12 months (OR 0.70, 95% CI 0.48 to 0.93) when compared with usual PSHE. However, there was also evidence that classroom-based CBT was less useful than usual PSHE for panic symptoms at 6 and 12 months, less useful than attention control PSHE for panic symptoms at 6 months and less useful than usual PSHE for CATS personal failure scores at 6 months and general anxiety at 12 months. Full details of adjusted differences, ORs and 95% CIs for this analysis are provided in Tables 13 and 14.
| Variable | Usual care | Adjusted difference (95% CI):a 6 months, 12 months | Classroom-based CBT | Adjusted difference (95% CI):a 6 months, 12 months | Attention control PSHE | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline, mean (SD) | 6 months, mean (SD) | 12 months, mean (SD) | Baseline, mean (SD) | 6 months, mean (SD) | 12 months, mean (SD) | Baseline, mean (SD) | 6 months, mean (SD) | 12 months, mean (SD) | |||
| SMFQ | 3.55 (4.73) | 3.60 (4.78) | 3.21 (4.50) | 0.22 (−0.09 to 0.53), 0.27 (−0.08 to 0.62) | 4.11 (4.95) | 4.24 (5.37) | 3.95 (5.44) | 0.06 (−0.30 to 0.42), −0.01 (−0.42 to 0.39) | 3.90 (4.81) | 4.28 (5.22) | 4.00 (5.21) |
| CATS | 4.07 (6.68) | 3.98 (6.53) | 3.47 (6.09) | 0.51 (0.06 to 0.96), 0.52 (−0.00 to 1.03) | 4.62 (7.08) | 4.86 (7.89) | 4.45 (7.68) | 0.40 (−0.13 to 0.94), 0.07 (−0.52 to 0.66) | 4.72 (7.14) | 4.82 (7.57) | 4.44 (7.44) |
| Self-esteem | 21.44 (5.23) | 21.42 (5.52) | 21.74 (5.43) | −0.07 (−0.39 to 0.24), 0.07 (−0.30 to 0.44) | 20.97 (5.41) | 20.97 (5.57) | 21.48 (5.71) | −0.15 (−0.52 to 0.22), 0.08 (−0.34 to 0.50) | 20.88 (5.31) | 20.97 (5.72) | 21.31 (5.74) |
| General anxiety | 3.11 (2.61) | 3.31 (2.70) | 2.93 (2.65) | 0.12 (−0.07 to 0.30), 0.23 (0.01 to 0.44) | 3.47 (2.71) | 3.66 (2.86) | 3.36 (2.96) | 0.05 (−0.17 to 0.26), −0.00 (−0.25 to 0.24) | 3.19 (2.74) | 3.54 (2.88) | 3.34 (2.86) |
| Separation anxiety | 1.06 (1.56) | 1.03 (1.81) | 0.89 (1.67) | 0.06 (−0.07 to 0.18), 0.04 (−0.10 to 0.19) | 1.21 (1.72) | 1.17 (1.89) | 1.06 (1.93) | 0.07 (−0.07 to 0.22), −0.04 (−0.20 to 0.12) | 1.21 (1.81) | 1.15 (1.89) | 1.12 (1.96) |
| Social phobia | 3.83 (2.88) | 4.10 (2.89) | 4.09 (2.93) | −0.03 (−0.22 to 0.16), −0.12 (−0.35 to 0.10) | 4.19 (3.09) | 4.32 (3.14) | 4.16 (3.27) | 0.11 (−0.12 to 0.33), −0.13 (−0.39 to 0.13) | 4.06 (2.99) | 4.36 (3.17) | 4.33 (3.25) |
| Panic | 1.63 (2.36) | 1.72 (2.49) | 1.49 (2.27) | 0.27 (0.10 to 0.43), 0.30 (0.12 to 0.49) | 1.90 (2.51) | 2.16 (2.74) | 1.95 (2.77) | 0.27 (0.07 to 0.46), 0.19 (−0.03 to 0.40) | 1.77 (2.39) | 1.96 (2.64) | 1.77 (2.52) |
| Depression | 2.17 (2.50) | 2.25 (2.56) | 2.07 (2.53) | 0.03 (−0.14 to 0.20), 0.15 (−0.05 to 0.35) | 2.62 (2.71) | 2.62 (2.81) | 2.54 (2.99) | −0.05 (−0.25 to 0.15), 0.10 (−0.14 to 0.33) | 2.44 (2.73) | 2.62 (2.86) | 2.40 (2.87) |
| RCADS | 11.80 (9.55) | 12.37 (9.88) | 11.48 (9.56) | 0.38 (−0.24 to 1.01), 0.52 (−0.23 to 1.28) | 13.33 (10.30) | 13.89 (10.85) | 13.08 (11.61) | 0.43 (−0.31 to 1.16) 0.06 (−0.81 to 0.94) | 12.63 (10.74) | 13.63 (10.81) | 12.96 (10.94) |
| School connectedness | 31.04 (6.11) | 30.07 (6.42) | 30.48 (6.33) | −0.05 (−0.45 to 0.35), 0.13 (−0.34 to 0.60) | 30.22 (6.29) | 29.63 (6.63) | 30.02 (6.77) | −0.12 (−0.58 to 0.34), 0.21 (−0.33 to 0.76) | 30.19 (6.39) | 29.27 (6.61) | 29.73 (6.79) |
| Variable | Usual PSHE | Adjusted OR (95% CI):a 6 months, 12 months | Classroom-based CBT | Adjusted OR (95% CI):a 6 months, 12 months | Attention control PSHE | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline, n (%) | 6 months, n (%) | 12 months, n (%) | Baseline, n (%) | 6 months, n (%) | 12 months, n (%) | Baseline, n (%) | 6 months, n (%) | 12 months, n (%) | |||
| SMFQ (< 5, ≥ 5) | 410 (26.61) | 399 (27.29) | 313 (22.93) | 1.07 (0.87, 1.32), 1.13 (0.91, 1.41) | 533 (32.09) | 495 (32.23) | 408 (29.10) | 0.91 (0.73, 1.15), 0.85 (0.67, 1.08) | 489 (30.91) | 493 (33.27) | 431 (31.39) |
| Bullying others | 215 (14.79) | 223 (15.58) | 161 (12.44) | 0.92 (0.72, 1.17), 0.91 (0.69, 1.20) | 258 (16.57) | 246 (16.67) | 178 (13.60) | 0.86 (0.65, 1.14), 0.69 (0.51, 0.94) | 312 (20.74) | 265 (18.48) | 209 (16.28) |
| Self-harm thoughts | 254 (17.43) | 259 (18.15) | 228 (17.52) | 0.84 (0.65, 1.08), 0.94 (0.73, 1.20) | 315 (20.27) | 274 (18.58) | 254 (19.36) | 0.78 (0.58, 1.05), 1.02 (0.78, 1.33) | 311 (20.66) | 304 (21.16) | 261 (20.17) |
| Self-harm behaviour | 113 (7.76) | 134 (9.42) | 110 (8.47) | 0.98 (0.72, 1.34), 1.20 (0.88, 1.65) | 162 (10.43) | 163 (11.06) | 161 (12.28) | 0.95 (0.67, 1.36), 1.34 (0.92, 1.95) | 160 (10.62) | 176 (12.32) | 139 (10.79) |
| Alcohol misuse | 294 (20.28) | 361 (25.26) | 370 (28.53) | 0.86 (0.68, 1.08), 0.87 (0.69, 1.10) | 328 (21.13) | 358 (24.34) | 375 (28.67) | 1.08 (0.82, 1.42), 1.00 (0.77, 1.30) | 247 (16.54) | 309 (21.64) | 316 (24.61) |
| Street drug misuse | 14 (0.97) | 28 (1.96) | 30 (2.31) | 1.18 (0.61, 2.30), 0.93 (0.50, 1.71) | 48 (3.10) | 45 (3.05) | 51 (3.89) | 1.48 (0.77, 2.86), 1.17 (0.65, 2.11) | 29 (1.93) | 41 (2.86) | 39 (3.02) |
| Cannabis misuse | 100 (6.89) | 143 (10.05) | 167 (12.88) | 0.56 (0.38, 0.82), 0.70 (0.48, 0.93) | 160 (10.33) | 159 (10.77) | 190 (14.48) | 0.71 (0.47, 1.07), 1.12 (0.79, 1.58) | 144 (9.59) | 169 (11.79) | 154 (11.96) |
Complier average causal effect
The instrumental variable analysis in high-risk participants did not alter the conclusions of the primary analysis for classroom-based CBT compared with attention control PSHE (adjusted difference −0.82, 95% CI −1.79 to 0.14; p = 0.093). However, the evidence was strengthened in that mean SMFQ score at 12 months in the classroom-based CBT group was higher (i.e. more symptoms of low mood) than in the usual PSHE group, although not exceeding clinically important levels (adjusted difference 1.43, 95% CI 1.22 to 1.64; p < 0.001).
Multiple imputations and missing data
Multiple imputations of 12-month SMFQ score for high-risk participants had no effect on the main conclusions (Table 15).
| Number of multiple imputations | Adjusted difference (95% CI)a | |
|---|---|---|
| Classroom-based CBT vs. usual PSHE at 12 months | Classroom-based CBT vs. attention control PSHE at 12 months | |
| 0 | 0.97 (−0.07 to 2.01); p = 0.067 | −0.63 (−1.71 to 0.44); p = 0.249 |
| 20 | 0.85 (−0.19 to 1.88); p = 0.110 | −0.56 (−1.64 to 0.52); p = 0.308 |
Comparison of baseline characteristics for participants categorised as high risk showed that individuals with missing primary outcome data tended on average to be slightly older; not living with both parents; using alcohol and cannabis; and bullying others. Within the usual PSHE arm in particular, those with missing primary outcome data were more likely to be engaging in regular self-harm thoughts and behaviour (Tables 16–18).
| Variable | Level | Trial arms | |||||
|---|---|---|---|---|---|---|---|
| Usual PSHE (N = 298) | Classroom-based CBT (N = 392) | Attention control PSHE (N = 374) | |||||
| Present (n = 242; 81%) | Missing (n = 56; 19%) | Present (n = 296; 76%) | Missing (n = 96; 24%) | Present (n = 308; 82%) | Missing (n = 66; 18%) | ||
| Sex | Male | 84 (34.7) | 17 (30.4) | 105 (35.5) | 27 (28.1) | 104 (33.8) | 31 (47.0) |
| Female | 158 (65.3) | 39 (69.6) | 191 (64.5) | 69 (71.9) | 204 (66.2) | 35 (53.0) | |
| Ethnicity | White | 198 (86.5) | 48 (87.3) | 245 (88.8) | 69 (84.1) | 239 (82.1) | 47 (79.7) |
| Non-white | 31 (13.5) | 7 (12.7) | 31 (11.2) | 13 (15.9) | 52 (17.9) | 12 (20.3) | |
| Living situation | Mother and father | 129 (57.3) | 20 (37.0) | 147 (53.8) | 39 (45.9) | 165 (56.1) | 24 (41.4) |
| Parent and partner | 36 (16.0) | 10 (18.5) | 49 (17.9) | 15 (17.6) | 56 (19.0) | 13 (22.4) | |
| Single parent | 53 (23.6) | 20 (37.0) | 69 (25.3) | 27 (31.8) | 66 (22.4) | 21 (36.2) | |
| Other | 7 (3.1) | 4 (7.4) | 8 (2.9) | 4 (4.7) | 7 (2.4) | 0 (0.0) | |
| Year group | 8 | 100 (41.3) | 12 (21.4) | 59 (19.9) | 7 (7.3) | 74 (24.0) | 5 (7.6) |
| 9 | 82 (33.9) | 7 (12.5) | 62 (20.9) | 19 (19.8) | 93 (30.2) | 9 (13.6) | |
| 10 | 13 (5.4) | 4 (7.1) | 124 (41.9) | 29 (30.2) | 129 (41.9) | 15 (22.7) | |
| 11 | 47 (19.4) | 33 (58.9) | 51 (17.2) | 41 (42.7) | 12 (3.9) | 37 (56.1) | |
| Age, mean (SD) | Years | 13.7 (1.1) | 14.7 (1.2) | 14.3 (1.0) | 14.9 (0.9) | 13.9 (0.9) | 14.9 (1.0) |
| Variable | Trial arm, mean (SD) | |||||
|---|---|---|---|---|---|---|
| Usual PSHE (N = 298) | Classroom-based CBT (N = 392) | Attention control PSHE (N = 374) | ||||
| Present (n = 242; 81%) | Missing (n = 56; 19%) | Present (n = 296; 76%) | Missing (n = 96; 24%) | Present (n = 308; 82%) | Missing (n = 66; 18%) | |
| SMFQ | 10.5 (4.8) | 10.9 (5.4) | 10.6 (4.9) | 10.8 (4.9) | 10.8 (4.1) | 10.6 (4.8) |
| CATS | 12.0 (9.1) | 13.2 (10.2) | 11.9 (9.0) | 14.0 (9.7) | 12.9 (8.0) | 13.4 (9.2) |
| Self-esteem | 16.2 (4.7) | 14.7 (5.1) | 15.7 (4.8) | 15.1 (4.4) | 15.7 (4.3) | 15.3 (4.4) |
| General anxiety | 5.7 (2.9) | 5.7 (2.6) | 5.8 (2.8) | 6.4 (3.1) | 5.3 (2.4) | 5.9 (2.9) |
| Separation anxiety | 2.3 (2.2) | 2.1 (2.2) | 2.3 (2.3) | 2.3 (2.2) | 2.3 (1.9) | 2.4 (2.4) |
| Social phobia | 6.6 (3.2) | 6.7 (3.3) | 6.8 (3.4) | 7.0 (3.2) | 6.9 (3.1) | 6.5 (3.2) |
| Panic | 4.1 (3.1) | 4.3 (3.4) | 4.3 (3.2) | 4.5 (3.0) | 4.2 (2.8) | 4.1 (3.2) |
| Depression | 5.2 (2.8) | 5.5 (3.0) | 5.6 (2.9) | 5.9 (2.9) | 6.1 (3.2) | 5.3 (3.1) |
| RCADS | 24.0 (10.8) | 24.4 (10.3) | 24.7 (10.8) | 26.1 (10.7) | 24.9 (9.5) | 24.2 (11.3) |
| School connectedness | 26.2 (6.2) | 26.2 (6.2) | 25.2 (6.2) | 25.9 (6.1) | 26.2 (6.7) | 25.0 (5.9) |
| Variable | Level | Trial arm | |||||
|---|---|---|---|---|---|---|---|
| Usual PSHE (N = 298) | Classroom-based CBT (N = 392) | Attention control PSHE (N = 374) | |||||
| Present (n = 242; 81%) | Missing (n = 56; 19%) | Present (n = 296; 76%) | Missing (n = 96; 24%) | Present (n = 308; 82%) | Missing (n = 66; 18%) | ||
| Self-harm thoughts | Never | 110 (48.7) | 20 (39.2) | 117 (42.7) | 43 (51.8) | 26 (46.4) | 134 (45.7) |
| Once or twice | 81 (35.8) | 21 (41.2) | 117 (42.7) | 27 (32.5) | 23 (41.1) | 109 (37.2) | |
| 3 or more times | 35 (15.5) | 10 (19.6) | 40 (14.6) | 13 (15.7) | 7 (12.5) | 50 (17.1) | |
| Self-harm behaviour | Never | 165 (72.7) | 36 (70.6) | 187 (68.8) | 62 (74.7) | 35 (62.5) | 205 (70.0) |
| Once or twice | 39 (17.2) | 11 (21.6) | 55 (20.2) | 13 (15.7) | 14 (25.0) | 48 (16.4) | |
| 3 or more times | 23 (10.1) | 4 (7.8) | 30 (11.0) | 8 (9.6) | 7 (12.5) | 40 (13.7) | |
| Alcohol consumption | Never drank alcohol | 69 (30.8) | 8 (15.7) | 70 (25.5) | 12 (14.5) | 9 (16.4) | 79 (27.1) |
| Once or twice | 99 (44.2) | 22 (43.1) | 126 (45.8) | 38 (45.8) | 26 (47.3) | 136 (46.6) | |
| More than 2–4 times a month | 49 (21.9) | 15 (29.4) | 59 (21.5) | 22 (26.5) | 13 (23.6) | 62 (21.2) | |
| More than once a week | 7 (3.1) | 6 (11.8) | 20 (7.3) | 11 (13.3) | 7 (12.7) | 15 (5.1) | |
| Street drug misuse | Never taken | 222 (98.7) | 46 (92.0) | 257 (93.8) | 75 (90.4) | 55 (98.2) | 278 (94.9) |
| Once or twice | 3 (1.3) | 2 (4.0) | 15 (5.5) | 5 (6.0) | 1 (1.8) | 14 (4.8) | |
| 2–4 times a month | 0 (0.0) | 1 (2.0) | 2 (0.7) | 3 (3.6) | 0 (0.0) | 0 (0.0) | |
| More than once a week | 0 (0.0) | 1 (2.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (0.3) | |
| Cannabis misuse | Never smoked | 207 (91.6) | 39 (78.0) | 243 (88.0) | 61 (75.3) | 36 (63.2) | 252 (85.7) |
| Once or twice | 14 (6.2) | 1 (2.0) | 21 (7.6) | 16 (19.8) | 17 (29.8) | 34 (11.6) | |
| 2–4 times a month | 5 (2.2) | 4 (8.0) | 7 (2.5) | 1 (1.2) | 1 (1.8) | 7 (2.4) | |
| More than once a week | 0 (0.0) | 6 (12.0) | 5 (1.8) | 3 (3.7) | 3 (5.3) | 1 (0.3) | |
| Bullying others | Never | 166 (73.5) | 31 (60.8) | 207 (75.5) | 55 (65.5) | 31 (54.4) | 201 (68.6) |
| Once or twice | 54 (23.9) | 20 (39.2) | 53 (19.3) | 22 (26.2) | 22 (38.6) | 77 (26.3) | |
| 2–3 times a month | 3 (1.3) | 0 (0.0) | 9 (3.3) | 3 (3.6) | 2 (3.5) | 11 (3.8) | |
| Once a week | 1 (0.4) | 0 (0.0) | 2 (0.7) | 2 (2.4) | 2 (3.5) | 1 (0.3) | |
| Several times a week | 2 (0.9) | 0 (0.0) | 3 (1.1) | 2 (2.4) | 0 (0.0) | 3 (1.0) | |
Comparison of baseline characteristics for all participants showed that those individuals with missing primary outcome data tended on average to be slightly older; to be living with a single parent or parent and their partner; to score noticeably worse on the psychometric scales; to be regularly using alcohol, street drugs and cannabis; and to be regularly bullying others. Within the usual PSHE arm in particular, those with missing primary outcome data were more likely to be engaging in regular self-harm thoughts and behaviour (Tables 19–21).
| Trial arm | |||||||
|---|---|---|---|---|---|---|---|
| Variable | Level | Usual PSHE (N = 1604) | Classroom-based CBT (N = 1753) | Attention control PSHE (N = 1673) | |||
| Present (n = 1365; 85%) | Missing (n = 239; 15%) | Present (n = 1402; 80%) | Missing (n = 351; 20%) | Present (n = 1373; 82%) | Missing (n = 300; 18%) | ||
| Sex | Male | 707 (51.8) | 127 (53.1) | 707 (50.4) | 173 (49.3) | 669 (48.7) | 180 (60.0) |
| Female | 658 (48.2) | 112 (46.9) | 695 (49.6) | 178 (50.7) | 704 (51.3) | 120 (40.0) | |
| Ethnicitya | White | 1085 (85.8) | 190 (88.4) | 1141 (88.2) | 231 (80.2) | 1074 (84.3) | 197 (79.8) |
| Non-white | 180 (14.2) | 25 (11.6) | 153 (11.8) | 57 (19.8) | 200 (15.7) | 50 (20.2) | |
| Living situationa | Mother and father | 874 (69.6) | 107 (50.7) | 828 (64.9) | 144 (50.2) | 898 (70.5) | 121 (49.0) |
| Parent and partner | 146 (11.6) | 47 (22.3) | 175 (13.7) | 49 (17.1) | 148 (11.6) | 41 (16.6) | |
| Single parent | 211 (16.8) | 51 (24.2) | 255 (20.0) | 88 (30.7) | 200 (15.7) | 83 (33.6) | |
| Other | 24 (1.9) | 6 (2.8) | 17 (1.3) | 6 (2.1) | 27 (2.1) | 2 (0.8) | |
| Year group | 8 | 529 (38.8) | 40 (16.7) | 432 (30.8) | 38 (10.8) | 346 (25.2) | 28 (9.3) |
| 9 | 440 (32.2) | 29 (12.1) | 322 (23.0) | 62 (17.7) | 468 (34.1) | 73 (24.3) | |
| 10 | 165 (12.1) | 14 (5.9) | 495 (35.3) | 88 (25.1) | 514 (37.4) | 48 (16.0) | |
| 11 | 231 (16.9) | 156 (65.3) | 153 (10.9) | 163 (46.4) | 45 (3.3) | 151 (50.3) | |
| Age, mean (SD) | Years | 13.7 (1.1) | 14.8 (1.2) | 13.9 (1.1) | 14.8 (1.0) | 13.8 (0.9) | 14.7 (1.1) |
| Variable | Trial arm, mean (SD) | |||||
|---|---|---|---|---|---|---|
| Usual PSHE (N = 1604) | Classroom-based CBT (N = 1753) | Attention control PSHE (N = 1673) | ||||
| Present (n = 1365; 85%) | Missing (n = 239; 15%) | Present (n = 1402; 80%) | Missing (n = 351; 20%) | Present (n = 1373; 82%) | Missing (n = 300; 18%) | |
| SMFQ | 3.3 (4.6) | 4.8 (5.5) | 3.9 (4.9) | 4.9 (5.2) | 3.8 (4.8) | 4.4 (4.8) |
| CATS | 3.8 (6.4) | 5.6 (8.1) | 4.2 (6.7) | 6.3 (8.3) | 4.6 (7.1) | 5.4 (7.2) |
| Self-esteem | 21.7 (5.1) | 19.7 (5.5) | 21.3 (5.3) | 19.6 (5.5) | 21.0 (5.3) | 20.0 (5.1) |
| General anxiety | 3.0 (2.6) | 3.6 (2.7) | 3.4 (2.6) | 3.9 (3.0) | 3.2 (2.8) | 3.3 (2.6) |
| Separation anxiety | 1.0 (1.5) | 1.3 (1.7) | 1.2 (1.7) | 1.2 (1.7) | 1.2 (1.8) | 1.4 (1.9) |
| Social phobia | 3.7 (2.9) | 4.5 (3.0) | 4.1 (3.1) | 4.7 (3.2) | 4.0 (3.0) | 4.4 (3.0) |
| Panic | 1.5 (2.2) | 2.1 (2.9) | 1.8 (2.5) | 2.3 (2.7) | 1.7 (2.4) | 2.1 (2.4) |
| Depression | 2.0 (2.4) | 3.0 (3.1) | 2.5 (2.6) | 3.2 (2.9) | 2.3 (2.7) | 3.0 (3.0) |
| RCADS | 11.3 (9.3) | 14.5 (10.4) | 12.9 (10.2) | 15.3 (10.7) | 12.4 (10.3) | 14.1 (10.3) |
| School connectedness | 31.3 (6.0) | 29.3 (6.3) | 30.5 (6.2) | 28.9 (6.6) | 30.4 (6.3) | 29.3 (6.7) |
| Variable | Level | Trial arm | |||||
|---|---|---|---|---|---|---|---|
| Usual PSHE (N = 1604) | Classroom-based CBT (N = 1753) | Attention control PSHE (N = 1673) | |||||
| Present (n = 1365; 85%) | Missing (n = 239; 15%) | Present (n = 1402; 80%) | Missing (n = 351; 20%) | Present (n = 1373; 82%) | Missing (n = 300; 18%) | ||
| Self-harm thoughts | Never | 1050 (84.1) | 153 (73.6) | 1024 (80.6) | 215 (76.0) | 1007 (79.2) | 187 (79.9) |
| Once or twice | 160 (12.8) | 38 (18.3) | 193 (15.2) | 51 (18.0) | 202 (15.9) | 36 (15.4) | |
| 3 or more times | 39 (3.1) | 17 (8.2) | 54 (4.2) | 17 (6.0) | 62 (4.9) | 11 (4.7) | |
| Self-harm behaviour | Never | 1162 (93.0) | 181 (87.4) | 1142 (89.9) | 249 (88.0) | 1141 (89.8) | 205 (87.2) |
| Once or twice | 58 (4.6) | 14 (6.8) | 89 (7.0) | 23 (8.1) | 82 (6.5) | 19 (8.1) | |
| 3 or more times | 29 (2.3) | 12 (5.8) | 39 (3.1) | 11 (3.9) | 48 (3.8) | 11 (4.7) | |
| Alcohol consumption | Never drank alcohol | 482 (38.8) | 36 (17.4) | 412 (32.4) | 59 (21.0) | 493 (39.1) | 47 (20.3) |
| Once or twice | 556 (44.7) | 82 (39.6) | 632 (49.7) | 121 (43.1) | 592 (46.9) | 114 (49.4) | |
| More than 2–4 times a month | 177 (14.2) | 69 (33.3) | 187 (14.7) | 70 (24.9) | 147 (11.6) | 55 (23.8) | |
| More than once a week | 28 (2.3) | 20 (9.7) | 40 (3.1) | 31 (11.0) | 30 (2.4) | 15 (6.5) | |
| Street drug misuse | Never taken | 1236 (99.4) | 197 (96.6) | 1240 (97.8) | 262 (92.9) | 1247 (98.3) | 224 (96.6) |
| Once or twice | 7 (0.6) | 4 (2.0) | 24 (1.9) | 15 (5.3) | 20 (1.6) | 6 (2.6) | |
| 2–4 times a month | 0 (0.0) | 1 (0.5) | 3 (0.2) | 4 (1.4) | 0 (0.0) | 1 (0.4) | |
| More than once a week | 0 (0.0) | 2 (1.0) | 1 (0.1) | 1 (0.4) | 1 (0.1) | 1 (0.4) | |
| Cannabis misuse | Never smoked | 1186 (95.2) | 165 (80.5) | 1176 (92.7) | 213 (75.8) | 1185 (93.5) | 172 (73.8) |
| Once or twice | 46 (3.7) | 20 (9.8) | 64 (5.0) | 43 (15.3) | 66 (5.2) | 43 (18.5) | |
| 2–4 times a month | 10 (0.8) | 8 (3.9) | 17 (1.3) | 14 (5.0) | 9 (0.7) | 8 (3.4) | |
| More than once a week | 4 (0.3) | 12 (5.9) | 11 (0.9) | 11 (3.9) | 8 (0.6) | 10 (4.3) | |
| Bullying others | Never | 1078 (86.5) | 161 (77.4) | 1087 (85.3) | 212 (74.9) | 1031 (81.2) | 161 (68.8) |
| Once or twice | 157 (12.6) | 45 (21.6) | 162 (12.7) | 52 (18.4) | 211 (16.6) | 62 (26.5) | |
| 2–3 times a month | 7 (0.6) | 0 (0.0) | 13 (1.0) | 6 (2.1) | 15 (1.2) | 6 (2.6) | |
| Once a week | 2 (0.2) | 0 (0.0) | 5 (0.4) | 7 (2.5) | 7 (0.6) | 4 (1.7) | |
| Several times a week | 2 (0.2) | 2 (1.0) | 7 (0.5) | 6 (2.1) | 6 (0.5) | 1 (0.4) | |
Acceptability
Evaluation questionnaire data
Questionnaires evaluating their PSHE lessons were completed by 482 boys and 506 girls from seven of the eight schools (Table 22). Of these, 386 (39.1%) received the classroom-based CBT programme (RAP-UK), 316 (32%) received attention control PSHE and 286 (28.9%) received usual PSHE.
