Notes
Article history
This issue of Health Technology Assessment contains a project originally commissioned by the MRC but managed by the Efficacy and Mechanism Evaluation Programme. The EME programme was created as part of the National Institute for Health Research (NIHR) and the Medical Research Council (MRC) coordinated strategy for clinical trials. The EME programme is funded by the MRC and NIHR, with contributions from the CSO in Scotland and NISCHR in Wales and the HSC R&D, Public Health Agency in Northern Ireland. It is managed by the NIHR Evaluation, Trials and Studies Coordinating Centre (NETSCC) based at the University of Southampton.
The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from the material published in this report.
Declared competing interests of authors
Cathy Creswell was supported by a Medical Research Council Clinician Scientist Fellowship (G0601874).
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Creswell et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Scientific background
Anxiety disorders are among the most common psychological disorders in childhood, affecting 2.6–5.2% of children under the age of 12 years. 1,2 These disorders adversely affect children’s functioning in personal, social and academic domains,3,4 raise the risk for disorders in adolescence and adulthood,5 and carry a substantial health and social cost. 6 Following advances in the development of successful cognitive–behavioural therapies (CBTs) for adult anxiety disorders,7 CBT for child anxiety disorders has now been developed. Although there is still some uncertainty over the optimal form of such an intervention, recent systematic reviews of outcome research indicate that the general CBT approach produces significant therapeutic benefit in this patient group, with, on average, 59% of anxious children no longer meeting criteria for their primary anxiety disorder following CBT. 8 However, it is clear from these reviews, and from the individual treatment trials, that the outcome is highly variable, with a significant proportion (40.6%) of patients retaining their anxiety diagnoses following treatment. 8
Parental anxiety disorders are associated with poor treatment outcomes
One way of further improving children’s responses to treatment is to identify predictors of poor outcome which are amenable to therapeutic change. One of these is parental emotional distress, in particular parental anxiety disorder, which has been found to be associated with up to a 50% reduction in child recovery following treatment. 6,9–13 This is of great significance given that the rate of anxiety disorder among the parents of anxious children is raised. 14,15 Indeed, in a consecutive series of children referred for treatment of an anxiety disorder in our clinic, two-thirds of the mothers were found to have a current Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)16 anxiety disorder (with no elevated rate of current disorder among the fathers), almost three times the base rate. 17
Two studies to date have examined whether or not targeting parental anxiety might benefit child treatment outcome. Cobham and colleagues9 found that supplementing child cognitive–behavioural therapy (CCBT) with parent anxiety management was associated with significantly improved diagnostic outcomes for children with anxiety disorders whose parents had elevated trait anxiety; however, this group did not maintain a specific benefit from the parent anxiety management treatment at a 3-year follow-up. 18 More recently, Hudson and colleagues19 used a similar design but classified groups according to parental anxiety disorder status. In this study, CCBT + parent anxiety management did not confer a significant benefit over CCBT post teatment or at a 6-month follow-up assessment. Notably, both studies administered brief treatments for parental anxiety which did not have an overall impact on parental anxiety symptoms or disorder. The question therefore remains open as to whether or not successful treatment of parental anxiety might benefit child outcome.
Other mechanisms associated with poor outcomes
An alternative possibility is that it might not be parental anxiety, per se, that is prognostically significant for child response to treatment but, rather, the parenting practices associated with high levels of parental anxiety that themselves reinforce or maintain the child disorder. Specific parenting responses have been implicated in the maintenance of child anxiety, in particular an overcontrolling and overprotective parental style, expressed anxiety when the child is faced with challenge, 20,21 and associated parental cognitions and expectations about child competence. 22 These behaviours are known to obtain significantly more in anxious than in non-anxious parents of children with anxiety disorder,23,24 as are associated cognitions characterised by elevated expectations that the child will be frightened and feel out of control in the face of a challenge. 23 Recent studies have suggested that targeting parental anxiety may be pertinent only insofar as it changes behaviours that are likely to interfere with the child’s treatment. 25 These studies suggest, therefore, that targeting parenting cognitions and behaviours, rather than parental anxiety, may be of most benefit in bringing about improvement in anxious children’s response to treatment in the context of parental anxiety disorders.
Implications for optimal treatment outcomes
Cognitive–behavioural therapy treatments of child anxiety disorder commonly require the day-to-day prosecution of treatment regimes to be managed by the parent (e.g. parents are typically required to model positive responses to fear provoking stimuli and to prompt and reinforce their child’s positive responses), so it is likely that the parent’s own anxiety and the associated disturbances in parenting responses may militate against optimal treatment delivery. Although the CBT treatments developed to date for the treatment of child anxiety do acknowledge the importance of both parental anxiety and parenting,26–29 there has been no systematic evaluation of an intervention in which both parental anxiety and parenting responses are specifically addressed. There is, therefore, a need for the development and evaluation of a CBT treatment for child anxiety disorder in which parental anxiety and associated patterns of parental responses to the child are systematically targeted.
Rationale for the research
The outcome from CBT for children with anxiety disorders is highly variable. Major factors contributing to this are likely to be the presence of parental anxiety and associated disturbances in how parents respond to their children when they are faced with challenges. Where parental anxiety has been addressed in treatment research,26–29 for several methodological reasons, it has been difficult to assess its contribution to child outcome. Two studies have systematically targeted parental anxiety in the treatment of child anxiety disorders. In one,9 child anxiety outcome was better where therapeutic measures to address parental anxiety symptoms were included, and in the other19 children’s outcomes were not improved. In both cases, as the treatment did not significantly alter levels of parental anxiety, it remains unclear what aspect of the treatment effected the clinical improvement in the children. Similarly, where therapeutic measures to address parenting responses have been included,30 it has not been possible to determine the specific role of such measures in the complex treatment package employed. A controlled trial in which both factors – treatment of parental anxiety and measures to alter parenting responses – are systematically varied, would produce data of both clinical utility and scientific importance. The study was determined on this basis, and there was no patient or public input at this stage.
Although paternal behaviours are likely to contribute to the maintenance of child anxiety disorder, this study focused on mothers for the following reasons: (i) it has been suggested that the parental responses that may promote anxiety among children differ for mothers and fathers;31 (ii) anxiety disorders are more common among women than men32 and, also, more common among mothers of children with anxiety disorders than fathers;17 (iii) mothers are most commonly the primary caregiving parent in the study region and are more likely to attend treatment sessions for their child (e.g. in a recent study in the same region, 98% of parents nominated as primary caregivers in order to attend treatment were mothers33).
Aims
The aim of the trial was to establish the relative clinical effectiveness and cost-effectiveness of treatments of (i) maternal anxiety and (ii) key maternal parenting responses for children with anxiety disorders who have a mother with current anxiety disorder.
Research questions
In a randomised controlled trial (RCT) for child anxiety occurring in the context of maternal anxiety, the principal questions are:
-
Is the impact of CCBT enhanced by first providing CBT to the mother for her own anxiety?
-
Is the impact of CCBT enhanced by the addition of therapeutic measures designed to address potentially anxiogenic maternal parenting responses?
Secondary questions are:
-
Is sustained improvement in child anxiety significantly associated with a reduction in maternal anxiety?
-
Is sustained improvement in child anxiety significantly associated with improvements in maternal modelling, encouragement, overcontrolling/overprotective behaviour and associated cognitions?
Chapter 2 Trial design and methods
Study design
The trial was set up to evaluate the benefit of supplementing individual CCBT with either treatment of maternal anxiety disorder or treatment that targeted maternal responses when interacting with her child, for children with anxiety disorders whose mothers also had a current anxiety disorder. A three-arm trial was conducted in which children received individual CCBT in all three arms, supplemented by either CBT for the maternal anxiety disorder [CCBT + maternal cognitive–behavioural therapy (MCBT)] or a mother–child interaction (MCI) focused intervention. Non-specific interventions were also delivered in all treatment arms in order to balance therapist contact. The main trial was supplemented with an economic evaluation to consider the cost-effectiveness of the CCBT and MCI interventions.
Ethical approval and research governance
Ethical approval for the study was given by Berkshire Research Ethics Committee (07/H0505/156) and the University of Reading Research Ethics Committee (07/48). The trial was registered with the International Standard Randomised Controlled Trial Register under the reference number 19762288.
Participants
Participants were 211 children, aged 7–12 years [mean age 10.22 years, standard deviation (SD) 1.58], with a current anxiety disorder, together with their mothers. As noted above, the study focused on mothers as (i) intergenerational associations for anxiety disorders are most commonly found between mothers and their children;17 (ii) mothers are most commonly the primary caregivers in the study region; and (iii) paternal behaviours may have different associations with childhood anxiety. 34 Participants were all referred to Berkshire Child Anxiety Clinic, run jointly by Berkshire Healthcare NHS Foundation Trust and the University of Reading, by a health or educational professional. Participants were recruited between June 2008 and May 2011, with the last follow-up assessment in February 2013.
Inclusion criteria
Child
-
Age 7–12 years.
-
Primary diagnosis of DSM-IV generalised anxiety disorder (GAD), social phobia, separation anxiety disorder (SAD), panic disorder (PD)/agoraphobia or specific phobia (if comorbid with another anxiety disorder).
Mother
-
Primary carer.
-
Current maternal DSM-IV anxiety disorder.
Exclusion criteria
Participants were not eligible if any of the following criteria are met.
Child
-
Significant physical (where it would impede treatment delivery) or intellectual impairment (including autistic spectrum disorders) (determined by registration with local learning disability services).
-
Current prescription of psychotropic medication that had not been at a stable dose for at least 1 month and without agreement to maintain that dose throughout the study.
-
Previously received six or more sessions of systematically administered CBT for an anxiety disorder.
Mother
-
Significant intellectual impairment (determined by registration with local learning disability services).
-
Severe comorbid disorder (e.g. severe major depressive disorder, psychosis, substance/alcohol dependence that would interfere with the mothers ability to participate in treatment).
-
Prescription of psychotropic medication that had not been at a stable dose for at least 1 month and without agreement to maintain that dose throughout the study.
If participating mothers were having any ongoing treatment, this did not preclude them from participating in the trial, but ideally, any psychotherapeutic treatment should have finished prior to initiating this trial.
Six children were recruited to the trial (two in each treatment arm) who were assigned a primary diagnosis of anxiety disorder not otherwise specified. Following consultation with the trial management team it was decided to include these children as the anxiety disorder not otherwise specified diagnosis reflected a slight variation from meeting diagnostic criteria for GAD. One child was recruited to the trial (CCBT + MCI arm) on the basis of having a primary diagnosis of selective mutism; and in this case the trial management group agreed to inclusion as the selective mutism was comorbid with, and was considered to be a manifestation of, social anxiety disorder. Four children were outside the specified age range at the point of randomisation. One child was 6 years old but was due to turn the age of 7 years before initiating treatment (CCBT + MCI arm); three turned 13 years of age between the initial assessment and randomisation.
Recruitment procedure
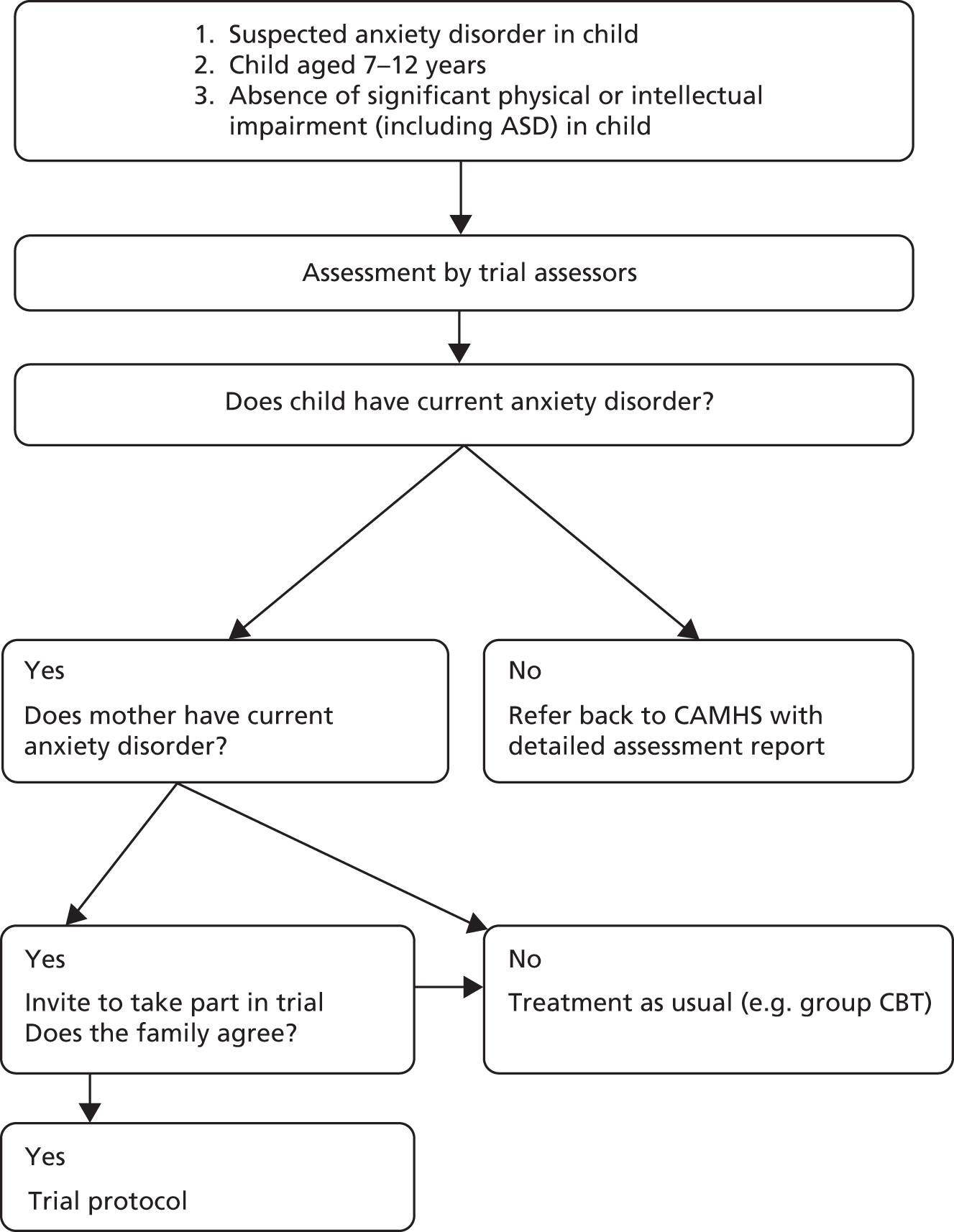
The recruitment schedule is shown in Figure 1.
FIGURE 1.
Flow chart outlining recruitment schedule. ASD, autistic spectrum disorder; CAMHS, Child and Adolescent Mental Health Services.
Informed consent
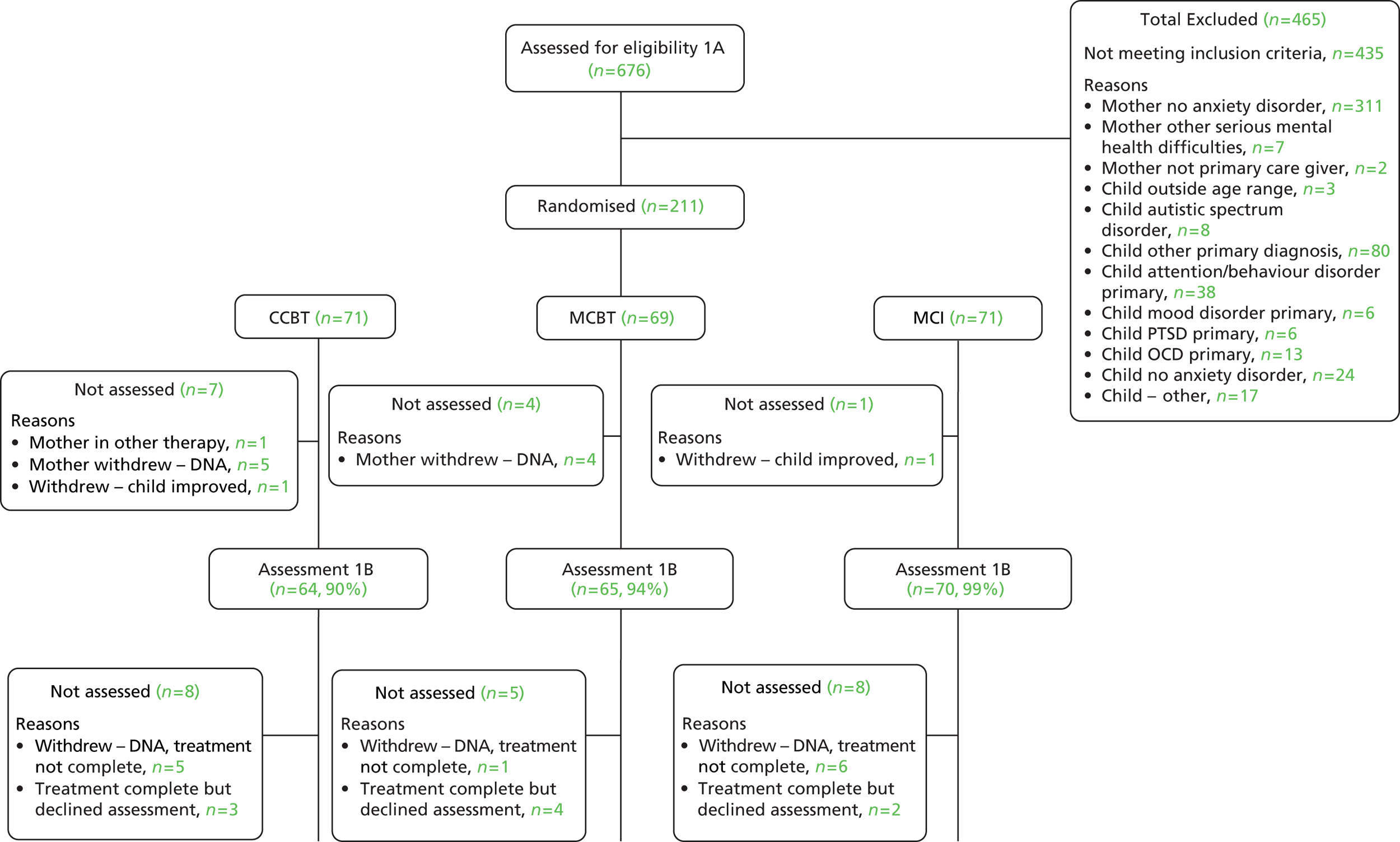
Participants were given a complete description of the study orally and in writing prior to written informed consent being obtained from participating mothers and assent from participating children. As shown in Figure 2, 676 children were referred and assessed for eligibility. A total of 435 families did not meet the inclusion criteria (24 children and 311 mothers because they did not meet criteria for a current anxiety disorder). Assent/consent was not given by 30 families.
FIGURE 2.
Consolidated Standards of Reporting Trials diagram. A3, assessment 3; A4, assessment 4. DNA, did not attend; OCD, obsessive–compulsive disorder; PTSD, post-traumatic stress disorder.

Randomisation, concealment and blinding
Participants were randomised to one of three treatment conditions: (i) CCBT; (ii) CCBT plus CBT for maternal anxiety disorder (CCBT + MCBT); or (iii) CCBT plus treatment focused on the MCI (CCBT + MCI). Each of the three conditions included non-specific therapeutic interventions to balance the treatment arms for therapist contact with both children and mothers. These were non-directive counselling (NDC; for mothers not receiving MCBT, i.e. groups i and iii) and a family health (FH) intervention (for those not receiving MCI, i.e. groups i and ii), see Table 1.
Randomisation was performed externally at the Centre for Statistics in Medicine (University of Oxford, UK) on receipt of anonymised participant information by fax. Patients were randomised with a 1 : 1 : 1 ratio and minimisation was used to ensure balanced allocation across the treatment groups for child age, gender and type of child anxiety disorder, and baseline severity of the child’s and mother’s primary anxiety disorder. The trial manager was informed of randomisation and allocated participants to therapists for treatment. All assessors and coders remained blind to treatment group for the duration of the study.
Treatment group allocation
The order of treatment delivery is shown in Table 1. MCBT/NDC was delivered first, then the CCBT and MCI/FH interventions were delivered in parallel. Each phase of treatment (MCBT/NDC, CCBT, MCI/FH) was delivered by a different therapist.
| Condition | CCBT | CCBT + MCBT | CCBT + MCI |
|---|---|---|---|
| Assessment 1: pre treatment | Diagnostic assessment (mother and child) + laboratory observation of MCI | ||
| Treatment 1 | NDC (8) | MCBT (8) | NDC (2) |
| Assessment 1B: mid-treatment (number of sessions) | Diagnostic assessment (mother and child) | ||
| Treatment 2 (number of sessions) | CCBT (8) + FH (mother: 2; child + mother: 2) | CCBT (8) + FH (mother: 2; child + mother: 2) | CCBT (8) + MCI (mother: 8; child + mother: 2) |
| Assessment 2: post treatment | Diagnostic assessment (mother and child) + laboratory observation of MCI | ||
| Assessment 3: 6 months post treatment | Diagnostic assessment (child) | ||
| Assessment 4: 12 months post treatment | Diagnostic assessment (child) | ||
| Total therapy sessions | Mother: 10 Child: 8 Child + mother: 2 |
Mother: 10 Child: 8 Child + mother: 2 |
Mother: 10 Child: 8 Child + mother: 2 |
Child cognitive–behavioural therapy
All children, in all treatment arms, received eight 1-hour weekly sessions of individual CBT delivered by 1 of 10 qualified clinical psychologists or cognitive–behaviour therapists (graduate therapists who held postgraduate certificates/diplomas in CBT), following a manual adapted from the widely used ‘Cool Kids’ programme35 to be used on an individual rather than group basis. Core components of the treatment include psychoeducation, identification and modification of anxious thoughts, and graded exposure to feared situations/stimuli. The adaptations involved reducing the number of sessions to eight (from nine) as the content could be covered more quickly on an individual basis, and altering exercises and practices so that they worked well on an individual basis using strategies from the ‘Coping Cat’ programme. 36 Sessions took place in the participants’ local Child and Adolescent Mental Health Services (CAMHS), at the University of Reading Child Anxiety Clinic or within the child’s home. The focus of treatment was on helping children to identify and challenge negative thinking styles, gradually increase exposure to feared stimuli and develop problem-solving skills. Mothers were included briefly in giving and receiving feedback at the beginning and end of each session (for approximately 5 minutes). To ensure therapist adherence to the CCBT treatment manual was equivalent across condition, 75 treatment sessions (25 from each condition) were rated for adherence to the manual (in terms of therapist stance, coverage of general and specific content) by blind raters (minimum Bachelor of Science psychology) trained to acceptable levels of reliability [therapist stance: intraclass correlation (ICC) = 0.76–76; general content: ICC = 0.73–0.82; specific content: ICC = 0.81–0.89]. Treatment adherence for CCBT did not differ across the three conditions [therapist stance: F(2,72) = 1.83, p = 0.17; general content: F(2,72) = 0.80, p = 0.92; specific content: F(2,72) = 0.23, p = 0.80].
Maternal cognitive–behavioural therapy
Maternal cognitive–behavioural therapy consisted of eight 1-hour weekly sessions delivered by one of seven clinical psychologists or cognitive–behaviour therapists (all supervised by a highly experienced clinical psychologist who was a British Association of Behavioural & Cognitive Psychotherapies-accredited cognitive–behaviour therapist) following a manualised transdiagnostic treatment for adult anxiety disorders. 37 A transdiagnostic approach was applied on the basis that mothers presented with various anxiety disorders; the effectiveness of a transdiagnostic approach to anxiety disorders has been established in similar contexts. 38 This treatment used cognitive–behavioural methods to reverse the putative maintaining mechanisms identified through individual formulation. Treatment was delivered in the participants’ local CAMHS, at the University of Reading Child Anxiety Clinic or within the family’s home.
Groups that did not receive MCBT received a non-specific intervention (NDC), in which mothers received a supportive individual intervention that was not focused specifically on reducing symptoms of anxiety but involved supportive non-directive listening for clients to facilitate self-reflection and to clarify and focus on feelings within an accepting, non-judgemental, empathic environment, following the manual of Borkovec and Costello. 39 NDC was provided by one of five qualified counsellors (all accredited by the British Association for Counselling & Psychotherapy), supervised by a highly experienced counsellor/psychotherapist with senior British Association for Counselling & Psychotherapy accreditation. 39 To ensure fidelity of the two treatments, the content of therapist utterances from 100 treatment sessions (50 MCBT, 50 NDC) was allocated by independent raters (psychology graduates), trained to a high level of reliability, to categories considered as allowed or not allowed within each treatment condition (reliability of proportion of allowable utterances, MCBT ICC = 0.73; NDC, ICC = 0.73). The proportion of MCBT allowable utterances was significantly higher in MCBT than in NDC [t(98) = 6.25; p < 0.001] and the proportion of NDC allowable utterances was significantly higher in NDC than in MCBT [t(98) = 4.40; p < 0.001], indicating that the content of the two treatments differed as intended. As shown in Table 1, MCBT and NDC were delivered first, before the delivery of CCBT.
Mother–child interaction treatment
The MCI intervention consisted of 10 sessions delivered over 8 weeks by one of seven qualified clinical psychologists or cognitive–behaviour therapists (supervised by an experienced clinical psychologist): eight sessions were with the mother alone and two were with the mother and child together. This was a novel intervention designed to target potentially anxiogenic maternal parenting behaviours. Specifically, it aimed to enhance maternal autonomy promoting cognitions (such as confidence in her child’s ability to face challenge) and behaviours and reduce potentially anxiogenic behaviours. This was achieved through a combination of specific strategies from existing family interventions for childhood anxiety,30,35 with the addition of video-feedback techniques developed and piloted by the trial investigators. 40,41 Sessions took place in the participants’ local CAMHS, at the University of Reading Child Anxiety Clinic or within the family’s home. The two mother and child sessions were conducted within the laboratory at the University of Reading, as these involved the mother and child completing structured tasks which were video-recorded for feedback purposes.
To balance therapist contact, those groups that did not receive the MCI intervention received sessions that focused on the promotion of a healthy lifestyle (see Table 1). A manual was developed for this intervention that principally focused on following a healthy diet and participating in regular exercise using a number of worksheets, games and activities based on existing interventions applied within school settings (FH). 42–54 The FH intervention was delivered by 1 of 10 therapists [qualified clinical psychologists, cognitive–behaviour therapists and one psychology graduate (Bachelor of Science) with extensive experience of delivering behavioural interventions, under supervision of an experienced clinical psychologist (LW)].
Mother–child interaction/FH were delivered in parallel with CCBT for all participants. To ensure treatment fidelity, raters who were blind to treatment condition rated audio-recordings of 40 therapy sessions on the degree to which session content focused on the MCI or FH. Inter-rater reliability was excellent (ICC = 0.98). MCI sessions were rated significantly higher than FH sessions on the degree to which sessions focused on MCI (Mann–Whitney U-test = 6.01; p < 0.0001), and FH sessions were rated significantly higher on the degree to which session focused on FH (Mann–Whitney U-test = 5.90; p < 0.0001) indicating that the content of the two treatments differed as intended.
Data collection and management
Trial data were entered into an International Business Machine Corporation Statistical Package for the Social Sciences database (IBM SPSS, version 17; IBM Corporation, Armonk, NY, USA) and monitoring and tracking information was entered onto a Microsoft Access 2003 database (Microsoft Corporation, Redmond, WA, USA). A range of data validation checks were carried out in Access, SPSS and Stata Software Release 12 (StataCorp LP, College Station, TX, USA) to minimise erroneous or missing data.
Assessments of maternal anxiety disorder and parenting were made before and immediately following the interventions. Assessments of child anxiety disorder status and severity were conducted before and following treatment, as well as at 6 and 12 months after treatment. All assessors were blind to treatment group allocation throughout the trial.
Baseline assessment
Baseline assessment for the trial comprised diagnostic interviews conducted with children and their mothers to ascertain whether or not both the child and his/her mother met diagnostic criteria for a current anxiety disorder. All of the follow-up measures were also administered at baseline. All baseline assessments were conducted between May 2008 and May 2011.
Follow-up
As shown in Table 1, follow-up data collection was scheduled to take place ‘mid-treatment’ [i.e. after the initial maternal intervention, MCBT/NDC (assessment 1B)], then ‘post treatment’ [i.e. after the CCBT and MCI/FH intervention (assessment 2)], and 6 and 12 months from the post-treatment assessment. Diagnostic assessments were conducted to establish whether or not interventions had successfully altered maternal anxiety at the ‘mid-treatment’ (1B) and ‘post-treatment’ (2) assessments. To establish whether or not the interventions had successfully altered maternal responses, observational and parent-reported measures were administered at the ‘post-treatment’ assessment. Child diagnostic and symptom outcomes were assessed at all time points.
All follow-up data were collected between September 2008 and February 2013. A flow chart showing all recruitment and retention is given in Figure 2.
Measures
Primary outcomes
The primary outcomes were (i) the status of the child’s primary anxiety disorder and (ii) the extent of child improvement at the post-treatment assessment. This second primary outcome was added to the primary outcomes identified in the original protocol following its inclusion as the primary outcome in a recent major multicentre trial for the treatment of anxiety disorders,55 with approval from the Trial Steering Committee (TSC).
Structured diagnostic interviews with children and parents
Children were assigned diagnoses on the basis of the Anxiety Disorder Interview Schedule for DSM-IV for children, child and parent versions (Anxiety Disorders Interview Schedule – child and parent report; ADIS-C/P). 56 For the ADIS-C/P, as is standard, overall diagnoses and clinical severity ratings (CSRs) were assigned if the child met diagnostic criteria on the basis of either the child or parent report, and the higher CSR of the two was taken. Following convention, only those with a CSR of ≥ 4 (moderate psychopathology) on a scale from 0 (complete absence of psychopathology) to 8 (severe psychopathology) were considered to meet diagnostic criteria. The assessors, all psychology graduates, were trained to administer and score the ADIS-C/P through verbal instruction, listening to assessment audio-recordings, role-play and participating in diagnostic consensus discussions. Each of the assessor’s first 20 interviews were discussed with a consensus team, led by a consultant clinical psychologist (LW). The assessor and the consensus team independently allocated diagnoses and CSRs. Once assessors achieved reliability of at least 0.85, they discussed one in six interviews with the consensus team (to prevent rater drift). Reliability for presence or absence of child diagnosis on the ADIS-C/P was κ = 0.98 (child report) and κ = 0.98 (mother report), and CSR ICC = 0.99 (child report) and CSR ICC = 0.99 (mother report).
Clinical Global Impression – Improvement scale57
Overall improvement in child anxiety was assessed using the Clinical Global Impression – Improvement (CGI-I) scale, a 7-point scale from 1 = very much improved to 7 = very much worse; scores of 1 and 2 are accepted to represent treatment success. Inter-rater reliability was established using the same procedures as for the ADIS-C/P. Overall mean inter-rater reliability for the assessment team was high (ICC = 0.96).
Secondary outcomes
Maternal anxiety and maternal interactive responses were assessed to establish whether or not MCI and MCBT effectively changed these factors. Secondary outcomes included (i) the severity of the child’s primary anxiety diagnosis; (ii) if the child was or was not free of all of their anxiety diagnoses (as assessed by the ADIS-C/P above); (iii) child- and mother-reported child anxiety symptoms and impact and comorbid difficulties; and (iv) teacher-reported symptoms of anxiety and adjustment to school at the post-treatment assessment. Finally, outcomes included all of the primary and secondary measures at the 6- and 12-month follow-up assessments.
Maternal anxiety disorder
The presence or absence of a current maternal anxiety disorder was assigned on the basis of the ADIS-IV,58 a structured diagnostic assessment designed to assess the presence and severity of DSM-IV anxiety, mood and somatoform disorders. CSRs for each disorder present are made and range from 0 (not at all severe) to 8 (extremely severe/distressing). A rating of 4 is considered to be the cut-off for a clinically significant disorder. Procedures for training assessors and ensuring inter-rater reliability followed those of the ADIS-C/P. Reliability for presence or absence of maternal diagnosis on the ADIS-IV was κ = 0.97; and for the CSR ICC = 0.99.
Maternal symptoms of anxiety and depression
The Depression Anxiety Stress Scale (DASS-21)59 was administered to all participating mothers to assess self-reported symptoms. The DASS-21 has demonstrated good internal consistency and concurrent validity. 60 Maternal symptoms of worry were assessed using the Penn State Worry Questionnaire (PSWQ),61 a 16-item self-report inventory designed to assess the pathological worry characteristic of GAD. Maternal symptoms of social anxiety were also measured using the Social Interaction Anxiety Scale (SIAS) and the Social Phobia Scale (SPS). 62 The SIAS is a 20-item self-report inventory designed to assess anxiety experienced while interacting with others. The SPS is a 20-item self-report inventory designed to assess fear of scrutiny when performing a task or being observed by others. Internal reliability for the scales was good across assessment time points (DASS-21 anxiety α = 0.80–0.87; DASS-21 depression α = 0.90–0.92; PSWQ α = 0.92–0.93; SIAS α = 0.92–0.93; SPS α = 0.91–0.94).
Maternal parenting and parental expectations
Maternal behaviours in interaction with the child was assessed by laboratory observation under conditions of mild social, performance and physical threat. 23 The social threat task involved the child preparing and delivering a speech to a research assistant with a hand-held video camera with their mother’s support. The performance task involved the child attempting difficult tangram puzzles following the procedure of Hudson and Rapee. 63 The physical threat task required children to investigate the content of four chambers within a mysterious ‘black box’. To account for prior experience, the assessment was modified at the post-treatment assessment point; for social stress the child was required to present to a panel rather than a single research assistant, the tangram puzzles were more difficult and the black box was accompanied by sound effects (e.g. rustling/scratching).
Observers who were blind to treatment condition coded parental behaviours on scales developed by Murray and colleagues64 and adapted by Creswell and colleagues23 to be suitable for children aged 7–12 years and for the specific tasks. Ratings were given for each minute of the interaction on 5-point scales (1 = none, 5 = pervasive/strong). As interactions varied somewhat in duration, mean scores for each task were summed to give total scores across the full range of tasks. For the current study the following behaviours were considered: maternal expressed anxiety; control (overprotection and intrusiveness); positivity (warmth and encouragement); promotion of avoidance; and the general quality of the relationship. See Table 2 for a description of each type of parenting behaviour. For each coder, in each task, a second coder independently scored a random sample of 25 videotapes. ICCs showed good agreement across all indices (range 0.60–1.00; mean 72). The constructs of encouragement and warmth overlap and these scales correlated highly (p = 0.56–0.58) so were combined to form as single measure of ‘positive behaviours’.
| Negative behaviour | |
|---|---|
| Expressed anxiety | Modelling of anxiety: anxiety in facial expression (e.g. fearful expression, biting lip), body movements (e.g. rigid posture, wringing hands), and speech (e.g. rapid, nervous, or inhibited) |
| Overprotection | Initiates emotional and/or practical support that is not required (stroking/kissing/offering unnecessary help while child manages independently) |
| Intrusiveness | Interferes, verbally or physically, cutting across child behaviour, attempts to take over and impose own agenda |
| Promotion of avoidance | Actively encourages/supports child avoidance of task (e.g. saying ‘you don’t have to do it’) |
| Positive behaviour | |
| Encouragement (autonomy–promotion) | Provides positive motivation to child to engage in the task, showing enthusiasm regarding both task and child capacity/efforts |
| Warmth | Affectionate, expresses positive regard for child, both verbally and physically |
| Quality of relationship | Sense of relatedness and mutual engagement between mother and child (e.g. talking, listening, laughing and joking with each other) |
Mothers also completed the parental overprotection measure (OP)65 to assess parenting behaviours that restrict a child’s exposure to perceived threat or harm (e.g. ‘when playing in the park I keep my child within a close distance of me’). This parent-reported measure has been found to correlate significantly with observations of parent behaviours,65,66 and has been found to be reliable and valid for children aged 7–12 years. 66 Internal consistency was good across the assessment time points (α = 0.87–0.89).
Maternal expectations were assessed before initiating the challenge tasks. Immediately after receiving the instructions for each task, mothers were taken to a separate room where they were asked to provide ratings regarding their child’s response. 23 In the current study we were interested in their responses regarding (a) how their child would feel about doing the task (0 not scared at all, 10 extremely scared); (b) how they would feel while their child was doing the task (0 not anxious at all, 10 extremely anxious); (c) how much their child could do about how the task went (0 nothing at all, 10 a lot); and (d) how much they could do about their child’s feelings and behaviours during the task (0 nothing at all, 10 a lot). Ratings were combined across the three tasks to represent their expectations across a range of challenge contexts.
Symptoms of child anxiety
The Spence Child Anxiety Scale (SCAS)29,67 assessed child- and parent-reported child anxiety symptoms. The child version [Spence Child Anxiety Scale – child report (SCAS-c)] requires children to rate how often they experience each of 38 anxiety symptoms, presented alongside six positive filler items. The SCAS-c and Spence Child Anxiety Scale – parent report (SCAS-p) have demonstrated high internal reliability and concurrent validity with other well-known anxiety measures. 29,67
Impact of child anxiety
The Child Anxiety Impact Scale (CAIS) was used to measure the extent to which anxiety interferes in a child’s life. 68 The Child Anxiety Impact Scale – child report (CAIS-c) and Child Anxiety Impact Scale – parent report (CAIS-p) covers three psychosocial domains (school, social activities and family functioning) and consists of 34 items, each rated on a 4-point scale to indicate how much anxiety has caused problems (not at all, just a little, pretty much, very much). The CAIS-c and CAIS-p have demonstrated good reliability and validity. 68,69
Symptoms of child comorbid difficulties
The Short Mood and Feelings Questionnaire (SMFQ)70 assessed child- and parent-reported symptoms of child low mood. The Short Mood and Feelings Questionnaire – child report (SMFQ-c) and Short Mood and Feelings Questionnaire – parent report (SMFQ-p) are brief, 13-item measures which require children or parents to report how often in the past 2 weeks they have experienced a number of symptoms. The SMFQ-c has demonstrated high internal reliability and concurrent validity with other well-known measures of symptoms of depression. 70 The conduct problems scale from the Strengths and Difficulties Questionnaire (SDQ)71 was used to assess child- and parent-reported behavioural disturbance. The Strengths and Difficulties Questionnaire – child report (SDQ-c) and Strengths and Difficulties Questionnaire – parent report (SDQ-p) are known to have good psychometric properties and scores correlate highly with other well-known scales. 71
Internal reliability for all these scales was good across assessment time points (SCAS-c α = 0.92–0.94; SCAS-p α = 0.88–0.93; CAIS-p α = 0.69–0.91; SMFQ-c α = 0.89–0.94; SMFQ-p α = 0.90–0.93), with the exception of the SDQ conduct scales where internal reliability was marginal (SDQ-p α = 0.54–0.68; SDQ-c α = 0.55–0.69), although this may reflect the relatively low number of items, and the CAIS-c at the initial assessment (α = 0.52), although for this scale internal reliability was higher at subsequent assessments (α = 0.88–0.96).
Teacher-reported child symptoms and adjustment
Teacher reports were collected in an attempt to provide an objective assessment of child adjustment in the school domain before and after treatment. To assess teacher perceptions of child anxiety symptoms they completed an adapted version of the SCAS (Spence Child Anxiety Scale – teacher report; SCAS-t). This comprised the 30 items that it was felt that teachers would be in a position to comment on (i.e. removing items about, for example, sleep, heights, animal fears). Teachers also completed the conduct scale of the parent/teacher report form of the SDQ (Strengths and Difficulties Questionnaire – teacher report; SDQ-t)71 which comprised five items. Finally, teachers completed a new measure of the child’s adjustment to school (Child Adjustment to School – teacher report; CAS-t), which focused on avoidance or worry about common school-based activities, such as showing things to the class, participating in group activities, speaking to the teacher. This comprised eight items that were rated on a 3-point scale from 0 (not true) to 2 (certainly true), see Appendix 4. Internal reliability for all these scales was acceptable across assessment time points (SCAS-t α = 0.91–0.96; SDQ-t α = 0.64–0.78; CAS-t α = 0.89–0.92).
Sample size
The study was powered to provide 90% power at the 5% (two-sided) significance level to detect a 30% difference in the proportion of children who recovered from their primary anxiety disorder post treatment in the CCBT + MCI or CCBT + MCBT conditions compared with the CCBT condition, with an estimated remission rate for the CCBT group of 40%. 9 Although the effects of the non-specific treatment on child outcomes were not clear, using the 40% remission rate from Cobham and colleagues9 was considered reasonable to account for the effect of CCBT plus any non-specific intervention, given the substantially briefer form of CCBT delivered in the current trial.
A difference of 30% in the proportion of anxiety-free children following completion of the treatment was considered to be the minimum that would be clinically worthwhile taking into account the increased resources required and change to service delivery that would be required if either of these interventions were found to be effective and implemented in practice. The required sample size of 56 children per group was increased to allow for an estimated 20% loss to follow-up. The sample size was estimated as if two independent trials were conducted, with no adjustment for multiple testing, as recommended by Machin and colleagues. 72
Statistical analysis
A comprehensive statistical analysis plan was prepared before embarking on the analysis. All primary and secondary analyses, apart from the per-protocol (PP) sensitivity analyses, were conducted on the intention-to-treat (ITT) population. The primary end points (recovery from primary diagnosis and overall improvement in anxiety (CGI-I ratings) at post treatment and other binary end points were analysed using a modified Poisson regression approach with robust error variance adjusting for the minimisation factors [child age, child gender, type of child anxiety disorder (GAD, social phobia, SAD, other)], baseline severity of the child’s and the mother’s primary anxiety disorder (ADIS-IV CSR). The modified Poisson regression approach described by Zou73 is an alternative to logistic regression which allows for estimation of risks ratios (RRs) rather than odds ratios. Sensitivity analyses of the primary end points included (i) no adjustment for minimisation criteria; (ii) PP population (this included those participants who had received at least half of the treatment sessions and had data for the post-treatment assessments, with the exception of one mother in the MCBT condition who also received the MCI intervention in error, rather than the FH control; data from this family was also removed for the PP analyses); and (iii) multiple imputation analysis. Missing data for the primary end points were multiply imputed by chained equations methods. 74 All results from sensitivity analyses were very similar to the primary results. Interim analyses were conducted by the trial statistician when 156 participants had been recruited following a request from the funders. The interim results were kept confidential from the trial manager, all assessors, therapists and their supervisors.
Questionnaire scores, maternal behaviours and maternal cognitions were modelled using linear regression models with the change from baseline as the dependent variable, adjusted for baseline score and minimisation factors. There were outliers present in some of the regression models; however, these were reviewed and were not considered to be due to incorrect completion of the questionnaires. Furthermore, their removal did not change the conclusions from the regression.
All analyses were conducted using Stata software.
Chapter 3 Trial results
Patient flow and numbers analysed
Patient flow is shown in Figure 2. The number of available participants for each treatment arm were as follows:
-
post treatment: CCBT n = 56 (79%), CCBT + MCBT n = 60 (87%), CCBT + MCI n = 62 (87%)
-
6 months post treatment: CCBT n = 49 (69%), CCBT + MCBT n = 53 (77%), CCBT + MCI n = 51 (72%)
-
12 months post treatment: CCBT n = 43 (61%), CCBT + MCBT n = 50 (70%), CCBT + MCI n = 46 (65%).
Baseline data
Baseline characteristics were well balanced across treatment groups (Table 3).
| Baseline characteristic | Category | CCBT, n (%) | CCBT + MCBT, n (%) | CCBT + MCI, n (%) |
|---|---|---|---|---|
| Child ethnicity | White British | 67 (94.4) | 58 (84.1) | 55 (77.5) |
| White Irish | 1 (1.4) | 1 (1.4) | ||
| Any other white background | 5 (7.2) | 7 (9.9) | ||
| White and black Caribbean | 1 (1.4) | |||
| White and black African | 1 (1.4) | |||
| White and Asian | 2 (2.9) | |||
| Any other mixed background | 1 (1.4) | |||
| Indian | 1 (1.4) | |||
| Pakistani | 2 (2.9) | 1 (1.4) | ||
| Any other Asian background | 1 (1.4) | 2 (2.8) | ||
| Caribbean | 1 (1.4) | |||
| Any other ethnic group | 1 (1.4) | |||
| Did not wish to state ethnicity | 1 (1.4) | |||
| Not recorded | 1 (1.4) | 1 (1.4) | ||
| Child gender | Male | 34 (47.9) | 35 (50.7) | 32 (45.1) |
| Female | 37 (52.1) | 34 (49.3) | 39 (54.9) | |
| Martial status | Single, never married | 2 (2.8) | 5 (7.2) | 5 (7.0) |
| Married (first time) | 28 (39.4) | 41 (59.4) | 38 (53.5) | |
| Remarried | 8 (11.3) | 3 (4.3) | 5 (7.0) | |
| Divorce/separated | 21 (29.6) | 11 (15.9) | 12 (16.9) | |
| Living with partner | 11 (15.5) | 9 (13.0) | 8 (11.3) | |
| Not recorded | 1 (1.4) | 3 (4.2) | ||
| Employment mother | Unemployed | 21 (29.6) | 23 (33.3) | 18 (25.4) |
| Part time | 33 (46.5) | 33 (47.8) | 37 (52.1) | |
| Full time | 14 (19.7) | 8 (11.6) | 13 (18.3) | |
| Not recorded | 3 (4.2) | 5 (7.2) | 3 (4.2) | |
| Employment father | Unemployed | 1 (1.4) | 6 (8.7) | 5 (7.0) |
| Part time | 1 (1.4) | 1 (1.4) | ||
| Full time | 50 (70.4) | 50 (72.5) | 53 (74.6) | |
| NA | 5 (7.0) | 1 (1.4) | 1 (1.4) | |
| Not recorded | 15 (21.1) | 11 (15.9) | 11 (15.5) | |
| Overall SES | Higher professional | 29 (40.8) | 39 (56.5) | 38 (53.5) |
| Other employed | 29 (40.8) | 16 (23.2) | 26 (36.6) | |
| Unemployed | 2 (2.8) | 1 (1.4) | ||
| Not recorded | 11 (15.5) | 14 (20.3) | 6 (8.5) | |
| Mother education | School completion | 21 (31.3) | 11 (17.7) | 22 (33.9) |
| Further education | 34 (50.8) | 32 (51.6) | 27 (41.5) | |
| Higher education | 7 (10.5) | 12 (19.4) | 12 (18.5) | |
| Postgraduate qualification | 5 (7.5) | 7 (11.3) | 4 (6.2) | |
| Father education | School completion | 17 (34.7) | 12 (22.6) | 23 (39.7) |
| Further education | 17 (34.7) | 20 (37.7) | 20 (34.5) | |
| Higher education | 9 (18.4) | 15 (28.3) | 11 (19.0) | |
| Postgraduate qualification | 6 (12.2) | 6 (11.3) | 4 (6.9) | |
| Child ADIS-C/P primary diagnosis | SAD | 19 (26.8) | 16 (23.2) | 21 (29.6) |
| Social phobia | 16 (22.5) | 18 (26.1) | 14 (19.7) | |
| GAD | 22 (31.0) | 20 (29.0) | 24 (33.8) | |
| Other | 14 (19.7) | 15 (21.7) | 12 (16.9) | |
| Specific phobia | 8 (11.3) | 11 (15.8) | 5 (7.0) | |
| PD without agoraphobia | 1 (1.4) | |||
| PD with agoraphobia | 1 (1.4) | |||
| Agoraphobia without PD | 3 (4.2) | 2 (2.9) | 3 (4.2) | |
| Selective mutism | 1 (1.4) | |||
| Anxiety disorder not otherwise specified | 2 (2.8) | 2 (2.9) | 2 (2.8) | |
| Child ADIS-C/P primary diagnosis CSR | Moderate 4 | 6 (8.5) | 5 (7.2) | 5 (7.0) |
| Moderate 5 | 21 (29.6) | 19 (27.5) | 19 (26.8) | |
| Severe 6 | 36 (50.7) | 37 (53.6) | 40 (56.3) | |
| Severe 7 | 8 (11.3) | 8 (11.6) | 7 (9.9) | |
| Child mood disorder (major depressive disorder/dysthymia) | No diagnosis | 62 (87.3) | 62 (89.9) | 67 (94.4) |
| Diagnosis | 9 (12.7) | 7 (10.1) | 4 (5.6) | |
| Child age (years) | 6 | 1 (1.4) | ||
| 7 | 4 (5.6) | 5 (7.2) | 7 (9.9) | |
| 8 | 12 (16.9) | 7 (10.1) | 13 (18.3) | |
| 9 | 9 (12.7) | 12 (17.4) | 12 (16.9) | |
| 10 | 17 (23.9) | 17 (24.6) | 13 (18.3) | |
| 11 | 18 (25.4) | 16 (23.2) | 13 (18.3) | |
| 12 | 10 (14.1) | 11 (15.9) | 11 (15.5) | |
| 13 | 1 (1.4) | 2 (2.8) | ||
| Mother’s ADIS-IV primary disorder | Specific phobia | 12 (16.9) | 17 (24.6) | 9 (12.7) |
| GAD | 37 (52.1) | 35 (50.7) | 40 (56.3) | |
| Social phobia | 9 (12.7) | 14 (20.3) | 11 (15.5) | |
| PD | 1 (1.4) | 1 (1.4) | ||
| Agoraphobia | 2 (2.8) | 1 (1.4) | 2 (2.8) | |
| OCD | 1 (1.4) | |||
| PTSD | 1 (1.4) | |||
| Major depressive disorder | 5 (7.0) | |||
| Hypochondriasis | 2 (2.8) | |||
| Anxiety disorder not otherwise specified | 1 (1.4) | 2 (2.9) | 8 (11.3) | |
| Mother ADIS-IV CSR of primary disorder | Moderate 4 | 20 (28.2) | 18 (26.1) | 18 (25.4) |
| Moderate 5 | 22 (31.0) | 25 (36.2) | 21 (29.6) | |
| Severe 6 | 22 (31.0) | 22 (31.9) | 24 (33.8) | |
| Severe 7 | 6 (8.5) | 4 (5.8) | 8 (11.3) | |
| Very severe 8 | 1 (1.4) | |||
| Mother mood disorder (major depressive disorder/dysthymia) | No diagnosis | 57 (80.3) | 58 (84.1) | 56 (78.9) |
| Diagnosis | 14 (19.7) | 11 (15.9) | 15 (21.1) |
Manipulation checks: effects of the interventions on maternal anxiety and responses
Manipulation checks were conducted to evaluate whether or not the MCBT and MCI interventions successfully altered maternal anxiety and maternal responses, respectively.
