Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 08/53/99. The contractual start date was in March 2011. The draft report began editorial review in June 2013 and was accepted for publication in November 2013. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
during this study Steve Iliffe was Associate Director of the Dementia and Neurodegenerative Diseases Research Network (DeNDRoN), responsible for promoting primary care research; Barbara Stephens was CEO of Dementia UK at the time of the project; and Louise Robinson was Chair of the Primary Care Clinical Studies Group of DeNDRoN at the time of the research.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2014. This work was produced by Iliffe et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background and rationale
In the UK, dementia is a key government priority for reseach, as outlined in the Prime Minister’s challenge. 1 Improving the health and social care of older people is also a priority for health and social care policy. 2,3 Changing demographics will lead to an increase in the prevalence of age-related illnesses, such as dementia, which will in turn present considerable challenges for families and health and social care providers. This will particularly be the case for primary and social care services following the recommendations of the White Paper, Our Heath, Our Care, Our Say, which stipulated that care for older people, and for other people with long-term conditions, should be delivered as close to their homes as possible. 4
The scale of the problem
Dementia is one of the main causes of disability in later life; in terms of global burden of disease, it contributes 11.2% of all years lived with disability, which is higher than stroke (9.5%), musculoskeletal disorders (8.9%), heart disease (5%) and cancer (2.4%). 5 One in 14 people aged > 65 years has a form of dementia, rising to one in six of those aged > 85 years. 5 Currently, around 800,000 people in the UK have dementia;6 this is estimated to rise to 1 million by 2020 and 1.7 million by 2050, an increase of over 150%. 5 The current costs of caring for people with dementia in the UK have been estimated at around £23B a year,6 which is far greater than the corresponding costs for heart disease, stroke and cancer. 1 Around two-thirds of people with dementia currently live at home, with the majority of their care provided by family members, with support from primary and social care teams. 2,5 It is estimated that family caregiving saves public expenditure on dementia of around £8B each year. 6
The rising number of older people will lead to an increasing number of frail older people requiring complex care packages if they are to continue to live independently and postpone or avoid moving into care homes. This will present considerable challenges for primary and social care. People with dementia aged > 65 years occupy one-quarter of NHS beds at any one time. 6 There has been a significant increase in the number of people with dementia entering the acute hospital system, which is an area of concern,7 particularly with regard to care and assessment practice. 8 The NHS Operating Framework for 2012/13 in England9 has emphasised the need for greater provision of care and support in the community to reduce unnecessary hospital admissions for people with dementia.
Current evidence suggests that dementia care is in urgent need of improvement,1,5 with frequent failure to deliver services in a timely, integrated or cost-effective manner. 10 General practitioners (GPs) in primary care experience and describe difficulties in diagnosing and managing dementia. 10 In the UK, educational interventions in primary care have been implemented to try and improve dementia diagnosis and management rates; however, these interventions have not significantly affected diagnosis or clinical management. 11 In an attempt to address this issue within primary care, the NHS Commissioning Board has recently developed guidance for GP practices to implement an enhanced service for detecting dementia in people who may be at risk. 12 The aims of this service are to increase rates of early dementia diagnosis and improve the care of people with dementia (including provision of appropriate treatment and signposting). The National Audit Office report of 200710 encouraged the use of case management by Community Mental Health Teams (CMHTs), believing it would reduce unnecessary hospital admissions of people with dementia.
Care co-ordination
Current national guidance13 on dementia care recommends the provision of co-ordinated health and social care, led by a single health or social care professional (often known as a ‘care manager’ in local authority adult services but as a ‘case manager’ in health care). This recommendation10,14 largely mirrors the views of people with dementia and their family carers. In NHS mental health services, case management is a particular type of collaborative care15 in which workers, known as ‘case managers’, systematically follow up patients under regular supervision and (usually) provide both brief psychological therapy and medication management. ‘Collaborative care’ has itself been variously defined to mean everything from collaboration between services, and ‘shared care’, to the more highly structured definition that is now becoming accepted internationally. 16
The components of a collaborative care model for depression are (1) a multiprofessional approach to patient care provided by a case manager working with the GP under supervision from specialist mental health medical and psychological therapies clinicians; (2) a structured management plan of medication support and brief psychological therapy; (3) scheduled patient follow-ups; and (4) enhanced interprofessional communication with patient-specific written feedback to GPs via electronic records and through personal contact. 17
In earlier studies of depression, mental health professionals provided the enhanced staff input to primary care settings and undertook a care co-ordinator role. 18,19 More recently, primary care nurses20,21 were used to fulfil the role of care co-ordinator. Most studies of collaborative care have taken place in the USA. In the UK, in one published study (carried out about 16 years ago) practice nurses undertook the care co-ordinator role but did not improve either patient antidepressant use or outcomes compared with usual GP care;21 however, more recently, Chew-Graham et al. 22 demonstrated an improvement in depression outcomes with the collaborative care approach and a flexible psychological intervention delivered by a mental health nurse. A systematic review of models of care for depression suggested that components that were found to significantly predict improvement were (1) the revision of professional roles; (2) the provision of a case manager who provided direct feedback and delivered a psychological therapy; and (3) an intervention that incorporated patient preferences into care. 23
The evidence base
A literature review24 published as part of the preliminary work for this study provided a commentary on case management interventions for people with dementia and a summary of its findings are provided here. The review set out to address (1) what are case managers and how do they relate to dementia care; (2) whether or not dementia care can be improved by case management; (3) what people with dementia and their carers want from a case manager and whether or not this can be provided; (4) whether or not we can measure the cost-effectiveness of case management; and (5) what direction research into case management needs to take.
A literature review,24 published as part of the preliminary work for the CARDEM study, provided a commentary on case management interventions for people with dementia and a summary of its findings are provided here. The review suggested that this diversity has led to difficulties in understanding the impact of the case manager role, who is most appropriate to undertake it, which populations may benefit most from it and what services should be offered as part of the case manager package. The review by Koch et al. 24 identified that many authors have suggested factors that may lead to a successful case manager approach. For example, Goodman et al. 25 proposed that successful case management requires:
-
a broad set of clinical skills
-
designated and protected time for case management
-
close involvement in multidisciplinary teamwork including a medical clinician and
-
having the mandate to undertake case management activities recognised by providers or commissioners or funders of services, especially if continuity of care and stability of services are to be assured.
Similarly, Minkman et al. 26 suggested that success factors for case management in dementia include the case manager having a wide knowledge base; working within a strong, local provider network that accepts case management; having effective multidisciplinary teams with medical input; and having a low threshold for accessing support services. Minkman et al. 26 also identified factors associated with failure, including a lack of investment, ill-defined patient inclusion criteria and an absence of involvement of primary care practitioners.
In addition to these findings, Verkade et al. 27 identified 44 essential components of case management and proposed that case management should be based on individual needs, should integrate management into the care chain, should offer a systematic active care approach and should provide information, support, co-ordination and monitoring roles. In our review24 we also reported the proposed theoretical framework of Connor et al. ,28 which identified 45 frequent case manager activities, which were further categorised into four main case management domains:
-
behaviour management
-
clinical strategies and caregiver support
-
community agency and
-
safety.
Connor et al. 28 commented that ad hoc but regular contact and the individualistic approach inherent in case management were responsible for the wide range of activities.
Impact of case management
Several empirical studies have illustrated the variety of roles that a case manager might undertake, including assessment, care planning, education, problem-solving, liaising, monitoring and counselling. 29–33 Overall, it was found that some studies showed positive results in the form of increased referrals to community services,29 fewer hospital and emergency admissions and less embarrassment, isolation and relationship strain,31 reduced stress30 and reduced risk of relocation to a care home,34 although few recorded a large effect. 24
The benefits associated with case management are variable and context specific. There is conflicting information about the duration of effects produced by case management, with some studies reporting a significant improvement in activities of daily living35 or reductions in relocation to care homes. 36 Additionally, our review24 found that case manager activities were being undertaken by a number of different professionals, to the extent that Newcomer et al. 37 concluded that there is currently no agreed choice of professional background for the role of case manager. Our review24 described how the level of heterogeneity of patients involved in case manager studies and the lack of subgroup analysis made it difficult to identify at what stage in the course of the illness patients and their carers would derive most benefit from a case management intervention.
Our review24 identified evidence that the needs of people with dementia and their caregivers revolve mainly around social networks, daytime activities, company and psychological distress,38,39 with behavioural and psychological symptoms of dementia (BPSD) and lack of social networks impacting indirectly on the person’s perceived quality of life. 38 These findings match the potential of aspects of various case management programmes well. As Mittelman et al. 40 suggested, there may be a direct association between quality of life and other measures such as time to institutionalisation, so that quality of life functions as an intermediate, early-changing, surrogate measurement for consequences that may take longer to appear. All this depends, of course, on regarding life in a care or nursing home as an undesirable outcome that leads to diminished quality of life, which may not always be the case.
Clinical and economic effectiveness
Verkade et al. 27 argued that, from the perspectives of clinical and economic effectiveness, there is little reason to promote case management programmes based on the current available evidence. Nevertheless, one could postulate that, because Mittelman et al. 40 – having followed participants for so long (17 years) – reported such convincing results, most of the trials described have failed to follow up participants for adequate periods of time to be able to demonstrate any outcome improvements or cost-effectiveness gains.
Our review24 suggested that the main limitation in these studies was the choice of outcome measures. It may be that aiming to delay a care home move may be an unrealistic or inappropriate goal, certainly in the short term, and the ambitions for case management therefore ought to be revisited. Most of the studies with positive findings report improvements in measures such as caregiver burden or stress,30,35,41 caregiver confidence,29 negative feelings about the patient,31 function35 and uptake of community services. 37,42 Moreover, in Mittelman’s study,40 spouse caregivers’ reactions to memory loss and challenging behaviour (BPSD), and satisfaction with social support, accounted for at least 30% of the effect of the intervention on nursing home admission. Reducing caregivers’ negative reactions to memory loss and BPSD accounted for 48.7% of the intervention’s impact, whereas depressive symptoms and frequency of BPSD were weaker (but still significant) mediators of the intervention effects. This subanalysis is pertinent as it seems to suggest that the intervention is more effective when it positively influences caregivers’ perceptions and reactions to the problems presented by dementia, rather than affecting any practical changes in their ability to manage the problems themselves. These findings corroborate the proposition that case management may affect the quality of life of both people with dementia and their carers.
The case management trials that we reviewed24 showed substantial heterogeneity in several domains: the number of activities or services offered, the length of the programme, the intensity of contact with the person with dementia or caregiver, and the personal and clinical characteristics of those individuals. Each of these could significantly affect the cost or cost-effectiveness of case management. Employing a case manager in primary care is likely to increase the use of other health and social care resources in the short term, which would need to be included in any economic evaluation. In many of the studies that attempted an economic evaluation and which concluded that using case management was too costly, the unfunded opportunity costs of caregivers’ and others’ inputs – whether for lost work time, lost leisure time or diminished caregiver health and well-being – were not considered. Case management should be costed from a societal perspective as well as the perspective of health and social care services if we are to understand its full impact and potential.
Our review24 suggested that case management does not need to reduce service costs to be cost-effective. It needs to demonstrate that any improvement in outcomes is worth any additional expenditure incurred. For example, Duru et al. 43 found that using internet-based case management software, developing a care plan and referring on to primary care and community agencies for specific treatment and care services were not cost-saving compared with standard care but were cost-effective because of improvements in patient and carer outcomes and because the quality of care of people with dementia was also significantly better. However, Pimouguet et al. 44 found only three randomised trials that included an explicit economic analysis and argued that no conclusion can be drawn about the economic impacts of case management. Nevertheless, some well-conducted long-term studies have demonstrated how case management can delay relocation to long-term care, with potentially important economic pay-offs. 40,45
Our review concluded by suggesting that there is a clear lack of UK-based research exploring the clinical effectiveness and cost-effectiveness of alternative models of service delivery in dementia care. It proposed that a detailed specification of the sorts of activities to be included in case management was required, including developing a better understanding of how case managers might tailor their support to the needs of the person with dementia and their family. 24 The review recommended that further questions to be addressed include:
-
determining which skills are most appropriate to the role
-
where these may be located
-
which cohort of patients with dementia would benefit most from case management and
-
the type and intensity of contact required to successfully carry out case management for people with dementia in primary care.
We embarked on the CAREDEM study to explore these issues, following discussions within the Dementia and Neurodegerative Diseases Research Network (DeNDRoN) Primary Care and Dementia Clinical Studies Groups. Our exploration began with an assessment of a successful case management trial conducted in the USA the PREVENT study. 30
Learning from the PREVENT study
The PREVENT study,30 a US-based trial of such a collaborative care model, led by a nurse practitioner working with a social worker in primary care, used evidence-based protocols to manage neuropsychiatric symptoms encountered by family carers of people with dementia. This study demonstrated significant improvements for both people with dementia (increased prescribing of cholinesterase medication, fewer behavioural and psychological symptoms) and their family carers (improved depression scores and higher carer satisfaction ratings). However, because of the limited follow-up period, effects on the rate of moves to long-term care facilities and cost-effectiveness could not be determined.
Following this positive US study, and the recommendations for primary care services from the World Alzheimer Report 2011,46 testing a case management approach for people with dementia in NHS primary care looked attractive. However, it quickly became apparent that there were grounds for being cautious. A recently completed critical review of nurse-led case management as a technique for supporting patients with complex needs warned against expecting substantial benefits from this approach. 25 Although a recent international systematic review of randomised controlled trials had identified studies of case management for people with dementia and their caregivers, with time to institutionalisation and cost as the main outcome variables, the authors of this study concluded that the evidence for the efficacy of case management in terms of cost and resource usage remains equivocal. 44 They highlighted that any further studies ought to consider which individuals might particularly benefit from case management. 44
Overview of the CAREDEM study
The CAREDEM study was a research and development project designed to (1) adapt the US-derived PREVENT intervention30 for use in English NHS contexts; (2) train primary care staff in the use of a culturally adapted intervention; and (3) test the acceptability and feasibility of this intervention in a pilot study in four general practices.
The full CAREDEM project as originally proposed consisted of four work packages; this report focuses on the pilot rehearsal trial and corresponding qualitative evaluation. The protocol for this study can be found at www.controlled-trials.com (ISRCTN74015152). Figure 1 shows the relationships between the work packages.
FIGURE 1.
Relationship between the four work packages of the CAREDEM study. RCT, randomised controlled trial.
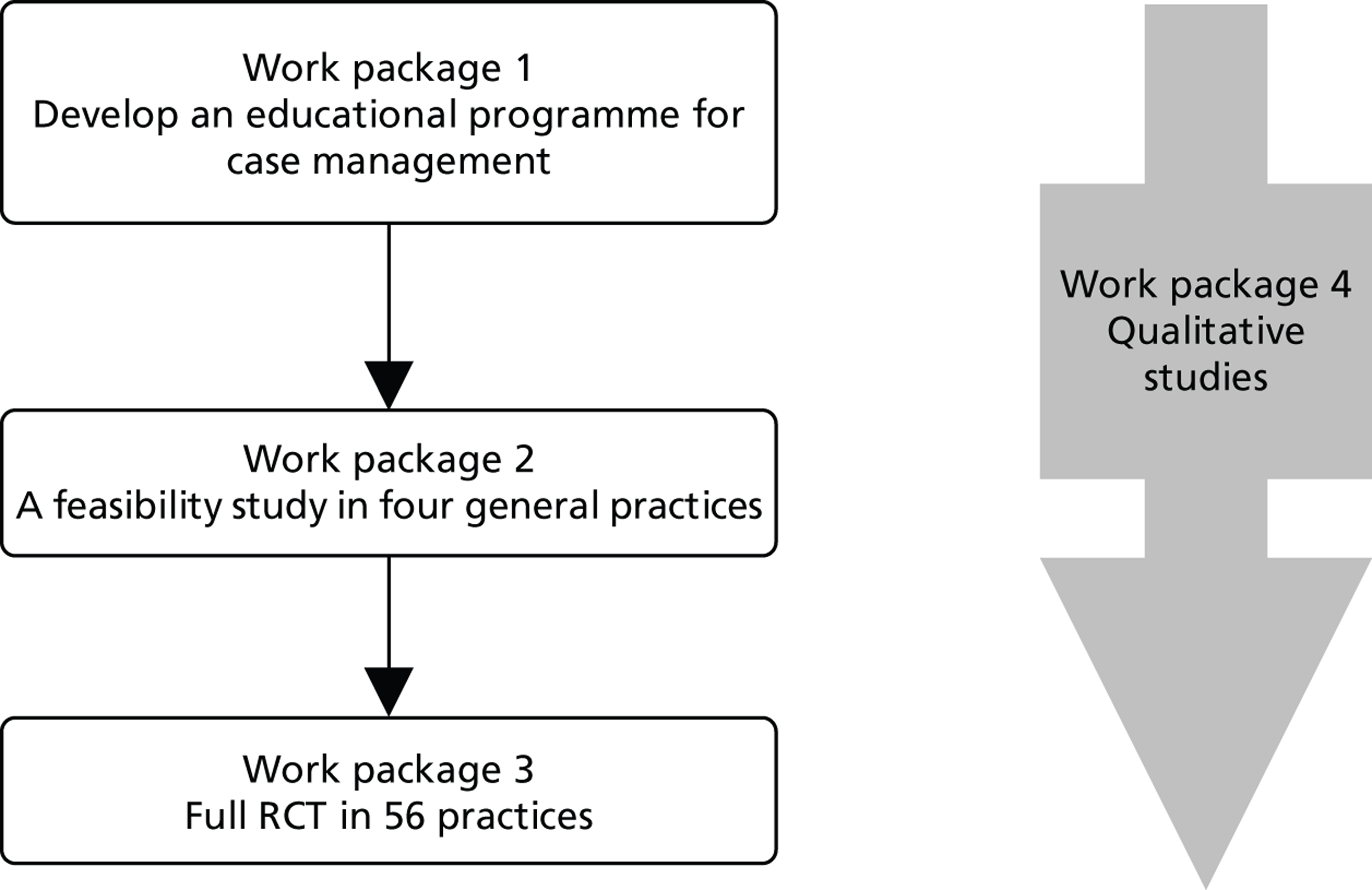
The aim of the full CAREDEM trial was to develop a collaborative case management approach that can be embedded into primary care, to enable better management of common problems in dementia. Work package 1 (WP1) involved the development of case management protocols and evidence-based care pathways. Work package 2 (WP2) assessed the feasibility and acceptability of the intervention developed in WP1. The study design was such that, if WP2 demonstrated that the case management programme fitted into everyday primary care practice and also showed positive benefits, it would then be evaluated in a large-scale randomised controlled trial [work package 3 (WP3)]. Work package 4 (WP4) was designed to provide a qualitative evaluation of each stage to gain a comprehensive and systematic evaluation of this project.
Following the development of WP1 materials, the CAREDEM pilot (WP2) took place in general practice-based primary care in three areas; London, Norfolk and Newcastle. During the final months of the pilot study the researchers engaged with whole Practice Based Commissioning (Clinical Commissioning Groups since 1 April 2013) localities and consortia. Based on the outcome of WP2, it was intended that the main trial (WP3) would take place in general practice-based primary care. For the main trial we estimated a target equivalent to 56 medium-sized general practices (with average list sizes of around 6000 patients). It was anticipated that each practice would recruit 11 patients to the main trial (WP3), with six retained at the 18-month follow-up; these rates of recruitment and retention would be reviewed and, if necessary, revised based on data from the pilot study (WP2).
Our proposed case manager role was designed to be carried out by practitioners located within primary care and working in liaison with secondary care services, to provide a multiprofessional care co-ordination approach. We anticipated providing training in collaborative care and case management techniques to a range of primary care practitioners as determined by the local skill mix and by local commissioning needs and intentions. Scheduled patient follow-ups were designed to be included as part of the case management process, with the frequency and location of meetings being client led. Enhanced interprofessional communication and liaison using patient-specific written feedback to GPs via electronic records as well as personal (face-to-face or telephone) contact were designed to be an integral part of the case management method.
We envisaged that professionals undertaking the case management role could be already in post within a community-based organisation [individual GP-based primary care team, primary care trust (PCT), CMHT or social worker], depending on existing local arrangements, interest and expertise. We anticipated that practitioners interested in taking on the case manager role might be nurses with the level of experience found at band 7, working in district nursing, as community psychiatric nurses or as practice nurses. It was planned that they would be able to undertake additional training (developed in WP1 and tested in WP2), provided through the Admiral Nurse organisation Dementia UK, with an induction period, periodic refresher days, experiential learning and mentoring and formal on-site supervision by Admiral nurses in the three planned study centres. Training was to be delivered by a regional senior clinician from the project team and an Admiral nurse, with other clinicians or allied medical professionals delivering specific training as required. In the PREVENT model, training takes place over eight 2-hour sessions and this study anticipated that at least this amount of time would be necessary. In addition to individual training and mentoring, a meeting of case managers was convened during the project to allow an opportunity for group reflection on the case management task and the research project. Details of this can be found in Appendix 6.
Patient and public involvement
The CAREDEM proposal arose from discussions within the DeNDRoN Primary Care and Dementia Clinical Studies Groups, both of which have public and patient involvement (PPI) representatives who contributed to the discussion about the intervention and desirable outcomes. The chief executive of Dementia UK (Barbara Stephens) drew on the expertise of carers in this organisation. The director of the Social Care Workforce Research Unit at King’s College London (Professor Manthorpe) was responsible for PPI in the management of the trial, at the trial steering committee, at trial management and site management committee levels and also in the PPI forum. A PPI forum was held after WP1 to enable individuals to participate in debates about the development of the case management training, the content of the care pathways, the optimal ways to engage people with dementia and their carers in the trial, the interpretation of the findings and the planning of dissemination. The invitation to join this group was extended to a carer representative from a local Alzheimer’s Society, the Greater London Forum for Older People, other relevant bodies such as Age UK and Pensioner Forum volunteers. This meeting was held in February 2012 and 11 lay experts attended.
In addition, preliminary findings from the whole study were presented to a PPI group assembled by DeNDRoN in March 2013, to obtain insights into the project’s outcomes. See Appendix 7 for further details of this consultation.
Data handling, record keeping and confidentiality
Throughout each stage of the CAREDEM study, data collection and transfer in this trial complied with the National Research Ethics Service (NRES), Caldicott principles47 and the Data Protection Act 1998. 48 All study documentation was held in secure offices and the research team operated to a written and signed code of confidentiality. A clinical data management software package was used for data entry and processing, allowing a full audit trail of any alterations made to the data post entry. Identifiable data will be kept for the duration of the trial and thereafter destroyed. All study documentation will be archived and held for 10 years by the study sponsor.
Ethics committee approval
The conduct of this study has been in accordance with the recommendations for physicians involved in research on human subjects adopted by the 18th World Medical Assembly (Helsinki, Finland, 1964) and later revisions. Ethical approval was successfully sought from an appropriate research ethics committee before the commencement of the work packages. Separate protocols were prepared and separate ethics applications were made for WP1 (North West London Research Ethics Committee 10/H0722/50) and WP2 (NRES Wandsworth 11/LO/1555).
Chapter 2 Work package 1
Changing clinical practice is difficult. Although some new and effective treatments are adopted quickly and diffuse across health-care systems, many do not. 49 The variability of general practice is a problem for those seeking to change it, but may be an asset for patients because it favours personalisation and tailoring of care. As Miller et al. 50 put it: ‘Standardising care without identifying desirable variation or unique adaptations that take advantage of local opportunities or strengths misses an opportunity to identify and investigate unanticipated circumstances or locally adapted practice configurations associated with better health care outcomes’ (p. 874).
The adoption of new ways of working depends on both the characteristics of the new approaches themselves and the characteristics of the professionals and patients who use them. Diffusion science, as summarised by Berwick,49 underpinned the development processes in WP1. The characteristics of innovations that favour their uptake and diffusion through clinical practice51,52 are shown in Table 1.
| Attribute | Description |
|---|---|
| Compatibility | Innovations that are compatible with the values, norms and perceived needs of intended adopters will be more easily adopted and implemented |
| Complexity/ease of use | The degree to which the innovation is expected to be free of effort. Innovations that are perceived by key players as simple to use will be more easily adopted and implemented. The perceived complexity of an innovation can be reduced by practical experience and demonstration |
| Relative advantage | Innovations that have a clear, unambiguous advantage in terms of either effectiveness or cost-effectiveness will be more easily adopted and implemented. This advantage must be recognised and acknowledged by all key players. If a potential user sees no relative advantage in the innovation, he or she does not generally consider it further; in other words, relative advantage is a sine qua non for adoption. Relative advantage is a socially constructed phenomenon. In other words, even so-called ‘evidence-based’ innovations go through a lengthy period of negotiation amongst potential adopters, in which their meaning is discussed, contested and reframed; such discourse can either increase or decrease the perceived relative advantage of the innovation |
| Trialability | Innovations that can be experimented with by intended users on a limited basis will be more easily adopted and implemented. Such experimentation can be supported and encouraged through provision of ‘trialability space’ |
| Observability/result demonstrability | If the benefits of an innovation are visible to intended adopters, it will be more easily adopted and implemented. Initiatives to make the benefits of an innovation more visible (e.g. through demonstrations) increase the chances of successful adoption |
| Reinvention | If a potential adopter can adapt, refine or otherwise modify the innovation to suit his or her own needs, it will be more easily adopted and implemented. Reinvention is a particularly critical attribute for innovations that arise spontaneously as ‘good ideas in practice’ and which spread primarily through informal, decentralised, horizontal social networks |
| Image and visibility | The degree to which it is seen as adding to the user’s social approval and the degree to which the use of the innovation is seen by others |
| ‘Voluntariness’ | The degree to which use of the innovation is controlled by the potential user’s free will |
A full discussion of the development of WP1 has been published. 53 WP1 was designed to review, adapt and customise the PREVENT intervention30 for implementation in the CAREDEM study within NHS general practice. Development of WP1 took place in the area covered by Kent and Medway NHS and Social Care Partnership Trust. This location allowed for good facilitation of meetings and covered a diverse population and different organisational boundaries. As noted, ethical committee permission for this part of the study was obtained successfully (NW London Rec1 10/H0722/50) and local research governance permissions were also obtained.
A co-design method was implemented to gain insight from a diverse range of experienced practitioners and carers54 (it was unfortunately not possible to recruit a person with dementia to this group). Following the development group meetings, the materials produced were reviewed and critiqued by two separate review groups, one a virtual group of practitioners and the other a forum of carers and older people with experience of using health and social care services. The virtual professional group responded to the output from the design group in a cyclic process, in which a series of prototypes were refined until the development group felt confident that it had produced a version of materials worth field-testing in WP2. Potential participants in the carers’ and older people‘s forum who were unable to attend a meeting were invited to contribute their comments by post or e-mail.
Development group
The research team invited an expert group of stakeholders including family carers as well as health and social care practitioners from the NHS, local authority and voluntary sectors to participate in the development group. Twelve people from a variety of backgrounds, including occupational therapy, social work, Admiral nursing, psychiatry, general practice and community mental health nursing, volunteered to join this core multidisciplinary development group. A family carer, an outreach worker from the local branch of the Alzheimer’s Society and an Age UK manager also joined the development group to ensure that a full range of perspectives were included during this process.
The group met six times (each meeting lasted half a day) with members of the research team (SI, JM and CF) from April 2010 to June 2011 to carry out the following tasks:
-
adapt the PREVENT intervention to meet service and cultural expectations in England
-
devise a job description and a list of desirable and essential attributes for a case manager
-
agree the contents of an educational needs assessment that would inform training and mentoring
-
produce written information designed to be used by the case managers with carers and people with dementia.
Review groups
The co-design process was extended by two further groups offering their comments on the materials produced by the development group. The research team recruited 10 professionals from different parts of England to provide comments by e-mail and, as noted earlier, also arranged a PPI forum of 11 older people with substantial experience of using health and social care services, including current and former carers of people with dementia. This was a diverse group including people from different ethnic and sociodemographic backgrounds and who held a variety of caregiving relationships (e.g. spouse/partner carers and adult/child carers). The forum membership was drawn from different locations from the development group to reflect a broader range of current service arrangements. During the forum a presentation was given on the objectives, activities and outputs of WP1 and the group was asked specific questions and for their general views. This forum served as a useful validation step, as participants’ comments helped to provide some assurance that the materials produced by the development group were suitable for other parts of England and for people with different experiences and circumstances.
Results/outputs
The development group agreed on the tasks that a case manager would carry out. That list of tasks was used to create a case manager job description (see Appendix 1), a person specification (see Appendix 2) and an educational needs assessment tool (see Appendix 3) to assist with recruitment, induction to the role and mentoring. A case management ‘manual’ (see Appendix 4) was also created (modified from materials used in the PREVENT study30). This manual included accessible leaflets for people with dementia and their carers, which could be used as an opportunity for information-giving and as talking points between case managers and their clients (both carers and people with dementia).
Job description and person specification
The development group was mindful to ensure that the job description and person specification did not overlap with existing roles. The group agreed that nurses would be a first obvious choice for this role (as in the PREVENT trial) but that other allied health and social care professionals might also be suitable. Therefore, the development of the job description focused on skills rather than specifying professional qualifications. The group was mindful that some professionals, for example doctors, were expensive and, therefore, possibly unaffordable. Important themes raised in the discussions included:
-
Interaction. Case managers would benefit from sharing knowledge and experiences with each other on a regular basis.
-
Mapping resources. Case managers would need to be proactive, ready to identify current resources to support people with dementia and their carers and able to identify gaps in the provision of services and the accessibility of resources.
-
Managing the risk of overload. There was a risk that the role might overwhelm the case manager (physically or emotionally) and the feasibility study (WP2) needed to highlight any such overload. This risk could be mitigated by developing close working relationships with specialist teams.
Educational needs assessment
The challenge for those seeking to change clinical performance is to find ways of working with the grain of professional knowledge and practice. One approach to working with the grain is to use educational needs assessments. 55 Assessment of educational needs has the potential to accommodate variations in individual understanding and competence, learning preferences and skill mix. Such tailoring of an educational ‘intervention’ to the specific identified needs of practitioners also draws on diffusion theory (as mentioned earlier) in that the ‘intervention’ itself can be modified in such a way as to make it more likely to be adopted. The educational needs assessment was constructed to take into account practitioners’ knowledge of the local health and social care systems, to reflect the complexity of the potential care processes for people with dementia, and to acknowledge the complexity of the disease process itself. 56 It was intended to foster reflection, allow practitioners to create time and space to plan changes and enable them to tolerate tension and discomfort. 57
During the development of the educational needs assessment, the group discussed case management tasks, competencies required or desirable for them, risks to minimise and tools required to undertake the case management role successfully. These conversations resulted in the production of a ‘task matrix’, which informed the job description (see Appendix 1) and person specification (see Appendix 2) as well as the educational needs assessment tool (see Appendix 3). This matrix was designed to be work in progress, with the expectation that some further risks and tools might emerge in WP2.
The overarching topics considered most important by the group were how existing competencies of case managers should be assessed in meeting the emotional needs of a person with dementia and their carers, and how to develop the skills of the case manager in areas where these could be improved. This was seen as important as each case manager was likely to bring different experiences and attributes and an adult learning approach would build on these and not assume that a common training package would suit all.
The competencies, risks and tools identified in the task matrix were used as the basis for an educational needs assessment tool. This mapped competencies onto the dementia disease trajectory under five headings:
-
supporting patients at the time of diagnosis
-
managing breakdown of support systems
-
managing acute illness and hospital admission
-
supporting decisions about relocation
-
supporting the person with dementia and his or her family at the end of life.
Subheadings were agreed for each of the five main headings (see Appendix 3). This educational needs assessment was designed not only to be used in the case manager induction process but also as a topic guide for mentoring during active case management.
The group viewed mentoring as essential to the introduction of case management approaches in primary care, as the new case managers would be learning through the experience of working with a diverse patient and carer group. The task of the mentor was to support the case manager in ‘absorbing’ the needs of people with dementia and their carers, ‘digesting’ these needs to understand what was tractable and needed solution and ‘providing’ where possible for unmet needs. 58
The manual
The manual focused on topics such as communication with the person with dementia, behaviour problems, mobility, personal care, sleep, legal and financial issues, physical health, depression and anxiety and how to respond to psychotic or distressing symptoms.
Rules were implemented in the adaptation of the PREVENT manual, to systematically alter the language and tone of the US version. These included:
-
Removal of all references to the person with dementia as the ‘loved one’ and replacement of this term with ‘relative’.
-
Use of words such as ‘try’, ‘consider’ and ‘may’ to make the manual less directive and prescriptive and deletion of phrases such as ‘instruct the carer’.
