Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 10/141/02. The contractual start date was in February 2012. The draft report began editorial review in November 2013 and was accepted for publication in March 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Professor Bhui is Director of Master of Science programmes in mental health including transcultural mental health care. Professor Weich is a member of the commissioning panel for the National Institute for Health Research Health Technology Assessment programme.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Bhui et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
The challenges faced by people from a black and minority ethnic (BME) group when they come into contact with psychiatric services are well documented. 1,2 Research reviews and evidence-based policies highlight ethnic inequalities in both experiences and outcomes. Indeed, in relation to BME people (relative to the white population), there are concerns about their worse record of patient safety, the disproportionate number of admissions and detentions in psychiatric hospitals, greater conflict with carers and staff, fear of services, lack of engagement with or poor access to effective services, fears about contact with the criminal justice system (principally the police), poorer access to psychological therapies and ethnic variations in the use of drug treatments. Recent data support differences in compulsory treatment, compulsory admissions, entry into primary care services, income and employment by ethnic groups. 3–5 Although BME is often used as a shorthand to represent minority ethnic groups in the UK owing to common linkages between histories of oppression, exclusion, vulnerability to psychiatric disorders and inequalities in outcomes and experiences,6 there are many subgroups and much heterogeneity within any ethnic group. 7 Furthermore, the over-representation of specific ethnic groups in specialist psychiatric services contrasts with their lesser use of primary care and public health interventions. Although this calls for a wider analysis, this report focuses on specialist psychiatric services only, irrespective of the disciplinary origins of staff in these services, given this has been the area generating most concern in previous policy reviews. 1,2
Culture and communication
The ability of mental health service staff to communicate effectively with any particular patient, and in a manner appropriate to that person’s culture, underpins successful diagnosis and therapy. The proposed value of understanding and evaluating communications is that they improve therapeutic outcomes through multiple mechanisms, hence the term therapeutic communications (TCs). For example, patients with a mental illness who cannot speak good (or perhaps any) English are likely to experience anxiety and uncertainty during assessment; moreover, diagnosis and clinical decision-making will be hampered. The use of family or friends as interpreters to address this issue is often inappropriate, and may undermine the clinical assessment. Instead, the use of bilingual professionals or interpreters with expertise in mental health is recommended. 8–10 Problems arise from language differences and the interconnection between language and concepts of health and illness (often called explanatory models or illness perceptions) that are used to communicate distress. These explanatory models vary across cultures, and this makes it difficult for the patient and professional to gather the same understanding of their cultural origins, and therefore concepts of health and illness, differ. These concepts may be expressed through particular idioms or metaphors, and these may differ across languages. The use of professional interpreters or other forms of formal language support is rare, but when the spoken word is the primary source of information for diagnosis and also the format of some forms of therapy, these cultural and linguistic influences on communication have a significant impact. 11,12 It is necessary to ensure that both aspects of diversity – language and culture – are addressed. 13 However, dissatisfaction and inequalities are also prominent among anglophone migrants and other people from BME groups who speak English. 9,10 There are wider issues of communication beyond translation and interpretation, and it is these that we focus on in this review.
Overall, BME groups are more likely than the white British population to report dissatisfaction with care, to fail to engage with services, to decline treatment and to have fears for their own safety while in treatment. This may be explained not only by inherent communication problems, but also by different (cultural) assumptions about the causes and treatments of mental and emotional distress. 14 Ineffective communication because of these differences may then lead to a feeling of not being understood, omissions of important information from the clinical assessment, conflict with staff, disengagement and/or a failure to take up interventions14,15 – sometimes termed failed negotiation. This may lead to more severe and more frequent episodes of illness and, in turn, the use of coercion, which is itself associated with a higher rate of adverse incidents. Such a cycle undermines the therapeutic potential of established care practices and processes, and further burdens BME users of mental health of services. Thus, improving TCs may permit maximum benefits to be realised from existing care and services, improve safety and avoid adverse incidents in care.
Effective communication is central to psychiatric assessment, diagnosis, engagement and treatment, and, ultimately, recovery. 14,15 Effective communication has proven more difficult to achieve where there are differences in culture or language between those delivering and receiving care. 6 Of course, communication difficulties might arise in any encounter between a patient and professional owing to differences in age, gender, social status or perceived power. However, cultural differences between patient and professional increase the challenges. For example, when attending to a patient from a different culture, the following abilities of a professional will be reduced:
-
the ability to identify with and empathise with the patient, and to assess that patient’s emotion accurately16–20
-
the ability to understand symbolic and metaphorical language, as this varies greatly across cultures21
-
the ability to understand the patient’s expectations of the health-care professional, as professional roles differ widely across countries and cultures (e.g. authoritarian versus egalitarian approaches and the preferential use of medication as opposed to ‘talking therapies’ to try to resolve emotional issues)22,23
-
the ability to appreciate the differences in illness perceptions and explanatory models of the illness. 14,24
Cultural factors amplify the limitations of TCs, and are of importance because they have the potential to compound inequalities in the social determinants of illness and to perpetuate inequalities in health-care outcomes following contact with health systems. 23,25,26 Conversely, good TC can reduce the inequalities. For example, Lorenz and Chillingerian27 argued that the use of visual supports to improve communication helps to address inequalities and gender disadvantage by introducing a more ‘fair process’ of assessment. They defined a fair process as one that involves patients in a collaborative approach to the exploration of diagnostic issues and treatments, explains the rationale for decisions, sets expectations about roles and responsibilities, and implements a core plan and ongoing evaluation. Fair process opens the door to bringing patient expertise into the clinical setting and the work of developing health-care goals and strategies. Although improved TC is at the heart of fair process, the evidence base to support its professional use is scattered across a number of disciplines, each of which uses a different theoretical model. There is therefore a need to pull together the evidence on interventions that improve TCs, appraise its quality and identify the components of effective interventions.
Cultural competency
One proposed solution to the problems stemming from poor communication between mental health services and their BME patients is the training of the professional in ‘cultural competency’. 28 A review of the international literature on cultural competency suggests that it is best conceptualised as a systemic and deep-seated process of change in both organisations and professional practice. 29 It often requires a change in the attitudes of staff, and a change in the way they assess, diagnose and treat people whose expectations and perceptions of both illness and recovery differ from their own. At an organisational level, the changes required include developing values that are more welcoming of culturally diverse populations and changes in management styles and human resource practices that reflect an understanding of the influence of culture on communication. Alongside these macro-level interventions, educational solutions have included training to address the attitudes and stereotypes held by individual members of staff. However, the introduction of long-term change at an individual and organisational level has not been widely achieved in the UK, perhaps because of the complexity of the task. Short-term educational solutions have been more popular and, therefore, more widely reported in the literature. These have varied in quality and focus, with some attending to communication; some to clinical skills and practices; some to the attitudes of practitioners and their cultural biases; and some to specific groups, such as faith groups, refugees, migrants, gypsies or other racialised groups. The lack of long-term programmes and the wide variability of the short-term interventions have made the development of a robust evidence base problematic.
Some cultural competency training has included information on race equality and compliance with recruitment legislation. The Department of Health rolled out a ‘race equality and cultural competency framework’ to address stigma, race equality and cultural factors. 30 This highlighted some of the communication issues that arise with BME patients and the need for sensitivity to stereotypes according to race and culture, but had rather little to say about clinical assessment, diagnosis or specific treatment strategies. Bennett and Keating28 mapped cultural competency training and its content in the UK and concluded there was insufficient attention to clinical interventions and to racial issues; they suggested instead that non-TC issues were more often reported. A systematic review of the international literature on cultural competency interventions in mental health settings similarly found few evaluations and none of these reported patient outcomes. 29 A systematic review of TCs with BME patients is necessary to synthesise the findings across the many approaches tried, and to identify lessons for policy, practice and research. Inevitably, such a systematic review will require characterisation of a wide range of interventions in diverse contexts and for diverse populations, rather than a meta-analysis of trials of a single intervention as there appears to be no single intervention that is known to be of superior efficacy.
Narratives, ethnography and diagnosis
The meaning a person assigns to an illness may be quite different from that assigned by the health professional. 31 This issue is not confined to the UK, and it reflects fundamental differences across national, cultural, ethnic and religious groups in the way mental distress and illness are understood and defined, and is related to expectations of recovery and treatment. 32,33 If psychiatric professionals have a good appreciation of a patient’s beliefs and expectations, then that can only be beneficial. Some pioneering services have sought to facilitate such an appreciation through, for example, the use of ‘patient narratives’ (the account of how the patient came to present to the professional, and what this might mean for the formulation of the treatment plan), what has been termed ‘ethnography’ (an understanding of, and sensitivity to, a patient’s ethnic background), and negotiations of meaning (the elucidation of the patient’s beliefs concerning the cause and likely outcome of the illness and, again, the account taken to inform the diagnosis and treatment plan).
Canales25 describes ‘narrative interaction’ – that is, the sharing of personal stories – as a form of TC that permits the inequalities by gender to be addressed in nursing practice. 25 Narratives and story-telling as part of assessment and treatment have a long history in cross-cultural psychology. 34 Narratives are ways of expressing and exploring personal identity, group histories and securing group cohesion35 that can influence the onset and course of psychiatric disorders. Assessing narratives in practice and research brings together idiographic and ethnographic methods of assessment and research. 36 Narrative methods are also valuable in addressing inequalities by engaging socially excluded groups, for example teenage mothers, so that they can receive nursing interventions,37 and in understanding challenges to the implementation of policy and practice. 38,39
A more detailed assessment of patients’ illness models is advocated by some medical anthropologists as a way of improving assessment; for example, ‘mini-ethnography’ has been used in the clinical assessment. 40 Studies of this approach have demonstrated improvements in diagnostic precision, diagnostic depth and care plans. Attempts to introduce ‘ethnography’ into the diagnostic process (i.e. to increase its ethnic sensitivity) have led to support for a ‘cultural formulation’, and indeed this has been highlighted in a previous and the most recent edition of the diagnostic manual produced by the American Psychiatric Association [Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (DSM-V)]. 41–43 This advocates that assessment includes ethnography and narrative, by the psychiatrist asking questions about cultural identity and explanatory models. Explanatory models in the anthropology literature are similar to illness perceptions reported in the psychology literature, as both refer to concepts about what causes illness, what it is called, who might help in recovery and what expectations there are of potential carers. 44 In addition, the cultural formulation covers psychosocial factors, and brings the clinician’s perspective into play by openly seeking the clinician’s reflections on interpersonal interactions before reaching an overall diagnosis and narrative about the problem and its resolution (also called a formulation). Although a cultural formulation has been reported to be helpful in clinical practice, the published papers have been mainly qualitative and descriptive, such as case reports; evaluative studies seem to appear only in the grey literature, although perhaps now just emerging in the scientific literature that tests effectiveness.
Other developments in the UK have included conflict resolution and mediation45 and a cultural consultation service (CCS) that is collecting pilot data on cultural competency and organisational narratives of care and communication with BME patients. 39
Chapter 2 Objectives
We conducted a systematic review and synthesis of the research evidence on interventions designed to improve TC between BME patients receiving specialist psychiatric care and the professionals who deliver that care.
Within this overall aim, our specific objectives were:
-
to review the published evidence as well as the unpublished grey literature and unreported research in order to identify promising interventions to improve TC for BME patients receiving specialist psychiatric care
-
to report evidence on the effectiveness, quality and cost-effectiveness of such interventions, using the following measures: patient-reported outcomes, symptoms, (dis)engagement with care, cost, safety and rates of adverse incidents (including the use of compulsion, such as being detained in hospital under the powers of the Mental Health Act (Mental Health Act 1983, www.legislation.gov.uk/ukpga/1983/20/contents; Mental Health Act Amendment 2007, www.legislation.gov.uk/ukpga/2007/12/contents), and treated compulsorily, including physical restraint)
-
to identify and describe the elements of interventions that show evidence of effectiveness, and list those that do not have a supportive evidence base
-
to produce recommendations for practitioners and policy-makers for different service contexts, patient groups and illnesses
-
to identify key gaps in the evidence and to highlight future primary research that would address these.
Chapter 3 Methods
Participants
We were interested in all studies that provide evidence on how to improve TC with BME psychiatric patients in the setting of specialist psychiatric care. Specialist psychiatric care is delivered by many professional disciplines. We adopt the term psychiatric services rather than mental health services as the latter is a very broad term that includes public health and social interventions in the community, for example housing and other services, that were not within the scope of the commissioned review.
Key populations included all age groups (young people, adults and the elderly) and all ethnic groups known to be prominent in health-care settings in the UK, i.e. people from Indian, Pakistani, Bangladeshi, Sri Lankan, black Caribbean, black British, black African, Irish and Chinese backgrounds. We used these terms in the search strategy but complemented them with other terms in order to identify the broadest literature of relevance to the UK. Although commissioned as a review of BME groups, our analysis specifies the groups of importance to the UK setting and reveals the ethnic and cultural specificity of interventions.
Although originally commissioned to include only UK studies of the larger ethnic groups, we amended this aspect of the protocol during the study wherever relevant as useful information might otherwise be overlooked, for example if a study included a diaspora population of relevance to the UK (e.g. east Europeans) or if an intervention was judged to be transferable to the UK (e.g. an intervention for African Americans). However, we included such studies only where the other inclusion criteria were met.
During the review we came across some studies located at the interface of specialist psychiatric care and other sectors of care, but requiring specialist input; we included those studies in the review.
Interventions
At the outset, we defined TC as:
[A]ny conversation (face-to-face or technology-assisted) that is undertaken using a pre-defined model that seeks to improve understanding, engagement and therapeutic outcomes. For communication in health care to be therapeutic, it must involve a relationship and exchange of ideas between a patient and professional helper, be patient centred and engaging in order to influence the patient’s emotional world, and directed by the professional using expertise and skill. Therapeutic communications include all interactions that enable people in distress to resolve conflicts, divergent expectations, traumatic histories and adverse life events, and to take up and to overcome distress and also take up offers of help.
Bhui et al. 46
In this review we were specifically interested in all interventions seeking to improve TC with BME patients receiving psychiatric care, and expected a broad range of such interventions, for example conflict resolution, cultural consultancy, cultural competence and others as yet undefined.
These interventions might be aimed at either individuals or populations.
Care could be delivered by psychiatrists, general practitioners (GPs), psychologists, nurses or any other professional as long as it was located in specialist psychiatric settings.
From existing knowledge of this field, interventions to promote TC include those that:
-
employ mediation to enhance mutual understanding and to improve engagement with care
-
seek to manage divergent views, conflict and differing explanatory models and illness perceptions through negotiation and mediation
-
include narrative-based interventions (i.e. that place the service user and patient perspectives at the heart of consultation, assessment and treatment)
-
employ cultural consultation as a process of gathering narratives
-
apply cultural competence interventions focused on communication
-
any other new method or process for improving TCs that is not captured by the above, but is suited for BME populations in psychiatric care.
Any of the above processes could be delivered face to face or through two-way real-time communication technologies (e.g. NHS Direct or other support systems, telemedicine or e-mail).
We did not review the literature on interventions that are considered to be (generic) TCs themselves, such as psychological therapies or music therapies, unless the research evidence focused on interventions that might improve TCs with the specified target group(s), while meeting the other inclusion criteria (see Box 2).
Furthermore, given the evidence base already available,13 we did not include studies that were purely testing models of translation or interpretation as an intervention. The reasons for this were twofold. First, there is already a concurrent enquiry into interpretation, translation and language support (ITALS) in mental health care;12 and, second, without a control group who are denied access to an interpreter (which itself would be deemed unethical), it is difficult to determine any effect on outcome that is produced by the interpretation as distinct from the effect of the psychiatric intervention of which the interpretation is a component.
Review procedures and processes
A systematic review was carried out in accordance with the methods outlined in guidance issued by the Centre for Reviews and Dissemination. The full peer-reviewed protocol submitted in the funding application has been published in an open access journal for scrutiny. 46 During the course of the review, the original protocol was changed in two ways, as indicated in Participants. First, we included studies from other countries of interventions that showed evidence of transferability to the UK and the ethnic groups were relevant to the UK (e.g. by being from the same diaspora), if other inclusion and exclusion criteria were met. Second, we discovered many studies that seemed not to include evaluations but only to describe an intervention; these were assessed more carefully for evaluative statements and conclusions to create a category of near misses (A– rather than A+).
Data sources and search strategy for published literature
The following databases were searched: MEDLINE, PsycINFO, EMBASE, Applied Social Sciences Index and Abstracts (ASSIA), Cochrane Database of Systematic Reviews, The Campbell Collaboration, ACP (American College of Physicians) Journal Club, The Cochrane Central Register of Controlled Trials, Cochrane Methodology Register, Allied and Complementary Medicine Database (AMED), Cumulative Index to Nursing and Allied Health Literature (CINAHL), British Nursing Index, Health Management Information Consortium, Social Science Citation Index (SSCI), Social Care Online (www.scie-socialcareonline.org.uk) and NHS Evidence collection on ethnicity and health. We also searched university databases for Doctor of Philosophy (PhD) theses (ProQuest assisted) and Master of Science theses from specialist centres on ethnicity and health.
The terms provided by Anderson et al. 47 to understand culturally competent care were adapted as a framework from which to generate search terms that might help identify publications on the effectiveness of interventions. Search strategies were constructed around BME groups using search terms refined through a number of systematic reviews29,48,49 and terms related to key descriptors of TCs: (1) aspect of TC; (2) types of mental disorder; (3) the professionals involved; and (4) aspects of clinical success.
These terms were tested and then applied to the electronic databases from database inception to 4 April 2012. All searches were rerun in early January and February 2013. The search strategy was designed to identify a broad range of literature on TC with BME patients and staff working in specialist psychiatric services (see Appendix 1 for the final search strategy). This strategy evolved as it was iteratively tested using a range of keywords and refined during pilot searches to provide a maximum yield.
The remit of the current systematic review is necessarily very broad: interventions for improving TC might be direct (i.e. between patient and professional) or indirect (through structural modifications to services to create more space for conflict to be resolved). Studies in both community and institutional settings were eligible. Studies of interventions designed to improve TC in our target population might not have been explicitly labelled as studies of TC. Indeed, relevant studies could be classified in many ways, for example as studies of communication, cultural competence or awareness, or just training to improve outcomes in ethnically diverse areas. Therefore, an inclusive strategy was felt most appropriate to capture all potentially relevant literature; specificity was sacrificed to maximise sensitivity.
The search strategy was iteratively developed to test its sensitivity to capture gold standard papers that were known to the research team. The final search strategy was settled following further discussion with the review management group (all investigators, listed as authors of this review) and carer representatives (Patrick Vernon/Afiya Trust). The complexity of the concept of TCs and the range of BME groups that might be relevant required us to develop this block search approach to ensure we captured all possible papers. The initial search strategy was trialled on different databases to assess the number of hits and relevant papers generated. We found a separate search strategy was needed to identify papers that included dementia, as these seemed not to be picked up by the generic search strategy. An example of the blocks of terms entered is shown in Box 1.
-
(BME or black ethnic minorit* or black minorit* ethnic*).mp.
-
asylum seeker*.ab,ti.
-
(migrant* or immigrant*).ab,ti.
-
race*.mp. or racial.ab,ti. [mp = title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier]
-
cultur*.ab,ti.
-
(multicultural or multi-cultural).ab,ti.
-
(cross-cultural or crosscultural).ab,ti.
-
(trans-cultural or transcultural).ab,ti.
-
(multi-rac* or multirac*).ab,ti.
-
(multiethnic or multi-ethnic).ab,ti.
-
refugee*.ab,ti.
-
(multi-lingu* or multilingu*).ab,ti.
-
(ethno-cultur* or ethnocultur*).ab,ti.
-
(socio-cultural or sociocultural).ab,ti.
-
(divers* or diverse population* or cultural diversity).ab,ti.
-
(south asian* or bangladeshi* or pakistani* or indian* or sri lankan*).mp.
-
(asian* or east asian* or chinese or taiwanese or vietnamese or korean* or japanese).mp.
-
(afro-caribbean* or african-caribbean* or caribbean or african* or black* or afro*).mp.
-
(islam* or hindu* or Sikh* or buddhis* or muslim* or moslem* or christian* or catholic* or jew*).ab,ti.
-
ethnic group*.mp.
-
((ethnic or linguistic) adj diversity).ab,ti.
-
(transient adj (group* or population*)).ab,ti.
-
acculturation.ab,ti.
-
(faith* or belief* or religion*).ab,ti.
-
ethnic minorit*.ab,ti.
-
minority ethnic.ab,ti.
-
hispanic.ab,ti.
-
(deprivation or low income).ab,ti.
-
or/1–28
-
mental disorders.mp. or exp Mental Disorders/
-
(psychosis or Psychotic or schizophr* or schizoaffective or delusional or depress* or dysthymi* or bipolar or cyclothymi* or panic or agoraphobia or phobia or “obsessive compulsive disorder” or “post-traumatic stress disorder” or stress or anxiety or dementia or ADHD or “attention deficit”).ab,ti.
-
30 or 31
-
Communication barriers.mp. or communication barriers/
-
(communicat* or talk* or interact* or “expressed emotion” or conversat* or discourse* or dialogue* or relationship* or alliance* or narrative* or “peer support”).ab,ti.
-
33 or 34
-
(adher* or complian* or concordan* or nonadher* or noncomplian* or persistence or “treatment usage”).ab,ti.
-
(attend* or engag* or “rejection of therapy”).ab,ti.
-
(“drop out” or “medication possession ratio”).ab,ti.
-
(service use* or pyschosocial intervention*).ab,ti.
-
(diagnosis or misdiagnosis).ab,ti.
-
36 or 37 or 38 or 39 or 40
-
Mental health services.mp. or exp Mental Health Services/
-
(psychiatr* or “mental health nurs* OR psychiatric nurs*” or “social work*” or psycholog* or “care coodinator*” or Counsel* or therapist* or “support work*” or “employment coach*” or “nurse practitioner*” or “case manager*” or “vocational rehab* specialist*” or “psych* tech*” or physician* or provider* or practitioner* or psychogeriatrician*).ab,ti.
-
42 or 43
-
29 and 32 and 35 and 41 and 44
-
limit 45 to (English language and humans)
Hand searches of the following journals were completed for the time period April 2007 to May 2012: Transcultural Psychiatry; Culture, Medicine and Psychiatry; International Journal of Social Psychiatry; Journal of Cross-Cultural Psychology; Ethnicity and Health; Ethnicity and Disease; and Diversity in Health & Care. In addition, two special issues of journals were also screened:
Grey literature: data sources and search strategy
An important body of relevant evidence was expected in the grey literature: unpublished reports and papers containing practice and community-based information on interventions. For this material, standard database searches were replaced by a variety of strategies: hand-searching more recent issues of journals on ethnicity and health (those that had appeared in the last 10 years), and journals on communications; cascade-searching; and searching specialist collections at the Centre for Evidence in Ethnicity, Health and Diversity, The King’s Fund, the NHS library on ethnicity and health, National Institute for Health Research (NIHR)’s Health Technology Assessment (HTA) programme, the National Institute for Health and Care Excellence (NICE), the Royal College of Psychiatrists and the Medical Foundation for the Care of Victims of Torture. We also made use of various web-based resources [e.g. Google (Google Inc., Menlo Park, CA, USA), NHS Evidence, JISCMail] to search for reports that were not published in conventional research or professional journals and research in progress.
Search strategies for these grey literature databases were also derived by an information scientist and researcher. They built on the terms used for searching the published literature (see Appendix 1). An initial stage consisted of testing several key terms and search strategies, followed by filtering by eye and then iterative refinement of the original searches.
Doctor of Philosophy or Doctor of Medicine theses
A search was undertaken of all dissertations and theses accepted for higher degrees by universities in Europe and North America up to February 2013. Examination of titles and abstracts (where available) identified six documents of potential importance. All were ordered; however, three had been lost by the originator universities52–54 and could not be assessed further. The other three were obtained,44,55,56 but the studies did not meet the criteria for inclusion (see Appendix 2 for details).
Conference papers
Conference papers were identified through key term searches of the ProQuest Conference Papers Index from June 2004 to February 2013. A total of 138 conference papers were identified and, following examination, 16 were selected as potentially relevant (see Appendix 3 for details). None of these papers, however, was included in the review after the full text had been read.
Bibliographies
Bibliographies of peer-reviewed articles short-listed for the main review were searched to identify any grey literature references. In total, 50 grey literature references were identified via this route; following examination, 32 were selected as likely to be relevant and a further 19 as possibly relevant (see Appendix 4 for details), but on testing against the inclusion and exclusion criteria, none was included in the review.
Websites and other electronic sources
Various electronic sources were searched using predefined search terms. Search strategies followed particular threads iteratively. A broad range of websites was searched systematically using key terms (see Appendix 5). Items identified were examined and short-listed by two reviewers. UK material was separated from non-UK material. A total of 97 items were short-listed: 86 from the UK and 11 from elsewhere (see Appendix 6). None was included in the final review.
Two further electronic sources were examined:
-
NHS Evidence: 380 items were identified; 34 were short-listed as relevant (see Appendix 7).
-
JISCMail archive: 29 items were identified and five were short-listed as relevant (see Appendix 8).
None of these entered the review after examination of the full text.
Other grey literature databases were considered but not searched, including the System for Information on Grey Literature (SIGLE), which was last updated in 2005, and the British National Bibliography for Report Literature, which ceased in 1998.
Research databases
Websites of research funding bodies were searched to identify projects in progress or those that had been completed. Intervention trials were distinguished from other studies. Potential items were examined and short-listed by two reviewers. This produced the following items for further examination:
-
UK Clinical Research Network (UKCRN) Study Portfolio: 15 projects of potential interest were short-listed; these include seven intervention trials, two of which focused on effective patient–clinician communication, but these specifically excluded non-English speakers (see Appendix 9).
-
NIHR Evaluation, Trials and Studies Coordinating Centre (NETSCC): 15 projects of potential interest were short-listed (see Appendix 9).
-
Research councils: no studies were identified on the Medical Research Council (MRC) website but five projects were short-listed from the Economic and Social Research Council (ESRC) website (see Appendix 9).
Following assessment of the full text, these searches did not yield studies beyond those identified in the published literature. Any completed project was tracked to identify outputs.
Economic literature
A series of systematic MEDLINE searches was undertaken by the information scientist to identify economic materials that were potentially relevant to interventions (see Appendix 10). Abstracts, were assessed and a total of 21 items were short-listed for full examination (see Appendix 10), as a result of which two studies with economic data were entered into the review; however, both had already been identified, one from the published literature search57 and one from the grey literature search. 58
Survey of experts
We consulted with experts, both those who are known in the field and those identified by asking service users about who they consider to have expertise in this area. We identified key researchers who had studied TCs. The applicants and collaborators drew on their networks in the UK, the European Union (EU) and beyond. Community groups and charities were also contacted to identify materials in community-based collections. All individuals so identified were invited to comment on omissions in the searches and to put forward candidate papers and to volunteer research work that was unpublished or in progress.
An online questionnaire59 was developed and a personal invitation sent to 37 experts in the field and to 75 organisations for circulation to their members (for list see Appendix 11). The questionnaire aimed to identify any additional grey literature, such as reports on projects, research in progress and resources or toolkits for mental health professionals (see Appendix 12). A reminder was sent to all non-responders after 2 weeks. This resulted in a total of 60 replies, of which 30 provided details of available materials. Finally, a request was posted on the ‘Minority-Ethnic-Health’ JISCMail discussion group with apologies for any cross-posting. This generated a further 10 replies, but no additional materials were identified. In total, these 70 respondents identified 30 separate grey literature items; 12 items were identified as relevant (see Appendix 13) but, after reading the full text, none was deemed to report sufficient evidence to meet our inclusion criteria.
Selecting appropriate sources
All databases searched (and number of hits retrieved from each) are shown in Table 1.
| Date of original search | Original search | Original results to 31 March 2012 (number of references) | Date of updated search | New search results |
|---|---|---|---|---|
| 3 April 2012 | MEDLINE: THERACOM 030412 – group 2. Expanded communication set | 597 | 4 February 2013 | 47 |
| 3 April 2012 | MEDLINE: THERACOM 030412 – group 3. Group 4 adapted | 538 | 4 February 2013 | 42 |
| 3 April 2012 | MEDLINE– THERACOM 030412 – group 5 | 1302 | 4 February 2013 | 119 |
| 3 April 2012 | ASSIA | 15 | 4 February 2013 | 1 |
| 3 April 2012 | The Cochrane Library | 111 | 4 February 2013 | 12 |
| 3 April 2012 | SSCI | 26 | 4 February 2013 | 3 |
| 3 April 2012 | AMED | 15 | 4 February 2013 | 0 |
| 3 April 2012 | PsycINFO | 238 | 4 February 2013 | 9 |
| 3 April 2012 | Dissertations and theses | 14 | 4 February 2013 | 0 |
| 3 April 2012 | Social Care Online | 7 | 4 February 2013 | 1 |
| 3 April 2012 | CINAHL | 20 | 4 February 2013 | 2 |
| 3 April 2012 | EMBASE | 515 | 4 February 2013 | 80 |
| 3 April 2012 | The Campbell Collaboration | 14 | 4 February 2013 | 12 |
Citations in the scientific literature were downloaded into an EndNote (version X5; Thomson Reuters, CA, USA) library. The relevance of all papers was assessed against the pre determined inclusion and exclusion criteria (Box 2) by two researchers, who inspected all the titles and abstracts. Each reviewer worked independently. Forward and backward citation tracking complemented the database searches.
Studies that report evaluations of:
-
models of TC designed to improve assessment, diagnosis, clinical decision-making, treatment and treatment adherence for BME patients
-
other aspects of direct communication, for example consensual/participatory activities, including participatory aspects of cultural consultation, conflict resolution, cultural competence, consent issues, complaints and grievances, drawing up care plans and crisis plans
-
teleconsultation services (e.g. NHS Direct, telemedicine, e-mail consultations, etc.)
-
psychiatric care which involved outreach or referral into services
-
service user interventions if they assisted with TCs in specialist mental health care.
-
Articles that simply report on translation or interpreter use in clinical assessment.
-
Studies of services for populations speaking diverse languages.
-
Studies that implemented a construct of TC without adapting it to local needs or conditions.
-
Evaluations of actual TCs (e.g. psychological therapies) rather than interventions that might improve TCs.
-
Articles in which ethnic minorities or ethnicity were ‘mentioned in passing’ and were not a significant focus.
-
Evaluations with no specific focus on interventions to improve TC with patients receiving psychiatric care.
-
Studies in settings or of groups not appropriate or not relevant to ethnic minorities in the UK. During the review we also decided to exclude alcohol-related treatments and treatments for drug misuse, as separate evidence reviews for these had been undertaken previously, and the nature of the interventions and the settings would not match our inclusion criteria.
-
The interventions were for the management of chronic diseases associated with mental distress or disorder, rather than the mental distress or disorder itself, such as attention deficit–hyperactivity disorder (ADHD) or human immunodeficiency virus (HIV) infection or smoking cessation.
-
Studies in which no intervention was evaluated, but analysis of routine data led to an inference that modifiable characteristics showing an association with a measure of TC or a proxy could be used as an intervention; for example, studies of ethnic matching as a derived variable in routine data were not included, whereas studies prospectively matching on an ethnic (or other) characteristic and testing the impact on the outcome were eligible for entry.
Full-text manuscripts of any titles/abstracts were obtained if these met the inclusion criteria or if there was uncertainty when reviewing the title and abstract. Any discrepancies were resolved by consensus and, if necessary, a third reviewer was consulted. The papers were classified into one of three groups: A+, A– and B. Only A+ papers entered the review.
The A+ papers met the original inclusion criteria and were entered into the review.
The A– papers:
-
Were descriptions of an intervention or elements of an intervention with no evaluation data.
-
Reported on studies that included patients from a group not relevant to the UK and held no immediate lessons for UK ethnic groups, for example they examined issues stemming from aboriginality or indigenousness. Transferability of the intervention to the UK context was a consideration.
Quality assessment
Core quality criteria
Different quality assessment tools had to be used because there were multiple research designs in the studies selected for review. Particular core criteria, though, were assessed for all studies. These were (1) the clarity with which the intervention was described as improving TC directly, by inference only, or not at all; (2) whether or not the outcomes (e.g. alliance, reduced conflict, greater trust) of a change in TC were directly measured using a reliable and valid scale; and (3) whether or not the ethnic groups would be of relevance to the UK and described in a manner consistent with a specific classification scheme for ethnicity (not just ‘race’). The last criterion was later relaxed where studies were of minorities and there were lessons that could be applied to ethnic minority groups in the UK. Core criteria scores ranged from 2 to 12 [scores of 0 on the intervention to improve TCs (1 above) and on outcome (2 above) would have led to exclusion of the study].
If there was an economic evaluation within a trial, this was separately scored. In addition, a quality-rating schema suited to different study types was used. This schema covered randomised controlled trials, case–control studies, observational quantitative studies, case studies and case series, and qualitative studies. The sources of our scoring scheme are presented in the following six sections. Copies of the full scoring scheme are presented in Appendix 14.
Quality criteria for randomised controlled trials
Through a brief review of the literature, Moncrieff et al. 76 developed a tool to assess the design of randomised controlled trials. Fifteen items could score 0, 1 or 2 (range of total score 0–30). Checklist items relate to the appropriateness and adequate description of the hypotheses, study design, intervention, main outcomes and methods of analysis. The checklist demonstrated good inter-rater reliability, and correlations between the three raters in the validation paper were high (r = 0.75–0.86).
Quality criteria for non-randomised observational quantitative studies
For the quality assessment of case–control or cohort studies, we used the evaluation of non-randomised observational studies by Deeks et al. 77 From the recommended scales, we selected that created by Reisch et al. 78 because it considers important confounding factors and differences between groups prior to the intervention, it has a good case-mix adjustment and it is a validated numeric scale (scores 0–34).
Quality criteria for case series
Through a brief literature review, we identified the NICE criteria for the assessment of case series. 79 However, with this quality assessment tool alone it was very difficult to discriminate between two studies that were similar in design or execution but that differed in the importance of the findings and their implications for practice. Furthermore, important characteristics that might better reflect quality in a case series – like length of follow-up and loss of clients over time – are not mentioned.
A previous HTA report indicated how difficult it is to use a specific system of quality ratings for case series, given that so little methodological research on quality ratings has taken place. 80 Consequently, we adopted the scoring system developed by the Canadian Institute of Health Economics (IHE). 81 This comprehensive 18-item checklist is based on quality criteria for assessment of case series from the Centre for Review and Dissemination. The inter-rater reliability of the checklist was based on the three reviewers, and has high kappa values. The IHE Delphi panel did not develop a scoring system for the checklist. According to the report, the quality of a study was assessed by counting the number of ‘yes’ responses to different criteria in the checklist. A study with 14 or more ‘yes’ responses was considered of acceptable quality. We decided to add the scoring system to the checklist; hence, a ‘yes’ to a criterion in the checklist would qualify for a score of 1 and ‘no’ would score 0 (scores range from 0 to 38).
Quality criteria for case studies, qualitative studies and studies from the grey literature
We chose the National Centre for Social Research (NATCEN) quality assessment criteria. 82 These criteria not only concentrate on the methodological quality of qualitative studies, but also highlight its conceptual quality. The NATCEN tool was based on 29 sets of previously suggested assessment criteria and consists of 18 appraisal questions underpinned by four guiding principles. We allocated a mark for each question asked and each of the items that might be endorsed to indicate quality and so the scale offers a range from 0 to 87.
Economic studies
These were rated 1–4 on the basis of the type of economic analysis. Cost-effectiveness studies scored 4, impact of interventions and cost–benefit studies scored 3, an intervention being costed scored 1, or the benefits being considered in terms of finances scored 1. A 0 was scored if there was no economic evaluation.
Overall quality score
The approach taken to quality rating was to use the core criteria and add the specialised criteria according to study design, and for the trials to include the economic score. For all other study types, the core and specialised criteria were used. The scores were summed and presented as percentages of the maximum score for each of the core items, the aggregated score of the specialised items and then as a total overall quality score. These were then categorised into low, medium or high quality on the basis of percentage of the maximum score (i.e. < 33% low, 33–66% medium and > 66% high). These are presented in Tables 2–5 to give an overall visual impression of the quality ratings according to study design, including how key elements of quality were rated, rather than relying only on a single total score. In undertaking the scoring, details about the methodological and design issues were evaluated using the scoring schedules. Specific methodological strengths or weaknesses were considered in the synthesis.
The B papers were:
-
reviews with no primary data
-
descriptions of potential interventions on theoretical grounds, but without an evaluation; often these were case studies for teaching purposes, without an evaluative and critical element or conclusion.
| Study | Does intervention improve TC? (1–4) | Outcome as a measure of TC (1–3) | Ethnic groups (0–5) | Quality of RCT (0–30) | Economic evaluation (0–4) | Total score (0–46) |
|---|---|---|---|---|---|---|
| Rathod et al., 201361 | 75 | 66.67 | 100 | 67.13 | 0 | 80.43a |
| Acosta, 198360 | 75 | 66.67 | 40 | 40.00 | 0 | 41.30b |
| Afuwape et al., 201057 | 100 | 66.67 | 100 | 56.67 | 75 | 67.39a |
| Alvidrez et al., 200966 | 75 | 66.67 | 20 | 50.00 | 0 | 45.65b |
| Chong and Moreno, 201265 | 50 | 100.00 | 20 | 53.33 | 0 | 47.83b |
| Grote et al., 200967 | 75 | 66.67 | 20 | 46.67 | 0 | 43.48b |
| Kanter et al., 201068 | 50 | 33.33 | 0 | 40.00 | 0 | 32.61c |
| Hinton et al., 200464 | 75 | 66.67 | 60 | 53.33 | 0 | 52.17b |
| Hinton et al., 200563 | 75 | 66.67 | 60 | 70.00 | 0 | 63.04b |
| Lambert and Lambert, 198469 | 50 | 66.67 | 0 | 26.67 | 0 | 26.09c |
| Tom, 198952 | 50 | 66.67 | 20 | 70.00 | 0 | 56.52b |
| Wissow et al., 200862 | 75 | 66.67 | 20 | 83.33 | 0 | 67.39a |
| Study | Does intervention improve TC? (1–4) | Outcome of TC (1–3) | Ethnic groups (0–5) | Quality assessment of quantitative studies (0–34) | Total score (0–46) |
|---|---|---|---|---|---|
| Alvidrez et al., 200571 | 75 | 66.67 | 20 | 26.47 | 32.61a |
| Kohn et al., 200270 | 75 | 66.67 | 60 | 29.65 | 19.57a |
| Study | Does intervention improve TC? (1–4) | Outcome of TC (1–3) | Ethnic groups (0–5) | Quality assessment for case series (0–38) | Total score (0–50) |
|---|---|---|---|---|---|
| Kirmayer et al., 200315 | 75 | 33.33 | 0 | 60.53 | 54a |
| Palinski et al., 201258 | 100 | 100 | 100.00 | 86.84 | 90b |
| Chow et al., 201072 | 75 | 66.67 | 20 | 78.95 | 72b |
| Study | Does intervention improve TC? (1–4) | Outcome of TC (1–3) | Ethnic groups (0–5) | Case study quality score (0–87) | Total score (0–99) |
|---|---|---|---|---|---|
| Bhui and Bhugra, 200414 | 75 | 33.33 | 100 | 63.22 | 64.65a |
| Chu et al., 201274 | 50 | 33.33 | 60 | 77.01 | 73.74b |
| Schouler-Ocak et al., 200875 | 50 | 33.33 | 60 | 50.57 | 50.51a |
| Grote et al., 200740 | 75 | 66.67 | 20 | 52.87 | 52.53a |
| Chow et al., 201072 | 75 | 66.67 | 20 | 64.37 | 72.73b |
Studies included
The database searches yielded 7329 hits, and 3733 records were found to be potentially relevant after removing duplicates. An extensive search for grey literature yielded 608 sources, including six PhD theses, two of which could not be located from the original universities. Figure 1 shows the selection of papers at each stage of the review.
FIGURE 1.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram showing selection of papers at each stage.
