Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 06/04/01. The contractual start date was in June 2007. The draft report began editorial review in May 2013 and was accepted for publication in February 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Dr Young was a Health Technology Assessment programme commissioning board member during the study and is currently a consultant advisor for the National Institute for Health Research Efficacy and Mechanism Evaluation programme. Professor Hulme is a Health Technology Assessment commissioning board member. Professor Lamb chairs the Health Technology Assessment Clinical Evaluation and Trials Board.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Lall et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction to the acute respiratory distress syndrome and the need for a trial of high-frequency oscillatory ventilation
The acute respiratory distress syndrome (ARDS) is a severe inflammatory lung condition that accompanies many critical illnesses. Though ARDS is reasonably uncommon, with an incidence estimated at 78–280 cases per million population per year, it is associated with a very high mortality (40% or greater). 1–9 Many of the deaths occur in young or middle-aged patients. In survivors, ARDS causes derangement of lung function for 2 years or more after hospital discharge,10,11 as well as marked reductions in quality of life (QoL). Although patients with ARDS only account for 8% of intensive care unit (ICU) admissions, because they have a long average stay in ICU they use up to a quarter of ICU bed-days. 5
To date, only two treatments, pressure- and volume-limited artificial ventilation and extracorporeal membrane oxygenation (ECMO), have been shown to decrease mortality in patients with ARDS. 12,13 These techniques reduce pressure swings and volume changes within the lung, and so reduce the secondary lung damage caused by artificial ventilation itself rather than influencing the disease process per se.
The benefits of tidal volume-limited artificial ventilation may increase as the tidal volume (volume of each breath delivered by an artificial ventilator) decreases. High-frequency oscillatory ventilation (HFOV) is a technique where tidal volumes can be reduced to the absolute minimum and so should provide the maximum protection against secondary lung damage. Yet, in spite of years of largely positive experimental studies, case series and small clinical trials, there were no adequate, large-scale randomised controlled trials (RCTs) to determine whether or not HFOV confers any advantage to patients requiring artificial ventilation for acute hypoxaemic respiratory failure when compared with conventional artificial ventilation. A Cochrane systematic review, also published as a journal paper,14,15 located only two methodologically sound RCTs in this area, one in children16 and one in adults. 17 A more recent systematic review of all of the eight clinical trials in children and adults18 published to date concluded that, in patients with acute lung injury (ALI) or ARDS, HFOV initially improved oxygenation {as measured by the ratio of the arterial oxygen partial pressure to the fractional inspired oxygen concentration [PaO2 : FiO2 ratio (P : F ratio); 7 trials, n = 323, ratio of means and 95% confidence interval (CI) 1.24 to 1.10–1.40]} but did not alter the duration of mechanical ventilation. Hospital or 30-day mortality was reduced (six trials, n = 365, risk ratio and 95% CI 0.77 to 0.61–0.98) and there was no increase in adverse events. The small size and poor quality of the trials reviewed, along with the heterogeneity of the populations studied, contrasted with the increasing use of HFOV in UK adult ICUs. This increasing use was occurring without any clear evidence of efficacy, in a patient population and setting where a trial to obtain this information was probably feasible.
In 2007, in part in response to the Cochrane review and associated review,14,15 the National Institute for Health Research (NIHR) [Health Technology Assessment (HTA) programme] in the UK commissioned the OSCAR (OSCillation in ARDS) study to determine if adult patients with ARDS who are treated with HFOV have a decreased mortality at 30 days compared with patients treated with conventional positive-pressure ventilation.
Overview of acute respiratory distress syndrome and acute lung injury
Acute hypoxaemic (‘type 1’) respiratory failure, where the patient is unable to maintain an adequate arterial oxygen partial pressure (PaO2) without high inspired oxygen concentrations, is a common reason for admission to an ICU. This type of respiratory failure is either due to a primary pulmonary condition or is secondary to the systemic inflammatory process caused by extrapulmonary pathology. The term ‘acute (or adult) respiratory distress syndrome’ was coined nearly 40 years ago19 to describe the acute respiratory failure that accompanies severe systemic disease, but over the years has expanded to cover virtually all causes of hypoxaemic respiratory failure other than those caused by cardiac failure.
To aid epidemiological and interventional studies of patients with acute hypoxaemic respiratory failure, a standard set of definitions were agreed at a consensus conference in 1994. 20 Two degrees of severity were recognised: ALI and the more severe ARDS. Features common to both were:
-
acute onset of impaired oxygenation
-
bilateral infiltrates on chest radiograph
-
pulmonary artery wedge pressure (an indirect measure of left atrial pressure) < 18 mmHg or exclusion of cardiogenic pulmonary oedema by other means
-
a known precipitant of acute respiratory failure.
The degree of severity was determined from the P : F ratio. If this was 26.7–40.0 kPa (200–300 mmHg), the patient had ALI. If it was < 26.7 kPa (200 mmHg), the patient had ARDS.
This common classification has allowed comparisons of the incidence of, and mortality from, ARDS, and, to a lesser extent, ALI, to be made over time within single populations,9 and between large national and subnational epidemiological studies. 1,3,4,7,8 There is now a large literature on the incidence and short-term outcome from ARDS.
While the OSCAR study was running, a different set of definitions for ALI and ARDS were developed at a consensus conference. The ‘Berlin Definition’21 defined three mutually exclusive categories of ARDS based on degree of hypoxaemia: mild [26.7 kPa (200 mmHg) < P : F ratio ≤ 40 kPa (300 mmHg)], moderate [13.3 kPa (100 mmHg) < P : F ratio ≤ 26.7 kPa (200 mmHg)], and severe [P : F ratio ≤ 13.3 kPa (100 mmHg)]. The ‘mild’ category is the group of patients previously categorised as ALI, otherwise the definitions are largely unchanged from those first proposed in 1994.
As ARDS almost never occurs in isolation and is secondary to another acute disease, the mortality attributable to the ARDS per se has been difficult to unpick from the mortality from the primary condition. For many years it was unclear if a treatment directed solely at ARDS, even if effective at improving gas exchange, would alter mortality. Treatments that clearly did improve arterial oxygenation, such as inhaled nitric oxide, prone positioning and high levels of positive end expiratory pressure (PEEP), proved ineffective when tested for an effect on mortality. However, in 2000, a large trial of limited tidal volume, pressure-controlled artificial ventilation compared with conventional artificial ventilation12 showed an 8.8% absolute reduction in mortality, confirming simultaneously that there was an attributable mortality to ARDS and that this could be reduced with treatments directed solely at the lungs. This study also confirmed the long-held view that artificial ventilation, while immediately life-saving, could in the longer term cause lung damage in addition to that caused by the primary disease. While the OSCAR study was running, the Conventional ventilation or ECMO for Severe Adult Respiratory failure (CESAR) study of ECMO, which allows respiratory failure to be treated with minimal ventilation of the lungs, reported a 12% absolute 6-month survival without disability benefit (relative risk 0.69, 95% CI 0.05 to 0.97; p = 0.03) for patients treated with ECMO. After recruitment had closed in OSCAR, a multicentre study reported a 16.8% absolute reduction in 28-day mortality by using prone positioning, which improves oxygenation by recruitment of collapsed lung [hazard ratio for death with prone positioning 0.39 (95% CI 0.25 to 0.63)]. 22 For these reasons, attention has again focused on artificial ventilation techniques like HFOV which, at least in experimental studies,23,24 minimise secondary lung injury.
Background to high-frequency ventilation
History of artificial ventilation
An artificial ventilator is essentially a device that replaces or augments the function of the inspiratory muscles, providing energy to ensure a flow of gas into the alveoli during inspiration. Exhalation during artificial ventilation is usually a passive process, so when this inspiratory assistance is removed the inspired gas is expelled as the lung and chest wall recoil to their original volume. In the earliest reports of artificial ventilation, the respiratory muscles of another person, as expired air resuscitation, provided this energy. Baker25 has traced references to expired air resuscitation in the newborn as far back as 1472, and in adults there is a report of an asphyxiated miner being revived with mouth-to-mouth resuscitation in 1744. In the eighteenth century, artificial ventilation became the accepted first-line treatment for drowning victims, although bellows replaced mouth-to-mouth resuscitation. 26 Automatic artificial ventilators which did not require a human as a power source were proposed by Fell 150 years later27 and made commercially available by Dräger in 1907. 28 These were still resuscitation devices as the Dräger company at that time made mine rescue apparatus not medical devices.
The introduction of artificial ventilators into anaesthetic practice proceeded slowly until surgical advances required surgeons to undertake thoracotomies. Without artificial ventilation during a thoracotomy, lung collapse and mediastinal movement made surgery difficult and anaesthesia hazardous. Mortality was markedly reduced with artificial ventilation. A further boost to the development of artificial ventilators occurred in 1952 when a catastrophic poliomyelitis epidemic struck Denmark. Although the combined use of tracheostomy and artificial ventilation reduced the mortality, especially in the patients with bulbar palsy, the artificial ventilation had to be provided entirely by hand and required 1400 university students working shifts. The fear of another epidemic expedited research into powered mechanical ventilators, leading to the development of the first modern ventilator, the Engström, in 1952. 29 Since the advent of microprocessors and computer-controlled gas valves, artificial ventilators have become increasingly sophisticated, though evidence of the effectiveness of any single ventilation mode or ventilator is often lacking.
During both spontaneous breathing and during artificial ventilation, tidal volumes (breaths) have to be greater than the volume of the trachea and conducting airways (the anatomical dead space). Tidal volumes less than the anatomical dead space move gas in and out of these airways but do not ventilate the alveoli, and so no gas exchange with blood in the pulmonary capillaries takes place. Anatomical dead space is usually about 2 ml/kg in adults, tidal volumes are usually set at about 10 ml/kg in anaesthetic practice and 6–8 ml/kg ideal body weight in adults artificially ventilated for acute lung conditions.
However, it has been known for many years that this ‘convective’ model of ventilation does not apply in all circumstances. As early as 1915, Henderson et al. 30 noted that panting dogs were able to eliminate carbon dioxide, even though the volume of each breath was less than their anatomical dead space. In 1954, Briscoe et al. 31 reported that in humans the anatomical dead space appears to be reduced at low tidal volumes, allowing more gas exchange than would be predicted using a convective model of ventilation. However, the absolute amount of carbon dioxide eliminated per breath is very small, so high respiratory frequencies are needed to clear metabolic carbon dioxide production.
The first description of high-frequency ventilation in a clinical setting is attributed to either Lunkenheimer et al. in 197232 or Jonzon et al. in 1971,33 both of whom used the technique to minimise the cyclical effects of intermittent positive-pressure ventilation on the cardiovascular system. Subsequent research into high-frequency ventilation initially concentrated on three techniques to deliver the breaths, HFOV, high-frequency positive-pressure ventilation (HFPPV) and high-frequency jet ventilation (HFJV). External HFOV (EHFOV) using either a cuirass ventilator34 or a pneumatic vest35 was also introduced but was mostly used as an adjunct to physiotherapy and as a research tool rather than a mode of ventilation for critically ill patients.
It became apparent that both HFJV and HFPPV probably had no special properties and conformed to the conventional, convective model of gas exchange. 36 However, it also became clear that carbon dioxide clearance could be achieved with HFOV in animals37 and humans38 with tidal volumes that were half the anatomical dead space or less. There are many theories to explain this phenomenon. All of them reject the simple anatomical (series) dead space concept, and assume there is no sharp cut-off between dead space and alveolar gas, and some form of mixing takes place. The most likely mechanism, termed ‘convective streaming’, is that the interaction of the gas-airway wall friction and the asymmetrical inspiratory-expiratory flow profiles lead to an inward movement of gas in the core of the large airways and an outward movement near the wall. 39 These theories have been extensively reviewed. 40,41
As tidal volumes during HFOV are very small, the peak pressures generated in the alveoli during artificial ventilation are correspondingly modest. Thus HFOV would seem an ideal technique to ventilate patients at risk from pressure-induced lung damage (‘barotrauma’) such as infants with the (infant) respiratory distress syndrome (RDS). This was the rationale behind the early trials of HFOV in infants.
Trials of high-frequency oscillatory ventilation in infants
In pre-term infants with immature lungs, (infant) RDS is a major cause of immediate mortality. In survivors there is also considerable long-term morbidity from bronchopulmonary dysplasia, a condition caused by the combination of high intrapulmonary pressures generated by artificial ventilators, and high concentrations of inspired oxygen. As case reports began to appear in the literature suggesting HFOV might benefit these patients, the National Institutes of Health (NIH) in the USA first convened a conference42 and then commissioned a randomised controlled study. The HiFi study, published in 1989,43 recruited 673 pre-term infants who were randomly assigned to either HFOV using a piston-driven ventilator or to conventional mechanical ventilation. This study showed no survival benefit or difference in the incidence of bronchopulmonary dysplasia in the HFOV group.
Since the HiFi study there have been have been a further 17 RCTs of HFOV in infants. These are described in a series of Cochrane reviews44–47 and independent48 reviews last updated in 2013. In general, though many studies showed more deaths in the conventional ventilation groups, either as individual studies or combined in a meta-analysis, no statistically significant difference could be detected. However, a repeated theme in both the commentaries in the meta-analyses, and in opinion pieces published alongside the trials,49 is that the negative results may be partially due to errors in trial design.
Trials of high-frequency oscillatory ventilation in adults
As part of the preparation for the OSCAR study, we undertook a systematic review of HFOV in patients with ARDS and ALI in July 2006 to update the 2004 Cochrane review. 14 Among the 319 papers identified, there were only two adequate-quality RCTs of HFOV in adults.
The first and largest RCT was published in 2002. 17 Recruitment took place between October 1997 and December 2000 in 13 university-affiliated medical centres in the USA and Canada. A total of 148 patients were recruited. The entry criteria were the ARDS consensus criteria,50 a PEEP of ≥ 10 cmH2O, and a predicted 6-month survival of 50% or greater. The investigators initially set the HFOV ventilator to a frequency of 5 Hz (breaths per second) and a mean pressure 5 cmH2O above the mean airway pressure on conventional ventilation, and the amplitude to ‘visible chest wall movement’. The conventional ventilation group were treated with pressure-controlled ventilation to a maximum tidal volume of 10 ml/kg. The HFOV group had better oxygen exchange as measured by P : F ratios, most notably in the first 24 hours of HFOV, though when corrected for the difference in mean airway pressure (which increases oxygen exchange) using the oxygenation index (OI) this difference disappeared. Although more deaths were seen in the control group, this was not statistically significant (see Figure 1, below).
The second study was published in 2005. 51 Recruitment took place in four university-affiliated hospitals in London, Cardiff, Mainz and Paris between October 1997 and March 2001. The entry criteria and HFOV management were virtually identical to the 2002 study. A total of 61 patients were recruited. This study showed a beneficial effect of HFOV on oxygenation, even when airway pressures were taken into account. There was an excess of deaths in the HFOV group which was not statistically significant.
The results for 30-day mortality from both studies have been combined in the forest plot in Figure 1. There is no statistically significant benefit for HFOV seen.
FIGURE 1.
Forest plot showing 30-day mortality in the two methodologically sound trials of HFOV in adult patients with ARDS identified at the start of the OSCAR study. OR, odds ratio.
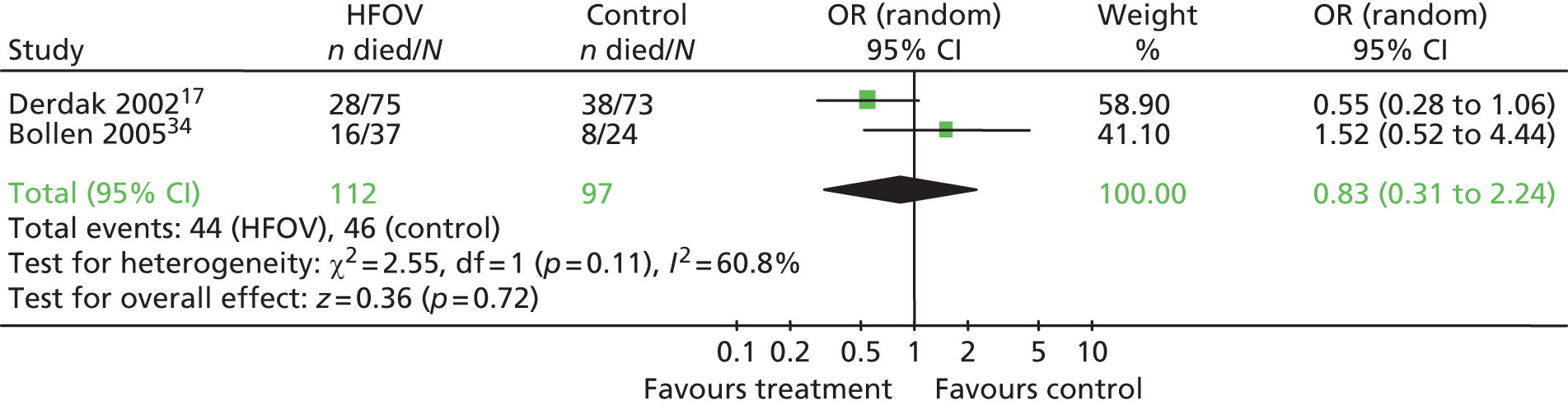
The report from Bollen et al. 51 contained a post-hoc analysis showing how the treatment effect on mortality varied with the severity of the initial lung damage as determined by the OI. As the OI (and hence the severity of the lung injury) worsened the odd ratios for survival increasingly favoured HFOV. The numbers in each OI band were very small, and there were corrections added to remove other known causes of mortality. There was a clear stepwise increase in treatment effect with increasing OI and hence disease severity, suggesting that HFOV might be more effective in patients with worse ARDS, either because these patients are more prone to secondary lung damage or simply because they have a higher mortality.
The original systematic reviews of HFOV by Wunsch et al. 14,15 reviewed as part of planning the OSCAR study predated the publication of the Bollen et al. 51 study, though the subsequent 2008 revision made no mention of the study. The systematic review published in 2010 while the OSCAR study was under way18 contained eight studies including the Bollen et al. 51 and Derdak et al. 17 studies, one study involving prone positioning which had been excluded from our original planning review, two studies undertaken in children and two studies published only as abstracts. The only fully reported study of 49 patients published since OSCAR started had no mortality data. 52
Current practice of high-frequency oscillatory ventilation
Patients on HFOV are all intubated or have a tracheostomy, this is not a ventilatory mode that can be used non-invasively with a face mask. Both of the adult HFOV ventilators available in the UK have no facility for the patient to take breaths (interbreathe) during HFOV and so the patients are usually sedated, and, in some cases, are treated with neuromuscular blocking agents (muscle relaxants) to prevent respiratory effort.
High-frequency oscillatory ventilation, much as conventional artificial ventilation, can be divided into components which maintain or improve oxygenation, and components that assist with carbon dioxide elimination. Patients on HFOV have their lungs maintained in an expanded (inflated) state by a standing pressure, usually termed the mean airway pressure. This pressure is maintained by passing a stream of warmed, humidified air and oxygen (the bias flow) across the top of the artificial airway to a valve that allows the mean airway pressure to be adjusted. The pressures used are typically about 5 cmH2O above the pressure used to inflate the lungs in conventional ventilation (the plateau pressure). The bias flow is typically 20 l/minute. The patients’ arterial oxygenation can be increased by increasing the mean airway pressure or by increasing the fractional concentration of oxygen in the bias flow gas.
To eliminate carbon dioxide, pressure fluctuations are superimposed around the mean airway pressure using an oscillating diaphragm. These pressure fluctuations cause small volumes of gas to move in and out of the lungs, removing carbon dioxide which is swept away in the bias flow. The superimposed pressure fluctuations are very rapid, typically 5–10 Hz (cycles/second). Although the fluctuations around the mean airway pressure, measured at the ventilator, can be large, these pressure oscillations are almost totally dissipated by a combination of gas inertia, gas compression and tubing expansion, such that the pressure changes at alveolar level are probably 5 cmH2O or less. 53 The relationship between carbon dioxide elimination and oscillatory frequency is the reverse of that seen in conventional ventilation. More carbon dioxide is eliminated at lower frequencies, because for a given superimposed pressure the volumes of gas moved in and out of the lungs are greater at lower frequencies.
High-frequency oscillatory ventilation cannot be used in patients with expiratory airflow limitation, as the short expiratory time does not allow the tidal volume to leave the lungs and so air-trapping occurs. The high intrathoracic pressures used in HFOV also impair venous return causing a reduction in stroke volume and hypotension.
Identification of data to inform the study design
Types of high-frequency oscillatory ventilators available
Although there is a wide range of high-frequency oscillatory ventilators available for neonatal use [e.g. SensorMedics 3100A® (SensorMedics Corporation, Yorba Linda, CA), Stefan SHF3000 (Fritz Stephan GmbH, Gackenbach, Germany), Hummingbird V (Metran Co. Ltd, Saitama, Japan), Dufour OHF1 (Dufour, Villeneuve d'Ascq, France)], there are only two commercially available positive-pressure HFOVs suitable for adults. The ventilator used in all of the studies in adults up to the start of the OSCAR study was the ‘SensorMedics Model 3100B® high-frequency oscillatory ventilator’ (SensorMedics Corporation, Yorba Linda, CA), manufactured by SensorMedics Corporation in California and distributed in the UK by Viasys Healthcare. This ventilator was approved by the US Food and Drug Administration (FDA) in 2001 for ventilation of selected patients over 35 kg in weight with acute respiratory failure. The second adult HFOV ventilator available is the ‘Novalung’ Metran R100® high-frequency ventilator (Metran Co. Ltd, Saitama, Japan) (also called the ‘Vision Alpha’) manufactured in Saitama, Japan by Metran Co. Ltd and distributed in the UK by Inspiration Healthcare, which has a long history of use in Japan but, at the time the OSCAR study was being planned, had only recently been CE (Conformité Européenne) marked for European use. A negative pressure external (cuirass) HFOV for adults [‘Hayek Oscillator’, United Hayek Industries (Medical) Ltd, London, UK] is also marketed in the UK and elsewhere.
Current users of high-frequency oscillatory ventilation in the UK
Viasys Healthcare provided us with details of all 3100B ventilators ever sold in the UK at the planning stage of the OSCAR study. A total of 38 ventilators have been sold by 2007 to 25 adult ICUs in England, Wales and the Isle of Man. Eighteen units had one ventilator; the remainder had two or three devices. No further data were obtained during the OSCAR study.
‘Substantial uncertainty’ within units already using high-frequency oscillatory ventilation
To run a RCT of HFOV in ICUs that already own one or more HFOV ventilators would require all clinicians caring for the patients to be substantially uncertain about which ventilation was best for their patients. As patients in the trial would be randomised in a 1 : 1 ratio to conventional positive-pressure ventilation or HFOV, up to 50% of the patients who the clinicians would treat with HFOV under their current protocols or guidelines would be randomised to conventional positive-pressure ventilation. In essence, the clinicians would have to withhold their standard treatment from half of the patients in the trial. The nature of medical care for patients in ICUs, where each consultant works for a block of time before handing onto a colleague, means that ‘substantial uncertainty’ would have to be present in the whole team to ensure the allotted trial treatment was continued throughout a patient’s ICU stay.
Lack of ‘substantial uncertainty’ would expose the study to a considerable risk of bias. Clinicians might elect not to enter the more severely ill patients in the study and treat them with HFOV outside of the trial. This would mean the trial population would not be representative of the UK patients with ARDS and would reduce the generalisability of the results. Crossover from the control to the treatment group might also occur, limiting the ability of the study to show an effect.
We tried to find evidence in the literature to determine whether or not these problems had occurred in previous trials. In the clinical trial of HFOV reported by Bollen et al. in 2005,51 61 patients were recruited from four major European ICUs in 41 months, or about one patient per centre per 3 months. This would be about 0.4% of total admissions. All of these ICUs had prior experience with HFOV. The inclusion criteria for the study were the standard consensus criteria for ARDS50 which include patients with a P : F ratio of < 26.7 kPa (200 mmHg). The mean P : F ratio in the treatment group was 12.6 kPa and in the control group was 16.0 kPa. No Consolidated Standards of Reporting Trials (CONSORT) diagram was published. From published data, we know that about 8% of admissions to general ICUs meet the consensus criteria for ARDS during their ICU stay. Therefore, both the low recruitment rate and the severity of the respiratory failure would suggest there was considerable case selection taking place, though whether or not patients received HFOV outside the study is not known. The trial was stopped prematurely because of ‘poor recruitment’ attributed, in the paper, to lack of local trial-dedicated staff. Crossovers (18%) occurred by protocol in this study.
The other clinical trial reported by Derdak et al. in 200217 took place in 13 university-affiliated medical centres in the USA and Canada over 38 months, a recruitment rate of one patient per centre per 3.6 months. There are no data on whether or not these centres had prior experience with HFOV but seven of the sites’ clinical leads had published on HFOV prior to the study. The inclusion criteria for the study were the standard consensus criteria for ARDS. The mean P : F ratio in the treatment group at enrolment was 15.0 kPa and in the control group 14.6 kPa. Again, no CONSORT diagram was published. Crossovers were 4/75 (5.3%) from HFOV to control, and 9/73 (12.3%) from control to HFOV. Again, these data suggest marked case selection was taking place, though again it is not known if HFOV was used outside of the trial.
We discussed the OSCAR trial with the clinical leads or senior clinicians in five UK ICUs where HFOV was used. Although all initially expressed interest in the study, when we explained that the study would require withholding HFOV in some patients, four of the clinicians suggested they could not take part in a trial under these circumstances.
Finally, we reviewed the experience gained by the Chief Investigator (DY) as a member of the management group for the PAC-Man study. 54,55 The clinicians in ICUs were asked to withhold a pulmonary artery catheter in half of the patients they would normally have used one in. Although the study was successful, a considerable effort was required in the early stages of the trial to generate equipoise. The trial probably only succeeded because it was a trial of a monitoring device, not a treatment, and nearly two-thirds of the ICUs used another monitoring method to generate at least some of the information a pulmonary artery catheter would have given them.
We concluded there are considerable risks to running the trial in centres which already used HFOVs. We believed the major risk was that HFOV would continue outside the trial as a rescue therapy and so the patients in the study would be an unrepresentative sample. The final trial design was a compromise; most ICUs were HFOV-naïve at study commencement, but two centres with HFOV experience did initially join the study and provided a pool of experienced health-care staff.
Identification of other trials of high-frequency oscillatory ventilation and trials competing for the same patient population
When the OSCAR trial was starting we were aware that Professor Meade and Dr Ferguson from the Canadian Critical Care Trials Group (CCCTG) had received funding for a national pilot study of HFOV [the Oscillation for Acute Respiratory Distress Syndrome Treated Early (OSCILLATE) study]. The OSCAR team contacted Professor Meade and agreed a common core data set to facilitate future meta-analyses should the pilot study progress to a full study. The OSCILLATE study did proceed to a full study and ceased recruitment just after the OSCAR study closed to recruitment. The OSCILLATE results56 are covered in Chapter 6.
The National Heart, Lung, and Blood Institute (NHLBI) in the USA funded a phase II study of HFOV using surrogate outcome measures (inflammatory cytokine concentrations in plasma) as a prelude to a full clinical trial (ClinicalTrials.gov identifier NCT00399581). This started in 2006 and was completed in 2009. The Chief Investigator was Dr Roy Brower. The results have not yet been published at the time of writing.
Identification of other trials in the UK competing for the same population
None of the ICUs we contacted as potential trial sites identified any studies of patients with ARDS that would compete for patients.
Three of the OSCAR investigators were on the management group of the Beta Agonist Lung Injury TrIal-2 (BALTI-2) study, a trial of intravenous salbutamol in ARDS. As the OSCAR study commenced, this was in a pilot phase in the West Midlands. It subsequently went to a full study57 and required the OSCAR study team and the BALTI-2 study team to communicate to prevent competition for patients as the entry criteria for the two studies were near identical.
There was a single-centre RCT of the effects of simvastatin in patients with ARDS under way in the Royal Victoria Hospital, Belfast as OSCAR started. This study became multicentre (HARP-2 study,58 ISRCTN88244364) but used different study centres.
Identification of data to inform estimates of the recruitment rate
A systematic review of all epidemiological studies of ALI and ARDS undertaken after the consensus criteria were formulated in 1994 was recently published. 7 The European and Australasian studies using consensus criteria to define ARDS cited in this review, along with additional studies identified from a systematic literature search undertaken in August 2006 by ourselves, are summarised in Table 1.
| Study | Population | Population incidence of ARDS (per 100,000 population per year) | Percentage of ICU admissions with ARDS | Mortality (%) for patients with ARDS |
|---|---|---|---|---|
| Brun-Buisson et al., 20043 | 78 ICUs across Europe | Not calculated | 6.1 | 49.4 (hospital) |
| Bersten et al., 20022 | 21 ICUs in Australia | 28.0 | Not calculated | 34.0 (time point not given) |
| Luhr et al., 19996 | 132 ICUs in Scandinavia | 13.5 | Not calculated | 41.2 (90 day) |
| Roupie et al., 199959 | 36 ICUs in France | Not calculated | 6.9 | 60.0 (28 day) |
| Monchi et al., 199860 | Single French ICU | Not calculated | 7.4 | 65.0 (28 day) |
| Sigvaldason et al., 20069 | All Icelandic ICUs | 7.8 | Not calculated | 40.0 (hospital) |
| Hughes et al., 20035 | 23 Scottish ICUs | 16.0 | 8.1 | 60.9 (hospital) |
From these studies, it would appear the incidence of ARDS in ICUs was about 6–8% of all admissions when OSCAR started.
Three estimates of the incidence of ARDS in UK ICUs were available. The Scottish Intensive Care Society Audit Group (SICSAG) published data from 23 of the 26 ICUs in Scotland for an audit run between May and December 1999. 5 They recorded patients meeting the diagnostic criteria for ARDS (including chest radiographs) on a daily basis. The results are in Table 1 (Hughes et al. 5).
Two other (unpublished) estimates of the number of cases of ARDS in UK ICUs were available. In both data sets, the diagnosis of ARDS is based on the P : F ratio only and did not include chest radiograph information or any clinician ‘filtering’.
The Intensive Care National Audit & Research Centre (ICNARC) reviewed 261,193 admissions to UK ICUs over a 10-year period to 2005 and found an incidence of ARDS, defined solely on the P : F ratio in the first 24 hours of ICU admission, of 49.3%. These data are unpublished.
We undertook a similar study using data on admissions to the adult ICU at the John Radcliffe Hospital, Oxford, for calendar year 2005. Of 973 admissions, 850 had simultaneous arterial blood gas analyses and FiO2 records which allowed P : F ratios to be calculated. The incidence of ARDS, defined on P : F ratio only at any point in the patient’s stay, was 78.9%. As the incidence was so high, we also searched the discharge summaries for any mention of ARDS. Only 2.5% of the patients had both a P : F ratio of < 26.7 kPa and any mention of ARDS in the discharge summary.
The true incidence of ARDS in ICU patients was almost certainly greater than the 2.5% we identified by retrospectively searching the Oxford database of discharge summaries because of errors of omission. However, it is also very clear that estimates of the incidence of ARDS based on the incidence of P : F ratios of < 26.7 kPa grossly overestimate the true incidence of ARDS.
As a result, the ICNARC and Oxford data on the incidence of ARDS were not used to inform recruitment rates or sample size calculations. The erroneously high incidence of ARDS identified in these databases presumably results from the loose definitions of ARDS used by ICNARC and at Oxford which did not include chest radiograph data, and because at least 50% of patients who meet the ARDS oxygenation criteria (P : F ratio of < 26.7 kPa) only have a very transient reduction in the P : F ratio which rapidly improves. 61
Selection of entry criteria, acute lung injury and acute respiratory distress syndrome or just acute respiratory distress syndrome?
As discussed above, acute hypoxaemic respiratory failure was divided into two severity bands by the consensus conference held in 1994. The less severe band was termed Acute Lung Injury or ALI, and includes patients with a P : F ratio of between 26.7 and 40.0 kPa. The more severe band, where the P : F ratio was < 26.7 kPa, was termed acute respiratory distress syndrome or ARDS.
There is often confusion over the terms ALI and ARDS. In some literature, the term ALI is incorrectly used to encompass all patients with a P : F ratio < 40 kPa, and the term ARDS is used to describe a subset of these with a P : F ratio of < 26.7 kPa. We did not use this convention and kept to the definitions published after the consensus conference in which ALI and ARDS are two discrete bands of severity of acute hypoxaemic respiratory failure with no overlap.
The commissioning brief from the HTA requested a study of HFOV in patients with ALI or ARDS. We elected to use ARDS only as an entry criterion for the trial. The reasons for this are as follows.
ALI represents a group of patients who will require between 30% and 45% inspired oxygen to maintain a normal PaO2 of 12 kPa. This degree of hypoxaemic respiratory failure would normally be managed with simple face mask oxygen as the patients do not require artificial ventilation. It follows from this that patients with ALI who are on artificial ventilators are probably ventilated as a result of non-pulmonary pathology which would not be improved by HFOV, and so would reduce the chance of seeing an effect of any ventilatory strategy if included in a clinical trial. Examples of such patients would be those with neurological conditions such as head injury, meningitis or similar. In a large study of 5183 mechanically ventilated patients in Europe and North America, patients with ALI had the same mortality as patients with no ALI at all. 62
The two RCTs of HFOV17,51 reviewed at the planning stage of OSCAR only recruited patients with ARDS. In the Bollen et al. study,51 a post-hoc analysis revealed that there might have been a treatment effect seen at the more severe end of the spectrum of ARDS. There was no treatment effect seen at the milder end of the ARDS severity spectrum. This suggests any benefit of HFOV would not be seen in patients with ALI.
As ALI is a relatively mild pulmonary insult and does not require artificial ventilation, most patients with this condition are managed on the general wards. In the Europe-wide epidemiological study of ALI and ARDS,3 only 62 out of 6522 ICU admissions (0.9%) had ALI against 6.1% with ARDS. More than half of the patients with ALI rapidly progressed to ARDS, leaving only 0.4% of admissions who had ALI alone. Only two-thirds of these patients with ALI alone were ventilated. By not including ALI patients, we are probably only excluding 0.1–0.2% of all admissions, many of whom will be ventilated for non-pulmonary reasons and could probably not benefit from HFOV. For all of these reasons, we believed it was inappropriate to undertake a study of HFOV that included patients with ALI.
As noted earlier, while the OSCAR study was running, a different set of definitions for ALI and ARDS were developed at a consensus conference. The ‘Berlin Definition’21 will have no effect on the interpretation of the results. The ‘mild’ category is the group of patients previously categorised as ALI, otherwise the definitions are largely unchanged from those first proposed in 1994.
Identification of data to inform the choice of measures used for long-term follow-up
The primary outcome for OSCAR was mortality, as specified in the commissioning brief. The brief also requested longer-term outcome measures. These were included in the OSCAR study, and are reported in this monograph for most, but not all, patients as data collection was still continuing at the monograph submission date.
The HTA commissioned a systematic review into outcome measures for adult critical care in 1998. The results were reported in 2000 both as a monograph and a paper. 63,64 At that time, the three measures of health-related QoL that had been most commonly used in follow-up studies of critically ill patients were the Sickness Impact Profile/Functional Limitations Profile (SIP/FLP), the Perceived Quality of Life (PQOL) and the Nottingham Health Profile (NHP). In addition, the Short Form questionnaire-36 items (SF-36) was increasingly being used.
At the time the review was undertaken, the European Quality of Life-5 Dimensions (EQ-5D) measure was not used in to any extent in critical care research and so did not feature in the reports, even though it was first developed in 1990. 65 However, it has since rapidly gained popularity in critical care research, to the extent that in 2004 a European consensus conference suggested that EQ-5D or SF-36 were the two preferred measures for health-related QoL in survivors of critical illness. 66
The SF-36 is a feasible and reliable instrument with sufficient discriminatory power to detect changes in the health-related QoL of ICU patients with different levels of chronic health and varied severity of their acute illness. 67 SF-36 contains 36 items to measure eight QoL domains: physical functioning, role limitations due to physical problems, bodily pain, general health perceptions, energy/vitality, social functioning, role limitations due to emotional problems, and mental health. 68
European Quality of Life-5 Dimensions is also a general health-related QoL measure that has also proven to be a useful tool in a mixed critical care population. 69 The EQ-5D comprises two parts: the EQ-5D self-classifier, a self-reported description of health problems according to a 5-dimensional classification (i.e. mobility, self-care, usual activities, pain/discomfort and anxiety/depression); and the European Quality of Life Visual Analogue Scale (EQ-VAS), a self-rated health status using a visual analogue scale, similar to a thermometer, to record perceptions of participants own current overall health. The scale is graduated from 0 (the worst imaginable health state) to 100 (the best imaginable state). 65
As part of the background work for the Intensive Care Outcome Network (ICON) studies (studies of long-term ICU survival and QoL being run by the OSCAR Chief Investigator), a systematic review of all of the ICU outcome studies that have used either EQ-5D, SF-36 or both was undertaken. Numerically there are more studies that use the SF-36, though there are eight high-quality studies using the EQ-5D. A similar systematic review was published in 2005 but this only identified five of the eight studies using EQ-5D. 70
A direct comparison of the EQ-5D and SF-36 as measures of health-related QoL in ICU survivors was undertaken in Sheffield in 2004. 71 The report came out strongly in favour of the EQ-5D, because it was simpler, had less floor and ceiling effects and so greater discrimination, and, if response rates were poor, follow-up using face-to-face or telephone interviews was easier.
There is only one published cost-effectiveness study of a treatment for ARDS. 72 This was a retrospective study using data from a large, long-term ICU outcome study undertaken in the USA (project SUPPORT). The treatment studied was artificial ventilation. Utilities were estimated using time-trade off questions and costs were from a hospital perspective.
The decision to use EQ-5D in the OSCAR study was made on a number of grounds. The EQ-5D serves both as a measure of health-related QoL and as a utility measure for calculating quality-adjusted life-years (QALYs). There is a large (3400) reference population database available, and the ICON study generated data on a population of mixed UK ICU survivors at the same time as the OSCAR trial was running, giving two appropriate reference populations. There is a large 11-centre study of survivors of ARDS planned in Baltimore, USA73 which will use EQ-5D as an outcome measure, allowing transatlantic comparisons.
We had originally planned to use formal, laboratory pulmonary function tests to determine residual respiratory dysfunction in survivors. However, two high-quality studies10,11 suggest this might not be cost-effective. The studies followed survivors of ARDS for up to 2 years. 10,11 At both 1 and 2 years, spirometry and lung volumes were normal. There was a reduction in carbon monoxide diffusing capacity (DLCO) compared with normal values, but, from the HTA review of outcome measures, this test is known to have poor measurement properties. 64 The 6-minute walking distance was also reduced compared with predicted values at both 1 and 2 years, but the patients attributed this to muscle weakness rather than cardio-pulmonary problems. The best measure of respiratory dysfunction was the physical problem domain of the SF-36. Thus if formal pulmonary function testing were to be used as an outcome measure, unless one of the treatments caused additional harm, spirometry and lung volumes would show no difference between groups (a ceiling effect). DLCO is probably not a valid measure of lung function after ARDS, and the 6-minute walk acts as a surrogate measure for muscle wasting. Thus the probability of distinguishing between treatment groups is very small, and, given both the burden to patients and the cost of transporting patients to pulmonary function laboratories, using laboratory pulmonary function tests as an outcome measure was abandoned.
Public and patient involvement
We used ‘CritPal’ (now the Patients and Relatives Committee of the UK Intensive Care Society) to provide advice and guidance on study documentation, consent procedures and publicity.
Health economics
The background to the health economic analysis is in Chapter 5.
Chapter 2 Methods (interventions)
Descriptions of interventions
The OSCAR study sought to answer the question ‘What effect would the introduction of high-frequency oscillation into the NHS have on the short-term mortality of patients artificially ventilated for ARDS?’. The study was a randomised controlled effectiveness study. The study groups which were compared in this trial were (a) HFOV versus (b) conventional positive-pressure ventilation (usual care). The detailed methodology for the study follows in Chapter 3, but as the experimental intervention is complex, the interventions are described separately in this chapter.
High-frequency oscillatory ventilation (experimental group)
In the original protocol, we had stipulated that the intervention would be HFOV, delivered using a SensorMedics 3100B ventilator ventilating at a rate of 5–15 Hz (breaths/second). When the study was designed this was the only commercially available high-frequency oscillatory ventilator for adult patients with CE marking marketed in the UK. Prior to the start of the study (early 2007), we became aware that a second CE-marked HFOV ventilator was due to come onto the UK market in May 2007. This ventilator is manufactured in Japan by Metran Co. Ltd (Kawaguchi, Saitama Prefecture, Japan) and marketed as the ‘R-100’ in the Asia-Pacific region. It is imported into Europe and rebadged as the ‘Novalung Vision Alpha’ by Novalung GmbH (Heilbronn, Germany) and distributed in the UK by Inspiration Healthcare Ltd (Leicester, UK). The SensorMedics 3100B was first released in 1993 and has a long history of use worldwide, but it uses analogue electronics, does not incorporate a conventional ventilator, and is noisier than the Vision Alpha device. The Vision Alpha is a digital device, which incorporates a conventional ventilator, but at the start of the study was little used outside Japan. The SensorMedics 3100B uses an electromechanical actuator to generate the oscillation, and, by modifying the driving signal, the ratio of inspiratory to expiratory time (I : E ratio) can be varied. The Vision Alpha uses a rotating mechanical valve and compressed gas to generate the oscillation and has a fixed 1 : 1 I : E ratio. Both ventilators have a frequency range of 5–15 Hz. After careful discussion, the investigators agreed that the study should proceed using the Vision Alpha ventilator, primarily because the transition from conventional ventilation to oscillatory ventilation and back was far simpler and the control interface was more intuitive which was felt to be important as many of the study sites would not have used HFOV prior to the study. The HTA was informed of the decision in June 2007.
The management of artificial ventilation with HFOV was based on two simple algorithms illustrated graphically in Figure 2, designed to allow arterial oxygen and carbon dioxide tensions (PaO2 and PaCO2) to be managed separately. The algorithms were derived from guidelines which had been used successfully at Addenbrooke’s Hospital ICU (Cambridge) and the University Hospitals Birmingham ICU for 5 years. The algorithms are virtually identical to the protocols used in the two published RCTs. 17,51
FIGURE 2.
The algorithms for managing HFOV. ABG, arterial blood gas analysis; BP, blood pressure; ETT, endotracheal tube; PAW¯, mean airway pressure; SpR, specialist registrar.
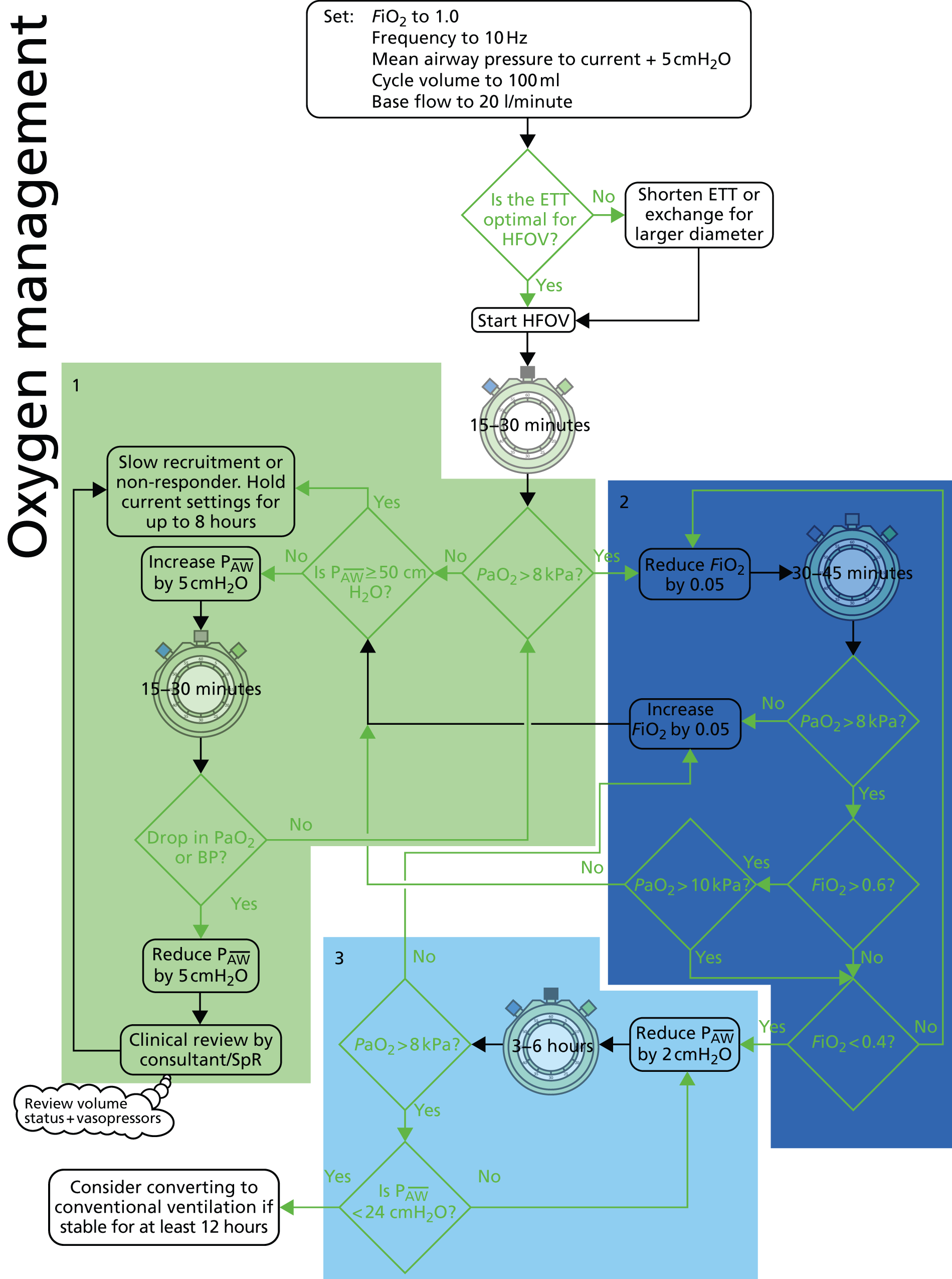

The algorithm for maintaining arterial oxygenation specified starting at a fractional concentration of inspired oxygen (FiO2) of 1.0, a frequency of 10 Hz, a mean airway pressure 5 cmH2O above the plateau or equivalent pressure on conventional ventilation, and a cycle volume of 100 ml (the cycle volume is the volume of gas displaced by the diaphragm, the volume reaching the alveoli is far less due to tubing expansion, gas compression and gas inertia). The starting bias flow was 20 l/minute. The target PaO2 was 8 kPa or greater. As the patient improved, the inspired oxygen was gradually reduced to 0.4 and then the mean airway pressure to 24 cmH2O. A ‘recruitment’ strategy was used for patients who did not demonstrate the expected improvement in P : F ratio after starting HFOV. When the patient had been stable on a FiO2 of 0.4 or less with a PaO2 in excess of 8 kPa, the patient was converted to conventional ventilation and weaned in the usual way. It is not possible to wean patients from artificial ventilation while on HFOV as the ventilator has no facility for spontaneous or patient-triggered breaths.
The algorithm for controlling arterial carbon dioxide tension (PaCO2) on HFOV involved a target arterial pH of 7.25–7.40, corresponding to a modest respiratory acidosis (mild permissive hypercapnia) in patients with normal metabolic acid-base status. To reduce PaCO2, the cycle volume was increased up to the maximum for the frequency (on the Vision Alpha ventilator cycle volume increases with decreasing frequency) and if that was insufficient the frequency was reduced. If the frequency was 5 Hz and the cycle volume maximised but the PaCO2 was still out of range, the on-call clinician was contacted for advice. Early experience with the ventilator identified a small number of patients in whom the PaCO2 increased rapidly (> 4 kPa rise) after starting on HFOV, and so the algorithm was modified to include a series of faster settings changes in these patients.
Training using the high-frequency oscillatory ventilation
In the original protocol it was anticipated that training would be carried out in the Netherlands and Germany. Before the study started it became clear this would not be practical. An amendment to the protocol was submitted (see Appendix 1, List 2: Substantial amendment 1, No. 5) which allowed training to be carried out in the UK (see Training in use of the ventilator and algorithms).
Troubleshooting with the high-frequency oscillatory ventilation ventilator
Troubleshooting notes prepared specifically for the study were supplied with the abbreviated operating manual. Clinical assistance was available from one of the principal investigators and technical assistance was available from Inspiration Healthcare by telephone at any time.
Supplying the Vision Alpha ventilators and associated disposables to collaborating centres
Collaborating ICUs were supplied with one Vision Alpha high-frequency oscillatory ventilator and humidifier. Inspiration Healthcare supplied service replacements within 48 hours if a ventilator or humidifier failed.
Centres were specifically told that the ventilator:
-
was not to be used until the trial office notified them that the appropriate national and local approvals were in place
-
was not to be used for treating patients outside of the OSCAR trial
-
would be removed from their ICU if there was evidence of violation of its use.
The Vision Alpha ventilators require a disposable ‘tubing set’ for each patient consisting of heated inspiratory and expiratory hoses, oscillator diaphragm assembly, the ‘wet’ assembly for the humidifier, pressure monitoring tubes and expiratory filter. Each patient also required a non-disposable sterile inspiratory valve, used to isolate the oscillator diaphragm from the breathing circuit during conventional ventilation. Each centre kept a stock of disposable tubing sets and sterile inspiratory valves. Used valves were returned to the study office and then sent to Novalung for cleaning and ethylene oxide sterilising. In 2009, the ventilators were retro-fitted with a ‘vent-protect’ heated filter assembly which prevented contact between the patient’s expiratory gases and the inspiratory valve and removed the requirement to sterilise the valves.
Training in use of the ventilator and algorithms
As HFOV had not been used previously in most of the ICUs in the study, a robust training/mentoring system was needed. Experience in neonatal trials where HFOV was introduced into special care baby units that had not previously used the technique suggested a major investment in training was required. 43,49
Before the study started, the clinicians in these units were trained to operate the HFOV ventilator and follow the treatment algorithms. Training was offered in various forms to suit the collaborating unit. During the first year of the study, a 2-day workshop-based course on the HFOV ventilator and how to manage ventilated patients was organised at each centre. In addition, follow-up ‘drop-in’ sessions were offered, usually on the ICU. These shorter sessions were to suit busy units and allow staff to dip in when possible during clinical shifts to top up their skills.
This training was to be backed up with centralised training programs run in Birmingham and Oxford for staff from each study site, targeting the ICU consultant medical staff, senior nursing staff and the local research nurses co-ordinating the OSCAR trial. These used the teaching suites equipped with patient simulators [Laerdal ‘SimMan®’ (Laerdal Medical Limited, Orpington, UK)] available at Birmingham and Oxford. The trial had a full-time, clinically trained research fellow in the team for the first year to lead and organise the training both centrally and locally, and two half-time senior nurse trainers for the next 3 years of the study. In addition, a member of the team regularly travelled to collaborating centres to support the use of the HFOV. Inspiration Healthcare also offered local training based on the need at individual centres.
Teaching material was prepared at the trial office and distributed to the ICUs taking part, both electronically and on paper. A newsletter was used to share any problems and solutions related to HFOV. We had planned to use a website to distribute information, but decided targeted e-mails with the information were more effective. The trial website held only contact details, details of regulatory approvals and the protocol.
Medical Devices Regulations 2002
As the trial employed a medical device (the Vision Alpha ventilator) for a purpose for which it was CE marked, approval from the competent authority [the Medicines and Healthcare Regulatory Authority (MHRA)] was not required.
Conventional ventilation (control group)
The control group received conventional positive-pressure ventilation using conventional pressure-controlled artificial ventilation.