-
Replacement of phrases with a negative tone (advising carers not to do things) with more positive actions or things to try. Here the group added explanations for why the person with dementia might behave in a certain way and tried to make the manual more person centred by explaining that symptoms and difficulties were likely to vary from time to time and from person to person.
Information about local NHS and social care services and about the Alzheimer’s Society and local support organisations was added to the manual. Suggestions that the carer should speak to the case manager were included to make the manual more interactive. ‘Key points’ boxes and subheadings were added and the order of the contents was changed to provide a more coherent structure. Images were removed when these were inappropriate for the English context and distracted from the content. The development group felt that the manual required some additional sections and so it added an introduction and contents page; it also developed pages on asking for help, looking after yourself, physical health, aggression and agitation, depression and anxiety, and planning for the future.
Chapter 3 Work package 2
This chapter describes the second work package (WP2) in the CAREDEM study, in which the previously developed case management programme (WP1) was tested in a feasibility trial. The primary objective for this pilot phase was to ensure that case management skills and the collaborative care model would be easy to acquire and implement in routine practice. The secondary objectives were to determine whether or not practices could recruit 11 patients into the study (depending on practice size), that nine could be contacted at 6 months and that stakeholders would find the brief intervention procedures acceptable and feasible within routine NHS practice. The researchers intended to check assumptions about practice and patient recruitment and retention and to ensure the feasibility (data yield and quality) of outcome measures; if necessary, the sample size calculation for WP3 would be adjusted based on these data. Practices that took part in the pilot study would not be able to participate in the main trial. Approval for WP2 was obtained from Wandsworth NRES (11/LO/1555).
Recruitment of practices and case managers
Practices were recruited from each site as detailed in the following sections. Data were obtained on practice population size, number of GPs and deprivation score. The average deprivation score in England is 21.5, with a higher value indicating greater deprivation.
London
In December 2011, the researchers wrote to 26 GP practices in Camden and Islington, inviting them to take part in the CAREDEM pilot study. Eight practices contacted the research team requesting more information; however, seven of these practices declined participation. Reasons given for declining participation were concerns about time, resources and current commitments, meaning that they were already very busy. One of these eight practices invited the researchers to present the proposed study at its practice meeting. After this meeting the practice agreed to participate in the study on the condition that the research team could guarantee Service Support Costs for a practice nurse, to backfill their time whilst working on CAREDEM.
Additionally, in January 2012 the researchers made contact with the North Central London Research Consortium (NoCLoR), which put them in touch with two further GP practices from NoCLoR’s local research clusters. One of these practices agreed to the researchers presenting the proposed study at its practice meeting in January 2012 and this practice subsequently agreed to take part in the research. At this point, as it was not possible to guarantee the Service Support funding, the practice that wished to take part unconditionally was recruited. During this process the researchers were further assisted by NoCLoR, whose staff negotiated with local commissioners on the study’s behalf to obtain Service Support funding for the CAREDEM study in London. This process facilitated engagement with the local research network and the researchers have retained the details of four GP practices who were interested in taking part in the main trial or in further research in this area but who could not commit to the pilot study. The list size of the recruited practice is 15,510 patients and the practice is served by 8.5 whole-time equivalent (WTE) GPs. The practice serves a population spread across two London boroughs, with deprivation scores of 21.5 and 27.
Norfolk
In Norfolk, 30 practices were contacted through the primary care research network and the DeNDRoN local research network and 12 expressed an interest in participating in the study. Practices were visited and the first to confirm involvement was recruited. The practice recruited covers a mainly rural setting with one large market town at the main practice and two satellite practices. The main practice was located adjacent to a community hospital. The practice had a list size of 14,400 patients and is served by 4.5 WTE GPs. Its deprivation score is 18.77.
Newcastle
Two GP practices were approached by the site lead and agreed to participate in the study. Adult services in one local authority were approached to assist with recruitment of the case manager and offered a seconded role of a full-time case manager to provide the intervention across the two GP practices. Funding for the role was brokered by the locality PCT. A social worker with considerable experience of working with people with dementia and their families was initially recruited but accepted another post at the beginning of the recruitment screening. A second experienced social worker with knowledge of dementia took over the role. Recipients of case management were unaffected by the change in personnel. The social worker was primarily located at the larger practice but also spent a significant proportion of time in adult services, which afforded access to social work systems.
Patients were recruited across the two sites. One was a large, two-centred practice with a central and a satellite practice covering the city centre plus a broad radius of suburbs; the other was a smaller practice covering one area of the city. The larger practice had a list size of 28,396 patients served by 15 WTE GPs, and the practice’s deprivation score was 27.8 (putting this practice in the fourth most deprived centile). The smaller practice had a list size of 6501 patients served by 4.25 WTE GPs, and its deprivation score was 29.7. Recruitment was more successful in the larger practice.
Recruitment of patient and carer dyads
Inclusion and exclusion criteria
The target patient population for the CAREDEM WP2 study was people of any age with a diagnosis of any type of dementia (confirmed by secondary care assessment). Potential participants had to be living in the community at the point of recruitment and to have a carer (spouse, close relative, friend or other informal carer) who maintained regular contact. Those resident in care homes or being seen regularly by specialist dementia services were deemed to be being case managed already and were therefore excluded. Those unable to read English language information sheets about the study were also excluded.
Delays in achieving approval from local PCT research and development departments meant that recruitment of patients could not begin before July 2012. Practices recruited people with dementia and their carers over a 6-month period between July and December 2012 and followed them up for 5 months, the last interview being on 31 May 2013.
The WP2 protocol stated that patients would be invited to take part by their GP; however, in the London and Norfolk practices this was not realistic and eligible patients were screened and invited to take part by the practice nurse working in the case manager role, with the agreement of their GP. In the Newcastle practices the invitations were offered by the patients’ GPs and followed up by the research team.
The case manager or GP sent the patient and carer an information sheet, an opt-in form and a prepaid envelope and followed this up with a telephone call. Once the opt-in form or verbal consent form had been received, the research team was informed and contacted potential participants to answer any questions that they may have had. If the patient and carer were happy to proceed, the researcher arranged a visit at home or in another place specified by them to obtain informed consent and collect the baseline data. At the end of the baseline interview the researcher explained the next stages of the process and agreed with the participants that they would contact them for a follow-up appointment.
Directly after the baseline appointment the researcher informed the local case manager that the baseline assessment had been completed so that they could commence the intervention and completed a reflection log on the informed consent form process. Mentoring was provided by an Admiral nurse seconded to the project from Dementia UK, who visited the practices, carried out joint assessments with the case managers, communicated by telephone and e-mail with case managers on a regular basis and used the educational needs assessment and task matrix as the framework for discussing the case management role. Patients were followed up at 5 months (instead of 6 months as specified in the protocol) to allow completion of the study.
Quantitative data collection methods
Following the process of informed consent, interviews were conducted with the carer and the person with dementia individually, unless either person preferred the interview to take place with their relative in the room.
Demographic details, including date of birth, gender, marital status, level of education, employment status, ethnicity and relationship to care recipient, were obtained from participants at the baseline interview.
The carer completed the following assessments:
-
The Neuropsychiatric Inventory (NPI)59 (on which the current sample size calculations are based). This is a validated instrument with 12 domains, completed in an interview with a carer to assess the prevalence of behavioural and psychological symptoms experienced by the person with dementia he or she is supporting.
-
The Bristol Activities of Daily Living Scale (BADLS)60 was used to assess the functional impairment of the person with dementia.
-
The 28-item General Health Questionnaire (GHQ-28)61 was used to provide a measure of the carers’ mood and quality of life.
-
The European Quality of Life-5 Dimensions (EQ-5D) (see www.euroqol.org/about-eq-5d.html; accessed 23 June 2014) was used to assess carer quality of life and to generate quality-adjusted life-years (QALYs).
-
The Client Service Receipt Inventory (CSRI)62 captures service utilisation data for the carer and the patient (including institutionalisation, extra patient care during therapy), unpaid carer support and other aspects relevant to health economics. The rates and dates of entry into institutional care are recorded.
The person with dementia was assessed in the following ways:
-
The Mini Mental State Examination (MMSE)63 was used as a measure of cognitive function.
-
The Dementia Quality of Life (DEMQOL) scale33 was completed if the patient scored ≥ 11 on the MMSE, in line with guidance. The DEMQOL scale is a generic measure from which it is possible to generate QALYs.
Discontinued measures
The decision was taken before recruitment of participants to remove two of the measures included in the original protocol. The scale measuring quality of life in Alzheimer’s disease (QoL-AD)64 was removed as we were already measuring quality of life with the EQ-5D and the DEMQOL scale; the researchers felt that the extra measure was excessive and therefore unnecessary. Similarly, the 12-item Health Status Questionnaire (HSQ-12)65 was removed and the GHQ-28 was retained.
Adverse events
The numbers and details of adverse events (e.g. emergency admission to hospital) or serious adverse events (e.g. deaths) were recorded.
Qualitative data collection
In-depth qualitative interviews were conducted with members of a range of stakeholder groups to explore different perspectives on case management. Those interviewed included people with dementia (patients), carers, case managers, the case manager mentor (hereafter ‘mentor’), health and social care professionals and members of the research team. Separate interview topic guides were developed for each stakeholder group to reflect different levels of engagement with case management. During data collection, interview topic guides for all stakeholder groups were adapted through an iterative process in light of low levels of intervention delivered in practice and emerging themes.
Interviews were conducted by members of the research team at various stages of the feasibility study to capture processes and experiences of case management at different time points and to capture key events such as case manager training. The majority of interviews were conducted face to face with individuals; however, when this was not practically feasible, a small number of interviews were conducted with two or three participants in a group or by telephone.
Patient and carer interviews
A purposive sample of patients and carers was invited to participate in a single in-depth qualitative interview to explore their experiences and views of case management (Table 2). Some interviews with patients and carers were carried out jointly at the request of the participants; however, when possible, interviews were conducted separately to enable exploration of potentially differing carer and patient experiences.
Case manager and mentor interviews
In total, there were four case managers throughout the pilot study. The views of the mentor were also sought through interview. Case managers and the mentor participated in several interviews throughout the study to explore changing expectations, the development of the role, training and supervision, the implementation of case management in practice and their views on the value of the case management approach. In total, 13 interviews were conducted (four with the mentor, two with each of three case managers and three with one case manager).
Research team interviews
Two members of the research team were interviewed and informal discussions were conducted with a further member of the team. These interviews/discussions explored the induction process, expectations of case management, barriers to implementation and their views on the value of the case management approach.
Health and social care professional interviews
In total, 18 in-depth interviews were conducted with a range of health and social care professionals (Table 3). Some practitioners reported direct interactions with the case managers whereas others gave a more theoretical perspective on case management (e.g. one of the commissioners). These are reported in Chapter 7.
| Profession | No. of participants |
|---|---|
| GP | 6 |
| Administrative practice staff | 5 |
| CMHT | 2 |
| Voluntary sector worker | 3 |
| Commissioner | 2 |
| Total | 18 |
Qualitative data management and analysis
All interviews were audio recorded, transcribed, checked and anonymised. In the initial stage of analysis individual team members (CB, KB, MP and LR) read and reread a number of transcripts to familiarise themselves with the data and identify preliminary themes. A series of data workshops were then held in which team members discussed these preliminary themes and developed a draft coding frame. This was then applied to a small number of transcripts and the findings were discussed in subsequent data workshops. Following a series of iterations, and informed by the theoretical domains framework,66 a final coding frame was agreed. All transcripts were coded in NVivo (version 9; QSR International, Warrington, UK) to facilitate data management using the final coding frame. In the next stage of analysis, the output for different stakeholder groups was reviewed. This led to the combination of some codes, the identification of new subcodes and the production of a narrative summarising the key themes for each group. These narratives were then compared and overarching themes identified across the stakeholder groups.
Confidentiality
Although we recruited both male and female case managers, to avoid identification we have referred to all case managers as female and we have not attributed quotes to individual case managers. By virtue of her role, the mentor was identifiable and she has reviewed and agreed to the use of all quotes attributed to her. Quotes from patient and carer interviews are identified by site (A, B or C) and unique identifier within each site.
The findings from WP2 are presented in the following four chapters:
-
Chapter 4 – recruitment to the study of practices and patient–carer dyads
-
Chapter 5 – implementation of the study including recruitment processes, acceptability and feasibility of outcome measures, patient and carer views on study participation and case manager and mentor views on study procedures
-
Chapter 6 – capturing what the case managers did during case management
-
Chapter 7 – stakeholder perceptions of case management for people with dementia.
Chapter 4 Recruitment to the study and characteristics of participants at baseline and follow-up
This chapter describes the recruitment and follow-up of study participants, by site, and provides a baseline description of participants’ characteristics as well as baseline and follow-up values for the following outcome measures: the NPI, the EQ-5D visual analogue scale, the BADLS, the GHQ-28 (total and domain scores), the MMSE and the DEMQOL scale (total and selected domain scores). We present the data primarily to characterise the sample and document the extent of follow-up. Finally, serious adverse events occurring during the study are described.
Recruitment
The recruitment target was 44 dyads (person with dementia plus a carer), 11 from each practice. The number of dyads recruited was 29; 14 were recruited from the two north-east practices, nine from the Norfolk practice and six from the London practice. Recruitment was halted at the Norfolk practice to deal with a backlog of case management work and this practice would probably have achieved its target had more time been available to the nurse case manager. Case identification using the Quality and Outcomes Framework (QOF) dementia register was supplemented by searches of electronic medical records to identify those taking cholinesterase inhibitors who were not on the QOF dementia register. Additional searches for patients with symptoms suggesting possible dementia (memory loss, confusion) allowed medical records to be checked for evidence that a formal diagnosis had been made but had not been added to the patient record. Figure 2 shows the derivation of the participant sample for the feasibility study.
FIGURE 2.
Recruitment flow diagram.
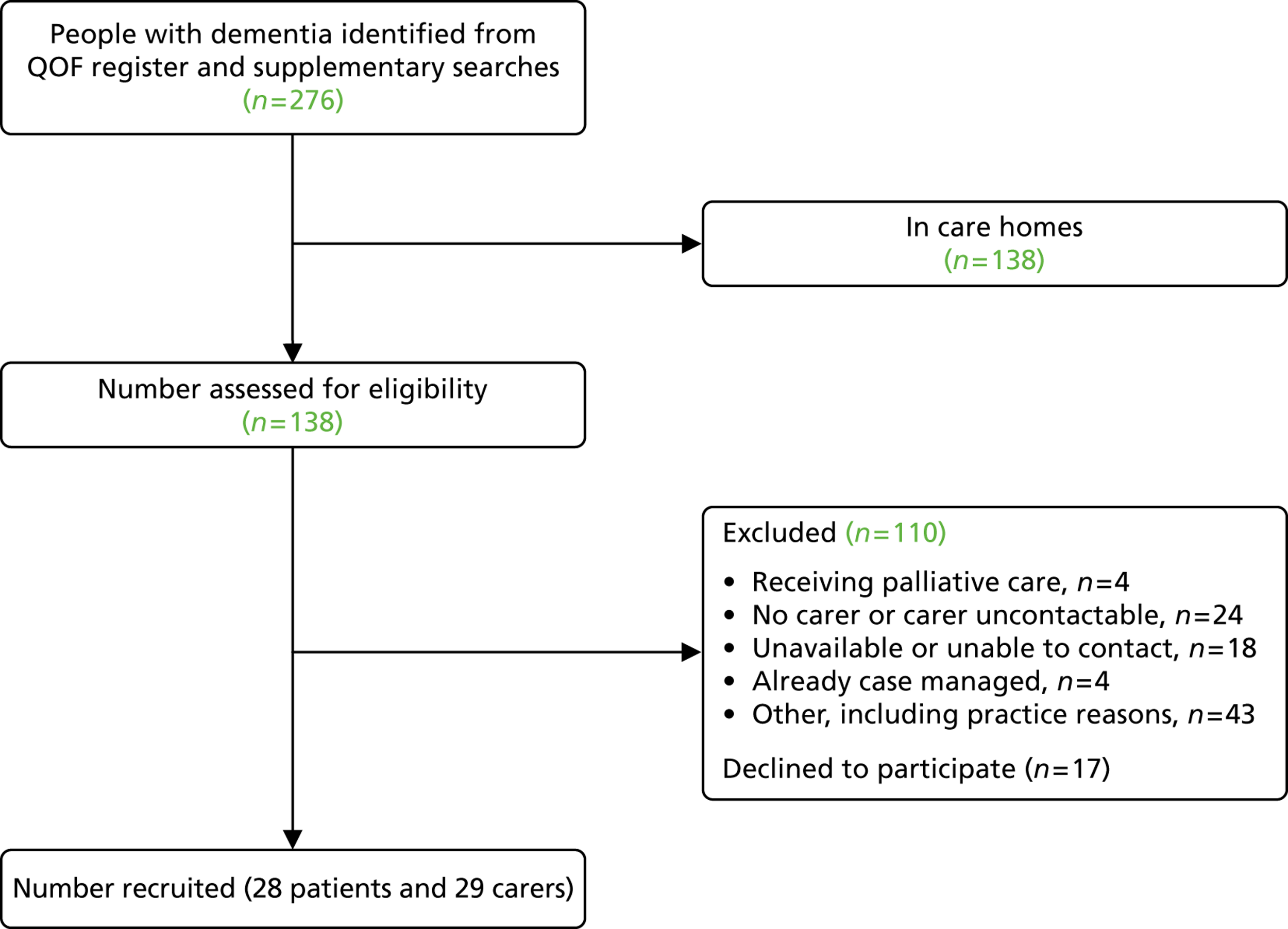
Of those patients not living in care homes, 45 [33%, 95% confidence interval (CI) 29% to 48%] met all of the criteria for inclusion in the study apart from providing informed consent. In total, 28 of these (62%, 95% CI 46% to 76%) agreed to participate.
Recruitment and follow-up by site
In London, six participant dyads (12 participants – six people with dementia and their main carer) were recruited between 17 August 2012 and 18 December 2012. Three potential participants agreed to speak with the researcher but declined to participate in the study. Reasons provided for this were not having the time to participate (two people) and not wanting their relative with dementia exposed to research questioning (one person). In London, a female patient was referred to the study and agreed to meet one of the researchers but it became apparent that she was unlikely to have dementia. The researcher checked with the surgery, which had placed her on the QOF dementia register without a diagnosis of dementia confirmed by secondary assessment. The researcher wrote to her to thank her for her time and withdrew her from the study. Follow-up appointments for the recruited participants in London were completed at 5 months. Six dyads were successfully contacted and follow-up data were collected.
In Norfolk, nine participant dyads (18 participants – nine people with dementia and their main carer) were recruited between 7 August 2012 and 24 September 2012. Three patients who were invited to participate returned the opt-in form stating that they would not be interested in taking part but gave no details about why they were declining participation. In Norfolk, all 18 participants recruited into the study completed a follow-up appointment at 5 months.
Thirteen dyads plus one carer-only participant were recruited in the north-east. Ten dyads were recruited through the larger practice. Recruitment took place between 30 July 2012 and 27 November 2012. Only one patient returned the opt-in form stating that she was not interested in participation.
A further four participants were agreeable to their details being passed to the researcher; however, either the patient or the nominated carer declined participation when approached by the researcher. Reasons for declining participation included patient illness/hospital admission and other family or care commitments. Despite multiple attempts, the researcher was unable to contact an additional two patients who had expressed an interest in participation through the GP contact. Table 4 shows the derivation of the denominator for outcome assessment at all sites.
| Area | Dyads recruited | Follow-up at 5 months | Denominator for outcome and quality of life data at 5 months | ||
|---|---|---|---|---|---|
| n | Rate (%) | 95% CI (%) | |||
| London | 6 | 6 | 100 | 54 to 100 | 4a |
| Norfolk | 9 | 9 | 100 | 66 to 100 | 9 |
| North-east | 13 | 10b | 77 | 46 to 95 | 4c |
| Total | 28 | 25 | 89 | 71 to 98 | 16 |
Baseline data collection
Baseline data were collected from all dyads (nine from Norfolk, six from London and 13 dyads and one carer from the north-east). All nine dyads from Norfolk and all six from London were followed up at 5 months, with complete data collection. Ten of the 13 dyads from the north-east were successfully followed up at 5 months (outcome data were collected from four and the other six indicated that they were willing to provide it). Two dyads in the north-east indicated that they were not willing to provide outcome data (one patient had moved into residential care and her carer felt that the patient was not capable of participating; one patient did not receive the intervention and the carer felt that data collection would be too upsetting for the patient) and one further patient was lost to follow-up.
Demographics of participants at baseline
Tables 5 and 6 show the characteristics at baseline of the carers and the people with dementia, respectively.
| Demographic | Centre | All (n = 29) | ||
|---|---|---|---|---|
| Norfolk (n = 9) | London (n = 6) | North-east (n = 14) | ||
| Age (years), mean (SD) | 71.2 (14.0) | 62.7 (13.6) | 64.1 (13.7) | 66.0 (13.8) |
| Gender female, n (%) | 5 (56) | 4 (67) | 10 (71) | 19 (66) |
| Marital status: married/partnered, n (%) | 6 (67) | 2 (33) | 10 (71) | 18 (62) |
| Level of education: no qualifications, n (%) | 3 (33) | 0 (0) | 6 (43) | 9 (31) |
| Work: retired, n (%) | 7 (78) | 3 (50) | 8 (57) | 18 (62) |
| Children at home, n (%) | 1 (11) | 0 (0) | 1 (7) | 2 (7) |
| Ethnicity: white British, n (%) | 9 (100) | 3 (50) | 14 (100) | 26 (90) |
| Demographic | Centre | All (n = 28) | ||
|---|---|---|---|---|
| Norfolk (n = 9) | London (n = 6) | North-east (n = 13) | ||
| Age (years), mean (SD) | 81.1 (3.5) | 79.8 (6.6) | 79.8 (11.6) | 80.2 (8.5) |
| Gender female, n (%) | 6 (67) | 5 (83) | 9 (69) | 20 (71) |
| Relationship to carer | ||||
| Cared for by a spouse/partner, n (%) | 7 (78) | 2 (33) | 6 (46) | 15 (54) |
| Cared for by a son or daughter, n (%) | 2 (22) | 3 (50) | 7 (54) | 12 (43) |
| Marital status: married, n (%) | 7 (78) | 2 (33) | 5 (38) | 14 (50) |
| Level of education: no qualifications, n (%) | 4 (44) | 3 (50) | 9 (69) | 16 (57) |
| Ethnicity: white British, n (%) | 9 (100) | 4 (67) | 13 (100) | 26 (93) |
Outcome measures
For each variable we provide an indication of the distribution of responses at baseline, usually in the form of a box and whiskers plot. Additionally, we present descriptive statistics for each of the measures of outcome and quality of life used in the pilot study. The purpose behind this is to facilitate the planning of any future studies. In particular, measures of variability are likely to inform sample size calculations; it is not intended that the data be used to make comparisons between the particular sites that participated in this study.
Neuropsychiatric Inventory
The NPI was chosen as the likely primary outcome measure for a definitive trial. The NPI assesses 10 behavioural disturbances occurring in dementia patients: delusions, hallucinations, dysphoria, anxiety, agitation/aggression, euphoria, disinhibition, irritability or emotional lability, apathy and aberrant motor activity. Higher scores suggest higher levels of disturbance. The distribution of total scores for the patients recruited to the feasibility study is provided in Table 7 and Figure 3.
| Time point | Centre | n | Minimum | Maximum | Median | Mean | SD |
|---|---|---|---|---|---|---|---|
| Baseline | Norfolk | 9 | 1 | 54 | 12.0 | 16.00 | 16.64 |
| London | 6 | 7 | 32 | 10.0 | 15.33 | 10.58 | |
| North-east | 14 | 1 | 85 | 19.0 | 25.43 | 24.63 | |
| Total | 29 | 1 | 85 | 13.0 | 20.41 | 20.13 | |
| 5-month follow-up | Norfolk | 8 | 5 | 40 | 20.0 | 19.62 | 11.33 |
| London | 4 | 2 | 13 | 8.5 | 8.00 | 4.97 | |
| North-east | 4 | 4 | 29 | 13.0 | 14.75 | 11.18 | |
| Total | 16 | 2 | 40 | 13.5 | 15.50 | 10.68 |
FIGURE 3.
Neuropsychiatric Inventory total scores: box and whiskers plot of baseline values.
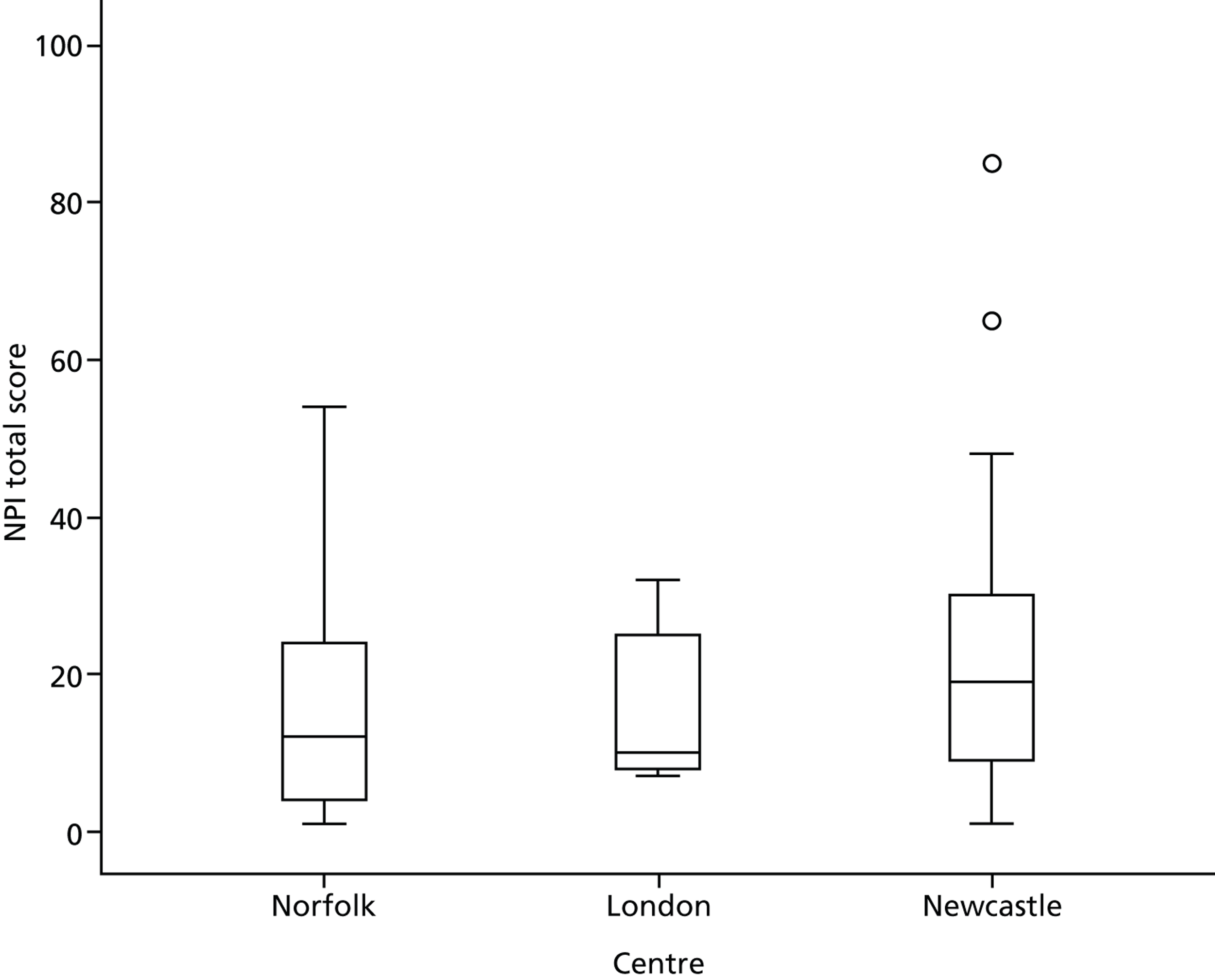
In Figure 3 (and subsequent box and whiskers plots), the horizontal line within each box corresponds to the median value, the lower and upper edges of the box correspond to the 25th and 75th percentiles and the whiskers indicate the range, except for any outlying values, which are indicated by circles and or stars. Figure 4 plots the NPI scores at 5 months against the baseline scores.
FIGURE 4.
Plot of NPI scores at 5 months against scores at baseline.
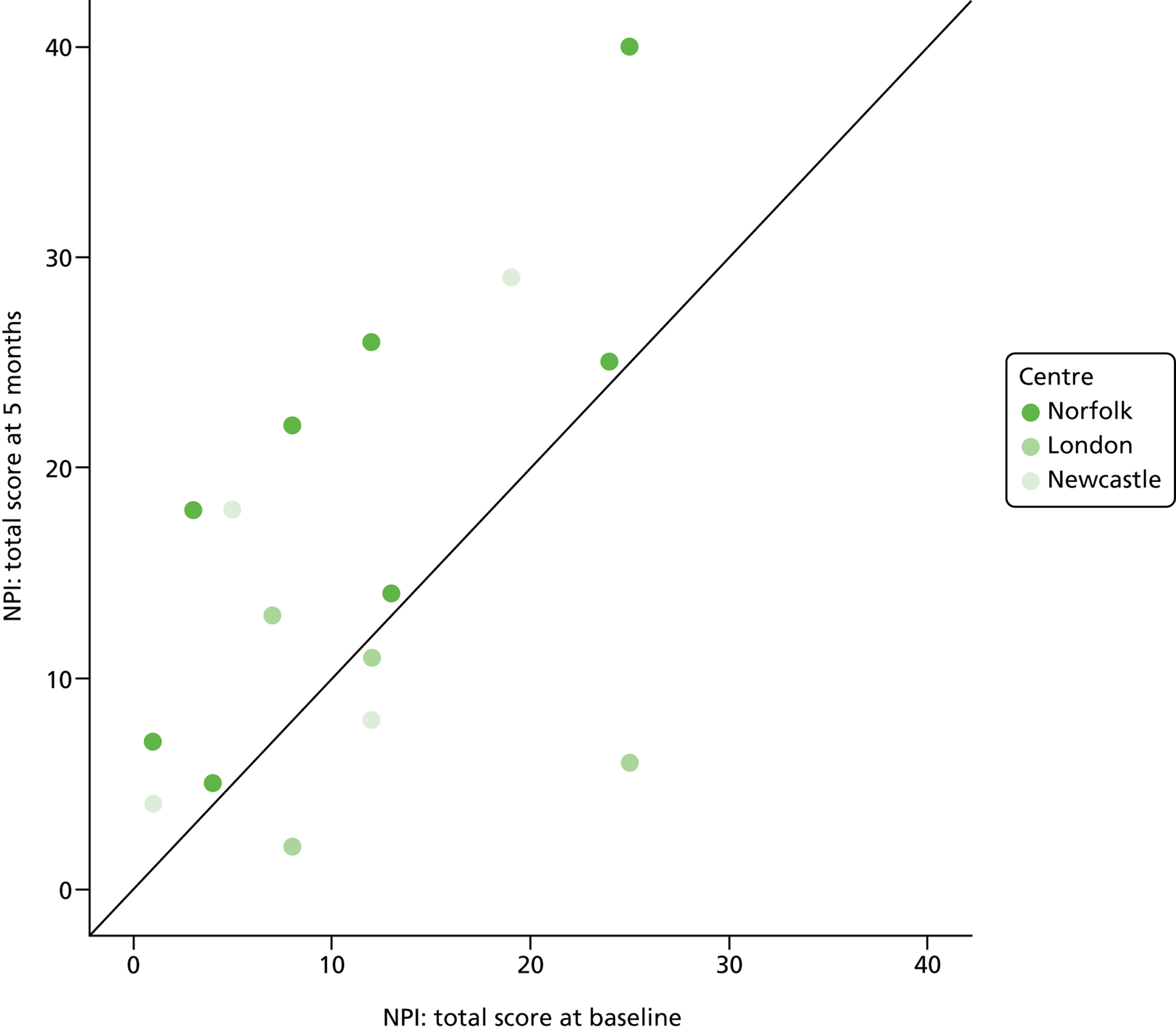
Most of the scores at 5 months are greater than the scores at baseline. There are four exceptions, three of which correspond to responses from London carers or patients. The mean increase in NPI total score is 4.3 (95% CI –0.31 to 8.56) (based on 50,000 bootstrap samples).