Change in maternal anxiety
Recovery from maternal primary diagnosis at assessment 1B
As shown in Table 4, from the CCBT group eight mothers had missing data for their primary ADIS-IV diagnosis at the mid-treatment assessment (assessment 1B, i.e. after the MCBT intervention), for the CCBT + MCBT group this was four mothers and for CCBT + MCI this was one mother.
| Treatment allocation | Missing, n (%) | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|---|
| CCBT | 8 (11.3) | 23 (32.4) | 40 (56.3) | 71 |
| CCBT + MCBT | 4 (5.8) | 38 (55.1) | 27 (39.1) | 69 |
| CCBT + MCI | 1 (1.4) | 30 (42.3) | 40 (56.3) | 71 |
| Total | 13 | 91 | 107 | 211 |
As shown in Table 5, at assessment 1B, 23 mothers (37%) in the control group had recovered from their primary diagnosis. In the CCBT + MCBT group 38 mothers (59%) had recovered and in the CCBT + MCI group 30 mothers (43%) had recovered.
| Treatment allocation | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|
| CCBT | 23 (36.5) | 40 (63.5) | 63 |
| CCBT + MCBT | 38 (58.5) | 27 (41.5) | 65 |
| CCBT + MCI | 30 (42.9) | 40 (57.1) | 70 |
| Total | 91 | 107 | 198 |
Mothers in the CCBT + MCBT group were 1.63 times more likely to recover from their ADIS-IV primary diagnosis by assessment 1B than those in the CCBT group [adjusted RR 1.63, 95% confidence interval (CI) 1.13 to 2.36; p = 0.009]. The adjusted RR for CCBT + MCI versus CCBT is 1.22 (95% CI 0.83 to 1.81; p = 0.314) (Table 6).
| Parameter | Adjusted RRa | 95% CI | p-valueb | |
|---|---|---|---|---|
| Treatment | CCBT | Ref. | ||
| CCBT + MCBT | 1.63 | 1.13 to 2.36 | 0.009 | |
| CCBT + MCI | 1.22 | 0.83 to 1.81 | 0.314 | |
Recovery from all anxiety diagnoses at assessment 1B
As shown in Table 7, the CCBT group had the largest per cent of missing data for mothers at assessment 1B with 13%, the CCBT + MCBT group had 6% and the CCBT + MCI group had 1%.
| Treatment allocation | Missing, n (%) | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|---|
| CCBT | 9 (12.7) | 10 (14.1) | 52 (73.2) | 71 |
| CCBT + MCBT | 4 (5.8) | 25 (36.2) | 40 (58.0) | 69 |
| CCBT + MCI | 1 (1.4) | 22 (31.0) | 48 (67.6) | 71 |
| Total | 14 | 57 | 140 | 211 |
As shown in Table 8, in the CCBT group 10 mothers (16%) had recovered from all anxiety diagnoses by assessment 1B. However, in the CCBT + MCBT group there were 25 recovered mothers (39%) and in the CCBT + MCI group there were 22 recovered mothers (31%).
| Treatment allocation | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|
| CCBT | 10 (16.1) | 52 (83.9) | 62 |
| CCBT + MCBT | 25 (38.5) | 40 (61.5) | 65 |
| CCBT + MCI | 22 (31.4) | 48 (68.6) | 70 |
| Total | 57 | 140 | 197 |
Mothers receiving CCBT + MCBT or CCBT + MCI were more than twice as likely to have recovered from all anxiety diagnoses by assessment 1B than mothers in the control group CCBT + MCBT (RR 2.51, 95% CI 1.43 to 4.40; p = 0.001) and CCBT + MCI (RR 2.15, 95% CI 1.21 to 3.81; p = 0.009) (Table 9).
| Parameter | RRa | 95% CI | p-valueb | |
|---|---|---|---|---|
| Treatment | CCBT | Ref. | ||
| CCBT + MCBT | 2.51 | 1.43 to 4.40 | 0.001 | |
| CCBT + MCI | 2.15 | 1.21 to 3.81 | 0.009 | |
Change in maternal self-reported symptoms at assessment 1B
Table 10 shows the results of analyses looking at the change from baseline to assessment 1B scores of questionnaires completed by mothers about themselves. There were no significant differences between treatment groups. Summary scores are shown in Appendix 5, Table 123.
| Questionnaire | Treatment | n | Adjusteda mean change (95% CI) | Adjusteda mean difference (95% CI) | p-value |
|---|---|---|---|---|---|
| PSWQ total score | CCBT | 40 | –2.91 (–5.91 to 0.10) | Ref. | |
| CCBT + MCBT | 42 | –4.96 (–7.90 to –2.01) | –2.05 (–6.31 to 2.21) | 0.342 | |
| CCBT + MCI | 44 | –3.72 (–6.59 to –0.84) | –0.81 (–5.03 to 3.40) | 0.704 | |
| SIAS total score | CCBT | 41 | –0.86 (–3.37 to 1.66) | Ref. | |
| CCBT + MCBT | 44 | –1.24 (–3.67 to 1.18) | –0.39 (–3.92 to 3.15) | 0.829 | |
| CCBT + MCI | 47 | –0.49 (–2.84 to 1.86) | 0.37 (–3.12 to 3.85) | 0.835 | |
| SPS total score | CCBT | 41 | –0.77 (–3.19 to 1.64) | Ref. | |
| CCBT + MCBT | 45 | –0.21 (–2.52 to 2.10) | 0.56 (–2.81 to 3.94) | 0.742 | |
| CCBT + MCI | 46 | 0.07 (–2.22 to 2.36) | 0.84 (–2.53 to 4.22) | 0.622 | |
| DASS-21 depression subscale | CCBT | 38 | –1.54 (–3.28 to 0.21) | Ref. | |
| CCBT + MCBT | 43 | –2.11 (–3.74 to –0.49) | –0.58 (–3.00 to 1.85) | 0.638 | |
| CCBT + MCI | 45 | –1.70 (–3.30 to –0.11) | –0.17 (–2.57 to 2.23) | 0.890 | |
| DASS-21 anxiety subscale | CCBT | 38 | –0.38 (–2.36 to 1.60) | Ref. | |
| CCBT + MCBT | 44 | –1.95 (–3.79 to –0.11) | –1.57 (–4.32 to 1.18) | 0.259 | |
| CCBT + MCI | 45 | –1.99 (–3.81 to –0.18) | –1.61 (–4.34 to 1.10) | 0.243 | |
| DASS-21 stress subscale | CCBT | 41 | –0.90 (–2.88 to 1.08) | Ref. | |
| CCBT + MCBT | 45 | –1.76 (–3.65 to 0.13) | –0.86 (–3.63 to 1.91) | 0.539 | |
| CCBT + MCI | 45 | –1.28 (–3.18 to 0.61) | –0.38 (–3.16 to 2.40) | 0.786 |
Recovery from maternal primary diagnosis at assessment 2 (end of all treatment)
As shown in Table 11, missing data was similar at the end of treatment (assessment 2) for mothers in the CCBT and CCBT + MCBT groups (24% and 20%, respectively). In the CCBT + MCI group it was 13%.
| Treatment allocation | Missing, n (%) | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|---|
| CCBT | 17 (23.9) | 28 (39.4) | 26 (36.6) | 71 |
| CCBT + MCBT | 14 (20.3) | 36 (52.2) | 19 (27.5) | 69 |
| CCBT + MCI | 9 (12.7) | 41 (57.8) | 21 (29.6) | 71 |
| Total | 40 | 105 | 66 | 211 |
As shown in Table 12, there were 36 mothers (66%) in the MCBT group and 41 mothers (66%) in the CCBT + MCI group who recovered from their primary diagnosis by assessment 2 compared with 28 mothers (52%) from the CCBT group.
| Treatment allocation | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|
| CCBT | 28 (51.9) | 26 (48.1) | 54 |
| CCBT + MCBT | 36 (65.5) | 19 (34.5) | 55 |
| CCBT + MCI | 41 (66.1) | 21 (33.9) | 62 |
| Total | 105 | 66 | 171 |
The results from log-linear regression of the mothers’ recovery from their primary ADIS-IV diagnosis by assessment 2, adjusted for minimisation factors, are shown in Table 13. There were no significant differences between CCBT + MCBT and CCBT or between CCBT + MCI and CCBT. The adjusted RR for the effect of CCBT + MCBT on recovery from maternal primary diagnosis was 1.23 (95% CI 0.90 to 1.68; p = 0.201). Similarly, the adjusted RR for the effect of CCBT + MCI on recovery was 1.27 (95% CI 0.93 to 1.74; p = 0.126).
| Parameter | Adjusted RRa | 95% CI | p-valueb | |
|---|---|---|---|---|
| Treatment | CCBT | Ref. | ||
| CCBT + MCBT | 1.23 | 0.90 to 1.68 | 0.201 | |
| CCBT + MCI | 1.27 | 0.93 to 1.74 | 0.126 | |
Recovery from all anxiety diagnoses at assessment 2
Missing data was similar at assessment 2 for mothers in the CCBT and CCBT + MCBT groups (24% and 20%, respectively). In the CCBT + MCI group it was 13% (Table 14).
| Treatment allocation | Missing, n (%) | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|---|
| CCBT | 17 (23.9) | 19 (26.8) | 35 (49.3) | 71 |
| CCBT + MCBT | 14 (20.3) | 26 (37.7) | 29 (42.0) | 69 |
| CCBT + MCI | 9 (12.7) | 29 (40.9) | 33 (46.5) | 71 |
| Total | 40 | 74 | 97 | 211 |
As can be seen in Table 15, 29 mothers (47%) in the CCBT + MCI group had recovered from all ADIS-IV anxiety diagnoses at assessment 2 and 26 (47%) from the CCBT + MCBT group. Nineteen mothers (35%) had fully recovered from the CCBT group.
| Treatment allocation | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|
| CCBT | 19 (35.2) | 35 (64.8) | 54 |
| CCBT + MCBT | 26 (47.3) | 29 (52.7) | 55 |
| CCBT + MCI | 29 (46.8) | 33 (53.2) | 62 |
| Total | 74 | 97 | 171 |
Table 16 shows the results from log-binomial regression of the mothers’ recovery from all ADIS-IV anxiety diagnoses adjusted for minimisation factors. There were no significant improvements for the CCBT + MCBT group (RR 1.32, 95% CI 0.85 to 2.04; p = 0.210) or the CCBT + MCI group (RR 1.35, 95% CI 0.87 to 2.10; p = 0.179).
| Parameter | RRa | 95% CI | p-valueb | |
|---|---|---|---|---|
| Treatment | CCBT | Ref. | ||
| CCBT + MCBT | 1.30 | 0.84 to 2.01 | 0.244 | |
| CCBT + MCI | 1.35 | 0.87 to 2.10 | 0.180 | |
Change in maternal self-reported symptoms at assessment 2
The regression results from the change in mothers’ self-report questionnaires can be seen in Table 17. There were no significant differences between the CCBT + MCBT and CCBT groups or between the CCBT + MCI and CCBT groups.
| Questionnaire | Treatment | n | Adjusteda mean change (95% CI) | Adjusteda mean difference (95% CI) | p-value |
|---|---|---|---|---|---|
| PSWQ total score | CCBT | 35 | –7.14 (–10.67 to –3.60) | Ref. | |
| CCBT + MCBT | 41 | –6.71 (–10.00 to –3.42) | 0.43 (–4.47 to 5.32) | 0.863 | |
| CCBT + MCI | 35 | –6.43 (–10.01 to –2.86) | 0.70 (–4.40 to 5.81) | 0.785 | |
| SIAS total score | CCBT | 34 | –3.52 (–6.77 to –0.27) | Ref. | |
| CCBT + MCBT | 40 | –4.80 (–7.82 to –1.79) | –1.28 (–5.79 to 3.22) | 0.574 | |
| CCBT + MCI | 36 | –4.75 (–7.93 to –1.58) | –1.23 (–5.84 to 3.37) | 0.597 | |
| SPS total score | CCBT | 35 | –3.91 (–6.15 to –1.67) | Ref. | |
| CCBT + MCBT | 41 | –4.03 (–6.12 to –1.94) | –0.12 (–3.24 to 2.99) | 0.937 | |
| CCBT + MCI | 36 | –2.20 (–4.65 to –2.16) | 1.71 (–1.49 to 4.91) | 0.291 | |
| DASS-21 depression subscale | CCBT | 32 | –2.83 (–5.11 to –0.55) | Ref. | |
| CCBT + MCBT | 36 | –3.89 (–6.05 to –1.73) | –1.06 (–4.24 to 2.13) | 0.511 | |
| CCBT + MCI | 33 | –2.59 (–4.87 to –0.31) | 0.24 (–3.05 to 3.54) | 0.884 | |
| DASS-21 anxiety subscale | CCBT | 32 | –0.62 (–2.80 to 1.57) | Ref. | |
| CCBT + MCBT | 36 | –2.75 (–4.85 to –0.65) | –2.13 (–5.21 to 0.94) | 0.171 | |
| CCBT + MCI | 33 | –2.40 (–4.61 to –0.19) | –1.79 (–4.95 to 1.38) | 0.266 | |
| DASS-21 stress subscale | CCBT | 34 | –3.60 (–5.82 to –1.39) | Ref. | |
| CCBT + MCBT | 41 | –2.45 (–4.48 to –0.42) | 1.15 (–1.88. 4.19) | 0.453 | |
| CCBT + MCI | 35 | –2.77 (–4.98 to –0.56) | 0.83 (–2.36 to 4.02) | 0.606 |
Change in parenting responses
Parenting behaviours
Change in maternal parenting behaviours was analysed using linear regression. Analysis in Table 18 shows the adjusted mean change from baseline to assessment 2, for each of the seven areas in each treatment group. The mean score over three tasks is used for each parenting behaviour. The adjusted mean difference compares the CCBT + MCBT group with CCBT and also the CCBT + MCI group with CCBT. A summary of scores is given in Appendix 5, Table 122.
The only significant difference was for CCBT + MCI versus CCBT in the ‘overprotection’ scores (p = 0.026). The difference between the CCBT + MCI and CCBT arms also approached significance for maternal self-report overprotection (p = 0.057).
| Questionnaire | Treatment | n | Adjusteda mean change (95% CI) | Adjusteda mean difference (95% CI) | p-value |
|---|---|---|---|---|---|
| Positive behaviour (–) | CCBT | 42 | 0.042 (–0.058 to 0.141) | Ref. | |
| CCBT + MCBT | 45 | –0.009 (–0.104 to 0.086) | –0.050 (–0.190 to 0.090) | 0.478 | |
| CCBT + MCI | 49 | 0.067 (–0.024 to 0.158) | 0.026 (–0.112 to 0.163) | 0.714 | |
| Over-protection (+) | CCBT | 42 | –0.016 (–0.036 to 0.005) | Ref. | |
| CCBT + MCBT | 45 | –0.035 (–0.055 to –0.016) | –0.020 (–0.048 to 0.009) | 0.174 | |
| CCBT + MCI | 49 | –0.048 (–0.066 to –0.029) | –0.032 (–0.060 to –0.004) | 0.026 | |
| Promotion of avoidance (+) | CCBT | 42 | –0.019 (–0.045 to 0.007) | Ref. | |
| CCBT + MCBT | 45 | –0.024 (–0.049 to 0.001) | –0.004 (–0.041 to 0.033) | 0.813 | |
| CCBT + MCI | 49 | –0.042 (–0.066 to –0.019) | –0.023 (–0.059 to 0.013) | 0.207 | |
| Intrusiveness (+) | CCBT | 42 | –0.058 (–0.163 to 0.046) | Ref. | |
| CCBT + MCBT | 45 | 0.015 (–0.085 to 0.116) | 0.074 (–0.074 to 0.221) | 0.324 | |
| CCBT + MCI | 49 | –0.108 (–0.205 to –0.012) | –0.050 (–0.195 to 0.195) | 0.499 | |
| Anxiety (+) | CCBT | 42 | –0.005 (–0.106 to 0.097) | Ref. | |
| CCBT + MCBT | 45 | 0.034 (–0.063 to 0.132) | 0.039 (–0.103 to 0.182) | 0.589 | |
| CCBT + MCI | 49 | –0.013 (–0.107 to 0.080) | –0.009 (–0.149 to 0.131) | 0.901 | |
| Quality of relationship (–) | CCBT | 42 | 0.023 (–0.074 to 0.121) | Ref. | |
| CCBT + MCBT | 45 | 0.050 (–0.044 to 0.142) | 0.026 (–0.111 to 0.163) | 0.712 | |
| CCBT + MCI | 49 | 0.003 (–0.086 to 0.092) | –0.020 (–0.155 to 0.114) | 0.763 | |
| POI total score ( + ) | CCBT | 34 | –5.83 (–9.07 to –2.59) | Ref. | |
| CCBT + MCBT | 38 | –6.41 (–9.51 to –3.31) | –0.58 (–5.06 to 3.89) | 0.7974 | |
| CCBT + MCI | 34 | –10.32 (–13.60 to –7.04) | –4.49 (–9.12 to 0.14) | 0.0573 |
Parenting cognitions
Maternal expectations were assessed before the behavioural tasks. These ratings were recorded at baseline and at assessment 2. The following analysis, shown in Table 19, looks at the change scores from baseline to assessment 2, analysed using adjusted linear regression.
For the pre-task ‘scared’ rating and pre-task ‘child in control’ rating there were significant differences between CCBT + MCI and CCBT (p = 0.029 and p = 0.046, respectively). A summary of mean scores is provided in Appendix 5, Table 125.
| Questionnaire | Treatment | n | Adjusteda mean change (95% CI) | Adjusteda mean difference (95% CI) | p-value |
|---|---|---|---|---|---|
| Pre-task ‘child scared’ (+) | CCBT | 40 | –0.69 (–1.12 to –0.26) | Ref. | |
| CCBT + MCBT | 45 | –1.22 (–1.62 to –0.82) | –0.53 (–1.12 to 0.07) | 0.083 | |
| CCBT + MCI | 46 | –1.36 (–1.76 to –0.96) | –0.67 (–1.26 to –0.07) | 0.029 | |
| Pre-task ‘mother anxious’ (+) | CCBT | 40 | –0.87 (–1.32 to –0.42) | Ref. | |
| CCBT + MCBT | 45 | –1.43 (–1.85 to –1.01) | –0.56 (–1.18 to 0.07) | 0.079 | |
| CCBT + MCI | 46 | –1.43 (–1.85 to –1.02) | –0.56 (–1.18 to 0.06) | 0.077 | |
| Pre-task ‘child in control’ (–) | CCBT | 40 | 0.25 (–0.12 to 0.63) | Ref. | |
| CCBT + MCBT | 45 | 0.75 (0.40 to 1.10) | 0.50 (–0.03 to 1.02) | 0.063 | |
| CCBT + MCI | 46 | 0.78 (0.44 to 1.13) | 0.53 (0.01 to 1.05) | 0.046 | |
| Pre-task ‘mother in control’ (+/–) | CCBT | 40 | –0.28 (–0.80 to 0.23) | Ref. | |
| CCBT + MCBT | 45 | –0.07 (–0.55 to 0.41) | 0.21 (–0.51 to 0.93) | 0.564 | |
| CCBT + MCI | 46 | –0.08 (–0.55 to 0.39) | 0.20 (–0.50 to 0.91) | 0.569 |
Primary outcomes
Missing data
Nine (13%) participants allocated to CCBT + MCBT and nine (13%) participants allocated to CCBT + MCI were not able to be measured for the primary end points. These rates of missing data were slightly lower than for participants allocated to CCBT (21%). Baseline characteristics of participants with or without missing primary outcomes are given in Tables 20–22.
| Treatment allocation | Missing, n (%) | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|---|
| CCBT | 15 (21.1) | 27 (38.0) | 29 (40.9) | 71 |
| CCBT + MCBT | 9 (13.0) | 35 (50.7) | 25 (36.2) | 69 |
| CCBT + MCI | 9 (12.7) | 37 (52.1) | 25 (35.2) | 71 |
| Total | 33 | 99 | 79 | 211 |
| Treatment allocation | Missing, n (%) | Much/very much improved, n (%) | Not much/very much improved, n (%) | Total, n (%) |
|---|---|---|---|---|
| CCBT | 15 (21.1) | 36 (50.7) | 20 (28.2) | 71 |
| CCBT + MCBT | 9 (13.0) | 48 (69.6) | 12 (17.4) | 69 |
| CCBT + MCI | 9 (12.7) | 47 (66.2) | 15 (21.1) | 71 |
| Total | 33 | 131 | 47 | 211 |
| Baseline characteristic | Category | Assessment 2 | |
|---|---|---|---|
| Completed, n (%) | Missing, n (%) | ||
| Gender | Male | 84 (83.2) | 17 (16.8) |
| Female | 94 (85.5) | 16 (14.5) | |
| Marital status | Single, never married | 7 (58.3) | 5 (41.7) |
| Married (first time) | 90 (84.1) | 17 (15.9) | |
| Remarried | 13 (81.3) | 3 (18.8) | |
| Divorce/separated | 39 (88.6) | 5 (11.4) | |
| Living with partner | 25 (89.3) | 3 (10.7) | |
| Not recorded | 4 (100.0) | ||
| Employment mother | Unemployed | 48 (77.4) | 14 (22.6) |
| Part time | 89 (86.4) | 14 (13.6) | |
| Full time | 30 (85.7) | 5 (14.3) | |
| Not recorded | 11 (100.0) | ||
| Employment father | Unemployed | 10 (83.3) | 2 (16.7) |
| Part time | 2 (100.0) | ||
| Full time | 128 (83.7) | 25 (16.3) | |
| NA | 4 (57.1) | 3 (42.9) | |
| Not recorded | 34 (91.9) | 3 (8.1) | |
| Overall SES | Higher professional | 93 (87.7) | 13 (12.3) |
| Other employed | 57 (80.3) | 14 (19.7) | |
| Unemployed | 3 (100.0) | ||
| Not recorded | 25 (80.6) | 6 (19.4) | |
| ADIS-C/P primary diagnosis (initial assessment) | SAD | 45 (80.4) | 11 (19.6) |
| Social phobia | 42 (87.5) | 6 (12.5) | |
| GAD | 51 (77.3) | 15 (22.7) | |
| Other | 40 (97.6) | 1 (2.4) | |
| ADIS-C/P primary diagnosis CSR (initial assessment) | Moderate 4 | 12 (75.0) | 4 (25.0) |
| Moderate 5 | 50 (84.7) | 9 (15.3) | |
| Severe 6 | 97 (85.8) | 16 (14.2) | |
| Severe 7 | 19 (82.6) | 4 (17.4) | |
| ADIS-C/P primary diagnosis CSR at assessment 1B | No diagnosis | 3 (100.0) | |
| Mild 3 | 6 (100.0) | ||
| Moderate 4 | 25 (92.6) | 2 (7.4) | |
| Moderate 5 | 52 (85.2) | 9 (14.8) | |
| Severe 6 | 86 (91.5) | 8 (8.5) | |
| Severe 7 | 5 (71.4) | 2 (28.6) | |
| Very severe 8 | 1 (100.0) | ||
| Not recorded | 12 (100.0) | ||
| Child age (years) | 6 | 1 (100.0) | |
| 7 | 11 (68.8) | 5 (31.3) | |
| 8 | 27 (84.4) | 5 (15.6) | |
| 9 | 28 (84.8) | 5 (15.2) | |
| 10 | 41 (87.2) | 6 (12.8) | |
| 11 | 43 (91.5) | 4 (8.5) | |
| 12 | 25 (78.1) | 7 (21.9) | |
| 13 | 3 (100.0) | ||
Unadjusted analyses: primary end points
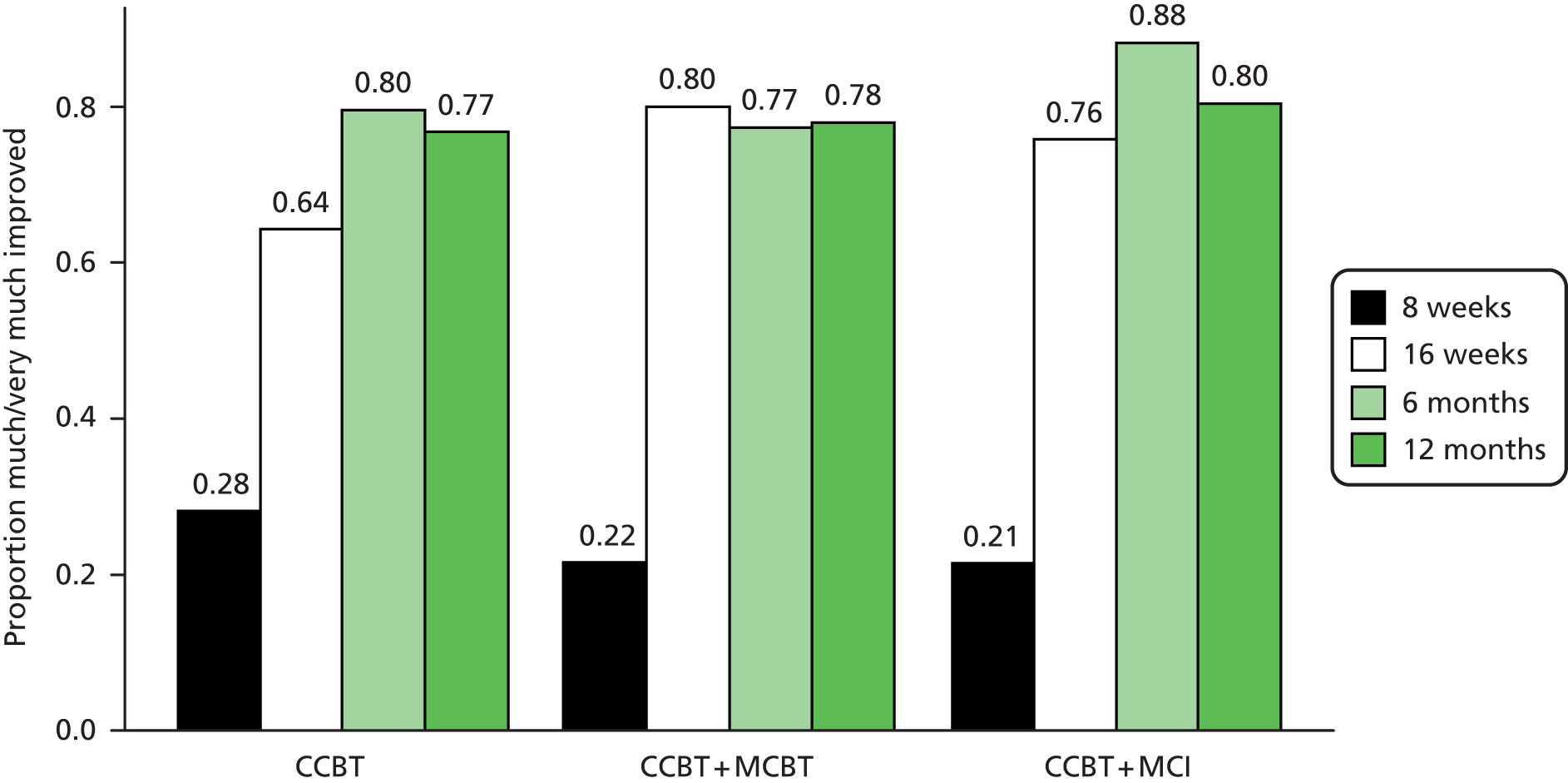
As shown in Table 23 and Figure 3, 48% of the children in the CCBT arm were free of their primary diagnosis status at assessment 2 compared with 58% of children in the CCBT + MCBT and 60% of children in the CCBT + MCI arms.
| Treatment allocation | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|
| CCBT | 27 (48.2) | 29 (51.8) | 56 |
| CCBT + MCBT | 35 (58.3) | 25 (41.7) | 60 |
| CCBT + MCI | 37 (59.7) | 25 (40.3) | 62 |
| Total | 99 | 79 | 178 |
FIGURE 3.
Presence of pre-treatment ADIS-C/P child primary diagnosis.

The unadjusted RR for the effect of CCBT + MCBT versus CCBT on recovery from primary ADIS-C/P diagnosis by assessment 2 was 1.21 (95% CI 0.86 to 1.71; p = 0.280). This was very similar to the unadjusted estimate of the effect of CCBT + MCI versus CCBT, RR 1.24 (95% CI 0.88 to 1.74; p = 0.219).
The unadjusted RR for the effect of CCBT + MCBT versus CCBT on CGI-I by assessment 2 was 1.24 (95% CI 0.99 to 1.57; p = 0.065) and for the effect of CCBT + MCI versus CCBT the RR was 1.18 (95% CI 0.93 to 1.50; p = 0.179). Frequencies are displayed in Table 24 and Figure 4.
| Treatment allocation | Much/very much improved, n (%) | Not much/very much improved, n (%) | Total, n (%) |
|---|---|---|---|
| CCBT | 36 (64.3) | 20 (35.7) | 56 |
| CCBT + MCBT | 48 (80.0) | 12 (20.0) | 60 |
| CCBT + MCI | 47 (75.8) | 15 (24.2) | 62 |
| Total | 131 | 47 | 178 |
FIGURE 4.
Child CGI-I.
Multiple imputation analyses
Multiple imputations were used to account for missing data for the two primary end points. Twenty imputed data sets were developed using the Stata ‘ice’ function for multiple imputation with chained equations. Imputation models were developed using variables for treatment allocation, minimisation factors [child age, child gender, type of child anxiety disorder (GAD, social phobia, SAD, other), baseline severity (ADIS-C/P CSR) of the child’s primary anxiety disorder and baseline severity (ADIS-IV mother self-report) of the mother’s primary anxiety disorder] as well as assessment of ADIS-C/P CSR at assessment 1B, assessment of ADIS-C/P primary diagnosis at assessment 1B, CGI-I at assessment 1B and baseline mother’s depression (DASS-21 – depression), child depression symptoms (SMFQ-c), child behavioural problems (SDQ-conduct) and presence of child social phobia.
Results from multiple imputation analyses, which were the primary analyses, along with adjusted RRs are presented in Table 25. Adjusted analyses for log-binomial regression models did not converge (as is often the case), therefore the modified Poisson regression framework with robust error variance was used as specified in the analysis plan, which gives almost identical CIs.
Confidence intervals for all estimates remained similar regardless of the method of analysis.
| Assessment 2 | RRa | 95% CI | p-value |
|---|---|---|---|
| ADIS-C/P primary diagnostic status: child | |||
| Unadjusted | |||
| CCBT | Ref. | ||
| CCBT + MCBT | 1.21 | 0.86 to 1.71 | 0.280 |
| CCBT + MCI | 1.24 | 0.88 to 1.74 | 0.219 |
| Adjusteda | |||
| CCBT | Ref. | ||
| CCBT + MCBT | 1.22 | 0.88 to 1.67 | 0.228 |
| CCBT + MCI | 1.21 | 0.88 to 1.65 | 0.243 |
| Multiple imputationa | |||
| CCBT | Ref. | ||
| CCBT + MCBT | 1.18 | 0.827 to 1.62 | 0.285 |
| CCBT + MCI | 1.22 | 0.90 to 1.67 | 0.203 |
| CGI-I: child | |||
| Unadjusted | |||
| CCBT | Ref. | ||
| CCBT + MCBT | 1.24 | 0.99 to 1.57 | 0.065 |
| CCBT + MCI | 1.18 | 0.93 to 1.50 | 0.179 |
| Adjusteda | |||
| CCBT | Ref. | ||
| CCBT + MCBT | 1.25 | 0.99 to 1.57 | 0.058 |
| CCBT + MCI | 1.18 | 0.93 to 1.50 | 0.173 |
| Multiple imputationa | |||
| CCBT | Ref. | ||
| CCBT + MCBT | 1.26 | 1.00 to 1.59 | 0.054 |
| CCBT + MCI | 1.20 | 0.95 to 1.53 | 0.133 |
Per-protocol analysis of primary outcomes at assessment 2
The PP population is a subset of the ITT population and excludes from the analysis participants who were ineligible or had significant non-compliance.
The CCBT arm PP population contained 58 children, the CCBT + MCBT arm contained 60 children and the CCBT + MCI arm contained 64 children. This is a total of 182 children in the PP population, whereas the ITT population contains 211 children.
Table 26 shows for each treatment group the proportion of children who had recovered from their primary diagnosis by assessment 2; in both the CCBT + MCBT and CCBT + MCI arms this was 59% and in the CCBT arm it was 49%.
| Treatment allocation | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|
| CCBT | 27 (49.09) | 28 (50.91) | 55 |
| CCBT + MCBT | 33 (58.93) | 23 (41.07) | 56 |
| CCBT + MCI | 36 (59.02) | 25 (40.98) | 61 |
| Total | 96 | 76 | 172 |
As shown in Table 27, the adjusted RR for the effect of CCBT + MCBT versus CCBT on recovery from primary ADIS-IV diagnosis by assessment 2 was 1.17 (95% CI 0.85 to 1.62; p = 0.328). This was very similar to the adjusted estimate of the effect of CCBT + MCI versus CCBT, RR 1.19 (95% CI 0.86 to 1.64; p = 0.288).
| Parameter | Adjusted RRa | 95% CI | p-valueb | |
|---|---|---|---|---|
| Treatment | CCBT | Ref. | ||
| CCBT + MCBT | 1.17 | 0.85 to 1.62 | 0.328 | |
| CCBT + MCI | 1.19 | 0.86 to 1.64 | 0.288 | |
The proportion of patients where the CGI-I rating improved by assessment 2 is shown in Table 28; in the CCBT arm this was 64%, in the CCBT + MCBT arm it was 80% and in the CCBT + MCI arm it was 75%.
| Treatment allocation | Much/very much improved, n (%) | Not much/very much improved, n (%) | Total, n (%) |
|---|---|---|---|
| CCBT | 35 (63.64) | 20 (36.36) | 55 |
| CCBT + MCBT | 45 (80.36) | 11 (19.64) | 56 |
| CCBT + MCI | 46 (75.41) | 15 (24.59) | 61 |
| Total | 126 | 46 | 172 |
As shown in Table 29, the adjusted RR for the effect of CCBT + MCBT versus CCBT on improvement in CGI-I by assessment 2 was 1.26 (95% CI 0.99 to 1.59); p = 0.056. The adjusted estimate of the effect of CCBT + MCI versus CCBT was RR 1.18 (95% CI 0.93 to 1.52; p = 0.170).
| Parameter | Adjusted RRa | 95% CI | p-valueb | |
|---|---|---|---|---|
| Treatment | CCBT | Ref. | ||
| CCBT + MCBT | 1.26 | 0.99 to 1.59 | 0.056 | |
| CCBT + MCI | 1.18 | 0.93 to 1.52 | 0.170 | |
Secondary outcomes
Severity of child’s primary Anxiety Disorder Interview Schedule diagnosis at assessment 2
By assessment 2, 59% of the CCBT arm, 73% of the CCBT + MCBT arm and 73% of the CCBT + MCI arm children had seen an improvement of at least 2 points (Figure 5 and Tables 30 and 31).
There were no significant differences between CCBT + MCBT and CCBT or between CCBT + MCI and CCBT (p = 0.101 and 0.118, respectively).
FIGURE 5.
Box plot of change in severity of child’s primary ADIS-C/P diagnosis at assessment 2 by treatment group.

| Treatment | –7 | –6 | –5 | –4 | –3 | –2 | –1 | 0 | 1 | Total |
|---|---|---|---|---|---|---|---|---|---|---|
| CCBT | 1 (1.8) | 9 (16.1) | 11 (19.6) | 2 (3.6) | 4 (7.1) | 6 (10.7) | 13 (23.2) | 9 (16.1) | 1 (1.8) | 56 |
| CCBT + MCBT | 2 (3.3) | 14 (23.3) | 9 (15.0) | 4 (6.7) | 4 (6.7) | 11 (18.3) | 7 (11.7) | 8 (13.3) | 1 (1.7) | 60 |
| CCBT + MCI | 2 (3.2) | 17 (27.4) | 8 (12.9) | 4 (6.5) | 2 (3.2) | 12 (19.4) | 14 (22.6) | 3 (4.8) | 0 (0.0) | 62 |
| Total | 5 | 40 | 28 | 10 | 10 | 29 | 34 | 20 | 2 | 178 |
| Treatment | n | n (%) with a 2 or more point reduction | p-valuea |
|---|---|---|---|
| CCBT | 56 | 33 (58.9) | |
| CCBT + MCBT | 60 | 44 (73.3) | 0.101 |
| CCBT + MCI | 62 | 45 (72.6) | 0.118 |
Presence of any Anxiety Disorder Interview Schedule anxiety diagnosis in children at assessment 2
As shown in Table 32, the proportion of children with missing data was higher in the CCBT arm (21%); the CCBT + MCBT arm (13%) and the CCBT + MCI arms (13%) were fairly similar.
| Treatment allocation | Missing, n (%) | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|---|
| CCBT | 15 (21.1) | 16 (22.5) | 40 (56.3) | 71 |
| CCBT + MCBT | 9 (13.0) | 18 (26.1) | 42 (60.9) | 69 |
| CCBT + MCI | 9 (12.7) | 25 (35.2) | 37 (52.1) | 71 |
| Total | 33 | 59 | 119 | 211 |
As can be seen in Table 33, in the CCBT + MCBT and CCBT + MCI arms 18 and 25 children (30% and 40%), respectively, had recovered from all ADIS-C/P anxiety diagnoses at assessment 2. From the CCBT arm, 16 participants (29%) had fully recovered.
| Treatment allocation | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|
| CCBT | 16 (28.6) | 40 (71.4) | 56 |
| CCBT + MCBT | 18 (30.0) | 42 (70.0) | 60 |
| CCBT + MCI | 25 (40.3) | 37 (59.7) | 62 |
| Total | 59 | 119 | 178 |
Table 34 shows the results from log-binomial regression of the children’s recovery from all ADIS-C/P anxiety diagnoses at assessment 2 adjusted for minimisation factors.
| Parameter | Adjusted RRa | 95% CI | p-valueb | |
|---|---|---|---|---|
| Treatment | CCBT | Ref. | ||
| CCBT + MCBT | 1.06 | 0.63 to 1.78 | 0.816 | |
| CCBT + MCI | 1.48 | 0.92 to 2.37 | 0.102 | |
The estimated effect of CCBT + MCBT on ADIS-C/P anxiety diagnoses at assessment 2 compared with the CCBT arm was RR 1.06 (0.63 to 1.78; p = 0.816). For those children receiving CCBT + MCI the adjusted RR was 1.48 (95% CI 0.92 to 2.37; p = 0.102).
Analysis of change in child-reported questionnaire scores at assessment 2
Analyses of questionnaire results were conducted on the change scores from baseline to assessment 2 owing to the skewed distribution of the raw scores at assessment 2. The change scores were more normally distributed.
The change scores were modelled using linear regression, adjusted for baseline scores and minimisation factors. There were some outliers in the regression models, but these were not thought to be due to incorrect completion of the questionnaires. Furthermore, their removal did not change the conclusions from the regression.
Table 35 shows the adjusted means of the children’s responses in each treatment arm along with the adjusted mean difference for CCBT + MCBT and CCBT + MCI in comparison with CCBT. For the SCAS-c a significant difference was seen between CCBT + MCBT and CCBT (p = 0.031), with the CCBT arm seeing a bigger reduction in total score on average. For the SMFQ-c a significant difference was seen between CCBT + MCBT and CCBT (p = 0.004) and also CCBT + MCI and CCBT (p = 0.012); in both cases the difference was in the opposite direction to what was expected, with the CCBT arm seeing a greater reduction in the children’s scores than the treatment arms.
| Questionnaire | Treatment | n | Adjusteda mean change (95% CI) | Adjusteda mean difference (95% CI) | p-value |
|---|---|---|---|---|---|
| SCAS-c total score | CCBT | 45 | –19.68 (–23.48 to –15.89) | Ref. | |
| CCBT + MCBT | 46 | –13.71 (–17.49 to –9.92) | 5.97 (0.54 to 11.41) | 0.031 | |
| CCBT + MCI | 52 | –15.73 (–19.27 to –12.19) | 3.96 (–1.28 to 9.19) | 0.137 | |
| CAIS-c total score | CCBT | 44 | –8.19 (–12.10 to –4.28) | Ref. | |
| CCBT + MCBT | 45 | –6.28 (–10.20 to –2.37) | 1.91 (–3.73 to 7.55) | 0.505 | |
| CCBT + MCI | 53 | –6.49 (–10.05 to –2.93) | 1.70 (–3.63 to 7.03) | 0.530 | |
| SMFQ-c total score | CCBT | 46 | –5.03 (–6.35 to –3.71) | Ref. | |
| CCBT + MCBT | 47 | –2.25 (–3.57 to –0.93) | 2.78 (0.88 to 4.68) | 0.004 | |
| CCBT + MCI | 54 | –2.70 (–3.92 to –1.48) | 2.33 (0.52 to 4.14) | 0.012 | |
| SDQ-c conduct subscale | CCBT | 47 | –0.61 (–1.08 to –0.14) | Ref. | |
| CCBT + MCBT | 47 | –0.52 (–1.00 to –0.05) | 0.09 (–0.59 to 0.76) | 0.803 | |
| CCBT + MCI | 55 | –0.50 (–0.94 to –0.07) | 0.10 (–0.54 to 0.75) | 0.748 |
Appendix 5, Table 126, presents the summary statistics for questionnaire scores at baseline and assessment 2, along with the difference between baseline and assessment 2, for only those participants with data at both time points who are included in Table 35.
Analysis of change in mother-reported child symptoms at assessment 2
The results from the regression of the mothers’ questionnaires for child symptoms/impact are shown in Table 36. There were no significant differences seen between the CCBT + MCBT and CCBT or between CCBT + MCI and CCBT. Appendix 5, Table 127, presents a summary of the descriptive statistics.
| Questionnaire | Treatment | n | Adjusteda mean change (95% CI) | Adjusteda mean difference (95% CI) | p-value |
|---|---|---|---|---|---|
| SCAS-c total score | CCBT | 36 | –18.00 (–21.09 to –14.88) | Ref. | |
| CCBT + MCBT | 39 | –16.77 (–19.75 to –13.78) | 1.22 (–3.15 to 5.59) | 0.581 | |
| CCBT + MCI | 38 | –18.30 (–21.35 to –15.25) | –0.32 (–4.77 to 4.14) | 0.888 | |
| CAIS-c total score | CCBT | 33 | –10.19 (–12.37 to –8.01) | Ref. | |
| CCBT + MCBT | 35 | –12.95 (–15.09 to –10.80) | –2.76 (–5.86 to 0.34) | 0.080 | |
| CCBT + MCI | 31 | –10.15 (–12.45 to –7.84) | 0.04 (–3.20 to 3.28) | 0.980 | |
| SMFQ-c total score | CCBT | 34 | –4.60 (–6.03 to –3.18) | Ref. | |
| CCBT + MCBT | 38 | –5.66 (–7.03 to –4.29) | –1.06 (–3.07 to 0.96) | 0.301 | |
| CCBT + MCI | 35 | –5.64 (–7.07 to –4.22) | –1.04 (–3.08 to 1.00) | 0.314 | |
| SDQ-c conduct subscale | CCBT | 37 | –0.65 (–1.06 to –0.24) | Ref. | |
| CCBT + MCBT | 41 | –0.74 (–1.12 to –0.35) | –0.09 (–0.66 to 0.49) | 0.763 | |
| CCBT + MCI | 40 | –0.84 (–1.23 to –0.45) | –0.19 (–0.77 to 0.39) | 0.515 |
Analysis of change in teacher-reported questionnaire scores at assessment 2
The analysis results of the change scores from the teachers’ questionnaires are shown in Table 37. The numbers of respondents were small and there were no significant differences in any of the comparisons. Appendix 5, Table 128, presents a summary of the descriptive statistics.
| Questionnaire | Treatment | n | Adjusteda mean change (95% CI) | Adjusteda mean difference (95% CI) | p-value |
|---|---|---|---|---|---|
| SCAS-t total score | CCBT | 7 | –4.02 (–11.27 to 3.23) | Ref. | |
| CCBT + MCBT | 14 | –4.94 (–9.90 to 0.03) | –0.92 (–10.69 to 8.85) | 0.847 | |
| CCBT + MCI | 12 | –5.31 (–10.53 to –0.10) | –1.29 (–10.86 to 8.27) | 0.782 | |
| CAS-t total score | CCBT | 18 | –0.86 (–2.32 to 0.60) | Ref. | |
| CCBT + MCBT | 24 | –1.96 (–3.22 to –0.70) | –1.10 (–3.11 to 0.90) | 0.275 | |
| CCBT + MCI | 25 | –1.26 (–2.48 to –0.04) | –0.40 (–2.37 to 1.57) | 0.684 | |
| SDQ-t conduct subscale | CCBT | 18 | 0.35 (–0.21 to 0.91) | Ref. | |
| CCBT + MCBT | 22 | –0.17 (–0.68 to 0.35) | –0.52 (–1.30 to 0.27) | 0.190 | |
| CCBT + MCI | 23 | –0.11 (–0.62 to 0.39) | –0.46 (–1.24 to 0.31) | 0.236 |
Post-treatment follow-up
Child outcomes at 6-month follow-up
Presence of child’s Anxiety Disorder Interview Schedule primary diagnosis at 6-month follow-up
Table 38 shows the proportion of missing data within each treatment arm for the assessment of the child’s primary diagnosis at 6 months post treatment. The CCBT arm has the highest proportion of missing data (31%).
| Treatment allocation | Missing, n (%) | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|---|
| CCBT | 22 (30.99) | 29 (40.85) | 20 (28.17) | 71 |
| CCBT + MCBT | 16 (23.19) | 34 (49.28) | 19 (27.54) | 69 |
| CCBT + MCI | 20 (28.17) | 38 (53.52) | 13 (18.31) | 71 |
| Total | 58 | 101 | 52 | 211 |
Table 39 shows the proportion of children who recovered from their primary ADIS-C/P anxiety diagnosis by 6 months. The CCBT + MCI arm had the highest proportion of recovered children (75%). The CCBT arm had the lowest proportion of recovered children (59%).
| Treatment allocation | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|
| CCBT | 29 (59.18) | 20 (40.82) | 49 |
| CCBT + MCBT | 34 (64.15) | 19 (35.85) | 53 |
| CCBT + MCI | 38 (74.51) | 13 (25.49) | 51 |
| Total | 101 | 52 | 153 |
Table 40 shows the results of the adjusted linear regression of the child’s primary diagnosis. The results show no statistically significant difference between CCBT + MCBT or CCBT + MCI treatment arms in comparison with CCBT.