Clinical management of patients in the control group (conventional ventilation)
When implementing the control intervention in the OSCAR trial, we suggested, but did not mandate, that the conventional ventilation strategy be based on limited tidal volume, pressure-controlled artificial ventilation using tidal volumes of 6–8 ml/kg, ideal body weight and fixed PEEP/FiO2 combinations as used in the ARDSnet study,74 the only ventilator mode for patients with ARDS with proven benefit. Most ICUs used pressure-controlled or pressure-supported ventilation modes. Two ICUs used airway pressure release ventilation (pressure-controlled ventilation with a very long inspiratory time and a very short expiratory time) on some of the control patients.
Other treatment
All patients were artificially ventilated at the point of randomisation, as this was one of the eligibility criteria. Both groups began the assigned treatment immediately following randomisation (or continued conventional ventilation if assigned to the control group). Patients in the experimental (HFOV) group remained on HFOV until the start of weaning from artificial ventilation. Weaning strategies were not specified by protocol, each unit followed its usual practice.
We recommended the following combinations of FiO2 and PEEP (Table 2).
| FiO2 | PEEP (cmH2O) |
|---|---|
| 0.3 | 5 |
| 0.4 | 5 |
| 0.4 | 8 |
| 0.5 | 8 |
| 0.5 | 10 |
| 0.6 | 10 |
| 0.7 | 10–14 |
| 0.8 | 12–14 |
| 0.9 | 12–16 |
| 1.0 | 12–18 |
This ventilation strategy was reported as normal practice in most UK ICUs.
Proposed duration of treatment and weaning
The patients continued on HFOV until they had recovered sufficiently to be weaned from artificial ventilation when their FiO2 was 0.4 or less, their mean airway pressure was 24 cmH2O or less, and the local clinician was satisfied that there were no non-pulmonary impediments to weaning. The HFOV ventilation mode does not allow any form of spontaneous (patient-triggered) ventilation which is normally required for weaning, so at this point the patients were placed back on conventional ventilation and weaned according to local protocols using inspiratory pressure support (Figure 3).
FIGURE 3.
Patient treatment and weaning flow chart.
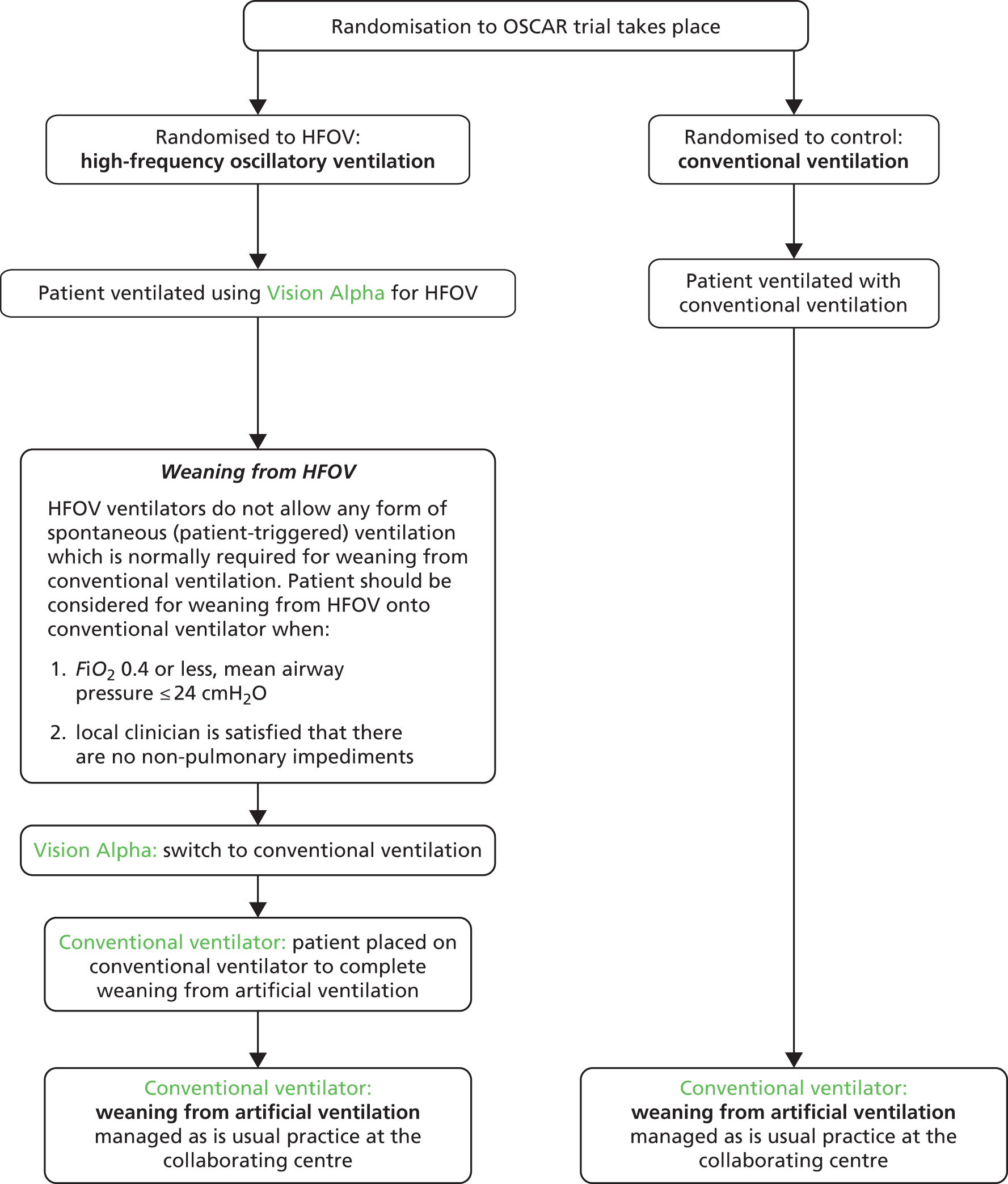
The point at which patients could be fully weaned from conventional artificial ventilation depended on a large number of factors that could not be protocolised.
Restarting high-frequency oscillatory ventilation
Patients who began weaning but then deteriorated could be restarted on HFOV for 48 hours after it was discontinued. If they deteriorated after 48 hours they were returned to conventional ventilation. This meant that for 48 hours after discontinuation of HFOV the HFOV ventilator was unavailable and so no recruitment of new patients could take place as each site only had one ventilator.
Health economics
The methods for health economic data collection are given in Chapter 5.
Chapter 3 Detailed methods
Hypothesis
The hypothesis for the OSCAR trial was that patients with ARDS who were treated with HFOV had a decreased mortality at 30 days following randomisation compared with patients treated with conventional positive-pressure ventilation (usual care).
Study design
OSCAR was a multicentre, open, randomised controlled effectiveness trial.
Setting
In the protocol, we planned to recruit patients in 12 ICUs in the NHS in the UK, which were able to care for Level 3 patients as defined by the Department of Health’s Comprehensive Critical Care: A Review of Adult Critical Care Services. 75 To achieve adequate recruitment, additional centres were added so a total of 30 ICUs had taken part by the end of the OSCAR trial.
Intensive care units
In the protocol, the timeline for the project was approximately 57 months. The anticipated start date for the project was 1 June 2007 and the completion date was 29 February 2012. In this timeline, it was anticipated that the first 6 months of the study would be allocated to ethic approvals, design and production of trial material and on-site training for the staff using ventilators.
Initially, 12 centres were recruited to the study: 10 were allocated the Vision Alpha ventilators which had been leased and two sites had their own ventilators. The John Radcliffe Hospital was the first site to recruit in December 2007. The remaining 11 sites were due to start shortly after this date. However, there were delays as the final Multicentre Research Ethics Committee (MREC) (ethics) approval was not obtained until October 2007, despite submitting to ethics in July 2007. Also, there was a delay in the delivery of the ventilators from Japan and Germany and therefore the ventilators were not available for a December 2007 start.
Recruitment was lower than anticipated and it was recognised very early on in the trial (May 2008) that the required number of patients would not be achieved in the original timescale and that an extension would be required. An application for this was submitted to the HTA. The decision was to award the funding, conditional on a HTA recruitment review visit which was scheduled for 18 December 2008.
Following the visit, a 13-month extension approval was confirmed in June 2009, moving the completion date of the project to the end of March 2013. Ten additional ventilators were purchased and this allowed an additional 10 new sites to collaborate (see Table 3). Allowing for the lead in time for arrival of the ventilators (12 weeks), it was estimated that the start date for recruitment for these new sites would be 1 October 2009. However, owing to a delay in arrival of the ventilators, setting up of new sites was not possible until end/beginning of 2009/2010. There were a further five sites which had their own ventilators and were approached and agreed to recruit patients into OSCAR.
In 2009/2010, some reallocation of the ventilators occurred:
-
Aberdeen Royal Infirmary closed for recruitment when the local Principal Investigator left in May 2009 and the ventilator was relocated to Stirling Royal Infirmary.
-
Royal United Hospital in Bath closed in June 2009 with the ventilator relocated firstly to the John Radcliffe Hospital to support HFOV training and then relocated to Queen Alexandra Hospital in Portsmouth once the new sites had all been set up.
-
University Hospital of Wales closed for recruitment in July 2010 owing to lack of recruitment and the ventilator from this site was sent to the highest recruiting site at the time, Queen Elizabeth Hospital in Birmingham, for use as a second ventilator.
In December 2010, the leasing period for the first 10 ventilators was coming to an end. Negotiations with Novalung led to the lease being extended to 3 March 2011, at no additional cost to the study. Also, there were enough additional funds to extend the lease on seven of these ventilators up to end of recruitment (August 2011). Thus, in the beginning of 2011, it was planned that four of the lowest recruiting sites would be closed so the lease could be extended for the remaining sites.
By the end of August 2011, 637 of the target of 802 patients had been recruited into the trial. It was decided to approach 17 sites (as indicated in Table 3) to see if they were prepared to continue recruiting patients into OSCAR until the end of July 2012 (when the last 12-month follow-up was due for the 637 patients). The sites were seven with their own ventilators and 10 which had a purchased (study) ventilator. A substantial amendment to the protocol was submitted to the MREC, as some documentation needed updating because follow-up might not be complete for all patients and this was approved (see Appendix 1, List 6: substantial amendment 5).
| Status of ventilator | Type of ventilator | Site code | Hospital name | Start date | End date | Number of recruits |
|---|---|---|---|---|---|---|
| Obtained from original funding | Leased | 6201 | John Radcliffe Hospitala | 3 December 2007 | 31 July 2012 | 15 |
| Leased | 6203 | Aberdeen Royal Infirmaryb | 3 December 2007 | 28 May 2009 | 15 | |
| Leased | 6204 | Medway Hospital | 7 January 2008 | 31 January 2011 | 27 | |
| Leased | 6202 | Derriford Hospitala | 7 January 2008 | 31 July 2012 | 46 | |
| Leased | 6206 | Royal Sussex County Hospitala | 14 January 2008 | 31 July 2012 | 46 | |
| Leased | 6210 | Manchester Royal Infirmary (General) | 11 February 2008 | 31 January 2011 | 24 | |
| 6220 | Manchester Royal Infirmary (Cardiac) | 7 September 2009 | 31 January 2011 | 1 | ||
| Leased | 6209 | Royal United Hospital, Bathb | 4 March 2008 | 26 June 2009 | 20 | |
| Leased | 6207 | University College Hospitala | 17 March 2008 | 31 July 2012 | 63 | |
| Leased | 6205 | Queen Elizabeth Hospital Birminghama | 25 March 2008 | 31 July 2012 | 102 | |
| Leased | 6208 | University Hospital of Wales | 9 June 2008 | 2 July 2010 | 16 | |
| Own | 6211 | Ysbyty Maelora | 21 April 2008 | 31 July 2012 | 32 | |
| Own | 6213 | Queen Elizabeth Hospital, Gatesheada | 1 December 2008 | 31 July 2012 | 14 | |
| Transferred | Leased | 6214 | Stirling Royal Infirmary (from Aberdeen) | 17 June 2009 | 31 August 2011 | 19 |
| Leased | 6222 | Queen Alexandra Hospital (from Bath/Oxford)a | 4 November 2009 | 31 July 2012 | 37 | |
| Funded: extension grant | Purchased | 6215 | Royal Cornwall Hospitala | 15 December 2008 | 31 July 2012 | 56 |
| Purchased | 6224 | Royal Blackburn Hospitala | 10 December 2009 | 31 July 2012 | 26 | |
| Purchased | 6216 | Wythenshawe Hospital | 4 January 2010 | 31 August 2011 | 15 | |
| Purchased | 6217 | University Hospital of North Staffordshire | 4 January 2010 | 31 August 2011 | 15 | |
| Purchased | 6218 | Ipswich Hospital | 4 January 2010 | 31 March 2011 | 5 | |
| Purchased | 6223 | Queen Margaret Hospital | 4 January 2010 | 31 January 2011 | 8 | |
| Purchased | 6227 | St James’s University Hospitala | 4 January 2010 | 31 July 2012 | 68 | |
| Purchased | 6228 | York Hospital | 4 January 2010 | 31 August 2011 | 13 | |
| Purchased | 6226 | Southampton General Hospital | 8 February 2010 | 31 August 2011 | 14 | |
| Purchased | 6229 | Victoria Hospital Blackpoola | 15 February 2010 | 31 July 2012 | 28 | |
| Own | 6230 | Southend Hospitala | 20 September 2010 | 7 November 2011 | 3 | |
| Own | 6221 | James Paget Hospitala | 2 November 2009 | 31 July 2012 | 23 | |
| Own | 6225 | Leeds General Infirmarya | 26 October 2009 | 31 July 2012 | 30 | |
| Own | 6231 | Royal Victoria Infirmarya | 11 October 2010 | 31 July 2012 | 8 | |
| Own | 6232 | James Cook University Hospitala | 17 January 2011 | 31 July 2012 | 6 |
Inclusion criteria for centres
An ICU was considered for collaboration in the trial if it met the following criteria:
-
The number of annual admissions to the ICU suggested patients with ARDS occurred sufficiently frequently (amended from the original protocol as stated in Appendix 1, List 2: substantial amendment 1, No. 1).
-
The ICU had a history of collaborating in research and staff members were keen to be involved.
-
All consultants in the ICU had ‘substantial uncertainty’ about the use of HFOV generally and were prepared to enter patients into a trial comparing HFOV with conventional treatment for patients with ARDS.
-
Consultants were willing to attend HFOV training.
-
The PI was prepared to negotiate the release of all other appropriate staff for HFOV training.
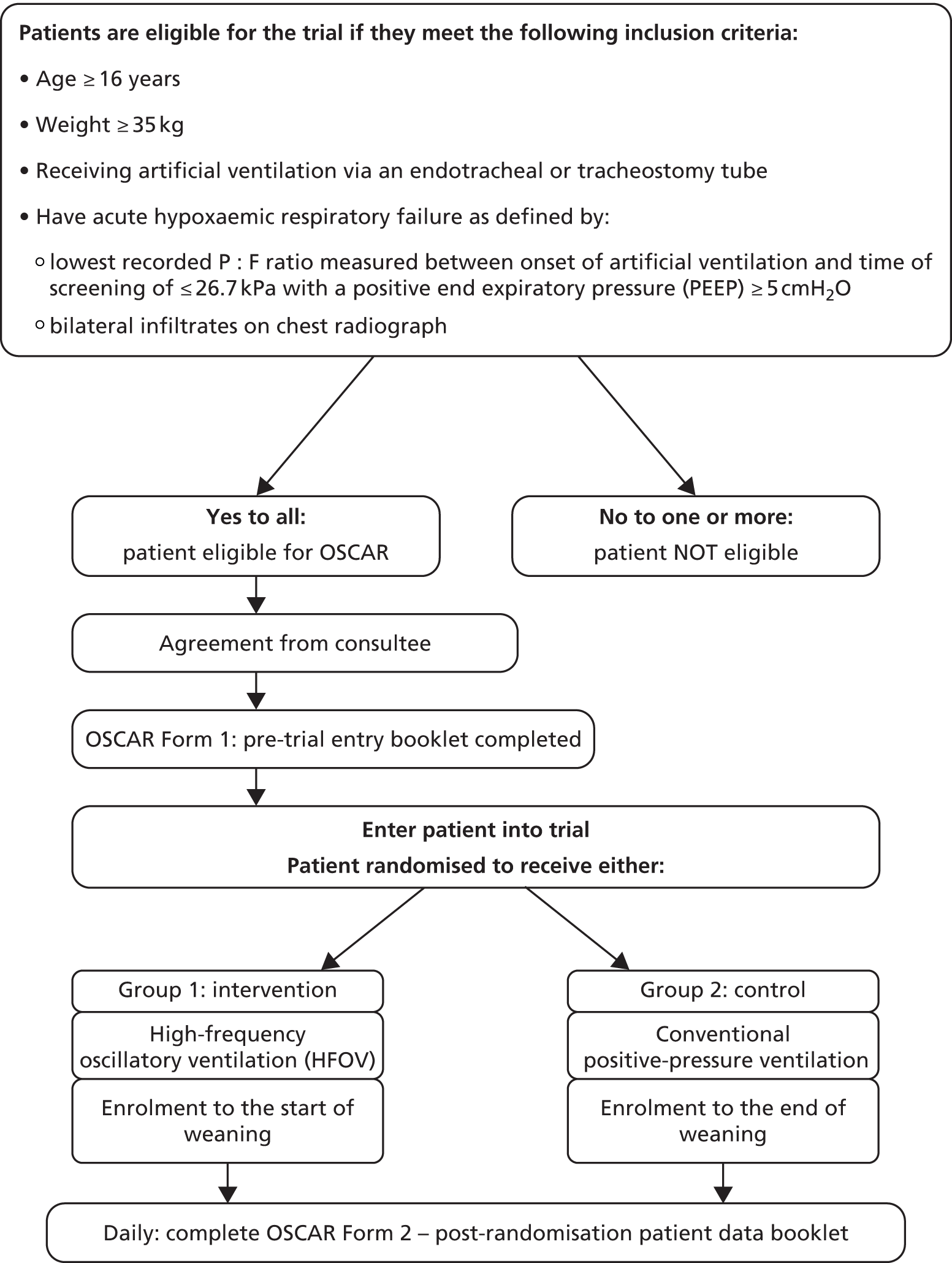
Inclusion criteria for patients
Our aim was to recruit adults (age ≥ 16 years old) admitted to an ICU with ARDS who were predicted to require artificial ventilation for 48 hours or greater. ARDS was defined using the American-European Consensus Committee definition of a P : F ratio of < 26.7 kPa51 from two arterial blood gas analyses 12 hours apart. We exclude patients who weighed < 35 kg as the ventilators were not CE approved for treatment of patients below this weight. Patients with obstructive lung pathologies and conditions in which HFOV might be hazardous were excluded.
Patients were therefore eligible for the trial if they met the following inclusion criteria:
-
age ≥ 16 years
-
weight ≥ 35 kg
-
was receiving artificial ventilation via an endotracheal or tracheostomy tube
-
had acute hypoxaemic respiratory failure as defined by:
-
– lowest recorded P : F ratio measured between onset of artificial ventilation and time of screening of ≤ 26.7 kPa with a PEEP ≥ 5 cmH2O
-
– bilateral infiltrates on chest radiograph
-
-
was not likely to be extubated by the following evening (predicted by attending clinician)
-
had been mechanically ventilated for < 7 consecutive days (≤ 168 hours) at the point of randomisation.
Exclusion criteria for patients prior to trial entry
Patients who were likely not to benefit from HFOV included the following:
-
Patients with left atrial hypertension from any cause, diagnosed clinically or with echocardiography or pulmonary artery catheterisation.
-
Patients who had been mechanically ventilated for more than 7 consecutive days at the point of enrolment.
-
Patients with moderate or severe airway disease expected to cause expiratory airflow limitation.
-
Patients who would have had a lung biopsy or resection during this hospital admission.
-
Patients with any other condition the clinician believed would make receiving HFOV hazardous.
Administrative, practical and ethical exclusions:
-
Patients who had previously enrolled in the OSCAR trial.
-
Patients (or their representative) who refused consent.
-
Patients (or their representative) who did not understand written or verbal information and for whom no interpreter was available.
-
Patients who had been enrolled in another therapeutic trial in the 30 days prior to randomisation.
-
Patients in whom active treatment had been withdrawn or withdrawal was planned.
Where a patient met one of the exclusion criteria, screening was stopped. Most patients were expected to be unable to give informed consent when recruited so patient representatives were used to provide an opinion/assent.
Conventional positive-pressure ventilation (control group)
Patients randomised to the control group received conventional positive-pressure ventilation using conventional pressure-controlled artificial ventilation (as detailed in Chapter 2).
High-frequency oscillatory ventilation
Patients randomised to the experimental group received (artificial) HFOV delivered using a Vision Alpha ventilator (as detailed earlier).
Patient flow
Figure 4 illustrates the flow of patients (screened and randomised) in the OSCAR trial.
FIGURE 4.
The flow of patients (screened and randomised) in the OSCAR trial.
Patient consent
Patients were almost invariably unable to give informed consent owing to alterations in conscious level caused by their illness and therapeutic sedation. As a result, assent from personal or professional consultees (a relative or a nominated health-care professional) was obtained in line with the legal requirements in England and Wales (Mental Capacity Act 200576), and in Scotland [Adults with Incapacity (Scotland) Act 200077]. See Appendix 2 for informed consent process, information and forms.
If a patient or their representative [‘Consultee’ (personal or nominated professional), in England and Wales; ‘Welfare Guardian/Nearest Relative’ in Scotland] refused assent, the patient received usual treatment as defined by the clinician responsible for their care.
Checking eligibility and ventilator availability
Prior to entry, the appropriate items on the eligibility checklist were ticked and the patient was assessed for suitability for entry into the OSCAR study.
Prior to randomisation, it was necessary to check the availability of the HFOV ventilator, in case it was in use treating another trial patient.
Pre randomisation
Patients who satisfied the eligibility criteria had their baseline data collected prior to randomisation.
The procedures for the data collected prior to randomisation are listed in Table 4. The use of antimicrobial drugs and sedatives was recorded. As an aide-memoire and because antimicrobial drugs are sometimes used for purposes other than treating infections (e.g. erythromycin used as a prokinetic agent), a table of antimicrobials was included in the case report form (CRF). Similarly, some drugs are variously used for their sedative or analgesic properties (e.g. morphine) so an explanatory table was included. These are given in Box 1 and Table 5.
| Time points | Measurement category | Measurements collected | Procedures and notes for data collection |
|---|---|---|---|
| Pre-randomisation/daily data in ICU/weaning off HFOV | Ventilation measurements: (these measurements had to relate to the arterial blood sample of ≤ 26.7 kPa with a PEEP ≥ 5 cmH2O) | Exhaled minute volume | This was the total volume of gas exhaled in 1 minute, as measured by the ventilator. It included both mandatory and spontaneous breaths |
| Total respiratory rate | This was the total respiratory rate per minute as measured by the ventilator. It included both mandatory and spontaneous breaths | ||
| PEEP | This was the set PEEP. No measured auto-PEEP was included. The measurements related to the required repeat arterial blood sample to confirm ARDS (taken at least 12 hours after the initial arterial blood sample) | ||
| Plateau pressure (cmH2O) | This was the plateau pressure on mandatory breaths. In a volume-controlled mode, the inspiratory pause was added to allow estimation of plateau pressure. In a pressure-controlled mode this was the set inspiratory pressure. In both cases, the value above PEEP was recorded, not the absolute value. If the patient had only received inspiratory pressure support, the support (inspiratory) pressure above PEEP was recorded | ||
| Arterial blood gases (PaCO2, pH, PaO2 and FiO2) | The PaO2 and FiO2 measurements related to the required repeat arterial blood sample to confirm ARDS (taken at least 12 hours after the initial arterial blood sample). The sample had to demonstrate a PaO2/FiO2 ratio of ≤ 26.7 kPa (200 mmHg) for eligibility | ||
| Pre-randomisation/daily data in ICU | Organ support: (during the last 24 hours had the patient received any of the following) | Advanced respiratory support | This was indicated by one or both of the following:
|
| Basic respiratory support | This was indicated by one or more of the following:
|
||
| Pre-randomisation/ICU data | Organ support: (during the last 24 hours had the patient received any of the following) | Advanced cardiovascular support | This was indicated by one or more of the following:
|
| Basic cardiovascular support | This was indicated by one or more of the following:
|
||
| Renal monitoring/support | This was indicated by acute renal replacement therapy (haemodialysis, haemofiltration, etc.) | ||
| Gastrointestinal support | This was indicated by feeding with parenteral or enteral nutrition via a feeding tube | ||
| Dermatological support | This was is indicated by one or more of the following:
|
||
| Liver support | This was indicated by extracorporeal liver replacement device such as a MARS device, bioartificial liver or charcoal haemoperfusion | ||
| Antimicrobial use | ‘Yes’ was ticked if the patient had received one or more doses of drugs primarily used for the treatment of bacterial, viral or fungal infections (as in Box 1). Drugs used to treat tuberculosis, HIV infection or parasitic diseases were excluded | ||
| Pre-randomisation/ICU data | Organ support: (during the last 24 hours had the patient received any of the following) | Sedative use | ‘Yes’ was ticked if (in the 24-hour period) the patient has received an intravenous bolus dose or an infusion of drugs primarily for sedation rather than for analgesia, treatment of insomnia, treatment of psychosis or antiepileptic actions. If patients were receiving opiates alone primarily for analgesia the ‘No’ box was ticked. See Table 5 |
| Muscle relaxants | If patient had received muscle relaxant drugs (neuromuscular junction blocking agent), then this was ticked ‘yes’ | ||
| Proned | Ventilation had to be in the prone position (fully prone – face down and no lateral tilt). Chest weighting in the supine position was not considered to be prone | ||
| Receiving inhaled nitric oxide | This was recorded as ‘yes’ if patient was receiving any concentration of therapeutic inhaled nitric oxide | ||
| Immediately post randomisation | Patient’s clinical data | Sex | |
| Age | |||
| Weight | |||
| ICU data | HFOV measurements | Frequency | The set HFOV oscillation frequency |
| Mean airway pressure | The set mean airway pressure | ||
| Amplitude | The measured amplitude in cmH2O | ||
| Arterial blood gases | Not venous gas results | ||
| Hours on HFOV | This is the total number of completed hours on HFOV since 8 a.m. the previous day | ||
| Cuff leak | Was a deliberate cuff leak introduced to improve CO2 clearance at any point in the last 24 hours? | ||
| Set cycle volume | This is set (not measured) volume | ||
| The set base flow | As recorded on the HFOV device |
Acyclovir.
Amikacin.
Amoxicillin.
Ampicillin.
Amphotericin.
Aztreonam.
Benzylpenicillin.
Caspofungin.
Cefamandole.
Cefazolin.
Cefotaxime.
Cefoxitin.
Cefpirome.
Cefradine (cephradine).
Ceftazidime.
Ceftriaxone.
Cefuroxime.
Chloramphenicol (i.v.).
Ciprofloxacin.
Clarithromycin.
Clindamycin.
Co-amoxiclav.
Colistin.
Co-trimaxazole.
Ertapenem.
Erythromycin (not prokinetic doses).
Flucloxacillin.
Fluconazole.
Flucytosine.
Foscarnet.
Ganiclovir.
Gentamicin.
Imipenem.
Itraconazole.
Ketoconazole.
Levofloxacin.
Linezolid.
Meropenem.
Metronidazole.
Netilmycin.
Ofloxacin.
Piperacillin.
Quinupristin/dalfopristin (Synercid®, Pfizer).
Sodium fusidate.
Sulfadiazine.
Teicoplanin.
Tazocin (piperacillin + tazobactam).
Ticarcillin.
Tigercycline.
Tobramycin.
Vancomycin.
Voriconazole.
i.v., intravenous.
| Drug class | Drug |
|---|---|
| Primarily used as sedative | Chlorpromazine |
| Chlordiazepoxide | |
| Diazepam | |
| Haloperidol | |
| Isoflurane | |
| Ketamine | |
| Lorazepam | |
| Methohexitone | |
| Midazolam | |
| Paraldehyde | |
| Phenobarbitone | |
| Promazine | |
| Propofol | |
| Thiopentone | |
| Opiates primarily used as sedative | Alfentanil |
| Diamorphine | |
| Fentanyl | |
| Morphine | |
| Remifentanil | |
| Papaveretum | |
| If used alone, these are not considered primarily sedative | Alpha 2-adrenoceptor agonists (clonidine, dexmedetomidine) |
| Buprenorphine | |
| Codeine phosphate | |
| Methadone | |
| Pethidine | |
| Tramadol |
The randomisation system
Randomisation was carried out by the Health Services Research Unit in Aberdeen. Randomisation was telephone based and was continuously available. Random allocation was generated by an independent programmer in an equal number assigned to each intervention.
Method of randomisation
We used stratified block randomisation. The randomisation was stratified by site, age of the patient (≤ 55 years and > 55 years) and P : F ratio (≤ 15 kPa and > 15 kPa). The block lengths were random so that prediction of intervention allocation could not be made.
Patients not in the trial
Brief details of patients initially eligible for the trial but not entered into the trial was recorded on a ‘Why not in trial’ log at each collaborating unit to monitor for bias in case selection and provide full reporting in accordance to the CONSORT statement. 78
Immediately post randomisation
Hospital admission date and time and reason for admission were recorded following randomisation. Data on the initial ventilation and the patient’s height (to allow calculation of ideal body weight) were also recorded.
For patients randomised to receive HFOV, the date and time the patient was connected onto the HFOV ventilator was recorded. In addition, the date/time the first FiO2 was reduced and the cause of the acute hypoxaemic respiratory failure were recorded.
First 24 hours in intensive care unit
The ICU date and time of entry and the details of the patient’s past medical history required to calculate the risk of in-hospital death using the Acute Physiology and Chronic Health Evaluation II (APACHE II) algorithm79 were recorded using definitions slightly modified from those used by the ICNARC Case Mix Programme, a UK-wide ICU audit programme (Box 2). The patient’s primary condition was also recorded using the ICNARC coding method convention. 80
-
Evidence of portal hypertension was the presence of oesophageal or gastric varices demonstrated by surgery, imaging or endoscopy or the demonstration of retrograde splenic venous flow by ultrasound.
-
Did not include gastrointenstinal bleeding without evidence of portal hypertension.
-
Episodes of hepatic encephalopathy, Grade 1 or greater.
-
Grade 0 No abnormality detected; Grade 1 Slowness in cerebration, intermittent mild confusion and euphoria; Grade 2 Confused most of the time, increasing drowsiness; Grade 3 Severe confusion, rousable, responds to simple commands; Grade 4 Unconscious, responds to painful stimuli.
-
Fatigue, claudication, dyspnoea or angina at rest, where any activity increased symptoms. Symptoms must have been attributable to myocardial or peripheral vascular disease. Functionally, this patient could not stand alone, walk slowly or dress without symptoms.
-
Had permanent shortness of breath with light activity attributable to pulmonary disease. Functionally, this patient was unable to work and has shortness of breath performing most normal activites of daily living (e.g. walking 20 metres on level ground, walking slowly in the house, climbing one flight of stairs, dressing or standing).
-
Had used or was using home ventilation.
-
Ventilation was defined where all or some of the breaths or a portion of the breaths (pressure support) were delivered by a mechanical device. Ventilation could be simply defined as a treatment where some or all of the energy required to increase lung volume during inspiration is supplied by a mechanical device.
-
CPAP is excluded.
-
Required chronic renal replacement therapy (either chronic haemodialysis, chronic haemofiltration or chronic peritoneal dialysis) for irreversible renal disease.
-
HIV-positive with clinical complications.
-
Clinical complications include Pneumocystis carinii (P. jirovecii) pneumonia, Karposi’s sarcoma, lymphoma, tuberculosis and toxoplasma infection.
-
Did not include AIDS-related complex or positive HIV test without clinical manifestations.
-
Had received ≥ 0.3 mg/kg prednisolone or an equivalent dosage of another corticosteroid, daily for the 6 months prior to admission to your unit.
-
Had received externally administered radiotherapy, excluding all of the following: radiotherapy for non-invasive skin tumours; enteral or parenteral radioisotope therapy; radioactive implants; radiotherapy for prevention of heterotopic bone formation.
-
Had received drug treatment resulting in a lower resistance to infection.
-
Examples include drug treatment malignancy, vasculitides, rheumatoid arthritis, inflammatory bowel disease, etc.
-
Had distant (not regional lymph node) metastates, documented by surgery, imaging or biopsy.
-
Acute myelogenous leukaemia, acute lymphocytic leukaemia or multiple myeloma must have been evident in the 6 months prior to admission to your ICU.
-
Chronic myelogenous leukaemia or chronic lymphocytic leukaemia must have been evident in the 6 months prior to admission to your unit.
-
Had active lymphoma, documented by surgery, imaging or biopsy.
-
Had documented congenital immunohumoral or congenital cellular immune deficiency state.
-
Examples include CVID, agammaglobulinaemia including XLA, SCID, chronic granulomatous disease, lgA deficiency, lgG deficiency, functional antibody deficiency, hyper lgE syndrome, Wiskott–Aldrich syndrome, CMCC, DiGeorge syndrome, ataxia telangiectasia, leucocyte adhesion defect, complement deficencies, C1 esterase inhibitor deficiency, Kostmann syndrome.
AIDS, acquired immunodeficiency syndrome; CMCC, chronic mucocutaneous candidiasis; CPAP, continuous positive airway pressure; CVID, common variable immunodeficiency; HIV, human immunodeficiency virus; IgA, immunoglobulin A; IgE, immunoglobulin E; IgG, immunoglobulin G; SCID, severe combined immunodeficiency; XLA, X-linked agammaglobulinemia.
Clinical data were also recorded to calculate the APACHE II score. The procedure for recording the data is listed in Box 3, which is an updated version of the definitions used in the original APACHE II study. 79
-
Tympanic membrane, nasopharyngeal, oesophageal, rectal, pulmonary artery, bladder are considered as central temperature measurement sites.
-
The readings at the most extreme. (If there was a decision to be made between two readings take the one that gave the most extreme MAP.)
-
For admissions who were paced, the actual measured ventricular rate is recorded.
-
Ventricular rate is not recorded for any admissions during periods of iatrogenic disturbance (e.g. physiotherapy, turning, periods of crying, etc.).
-
A respiratory rate is defined as ventilated when all or some of the breaths or a portion of the breaths (pressure support) are delivered by a mechanical device. Ventilation can be simply defined as a treatment where some or all of the energy required to increase lung volume during inspiration is supplied by a mechanical device.
-
High-frequency and jet ventilators, negative pressure ventilators and BIPAP are considered as ventilated.
-
Hand ventilation by a member of your team is considered as ventilated.
-
CPAP and ECMO are considered as not ventilated.
-
For admissions who were ventilated, the respiratory rate is to be the sum of both ventilated and spontaneous breaths in a minute.
-
A patient is considered intubated if they have a laryngeal mask or an endotracheal, endobronchial or tracheostomy tube in place.
-
Laboratory results only, performed either in the departments of clinical chemistry or haematology or in near patient testing laboratories with formal quality control programmes in operation. For white blood cell count, the effects of steroids, inotropes and splenectomy are ignored.
-
No account is taken of the effect of diuretics.
Glasgow Coma Scale scores assessed only when the patient was free from the effects of sedative and/or paralysing or neuromuscular blocking agents are valid (Table 6). For patients sedated or paralysed for part of the first 24 hours, the lowest Glasgow Coma Scale score is during the periods they are free of drug effects.
BIPAP, biphasic positive airway pressure; CPAP, continuous positive airway pressure; MAP, mean arterial pressure.
| Feature | Response | Score |
|---|---|---|
| The best eye opening response | Spontaneous | 4 |
| To verbal command | 3 | |
| To pain | 2 | |
| No response | 1 | |
| The best verbal response | Orientated and converses | 5 |
| Disorientated and converses | 4 | |
| Inappropriate words | 3 | |
| Incomprehensible sounds | 2 | |
| The best motor response | Obeys verbal command | 6 |
| Localises pain | 5 | |
| Flexion withdrawal | 4 | |
| Flexion-abnormal/decorticate rigidity | 3 | |
| Extension/decerebrate rigidity | 2 | |
| No response | 1 | |
| If a patient is intubated, use clinical judgement to score verbal response as follows | Appears orientated | 5 |
| Responsive but ability to converse questionable | 3 | |
| Generally unresponsive | 1 |
Daily data in intensive care unit
Following ICU admission, data were collected every morning, starting at 8 a.m. (or as near as possible) the day after randomisation.
The data collected on all patients were details of organ support, antimicrobial use, sedative use, muscle relaxant use, nitric oxide use and information on prone positioning. For patients on conventional ventilation, exhaled minute volume, total respiratory rate (and hence tidal volume), PEEP and plateau pressures, blood gases and inspired oxygen were recorded. For the patients on HFOV, the frequency, mean airway pressure, measured amplitude, cycle volume, bias flow, completed hours on HFOV and the use of a cuff leak were recorded, along with arterial blood gases and inspired oxygen.
Transition from high-frequency oscillatory ventilation to conventional ventilation for weaning
As noted earlier, there is no facility for spontaneous breaths while a patient is receiving HFOV. As weaning from artificial ventilation back to spontaneous (unassisted) breathing involves a gradual removal of artificial ventilator support with a concomitant increase in spontaneous breathing, this could not be undertaken on the HFOV ventilator. When a patient randomised to HFOV had improved sufficiently (i.e. FiO2 was ≤ 0.4 or less and the mean airway pressure was ≤ 25 cmH2O) the patient was switched to conventional ventilation, initially using the conventional ventilation mode on the Vision Alpha ventilator for up to 48 hours and then using the ICU’s normal ventilators. If, during the first 48 hours on conventional ventilation (either Vision Alpha or standard conventional ventilator), the consultant had decided that the patient might benefit from further high-frequency ventilation, the patient was placed back on HFOV and this was recorded accordingly. Figure 3 summarises the patient treatment and weaning flow chart.
The point at which patients could be fully weaned from conventional artificial ventilation depended on a large number of factors that could not be protocolised. The assessments made whilst weaning a patient off HFOV are illustrated in Figure 3.
Hospital stay and after hospital discharge
Patients either died on the ICU or survived and were transferred to a hospital ward. The date, time and vital status at ICU discharge were recorded. No data were collected while in the hospital ward, except the hospital discharge date.
Patients were ‘flagged’ on the Office for National Statistics (ONS) database to ensure reliable collection of the survival data. Lists of survivors to hospital discharge were sent to the ONS regularly where two checks were carried out. The first was list cleaning, which maximised the chances of identifying individual patients on the ONS databases. The second check was to reveal any patients who have died after hospital discharge to ensure follow-up questionnaires were not posted out to deceased patients. For some patients it was necessary to contact the patient’s general practitioner to obtain the patient’s vital status.
Follow-up assessments
This section describes the methods used for patient follow-up to 1 year after randomisation, to obtain data on health-related QoL and health-care costs. As the trial recruitment period was extended into the period planned for follow-up, the follow-up data are incomplete at the time of writing, and so only a limited number of results are reported in Chapter 4.
Patients were followed up at 6 and 12 months after randomisation using self-completed postal questionnaires. Return of questionnaires was tracked carefully by the OSCAR trial office. Patients who died after hospital discharge but prior to the mailing were identified from the ONS returns and removed from the mailing list. The questionnaire included standard instruments to measure health-related QoL and calculate utility indices for the first year after ICU discharge [Short Form questionnaire-12 items (SF-12) and EQ-5D, see Chapter 1]. Questions on social- and health-service use were included to allow a health economic analysis. Freepost envelopes were provided to maximise the response rate.
A letter was sent out to survivors 2 weeks ahead of the first follow-up questionnaire at 6 months and the second questionnaire at 12 months. This letter was added in as a substantial amendment to the protocol (see Appendix 1, List 5: substantial amendment 4) as a reminder to the participant that they would be receiving a questionnaire related to their health in the near future, in an attempt to maximise the response rate. If the questionnaire was not returned a month after it was posted, the vital status of the patient was rechecked using ONS and a reminder letter and another questionnaire were posted. This reminder letter was added in as a substantial amendment to the protocol (see Appendix 1, List 3: substantial amendment 2).
A carer’s questionnaire was also included as part of the follow-up package. This was added in as a substantial amendment to the protocol (see Appendix 1, List 2: substantial amendment 1, No. 9), as part of the study involved learning about the carers and the financial impact on them as a result of providing care to someone who has been treated on an ICU. Collecting the data on carers allowed an insight into the cost of the interventions not just to the NHS but to the wider society.
Outcomes
The outcomes are listed in Table 7.
| Type of outcome | Time point | Outcome | Derived | |
|---|---|---|---|---|
| Primary | Post randomisation | Mortality (all cause) at 30 days | Status of the patient at 30 days (dead/alive) | |
| Safety | Throughout the trial | SAEs | – | |
| Secondary | ICU | Mortality rate at first discharge from ICU | Mortality rate from randomisation to first ICU discharge | |
| ICU length of stay | Discharged from ICU/death date | |||
| Number of ventilator-free days (up to 30 days) | Number of days free of advanced respiratory support up to day 30, ICU discharge if prior to day 30 or death | |||
| Advanced respiratory support-free days | Number of ‘no’ responses for advanced respiratory support from ICU entry to ICU discharge | |||
| Basic respiratory support-free days | Number of ‘no’ responses for basic respiratory support from ICU entry to ICU discharge | |||
| Number of days on renal support | Number of ‘yes’ responses for renal support from ICU entry to ICU discharge | |||
| Number of days on gastrointestinal support | Number of ‘yes’ responses for gastrointestinal support from ICU entry to ICU discharge | |||
| Number of days on dermatological support | Number of ‘yes’ responses for dermatological support from ICU entry to ICU discharge | |||
| Number of days on liver support | Number of ‘yes’ responses for liver support from ICU entry to ICU discharge | |||
| Exhaled minute volume | – | |||
| Total respiratory rate | – | |||
| PEEP | – | |||
| Plateau pressure | – | |||
| Arterial blood gas | PaO2 | – | ||
| PaCO2 | – | |||
| pH | – | |||
| FiO2 | – | |||
| Hospital discharge | Mortality rate at first discharge from hospital | Mortality rate from randomisation to first hospital discharge | ||
| Length of acute hospital stay | Date of discharge from hospital/death | |||
| Follow-up (6 months after randomisation) | SF-12 Health Survey questionnaire (version 2) | Scoring of the SF-12 was carried out using the How to Score Version 2 of the SF-12 Health Survey: With a Supplement Documenting Version 1 manual81 | ||
| EQ-5D scale | ED-5D was scored using the devised algorithm and summarised as detailed in the EQ-5D-3L User Guide version 4.082 | |||
| Follow-up (12 months after randomisation) | Mortality rate 1 year after randomisation | – | ||
| Respiratory function (SGRQ) | This was scored as outlined in the text | |||
| EQ-5D scale | As at 6 months | |||
| SF-12 Health Survey questionnaire (version 2) | As at 6 months | |||
| ICU | Number of days antimicrobial use: received in past 24 hours | Number of ‘yes’ responses on this variable from ICU entry to ICU discharge | ||
| Number of days antimicrobial use: treating pulmonary infection | Number of ‘yes’ responses on this variable from ICU entry to ICU discharge | |||
| Number of days antimicrobial use: given intravenously | Number of ‘yes’ responses on this variable from ICU entry to ICU discharge | |||
| Number of days for sedative use: received in past 24 hours | Number of ‘yes’ responses on this variable from ICU entry to ICU discharge | |||
| Number of days for sedative use: given as an intravenous bolus dose | Number of ‘yes’ responses on this variable from ICU entry to ICU discharge | |||
| Number of days for sedative use: given by infusion | Number of ‘yes’ responses on this variable from ICU entry to ICU discharge | |||
| Number of days for sedative use: more than one class of sedative | Number of ‘yes’ responses on this variable from ICU entry to ICU discharge | |||
| Number of days for sedative use: more than two classes of sedative | Number of ‘yes’ responses on this variable from ICU entry to ICU discharge | |||
| Number of days for sedative use: more than three classes of sedative | Number of ‘yes’ responses on this variable from ICU entry to ICU discharge | |||
Primary outcome
The primary outcome was all-cause mortality 30 days after randomisation. This allows comparison with previous studies and is the FDA’s preferred ICU mortality outcome. Most deaths in observational/interventional studies of ARDS occur within 30 days.
Secondary outcomes
Prior to hospital discharge
In the original protocol, the secondary effectiveness outcomes which were to be assessed prior to follow-up included:
-
mortality at ICU discharge
-
mortality at hospital discharge
-
non-respiratory organ failure during intensive care treatment (measured using the Critical Care Minimum Data Set which all ICUs in the UK collect).
An amendment to the protocol was added in (see Appendix 1, Listing 2: Substantial amendment 1, No. 2) to allow for ventilation-free days, antimicrobial-free and sedative-free days to be secondary outcome measures.
The amendment to change to organ or treatment-free days was felt necessary because differing total mortality, or differing patterns of mortality over time, interacts with the number of days of organ failure or treatment. Early deaths decrease the interval available to accrue days of organ failure or treatment. Ventilation-free days are calculated by assigning a census day (day 28 post randomisation) and all patients who die before that date are assigned 28 days of ventilation. All survivors at day 28 are assigned the actual number of days they received ventilation. Other treatment-free days are calculated in the same way.
Follow-up at 6 and 12 months
-
Mortality 1 year after randomisation.
-
Health-related QoL (at 6 months and 12 months) using SF-12 and EQ-5D.
-
Respiratory function questionnaires [St. George’s Respiratory Questionnaire (SGRQ)] to measure long-term lung damage.
-
Cognitive function.
It was originally anticipated that we would use the SF-36 health-related QoL questionnaire. However, amendments to the protocol were made (see Appendix 1, Listing 2: Substantial amendment 1, No. 3 and No. 7) which allowed us to use the SF-12 questionnaire. The reasons for the change were that it would reduce responder burden and many ARDS studies were using SF-12 which would make pooling of results easier.
Respiratory function was measured using the SGRQ. 83
Cognitive function was not measured in this study. After an extensive literature review, no self-completed questionnaire was found which could be used to adequately record cognitive function at the follow-up times. An amendment (see Appendix 1, Listing 2: substantial amendment 3) was submitted to remove this from the protocol.
Short-Form questionnaire-12 items health-related quality-of-life instrument
Scoring
The SF-12 manual84 was used to score the eight concepts included in the SF-12: general health, vitality, social functioning, role functioning physical, role functioning emotional, mental health, physical functioning, and bodily pain. Results were expressed in terms of two meta-scores: physical and mental components.
Interpretation
The SF-12 is scored so that a high score indicates better physical functioning. The physical and mental scores have a range of 0 to 100 and were designed to have a mean score of 50 and a standard deviation (SD) of 10 in a representative sample of the US population. A SF-12 score that is > 50 represents above-average health status. On the other hand, people with a score of 40 function at a level lower than 84% of the population (1 SD) and people with a score < 30 function at a level lower than approximately 98% of the population (2 SDs). An example of the scores recorded in a mixed population in the USA is shown in Table 8.
| Age (years) | Mean physical component score | Mean mental component score |
|---|---|---|
| 45–54 | 50 | 50 |
| 55–64 | 47 | 51 |
| 65–74 | 44 | 52 |
| > 75 | 39 | 50 |
European Quality of Life-5 Dimensions
In order to conduct an economic evaluation, it was also necessary to have a single index measure of health status differences. The EQ-5D is one of the most commonly used tools. It measures health on five dimensions and a tariff is available for deriving a single utility score. Completion takes < 5 minutes. We used the three-level version of the instrument.
Scoring
The instrument contains a description of the health state in five dimensions or items: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression.
The items are always presented in the same order and there are three levels of severity for each item: 1 (no problems), 2 (some problems) and 3 (unable to do/extreme problems). For each item, the respondent must indicate the level of severity that best describes his/her personal health state at the time of giving the answers. The subject’s global health state is defined as the combination of the level of problems described for each of the five dimensions contained in the EQ-5D. Health states defined by the EQ-5D can be converted to a single summary by applying scores from a standard set of values (or preferences) derived from general population samples. 84
Interpretation
The numbers or weightings representing the strength of society’s preferences for an experienced or described health state are scored between 0 (death or worst imaginable health state) and 1 (full health or best imaginable health state). The quality adjustment is then multiplied by the expected life-years (LYs) in the assessed health state to arrive at the number of QALYs achieved. The expected utility associated with a health-care intervention is then the sum of the probability of entering a health state multiplied by the utility (QALY) associated with that state.
St. George’s Respiratory Questionnaire
The SGRQ is a self-reported, disease-specific, health-related QoL questionnaire. 83 It was originally developed to measure the impact of chronic obstructive pulmonary disease (COPD) on a person’s life, but has also been studied and applied to non-COPD pulmonary disease populations.
Scoring
Each of the questionnaire responses has a unique empirically derived weight. The lowest possible weight is 0 and the highest is 100.
Each component of the questionnaire is scored as follows:
-
The weights for all items with a positive response are summed.
-
The weights for all missed items are deducted from the maximum possible weight for the total score.
-
The total score is calculated by:
Interpretation
A total score is calculated which summarises the impact of the disease on overall health status. Scores are expressed as a percentage of overall impairment where 100 represents worst possible health status and 0 indicates best possible health status.
Tertiary outcomes and process variables
Other outcome measures and process variables were collected and are listed in Table 9. Oxygenation is not listed as a process variable because, as expected, the patients receiving HFOV initially had an improved oxygenation compared with conventionally ventilated patients (mean P : F ratio 25.8 kPa vs. 20.9 kPa) which persisted for the first 4 days. It then declined as the recovering patients were converted to conventional ventilation and so, over time, only the ‘sicker’ patients who are not responding to HFOV dominated the results.
| Type of outcome | Time point | Outcome | Derived |
|---|---|---|---|
| Tertiary outcomes | ICU | APACHE II score | APACHE II score and associated predicted mortality was derived using the specified algorithm79 |
| Number of days for muscle relaxants use: received in past 24 hours | Number of ‘yes’ responses on this variable from ICU entry to ICU discharge | ||
| Number of days for muscle relaxants use: given as an intravenous bolus dose | Number of ‘yes’ responses on this variable from ICU entry to ICU discharge | ||
| Number of days for muscle relaxants use: given by infusion | Number of ‘yes’ responses on this variable from ICU entry to ICU discharge | ||
| Number of days prone in last 24 hours | Number of ‘yes’ responses on this variable from ICU entry to ICU discharge | ||
| Number of days patient received inhaled nitric oxide in past 24 hours | Number of ‘yes’ responses on this variable from ICU entry to ICU discharge | ||
| Process | Hospital admission/ICU | Time from hospital admission to ICU admission | Time (date and time) of ICU admission |
| Hospital admission/randomisation | Time from hospital admission to randomisation | Time (date and time) of randomisation – time (date and time) of hospital admission | |
| ICU/randomisation | Time from ICU to randomisation | Time (date and time) of randomisation – time (date and time) of ICU admission | |
| ICU | Exhaled minute volume (conventional ventilation only) | – | |
| Total respiratory rate (conventional ventilation only) | – | ||
| PEEP level (conventional ventilation only) | – | ||
| Plateau pressure (conventional ventilation only) | – | ||
| HFOV settings on ventilation | – |
Health economic outcomes
The EQ-5D was the main measure of health economics and it was planned to collect data on non-public sector resource utilisation. 85
However, an amendment submitted (see Appendix 1, Listing 2: substantial amendment 1, No. 4 and No. 8) also allowed the data collection on social- and health-service use and care both from a patient’s point of view as well as the carer’s.
Quality assurance
There was no formalised quality assurance check of individual site delivery of the protocol but two OSCAR research nurses continually visited sites both to train staff and discuss the operational aspects of the trial with local staff.