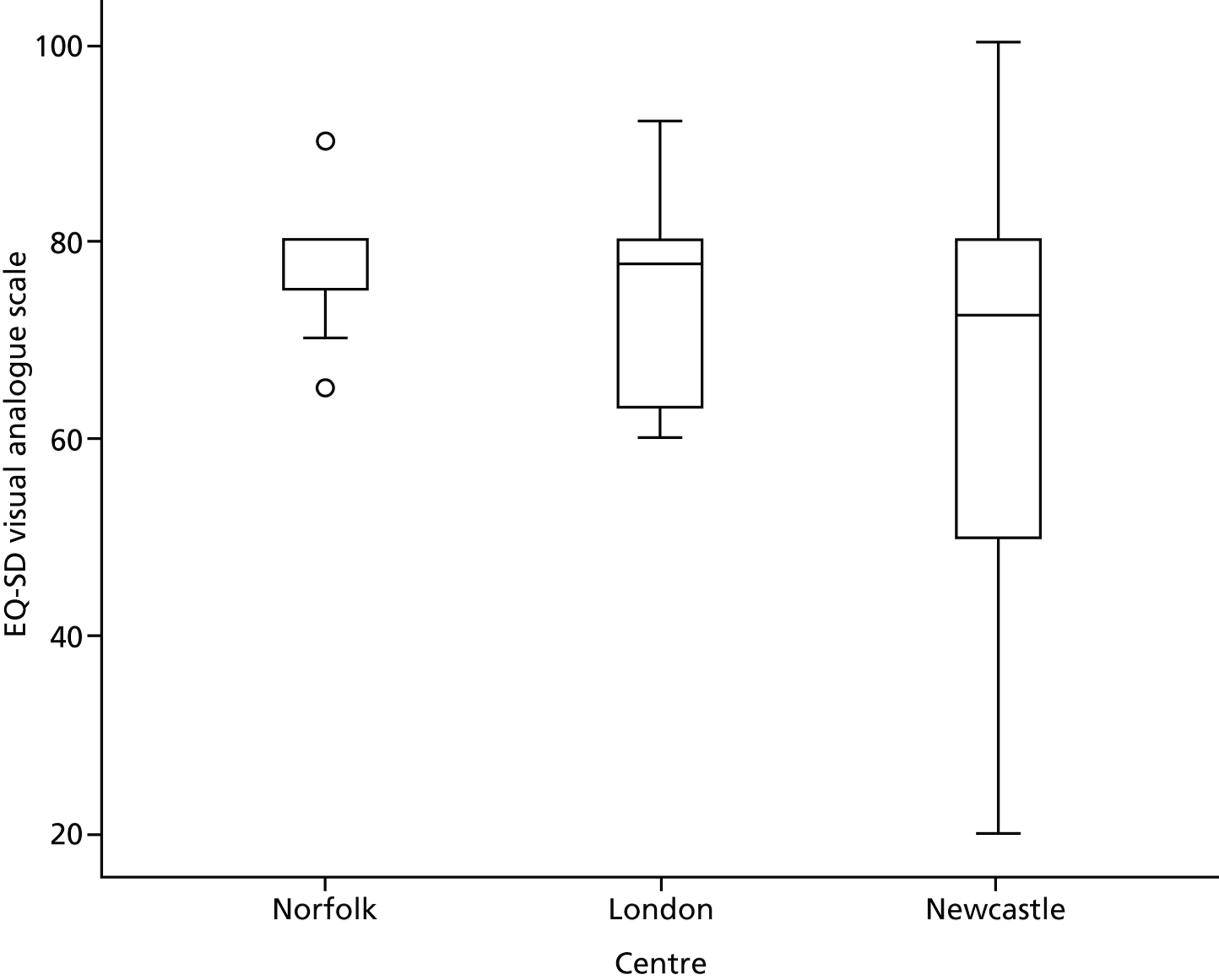
European Quality of Life-5 Dimensions visual analogue scale
This general health rating scale (0–100) was completed by carers. Higher values suggest a higher quality of life. Table 8 shows the descriptive statistics for the EQ-5D visual analogue scale at baseline and at the 5-month follow-up and Figure 5 shows a box and whiskers plot of baseline values.
| Time point | Centre | n | Minimum | Maximum | Median | Mean | SD |
|---|---|---|---|---|---|---|---|
| Baseline | Norfolk | 9 | 65 | 90 | 80.0 | 77.22 | 7.120 |
| London | 6 | 60 | 92 | 77.5 | 75.00 | 11.900 | |
| North-east | 14 | 20 | 100 | 72.5 | 68.57 | 21.700 | |
| Total | 29 | 20 | 100 | 75.0 | 72.59 | 16.571 | |
| 5-month follow-up | Norfolk | 9 | 40 | 95 | 75.0 | 72.78 | 18.047 |
| London | 4 | 40 | 80 | 69.5 | 64.75 | 17.231 | |
| North-east | 4 | 70 | 95 | 80.0 | 81.25 | 10.308 | |
| Total | 17 | 40 | 95 | 75.0 | 72.88 | 16.507 |
FIGURE 5.
European Quality of Life-5 Dimensions visual analogue scale: box and whiskers plot of baseline values.
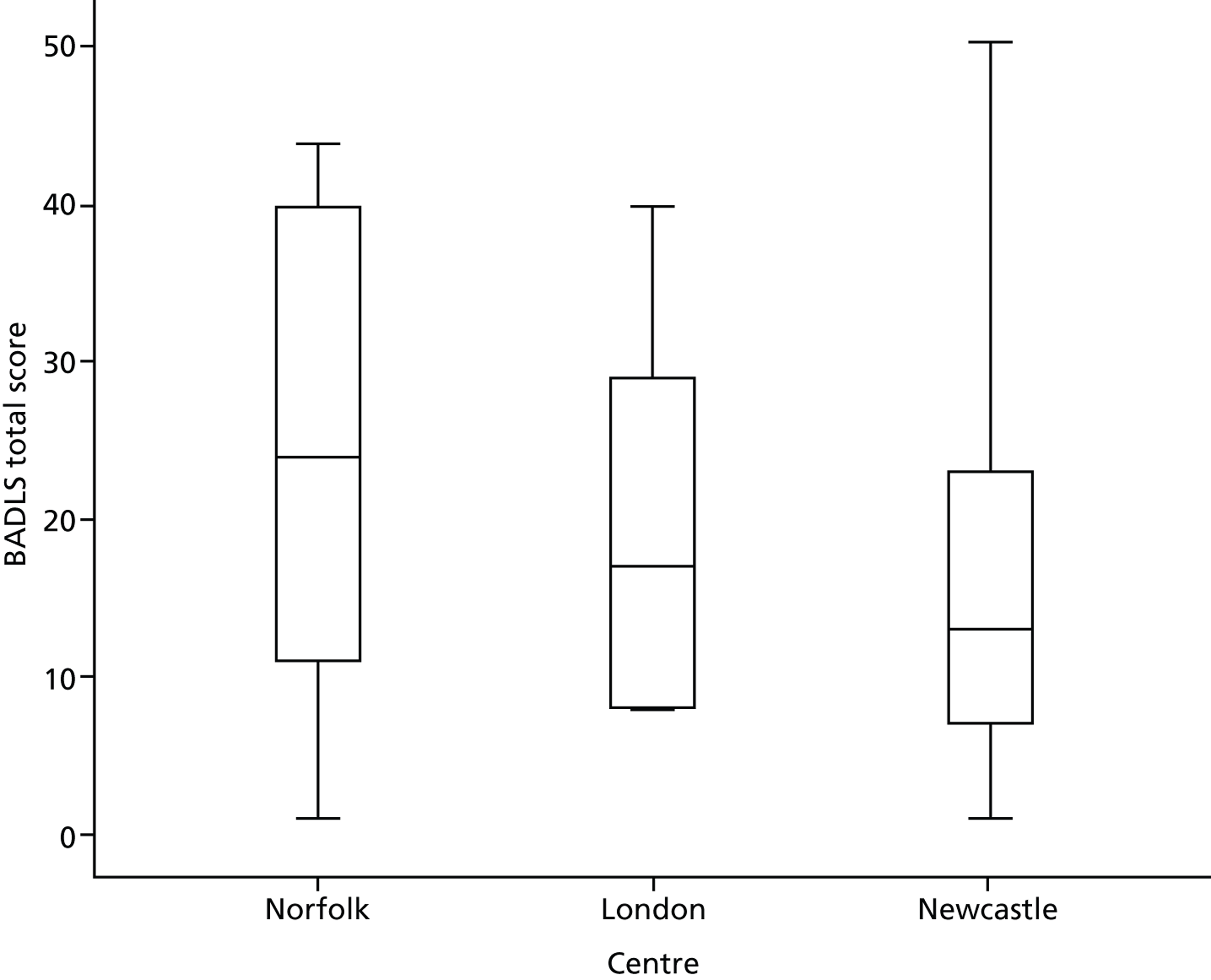
Bristol Activities of Daily Living Scale
The BADLS was designed specifically for use in patients with dementia and assesses 20 daily living abilities. A score of 0 suggests total independence and a score of 60 suggests total dependence. Table 9 shows the BADLS scores at baseline and at 5 months’ follow-up and Figure 6 shows baseline values as a box and whiskers plot.
| Time point | Centre | n | Minimum | Maximum | Median | Mean | SD |
|---|---|---|---|---|---|---|---|
| Baseline | Norfolk | 9 | 1 | 44 | 24.0 | 22.78 | 17.548 |
| London | 6 | 8 | 40 | 17.0 | 19.83 | 12.937 | |
| North-east | 14 | 1 | 32 | 13.0 | 15.00 | 10.720 | |
| Total | 29 | 1 | 44 | 15.0 | 18.41 | 13.550 | |
| 5-month follow-up | Norfolk | 8 | 4 | 48 | 23.0 | 24.00 | 15.381 |
| London | 4 | 8 | 30 | 14.5 | 16.75 | 10.372 | |
| North-east | 4 | 1 | 29 | 4.0 | 9.50 | 13.178 | |
| Total | 16 | 1 | 48 | 17.5 | 18.56 | 14.325 |
FIGURE 6.
Bristol Activities of Daily Living Scale total scores: box and whiskers plot of baseline values.
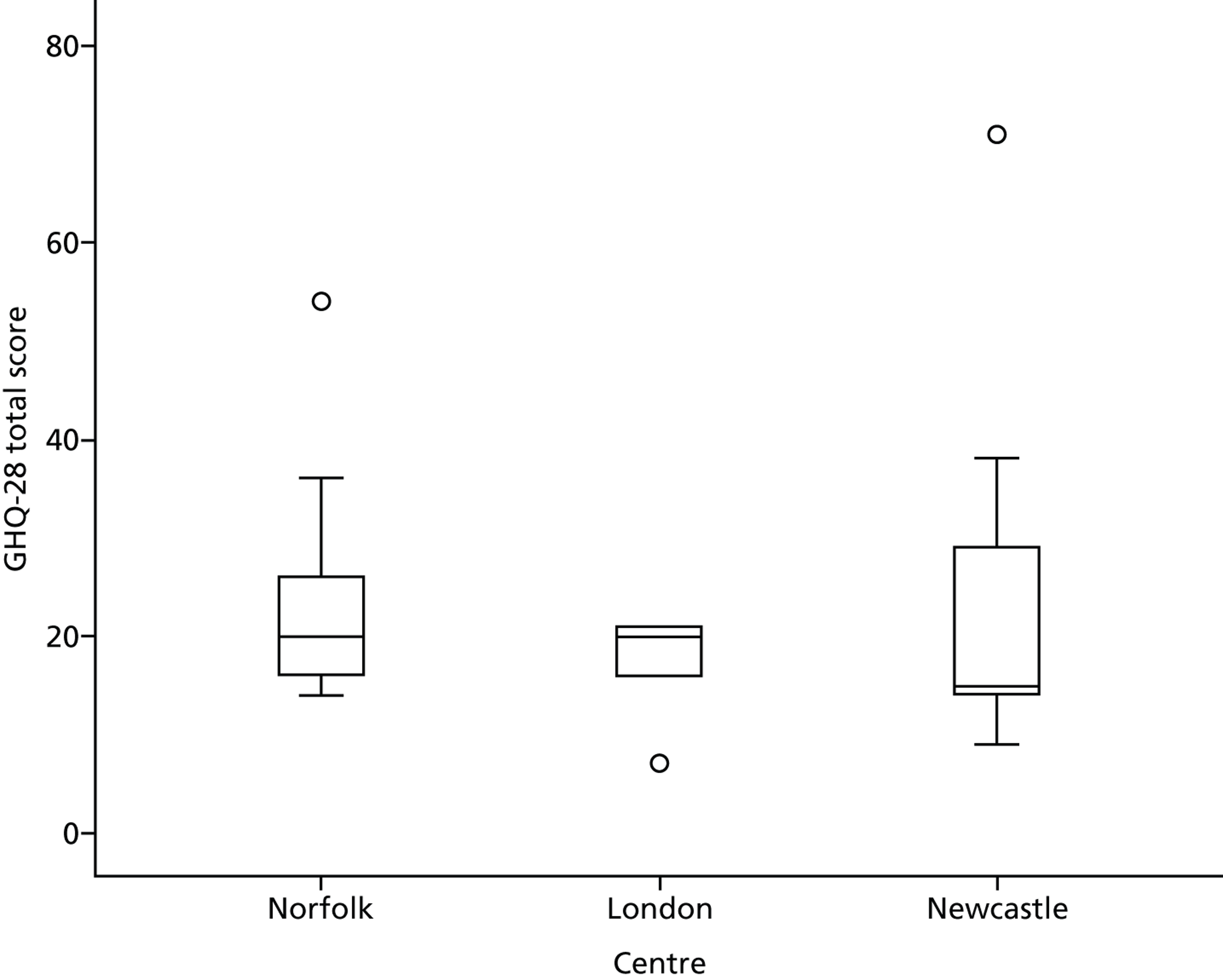
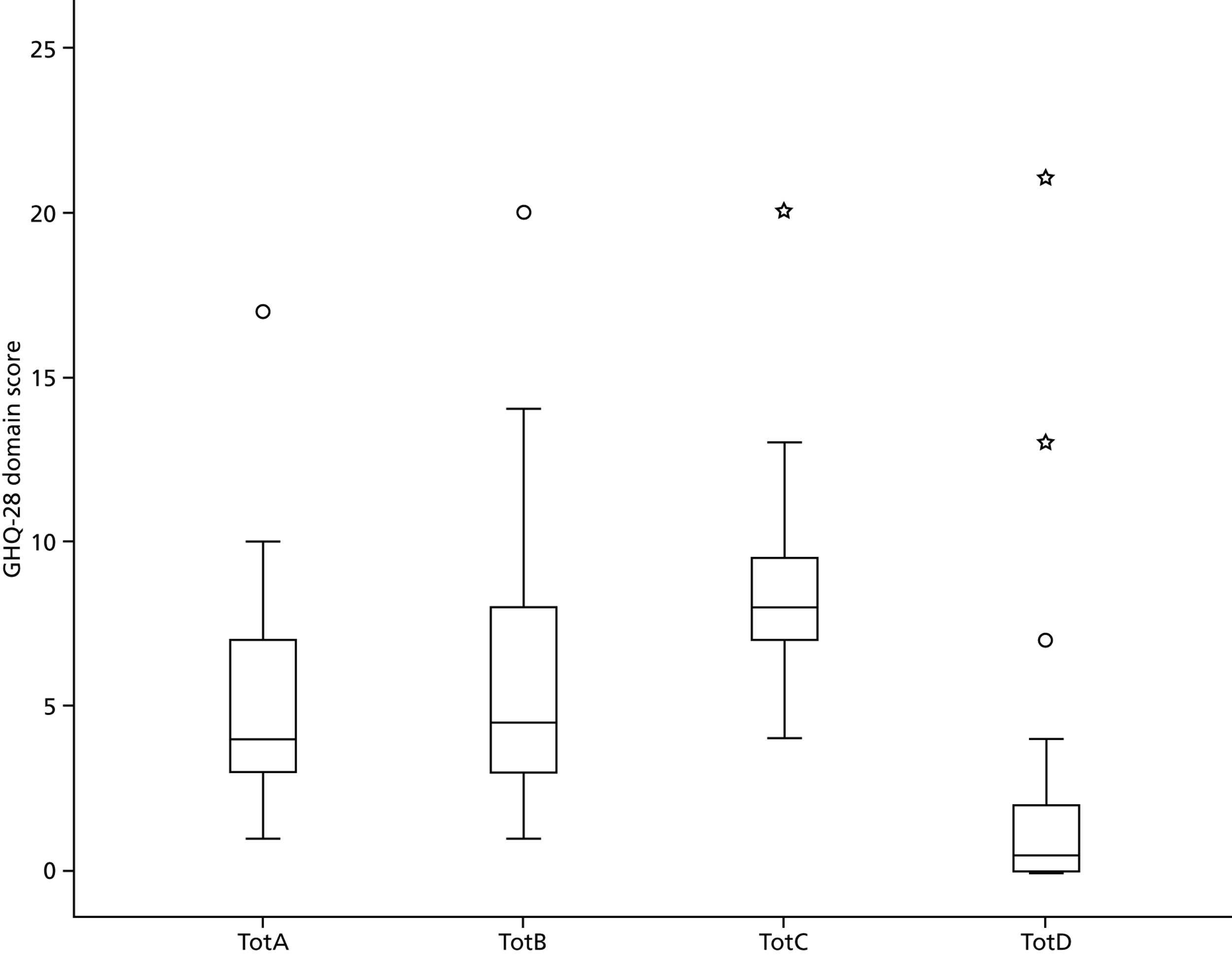
General Health Questionnaire
The GHQ-28 has possible scores across four domains in the range from 0 to 84, with higher scores suggesting higher levels of psychological disorder. The four domains are (A) somatic symptoms, (B) anxiety and insomnia, (C) social dysfunction and (D) severe depression. Table 10 shows the GHQ-28 total scores at baseline and at 5 months’ follow-up and Figure 7 shows the GHQ-28 total scores at baseline as a box and whiskers plot. Table 11 shows the domain scores at both time points and Figure 8 shows the baseline domain scores as a box and whiskers plot.
| Time point | Centre | n | Minimum | Maximum | Median | Mean | SD |
|---|---|---|---|---|---|---|---|
| Baseline | Norfolk | 9 | 14 | 54 | 20.0 | 24.44 | 13.182 |
| London | 5 | 7 | 21 | 20.0 | 17.00 | 5.958 | |
| North-east | 14 | 9 | 71 | 15.0 | 23.00 | 16.530 | |
| Total | 28 | 7 | 71 | 17.5 | 22.39 | 13.974 | |
| 5-month follow-up | Norfolk | 7 | 8 | 45 | 18.0 | 21.00 | 12.728 |
| London | 3 | 11 | 32 | 16.0 | 19.67 | 10.970 | |
| North-east | 4 | 9 | 28 | 11.0 | 14.75 | 8.921 | |
| Total | 14 | 8 | 45 | 15.5 | 18.93 | 10.930 |
FIGURE 7.
General Health Questionnaire total scores: box and whiskers plot of baseline values.
| Time point | Centre | Section A | Section B | Section C | Section D | |
|---|---|---|---|---|---|---|
| Baseline | Norfolk | n | 9 | 9 | 9 | 9 |
| Mean | 5.56 | 6.44 | 9.44 | 3.00 | ||
| SD | 2.455 | 3.712 | 4.157 | 4.416 | ||
| London | n | 5 | 5 | 5 | 5 | |
| Mean | 3.20 | 5.60 | 8.00 | 0.20 | ||
| SD | 1.789 | 2.510 | 2.915 | 0.447 | ||
| North-east | n | 14 | 14 | 14 | 14 | |
| Mean | 5.79 | 6.29 | 8.43 | 2.50 | ||
| SD | 4.264 | 5.902 | 2.503 | 5.460 | ||
| Total | n | 28 | 28 | 28 | 28 | |
| Mean | 5.25 | 6.21 | 8.68 | 2.25 | ||
| SD | 3.460 | 4.677 | 3.116 | 4.600 | ||
| 5-month follow-up | Norfolk | n | 9 | 7 | 9 | 8 |
| Mean | 7.22 | 6.57 | 7.22 | 2.13 | ||
| SD | 3.898 | 4.036 | 2.682 | 3.643 | ||
| London | n | 3 | 3 | 3 | 3 | |
| Mean | 4.33 | 6.67 | 8.00 | 0.67 | ||
| SD | 4.041 | 4.509 | 2.646 | 0.577 | ||
| North-east | n | 4 | 4 | 4 | 4 | |
| Mean | 3.25 | 4.75 | 6.75 | 0.00 | ||
| SD | 2.872 | 6.850 | 0.500 | 0.000 | ||
| Total | n | 16 | 14 | 16 | 15 | |
| Mean | 5.69 | 6.07 | 7.25 | 1.27 | ||
| SD | 3.911 | 4.714 | 2.236 | 2.764 | ||
FIGURE 8.
General Health Questionnaire domain scores: box and whiskers plot. A, somatic symptoms; B, anxiety and insomnia; C, social dysfunction; D, severe depression; and Tot, total.
Mini Mental State Examination
The range of scores on the MMSE is from 0 to 30, with lower scores suggesting worse cognitive impairment. Table 12 shows the MMSE scores at baseline and at 5 months’ follow-up and Figure 9 shows the baseline MMSE scores as a box and whiskers plot. A MMSE score of < 10 suggests advanced dementia (Table 13).
| Time point | Centre | n | Minimum | Maximum | Median | Mean | SD |
|---|---|---|---|---|---|---|---|
| Baseline | Norfolk | 7 | 9 | 27 | 19.00 | 17.57 | 7.786 |
| London | 5 | 12 | 29 | 23.00 | 20.20 | 7.050 | |
| North-east | 13 | 4 | 26 | 21.00 | 20.15 | 5.757 | |
| Total | 25 | 4 | 29 | 21.00 | 19.44 | 6.436 | |
| 5-month follow-up | Norfolk | 6 | 7 | 24 | 20.00 | 17.17 | 7.548 |
| London | 3 | 22 | 29 | 23.00 | 24.67 | 3.786 | |
| North-east | 4 | 15 | 27 | 20.00 | 20.50 | 5.196 | |
| Total | 13 | 7 | 29 | 22.00 | 19.92 | 6.512 |
FIGURE 9.
Mini Mental State Examination scores: box and whiskers plot.
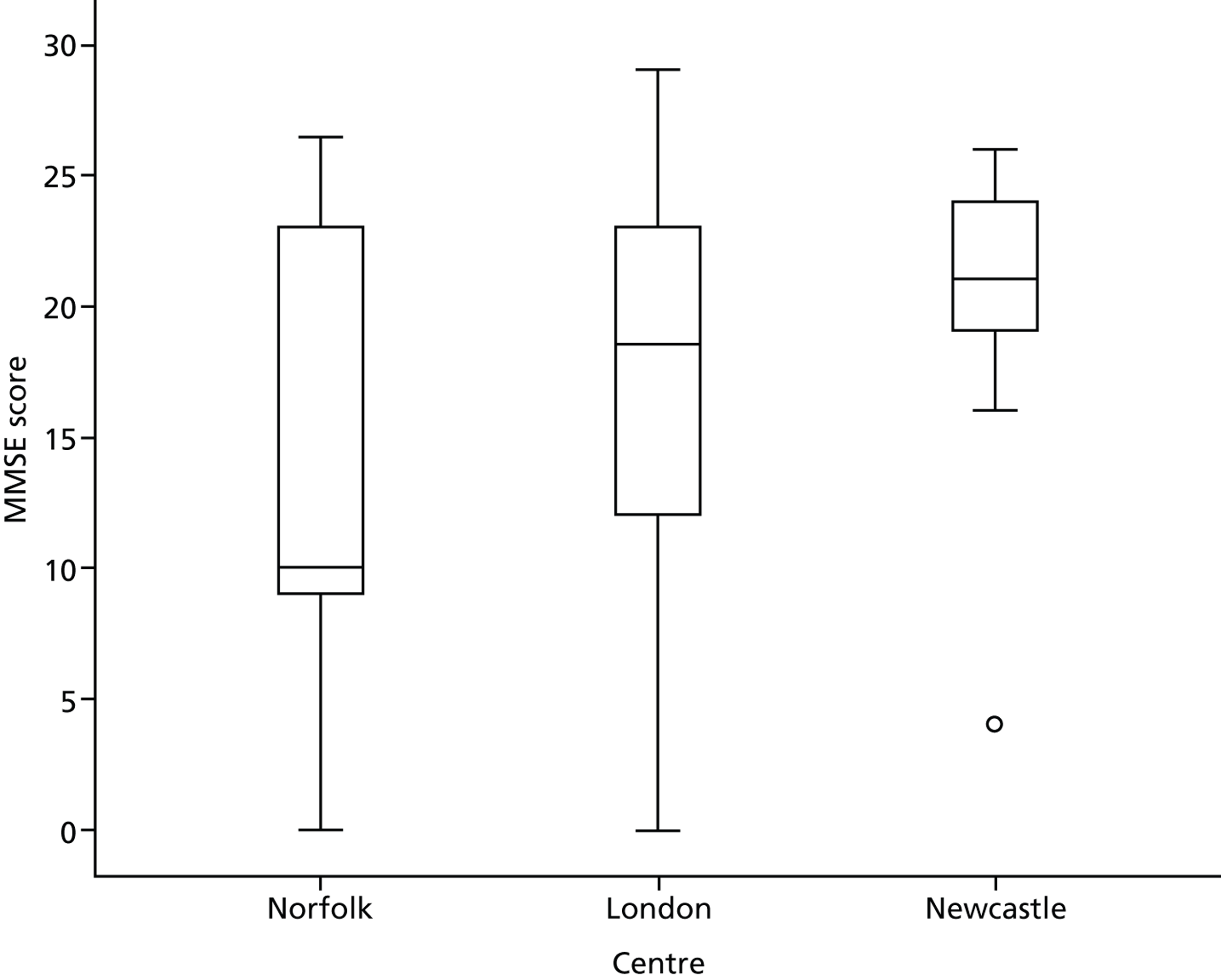
| MMSE category | Centre | Total | ||
|---|---|---|---|---|
| Norfolk | London | North-east | ||
| ≥ 10 | 6 | 5 | 12 | 23 |
| < 10 | 3 | 1 | 1 | 5 |
| Total | 9 | 6 | 13 | 28 |
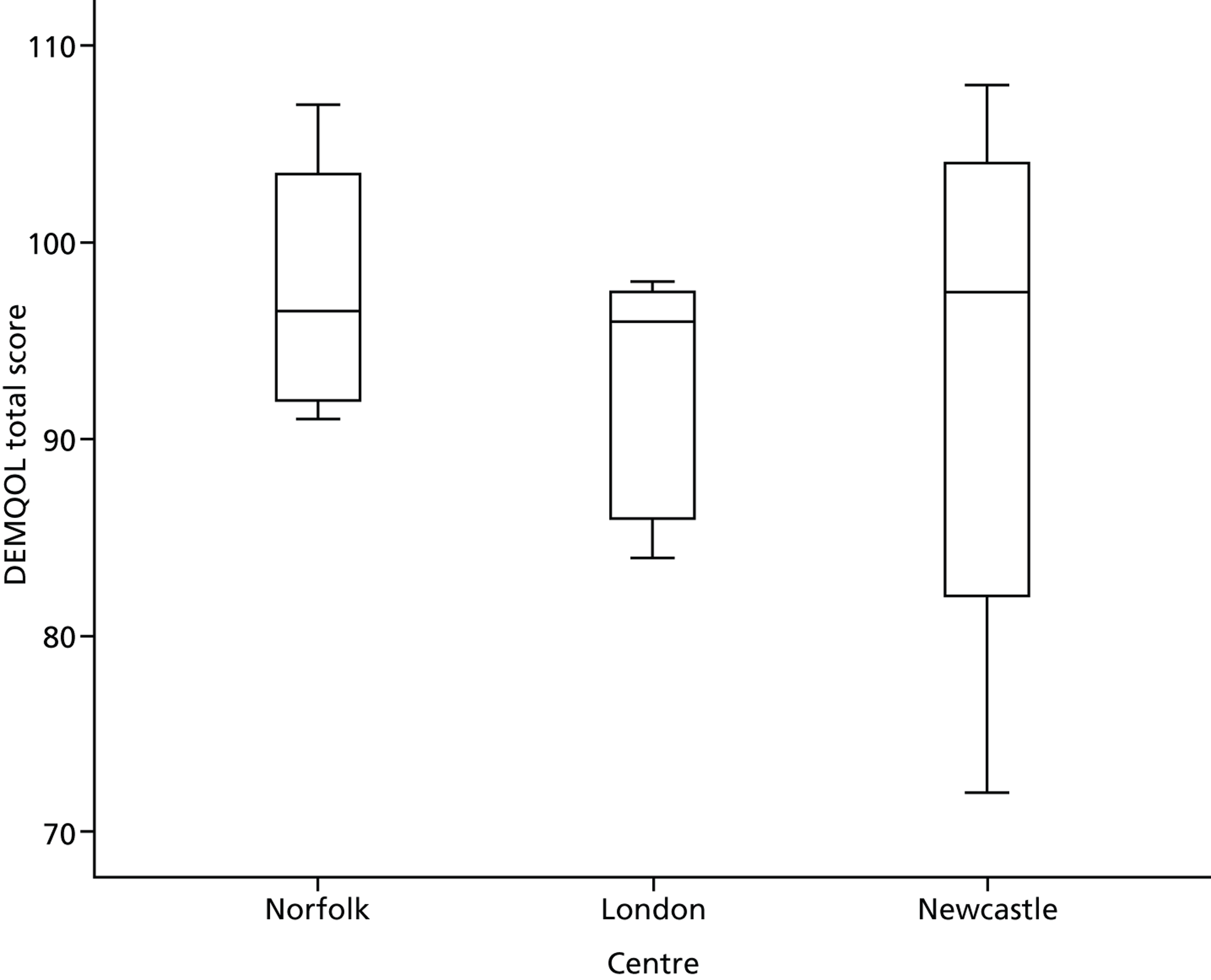
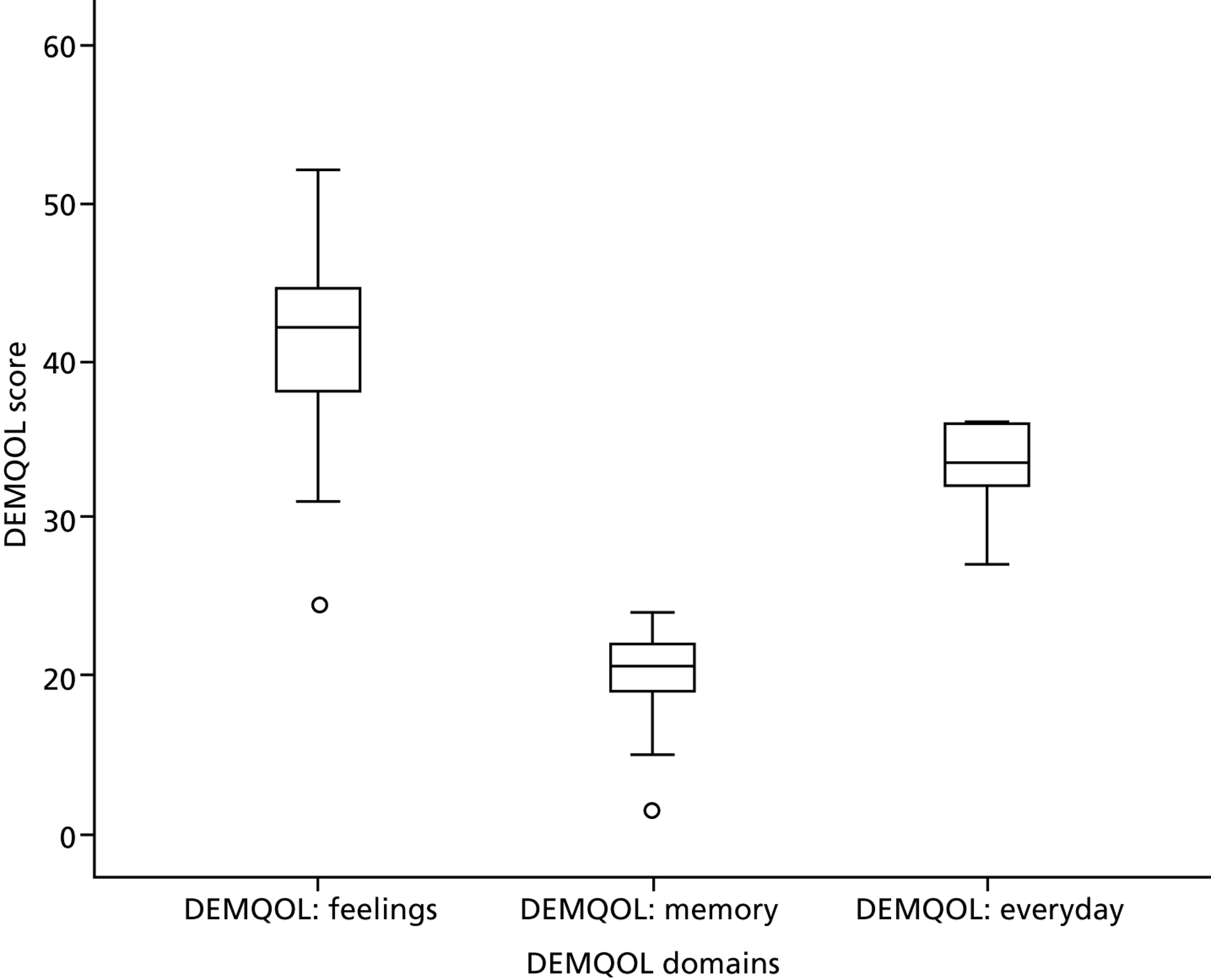
Dementia Quality of Life scale
The DEMQOL is a quality of life measure in which higher scores imply better quality of life. Participant total scores at baseline and at 5 months’ follow-up are shown in Table 14; Figure 10 displays baseline values as a box and whiskers plot. The DEMQOL scale includes five domains, three of which are reported in Table 15 (‘feelings’ = health and well-being; ‘memory’ = cognitive function; and ‘everyday’ = daily activities and looking after yourself). Baseline domain scores are provided in Figure 11 as a box and whiskers plot.
| Time point | Centre | n | Minimum | Maximum | Median | Mean | SD |
|---|---|---|---|---|---|---|---|
| Baseline | Norfolk | 4 | 91 | 107 | 96.50 | 97.75 | 7.274 |
| London | 4 | 84 | 98 | 96.00 | 93.50 | 6.455 | |
| North-east | 12 | 72 | 108 | 97.50 | 92.67 | 13.282 | |
| Total | 20 | 72 | 108 | 97.00 | 93.85 | 11.008 | |
| 5-month follow-up | Norfolk | 4 | 90 | 111 | 98.00 | 99.25 | 9.979 |
| London | 3 | 80 | 103 | 84.00 | 89.00 | 12.288 | |
| North-east | 4 | 75 | 111 | 92.50 | 92.75 | 17.017 | |
| Total | 11 | 75 | 111 | 92.00 | 94.09 | 12.888 |
FIGURE 10.