As in all of the analyses reporting RRs in this report, a value > 1 implies a better outcome for the index treatment arm compared with the control (CCBT) arm, if the value is < 1, the outcome is better for the CCBT arm.
| Parameter | Adjusted RRa | 95% CI | p-valueb | |
|---|---|---|---|---|
| Treatment | CCBT | Ref. | ||
| CCBT + MCBT | 1.09 | 0.81 to 1.46 | 0.566 | |
| CCBT + MCI | 1.26 | 0.97 to 1.64 | 0.077 | |
Child’s Clinical Global Impression – Improvement at 6 months
The proportion of missing data for child’s CGI-I assessment at 6 months was lower in the CCBT + MCBT arm (23%) and similar in the CCBT (31%) and CCBT + MCI arms (28%) (Table 41).
| Treatment allocation | Missing, n (%) | Much/very much improved, n (%) | Not much/very much improved, n (%) | Total, n (%) |
|---|---|---|---|---|
| CCBT | 22 (30.99) | 39 (54.93) | 10 (14.08) | 71 |
| CCBT + MCBT | 16 (23.19) | 41 (59.42) | 12 (17.39) | 69 |
| CCBT + MCI | 20 (28.17) | 45 (63.38) | 6 (8.45) | 71 |
| Total | 58 | 125 | 28 | 211 |
The proportion of children who were ‘much/very much improved’ at 6 months is shown in Table 42. The CCBT + MCI arm had the highest proportion (88%). CCBT and CCBT + MCBT were similar (80% and 77%, respectively).
| Treatment allocation | Much/very much improved, n (%) | Not much/very much improved, n (%) | Total, n (%) |
|---|---|---|---|
| CCBT | 39 (79.59) | 10 (20.41) | 49 |
| CCBT + MCBT | 41 (77.36) | 12 (22.64) | 53 |
| CCBT + MCI | 45 (88.24) | 6 (11.76) | 51 |
| Total | 125 | 28 | 153 |
The linear regression results in Table 43 show that there are no statistically significant differences between treatment arms.
| Parameter | Adjusted RRa | 95% CI | p-valueb | |
|---|---|---|---|---|
| Treatment | CCBT | Ref. | ||
| CCBT + MCBT | 0.97 | 0.79 to 1.19 | 0.771 | |
| CCBT + MCI | 1.16 | 0.94 to 1.33 | 0.216 | |
Presence of any Anxiety Disorder Interview Schedule anxiety diagnosis in children at 6 months
As shown in Table 44, the proportion of missing data for any ADIS-C/P anxiety diagnosis was similar in CCBT (31%) and CCBT + MCI (28%), but lower in MCBT (23%) children.
| Treatment allocation | Missing, n (%) | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|---|
| CCBT | 22 (30.99) | 23 (32.39) | 26 (36.62) | 71 |
| MCBT | 16 (23.19) | 25 (36.23) | 28 (40.58) | 69 |
| CCBT + MCI | 20 (28.17) | 24 (33.80) | 27 (38.03) | 71 |
| Total | 58 | 72 | 81 | 211 |
Table 45 shows the proportion of children recovering from all anxiety diagnoses by 6 months; and this is the same in each group (47%).
| Treatment allocation | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|
| CCBT | 23 (46.94) | 26 (53.06) | 49 |
| CCBT + MCBT | 25 (47.17) | 28 (52.83) | 53 |
| CCBT + MCI | 24 (47.06) | 27 (52.94) | 51 |
| Total | 72 | 81 | 153 |
The results of the linear regression of recovery from all ADIS-C/P anxiety diagnoses by 6 months are shown in Table 46; there are no statistically significant differences between treatment groups.
| Parameter | Adjusted RRa | 95% CI | p-valueb | |
|---|---|---|---|---|
| Treatment | CCBT | Ref. | ||
| CCBT + MCBT | 1.04 | 0.70 to 1.53 | 0.860 | |
| CCBT + MCI | 1.04 | 0.71 to 1.55 | 0.814 | |
Severity of child’s primary Anxiety Disorder Interview Schedule diagnosis at 6 months
Figure 6 and Table 47 show the distribution of the change scores from baseline to 6 months for the severity rating of the child’s primary diagnosis. As shown in Table 48, the proportion of children with a reduction of 2 or more points is 74% in the CCBT arm, 70% in the CCBT + MCBT arm and 92% in the CCBT + MCI arm. When comparing the CCBT + MCBT arm with CCBT there is no significant difference. However, there is a significant difference between CCBT + MCI and CCBT (p = 0.013).
FIGURE 6.
Box plot of change in severity of child’s pre-treatment ADIS-C/P primary anxiety diagnosis at 6 months.
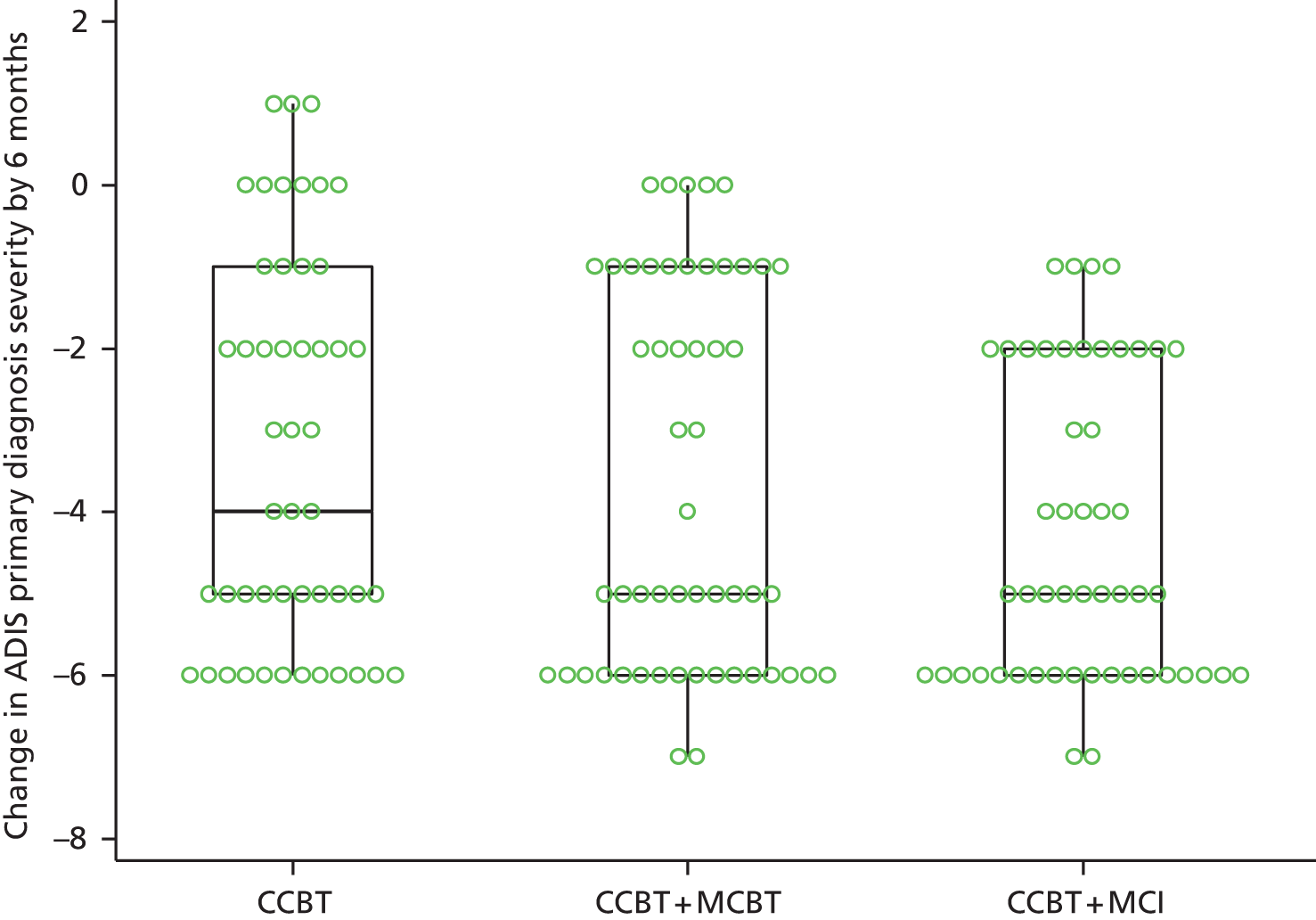
| Treatment allocation | –7 | –6 | –5 | –4 | –3 | –2 | –1 | 0 | 1 | Total |
|---|---|---|---|---|---|---|---|---|---|---|
| CCBT | 0 (0.0) | 12 (24.5) | 10 (20.4) | 3 (6.1) | 3 (6.1) | 8 (16.3) | 4 (8.2) | 6 (12.2) | 3 (6.1) | 49 |
| CCBT + MCBT | 2 (3.8) | 16 (30.2) | 10 (18.9) | 1 (1.9) | 2 (3.8) | 6 (11.3) | 11 (20.8) | 5 (9.4) | 0 (0.0) | 53 |
| CCBT + MCI | 2 (3.9) | 18 (35.3) | 9 (17.7) | 5 (9.8) | 2 (3.9) | 11 (21.6) | 4 (7.8) | 0 (0.0) | 0 (0.0) | 51 |
| Total | 4 | 46 | 29 | 9 | 7 | 25 | 19 | 11 | 3 | 153 |
| Treatment | n | n (%) with a 2 or more point reduction | p-valuea |
|---|---|---|---|
| CCBT | 49 | 36 (73.5) | |
| CCBT + MCBT | 53 | 37 (69.8) | 0.682 |
| CCBT + MCI | 51 | 47 (92.2) | 0.013 |
Analysis of questionnaire data at 6 month follow-up assessments
Analyses of questionnaire results were conducted on the change scores from baseline to the relevant time point. The change scores were more normally distributed. The change scores were modelled using linear regression, adjusted for baseline scores and minimisation factors.
In this section, only patients who are included in the analysis are included in the summary tables.
Adjusted analysis of change in child-reported questionnaire scores at 6 months (intention-to-treat analysis)
Table 49 shows the results for the analysis of the child-reported questionnaire scores, and the change in scores from baseline to 6 months. For all four of the questionnaires there were no significant differences between CCBT + MCBT and CCBT or between CCBT + MCI and CCBT. The adjusted mean scores for each treatment group and every questionnaire are negative, which shows that all groups improved. A summary of the descriptive statistics is given in Appendix 5, Table 136.
| Variable name | Treatment | n | Adjusteda mean change (95% CI) | Adjusteda mean difference (95% CI) | p-value |
|---|---|---|---|---|---|
| CAIS-c total score | CCBT | 38 | –12.45 (–15.06 to –9.84) | Ref. | – |
| CCBT + MCBT | 43 | –11.02 (–13.50 to –8.54) | 1.43 (–2.21 to 5.07) | 0.4374 | |
| 41 | –10.75 (–13.29 to –8.21) | 1.70 (–1.97 to 5.37) | 0.3614 | ||
| SCAS-c total score | CCBT | 41 | –17.85 (–22.73 to –12.98) | Ref. | – |
| CCBT + MCBT | 43 | –16.59 (–21.35 to –11.83) | 1.26 (–5.56 to 8.08) | 0.7146 | |
| CCBT + MCI | 41 | –17.60 (–22.52 to –12.67) | 0.26 (–6.77 to 7.28) | 0.9427 | |
| SDQ-c conduct subscale | CCBT | 42 | –0.88 (–1.35 to –0.42) | Ref. | – |
| CCBT + MCBT | 44 | –0.91 (–1.37 to –0.46) | –0.03 (–0.68 to 0.62) | 0.9245 | |
| CCBT + MCI | 42 | –0.81 (–1.28 to –0.34) | 0.07 (–0.60 to 0.74) | 0.8317 | |
| SMFQ-c total score | CCBT | 40 | –3.81 (–5.33 to –2.29) | Ref. | – |
| CCBT + MCBT | 44 | –3.52 (–4.97 to –2.06) | 0.30 (–1.82 to 2.42) | 0.7828 | |
| CCBT + MCI | 39 | –3.97 (–5.52 to –2.41) | –0.16 (–2.36 to 2.04) | 0.8872 |
Adjusted analysis of change in mother-reported questionnaire scores at 6 months (intention-to-treat analysis)
Table 50 shows results of linear regression looking at mother-reported questionnaires about child symptoms/impact. For the SDQ-p conduct subscale a significant difference was seen between the CCBT + MCI and the CCBT arms (p = 0.022), with the CCBT + MCI arm seeing a bigger reduction in score on average. A summary of the descriptive statistics is given in Appendix 5, Table 137.
| Variable name | Treatment | n | Adjusteda mean change (95% CI) | Adjusteda mean difference (95% CI) | p-value |
|---|---|---|---|---|---|
| CAIS-p total score | CCBT | 35 | –9.25 (–12.12 to –6.37) | Ref. | – |
| CCBT + MCBT | 37 | –12.13 (–14.95 to –9.31) | –2.88 (–6.92 to 1.16) | 0.1599 | |
| CCBT + MCI | 34 | –9.69 (–12.68 to –6.70) | –0.44 (–4.61 to 3.73) | 0.8348 | |
| SCAS-p total score | CCBT | 36 | –17.44 (–21.03 to –13.84) | Ref. | – |
| CCBT + MCBT | 41 | –16.62 (–20.00 to –13.25) | 0.82 (–4.11 to 5.74) | 0.7432 | |
| CCBT + MCI | 38 | –19.17 (–22.72 to –15.61) | –1.73 (–6.86 to 3.40) | 0.5050 | |
| SDQ-p conduct subscale | CCBT | 39 | –0.47 (–0.86 to –0.09) | Ref. | – |
| CCBT + MCBT | 42 | –0.99 (–1.36 to –0.62) | –0.51 (–1.05 to 0.02) | 0.0600 | |
| CCBT + MCI | 41 | –1.11 (–1.49 to –0.73) | –0.64 (–1.19 to -0.09) | 0.0224 | |
| SMFQ-p total score | CCBT | 36 | –4.25 (–5.82 to –2.67) | Ref. | – |
| CCBT + MCBT | 38 | –5.86 (–7.40 to –4.32) | –1.61 (–3.83 to 0.61) | 0.1542 | |
| CCBT + MCI | 36 | –4.90 (–6.49 to –3.30) | –0.65 (–2.91 to 1.61) | 0.5701 |
Adjusted analysis of change in teacher-reported questionnaire scores at 6 months (intention-to-treat analysis)
The number of respondents was low. As shown in Table 51, no significant differences were seen. A summary of descriptive statistics are given in Appendix 5, Table 138.
| Variable name | Treatment | n | Adjusteda mean change (95% CI) | Adjusteda mean difference (95% CI) | p-value |
|---|---|---|---|---|---|
| CAS-t total score | CCBT | 11 | –1.43 (–3.85 to 0.99) | Ref. | – |
| CCBT + MCBT | 17 | –2.92 (–4.91 to –0.94) | –1.50 (–4.65 to 1.66) | 0.3432 | |
| CCBT + MCI | 23 | –1.40 (–3.02 to 0.23) | 0.03 (–2.92 to 2.98) | 0.9845 | |
| SCAS-t total score | CCBT | 4 | –1.88 (–15.75 to 12.00) | Ref. | – |
| CCBT + MCBT | 9 | –15.07 (–22.85 to –7.29) | –13.19 (–30.33 to 3.94) | 0.1227 | |
| CCBT + MCI | 15 | –10.26 (–15.89 to –4.64) | –8.39 (–24.79 to 8.01) | 0.2955 | |
| SDQ-t conduct subscale | CCBT | 12 | 0.57 (–0.36 to 1.50) | Ref. | – |
| CCBT + MCBT | 18 | –0.21 (–0.98 to 0.57) | –0.78 (–1.98 to 0.42) | 0.1961 | |
| CCBT + MCI | 22 | 0.31 (–0.37 to 1.00) | –0.26 (–1.42 to 0.90) | 0.6540 |
Child outcomes at 12-month follow-up
Presence of child’s Anxiety Disorder Interview Schedule primary diagnosis at 12 months
Table 52 shows that the proportion of missing data for the assessment of the child’s primary diagnosis at 12 months is very similar in the CCBT (39%) and CCBT + MCI (35%) arms, but lower in the CCBT + MCBT arm (28%).
| Treatment allocation | Missing, n (%) | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|---|
| CCBT | 28 (39.44) | 31 (43.66) | 12 (16.90) | 71 |
| CCBT + MCBT | 19 (27.54) | 30 (43.48) | 20 (28.99) | 69 |
| CCBT + MCI | 25 (35.21) | 34 (47.89) | 12 (16.90) | 71 |
| Total | 72 | 95 | 44 | 211 |
Table 53 shows that recovery from primary diagnosis is very similar in the CCBT (72%) and CCBT + MCI arms (74%), whereas in the CCBT + MCBT group it is lower (60%).
| Treatment allocation | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|
| CCBT | 31 (72.09) | 12 (27.91) | 43 |
| CCBT + MCBT | 30 (60.00) | 20 (40.00) | 50 |
| CCBT + MCI | 34 (73.91) | 12 (26.09) | 46 |
| Total | 95 | 44 | 139 |
The results of the linear regression are shown in Table 54. The results show no statistically significant difference between the CCBT + MCBT or CCBT + MCI treatment arms in comparison with CCBT.
| Parameter | Adjusted RRa | 95% CI | p-valueb | |
|---|---|---|---|---|
| Treatment | CCBT | Ref. | ||
| CCBT + MCBT | 0.85 | 0.65 to 1.12 | 0.257 | |
| CCBT + MCI | 1.04 | 0.82 to 1.30 | 0.766 | |
Child’s Clinical Global Impression – Improvement at 12 months
The proportion of 12-month CGI-I assessments that were missing is shown in Table 55. The CCBT arm had 39% missing, CCBT + MCI had 35% missing and CCBT + MCBT had 28% missing.
| Treatment allocation | Missing, n (%) | Much/very much improved, n (%) | Not much/very much improved, n (%) | Total, n (%) |
|---|---|---|---|---|
| CCBT | 28 (39.44) | 33 (46.48) | 10 (14.08) | 71 |
| CCBT + MCBT | 19 (27.54) | 39 (56.52) | 11 (15.94) | 69 |
| CCBT + MCI | 25 (35.21) | 37 (52.11) | 9 (12.68) | 71 |
| Total | 72 | 109 | 30 | 211 |
As shown in Table 56, the proportion of children who were ‘much/very much improved’ was similar between treatment groups; between 77% and 80%.
| Treatment allocation | Much/very much improved, n (%) | Not much/very much improved, n (%) | Total, n (%) |
|---|---|---|---|
| CCBT | 33 (76.74) | 10 (23.26) | 43 |
| CCBT + MCBT | 39 (78.00) | 11 (22.00) | 50 |
| CCBT + MCI | 37 (80.43) | 9 (19.57) | 46 |
| Total | 109 | 30 | 139 |
The results of the linear regression of CGI-I at 12 months are shown in Table 57; there are no statistically significant differences between treatment groups.
| Parameter | Adjusted RRa | 95% CI | p-valueb | |
|---|---|---|---|---|
| Treatment | CCBT | Ref. | ||
| CCBT + MCBT | 1.02 | 0.82 to 1.27 | 0.834 | |
| CCBT + MCI | 1.05 | 0.85 to 1.30 | 0.628 | |
Presence of any Anxiety Disorder Interview Schedule anxiety diagnosis in children at 12 months
As shown in Table 58, the proportion of missing data for all anxiety diagnoses at 12 months was lowest in the CCBT + MCBT arm (28%). In the CCBT + MCI arm it is 35% and in the CCBT arm 39%.
| Treatment allocation | Missing, n (%) | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|---|
| CCBT | 28 (39.44) | 23 (32.39) | 20 (28.17) | 71 |
| CCBT + MCBT | 19 (27.54) | 23 (33.33) | 27 (39.13) | 69 |
| CCBT + MCI | 25 (35.21) | 24 (33.80) | 22 (30.99) | 71 |
| Total | 72 | 70 | 69 | 211 |
The proportion of recovered children was similar in the CCBT arm (53%) and the CCBT + MCI arm (52%). In the CCBT + MCBT arm the proportion was slightly lower at 46% (Table 59).
| Treatment allocation | No diagnosis, n (%) | Diagnosis, n (%) | Total, n (%) |
|---|---|---|---|
| CCBT | 23 (53.49) | 20 (46.51) | 43 |
| CCBT + MCBT | 23 (46.00) | 27 (54.00) | 50 |
| CCBT + MCI | 24 (52.17) | 22 (47.83) | 46 |
| Total | 70 | 69 | 139 |
The results of the linear regression of recovery from all ADIS-C/P anxiety diagnoses by 12 months are shown in Table 60. There are no statistically significant differences between treatment groups.
| Parameter | Adjusted RRa | 95% CI | p-valueb | |
|---|---|---|---|---|
| Treatment | CCBT | Ref. | ||
| CCBT + MCBT | 0.89 | 0.61 to 1.31 | 0.569 | |
| CCBT + MCI | 1.01 | 0.70 to 1.45 | 0.972 | |
Severity of child’s pre-treatment Anxiety Disorder Interview Schedule primary diagnosis at 12 months
By 12 months 77% of the control group, 74% of the CCBT + MCBT group and 87% of the CCBT + MCI group children had seen an improvement of at least 2 points (Figure 7 and Tables 61 and 62).
There were no significant differences between the CCBT + MCBT and CCBT arms or between the CCBT + MCI and CCBT arms (p = 0.760 and p = 0.210, respectively).
FIGURE 7.
Box plot of change in severity of child’s primary ADIS-C/P anxiety diagnosis at 12 months.

| Treatment allocation | –7 | –6 | –5 | –4 | –3 | –2 | –1 | 0 | 1 | Total |
|---|---|---|---|---|---|---|---|---|---|---|
| CCBT | 3 (6.98) | 10 (23.26) | 9 (20.93) | 5 (11.63) | 2 (4.65) | 4 (9.30) | 7 (16.28) | 1 (2.33) | 2 (4.65) | 43 |
| CCBT + MCBT | 3 (6.00) | 10 (20.00) | 12 (24.00) | 1 (2.00) | 3 (6.00) | 8 (16.00) | 6 (12.00) | 7 (14.00) | 0 (0.00) | 50 |
| CCBT + MCI | 1 (2.17) | 18 (39.1) | 8 (17.39) | 4 (8.70) | 3 (6.52) | 6 (13.04) | 6 (13.04) | 0 (0.00) | 0 (0.00) | 46 |
| Total | 7 | 38 | 29 | 10 | 8 | 18 | 19 | 8 | 2 | 139 |
| Treatment | n | n (%) with 2 or more point reduction | p-valuea |
|---|---|---|---|
| CCBT | 43 | 33 (76.7) | |
| CCBT + MCBT | 50 | 37 (74.0) | 0.760 |
| CCBT + MCI | 46 | 40 (87.0) | 0.210 |
Analysis of questionnaire data at 12-month follow-up assessments
Analyses of questionnaire results were conducted on the change scores from baseline to the relevant time point owing to the skewed distribution of the raw scores at each time point. The change scores were more normally distributed. The change scores were modelled using linear regression, adjusted for baseline scores and minimisation factors.
In this section, only patients who are included in the analysis are included in the summary tables.
Adjusted analysis of change in child-reported questionnaire scores at 12 months (intention-to-treat analysis)
As shown in Table 63, no significant differences were seen. A summary of the descriptive statistics is given in Appendix 5, Table 139.
| Variable name | Treatment | n | Adjusteda mean change (95% CI) | Adjusteda mean difference (95% CI) | p-value |
|---|---|---|---|---|---|
| CAIS-c total score | CCBT | 29 | –12.83 (–17.14 to –8.51) | Ref. | – |
| CCBT + MCBT | 33 | –9.25 (–13.41 to –5.09) | 3.57 (–2.59 to 9.74) | 0.2525 | |
| CCBT + MCI | 37 | –11.71 (–15.48 to –7.93) | 1.12 (–4.59 to 6.83) | 0.6978 | |
| SCAS-c total score | CCBT | 31 | –18.11 (–23.18 to –13.03) | Ref. | – |
| CCBT + MCBT | 34 | –18.92 (–23.82 to –14.01) | –0.81 (–7.96 to 6.34) | 0.8225 | |
| CCBT + MCI | 37 | –17.98 (–22.59 to –13.38) | 0.12 (–6.73 to 6.97) | 0.9718 | |
| SDQ-c conduct subscale | CCBT | 31 | –1.21 (–1.87 to –0.55) | Ref. | – |
| CCBT + MCBT | 34 | –0.94 (–1.58 to –0.30) | 0.27 (–0.65 to 1.18) | 0.5622 | |
| CCBT + MCI | 38 | –1.00 (–1.59 to –0.40) | 0.21 (–0.68 to 1.10) | 0.6373 | |
| SMFQ-c total score | CCBT | 28 | –4.08 (–5.95 to –2.21) | Ref. | – |
| CCBT + MCBT | 35 | –4.20 (–5.91 to –2.49) | –0.12 (–2.71 to 2.48) | 0.9284 | |
| CCBT + MCI | 37 | –2.09 (–3.72 to –0.47) | 1.99 (–0.48 to 4.46) | 0.1132 |
Adjusted analysis of change in mother-reported questionnaire scores at 12 months (intention-to-treat analysis)
As shown in Table 64, no significant differences were seen. A summary of descriptive statistics is given in Appendix 5, Table 140.
| Variable name | Treatment | n | Adjusteda mean change (95% CI) | Adjusteda mean difference (95% CI) | p-value |
|---|---|---|---|---|---|
| CAIS-p total score | CCBT | 28 | –9.50 (–12.44 to –6.56) | Ref. | – |
| CCBT + MCBT | 27 | –12.11 (–15.19 to –9.04) | –2.61 (–6.88 to 1.66) | 0.2270 | |
| CCBT + MCI | 31 | –12.15 (–14.99 to –9.32) | –2.65 (–6.72 to 1.42) | 0.1985 | |
| SCAS-p total score | CCBT | 30 | –22.37 (–26.62 to –18.12) | Ref. | – |
| CCBT + MCBT | 31 | –16.36 (–20.58 to –12.15) | 6.01 (–0.01 to 12.02) | 0.0502 | |
| CCBT + MCI | 33 | –20.74 (–24.78 to –16.71) | 1.62 (–4.27 to 7.51) | 0.5850 | |
| SDQ-p conduct subscale | CCBT | 32 | –1.04 (–1.56 to –0.53) | Ref. | – |
| CCBT + MCBT | 32 | –0.89 (–1.40 to –0.38) | 0.16 (–0.57 to 0.89) | 0.6685 | |
| CCBT + MCI | 38 | –0.85 (–1.31 to –0.38) | 0.20 (–0.50 to 0.89) | 0.5755 | |
| SMFQ-p total score | CCBT | 30 | –5.14 (–6.81 to –3.48) | Ref. | – |
| CCBT + MCBT | 29 | –4.54 (–6.25 to –2.82) | 0.61 (–1.82 to 3.04) | 0.6194 | |
| CCBT + MCI | 33 | –5.97 (–7.55 to –4.39) | –0.83 (–3.11 to 1.46) | 0.4739 |
Adjusted analysis of change in teacher-reported questionnaire scores at 12 months (intention-to-treat analysis)
As shown in Table 65, no significant differences were seen. A summary of descriptive statistics is given in Appendix 5, Table 141.
Note the small number of observations when looking at these results.
| Variable name | Treatment | n | Adjusteda mean change (95% CI) | Adjusteda mean difference (95% CI) | p-value |
|---|---|---|---|---|---|
| CAS-t total score | CCBT | 9 | –2.56 (–4.76 to –0.37) | Ref. | – |
| CCBT + MCBT | 10 | –0.04 (–2.23 to 2.14) | 2.52 (–0.62 to 5.66) | 0.1099 | |
| CCBT + MCI | 12 | –0.40 (–2.29 to 1.48) | 2.16 (–0.77 to 5.09) | 0.1391 | |
| SCAS-t total score | CCBT | 4 | –7.90 (–17.17 to 1.37) | Ref. | – |
| CCBT + MCBT | 4 | –0.04 (–18.30 to 18.22) | 7.86 (–12.83 to 28.55) | 0.2437 | |
| CCBT + MCI | 5 | –11.90 (–23.14 to –0.66) | –4.00 (–18.25 to 10.25) | 0.3510 | |
| SDQ-t conduct subscale | CCBT | 9 | –0.09 (–1.21 to 1.03) | Ref. | – |
| CCBT + MCBT | 11 | –0.27 (–1.30 to 0.75) | –0.18 (–1.71 to 1.34) | 0.8051 | |
| CCBT + MCI | 12 | 0.41 (–0.54 to 1.36) | 0.50 (–0.99 to 2.00) | 0.4903 |
Secondary research questions
The extent to which improvement in child anxiety was associated with changes in maternal anxiety and parenting responses is shown in the following tables of correlations (see Tables 66–75). In each case Pearson’s correlation coefficient (r), the p-value and the number of observations are shown. For each of the three child anxiety variables that are used to correlate with other variables, a higher score implies a worse outcome for the child (as we are looking at the change from baseline).
Associations between change in maternal anxiety and child anxiety outcomes immediately post treatment (assessment 2)
Table 66 (assessment 1B) and Table 67 (assessment 2) show the correlations between child anxiety (change in SCAS-c total score, change in CSR of primary diagnosis and CGI-I) and maternal anxiety (change in CSR of primary diagnosis). In these tables none of the correlations are statistically different from zero.
| Mother anxiety change scores (baseline to assessment 1B) | Child anxiety change scores (baseline to assessment 1B) | |||
|---|---|---|---|---|
| SCAS-c | CSR of primary diagnosis | CGI-I | ||
| Change in CSR | r | 0.03295 | 0.06790 | 0.05102 |
| p-value | 0.6642 | 0.3419 | 0.4753 | |
| n | 176 | 198 | 198 | |
| Mother anxiety change scores (baseline to assessment 2) | Child anxiety change scores (baseline to assessment 2) | |||
|---|---|---|---|---|
| SCAS-c | CSR of primary diagnosis | CGI-I | ||
| Change in CSR | r | 0.01689 | 0.03667 | 0.09354 |
| p-value | 0.8447 | 0.6339 | 0.2237 | |
| n | 137 | 171 | 171 | |
Similarly to before, the following table (Table 68) shows the correlations between the change in child anxiety scores from baseline to assessment 2 (SCAS-c, CSR and CGI-I) and mother anxiety questionnaire change scores (DASS-21).
| Mother anxiety change scores (baseline to assessment 2) | Change in child anxiety (baseline to assessment 2) | |||
|---|---|---|---|---|
| SCAS-c | CSR of primary diagnosis | CGI-I | ||
| DASS-21 anxiety | r | –0.06825 | –0.0036 | 0.05363 |
| p-value | 0.5227 | 0.9710 | 0.5943 | |
| n | 90 | 101 | 101 | |
Associations between change in maternal parenting responses and child anxiety outcomes
Table 69 shows the correlations between the same child anxiety ratings and each of the behavioural change scores at assessment 2. There are significant correlations between change in CSR and change in overprotection (r = –0.1956; p = 0.0225), CGI-I and change in overprotection (r = –0.3123; p = 0.0002), CGI-I and change in quality of relationship (r = –0.1097; p = 0.0450).
| Mother–child behavioural change scores (baseline to assessment 2) | Child anxiety change scores (baseline to assessment 2) | |||
|---|---|---|---|---|
| SCAS-c | CSR of primary diagnosis | CGI-I | ||
| Positive behaviour | r | 0.00914 | –0.01251 | –0.06857 |
| p-value | 0.9220 | 0.8851 | 0.4294 | |
| n | 117 | 136 | 135 | |
| Overprotection | r | 0.03525 | –0.19558 | –0.31226 |
| p-value | 0.7059 | 0.0225 | 0.0002 | |
| n | 117 | 136 | 135 | |
| Promotion of avoidance | r | 0.02498 | –0.04638 | 0.07694 |
| p-value | 0.7892 | 0.5918 | 0.3751 | |
| n | 117 | 136 | 135 | |
| Intrusiveness | r | 0.14039 | –0.01128 | –0.02442 |
| p-value | 0.1311 | 0.8963 | 0.7786 | |
| n | 117 | 136 | 135 | |
| Anxiety | r | –0.06341 | –0.00024 | –0.10791 |
| p-value | 0.4970 | 0.9978 | 0.2129 | |
| n | 117 | 136 | 135 | |
| Quality of relationship | r | –0.03089 | –0.15215 | –0.17282 |
| p-value | 0.7409 | 0.0770 | 0.0450 | |
| n | 117 | 136 | 135 | |
| POI | r | 0.17777 | –0.00642 | 0.07565 |
| p-value | 0.0848 | 0.9479 | 0.4409 | |
| n | 95 | 106 | 106 | |
Similarly, Table 70 shows the correlations between the same child anxiety change scores and each of the cognition change scores at assessment 2. None of the correlations are statistically different from zero.
| Mother–child cognition change scores (baseline to assessment 2) | Child anxiety change scores (baseline to assessment 2) | |||
|---|---|---|---|---|
| SCAS-c | CSR of primary diagnosis | CGI-I | ||
| Pre-task ‘scared’ | r | 0.15092 | 0.00701 | 0.16665 |
| p-value | 0.1122 | 0.9367 | 0.0581 | |
| n | 112 | 131 | 130 | |
| Pre-task ‘anxious’ | r | –0.02832 | 0.01928 | 0.07960 |
| p-value | 0.7669 | 0.8270 | 0.3680 | |
| n | 112 | 131 | 130 | |
| Pre-task ‘child in control’ | r | –0.03400 | –0.04478 | –0.08487 |
| p-value | 0.7219 | 0.6115 | 0.3370 | |
| n | 112 | 131 | 130 | |
| Pre-task ‘mother in control’ | r | 0.17628 | 0.04862 | 0.04707 |
| p-value | 0.0630 | 0.5813 | 0.5949 | |
| n | 112 | 131 | 130 | |
Associations between change in maternal anxiety and child anxiety outcomes 6 and 12 months post treatment (assessments 3 and 4)
Tables 71 and 72 show correlations between change in child anxiety scores and change in mother anxiety questionnaire scores from baseline to the 6- and 12-month post-treatment follow-up assessment. At the 6-month time point none of the correlations were statistically significant. At 12 months, maternal general anxiety (DASS-21) was significantly associated with change in the CSR of the child’s primary diagnosis (p = 0.0195).
| Mother change scores (baseline to 6 months) | Child change scores (baseline to 6 months) | |||
|---|---|---|---|---|
| SCAS-c | CSR of primary diagnosis | CGI-I | ||
| DASS-21 anxiety | r | 0.08825 | –0.06079 | 0.06979 |
| p-value | 0.3875 | 0.5359 | 0.4772 | |
| n | 98 | 106 | 106 | |
| Mother change scores (baseline to 12 months) | Child change scores (baseline to 12 months) | |||
|---|---|---|---|---|
| SCAS-c | CSR of primary diagnosis | CGI-I | ||
| DASS-21 anxiety | r | –0.05089 | –0.25755 | –0.05375 |
| p-value | 0.6624 | 0.0195 | 0.6315 | |
| n | 76 | 82 | 82 | |
Observations of parental behaviours and cognitions were not made at the 6- and 12-month follow-up assessments, so associations between change in these variables and longer-term outcomes were assessed on the basis of maternal behavioural and cognition change scores at assessment 2 and child anxiety outcomes at 6 and 12 months (Tables 73 and 74). Change in maternal overprotection at assessment 2 was associated with CGI-I at 6 months (p = 0.044) and change in child anxiety symptoms (SCAS-c) at 12 months (p = 0.004). Change in maternal intrusiveness was significantly associated with child CGI-I at 12 months (p = 0.009). In relation to maternal cognitions, change in pre-task expectations of how much the mother would be in control of her child’s response was significantly associated with change in child anxiety symptoms at 6 months (SCAS-c) (p = 0.022).
| Mother–child behavioural change scores (baseline to assessment 2) | Child anxiety change scores (baseline to 6 months) | Child anxiety change scores (baseline to 12 months) | |||||
|---|---|---|---|---|---|---|---|
| SCAS-c | CSR of primary diagnosis | CGI-I | SCAS-c | CSR of primary diagnosis | CGI-I | ||
| Positive behaviour | r | 0.14050 | –0.02741 | 0.02782 | –0.00056 | 0.00176 | 0.03081 |
| p-value | 0.1489 | 0.7615 | 0.7581 | 0.9958 | 0.9850 | 0.7416 | |
| n | 107 | 125 | 125 | 90 | 117 | 117 | |
| Overprotection | r | 0.12875 | 0.05708 | –0.18019 | 0.30408 | 0.03819 | –0.09012 |
| p-value | 0.1863 | 0.5272 | 0.0443 | 0.0036 | 0.6827 | 0.3339 | |
| n | 107 | 125 | 125 | 90 | 117 | 117 | |
| Promotion of avoidance | r | 0.01996 | –0.05951 | 0.03262 | –0.02830 | 0.03669 | 0.05961 |
| p-value | 0.8383 | 0.5098 | 0.7180 | 0.7912 | 0.6945 | 0.5232 | |
| n | 107 | 125 | 125 | 90 | 117 | 117 | |
| Intrusiveness | r | 0.03897 | 0.11560 | –0.05094 | –0.05594 | –0.07602 | –0.24017 |
| p-value | 0.6902 | 0.1992 | 0.5726 | 0.6005 | 0.4153 | 0.0091 | |
| n | 107 | 125 | 125 | 90 | 117 | 117 | |
| Expressed anxiety | r | –0.09444 | –0.10867 | –0.11103 | –0.14463 | –0.02053 | –0.16905 |
| p-value | 0.3333 | 0.2277 | 0.2177 | 0.1738 | 0.8261 | 0.0685 | |
| n | 107 | 125 | 125 | 90 | 117 | 117 | |
| Quality of relationship | r | –0.03542 | –0.09344 | –0.06767 | 0.00020 | –0.10428 | –0.11616 |
| p-value | 0.7172 | 0.3000 | 0.4534 | 0.9985 | 0.2632 | 0.2123 | |
| n | 107 | 125 | 125 | 90 | 117 | 117 | |
| Mother–child cognition change scores (baseline to assessment 2) | Child anxiety change scores (baseline to 6 months) | Child anxiety change scores (baseline to 12 months) | |||||
|---|---|---|---|---|---|---|---|
| SCAS-c | CSR of primary diagnosis | CGI-I | SCAS-c | CSR of primary diagnosis | CGI-I | ||
| Pre-task ‘scared’ | r | 0.05618 | 0.13760 | 0.06005 | 0.14249 | –0.05847 | –0.02565 |
| p-value | 0.5711 | 0.1323 | 0.5129 | 0.1906 | 0.5384 | 0.7874 | |
| n | 104 | 121 | 121 | 86 | 113 | 113 | |
| Pre-task ‘anxious’ | r | 0.00674 | 0.07552 | –0.00865 | –0.04708 | –0.02433 | –0.06011 |
| p-value | 0.9458 | 0.4103 | 0.9249 | 0.6669 | 0.7981 | 0.5271 | |
| n | 104 | 121 | 121 | 86 | 113 | 113 | |
| Pre-task ‘child in control’ | r | 0.06490 | –0.16300 | –0.05574 | 0.12284 | 0.00607 | –0.01974 |
| p-value | 0.5127 | 0.0740 | 0.5437 | 0.2598 | 0.9492 | 0.8356 | |
| n | 104 | 121 | 121 | 86 | 113 | 113 | |
| Pre-task ‘mother control’ | r | 0.22508 | 0.06698 | 0.03040 | 0.20293 | –0.05837 | 0.01778 |
| p-value | 0.0216 | 0.4654 | 0.7406 | 0.0609 | 0.5391 | 0.8517 | |
| n | 104 | 121 | 121 | 86 | 113 | 113 | |
Parent-reported overinvolvement was assessed at all assessments so concurrent change in this variable could be correlated with child outcomes at the 6- and-12 month assessments, as shown in Table 75. There were no significant correlations.
| POI change scores | SCAS-c | CSR of primary diagnosis | CGI-I | |
|---|---|---|---|---|
| Baseline to 6-month follow-up | r | 0.11522 | –0.05258 | 0.07649 |
| p-value | 0.2488 | 0.5854 | 0.4270 | |
| n | 102 | 110 | 110 | |
| Baseline to 12-month follow-up | r | 0.09522 | –0.06828 | 0.04747 |
| p-value | 0.3860 | 0.5201 | 0.6568 | |
| n | 85 | 91 | 90 | |
Adverse events
Adverse events were defined as follows:
Adverse or unexpected events resulting in physical or psychological injury that arise from the administration of research procedures or the provision of treatment within the trial. This will include events such as breach of confidentiality, adverse therapeutic interventions, diagnostic error, improper staff behaviour, falls and injury.
There were no adverse events.
Chapter 4 Economic evaluation: cost–utility analysis of treatment of childhood anxiety disorder in the context of maternal anxiety disorder
Introduction
The aim of the economic evaluation was to assess the cost-effectiveness of the CCBT + MCBT and CCBT + MCI treatment arms compared with the CCBT treatment arm. This design mirrored the study research questions, and hence was equivalent to conducting two separate economic evaluations, that is CCBT + MCBT versus CCBT, and CCBT + MCI versus CCBT. An incremental comparison between CCBT + MCBT and CCBT + MCI was not a research question and the statistical and economic analyses were not powered for this comparison. The primary economic analyses followed an ITT approach and adopted a health service provider perspective. The economic analyses aligned with the primary aim of the trial, namely to evaluate whether or not the CCBT treatment arm could be improved by the addition of (i) treatment of maternal anxiety disorders (MCBT), or (ii) treatment focused on maternal responses (MCI). Secondary economic analyses complemented the results of the primary analyses by measuring additional mother and child resource use of health and personal social services beyond the main costs of the treatment. Broader impacts on other sectors, including education and employment, were also measured. Data were collected on time off school for children and time off work and usual activities for mothers/carers.
Methods
The primary economic analyses for both comparisons consisted of a cost–utility analysis (CUA) conducted from a health service provider perspective. Secondary economic analyses supplemented the primary results by identifying, measuring and valuing resource use impacts from a wider social and personal social service perspective in addition to measuring the impact on the education and employment sectors. Recent methods guidance on the conduct, reporting and presentation of economic evaluations were adhered. 75–77 Costs and outcomes were combined within a CUA framework and presented using incremental cost-effectiveness ratios (ICERs) with uncertainty represented using the cost-effectiveness plane. The results were also reported using net monetary benefit (NMB). Prices were reported in 2011/12 as the base year, adjusted for inflation using Retail Price Index (RPI) 201278 or Hospital and Community Health Service (HCHS) index 2011/1279 as appropriate. All statistical analyses were performed using Stata version 12.1. Statistical significance was set at p-values < 0.05.
Identification and measurement of health and social care resource use
Patient-level resource use data, including all associated treatment costs, additional health and personal social service costs, were identified and measured as an integral part of the trial data collection process. Resource use data were collected via a ‘bottom up’ approach where detail on the intervention and control resources used to deliver the CCBT + MCBT, CCBT + MCI and CCBT treatment arms were identified and measured via the use of a specially designed ‘therapist resource use log’. This log was designed for trial therapists to complete every time a contact was made. Details for all types of visit (e.g. client face-to-face visit, phone contact, school visit) were collected by recording all resources used, duration of any contact with the patient as well as other resources such as travel mileage, rail fares or other expenses incurred during the contact. See Appendix 3, Health economic logs, for a copy of the therapist resource use log.
A patient-held ‘resource use’ diary was developed to capture any additional health and social care resources used by the mother and child beyond the therapy sessions (see Appendix 3, Health economics diary/patient-held resource use diary). The aim of the diary was to aid recall, that is for the use of mothers as a means of recording relevant resource use information for them and their children during the time between assessments (baseline to assessment 1B for mid-intervention; assessment 1B to assessment 2 for post intervention; assessment 2 to 6 months for the 6-month follow-up; 6 months to 12 months for the 12-month follow-up), so that they might be able to complete the mid- and post-intervention questionnaires more efficiently. The resource use diaries comprised three sections. The first section included questions on use of primary and secondary care health services (except the main anxiety intervention), of other social services (e.g. social worker contacts) and of services provided by government bodies other than the NHS (e.g. education department). The second section aimed to collect information on drug treatment by asking mothers whether or not they and/or their children made use of medications and if the latter were GP prescribed or purchased ‘over-the-counter’. Finally, in a bid to capture broader societal impacts on employment and education, the third section asked mothers to report how much time they had to take off work and/or usual activities owing to ill health and how many days off school their children had taken owing to ill health.
Valuation of health and social care resource use
For each trial participant (mother and child), all components of treatment costs stratified by category of resource use were computed by multiplying units of resource use by their unit costs. These were then summed over all resource use categories to obtain a total annual cost for each participant. Unit cost sources included NHS reference costs and unit costs of community care. 79–86 Unit costs can be found in Appendix 3, Table 89. Primary economic analyses focused only on the NHS cost of the alternative anxiety treatments; preliminary secondary analyses included also wider societal and further health and social care costs and will be developed further to include cost of medications and time off work. Prescription cost analysis87 and published literature will be used to identify unit costs of prescribed and ‘over-the-counter’ drugs, respectively, whereas time off work will be valued using the human capital approach, using the median gross weekly earnings by age and sex. 88 Values are expressed in 2011/12 UK pounds sterling (£). Values available only in 2010/11 or earlier prices were adjusted for inflation using RPI 201278 or the HCHS pay and price inflation index 2011/12. 79 As the duration of the study was 12 months, discounting of future costs and benefits was not required.