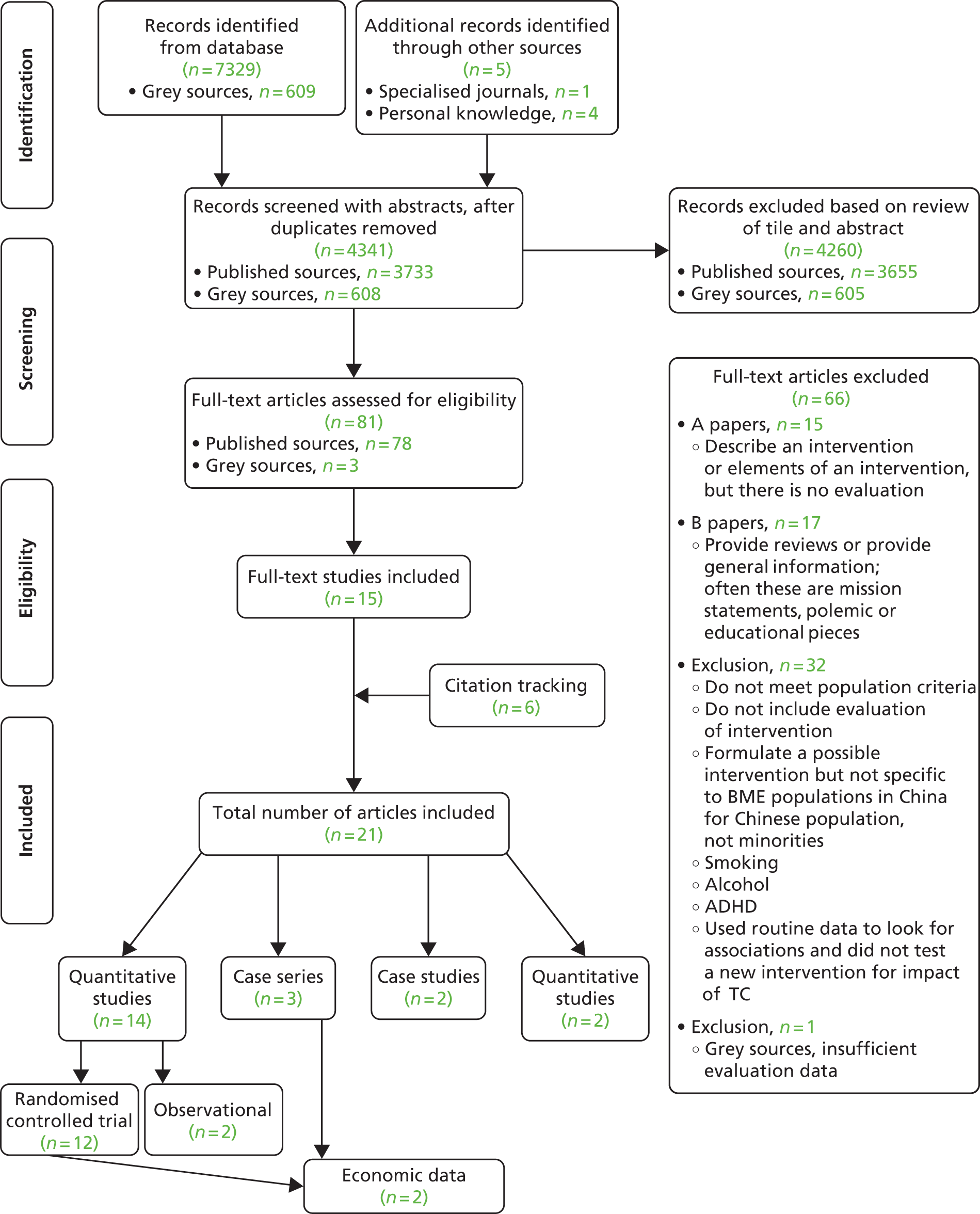
A total of 21 publications were deemed to be relevant and met all the inclusion criteria. These comprised 12 trials52,57,60–69 one of which was from the grey literature,52 two observational studies,70,71 three case series58,72,73 (one of which was from the grey literature58 and one of which had a qualitative component that was separately extracted72), two qualitative studies40,74 (which included a case study in each) and two pure case studies. 14,75
Methods of analysis and synthesis
The findings are presented below in two groups (trials and non-trials) given that within the hierarchies of evidence it is the trials that provide the most definitive evidence of effectiveness. 83 We set out the interventions, study design, ethnic groups and service setting, and outcomes. Given the diversity of study settings, interventions and outcomes, the studies were not suitable for a meta-analysis and thus the data were subjected to a narrative synthesis. Popay et al. 84 define narrative synthesis as:
[A]n approach to the systematic review and synthesis of findings from multiple studies that relies primarily on the use of words and text to summarise and explain the findings of the synthesis. Whilst narrative synthesis can involve the manipulation of statistical data, the defining characteristic is that it adopts a textual approach to the process of synthesis to ‘tell the story’ of the findings from the included studies. As used here ‘narrative synthesis’ refers to a process of synthesis that can be used in systematic reviews focusing on a wide range of questions, not only those relating to the effectiveness of a particular intervention.
It is part of a larger review process that includes a systematic approach to searching for and quality[-]appraising research[-]based evidence as well as the synthesis of this evidence. 84
Narrative synthesis includes the following elements: textual description, tabulation, grouping and thematic analysis. We undertook this process and by thematic analysis contrasted, within- and non-trial designs, elements of intervention, the outcomes used in studies, and direct or indirect measures of effectiveness, taking account of the elements contributing to the quality score and the perspectives of patients and carers who reviewed the emergent evidence (see Patients’ and carers’ views).
Data extraction
Quantitative studies
An electronic version of a quantitative data extraction form was circulated to all members of the review group for comments and revision as appropriate. The two main reviewers used an Excel (Microsoft Corporation, Redmond, WA, USA) spreedsheet to help ensure the consistency of the extracted data by allowing only certain types of options to be entered in any one field, thus ensuring that all data were categorised in a similar way. In the first stage, detailed information relating to study methods was extracted concerning the interventions (e.g. whether the effect of the change in TC was inferred or directly measured), size of the population, ethnic group, setting, timeline of intervention and of follow-up, and the outcomes that were measured (including the tool used to measure each outcome).
The second stage involved more detailed extraction of appropriate numerical data for all studies categorised as either randomised trials or quasi-experimental designs. This too was recorded in an Excel spreadsheet. The effect sizes of the various studies were extracted to judge whether or not a meta-analysis could be performed.
Qualitative studies
A similar pattern was followed with the qualitative studies. Data were extracted into a summary table in Excel. Data extracted comprised the concepts identified and evaluation methods of studies and narrative findings.
Patients’ and carers’ views
A key element of the study was to ascertain user views from the outset; in the design and operation of the literature review, as well as in the evaluation of the interventions and themes identified as having potential to improve TC. In other words, we asked service users and their carers what they regarded (or would regard) as TC and what they would see as better practice. The involvement of minority ethnic users (i.e. BME people currently using health services for mental health needs, or significantly involved as carers of such patients) was operationalised by a collaboration with the national charity The Afiya Trust (www.afiya-trust.org) and its links to the National Black Carers Workers Network (NWBCN), CatchAFiya, and the National Survivor User Network, which support and enable the voices of such individuals through a panel of users who have had basic training in self-representation and some experience of supporting similar research and service development.
The Afiya Trust circulated a call for expressions of interest and selected a panel of eight people who had relevant experience and covered a range of ethnicities and mental health needs. The panel members, chaired by an Afiya Trustee, then worked closely with the research team in advising on the literature search, considering the emergent themes and assisting with the rating, validation and dissemination of the emergent models of good practice.
The core user panel comprised two men and six women. Three self-identified as being of African/Caribbean/black British origin and five were of South Asian background, with Hindu, Sikh, Muslim and other religious affiliations, and from a variety of the major South Asian national/linguistic groups. Three had experience as carers of mental health service users (some having also been patients themselves) and most had also some experience of working with community-based third-sector support groups.
Initially, a series of three user workshops were held, to elicit key themes and to discuss perspectives on TC as a process and what issues were seen as likely to be of concern. The panel’s views were then compared and contrasted with those emerging from the review of the published scientific literature and the grey literature. This background exploration was important for the patients and carers in order to prepare themselves to consider the outputs from the review, so that they were more active in deliberating the value of the interventions identified in the review.
The interventions or other solutions identified by the literature review were grouped and presented as model responses, using a technique of vignettes that included quotes from the publications and a brief description of key elements. A series of Delphi technique consultation rounds were engaged in using e-mail and workshops to highlight the most significant issues and to draw up a list of priorities for desired changes or best practice, as well as a list of issues of concern, responding to the research team’s initial questions and planned recommendations. Although overall agreement did emerge, there was a degree of variation between panel members, and many of the model interventions were ranked as ‘most desirable’ by some members but ‘least important’ by one or more others, illustrating the heterogeneity of need and the requirement for a variety of options to be available to service providers and users.
The patient and carers commented on the proposed interventions and ranked them as high or low priority, and these judgements were included in the synthesis alongside the quality of design and methodological issues, and the strength of the findings.
Chapter 4 Results and synthesis
A total of 21 publications were deemed to be relevant and met all the inclusion criteria. These comprised 12 trials52,57,60–69 (one of which was from the grey literature52), two observational studies,70,71 three case series58,72,73 (one of which was from the grey literature58 and one of which had a qualitative component that was separately extracted72), two qualitative studies (which included a case study in each)40,74 and two pure case studies. 14,75 Two studies included economic information (see Figure 1). 57,58 The data from extractions were tabulated separately for trials and the more varied non-trial designs. The findings for trials were stratified by the quality banding (upper, middle, lower third). Within each group, we first describe the intervention and its components, and the outcomes assessed in these studies. We then synthesise the findings and conclude with a summary of that synthesis. The purpose of the groups by which the results are presented is that due weight can be given to the trials over other designs, and specifically the high-quality trials. We did not wish to overlook potential interventions that did not fall within this high-quality trials group, and so have included all trials and non-trials with evidence of effectiveness on any proxy measure. This synthesis takes account of methodological insights during the extraction and analysis process, the broad quality bandings and, where significant, particular elements contributing to quality scores.
The trials
For trials Table 6 includes details of the study authors, title, intervention and the country, ethnic groups and sample sizes, diagnostic groups and service settings, and details on the professionals involved and the outcome measures used. The findings of the trials are presented in Table 7, which gives both the statistical details against each of the main outcomes used and a narrative summary of the findings for each study.
| Study | Title | Country | Intervention | Study design | Sample size (number of individuals) and ethnic groups | Diagnostic groups | Service setting | Professional groups | Outcome measures |
|---|---|---|---|---|---|---|---|---|---|
| Rathod et al., 201361 | Cognitive–behaviour therapy for psychosis can be adapted for minority ethnic groups: a RCT | UK | CaCBTp. Tseng’s framework of philosophical, practical, technical and theoretical adaptation | RCT in two centres. Thirty-five participants with a diagnosis from schizophrenia group of disorders. CaCBTp participants were offered 16 sessions of CaCBTp with a trained therapist and compared with standard treatment | African Caribbean: CaCBTp = 5, TAU = 4, Black African: CaCBTp = 1, TAU = 4 Mixed race: CaCBTp = 4, TAU = 6 Pakistani: CaCBTp = 3, TAU = 3 Bangladesh: CaCBTp = 2, TAU = 0 Other (Iranian): CaCBTp = 1, TAU = 0 |
Schizophrenia, schizoaffective disorder or delusional disorders (ICD-10 criteriaa) | Inpatient forensic: CaCBTp = 3, TAU = 4 Rehabilitation: CaCBTp = 1, TAU = 0 Assertive outreach: CaCBTp = 1, TAU = 0 EIP: CaCBTp = 7, TAU = 4 CMHT: CaCBTp = 4, TAU = 8 Other (immigration centre) CaCBTp = 0, TAU = 1 |
Psychotherapists registered with BABCP; all therapists received ongoing supervision | Primary outcome: CPRS. Several subscales were derived and analysed: MADRAS, SCS, BRAINS Secondary outcome: Insight in Psychosis scale, PEQ, medication |
| Wissow et al., 200862 | Improving child and parent mental health in primary care: a cluster randomised trial of communication skills training | USA | Brief communication training of three, 1-hour discussions structured around video examples of family/provider communication. Each was followed by practice with standardised patients and self-evaluation. Skills encouraged were eliciting parent and child concerns, partnering with families, and increasing expectations that treatment would help. Psychiatrists training primary care professionals to work with family, negotiate treatment choice and expectations of treatment | Cluster randomised trial. The training was tested with providers at 13 sites. Children (5–16 years of age) on a routine visit were enrolled if they screened ‘possible’ or ’probable’ for mental disorders on a questionnaire, or if their provider said they were likely to have an emotional or behavioural problem | 418 children: 54% were white, 30% black, 12% Latino and 4% other ethnicities | On the basis of SDQ 39% had possible or probable disorder related to hyperactivity, 51% conduct difficulties and 31% emotional difficulties | Participating rural sites (n = 7) included a solo paediatric practice, a hospital-based, multimember, paediatric practice, four freestanding multispecialty offices and a practice staffed by two family nurse practitioners. Urban sites (n = 6) included three community medical centres (two multispecialty and one paediatric), a private paediatric practice, a hospital-based family practice and a community centre serving Latino immigrants | Paediatric primary care, no site had formal arrangements with psychiatrists or psychologists. Providers had practised for an average of 15 years since obtaining their degree (range 2–40 years; median 13 years); 85% had been at their site for 1 year, and 60% were female. Sixty per cent were trained in paediatrics, and 38% in family practice. Eighty-three per cent were physicians, 16% were nurse practitioners and one was a physician’s assistant. Twenty-one per cent had additional training in child behaviour | Parent mental health symptoms – rated on GHQ-28. Child symptoms and functional impairment-computed total symptom (range 0–40) and impairment (range 0–10) scores from the parent-rated SDQ |
| Afuwape et al., 201057 | The Cares of Life Project (CoLP): an exploratory RCT of a community-based intervention for black people with common mental disorders | UK | Needs-led stepped-care approach by six community health workers with a more experienced therapist. Practical advice, assistance, advocacy for social needs, health education, mentoring, brief therapies based on CBT and brief work focused on solutions. CBT with ethnically matched therapists (black African and black Caribbean origin), delivered through multiple social sites with significant flexibility | RCT: individuals were randomised to a needs-led package of care (rapid access) or to a 3-month waiting list control with information on local mental health services (standard access). The needs-led package involved practical advice and assistance, advocacy for social needs, health education and mentoring as well as one-to-one brief therapies based on principles of CBT and brief solution by ethnically matched therapists | 40 individuals of black African origin (black African individuals born in sub-Saharan Africa or born in the UK with at least one parent of sub-Saharan descent) and of black Caribbean origin (black patients born in the Caribbean or born in the UK with at least one parent of Caribbean descent) | WHO diagnostic criteriaa for anxiety (generalised anxiety, panic, social disorder or agoraphobia) and/or depression | Separate service at the interface between statutory agencies and the local black community organisations. Community, referrals for service users, services, and self-referral or referral by friend (37%) | Community health workers (psychology graduates with a minimum of 2-months’ training in the delivery of the intervention). There was backup of a more experienced therapist with access to a psychiatrist for individuals with more complex needs | Primary outcome: At 3 months, GHQ-28 total scores. Secondary outcome: transformed sub-scales of the GHQ-28; Physical Functioning, Role-Physical, Bodily Pain, General Health, Vitality, Social Functioning, Role-Emotional, Mental Health, Experience of a severe difficulty from the Life Events and Difficulty. General psychosocial functioning using the GAF; eight transformed scales of the SF-36 and the Mental and Physical component summary scores; ‘fresh start’ events and cost of service use |
| Hinton et al., 200563 | A RCT of CBT for Cambodian refugees with treatment-resistant PTSD and panic attacks: a crossover design | USA | Culturally adapted CBT for Vietnamese refugees with treatment-resistant PTSD and panic attacks. Information about PTSD and PD, muscle relaxation and diaphragmatic breathing, culturally appropriate visualisation, relaxation techniques/mindfulness; cognitive restructuring of fear networks; exposure to anxiety-related sensation alongside reassociation to positive images to treat panic attacks generated by sensation-activated fear networks. Exposure to, and narrativisation of, trauma-related memories. Teaching cognitive flexibility by lotus visualisation and enactment and by a flexibility protocol. Practice set shifting, during the emotional processing protocol: shifting from acknowledgement of trauma to self and other pity, to kindness and to mindfulness | RCT: individual CBT was offered across 11 weekly sessions. Vietnamese social workers and staff provided translation and cultural consultation | Cambodian refugees (n = 40): 20 patients in the IT condition and 20 in DT | PTSD and panic attacks | Two community-based outpatient clinics that provided specialised services to non-English speaking Cambodian and Vietnamese refugees | Therapist (fluent in Cambodian). All outcomes were measured by a Cambodian bicultural worker (D.C., V.P.) with over 2 years of mental health experience; blind to treatment condition |
|
| Hinton et al., 200464 | CBT for Vietnamese refugees with treatment-resistant PTSD and panic attacks: a pilot study | USA | Culturally adapted CBT for Vietnamese refugees with treatment-resistant PTSD and panic attacks. Eight core elements highlighted in the sessions: providing information about the nature of PTSD and panic disorder; training in muscle relaxation and diaphragmatic breathing procedures, including the use of applied relaxation techniques; instruction in a culturally appropriate visualisation; framing relaxation techniques as a form of mindfulness; cognitive restructuring of fear networks; exposure to sensations that induce panic; providing an emotional processing protocol; and exploring panic | Pilot of RCT: individual CBT was offered across 11 weekly sessions. Vietnamese social workers and staff provided translation and cultural consultation. Pilot RCT and cohort study | (n = 12) non-English speaking Cambodian and Vietnamese refugees | PTSD and panic attacks | Two community-based outpatient clinics that provided specialised services to non-English speaking Cambodian and Vietnamese refugees | Therapist | HTQ, translated and validated for the Vietnamese population HSCL-25, translated and validated for the Vietnamese population ASI, translated and validated for the Vietnamese population H-PASS O-PASS Outcomes from HTQ, HSCL-25 and ASI were measured (a) at pre-treatment (first assessment); (b) after group 1 had undergone 11 sessions of CBT (second assessment); and (c) after group 2 had undergone 11 sessions of CBT (third assessment). Outcomes from H-PASS and O-PASS were measured every 2 weeks |
| Chong and Moreno, 201265 | Feasibility and acceptability of clinic-based telepsychiatry for low-income Hispanic primary care patients | USA | Telepsychiatry intervention for Hispanic patients. Online meeting programme between Hispanic psychiatrists and Hispanic low-income primary care patients seeking consultation. Two Hispanic psychiatrists fluent in English and Spanish; organisational readiness concept; importance of mental health treatment accepted; payment not expected of either group. Patient and psychiatrists sit in front of respective PC using webcam | RCT: eligible subjects were randomly assigned to telepsychiatry using WEB or TAU. Those assigned to the WEB condition agreed to arrive for telepsychiatry sessions once a month for 6 months (1 hour for intake and six 30-minute follow-ups). Those assigned to TAU were told that their provider would be responsible for their mental health needs | 80 intervention and 89 TAU Hispanic patients | Depression | Primary care referred for telepsychiatry specialist consultation | Hispanic psychiatrists | PHQ-9: WEB – each session (for 6 months); TAU – baseline, 3 and 6 months post baseline MINI: only once for exclusion and inclusion ARSMA II SDS: patients baseline and 3 and 6 months post baseline. WEB – monthly. TAU – baseline and 3 and 6 months post baseline VSQ-9 was developed from Rand’s Medical Outcomes Study. The VSQ-9 was found to reflect patient–doctor communication if used immediately after the clinical visit Working Alliance Inventory Short Form rate questions regarding the working relationship between them and the clinician/therapist during the specific clinic visit. It measures three subscales of the alliance that are related to the goal, task, and client–therapist bond. VSQ-9 (doctor patient communication) satisfaction ratings, proportion of completed primary care appointments |
| Alvidrez et al., 200966 | Psychoeducation to address stigma in black adults referred for mental health treatment: a randomised pilot study | USA | Psychoeducation booklet to tackle stigma. Booklet based on peers’ experiences of services to reduce stigma – preparatory to treatment in mental health services/engagement. Getting Mental Health Treatment: Advice from People Who’ve Been There was a psychoeducation booklet developed from qualitative interviews revealing black patients’ experiences with mental health treatment and stigma. The booklet included information on what consumers wished they had before entering mental health treatment, challenges faced, getting or staying in treatment and the strategies to deal with challenges, and advice on making treatment work better | RCT: comparison with information in two existing brochures on local mental health services and the services in the outpatient clinic. Twenty-two of 42 participants assigned to psychoeducation and 20 to general information | 42 clients self-identified as black/African Americans, first time clients of the clinic | DSM-IV, diagnosis made by clinician. Depression, PSTD, stress and anxiety disorders were most common. Forty per cent co-occurring substance misuse, 40% had treatment previously in another setting | County hospital-based outpatient mental health service | Clinicians diagnosed conditions | Symptom severity based on Global Severity Score of Brief Symptom Inventory Perceived need for treatment. Treatment concerns. Diagnosis. Stigma-discrimination (devaluation-discrimination scale). Helpfulness of information (questionnaire). Treatment entry and attendance |
| Grote et al., 200967 (pilot data reported in 200740 and included in this paper) | A RCT of culturally relevant, brief interpersonal psychotherapy for perinatal depression | USA | Short, enhanced culturally relevant interpersonal therapy. IPT-B delivered as part of multicomponent care for antenatal depression; engagement sessions were followed by eight IPT-B sessions before the birth and maintenance IPT up to 6 months post partum. IPT was combined with motivational and ethnographic interviews taking account of social isolation, vulnerability and financial strain | RCT: 53 non-treatment seeking, pregnant African American and white patients receiving prenatal services were randomly assigned to receive either enhanced IPT-B (n = 25) or enhanced usual care (n = 28). Participants were assessed before and after treatment | 53 non-treatment seeking pregnant African American women (n = 33) and white counterparts (n = 20) | Depression on EPDS, score of > 12 | Obstetrics and gynaecology clinic in an urban setting | Therapists | Baseline, 3 months post baseline, 6 months post partum: depression diagnoses, symptoms (EPND scale for screening post-natal depression). Beck 21 item for depression diagnosis if cut off > 10; BAI-21 anxiety measure; social functioning on Social Adjustment Scale’s social and leisure domain |
| Acosta, 198360 | Preparing low-income Hispanic, black, and white patients for psychotherapy: evaluation of new orientation programme | USA | Audiovisual programme instructing patients about psychotherapy. The control patients saw a programme that was neutral with regard to psychotherapy. Orientation, role induction, management of expectations assuming knowledge is limiting factor. An audiovisual slide/cassette programme titled ‘Tell It Like It Is’ designed to inform patients from widely diverse ethnic, language and cultural backgrounds about verbal psychotherapy. Combined simple explanations of the therapy process with presentations of vignettes that model helpful patient behaviours such as self-disclosures and direct statements of patient expectations | RCT: patients in each of the three ethnic groups were assigned randomly to one of two experimental groups: (1) oriented or (2) not oriented. The study employed a 2 × 3 × 2 factorial design, with two levels of patient orientation (oriented and not oriented). Three levels of patient ethnicity (Hispanic, black and white) and two levels of patient sex (male and female) | 62 Hispanic, 51 black and 60 white participants (n = 173) | Most frequent diagnoses: Hispanics: 27.8% transient situational disturbance, black: 34.1% psychoses, white: 37% neuroses | Psychiatric outpatients | Adult psychiatric outpatient clinic | Attitude Towards Psychotherapy; questionnaire is an 8-item questionnaire on 6-point Likert-type scales that ranged from ‘agree strongly’ to ‘disagree strongly’. Knowledge Questionnaire, 10 items with multiple-choice questions |
| Kanter et al., 201068 | Initial outcomes of a culturally adapted behavioural activation for Latinas diagnosed with depression at a community clinic | USA | Behavioural activation therapy adapted for Latino patients. Less individual, more family/community focused. More practical rather than psychological. Language matching in some cases. Adaptations account for the clients’ circumstances, and sensitivity to the support resources, including the local community, spiritual traditions, and the extended family. Specific set of modifications including specification of culturally sensitive activation targets, incorporation of Latino-specific cultural values and beliefs, addition of specific strategies to address treatment engagement and retention in the first session, and inclusion of tips for incorporating family, social and community resources into treatment | RCT: 10 people randomly assigned to BAL and 12 to a control condition | Total = 10 Latino clients. Country of origin: 60% Mexico, 30% Puerto Rico and 10% the USA | Depressive symptoms (score of ≥ 16 HRSD), score of ≥ 20 on BDI and diagnosis of major depressive disorder on PRIME-MD, and presenting to centre’s primary care or mental health clinic | Mental health clinic of a large community health centre that provides comprehensive medical, dental, and mental health care and is the only community-based agency in the area with a full-service bilingual (English–Spanish) mental health clinic. The centre serves a client population that is 80% Latino, the majority monolingual Spanish speakers | Psychiatrists, psychologists, psychiatric nurse, masters-level clinicians, graduate intern for total of seven providers, of which 11 were bilingual. – BAL bilingual Latina MSc, one English speaking white male doctoral student in psychology. Training included 2-day workshop by a national expert, training cases and weekly supervision | 17-item HSRD, a Spanish-speaking version; Spanish BDI-ii, Spanish PRIME-MD. Pan-Hispanic familialism scale, short acculturation scale, multidimensional acculturative stress inventory, and a treatment adherence checklist |
| Lambert and Lambert, 198469 | Effects of role preparation for psychotherapy on immigrant clients seeking mental health services in Hawaii | USA | Role induction involved therapy preparation intervention consisting of role preparation interview. Role induction to inform and manage expectations, clarify client and therapist roles, provide rational basis for patient to accept therapy to deal with problems, provide a general outline for the course of therapy with particular emphasis on the clarification of hostile and negative feelings; and convey information designed to create ‘more positive and realistic’ attitudes | RCT: 30 immigrant clients were assigned to either role induction (therapy preparation intervention) or a placebo intervention prior to receiving therapy | Matching not expected to improve potency, but if it took place would work against finding significant effects. Ethnic background decided on the basis of 11-item questionnaire (n = 30) | 10 therapists; one psychiatry, two psychology, five social work, five nursing. Six of the ten therapists came from Asian backgrounds; four were Caucasians | Patient admission form, background information – client; background information – therapist; revised client expectancy inventory, approval-seeking, advice-seeking; audience-seeking; relationship-seeking; psychotherapy questionnaire – Therapy Evaluation Inventory; premature termination; attendance rate measured by the number of scheduled sessions a client failed to attend from the time of assignment to a therapist through the sixth therapy session | ||
| Tom, 198952 | Psychoeducational approach with chronically mentally ill Chinese Americans: a cultural framework | USA | Formation and application of a culturally relevant psychoeducation programme. Incorporated relevant cultural issues including Chinese perceptions of illness, concepts and terms. A lecture format was used with slide show and handouts, followed by a question and answer period. Topics included the disparity between Chinese and American views on mental disorders, the major diagnostic categories of mental disorders, symptoms of psychosis, the purpose of medication in treatment, warning signals of relapse, modalities and settings for treatment and roles of mental health professionals Increase knowledge of western concepts of mental illness and treatment |
RCT and post test Control group design: 30 Chinese American clients were assigned to psychoeducation or a regularly scheduled group. Twenty-four participated in the trial. On trial completion, control group clients were given the option to receive the intervention |
Chinese Americans: 12 in experimental and 12 in continuing treatment group | Schizophrenia was the most common diagnosis (experimental = 10: control = 9), followed by schizoaffective disorder and bipolar disorders | Outpatient chinese unit of the Asian American mental health services located in New York’s Chinatown | The continuing treatment programme was staffed by two social workers with Master’s degrees, two paraprofessionals, a kitchen service worker and a part-time consulting psychiatrist. All staff were Chinese-speaking The psychoeducation programme was conducted by two Chinese-speaking psychiatric social workers with Master’s degrees. Staff received three training sessions. A social worker and paraprofessional administered the questionnaires |
Knowledge of mental illness and treatment using modified KSQ Attitude towards mental illness using modified Opinions about mental illness Instrument Satisfaction with services using Client Satisfaction Questionnaire Motivation for treatment using staff completed modified Task Check List Questionnaires were administered in a group setting. Oral administration in order to minimise the number of unanswered items |
| Study | Intervention | Main findings | Narrative summary |
|---|---|---|---|
| Rathod et al., 201361 | Culturally adapted CBT for psychosis | Symptoms Post treatment, the intervention group showed statistically significant reduction in symptoms on overall CPRS scores [CaCBTp group mean (SD) = 16.23 (10.77), TAU group mean (SD) = 18.60 (14.84); p = 0.047] and a change of 11.31 (95% CI 0.14 to 22.49). At the 6-month follow-up, MADRAS score change = 5.6 (95% CI 2.92 to 7.60; p < 0.001) Insight Insight domains 2 (acceptance of illness) and 3 (relabelling of psychotic experiences) – when adjusted for baseline scores – post-treatment scores were statistically significant at p = 0.001 and p = 0.001, respectively. A 0.11-unit improvement was observed in CaCBTp group than in the TAU group Patient experience Post treatment, overall satisfaction with treatment experience was based on PEQ item 10 score (overall satisfaction with service). PEQ n = 14 patients mean (SD) = 4.36 patients (1.082 patients; 88.2% CI 3.71 to 4.71 patients). Overall satisfaction was significantly correlated with the number of sessions attended (r = 0.563; p = 0.003). PEQ item 10 (overall satisfaction with service) and item 8 (perception of involvement with treatment decisions) were significantly correlated (r = 0.563; p = 0.003). There was also a significant correlation between PEQ item 10 and item 5 (satisfaction with therapist) (r = 0.78; p = 0.001) Medication At the 6-month follow-up, the mean medication change for the TAU group was mean (SD) = 2.29 (1.10) and 3.13 (0.61) for the CaCBTp group. There was a statistically significant difference between the two groups (β = −0.83; p = 0.001) |
CaCBTp was acceptable and effective as evidenced by a significant reduction of symptomatology on CPRS score total and subscales scores post treatment. The only gains maintained at follow-up were in the MADRAS subscale, although a positive trend towards reduction was noted overall. A subanalysis from the study revealed change in domains 2 and 3 (acceptance of illness and relabelling of psychotic symptoms) as statistically significant when adjusted for baseline scores. The CaCBTp group engaged well when judged by attrition rates, mean number of sessions attended and the scores on the PEQ questionnaire. Overall satisfaction was associated with accessibility, type of therapy, therapist and involvement in decision-making process. The CaCBTp group presented with a significantly higher rate of medication change than the TAU group at the 6-month follow-up |
| Wissow et al., 200862 | Brief communication training for primary care providers led by psychiatrists. Skills targeted were related to eliciting child and parent concerns about mental health, partnering with parents, and increasing expectations that therapy would be helpful | Symptoms Child symptoms: no statistical evidence of impact or differential effects on minority vs. white children Parent’s symptoms: trained providers were associated with a significantly greater decrease in parent symptoms compared with control providers (on average, –1.7 GHQ points, 95% CI –3.2 to –0.11 points; p = 0.035; effect size: 1.7/5.4 = 0.31) Seeing a trained provider did not result in different effects on minority compared with white parents. Effect sizes were calculated to compare the impact of training with other child mental health interventions The estimated size of the sample at follow-up evaluations, based on Monte Carlo simulations and a range of possible intracluster and intercluster correlations, was ≈ 350 to detect effect sizes ranging from 0.2 to 0.4 by using two-tailed tests with alpha = 0.05 and power = 0.80 In an analysis for children with different SDQ ratings at enrolment, trained providers were associated with a significantly greater decrease in parent symptoms for children rated as possibly having a mental disorder (mean difference for parents seeing trained vs. control providers: –1.6 GHQ points, 95% CI –2.9 to –0.25 points; p = 0.019) but not for children rated as probable (mean difference –0.7 GHQ points, 95% CI –2.6 to –1.2 points; p = 0.47) or unlikely to have a disorder (mean difference: 0.79 GHQ points; 95% CI –0.95 to 2.5 points; p = 0.38) Impairment Child functional impairment: minority children (black and Latino combined) seen by trained providers showed a decrease in impairment (mean = –0.91 points, 95% CI: –1.8 to –0.01 points) compared with white children (p = 0.049) Separate regression analyses indicated that, for black children, seeing a trained provider was associated with a significantly greater decrease in impairment compared with children seeing control providers (mean difference = –1.1 points, 95% CI –2.0 to –0.24 points; p = 0.012; effect size: 1.1/2.5 = 0.44). For Latino children, there was a trend towards greater reduction among those seeing a trained provider (treatment/control difference in impairment changes for Latino children = –0.40, 95% CI –1.5 to 0.66; p = 0.46; no effect size) |
Minority children (black and Latino combined) seeing trained providers had a decrease in impairment compared with white children. For black children, seeing a trained provider was associated with a significantly greater decrease in impairment compared with children seeing control providers. For Latino children, there was a trend towards greater reduction in impairment among those seeing a trained provider. Training was associated with a significantly greater decrease in parent symptoms across ethnicities, compared with seeing a control provider. Seeing a trained provider was associated with a significant decrease in symptoms for the parents of children with an enrolment SDQ rating indicating the possibility of having a mental disorder, but not for parents of children rated as probable or unlikely to have a mental disorder |
| Afuwape et al., 201057 | A needs-led stepped care approach providing practical advice, assistance, advocacy for social needs, health education and mentoring. CBT and brief solution therapy were delivered by ethnically matched therapists (black African and black Caribbean origin) | Symptoms Baseline mean GHQ-28 score was 16 with 95% of participants scoring above the cut-off of 5. Means in the standard access and rapid access groups were 14.10 and 18.30 dropping to 12.25 and 8.06 at the 3-month follow-up, respectively Adjusting for baseline score, age and psychiatric history, the adjusted mean difference was 7.76 (95% CI 0.86 to 14.65; p = 0.03), with the participants in the intervention group showing improved mental health. Analysis of the GHQ-28 subscale severe depression indicated that participants in the intervention group were significantly less severely depressed compared with those in the control group at 3 months (adjusted mean difference 2.20, 95% CI 0.07 to 4.32; p = 0.04). There was a trend towards the intervention group demonstrating better outcomes on the anxiety and insomnia subscale (adjusted mean difference 2.08, 95% CI −0.10 to 4.26; p = 0.06). RA led to significantly better outcomes than the SA group for two of the SF-36 scales: mental health (p = 0.04) and vitality (p = 0.01). The overall mental health component score also showed improvement (p = 0.02) Fresh start events during 3-month follow-up were significantly associated with symptom improvement as measured by the GHQ-28. Moreover, more often than not these fresh starts had been facilitated by the community health worker (7 out of a total of 11). Multiple regression analysis suggested that group assignment and fresh start experience each contributed independently to outcome (p = 0.043 and p < 0.045, respectively) Functioning No evidence of difference between groups |
Access to a needs-led package of care significantly improved mental health among black individuals with depression and anxiety with limited additional cost implications. There was a significant decrease in depression for the rapid access group compared with the control group and positive trends in outcomes for anxiety and insomnia for the rapid assessment group compared with the control group. Fresh start events were significantly associated with symptom improvement. These results were achieved with a study sample consisting of individuals with moderately severe levels of untreated mental illness despite most having contact with some form of NHS service in the 3 months prior to baseline |
| Hinton et al., 200563 | Culturally adapted CBT for Cambodian refugees with treatment-resistant post-traumatic stress disorder and panic attacks | Symptoms Between-group effect sizes, comparing the IT and DT groups at the second assessment, were computed using Cohen’s d. Large effect sizes (Cohen’s d) were found for all outcome measures: ASI (d = 3.78), CAPS (d = 2.17) and SCL-90R subscales (d = 2.77) To evaluate the effects of treatment on symptom change, a 2 by 4 repeated-measures MANOVA (group: initial vs. delayed treatment; time: first, second, third and follow-up assessments) was conducted with the following dependent variables: ASI, CAPS, N-PASS, O-PASS, N-FSS, O-FSS, and SCL-90R scales. The results showed a significant group effect, F7,32 = 5.29 (p < 0.001); time effect, F21,18 = 42.97 (p < 0.001); and group by time interaction, F21,18 = 25.75 (p <0.001) Follow-up analyses of repeated-measures ANOVAs showed that, for all dependent variables, there was a significant time effect (F > 79.90; p < 0.001), group effect (F > 8.40; p < 0.01) and time by group interaction (F > 17.38; p < 0.001) To examine group differences in the various assessment points, we conducted unpaired t-tests. The IT group had significantly lower scores at the second assessment on the ASI, CAPS, O-PASS, O-FSS, N-PASS, N-FSS, and SCL-90R scales (p < 0.001). No group differences were observed on any of the outcome variables at the first, third, or follow-up assessment (NS). The categorical data for PTSD and GAD were analysed by 2 × 2 chi-squared tests to assess changes across treatment. Before treatment, all patients had PTSD. After the first course of CBT (second assessment), 12 (60%) IT patients no longer met PTSD criteria, whereas all DT patients still did, [χ2(1,40) = 17.14; p < 0.001] Before treatment, all participating patients met GAD criteria. After the first course of treatment (second assessment), 11 (60%) IT patients no longer met GAD criteria, whereas all DT patients did, [χ2(1, 40) = 15.17; p < 0.001] Likewise, the DT group improved across treatment, with, at the third assessment 10 (50%) DT patients no longer having PTSD [χ2(1, 20) = 13.33; p < 0.001] and nine (45%) DT patients no longer having GAD [χ2(1, 40) = 11.61; p < 0.01)] |
Culturally adapted CBT targeting PTSD and comorbid panic attacks for traumatised Cambodian refugees was well accepted and efficacious. This was evidenced by a significant reduction in PTSD and GAD symptomatology post intervention. Observed improvements may have been influenced by a therapist effect rather than a treatment effect as the same therapist provided all treatment |
| Hinton et al., 200464 | Culturally adapted CBT for Vietnamese refugees with treatment-resistant post-traumatic stress disorder and panic attacks | Symptoms Between-group effect sizes (mean wait list – mean CBT)/SD pooled) were computed to illustrate the magnitude of treatment benefits relative to other studies (Otto et al., 1996)85 Large effect sizes (Cohen’s d) were calculated for all outcome measures: HTQ (d = 2.5; ASI (d = 4.3); HSCL-25 (d = 2.2); and HSCL-25, depression subscale (d = 2.0) scores Authors conducted 2 × 3 repeated-measures ANOVA (initial wait list vs. initial treatment; and first, second, and third assessments) on each of the outcome variables. The overall interaction was significant for each of the outcome variables:
|
Culturally adapted CBT targeting PTSD and comorbid panic attacks for traumatised Vietnamese refugees was well accepted and efficacious. This was evidenced by a significant reduction in PTSD and GAD symptomatology post intervention. Observed improvements may have been influenced by a therapist effect rather than a ‘treatment effect’ as the same therapist provided all treatment It was not possible to determine whether or not this combined treatment as opposed to other treatments would be more efficacious as this was a low-powered study |
| Chong and Moreno, 201265 | Telepsychiatry intervention for Hispanic patients | Attendance No significant difference in completion of appointments Working alliance By the Working Alliance Inventory Short Form. Assignment (WEB vs. TAU), F1,94 = 31.6 (p < 0.01); time, F2,188 = 87.4 (p < 0.001); and time × assignment, F2,188 = 2.1 (NS) Antidepressant use: WEB 7% vs. TAU 54.8.%. By chi-squared test: χ2(1,152) = 3.8 (p < 0.05) Satisfaction How pleased they are with depression care. A 0–10 scale was used, where a higher score reflects greater satisfaction. TAU mean (SD): 8.8 (2.4); and WEB mean (SD): 9.4, (1.1) By the nine-item Visit Specific Satisfaction Questionnaire. Assignment (WEB vs. TAU): F1,97 = 6.9 (p < 0.01); time (baseline, 3 and 6 months): F2,194 = 46.6 (p < 0.001); and time × assignment: F2,194 = 10.8 (p < 0.05) 76% of patients in the TAU group and 46% in the WEB group were willing to pay the same for a mental health session as for primary care visit, while 12% of patients in the TAU group and 50% in the WEB group were willing to pay more Symptoms No significant difference observed in depression scores; however, a higher rate of improvement observed in WEB vs. TAU. By Personal Health Questionnaire 9. Assignment (WEB vs. TAU): F1,130 = 1.1 (NS); time F2,260 = 254.4 (p < 0.001); and time × assignment F2,260 = 4.4 (p < 0.05) Functional days No significant difference in number of days lost or unproductive days due to depression |
Working alliance and visit satisfaction rated as higher for WEB than TAU. More WEB patients used antidepressants. Although there was no difference in overall depression score, WEB depression scores improved at a faster rate than TAU. Twice as many WEB patients were willing to pay more for telepsychiatry than TAU patients. WEB patients wanted longer sessions, reporting 30 minutes as too short and TAU patients wanted more sessions |
| Alvidrez et al., 200966 | Psychoeducation booklet to tackle stigma | Treatment entry and attendance There were no significant differences between the types of information on treatment entry or attendance. Entered treatment: PG 76%, GIG 71%. Sessions attended (mean): PG 4.9 sessions, GIG 4.7 sessions Perceived helpfulness Both types of information were rated as helpful and relevant on a scale from 1 (not at all helpful) to 4 (very helpful). Mean scores: PG 3.4, GIG 3.0 (p = 0.35) Perceived stigma There was no significant difference between overall perceived stigma between the groups. However, there were two significant interactions between the type of information and the client-perceived stigma. The data for these interactions were not reported |
Interactions revealed that individuals perceiving themselves to have a greater treatment need and individuals expressing more uncertainty about treatment had greater stigma reduction if they received psychoeducation. Individuals with lesser perceived treatment need and individuals with less uncertainty about treatment showed greater stigma reduction if they received general information not psychoeducation |
| Grote et al., 200967 | Short enhanced culturally relevant interpersonal therapy incorporating ethnographic and motivational interviewing | Treatment adherence 68% (n = 17) of the IPT-B group compared with 7% (n = 2) in usual care completed a full course of treatment (seven or eight sessions) Change in clinical and social functioning symptom scores Baseline and before childbirth: EPDS score of 71, BDI score of 0.33, BAI score of 0.27, social and leisure score of 0.26. Baseline and 6 months post partum: EPDS score of 0.89, BDI score of 0.47, BAI score of 0.24, and social and leisure score of 0.46. There was a trend showing that social functioning and anxiety symptoms also improved more in the IPT-B group than in the usual care group between baseline and time 2, but these findings were not significant (p = 0.063 and p = 0.051, respectively) |
Treatment adherence: patients in the IPT-B group showed significantly higher rates of treatment engagement and retention than patients in the usual care group. Intention-to-treat analyses showed that participants in enhanced IPT-B, compared with those receiving enhanced usual care, displayed significant reductions in depressive symptoms before childbirth (3 months post baseline) and at 6 months post partum, and showed significant improvements in social functioning at 6 months post partum |
| Acosta, 198360 | Universal audiovisual programme instructing patients about psychotherapy. The control patients saw a programme that was neutral with regard to psychotherapy | Knowledge about psychotherapy A 2 × 3 × 2 ANOVA (patient orientation × ethnicity × sex) showed a significant main effect for patient orientation [F1,149 = 9.44 (p < 0.01)]. There were no interactions between ethnicity and the orientation main effect observed The ANOVA did show a significant main effect for ethnicity when oriented and non-oriented patient groups were combined, F1,149 = 3.06 (p < 0.05). White patients were rated as most knowledgeable about psychotherapy (χ2 = 6.42), followed by Hispanic patients (χ2 = 6.16) and black patients (χ2 = 5.61). There were no sex differences in knowledge about psychotherapy Attitudes towards psychotherapy The items on the Attitude Towards Psychotherapy Questionnaire were combined to form an index for the pre and post orientation. An analysis of covariance was performed on the post-orientation data that used the pre-orientation data as the covariate. This analysis showed a significant main effect for orientation, F1,148 = 4.38 (p < 0.05), such that patients who had been oriented by exposure to ‘Tell It Like It Is’ were more positive in their attitudes towards psychotherapy (χ2 = 2.03) than were patients who had not been oriented (χ2 = 2.19) |
The orientation programme was successful in increasing a patient’s information about psychotherapy and a patient’s role in that process Although there were no interactions between ethnicity and the orientation main effect, across the groups knowledge of psychotherapy was found to be related to ethnicity, with white patients scoring as most knowledgeable, followed by Hispanic and then black patients Oriented patients were significantly more positive towards psychotherapy than non-oriented patients. More specifically, oriented patients indicated that they were more willing to make self-disclosures and to discuss problems with their therapists, more willing to be assertive in telling the therapist when they disagreed with him/her, more willing to be direct with the therapist with regard to how many sessions they were willing to attend, and more accepting of the concept that talking about problems would be helpful to them |
| Kanter et al., 201068 | Behavioural activation therapy adapted for Latino patients | Treatment adherence 3.24 of four BA techniques per session were implemented by therapists and activation assignments were scheduled for 93% of sessions. Therapists reported most homework partially completed, 84%; fully completed, 12%; or not completed, 4% Retention Averaging across clients, a mean of 7.7 sessions (median 10 sessions) were completed over a mean of 12.4 weeks (median 16 weeks) Symptoms Completers sample: significant decrease in depression severity on the BDI-II from pre to post treatment for completers [t = 5.69; p = 0.002, representing a large effect size (d = 1.67)]. Similar results were found with the HRSD from pre to post treatment [t = 12.77; p < 0.001, representing a large effect size (d = 1.57)] Intent-to-treat sample: decrease in depression severity was significant for the BDI-II (t = 5.62; p < 0.001). The final session was used for clients who did not complete treatment, and HRSD (t = 8.31; p < 0.001, representing large effect sizes (BDI-II, d = 1.07; HRSD, d = 1.43). The response was defined as a 50% reduction in symptoms and remission as a BDI-II score of < 10 or a HRSD score of < 7. Six of 10 participants achieved response according to the BDI-II and 7 of 9 participants achieved response according to the HRSD. For remission, 6 of 10 participants achieved remission according to the BDI-II and 4 of 9 participants achieved remission according to the HRSD. The reliable change index was calculated for BDI-II and HRSD scores using the formula of 1.96 times the standard error of change. Given that the sample was small, the required estimates of SD and internal consistency for this formula were drawn from the two previous validation studies of the Spanish BDI-II. To be most conservative the lowest reported reliability (0.91) and highest reported SD (13.62), were used, resulting in a RCI threshold of 11.33 BDI-II points. Only one participant failed to meet this criterion; thus, 9 of 10 participants experienced a reliable change in depression according to the BDI-II. Regarding reliable change on the HRSD, a reliability estimate of 0.72 and SD of 6.13 from Ramos-Brieva and Cordero-Villafafila 198886 were used to estimate standard error of change scores. This resulted in an RCI threshold of 8.99 points. Eight of the nine participants with valid follow-up HRSD scores experienced a reliable change in depression according to this threshold |
BAL did well with respect to treatment adherence, engagement and retention. BAL was effective in decreasing depression severity evidenced by a significant decrease in symptoms for both completers and intent to treat groups on BDI-II and HRSD scales |
| Lambert and Lambert, 198469 | Role induction involved therapy preparation intervention consisting of role preparation interview | Attendance No significant difference in attendance rates: EPs 90% and CPs 69% Premature termination: 87% EPs and 53% of CPs completed all six sessions. [t-Test for independent samples was calculated on dropout data; difference in dropout rate between the experimental and control group was significant (t = 2.05, df = 28; p = 0.05)] Satisfaction EPs perceived themselves as experiencing significantly more change than CPs (amount of change t = 3.71; p = 0.00; present adjustment t = 2.53; p = 0.017; change apparent to others t = 2.52; p = 0.018) EPs also perceived their therapists as significantly more interested and respectful than the CPs (t = 2.43; p = 0.028) Expectancy There was a significant improvement in expectancy scores for the EPs when compared with the CPs (advice-seeking, audience-seeking, and relationship-seeking) |
Role preparation intervention has impact for high-risk clients such as immigrants. There was a reduction in premature termination for the EP group compared with the CP group. EP reported greater satisfaction and perceived change in self. Compared with the CP group, the EP group saw therapists as more interested, respectful and accepting Both groups had entered treatment expecting unrealistically high levels of rational guidance, structure and direction, to have difficulty with verbalising, difficulty in spontaneous self-disclosure and with developing an egalitarian relationship. In comparison with the CP group, the EP group significantly improved their expectancy scores in relation to advice-seeking, audience-seeking, and relationship-seeking |
| Tom, 198952 | Formation and application of a culturally relevant psychoeducation programme | Knowledge The experimental group (mean 23.58, SD 8.19) demonstrated a significantly greater knowledge of mental illness than the control group (mean 16.83, SD 8.12) df = 22, t = 2.03, one-tailed; p < 0.05 Attitude No significant difference observed: experimental group mean 25.67, SD 5.41; control group mean score on KSQ 25.83, SD 5.06 (df = 22, t = –0.75) Satisfaction No significant difference observed: experimental group mean 24.58, SD 1.85; control group mean score on KSQ 23.42, SD 3.75, df = 22, t = 0.96 Motivation No significant difference observed: experimental group mean score on KSQ 6.6, SD 6.14; control group mean 23.42, SD 3.75 (df = 22, t = 0.58) |
The psychoeducation enhances knowledge of western concepts of mental illness and treatment methods. The experimental group had a greater number of years of education than the control group, potentially contributing to their higher mean score on KSQ. In the experimental group, individuals who were younger or better educated or had a longer duration of illness were most knowledgeable about concepts of mental illness and treatment. This suggests that younger patients with more chronic disease and at least a high-school level of education would benefit most from psychoeducation |
Description of interventions
The studies included in the review had interventions that could be broadly categorised as seven types:
-
preparing patients beforehand for their expected role in a psychiatric therapy before they received a therapeutic intervention60,69
-
enhancements of existing therapies in terms of technical content and attention to beliefs57,61,62,64,68
-
influencing wider social systems before and during therapy57,67
-
peer or professional to patient psychoeducation to encourage acceptability and effective use of therapy52,66
-
communication training for professionals to partner better with families, and increase expectations62
-
an audiovisual pre-therapy training to help patients make best use of the therapy, described as role induction60
-
the ethnic matching of the psychiatrist to the patient, achieved through the use of telepsychiatry. 65
The various components of each intervention were subjected to thematic analysis in order to capture the proposed effective elements. These are tabulated in Table 8. We also applied the framework for cultural adaptations of psychotherapies proposed by Tseng to assess if the following types of cultural adaptation were evident: philosophical, technical, theoretical or practical alternatives. 82
| Themes | Study | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Rathod et al., 201361 | Wissow et al., 200862 | Afuwape et al., 201057 | Hinton et al., 200563 | Hinton et al., 200464 | Chong and Moreno, 201265 | Alvidrez et al., 200966 | Grote et al., 200967 (pilot data reported in 200740 and included in this paper) | Acosta, 198360 | Kanter et al., 201068 | Lambert and Lambert, 1984,69 Tom, 198952 |
|
| Patient | |||||||||||
| Causal explanations | ✗ | ✗ | ✗ | ✗ | |||||||
| Beliefs | ✗ | ✗ | ✗ | ✗ | ✗ | ✗✗ | |||||
| Pre-therapy preparation | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||
| Accessibility | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||
| Training | ✗ | ✗ | ✗ | ✗ | |||||||
| Ethnic group specific | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||
| Professional | |||||||||||
| Matching | ✗ | ✗ | |||||||||
| Patient and professional | ✗ | ||||||||||
| Interview structure and content | |||||||||||
| Adaptation of therapy | |||||||||||
| Modify content of materials | ✗ | ✗ | ✗ | ✗ | ✗ | ||||||
| Adapt technical delivery/structure of therapy | ✗ | ✗ | ✗ | ✗ | |||||||
| Wider social systems | ✗ | ✗ | |||||||||
| Empowerment | ✗ | ✗ | ✗ | ||||||||
| Engagement | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||||
| Components according to Tseng, 200187 | Ph, Te, Th, Pr | Pr | Ph, Te, Th, Pr | Ph, Th, Te | Ph, Th, Te | Pr | Te | Ph, Te, Pr, Th | Te, Pr | Te, Pr | Te, Pr |
Outcomes
Symptoms were assessed as outcomes by 8 of the 11 trials. 57,61–68 One study included insight,61 one impairment,62 two functioning,57,67 six studies medication use and adherence,61,65–69 one patient experience,57 one perceived helpfulness,66 two patient satisfaction,65,69 one knowledge and attitude towards treatment,60 and one perceived stigma. 66 All of these outcomes can be understood as reflecting an inferred relationship between the intervention and improved TCs, rather than a direct measure of TC. Only one study included working alliance as an outcome. 65
Synthesis of findings
The trials did not exhibit sufficient similarity of diagnostic groups, samples, contexts or settings (see Tables 7 and 8), outcomes or interventions to warrant a meta-analysis that would provide meaningful pooling of data. They are briefly described below, categorised by their quality rating.