| Items (Rated 0 – not at all to 10 – a great deal) | Classroom-based CBT (n = 386), mean (SD) | Usual PSHE (n = 286), mean (SD) | Attention control PSHE (n = 316), mean (SD) |
|---|---|---|---|
| How much did you like your PSHE lessons? | 4.38 (2.81) | 5.06 (2.54) | 4.33 (2.49) |
| How relevant were your lessons for people of your age? | 5.23 (2.76) | 5.92 (2.45) | 5.24 (2.81) |
| How useful was what you learnt in PSHE to your everyday life? | 4.22 (2.94) | 5.13 (2.85) | 4.36 (2.77) |
| How much did PSHE help you to feel happier in your mood? | 3.62 (3.01) | 3.81 (3.12) | 3.44 (2.89) |
| How much did your PSHE help you to worry less? | 3.34 (3.07) | 3.31 (3.04) | 3.22 (2.85) |
| How much did your PSHE help you to cope with worries when you have them? | 3.71 (3.15) | 3.61 (3.11) | 3.37 (3.00) |
| How much did PSHE help you to solve problems? | 3.81 (3.22) | 3.92 (3.18) | 3.40 (2.93) |
| How much did your PSHE help you to recognise your strengths? | 4.44 (3.40) | 4.62 (3.32) | 4.13 (3.18) |
| How much did your PSHE help stop disagreements turning into arguments? | 3.96 (3.20) | 3.96 (3.19) | 3.43 (2.92) |
| How much did your PSHE help you to get on better with people? | 4.24 (3.38) | 4.44 (3.38) | 3.83 (3.19) |
| How much did your PSHE help you to ask for help when you need it? | 4.17 (3.44) | 4.41 (3.42) | 4.03 (3.28) |
Taking the sample overall, the majority of young people did not rate their PSHE lessons positively, with only 38.3% of the usual PSHE group and 36.5% of those who received classroom-based CBT positively rating PSHE (6 or more out of 10 for liking their lessons). Similarly, 42.1% of those in the usual PSHE group and 35.4% of those who received classroom-based CBT rated the usefulness of PSHE in everyday life as 6 or more out of 10. Approximately half felt that their lessons were relevant for their age (usual PSHE, 53.7%; classroom-based CBT, 49.6%). Usual PSHE was rated more positively than both classroom-based CBT and attention control PSHE for liking (F = 7.11, df 2,970; p < 0.01), usefulness (F = 6.46, df 2,966; p < 0.01) and relevance for their age (F = 8.84, df 2,963; p < 0.01).
In the high-risk group, no differences were found in the ratings of the three trial arms (n = 203). Further, when the analysis was split by sex, there were no differences between trial arms in girls' ratings of PSHE, but boys preferred usual PSHE to either classroom-based CBT or attention control PSHE (liking F = 5.49, df 2,469; p < 0.01; usefulness F = 7.26, df 2,465; p < 0.01; relevance for their age F = 7.72, df 2,465; p < 0.01).
Project facilitator views
Feedback was obtained from 46 of the facilitators providing the PSHE sessions. Of these, 29 (63%) led the classroom-based CBT and 17 (37%) supported the teacher in delivering attention control PSHE. In general, facilitators felt sufficiently trained (65.5% agree/strongly agree) and supported (71.5% agree/strongly agree), and enjoyed their work (86.2% agree/strongly agree). Those supporting the attention control PSHE reported higher levels of student engagement (58.8% attention control PSHE vs. 48.2% classroom-based CBT). Those delivering classroom-based CBT were more likely to feel that the programme would have a positive effect on the mental health of students (55.1% agree as opposed to 35.3% for attention control PSHE). A comparison of average scores for classroom-based CBT and attention control PSHE facilitators revealed that the classroom-based CBT group found their role more challenging (t = 2.92, df 44; p = 0.005) and would have liked more supervision (t = 2.99, df 42; p = 0.005).
Teacher views
The views of 56 of the 73 (76.7%) teachers who took part in the study were obtained. Of these, 36 were involved in the classroom-based CBT programme, with the remaining 20 providing the attention control PSHE. This section provides a summary of the data for the classroom-based CBT group only. In terms of delivery, content and materials, 24 (66.7%) thought that classroom-based CBT sessions were well or very well organised, 22 (66.1%) thought that the content was relevant and 22 (66.1%) felt that the content was age appropriate. Teachers were less sure about the number of sessions, with seven (20%) feeling that there were not enough, 14 (40%) feeling that the number was right and 14 (40%) feeling that there were too many.
Only 10 (27.8%) of the teachers felt that the classroom-based CBT would be helpful or very helpful in improving children's mood. Similarly, only 12 (33.3%) rated classroom-based CBT as useful or very useful in terms of helping children cope with future challenges. In terms of maintenance after the end of the clinical trial, of the 33 teachers who answered, most (n = 24, 72.7%) thought they would use some of the ideas from RAP-UK after the programme had finished, although seven teachers (21.1%) did not think they would use any of the ideas from RAP-UK after the programme had finished and only two (6.1%) felt they would use quite a lot of the ideas. Around half (n = 19/35, 54.3%) of teachers involved with the classroom-based CBT felt that they would be comfortable or very comfortable delivering it on their own.
Qualitative feedback
The main themes emerging from the qualitative data are summarised in Table 23.
| Main theme | Subtheme | Key points |
|---|---|---|
| Structure and content of RAP | Types of teaching | ‘Hands-on’ and interactive activities preferred |
| Usefulness | Useful aspects of the programme were highlighted, e.g. sessions on resolving conflict, recognising body signals and problem solving | |
| Length of the programme | Shorter faster-paced programme would have been preferred | |
| Delivery | Quality of delivery | Variable. Experience, confidence and reliance on scripts for facilitators and teacher engagement and support were important |
| Classroom management | Teachers and facilitators found this challenging and were unsure of their roles | |
| Rapport with young people | Success in achieving this was variable, particularly where classes did not have the same facilitators throughout the programme | |
| Flexibility and differentiation | Age | The classroom-based CBT programme (RAP-UK) seemed to be more appropriate for year 8 than for older year groups |
| Involvement of teachers | Teachers wanted more flexibility and involvement in development of the classroom-based CBT programme | |
| Targeting the intervention | Some young people, teachers and facilitators felt that a targeted intervention may have been more useful | |
| Sustainability | Resources | Cost and time involved meant the classroom-based CBT would not be sustainable in its current form |
| Future use of the programme | Teachers generally felt that they could deliver the programme alone with the right training, although they would be most likely to adapt it and select some parts only | |
| Implementation in the school context | Value of PSHE | PSHE was perceived to be undervalued and under-resourced |
| Busy school environment | Insufficient lead-in time, communication within schools and lack of time for contact between teachers and facilitators were problematic |
There was evidence that aspects of RAP-UK were well received and perceived to be useful, particularly those that involved interactive activities:
You've got a really good little connect activity actually here, this ‘two sides’ of things ... And they love that.
Teacher
I thought the body signals one was handy... I think that's something that works across the age range.
Teacher
You could see the light going on for so many of them… it was almost like it was news to them … that we don't have to think like this. I saw it happening with a lot of them, that they embraced it … you could see it working.
Teacher
The content and structure of RAP-UK was generally felt to be good, although the programme was perceived to be a little repetitive in places and teachers felt it could have been condensed into a shorter and faster-paced programme.
Teachers reported that the quality of the delivery of the classroom-based CBT by the facilitators was variable:
Some of the people who delivered were quite comfortable and I felt quite successful in what they did. Whereas I got the impression from some of my colleagues that some of the people who came to teach it struggled really, and found it hard to deliver the materials in the way they needed to be delivered.
Teacher
Similarly, facilitators felt that active teacher engagement and support was imperative for the delivery of a successful session:
That made such a crucial difference with the teacher's attitude, just … make or break … whether it went … how the class reacted to it.
Facilitator
Experience and confidence of facilitators were perceived to be important, and facilitators reported finding it much easier to deliver RAP-UK after a period of familiarisation:
It definitely got easier the more you did the sessions 'cos you just obviously knew them more by heart and didn't have to rely on the script so much and you can just take the lead.
Facilitator
While RAP-UK was felt to be appropriate and was well received by younger students (year 8), feedback was less positive in relation to the older year groups, and insufficient differentiation was raised as an issue:
All the sessions were the same ... for year 9 and 10 they were identical. It wasn't age appropriate, I don't think.
Teacher
I think the idea of Key Stages is really important … we're going in and aiming it at year 8 who are 13 to year 11 who are 16.
Facilitator
In terms of sustainability, all of the teachers interviewed stated that it would not be possible to run RAP-UK in its current format because of timetabling restrictions and budgetary constraints, particularly as PSHE was seen to be undervalued and under-resourced:
That's the sad thing about our PSHE, unfortunately we don't have a designated team... it is squeezed on the timetable, it's not given the proper priority it should be.
Teacher
It's always one of the least funded departments, PSHE.
Teacher
The fact that the RAP sessions were in PSHE, a lesson that isn't taken particularly seriously, I think that really affected how people came into the class.
Facilitator
Teachers felt they would have liked to have been more involved in the development of the classroom-based CBT programme and believed that it could be successfully delivered by school staff if enough guidance was provided, although the quality would depend on individual teachers:
I don't think there's anything about the way it's (RAP-UK) been structured or put together, the subject matter, that makes it difficult for a teacher to pick up and go with. But again, I think it's down to that person.
Teacher
Some facilitators and young people suggested that a targeted (rather than universal) approach to delivering classroom-based CBT might be preferable, particularly as some young people did not feel the programme was relevant to them:
I'm not depressed or anything, so why do I need to learn about this?
Year 9 male
Schools are complex and busy organisations where there are many competing demands on time and resources. Teachers and facilitators acknowledged that more lead-in time and planning should have taken place, but that competing activities made it impossible to free up sufficient time to meet before or after lessons to do this. Facilitators and teachers alike highlighted that implementing the classroom-based CBT in schools was immensely challenging:
I think the length of time that you're here is quite challenging for us … it's just trying to fit that in with our curriculum, it's really hard.
Teacher
I think it's difficult bringing mental health programmes into a school environment and it's a massive job to integrate that kind of clinical [programme] into everyday school.
Facilitator
Cost-effectiveness
Costing the intervention
Table 24 shows the key data and costs that were used to calculate the mean intervention cost per student.
| Type of cost or data | Classroom-based CBT | Attention control PSHE |
|---|---|---|
| Total salary cost of those providing the intervention | £59,621 | £51,267 |
| Total cost of training facilitators | £18,418 | £11,099 |
| Hours of coordinator time to organise staff | 150 | 150 |
| Total number of classes receiving the intervention | 79 | 72 |
| Total number of students on the programmea | 2030 | 1915 |
| Mean number of students per class (all on roll) | 25.7 | 26.6 |
| Total number of sessions delivered | 787 | 648 |
| Mean number of sessions received per class | 9.96 | 9.00 |
| Total number of facilitators who delivered sessions | 39 | 35 |
| Number of sessions delivered per school visit (to estimate travel costs) | 3 | 3 |
| Cost of staff time recruiting each school to the programme | £60 | £60 |
| Cost of travel for recruiting each school to the programme | £20 | £20 |
The classroom-based CBT intervention cost an estimated £41.96 per child, while attention control PSHE cost an estimated £34.45 per child (Table 25). These costs exclude the costs of developing or adapting the new materials (these are ‘sunk costs’ and it is assumed that they would not be incurred again) or the estimated proportions of people's time, which are as a result of the research/trial context of programme delivery. The costs do, however, include a share of the initial training costs of the facilitators (time of trainers and facilitators, room hire and subsistence). Therefore, they do reflect the relatively high ratio of facilitators to total number of classes delivered, which might not be as high if the classroom-based CBT or attention control PSHE was rolled out on a larger scale and for longer. These ratios were 39 facilitators to 79 classes for classroom-based CBT, and 35 to 72 for attention control PSHE. Furthermore, with attention control PSHE there are no booklet costs and outside of a randomised controlled trial we assume that there would also be no costs associated with school recruitment to such a programme.
| Type of cost | Classroom-based CBT (£) | Attention control PSHE (£) |
|---|---|---|
| Cost of training and managing facilitators | 9.84 | 6.61 |
| Cost of facilitator time delivering the intervention | 29.37 | 26.77 |
| Booklet (printing) cost per child | 1.41 | NA |
| Travel cost of facilitators | 1.23 | 1.07 |
| Allocation of school recruitment cost | 0.12 | NA |
| Cost per child receiving intervention | 41.96 | 34.45 |
Cost of health and social care usage
Table 26 (hospital health care costs) and Table 27 (community-based care costs) show the health and social care service and resources data and costs that were used to calculate the mean service user cost per student in the cost-effectiveness analysis (i.e. for the subsample with complete EQ-5D responses and costs at all three study time points). Overall, these data show that the total care costs for adolescents were similar across the three trial arms at all three time points. Between 26% and 33% of adolescents in each trial arm had hospital care and between 37% and 45% had seen a general practitioner (GP) during the previous 6 months for any health reason. However, rates of service use or seeing care professionals for worry, anxiety or unhappiness were much lower: 1.6–4.6% of adolescents saw a GP for such problems; 0.5–3.0% saw a school nurse; and < 1% saw either the Child Mental Health Service or a child psychologist during a 6-month period. Of the 4.0–6.7% who saw ‘someone else’ for their psychological problems, most reported seeing or talking to their parents or other close relatives; teachers; friends; other doctors; youth workers; or a mentor/counsellor.
In total, over the 18 months for which service use data were collected, the per-person cost of services used by adolescents in each trial arm were £484 (SD £1294) for classroom-based CBT, £385 (SD £1169) for usual PSHE and £483 (SD £1294) for attention control PSHE. We did not test for the statistical significance of any service use cost differences between trial arms both because the study was not powered to detect such differences and because, in a cost-effectiveness analysis, it is more important to estimate the CIs around the joint distribution of cost and effectiveness differences.
| Hospital services | Classroom-based CBT (N = 1006) | Usual PSHE (N = 1067) | Attention control PSHE (N = 1044) | |||
|---|---|---|---|---|---|---|
| n (%)a | Mean cost, £ (SE) | n (%)a | Mean cost, £ (SE) | n (%)a | Mean cost, £ (SE) | |
| In the 6 months up to baseline | ||||||
| Inpatient stays | 45 (4.5) | 72.09 (16.43) | 33 (3.1) | 50.48 (14.77) | 33 (3.2) | 56.43 |
| A&E attendances | 167 (16.6) | 26.93 (2.60) | 169 (15.8) | 25.19 (2.16) | 183 (17.5) | 29.80 (2.97) |
| Outpatient visits | 226 (22.5) | 46.25 (3.86) | 234 (21.9) | 37.21 (3.36) | 226 (21.6) | 39.45 (3.23) |
| Total hospital use/costs | 328 (32.6) | 145.27 (18.82) | 335 (31.4) | 112.89 (16.63) | 327 (31.3) | 125.67 (16.84) |
| In the period between baseline and 6 months' follow-up | ||||||
| Inpatient stays | 36 (3.6) | 43.62 (9.13) | 27 (2.5) | 52.66 (16.28) | 29 (2.8) | 31.07 (7.41) |
| A&E attendances | 158 (15.7) | 22.93 (2.06) | 144 (13.5) | 21.43 (2.18) | 176 (16.9) | 28.02 (2.61) |
| Outpatient visits | 212 (21.1) | 47.93 (4.84) | 227 (21.3) | 39.80 (3.58) | 255 (24.4) | 50.73 (4.03) |
| Total hospital use/costs | 309 (30.7) | 114.48 (12.51) | 311 (29.1) | 113.89 (17.96) | 346 (33.1) | 109.82 (10.40) |
| In the period between 6 months' and 12 months' follow-up | ||||||
| Inpatient stays | 30 (3.0) | 59.71 (19.78) | 20 (1.9) | 21.78 (6.91) | 34 (3.3) | 62.87 (33.28) |
| A&E attendances | 145 (14.4) | 21.30 (2.16) | 126 (11.8) | 16.12 (1.75) | 167 (16.0) | 28.51 (4.15) |
| Outpatient visits | 179 (17.8) | 36.41 (3.50) | 198 (18.6) | 33.68 (3.14) | 234 (22.4) | 49.41 (5.20) |
| Total hospital use/costs | 275 (27.3) | 117.42 (21.82) | 273 (25.6) | 71.58 (8.47) | 338 (32.4) | 140.79 (39.85) |
| Community services | Classroom-based CBT (N = 1006) | Usual PSHE (N = 1067) | Attention control PSHE (N = 1044) | |||
|---|---|---|---|---|---|---|
| n (%)a | Mean cost, £ (SE) | n (%)a | Mean cost, £ (SE) | n (%)a | Mean cost, £ (SE) | |
| In the 6 months up to baseline | ||||||
| GP (for any reason) | 448 (44.5) | 28.76 (1.67) | 440 (41.2) | 25.49 (1.59) | 449 (43.0) | 26.57 (1.74) |
| GP (for psychological problems) | 33 (3.3) | 1.94 (0.39) | 29 (2.7) | 1.41 (0.30) | 27 (2.6) | 1.04 (0.21) |
| GP nurse | 26 (2.6) | 0.51 (0.13) | 12 (1.1) | 0.17 (0.05) | 24 (2.3) | 0.37 (0.11) |
| School nurse | 30 (3.0) | 0.76 (0.17) | 18 (1.7) | 0.97 (0.41) | 31 (3.0) | 1.03 (0.24) |
| Counsellor | 14 (1.4) | 2.80 (0.98) | 7 (0.7) | 1.07 (0.53) | 13 (1.2) | 2.61 (1.26) |
| CMHS | 6 (0.6) | 0.81 (0.37) | 5 (0.5) | 0.81 (0.39) | 6 (0.6) | 0.46 (0.25) |
| Child psychologist | 7 (0.7) | 3.06 (1.68) | 2 (0.2) | 1.14 (1.00) | 6 (0.6) | 2.72 (1.49) |
| Social worker | 4 (0.4) | 1.63 (0.92) | 6 (0.6) | 0.70 (0.31) | 7 (0.7) | 1.73 (0.91) |
| Someone else | 64 (6.4) | 9.58 (2.47) | 43 (4.0) | 4.86 (1.50) | 70 (6.7) | 9.25 (2.25) |
| Total: all service use/costsb | 607 (60.3) | 183.61 (19.64) | 615 (57.6) | 143.24 (17.01) | 626 (60.0) | 161.50 (17.71) |
| In the period between baseline and 6 months' follow-up | ||||||
| GP (for any reason) | 404 (40.2) | 26.24 (1.86) | 445 (41.7) | 25.70 (1.44) | 469 (44.9) | 28.20 (1.48) |
| GP (for psychological problems) | 35 (3.5) | 1.92 (0.40) | 27 (2.5) | 1.78 (0.50) | 34 (3.3) | 1.99 (0.45) |
| GP nurse | 21 (2.1) | 0.46 (0.12) | 11 (1.0) | 0.25 (0.11) | 27 (2.6) | 0.53 (0.13) |
| School nurse | 15 (1.5) | 0.39 (0.11) | 5 (0.5) | 0.24 (0.13) | 22 (2.1) | 1.18 (0.42) |
| Counsellor | 17 (1.7) | 4.37 (1.46) | 10 (0.9) | 2.60 (1.18) | 14 (1.3) | 3.03 (1.18) |
| CMHS | 5 (0.5) | 1.24 (0.80) | 4 (0.4) | 0.45 (0.25) | 5 (0.5) | 0.32 (0.15) |
| Child psychologist | 4 (0.4) | 2.62 (1.52) | 1 (0.1) | 0.08 (0.08) | 3 (0.3) | 0.47 (0.29) |
| Social worker | 4 (0.4) | 1.53 (1.06) | 3 (0.3) | 0.35 (0.23) | 8 (0.8) | 0.86 (0.32) |
| Someone else | 51 (5.1) | 11.50 (3.58) | 27 (2.5) | 4.01 (1.26) | 67 (6.4) | 6.64 (1.56) |
| Total: all service use/costsb | 579 (57.6) | 152.22 (13.59) | 608 (57.0) | 143.60 (18.17) | 641 (61.4) | 144.65 (11.14) |
| In the period between 6 months' and 12 months' follow-up | ||||||
| GP (for any reason) | 368 (36.6) | 22.30 (1.49) | 427 (40.0) | 21.89 (1.14) | 402 (38.5) | 24.12 (1.40) |
| GP (for psychological problems) | 36 (3.6) | 2.35 (0.53) | 17 (1.6) | 0.97 (0.28) | 48 (4.6) | 2.90 (0.55) |
| GP nurse | 28 (2.8) | 0.46 (0.11) | 19 (1.8) | 0.40 (0.11) | 23 (2.2) | 0.52 (0.15) |
| School nurse | 14 (1.4) | 0.65 (0.27) | 18 (1.7) | 0.43 (0.11) | 26 (2.5) | 1.35 (0.41) |
| Counsellor | 21 (2.1) | 4.42 (1.21) | 14 (1.3) | 2.43 (0.79) | 5 (0.5) | 6.45 (2.72) |
| CMHS | 10 (1.0) | 0.72 (0.26) | 2 (0.2) | 0.22 (0.16) | 7 (0.7) | 0.74 (0.49) |
| Child psychologist | 2 (0.2) | 0.40 (0.33) | 3 (0.3) | 1.21 (0.82) | 7 (0.7) | 1.94 (1.03) |
| Social worker | 4 (0.4) | 0.26 (0.14) | 4 (0.4) | 0.20 (0.10) | 8 (0.8) | 0.81 (0.34) |
| Someone else | 56 (5.6) | 8.94 (2.55) | 39 (3.7) | 4.91 (1.43) | 67 (6.4) | 11.80 (3.32) |
| Total: all service use/costsb | 529 (52.6) | 148.66 (22.26) | 585 (54.8) | 98.38 (8.81) | 595 (57.0) | 176.71 (40.46) |
Impacts on health-related quality of life (European Quality of Life-5 Dimensions)
Figure 3a shows the EQ-5D index scores by trial arm and time point that were used to calculate incremental effectiveness in relation to health-related quality of life, and used in the cost-effectiveness analysis. For completeness, Figure 3b shows the equivalent results for the EQ-5D visual analogue scale scores.