Compliance
The primary responsibility for the care of ventilated patients on ICUs passed from one consultant to the next on a daily or weekly basis depending on the type of duty roster. To ensure that there was compliance with the trial protocol throughout a patient’s stay, and to avoid crossover after allocation, units were only signed up to the trial if all the consultant staff agreed to abide by the randomisation for study patients under their care.
Adverse events
Serious adverse events
The reporting guidelines from the National Research Ethics Service (NRES) for safety reporting in research other than clinical trials of investigational medicinal products were used for serious adverse events (SAEs).
A SAE was considered as an untoward and unexpected occurrence that a research participant experienced which: (i) resulted in death; (ii) was life-threatening; (iii) required hospitalisation or prolongation of existing hospitalisation; (iv) resulted in persistent or significant disability or incapacity; (v) consisted of a congenital anomaly or birth defect.
A SAE was recorded on the appropriate trial form by the clinician caring for the patient and reported immediately to the Principal Investigator at that centre. The Principal Investigator then reported the SAE to the Chief Investigator of the OSCAR trial. The Chief Investigator gave an opinion on whether or not the event was:
-
‘related’ (resulted from administration of any of the research procedures), and
-
‘unexpected’ (the type of event was not listed in the protocol as an expected occurrence).
A confirmed, related SAE was submitted to a MREC (England or Scotland) within 15 days of the Chief Investigator becoming aware of the event using the NRES report of SAE form. Events were also reported to the Data Monitoring and Ethics Committee (DMEC).
Expected events
Most known events related to artificial ventilation should occur equally in both groups. Exceptions that were noted that might occur more frequently in the HFOV group were:
-
air trapping
-
secondary effects of air trapping such as reduced carbon dioxide clearance, and impaired venous return to the thorax.
Sample size
In the original protocol, the sample size was 1006 patients randomised in equal allocation to either group.
The sample size calculations were based on the primary outcome measure, 30-day all-cause mortality. Data to inform the sample size estimation were available for all-cause mortality in patients meeting the entry criteria for the proposed study from a number of sources, to assist with sample size calculations.
Large epidemiological studies of ARDS in Europe had been undertaken at regular intervals over the last decade. The most recent was the ALIVE study,3 which collected data from February 1999 to March 1999 from 78 ICUs across Europe. Cases of ARDS were identified at any point in the ICU stay using the American-European consensus conference criteria. A total of 401 cases of ARDS were identified among 6522 admissions. Hospital mortality was 57.9% but 30-day mortality was not recorded. These data were robust but were an average across multiple European ICUs. However, they were outdated (7 years old at the study start) and the 30-day mortality was not known.
Data collected and analysed by the ICNARC were presented at the US Society of Critical Care Medicine in January 2006. The data came from 261,193 cases admitted to 174 adult, general ICUs in England, Wales and Northern Ireland, from December 1995 to July 2005. Cases were identified using the lowest P : F ratio recorded in the first 24 hours after ICU admission, and categorised into ALI and ARDS using the American-European Consensus Conference on ARDS definitions20 but excluding the chest radiograph requirement. Overall (patients with either ALI or ARDS) the hospital mortality was 44%, but only 61% of these patients were artificially ventilated on ICU admission. For those with ARDS who required artificial ventilation at the time of admission the hospital mortality was 42.4%. The 30-day mortality was not presented and median length of hospital stay was 16 days.
The main drawbacks with the ICNARC data were that they only identify patients who meet the study entry criteria in the first 24 hours following ICU admission, they were based on single blood gas estimation, there was no chest radiograph data, and the quoted mortality was hospital, not 30-day mortality.
The Chief Investigator of the OSCAR trial undertook a similar study using data on admissions to the adult ICU at the John Radcliffe Hospital, Oxford, for the calendar year 2005. Of 973 admissions, 850 had simultaneous arterial blood gas analyses and FiO2 records which allowed P : F ratios to be calculated. The incidence of ARDS, defined using a P : F ratio of < 23.7 kPa at any point during the patient’s stay, was 78.9%. However, only 2.5% of the patients had both a P : F ratio of < 26.7 kPa and any mention of ARDS in the discharge summary. These patients had a 38% 30-day mortality.
The limitation of the Oxford data was that true incidence of ARDS in ICU patients was almost certainly greater than the 2.5% we identified by retrospectively searching the database of discharge summaries. As a result the mortality estimate may be erroneous.
The SICSAG published data from 23 of the 26 ICUs in Scotland for an audit run between May 1999 and December 1999. 5 They only recorded patients meeting the diagnostic criteria for ARDS, but unlike ICNARC determined whether or not patents had ARDS on a daily basis, rather than only on admission, and included chest radiographs in the inclusion criteria. They reported 61% hospital mortality for patients meeting the ARDS criteria at any point in their ICU stay. The main drawbacks of the SICSAG data were that they were outdated (7 years old) and the data were hospital not 30-day mortality.
In calculating the original sample size, we assumed that hospital mortality was close to 30-day mortality, and chose a middle value from the available data, namely 45%. We had used the effect size from the only intervention known to alter mortality in ARDS12 as our predicted effect size (9% absolute mortality reduction). This was close to the effect size in the unweighted pooled data from the two RCTs performed to date at the time (8.1% absolute mortality reduction). We knew that the loss of patients to the PAC-Man study54 owing to withdrawals was in the order of 3%. Crossovers were to be analysed on an intention-to-treat basis and so no correction was required. Using an 80% certainty of detecting this difference at p = 0.05 with a control group mortality of 45% required 503 patients in each group, a total study size of 1006.
Planned recruitment rate
Recruiting patients from 12 large UK ICUs admitting at least 650 patients per year each allowed a potential pool of patients of 7800 admissions per annum or 23,400 in the 36 months OSCAR was planned to recruit over. Based on the incidence of ARDS found in Scotland5 of 8.1%, this gave a potential pool to recruit from of 1895 patients. From previous studies in ICU (the completed PAC-Man study54 and the then ongoing TracMan,86 PERMIT and SimSepT studies) we knew that the refusal rate for consent to research in ICU was approximately 30%. This would leave about 1320 potential patients for the OSCAR study, about 30% more than required. The required recruitment rate was just over two patients per month per site.
Revised recruitment target
From 1 December 2007 (start of recruitment) to 1 April 2009, the observed rate of recruitment had averaged to 1.01 per centre per month, approximately half of what was expected and thus the trial was severely underrecruiting.
After reviewing various strategies of increasing recruitment with experts in this research field, the DMEC and the Trial Steering Committee (TSC), it was agreed that the effect size based on the clinical relevant difference should be revisited and closely assessed. In addition, the assumptions around control group mortality should be checked by the study statistician reviewing the control group 30-day mortality. It was agreed that this information should be shared with the trial statistician and the HTA only. The sample size was recalculated using a 10% absolute change in mortality, with 80% power and 5% significance level and the control group mortality, giving a total of 802 patients (with 401 per treatment group), allowing for a 3% withdrawal rate. This recalculated sample size was discussed with clinical members of the TSC, who felt this represented a reasonable compromise between an achievable and clinically credible improvement in mortality, and the need to reduce the sample size and hence costs.
Data management
Before the start of the trial, data collection forms were piloted to determine ease of use and other practical issues.
Electronic databases were developed using specialised software. These were developed by the programmers at the Warwick Clinical Trials Unit, in collaboration with the trial manager and statistician. Computerised validation checks were incorporated into the databases to minimise data entry errors.
Validation checks were conducted at every interim analysis (once per year) and once the data had started to accumulate at a rapid rate (i.e. after January 2011), the validation checks were carried out every 6 months, until a final completely validated data set was produced. All items from the CRFs and as entered on the database were checked in the validation process.
Statistical analysis
The trial has been reported in accordance with the CONSORT78 guidelines. All statistical tests were two-sided. The statistical analysis was carried out in SAS 9.3 (SAS Institute Inc., Cary, NC, USA) and Stata 9 (StataCorp LP, College Station, TX, USA).
Formal interim analyses
At the request of the DMEC, the following were pre-specified:
-
Two definite equally spaced formal interim analyses (one approximately 1/3 of the way and another 2/3 of the way through the trial).
-
It was decided a priori that if any of the stopping guidelines (detailed in Table 10) were met at the first interim analysis, then the DMEC decided whether or not a closer monitoring of the trial was required. In this case, it was anticipated that another interim analysis would be planned half way through recruitment.
-
It was not appropriate to specify fixed stopping rules, but the p-values given in Table 10 were used as guidance for reviewing the primary end point, to assist decision-making around stopping or modifying the trial prematurely. Table 10 illustrates the p-values if the data were reviewed three times (at equal time intervals), or four times (with unequal time spacing). The pre-specified reasons for stopping/modifying the trial were:
-
treatments were convincingly different in terms of mortality at 30 days
-
there were an unacceptable number of SAEs.
-
-
Two formal interim analyses were conducted as detailed above and at each stage there was no cause for concern to stop or modify the trial.
| Number of planned interim analysis | Interim analysis | O’Brien–Fleming | Alpha spending function (Lan-DeMets) |
|---|---|---|---|
| 3 | 1 | 0.00021 | – |
| 3 | 2 | 0.01210 | – |
| 3 | 3 (final) | 0.05000 | – |
| 4 | 1 | – | 0.00019 |
| 4 | 2 | – | 0.00305 |
| 4 | 3 | – | 0.01235 |
| 4 | 4 (final) | – | 0.05000 |
Final statistical analyses
Data sets used for the analysis
Intention to treat (observed data set)
The primary data analysis was ‘intention to treat’ (effectiveness analysis), using the observed data. The patients were analysed according to the intervention they had been randomised to, irrespective of the treatment they actually received.
Intention to treat (imputed data set)
A sensitivity analysis to assess the impact of missing data was carried out on the main observed data. The ICU data were not imputed as the assumption ‘missing completely at random’ could not be made due to the nature of the trial – missing data may be a result of poor prognosis of a patient in ICU.
However, questionnaire data at follow-up, in particular the items on a questionnaire, were imputed. Multiple imputation methods were used to impute missing data. Prior to an imputation, the data mechanisms (MAR – missing at random; NMAR – not missing at random; MCAR – missing completely at random) were assessed to make sure that multiple imputation was viable. This was done by looking at any patterns of missingness and only data that were validly missing were imputed. In the case of multivariate normal data, the multiple imputation methods assuming normality was used. In the case where we could not assume a distribution of the data, the ICE procedure87 was used.
Per protocol
A secondary analysis was an efficacy analysis, which was restricted to patients who fulfilled the protocol and adhered perfectly to the clinical trial instructions as stipulated in the protocol.
Patients who were excluded from this analysis were:
-
those who had ventilator problems
-
those who were randomised to HFOV and crossed over to conventional ventilation within 30 days of randomisation
-
those who were randomised to conventional ventilation but crossed over to HFOV within 30 days of randomisation
-
those who received less than the protocol 12 hours of HFOV
-
those that were taken off the ventilator due to clinical concerns
-
those that were taken off the ventilator as staff were not confident with the ventilator.
CONSORT flow chart
The CONSORT flow chart details the number of patients who were recruited into the trial and the passage of patients through the trial (randomisation, ICU, follow-up and primary data analysis).
Details of patient withdrawal, those not responding at follow-up and patients who deviated from the protocol are also given (number and percentage based on those randomised within intervention group).
Serious adverse events
The number (and percentage) of SAEs which have occurred within each intervention group and at each time point (in ICU, from ICU to hospital discharge, hospital discharge to 6 months, 6 months to 12 months) were summarised. The details of each SAE were described in a listing.
Not in the trial patients
A patient who was not eligible for the trial could fall into one of the categories detailed in Table 11.
| Reasona | Reason |
|---|---|
| A | Another trial patient is already on the Vision Alpha |
| B | Another non-trial patient is on the Vision Alpha |
| C | Oscillator not working/technical failure |
| D | Patient has been ventilated for > 7 days |
| E | Consultant predicts patient will need > 48 hours of artificial ventilation |
| F | Consultant not ‘substantially uncertain’/wants to continue only with conventional ventilation |
| G | PERSONAL consultee refused agreement |
| H | Nominated PROFESSIONAL consultee refused agreement |
| I | Excluded as welfare guardian/nearest relative refused consent |
| J | Exclusion criteria: previously in OSCAR |
| K | Exclusion criteria: in another trial |
| L | Exclusion criteria: interpreter not available |
| M | Exclusion criteria: treatment withdrawal is planned |
| N | Exclusion criteria: left atrial hypertension from any cause |
| O | Exclusion criteria: moderate or severe airway disease |
| P | Exclusion criteria: lung biopsy or resection |
| Q | Exclusion criteria: patient has condition clinician believes would make HFOV hazardous |
| Z | Other reasons |
For the CONSORT diagram, we could summarise these into the following:
| Reasons from Table 11 | Categories for exclusion |
|---|---|
| D + E | Not meeting all inclusion criteria |
| A + B + C | Meeting all the inclusion criteria but ventilator not available |
| F + G + H | Meeting all the inclusion criteria but also met one or more of the exclusion criteria |
| I through to Z | Meeting all the inclusion criteria but excluded due to other reasons |
The demography details (i.e. age and sex) of patients, who were not entered into the trial and those who were entered into the trial were assessed statistically, using t-tests and chi-squared tests, respectively. This was to ensure that those in the trial were similar in characteristics to patients from a large population.
Pre-randomisation, randomisation and immediately post-randomisation assessment
The categorical variables were summarised using number of patients and percentages and the continuous variables were summarised using mean, SD, median, range (minimum and maximum) and number of patients with data prior and after randomisation.
No formal statistical testing was carried out on these data.
First 24 hours in intensive care unit
Data collected in the first 24 hours in ICU were summarised in a similar way to the above. In addition, comparison of interventions was carried out and the ‘unadjusted estimates’ were obtained using analysis of variance. The ‘adjusted estimates’ were obtained using analysis of covariance, with adjustments made for centre, P : F ratio and sex.
Intensive care unit and hospital stay data
These data were presented as tables and analysed using a linear regression model. The data were not split into survivors and non-survivors.
Primary outcome measure
For mortality at 30 days post-randomisation frequencies and percentages per intervention group were presented in a table. Mortality at 30 days was compared between treatment groups using chi-squared test (for an unadjusted estimate) and logistic regression model (for the adjusted estimates). For the latter model, the dependent variable was survived/died and independent variables were treatment and other important predictors (e.g. centre, age, P : F ratio and APACHE II score). An odds ratio measuring the treatment effect and its 95% CI was reported.
Survival time from randomisation to 30 days was analysed using a log-rank test. The event here was ‘death up to 30 days’. Thus, any patient who was alive up to day 30 or after or had withdrawn prior to day 30 (after randomisation) was censored. The proportion dying over time was illustrated using a Kaplan–Meier curve for each of the ventilator groups. The p-values and a hazard ratio with its 95% CI obtained from a Cox-proportional hazards model were also presented (adjusted for centre, age, P : F ratio and APACHE II score). The proportional hazard assumption across treatment groups was checked graphically using a log-cumulative hazard plot.
The Kaplan–Meier curve with the probability of survival up to 30 days post randomisation, for each intervention was plotted. For this plot, the event was ‘mortality up to 30 days post randomisation’. In the case where the event did not occur (i.e. where patients lived beyond 30 days or had any withdrew prior to 30 days), the observations were censored (i.e. the event was not observed). Thus, at the end of each day, taking account of all those who have died in the study to that day, the probability of death is computed, and from that the probability of survival is obtained [i.e. 1 – Pr(dying)].
Secondary and tertiary outcomes and process variables (during intensive care unit and follow-up)
In terms of other outcomes and variables, three different types of data were presented:
-
Categorical data Categorical data were analysed using logistic regression models, with intervention as an independent variable with other important predictors (e.g. centre, age, P : F ratio and APACHE II score). The summary statistics were based on proportions and the 95% CI.
-
Continuous data Continuous data were analysed using linear regression models, with intervention as an independent variable with other important predictors (e.g. centre, age and P : F ratio and APACHE II score). Intervention difference was based on adjusted mean estimates (and 95% CIs).
-
Time to an event Time to ICU discharge from randomisation (i.e. length of intensive care stay), time to hospital discharge from randomisation (i.e. length of acute hospital stay) and ‘survival time to 12 months’ were summarised in tables. The analysis based on the comparison of the ventilation groups was done using survival analysis (in a similar way stated for the ‘Primary outcome’ above). The events of interest were ‘died during ICU stay’, ‘died during hospital stay’ and ‘died by 12 months’. Thus, any patients who did not have the event (e.g. alive or withdrew prior to the event or non-responders) were treated as censored observations in the survival analysis.
Subgroup analyses
The most scientifically robust method of subgroup analysis is a test of interaction between treatment and outcome that has been appropriately powered. It is widely recognised that powering a study for subgroup analysis can dramatically increase sample size requirement. A rough rule is that detection of interactions approximately twice the size of the main effect requires no increase in the sample size, provided that the subgroups are of equal size, the subgroup comparisons are limited and pre-specified, and the results are considered hypotheses generating as opposed to confirmatory. 88 Three pre-specified analyses were alongside the main trial results. For each of these, the outcome was modelled with the intervention, subgroupings and interaction of intervention and subgroups. These analyses explored:
-
The effect of HFOV on length of acute hospital stay, 30-day and hospital mortality in subgroups with different severity of illness determined by APACHE II scoring on ICU admission.
-
The effect of HFOV on length of acute hospital stay, 30-day and hospital mortality in broad ARDS subgroups (pulmonary or extrapulmonary cause, sepsis, trauma, burns).
-
The effect of HFOV on length of acute hospital stay, 30-day and hospital mortality in patients with differing severity of lung injury determined from their P : F ratio.
For each subgroup analysis, the Cox’s proportional hazard’s model and Kaplan–Meier plots were used to assess the difference in treatment effect and each subgrouping.
Health economic analysis
As noted above, data collection for the health economic analysis is ongoing.
In the original protocol, the primary measure of health-care system benefit was within-trial cost-effectiveness analysis (CEA) to estimate the cost per QALY gained for HFOV compared with conventional ventilation at 1 year. A long-term CEA was planned by implementing a decision analytic cost-effectiveness model with a lifetime time horizon. The parameters for the CEA were obtained by a Bayesian synthesis of the trial evidence with evidence identified by a systematic review and a costing study in a guided sample of ICUs. The primary analysis followed National Institute for Health and Care Excellence (NICE) guidance. Secondary analysis adopted a full societal perspective. Data on non-public sector resource utilisation was being collected from the patients at 6 and 12 months.
Analyses for this study was undertaken from a NHS perspective. The main health economic outcome was the health status of survivors of ARDS at 6 months (from EQ-5D data) which were converted into QALYs to allow cost-utility modelling. Additionally, a range of modelling techniques was used to estimate longer-term cost-utility from 1-year follow-up data. Epidemiological and economic models were used to estimate lifetime gains or losses in QALYs from HFOV and savings in health-care expenditures. A full literature review was undertaken to explore the potential for providing monetary estimates of the long-term impacts of HFOV. This work was being undertaken at the University of Leeds.
To inform the economic analysis, a representative sampling framework for UK ICUs based on size (number of beds), consultant/bed ratio, nurse/bed ratio; and median APACHE II score of admissions was prepared, and in at least one unit from each cell in the sampling frame we undertook a micro costing study for patients with ARDS.
A research assistant visited these units to observe the care patients with ARDS receive and then cost it, along with representative patients not suffering from ARDS. The units did not have to be the same as those recruiting patients to the trial to obtain data on resource use in patients not receiving HFOV. Trial units, and in addition some non-trial ICUs undertaking HFOV, were used to determine resource use for HFOV in both the trial setting and in the more ‘mature’ use of HFOV in ARDS.
To provide some estimate of QoL beyond 12 months, patients recruited in the first year received an additional EQ-5D questionnaire and questions concerning social and health service use at 24 and 30 months. The patients recruited in the second year received an additional EQ-5D questionnaire and questions concerning social and health service use at 18 months. This allowed us to model the time for health-related QoL to return to population normal levels after ICU by group.
Trial organisation
The Data Monitoring and Ethics Committee
The DMEC comprised a senior statistician, a senior clinician and a senior triallist (chairperson); see Appendix 4 for membership details.
Standard operating procedures for the DMEC were:
-
During the period of recruitment into the study, interim analyses of the proportion of patients alive at 30 days and analyses of deaths from all causes at 30 days were supplied, in strict confidence, to the chairperson of the DMEC, along with any other analyses that the committee requested.
-
In the light of these analyses, the DMEC advised the chairperson of the Steering Committee if, in their view, the randomised comparisons provided both (i) ‘proof beyond reasonable doubt’ that for all, or some, the treatment was clearly indicated or clearly contra-indicated and (ii) evidence that might reasonably be expected to materially influence future patient management.
-
Data relating to the safety of patients were reviewed by the Chair of the DMEC. The data reviewed were specifically related to:
-
– procedure related ‘serious, unanticipated adverse events’ (death or serious disability)
-
– procedure related adverse events/complications
-
– deaths at 30 days (any cause).
-
The DMEC met to review progress at 1 year and when a formal interim analysis was due.
The Trial Steering Committee
The trial was guided by a group of respected and experienced critical care personnel and triallists as well as a public and patient representative. Face-to-face meetings were held at regular intervals determined by need but not less than once a year.
Standard operating procedures for the TSC were:
The TSC, in the development of this protocol and throughout the trial, was responsible for:
-
major decisions such as a need to change the protocol for any reason
-
monitoring and supervising the progress of the trial
-
reviewing relevant information from other sources
-
considering recommendations from the DMEC
-
informing and advising on all aspects of the trial.
Project management groups’ responsibilities
This group was made up of the investigators on the grant application to the HTA programme plus the OSCAR co-ordinating team (see Appendix 3 for membership details). They were responsible for:
-
monitoring the progress of the trial and discussing project milestones
-
reviewing centre and patient recruitment to the trial
-
discussing day-to-day management issues that arise.
Collaborators’ responsibilities
Co-ordination within each participating hospital was through a local collaborator who:
-
complied with the protocol at all times
-
discussed the trial with medical and nursing staff who treated ICU patients and ensured that they remained aware of the state of the current knowledge, the trial and its procedures (posters and other ‘reminders’ were provided by the trial office)
-
ensured that patients in the ICU were considered promptly for the trial
-
ensured that the trial CRFs and consent forms were completed in full
-
ensured the trial was conducted in accordance with the Research Governance Framework and Good Clinical Practice (GCP) and fulfilled all national and local regulatory requirements
-
allowed access to source data for audit and verification.
Co-ordinating centre responsibilities
The trial was co-ordinated by the Intensive Care Society (ICS) Trials Group based at the Kadoorie Centre for Critical Care Research and Education at the John Radcliffe Hospital in Oxford. Administrative support was supplied by the Nuffield Department of Anaesthetics, University of Oxford. Assistance with trial management and the statistical elements of the trial was supplied by the Clinical Trials Unit at Warwick University. Health economic support and analysis was provided by the Academic Unit of Health Economics at the University of Leeds. Randomisation services were provided by the University of Aberdeen.
The co-ordinating centre had the responsibility to:
-
assist and facilitate the setting up of centres wishing to collaborate
-
organise training in the use of the Vision Alpha high-frequency oscillatory ventilator
-
provide study materials and organise a 24-hour randomisation service
-
respond to any questions from collaborators about the trial
-
give collaborators regular information about the progress of the study
-
monitor the collection of data, process and seek missing data
-
assure data security and quality
-
organise any interim and main analyses
-
organise TSC, DMEC and collaborators meetings
-
carry out the trial according to the Research Governance Framework and GCP.
Good Clinical Practice and research governance
The OSCAR trial did not fall under the EU Clinical Trials Directive (Directive 2001/20/EC) as it was not a medicinal product trial (Clinical Trial of an Investigational Medicinal Product). It was therefore not required by law to work to International Conference on Harmonisation (ICH) of Technical Requirements for Registration of Pharmaceuticals for Human Use GCP although we worked to the principles outlined in ICH GCP, as well as following the Medical Research Council’s GCP guidelines and the Department of Health’s Research Governance Framework.
Health economics methods
The health economics methods are given in Chapter 5.
Chapter 4 Results
The OSCAR trial was generally complex, used different sites for different periods of the study, useda combination of unit- and study-owned ventilators, and recruited patients with a condition which is known to vary in incidence over the year. A figure summarising active sites and recruitment rates month-by-month in the study is shown in Figure 5, with periods of peak H1N1 influenza infection incidence marked. The overall recruitment/retention is listed in Table 13.
FIGURE 5.
Recruitment summary for the study.
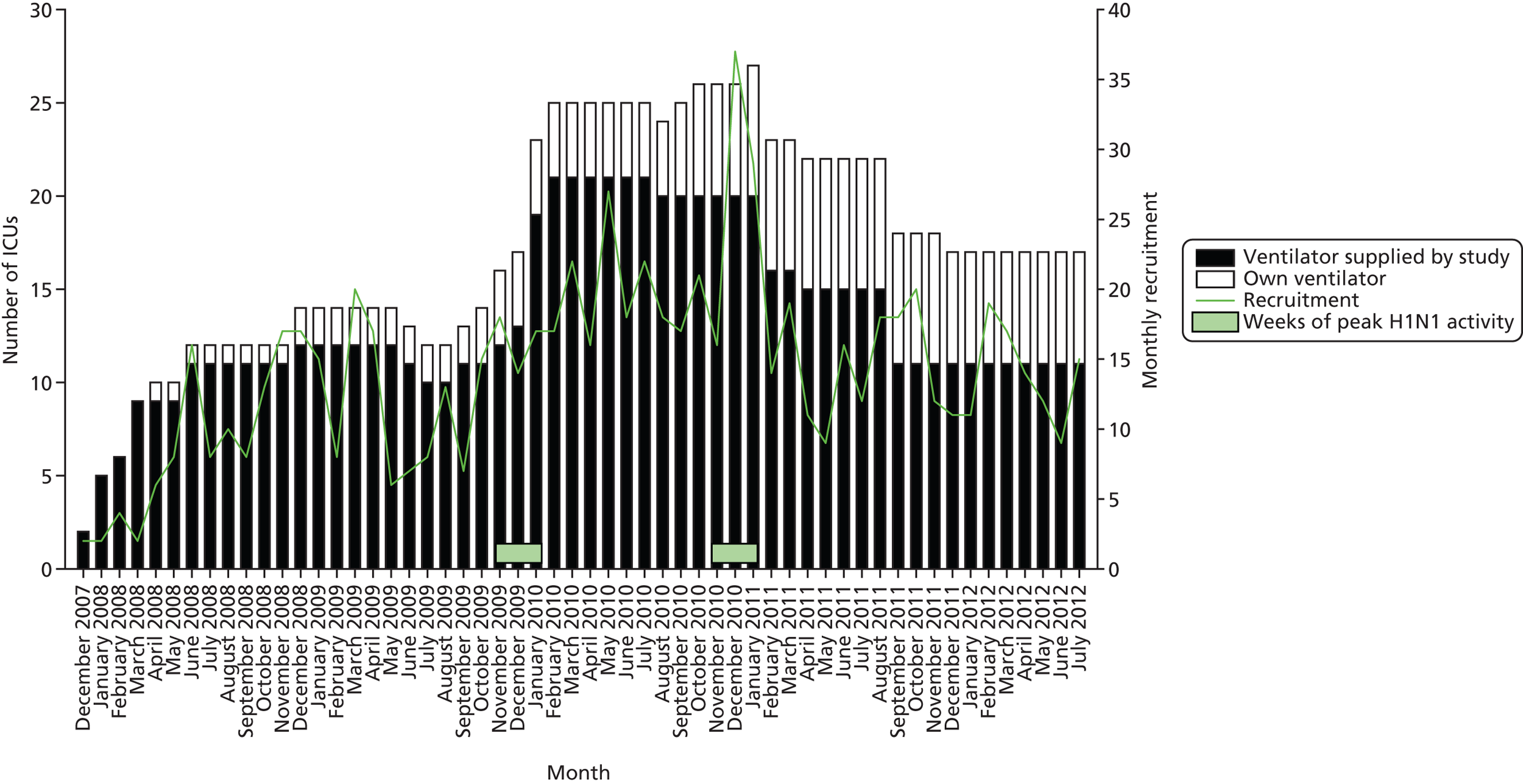
| Stage | Category | Total |
|---|---|---|
| From screening to pre randomisation | All patients approached (on the not in the trial and those randomised) | 2769 |
| Excluded patients: not in the trial | 1974 | |
| Pre randomisation | Patients with pre-randomisation baseline data (form) | 795 |
| Randomised | Patients satisfying the entry inclusion criteria – randomised | 795 |
| Patients satisfying the entry inclusion criteria – not randomised | 0 | |
| Patients randomised but ineligible | 0 | |
| Died | From randomisation to first discharge ICU | 342 (43.1%) |
| 30 days post randomisation | 329 (41.4%) | |
| From randomisation to hospital discharge | 388 (48.8%) | |
| 6 months follow-up | 395 (49.7%) | |
| 12 months follow-up | 405 (50.9%) | |
| Survivors (in trial) | From randomisation to first discharge ICU | 452 (56.9%) |
| 30 days post randomisation | 466 (58.6%) | |
| From randomisation to hospital discharge | 400 (50.3%) | |
| 6 months follow-up | 400 (50.3%) | |
| 12 months follow-up | 390 (49.1%) | |
| Withdrawals | In ICU (immediately post randomisation to ICU discharge) | 0 (0.0%) |
| From 6 months follow-up | 1 (0.1%) | |
| From 12 months follow-up | 3 (0.4%) | |
| Follow-up | Follow-up data at 6 months | 215 (27.0%) |
| Follow-up data at 12 months | 179 (22.5%) | |
| Non-responders (follow-up) | Up to 6 months follow-up | 123 (15.5%) |
| 6–12 months follow-up | 118 (14.8%) |
CONSORT flow chart
Summary of CONSORT flow chart
Figure 6 illustrates the CONSORT diagram78 of the OSCAR trial.
FIGURE 6.
The CONSORT flow chart for the OSCAR trial. ‘Not meeting all inclusion criteria’ are reasons D + E in Table 12; ‘meeting all inclusion criteria but ventilator not available’ are reasons A + B + C in Table 12; ‘meeting all the inclusion criteria but also met one of more of the exclusion criteria’ are reasons F + G + H in Table 12 and ‘meeting all the inclusion criteria but excluded due to the other reasons’ are reasons I to Z in Table 12.
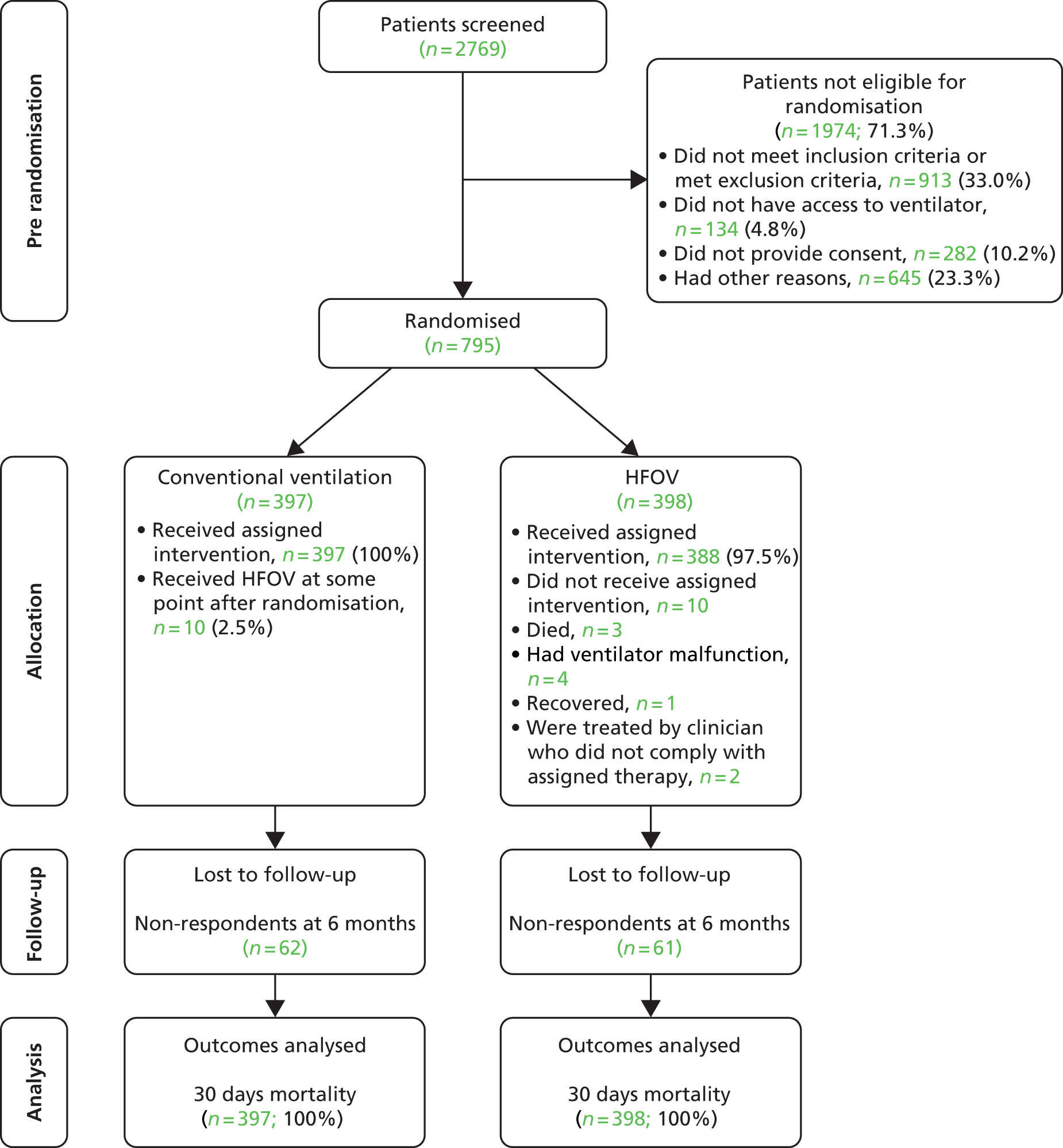
In brief:
-
Two thousand seven hundred and sixty-nine patients were screened for the OSCAR trial.
-
Of these, 1974 (71.4% of those screened) did not meet the inclusion criteria or met the inclusion criteria and were excluded for another reason.
-
The total number randomised was 795 (28.7% of those screened).
-
Of these, one patient remained in ICU and six patients were in hospital when the database was closed for the analysis for this report (14 October 2012).
-
Of the patients randomised, three withdrew from follow-up (one who had received HFOV and two who had received conventional ventilation). The withdrawal rate was 0.3% of those randomised (the anticipated withdrawal rate used for the sample size calculation was 3%).
-
The number of patients who did not receive the randomised intervention was very similar between the two intervention groups.
-
Follow-up data have been collected on 215 patients (64% of those approached for follow-up) at 6 months and on 179 patients (60% of those approached for follow-up) at 12 months (as of database closure on 14 October 2012). Follow-up of the remaining patients continues but the results will not be included in this report.
-
All randomised patients had the primary outcome data recorded.
Patient flow in the trial
Of the 795 patients randomised, at database closure (14 October 2012) there was one patient in ICU [trial number (TNO) = 22035] and there were six patients who were in hospital and had not been discharged (TNO = 7043, 8005, 25030, 27021, 27054, 27037).
Withdrawals
There were three patients who withdrew during the trial from follow-up (as in Tables 14 and 15) as follows:
-
One patient (TNO = 8011: allocated conventional ventilation) withdrew in ICU from all follow-up (both 6 and 12 months).
-
Two patients withdrew after 6 months follow-up from any further follow-up (TNO = 5022 allocated conventional ventilation; TNO = 6002 allocated HFOV).
All three patients provided data from randomisation to hospital discharge.
| Time period | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| In ICU (immediately post randomisation to ICU discharge) | 0 (0.0%) | 0 (0.0%) | 0 |
| From 6-month follow-up | 1 (0.3%) | 0 (0.0%) | 1 |
| From 6- and 12-month follow-up | 1 (0.3%) | 1 (0.3%) | 2 |
| Time period | Initiator of withdrawal | Conventional ventilation (n = 397) | HFOV (n = 398) | Total |
|---|---|---|---|---|
| Patients allocated treatment withdrawn | Patient | 0 (0.0%) | 0 (0.0%) | 0 |
| Consultee | 0 (0.0%) | 0 (0.0%) | 0 | |
| Permission withdrawn to allow trial to use ICU data | Patient | 0 (0.0%) | 0 (0.0%) | 0 |
| Consultee | 0 (0.0%) | 0 (0.0%) | 0 | |
| Permission withdrawn to allow follow-up (by questionnaires) | Patient | 1 (0.3%) | 0 (0.0%) | 0 |
| Consultee | 0 (0.0%) | 0 (0.0%) | 0 |
Responders at follow-up
The responders are detailed in Table 16.
| Non-responders | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| Up to 6 months follow-up | 62 (15.6%) | 61 (15.3%) | 123 |
| Up to 12 months follow-up | 62 (15.6%) | 56 (14.1%) | 118 |
Protocol deviations
There were, in total, 84 deviations from the protocol.
Eleven patients (2.8% of those randomised to conventional ventilation) received HFOV. Nine patients (2.3% of those randomised to HFOV) did not receive HFOV. The breakdown of these nine patients is illustrated in Table 17. There were 64 patients (16.1%) who were randomised to HFOV but had some problem with the ventilator during weaning or received < 12 hours of HFOV that was required (see Table 17 for details).
| Category | Reasons | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| Randomised to HFOV but did not receive it | Patient recovered before HFOV used | N/A | 1 (0.3%) | 1 |
| Patient died before HFOV used | N/A | 2 (0.5%) | 2 | |
| Transferred out of unit before treatment | N/A | 0 (0.0%) | 0 | |
| Oscillator being used for non-trial patient | N/A | 0 (0.0%) | 0 | |
| Oscillator being used for another trial patient | N/A | 0 (0.0%) | 0 | |
| Failure to recruit lung | N/A | 0 (0.0%) | 0 | |
| Failure attributable to haemodynamic compromise | N/A | 0 (0.0%) | 0 | |
| Clinician’s instruction not to use | N/A | 2 (0.5%) | 2 | |
| Oscillator technical failure | N/A | 4 (1.0%) | 4 | |
| Others | N/A | 0 (0.0%) | 0 | |
| Randomised to HFOV but received < 12 hours of HFOV | – | N/A | 33 (8.3%) | 33 |
| Problems with ventilator when HFOV weaning | – | N/A | 16 (4.0%) | 16 |
| Other reasons | – | N/A | 15 (3.8%) | 15 |
| Randomised to conventional ventilation but received HFOV | – | 11 (2.8%) | – | 11 |
| Total | – | 11 | 73 | 84 |
Serious adverse events
There are four SAEs recorded for four patients in the trial. All of these were in ICU while on HFOV. All of these events were thought to be related to the trial treatment and they were life-threatening. Details are in Table 18.
| Location | Category | SAE subgroup | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|---|
| In ICU | SAE details | Unexpected for the treatments offered | 0 (0.0%) | 3 (0.8%) | 3 |
| Related directly to the treatments offered | 0 (0.0%) | 4 (1.0%) | 4 | ||
| Unexpected and related to the treatments offered | 0 (0.0%) | 3 (0.8%) | 3 | ||
| SAEs | Patient died | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| Event was life-threatening | 0 (0.0%) | 4 (1.0%) | 4 | ||
| Event involved prolonged hospitalisation | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Event involved persistent or significant disability/incapacity | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Others | 0 (0.0%) | 2 (0.5%) | 0 (0.0%) | ||
| SAE was caused by OSCAR trial participation | Yes | 0 (0.0%) | 4 (1.0%) | 4 | |
| No | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| From ICU to hospital discharge | SAE details | Unexpected for the treatments offered | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Related directly to the treatments offered | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Unexpected and related to the treatments offered | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| SAEs | Patient died | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| Event was life-threatening | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Event involved prolonged hospitalisation | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Event involved persistent or significant disability/incapacity | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Others | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| SAE was caused by OSCAR trial participation | Yes | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| No | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Hospital discharge to 6 months | SAE details | Unexpected for the treatments offered | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Related directly to the treatments offered | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Unexpected and related to the treatments offered | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| SAEs | Patient died | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| Event was life-threatening | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Event involved prolonged hospitalisation | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Event involved persistent or significant disability/incapacity | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Others | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| SAE was caused by OSCAR trial participation | Yes | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| No | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| 6 to 12 months | SAE details | Unexpected for the treatments offered | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Related directly to the treatments offered | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Unexpected and related to the treatments offered | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| SAEs | Patient died | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| Event was life-threatening | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Event involved prolonged hospitalisation | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Event involved persistent or significant disability/incapacity | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Others | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| SAE was caused by OSCAR trial participation | Yes | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | |
| No | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
Serious adverse event details are listed as reported to the trial office in Table 19.
| Reporting heading | Data supplied |
|---|---|
| Patient | ID = 2002 |
| Centre | Derriford Hospital |
| Age | 36 years |
| Sex | [Sex removed] |
| Event details | Difficulty in reintubating patient at time of ETT change owing to oropharyngeal swelling |
| Event caused by trial? | Patient was grade 1 intubation grade at intubation initially. At time of ETT change, 36 hours later the view was significantly reduced by oropharyngeal oedema |
| Patient | ID = 7036 |
| Centre | University College Hospital |
| Age | 63 years |
| Sex | [Sex removed] |
| Event details | Nurse deviated from protocol by progressively increasing mean airway pressure despite acceptable oxygenation, pressure up 28 cmH2O to 38 cmH2O. The higher pressure impaired the patient’s right ventricle |
| Other event details | Atrial fibrillation was associated with loss of blood pressure requiring cardiopulmonary resuscitation at [date/time removed] |
| Event caused by trial? | Raised intrathoracic pressure impaired right ventricular function leading to cardiovascular collapse – this occurred as a deviation from protocol |
| Patient | ID = 18004 |
| Centre | Ipswich Hospital |
| Age | 38 years |
| Sex | [Sex removed] |
| Event details | PEA cardiac arrest – drop in blood pressure and heart rate leading to loss of cardiac output. HFOV stopped, CPR commenced. CXR no pneumothorax. Oscillation restarted |
| Other event details | Second arrest at [date/time removed]. Again PEA arrest. Shocked – resuscitated. Decision made by resident doctor to discontinue oscillation. CXR no pneumothorax |
| Event caused by trial? | Probable combination of high acidosis from ineffective CVVHDF (haemofilter clotting off) and high PaCO2 since being on oscillation despite ‘accelerated’ changes |
| Patient | ID = 24015 |
| Centre | Royal Blackburn Hospital |
| Age | 47 years |
| Sex | [Sex removed] |
| Event details | Patient on HFOV, arterial blood gas pH 6.8 PaCO2 off the measurable scale of blood gas machine. O2 4 kPa. Periarrest. Life-threatening? Bronchospasm? ETT problem |
| Event caused by trial? | Patient was randomised to HFOV group of trial. The above problem only occurred post randomisation once the patient was on HFOV |
Not in trial patients
From Table 20, of the 1974 patients not taking parting in the trial:
-
University College Hospital had the highest proportion of patients who were not randomised into the study (n = 307; 15.6%).
-
Queen Margaret Hospital and York Hospital had the lowest proportion of patients who were not randomised into the study (each had n = 6; 0.3%).
-
The single most common reason for not including patients into the study was ‘consultant predicts patient will need < 48 hours artificial ventilation’ (n = 195; 9.9%).
-
The single least common reason for not including patients into the study was ‘another non-trial patient is on the Vision Alpha’ (n = 2; 0.1%).
-
The ‘others’ category made up for 32.7% (n = 645) of the patients who were not included into the study.
| Centre | Reasons for patients not in the trial | Total (within centre) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | ||||
| John Radcliffe, Oxford | 2 (2.2%) | 0 (0.0%) | 0 (0.0%) | 7 (7.7%) | 25 (27.5%) | 0 (0.0%) | 6 (6.6%) | 0 (0.0%) | 91 | ||
| Derriford Hospital, Plymouth | 13 (9.2%) | 0 (0.0%) | 0 (0.0%) | 9 (6.4%) | 2 (1.4%) | 0 (0.0%) | 10 (7.1%) | 0 (0.0%) | 141 | ||
| Aberdeen Royal Infirmary | 1 (1.3%) | 1 (1.3%) | 0 (0.0%) | 7 (9.0%) | 6 (7.7%) | 8 (10.3%) | 0 (0.0%) | 0 (0.0%) | 78 | ||
| Medway Maritime Hospital | 6 (4.1%) | 0 (0.0%) | 1 (0.7%) | 2 (1.4%) | 18 (12.2%) | 12 (8.2%) | 11 (7.5%) | 5 (3.4%) | 147 | ||
| Selly Oak/Queen Elizabeth, Birmingham | 13 (12.4%) | 0 (0.0%) | 5 (4.8%) | 4 (3.8%) | 5 (4.8%) | 4 (3.8%) | 26 (24.8%) | 14 (13.3%) | 105 | ||
| Royal Sussex County Hospital | 5 (2.9%) | 0 (0.0%) | 3 (1.7%) | 8 (4.6%) | 7 (4.0%) | 3 (1.7%) | 12 (6.9%) | 1 (0.6%) | 175 | ||
| University College Hospital | 15 (4.9%) | 0 (0.0%) | 0 (0.0%) | 26 (8.5%) | 8 (2.6%) | 4 (1.3%) | 28 (9.1%) | 37 (12.1%) | 307 | ||
| University Hospital of Wales | 9 (7.9%) | 0 (0.0%) | 0 (0.0%) | 5 (4.4%) | 11 (9.7%) | 0 (0.0%) | 8 (7.0%) | 0 (0.0%) | 114 | ||
| Royal United Hospital | 3 (6.8%) | 0 (0.0%) | 3 (6.8%) | 4 (9.1%) | 1 (2.3%) | 0 (0.0%) | 6 (13.6%) | 0 (0.0%) | 44 | ||
| Manchester Royal Infirmary | 16 (9.6%) | 0 (0.0%) | 0 (0.0%) | 4 (2.4%) | 20 (12.0%) | 1 (0.6%) | 28 (16.8%) | 1 (0.6%) | 167 | ||
| Ysbyty Maelor Hospital | 5 (5.0%) | 0 (0.0%) | 0 (0.0%) | 2 (2.0%) | 10 (10.0%) | 6 (6.0%) | 7 (7.0%) | 0 (0.0%) | 100 | ||
| Queen Elizabeth Hospital, Gateshead | 1 (11.1%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 9 | ||
| Royal Cornwall Hospital | 5 (7.4%) | 0 (0.0%) | 0 (0.0%) | 2 (2.9%) | 8 (11.8%) | 0 (0.0%) | 5 (7.4%) | 0 (0.0%) | 68 | ||
| Stirling Royal Hospital | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (5.0%) | 1 (5.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 20 | ||
| James Paget University Hospital | 1 (1.9%) | 0 (0.0%) | 0 (0.0%) | 4 (7.6%) | 10 (18.9%) | 0 (0.0%) | 6 (11.3%) | 3 (5.7%) | 53 | ||
| Queen Alexandra Hospital | 9 (14.5%) | 0 (0.0%) | 0 (0.0%) | 1 (1.6%) | 8 (12.9%) | 0 (0.0%) | 8 (12.9%) | 1 (1.6%) | 62 | ||
| Wythenshawe Hospital | 4 (5.3%) | 1 (1.3%) | 0 (0.0%) | 10 (13.3%) | 16 (21.3%) | 0 (0.0%) | 5 (6.7%) | 0 (0.0%) | 75 | ||
| University Hospital, North Straffordshire | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (4.4%) | 0 (0.0%) | 2 (8.7%) | 12 (52.2%) | 0 (0.0%) | 23 | ||
| Ipswich Hospital | 2 (20.0%) | 0 (0.0%) | 0 (0.0%) | 1 (10.0%) | 1 (10.0%) | 0 (0.0%) | 1 (10.0%) | 0 (0.0%) | 10 | ||
| Queen Margaret Hospital | 1 (16.7%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 6 | ||
| Southampton General Hospital | 2 (4.9%) | 0 (0.0%) | 0 (0.0%) | 2 (4.9%) | 8 (19.5%) | 0 (0.0%) | 2 (4.9%) | 0 (0.0%) | 41 | ||
| York Hospital | 1 (16.7%) | 0 (0.0%) | 0 (0.0%) | 2 (33.3%) | 2 (33.3%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 6 | ||
| Victoria Hospital Blackpool | 4 (5.1%) | 0 (0.0%) | 1 (1.3%) | 2 (2.6%) | 21 (26.9%) | 0 (0.0%) | 7 (9.0%) | 0 (0.0%) | 78 | ||
| Newcastle upon Tyne Hospital | 1 (2.3%) | 0 (0.0%) | 0 (0.0%) | 2 (4.6%) | 6 (13.6%) | 1 (2.3%) | 2 (4.6%) | 0 (0.0%) | 44 | ||
| James Cook University Hospital | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (10.0%) | 1 (10.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 10 | ||
| Total (of each reason) | 119 | 2 | 13 | 107 | 195 | 41 | 190 | 62 | 1974 | ||
| I | J | K | L | M | N | O | P | Q | Z | ||
| John Radcliffe, Oxford | 0 (0.0%) | 0 (0.0%) | 2 (2.2%) | 0 (0.0%) | 15 (16.5%) | 2 (2.2%) | 1 (1.1%) | 0 (0.0%) | 7 (7.7%) | 24 (26.4%) | 91 |
| Derriford Hospital, Plymouth | 0 (0.0%) | 1 (0.7%) | 7 (5.0%) | 0 (0.0%) | 3 (2.1%) | 5 (3.6%) | 5 (3.6%) | 1 (0.7%) | 33 (23.4%) | 52 (36.9%) | 141 |
| Aberdeen Royal Infirmary | 20 (25.6%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 11 (14.1%) | 6 (7.7%) | 2 (2.6%) | 0 (0.0%) | 5 (6.4%) | 11 (14.1%) | 78 |
| Medway Maritime Hospital | 0 (0.0%) | 2 (1.4%) | 2 (1.4%) | 0 (0.0%) | 23 (15.7%) | 2 (1.4%) | 13 (8.8% | 1 (0.7%) | 21 (14.3%) | 28 (19.1%) | 147 |
| Selly Oak/Queen Elizabeth, Birmingham | 0 (0.0%) | 2 (1.9%) | 5 (4.8%) | 0 (0.0%) | 2 (1.9%) | 0 (0.0%) | 1 (1.0%) | 2 (1.9%) | 0 (0.0%) | 22 (21.0%) | 105 |
| Royal Sussex County Hospital | 0 (0.0%) | 0 (0.0%) | 2 (1.1%) | 0 (0.0%) | 19 (10.9%) | 18 (10.3%) | 15 (8.6%) | 0 (0.0%) | 21 (12.0%) | 61 (34.9%) | 175 |
| University College Hospital | 0 (0.0%) | 0 (0.0%) | 40 (13.0%) | 0 (0.0%) | 6 (2.0%) | 6 (2.0%) | 6 (2.0%) | 0 (0.0%) | 1 (0.3%) | 130 (42.4%) | 307 |
| University Hospital of Wales | 0 (0.0%) | 0 (0.0%) | 1 (0.9%) | 2 (1.8%) | 11 (9.7%) | 10 (8.8%) | 2 (1.8%) | 3 (2.6%) | 8 (7.0%) | 44 (38.6%) | 114 |
| Royal United Hospital | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 5 (11.4%) | 3 (6.8%) | 3 (6.8%) | 1 (2.3%) | 7 (15.9%) | 8 (18.2%) | 44 |
| I | J | K | L | M | N | O | P | Q | Z | ||
| Manchester Royal Infirmary | 0 (0.0%) | 0 (0.0%) | 2 (1.2%) | 3 (1.8%) | 37 (22.2%) | 3 (1.8%) | 6 (3.6%) | 0 (0.0%) | 21 (15.6%) | 25 (15.0%) | 167 |
| Ysbyty Maelor Hospital | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 12 (12.0%) | 1 (1.0%) | 11 (11.0%) | 0 (0.0%) | 3 (3.0%) | 43 (43.0%) | 100 |
| Queen Elizabeth Hospital, Gateshead | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 2 (22.2%) | 0 (0.0%) | 1 (11.1%) | 5 (55.6%) | 9 |
| Royal Cornwall Hospital | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 8 (11.8%) | 2 (2.9%) | 7 (10.3%) | 0 (0.0%) | 2 (2.9%) | 29 (42.7%) | 68 |
| Stirling Royal Hospital | 9 (45.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 9 (45.0%) | 20 |
| James Paget University Hospital | 0 (0.0%) | 0 (0.0%) | 2 (3.8%) | 0 (0.0%) | 5 (9.4%) | 0 (0.0%) | 2 (3.8%) | 0 (0.0%) | 2 (3.8%) | 18 (34.0%) | 53 |
| Queen Alexandra Hospital | 0 (0.0%) | 0 (0.0%) | 2 (3.2%) | 0 (0.0%) | 3 (4.8%) | 1 (1.6%) | 1 (1.6%) | 0 (0.0%) | 2 (3.2%) | 26 (41.9%) | 62 |
| Wythenshawe Hospital | 0 (0.0%) | 1 (1.3%) | 0 (0.0%) | 0 (0.0%) | 10 (13.3%) | 4 (5.3%) | 2 (2.7%) | 0 (0.0%) | 3 (4.0%) | 19 (25.3%) | 75 |
| University Hospital, North Straffordshire | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 2 (8.7%) | 1 (4.4%) | 1 (4.4%) | 0 (0.0%) | 1 (4.4%) | 3 (13.0%) | 23 |
| Ipswich Hospital | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 5 (50.0%) | 10 |
| Queen Margaret Hospital | 1 (16.7%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 4 (66.7%) | 6 |
| Southampton General Hospital | 0 (0.0%) | 0 (0.0%) | 2 (4.9%) | 0 (0.0%) | 7 (17.1%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 2 (4.9%) | 16 (39.0%) | 41 |
| York Hospital | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (16.7%) | 6 |
| Victoria Hospital Blackpool | 0 (0.0%) | 1 (1.3%) | 7 (9.0%) | 0 (0.0%) | 2 (2.6%) | 0 (0.0%) | 1 (1.3%) | 0 (0.0%) | 1 (1.3%) | 31 (39.7%) | 78 |
| Newcastle upon Tyne Hospital | 0 (0.0%) | 0 (0.0%) | 4 (9.1%) | 0 (0.0%) | 3 (6.8%) | 0 (0.0%) | 1 (2.3%) | 0 (0.0%) | 0 (0.0%) | 24 (54.6%) | 44 |
| James Cook University Hospital | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (10.0%) | 7 (70.0%) | 10 |
| TOTAL (of each reason) | 30 | 7 | 78 | 5 | 184 | 64 | 82 | 8 | 142 | 645 | 1974 |
Patients who were not randomised to the trial
-
Patients who are not in the trial are statistically significantly (p < 0.0001; based on a two-sample t-test) older than those randomised into the trial.