High-quality trials
Three trials were of high quality. 57,61,62 Afuwape et al. ,57 in an exploratory randomised trial, showed improved symptom improvement on the 28-item General Health Questionnaire, following a community-based intervention for black people with common mental disorders in London; this was delivered by flexible outreach from psychiatric services into community venues. The intervention used principles of cognitive–behavioural therapy (CBT), ethnically matched therapists, advocacy and mentoring, and rapid access. 57 Rathod et al. 61 adapted CBT for black British, African Caribbean and South Asian Muslim people with psychosis in the UK. Benefits were found on completing therapy for all symptoms (as assessed using the Comprehensive Psychopathological Rating Scale) and for delusions but not for hallucinations; symptom improvement was maintained at 6-month follow-up (measured on the Montgomery–Åsberg Depression Rating Scale). Wissow et al. 62 adopted a different approach and offered communication training to professionals. Training involved three 1-hour discussions structured around video examples of family/provider communication skills, followed by practice with standardised patients and self-evaluation. Skills were to elicit parent and child concerns, partnerships with families, and increasing expectations of helpful treatment. They recruited people of black, white Latino and other ethnicities and reported that minority children had less impairment at 6-month follow-up, but no change in symptoms.
Synthesis summary of high-quality trials
Although all three of these high-quality trials reported some benefits from their different interventions to improve communication between psychiatric professionals and BME patients, the service user reviews of the evidence did not favour that conducted by Afuwape et al. ,57 as that study seemed over-complex and not easily generalisable. This leaves adapted CBT and communication training as the most well evidenced and favoured interventions.
Medium-quality trials
Six trials were of medium quality. Two trials of a model of CBT for treatment-resistant post-traumatic stress disorder (PTSD) and panic attacks, specially adapted for Vietnamese and Cambodian refugees,63,64 showed significant improvement in symptoms on the Harvard Trauma Questionnaire and the Hopkins Symptoms Checklist and its depression subscale. Culturally shaped symptoms of headache and orthostatic symptoms that induced panic (a culturally specific syndrome) also improved. These interventions incorporated cultural unique concepts of distress and illness. Including them in the content of the therapy enabled the approach to appear more relevant and culturally embedded rather than something being applied or borrowed from outside the culture of the patients. However, a clinician who is unfamiliar with this cultural expression of distress will not recognise it and may not be able to understand it or use it in the therapeutic process. In a paper by Hinton et al. ,63 published in 2005, symptoms improved on self-report and clinician-administered scales, suggesting not only that improvements are subjective but also that a true, shared assessment of distress is possible if our assessment methods and interventions are adapted.
A multicomponent intervention involved African American and white pregnant women in contact with prenatal services who had been shown to have depression on routine screening. Motivational and ethnographic interviewing was used to empower these women to receive interpersonal therapy for depression. 67 The approach included assessment methods that allowed their true cultural identity and their priorities to be understood, before they were then offered further intervention. The emphasis on exercising choice, and being informed of their options, coupled with the confidence in being understood, were felt to be empowering and minimised any miscommunications that might lead to treatment breakdown or misunderstandings. Those receiving the intervention had less severe depressive symptoms and fewer of them received a formal diagnosis of depression during the 6 months after birth. The empowering nature of this approach, which permitted a better understanding of the social and urban contexts in which patients lived, was favoured by service users in their review of the studies.
A pilot randomised trial66 of a psychoeducation intervention – essentially, the provision of a new information sheet for black mental health service users – found it had no effect on symptoms, attendance or stigma. This new information sheet specifically included knowledge from previous service users about how to improve service use and gain benefit and overcome obstacles in therapy. The aim was to reduce stigma and so encourage help-seeking. Although this was a disappointing overall result, when the sample was divided into two groups according to perceived treatment need and uncertainty about treatment, those with high perceived need and the most uncertainty about treatment reported lower levels of stigma when they received the new sheet; in contrast, those with low perceived treatment need and uncertainty about treatment had lower stigma scores after receiving the usual information sheet and so did not benefit from the new sheet.
A trial that included a sample of Chinese Americans with chronic mental disorders52 found that psychoeducation improved their knowledge about Western concepts of mental disorder, treatment and professional roles, but there was no impact on stigma (measured by attitudes towards mental illness), satisfaction with services or motivation. Those more likely to show improvements in knowledge were younger and better educated and slightly over-represented in the intervention group.
Another pre-therapy trial used an audiovisual orientation programme of instruction to prepare low-income, black, Hispanic and white outpatients to enter therapy. This was to instruct them about psychotherapy, before their assessment interview. This generic, not ethnically adapted programme, showed that oriented patients were more knowledgeable and more positive about therapy before starting therapy. 60
In a feasibility trial of telepsychiatry for low-income Hispanic patients in primary care, ethnically matched psychiatrists produced greater satisfaction. 65 The intervention did not affect the number of appointments patients attended, but it did improve ratings of the working alliance and satisfaction, and patients showed more use of antidepressants (i.e. compliance with treatment was better). There was no effect on the patients’ number of unproductive days due to depression, and more patients using telepsychiatry were willing to pay for care.
Synthesis summary of medium-quality trials
The synthesis suggests that culturally adapted CBT that takes account of histories and beliefs and philosophies of care was attractive and effective, as were complex interventions embedded in the community; these were effective at engaging marginalised groups and also favoured by service users. Part of the effectiveness may be explained by the adoption of and understanding of cultural concepts and language within the intervention, and locating the intervention with some flexibility within the community and cultural contexts that affect the lives of the participants in these studies. These culturally embedded interventions contrasted with the interventions that provided education or role induction, which seemed to improve knowledge but were not favoured by the patients and carers who reviewed the evidence, perhaps as they showed less flexible services and required passive take-up of knowledge by the patient. One study66 showed that the effect of educational interventions was contingent on expectations. High-perceived treatment need accompanied by uncertainty led to less stigma following the intervention, whereas those with low-perceived need did better with treatment as usual. Technology-based interventions seem acceptable but of variable effectiveness, with telepsychiatry and ethnic matching leading to an improved working alliance, if not improved attendance.
Poorer-quality trials
Two trials were rated as being of low quality, and both offered an intervention to help patients adapt and make full use of therapeutic interventions. Thus, Lambert and Lambert69 used a pre-therapy role preparation procedure on immigrants in Hawaii. The role-prepared patients became less dependent on their therapists, changed their expectations ‘in an appropriate way’, were more satisfied and were less likely to drop out. However, the service users who reviewed the evidence felt this intervention was too inflexible and not patient centred and was not favoured by them.
Kanter et al. ’s trial68 was a pilot study of a culturally and linguistically adapted version of a cognitive–behaviour technique that targets behaviour change to drive emotional change (called behavioural activation) as an intervention for Latino patients attending a bilingual clinic in the USA, but close to the border with Mexico. The intervention was to be applied during the course of the therapy. 68 This reported favourable results on symptoms and adherence and retention in the study, but it was not well rated by the service user review group.
Summary synthesis of low-quality trials
Role induction and behavioural activation seemed to be effective in improving adherence, symptoms and satisfaction, but were less valued by patients and carers who reviewed these interventions. This was perhaps because they perceived them to be pre-formed and lacking adaptation, although in fact in both trials efforts were made to adapt the treatments.
Non-trial designs
The data from the non-trial designs were extracted and tabulated (Table 9). Details extracted were the study title, design, country, interventions, sample sizes, ethnic groups, settings, professional groups and the outcomes used. In addition, a summary of findings with statistical and narrative conclusions is included.
| Study | Title | Country | Study type | Detail of intervention | Sample size and ethnic groups | Service setting | Professional groups | Outcomes | Main findings |
|---|---|---|---|---|---|---|---|---|---|
| Kohn et al., 200270 | Adapted cognitive–behavioural group therapy for depressed low-income African American women | USA | Observational studies | Culturally adapted cognitive–behavioural group therapy for depressed African American women. The CBT consists of three four-session cognitive–behavioural modules. After completing each of the three modules patients repeat the first module for a total of 16 sessions. These modules focus on cognitions, activities and relationship: based on cognitive–behavioural treatment for depression. Structural adaptations include limiting the group to African American women, any age, with a diagnosis of major depressive disorder; keeping the group closed to facilitate cohesion; adding experiential meditative exercises during treatment and a termination ritual at the end of the 16-week intervention; and changes in some of the language used to describe cognitive–behavioural techniques. For example, rather than using the term homework the group members were asked for suggestions and agreed upon a preferred term therapeutic exercises. Whenever possible, African American individuals and anecdotes from African American literature were used as examples to illustrate concepts. Didactic adaptations of materials, creating healthy relationships, spirituality, African American family issue and African American female identity. These adaptations represent our attempt to contextualise the therapy manual to address issues relevant to African American women in treatment for depression | 20 African American women: 10 in AACBT group. Comparator group consisted of 10 demographically matched women who had been treated with CBT Approximately 83% of these patients (10/12) offered CBT or AACBT opted for treatment in the AACBT group. One woman preferred individual treatment to group treatment; and another woman preferred the CBT group. Of the 10 African American women who agreed to enter the AACBT, eight completed therapy and were compared with 10 women who were demographically matched on race, age, education, income, diagnosis, referral source and who had been previously treated in the CBT group |
Referred by primary care doctor, to outpatient service. Depression Clinic at San Francisco General Hospital | Therapists? Not reported | The BDI was used to assess the level of symptom intensity during the first and last weeks of treatment | The intervention was acceptable and effective. Women in the culturally adapted (AACBT) group exhibited alleviation of twice the magnitude of women in the usual (CBT) treatment group. Both groups’ scores suggested a need for further treatment. In Nietzel’s meta-analysis,88 with a predominantly white, middle-class population (n = 28 studies), the post-treatment BDI score was 12.0; in Organista’s outcome study,89 with a predominantly low-income, public-sector population (n = 70), the post-treatment BDI score was 18.0. For low-income, African American women, the post-treatment score was 21.8 in the AACBT condition (n = 8) and 24.4 in the regular CBT condition (n = 10). This suggests that CBT for depression may work best in the population for which it was developed, and becomes less effective as groups differ |
| Alvidrez et al., 200566 | Psychoeducation to increase psychotherapy entry for older African Americans | USA | Observational study | Descriptive pre and post comparison. Historical comparison (historical control group). The psychoeducation script begins with a brief description of psychotherapy and specific services offered; this is followed by six topics which were concerns identified by the focus groups: (1) how a medical model of psychiatric disorders reduces stigma; (2) illnesses leading to involuntary hospitalisation; (3) the importance of the patient’s input in therapy goals and topics; (4) the importance of talking about conflicts, misunderstandings, or dissatisfaction with treatment; (5) differences between therapists and patients and how these can be helpful; and (6) receptivity of therapists to discuss religion/spirituality and incorporating into treatment. In the psychoeducation session, the psychoeducation material read from the script while the participant followed along with a large-print handout summarising the major points. The session was didactic; participants were encouraged to ask questions and raise concerns about treatment. Psychoeducation intervention is a 15-minute, scripted individual session. Content was developed by 22 participants in three focus groups, discussing barriers to mental health treatment for older African Americans. Barriers included stigma of receiving mental health care; fear of hospitalisation or institutionalisation; reluctance to work with a non-African American therapist; feeling pressure to divulge personal information or discuss irrelevant material; the lack of attention to religious beliefs/spirituality by therapists; and dissatisfaction when the therapist does not provide solutions | 32 African American patients were recruited to the intervention. A historical control group of 37 consecutive African American patients who were referred to on-site clinic psychologists for psychotherapy in the 12-month period prior to study initiation was used for comparison. Thirty-nine patients were identified for the historical control group; however, two patients were already enrolled in the current study and were excluded 31 participants (97%) completed follow-up interviews. The 32 participants did not differ significantly from the 12 patients who were not enrolled in the study |
Neighbourhood geriatric health clinic with on-site social services. Primary care providers referred patients to the geriatric clinic for psychotherapy or psychosocial services | Psychologists, social workers and PhD-level workers | Number of sessions attended in the 3 months following psychoeducation intervention; historical cohort information obtained from computerised records: age, gender, diagnosis, insurance, dates of therapy appointments and number of sessions in 3 months following referral | An equal proportion (75%) of patients in each group started therapy Therapy entry and attendance, in the 3-month period after the psychoeducation session: 24 of the 32 study participants (75%) attended at least one psychotherapy session (range 1–0). Therapy entry was not related to an African American psychoeducation (71%) or not (76%; p = 0.8), nor were there significant differences in the number of sessions attended (mean 3.3, SD 2.9 vs. mean 4.2, SD 1.9; Mann–Whitney U-test 36.0; exact p = 0.45). In the historical comparison group, 28 of the 37 (76%) attended at least one session (range 1–8). In the 3-month period after referral, the proportion of participants who attended at least one session did not differ by intervention status. Psychoeducation participants who started therapy attended significantly more sessions. In the follow-up interviews, 25 of the 31 participants reported attending at least one psychotherapy session in the 3-month period after the psychoeducation session. The majority of participants (84%) found the psychoeducation to be very or somewhat helpful. Just over half (52%) of those who began therapy said that the psychoeducation influenced their decision to begin therapy ‘a great deal’. When six who did not begin therapy were asked if the psychoeducation influenced their decision, all said no except one who reported that the psychoeducation influenced her decision ‘somewhat’. Twenty-nine of 31 respondents (94%) said ethnicity of psychoeducation made no difference to perceived helpfulness. One respondent who had an African American psychoeducation said the session was more helpful and another who had a non-African American psychoeducation said the session was less helpful because of the ethnicity of the psychoeducation Experience in therapy: among the 24 patients starting therapy, 60% said the psychoeducation addressed many or all of their concerns about treatment Helpfulness for ongoing therapy issues: the majority of patients indicated at least slight helpfulness in all areas. The strongest ratings were given for the role of psychoeducation in helping the patient to bring up concerns about treatment and discussing ethnic, cultural or religious issues with the therapist. Although the majority of patients indicated that the psychoeducation helped them deal with stigma concerns, this was endorsed less frequently and less strongly than the other topics |
| Chow et al., 201072 | Multifamily psychoeducation group for assertive community treatment clients and families of culturally diverse background: a pilot study | Canada | Case series | Psychosocial conference that began at a local restaurant to introduce the study, then transport was provided to attend MFPG; meetings were held at preferred community venues, and those meetings at weekends were followed by lunch. A 2-hour session was held once a month, for a period of 12 months Two sessions involved listening to concerns around medication and any chronic disease needing medication Provider and client stakeholder input with iterative testing process within a FMAP was used to create problem-solving therapy for older Chinese clients The use of community venues, transport and engagement to recruit to the study are part of the adaptation Cultural adaptation using evidence-based practice using an interactive stakeholder process and theoretical framework: problem-solving therapy for Chinese older adults. Focus groups and interviews with community providers and a depressed 60-year-old Chinese elder to assess feasibility of modification to PST; community providers included 31 paraprofessionals, or doctoral- or masters-level clinicians or trainees. Focus groups and interviews 1.5–2 hours each |
Seven Chinese clients with mean age (SD) of 38.6 years (6.5 years), two of whom were women (29%). Mean age (SD) of 11 Chinese family members was 64.3 years (11.6 years), seven of whom were women (64%) Seven Tamil clients with mean age (SD) of 37.6 years (6.4 years), one of whom was a woman (14%). Nine Tamil family members with mean age (SD) of 55.1 years (17.9 years), 6 of whom were women (67%) |
ACT | Team, with psychiatrist lecturing in one session | Social Adjustment Scale | Participation: 57% families in study attended at least half of the sessions. The mean score of family members’ acceptance was significantly increased (64.20, SD 13.90 vs. 76.30, SD 14.72, df = 13; p = 0.01). This acceptance was more pronounced in families who participated in > 50% of the sessions (n = 8, mean 61.38, SD 16.54 vs. mean 80.05, SD 17.02, df = 7; p = 0.01). A rank order correlation analysis found that attendance was associated with greater reduction in family burden (r = 0.5; p = 0.05). No significant changes were found in other SAS variables, but some positive trends were noted, i.e. the family members’ perceived burden of the client, family members’ satisfaction with their own physical health, mental health and health in general |
| Kirmayer et al., 200315 | Cultural consultation: a model of mental health service for multicultural societies | Canada | Case series | Cultural consultation of referred patients comprised three types of activity: (1) consultant with relevant cultural expertise assessed the patient, preferably with the participation of the referring person over 1–3 meetings; (2) brief written report; and (3) telephone call or case conference | Descriptive pre and post assessments in a case series with some case studies. About 60% were women, 44% had only elementary school education, 9% had high-school education, 47% had some college or university education, 65% were unemployed, 27% Canadians, 24% were landed immigrants and 41% refugees or asylum seekers. Fifty ethnocultural groups (undifferentiated). Four cases involved requests from organisations to discuss issues related to their work with a whole ethnocultural group or community | General hospital | Mental health team, bank of culture brokers and consultants included 73 professionals who were predominantly psychologists, psychiatrists and social workers | Service evaluation questionnaires, satisfaction questionnaire, types of referral, types of problems solved and participant observation of experience | Twenty-nine referring clinicians (representing 47 cases) completed service evaluation questionnaires. Eighty-six per cent reported that they were satisfied with the consultation and that it had helped them manage their patients. Useful aspects of the consultation included increased knowledge of the social, cultural or religious aspects of their cases (41%); increased knowledge of the psychiatric or psychological aspects of their cases (21%); improved treatment (48%); improved communication, empathy, understanding, or therapeutic alliance (31%); and increased confidence in diagnosis or treatment (14%) The major difficulties or dissatisfactions with the cultural consultation were the lack of treatment or more intensive follow-up (14%), unavailability or inappropriateness of recommended resources (14%), concerns about the competence of the culture broker (10%), and the impression that there was too much focus on social context, rather than on psychiatric issues (10%). All said they would use the service again and would recommend that their colleagues use it. They reported high rates of concordance with recommendations. In 21 cases, some aspect of the CCS recommendations was not implemented. Reasons for this included patient non-compliance (n = 13), lack of staff or other resources (n = 9) and spontaneous improvement (n = 7). Language barriers and cultural complexity prevent adequate diagnosis and treatment for a significant number of patients, including refugees, new immigrants, and members of established ethnocultural communities. A CCS can respond to these needs in most cases. Assessments, treatment plans, and interventions are well received by referring clinicians. There is a need to train clinicians systematically in the effective use of interpreters, culture brokers and the cultural formulation |
| Palinski et al., 201258 | A cultural consultation service in east London: experiences and outcomes from implementation of an innovative service | UK | Case series | Cultural consultation model adapted to elicit narratives from service users, carers, staff and organisational managers. These reconciled to support clinical decisions for patient care. Adapted from Kirmayer et al.15 to include the organisational narratives, team narratives and staff narratives. Specialist CCS staff worked alongside existing staff rather than take referrals. The cultural consultants and the team provided a report and advice on management based on documentary analysis, narrative information, and participant and non-participant observations | 46 in-depth consultations: white British (15%), white other (4%), Asian or Asian British Pakistani (4%), Asian or Asian British Bangladeshi (40%), other Asian background (2%), black or black British Caribbean (4%), black or black British African (9%), black or black British Somali (15%), mixed white and black Caribbean (2%) and other ethnic background (18%) | Referrals from assertive outreach, CMHTs and home treatment teams in a specific London borough | GAF, CANSAS, recovery STAR,90 HoNOS, qualitative reports and TACCT measure of cultural competency | Response rate from clinicians: 78% at baseline and 46% at follow-up Response rate from service users: 61% at baseline and 35% at follow-up. Service-level outcomes collected at baseline and follow-up for 36 patients. Clinician-rated clinical outcomes: 36 at baseline and 20 at follow-up. After the cultural consultation process clinicians rated service users as having significantly higher overall functioning compared with ratings before the CCS work, on the GAF (p < 0.02). No significant changes were found for CANSAS-rated needs of service users, nor the clinicians’ rating of the therapeutic relationship (measured using the STAR). Non-significant trends include more met needs on the CANSAS and a lower score on the CORE91 Quantitative cultural competence assessment: 67 clinicians completed the TACCT questionnaire at baseline and 28 at follow-up. The change between baseline (mean 90.21, SD 19.11) and follow-up (mean 95.4, SD = 18.87) (Mann–Whitney U-test 635.5; p < 0.02) was significant. Service-level outcomes (n = 36 at baseline and follow-up): the level of service receipt (and associated costs) significantly reduced after CCS intervention, with a significant reduction in use of A&E (p < 0.02), psychiatrists baseline (p < 0.001), and CPNs and case managers (p < 0.001). No significant difference in hospital admissions were found. Referrals were for perplexing and complex clinical presentations, lack of sufficient knowledge or lack of comprehensive understanding about the cases; concerns about racism and discrimination; lack of engagement or progress and failed treatment alliance; exploration, and resolution of cultural conflicts, and the impact of social changes on service user’s recovery; information requests; and defensive practices. The focus of interventions was to minimise miscommunication; provide links with third-sector and statutory bodies for support; offer and suggest new interventions/assessments; suggest psychological interventions and services with suitable culturally appropriate models; offer education, empowerment, autonomy and choice; and, interventions include family engagement, mediation and diagnostic clarification |
|
| Chu et al., 201274 | Cultural adaptation of evidence-based practice utilising an iterative stakeholder process and theoretical framework: problem-solving therapy for Chinese older adults | USA | Qualitative | Provider and client stakeholder input combined with an iterative testing process within the FMAP framework was utilised to create the Problem Solving Therapy – Chinese Older Adult (PSTCOA) manual for depression. Data from pilot testing the intervention with a clinically depressed Chinese elderly woman are reported | Case study; participant recruited from primary care setting. Single Chinese older woman to test intervention | Chinese elderly clients at three community mental health organisations in northern California, USA. Ten providers provide care in Mandarin and eight in Cantonese | Focus group: 31 mental health paraprofessionals, doctoral- or masters-level clinicians or trainees | Qualitative, but used PHQ-9 in testing intervention | Themes emerging from stakeholder feedback, literature review, and pilot testing: a need for flexibility; psychoeducation and destigmatising language; managing expectations of the provider–client relationship involving attention to hierarchy, respect, case management, and providing suggestions; visual aids and measurement; and incorporation of acculturative processes. The adapted intervention resulted in a decrease in depressive symptoms for the test participant and improved mood. Community providers evaluated the intervention as culturally appropriate and the pilot participant rated the intervention as satisfactory and effective |
| Chow et al., 201072 | Multifamily psychoeducation group for assertive community treatment clients and families of culturally diverse background: a pilot study | Canada | Qualitative | Psychosocial conference at a local restaurant to introduce the study, then transport provided to attend MFPG; meetings held at preferred community venues; meetings at weekends following by lunch. Two-hour session once a month for 12 months. Each session led by a supervisor supported by two group facilitators who spoke the participants’ language. Two sessions were dedicated to listening to concerns around medication and chronic disease needing medication. Ten sessions followed a slightly modified MFPG model | As above for Chow et al., 201072 case series | Assertive community treatment | As above for Chow et al., 201072 case series | Understanding of clients’ condition; client family relationships; support from family; and, decrease in helplessness and hopelessness | Key themes from content analysis from focus group transcripts: reduced stigma and shame, less isolation among family; increase in understanding of client’s condition more support from family; reduced helplessness and hopelessness; improvement in client–family relationships; mutual enhancement of MFPG and ACT; and, importance of cultural and linguistic matching between clients/family and clinicians |
| Grote et al., 200967 (pilot trial data reported in Grote et al., 200740) | Engaging women who are depressed and economically disadvantaged in mental health treatment | USA | Case study | Enhanced, culturally relevant IPT-B is a multicomponent model of care designed to treat antenatal depression and consists of an engagement session, followed by eight IPT-B sessions before the birth and maintenance IPT up to 6 months post partum. Engagement interview includes ethnographic interviewing and motivational interviewing. The use of ethnography in assessment was a way of engagement and empowers the patient as it includes taking account of the person’s biography, heritage, power relations and dilemmas from their perspective. The process elicits narratives of patient experience and meaning-making, and negotiates the treatment, taking account of social systems and resources in the community. The intervention changes the type of interview, in order to improve engagement and better inform the discussion about treatment. The interview elicits the patient’s story, promotes interest in treatment, provides hope, and offers feedback and psychoeducation, so leading to commitment to receive treatment | A 33-year-old unmarried African American woman who lived with her 7-year-old son and her physically disabled unemployed boyfriend. Is the primary breadwinner in the family, working at night at a low-wage job in the inventory department of a large store. At the initial intake interview, she was diagnosed with moderately severe level of depressive symptoms on the BDI. She was 28 weeks’ pregnant when she came to the engagement interview | Obstetrics and gynaecology clinics in urban setting | Psychotherapist | Depression on EPDS, score of > 12 | Patient engaged, motivated and completed therapy sessions, with improvements in mood, despite social circumstances |
| Bhui et al., 200414 | Communication with patients from other cultures: the place of explanatory models | UK | Case study | Two case histories were included. Negotiations of explanatory models were used to aid in assessment, and also to facilitate delivery of CBT, including a negotiated agreement, but not were not adapted to the CBT content | Psychiatrist and two patients in mental health services in the UK | Psychiatric outpatients and general medical hospital | Psychiatrist | Narrative evaluation | Patient recovery through partial adoption of understanding patient’s explanatory model, leading to a jointly formed treatment plan. Consultations that involve culturally grounded explanatory models of illness challenge the professional. Through case studies, a method of reconciling different explanatory models is evaluated |
| Schouler-Ocak, 200875 | Cultural factors in the diagnosis and treatment of traumatised migrant patients from Turkey | Germany | Case study | Clinical ethnography used in order to influence decision-making. Trauma-focused transference-based psychotherapy was used; this was informed by cultural perspectives on coping and an understanding of religious perspectives | Outpatient trauma clinic | Hospital case study | Psychiatrist and therapist | Narrative evaluation | The strategies used to deal with symptoms induced by trauma are often culture specific. There are unique aspects of trauma-focused psychotherapy in patients with a history of migration (trauma-focused therapy + explanatory models). Approaches included combining trauma-focused therapy including visualisation and reliving experience with massage, physiotherapy, swimming, exercise groups, all used to improve overall well-being and develop self-help skills. Religion became important too in one patient’s therapy, given its role in preventing suicide, so religious prescriptions were encouraged |
Description of interventions tested in non-trial designs
The non-trial trial designs (see Table 11) included two observational studies:70,92 an intervention involving the enhancement of an existing CBT in terms of technical content and attention to beliefs for African American depressed women, and drawing in elements of female gender identity and appropriate vocabulary to engage women, for example using ‘therapeutic exercises’ as a term rather than ‘homework tasks’;70 and an intervention focused on peer-based psychoeducation before therapy to improve the acceptability of and effective use of therapy. 92 Both scored in the lower tertile on quality.
There were three case series:15,58,72 one offered peer-based psychoeducation;72 and two offered cultural consultation, a process that elicits illness narratives and training staff to elicit and assess these. 15,58
The two case studies14,75 reported enhancements of existing therapies in terms of technical content and attention to beliefs for trauma symptoms among Turkish patients,75 and the incorporation of assessment of health beliefs (explanatory models) into the assessment process for Bangladeshi patients. 14
Two qualitative studies included an evaluative case study. Grote et al. 40,67 evaluated an evolving model of ethnographic and motivational interviewing using qualitative data but mainly with a single case study40 that then informed the trial also reported in this review. 67 Chu et al. 74 included qualitative focus groups to iteratively adapt problem-solving therapy for older Chinese adults and tested this with a single case study.
Outcome measures
Obviously, the outcome measures used in the non-trial designs included a mixture of standardised instruments, evaluation questionnaires, evaluative statements and narrative findings. It was difficult to ensure there was some measure of evaluation or data in the qualitative studies, so our minimum criterion for the inclusion of a qualitative study was an evaluative narrative or statement. The outcome measures are listed more fully in Table 9, and include the Beck Depression Inventory (BDI), the number of sessions attended, the Social Adjustment Scale, the Global Assessment of Function, a measure of service need [Camberwell Assessment of Need Short Appraisal Schedule (CANSAS)], the recovery star, the Health of the Nation Outcome Scales (HoNOS), the nine-item Patient Health Questionnaire (PHQ-9), Edinburgh Postnatal Depression Scale (EPDS), a measure of cultural competency [Tool for Assessing Cultural Competence Training (TACCT)] and narrative findings.
Synthesis of findings from the non-trial designs
The two observational studies scored as low-quality studies. 70,71 The first was an adapted CBT for depressed, low-income African American women; this study included a historical cohort and a prospective series. 70 The CBT, which was adapted by including quotes from African American literature on issues such as family, gender, identity and experiential meditative exercises, and using terms such as ‘therapeutic exercises’ instead of ‘homework tasks’, was effective in engaging in treatment and, then, decreasing depressive symptoms in low-income African American women. Although there was an improvement in symptoms, the African American women’s post-treatment scores remained higher than those recorded for white middle-class and low-income women after CBT.
The second study involved a psychoeducational package for older African American medical patients referred to psychotherapy, and took the form of a 15-minute individual psychoeducation session about psychotherapy that was specifically tailored for older African Americans. This was constructed using information from a focus group that explored barriers to treatment. The session was didactic, with a question and answer session. 71 Although psychoeducation did not seem to have an effect on the numbers of patients starting therapy, it did significantly increase the overall attendance of those who received the intervention compared with those who did not.
One of the three case series was graded medium quality15 and the other two were graded as high quality. 58,72 Kirmayer et al. 15 tested a CCS into which other professionals referred patients for assessment and recommendations. This developed from anthropological methods and ethnography, and was adapted for use in hospital settings. The intervention involved meetings with the referrer, then the patient, and a report to the referrer. A high percentage of clinicians who used the service reported that they were satisfied with the consultation and that it had helped them manage their patients. Helpful results from the intervention included increased knowledge of the social, cultural, or religious aspects of their cases, increased knowledge of the psychiatric or psychological aspects of their cases, improved treatment, improved communication, empathy understanding, or therapeutic alliance and increased confidence in diagnosis or treatment. All clinicians said they would use the service again and would recommend that their colleagues use it. They reported high rates of concordance with the advice offered to the clinicians.
Palinski et al. 58 further developed the cultural consultation model and applied it to Community Mental Health Teams, involving patients, carers and staff in the consultation process, and also permitted concerns to be communicated to commissioners. The service included educational events, and work alongside staff rather than referral into the service. A report with recommendations was coconstructed with the referring staff, patients and carers, if appropriate. After the cultural consultation process, clinicians rated service users as having significantly higher overall functioning compared with ratings before the cultural consultation work. Staff also exhibited a significant increase in overall cultural competence after the cultural consultation. In a small number of highly complex patients, the intervention also impacted on the level of service receipt, with a reduction in use of accident and emergency services, psychiatrists, community psychiatric nurses and case managers after consultation.
Chow et al. tested an intervention they called the MFPG (Multi-Family Psycho-Education Group) for assertive community treatment (ACT) clients and families of culturally diverse background. 72 This was delivered to participants in the community before referral into the service, including meetings at a community restaurant in order to encourage discussion and then recruitment and transport to and from the services where the intervention was provided. The barriers to care and culturally relevant concerns were discussed, while the MFPG was delivered. Participating families experienced a significant increase in their acceptance of their client relatives, and this increase was more profound for families who attended more than half the sessions. Family attendance was also correlated with a greater reduction in family burden.
There were four studies with qualitative data or case studies;14,40,74,76 one of the case series also included a focus group evaluation of the adapted MFPG. 72 The qualitative component of the MFPG and the case study on the cultural adaptation of a problem-solving approach for Chinese older adults (single case study74) were reported as effective. Other key themes were raised by focus group participants. MFPG participants reported experiencing reduced stigma and shame; less isolation among family; an increase in understanding of the client’s condition; more support for family; reduced helplessness and hopelessness; improvement in client–family relationships; and, mutual enhancement of MFPG and ACT. A theme raised by participants was the importance of cultural and linguistic matching between clients/family and clinicians. 72 The problem-solving therapy for Chinese older adults piloted on a single patient resulted in a decrease in depressive symptoms and improved mood. 74 Analysis of stakeholder feedback, a literature review and pilot testing yielded five recurrent themes of cultural modifications for the intervention, including a need for (1) flexibility; (2) psychoeducation and destigmatising language; (3) managing expectations of the provider–client relationship, involving attention to hierarchy, respect, case management and providing suggestions; (4) visual aids and measurement; and (5) incorporation of acculturative processes.
The remaining case studies illustrated the use of explanatory models as an intervention for Bangladeshi people with depression,14 trauma-focused psychotherapy using clinical ethnography for Turkish patients with PTSD,75 and an enhanced, culturally relevant, brief interpersonal therapy (IPT-B). 40
In a case study presented by Bhui and Bhugra,14 explanatory models were evaluated as facilitating patient recovery through the mutual increase in understanding and negotiation of explanatory models between psychiatrist and patient. This process was observed to lead to a jointly formed treatment plan and was also assessed as challenging to professionals. 14
Schouler-Ocak et al. 75 highlighted the need for culture-specific strategies in treating trauma symptoms. Analysis of the case studies indicated the importance of combining trauma-focused therapy with patient explanatory models. 75 This allowed for an enhanced trauma-focused therapy incorporating approaches such as visualisation and reliving experience, with massage, physiotherapy, swimming, exercise groups and religious prescription to improve overall well-being and self-help skills.