FIGURE 3.
(a) European Quality of Life-5 Dimensions index scores; and (b) visual analogue scale scores by time point and trial arm.
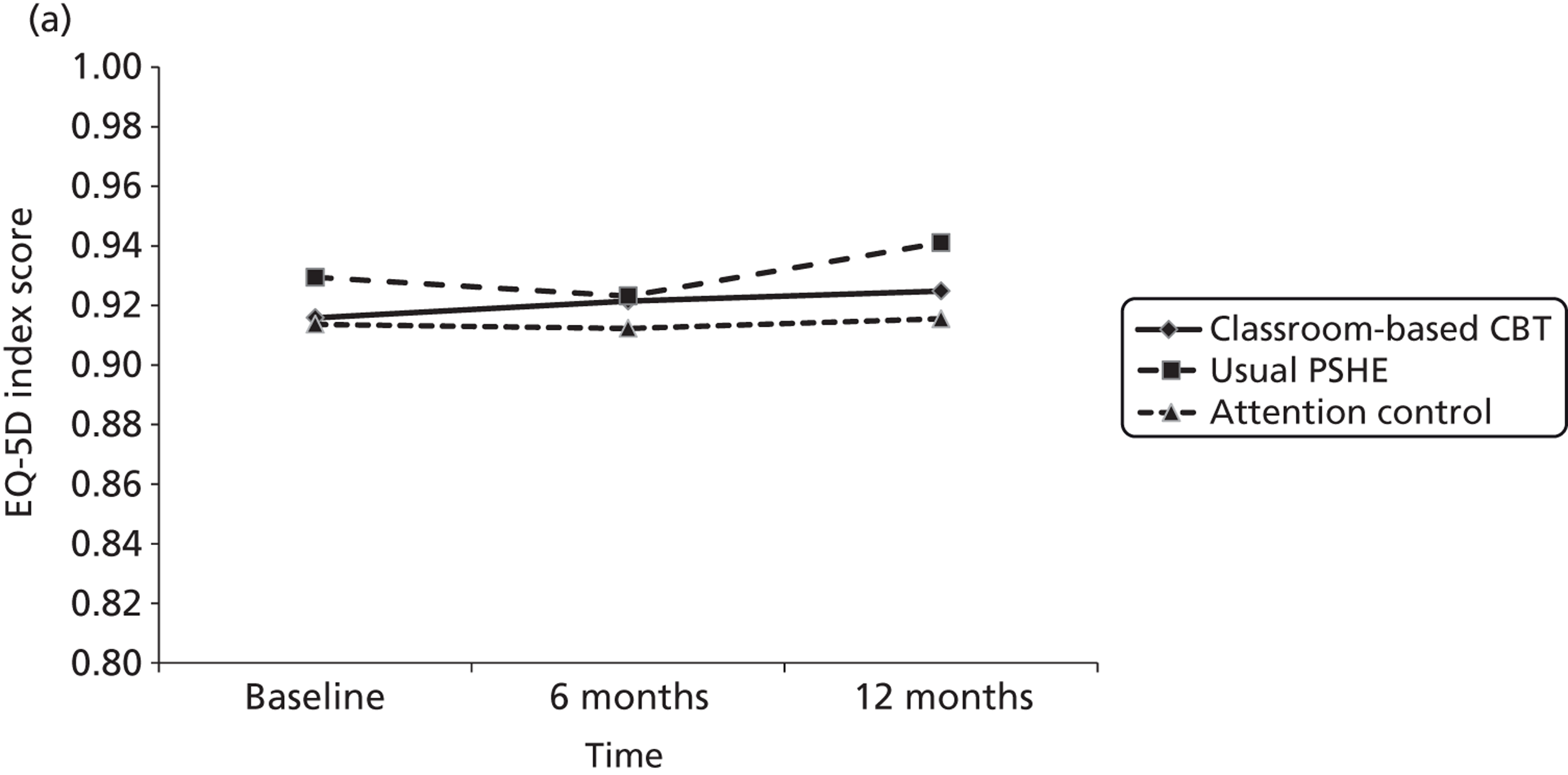
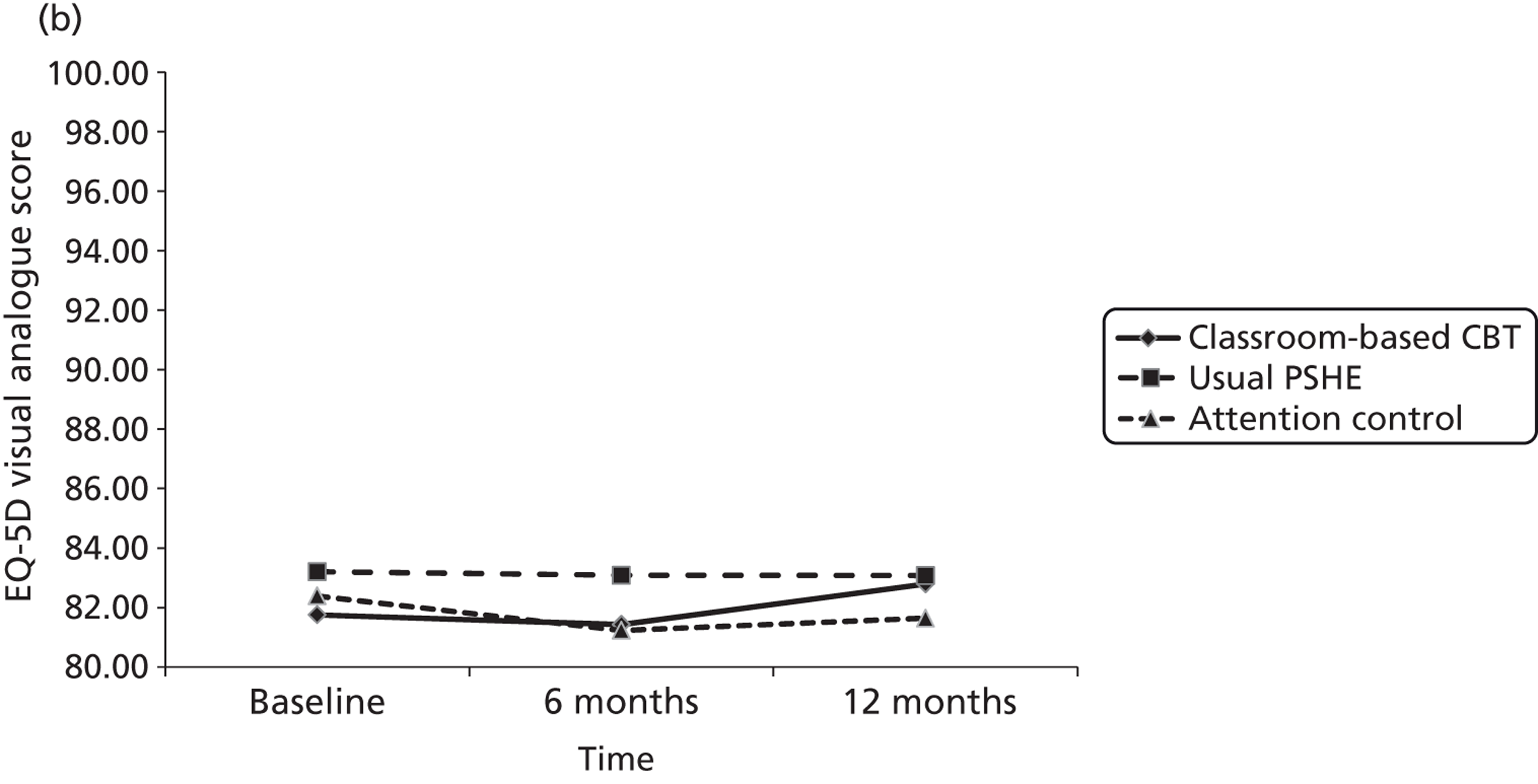
Both these figures and the data on which they are based (Table 28) show that any mean changes over time or mean differences between trial arms in either of these scores were minimal [varying less than 0.03 (EQ-5D index) or less than 2 points (EQ-5D visual analogue scale) over time or between trial arms]. As with the cost data, we did not test for the statistical significance of any service use cost differences between trial arms both because the study was not powered to detect such differences and because, in cost-effectiveness analysis, it is more important to estimate the CIs around the joint distribution of cost and effectiveness differences.
| Trial arm | EQ-5D preference-based index (possible range −0.594 to 1.0) | EQ-5D visual analogue scale score (possible range 0 to 100) | ||||
|---|---|---|---|---|---|---|
| Baseline | 6 months | 12 months | Baseline | 6 months | 12 months | |
| Classroom-based CBT | ||||||
| n | 1006 | 1006 | 1006 | 973 | 985 | 992 |
| Mean | 0.916 | 0.921 | 0.925 | 81.8 | 81.4 | 82.8 |
| SD | 0.1484 | 0.1578 | 0.1585 | 16.18 | 17.26 | 16.70 |
| Median | 1.000 | 1.000 | 1.000 | 85.0 | 85.0 | 90.0 |
| 25th percentile | 0.848 | 0.848 | 0.850 | 75.0 | 75.0 | 75.0 |
| Usual PSHE | ||||||
| n | 1067 | 1067 | 1067 | 1050 | 1054 | 1053 |
| Mean | 0.929 | 0.923 | 0.941 | 83.2 | 83.1 | 83.1 |
| SD | 0.1348 | 0.1685 | 0.1291 | 15.56 | 14.76 | 15.00 |
| Median | 0.848 | 0.848 | 1.000 | 75.0 | 76.8 | 75.5 |
| 25th percentile | 0.848 | 0.848 | 0.850 | 75.0 | 75.0 | 75.0 |
| Attention control PSHE | ||||||
| n | 1044 | 1044 | 1044 | 1017 | 1025 | 1028 |
| Mean | 0.914 | 0.912 | 0.915 | 82.4 | 81.2 | 81.6 |
| SD | 0.1464 | 0.1632 | 0.1656 | 15.24 | 16.88 | 16.54 |
| Median | 1.000 | 1.000 | 1.000 | 85.0 | 85.0 | 85.0 |
| 25th percentile | 0.848 | 0.848 | 0.848 | 75.0 | 75.0 | 75.0 |
The detailed profiles of health-related quality of life by individual EQ-5D question and response level, by both trial arm and study time point, are shown in Tables 29 and 30. These tables show that the vast majority of self-reported health problems (affecting between 15% and 20% of adolescents) related to either pain/discomfort or anxiety/depression, while relatively few reported health problems impacting on mobility, self-care or usual activities.
| Question | Baseline, % (n) | 6 months, % (n) | 12 months, % (n) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Classroom-based CBT (n = 1539) | Usual PSHE (n = 1432) | Attention control PSHE (n = 1492) | Classroom-based CBT (n = 1447) | Usual PSHE (n = 1411) | Attention control PSHE (n = 1424) | Classroom-based CBT (n = 1271) | Usual PSHE (n = 1275) | Attention control PSHE (n = 1270) | |
| Mobility | |||||||||
| No problems walking | 94.5 (1454) | 96.0 (1375) | 94.7 (1413) | 94.3 (1364) | 94.8 (1337) | 93.5 (1332) | 94.6 (1202) | 95.8 (1222) | 94.5 (1200) |
| Some problems | 4.9 (76) | 3.3 (47) | 4.8 (72) | 4.9 (71) | 4.2 (59) | 5.6 (80) | 4.9 (62) | 3.8 (48) | 5.0 (64) |
| Confined to bed | 0.6 (9) | 0.7 (10) | 0.5 (7) | 0.8 (12) | 1.1 (15) | 0.8 (12) | 0.6 (7) | 0.4 (5) | 0.5 (6) |
| Self-care | |||||||||
| No problems | 98.8 (1521) | 99.1 (1419) | 99.1 (1479) | 98.5 (1426) | 99.0 (1397) | 98.4 (1401) | 99.0 (1258) | 99.3 (1266) | 98.7 (1253) |
| Some problems | 0.9 (14) | 0.8 (11) | 0.7 (11) | 0.7 (10) | 0.6 (9) | 1.1 (15) | 0.6 (8) | 0.5 (7) | 0.7 (9) |
| Unable to wash or dress myself | 0.3 (4) | 0.1 (2) | 0.1 (2) | 0.8 (11) | 0.4 (5) | 0.6 (8) | 0.4 (5) | 0.2 (2) | 0.6 (8) |
| Usual activities | |||||||||
| No problems | 91.4 (1407) | 93.3 (1336) | 90.5 (1350) | 93.4 (1351) | 93.6 (1320) | 91.3 (1300) | 92.8 (1179) | 94.7 (1208) | 93.3 (1185) |
| Some problems | 8.2 (126) | 6.2 (89) | 9.3 (139) | 5.8 (84) | 5.7 (81) | 7.6 (108) | 7.0 (89) | 4.9 (62) | 5.8 (74) |
| Unable to perform usual activities | 0.4 (6) | 0.5 (7) | 0.2 (3) | 0.8 (12) | 0.7 (10) | 1.1 (16) | 0.2 (3) | 0.4 (5) | 0.9 (11) |
| Pain/discomfort | |||||||||
| No pain or discomfort | 77.8 (1198) | 81.9 (1173) | 76.9 (1147) | 80.6 (1166) | 81.5 (1150) | 77.2 (1100) | 81.3 (1033) | 85.2 (1086) | 80.4 (1021) |
| Moderate | 21.4 (329) | 17.6 (252) | 22.5 (335) | 18.2 (264) | 17.6 (249) | 21.2 (302) | 17.9 (228) | 14.4 (184) | 18.7 (237) |
| Extreme | 0.8 (12) | 0.5 (7) | 0.7 (10) | 1.2 (17) | 0.9 (12) | 1.5 (22) | 0.8 (10) | 0.4 (5) | 0.9 (12) |
| Anxiety/depression | |||||||||
| Not anxious or depressed | 80.6 (1241) | 83.8 (1200) | 79.0 (1178) | 83.2 (1204) | 84.1 (1186) | 79.1 (1126) | 85.2 (1083) | 84.5 (1078) | 81.0 (1029) |
| Moderately | 17.2 (264) | 15.2 (218) | 19.4 (290) | 14.8 (214) | 14.4 (203) | 19.2 (273) | 12.7 (162) | 14.4 (183) | 17.4 (221) |
| Extremely | 2.2 (34) | 1.0 (14) | 1.6 (24) | 0.1 (1) | 0.0 (0) | 0.0 (0) | 2.0 (26) | 1.1 (14) | 1.6 (20) |
| Question | Baseline | 6 months | 12 months | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Classroom-based CBT (n = 1539) | Usual PSHE (n = 1432) | Attention control PSHE (n = 1492) | Classroom-based CBT (n = 1447) | Usual PSHE (n = 1411) | Attention control PSHE (n = 1424) | Classroom-based CBT (n = 1271) | Usual PSHE (n = 1275) | Attention control PSHE (n = 1270) | |
| Mobility, % (n) | |||||||||
| No problems walking | 94.9 (955) | 96.6 (1031) | 95.6 (998) | 94.4 (950) | 94.9 (1013) | 94.4 (986) | 95.3 (959) | 96.4 (1029) | 94.4 (986) |
| Some problems | 4.8 (48) | 2.8 (30) | 4.3 (45) | 5.0 (50) | 4.0 (43) | 5.2 (54) | 4.1 (41) | 3.5 (37) | 5.1 (53) |
| Confined to bed | 0.3 (3) | 0.6 (6) | 0.1 (1) | 0.6 (6) | 1.0 (11) | 0.4 (4) | 0.5 (6) | 0.1 (1) | 0.5 (5) |
| Self-care, % (n) | |||||||||
| No problems | 99.2 (98) | 99.3 (1059) | 99.5 (1039) | 98.9 (995) | 99.1 (1057) | 98.9 (1032) | 99.3 (999) | 99.3 (1060) | 98.8 (1031) |
| Some problems | 0.6 (6) | 0.7 (8) | 0.4 (4) | 0.7 (7) | 0.6 (6) | 0.8 (8) | 0.4 (4) | 0.5 (5) | 0.6 (6) |
| Unable to wash or dress myself | 0.2 (2) | 0 (0) | 0.1 (1) | 0.4 (4) | 0.4 (4) | 0.4 (4) | 0.3 (3) | 0.2 (2) | 0.7 (7) |
| Usual activities, % (n) | |||||||||
| No problems | 92.3 (929) | 93.9 (1002) | 91.2 (952) | 94.0 (946) | 93.8 (1001) | 92.3 (964) | 93.5 (941) | 95.1 (1015) | 93.44 (975) |
| Some problems | 7.4 (74) | 5.9 (63) | 8.6 (90) | 5.4 (54) | 5.3 (57) | 7.1 (74) | 6.4 (64) | 4.6 (49) | 5.7 (60) |
| Unable to perform usual activities | 0.3 (3) | 0.2 (2) | 0.2 (2) | 0.6 (6) | 0.8 (9) | 0.6 (6) | 0.1 (1) | 0.3 (3) | 0.9 (9) |
| Pain/discomfort, % (n) | |||||||||
| No pain or discomfort | 78.4 (789) | 81.3 (868) | 78.4 (818) | 81.0 (815) | 81.9 (874) | 79.2 (827) | 82.4 (829) | 85.5 (912) | 80.4 (839) |
| Moderate | 20.9 (210) | 18.5 (197) | 21.0 (219) | 18.4 (185) | 17.2 (184) | 19.9 (208) | 17.0 (171) | 14.2 (151) | 18.8 (196) |
| Extreme | 0.7 (7) | 0.2 (2) | 0.7 (7) | 0.6 (6) | 0.8 (9) | 0.9 (9) | 0.6 (6) | 0.4 (4) | 0.9 (9) |
| Anxiety/depression, % (n) | |||||||||
| Not anxious or depressed | 83.8 (843) | 84.8 (905) | 80.6 (841) | 84.9 (854) | 85.3 (910) | 81.2 (848) | 86.3 (868) | 85.2 (909) | 81.5 (851) |
| Moderately | 14.8 (149) | 14.2 (152) | 18.0 (188) | 13.8 (139) | 13.4 (143) | 17.2 (180) | 11.5 (116) | 14.0 (149) | 17.2 (180) |
| Extremely | 1.4 (14) | 0.9 (10) | 1.4 (15) | 1.3 (13) | 0 (0) | 0 (0) | 2.2 (22) | 0.8 (9) | 1.2 (13) |
Incremental cost-effectiveness
Tables 31 and 32 show the incremental cost-effectiveness for each of classroom-based CBT and attention control PSHE per person compared with usual PSHE for the 12-month period of the trial. This includes SMFQ score at 12 months and QALYs from baseline to 12 months as outcomes, and adjusted and unadjusted analyses are shown. Attention control PSHE was both less effective and more costly than usual PSHE; that is to say, both the point estimate ICER and most of the joint distribution of incremental costs and effects are in the north-west quadrant of the cost-effectiveness plane. All of the analyses except one found classroom-based CBT to be both less effective and more costly than the usual PSHE control. For the adjusted analysis of the incremental cost per QALY of classroom-based CBT compared with controls there is a very small estimated per person QALY gain (0.00054) for the additional cost of £100 per person.
| n | Costs (£) | SMFQ | Difference in costs | Difference in SMFQ | ICER unadjusted (95% CI) | Difference in costs adjusted | Difference in SMFQ adjusted | ICER adjusted (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|
| Classroom-based CBT vs. usual PSHE | |||||||||
| Usual PSHE | 1140 | 406 (1240) | 3.18 (4.46) | NA | NA | ||||
| Classroom-based CBT | 1096 | 553 (1392) | 3.73 (5.34) | 147 | −0.58 | Dominateda | 106 | −0.29 | Dominateda |
| Attention control PSHE vs. usual PSHE | |||||||||
| Usual PSHE | 1140 | 406 (1240) | 3.18 (4.46) | NA | NA | ||||
| Attention control PSHE | 1108 | 539 (1572) | 3.89 (5.12) | 133 | −0.74 | Dominateda | 160 | −0.37 | Dominateda |
| n | Costs (£) | QALYs | Difference in costs | Difference in QALYs | ICER unadjusted (95% CI) | Difference in costs adjusted | Difference in QALYs adjusted | ICER adjusted (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|
| Classroom-based CBT vs. usual PSHE | |||||||||
| Usual PSHE | 1067 | 385 (1169) | 0.91 (0.12) | NA | NA | ||||
| Classroom-based CBT | 1006 | 526 (1294) | 0.90 (0.12) | 141 | −0.009 | Dominateda | 100 | 0.00054 | 185,338 (95% CI undefinedb) |
| Attention control PSHE vs. usual PSHE | |||||||||
| Usual PSHE | 1067 | 385 (1169) | 0.91 (0.12) | NA | NA | ||||
| Attention control PSHE | 1044 | 517 (1553) | 0.89 (0.12) | 132 | −0.016 | Dominateda | 177 | −0.017 | Dominateda |
Scatterplots of incremental costs and QALYs (Figures 4 and 5) and the related cost-effectiveness acceptability curve (Figure 6) were produced. The cost-effectiveness acceptability curve shows that there is an approximately 5% probability that classroom-based CBT is less costly than usual PSHE, and a 46% probability that it is less effective than usual PSHE. An incremental cost per QALY gained of £185,000 (95% CI is undefined) was estimated for classroom-based CBT in the adjusted analysis. This is both higher than the normally accepted willingness to pay for QALYs when they relate to the adoption of health technologies within the NHS58 and highly uncertain. Further to the statistically non-significant effectiveness results for nearly all comparisons and analyses conducted, it can also be concluded that neither classroom-based CBT nor attention control PHSE would be cost-effective compared with usual PSHE. Given the small and highly uncertain differences in cost and effectiveness (SMFQ or QALYs) between classroom-based CBT and attention control PHSE, it would not be informative to estimate the incremental cost-effectiveness of these comparisons.