-
The proportion within each sex group was found to be similar across for those that were randomised and not randomised (p = 0.2971; based on chi-squared test).
-
Almost two-thirds of the patients approached for the trial were male.
| Category | Mean | n | Median | SD | Minimum | Maximum | Missing |
|---|---|---|---|---|---|---|---|
| Randomised | 55.4 | 795 | 57.2 | 16.8 | 16.2 | 90.1 | 0 |
| Not in the trial | 58.6 | 1720 | 61.1 | 16.9 | 16.1 | 95.1 | 254 |
| Total | 57.6 | 2515 | 59.9 | 16.9 | 16.1 | 95.1 | 254 |
| Sex | Randomised | Not in the trial | Total |
|---|---|---|---|
| Missing | 0 (0.0%) | 18 (0.9%) | 18 (0.7%) |
| Male | 495 (62.3%) | 1176 (59.6%) | 1671 (60.3%) |
| Female | 300 (37.7%) | 780 (39.5%) | 1080 (39.0%) |
| Total | 795 | 1974 | 2769 |
Pre-randomisation assessments
All potential patients who were eligible for randomisation had pre-randomisation assessments completed (i.e. n = 795).
From Table 23, there is indication that the assessments are similar across the two intervention groups.
| Ventilation | Measure | Exhaled minute volume (l/minute) | Total respiratory rate (breaths/minute) | PEEP (cmH2O) | Plateau pressure (cmH2O) | Arterial blood gas | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| PaO2 (kPa) | PaCO2 (kPa) | pH | Hydrogen ion concentration (nmol) | Associated FiO2 | ||||||
| Conventional ventilation | Mean | 10.2 | 21.1 | 11.3 | 22.3 | 10.4 | 6.9 | 7.3 | 49.4 | 0.7 |
| n | 396 | 397 | 391 | 381 | 397 | 397 | 392 | 5 | 397 | |
| SD | 3.5 | 8.2 | 3.3 | 9.1 | 2.5 | 1.8 | 0.1 | 6.5 | 0.2 | |
| Median | 9.9 | 20.0 | 10.0 | 24.0 | 10.0 | 6.7 | 7.3 | 49 | 0.7 | |
| Minimum | 0.3 | 8.0 | 5.0 | 0.0 | 5.0 | 3.5 | 7.0 | 43 | 0.4 | |
| Maximum | 33.4 | 70.0 | 36.0 | 48.0 | 24.2 | 16.3 | 7.5 | 57 | 1.0 | |
| Missing | 1 | 0 | 6 | 16 | 0 | 0 | 5 | 392 | 0 | |
| HFOV | Mean | 10.4 | 20.8 | 11.4 | 22.1 | 10.3 | 6.9 | 7.3 | 47.8 | 0.7 |
| n | 398 | 398 | 391 | 386 | 398 | 398 | 390 | 8 | 398 | |
| SD | 3.3 | 7.9 | 3.5 | 9.1 | 2.3 | 1.9 | 0.1 | 11.0 | 0.2 | |
| Median | 10.1 | 20.0 | 10.0 | 23.0 | 10.0 | 6.6 | 7.3 | 47 | 0.7 | |
| Minimum | 3.0 | 0.0 | 5.0 | 0.0 | 5.9 | 3.6 | 6.9 | 31 | 0.4 | |
| Maximum | 30.8 | 69.0 | 33.0 | 43.0 | 23.6 | 19.6 | 7.7 | 67 | 1.0 | |
| Missing | 0 | 0 | 7 | 12 | 0 | 0 | 8 | 390 | 0 | |
| Total | Mean | 10.3 | 21.0 | 11.4 | 22.2 | 10.4 | 6.9 | 7.3 | 48.4 | 0.7 |
| n | 794 | 795 | 782 | 767 | 795 | 795 | 782 | 13 | 795 | |
| SD | 3.4 | 8.0 | 3.4 | 9.1 | 2.4 | 1.9 | 0.1 | 9.2 | 0.2 | |
| Median | 10.0 | 20.0 | 10.0 | 23.0 | 10.0 | 6.7 | 7.3 | 49 | 0.7 | |
| Minimum | 0.3 | 0.0 | 5.0 | 0.0 | 5.0 | 3.5 | 6.9 | 31 | 0.4 | |
| Maximum | 33.4 | 70.0 | 36.0 | 48.0 | 24.2 | 19.6 | 7.7 | 67 | 1.0 | |
| Missing | 1 | 0 | 13 | 28 | 0 | 0 | 13 | 782 | 0 | |
From Table 24:
Organ support:
-
Almost all patients (99.6%) randomised received advanced respiratory support, as would be expected from the inclusion criteria. The proportion of patient receiving advanced respiratory support was similar across the two interventions.
-
Most of the patients had basic cardiovascular support (as opposed to advanced cardiovascular support) and the proportion getting this support was similar across the intervention groups.
-
Most of the patients required gastrointestinal support, with very few patients requiring renal, dermatological or liver support.
Antimicrobial use:
-
Almost all patients received intravenous antimicrobial drugs for pulmonary infection. The proportions receiving these drugs were similar across the two interventions.
Sedation use:
-
Almost all patients received sedation by infusion. Where sedation was given, a single sedative (as opposed to multiple drugs) was used in the majority of the patients. Again the proportions receiving sedation were similar across the interventions.
Muscle relaxants:
-
These were used on a small proportion of patients and the proportions were similar across the interventions.
Prone position ventilated and nitric oxide received:
-
Nearly all patients were ventilated in the supine position and very few received inhaled nitric oxide. This again was similar across the interventions.
| Monitoring category | Response | Conventional ventilation | HFOV | Total | |
|---|---|---|---|---|---|
| Organ support | Advanced respiratory support | No | 2 (0.5%) | 1 (0.3%) | 3 (0.4%) |
| Yes | 395 (99.5%) | 397 (99.7%) | 792 (99.6%) | ||
| Basic respiratory support | No | 334 (84.1%) | 341 (85.7%) | 675 (84.9%) | |
| Yes | 63 (15.9%) | 57 (14.3%) | 120 (15.1%) | ||
| Advanced cardiovascular support | No | 211 (53.1%) | 231 (58.0%) | 442 (55.6%) | |
| Yes | 186 (46.9%) | 167 (42.0%) | 353 (44.4%) | ||
| Basic cardiovascular support | No | 149 (37.5%) | 135 (33.9%) | 284 (35.7%) | |
| Yes | 248 (62.5%) | 263 (66.1%) | 511 (64.3%) | ||
| Renal support | No | 326 (82.1%) | 311 (78.1%) | 637 (80.1%) | |
| Yes | 71 (17.9%) | 87 (21.9%) | 158 (19.9%) | ||
| Gastrointestinal support | No | 88 (22.2%) | 90 (22.6%) | 178 (22.4%) | |
| Yes | 309 (77.8%) | 308 (77.4%) | 617 (77.6%) | ||
| Dermatological support | No | 384 (96.7%) | 380 (95.5%) | 764 (96.1%) | |
| Yes | 13 (3.3%) | 18 (4.5%) | 31 (3.9%) | ||
| Liver support | No | 392 (98.7%) | 397 (99.7%) | 789 (99.2%) | |
| Yes | 5 (1.3%) | 1 (0.3%) | 6 (0.8%) | ||
| Antimicrobial use | Antimicrobial drug received | No | 12 (3.0%) | 16 (4.0%) | 28 (3.5%) |
| Yes | 385 (97.0%) | 382 (96.0%) | 767 (96.5%) | ||
| Antimicrobial for pulmonary infection | No | 62 (15.6%) | 63 (15.8%) | 125 (15.7%) | |
| Yes | 323 (81.4%) | 319 (80.2%) | 642 (80.8%) | ||
| Missing | 12 (3.0%) | 16 (4.0%) | 28 (3.5%) | ||
| Antimicrobial intravenous | No | 3 (0.8%) | 2 (0.5%) | 5 (0.6%) | |
| Yes | 382 (96.2%) | 380 (95.5%) | 762 (95.9%) | ||
| Missing | 12 (3.0%) | 16 (4.0%) | 28 (3.5%) | ||
| Sedation use | Sedation received | No | 7 (1.8%) | 8 (2.0%) | 15 (1.9%) |
| Yes | 390 (98.2%) | 390 (98.0%) | 780 (98.1%) | ||
| Sedation intravenous | No | 352 (88.7%) | 339 (85.2%) | 691 (86.9%) | |
| Yes | 38 (9.6%) | 51 (12.8%) | 89 (11.2%) | ||
| Missing | 7 (1.8%) | 8 (2.0%) | 15 (1.9%) | ||
| Sedation infusion | No | 2 (0.5%) | 4 (1.0%) | 6 (0.8%) | |
| Yes | 388 (97.7%) | 386 (97.0%) | 774 (97.4%) | ||
| Missing | 7 (1.8%) | 8 (2.0%) | 15 (1.9%) | ||
| Sedation, more than one class of drug used | No | 47 (11.8%) | 54 (13.6%) | 101 (12.7%) | |
| Yes | 343 (86.4%) | 336 (84.4%) | 679 (85.4%) | ||
| Missing | 7 (1.8%) | 8 (2.0%) | 15 (1.9%) | ||
| Sedation, more than two classes of drugs used | No | 339 (85.4%) | 342 (85.9%) | 681 (85.7%) | |
| Yes | 51 (12.9%) | 48 (12.1%) | 99 (12.5%) | ||
| Missing | 7 (1.8%) | 8 (2.0%) | 15 (1.9%) | ||
| Sedation, more than three classes of drugs used | No | 387 (97.5%) | 386 (97.0%) | 773 (97.2%) | |
| Yes | 3 (0.8%) | 4 (1.0%) | 7 (0.9%) | ||
| Missing | 7 (1.8%) | 8 (2.0%) | 15 (1.9%) | ||
| Muscle relaxant drug use | Muscle relaxants received | No | 223 (56.2%) | 223 (56.0%) | 446 (56.1%) |
| Yes | 174 (43.8%) | 175 (44.0%) | 349 (43.9%) | ||
| Muscle relaxants primarily by intravenous bolus | No | 89 (22.4%) | 80 (20.1%) | 169 (21.3%) | |
| Yes | 85 (21.4%) | 95 (23.9%) | 180 (22.6%) | ||
| Missing | 223 (56.2%) | 223 (56.0%) | 446 (56.1%) | ||
| Muscle relaxants primarily by intravenous infusion | No | 72 (18.1%) | 69 (17.3%) | 141 (17.7%) | |
| Yes | 102 (25.7%) | 106 (26.6%) | 208 (26.2%) | ||
| Missing | 223 (56.2%) | 223 (56.0%) | 446 (56.1%) | ||
| Others | Ventilated in the prone position | No | 378 (95.2%) | 378 (95.0%) | 756 (95.1%) |
| Yes | 19 (4.8%) | 20 (5.0%) | 39 (4.9%) | ||
| Inhaled nitric oxide treatment | No | 389 (98.0%) | 386 (97.0%) | 775 (97.5%) | |
| Yes | 8 (2.0%) | 12 (3.0%) | 20 (2.5%) | ||
Time to randomisation
-
The times from hospital to ICU admission, and ICU admission to randomisation are given in Table 25.
| Interval | Measure | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| Time from hospital admission to ICU admission (days) | Mean | 3.8 | 5.0 | 4.4 |
| n | 397 | 398 | 795 | |
| SD | 7.5 | 19.3 | 14.6 | |
| Median | 1 | 1 | 1 | |
| Minimum | 0 | 0 | 0 | |
| Maximum | 80 | 334 | 334 | |
| Time from hospital admission to randomisation (days) | Mean | 8.3 | 7.9 | 8.1 |
| n | 397 | 398 | 795 | |
| SD | 37.3 | 19.8 | 29.8 | |
| Median | 4 | 4 | 4 | |
| Minimum | 0 | 0 | 0 | |
| Maximum | 732 | 340 | 732 | |
| Time from ICU to randomisation (days) | Mean | 4.5 | 2.9 | 3.7 |
| n | 397 | 398 | 795 | |
| SD | 36.7 | 2.6 | 26.0 | |
| Median | 2 | 2 | 2 | |
| Minimum | 0 | 0 | 0 | |
| Maximum | 732 | 22 | 732 |
Randomisation
Table 26 illustrates the randomised patients by each centre. There is evidence in this table that the proportion of patients recruited on each intervention is approximately the same within a centre.
| Centre | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| John Radcliffe, Oxford | 8 (53.3%) | 7 (46.7%) | 15 |
| Derriford Hospital, Plymouth | 22 (47.8%) | 24 (52.2%) | 46 |
| Aberdeen Royal Infirmary | 8 (53.3%) | 7 (46.7%) | 15 |
| Medway Maritime Hospital | 14 (51.9%) | 13 (48.2%) | 27 |
| Selly Oak/Queen Elizabeth, Birmingham | 50 (49.0%) | 52 (51.0%) | 102 |
| Royal Sussex County Hospital | 22 (47.8%) | 24 (52.2%) | 46 |
| University College Hospital | 33 (52.4%) | 30 (47.6%) | 63 |
| University Hospital of Wales | 9 (56.3%) | 7 (43.8%) | 16 |
| Royal United Hospital | 11 (55.0%) | 9 (45.0%) | 20 |
| Manchester Royal Infirmary | 12 (50.0%) | 12 (50.0%) | 24 |
| Ysbyty Maelor Hospital | 17 (53.1%) | 15 (46.9%) | 32 |
| Queen Elizabeth Hospital, Gateshead | 7 (50.0%) | 7 (50.0%) | 14 |
| Royal Cornwall Hospital | 28 (50.0%) | 28 (50.0%) | 56 |
| Stirling Royal Hospital | 8 (42.1%) | 11 (57.9%) | 19 |
| Manchester Royal Infirmary, Cardiac ICU | 1 (100.0%) | 0 (0.0%) | 1 |
| Leeds General Infirmary | 14 (46.7%) | 16 (53.3%) | 30 |
| James Paget University Hospital | 12 (52.2%) | 11 (47.8%) | 23 |
| Queen Alexandra Hospital | 18 (48.7%) | 19 (51.4%) | 37 |
| Royal Blackburn Hospital | 13 (50.0%) | 13 (50.0%) | 26 |
| Wythenshawe Hospital | 7 (46.7%) | 8 (53.3%) | 15 |
| University Hospital of North Staffordshire | 7 (46.7%) | 8 (53.3%) | 15 |
| Ipswich Hospital | 1 (20.0%) | 4 (80.0%) | 5 |
| Queen Margaret Hospital | 5 (62.5%) | 3 (37.5%) | 8 |
| Southampton General Hospital | 8 (57.1%) | 6 (42.9%) | 14 |
| St James’s University Hospital | 34 (50.0%) | 34 (50.0%) | 68 |
| York Hospital | 7 (53.8%) | 6 (46.2%) | 13 |
| Victoria Hospital Blackpool | 13 (46.4%) | 15 (53.6%) | 28 |
| Southend Hospital | 1 (33.3%) | 2 (66.7%) | 3 |
| Newcastle upon Tyne Hospital | 4 (50.0%) | 4 (50.0%) | 8 |
| James Cook University Hospital | 3 (50.0%) | 3 (50.0%) | 6 |
| Total | 397 | 398 | 795 |
Appendix 6 shows the allocation of patients within each of the randomisation strata (age and P : F ratio) within each centre. Again, there is an indication that the allocation of the proportion of patients within a centre is similar within a treatment group.
There were 31 patients who were randomised ‘incorrectly’ because their age or P : F ratio entered into the randomisation system did not match that recorded on the Case Report Form. There were eight patients who had their age group recorded as ‘> 55 years old’, when in fact their date of birth indicated they were ‘< 55 years old’. There were 23 patients who had a P : F ratio recorded as ‘< 15 kPa’, when their P : F ratio was ‘> 15 kPa’.
Tables 27–32 illustrate the demographic variables and those measured immediately post randomisation. In general, the variables presented in these tables are similar across the two treatment groups.
| Classifier | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| Age group (years) | |||
| ≤ 55 | 174 (43.8%) | 178 (44.7%) | 352 (44.3%) |
| > 55 | 223 (56.2%) | 220 (55.3%) | 443 (55.7%) |
| Sex | |||
| Male | 239 (60.2%) | 256 (64.3%) | 495 (62.3%) |
| Female | 158 (39.8%) | 142 (35.7%) | 300 (37.7%) |
| P : F ratio (kPa) | |||
| ≤ 15 | 234 (58.9%) | 227 (57.0%) | 461 (58.0%) |
| > 15 | 163 (41.1%) | 171 (43.0%) | 334 (42.0%) |
| Weight (kg) | |||
| Mean | 78.60 | 80.79 | 79.70 |
| n | 397 | 398 | 795 |
| SD | 20.9 | 21.7 | 21.4 |
| Median | 76.0 | 79.5 | 78.0 |
| Minimum | 37.0 | 35.0 | 35.0 |
| Maximum | 215.0 | 186.0 | 215.0 |
| Patient’s height or heel/crown measurement (m) | |||
| Mean | 1.7 | 1.7 | 1.7 |
| n | 386 | 383 | 769 |
| SD | 0.1 | 0.1 | 0.1 |
| Median | 1.7 | 1.7 | 1.7 |
| Minimum | 1.4 | 1.2 | 1.2 |
| Maximum | 2.0 | 2.0 | 2.0 |
| Associated FiO2 | |||
| Mean | 0.7 | 0.7 | 0.7 |
| n | 397 | 398 | 795 |
| SD | 0.2 | 0.2 | 0.2 |
| Median | 0.7 | 0.7 | 0.7 |
| Minimum | 0.4 | 0.4 | 0.4 |
| Maximum | 1.0 | 1.0 | 1.0 |
| Cause | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| Pulmonary | 304 (76.6%) | 302 (75.9%) | 606 (76.2%) |
| Extrapulmonary | 93 (23.4%) | 96 (24.1%) | 189 (23.8%) |
| Initiation of ventilation | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| Ventilated before hospital admission | 20 (5.0%) | 13 (3.3%) | 33 (4.2%) |
| Ventilated after hospital admission but prior to ICU admission | 119 (30.0%) | 118 (29.6%) | 237 (29.8%) |
| First ventilated during ICU stay | 257 (64.7%) | 267 (67.1%) | 524 (65.9%) |
| Where first ventilated not known | 1 (0.3%) | 0 (0.0%) | 1 (0.1%) |
First 24 hours in intensive care unit
| Surgical filters | Classifier | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| Was the patient admitted to your ICU directly from the operating theatre/recovery area in your hospital? | No | 347 (87.4%) | 340 (85.4%) | 687 (86.4%) |
| Yes | 50 (12.6%) | 58 (14.6%) | 108 (13.6%) | |
| If ‘yes’,a was the surgery | Emergency? | 21 (42.0%) | 29 (50.0%) | 50 (46.3%) |
| Urgent? | 17 (34.0%) | 19 (32.8%) | 26 (33.3%) | |
| Scheduled? | 2 (4.0%) | 3 (5.2%) | 5 (4.6%) | |
| Elective? | 10 (20.0%) | 7 (12.1%) | 17 (15.7%) |
| Status | Past medical history | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| No past history | Yes | 90 (22.7%) | 74 (18.6%) | 164 (20.6%) |
| No | 307 (77.3%) | 324 (81.4%) | 631 (79.4%) | |
| Past history | ||||
| Biopsy-proven cirrhosis | Yes | 6 (6.7%) | 8 (10.8%) | 14 (8.5%) |
| No | 84 (93.3%) | 66 (89.2%) | 150 (91.5%) | |
| Portal hypertension | Yes | 8 (8.9%) | 11 (14.9%) | 19 (11.6%) |
| No | 82 (91.1%) | 63 (85.1%) | 145 (88.4%) | |
| Hepatic encephalopathy | Yes | 7 (7.8%) | 7 (9.5%) | 14 (8.5%) |
| No | 83 (92.2%) | 67 (90.5%) | 150 (91.5%) | |
| Very severe cardiovascular disease | Yes | 6 (6.7%) | 1 (1.4%) | 7 (4.3%) |
| No | 84 (93.3%) | 73 (98.7%) | 157 (95.7%) | |
| Severe respiratory disease | Yes | 6 (6.7%) | 7 (9.5%) | 13 (7.9%) |
| No | 84 (93.3%) | 67 (90.5%) | 151 (92.1%) | |
| Home ventilation | Yes | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| No | 90 (100.0%) | 74 (100.0%) | 164 (100.0%) | |
| Chronic renal replacement | Yes | 4 (4.4%) | 2 (2.7%) | 6 (3.7%) |
| No | 86 (95.6%) | 72 (97.3%) | 158 (96.3%) | |
| AIDS | Yes | 3 (3.3%) | 5 (6.8%) | 8 (4.9%) |
| No | 87 (96.7%) | 69 (93.2%) | 156 (95.1%) | |
| Steroid treatment | Yes | 15 (16.7%) | 8 (10.8%) | 23 (14.0%) |
| No | 75 (83.3%) | 66 (89.2%) | 141 (86.0%) | |
| Radiotherapy | Yes | 9 (10.0%) | 7 (9.5%) | 16 (9.8%) |
| No | 81 (90.0%) | 67 (90.5%) | 148 (90.2%) | |
| Chemotherapy | Yes | 39 (43.3%) | 27 (36.5%) | 66 (40.2%) |
| No | 51 (56.7%) | 47 (63.5%) | 98 (59.8%) | |
| Metastatic disease | Yes | 10 (11.1%) | 4 (5.4%) | 14 (8.5%) |
| No | 80 (88.9%) | 70 (94.6%) | 150 (91.5%) | |
| Acute myelogenous/lymphocytic leukaemia or multiple myeloma | Yes | 16 (17.8%) | 8 (10.8%) | 24 (14.6%) |
| No | 74 (82.2%) | 66 (89.2%) | 140 (85.4%) | |
| Chronic myelogenous/lymphocytic leukaemia | Yes | 4 (4.4%) | 7 (9.5%) | 11 (6.7%) |
| No | 86 (95.6%) | 67 (90.5%) | 153 (93.3%) | |
| Lymphoma | Yes | 10 (11.1%) | 12 (16.2%) | 22 (13.4%) |
| No | 80 (88.9%) | 62 (83.8%) | 142 (86.6%) | |
| Congenital immunohumoral or cellular immune deficiency state | Yes | 2 (2.2%) | 4 (5.4%) | 6 (3.7%) |
| No | 88 (97.8%) | 70 (94.6%) | 158 (96.3%) | |
| Measure | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| Mean | 21.7 | 21.8 | 21.8 |
| n | 383 | 382 | 765 |
| SD | 6.1 | 6.0 | 6.1 |
| Median | 21.0 | 22.0 | 22.0 |
Daily data in intensive care unit
There are 792 patients with ICU data – of the 795 patients randomised, three patients died on the same day as the randomisation day and therefore have no ICU data. Tables 33–37 provide details of the daily data collected by group.
| Organ support | Measure | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| Ventilation-free (days) up to 30 days post randomisation | Mean | 2.3 | 2.6 | 2.5 |
| n | 397 | 395 | 792 | |
| SD | 3.5 | 3.5 | 3.5 | |
| Median | 0 | 1 | 1 | |
| Range | 0–21 | 0–20 | 0–21 | |
| Advanced respiratory support-free days | Mean | 3.1 | 3.8 | 3.8 |
| n | 397 | 395 | 792 | |
| SD | 4.7 | 5.9 | 5.3 | |
| Median | 2 | 2 | 2 | |
| Range | 0–32 | 0–57 | 0–57 | |
| Days on advanced cardiovascular support | Mean | 2.8 | 2.9 | 2.9 |
| n | 397 | 395 | 792 | |
| SD | 5.6 | 4.5 | 5.1 | |
| Median | 1 | 1 | 1 | |
| Range | 0–75 | 0–35 | 0–75 | |
| Days on basic cardiovascular support | Mean | 11.8 | 12.5 | 12.1 |
| n | 397 | 395 | 792 | |
| SD | 10.7 | 11.5 | 11.1 | |
| Median | 10 | 10 | 10 | |
| Range | 0–73 | 0–85 | 0–85 | |
| Days on renal support | Mean | 2.6 | 4.5 | 3.5 |
| n | 397 | 395 | 792 | |
| SD | 5.1 | 7.7 | 6.6 | |
| Median | 0 | 0 | 0 | |
| Range | 0–34 | 0–52 | 0–52 | |
| Days on gastrointestinal support | Mean | 16.0 | 17.4 | 16.7 |
| n | 397 | 395 | 792 | |
| SD | 15.1 | 16.7 | 15.9 | |
| Median | 12 | 13 | 12 | |
| Range | 0–113 | 0–114 | 0–114 | |
| Days on dermatological support | Mean | 1.0 | 0.9 | 1.0 |
| n | 397 | 395 | 792 | |
| SD | 5.3 | 4.6 | 5.0 | |
| Median | 0 | 0 | 0 | |
| Range | 0–59 | 0–47 | 0–59 | |
| Days on liver support | Mean | 0.04 | 0.03 | 0.03 |
| n | 397 | 395 | 792 | |
| SD | 0.4 | 0.2 | 0.3 | |
| Median | 0 | 0 | 0 | |
| Range | 0–5 | 0–2 | 0–5 |
| Antimicrobial use | Measure | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| Number of days free from antimicrobial use | Mean | 4.9 | 5.9 | 5.4 |
| n | 397 | 395 | 792 | |
| SD | 8.2 | 9.2 | 8.7 | |
| Median | 1 | 2 | 2 | |
| Range | 0–60 | 0–63 | 0–63 | |
| Number of days antimicrobial used | Mean | 12.4 | 12.8 | 12.6 |
| n | 397 | 395 | 792 | |
| SD | 10.3 | 12.0 | 11.2 | |
| Median | 10 | 10 | 10 | |
| Range | 0–68 | 0–111 | 0–111 | |
| Number of days antimicrobial used to treat pulmonary infection | Mean | 9.8 | 9.9 | 9.8 |
| n | 397 | 395 | 792 | |
| SD | 9.3 | 9.7 | 9.5 | |
| Median | 8 | 8 | 8 | |
| Range | 0–54 | 0–68 | 0–68 | |
| Number of days antimicrobial given intravenously | Mean | 11.7 | 11.9 | 11.8 |
| n | 397 | 395 | 792 | |
| SD | 9.6 | 10.7 | 10.1 | |
| Median | 9 | 10 | 10 | |
| Range | 0–60 | 0–86 | 0–86 |
| Sedative use | Measure | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| Number of days free from sedative received primarily for sedation | Mean | 8.8 | 9.4 | 9.1 |
| n | 397 | 395 | 792 | |
| SD | 12.6 | 14.6 | 13.6 | |
| Median | 5 | 4 | 4 | |
| Range | 0–108 | 0–97 | 0–108 | |
| Number of days sedative received primarily for sedation | Mean | 8.5 | 9.4 | 8.9 |
| n | 397 | 395 | 792 | |
| SD | 6.9 | 7.2 | 7.0 | |
| Median | 7 | 8 | 7 | |
| Range | 0–39 | 0–50 | 0–50 | |
| Number of days an intravenous bolus dose used | Mean | 0.5 | 0.4 | 0.5 |
| n | 397 | 395 | 792 | |
| SD | 2.1 | 1.4 | 1.8 | |
| Median | 0 | 0 | 0 | |
| Range | 0–30 | 0–13 | 0–30 | |
| Number of days sedative given by infusion | Mean | 8.3 | 9.1 | 8.7 |
| n | 397 | 395 | 792 | |
| SD | 6.8 | 7.0 | 6.9 | |
| Median | 7 | 8 | 7 | |
| Range | 0–39 | 0–50 | 0–50 | |
| Number of days patient on more than one class of sedative | Mean | 6.6 | 7.3 | 7.0 |
| n | 397 | 395 | 792 | |
| SD | 5.9 | 5.7 | 5.8 | |
| Median | 5 | 6 | 6 | |
| Range | 0–36 | 0–44 | 0–44 | |
| Number of days patient on more than two classes of sedative | Mean | 1.4 | 1.4 | 1.4 |
| n | 397 | 395 | 792 | |
| SD | 3.2 | 3.0 | 3.1 | |
| Median | 0 | 0 | 0 | |
| Range | 0–28 | 0–26 | 0–28 | |
| Number of days patient on more than three classes of sedative | Mean | 0.1 | 0.2 | 0.2 |
| n | 397 | 395 | 792 | |
| SD | 0.8 | 0.8 | 0.8 | |
| Median | 0 | 0 | 0 | |
| Range | 0–11 | 0–9 | 0–11 |
| Muscle relaxant use | Measure | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| Number of days patient received muscle relaxant drugs to aid artificial ventilation | Mean | 2.1 | 2.5 | 2.3 |
| n | 397 | 395 | 792 | |
| SD | 3.4 | 3.5 | 3.5 | |
| Median | 1 | 1 | 1 | |
| Range | 0–22 | 0–25 | 0–25 | |
| Number of days an intravenous bolus dose used | Mean | 0.5 | 0.5 | 0.5 |
| n | 397 | 395 | 792 | |
| SD | 1.0 | 0.9 | 1.0 | |
| Median | 0 | 0 | 0 | |
| Range | 0–6 | 0–5 | 0–6 | |
| Number of days an muscle relaxants given by infusion | Mean | 1.7 | 2.0 | 1.9 |
| n | 397 | 395 | 792 | |
| SD | 3.3 | 3.4 | 3.3 | |
| Median | 0 | 0 | 0 | |
| Range | 0–22 | 0–24 | 0–24 |
| Treatment | Measure | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| Number of days patient ventilated prone | Mean | 0.5 | 0.2 | 0.3 |
| n | 397 | 395 | 792 | |
| SD | 1.3 | 0.7 | 1.1 | |
| Median | 0 | 0 | 0 | |
| Range | 0–12 | 0–8 | 0–12 | |
| Number of days patient received inhaled nitric oxide | Mean | 0.4 | 0.2 | 0.3 |
| n | 397 | 395 | 792 | |
| SD | 2.1 | 0.9 | 1.6 | |
| Median | 0 | 0 | 0 | |
| Range | 0–23 | 0–12 | 0–23 |
Table 38 details the statistical analysis in terms of model fitting.
| Organ support | Means estimate | Conventional ventilation (95% CI) | HFOV (95% CI) | Difference (95% CI) | p-valuea |
|---|---|---|---|---|---|
| Ventilation-free days (up to 30 days post randomisation) | Unadjusted | 2.3 (2.0 to 2.6) | 2.6 (2.3 to 3.0) | 0.3 (–0.2 to 0.8) | 0.1731 |
| Adjusted | 2.3 (1.9 to 2.8) | 2.6 (2.2 to 3.1) | 0.3 (–0.2 to 0.7) | 0.2483 | |
| Advanced respiratory support-free days (up to 30 days post randomisation) | Unadjusted | 3.1 (2.7 to 3.6) | 3.8 (3.2 to 4.4) | 0.6 (–0.1 to 1.4) | 0.0888 |
| Adjusted | 3.1 (2.4 to 3.8) | 3.7 (3.0 to 4.4) | 0.6 (–0.1 to 1.4) | 0.0962 | |
| Basic respiratory support-free days (up to 30 days post randomisation) | Unadjusted | 14.7 (13.3 to 16.1) | 15.6 (14.1 to 17.1) | 0.9 (–1.1 to 2.9) | 0.3780 |
| Adjusted | 14.0 (12.1 to 15.9) | 15.0 (13.0 to 16.9) | 1.0 (–1.0 to 2.9) | 0.3430 | |
| Days on advanced cardiovascular support | Unadjusted | 2.8 (2.3 to 3.7) | 2.9 (2.5 to 3.4) | 0.1 (–0.6 to 0.8) | 0.7446 |
| Adjusted | 3.0 (2.3 to 3.6) | 3.2 (2.5 to 3.9) | 0.2 (–0.4 to 0.9) | 0.4966 | |
| Days on basic cardiovascular support | Unadjusted | 11.8 (10.7 to 12.9) | 12.5 (11.4 to 13.6) | 0.7 (–0.9 to 2.2) | 0.3853 |
| Adjusted | 11.5 (10.0 to 13.0) | 12.2 (10.7 to 13.7) | 0.7 (–0.9 to 2.3) | 0.3802 | |
| Days on renal support | Unadjusted | 2.6 (2.1 to 3.1) | 4.5 (3.7 to 5.2) | 1.8 (0.9 to 2.7) | 0.0001 |
| Adjusted | 2.5 (1.6 to 3.4) | 4.3 (3.4 to 5.2) | 1.8 (0.9 to 2.7) | 0.0001 | |
| Days on gastrointestinal support | Unadjusted | 16.0 (14.5 to 17.5) | 17.4 (15.7 to 19.0) | 1.3 (–0.9 to 3.6) | 0.2382 |
| Adjusted | 15.3 (13.2 to 17.5) | 16.7 (14.6 to 18.9) | 1.4 (–0.8 to 3.6) | 0.2193 | |
| Dermatological support days | Unadjusted | 1.0 (0.5 to 1.6) | 0.9 (0.5 to 1.4) | –0.1 (–0.8 to 0.6) | 0.7037 |
| Adjusted | 0.9 (0.2 to 1.6) | 0.8 (0.1 to 1.5) | –0.1 (–0.8 to 0.6) | 0.7330 | |
| Liver support days | Unadjusted | 0.040 (–0.001 to 0.100) | 0.03 (0.01 to 0.10) | –0.002 (–0.040 to 0.040) | 0.9127 |
| Adjusted | 0.03 (–0.01 to 0.10) | 0.03 (–0.01 to 0.10) | –0.001 (–0.040 to 0.040) | 0.9501 | |
| Number of days free of antimicrobial use | Unadjusted | 4.9 (4.1 to 5.7) | 5.9 (5.0 to 6.8) | 1.0 (–0.2 to 2.2) | 0.1109 |
| Adjusted | 4.5 (3.3 to 5.6) | 5.5 (4.3 to 6.7) | 1.0 (–0.2 to 2.2) | 0.1030 | |
| Number of days free of drugs received primarily for sedation | Unadjusted | 8.8 (7.6 to 10.0) | 9.4 (7.9 to 10.8) | 0.6 (–1.3 to 2.5) | 0.5628 |
| Adjusted | 7.7 (5.9 to 9.6) | 8.3 (6.5 to 10.2) | 0.6 (–1.3 to 2.5) | 0.5435 |
Plots of daily percentage of patients on each type of support
The daily counts of number patients for all percentage plots are shown in Table 39.
| Day | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Conventional ventilation (n) | 397 | 381 | 369 | 356 | 337 | 328 | 308 | 290 | 273 | 259 | 246 | 227 | 205 | 192 | 173 | 155 | 147 | 132 | 124 | 117 |
| HFOV (n) | 395 | 379 | 362 | 350 | 343 | 332 | 321 | 306 | 290 | 271 | 258 | 241 | 227 | 208 | 189 | 167 | 157 | 145 | 139 | 131 |
| Total (n) | 792 | 760 | 731 | 706 | 680 | 660 | 629 | 596 | 563 | 530 | 504 | 468 | 432 | 400 | 362 | 322 | 304 | 277 | 263 | 248 |
| Day | 21 | 22 | 23 | 24 | 25 | 26 | 27 | 28 | 29 | 30 | 31 | 32 | 33 | 34 | 35 | 36 | 37 | 38 | 39 | 40 |
| Conventional ventilation (n) | 110 | 102 | 96 | 89 | 82 | 79 | 77 | 69 | 44 | 60 | 55 | 54 | 52 | 48 | 45 | 41 | 38 | 38 | 36 | 34 |
| HFOV (n) | 122 | 117 | 107 | 99 | 91 | 88 | 86 | 77 | 69 | 65 | 64 | 60 | 58 | 54 | 48 | 44 | 42 | 40 | 38 | 35 |
| Total (n) | 232 | 219 | 203 | 188 | 173 | 167 | 163 | 146 | 113 | 125 | 119 | 114 | 110 | 102 | 93 | 85 | 80 | 78 | 74 | 69 |
Primary outcome
The primary outcome was all-cause mortality at 30 days following randomisation.
In the protocol, the original sample size of 1006 randomised patients was based on reducing mortality by 9% from 45% (on control group). In an early formal interim analysis, it was decided to change the effect size, in agreement with the HTA. At that point in the trial, the control group illustrated a higher proportion of mortality and difference of 10% required 802 patients.
Table 40 illustrates the results for mortality at 30 days post randomisation.
| Status | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| Alive | 234 (58.9%) | 232 (58.3%) | 466 (58.6%) |
| Died | 163 (41.1%) | 166 (41.7%) | 329 (41.4%) |
| Total | 397 | 398 | 795 |
No statistically significant difference in mortality rates at 30 days post randomisation was found between the two interventions (chi-squared test: p = 0.8523). The absolute difference in mortality rates between the two interventions was 0.65% (95% CI –6.17% to 7.46%).
No statistically significant difference in mortality rates at 30 days post randomisation was found between the two interventions when adjusting for centre, sex, P : F ratio and APACHE II score (logistic regression: p-value 0.8674). The odds of being alive (as opposed to dying) were 1.03 (95% CI 0.75 to 1.40) when on conventional ventilation compared with HFOV.
Figure 7 illustrates the Kaplan–Meier curve with the probability of survival up to 30 days post randomisation for each intervention. There is evidence from this plot that, on some days, HFOV did marginally worse than the conventional ventilator with respect to survival of patients over time.
FIGURE 7.
Kaplan–Meier curves for survival to day 30 post randomisation.

Secondary outcomes
Mortality rate at first discharge from intensive care unit/intensive care unit length of stay
The number (and percentage) of patients who died in ICU or were alive at discharge from ICU are summarised in Table 41 by each intervention. Note that there are 794 patients in total with ICU data, as one patient was still in an ICU when the database was analysed.
| Status | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| Alive | 230 (57.9%) | 222 (55.9%) | 452 (56.9%) |
| Died | 167 (42.1%) | 175 (44.1%) | 324 (43.1%) |
| Total | 397 | 397 | 794 |
No statistically significant difference in mortality rates at first discharge from ICU was found between the two interventions (chi-squared test: p = 0.5664). The difference in mortality rates between the two interventions was 2.02% (95% CI –4.85% to 8.86%).
For the survival analysis, patients who died up to first discharge from ICU were uncensored, and all others (including the one patient in ICU) were uncensored. No statistically significant difference in mortality rates at first discharge from ICU was found between the two interventions when adjusting for centre, sex, P : F ratio and APACHE II score (logistic regression: p-value 0.5400). The odds of being alive (as opposed to dying) at first discharge from ICU were 1.102 (95% CI 0.807 to 1.505) when on conventional ventilation compared with HFOV.
Table 42 details the summary statistic for the length of stay in ICU (from randomisation to first discharge). No significant difference was found in the length of stay in ICU between the interventions. Using a linear regression model and adjusting for centre, sex, P : F ratio and APACHE II score, the mean [standard error (SE)] estimates were conventions: 15.8 (1.1) days; HFOV 17.5 (1.1) days and a difference of 1.8 (1.2) days: p-value for difference = 0.1314.
| Measure | Conventional ventilation | HFOV | Total | |
|---|---|---|---|---|
| Time from ICU admission to ICU discharge (days) | Mean | 16.2 | 17.6 | 16.9 |
| n | 397 | 397 | 794 | |
| SD | 15.2 | 16.6 | 15.9 | |
| Median | 12 | 13 | 13 | |
| Range | 0–112 | 0–114 | 0–114 |
Figure 8 illustrates the Kaplan–Meier curve for the probability of survival in ICU against the number of days in ICU (with the number of patients at risk). The event here was mortality from randomisation to first discharge from ICU. Thus all patients who did not die in ICU and were discharged alive are censored (as their death date was beyond that of discharge from ICU date).
FIGURE 8.
Kaplan–Meier curves displaying the probability of survival in ICU over the time in ICU for both interventions.

From Table 42, it is evident that the number of days in ICU range from 0 to 114 over both intervention groups. From Figure 8, we can see that the probability of survival in ICU appears to increase for patients on HFOV from day 50 (in ICU) to just beyond day 75. However, this is based on a small sample of patients at risk.
Mortality rate at first discharge from hospital/hospital length of stay
The number (and percentage) of patients who died prior to hospital discharge or were alive at hospital discharge are summarised in Table 43 by each intervention. Note that there are 788 patients in total with hospital data – one patient was still in ICU and the other six patients were in hospital and had not been discharged.
| Status | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| Alive | 204 (51.7%) | 196 (49.9%) | 400 (50.8%) |
| Died | 191 (48.4%) | 197 (50.1%) | 388 (49.2%) |
| Total | 395 | 393 | 788 |
No statistically significant difference in mortality rates at first discharge from hospital was found between the two interventions (chi-squared test: p = 0.6187). The difference in mortality rates between the two interventions was 1.77% (95% CI –5.19% to 8.71%).
No statistically significant difference in mortality rates at first discharge from hospital was found between the two interventions when adjusting for centre, sex, P : F ratio and APACHE II score (logistic regression: p-value 0.5276). The odds of being alive (as opposed to dying) at first discharge from ICU were 1.104 (95% CI 0.812 to 1.501) when on conventional ventilation compared with HFOV.
Table 44 details the summary statistics for the length of stay in hospital (from randomisation to first discharge from hospital). No significant difference was found in the length of stay in hospital between the interventions. Using a linear regression model and adjusting for centre, sex, P : F ratio and the APACHE II score, the mean (SE) estimates were conventions: 31.0 (3.0) days; HFOV 32.8 (3.1) days and a difference of 1.9 (3.2) days: p-value for difference = 0.5426.
| Measure | Conventional ventilation | HFOV | Total | |
|---|---|---|---|---|
| Number of days from randomisation to first discharge from hospital | Mean | 33.1 | 33.9 | 33.5 |
| n | 395 | 393 | 788 | |
| SD | 44.3 | 41.6 | 43.0 | |
| Median | 21 | 21 | 21 | |
| Range | 0–584 | 0–280 | 0–584 |
Figure 9 illustrates the Kaplan–Meier curve for the probability of survival in hospital against the number of days in hospital (with the number of patients at risk).
FIGURE 9.
Kaplan–Meier curves displaying the probability of survival in hospital over the time in hospital for both interventions.

Mortality rate one year after randomisation
The number (and percentage) of patients who were alive/died on year after randomisation are summarised in Table 45 by each intervention. An assumption that all of those who have not reached 12-month follow-up are alive has been made for the survival analysis. The uncensored observations are all of those who died prior to 12 months and the censored are all other subjects.
| Status | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| Alive (or assumed alive) | 194 (48.9%) | 196 (49.2%) | 390 |
| Died | 203 (51.1%) | 202 (50.8%) | 405 |
| Total | 397 | 398 | 795 |
Allowing for the censoring, no statistically significant difference in mortality rates at 12 months post randomisation were found between the two interventions (log-rank test: p = 0.2419). The difference in mortality rates between the two interventions was 0.38% (95% CI –6.54% to 7.29%).
No statistically significant difference in mortality rates at 12 months post randomisation from hospital was found between the two interventions when adjusting for centre, sex, P : F ratio and APACHE II score (Cox’s regression model: p-value = 0.1781). The odds of being alive (as opposed to dying) at 12 months post randomisation were 1.148 when on conventional ventilation compared with HFOV.
Figure 10 illustrates the Kaplan–Meier curve for the probability of survival up to 12 months post randomisation (with the number of patients at risk).
FIGURE 10.
Kaplan–Meier curves displaying the probability of survival up to 12 months post randomisation for both interventions.
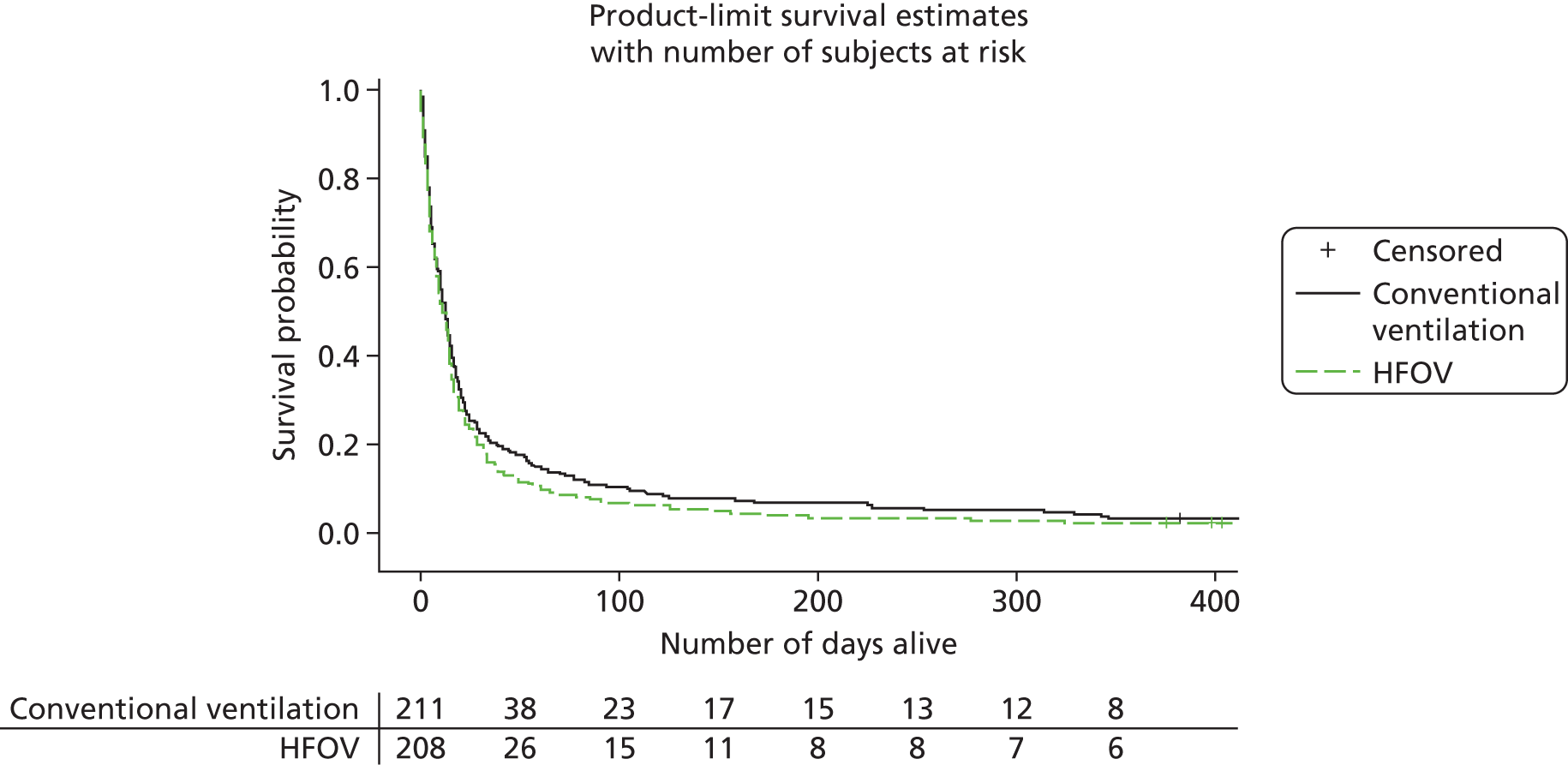
Follow-up
As the study recruitment period was extended, the longer-term follow-up for this study was not complete when this report was written. Data available up to 14 October 2012 are reported here. These results should be interpreted with considerable caution as they are not complete.
Six-month follow-up
From Table 43, there are 400 patients who are alive at hospital discharge.
From Table 46, there were 15 patients who died from hospital discharge to the 6-month follow-up time point and one patient withdrew from their 6 month follow-up. Also, there are 37 patients who are not due for their 6-month follow-up questionnaire. Thus, 53 patients will not have had their 6-month follow-up.
| Time point | Status | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| 6-month follow-up | Died prior to 6-month follow-up | 196 (49.6%) | 199 (50.4%) | 395 |
| Known to be alive at 6-month follow-up | 201 (50.3%) | 199 (49.8%) | 400 | |
| Not due their 6-month questionnaire | 17 (45.9%) | 20 (54.1%) | 37 | |
| Withdrawn from 6-month follow-up | 1 (100.0%) | 0 (0.0%) | 1 | |
| Not sent questionnairea | 1 (33.3%) | 2 (66.7%) | 3 | |
| Follow-up questionnaire sent out | 176 (51.2%) | 221 (64.2%) | 344 | |
| Overdue their 6-month questionnaire (non-responders) | 62 (50.4%) | 61 (49.6%) | 123 | |
| Received completed follow-up questionnaire (on database) | 110 (51.2%) | 105 (48.8%) | 215 | |
| Received follow-up questionnaire, but blank | 6 (100.0%) | 0 (0.0%) | 6 | |
| 12-month follow-up | Died prior to 12-month follow-up | 203 (50.1%) | 202 (49.9%) | 405 |
| Known to be alive at 12-month follow-up | 194 (49.7%) | 196 (50.3%) | 390 | |
| Not due their 12-month questionnaire | 44 (53.0%) | 39 (47.0%) | 83 | |
| Withdrawn from 12-month follow-up | 2 (66.7%) | 1 (33.3%) | 3 | |
| Not sent questionnaire | 1 (50.0%) | 1 (50.0%) | 2 | |
| Follow-up questionnaire sent out | 147 (48.8%) | 155 (51.3%) | 302 | |
| Overdue their 6-month questionnaire (non-responders) | 62 (52.1%) | 57 (47.9%) | 119 | |
| Received completed follow-up questionnaire (on database) | 84 (46.9%) | 95 (53.1%) | 179 | |
| Received follow-up questionnaire, but blank | 1 (25.0%) | 3 (75.0%) | 4 |
In total, 347 patients (86.8% of those discharged) were sent the 6-month questionnaire.