Grote et al. 40 reported that interpersonal therapy, adapted for use in low-income black women (IPT-B), enhanced by ethnographic and motivational components, facilitated patient engagement and completion of therapy sessions, increased motivation and improved mood. 40
Synthesis summary of non-trial designs
Although of mixed quality, the findings of the non-trial studies provide evidence to direct the further development of interventions designed to improve TC. The observational studies are the weakest of those reviewed. 70,92 The studies were not only of low quality, but were rated as low priority by service users. The case series studies were of higher quality and described interventions most suitable for future trials. 15,58,72 The three interventions evaluated achieved positive outcomes. They were aimed at populations with serious mental illness and shared key components, including attention to patient attributes and beliefs, and constructive dialogue between patients and professionals, facilitated by technical adaptations to the psychiatric interview and to the structure of sessions. Key differences between the interventions included the cultural consultation intervention’s focus on the tailoring of treatment to meet client needs versus the psychoeducational interventions’ focus on increasing service user and family understating of illness and care. This may account for the surveyed service users viewing the cultural consultation intervention more favourably. However, in contrast to Kirmayer et al. ’s intervention,15 Palinski et al. ’s58 and Chow et al. ’s72 interventions engaged with service users’ wider community; these were given a high priority as a component of interventions by service users.
Finally, the qualitative study and case studies present innovative modifications and interventions in need of further piloting. 14,40,74,75 The elements of intervention identified as valuable from the qualitative studies that were also highlighted as priorities by service users included respect, clear expectations and flexibility. Although ethnic and cultural matching (i.e. of patient to professional) were not rated as a high priority by service users, its importance was a key theme to emerge from Chow et al. ’s study. 72 The case studies reported positive results. Three of the four incorporated the elicitation of and engagement with explanatory models into their intervention modifications. 14,74,75 Engagement with explanatory models received the highest priority rating from service users.
Thematic analysis of interventions
The evidence on the interventions and how they were constructed as set out in Tables 6–8, and detailed in terms of components in Tables 8 and 10, was synthesised using thematic analysis. This analysis had a particular focus on the aims and components of different interventions. Overwhelmingly, interventions aimed to improve engagement of the patient in treatment, while some also explicitly aimed to empower patients. These empowering interventions were especially valued when our patient and carer group reviewed the interventions. Most interventions aimed to engage or empower by increasing professional understanding of patients’ belief systems about illness, either through formal training or through adapting the content and/or structure of treatment to accommodate differences arising from ethnic diversity. A minority of interventions focused rather on patients’ expectations of treatment. Compared with interventions evaluated in non-trials, those evaluated in trials were less likely to be specific to a single ethnic group (8/10 and 5/12, respectively) and were more likely to focus on accessibility of treatment for patients (1/10 vs. 4/12). In two of the trials57,67 and two of the non-trials,40,58 the wider social system was also considered in the intervention. The elements of the interventions that we have isolated might also be valuable in future evaluations of complex interventions, where these might be adaptations of the interventions we have identified or composite interventions that combined the best of the interventions we have identified with new approaches to improve TC.
| Themes | Study | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Kohn et al., 200270 | Alvidrez et al., 200571 | Chow et al., 201072 | Kirmayer et al., 200315 | Palinski et al. 201258 | Chu et al., 201274 | Chow et al., 201072 | Grote et al., 200967 (pilot data reported in 200740 and included in this paper) | Bhui et al. 200414 | Schouler-Ocak et al., 200875 | |
| Patient | ||||||||||
| Causal explanations | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| Beliefs | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| Pre-therapy preparation | ✗ | ✗ | ✗ | |||||||
| Accessibility | ✗ | |||||||||
| Training | ||||||||||
| Ethnic group specific | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| Professional | ||||||||||
| Matching | ||||||||||
| Patient and professional | ||||||||||
| Interview structure and content | ✗ | |||||||||
| Adaptation of therapy | ||||||||||
| Modify content of materials | ✗ | ✗ | ✗ | ✗ | ✗ | |||||
| Adapt technical delivery/structure of therapy | ✗ | ✗ | ✗ | ✗ | ||||||
| Wider social systems | ✗ | ✗ | ||||||||
| Empowerment | ✗ | ✗ | ||||||||
| Engagement | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |||
There were some studies that included a description of an intervention and did not include an evaluation, or the populations of interest were not relevant to the UK context and there was not any obvious transferability of the knowledge; these did not enter the review and were assessed as meeting our A– criteria. These included the following interventions: cultural formulation,93 restructuring illness narratives,94 cultural sensitivity,95 multicultural competence and evidence-based group therapy practice,96 a community-based treatment for Native Americans,97 adapted CBT for traumatised refugees (other papers from the same author were included in the review as they provided evidence),98 culturally sensitive CBT for psychosis in ethnic minorities (other papers from the same author were included in the review as those provided evidence for this intervention),99 components of cultural competence in three mental health programmes (service intervention across programmes and not focused on the TCs),100 culturally relevant psychoeducation for Korean American families,101 psychosocial counselling in Nepal,102 cultural considerations in CBT with Chinese people,103 and adaptation of solution-focused therapy in Chinese culture. 102 These interventions were described often as serving an educative role about constructing interventions or sharing how to deliver an intervention and so did not enter the review. A full reference list is available in Appendix 16.
Patients’ and carers’ ranking of interventions
This broader discussion served to contexualise the work and provide insights about interventions that patients and carers valued. This seeking of views from a general discussion, to grade and then to comment on the evidenced interventions, was considered the most useful and creative process to engage patients and carers, rather than just presenting them with a set of outcomes and expecting a passive approval or disapproval of identified interventions. In initial discussions, a number of aspects of TC and experience of mental health services were discussed and some key ‘likes’ and ‘dislikes’ were identified (Tables 11 and 12). In all cases, it was clear that a personalised experience was being sought and that tokenism or being reduced to stereotypical categories was an experience that had adverse effects. Some possible actions or solutions to a failure of communication were also discussed, and the panel members were able to identify some ideas which they were aware of, or which emerged in discussion, and which were felt to be less helpful, while greater enthusiasm was expressed for other ideas which reflected a degree of interest in their community, culture or situation, and which they regarded as being general good practice. This included choice and continuity of care, and attention to human rights and patient rights approaches.
| Good | Bad |
|---|---|
| Spending time with patient | No acknowledgement |
| Constructive time | Inappropriate, unwanted or invasive support, e.g. on telephone or telephone calls |
| Peer support – lived experience of mental health; mutual support; not tokenistic | Inability to relate |
| Rapport | Lack of empathy |
| Validate experience | Biomedical focus, e.g. not holistic or psychosocial |
| Multidisciplinary communication, e.g. between GPs and psychiatrists | Making assumptions about your state of mind |
| Ticking boxes when making ‘contract’ regarding engagement |
| Good | Bad |
|---|---|
| Going into community, e.g. sharing food, using herbal remedies | Lack of intervention by professionals, e.g. when in mainstream hospitals |
| Good social worker | Need independent advocate to arbitrate between psychiatrist and patient, e.g. when patient wants to stop taking medication |
| Advocates (however, patient advice and liaison service is not very good) | |
| Communication and explanation about use of medication | Gender – is it important? Depends |
| Full information about legal rights | Legal stuff is complicated |
| Facilitating finding the right person | Equality and diversity (as a tick-box issue) |
| People (staff administration) in communication, e.g. structural issue | Limited access to social worker |
| Interprofessional communication | Multiple diagnosis and confusion |
| Surveys or use mystery shoppers to test quality | Lack of system cohesion |
| Money for holidays | Not knowing who to approach |
| More time dedicated to training to communicate with patients | Criticism from nurses |
| Opportunities to identify and work with someone of your choice, e.g. mentor |
Subsequently, the panel members were presented with the key emergent themes from the grey literature, which had been published on the subject of access to, and improvement of, mental health communication with BME communities. A list of the emergent themes is provided in Box 3.
-
An integrated understanding of well-being commonly held among BME communities, i.e. that mental, physical, emotional and spiritual welfare go together.
-
The centrality of practical, non-clinical support, for example housing, benefits, etc. (not just mental health treatment and advice) and opportunities for relaxation and social life.
-
Stigma – shame and finding it hard to ‘share’ or reveal mental distress.
-
A wish to work with ‘staff with the right attitude’ – looking for
-
respect
-
empathy and understanding
-
people who are caring and supportive
-
confidential and trustworthy relationships
-
an example phrase was ‘asking me what I want and then doing it! – working with me to tailor-make a plan’.
-
Particular value was placed on staff’s understanding and valuing community and cultural/religious connections/sensitivities – examples given being:
-
being aware of culture-bound issues such as honour and witchcraft
-
gender relations, domestic violence (potential) – and confidentiality
-
issues of ‘double discrimination’ feelings (racism plus . . .)
-
knowledge of where to refer to/find culturally specific support
-
single-sex arrangements where gender separation was practised in the community
-
valuing prayer/meditation/spiritual issues
-
language and unfamiliarity with systems and ability to provide interpreters, translation or other forms of language support.
In addition to these, the literature reported a number of concerns apparently specific to particular ethnic groups, noting in particular:
-
African Caribbean community members fear medication or ‘strong drugs’ which may alter personality.
-
Men want to see male practitioners where issues to do with masculinity are valued.
-
Chinese people have very culturally specific understandings of needs and a specific world view.
-
South Asian people have commonly reported concerns about three main issues: languages, stigma (or shame) and effects on family status (referred to as Izzat).
-
Asylum seekers were reported to avoid contact with services and to suffer additional ill health because of stresses arising from their contacts with the UK Borders Agency and others in connection with their immigration status.
-
Migrants of Eastern European origin (of recent years) are known to have increased health needs owing to the long and unsocial hours typically worked by members of such groups.
-
Religious Jews are also reported to wish for Kosher (Kishrut) rules to be observed, in particular around diet, but also want their support to be from people who are not members of their religious community, to preserve confidentiality.
The panel discussed these matters and applied the model to their own experiences, understanding and community concerns. There was some agreement on these, and also recognition that many of them were reflected in each other’s cultural setting and were not as restricted to one cultural group as initially perceived, especially issues in relation to shame and cultural rules. However, they were adamant that these rules should not become accommodated in new fixed guidelines that might imprison people within a stereotypical culture-bound set of behaviours and treatments, but people should have the ability to choose a level of observance or derogation from such ‘norms’ and not to be treated ‘as if’ without their explicit agreement. In other words, practitioners should be aware and informed about these matters, but to ask before acting on the basis of perceived cultural norms. Their key principles are listed in the next section, Users’ final perspective. Solutions that were proposed in the grey literature included Box 4, which were again subjected to a critique by the panel members.
-
Use experience as evidence of service needs and gaps.
-
Combine and project from a mixture of local and national evidence.
-
Partnership between user-based groups and practitioners.
-
Perseverance.
-
Make it easy to access and self-refer or be signposted through community sector – there being an apparent preference for services provided through the voluntary sector, as long as this also ensures confidentiality.
-
A non-clinical feel to the setting – but a clinician/qualified supporter.
-
Consistency and continuity: stable patient–clinician relationships.
-
Development of appropriate/additional pathways of referral and recommendation – people unfamiliar with the options need to be signposted into services.
-
Home visits and befriender support and regular follow-up.
Users’ final perspectives
The following were the issues identified from our workshops and presented as a set of ‘key recommendations’ by the panel members that might be central to TCs:
-
acknowledgement of pain and hurt, and encouragement to share through talking
-
‘ask me what I want and work with me to tailor-make a plan’
-
stable, consistent relationships between patient and clinician.
These three themes appear to be universal truths appropriate to all service users, but were stated to have additional salience and cultural specificity for BME populations, in which pain and distance between user and provider may be greater and there is a friction or strain involved in having to explain the additional issues of cultural identity ‘again and again’. As suggested in some of the ‘grey literature’, the panel members noted the importance of care plans, including attention to housing and financial benefits (i.e. not just mental health treatment and advice) and opportunities for relaxation and social life. It was noted that users may need to be helped to know what forms of additional support are available, but clinicians need to be open to the user’s own solutions, even if these are not in the NICE guidelines. In addition, the following suggestions and understandings were offered as guidelines for training and improved practice:
-
Good listening skills and reassuring body language.
-
Different ethnic groups have different attitudes towards looking steadfastly in the eyes, touch and gaze, and clinicians should be aware of these matters.
-
How do people show attention and respect?
-
‘Don’t lean and gesticulate!’
-
The centrality of practical, non-clinical support.
-
The treatment needs to be looked at as a whole, over a long-term ‘recovery relationship’, not a single episode.
-
Equally, training and growth by experience cannot be achieved by a one-off training course but comes from sustained immersion in working with difference.
-
Respect – non-critical listening is crucial – don’t send out signals of alarm or startle or even dismissal – this can close down the conversation.
-
Characteristics that might help:
-
‘someone like me’ may mean ‘not too much like me’, as it could lead to assumptions
-
someone who understands and can show it!
-
someone ‘who likes me’
-
signalling some prior knowledge of culture.
-
One African-heritage member of the group noted that some white professionals had been very helpful, and showed they were ‘trying to understand’, but her current Asian professional was even better, in showing a caring attitude and calling back (by telephone) to ask about any side-effects of treatment (outside consultation).
Prioritisation of ‘good practice’ models and interventions
The panel was finally presented with vignettes based on the 10 main types of intervention identified in the literature review, and a brief description of each. These are included in Table 13.
| Study | Intervention | Outline description |
|---|---|---|
|
Communication training for doctors and patients | Training contained communication skills that built on providers (doctors) existing knowledge of child behaviour and development. Skills were drawn from patient-centred care, family therapy, solution-focused cognitive therapy, etc. Training methods mixed structure with opportunities for active learning and locally relevant content. Each session began with a 60-minute, small-group discussion, held on-site during work hours and led by a child psychiatrist Immediately after each discussion, providers practised skills in a 10-minute, standardised, patient visit |
|
Community workers practical advice and advocacy | Based on comparison of a needs-led package of care to the ‘standard access’ of 3-month waiting list control with information on local mental health in the UK. The package included practical advice and assistance, advocacy for social needs, health education and mentoring delivered by six community health workers with access to a psychiatrist for individuals with more complex needs |
|
Cultural consultation team assessment | A consultant with relevant cultural expertise assessed the patient, preferably with the participation of the doctor or professional who made the referral. One to three meetings with patient, brief written report, and a telephone call for discussion or case conference for discussion Two vignette examples were discussed with users: first a 21-year-old, recently married woman from India, referred for anorexia unresponsive to treatment. The consultation focused on supporting mother and daughter in dealing with multiple stressors that included feelings of shame and family dishonour; and, secondly, a 22-year-old man from the Caribbean, with a diagnosis of brief psychotic episode with symptoms of depression and anxiety, whose family to had hopes for traditional healing. The patient went to his country of origin and, following treatment by a healer, was greatly improved |
|
Explanatory models of mental illness | By trying to understand the patients understanding of his/her illness, patient and physician negotiate a treatment plan. A vignette was presented to users: an 18-year-old Bangladeshi man under investigation for unexplained stomach and other physical symptoms had a belief that there was a mass in his stomach, which resonated with the phenomenon of Tharan, which the psychiatrist had previously encountered among patients of Indian origin. The psychiatrist was then able to instigate a series of CBT sessions |
|
Telepsychiatry (skype™, Microsoft Corporation, Redmond, WA, USA) by language-competent staff | An approach used in the USA for rural patients by providing an online meeting between Hispanic psychiatrists and Hispanic, low-income, primary care patients seeking consultation. Psychiatrist and patient sit in front of computers with webcams in locations convenient to themselves |
|
Role induction | Offered prior to first therapy session when the client can be given information, including a description of appropriate client/therapist behaviours, and explanation of typical problems encountered in therapy (e.g. resistance)
|
Kanter et al., 201068 Kohn 200270 |
Cultural adaptation, e.g. CBT to specific cultures | CBT modified to clients circumstances with sensitivity to the support available, including the local community, spiritual traditions, and the extended family and elements of destigmatising language – used with Chinese and Latino clients. Treatment involves active collaboration between patient and therapist |
Grote et al., 200740 |
Ethnographic and motivational interviewing | An interviewing technique to ensure treatment follow-up by seeking to understand the client’s cultural view of depression and the acute and chronic stressors linked to it; previous coping mechanisms, including spirituality and prayer; and integrating psychoeducation about depression and its treatment into the engagement. A vignette was presented based on an unmarried African American woman and her physically disabled, unemployed boyfriend |
|
Ethnic matching of client and service provider | A commonly recommended strategy for transcultural working – to deal with the problem encapsulated in the following comment: ‘I would say there are more white psychotherapists out there than blacks. You know if you made an appointment to see a therapist, more likely than not you are going to be sitting down talking to someone who can’t relate to you’ |
|
MFPG | A monthly 2-hour session over 12 months led by a supervisor and two group facilitators who spoke the participants’ language. These sessions were modified to meet the specific needs of ethnocultural clients and family members, addressing issues such as stigma and frustration over long-term pharmacological management. They included ‘learning from each other’ (opportunity to share his/her family’s personal story) and a ‘problem-solving skills workshop’, medication review, and communication skills |
Following two workshops in which these themes and interventions were discussed and described, the users were asked to ‘rate’ each of the proposed interventions, and to make any comments that would explain their judgement. Then, in a final round, they were asked specifically to select the three they most felt worthy of investment and development or implementation, and the three they regarded as being of least interest or value. The ratings, and some key comments, are shown in Table 14.
| Intervention | Highest priority | Lowest priority | Selected comments by users |
|---|---|---|---|
| Communication training for doctors and patients | a | . . . this is the first access point and if this is done right, pathways to appropriate support can followHad some trouble understanding this intervention: what is meant by ‘mixed structure’ (anti) | |
| Community workers practical advice and advocacy | b | Seems crisis oriented – too many professionalsHow serious or unwell does one really have to be before you get to see the ‘backups of more experienced therapist and access to psychiatrist’? | |
| ‘Cultural consultation’ team assessment | a | I think I dislike the phrase ‘consultant with cultural expertise’ | |
| ‘Explanatory models’ of mental illness | a | This knowing of what is best must arise out of a dialogue between patient and professional, which is respectful, mutually intelligible, culturally sensitive, and open enough to engage with a wide range of explanatory models and ideas for recoveryPeople are not afraid of what they know: more information . . . is a must | |
| Telepsychiatry (via Skype) to language competent staff | Telepsychiatry is important for a client who doesn’t want to go out or see anyone face to face | ||
| ‘Role induction’ briefing the user first | b | This intervention sounds like marketing therapy to patientsVery important to clarify what to expect. Not in a crisis situation though (pro) | |
| Culturally adapting, e.g. CBT to specific cultures | b | This still won’t work if the people running it are culturally incompetent | |
| Ethnographic and motivational interviewing | a | A way of validating and working empathetically with individualsVery compelling, but is this interventionist ‘style’ not what most people expect from ALL therapy and all interviews? | |
| ‘Ethnic matching’ of client and service provider | b | Similar to #3 – which would be more desirableYes, bi-lingual and bi-cultural (and gender) ethnic matching is important, necessary, and helpful for some. But in other cases, it makes no difference, and for others, it is not appropriate because the therapist is culturally too close to the patient. Must resist simplistic assumptions and generalisationsThis has helped me: I know it works (pro) | |
| MFPG | b | Allows in-depth work with user/family and chances for identifying with others to create opportunity to build connections (pro)The multi-family education group is not for me because my family believe mental health is a cursePeople don’t always have families |
It is clear that there was a degree of consensus on the top four ideas, while some were agreed to be of less salience from the point of view of service users and their carers. There was not, though, total agreement, since some models were rated by different members of the panel as both ‘top priority’ and ‘least value’. As one of the members of the group commented:
In general, the ranking exercise was more challenging than I anticipated because no single intervention is perfect, and even the worst interventions have at least one positive attribute.
Overall, there was a strong feeling of support for both the need for health-care professionals to learn more about how to communicate with BME patients, and for the use of consultation approaches that were modified to take account of specific cultural sensitivities (such as stigma, language and somatisation).
There was less support for approaches which were seen as ignoring the skills or insights of the user, and providing ‘briefing’ or training in ‘how to be a patient’, but this may have depended on how far such support was deemed to be sympathetic to their expertise and culture: some of the examples found reported in the professional literature had quite detailed vignettes or descriptions of case studies which provide a more accessible way to understand how the intervention was put into practice.
Somewhat unexpectedly, the use of community workers providing advocacy (see Community workers practical advice and advocacy in Table 14), despite its attention to practical needs such as entitlement to benefits, was not well regarded, even though this was a theme that had been highlighted in earlier discussions. It may be that the specific study was felt to be less applicable to the situation of the panel members, or that it did not show enough care to provide confidentiality and protection against community spread of ‘gossip’, which was another very real concern. Members of the group certainly felt it was overcomplicated in practice and might lead to problems in communication or leadership between different professionals. A degree of medical professionalism was seen as appropriate, in addition to ‘cultural competence’ – which they felt should be expected of any professional, and not seen as an ‘add-on’ capability.
None of the proposed models of service development achieved total support, and there were a number of issues – such as public perceptions of communities and the impact of racism or media coverage of ‘immigrant concerns’ – that were not addressed by any of the proposed solutions located in the published papers reviewed. Some of these issues are addressed in the next section, User priorities.
User priorities
Many of the points raised in the user group discussions incorporated several elements of the suggested ‘model’ interventions located in the published literature. A key theme was: ‘asking me what I want and then doing it! Working with me to tailor-make a plan.’ Many participants had had negative experiences of treatment:
It stays with and changes you. Staff with the right attitude – [we are] looking for . . . respect.
It was noted that empathy and understanding need to be unconditional and not subject to imposed rules and the assertion of dominance by professionals. Clients were looking for flexibility in application of rules and standards. Some expressed the feeling that professionals selected ‘good’ clients and that people have to ‘merit’ help. This was related often in terms of cultural attitudes to timekeeping and authority: people find having to conform to ‘being here at a fixed time/place’ hard, even punitive. This was said by more than one user to have caused them distress and got in the way of therapy. As one of the group noted:
Staff often speak to you and treat you like a child. Over time, this has the effect of disempowering you and reduces your ability to trust yourself. When staff complain about people being dependent, they don’t acknowledge then they in fact created this dependency by taking away free will and choice.
An element of ‘the right attitude’ was ‘understanding and valuing community and cultural and religious connections and sensitivity.’ It was expected that (or at least hoped that) professionals would have some sensitivity to, and prior knowledge of, the communities of origin of their clients, and be aware of culturally influenced issues such as honour and witchcraft, as well as of gender relations (including the risks of domestic violence) and expectations and fears around confidentiality and stigma. Users reported sensitivity to issues of ‘double discrimination’ where, on top of the stigma of mental illness, they might be discriminated against on the grounds of their culture or religion, or their ‘colour’ or race. Such processes were noted also to occur within minority communities. Consequently, it was felt that professionals should have some knowledge of where to refer clients in order to find culturally specific support from appropriate and supportive community-based organisations, while avoiding those which would be judgemental or which would otherwise expose the community member to disapprobation and stigma.
Finally, people in BME groups – especially but not exclusively those of recent migrant origin – pleaded for professionals to: ‘be patient when I don’t understand things – language, forms and entitlement.’ They reported the stress of trying to fit into checklists of symptoms, noting that people have different ways of expressing themselves – but also were anxious to be seen to be showing respect to doctors and other important persons. ‘Not being able to express myself makes me feel there is something wrong with me’. This was exacerbated by frequent changes in personnel and referral between teams.’ Overall, there was a strong wish for ‘consistency and continuity and stable patient–clinician relationships.’
Discussion
This review identified several types of effective interventions in trial designs, including adapted cognitive–behavioural treatments,61,63,64 adapted psychotherapies more generally,57,67,68 complex interventions that engage with social systems and stepped care,57 different interviewing techniques like ethnographic and motivational interviewing,67 behavioural activation within an adapted cognitive–behaviour paradigm,68 and role adoption that included information and training for patients to make best use of their services and better use of encounters with professionals. 60,69 The telepsychiatry intervention65 showed a favourable response in that patients were willing to pay more for it than the standard treatment, although there was not much evidence of advantage in term of symptoms.
Each of these showed benefits in terms of an improvement in outcomes.
Adapted cognitive–behavioural therapy
What these studies offer is a range of effective interventions with differing emphases all showing benefit. Thus adapted CBT for several ethnic groups61 worked as well as CBT adapted for a single ethnic group. 64 Service users reviewing the evidence were supportive of these. Importantly, the methods of adaptation paid attention to technical, theoretical, philosophical and practical aspects,87 and in that respect both Rathod et al. 61 and Hinton et al. 63,64 were similarly adapted. These adapted interventions were promising as they showed benefit in terms of both symptoms and patient-reported outcomes, and were evolved by including elements of culturally determined communication of distress in the CBT manual; Rathod et al. ’s61 study contrasted with Hinton et al. ’s63,64 studies as the former was applied across ethnic groups in the UK, whereas Hinton et al. 63,64 offered a more profound adaptation for specific East Asian ethnic/cultural groups with PTSD, where these populations held markedly contrasting beliefs and practices regarding health and illness when compared with the majority US population. We omitted from our review studies that applied a non-adapted CBT intervention in other countries, as the concept of ‘improving the intervention’ was not visible and the attention to cultural or ethnic groups was minimal other than recruiting a sample in another country; some of these excluded studies, even if of high quality, paid little attention to therapeutic relationships and so do not feature in our review.
Complex interventions
There were two trials that included a complex intervention based on social systems in the community. 57,67 One of these engaged ethnographic and motivational interviewing as part of the assessment to empower pregnant African American single women who were depressed,67 and this preceded interpersonal therapy. One of the key components of this intervention was the emphasis on empowerment through personal stories being understood. This contrasted with another complex intervention: a stepped care model of community social venues acting as points of access to an adapted CBT intervention for black African, black Caribbean and black British people living in south London. 57 Both of these were effective at reducing symptom outcomes, yet service users in our review of the evidence favoured the US intervention, perhaps because of its emphasis on belief systems, ethnography and empowering interviews, which gathered knowledge and stories from participants in their community contexts before recommending an intervention. They were less keen on a stepped care approach or too complex a system of health care, which they felt they would find difficult to negotiate. The trial by Afuwape et al. 57 was the only one to include an economic evaluation suggesting the cost-effectiveness of the approach. The economic review indicated this evidence to be weak given the small samples and single centre in a pilot study. These studies emphasising the patients’ perspectives share the empowerment and motivational elements with other non-trial designs, specifically the small case series on cultural consultation,58 more details of which were published in an educational paper following the completion of our review. 104
Training, education and communications skills
There were a few studies of training and education for professionals, including on communication skills with family members. One study of specialist psychiatric services outreach focused on the treatment of children62 and showed less impairment in black compared with white children for the sites in which training took place, but there were no differences in symptoms, and the training also led to fewer parent symptoms, irrespective of ethnicity. White parent symptoms diminished while ethnic minority parent symptoms increased. Of the two other trials that included an educational intervention, one tested role induction69 and the other an audiovisual programme that prepared patients for psychotherapy. 60 The first of these, scoring low on quality, was associated with higher premature dropout, but more satisfaction in the intervention group and greater expectancy of what therapy might offer which is a positive sign when approaching a therapy. 69 The second of these, a medium-quality study, increased patients’ information about psychotherapy and improved attitudes so they expected more from therapy. 60 Although less favoured by patients who commented on the evidence we generated, these preparatory interventions seem attractive to practitioners as a way of enhancing the benefit patients receive from interventions that are already provided. Yet, these have not been assessed for cost-effectiveness and value to a wider range of patients; these may be especially unhelpful for those who are socially isolated or who have difficulty seeing the value of travelling to a hospital or therapy centre, where the more complex ethnographic and motivational interview-based interventions may achieve more success.
Despite the body of literature on cultural competence29 of professionals as a key way of improving health outcomes and communication between BME patients and professionals, none of our trials tested a specific model of cultural competence, or at least that is not what the authors called their interventions. Given the nature of the review, we may be demonstrating that cultural competence is too broad a framework, better suited to policy and aspirations for practitioners, while more concrete and specific examples of interventions are needed. This review illustrates just that. Tables 6 and 8 show the shared and non-shared components across the interventions. Future interventions might select particular components and test them either individually or be able to discern which are more important for a positive care experience and a positive health outcome (the two may not always be closely linked).
Only one study included telepsychiatry; this was of Mexican patients and psychiatrists living in the USA close to the Mexican border, and essentially relied on ethnic matching and the telepsychiatry intervention. 65 This showed more antidepressant use, and greater working alliance and satisfaction, but no difference in depressive symptoms. Patients were willing to pay more for this intervention, which suggests its convenience was valued, but the relative benefits of ethnic matching and a telepsychiatry intervention cannot be disentangled. Although many studies of ethnic matching can be found in the literature, these are often observational and show an association between ethnic matching and outcomes in administrative data sets rather than testing an intervention in a trial. 105,106 However, this study does illustrate how just a few psychiatrists can provide services to geographically remote or scattered populations who need a mental health professional with a similar ethnic background, or, for that matter, linguistic skills. The wider issue of using e-technology and social media as a way of encouraging engagement and delivering interventions was not investigated in the studies that entered the review.
Other study designs
The studies with a non-trial design did not add more to the evidence base. They assessed psychoeducation, ways of adapting psychotherapies, including a family orientated intervention, ethnographic interviewing and case studies concerning ethnographic principles. Given that these interventions were at an earlier stage of development, it is reasonable to suggest that their elements, especially their ethnographic elements, may prove suitable for testing in trials. 14,15,40,58,75 Two of these studies nicely showed how to involve the community before adapting an intervention. 72,74 Many excluded papers presented accounts of the cultural formulation, and its use as part of the formal psychiatric assessment process, yet none evaluated the cultural formulation, or offered a sufficiently critical evaluative statement. 87,107 In the new edition of its diagnostic manual Diagnostic and Statistical Manual of Mental Illness-Fifth Edition (DSM-V),108 the American Psychiatric Association has included a section on the ‘Cultural Interview’ that promotes the assessment of cultural factors (at least this area is no longer in an appendix, as it was in previous editions of the manual) and sets out guidelines. However, this approach needs evaluation and some have expressed a concern that the approach will not be well known or widely adopted by practitioners. 43
UK compared with US studies
Two trials,57,61 one case series58 and one case study14 were based in the UK. All the remaining studies were based in the USA. Given the differences in the cultural heritage and history of migrant groups in the UK and the USA, we were careful not to include studies that did not hold lessons for UK populations. Otherwise, where important principles of adaptation were studied, and where the US populations had similar ancestry, cultural history, or experiences of racial and ethnic discrimination and social exclusion, studies were included. All studies need to consider adaptations if the proposed interventions have not previously been used; usefully, the studies reviewed included the adaptation method for a range of study designs which are useful for future researchers working on new health outcomes or ethnic or culturally distinct populations for which little evidence exists. Although we have focused here on USA versus UK comparisons, this was not the original intention. The studies that met our inclusion criteria happened to be from the USA or the UK, reflecting the attention given to this in these countries and that more work is needed from other countries.
Economic evaluations
The review found only two studies offering economic evidence: a report on the CCS commissioned by the NHS in part of London,58 and a pilot trial of a community-based intervention for individuals from BME groups with common mental disorders. 57 The initial economic analysis of the CCS in Tower Hamlets suggested that there could be service use-related cost savings over a 3-month period following a clinical cultural consultation. And there was less emergency care needed in the intervention group. The Cares of Life Project (CoLP)57 was a small randomised controlled trial comparing rapid access and delayed access (by 3 months) to a pragmatic, needs-led care package consisting of practical advice and assistance, advocacy for social needs, health education, mentoring and one-to-one brief therapies based on principles of CBT and brief solution-focused therapy.
The rapid-access group had better depression outcomes, and the service was found to be more culturally appropriate and acceptable among users, and costs were slightly higher, but not statistically significantly for the rapid-access group. Both of these studies can be described as exploratory rather than definitive – partly because of their small sample sizes, short follow-up periods, and recruitment from a single locality – but both studies offer encouraging economic evidence. The stronger message coming from this review, however, is the absence of economic evidence in this area, making it impossible at this stage to draw conclusions as to cost-effectiveness.
Intervention elements
Many elements of the interventions were not dissimilar when the trials and non-trials were compared (see Tables 6 and 9). The elements following thematic analysis fell into the following groups: patient centred, professional centred, adaptation of a specific established intervention, involvement of social systems and the community, empowerment and engagement. The adaptation process can also be guided by the work of Tseng, which emphasises philosophical, technical, theoretical, and practical adaptation. 87 The patient and carer rankings of interventions was instructive, in that these added an additional source of valuable information to the synthesis, alongside the effectiveness data, and methodological strengths and weaknesses of each study. The patient and carer perspectives also combated to some extent the very focused research questions and setting; service users emphasised the personal experience and journey, giving a clear indication that the ways professionals communicate and interact are as important as the intervention itself. Therefore, the interventions that encouraged understanding of patient beliefs and causal explanations about illness may not always lead to a direct symptomatic benefit, but nonetheless seem to be important in a recovery-orientated approach. In particular, ethnography, motivational interviewing, engaging with social systems, before and during therapy, and professional-centred interventions seem to be preferable and essential considerations to research.
Strengths and weaknesses
The scope of the review was broad, and so it included many interventions and many outcomes, and considered studies of any design. Yet, despite this broad scope, the setting being examined was very specific, namely communications between psychiatric services and BME patients using these services; further, we were looking for evidence that interventions improved communications, rather than assessing the efficacy and effectiveness of good communications in themselves. Therefore, many studies that might prove of interest for adapting interventions were outside the scope of our review and, similarly, we did not address the effectiveness or efficacy of established psychological interventions, unless there was an additional component to improve communications alongside some measure of improved health outcome or a direct measure of communications. Furthermore, we excluded specific conditions (see Figure 1) if these were likely to be ultra-specialist services (ADHD for example) or where there were established reviews already (e.g. smoking, alcohol use and drug addiction) and they were not necessarily linked to mental health problems.
It should be noted, though, that the outcome measures used in the trials were essentially proxy measures of TCs. The concept of TC is broad, and thus included many interventions designed to improve clinical outcomes for patients; sometimes these were assessed using symptom measures, self-report symptom measures or measures of function and quality of life. Rarely was there a unified concept of ‘TC’ anchored to a single outcome. The concept of therapeutic alliances has been given great emphasis in the psychotherapeutic literature and perhaps comes closest to the concept of a TC; however, ‘therapeutic alliance’ does not automatically imply improved symptoms or functional outcomes but is a theoretical mechanism by which improved outcomes are anticipated. As a consequence, the reviewed studies and the interventions used were varied, and the mechanisms of benefit warrant greater attention. Given the range of interventions, outcomes and study designs, we were unable to undertake a meta-analysis. However, for the trial designs, given there were measurable outcomes, even if proxy outcomes, we were able to undertake a comparative synthesis of the literature (the non-trial designs were less comparable and so are only described here and the elements of shared interest drawn out). Given the nature of the evidence, the quality scores had to reflect many study designs and could not be easily read across study designs. The quality scores were helpful but gave a summary of a complex set of strengths and weaknesses in each study. However, in the synthesis, we kept in mind the strengths of each study and reflected this in our overall conclusions. The economic elements were uncommon and then judged to be relatively weak; there was only one trial that included an economic element and so the economic quality scoring contributed little to the overall findings, except to indicate a need for more economic research.
The review was successful in identifying many more trials than originally expected, albeit these were mainly from the USA; these still hold lessons for practice in the NHS in the UK. We specifically explored the components of interventions, and the methods of adaptation that can be replicated in future studies. Only two trials were located in the UK, suggesting there is scope for more studies that specifically aim to improve existing interventions by adaptation; however, the components are extensive and we require further studies to unpack which of these are critical, alongside economic evaluations of these. The comments of the patient and carer group were valuable in helping us rank the interventions, and to discern interventions that had similar apparent levels of efficacy, but components which were more or less acceptable and attractive to patients and carers.
Conclusions and future research
Research
There were three types of interventions that seem promising and warrant further research and evaluation, alongside hybrid interventions that might be developed on the basis of this review.
Adapted cognitive–behavioural therapy
Adapted CBT61 seems effective for the treatment of psychosis (for African Caribbean, black African, Pakistani and Bangladeshi patients and those of mixed ethnicities), and for the treatment of post-traumatic stress symptoms in Vietnamese and Cambodian refugees,63,64 including depressive affect. Future trials might include adaptations to other populations, taking account of the technical, philosophical, practical and theoretical limitations of existing models of interventions for any ethnic group.
Complex community interventions
Two complex interventions showed most promise, and might be used to develop a new intervention: an adapted CBT57 and an interpersonal therapy. 40,67 The fact that these interventions were delivered in community social venues (the ‘access points’) encouraged socially excluded populations to access the service for the treatment of depression. These helped to destigmatise mental health intervention, encourage community recruitment and assessment, and then progression into specific mental health services for intervention (interpersonal therapy) for the treatment of depression.
Ethnographic interventions
Grote et al. 67 included a third element not present in Afuwape et al. ’s study. 57 This ethnographic element involved motivational and ethnographic interviewing to better ground the assessment within the social and cultural context. This ethnographic element was also found in two of the case series of hospital-based and community-team referrals,15,58 and one outpatient case study. 14 This group of studies highlights a third set of future studies (case studies, case series, right through to trials): ones that integrate ethnography in the development of interventions.
There is a need for cost-effectiveness studies within future research designs, and designs that include a full range of intervention development right through to trials of interventions. Future studies might also test the different components of the interventions we have presented. Patients and carers preferred the adapted CBT interventions and community-based interventions, and commented that stepped care was too complicated; they also preferred the studies that made use of ethnographic methods which enabled more authentic assessment, grounded in the cultural background of the individual. These were interventions that were perceived to empower patients and carers rather than expect them to be passive recipients of knowledge to improve their use of existing services.
Implications for clinical practice
Our review found a range of interventions designed to improve TCs with BME patients in psychiatric services. Furthermore, we identified specific elements of these interventions that are likely to prove amenable to incorporation with clinical practice and to be effective. Practitioners might map their existing provision against these. They are:
-
patient centred
-
professional centred
-
cultural adaptation of established therapies
-
the involvement of social systems and the community in the patient’s care
-
patient empowerment and engagement.
Clinicians may wish to adapt interventions, and our evidence gives examples of the processes by which this can be undertaken with families and individuals. Two issues were emphasised in our consultations with patients and carers: they didn’t like it when they were passive recipients of information in an impersonal service; and communications matter, even if these are not directly related to therapy. If professionals better understand patients’ causal explanations and health beliefs, they will be better able to assess patients and to deliver effective information to patients and carers. In particular, pre-therapy education can improve therapeutic outcomes for people from diverse cultural and ethnic backgrounds when it is tailored to their needs and expectations. Given the emphasis in policy and practice on equity and reducing inequalities, commissioners and policy-makers need to consider the recommendations set out here on what types of interventions are helpful. In summary, interventions that include outreach and engagement with the patients’ social world, cultural beliefs about health and illness, overcoming difficulties accessing services and stigma, motivational and ethnographic interview and cultural consultation processes are important foundations that empower and offer a more flexible experience that is tailored to individual patients. The may wish to map existing provisions, taking more notice of specific types of services and whether or not they offer effective intervention and service models that are acceptable and attractive for ethnically and culturally diverse populations.
Acknowledgements
We would like to acknowledge the Afiya Trust for organising the Patient and Public Involvement group: Patrick Vernon, former Chief Executive Officer of Afiya; Rampaul Chamba, former trustee at Afiya and chair of Patient and Public Involvement group; Sola Afuape, Chair of Afiya. We also thank the service users and members of the public who commented, returned survey responses and participated in discussions and critical feedback over the lifetime of the project. We are grateful to Diana Clay (information scientist at Warwick Medical School) for constructing, testing and running the searches of the peer-reviewed literature; Josh Elliot (research assistant, Institute of Digital Healthcare, University of Warwick) for undertaking the grey literature and web searches, and running the survey of experts; and Ralph Footring, freelance production editor, for proofing and formatting advice and assistance.
Author contributions
Kamaldeep Bhui was the principal investigator, managed the project, was lead on the analyses and writing of the report, and responsible for sharing consecutive drafts with the team. Kamaldeep Bhui supervised the research fellow at Queen Mary University of London, extracted data with Rabbea’h W Aslam and Andrea Palinski, and was lead on writing the final report.
Rabbea’h W Aslam was a research fellow on the project, collected the publications, acted as second searcher and first extractor.
Andrea Palinski appraised the grey literature, assessed against criteria, extracted data, and prepared tables for the report with Kamaldeep Bhui and Rabbea’h W Aslam.
Rose McCabe was an applicant, helped extract some papers, assess against inclusion and exclusion criteria and adjudicate on disagreements on meeting inclusion criteria and characterised interventions with Kamaldeep Bhui and Rabbea’h W Aslam.
Mark RD Johnson was an applicant, assembled and helped facilitate the service user group, helped identify grey literature sources, and web resources, and supervised the survey of experts.
Scott Weich was an applicant, critiqued research processes, clarified methods and inclusion and exclusion criteria, and reviewed outputs with Kamaldeep Bhui.
Swaran Preet Singh was an applicant and reviewed outputs.
Martin Knapp critiqued economic outputs, prepared economics sections of text, and reviewed outputs.
Vittoria Ardino critiqued economic outputs, prepared economics text and reviewed outputs.
Ala Szczepura was an applicant, managed grey literature and web searches, early economic searches and helped facilitate the service user group.
All authors commented on consecutive drafts and reviewed the final draft.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Inside Outside: Improving Mental Health Services for Black and Minority Ethnic Communities in England. Leeds: National Institute for Mental Health in England; 2003.
- Delivering Race Equality in Mental Health Care. An Action Plan for Reform Inside and Outside Services and the Government’s Response to the Independent Inquiry into the Death of David Bennett. London: Department of Health; 2005.
- Bansal N, Bhopal R, Netto G, Lyons D, Steiner MF, Sashidharan SP. Disparate patterns of hospitalisation reflect unmet needs and persistent ethnic inequalities in mental health care: the Scottish health and ethnicity linkage study. Ethn Health 2014;19:217-39. http://dx.doi.org/10.1080/13557858.2013.814764.
- Cooper C, Spiers N, Livingston G, Jenkins R, Meltzer H, Brugha T, et al. Ethnic inequalities in the use of health services for common mental disorders in England. Soc Psychiatry Psychiatr Epidemiol 2013;48:685-92. http://dx.doi.org/10.1007/s00127-012-0565-y.
- Mangalore R, Knapp M. Income-related inequalities in common mental disorders among ethnic minorities in England. Soc Psychiatry Psychiatr Epidemiol 2012;47:351-9. http://dx.doi.org/10.1007/s00127-011-0345-0.