Identifying and measuring outcomes: quality-adjusted life-years
In line with National Institute for Health and Care Excellence (NICE) recommendations, outcomes in the economic analyses were identified and measured using quality-adjusted life-years (QALYs). Data to estimate QALYs for mothers were collected through the European Quality of Life-5 Dimensions (EQ-5D) self-completion questionnaire,89 which was administered to mothers at baseline, assessment 1B (mid-treatment), assessment 2 (post treatment), and at 6- and 12-month follow-ups. For children the EQ-5D child-friendly version was used. 90 The EQ-5D is a generic measure of health-related quality of life, designed to estimate QALYs and widely used across disease areas. It contains five questions each concerned with a different area or ‘domain’ of everyday life: mobility; self-care; usual activities such as work, study, housework and leisure activities; pain/discomfort; and anxiety/depression. The answers to these questions provide a description or profile of the respondent’s quality of life and a value is then attached to each profile using the results of a large UK general population survey. 91 The tariff was used to estimate health-related quality of life (EQ-5D scores) for each child and mother at baseline, assessment 1B (mid-treatment), assessment 2 (post treatment), and at 6- and 12-month follow-ups. These EQ-5D utilities were then combined with duration spent in each health state to estimate QALY gain over the 12-month period of the study, assuming linear changes of utility between measurements and linear interpolation to identify the area under the curve for the 12-month period. 92 QALYs were computed using the area under the curve approach, weighting the 12-month period by utility measured on a scale from 0 to 1. 92
Reporting and presenting results
Within the primary economic analyses the mean volume of health-care resources associated with each arm were estimated and reported together with their standard errors (CCBT + MCBT, CCBT + MCI and CCBT). Mean differences were calculated using ordinary least squares (OLS) regression to reflect the trial comparisons: first the incremental resources used by the CCBT + MCBT arm versus the CCBT arm, and second the incremental resources used by the CCBT + MCI arm versus the CCBT arm. Differences in resource use are reported alongside 95% CIs.
Within the secondary economic analyses, health-care services other than those associated with the intervention, other personal social services, non-NHS resources and medication use, were investigated both for the mother and the child in each arm using descriptive statistics on the available data. More specifically, mean resource use volumes were reported with their SDs for mother and child separately over the following periods: baseline to assessment 1B (mid-treatment); assessment 1B to assessment 2 (post treatment); assessment 2 to 6 months follow-up; and from 6 months to 12 months follow-up.
In the primary analyses the total intervention cost per participant (mother and child) was estimated by multiplying the volume of each item of resource used by the unit cost of that item, then summing each item cost for each participant. Mean costs were estimated and reported together with their standard errors for each trial arm. Statistical differences in mean cost estimates across trial arms (CCBT + MCBT vs. CCBT; and CCBT + MCI vs. CCBT) were evaluated using OLS regression. Robustness checks were conducted using generalized linear modelling estimates to account for skewedness of cost data. Similar analyses were conducted in relation to wider health and social care costs in the preliminary secondary analyses. In those cases, however, total cost per patient was first calculated over each period between measurements, namely from baseline to assessment 1B (mid-treatment); from assessment 1B to assessment 2 weeks (post treatment); from assessment 2 to 6 months follow-up; and from 6 months to 12 months follow-up, and then summed for each patient in order to obtain a total cost over the 12-month period. Cost estimates were calculated for mother and child separately and then combined into one variable.
In order to inform whether or not either intervention is cost-effective, current methods recommended by NICE technology assessment guidance have been adopted to report and present the results of the incremental costs and QALYs for each comparison (CCBT + MCBT vs. CCBT; CCBT + MCI vs. CCBT). The methods recommended by NICE are to combine incremental costs and outcomes within an ICER and to report the joint distribution of the bootstrapped ICERs on a cost-effectiveness plane to provide information on the associated uncertainty around this point estimate. Currently NICE uses a threshold range of £20,000–30,000 per QALY gained (i.e. any ICER within or below this range would be deemed a cost-effective use of resources). Mean incremental cost of the intervention and mean child QALYs were combined within an ICER for CCBT + MCBT versus CCBT and CCBT + MCI versus CCBT, respectively. Uncertainty around matched costs and QALY dyads were explored using both a parametric (Fieller’s theorem93,94) and non-parametric (bootstrap method95,96) approach. Within the bootstrap approach, uncertainty was investigated using 1000 bootstrapped samples to generate multiple cost–effect pairs, and displayed and analysed using cost-effectiveness acceptability curves (CEACs). 97 CEACs show the probability of a treatment being cost-effective given a wide range of willingness-to-pay threshold values for health gains. In addition, a linear representation of the CEAC, incorporating values for societal willingness to pay, NMB, was calculated for CCBT + MCBT and CCBT + MCI versus CCBT, respectively, as:
where Ei and Ci are the observed differences in effects (E) and costs (C), respectively, for patient ‘i’ and λ is the societal willingness to pay for a health gain. Where NMB is positive, this suggests the intervention is a worthwhile use of resources. The NMB framework can be seen as an alternative way of representing the ICER.
In the secondary analyses, days off school for the child and days off work and/or usual activities for the mother due to ill health were investigated using descriptive statistics. Further analyses will be developed to explore mean differences statistically and to include a valuation of lost productivity using the human capital approach with standard valuations to avoid bias. 98
Sensitivity analysis
Sensitivity analysis around key variables is performed in a bid to determine the key factors influencing cost-effectiveness. A key question is uncertainty in the cost-effectiveness analysis related to the impact of reducing the treatment costs of non-specific interventions. Hence, sensitivity analysis was conducted by setting the treatment costs related to non-specific interventions to zero. Treatment costs related to non-specific interventions included NDC and the FH control delivered to balance groups for therapist contact. Exploring the impact of reducing these costs was intended to reflect what would happen in reality if the interventions were adopted in current practice. Further sensitivity analysis will be developed by altering other key assumptions to explore their consequences for the results at the 12-month follow-up. In particular, an exploration of the incorporation of broader societal impacts on the cost-effectiveness results will be carried out, as well as further exploration of the results of the cost-effectiveness analysis to include combined child and maternal QALYs in the full CUA. The latter were not included in the primary analyses (only the child QALYs) in order to mirror the main trial outcomes.
Handling missing data
The primary economic evaluation adopted an ITT approach and missing data on resource use and health outcomes were imputed using two different methods. For face-to-face therapist contacts, where missing data values were highly deterministic (i.e. readily identifiable and standardised given observed practice), a conditional imputation method was conducted whereby missing data were estimated as an average of know durations for that client and session type. For the other resource use (mainly supervision time), costs (i.e. reward costs) and health outcomes (EQ-5D), where missing data were presented in higher percentages, multiple imputation was performed using a chained equation procedure99 and 20 imputed data sets were generated using the Stata command ‘mi impute chained’. Prediction equations for each imputation variable were customised and allowed to differ. Conditional models for imputed variables are specified in Appendix 3, Health economic supplementary material section 1.
Results
Data completeness
Data were missing because questionnaires were not fully completed at all time points. However, a high percentage of complete data were obtained from the likely key drivers, the therapist log for the intervention and control service costs (e.g. 76.8% complete for MCBT contact time). Complete EQ-5D data from mothers and child-friendly EQ-5D data for children ranged from 47.9% to 91.3% for mother and from 46.5% to 98.6% for children. Detailed percentages of missing data are presented in Appendix 3, Tables 90 and 91 to maximise transparency and aid interpretation of results. A complete case analysis was not possible owing to the high percentage of missing data across resource use and health outcomes. Restricting the sample to those children who had the EQ-5D measured at each assessment reduced the sample size to just above one-third of the initial sample (77 vs. 211). These results were underpowered and are therefore unreliable hence not reported, but they are available from the authors on request.
Resource use: therapy time
Utilising data obtained from the therapists’ log, Table 76 provides a detailed descriptive breakdown of the specific components of health-care resources used across each trial’s arm (face-to-face contact with patients, supervision time, preparation time, travel time and mileage). The principal resource used for the intervention was the staff time that the therapists spent directly with the patient, preparation time and travelling time.
| Resource use item | CCBT + MCBT (n = 69), mean (SD) (minutes) | CCBT + MCI (n = 71), mean (SD) (minutes) | CCBT (n = 71), mean (SD) (minutes) |
|---|---|---|---|
| CCBT | 423.95 (143.26) | 454.31 (147.13) | 391.74 (183.95) |
| MCBT | 380.79 (106.30) | NA | NA |
| Maternal counselling (NDC) | NA | 108.77 (20.27) | 329.73 (110.05) |
| MCI treatment (MCI; mother only)a | NA | 399.79 (132.24) | NA |
| MCI treatment (MCI; mother and child)a | NA | 58.94 (37.56) | NA |
| FH | 143.41 (65.11) | NA | 138.61 (70.85) |
| Supervision time for CCBT (therapist time) | 26.22 (3.42)b | 30.43 (3.77)b | 26.22 (3.55)b |
| Supervision time for CCBT (supervisor time) | 26.22 (3.42)b | 30.43 (3.77)b | 26.22 (3.55)b |
| Supervision time for MCBT/NDC (therapist time) | 46.03 (4.59)b | 35.50 (5.09)b | 52.21 (6.62)b |
| Supervision time for MCBT/NDC (supervisor time) | 46.03 (4.59)b | 35.50 (5.09)b | 52.21 (6.62)b |
| Supervision time for MCI/FH (therapist time) | 8.77 (2.36)b | 24.99 (2.55)b | 9.09 (2.06)b |
| Supervision time for MCI/FH (supervisor time) | 8.77 (2.36)b | 24.99 (2.55)b | 9.09 (2.06)b |
| Travel (duration) | 317.13 (437.18) | 221.48 (379.50) | 191.08 (298.52) |
| Travel (mileage) | 181.31 (260.03) | 127.73 (231.39) | 105.69 (180.75) |
| Other | 33.04 (48.06) | 20.61 (49.35) | 30.26 (86.41) |
| Extra time associated to ‘not attended’ sessions (e.g. waiting time, phone call, etc.) | 0.80 (4.67) | 3.52 (17.14) | 0.42 (3.56) |
| Reward (monetary only) | £0.97 (2.14) | £1.07 (2.34) | £0.86 (2.14) |
| Parking (monetary only) | £0.10 (0.84) | £0.03 (0.24) | £0 |
Table 77 reports the incremental mean time differences in minutes between CCBT + MCBT and CCBT. Although the total time difference between the groups is not statistically significant, individual items including duration of treatment for maternal anxiety, travel time and mileage are all significantly higher in the CCBT + MCBT arm.
| Resource use item | CCBT + MCBT (n = 69), mean (SD) (minutes) | CCBT (n = 71), mean (SD) (minutes) | Mean differences (minutes): CCBT + MCBT – CCBT (95% CI) | p-value |
|---|---|---|---|---|
| CCBT | 423.95 (143.26) | 391.74 (183.95) | 32.21 (–22.99 to 87.41) | 0.251 |
| MCBT/NDC | 380.79 (106.30) | 329.73 (110.05) | 51.06 (14.89 to 87.24) | 0.006 |
| MCI/FH | 150.00 (72.94) | 138.61 (70.85) | 11.39 (–12.63 to 35.43) | 0.350 |
| Supervision time for CCBT (therapist time) | 26.22 (3.42)a | 26.22 (3.55)a | 0.0019596 (–9.10 to 9.10) | 1.000 |
| Supervision time for CCBT (supervisor time) | 26.22 (3.42)a | 26.22 (3.55)a | 0.0019596 (–9.10 to 9.10) | 1.000 |
| Supervision time for MCBT/NDC (therapist time) | 46.03 (4.59)a | 52.21 (6.62)a | –6.18 (–22.77 to 10.42) | 0.456 |
| Supervision time for MCBT/NDC (supervisor time) | 46.03 (4.59)a | 52.21 (6.62)a | –6.18 (–22.77 to 10.42) | 0.456 |
| Supervision time for MCI/FH (therapist time) | 8.77 (2.36)a | 9.09 (2.06)a | –0.32 (–5.88 to 5.24) | 0.905 |
| Supervision time for MCI/FH (supervisor time) | 8.77 (2.36)a | 9.09 (2.06)a | –0.32 (–5.88 to 5.24) | 0.905 |
| Preparation time and record keeping | 376.22 (192.47) | 404.28 (191.75) | –28.06 (–92.27 to 36.15) | 0.39 |
| Travel (duration) | 317.13 (437.18) | 191.08 (298.52) | 126.05 (1.25 to 250.84) | 0.048 |
| Travel (mileage) | 181.31 (260.03) | 105.69 (180.75) | 75.63 (0.97 to 150.29) | 0.047 |
| Other | 33.04 (48.06) | 30.26 (86.41) | 2.78 (–20.68 to 26.24) | 0.815 |
| Extra time associated to ‘not attended’ sessions (e.g. waiting time, phone call, etc.) | 0.80 (4.67) | 0.42 (3.56) | 0.37 (–1.01 to 1.76) | 0.594 |
| Total therapy resource useb (minutes) | 1843.98 (81.78)a | 1661.18 (78.67)a | 182.79 (–40.92 to 406.51) | 0.108 |
Table 78 reports incremental differences between the CCBT + MCI and CCBT treatment arms. Total time differences between the arms are not statistically significant; however, there are statistically significant differences among individual items including time spent providing CCBT, MCBT/NDC, MCI/FH; treatment and supervision time for MCBT/NDC; and treatment and supervision time for MCI/FH.
| Resource use item | CCBT + MCI (n = 71), mean (SD) (minutes) | CCBT (n = 71), mean (SD) (minutes) | Mean differences (minutes): CCBT + MCI – CCBT (95% CI) | p-value |
|---|---|---|---|---|
| CCBT | 454.31 (147.13) | 391.74 (183.95) | 62.57 (7.30 to 117.84) | 0.027 |
| MCBT/NDC | 108.77 (20.27) | 329.73 (110.05) | –220.97 (–247.22 to –194.71) | 0.000 |
| MCI/FH | 458.73 (148.85) | 138.61 (70.85) | 320.12 (281.45 to 358.80) | 0.000 |
| Supervision time for CCBT (therapist time) | 30.43 (3.77)a | 26.22 (3.55)a | 4.21 (–6.52 to 14.94) | 0.436 |
| Supervision time for CCBT (supervision time) | 30.43 (3.77)a | 26.22 (3.55)a | 4.21 (–6.52 to 14.94) | 0.436 |
| Supervision time for MCBT/NDC (therapist time) | 35.50 (5.09)a | 52.21 (6.62)a | –16.72 (–32.21 to –1.22) | 0.035 |
| Supervision time for MCBT/NDC (supervision time) | 35.50 (5.09)a | 52.21 (6.62)a | –16.72 (–32.21 to –1.22) | 0.035 |
| Supervision time for MCI/FH (therapist time) | 24.99 (2.55)a | 9.09 (2.06)a | 15.90 (9.30 to 22.49) | 0.000 |
| Supervision time for MCI/FH (supervision time) | 24.99 (2.55)a | 9.09 (2.06)a | 15.90 (9.30 to 22.49) | 0.000 |
| Preparation time and record keeping | 346.93 (157.95) | 404.28 (191.75) | –57.36 (–115.64 to 0.93) | 0.054 |
| Travel (duration) | 221.48 (379.50) | 191.08 (298.52) | 30.39 (–82.89 to 143.68) | 0.597 |
| Travel (mileage) | 127.73 (231.39) | 105.69 (180.75) | 22.05 (–46.85 to 90.94) | 0.528 |
| Other | 20.61 (49.35) | 30.26 (86.41) | –9.65 (–32.99 to 13.70) | 0.415 |
| Extra time associated to ‘not attended’ sessions (e.g. waiting time, phone call, etc.) | 3.52 (17.14) | 0.42 (3.56) | 3.10 (–1.01 to 7.21) | 0.138 |
| Total therapy resource useb (minutes) | 1796.18 (75.27)a | 1661.18 (78.67)a | 134.99 (–79.71 to 349.69) | 0.216 |
Cost of therapy
Resource differences in time for CCBT + MCBT versus CCBT are translated into cost differences in Table 79 below and reveal a borderline statistically significant difference in total cost between the groups, with CCBT + MCBT being £233.55 more expensive than the CCBT arm.
| Costa | CCBT + MCBT (n = 69), mean (SD) | CCBT (n = 71), mean (SD) | Mean differences: CCBT + MCBT – CCBT (95% CI) | p-value |
|---|---|---|---|---|
| CCBT | £621.65 (210.07) | £574.42 (269.72) | £47.23 (–£33.72 to £128.17) | 0.251 |
| MCBT/NDC | £558.37 (155.87) | £483.50 (161.38) | £74.87 (£21.83 to £127.91) | 0.006 |
| MCI/FH | £219.96 (106.96) | £203.24 (103.88) | £16.71 (–£18.52 to £51.95) | 0.350 |
| Supervision time for CCBT (therapist time) | £17.11 (2.23)b | £17.11 (2.32)b | £0.001 (–£5.94 to £5.94) | 1.000 |
| Supervision time for CCBT (supervision time) | £30.93 (4.03)b | £30.92 (4.19)b | £0.002 (–£10.73 to £10.74) | 1.000 |
| Supervision time for MCBT/NDC (therapist time) | £30.04 (2.99)b | £34.07 (4.32)b | –£4.03 (–£14.87 to £6.80) | 0.456 |
| Supervision time for MCBT/NDC (supervision time) | £54.29 (5.41)b | £61.59 (7.80)b | –£7.29 (–£26.88 to £12.29) | 0.456 |
| Supervision time for MCI/FH (therapist time) | £5.72 (1.54)b | £5.93 (1.35)b | –£0.21 (–£3.84 to £3.42) | 0.905 |
| Supervision time for MCI/FH (supervision time) | £10.34 (2.79)b | £10.72 (2.43)b | –£0.38 (–£6.94 to £6.18) | 0.905 |
| Preparation time and record keeping | £245.49 (125.58) | £263.80 (125.11) | –£18.31 (–£60.21 to £23.59) | 0.389 |
| Travel (duration) | £206.93 (285.26) | £124.68 (194.78 | £82.24 (£0.82 to £163.67) | 0.048 |
| Travel (mileage) | £97.91 (140.42) | £57.07 (97.60) | £40.84 (£0.52 to £81.16) | 0.047 |
| Other | £21.56 (31.36) | £19.75 (56.39) | £1.81 (–£13.50 to £17.12) | 0.815 |
| Extra time associated to ‘not attended’ sessions (e.g. waiting time, phone call, etc.) | £0.52 (3.05) | £0.28 (2.32) | £0.24 (–£0.66 to £1.15) | 0.594 |
| Rewards | £3.95 (0.46)b | £4.22 (0.48)b | –£0.27 (–£1.72 to £1.18) | 0.763 |
| Parking | £0.10 (0.84) | £0 NA | £0.10 (–£0.10 to £0.30) | 0.312 |
| Treatment total cost | £2124.85 (84.98)b | £1891.30 (87.14)b | £233.55 (–£6.81 to £473.92) | 0.057 |
Resource differences in time for CCBT + MCI versus CCBT are translated into cost differences in Table 80 and reveal a borderline statistically significant difference in total cost between the groups, with the CCBT + MCI arm being £233.16 more expensive that the CCBT arm.
| Costa | CCBT + MCI (n = 71), mean (SD) | CCBT (n = 71), mean (SD) | Mean differences: CCBT + MCI – CCBT + MCBT (95% CI) | p-value |
|---|---|---|---|---|
| CCBT | £666.18 (215.74) | £574.42 (269.72) | £91.75 (£10.71 to £172.80) | 0.027 |
| MCBT/NDC | £159.49 (29.72) | £483.50 (161.38) | –£324.01 (–£362.51 to –£285.51) | 0.000 |
| MCI/FH | £672.65 (218.26) | £203.24 (103.88) | £469.41 (£412.69 to £526.13) | 0.000 |
| Supervision time for CCBT (therapist time) | £19.85 (2.46)b | £17.11 (2.32)b | £2.75 (–£4.25 to £9.75) | 0.436 |
| Supervision time for CCBT (supervision time) | £35.89 (4.44)b | £30.92 (4.19)b | £4.96 (–£7.69 to £17.62) | 0.436 |
| Supervision time for MCBT/NDC (therapist time) | £23.16 (3.32)b | £34.07 (4.32)b | –£10.91 (–£21.02 to –£0.80) | 0.035 |
| Supervision time for MCBT/NDC (supervision time) | £41.87 (6.00)b | £61.59 (7.80)b | –£19.72 (–£37.99 to–£1.44) | 0.035 |
| Supervision time for MCI/FH (therapist time) | £16.31 (1.66)b | £5.93 (1.35)b | £10.37 (£6.07 to £14.68) | 0.000 |
| Supervision time for MCI/FH (supervision time) | £29.48 (3.01)b | £10.72 (2.43)b | £18.75 (£10.97 to £26.53) | 0.000 |
| Preparation time and record keeping | £226.37 (103.06) | £263.80 (125.11) | –£37.42 (–£75.46 to £0.61) | 0.054 |
| Travel (duration) | £144.52 (247.62) | £124.68 (194.78) | £19.83 (–£54.09 to £93.75) | 0.597 |
| Travel (mileage) | £68.97 (124.95) | £57.07 (97.60) | £11.90 (–£25.30 to £49.11) | 0.528 |
| Other | £13.45 (32.20) | £19.75 (56.39) | –£6.30 (–£21.53 to £8.94) | 0.415 |
| Extra time associated to ‘not attended’ sessions (e.g. waiting time, phone call, etc.) | £2.30 (11.19) | £0.28 (2.32) | £2.02 (–£0.66 to £4.70) | 0.138 |
| Reward | £3.96 (0.49)b | £4.22 (0.48)b | –£0.26 (–£1.77 to £1.25) | 0.727 |
| Parking | £0.03 (0.24) | £0 | £0.03 (–£0.03 to £0.08) | 0.319 |
| Treatment total cost | £2124.46 (83.06)b | £1891.30 (87.14)b | £233.16 (–£6.81 to £473.92) | 0.054 |
Cost of additional health, personal social and non-NHS services
The total cost variable for use in the CUA comparing CCBT + MCBT with CCBT and CCBT + MCI with CCBT was derived using the treatment costs only. Limited data were available from the additional health and social service use patient diaries and three monthly resource use questionnaires (see Appendix 3, Tables 92–115) owing to small numbers completed (reported in Appendix 3, Table 91). The results from these analyses provide an indication of the broad health and social care resources used by this group. Tables 81 and 82 report a summary of these results for CCBT + MCBT versus CCBT and for CCBT + MCI versus CCBT. Further, detailed sensitivity analyses using chained equations to impute missing data will consider this wider societal perspective. The analyses will include these health and social care resources and costs beyond the resources/cost of the treatment, as well as resource use/cost from other sectors of the economy (e.g. education). Furthermore, additional information on productivity loss (i.e. days off school for children, and days off work and usual activities for mothers) will be included in these sensitivity analyses (see Appendix 3, Tables 112–115).
| Cost | n | CCBT + MCBT, mean (SD) | n | CCBT, mean (SD) | Mean differences: CCBT + MCBT – CCBT (95% CI) | p-value |
|---|---|---|---|---|---|---|
| Child | ||||||
| Baseline to assessment 1B | 35 | £191.10 (281.97) | 32 | £148.01 (302.32) | £43.10 (–£99.46 to £185.66) | 0.548 |
| Assessment 1B to assessment 2 | 17 | £202.02 (648.96) | 20 | £121.76 (369.93) | £80.25 (–£265.66 to £426.18) | 0.641 |
| Assessment 2 to assessment 3 | 32 | £161.53 (267.83) | 30 | £385.78 (1043.20) | –£224.25 (–£605.70 to £157.19) | 0.244 |
| Assessment 3 to assessment 4 | 23 | £103.47 (158.66) | 30 | £327.45 (1178.54) | –£223.98 (–£721.84 to £273.88) | 0.371 |
| Total over 12 months (child) | 54 | £327.26 (546.50) | 51 | £560.16 (1803.80) | –£232.90 (–£742.72 to £276.90) | 0.367 |
| Mother | ||||||
| Baseline to assessment 1B | 35 | £145.32 (189.04) | 32 | £223.66 (429.56) | –£78.33 (–£237.89 to £81.22) | 0.330 |
| Assessment 1B to assessment 2 | 17 | £202.95 (272.91) | 20 | £382.62 (867.47) | –£179.66 (–£625.18 to £265.85) | 0.418 |
| Assessment 2 to assessment 3 | 32 | £194.44 (323.03) | 30 | £313.20 (886.12) | –£118.76 (–£453.43 to £215.91) | 0.481 |
| Assessment 3 to assessment 4 | 23 | £299.35 (537.12) | 30 | £206.27 (614.93) | £93.09 (–231.09 to 417.27) | 0.567 |
| Total over 12 months (mother) | 54 | £400.81 (622.99) | 51 | £595.95 (1987.14) | –£195.13 (–£758.53 to £368.25) | 0.494 |
| Child and mother | ||||||
| Total over 12 months (child and mother) | 54 | £728.07 (860.19) | 51 | £1156.11 (281.97) | –£428.048 (–£1453.25 to £597.16) | 0.410 |
| Cost | n | CCBT + MCI, mean (SD) | n | CCBT, mean (SD) | Mean differences: CCBT + MCI – CCBT (95% CI) | p-value |
|---|---|---|---|---|---|---|
| Child | ||||||
| Baseline to assessment 1B | 47 | £172.17 (390.05) | 32 | £148.01 (302.32) | £24.16 (–£138.91 to £187.24) | 0.769 |
| Assessment 1B to assessment 2 | 25 | £120.25 (330.03) | 20 | £121.76 (369.93) | –£1.51 (–£212.19 to £209.17) | 0.989 |
| Assessment 2 to assessment 3 | 31 | £89.51 (169.73) | 30 | £385.78 (1043.20) | –£296.28 (–£676.18 to £83.63) | 0.124 |
| Assessment 3 to assessment 4 | 23 | £132.54 (258.41) | 30 | £327.45 (1178.54) | –£194.90 (–£698.31 to £308.51) | 0.441 |
| Total over 12 months (child) | 60 | £282.03 (586.32) | 51 | £560.16 (1803.80) | –£278.139 (–£767.21 to £210.93) | 0.262 |
| Mother | ||||||
| Baseline to assessment 1B | 47 | £122.15 (232.82) | 32 | £223.66 (429.56) | –£101.512 (–£250.56 to £47.54) | 0.179 |
| Assessment 1B to assessment 2 | 25 | £129.19 (259.35) | 20 | £382.62 (867.47) | –£253.42 (–£621.46 to £114.61) | 0.172 |
| Assessment 2 to assessment 3 | 31 | £82.67 (127.86) | 30 | £313.20 (886.12) | –£230.53 (–£552.31 to £91.25) | 0.157 |
| Assessment 3 to assessment 4 | 23 | £151.26 (213.60) | 30 | £206.27 (614.93) | –£55.01 (–£324.56 to £214.55) | 0.684 |
| Total over 12 months (mother) | 60 | £250.21 (311.15) | 51 | £595.95 (1987.14) | –£345.74 (–£861.08 to £169.59) | 0.186 |
| Child and mother | ||||||
| Total over 12 months (child and mother) | 60 | £311.15 (814.58) | 51 | £1156.11 (281.97) | –£623.88 (–£1595.28 to £347.52) | 0.206 |
Quality-adjusted life-years
Table 83 reports the results of the child EQ-5D utility values and QALYs for CCBT + MCBT versus CCBT. There are no statistically significant differences in QALYs at 12 months.
| Time of assessment | CCBT + MCBT (n = 69), mean (SE) | CCBT (n = 71), mean (SE) | Mean differences: CCBT + MCBT – CCBT (95% CI) | p-value |
|---|---|---|---|---|
| EQ-5D utility values | ||||
| Baseline | 0.706 (0.028) | 0.684 (0.036) | 0.022 (–0.070 to 0.113) | 0.641 |
| Assessment 1B | 0.727 (0.030) | 0.773 (0.034) | –0.046 (–0.135 to 0.042) | 0.300 |
| Assessment 2 | 0.798 (0.028) | 0.862 (0.028) | –0.065 (–0.144 to 0.015) | 0.108 |
| 6-month follow-up | 0.823 (0.033) | 0.840 (0.034) | –0.018 (–0.116 to 0.081) | 0.723 |
| 12-month follow-up | 0.821 (0.038) | 0.862 (0.034) | –0.042 (–0.150 to 0.067) | 0.440 |
| QALYs gained | ||||
| Baseline to assessment 1B | 0.110 (0.004) | 0.112 (0.004) | –0.002 (–0.013 to 0.009) | 0.741 |
| Assessment 1B to assessment 2 | 0.117 (0.004) | 0.126 (0.004) | –0.009 (–0.019 to 0.002) | 0.097 |
| Assessment 2 to 6 months | 0.156 (0.005) | 0.164 (0.005) | –0.008 (–0.023 to 0.007) | 0.291 |
| 6–12 months | 0.411 (0.015) | 0.426 (0.015) | –0.015 (–0.059 to 0.030) | 0.508 |
| Total over 12 months | 0.794 (0.022) | 0.827 (0.024) | –0.033 (–0.101 to 0.035) | 0.332 |
Table 84 reports the results of the child EQ-5D utility values and QALYs for CCBT + MCI versus CCBT. There are no statistically significant differences in QALYs at 12 months.
| Time of assessment | CCBT + MCI (n = 71), mean (SE) | CCBT (n = 71), mean (SE) | Mean differences: CCBT + MCI – CCBT (95% CI) | p-value |
|---|---|---|---|---|
| EQ-5D utility values | ||||
| Baseline | 0.729 (0.036) | 0.684 (0.036) | 0.045 (–0.058 to 0.147) | 0.393 |
| Assessment 1B | 0.798 (0.026) | 0.773 (0.034) | 0.025 (–0.059 to 0.109) | 0.559 |
| Assessment 2 | 0.867 (0.023) | 0.862 (0.028) | 0.004 (–0.068 to 0.076) | 0.904 |
| 6-month follow-up | 0.897 (0.023) | 0.840 (0.034) | 0.057 (–0.026 to 0.139) | 0.175 |
| 12-month follow-up | 0.864 (0.031) | 0.862 (0.034) | 0.001 (–0.083 to 0.086) | 0.973 |
| QALYs gained | ||||
| Baseline to assessment 1B | 0.118 (0.004) | 0.112 (0.004) | 0.005 (–0.006 to 0.017) | 0.370 |
| Assessment 1B to assessment 2 | 0.128 (0.003) | 0.126 (0.004) | 0.002 (–0.007 to 0.012) | 0.637 |
| Assessment 2 to 6 months | 0.170 (0.004) | 0.164 (0.005) | 0.006 (–0.007 to 0.018) | 0.358 |
| 6–12 months | 0.440 (0.012) | 0.426 (0.015) | 0.015 (–0.021 to 0.050) | 0.424 |
| Total over 12 months | 0.855 (0.018) | 0.827 (0.024) | 0.028 (–0.030 to 0.086) | 0.342 |
Table 85 reports the results of the mother EQ-5D utility values and QALYs for CCBT + MCBT versus CCBT. There are no statistically significant differences in QALYs at 12 months.
| Time of assessment | CCBT + MCBT (n = 69), mean (SE) | CCBT (n = 71), mean (SE) | Mean differences: CCBT + MCBT – CCBT (95% CI) | p-value |
|---|---|---|---|---|
| EQ-5D utility values | ||||
| Baseline | 0.833 (0.022) | 0.816 (0.025) | 0.017 (–0.050 to 0.084) | 0.613 |
| Assessment 1B | 0.848 (0.022) | 0.810 (0.036) | 0.038 (–0.044 to 0.120) | 0.358 |
| Assessment 2 | 0.865 (0.026) | 0.842 (0.030) | 0.022 (–0.060 to 0.103) | 0.597 |
| 6-month follow-up | 0.861 (0.026) | 0.855 (0.026) | 0.007 (–0.069 to 0.082) | 0.860 |
| 12-month follow-up | 0.824 (0.030) | 0.841 (0.034) | –0.017 (–0.101 to 0.067) | 0.689 |
| QALYs gained | ||||
| Baseline to assessment 1B | 0.129 (0.003) | 0.125 (0.004) | 0.004 (–0.005 to 0.014) | 0.384 |
| Assessment 1B to assessment 2 | 0.132 (0.003) | 0.127 (0.004) | 0.005 (–0.006 to 0.015) | 0.381 |
| Assessment 2 to 6 months | 0.166 (0.004) | 0.163 (0.004) | 0.003 (–0.011 to 0.016) | 0.690 |
| 6–12 months | 0.421 (0.011) | 0.424 (0.013) | –0.003 (–0.036 to 0.031) | 0.878 |
| Total over 12 months | 0.848 (0.019) | 0.839 (0.023) | 0.009 (–0.050 to 0.068) | 0.763 |
Table 86 reports the results of the mother EQ-5D utility values and QALYs for CCBT + MCI versus CCBT. There are no statistically significant differences in QALYs at 12 months.
| Time of assessment | CCBT + MCI (n = 71), mean (SE) | CCBT (n = 71), mean (SE) | Mean differences: CCBT + MCI – CCBT (95% CI) | p-value |
|---|---|---|---|---|
| EQ-5D utility values | ||||
| Baseline | 0.799 (0.028) | 0.816 (0.025) | –0.017 (–0.091 to 0.058) | 0.655 |
| Assessment 1B | 0.822 (0.027) | 0.810 (0.036) | 0.012 (–0.079 to 0.104) | 0.789 |
| Assessment 2 | 0.843 (0.027) | 0.842 (0.030) | 0.0003 (–0.082 to 0.083) | 0.995 |
| 6-month follow-up | 0.829 (0.026) | 0.855 (0.026) | –0.026 (–0.097 to 0.045) | 0.474 |
| 12-month follow-up | 0.857 (0.029) | 0.841 (0.034) | 0.016 (–0.067 to 0.100) | 0.696 |
| QALYs gained | ||||
| Baseline to assessment 1B | 0.125 (0.004) | 0.125 (0.004) | –0.0003 (–0.011 to 0.010) | 0.950 |
| Assessment 1B to assessment 2 | 0.128 (0.004) | 0.127 (0.004) | 0.001 (–0.011 to 0.013) | 0.869 |
| Assessment 2 to 6 months | 0.161 (0.004) | 0.163 (0.004) | –0.002 (–0.015 to 0.010) | 0.705 |
| 6–12 months | 0.422 (0.012) | 0.424 (0.013) | –0.002 (–0.036 to 0.032) | 0.893 |
| Total over 12 months | 0.835 (0.021) | 0.839 (0.023) | –0.004 (–0.065 to 0.057) | 0.894 |
Cost–utility analysis
Table 87 and Figures 8–10 report the results of the CUA from a health-care perspective for CCBT + MCBT compared with CCBT. The bootstrapped ICERs for this comparison are shown in the cost-effectiveness plane in Figure 8. With higher mean costs (albeit statistically insignificant) and lower mean utility (albeit statistically insignificant) differences between the groups, Figure 8 reveals that, given current thresholds for commonly accepted levels of cost-effectiveness (£20,000–30,000), CCBT + MCBT is not likely to be a cost-effective alternative to CCBT. The CEAC shown in Figure 9 reveals that the probability that CCBT + MCBT will be cost-effective in comparison with CCBT is < 10%. The NMB curve (see Figure 10) confirms that CCBT + MCBT confers no monetary benefit over CCBT for a broad range of societal willingness-to-pay thresholds and would not be deemed cost-effective given commonly accepted threshold values representing value for money.
| CUA results | CCBT + MCBT (n = 69), mean (SE) | CCBT (n = 71), mean (SE) |
|---|---|---|
| Cost of intervention | £2124.85 (84.98) | £1891.30 (87.14) |
| QALY gain | 0.794 (0.022) | 0.827 (0.024) |
| Incremental cost (95% CI) | £233.55 (–£6.81 to £473.92) | |
| Incremental QALY gain (95% CI) | –0.033 (–0.101 to 0.035) | |
| ICER, incremental cost per QALY gain | –£7077 | |
| (95% CI) bootstrap method | Lower limit, £12,373; upper limit, –£91 | |
| (95% CI) Fieller’s method | Lower limit, £10,000; upper limit, £187 | |
| NMB for WTP = £20,000 | –0.033 × £20,000 – £233.55 = –£893.55 | |
| NMB for WTP = £30,000 | –0.033 × £30,000 – £233.55 = –£1223.55 | |
FIGURE 8.
Cost-effectiveness plane showing bootstrapped replicates of the ICER: CCBT + MCBT vs. CCBT. LL, lower limit; PE, point estimate; UL, upper limit.

FIGURE 9.
Cost-effectiveness acceptability curve showing the probability that the intervention is cost-effective at different willingness-to-pay thresholds: CCBT + MCBT vs. CCBT.
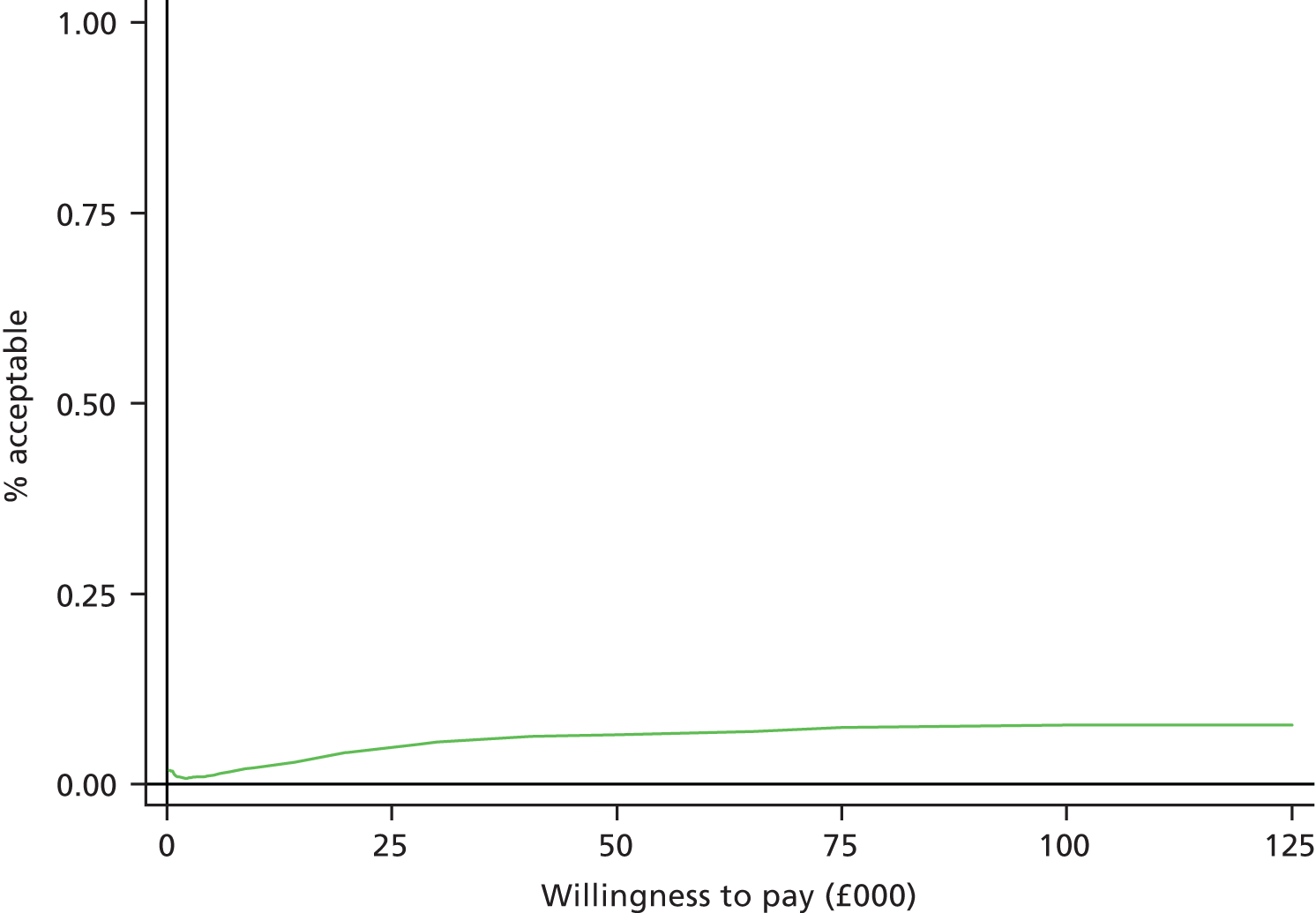
FIGURE 10.
Net monetary benefit curve and limit curves: CCBT + MCBT vs. CCBT. LL, lower limit; UL, upper limit.
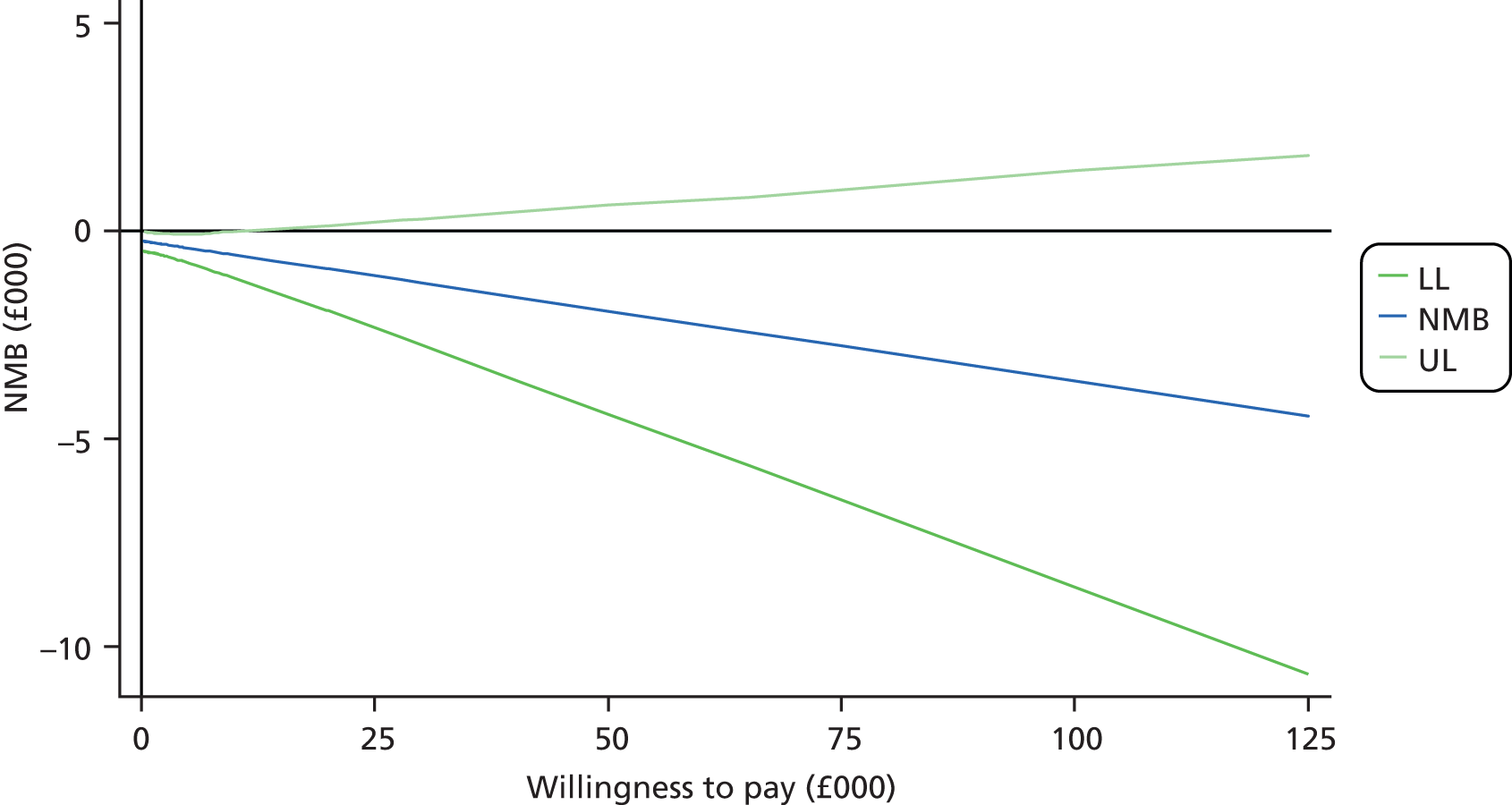
Table 88 and Figures 11–13 present the results of the CUA from a health-care perspective for CCBT + MCI compared with CCBT. The bootstrapped ICERS for this comparison are shown in the cost-effectiveness plane in Figure 11. With higher mean costs (albeit statistically insignificant) and higher mean utility (albeit statistically insignificant) differences between the groups, Figure 11 reveals that, given the distribution of the ICERS, CCBT + MCI is highly likely to be a cost-effective alternative to CCBT. The CEAC shown in Figure 12 reveals that, given current NICE thresholds for accepted levels of willingness to pay for an extra QALY (£20,000–30,000), the probability that CCBT + MCI will be cost-effective in comparison with CCBT is around 75%. The NMB curve (see Figure 13) confirms that CCBT + MCI confers additional monetary benefit over CCBT alone and would be deemed a cost-effective alternative given commonly accepted threshold values representing value for money.
| CUA results | CCBT + MCI (n = 71), mean (SE) | CCBT (n = 71), mean (SE) |
|---|---|---|
| Cost of intervention | £2124.46 (83.06) | £1891.30 (87.14) |
| QALYs | 0.855 (0.018) | 0.827 (0.024) |
| Incremental cost (95% CI) | £233.16 (–£6.81 to £473.92) | |
| Incremental benefit, QALY gain (95% CI) | 0.028 (–0.030 to 0.086) | |
| ICER, incremental cost per QALY gain | £8327 | |
| (95% CI) bootstrap method | Lower limit, –£173; upper limit, –£11,021 | |
| (95% CI) Fieller’s method | Lower limit, –£95; upper limit, –£8881 | |
| NMB for WTP = £20,000 | 0.028 × £20,000 – £233.16 = £326.84 | |
| NMB for WTP = £30,000 | 0.028 × £30,000 – £233.16 = £606.84 | |
FIGURE 11.
Cost-effectiveness plane showing bootstrapped replicates of the ICER: CCBT + MCI vs. CCBT. LL, lower limit; PE, point estimate; UL, upper limit.

FIGURE 12.
Cost-effectiveness acceptability curve showing the probability that the intervention is cost-effective at different willingness-to-pay thresholds: CCBT + MCI vs. CCBT.

FIGURE 13.
Net monetary benefit curve and limit curves: CCBT + MCI vs. CCBT. LL, lower limit; UL, upper limit.