In total, we received back 221 questionnaires (63.6% of those sent). Thus, our follow-up rate at 6 months is currently 64%. Of these 221 questionnaires, 6 were returned blank and 215 were returned with data. There are 126 (36.3%) non-responders at 6 months. Table 46 lists the numbers sent the questionnaires and followed up at 6 months by treatment group.
The statistical results from the linear regression models (unadjusted estimates and adjusted for centre, sex, APACHE II score and P : F ratio) are given in Table 47. The outcomes for the 6 months are in Tables 48–50.
| Score and time | Means estimates | Conventional ventilation (95% CI) | HFOV (95% CI) | Difference (95% CI) | p-valuea |
|---|---|---|---|---|---|
| SF-12 (mental) 6 months | Unadjusted | 45.2 (42.6 to 47.8) | 46.5 (43.8 to 49.2) | 1.3 (–2.4 to 5.0) | 0.4760 |
| Adjusted | 44.8 (41.7 to 47.9) | 46.5 (43.1 to 49.8) | 1.7 (–2.1 to 5.4) | 0.3890 | |
| SF-12 (mental) 12 months | Unadjusted | 45.5 (42.6 to 48.3) | 48.0 (45.3 to 50.7) | 2.56 (–1.30 to 6.40) | 0.1956 |
| Adjusted | 45.3 (41.8 to 48.9) | 46.8 (43.3 to 50.3) | 1.5 (–2.9 to 5.8) | 0.5089 | |
| SF-12 (physical) 6 months | Unadjusted | 36.9 (34.5 to 39.3) | 38.2 (35.4 to 40.9) | 1.3 (–2.3 to 4.9) | 0.4777 |
| Adjusted | 36.3 (33.2 to 39.4) | 38.5 (35.2 to 41.9) | 2.2 (–1.6 to 6.1) | 0.2470 | |
| SF-12 (physical) 12 months | Unadjusted | 38.7 (35.8 to 41.6) | 41.6 (38.6 to 44.5) | 2.9 (–1.3 to 6.9) | 0.1723 |
| Adjusted | 38.0 (34.3 to 41.7) | 41.5 (37.9 to 45.0) | 3.5 (–1.0 to 7.9) | 0.1309 | |
| SGRQ 6 months | Unadjusted | 33.3 (28.1 to 38.6) | 30.7 (25.3 to 36.1) | –2.6 (–10.1 to 4.9) | 0.4874 |
| Adjusted | 34.3 (27.3 to 41.3) | 29.5 (22.6 to 36.5) | –4.8 (–12.9 to 3.4) | 0.2499 | |
| SGRQ 12 months | Unadjusted | 33.6 (27.2 to 40.0) | 27.9 (21.8 to 34.1) | –5.7 (–14.4 to 3.1) | 0.2037 |
| Adjusted | 35.2 (27.0 to 43.4) | 30.0 (22.5 to 37.6) | –5.2 (–14.8 to 4.5) | 0.2918 |
| Domain | Level | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| Mobility | I have no problems in walking about | 44 (40.0%) | 45 (42.9%) | 89 |
| I have some problems in walking about | 61 (55.5%) | 57 (54.3%) | 118 | |
| I am confined to bed | 2 (1.8%) | 2 (1.9%) | 4 | |
| Missing | 3 (2.7%) | 1 (1.0%) | 4 | |
| Self-care | I have no problems with self-care | 69 (62.7%) | 75 (71.4%) | 144 |
| I have some problems with washing and dressing myself | 29 (26.4%) | 26 (24.8%) | 55 | |
| I am unable to wash and dress myself | 6 (5.5%) | 3 (2.9%) | 9 | |
| Missing | 6 (5.5%) | 1 (1.0%) | 7 | |
| Usual activities | I have no problems with performing my usual activities | 37 (33.6%) | 43 (41.0%) | 80 |
| I have some problems with my usual activities | 55 (50.0%) | 50 (47.6%) | 105 | |
| I am unable to perform by usual activities | 17 (15.5%) | 10 (9.5%) | 27 | |
| Missing | 1 (0.9%) | 2 (1.9%) | 3 | |
| Pain/discomfort | I have no pain or discomfort | 40 (36.4%) | 54 (51.4%) | 94 |
| I have moderate pain or discomfort | 54 (49.1%) | 40 (38.1%) | 94 | |
| I have extreme pain or discomfort | 14 (12.7%) | 10 (9.5%) | 24 | |
| Missing | 2 (1.8%) | 1 (1.0%) | 3 | |
| Anxiety | I am not anxious or depressed | 48 (43.6%) | 58 (55.2%) | 106 |
| I am moderately anxious or depressed | 52 (47.3%) | 34 (32.3%) | 86 | |
| I am extremely anxious or depressed | 9 (8.2%) | 13 (12.4%) | 22 | |
| Missing | 1 (1.0%) | 0 (0.0%) | 1 |
| Domain | Level | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| Mobility | I have no problems in walking about | 29 (34.5%) | 45 (47.4%) | 74 |
| I have some problems in walking about | 49 (58.3%) | 44 (46.3%) | 93 | |
| I am confined to bed | 2 (2.4%) | 2 (2.1%) | 4 | |
| Missing | 4 (4.8%) | 4 (4.2%) | 8 | |
| Self-care | I have no problems with self-care | 50 (59.5%) | 65 (68.4%) | 115 |
| I have some problems with washing and dressing myself | 28 (33.3%) | 26 (27.4%) | 54 | |
| I am unable to wash and dress myself | 4 (4.8%) | 1 (1.1%) | 5 | |
| Missing | 2 (2.4%) | 3 (3.2%) | 5 | |
| Usual activities | I have no problems with performing my usual activities | 30 (35.7%) | 42 (44.2%) | 72 |
| I have some problems with my usual activities | 40 (47.6%) | 44 (46.3%) | 84 | |
| I am unable to perform by usual activities | 10 (11.9%) | 7 (7.4%) | 17 | |
| Missing | 4 (4.8%) | 2 (2.1%) | 6 | |
| Pain/discomfort | I have no pain or discomfort | 31 (36.9%) | 44 (46.3%) | 75 |
| I have moderate pain or discomfort | 44 (52.4%) | 41 (43.2%) | 85 | |
| I have extreme pain or discomfort | 6 (7.1%) | 9 (9.5%) | 15 | |
| Missing | 3 (3.6%) | 1 (1.0%) | 4 | |
| Anxiety | I am not anxious or depressed | 32 (38.1%) | 48 (50.5%) | 80 |
| I am moderately anxious or depressed | 43 (51.2%) | 34 (35.8%) | 77 | |
| I am extremely anxious or depressed | 8 (9.5%) | 11 (11.6%) | 19 | |
| Missing | 1 (1.2%) | 2 (2.1%) | 3 |
| Assessment point | Summary measure | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| 6 months | Mean | 33.3 | 30.7 | 32.0 |
| n | 86 | 80 | 163 | |
| SD | 24.5 | 23.9 | 24.2 | |
| Median | 28.4 | 26.2 | 27.2 | |
| Range | 0.0–88.9 | 0.0–90.3 | 0.0–90.3 | |
| 12 months | Mean | 32.6 | 27.9 | 30.6 |
| n | 59 | 67 | 126 | |
| SD | 24.4 | 25.1 | 24.9 | |
| Median | 30.3 | 22.2 | 28.4 | |
| Range | 0.0–79.8 | 0.0–89.4 | 0.0–89.4 |
Twelve-month follow-up
-
Similar to the 6-month flow of patients, the 12-month rates are displayed in Table 51.
-
The follow-up rate at 12 months is currently 60%.
| Score | Time | Measure | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|---|
| SF-12 (mental) | 6 months | Mean | 45.2 | 46.5 | 45.8 |
| n | 98 | 94 | 192 | ||
| SD | 12.7 | 13.2 | 13.0 | ||
| Median | 44.9 | 50.7 | 47.1 | ||
| Range | 18.4–72.0 | 15.8–67.1 | 15.8–72.0 | ||
| 12 months | Mean | 45.5 | 48.0 | 46.8 | |
| n | 73 | 80 | 153 | ||
| SD | 12.1 | 12.2 | 12.2 | ||
| Median | 44.3 | 51.1 | 47.7 | ||
| Range | 19.7–68.3 | 15.6–64.9 | 15.6–68.3 | ||
| SF-12 (physical) | 6 months | Mean | 36.9 | 38.2 | 37.5 |
| n | 98 | 94 | 192 | ||
| SD | 11.9 | 13.4 | 12.6 | ||
| Median | 35.8 | 39.4 | 36.8 | ||
| Range | 11.1–61.9 | 8.2–66.1 | 8.2–66.1 | ||
| 12 months | Mean | 38.7 | 41.6 | 40.2 | |
| n | 73 | 80 | 153 | ||
| SD | 12.5 | 13.2 | 12.9 | ||
| Median | 37.4 | 40.8 | 39.0 | ||
| Range | 12.2–63.9 | 18.9–65.5 | 11.9–65.5 | ||
| SGRQ | 6 months | Mean | 33.30 | 30.68 | 32.10 |
| n | 86 | 77 | 163 | ||
| SD | 24.5 | 23.9 | 24.2 | ||
| Median | 28.4 | 26.2 | 27.2 | ||
| Range | 0.0–88.9 | 0.0–90.3 | 0.0–90.3 | ||
| 12 months | Mean | 33.6 | 27.9 | 30.6 | |
| n | 59 | 67 | 126 | ||
| SD | 24.4 | 25.1 | 24.9 | ||
| Median | 30.3 | 22.2 | 28.4 | ||
| Range | 0.0–79.7 | 0.0–89.4 | 0.0–89.4 |
Subgroup analysis
Severity of illness
The APACHE II score was used to compute the risk of dying and thus the severity of illness. For the calculation, the diagnostic coefficient was set to 0 (i.e. all the patients were given a respiratory infection diagnosis). A logistic regression model was set up to assess the risk of dying, with the APACHE II score as the independent variable. The cut-off point of a score of 26 for the APACHE II score was chosen, as this divided patients into equal risk groups [patients with a score of < 26 (N = 607) had more than 50% risk of survival, whereas those with a score of ≥ 26 (N = 188) had less than 50% risk of survival]. Thus, those in the latter category were more severely ill. The 50% risk cut off was selected during study design.
There is an indication that the interaction term for the subgroupings of illness and intervention is significant, with patients who are more ill likely to survive (up to 30 days) on the conventional ventilation group and patients who are less ill likely to survive (up to 30 days) on the intervention group (Table 52 and Figure 11).
| Illness | Treatment | Median (quartile range) | n | Died | Hazard ratio (risk of dying) | p-value (interaction) |
|---|---|---|---|---|---|---|
| Less | Conventional ventilation | 30 (12–30) | 304 | 116 | 1.2 (0.9 to 1.5) | 0.0104 |
| Less | HFOV | 30 (14–30) | 303 | 103 | ||
| More | Conventional ventilation | 28 (8–30) | 93 | 47 | 0.6 (0.4 to 0.9) | |
| More | HFOV | 30 (4–30) | 95 | 63 |
FIGURE 11.
Subgroup analysis: Kaplan–Meier curve for number of days survived (up to 30 days) with subgroups of severity of illness (n = 795).

The statistical significance of the interaction term (p = 0.0104) indicates the need for caution in interpreting these findings.
The interaction of intervention and the two groups of illness for the number of days in ICU (Table 53 and Figure 12) and number of days in hospital (Table 54 and Figure 13) were not significant.
| Illness | Treatment | Median (quartile range) | n | Died | Hazard ratio (risk of dying) | p-value (interaction) |
|---|---|---|---|---|---|---|
| Less | Conventional ventilation | 12 (6.5–20.0) | 304 | 114 | 0.7 (0.5 to 1.1) | 0.0637 |
| Less | HFOV | 14 (8–23) | 302 | 113 | ||
| More | Conventional ventilation | 12 (6–40) | 93 | 53 | 1.4 (0.9 to 1.5) | |
| More | HFOV | 9 (4–19) | 95 | 95 |
FIGURE 12.
Subgroup analysis: Kaplan–Meier curve for number of days in ICU with subgroups of severity of illness (n = 794).
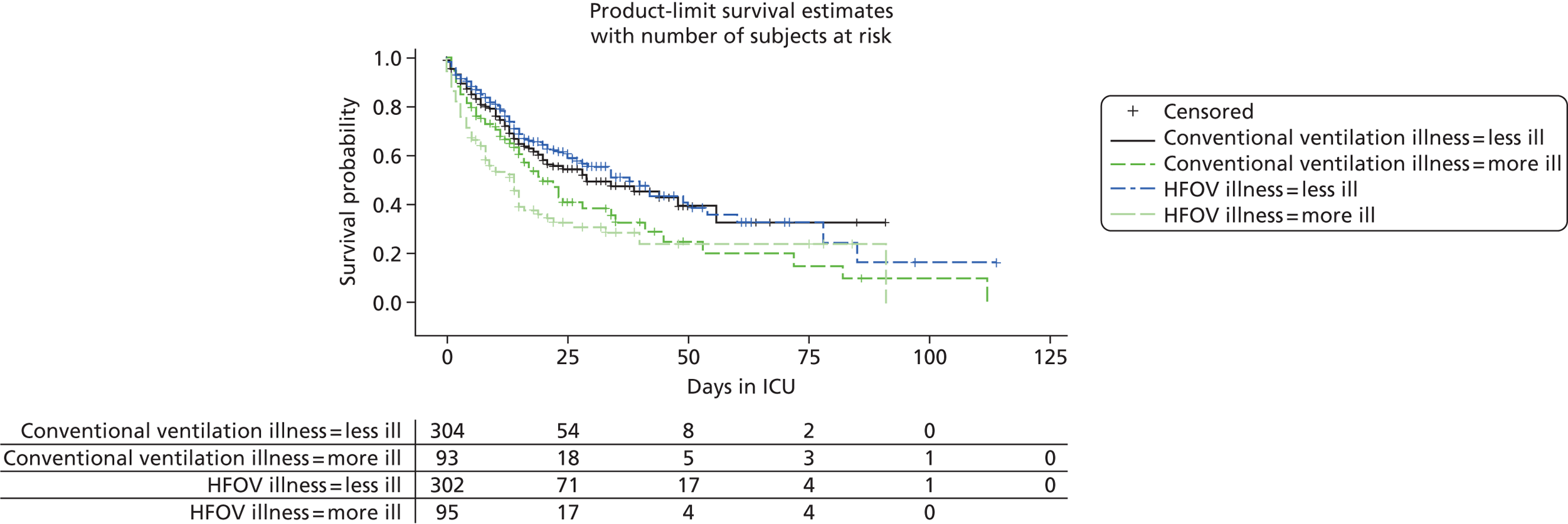
| Illness | Treatment | Median (quartile range) | n | Died | Hazard ratio (risk of dying) | p-value (interaction) |
|---|---|---|---|---|---|---|
| Less | Conventional ventilation | 21 (10–44) | 303 | 133 | 1.1 (0.8 to 1.4) | 0.1085 |
| Less | HFOV | 23 (12–42) | 299 | 129 | ||
| More | Conventional ventilation | 18 (7.5–40.0) | 92 | 58 | 0.75 (0.50 to 1.10) | |
| More | HFOV | 13 (4–13) | 94 | 68 |
FIGURE 13.
Subgroup analysis: Kaplan–Meier curve for number of days up to hospital discharge with subgroups of severity of illness (n = 788).
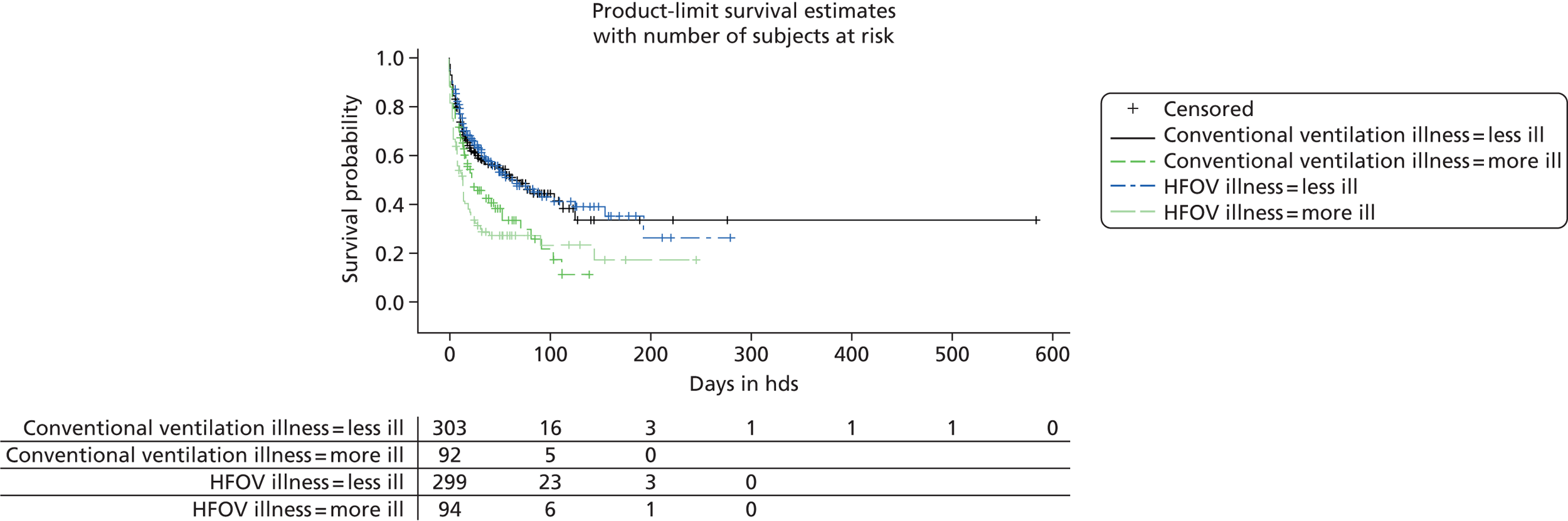
P : F ratio
The cut-off point for the P : F ratio was based on the median value of 15 kPa (i.e. the value where 50% of the data fall above and below 15 kPa).
There was no indication of an interaction between intervention and the categories of P : F ratio for any of the outcomes (Tables 55–57 and Figures 14–16).
| Illness | Treatment | Median (quartile range) | n | Died | Hazard ratio (risk of dying) | p-value (interaction) |
|---|---|---|---|---|---|---|
| < 15 kPa | Conventional ventilation | 30 (6–30) | 221 | 110 | 0.8 (0.6 to 1.2) | 0.3906 |
| < 15 kPa | HFOV | 30 (7–30) | 211 | 102 | ||
| ≥ 15 kPa | Conventional ventilation | 30 (19–30) | 176 | 53 | 1.0 (0.8 to 1.4) | |
| ≥ 15 kPa | HFOV | 30 (14–30) | 187 | 64 |
| Illness | Treatment | Median (quartile range) | n | Died | Hazard ratio (risk of dying) | p-value (interaction) |
|---|---|---|---|---|---|---|
| < 15 kPa | Conventional ventilation | 12 (5–18) | 221 | 109 | 0.9 (0.6 to 1.3) | 0.4863 |
| < 15 kPa | HFOV | 13 (6–22) | 210 | 109 | ||
| ≥ 15 kPa | Conventional ventilation | 13 (7–22) | 176 | 58 | 1.1 (0.8 to 1.4) | |
| ≥ 15 kPa | HFOV | 14 (9–23) | 187 | 66 |
| Illness | Treatment | Median (quartile range) | n | Died | Hazard ratio (risk of dying) | p-value (interaction) |
|---|---|---|---|---|---|---|
| < 15 kPa | Conventional ventilation | 15 (6–33) | 280 | 181 | 1.0 (0.8 to 1.2) | 0.7739 |
| < 15 kPa | HFOV | 14 (6–33) | 276 | 185 | ||
| ≥ 15 kPa | Conventional ventilation | 33 (21–65) | 115 | 10 | 0.9 (0.4 to 2.0) | |
| ≥ 15 kPa | HFOV | 32 (22–52) | 117 | 12 |
FIGURE 14.
Subgroup analysis: Kaplan–Meier curve for number of days survived (up to 30 days) with subgroups based on P : F ratio (n = 795).
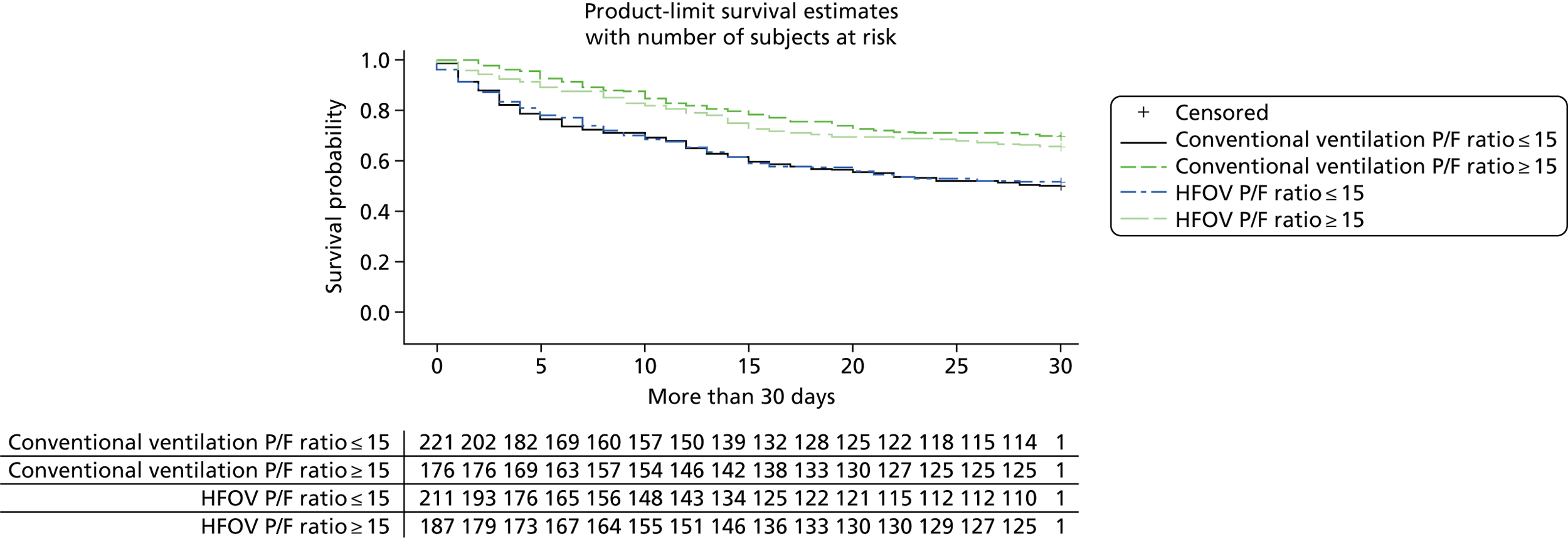
FIGURE 15.
Subgroup analysis: Kaplan–Meier curve for number of days in ICU with subgroups based on P : F ratio (n = 795).

FIGURE 16.
Subgroup analysis: Kaplan–Meier curve for number of days in hospital with subgroups based on P : F ratio (n = 788).

Causes of hypoxaemic respiratory failure
The two categories for the cause of hypoxaemic respiratory failure were pulmonary and extrapulmonary.
There was no indication of an interaction between intervention and the categories of hypoxaemic respiratory failure for any of the outcomes (Tables 58–60 and Figures 17–19).
| Illness | Treatment | Median (quartile range) | n | Died | Hazard ratio (risk of dying) | p-value (interaction) |
|---|---|---|---|---|---|---|
| Pulmonary | Conventional ventilation | 30 (11.5–30.0) | 304 | 131 | 0.9 (0.6 to 1.5) | 0.8096 |
| Pulmonary | HFOV | 30 (9–30) | 302 | 130 | ||
| Extrapulmonary | Conventional ventilation | 30 (10–30) | 93 | 32 | 1.0 (0.8 to 1.3) | |
| Extrapulmonary | HFOV | 30 (13.5–30.0) | 96 | 36 |
| Illness | Treatment | Median (quartile range) | n | Died | Hazard ratio | p-value (interaction) |
|---|---|---|---|---|---|---|
| Pulmonary | Conventional ventilation | 13 (6–21) | 304 | 134 | 1.0 (0.6 to 1.3) | 0.8293 |
| Pulmonary | HFOV | 13 (7–23) | 301 | 137 | ||
| Extrapulmonary | Conventional ventilation | 11 (7–20) | 93 | 33 | 1.0 (0.8 to 1.3) | |
| Extrapulmonary | HFOV | 13 (8.5–22.0) | 96 | 38 |
| Illness | Treatment | Median (quartile range) | n | Died | Hazard ratio | p-value (interaction) |
|---|---|---|---|---|---|---|
| Pulmonary | Conventional ventilation | 19 (9–41) | 303 | 155 | 0.9 (0.6 to 1.4) | 0.6678 |
| Pulmonary | HFOV | 18 (9–37) | 298 | 153 | ||
| Extrapulmonary | Conventional ventilation | 23.5 (10.0–51.0) | 92 | 36 | 1.0 (0.8 to 1.2) | |
| Extrapulmonary | HFOV | 28 (2–52) | 95 | 44 |
FIGURE 17.
Subgroup analysis: Kaplan–Meier curve for number of days survived (up to 30 days) with subgroups based on the cause of hypoxaemic respiratory failure (n = 795).

FIGURE 18.
Subgroup analysis: Kaplan–Meier curve for number of days in ICU with subgroups based on the cause of hypoxaemic respiratory failure (n = 794).

FIGURE 19.
Subgroup analysis: Kaplan–Meier curve for number of days in hospital with subgroups based on the cause of hypoxaemic respiratory failure (n = 794).
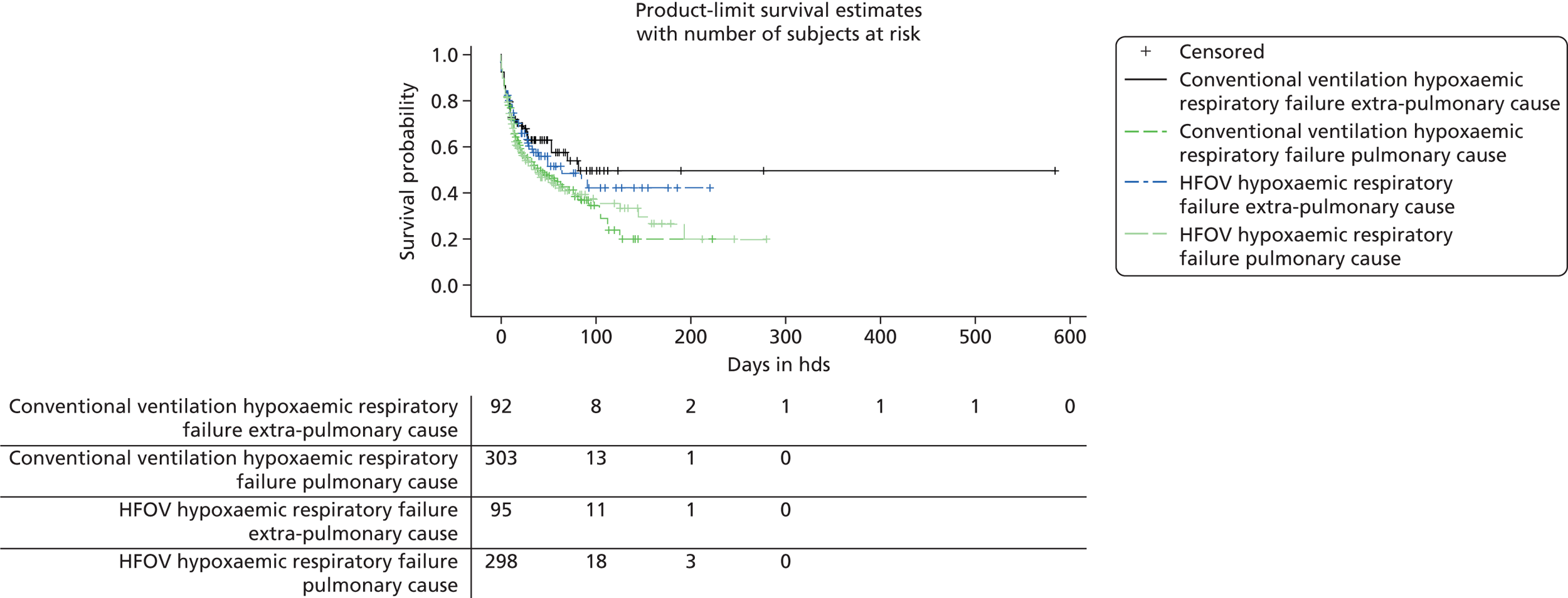
Per-protocol analysis
There are 84 patients who had a protocol violation (as detailed in Table 17). These patients were as follows:
-
Randomised to HFOV but did not receive it: 8.
-
Randomised to HFOV but received < 12 hours of HFOV: 25.
-
Randomised to HFOV but did not receive it and received < 12 hours of HFOV: 2.
-
Randomised to HFOV but received < 12 hours of HFOV and classified as protocol violator: 3.
-
Randomised to HFOV but received < 12 hours of HFOV and recorded as ventilator problems on HFOV weaning: 3.
-
Randomised to conventional ventilation but received HFOV: 11.
-
Classified as protocol violator: 15.
-
Classified as protocol violator and recorded as ventilator problems: 1.
-
Recorded as ventilator problems on HFOV weaning: 16.
Table 61 illustrates the distribution of patients who violated the protocol and the randomised treatment allocations.
| Compliance | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| Violation of the protocol | 11 (2.8%) | 73 (18.3%) | 84 (10.6%) |
| Complied with the protocol | 386 (97.2%) | 325 (81.7%) | 711 (89.4%) |
| Total | 397 | 398 | 795 |
The following tables contain patients who complied with the protocol (n = 711, Tables 62–81).
| Ventilation | Summary measure | Exhaled minute volume (l/minute) | Total respiratory rate (breaths/minute) | PEEP (cmH2O) | Plateau pressure (cmH2O) | Arterial blood gas | |||
|---|---|---|---|---|---|---|---|---|---|
| PaO2 (kPa) | PaCO2 (kPa) | pH | FiO2 | ||||||
| Conventional ventilation | Mean | 10.20 | 21.20 | 11.33 | 22.33 | 10.47 | 6.88 | 7.32 | 0.74 |
| n | 385 | 386 | 380 | 370 | 386 | 386 | 381 | 386 | |
| SD | 3.47 | 8.23 | 3.31 | 9.17 | 2.52 | 1.84 | 0.10 | 0.18 | |
| Median | 9.90 | 20.00 | 10.00 | 24.00 | 10.00 | 6.70 | 7.32 | 0.70 | |
| Minimum | 0.30 | 8.00 | 5.00 | 0.00 | 5.00 | 3.50 | 7.00 | 0.35 | |
| Maximum | 33.40 | 70.00 | 36.00 | 48.00 | 24.20 | 16.30 | 7.53 | 1.00 | |
| Missing | 1 | 0 | 6 | 16 | 0 | 0 | 5 | 0 | |
| HFOV | Mean | 10.38 | 20.96 | 11.28 | 21.58 | 10.23 | 6.87 | 7.32 | 0.72 |
| n | 325 | 325 | 320 | 315 | 325 | 325 | 319 | 325 | |
| SD | 3.34 | 8.22 | 3.29 | 9.08 | 2.19 | 1.81 | 0.11 | 0.18 | |
| Median | 10.10 | 20.00 | 10.00 | 22.00 | 9.90 | 6.70 | 7.33 | 0.70 | |
| Minimum | 3.04 | 0.00 | 5.00 | 0.00 | 5.90 | 3.60 | 6.86 | 0.35 | |
| Maximum | 30.8 | 69.0 | 33.0 | 43.0 | 23.6 | 15.9 | 7.7 | 1.0 | |
| Missing | 0 | 0 | 5 | 10 | 0 | 0 | 6 | 0 | |
| Total | Mean | 10.28 | 21.09 | 11.31 | 21.00 | 10.36 | 6.90 | 7.32 | 0.73 |
| n | 710 | 711 | 700 | 685 | 711 | 711 | 700 | 711 | |
| SD | 3.41 | 8.22 | 3.30 | 9.13 | 2.37 | 1.82 | 0.10 | 0.18 | |
| Median | 9.93 | 20.00 | 10.00 | 23.00 | 10.00 | 6.70 | 7.32 | 0.70 | |
| Minimum | 0.30 | 0.00 | 5.00 | 0.00 | 5.00 | 3.50 | 6.86 | 0.35 | |
| Maximum | 33.4 | 70.0 | 36.0 | 48.0 | 24.2 | 16.3 | 7.7 | 1.0 | |
| Missing | 1 | 0 | 11 | 26 | 0 | 0 | 11 | 0 | |
| Treatment or organ support | Response | Conventional ventilation | HFOV | Total | |
|---|---|---|---|---|---|
| Support organ monitoring | Advanced respiratory support | No | 1 (0.3%) | 1 (0.3%) | 2 (0.3%) |
| Yes | 385 (99.7%) | 324 (99.7%) | 709 (99.7%) | ||
| Basic respiratory support | No | 325 (84.2%) | 282 (86.8%) | 607 (85.4%) | |
| Yes | 61 (15.8%) | 43 (13.2%) | 104 (14.6%) | ||
| Advanced cardiovascular support | No | 205 (53.1%) | 201 (61.8%) | 406 (57.1%) | |
| Yes | 181 (46.9%) | 124 (38.2%) | 305 (42.9%) | ||
| Basic cardiovascular support | No | 142 (36.8%) | 104 (32.0%) | 246 (34.6%) | |
| Yes | 244 (63.2%) | 221 (68.0%) | 465 (65.4%) | ||
| Renal support | No | 316 (81.9%) | 261 (80.3%) | 577 (81.2%) | |
| Yes | 70 (18.1%) | 64 (19.7%) | 134 (18.8%) | ||
| Gastrointestinal support | No | 84 (21.8%) | 65 (20.0%) | 149 (21.0%) | |
| Yes | 302 (78.2%) | 260 (80.0%) | 562 (79.0%) | ||
| Dermatological support | No | 373 (96.6%) | 312 (96.0%) | 685 (96.3%) | |
| Yes | 13 (3.4%) | 13 (4.0%) | 26 (3.7%) | ||
| Liver support | No | 381 (98.7%) | 325 (100.0%) | 706 (99.3%) | |
| Yes | 5 (1.3%) | 0 (0.0%) | 5 (0.7%) | ||
| Antimicrobial use | Antimicrobial drug received | No | 12 (3.1%) | 13 (4.0%) | 25 (3.5%) |
| Yes | 374 (96.9%) | 312 (96.0%) | 686 (96.5%) | ||
| Antimicrobial for pulmonary infection | No | 59 (15.8%) | 54 (17.3%) | 113 (16.5%) | |
| Yes | 315 (84.2%) | 258 (82.7%) | 573 (83.5%) | ||
| Antimicrobial intravenous | No | 3 (0.8%) | 2 (0.6%) | 5 (0.7%) | |
| Yes | 371 (99.2%) | 310 (99.4%) | 681 (99.3%) | ||
| Sedation use | Sedation received | No | 7 (1.8%) | 7 (2.2%) | 14 (2.0%) |
| Yes | 379 (98.2%) | 318 (97.8%) | 697 (98.0%) | ||
| Sedation intravenous | No | 342 (90.2%) | 278 (87.4%) | 620 (89.0%) | |
| Yes | 37 (9.8%) | 40 (12.6%) | 77 (11.0%) | ||
| Sedation infusion | No | 2 (0.5%) | 2 (0.6%) | 4 (0.6%) | |
| Yes | 377 (99.5%) | 316 (99.4%) | 693 (99.4%) | ||
| Sedation one class | No | 45 (11.9%) | 41 (12.9%) | 86 (12.3%) | |
| Yes | 334 (88.1%) | 277 (87.1%) | 611 (87.7%) | ||
| Sedation two classes | No | 329 (86.8%) | 283 (89.0%) | 612 (87.8%) | |
| Yes | 50 (13.2%) | 35 (11.0%) | 85 (12.2%) | ||
| Sedation three or more classes | No | 376 (99.2%) | 315 (99.1%) | 691 (99.1%) | |
| Yes | 3 (0.8%) | 3 (0.9%) | 6 (0.9%) | ||
| Muscle relaxants | Muscle relaxants received | No | 218 (56.5%) | 180 (55.4%) | 398 (56.0%) |
| Yes | 168 (43.5%) | 145 (44.6%) | 313 (44.0%) | ||
| Muscle relaxants intravenous | No | 87 (51.8%) | 66 (45.5%) | 153 (48.9%) | |
| Yes | 81 (48.2%) | 79 (54.5%) | 160 (51.1%) | ||
| Muscle relaxants infusion | No | 68 (40.5%) | 58 (40.0%) | 126 (40.3%) | |
| Yes | 100 (59.5%) | 87 (60.0%) | 187 (59.7%) | ||
| Others | Prone position ventilated | No | 153 (91.1%) | 130 (89.7%) | 283 (90.4%) |
| Yes | 15 (8.9%) | 15 (10.3%) | 30 (9.6%) | ||
| Nitric oxide received | No | 378 (97.9%) | 316 (97.2%) | 694 (97.6%) | |
| Yes | 8 (2.1%) | 9 (2.8%) | 17 (2.4%) | ||
| Interval | Summary measure | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| Time from hospital admission to ICU admission (days) | Mean | 3.86 | 4.19 | 4.01 |
| n | 386 | 325 | 711 | |
| SD | 7.57 | 10.31 | 8.92 | |
| Median | 1 | 1 | 1 | |
| Minimum | 0 | 0 | 0 | |
| Maximum | 80 | 108 | 108 | |
| Time from hospital admission to randomisation (days) | Mean | 8.38 | 7.07 | 7.78 |
| n | 386 | 325 | 711 | |
| SD | 37.78 | 11.18 | 28.83 | |
| Median | 4 | 4 | 4 | |
| Minimum | 0 | 0 | 0 | |
| Maximum | 732 | 130 | 732 | |
| Time from ICU to randomisation (days) | Mean | 4.53 | 2.88 | 3.77 |
| n | 386 | 325 | 711 | |
| SD | 37.20 | 2.61 | 27.46 | |
| Median | 2 | 2 | 2 | |
| Minimum | 0 | 0 | 0 | |
| Maximum | 732 | 22 | 732 |
| Demographic | Summary measure | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| Age group (years) | ≤ 55 | 168 (43.5%) | 148 (45.5%) | 316 (44.4%) |
| > 55 | 218 (56.5%) | 177 (54.5%) | 395 (55.6%) | |
| Sex | Male | 230 (59.6%) | 207 (63.7%) | 437 (61.5%) |
| Female | 156 (40.4%) | 118 (36.3%) | 274 (38.5%) | |
| P : F ratio | ≤ 15 | 227 (58.8%) | 188 (57.8%) | 415 (58.4%) |
| > 15 | 159 (41.2%) | 137 (42.2%) | 296 (41.6%) | |
| Weight (kg) | Mean | 78.70 | 81.23 | 79.86 |
| n | 386 | 325 | 711 | |
| SD | 20.98 | 21.91 | 21.43 | |
| Median | 76 | 80 | 78 | |
| Minimum | 37 | 40 | 37 | |
| Maximum | 215 | 186 | 215 | |
| PaO2 (kPa) | Mean | 10.47 | 10.23 | 10.36 |
| n | 386 | 325 | 711 | |
| SD | 2.52 | 2.18 | 2.37 | |
| Median | 10.0 | 9.9 | 10.0 | |
| Minimum | 5.0 | 5.9 | 5.0 | |
| Maximum | 24.2 | 23.6 | 24.2 | |
| Associated FiO2 | Mean | 0.74 | 0.73 | 0.73 |
| n | 386 | 325 | 711 | |
| SD | 0.18 | 0.18 | 0.18 | |
| Median | 0.70 | 0.70 | 0.70 | |
| Minimum | 0.35 | 0.35 | 0.35 | |
| Maximum | 1.00 | 1.00 | 1.00 |
| Cause of respiratory failure | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| Pulmonary | 298 (77.2%) | 248 (76.3%) | 546 (76.8%) |
| Extrapulmonary | 88 (22.8%) | 77 (23.7%) | 165 (23.2%) |
| Ventilation start | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| Before hospital admission | 20 (5.2%) | 11 (3.4%) | 31 (4.4%) |
| Prior to ICU admission | 116 (30.0%) | 96 (29.5%) | 212 (29.8%) |
| During ICU stay | 249 (64.5%) | 218 (67.1%) | 467 (65.7%) |
| Where first ventilated not known | 1 (0.3%) | 0 (0.0%) | 1 (0.1%) |
| Patient height or heel/crown (m/cm) | Conventional ventilation | HFOV | Total |
| Mean | 1.68 | 1.69 | 1.69 |
| n | 376 | 316 | 692 |
| SD | 0.11 | 0.11 | 0.11 |
| Median | 1.68 | 1.70 | 1.69 |
| Minimum | 1.40 | 1.21 | 1.21 |
| Maximum | 2.01 | 1.97 | 2.01 |
| Summary measure | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| Mean | 21.9 | 21.6 | 21.8 |
| n | 372 | 313 | 685 |
| SD | 6.07 | 5.87 | 5.97 |
| Median | 22 | 22 | 22 |
| Minimum | 5 | 7 | 5 |
| Maximum | 45 | 39 | 45 |
| Surgical status | NCEPOD classification | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| Was the patient admitted to your ICU directly from the operating theatre/recovery area in your hospital? | No | 338 (87.6%) | 282 (88.8%) | 620 (87.2%) |
| Yes | 48 (12.4%) | 43 (13.2%) | 91 (12.8%) | |
| If ‘yes’ | Emergency | 19 (39.6%) | 19 (44.2%) | 38 (41.8%) |
| Urgent | 17 (35.4%) | 17 (39.5%) | 34 (37.4%) | |
| Scheduled | 2 (4.2%) | 1 (2.3%) | 3 (3.3%) | |
| Elective | 10 (20.8%) | 6 (14.0%) | 16 (17.6%) |
| Support | Summary measure | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| Ventilation-free days up to 30 days post randomisation | Mean | 2.3 | 2.8 | 2.6 |
| n | 386 | 325 | 711 | |
| SD | 3.5 | 3.5 | 3.5 | |
| Median | 1 | 2 | 1 | |
| Range | 0–21 | 0–20 | 0–21 | |
| Advanced respiratory support-free days | Mean | 3.2 | 3.9 | 3.5 |
| n | 386 | 325 | 711 | |
| SD | 4.7 | 6.1 | 5.4 | |
| Median | 2 | 2 | 2 | |
| Range | 0–32 | 0–57 | 0–57 | |
| Basic respiratory support-free days | Mean | 14.5 | 16.0 | 15.2 |
| n | 386 | 325 | 711 | |
| SD | 13.8 | 15.5 | 14.4 | |
| Median | 11 | 12 | 11 | |
| Range | 0–91 | 0–106 | 0–106 | |
| Days on advanced cardiovascular support | Mean | 2.8 | 2.7 | 2.8 |
| n | 386 | 325 | 711 | |
| SD | 5.7 | 4.1 | 5.0 | |
| Median | 1 | 1 | 1 | |
| Range | 0–75 | 0–28 | 0–75 | |
| Days on basic cardiovascular support | Mean | 11.6 | 13.1 | 12.3 |
| n | 386 | 325 | 711 | |
| SD | 10.6 | 11.8 | 11.2 | |
| Median | 10 | 11 | 10 | |
| Range | 0–73 | 0–85 | 0–85 | |
| Days on renal support | Mean | 2.57 | 4.5 | 3.5 |
| n | 386 | 325 | 711 | |
| SD | 5.0 | 8.1 | 6.7 | |
| Median | 0 | 0 | 0 | |
| Range | 0–34 | 0–52 | 0–52 | |
| Days on gastrointestinal support | Mean | 15.9 | 17.7 | 16.7 |
| n | 386 | 325 | 711 | |
| SD | 15.1 | 16.6 | 15.8 | |
| Median | 12 | 13 | 13 | |
| Range | 0–113 | 0–114 | 0–114 | |
| Days on dermatological support | Mean | 1.1 | 0.9 | 1.0 |
| n | 386 | 325 | 711 | |
| SD | 5.4 | 4.2 | 4.9 | |
| Median | 0 | 0 | 0 | |
| Range | 0–59 | 0–31 | 0–59 | |
| Days on liver support | Mean | 0.04 | 0.02 | 0.03 |
| n | 386 | 325 | 711 | |
| SD | 0.37 | 0.15 | 0.29 | |
| Median | 0 | 0 | 0 | |
| Range | 0–5 | 0–2 | 0–5 |
| Antimicrobial use | Summary measure | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| Number of days free from antimicrobial used | Mean | 4.9 | 5.8 | 5.3 |
| n | 386 | 325 | 711 | |
| SD | 8.2 | 8.9 | 8.5 | |
| Median | 1 | 2 | 2 | |
| Range | 0–60 | 0–63 | 0–63 | |
| Number of days antimicrobial used | Mean | 12.2 | 13.3 | 12.7 |
| n | 386 | 325 | 711 | |
| SD | 10.3 | 12.5 | 11.4 | |
| Median | 10 | 10 | 10 | |
| Range | 0–68 | 0–111 | 0–111 | |
| Number of days antimicrobial used to treat pulmonary infection | Mean | 9.7 | 10.4 | 10.0 |
| n | 39 | 325 | 711 | |
| SD | 9.3 | 10.2 | 9.7 | |
| Median | 8 | 8 | 8 | |
| Range | 0–54 | 0–68 | 0–68 | |
| Number of days antimicrobial given intravenously | Mean | 11.5 | 12.4 | 11.9 |
| n | 386 | 325 | 711 | |
| SD | 9.5 | 11.1 | 10.3 | |
| Median | 9 | 10 | 10 | |
| Range | 0–60 | 0–86 | 0–86 |
| Sedative use | Summary measure | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| Number of days free from sedative received primarily for sedation | Mean | 8.9 | 9.5 | 9.2 |
| n | 386 | 325 | 711 | |
| SD | 12.7 | 14.7 | 13.6 | |
| Median | 5 | 5 | 5 | |
| Range | 0–108 | 0–97 | 0–97 | |
| Number of days sedative received primarily for sedation | Mean | 8.2 | 9.7 | 8.9 |
| n | 386 | 325 | 711 | |
| SD | 6.4 | 7.4 | 6.9 | |
| Median | 7 | 8 | 7 | |
| Range | 0–38 | 0–50 | 0–50 | |
| Number of days an intravenous bolus dose used | Mean | 0.5 | 0.4 | 0.4 |
| n | 386 | 325 | 711 | |
| SD | 2.1 | 1.2 | 1.7 | |
| Median | 0 | 0 | 0 | |
| Range | 0–30 | 0–13 | 0–30 | |
| Number of days sedative given by infusion | Mean | 8.1 | 9.4 | 8.7 |
| n | 386 | 325 | 711 | |
| SD | 6.4 | 7.2 | 6.8 | |
| Median | 6.5 | 8.0 | 7.0 | |
| Range | 0–38 | 0–50 | 0–50 | |
| Number of days patient on more than one class of sedative | Mean | 6.4 | 7.6 | 7.0 |
| n | 386 | 325 | 711 | |
| SD | 5.6 | 5.9 | 5.8 | |
| Median | 5 | 6 | 6 | |
| Range | 0–36 | 0–44 | 0–44 | |
| Number of days patient on more than two classes of sedative | Mean | 1.3 | 1.4 | 1.4 |
| n | 386 | 325 | 711 | |
| SD | 2.9 | 3.0 | 3.0 | |
| Median | 0 | 0 | 0 | |
| Range | 0–28 | 0–26 | 0–28 | |
| Number of days patient on more than three classes of sedative | Mean | 0.1 | 0.2 | 0.1 |
| n | 386 | 325 | 711 | |
| SD | 0.8 | 0.9 | 0.8 | |
| Median | 0 | 0 | 0 | |
| Range | 0–11 | 0–9 | 0–11 |
| Muscle relaxant | Summary measure | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| Number of days patient received muscle relaxant drugs to aid artificial ventilation | Mean | 2.0 | 2.5 | 2.2 |
| n | 386 | 325 | 711 | |
| SD | 3.0 | 3.6 | 3.3 | |
| Median | 1 | 1 | 1 | |
| Range | 0–22 | 0–25 | 0–25 | |
| Number of days an intravenous bolus dose use | Mean | 0.5 | 0.6 | 0.5 |
| n | 386 | 325 | 711 | |
| SD | 1.0 | 0.9 | 1.0 | |
| Median | 0 | 0 | 0 | |
| Range | 0–6 | 0–5 | 0–6 | |
| Number of days muscle relaxants given by infusion | Mean | 1.6 | 2.0 | 1.8 |
| n | 386 | 325 | 711 | |
| SD | 2.8 | 3.4 | 3.1 | |
| Median | 0 | 0 | 0 | |
| Range | 0–20 | 0–24 | 0–24 |
| Treatment | Summary measure | Conventional ventilation | HFOV | Total |
|---|---|---|---|---|
| Number of days patient been placed prone | Mean | 0.5 | 0.2 | 0.3 |
| n | 386 | 325 | 711 | |
| SD | 1.3 | 0.7 | 1.0 | |
| Median | 0 | 0 | 0 | |
| Range | 0–12 | 0–8 | 0–12 | |
| Number of days patient received inhaled nitric oxide | Mean | 0.30 | 0.20 | 0.26 |
| n | 386 | 325 | 711 | |
| SD | 1.9 | 0.9 | 1.5 | |
| Median | 0 | 0 | 0 | |
| Range | 0–23 | 0–12 | 0–23 |
| Variable | Means estimates | Conventional ventilation (95% CI) | HFOV (95% CI) | Difference (95% CI) | p-valuea |
|---|---|---|---|---|---|
| Ventilation-free days up to 30 days post randomisation | Unadjusted | 2.30 (2.00 to 2.69) | 2.80 (2.44 to 3.21) | 0.50 (–0.04 to 1.00) | 0.0696 |
| Adjusted | 2.40 (1.91 to 2.86) | 2.70 (2.23 to 3.24) | 0.40 (–0.16 to 0.86) | 0.1757 | |
| Advanced respiratory support-free days | Unadjusted | 3.20 (2.71 to 3.65) | 3.90 (2.25 to 4.57) | 0.70 (–0.07 to 1.52) | 0.0735 |
| Adjusted | 3.10 (2.38 to 3.87) | 3.80 (2.96 to 4.55) | 0.60 (–0.17 to 1.43) | 0.1226 | |
| Basic respiratory support-free days | Unadjusted | 14.50 (13.15 to 15.91) | 16.00 (14.40 to 17.67) | 1.50 (–0.62 to 3.63) | 0.1646 |
| Adjusted | 13.60 (11.66 to 15.58) | 15.00 (12.92 to 17.12) | 1.40 (–0.71 to 3.52) | 0.1937 | |
| Days on advanced cardiovascular support | Unadjusted | 2.80 (2.25 to 3.39) | 2.70 (2.40 to 3.14) | –0.10 (–0.85 to 0.63) | 0.7635 |
| Adjusted | 3.00 (2.31 to 3.62) | 3.00 (2.33 to 3.73) | 0.10 (–0.63 to 0.78) | 0.8417 | |
| Days on basic cardiovascular support | Unadjusted | 11.60 (10.58 to 12.70) | 13.10 (11.78 to 13.11) | 1.40 (–0.22 to 3.07) | 0.0903 |
| Adjusted | 11.20 (9.62 to 12.71) | 12.40 (10.77 to 14.08) | 1.30 (–0.41 to 2.93) | 0.1378 | |
| Days on renal support | Unadjusted | 2.60 (2.07 to 3.08) | 4.50 (3.63 to 5.40) | 1.90 (0.97 to 2.92) | 0.0001 |
| Adjusted | 2.20 (1.32 to 3.15) | 4.20 (3.19 to 5.15) | 1.90 (0.95 to 2.92) | 0.0001 | |
| Days on gastrointestinal support | Unadjusted | 15.90 (14.41 to 17.43) | 17.70 (15.91 to 19.55) | 1.80 (–0.53 to 4.14) | 0.1286 |
| Adjusted | 15.00 (12.86 to 17.21) | 16.70 (14.40 to 19.06) | 1.70 (–0.66 to 4.04) | 0.1577 | |
| Days on dermatological support | Unadjusted | 1.10 (0.53 to 1.61) | 0.90 (0.42 to 1.34) | –0.20 (–0.91 to 0.53) | 0.6054 |
| Adjusted | 0.90 (0.24 to 1.58) | 0.70 (–0.01 to 1.44) | –0.20 (–0.92 to 0.53) | 0.5963 | |
| Days on liver support | Unadjusted | 0.040 (–0.001–0.070) | 0.020 (–0.001 to 0.030) | –0.02 (–0.06 to 0.02) | 0.3423 |
| Adjusted | 0.03 (–0.01 to 07) | 0.01 (–0.03 to 0.05) | –0.02 (–0.06 to 0.02) | 0.3562 | |
| Number of days free of antimicrobial use | Unadjusted | 4.90 (4.06 to 5.70) | 5.80 (4.86 to 6.81) | 1.00 (–0.31 to 2.21) | 0.1398 |
| Adjusted | 4.40 (3.20 to 5.57) | 5.40 (4.09 to 6.63) | 1.00 (–0.29 to 2.26) | 0.1314 | |
| Number of days free of drugs used primarily for sedation | Unadjusted | 8.90 (7.68 to 10.22) | 9.50 (7.86 to 11.08) | 0.50 (–1.49 to 2.54) | 0.6111 |
| Adjusted | 7.80 (5.90 to 9.69) | 8.20 (6.21 to 10.25) | 0.40 (–1.60 to 2.47) | 0.6737 |
Primary outcome
Table 76 illustrates the results for mortality at 30 days post randomisation. No statistically significant difference in mortality rates at 30 days post randomisation was found between the two interventions (chi-squared test: p = 0.6053). The absolute difference in mortality rates between the two interventions was 1.90% (95% CI –5.35% to 9.05%). No statistically significant difference in mortality rates at 30 days post randomisation was found between the two interventions when adjusting for centre, sex, P : F ratio and APACHE II score (logistic regression: p-value = 0.8536). The odds of being alive (as opposed to dying) were 0.97 (95% CI 0.69 to 1.36) when on conventional ventilation compared with HFOV. Figure 20 illustrates the Kaplan–Meier curve with the probability of survival up to 30 days post randomisation for each intervention. There is essentially no separation between the curves.
| Status | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| Alive | 229 (59.3%) | 199 (61.2%) | 428 (60.2%) |
| Died | 157 (40.7%) | 126 (38.8%) | 283 (39.8%) |
| Total | 386 | 325 | 711 |
FIGURE 20.