- Rentmeester CA. Postcolonial bioethics – a lens for considering the historical roots of racial and ethnic inequalities in mental health. Camb Q Healthc Ethics 2012;21:366-74. http://dx.doi.org/10.1017/S0963180112000084.
- Bhopal R. Glossary of terms relating to ethnicity and race: for reflection and debate. J Epidemiol Community Health 2004;58:441-5. http://dx.doi.org/10.1136/jech.2003.013466.
- Kai J, Beavan J, Faull C. Challenges of mediated communication, disclosure and patient autonomy in cross-cultural cancer care. Br J Cancer 2011;105:918-24. http://dx.doi.org/10.1038/bjc.2011.318.
- Johnson MRD, Clark MD, Owen D, Szczepura A. The Unavoidable Costs of Ethnicity: A Review of Evidence on Health Costs. Coventry: Centre for Health Services Studies, University of Warwick; 1999.
- Szczepura A. Access to health care for ethnic minority populations. Postgrad Med J 2005;81:141-7. http://dx.doi.org/10.1136/pgmj.2004.026237.
- Taggart F, Friede T, Weich S, Clarke A, Johnson M, Stewart-Brown S. Cross cultural evaluation of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS) – a mixed methods study. Health Qual Life Outcomes 2013;11. http://dx.doi.org/10.1186/1477-7525-11-27.
- Cambridge J, Johnson M, Singh S. The need for measurable standards in mental health interpreting: a neglected area. Psychiatrist 2012;36:121-4. http://dx.doi.org/10.1192/pb.bp.110.031211.
- Liu J, Davidson E, Bhopal R, White M, Johnson M, Netto G, et al. Adapting health promotion interventions to meet the needs of ethnic minority groups: mixed-methods evidence synthesis. Health Technol Assess 2012;16. http://dx.doi.org/10.3310/hta16440.
- Bhui K, Bhugra D. Communication with patients from other cultures: the place of explanatory models. Adv Psychiatr Treat 2004;10:474-8. http://dx.doi.org/10.1192/apt.10.6.474.
- Kirmayer LJ, Groleau D, Guzder J, Blake C, Jarvis E. Cultural consultation: a model of mental health service for multicultural societies. Can J Psychiatry 2003;48:145-53.
- Shioiri T, Someya T, Helmeste D, Tang SW. Cultural difference in recognition of facial emotional expression: contrast between Japanese and American raters. Psychiatry Clin Neurosci 1999;53:629-33. http://dx.doi.org/10.1046/j.1440-1819.1999.00617.x.
- Shioiri T, Someya T, Helmeste D, Tang SW. Misinterpretation of facial expression: a cross-cultural study. Psychiatry Clin Neurosci 1999;53:45-50. http://dx.doi.org/10.1046/j.1440-1819.1999.00469.x.
- Elfenbein HA, Ambady N. On the universality and cultural specificity of emotion recognition: a meta-analysis. Psychol Bull 2002;128:203-35. http://dx.doi.org/10.1037/0033-2909.128.2.203.
- Elfenbein HA, Ambady N. When familiarity breeds accuracy: cultural exposure and facial emotion recognition. J Pers Soc Psychol 2003;85:276-90. http://dx.doi.org/10.1037/0022-3514.85.2.276.
- Elfenbein HA, Mandal MK, Ambady N, Harizuka S, Kumar S. Cross-cultural patterns in emotion recognition: highlighting design and analytical techniques. Emotion 2002;2:75-84. http://dx.doi.org/10.1037/1528-3542.2.1.75.
- Tesone JE. Multi-lingualism, word-presentations, thing-presentations and psychic reality. Int J Psychoanal 1996;77:871-81.
- Rogers A, Day JC, Williams B, Randall F, Wood P, Healy D, et al. The meaning and management of neuroleptic medication: a study of patients with a diagnosis of schizophrenia. Soc Sci Med 1998;47:1313-23. http://dx.doi.org/10.1016/S0277-9536(98)00209-3.
- Williams B, Healy D. Disclosure of minor mental health problems: an exploratory theoretical study. J Adv Nurs 2001;35:108-16. http://dx.doi.org/10.1046/j.1365-2648.2001.01827.x.
- Rudell K, Bhui K, Priebe S. Concept, development and application of a new mixed method assessment of cultural variations in illness perceptions: Barts Explanatory Model Inventory. J Health Psychol 2009;14:336-47. http://dx.doi.org/10.1177/1359105308100218.
- Canales M. Narrative interaction: creating a space for therapeutic communication. Issues Ment Health Nurs 1997;18:477-94. http://dx.doi.org/10.3109/01612849709009425.
- Drennan G, Swartz L. The paradoxical use of interpreting in psychiatry. Soc Sci Med 2002;54:1853-66. http://dx.doi.org/10.1016/S0277-9536(01)00153-8.
- Lorenz LS, Chilingerian JA. Using visual and narrative methods to achieve fair process in clinical care. J Vis Exp 2011;48. http://dx.doi.org/10.3791/2342.
- Bennett J KJ, Keating F. Race Equality Training in Mental Health Services in England. Does One Size Fit All?. London: The Sainsbury Centre for Mental Health; 2011.
- Bhui K, Warfa N, Edonya P, McKenzie K, Bhugra D. Cultural competence in mental health care: a review of model evaluations. BMC Health Serv Res 2007;7. http://dx.doi.org/10.1186/1472-6963-7-15.
- Ferns P, Stickley T, Bassett T. Teaching Mental Health. Chichester: John Wiley & Sons Ltd; 2008.
- Kleinman A. Patients and Healers in the Context of Culture: An Exploration of the Borderland Between Anthropology, Medicine, and Psychiatry. Berkley, CA: Universtiy of California Press; 1980.
- Sargent C, Larchanche S. The construction of “cultural difference” and its therapeutic significance in immigrant mental health services in France. Cult Med Psychiatry 2009;33:2-20. http://dx.doi.org/10.1007/s11013-008-9115-1.
- Caroppo E, Muscelli C, Brogna P, Paci M, Camerino C, Bria P. Relating with migrants: ethnopsychiatry and psychotherapy. Ann Ist Super Sanita 2009;45:331-40.
- Howard GS. Culture tales. A narrative approach to thinking, cross-cultural psychology, and psychotherapy. Am Psychol 1991;46:187-97. http://dx.doi.org/10.1037/0003-066X.46.3.187.
- Jovchelovitch S. Narrative, memory and social representations: a conversation between history and social psychology. Integr Psychol Behav Sci 2012;46:440-56. http://dx.doi.org/10.1007/s12124-012-9217-8.
- Hammack PL. Narrative and the cultural psychology of identity. Pers Soc Psychol Rev 2008;12:222-47. http://dx.doi.org/10.1177/1088868308316892.
- Smithbattle L, Lorenz R, Leander S. Listening with care: using narrative methods to cultivate nurses’ responsive relationships in a home visiting intervention with teen mothers. Nurs Inq 2013;20:188-98. http://dx.doi.org/10.1111/j.1440-1800.2012.00606.x.
- Bhui K, Ascoli M, Nuamh O. The place of race and racism in cultural competence: what can we learn from the English experience about the narratives of evidence and argument?. Transcult Psychiatry 2012;49:185-20. http://dx.doi.org/10.1177/1363461512437589.
- Ascoli M, Palinski A, Owiti JA, De Jongh B, Bhui KS. The culture of care within psychiatric services: tackling inequalities and improving clinical and organisational capabilities. Philos Ethics Humanit Med 2012;7. http://dx.doi.org/10.1186/1747-5341-7-12.
- Grote N, Zuckoff A, Swartz H, Bledsoe SE, Geibel S. Engaging women who are depressed and economically disadvantaged in mental health treatment. Soc Work 2007;52:295-308. http://dx.doi.org/10.1093/sw/52.4.295.
- Cultural Assessment in Clinical Psychiatry. Washington, DC: American Psychiatric Publishing; 2002.
- Aggarwal NK. Cultural psychiatry, medical anthropology, and the DSM-5 field trials. Med Anthropol 2013;32:393-8. http://dx.doi.org/10.1080/01459740.2013.776047.
- Aggarwal NK, Nicasio AV, DeSilva R, Boiler M, Lewis-Fernandez R. Barriers to implementing the DSM-5 cultural formulation interview: a qualitative study. Cult Med Psychiatry 2013;37:505-33. http://dx.doi.org/10.1007/s11013-013-9325-z.
- Rudell K. Barts Explanatory Model Inventory: The Development of an Instrument and the Exploration of Cross-Cultural Variations in Perceptions of Distress 2006.
- Kilshaw S, Ndgewa D, Curran J. Between Worlds – Interpreting Conflict Between Black Patients and Their Clinicians. London: Southwark & Lewisham Health Action Zone; 2002.
- Bhui K, McCabe R, Weich S, Singh S, Johnson M, Szczepura A. THERACOM: a systematic review of the evidence base for interventions to improve Therapeutic Communications between black and minority ethnic populations and staff in specialist mental health services. Syst Rev 2013;2. http://dx.doi.org/10.1186/2046-4053-2-15.
- Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Normand J. Culturally competent healthcare systems. A systematic review. Am J Prev Med 2003;24:68-79. http://dx.doi.org/10.1016/S0749-3797(02)00657-8.
- Szczepura A, Clark MD, Johnson MRD, Owen D. Assessment of the Costs To The NHS Arising from the Need for Interpreter, Advocacy And Translation Services. Coventry: Centre for Health Services Studies, Warwick Business School, University of Warwick; 1999.
- Bhui K, Stansfeld S, Hull S, Priebe S, Mole F, Feder G. Ethnic variations in pathways to and use of specialist mental health services in the UK. Systematic review. Br J Psychiatry 2003;182:105-16. http://dx.doi.org/10.1192/bjp.182.2.105.
- A special issue on culture, race, and ethnicity in psychotherapy. Psychother Theory Res Prac Train 2006;43:377-560.
- J Counsel Psychol 2011;58:457-646. http://dx.doi.org/10.1037/a0024937.
- Tom LM. Psychoeducational Approach With Chronically Mentally Ill Chinese Americans: A Cultural Special Issue – Cultural Adaptions Framework 1989.
- Schwarz D. The Effect of a Spanish Pre-Therapy Orientation Videotape on Puerto Rican Clients’ Knowledge about Psychotherapy, Improvement in Therapy, Attendance Patterns and Satisfaction With Services 1989.
- Mickens-English P. The Efficacy of an Afrocentric Holistic Group Psychotherapy Approach for Black Women 1996.
- Raymond MJ . Analysis of Native American Cultural Practices Used As a Treatment Modality for Alcohol Addiction 1996.
- Hines A. Perceptions, Preferences, and Partnerships: A Patient-centered Approach to Understanding Racial and Ethnic Differences in Mental Healthcare. Baltimore, MD: Johns Hopkins University; 2010.
- Afuwape SA, Craig TK, Harris T, Clarke M, Flood A, Olajide D, et al. The Cares of Life Project (CoLP): an exploratory randomised controlled trial of a community-based intervention for black people with common mental disorder. J Affect Disord 2010;127:370-4. http://dx.doi.org/10.1016/j.jad.2010.05.017.
- Palinski A, Owiti JA, Ascoli M, De Jongh B, Archer J, Staples P, et al. A Cultural Consultation Service in East London: Experiences and Outcomes from Implementation of an Innovative Service. London: Queen Mary University of London; 2012.
- Szczepura A, Johnson M. Theracom Project Survey n.d. www.surveymonkey.com/s/TheracomSurvey (accessed 5 March 2015).
- Acosta F. Preparing low-income hispanic, black, and white patients for psychotherapy. J Clin Psychol 1983;39:872-7. http://dx.doi.org/10.1002/1097-4679(198311)39:6<872::AID-JCLP2270390610>3.0.CO;2-X.
- Rathod S, Phiri P, Harris S, Underwood C, Thagadur M, Padmanabi U, et al. Cognitive behaviour therapy for psychosis can be adapted for minority ethnic groups: a randomised controlled trial. Schizophr Res 2013;143:319-26. http://dx.doi.org/10.1016/j.schres.2012.11.007.
- Wissow LS, Gadomski A, Roter D, Larson S, Brown J, Zachary C, et al. Improving child and parent mental health in primary care: a cluster-randomized trial of communication skills training. Pediatrics 2008;121:266-75. http://dx.doi.org/10.1542/peds.2007-0418.
- Hinton DE, Chhean D, Pich V, Safren SA, Hofmann SG, Pollack MH. A randomized controlled trial of Cognitive–behavior therapy for Cambodian refugees with treatment-resistant PTSD and panic attacks: a cross-over design. J Trauma Stress 2005;18:617-29. http://dx.doi.org/10.1002/jts.20070.
- Hinton DE, Pham T, Tran M, Safren SA, Otto MW, Pollack MH. CBT for Vietnamese refugees with treatment-resistant PTSD and panic attacks: a pilot study. J Trauma Stress 2004;17:429-33. http://dx.doi.org/10.1023/B:JOTS.0000048956.03529.fa.
- Chong J, Moreno F. Feasibility and acceptability of clinic-based telepsychiatry for low-income Hispanic primary care patients. Telemed J E Health 2012;18:297-304. http://dx.doi.org/10.1089/tmj.2011.0126.
- Alvidrez J, Snowden LR, Rao SM, Boccellari A. Psychoeducation to address stigma in black adults referred for mental health treatment: a randomized pilot study. Community Ment Health J 2009;45:127-36. http://dx.doi.org/10.1007/s10597-008-9169-0.
- Grote NK, Swartz HA, Geibel SL, Zuckoff A, Houck PR, Frank E. A randomized controlled trial of culturally relevant, brief interpersonal psychotherapy for perinatal depression. Psychiatr Serv 2009;60:313-21. http://dx.doi.org/10.1176/ps.2009.60.3.313.
- Kanter JW, Santiago-Rivera AL, Rusch LC, Busch AM, West P. Initial outcomes of a culturally adapted behavioral activation for Latinas diagnosed with depression at a community clinic. Behav Modif 2010;34:120-44. http://dx.doi.org/10.1177/0145445509359682.
- Lambert R, Lambert M. The effects of role preparation for psychotherapy on immigrant clients seeking mental health services in Hawaii. J Community Psychol 1984;12:263-75. http://dx.doi.org/10.1002/1520-6629(198407)12:3<263::AID-JCOP2290120310>3.0.CO;2-J.
- Kohn LP, Oden T, Muñoz RF, Robinson A, Leavitt D. Adapted Cognitive Behavioral Group Therapy for Depressed Low-Income African American Women. Community Ment Health J 2002;38:497-504. http://dx.doi.org/10.1023/A:1020884202677.
- Alvidrez J, Arean P, Stewart A. Psychoeducation to increase psychotherapy entry for older African Americans. Am J Geriatr Psychiatry 2005;13:554-61. http://dx.doi.org/10.1097/00019442-200507000-00003.
- Chow W, Law S, Andermann L, Yang J, Leszcz M, Wong J, et al. Multi-family psycho-education group for assertive community treatment clients and families of culturally diverse background: a pilot study. Community Ment Health J 2010;46:364-71. http://dx.doi.org/10.1007/s10597-010-9305-5.
- Kirmayer LJ, Groleau D, Guzder J, Blake C, Jarvis E. Cultural consultation: a model of mental health service for multicultural societies. Can J Psychiatry 2003;48:145-53.
- Chu JP, Huynh L, Arean P. Cultural adaptation of evidence-based practice utilizing an iterative stakeholder process and theoretical framework: problem solving therapy for Chinese older adults. Int J Geriatr Psychiatry 2012;27:97-106. http://dx.doi.org/10.1002/gps.2698.
- Schouler-Ocak M, Reiske SL, Rapp MA, Heinz A. Cultural factors in the diagnosis and treatment of traumatised migrant patients from Turkey. Transcult Psychiatry 2008;45:652-70. http://dx.doi.org/10.1177/1363461508100787.
- Moncrieff J, Drummond DC. The quality of alcohol treatment research: an examination of influential controlled trials and development of a quality rating system. Addiction 1998;93:811-23. http://dx.doi.org/10.1046/j.1360-0443.1998.9368113.x.
- Deeks J, Dinnes J, D’Amico R, Sowden A, Sakarovitch C, Song F, et al. Evaluating non-randomised intervention studies. Health Technol Assess 2003;7. http://dx.doi.org/10.3310/hta7270.
- Reisch JS, Tyson JE, Mize SG. Aid to the evaluation of therapeutic studies. Pediatrics 1989;84:815-27.
- Quality Appraisal of Case Series Form. London: NICE; 2013.
- Dalziel K, Round A, Stein K, Garside R, Castelnuovo E, Payne L. Do the findings of case series studies vary significantly according to methodological characteristics?. Health Technol Assess 2005;9. http://dx.doi.org/10.3310/hta9020.
- Moga C, Guo B, Schopflocher D, Harstall C. Development of a Quality Appraisal Tool for Case Series Studies Using a Modified Delphi Technique. Edmonton, AB, Canada: Institute of Health Economics; 2012.
- Spencer L, Ritchie J, Lewis J, Dillon L. Quality in Qualitative Evaluation: A Framework for Assessing Research Evidence. London: Chief Social Researcher’s Office, Cabinet Office; 2003.
- Concato J, Shah N, Horwitz RI. Randomized, controlled trials, observational studies, and the hierarchy of research designs. N Engl J Med 2000;342:1887-92. http://dx.doi.org/10.1056/NEJM200006223422507.
- Popay J, Roberts H, Sowden A, Petticrew M, Arai A, Rodgers R, et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. Lancaster: Lancaster University; 2006.
- Otto MW, Penava SJ, Pollack RA, Smoller JW, Pollack M, Otto M, et al. Challenges in Clinical Practice: Pharmacologic and Psychosocial Strategies. New York, NY: Guilford Press; 1996.
- Ramos-Brieva JA, Cordero-Villafáfila A. A new validation of the Hamilton Rating Scale for Depression. J Psychiatr Res 1988;22:21-8. http://dx.doi.org/10.1016/0022-3956(88)90024-6.
- Tseng W. Handbook of Cultural Psychiatry. San Diego, CA: Academic Press; 2001.
- Nietzel MT, Russell RL, Hemmings KA, Gretter ML. Clinical significance of psychotherapy for unipolar depression: a meta-analytic approach to social comparison. J Consult Clin Psychol 1987;55:156-61. http://dx.doi.org/10.1037/0022-006X.55.2.156.
- Organista KC, Muñoz RF, González G. Cognitive–behavioral therapy for depression in low-income and minority medical outpatients: Description of a program and exploratory analyses. Cognit Ther Res 1994;18:241-59. http://dx.doi.org/10.1007/BF02357778.
- McGuire-Snieckus R, McCabe R, Catty J, Hansson L, Priebe S. A new scale to assess the therapeutic relationship in community mental health care: STAR. Psychol Med 2007;37:85-9. http://dx.doi.org/10.1017/S0033291706009299.
- Evans C, Mellor-Clark J, Margison F, Barkham M, McGrath G, Connell J, et al. Clinical Outcomes in Routine Evaluation: The CORE-OM. J Ment Health 2000;9:247-55. http://dx.doi.org/10.1080/713680250.
- Alvidrez J, Arean PA, Stewart AL. Psychoeducation to increase psychotherapy entry for older African Americans. Am J Geriatr Psychiatry 2005;13:554-61. http://dx.doi.org/10.1097/00019442-200507000-00003.
- Baarnhielm S. The meaning of pain: a cultural formulation of a Syrian woman in Sweden. Transcult Psychiatry 2012;49:105-20. http://dx.doi.org/10.1177/1363461511427781.
- Bäärnhielm B. Restructuring illness meaning through the clinical encounter: a process of disruption and coherence. Cult Med Psychiatry 2004;28:41-65. http://dx.doi.org/10.1023/B:MEDI.0000018097.31002.79.
- Baker KA. The importance of cultural sensitivity and therapist self-awareness when working with mandatory clients. Fam Process 1999;38:55-67. http://dx.doi.org/10.1111/j.1545-5300.1999.00055.x.
- Chen EC, Kakkad D, Balzano J. Multicultural competence and evidence-based practice in group therapy. J Clin Psychol 2008;64:1261-78. http://dx.doi.org/10.1002/jclp.20533.
- Gone JP. A community-based treatment for Native American historical trauma: prospects for evidence-based practice. J Consult Clin Psychol 2009;77:751-62. http://dx.doi.org/10.1037/a0015390.
- Hinton DE, Rivera EI, Hofmann SG, Barlow DH, Otto MW. Adapting CBT for traumatized refugees and ethnic minority patients: examples from culturally adapted CBT (CA-CBT). Transcult Psychiatry 2012;49:340-65. http://dx.doi.org/10.1177/1363461512441595.
- Rathod S, Kingdon D, Phiri P, Gobbi M. Developing culturally sensitive cognitive behaviour therapy for psychosis for ethnic minority patients by exploration and incorporation of service users’ and health professionals’ views and opinions. Behav Cogn Psychother 2010;38:511-33. http://dx.doi.org/10.1017/S1352465810000378.
- Siegel C, Haugland G, Reid-Rose L, Hopper K. Components of cultural competence in three mental health programs. Psychiatr Serv 2011;62:626-31. http://dx.doi.org/10.1176/ps.62.6.pss6206_0626.
- Shin SK, Lukens EP. Effects of psychoeducation for Korean Americans with chronic mental illness. Psychiatr Serv 2002;53:1125-31. http://dx.doi.org/10.1176/appi.ps.53.9.1125.
- Tol WA, Jordans MJ, Regmi S, Sharma B. Cultural challenges to psychosocial counselling in Nepal. Transcult Psychiatry 2005;42:317-33. http://dx.doi.org/10.1177/1363461505052670.
- Williams MW, Foo KH, Beverley H. Cultural considerations in using cognitive behaviour therapy with Chinese people: a case study of an elderly Chinese woman with generalised anxiety disorder. NZ J Psychol 2006;35:153-62.
- Owiti J, Bhui KS. The reciprocal relationship between physical activity and depression in older European adults. Evid Based Nurs 2012;15. http://dx.doi.org/10.1136/ebnurs-2011-100294.
- Cabral RR, Smith TB. Racial/ethnic matching of clients and therapists in mental health services: a meta-analytic review of preferences, perceptions, and outcomes. J Couns Psychol 2011;58:537-54. http://dx.doi.org/10.1037/a0025266.
- Maramba GG, Hall GC. Meta-analyses of ethnic match as a predictor of dropout, utilization, and level of functioning. Cultur Divers Ethnic Minor Psychol 2002;8:290-7. http://dx.doi.org/10.1037/1099-9809.8.3.290.
- Fortuna LR, Porche MV, Alegria M. A qualitative study of clinicians’ use of the cultural formulation model in assessing posttraumatic stress disorder. Transcult Psychiatry 2009;46:429-50. http://dx.doi.org/10.1177/1363461509342948.
- Diagnostic and Statistical Manual of Mental Illness. Arlington, VA: American Psychiatric Publishing; 2013.
Appendix 1 Published literature: search terms
| Aspect of TC | Descriptor of mental disorder | Descriptor of professionals involved | Aspects of clinical success |
|---|---|---|---|
| communicat* | psychosis | psychiatr* | adher* |
| talk* | psychotic | doctor | complian* |
| interact* | schizophr* | psychoger* | concordan* |
| expressed emotion | schizoaffective | mental health nurs* | nonadher* |
| conversat* | delusional | psychiatric nurs* | noncomplian* |
| discourse* | depress* | social work* | concordan* |
| dialogue* | dysthymi* | psycholog* | persistence |
| relationship* | bipolar | care coordinator | treatment usage |
| alliance* | cyclothymi* | counsel* | Attendance |
| narrative* | panic | therapist | engag* |
| peer support | agoraphobia | support work* | rejection of therapy |
| psychosocial intervention* | phobia | employment coach | drop out |
| OCD | nurse practitioner | medication possession ratio | |
| PTSD | case manager | service use | |
| stress | vocational rehab specialist | diagnos*/ misdiagnos* | |
| anxiety | psych tech | ||
| dementia/ Alzheimer’s | physician | ||
| ADHD (adult) | provider | ||
| practitioner |
Sample search strategy run on Ovid MEDLINE and adapted for other databases
Searched: 31 March 2012.
Date range of searches: from inception until 31 March 2012.
THERACOM final strategy
-
(BME or black ethnic minorit* or black minorit* ethnic*).mp.
-
asylum seeker*.ab,ti.
-
(migrant* or immigrant*).ab,ti.
-
race*.mp. or racial.ab,ti. [mp = title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier]
-
cultur*.ab,ti.
-
(multicultural or multi-cultural).ab,ti.
-
(cross-cultural or crosscultural).ab,ti.
-
(trans-cultural or transcultural).ab,ti.
-
(multi-rac* or multirac*).ab,ti.
-
(multiethnic or multi-ethnic).ab,ti.
-
refugee*.ab,ti.
-
(multi-lingu* or multilingu*).ab,ti.
-
(ethno-cultur* or ethnocultur*).ab,ti.
-
(socio-cultural or sociocultural).ab,ti.
-
(divers* or diverse population* or cultural diversity).ab,ti.
-
(south asian* or bangladeshi* or pakistani* or indian* or sri lankan*).mp.
-
(asian* or east asian* or chinese or taiwanese or vietnamese or korean* or japanese).mp.
-
(afro-caribbean* or african-caribbean* or caribbean or african* or black* or afro*).mp.
-
(islam* or hindu* or Sikh* or buddhis* or muslim* or moslem* or christian* or catholic* or jew*).ab,ti.
-
ethnic group*.mp.
-
((ethnic or linguistic) adj diversity).ab,ti.
-
(transient adj (group* or population*)).ab,ti.
-
acculturation.ab,ti.
-
(faith* or belief* or religion*).ab,ti.
-
ethnic minorit*.ab,ti.
-
minority ethnic.ab,ti.
-
hispanic.ab,ti.
-
(deprivation or low income).ab,ti.
-
or/1-28
-
mental disorders.mp. or exp Mental Disorders/
-
(psychosis or Psychotic or schizophr* or schizoaffective or delusional or depress* or dysthymi* or bipolar or cyclothymi* or panic or agoraphobia or phobia or “obsessive compulsive disorder” or “post-traumatic stress disorder” or stress or anxiety or dementia or ADHD or “attention deficit”).ab,ti.
-
30 or 31
-
Communication barriers.mp. or communication barriers/
-
(communicat* or talk* or interact* or “expressed emotion” or conversat* or discourse* or dialogue* or relationship* or alliance* or narrative* or “peer support”).ab,ti.
-
33 or 34
-
(adher* or complian* or concordan* or nonadher* or noncomplian* or persistence or “treatment usage”).ab,ti.
-
(attend* or engag* or “rejection of therapy”).ab,ti.
-
(“drop out” or “medication possession ratio”).ab,ti.
-
(service use* or pyschosocial intervention*).ab,ti.
-
(diagnosis or misdiagnosis).ab,ti.
-
36 or 37 or 38 or 39 or 40
-
Mental health services.mp. or exp Mental Health Services/
-
(psychiatr* or “mental health nurs* OR psychiatric nurs*” or “social work*” or psycholog* or “care coodinator*” or Counsel* or therapist* or “support work*” or “employment coach*” or “nurse practitioner*” or “case manager*” or “vocational rehab* specialist*” or “psych* tech*” or physician* or provider* or practitioner* or psychogeriatrician*).ab,ti.
-
42 or 43
-
29 and 32 and 35 and 41 and 44
Appendix 2 Survey of experts
Organisations contacted
-
Advocacy Project.
-
African Caribbean Mental Health Services.
-
AnxietyUK (formerly the National Phobics Society).
-
Asian Family Counselling Service.
-
Asian Resource Centre.
-
B-eat.
-
Better Health.
-
BHA.
-
Black and Asian Therapists Online.
-
Black Orchid.
-
Breathing Space Scotland.
-
British Association for Behavioural and Cognitive Psychotherapies.
-
British Association for Counselling and Psychotherapy.
-
British Association of Psychotherapists.
-
British Psychoanalytic Council.
-
British Psychological Society.
-
Care Quality Commission.
-
Carers Northern Ireland.
-
Carers Scotland.
-
Carers UK.
-
Carers Wales.
-
CAUSE (Carers and Users Support Enterprise).
-
Centre for Mental Health (Sainsbury).
-
Chinese Mental Health Association.
-
Confederation of Indian Organisations (UK).
-
Cruse Bereavement Care.
-
Depression Alliance Scotland.
-
Depression UK.
-
Equilibrium.
-
Fanon Women’s Centre.
-
Greenwich Mind.
-
ICAP.
-
Institute of Family Therapy.
-
Jewish Association for the Mentally Ill.
-
Kuumba Centre.
-
MDF – The BiPolar Organisation.
-
MECOPP (Minority Ethic Carers of Older People Project).
-
Mental Health Foundation.
-
Mental Health Shop.
-
MIND.
-
Muslim Youth Helpline.
-
Nafsiyat – The Intercultural Therapy Centre.
-
Narcotics Anonymous.
-
Narcotics Anonymous Northern Ireland.
-
National Mental Health Development Unit.
-
National Self-Harm Network.
-
Northern School of Child and Adolescent Psychotherapy.
-
OCD-UK.
-
Pakistani Resource Centre.
-
Qualb Centre.
-
Recovery Research Network.
-
Refugee Council.
-
Rethink Mental Illness.
-
Royal College of Psychiatrists.
-
Sahara – Asian Women’s Group.
-
Samaritans.
-
Sane.
-
Sathi – Asian Men’s Group.
-
Savera.
-
Scottish Association for Mental Health.
-
Sheffield African Caribbean Mental Health Association.
-
Society of Analytical Psychology.
-
South London Family Centre.
-
Southall Black Sisters.
-
Tamarind Centre.
-
The Afiya Trust.
-
The Black Women’s Mental Health Project.
-
The Harmony Family Centre.
-
The Naz Project.
-
Triumph Over Phobia (TOP UK).
-
Tulip Mental Health Group.
-
UK Council for Psychotherapy.
-
Waltham Forest Black People’s Mental Health Association.
-
Women’s Therapy Centre.
Experts found in ongoing research
| Name | Organisation |
|---|---|
| Cheryl Pugh | Medical Research Council |
| Ksenija Yeeles | Newham Centre for Mental Health |
| Jo Dixon | University of York |
| Jayne Hill | Leicester Royal Infirmary |
| Emer Brady | Leicester Royal Infirmary |
| Dr Paul Fearon | King’s College London |
| Simone Farrelly | King’s College London |
| Professor Til Wykes | King’s College London |
| Alexandra Gardiner | University of Oxford |
| Professor Martin Knapp | PSSRU London School of Economics |
| Dr Zoebia Islam | Warwick Medical School |
| Luke Brown | Birmingham and Solihull Mental Health NHS Foundation Trust |
| Peter Phiri | Royal South Hants Hospital |
| Dr Karen Ersche | Addenbrooke’s Hospital |
| Professor Swaran Singh | University of Warwick |
| Nicola Bailey | University of Warwick |
| Dr Lynn Legg | Glasgow Royal Infirmary |
| Dr Rachel Hayes | University of Exeter |
| Dr James Kirkbride | Addenbrooke’s Hospital |
| Peter Phiri | Royal South Hants Hospital |
| Dr Richard Kyle | University of Manchester |
| Professor Allan House | University of Leeds |
| Dr Rosemarie McCabe | Newham Centre for Mental Health |
| Dr Ian C Scott | King’s College London |
| Dr Andreas Roposch | Institute of Child Health, Department of Orthopaedic Surgery, Great Ormond Street |
| Dr Maria Zubair | University of Manchester |
| Professor Alys Young | University of Manchester |
| Dr Ghazala Mir | University of Leeds |
| Stuart Gormley | Imperial College London |
| Dr Lisa Edwards | Salford Royal NHS Foundation Trust, Photobiology Unit |
| Dr Dana Rosenfeld | Keele University |
| Dr Clare Relton | University of Sheffield |
| Dr Chris McKevitt | King’s College London |
| Dr Rachel Byng-Maddick | University College London |
| Dr Michael Larkin | University of Birmingham |
| Lauren Kelley | Newham Centre for Mental Health |
| Patricia Jessiman | University of Bristol |
Appendix 3 Survey questionnaire
Therapeutic communications in black and minority ethnic populations (THERACOM)
Questionnaire for experts
We are undertaking a systematic HTA review of the evidence on:
-
interventions/initiatives aimed at improving ‘TC’ between BME patients receiving specialist psychiatric care and the professionals who deliver that care.
By ‘TC’ we mean any ways of improving practice to ensure the ability of clinicians and service users to communicate effectively and in a culturally appropriate manner in order to achieve successful assessment, diagnosis and therapy. For communication in health care to be therapeutic, it must involve a relationship and exchange of ideas between a patient and professional helper, be patient centred and engaging in order to influence the patient’s emotional worlds and directed by the professional using expertise and skill. TCs include all interactions that enable people in distress to resolve conflicts, divergent expectations, traumatic histories, adverse life events, and to overcome distress and also take up offers of help.
As well as peer-reviewed articles, we are trying to identify examples of good practice and grey literature, i.e. reports/unpublished papers and research/development work in progress, since much good work may not yet be available in peer-reviewed journals!
If you know of such material, or have been responsible for developments in this area, please can you let us know of it – and how to access the reports, by filling in the attached questionnaire and e-mailing it back to us.
| TITLE OF PROJECT/REPORT (include date if possible) | NAME OF AUTHOR/ORGANISATION | WEBSITE/LINK (or where it can be obtained) |
|---|---|---|
Appendix 4 Survey responses
Name: Rotimi Akinsete.
E-mail address:
Title of project: Black Men on the Couch (has been running for last 18 months).
Author: Rotimi Akinsete, Project 20:20, UK Council of Psychotherapy.
Website link: www.psychotherapy.org.uk/project_2020.html.
Description: Series of events aiming to change the status quo surrounding counselling and psychotherapy and open it up to those who would have never considered either undergoing it themselves or as a profession. Special guests are invited to take part in a live therapy session with a professional psychotherapist on stage, to discuss their challenges, successes and views on the value of talking therapy. Guests so far include Lemn Sissay, Benjamin Zephaniah, David Lammy, Stuart Lawrence and Ashley Walters. Black Men on the Couch aims to show that even those we look up to sometimes need to turn to others to help them to achieve their goals in life.
Name: Dr Aida Alayarian.
E-mail address:
Title of project: Resilience, Trauma, Torture and Dissociations; a Psychoanalytic view.
Author: Dr Aida Alayarian, The Refugee Therapy Centre.
Website link: www.refugeetherapy.org.uk.
Description: Looking into resilience and vulnerability in traumatised people and specifically refugee and asylum seekers.
Name: Eugene Ellis.
E-mail address:
Title of project: The Black and Asian Therapist Network – started in 2005.
Author: The resources section of the website has many articles written by prominent therapists about black and Asian mental health.
Website link: www.baatn.org.uk/articles.asp.
Description: This section of the website has a selection of various articles. www.baatn.org.uk/articles.asp.
Name: Pauline Clear.
E-mail address:
Title of project: The African and Caribbean Mental Health Services.
Author: Pauline Clear.
Website link: www.acmhs-blackmentalhealth.org.uk.
Description: A cultural appropriate service providing care for those with a severe and enduring diagnosis, in hospital and in the community. We also support those with common mental health issues in the community as well as their carers. We provide short interventions (6–8) sessions within a stepped care model of 1–1 sessions, counselling, CBT counselling, groups, telephone sessions, Rethink Physical Health Toolkit, PHQ-9, etc.
Name: Tricia Jessiman
E-mail address:
Title of project: Letting the Future In: evaluation of a therapeutic intervention for children affected by sexual abuse Finish date – June 15.
Author: Professor John Carpenter and Tricia Jessiman, University of Bristol; Professor Simon Hackett and Josie Phillips, University of Durham.
Website link: www.bristol.ac.uk/news/2013/9202.html.
Description: Randomised controlled tirial with a waiting list control of a therapeutic intervention for children affected by SA delivered by the NSPCC. Also qualitative process evaluation and PhD project on therapeutic alliance.
Name: Jayasree Kalathil.
E-mail address:
Title of project: Recovery and Resilience: African, African Caribbean and South Asian Women’s Stories of Recovering from Mental Distress (2011).
Author: Kalathil, J Published by Mental Health Foundation and Survivor Research.
Website link: www.survivor-research.com/images/documents/black%20women%20recovery%20and%20resilience%20final%20report.pdf.
Description: User-controlled narrative research using a reflexive methodology. Explores how black women make meaning of their madness and places their definitions of recovery within the contexts of those meanings.
Name: Shaista Meer.
E-mail address:
Title of Project: Addressing depression in Muslim communities: development of a treatment manual for professionals.
Author: Dr Ghazala Mir, Leeds Institute of Health Sciences.
Website link: Pilot report: www.leeds.ac.uk/hsphr/research/AUPBS/addressing-depression.html.
Description: The study piloted an adapted therapy manual based on the psychological approach behavioural activation. The manual was adapted to be sensitive to the needs of Muslims with depression and allowed for the inclusion of their beliefs and values, should they choose to. It was designed to be used by practitioners of any background with clients who identified themselves as Muslim.
Name: Peter Phiri.
E-mail address:
Title of project: Developing culturally sensitive CBT for psychosis for ethnic minority patients by exploration and incorporation of service users’ and health professionals’ views and opinions.
Author: Rathod, Kingdon, Phiri and Gobbi (2010), Southern Health NHS Foundation Trust and University of Southampton.
Website link: http://journals.cambridge.org/action/displayAbstract?fromPage=online&aid=7873664.
Description: The main aim of the study was to produce a culturally sensitive adaption of an existing CBT manual for therapists working with patients with psychosis from specified ethnic minority communities (African Caribbean, black African/black British and South Asian Muslims). Based on gaining meaningful understanding of the way members (lay and service users) of these minority communities typically view psychosis, its origin and management including their cultural influences, values and attitudes. Two-centre (Hampshire and west London) qualitative study; semistructured interviews with patients with schizophrenia (n = 15); focus groups with lay members from selected ethnic communities (n = 52); focus groups or semistructured interviews with CBT therapists (n = 22); and mental health practitioners who work with patients from the ethnic communities (n = 25).
Conclusion: While individualisation of therapy is generally accepted as a principle, in practice therapists require an understanding of patient-related factors that are culturally bound and influence the way the patient perceives or responds to therapy.
Name: Peter Phiri.
E-mail address:
Title of project: Feasibility of culturally adapted CBT for psychosis for ethnic groups.
Author: Rathod, Phiri and Kingdon.
Website link: Schizophrenia Research (1–2) 2013.
Description: Entered review by end of project as published.
Name: Peter Phiri.
E-mail address:
Title of project: Adapting Cognitive–behavioural Therapy for Psychosis for Black and Minority Ethnic Communities.
Author: Rathod et al.
Website link:
Description: Relates to Rathod et al. 201390 above.
Name: Natasha Sackey.
E-mail address:
Title of project: Searching for Motherland: An Exploration of Envy, Culture, Similarity and Difference in Dance Movement Psychotherapy with a female out-patient with Paranoid Schizophrenia. (Final Clinical Report 2012).
Author: Natasha Sackey Dance Movement Psychotherapist.
Description: This report is currently unpublished. It pertains to good working practices intrinsic to dance movement therapy’s multisystem approach which holistically interlinks the cultural and social context of an individual. The case study is with a BME outpatient in an acute psychiatry setting, who has been diagnosed with paranoid schizophrenia and is on the pathway to recovery. Approach includes a journey that encounters the complexities of working in the context of envy, cultural issues and schizophrenia. Subsequently this encounters difficulties in managing the tension of our differences and sameness, within the therapeutic process. My objective is to determine, by what means fostering a therapeutic relationship in the context of short term dance movement psychotherapy (DMP), can effectively assist in promoting a sense of restoration and recovery with patients.
Name: Olatunde Spence.
E-mail address:
Title of project: Musings on the impact of aniconism and the practice of art therapy within a Muslim community.
Author: Talid Khan.
Website link: Art Therapy Online – British Association of Art Therapists; http://eprints-gojo.gold.ac.uk/459/.
Description: This article puts forward an understanding of aniconism within Islam and the implications for art therapy practice within a Muslim community. As a non-practising Muslim, the author describes his experience of aniconsim. Aniconism is considered to be a custom or belief of avoiding graphic representation of any godly beings or religious figures. This belief system also extends to the graphic representation of all human beings and living animals. Representations of god, divine beings and religious figures are all subject matters that could potentially arise in an art therapy context. However, the aspect of aniconism of most relevance and concern to this article is the representation of any living beings, i.e. human beings and animals. [Oxford English Dictionary (1992).]
Appendix 5 Theses, conference papers and bibliographies
Searches of index to theses
A search of the index of all doctoral dissertations and some master’s theses from most North American and many European colleges and universities was undertaken covering nearly 3 million searchable citations to dissertation and theses from around the world to 4 February 2013. The search used the terms Psychiatr* AND Communication AND Ethnic.
Rudell K. Bart’s Explanatory Model Inventory – The Exploration of Cross-cultural Variations in Perceptions of Mental Distress. PhD thesis. London: Queen Mary University of London; 2006.
Outcome: A study of explanatory models in primary care and in the population, not in specialist-psychiatric care. And did not assess TCs or outcomes therefore does not meet inclusion criteria.
Hines AL. Perceptions, Preferences, and Partnerships: A Patient-Centred Approach to Understanding Racial and Ethnic Differences in Mental Healthcare. PhD thesis. Baltimore, MD: The Johns Hopkins University; 2010.
Outcome: This thesis uses routine data from the collaborative psychiatric epidemiology studies, including the national comorbidity survey replication, the national survey of American life and the national Latino and Asian American study and patient-centred care for African Americans and depression study. There is no intervention or any evaluation of an intervention so it does not meet inclusion criteria.
Mickens-English P. The Efficacy of an Afrocentric/Holistic Group Psychotherapy Approach for Black Women. PhD thesis. Kent, OH; Kent State University; 1996.
Outcome: Not available for order or from originator university.
Tom LM. Psychoeducational Approach With Chronically Mentally Ill Chinese Americans: A Cultural Special Issue: Cultural Adaptions 547 Framework. PhD thesis. New York, NY: The City University of New York; 1989.
Outcome: Not available from originator university.
Raymond MJ. Analysis of Native American Cultural Practices Used as a Treatment Modality for Alcohol Addiction. PhD thesis. Palo Alto, CA: Pacific Graduate School of Psychology; 1996.