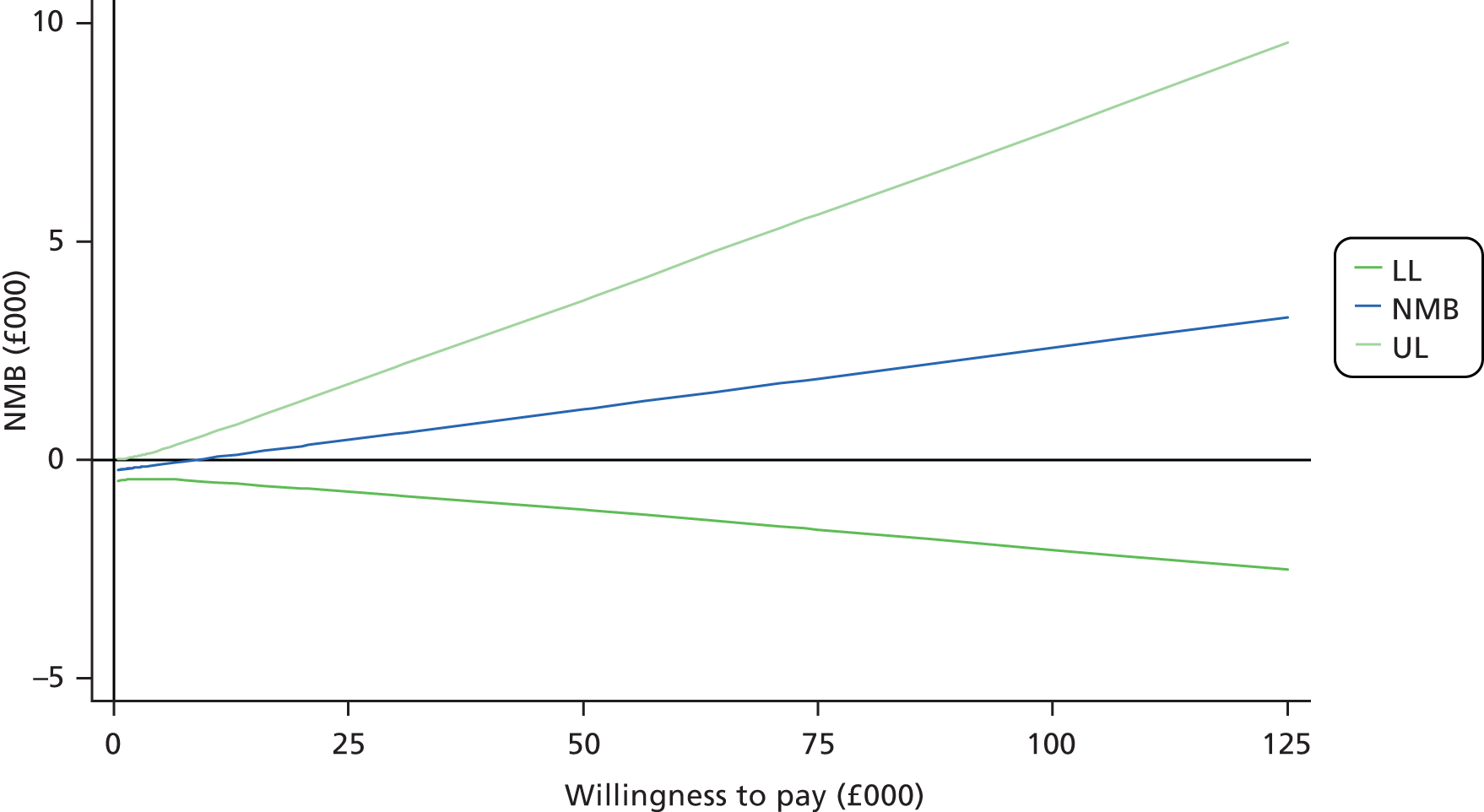
Sensitivity analysis
A key question of uncertainty in the cost-effectiveness analysis related to the impact of reducing the treatment costs of non-specific interventions. Hence, sensitivity analysis was conducted by setting the treatment costs related to non-specific interventions to zero. Treatment costs related to non-specific interventions included NDC and a generic FH control intervention delivered to balance groups for therapist contact. Although this analysis was conducted with the intention to reflect what would happen in reality if the interventions were adopted in current practice, it relied on the strong assumption that the non-specific interventions had no impact at all on the child anxiety outcomes. By increasing the cost difference between interventions and control, but maintaining the difference in effects invariant (as counterfactual outcomes in absence of non-specific interventions could not be measured), no evidence was found that either CCBT + MCBT or CCBT + MCI would offer any added value for money in improving child anxiety outcomes beyond what was already suggested in the primary analyses. Detailed results are reported in Appendix 3, Tables 116 and 117, and Figures 14–19.
Further sensitivity analysis will be developed by altering other key assumption to explore their consequences for the results at 12 months follow-up. In particular, an exploration of the incorporation of broader societal impacts and of the combined child and maternal QALYs on the cost-effectiveness results will be carried out.
Limitations of the data
The high level of missing data in the follow-up health and social care resource use beyond the treatment costs is a limitation for this economic evaluation. If the health and personal social service costs reported for the CCBT + MCBT versus CCBT comparison were representative of this population and included in the ICER, as they typically would be, the costs in the CCBT arm would increase by £428, thereby placing CCBT + MCBT into the lower cost/lower effectiveness zone of the cost-effectiveness plane (south west) and a different scenario to the cost-ineffective scenario arising when treatment only costs were included in the ICER. If the health and social care resources reported for the CCBT + MCI versus CCBT comparison were representative of this population and included in this analysis, the costs in the control arm would increase by £624. This would have placed the CCBT + MCI arm in the realms of being highly cost-effective (south-east quadrant of the cost-effectiveness place), that is dominating the CCBT arm and being both less costly and more effective, a clear win–win scenario. Another limitation of the data was the high percentage of missing data. This was dealt with using appropriate data imputation techniques; however, imputation cannot account for potentially non-random reasons for missing data.
Discussion
The aim of the economic evaluation was to assess the cost-effectiveness of the CCBT + MCBT and CCBT + MCI treatment arms in relation to the CCBT treatment arm from a health service perspective. The economic analyses aligned with the primary aim of the trial, namely to evaluate whether or not CCBT could be improved by the addition of (i) treatment of maternal anxiety disorders (MCBT), or (ii) treatment focused on maternal responses (MCI). Combining the total treatment costs with maternal and child QALYs revealed that, within commonly accepted levels of value for money (i.e. £20,000–30,000 per extra QALY gained), CCBT + MCBT was not likely to be a cost-effective alternative to CCBT. However, combining the total treatment costs with child QALYs revealed that in the comparison of the CCBT + MCI with CCBT treatment arms, the CCBT + MCI treatment arm was highly likely to be a cost-effective alternative to the CCBT arm. A limitation of these analyses, however, was that the resource use and costs of additional health and personal social services, beyond the current treatment costs, were not included in the primary analyses owing to very small sample sizes for these data components. Insufficient statistical power meant that conclusions could not be drawn about the impact of these additional costs on the overall cost-effectiveness. These additional data, however, do provide insights about the type and range of services this group of children and mothers use. Children undergoing treatment for anxiety disorders can be seen to be accessing a broad range of services beyond treatment from GPs, including social workers, psychologists, psychiatrists, education welfare officers, family liaison officers, teachers, paediatricians, audiologists, ophthalmology, accident and emergency (A&E), dieticians, physiotherapists, mental health workers and ‘other services’. Notwithstanding the limited evidence these small sample sizes convey, comparisons of CCBT + MCBT and CCBT + MCI with the CCBT treatment arm reveal increasing costs prevalent in the CCBT arm in the majority of the assessment periods. Furthermore, counting the number of services accessed by each group it can be seen that overall participants in the CCBT arm were accessing approximately one-third more services than those in the CCBT + MCBT and CCBT + MCI arms. In addition, the total costs are always higher in the CCBT arm for both comparisons. If these differences translated into actual differences then this would only increase the likelihood of the CCBT + MCBT and CCBT + MCI arms being more cost-effective than the CCBT arm. It is only by replicating these data collection exercises with larger samples that these results can be confirmed or refuted. On a cautionary note, however, it is important to outline that increased use of services may not represent an inferior quality-of-life outcome owing to the benefits of increased awareness about the health and well-being advantages of accessing additional services.
Broader impacts on other sectors, including impacts on education, employment and impacts on leisure time including time off school for children and time off work and usual activities for their mothers, were also presented but not included in the primary analyses. Further analyses will explore the impact of these effects on a broader societal perspective.
Conclusions
These CUAs have shown that when adopting a health service perspective, only the addition of MCI to standard CCBT is highly likely to represent a cost-effective use of resources for these mother/child pairs within commonly accepted thresholds of cost-effectiveness. Further, analyses reveal that when adopting a health service perspective only the addition of MCBT to standard CCBT is unlikely to be a cost-effective use of resources for these mother/child pairs. However, the latter result should be interpreted with caution because of the high percentage of missing data in some variables which, despite being dealt with using appropriate imputation techniques, may still be viewed as a shortcoming. However, further analysis incorporating the additional health and social care costs has indicated that, depending on the representativeness of these data, there are possible improvements in the cost-effectiveness of both CCBT + MCBT and CCBT + MCI depending on the assumptions made about these costs. Further analysis of the data exploring inclusion of the additional health and personal social service costs and employment and educational impacts using multiple imputations within sensitivity analyses may provide further insight to the cost-effectiveness of these interventions. This economic evaluation provides insight to the broad range of services accessed by this client group, hence it is recommended that future economic evaluations in this area incorporate data collection on this full range of services to fully capture the impact of new interventions.
Chapter 5 Discussion and conclusions
Summary of findings
Children with anxiety disorders whose mothers are also highly anxious have been shown to have a poorer response to treatment than those whose mothers are not anxious,9,100 yet the impact on children of treating the maternal anxiety has been unclear. Further, the clinical impact on children with anxiety disorders of targeting potentially anxiogenic maternal behaviours has not previously been evaluated systematically. The current study set out to address both these issues in a large RCT.
There was some evidence that the MCBT and MCI treatments were successful in altering the maternal factors which they were designed to address. Specifically, MCBT conferred short-term benefits in maternal recovery from primary diagnoses. However, by the post-treatment assessment, when children in all treatment arms had received CCBT, mothers in all arms had experienced a good level of recovery from their primary disorder and differences between treatment arms were no longer apparent. It is important to note that there were no significant differences between treatment arms on maternal-reported symptoms of anxiety at any time point. For the CCBT + MCI treatment arm there was evidence of change in maternal overprotection and expectations relating to a lack of child coping with challenge. There were no differences between treatment arms in change in other potentially anxiogenic parenting responses (such as expressed anxiety and positive behaviours).
Despite the success in changing some aspects of maternal anxiety and parenting responses, adding neither treatment of maternal anxiety (MCBT) nor treatment of maternal responses (MCI) conferred a significant benefit on children on the basis of the primary child treatment outcomes. Although both adjunct treatments achieved higher child recovery and global improvement rates post treatment than the group in which neither maternal anxiety nor potentially anxiogenic parenting received specific therapeutic attention, the advantages were neither statistically significant nor consistent across treatment arms and outcome measures.
There was some evidence of an advantage for the CCBT + MCI treatment arm on the primary outcomes at the 6-and 12-month follow-up assessments, but this did not reach statistical significance. There was a significant advantage of CCBT + MCI over CCBT on change in child anxiety severity at the 6-month follow-up, and a similar pattern existed at the 12-month follow-up (although it was no longer statistically significant). There was a general lack of significant differences between treatment arms on child-, mother- and teacher-reported anxiety symptom questionnaires. Where statistically significant differences did exist, these were contrary to expectations, with children in the CCBT group reporting a greater reduction in symptoms of anxiety and low mood than children in the CCBT + MCI arm at the post-treatment assessment. In contrast, mothers in the CCBT + MCI arm reported a greater reduction in child conduct problems at the 12-month follow-up assessment than mothers in the CCBT arm.
The secondary research questions considered whether or not improvement in child anxiety was significantly associated with change in (i) maternal anxiety, and (ii) maternal parenting responses. No significant associations were found between change in maternal anxiety and change in child anxiety symptoms, severity or improvement at the mid-treatment, post-treatment and 6-month follow-up assessments. Contrary to expectations, greater change in maternal anxiety symptoms was associated with less change in the severity of the child’s primary anxiety diagnosis. It is important to note that a large number of correlations were conducted to examine this research question and the lack of a consistent pattern of results highlights the fact that no clear conclusions can be drawn. In relation to maternal parenting responses, significant associations were found between change in maternal behaviours and change in child anxiety, most commonly for maternal overprotection. Specifically, and contrary to expectations, a greater increase in overprotection was associated with a greater reduction in the severity of the child’s primary anxiety diagnosis post treatment and global improvement at both the post-treatment and the 6-month follow-up assessments. These indices are both assessor rater; when child symptom ratings were used the opposite pattern was found, with a greater reduction in maternal overprotection being associated with greater reduction in child anxiety symptoms. The difference in the pattern of findings according to who is reporting on child anxiety is interesting and warrants further investigation, but for now clear conclusions about mechanisms of change cannot be drawn.
Economic evaluation
The CUAs demonstrated that, when adopting a health service perspective, the addition of MCI to standard CCBT is highly likely to represent a cost-effective use of resources for these mother/child pairs within commonly accepted thresholds of cost-effectiveness. Further, analyses reveal that when adopting a health service perspective the addition of MCBT to standard CCBT is unlikely to be a cost-effective use of resources for these mother/child pairs. Those cost-effectiveness results should be interpreted with caution owing to the high percentage of missing data on some variables which, despite being dealt with using appropriate imputation techniques, may still be viewed as a shortcoming. Furthermore, analysis incorporating the additional health and social care costs has indicated that, depending on the representativeness of these data, there are possible improvements in the cost-effectiveness of both CCBT + MCBT and CCBT + MCI depending on the assumptions made about these costs. Further analysis of the data exploring inclusion of the additional health and personal social service costs and employment and educational impacts using multiple imputations within sensitivity analyses may provide further insight to the cost-effectiveness of these interventions. The economic evaluation provides insight into the broad range of services accessed by this client group; hence, it is recommended that future economic evaluations in this area incorporate data collection on this full range of services when evaluating new interventions.
Strengths and limitations
The study had several notable strengths, including the referred clinical sample, the use of reliable, blind raters to make assessments of child and maternal anxiety and maternal behaviours before and after treatment, and a design which allowed for isolating the effects of specifically targeting maternal anxiety and parenting responses. A further strength of the study was the inclusion of non-specific interventions designed to balance therapist contact. However, the data collected for health economic analyses indicated that therapist contact did not end up entirely balanced within each phase of treatment. Most notably, more therapist time was spent delivering the eight sessions of MCBT treatment than the eight sessions of NDC that were delivered in the CCBT arm. Similarly, the MCI treatment took more time to deliver than the FH-oriented control. In both cases this may have resulted from the more directive treatment manuals in the MCBT and MCI treatments requiring longer sessions, or from therapist difficulties in maintaining engagement in the NDC and FH treatments so moving through the material more quickly. This suggestion is consistent with the fact that the highest rate of dropout was found during the eight-session NDC phase of treatment. Despite these differences, the overall time and cost of interventions across the entire treatment period was not significantly different across arms, supporting a good balance overall in therapist contact across treatment arms.
The strengths of the study need to be considered in the light of various other limitations. Although we allowed for 20% loss to follow-up, by the 1-year post-treatment assessment retention was down to 61% in the CCBT condition. This limits the conclusions that can be drawn about differences between treatment conditions in the longer term. Although there were no clear baseline differences between completers and those who dropped out, it is of concern that the greatest amount of dropout occurred during the eight-session maternal counselling phase. Therefore, this form of intervention appears not to have been an acceptable treatment approach for some families. This finding presents a challenge for future research; the inclusion of non-specific interventions presents a conservative test of the specific effects of particular interventions but requires the delivery of credible, alternative interventions. Whether longer-term dropouts over-represented those with good or bad treatment outcomes cannot be determined, although the sensitivity analyses that were conducted suggest that this was not the case. Our impression was that, in some cases, those that dropped out from follow-up assessments did so because they felt that their child had made a good recovery and had ‘moved on’ (and so did not want them to have to take part in a long diagnostic assessment). Future studies might benefit from an abridged follow-up assessment which places a minimal burden on participants. The degree to which long-term outcome was also influenced by involvement with help seeking elsewhere is also unclear. Although families agreed not to initiate any other treatment during the course of the intervention, they may have sought help elsewhere during the follow-up period. However, as indicated in the economic analyses (see Appendix 3, Tables 91–111), use of other resources was low across all treatment arms.
The lack of additional health and social care resource use beyond the treatment costs is a limitation for the economic evaluation presented here. Unfortunately there was a large amount of missing data on this measure which precluded its inclusion in these analyses. However, preliminary analysis incorporating the limited data available on the additional health and social care costs has indicated that, depending on the representativeness of these data, there are possible improvements in the cost-effectiveness of both CCBT + MCBT and CCBT + MCI depending on the assumptions made about these costs. Further analysis of the data exploring inclusion of the additional health and personal social service costs and employment and educational impacts using multiple imputations within sensitivity analyses may provide further insight to the cost-effectiveness of these interventions.
Other limitations include the relatively restricted demographic characteristics of the participating group, who were predominantly of non-minority ethnicity and relatively high socioeconomic status (SES), although this was lower than in a comparable trial on the basis of parent education. 19 Our study population also had somewhat higher rates of child- and parent-rated anxiety levels than in similar studies. 19 In terms of marital status, the population was representative of the wider population. 101 We elected to focus on middle childhood (ages 7–12 years) and intervening with mothers as a methodological expediency as it is likely that the nature of parental influences on child anxiety varies with child age102,103 and parent gender;34 however, as a result, the findings cannot be generalised to young children or adolescents or to interventions with fathers or other caregivers. The extent to which characteristics of other parental figures (e.g. paternal anxiety and parenting responses) moderate treatment outcomes warrants further examination. In our trial each phase of treatment was delivered by a different therapist, this meant that there was a very large number of different combinations of therapists (116 combinations) which precluded us from examining therapist effects.
The study also included children and mothers with a broad range of anxiety disorders. There is emerging evidence that generic treatment approaches, of the sort provided in the study, may be more beneficial for some child anxiety disorders than others104 and that particular potentially anxiogenic parental responses may be disorder specific. 64,105 Both of these sets of findings suggest that further work needs to be done which takes account of the precise form of parental and child anxiety, as well as particular forms of parenting responses. The inclusion of mothers with a broad range of disorders also meant that it was most appropriate for a transdiagnostic anxiety treatment to be delivered. Although there is evidence for the effectiveness of this approach (both here and in previous studies),38 it is unclear if disorder-specific treatments would have conferred greater benefits in terms of maternal anxiety. Furthermore, anxiety disorders are commonly comorbid with depression;32 the extent to which maternal depression moderates treatment outcomes in the context of maternal anxiety disorders warrants further attention. Finally, although we recruited a referred clinical population, their experience of treatment will have been very different from routine child mental health services because of the intensive research assessments and the adjunct interventions that were essential for our research purposes. Further insights in to the experiences of patients and therapists participating in this trial would be of value.
Interpretation of results
The findings suggest that adding specific interventions targeting maternal anxiety or the MCIs to individual CBT for children with anxiety disorders in the context of maternal anxiety disorder do not confer significant benefits in terms of child outcomes when compared with individual CBT (supplemented with non-specific therapist support); although some cost–benefit may obtain from the addition of an intervention to target the MCI.
Our findings, in relation to the treatment of parental anxiety disorder, are consistent with those obtained in a recent study by Hudson and colleagues. 19 Their study also specifically focused on children with anxiety disorders who had a parent with an anxiety disorder, and they also failed to find a significant benefit of the addition of parental anxiety management to CCBT. The findings also run contrary to the idea that changing parental responses is necessary for successful treatment of child anxiety disorder in the context of parental anxiety disorder. 23 Notably, however, the CCBT treatment arm in the current study performed considerably better than expected: immediately post treatment, 48% of children were free of their primary anxiety disorder, and 64% were ‘much’ or ‘very much’ improved; a year after treatment, 72% were free of their primary diagnosis and 77% were ‘much’/‘very much’ improved. These outcomes are particularly notable given the relatively brief nature of the CCBT intervention. 106 They are also higher than the 33% of children (with a parent with an anxiety disorder) who were free of their primary anxiety disorder in the study reported by Hudson and colleagues. 19 Indeed, the success rates reported here are similar to those found from more intensive (14-session) CBT for children with anxiety disorders, regardless of parental anxiety disorder status, where 60% and 72% were ‘much’/’very much’ improved at post treatment55 and 6-month follow-up,107 respectively. The lack of consistent differences between groups on clinical outcomes and the failure to find consistent, significant associations between the hypothesised mechanisms of change and child outcomes, may suggest that the association that has been commonly found between maternal anxiety disorder and child treatment outcomes may be the result of some third factor, for example other stressors experienced by the family, or shared associations with particular child or maternal comorbidities. The fact that we obtained higher child outcomes than expected following CCBT suggests that it is possible that this third factor variable was addressed to some extent by the generic support received by all mothers in this trial.
One consideration in making sense of the lack of main effects of the two active adjunct interventions (MCI/MCBT) is statistical power, given the higher than anticipated success rate on the CCBT arm. However, the extent of differences found between our treatment arms was below our a priori criteria for clinical significance (30% more children free of their anxiety diagnoses). The unexpectedly high rate of recovery within the CCBT group in the current study is unlikely to be a function of particular features of our sample, as our study population was a referred sample with systematically confirmed anxiety diagnoses, comparable to other clinic samples in the literature. One possible explanation may lie in the potential added value of the non-specific interventions. These both provided some level of parental support. Although the design used for the current study was appropriate for determining whether or not the MCBT and MCI interventions conferred specific benefits, controlling for therapist contact time using non-specific interventions is a conservative approach and the effects of the non-specific treatments are unclear. The absence of a significant main effect of either CCBT + MCBT or CCBT + MCI also needs to be considered in the light of the degree to which the adjunctive interventions were successful in altering their respective targets. In the one previous study that assessed the impact of adding CBT for parental anxiety disorders to CBT for child anxiety disorders,12 the failure to find differences in child outcomes was attributed to the fact that the parental CBT did not confer a benefit in terms of reducing parental anxiety compared with when only the children received CBT (i.e. 35.5% vs. 32.7% of mothers were free of their primary anxiety disorder, respectively). In the current study, a more intensive CBT intervention was delivered to the mothers and, as predicted, CCBT + MCBT was associated with a significant reduction in the frequency of maternal anxiety disorder compared with when mothers received NDC (58.5% vs. 36.5% diagnosis free). However, by the end of the CCBT treatment phase there were no group differences in maternal anxiety disorder, with all groups showing high rates of recovery from maternal anxiety disorder (52–66%). The fact that a marked reduction in anxiety disorders across all groups was found following CCBT is consistent with recent findings indicating that reduction in child anxiety promotes reduction in parental anxiety. 25
This study is the first of which we are aware to report on observational assessments of parental responses before-and-after treatment for child anxiety disorders. We were able to rigorously evaluate the extent to which the MCI intervention successfully altered maternal responses to her child when confronted with a challenge. These assessments provided evidence that, in terms of a reduction in overprotective behaviours, the MCI treatment was indeed successful. It is notable that this observation-based finding was confirmed by maternal self-report data. The MCI intervention was also associated with change in maternal cognitions associated with confidence in child coping (i.e. reduced predictions regarding child fear and increased predictions regarding child control). Despite these positive benefits of the MCI intervention, no significant benefit to child outcomes was conferred on primary outcome measures (although MCI added to CCBT seemed to represent good value for money). One possible reason for this may be that the changes were not of sufficient magnitude to be of benefit in terms of the clinical outcomes. Another possibility is that the factors that did change are not central to the maintenance of child anxiety. Indeed, although scores on the self-report maternal overprotection scale used have been found to be associated with the development of child anxiety,108 others have found that they do not discriminate clinically anxious children from their non-anxious peers. 66 It will be important to evaluate whether the association between maternal anxiety disorder and child treatment outcomes is in fact mediated by other shared factors, for example other stressors experienced by the family, which might have been addressed to some extent by the generic support received by all mothers in this trial. It is of interest that no specific benefit was apparent for the MCI intervention on the measures of maternal expressed anxiety, intrusiveness or positive behaviours. Although it is, of course, possible that the intervention was ineffective with respect to these dimensions, it is also possible that these findings reflect a lack of sensitivity of the laboratory-based observational tasks. It is also possible that these parental behaviours changed equally across groups in response to improvements in child anxiety. 13
Although there were no significant differences between treatment arms on the primary outcome measures at the post-treatment assessment, an advantage for CCBT + MCI was found on indices of change in anxiety disorders severity and an advantage which approached significance in terms of being free of the primary anxiety diagnosis at the 6-month follow-up assessment. There was also a trend for an advantage of CCBT + MCI over the CCBT arm in terms of the proportion of children who were free of all their anxiety diagnoses. These findings are consistent with the health economic outcomes which suggest that the CCBT + MCI is a cost-effective use of resources in comparison with the CCBT intervention. As the inclusion of two non-specific interventions within the CCBT arm would be expected to reduce its cost-effectiveness, sensitivity analyses were conducted in which zero costs were attributed to the non-specific interventions. This is a conservative test given that the non-specific interventions might be expected to confer some benefit to children and mothers, yet there was still evidence to support the cost-effectiveness of the CCBT + MCI intervention in this context. As noted above, the mechanisms by which CCBT + MCI conferred a cost–benefit advantage remain unclear.
It is notable that there was also a trend for CCBT + MCBT to have an advantage over CCBT in terms of general improvement post treatment. However, differences between arms were not consistent across time points or measures. Thus, although there is a possibility that MCBT helped support the generalisation of benefits in the short term, this speculation received only weak support.
Some unexpected findings should also be noted. In particular, on the basis of child self-reported anxiety symptoms, the CCBT + MCBT group did less well than the CCBT group at the post-treatment assessment. Both the CCBT + MCI and CCBT + MCBT groups also reported less of a reduction in low mood than the CCBT groups. None of these findings were maintained at the later assessment (although CCBT + MCBT had the poorest overall outcomes by the 12-month assessment); however, they are surprising given the content of the child treatment was the same across groups. Whether or not the full course of NDC (eight sessions) received by the mothers in the CCBT group led to some short-term benefit in terms of children’s perceptions of their symptoms remains unclear. There were also some unexpected findings in relation to the secondary research questions, which addressed the extent to which change in maternal anxiety and parenting responses was associated with change in child anxiety. However, as the pattern of findings was not consistent across measures and assessment time points no clear conclusions can be drawn. It is important to note that the sample size for this study was based on providing enough power to assess the primary outcomes. Other outcomes are secondary and, owing to the large number of tests, the results must be interpreted with caution.
Implications for health care
-
The novel intervention that focused on modifying maternal parenting responses was associated with some benefit to children and mothers with anxiety disorders, and is likely to be cost-effective (although the latter result needs to be considered with caution because of the high percentage of missing data in the economic analyses). Incorporating effective measures to address maternal cognitions and behaviours when interacting with her child may improve health outcomes for children with anxiety disorders in the context of maternal anxiety disorder.
-
We can be confident that supplementing individual CCBT with CBT to target the maternal anxiety disorder is unlikely to confer substantial health benefits and is unlikely to be cost-effective (although the latter result needs to be considered with caution owing to the high percentage of missing data in the economic analyses). Given the intensity of this intervention and its general lack of effectiveness we think it is unlikely that supplementing CCBT with this intervention will improve child outcomes.
Implications for future research
-
Given that CCBT alone was sufficient for a good number of patients, it is possible that a benefit of the CCBT + MCI and CCBT + MCBT interventions may be enhanced in particular contexts, for example in the context of particular maternal or child anxiety disorders or high levels of severity. Future research that directly addresses these possibilities is warranted.
-
The relatively low level of association between change in parental anxiety and responses and child anxiety may suggest that other factors may account for the modest treatment outcomes typically found among children with anxiety disorders who have mothers with anxiety disorders (such as genetic or broader social/environmental factors). Future research is warranted to address these issues.
-
The economic evaluation provides insight as to the broad range of services accessed by this client group, hence it is recommended that future economic evaluations in this area incorporate data collection on this full range of services when evaluating new interventions.
Acknowledgements
We thank the children and their mothers who took part in this research for their help. We also thank the external members of the Steering Committee [Jonathan Hill (Chair), Sara Ingham, Pasco Fearon, Paul Stallard and Natasha Connor] and the Data Management and Ethics Committee [John Geddes (Chair) and Max Parmar] for their support and guidance; Jeff Wood for providing consultation on the development of the MCI intervention; and Ron Rapee for making the Cool Kids programme available free of charge. We thank Patricia Howard, Monika Parkinson, Katherine Lawrence, Kerstin Thirwall, Lorraine Carpenter-Emory, Kate Moberley, Laura Wheen, Sarah Cook, Zoe Hughes, Katie Adolphus, Polly Waite, Jill Fletcher and Sally Greenfield for assistance in delivering the therapy; Jenny Crosby, Rebecca O’Grady, Sarah Cook, Amy Corcoran, Ray Percy, Anna Alkozei, Sarah Shildrick, Ray Percy, Zoe Hughes and Jessica Karalus for assistance with carrying out assessments; Kiri Clarke, Nina Melunsky, Elizabeth Houghton, Jennifer Bradbury, Adela Apetroaia, Mandy Lau, Emma Cosham, Lucy Foulkes, Michaela Muggeo, Ashton Kissoon, Joanne Priestly, Sara Andergachew, Catherine Broadway, Ruth Hammond, Richard Bushell, Gemma Denton and Kelsey Heard for assistance with coding parental behaviours and therapy sessions; and Jackie Barton, Susie Fornby, Ian Gallimore and Brendan Lawrence for administrative assistance. We are grateful to Meriel Powell for providing clinical supervision. We are also grateful to Marie Weber and Katie Hobbs for their help formatting the manuscript.
Contribution of authors
Cathy Creswell and Peter J Cooper had overall responsibility for the study.
Cathy Creswell was responsible for the day-to-day operationalisation and of the study and drafting the final report.
Susan Cruddace and Rachel Gitau were responsible for day-to-day management of the research and Lucy Willetts was responsible for clinical management.
Stephen Gerry was responsible for the final statistical analysis of the clinical outcomes, under supervision of Merryn Voysey and Ly-Mee Yu.
Emma McIntosh led on the design of the economic analysis.
The initial statistical analyses were designed by Jill Mollison.
Lynne Murray and Alan Stein were involved in the design, monitoring the trial and interpretation of results.
Rosamund Shafran was responsible for developing and overseeing the MCBT intervention.
Mara Violato led on the analysis and drafting of the economic results in collaboration with Emma McIntosh.
Lucy Willetts and Cathy Creswell were responsible for developing the MCI intervention.
Nicola Williams was responsible for monitoring of randomisation and interim data monitoring.
All authors contributed to drafting the final report.
Ethical approval
The study was approved by the Berkshire Research Ethics Committee (07/H0505/156) and the University of Reading Research Ethics Committee (07/48).
Publications
Data from initial assessments of subgroups of participants included in this trial were included in the following papers:
Creswell C, Apetroaia A, Murray L, Cooper P. Cognitive, affective, and behavioural characteristics of mothers with anxiety disorders in the context of child anxiety disorder. J Abnorm Psychol 2013;122:26.
Clarke K, Cooper P, Creswell C. The Parental Over-protection Scale: associations with child and parental anxiety. J Affect Disord 2013;151:618–24.
Orchard F, Cooper PJ, Creswell C. Interpretation and expectations among mothers of children with anxiety disorders: associations with maternal anxiety disorder. Depress Anxiety 2015;32:99–107.
Publication reporting on trial outcomes
Creswell C, Cruddace S, Gerry S, Murray L, Stein A, Willetts L, et al. Treatment of childhood anxiety disorder in the context of maternal anxiety disorder: A randomised controlled trial. In preparation.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the MRC, NETSCC, the HTA programme, the EME programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme, the EME programme or the Department of Health.
References
- Costello EJ, Egger HL, Angold A, Costello EJ, Egger HL, Angold A, et al. Phobic and Anxiety Disorders in Children and Adolescents: A Clinician’s Guide to Effective Psychosocial and Pharmacological Interventions. New York, NY: Oxford University Press; 2004.
- Ford T, Goodman R, Meltzer H. The British child and adolescent mental health survey 1999: the prevalence of DSM-IV disorders. J Am Acad Child Adolesc Psychiatry 2003;42:1203-11. http://dx.doi.org/10.1097/00004583-200310000-00011.
- Ezpeleta L, Keeler G, Erkanli A, Costello EJ, Angold A. Epidemiology of psychiatric disability in childhood and adolescence. J Child Psychol Psychiatry 2001;42:901-14. http://dx.doi.org/10.1111/1469-7610.00786.
- Essau CA, Conradt J, Petermann F. Frequency, comorbidity and psychosocial impairment of anxiety disorders in German adolescents. J Anxiety Disord 2000;14:263-79. http://dx.doi.org/10.1016/S0887-6185(99)00039-0.
- Woodward LJ, Fergusson DM. Life course outcomes of young people with anxiety disorders in adolescence. J Am Acad Child Adolesc Psychiatry 2001;40:1086-93. http://dx.doi.org/10.1097/00004583-200109000-00018.
- Bodden D, Dirksen CD, Bogels SM. Societal burden of clinically anxious youth referred for treatment: a cost-of-illness study. J Abnorm Child Psychol 2008;36:487-97. http://dx.doi.org/10.1007/s10802-007-9194-4.
- Clark DME, Fairburn CG. Science and Practice of Cognitive Behaviour Therapy. Oxford: Oxford University Press; 1997.
- James AC, James G, Cowdrey FA, Soler A, Choke A. Cognitive Behavioural Therapy for Anxiety Disorders in Children and Adolescents (Review) 2013. www.bibliotecacochrane.com/pdf/CD004690.pdf (accessed 21 April 2015).
- Cobham VE, Dadds MR, Spence SH. The role of parental anxiety in the treatment of childhood anxiety. J Consult Clin Psychol 1998;66:893-905. http://dx.doi.org/10.1037/0022-006X.66.6.893.
- Cooper PJ, Gallop C, Willetts L, Creswell C. Treatment response in child anxiety is differentially related to the form of maternal anxiety disorder. Behav Cogn Psychother 2008;36:41-8. http://dx.doi.org/10.1017/S1352465807003943.
- Crawford AM, Manassis K. Familial predictors of treatment outcome in childhood anxiety disorders. J Am Acad Child Adolesc Psychiatry 2001;40:1182-9. http://dx.doi.org/10.1097/00004583-200110000-00012.
- Hudson JL, Lester KJ, Lewis CM, Tropeano M, Creswell C, Collier DA, et al. Predicting outcomes following cognitive behaviour therapy in child anxiety disorders: the influence of genetic, demographic and clinical information. J Child Psychol Psychiatry 2013;54:1086-94. http://dx.doi.org/10.1111/jcpp.12092.
- Silverman WK, Kurtines WM, Jaccard J, Pina AA. Directionality of change in youth anxiety treatment involving parents: an initial examination. J Consult Clin Psychol 2009;77:474-85. http://dx.doi.org/10.1037/a0015761.
- Last CG, Hersen M, Kazdin AE, Francis G, Grubb HJ. Psychiatric illness in the mothers of anxious children. Am J Psychiatry 1987;144:1580-3. http://dx.doi.org/10.1176/ajp.144.12.1580.
- Last CG, Hersen M, Kazdin A, Orvaschel H, Perrin S. Anxiety disorders in children and their families. Arch Gen Psychiatry 1991;48:928-34. http://dx.doi.org/10.1001/archpsyc.1991.01810340060008.
- Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association; 2000.
- Cooper PJ, Fearn V, Willetts L, Seabrook H, Parkinson M. Affective disorder in the parents of a clinic sample of children with anxiety disorders. J Affective Disord 2006;93:205-12. http://dx.doi.org/10.1016/j.jad.2006.03.017.
- Cobham VE, Dadds MR, Spence SH, McDermott B. Parental anxiety in the treatment of childhood anxiety: a different story three years later. J Clin Child Adolesc Psychol 2010;39:410-20. http://dx.doi.org/10.1080/15374411003691719.
- Hudson JL, Newall C, Rapee RM, Lyneham HJ, Schniering CC, Wuthrich VM, et al. The impact of brief parental anxiety management on child anxiety treatment outcomes: a controlled trial. J Clin Child Adolesc Psychol 2014;43:370-80. http://dx.doi.org/10.1080/15374416.2013.807734.
- Rapee RM. Potential role of childrearing practices in the development of anxiety and depression. Clin Psychol Rev 1997;17:47-6. http://dx.doi.org/10.1016/S0272-7358(96)00040-2.
- Wood JF, McLeod BD, Sigman M, Hwang W, Chu BC. Parenting and childhood anxiety: theory, empirical findings, and future directions. J Child Psychol Psychiatry 2003;44:134-51. http://dx.doi.org/10.1111/1469-7610.00106.
- Creswell C, O’Connor TG. Anxious cognitions’ in children: an exploration of associations and mediators. Br J Dev Psychol 2006;24:761-6. http://dx.doi.org/10.1348/026151005X70418.
- Creswell C, Apetroaia A, Murray L, Cooper P. Cognitive, affective, and behavioral characteristics of mothers with anxiety disorders in the context of child anxiety disorder. J Abnorm Psychol 2013;122. http://dx.doi.org/10.1037/a0029516.
- Moore PS, Whaley SE, Sigman M. Interactions between, mothers and children: impacts of maternal and child anxiety. J Abnorm Psychol 2004;113:471-6. http://dx.doi.org/10.1037/0021-843X.113.3.471.
- Settipani A, O’Neil A, Podell L, Beidas S, Kendall PC. Youth anxiety and parent factors over time: directionality of change among youth treated for anxiety. J Clin Child Adolesc Psychol 2013;42:9-21. http://dx.doi.org/10.1080/15374416.2012.719459.
- Barrett PM, Rapee RM, Dadds MR. Family treatment of childhood anxiety: a controlled trial. J Consult Clin Psychol 1996;64:333-42. http://dx.doi.org/10.1037/0022-006X.64.2.333.
- Mendlowitz SL, Manassis K, Bradley S, Scapillato D, Miezitis S, Shaw BE. Cognitive-behavioral group treatments in childhood anxiety disorders: the role of parental involvement. J Am Acad Child Adolesc Psychiatry 1999;38:1223-9. http://dx.doi.org/10.1097/00004583-199910000-00010.
- Spence SH, Donovan C, Brechman-Toussaint M. The treatment of childhood social phobia: the effectiveness of a social skills training-based, cognitive-behavioural intervention, with and without parental involvement. J Child Psychol Psychiatry 2000;41:713-26. http://dx.doi.org/10.1111/1469-7610.00659.
- Nauta MH, Scholing A, Emmelkamp PM, Minderaa RB. Cognitive-behavioral therapy for children with anxiety disorders in a clinical setting: no additional effect of a cognitive parent training. J Am Acad Child Adolesc Psychiatry 2003;42:1270-8. http://dx.doi.org/10.1097/01.chi.0000085752.71002.93.
- Wood JJ. Parental intrusiveness and children’s separation anxiety in a clinical sample. Child Psychiatry Hum Dev 2006;37:73-87. http://dx.doi.org/10.1007/s10578-006-0021-x.
- Majdandžić M, Möller EL, de Vente W, Bögels SM, van den Boom DC. Fathers’ challenging parenting behavior prevents social anxiety development in their 4-year-old children: a longitudinal observational study. J Abnorm Child Psychol 2014;42:301-10. http://dx.doi.org/10.1007/s10802-013-9774-4.
- Kessler RC, McGonagle KA, Zhao SY, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States – results from the National Comorbidity Survey. Arch Gen Psychiatry 1994;51:8-19. http://dx.doi.org/10.1001/archpsyc.1994.03950010008002.
- Thirlwall K, Cooper PJ, Karalus J, Voysey M, Willetts L, Creswell C. Treatment of child anxiety disorders via guided parent-delivered cognitive–behavioural therapy: a randomised controlled trial. Br J Psychiatry 2013;203:436-44. http://dx.doi.org/10.1192/bjp.bp.113.126698.
- Bögels SM, Perotti EC. Does father know best? A formal model of the paternal influence on childhood social anxiety. J Child Family Stud 2011;20:171-81. http://dx.doi.org/10.1007/s10826-010-9441-0.
- Lyneham H, Abbott M, Wignall A, Rapee R. The Cool Kids Family Program—Therapist Manual. Sydney, Australia: Macquarie University; 2003.
- Kendall PC, Hedtke KA. Cognitive-Behavioral Therapy for Anxious Children: Therapist Manual. Ardmore, PA: Workbook Publishing; 2006.
- McManus F, Shafran R, Cooper Z. What does a transdiagnostic approach have to offer the treatment of anxiety disorders?. Br J Clin Psychol 2010;49:491-505. http://dx.doi.org/10.1348/014466509X476567.
- Norton PJ, Barrera TL. Transdiagnostic versus diagnosis-specific CBT for anxiety disorders: a preliminary randomized controlled noninferiority trial. Depress Anxiety 2012;29:874-82. http://dx.doi.org/10.1002/da.21974.
- Borkovec T, Costello E. Efficacy of applied relaxation and cognitive-behavioral therapy in the treatment of generalized anxiety disorder. J Consult Clin Psychol 1993;61. http://dx.doi.org/10.1037/0022-006X.61.4.611.
- Stein A, Woolley H, Senior R, Hertzmann L, Lovel M, Lee J, et al. Treating disturbances in the relationship between mothers with bulimic eating disorders and their infants: a randomized, controlled trial of video feedback. Am J Psychiatry 2006;163:899-906. http://dx.doi.org/10.1176/ajp.2006.163.5.899.
- Creswell C, Willetts L, Murray L, Singhal M, Cooper P. Treatment of child anxiety: an exploratory study of the role of maternal anxiety and behaviours in treatment outcome. Clin Psychol Psychother 2008;15:38-44. http://dx.doi.org/10.1002/cpp.559.
- Good Grub Game, Set & Match. London: Comic Company; 2006.
- ‘Give Me 5’ Factsheets. London: Comic Company; 2001.
- NHS Direct . Common Health Questions n.d. www.nhsdirect.uk/articles/article.aspx?articleld+819 (accessed 5 December 2007).
- Why Your Child’s Weight Matters. London: DH; 2007.
- President’s Council on Physical Fitness and Sport. Washington, DC; 1996.
- EmaxHealth . 50 Ways for Kids to Exercise – Indoors or Out n.d. www.emaxhealth.com/43/6031.html (accessed 5 December 2007).
- Patz A. 10 Ways to Exercise As a Family n.d. http://lifestyle.msn.com/FamilyandParenting/RaisingKids/Article (accessed 5 December 2007).
- Kellow J. Fit Kids n.d. www.weightlossresources.co.uk/children/fit-kids.htm (accessed 28 November 2007).
- Promoting Physical Activity and Exercise Among Children n.d. www.kidsource/content4/promote.phyed.html (accessed 5 December 2007).
- MayoClinic . Fitness for Kids: Getting Your Children off the Couch n.d. www.mayoclinic.com/print/fitness/FL00030/METHOD=print (accessed 5 December 2007).
- Basile H. Benefits of Exercise for Children n.d. http://ezinearticles.com/?Fitness-Benefits-of-Exercise-for-Children (accessed 5 December 2007).
- KidsHealth . Kids and Exercise n.d. www.kidshealth.org/parent/nutrition_fit/fitness/exercise.html (accessed 5 December 2007).
- Your Body and Activity n.d. www.galaxy-h.gov.uk/teacher_your-body-and-activity.html (accessed 28 November 2007).
- Walkup J, Albano A, Piacentini J, Birmaher B, Compton S, Sherill J, et al. Cognitive behavioural therapy, sertraline, or a combination in childhood anxiety. N Engl J Med 2009;359:2753-66. http://dx.doi.org/10.1056/NEJMoa0804633.
- Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for DSM-IV – Child and Parent Versions. San Antonio, TX: Psychological Corporation; 1996.
- Guy W. ECDEU Assessment Manual for Psychopharmacology-Revised. Rockville, MD: US Department of Health, Education, Welfare and Public Health Services; 1976.
- Brown TA, DiNardo P, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV: Client Interview Schedule. Oxford: Oxford University Press; 1994.
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. Sydney, NSW: Psychology Foundation; 1995.
- Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychol Assess 1998;10:176-81. http://dx.doi.org/10.1037/1040-3590.10.2.176.
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behav Res Ther 1990;28:487-95. http://dx.doi.org/10.1016/0005-7967(90)90135-6.
- Mattick RP, Clarke AC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behav Res Ther 1998;36:455-70. http://dx.doi.org/10.1016/S0005-7967(97)10031-6.
- Hudson JL, Rapee RM. Parent–child interactions and anxiety disorders: an observational study. Behav Res Ther 2001;39:1411-27. http://dx.doi.org/10.1016/S0005-7967(00)00107-8.
- Murray L, Lau PY, Arteche A, Creswell C, Russ S, Zoppa LD, et al. Parenting by anxious mothers: effects of disorder subtype, context and child characteristics. J Child Psychol Psychiatry 2012;53:188-96. http://dx.doi.org/10.1111/j.1469-7610.2011.02473.x.
- Edwards SL, Rapee RM, Kennedy SJ. Psychometric Properties of a Parent Report Measure of Overprotection in Preschool-Aged Children 2008.
- Clarke K, Cooper P, Creswell C. The Parental Overprotection Scale: associations with child and parental anxiety. J Affect Disord 2013;151:618-24. http://dx.doi.org/10.1016/j.jad.2013.07.007.
- Spence SH. A measure of anxiety symptoms among children. Behav Res Ther 1998;36:545-66. http://dx.doi.org/10.1016/S0005-7967(98)00034-5.
- Langley AK, Bergman RL, McCracken J, Piacentini JC. Impairment in childhood anxiety disorders: preliminary examination of the child anxiety impact scale-parent version. J Child Adolesc Psychopharmacol 2004;14:105-14. http://dx.doi.org/10.1089/104454604773840544.
- Langley AK, Falk A, Peris T, Wiley JF, Kendall PC, Ginsburg G, et al. The child anxiety impact scale: examining parent- and child-reported impairment in child anxiety disorders. J Clin Child Adolesc Psychol 2014;43:579-91. http://dx.doi.org/10.1080/15374416.2013.817311.
- Angold A, Costello EJ, Messer SC, Pickles A, Winder F, Silver D. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Int J Methods Psychiatr Res 1995;5:237-49.
- Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry 1997;38:581-6. http://dx.doi.org/10.1111/j.1469-7610.1997.tb01545.x.
- Machin D, Campbell MJ, Fayers PM, Alain P. Sample Size Tables For Clinical Studies. Oxford: Blackwell Science Ltd; 1997.
- Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702-6. http://dx.doi.org/10.1093/aje/kwh090.
- Royston P. Multiple imputation of missing values: update of ice. Stata J 2005;5.
- Guide to the Methods of Technology Appraisal. London: NICE; 2009.
- Petrou S, Gray A. Economic evaluation alongside randomised controlled trials: design, conduct, analysis, and reporting. BMJ 2011;342. http://dx.doi.org/10.1136/bmj.d1548.
- Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) statement. BMC Med 2013;11. http://dx.doi.org/10.1186/1741-7015-11-80.
- Office for National Statistics . Consumer Price Indices – RPI Indices: 1987 to 2015: Jan 1987=100 n.d. www.ons.gov.uk/ons/datasets-and-tables/data-selector.html?cdid=CHAW&dataset=mm23&table-id=2.1 (accessed 13 May 2015).
- Curtis L. Unit Costs of Health and Social Care 2012. Canterbury: University of Kent at Canterbury: Personal Social Services Research Unit; 2012.
- Department of Health . National Schedule of Reference Costs Year: ‘2011–2012’ 2012. www.gov.uk/government/publications/nhs-reference-costs-financial-year-2011-to-2012 (accessed 18 April 2013).
- NHS Staff Council . NHS Terms and Conditions of Service Handbook. Amendment Number 25- Pay Circular (AforC) 1 2012 2012. www.nhsemployers.org/∼/media/Employers/Documents/Pay%20and%20reward/AfC%20Handbook%20Version%2027.pdf (accessed 12 November 2013).
- Local Government Association . Local Government Earnings Survey 2011 12 – Observed Pay Rates 2012. www.local.gov.uk/web/guest/local-government-intelligence/-/journal_content/56/10171/3015313/ARTICLE-TEMPLATE (accessed 22 April 2013).
- Department of Education . Statistical First Release. School Workforce in England, November 2011 2012. www.education.gov.uk/rsgateway/DB/SFR/s001062/sfr06–2012v7.pdf (accessed 16 April 2013).
- Office for National Statistics (UK) . Labour Market, Earnings by Industry. Patterns of Pay: Results from the Annual Survey of Hours and Earnings, 1997–2012 2013. www.ons.gov.uk/ons/taxonomy/search/index.html?nscl=Earnings+by+Industry&nscl-orig=Earnings+by+Industry&content-type=Dataset&content-type=Reference+table&sortDirection=DESCENDING&sortBy=pubdate (accessed 19 April 2013).
- McIntosh E, Barlow J, Davis H, Stewart-Brown S. Economic evaluation of an intensive home visiting programme for vulnerable families: a cost-effectiveness analysis of a public health intervention. J Public Health 2009;31:423-33. http://dx.doi.org/10.1093/pubmed/fdp047.
- Health and Social Care Information Centre . April–June 2012 NHS Staff Earnings Estimates 2012. www.hscic.gov.uk/catalogue/PUB07388 (accessed 23 April 2013).
- Health and Social Care Information Centre . Prescription Cost Analysis – England 2012 2013. www.hscic.gov.uk/catalogue/PUB10610 (accessed 25 March 2014).