Dementia Quality of Life scale total scores: box and whiskers plot.
| Time point | Centre | DEMQOL: feelings | DEMQOL: memory | DEMQOL: everyday | |
|---|---|---|---|---|---|
| Baseline | Norfolk | n | 4 | 4 | 4 |
| Mean | 42.75 | 20.25 | 34.75 | ||
| SD | 6.397 | 1.500 | 1.500 | ||
| London | n | 4 | 4 | 4 | |
| Mean | 42.25 | 19.50 | 31.75 | ||
| SD | 1.708 | 3.109 | 3.686 | ||
| North-east | n | 12 | 12 | 12 | |
| Mean | 39.42 | 19.92 | 33.33 | ||
| SD | 8.372 | 3.848 | 2.674 | ||
| Total | n | 20 | 20 | 20 | |
| Mean | 40.65 | 19.90 | 33.30 | ||
| SD | 7.066 | 3.243 | 2.755 | ||
| 5-month follow-up | Norfolk | n | 4 | 4 | 4 |
| Mean | 44.00 | 20.00 | 35.25 | ||
| SD | 5.715 | 4.082 | 1.500 | ||
| London | n | 3 | 3 | 3 | |
| Mean | 38.67 | 17.67 | 32.67 | ||
| SD | 6.351 | 4.726 | 3.215 | ||
| North-east | n | 4 | 4 | 4 | |
| Mean | 38.75 | 21.00 | 33.00 | ||
| SD | 10.532 | 2.944 | 3.830 | ||
| Total | n | 11 | 11 | 11 | |
| Mean | 40.64 | 19.73 | 33.73 | ||
| SD | 7.632 | 3.744 | 2.936 | ||
FIGURE 11.
Dementia Quality of Life scale domain scores: box and whiskers plot.
Safety: serious adverse events
In London, two serious adverse events were reported. One involved a carer being admitted to hospital and one involved a patient (from a separate dyad) being admitted to hospital. These admissions were the result of falls and were unrelated to the study but were expected because of the nature of the patient and carer population. In the north-east, four serious adverse events were reported. One patient was hospitalised twice, both times because of a fall. Another patient suffered a fall and one patient was hospitalised with suspected pneumonia. Again, these serious adverse events were expected because of the age of the patients recruited. No serious adverse events were reported in Norfolk.
Costs
Case management salary costs for WP2 amounted to £52,890 across all sites. Training and mentoring by an Admiral nurse cost £5201 and £6273, respectively.
Chapter 5 Implementing the pilot study: review of processes and procedures
As part of the embedded qualitative study, data were collected on a number of aspects of study processes and procedures, including:
-
recruitment processes
-
acceptability and feasibility of outcome measures
-
patient and carer views on study participation
-
case manager and mentor views on study procedures.
Data on study processes and procedures were obtained through interviews with stakeholders and from reflective field notes made by the researchers responsible for conducting the baseline assessments. Although all researchers recorded whether or not there had been any problems relating to consent, detailed field notes on the conduct of the baseline assessments were kept for only one site.
Recruitment processes
One aim of the feasibility study was to explore whether or not it was possible to recruit 11 patient–carer dyads from each of the four participating practices. As described earlier, none of the participating practices succeeded in recruiting the target number of dyads. Factors influencing recruitment, explored through the qualitative interviews and documentation on the consent process, are summarised below:
-
the user-friendliness of the information provided to patients and carers
-
the extent to which practice dementia registers were comprehensive and up to date
-
the introduction of additional screening criteria by the case managers and other professionals within the practice
-
the complexity of the recruitment process, which involved a series of contacts by up to three different individuals (GP, case manager and researcher).
Accessibility of patient and carer information sheets
Both the mentor and the case managers expressed concern over the language used within the recruitment letter and information sheets:
I suppose for me at the beginning, we’ve got the title ‘effectiveness of collaborative care’ and straightaway I’m thinking that’s going to exclude quite a lot of people straight away you know if they’re reading that, they might go, ‘oh well what do those words mean?’
Case manager
The failure to provide information in appropriate community languages was criticised, and it was thought that the information was inaccessible to many people for whom English was not their first language (participants who could not read English were excluded from this study):
There are issues around the documentation not being user-friendly for those where English is not their first language. And there was a delay, there was this one particular gentleman who has dementia where he was put to one side because he didn’t understand the wording and he had to wait until his son could read and interpret it for him.
Mentor
Although none of the patients or carers recruited to the study commented on the documentation, this may reflect the possibility that only those people who understood the participant information sheet agreed to take part in the study.
Problems with practice dementia registers
The practice QOF dementia registers were used to identify potential participants. However, additional searches of electronic medical records indicated that several patients being treated with cholinesterase inhibitors had not been included in these registers. Careful review of their medical records indicated that in some cases a formal diagnosis of dementia had not been made; instead, terms such as ‘cognitive impairment’ or ‘memory problems’ had been used as diagnostic labels in the letters received from secondary care specialists. At other times, patients were not included on the practice dementia registers because, although they had been given a formal diagnosis, the initial Read Code used to describe their symptoms (e.g. ‘memory problems’) had never been updated. It was therefore necessary to use different search strategies to identify patients with dementia:
There was a list of ‘possibles’ with those who may have had medication for dementia but were not coded as being a dementia patient. So she [case manager] went through those . . . and found some more.
Practice administrative staff
Discussions with GPs within the practices also highlighted other potentially eligible patients who were not included on the practice dementia registers:
I have been in a couple of the GP meetings . . . and the GPs were in fairness, they were very keen, they were very enthusiastic and they were all shooting names out of patients . . . ‘oh you know I think Mr and Mrs Anybody here or bla bla bla there, they would be perfect, could you look at them?’ . . . but it was interesting these people they were suggesting weren’t on the list [the QOF dementia register].
Case manager
The patients identified by the GPs could have been added to the practice dementia registers and thereby become eligible for inclusion in the study, providing that a formal diagnosis of dementia had been made and communicated, but this opportunity to increase recruitment was not explored. The failure to capitalise on the interest shown by the GPs in referring patients may have affected recruitment within these practices, as the following suggests:
I mean they showed some initial interest in referring cases and I think if they could have done that it would have been very different but obviously they couldn’t, we weren’t open to the GPs referring people in so I think . . . that they really didn’t bond with it.
Case manager
A further shortcoming of the practice dementia registers was that information on place of residence was not always up to date, meaning that patients on the register were not always eligible for the study:
It’s been very difficult to recruit because the last time I was sat in her [case manager’s] office we went through the QOF register together and it’s not up to date enough, so by the time she gets to actually ringing and doing follow-ups people have either gone into residential care or the situation has changed, they’re in hospitals, they’re acutely ill and it’s not appropriate to approach them.
Mentor
Information on carers was not always clearly recorded in the records, adding to the difficulties of identifying eligible patients:
To be honest for some of the records they didn’t have a next of kin on, it was blank. For example, I remember a lady who’s 69, diagnosed with Alzheimer’s disease . . . and there was no next of kin. I didn’t know if she lived alone and I didn’t know if she had any daughters, any other family but it was only when I went into the consultations [section], there was a little message to say ‘attended with husband’.
Case manager
Introduction of additional screening criteria
In some instances the inclusion/exclusion criteria from the study protocol had been modified or amended during the process of screening patients for the study. For example, one case manager excluded patients aged < 65 years and in another practice the requirement for patients to have a family carer became the perceived need for a co-resident carer:
I think the goal post kept shifting a little bit as well as to who was eligible and who wasn’t eligible. To begin with they had to live with a carer and then it wasn’t necessarily that they had to live with a carer, the carer could live miles away.
Case manager
Although both of these errors were identified and corrected, the potential for misinterpreting the inclusion/exclusion criteria was clear. The issue of whether or not patients who were already receiving a form of case management should be excluded was an ongoing source of confusion for both research team members and the case managers themselves. It also became apparent that in most practices there were multiple layers of ‘informal screening’ by other members of practice staff, during which patients who (for unspecified reasons) were ‘not suitable’ or ‘not amenable’ were excluded, as the following extract illustrated:
Straightaway I was with my nurse manager who could say yes, no, yes, no, yes, no.
So how could she say yes, no, yes, no?
Because she knows them, she’s been in the surgery for 15 years she knows lots of patients very well.
But on what basis is she saying yes or no?
From the criteria.
Oh right ok so we have the criteria.
It was housebound and living in residential or being too mad, too ‘past it’ to actually benefit.
Was it housebound? Is housebound in there?
Well she was putting housebound by lots of them so no but it was if they could come to surgery we were looking at it from that perspective or how long ago she had seen them.
I see, right.
So she was looking at it from a practical point of view without knowing all the variables I suppose and then I spoke to one of the senior partners who had another spin on who would be amenable.
Right.
Because obviously some families as a feasibility it probably wouldn’t work with and of course they have the right to refuse which is fine.
Complexity of the recruitment process
A final barrier to recruitment was the complexity of the recruitment process; patients and carers were initially sent a letter and were then telephoned by either the case manager (when this was a practice nurse) or a GP and contacted by a researcher, who then completed a baseline assessment before any contact was made by the case manager. As well as possibly being off-putting to patients and carers, delays between contacts and a potential lack of consistency between the various members of the practice making the telephone calls were identified as potential barriers to recruitment:
There’s also, in terms of consistency of approach that’s diluted isn’t it because you may have one person with a particular approach doing a follow-up call and somebody else in the practice doing the next follow-up call.
Mentor
Even when details had been passed on to the research team, it was not always straightforward to make contact with patients and carers. Multiple telephone contacts had to be made with many participants to arrange an appointment. Carers were sometimes not able to speak on the telephone because they were busy with other commitments, for example work or care of grandchildren; the telephone numbers provided by the GP practices were not always up to date; participants did not always answer the telephone (either because they were not at home or they picked up the telephone only when they recognised the number of the person calling); participants did not always respond to telephone messages left by the researchers, necessitating further calls; and sometimes participants reported that because of hospitalisation or family problems they were not able to take part at the moment but would like to be contacted again in the near future.
There were also tensions over whether it would be more appropriate to call the patient or carer first when they did not live together. Some patients asked us to contact their relative instead; others were happy to be called but clearly experienced difficulties with short-term recall and retaining information about the purpose of the call. One perceived consequence of this approach to recruitment was that study participants were not representative of the broad group of community-dwelling people with dementia, with the complex recruitment process off-putting to those people in greatest need of support:
I think there is a concern, for me anyway, that the people we’re getting are quite well educated, quite middle class, quite skilled, resourceful client group. . . . I think it is a little alarming that we’re not getting the people who are from a lower socioeconomic class who maybe don’t have the skills and resources and who maybe are in a bit more crisis.
Case manager
Process of seeking informed consent
A structured form was produced on which the researchers recorded their experiences of obtaining informed consent from patients and carers. Information on the process of recruitment was available for 23 patients and 23 carers. In nearly all cases consent was obtained from the patient and carer at the same visit. When two researchers attended, typically the process of explaining the study was carried out with the patient and carer together; one researcher would then focus on taking consent from the patient and one would focus on taking consent from the carer. Three carers were seen by themselves and one couple was seen with their daughter. Typically, the process of explaining the study and seeking consent took about 20 minutes, although in two cases it took > 25 minutes. One person with dementia seemed very acquiescent and it was difficult for the researcher to gauge her level of understanding; following discussion she was thought to lack capacity to consent and a personal consultee form was completed. The second very long consent process was with a couple; in this case, the patient wished to discuss every aspect of participation in detail, often losing track of the discussion.
Clarification of the patient information sheet was required by five patients and four carers; most of the queries related to issues that were of particular relevance to individual participants (e.g. arrangements for accessing usual care, reassurance regarding confidentiality and questions about the case manager). One carer requested that the patient information sheet was not used with her mother because it included the term ‘memory problems’. Clarification of the consent form was required more frequently (for 10 patients and seven carers). Typical issues noted by the researchers were the need to remind participants to initial rather than tick the boxes; to provide assistance to patients; or to explain the sections relating to a personal consultee and the qualitative interviews. Two patients had difficulties completing the form because of problems with fine motor co-ordination; others had difficulties with writing their initials:
The patient found it very difficult to complete information due to his ability to write and hold a pen. Made him slightly embarrassed, I completed some of the form for him.
Referring to patient B12
The consent form seemed too long and complex for someone with memory problems. Whilst cognitively capable of understanding the form, the patient was quite slow signing her initials and it felt quite uncomfortable having to keep asking her to sign the various boxes. She was aware that she was quite slow and made some self-detrimental comments (e.g. about being ‘useless’).
Referring to patient B03
The most frequent comment made by the researchers about the process of consent was that the form was too long for people with dementia; the fact that it ran over two pages was thought to generate confusion.
Acceptability and feasibility of the outcome measures
Details of completion rates of outcome measures are reported in Chapter 4. The data suggest some blurring of boundaries between the assessments carried out by the researchers and the work with case managers. Participants sometimes perceived members of the research team to be a source of support and someone to ‘open up to’, with assessments and interviews being perceived to have therapeutic value:
She was really putting on a brave face . . . and clearly seeking reassurance and comfort. She said I was the only person she had spoken to about this, and she normally hides herself away in her room or throws herself into something like decorating as a distraction.
Field notes, B10
Specific issues relating to the outcome measures for patients are described first, followed by a description of problems noted with the outcome measures for carers.
Outcome measures for patients
Only two outcome measures were administered to patients: the MMSE and the DEMQOL scale (a measure of health-related quality of life for people with dementia). The MMSE was administered first as the DEMQOL scale is not appropriate for people with severe dementia (MMSE score < 10). In general, the assessment with patients took between about 30 and 60 minutes. Although some patients seemed to take the assessment in their stride, it was clear that others became anxious and, at times, seemed stressed by the questions:
After the assessment, I asked the patient how he had felt about answering all of these questions. He said that there were quite a lot and he was worried that he hadn’t done very well. I reassured him that he had done well.
Field notes, B04
Mini Mental State Examination
The MMSE was abandoned with three participants as the researcher considered them too cognitively impaired to continue. Some practical issues with completing the MMSE emerged for patients who had difficulty writing because of other conditions such as arthritis or Parkinson’s disease:
The participant had struggled to sign his name on the consent form and I was unsure whether or not to ask him to write the sentence. I gave him the option and said he should stop at any time if he wanted to. He really gave this a good attempt despite his significant tremor but was unable to complete it. When he really started to shake I asked if I could complete if for him. It was clear that he was trying to write ‘wish you were here’ and understood the concept of a sentence but lacked the motor skills to be able to complete it. I did not ask the participant to attempt the intersecting pentagons as he had commented on how he was ‘hopeless’ and the writing task had clearly made him upset.
Field notes, B04
Some patients were familiar with the MMSE (having previously completed it at the memory clinic). Knowing what to expect was comforting for some participants but created anxiety for others. ‘Serial sevens’ (in which participants are asked to deduct seven from 100 and then to keep subtracting sevens from their answers) seemed to cause respondents the greatest anxiety, regardless of overall score or performance:
B51 commented that she was pleasantly surprised that the questions were OK – and they weren’t too personal. During the MMSE, she commented on her lack of arithmetic skills (and serial 7’s was the only question she really seemed to struggle with).
Field notes, B51
Some patients expressed an awareness of being ‘tested’, which made them defensive or concerned about getting the right answers:
MMSE – PWD [person with dementia] wasn’t particularly happy about doing this, and I said that she didn’t have to do anything she wasn’t happy with. Husband was still present and encouraged her to have a go at least. She warned me that she hated maths and wouldn’t do those (but she did and got 5/5). It was quite amusing when she wrote what she thought about doing the assessment in the ‘write a sentence task’ (I am sick of this test!). She was jokingly defiant with me when she handed it back and was laughing.
Field notes, B09
Dementia Quality of Life scale
All researchers involved in baseline assessments highlighted problems with the wording of the DEMQOL scale. The initial questions of the DEMQOL scale, which focus on feelings, begin with the stem, ‘In the last week, have you felt . . .’ and were generally straightforward to administer. However, the questions relating to memory and everyday life start with the stem, ‘In the last week, how worried have you been about . . .’. Several patients responded that they ‘never worried’ or that they were ‘not a worrier’ when asked the first question in these sections; but we then had to ask a further 14 questions asking how worried they had been about various aspects of their life. Ironically, one of the later questions asks, ‘how worried have you been about people not listening to you’. The extract from field notes in Table 16 illustrates the verbatim responses spontaneously given by one patient (B06).
| In the last week how worried have you been about: | Response |
|---|---|
| Difficulty making decisions |
|
| Not having enough company |
|
| How you get on with people close to you |
|
| Getting help when you need it |
|
| Getting to the toilet on time |
|
A further concern was that a small number of patients asked us ‘whether I should be worried’, suggesting that we were potentially creating anxiety. Even when the specific issue was a problem for patients, they did not always ‘worry’ about it, as in the example below:
The patient’s main comments were that he experienced problems with his memory – but he wasn’t really worried about them. He said that because of this, he found it hard to choose a response.
Field notes, B02
These problems with the DEMQOL scale were not universal; however, eight of the 12 patients for whom detailed field notes were made and who completed the DEMQOL scale reported that they did not worry. This suggests that this was not an isolated issue relevant to one or two patients. For other patients administration of the measure was straightforward:
The patient had no problems in understanding any of the questions, and seemed to understand and apply the appropriate response options. The options seemed unproblematic, and only a few times did I have to clarify which response would be most appropriate based on her verbatim responses.
Field notes, B10
Other participants found the response categories problematic, explaining that they did not capture their perceptions and experiences:
It was a real challenge (understatement), to get the respondent to use the four response options to the questions. He would discuss at length how inadequate each response option was and how this did not reflect his experiences. This was not a case of the patient being unable to grasp the concepts – anything but. He fully understood them, but found them unrepresentative and ‘badly phrased’ – he particularly took umbrage with the phrase ‘quite a bit’ – stating that this wasn’t particularly positive and ‘bit’ meant only a small amount. . . . The tack I found effective was to get the patient to respond in a way he felt was relevant, note these verbatim, and then choose an appropriate response. I explained this to him and put it to him that the only other alternative would be to abandon the questionnaire. He was keen to keep going and commented that this would end his sport for the afternoon!
Field notes, B05
Some patients also commented that basing their responses on the previous week would not be representative as that week had been atypical:
The first 5 questions about feelings in particularly prompted her to give a lot of context to her feelings and how this was not a typical week (as she had a visit to her sister who lives at the other end of the country) and how she was more likely to rate things positively in some ways, but then felt a bit down and tired on return – so there could be a negative influence on some questions too.
Field notes, B09
The guidance on the DEMQOL scale suggests that it is not suitable for patients with severe dementia (MMSE score < 10). However, one participant with an MMSE score of 14 was considered unable to grasp the concept of the assessment and the DEMQOL scale was abandoned.
Outcome measures for carers
Given the option, carers generally preferred the self-completion questionnaires to be administered by the researcher rather than completing them independently.
Neuropsychiatric Inventory
The main problem with administering the NPI was that carers sometimes found it difficult to quantify aspects of patients’ behaviours, particularly in terms of frequency rather than severity.
She found some aspects of the NPI hard to quantify in terms of frequency. Specifically in relation to certain behaviours (G – apathy/indifference; L – appetite and eating). She felt that these weren’t ‘one off or individual’ episodes, but things that were either present or not.
Field notes, B01
Carers who did not live with the patient understandably found it difficult to answer questions about sleeping habits.
Bristol Activities of Daily Living Scale
Although the BADLS was considered relatively straightforward by most participants, some carers felt that the response categories did not fit well, especially around finance. This is perhaps complicated by matters such as power of attorney and may not reflect the severity of functional impairment:
The question about finance was problematic; she described how mother repeatedly sits and counts money and can sign her name but doesn’t need to deal with money since her daughter deals with it all.
Field notes, B10
General Health Questionnaire
This questionnaire caused considerable distress for several participants. Section D – relating to negative aspects of mental well-being and including issues such as suicidal thoughts – proved particularly emotionally challenging and resulted in several carers becoming tearful and upset:
GHQ – Question D1 caused the carer to break down. This came from the left-field as, up until then, she had shown no signs of being distressed or stressed either when completing the questionnaires or in our general discussions. We took a small break; I reassured the carer and asked if she wanted to get a drink/tissue etc. I asked her if she was fine to continue and she said she was. I reassured her that lots of people found this section difficult and she said she was fine to continue and suggested we just ‘blasted through them’!
Field notes, B06
The wording of some questions was unfamiliar; in particular, some participants were unsure of the meaning of to ‘make away with yourself’.
European Quality of Life-5 Dimensions
Respondents generally found this measure straightforward and easy to complete (including the visual analogue scale).
Client Service Receipt Index
Although the researchers who were familiar with the CSRI from earlier research studies found this measure straightforward to complete, those who had not previously used this measure experienced a number of problems. The design of the CSRI could be improved to facilitate data entry for analysis; for example, the addition of a column indicating whether or not services had been used would eliminate the need to record that the frequency of service use was ‘zero’ for services with which there had not been any contact.
Overall, carers often found events over a 6-month period difficult to recall. This particularly related to service use for themselves and patients. Carers often relied on secondary sources such as diaries and care plans to facilitate accuracy. Carers lacked confidence in reporting financial benefits; although they could describe receiving benefits, they were often unsure of the official name.
Other areas of difficulty related to quantifying the length of time that patients could be left alone (for those who lived with the patient) and quantifying how much support they provided (for carers who did not live with the patient). Husbands and wives of patients sometimes reported that they had always done everything together and so did not spend time apart; non-co-resident carers sometimes reported that family members provided a network of support:
The carer struggled to quantify one particular question on CSRI (about the amount of time he is able to leave his wife for), as he doesn’t really do this. He wanted to give a ‘not applicable’ response (however this is not an option). He recounted a couple of rare examples when he would leave his wife but how it was impossible to put a time on this as he would never leave her so long that she would become distressed, and this hasn’t happened yet ‘touching wood’.
Field notes, B11
The range of response options was also queried in relation to other questions on the CSRI. For example, the daughter of one couple organised all of their finances. Neither the patient nor the carer knew which benefits they received but there was not a ‘do not know’ response option.
Patient and carer views on study participation
This study explored the feasibility and acceptability of case management delivered as part of a research study rather than as part of an established service. Many of the patients and carers participated in the study because of their desire to support research, rather than because of their need for case management. Although some participants identified personal benefits from case management, this was perceived as a bonus. Altruistic drivers for participation include a desire to help others through improving services; to more broadly raise awareness about dementia and its effects on patients and carers; and to contribute to research in general:
I think it’s been good. Like I say, when we were first offered it from the doctor we didn’t even know what it was. She just said, ‘It’s CAREDEM research . . . something to work out of the doctors’ surgeries.’ I said, ‘Yes. Anything to make people aware; I think it’s a good thing. Really.’
B02, carer
One dyad in particular felt empowered by participation in the research and felt that they may now be in a position to help others in a similar situation and described how they might like to take on a supporting role. Other participants expressed how participating had made them ‘visible’ again and ‘got the ball rolling’ in terms of access to services. As mentioned earlier, some participants found participation in the baseline assessments and qualitative interviews useful for airing issues that might otherwise not have been identified, as the following extract illustrates:
just hold on a second, the fact that you are here has brought up issues that we’ve discussed while you have been here about you know obviously mum’s feelings have changed about going to the . . .
Alzheimer Society.
Alzheimer’s meeting you know, so the fact that you are here has addressed that again which I’ll now . . .
Well I think you have to face the situation you are in and help yourself the best you can.
But last time we did have the conversation you didn’t feel that way mum, so you know that’s good you know and I know.
Well that’s cleared the air isn’t it?
Patient and carer, C04
Case manager and mentor views on study procedures
In addition to identifying, recruiting and case managing people with dementia and carers, the case managers were also expected to undertake a range of research activities (e.g. completing a recruitment log, allowing members of the research team to observe assessments and participating in interviews and informal discussions). When members of the research team were based in the same geographical area there were more opportunities to build relationships and to have informal meetings; however, the multiple demands on the case managers could lead to tensions over workload:
I felt that sometimes I was getting lots of emails from people saying ‘could I do this, could I do that, have you done the log, have you done this paperwork’ . . . I didn’t think people really understood the role of a practice nurse.
Case manager
I wish your research team would see that as a whole afternoon, that it isn’t just the assessment, you don’t just write. If you see a couple in an assessment then you have to formulate what their needs are, that all has to be done in the office.
Mentor
There could also be tension between the requirements of the research team to collect data, for example by observing the case manager undertaking assessments, and a case manager’s desire to prioritise patient and carer needs:
I think it’s been quite hard to avoid the fact that ultimately this has been for the benefit of the study not for the service users or patients and carers etc. And I think . . . there has been a feeling that the participants don’t really matter and that they are just tools to gather this information to get a research paper out of it.
Case manager
At other times, members of the research team were regarded as a key source of support by case managers, providing a sounding board or an opportunity to discuss issues arising with the practices or clients:
You’ve been very supportive and helpful throughout which I appreciate isn’t really part of your role . . . I think certainly for day-to-day support, discussing cases, discussing where the project is going, you’ve been the main link really and again you’ve been absolutely fantastic.
Case manager
The expectations placed on the case managers at the outset of the project (particularly the practice nurses) were articulated by a team member:
These poor case managers have half a day a week to get their heads round dementia, recruitment, case management, research, mentor’s training; so many new elements are thrown at them at once.
Team member
The familiarity of the research team with recruitment processes, in particular applying inclusion and exclusion criteria, meant that the difficulties that the case managers experienced with these research tasks were underestimated. Although the mentor was in regular contact with the site principal investigator, more formal links and systematic communication between the research team, mentor and case managers may have helped develop a better understanding of the research process:
Where I think it would have been so much better was if communication all round had been better . . . I don’t think we ever had the time to do all of that but you know part of, it’s all that soft intelligence that comes out of informal conversations and things that perhaps wouldn’t be recorded on a documentation or in an email which is really helpful to keep in touch and have that continuity which I feel I was sort of out of the loop really.
Mentor
Chapter 6 Capturing what case managers do
Case notes and data extraction
Structured forms were provided for data collection but were underused by case managers who generally preferred to write freehand notes. To provide a description of case management in practice, two researchers (CB and AW) jointly reviewed all available documentation for each participant and systematically coded the information for analysis. Documentation included:
-
the formal paperwork provided
-
freehand notes produced by the case managers
-
correspondence sent to GPs to summarise the case management intervention.
To illustrate this process, Table 17 provides an extract from the case manager notes and the way in which this was coded.
| Extract from case manager notes | Researcher coding |
|---|---|
|
PWD unmet need relating to coping with dementia-related problems |
|
PWD unmet need relating to physical well-being |
|
PWD unmet need relating to emotional well-being; carer unmet need relating to emotional well-being |
Actions taken were similarly coded; a code was included to indicate when investigations were already under way by another professional. The full coding frame was a slightly modified version of the documentation provided to case managers.
Limitations of the data
The lack of consistent use of the formal documentation was not ideal as the researchers had to rely largely on the narrative accounts provided by the case managers. The researchers’ interpretation of needs was not necessarily consistent with that of the case managers. For example, one case manager recorded that a couple had ‘no unmet needs’ despite documenting that the husband’s (carer’s) sleep was disrupted to the extent that he is ‘frequently tired during the day’. Any statements that seemed to indicate an underlying need were coded.
Through informal discussions with case managers, observations of case management and contact with patients and carers, the researchers were aware that contacts and actions were under-reported by all of the case managers.
The researchers were also aware of the potential for introducing bias when they had previous knowledge of the patients and carers (either through baseline assessments or qualitative interviews). By undertaking the coding jointly, the two researchers working from different research sites were able to ensure that they relied solely on what was recorded in the paperwork provided by the case managers.
Demographic information on patients and carers
In designing the paperwork the team was mindful of the need to avoid unnecessary duplication of information; however, a section on demographic information was included as not all of this information was always readily available in the GP records. Table 18 shows the documentation of participants’ demographic information by case managers.
| Information | Recorded | Not recorded |
|---|---|---|
| Age/date of birth | 19 | 5 |
| Gender | 24 | 0 |
| Living arrangements | 22 | 2 |
| Diagnosis (type of dementia) | 19 | 5 |
| Year of diagnosis | 17 | 7 |
| Preferred language | 12 | 12 |
| Religiona | 12 | 12 |
| Ethnicity | 18 | 6 |
| Number of informal carers | 11 | 13 |
Although the case manager working in the most multicultural area always recorded religion and ethnicity, those based in more culturally homogeneous environments were less likely to consistently record this information. Whether or not a patient’s religion had implications for the way in which services were provided was noted for only around half of those patients (n = 7) whose religion was recorded. One case manager recorded no information on the number of informal carers; this appeared to be because of a photocopying or printing error on the recording sheets used.
Although worksheets were available for recording information on more than one carer these were so rarely used that we focus only on information relating to the main carer. In general, case managers were less likely to record information relating to the main carer than information on the person with dementia (Table 19). Whether or not a statutory carer’s assessment had been undertaken was documented for only half of the carers and this varied significantly between case managers.
| Information | Recorded | Not recorded |
|---|---|---|
| Age | 15 | 9 |
| Gender | 23 | 1 |
| Relationship to patient | 23 | 1 |
| Employment status | 15 | 9 |
| Statutory carer’s assessmenta | 13 | 11 |
| Preferred language | 11 | 13 |
| Religion | 7 | 17 |
| Ethnicity | 13 | 11 |
| Whether or not registered with the same GP practice | 17 | 7 |
We also compared the recording of demographic details according to the professional background of the case managers, but there were no differences in the amount of missing data between the case managers who were practice nurses and the case manager from a social work background.
Type and frequency of contact
Details were recorded for 63 contacts, the majority of which were with patients and/or carers (n = 59); it was not clear whether the case manager had seen the patient, the carer or both for 15 contacts. Only four contacts with other professionals were recorded: two with GPs, one with an old age psychiatrist and one with staff from the local Alzheimer’s Society.