Outcome: This was an observational study on retrospective data on treatment outcomes following alcohol programme, with a newly constructed variable of traditionalism assessed against outcomes: physical health, alcohol use, emotional status, cultural status, spiritual status. There was no intervention to improve TCs between ethnic minority populations and specialist psychiatric staff; indeed this was a study of indigenous groups in the population. Thus the thesis did not meet criteria for inclusion.
Schwarz DA. The Effect of a Spanish Pre-Therapy Orientation Videotape on Puerto Rican Clients’ Knowledge About Psychotherapy, Improvement in Therapy, Attendance Patterns and Satisfaction with Services. PhD thesis. Philadelphia, PA: Temple University; 1989.
Outcome: Originator university unable to locate microfiche of thesis.
Appendix 6 Searches of ProQuest COS Conference Papers Index
Source: http://search.proquest.com/cpi?accountid=14888.
Title: What Would a Mental Health System that was Responsive to People from Ethnic Communities Look Like?
Author: Desouza, Ruth; Singham, Mervin; Gavriel, Athena; Wong, Kirsten; and Lallu, Nemu.
Conference: 2010 Conference on Building Bridges National Community Mental Health and Addictions, 14 April 2010.
Title: Culturally Relevant Psychotherapy in Singapore, a Multi-Ethnic and Multi-Religious Nation.
Author: Chang, Lyn.
Conference: Fifth World Congress for Psychotherapy (WCP 2008), 12 October 2008.
Title: Business Case for Eliminating Health Disparities: A “Cost of Disparity” Methodology for State Health Departments.
Author: Mann, David; and Hussein, Carlessia.
Conference: 136th American Public Health Association Annual Meeting and Exposition (APHA 2008), 25 October 2008.
Title: Do Health Preferences Vary Across Racial and Ethnic Minority Populations with Mental Health Disorders? An Exploratory Study.
Author: Mulvaney-Day, Norah; Horvitz-Lennon, Marcela; Chen, Chih-nan; Laderman, Mara; and Alegria, Margarita.
Conference: 136th American Public Health Association Annual Meeting and Exposition (APHA 2008), 25 October 2008.
Title: A New Paradigm and Skills Base for Psychotherapy in Our Multi Cultural World.
Author: Bowden, Roy.
Conference: 5th World Congress for Psychotherapy (WCP 2008), 12 October 2008.
Title: Building Evidence for Better Practice in Support of Asian Refugee and Migrant Mental Wellbeing.
Author: Wong, Anita; Sobrun-Maharaj, Amritha.
Conference: Fourth International Asian Health and Wellbeing Conference, 5 July 2010.
Title: Mental Health, Social Relations and Quality of Life Among Refugees Before During and After Treatment at the Rehabilitation and Research Centre for Torture Victims.
Author: Carlsson, JM.
Conference: 12th Association of European Psychiatrists Congress, Geneva (Switzerland), 14–18 April 2004.
Title: Beyond Language Barriers and Access to Care: Less Mental Health Care Utilization by Immigrants in Primary Care.
Author: Jabbar, Khelda S; Tran, Jennifer; Averbuch, Tali; Liebschutz, Jane M; Samet, Jeffrey H; and Saitz, Richard.
Conference: 135th Annual Meeting and Exposition of the American Public Health Association (APHA 2007), 3 November 2007.
Title: Researching Interventions in Refugee Mental Health.
Author: Raina, D.
Conference: 16th Annual Meeting of the International Society for Traumatic Stress Studies, San Antonio, TX, USA, 16–19 November 2000.
Title: Engaging Chinese Immigrant Communities to Counter the Stigma and Discrimination Surrounding Mental Illness.
Author: Tang, Charlie.
Conference: Fourth International Asian Health and Wellbeing Conference, 5 July 2010.
Title: Immigrant Mental Health: Overcoming Health Disparities.
Author: Khanlou, Nazilla.
Conference: 100th Annual Conference of the Canadian Public Health Association, 13 June 2010.
Title: Participatory Approaches to Community Mobilization Around Mental Health and Chronic Disease Among Rural Hispanic Immigrants.
Author: Peters, Karen.
Conference: 2010 Conference of the Institute on Social Exclusion (ISE 2010), 3 June 2010.
Title: Mental Health Services: Improving Access to Sociopsychiatric Care for Immigrants (Regional Analysis).
Author: Kimil, Ahmet.
Conference: 17th European Conference on Public Health (EUPHA 09), 25 November 2009.
Title: La Maestra Enhanced Psychosocial Program: An Educational, Preventive, Early Intervention and Treatment Mental Health Model Addressing the Mental Health Needs of Immigrants and Refugees of Central San Diego.
Author: Carbonell, Sonia.
Conference: 136th American Public Health Association Annual Meeting and Exposition (APHA 2008), 25 October 2008.
Title: Patients’ Narratives of Cross-Racial Therapy: Implications for Bridging Cultural Distance in Multicultural Counseling Contexts.
Author: Chang, Doris F.
Conference: Fifth World Congress for Psychotherapy (WCP 2008), 12 October 2008.
Appendix 7 Bibliographies of published articles selected for review
| Peer-reviewed article | Number of grey literature references | Bibliography: grey literature references selected. (R) = selected as relevant; and (P) = identified as potentially relevant |
|---|---|---|
| A-rated articles: systematic search | ||
| Zayas LH, Cabassa LJ, Perez MC, Howard MO. Clinician-Patient Ethnicity in Psychiatric Diagnosis. J Ethn Cult Divers Soc Work 2005;14:93–109 | 1 | (P) Cooper LA, Roter DL, Rockeymoore MB, Johnson RL, Ford D. Are There Racial Differences in Primary Care Patient–Physician Communication About Depression? Paper presented at the 15th Biennial International Conference on Mental Health Services Research, Washington, DC, April 2002 |
| Bultman DC, Svarstad BL. Effects of physician communication style on client medication beliefs and adherence with antidepressant treatment. Patient Educ Couns 2000;40:173–85 | 2 | None |
| Pugh MA, Vetere A. Lost in translation: an interpretative phenomenological analysis of mental health professionals’ experiences of empathy in clinical work with an interpreter. Psychol Psychother 2009;82:305–21 | 1 | (P) Raval H. Therapists’ Experiences of Working with Interpreters. PhD thesis. Guildford: University of Surrey; 2000 |
| Simpson D, Rowan-Szal GA, Joe GW, Best D, Day E, Campbell A. Relating counselor attributes to client engagement in England. J Subst Abuse Treat 2009;36:313–20 | 7 | National Treatment Agency. Engaging and Retaining Clients in Drug Treatment. London: NHS National Treatment Agency for Substance Misuse; 2004. URL: www.dldocs.stir.ac.uk/documents/briefings5.pdf |
| Allan J, Campbell M. Improving access to hard-to-reach services: a soft entry approach to drug and alcohol services for rural Australian Aboriginal communities. Soc Work Health Care 2011;50:443–65 | 14 | None |
| Flynn WR. Review of Ethnicity and substance abuse: Prevention and intervention. Am J Psychiatry 2004;161:1514–15 | 5 | None |
| Kim MS. Perspectives on human communication: implications for transculture theory. In Milhouse VH, Asante MK, Nwosu P, editors. Transcultural Realities: Interdisciplinary Perspectives on Cross-Cultural Relations. Thousand Oaks, CA: Sage Publications; 2001. pp. 3–32 | 2 | Cross SE, Markus HR. Cultural Adaptation and the Self: Self-Construal, Coping and Stress. Paper presented at the 99th annual convention of the American Psychological Association, San Francisco, CA, July 1991 Iwao S. Social Psychology’s Models of Man: Isn’t it Time for East to Meet West? Invited address to the International Congress of Scientific Psychology, Sydney, Australia, August 1988 |
| Storck M, Csordas TJ, Strauss M. Depressive illness and Navajo healing. Med Anthropol Q 2000;14:571–97 | 5 | None |
| Dominguez J. Effect of culture and language in the adaptation of the Montreal cognitive assessment (MOCA) in the Philippines. Alzheimers Dement 2011;7:S450 | 0 | N/A |
| Ruiz P, Langrod J. The role of folk healers in community mental health services. Community Ment Health J 1976;12:392–8 | 0 | N/A |
| Yen J, Wilbraham L. Discourses of culture and illness in South African mental health care and indigenous healing, Part I: Western psychiatric power. Transcult Psychiatry 2003;40:542–61 | 5 | None |
| Baker KA. The importance of cultural sensitivity and therapist self-awareness when working with mandatory Clients. Fam Process 1999;38:55–67 | 0 | N/A |
| Chen EC, Kakkad D, Balzano J. Multicultural competence and evidence-based practice in group therapy. J Clin Psychol 2008;64:1261–78 | 0 | N/A |
| Gil AG, Wagner EF, Tubman JG. Culturally sensitive substance abuse intervention for Hispanic and African American adolescents: empirical examples from the Alcohol Treatment Targeting Adolescents in Need (ATTAIN) Project. Addiction 2004:99(Suppl. 2):140–50 | 0 | N/A |
| Hinton DE, Rivera EI, Hofmann SG, Barlow DH, Otto MW. Adapting CBT for traumatized refugees and ethnic minority patients: examples from culturally adapted CBT (CA-CBT). Transcult Psychiatry 2012;49:340–65 | 1 | (P) Hinton DE. Musical Healing and Cultural Syndromes in Isan: Landscape, Conceptual Metaphor, and Embodiment. PhD thesis. Cambridge, MA: Harvard University; 2000 |
| Ito KL, Maramba GG. Therapeutic Beliefs of Asian American Therapists: Views from an Ethnic-Specific Clinic. Transcult Psychiatry 2002;39:33–73 | 3 | None |
| Zheng L, Arthur D. Family education for people with schizophrenia in Beijing, China: randomised controlled trial. Br J Psychiatry 2005;187:339–45 | 1 | (R) Li Z. The Effect of a Nurse-initiated Patient/Family Education Strategy on People with Schizophrenia in Beijing. PhD Thesis. Hong Kong: Hong Kong Polytechnic University; 2003 |
| Rahman A, Malik A, Sikander S, Roberts C, Creed F. Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster-randomised controlled trial. Lancet 2008;372:902–9 | 0 | N/A |
| Rathod S, Kingdon D, Phiri P, Gobbi M. Developing culturally sensitive cognitive behaviour therapy for psychosis for ethnic minority patients by exploration and incorporation of service users’ and health professionals’ views and opinions. Behav Cogn Psychother 2010;38:511–33 | 3 | (R) Rathod S, Kingdon D, Phiri P, Gobbi M. Developing Culturally Sensitive Cognitive Behaviour Therapy for Psychosis For Ethnic Minority Groups By Exploration And Incorporation Of Service User’s And Health Professionals Views And Opinions. Report to the Department of Health, Delivering Race Equality, Clinical Trailblazers programme; 2009 |
| Sturm G, Nadig M, Moro MR. Current developments in French ethnopsychoanalysis. Transcult Psychiatry 2011;48:205–27 | 1 | (R) Sturm G, Nadig M, Moro MR. Writing therapies – An ethnographic approach to transcultural therapies. Forum Qualitative Sozialforschung/Forum: Qualitative Social Research 2010;11:art 1. URL: www.qualitative-research.net/index.php/fqs/issue/view/35 (accessed 6 March 2015) |
| Williams MW, Foo KH, Haarhoff B. Cultural considerations in using cognitive behaviour therapy with Chinese people: A case study of an elderly Chinese woman with generalised anxiety disorder. NZ J Psychol 2006;35:3 | 0 | N/A |
| Xiang M, Ran M, Li S. A controlled evaluation of psychoeducational family intervention in a rural Chinese community. Br J Psychiatry 1994:165:544–8 | 0 | N/A |
| A-rated articles: hand search | ||
| Bäärnhielm S. The meaning of pain: A cultural formulation of a Syrian woman in Sweden. Transcult Psychiatry 2012;49:105–20 | 1 | None |
| Leavey G. UK clergy and people in mental distress: community and patterns of pastoral care. Transcult Psychiatry 2008;45:79–104 | 0 | N/A |
| Ullrich HE. The peripatetic cultural psychiatrist: reflections on a forty-five year longitudinal study of a South India village. Transcult Psychiatry 2011;48:146–59 | 1 | (P) Ullrich HE. The impact of environment on learned helplessness: Research from a South India Village. Society for the Study of Psychiatry and Culture Annual Meeting, 15–17 May 2009, San Francisco, CA, USA |
| Yeung A, Kam R. Ethical and cultural considerations in delivering psychiatric diagnosis: reconciling the gap using MDD diagnosis delivery in less-acculturated Chinese patients. Transcult Psychiatry 2008;45:531–52 | 0 | N/A |
| B-rated articles: systematic search | ||
| Eguchi, S. Between folk concepts of illness and psychiatric diagnosis: Kitsune-Tsuki (fox possession) in a mountain village of western Japan. Cult Med Psychiatry 1991;15:421–51 | 0 | N/A |
| Eley D, Hunter K, Young L, Baker P, Hunter E, Hannah D. Tools and methodologies for investigating the mental health needs of Indigenous patients: it’s about communication. Australas Psychiatry 2006;14:33–7 | 1 | None |
| Eley D, Young L, Hunter K, Baker P, Hunter E, Hannah D. Perceptions of mental health service delivery among staff and Indigenous consumers: it’s still about communication. Australas Psychiatry 2007;15:130–4 | 2 | None |
| Gone JP. A community-based treatment for Native American historical trauma: prospects for evidence-based practice. J Consult Clin Psychol 2009;77:751–62 | 3 | None |
| Lykes MB. Terror, silencing and children: international, multidisciplinary collaboration with Guatemalan Maya communities. Soc Sci Med 1994;38:543–52 | 2 | None |
| Tseng WS, editor. Culture and Psychotherapy: A Guide to Clinical Practice. Arlington, VA: American Psychiatric Publishing, Inc.; 2001 | 0 | N/A |
| B-rated articles: hand search | ||
| Aggarwal NK. Hybridity and intersubjectivity in the clinical encounter: Impact on the Cultural Formulation. Transcult Psychiatry 2012;49:121–39 | 0 | |
| Curran C, Ndegwa D, Kilshaw S. Between Worlds: Interpreting Conflict Between Black Patients and Their Clinicians. URL: www.lho.org.uk/Download/Public/8748/1/Between_Worlds_Report_3.pdf (accessed 18 December 2014) | 3 | None |
| Griner D, Smith TB. Culturally adapted mental health intervention: a meta-analytic review. Psychotherapy 2006;43:531–48 | 18 | Jackson PA. The Effect of Exposure to Culturally Relevant/Historically Based Material on Level of Frustration Tolerance, Level of Depression, and Mediation of anger in African-American Young Males. PhD Thesis. Alameda, CA: The California School of Professional Psychology; 1997 Mickens-English P. The Efficacy of an Afrocentric/Holistic Group Psychotherapy Approach for Black Women. PhD thesis. Kent, OH: Kent State University; 1996 Raymond MJ. Analysis of Native American Cultural Practices Used as a Treatment Modality for Alcohol Addiction. PhD Thesis. Palo Alto, CA: Pacific Graduate School of Psychology; 1996 Schwarz DA. The Effect of a Spanish Pretherapy Orientation Videotape on Puerto Rican Clients’ Knowledge About Psychotherapy, Improvement in Therapy, Attendance Patterns and Satisfaction with Services. PhD Thesis. Philadelphia, PA: Temple University; 1989 Tom LM. Psychoeducational Approach with Chronically Mentally Ill Chinese Americans: A Cultural Special Issue: Cultural Adaptions 547 framework. PhD Thesis. New York, NY: The City University of New York; 1989 |
| Zhang Y. Negotiating a path to efficacy at a clinic of traditional Chinese medicine. Cult Med Psychiatry 2007;31:73–100 | 0 | N/A |
| Arpin J. Masters of their conditions II: intercultural theatre, narration and stage work with patients and healers. Transcult Psychiatry 45:355–78 | 0 | N/A |
| BenEzer G. From Winnicott’s potential space to mutual creative space: a principle for intercultural psychotherapy. Transcult Psychiatry 2012;49:323–39 | 2 | None |
| Scuglik DL, Alarcón RD, Lapeyre AC, III, Williams MD, Logan KM. When the poetry no longer rhymes: mental health issues among Somali Immigrants in the USA. Transcult Psychiatry 2007:44:581–95 | 3 | None |
Appendix 8 Websites and other sources
Health, health policy, evidence-based medicine and health services research websites searched
A wide array of health, health policy, evidence-based medicine, health services research and other websites were searched in November 2013. These included the following:
-
BME Health Forum. URL: www.bmehf.org.uk
-
Bristol Mind. URL: www.bristolmind.org.uk
-
Centre for Mental Health. URL: www.centreformentalhealth.org.uk
-
Healing Circles. URL: www.healingcircles.org
-
Hogg Foundation for Mental Health. URL: www.hogg.utexas.edu
-
Mental Health Commission of Canada. URL: www.mentalhealthcommission.ca
-
Mental Health Foundation. URL: www.mentalhealth.org.uk
-
Mind. URL: www.mind.org.uk
-
Mind in Croydon. URL: www.mindincroydon.org.uk
-
National Alliance on Mental Illness. URL: www.nami.org
-
National Mental Health Development Unit. URL: www.nmhdu.org.uk
-
Network for Mental Health. URL: www.nsun.org.uk
-
Race Equality Foundation. URL: www.raceequalityfoundation.org.uk
-
Rethink Mental Illness. URL: www.rethink.org
-
Social Care Institute for Excellence. URL: www.scie.org.uk/
-
World Federation for Mental Health. URL: www.wfmh.org
Black or minority ethic-relevant websites searched
-
The Afiya Trust. URL: www.afiya-trust.org
-
Better Health. URL: www.better-health.org.uk/
-
The Black and Asian Therapist Network. URL: www.baatn.org.uk/
-
Bolton Council of Mosques. URL: www.thebcom.org
-
British Asian Medical Association. URL: www.thebama.co.uk/
-
Friends, Families and Travellers. URL: www.gypsy-traveller.org
-
Health Development Authority (HDA) – closed 2007. URL: www.nice.org.uk/aboutnice/whoweare/aboutthehda/hdapublications/hda_publications.jsp
-
Institute of Race Relations. URL: www.irr.org.uk
-
The King’s Fund. URL: www.kingsfund.org.uk
-
Meri Yaadain – Recognising Dementia in South Asian Communities. URL: www.meriyaadain.co.uk
-
Migrant Health. URL: http://mighealth.net
-
Minority Fellowship Programme. URL: www.emfp.org
-
Mosaics of Meaning. URL: www.mosaicsofmeaning.info
-
MultiKulti – closed 2008. URL: www.multikulti.org.uk/
-
Race Equality Foundation. URL: www.raceequalityfoundation.org.uk/
-
South Asian Health Foundation (SAHF). URL: www.sahf.org.uk/
-
South East and Migrant Health (SEMH) Network. URL: www.migranthealthse.co.uk
-
The Urban Indian Health Institute. URL: www.uihi.org/
Other websites searched
-
Aethos Consultancy and Training. URL: www.aethos.org.uk
-
Care Quality Commission. URL: www.cqc.org.uk
-
Child and Maternal Health Observatory. URL: www.chimat.org.uk
-
CLAHRC (Collaboration for Leadership in Applied Health Research and Care) for South Yorkshire. URL: http://clahrc-sy.nihr.ac.uk/
-
The College of Emergency Medicine. URL: www.collemergencymed.ac.uk
-
Department of Health. URL: www.dh.gov.uk
-
Economic and Social Data Service. URL: www.esds.ac.uk/
-
Health Services Research and Development Service (HSR&D). URL: www.hsrd.research.va.gov
-
Health Talk Online. URL: www.healthtalkonline.org
-
Informa Healthcare. URL: http://informahealthcare.com/
-
Joseph Rowntree Foundation. URL: www.jrf.org.uk
-
National Association of Social Workers. URL: www.socialworkers.org
-
National Center for Biotechnology Information. URL: www.ncbi.nlm.nih.gov
-
NHS Camden. URL: www.camden.nhs.uk/
-
NHS Confederation. URL: www.nhsconfed.org
-
NHS Norfolk. URL: www.norfolk.nhs.uk
-
NHS North West. URL: www.northwest.nhs.uk
-
Offender Health Research Network. URL: www.ohrn.nhs.uk
-
The Psychologist. URL: www.thepsychologist.org.uk
-
Scope. URL: www.scope.org.uk
-
UC Davis Health System. URL: www.ucdmc.ucdavis.edu
Closed websites
Health Development Authority (HDA)
www.nice.org.uk/aboutnice/whoweare/aboutthehda/hdapublications/hda_publications.jsp
MultiKulti
Appendix 9 Items identified
UK sources
All websites were accessed in November 2013.
| ID (C)a | Author/source | Title | Relevance | BME group(s) | Date | URL |
|---|---|---|---|---|---|---|
| AA1 (NR) | Care Quality Commission | Monitoring the Mental Health Act in 2011/12 | Not service delivery | None | 2013 | www.google.co.uk/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=0CDwQFjAA&url=http%3A%2F%2Fwww.cqc.org.uk%2Fsites%2Fdefault%2Ffiles%2Fmedia%2Fdocuments%2Fcqc_mha_report_2011_main_final.pdf&ei=Xo8PUZj4OenJ0AXVi4CwAQ&usg=AFQjCNHnrVqp1bQgs8JlwCT5aPsOswMumQ&bvm=bv.41867550,d.d2k&cad=rja |
| A1 (GR) | Sewell H, Waterhouse S. (HS Consultancy) | Making progress on race equality | Evaluation of learning from DRE. Provider and commissioner views – no interventions | Black African, black Caribbean, black other | 2012 March | www.nhsconfed.org/Publications/Documents/Making%20Progress%20on%20Race%20Equality%20in%20Mental%20Health%20FINAL%20SUBMITTED%2014%2005%2012.pdf |
| A3 (NR) | Liu J, Davidson J, Bhopal E, White RS, Johnson M, Netto MRD, et al. (Health Technology Assessment) | Adapting health promotion interventions to meet the needs of ethnic minority groups: mixed-methods evidence synthesis | Not mental health | African, Chinese and South Asian | 2012 | https://amsprd0104.outlook.com/owa/attachment.ashx?attach=1&id=RgAAAACi%2fBhVooZXRadNzVMdVbEmBwCkg3ZebfYETpwCsQtcVAN1AAAAoZr7AACkg3ZebfYETpwCsQtcVAN1AAAAo04ZAAAJ&attid0=BAAAAAAA&attcnt=1 |
| A5 (GR) | Turner D, Salway S, Chowbey P, Mir G, (Evidence and Ethnicity in Commissioning) | Mini case study book – real world examples of using evidence to improve health services for minority ethnic people | Wakefield (Yorkshire) – case study of project | BME various | 2012 | http://clahrc-sy.nihr.ac.uk/images/health%20inequalities/resources/EEiC_mini_case_study_book.pdf |
| A7 (GR) | Ahmed S, Amer MM | Counseling muslims – handbook of mental health issues and interventions | Focus on clinician, culture and guidance to intervene. Not evidence based. Expert opinion | Muslim | 2012 | www.guilfordpress.co.uk/common/sample-chapters/9780415988605.pdf |
| A8 (GR) | Ennis L, Rose D, Denis M, Pandit N, Wykes T. (Journal of Mental Health) | Can’t surf, won’t surf: the digital divide in mental health | Background (limitations to use of media). May be out of date | BME Various | 2012 | http://informahealthcare.com/doi/pdf/10.3109/09638237.2012.689437 |
| A7 (NR) | The King’s Fund | Reading list – mental health – BME communities | Provides a comprehensive list of grey literature and other material | BME various | 2012 | www.kingsfund.org.uk/sites/files/kf/field/field_pdf/Library-reading-list-bme-mental-health-Apr2012–1.pdf |
| A11 (NR) | All Party Parliamentary Group on Mental Health | Health and social care reform: making it work for mental health | Nothing specific to BME or case interventions | None | 2012 | www.mind.org.uk/assets/0001/8974/APPGMH_Report_Health_and_Social_Care_Reform_Making_it_work_for_Mental_Health.pdf |
| B1 (NR) | Malek, M. (The Afiya Trust) | Enjoy, achieve and be healthy | Children and Young People | BME young people | 2011 | www.developbromley.com/public/SocialInclusion/EvidenceandPolicy/Enjoy-achieve-and-be-healthy.pdf |
| B2 (NR) | The University of Nottingham | Investigation into the mental health support needs of international students with particular reference to Chinese and Malaysian students | Not about treatment | Chinese and Malaysian | 2011 | www.nottingham.ac.uk/studentservices/documents/investigation-into-the-mental-health-support--needs-of-international-students-with-particular-reference-to-chinese-and-malaysian-students.pdf |
| B3 (GR) | Moriarty J, Sharif N, Robinson J. (Social Care Institute for Excellence) | Black and minority ethnic people with dementia and their access to support and services | Comprehensive review of dementia – few examples of good practice but evidence of some effective practices | BME people with dementia | 2011 | www.scie.org.uk/publications/briefings/files/briefing35.pdf |
| B4 (GR/UV) | Kalathil J. (Mental Health Foundation) | Recovery and resilience – African, African Caribbean and South Asian women’s narratives of recovering from mental distress | User narratives. Includes references to racism and spiritual issues | African, African Caribbean and South Asian | 2011 | www.mentalhealth.org.uk/content/assets/PDF/publications/recovery_and_resilience.pdf?view=Standard |
| B5 (SE) | Neblett A | Psychological therapies draft service specification | Related to economic models. Nothing on culture competence therapy. But numbers expected | None | 2011 | www.camden.nhs.uk/downloads/Psychological%20Therapies%20Spec.pdf |
| B6 (GR/UV) | Pacitti R, Hughes J, Statter C, Alvarado-Rivero K, Chaddha R. (Mind in Croydon) | THE FIRST STEP: an exploration of how Croydon’s black and minority ethnic communities access counselling services | Evaluation of a successful service. Why BME patients felt confident to access | BME British | 2011 | www.mindincroydon.org.uk/DocumentStore/BME%20Report%20-%20The%20First%20Step%20-%20WEB.pdf |
| C1 (GR) | Wilkinson S, Lane K, Stockl A. (Centre for Applied Research in Education) | A survey of the health needs of black and minority ethnic groups in Norfolk | Background on needs assessment. Largely epidemiology | BME Norfolk | 2010 | www.norfolk.nhs.uk/sites/default/files/BME%20Health%20Needs%20Survey%20for%20NHS%20Norfolk-1.pdf |
| C2 (GR) | Rotondi AJ, Anderson CM, Haas GL, Eack SM, Spring MB, Ganguli R, et al. (Psychiatric Services) | Web-based psychoeducational intervention for persons with schizophrenia and their supporters: one-year outcomes | USA – background, no racial ethnic effects. Concludes more research needed | None | 2010 | ps.psychiatryonline.org/article.aspx?articleid=101634 |
| C3 (SE) | Care Quality Commission, National Mental Health Development Unit | Count me in census 2010 | Census data, epidemiology. Basic background | BME various | 2010 | www.cqc.org.uk/sites/default/files/media/documents/count_me_in_2010_final_tagged.pdf |
| C4 (GR/UV) | Edge D. (National Mental Health Development Unit) | National perinatal mental health project report | Practitioners concerns about own cultural competence. Supports user views | BME women | 2010 | www.nmhdu.org.uk/silo/files/national-perinatal-mental-health-project-report-.pdf |
| C5 (GR/UV) | Rights and Wellbeing of Racialised Groups | The end of delivering race equality? | User views, perspectives on end of DRE programme | BME various | 2010 | www.mind.org.uk/assets/0001/3140/DRE_LZ.pdf |
| C6 (GR/SE) | Health protection Agency, Department of Health. Understanding the Health needs of Migrants in the South East Regions: A Report By the South East Migrant Health Study Group on Behalf of the Department of Health. URL www.sepho.org.uk/Download/Public/13743/1/migrant_health_report_Oct10.pdf (accessed November 2013) | Chapter 5: Mental health needs of migrants in the South East region | Needs assessment (epidemiological). Useful for economic model. Good practice examples, not strong on evaluation | BME south-east England | Up to and including 2010 | www.migranthealthse.co.uk/sites/default/files/report/Migrant%20Health%20Report%20-%20Chapter%20Five:%20Mental%20health%20needs%20of%20migrants%20in%20the%20South%20East%20region.pdf |
| D1 (GR) | Moffat J, Sass B, McKenzie K, Bhui K. (Queen Mary’s School of Medicine and Dentistry) | Improving pathways into mental health care for black and ethnic minority groups: a systematic review of the grey literature | Access | BME various | 2009 | www.nmhdu.org.uk/silo/files/improving-pathways-into-mental-health-care-for-black-and.pdf |
| D2 (SE) | Shah A, Adelman S and Ong YL. (Royal College of Psychiatrists) | Psychiatric services for black and minority ethnic older people | Some costs, update of 2001. Not much improvement | BME various, aged ≥ 65 years | 2009 | www.rcpsych.ac.uk/files/pdfversion/CR156.pdf |
| D3 (NR) | Mind | Psychiatry, race and culture – a challenge for the mental health professions – Mind Think Report 4 | Consensus discussion only | BME various | 2009 | www.mind.org.uk/assets/0000/4965/mind_think_report_4.pdf |
| D4 (NR) | Meriden – The West Midlands Family Programme | References on family work black and minority ethnic (BME) | Document is dated, nothing obviously new | BME various | 2009 | www.meridenfamilyprogramme.com/docs/BME%20Reference%20List%20-%20Jan%2009.pdf |
| D5 | Fernando S, Keating F | Mental health in a multi-ethnic society: a multidisciplinary handbook (not available to download) | BME various | 2009 | books.google.ca/books?id=110bqd4nEcYC&printsec=frontcover&source=gbs_ge_summary_r&cad=0#v=onepage&q&f=false | |
| D7 (GR/SE) | Mind | Improving mental health support for refugee communities – an advocacy approach | Largely anecdotal but valuable case studies of role of community advocacy. Training model, (value for costs of training) | Refugees and asylum seekers in UK | 2009 | www.mind.org.uk/assets/0000/5696/Refugee_Report_1.pdf |
| D8 (GR) | Farmer H. (Black and minority ethnic working group) | Mental health conference: addressing the needs of refugees and asylum seekers in City and Hackney conference report | Little on TC. More on the need for training providers in cultural competence. Background | Refugees and asylum seekers in City and Hackney, London. | 2009 | www.hackneycen.org.uk/resources/CEN_BEMWG_report_nov09.pdf |
| D9 (GR) | NHS West Midlands – Regional Development Centre | Briefing paper on models of mental health care for black African Caribbean communities | Good examples of case studies and approaches. No formal evaluation | Black African Caribbean | 2009 | www.wmrdc.org.uk/silo/files/moc-african-caribbean-final.pdf |
| D10 (GR) | Mind | A civilised society mental health provision for refugees and asylum-seekers in England and Wales | Training service provider, collaborative, working with charitable organisations | Refugees and asylum seekers in England and Wales | 2009 | www.mind.org.uk/assets/0000/5695/refugee_report_2.pdf |
| E1 (GR) | Dowrick C, Chew-Graham C, Lovell K, Lamb J, Aseem, Beatty S, et al. Increasing equity of access to high-quality mental health services in primary care: a mixed-methods study. Programme Grants Appl Res 2013;1(2) | Access to high quality mental health services by hard-to-reach groups: a grey literature review (final) | Check, very low level of evidence relevant to BME groups | BME various | 2008 | www.liv.ac.uk/amp/greyliteraturereview.pdf |
| E2 (GR) | Mathews Z. (Race Equality Foundation) | The health of Gypsies and Travellers in the UK | Background, lack of evidence of interventions relevant to most in this group | Gypsies and Travellers in UK | 2008 | www.gypsy-traveller.org/wp-content/uploads/health-brief.pdf |
| E3 (GR) | Bristol Mind | Do Gypsies, Travellers and Show-people get the support they need with stress, depression and nerves? | Background, very small study, not receiving care | Gypsies, Travellers and Show people | 2008 | www.bristolmind.org.uk/files/docs/research/gypsy-traveller-research-summary.pdf |
| E4 (UV) | Kalathil J. (National Survivor User Network) | Dancing to our own tunes: reassessing black and minority ethnic mental health service user involvement | User views, strong voices on involvement and racism and social determinants and issues | BME various | 2008 | www.nsun.org.uk/modules/downloadable_files/assets/dancing-to-our-own-tunes---report.pdf |
| E5 (NR) | Greene R, Pugh R. and Roberts D. (Social Care and Institute for Excellence) | Black and minority ethnic parents with mental health problems and their children | No, effects of parenting, access issues, not TC | BME parents | 2008 | www.scie.org.uk/publications/briefings/files/briefing29.pdf |
| E6 (GR/UV) | Howard P, Buffin J, Bashford J, Heginbotham C. (University of Central Lancashire) | Engaging local communities: reaching seldom heard groups | User consultation, focus on the more professional support, i.e. community and family networks and communication | BME and marginalised groups | 2008 | www.northwest.nhs.uk/document_uploads/Mental_Health_in_the_North_West/NW_UCLANCommission_Hard_to_Reach_groups_Final_Report010408%282%29.pdf |
| E7 (NR) | David Ingleby | New perspectives on migration, ethnicity and schizophrenia | No, background discussion | BME various | 2008 | http://mighealth.net/eu/images/a/ad/Ingle.doc |
| E8 (NR) | Royal College of Psychiatrists | Standards on the use of Section 136 of the Mental Health Act 1983 (2007) | No, focus on place of safety, not on cultural communication | BME various | 2008 | www.collemergencymed.ac.uk/code/document.asp?ID=4572 |
| E10 (GR/UV) | NHS Health Scotland, Scottish Recovery Network, Health in Mind, NHS Lothian Minority Ethnic Mental Health Project, Saheliya and Outside the Box | Finding strength from within | User perspectives in three intervention projects, not formal evaluation – family and community life | BME people in Edinburgh | 2008 | www.intute.ac.uk/cgi-bin/redir.pl?url2=http://www.scottishrecovery.net/Download-document/68-Finding-Strength-From-Within.html&handle=20090913–17071797 |
| E11 (NR) | Salisbury Centre for Mental Health | Evening the odds – employment support, mental health and [\2] and minority ethnic communities | Not about mental health service but employment | BME various | 2008 | www.centreformentalhealth.org.uk/pdfs/Briefing35_Evening_the_Odds.pdf |
| E12 (NR) | Tobert N. (Harrow Primary Care Trust) | Mental health needs assessment with black and minority ethnic (BME) communities | Not about actual delivery of services, and focus on health promotion | BME people in Harrow | 2008 | www.aethos.org.uk/PDF%27s/BME%20Needs%20Assessment.pdf |
| F1 (GR) | Newbigging K, McKeown M, Hunkins-Hutchinson EA, French B. (Social Care and Institute for Excellence) | Developing mental health advocacy with African and Caribbean men | Genuine high-grade evaluation of a project | African and Caribbean men | 2007 | www.scie.org.uk/publications/knowledgereviews/kr15.pdf |
| F2 (GR) | Glasgow Anti Stigma Partnership | Mosaics of meaning – full report. Exploring stigma and discrimination towards mental health problems with black and minority ethnic communities in Glasgow | More on community perceptions and health promotion, treatment | BME people in Glasgow | 2007 | www.mosaicsofmeaning.info/sites/default/files/mosaics_full_research_report_0.pdf |
| F3 (NR) | Nacro Mental Health Unit | Black communities, mental health and the criminal justice system | Not about TC | Black people in Britain | 2007 | www.ohrn.nhs.uk/resource/policy/Nacroblackcommunities.pdf |
| F4 (SE) | Ponte P, Jacobson B. (Care Services Improvement Partnership) | Commissioning for equity series: equal access, equal care? Can London deliver the race equality action plan for mental health? | Statistics (activity analysis) | BME people in London | 2007 | www.lho.org.uk/Download/Public/11962/1/Commissioning%20for%20Equity_Equal%20access%20equal%20care_revised%20June%202007.pdf |
| F5 (GR/UV) | Rabiee F, Smith P. (Department of Health) | Being understood, being respected: an evaluation of the statutory and voluntary mental health service provision in Birmingham for members of the black African and black African-Caribbean communities | User views | Black African and black African Caribbean people in Birmingham | 2007 | http://bcu.ac.uk/_media/docs/ccmh_bme_full_report.pdf |
| F6 (NR) | Lane P, Hearsum S. (CSIP West Midlands) | The mental health and well being of black and minority ethnic elders: a foundational report on the research literature and a mapping of national resources | General | BME various, aged ≥ 65 years | 2007 | www.nmhdu.org.uk/silo/files/bme-report.pdf |
| F7 (NR) | Lane P, Hearsum S. (CSIP West Midlands) | Part 4: a national mapping of projects for BME elders to support their mental health well-being | Catalogue of projects, not evaluation (many now defunct) | BME various aged ≥ 65 years | 2007 | www.nmhdu.org.uk/silo/files/bme-mapping-doc.pdf |
| F8 (NR) | Bennett J, Kalathil J, Keating F. (The Sainsbury Centre for Mental Health) | Race equality training in mental health services in England – does one size fit all? | Staff training | BME people in England | 2007 | www.centreformentalhealth.org.uk/pdfs/sainsbury_centre_race_equality_training_report.pdf |
| F9 (NR) | Frank Keating. (Race Equality Foundation) | African and Caribbean men and mental health | Overview – all been covered | African and Caribbean men | 2007 | www.better-health.org.uk/sites/default/files/briefings/downloads/health-brief5.pdf |
| F10 (NR) | NHS Department of Mental Health | Positive steps: supporting race equality in mental health care | Case study descriptions – no evaluation evidence | South Asian and African Caribbean people in Britain | 2007 | www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_066061.pdf |
| F11 (NR) | Wazir Muhammed | Community engagement project | Description of project. Not about TC | South Asian, asylum seekers and refugees | 2007 | www.nmhdu.org.uk/silo/files/cdw-work-with-service-users-and-carers-wazir-muhammad.pdf |
| F12 (UV) | Jim J, Pistrang N | Running head: culture and the therapeutic relationship | Rare group | Chinese people in the UK and USA | 2007 | http://eprints.ucl.ac.uk/2495/1/2495.pdf |
| F13 (UV) | Rethink | Our voice: the Pakistani community’s view of mental health and mental health services in Birmingham | Overview of user views of mental health services – little on specific communication improvements | Pakistani people in Birmingham | 2007 | www.rethink.org/document.rm?id=5128 |
| G1 (NR) | Palmer D, Ward K. (Shaping Health, Commission for Patient and Public Involvement in Health) | ‘Unheard voices’: listening to refugees and asylum seekers in the planning and delivery of mental health service provision in London | Not evaluation of intervention | Refugees and asylum seekers in London | 2006 | www.irr.org.uk/pdf/Unheard_Voices.pdf |
| G2 (GR/UV) | Netto G, Gang S, Thanki M | Increasing access to appropriate counselling services for Asian people: the role of primary care services | Some evidence of what made users feel happy to use a service | Asian people in UK | 2006 | www.priory.com/psych/counselling.htm |
| G3 (NR) | African and Caribbean Mental Health Commission | Improving the mental health of the population. Towards a strategy on mental health for the European Union | Critique of EU policy paper | African Caribbean and BME various | 2006 | http://ec.europa.eu/health/archive/ph_determinants/life_style/mental/green_paper/mental_gp_co001.pdf |
| G4 (SE) | Moreland N. (DementiaPlus West Midlands) | Current research relating to minority ethnic groups and mental health | Funding of research projects, explains lack of research evidence | BME various | 2006 | www.nmhdu.org.uk/silo/files/current-research-relating-to-minority-ethnic-groups-and-mental-health.doc |
| G6 (NR) | Greenhalgh T, Robb N, and Scambler G. (University College, London) | Communicative and strategic action in interpreted consultations in primary health care: a Habermasian perspective | Background – theory about role of interpreter | BME people in UK | 2006 | http://pdn.sciencedirect.com/science?_ob=MiamiImageURL&_cid=271821&_user=11804549&_pii=S0277953606001766&_check=y&_origin=article&_zone=toolbar&_coverDate=30-Sep-2006&view=c&originContentFamily=serial&wchp=dGLbVlS-zSkWz&md5=30bcd2daa13809315770be86ec36115e&pid=1-s2.0-S0277953606001766-main.pdf&sqtrkid=0.9348358417375502 |
| G7 (SE) | The Sainsbury Centre for Mental Health | POLICY PAPER 6 – The Costs of Race Inequality | Costs | Black African and Caribbean people in UK | 2006 | www.centreformentalhealth.org.uk/pdfs/costs_of_race_inequality_policy_paper_6.pdf |
| G8 (NR) | Child and Adolescent Mental Health Services (CAMHS) | Cracking Cultural Competence in CAMHS | Children and young people | BME people in UK | 2006 | www.chimat.org.uk/resource/view.aspx?RID=82882 |
| G9 (NR) | Sooch R, Kaylan G, Rai J. (Rethink Sahayak Community Engagement Project) | Oppressed voices: understanding the effects of domestic violence on mental health for South Asian women in north-west Kent | Not actively focusing on treating mental health | South Asian women | 2006 | www.rethink.org/search_clicks.rm?id=2060&destinationtype=2&instanceid=744886 |
| H1 (NR) | BME Health Forum and Migrant & Refugee Communities’ Forum | Caught between stigma and inequality | Health promotion and access, not treating | BME people in Kensington, Chelsea and Westminster | 2005 | www.bmehf.org.uk/media/publications/research/caught_between_stigma_and_inequality.pdf |
| H2 (GR) | Department of Health | Delivering race equality in mental health care: An action plan for reform inside and outside services (Government response to the enquiry into the death of David Bennett) | Basic background | BME various | 2005 | www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4100775.pdf |
| H3 (SE) | McCrone P, et al. (Acta Psychiatrica Scandinavia) | Mental health needs, service use and costs among Somali refugees in the UK | Costs | Somali Refugees in UK | 2005 | http://onlinelibrary.wiley.com/doi/10.1111/j.1600–0447.2004.00494.x/pdf |
| H4 (NR) | Street C, Stapelkamp C, Taylor E, Malek M, Kurtz, Z. (Young Minds Research) | Minority voices: research into the access and acceptability of services for the mental health of young people from black and minority ethnic groups | Children and young people | BME young people | 2005 | www.dawsonmarketing.co.uk/youngminds/shop/PDF/MV.pdf |
| H5 (GR) | Seebohm P, Henderson P, Munn-Giddings C, Thomas P, Yasmeen S. (The Sainsbury Centre for Mental Health) | Together we will change – community development, mental health and diversity | Community development interventions | BME various | 2005 | www.centreformentalhealth.org.uk/pdfs/Together_we_will_change_report.pdf |
| I1 (NR) | The Sainsbury Centre for Mental Health | Acute Care 2004: A national survey of adult psychiatric wards in England | Not clear ethnicity | None | 2004 | www.centreformentalhealth.org.uk/pdfs/briefing_28.pdf |
| I2 (GR) | Seabrooke V, Milne A. (The Mental Health Foundation) | Culture and care in dementia | Background, not specifically TC | Asian people in north-west Kent | 2004 | www.mentalhealth.org.uk/content/assets/PDF/publications/culture_care_dementia.pdf?view = Standard |
| J1 (NR) | Department of Health | Delivering race equality: A framework for action | Policy document | BME various | 2003 | www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4069427.pdf |
| J2 (GR) | Christie Y, Hill N. (The Mental Health Foundation) | Black spaces project | Good practice case studies | Black African Caribbean and BME various | 2003 | www.mentalhealth.org.uk/content/assets/PDF/publications/black_spaces.pdf?view=Standard |
| J3 (NR) | National Institute for Mental Health in England | Improving mental health services for black and minority ethnic communities in England | Policy foundation document (policy) for this whole project | BME people in England | 2003 | www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4019452.pdf |
| J4 (NR) | Shields M, Price S. (Home Office) | The labour market outcomes and psychological well-being of ethnic minority migrants in Britain | Jobs and well-being | BME migrants | 2003 | webarchive.nationalarchives.gov.uk/20110218135832/rds.homeoffice.gov.uk/rds/pdfs2/rdsolr0703.pdf |
| J5 (GR) | Keating F, Robertson D, Kotecha N. (The King’s Fund) | Ethnic diversity and mental health in London | Recommendations for service delivery, improvements based on projects and case studies – low evaluation content | BME people in London | 2003 | www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/ethnic-diversity-mental-health-london-recent-developments-frank-keating-david-robertson-nutan-kotecha-kings-fund-1-august-2003.pdf |
| K1 (GR) | Asha Rai-Atkins | Best practice in mental health advocacy for African, Caribbean and South Asian communities | Background, case studies and projects. Does include reference to faith-based organisations | African, Caribbean and South Asian | 2002 | www.jrf.org.uk/sites/files/jrf/jr109-mental-health-advocacy.pdf |
| K2 (GR) | Bhui K, Fenton S, Grewal I, Karlsen S, Lloyd K, Nazroo J, et al. (National Centre for Social Research) | Ethnic differences in the context and experience of psychiatric illness: a qualitative study | How to understand clients’ self-descriptions of mental health | Bangladeshi, Caribbean, Indian, Irish, Pakistani and white | 2002 | www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4023952.pdf |
| K3 (GR) | The Sainsbury Centre for Mental Health | Breaking the circles of fear – a review of the relationship between mental health services and African and Caribbean communities | The consensus model of good practice | African and Caribbean | 2002 | www.centreformentalhealth.org.uk/pdfs/breaking_the_circles_of_fear.pdfM |
| K4 (SE/UV) | Lee J, McCrone P, Ford R. (The King’s Fund, Sainsbury Centre for Mental Health) | Independent and able to cope: Evaluation of Working Together in London: An integrated mental health initiative | Costs, social supports and moving out of health-care model | BME various | 2002 | www.centreformentalhealth.org.uk/pdfs/independent_and_able_to_cope.pdf |
| L1 (UV) | The Sainsbury Centre for Mental Health | Cultural sensitivity audit tool for mental health services – case study 2001 | User views of what a good service looks like (not an evaluation of intervention) | BME various | 2001 | www.centreformentalhealth.org.uk/pdfs/Cultural_Sensitivity_Booklet2_CaseStudy.pdf |
| L2 (GR) | Nigel Copsey. (The Sainsbury Centre for Mental Health) | Forward in Faith – An experiment in building bridges between ethnic communities and mental health services in East London | Pilot project, no evaluation, describes ‘what will be’ | BME people in east London | 2001 | www.centreformentalhealth.org.uk/pdfs/scmh_forward_in_faith.pdf |
| L3 (NR) | Silveira E, Allebeck P. (International Journal of Social Welfare) | Migration, ageing and mental health | Coping strategies, not about service delivery | Somali men in east London | 2001 | http://onlinelibrary.wiley.com/doi/10.1111/1468–2397.00188/pdf |
| M2 (GR) | Warner L, Nicholas S, Patal K, Harris J, Ford R. (The Sainsbury Centre for Mental Health) | Improving care for detained patients from black and minority ethnic communities – preliminary report | Background on provision, covers detained patients | Detained BME patients | 2000 | www.centreformentalhealth.org.uk/pdfs/national_visit_2.pdf |
| M3 (NR) | UK Data Archive | Ethnic minority psychiatric illness rates in the community (EMPIRIC) | Reference to EMPIRIC study. (Peer reviewed papers) | BME people in UK | 2000 | www.esds.ac.uk/doc/4685%5Cmrdoc%5Cpdf%5C4685userguide.pdf |
| M4 (GR) | Al-Krenawi A, Graham JR. (National Association of Social Workers) | Culturally sensitive social work practice with Arab clients in mental health settings | Descriptive and prescriptive but social work focus. Arabic – highlighted – rare group | Ethnic Arab people | 2000 | www.socialworkers.org/pressroom/events/911/alkrenawi.asp |
| O1 (SE) | The Sainsbury Centre for Mental Health | Keys to engagement – review of care for people with severe mental illness who are hard to engage with services | Old background, some case studies. Cost data | BME people in UK | 1998 | www.centreformentalhealth.org.uk/pdfs/keys_to_engagement.pdf |
| P1 (GR/UV) | Nigel Copsey. (The Sainsbury Centre for Mental Health) | Keeping faith – the provision of community mental health services within a multi-faith context | Largely obsolete by later report but worth considering to compare if changes in user views. Description of prayer | BME people in London | 1997 | www.centreformentalhealth.org.uk/pdfs/keeping_faith.pdf |
| Q1 (NR) | Social Care Research | Housing and mental health care needs of Asian people | Old | Asian people in London | 1996 | www.jrf.org.uk/sites/files/jrf/sc79.pdf |
Non-UK sources
| ID (C)a | Author/Source | Country | Title | Relevanceb | BME group(s) | Date | URL | |||
|---|---|---|---|---|---|---|---|---|---|---|
| A2 (GR) | Sanchez K, Chapa T, Ybarra R, Martinez ON. (US Department of Health and Human Services, Office of Minority Health and Hogg Foundation for Mental Health) | USA | Eliminating disparities through the integration of behavioural health and primary care services for racial and ethnic minority populations, including individuals with limited English proficiency – literature review | Grey literature review, USA – recommendations (evidence based) on culturally competent care (clinicians) | BME people in the USA | 2012 September | www.hogg.utexas.edu/uploads/documents/OMH%20Report_FINAL-FINAL.pdf | |||
| A4 (GR) | Ward EC. (National Institute for Health Research) | USA | Examining differential treatment effects for depression in racial and ethnic minority women: a qualitative systematic review | Review USA/critique, good summary | African American, Native American, Latina, Hispanic or Asian American | 2012 | http://update-sbs.update.co.uk/CMS2Web/tempPDF/12007005318.pdf | |||
| A6 (GR) | US Davis Centre for Reducing Health Disparities | USA | Community-defined solutions for Latino mental health care disparities | USA – issues of service accountability/monitoring | African American, Asian/Pacific Islander, LGBTQ strategic planning workgroups, Native American, Latino | 2012 | www.ucdmc.ucdavis.edu/newsroom/pdf/Latino_mental_health_report-6–25–2012–1.pdf | |||
| A10 (GR) | Urban Indian Health Institute | USA | Addressing depression among American Indians and Alaska natives: a literature review | US literature review, includes grey literature and recommendations | American Indian and Alaska native | 2012 | www.uihi.org/wp-content/uploads/2012/08/Depression-Environmental-Scan_Complete_2012–08–22_ER.pdf | |||
| B7 (NR) | Quinones AR. (Health Services Research and Development) | USA | Interventions to improve minority health care and reduce racial and ethnic disparities – table of interventions | This is all about the quality of the review (US based) | BME various | 2011 | www.hsrd.research.va.gov/publications/esp/healthcare-disparities-APP.pdf | |||
| B8 (NR) | Quinones AR. (Health Services Research and Development) | USA | Interventions to Improve Minority Health Care and Reduce Racial and Ethnic Disparities – full article | No, veterans in the USA | BME various | 2011 | www.ncbi.nlm.nih.gov/pubmedhealth/PMH0033373/pdf/TOC.pdf | |||
| D6 (NR) | Centre for Addiction and Mental Health, Mental Health Commission of Canada | Canada | Improving mental health services for immigrant, refugee, ethnocultural and racialised groups – issues and options for service improvement | Policy and review – mostly on Canadian structures | Immigrant, refugee, ethno-cultural and racialised groups (IRER) in Canada | 2009 | www.mentalhealthcommission.ca/SiteCollectionDocuments/Key_Documents/en/2010/Issues_Options_FINAL_English%2012Nov09.pdf | |||
| E9 (NR) | National Alliance on Mental Health | USA | Evidence-based practices and multicultural mental health | Providing a critique of the quality of the evidence base | BME people in the USA | 2008 | www.nami.org/Template.cfm?Section = Fact_Sheets1&Template=/ContentManagement/ContentDisplay.cfm&ContentID = 63974 | |||
| G5 (GR) | Bernal G, Saez-Santiago E. (University of Puerto Rico) | USA | Culturally centred psychological interventions | Describes a system for Latin American practice. Transferable? | Latino and various BME people in the USA | 2006 | www.utaccs.org/docs/bernal%20et%20al%20.pdf | |||
| G10 (NR) | Bernal G. (University of Puerto Rico) | USA | Beyond ‘one size fits all’: adapting evidence-based interventions for ethnic minorities | Refers to peer-reviewed literature and US-based models | BME various | Up to and including 2006 | www.hogg.utexas.edu/uploads/documents/rls14_GuillermoBernal.pdf | |||
| M1 (NR) | Williams D, Williams-Morris R. (University of Michigan) | USA | Racism and mental health – the African American experience | Useful background on role of racism, US based | African American people in the USA | 2000 | www.isr.umich.edu/williams/All%20Publications/DRW%20pubs%202000/racism%20and%20mental%20health.%20the%20African%20American%20experience.pdf | |||
Appendix 10 Other source: NHS Evidence
Search terms used included: ‘Ethnic’ ‘Mental’/’Therapeutic Communication’ AND ‘ethnic’/’therapeutic communication’ ‘ethnic’ ‘mental’/’therapeutic communication’ ‘ethnic mental’.