Kaplan–Meier curves for survival to day 30 post randomisation.

Secondary outcomes
Mortality rate at first discharge from intensive care unit/intensive care unit length of stay
The number (and percentage) of patients who died in ICU or were alive at discharge from ICU are summarised in Table 77 by each intervention. Note that there are 710 patients in total with ICU data, as one patient was still in an ICU when the database was analysed. No statistically significant difference in mortality rates at first discharge from ICU was found between the two interventions (chi-squared test: p = 0.9801). The difference in mortality rates between the two interventions was 0.1% (95% CI –7.2% to 7.3%). For the survival analysis, patients who died up to first discharge from ICU were uncensored and all others (including the one patient in ICU) were uncensored. No statistically significant difference in mortality rates at first discharge from ICU was found between the two interventions when adjusting for centre, sex, P : F ratio and APACHE II score (logistic regression: p-value = 0.7126). The odds of being alive (as opposed to dying) at first discharge from ICU were 1.07 (95% CI 0.76 to 1.49) when on conventional ventilation compared with HFOV.
| Status | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| Alive | 226 (58.6%) | 190 (58.6%) | 416 (58.6%) |
| Died | 160 (41.5%) | 134 (41.4%) | 294 (41.1%) |
| Total | 386 | 324 | 710 |
Table 78 details the summary statistic for the length of stay in ICU (from randomisation to first discharge). No significant difference was found in the length of stay in ICU between the interventions. Using a linear regression model, and adjusting for centre, sex, P : F ratio and APACHE II score, the mean (SE) estimates were conventions: 15.4 (1.4) days; HFOV 17.4 (1.4) days and a difference of 2.3 (1.2) days: p-value for difference = 0.0643.
| Summary measure | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| Mean | 16.0 | 18.1 | 16.9 |
| n | 386 | 324 | 710 |
| SD | 15.1 | 16.5 | 15.8 |
| Median | 12.0 | 13.5 | 13.0 |
| Range | 0–112 | 0–114 | 0–114 |
Figure 21 illustrates the Kaplan–Meier curve for the probability of survival in ICU against the number of days in ICU (with the number of patients at risk). The event here was mortality from randomisation to first discharge from ICU. Thus all patients who did not die in ICU and were discharged alive are censored (as their death date was beyond that of discharge from ICU date).
FIGURE 21.
Kaplan–Meier curves for survival to first discharge from ICU mortality rate at first discharge from hospital/hospital length of stay.
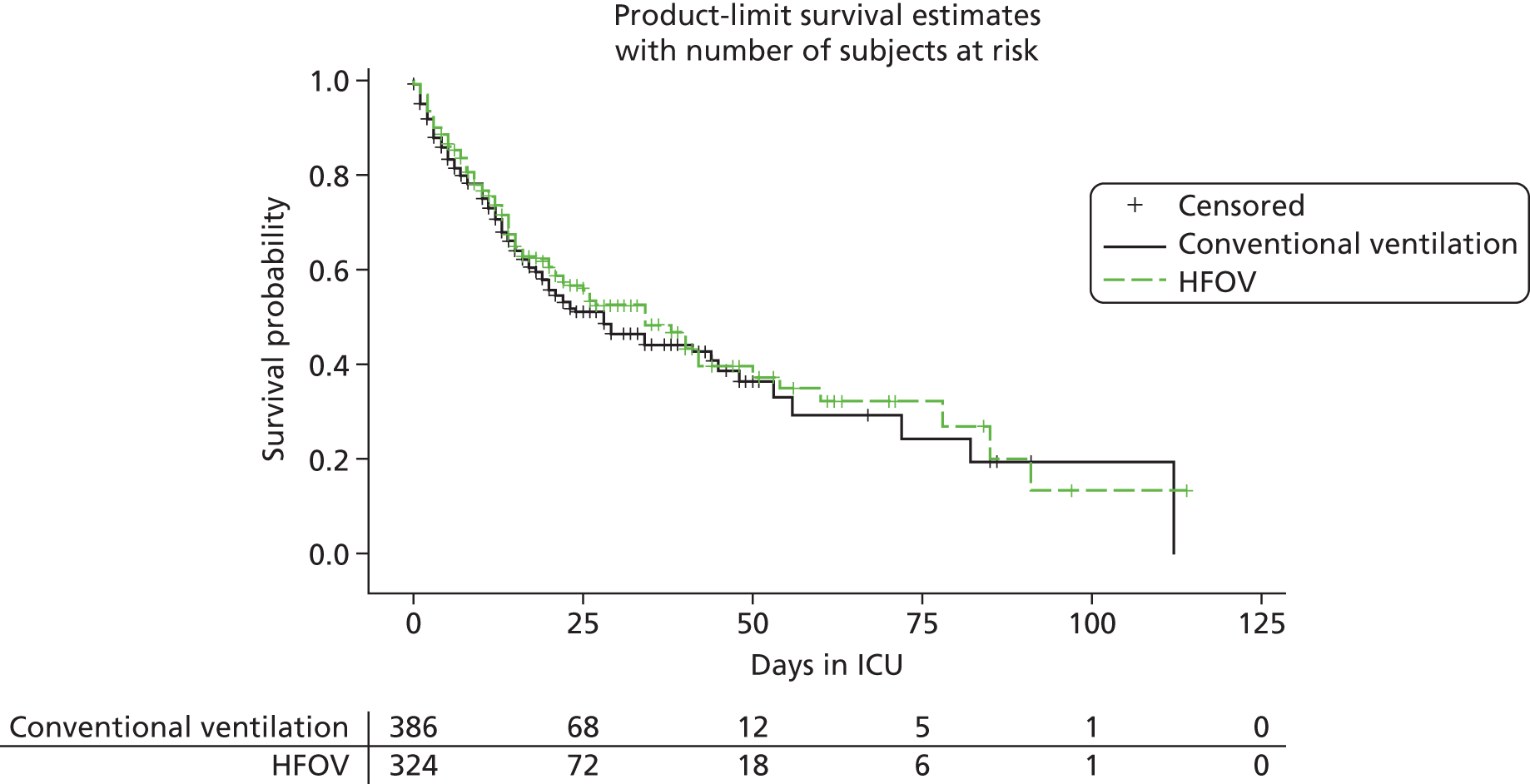
The numbers (and percentage) of patients who died prior to hospital discharge or were alive at hospital discharge are summarised in Table 79 by each intervention. Note that there are 706 patients in total with hospital data for the per protocol analysis. This is because, of the 795 randomised patients, two patients were in hospital and are also protocol violators. Thus, of the 711 patients, only five (not seven patients) would be excluded from the hospital stay data as these five have not reached end of hospital discharge.
| Status | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| Alive | 204 (51.7%) | 196 (49.9%) | 400 (50.8%) |
| Died | 191 (48.4%) | 197 (50.1%) | 388 (49.2%) |
| Total | 395 | 393 | 788 |
No statistically significant difference in mortality rates at first discharge from hospital was found between the two interventions (chi-squared test: p = 0.9641). The difference in mortality rates between the two interventions was 0.2% (95% CI –7.2% to 7.5%). No statistically significant difference in mortality rates at first discharge from hospital was found between the two interventions when adjusting for centre, sex, P : F ratio and APACHE II score (logistic regression: p-value = 0.5872). The odds of being alive (as opposed to dying) at first discharge from ICU were 1.10 (95% CI 0.79 to 1.53) when on conventional ventilation compared with HFOV.
Table 80 details the summary statistic for the length of stay in hospital (from randomisation to first discharge from hospital). No significant difference was found in the length of stay in hospital between the interventions. Using a linear regression model and adjusting for centre, sex, P : F ratio and the APACHE II score, the mean (SE) estimates were conventions: 31.1 (3.1) days; HFOV 33.6 (3.4) days and a difference of 2.5 (3.6) days: p-value for difference = 0.4563.
| Summary measure | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| Mean | 33.1 | 33.9 | 33.5 |
| n | 395 | 393 | 788 |
| SD | 44.3 | 41.6 | 43.0 |
| Median | 21 | 21 | 21 |
| Range | 0–584 | 0–280 | 0–584 |
Figure 22 illustrates the Kaplan–Meier curve for the probability of survival in hospital against the number of days in hospital (with the number of patients at risk).
FIGURE 22.
Kaplan–Meier curves displaying the probability of survival in hospital over the time in hospital for both interventions.
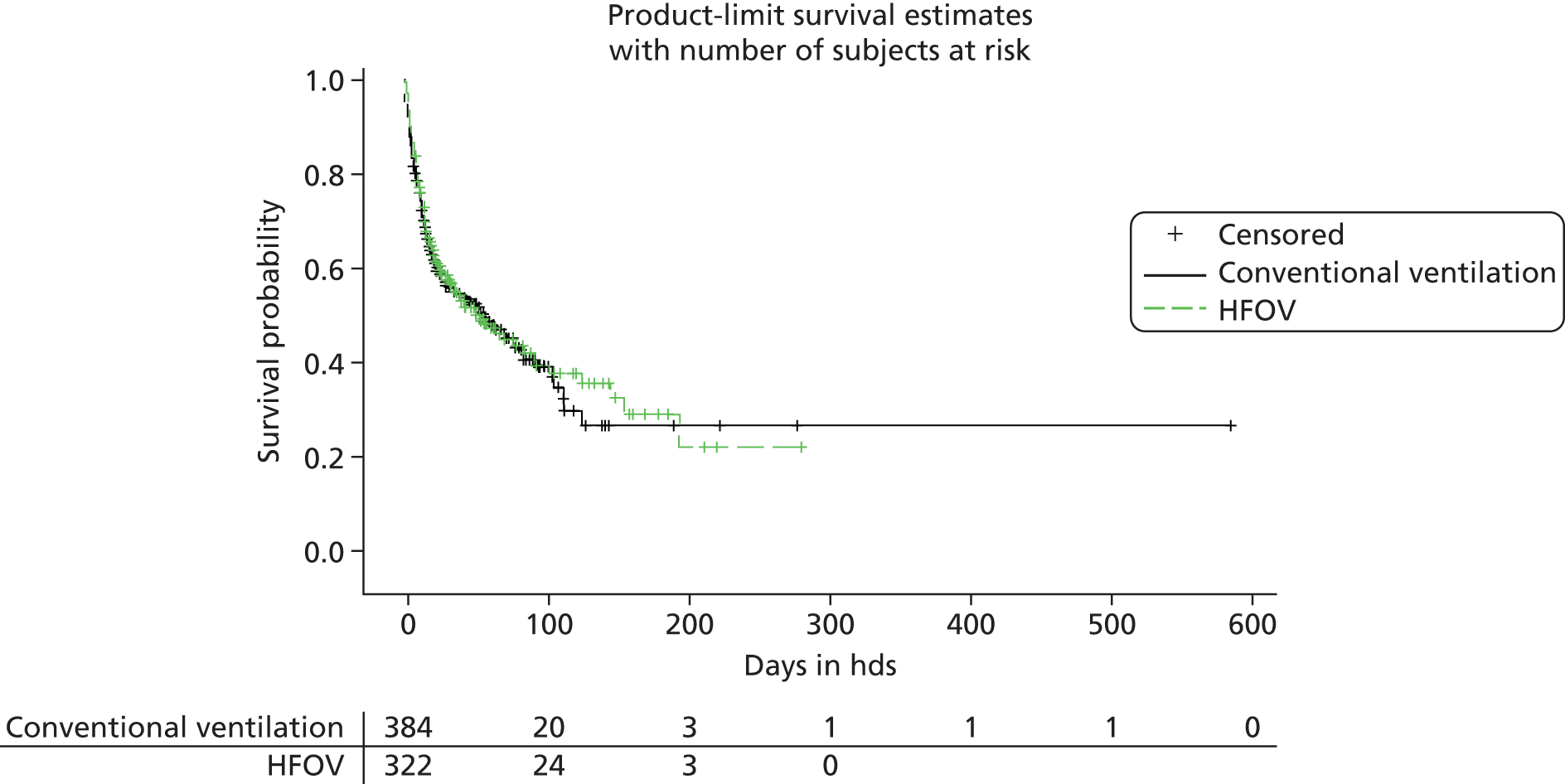
Mortality rate one year after randomisation
The number (and percentage) of patients who were alive/died 1 year after randomisation are summarised in Table 81 by each intervention. An assumption that all those who have not reached 12-month follow-up are alive has been made for the survival analysis. The uncensored observations are all those who died prior to 12 months and the censored are all other subjects.
| Status | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| Alive (or assumed alive) | 191 (49.5%) | 167 (51.4%) | 358 |
| Died | 195 (50.2%) | 158 (48.6%) | 353 |
| Total | 386 | 325 | 711 |
Allowing for the censoring, no statistically significant difference in mortality rates at 12 months post randomisation were found between the two interventions (log-rank test: p = 0.5702). The difference in mortality rates between the two interventions was 1.90% (95% CI –5.45% to 9.22%).
No statistically significant difference in mortality rates at 12 months post randomisation from hospital was found between the two interventions when adjusting for centre, sex, P : F ratio and APACHE II score (Cox’s regression model: p-value = 0.6539). The odds of being alive (as opposed to dying) at 12 months post randomisation is 1.051 when on conventional ventilation compared with HFOV.
Figure 23 illustrates the Kaplan–Meier curve for the probability of survival up to 12 months post randomisation (with the number of patients at risk).
FIGURE 23.
Kaplan–Meier curves displaying the probability of survival up to 12 months post randomisation for both interventions.
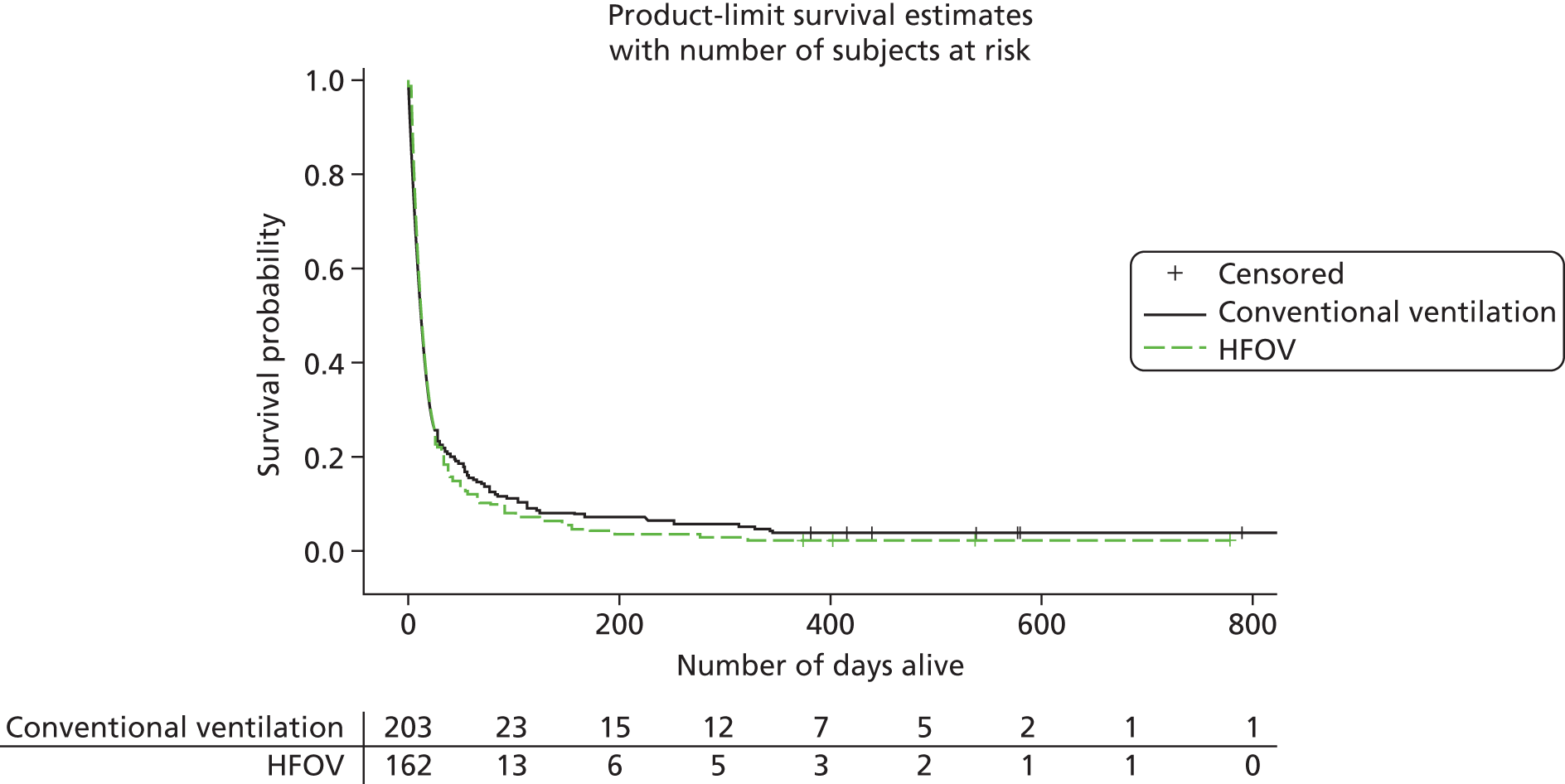
The results for the health economics analysis are given in Chapter 5.
Chapter 5 OSCillation in ARDS trial economic analysis
Methods
The economic evaluation was carried out alongside the trial using recommended methods. 90 An additional model-based analysis was used to extrapolate the results over the expected lifetime of the trial participants. The perspective of the NHS and personal social services was undertaken for the main analysis with an additional analysis from a societal perspective. Other methods were in line with NICE Technology Appraisal Guidelines. 91
The primary health economic outcome is the cost per QALY gained 1 year after randomisation. The primary outcome for the clinical analysis was mortality at 30 days and the economic analysis therefore also used cost per life saved at 30 days and cost per LY gained at 30 days. Cost analysis was undertaken to present costs at 30 days, costs at ICU discharge, costs at hospital discharge and costs over 1 year from randomisation.
Cost estimation
Resource use was collected during the trial and unit costs were assigned at the time of analysis. Patients were randomised after up to 7 days on ventilation and only resources used from the date of randomisation were included. These included the resources used on the initial ICU admission; the costs of subsequent ICU admissions were based solely on the number of days admitted to ICU (a per day cost). The cost post CU was based on the number of days on the step down ward until death or hospital discharge. If a patient was discharged to another hospital after ICU, the cost of transport was taken as that of an emergency transfer. SAEs were costed on an individual basis. After discharge, the resources used included the use of aids and devices, use of medical services including residential care, cost of travel for the patient and carers, loss of earnings and patient out of pocket expenses. Tables 82–84 list the costs of resources used.
| Resource used | Cost (£) | Reference |
|---|---|---|
| Number of organs supported in ICU | NHS Reference Costs 2011–1292 | |
| 0 | 631.00 | |
| 1 | 868.00 | |
| 2 | 1223.00 | |
| 3 | 1401.00 | |
| 4 | 1586.00 | |
| 5 | 1745.00 | |
| Renal replacement therapy | 156.00 | NHS Reference Costs 2011–1292 |
| Chest X-ray (evidence for barotrauma) | 30.00 | NHS Reference Costs 2011–1292 |
| Cost of pneumothorax | 1773.00 | NHS Reference Costs 2011–1292 |
| Intravenous antibiotics (per dose) | BNF 201293 | |
| Tazocin | 42.63 | |
| Ciprofloxacin | 44.00 | |
| Levofloxacin | 50.20 | |
| Antibiotics in renal failure (per dose) | BNF 201293 | |
| Tazocin | 28.42 | |
| Ciprofloxacin | 22.00 | |
| Levofloxacin | 12.60 | |
| Oral antibiotics (per dose) | BNF 201293 | |
| Augmentin | 1.14 | |
| Ciprofloxacin | 0.14 | |
| Levofloxacin | 5.18 | |
| Sedation (per dose) | BNF 201293 | |
| Propofol (bolus) | 0.73 | |
| Propofol (infusion) | 65.18 | |
| Alfentanyl | 25.00 | |
| Midazolam | 8.40 | |
| Haloperidol | 0.07 | |
| Muscle relaxants (per dose) | BNF 201293 | |
| Atracurium (infusion) | 63.12 | |
| Atracurium (bolus) | 1.51 | |
| Palliative care (per day) | 113.00 | NHS Reference Costs 2011–1292 |
| Level 3 care (per day) | 1476.07 | NICE – Critical illness rehabilitation (CG83)91 |
| Level 2 care (per day) | 1476.07 | NICE – Critical illness rehabilitation (CG83)91 |
| Level 1 care (per day) | 297.00 | NHS Reference Costs 2011–1292 |
| Emergency transport | 261.35 | PSSRU – Unit Costs of Health and Social Care 201194 |
| Rehabilitation (per day) | 297.00 | NHS Reference Costs 2011–1292 |
| Nursing home (per day) | 106.10 | PSSRU – Unit Costs of Health and Social Care 201194 |
| Resource used | Unit of measure | Cost (£) | Reference |
|---|---|---|---|
| Primary and community-based health and social services | |||
| GP | PSSRU – Unit Costs of Health and Social Care 201194 | ||
| Surgery visit | 37.19 | ||
| Telephone consultation | 22.73 | ||
| Home visit | 125.00 | ||
| Practice nurse | Per appointment | 52.68 | |
| District nurse | NHS Reference Costs 2011–1292 | ||
| Face to face | 38.00 | ||
| Telephone consultation | 14.00 | ||
| Health visitor | NHS Reference Costs 2011–1292 | ||
| Face to face | 46.00 | ||
| Telephone consultation | 21.00 | ||
| Social worker | PSSRU – Unit Costs of Health and Social Care 201194 | ||
| Face to face | 219.00 | ||
| Telephone consultation | 76.44 | ||
| Support worker | PSSRU – Unit Costs of Health and Social Care 201194 | ||
| Face to face | 29.96 | ||
| Telephone consultation | 24.79 | ||
| Addiction services | PSSRU – Unit Costs of Health and Social Care 201194 | ||
| Face to face | 141.52 | ||
| Telephone consultation | 48.55 | ||
| Physiotherapy | Per session | 46.00 | NHS Reference Costs 2011–1292 |
| Occupational therapy | Per session | 71.00 | NHS Reference Costs 2011–1292 |
| Dietitian | Per session | 71.00 | NHS Reference Costs 2011–1292 |
| Phlebotomy | Per visit | 3.00 | NHS Reference Costs 2011–1292 |
| Home help | Per session | 22.73 | PSSRU – Unit Costs of Health and Social Care 201194 |
| NHS walk-in centre | Per visit | 42.35 | PSSRU – Unit Costs of Health and Social Care 201194 |
| NHS Direct | Per call | 8.00 | NHS Reference Costs 2011–1292 |
| Meals on wheels | Per day | 25.83 | PSSRU – Unit Costs of Health and Social Care 201194 |
| Family support | Per session | 27.89 | PSSRU – Unit Costs of Health and Social Care 201194 |
| Respite care | Per day | 68.00 | NHS Reference Costs 2011–1292 |
| Tuberculosis specialist nurse | Per appointment | 60.00 | NHS Reference Costs 2011–1292 |
| Palliative care specialist nurse | Per appointment | 86.00 | NHS Reference Costs 2011–1292 |
| Stoma care nurse | Per appointment | 43.00 | NHS Reference Costs 2011–1292 |
| Critical care nurse | Per appointment | 86.00 | NHS Reference Costs 2011–1292 |
| Upper GI specialist nurse | Per appointment | 86.00 | NHS Reference Costs 2011–1292 |
| Rapid response team | Per appointment | 36.16 | NHS Reference Costs 2011–1292 |
| Cardiology nurse specialist | Per appointment | 73.00 | NHS Reference Costs 2011–1292 |
| Macmillan nurse specialist | Per appointment | 66.00 | NHS Reference Costs 2011–1292 |
| Magnetic resonance imaging | Per scan | 145.00 | NHS Reference Costs 2011–1292 |
| Hospital and residential care services | |||
| Hospital inpatient stay | Per day | 297.00 | NHS Reference Costs 2011–1292 |
| Hospital day centre | Per day | 148.00 | NHS Reference Costs 2011–1292 |
| Hospital outpatient clinic | Per appointment | 150.00 | NHS Reference Costs 2011–1292 |
| Psychiatry | Per appointment | 136.36 | NHS Reference Costs 2011–1292 |
| Respiratory outpatients clinic | Per appointment | 143.00 | NHS Reference Costs 2011–1292 |
| Nephrology outpatients clinic | Per appointment | 164.00 | NHS Reference Costs 2011–1292 |
| Diabetic outpatients clinic | Per appointment | 130.00 | NHS Reference Costs 2011–1292 |
| Stoma outpatients clinic | Per appointment | 105.00 | NHS Reference Costs 2011–1292 |
| Pain management | Per appointment | 125.00 | NHS Reference Costs 2011–1292 |
| Hospital A&E visit | Per visit | 151.85 | PSSRU – Unit Costs of Health and Social Care 201194 |
| Local authority day centre | Per day | 37.19 | PSSRU – Unit Costs of Health and Social Care 201194 |
| Residential care home | Per day | 148.31 | PSSRU – Unit Costs of Health and Social Care 201194 |
| Rehabilitation centre | Per day | 98.87 | PSSRU – Unit Costs of Health and Social Care 201194 |
| Warden controlled residence | Per day | 61.68 | PSSRU – Unit Costs of Health and Social Care 201194 |
| Resource used | Cost (£) | Reference |
|---|---|---|
| Commode | 81.70 | NHS supply chain95 |
| Mowbray frame | 21.49 | |
| Combiframe | 27.37 | |
| Free-standing toilet frame | 27.37 | |
| Raised toilet seat | 27.81 | |
| Urine bottle | 14.79 | |
| Bed pan | 27.11 | |
| Chair raisers | 83.21 | |
| Bed sitting support | 144.74 | |
| Bed leaver/grab rail | 94.00 | |
| Transfer board | 190.00 | |
| Banana board | 58.72 | |
| Slide sheet | 3.96 | |
| Walking frame | 17.34 | |
| Mobilator | 91.67 | |
| Walking frame with wheels | 70.79 | |
| Walking stick | 4.02 | |
| Quad stick | 11.82 | |
| Perching stool | 28.80 | |
| Leg lifter | 5.81 | |
| Bottom wipers | 25.28 | |
| Buckingham caddy | 24.71 | |
| Hospital bed | 348.15 | |
| Petrol | 0.45 | HMRC96 |
Measuring resources
During the patients’ initial ICU stay, daily CRFs were completed by the medical and nursing staff. These included data on the organs supported and for the use of antibiotics, sedatives and muscle relaxants. The CRF was also used to collect data on discharge from the ICU and from hospital; death was recorded in the same CRF. The data collected at this stage included date and time of discharge from the ICU or death, where the patient was discharged to and whether or not discharge was to the same hospital. It contained information on readmissions to ICU, whether or not the patient required a chest drain or if there was any radiological evidence of barotrauma while on ICU.
Once discharged, questionnaires were sent to surviving patients and their carers at 6 and 12 months with follow-up questionnaires 1 month later if there was no response. The patient questionnaires contained questions relating to the cost for the patients themselves, and to the NHS, of aids and devices. Patients were asked about their use of medical services including residential inpatient stays, major expenses and their gross loss of earnings. The questionnaires also included the EQ-5D. The carers’ questionnaires included questions regarding the cost of travel to and from medical services, major expenses and loss of earnings.
Estimating unit costs
Total costs per patient while in ICU were calculated on a daily basis using the individual unit costs per resource used and the sum per patient was calculated. The costs of medicines used were taken from the British National Formulary (BNF) 64. 93 The CRFs provided information on whether the patient had oral or intravenous antibiotics and whether these were for sepsis relating to the lung or another source. The choice of antibiotic was not standardised across centres and therefore the costs had to be estimated, and for this we took those antibiotics that are recommended by the British Thoracic Society guidelines for the treatment of community-acquired pneumonia97 and the Scottish Intercollegiate Guidelines Network guidelines for the management of suspected bacterial urinary tract infections in adults. 98 For sepsis secondary to a pulmonary source we used co-amoxiclav orally, with piperacillin and tazobactam if given intravenously. Despite pneumonia being both the leading cause of sepsis leading to ICU admission99 and sepsis causing ARDS,100 urinary tract infection (UTI) remains the most prevalent bacterial infection in hospitals and in the community with a high incidence in the critically ill. 101–104 We therefore assumed that the majority of patients requiring antibiotics for an extrapulmonary cause would be due to a UTI and used the cost for ciprofloxacin either orally or intravenously (based on the CRF) in this cohort.
In the case of penicillin allergy we were not provided with patient-specific information. Patient self-reported rates for penicillin allergy can be as high as 15% with 10% a generally accepted figure,105–108 with true rates of penicillin allergy likely to be much lower. 105,106,109 We therefore used the cost of levofloxacin either orally or intravenously for 10% of patients who required antibiotics. The unit costs per medication are provided in Table 83. For patients on dialysis, we adjusted the costs accordingly in those antibiotics which are renally excreted. The costs of ICU resources including radiology and the cost of pneumothorax were taken from the National Schedule of Reference Costs. 92
The added cost of the HFOV machine was calculated based on the cost of the Novalung Vision Alpha High-frequency Oscillator. The difference in price between the HFOV and conventional ventilation machines was calculated based on the machines being used for 5 years with annual maintenance. The costs of single-use circuits for were also included for each patient. The purchase cost of the Novalung Vision Alpha High-frequency Oscillator was £45,000, with an annual maintenance cost of £840. A single-use circuit was £400. The price for conventional ventilation was a Covidien (Puritan Bennett/Tyco) Ventilator (Covidien plc, Mansfield, MA) at £23,000 with an annual maintenance cost of £1300 and a single-use circuit per patient of £100. Once patients were discharged from ICU, the cost of step down was calculated using the number of days until death or discharge multiplied by the cost of the level of care required. The costs for the step down care were taken from various nationally available references. 92,94,110
Once discharged from hospital, the costs of attendance at medical services were calculated using national reference costs multiplied by the number of times a patient attended. Inpatient stays were based on the number of days admitted multiplied by the cost for each resource taken from the unit costs of health and social care. 94 The questionnaire sent to each patient at 6 and 12 months provided a list of individual aids or devices available to them. If a patient used one of these but did not pay for it, the cost was taken from the NHS supply chain cost for each individual item. 95 If a patient bought an item themselves, then the actual cost provided by the patient in the questionnaire was used. The cost of travel for both carers and patients was based on the distance in miles provided in the questionnaires multiplied by the cost per petrol mile as provided by Her Majesty’s Revenue and Customs (HMRC). 96 Patients and carers were asked to give the gross amount lost in earnings in the 6 months covered by each questionnaire. Patients who had died at the 6- and 12-month time points were considered to have incurred no costs and were included in all calculations.
All costs were adjusted to 2012 prices using the Hospital and Community Healthcare Services (HCHS) Index published by Personal Social Services Research Unit (PSSRU). 94
Quality of life
The quality-adjusted survival was estimated from the Kaplan–Meier survival function to 1 year from randomisation and the questionnaires sent to patients at 6 and 12 months, which contained the EQ-5D questionnaire. For the time that patients were intubated until extubation, their scores were taken as those for an unconscious patient (–0.40) reported in the EQ-5D scoring manual. 65 From the day following successful weaning from ventilation to day 240, the QoL score was measured using the mean EQ-5D score from the patient questionnaires sent out at the 6 month period. As patients only fill in the EQ-5D questionnaires at 6-monthly intervals, we used the 6-month questionnaires to day 240 in order to reflect the fact that patients QoL is unlikely to change immediately after completing the 6-month questionnaire to the score on the 12-month questionnaire. From day 241 to 1 year, the score was taken as the mean EQ-5D from the 12-month questionnaires. The mean QALYs per patient were estimated by multiplying the EQ-5D score by the area under the survival curve to 1 year from randomisation. 65,111
Analysis and reporting
The cost for each patient was calculated using the unit cost of each resource used as described above. The costs and QALYs are presented as means with 95% CIs calculated by bootstrapping. 112 All costs are presented as the mean cost per patient. The cost-effectiveness acceptability curve (CEAC) and the cost-effectiveness acceptability plane were generated following the recommendations of Briggs and Fenn. 113 Mean costs from the 6- and 12-month questionnaires were calculated separately with the means from each time point being summed to provide an estimate of mean costs to 1 year post discharge.
Cost-effectiveness outcome measures are:
-
30-day cost per life saved (NHS perspective)
-
30-day cost per LY (NHS perspective)
-
1-year cost per QALY (NHS and societal perspectives).
To assess cost-effectiveness over the lifetime horizon a Markov model was constructed114 (Figure 24). The parameters for the model, and their sources, are listed in Table 85. The long-term survival of patients following discharge from ICU has been shown to be lower than that of the general population. 115 For years 2 to 9 post randomisation, we therefore used the relative survival rates from an observational study of long-term survival following ICU discharge in an Australian population. 115 This study presented relative survival data for four subsets: hospitalised patients with either sepsis or not and ICU patients with sepsis or no evidence of sepsis; each of these was presented separately by sex. Only the data for the ICU patient subsets were used. If an OSCAR patient required antibiotics at any point during their ICU stay, they were included in the septic cohort of ICU survivors. The relative survival effects from this study, weighted by the proportion of each subgroup in OSCAR were then applied to age and sex matched UK population reference mortality published by the ONS. 116 From year 10 onwards, as there are no data available for the survival of patients post ICU, unadjusted age- and sex-matched mortality rates were therefore used. With limited data on the long-term effects on EQ-5D scores following ARDS, the age and sex matched EQ-5D norms for the UK general population for the QoL weight were used from 1 year post randomisation onwards117 (see Table 88).
FIGURE 24.
Markov model. Year 1 – data from study.
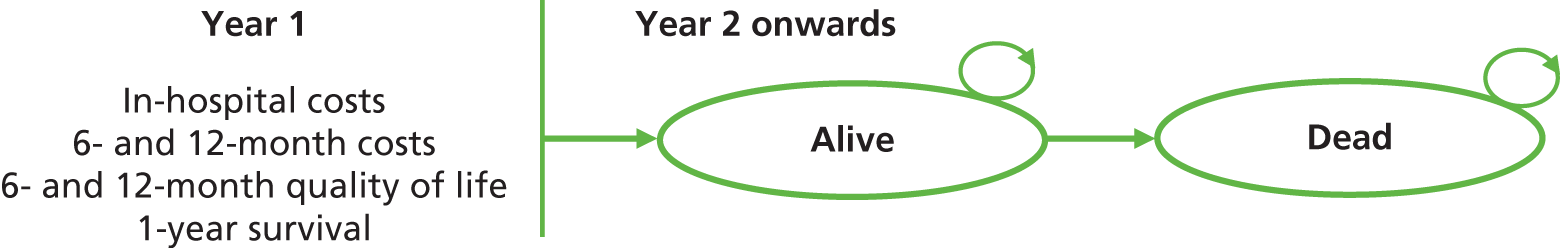
| Parameters | Conventional ventilation | HFOV | Reference | |
|---|---|---|---|---|
| Year 0–1 | ||||
| Mean LYs saved | 0.5578547 | 0.5232611 | Trial data | |
| Mean QALY | 0.2456425 | 0.3021253 | Trial data | |
| Mortality | 0.5113 | 0.5101 | Trial data | |
| Cost (£) | 40,129.87 | 44,550.26 | Trial data | |
| Year 2 onwards | ||||
| Mortality rate | Year | Age- and sex-matched norms | ONS116 | |
| Relative survival | 2 | 0.864665 | 0.864665 | Ghelani et al.115 and ONS116 |
| 3 | 0.950213 | 0.950213 | ||
| 4 | 0.981684 | 0.981684 | ||
| 5 | 0.993262 | 0.993262 | ||
| 6 | 0.997521 | 0.997521 | ||
| 7 | 0.999088 | 0.999088 | ||
| 8 | 0.999665 | 0.999665 | ||
| 9 | 0.999877 | 0.999877 | ||
| > 9 | Unadjusted | |||
| Utility | Age- and sex-matched norms | |||
Missing data
Analysis of the 6- and 12-month questionnaires used complete case analysis for costs and QoL. Mean values for QoL and cost were calculated separately from returned questionnaires at the 6- and 12-month time points. A sensitivity analysis was conducted using multiple imputations (chained equation method) for missing questionnaire-derived costs and utility values at 6 and 12 months. 118
Results
There were 795 patients randomised, although 3 died prior to initiation of treatment and were excluded from the analysis (Table 86). Data for inpatient resources were therefore collected on 792 patients: 397 in the conventional ventilation group and 398 in the HFOV group. Once discharged, a total of 226 patients completed the 6-month questionnaires: 116 in the conventional ventilation group and 110 in the HFOV group. One hundred and eighty-six patients completed the 12-month questionnaires; 89 in the conventional ventilation group and 97 in the HFOV group. One hundred and fifty-six patients completed both the 6- and the 12-month questionnaires, with 78 in each group. One hundred and fifty-four carers completed the 6-month questionnaires with 79 in the conventional ventilation group and 75 in the HFOV group. At 12 months, 108 carers had completed the questionnaires with 53 in the conventional ventilation group versus 55 in the HFOV group. A total of 76 carers completed both the 6- and 12-month questionnaires with 38 in each group.
| Data source | Number of complete data sets | Number of complete data sets | Number of complete data sets |
|---|---|---|---|
| Inpatient data sheets | 795a | 397 | 398 |
| Patient questionnaire at 6 months | 226 | 116 | 110 |
| Patient questionnaire at 12 months | 186 | 89 | 97 |
| Patient questionnaire at both 6 and 12 months | 156 | 78 | 78 |
| Carer questionnaire at 6 months | 154 | 79 | 75 |
| Carer questionnaire at 12 months | 108 | 53 | 55 |
| Carer questionnaire at both 6 and 12 months | 76 | 38 | 38 |
Cost analysis 1 – NHS and personal social services perspective
Thirty-day costs
The primary end point for costs was 30-day costs (Table 87). The total cost for patients in the HFOV group at 30 days is more expensive at £30,889.30 compared with £29,064.00 in the conventional ventilation group with an incremental cost of £1825.30. At 30 days, the cost of the initial ICU admission was more expensive for those patients on HFOV at £27,769.47 versus £25,279.65 giving an incremental cost of £2489.83. Even without accounting for the higher cost of the HFOV machine compared with conventional ventilation, it was more expensive in the HFOV group. Total cost for the first 30 days without the cost of the HFOV machines was £27,327.58 versus £25,279.65 in the conventional ventilation group with an incremental cost of £2047.92.
| Arm | Mean (£) | Lower CI 95% (£) | Upper CI 95% (£) |
|---|---|---|---|
| Total cost to day 30 | |||
| Conventional ventilation | 29,064.00 | 27,280.62 | 30,780.85 |
| HFOV | 30,889.30 | 29,069.11 | 33,999.24 |
| Incremental cost | 1825.30 | –1006.24 | 4818.91 |
| Cost of initial ICU admission to day 30 | |||
| Conventional ventilation | 25,279.65 | 23,183.81 | 27,490.50 |
| HFOV | 27,769.47 | 25,412.51 | 30,228.39 |
| Incremental cost | 2489.82 | –749.90 | 5728.20 |
| Cost of initial ICU admission excluding the cost of HFOV equipment to day 30 | |||
| Conventional ventilation | 25,279.65 | 23,183.23 | 27,491.39 |
| HFOV | 27,327.58 | 24,957.11 | 29,809.61 |
| Incremental cost | 2047.92 | –1197.91 | 5288.84 |
| Cost of ICU readmissions to day 30 | |||
| Conventional ventilation | 6642.33 | 738.04 | 14,760.74 |
| HFOV | 6425.26 | 2604.84 | 10,766.66 |
| Incremental cost | –217.07 | –8639.38 | 7380.37 |
| Post-ICU costs to day 30 | |||
| Conventional ventilation | 3784.35 | 3216.28 | 4203.94 |
| HFOV | 3119.83 | 2641.66 | 3588.74 |
| Incremental cost | –664.51 | –1246.51 | –251.42 |
The cost of readmission to ICU was marginally more expensive in the conventional ventilation group, but patients in the HFOV were more than twice as likely to be readmitted to the ICU. In total there were 22 patients readmitted once (7 in the conventional ventilation group and 15 in the HFOV group), and 3 patients readmitted twice (1 in the conventional ventilation group compared with 2 in the HFOV group). The cost of readmission to ICU up to day 30 in the conventional ventilation group was £6642.33 compared with £6425.26 giving an incremental cost of –£217.07.
The cost post ICU was also marginally more expensive in the conventional ventilation group at a cost of £3784.35 versus £3119.83 in the HFOV group. This gives an incremental cost of –£664.51.
Total NHS and Personal Social Services costs to 1 year following discharge
The total NHS and Personal Social Services (PSS) costs to 1 year were dominated by the NHS cost during the patients ICU stay.
Total cost to the NHS over 1 year
At 1 year following randomisation, the total cost to the NHS including inpatient stay and resources used following discharge was higher in the HFOV group at £44,550.26 compared with £40,129.87 in those patients on conventional ventilation. This gives an incremental cost of £4420.39 (Table 88).
| Arm | Mean (£) | Lower CI 95% (£) | Upper CI 95% (£) |
|---|---|---|---|
| Total cost to the NHS over 1 year | |||
| Conventional ventilation | 40,129.87 | 36,489.31 | 43,960.34 |
| HFOV | 44,550.26 | 40,375.16 | 48,989.02 |
| Incremental cost | 4420.39 | –2044.65 | 9239.74 |
| Total cost of inpatient stay | |||
| Conventional ventilation | 36,101.77 | 32,913.81 | 39,919.86 |
| HFOV | 38,997.20 | 34,742.45 | 43,620.86 |
| Incremental cost | 2895.43 | –2732.54 | 8508.93 |
| Cost of initial ICU admission | |||
| Conventional ventilation | 25,279.65 | 23,183.81 | 27,490.50 |
| HFOV | 27,769.47 | 25,412.51 | 30,228.39 |
| Incremental cost | 2489.82 | –749.90 | 5728.20 |
| Total cost of initial ICU admission excluding the cost of HFOV equipment | |||
| Conventional ventilation | 25,279.65 | 23,183.23 | 27,491.39 |
| HFOV | 27,327.58 | 24,957.11 | 29,809.61 |
| Incremental cost | 2047.92 | –1197.91 | 5288.84 |
| Cost of readmission to ICU | |||
| Conventional ventilation | 19,557.99 | 5904.30 | 36,901.86 |
| HFOV | 17,018.27 | 10,766.66 | 23,790.85 |
| Incremental cost | –2539.72 | –21,186.01 | 12,893.94 |
| Total cost post ICU | |||
| Conventional ventilation | 10,822.12 | 8798.29 | 13,250.11 |
| HFOV | 11,227.73 | 8504.71 | 14,347.87 |
| Incremental cost | 405.61 | –3076.64 | 4141.05 |
Total cost of inpatient stay
When looking at the total cost of a patient’s inpatient stay, similar results are found. With all inpatient resources considered, the total cost for patients in the HFOV group comes to £38,997.20 compared with £36,101.77 for patients in the conventional ventilation group with an incremental cost of £2895.43. The initial ICU admission was more expensive for patients in the HFOV group at £27,769.47 versus £25,279.65 in the conventional ventilation group, with an incremental cost of £2489.82. If the added cost of HFOV is removed, the initial ICU admission still remains more expensive for those patients in the HFOV group of the trial at £27,327.58 compared with £25,279.58 in the conventional ventilation group, with an incremental cost of £2047.92. If a patient required readmission to ICU (numbers are the same as in the 30 day analysis) then the cost in the conventional ventilation group was markedly higher than those patients in the HFOV group at £19,557.99 and £17,018.72, respectively, with an incremental cost of –£2539.72. Even with the increased cost of readmission to ICU in the HFOV group, when the total cost for a patient post ICU is considered, it is still marginally more expensive in the HFOV group at £11,227.73 compared with £10,822.12 giving an incremental cost of £405.61.
Cost analysis 2 – societal perspective
Total cost to society over 1 year
Taking into consideration the cost to the NHS, patient and carers out-of-pocket expenses and the loss of earnings over 1 year post randomisation, the total cost to society was higher in the HFOV group at £50,583.31 compared with £45,568.12 with an incremental cost of £5015.19 (Table 89).
| Arm | Mean (£) | Lower CI 95% (£) | Upper CI 95% (£) |
|---|---|---|---|
| Total cost to society over 12 months | |||
| Conventional ventilation | 45,568.12 | 41,610.63 | 49,805.00 |
| HFOV | 50,583.31 | 44,427.88 | 54,057.85 |
| Incremental cost | 5015.19 | –2985.68 | 9817.05 |
| Patient out-of-pocket expenses | |||
| Conventional ventilation | 183.64 | 64.57 | 356.52 |
| HFOV | 54.83 | 19.39 | 104.63 |
| Incremental | –128.81 | –306.39 | 0.87 |
| Total cost for carers to 1 year post randomisation | |||
| Conventional ventilation | 926.71 | 500.76 | 1454.80 |
| HFOV | 1100.25 | 596.43 | 1705.79 |
| Incremental | 173.54 | –561.09 | 924.85 |
| Loss of earnings for patients | |||
| Conventional ventilation | 4576.81 | 3500.92 | 5730.82 |
| HFOV | 2993.74 | 1981.37 | 4143.27 |
| Incremental | –1583.08 | –3117.80 | –8.30 |
| Loss of earnings for carers | |||
| Conventional ventilation | 516.68 | 310.18 | 768.28 |
| HFOV | 758.64 | 460.97 | 1108.09 |
| Incremental | 241.96 | –148.20 | 648.29 |
| Total loss of earnings for patients and carers | |||
| Conventional ventilation | 5093.49 | 3988.15 | 6278.49 |
| HFOV | 3752.37 | 2689.52 | 4937.84 |
| Incremental | –1341.12 | –2926.31 | 282.55 |
Patient out-of-pocket expenses
Once patients were discharged, we estimated the cost to the patient over the first year post randomisation based on the questionnaires. In the conventional ventilation group, patients on average had to spend £183.64 of their own money; this included travel to and from medical services and the cost of aids and devices that they paid for themselves. In the HFOV group, this was lower at £54.83 giving an incremental cost of –£128.81.
Total cost for carers 1 year post randomisation
At 1 year post randomisation there was a slightly higher cost to the carers of patients in the HFOV group at £1100.25 compared with £926.71 with an incremental cost of £173.54.
Loss of earnings
Following discharge, patients in the conventional ventilation group have a higher loss of earnings at 1 year post randomisation at £4576.81 compared with £2993.74 in the HFOV group with an incremental cost of –£1583.08.
For carers, there was a slightly higher loss of earnings in the HFOV group; in this group the carers lost £758.64 over the course of the year compared with £516.68 in the conventional ventilation group, giving an incremental cost of £241.96. The total loss of earnings over the first year following randomisation is therefore £5093.49 in the conventional ventilation group and £3752.37 in the HFOV group with an incremental cost of –£1341.12.
Cost-effectiveness
30-day cost-effectiveness
At 30 days, the incremental lives saved is –0.0041 (Table 90) and with an incremental cost of £1825.30, the incremental cost-effectiveness ratio (ICER) is –£445,195.12 (see Table 94). The incremental cost per life saved at 1 year for HFOV is therefore –£47,487,837.
| Arm | Lives saved at day 30 | Cost (£) | ICER |
|---|---|---|---|
| Conventional ventilation | 0.4106 | 28,923.87 | |
| HFOV | 0.4065 | 30,613.80 | |
| Incremental | –0.0041 | 1825.30 | Conventional ventilation dominates HFOV |
Figure 25 is a scatterplot of incremental costs versus number of lives saved at 30 days showing a right and left upper quadrant distribution, indicating that HFOV is more expensive than conventional ventilation.
FIGURE 25.
Incremental costs vs. lives saved at 30 days.