- Office for National Statistics . Annual Survey of Hours and Earnings. Office for National Statistics; 2012 2012. www.ons.gov.uk/ons/rel/ashe/annual-survey-of-hours-and-earnings/2012-provisional-results/stb-ashe-statistical-bulletin-2012.html (accessed 25 March 2014).
- Euroqol . European Quality of Life-5 Dimension (EQ-5D) 2009. www.euroqol.org/about-eq-5d.html (accessed July 2008).
- Wille N, Badia X, Bonsel G, Burström K, Cavrini G, Devlin N, et al. Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Qual Life Res 2010;19:875-86. http://dx.doi.org/10.1007/s11136-010-9648-y.
- Dolan P, Gudex C, Kind P, Williams A. A Social Tariff for EuroQol: Results From a UK General Population Survey. York: Centre for Health Economics University of York; 1995.
- Torrance GW, Drummond MF. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2005.
- Chaudhary MA, Stearns SC. Estimating confidence intervals for cost-effectiveness ratios: an example from a randomized trial. Stat Med 1996;15:1447-58. http://dx.doi.org/10.1002/(SICI)1097-0258(19960715)15:13<1447::AID-SIM267>3.0.CO;2-V.
- Willan AR, O’Brien BJ. Confidence intervals for cost-effectiveness ratios: an application of Fieller’s theorem. Health Econ 1996;5:297-305. http://dx.doi.org/10.1002/(SICI)1099-1050(199607)5:4<297::AID-HEC216>3.0.CO;2-T.
- Briggs AH, Wonderling DE, Mooney CZ. Pulling cost-effectiveness analysis up by its bootstraps: a non-parametric approach to confidence interval estimation. Health Econ 1997;6:327-40. http://dx.doi.org/10.1002/(SICI)1099-1050(199707)6:4<327::AID-HEC282>3.0.CO;2-W.
- O’Hagan A, Stevens JW. Assessing and comparing costs: how robust are the bootstrap and methods based on asymptotic normality?. Health Econ 2003;12:33-49. http://dx.doi.org/10.1002/hec.699.
- Briggs A, Fenn P. Confidence intervals or surfaces? Uncertainty on the cost-effectiveness plane. Health Econ 1998;7:723-40. http://dx.doi.org/10.1002/(SICI)1099-1050(199812)7:8<723::AID-HEC392>3.0.CO;2-O.
- McIntosh E, Clarke P, Frew E, Louviere JJ. Applied Methods of Cost Benefit Analysis in Health Care. Oxford: Oxford University Press; 2010.
- White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med 2011;30:377-99. http://dx.doi.org/10.1002/sim.4067.
- Bodden D, Bögels S, Nauta M, de Hann E, Ringrose J, Appelboom C, et al. Child versus family cognitive behavioural therapy in clinically anxious youth: an efficacy and partial effectiveness study. J Clin Child Adolesc Psychol 2008;47:1384-94. http://dx.doi.org/10.1097/CHI.0b013e318189148e.
- Office for National Statistics . Infographic Showing the Number and Type of Households in the UK 2013 n.d. www.ons.gov.uk/ons/rel/family-demography/families-and-households/2013/info-uk-households.html (accessed 23 April 2015).
- Connell AM, Goodman SH. The association between psychopathology in fathers versus mothers and children’s internalizing and externalizing behavior problems: a meta-analysis. Psychol Bull 2002;128:746-73. http://dx.doi.org/10.1037/0033-2909.128.5.746.
- Maccoby EE. The role of parents in the socialization of children: an historical overview. Dev Psychol 1992;28. http://dx.doi.org/10.1037/0012-1649.28.6.1006.
- Ginsburg GS, Sakolsky D, Piacentini J, Walkup JT, Coffey KA, Keeton CP, et al. Remission after acute treatment in children and adolescents with anxiety disorders: findings from the CAMS. J Consult Clin Psychol 2011;79:806-13. http://dx.doi.org/10.1037/a0025933.
- Budinger MC, Drazdowski TK, Ginsburg GS. Anxiety-promoting parenting behaviors: a comparison of anxious parents with and without social anxiety disorder. Child Psychiatry Hum Dev 2013;44:412-18. http://dx.doi.org/10.1007/s10578-012-0335-9.
- Crawley SA, Kendall PC, Benjamin CL, Brodman DM, Wei C, Beidas RS, et al. Brief cognitive-behavioral therapy for anxious youth: feasibility and initial outcomes. Cogn Behav Pract 2013;20:123-33. http://dx.doi.org/10.1016/j.cbpra.2012.07.003.
- Piacentini J, Bennett S, Compton S, Kendall PC, Birmaher B, Albano AM, et al. 24- and 36-week outcomes for the Child/Adolescent Anxiety Multimodal Study (CAMS). J Am Acad Child Adolesc Psychiatry 2014;53:297-310. http://dx.doi.org/10.1016/j.jaac.2013.11.010.
- Edwards SL, Rapee RM, Kennedy S. Prediction of anxiety symptoms in preschool-aged children: examination of maternal and paternal perspectives. J Child Psychol Psychiatry 2010;51:313-21. http://dx.doi.org/10.1111/j.1469-7610.2009.02160.x.
Appendix 1 Patient and public involvement
Public involvement in the conduct of the research
A member of the public was a full member of the TSC from initiation to completion of the trial. This lay member was identified by contacting parents of children that had received treatment for anxiety disorders at the University of Reading/Berkshire Healthcare NHS Foundation Trust/Berkshire Child Anxiety Clinic. The individual appointed was the only parent to express an interest who was available to commit to ongoing participation and so no selection process was needed. The lay member’s contributions to the conduct of the trial included reviewing information sheets for children and parents, providing feedback on the study protocol and providing guidance on strategies for successful recruitment. This proved invaluable, particularly in providing advice on how to best inform potential participants about the trial and recruitment strategies.
Lessons learned
We benefited from the commitment of our one lay representative; however, we were unable to secure a commitment from other potential lay members, and two general practitioners who gave agreement to join the TSC were ultimately unable to attend meetings. We clearly recognise the value of patient and public involvement at all stages of the research process so will include more comprehensive costings to cover the expenses/lost earnings associated with patient and public involvement and will be more explicit in forming patient and public involvement relationships (e.g. through honorary appointments) in future grants.
Appendix 2 Mother and child anxiety trial study protocol
Appendix 3 Health economic measures
Health economic logs
Health economics diary/patient-held resource use diary
| Item | Unit cost (£) | Source | Notes |
|---|---|---|---|
| Family doctor (GP consultation in surgery) | 40 | Personal Social Services Research Unit. Unit Costs of Health and Social Care 2012. Kent: University of Kent; 2012 | Table 10.8b. Cost including qualifications, excluding other direct care staff costs |
| Social worker | 74 | Personal Social Services Research Unit. Unit Costs of Health and Social Care 2012. Kent: University of Kent; 2012 | Table 11.3. Cost per hour of face-to-face contact, including qualifications |
| Practice nurse (nurse consultation in surgery) | 13.69 | Personal Social Services Research Unit. Unit Costs of Health and Social Care 2012. Kent: University of Kent; 2012 | Table 10.6. Cost including qualifications, excluding other direct care staff costs and based on duration of contact of 15.5 minutes |
| Psychologist | 136 | Personal Social Services Research Unit. Unit Costs of Health and Social Care 2012. Kent: University of Kent; 2012 | Table 9.5. Cost per hour of client contact (includes A to E: A = wages/salary; B = salary oncosts; C = qualifications; D = overheads; E = capital overheads) |
| Consultant: psychiatrist | 383 | Personal Social Services Research Unit. Unit Costs of Health and Social Care 2012. Kent: University of Kent; 2012 | Table 15.7. Cost per face-to-face contact, including qualifications |
| Community psychiatrist nurse (nurse – mental health) | 76 | Personal Social Services Research Unit. Unit Costs of Health and Social Care 2012. Kent: University of Kent; 2012 | Table 10.2. Cost per hour of face-to-face contact (including qualifications) |
| Education welfare officer | 20.44 | Local Government Earnings Survey 2011/12 – Observed Pay Rates. URL: www.local.gov.uk/web/guest/local-government-intelligence/-/journal_content/56/10171/3015313/ARTICLE-TEMPLATE (accessed 22 April 2013) | Education welfare officer, median annual gross pay (FTE). Unit cost calculated using information on local government pension schemes and employer National Insurance contributions. Adjusted for inflation using RPI |
| Educational psychologist | 37.29 | Local Government Earnings Survey 2011/12 – Observed Pay Rates. URL: www.local.gov.uk/web/guest/local-government-intelligence/-/journal_content/56/10171/3015313/ARTICLE-TEMPLATE (accessed 22 April 2013) | Educational psychologist, median annual gross pay (FTE). Unit cost calculated using information on local government pension schemes and employer National Insurance contributions. Adjusted for inflation using RPI |
| Family liaison officer (school) (approximated with family support worker) | 49 | Personal Social Services Research Unit. Unit Costs of Health and Social Care 2012. Kent: University of Kent; 2012 | Table 11.8. Costs per hour of client-related work |
| Teacher | 35.41 | Department of Education. Statistical First Release. School Workforce in England, November 2011. URL: www.education.gov.uk/rsgateway/DB/SFR/s001062/sfr06–2012v7.pdf (accessed 16 April 2013) | Table 9a. Average salary (£) in total, publicly funded school. Salary oncosts have been included in the calculation of the unit cost. Adjusted for inflation using RPI |
| Paediatrician: outpatient department – paediatrics | 225 | National Schedule of Reference Costs Year: ‘2011–2012’. URL: www.gov.uk/government/publications/nhs-reference-costs-financial-year-2011-to-2012 (accessed 18 April 2013) | NHS trusts. Consultant led, first attendance, non-admitted, face to face. Service code: 420 |
| Audiology: outpatient department – paediatric audiological medicine (A), audiological medicine (B), audiology (C) | 110 | National Schedule of Reference Costs Year: ‘2011–2012’. URL: www.gov.uk/government/publications/nhs-reference-costs-financial-year-2011-to-2012 (accessed 18 April 2013) | As above. Weighted average of (A), (B) and (C). (A) service code 254; (B) service code 310; (C) service code 840 |
| Speech and language (community speech and language therapist) | 33 | Personal Social Services Research Unit. Unit Costs of Health and Social Care 2012. Kent: University of Kent; 2012 | Table 9.3. Cost including qualifications |
| Ophthalmology: outpatient department –ophthalmology (A), paediatric ophthalmology (B), medical ophthalmology (C), orthoptics (D), optometry (E) | 107 | Personal Social Services Research Unit. Unit Costs of Health and Social Care 2012. Kent: University of Kent; 2012 | As above. Weighted average of (A), (B), (C) and (D). (A) service code 130; (B) service code 216; (C) service code: 460; (D) service code 655; (E) service code 662 |
| Hospital A&E department | 108 | National Schedule of Reference Costs Year: ‘2011–2012’. URL: www.gov.uk/government/publications/nhs-reference-costs-financial-year-2011-to-2012 (accessed 18 April 2013) | A&E services: no leading to admitted. Weighted average of all services in the category |
| Occupational therapist | 33 | Personal Social Services Research Unit. Unit Costs of Health and Social Care 2012. Kent: University of Kent; 2012 | Table 9.2. Cost including qualifications |
| Paediatric dietitian | 34 | Personal Social Services Research Unit. Unit Costs of Health and Social Care 2012. Kent: University of Kent; 2012 | Table 13.4. Cost including qualifications |
| Paediatric physiotherapist | 74 | National Schedule of Reference Costs Year: ‘2011–2012’. URL: www.gov.uk/government/publications/nhs-reference-costs-financial-year-2011-to-2012 (accessed 18 April 2013) | Community physiotherapy services: child, one-to-one services, service code N5C1 |
| Paediatric play specialist | 11.55 | Local Government Earnings Survey 2011/12 – Observed Pay Rates. URL: www.local.gov.uk/web/guest/local-government-intelligence/-/journal_content/56/10171/3015313/ARTICLE-TEMPLATE (accessed 22 April 2013) | Playworker, median annual gross pay (FTE). Unit cost calculated using information on local government pension schemes and employer National Insurance contributions. Adjusted for inflation using RPI |
| Family therapist (family support worker) | 49 | Personal Social Services Research Unit. Unit Costs of Health and Social Care 2012. Kent: University of Kent; 2012 | Table 11.8. Costs per hour of client-related work |
| Community children’s nurse | 93 | National Schedule of Reference Costs Year: ‘2011–2012’. URL: www.gov.uk/government/publications/nhs-reference-costs-financial-year-2011-to-2012 (accessed 18 April 2013) | Community nursing services: nursing services for children, service code CN101 |
| Child and adolescent mental health worker | 68 | Personal Social Services Research Unit. Unit Costs of Health and Social Care 2012. Kent: University of Kent; 2012 | Table 12.6. Generic single-disciplinary CAMHS |
| Primary mental health worker | 68 | Personal Social Services Research Unit. Unit Costs of Health and Social Care 2012. Kent: University of Kent; 2012 | Table 12.6. Generic single-disciplinary CAMHS |
| Housing department | 19.81 | Local Government Earnings Survey 2011/12 – Observed Pay Rates. URL: www.local.gov.uk/web/guest/local-government-intelligence/-/journal_content/56/10171/3015313/ARTICLE-TEMPLATE (accessed 22 April 2013) | Housing officer, median annual gross pay (FTE) England. Unit cost calculated using information on local government pension schemes and employer National Insurance contributions. Adjusted for inflation using RPI |
| Citizens advice bureau | 15.50 | Office for National Statistics (UK). Labour Market, Earnings by Industry. Patterns of Pay: Results from the Annual Survey of Hours and Earnings, 1997–2012. URL: www.ons.gov.uk/ons/taxonomy/search/index.html?nscl=Earnings+by+Industry&nscl-orig=Earnings+by+Industry&content-type=Dataset&content-type=Reference+table&sortDirection=DESCENDING&sortBy=pubdate (accessed on 19 April 2013) | Table 5_SIC07. Full-time employees’ pay by industry sector (SIC 2007), United Kingdom, April 2008–12. Industry sector: other service activities. Unit cost calculated using information on stakeholders pension schemes and employer National Insurance contributions |
| Family centre (family support worker | 49 | Personal Social Services Research Unit. Unit Costs of Health and Social Care 2012. Kent: University of Kent; 2012 | Table 11.8. Costs per hour of client-related work |
| Home-Start | 95.59 | McIntosh E, Barlow J, Davis H, Stewart-Brown. Economic evaluation of an intensive home visiting programme: a cost-effectiveness analysis from a societal perspective. J Publ Health 2009;3:423–33 | Table 1, p. 427. Price inflated to 2011/12 prices using the HCHS index |
| Other health and social care resource use | 81.12 | Authors’ calculations | Average of all other unit costs |
| Therapist: newly qualified clinical psychologist | 39.15 (per hour); 87.98 (per hour of client contact) | Health & Social Care Information Centre. NHS Staff Earnings, Estimates – April–June 2012. URL: www.hscic.gov.uk/catalogue/PUB07388 (accessed 23 April 2013) | Table 3. Basic pay and earnings for Agenda for Change Band 7 (spine point 26), and calculated according to the methodology adopted in Personal Social Services Research Unit. Unit Costs of Health and Social Care 2012. Kent: University of Kent; 2012. Table 9.5 |
| Supervisor | £70.77 (per hour) £159.03 (per hour of client contact) | Health & Social Care Information Centre. NHS Staff Earnings, Estimates – April–June 2012. URL: www.hscic.gov.uk/catalogue/PUB07388 (accessed 23 April 2013) | Table 3. Basic pay and earnings for Agenda for Change Band 8b (spine point 41), and calculated according to the methodology adopted in Personal Social Services Research Unit. Unit Costs of Health and Social Care 2012. Kent: University of Kent; 2012. Table 9.5 |
| Mileage allowance | £0.54 per mile | NHS Employers. NHS Terms and conditions of service handbook. Amendment number 25 – Pay Circular (AforC) 1/2012. URL: www.nhsemployers.org/∼/media/Employers/Documents/Pay%20and%20reward/AfC_tc_of_service_handbook_fb.pdf (accessed 12 November 2013) | Car (all types of fuel), annual mileage up to 3500 miles (standard rate) |
Health economic supplementary material section 1
Conditional models for multiple imputation using chained equations
Variable imputed: each category of supervision time.
Covariates in the model:
-
treatment allocation
-
minimisation factors, that is child age, child gender, type of child anxiety disorder (GAD, social phobia, SAD, other)
-
baseline severity (ADIS-IV CSR) of the child’s primary anxiety disorder
-
baseline severity (ADIS-IV mother self-report) of the mother’s primary anxiety disorder
-
mothers’ baseline depression (DASS-21 – depression)
-
child baseline depression symptoms (SMFQ-c, child-reported)
-
child behavioural problems (SDQ conduct, mother-reported)
-
baseline presence of child social phobia
-
all other categories of supervision time.
Variable imputed: total rewards.
Covariates in the model:
-
treatment allocation
-
minimisation factors, that is child age, child gender, type of child anxiety disorder (GAD, social phobia, SAD, other).
Variable imputed: baseline EQ-5D for child and mother.
Covariates in the model:
-
treatment allocation
-
minimisation factors, that is child age, child gender, type of child anxiety disorder (GAD, social phobia, SAD, other)
-
baseline severity (ADIS-IV CSR) of the child’s primary anxiety disorder
-
baseline severity (ADIS-IV mother self-report) of the mother’s primary anxiety disorder
-
mothers’ baseline depression (DASS-21 – depression)
-
child baseline depression symptoms (SMFQ-c, child-reported)
-
child behavioural problems (SDQ conduct, mother-reported)
-
baseline presence of child social phobia.
Variable imputed: follow-up measurements of child and mother EQ-5D.
Covariates in the model:
-
treatment allocation
-
minimisation factors, that is child age, child gender, type of child anxiety disorder (GAD, social phobia, SAD, other)
-
measurement of outcomes at previous time points.
| Item | CCBT + MCBT, %a | CCBT + MCI, %b | CCBT, %c |
|---|---|---|---|
| CCBT time | 34.8 | 25.4 | 38 |
| MCBT time | 23.2 | NA | NA |
| MCI time | NA | 33.8 | NA |
| NDC time | NA | 2.8 | 8.5 |
| FH time | 27.5 | NA | 11.3 |
| Supervision time for CCBT | 42.03 | 47.89 | 33.80 |
| Supervision time for CCBT | 13.04 | NA | NA |
| Supervision time for MCI | NA | 42.25 | NA |
| Supervision time for NDC time | NA | 73.24 | 59.15 |
| Supervision time for FH | 79.71 | NA | 74.65 |
| Total cost rewards | 75.36 | 70.42 | 81.69 |
| Child: EQ-5D score – baseline | 1.45 | 2.82 | 5.63 |
| Child: EQ-5D score – assessment 1B | 13.04 | 8.45 | 21.13 |
| Child: EQ-5D score – assessment 2 | 33.33 | 21.13 | 32.39 |
| Child: EQ-5D score – 6-month follow-up | 36.23 | 39.44 | 40.85 |
| Child: EQ-5D score – 12-month follow-up | 50.72 | 46.48 | 53.52 |
| Mother: EQ-5D score – baseline | 8.70 | 9.86 | 15.49 |
| Mother: EQ-5D score – assessment 1B | 33.33 | 28.17 | 38.03 |
| Mother: EQ-5D score – assessment 2 | 37.68 | 40.85 | 43.66 |
| Mother: EQ-5D score – 6-month follow-up | 37.68 | 40.85 | 43.66 |
| Mother: EQ-5D score – 12-month follow-up | 50.72 | 46.48 | 52.11 |
| Section | CCBT + MCBT, %a | CCBT + MCI, %b | CCBT, %c |
|---|---|---|---|
| Other health and social care resources: child and mother – period ‘baseline to assessment 1B’ | 50.7 | 66.2 | 45.1 |
| Medication use: child and mother – period ‘baseline to assessment 1B’ | 39.1 | 39.4 | 32.4 |
| Other health and social care resources: child and mother – period ‘assessment 1B to assessment 2’ | 24.6 | 35.2 | 28.2 |
| Medication use: child and mother – period ‘assessment 1B to assessment 2’ | 18.8 | 32.4 | 26.8 |
| Other health and social care resources: child and mother – period ‘assessment 2- to 6-month follow-up’ | 46.4 | 43.6 | 42.3 |
| Medication use: child and mother – period ‘assessment 2- to 6-month follow-up’ | 46.4 | 43.6 | 42.3 |
| Other health and social care resources: child and mother – period ‘6–12 months follow-up’ | 28.9 | 26.8 | 29.6 |
| Medication use: child and mother – period ‘6–12 months follow-up’ | 33.3 | 32.4 | 42.3 |
| Resource use (contacts): child | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Family doctor | 1.11 (1.59) | 0.36 (0.76) | 0.5 (0.80) |
| Social worker | 0.13 (0.88) | 0.25 (1.41) | |
| Practice nurse | 0.03 (0.17) | 0.09 (0.28) | 0.06 (0.25) |
| Psychologist | 0.09 (0.50) | 0.13 (0.74) | 0.06 (0.25) |
| Education welfare officer | 0.021 (0.15) | 0.13 (0.71) | |
| Educational psychologist | 0.06 (0.34) | 0.04 (0.21) | |
| Family liaison officer | 0.11 (0.68) | 0.04 (0.29) | |
| Teacher | 0.34 (1.21) | 0.62 (3.10) | 0.66 (2.50) |
| Paediatrician | 0.2 (0.63) | 0.15 (0.47) | |
| Audiology | 0.06 (0.34) | ||
| Speech and language | 0.03a (0.17) | 0.02 (0.15) | 0.06 (0.25) |
| Ophthalmology | 0.06 (0.24) | 0.04 (0.20) | |
| Hospital A&E department | 0.11 (0.47) | 0.09 (0.28) | 0.06 (0.35) |
| Occupational therapist | 0.09 (0.51) | ||
| Paediatric physiotherapist | 0.06 (0.32) | ||
| Community children’s nurse | 0.14 (0.85) | ||
| Child and adolescent mental health worker | 0.02 (0.15) | ||
| Primary mental health worker | 0.03 (0.18) | ||
| Other | 0.57b (1.03) | 0.79c (1.59) | 0.71c (1.36) |
| Observations | 35 | 47 | 32 |
| Resource use (contacts): mother | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Family doctor | 1.74 (2.19) | 1.04 (1.52) | 1.41 (3.24) |
| Social worker | 0.13 (0.88) | 0.09 (0.53) | |
| Practice nurse | 0.23 (0.49) | 0.11 (0.31) | 0.22 (0.75) |
| Psychologist | 0.16 (0.57) | ||
| Psychiatrist | 0.04 (0.29) | 0.03 (0.18) | |
| Community psychiatrist nurse | 0.22 (1.24) | ||
| Education welfare officer | 0.02 (0.15) | 0.03 (0.18) | |
| Family liaison officer | 0.22(1.24) | ||
| Teacher | 0.23 (0.60) | 0.15 (0.72) | 0.28 (0.81) |
| Paediatrician | 0.06 (0.25) | ||
| Ophthalmologist | 0.14 (0.60) | ||
| Hospital A&E department | 0.09 (0.28) | 0.11 (0.37) | 0.03 (0.18) |
| Family therapist | 0.06 (0.35) | ||
| Community children nurse | 0.13 (0.88) | ||
| Primary mental health worker | 0.03 (0.18) | ||
| Housing department | 0.02 (0.15) | 0.03 (0.18) | |
| Citizens Advice Bureau | 0.03 (0.17) | ||
| Other | 0.77a (1.54) | 0.14b (0.58) | 0.91c (1.85) |
| Observations | 35 | 47 | 32 |
| Resource use: medications | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Mother’s consumption of prescription medications | 0.70 (1.10) | 0.89 (1.20) | 0.78 (1.28) |
| Mother’s consumption of ‘over-the-counter’ medications | 0.15 (0.46) | 0.18 (0.55) | 0 |
| Child’s consumption of prescription medications | 0.48 (0.89) | 0.46 (0.84) | 0.35 (0.49) |
| Child’s consumption of ‘over-the-counter’ medications | 0.11 (0.32) | 0.36 (0.62) | 0.22 (0.85) |
| Observations | 27 | 28 | 23 |
| Resource use (contacts): child | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Family doctor | 0.24 (0.44) | 0.64 (1.04) | 0.3 (0.47) |
| Social worker | 0.76 (3.15) | 0.4 (1.8) | |
| Practice nurse | 0.12 (0.49) | 0.08 (0.28) | |
| Psychologist | 0.32 (1.6) | ||
| Education welfare officer | 0.18 (0.73) | ||
| Family liaison officer | 0.04 (0.2) | ||
| Teacher | 0.24 (0.56) | 0.24 (0.83) | 0.2 (0.70) |
| Paediatrician | 0.06 (0.24) | 0.08 (0.4) | |
| Speech and language | 0.06 (0.24) | ||
| Ophthalmology | 0.04 (0.2) | ||
| Hospital A&E department | 0.06 (0.24) | 0.04 (0.2) | |
| Other | 0.25a (0.77) | 0.29b (0.77) | |
| Observations | 17 | 25 | 20 |
| Resource use (contacts): mother | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Family doctor | 1.06 (1.71) | 0.8 (0.96) | 1.9 (4.94) |
| Social worker | 0.25 (0.79) | ||
| Practice nurse | 0.06 (0.24) | 0.12 (0.33) | 0.1 (0.45) |
| Psychologist | 0.4 (1.63) | ||
| Community psychiatrist nurse | 0.04 (0.2) | 1.05 (4.70) | |
| Education welfare officer | 0.29 (0.85) | ||
| Educational psychologist | 0.04 (0.2) | ||
| Family liaison officer | 0.04 (0.2) | 1.2 (4.71) | |
| Teacher | 0.12 (0.49) | 0.08 (0.4) | 0.1 (0.31) |
| Audiology | 0.24 (0.66) | ||
| Ophthalmology | 0.04 (0.2) | ||
| Hospital A&E department | 0.2 (0.89) | ||
| Occupational therapist | 0.18 (0.73) | ||
| Housing department | 0.41 (1.70) | 0.08 (0.28) | |
| Citizens Advice Bureau | 0.05 (0.22) | ||
| Other | 1.77a (3.32) | 0.38b (1.53) | 1.16c (2.36) |
| Observations | 17 | 25 | 20 |
| Resource use: medications | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Mother’s consumption of prescription medications | 0.46 (0.78) | 0.96 (1.46) | 0.63 (1.38) |
| Mother’s consumption of ‘over-the-counter’ medications | 0.31 (0.63) | 0.17 (0.39) | 0.05 (0.23) |
| Child’s consumption of prescription medications | 0.38 (0.65) | 0.30 (0.63) | 0.11 (0.32) |
| Child’s consumption of ‘over-the-counter’ medications | 0.31 (0.48) | 0.17 (0.39) | 0.05 (0.23) |
| Observations | 13 | 23 | 19 |
| Resource use (contacts): child | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Family doctor | 0.66 (1.10) | 0.45 (0.77) | 0.93 (1.80) |
| Social worker | 0.73 (2.90) | ||
| Practice nurse | 0.13 (0.43) | 0.07 (0.37) | |
| Psychologist | 0.13 (0.71) | 0.17 (0.75) | |
| Psychiatrist | 0.03 (0.18) | ||
| Education welfare officer | 0.19 (0.90) | ||
| Educational psychologist | 0.07 (0.37) | ||
| Family liaison officer | 0.03 (0.18) | 0.87 (3.88) | |
| Teacher | 0.38 (1.13) | 0.35 (1.14) | 0.6 (2.43) |
| Paediatrician | 0.19 (0.60) | 0.13 (0.50) | 0.10 (0.55) |
| Audiology | 0.03 (0.18) | 0.10 (0.40) | |
| Ophthalmology | 0.03 (0.18) | 0.1 (0.40) | |
| Hospital A&E department | 0.16 (0.37) | 0.06 (0.25) | 0.07 (0.25) |
| Paediatric dietitian | 0.03 (0.18) | 0.27 (1.46) | |
| Paediatric physiotherapist | 0.03 (0.18) | 0.03 (0.18) | |
| Paediatric play specialist | 0.19 (1.06) | ||
| Community children’s nurse | 0.03 (0.18) | ||
| Child and adolescent mental health worker | 0.23 (1.10) | ||
| Other | 0.83a (1.53) | 0.36b (0.92) | 0.63c (1.63) |
| Observations | 32 | 31 | 30 |
| Resource use (contacts): mother | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Family doctor | 1.34 (1.75) | 0.81 (1.05) | 1.77 (3.94) |
| Social worker | 0.4 (2.19) | ||
| Practice nurse | 0.16 (0.45) | 0.26 (0.58) | 0.13 (0.43) |
| Psychologist | 0.17 (0.75) | ||
| Psychiatrist | 0.06 (0.25) | 0.03 (0.18) | |
| Community psychiatrist nurse | 0.31 (1.77) | 0.2 (1.10) | |
| Education welfare officer | 0.25 (0.92) | 0.07 (0.7) | |
| Educational psychologist | 0.03 (0.18) | ||
| Family liaison officer | 0.03 (0.17) | 0.73 (3.83) | |
| Teacher | 0.41 (1.50) | 0.16 (0.73) | 0.07 (0.37) |
| Audiology | 0.13 (0.50) | 0.10 (0.54) | 0.13 (0.73) |
| Ophthalmology | 0.06 (0.25) | ||
| Hospital A&E department | 0.13 (0.42) | 0.06 (0.25) | 0.07 (0.26) |
| Occupational therapist | 0.17 (0.91) | ||
| Paediatric dietitian | 0.06 (0.35) | ||
| Family therapist | 0.03 (0.18) | ||
| Community children’s nurse | 0.03 (0.18) | ||
| Citizens Advice Bureau | 0.09 (0.53) | 0.1 (0.55) | |
| Other | 0.53a (1.67) | 0.69b (1.70) | 0.93c (2.28) |
| Observations | 32 | 31 | 30 |
| Resource use: medications | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Mother’s consumption of prescription medications | 0.85 (1.23) | 0.69 (0.75) | 0.95 (1.24) |
| Mother’s consumption of ‘over-the-counter’ medications | 0.15 (0.49) | 0.11 (0.32) | 0.05 (0.22) |
| Child’s consumption of prescription medications | 0.60 (0.75) | 0.53 (0.84) | 0.38 (0.81) |
| Child’s consumption of ‘over-the-counter’ medications | 0.11 (0.46) | 0.21 (0.42) | 0.05 (0.22) |
| Observations | 20 | 19 | 21 |
| Resource use (contacts): child | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Family doctor | 0.96 (1.02) | 0.35 (0.65) | 0.60 (1.00) |
| Social worker | 0.04 (0.21) | 0.53 (2.92) | |
| Practice nurse | 0.22 (0.85) | 0.27 (0.78) | |
| Psychologist | 0.04 (0.21) | 0.09 (0.42) | 0.57 (2.46) |
| Psychiatrist | 0.03 (0.18) | ||
| Education welfare officer | 0.03 (0.18) | ||
| Educational psychologist | 0.04 (0.21) | 0.04 (0.21) | |
| Family liaison officer | 0.13 (0.63) | 0.77 (3.84) | |
| Teacher | 0.04 (0.21) | 0.17 (0.58) | 0.13 (0.43) |
| Paediatrician | 0.13 (0.63) | 0.35 (0.93) | 0.07 (0.37) |
| Audiology | 0.09 (0.42) | ||
| Ophthalmology | 0.07 (0.37) | ||
| Hospital A&E department | 0.04 (0.21) | 0.04 (0.2085144) | 0.03 (0.18) |
| Paediatric dietitian | 0.23 (1.28) | ||
| Paediatric physiotherapist | 0.04 (0.21) | ||
| Child and adolescent mental health worker | 0.03 (0.18) | ||
| Primary mental health worker | 0.03 (0.18) | ||
| Other | 0.05a (0.23) | 0.05b (0.23) | 0.30c (0.93) |
| Observations | 23 | 23 | 30 |
| Resource use (contacts): mother | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Family doctor | 2.39 (3.49) | 1.52 (1.98) | 1.37 (1.97) |
| Social worker | 0.22 (1.04) | 0.33 (1.83) | |
| Practice nurse | 0.04 (0.21) | 0.35 (1.27) | 0.10 (0.31) |
| Psychologist | 0.39 (1.88) | 0.17 (0.83) | |
| Psychiatrist | 0.04 (0.21) | ||
| Education welfare officer | 0.03 (0.18) | ||
| Educational psychologist | 0.04 (0.21) | 0.03 (0.18) | |
| Family liaison officer | 0.09 (0.29) | 0.73 (3.83) | |
| Teacher | 0.13 (0.46) | 0.74 (2.53) | 0.13 (0.43) |
| Ophthalmology | 0.033 (0.18) | ||
| Hospital A&E department | 0.17 (0.49) | 0.09 (0.42) | 0.07 (0.37) |
| Occupational therapist | 0.04 (0.21) | ||
| Housing department | 0.09 (0.42) | 0.03 (0.18) | |
| Citizens Advice Bureau | 0.04 (0.21) | 0.03 (0.18) | |
| Family centre | 0.04 (0.21) | 0.07 (0.37) | |
| Home-Start | 0.04 (0.21) | ||
| Other | 0.71a (1.23) | 0.37b (1.01) | 0.43c (1.04) |
| Observations | 23 | 23 | 30 |
| Resource use: medications | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Mother’s consumption of prescription medications | 0.65a (0.93) | 0.45a (0.89) | 0.54b (1.07) |
| Mother’s consumption of ‘over-the-counter’ medications | 0.14c (0.35) | 0.41 (0.96) | 0.26d (0.71) |
| Child’s consumption of prescription medications | 0.52 (0.67) | 0.18 (0.50) | 0.17 (0.38) |
| Child’s consumption of ‘over-the-counter’ medications | 0.22 (0.67) | 0.23 (0.53) | 0.21 (0.62) |
| Observations | 23 | 22 | 29 |
| Cost: child | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Family doctor | £44.57 (63.45) | £14.46 (30.56) | £20.00 (32.12) |
| Social worker | £26.30 (180.29) | £51.50 (291.33) | |
| Practice nurse | £0.39 (2.31) | £1.16 (3.86) | £0.86 (3.37) |
| Psychologist | £11.66 (68.96) | £17.36 (100.73) | £8.50 (33.45) |
| Education welfare officer | £0.43 (2.98) | £2.56 (14.45) | |
| Educational psychologist | £2.13 (12.61) | £1.62 (7.69) | |
| Family liaison officer | £5.60 (33.13) | £2.09 (14.29) | |
| Teacher | £12.14 (42.89) | £21.85 (109.90) | £23.24 (88.40) |
| Paediatrician | £45.00 (142.30) | £33.51 (104.68) | |
| Audiology | £6.29 (37.19) | ||
| Speech and language | £0.97a (5.65) | £0.70 (4.81) | £2.06 (8.12) |
| Ophthalmology | £6.11 (25.20) | £4.55 (21.83) | |
| Hospital A&E department | £12.34 (50.87) | £9.19 (30.46) | £6.75 (38.18) |
| Occupational therapist | £2.83 (16.73) | ||
| Paediatric physiotherapist | £4.72 (23.93) | ||
| Community children’s nurse | £13.28 (78.60) | ||
| Child and adolescent mental health worker | £1.44 (9.92) | ||
| Primary mental health worker | 2.13 (12.02) | ||
| Other | £46.35b (83.41) | £64.22c (128.77) | £57.26d (110.20) |
| Observations | 35 | 47 | 32 |
| Cost: mother | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Family doctor | £69.71 (87.50) | £41.70 (60.70) | £56.25 (129.66) |
| Social worker | £26.30 (180.28) | £19.31 (109.25) | |
| Practice nurse | £3.13 (6.71) | £1.45 (4.27) | £2.99 (10.28) |
| Psychologist | £21.25 (78.08) | ||
| Psychiatrist | £16.30 (111.73) | £11.97 (67.71) | |
| Community psychiatrist nurse | £16.63 (94.05) | ||
| Education welfare officer | £0.43 (2.98) | £0.64 (3.61) | |
| Family liaison officer | £10.71 (60.63) | ||
| Teacher | £8.09 (21.19) | £5.27 (25.55) | £9.96 (28.77) |
| Paediatrician | £14.06 (55.34) | ||
| Ophthalmologist | £15.20 (64.32) | ||
| Hospital A&E department | £9.26 (30.68) | £11.49 (40.50) | £3.38 (19.09) |
| Family therapist | £3.06 (17.32) | ||
| Community children nurse | £11.87 (81.39) | ||
| Primary mental health worker | £2.12 (12.02) | ||
| Housing department | £0.42 (2.89) | £0.619 (3.50) | |
| Citizens Advise Bureau | £0.44 (2.62) | ||
| Other | £62.68a (125.00) | £11.19b (47.12) | £73.75c (150.02) |
| Observations | 35 | 47 | 32 |
| Cost: child | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Family doctor | £9.41 (17.49) | £25.60 (41.44) | £12.00 (18.81) |
| Social worker | £157.53 (649.51) | £82.40 (368.50) | |
| Practice nurse | £1.61 (6.64) | £1.10 (3.79) | |
| Psychologist | £43.52 (217.6) | ||
| Education welfare officer | £3.61 (14.87) | ||
| Family liaison officer | £1.96 (9.8) | ||
| Teacher | £8.33 (19.91) | £8.50 (29.41) | £7.08 (24.64) |
| Paediatrician | £13.24 (54.57) | £18 (90.00) | |
| Speech and language | £1.94 (8.00) | ||
| Ophthalmology | £4.28 (21.4) | ||
| Hospital A&E department | £6.35 (26.19) | £4.32 (21.6) | |
| Other | £20.28a (62.84) | £23.86b (62.60) | |
| Observations | 17 | 25 | 20 |
| Cost: mother | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Family doctor | £42.35 (68.51) | £32.00 (38.30) | £76.00 (197.63) |
| Social worker | £51.50 (161.99) | ||
| Practice nurse | £0.81 (3.32) | £1.64 (4.54) | £1.37 (6.12) |
| Psychologist | £54.4 (222.09) | ||
| Community psychiatrist nurse | £3.04 (15.20) | £79.80 (356.88) | |
| Education welfare officer | £6.01 (17.35) | ||
| Educational psychologist | £1.49 (7.46) | ||
| Family liaison officer | £1.96 (9.80) | £58.8 (230.71) | |
| Teacher | £4.17 (17.17) | £2.83 (14.16) | £3.54 (10.90) |
| Audiology | £25.88 (73.06) | ||
| Ophthalmology | £4.28 (21.40) | ||
| Hospital A&E department | £21.6 (96.60) | ||
| Occupational therapist | £5.82 (24.01) | ||
| Housing department | £8.16 (33.63) | £1.58 (5.49) | |
| Citizens Advice Bureau | £0.78 (3.47) | ||
| Other | £143.52a (269.36) | £30.90b (124.29) | £93.93c (191.70) |
| Observations | 17 | 25 | 20 |
| Cost: child | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Family doctor | £26.25 (43.83) | £18.06 (30.70) | £37.33 (71.96) |
| Social worker | £151.07 (597.37) | ||
| Practice nurse | £1.77 (5.85) | £0.91 (5.00) | |
| Psychologist | £17.00 (96.17) | £22.67 (101.54) | |
| Psychiatrist | £12.76 (69.93) | ||
| Education welfare officer | £3.83 (18.31) | ||
| Educational psychologist | £2.49 (13.62) | ||
| Family liaison officer | £1.53 (8.66) | £42.47 (189.88) | |
| Teacher | £13.28 (39.97) | £12.56 (40.42) | £21.25 (86.04) |
| Paediatrician | £42.19 (133.27) | £29.03 (112.38) | £22.50 (123.24) |
| Audiology | £3.44 (19.45) | £10.65 (43.58) | |
| Ophthalmology | £3.34 (18.92) | £10.70 (43.08) | |
| Hospital A&E department | £16.88 (39.84) | £6.97 (26.97) | £7.20 (27.40) |
| Occupational therapist | |||
| Paediatric dietitian | £1.06 (6.01) | £9.07 (49.66) | |
| Paediatric physiotherapist | £2.31 (13.08) | £2.47 (13.51) | |
| Paediatric play specialist | £2.17 (12.25) | ||
| Community children’s nurse | £2.91 (16.44) | ||
| Child and adolescent mental health worker | £15.87 (75.09) | ||
| Other | £67.60a (123.91) | £29.50b (74.99) | £50.70c (132.05) |
| Observations | 32 | 31 | 30 |
| Cost: mother | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Family doctor | £53.75 (70.10) | £32.26 (41.85) | £70.67 (157.46) |
| Social worker | £82.40 (451.32) | ||
| Practice nurse | £2.14 (6.13) | £3.53 (7.88) | £1.83 (5.94) |
| Psychologist | £22.67 (101.54) | ||
| Psychiatrist | £23.94 (94.19) | £12.77 (69.93) | |
| Community psychiatrist nurse | £23.75 (134.35) | £15.2 (83.25) | |
| Education welfare officer | £5.11 (18.72) | £1.36 (7.46) | |
| Educational psychologist | £1.24 (6.81) | ||
| Family liaison officer | £1.53 (8.66) | £35.93 (187.77) | |
| Teacher | £14.39 (53.10) | £5.71 (26.02) | £2.36 (2.93) |
| Audiology | £13.75 (54.11) | £10.65 (59.27) | £14.67 (80.33) |
| Ophthalmology | £6.69 (26.32) | ||
| Hospital A&E department | £13.50 (45.49) | £6.97 (26.97) | £7.20 (27.40) |
| Occupational therapist | £5.50 (30.12) | ||
| Paediatric dietitian | £2.13 (12.02) | ||
| Family therapist | £1.53 (8.66) | ||
| Community children’s nurse | £2.91 (16.44) | ||
| Citizens Advice Bureau | £1.45 (8.22) | £1.55 (8.49) | |
| Other | £81.12a (135.73) | £56.16b (138.08) | £75.71c (185.15) |
| Observations | 32 | 31 | 30 |
| Cost: child | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Family doctor | £38.26 (40.86) | £13.91 (25.89) | £24 (40.14) |
| Social worker | £8.96 (42.95) | £109.87 (601.76) | |
| Practice nurse | £2.98 (11.64) | £3.65 (10.75) | |
| Psychologist | £5.91 (28.36) | £11.83 (56.72) | £77.07 (334.44) |
| Psychiatrist | £12.77 (69.93) | ||
| Education welfare officer | £0.68 (3.73) | ||
| Educational psychologist | £1.62 (7.78) | £1.62 (7.78) | |
| Family liaison officer | £6.39 (30.65) | £37.57 (188.10) | |
| Teacher | £1.54 (7.38) | £6.16 (20.40) | £4.72 (15.37) |
| Paediatrician | £29.35 (140.75) | £78.26 (210.29) | £15.00 (82.16) |
| Audiology | £9.57 (45.87) | ||
| Ophthalmology | £7.13 (39.07) | ||
| Hospital A&E department | £4.70 (22.52) | £4.70 (22.52) | £3.60 (19.72) |
| Paediatric dietitian | £7.93 (43.45) | ||
| Paediatric physiotherapist | £3.22 (15.43) | ||
| Child and adolescent mental health worker | £2.27 (12.42) | ||
| Primary mental health worker | £2.27 (12.42) | ||
| Other | £4.27a (18.61) | £4.27b (18.61) | £24.69c (75.13) |
| Observations | 23 | 23 | 30 |
| Cost: mother | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Family doctor | £95.65 (139.47) | £60.87 (78.97) | £54.67 (78.95) |
| Social worker | £44.78 (214.77) | £68.67 (376.10) | |
| Practice nurse | £0.60 (2.85) | £4.76 (17.32) | £1.37 (4.18) |
| Psychologist | £53.22 (255.22) | £23.65 (113.43) | |
| Psychiatrist | £16.65 (79.86) | ||
| Education welfare officer | £0.68 (3.73) | ||
| Educational psychologist | £1.62 (7.78) | £1.24 (6.81) | |
| Family liaison officer | £4.26 (14.12) | £35.93 (187.77) | |
| Teacher | £4.62 (16.21) | £26.17 (89.46) | £4.72 (15.37) |
| Ophthalmology | £3.57 (19.54) | ||
| Hospital A&E department | £18.78 (53.03) | £9.39 (45.04) | £7.20 (39.44) |
| Occupational therapist | £1.43 (6.88) | ||
| Housing department | £1.72 (8.26) | £0.66 (3.62) | |
| Citizens Advice Bureau | £0.67 (3.23) | £0.52 (2.83) | |
| Family centre | £2.13 (10.22) | £3.27 (17.89) | |
| Home-Start | £4.16 (19.93) | ||
| Other | £57.94a (103.07) | £29.89b (82.06) | £35.27c (84.11) |
| Observations | 23 | 23 | 30 |
| Time off (days) | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Time off school (days): child | 1.46 (1.97) | 0.28 (0.92) | 1.88 (2.91) |
| Time off work (days): mother | 0.50a (1.38) | 0.28b (0.92) | 2.00 (6.42) |
| Time off usual activities (days): mother | 1.14 (3.04) | 0.57 (2.38) | 0.78 (2.76) |
| Observations | 35 | 47 | 32 |
| Time off (days) | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Time off school (days): child | 2.12 (4.09) | 1.84 (2.64) | 3.38 (10.02) |
| Time off work (days): mother | 0.41 (1.70) | 0.72 (1.74) | 2.65 (8.29) |
| Time off usual activities (days): mother | 0.06 (0.24) | 1.96 (6.09) | 0.65 (2.68) |
| Observations | 17 | 25 | 20 |
| Time off (days) | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Time off school (days): child | 3.38 (6.74) | 1.32 (2.28) | 2.55 (4.69) |
| Time off work (days): mother | 0.59 (1.62) | 0.42 (1.12) | 3.03 (8.66) |
| Time off usual activities (days): mother | 1.00 (2.75) | 1.06 (3.72) | 0.23 (1.28) |
| Observations | 32 | 31 | 30 |
| Time off (days) | Mean (SD) | ||
|---|---|---|---|
| CCBT + MCBT | CCBT + MCI | CCBT | |
| Time off school (days): child | 3.23 (4.82) | 0.61 (1.53) | 3.15 (6.34) |
| Time off work (days): mother | 1.45 (3.29) | 1.00 (3.12) | 1.03a (2.38) |
| Time off usual activities (days): mother | 0.64 (2.98) | 1.68 (1.99) | 1.69a (6.43) |
| Observations | 22 | 23 | 30 |
| CUA results | CCBT + MCBT (n = 69), mean (SE) | CCBT (n = 71), mean (SE) |
|---|---|---|
| Cost of intervention | £1888.84 (78.65) | £1092.25 (61.88) |
| QALY gain | 0.794 (0.022) | 0.827 (0.024) |
| Incremental cost (95% CI) | £796.59 (£599.48 to £993.70) | |
| Incremental benefit, QALY gain (95% CI) | –0.033 (–0.101 to 0.035) | |
| ICER, incremental cost per QALY gain | –£24,139 | |
| (95% CI) bootstrap method | Lower limit, £47,106; upper limit, –£10,094 | |
| (95% CI) Fieller’s method | Lower limit, –£9251; upper limit, £46,271 | |
| NMB for WTP = £20,000 | –0.033 × £20,000 – £796.59 = –£1456.00 | |
| NMB for WTP = £30,000 | –0.033 × £30,000 – £796.59 = –£1786.59 | |
| CUA results | CCBT + MCI (n = 71), mean (SE) | CCBT (n = 71), mean (SE) |
|---|---|---|
| Cost of intervention | £1899.95 (80.72) | £1891.30 (87.14) |
| QALY gain | 0.855 (0.018) | 0.827 (0.024) |
| Incremental cost (95% CI) | £807.70 (£606.55 to £1008.85) | |
| Incremental benefit, QALY gain (95% CI) | 0.028 (–0.030 to 0.086) | |
| ICER, incremental cost per QALY gain | £28,846 | |
| (95% CI) bootstrap method | Lower limit, £10,129; upper limit, –£41,264 | |
| (95% CI) Fieller’s method | Lower limit, £10,207; upper limit, –£41,499 | |
| NMB for WTP = £20,000 | 0.028 × £20,000 – £807.70 = –£247.70 | |
| NMB for WTP = £30,000 | 0.028 × £30,000 – £807.70 = £32.30 | |
FIGURE 14.