Search strategy for NHS Evidence
URL: www.evidence.nhs.uk/
Date of search: January 2012.
| Search term | Number of results |
|---|---|
| Ethnic mental | 9108 |
| Ethnic mental communication | 4508 |
| Ethnic mental psychiatrist | 1905 |
| Ethnic mental intervention | 5216 |
| Ethnic mental therapy | 3922 |
| Minority mental | 9830 |
| Minority mental communication | 5062 |
| Minority mental relationship | 5985 |
| Minority mental intervention | 6041 |
| Multi ethnic mental | 3672 |
| Multi ethnic mental therapy | 2353 |
| Multi cultural mental | 3861 |
| Multi cultural mental psychology | 2690 |
| Black mental | 9321 |
| Black mental communication | 4828 |
| Black mental psychiatrist | 1955 |
| Black mental counselling | 3414 |
| BME mental | 1243 |
| Refugee mental | 1438 |
| Refugee mental communication | 1034 |
| Refugee mental psychiatrist | 406 |
| Refugee mental psychologist | 405 |
| Refugee mental intervention | 1085 |
| Refugee mental therapy | 709 |
| Immigrant mental | 1044 |
| Immigrant mental communication | 695 |
| Immigrant mental psychiatrist | 271 |
| Immigrant mental intervention | 780 |
| Immigrant mental therapy | 552 |
| Racial mental | 1927 |
| Racial mental relationship | 1645 |
| Racial mental minority | 1366 |
| Racial mental therapy | 1014 |
| Racial mental counselling | 987 |
| Therapeutic communication | 16,924 |
| Therapeutic communication ethnic mental | 2055 |
| Therapeutic communication BME | 362 |
| Therapeutic mental ethnic | 2647 |
All URLs were accessed in November 2013.
| ID number | Country | Title | Date | URL/reference | BME group(s) | ||
|---|---|---|---|---|---|---|---|
| (R) Selected as relevant | |||||||
| NHSE-1 | UK | Improving pathways into mental health care for black and ethnic minority groups: a systematic review of the grey literature | 1 January 2009 | www.ncbi.nlm.nih.gov/pubmed/20374159 | BME various | ||
| NHSE-2 | UK | Ethnic variations in pathways to and use of specialist mental health services in the UK: systematic review | 1 January 2003 | www.scie-socialcareonline.org.uk/profile.asp?guid=54E2F355-BBE2-4850-B7EC-581BB2678FFF | BME various | ||
| NHSE-3 | Scotland | Scoping exercise with black and minority ethnic groups on perceptions of mental well-being in Scotland | 1 January 2008 | www.scie-socialcareonline.org.uk/profile.asp?guid=FFCF370D-CCED-44E2-A10D-CE8BFCF999F0 | Chinese and Pakistani | ||
| NHSE-4 | UK | Dancing to our own tunes: reassessing black and minority ethnic mental health service user involvement | 1 January 2008 | www.scie-socialcareonline.org.uk/profile.asp?guid=DADB0CEB-3046-4D2C-BB6C-99758409416F | BME various | ||
| NHSE-5 | UK | Ethnic variations in the experiences of mental health service users in England: results of a national patient survey programme | 1 January 2007 | www.scie-socialcareonline.org.uk/profile.asp?guid=FEC9DAC4-9C96-4EDF-98E1-56CDBA96D3D9 | BME various | ||
| NHSE-6 | Scotland – Glasgow | Mosaics of meaning – partnerships with black and minority ethnic communities to promote mental health | 3 May 2010 | www.healthscotland.com/uploads/documents/12843-Mosaics of Meaning Handbook 2010.pdf | BME various | ||
| NHSE-7 | England | Race equality action plan: a 5-year review | 1 January 2010 | www.scie-socialcareonline.org.uk/profile.asp?guid=6C6EEBBF-E39E-4AF8-951F-2003D19CC294 | BME various | ||
| NHSE-8 | Austria and the rest of the world | Therapeutic conversation: expectations and results with regard to intensified physician-patient communication | 26 March 2007 | www.crd.york.ac.uk/crdweb/ShowRecord.asp?LinkFrom=OAI&ID=32007000103 | BME various | ||
| NHSE-9 | UK – London | ‘Unheard voices’: listening to refugees and asylum seekers in the planning and delivery of mental health service provision in London | 1 January 2006 | www.scie-socialcareonline.org.uk/profile.asp?guid=7565196A-6030-47C3-8046-206204A5B722 | Refugees and asylum seekers | ||
| NHSE-10 | Scotland | National programme for improving mental health and well-being: addressing mental health inequalities in Scotland: equal minds | 1 January 2005 | www.scie-socialcareonline.org.uk/profile.asp?guid=8B27ED62-B327-4A17-8F23-9047548DCDDC | BME various | ||
| NHSE-11 | USA | Examining differential treatment effects for depression in racial and ethnic minority women: a qualitative systematic review | 16 May 2008 | www.crd.york.ac.uk/crdweb/ShowRecord.asp?LinkFrom=OAI&ID=12007005318 | African American, Latinos and Asians | ||
| NHSE-12 | USA | Racial differences in attitudes toward professional mental health treatment: the mediating effect of stigma | 1 January 2009 | www.scie-socialcareonline.org.uk/profile.asp?guid=84A97B11-2640-4FEE-A8DD-640D644EFEB6 | African American | ||
| NHSE-13 | UK | Training to redress racial disadvantage in mental health care; race equality or cultural competence? | 1 January 2009 | www.scie-socialcareonline.org.uk/profile.asp?guid=0E16126F-F1CB-4B46-806F-95B6F0570AB4 | BME various | ||
| NHSE-14 | USA | Cognitive behavior therapy: a potential treatment for depression among Asian Indian immigrant women in the United States | 1 January 2012 | www.scie-socialcareonline.org.uk/profile.asp?guid=D9B6DD71-406E-416A-9D4D-5AA27D916104 | Asian Indian women | ||
| NHSE-15 | UK – London | ‘Unheard voices’: listening to refugees and asylum seekers in the planning and delivery of mental health service provision in London | 3 April 2006 | www.irr.org.uk/pdf/Unheard_Voices.pdf | Refugees and asylum seekers | ||
| NHSE-16 | UK – Birmingham | Irish mental health in Birmingham: what is appropriate and culturally competent primary care? | 1 January 2008 | www.scie-socialcareonline.org.uk/profile.asp?guid=C0BA4811-8284-4948-98A3-26DB5DB0E077 | Irish | ||
| NHSE-17 | UK | Breaking the circles of fear | 28 June 2002 | www.centreformentalhealth.org.uk/pdfs/Breaking_the_Circles_of_Fear.pdf | African Caribbean | ||
| NHSE-18 | UK | An overview of the research evidence on ethnicity and communication in health care | 1 October 2005 | www2.warwick.ac.uk/fac/med/research/csri/ethnicityhealth/research/communicationsreview.pdf | BME various | ||
| NHSE-19 | Various | Cultural competence in the mental health treatment of immigrant and ethnic minority clients | 1 December 2005 | www.ingentaconnect.com/content/rmp/dhsc/2005/00000002/00000004/art00008 | BME various | ||
| NHSE-20 | England and Wales | A civilised society: mental health provision for refugees and asylum seekers in England and Wales. (Also found in grey literature search) | 5 November 2009 | www.mind.org.uk/assets/0000/5695/refugee_report_2.pdf | Refugees and asylum seekers | ||
| NHSE-21 | UK | Improving mental health support for refugee communities: an advocacy approach | 1 January 2009 | www.scie-socialcareonline.org.uk/profile.asp?guid=411BE09E-65D9-43E6-9326-F7148D73BC26 | Refugees and asylum seekers | ||
| NHSE-22 | England and Wales | A civilised society: mental health provision for refugees and asylum seekers in England and Wales (repeat of NHSE-20) | 1 January 2009 | www.scie-socialcareonline.org.uk/profile.asp?guid=7C52D3F2-7B27-43A4-93FD-ED4F9219AADF | Refugees and asylum seekers | ||
| NHSE-23 | UK | Improving mental health support for refugee communities: an advocacy approach | 5 November 2009 | www.mind.org.uk/assets/0000/5696/Refugee_Report_1.pdf | Refugees and asylum seekers | ||
| NHSE-24 | UK | Liaison and diversion for BME service users: a good practice guide for court diversion and criminal justice mental health liaison schemes | 1 January 2009 | www.scie-socialcareonline.org.uk/profile.asp?guid=338BE3DA-A039-4D73-9690-FE23F4975D22 | BME various | ||
| NHSE-25 | UK | Voices for change – involving BME groups in commissioning mental health services | 1 January 2009 | www.scie-socialcareonline.org.uk/profile.asp?guid=E91D688F-A894-4A3D-AF12-76922F3C8D43 | BME various | ||
| NHSE-26 | England and Wales | Managed care networks improve perinatal mental health care for black and minority ethnic (BME) women? | 1 January 2011 | www.scie-socialcareonline.org.uk/profile.asp?guid=E1AE92B7-1B54-44C9-894A-4CBF0CD3F64D | BME women | ||
| NHSE-27 | UK – Sheffield | Improving quality of mental health care for BME clients | 1 January 2008 | www.scie-socialcareonline.org.uk/profile.asp?guid=EDC63035-4494-4366-94AB-410CF4AF8F5F | Pakistani | ||
| NHSE-28 | UK | Independent mental health advocacy | 1 January 2011 | www.scie-socialcareonline.org.uk/profile.asp?guid=9A11711D-4958-4C89-A4D1-0E6AC4F41B4A | BME various | ||
| NHSE-29 | UK – Birmingham | Being understood, being respected: an evaluation of the statutory and voluntary mental health service provision in Birmingham for members of the black African and black African-Caribbean communities | 1 January 2007 | www.scie-socialcareonline.org.uk/profile.asp?guid=5C95D458-63D0-4477-AB8F-DA491EFF9A74 | Black African and black African Caribbean people | ||
| NHSE-30 | England and Wales | The early experience of consultant psychiatrists in application of the Mental Capacity Act: issues for black and minority individuals | 1 January 2009 | www.scie-socialcareonline.org.uk/profile.asp?guid=F2F31332-EEFB-46B7-A118-1BE6B25A308B | BME various | ||
| NHSE-31 | UK | The Cares of Life Project (CoLP): an exploratory randomised controlled trial of a community-based intervention for black people with common mental disorder | 1 December 2010 | www.jad-journal.com/article/S0165-0327(10)00402-7/abstract | BME various | ||
| NHSE-32 | UK – Birmingham and Solihull | Faith in one city: exploring religion, spirituality and mental well-being in urban UK | 1 January 2011 | www.scie-socialcareonline.org.uk/profile.asp?guid=A9F911DD-D602-47AC-8CF0-C9158E760D4D | BME various | ||
| NHSE-33 | UK | Dancing to our own tunes: reassessing black and minority ethnic mental health service user involvement | 1 January 2008 | www.survivor-research.com/images/reports/nsun_report.pdf | BME various | ||
| NHSE-34 | UK | Ethnic variations in pathways to and use of specialist mental health services in the UK: systematic review | 1 February 2003 | http://bjp.rcpsych.org/cgi/reprint/182/2/105.pdf | BME various | ||
| (P) Identified as possibly relevant | |||||||
| NHSE-B1 | UK | The mental health and well-being of black and minority ethnic elders: a foundational report on the research literature and a mapping of national resources | 1 January 2007 | www.scie-socialcareonline.org.uk/profile.asp?guid=08095F4B-C147-48DF-872B-3302C82D6CEA | BME various. Aged ≥ 65 years | ||
| NHSE-B2 | UK – Manchester | Evaluation of day services run by agency partnerships and Therapeutic Community Service North | 1 January 2008 | www.scie-socialcareonline.org.uk/profile.asp?guid=14D20D5A-C726-48FB-BC15-4B6DC4FC8FF9 | BME various | ||
| NHSE-B3 | UK | Structured patient–clinician communication and 1-year outcome in community mental health care: cluster randomised controlled trial | 1 January 2007 | www.scie-socialcareonline.org.uk/profile.asp?guid=AC946F22-6E11-4C21-9E2E-F19B7C81FF50 | N/A | ||
| NHSE-B4 | England | Race equality training in mental health services in England | 6 September 2007 | www.centreformentalhealth.org.uk/pdfs/sainsbury_centre_race_equality_training_report.pdf | BME various | ||
| NHSE-B5 | UK | Ethnic minority parents with mental health problems. | 1 January 2008 | www.scie-socialcareonline.org.uk/profile.asp?guid=0DE81C7D-CFCF-4950-9433-20EFDA34B394 | BME various | ||
| NHSE-B6 | UK | The mental well-being impact assessment toolkit | 1 January 2010 | www.scie-socialcareonline.org.uk/profile.asp?guid=57EB84EE-65A4-4495-9E78-B4E8122E9CE6 | N/A | ||
| NHSE-B7 | European countries | Policies and practices for mental health in Europe: meeting the challenges | 1 January 2008 | www.scie-socialcareonline.org.uk/profile.asp?guid=05A0D61F-47E9-4788-A046-FC1C3B92FD89 | N/A | ||
| NHSE-B8 | Spain | Duration and compliance with antidepressant treatment in immigrant and native-born populations in Spain: a 4-year follow-up descriptive study | 11 April 2012 | www.biomedcentral.com/content/pdf/1471-2458-12-256.pdf | Immigrants | ||
| NHSE-B9 | UK | An evidence synthesis of qualitative and quantitative research on component intervention | 25 February 2011 | www.hta.ac.uk/fullmono/mon1509.pdf | N/A | ||
| NHSE-B10 | N/A | Forced migration and mental health: rethinking the care of refugees and displaced persons | 1 January 2005 | www.scie-socialcareonline.org.uk/profile.asp?guid=E28F5122-07FE-40E4-AE78-95494C82DBEF | Asylum seekers, refugees and displaced persons | ||
| NHSE-B11 | England | Perinatal mental health care for black and minority ethnic (BME) women: a scoping review of provision in England | 1 January 2010 | www.scie-socialcareonline.org.uk/profile.asp?guid=79B1A747-A16E-4D84-8C37-C38796016885 | BME women | ||
| NHSE-B12 | UK | Psychiatric services for black and minority ethnic older people | 1 January 2009 | www.scie-socialcareonline.org.uk/profile.asp?guid=9506188C-5EF0-4917-9F32-74C0BB3BCF01 | BME various. Aged ≥ 65 years | ||
| NHSE-B13 | UK | Delivering male: effective practice in male mental health | 1 January 2011 | www.scie-socialcareonline.org.uk/profile.asp?guid=36E3BA0E-8FF1-4C79-B10B-0C84C96FF891 | N/A | ||
| NHSE-B14 | N/A | Black and minority ethnic people are more likely to be detained under the Mental Health Act 1983 – no clear evidence why: a systematic review | 1 May 2008 | http://ebmh.bmj.com/cgi/content/extract/11/2/61?maxtoshow=&HITS=10&hits=10&RESULTFORMAT=&titleabstract=minority+ethnic&searchid=1&FIRSTINDEX=0&resourcetype=HWCIT | BME various | ||
| NHSE-B15 | UK | Talking therapies; ECT – ethnic minority experiences, black and ethnic minority mental health, anxiety, mania, hallucinations, discrimination, being sectioned, diagnosis: Healthtalkonline | 1 February 2013 | www.healthtalkonline.org/mental_health/mentalhealthserviceusers/Topic/3414/ | BME various | ||
Appendix 11 Other source: JISCMail archive
The archives of the Minority-Ethnic-Health discussion group (minority-ethnic-health@jiscmail.ac.uk) were searched (April 2013) and any relevant postings relating to reports or projects identified.
Search terms used
Search terms used (always used in pairs both ways if two given).
-
Mental and communication.
-
Therapeutic and mental.
-
Therapeutic and communication.
-
Mental and counselling.
-
Mental and therapy.
-
Mental and intervention.
-
Advocacy.
Items identified
| ID number | Author | Title | URL/reference (accessed November 2013) |
|---|---|---|---|
| JMA-1 | Beverley Costa | Language support: challenges and benefits for users and providers of health and social care services (briefing paper) | www.better-health.org.uk |
| JMA-2 | Dr Gavin Miller | Debating the first principles of transcultural psychiatry (summary document, position papers, podcasts) | http://transculturalpsychiatry.gla.ac.uk/ |
| JMA-3 | Posted by Ghazala Mir | A systematic review of interventions for treating depression in Muslim clients | http://dx.doi.org/10.1016/j.jad.2012.06.035 |
| JMA-4 | Jane Fountain and Joanna Hicks | Delivering race equality in mental health care: report on the findings and outcomes of the community engagement programme 2005–2008 | www.better-health.co.uk |
Appendix 12 Research databases
Projects identified in UK Clinical Research Network study portfolio
| ID (type) | Acronym | Title | Status | Closure date | URL (accessed November 2013) |
|---|---|---|---|---|---|
| 2145 (context) | InvolvE | Outcomes of involuntary hospital admission in England | Closed | 8 July 2005 | Authors: Priebe S and Yeeles K http://public.ukcrn.org.uk/Search/StudyDetail.aspx?StudyID=2145 |
| 4010 (context) | AESOP | The causes of ethnic differences in the course and outcome of psychosis | Closed | 31 August 2011 | Authors: Murray R, Fearon P and Morgan C http://public.ukcrn.org.uk/Search/StudyDetail.aspx?StudyID=4010 |
| 4011 (intervention) | CRIMSON | RCT of joint crisis plans to reduce compulsory admission for people with psychosis | Closed | 6 April 2010 | Authors: Thornicroft G and Farrelly S http://public.ukcrn.org.uk/Search/StudyDetail.aspx?StudyID=4011 |
| 4237 (intervention) | Patient involvement – inpatient care (WP3) | Patient involvement in improving the evidence base on inpatient care – increasing the therapeutic activities on wards (WP3) – doorways | Open | 30 March 2013 | Authors: Csipke E and Wykes T http://public.ukcrn.org.uk/Search/StudyDetail.aspx?StudyID=4237 |
| 4238 (qualitative) | Patient involvement – inpatient care (WP4) | Patient involvement in improving the evidence base on inpatient care (WP4) – better pathway | Closed | 30 November 2010 | Author: Wykes T http://public.ukcrn.org.uk/Search/StudyDetail.aspx?StudyID=4238 |
| 5170 (context) | ENRICH 1: ethnic differences in pathways to care for FEP patients | Ethnicity, detention and early intervention: reducing inequalities and improving outcomes for black and ethnic minority (BME) patients | Closed | 15 April 2011 | Author: Islam Z http://public.ukcrn.org.uk/Search/StudyDetail.aspx?StudyID=5170 |
| 5171 (context) | ENRICH 2: Ethnicity and the Mental Health Act | An exploration of the determinants of ethnic differences in detention rates under the Mental Health Act | Closed | 31 March 2010 | Authors: Singh S, Brown L and Islam Z http://public.ukcrn.org.uk/Search/StudyDetail.aspx?StudyID=5171 |
| 5172 (intervention) | ENRICH 3: evaluating EIS services for the BME communities | Appropriateness, accessibility and acceptability of generic early intervention (EI) services in meeting the specific needs of BME patients | Closed | 21 July 2011 | Authors: Singh S, Brown L and Islam Z http://public.ukcrn.org.uk/Search/StudyDetail.aspx?StudyID=5172 |
| 5315 (intervention) | CBTP BME | Developing culturally sensitive cognitive therapy for psychosis | Closed | 31 December 2008 | Authors: Kingdon D, Rathod S, Peter Phiri P and Price J http://public.ukcrn.org.uk/Search/StudyDetail.aspx?StudyID=5315 |
| 6286 (context) | AMEND | Assessing the Impact of the Mental Health Act (2007) | Closed | 31 March 2012 | Author: Singh S http://public.ukcrn.org.uk/Search/StudyDetail.aspx?StudyID=6286 |
| 6436 (intervention) | An evaluation of the focused implementation site (FIS) programme | An evaluation of the focused implementation site (FIS) programme | Closed | 30 July 2008 | Authors: Singh S and Bailey N http://public.ukcrn.org.uk/Search/StudyDetail.aspx?StudyID=6436 |
| 7499 (intervention) | CaCBTp | Feasibility study of culturally adapted cognitive–behaviour therapy for psychosis for ethnic minority groups | Closed | 31 January 2011 | Authors: Rathod S and Phiri P http://public.ukcrn.org.uk/Search/StudyDetail.aspx?StudyID=7499 |
| 8018 (intervention) (Excludes non-English speakers) |
An intervention to improve psychiatrist patient communication | Developing and piloting a new intervention to improve psychiatrist patient communication about psychosis: an exploratory cluster randomised controlled trial | Open | 1 December 2012 | Authors: McCabe R and Hermann P http://public.ukcrn.org.uk/Search/StudyDetail.aspx?StudyID=8018 |
| 11,980 (models) | South Asian Voices Enabling Dementia (SAVE-D) care version | South Asian Voices Enabling Dementia (SAVE-D) care recognition of and consultation for memory problems among South Asian elders: a literature review and face to face interviews to study explanatory models | Open | 4 July 2013 | Authors: McCabe R and Hermann P http://public.ukcrn.org.uk/Search/StudyDetail.aspx?StudyID=11980 |
| 13,516 (intervention) | The EPOS trial | The EPOS trial: effective patient–clinician communication in community mental health care | Open | 1 July 2014 | Authors: Priebe S and Golden E http://public.ukcrn.org.uk/Search/StudyDetail.aspx?StudyID=13516 |
Projects identified on the National Institute for Health Research Evaluation, Trials and Studies Coordinating Centre website
| Title | Author | Date | URL (accessed November 2013) |
|---|---|---|---|
| Services to support carers of people with mental health problems | Arksey H, O’Malley L, Baldwin S, Harris J, Mason A and Golder S | July 2002 | www.netscc.ac.uk/hsdr/projdetails.php?ref=08–1109–015 |
| Promoting continuity of care for people with severe mental illness whose needs span primary, secondary and social care. A multi-method investigation of relevant mechanisms and contexts | Freeman G, Crawford M, Ferlie E, Renton A, Robinson I, Schneider J, et al. | June 2002 | www.netscc.ac.uk/hsdr/projdetails.php?ref=08–1109–009 |
| User and carer involvement in change management in a mental health context: review of the literature | Rose R, Fleischmann P, Hogman G, Tonkiss F, and Wykes T | May 2005 | www.netscc.ac.uk/hsdr/projdetails.php?ref=08–1201–017 |
| Seeking users’ views in service delivery and organisation research | Innes A, Archibald C, Brownlie J, Ferguson I, Simmons R and Stalker K | August 2003 | www.netscc.ac.uk/hsdr/projdetails.php?ref=08–1217–019 |
| Positive and Inclusive? Effective ways for professionals to involve carers in information sharing | Farmer P, Rapaport J, Bellringer S, Murray J, Huxley P, Banerjee S, et al. | January 2005 | www.netscc.ac.uk/hsdr/projdetails.php?ref=08–1309–054 |
| Research priorities for service user and carer-centred mental health services: A consultation report | Naylor C, Wallcraft J, Samele C and Greatley A | March 2007 | www.netscc.ac.uk/hsdr/projdetails.php?ref=08–1514–086 |
| Research priorities for service user and carer-centred mental health services: A synthesis of the literature | Keating F, Samele C, Furnish K and Greatley A | March 2007 | www.netscc.ac.uk/hsdr/projdetails.php?ref=08–1514–085 |
| Experiences of continuity of care and health social outcomes: the ECHO study | Burns T, Catty J, Clement S, Harvey K, Holloway F, et al. | March 2008 | www.netscc.ac.uk/hsdr/projdetails.php?ref=08–1509–088 |
| The development of an online training resource for mental health professionals to involve carers in information sharing | Pinfold V, Duggan Á, Huxley P, Tomlin A and Rapaport J | June 2010 | www.netscc.ac.uk/hsdr/projdetails.php?ref=08–1711–160 |
| How do managers and leaders in the National Health Service and social care respond to service user involvement in mental health services in both its traditional and emergent forms? (ENSUE) | Rose D, Barnes M, Crawford M, Omeni E, MacDonald D and Wilson A | Estimated: November 2013 | www.netscc.ac.uk/hsdr/projdetails.php?ref=10–1008–09 |
| An investigation of therapeutic alliance and its relationship to service user satisfaction in acute psychiatric wards and crisis residential alternatives | Johnson S, Flach C, Gilburt H, Lloyd-Evans B, McCabe R, Morant N, et al. | Estimated: June 2013 | www.netscc.ac.uk/hsdr/projdetails.php?ref=09–1001–51 |
| New ways of working in mental health services: assessing and informing the emergence of peer worker roles in mental health service delivery | Gillard S, Beales A, Cheeseman K, Edwards C, Lucock M, McKenzie J, et al. | Estimated: October 2013 | www.netscc.ac.uk/hsdr/projdetails.php?ref=10–1008–15 |
| Understanding the increasing rate of involuntary admissions in NHS mental health care | Weich S, Bhui K, Scott J, Twigg L and Crepaz-Keay D | Estimated: December 2013 | www.netscc.ac.uk/hsdr/projdetails.php?ref=10–1011–70 |
| Cross-national comparative study of recovery-focused mental health care planning and coordination | Simpson A, Coffey M, Hannigan B and Jones A | Estimated: April 2015 | www.netscc.ac.uk/hsdr/projdetails.php?ref=11–2004–12 |
Projects identified on the Economic and Social Research Council website
| Title | Author | Date | URL (accessed November 2013) |
|---|---|---|---|
| East London Bangladeshis and mental health: relationships between religious and professional health sectors | Dein S and Alexander M | December 2009 | www.esrc.ac.uk/my-esrc/grants/RES-000–22–3074/read |
| Exploring trust between service-users and professionals in acute mental health services | Calnan M and Brown P | November 2010 | www.esrc.ac.uk/my-esrc/grants/RES-000–22–3535/read |
| ESRC/NIH health disparities – understanding social contributions to disparities in depression care: USA and UK | Adams A, Kidd J, Nanton V, Roter D, Weich S and Buckingham C | Estimated: December 2014 | www.esrc.ac.uk/my-esrc/grants/RES-177–25–0014/read |
| Social science approaches to the study of mental health | Freestone M, Larsen J, Parr H, Woodward L, Speed E and Rogers A | May 2008 | www.esrc.ac.uk/my-esrc/grants/RES-451–25–4233/read |
Outputs identified for completed projects From UK Clinical Research Network study search
| Title | Author | Project | Date | URL (accessed November 2013) |
|---|---|---|---|---|
| Clinical and social determinants of duration of untreated psychosis in the AESOP first-episode psychosis study | Morgan C, Abdul-Al R, Lappin JM, Jones P, Fearon P, Leese M, et al. | AESOP | 2006 | www.ncbi.nlm.nih.gov/pubmed/17077436 |
| Neurological abnormalities and cognitive ability in first-episode psychosis | Dazzan P, Lloyd T, Morgan KD, Zanelli J, Morgan C, Orr K, et al. | AESOP | 2008 | www.ncbi.nlm.nih.gov/pubmed/18757976 |
| Self-harm in first-episode psychosis | Harvey SB, Dean K, Morgan C, Walsh E, Demjaha A, Dazzan P, et al. | AESOP | 2008 | www.ncbi.nlm.nih.gov/pubmed/18310576 |
| Gender differences in the association between childhood abuse and psychosis | Fisher H, Morgan C, Dazzan P, Craig TK, Morgan K, Hutchinson G, et al. | AESOP | 2009 | www.ncbi.nlm.nih.gov/pubmed/19336782 |
| Insight, grey matter and cognitive function in first-onset psychosis | Morgan K, Dazzan P, Morgan C, Lappin J, Hutchinson G, Suckling J, et al. | AESOP | 2010 | www.ncbi.nlm.nih.gov/pubmed/20679268 |
| Selective deficits in semantic verbal fluency in patients with a first affective episode with psychotic symptoms and a positive history of mania | Kravariti E, Reichenberg A, Morgan K, Dazzan P, Morgan C, Zanelli JW, et al. | AESOP | 2009 | www.ncbi.nlm.nih.gov/pubmed/19419389 |
| Incidence of schizophrenia and other psychoses in ethnic minority groups: results from the MRC AESOP Study | Fearon P, Kirkbride JB, Morgan C, Dazzan P, Morgan K, Lloyd T, et al. | AESOP | 2006 | www.ncbi.nlm.nih.gov/pubmed/16938150 |
| Neighbourhood-level effects on psychoses: re-examining the role of context | Kirkbride J, Morgan C, Fearon P, Dazzan P, Murray RM, Jones PB, et al. | AESOP | 2007 | www.ncbi.nlm.nih.gov/pubmed/17472758 |
| Individualized prediction of illness course at the first psychotic episode: a support vector machine MRI study | Mourao-Miranda J, Reinders AA, Rocha-Rego V, Lappin J, Rondina J, Morgan C, et al. | AESOP | 2012 | www.ncbi.nlm.nih.gov/pubmed/22059690 |
| Reliability and comparability of psychosis patients’ retrospective reports of childhood abuse | Fisher L, Craig TK, Fearon P, Morgan K, Dazzan P, Lappin J, et al. | AESOP | 2011 | www.ncbi.nlm.nih.gov/pmc/articles/PMC3080697/ |
| Migration, ethnicity, and psychosis: toward a sociodevelopmental model | Morgan C, Charalambides M, Hutchinson G and Murray RM | AESOP | 2010 | www.ncbi.nlm.nih.gov/pubmed/20513653 |
| Heterogeneity in incidence rates of schizophrenia and other psychotic syndromes | Kirkbride JB, Fearon P, Morgan C, Dazzan P, Morgan K and Tarrant J | AESOP | 2006 | www.ncbi.nlm.nih.gov/pubmed/16520429 |
| Developing culturally sensitive cognitive–behavioural therapy for psychosis for ethnic minority patients by exploration and incorporation of service users and health professionals views and opinions | Rathod S, Kingdon D, Phiri P and Gobbi M | CBTP BME | 2010 | www.ncbi.nlm.nih.gov/pubmed/20630118 |
| Clinical outcomes of Joint Crisis Plans to reduce compulsory treatment for people with psychosis: a randomised controlled trial | Thronicroft G, Farrelly S, Szmukler G, Birchwood M, Waheed W, Flach C, et al. | CRIMSON | 2013 | www.ncbi.nlm.nih.gov/pubmed/23537606 |
| Cultural attributions in help seeking during first episode psychosis (FEP) | Brown L, Rubibna J, Gajwani R, Islan Z and Singh S | ENRICH 1 | 2012 | www.rcpsych.ac.uk/pdf/17%20Brown%20L%20IC2012.pdf |
| Ethnicity and the Mental Health Act 1983 | Singh, S, Greenwood N, White S and Churchill R | ENRICH 2 | 2007 | http://bjp.rcpsych.org/content/191/2/99.abstract |
| Outcomes of involuntary hospital admission – a review | Katsakou C and Priebe S | INVOLVE | 2006 | www.ncbi.nlm.nih.gov/pubmed/16968360 |
| South Asian voices enabling dementia care (SAVE-D) factors influencing recognition of symptoms of dementia in South Asian elders: equipping families and professionals to provide sensitive responses and early intervention | Giebel CM, Jolley D, Zubair M, Worden, A, Challis D, Lambat, A, Kanani C, et al. | SAVE-D | 2013 |
Outputs identified from National Institute for Health Research Evaluation, Trials and Studies Coordinating Centre search
| Title | Author | Date | URL (accessed November 2013) |
|---|---|---|---|
| Research priorities for service user and carer-centred mental health services: a synthesis of the literature | Keating F, Samele C, Furnish K and Greatley A | July 2006 | www.netscc.ac.uk/hsdr/projdetails.php?ref=08–1514-085 |
| Research priorities for service user and carer-centred mental health services: consultation report | Naylor C, Wallcraft J, Samele C and Greatley A | January 2007 | www.netscc.ac.uk/hsdr/projdetails.php?ref=08–1514-086 |
| User and carer involvement in change management in a mental health context: review of the literature | Rose D, Fleischmann P, Tonkiss F, Campbell P and Wykes T | November 2002 | www.netscc.ac.uk/hsdr/projdetails.php?ref=08–1201-017 |
| Promoting continuity of care for people with severe mental illness | Freeman G, Crawford M, Ferlie E, Renton A, Robinson I, Schneider J, et al. | October 2001 | www.netscc.ac.uk/hsdr/projdetails.php?ref=08–1109-009 |
| Services to support carers of people with mental health problems | Arksey H, O’Malley L, Baldwin S, Harris J, Mason A and Golder S | March 2002 | http://php.york.ac.uk/inst/spru/research/summs/carers_mhprobs.php |
| Positive and Inclusive? Effective ways for professionals to involve carers in information sharing | Farmer P, Rapaport J, Bellringer S, Murray J, Huxley P, Banerjee S, et al. | Autumn 2004 | www.netscc.ac.uk/hsdr/projdetails.php?ref=08–1309-054 |
| Experiences of continuity of care and health and social outcomes: the ECHO study | Burns T, Catty C, Clement S, Harvey K, Holloway F, et al. | December 2007 | www.nets.nihr.ac.uk/__data/assets/pdf_file/0004/64507/FR-08-1509-088.pdf |
| The development of an online training resource for mental health professionals to involve carers in information sharing | Pinfold V, Huxley P, Rapaport J and Teasdale M | June 2010 | www.netscc.ac.uk/hsdr/projdetails.php?ref=08–1711-160 |
Outputs identified from Economic and Social Research Council search
| Title | Author | Date | URL (accessed November 2013) |
|---|---|---|---|
| Exploring trust between service-users and professionals in acute mental health services – economic and social research council end of award report | Calnan M and Brown P | 2011 | www.esrc.ac.uk/my-esrc/grants/RES-000-22-3535/outputs/Download/22311092-c958–407a-958d-618c5e2396e9 |
| East London Bangladeshis and mental health relationships between religious and professional sectors | Dein S and Alexander M | 2010 | www.esrc.ac.uk/my-esrc/grants/RES-000-22-3074/outputs/Download/1dc1cf25–2f2a-43c7-b5f8-8ae81c019558 |
Appendix 13 Economic evidence
Search strategies
Sample search strategy run on Ovid MEDLINE and adapted for other mental disorders.