The number of contacts with patients (either alone or with the carer) ranged from zero to eight (mean 1.08) whereas the number of contacts with carers (either alone or with the patient) ranged from zero to six (mean 1.42). The median number of contacts per patient–carer dyad differed significantly by case manager (independent samples median test p < 0.001) (Table 20). Although two of the case managers predominantly had a single contact with each of the patient–carer dyads recruited to the study, one case manager had an average of just over five contacts per patient–carer dyad. This case manager was also the only one to record any contacts with patients only (see Table 20). It is noteworthy that the case manager with the greatest number of contacts was one of the practice nurses who had only half a day per week allocated to case management.
| Case manager | Number of patients | With patient and/or carer | Other | All | |||
|---|---|---|---|---|---|---|---|
| Patient only | Carer only | Together | Not specified | ||||
| 1 | 9 | 10 | 17 | 10 | 6 | 3 | 46 |
| 2 | 6 | 0 | 0 | 3 | 4 | 1 | 8 |
| 3 | 9 | 0 | 1 | 3 | 5 | 0 | 9 |
| Total | 24 | 10 | 18 | 16 | 15 | 4 | 63 |
To achieve this number of contacts within the allocated hours, the case manager relied extensively on telephone follow-ups, although she also had an initial face-to-face meeting with each patient–carer dyad. The type of contact varied significantly by case manager (applying an extension of Fisher’s exact test p < 0.001) (Table 21).
| Case manager | Number of patients | Type of contact | Total | |||
|---|---|---|---|---|---|---|
| Face-to-face | Telephone | Letter/e-mail | Not specified | |||
| 1 | 9 | 10 | 26 | 0 | 10 | 46 |
| 2 | 6 | 3 | 0 | 2 | 3 | 8 |
| 3 | 9 | 3 | 0 | 0 | 6 | 9 |
| Total | 24 | 16 | 26 | 2 | 19 | 63 |
Needs identified
The 14 areas of need included in the paperwork were grouped into five broad areas for analysis: daily living and routines (including informal or social networks); physical well-being and medication; emotional well-being and support (including willingness to accept help, adjusting to diagnosis and managing transitions); coping with dementia-related problems (including behavioural and psychological symptoms); and financial and legal needs (including access to benefits and lasting power of attorney). The frequency with which needs in each of these areas were identified for patients and carers is shown in Table 22. Case managers were more likely to document unmet needs than met needs or areas in which there were currently no needs for both patient and carer. Unmet needs were more likely to be recorded for patients than for carers in all areas with the exception of financial and legal needs, which were documented more frequently for carers (see Table 22).
| Area of need | Patient | Carer | ||||
|---|---|---|---|---|---|---|
| No need | Met need | Unmet need | No need | Met need | Unmet need | |
| Daily living | 8 | 10 | 20 | 1 | 0 | 10 |
| Physical well-being and medication | 0 | 5 | 22 | 1 | 2 | 3 |
| Emotional well-being and support | 6 | 2 | 15 | 6 | 2 | 10 |
| Coping with dementia-related problems | 5 | 2 | 20 | 0 | 2 | 5 |
| Financial and legal needs | 1 | 4 | 3 | 0 | 2 | 8 |
| All needs | 20 | 23 | 80 | 8 | 8 | 36 |
Examining the needs identified by different case managers indicated that, although they identified a similar range of needs in relation to patients, there were significant differences in the types of carer needs identified (p < 0.01). The areas of need with most variation between case managers were daily living and routines (which accounted for between 9.1% and 50.0% of carer needs identified); emotional support and well-being (accounting for between 0% and 47.1% of carer needs identified); and financial and legal needs (accounting for between 5.9% and 54.5% of carer needs identified). When examined by the professional background of the case managers, there were no significant differences in the areas of need identified, suggesting that the variation reflected personal differences in style rather than professional training.
Actions taken
The actions taken for unmet needs are summarised in Table 23; as can be seen there was a discrepancy between the number of unmet needs identified (n = 116) and the number of actions recorded to address these (n = 58). Although a small number of actions were recorded that were not specifically linked to unmet needs, there was no documented evidence of any action being taken for almost half of the unmet needs identified. There was only one recorded instance of a case manager giving a patient–carer dyad one of the leaflets produced in WP1.
| Action | n |
|---|---|
| Provision of written information | 6 |
| Provision of verbal advice/information | 16 |
| Advocating | 1 |
| Identify appropriate services | 3 |
| Liaise with professionals | 6 |
| Monitoring | 2 |
| Referral | 10 |
| Other | 6 |
| No action, being addressed by other professional | 8 |
| All actions | 58 |
The extent to which actions were taken by area of need is summarised in Table 24. Seven unmet needs that were being addressed by another professional have been excluded. Overall, at least one action was recorded for 25.7% of patient unmet needs and for 48.6% of carer unmet needs. The proportion of needs for which actions were recorded varied significantly by area of need for carers (p < 0.001) but not for patients. Actions were most likely to be recorded for financial and legal unmet needs; this may reflect the clear referral pathway for such needs.
| Area of unmet need | Patients | Carers | All | |||
|---|---|---|---|---|---|---|
| No action recorded | Action recorded | No action recorded | Action recorded | No action recorded | Action recorded | |
| Daily living | 13 | 7 | 9 | 1 | 22 | 8 |
| Physical well-being and medication | 12 | 5 | 3 | 0 | 15 | 5 |
| Emotional well-being and support | 13 | 2 | 4 | 5 | 17 | 7 |
| Coping with dementia-related problems | 16 | 3 | 2 | 3 | 18 | 6 |
| Financial and legal | 1 | 2 | 0 | 8 | 1 | 10 |
| All unmet needs | 55 | 19 | 18 | 17 | 73 | 36 |
There were significant differences between case managers in the likelihood of some actions being recorded for unmet needs (range 25.0–51.8%, p = 0.05); further analysis indicated that the proportion of patient unmet needs with actions was similar for all case managers, whereas the proportion of carer unmet needs with actions varied significantly (from 25.0% to 81.8%, p < 0.05). The differences between case managers were not linked to their professional background. Case managers were equally likely to record actions for patient and carer unmet needs in all areas of need with the exception of needs relating to emotional well-being and support, which were more likely to be addressed when identified for carers than for patients (p < 0.05).
The discrepancy between unmet needs and actions recorded may in part reflect the different judgements of the researchers and case managers, as in several sets of notes the case manager explicitly stated that the patient and carer had ‘no unmet needs’ despite having clearly documented a number of areas in which there appeared to be unmet need. One example of such a discrepancy, mentioned earlier, is illustrated in Table 25.
| Extract from case manager notes | Researcher coding |
|---|---|
|
PWD unmet need relating to physical well-being PWD unmet need relating to emotional well-being |
|
PWD unmet need relating to daily routines |
|
PWD unmet need relating to coping with dementia-related problems Action – physical well-being being addressed by other professional |
|
PWD unmet need relating to coping with dementia-related problems Carer unmet need relating to daily routines Carer unmet need relating to physical well-being |
Views on the documentation
During interviews and informal discussions with case managers and other team members we explored the reasons for the limited use of the documentation and lack of systematic recording of activities. Given that the case managers were experienced professionals within their own disciplines and were used to the requirement to record contact with patients/clients, we had not anticipated the problems with documentation. Key reasons for the limited use of the documentation are summarised in Box 1 and explored in detail below.
-
Lack of ownership.
-
Inadequate training.
-
Resource issues (time, access to printer/computer).
-
Lack of supervision.
-
Problems with the documentation provided.
-
Lack of familiarity with research.
Lack of ownership
Much of the work on developing the documentation had to take place before the appointment of the case managers. Once the case managers were in post, the emphasis initially was on providing induction and on identifying potential study participants. As a result, there was little opportunity for the case managers to contribute to the refinement of the documentation. The lack of clarity over the role of case management added to the difficulties in co-designing the paperwork. One case manager reviewed the documentation and felt that it was workable; however, she then resigned. As a result of the lack of involvement of the other case managers in designing the paperwork, they may have had little sense of ownership or commitment to using the documentation.
Although increased ownership may have improved both the paperwork and compliance with recording, within statutory services staff are expected to comply with existing recording systems without having ownership over them. Such discrepancy may need to be further explored in other studies.
Training in research instrument use
A brief session to introduce the documentation was included in the first meeting of the case managers, which took place in May 2012. Unfortunately, one of the case managers was unable to attend this meeting; for this case manager the introduction to the documentation was limited to sessions with the case manager mentor, which were already time pressured. The poor completion of the documentation and confusion over certain sections, in particular the log of contacts, reflected the case managers’ lack of understanding and familiarity with the paperwork:
[Case manager] asked if s/he should set up a log of contacts to share with the research team. I suggested that this would already be captured via the paperwork but s/he didn’t think this would be.
Field notes of telephone conversation with case manager
Resource issues
Time pressures were a recurrent problem for those case managers whose input was limited to one session per week. The perceived time required to complete the paperwork was highlighted as a key barrier:
I’m finding in my visits, documenting everything I want is really difficult . . . I do use the pack the 11 pages that you’ve given me. Do I fill everything out beautifully? No. Do I get back to it when I want to all the time? No. Have I got a good sense of what happened in that meeting? Yes. What I’ve worked out is that I need to have time fairly soon after that meeting to write more coherent notes, have I been able to do that every time? No I haven’t. It’s time.
Case manager
In addition to the time requirements, concerns were also raised about the potential duplication of work if the case managers had to record their work in both the practice electronic record system and the separate documentation for the research project. Although concerns were raised over the time required to complete the documentation, the paperwork requirements were seemingly far less stringent than those within statutory services. One of the case managers estimated that approximately 80% of social worker time was spent on documentation. The small numbers of cases and resistance to using the study documentation may have had the effect that the case managers never fully familiarised themselves with the paperwork, which would have made the process of completing the documentation less time-consuming.
Lack of clarity over responsibility for documentation
Although the paperwork was primarily designed by members of the research team, responsibility for monitoring how it was used was never formally agreed. Furthermore, the use of a paper-based rather than an electronic system meant that it was difficult for the research team to gain access to the paperwork and therefore provide feedback on how the case managers were documenting their work. Although existing line management arrangements were intended to continue throughout the project, the value of such arrangements was questioned:
I mean technically I get supervision from my [line] manager . . . she’s great but at the end of the day she doesn’t know anything about CAREDEM, she isn’t involved in CAREDEM, doesn’t know any of the patients, any of the cases. So with the best will of the world you know there’s nothing really she can do which, you know, isn’t her fault but it’s not really an ideal set up.
Case manager
Problems with the documentation
An electronic version of the documentation would have been (from the research team’s perspective) preferable in terms of ease of transfer and analysis of data, but also ease of data entry, as a well-designed system would have prompted the case managers for key information and would have facilitated consistent data entry through the use of drop-down menus. However, before the production of an electronic version there was a need to field test the content of the documentation to make sure that it captured the key elements of case management. Issues relating to access to computers and printers and a lack of confidence with information technology (IT) were also raised as potential barriers to the introduction of an electronic version of the paperwork:
[Researcher] felt that the case managers just didn’t have time to learn how to manage the [IT] systems, even if these were set up and this was no reflection on them or their skills.
Researcher
It seemed that aspects of the documentation did not work and that some of the case managers found this very frustrating:
It was so un-user-friendly; I tried my level best to use it, I really, really did, but it just got so tedious at the end.
Case manager
One case manager, however, found the paperwork a useful tool for structuring assessments:
It’s really useful to have such a clear structure because you can come back. If you don’t have a structure, you can go off wherever you want, but it’s quite difficult to come back. I’m sure the paperwork could be improved upon but I find it very easy to work through.
Case manager
Other criticisms of the paperwork related to the order or sequencing as the sections were not perceived as logical in flow. As the paperwork was provided as loose leaves, it could have easily been reorganised to suit case manager preferences; however, their difficulty in engaging in general with the paperwork meant that such options were not explored. The research team had hoped that the paperwork would facilitate the process of case management through systematically linking needs, desired outcomes and actions; however, this was rarely evident in practice. Desired outcomes were rarely explicitly recorded and, as illustrated earlier, actions were not always linked to areas of need.
Lack of familiarity with research
Although all three case managers were experienced in keeping records of work with clients/patients, this had previously been in the context of routine work. To provide a detailed description of the intervention provided we wanted to capture their activities more systematically. However, this was not successfully communicated to the case managers and their commitment to documenting their work varied.
Chapter 7 Implementing case management for people with dementia in general practice: views of key stakeholders
This chapter summarises the results of the nested qualitative study and presents the views of key stakeholders. Participants’ perspectives are presented in terms of three stakeholder groupings:
-
patients and carers
-
health and social care professionals from participating GP practices and associated voluntary sector services
-
case managers, case manager mentor and members of the research team.
For all three stakeholder groups, key findings were amalgamated into three specific themes:
-
knowledge and skills that they felt were required for case management
-
practical delivery of case management compared with the theoretical concept, including the perceived and actual benefits of case management and clarity, or lack of it, over the case manager role
-
delivery of case management through primary care.
Knowledge and skills required for case management: patient and carer perspectives
Core knowledge and skills
In terms of knowledge and skills required by case managers, participants expected them to be able to provide information around dementia and local services. Participants felt that case managers should have sufficient knowledge to signpost people to appropriate services and provide information. Access to information about dementia was crucial in enabling participants to manage the practicalities and uncertainties of the condition and to empower patients and carers to understand their condition and plan for the future:
Professional carers that’s their vocation they understand it, they’ve been trained for it. If you’re a son, the child, who’s been doing something else you don’t know what the nature of the beast is and if you misunderstand it you can say ‘well that person is just being difficult’ even though they’ve never, they’ve been a beautifully loving person up until that point when they sort of change. If you don’t, if you haven’t been counselled, it hasn’t been explained to you, you misinterpret that can cause for stress. The more you understand this disease and the behavioural symptoms then the better you are to deal with it. So again somebody like [case manager] you know being a point of contact.
Care, A04
Professional background
Most patients and carers expressed no strong preference regarding the professional background of case managers. Although one participant felt that the nursing/medical status was important, another patient–carer dyad felt more comfortable with a non-medical professional as so much of their life was already medicalised. Benefits of both a nursing and social work background were identified, but neither was seen as a core requirement. From the perspectives of patients and carers, nurses were perceived as providing a more direct link to the GP and advice and support around comorbidities and minor ailments:
And obviously [case manager] is a nurse and is that important to you that she’s got a nursing background, a medical background?
Yes, oh yes it’s always very important, yes it’s because as I say I have got different things wrong with me but I feel pretty good most of the time, I don’t feel like an invalid, not yet anyway.
Patient, A02
In contrast, social workers were seen as closely linked to formal or paid support services. There was also a feeling that there were established routes for seeking help with medical issues, whereas patients and carers were less familiar with where and how to seek help for social problems and therefore valued the specialist knowledge of case managers with a social work background:
I don’t think the clinical side probably comes into it, it’s probably more having access to knowing what services are available and more helpful in that way. I mean obviously the doctors would be the ones that would be doing the medical side of things as regards the illness, but it’s more about managing the problem and it wouldn’t make any difference to me where it came from, and what department or whatever, so no, it’s not a problem.
Carer, B01
Interpersonal skills
In describing the skills needed for case management, patients and carers emphasised interpersonal skills such as empathy, the ability to listen, making people feel at ease and not rushing people. Advocacy was also suggested as an important professional skill by one carer. In addition to skills, personal attributes of case managers were considered important. Case managers were described positively and adjectives were used such as ‘nice’, ‘pleasant’, ‘bubbly’, ‘lovely’, ‘easy to talk to’, ‘a friendly face’, ‘comforting’ and ‘supportive’:
I think the most important thing is the care. That’s what I think. Because having worked in that sort of industry there were people who came along that obviously had fantastic qualifications to see the people that I was looking after but they didn’t seem to have any empathy.
Carer, A02
Case management in theory and practice: patient and carer perspectives
Potential and actual benefits of case management
The perceived and actual benefits of a case manager from the patient and carer perspective included acting as a first point of contact and also as a ‘safety net’ for all concerns, potentially providing a one-to-one, therapeutic relationship for future ongoing support and offering information and direct links to the practice and other services. Some participants suggested that the case managers should also be able to take on a more active role in negotiating or brokering with local services. Participants valued the ability of case managers to address both health-care and social care problems. Patients and carers were generally satisfied with their experience of case management and several participants were clear that they wished the service to remain in place (both for their own benefit and to benefit others). The service created feelings of security or comfort for some patients and carers. In addition, a number of practical benefits were reported, including easier access to GP appointments, benefit checks and links with other services:
What was very useful was when I told her that trying to get appointments is really difficult; she’s actually used a pop-up system now in the surgery to get the earliest appointment without me having to say ‘is it possible, can you bring the appointment a bit forward?’ Because I might be off on a particular day. She used the pop-up system so it comes up on the screen to let us have, without debating, the earliest appointment in view of my being a carer and at work and mum being not been able to wait a long time for an appointment.
Carer, A06
At the minute, we’re going through a care plan [for a personal budget], and that’s where you get an amount of money and it’s done through the council, which we never know about. It was [case manager] who directed us in that way and we can go and spend it like – [patient], basically, can go out and spend it. It covers your care needs and everything, and that’s something we never knew about. It was just [case manager] directed us in that, and checking that our benefits were in place.
Carer, B02
However, outcomes were less positive for some patients and carers. For example, one carer was waiting for information on whether or not her mother could keep a cat in sheltered accommodation:
It’s the one thing that my mum said that she really, really would love to happen but as I say I don’t know whether it would be possible.
And has there been any follow up with [case manager]?
We haven’t heard anything. No we haven’t heard anything yet. But it wasn’t that long ago so maybe she’s tried to get in touch with them.
Carer, A02
A key aspect of case management valued by patients and carers was the idea of background support that could easily be called on at a time of need. This was described as providing a sense of back-up, a safety net, security and knowledge that help was available if needed. This concept of contingency was considered key to avoiding or averting crisis:
She [case manager] was good. She said if there was anything, ‘Don’t sit there worrying. Pick up the phone and we’ll sort something out.’
Did you ever have the opportunity to pick up the phone and call her?
No, no, but it was just nice to have that safety blanket there, because I’ve got her number in my phone now, so if there’s anything that comes up, or anything like that, I know the phone number is there to get in touch with [case manager]. So it’s really good.
Carer, B02
For patients and carers to feel comfortable about contacting the case manager in the event of difficulties, there needed to be time and opportunities to develop a deeper relationship. Regular contact, the provision of case management from the early stages of the condition and continuity were seen as crucial for establishing a good relationship:
I think it needs to be regular […]
Right, even from that early stage?
I think so.
Yes.
So that then when it gets to a stage when we really do need help we’ve got the confidence in the person you’ve been seeing all along.
PWD and carer, C04
Face-to-face and telephone contact were both considered acceptable, although face-to-face contact was often preferred as it facilitated relationship building better than telephone contact. One participant would have preferred more face-to-face visits at regular intervals rather than just telephone follow-ups:
I was hoping that we’ll get regular support and I think visits on a regular basis . . . it would be nice to think that I know that we are going to have another visit say every 3 months or something like that.
Carer, C04
Clarity over the case manager role
The remit of case managers was unclear to some patients and carers and there was a degree of uncertainty about the specific areas of support available:
Do you think a case manager could have helped to support you in that role, or . . .
Eeh, I don’t know, is it their job to do that is it?
Well, case managers can support the carer and the person with dementia as well, so, or did you feel that you navigated it fine by yourself?
Well no, I didn’t – I had to go to the, I’m still going to the council, I was there yesterday.
Carer, B13
In addition, there was some overlap of roles, with dementia advisors (piloted in one site) and case managers being perceived as offering similar types of support. The potential for case management to offer continuity of care was one aspect of case management that was potentially distinct from other services. Participants reported having been discharged from other services and even in primary care found it difficult to consistently see the same GP unless they were prepared to wait for an appointment:
We never had that [ongoing contact] before. It was just like, we’d got the diagnosis, go to the doctors’ appointments and things, and then that was it; we were just sort of left.
Carer, B02
Because very often you can’t get in to see a doctor
Right, is it difficult?
It can be. It is yes. I mean I just see whoever, not like the old days when you used to see your doctor.
Patient, C02
Implementing case management in practice
Key issues for patients and carers included access to and availability of the case manager, the most appropriate time for them to access case management and the perceived severity of the problems that the case manager would deal with.
Access and availability
Although all carers in one area were aware of the case manager’s time constraints, often spontaneously mentioning how busy she was, they reported that she had nonetheless made time for them during assessment visits. They also reported that they would have no qualms in contacting her should the need arise:
I think [case manager] is a very busy woman so to pile things onto her would be wrong but it’s lovely knowing she’s there if I need her, I can pick that phone up, I can even ring her at the surgery and she’d listen which is nice, but I wouldn’t want to say to you ‘oh I’d like to see her two more times a week’ or something like that where at the moment she’s running, she’ll get here at a gallop won’t she, if I want to see her too much, so it’s just nice her being there so I can ring.
Carer, C03
One issue that arose for patients and carers recruited later in the study was the lack of time to build up a relationship with the case manager, although first impressions had generally been very positive:
She is . . . very nice, I could only say as I, she’s amazing, she’s nice, she’s a lovely person, well she came over as lovely to me. As I say I don’t know her very well, sometimes it does take a while to get to know people.
Patient, A02
The relatively short duration of the pilot study meant that relatively few changes occurred and the situation of most patients and carers remained stable. Contingency therefore remained a hypothetical concept rather than one that participants had personally experienced. It was also clear that there were some tensions and inconsistencies around the concept of contingency. Despite their apparent enthusiasm for flexibility and responsiveness, participants frequently expressed a reluctance to initiate contact with the case manager, somewhat undermining the idea that they could ask for help when needed:
I wouldn’t personally ask. I’m happy to accept it all, if somebody points me in the right direction, I just won’t initially ask. I mean I wouldn’t say to you, ‘I’m struggling with this. Can you help me with that?’ I just wouldn’t do it. I’ve never done it. I just don’t feel comfortable with it.
Patient, B02
Timing of case management
Many participants reported that their greatest need for information was at the point of diagnosis and in the early phases of the condition when they had been faced with navigating the system without any support. They felt that the lack of information at this point had compounded the difficulties of coming to terms with the diagnosis. However, those patients and carers who were still at the early stages often felt that they did not need any support at the moment but could see a point in the future when they might have needs requiring input. This mismatch in the views of people in the early and later stages of the illness trajectory may reflect the possibility that patients and carers are able to see their needs more clearly retrospectively than at the time.
In the light of these difficulties in recognising and articulating needs, it was interesting that some participants explicitly commented on the problems of identifying their own needs. Whereas they were too immersed in the situation, they felt that a case manager might bring a more detached perspective and could be in a better position to identify needs through regular contact and monitoring:
You need somebody to be able to look at the bigger picture, who knows where you’re going, who’s seen it before and [who could] deem and assess your situation to be stable and tenable or not and either talk to you about it, get you the right support or what have you but you can’t be the judge of your own situation. I mean obviously you know it’s bad but sometimes you just don’t know what to do.
Carer, A04
Although early intervention was considered to be the optimal way of identifying and addressing needs, this was somewhat at odds with the ability of patients and carers to identify low-level needs and to initiate contact with the case manager. Achieving the benefits of case management in practice may require a more structured, formal approach in which the case manager initiates regular contact with patients and carers.
Identification of patient and carer concerns about case management: major problems compared with ‘day-to-day’ issues
A further barrier was the difficulty that patients and carers appeared to have in identifying their needs, with many having few or no needs (any identified were considered low level). Both patients and carers frequently stated that they did not have any needs:
And she also rang me since she came to say ‘have you got any problems?’ At that stage we haven’t got really anything to report.
Carer, C04
We haven’t, luckily we haven’t had any major problems; it’s just day-to-day things.
Carer, C02
It appeared that many patients and carers seemed to associate case management with ‘major’ problems, with input being seen as most relevant in times of significant change (e.g. move to a care home). The ‘day-to-day things’ described above may have been a legitimate focus of attention for the case manager but tended not to be raised by patients and carers. This limited the ability of the case manager to provide a preventative, proactive service. Rather than focusing on current needs, participants tended to emphasise past and future needs, for example describing how case management either would have been helpful in the past or would be helpful in the future:
The things that [case manager] had to offer were perhaps something that I would have found very useful at the beginning of my mum’s Alzheimer’s and not so much [now] because I’ve learnt by trial and error on how to deal with it.
Carer, B01
At the moment you see with my wife things are in early stage, aren’t they? [mmh mmh] so you know we might be very, very glad of [case manager] in months, years, a couple of years to come you know, I hope she’s still about to help us, of course with her doing this she’s the person you want to help you.
Carer, C03
Delivery of case management through primary care: patient and carer perspectives
For most people, going to the GP surgery is an ordinary thing that ordinary people do in their everyday lives. It is not a new experience or a ‘special’ experience such as a hospital attendance or intervention through another agency such as social work. Neither patients nor carers expressed any concerns about going to their surgery, which was an accepted activity for many because of their management of other conditions.
Participants often described general practice as the ‘gateway’ to the ‘formal’ system of care and support. The GP was considered as the first point of contact for participants. The most appropriate way to access case management was thought to be through the GP around the time of diagnosis. This would ensure support at a time when participants have identified that it would be most beneficial. It would also avoid the difficulties that carers reported in negotiating support systems and allow people to ‘seamlessly’ access the service, as the following interview extract illustrates:
How important is it to you that [case manager] is based at the medical practice?
Because it’s more linked with doctors and any service that I need it’s all linked through the GP. So [case manager] will know us and they must have meetings there if there’s anything that sort of crops up she can say that she knows us and can actually trace things happening through the system if she feels there is a need for that and it’s the centre rather than have her placed in a different area. [. . .] It’s the most appropriate place that she’s there attached to the GP and let’s face it I can’t get any service for mum or any care unless I go through that point so it’s very important.
Carer, A06
Another aspect of being in primary care was the perception that this would provide a ‘one-stop shop’ in the sense that other conditions as well as dementia could be managed through the practice rather than having to engage with multiple agencies, as this carer suggested:
What are the advantages [of case manager being based at the surgery]?
Well probably because she’s got other medical staff there that she can, if there’s a bigger problem, then she can discuss it with them and then.
Carer, C02
Although the case manager was located within the practice, participants generally thought home visits were the most appropriate way of engaging with the case manager. Given the choice, patients tended to opt for a home visit rather than arrange to see the case manager at the practice. Aside from the logistics of organising an appointment, some carers also acknowledged the broader benefits of home visits in relation to assisting with assessing need. The option of surgery appointments was valued when the carer wished to see the case manager in private. The primary care setting was seen as offering a range of opportunities for contact, some serendipitous and some organised more formally:
At the moment I can just ring [case manager], you know we’ve got so used to [case manager] now, seeing her at the surgery, seeing her coming here, I think she’s going to come round and see us again which she said yesterday didn’t she? She said ‘I’m going to pop round and see you’, so another little moment I can have you see, so this is handy isn’t it?
Carer, C03
The only potential disadvantage of case management being delivered through primary care related to the issue of ‘medicalisation’, which was raised by one couple.
Knowledge and skills required for case management: perspectives of health and social care professionals
Professionals felt that a core knowledge of dementia and excellent interpersonal skills were essential attributes for case management; the professional background of case managers, either social work or nursing, was felt on the whole not to be important. Having the ability to adopt a holistic approach to care was also fundamental.
Core knowledge and skills
Participants generally felt that having an interest in working with people with dementia was the most important aspect of the role:
I think it’s knowing something about dementia and handling dementia.
GP
It seems to me that you need to be a dementia specialist but you don’t necessarily need to be a nurse.
Voluntary sector worker
It was suggested that knowledge about dementia was crucial for supporting carers, who often had limited understanding about the behavioural changes and illness trajectory of dementia. For carers, an empathic approach and practical strategies were seen as more important than medical knowledge:
So a lot of carers who come to us are struggling with coming to terms with how different that person has become, with perhaps that they’re beginning not to recognise them, that they are in some cases quite difficult, their behaviour is difficult at times. So it’s about information but also a discussion then around how that impacts and kind of validating how that person feels about that and helping them to think about strategies and communication techniques that will improve that, because they’re dealing with it all day every day. So slightly the medical knowledge is almost less important than how you deal with that day in and day out.
Voluntary sector worker
Professional background
The professional background of the case manager was not felt to be crucial to adopting a case manager role.
Well I think that the important thing is really the background of the worker and the fact that they’ve got experience in working with people with dementia and an interest in continuing to do so. So their professional background is less important I think than that. But I wouldn’t have said that it needed to be a role that any particular profession is best at, I think it very much depends on the individual rather than what their background is.
CMHT worker
Although many respondents felt that a clinical background was not important, some professionals thought that a nursing background would equip case managers with appropriate skills:
I do think the nursing team are the place where most of the skills are to help to do things like case management. Yes, there’s the medical and there’s tablets now so doctors suddenly and neurologists suddenly get all excited about dementia, but actually a lot of it is to do with a more nursing perspective and looking at problem-solving around practical things a lot of the time.
GP
One participant thought that the stigma associated with having a social worker might prove to be a barrier to accepting case management in the early stages of dementia and suggested that a nurse might be more acceptable to patients and carers:
We do get people who find it very difficult to feel that they’ve got social workers involved, there’s still that certain stigma involved isn’t there? Having you know, in your family, having a social worker. So I can see that particularly at an early stage there could be some advantages in it being a practice nurse.
Voluntary sector worker
Interpersonal skills
Some participants identified the importance of good interpersonal skills and the need to build up the relationship with the patient and carer over time:
Going into someone’s home and assessing the situation fully takes a lot of time and my own experience is that carers are often a little bit anxious about what you’re going to suggest and what you’re going to try and do and whether you’re going to be critical of – they might know that their care is falling short of the ideal a lot of the time but it’s their husband or their wife and they want to carry on. I think people are very scared and it takes a while to build up a relationship, to actually develop that – so I think half a day a week in a practice like this which has got a large elderly population, you could easily use that and double it and possibly more.
GP
Although some professionals recognised the value of a series of face-to-face contacts, they suggested that telephone calls could also be an effective way of maintaining links with patients and carers:
Well I think it depends on the patient but . . . I don’t think it has to be a rigid structure. I think it doesn’t necessarily have to be visits; I’m a big fan of the phone call. I think because they take two minutes, you know, but actually people just really appreciate the ringing up to say ‘oh you know we talked about this last time, how’s it going?’ and ‘oh it’s great!’ or ‘no it’s not quite working’ or ‘we’ll do some tests’. It takes no time at all but patients really appreciate it, or patients and carers.
GP
Holistic approach
Professionals thought that case managers needed to use a holistic approach that allowed them to ‘see the bigger picture’. Rather than a medical focus an in-depth exploration of the impact of the disease was required:
If there were specific medical questions they [case managers] would be able to direct somebody to whoever could give them those answers. It’s more important from our point that it’s a sensitive discussion around ‘how does that feel for you?’ ‘Do you feel you are going to be able to look after, is the family going to be able to do some of this looking after?’ ‘What impact is that going to have on you, do you need some support around you?’ That sort of thing. In a, you know [laughs] a more sensitive way maybe than I’ve just done but that’s the discussion that we need somebody to have and I think that’s about the way you have that discussion rather than a particular expertise around the medical side of dementia. I can’t see that that would make that much difference.
Voluntary sector worker
The lack of attention of existing services to the psychosocial aspects of diagnosis was highlighted by the recent professional experience of a dementia support worker:
I saw a couple in [place] last week and it’s a recent diagnosis. She said, ‘of all the medical professionals, no one has asked me how I feel about it’. This had been going on 2 months. Had the diagnosis, she was seeing someone about medication. ‘Nobody has said to me, except for you, how are you feeling?’
Voluntary sector worker
Case management in theory and practice: perspectives of health and social care professionals
Potential and actual benefits of case management
Professionals focused on potential benefits to those with dementia, their carers and then finally the GP practice. Case management was seen as potentially benefiting the person with dementia by providing continuing care, with an individual maintaining contact over a long period of time and dealing with problems at an early stage. It was seen as complementary to existing secondary care and social services, neither of which had the capacity to monitor patients and carers nor to provide support at an early stage in the illness trajectory:
We do know that people with dementia, their needs change dramatically over time in different ways and ideally we would keep them on and monitor and follow up and provide support as their needs do change, but that’s impossible. So they have to be discharged, and then hopefully are re-referred before a crisis occurs but sadly it’s often at the point of crisis so, that’s one area where the case manager in primary care can plug that gap.
CMHT worker
So people at the beginning of their dementia actually don’t come to us. It’s when they’re wandering or they’re not safe or if they’re a risk to themselves.”
Commissioner
The lack of routine reviews for people with dementia was highlighted as a shortcoming of existing services (although the introduction of the dementia reviews within primary care will ensure at least annual follow-up):
That would be great if everybody who was given a diagnosis had a review a year later because they don’t at the moment. . . . I sit there at these multidisciplinary team meetings, and people write in and say: ‘Mr Bloggs has got dementia and it’s got worse. Can he be re-reviewed?’ Basically, the mental health team will say, well, unless there are any specific behavioural problems, unless there are any other particular problems, and something has changed; if it’s just the fact the dementia’s got worse, they won’t pick them up.