FIGURE 4.
Cost-effectiveness plane. Classroom-based CBT vs. usual PSHE, ratio of incremental cost to QALYs gained (adjusted analysis).
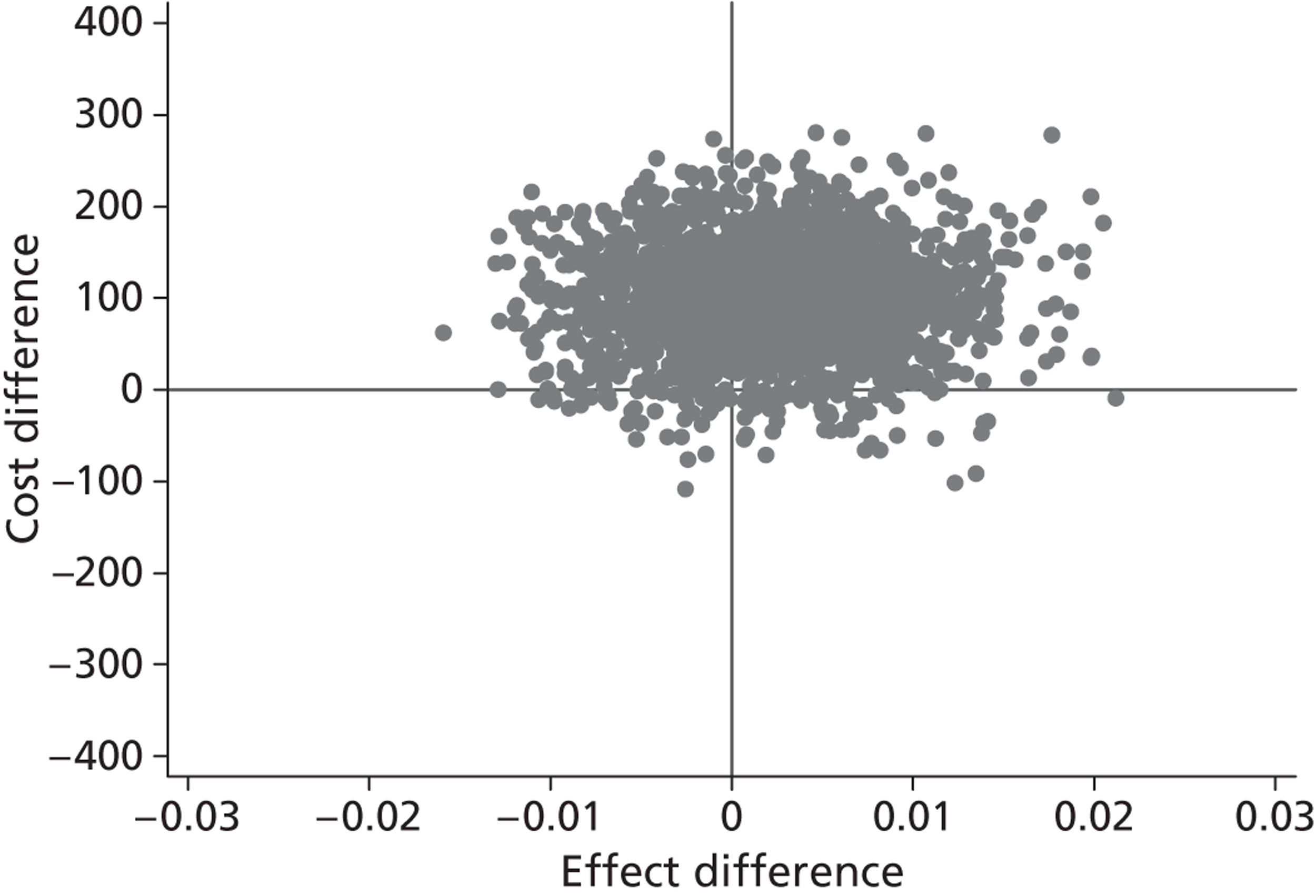
FIGURE 5.
Scatterplots of incremental costs and effects for the adjusted analyses. (a) Classroom-based CBT vs. usual PSHE: SMFQ; (b) attention control PSHE vs. usual PSHE: SMFQ; (c) classroom-based CBT vs. usual PSHE: QALYs; and (d) attention control PSHE vs. usual PSHE: QALYs.
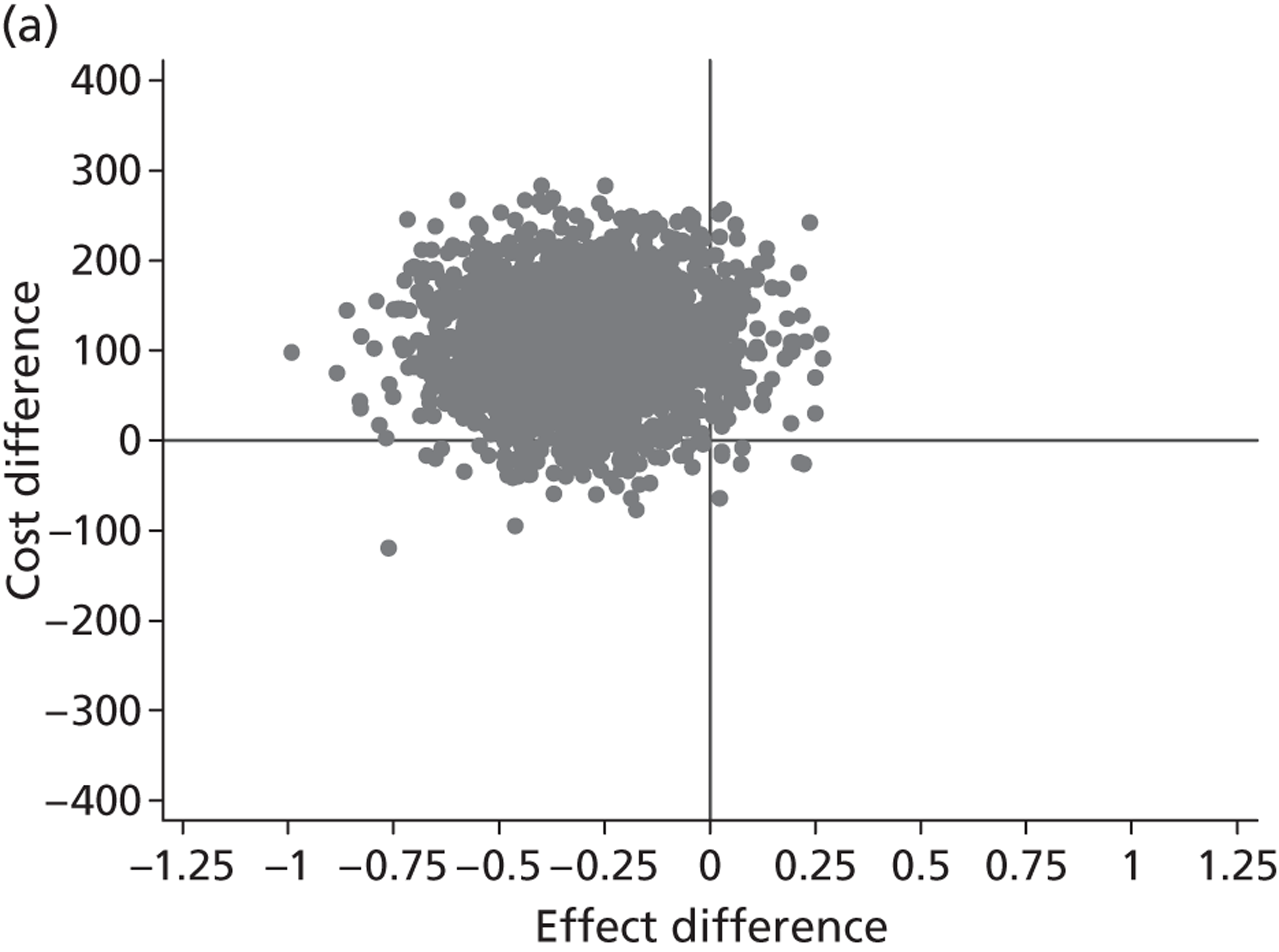
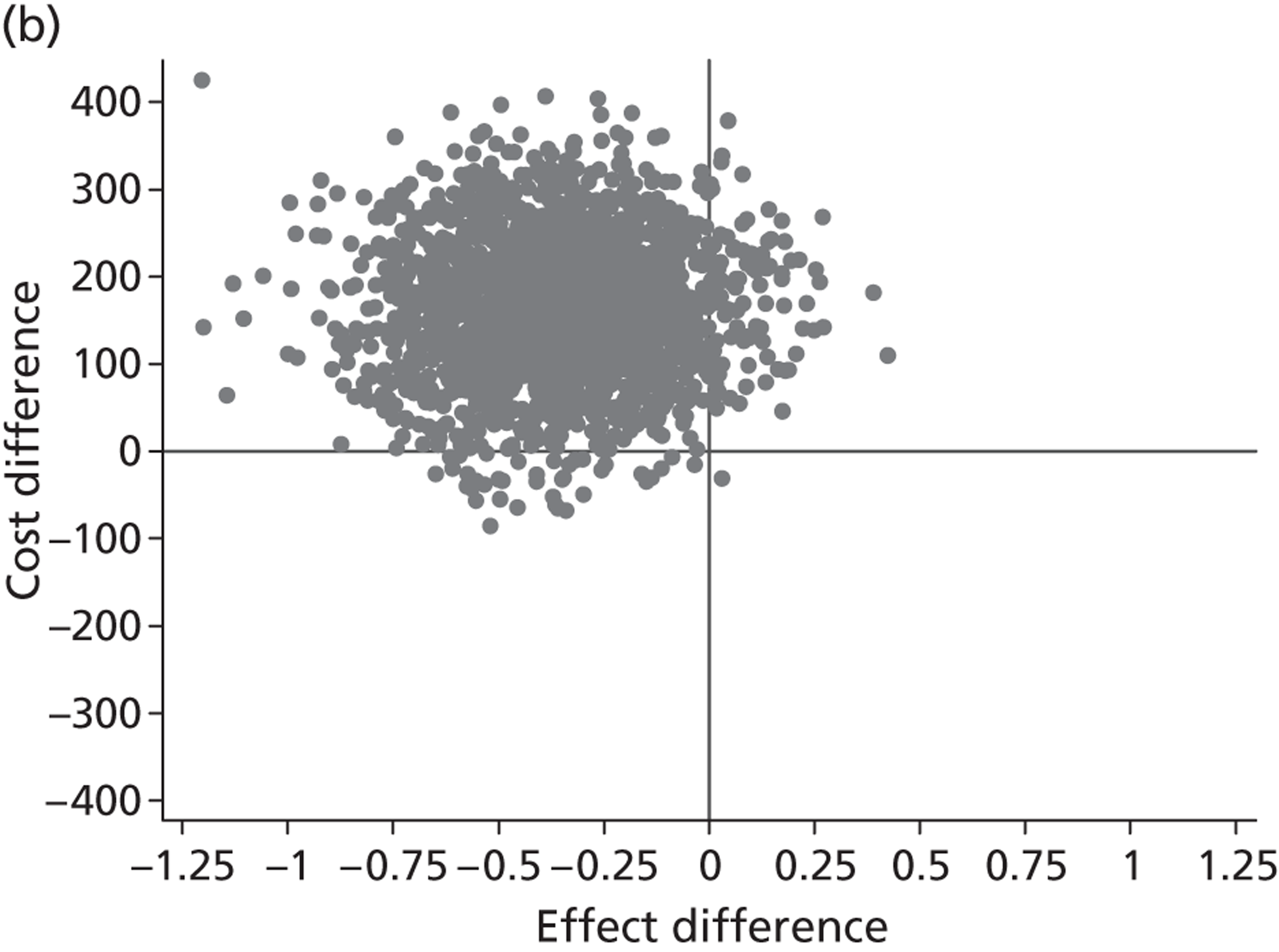
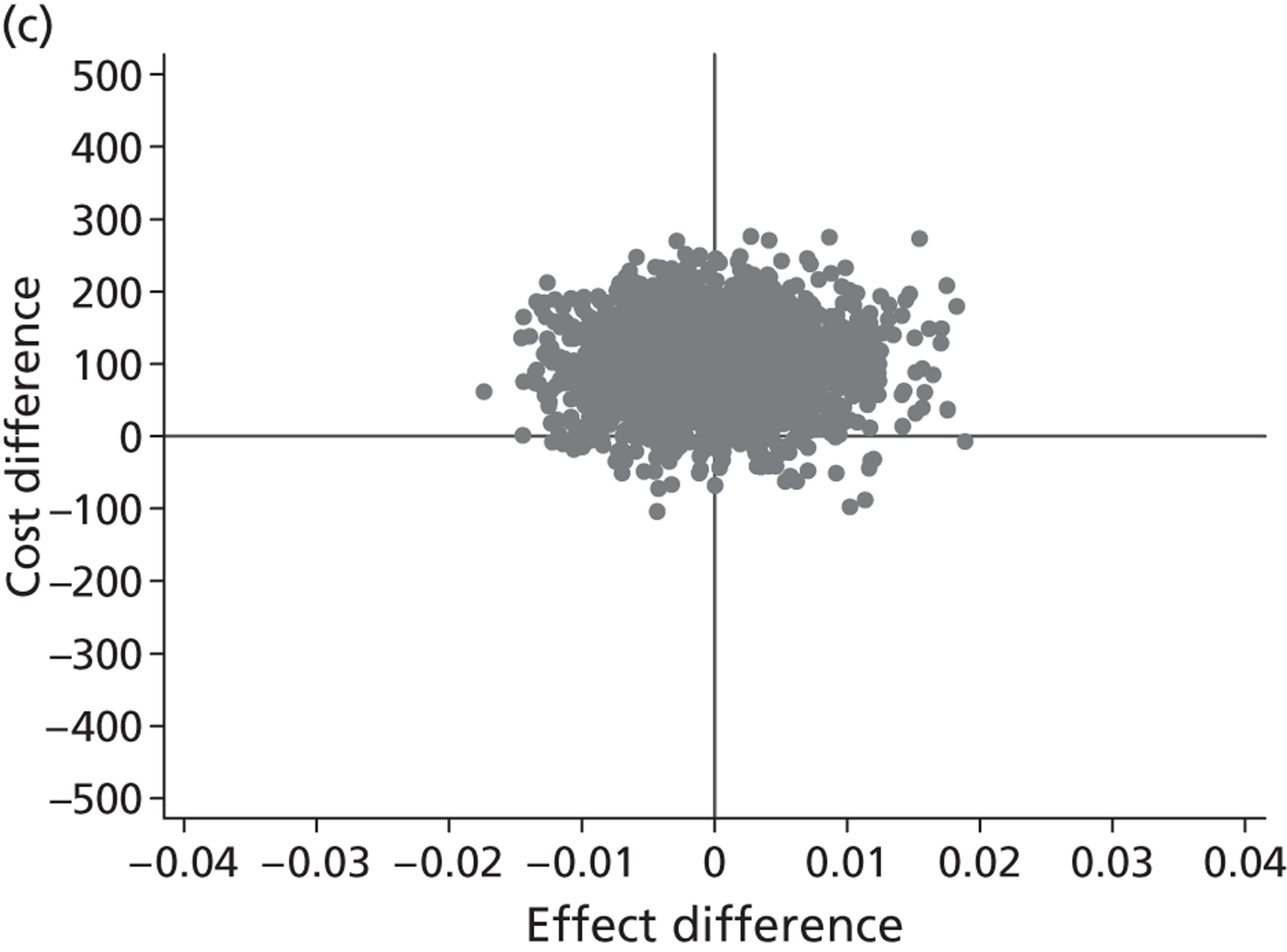
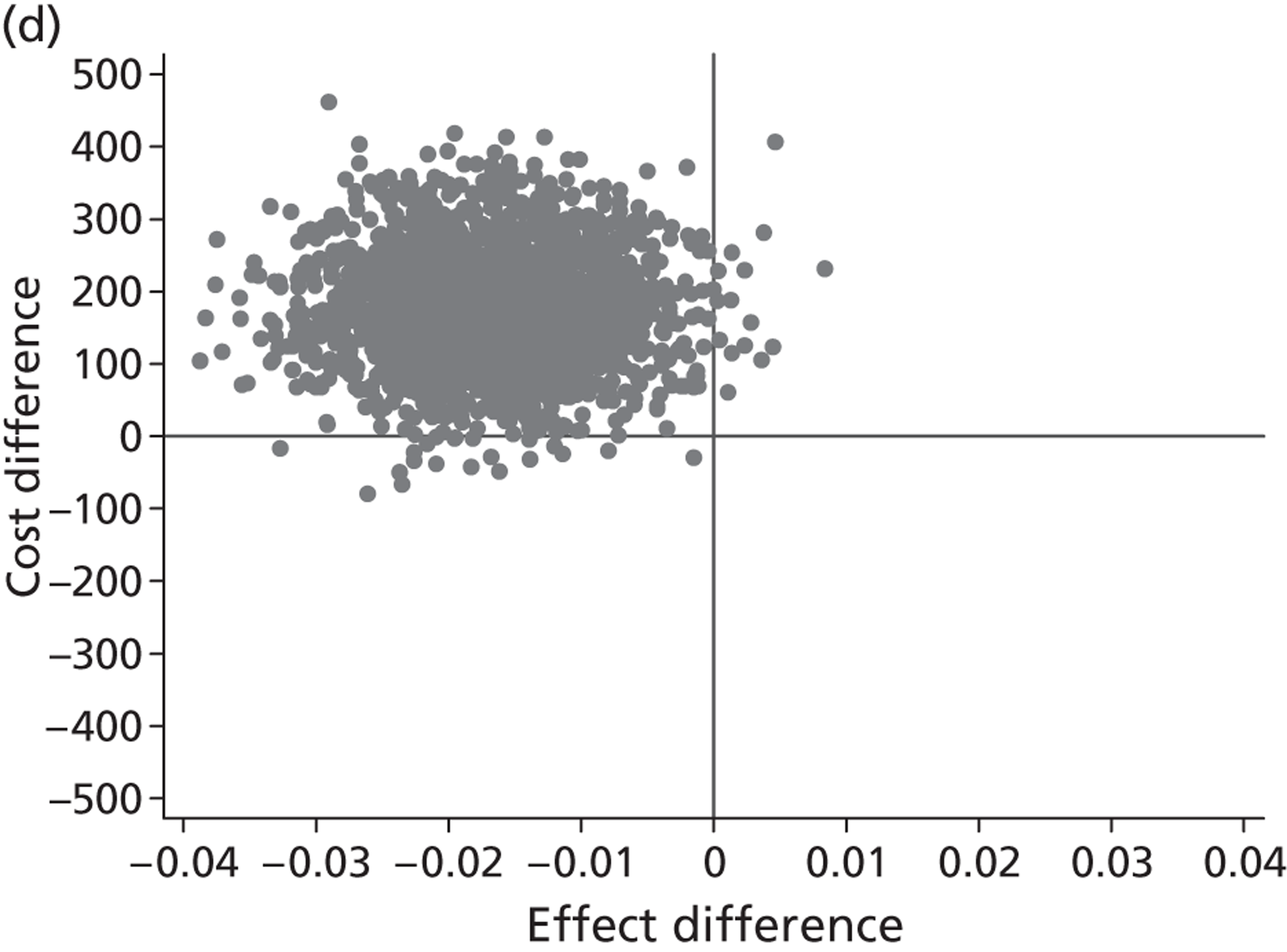
FIGURE 6.
Probability that classroom-based CBT is cost-effective compared with usual PSHE based on cost per QALY (adjusted analysis).
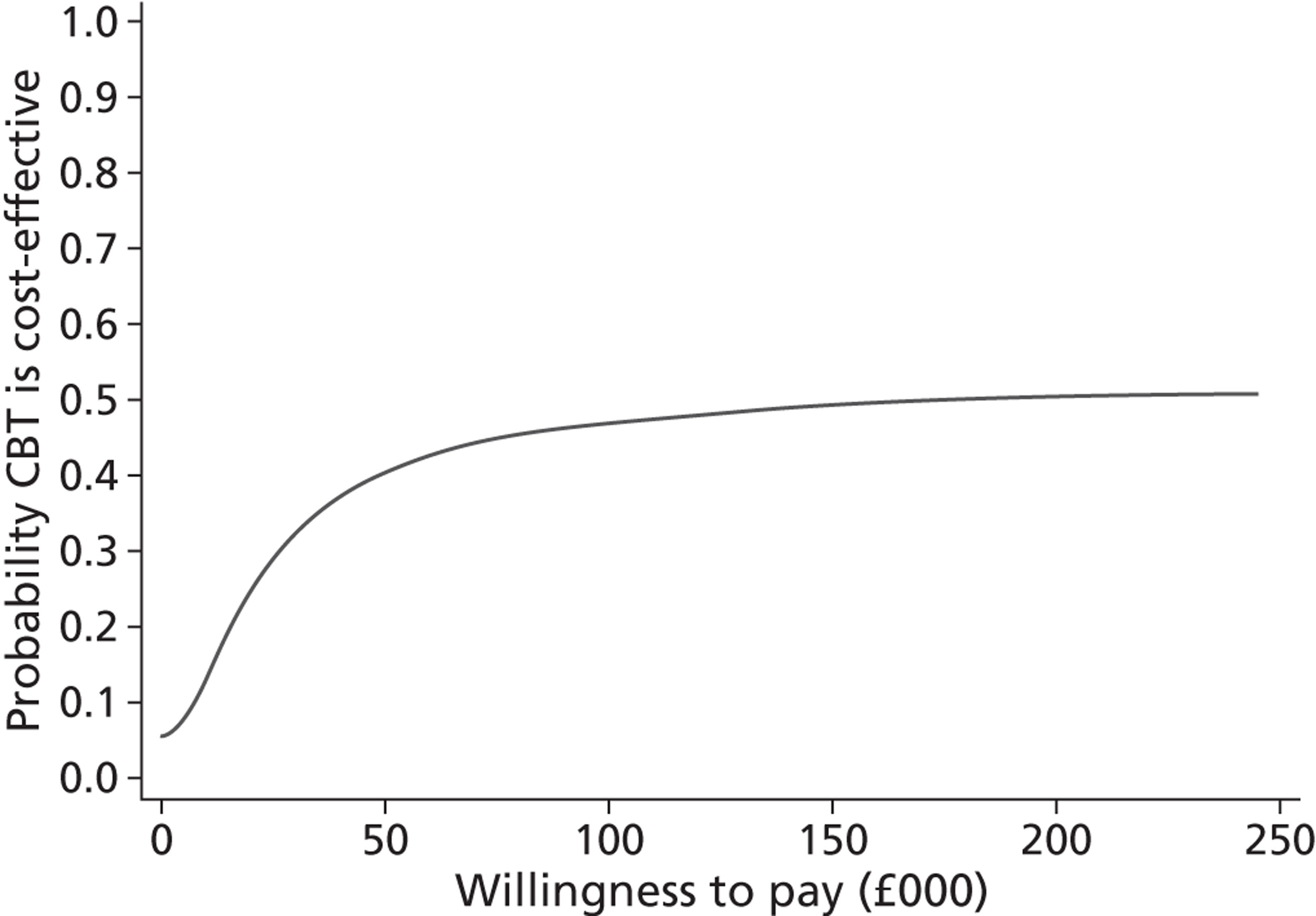
Chapter 5 Discussion
Principal findings
This is the first large-scale pragmatic cluster randomised controlled trial to compare the effects of a focused classroom-based CBT programme (RAP-UK) on symptoms of depression in adolescents with both usual school PSHE provision group and an attention control group, and incorporating a long-term follow-up (12 months from baseline). We found no evidence that classroom-based CBT reduced symptoms of depression in the high-risk group of adolescents when implemented under diverse everyday conditions, despite high levels of treatment fidelity and adherence. Having adjusted for variables that were imbalanced at baseline, there was some evidence of increased reporting of symptoms of depression in the high-risk group at 12-month follow-up. Classroom-based CBT was not cost-effective and there was a high probability that it was both less effective and more expensive than usual PSHE. Furthermore, there were a number of challenges associated with implementing classroom-based CBT within schools, particularly with regard to fitting classroom-based CBT into a busy timetable, the lack of value placed on PSHE in schools and difficulties engaging with teachers and young people.