Searched: inception to 4 April 2012 (re-run January/February 2013).
THERACOM economics – 150,512 (psychosis)
Search strategy
-
ethnic*.mp.
-
minorit*.mp.
-
(Multicultural or multi-cultural).mp.
-
(crosscultural or cross-cultural).mp.
-
(transcultural or trans-cultural).mp.
-
(multiethnic or multi-ethnic).mp.
-
(multiracial or multi-racial).mp.
-
(migrant* or immigrant*).mp.
-
refugee*.mp.
-
cultural diversity.mp.
-
(multilingual or multi-lingual).mp.
-
or/1-11
-
(cost or costs or costing*).ab,ti.
-
cost analysis.mp. or exp “Costs and Cost Analysis”/
-
cost effective*.ab,ti.
-
Cost-benefit analysis.mp. or exp Cost-Benefit Analysis/
-
(economic and (assessment$or evaluation$)).ab,ti.
-
13 or 15 or 14 or 17 or 16
-
mental disorders.mp. or exp Mental Disorders/
-
(psychosis or Psychotic or schizophr* or schizoaffective or delusional or depress* or dysthymi* or bipolar or cyclothymi* or panic or agoraphobia or phobia or “obsessive compulsive disorder” or “post-traumatic stress disorder” or stress or anxiety or dementia or ADHD or “attention deficit”).ab,ti.
-
19 or 20
-
12 and 18 and 21
-
limit 22 to (english language and humans)
Shortlisted economic articles
Brazier J, Tumur I, Holmes M, Ferriter M, Parry G, Dent-Brown K, et al. Psychological therapies including dialectical behaviour therapy for borderline personality disorder: a systematic review and preliminary economic evaluation. Health Technol Assess 2006;10(35).
Frank RG, Huskamp HA, McGuire TG, Newhouse JP. Some economics of mental health ‘carve-outs’. Arch Gen Psychiatry 1996;53:933–7.
Gitlin LN, Fields Harris L, McCoy M, Chernett NL, Jutkowitz E, Pizzi LT, et al. A community-integrated home-based depression intervention for older African Americans: description of the Beat the Blues randomized trial and intervention costs. BMC Geriatr 2012;12:4.
Gutierrez-Recacha P, Chisholm D, Haro JM, Salvador-Carulla L, Ayuso-Mateos JL. Cost-effectiveness of different clinical interventions for reducing the burden of schizophrenia in Spain. Acta Psychiatr Scand Suppl 2006;432:29–38.
Haby MM, Carter R, Mihalopoulos C, Magnus A, Sanderson K, Andrews G, et al. Assessing cost-effectiveness – mental health: introduction to the study and methods. Aust N Z J Psychiatry 2004;38:569–78.
Hong J, Windmeijer F, Novick D, Haro JM, Brown J. The cost of relapse in patients with schizophrenia in the European SOHO (Schizophrenia Outpatient Health Outcomes) study. Prog Neuropsychopharmacol Biol Psychiatry 2009;33:835–41.
Howard K, Marinovitch Z. Costs and benefits of psychotherapy. Acta Psychiatr Belg 1996;96:154–70.
Knapp M, Mangalore R, Simon J. The global costs of schizophrenia. Schizophr Bull 2004;30:279–93.
McCrone P, Knapp M. Economic evaluation of early intervention services. Br J Psychiatry 2007;51:s19–22.
McEvoy JP. The costs of schizophrenia. J Clin Psychiatry 2007;68(Suppl. 14):4–7.
Miklowitz DJ, Scott J. Psychosocial treatments for bipolar disorder: cost-effectiveness, mediating mechanisms, and future directions. Bipolar Disord 2009;11(Suppl. 2):110–22.
Morreim EH. The new economics of medicine: special challenges for psychiatry. J Med Philos 1990;15:97–119.
Noordik E, van Dijk FJ, Nieuwenhuijsen K, van der Klink JJ. Effectiveness and cost-effectiveness of an exposure-based return-to-work programme for patients on sick leave due to common mental disorders: design of a cluster-randomized controlled trial. BMC Public Health 2009;9:140.
Payton FC, Brennan PF, Silvers JB. Cost justification of a community health information network: the ComputerLink for AD caregivers. Proc Ann Symp Comput Appl Med Care 1995:566–70.
Serretti A, Mandelli L, Bajo E, Cevenini N, Papili P, Mori E. The socio-economical burden of schizophrenia: a simulation of cost-offset of early intervention program in Italy. Eur Psychiatry 2009;24:11–16.
Smoot SL, Gonzales JL. Cost-effective communication skills training for state hospital employees. Psychiatr Serv 1995:46:819–22.
Gray B, Hilder J, Stubbe M. How to use interpreters in general practice: the development of a New Zealand toolkit. J Prim Health Care 2012;4:52–61.
Klug MG, Muus K, Volkov B, Halaas GW. Reducing health care costs for dementia patients: estimating savings from a caregiver support program. J Aging Health 2012;24:1470–85.
Calvert M, Duffy H, Freemantle N, Davis R, Lip GY, Gill P. Population health status of South Asian and African-Caribbean communities in the United Kingdom. BMC Health Serv Res 2012;12:101.
Dalky HF. Mental illness stigma reduction interventions: review of intervention trials. West J Nurs Res 2012;34:520–47.
Gitlin LN, Harris LF, McCoy M, Chernett NL, Jutkowitz E, Pizzi LT; Beat the Blues Team. A community-integrated home-based depression intervention for older African Americans: [corrected] description of the Beat the Blues randomized trial and intervention costs. BMC Geriatr 2012;12:4.
Other economic articles shortlisted
Searched for: cost of illness and stress
Walker EA, Katon W, Russo J, Ciechanowski P, Newman E, Wagner AW. Health care costs associated with posttraumatic stress disorder symptoms in women. Arch Gen Psychiatry 2003;60:369–74.
Searched for: cost of illness and anxiety
Rovira J, Albarracin G, Salvador L, Rejas J, Sánchez-Iriso E, Cabasés JM. The cost of generalized anxiety disorder in primary care settings: results of the ANCORA study. Community Ment Health J 2012;48:372–83.
Hodgkins P, Montejano L, Sasané R, Huse D. Cost of illness and comorbidities in adults diagnosed with attention-deficit/hyperactivity disorder: a retrospective analysis. Prim Care Companion CNS Disord 2011;13:e1–12.
Hedman E, Ljótsson B, Andersson E, Rück C, Andersson G, Lindefors N. Effectiveness and cost offset analysis of group CBT for hypochondriasis delivered in a psychiatric setting: an open trial. Cogn Behav Ther 2010;39:239–50.
Johnston K, Westerfield W, Momin S, Phillippi R, Naidoo A. The direct and indirect costs of employee depression, anxiety, and emotional disorders – an employer case study. J Occup Environ Med 2009;51:564–77.
Bodden DH, Dirksen CD, Bögels SM, Nauta MH, De Haan E, Ringrose J. Costs and cost-effectiveness of family CBT versus individual CBT in clinically anxious children. Clin Child Psychol Psychiatry 2008;13:543–64.
Soeteman DI, Hakkaart-van Roijen L, Verheul R, Busschbach JJ. The economic burden of personality disorders in mental health care. J Clin Psychiatry 2008;69:259–65.
Dozeman E, van Schaik DJ, Beekman AT, Stalman WA, Bosmans JE, van Marwijk HW. Depression and anxiety, an indicated prevention (DIP) protocol in homes for the elderly: feasibility and (cost) effectiveness of a stepped care programme. BMC Geriatr 2007;7:6.
Hoffman DL, Dukes EM, Wittchen HU. Human and economic burden of generalized anxiety disorder. Depress Anxiety 2008;25:72–90.
Löthgren M. Economic evidence in anxiety disorders: a review. Eur J Health Econ 2004;5(Suppl. 1):S20–5.
McCrone P, Knapp M, Proudfoot J, Ryden C, Cavanagh K, Shapiro DA, et al. Cost-effectiveness of computerised cognitive–behavioural therapy for anxiety and depression in primary care: randomised controlled trial. Br J Psychiatry 2004;185:55–62.
Marciniak M, Lage MJ, Landbloom RP, Dunayevich E, Bowman L. Medical and productivity costs of anxiety disorders: case control study. Depress Anxiety 2004;19:112–20.
Issakidis C, Sanderson K, Corry J, Andrews G, Lapsley H. Modelling the population cost-effectiveness of current and evidence-based optimal treatment for anxiety disorders. Psychol Med 2004;34:19–35.
Wittchen HU. Generalized anxiety disorder: prevalence, burden, and cost to society. Depress Anxiety 2002;16:162–71.
Searched for: cost of illness and post-traumatic stress disorder
Zhu B, Ascher-Svanum H, Faries DE, Peng X, Salkever D, Slade EP. Costs of treating patients with schizophrenia who have illness-related crisis events. BMC Psychiatry 2008;8:72.
Marciniak MD, Lage MJ, Dunayevich E, Russell JM, Bowman L, Landbloom RP, et al. The cost of treating anxiety: the medical and demographic correlates that impact total medical costs. Depress Anxiety 2005;21:178–84.
Joesch JM, Sherbourne CD, Sullivan G, Stein MB, Craske MG, Roy-Byrne P. Incremental benefits and cost of coordinated anxiety learning and management for anxiety treatment in primary care. Psychol Med 2012;42:1937–48.
Searched for: cost of illness and obsessive–compulsive disorder
Diefenbach GJ, Tolin DF. The cost of illness associated with stepped care for obsessive-compulsive disorder. J Obsessive Compuls Relat Disord 2013;2:144–8.
Tolin DF, Frost RO, Steketee G, Gray KD, Fitch KE. The economic and social burden of compulsive hoarding. Psychiatry Res 2008;160:200–11.
Searched for: cost of illness and bipolar
Jones S, McGrath E, Hampshire K, Owen R, Riste L, Roberts C, et al. A randomised controlled trial of time limited CBT informed psychological therapy for anxiety in bipolar disorder. BMC Psychiatry 2013;13:54.
Wolff N, Perlick DA, Kaczynski R, Calabrese J, Nierenberg A, Miklowitz DJ. Modeling costs and burden of informal caregiving for persons with bipolar disorder. J Ment Health Policy Econ 2006;9:99–110.
Kleinman L, Lowin A, Flood E, Gandhi G, Edgell E, Revicki D. Costs of bipolar disorder. Pharmacoeconomics 2003;21:601–22.
Simon GE. Social and economic burden of mood disorders. Biol Psychiatry 2003;54:208–15.
Das Gupta R, Guest JF. Annual cost of bipolar disorder to UK society. Br J Psychiatry 2002;180:227–33.
Searched for: cost of illness and agoraphobia
Batelaan N, Smit F, de Graaf R, van Balkom A, Vollebergh W, Beekman A. Economic costs of full-blown and subthreshold panic disorder. J Affect Disord 2007;104:127–36.
Searched for: cost of illness and schizophrenia
Vanmeerten NJ, Harris JI, Nienow TM, Hegeman BM, Sherburne A, Winskowski AM, et al. Inpatient utilization before and after implementation of psychosocial rehabilitation programs: analysis of cost reductions. Psychol Serv 2013;10:402–7.
Centorrino F, Mark TL, Talamo A, Oh K, Chang J. Health and economic burden of metabolic comorbidity among individuals with bipolar disorder. J Clin Psychopharmacol 2009;29:595–600.
Fitzgerald PB, Montgomery W, de Castella AR, Filia KM, Filia SL, Christova L, et al. Australian Schizophrenia Care and Assessment Programme: real-world schizophrenia: economics. Aust N Z J Psychiatry 2007;41:819–29.
Vázquez-Polo FJ, Negrín M, Cabasés JM, Sánchez E, Haro JM, Salvador-Carulla L. An analysis of the costs of treating schizophrenia in Spain: a hierarchical Bayesian approach. J Ment Health Policy Econ 2005;8:153–65.
Garattini L, Barbui C, Clemente R, Cornago D, Parazzini F; Study Group SCORE. Direct costs of schizophrenia and related disorders in Italian community mental health services: a multicenter, prospective 1-year follow up study. Schizophr Bull 2004;30:295–302.
Almond S, Knapp M, Francois C, Toumi M, Brugha T. Relapse in schizophrenia: costs, clinical outcomes and quality of life. Br J Psychiatry 2004;184:346–51.
Andrews G, Sanderson K, Corry J, Issakidis C, Lapsley H. Cost-effectiveness of current and optimal treatment for schizophrenia. Br J Psychiatry 2003;183:427–35.
Percudani M, Fattore G, Belloni GC, Gerzeli S, Contini A. Service utilisation and costs of first-contact patients in a community psychiatric service in Italy. Eur Psychiatry 2002;17:434–42.
Knapp M. Schizophrenia costs and treatment cost-effectiveness. Acta Psychiatr Scand 2000;407:15–18.
Kemp R, Kirov G, Everitt B, David A. A randomised controlled trial of compliance therapy: 18 month follow up. Br J Psychiatry 1998;172:413–19.
Woods SW. The economic burden of bipolar disease. J Clin Psychiatry 2000;61(Suppl. 1):38–41.
Tarricone R, Gerzeli S, Montanelli R, Frattura L, Percudani M, Racagni G. Direct and indirect costs of schizophrenia in community psychiatric services in Italy. The GISIES study. Interdisciplinary Study Group on the Economic Impact of Schizophrenia. Health Policy 2000;51:1–18.
Guest JF, Cookson RF. Cost of schizophrenia to UK Society. An incidence-based cost-of-illness model for the first 5 years following diagnosis. Pharmacoeconomics 1999;15:597–610.
Searched for: cost of illness and psychosis
Gilden J, Staring AB, der Gaag Mv, Mulder CL. Does treatment adherence therapy reduce expense of healthcare use in patients with psychotic disorders? Cost-minimization analysis in a randomized controlled trial. Schizophr Res 2011;133:47–53.
Mihalopoulos C, Harris M, Henry L, Harrigan S, McGorry P. Is early intervention in psychosis cost-effective over the long term? Schizophr Bull 2009;35:909–18. [Erratum published in Schizophr Bull 2011;37:651.]
Insel TR. Assessing the economic costs of serious mental illness. Am J Psychiatry 2008;165:663–5.
Byford S, Barber JA, Fiander M, Marshall S, Green J. Factors that influence the cost of caring for patients with severe psychotic illness: report from the UK 700 trial. Br J Psychiatry 2001;178:441–7.
Other papers
Brown SD, Lee K, Schoffman DE, King AC, Crawley LM, Kiernan M. Minority recruitment into clinical trials: Experimental findings and practical implications. Contemp Clin Trials 2012;33:620–3.
Keane MM, Martin E, Verfaellie M. Performance benefits and costs in forced choice perceptual identification in amnesia: Effects of prior exposure and word frequency. Mem Cognit 2009;37:655–66.
Williams MT, Domanico J, Marques L, Leblanc NJ, Turkheimer E. Barriers to treatment among African Americans with obsessive-compulsive disorder. J Anxiety Disord 2012;26:555–63.
Williams MT, Proetto D, Casiano D, Franklin ME. Recruitment of a hidden population: African Americans with obsessive-compulsive disorder. Contemp Clin Trials 2012;33:67–75.
Appendix 14 Core quality score for all quantitative studies (0–12)
Numbers in brackets refer to quality score.
How clearly each study indicates that there is an intervention to improve therapeutic communication could be a quality indicator (1–4)
-
Intervention clearly shown, and it clearly is to improve TC, for relevant outcomes of interest. (4)
-
Intervention clearly shown and relevant to outcomes of interest. (3)
-
Intervention vague and or multicomponent, so difficult to discern whether the mediating effect is truly through improved TC. (2)
-
Inferred by reviewer given elements of decision-making, assessment and conversation needed and efforts to improve these through adaptation of interventions. (1)
Outcome of therapeutic communication (1–3)
-
Direct measure of TC by a reliable and valid scale, for example alliance, reduced conflict, greater trust. (3)
-
Proxy measure: attendance, premature termination. (2)
-
Narrative outcome. (1)
-
No outcome: exclude study.
Ethnic groups (0–5)
-
Groups of relevance to the UK and described in a manner consistent with a specific classification scheme for ethnicity (not just race). (5)
-
Groups of relevance to the UK. (3)
-
Not of relevance to the UK but well described in terms of ethnicity. (1)
-
Not of relevance not the UK. (0)
Types of study: (1–4)
-
Quantitative: randomised controlled trial. (4)
-
Observational: a series, or service evaluation data, or pre–post type evaluations. (3)
-
Qualitative/narrative evaluation of a series. (2)
-
Case study/studies: in-depth narrative information. (1)
-
Experiences and personal reports with no methodological framework. (0)
Economic evaluation (0–4)
-
Cost-effectiveness. (4)
-
Impact and interventions cost/benefits. (3)
-
Intervention costs. (1)
-
Financial gains and losses. (1)
Quality of randomised controlled trial (0–30)
-
Adequate sample size (n per group): 0 = inadequate, 1 = moderate and 2 = large or specified by power calculations.
-
Appropriate duration of trial including follow up: 0 = too short, 1 = reasonable length and 2 = long enough for assessment of long-term outcomes.
-
Power calculation: 0 = not reported, 1 = mentioned without details and 2 = details of calculations provided.
-
Method of allocation: 0 = unrandomised and likely to be biased, 1 = partially or quasi-randomised with some bias possible and 2 = randomised allocation.
-
Source of subjects described and representative sample recruitment: 0 = source of subjects not described, 1 = source of subjects given but no information on sampling or use of unrepresentative sample (e.g. volunteers) and 2 = source of subjects described plus representative sample taken (e.g. all consecutive admissions or referrals, or random sample taken).
-
Use of diagnostic criteria (or clear specification of inclusion criteria): 0 = none, 1 = diagnostic criteria or clear inclusion criteria and 2 = diagnostic criteria plus specification of severity.
-
Record of exclusion criteria and number of exclusions and refusals reported: 0 = criteria and number not reported, 1 = criteria or number of exclusions and refusals not reported and 2 = criteria and number of exclusions and refusals reported.
-
Blinding of assessor: 0 = not done, 1 = done but no test of blind and 2 = done and integrity of blind tested.
-
Assessment of compliance with experimental treatments (including attendance for therapy): 0 = not assessed, 1 = assessed for some experimental treatments and 2 = assessed for all experimental treatments.
-
Record of number and reasons for withdrawal: 0 = no information on withdrawals by group, 1 = withdrawals by group reported without reason and 2 = withdrawals and reason by group reported.
-
Information on comparability and adjustment for differences in analysis: 0= no information on comparability, 1 = some information on comparability with appropriate adjustment and 2 = sufficient information on comparability with appropriate adjustment.
-
Inclusion of all subjects in analyses: 0 = less than 95% of subjects included (intention-to-treat analysis) and 2 = 95% or more included.
-
Presentation of results with inclusion of data for re-analysis of main outcomes (e.g. standard deviations): 0 = little information presented, 1 = adequate information and 2 = comprehensive.
-
Appropriate statistical analysis (including correction for multiple tests where applicable): 0 = inadequate, 1 = adequate and 2 = comprehensive and appropriate.
-
Conclusions justified: 0 = no, 1 = partially and 2 = yes.
Quality assessment for case series
Scoring: yes = 2, unclear = 1 and no = 0 (total score = 0–38).
-
Is the hypothesis/aim/objective of the study clearly described?
-
Yes: the hypothesis/aim/objective of the study is clearly reported.
-
Unclear: the hypothesis/aim/objective of the study is vague or unclearly reported.
-
No: the hypothesis/aim/objective is not reported.
-
-
Are the characteristics of the participants included in the study described?
-
Yes: the most relevant characteristics of the participants are reported (e.g. the total number, age, and gender distribution). Ethnicity, severity of disease/condition, comorbidity, or aetiology should also be included, if relevant.
-
Partially reported: only the number of participants was reported.
-
No: none of the relevant characteristics of the participants is reported.
-
-
Were the cases collected in more than one centre?
-
Yes: cases are collected in more than one centre (multicentre study).
-
Unclear: unclear where the patients come from (i.e. single or multicentre study).
-
No: cases are collected from one centre.
-
-
Are the eligibility criteria (i.e. inclusion and exclusion criteria) for entry into the study clearly stated?
-
Yes: both inclusion and exclusion criteria are reported.
-
Partially reported: only one, the inclusion or exclusion criteria are reported.
-
No: neither inclusion nor exclusion criteria are reported.
-
-
Were participants recruited consecutively?
-
Yes: there is a clear statement or it is clear from the context that the participants were recruited consecutively or study stated that all eligible patients were recruited.
-
Unclear: the method used to recruit participants is not clearly stated or no information is provided about the method used to recruit participants in the study.
-
No: the cases studied were a subgroup of those treated with no evidence to show that they were selected consecutively. The participants were recruited based on other criteria such as access to intervention determined by the distance or availability of resources.
-
-
Did participants enter the study at a similar point in the disease?
-
Yes: there is a clear description about all participants entering the study at a similar point in the condition/disease based on their clinical status, duration of condition or exposure before the intervention, severity of disease, and presence of comorbidities or complications.
-
Unclear: there is no description of the characteristics of participants before entering the study or there is no statement about entering the study at a similar point in the disease.
-
No: participants did not enter the study at a similar point in the condition/disease. This can be revealed by a wide range of disease durations before entering the study or different levels of severities or comorbidities or complications due to progression of their condition/disease.
-
-
Were additional interventions (co-interventions) reported in the study?
-
Yes: participants received additional co-intervention(s).
-
Unclear: it is suspected that a co-intervention was administered but the information is not reported.
-
No: there is a clear statement or it is clear from the context that a co-intervention was not administered.
-
-
Are the outcome measures established a priori?
-
Yes: all relevant outcome measures are reported in the introduction or methods section (e.g. accomplished, measurable improvements or effects, symptoms relieved, improved function, improved test scores, and quality-of-life measures).
-
Partially reported: some of the relevant outcomes are briefly reported in the introduction or methods section.
-
No: the outcome measures are reported for the first time in the results, discussion, or conclusion section of the study.
-
-
Were the relevant outcomes measured with appropriate objective and/or subjective methods?
-
Yes: all relevant outcomes are measured with appropriate methods, which are described in the methods section. These measures might be objective (e.g. gold standard tests or standardised clinical tests), subjective (e.g. self-administered questionnaires, standardised forms, or patient symptoms interview forms), or both.
-
Unclear: it is unclear how the relevant outcomes were measured. No information is provided on the methods used to measure the study’s relevant outcomes.
-
No: the methods used to measure outcomes were inappropriate.
-
-
Were the relevant outcomes measured before and after the intervention?
-
Yes: the relevant outcomes are measured before and after applying the intervention.
-
Unclear: it is unclear when the outcomes were measured.
-
No: the study reported only outcomes measured after applying the intervention.
-
-
Was the study conducted prospectively?
-
Yes: it is clearly stated that the study was conducted prospectively.
-
Unclear: the design of the study is not mentioned or it is unclear if the study was conducted prospectively.
-
No: the authors clearly stated that it was a retrospective study.
-
-
Were the relevant outcomes assessed blinded to intervention status?
-
Yes: the relevant outcomes were analysed by individuals who were not aware of the intervention status.
-
Unclear: the study did not report whether the outcome assessors were aware of the intervention status.
-
No: it is clearly stated or obvious that the relevant outcomes were analysed by individuals who were aware of the intervention status.
-
-
Were the statistical tests used to assess the relevant outcomes appropriate?
-
Yes: the statistical tests are clearly described in the methods section of the study and are used appropriately (e.g. parametric test for normally distributed population vs. nonparametric test for non-Gaussian population). The reviewer should assign a yes score if no statistical analysis was performed but reasons for this were stated.
-
Unclear: the statistical tests are not described in the methods section of the study or there is no information about the statistical analysis.
-
No: the statistical tests were used inappropriately.
-
-
Was the length of follow-up reported?
-
Yes: the length of follow-up is clearly reported (mean, median, range, standard deviation).
-
Unclear: the duration of follow-up is not clearly reported.
-
No: the length of follow-up is not reported.
-
-
Was the loss to follow-up reported?
-
Yes: the number or proportion of participants lost to follow-up is clearly reported or authors report outcome results on all participants included initially, or number lost to follow-up can be subtracted from the number enrolled and number analysed.
-
Unclear: it is not clear from the information provided how many participants were lost to follow-up or it is an inconsistence of reporting lost to follow-up (e.g. discrepancies between information from tables and text).
-
No: the number or proportion of participants lost to follow-up is not reported.
-
-
Does the study provide estimates of the random variability in the data analysis of relevant outcomes?
-
Yes: the study reports estimates of the random variability (e.g. standard error, standard deviation, confidence interval for parametric data, and range and interquartile range for nonparametric data) for all relevant outcomes.
-
Unclear or partially reported: the presentation of the random variability is unclear (e.g. the measure of dispersion is reported without indicating if it is a standard deviation or standard error). Estimates of the random variability are not reported for all relevant outcomes.
-
No: the study does not report estimates of the random variability.
-
-
Are the adverse events related with the intervention reported?
-
Yes: the undesirable or unwanted consequences of the intervention during the study period or within a pre-specified time period are reported. The absence of adverse event(s) is acknowledged in the study.
-
Partially reported: it is deducible that only some but not all potential adverse events are reported.
-
No: there is no statement about the presence or absence of adverse events.
-
-
Are the conclusions of the study supported by results?
-
Yes: the conclusions of the study (in terms of patient, intervention, outcomes) are supported by the evidence presented in the results and discussion sections.
-
Partially reported: not all components of the patient, intervention, outcomes are supported by the evidence presented in the results and discussion section.
-
No: the conclusions are not supported by the evidence presented in the results and discussion section.
-
-
Are both competing interests and sources of support for the study reported?
-
Yes: both competing interests and sources of support (financial or other) received for the study are reported, or the absence of any competing interest and source of support is acknowledged.
-
Partially reported: only one of these elements is reported.
-
No: neither competing interests nor sources of support were reported.
-
Quality score for qualitative studies
One point for each endorsed statement based on judgement (total score = 0–87).
-
Findings: how credible are the findings?
-
Findings/conclusions are supported by data/study evidence (i.e. the reader can see how the researcher arrived at his/her conclusions; the ‘building blocks’ of analysis and interpretation are evident).
-
Findings/conclusions ‘make sense’/have a coherent logic.
-
Findings/conclusions are resonant with other knowledge and experience (this might include peer or member review).
-
Use of corroborating evidence to support or refine findings (i.e. other data sources have been used to examine phenomena; other research evidence has been evaluated: see also statement 14, Reporting: how clear are the links between data, interpretation and conclusions, i.e. how well can the route to any conclusions be seen?).
-
-
Findings: how has knowledge/understanding been extended by the research?
-
Literature review (where appropriate) summarising knowledge to date/key issues raised by previous research aims and design of study set in the context of existing knowledge/understanding; identifies new areas for investigation (for example, in relation to policy/practice/substantive theory).
-
Credible/clear discussion of how findings have contributed to knowledge and understanding (e.g. of the policy, programme or theory being reviewed); might be applied to new policy developments, practice or theory.
-
Findings presented or conceptualised in a way that offers new insights/alternative ways of thinking.
-
Discussion of limitations of evidence and what remains unknown/unclear or what further information/research is needed.
-
-
Findings: how well does the evaluation address its original aims and purpose?
-
Clear statement of study aims and objectives; reasons for any changes in objectives.
-
Findings clearly linked to the purposes of the study – and to the initiative or policy being studied.
-
Summary or conclusions directed towards aims of study.
-
Discussion of limitations of study in meeting aims (e.g. are there limitations because of restricted access to study settings or participants, gaps in the sample coverage, missed or unresolved areas of questioning; incomplete analysis; time constraints?).
-
-
Findings: scope for drawing wider inference – how well is this explained?
-
Discussion of what can be generalised to wider population from which sample is drawn/case selection has been made.
-
Detailed description of the contexts in which the study was conducted to allow applicability to other settings/contextual generalities to be assessed.
-
Discussion of how hypotheses/propositions/findings may relate to wider theory; consideration of rival explanations.
-
Evidence supplied to support claims for wider inference (either from study or from corroborating sources).
-
Discussion of limitations on drawing wider inference (e.g. re-examination of sample and any missing constituencies: analysis of restrictions of study settings for drawing wider inference).
-
-
Findings: how clear is the basis of evaluative appraisal?
-
Discussion of how assessments of effectiveness/evaluative judgements have been reached (i.e. whose judgements are they and on what basis have they been reached?).
-
Description of any formalised appraisal criteria used, when generated and how and by whom they have been applied.
-
Discussion of the nature and source of any divergence in evaluative appraisals.
-
Discussion of any unintended consequences of intervention, their impact and why they arose.
-
-
Design: how defensible is the research design?
-
Discussion of how overall research strategy was designed to meet aims of study.
-
Discussion of rationale for study design.
-
Convincing argument for different features of research design (e.g. reasons given for different components or stages of research; purpose of particular methods or data sources, multiple methods, time frames, etc.).
-
Use of different features of design/data sources evident in findings presented.
-
Discussion of limitations of research design and their implications for the study evidence.
-
-
Sample: how well defended is the sample design/target selection of cases/documents?
-
Description of study locations/areas and how and why chosen.
-
Description of population of interest and how sample selection relates to it (e.g. typical, extreme case, diverse constituencies, etc.).
-
Rationale for basis of selection of target sample/settings/documents (e.g. characteristics/features of target sample/settings/documents, basis for inclusions and exclusions, discussion of sample size/number of cases/setting selected, etc.).
-
Discussion of how sample/selections allowed required comparisons to be made.
-
-
Sample: sample composition/case inclusion – how well is the eventual coverage described?
-
Detailed profile of achieved sample/case coverage.
-
Maximising inclusion (e.g. language matching or translation; specialised recruitment; organised transport for group attendance).
-
Discussion of any missing coverage in achieved samples/cases and implications for study evidence (e.g. through comparison of target and achieved samples, comparison with population, etc.).
-
Documentation of reasons for non-participation among sample approached/non-inclusion of selected cases/documents.
-
Discussion of access and methods of approach and how these might have affected participation/coverage.
-
-
Data collection: how well was the data collection carried out?
-
Discussion of:
-
– who conducted data collection.
-
– procedures/documents used for collection/recording.
-
– checks on origin/status/authorship of documents.
-
-
Audio or video recording of interviews/discussions/conversations (if not recorded, were justifiable reasons given?).
-
Description of conventions for taking field notes (e.g. to identify what form of observations were required/to distinguish description from researcher commentary/analysis).
-
Discussion of how fieldwork methods or settings may have influenced data collected.
-
Demonstration, through portrayal and use of data, that depth, detail and richness were achieved in collection.
-
-
Analysis: how well has the approach to and formulation of the analysis been conveyed?
-
Description of form of original data (e.g. use of verbatim transcripts, observation or interview notes, documents, etc.).
-
Clear rationale for choice of data management method/tool/package Evidence of how descriptive analytic categories, classes, labels, etc., have been generated and used (i.e. either through explicit discussion or portrayal in the commentary).
-
Discussion, with examples, of how any constructed analytic concepts/typologies, etc. have been devised and applied.
-
Discussion, with examples, of how any constructed analytic concepts/typologies, etc., have been devised and applied.
-
-
Analysis: contexts of data sources – how well are they retained and portrayed?
-
Description of background or historical developments and social/organisational characteristics of study sites or settings.
-
Participants’ perspectives/observations placed in personal context (e.g. use of case studies/vignettes/individual profiles, textual extracts annotated with details of contributors).
-
Explanation of origins/history of written documents.
-
Use of data management methods that preserve context (i.e. facilitate within case description and analysis).
-
-
Analysis: how well has diversity of perspective and content been explored?
-
Discussion of contribution of sample design/case selection in generating diversity.
-
Description and illumination of diversity/multiple perspectives/alternative positions in the evidence displayed.
-
Evidence of attention to negative cases, outliers or exceptions.
-
Typologies/models of variation derived and discussed.
-
Examination of origins/influences on opposing or differing positions.
-
Identification of patterns of association/linkages with divergent positions/groups.
-
-
Analysis: how well has detail, depth and complexity (i.e. richness) of the data been conveyed?
-
Use and exploration of contributors’ terms, concepts and meanings.
-
Unpacking and portrayal of nuance/subtlety/intricacy within data.
-
Discussion of explicit and implicit explanations.
-
Detection of underlying factors/influences.
-
Identification and discussion of patterns of association/conceptual linkages within data.
-
Presentation of illuminating textual extracts/observations.
-
-
Reporting: how clear are the links between data, interpretation and conclusions, i.e. how well can the route to any conclusions be seen?
-
Clear conceptual links between analytic commentary and presentations of original data (i.e. commentary and cited data relate; there is an analytic context to cited data, not simply repeated description).
-
Discussion of how/why particular interpretation/significance is assigned to specific aspects of data – with illustrative extracts of original data.
-
Discussion of how explanations/theories/conclusions were derived – and how they relate to interpretations and content of original data (i.e. how warranted); whether alternative explanations explored.
-
Display of negative cases and how they lie outside main proposition/theory/hypothesis, etc.; or how proposition, etc. revised to include them.
-
-
Reporting: how clear and coherent is the reporting?
-
Demonstrates link to aims of study/research questions.
-
Provides a narrative/story or clearly constructed thematic account.
-
Has structure and signposting that usefully guide reader through the commentary.
-
Provides accessible information for intended target audience(s).
-
Key messages highlighted or summarised.
-
-
Reflexivity and neutrality: how clear are the assumptions/theoretical perspectives/values that have shaped the form and output of the evaluation?
-
Discussion/evidence of the main assumptions/hypotheses/theoretical ideas on which the evaluation was based and how these affected the form, coverage or output of the evaluation (the assumption here is that no research is undertaken without some underlying assumptions or theoretical ideas).
-
Discussion/evidence of the ideological perspectives/values/philosophies of research team and their impact on the methodological or substantive content of the evaluation (again, may not be explicitly stated).
-
Evidence of openness to new/alternative ways of viewing subject/theories/assumptions (e.g. discussion of learning/concepts/constructions that have emerged from the data; refinement and restatement of hypotheses/theories in light of emergent findings; evidence that alternative claims have been examined).
-
Discussion of how error or bias may have arisen in design/data collection/analysis and how addressed, if at all.
-
Reflections on the impact of the researcher on the research process.
-
-
Ethics: what evidence is there of attention to ethical issues?
-
Evidence of thoughtfulness/sensitivity about research contexts and participants.
-
Documentation of how research was presented in study settings/to participants (including, where relevant, any possible consequences of taking part).
-
Documentation of consent procedures and information provided to participants.
-
Discussion of confidentiality of data and procedures for protecting.
-
Discussion of how anonymity of participants/sources was protected.
-
Discussion of any measures to offer information/advice/services, etc. at end of study (i.e. where participation exposed the need for these).
-
Discussion of potential harm or difficulty through participation, and how avoided (guides, observation templates, data management frameworks, etc.).
-
-
Auditability: how adequately has the research process been documented?
-
Discussion of strengths and weaknesses of data sources and methods.
-
Documentation of changes made to design and reasons; implications for study coverage.
-
Documentation and reasons for changes in sample coverage/data collection/analytic approach; implications.
-
Reproduction of main study documents (e.g. letters of approach, topic guides, observation templates, data management frameworks, etc.).
-
Criteria for quantitative observational studies (0–34)
Published in Reisch JS, Tyson JE, Mize SG. Aid to the evaluation of therapeutic studies. Pediatrics 1989;84:815–27. 78
Appendix 15 Web address to full published protocol
URL: www.systematicreviewsjournal.com/content/pdf/2046-4053-2-15.pdf
Last accessed date: 5 March 2015
Appendix 16 List of papers rated as A: including intervention without evaluation or not transferable to UK
| First author and date | Reference | Reason for exclusion |
|---|---|---|
| Aggarwal (2012) | Hybridity and intersubjectivity in the clinical encounter: Impact on the Cultural Formulation. Transcult Psychiatry 2012:49:121–39 | Case study without evaluative conclusion |
| Bäärnhielm (2004) | Restructuring illness meaning through the clinical encounter: a process of disruption and coherence. Cult Med Psychiatr 2004;28:41–5 | Case study without evaluative conclusion |
| Bäärnhielm (2012) | The meaning of pain: a cultural formulation of a Syrian woman in Sweden. Transcult Psychiatry 2012;49:105–20 | Case study without evaluative conclusion |
| Baker (1999) | The importance of cultural sensitivity and therapist self-awareness when working with mandatory clients. Fam Process 1999;38:55–67 | No evaluation of intervention |
| Bucardo (2008) | Cultural formulation with attention to language and cultural dynamics in a mexican psychiatric patient treated in San Diego, California. Cult Med Psychiatr 2008;3:102–21 | Case study without evaluative conclusion |
| Chen (2008) | Multicultural competence and evidence-based practice in group therapy. J Clin Psychol 2008;64:1261–78 | No evaluation of intervention |
| Gone (2009) | A community-based treatment for Native American historical trauma: prospects for evidence-based practice. J Consult Clin Psychol 2009;77:751–62 | No evaluation of intervention, just description |
| Hinton (2012) | Adapting CBT for traumatized refugees and ethnic minority patients: examples from culturally adapted CBT (CA-CBT). Transcult Psychiatry 2012;49:340–65. | No evaluation of intervention |
| Rai-Atkins (2002) | Best practice in mental health advocacy for African, Caribbean and South Asian communities. URL: www.jrf.org.uk/sites/files/jrf/jr109-mental-health-advocacy.pdf | No evaluative conclusion |
| Rathod (2010) | Developing culturally sensitive cognitive behaviour therapy for psychosis for ethnic minority patients by exploration and incorporation of service users’ and health professionals' views and opinions. Behav Cogn Psychother 2010;38:511–33 | No evaluation of intervention |
| Siegel (2011) | Components of cultural competence in three mental health programs. Psychiatr Serv 2011;62:626–31 | No evaluation of intervention, just description |
| Sun-Kyung Shin (2004) | Effects of culturally relevant psychoeducation for Korean American families of persons with chronic mental illness. Res Soc Work Pract 2004;14:231–9 | There is cultural adaptation which is compared with social support, i.e. informs development of intervention but no relevant outcome data |
| Tol (2005) | Cultural challenges to psychosocial counselling in Nepal. Transcult Psychiatry 2005;42:317–33 | No evaluation of intervention, some case histories |
| Williams (2006) | Cultural considerations in using cognitive behaviour therapy with Chinese people: a case study of an elderly Chinese woman with generalised anxiety disorder. N Z J Psychol 2006;35:153–62 | Case study without evaluative conclusion |
| Yeung (1999) | The adaptation of solution-focused therapy in Chinese culture: a linguistic perspective. Transcult Psychiatry 1999;36:477–89 | No evaluation of intervention, use of a case study to illustrate an approach |
List of abbreviations
- ACT
- assertive community treatment
- ADHD
- attention deficit–hyperactivity disorder
- AMED
- Allied and Complementary Medicine Database
- ASSIA
- Applied Social Sciences Index and Abstracts
- BME
- black and minority ethnic
- CBT
- cognitive–behavioural therapy
- CCS
- cultural consultation service
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- DSM-V
- Diagnostic and Statistical Manual of Mental Illness–Fifth Edition
- EU
- European Union
- GP
- general practitioner
- HTA
- Health Technology Assessment
- IHE
- Institute of Health Economics
- IPT-B
- brief interpersonal psychotherapy
- MFPG
- Multi-Family Psycho-Education Group
- MRC
- Medical Research Council
- NATCEN
- National Centre for Social Research
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- PhD
- Doctor of Philosophy
- PHQ-9
- nine-item Patient Health Questionnaire
- PTSD
- post-traumatic stress disorder
- SSCI
- Social Science Citation Index
- TC
- therapeutic communication