Voluntary sector worker
By introducing regular, informal contact with patients and carers, case management was seen as having the potential to identify problems at an early stage and facilitate appropriate support:
I think that if you can induce sort of joined up care and if you can almost form a circle around a patient, these vulnerable people and if something happens or you’re worried or something goes wrong or they’re not quite so well, if you can communicate with other people involved often you can catch them. Whereas if you don’t know who’s involved it can take you ages or it can send you off on another referral pathway or get too many cooks involved and I think that’s the secret of looking after these people – is to have a few people involved but who are involved all of the time. The advantage of it is that I think the patient gets better care, things get picked up sooner, there’s less upheaval for them if they’re moved from one person to the other, there’s less duplication of investigations and possibly conflict even of treatments and from a personal point of view as a GP it’s actually less hard work if you know who to ring and you’re all on the same page.
GP
It was also suggested that carers would benefit from early and ongoing support:
From our point of view, the earlier that the carer is recognised as part of the care that needs to be given, the better, so if they’re part of care planning right from the beginning then they’re going to feel recognised and valued. They’re also going to recognise some of the stresses on themselves and be able to make informed decisions about how much care they want to give and how much they want to ensure is given by other services. So you just get a more balanced development in terms of a caring role. I think unfortunately what quite often happens is that carers arrive here at the point where they’ve hit a brick wall.
Voluntary sector worker
There were also perceived to be benefits for the practice, in terms of potentially saving appointment time, having a specialist in dementia within the practice and, on a personal level, the opportunities for professional development for any practice nurse who took on the role of case management:
I think several things for the patients and their carers, someone in the practice who was known to them as having an interest in dementia and would be a point of contact for them. And also some professional, not, professional development is not quite the right word, but some increasing professional self-esteem really for [case manager] who was doing it.
GP
All participants found it difficult to evaluate the extent to which these potential benefits of case management had been realised in practice. The lack of feedback from case managers about their work with patients meant that GPs were often unaware of which patients and carers had received the service:
To tell you truthfully, I have no idea if you had picked the two, the people up that I referred and I have no idea what has been done with them on behalf of the project and I have no idea if it’s made a difference.
GP
Health and social care professionals beyond primary care similarly found it difficult to assess the impact of case management other than having received a small number of referrals or requests for information from the case manager. Even when positive feedback from patients and carers had been received, there was recognition that they were often very grateful for help and that it was often difficult to get anything other than positive feedback:
Certainly one or two, and certainly good feedback, they like her . . . I think patients and carers obviously kind of value almost anything that’s offered and that they’re very grateful for any additional support that can be provided and particularly if it’s just on their doorstep . . . you get good feedback, but actually in terms of being constructively critical you need to actually dig a bit deeper don’t you?
CMHT worker
Clarity over the case manager role
Although, in theory, professionals could see that case management potentially ‘plugged a gap’ in services, in practice there was confusion over the boundaries between case management and other professional roles. Concerns were expressed over potential duplication of roles and the difficulties of identifying the most appropriate referral pathway:
I just remember at the time we all sat there and said, ‘Well, where do you fit in?’ This was the mental health nurses and myself: ‘Where do you fit in compared to all the people who are already visiting these people with dementia?’ . . . I think it was felt that there was going to be some duplication.
Voluntary sector worker
The provision of support for people with dementia and their care is so stretched that somebody else providing a kind of direct link between if you like the primary care and other services would be a good idea. So yes, I was very supportive of the plan . . . I think that the problem sometimes is that roles aren’t clearly, or maybe not clearly defined enough, between for example our community mental health nurses, the dementia advisor that we work with and the case manager. And I do admit sometimes that, when I’ve got somebody who I know needs support, I’m not at all sure necessarily who would be best to refer to. And so, if I think if anything I think the definition of roles and responsibilities needs to be much clearer for it to be most effective.”
CMHT worker
Implementing case management in practice
Several practical issues were raised about the implementation of case management in practice. The time required for the role was identified as a potential issue by several professionals:
I know [case manager]’s feeling quite pressured in actually trying to find the time to do this – my impression was that this was feeling like something additional that had to and I think it’s just that whole thing of having to, even if you’ve got funding for something, you still have to fight for the time and fight for other people to recognise it as being important, and that’s quite hard sometimes.
GP
Although home visits were recognised as taking significant time, there was a strong view that the ability to offer home visits was essential with this client group, partly because of mobility issues for older people but also to gain a better understanding of their social environment:
You know you see the nicest turned out people who they make an effort, they come into the doctors but you go home and then you realise there’s mouldy food in the fridge and the milk’s still on the doorstep or they’re sleeping downstairs or you walk in and you get a picture straight away usually, particularly about circumstances. . . . If they know they’re coming to the doctors, often you dress and think appropriately and plan that out. Also, the other thing is quite often if they do have dementia and unfortunately they quite often forget their appointment and it means that you don’t get any follow-up anyway.
GP
For the purposes of the feasibility study, patients with dementia were identified from the practice dementia registers and so the patients who were included were at different points on the illness trajectory. We asked professionals when they felt that case management should be provided. Overall, early intervention was seen as the best practice, although views varied whether it should be offered at diagnosis or slightly after diagnosis (e.g. on discharge from the CMHT at the memory service):
Probably it should happen at diagnosis so that the patient and the carers are aware that the service is there without being awfully intrusive, so that they get used to the idea. So I would have thought from the word go . . . and then we go in say once every 3 months or if there’s a crisis, or even once every 6 months depending on what they’re like.
GP
I don’t think it should be offered at diagnosis, because I think that’s where in fact patients get the most contact from us, and in particular if somebody is starting on Alzheimer meds [medication] then they’re seen sort of fairly regularly by ourselves. I think what would be helpful would be for us to be able to offer the case manager at the point of discharge from ourselves and . . . maybe we’ll arrange for you to see her once just so you can say ‘hello’ and then you know that she’s there if you’ve got any concerns. I think that as I said before, I think that would kind of plug the gap really, and to some extent at least, rather than people feel they’ve been discharged so they’re not quite sure where they can go now to get help.
CMHT worker
Some of the GPs noted that similar systems of providing a contact for a known person within the primary care team were already in place for other patient groups, such as those with cancer:
We’ll have a cancer watch list so as soon as they’re diagnosed there may be absolutely no need at that time but I’ll make contact and the district nurse will make contact so at that point there might be nothing, but at least they’ve met us, we’ve said ‘hello, we’re available get in touch’.
GP
Potential barriers to case management were that some people often do not identify themselves as a ‘carer’, particularly in the early stages of their relative’s dementia, and that people from some minority ethnic groups were reluctant to be diagnosed because of the perceived stigma:
So if you look at some of the minority ethnic communities often there’s a reluctance to get a diagnosis for dementia; there’s still a lot of stigma attached to it . . . and even more of a difficulty in terms of people recognising themselves as a carer because it’s just seen as the role within the family. I’ve done some work with older Bangladeshi women . . . and one of the things that that you discover is that there isn’t a word in their language that directly translates the word carer because there isn’t that concept. Do you see what I mean? It’s just seen as within the family, that’s what happens.
Voluntary sector worker
Delivery of case management through primary care: perspectives of health and social care professionals
Advantages and disadvantages of siting case management in primary care
A range of advantages and disadvantages of case management being based in primary care was identified (Box 2). Ease of access was identified as a key benefit; professionals working for a local voluntary service felt that being based at the GP surgery would facilitate uptake of support:
If we sat in a surgery we’d pick up a lot more trade, wouldn’t we? We’d have a lot more people than we do at the minute, if we were based in the surgery.
Voluntary sector worker
I think a lot of people feel that going to the GP practice is more, it’s kind of more normal for them isn’t it? Everybody has a GP; everybody goes along, so being involved in some ways is easier particularly at an early stage.
Voluntary sector worker
Opportunity for ad hoc contacts
To use the fact that people go into that surgery for other purposes but to take the opportunity to discuss their dementia and the problems associated with it at that time.
CMHT worker
Links to GPs and practice nurses
We will catch things and we will pick things up sooner because they notice when things change. Or they might share and say to a GP, ‘have you seen so and so yet, have you noticed?’ or ‘oh I’m a bit worried about so and so’.
GP
Creation of expertise within primary care
I think somebody who deals with a lot of dementia tends to get good at their job too. So I think I kind of thought there was a level of expertise there that would be good for us.
GP
Fit with long-term focus of primary care
I think that’s where general practice – and obviously I’m going to say this because I’m a GP – so I think it always trumps secondary care, is that it does have that long-term view and a long-term commitment to patients and their carers which the secondary services because of their constant reorganisations, they don’t have that same focus on the long term and being there and just raising things early on about changing needs and still being there to actually address those.
GP
Disadvantages
Patients and carers may prefer to keep issues confidential from their GP
Where patients are already relatively well known we know their social context we’ve often, we know the family quite often. We’ve kind of had some sort of continuity but we certainly don’t know everything about them and you do come across situations where people definitely don’t want their GP to know because they’re afraid they will get put in a home or taken to hospital . . . the neighbours and the family and social workers may well know things that we don’t.
Commissioner
Issues with backfilling posts and nursing capacity
It’s impacted a little bit on my colleague who’s helped [case manager] get her appointments organised and home visits organised and telephone consultation organised because obviously that’s taken her out of her practice nurse sessions.
Administrative staff
Overall, the benefits of being based in primary care far outweighed the disadvantages identified.
Although primary care was seen as the most appropriate site for case management, the importance of being linked with other local services (either the voluntary sector or CMHTs) was highlighted. It was thought that this would help clarify role boundaries and facilitate joint case work. One suggestion was for the case manager to attend CMHT meetings:
I know she’s on the end of the phone but . . . maybe not weekly, but maybe every now and again [she could come to the CMHT meeting] to discuss the people that she’s got on her caseload and the people we’ve got on our caseload, and in particular the ones that are shared.
CMHT worker
Embedding case management in primary care
A key advantage of being based in primary care was the potential for the case manager to liaise with colleagues in the event of concerns about individual patients and carers. The extent to which these links were enacted in practice varied considerably. There seemed to be particular challenges in developing effective working relationships for the case manager from a social work background who had not previously been known to the practices. From the GPs’ perspectives, the lack of visibility of the case manager, together with the lack of feedback on work carried out with patients and carers, meant that liaison had been minimal:
If I’m honest we hardly ever saw [case manager] within the practice. We only saw the person twice, once at the very start and once after I think I’d met with you and said we haven’t heard or seen her and she then turned up once again.
GP
Two participants suggested that the lack of embeddedness of this particular case manager was perhaps more to do with the individual than the role:
That might be an issue with her rather than the role as a whole.
GP
Even in practices in which existing practice nurses took on the role of case manager, it was unclear exactly how familiar their colleagues were with their activities:
Do you think the other practice staff knew what [case manager]’s role was when she was doing this other role?
I don’t think they did necessarily because you are right, we are a large practice. We’ve got 15,500 patients. We’ve got 19 doctors, three nurses, etc. Nine or eight loads of people to staff, receptionists, etc. So I don’t think, everyone just gets on with their parts of the work and one or two might decide to find out and so on. But we might have mentioned it in the newsletter or one of the staff meetings on a couple of occasions last year, but I don’t think anyone really knows. But then if you ask me ‘do they know that there’s a midwifery service?’ I don’t think they know what’s on here. Do you see what I mean?
In general, primary care staff had little knowledge of what was actually being delivered to patients. This was compounded by different approaches to recording case management work in the primary care notes. Only one case manager made detailed entries; one simply noted times and dates of contacts; and the final case manager felt that it was inappropriate to record any details in the GP notes. Instead, a summary of the work with each patient–carer dyad was sent to the GPs at the end of the project; however, although the GPs found this very useful, they would have preferred more timely feedback.
A number of participants felt that having a summary or key points recorded in the patients’ notes would facilitate communication; it was suggested that the model of recording used by counsellors attached to GP practices would be ideal. It was also suggested that regular feedback through practice meetings would have been beneficial. Furthermore, appropriate meetings were identified that a case manager might usefully attend, including CMHT meetings, district nurse meetings or the multidisciplinary team meeting:
Every 3 months we have a meeting with [name] who is our consultant psychiatrist and I think that could be a useful tag on to that. It could be, if that was inconvenient, it could be a tag on to our regular meetings with the district nurses.
GP
I think for benefit further would be for [case manager], and maybe [mentor], to host an education meeting for the GPs, and to cascade what they’ve learnt. I know we do have, every Friday lunchtime, an education meeting and . . . if it wasn’t ever discussed, it’s a route that we ought to go, so the nurses, peers and the GPs, they all can learn.
Administrative staff
The value of informal ad hoc meetings was also mentioned:
I think if it could be from somebody who was in and around the building who you bumped into or who you could have internal e-mail contact with that would be the ideal.
GP
The extent to which the practice nurses engaged in these meetings within their own practices was unclear, although no comments were made about their integration (or lack of it) in the interviews with their primary care colleagues. Although the practice nurses had the advantage of already being embedded within the practice, the potential difficulties of integrating an ‘outsider’ were not seen as insurmountable, provided that they had the necessary communication skills and desire to link with the primary care team. There were, however, other advantages to having existing members of the team act as case managers. These included their existing knowledge of patients and practice information systems, the benefits to the practice of developing the skills and roles of existing team members and the perception that using an existing member of staff was somehow more holistic:
But how would she know how to use the system? Time wise because obviously she’d have to go to someone to find out, how do I source these patients, how do I go through their records, just to get to know a medical system I know from just my experience here that you know it isn’t just a quick lesson, there really isn’t. My gut feeling would say it’s a downside. I would think it’s far better where people are familiar with the system.
Administrative staff
I think it makes her work seem more valid, rather than just being an add-on. And I think for patients it feels – I think for our patients, we know our patients, they like the surgery here, they like the nursing team, and it feels more solid, it feels more a part of their overall health care and their overall, that they’re being looked after holistically rather someone else coming in and doing an add-on.
GP
The one benefit of being an ‘outsider’ to the practice and coming in to the case manager role was the perceived ability to legitimately ‘ring fence’ one’s time. Professionals working in small practices felt that it would not be appropriate to have a case manager embedded within their practice, but suggested that a different model was needed, such as a mobile service that could attach itself to the practice at certain times:
You can’t have an embedded person because actually they haven’t got the resources to do it so you’re probably looking at a model where you do have one person covering several practices. So for example we have, I know it’s not the same thing but one of the things that’s come up, is the 24-hour blood pressure monitoring which is a new NICE [National Institute for Health and Care Excellence] guideline. We have a lady who comes in every two weeks because our population’s smaller and that suits our population so they get seen quickly and efficiently and it actually only takes one afternoon a week to cover our patient load.
GP
Supervision and support of case managers
Although existing line management arrangements continued for all case managers, there was little evidence that this had included any detailed discussion of work with clients for the practice nurses involved. Only minimal contact between the lead GP and case managers was reported in three of the four participating practices:
But I’ve just let her get on with things really, and I sought her out I don’t know, probably end of November time, a bit before Christmas just to see how things were going and touch base at that point.
GP
The extent and form of supervision provided by existing line managers seemed inadequate to support the case managers in their new role. There was no evidence that line managers facilitated or encouraged case managers to participate in relevant practice meetings, checked that work was being recorded in the primary care notes, helped them to ring fence the time available for case management or reviewed their work with individual clients:
So what [case manager] was doing was she was also going on home visits to meet these patients on our register. When she went on these visits she’d either let me or her colleagues and the nursing team know that she’s on these visits. I think they took about over an hour or so, a long time for a consultation. She’d come back and do the documentation, etc. and so on. My question with her was ‘Do you need as much time as you’re spending for six patients?’ . . . I always received the answer ‘Yes’. I didn’t bother going beyond that really.
Administrative staff
With more robust practice-based support and supervision, it is possible that the case managers could have achieved more within the time and resources available.
Knowledge and skills required for case management: perspectives of case managers, the mentor and the research team
The case managers brought different skills, professional backgrounds and experiences to their role (Table 26), which impacted on their training needs and the implementation of case management. In addition, the dedicated time available for case management varied between practices. Although there were only three case manager posts, with one post designed to cover both of the north-east GP practices, these were covered by four case managers as one resigned to take up a new post and was replaced during the period when patients and carers were still being recruited. The case manager who resigned and the replacement were similar in terms of gender, professional background (social work) and experience, with the exception that one had more experience of working with people with dementia. The details in Table 26 are for the case manager who was in post for the majority of the feasibility study. To maintain confidentiality, quotes from interviews are not attributed to individual case managers.
| Characteristic | Details |
|---|---|
| Gender | Female n = 2, male n = 1 |
| Professional background | Practice nurses n = 2, social worker n = 1 |
| Experience of working with people with dementia | None n = 1, limited experience n = 1, significant experience n = 1 |
| Experience of case management | No experience n = 1, experience of care/case management n = 2 |
| Experience of community-based assessments | None n = 1, significant experience n = 2 |
| Dedicated time for case management (per practice) | One session per week n = 2, five sessions per week n = 1 |
Core knowledge and skills
There was recognition by the mentor and members of the research team of the range of knowledge and skills required by the case managers. Knowledge of dementia and available interventions and awareness of local services were highlighted as core skills. Existing knowledge of dementia varied significantly between case managers; although one person had no direct experience of working with people with dementia, two case managers had a specific interest in dementia and were keen to develop or utilise their skills in this new role:
Dementia’s my special interest anyway; I’ve worked for many, many years in dementia care. I’ve got a diploma in dementia care as well.
Case manager
The process of recruiting case managers varied between sites; whereas the social workers had to formally apply for secondment to the role, arrangements for the practice nurses were less formal:
I was nominated and I had the right to refuse but I was nominated . . . I suppose as soon as they got a whiff of my case management experience my fate was sealed.
Case manager
Although this practice nurse had extensive case management experience (in paediatrics), she had little knowledge or experience of dementia. The feasibility of developing sufficient expertise within the time available was questioned and it was suggested that a more formal interview process, perhaps including discussion of scenarios, would be useful in ensuring that the case managers had core knowledge and skills relating to dementia:
For me one of the fundamental flaws was perhaps recruiting people into a dementia case management role where not everyone had a basic understanding around dementia.
Mentor
The value of knowledge of local services was emphasised by the case managers and mentor, who saw signposting as a key part of their role:
I think families will want to know about ‘what’s the name of that day centre, two streets away?’ but I think that will come with the practitioner’s knowledge and I think that’s when I would say ‘well actually I’ve got a leaflet on [a particular] day centre, here it is’ or ‘I can talk about that’.
Case manager
Although the case manager with a social work background had a good knowledge of local services (and often had contacts within such services that further facilitated the process of referral and liaison), developing this knowledge was challenging for practice nurses, particularly in one setting where the practice population spanned two local authorities:
I’ve learnt a lot about different services and networking and I feel like there’s a lot to learn still, loads and loads and loads, I still feel ‘oh, I don’t know who to turn to with this’.
Case manager
Professional background
Views on the relative merits of different professional backgrounds for case management varied. In addition to their knowledge of local services and their skill set, social workers were also more familiar with working independently in the community, visiting people at home and working within existing policies for activities such as out-of-hours working. Practice nurses were used to working within the GP surgery and had some concerns about home visits:
They [practice nurses] don’t see themselves as doing many home visits and they are concerned about insurance cover for doing that.
Team member
Whereas the practice nurses were familiar with the primary care environment and culture, being based in primary care was a significant shift for the social worker, in terms of both the physical environment and the lack of formal structure for their work:
I suppose it’s quite a unique situation where you’re not tied down by statutory frameworks, I suppose what I’m conscious of is that sort of freedom, that flexibility that’s quite a unique situation to be in; I don’t need to see the person every 6 weeks, I don’t have to make sure that I’ve done that document in time and I’ve done particular things. I suppose I’ve just absorbed so much organisational policy that I’m so used to and it’s just putting that different hat on, that’s going to be hard.
Case manager
In addition to bringing their own professional knowledge and expertise, the case managers also brought their preconceptions about other agencies to the role. The views expressed by one case manager from a social work background may have impacted on her ability to work effectively with primary care colleagues:
I think medics have a very different approach from social workers. Obviously medics are quite problem orientated there is something wrong, we shall fix that, move on. Whereas obviously adult services, social services are more looking at the wider aspects, the bigger picture, more long-term changes which is certainly the way I see the care manager’s role. It’s [a] more holistic approach; it’s not about there’s a problem, diagnose it, cure it.
Case manager
Although one of the social workers argued that a social work background was essential for case management, none of the other case managers had a strong view on the relative values of different professional backgrounds.
Interpersonal skills
Developing relationships with people with dementia and their carers, and managing potentially conflicting needs, were seen as key skills for the case managers. Again, case managers with a social work background felt that their training had equipped them with the necessary interpersonal skills:
The core social work skill is in communication, it’s in observing, reflecting, evaluating information, being analytical with information, being able to probe deeper into systems, into relationships and from that being able to problem solve a situation.
Case manager
She knows how to think about information, synthesise it, check it with people and so on. She’s aware of a lot of the issues around things like capacity and engaging family and social networks, managing the dynamics that can emerge.
Team member
Case management in theory and practice: perspectives of case managers, the mentor and the research team
Potential and actual benefits of case management
Among the case managers and members of the research team there was strong commitment in theory to the case management approach. A range of potential benefits of case management was identified (Box 3). The key differences between case management and other services related to continuity of care and flexibility over input:
It would be supporting people across the whole journey, and that’s what families need and that’s what they ask for, and they’ve been asking for it repeatedly for many, many years.
Team member
you see the patient and it’s for a short, predictable space of time. An allotted space of time so it will be nice to get back into people’s lives rather than just what they’ve come to you for.
A named contact who provides continuity
sometimes having an identified person as your first port of call solves three quarters of the problems.
So it’s not a case of having to go through the GP and arrange an appointment and all that rigmarole – which can be really off putting – it’s quite an easy opening point of contact where you can just call up and say ‘look mum or dad whoever they’re exhibiting this new behaviour, they are really not settling at night – what can I do?’
People relate best having one key person wherever possible and a consistent approach. Apart from anything that way the worker will get to know the people involved and they will be best placed to know how things change.
Provision of different levels of input as needed
you’ve got continuity, longevity, you’ve got an appointed person who can hold a case . . . you’ve got that capacity . . . so the carer or the person with dementia can call you and you can be involved in small level or big level.
the range of what the case managers can do is massive. You’ve got everything from full-on interventions to very mild kind of therapeutic interventions to more intensive CBT [cognitive–behavioural therapy] to the signposting element.
A proactive, rather than reactive, approach
I think so many people just manage or manage enough to not be at the A&E (Accident and Emergency) all the time but I don’t think that means it’s a constructive experience for them and that’s what’s got to change and I think that’s the whole point of this.
potential outcomes for the patient, the carer, the NHS and adult services – from a budget point of view is awesome, because I think potentially you will avoid so much crisis, so much early admissions to hospitals or to residential care. And deteriorations in health . . . we know for a fact if people don’t get appropriate help early enough, it adds to stress, anxiety.
Support with navigating services
I mean just myself trying to navigate all the different services and financial aspects and benefits and things like that em, you know, what must it be like if you’re older and feeling muddled?
I would like to think that they have become aware of the different support there whether it’s the Alzheimer’s Society or the carer centre or social services and they’ve kept the numbers and they will feel more likely and be more knowledgeable about who to contact should things change, which they will, for them and they need that support.
The opportunity for longer-term therapeutic work when needed
And I think that’s what case managing is all about; it’s having that therapeutic assessment, it’s really getting to the nitty gritty of what’s going on here we’ve got a family situation, the carer’s stressed, why is she stressed? What is she saying? How is she saying, how is she describing her loved one? . . . it’s being able to have that time to say how long we can manage this? What’s going on here? Have you thought about this?
Only one potential negative consequence of case management was identified and this was the risk of creating dependency and disempowering patients and carers:
certain people will hold on too long and do too much for people and with the best will in the world, the best intentions will foster dependency . . . the potential [is] there for crossing a boundary of being too close, of de-skilling people and making people dependent.
Case manager
There was a sense of frustration among the case managers and mentor that there had been insufficient time in the feasibility study to really demonstrate the potential of case management. The time available for case management had been curtailed by the considerable delay (of almost 5 months) in obtaining ethical approval for a substantial amendment relating to recruitment and slow recruitment. As a result, the case managers had had relatively little time to develop their work with patients and carers and could identify relatively few concrete benefits for participating patients and carers. Several participants had gained financially through claiming benefits or a council tax reduction, and feedback from patients and carers to the case managers had generally been positive.
I mean all I’ve really been able to put in has been a few sort of like basic stuff things like welfare rights checks, benefits checks, some equipment like grab rails.
Case manager
they [patients and carers] all said the same thing to me anyway that it was nice to know somebody was there and they all kind of appreciated that although I wasn’t there 24/7 I was still a name and they could put a face to the name as well and they weren’t always expecting me to know all the answers but they knew that I would do my level best to help them find the answer to whatever that may be.
Case manager
it was such a short project I feel almost frustrated we didn’t have a bit more time to get through what I think are natural initial hurdles and actually get our teeth stuck in and make a proper go of it, so that’s just a sense of frustration.
Mentor
Although the primary focus was on the benefits for participating patients and carers, there were also benefits for the case managers and their practices:
I think it’s just flagged me up as being a member of the team who does have the special interest, does have some skills that I can bring to the practice concerning dementia care and now that’s got the ball rolling with me doing the dementia QOF and reviewing patients that way.
Case manager
Clarity over the case manager role
A key issue for case managers (and team members) concerned the lack of understanding over what case management involved and how it differed from existing services such as Admiral nursing and dementia advisors:
Well I think there’s a big question about what we mean by case management. I don’t think there’s any kind of real clarity about what the term means.
Team member
Certainly in the early stages it didn’t seem very clear at all to me what was expected or what I was supposed to be doing, or how I was supposed to go about it. And I was relying on [mentor] a lot more, I didn’t really fully understand what I was doing. But, now that I’m kind of on the road as it were, I feel, yes, a bit more confident in my own skills really.
Case manager
This lack of clarity occasionally led to case managers having misconceptions about their role. For example, one case manager carried out some ‘informal’ assessments with carers. When asked how these ‘informal’ assessments differed from the more usual assessments, the case manager explained:
I mean obviously the project is designed to work with the patient as opposed to the carer, so the informal ones have been basically where the patient hasn’t wanted to be involved.
Case manager
Even towards the end of the project, case managers still expressed confusion about their role. The situation may have been compounded by the interest/background in Admiral nursing among some members of the research team and the mentor. This led to some concepts from Admiral nursing being incorporated into the project and also to inappropriate comparisons of case managers with their own role and that of the mentor:
I mean I don’t really still understand the role of a case manager anyway I don’t feel, I feel like I’m still learning because I’m not a case manager, I feel like I’m probably just giving people advice, I don’t see it as case managing as such, not like [mentor] does.
Case manager
In contrast to the other case managers, the practice nurse with previous experience of case management felt that there was ‘clear guidance’ about her role.
Implementing case management in practice
A range of issues concerning the practical implementation of case management was highlighted, including time constraints for case management, the timing of the intervention and identification of needs. Issues relating to the documentation of case management activities have been explored in Chapter 6.
Time available for case management
As already described, the practice nurses had one session a week (4 hours) available for case management; in contrast, the social worker was full-time but covered two practices (equivalent to five sessions per week per practice). Although discussions with practice managers suggested that cover had been arranged for the practice nurses, neither of the practice nurses was aware of any additional staffing. The feasibility of effectively case-managing clients in the available time was repeatedly questioned:
How was I going to case manage 11 patients in 4 hours a week? . . . how was I going to manage with them if they were phoning me up and it was not Monday afternoon? . . . and anyway I kind of grew with it and said ‘well you know I won’t be able to answer you straight away but I will get back to you’.
Case manager
The time constraints for practice nurses were exacerbated by interruptions during the dedicated sessions:
The last time I went to see her, she was pulled out to do two practical procedures in the middle of our meeting.
Mentor
After several months, the situation was partially resolved by a member of the research team visiting one case manager each week to facilitate the process of recruitment and to discourage the frequent interruptions from colleagues:
I can’t do without it. You can’t do the project without it. So she’s [researcher] been able to really be my bodyguard so I’ve had time to do things. That’s been very, very helpful.
Case manager
Although the other practice nurse experienced similar problems initially, she was more successful in preserving the time allocated. By the end of the feasibility study, she was negotiating with the practice to take over responsibility for the QOF dementia register and annual dementia reviews:
Well I’ve suggested actually that because everybody is now used to me having Monday afternoons for dementia that we keep that as a dementia afternoon so I can focus on all my reviews and the patients within the practice who have got ongoing problems.
Case manager
For both of the practice nurses, a period of reacclimatising to CAREDEM work was needed at the beginning of each session. One potential difficulty of confining the case manager role to one afternoon per week was managing both routine follow-ups and urgent requests from patients and carers. The situation was further exacerbated by the time required for travelling to home visits for the practice nurse working in a rural area. Concerns about access to the case managers were raised by the mentor and members of the research team after experiencing difficulties in getting through to the case managers by telephone:
From a patient perspective I could perceive problems with some practices in actually accessing the case manager because of the other responsibilities they have . . . when I’ve tried to get hold of case managers I’ve thought well I could be a patient trying to get hold of them and I’ve left three messages, they’ve got clinics back to back for example, when am I going to get my call back?
Mentor
Despite these concerns, access to the case managers did not emerge as a significant problem in the interviews with patients and carers. To some extent, expectations were carefully managed by one of the case managers and, following discussions with the mentor, the case managers set aside 30 minutes at the start of their dedicated afternoon for telephone calls:
They have both allocated half an hour at the beginning of the session where they can be contacted by families who know they’re there. So that’s a dedicated slot and if this family have had to call someone in practice on a non-CAREDEM day, the case manager in the practice will have to use that slot to do a follow-up call.
Mentor
To some extent, the potential difficulties with access were offset by either serendipitous or planned meetings at the surgery. One carer arranged a long appointment with the case manager during one of her normal clinics at which she had the opportunity to speak at length about her difficulties in managing the patient’s repetitive questions. At other times the practice nurses were able to quickly catch up with patients and carers when they attended the surgery for other reasons:
one of the ladies that’s a carer, she came to see me outwith CAREDEM, she left her husband at home and came to see me in a practice nurse appointment and we were able to talk about how to sort of understand repetitive behaviours and forgetfulness and things like that.
Case manager
I’ve done flu jabs for some of the people . . . so there’s been continuity but I haven’t done any second home visits but it’s been corridor catch ups which can be very, very powerful.
Case manager
To manage the time constraints, one case manager relied on telephone contact rather than face-to-face follow-up visits, but recognised that this was not always ideal:
actually quite often if I’ve got a carer on the phone they were clearly trying to choose their words very carefully and I would be left saying ‘I can see that it’s difficult for you to talk to me at the moment’.
Case manager
Timing of the intervention
It was generally agreed that the best time to offer case management was at the point of diagnosis, although there was also recognition that some patients and carers would not be ready to engage with the service at that point. One of the case managers felt that there had been limited opportunities for case management with the patients and carers participating in the study:
We’ve either got people who are very, very highly functioning still who are still going out on their own, who are still doing their own housework, who are still going to the pub every other night in some cases on their own. Or we’ve got people who are a lot more incapacitated but have . . . carers going in four times a day and the sons and daughters have a very clear schedule of visiting their mum and dad. There’s not so far the unmet needs which we need for people to be contacting us, which again is quite frustrating.
Case manager
For some of the clients, it was felt that the service was offered too late to be of benefit as the carers had already single-handedly negotiated services and support:
At the end of the assessment with her mum and with her, she was like . . . ‘this would have been a godsend two or three years ago. It’s exactly what I wanted, someone like you to come out and discuss and go through stuff, have time to discuss it, tell us what help is available and just to have someone to listen to us’.
Case manager
The recruitment process was thought to have influenced the types of participants recruited. A situation in which patients and carers self-referred to the service was thought to facilitate the provision of case management:
This wouldn’t be the approach we’d have in normal case management engaging with families, we may have a different referral process or people could readily access or self-refer or relatives could self-refer, and then I think you’d probably have a more realistic cohort of people who would have already engaged through actually approaching and asking to speak to the case manager and be halfway there already into identifying the needs.
Mentor
Other case managers also felt that the clients involved were generally at a fairly stable stage in the illness trajectory and only in need of ‘light touch’ support. However, it is not clear to what extent the apparent low needs of participating patients and carers reflected the stage in the illness trajectory or the difficulties in identifying unmet needs, described in the following section.
Identification of needs
The time constraints of two of the case managers were a key factor influencing the scope to spread the assessment over a number of visits, and concerns were expressed that this may have impacted on their ability to gain an accurate picture of patient and carer needs:
The potential for patient and carers’ needs to naturally emerge over time was lost. In addition, as the main assessment took place over one visit, there was little opportunity to see either the patient or family carer on their own, which may have facilitated a more open discussion as to what the main concerns were.