Nonetheless, in this unreferred community sample, around one in five adolescents reported elevated depressive symptoms on two separate occasions prior to the interventions. This high-risk group showed modest improvements in symptoms of depression over the following year that may reflect regression to the mean regardless of which trial arm they were in. However, around two-thirds of these high-risk participants continued to be at risk of depression at 12-month follow-up. Our data provide further evidence of a need for clinically effective and cost-effective community-based depression prevention and early intervention programmes for adolescents.
Pilot phase
The pilot study demonstrated that the delivery and evaluation of classroom-based CBT in the UK school context was feasible. Ninety-six per cent of students on roll were actually attending school and able to access and potentially benefit from the interventions. The complete nine-session classroom-based CBT programme was delivered to all but one class, with 95% of sessions being delivered as intended by two trained facilitators. Of those students who received classroom-based CBT, almost 90% attended seven or more sessions. However, classroom-based CBT was delivered to only two of the school year groups and it was unclear whether or not delivery and attendance rates would be similar for the other year groups. Delivering to year 11 students may be particularly problematic as the main focus for these students is on preparing for their General Certificate of Secondary Education (GCSE) examinations. Nonetheless, these results were encouraging and suggested that the majority of students in secondary school would be able to access and receive sufficient dosage from classroom-based CBT.
The consent process was both practical and acceptable, with consent to complete study assessments approaching 90%. At the 12-month follow-up, 78% of participants were retained. Retention rates of year 11 students were the lowest (45%) as many had left school. This highlighted the need to investigate ways of improving retention in this group in the main trial, including ensuring that there were alternative ways of contacting older students (e.g. mobile telephones, e-mail, putting the assessments online). The classroom-based CBT programme (RAP-UK) content and exercises were also modified for the main trial in the light of the qualitative feedback from the pilot study to try to make materials more engaging, appealing and relevant to all age groups. The training for facilitators was revised to incorporate information on working within the school environment, including discussion of issues around classroom management and working alongside teachers. These issues were also discussed and reviewed during the ongoing supervision sessions for facilitators in the main trial.
Main trial
Reach and effectiveness
The reach of classroom-based CBT within participating schools was good, with the vast majority of young people on roll attending PSHE and therefore being able to access the intervention. Over 90% of eligible young people assented to complete assessments, and over 80% of young people completing baseline were retained at 12-month follow-up. Attendance of PSHE was good and attrition from the PSHE programmes was low. Nonetheless, initial recruitment of schools to the trial was challenging, with only 9 of the 66 schools approached agreeing to take part. This was partly due to other pressures on schools [e.g. Ofsted (Office for Standards in Education, Children's Services and Skills) inspections, staffing changes, participation in other projects]. It may have also been due to the additional demands of a research trial in terms of assessments and research procedures (e.g. randomisation, consent/assent, assessments). However, this may have been indicative of a wider lack of engagement with the project, particularly given other pressures on their time and resources and the general emphasis on academic targets within the UK education system.
The classroom-based CBT programme used (RAP-UK) specifically targeted factors reported to protect against the development of depression, that is thinking styles, emotional recognition and regulation and coping skills. 59 However, we observed that when variables that were imbalanced at baseline had been adjusted for, there was some evidence that classroom-based CBT could have had a small but potentially harmful effect on symptoms of depression compared with usual PSHE in the high-risk group. Furthermore, the high-risk group receiving classroom-based CBT reported more feelings of personal failure at 12 months than those who received usual PSHE. This may indicate a detrimental effect, reflecting limited improvement in mood over time in the high-risk group. While the possibility of a small harmful effect needs to be acknowledged, higher rates of symptoms may reflect greater self-recognition and acknowledgement of exisiting symptoms of depression and negative thinking styles. Furthermore, there was some evidence of potentially beneficial effects of classroom-based CBT on some of the secondary outcomes (i.e. RCADS depression at 12 months compared with usual PSHE, self-harm thoughts at 6 months, and SMFQ as a binary outcome at 12 months compared with attention control PSHE). Similarly, when all participants were included in the analysis regardless of risk status, both potential benefits and potential harms of classroom-based CBT were identified, although all effects were modest and unlikely to be clinically significant.
Unfortunately, our data do not extend beyond 12 months so the longer-term effects of the interventions are not known. Nonetheless, in the short term, our results suggested that, compared with no intervention, classroom-based CBT targeting symptoms of depression in high-risk adolescents was associated with increased levels of self-reported depressive symptoms. The possibility of worse outcomes following school-based intervention programmes has also been found for other mental health disorders such as attention-deficit hyperactivity disorder, and an improved understanding of the mechanisms underlying possible adverse outcomes merits further investigation. 60
Adoption and implementation
Classroom-based CBT was adopted and successfully implemented in the participating schools, but this process proved to be immensely challenging. Schools are very busy and complex environments where there are many competing demands. Furthermore, PSHE is generally undervalued, under-resourced and not prioritised in secondary schools. Finding time, resources and the enthusiasm required to implement a focused mental health programme in this context is difficult. RAP-UK was designed to fit in with existing school structures and enormous flexibility was required to attempt to fit the programme into schools. To accommodate this, a team of over 70 trained facilitators was required to deliver the interventions, predominantly owing to timetabling issues. This posed a major challenge in terms of training and co-ordination of the intervention delivery.
Our experience was that successful delivery of the interventions required a great deal of organisation on the part of schools and the research team, involving regular communication, fitting in around timetables and other demands (e.g. examinations, sports days, work experience) and managing unexpected events (e.g. school closures due to adverse weather). In cases where lessons were cancelled, it could be very difficult to rearrange these. For example, the classroom-based CBT intervention was terminated after session 4 in a whole year group in one school because the school had lost several days to closures during adverse weather and they needed the time allocated to the programme to catch up on examined subjects. Therefore, despite having agreed the best way of implementing the programme with PSHE co-ordinators in schools, we experienced regular ongoing difficulties with delivery because of competing pressures.
Feedback from teachers and facilitators indicated that a shorter and more fast-paced programme might have been more engaging and easier to implement. However, reviews of depression prevention programmes in adolescents indicate that between 8 and 12 sessions are required for these to be effective. 8,9 Part of the issue for teachers appeared to be insufficient content in the RAP-UK programme given the amount of time allocated to the classroom-based CBT intervention; therefore, including more materials and activities to ensure that the students remained engaged and time was used constructively might have been helpful, rather than reducing the programme in length. Alternatively, Wolfe et al. 61 have argued that, to enhance maintenance, shorter programmes should be considered. Programmes could potentially be delivered more flexibly over a longer period of time. Continuous and extended programmes are advocated by Wells et al. 62 and may help to sustain a given programme's benefit. 63 Nonetheless, the current format of delivering nine classroom-based CBT sessions within an academic year was difficult to implement and it is unlikely that this could be sustained outside the context of a research trial.
Engagement with and sustainability of school-based intervention programmes is likely to be strongly influenced by levels of teacher and pupil satisfaction. 64 A number of previous studies have reported that RAP was positively received and perceived to be useful by teachers and young people,16,61,65 and this was our experience in the pilot study. However, in the main trial where the interventions were implemented under more diverse conditions, the feedback was more mixed. In the main trial, a number of positive aspects of the classroom-based CBT were noted in the feedback received from young people and teachers, particularly relating to the content and structure of the RAP-UK sessions, the use of hands-on and interactive tasks, and the usefulness of some of the components of the programme (e.g. recognising body signals and problem solving). Nonetheless, the feedback relating to the acceptability and sustainability of classroom-based CBT was not generally very positive, despite us having revised the intervention and training for facilitators following the feedback from the pilot study.
One of the major challenges faced was that PSHE in general was not positively rated by students regardless of trial arm, and teachers noted that it was an undervalued subject in schools. Given that PSHE is a mandatory part of the school curriculum and deals with issues that are central to the health and well-being of young people, further work needs to be undertaken to make PSHE more engaging, useful and relevant for students. This seems especially important, as fitting programmes into a curriculum that is already so negatively viewed is unlikely to be useful. The feedback questionnaires indicated that classroom-based CBT was more negatively rated than usual PSHE by boys and by the low-risk group, but that there was little difference in the way the programmes were rated in the high-risk group and by girls. Based on the qualitative data, the classroom-based CBT programme appeared to be more acceptable to younger students (year 8) but was less well received in the older year groups, and it was suggested that there was a need for greater differentiation and flexibility, and more emphasis on hands-on tasks.
Overall, teachers were not positive about classroom-based CBT in terms of helping students with their mood. This may reflect a lack of general understanding about childhood depression or a failure to clearly communicate the purpose and aims of the classroom-based CBT programme. Although the research team invested considerable time engaging with the senior management teams and PSHE coordinators at participating schools, interacting with individual teachers proved more difficult. Schools are very busy places, and it was not always possible to find an opportunity at the start of the project for either the research team or facilitators to meet and discuss the project with individual PSHE teachers. Teachers were consulted during the pilot phase of this study to gather feedback and inform the development of the programme before it was rolled out for the main trial. However, it became evident that the teachers involved in the main trial would have liked to be more directly involved in developing the programmes and tailoring them to their students. Teachers in a study of RAP in New Zealand also felt that they could have delivered the programme more effectively if they had been able to deviate from the manual and adapt the way some of the concepts were taught. 25 Involving teachers in programme development and planning may have improved engagement with teachers and young people, but this process would affect treatment fidelity unless all the key active elements were retained, so care would need to be taken with this approach. Furthermore, our experience was that teachers were very busy and had many demands on their time. Finding time to work with facilitators on planning, preparation and reviewing progress often proved impossible in reality, even when teachers were very motivated and engaged with the programme.
The majority of classroom-based CBT facilitators felt positive about their role, enjoyed their work and felt they had sufficient training in general. However, almost half of the facilitators did not feel that the classroom-based CBT would improve mental health, with similar numbers feeling that young people were not engaged with the programme. Facilitators' knowledge and confidence have been identified as important factors in relation to the effectiveness of a programme. 66 Providing more training, including an acclimatisation period in schools, allowing more time for facilitators and teachers to work together and develop a relationship and providing more time to familiarise with the programme could have improved acceptability for classroom-based CBT facilitators. However, this may have been less of an issue outside the confines of a research trial if facilitators were able to work regularly with a group of schools over a longer period of time.
Maintenance
Feedback from teachers and PSHE co-ordinators indicated that delivering classroom-based CBT in secondary schools in its current form would not be sustainable. During interviews, teachers unanimously felt that the classroom-based CBT would be too expensive and lengthy to deliver. Training school staff in mental health programmes provides an alternative and potentially more cost-effective model, although school staff tend to be less effective than trained facilitators or health professionals. 9,19 Around half of the teachers involved in classroom-based CBT did not feel confident that they could deliver the programme on their own, suggesting the need for a significant teacher training and support programme if all teachers were expected to deliver it. Teacher feedback also suggested that if they were to deliver the RAP-UK programme used in the current study, it would be reduced and amended, indicating that treatment fidelity would be compromised. Furthermore, enthusiasm and motivation from teachers would be required to engage with young people in delivering classroom-based CBT, and this was not always present. Therefore, neither delivery by external facilitators (more expensive) nor delivery by teachers (likely to be less effective) appeared to represent sustainable models for delivering classroom-based CBT in schools in its current form.
Economic evaluation
Whether based on estimated differences in QALYs or on differences in SMFQ scores, this research provides no evidence that either classroom-based CBT or attention control PSHE is a cost-effective way of reducing symptoms of depression in adolescents in schools. For all of the analyses bar one, the point estimate of the ICER was in the upper-left quadrant and so it would not be a meaningful number to report. The probability that classroom-based CBT or attention control PSHE were both less effective and more costly than usual PSHE ranged from 43% to 98% in the adjusted analyses. Although the adjusted estimate of the mean incremental cost per QALY of classroom-based CBT compared with usual PSHE is about £185,000 per QALY, the 95% CI surrounding this ratio is not definable. The very small estimated QALY gain and the considerable uncertainty surrounding this estimate are consistent with the overall effectiveness results of the trial in relation to the SMFQ outcome. Even for this analysis, however, there is still a 43% estimated probability that classroom-based CBT is both more costly and less effective than usual PSHE, and only a 25% probability that the cost-effectiveness ratio is less than £20,000 per QALY, which is the current threshold below which the National Institute for Health and Care Excellence is likely to recommend treatments on the basis of value for money.
There are currently very few economic evaluations of similar group-CBT programmes for low mood or depression, and none that is for depression prevention trials targeting school children. However, a study comparing individual versus family CBT for children with anxiety disorders in the Netherlands similarly found no significant differences in costs or effectiveness (QALYs). 67 However, individual CBT was found to be both more effective and less costly than family CBT in most sensitivity analyses. 67 In contrast, an earlier modelling-based cost-effectiveness study in Australia, comparing individual CBT with ‘current practice’ to treat major depression in children and adolescents (aged 6–17 years), estimated that CBT saved disability-adjusted life-years (DALYs) at a cost of A$9000 per DALY saved. 68 Therefore, it is not possible to judge whether or not our findings are consistent with those of similar studies because of the lack of trial-based economic evaluations of group CBT to prevent depression, low mood and anxiety in children.
Implications
Our findings suggest that a more cautious approach is required to the widespread implementation of depression prevention programmes in schools. To maximise the potential for effectiveness of the depression prevention intervention, we selected an efficacious CBT-based programme, the RAP,24,25 and adapted this for the UK (RAP-UK). We ensured that there was a sufficient number of sessions, delivery was by trained facilitators rather than teachers and the majority of content was delivered in small groups within classes, as these factors are usually associated with larger effects. 8,9 The pilot study described above assessed feasibility and provided an opportunity to refine and adapt the RAP-UK programme before commencing the main trial. Despite this, the findings indicated that classroom-based CBT had very little effect on outcomes either in the high-risk group or for all participants. Where effects were observed, these were typically small and were mixed in terms of indicating possible benefits or harms.
While secondary schools provide a convenient focus for mental health interventions, the suitability of this setting for depression-focused interventions cannot be assumed. The success and sustainability of mental health interventions within this setting will be determined by a number of factors other than programme efficacy, including compatibility with organisational objectives, perceived relevance, programme flexibility and fit within existing structures. 69 Secondary schools are organisationally complex and, while the importance of developing social and emotional awareness is increasingly being recognised, the primary objective of schools is to develop academic skills. While we addressed this issue by using a dedicated team of trained facilitators to deliver the intervention, the absence of a positive effect and the feedback from teachers suggested that this is not a sustainable or viable option.
Systematic reviews of programmes designed to reduce symptoms of depression in adolescents have noted considerable variability in results but remain supportive of prevention and early intervention approaches delivered in schools. 8,9 Significant methodological shortfalls, limited follow-up and absence of attention control or placebo comparisons have been noted as important omissions in previous studies and the current study has addressed some of these issues. Although previous studies have succeeded in showing that classroom-based CBT can be efficacious in the short term,16,24,25 effects appear to be diluted when rolled out under more diverse conditions. The lack of clinical effectiveness of classroom-based depression prevention programmes has also been observed in other recent large-scale trials. The long-term follow-up of a large-scale trial (n = 5633) of the Beyondblue intervention failed to show clinical effectiveness of the programme in preventing depression, despite having taken an integrative approach and working on a whole-school as well as an individual level. 19,20 Likewise, in a recent evaluation of the UK Resilience Programme with year 7 students across 22 schools under ‘everyday’ conditions, no sustained effect of the programme was found at 1 year. 70 It has been suggested that classroom-based CBT may be better at promoting positive mental health rather than having an effect on clinical problems. 65 However, no effect was found on self-esteem in the current study, and so our data do not support this view.
Universally delivered classroom-based CBT programmes may not be sufficiently focused and intensive to support high-risk adolescents. They may even pose a small risk of harm, which needs to be considered if further investigation of this approach is to be carried out to ensure that the benefits of such interventions outweigh any risks. Indicated interventions for depression typically have larger effects than universally delivered programmes,9 although issues around identifying young people and improving compliance would need to be addressed. Lower intensity and more cost-effective models of delivery could also be employed. For example, using an indicated approach, brief group CBT, bibliotherapy and group supportive-expressive interventions have all been found to have long-term benefits (1- and 2-year follow-up) in high-risk adolescents, with bibliotherapy being a particularly economical approach. 71 Internet-based depression prevention interventions have been shown to have short-term benefits, although evidence of long-term effects using this approach is inconsistent. 72 Given the popularity of the internet and social-networking websites among young people, internet-assisted delivery would be worth investigating further.
The age at which depression prevention programmes are introduced also needs to be considered. Symptoms of depression were already common in the year 8 students in the current study and it may be necessary to start prevention programmes at a younger age. It has been suggested that preventative interventions should occur before the general increase in depressive symptoms at about age 13–14 years, and continue during the time when rates and symptoms would be expected to rise, at about age 15–18 years. 73 However, others have suggested that the optimal time for depression prevention programmes may actually be in late childhood (9–10 years of age). 74–76
Finally, preventing depression in adolescents is challenging. It is a complex problem, in which genetic and developmental factors, the role of puberty and sex hormones, and psychosocial stress and adversity all play an important role. 59 CBT-based prevention and early intervention programmes may have an important role to play in community settings if these can be refined and effects consistently demonstrated. However, a broader approach is likely to be required to preventing depression in young people that takes into account factors such as their school and home environment and facilitates timely access to effective health-care services when necessary.
Strengths and limitations
This study involved a large cohort, with an excellent response rate, low attrition from interventions and good treatment fidelity within participating schools. Furthermore, this was a multicentre study including a range of schools in terms of size, demographics and location (urban, suburban, semi-rural). These data therefore provide a strong profile of mental health in this age group in the UK. We also sought to maximise the clinical effectiveness of the intervention by selecting a programme that had been shown to be efficacious in smaller trials, providing external facilitators to deliver the programmes, ensuring that they had sufficient training and ongoing supervision and assessing treatment fidelity. The inclusion of both 6- and 12-month follow-up assessments with good retention rates (> 80%) provided high-quality data for the longitudinal analysis and the trial had sufficient power for the planned analysis.
Limitations included some sampling biases that need to be considered when generalising from the findings. There were initial difficulties in recruiting schools for the trial, and the participating schools had a greater percentage of white students, were more academically able and had fewer students eligible for free school meals than UK national averages. There was also selective drop-out in those who were slightly older, not living with both parents, using alcohol and cannabis and bullying others at baseline, although multiple imputation of missing data did not have any impact on the main conclusions of the trial. The assessments relied on self-report and no clinical or diagnostic interviews were used, although this was because we were interested in symptoms of and risk for depression rather than identifying established clinical cases of depressive disorder. Young people were not blinded to trial allocation after randomisation as this was not feasible, but assessments were self-completed by young people in classes so the potential for researchers to influence responses was minimal.
The collection of cost data and cost-effectiveness analysis were carried out according to current best practice methods for conducting economic evaluation alongside randomised trials. 49,58 Analysis was based on effectiveness measures of established validity and reliability and the self-report data were relatively complete. It incorporated a relatively detailed ‘bottom-up’ costing of classroom-based CBT and attention control PSHE, based on accurate records of staffing, resources and other activities required. Efforts have been made to adjust for or omit those intervention costs (sometimes called ‘protocol-driven’ costs) which would, in all likelihood, not be incurred outside of a research trial context, or those which would not be incurred with the widespread roll-out of such interventions (e.g. adaptation of course materials). The statistical methods of the cost-effectiveness analysis have accounted for the clustered nature of the data and correlation between costs and effects. Sensitivity analyses, using the bootstrap, were also used to validate the estimates from the parametric methods, given the skewness that is typical of cost and resource use data.
There are some limitations to the cost-effectiveness analysis that should be acknowledged. Individuals with relevant cost and effectiveness data at all three assessment time points (which are necessary for calculating both the costs and the QALYs) inevitably represent a smaller proportion of all those randomised than those with an assessment for the primary end point only. However, given the level of completeness of the data collection relative to that for the primary outcome (SMFQ), and the overall similarity of the subsample characteristics of those used in the cost-effectiveness analysis, the cost and EQ-5D data were still adequately complete and representative to justify a complete case analysis. As with the SMFQ data at 12 months, those who were in the younger year groups at baseline (8, 9 and 10) and those living with both parents tended to have more complete data for the cost and EQ-5D questions. In addition, while the EuroQol Group endorses the use of the EQ-5D in people down to the age of 12 years, its reliability and interpretation in this age group (e.g. in relation to what constitutes usual activities) is not well researched. The fact that the recently developed EQ-5D-Youth instrument yields different frequencies of reported problems from the EQ-5D supports the view that the dimensions of quality of life and problem levels may have different meanings in younger age groups. 77 Moreover, for the preference-based EQ-5D index scores, adult valuations have been used, implicitly assessing how these health states would be valued when experienced by adults.
Service use questions mostly sought data on health service use for any health reason (whether or not related to mental health issues), which is standard best practice for data collection alongside trials. However, to limit the size of the questionnaire, questions about support or care provided outside hospitals asked this only in relation to seeing professionals about psychological problems (i.e. for ‘problems such as worry, anxiety or unhappiness’). Despite the pilot work, some questions relating to service use could have been more clearly worded or laid out. Children had difficulty clearly recalling and spelling the names of drugs that they were taking for anxiety or depression and these data had to be omitted from the cost and cost-effectiveness analyses owing to poor quality. Lastly, without linked data collection from health or other support services, it is not possible to assure the validity and reliability of the self-report of service use data from children of these ages. Other research, in adults, suggests that patient self-report agrees closely with service/provider records for hospital use, with recall periods of up to 6 months, but that for medication and other care products patient recall can be quite incomplete. 78 However, as we were mainly interested in differences in service use between the trial arms, these issues would affect all trial arms fairly equally and only modestly affect the size of any estimated cost differences.
Research recommendations
The null effect reported in this study leaves unanswered the key question of how depression in children and adolescents can be prevented. Despite the appeal and reach of universal prevention programmes, those delivered in secondary schools have little effect on reducing symptoms of depression in adolescents.
-
If universal approaches are to be pursued then the clinical effectiveness and cost-effectiveness of universal prevention programmes with younger children (aged 10–11 years) before the incidence of depression increases should be investigated.
-
The clinical effectiveness and cost-effectiveness of alternative preventative approaches should be investigated; for example, indicated programmes targeting those who already have increased symptoms or are at high risk (e.g. mother has depression).
-
Indicated approaches should report upon reach and acceptability as well as clinical effectiveness and cost-effectiveness.
-
Current preventative models involve the delivery of a single intervention at one point of time. The development and clinical effectiveness of alternative approaches, for example brief interventions woven throughout school life designed to enhance psychological resilience over time, should be assessed.