Cost-effectiveness plane showing bootstrapped replicates of the ICER: ITT analysis – CCBT + MCBT vs. CCBT. LL, lower limit; PE, point estimate; UL, upper limit.

FIGURE 15.
Cost-effectiveness acceptability curve showing the probability that the intervention is cost-effective at different willingness-to-pay thresholds: ITT analysis – CCBT + MCBT vs. CCBT.

FIGURE 16.
Net monetary benefit curve and limit curves: ITT analysis – CCBT + MCBT vs. CCBT. LL, lower limit; UL, upper limit.

FIGURE 17.
Cost-effectiveness plane showing bootstrapped replicates of the ICER: ITT analysis – CCBT + MCI vs. CCBT. LL, lower limit; PE, point estimate; UL, upper limit.

FIGURE 18.
Cost-effectiveness acceptability curve showing the probability that the intervention is cost-effective at different willingness-to-pay thresholds: ITT analysis – CCBT + MCI vs. CCBT.

FIGURE 19.
Net monetary benefit curve and limit curves: ITT analysis – CCBT + MCI vs. CCBT. LL, lower limit; UL, upper limit.

Appendix 4 Teacher-reported questionnaire
Child adjustment to school: teacher report
Instructions
For each item mark the box for not true, somewhat true or certainly true. It would help us if you answered all items as best you can, even if you are not absolutely certain or the item seems daft! Please give your answers on the basis of the child’s behaviour over the previous 2 weeks of school.
| Not true | Somewhat true | Certainly true | |
|---|---|---|---|
| Avoids or gets worried about presenting work or showing things to the class | |||
| Avoids or gets worried about participating in group or sports activities | |||
| Avoids or gets worried about approaching a group of children to ask to join in | |||
| Avoids or gets worried about standing up for him/herself with peers | |||
| Avoids or gets worried about answering questions in class | |||
| Avoids or gets worried about speaking in class | |||
| Avoids or gets worried about asking questions in class | |||
| Avoids or gets worried about telling a teacher if he/she doesn’t understand something |
Appendix 5 Summary statistics
| Questionnaire | Treatment | n | n missing | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|---|
| SCAS-c | |||||||
| Total score baseline | CCBT | 67 | 4 | 40.24 (21.29) | 35.0 (24.0–53.0) | 2 | 105 |
| CCBT + MCBT | 67 | 2 | 41.33 (18.26) | 41.0 (29.0–56.0) | 7 | 80 | |
| CCBT + MCI | 69 | 2 | 39.16 (17.38) | 39.0 (29.0–47.0) | 4 | 92 | |
| Total score 6 months | CCBT | 44 | 27 | 21.05 (16.24) | 18.0 (8.0–28.5) | 0 | 73 |
| CCBT + MCBT | 43 | 26 | 24.42 (17.41) | 19.0 (12.0–39.0) | 0 | 63 | |
| CCBT + MCI | 43 | 28 | 23.88 (17.37) | 22.0 (9.0–35.0) | 1 | 67 | |
| Total score 12 months | CCBT | 33 | 38 | 18.24 (13.31) | 16.0 (9.0–27.0) | 1 | 54 |
| CCBT + MCBT | 34 | 35 | 23.09 (14.92) | 21.0 (10.0–34.0) | 0 | 52 | |
| CCBT + MCI | 39 | 32 | 21.15 (18.65) | 15.0 (9.0–34.0) | 0 | 68 | |
| SCAS-c/p | |||||||
| Total score baseline | CCBT | 64 | 7 | 43.17 (15.64) | 43.0 (32.5–50.0) | 16 | 94 |
| CCBT + MCBT | 63 | 6 | 42.19 (15.53) | 39.0 (32.0–50.0) | 17 | 82 | |
| CCBT + MCI | 65 | 6 | 41.60 (16.75) | 40.0 (29.0–52.0) | 16 | 94 | |
| Total score 6 months | CCBT | 40 | 31 | 22.40 (16.33) | 19.0 (14.0–27.5) | 1 | 93 |
| CCBT + MCBT | 43 | 26 | 23.21 (13.53) | 19.0 (14.0–31.0) | 3 | 61 | |
| CCBT + MCI | 39 | 32 | 22.26 (11.19) | 22.0 (14.0–28.0) | 5 | 51 | |
| Total score 12 months | CCBT | 34 | 37 | 19.44 (13.14) | 15.5 (10.0–29.0) | 1 | 51 |
| CCBT + MCBT | 32 | 37 | 24.63 (15.37) | 25.0 (12.0–32.5) | 1 | 66 | |
| CCBT + MCI | 36 | 35 | 18.28 (12.80) | 17.0 (9.0–24.0) | 2 | 58 | |
| CCBT + MCBT | 20 | 49 | 4.05 (3.02) | 3.5 (2.0–5.5) | 0 | 12 | |
| CCBT + MCI | 26 | 45 | 5.04 (3.46) | 5.0 (3.0–7.0) | 0 | 13 | |
| SCAS-t | |||||||
| Total score baseline | CCBT | 25 | 46 | 17.60 (13.39) | 15.0 (10.0–22.0) | 0 | 49 |
| CCBT + MCBT | 37 | 32 | 14.38 (14.57) | 9.0 (5.0–16.0) | 1 | 66 | |
| CCBT + MCI | 42 | 29 | 18.67 (12.98) | 15.0 (10.0–26.0) | 0 | 47 | |
| Total score 6 months | CCBT | 11 | 60 | 11.91 (13.16) | 6.0 (1.0–15.0) | 0 | 43 |
| CCBT + MCBT | 16 | 53 | 8.63 (7.05) | 6.5 (3.5–12.0) | 2 | 29 | |
| CCBT + MCI | 22 | 49 | 11.68 (11.51) | 7.0 (4.0–16.0) | 0 | 46 | |
| Total score 12 months | CCBT | 9 | 62 | 9.44 (9.86) | 6.0 (5.0–8.0) | 1 | 32 |
| CCBT + MCBT | 8 | 61 | 15.75 (11.51) | 14.0 (8.0–20.5) | 2 | 39 | |
| CCBT + MCI | 10 | 61 | 7.70 (5.19) | 7.5 (3.0–11.0) | 0 | 17 | |
| Questionnaire | Treatment | n | n missing | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|---|
| CAIS-c | |||||||
| Total score baseline | CCBT | 66 | 5 | 18.29 (12.83) | 16.5 (9.0–24.0) | 1 | 58 |
| CCBT + MCBT | 67 | 2 | 23.15 (16.34) | 20.0 (10.0–37.0) | 0 | 70 | |
| CCBT + MCI | 68 | 3 | 18.91 (14.02) | 15.0 (7.5–28.0) | 0 | 63 | |
| Total score 6 months | CCBT | 42 | 29 | 7.48 (7.39) | 5.0 (2.0–11.0) | 0 | 27 |
| CCBT + MCBT | 43 | 26 | 10.02 (8.56) | 8.0 (3.0–14.0) | 0 | 29 | |
| CCBT + MCI | 43 | 28 | 9.74 (9.39) | 7.0 (2.0–16.0) | 0 | 39 | |
| Total score 12 months | CCBT | 32 | 39 | 6.75 (7.36) | 4.0 (1.0–11.0) | 0 | 29 |
| CCBT + MCBT | 33 | 36 | 11.82 (15.16) | 7.0 (2.0–18.0) | 0 | 78 | |
| CCBT + MCI | 38 | 33 | 7.82 (11.23) | 3.5 (1.0–10.0) | 0 | 49 | |
| CAIS-c/p | |||||||
| Total score baseline | CCBT | 58 | 13 | 23.17 (16.04) | 18.5 (11.0–32.0) | 1 | 66 |
| CCBT + MCBT | 56 | 13 | 25.46 (15.07) | 25.0 (15.0–34.5) | 0 | 60 | |
| CCBT + MCI | 58 | 13 | 20.55 (12.66) | 17.0 (10.0–28.0) | 1 | 58 | |
| Total score 6 months | CCBT | 40 | 31 | 13.18 (12.87) | 9.0 (3.0–22.0) | 0 | 54 |
| CCBT + MCBT | 43 | 26 | 11.65 (9.67) | 9.0 (5.0–16.0) | 1 | 44 | |
| CCBT + MCI | 42 | 29 | 11.17 (9.17) | 9.0 (4.0–18.0) | 0 | 38 | |
| Total score 12 months | CCBT | 33 | 38 | 11.48 (12.14) | 9.0 (3.0–16.0) | 0 | 58 |
| CCBT + MCBT | 33 | 36 | 14.39 (12.15) | 14.0 (6.0–19.0) | 0 | 45 | |
| CCBT + MCI | 38 | 33 | 7.92 (6.58) | 7.0 (3.0–13.0) | 0 | 24 | |
| Questionnaire | Treatment | n | n missing | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|---|
| SDQ-c conduct | |||||||
| Score baseline | CCBT | 68 | 3 | 2.97 (2.01) | 3.0 (1.0–4.0) | 0 | 8 |
| CCBT + MCBT | 66 | 3 | 3.05 (1.88) | 3.0 (2.0–4.0) | 0 | 8 | |
| CCBT + MCI | 70 | 1 | 2.84 (1.72) | 3.0 (2.0–4.0) | 0 | 8 | |
| Score 6 months | CCBT | 44 | 27 | 2.07 (1.61) | 2.0 (1.0–3.0) | 0 | 6 |
| CCBT + MCBT | 44 | 25 | 2.05 (1.38) | 2.0 (1.0–3.0) | 0 | 6 | |
| CCBT + MCI | 43 | 28 | 2.14 (1.93) | 2.0 (1.0–3.0) | 0 | 6 | |
| Score 12 months | CCBT | 33 | 38 | 1.64 (1.48) | 2.0 (0.0–3.0) | 0 | 5 |
| CCBT + MCBT | 35 | 34 | 2.06 (1.66) | 2.0 (1.0–2.0) | 0 | 8 | |
| CCBT + MCI | 39 | 32 | 1.95 (2.31) | 1.0 (0.0–3.0) | 0 | 8 | |
| SDQ-c/p conduct | |||||||
| Score baseline | CCBT | 65 | 6 | 2.46 (1.96) | 2.0 (1.0–3.0) | 0 | 8 |
| CCBT + MCBT | 65 | 4 | 3.05 (1.82) | 3.0 (2.0–4.0) | 0 | 9 | |
| CCBT + MCI | 70 | 1 | 2.57 (1.88) | 2.0 (1.0–4.0) | 0 | 8 | |
| Score 6 months | CCBT | 41 | 30 | 2.00 (1.90) | 2.0 (1.0–3.0) | 0 | 8 |
| CCBT + MCBT | 43 | 26 | 1.77 (1.62) | 1.0 (1.0–3.0) | 0 | 6 | |
| CCBT + MCI | 42 | 29 | 1.45 (1.40) | 1.0 (0.0–2.0) | 0 | 6 | |
| Score 12 months | CCBT | 34 | 37 | 1.26 (1.64) | 1.0 (0.0–2.0) | 0 | 8 |
| CCBT + MCBT | 34 | 35 | 1.97 (1.47) | 2.0 (1.0–3.0) | 0 | 5 | |
| CCBT + MCI | 38 | 33 | 1.82 (2.04) | 1.0 (0.0–3.0) | 0 | 8 | |
| Questionnaire | Treatment | n | n missing | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|---|
| SMFQ-c | |||||||
| Total score baseline | CCBT | 67 | 4 | 7.81 (6.76) | 5.0 (2.0–13.0) | 0 | 24 |
| CCBT + MCBT | 68 | 1 | 9.03 (5.52) | 8.5 (5.0–12.0) | 0 | 24 | |
| CCBT + MCI | 69 | 2 | 7.42 (5.70) | 6.0 (3.0–10.0) | 0 | 23 | |
| Total score 6 months | CCBT | 43 | 28 | 4.51 (5.29) | 3.0 (0.0–7.0) | 0 | 19 |
| CCBT + MCBT | 44 | 25 | 5.20 (4.99) | 4.5 (0.5–10.0) | 0 | 16 | |
| CCBT + MCI | 41 | 30 | 4.00 (5.17) | 1.0 (0.0–7.0) | 0 | 22 | |
| Total score 12 months | CCBT | 31 | 40 | 3.00 (3.91) | 1.0 (0.0–5.0) | 0 | 12 |
| CCBT + MCBT | 35 | 34 | 4.31 (5.42) | 3.0 (0.0–6.0) | 0 | 25 | |
| CCBT + MCI | 38 | 33 | 4.61 (6.74) | 1.0 (0.0–6.0) | 0 | 26 | |
| SMFQ-c/p | |||||||
| Total score baseline | CCBT | 59 | 12 | 9.39 (6.61) | 7.0 (4.0–14.0) | 0 | 24 |
| CCBT + MCBT | 58 | 11 | 10.74 (7.24) | 10.0 (5.0–15.0) | 0 | 26 | |
| CCBT + MCI | 62 | 9 | 8.79 (7.25) | 7.0 (3.0–14.0) | 0 | 25 | |
| Total score 6 months | CCBT | 41 | 30 | 5.12 (5.81) | 3.0 (1.0–9.0) | 0 | 25 |
| CCBT + MCBT | 43 | 26 | 4.65 (5.25) | 3.0 (1.0–7.0) | 0 | 20 | |
| CCBT + MCI | 42 | 29 | 4.33 (4.74) | 3.5 (1.0–7.0) | 0 | 23 | |
| Total score 12 months | CCBT | 34 | 37 | 4.06 (5.43) | 1.5 (0.0–6.0) | 0 | 20 |
| CCBT + MCBT | 34 | 35 | 6.29 (5.84) | 5.0 (1.0–10.0) | 0 | 22 | |
| CCBT + MCI | 38 | 33 | 3.71 (4.78) | 1.0 (0.0–6.0) | 0 | 18 | |
| Questionnaire | Treatment | n | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|
| Positive behaviour | ||||||
| Difference baseline–assessment 2 | CCBT | 42 | 0.01 (0.40) | –0.01 (–0.26 to 0.35) | –1.20 | 0.75 |
| CCBT + MCBT | 45 | 0.01 (0.33) | 0.02 (–0.28 to 0.24) | –0.57 | 0.94 | |
| CCBT + MCI | 49 | 0.08 (0.42) | 0.10 (–0.19 to 0.37) | –1.19 | 1.04 | |
| Score 2 | CCBT | 42 | 3.17 (0.36) | 3.22 (2.93 to 3.43) | 2.32 | 3.82 |
| CCBT + MCBT | 45 | 3.07 (0.36) | 3.04 (2.86 to 3.31) | 2.30 | 3.96 | |
| CCBT + MCI | 49 | 3.16 (0.47) | 3.17 (2.95 to 3.49) | 1.81 | 4.34 | |
| Total score baseline | CCBT | 42 | 3.16 (0.45) | 3.14 (2.88 to 3.47) | 2.08 | 4.03 |
| CCBT + MCBT | 45 | 3.06 (0.39) | 3.04 (2.75 to 3.38) | 2.29 | 4.03 | |
| CCBT + MCI | 49 | 3.08 (0.55) | 3.11 (2.74 to 3.39) | 1.89 | 4.33 | |
| Overprotection | ||||||
| Difference baseline–assessment 2 | CCBT | 42 | –0.04 (0.18) | 0.00 (–0.07 to 0.00) | –1.00 | 0.28 |
| CCBT + MCBT | 45 | –0.03 (0.10) | 0.00 (–0.02 to 0.00) | –0.33 | 0.22 | |
| CCBT + MCI | 49 | –0.04 (0.09) | 0.00 (–0.07 to 0.00) | –0.33 | 0.07 | |
| Score 2 | CCBT | 42 | 1.04 (0.10) | 1.00 (1.00 to 1.00) | 1.00 | 1.50 |
| CCBT + MCBT | 45 | 1.02 (0.05) | 1.00 (1.00 to 1.00) | 1.00 | 1.22 | |
| CCBT + MCI | 49 | 1.01 (0.03) | 1.00 (1.00 to 1.00) | 1.00 | 1.11 | |
| Total score baseline | CCBT | 42 | 1.08 (0.17) | 1.00 (1.00 to 1.11) | 1.00 | 2.00 |
| CCBT + MCBT | 45 | 1.05 (0.09) | 1.00 (1.00 to 1.08) | 1.00 | 1.33 | |
| CCBT + MCI | 49 | 1.05 (0.09) | 1.00 (1.00 to 1.07) | 1.00 | 1.33 | |
| Promotion of avoidance | ||||||
| Difference baseline–assessment 2 | CCBT | 42 | –0.04 (0.13) | 0.00 (–0.11 to 0.00) | –0.47 | 0.28 |
| CCBT + MCBT | 45 | –0.01 (0.13) | 0.00 (–0.07 to 0.00) | –0.53 | 0.33 | |
| CCBT + MCI | 49 | –0.04 (0.11) | 0.00 (–0.07 to 0.00) | –0.40 | 0.13 | |
| Score 2 | CCBT | 42 | 1.06 (0.10) | 1.00 (1.00 to 1.08) | 1.00 | 1.44 |
| CCBT + MCBT | 45 | 1.05 (0.09) | 1.00 (1.00 to 1.07) | 1.00 | 1.33 | |
| CCBT + MCI | 49 | 1.03 (0.06) | 1.00 (1.00 to 1.07) | 1.00 | 1.33 | |
| Total score baseline | CCBT | 42 | 1.10 (0.12) | 1.08 (1.00 to 1.13) | 1.00 | 1.47 |
| CCBT + MCBT | 45 | 1.06 (0.09) | 1.00 (1.00 to 1.08) | 1.00 | 1.53 | |
| CCBT + MCI | 49 | 1.06 (0.10) | 1.00 (1.00 to 1.11) | 1.00 | 1.40 | |
| Intrusiveness | ||||||
| Difference baseline–assessment 2 | CCBT | 42 | –0.06 (0.47) | –0.04 (–0.28 to 0.13) | –1.45 | 1.28 |
| CCBT + MCBT | 45 | 0.01 (0.46) | 0.05 (–0.14 to 0.28) | –1.08 | 1.00 | |
| CCBT + MCI | 49 | –0.10 (0.46) | –0.05 (–0.27 to 0.13) | –1.43 | 0.87 | |
| Score 2 | CCBT | 42 | 1.52 (0.44) | 1.48 (1.20 to 1.84) | 1.00 | 2.88 |
| CCBT + MCBT | 45 | 1.60 (0.39) | 1.47 (1.31 to 1.84) | 1.00 | 2.45 | |
| CCBT + MCI | 49 | 1.48 (0.38) | 1.41 (1.13 to 1.78) | 1.00 | 2.43 | |
| Total score baseline | CCBT | 42 | 1.58 (0.52) | 1.48 (1.16 to 1.88) | 1.00 | 2.93 |
| CCBT + MCBT | 45 | 1.60 (0.50) | 1.40 (1.20 to 1.87) | 1.00 | 2.86 | |
| CCBT + MCI | 49 | 1.58 (0.49) | 1.51 (1.16 to 1.80) | 1.00 | 2.99 | |
| Expressed anxiety | ||||||
| Difference baseline–assessment 2 | CCBT | 42 | 0.03 (0.34) | 0.04 (–0.23 to 0.22) | –0.64 | 0.96 |
| CCBT + MCBT | 45 | 0.02 (0.38) | –0.01 (–0.17 to 0.24) | –1.16 | 0.94 | |
| CCBT + MCI | 49 | –0.04 (0.40) | –0.04 (–0.26 to 0.19) | –1.03 | 1.43 | |
| Score 2 | CCBT | 42 | 1.61 (0.36) | 1.59 (1.37 to 1.73) | 1.07 | 2.74 |
| CCBT + MCBT | 45 | 1.64 (0.41) | 1.56 (1.33 to 1.92) | 1.00 | 2.66 | |
| CCBT + MCI | 49 | 1.59 (0.36) | 1.57 (1.41 to 1.79) | 1.00 | 2.96 | |
| Total score baseline | CCBT | 42 | 1.58 (0.27) | 1.49 (1.37 to 1.75) | 1.18 | 2.23 |
| CCBT + MCBT | 45 | 1.62 (0.33) | 1.54 (1.40 to 1.86) | 1.11 | 2.62 | |
| CCBT + MCI | 49 | 1.63 (0.38) | 1.53 (1.36 to 1.83) | 1.00 | 2.60 | |
| Quality of relationship | ||||||
| Difference baseline–assessment 2 | CCBT | 42 | 0.00 (0.36) | 0.05 (–0.20 to 0.22) | –0.83 | 0.87 |
| CCBT + MCBT | 45 | 0.06 (0.37) | 0.04 (–0.13 to 0.30) | –0.72 | 0.83 | |
| CCBT + MCI | 49 | 0.01 (0.44) | –0.02 (–0.33 to 0.31) | –0.95 | 1.42 | |
| Score 2 | CCBT | 42 | 3.37 (0.33) | 3.38 (3.17 to 3.63) | 2.40 | 3.93 |
| CCBT + MCBT | 45 | 3.36 (0.42) | 3.38 (3.13 to 3.67) | 2.36 | 4.32 | |
| CCBT + MCI | 49 | 3.34 (0.39) | 3.33 (3.20 to 3.60) | 2.36 | 4.13 | |
| Total score baseline | CCBT | 42 | 3.37 (0.40) | 3.44 (3.04 to 3.67) | 2.53 | 4.07 |
| CCBT + MCBT | 45 | 3.30 (0.42) | 3.37 (2.93 to 3.56) | 2.27 | 4.00 | |
| CCBT + MCI | 49 | 3.33 (0.51) | 3.40 (3.08 to 3.56) | 1.91 | 4.55 | |
| POI | ||||||
| Difference baseline–assessment 2 | CCBT | 34 | –5.94 (10.15) | –6.0 (–11.0 to 2.0) | –36 | 9 |
| CCBT + MCBT | 38 | –6.53 (11.26) | –6.0 (–15.0 to 0.0) | –32 | 35 | |
| CCBT + MCI | 34 | –10.35 (10.22) | –8.5 (–15.0 to 4.0) | –41 | 7 | |
| Score 2 | CCBT | 34 | 21.74 (13.27) | 20.0 (12.0 to 32.0) | 2 | 56 |
| CCBT + MCBT | 38 | 21.82 (13.87) | 20.0 (10.0 to 28.0) | 3 | 59 | |
| CCBT + MCI | 34 | 17.76 (9.18) | 16.5 (10.0 to 25.0) | 1 | 39 | |
| Total score baseline | CCBT | 34 | 27.68 (13.45) | 27.0 (17.0 to 40.0) | 5 | 49 |
| CCBT + MCBT | 38 | 28.34 (11.58) | 29.5 (20.0 to 35.0) | 8 | 54 | |
| CCBT + MCI | 34 | 28.12 (11.99) | 27.5 (19.0 to 36.0) | 4 | 54 | |
| Questionnaire | Treatment | n | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|
| PSWQ | ||||||
| Difference baseline–assessment 1B | CCBT | 40 | –3.4 (10.2) | –2.5 (–7.0 to 2.5) | –37 | 18 |
| CCBT + MCBT | 42 | –5.3 (12.5) | –1.5 (–12.0 to 3.0) | –41 | 17 | |
| CCBT + MCI | 44 | –3.0 (8.0) | –3.0 (–8.0 to 4.5) | –20 | 9 | |
| Self-report total score assessment 1B | CCBT | 40 | 35.9 (13.8) | 38.0 (25.0 to 47.0) | 9 | 64 |
| CCBT + MCBT | 42 | 35.6 (14.3) | 36.0 (25.0 to 45.0) | 12 | 64 | |
| CCBT + MCI | 44 | 33.9 (13.5) | 35.0 (22.0 to 46.0) | 3 | 59 | |
| Self-report total score baseline | CCBT | 40 | 39.2 (13.7) | 41.5 (28.5 to 49.5) | 15 | 64 |
| CCBT + MCBT | 42 | 40.9 (13.4) | 42.0 (34.0 to 52.0) | 6 | 62 | |
| CCBT + MCI | 44 | 36.8 (13.2) | 36.5 (28.5 to 45.5) | 8 | 62 | |
| SIAS | ||||||
| Difference baseline–assessment 1B | CCBT | 41 | –0.9 (8.4) | –1.0 (–4.0 to 2.0) | –23 | 22 |
| CCBT + MCBT | 44 | –1.6 (8.7) | –1.5 (–6.0 to 4.5) | –28 | 15 | |
| CCBT + MCI | 47 | –0.1 (8.3) | 0.0 (–6.0 to 5.0) | –21 | 16 | |
| Self-report total score assessment 1B | CCBT | 41 | 22.9 (14.2) | 21.0 (12.0 to 30.0) | 3 | 67 |
| CCBT + MCBT | 44 | 25.0 (13.5) | 25.0 (14.5 to 31.5) | 4 | 63 | |
| CCBT + MCI | 47 | 23.5 (14.6) | 18.0 (13.0 to 36.0) | 0 | 62 | |
| Self-report total score baseline | CCBT | 41 | 23.8 (12.8) | 23.0 (14.0 to 31.0) | 1 | 55 |
| CCBT + MCBT | 44 | 26.5 (15.4) | 24.0 (13.5 to 38.5) | 6 | 66 | |
| CCBT + MCI | 47 | 23.7 (13.7) | 22.0 (15.0 to 31.0) | 0 | 61 | |
| SPS | ||||||
| Difference baseline–assessment 1B | CCBT | 41 | –0.9 (9.5) | 0.0 (–5.0 to 2.0) | –31 | 26 |
| CCBT + MCBT | 45 | –0.6 (7.2) | 0.0 (–6.0 to 3.0) | –16 | 18 | |
| CCBT + MCI | 46 | 0.5 (7.3) | 0.5 (–3.0 to 2.0) | –22 | 22 | |
| Self-report total score assessment 1B | CCBT | 41 | 13.5 (12.4) | 9.0 (4.0 to 20.0) | 0 | 53 |
| CCBT + MCBT | 45 | 16.6 (14.1) | 14.0 (6.0 to 26.0) | 0 | 65 | |
| CCBT + MCI | 46 | 13.7 (12.7) | 10.0 (4.0 to 18.0) | 0 | 47 | |
| Self-report total score baseline | CCBT | 41 | 14.4 (11.5) | 12.0 (5.0 to 21.0) | 0 | 42 |
| CCBT + MCBT | 45 | 17.2 (13.0) | 15.0 (7.0 to 26.0) | 0 | 47 | |
| CCBT + MCI | 46 | 13.2 (11.7) | 9.0 (4.0 to 22.0) | 0 | 45 | |
| DASS-21 | ||||||
| Depression score difference baseline–assessment 1B | CCBT | 38 | –1.7 (6.9) | –1.0 (–6.0 to 0.0) | –20 | 18 |
| CCBT + MCBT | 43 | –1.9 (5.2) | –2.0 (–6.0 to 0.0) | –10 | 10 | |
| CCBT + MCI | 45 | –1.7 (5.6) | –2.0 (–6.0 to 2.0) | –16 | 10 | |
| Self-report depression score assessment 1B | CCBT | 38 | 10.0 (9.6) | 8.0 (4.0 to 14.0) | 0 | 42 |
| CCBT + MCBT | 43 | 9.8 (9.7) | 8.0 (2.0 to 14.0) | 0 | 36 | |
| CCBT + MCI | 45 | 10.2 (8.0) | 8.0 (4.0 to 14.0) | 0 | 32 | |
| Self-report depression score baseline | CCBT | 38 | 11.7 (8.8) | 10.0 (6.0 to 14.0) | 0 | 40 |
| CCBT + MCBT | 43 | 11.7 (9.2) | 8.0 (6.0 to 18.0) | 0 | 40 | |
| CCBT + MCI | 45 | 11.9 (10.3) | 10.0 (4.0 to 16.0) | 0 | 42 | |
| Anxiety score difference baseline–assessment 1B | CCBT | 38 | –0.3 (6.1) | 0.0 (–2.0 to 2.0) | –16 | 16 |
| CCBT + MCBT | 44 | –2.3 (6.7) | –2.0 (–6.0 to 2.0) | –22 | 12 | |
| CCBT + MCI | 45 | –1.7 (6.8) | –2.0 (–4.0 to 2.0) | –30 | 12 | |
| Self-report anxiety score assessment 1B | CCBT | 38 | 7.3 (9.0) | 6.0 (0.0 to 8.0) | 0 | 40 |
| CCBT + MCBT | 44 | 8.2 (8.2) | 6.0 (2.0 to 12.0) | 0 | 36 | |
| CCBT + MCI | 45 | 7.1 (8.1) | 4.0 (2.0 to 8.0) | 0 | 32 | |
| Self-report anxiety score baseline | CCBT | 38 | 7.6 (7.3) | 5.0 (0.0 to 14.0) | 0 | 24 |
| CCBT + MCBT | 44 | 10.5 (8.0) | 9.0 (4.0 to 16.0) | 0 | 34 | |
| CCBT + MCI | 45 | 8.8 (8.4) | 6.0 (2.0 to 14.0) | 0 | 34 | |
| Stress score difference baseline–assessment 1B | CCBT | 41 | –1.4 (6.7) | –2.0 (–6.0 to 2.0) | –16 | 14 |
| CCBT + MCBT | 45 | –1.9 (9.1) | –2.0 (–8.0 to 2.0) | –20 | 28 | |
| CCBT + MCI | 45 | –0.7 (5.9) | –2.0 (–4.0 to 2.0) | –16 | 16 | |
| Self-report stress score assessment 1B | CCBT | 41 | 16.0 (9.9) | 16.0 (10.0 to 22.0) | 0 | 42 |
| CCBT + MCBT | 45 | 16.0 (9.3) | 14.0 (8.0 to 22.0) | 0 | 40 | |
| CCBT + MCI | 45 | 15.4 (8.2) | 16.0 (8.0 to 22.0) | 0 | 32 | |
| Self-report stress score baseline | CCBT | 41 | 17.3 (10.1) | 16.0 (10.0 to 22.0) | 0 | 42 |
| CCBT + MCBT | 45 | 17.9 (9.9) | 18.0 (10.0 to 22.0) | 2 | 42 | |
| CCBT + MCI | 45 | 16.1 (9.0) | 14.0 (10.0 to 22.0) | 0 | 40 | |
| Questionnaire | Treatment | n | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|
| PSWQ | ||||||
| Difference baseline–assessment 2 | CCBT | 35 | –6.9 (12.0) | –6.0 (–13.0 to –1.0) | –40 | 21 |
| CCBT + MCBT | 41 | –7.3 (12.5) | –5.0 (–14.0 to 1.0) | –37 | 13 | |
| CCBT + MCI | 35 | –6.0 (9.3) | –8.0 (–11.0 to –2.0) | –23 | 16 | |
| Self-report total score 2 | CCBT | 35 | 31.5 (13.7) | 29.0 (19.0 to 42.0) | 10 | 59 |
| CCBT + MCBT | 41 | 33.3 (15.2) | 33.0 (23.0 to 43.0) | 1 | 64 | |
| CCBT + MCI | 35 | 30.9 (12.9) | 30.0 (22.0 to 43.0) | 2 | 54 | |
| Self-report total score baseline | CCBT | 35 | 38.4 (13.2) | 41.0 (29.0 to 49.0) | 15 | 60 |
| CCBT + MCBT | 41 | 40.6 (12.9) | 42.0 (34.0 to 50.0) | 6 | 64 | |
| CCBT + MCI | 35 | 36.9 (13.7) | 36.0 (28.0 to 47.0) | 8 | 64 | |
| SIAS | ||||||
| Difference baseline–assessment 2 | CCBT | 34 | –2.9 (10.8) | –4.0 (–8.0 to –1.0) | –35 | 28 |
| CCBT + MCBT | 40 | –5.5 (13.5) | –2.0 (–11.5 to 3.0) | –41 | 17 | |
| CCBT + MCI | 36 | –4.5 (8.0) | –5.5 (–10.0 to 0.0) | –29 | 16 | |
| Self-report total score 2 | CCBT | 34 | 20.5 (14.7) | 17.0 (11.0 to 30.0) | 0 | 66 |
| CCBT + MCBT | 40 | 22.3 (14.5) | 16.5 (12.5 to 29.0) | 3 | 65 | |
| CCBT + MCI | 36 | 19.1 (12.8) | 17.0 (10.5 to 29.0) | 0 | 48 | |
| Self-report total score baseline | CCBT | 34 | 23.4 (13.4) | 31.0 (22.5 to 31.0) | 1 | 55 |
| CCBT + MCBT | 40 | 27.9 (15.8) | 26.5 (14.0 to 39.0) | 6 | 66 | |
| CCBT + MCI | 36 | 23.7 (14.4) | 22.5 (14.0 to 29.0) | 0 | 61 | |
| SPS | ||||||
| Difference baseline–assessment 2 | CCBT | 35 | –3.6 (8.0) | –3.0 (–8.0 to –1.0) | –21 | 18 |
| CCBT + MCBT | 41 | –4.7 (7.9) | –3.0 (–9.0 to 0.0) | –28 | 12 | |
| CCBT + MCI | 36 | –1.8 (7.1) | –2.0 (–7.0 to 1.0) | –16 | 28 | |
| Self-report total score 2 | CCBT | 35 | 9.7 (9.7) | 7.0 (2.0 to 13.0) | 0 | 45 |
| CCBT + MCBT | 41 | 11.8 (11.5) | 8.0 (3.0 to 16.0) | 0 | 52 | |
| CCBT + MCI | 36 | 11.0 (10.9) | 6.0 (3.0 to 19.5) | 0 | 43 | |
| Self-report total score baseline | CCBT | 35 | 13.3 (10.9) | 12.0 (5.0 to 18.0) | 0 | 42 |
| CCBT + MCBT | 41 | 16.5 (12.7) | 14.0 (7.0 to 23.0) | 0 | 47 | |
| CCBT + MCI | 36 | 12.8 (11.3) | 9.5 (3.5 to 19.0) | 0 | 45 | |
| DASS-21 | ||||||
| Depression score difference baseline–assessment 2 | CCBT | 32 | –3.2 (8.8) | –4.0 (–1.00 to 1.0) | –24 | 18 |
| CCBT + MCBT | 36 | –4.0 (7.0) | –4.0 (–6.0 to 0.0) | –20 | 14 | |
| CCBT + MCI | 33 | –2.1 (5.2) | –2.0 (–4.0 to 0.0) | –14 | 8 | |
| Self-report depression score assessment 2 | CCBT | 32 | 8.9 (10.6) | 4.0 (2.0 to 14.0) | 0 | 42 |
| CCBT + MCBT | 36 | 8.2 (8.8) | 6.0 (2.0 to 12.0) | 0 | 40 | |
| CCBT + MCI | 33 | 7.8 (7.3) | 6.0 (2.0 to 14.0) | 0 | 26 | |
| Self-report depression score baseline | CCBT | 32 | 12.1 (10.2) | 10.0 (4.0 to 17.0) | 0 | 40 |
| CCBT + MCBT | 36 | 12.1 (8.8) | 9.0 (6.0 to 17.0) | 2 | 40 | |
| CCBT + MCI | 33 | 9.9 (8.2) | 10.0 (4.0 to 14.0) | 0 | 28 | |
| Anxiety score difference baseline–assessment 2 | CCBT | 32 | –0.6 (7.4) | –2.0 (–4.0 to 2.0) | –20 | 18 |
| CCBT + MCBT | 36 | –3.1 (6.8) | –4.0 (–7.0 to 0.0) | –14 | 26 | |
| CCBT + MCI | 33 | –2.0 (5.0) | –2.0 (–4.0 to 0.0) | –14 | 12 | |
| Self-report anxiety score assessment 2 | CCBT | 32 | 7.3 (10.3) | 3.0 (0.0 to 9.0) | 0 | 42 |
| CCBT + MCBT | 36 | 6.7 (8.0) | 5.0 (0.0 to 11.0) | 0 | 40 | |
| CCBT + MCI | 33 | 4.5 (5.3) | 2.0 (0.0 to 8.0) | 0 | 16 | |
| Self-report anxiety score baseline | CCBT | 32 | 7.9 (8.0) | 5.0 (2.0 to 14.0) | 0 | 30 |
| CCBT + MCBT | 36 | 9.8 (6.8) | 9.0 (4.0 to 15.0) | 0 | 24 | |
| CCBT + MCI | 33 | 6.5 (5.0) | 6.0 (2.0 to 10.0) | 0 | 18 | |
| Stress score difference baseline–assessment 2 | CCBT | 34 | –3.8 (8.0) | –4.0 (–8.0 to 0.0) | –22 | 14 |
| CCBT + MCBT | 41 | –2.5 (6.5) | –4.0 (–6.0 to 0.0) | –14 | 12 | |
| CCBT + MCI | 35 | –2.5 (6.7) | –2.0 (–6.0 to 0.0) | –16 | 12 | |
| Self-report stress score assessment 2 | CCBT | 34 | 12.9 (9.2) | 11.0 (6.0 to 20.0) | 0 | 32 |
| CCBT + MCBT | 41 | 14.7 (9.4) | 14.0 (10.0 to 18.0) | 0 | 42 | |
| CCBT + MCI | 35 | 12.1 (8.8) | 12.0 (4.0 to 20.0) | 0 | 28 | |
| Self-report stress score baseline | CCBT | 34 | 16.7 (9.7) | 16.0 (10.0 to 22.0) | 0 | 40 |
| CCBT + MCBT | 41 | 17.2 (8.4) | 18.0 (12.0 to 22.0) | 2 | 36 | |
| CCBT + MCI | 35 | 14.6 (8.2) | 12.0 (8.0 to 20.0) | 0 | 32 | |
| Questionnaire | Treatment | n | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|
| Pre-task ‘child scared’ | ||||||
| Difference baseline–assessment 2 | CCBT | 40 | –0.70 (1.78) | –0.67 (–2.00 to 0.33) | –3.67 | 4.00 |
| CCBT + MCBT | 45 | –1.10 (1.62) | –1.00 (–1.67 to 0.00) | –6.33 | 1.67 | |
| CCBT + MCI | 46 | –1.47 (1.55) | –1.33 (–2.33 to –0.33) | –5.33 | 1.00 | |
| Score post treatment | CCBT | 40 | 3.62 (1.58) | 3.33 (2.50 to 5.00) | 1.00 | 7.67 |
| CCBT + MCBT | 45 | 3.10 (1.57) | 3.00 (1.67 to 4.33) | 0.00 | 7.00 | |
| CCBT + MCI | 46 | 3.18 (1.69) | 3.33 (2.00 to 4.33) | 0.00 | 6.67 | |
| Total score baseline | CCBT | 40 | 4.31 (1.86) | 4.33 (3.00 to 5.50) | 0.50 | 8.33 |
| CCBT + MCBT | 45 | 4.21 (1.81) | 4.00 (3.00 to 5.33) | 0.33 | 8.33 | |
| CCBT + MCI | 46 | 4.65 (1.82) | 4.67 (3.67 to 6.00) | 0.00 | 8.33 | |
| Pre-task ‘mother anxious’ | ||||||
| Difference baseline–assessment 2 | CCBT | 40 | –0.85 (1.63) | –1.00 (–2.33 to 0.00) | –3.33 | 3.33 |
| CCBT + MCBT | 45 | –1.46 (1.95) | –1.33 (–2.67 to 0.00) | –7.00 | 2.33 | |
| CCBT + MCI | 46 | –1.42 (1.73) | –1.33 (–2.67 to –0.33) | –5.67 | 2.33 | |
| Score post treatment | CCBT | 40 | 3.03 (1.41) | 3.00 (2.00 to 4.00) | 0.00 | 6.67 |
| CCBT + MCBT | 45 | 2.56 (1.89) | 2.33 (1.33 to 3.33) | 0.00 | 8.67 | |
| CCBT + MCI | 46 | 2.52 (1.81) | 2.50 (1.00 to 3.67) | 0.00 | 7.00 | |
| Total score baseline | CCBT | 40 | 3.88 (1.74) | 4.17 (3.00 to 5.17) | 0.00 | 7.67 |
| CCBT + MCBT | 45 | 4.02 (1.91) | 4.33 (2.67 to 5.33) | 0.00 | 8.00 | |
| CCBT + MCI | 46 | 3.95 (2.05) | 3.83 (2.00 to 5.67) | 0.33 | 8.00 | |
| Pre-task ‘child in control’ | ||||||
| Difference baseline–assessment 2 | CCBT | 40 | 0.16 (1.04) | 0.33 (–0.42 to 0.92) | –2.17 | 1.83 |
| CCBT + MCBT | 45 | 0.83 (1.55) | 0.83 (0.17 to 1.50) | –5.50 | 4.50 | |
| CCBT + MCI | 46 | 0.78 (1.41) | 1.00 (–0.17 to 1.67) | –4.17 | 4.17 | |
| Score post treatment | CCBT | 40 | 6.93 (1.47) | 7.08 (6.33 to 8.00) | 3.17 | 10.00 |
| CCBT + MCBT | 45 | 7.32 (1.36) | 7.50 (6.83 to 8.17) | 3.00 | 9.50 | |
| CCBT + MCI | 46 | 7.49 (1.22) | 7.42 (7.00 to 8.50) | 4.33 | 9.83 | |
| Total score baseline | CCBT | 40 | 6.77 (1.26) | 6.83 (6.17 to 7.50) | 4.00 | 9.33 |
| CCBT + MCBT | 45 | 6.49 (1.58) | 6.33 (5.50 to 7.67) | 2.17 | 9.17 | |
| CCBT + MCI | 46 | 6.71 (1.13) | 6.67 (5.83 to 7.50) | 4.67 | 9.17 | |
| Pre-task ‘mother in control’ | ||||||
| Difference baseline–assessment 2 | CCBT | 40 | –0.18 (1.52) | –0.17 (–1.08 to 0.58) | –3.83 | 3.00 |
| CCBT + MCBT | 45 | –0.19 (1.73) | 0.00 (–1.50 to 0.67) | –3.67 | 3.17 | |
| CCBT + MCI | 46 | –0.06 (1.92) | 0.17 (–1.33 to 1.17) | –4.00 | 3.67 | |
| Score post treatment | CCBT | 40 | 4.61 (1.60) | 4.83 (3.33 to 5.58) | 1.00 | 7.50 |
| CCBT + MCBT | 45 | 5.15 (2.48) | 5.67 (2.83 to 7.17) | 0.33 | 8.67 | |
| CCBT + MCI | 46 | 4.91 (1.69) | 5.21 (3.67 to 6.17) | 0.83 | 8.33 | |
| Total score baseline | CCBT | 40 | 4.79 (1.65) | 5.08 (3.75 to 6.00) | 0.50 | 7.67 |
| CCBT + MCBT | 45 | 5.33 (1.96) | 5.17 (4.00 to 6.83) | 1.17 | 10.00 | |
| CCBT + MCI | 46 | 4.98 (1.73) | 5.25 (3.67 to 6.33) | 1.25 | 7.83 | |
| Questionnaire | Treatment | n | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|
| SCAS-c | ||||||
| Difference baseline–assessment 2 | CCBT | 45 | –19.5 (17.2) | –17.0 (–29.0 to –8.0) | –68 | 13 |
| CCBT + MCBT | 46 | –15.0 (11.6) | –16.0 (–23.0 to –8.0) | –37 | 12 | |
| CCBT + MCI | 52 | –14.7 (20.0) | –14.5 (–24.5 to –2.5) | –72 | 20 | |
| Total score post treatment | CCBT | 45 | 21.0 (15.3) | 15.0 (11.0 to 30.0) | 0 | 86 |
| CCBT + MCBT | 46 | 28.3 (15.2) | 25.5 (16.0 to 41.0) | 0 | 69 | |
| CCBT + MCI | 52 | 24.9 (15.2) | 23.0 (13.5 to 34.5) | 0 | 65 | |
| Total score baseline | CCBT | 45 | 40.4 (21.7) | 35.0 (24.0 to 53.0) | 2 | 105 |
| CCBT + MCBT | 46 | 43.3 (17.6) | 40.0 (31.0 to 58.0) | 8 | 80 | |
| CCBT + MCI | 52 | 39.6 (18.9) | 40.0 (29.0 to 48.5) | 4 | 92 | |
| CAIS-c | ||||||
| Difference baseline–assessment 2 | CCBT | 44 | –7.0 (17.3) | –8.0 (–17.0 to –1.0) | –35 | 52 |
| CCBT + MCBT | 45 | –8.4 (15.9) | –7.0 (–11.0 to –2.0) | –49 | 53 | |
| CCBT + MCI | 53 | –5.6 (15.9) | –6.0 (–14.0 to 0.0) | –48 | 70 | |
| Total score post treatment | CCBT | 44 | 10.8 (12.2) | 8.0 (3.0 to 13.0) | 0 | 58 |
| CCBT + MCBT | 45 | 13.8 (13.2) | 11.0 (4.0 to 21.0) | 0 | 58 | |
| CCBT + MCI | 53 | 12.4 (14.4) | 8.0 (3.0 to 16.0) | 0 | 78 | |
| Total score baseline | CCBT | 44 | 17.8 (12.5) | 18.0 (8.5 to 24.5) | 1 | 58 |
| CCBT + MCBT | 45 | 22.2 (15.9) | 17.0 (10.0 to 32.0) | 1 | 60 | |
| CCBT + MCI | 53 | 18.1 (13.2) | 15.0 (7.0 to 27.0) | 0 | 63 | |
| SMFQ-c | ||||||
| Difference baseline–assessment 2 | CCBT | 46 | –4.9 (6.0) | –3.0 (–7.0 to –1.0) | –20 | 2 |
| CCBT + MCBT | 47 | –2.8 (4.7) | –3.0 (–5.0 to –1.0) | –12 | 12 | |
| CCBT + MCI | 54 | –2.3 (5.7) | –2.0 (–5.0 to 1.0) | –15 | 15 | |
| Total score post treatment | CCBT | 46 | 2.7 (4.0) | 1.5 (0.0 to 4.0) | 0 | 23 |
| CCBT + MCBT | 47 | 6.0 (5.5) | 4.0 (1.0 to 9.0) | 0 | 24 | |
| CCBT + MCI | 54 | 5.0 (5.7) | 3.0 (0.0 to 8.0) | 0 | 25 | |
| Total score baseline | CCBT | 46 | 7.6 (6.6) | 5.0 (2.0 to 11.0) | 0 | 24 |
| CCBT + MCBT | 47 | 8.8 (4.9) | 8.0 (5.0 to 12.0) | 0 | 22 | |
| CCBT + MCI | 54 | 7.3 (5.6) | 7.0 (3.0 to 11.0) | 0 | 23 | |
| SDQ-c conduct problems scale | ||||||
| Difference baseline–assessment 2 | CCBT | 47 | –0.6 (1.6) | –1.0 (–2.0 to 0.0) | –4 | 1 |
| CCBT + MCBT | 47 | –0.6 (2.0) | 0.0 (–2.0 to 1.0) | –5 | 3 | |
| CCBT + MCI | 55 | –0.5 (1.8) | –1.0 (–1.0 to 0.0) | –4 | 5 | |
| Total score post treatment | CCBT | 47 | 2.2 (1.6) | 2.0 (1.0 to 3.0) | 0 | 8 |
| CCBT + MCBT | 47 | 2.4 (2.0) | 2.0 (1.0 to 4.0) | 0 | 8 | |
| CCBT + MCI | 55 | 2.3 (2.0) | 2.0 (0.0 to 3.0) | 0 | 7 | |