Mentor
The case managers acknowledged that most of their work had consisted of one-off assessment visits, but they were less likely to perceive this as a problem than the mentor:
My second visits have not actually been at people’s homes. They’ve been much more I’ve seen people or I’ve spoken to people [in the surgery]. I don’t think I’ve actually been back to anyone’s house again, which feels okay because I haven’t had to do tasks that need me to go back to the homes. I think if I was staying on longer I probably would, as a matter of not routine but standard follow-up, because you need to see people. Actually they need to see you as well.
Case manager
Well really it’s been an assessment role. I was hoping it would be a therapeutic role and I think there are certain elements of that in the assessment process but mostly it’s been assessing people’s needs and finding very surprisingly that there weren’t really any needs there to be met, or if there were needs that they already are being met.
Case manager
Despite the apparent enthusiasm to deliver interventions to patients and carers, there was little evidence of such work in practice. This was justified in terms of the needs of the clients:
I’m dying to do a bit of CBT [cognitive–behavioural therapy] with someone . . . I love the psychosocial interventions, but no-one wants or needs them at the moment.
Case manager
However, analysis of the documentation seemed to indicate scope for therapeutic work. The reasons for this mismatch are unclear. Two of the case managers emphasised the need for patients and carers to be willing to engage, but did not seem to see it as part of their role to help people to move towards the stage of accepting help:
I think they probably need rehousing, but it’s privately rented. It’s a big choice for them. I suppose for [one patient], who rents it, it’s about his independence even though I think his independence is so compromised and challenged. But I’m sure a lot more could be done for them. But they’ve got to want it. They’ve got to be willing to be scrutinised before anything will change.
Case manager
Even when one of the case managers acknowledged that it would fall within the remit of her role to encourage openness about the diagnosis in a family in which the person with dementia had not been told the diagnosis at her husband’s request, this had not followed up:
The fact that he’s not willing to admit it says as much about how he’s dealing with it as she potentially would. So I would think that’s exactly the kind of thing a case manager would do, but of course it depends on whether or not they let you, if they’re willing to take part or not. But I think that kind of thing over time when you work with someone is probably one of the key things you would do.
Case manager
The fact that social workers were used to working within Fair Access to Care Services (FACS) criteria and focusing on people with substantial and critical needs may have influenced their ability to identify low level of needs when working with patients and carers. This may particularly have affected the case manager who had been working as a duty social worker, to whom calls were typically from people in crisis:
They end up coming to social services because they’re reaching absolute point of crisis where they literally can’t cope and end up phoning up the GP and saying ‘the carer has walked out or had a nervous breakdown’.
Case manager
Delivery of case management through primary care: perspectives of case managers, the mentor and the research team
Advantages and disadvantages of primary care
Views varied on whether or not primary care was the most appropriate place for case management and a range of advantages and disadvantages were identified (Box 4). Although the key task for the social worker was to become integrated and embedded into the primary care team, the challenge for the practice nurses was to have their new role recognised and to be given the time to do it. The importance of support from the practice to enable the practice nurses to have protected time for case management was highlighted:
They need to be fully supported by the practice and I don’t see that happening. It seems to be a bit tokenistic to me. They need that dedicated time and everything to be in place to support them in their role.
Mentor
People come to the doctor for all sorts of things . . . It’s not like having to go to see the psychiatrist or it’s not like having to go and see the Alzheimer’s Society people or all those other funny words that people use, the cognitive stimulation and all that sort of stuff. People go to the doctors for all sorts of things . . . I think it’s the best place.
Case manager
Opportunity for ad hoc contacts
Because I see people coming in for maybe a warfarin test or a leg dressing or I can see people on other people’s lists and think ‘oh I haven’t seen them for a little while’, I can pop my head round the door and just check they’re ok.
Case manager
Creation of expertise within primary care
There’s something about bringing this expertise closer to people, closer to the community, closer to the coalface. And certainly for Admiral nurses who are all mental health specialist, they are all mental health nurses, we’ve found that actually putting mental health specialists into primary care has been very welcomed because it’s expertise that doesn’t exist within primary care.
Team member
Potential for early involvement
Case finding absolutely has to happen there [primary care] because that’s where the journey starts . . . a lot of people never get to secondary mental health services, they never get as far as the memory clinic.
Team member
Disadvantages
Conflicting roles (for practice nurses)
Our hypothesis was actually having somebody who was part of the practice team would be really best placed to kind of do this work but in reality what seems to have emerged is a picture whereby the immediacy, the immediate issues of a GP practice, and working in a GP practice always takes precedence to some of this other work, and maybe that’s de-railed it.
Team member
Space limitations
At [practice 2] I stopped booking rooms there because it was inappropriate, they have a limited amount of rooms, I had to book rooms which was taking rooms away from other people just to be you know just to be sitting there with not a great deal to do in the surgery.
Case manager
Culture clash
The surgery is set up for everybody to have 10- to 15-minute appointments with however many people you can cram into your day, it’s not about sitting and reflecting and analysing and spending a lot of time on a person and within that person a particular problem for that particular person or the dynamic of whatever; it’s not how a GP’s surgery functions.
Case manager
The potential difficulties for the social workers of integrating into the primary care team were recognised by members of the research team:
My experience of working with multidisciplinary teams is that’s it’s been really very hard for social workers to become part of the system in that way.
Team member
Embedding case management in primary care
All of the participating practices had identified a lead GP with a particular interest in dementia; however, the contact between the lead GP and case manager varied between practices. Although one lead GP held regular meetings with the case manager, in other practices contact was limited, typically to one or two meetings to discuss case management throughout the whole period of implementation:
I think people are interested but people have to have the head space to be interested and yes they know I’m doing it but it’s probably not that relevant to them on a daily [basis].
Case manager
It’s been challenging to be honest. I’m quite confused over the reaction from the surgeries. . . . I don’t know, it’s whether it’s a priority or whether it’s been lost in the mix, or people just don’t know, quite know what expectations of roles are, but they don’t seem as involved as I would desire . . . there doesn’t really seem a huge interest in it through some quarters.
Case manager
One case manager was proactive in taking on the dementia reviews and thereby created a continuing specialist role within the practice. However, there was little evidence that either of the other case managers thought strategically about their role or sought to create structures to support their activities within the practice:
I would imagine if the role became a permanent one, case managers and the GPs would have regular meetings and they would go through the lists, and discuss people, not just reliant on the QOF but a much more robust examination of who’s on the books, as it were. And you know targeting people that way.
Case manager
Although this would have been a useful way of increasing the case manager’s profile within the practice, there was no attempt to arrange any such meetings or to become involved in existing meetings within the practice that might have been relevant. The lack of involvement of other members of the primary care team became clear towards the end of the project when we asked case managers to suggest colleagues whom we could interview about their perspectives on case management:
Regarding the interviews – I’m not sure who to suggest really. I doubt if anyone here at the surgery would have any inkling of how the case management I have done will have impacted (or not) on the practice as a whole.
E-mail from case manager
Supervision and support of case managers
Developing case management skills
Each case manager received an induction session, lasting between 90 minutes and 3 hours, to orient them to the project, clarify their role and enable them to complete and discuss an educational needs assessment form. The variation in time was, in part, because of the different needs of the case managers and, in part, because of the time available, highlighting some of the difficulties encountered in preserving the nurse case managers’ dedicated time in practices. The induction was supplemented by individual meetings with the mentor, the provision of the CAREDEM manual (developed in WP1; see Chapter 2), additional tailored materials provided by the mentor and self-directed learning. The educational needs assessment enabled the mentor to provide individualised training and support to each case manager:
What it [educational needs assessment] did do for me, is where there was an identified need it helped frame how I would support or ensure that need was met for that case manager either through training that I would deliver or direct them to access that training elsewhere but it was a document where we had written and agreed before we left about what the needs were and what we would do next, so I found that helpful.
Mentor
The educational needs assessment tool developed in WP1 focused on dementia-specific knowledge; one result of this may have been that there was less emphasis on assessing and developing the other skills outlined earlier:
[The] needs assessment’s built around the trajectory of dementia, loosely speaking, so it starts with working with the person who has recently acquired or is just about to acquire the diagnosis and coping with the confusion that arises then and the other types of psychological responses you can encounter, managing that and then working through crisis in the support system, admission to hospitals and having some hospital in-reach function, advocating for the patient in the hospital. Relocation to a nursing home and the issues that arise there and end of life care so those are the five components of the needs assessment tool and we go through them.
Team member
Some reservations were expressed about self-identification of needs. There was a potential for training needs to be missed if the case manager was either unaware of her training needs or was reluctant to voice them at the induction meeting, which took place at an early stage in the project. Although in the current project the induction sessions were individual, this was not seen as viable for a larger project. Views varied on whether case managers would be more or less willing to voice their training needs in a group session. A more rigorous interview process was suggested as an alternative way of assessing the extent to which the case managers possessed the required skill set:
You’re very reliant on the openness of the case manager and I’m not sure how you would assess for that; my own feelings are that some of those things could be assessed at interview.
Mentor
Interestingly, the documentation provided (the CAREDEM manual and supplementary materials) seemed to be valued most by those case managers with an existing interest in dementia; in particular, some of the assessment tools and information provided by the mentor were seen as potentially useful:
[They] are going to be very useful in the future, so I’m going to get a lot out of it, lots of assessment tools and things like that . . . I’ll be able to see myself using these in the future, I’m very pleased with that.
Case manager
I’ve used a document that [mentor] gave me which is a summary, like a leaflet/pamphlet that she has produced, and there are just some really good ways of talking about dementia, that are accessible to older people.
Case manager
The leaflets for patients and carers produced as part of WP1 were seen as a useful resource for the case managers, particularly when they first started out in the role, but were rarely given to patients or carers. This seemed to be because they were not currently perceived to be relevant to the patients and carers recruited.
Although the intention was to provide on-the-job training, opportunities for training were limited by the time restrictions of the mentor and practice nurses. It was suggested that more time should be made available at the beginning to ensure that case managers had the basic skills:
I discussed some more front-loading of support and induction because all they’ve had is a couple of hours on MCA [Mental Capacity Act 2005] as part of the provision of the assessment.
Mentor
Support networks of case managers
The existing line management arrangements for all of the case managers continued throughout the study. In addition, a mentor was available to provide training and support with case management. It was clear that case managers also derived support from other sources:
I’ve got obviously support from yourselves, support from [mentor] and there’s (lead GP) if I need to speak to her and there’s that network of other case managers on e-mail . . . and I’ve also got my adult services’ supervision as well so there’s lots of different kinds of support that I can access which is good.
Case manager
Chapter 8 Conclusions and future work
Did the case manager role, as developed in WP1, fit within the routine processes of care of the four practices recruited to the pilot study? One way to answer that question is to compare the quantitative and qualitative findings of WP2 with the desirable characteristics of a diffusible innovation shown in Table 1:
-
Compatibility. Case management did appear to be compatible with the values, norms and perceived needs of the practices, the case managers and the recipients of case management, although the compatibility was perhaps more evident at the conceptual level than at the practical level.
-
Complexity/ease of use. The degree to which an innovation is expected to be free of effort influences its uptake and diffusion. The case management role was not seen as complex and difficult by all case managers, one of whom had previous experience of it with a different patient group; nonetheless, the other case managers experienced some lack of clarity about case management and concern was expressed about potential duplication of existing roles. The case managers’ difficulties also arose from time constraints and unfamiliarity with dementia as well as from the demands of the research process. Although the perceived complexity of an innovation can be reduced by practical experience and demonstration, it was not clear that this occurred within the time frame of the pilot study.
-
Relative advantage. The evidence from the pilot study does not suggest a clear, unambiguous advantage of case management in terms of effectiveness for patients.
-
Trialability. Innovations that can be experimented with by intended users on a limited basis will be more easily adopted and implemented. The pilot study provided a ‘trialability space’ for the idea of case management for people with dementia in primary care, but the findings from interviews and the case manager group discussion suggest that the role as conceived and constructed was difficult to implement.
-
Observability/result demonstrability. Positive patient and carer feedback, and the equally positive response from a PPI panel at the end of the project, may reflect the perceived value of the case manager role, but the low level of activity with dyads makes it difficult to be certain about observable gains.
-
Reinvention. Adoption and implementation of an innovation are increased if the potential adopter can adapt, refine or otherwise modify the innovation to suit his or her own needs. Flexibility was built into the case management role, which was tailored to discipline (nurses, social worker), practice and individual, and one of the mentor’s functions was to support that tailoring. However, such flexibility interferes with the research function, which needs to standardise measures and processes as much as possible – hence, the difficulties with modifying inclusion and exclusion criteria and incomplete research documentation.
-
Image and visibility. We have no evidence that the case manager role added to the user’s social approval (other than patient and carer feedback) or enhanced the practices’ standing within their clinical communities.
-
‘Voluntariness’. The degree to which the adoption of the case manager role was controlled by the potential user’s free will varied between settings. Senior staff in practices made decisions about participation, encouraging their staff to take up the case manager role, but did not necessarily support them in the new role.
Implications for further research and development
From a theoretical perspective, the concept of case management potentially affords considerable benefit to patients, their carers and community-based professionals to improve the quality of dementia care through continuity of care with a named, trusted individual and the ability to provide proactive care to prevent a crisis. However, the findings of the feasibility study suggest that the actual need for this way of working in this population needs to be established. If the need is substantial then a number of changes are needed to the model of case management implemented in this pilot study before these potential benefits could be achieved in practice. These changes are discussed in the following sections.
Clarifying the purpose of case management
The uncertainty expressed by professionals, people with dementia, carers and case managers themselves indicates the need for a clear definition of the theoretical concept of case management and hence the case manager role, as suggested by our review. 24 This study provides empirical evidence about the limitations of implementing a case management approach in primary care for people with dementia, which can inform the theoretical debate that is needed. One aspect of this debate might involve establishing the boundaries between a practice-based case manager and existing professional roles within the NHS, for example Admiral nurses and social services care managers.
Revisiting which skills and attributes are required for case management
Specific experience of working with people with dementia and with local service and support networks, and understanding how dementia impacts both patients and their families is essential. In addition, good interpersonal skills and the ability to work holistically, proactively seeking out ‘day-to-day’ issues that may become tomorrow’s crisis, are required. For practice staff seconded to the case management role, time management skills were required to balance competing demands and protect time for delivering the intervention. Professional background is less important than the above skills and a positive attitude and enthusiasm to work with patients and families living with dementia. Practice nursing experience may facilitate links with GPs but social workers have experience of independent working in the community. The feasibility study highlighted the need for robust line management arrangements, peer support and supervision for case managers, especially in the early stages of implementation.
Embedding delivery of case management
Primary care is the preferred environment for implementation and contact with patients; this was thought to ‘normalise’ case management and provide opportunities for ad hoc proactive care. The primary care QOF dementia annual review provides further opportunities for case manager contact with those with dementia and their carers along the disease trajectory if, for example, patients or their families are not ready to engage at the time of diagnosis. However, for primary care-based case management to succeed, the practice must be supportive of the case manager role and allow protected time from other conflicting duties. When case managers work part-time, flexible arrangements are needed to enable a timely response if patients or carers need assistance outside the formally agreed hours.
Even when existing practice staff took on the role of case management, time and effort were required to ‘embed’ the case manager within the practice team and local mental health services. Attendance at joint meetings (e.g. district nurse meetings in primary care and CMHT meetings) was seen as a possible way of embedding case management in practice. Recording case management activities in primary care notes was seen as essential to ensure that colleagues were aware that the case manager was involved and to build links within the practice. An alternative model of case management (suitable for smaller practices) would be to have one case manager covering a number of practices. The most appropriate alternative site proposed for case management was within secondary care memory clinics as this would ensure that the service was available at diagnosis. Regardless of location, the ability to visit patients and family carers at home was seen as essential to facilitate detailed assessment of patients and their environment.
Establishing when case management is likely to have maximum effect
The timing of the introduction of case management may matter. If case management were available from the point of diagnosis, it might help establish a relationship and let people with dementia and their carers know that they have a named contact for future support; this is similar to the current primary care management of newly diagnosed cancer patients. Although patients and carers valued the idea of a ‘safety net’, it was clear that they would not necessarily seek help; this was partly because of an unwillingness to make demands on busy professionals but also reflected their lack of knowledge of the range of support available. Regular informal contact between case managers and patients and carers, case manager led but negotiated with clients, is required to facilitate identification of areas of low-level need and allow proactive intervention to prevent future crises and/or reduce family stress. It is difficult to make recommendations about the time required for case management given the low rates of contact and intervention observed in the present study. It was clear that one session a week was not sufficient to deliver anything beyond signposting and brief follow-up telephone calls. Within the context of future research trials, adequate time needs to be allowed for research-related tasks, training, supervision and completion of any study-specific documentation.
Key issues for any future trial of case management
The findings of this feasibility study suggest that the model of case management developed in the CAREDEM study is not suitable for testing in a randomised controlled trial within the NHS as currently organised. Different approaches to recruiting GP practices, training and employing case managers and identifying people with dementia who might benefit from case management are needed. We encountered particular difficulties in recruitment and follow-up of people with dementia and their families and with applying case management methods.
Recruitment and follow-up
A complex, co-designed induction and training programme on case management for primary care workers can be embedded in practice, but the amount of time needed to fulfil the role is greater than we anticipated and the rate of case identification is slow. Delays in recruitment partly reflected the need to balance case finding with case management tasks and partly reflected the inconsistent recording of dementia diagnoses in electronic medical records in general practice. In some sites the recruitment of practices willing to take part in this study was more challenging than we anticipated; this experience alone suggests that a full-scale trial (initially anticipated as involving 56 practices) would be time-consuming and expensive to carry out, at least using the model of case management that we have evaluated. The recruitment target of 11 patients per practice was nearly achieved in two of the four participating practices and one practice would probably have achieved the target had the nurse case manager had more time available each week. Overall, we recruited 28 of the planned 44 dyads, a recruitment rate of 64%.
The inclusion criteria tested in this project were narrow. Our original assumptions about those attending specialist clinics or living in care homes not needing case management were generous; these two patient groups could be included among those invited to take up primary care-based case management in future studies although the case management intervention may need modification. Recruitment periods would need to be extended to > 6 months to reach the targets proposed in the original study protocol.
Follow-up rates were good. In total, 24 out of 29 patients (83%) were successfully followed up at 5 months (either by providing data or indicating a willingness to provide data), which was consistent with the retention target of nine out of 11 (82%). The response to the evaluation of the intervention, and to the idea of case management, was largely positive among people with dementia and their carers. However, the actual collection of data was variable. For example, the NPI outcome at 5 months was missing for 13 out of 29 (55%) overall but for only four out of 14 (29%) in the north-east. Likewise, follow-up data collection for secondary outcomes ranged between 50% and 59%.
Case management intervention
Only one of the four practices achieved a level of case management activity that might have had an impact on outcomes, with nine dyads recruited (and recruitment stopped to concentrate on follow-up work). There was an average of five contacts per dyad (compared with contact rates of less than two in the other practices) although most of these contacts were by telephone. In this practice the nurse acting as the case manager had a background in care work with people with dementia, but no previous experience of case management methods.
There was evidence that the threshold for identification of unmet needs was high, that identification of unmet needs did not necessarily lead to action and that data capture for research purposes was burdensome to the case managers, who had not had previous experience of research.
Conclusions and recommendations
In conclusion, the key lessons learned from the feasibility study to be taken forward in any future trial of implementation of case management for people with dementia are summarised below:
-
The case managers in the present study had little research experience and found tasks relating to recruitment and recording their case management activities onerous. In any future trial we suggest that the research team provides a brief introduction to research, and the individual research study, for those responsible for delivering interventions, to enhance their understanding of the rationale behind research tasks such as data capture.
-
It may be that case management for people with dementia is unlikely to work without substantially more time being allocated to it (as in the Netherlands and Finland) by dedicated practitioners who have had more training than we could provide in the pilot study. The overall experience of NHS case management (not for people with dementia necessarily) is not positive and so this type of intervention would still need to be tested in a randomised controlled trial.
-
Dementia syndrome may be too narrow a clinical problem for case management in primary care; frailty might be a broader and potentially more tractable clinical target.
-
Allowing time for research team members to develop an understanding of the context and day-to-day routines of those delivering the intervention (e.g. by shadowing professionals) is also recommended. This would help the research team to gain insight into the realities of the work of staff delivering the intervention, which is particularly important when this is combined with an existing role. This could lead to further simplification of the research data capture methods. Developing clear lines of communication and co-ordination of research activities would ensure that professionals are not overwhelmed by requests. Regular opportunities for links and communication between those delivering the intervention and the research team would also help to build mutual understanding.
-
To specifically facilitate the process of recruitment in future research studies it is essential to ensure either that practice staff responsible for recruitment have a good understanding of the inclusion/exclusion criteria or that they devolve recruitment to research network staff or the research team. When practice staff are tasked with recruiting patients, we suggest that all exclusions are reviewed by the research team to ensure that the criteria have been appropriately used.
-
It was clear that the current dementia registers do not provide a comprehensive list of patients with dementia in general practice. Multiple strategies for identifying patients with dementia, for example informal discussions with primary care staff and systematic searches of electronic patient records for specific dementia-related drugs and terms that may be used as synonyms for dementia (e.g. ‘memory problems’, ‘cognitive impairment’), could be used to ensure that dementia registers are up-to-date before recruitment.
-
Family carers were not systematically recorded in primary care records. Again, a range of strategies may be required to identify family members, for example searching on address (for co-resident carers), reviewing recent consultations for mention of family members and informal discussions with primary care staff may be helpful.
-
In the present study, case management was offered only to patients with informal carers – approximately one-third of people with dementia in the UK live alone in their own homes;6 offering the service to patients who do not have family carers or informal support networks may ensure that the service reaches those in greatest need.
-
Consideration should be given to ways of increasing the image and visibility of any future case management study and of making any benefits from case management widely known. Practices (and other local services) need to be included in discussions about the implementation of case management, to maintain the profile of the intervention. This could extend as far as having a formal, written contract with participating organisations to clarify expectations and roles.
-
There may be advantages in working with Clinical Commissioning Groups to incorporate case management into a locally or directly enhanced service (L/DES) so that practices are reimbursed for the extra workload. Similarly, case management innovations could be incorporated into integrated care initiatives.
-
Developing a system for recording intervention-related activity that was acceptable to the case managers, facilitating the process of case management and providing sufficient detail for the research team to be able to adequately describe the intervention proved challenging. Possible strategies for improving record-keeping in future studies include:
-
making time to co-design the research paperwork to ensure that it meets the needs of the research team and also the practitioners, and deliberately involving inexperienced researchers in this process to reduce later risks of poor data capture
-
ensuring adequate time for initial and ongoing training
-
implementing robust systems for ongoing monitoring and review of documentation (which informs additional training needs)
-
providing early interim analyses of completed documentation to illustrate how the information will be used (and the consequences of inadequate documentation).
-
Further thoughts on methodological problems and their solutions can be found in Appendix 8.
Our findings and arguments need to be considered in the light of the limitations of the study’s methods. The interviews with case managers, the mentor and team members were, in general, based on first-hand experience of case management (or an aspect of case management of which the respondent had specific knowledge). In contrast, the limited case management provided and the lack of visibility of case management to colleagues both within and outside the primary health care team meant that other stakeholders had limited practical knowledge of case management. Patients and carers were able to describe their experiences of assessment and any subsequent contacts with the case manager. However, many of their comments on the value of case management relate to hypothetical or potential benefits of this approach rather than personal experiences. Health and social care professionals, even those within participating practices, also reported a lack of contact with case managers and limited knowledge of their work. The data therefore are skewed towards views of case management in the abstract, rather than being based on practical experience of this approach.
In conclusion, although the feasibility study demonstrated that the concept of case management was valued by patients, family carers and professionals, there were significant difficulties in delivering the case management intervention. A range of factors influencing implementation was identified, which need to be addressed in any future trial of case management for people with dementia.
Acknowledgements
This study was funded by the National Institute for Health Research Health Technology Assessment (HTA) programme (08/53/99) and we are grateful for the support given by HTA programme staff.
We thank all the members of the WP1 development group in East Kent who gave their time and expertise in the development of the case manager role, practices and materials, and the members of the review and PPI groups who critiqued the work carried out in this work package.
We are grateful to the case managers for their efforts, to the general practices that took part in the feasibility study and to the people with dementia and their carers who participated in WP2.
The CAREDEM study benefited from the advice of its trial steering committee and its data management committee. The trial steering committee members were Professor Bob Woods (chair), Dr Zuzana Walker, Dr David Smithard and Ken and Janet Clasper (PPI representatives). The data management committee members were Professor James Lindesay (chair), Professor Murna Downs and Dr Mona Kanaan.
Contributions of authors
The CAREDEM research team was drawn from seven academic institutions and one charity.
University College London
Steve Iliffe led the funding application, was co-chief investigator and finalised this report.
Amy Waugh and Allana Austin were research assistants working with the London and Norfolk practices respectively. Amy Waugh drafted Chapters 1–3 of this report
Cornelius Katona was a co-applicant, chaired the study management committee and contributed to this report.
Gill Livingston was a co-applicant and site principal investigator for London and contributed to this report.
University of Newcastle
Louise Robinson led the funding application, was co-chief investigator and site principal investigator for the north-east and contributed to this report.
Katie Brittain was a co-applicant and was responsible for the qualitative research (with support from John Bond) and contributed to this report.
Claire Bamford and Marie Poole were a senior research associate and research associate, respectively, working with the north-east practices, and were also responsible for carrying out the qualitative research. They drafted Chapters 5–7 of this report.
Nick Steen was a co-applicant and the study statistician and drafted Chapter 4 of this report.
Elaine McColl and Chris Speed of the Newcastle Clinical Trials Unit advised on study design.
Vanessa Hogan of the Newcastle Clinical Trials Unit administered the study and contributed to this report.
Dementia UK
Barbara Stephens was a co-applicant, worked on WP1 and contributed to this report.
Pat Brown was the mentor for the case managers in WP2.
University of East Anglia
Chris Fox was a co-applicant and site principal investigator for Norfolk and contributed to this report.
King’s College London
Jill Manthorpe was a co-applicant, helped co-ordinate WP1 and PPI involvement and contributed to this report.
Keele University
Carolyn Chew-Graham was a co-applicant and the study’s expert on care co-ordination and contributed to this report.
University of Kent
Simon Coulton was a co-applicant and advisor on service modelling for the intended full trial.
London School of Economics and Political Science
Martin Knapp was a co-applicant and advised the study on economic evaluation methods.
Publication
Koch T, Iliffe S, Manthorpe J, Stephens B, Fox C, Robinson L, et al. (2012) The potential of case management for people with dementia: a commentary. Int J Geriatr Psychiatry 2012:27:1305–14.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Prime Minister’s Challenge on Dementia – Delivering Major Improvements in Dementia Care and Research by 2015. London: Department of Health; 2012.
- NHS R&D Strategic Review: Ageing and Age-Associated Disease and Disability. London: Department of Health; 1999.
- National Service Framework for Older People. London: Department of Health; 2001.
- Our Health, Our Care, Our Say: a New Direction for Community Services. London: Department of Health; 2006.
- Knapp M, Prince M, Albanese E, Banerjee S, Dhanasiri S, Fernandez JL, et al. Dementia UK. London: Alzheimer’s Society; 2007.
- Dementia 2012: a National Challenge. London: Alzheimer’s Society; 2012.
- Smith T, Hameed Y, Cross J, Sahota O, Fox C. Assessment of people following hip fracture with cognitive impairment: a systematic review and meta-analysis. Arch Gerontol Geriatr 2013;57:117-26. http://dx.doi.org/10.1016/j.archger.2013.04.009.
- Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery Office; 2013.
- The Operating Framework for the NHS in England 2012/13. London: Department of Health; 2011.
- Improving Services and Support for People with Dementia. London: National Audit Office; 2007.
- Downs M, Turner S, Bryans M, Wilcock J, Keady J, Levin E, et al. Effectiveness of educational interventions in improving detection and management of dementia in primary care: cluster randomised controlled study. BMJ 2006;332:692-5. http://dx.doi.org/10.1136/bmj.332.7543.692.
- Facilitating Timely Diagnosis and Support for People with Dementia. London: NHS England; 2013.
- Dementia: Supporting People with Dementia and their Carers in Health and Social Care. London: NICE; 2006.
- Improving Services and Support for People with Dementia: Sixth Report of Session 2007–2008. London: The Stationery Office; 2008.
- Richards DA, Lankshear AJ, Fletcher J, Rogers A, Barkham M, Bower P, et al. Developing a UK protocol for collaborative care: a qualitative study. Gen Hosp Psychiatry 2006;28:296-305. http://dx.doi.org/10.1016/j.genhosppsych.2006.03.005.
- Bower P, Gilbody S, Richards D, Fletcher J, Sutton A. Collaborative care for depression in primary care – making sense of a complex intervention: systematic review and meta-regression. Br J Psychiatry 2006;189:484-93. http://dx.doi.org/10.1192/bjp.bp.106.023655.
- Gunn J, Diggens J, Hegarty K, Blashki G. A systematic review of complex system interventions designed to increase recovery from depression in primary care. BMC Health Serv Res 2006;6. http://dx.doi.org/10.1186/1472-6963-6-88.
- Katon W, Von Korff M, Lin E, Walker E, Simon GE, Bush T, et al. Collaborative management to achieve treatment guidelines. Impact on depression in primary care. JAMA 1995;273:1026-31. http://dx.doi.org/10.1001/jama.1995.03520370068039.
- Unutzer J, Katon W, Callahan CM, Williams JW, Hunkeler E, Harpole L, et al. Collaborative care management of late-life depression in the primary care setting – a randomized controlled trial. JAMA 2002;288:2836-45. http://dx.doi.org/10.1001/jama.288.22.2836.
- Hunkeler EM, Meresman JF, Hargreaves WA, Fireman B, Berman WH, Kirsch AJ, et al. Efficacy of nurse telehealth care and peer support in augmenting treatment of depression in primary care. Arch Fam Med 2000;9:700-8. http://dx.doi.org/10.1001/archfami.9.8.700.
- Mann AH, Blizard R, Murray J, Smith JA, Botega N, MacDonald E, et al. An evaluation of practice nurses working with general practitioners to treat people with depression. Br J Gen Pract 1998;48:875-9.
- Chew-Graham CA, Lovell K, Roberts C, Baldwin R, Morley M, Burns A, et al. A randomised controlled trial to test the feasibility of a collaborative care model for the management of depression in older people. Br J Gen Pract 2007;57:364-70.
- Christensen H, Griffiths KM, Gulliver A, Clack D, Kljakovic M, Wells L. Models in the delivery of depression care: a systematic review of randomised and controlled intervention trials. BMC Fam Pract 2008;9. http://dx.doi.org/10.1186/1471-2296-9-25.
- Koch T, Iliffe S, Manthorpe J, Stephens B, Fox C, Robinson L, et al. The potential of case management for people with dementia: a commentary. Int J Geriatr Psychiatry 2012;27:1305-14. http://dx.doi.org/10.1002/gps.3783.
- Goodman C, Drennan V, Davies S, Massey H, Gage H, Scott C, et al. Nurses as Case Managers in Primary Care: the Contribution to Chronic Disease Management. Southampton: NIHR; 2010.
- Minkman MMN, Ligthart SA, Huijsman R. Integrated dementia care in the Netherlands: a multiple case study of case management programmes. Health Soc Care Community 2009;17:485-94. http://dx.doi.org/10.1111/j.1365-2524.2009.00850.x.
- Verkade PJ, van Meijel B, Brink C, van Os-Medendorp H, Koekkoek B, Francke AL. Delphi research exploring essential components and preconditions for case management in people with dementia. BMC Geriatr 2010;10. http://dx.doi.org/10.1186/1471-2318-10-54.
- Connor K, McNeese-Smith D, van Servellen G, Chang B, Lee M, Cheng E, et al. Insight into dementia care management using social-behavioral theory and mixed methods. Nurs Res 2009;58:348-58. http://dx.doi.org/10.1097/NNR.0b013e3181b49910.
- Vickrey BG, Mittman BS, Connor KI, Pearson ML, Della Penna RD, Ganiats TG, et al. The effect of a disease management intervention on quality and outcomes of dementia care – a randomized, controlled trial. Ann Intern Med 2006;145:713-26. http://dx.doi.org/10.7326/0003-4819-145-10-200611210-00004.
- Callahan CM, Boustani MA, Unverzagt FW, Austrom MG, Damush TM, Perkins AJ, et al. Effectiveness of collaborative care for older adults with Alzheimer disease in primary care – a randomized controlled trial. JAMA 2006;295:2148-57. http://dx.doi.org/10.1001/jama.295.18.2148.
- Clark PA, Bass DM, Looman WJ, McCarthy CA, Eckert S. Outcomes for patients with dementia from the Cleveland Alzheimer’s Managed Care Demonstration. Aging Ment Health 2004;8:40-51. http://dx.doi.org/10.1080/13607860310001613329.