Chapter 6 Conclusions
Universally delivered classroom-based prevention programmes to reduce symptoms of depression in adolescents are an appealing concept in terms of their potential convenience and reach. However, our study indicates that classroom-based CBT programmes aiming to prevent depression delivered in schools may not be clinically effective and indeed may increase reporting of symptoms.
Acknowledgements
This research was funded by a National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme grant (06/37/04). The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the HTA programme, NIHR, NHS or the Department of Health.
The authors would like to thank the schools and students who participated in this project, the facilitators who helped with intervention delivery and the East Midlands Hub of the NIHR Mental Health Research Network for their administrative and research support. We are grateful for the advice of Professor Ian Shochet, who developed the Resourceful Adolescent Programme. We acknowledge the support and guidance of the Trial Steering Committee and Data Monitoring Ethics Committee and in particular their respective chairs, Professor Laurence Moore and Professor David Gunnell.
Author contributions
PS was the principal investigator for the project and led on developing the rationale and design for the study and interpretation of findings. RP was the trial manager. KS led the trial team in the East Midlands. AAM and MS carried out the statistical analysis. RA and OCU carried out the economic analysis. JT, EC and LG carried out the qualitative analysis. These co-authors also drafted specific sections of the results for this report relating to their areas of expertise, which were collated and edited by RP. KS, RA and GL provided guidance throughout the project on design, analysis and interpretation. All authors had access to all study data and participated in interpretation of the findings, contributed core ideas and were involved in critically revising the report for important intellectual content. All authors read and approved the final report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
Publications
Millings A, Buck R, Montgomery A, Spears M, Stallard P. School connectedness, peer attachment, and self esteem as predictors of adolescent depression. J Adolesc 2012;35:1061–7.
Stallard P, Buck R. Preventing depression and promoting resilience through CBT-based school interventions: a feasibility study of a school based depression prevention programme (PROMISE). Br J Psychiatr 2012;201:518–23.
Stallard P, Sayal K, Phillips R, Taylor JA, Spears M, Anderson R, et al. Classroom based cognitive behaviour therapy in reducing symptoms of depression in high risk adolescents: a pragmatic cluster randomised controlled trial. BMJ 2012;345:e6058.
Phillips R, Spears MR, Montgomery AA, Millings A, Sayal K, Stallard P. Could a brief assessment of negative emotions and self-esteem identify adolescents at current and future risk of self-harm in the community? A prospective cohort analysis. BMC Public Health 2013;13:604.
Stallard P, Montgomery AA, Araya R, Anderson R, Lewis G, Sayal K, et al. Protocol for a randomised controlled trial of a school based cognitive behaviour therapy (CBT) intervention to prevent depression in high risk adolescents (PROMISE). Trials 2010;11:114.
References
- Merry S, McDowell H, Hetrick S, Bir J, Muller N. Psychological and/or educational interventions for the prevention of depression in children and adolescents. Cochrane Database Syst Rev 2004;1. http://dx.doi.org/10.1002/14651858.CD003380.
- Birmaher B, Ryan ND, Williamson DE, Brent DA, Kaufman J, Dahl RE, et al. Childhood and adolescent depression: a review of the past 10 years. Part 1. J Am Acad Child Adolesc Psychiatry 1996;35:1427-39. http://dx.doi.org/10.1097/00004583-199611000-00011.
- Harrington R, Fudge H, Rutter M, Pickles A, Hill J. Adult outcomes of child and adolescent depression, part 1: psychiatric status. Arch Gen Psychiatry 1990;47:465-73.
- Lewinsohn PM, Clarke GN. Psychosocial treatments for adolescent depression. Clin Psychol Rev 1999;19:329-42. http://dx.doi.org/10.1016/S0272-7358(98)00055-5.
- Vernberg EM. Psychological adjustment and experiences with peers during early adolescence – reciprocal, incidental, or unidirectional relationships. J Abnorm Child Psychol 1990;18:187-98. http://dx.doi.org/10.1007/BF00910730.
- Logan DE, King CA. Parental identification of depression and mental health service use among depressed adolescents. J Am Acad Child Adolesc Psychiatry 2002;41:296-304. http://dx.doi.org/10.1097/00004583-200203000-00009.
- Moor S, Maguire A, McQueen H, Wells JE, Elton R, Wrate R, et al. Improving the recognition of depression in adolescence: can we teach the teachers?. J Adolesc 2007;30:81-95. http://dx.doi.org/10.1016/j.adolescence.2005.12.001.
- Merry SN, Hetrick SE, Cox GR, Brudevold-Iversen T, Bir JJ, McDowell H. Psychological and educational interventions for preventing depression in children and adolescents (Review). Cochrane Database Syst Rev 2011;12. http://dx.doi.org/10.1002/14651858.CD003380.
- Calear AL, Christensen H. Systematic review of school-based prevention and early intervention programs for depression. J Adolesc 2010;33:429-38. http://dx.doi.org/10.1016/j.adolescence.2009.07.004.
- Spence SH, Shortt AL. Research review: can we justify the widespread dissemination of universal, school-based interventions for the prevention of depression among children and adolescents?. J Child Psychol Psychiatry 2007;48:526-42. http://dx.doi.org/10.1111/j.1469-7610.2007.01738.x.
- Gillham JE, Hamilton J, Freres DR, Patton K, Gallop R. Preventing depression among early adolescents in the primary care setting: a randomized controlled study of the Penn Resiliency Program. J Abnorm Child Psychol 2006;34:203-19. http://dx.doi.org/10.1007/s10802-005-9014-7.
- Brunwasser SM, Gillham JE, Kim ES. A meta-analytic review of the Penn Resiliency Program's effect on depressive symptoms. J Consult Clin Psychol 2009;77:1042-54. http://dx.doi.org/10.1037/a0017671.
- Clarke GN, Hawkins W, Murphy M, Sheeber LB, Lewinsohn PM, Seeley JR. Targeted prevention of unipolar depressive disorder in an at-risk sample of high-school adolescents – a randomized trial of group cognitive intervention. J Am Acad Child Adolesc Psychiatry 1995;34:312-21. http://dx.doi.org/10.1097/00004583-199503000-00016.
- Spence SH, Sheffield JK, Donovan CL. Preventing adolescent depression: an evaluation of the problem solving for life program. J Consult Clin Psychol 2003;71:3-13. http://dx.doi.org/10.1037//0022-006X.71.1.3.
- Lowry-Webster HM, Barrett PM, Dadds MR. A universal prevention trial of anxiety and depressive symptomatology in childhood: preliminary data from an Australian study. Behav Change 2001;18:36-50. http://dx.doi.org/10.1375/bech.18.1.36.
- Shochet IM, Dadds MR, Holland D, Whitefield K, Harnett PH, Osgarby SM. The efficacy of a universal school-based program to prevent adolescent depression. J Clin Child Psychol 2001;30:303-15. http://dx.doi.org/10.1207/S15374424JCCP3003_3.
- Seligman M, Schulman P, DeRubies R, Hollon S. The prevention of depression and anxiety. Prevention Treatment 1999;2. http://dx.doi.org/10.1037//1522-3736.2.1.28a.
- Spence SH, Sheffield JK, Donovan CL. Long-term outcome of a school-based, universal approach to prevention of depression in adolescents. J Consult Clin Psychol 2005;73:160-7. http://dx.doi.org/10.1037/0022-006X.73.1.160.
- Sawyer MG, Harchak TF, Spence SH, Bond L, Graetz B, Kay D, et al. School-based prevention of depression: a 2-year follow-up of a randomized controlled trial of the beyondblue schools research initiative. J Adolesc Health 2010;47:297-304. http://dx.doi.org/10.1016/j.jadohealth.2010.02.007.
- Sawyer MG, Pfeiffer S, Spence SH, Bond L, Graetz B, Kay D, et al. School-based prevention of depression: a randomised controlled study of the beyondblue schools research initiative. J Child Psychol Psychiatry 2010;51:199-20.
- Clarke GN, Hornbrook M, Lynch F, Polen M, Gale J, Beardslee W, et al. A randomized trial of a group cognitive intervention for preventing depression in adolescent offspring of depressed parents. Arch Gen Psychiatry 2001;58:1127-34. http://dx.doi.org/10.1001/archpsyc.58.12.1127.
- Kowalenko N, Rapee R, Simmons J, Wignall A, Hoge R, Whitefield K, et al. Short-term effectiveness of a school based early intervention program for adolescent depression. Clin Child Psychol Psychiatry 2005;10:493-507. http://dx.doi.org/10.1177/1359104505056311.
- Possel P, Horn AB, Groen G, Hautzinger M. School-based prevention of depressive symptoms in adolescents: a 6-month follow-up. J Am Acad Child Adolesc Psychiatry 2004;43:1003-10. http://dx.doi.org/10.1097/01.chi.0000126975.56955.98.
- Shochet I, Ham D. Universal school-based approaches to preventing adolescent depression: past findings and future directions of the Resourceful Adolescent Program. Int J Mental Health Promotion 2004;6:17-25. http://dx.doi.org/10.1080/14623730.2004.9721935.
- Merry S, McDowell H, Wild CJ, Bir J, Cunliffe R. A randomized placebo-controlled trial of a school-based depression prevention program. J Am Acad Child Adolesc Psychiatry 2004;43:538-47. http://dx.doi.org/10.1097/00004583-200405000-00007.
- Brown C, Liao J. Principles for designing randomised preventive trials in mental health: an emerging developmental epidemiology paradigm. Am J Comm Psychol 1999;27:673-710.
- Angold A, Costello E, Messer S, Pickles A, Winder F, Silver D. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Int J Methods Psychiatr Res 1995;5:237-49.
- Raab GM, Butcher I. Balance in cluster randomized trials. Stat Med 2001;20:351-65. http://dx.doi.org/10.1002/1097-0258(20010215)20:3<351::AID-SIM797>3.3.CO;2-3.
- Shapiro A, Shapiro E. The powerful placebo: from ancient priest to modern physician. Baltimore, MD: Johns Hopkins University Press; 1997.
- Costello E, Angold A. Scales to assess child and adolescent depression: checklist, screens and nets. J Am Acad Child Adolesc Psychiatry 1988;27:726-37. http://dx.doi.org/10.1097/00004583-198811000-00011.
- Angold A, Costello EJ, Messer SC, Pickles A, Winder F, Silver D. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Int J Methods Psychiatr Res 1995;5:237-49.
- Kent L, Vostanis P, Feehan C. Detection of major and minor depression in children and adolescents: evaluation of the mood and feelings questionnaire. J Child Psychol Psychiatry 1997;38:565-73. http://dx.doi.org/10.1111/j.1469-7610.1997.tb01543.x.
- Thapar A, McGuffin P. Validity of the shortened Mood and Feelings Questionnaire in a community sample of children and adolescents: a preliminary research note. Psychiatry Res 1998;81:259-68. http://dx.doi.org/10.1016/S0165-1781(98)00073-0.
- Schniering CA, Rapee RM. Development and validation of a measure of children's automatic thoughts: the children's automatic thoughts scale. Behav Res Ther 2002;40:1091-109. http://dx.doi.org/10.1016/S0005-7967(02)00022-0.
- Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965.
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, Francis SE. Assessment of symptoms of DSM-IV anxiety and depression in children: a revised child anxiety and depression scale. Behav Res Ther 2000;38:835-55. http://dx.doi.org/10.1016/S0005-7967(99)00130-8.
- Shochet IM, Dadds MR, Ham D, Montague R. School connectedness is an underemphasized parameter in adolescent mental health: results of a community prediction study. J Clin Child Adolesc Psychol 2006;35:170-9. http://dx.doi.org/10.1207/s15374424jccp3502_1.
- Sharpe TM, Killen JD, Bryson SW, Shisslak CM, Estes LS, Gray N, et al. Attachment style and weight concerns in preadolescent and adolescent girls. Int J Eat Disord 1998;23:39-44. http://dx.doi.org/10.1002/(SICI)1098-108X(199801)23:1<39::AID-EAT5>3.3.CO;2-S.
- Solberg ME, Olweus D. Prevalence estimation of school bullying with the Olweus Bully Victim Questionnaire. Aggress Behav 2003;29:239-68. http://dx.doi.org/10.1002/ab.10047.
- The EuroQol Group . EuroQol – a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208.
- Beecham J, Knapp M, Thorncroft G. Measuring mental health needs. London: Gaskell; 2001.
- Boyce W, Torsheim T, Currie C, Zambon A. The family affluence scale as a measure of national wealth: validation of an adolescent self-report measure. Soc Indic Res 2006;78:473-87. http://dx.doi.org/10.1007/s11205-005-1607-6.
- Glasgow RE. RE-AIMing research for application: ways to improve evidence for family medicine. J Am Board Fam Med 2006;19:11-9. http://dx.doi.org/10.3122/jabfm.19.1.11.
- Stallard P, Montgomery A, Araya R, Anderson R, Lewis G, Sayal K, et al. Protocol for a randomised controlled trial of a school based cognitive behaviour therapy (CBT) intervention to prevent depression in high risk adolescents (PROMISE). Trials 2010;11. http://dx.doi.org/10.1186/1745-6215-11-114.
- Sterne J, White I, Carlin J, Spratt M, Royston P, Kenward M, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.b2393.
- Dunn G, Maracy M, Tomenson B. Estimating treatment effects from randomized clinical trials with noncompliance and loss to follow-up: the role of instrumental variable methods. Stat Methods Med Res 2005;14:369-95. http://dx.doi.org/10.1191/0962280205sm403oa.
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol 2006;3:77-101. http://dx.doi.org/10.1191/1478088706qp063oa.
- Joffe H, Yardley L, Marks DF, Yardley L. Research methods for clinical and health psychology. London: Sage; 2004.
- Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic Evaluation in Clinical Trials. Oxford: Oxford University Press; 2007.
- Gomes M, Grieve, R, Nixon R, Edmunds WJ. Statistical methods for cost-effectiveness analyses that use data from cluster randomized trials: a systematic review and checklist for critical appraisal. Med Decis Making 2011;12:209-20. http://dx.doi.org/10.1177/0272989X11407341.
- NHS reference costs 2009–10. London: Department of Health; 2011.
- Curtis L. Unit costs of health and social care 2010. Canterbury: PSSRU, University of Kent; 2011.
- Kind P, Hardman G, Macran S. UK population norms for EQ-5D. York: Centre for Health Economics, University of York; 1999.
- Goldstein H. Multilevel statistical models. London: Arnold; 2003.
- Schools, pupils and their characteristics. London: Department for Education; 2010.
- Pupil absence in schools in England, including pupil characteristics: 2009 to 2010. London: Department for Education; 2011.
- Secondary school (key stage 4) performance tables in England: 2009 to 2010 (formerly achievement and attainment tables). London: Department for Education; 2011.
- Guide to the methods of technology appraisal. London: NICE; 2008.
- Thapar A, Collishaw S, Pine D, Thapar A. Depression in adolescence. Lancet 2012;379:1056-67.
- Sayal K, Owen V, White K, Merrell C, Tymms P, Taylor E. The impact of early school-based screening and intervention programs for ADHD on children's outcomes and access to services – follow-up of a school-based trial at age 10 years. Arch Pediatr Adolesc Med 2010;164:462-9. http://dx.doi.org/10.1001/archpediatrics.2010.40.
- Wolfe VV, Dozois DJA, Fisman S, DePace J. Preventing depression among adolescent girls: pathways toward effective and sustainable programs. Cogn Behav Pract 2008;15:36-4. http://dx.doi.org/10.1016/j.cbpra.2007.01.001.
- Wells J, Barlow J, Stewart-Brown S. A systematic review of universal approaches to mental health promotion in schools. Health Educ 2003;103:197-220. http://dx.doi.org/10.1108/09654280310485546.
- Horowitz JL, Garber J, Ciesla JA, Young JF, Mufson L. Prevention of depressive symptoms in adolescents: a randomized trial of cognitive–behavioral and interpersonal prevention programs. J Consult Clin Psychol 2007;75:693-706. http://dx.doi.org/10.1037/0022-006X.75.5.693.
- Rapee RM, Wignall A, Sheffield J, Kowalenko N, Davis A, McLoone J, et al. Adolescents' reactions to universal and indicated prevention programs for depression: perceived stigma and consumer satisfaction. Prevent Sci 2006;7:167-77. http://dx.doi.org/10.1007/s11121-006-0035-4.
- Rivet-Duval E, Heriot S, Hunt C. Preventing adolescent depression in Mauritius: a universal school-based program. Child Adolesc Mental Health 2011;16:86-91. http://dx.doi.org/10.1111/j.1475-3588.2010.00584.x.
- Dane AV, Schneider BH. Program integrity in primary and early secondary prevention: are implementation effects out of control?. Clin Psychol Rev 1998;18:23-45. http://dx.doi.org/10.1016/S0272-7358(97)00043-3.
- Bodden DHM, Dirksen CD, Bögels SM, Nauta MH, De Haan E, Ringrose I, et al. Costs and cost-effectiveness of family CBT versus individual CBT in clinically anxious children. Clin Child Psychol Psychiatry 2008;13:543-64. http://dx.doi.org/10.1177/1359104508090602.
- Haby MM, Tonge B, Littlefield L, Carter R, Vos T. Cost-effectiveness of cognitive behavioural therapy and selective serotonin reuptake inhibitors for major depression in children and adolescents. Aus N Z J Psychiatry 2004;38:579-91. http://dx.doi.org/10.1111/j.1440-1614.2004.01421.x.
- Giesen F, Searle A, Sawyer M. Identifying and implementing prevention programmes for childhood mental health problems. J Paediatr Child Health 2007;43:785-9. http://dx.doi.org/10.1111/j.1440-1754.2007.01196.x.
- Challen A, Noden P, West A, Machin S. UK Resilience Programme Evaluation: final report. London: London School of Economics; 2010.
- Stice E, Rohde P, Gau JM, Wade E. Efficacy trial of a brief cognitive–behavioral depression prevention program for high-risk adolescents: effects at 1- and 2-year follow-up. J Consult Clin Psychol 2010;78:856-67. http://dx.doi.org/10.1037/a0020544.
- Calear AL, Christensen H. Review of internet-based prevention and treatment programs for anxiety and depression in children and adolescents. Med J Aust 2010;192:S12-14.
- Horowitz JL, Garber J. The prevention of depressive symptoms in children and adolescents: a meta-analytic review. J Consult Clin Psychol 2006;74:401-15. http://dx.doi.org/10.1037/0022-006X.74.3.401.
- Farell L, Barrett P. Prevention of childhood emotional disorders: reducing the burden of suffering associated with anxiety and depression. J Child Adolesc Mental Health 2007;12:58-65. http://dx.doi.org/10.1111/j.1475-3588.2006.00430.x.
- Jones SM, Brown JL, Aber JL. Two-year impacts of a universal school-based social-emotional and literacy intervention: an experiment in translational developmental research. Child Dev 2011;82:533-54. http://dx.doi.org/10.1111/j.1467-8624.2010.01560.x.
- Jones SM, Brown JL, Hoglund WLG, Aber JL. A school-randomized clinical trial of an integrated social-emotional learning and literacy intervention: impacts after 1 school year. J Consult Clin Psychol 2010;78:829-42. http://dx.doi.org/10.1037/a0021383.
- Wu P, Bird HR, Liu XH, Fan B, Fuller C, Shen S, et al. Childhood depressive symptoms and early onset of alcohol use. Pediatrics 2006;118:1907-15.
- van den Brink M, van den hout WB, Stigglebout AM, van de Velde CJH, Kievit J. Cost measurement in economic evaluations of health care: whom to ask?. Med Care 2004;42:740-6. http://dx.doi.org/10.1097/01.mlr.0000132351.78009.a1.
- Compton SN, March JS, Brent D, Albano AM, Weersing VR, Curry J. Cognitive–behavioral psychotherapy for anxiety and depressive disorders in children and adolescents: an evidence-based medicine review. J Am Acad Child Adolesc Psychiatry 2004;43:930-59. http://dx.doi.org/10.1097/01.chi.0000127589.57468.bf.
- Durlak JA, Wells AM. Primary prevention mental health programs for children and adolescents: a meta-analytic review. Am J Comm Psychol 1997;25:115-52.
- Harrington R, Whittaker J, Shoebridge P, Campbell F. Systematic review of efficacy of cognitive behaviour therapies in childhood and adolescent depressive disorder. BMJ 1998;316:1559-63. http://dx.doi.org/10.1136/bmj.316.7144.1559.
- Depression in children and young people: identification and management in primary, community and secondary care. Leicester: British Psychological Society and Royal College of Psychiatrists; 2005.
- Kramer T, Garralda ME. Psychiatric disorders in adolescents in primary care. Br J Psychiatry 1998;173:508-13. http://dx.doi.org/10.1192/bjp.173.6.508.
- Green H, McGinnity A, Meltzer H, Ford T, Goodman R. Mental health of children and young people in Great Britain. Cardiff: Palgrave MacMillan; 2005.
- Fergusson DM, Horwood LJ, Ridder EM, Beautrais AL. Subthreshold depression in adolescence and mental health outcomes in adulthood. Arch Gen Psychiatry 2005;62:66-72. http://dx.doi.org/10.1001/archpsyc.62.1.66.
- Rose G. The strategy of preventative medicine. New York, NY: Oxford University Press; 1992.
- Angold A, Erkanli A, Silberg J, Eaves L, Costello EJ. Depression scale scores in 8–17-year-olds: effects of age and gender. J Child Psychol Psychiatry 2002;43:1052-63. http://dx.doi.org/10.1111/1469-7610.00232.
- Stallard P, Simpson N, Anderson S, Carter T, Osborn C, Bush S. An evaluation of the FRIENDS programme – a cognitive behaviour therapy intervention to promote emotional resilience. Arch Dis Child 2005;90:1016-19. http://dx.doi.org/10.1136/adc.2004.068163.
- Junghans C, Feder G, Hemingway H, Timmis A, Jones M. Recruiting patients to medical research: double blind randomised trial of ‘opt-in’ versus ‘opt-out’ strategies. BMJ 2005;331:940-2. http://dx.doi.org/10.1136/bmj.38583.625613.AE.
- Costello EJ, Benjamin R, Angold A, Silver D. Mood variability in adolescents – a study of depressed, nondepressed and comorbid patients. J Affect Disord 1991;23:199-212. http://dx.doi.org/10.1016/0165-0327(91)90101-W.
- Messer SC, Angold A, Costello EJ, Loeber R, VanKammen W, StouthamerLoeber M. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents: factor composition and structure across development. Int J Methods Psychiatr Res 1995;5:251-62.
- Sharp C, Goodyer IM, Croudace TJ. The Short Mood and Feelings Questionnaire (SMFQ): a unidimensional item response theory and categorical data factor analysis of self-report ratings from a community sample of 7- through 11-year-old children. J Abnorm Child Psychol 2006;34:379-91. http://dx.doi.org/10.1007/s10802-006-9027-x.
- Schniering CA, Rapee RM. The structure of negative self-statements in children and adolescents: a confirmatory factor-analytic approach. J Abnorm Child Psychol 2004;32:95-109.
- Schniering CA, Rapee RM. The relationship between automatic thoughts and negative emotions in children and adolescents: a test of the cognitive content-specificity hypothesis. J Abnorm Child Psychol 2004;113:464-70. http://dx.doi.org/10.1037/0021-843X.113.3.464.
- Spence S, Sclare I. Child psychology portfolio. Windsor: NFER-Nelson; 1997.
- Muris P, Meesters C, Schouten E. A brief questionnaire of DSM-IV-defined anxiety and depression symptoms among children. Clin Psychol Psychother 2002;9:430-42. http://dx.doi.org/10.1002/cpp.347.
- Chorpita BF, Moffitt CE, Gray J. Psychometric properties of the revised child anxiety and depression scale in a clinical sample. Behav Res Ther 2005;43:309-22.