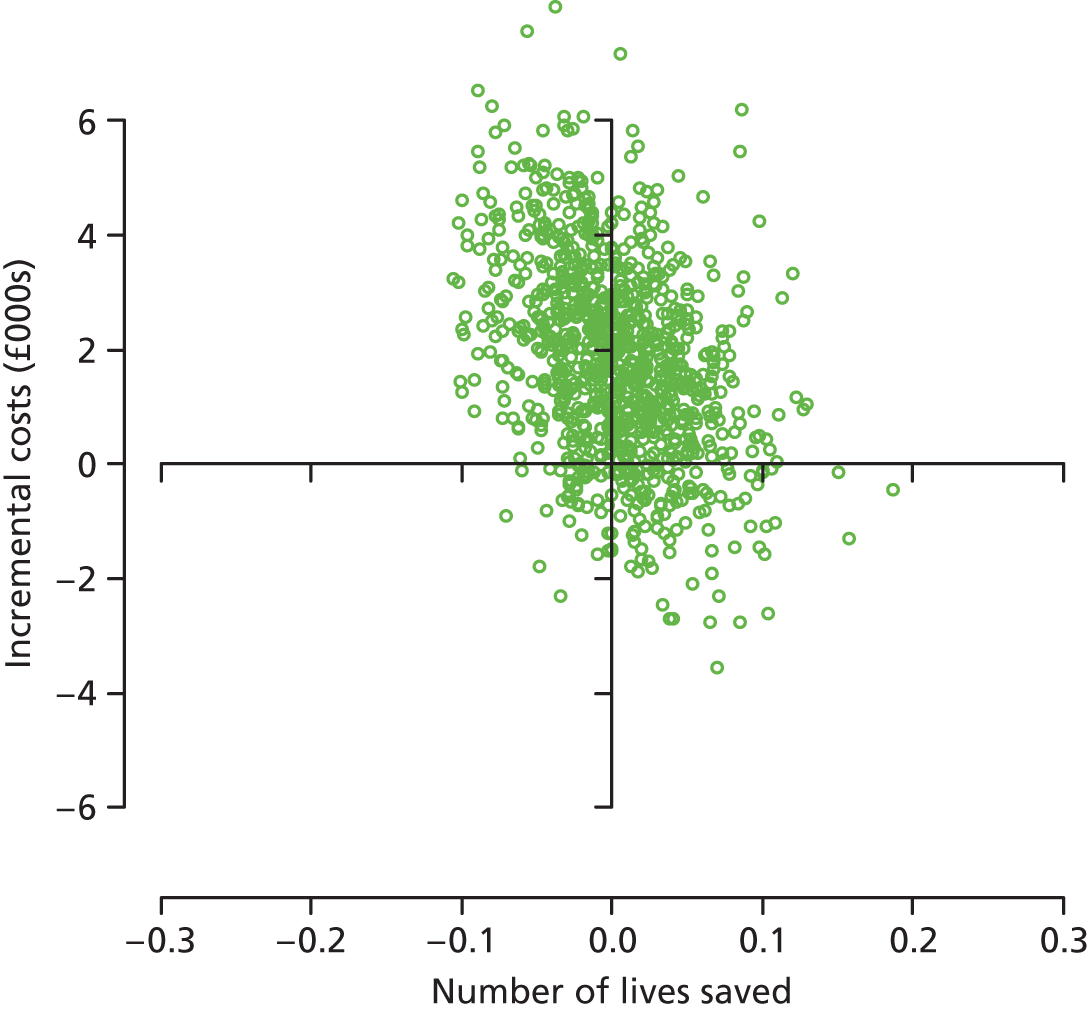
Cost-effectiveness at 1 year
At 1 year, the cost to both the NHS and to society is more in the HFOV group of the trial at £40,129.87 and £45,568.12, respectively, with an incremental cost of £4420.39 and £5015.14, respectively. There was however a higher QALY at 1 year in the HFOV group at 0.302 compared with those patients in the conventional ventilation group at 0.246 with an incremental QALY of 0.056. This gives an ICER for the cost to society per QALY of £88,790.57 and an ICER for the cost to the NHS per QALY of £78,260.82.
Figures 26 and 27 show scatterplot diagrams for the incremental cost to the NHS and to society per QALY respectively, with the diagonal at the threshold of £20,000 per QALY. Both show a right upper quadrant dominant pattern with the majority above the diagonal.
FIGURE 26.
Cost-effectiveness plane for the incremental cost to the NHS per QALY with the diagonal at the threshold of £20,000 per QALY. Right upper quadrant dominant pattern.
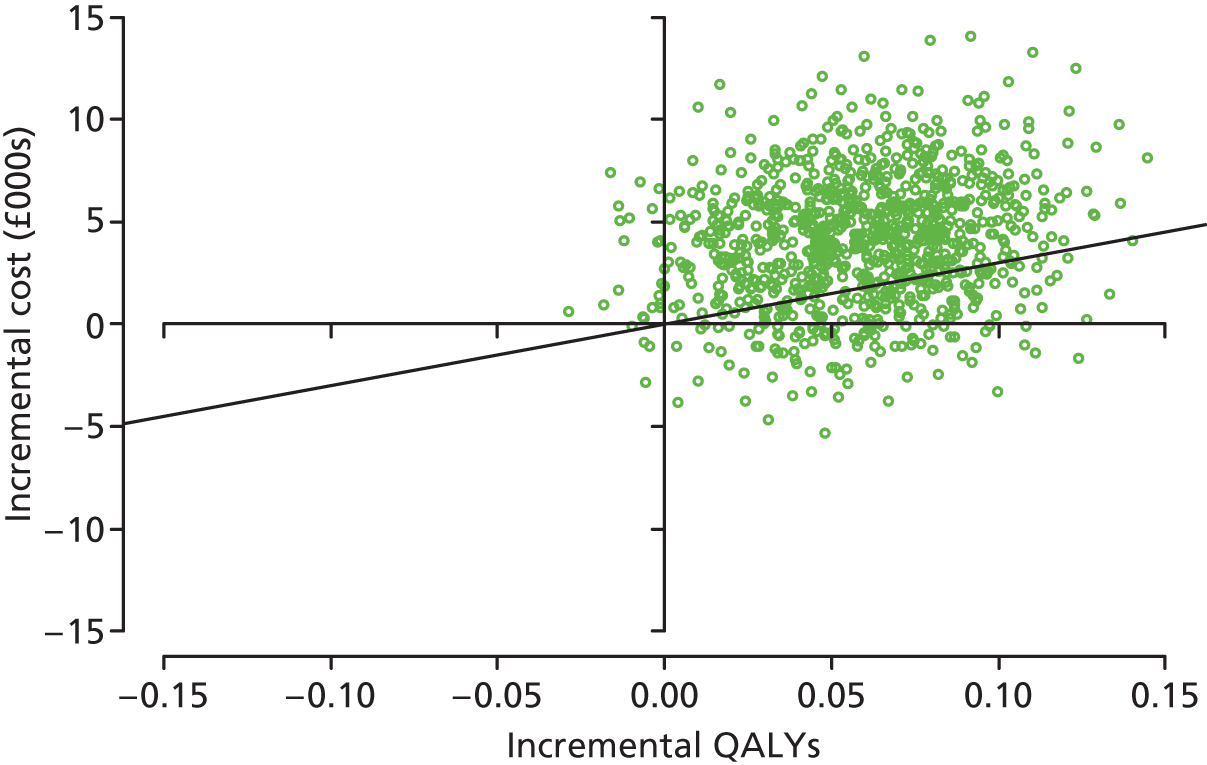
FIGURE 27.
Cost-effectiveness plane for the incremental cost to society per QALY, again with the diagonal at the threshold of £20,000 per QALY. Right upper quadrant dominant pattern.

Figures 28 and 29 show the CEAC for the cost to the NHS and to society, respectively.
FIGURE 28.
Cost-effectiveness acceptability curve for the cost to the NHS.
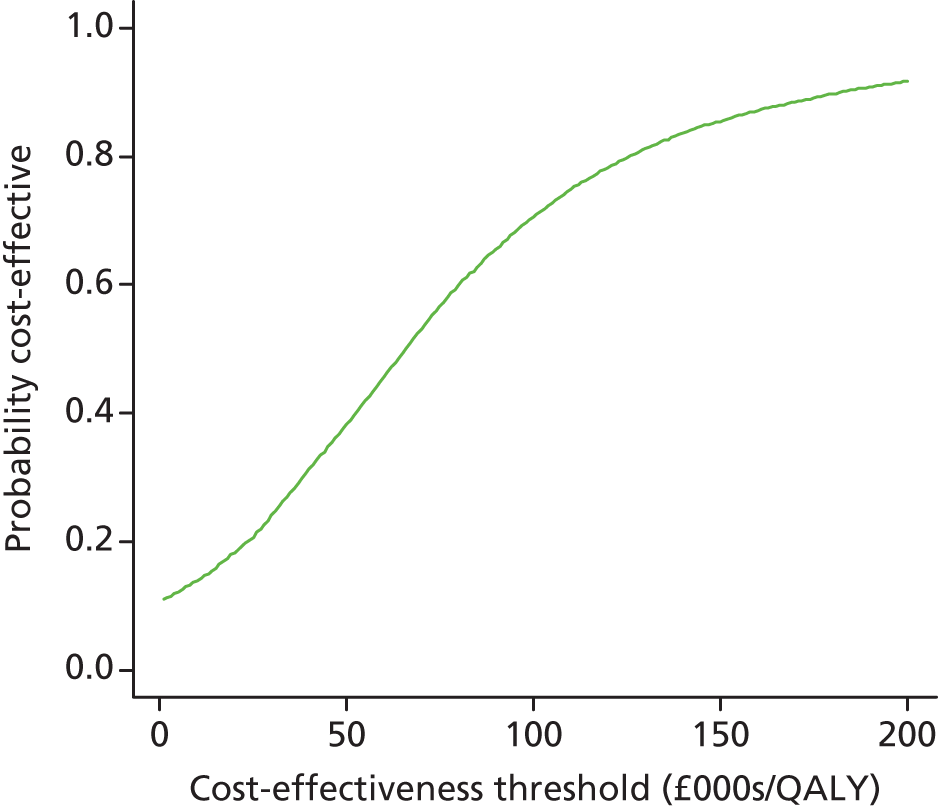
FIGURE 29.
Cost-effectiveness acceptability curve for the cost to society.
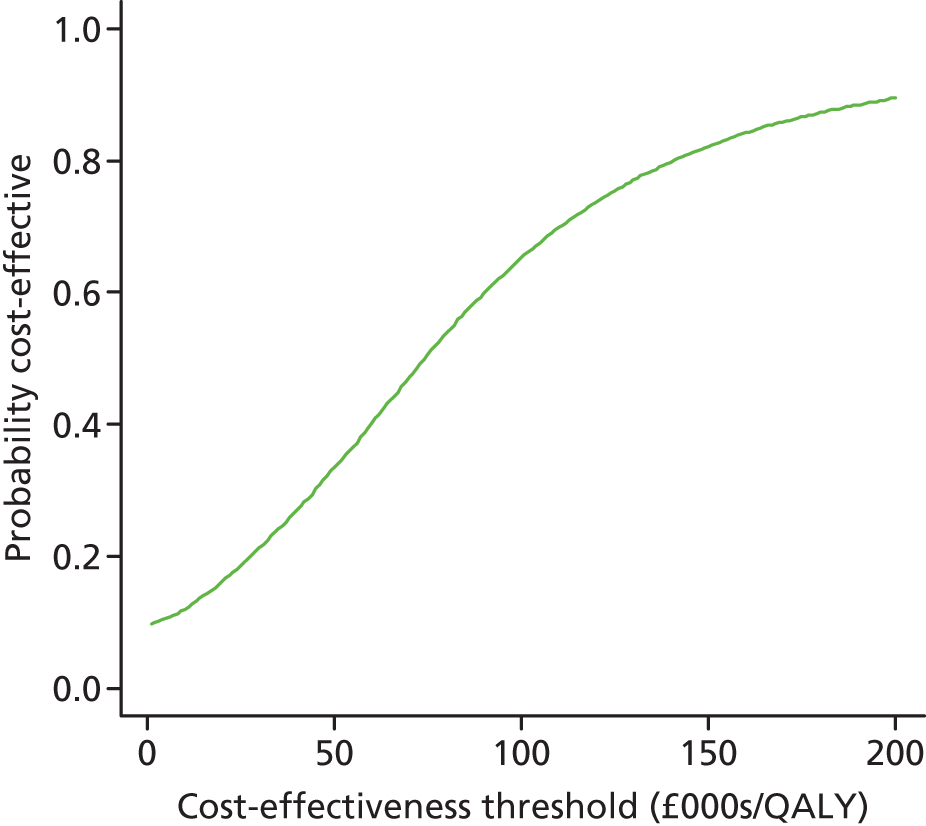
There were 0.558 LYs saved in the conventional ventilation group compared with the 0.523 in the HFOV group of the trial. This gives an incremental LYs saved of –0.035. The cost to society per LY saved is therefore –£144,973.06 and the cost to the NHS per LY saved is –£127,780.57 (Table 91).
| Costs | Conventional ventilation | HFOV | Incremental |
|---|---|---|---|
| Societal costs (95% CI) | £45,568.12 (£41,811.72 to £49,805.00) | £50,583.31 (£44,427.88 to £54,057.85) | £5015.14 (–£2985.68 to £9817.05) |
| Cost to NHS (95% CI) | £40,129.87 (£36,679.95 to £43,869.53) | £44,550.26 (£40,375.16 to £48,989.02) | £4420.39 (–£2044.65 to £9239.74) |
| LYs (95% CI) | 0.5578547 (0.5253814 to 0.5861216) | 0.5232611 (0.4849942 to 0.5481074) | –0.0345936 (–0.0403872 to –0.0380142) |
| QALYs (95% CI) | 0.2456425 (0.2242694 to 0.2668142) | 0.3021253 (0.2819215 to 0.3184306) | 0.0564828 (0.0576521 to 0.0516164) |
| ICER | |||
| Cost to society/LY | – | – | Conventional ventilation dominates HFOV |
| Cost to society/QALY | – | – | £88,790.57 |
| Probability of cost-effectiveness at £20,000/QALY | 0.1632 | ||
| Probability of cost-effectiveness at £30,000/QALY | 0.2130 | ||
| Cost to NHS/LY | – | – | Conventional ventilation dominates HFOV |
| Cost to NHS/QALY | – | – | £78,260.82 |
| Probability of cost-effectiveness at £20,000/QALY | 0.1837 | ||
| Probability of cost-effectiveness at £30,000/QALY | 0.2415 | ||
| Imputation | |||
| Societal costs (95% CI) | £39,553.67 (£35,964.98 to £43,419.66) | £43,445.121 (£38,832.11 to £48,317.78) | £3878.31 (–£2360.46 to £9713.41) |
| LYs (95% CI) | 0.5508081 (0.5050072 to 0.5988424) | 0.5472963 (0.5003348 to 0.5944412) | –0.0035118 (–0.0691065 to 0.0608372) |
| QALYs (95% CI) | 0.1874296 (0.1609454 to 0.2190520) | 0.2010838 (0.1723002 to 0.2334543) | 0.0136542 (–0.0295872 to 0.0515767) |
| Cost to society/LY | – | – | Conventional ventilation dominates HFOV |
| Cost to society/QALY | – | – | £284,037.88 |
| Probability of cost-effectiveness at £20,000/QALY | 0.2357 | ||
| Probability of cost-effectiveness at £30,000/QALY | 0.2605 | ||
Lifetime cost-effectiveness
The cost-effectiveness extrapolated to the lifetime time horizon using the Markov model gives the mean LYs per patient for the conventional ventilation group as 8.27 compared with the HFOV group whose mean LYs per patient was 8.39. The mean QALY is slightly higher in the HFOV group at 6.60 compared with 6.21 and it remains more expensive at £44,550.26 versus £40,129.87 in the conventional ventilation group. This results in an ICER of £11,334 per QALY (Table 92).
| Arm | Mean LYs saved | Mean QALY | Mean cost (£) | ICER (£) |
|---|---|---|---|---|
| Conventional ventilation | 8.27 | 6.21 | 40,129.87 | – |
| HFOV | 8.39 | 6.60 | 44,550.26 | – |
| Incremental | – | 0.39 | 4420.39 | 11,334.33 |
Sensitivity analysis
Thirty-day sensitivity analysis
The sensitivity analysis for the cost to the NHS by day is shown in Table 93 and graphically in Figures 30 and 31 as tornado charts.
| Variable | Cost to NHS at day 30 (£) | ICER (£) | ||
|---|---|---|---|---|
| 25th centile | 75th centile | 25th centile | 75th centile | |
| Cost of initial ICU stay (IQR) | –10,232.04 | 11,748.69 | 2,495,619.51 | –2,865,534.15a |
| Cost of renal replacement therapy (IQR) | –4200.15 | 6132.37 | 1,024,426.10 | –1,495,700.73a |
| Cost of readmission to ICU (IQR) | –3696.57 | 6635.95 | 901,602.44 | –1,618,524.63a |
| Cost of hospital stay following discharge from ICU (IQR) | 488.80 | 3161.80 | –119,220.10a | –771,171.22a |
| Cost of number of organs supported (2–3) | 23.21 | 2399.53 | –5659.87a | –585,250.73a |
| Cost of HFOV (no extra cost – +£1000 per patient) | 1270.71 | 2270.71 | –309,929.49a | –553,831.93a |
FIGURE 30.
Tornado chart for sensitivity analysis of cost to the NHS to day 30: mean cost.

FIGURE 31.
Tornado chart for sensitivity analysis of cost to the NHS to day 30: ICER.
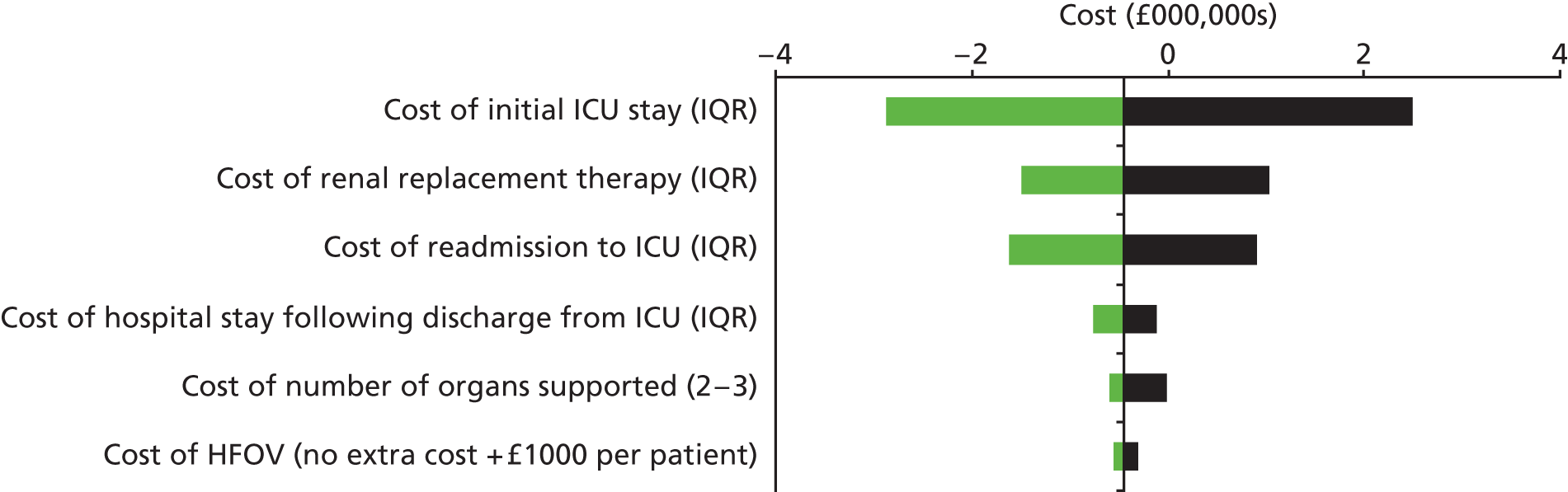
One-year sensitivity analysis
Table 94 shows the sensitivity analysis for the cost per patient to the NHS out to 1 year. Figure 32 shows the associated tornado chart for mean cost and Figure 33 shows the tornado plot for the ICER.
| Variable | Cost to NHS at 1 year (£) | ICER (£) | ||
|---|---|---|---|---|
| 25th centile | 75th centile | 25th centile | 75th centile | |
| Cost of hospital stay (IQR) | –11,254.40 | 20,095.07 | 199,253.58 | 355,773.26 |
| Cost following discharge from hospital (IQR) | 2281.73 | 6558.94 | 40,396.81 | 116,122.82 |
| Use of primary- and community-based health and social services (IQR) | 4063.24 | 5416.56 | 71,937.72 | 95,897.55 |
| Use of hospital and residential care services (IQR) | 3279.90 | 5404.35 | 58,068.95 | 95,681.41 |
| Use of equipment and aids (IQR) | 4578.40 | 4657.40 | 81,058.27 | 82,456.92 |
FIGURE 32.
Tornado chart for sensitivity analysis of cost to the NHS to 1 year – mean cost.

FIGURE 33.
Tornado chart for sensitivity analysis of cost to the NHS to 1 year – ICER.

Discussion
The clinical results for the OSCAR trial shows that there was no significant difference between the two groups for the primary end point of mortality at 30 days and found no benefit or harm to patient outcomes in using HFOV in adults with ARDS. 119 The economic analysis shows that the mean cost of HFOV is overall more expensive than conventional ventilation. Given this, there would be no economic justification for recommending HFOV over conventional ventilation in the treatment of ARDS. Perhaps of more importance is the certainty with which this statement can be made. Figure 26 shows a large overlap with both the x- and y-axes on the cost-effectiveness plane, implying substantial uncertainty about the true balance of costs and benefits, with the difference between the two trial groups likely to be small.
Breaking down the costs that comprise the overall 30-day totals: the costs of initial ICU admission, and of the initial ICU admission accounting for the increased cost of the HFOV machine, are both more expensive in the HFOV group. The cost per ICU readmissions are slightly cheaper in the conventional ventilation group but in the HFOV group, patients are more than twice as likely to be readmitted in the first place and more likely to be readmitted for a second time. The cost of the post-ICU stay to 30 days was also more expensive in the conventional ventilation group. The ICER shows that conventional ventilation dominates HFOV, implying that HFOV is more expensive and less effective up to the 30-day point.
More relevant to reimbursement decision-making is the 1-year cost and QALY differences. At 1 year the costs to the NHS and to society remain more expensive in the HFOV group and the cost of the post-ICU stay has reverted to being more expensive in the HFOV group. For carers, it appears that the cost in the HFOV group is also more expensive but the patients themselves have more out-of-pocket expenses and loss of earnings in the conventional ventilation group. Their QoL is also slightly better in the HFOV at both 6 and 12 months. At 1 year, the cost to society and to the NHS per LYs saved still shows conventional ventilation dominating HFOV and the ICER for the cost per QALY does not fall below the established range for cost-effectiveness in the UK.
Perhaps the most important message to be gleaned from the 1-year cost-effectiveness results is the level of uncertainty around these. With a probability of being cost-effective at a threshold of £20,000 per QALY of 0.18 the chance of HFOV ever being cost-effective must be considered low, although the uncertainty about this grows as the threshold increases.
The imputed results for the missing data show that there is a smaller incremental QALY and a smaller incremental cost to society for the HFOV at 1 year but the conventional ventilation still dominates the HFOV in the ICER. The imputation is most likely alluding to the likelihood for missing QoL data to be due to poor questionnaire return in patients experiencing a worse QoL. Extrapolation based on the sensitivity analysis at both 30 days and 1 year the most important consideration for the cost of intervention is the cost of the initial ICU admission and the cost of the total hospital stay, respectively.
There are a number of limitations in this study brought about by the inevitable shortfall in information retrieval in a clinical trial setting. For example, patients were separated into those requiring antibiotics based on whether they experienced pulmonary symptoms or non-pulmonary symptoms. We therefore had to assume that those in the non-pulmonary group were using them for a UTI as this is the most common cause of sepsis in hospital and the community. 101–105 We also had no information about which antibiotics were in use or patient allergies and therefore based our costing on antibiotics in common use and assumed a similar rate of allergy to penicillin as the normal population. We had to assume which types of muscle relaxants and sedation were in use as there was no standard protocol in place. It should be noted that the QoL data were based on incomplete follow-up for some patients. We therefore used complete-case analysis followed by a second analysis using imputation for missing values. A subsequent analysis will update the 1-year cost-effectiveness.
Markov modelling shows that over a lifetime horizon the cost of HFOV remains higher than conventional ventilation and with a continuation of the small improvement in QALYs. The ICER reported from the model suggests that HFOV is cost-effective, which is a surprise given the within-trial analysis results. This appears to be driven by the slightly greater proportion of patients surviving at the end of 1-year follow-up in the HFOV group of the trial. More complete trial follow-up is required in order to make reliable inference from this analysis. It should also be noted that we have not adjusted for baseline characteristics or stratification factors. We did not have evidence that this increased mortality continues past 9 years but it is unlikely to revert to that of the normal population and more data would be required to make this a robust analysis. However, as there was no evidence available we used the mortality rate for the normal population after this. The evidence for the increased mortality up to 9 years post-ICU discharge was based on an Australian population and we assumed there would be a high correlation with that of our UK population. Another limitation was the lack of long-term data for utility values associated with ARDS and ICU admission available and we therefore assumed that once patients were 1 year post randomisation, their utility value reverted back to that of the normal population.
Conclusion
A number of uncertainties in the evidence for cost-effectiveness remain but at present there is no economic justification for the use of HFOV over conventional ventilation in the setting of ARDS.
Chapter 6 Discussion
The design of the OSCAR study
The OSCAR study was a randomised, open, effectiveness study of HFOV in patients with ARDS. It was primarily designed to answer the question ‘what would be the effect of introducing high-frequency oscillatory ventilation into the NHS?’. It was a largely pragmatic study, meeting 7 of the 10 criteria of the Pragmatic–Explanatory Continuum Indicator Summary (PRECIS). 120 The study was not totally pragmatic because of the tight protocol-specified restrictions on the use of HFOV, protocol-compliance monitoring and follow-up beyond that required clinically.
The patients we recruited all had ARDS as determined by the internationally agreed definitions current when the study was planned,20 and by the revised definitions published as the study was finishing. 21,121 However, these definitions alone are insufficient as study entry criteria, largely because they do not specify a duration during which the P : F ratio needs to be below a threshold value. As the P : F ratio has a non–linear relationship with inspired oxygen, PEEP, patient position and ventilation mode, a patient may be eligible on one blood gas estimation but with a change in treatment but no real change in the severity of their ARDS be ineligible on the next. In addition, for HFOV to have any effect, it would have to be in use long enough to avoid lung damage caused by the alternative conventional ventilation. This is not a problem unique to OSCAR, it applies to all other studies of lung-protective ventilation. Thus, we additionally specified that the patient should be expected to be ventilated for a further 48 hours. During the study we were asked by collaborators for guidelines on how to predict expected duration of ventilation other than with clinical skills. We systematically searched the literature to find a prediction tool that was useable during the first 7 days of artificial ventilation, which had been validated, which was applicable to a wide range of causes of ARDS, and was sufficiently sensitive and specific to be used on individual patients. We were unable to find such a tool. To try to ensure the maximum benefit from HFOV we used it as long as possible, up to the point at which the mechanics of the HFOV ventilator hindered weaning.
We recruited patients with moderate-to-severe ARDS, with an average P : F ratio of 15.1 kPa. The study entry criterion was a P : F ratio of < 26.7 kPa, which was in line with the agreed definitions of ARDS but the additional requirement of a further 48 hours or more of mechanical ventilation may have excluded milder cases of ARDS. The average P : F ratio is nearly identical to the mean of 14.9 kPa reported in the recent systematic review of HFOV18 and is similar to the mean values reported in studies of other treatments for ARDS. 122–124
To deliver HFOV in our study, we used the Novalung (Metran) R100 ventilator, a device that had not been used before in clinical trials. To date, all other studies of HFOV in adults have used the SensorMedics 3100B ventilator. The differences in the techniques used to generate HFOV between the machines were not believed to be important when the study was designed, as both were CE marked and reported to improve oxygenation. No additional data emerged during the study to suggest one device was superior to the other. As the SensorMedics 3100B ventilator has a diaphragm that is electrically driven it is possible to vary the inspiratory to expiratory time ratio, an adjustment not possible on the pneumatically driven diaphragm in the R100. This probably had little effect, as in studies on model lungs using both ventilators the 1 : 1 ratio that the R100 uses caused greatest gas movement. 125 However, the R100 did have the facility to perform conventional ventilation, which made protocol design and training considerably easier, and it was this that largely determined our choice of ventilator.
Our study specified a higher starting frequency than most other studies. Most studies used 5 Hz as the starting frequency,17,51 with only the OSCILLATE56 study allowing high starting frequencies. We chose the 10 Hz starting frequency because higher frequencies are thought to offer more lung protection, although carbon dioxide clearance becomes less efficient at higher frequencies. As noted in Chapter 3, this choice of starting frequency did cause problems with hypercarbia in some patients, including one patient in whom the local investigator raised a SAE, and the algorithms required a modification to deal with this. Other than the higher starting frequency, our algorithms were similar to those used in other studies and were based on algorithms used clinically in Addenbrooke’s Hospital (Cambridge), the University of Wales Hospital (Cardiff) and Queen Elizabeth Hospital (Birmingham).
Early in the study design process we had to decide whether to use centres ‘experienced’ in HFOV or HFOV-naïve centres. The advantages of using experienced centres include reduced training requirements, the possibility of using their own equipment thereby reducing study costs, and the availability of experienced clinicians for advice on trial design and execution. However, centres with HFOV already in use as part of their clinical management of ARDS were unlikely to have equipoise, and when asked were not willing to undertake conventional ventilation in half the patients they would previously have treated with HFOV. In addition, there were simply not enough experienced centres in the UK to run the study. We therefore chose to base the study on HFOV-naïve centres and put a comprehensive training package in place.
However, the need for experienced clinicians remained. Three of the applicants on the grant (Shah, Tunnecliffe and MacKenzie) had experience with HFOV, and convinced their centres (Queen Elizabeth Hospital, Birmingham and University Hospital of Wales, Cardiff) to take part. As they had SensorMedics 3100B ventilators, the study supplied leased R100 ventilators. In addition, two hospitals who bought R100 ventilators as the study started [Ysbyty (Wrexham) Maelor Hospital and Queen Elizabeth Hospital, Gateshead] agreed to join the study using their own ventilators. The ventilator suppliers kept us appraised of all new orders so we could approach centres buying R100 ventilators to join the study. The hospitals who agreed to join the study using their own new ventilators were Southend Hospital, Royal Victoria Hospital (Newcastle), James Cook University Hospital (Middlesbrough) and the James Paget Hospital (Great Yarmouth). Later in the study the Leeds hospitals, also experienced in HFOV, joined the study. Thus though the majority of recruited patients came from HFOV-naïve centres, three major centres with HFOV experience also took part.
The original recruitment rate estimate was 2 patients per centre per month. The final figure was less than half of this (0.82 patients per centre per month), and as a result the recruitment period had to be extended and took 56 months rather than the planned 36 months. Overall, we recruited for 80.7 centre-years. The usual checks and inducements were used to monitor and increase the recruitment rate, including a formal review of barriers to recruitment, ‘Not in trial’ log reviews, publicity at professional meetings, site visits, newsletters, recruitment prizes, a study nurses’ network, and repeated training sessions. With one ventilator per site recruitment could only take place when the ventilator was not in use, but the ‘Not in trial’ logs suggested this was not a practical problem. In some trials, in-critical-care patients are lost when they present out-of-hours, but in OSCAR the study recruitment window allowed office hours recruitment. We believe part of the problem was the original recruitment estimates were too optimistic. The estimates were largely based on epidemiological studies, which record the incidence of ARDS in ICUs. As noted above, this incidence could be based on patients with only one blood gas estimation in the required range, and so the epidemiological studies took no account of the duration of illness. In addition, we were unable to estimate the number of ineligible patients. In hindsight, there were indications that recruitment might be difficult. The discrepancy between the number of patients in Oxford with abnormal blood gas readings on at least one occasion and the clinically recorded incidence of ARDS might have alerted us. The problem of recruitment to studies of ARDS in the UK was not limited to the OSCAR study. The BALTI-2 study122 which ran simultaneously with the OSCAR study and had similar entry criteria recruited at about 0.2 patients per centre per month.
The limitations of the OSCillation in ARDS study
The study was powered on the primary outcome, 30-day all-cause mortality. Although planned subgroup analyses were performed, the study was not powered for these analyses and so the results should be interpreted with caution. The study group allocation was necessarily open to study staff, clinical staff, patients and their relatives, and so there is a risk of bias in reported subjective secondary outcomes. We believe that this may be one explanation for the modestly improved QoL reported to date (full follow-up is not complete) in the patients who received HFOV. Similarly, treatments other than ventilation may have differed between groups, either as a result of different effects of HFOV and conventional ventilation or differing decision making in the presence of unblinded allocation. The generous page count for this report enabled us to report all the analyses in our predefined analysis plan, which minimises the chance of reporting bias, but even so we cannot report every nuance of the study
The validity of the OSCillation in ARDS study
The study has good internal and external validity. Bias was minimised by using centres with equipoise (see above), by concealing treatment assignments before randomisation by using random block sizes, by concealing interim analysis results from all study investigators except for the DMEC, and by using an analysis plan that was agreed on before study closure and before any results were available. There was no loss to follow-up, crossovers were minimal, and the study recruited 99.1% of the planned sample size.
External validity was maintained by using a large number of different-sized ICUs spread across the UK. Most of the centres in this trial were inexperienced with the intervention at the start, but this was unavoidable, since few centres in the United Kingdom had experience with the use of HFOV. We invested heavily in training at each study centre. The consent refusal rate was low, as was the dropout rate.
The study showed no survival benefit from HFOV in a group of adult patients with moderate to severe ARDS. The 95% confidence limits for the risk ratio were –6.1% to 7.5%, indicating that the effect size, if any, was less than the 10% absolute reduction in 30-day mortality the study was powered to detect, and less than the 9% that the study was originally powered for. The two Kaplan–Meier survival probability curves essentially overlay each other to 30 days, indicating both the number and timing of deaths were similar in both groups. Thus, this study does not show a short-term survival benefit for HFOV seen in the systematic review,18 where patients randomised to high-frequency oscillation, mortality was significantly reduced (risk ratio 0.77, 95% CI 0.61 to 0.98; p = 0.03; six trials, 365 patients, 160 deaths).
The CCCTG were running a similar study in Canada during the period OSCAR was recruiting. The OSCILLATE study (ISRCTN42992782 and ISRCTN87124254) took place from July 2007 to August 2012 in 39 ICUs in five countries, but was primarily run in Canada. The entry criteria were similar, using standard definitions of ARDS. The HFOV was delivered using the SensorMedics 3100B ventilator, and most centres were already experienced in HFOV and had their own ventilators. The design was closer to an efficacy study than OSCAR, with a tightly protocolised ventilation strategy for the control group. The study was stopped by the DMEC at 500 recruited patients, when the treatment (HFOV) group mortality was 47% and the control group mortality was 35% (RR 1.33, 95% CI 1.09 to 1.64). The Kaplan–Meier survival curves suggest the excess mortality occurred in the first 20–25 days after randomisation. The primary study results were published alongside the headline clinical result of the OSCAR study in the same edition of the New England Journal of Medicine. 56,119
The OSCILLATE investigators suggested some mechanisms which may have contributed to the increased mortality with HFOV seen in their study. Higher mean airway (and hence intrathoracic) pressures in the HFOV group may have resulted in haemodynamic compromise by decreasing venous return or directly affecting right ventricular function and thereby reducing cardiac output. Increased use of vasodilating sedative agents in the HFOV group may also have contributed to haemodynamic compromise. The study could not exclude the possibility of increased barotrauma in association with HFOV.
There was little evidence of harm caused by haemodynamic compromise in the OSCAR study. There was increased use of renal support in the HFOV group. We do not know the reason for this, it may represent a true effect of HFOV on renal function, possibly mediated via haemodynamic changes, or it may be that the respiratory acidosis seen early in the HFOV group altered clinicians’ decision making about the timing of renal replacement.
The OSCILLATE HFOV group, and both the OSCAR groups had broadly similar hospital mortality (47% in the OSCILLATE HFOV group, 50.1% in the OSCAR HFOV group and 48.4% in the OSCAR control group). In the OSCILLATE paper, the authors suggest that one possible explanation for the discordant results in the two studies relates to the control group treatment. In OSCILLATE, tidal volumes were lower and PEEP greater in the control groups. It is possible that ‘better’ treatment of the control group in the OSCILLATE study ‘unmasked’ the harm the HFOV was causing, an effect not seen in OSCAR because of the higher control group mortality.
While superficially attractive, this theory really only applies if both studies had similar populations. When compared with the OSCAR study, the patients in OSCILLATE had a much higher APACHE II score (29 compared with OSCAR 22, though the OSCILLATE patients had the APACHE II score calculated at enrolment not ICU admission). OSCILLATE patients were treated earlier in their illness. To try and understand the differences in the studies the results are being pooled in a meta-analysis, which may reveal results in subgroups too small to be analysed if only one set of patients were available. This work is ongoing at the time of writing.
Conclusions
The major conclusion is that, in the NHS in England, Wales, Scotland and Northern Ireland, the introduction of HFOV as a treatment for ARDS would not result in an improved survival for patients or a reduction in resource use as measured by treatment duration in acute health-care facilities.
The study was not powered for equivalence, and the result should not be interpreted as indicating that HFOV does not cause harm, especially in light of the results from the OSCILLATE study.
The OSCAR and OSCILLATE studies were expensive and took a long time to complete. Unless the meta-analysis of OSCAR and OSCILLATE suggests a subset of patients in whom HFOV has a major benefit, we suggest further large studies of HFOV in patients for ARDS should not be a priority for health-care research.
The control group treatment in OSCAR suggests that ‘best practice’ of low tidal volume ventilation is not occurring in ICUs in the UK. The reasons for this require further investigation, as to date low tidal volume ventilation is the only commonly available intervention with proven efficacy in patients with ARDS.
Acknowledgements
Dr Ranjit Lall (Senior Statistician, Warwick Clinical Trials Unit, Warwick, UK) participated in the design and running of the study, performed all statistical analyses except the health economics, and prepared this report.
Dr Patrick Hamilton (Clinical Researcher, Academic Unit of Health Economics, University of Leeds, Leeds, UK) participated in analysing the health economics data and writing the chapter on health economics.
Dr Duncan Young (Consultant and Senior Lecturer in Intensive Care, John Radcliffe Hospital and University of Oxford, Oxford, UK) participated in the design and running of the study as Chief Investigator, and edited the final version of this report.
Professor Claire Hulme (Professor of Health Economics, Academic Unit of Health Economics, University of Leeds, Leeds, UK) participated in the design and running of the study, oversaw the health economics analysis and the chapter on health economics.
Dr Peter Hall (NIHR Clinical Lecturer, Academic Unit of Health Economics, University of Leeds, Leeds, UK) participated in analysing the health economics data and writing the chapter on health economics.
Dr Sanjoy Shah (Consultant in Intensive Care, Bristol Royal Infirmary, Bristol, UK) participated in the design and running of the study.
Dr Iain MacKenzie (Consultant in Intensive Care, Queen Elizabeth Hospital, Birmingham, UK) participated in the design and running of the study.
Dr William Tunnicliffe (Consultant in Intensive Care, Queen Elizabeth Hospital, Birmingham, UK) participated in the design and running of the study.
Professor Kathy Rowan (Director, ICNARC, London, UK) participated in the design and running of the study.
Professor Brian Cuthbertson (Chief of Critical Care, Sunnybrook Health Sciences Centre, Toronto, ON, Canada) participated in the design and running of the study.
Professor Chris McCabe (Capital Health Research Chair, University of Alberta, AB, Canada) participated in the design and running of the study, oversaw the health economics analysis and the chapter on health economics.
Professor Sallie Lamb (Director, Warwick Clinical Trials Unit, University of Warwick, Warwick, UK; Professor of Trauma Rehabilitation, University of Oxford, Oxford, UK) participated in the design and running of the study, and oversaw study activities at Warwick.
The OSCAR collaborators are listed in Appendix 5. They were the principal investigators who ran the study at their local hospitals.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
Publication
Young D, Lamb SE, Shah S, MacKenzie I, Tunnicliffe W, Lall R, et al. High-Frequency Oscillation for Acute Respiratory Distress Syndrome. N Engl J Med 2013;368:806–13.
References
- Arroliga AC, Ghamra ZW, Perez Trepichio A, Perez Trepichio P, Komara JJ, Smith A, et al. Incidence of ARDS in an adult population of northeast Ohio. Chest 2002;121:1972-6. http://dx.doi.org/10.1378/chest.121.6.1972.
- Bersten AD, Edibam C, Hunt T, Moran J. Australian New Zealand Intensive Care Society Clinical Trials Group . Incidence and mortality of acute lung injury and the acute respiratory distress syndrome in three Australian states. Am J Respir Crit Care Med 2002;165:443-8. http://dx.doi.org/10.1164/ajrccm.165.4.2101124.
- Brun-Buisson C, Minelli C, Bertolini G, Brazzi L, Pimentel J, Lewandowski K, et al. Epidemiology and outcome of acute lung injury in European intensive care units. Results from the ALIVE study. Intensive Care Med 2004;30:51-6. http://dx.doi.org/10.1007/s00134-003-2136-x.
- Goss CH, Brower RG, Hudson LD, Rubenfeld GD. ARDS Network . Incidence of acute lung injury in the United States. Crit Care Med 2003;31:1607-11. http://dx.doi.org/10.1097/01.CCM.0000063475.65751.1D.
- Hughes M, MacKirdy FN, Ross J, Norrie J, Grant IS. Scottish Intensive Care Society . Acute respiratory distress syndrome: an audit of incidence and outcome in Scottish intensive care units. Anaesthesia 2003;58:838-45. http://dx.doi.org/10.1046/j.1365-2044.2003.03287.x.
- Luhr OR, Antonsen K, Karlsson M, Aardal S, Thorsteinsson A, Frostell CG, et al. Incidence and mortality after acute respiratory failure and acute respiratory distress syndrome in Sweden, Denmark, and Iceland. Am J Respir Crit Care Med 1999;159:1849-61. http://dx.doi.org/10.1164/ajrccm.159.6.9808136.
- MacCallum NS, Evans TW. Epidemiology of acute lung injury. Curr Opin Crit Care 2005;11:43-9. http://dx.doi.org/10.1097/00075198-200502000-00007.
- Roca O, Sacanell J, Laborda C, Pérez M, Sabater J, Burgueño MJ, et al. Cohort study on incidence of ARDS in patients admitted to the ICU and prognostic factors of mortality. Med Intensiva 2006;30:6-12. http://dx.doi.org/10.1016/S0210-5691(06)74455-2.
- Sigvaldason K, Thornormar K, Bergmann JB, Reynisson K, Magnúsdóttir H, Stefánsson TS, et al. The incidence and mortality of ARDS in Icelandic intensive care units 1988–1997. Laeknabladid 2006;92:201-7.
- Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med 2003;348:683-93. http://dx.doi.org/10.1056/NEJMoa022450.
- Cheung AM, Tansey CM, Tomlinson G, Diaz-Granados N, Matte A, Barr A, et al. Two-year outcomes, health care use and costs in survivors of ARDS. Am J Respir Crit Care Med 2006;174:538-44. http://dx.doi.org/10.1164/rccm.200505-693OC.
- The Acute Respiratory Distress Syndrome Network . Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000;342:1301-8. http://dx.doi.org/10.1056/NEJM200005043421801.
- Peek GJ, Mugford M, Tiruvoipati R, Wilson A, Allen E, Thalanany MM, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet 2009;374:1351-63. http://dx.doi.org/10.1016/S0140-6736(09)61069-2.
- Wunsch H, Mapstone J. High-frequency ventilation versus conventional ventilation for treatment of acute lung injury and acute respiratory distress syndrome. Cochrane Database Syst Rev 2004;1.
- Wunsch H, Mapstone J, Takala J. High-frequency ventilation versus conventional ventilation for the treatment of acute lung injury and acute respiratory distress syndrome: a systematic review and cochrane analysis. Anesth Analg 2005;100:1765-72. http://dx.doi.org/10.1213/01.ANE.0000145070.52315.F2.
- Arnold JH, Hanson JH, Toro-Figuero LO, Gutiérrez J, Berens RJ, Anglin DL. Prospective, randomized comparison of high-frequency oscillatory ventilation and conventional mechanical ventilation in pediatric respiratory failure. Crit Care Med 1994;22:1530-9. http://dx.doi.org/10.1097/00003246-199422100-00006.
- Derdak S, Mehta S, Stewart TE, Smith T, Rogers M, Buchman TG, et al. High-frequency oscillatory ventilation for acute respiratory distress syndrome in adults: a randomized, controlled trial. Am J Respir Crit Care Med 2002;166:801-8. http://dx.doi.org/10.1164/rccm.2108052.
- Sud S, Sud M, Friedrich JO, Meade MO, Ferguson ND, Wunsch H, et al. High frequency oscillation in patients with acute lung injury and acute respiratory distress syndrome (ARDS): systematic review and meta-analysis. BMJ 2010;340. http://dx.doi.org/10.1136/bmj.c2327.
- Ashbaugh DG, Bigelow DB, Petty TL, Levine BE. Acute respiratory distress in adults. Lancet 1967;2:319-23. http://dx.doi.org/10.1016/S0140-6736(67)90168-7.
- Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, et al. Report of the American-European consensus conference on ARDS: definitions, mechanisms, relevant outcomes and clinical trial coordination. The Consensus Committee. Intensive Care Med 1994 1994;20:225-32. http://dx.doi.org/10.1007/BF01704707.
- Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, . ARDS Definition Task Force . Acute respiratory distress syndrome: the Berlin Definition. JAMA 2012;307:2526-33.
- Guérin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 2013;368:2159-68. http://dx.doi.org/10.1056/NEJMoa1214103.
- Imai Y, Kawano T, Miyasaka K, Takata M, Imai T, Okuyama K. Inflammatory chemical mediators during conventional ventilation and during high frequency oscillatory ventilation. Am J Respir Crit Care Med 1994;150:1550-4. http://dx.doi.org/10.1164/ajrccm.150.6.7952613.
- Imai Y, Nakagawa S, Ito Y, Kawano T, Slutsky AS, Miyasaka K. Comparison of lung protection strategies using conventional and high-frequency oscillatory ventilation. J Appl Physiol 2001;91:1836-44.
- Baker AB, Atkinson RS, Boulton TB. The History of Anaesthesia. London: Royal Society of Medicine; 1987.
- Kite C. An Essay on the Recovery of the Apparently Dead. London: C. Dilly; 1788.
- Goerig M, Filos K, Ayisi KW, Atkinson RS, Boulton TB. The History of Anaesthesia. London: Royal Society of Medicine; 1987.
- Redell-Baker L, Pettis JL, Atkinson RS, Boulton TB. The History of Anaesthesia. London: Royal Society of Medicine; 1987.
- Mushin WW, Rendell-Baker L, Thompson PW, Mapleson WW. Automatic Ventilation of the Lungs. Oxford: Blackwell; 1980.
- Henderson Y, Chillingsworth F, Whitney J. The respiratory dead space. Am J Physiol 1915;38:1-9.
- Briscoe WA, Forster RE, Comroe JH. Alveolar ventilation at very low tidal volumes. J Appl Physiol 1954;17:27-30.
- Lunkenheimer PP, Rafflenbeul W, Keller H, Frank I, Dickhut HH, Fuhrmann C. Application of transtracheal pressure oscillations as a modification of ‘diffusing respiration’. Br J Anaesth 1972;44. http://dx.doi.org/10.1093/bja/44.6.627.
- Jonzon A, Oberg PA, Sedin G, Sjostrand U. High-frequency positive-pressure ventilation by endotracheal insufflation. Acta Anaesthesiol Belg 1971;43:1-43. http://dx.doi.org/10.1111/j.1399-6576.1971.tb05463.x.
- Hardinge FM, Davies RJ. Stradling Alveolar ventilation at very low tidal volumes . Effects of short term high frequency negative pressure ventilation on gas exchange using the Hayek oscillator in normal subjects. Thorax 1995;50:44-9. http://dx.doi.org/10.1136/thx.50.1.44.
- Piquet J, Brochard L, Isabey D, de Cremoux H, Chang HK, Bignon J, et al. High frequency chest wall oscillation in patients with chronic air-flow obstruction. Am Rev Respir Dis 1987;136:1355-9. http://dx.doi.org/10.1164/ajrccm/136.6.1355.
- Young JD. Gas movement during jet ventilation. Acta Anaesthesiol Scand Suppl 1989;90:72-4. http://dx.doi.org/10.1111/j.1399-6576.1989.tb03008.x.
- Bohn DJ, Miyasaka K, Marchak BE, Thompson WK, Froese AB, Bryan AC. Ventilation by high-frequency oscillation. J Appl Physiol 1980;48:710-6.
- Butler WJ, Bohn DJ, Bryan AC, Froese AB. Ventilation by high-frequency oscillation in humans. Anesth Analg 1980;59:577-84. http://dx.doi.org/10.1213/00000539-198008000-00002.
- Isabey D, Harf A, Chang HK. Alveolar ventilation during high-frequency oscillation: core dead space concept. J Appl Physiol Respir Environ Exerc Physiol 1984;56:700-7.
- Chang HK, Harf A. High-frequency ventilation: a review. Respir Physiol 1984;57:135-52. http://dx.doi.org/10.1016/0034-5687(84)90089-6.
- Drazen JM, Kamm RD, Slutsky AS. High-frequency ventilation. Physiol Rev 1984;64:505-43.
- High frequency ventilation for immature infants . Pediatrics 1983;71:280-7.
- High-frequency oscillatory ventilation compared with conventional mechanical ventilation in the treatment of respiratory failure in preterm infants . The HIFI Study Group. N Engl J Med 1989;320:88-93. http://dx.doi.org/10.1056/NEJM198901123200204.
- Bhuta T, Clark RH, Henderson-Smart DJ. Rescue high frequency oscillatory ventilation vs conventional ventilation for infants with severe pulmonary dysfunction born at or near term. Cochrane Database Syst Rev 2001;1.
- Bhuta T, Henderson-Smart DJ. Rescue high frequency oscillatory ventilation versus conventional ventilation for pulmonary dysfunction in preterm infants. Cochrane Database Syst Rev 2000;2.
- Cools F, Henderson-Smart DJ, Offringa M, Askie LM. Elective high frequency oscillatory ventilation versus conventional ventilation for acute pulmonary dysfunction in preterm infants. Cochrane Database Syst Rev 2009;3.
- Henderson-Smart DJ, Bhuta T, Cools F, Offringa M. Elective high frequency oscillatory ventilation versus conventional ventilation for acute pulmonary dysfunction in preterm infants. Cochrane Database Syst Rev 2003;1.
- Soll RF. Elective high-frequency oscillatory ventilation versus conventional ventilation for acute pulmonary dysfunction in preterm infants. Neonatology 2013;103:7-9. http://dx.doi.org/10.1159/000338553.
- Bryan AC, Froese AB. Reflections on the HiFi trial. Pediatrics 1991;87:565-7.
- Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, et al. Report of the American-European Consensus conference on acute respiratory distress syndrome: definitions, mechanisms, relevant outcomes, and clinical trial coordination. Consensus Committee. J Crit Care 1994;9:72-81. http://dx.doi.org/10.1016/0883-9441(94)90033-7.
- Bollen CW, van Well GT, Sherry T, Beale RJ, Shah S, Findlay G, et al. High frequency oscillatory ventilation compared with conventional mechanical ventilation in adult respiratory distress syndrome: a randomized controlled trial [ISRCTN24242669]. Crit Care 2005;9:R430-9. http://dx.doi.org/10.1186/cc3737.