- Fortinsky RH, Kulldorff M, Kleppinger A, Kenyon-Pesce L. Dementia care consultation for family caregivers: collaborative model linking an Alzheimer’s association chapter with primary care physicians. Aging Ment Health 2009;13:162-70. http://dx.doi.org/10.1080/13607860902746160.
- Smith SC, Lamping DL, Banerjee S, Harwood RH, Foley B, Smith P, et al. Development of a new measure of health-related quality of life for people with dementia: DEMQOL. Psychol Med 2007;37:737-46. http://dx.doi.org/10.1017/S0033291706009469.
- Pinquart M, Sorensen S. Helping caregivers of persons with dementia: which interventions work and how large are their effects?. Int Psychogeriatr 2006;18:577-95. http://dx.doi.org/10.1017/S1041610206003462.
- Specht J, Bossen A, Hall GR, Zimmerman B, Russell J. The effects of a dementia nurse care manager on improving caregiver outcomes. Am J Alzheimers Dis Other Dementia 2009;24:193-207. http://dx.doi.org/10.1177/1533317508330466.
- Spijker A, Vernooij-Dassen M, Vasse E, Adang E, Wollersheim H, Grol R, et al. Effectiveness of nonpharmacological interventions in delaying the institutionalization of patients with dementia: a meta-analysis. J Am Geriatr Soc 2008;56:1116-28. http://dx.doi.org/10.1111/j.1532-5415.2008.01705.x.
- Newcomer R, Spitalny M, Fox P, Yordi C. Effects of the Medicare Alzheimer’s disease demonstration on the use of community-based services. Health Serv Res 1999;34:645-67.
- Miranda-Castillo C, Woods B, Galboda K, Oomman S, Olojugba C, Orrell M. Unmet needs, quality of life and support networks of people with dementia living at home. Health Qual Life Outcomes 2010;8. http://dx.doi.org/10.1186/1477-7525-8-132.
- van der Roest HG, Meiland FJM, Comijs HC, Derksen E, Jansen APD, van Hout HPJ, et al. What do community-dwelling people with dementia need? A survey of those who are known to care and welfare services. Int Psychogeriatr 2009;21:949-65. http://dx.doi.org/10.1017/S1041610209990147.
- Mittelman MS, Haley WE, Clay OJ, Roth DL. Improving caregiver well-being delays nursing home placement of patients with Alzheimer disease. Neurology 2006;67:1592-9. http://dx.doi.org/10.1212/01.wnl.0000242727.81172.91.
- Challis D, von Abendorff R, Brown P, Chesterman J, Hughes J. Care management, dementia care and specialist mental health services: an evaluation. Int J Geriatr Psychiatry 2002;17:315-25. http://dx.doi.org/10.1002/gps.595.
- Lam LC, Lee JS, Chung JC, Lau A, Woo J, Kwok TC. A randomized controlled trial to examine the effectiveness of case management model for community dwelling older persons with mild dementia in Hong Kong. Int J Geriatr Psychiatry 2010;25:395-402. http://dx.doi.org/10.1002/gps.2352.
- Duru OK, Ettner SL, Vassar SD, Chodosh J, Vickrey BG. Cost evaluation of a coordinated care management intervention for dementia. Am J Manag Care 2009;15:521-8.
- Pimouguet C, Lavaud T, Dartigues JF, Helmer C. Dementia case management effectiveness on health care costs and resource utilization: a systematic review of randomized controlled trials. J Nutr Health Aging 2010;14:669-76. http://dx.doi.org/10.1007/s12603-010-0314-4.
- Chien WT, Lee YM. A disease management program for families of persons in Hong Kong with dementia. Psychiatr Serv 2008;59:433-6. http://dx.doi.org/10.1176/appi.ps.59.4.433.
- World Alzheimer Report 2011: The Benefits of Early Diagnosis and Intervention. London: Alzheimer’s Disease International; 2011.
- Department of Health . Report on the Review of Patient-Identifiable Information n.d. http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4068403 (accessed 20 June 2014).
- Data Protection Act 1988. London: The Stationery Office; 1988.
- Berwick D. Disseminating innovations in health care. JAMA 2003;289:1969-75. http://dx.doi.org/10.1001/jama.289.15.1969.
- Miller WL, McDaniel RR, Crabtree BF, Stange KC. Practice Jazz: understanding variation in family practices using complexity science. J Fam Pract 2001;50:872-80.
- Moore GC, Benbasat I. Development of an instrument to measure the perception of adopting an information technology innovation. Inform Syst Res 1991;2:172-91. http://dx.doi.org/10.1287/isre.2.3.192.
- Rogers EM. Diffusion of Innovation. New York, NY: New York Free Press; 2003.
- Waugh A, Austin A, Manthorpe J, Fox C, Stephens B, Robinson AL, et al. Designing a complex intervention for dementia case management in primary care. BMC Fam Pract 2013;14. http://dx.doi.org/10.1186/1471-2296-14-101.
- Kaulio MA. Customer, consumer and user involvement in product development: a framework and a review of selected methods. Total Qual Manag 1998;9:141-9. http://dx.doi.org/10.1080/0954412989333.
- Grant J. Learning needs assessment: assessing the need. BMJ 2002;324:156-9. http://dx.doi.org/10.1136/bmj.324.7330.156.
- Kochevar L, Yano E. Understanding health care organisations needs: beyond performance gaps. J Gen Intern Med 2006;21:S25-9.
- Cohen D, McDaniel R, Crabtree B, Ruhe M, Weyer S, Tallia A, et al. A practice change model for quality improvement in primary care practice. J Healthcare Manag 2004;49:155-68.
- Kahn WA. Holding Fast: the Struggle to Create Resilient Caregiving Organisations. New York, NY: Brunner-Routledge; 2005.
- Cummings JL, Mega M, Grey K, Rosenberg-Thomas S, Carusi DA. The Neuropsychiatric Inventory: a comprehensive assessment of psychopathology in dementia. Neurology 1994;44:2308-14. http://dx.doi.org/10.1212/WNL.44.12.2308.
- Byrne LM, Wilson PM, Bucks RS, Hughes AO, Wilcock GK. The sensitivity to change over time of the Bristol Activities of Daily Living in Alzheimer’s disease. Int J Geriatr Pscyhiatry 2000;15:656-61. http://dx.doi.org/10.1002/1099-1166(200007)15:7<656::AID-GPS163>3.0.CO;2-Q.
- Goldberg D. Manual of the General Health Questionnaire. Windsor: NEFR-Nelson; 1978.
- Beecham J, Knapp M, Thornicroft G. Measuring Mental Health Needs. London: Gaskell; 2001.
- Folstein MF, Folstein SE, McHugh PR. The ‘mini-mental state’: a practical method for grading the cognitive state of patients for the clinician. J Psychiatric Res 1975;12:189-98. http://dx.doi.org/10.1016/0022-3956(75)90026-6.
- Logsdon RG, Gibbons LE, McCurry SM, Teri L. Assessing quality of life in older adults with cognitive impairment. Psychosom Med 2002;64:510-19. http://dx.doi.org/10.1097/00006842-200205000-00016.
- Barry TL, Kaiser KL, Atwood JR. Reliability, validity, and scoring of the Health Status Questionnaire-12 version 2.0. J Nurs Meas 2007;15:24-35. http://dx.doi.org/10.1891/106137407780851778.
- Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012;7. http://dx.doi.org/10.1186/1748-5908-7-37.
Appendix 1 Case manager job description
Case management is the provision of co-ordinated health and social care by a single health or social care professional.
The CAREDEM study is a randomised controlled trial of case managment for people with dementia and their carers, conducted in primary care.
Case managers in the CAREDEM trial will be employed by NHS organisations and will work under the supervision of a GP or other clinical lead and a NHS line manager.
The case manager in the CAREDEM trial will undertake the following tasks:
-
Identify people with dementia from general practice lists.
-
Review medical records of people with dementia ± their carers, noting any gaps in the record and also the involvement of other possible sources of support.
-
Liaise with other professionals who know the people with dementia to learn their perspectives on individual or family needs.
-
Engage with the people with dementia ± their carers to identify their main concerns or unmet needs.
-
Update or fill in gaps in GP medical records and when appropriate update social care records.
-
Analyse information obtained from the people with dementia and their carers.
-
Map support available to and wanted by people with dementia and their carers. Create a personal care or support plan with each person with dementia and his or her carer and initiate actions that will provide that support [e.g. help with seeking advice about benefits, liaising with the GP about treatment of other conditions and discussion of plans around finance, health and welfare decisions (details inserted here to limit the scope for interpretation of the job by those doing it).
-
Analyse information obtained by other relevant practitioners (e.g. GP, social worker, care home key worker).
-
Prioritise individual people with dementia and their carers: assess need for action in terms of ‘intensive’, ‘maintenance’ and ‘holding’ (for those already being case managed by other agencies).
-
Build the care plan into the GP medical records and share it with other disciplines and agencies as needed.
-
Organise systematic follow-up to review the outcomes of actions taken, meet regularly with the GP or other relevant clinical leads and act as an advocate for the people with dementia and their carers.
-
Meet regularly with his/her mentor to discuss the people with dementia and their carers with whom they are working, review prioritisation, resolve any problems that have arisen and plan the end of their role with the people with dementia and their carers, as appropriate.
-
Undertake professional updating and top-up training, as needed.
-
Meet with and communicate with members of the research team to discuss the case manager role as it develops.
Appendix 2 Case manager person specification
Applicants for the case manager roles in CAREDEM should have the following attributes and skills.
| Attribute/skill | Desirable (D) or essential (E) | Assessed by |
|---|---|---|
| Already working in local NHS or adult services | D (could be a returner, etc.) | CV |
| Hold a relevant qualification for their discipline | E | CV |
| Basic IT skills, knowledge of local IT systems and experience in recording information electronically | E | CV and reference |
| Interpretation of medical and nursing records | E | CV, interview and reference |
| Knowledge of local dementia and older people’s and carers’ services | D | CV and interview |
| Communication skills, particularly with difficult topics (diagnosis itself, prognosis, BPSD, continence, anxiety) | E | CV, interviewa and reference |
| Person centred (respects autonomy), non-judgemental attitudes and values | E | CV, interviewb and reference |
| Capable of system-building, networking and increasing efficiency within services | D | CV, interview and reference |
| Awareness of confidentiality, family dynamics, adult safeguarding, sensitivity of financial issues, taboos (e.g. continence) | E | Covering letter, interview and reference |
| Skilled in maintaining dialogue, shared decision-making and interagency communication; ability to seek agreements on data sharing | E | Interview and reference |
| Experience in decision-making, risk assessment, prioritisation | E | CV, interview and reference |
| Skills in empowering PWD and their carers to identify and solve problems | D | Interview and reference |
| Verbal and written communication skills, ability to negotiate, able to create relationships and respect boundaries | E | CV, interview and reference |
| Able to vary involvement according to needs of PWD and their carers | D | Interview and reference |
| Openness to learning, prepared to develop skills | E | Interview and reference |
| Good at managing tensions and contradictory demands, good time and stress management skills | E | Covering letter, interview and reference |
Appendix 3 Educational needs assessment tool
Educational needs assessment for CAREDEM case managers’ learning, induction and refresher courses
| Thinking about . . . | Themes | Confident about this | Need to learn about this |
|---|---|---|---|
| 1. People who are acquiring or who have just received a dementia diagnosis | Able to establish relationship with the individual and their family that is at the levels and intensity of the protocol | ||
| Informed about sources of support locally (and beyond), including peer support | |||
| Able to inform practice with knowledge of memory aids and techniques | |||
| Able to reframe dementia as a disability | |||
| Able to assess individual/family adjustment to and assimilation of the diagnosis, able to set assessments in interprofessional and multiagency frameworks | |||
| Able to reinforce resilience | |||
| Aware of how to introduce advance care planning and other possible planning/decisions | |||
| Aware of psychosocial interventions and their availability, effectiveness and cost | |||
| 2. Managing breakdown of support systems | Able to analyse and respond to behavioural and psychological symptoms | ||
| Able to support person/carer to access sources of support for crisis and ensure that these are as effective as possible | |||
| Able to identify and analyse support networks and to develop or sustain support | |||
| Know how to advise about incontinence/aids and equipment/safeguarding/housing/community-based social care and other opportunities | |||
| 3. Managing acute illness and hospital admission | Able to command confidence and exhibit negotiation skills in liaison with multidisciplinary team. Able to advocate on the person’s behalf or support them in self-advocacy. Able to advise on re-ablement | ||
| 4. Supporting decisions about relocation | Aware of resources and implications of relocation and able to discuss them with the individual to assist in considered decision-making | ||
| 5. Supporting the person with dementia and his or her family at the end of life | Able to command confidence that support will be available and that decision-making will be personalised. Able to elicit fears and concerns about the management of crisis, distress and pain. Able to offer support to bereaved carers and other members of the support network |
Appendix 4 The CAREDEM case manager’s manual
Appendix 5 Notes abstraction form
1. Patient details
| Age (years) | ||
| Gender | Female | 1 |
| Male | 2 | |
| Living arrangements | Lives alone | 1 |
| Lives with main carer | 2 | |
| Lives with main carer and other(s) | 3 | |
| Lives with other(s) (please specify) | 4 | |
| Other (please specify) | 5 | |
| Diagnosis | Alzheimer’s disease | 1 |
| Vascular dementia | 2 | |
| Frontal lobe dementia | 3 | |
| Dementia with Lewy bodies | 4 | |
| Mixed dementia | 5 | |
| Other | 6 | |
| Date of diagnosis | dd/mm/yy | |
| Preferred language | English | 1 |
| Other | 2 | |
| Religion | None | 1 |
| Church of England | 2 | |
| Catholic | 3 | |
| Muslim | 4 | |
| Does the service user’s religion influence the way in which their service should be provided? | Yes | 1 |
| No | 2 | |
| Ethnicity | White | 1 |
| Mixed/multiple ethnic groups | 2 | |
| Asian/Asian British | 3 | |
| Black/African/Caribbean/black British | 4 | |
| Other ethnic group (including Arab) | 5 | |
| Number of informal carers | Number |
2. Main carer details
| Age (years) | ||
| Gender | Female | 1 |
| Male | 2 | |
| Relationship to person with dementia | Friend | 1 |
| Husband/wife | 2 | |
| Partner | 3 | |
| Parent | 4 | |
| Sibling | 5 | |
| Other relative | 6 | |
| Other (please specify) | 7 | |
| Employment status | Working full-time | 1 |
| Working part-time | 2 | |
| Retired | 3 | |
| Long-term sick or disabled | 4 | |
| Looking after home or family | 5 | |
| In full-time or part-time education | 6 | |
| Has a formal carer assessment been completed? | Yes | 1 |
| No | 2 | |
| Preferred language | English | 1 |
| Other | 2 | |
| Religion | None | 1 |
| Church of England | 2 | |
| Catholic | 3 | |
| Muslim | 4 | |
| Does the carer’s religion influence the way in which their service should be provided? | Yes | 1 |
| No | 2 | |
| Ethnicity | White | 1 |
| Mixed/multiple ethnic groups | 2 | |
| Asian/Asian British | 3 | |
| Black/African/Caribbean/Black British | 4 | |
| Other ethnic group (including Arab) | 5 | |
| Registered with practice | Yes | 1 |
| No | 2 | |
Appendix 6 Notes from the case manager meeting
London, Monday 26 November 2012
Present: Steve Iliffe (co-chair), Pat Brown (co-chair), Claire Bamford, case managers, Marie Poole, Barbara Stephens, Amy Waugh
Session 1: Where we are now?
No researchers were present at this session to allow case managers and Pat Brown an opportunity to confidentially discuss their experiences of case management. The mentor and case managers then summarised their discussions to feed back to the wider group in session 2.
Session 2: Discussions of lessons learned (all)
Pat Brown summarised the key points of the discussion of what had worked well and not so well in case management. She encouraged the case managers to contribute to the discussion. The following key points were included.
Positive feedback from patients and carers
Informal feedback to the case managers indicated that patients and carers valued the continuity and consistency of having a named case manager. Other positive feedback to case managers related to ease of access to case management and being able to contact the case manager directly as and when needed rather than having to deal with appointment systems. The service could also react quickly when needed.
Issues with recruitment and identification of eligible patients
The process of identifying potential participants using the QOF register had highlighted a number of issues and areas for improvement. The Norfolk and Newcastle case managers had conducted additional searches to identify any patients with dementia who were not on the QOF register. One case manager described how some patient records included symptom codes only (e.g. memory problems/disturbance; cognitive impairment) rather than a formal diagnosis despite general recognition within the practice that the patient had dementia. The lack of formal diagnosis meant that these patients were not included in the QOF register. Another had identified a significant number of patients receiving anti-dementia drugs who were not included on the QOF register. A detailed review of their notes indicated that the majority of these patients had a diagnosis of dementia but this information had either not been added to the patient summary or not been properly coded and therefore the patient had not been added to the QOF register. Diagnoses were often included in correspondence, suggesting that data from incoming letters are not systematically coded. Because the diagnosis had often been made some years earlier and was often in correspondence (e.g. from old age psychiatry), the process of reviewing the notes to check for a diagnosis had been a lengthy and intensive process.
There was some discussion of the inclusion criteria for the study, in particular the issue of whether patients using secondary mental health services should be included. It was agreed that only patients being actively managed by the CMHT should be excluded.
Need for culturally appropriate recruitment processes
The need for culturally appropriate documentation was emphasised, together with detailed knowledge of specific local services for minority ethnic groups. The existing documentation was identified as a significant barrier to recruitment in the London practice, which serves a multiethnic population.
Whether the ‘right’ patients and carers are being recruited
The north-east case manager felt that in Newcastle only patients and carers whose situation was relatively stable were accessing the service. There was concern that those with high levels of unmet need were not engaging with the study. Possible reasons for this related to the research aspects of the study, accessibility of the information and the lack of emotional energy and time to get involved. Given that people with most needs may not be participating, it is difficult to gain an accurate picture of the time allocation required to fulfil the case manager role.
The approach to recruitment means that patients and carers are being offered case management at different points on their illness trajectory. Some cases had reported that the service would have been useful earlier, particularly when they had recently negotiated substantial care packages. However, some people offered the service shortly after diagnosis felt that they did not need any input yet. Barbara Stephens felt that people are not always aware of their needs and only realise with hindsight that some help would have been useful. However, increased awareness of current needs should be facilitated by good assessment and engagement with patients and carers.
Concerns over future management of patients and carers
Although one case manager felt that she would be able to continue to support patients and carers after the end of CAREDEM as part of the QOF reviews, the other case managers were concerned that families would be left in ‘limbo’ once the intervention is withdrawn.
Time allocated to case management
There was a clear message that half a day per week is not sufficient to fulfil the role, particularly when travelling time for home-based assessments is considered. The case managers and mentor did not think that a varied-enough caseload had been encountered (e.g. people with high levels of need or in crisis) to be able to accurately estimate the time required. One case manager felt that patients recruited to date in Newcastle were very homogeneous in terms of social class, education and cultural background, which may also give a skewed picture of workload. Although the case manager role allows time to build therapeutic relationships, the time constraints of the case managers limited the extent to which this was possible. Time is also needed by sessional case managers to ‘pick up where you left off’, and also to reflect on sometimes intense experiences within case management.
Case management as a distinct role
The case managers felt that the case management role should be a role with its own identity, rather than an add-on to another role, for example practice nurse. This was considered important as a message to others in the practice and for delivering a high-quality service. Even with additional time (e.g. 50% clinical management and 50% case management), the clinical case managers did not think that the two roles would ‘sit’ together well.
Boundaries between research and case management
Marie Poole raised the additional difficulties created by the embedding of case management within a feasibility study. Patients and carers in Newcastle seemed to focus more on the research element than case management, despite an emphasis on the service element. In contrast, participants in Norfolk seemed more tuned into case management than the research elements. Possible reasons for this were discussed such as a different relationship between the participants and practice nurses.
There was felt to be an overlap between the baseline assessment conducted by the research team and the initial assessment by case managers. Outside the trial the case managers were keen to develop assessment skills (e.g. in using the MMSE) and this could be a useful outcome for practices as well. Steve Iliffe will investigate possible training opportunities for the case managers.
Some of the problems with recruitment may reflect a reluctance to engage with the research aspects of the study rather than a lack of interest in case management.
Location of case managers
One case manager queried the feasibility of delivering case management in GP practices. Colleagues in general practice tended to assume that the case managers were available for other work during their CAREDEM time, resulting in frequent interruptions. The extent to which the practice nurses were supported by their practices varied. One case manager had been asked to take on the QOF register and the dementia reviews, which would build on the experience and knowledge of local services she had developed in the project. Another reported being under pressure to ‘give something back’ to the practice, suggesting that case management is not valued in its own right and consideration needs to be given to ways of quantifying the benefits of case management to individual patients and carers and the practice.
A further issue with being based in general practice was the difficulty in getting through to the surgery by telephone if patients or carers wished to contact the case manager. One case manager suggested a work mobile and the possible use of texting (if acceptable to patients and carers); however, others did not think that this would be logistically possible as they may be undertaking clinical work and unable to respond. One case manager was concerned about her ability to offer a quality service outside of her allocated time (although as yet no participants had attempted to contact her out of hours).
Induction of case managers
Pat Brown suggested that the induction process could be improved, particularly as the case managers had variable knowledge of dementia and local services. A longer induction time could ensure that case managers were better equipped to deliver case management and help them get into their new role. Although the delays in recruitment created some additional time for training, they also resulted in a backlog of cases waiting for initial case manager assessment and limited opportunities for following up cases. PB felt more active support from the mentor would be helpful.
The north-east case manager felt that a background in adult services was an advantage, partly as existing knowledge of services and personal working relationships/contacts facilitated speedy referral, but also because access to social care records provided a more detailed and holistic picture of patients and carers. Another case manager commented that she would benefit from increased knowledge of social services provision.
Preparation of and liaison with existing services
A number of issues had arisen concerning boundaries and perceived overlap of roles with existing services. These concerns are likely to be heightened in the current climate of primary care services. Building up networks, developing knowledge of local services and liaising with colleagues are a key part of the case manager role and sufficient time needs to be allocated to these activities. One case manager had met with CMHTs to try to allay their suspicions about her role and potential overlap with their remit. PB reported that case management had been received positively by social work teams.
Steve Iliffe asked the group for suggestions as to how some of the issues could be addressed.
Recruitment
Possible strategies to recruit the most appropriate participants were:
-
to link to memory clinics or secondary mental health services with newly diagnosed patients automatically being referred for case management
-
to alert GPs to involve case managers when concerns are first raised, at the same time as the process of diagnosis
-
to offer a self-referral system so that relatives could approach a key person in the practice
-
to have an aggressive information campaign with other community-based services to encourage referrals (e.g. from wardens, housing, banks, police and adult services).
Most of the proposed strategies focused on identifying people early in the illness trajectory. If a prospective approach was used, we would anticipate that one new case of dementia would be identified each year per 1000 patients registered with a practice. Although some patients and carers might require intensive intervention early on (e.g. daily contact in some cases), a staggered approach to recruitment might be easier to manage than the approach that we had used, in which numerous cases were identified at the same time, leading to problems with following up patients and carers in a timely manner. It was important to ensure that recruitment strategies included people with vascular dementia as this group often receive fewer services than people with Alzheimer’s disease.
Location
The team discussed the benefits and disadvantages of working in another environment. Some of the key disadvantages were constant interruptions by colleagues and systems-based pop-up messages. One case manager thought that being located elsewhere would increase efficiency. Possible alternatives were:
-
Multiagency settings, which could enhance opportunities for liaison with other practitioners and raise the profile of the case managers. One potential difficulty might be remote access to GP notes. A specific issue for one case manager was the need to work across two local authorities.
-
Home working or hot desking in Age UK offices might minimise the potential for mission creep but could also reduce the visibility of the service.
-
Memory clinics (currently where Admiral Nurses are based).
Steve Iliffe suggested that there may be the same scope for interruptions and mission creep in other locations.
Time required
Cross-practice working was discussed in the light of one case manager’s experience on CAREDEM and another’s previous role as a paediatric case manager. We explored typical caseloads of case managers in other contexts. One case manager had a caseload of approximately 150, as do Admiral nurses. Community matrons were thought to have a similar case load. If we were recruiting prospectively, a typical practice of 12,000–14,000 patients would expect to have around 12 patients with a new diagnosis of dementia per year. Based on a caseload of approximately 150, a full-time case manager would be able to cover approximately 12 practices. The capacity of the case manager would depend on the availability of other services, which would determine whether the case manager primarily had a co-ordinating role or was providing direct help to patients and carers.
Session 3: Case managers’ input into practice records (all except Amy Waugh)
Marie Poole asked the case managers to describe how they were documenting case management. There was consensus that the paperwork designed for the study was not user-friendly and, as a result, each case manager had developed her own approach.
One case manager had recorded the initial assessment in the study documentation and the GP notes but felt that this was an inefficient use of time. Subsequently, she had written a narrative summary of each contact in the practice notes and then cut and pasted this and kept a copy in a Word document for each patient and carer. This enabled her to quickly review her caseload each Monday. Although another queried whether it was appropriate to record case management in the GP records, this case manager felt that it was helpful for her colleagues.
Two case managers were not inputting any data on to the practice systems (EMIS; Egton Medical Information Systems), with the exception of one noting when telephone calls were anticipated. The other raised the issue of patient confidentiality as one patient had specifically requested that certain information not be shared with the GP. Pat Brown suggested that this could be managed by noting brief details of the contact in the GP notes but writing fuller notes elsewhere (perhaps even omitting details from these notes but including sufficient information to act as an aide memoire).
Marie Poole asked whether there should be some standardisation of recording data in the practice systems. It was agreed that at a minimum the GP notes should indicate that the patient was involved in the CAREDEM study. Steve Iliffe suggested that, if there was a READ code for case management, this could be used to code each contact with the patient.
Marie Poole had drafted a QOF letter and proforma that could be completed by case managers and used to meet the requirement for annual review of patients on the dementia register. None of the case managers had used these to date. One case manager had now taken over responsibility for the annual reviews in her practice; however, these documents may still be relevant to the other practices. Another had discussed with the general practitioner adding scanned versions of case manager assessment documents to the patient notes, but had not yet done this.
Pat Brown raised issues around the practicalities of using paper compared with electronic documentation.
Session 4: Identification of cases for interview and observation (all except Amy Waugh and one case manager)
Claire Bamford asked the case managers about opportunities to carry out observations and interviews in London and Norfolk. She emphasised the value of including patients and carers with different characteristics in terms of the relationship between patient and carer (e.g. spouse vs. adult child), level of need, availability of social support and stage of dementia. She clarified that it is important to include cases in which the case manager had limited input rather than ‘cherry-picking’ cases with more substantial involvement that would demonstrate the positive impact of CAREDEM.
Claire Bamford and Marie Poole will liaise with case managers to arrange observations and interviews.
Session 5: Summary of the day and moving forward (all except Amy Waugh and one case manager)
Steve Iliffe summarised the key discussion points of the day:
-
the utility of this meeting in terms of discovering important ‘lessons learned’ for case management in practice and the trial phase
-
whether GP practice is the ideal setting for the delivery of case management and what the alternatives are
-
whether case management can be an additional role or should be a distinct role, perhaps covering a broader practice base
-
whether a second feasibility study is required to specifically focus on the outcomes of case management.
Appendix 7 Dementia and Neurodegerative Diseases Research Network public and patient involvement review
We really appreciate what you are trying to do
The first statement on the notes written by group members after the discussion
Seven members of the DeNDRoN PPI Forum took part in a group discussion of the CAREDEM project on 19 March 2013. They were provided with a briefing document at the group discussion, which lasted 1.5 hours.
The discussion was organised within a modified nominal group format, with a specific task – the identification of lessons to be learned from CAREDEM – and with time to clarify answers and reach agreement on key topics (the modification was not prioritising answers or topics).
Steve Iliffe facilitated the discussion, took notes and attempted to sum up the topics discussed. The next day written notes from a further discussion were given to the research team and these have incorporated into this report. This report will be sent to the group members to verify and validate the topics.
The group’s response to the briefing document ranged across three main topics: the nature of the illness pathway in dementia and the implications for the timing and conduct of case management; the nature of existing services for people with dementia; and the attributes needed by case managers working with people with dementia and their carers.
1. Illness processes
Two things matter here. Comorbidities have an impact on the illness pathway and the case manager needs to understand them and their interactions with dementia. Conflict is common and the case manager has to be able to deal with it – the most difficult conflicts are those that develop between the person with dementia and their carers.
Timing of case management may be critical and it should begin around the time of diagnosis (to start the development of care plans early) whilst allowing for other and later routes of entry.
2. Services for people with dementia
The fragmentation of care is long-standing and will not easily be resolved by case management. The development time for case management may need to be longer than the 5 or 6 months allowed in the CAREDEM project – but one practice nearly reached its recruitment target (this practice would have reached its recruitment target if case management work had not taken precedence over recruitment in the one session per week allocated to case management), so perhaps the time needed will vary from one community to another. Services are very variable across the country, so localising case management will be important.
Existing services mostly do not do case management as defined in CAREDEM – this is true of most specialist mental health services, and most care homes – so their users should not be excluded from a future trial. However, clinicians need to be engaged with case management, both in the general practices and in local specialist services, both to assist the case manager and to avoid conflicts of interest, duplication of effort and misunderstandings about respective roles.
The demand for nursing skills is high, especially in general practice, so it may not be realistic to expect practice nurses to take on case management tasks.
3. Attributes of the case manager
These were summed up as authority, flexibility and being skilled in project management. The variability and high turnover of case managers were also mentioned (based in part on the personal experience of a group member from Northumberland, where there are case managers for people with dementia), and it was argued that the best case manager is a family member.
Authority was seen as necessary to make case management happen, partly through negotiation with senior managers in other services. Flexibility (and functioning in ‘catch-up mode’) is necessary for the case manager’s response to (sometimes rapidly) changing needs in the person with dementia – described by one participant as ‘a moving target’ – and their carers. Project management skills were suggested as the core components of case management, rather than clinical skills, within an ‘ambassadorial’ role that had authority.
Appendix 8 Design lessons for a definitive trial
| Challenges | Potential solutions | |
|---|---|---|
| Recruitment of practices | Recruitment of practices is difficult in the present primary care environment | Consider how any new intervention will fit alongside Direct Enhanced Services for dementia, changes in the GP contract and the emergence of Any Willing Providers |
| Recruitment | How familiar are the case managers with recruitment? (e.g. follow-up calls, having to be proactive, importance of documentation during recruitment, etc.) | Can research assistants or research network staff be of further assistance?
|
| Case managers’ knowledge of inclusion/exclusion criteria needs to be accurate (e.g. all people with dementia – all ages and types – must have a family carer, etc.) | ||
| Few people on the QOF dementia register |
|
|
| Not having carer details on GP record, especially if carer not registered with the same practice | Make sure case managers seek details of a family carer from the outset of screening – screen potential participants as dyads not individuals | |
| Time limits in the south | Half a day per week is not enough time for all of the case manager tasks if carried out by practitioners without experience of dementia care:
|
|
| Time is not dedicated to case management/interruptions from colleagues during case management work |
|
|
Having a fixed case management time period means:
|
|
|
| Other | Various requests from research team members who are unaware that colleagues have also contacted the case manager | Nominate only one member of the research team to contact the case manager plus the mentor in regular contact with the case manager to reduce excess demands on the case manager. Information can then be cascaded to the rest of the research team instead of the same information being requested from different members of the team. This should reduce the burden on the case managers |
List of abbreviations
- BADLS
- Bristol Activities of Daily Living Scale
- BPSD
- behavioural and psychological symptoms of dementia
- CI
- confidence interval
- CMHT
- Community Mental Health Team
- CSRI
- Client Service Receipt Inventory
- DEMQOL
- Dementia Quality of Life
- DeNDRoN
- Dementia and Neurodegerative Diseases Research Network
- EQ-5D
- European Quality of Life-5 Dimensions
- GHQ-28
- 28-item General Health Questionnaire
- GP
- general practitioner
- HTA
- Health Technology Assessment
- IT
- information technology
- MMSE
- Mini Mental State Examination
- NoCLoR
- North Central London Research Consortium
- NPI
- Neuropsychiatric Inventory
- NRES
- National Research Ethics Service
- PCT
- primary care trust
- PPI
- public and patient involvement
- PWD
- person with dementia
- QALY
- quality-adjusted life-year
- QOF
- Quality and Outcomes Framework
- WP1
- work package 1 of the CAREDEM project
- WP2
- work package 2 of the CAREDEM project
- WP3
- work package 3 of the CAREDEM project
- WP4
- work package 4 of the CAREDEM project
- WTE
- whole-time equivalent