- Boys A, Farrell M, Taylor C, Marsden J, Goodman R, Brugha T, et al. Psychiatric morbidity and substance use in young people aged 13–15 years: results from the Child and Adolescent Survey of Mental Health. Br J Psychiatry 2003;182:509-17. http://dx.doi.org/10.1192/bjp.182.6.509.
- Muris P, Mayer B, Meesters C. Self-reported attachment style, anxiety, and depression in children. Soc Behav Personality 2000;28:157-62. http://dx.doi.org/10.2224/sbp.2000.28.2.157.
- Muris P, Meesters C, Merckelbach H, Hulsenbeck P. Worry in children is related to perceived parental rearing and attachment. Behav Res Ther 2000;38:487-97. http://dx.doi.org/10.1016/S0005-7967(99)00072-8.
- Wille N, Badia X, Bonsel G, Burström K, Cavrini G, Devlin N, et al. Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Qual Life Res 2010;19:875-86. http://dx.doi.org/10.1007/s11136-010-9648-y.
Appendix 1 Assessments
Appendix 2 PROMISE trial protocol
Promoting Mental Health in Schools Through Education (PROMISE) Project Protocol, HTA: 06/37/04
1. Project Title
A single blind randomised controlled trial to determine the effectiveness of group cognitive behaviour therapy (CBT) in the prevention of depression in high risk adolescents.
1.1. Acronym
PROMISE: PROmoting Mental health In Schools through Education
2. Planned Investigation:
2.1. Research Objectives
A number of systematic and meta-reviews have highlighted the potential efficacy of CBT in the prevention and treatment of depression in children. 1,79–82 Although these reviews have been positive a number of issues have been identified including the absence of comparisons with appropriate placebo groups, the need for longer term follow-up and the absence of randomised controlled trails within a UK context. This study aims to address these issues and in particular will:
-
Examine the effectiveness of school based CBT Personal Social and Health Education (PSHE) vs. an attention PSHE (delivered by people external to the school) vs. usual PSHE (school delivered) on the prevention of depressive symptoms in high risk adolescents aged 13-16 as assessed by the Short Mood and Feelings Questionnaire at 6 and 12 months. Our primary follow-up will be 6 months after completing the intervention.
-
Examine the effectiveness of CBT (6 & 12 months) on the secondary outcomes of negative thoughts, self-esteem and anxiety.
-
To undertake a secondary sub-group analysis to investigate the effect modification by school connectedness, bullying, self harm, alcohol and drug misuse on treatment outcome (6 months).
-
Assess the cost-effectiveness of the intervention in terms of health-related quality of life (and cost-utility) at 6 months.
-
To undertake a process evaluation to assess factors associated with adherence and acceptability of the intervention including participant perception of usefulness, examples of on-going skill usage, and satisfaction (6 & 12 months).
3.2. Existing Research
Epidemiological studies suggest that over a six month period up to 2.5% of children and 8.3% of adolescents suffer from a major depressive disorder. 2 Cumulative rates indicate that up to 20% will suffer at least one clinically depressive episode by the age of 18. 1 In the UK prevalence estimates are 1.4% amongst 11–16 year olds in the community and around 20% amongst 13–16 year olds attending primary care. 83,84 Adolescent depression causes significant impairment, impacts on developmental trajectories, interferes with educational attainment and increases the risk of attempted and completed suicide as well as major depressive disorder in adulthood. 2–5 In addition, sub-threshold depressive symptoms in adolescence carry a similar risk to major depression for developing depression and suicidal behaviours later in life. 85 Whilst approximately 50% of children are estimated to spontaneously recover for the remaining half symptoms persist and significantly impair functioning. 82 It is therefore particularly concerning to note that depression in adolescents often remains unrecognised and untreated. 6,7
Depression is an important public health issue and, in view of the above, there has been growing interest in the development of interventions designed to prevent depression in adolescents. The better evaluated depression prevention programmes have tended to be based upon cognitive behavioural therapy (CBT). These include the Penn Resiliency Programme,14 Coping with Stress,16 Problem Solving for Life,17 FRIENDS,18 Resourceful Adolescent Programme10 and other CBT programmes. 19 Some have been delivered as selective interventions to adolescents with elevated symptoms of depression23,24 whilst others have been delivered as universal interventions to whole populations. 10,25 Most preventative CBT interventions have produced immediate short term gains in terms of reductions in depression scores although these are not always maintained at follow-up. For example, Spence, Sheffield and Donovan17 published the largest study to date which involved 1500 children aged 12–14 .The 8-session Problem Solving for Life programme resulted in significant post-treatment reductions in symptoms of depression and an increase in problem solving skills compared to a non-intervention comparison group. However, when assessed at 12 month follow-up this difference was no longer significant. 20
The Cochrane review notes that targeted preventative interventions result in marginally greater reductions in depressive symptoms. 1 This may partly be explained by initial levels of depressive symptoms in the control groups. 71 In targeted interventions the sample is chosen on the basis of risk status and the control group is therefore likely to have higher levels of depressive symptoms at baseline and follow-up. This is in contrast to universal interventions where initial levels of symptoms are lower and may not therefore be high enough to demonstrate a preventative effect at follow-up. However targeted approaches encounter significant recruitment problems that severely limit their potential impact and use. For example, in one targeted study 3935 parents with depression or depressive symptoms were identified. 23 Of these, 2995 were judged appropriate for the study although baseline interviews were conducted with only 551 youth parent dyads, 18% of the eligible sample. Similarly, in a recent study only 271 out of a total population of 6000 responded or were eligible to receive the preventative intervention and of the 147 young people allocated to the active intervention 41 (29%) did not attend. 14 Other reviewers have noted recruitment rates of less than 50% and attrition rates of approximately 30% in targeted preventative studies. 12 A further limitation of targeted approaches is their failure to provide any input to low risk children that would prevent low level symptoms escalating. In a study involving 260 adolescents, 1.2% of the healthy adolescents receiving a preventative intervention moved into the high risk group at follow-up compared with 10.1% in the control group. 10 Selective depression preventative programmes therefore have a limited effect and reach and engage only a small proportion of adolescents who are identified as at risk for depression.
Universal prevention programmes provide an alternative approach. Whilst not all recipients of universal approaches present with elevated depressive symptoms they nonetheless provide a pragmatic alternative, reduce possible negative effects of stigma and labelling, result in lower rates of dropout and greater participation rates. 10,16,17 Indeed, universal approaches achieve recruitment rates of 67%–88%. 10,11,17 Proponents of universal population based approaches argue that whilst they might have a more limited effect on individuals they will nonetheless reduce far more disorders in the population as a whole than a highly effective targeted approach. 26 Indeed, Rose86 argues that a large group of people exposed to a low risk (e.g. minor depressive symptoms) will ultimately generate more clinical cases than a small group of people exposed to a high risk. There is therefore a strong rationale for pursuing universal approaches for the prevention of depression in adolescents.
Of the evaluated universal depression prevention programmes the Resourceful Adolescent Programme (RAP) appears particularly promising. In the initial efficacy study, 260 adolescents were assigned to RAP, RAP plus family involvement or a no intervention group. 10 In terms of reach 85% of the eligible cohort took part and attrition was 5.8%. Adolescents who received either version of RAP reported significantly lower levels of depressive symptomatology at post intervention and 10 month follow-up compared with the no intervention group. In terms of health status, 71% of the RAP group who were classified as “at risk” on the basis of initial depression scores had moved into the healthy range when assessed at post intervention compared with 31% in the control condition. This was maintained at 10 month follow-up where 75% of the RAP high risk group and 41% of the control high risk group scored within the normal range on measures of depression. There was also evidence of a preventative effect since none of the “healthy” adolescents in the RAP group moved into the “at risk” range at follow-up compared to 10.5% of those in the control condition.
In a New Zealand adaptation of the programme, RAP-Kiwi, 392 students were assigned to either RAP-Kiwi or an attention placebo condition. 11 Once again recruitment rates were high (73%) and attrition low (9% attrition at 6 months). Depression scores were significantly lower in the RAP group post intervention. In clinical terms, sixteen students in the RAP group, as determined by scores on the Beck Depression Inventory moved from the moderate/severe to the minimal/mild category at post-test compared to six in the placebo group. The results were less conclusive at 18 month follow-up where although the difference on the Reynolds Adolescent Depression Scale remained significant scores on the Beck Depression Inventory were not.
A large multi-site randomised controlled effectiveness trial in Australia of RAP involving 2664 students from 12 schools has recently been undertaken. 12 RAP participants recorded significantly lower levels of depressive symptoms than those in the control condition at both post-intervention and 12-month follow-up. Based on initial depression scores, significantly more (49.1%) of the at-risk students in the RAP condition moved into the healthy category at post-intervention compared with 35.3% in the control group. This difference was maintained at 12 month follow-up. In a subsequent qualitative evaluation with 109 young people, 61.2% of girls and 46.6% of boys were able to identify specific examples where they had used skills learned during RAP. 12 The authors concluded that within the context of a real world effectiveness study RAP appears to positively affect the health status of “at risk” students.
The absence of long term follow-up and the tendency for post-intervention effects of depression prevention programmes to diminish after 6 months have been noted. 1,20 It would therefore seem important for preventative interventions to include additional booster sessions in order to maintain short term benefits. In addition, there is a need to determine whether improvements are due to the specific treatment components of the intervention or the non-specific factors associated with therapy and whether these improvements are significantly greater than would normally occur over time. Active interventions therefore need to be compared with placebo conditions and usual care. In view of the promising results from RAP this project intends to undertake a pragmatic trial to evaluate the effectiveness of the universal group RAP CBT programme in the UK context. RAP will be delivered via PSHE in schools by trained mental health professionals and will be compared over a 12 month period with an attention PSHE and usual PSHE (treatment as usual).
3.3. Research Methods
3.3.1. Design:
A cluster randomised controlled treatment trial comparing the effectiveness and cost effectiveness of group CBT PSHE versus attention PSHE versus usual PSHE in the prevention of depression in high risk adolescents in UK school years 8 to 11 (aged 12–16).
3.3.2. Setting:
8 mixed sex comprehensive schools in Bath and North East Somerset, Bristol, Nottingham & Wiltshire.
3.3.3. Recruitment of schools:
A list of 66 mixed comprehensive secondary schools in Nottingham, Wiltshire, Bath and North East Somerset and Bristol was compiled from local authority information. Letters were sent to the Head Teachers and PSHE leads at each of these schools. The schools that did not respond were sent a reminder e-mail and were contacted by telephone. Schools that expressed an interest were contacted by the research team and a meeting was arranged to discuss the project. The schools were asked to return a form to confirm they were willing to participate by May 2009. They were also asked to indicate at this stage if there were any year groups that they would not be able to include in the study (i.e. those who did not have discrete PSHE lessons).
8 schools agreed to take part. One of these schools did not have a Year 11 group as they were a new school. A further three schools could not include their Year 11 groups and one of these was also unable to include their Year 10 group as these year groups did not have discrete PSHE lessons within which the program could be accommodated were they allocated to the active intervention arm. A total of 28 year groups, with 222 classes, and approximately 5,708 young people were included in the randomisation process.
Of the remaining 58 schools who were initially contacted, 5 declined without giving a reason, 2 did not teach PSHE as a discrete lesson, 5 were unable to participate at the present time due to other commitments (e.g. major changes in staffing, school buildings, responding to OFSTED), and 2 of the schools were closing down. Initial meetings were held with 3 schools who expressed an interest initially, but two of these later declined due to staffing changes and we were unable to get a response from one school when we asked them to confirm whether they would like to participate.
3.3.4. Group classification:
Our target population will be boys and girls in years 8–11 (aged 12–16). The Short Mood and Feelings Questionnaire (SMFQ) completed on two separate occasions will be used to categorise the cohort. The ideal interval between SMFQ completion would be two weeks. However, some flexibility in this interval will be required to fit in with the school timetable. The primary aim of the present study is examine the effect of the interventions on children at “high risk” of developing depression. This study is not concerned with whether or not children present with a clinical diagnosis of depression but is concerned with identifying children with elevated symptoms of low mood. To account for transient changes in mood, in the current study SF-MFQ scores will be collected on two separate occasions to allow for the identification of those with more persistent low mood. Furthermore, it is a level of low mood above community population means rather than clinical ‘caseness’ cut-off points that are of interest. Research with clinical and community samples demonstrates that young people who fulfill DSM diagnostic criteria for depression achieve mean scores on short forms of the MFQ ranging between 7.01–11.95 compared with 3.24–4.68 for those who are not depressed. 27,32,33,87 Approx 6% of a community sample achieved a total cut-off score of 11 or more. 85 On this basis, we intend to use total SMFQ scores to categorise young people as follows: Low Risk of depression < 5; High Risk of depression, ≥ 5; Probably Clinically Depressed > 11. Those with persistent symptoms (scoring ≥ 5 on both occasions) will become our high risk group. We expect 77% of the cohort will be categorised as low risk group; 20% high risk and 3% as probably clinically depressed. In a class of 30 this would equate to 23; 6; and 1 child respectively.
3.3.5. Method of randomisation:
Individual randomisation is not practical and would create insurmountable timetabling and organisational difficulties for the school. The intervention will be delivered as part of the PSHE curriculum and as such it is important that the intervention fits within the existing school structures. Minimising contamination between the three arms of the trial is an important consideration. The cluster unit will therefore be year groups and whilst it is recognised that there is a risk of between group contamination, this is considered to be minimal. Firstly, the main friendship groups for the majority of young people will be within their year group. Between year group discussions are generally limited and as such it is unlikely that they will focus upon the specific content of these sessions. Secondly, it is doubtful whether any brief discussions that might occur would be sufficient to bring about any significant change or on-going skill usage. Within the existing school structure young people are assigned to a tutor group and it is usually within these groups that PSHE is undertaken. These may be different from registration classes and classes for core subjects, which are streamed by ability and therefore randomising by class would pose a greater risk of contamination. Classes within a year group typically follow the same scheme of work for PSHE and therefore randomisation by year group makes delivery of the intervention more convenient for participating schools.
Allocation of year groups will take place once all schools have been recruited. Balance between trial arms with respect to key characteristics of year groups will be achieved by calculating an imbalance statistic for a large random sample of possible allocation sequences. 28 The variables used for balancing will be numbers of students, number of classes, the way in which PSHE is delivered (i.e. weekly, fortnightly, or other) for each year group. The number of clashes (i.e. classes having PSHE at the same time) will also be included when balancing to ensure that delivery of the interventions is feasible. A statistician with no other involvement in the study will then randomly select one sequence from a subset with the most desirable balance properties. Generation of possible allocation sequences and selection of one sequence will be conducted using computer-generated random numbers.
3.4. Planned Interventions
-
Active Intervention – CBT PSHE
This study will evaluate the Australian developed Resourceful Adolescent Programme (RAP) CBT programme in a UK context. RAP is a group based depression prevention programme designed for young people aged 12–16. The intervention is manualised and is provided by trainers external to the school. Students complete their own workbook and group leaders have a detailed manual specifying key learning points and objectives. Detailed content for each of the 11 sessions is summarised below. It is intended that participating schools would hold the RAP sessions within their normal PSHE sessions. The programme developer, Professor Ian Shochet, notes that the programme can be adapted to fit with the time restraints of the school. Sessions can be combined and delivered over six, 75–90 minute sessions if the school has double periods of PSHE. In this eventuality, the attention placebo condition would also be modified to ensure that number of sessions and contact time matched RAP.
RAP is based upon a cognitive behavioural theoretical (CBT) model. CBT recognises the importance of negative thoughts and low self-worth/image in the onset and maintenance of depression. These are therefore actively targeted during CBT with core treatment components including psycho education, identifying and challenging negative/dysfunctional thoughts, identifying personal strengths (thereby enhancing self-esteem/image), managing social problems, and learning to problem solve.
For the purposes of this study, the original RAP program has been modified for use in the UK (RAP-UK). Whilst the content, key messages and goals remain consistent with the original program, the structure and method of delivery have been revised to fit in with the UK state secondary education system. The key elements of the RAP-UK program are:
-
Personal Strengths
Young people are helped to recognize and reinforce their existing strengths and personal resources. The aim of this part of the programme is to help adolescents focus upon the importance of developing and maintaining good self-esteem.
-
Helpful Thinking
Young people are helped to recognize and challenge unhelpful ways of thinking and to develop more balanced and helpful thinking (cognitive restructuring).
-
Keeping Calm
Young people are helped to discover ways in which they can manage unpleasant feelings. This involves learning to recognize physical symptoms such as butterflies in the stomach or tense muscles and how to manage these (e.g. through relaxation, humour and other stress reduction techniques).
-
Problem Solving
Young people are encouraged to define their problems, consider alternative solutions and to use a stepped approach to carry out and evaluate the solution.
-
Support Networks
Young people are helped to acknowledge the importance of developing a support network and are encouraged to seek help, when necessary.
-
Keeping the Peace
Young people are helped to consider how growing older and becoming more responsible can lead to disputes with peers and adults. Strategies for interpersonal problem solving designed to promote harmony and to avoid escalation of conflicts are considered. Similarly, during the programme young people are helped to examine the value of empathy in keeping the peace. They are encouraged to understand that getting along with people is easier if we can acknowledge and see things from the other person's perspective.
These key elements are of the RAP-UK program are organised over the following 9 sessions:
-
Find your strengths
-
Thoughts, feelings and behaviour
-
Feelings and body signals
-
I am what I think
-
You can change the way you think
-
Problems can be solved
-
There is always help at hand
-
There are two sides to every story
-
Keep the peace
Each session is designed to be delivered in approximately 50 to 60 minutes. However, the method of delivery of PSHE in the UK varies widely (e.g. regular weekly or fortnightly lessons, project days, or condensed courses over a number of weeks). Therefore, the revised program has been designed with a flexible method of delivery in mind to ensure that it is possible to fit the program in to school curricula while retaining the core content and key elements of the program. Two additional booster sessions will be provided approximately 6 months later. These will provide opportunities to review RAP skills and to practice applying them to current difficulties.
-
-
Attention Placebo Intervention
The attention placebo intervention will involve similar time and contact with external providers, but will not include the active components of the CBT intervention identified above. The school will deliver their usual PSHE curriculum, but the class teacher will be joined by two researchers from outside of the school who will assist with delivering the lessons and engaging with young people. This will therefore control for the non-specific effects of interventions that are considered important in studies of depression. 29 In the same way as the RAP program, the delivery of the Attention Placebo intervention will be flexible to fit in with existing school PSHE programs.
-
Usual PSHE
In this group young people will participate in the usual personal health and social education (PSHE) sessions provided by the school. This is therefore “treatment” as usual provided by the school staff and does not involve any external input from the research team. Records summarising the content of each session will be kept so that any potential overlap with the active intervention can be determined.
3.4.1. Intervention Leaders:
The intervention leaders will be Psychology Assistants who will have completed an undergraduate degree. The active and placebo interventions will be delivered by two Psychology Assistants with the tutor group teacher being present to manage the class. Psychology Assistant posts are very popular and we would not expect any recruitment problems. In order to avoid therapist contamination different leaders will deliver each intervention. The leaders will receive a minimum of two days of initial training, which will cover the identification and management of mental health concerns, group management techniques, as well as training them to deliver the specific intervention. The active intervention is manualised and each leader will have a trainer's manual. During the course of delivery, regular separate supervision groups will be provided for the active and attention placebo intervention group leaders. The supervision sessions will take place at least once a month and will require a minimum of 9 hours (equivalent to 1 hour for each session of RAP). Notes will be taken during these sessions to provide a record of content.
3.4.2. Treatment Fidelity:
Independent observers will attend randomly selected sessions (5%) and rate the content against the key learning points and exercises detailed in the manual. The intervention leaders in the Attention Placebo and Active Intervention groups will also record the content of each lesson using a standardised checklist such that comparisons between the content of the Active Intervention and Attention Placebo can be made.
3.4.3. Attrition:
An attendance register will be kept to monitor attendance and attrition during the course of delivering the intervention and placebo PSHE sessions.
3.4.4. Recruitment rates and loss to follow-up:
Universal depression prevention programmes tend to achieve recruitment rates of 67-88%. 14,16,25 Our local experience of running a universal emotional health prevention programme in 30 junior schools has resulted in recruitment rates in excess of 95%. 81 Our predictions for this study are more conservative and we predict a recruitment rate of 70%. Of those who consent to assessments, we predict that 20% will become lost by the end of the 12 month follow-up. We are expecting differential dropout for the Year 11 students for their 12 month follow-up, many of whom will have left school by this time. To maximise response rates in this group, they will be offered an option to fill the questionnaire in either online at a secure website (surveymonkey.com) or using the paper version. As they will be required to complete the survey in their own time rather than during lesson time, an incentive of a prize draw will be offered with a number of small gift vouchers offered as a prize (Love2Shop vouchers or other appropriate high street stores, values 10 × £10, 20 × £5).
3.5. Planned inclusion/exclusion criteria:
3.5.1. Inclusion:
Interventions will be provided during the school day as part of the school PSHE curriculum. All eligible children, i.e. years 8–11 (12–16 years old) will be expected to participate. There will be some occasions when young people do not participate in PSHE for religious reasons or due to absence but it is expected that these will be limited. Attendance at each session during the study will be monitored.
3.5.2. Exclusion:
Young people who do not attend PSHE lessons will be the only exclusion in this study (e.g. if they are on technical training courses off site, on long term sickness absence, homeschooled). Children, identified during the study with possible clinical depression, and their carers will be contacted and advised to seek further help. They will continue to participate in the programmes running in the schools.
3.6. Ethical arrangements
3.6.1. Ethical Approval:
An application was made to NHS MREC and was considered by the South West committee. They felt unable to offer a view feeling since the study was not concerned with NHS clients and was conducted in schools not NHS settings. An application was therefore submitted to the University of Bath ethics committee who reviewed and approved the study.
3.6.2. Research Governance:
The study will comply and be conducted in accordance with NHS Trust Research Governance requirements. This will include storage & retention of confidential research data. and the establishment of a Trial Steering Committee (TSC) and a Data and Ethics Monitoring Committee (DMEC). Avon and Wiltshire Partnership NHS Trust have agreed to act as the sponsor of the study.
3.6.3. Consent/Assent:
Evaluation of opt-in and opt-out recruitment strategies suggest that opt in strategies result in lower recruitment rates and healthier participants. 89 This led the authors to suggest that opt-out approaches for obtaining parental consent should be the default recruitment strategy for interventions that pose a low risk to participants. The participants in this study are not referred NHS patients, the intervention is low risk, and as such we propose an opt-out approach. At the start of the project a letter will be posted to the carers of all eligible young people informing them about the study. Although all young people will be expected to participate in the interventions only those who opt-in and provide signed consent/assent will complete the assessments. The letter will therefore inform carers that they can opt out of the assessments if they do not wish their child to complete the questionnaires. In addition, the project information sheet will be read to the young people and child consent/assent obtained before completing the questionnaires i.e. dual carer/child consent/assent will be required. Young people will be asked for alternative contact details (i.e. e-mail address/mobile number/home address) in case the research team should need to contact them in relation to the project. This is particularly relevant for Year 11 students who may have left the school before the 12-month follow up.
3.7. Risk and Benefits
The risks of participating in this study are considered to be small. At worse, the proposed interventions may not result in any additional lasting benefits although it is considered highly unlikely that they will have any detrimental effects. A study information sheet, provided at the outset of the study, will be prepared for participants informing them of risks and benefits. If the intervention is shown to have a positive effect then the potential to promote positive mental health in adolescents is a significant benefit to society and the individuals who took part.