- Demory D, Michelet P, Arnal JM, Donati S, Forel JM, Gainnier M, et al. High-frequency oscillatory ventilation following prone positioning prevents a further impairment in oxygenation. Crit Care Med 2007;35:106-11. http://dx.doi.org/10.1097/01.CCM.0000251128.60336.FE.
- Frantz ID, Close RH. Alveolar pressure swings during high frequency ventilation in rabbits. Pediatr Res 1985;19:162-6. http://dx.doi.org/10.1203/00006450-198502000-00002.
- Harvey S, Harrison DA, Singer M, Ashcroft J, Jones CM, Elbourne D, et al. Assessment of the clinical effectiveness of pulmonary artery catheters in management of patients in intensive care (PAC-Man): a randomised controlled trial. Lancet 2005;366:472-7. http://dx.doi.org/10.1016/S0140-6736(05)67061-4.
- Harvey S, Stevens K, Harrison D, Young D, Brampton W, McCabe C, et al. An evaluation of the clinical and cost-effectiveness of pulmonary artery catheters in patient management in intensive care: a systematic review and a randomised controlled trial. Health Technol Assess 2006;10. http://dx.doi.org/10.3310/hta10290.
- Ferguson ND, Cook DJ, Guyatt GH, Mehta S, Hand L, Austin P, et al. High-frequency oscillation in early acute respiratory distress syndrome. N Engl J Med 2013;368:795-80. http://dx.doi.org/10.1056/NEJMoa1215554.
- Gao Smith F, Perkins GD, Gates S, Young D, McAuley DF, Tunnicliffe W, et al. Effect of intravenous β-2 agonist treatment on clinical outcomes in acute respiratory distress syndrome (BALTI-2): a multicentre, randomised controlled trial. Lancet 2012;379:229-35. http://dx.doi.org/10.1016/S0140-6736(11)61623-1.
- McAuley DF, Laffey JG, O’Kane CM, Perkins GD, Mullan B, Trinder TJ, et al. Simvastatin in the acute respiratory distress syndrome. N Engl J Med 2014;371:1695-703. http://dx.doi.org/10.1056/NEJMoa1403285.
- Roupie E, Lepage E, Wysocki M, Fagon JY, Chastre J, Dreyfuss D, et al. Prevalence, etiologies and outcome of the acute respiratory distress syndrome among hypoxemic ventilated patients. SRLF Collaborative Group on Mechanical Ventilation. Société de Reanimation de Langue Française. Intensive Care Med 1999;25:920-9. http://dx.doi.org/10.1007/s001340050983.
- Monchi M, Bellenfant F, Cariou A, Joly LM, Thebert D, Laurent I, et al. Early predictive factors of survival in the acute respiratory distress syndrome. A multivariate analysis. Am J Respir Crit Care Med 1998;158:1076-81. http://dx.doi.org/10.1164/ajrccm.158.4.9802009.
- Ferguson ND, Kacmarek RM, Chiche JD, Singh JM, Hallett DC, Mehta S, et al. Screening of ARDS patients using standardized ventilator settings: influence on enrollment in a clinical trial. Intensive Care Med 2004;30:1111-16. http://dx.doi.org/10.1007/s00134-004-2163-2.
- Esteban A, Anzueto A, Frutos F, Alia I, Brochard L, Stewart TE, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA 2002;287:345-55. http://dx.doi.org/10.1001/jama.287.3.345.
- Black NA, Jenkinson C, Hayes JA, Young D, Vella K, Rowan KM, et al. Review of outcome measures used in adult critical care. Crit Care Med 2001;29:2119-24. http://dx.doi.org/10.1097/00003246-200111000-00012.
- Hayes JA, Black NA, Jenkinson C, Young JD, Rowan KM, Daly K, et al. Outcome measures for adult critical care: a systematic review. Health Technol Assess 2000;4.
- EuroQol Group . EuroQol – a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199-208. http://dx.doi.org/10.1016/0168-8510(90)90421-9.
- Angus DC, Carlet J. 2002 Brussels Roundtable Participants . Surviving intensive care: a report from the 2002 Brussels Roundtable. Intensive Care Med 2003;29:368-77.
- Wehler M, Geise A, Hadzionerovic D, Aljukic E, Reulbach U, Hahn EG, et al. Health-related quality of life of patients with multiple organ dysfunction: individual changes and comparison with normative population. Crit Care Med 2003;31:1094-101. http://dx.doi.org/10.1097/01.CCM.0000059642.97686.8B.
- Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey: Manual and Interpretation Guide. Boston, MA: The Health Institute; 1993.
- Badia X, Diaz-Prieto A, Gorriz MT, Herdman M, Torrado H, Farrero E, et al. Using the EuroQol-5D to measure changes in quality of life 12 months after discharge from an intensive care unit. Intensive Care Med 2001;27:1901-7. http://dx.doi.org/10.1007/s00134-001-1137-x.
- Dowdy DW, Eid MP, Dennison CR, Mendez-Tellez PA, Herridge MS, Guallar E, et al. Quality of life after acute respiratory distress syndrome: a meta-analysis. Intensive Care Med 2006;32:1115-24. http://dx.doi.org/10.1007/s00134-006-0217-3.
- Smith S, Brazier JE, Parry G, Edbrooke DL, Rantaell K. Measuring the Outcomes of Adult Intensive Care Patients. Trent; 2004.
- Covinsky KE, Fuller JD, Yaffe K, Johnston CB, Hamel MB, Lynn J, et al. Communication and decision-making in seriously ill patients: findings of the SUPPORT project. The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Am Geriatr Soc 2000;48:S187-93.
- Needham DM, Dennison CR, Dowdy DW, Mendez-Tellez PA, Ciesla N, Desai SV, et al. Study protocol: The Improving Care of Acute Lung Injury Patients (ICAP) study. Crit Care 2005;10. http://dx.doi.org/10.1186/cc3948.
- Acute Respiratory Distress Syndrome N . Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000;342:1301-8. http://dx.doi.org/10.1056/NEJM200005043421801.
- Comprehensive Critical Care: A Review of Adult Critical Care Services. London: DH; 2000.
- Mental Capacity Act 2005. London: The Stationery Office; 2005.
- Adults with Incapacity (Scotland) Act 2000. Edinburgh: The Scottish Government; 2000.
- Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. PLOS Med 2010;7. http://dx.doi.org/10.1371/journal.pmed.1000251.
- Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med 1985;13:818-29. http://dx.doi.org/10.1097/00003246-198510000-00009.
- Young JD, Goldfrad C, Rowan K. Development and testing of a hierarchical method to code the reason for admission to intensive care units: the ICNARC Coding Method. Intensive Care National Audit & Research Centre. Br J Anaesth 2001;87:543-8. http://dx.doi.org/10.1093/bja/87.4.543.
- Ware JE, Kosinski M, Turner-Bowker D, Gandek B. How to Score Version 2 of the SF-12 Health Survey: With a Supplement Documenting Version 1. Boston: QualityMetric Incorporated; 2002.
- Rabin R, Oemar M, Oppe M. EQ-5D-3L User Guide Version 4.0: EuroQol Group Executive Office; 2011 n.d. www.euroqol.org/fileadmin/user_upload/Documenten/PDF/Folders_Flyers/UserGuide_EQ-5D-3L.pdf (accessed 14 February 2013).
- Jones PW, Quirk FH, Baveystock CM. The St George’s Respiratory Questionnaire. Respir Med 1991;85:3-7.
- QualityMetric . The SF-12®: An Even Shorter Health Survey 2013 n.d. www.sf-36.org/tools/sf12.shtml (accessed 6 February 2013).
- Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2005.
- Young D, Harrison DA, Cuthbertson BH, Rowan K. TracMan Collaborators . Effect of early vs late tracheostomy placement on survival in patients receiving mechanical ventilation: the TracMan randomized trial. JAMA 2013;309:2121-9. http://dx.doi.org/10.1001/jama.2013.5154.
- Royston P. Multiple imputation of missing values: Update of ice. Stata J 2005;5:527-36.
- Brookes ST, Whitley E, Peters TJ, Mulheran PA, Egger M, Davey Smith G. Subgroup analyses in randomised controlled trials: quantifying the risks of false-positives and false-negatives. Health Technol Assess 2001;5. http://dx.doi.org/10.3310/hta5330.
- Campling EA, Devlin HB, Hoile RW, Lunn JN. National Confidential Enquiry into Perioperative Deaths 1990. London: National Confidential Enquiry into Perioperative Death; 1992.
- Ramsey S, Willke R, Briggs A, Brown R, Buxton M, Chawla A, et al. Good research practices for cost-effectiveness analysis alongside clinical trials: the ISPOR RCT-CEA Task Force report. Value Health 2005;8:521-33. http://dx.doi.org/10.1111/j.1524-4733.2005.00045.x.
- Guide to the Methods of Technology Appraisal. London: NICE; 2004.
- NHS Reference Costs 2011 to 2012. London: (DH); 2013.
- British National Formulary. London: BMA and RPS; 2012.
- Curtis L. Unit Costs of Health and Social Care 2011. Canterbury: PSSRU, University of Kent; 2011.
- NHS . NHS Supply Chain n.d. www.supplychain.nhs.uk/ (accessed 7 February 2014).
- Approved Mileage Rates 2011/2012. London: HMRC; 2012.
- Lim WS, Baudouin SV, George RC, Hill AT, Jamieson C, Le Jeune I, et al. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax 2009;64:iii1-55. http://dx.doi.org/10.1136/thx.2009.121434.
- Management of Suspected Bacterial Urinary Tract Infection in Adults. Edinburgh: SIGN; 2012.
- Harrison DA, Welch CA, Eddleston JM. The epidemiology of severe sepsis in England, Wales and Northern Ireland, 1996 to 2004: secondary analysis of a high quality clinical database, the ICNARC Case Mix Programme Database. Crit Care 2006;10. http://dx.doi.org/10.1186/cc4854.
- Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, et al. Incidence and outcomes of acute lung injury. N Engl J Med 2005;353:1685-93. http://dx.doi.org/10.1056/NEJMoa050333.
- Foxman B. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med 2002;113:5S-13S. http://dx.doi.org/10.1016/S0002-9343(02)01054-9.
- Laupland KB, Zygun DA, Davies HD, Church DL, Louie TJ, Doig CJ. Incidence and risk factors for acquiring nosocomial urinary tract infection in the critically ill. J Crit Care 2002;17:50-7. http://dx.doi.org/10.1053/jcrc.2002.33029.
- Stamm WE, Hooton TM. Management of urinary tract infections in adults. N Engl J Med 1993;329:1328-34. http://dx.doi.org/10.1056/NEJM199310283291808.
- Vincent JL, Bihari DJ, Suter PM, Bruining HA, White J, Nicolas-Chanoin MH, et al. The prevalence of nosocomial infection in intensive care units in Europe. Results of the European Prevalence of Infection in Intensive Care (EPIC) Study. EPIC International Advisory Committee. JAMA 1995;274:639-44. http://dx.doi.org/10.1001/jama.1995.03530080055041.
- Joint Task Force on Practice Parameters; American Academy of Allergy, Asthma and Immunology; American College of Allergy, Asthma and Immunology; Joint Council of Allergy, Asthma and Immunology . Drug allergy: an updated practice parameter. Ann Allergy Asthma Immunol 2010;105:259-73. http://dx.doi.org/10.1016/j.anai.2010.08.002.
- Kerr JR. Penicillin allergy: a study of incidence as reported by patients. Br J Clin Pract 1994;48:5-7.
- Lee CE, Zembower TR, Fotis MA, Postelnick MJ, Greenberger PA, Peterson LR, et al. The incidence of antimicrobial allergies in hospitalized patients: implications regarding prescribing patterns and emerging bacterial resistance. Arch Intern Med 2000;160:2819-22. http://dx.doi.org/10.1001/archinte.160.18.2819.
- Wyatt JP. Patients’ knowledge about their drug allergies. J Accid Emerg Med 1996;13:114-15. http://dx.doi.org/10.1136/emj.13.2.114.
- Gadde J, Spence M, Wheeler B, Adkinson NF. Clinical experience with penicillin skin testing in a large inner-city STD clinic. JAMA 1993;270:2456-63. http://dx.doi.org/10.1001/jama.1993.03510200062033.
- Rehabilitation After Critical Illness. London: NICE; 2009.
- Brooks R. EuroQol: the current state of play. Health Policy 1996;37:53-72. http://dx.doi.org/10.1016/0168-8510(96)00822-6.
- Efron B, Tibshirani R. An Introduction to the Bootstrap. London: Chapman & Hall; 1993.
- Briggs A, Fenn P. Confidence intervals or surfaces? Uncertainty on the cost-effectiveness plane. Health Econ 1998;7:723-40. http://dx.doi.org/10.1002/(SICI)1099-1050(199812)7:8<723::AID-HEC392>3.0.CO;2-O.
- Sonnenberg FA, Beck JR. Markov models in medical decision making: a practical guide. Med Decis Making 1993;13:322-38. http://dx.doi.org/10.1177/0272989X9301300409.
- Ghelani D, Moran JL, Sloggett A, Leeson RJ, Peake SL. Long-term survival of intensive care and hospital patient cohorts compared with the general Australian population: a relative survival approach. J Eval Clin Pract 2009;15:425-35. http://dx.doi.org/10.1111/j.1365-2753.2008.01030.x.
- Historic and Projected Mortality Data (1951 to 2060) from the UK Life Tables, 2010-Based (March 2012). London: ONS; 2012.
- Kind P, Hardman G, Macran S. UK Population Norms for EQ-5D. York: York Centre for Health Economics, University of York; 1999.
- van Buuren S, Groothuis-Oudshoorn K. MICE: Multivariate Imputation by Chained Equations in R. J Statistical Software 2011;45:1-67.
- Young D, Lamb SE, Shah S, MacKenzie I, Tunnicliffe W, Lall R, et al. High-frequency oscillation for acute respiratory distress syndrome. N Engl J Med 2013;368:806-13. http://dx.doi.org/10.1056/NEJMoa1215716.
- Thorpe KE, Zwarenstein M, Oxman AD, Treweek S, Furberg CD, Altman DG, et al. A pragmatic-explanatory continuum indicator summary (PRECIS): a tool to help trial designers. J Clin Epidemiol 2009;62:464-75. http://dx.doi.org/10.1016/j.jclinepi.2008.12.011.
- Ferguson ND, Fan E, Camporota L, Antonelli M, Anzueto A, Beale R, et al. The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive Care Med 2012;38:1573-82. http://dx.doi.org/10.1007/s00134-012-2682-1.
- Perkins GD, Gates S, Lamb SE, McCabe C, Young D, Gao F. Beta Agonist Lung Injury TrIal-2 (BALTI-2) trial protocol: a randomised, double-blind, placebo-controlled of intravenous infusion of salbutamol in the acute respiratory distress syndrome. Trials 2011;12. http://dx.doi.org/10.1186/1745-6215-12-113.
- Villar J, Blanco J, Anon JM, Santos-Bouza A, Blanch L, Ambros A, et al. The ALIEN study: incidence and outcome of acute respiratory distress syndrome in the era of lung protective ventilation. Intensive Care Med 2011;37:1932-41. http://dx.doi.org/10.1007/s00134-011-2380-4.
- Villar J, Pérez-Méndez L, Basaldúa S, Blanco J, Aguilar G, Toral D, et al. A risk tertiles model for predicting mortality in patients with acute respiratory distress syndrome: age, plateau pressure, and PaO2FIO2 at ARDS onset can predict mortality. Respir Care 2011;56:420-8. http://dx.doi.org/10.4187/respcare.00811.
- Iguchi N, Hirao O, Uchiyama A, Mashimo T, Nishimura M, Fujino Y. Evaluation of performance of two high-frequency oscillatory ventilators using a model lung with a position sensor. J Anesth 2010;24:888-92. http://dx.doi.org/10.1007/s00540-010-1032-0.
Appendix 1 Substantial and non-substantial amendments to the OSCAR protocol
List 1: non-substantial amendments
| Date of amendment | Non-substantial amendment |
|---|---|
| 12 June 2007 | Ensuring all inclusion criteria in box Expanding ventilator criteria Updating ‘consent refused’ in line with Mental Capacity Act 200576 (and broken down into who is refusing Professional or Personal consultee) |
| 17 October 2007 | Page 21: Eligibility of patients A) Clinician is ‘substantially uncertain’ as to the utility of HFOV in this patient Remains the same just a re-ordering of points: point ‘v’ moved down to become point ‘vii’ keeping all clinical points together B) Predicted by the attending clinician likely to require at least 48 hours of artificial ventilation from the time of randomisation Word ‘likely’ added to reinforce this is a prediction not exact C) Have been mechanically ventilated for LESS than 7 consecutive days (≤ 168 hours) at the point of randomisation 7 days clarified by ‘consecutive’ being included and the number of hours indicated to ease calculating time frame |
| Page 21: Patients excluded D) Patients in whom HFOV might be hazardous: patients with moderate or severe airway disease expected to cause expiratory airflow limitation. ‘Moderate or severe’ added to aid definition of patient group E) Addition to exclusion criteria: ‘Patients with any other condition the clinician believes would make receiving HFOV hazardous.’ We had seen this as obvious but some clinicians asked for clarification hence now including it |
|
| Page 22: Screening and recruitment flow chart F) Eligibility box has been updated in line with (A) to (C) above G) Consent box wording changed to match England/Scotland Acts re. incapacity wording in other parts of Protocol Now: ‘Agreement from Consultee (Scotland: Consent from Welfare Guardian/Nearest Relative)’ Continue over/. . . H) ‘Trial Entry form’ box wording changed to match name of form used Now: ‘OSCAR Form 1: Pre-trial Entry Booklet completed’ I) ‘ICU/30 DAY/HOSPITAL DATA COLLECTED’ box wording changed to match name of form used to collect data. Now: ‘Daily: complete OSCAR Form 2: Post-Randomisation Patient Data Booklet’ |
|
| Page 25: Figure 3: The algorithm for managing HFOV J) This flow chart is used for training clinicians in the use of the oscillator and has been expanded to aid training in the use of the Vision Alpha ventilator The adjustments have been made to match the controls on the Vision Alpha machine which were not available until the new machine was delivered |
|
| New page 27 (was page 26): 4.9.2. Clinical management of patients in the control arm (conventional ventilation) K) Update to 4.9.2 text and accompanying chart More recent data have become available so minor changes have been made that is a synthesis of all available data |
|
| 4.9.3 Proposed duration of treatment and weaning L) Typo – 0.5 should have been 0.4. This has now been changed |
|
| Page 28: Figure 4: Patient treatment and weaning flow chart M) FiO2 chart box removed as duplicate of what on page 27 and is unnecessary in flow chart |
|
| 17 October 2007 | Page 2: Changes to wording (bold below) in numbers v and vi. Non-substantial amendment to Protocol led to this Summary Protocol being amended to ensure consistency: v Predicted by the attending clinician likely to require at least 48 hours of artificial ventilation from the time of randomisation vi Have been mechanically ventilated for LESS than 7 consecutive days (≤ 168 hours) at the point of randomisation |
| 7 March 2008 | A minor clarification of the protocol has been made The wording of one of the inclusion criteria has changed from: Patient: v Predicted by the attending clinician likely to require at least 48 hours of artificial ventilation from the time of randomisation. To: Patient: Will not be extubated by tomorrow evening (predicted by attending clinician) The justification for this clarification is based on feedback from sites who find the 48 hours of ventilation prediction difficult. Therefore this has been turned into a practical question they can relate to Patients are generally screened for suitability for the trial on the morning ward rounds once a day therefore the time frame still applies. Pages affected: 5, 21, 22 (Appendices: 107, 110) |
| 25 April 2008 | A minor clarification of admission criteria has been made relating to the hypoxaemia criterion. The new criterion is: ‘Lowest recorded PaO2/FiO2 ratio measured between onset of artificial ventilation and time of screening of ≤ 26.7 kPa with a positive end expiratory pressure (PEEP) ≥5 cmH20’ The requirement for a specific cause and a second test are removed |
| 1 October 2008 | A more manageable size of protocol is required. Therefore the full protocol that is currently approved (Version 5.1, 4 March 2008) has been split into two documents – Working Protocol (Version 1 – 1 October 2008) and Background Information (Version 1 – 1 October 2008) |
| The working protocol has been slimmed down from the original full protocol by removing the background information and copies of other trial documentation (already approved by MREC in their own right). The background information document (Version 1 – 1 October 2008) has been created from the information removed from the protocol | |
| A full protocol will still be maintained for the trial, the approved version 5.1, 4 March 2008, has been updated in section 5.8.2 and 5.13, as initially units collaborating the trial would receive a ventilator from the trial group and have the opportunity to potentially purchase it at the end of the trial, now however units are collaborating who already have their own ventilator and therefore they will not receive a ventilator from the trial group and have the opportunity to potentially purchase it | |
| As these changes do not alter the studies design, methodology, background or its scientific value, the Chief Investigator considers these are not significant changes to the protocol, nor do they alter any of the procedures undertaken by participants or alter the documentation participants receive, and these changes do not include a new site or a new Principal Investigator at an existing site, and this is therefore thought to be an non-substantial amendment | |
| 12 February 2009 | Page 26 of current protocol: additional detail added to carbon dioxide algorithm We know that some patients experience a significant rise in carbon dioxide levels on initiation of HFOV, this has always been known. However, as we have received enquiries about such cases, we felt the advice we give should be incorporated into the algorithm. Hence, we have added more detail. This is a minor clarification of the protocol |
| 22 January 2010 | The 24-month questionnaires are sent out to patients recruited in the first year of the study only. Due to an administrative oversight, the questionnaires were printed with questions relating to the previous 6 months. In order to calculate QALYs, we need information for the previous 12 months not 6 as in the questionnaire. We have therefore amended the questionnaires we send to patients or carers as appropriate. The changes are almost entirely simple substitution of ‘12’ for ‘6’ months. Each questionnaire is accompanied by a covering letter which has also been changed as appropriate. Copies showing the changes using the Track Changes facility in Microsoft Word (Microsoft Corporation, Redmond, WA, USA) is attached. In addition, the questionnaire we sent to the patients recruited in the first year of the study at 24 months contained a section on the burden of illness and, specifically, respiratory morbidity. It became apparent during the preparation of the analysis plan that these data would not produce useful results. Therefore, to reduce the burden on the patients we have removed this section. These changes are judged as non-substantial amendments by the Chief Investigator as: as these changes do not alter the study design, methodology, background or its scientific value, the Chief Investigator considers these are not significant changes to the protocol, nor do they alter any of the procedures undertaken by participants and these changes do not include a new site or a new Principal Investigator at an existing site. They consist of simple changes to questions which do not significantly alter the content and a change that reduces the data burden to the patient |
| 6 May 2011 | Creation of a pre-questionnaire warning letter for participants. This letter will be sent out 2 weeks ahead of the first questionnaire at 6 months and the second questionnaire at 12 months following randomisation. It does not alter any of the previously approved documentation that participants receive as it will be sent solely as a reminder to participants that they are taking part in the study and are due to receive a questionnaire and will prepare them for the types of questions we are asking them to answer |
List 2: substantial amendment 1, OSCAR trial – substantial amendment no. 1, 4 March 2008 summary of changes
| Document name | No. | Page number | Subsection | Changed from | Updated to |
|---|---|---|---|---|---|
| Full Protocol | Front sheet | Version 4 – 12 June 2007 | Version 5 – 4 March 2008 | ||
| 1 | 20 | 4.3.1 Centres | First bullet point: we have amended the first criteria as the number of ICU admissions alone does not always reflect the case mix of the unit. It may therefore be necessary to take on sites with a lower admission rate (< 650 per year), but who have more ARDS cases | ||
| 2 | 30 | 4.12 Secondary outcome measures | N/A | Addition of ventilator-free, antimicrobial-free and sedative-free days to Secondary outcome measures. These should have been included in the protocol from the outset. This information is required for both economic analysis (to ensure we can calculate the true cost of either treatment), and is required by clinicians for an all round knowledge of the effect of HFOV vs. conventional ventilation | |
| 3 | 31 | 4.13 Data collection | N/A | Final paragraph: the added text indicates the use of the SF-12 version 2 questionnaire and questions concerning social and health service use (see Patient Questionnaire Section below, 2 & 3) | |
| 4 | 31 | 4.14 Health economics | N/A | Final paragraph: added text indicates use of questions concerning social and health service use | |
| 5 | 39 | 5.13.2 Vision Alpha HFOV training | N/A | Second paragraph: this has been amended to reflect the way training has evolved during the initial phases of the trial. It was not possible for groups of individuals from busy ICUs to attend training in the Netherlands | |
| FOLLOW-UP QUESTIONNAIRES TO PATIENTS | 6 | Front page | Identifying when another individual has completed the questionnaire for the patient. The front page of the questionnaire has a small change in the box (in bold), identifying when another individual has completed the questionnaire on the patient’s behalf | ||
| 7 | Page 8/9 | Questions 25–31 | Adding questions to the questionnaire: SF-12 Validated Questionnaire. In the original protocol we had proposed and justified using a 36-item questionnaire to measure quality of life – called the Short Form 36 (SF-36). This is a well-validated questionnaire, which is widely used. It has proven efficacy in the intensive care population. However, over the last 5 years, it has been recognised that the instrument is long, and newer version have been developed which retain all of the original features, but with less items [known as the Short Form 12 (SF-12)]. We are now proposing to utilise the SF-12 (version 2) as the respondent burden is considerably less. The SF-12 is currently being used in other ARDS trials, which will facilitate pooling of results in meta-analyses. It has proved a good measure of the quality of life for patients who have suffered from ARDS | ||
| 8 | Pages 10–21 | Questions 32–47 | Adding questions to the questionnaire: Health Economic questions. The health economic questions have now been added. This is to establish an unbiased estimate of the long-term cost-effectiveness of HFOV vs. conventional ventilation. It is important to collect data on the patients’ long-term health and social care utilisation and their expenditure as a result of their stay in the ICU. It is important that the study does not just provide information about the short-term health benefits and that any increased burden on the NHS and on the patients themselves is identified so that the overall value of this technology can be assessed | ||
| CARERS QUESTIONNAIRE | 9 | We have created a questionnaire for carers which will be sent with the patients follow-up questionnaires. Informal carers are estimated to save the NHS billions of pounds and although informal carers are not typically paid for their work, in some instances they are entitled to benefits from the state. In this study we are interested in learning about the impact on the resources of these informal carers as a result of providing care to someone who has been in the ICU. Collecting this information from carers allows us to gain a complete picture of the cost of the interventions not just to the NHS but to wider society |
List 3: substantial amendment 2
Summary of changes
We would like the committee to approve the content of a follow-up reminder letter to participants. Our proposed letter is attached and is based on the wording in the initial follow-up letter sent to participants (approved by MREC).
The process:
Surviving patients are sent a follow-up letter/questionnaire, etc. (process and content already approved by MREC).
Non-responders 1 month later: status checked via ONS re: alive/deceased (process approved by MREC).
Those surviving are sent a reminder letter/questionnaire, etc. (process and questionnaire, etc. already approved by MREC, content of reminder letter not yet approved).
For your information, the relevant section of our approved protocol (page 30, section 4.13) is detailed below. This remains unchanged. ‘The trial office will send self-administered questionnaires to determine health-related quality of life (EQ-5D and SF-12 version 2) and specifically respiratory function (St George’s Respiratory Questionnaire) to all survivors at 6 months and 1 year after hospital discharge, with follow-up letters one month after the original mailing. These questionnaires also include questions on social and health service use. Freepost envelopes will be provided. Patients who have died after hospital discharge but prior to the mailing will be identified from the ONS returns and removed from the mailing list.’
List 4: substantial amendment 3
| Document name | Page number | Subsection | Changed from | Updated to |
|---|---|---|---|---|
| Full Protocol | Front sheet | Version 6.1 – 1 October 2008 | Version 7 – 19 October 2009 | |
| 5 | Sample size: 1006 and 3-year recruitment period | Sample size: 802 | ||
| 29 | Outcome measures | Cognitive function 1 year after randomisation | Removal of cognitive function from outcome measures | |
| 30 | Sample size | 1006 | 802 – plus explanation of change | |
| 31 | Sample size/justification for sample size | N/A | Inserted note to see update in section 4.15 | |
| 33 | Planned recruitment rate | N/A | Inserted note to see update in section 4.15 | |
| Working Protocol | Front sheet | Version 1 – 1 October 2008 | Version 2 – 19 October 2009 | |
| 2 | Outcome measures | Cognitive function 1 year after randomisation | Removal of cognitive function from outcome measures | |
| Sample size | 1006 | 802 | ||
| Planned recruitment period | November 2010 | August 2011 | ||
| Background Information | Front sheet | Version 1 – 1 October 2008 | Version 2 – 19 October 2009 | |
| 17 | Sample size | 1006 | 802 – plus explanation of change (as in full protocol) | |
| 18 | Sample size/justification for sample size | N/A | Inserted note to see update in section 5 | |
| Planned recruitment rate | N/A | Inserted note to see update in section 5 | ||
| Summary Protocol | 1 | Outcome measures | Cognitive function 1 year after randomisation | Removal of cognitive function from outcome measures |
| 2 | Sample size | 1006 | 802 | |
| 2 | Planned recruitment period | November 2010 | August 2011 |
List 5: substantial amendment 4
Creation of a pre-questionnaire warning letter for participants. This letter may be sent out 2 weeks ahead of the first questionnaire at 6 months and the second questionnaire at 12 months following randomisation.
It does not alter any of the previously approved documentation that participants receive as it will be sent solely as a reminder to participants that they are taking part in the study and are due to receive a questionnaire and will prepare them for the types of questions we are asking them to answer.
The letter has been modified as suggested by the Sub Committee (letter dated 27 June 2011) to avoid anxiety in participants who may not have realised they were in the study.
List 6: substantial amendment 5
In order to maximise recruitment, it has been proposed that a subset of centres will continue to randomise patients to the OSCAR trial until such time that follow-up to 30 days (the primary outcome) is no longer possible. We anticipate that the last patients will be recruited to the trial in July 2012. To maintain the current end of trial date, the final follow-up for any patient will be October 2012; therefore additional follow-up will be limited based on individual randomisation dates. This will be explained in an addendum to both the protocol and informed consent documents.
Appendix 2 Consent process for the OSCAR trial by country
1. England and Wales OSCAR trial agreement processes
England and Wales – Mental Capacity Act 200576 (relates to collaborating hospitals in England and Wales)
Multicentre Research Ethics Committee: 07/H0502/98/version 2 – 3 September 2007
The Mental Capacity Act 200576 comes into force on 1 October 2007. This Act is relevant to research involving adults over the age of 16 years in England and Wales (except Clinical Trials of Investigational Medicinal Products).
The Act provides the legal arrangements (1) to enable adults lacking capacity to consent to take part in research that would otherwise require the participant’s consent, and (2) it enables adults with capacity to specify, in advance, their wishes should they lose capacity in the future with regard to taking part in research.
In the OSCAR trial, patients will usually be unable to give consent prior to trial entry owing to alternations in consciousness. The diagram below specifies the process, approved by the Research Ethics Committee, that must be followed with regard to obtaining consent to take part in the OSCAR trial.
The following has been guided by the Department of Health’s document {issued by the Secretary of State and National Assembly for Wales in accordance with section [32(3)] of the Mental Capacity Act 200576; URL: www.dh.gov.uk/en/Consultations/Liveconsultations/DH_076216} published 22 June 2007. This draft guidance is for consultation on how to identify an appropriate ‘consultee’ for the purposes of section 32 of the Mental Capacity Act 200576. The guidance indicates how researchers should go about identifying an appropriate person to consult when they wish to carry out research which involves someone who lacks capacity to consent to take part.
2. Scotland OSCAR trial consent processes
Scotland – Adults with Incapacity (Scotland) Act 200077 (relates to collaborating hospitals in England and Wales)
Multicentre Research Ethics Committee: 07/MRE00/73/version 2 – 3 September 2007
Scottish collaborators should follow the table:
Appendix 3 OSCAR Trial Steering Committee
Professor Deborah Ashby (chairperson)
Professor of Medical Statistics and Clinical Trials
Department of Epidemiology and Public Health
Imperial College London
Faculty of Medicine, St Mary’s Campus
Norfolk Place
Paddington
London
W2 1PG
Dr Steve Drage
Consultant in Intensive Care Medicine
Adult Intensive Care Unit
Royal Sussex County Hospital
Eastern Road
Brighton
BN2 5BE
Mr Barry Williams
Critical Care Patient Liaison Committee (CritPal)
12 Church Green
Bishops Caundle
Sherborne
Dorset
DT9 5NN
Professor Brian H Cuthbertson
Chief of Critical Care
Sunnybrook Health Sciences Centre
Toronto
Canada
ON M4N 3M5
Dr Ranjit Lall
Senior Statistician
Warwick Clinical Trials Unit
Warwick Medical School
University of Warwick
Gibbet Hill Road
Coventry
CV4 7AL
Professor Kathy Rowan
Director
Intensive Care National Audit & Research Centre (ICNARC)
Napier House
24 High Holborn
London
WC1V 6AZ
Professor Tim Walsh
Consultant in Anaesthesia and Intensive Care
Ward 118 (ICU)
Royal Infirmary
51 Little France Crescent
Edinburgh
EH16 4SA
Mrs Heather House
University of Oxford Clinical Trials and Research Governance
Manor House
John Radcliffe Hospital
Headington
Oxford
OX3 9DU
Professor Sallie Lamb
Director
Warwick Clinical Trials Unit
Warwick Medical School
University of Warwick
Gibbet Hill Road
Coventry
CV4 7AL
Professor Chris McCabe
Professor of Health Economics
University of Alberta
116 St. and 85
Avenue Edmonton
Alberta
Canada
T6G 2R3
Antonia Perez/Lesley Dodd
Monitoring and Contracts Administrator
HTA
Alpha House
Enterprise Road
Southampton Science Park
Chilworth
Southampton
SO16 7NS
Appendix 4 OSCAR Trial Data Monitoring and Ethics Committee
Professor David Torgerson (chairperson)
Director
York Trials Unit
Area 4 – Second Floor
Seebohm Rowntree Building
University of York
Heslington
York
YO10 5DD
Professor David K Menon
Professor of Anaesthesia
University of Cambridge
Box 93 – Level 4
E Block
Addenbrooke’s Hospital
Hills Road
Cambridge
CB2 2QQ
Dr Peter Nightingale
ICU Acute Block
Wythenshawe Hospital
Southmoor Road
Wythenshawe
Manchester
M23 9LT
Appendix 5 OSCAR collaborators
Sites and principal investigators
John Radcliffe Hospital, Oxford: Dr Duncan Young. Derriford Hospital, Plymouth: Dr Peter MacNaughton. Aberdeen Royal Infirmary, Aberdeen: Professor Brian Cuthbertson. Medway Hospital, Gillingham: Mrs Catherine Plowright. Queen Elizabeth Hospital, Birmingham: Dr Bill Tunnicliffe. Royal Sussex County Hospital, Brighton: Dr Steve Drage. University College Hospital, London: Dr Geoff Bellingan. University Hospital of Wales, Cardiff: Dr Sanjoy Shah. Royal United Hospital, Bath: Dr Andrew Padkin. Manchester Royal Infirmary, Manchester: Dr Bernard Foex. Ysbyty Maelor Hospital, Wrexham: Dr Paul Hughes/Dr Khalid Elfituri. Queen Elizabeth Hospital, Gateshead: Dr Frank McAuley. Stirling Royal Infirmary, Stirling: Dr Chris Cairns. Royal Cornwall Hospital, Truro: Dr Jonathan Paddle. Wythenshawe Hospital, Manchester: Dr Huw Maddock. University Hospital of North Staffordshire, Stoke-on-Trent: Dr Nick Coleman. Ipswich Hospital, Ipswich: Dr Andy Kong/Dr Robert Lewis. Manchester Royal Infirmary (Cardiac), Manchester: Dr Martin Bewsher. James Paget Hospital, Great Yarmouth: Dr Andreas Brodbeck. Queen Alexandra Hospital, Portsmouth: Dr David Pogson. Queen Margaret Hospital, Dunfermline: Dr Martin Clark. Royal Blackburn Hospital, Blackburn: Dr Stephen Mousdale. Leeds General Infirmary, Leeds: Dr Andrew Bodenham. Southampton General Hospital, Southampton: Dr Rebecca Cusack. St James’s University Hospital, Leeds: Professor Mark Bellamy. York Hospital, York: Dr Henry Paw. Victoria Hospital, Blackpool: Dr Jason Cupitt. Southend Hospital, Westcliff-on-Sea: Dr David Higgins. Royal Victoria Infirmary, Newcastle: Dr Cait Searl. James Cook University Hospital, Middlesbrough: Dr Judith Wright.
Appendix 6 Details of randomisation by centre
| Age (years) | ≤ 55 | > 55 | ||||||
|---|---|---|---|---|---|---|---|---|
| P : F ratio (kPa) | ≤ 15 | > 15 | ≤ 15 | > 15 | ||||
| Intervention/centre | Conv. | HFOV | Conv. | HFOV | Conv. | HFOV | Conv. | HFOV |
| John Radcliffe, Oxford | 1 (50.0) | 1 (50.0) | 1 (50.0) | 1 (50.0) | 3 (60.0) | 2 (40.0) | 3 (50.0) | 3 (50.0) |
| Derriford Hospital, Plymouth | 4 (44.4) | 5 (55.6) | 5 (41.7) | 7 (58.3) | 10 (47.6) | 11 (52.4) | 3 (75.0) | 1 (25.0) |
| Aberdeen Royal Infirmary | 1 (100.0) | 0 (0.0) | 1 (50.0) | 1 (50.0) | 3 (50.0) | 3 (50.0) | 3 (50.0) | 3 (50.0) |
| Medway Maritime Hospital | 4 (66.7) | 2 (33.3) | 1 (33.3) | 2 (66.7) | 5 (45.5) | 6 (54.5) | 4 (57.1) | 3 (42.9) |
| Selly Oak/Queen Elizabeth, Birmingham | 7 (50.0) | 7 (50.0) | 18 (48.6) | 19 (51.4) | 11 (47.8) | 12 (52.2) | 14 (50.0) | 14 (50.0) |
| Royal Sussex County Hospital, Brighton | 4 (40.0) | 6 (60.0) | 3 (42.9) | 4 (57.1) | 4 (66.7) | 2 (33.3) | 11 (47.8) | 12 (52.2) |
| University College Hospital, London | 15 (51.7) | 14 (48.3) | 5 (50.0) | 5 (50.0) | 10 (52.6) | 9 (47.4) | 3 (60.0) | 2 (40.0) |
| University Hospital of Wales, Cardiff | 1 (100.0) | 0 (0.0) | 3 (50.0) | 3 (50.0) | 2 (66.7) | 1 (33.3) | 3 (50.0) | 3 (50.0) |
| Royal United Hospital, Bath | 0 (0.0) | 1 (100.0) | 3 (75.0) | 1 (25.0) | 3 (60.0) | 2 (40.0) | 5 (50.0) | 5 (50.0) |
| Manchester Royal Infirmary | 4 (57.1) | 3 (42.9) | 2 (50.0) | 2 (50.0) | 1 (50.0) | 1 (50.0) | 5 (45.5) | 6 (54.5) |
| Ysbyty Maelor, Wrexham | 3 (60.0) | 2 (40.0) | 4 (50.0) | 4 (50.0) | 7 (58.3) | 5 (41.7) | 3 (42.9) | 4 (57.1) |
| Queen Elizabeth Hospital, Gateshead | 2 (50.0) | 2 (50.0) | 0 (0.0) | 0 (0.0) | 3 (50.0) | 3 (50.0) | 2 (50.0) | 2 (50.0) |
| Royal Cornwall Hospital, Treliske | 7 (53.8) | 6 (46.2) | 4 (50.0) | 4 (50.0) | 12 (50.0) | 12 (50.0) | 5 (45.5) | 6 (54.5) |
| Stirling Royal Infirmary | 3 (42.9) | 4 (57.1) | 1 (33.3) | 2 (66.7) | 2 (40.0) | 3 (60.0) | 2 (50.0) | 2 (50.0) |
| Manchester Royal Infirmary, Cardiac ICU | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (100.0) | 0 (0.0) |
| Leeds General Infirmary | 4 (44.4) | 5 (55.6) | 2 (40.0) | 3 (60.0) | 6 (50.0) | 6 (50.0) | 2 (50.0) | 2 (50.0) |
| James Paget Hospital, Great Yarmouth | 3 (75.0) | 1 (25.0) | 2 (40.0) | 3 (60.0) | 3 (37.5) | 5 (62.5) | 4 (66.7) | 2 (33.3) |
| Queen Alexandra Hospital, Portsmouth | 4 (40.0) | 6 (60.0) | 3 (60.0) | 2 (40.0) | 9 (52.9) | 8 (47.1) | 2 (40.0) | 3 (60.0) |
| Royal Blackburn Hospital | 3 (50.0) | 3 (50.0) | 2 (66.7) | 1 (33.3) | 5 (41.7) | 7 (58.3) | 3 (60.0) | 2 (40.0) |
| Wythenshawe Hospital, Manchester | 2 (50.0) | 2 (50.0) | 1 (33.3) | 2 (66.7) | 3 (50.0) | 3 (50.0) | 1 (50.0) | 1 (50.0) |
| University Hospital of North Staffordshire, Stoke-on-Trent | 3 (60.0) | 2 (40.0) | 1 (50.0) | 1 (50.0) | 0 (0.0) | 1 (100.0) | 3 (42.9) | 4 (57.1) |
| Ipswich Hospital | 1 (33.3) | 2 (66.7) | 0 (0.0) | 1 (100.0) | 0 (0.0) | 1 (100.0) | 0 (0.0) | 0 (0.0) |
| Queen Margaret Hospital, Dunfermline | 1 (50.0) | 1 (50.0) | 1 (100.0) | 0 (0.0) | 1 (100.0) | 0 (0.0) | 2 (50.0) | 2 (50.0) |
| Southampton General Hospital | 3 (60.0) | 2 (40.0) | 0 (0.0) | 0 (0.0) | 5 (71.4) | 2 (28.6) | 0 (0.0) | 2 (100.0) |
| St James’s University Hospital, Leeds | 14 (51.9) | 13 (48.1) | 4 (44.4) | 5 (55.6) | 13 (50.0) | 13 (50.0) | 3 (50.0) | 3 (50.0) |
| York Hospital | 2 (50.0) | 2 (50.0) | 2 (50.0) | 2 (50.0) | 2 (66.7) | 1 (33.3) | 1 (50.0) | 1 (50.0) |
| Victoria Hospital, Blackpool | 5 (50.0) | 5 (50.0) | 1 (25.0) | 3 (75.0) | 4 (44.4) | 5 (55.6) | 3 (60.0) | 2 (40.0) |
| Southend Hospital | 0 (0.0) | 1 (100.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (50.0) | 1 (50.0) |
| Royal Victoria Infirmary, Newcastle | 1 (100.0) | 0 | 1 (50.0) | 1 (50.0) | 2 (50.0) | 2 (50.0) | 0 (0.0) | 1 (100.0) |
| James Cook University Hospital, Middlesbrough | 1 (50.0) | 1 (50.0) | 0 (0.0) | 0 (0.0) | 2 (50.0) | 2 (50.0) | 0 (0.0) | 0 (0.0) |
| Total | 103 (51.0) | 99 (49.0) | 71 (47.3) | 79 (52.7) | 131 (50.6) | 128 (49.4) | 92 (50.0) | 92 (50.0) |
| Intervention/centre | Conventional ventilation | HFOV | Total |
|---|---|---|---|
| John Radcliffe, Oxford | 8 (66.7%) | 4 (33.3%) | 12 |
| Derriford Hospital, Plymouth | 22 (47.8%) | 24 (52.2%) | 46 |
| Aberdeen Royal Infirmary | 8 (61.5%) | 5 (38.5%) | 13 |
| Medway Maritime Hospital | 13 (72.2%) | 5 (27.8%) | 18 |
| Selly Oak/Queen Elizabeth, Birmingham | 47 (51.6%) | 44 (48.4%) | 91 |
| Royal Sussex County Hospital | 22 (55.0%) | 18 (45.0%) | 40 |
| University College Hospital | 33 (62.3%) | 20 (37.7%) | 53 |
| University Hospital of Wales | 9 (64.3%) | 5 (35.7%) | 14 |
| Royal United Hospital | 11 (64.7%) | 6 (35.3%) | 17 |
| Manchester Royal Infirmary | 12 (52.2%) | 11 (47.8%) | 23 |
| Ysbyty Maelor | 15 (53.6%) | 13 (46.4%) | 28 |
| Queen Elizabeth Hospital, Gateshead | 5 (45.5%) | 6 (54.5%) | 11 |
| Royal Cornwall Hospital (Treliske) | 28 (53.8%) | 24 (46.2%) | 52 |
| Stirling Royal Infirmary | 8 (50.0%) | 8 (50.0%) | 18 |
| Manchester Royal Infirmary, Cardiac ICU | 1 (100.0%) | 0 (0.0%) | 1 |
| Leeds General Infirmary | 14 (56.0%) | 11 (44.0%) | 25 |
| James Paget Hospital | 11 (50.0%) | 11 (50.0%) | 22 |
| Queen Alexandra Hospital | 18 (48.6%) | 19 (51.4%) | 37 |
| Royal Blackburn Hospital | 13 (54.2%) | 11 (45.8%) | 24 |
| Wythenshawe Hospital | 7 (46.7%) | 8 (53.3%) | 15 |
| University Hospital of North Staffordshire | 7 (46.7%) | 8 (53.3%) | 15 |
| Ipswich Hospital | 1 (25.0%) | 3 (75.0%) | 4 |
| Queen Margaret Hospital | 5 (62.5%) | 3 (37.5%) | 8 |
| Southampton General Hospital | 8 (57.1%) | 6 (42.9%) | 14 |
| St James’s University Hospital | 33 (54.1%) | 28 (45.9%) | 61 |
| York Hospital | 7 (63.6%) | 4 (36.4%) | 11 |
| Victoria Hospital Blackpool | 13 (50.0%) | 13 (50.0%) | 26 |
| Southend Hospital | 1 (33.3%) | 2 (66.7%) | 3 |
| Royal Victoria Infirmary | 4 (50.0%) | 4 (50.0%) | 8 |
| James Cook University Hospital | 2 (66.7%) | 1 (33.3%) | 3 |
| Total | 386 (54.3%) | 325 (45.7%) | 711 |
Glossary
- Acute Physiology and Chronic Health Evaluation II
- A scoring system originally used to predict mortality in patients admitted to intensive care units but now widely used as a measure of severity of acute illness.
- Centimetres of water (cmH2O)
- A unit of pressure measurement used in respiratory measurement.
- Consolidated Standards of Reporting Trials
- A standardised format for reporting clinical trials.
- Conventional ventilation or ECMO for Severe Adult Respiratory failure (CESAR)
- A clinical trial of extracorporeal membrane oxygenation in patients with acute respiratory distress syndrome.
- European Quality of Life-5 Dimensions
- A measure of health-related quality of life.
- European Quality of Life Visual Analogue Scale
- A single dimension measure of recalled health-related quality of life.
- Extracorporeal membrane oxygenation
- A technique to oxygenate blood outside the body in patients with severe respiratory failure.
- Health Technology Assessment programme
- Part of the National Institute for Health Research.
- Hertz (Hz)
- A unit of measurement of cycles per second.
- HiFi trial
- An early randomised controlled trial of high-frequency ventilation in newborn children.
- Kilopascal
- Unit of pressure measurement used in respiratory medicine to describe the partial pressure of (kPa) gases in the blood.
- Millimetres of mercury (mmHg)
- A non-SI unit used in respiratory medicine to describe the partial pressure of gases in the blood and intravascular/intracavity pressures.
- National Heart, Lung and Blood Institute
- Part of the US National Institutes of Health.
- National Institutes of Health
- A US Government medical research funder.
- Oxygenation index
- A measure of the effectiveness of oxygen exchange in the lung that takes account of pressures in the lung.
- P : F ratio
- The ratio of the partial pressure of oxygen in the arterial blood to the fractional inspired oxygen concentration, a measure of the effectiveness of oxygen exchange in the lung.
- Short Form questionnaire-12 items
- A measure of health-related quality of life.
- Short Form questionnaire-36 items
- A more detailed measure of health-related quality of life.
List of abbreviations
- ALI
- acute lung injury
- APACHE II
- Acute Physiology and Chronic Health Evaluation II
- ARDS
- acute respiratory distress syndrome
- BALTI-2
- Beta Agonist Lung Injury TrIal-2
- BNF
- British National Formulary
- CCCTG
- Canadian Critical Care Trials Group
- CE
- Conformité Européenne
- CEA
- cost-effectiveness analysis
- CEAC
- cost-effectiveness acceptability curve
- CESAR
- Conventional ventilation or ECMO for Severe Adult Respiratory failure
- CI
- confidence interval
- cmH2O
- centimetres of water
- CONSORT
- Consolidated Standards of Reporting Trials
- COPD
- chronic obstructive pulmonary disease
- CRF
- case report form
- DLCO
- carbon monoxide diffusing capacity
- DMEC
- Data Monitoring and Ethics Committee
- ECMO
- extracorporeal membrane oxygenation
- EQ-5D
- European Quality of Life-5 Dimensions
- EQ-VAS
- European Quality of Life Visual Analogue Scale
- FDA
- US Food and Drug Administration
- FiO2
- fractional concentration of inspired oxygen
- GCP
- Good Clinical Practice
- HFJV
- high-frequency jet ventilation
- HFOV
- high-frequency oscillatory ventilation
- HFPPV
- high-frequency positive-pressure ventilation
- HMRC
- Her Majesty’s Revenue and Customs
- HTA
- Health Technology Assessment
- Hz
- hertz
- ICER
- incremental cost-effectiveness ratio
- ICH
- International Conference on Harmonisation
- ICNARC
- Intensive Care National Audit & Research Centre
- ICON
- Intensive Care Outcome Network study
- ICS
- Intensive Care Society
- ICU
- intensive care unit
- I : E
- inspiratory : expiratory
- LY
- life-year
- MHRA
- Medicines and Healthcare Regulatory Authority
- mmHg
- millimetres of mercury
- MREC
- Multicentre Research Ethics Committee
- NCEPOD
- National Confidential Enquiry into Peri-Operative Deaths
- NHLBI
- National Heart, Lung and Blood Institute
- NHP
- Nottingham Health Profile
- NICE
- National Institute for Health and Care Excellence
- NIH
- National Institutes of Health
- NIHR
- National Institute for Health Research
- NRES
- National Research Ethics Service
- OI
- oxygenation index
- ONS
- Office for National Statistics
- OSCAR
- OSCillation in ARDS
- OSCILLATE
- Oscillation for Acute Respiratory Distress Syndrome Treated Early
- PaCO2
- partial pressure of carbon dioxide in arterial blood
- PaO2
- partial pressure of oxygen in arterial blood
- PEEP
- positive end expiratory pressure
- P : F ratio
- partial pressure of oxygen in arterial blood/fractional concentration of inspired oxygen ratio
- PQOL
- Perceived Quality of Life Scale
- PSS
- Personal Social Services
- PSSRU
- Personal Social Services Research Unit
- QALY
- quality-adjusted life-year
- QoL
- quality of life
- RCT
- randomised controlled trial
- SAE
- serious adverse event
- SD
- standard deviation
- SE
- standard error
- SF-12
- Short Form questionnaire-12 items
- SF-36
- Short Form questionnaire-36 items
- SGRQ
- St. George’s Respiratory Questionnaire
- SICSAG
- Scottish Intensive Care Society Audit Group
- SIP/FLP
- Sickness Impact Profile/Functional Limitations Profile
- TNO
- trial number
- TSC
- Trial Steering Committee
- UTI
- urinary tract infection