Young People with possible depression:
We expect that 3% of the young people will achieve very high scores on depression measures suggesting possible clinical depression. These young people and their carers will be contacted and advised to contact either their GP or the local mental health contact if they would like further help. In exceptional circumstances, a young person may request that there be no home contact. When this occurs, a suitably qualified member of the research team will contact the young person either directly via e-mail or via an appropriate member of staff at the school involved in student welfare (e.g. school nurse, counsellor, head of pastoral care) so that they can be provided with the relevant information and sources of support. The well-being of the young person is the main priority in this situation and therefore it may be necessary to breach confidentiality in order to ask an appropriate person at the school to contact the young person. In each study locality (Bath and North East Somerset, Bristol, Wiltshire, and Nottingham) there will be a qualified mental health expert who will be the identified point of contact for young people, teachers, researchers and programme leaders who have concerns about significant mental health issues. These young people will still participate in the interventions provided in school.
3.8. Proposed sample size
The HTA commissioning brief (06/37) specifies a shift in the distribution of depression scores as an important outcome. The primary outcome for this trial will therefore be score on the SMFQ as a continuous measure. The pilot study (n = 711) provided estimates of ICC (0.025), mean year group size (n = 203) and consent rate (at least 80%). A range of target differences for effect sizes of 0.36–0.42 SDs are detectable with 80% power and 5% two-sided alpha with 20–27 year groups. The eight participating schools have a total of 28 participating year groups, meaning that the study will have > 80% power at the 5% alpha level to detect a planned minimum difference of 0.36 SDs.
3.8.1. Assessment Schedule:
Figure 1 provides an overview of the consent/assent and assessment process and indicates how this fits in with intervention delivery. Initial screen with the Short form Mood and Feelings Questionnaire (SMFQ) will be carried out prior to the start of interventions in addition to the baseline assessment to identify individuals with consistent low mood who would be classified as high risk. Baseline assessment T1: pre-intervention completed during first session; Assessment T2: 6 month follow-up; Assessment T3: 12 month follow-up. At each assessment point young people will complete the following psychological measures designed to assess outcomes that the intervention is expected to achieve, i.e. improvements in mood (SMFQ), reductions in negative depressive thoughts (Children's Automatic Thoughts Scale), enhanced self-esteem (Rosenberg Self-esteem Scale) and reduction in anxiety symptoms (Revised Child Anxiety and Depression Scale). Continuous scores on the SMFQ will be our primary outcome measure of depressive symptoms. Secondary psychological outcomes will be assessed by examining continuous scores on the Children's Automatic Thoughts Scale, Rosenberg self-esteem scale and Revised Child Anxiety and Depression scale.
3.8.2. Research Assistants:
Individually administered assessments are not feasible in this study, therefore group administered self-completed questionnaires will be used. For practical reasons, schools may only be able to arrange for these assessments to be carried out in large groups or with several classes running at the same time. Therefore, a large number of researchers are needed to carry out these assessments and the assistants delivering the interventions are ideally positioned to assist with this. All research assistants will receive a full day of training to ensure data collection is fully standardised. It is virtually impossible to blind research assistants completely in a study of this kind, although observer bias will be minimised by the use of self-completed assessments. The assistants will not be made aware of group allocation until baseline assessments have been completed. Following intervention delivery, they will be rotated to different year groups so that they will not be involved in assessments with the classes they have been working with.
3.9. Proposed Outcome measures
3.9.1. Psychological Functioning
-
Primary Outcome Measure – Short Form Mood and Feelings Questionnaire (SMFQ;27 This 13 item scale is derived from the long form (33 item) Moods and Feeling Questionnaire 30. Each item consists of a simple statement (e.g. I didn't enjoy anything at all) which is rated as being either “true” (scores 2), “sometimes true” (scores 1) or “not true” (scores 0). The short form is designed as a brief self-report screening instrument that can be used to assess severity of depression in community samples 31. The SMFQ is a unifactorial scale with a robust single factor structure. 90,91 Criterion validity (i.e. ability to predict clinical diagnosis) has been established within both clinical27 and community samples33,92 and with children ranging in age from 7–16. The scale correlates well with other measures of depression, has good test/re-test reliability with higher scores tending to be associated with children who fulfill diagnostic criteria for clinical depression. 31–33
-
Secondary Outcome Measure – Children's Automatic Thoughts Scale (CATS;34 This self completed scale assesses a range of negative self statements in children and young people aged 7-16. For each item the child is asked to rate whether they have had a similar thought over the past week. Each item is rated as “not at all” (scores 0), “sometimes” (scores 1), “fairly often” (scores 2), “often” (scores 3) or “all the time” (scores 4). Confirmatory factor analysis identified 4 distinct but correlated factors relating to thoughts about physical threat, social threat, personal failure and hostility. 93 Internal consistency for the total score was high (Cronbach Alpha = 0.95) with acceptable test–retest reliability (0.79). The scale has been found to effectively discriminate between a community and clinical sample with the personal failure sub-scale being the strongest predictor of depressive symptoms. 94 The 10 item personal failure sub-scale will be used.
-
Secondary Outcome Measure – Rosenberg Self-Esteem Inventory35 The Rosenberg Self-Esteem Scale is a 10-item self-report measure of global self-esteem. It consists of 10 statements related to overall feelings of self-worth or self-acceptance. The items are answered on a four-point scale ranging from, strongly agree to strongly disagree. The Rosenberg Self-Esteem Scale has demonstrated good reliability and validity across a large number of different sample groups and has been validated for use with male and female adolescents as well as substance abusers and other clinical groups, and is regularly used in treatment outcome studies.
-
Secondary Outcome – Revised Child Anxiety and Depression Scale (RCADS;36 This self-report scale assesses symptoms of DSM-defined anxiety disorders and major depression in children aged 9–16. The scale is an adapted version of the Spence Children's Anxiety Scale95 and after psychometric evaluation was reduced to 25 items. 96 Each item is rated on a 5 point scale to indicate frequency and can be combined to form 5 sub-scales assessing symptoms of generalised anxiety disorder, separation anxiety disorder, social phobia, panic disorder and major depressive disorder. The scale has good internal consistency, test-re-test stability, and good convergent and divergent validity. 97
FIGURE 1.
PROMISE Procedure Flowchart.
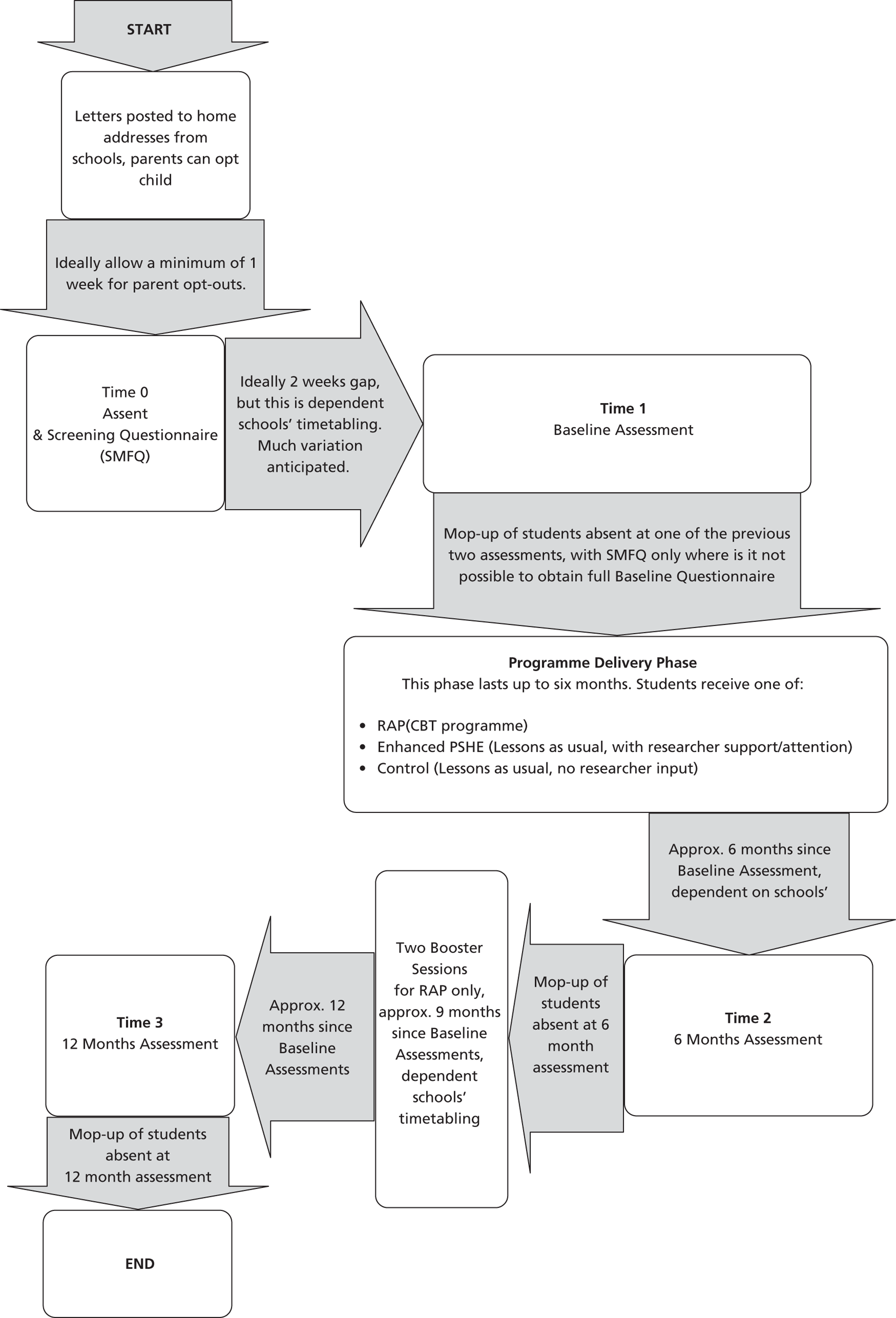
3.9.2. School environment and bullying
-
School Connectedness Scale. 37
The 8-item scale assesses the extent to which students feel accepted, valued, respected, and included in their school. Each item is rated in a 5 point scale to indicate how strongly they endorse each item. School connectedness correlated extensively with concurrent mental health symptoms when assessed 12 months apart (between 38% and 55% covariation with depression, 26% to 46% with general functioning, and 9% and 16% for anxiety symptoms). Results suggest a strong association between school connectedness and adolescent depressive symptoms.
-
Olweus Bully/Victim Questionnaire. 39
The Olweus Bully/Victim Questionnaire is the most widely used questionnaire to assess the nature and extent of bullying amongst school children. The two global items assessing the frequency of self reported bullying and being the victim of bullying will be used.
3.9.3. Economic Evaluation
-
Quality of Life: EQ-5D is a standardised instrument for use as a measure of health outcome.
Applicable to a wide range of health conditions and treatments, it provides a simple descriptive profile and a single index value for health status. The EQ-5D comprises 5 dimensions of health (mobility, self-care, usual activities, pain/discomfort anxiety/depression) and each consists of three levels (no problems, some/moderate problems/extreme problems). The EQ-5D will be completed twice by the adolescents, once at baseline (T1) and at the six month assessment (T2).
Additional data
-
Socio-demographic data: will be collected at baseline (T1). Participants will complete a modified version of the Client Service Receipt Inventory (CSRI)41 to retrospectively assess receipt of mental health or other health services; educational support; anti-psychotropic medication i.e. depressants or others; social work/care services at baseline (T1) and six (T2) month follow-up. Basic demographic data will also be collected (gender, age, who you usually live with, ethnicity, affluence/socio-economic status).
-
Self-harm, drug and alcohol misuse: Although high levels of depression are associated with self-harm and regular alcohol use and precede the onset of alcohol use;98,99 it is unlikely that either of these factors will act as mediators or mechanisms through which the intervention influences the main outcome of reduction in depressive symptoms. However, there might be a sub-group of young people with these problems for whom the intervention has limited effectiveness i.e. the presence or absence of self-harm or regular alcohol use may moderate the effectiveness of the intervention. In order to asses this possibility participants will complete Likert measures at baseline (T1) and six months (T2) detailing the extent to which they have engaged in harmful behaviours including self-harm, alcohol, cannabis and drug misuse over the past 6 months.
-
Attachment style: Because attachment style is known to be a significant predictor of both depression and anxiety in adolescents100,101 peer attachment will be captured at baseline, 6 months, and 12 months using the Attachment Questionnaire for Children. 38 This is a single-item measure whereby respondents select one of three statements to best describe how they feel in their friendships. This measure was selected due to its use in previous studies. 100,101 It is anticipated that adolescents who self report insecure peer attachment styles will have higher depression and anxiety scores than those who self report secure peer attachment styles. If this result is present, subsequent analyses can control for attachment style at baseline. It is also anticipated that the intervention might be seen to have an effect on changes from insecure to secure attachment styles.
3.9.4. Process Evaluation
Participants: A semi-structured assessment using qualitative and quantitative methods will be undertaken at the end of each programme to assess participants' perception of: (a). the intervention, usefulness, what they had learned and evidence of on-going skill usage; (b). the extent of possible between group contamination by exploring discussions about session content between classes. Semi-structured interviews will be conducted with 24 young people (2 from each of the 3 study groups, male/female, high risk/low risk). A topic guide for the interviews will be developed and will alter in response to the content of the interviews and in order to clarify emerging themes. Analysis will go on in parallel to the fieldwork. When young people are required to give up their own time to take part in the interviews (e.g. after school or during lunch time), they will be offered a small gift voucher as recompense for their time (£5 Love2Shop vouchers or similar appropriate high street stores).
Group Leaders: At the end of each programme a randomly selected one in five sample of group leaders will participate in a brief semi-structured interview to assess their views of the programme. Interviews will be tape recorded and will cover a range of factors including participant engagement, school/class teacher support, leader confidence and effectiveness in delivering the programme and perception of participant usefulness.
Tutor Group Teachers: Before commencing the study form tutors will be asked to indicate on the class list which students they think possibly or probably has a depressive disorder. At the end of each programme the class teacher will participate in a semi-structured interview to assess their general views about the usefulness and relevance of the programme and any observations both positive and negative about participants' behaviour. Teachers will be asked to re-assess their perception of the status of those young people they initially identified as possible depressed and whether any other students now present as “at risk”.
3.10. Data analysis and management
3.10.1.
Analysis and presentation of data will be in accordance with CONSORT guidelines, with the primary comparative analyses being conducted on an intention-to-treat basis and due emphasis placed on confidence intervals for the between-arm comparisons. Descriptive student- and class-level statistics will be used to ascertain any marked imbalance between the arms at baseline. The primary analysis will employ multi-level linear regression to compare intervention versus each of the two control groups, adjusting for stratification variables and baseline SMFQ score, and taking appropriate account of the hierarchical nature of the data (repeated measures, students, classes and schools). Sensitivity analyses making different assumptions will be conducted to investigate the potential effects of missing data.
Secondary analyses will include: 1) repeating the primary analysis adjusting also for any variables exhibiting marked imbalance at baseline to examine whether this influences the findings; 2) comparison of SMFQ as binary outcome among high risk students; 3) comparison of SMFQ as a continuous outcome using all students in the study; 4) similar analyses for other secondary outcomes (using appropriate regression models and adjusting p-values for multiple testing); 5) investigation of process measures such as number of sessions attended; 6) investigation of patterns (for example, divergent or convergent) of SMFQ scores at repeated follow ups. Finally appropriate interaction terms will be entered into the primary regression analyses in order to conduct pre-specified subgroup analyses according to depression risk at baseline (SMFQ < 7 vs. ≥ 7), self-harm, drug and alcohol misuse. Since the trial is powered to detect overall differences between the groups rather than interactions of this kind, the results of these essentially exploratory analyses will be presented using confidence intervals as well as p-values, and interpreted with due caution.
3.10.2. Economic Evaluation.
We will perform incremental cost-effectiveness analysis (on the basis of score changes in the primary clinical outcome, SMFQ) and cost-utility analysis (i.e. cost per QALY, on the basis of utility estimates derived from EQ-5D scores) for all included comparators. These analyses will be from a societal perspective, capturing and where possible valuing cost and other potential impacts of the intervention across the health, education and social care sectors.
In addition to detailed recording of the staff time and other resources used in adapting and delivering the intervention(s), we will collect individual-level data on: use of extra educational support; use of mental or other health services; use of anti-psychotropic medication i.e. depressants or others; use of social work/care services; use of voluntary/advice services and informal care. Resource use data will be collected directly from participants at baseline (T1) and 6 month follow-up (T2). An adapted version of the parent-completed Client Service Receipt Inventory (46) will be used to assess frequency and duration of use of health, education and social care services and informal care. Resources will be valued using national unit cost information, such as the PSSRU's Unit Costs for Health and Social Care, or local unit costs from the four study areas where national costs are unavailable. For the trial-based analysis (6 month follow-up T2) no discounting will be used.
In the base case analysis we will compare the whole cost of the intervention(s), with outcomes for all recruited adolescents. Cost-effectiveness in relation to baseline high-risk and low-risk status will be explored in a sub-group analysis. Uncertainty will primarily be expressed through the calculation of confidence intervals for the incremental cost-effectiveness ratios (using non-parametric Bootstrapping). If appropriate the trial-based cost-utility results will also be extended beyond 12 months, and key uncertainties further explored, using a simple decision model.
3.10.3. Qualitative data:
Will be analysed using the latest version of NUD*IST a software programme for analysing text-based data. Tapes will be transcribed and codebooks will be generated. Insights from these data will inform data analysis of the quantitative data on attrition and perceived feasibility and acceptability of the intervention in different schools.
3.11. Research governance
There will be three main management committees: 1) Trial Steering Committee (TSC) This will provide overall supervision of the trial. It will meet at least once a year and its role will be to monitor and supervise the progress of the trial towards achieving its goals; to advise the investigators in general scientific and management issues; and to ensure that there are no major deviations from the trail protocol. The Lead applicant will inform the Chair of the TSC who may call additional meetings when there are matters arising from the conduct or management of the trial that might require their advice. 2) Data Monitoring and Ethics Committee (DMEC). This will monitor data and advise the TSC on whether there are any ethical or safety reasons why the trial should not continue. This will have access to unblinded data and will consider the need for any interim analysis. The DMEC will meet at least annually. 3) Trial Management Group: A separate Trial Management Group will be established to oversee the operational running and progress of the project. This will be chaired by the Lead Applicant and will include the senior researcher and researchers, and other co-applicants as appropriate. The meeting will involve monthly teleconferencing as well as 3 monthly face to face meetings.
In addition, local monthly supervision groups will be established in each of the 4 localities for the psychology assistants delivering the interventions. Separate groups will be established for the RAP and the attention interventions. Each group will meet monthly for 2 hours. Supervisors will be experienced Senior Clinicians from the local CAMHS teams. They will participate in the initial intervention training sessions so that they are familiar and knowledgeable about the intervention. The Lead applicant will offer support and advice to the group supervisors.
3. Project timetable and milestones
Month 1–4 (Sept–Dec 08): Recruitment, induction, establishment of project infra-structure, links with project schools. Training of intervention leaders and research assistants for pilot.
Month 5–10: (Jan–June 09): Feasibility and piloting of recruitment, assessments, randomisation, RAP and attention placebo intervention and process evaluation in 1 school (n = 711).
Month 11–12 (July–August 09): Training of intervention leaders and research assistants for main trial.
Month 13 (Sept 09–January 10): Initial screening and baseline assessments of study cohort (T1).
Month 13–22 (Sep 09–June 10): Intervention starts and is provided across study schools during the next 3 terms (9 months).
Month 22–31 (March–July 10): 6 month (T2) assessments.
Month 28–37 (Sept 10–January 11): Final 12 month (T3) assessment.
Months 31–38 (February 11–June 11): Complete data entry/database cleaning.
Months 38–40 (July–December 11): Data analysis, final project report, preparation of papers for publication.
4. Expertise
Professor Paul Stallard is regarded as a National expert on the use of CBT with children and young people and is leading a school based CBT anxiety prevention programme in 30 local junior schools. Professor Ricardo Araya is a practising CBT therapist and has conducted several trials with CBT components for groups of depressed adults and is currently undertaking research in schools overseas. Professor Glyn Lewis is leading a number of projects examining the treatment of depression in primary care. Dr Alan Montgomery has particular expertise in medical statistics and the design, conduct and analysis of pragmatic, community-based randomised trial, and works in the Bristol Randomised Trials Collaboration at the University of Bristol. Dr Kapil Sayal has led school-based child mental health projects aimed at improving identification and access to health services. Dr Rob Anderson, a health economist based in the Peninsula Technology Assessment Group, Universities of Exeter & Plymouth, will lead the cost and cost effectiveness analysis and has previously evaluated the cost-effectiveness of school-based screening programmes. Dr Moldavsky, Dr Phil Shoebridge and Dr Wendy Woodhouse are the school links for Nottingham, Bristol and Swindon respectively. Finally, Ms. Rose Stevens is a mental health service user with interest in child mental health who will provide service user input for the project. Professor Ian Shochet, the developer of RAP, has agreed to provide training in the intervention and advice on delivery.
5.1. Dissemination
The results of this study will be of national and international significance for policy makers and academics and will therefore be widely disseminated.
Funders: Project reports will be prepared for the funding body according to their requirements. Key reports will be after the feasibility and piloting stage (month 8), after completion of the 6 month follow-up (month 24) and after the 12 month follow-up (month 36). Participants: The results will be presented to all participating schools and a project summary provided. This will be distributed to parents through the school newsletter and posters summarising the study will be prepared for each participating school to display. Academic: The results will be published in high impact peer review journals. The results will be presented at local, national, European and International meetings of appropriate professionals including policy planners and developers, educationalists and child health professionals. Service Improvement: If the intervention proves effective then a cascading National training programme could be implemented. This will be informed by contextual data collected during the study about the process of implementation, types of schools and provider-specific effects that make the intervention more or less likely to be effective/cost-effective. Recommendations about school and leader characteristics that appear to mediate the effects of RAP will be embedded in the training programme.
5. Service Users
RAP is an established manualised programme and thus the content and structure is already determined. However we intend to involve young people to ensure that the content and wording is appropriate for the UK and in seeking their advice and guidance about our proposed process evaluations. We therefore plan to work with young people in two main ways:
Consultation: during the pilot and feasibility stage we will establish 4 focus groups within the pilot school (one for each year group). These will provide opportunities to discuss with young people issues of implementation, ways of maintaining the profile of the project, ideas to maximise assessment completion, their views about the content and wording of the interventions and assessments and how sensitive issues such as deliberate self-harm, drug and alcohol misuse can be presented in a clear and acceptable way.
Collaboration: two young people from the pilot schools will be recruited to become members of the project steering group. The user researcher for this project, Ms Stevens, will be instrumental in recruiting and promoting the importance of this to young people and will undertake a promotion exercise in which research is demystified and their important role and contribution highlighted. They will be supported by the user researcher to attend and participate in the Trial Steering Committee and will therefore be active partners in the management of the project including monitoring progress and potential difficulties, interpretation of findings summarising conclusions & identifying key lessons. An allowance has been made to pay for their time and to support their travel and attendance at meetings.
List of abbreviations
- CATS
- Children's Automatic Thoughts Scale
- CBT
- cognitive–behavioural therapy
- CEAC
- cost-effectiveness acceptability curve
- CI
- confidence interval
- CSRI
- Client Services Receipt Inventory
- DALY
- disability-adjusted life-year
- EQ-5D
- European Quality of Life-5 Dimensions
- FAS
- Family Affluence Scale
- GP
- general practitioner
- HTA
- Health Technology Assessment
- ICC
- intraclass correlation coefficients
- ICER
- incremental cost-effectiveness ratio
- NIHR
- National Institute for Health Research
- OR
- odds ratio
- PCT
- primary care trust
- PSHE
- Personal, Social and Health Education
- QALY
- quality-adjusted life-year
- RAP
- Resourceful Adolescent Programme
- RCADS
- Revised Child Anxiety and Depression Scale
- SD
- standard deviation
- SMFQ
- Short Mood and Feelings Questionnaire