| Total score baseline | CCBT | 47 | 2.8 (1.8) | 3.0 (1.0 to 4.0) | 0 | 7 |
| CCBT + MCBT | 47 | 3.0 (1.9) | 3.0 (2.0 to 4.0) | 0 | 8 | |
| CCBT + MCI | 55 | 2.8 (1.6) | 3.0 (2.0 to 4.0) | 0 | 7 | |
| Questionnaire | Treatment | n | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|
| SCAS-p | ||||||
| Difference baseline–assessment 2 | CCBT | 36 | –18.3 (10.9) | –16.5 (–27.0 to –11.5) | –36 | 12 |
| CCBT + MCBT | 39 | –17.5 (12.2) | –21.0 (–25.0 to –7.0) | –38 | 10 | |
| CCBT + MCI | 38 | –17.3 (11.5) | –16.0 (–24.0 to –9.0) | –46 | 5 | |
| Total score post treatment | CCBT | 36 | 23.8 (14.5) | 20.0 (14.0 to 29.0) | 3 | 80 |
| CCBT + MCBT | 39 | 26.0 (15.0) | 24.0 (14.0 to 33.0) | 2 | 62 | |
| CCBT + MCI | 38 | 23.8 (8.7) | 23.5 (19.0 to 28.0) | 6 | 41 | |
| Total score baseline | CCBT | 36 | 42.0 (15.3) | 41.5 (32.0 to 47.0) | 16 | 94 |
| CCBT + MCBT | 39 | 43.5 (17.2) | 38.0 (32.0 to 57.0) | 17 | 82 | |
| CCBT + MCI | 38 | 41.1 (13.3) | 41.0 (30.0 to 50.0) | 17 | 81 | |
| CAIS-p | ||||||
| Difference baseline–assessment 2 | CCBT | 33 | –10.5 (8.9) | –9.0 (–15.0 to –5.0) | –34 | 5 |
| CCBT + MCBT | 35 | –14.5 (10.5) | –16.0 (–19.0 to –6.0) | –45 | 2 | |
| CCBT + MCI | 31 | –8.1 (8.5) | –8.0 (–14.0 to 0.0) | –26 | 8 | |
| Total score post treatment | CCBT | 33 | 12.6 (12.0) | 8.0 (3.0 to 18.0) | 0 | 48 |
| CCBT + MCBT | 35 | 11.2 (10.7) | 9.0 (4.0 to 14.0) | 0 | 38 | |
| CCBT + MCI | 31 | 11.4 (8.2) | 11.0 (4.0 to 15.0) | 1 | 33 | |
| Total score baseline | CCBT | 33 | 23.1 (16.7) | 18.0 (10.0 to 32.0) | 1 | 66 |
| CCBT + MCBT | 35 | 25.7 (16.2) | 25.0 (12.0 to 35.0) | 0 | 60 | |
| CCBT + MCI | 31 | 19.5 (11.9) | 17.0 (10.0 to 28.0) | 2 | 52 | |
| SMFQ-p | ||||||
| Difference baseline–assessment 2 | CCBT | 34 | –4.1 (7.4) | –4.0 (–6.0 to 0.0) | –23 | 8 |
| CCBT + MCBT | 38 | –6.8 (5.6) | –6.0 (–10.0 to –3.0) | –23 | 5 | |
| CCBT + MCI | 35 | –4.9 (6.6) | –3.0 (–9.0 to 0.0) | –23 | 5 | |
| Total score post treatment | CCBT | 34 | 4.7 (5.1) | 2.5 (1.0 to 8.0) | 0 | 19 |
| CCBT + MCBT | 38 | 4.6 (5.7) | 2.5 (0.0 to 6.0) | 0 | 22 | |
| CCBT + MCI | 35 | 3.9 (4.1) | 2.0 (0.0 to 8.0) | 0 | 14 | |
| Total score baseline | CCBT | 34 | 8.8 (7.3) | 6.0 (4.0 to 14.0) | 0 | 24 |
| CCBT + MCBT | 38 | 11.3 (7.7) | 10.0 (5.0 to 16.0) | 0 | 26 | |
| CCBT + MCI | 35 | 8.9 (7.3) | 7.0 (2.0 to 14.0) | 0 | 23 | |
| SDQ-p conduct problems scale | ||||||
| Difference baseline–assessment 2 | CCBT | 37 | –0.5 (1.6) | –1.0 (–1.0 to 0.0) | –6 | 3 |
| CCBT + MCBT | 41 | –0.9 (1.3) | –1.0 (–2.0 to 0.0) | –4 | 3 | |
| CCBT + MCI | 40 | –0.9 (1.4) | –1.0 (–1.0 to 0.0) | –6 | 1 | |
| Total score post treatment | CCBT | 37 | 1.7 (1.6) | 1.0 (1.0 to 2.0) | 0 | 8 |
| CCBT + MCBT | 41 | 1.9 (1.7) | 2.0 (0.0 to 3.0) | 0 | 6 | |
| CCBT + MCI | 40 | 1.7 (1.8) | 1.0 (0.0 to 2.5) | 0 | 7 | |
| Total score baseline | CCBT | 37 | 2.2 (1.7) | 2.0 (1.0 to 3.0) | 0 | 8 |
| CCBT + MCBT | 41 | 2.8 (1.9) | 3.0 (2.0 to 4.0) | 0 | 9 | |
| CCBT + MCI | 40 | 2.6 (2.0) | 2.0 (1.0 to 4.0) | 0 | 8 | |
| Questionnaire | Treatment | n | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|
| SCAS-t | ||||||
| Difference baseline–assessment 2 | CCBT | 7 | –6.1 (9.4) | –8.0 (–16.0 to 0.0) | –18 | 8 |
| CCBT + MCBT | 14 | –3.3 (12.1) | –2.5 (–9.0 to 4.0) | –34 | 21 | |
| CCBT + MCI | 12 | –6.0 (11.7) | –5.0 (–7.0 to –0.5) | –30 | 14 | |
| Total score post treatment | CCBT | 7 | 13.4 (11.5) | 10.0 (7.0 to 25.0) | 0 | 33 |
| CCBT + MCBT | 14 | 10.7 (9.4) | 8.0 (7.0 to 10.0) | 0 | 37 | |
| CCBT + MCI | 12 | 12.4 (11.9) | 9.0 (5.5 to 16.0) | 1 | 46 | |
| Total score baseline | CCBT | 7 | 19.6 (19.5) | 15.0 (2.0 to 43.0) | 0 | 49 |
| CCBT + MCBT | 14 | 14.0 (12.2) | 9.5 (5.0 to 16.0) | 3 | 42 | |
| CCBT + MCI | 12 | 18.4 (13.2) | 11.5 (8.0 to 29.0) | 4 | 40 | |
| CAS-t | ||||||
| Difference baseline–assessment 2 | CCBT | 18 | –1.6 (3.8) | –1.0 (–3.0 to 0.0) | –11 | 5 |
| CCBT + MCBT | 24 | –1.3 (4.6) | –2.0 (–3.0 to 1.0) | –16 | 8 | |
| CCBT + MCI | 25 | –1.4 (4.2) | –2.0 (–4.0 to 2.0) | –9 | 7 | |
| Total score post treatment | CCBT | 18 | 5.3 (4.3) | 5.0 (2.0 to 8.0) | 0 | 15 |
| CCBT + MCBT | 24 | 3.4 (2.9) | 3.0 (0.5 to 6.0) | 0 | 9 | |
| CCBT + MCI | 25 | 3.8 (3.8) | 3.0 (1.0 to 5.0) | 0 | 16 | |
| Total score baseline | CCBT | 18 | 6.9 (5.2) | 5.5 (3.0 to 10.0) | 0 | 16 |
| CCBT + MCBT | 24 | 4.7 (4.2) | 4.5 (1.0 to 6.0) | 0 | 16 | |
| CCBT + MCI | 25 | 5.1 (4.3) | 5.0 (2.0 to 8.0) | 0 | 14 | |
| SDQ-t conduct problems scale | ||||||
| Difference baseline–assessment 2 | CCBT | 18 | 0.4 (0.7) | 0.0 (0.0 to 1.0) | 0 | 2 |
| CCBT + MCBT | 22 | –0.3 (1.5) | 0.0 (–1.0 to 1.0) | –4 | 3 | |
| CCBT + MCI | 23 | –0.1 (1.2) | 0.0 (0.0 to 0.0) | –3 | 3 | |
| Total score post treatment | CCBT | 18 | 1.2 (1.8) | 0.5 (0.0 to 2.0) | 0 | 7 |
| CCBT + MCBT | 22 | 1.1 (2.1) | 0.0 (0.0 to 1.0) | 0 | 8 | |
| CCBT + MCI | 23 | 0.8 (1.7) | 0.0 (0.0 to 1.0) | 0 | 7 | |
| Total score baseline | CCBT | 18 | 0.7 (1.2) | 0.0 (0.0 to 1.0) | 0 | 5 |
| CCBT + MCBT | 22 | 1.4 (2.3) | 0.5 (0.0 to 2.0) | 0 | 10 | |
| CCBT + MCI | 23 | 0.9 (1.7) | 0.0 (0.0 to 1.0) | 0 | 6 | |
Questionnaires: assessment 2 – data summaries by treatment arm (all available participants)
| Questionnaire subscale | Treatment | n | n missing | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|---|
| SCAS-c total score post treatment | CCBT | 49 | 22 | 21.0 (15.6) | 15.0 (10.0–30.0) | 0 | 86 |
| CCBT + MCBT | 47 | 22 | 29.1 (16.0) | 26.0 (16.0–42.0) | 0 | 69 | |
| CCBT + MCI | 54 | 17 | 25.3 (15.5) | 23.0 (14.0–35.0) | 0 | 65 | |
| SCAS-p total score post treatment | CCBT | 40 | 31 | 23.3 (13.8) | 20.0 (14.5–28.5) | 3 | 80 |
| CCBT + MCBT | 41 | 28 | 25.5 (14.8) | 22.0 (14.0–32.0) | 2 | 62 | |
| CCBT + MCI | 40 | 31 | 23.9 (8.7) | 23.5 (19.0–28.0) | 6 | 41 | |
| SCAS-t total score post treatment | CCBT | 18 | 53 | 11.9 (10.3) | 8.5 (5.0–16.0) | 0 | 36 |
| CCBT + MCBT | 22 | 47 | 12.2 (9.1) | 9.0 (7.0–17.0) | 0 | 37 | |
| CCBT + MCI | 19 | 52 | 15.7 (12.8) | 9.0 (7.0–20.0) | 1 | 46 |
| Questionnaire subscale | Treatment | n | n missing | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|---|
| CAIS-c total score post treatment | CCBT | 49 | 22 | 10.9 (12.5) | 8.0 (2.0–13.0) | 0 | 58 |
| CCBT + MCBT | 45 | 24 | 13.8 (13.2) | 11.0 (4.0–21.0) | 0 | 58 | |
| CCBT + MCI | 56 | 15 | 12.5 (14.1) | 9.5 (3.0–16.0) | 0 | 78 | |
| CAIS-p total score post treatment | CCBT | 39 | 32 | 12.3 (11.3) | 8.0 (4.0–19.0) | 0 | 48 |
| CCBT + MCBT | 42 | 27 | 12.5 (10.9) | 10.0 (5.0–16.0) | 0 | 38 | |
| CCBT + MCI | 41 | 30 | 10.9 (8.2) | 11.0 (4.0–15.0) | 1 | 33 |
| Questionnaire subscale | Treatment | n | n missing | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|---|
| SDQ-c conduct problems scale post treatment | CCBT | 50 | 21 | 2.2 (1.6) | 2.0 (1.0–3.0) | 0 | 8 |
| CCBT + MCBT | 48 | 21 | 2.4 (2.0) | 2.0 (1.0–4.0) | 0 | 8 | |
| CCBT + MCI | 56 | 15 | 2.3 (2.0) | 2.0 (0.5–3.0) | 0 | 7 | |
| SDQ-p conduct problems scale post treatment | CCBT | 40 | 31 | 1.7 (1.6) | 1.5 (0.5–2.0) | 0 | 8 |
| CCBT + MCBT | 44 | 25 | 2.0 (1.7) | 2.0 (0.5–3.0) | 0 | 6 | |
| CCBT + MCI | 41 | 30 | 1.7 (1.8) | 1.0 (0.0–2.0) | 0 | 7 | |
| SDQ-t conduct problems scale post treatment | CCBT | 23 | 48 | 1.1 (1.7) | 0.0 (0.0–2.0) | 0 | 7 |
| CCBT + MCBT | 27 | 42 | 1.0 (2.0) | 0.0 (0.0–1.0) | 0 | 8 | |
| CCBT + MCI | 31 | 40 | 0.9 (1.6) | 0.0 (0.0–2.0) | 0 | 7 | |
| SMFQ-c total score post treatment | CCBT | 50 | 21 | 3.1 (4.4) | 1.5 (0.0–5.0) | 0 | 23 |
| CCBT + MCBT | 48 | 21 | 6.3 (5.8) | 4.0 (1.5–9.5) | 0 | 24 | |
| CCBT + MCI | 56 | 15 | 4.9 (5.6) | 3.0 (0.0–8.0) | 0 | 25 | |
| SMFQ-p total score post treatment | CCBT | 40 | 31 | 4.2 (4.9) | 2.0 (0.0–6.5) | 0 | 19 |
| CCBT + MCBT | 43 | 26 | 5.3 (5.9) | 3.0 (1.0–8.0) | 0 | 22 | |
| CCBT + MCI | 42 | 29 | 4.0 (4.5) | 2.0 (0.0–7.0) | 0 | 18 |
Missing data for different variables
| Baseline characteristic | Category | At least one missing at assessment 2 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Primary outcome | Child questionnaires | Parent questionnaires | Teacher questionnaires | Behavioural | Cognitions | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | ||
| Gender | Male | 18 | 17.8 | 35 | 34.7 | 72 | 71.3 | 75 | 74.3 | 40 | 39.6 | 40 | 39.6 |
| Female | 16 | 14.5 | 29 | 26.4 | 72 | 65.5 | 81 | 73.6 | 35 | 31.8 | 38 | 34.5 | |
| Status | Single, never married | 6 | 50.0 | 7 | 58.3 | 10 | 83.3 | 10 | 83.3 | 6 | 50.0 | 7 | 58.3 |
| Married (first time) | 17 | 15.9 | 33 | 30.8 | 62 | 57.9 | 72 | 67.3 | 34 | 31.8 | 34 | 31.8 | |
| Remarried | 3 | 18.8 | 3 | 18.8 | 6 | 37.5 | 12 | 75.0 | 4 | 25.0 | 4 | 25.0 | |
| Divorce/separated | 5 | 11.4 | 9 | 20.5 | 41 | 93.2 | 34 | 77.3 | 16 | 36.4 | 18 | 40.9 | |
| Living with partner | 3 | 10.7 | 11 | 39.3 | 21 | 75.0 | 25 | 89.3 | 15 | 53.6 | 15 | 53.6 | |
| Not recorded | 0 | 0.0 | 1 | 25.0 | 4 | 100.0 | 3 | 75.0 | 0 | 0.0 | 0 | 0.0 | |
| Employment mother | Unemployed | 15 | 24.2 | 20 | 32.3 | 43 | 69.4 | 48 | 77.4 | 26 | 41.9 | 29 | 46.8 |
| Part time | 14 | 13.6 | 31 | 30.1 | 71 | 68.9 | 77 | 74.8 | 38 | 36.9 | 38 | 36.9 | |
| Full time | 5 | 14.3 | 9 | 25.7 | 22 | 62.9 | 22 | 62.9 | 8 | 22.9 | 8 | 22.9 | |
| Not recorded | 0 | 0.0 | 4 | 36.4 | 8 | 72.7 | 9 | 81.8 | 3 | 27.3 | 3 | 27.3 | |
| Employment father | Unemployed | 3 | 25.0 | 4 | 33.3 | 8 | 66.7 | 8 | 66.7 | 3 | 25.0 | 3 | 25.0 |
| Part time | 0 | 0.0 | 0 | 0.0 | 1 | 50.0 | 2 | 100.0 | 0 | 0.0 | 0 | 0.0 | |
| Full time | 25 | 16.3 | 49 | 32.0 | 94 | 61.4 | 112 | 73.2 | 55 | 35.9 | 55 | 35.9 | |
| NA | 3 | 42.9 | 4 | 57.1 | 7 | 100.0 | 5 | 71.4 | 4 | 57.1 | 4 | 57.1 | |
| Not recorded | 3 | 8.1 | 7 | 18.9 | 34 | 91.9 | 29 | 78.4 | 13 | 35.1 | 16 | 43.2 | |
| Overall SES | Higher professional | 13 | 12.3 | 28 | 26.4 | 63 | 59.4 | 75 | 70.8 | 34 | 32.1 | 34 | 32.1 |
| Other employed | 14 | 19.7 | 24 | 33.8 | 53 | 74.6 | 54 | 76.1 | 26 | 36.6 | 26 | 36.6 | |
| Unemployed | 0 | 0.0 | 0 | 0.0 | 3 | 100.0 | 2 | 66.7 | 0 | 0.0 | 1 | 33.3 | |
| Not recorded | 7 | 22.6 | 12 | 38.7 | 25 | 80.6 | 25 | 80.6 | 15 | 48.4 | 17 | 54.8 | |
| ADIS-C/P primary diagnosis | SAD | 1 | 2.4 | 6 | 14.6 | 21 | 51.2 | 24 | 58.5 | 10 | 24.4 | 10 | 24.4 |
| Social phobia | 11 | 19.6 | 18 | 32.1 | 37 | 66.1 | 44 | 78.6 | 22 | 39.3 | 22 | 39.3 | |
| GAD | 7 | 14.6 | 17 | 35.4 | 32 | 66.7 | 35 | 72.9 | 15 | 31.3 | 17 | 35.4 | |
| Other | 15 | 22.7 | 23 | 34.8 | 54 | 81.8 | 53 | 80.3 | 28 | 42.4 | 29 | 43.9 | |
| ADIS-C/P primary diagnosis CSR (initial assessment) | Moderate 4 | 4 | 25.0 | 9 | 56.3 | 14 | 87.5 | 13 | 81.3 | 9 | 56.3 | 9 | 56.3 |
| Moderate 5 | 9 | 15.3 | 14 | 23.7 | 40 | 67.8 | 36 | 61.0 | 18 | 30.5 | 18 | 30.5 | |
| Severe 6 | 16 | 14.2 | 35 | 31.0 | 74 | 65.5 | 88 | 77.9 | 37 | 32.7 | 39 | 34.5 | |
| Severe 7 | 5 | 21.7 | 6 | 26.1 | 16 | 69.6 | 19 | 82.6 | 11 | 47.8 | 12 | 52.2 | |
| ADIS-C/P primary diagnosis CSR at assessment 1B | No diagnosis | 0 | 0.0 | 2 | 66.7 | 2 | 66.7 | 2 | 66.7 | 2 | 66.7 | 2 | 66.7 |
| Mild 3 | 0 | 0.0 | 2 | 33.3 | 4 | 66.7 | 4 | 66.7 | 2 | 33.3 | 2 | 33.3 | |
| Moderate 4 | 2 | 7.4 | 10 | 37.0 | 18 | 66.7 | 21 | 77.8 | 7 | 25.9 | 7 | 25.9 | |
| Moderate 5 | 9 | 14.8 | 14 | 23.0 | 40 | 65.6 | 42 | 68.9 | 21 | 34.4 | 23 | 37.7 | |
| Severe 6 | 8 | 8.5 | 21 | 22.3 | 63 | 67.0 | 69 | 73.4 | 29 | 30.9 | 30 | 31.9 | |
| Severe 7 | 2 | 33.3 | 2 | 33.3 | 4 | 66.7 | 4 | 66.7 | 2 | 33.3 | 2 | 33.3 | |
| Very severe 8 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 100.0 | 0 | 0.0 | 0 | 0.0 | |
| Not recorded | 13 | 100.0 | 13 | 100.0 | 13 | 100.0 | 13 | 100.0 | 12 | 92.3 | 12 | 92.3 | |
| Child age (years) | 6 | 1 | 100.0 | 1 | 100.0 | 1 | 100.0 | 1 | 100.0 | 1 | 100.0 | 1 | 100.0 |
| 7 | 5 | 31.3 | 7 | 43.8 | 11 | 68.8 | 13 | 81.3 | 8 | 50.0 | 9 | 56.3 | |
| 8 | 5 | 15.6 | 10 | 31.3 | 19 | 59.4 | 19 | 59.4 | 10 | 31.3 | 10 | 31.3 | |
| 9 | 5 | 15.2 | 11 | 33.3 | 17 | 51.5 | 24 | 72.7 | 10 | 30.3 | 10 | 30.3 | |
| 10 | 6 | 12.8 | 16 | 34.0 | 38 | 80.9 | 35 | 74.5 | 15 | 31.9 | 16 | 34.0 | |
| 11 | 4 | 8.5 | 7 | 14.9 | 29 | 61.7 | 35 | 74.5 | 14 | 29.8 | 14 | 29.8 | |
| 12 | 8 | 25.0 | 12 | 37.5 | 27 | 84.4 | 26 | 81.3 | 16 | 50.0 | 17 | 53.1 | |
| 13 | 0 | 0.0 | 0 | 0.0 | 2 | 66.7 | 3 | 100.0 | 1 | 33.3 | 1 | 33.3 | |
Questionnaire baseline results by treatment arm (all available participants)
| Questionnaire subscale | Treatment | n | n missing | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|---|
| SCAS-c total score post baseline | CCBT | 67 | 4 | 40.2 (21.3) | 35.0 (24.0–53.0) | 2 | 105 |
| CCBT + MCBT | 67 | 2 | 41.3 (18.3) | 41.0 (29.0–56.0) | 7 | 80 | |
| CCBT + MCI | 69 | 2 | 39.2 (17.4) | 39.0 (29.0–47.0) | 4 | 92 | |
| SCAS-p total score baseline | CCBT | 64 | 7 | 43.2 (15.6) | 43.0 (32.5–50.0) | 16 | 94 |
| CCBT + MCBT | 63 | 6 | 42.2 (15.5) | 39.0 (32.0–50.0) | 17 | 82 | |
| CCBT + MCI | 65 | 6 | 41.6 (16.7) | 40.0 (29.0–52.0) | 16 | 94 | |
| SCAS-t total score baseline | CCBT | 25 | 46 | 17.6 (13.4) | 15.0 (10.0–22.0) | 0 | 49 |
| CCBT + MCBT | 37 | 32 | 14.4 (14.6) | 9.0 (5.0–16.0) | 1 | 66 | |
| CCBT + MCI | 42 | 29 | 18.7 (13.0) | 15.0 (10.0–26.0) | 0 | 47 |
| Questionnaire subscale | Treatment | n | n missing | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|---|
| CAIS-c total score baseline | CCBT | 66 | 5 | 18.3 (12.8) | 16.5 (9.0–24.0) | 1 | 58 |
| CCBT + MCBT | 67 | 2 | 23.1 (16.3) | 20.0 (10.0–37.0) | 0 | 70 | |
| CCBT + MCI | 68 | 3 | 18.9 (14.0) | 15.0 (7.5–28.0) | 0 | 63 | |
| CAIS-p total score baseline | CCBT | 58 | 13 | 23.2 (16.0) | 18.5 (11.0–32.0) | 1 | 66 |
| CCBT + MCBT | 56 | 13 | 25.5 (15.1) | 25.0 (15.0–34.5) | 0 | 60 | |
| CCBT + MCI | 58 | 13 | 20.6 (12.7) | 17.0 (10.0–28.0) | 1 | 58 |
| Questionnaire subscale | Treatment | n | n missing | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|---|
| SDQ-c conduct problems scale baseline | CCBT | 68 | 3 | 3.0 (2.0) | 3.0 (1.0–4.0) | 0 | 8 |
| CCBT + MCBT | 66 | 3 | 3.0 (1.9) | 3.0 (2.0–4.0) | 0 | 8 | |
| CCBT + MCI | 70 | 1 | 2.8 (1.7) | 3.0 (2.0–4.0) | 0 | 8 | |
| SDQ-p conduct problems scale baseline | CCBT | 65 | 6 | 2.5 (2.0) | 2.0 (1.0–3.0) | 0 | 8 |
| CCBT + MCBT | 65 | 4 | 3.0 (1.8) | 3.0 (2.0–4.0) | 0 | 9 | |
| CCBT + MCI | 70 | 1 | 2.6 (1.9) | 2.0 (1.0–4.0) | 0 | 8 | |
| SDQ-t conduct problems scale baseline | CCBT | 44 | 27 | 0.9 (1.5) | 0.0 (0.0–1.0) | 0 | 6 |
| CCBT + MCBT | 54 | 15 | 1.2 (1.9) | 0.0 (0.0–2.0) | 0 | 10 | |
| CCBT + MCI | 56 | 15 | 1.8 (1.5) | 0.0 (0.0–1.0) | 0 | 6 | |
| SMFQ-c total score baseline | CCBT | 67 | 4 | 7.8 (6.8) | 5.0 (2.0–13.0) | 0 | 24 |
| CCBT + MCBT | 68 | 1 | 9.0 (5.5) | 8.5 (5.0–12.0) | 0 | 24 | |
| CCBT + MCI | 69 | 2 | 7.4 (5.7) | 6.0 (3.0–10.0) | 0 | 23 | |
| SMFQ-p report total score baseline | CCBT | 59 | 12 | 9.4 (6.6) | 7.0 (4.0–14.0) | 0 | 24 |
| CCBT + MCBT | 58 | 11 | 10.7 (7.2) | 10.0 (5.0–15.0) | 0 | 26 | |
| CCBT + MCI | 62 | 9 | 8.8 (7.2) | 7.0 (3.0–14.0) | 0 | 25 |
Summary of questionnaire scores at different time points by treatment arm
| Questionnaire | Treatment | n | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|
| CAIS-c | ||||||
| Total score difference baseline–6 months | CCBT | 38 | –10.87 (13.07) | –11.0 (–20.0 to 1.0) | –37 | 15 |
| CCBT + MCBT | 43 | –13.86 (15.74) | –11.0 (–21.0 to –5.0) | –62 | 13 | |
| CCBT + MCI | 41 | –9.56 (13.48) | –9.0 (–17.0 to 0.0) | –47 | 13 | |
| Total score 6 months | CCBT | 38 | 7.37 (7.01) | 5.5 (2.0 to 11.0) | 0 | 27 |
| CCBT + MCBT | 43 | 10.02 (8.56) | 8.0 (3.0 to 14.0) | 0 | 29 | |
| CCBT + MCI | 41 | 9.63 (9.35) | 7.0 (2.0 to 15.0) | 0 | 39 | |
| Total score baseline | CCBT | 38 | 18.24 (13.10) | 18.0 (9.0 to 25.0) | 1 | 58 |
| CCBT + MCBT | 43 | 23.88 (16.41) | 21.0 (11.0 to 37.0) | 1 | 70 | |
| CCBT + MCI | 41 | 19.20 (13.44) | 18.0 (8.0 to 27.0) | 0 | 63 | |
| SCAS-c | ||||||
| Total score difference baseline–6 months | CCBT | 41 | –17.80 (17.91) | –15.0 (–28.0 to –6.0) | –61 | 13 |
| CCBT + MCBT | 43 | –17.47 (16.35) | –18.0 (–26.0 to –6.0) | –51 | 29 | |
| CCBT + MCI | 41 | –16.83 (21.80) | –13.0 (–28.0 to –5.0) | –70 | 22 | |
| Total score 6 months | CCBT | 41 | 22.20 (16.22) | 19.0 (10.0 to 30.0) | 0 | 73 |
| CCBT + MCBT | 43 | 24.42 (17.41) | 19.0 (12.0 to 39.0) | 0 | 63 | |
| CCBT + MCI | 41 | 23.73 (17.51) | 22.0 (9.0 to 30.0) | 1 | 67 | |
| Total score baseline | CCBT | 41 | 40.00 (21.60) | 35.0 (24.0 to 53.0) | 2 | 105 |
| CCBT + MCBT | 43 | 41.88 (16.63) | 39.0 (31.0 to 54.0) | 10 | 80 | |
| CCBT + MCI | 41 | 40.56 (18.60) | 42.0 (30.0 to 48.0) | 11 | 92 | |
| SDQ-c conduct subscale | ||||||
| Total score difference baseline–6 months | CCBT | 42 | –0.86 (1.76) | –1.0 (–2.0 to 0.0) | –4 | 3 |
| CCBT + MCBT | 44 | –0.89 (2.08) | –1.0 (–2.0 to 1.0) | –6 | 3 | |
| CCBT + MCI | 42 | –0.86 (1.47) | –1.0 (–2.0 to 0.0) | –4 | 2 | |
| Total score 6 months | CCBT | 42 | 2.10 (1.64) | 2.0 (1.0 to 3.0) | 0 | 6 |
| CCBT + MCBT | 44 | 2.05 (1.38) | 2.0 (1.0 to 3.0) | 0 | 6 | |
| CCBT + MCI | 42 | 2.17 (1.95) | 2.0 (1.0 to 3.0) | 0 | 6 | |
| Total score baseline | CCBT | 42 | 2.95 (1.82) | 3.0 (1.0 to 4.0) | 0 | 8 |
| CCBT + MCBT | 44 | 2.93 (1.90) | 3.0 (1.5 to 4.5) | 0 | 8 | |
| CCBT + MCI | 42 | 3.02 (1.79) | 3.0 (2.0 to 4.0) | 0 | 8 | |
| SMFQ-c | ||||||
| Total score difference baseline–6 months | CCBT | 40 | –3.45 (6.49) | –2.0 (–5.5 to 1.0) | –23 | 7 |
| CCBT + MCBT | 44 | –4.25 (6.03) | –3.0 (–6.0 to –0.5) | –24 | 7 | |
| CCBT + MCI | 39 | –3.51 (6.12) | –4.0 (–7.0 to 0.0) | –20 | 15 | |
| Total score 6 months | CCBT | 40 | 4.18 (5.01) | 3.0 (0.0 to 6.0) | 0 | 19 |
| CCBT + MCBT | 44 | 5.20 (4.99) | 4.5 (0.5 to 10.0) | 0 | 16 | |
| CCBT + MCI | 39 | 4.03 (5.24) | 1.0 (0.0 to 8.0) | 0 | 22 | |
| Total score baseline | CCBT | 40 | 7.63 (6.93) | 5.0 (2.5 to 11.5) | 0 | 24 |
| CCBT + MCBT | 44 | 9.45 (5.94) | 8.5 (5.0 to 13.0) | 0 | 24 | |
| CCBT + MCI | 39 | 7.54 (5.88) | 5.0 (3.0 to 11.0) | 0 | 23 | |
| Questionnaire | Treatment | n | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|
| CAIS-c/p | ||||||
| Total score difference baseline–6 months | CCBT | 35 | –9.40 (10.26) | –7.0 (–17.0 to –1.0) | –33 | 8 |
| CCBT + MCBT | 37 | –13.78 (13.07) | –12.0 (–21.0 to –4.0) | –47 | 4 | |
| CCBT + MCI | 34 | –8.47 (10.71) | –9.0 (–14.0 to 0.0) | –29 | 11 | |
| Total score 6 months | CCBT | 35 | 13.51 (13.24) | 9.0 (3.0 to 22.0) | 0 | 54 |
| CCBT + MCBT | 37 | 11.46 (10.00) | 9.0 (5.0 to 16.0) | 1 | 44 | |
| CCBT + MCI | 34 | 11.24 (9.24) | 9.0 (5.0 to 17.0) | 0 | 38 | |
| Total score baseline | CCBT | 35 | 22.91 (15.48) | 20.0 (11.0 to 30.0) | 1 | 66 |
| CCBT + MCBT | 37 | 25.24 (16.00) | 25.0 (12.0 to 35.0) | 0 | 60 | |
| CCBT + MCI | 34 | 19.71 (11.13) | 17.0 (11.0 to 26.0) | 2 | 52 | |
| SCAS-c/p | ||||||
| Total score difference baseline–6 months | CCBT | 36 | –17.81 (11.43) | –19.0 (–25.5 to –11.5) | –44 | 3 |
| CCBT + MCBT | 41 | –17.32 (12.64) | –18.0 (–24.0 to –10.0) | –45 | 13 | |
| CCBT + MCI | 38 | –18.29 (13.59) | –16.0 (–27.0 to –9.0) | –44 | 15 | |
| Total score 6 months | CCBT | 36 | 23.11 (16.89) | 20.0 (14.0 to 28.5) | 1 | 93 |
| CCBT + MCBT | 41 | 23.66 (13.68) | 20.0 (14.0 to 31.0) | 3 | 61 | |
| CCBT + MCI | 38 | 22.68 (11.01) | 22.0 (15.0 to 28.0) | 5 | 51 | |
| Total score baseline | CCBT | 36 | 40.92 (14.95) | 39.0 (31.0 to 46.0) | 20 | 94 |
| CCBT + MCBT | 41 | 40.98 (15.15) | 38.0 (32.0 to 49.0) | 17 | 82 | |
| CCBT + MCI | 38 | 40.97 (14.64) | 41.0 (29.0 to 52.0) | 16 | 81 | |
| SDQ-c/p conduct subscale | ||||||
| Total score difference baseline–6 months | CCBT | 39 | –0.36 (1.50) | 0.0 (–1.0 to 0.0) | –5 | 3 |
| CCBT + MCBT | 42 | –1.12 (1.21) | –1.0 (–2.0 to 0.0) | –4 | 2 | |
| CCBT + MCI | 41 | –1.12 (1.50) | –1.0 (–2.0 to 0.0) | –4 | 1 | |
| Total score 6 months | CCBT | 39 | 2.05 (1.92) | 2.0 (1.0 to 3.0) | 0 | 8 |
| CCBT + MCBT | 42 | 1.79 (1.63) | 1.0 (1.0 to 3.0) | 0 | 6 | |
| CCBT + MCI | 41 | 1.44 (1.42) | 1.0 (0.0 to 2.0) | 0 | 6 | |
| Total score baseline | CCBT | 39 | 2.41 (1.98) | 2.0 (1.0 to 3.0) | 0 | 8 |
| CCBT + MCBT | 42 | 2.90 (1.69) | 3.0 (2.0 to 4.0) | 0 | 9 | |
| CCBT + MCI | 41 | 2.56 (1.90) | 2.0 (1.0 to 4.0) | 0 | 8 | |
| SMFQ-c/p | ||||||
| Total score difference baseline–6 months | CCBT | 36 | –3.56 (6.53) | –2.5 (–5.5 to 1.0) | –21 | 10 |
| CCBT + MCBT | 38 | –6.76 (6.66) | –6.0 (–9.0 to –2.0) | –25 | 3 | |
| CCBT + MCI | 36 | –4.64 (6.33) | –3.0 (–9.0 to –0.5) | –19 | 8 | |
| Total score 6 months | CCBT | 36 | 5.31 (5.95) | 3.0 (0.5 to 9.0) | 0 | 25 |
| CCBT + MCBT | 38 | 4.61 (5.53) | 2.0 (0.0 to 6.0) | 0 | 20 | |
| CCBT + MCI | 36 | 4.56 (4.87) | 4.0 (1.0 to 7.5) | 0 | 23 | |
| Total score baseline | CCBT | 36 | 8.86 (6.86) | 6.0 (4.0 to 13.0) | 0 | 24 |
| CCBT + MCBT | 38 | 11.37 (7.72) | 10.0 (6.0 to 17.0) | 0 | 26 | |
| CCBT + MCI | 36 | 9.19 (6.86) | 8.5 (2.5 to 14.0) | 0 | 23 | |
| Questionnaire | Treatment | n | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|
| CAS-t | ||||||
| Total score difference baseline–6 months | CCBT | 11 | –2.55 (5.82) | –1.0 (–9.0 to 1.0) | –13 | 5 |
| CCBT + MCBT | 17 | –2.35 (5.15) | –2.0 (–5.0 to 2.0) | –16 | 5 | |
| CCBT + MCI | 23 | –1.30 (3.94) | 0.0 (–5.0 to 1.0) | –9 | 5 | |
| Total score 6 months | CCBT | 11 | 4.82 (5.08) | 2.0 (0.0 to 8.0) | 0 | 14 |
| CCBT + MCBT | 17 | 3.35 (3.32) | 2.0 (1.0 to 5.0) | 0 | 10 | |
| CCBT + MCI | 23 | 4.74 (4.54) | 4.0 (1.0 to 8.0) | 0 | 16 | |
| Total score baseline | CCBT | 11 | 7.36 (5.26) | 6.0 (3.0 to 13.0) | 0 | 16 |
| CCBT + MCBT | 17 | 5.71 (5.58) | 6.0 (0.0 to 10.0) | 0 | 16 | |
| CCBT + MCI | 23 | 6.04 (4.72) | 7.0 (1.0 to 9.0) | 0 | 16 | |
| SCAS-t | ||||||
| Total score difference baseline–6 months | CCBT | 4 | –1.25 (4.99) | –0.5 (–4.5 to 2.0) | –8 | 4 |
| CCBT + MCBT | 9 | –12.22 (12.28) | –9.0 (–13.0 to –8.0) | –37 | 4 | |
| CCBT + MCI | 15 | –11.73 (11.63) | –9.0 (–24.0 to –3.0) | –36 | 1 | |
| Total score 6 months | CCBT | 4 | 15.75 (19.05) | 10.0 (3.0 to 28.5) | 0 | 43 |
| CCBT + MCBT | 9 | 5.56 (4.07) | 4.0 (3.0 to 7.0) | 2 | 15 | |
| CCBT + MCI | 15 | 10.73 (9.04) | 7.0 (4.0 to 16.0) | 0 | 31 | |
| Total score baseline | CCBT | 4 | 17.00 (16.19) | 14.5 (7.0 to 27.0) | 0 | 39 |
| CCBT + MCBT | 9 | 17.78 (13.23) | 16.0 (12.0 to 17.0) | 3 | 40 | |
| CCBT + MCI | 15 | 22.47 (13.08) | 20.0 (10.0 to 36.0) | 6 | 44 | |
| SDQ-t conduct subscale | ||||||
| Total score difference baseline–6 months | CCBT | 12 | 0.58 (2.11) | 0.0 (0.0 to 0.5) | –1 | 7 |
| CCBT + MCBT | 18 | –0.06 (1.70) | 0.0 (0.0 to 0.0) | –2 | 6 | |
| CCBT + MCI | 22 | 0.41 (1.37) | 0.0 (0.0 to 0.0) | –1 | 5 | |
| Total score 6 months | CCBT | 12 | 1.25 (2.18) | 0.0 (0.0 to 1.5) | 0 | 7 |
| CCBT + MCBT | 18 | 0.61 (1.54) | 0.0 (0.0 to 0.0) | 0 | 6 | |
| CCBT + MCI | 22 | 0.86 (1.70) | 0.0 (0.0 to 1.0) | 0 | 5 | |
| Total score baseline | CCBT | 12 | 0.67 (1.44) | 0.0 (0.0 to 1.0) | 0 | 5 |
| CCBT + MCBT | 18 | 0.67 (1.08) | 0.0 (0.0 to 1.0) | 0 | 3 | |
| CCBT + MCI | 22 | 0.45 (1.14) | 0.0 (0.0 to 0.0) | 0 | 5 | |
| Questionnaire | Treatment | n | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|
| CAIS-c | ||||||
| Total score difference baseline–12 months | CCBT | 29 | –8.41 (12.18) | –6.0 (–15.0 to 0.0) | –34 | 16 |
| CCBT + MCBT | 33 | –15.24 (23.01) | –14.0 (–29.0 to –6.0) | –51 | 77 | |
| CCBT + MCI | 37 | –9.86 (10.88) | –8.0 (–19.0 to –1.0) | –36 | 13 | |
| Total score 12 months | CCBT | 29 | 6.38 (6.30) | 4.0 (1.0 to 10.0) | 0 | 25 |
| CCBT + MCBT | 33 | 11.82 (15.16) | 7.0 (2.0 to 18.0) | 0 | 78 | |
| CCBT + MCI | 37 | 8.00 (11.33) | 4.0 (1.0 to 10.0) | 0 | 49 | |
| Total score baseline | CCBT | 29 | 14.79 (11.48) | 14.0 (3.0 to 22.0) | 1 | 40 |
| CCBT + MCBT | 33 | 27.06 (17.26) | 22.0 (14.0 to 41.0) | 1 | 60 | |
| CCBT + MCI | 37 | 17.86 (14.00) | 15.0 (6.0 to 26.0) | 0 | 63 | |
| SCAS-c | ||||||
| Total score difference baseline–12 months | CCBT | 31 | –14.68 (17.11) | –12.0 (–25.0 to 0.0) | –52 | 21 |
| CCBT + MCBT | 34 | –21.44 (15.86) | –22.5 (–27.0 to –13.0) | –59 | 12 | |
| CCBT + MCI | 37 | –17.78 (19.53) | –20.0 (–28.0 to –4.0) | –58 | 22 | |
| Total score 12 months | CCBT | 31 | 18.94 (13.34) | 18.0 (9.0 to 29.0) | 1 | 54 |
| CCBT + MCBT | 34 | 23.09 (14.92) | 21.0 (10.0 to 34.0) | 0 | 52 | |
| CCBT + MCI | 37 | 20.78 (19.04) | 13.0 (9.0 to 33.0) | 0 | 68 | |
| Total score baseline | CCBT | 31 | 33.61 (18.20) | 30.0 (22.0 to 45.0) | 2 | 88 |
| CCBT + MCBT | 34 | 44.53 (17.52) | 42.5 (31.0 to 59.0) | 10 | 80 | |
| CCBT + MCI | 37 | 38.57 (19.17) | 41.0 (29.0 to 47.0) | 4 | 92 | |
| SDQ-c conduct subscale | ||||||
| Total score difference baseline–12 months | CCBT | 31 | –1.06 (1.73) | –1.0 (–2.0 to 0.0) | –5 | 3 |
| CCBT + MCBT | 34 | –0.97 (2.12) | –1.0 (–2.0 to 0.0) | –7 | 3 | |
| CCBT + MCI | 38 | –1.08 (2.50) | –1.0 (–2.0 to 0.0) | –8 | 8 | |
| Total score 12 months | CCBT | 31 | 1.65 (1.52) | 2.0 (0.0 to 3.0) | 0 | 5 |
| CCBT + MCBT | 34 | 2.03 (1.68) | 2.0 (1.0 to 2.0) | 0 | 8 | |
| CCBT + MCI | 38 | 1.97 (2.33) | 1.0 (0.0 to 3.0) | 0 | 8 | |
| Total score baseline | CCBT | 31 | 2.71 (1.81) | 3.0 (1.0 to 4.0) | 0 | 7 |
| CCBT + MCBT | 34 | 3.00 (2.09) | 3.0 (1.0 to 4.0) | 0 | 8 | |
| CCBT + MCI | 38 | 3.05 (1.84) | 3.0 (2.0 to 4.0) | 0 | 8 | |
| SMFQ-c | ||||||
| Total score difference baseline–12 months | CCBT | 28 | –2.89 (6.11) | –2.0 (–5.0 to 1.0) | –24 | 5 |
| CCBT + MCBT | 35 | –5.51 (5.73) | –6.0 (–11.0 to –2.0) | –13 | 9 | |
| CCBT + MCI | 37 | –1.95 (5.68) | –2.0 (–5.0 to 1.0) | –20 | 12 | |
| Total score 12 months | CCBT | 28 | 2.86 (3.67) | 1.0 (0.0 to 5.0) | 0 | 12 |
| CCBT + MCBT | 35 | 4.31 (5.42) | 3.0 (0.0 to 6.0) | 0 | 25 | |
| CCBT + MCI | 37 | 4.73 (6.78) | 1.0 (0.0 to 6.0) | 0 | 26 | |
| Total score baseline | CCBT | 28 | 5.75 (5.69) | 4.5 (1.5 to 8.0) | 0 | 24 |
| CCBT + MCBT | 35 | 9.83 (5.39) | 11.0 (5.0 to 14.0) | 0 | 22 | |
| CCBT + MCI | 37 | 6.68 (5.47) | 5.0 (3.0 to 9.0) | 0 | 23 | |
| Questionnaire | Treatment | n | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|
| CAIS-c/p | ||||||
| Total score difference baseline–12 months | CCBT | 28 | –9.32 (10.99) | –7.5 (–15.5 to –1.0) | –37 | 6 |
| CCBT + MCBT | 27 | –15.07 (11.07) | –16.0 (–22.0 to –5.0) | –37 | 2 | |
| CCBT + MCI | 31 | –9.90 (10.31) | –8.0 (–16.0 to –1.0) | –39 | 5 | |
| Total score 12 months | CCBT | 28 | 11.57 (12.64) | 8.0 (3.5 to 15.5) | 0 | 58 |
| CCBT + MCBT | 27 | 12.74 (11.72) | 8.0 (4.0 to 17.0) | 0 | 42 | |
| CCBT + MCI | 31 | 8.03 (6.79) | 7.0 (1.0 to 13.0) | 0 | 24 | |
| Total score baseline | CCBT | 28 | 20.89 (15.12) | 17.0 (10.5 to 26.5) | 1 | 66 |
| CCBT + MCBT | 27 | 27.81 (16.82) | 25.0 (16.0 to 44.0) | 0 | 60 | |
| CCBT + MCI | 31 | 17.94 (11.52) | 15.0 (10.0 to 24.0) | 1 | 52 | |
| SCAS-c/p | ||||||
| Total score difference baseline–12 months | CCBT | 30 | –21.97 (13.18) | –23.5 (–31.0 to –11.0) | –48 | 3 |
| CCBT + MCBT | 31 | –16.26 (14.23) | –15.0 (–26.0 to –6.0) | –43 | 12 | |
| CCBT + MCI | 33 | –20.85 (15.57) | –19.0 (–29.0 to –12.0) | –59 | 6 | |
| Total score 12 months | CCBT | 30 | 18.67 (13.68) | 14.0 (9.0 to 29.0) | 1 | 51 |
| CCBT + MCBT | 31 | 24.90 (15.55) | 25.0 (12.0 to 33.0) | 1 | 66 | |
| CCBT + MCI | 33 | 19.12 (12.99) | 17.0 (13.0 to 24.0) | 2 | 58 | |
| Total score baseline | CCBT | 30 | 40.63 (14.09) | 39.5 (32.0 to 46.0) | 16 | 74 |
| CCBT + MCBT | 31 | 41.16 (17.02) | 37.0 (29.0 to 55.0) | 17 | 75 | |
| CCBT + MCI | 33 | 39.97 (14.44) | 42.0 (29.0 to 50.0) | 16 | 81 | |
| SDQ-c/p conduct subscale | ||||||
| Total score difference baseline–12 months | CCBT | 32 | –0.75 (1.74) | 0.0 (–2.0 to 0.0) | –6 | 2 |
| CCBT + MCBT | 32 | –1.13 (1.50) | –1.0 (–2.0 to 0.0) | –4 | 1 | |
| CCBT + MCI | 38 | –0.95 (1.66) | –1.0 (–2.0 to 0.0) | –4 | 3 | |
| Total score 12 months | CCBT | 32 | 1.25 (1.65) | 1.0 (0.0 to 2.0) | 0 | 8 |
| CCBT + MCBT | 32 | 1.91 (1.47) | 2.0 (0.5 to 3.0) | 0 | 5 | |
| CCBT + MCI | 38 | 1.82 (2.04) | 1.0 (0.0 to 3.0) | 0 | 8 | |
| Total score baseline | CCBT | 32 | 2.00 (1.95) | 2.0 (1.0 to 3.0) | 0 | 8 |
| CCBT + MCBT | 32 | 3.03 (1.82) | 3.0 (2.0 to 4.0) | 0 | 7 | |
| CCBT + MCI | 38 | 2.76 (2.03) | 2.0 (1.0 to 4.0) | 0 | 8 | |
| SMFQ-c/p | ||||||
| Total score difference baseline–12 months | CCBT | 30 | –4.00 (6.37) | –3.0 (–5.0 to –1.0) | –24 | 8 |
| CCBT + MCBT | 29 | –6.31 (6.20) | –5.0 (–9.0 to –1.0) | –24 | 4 | |
| CCBT + MCI | 33 | –5.64 (6.95) | –3.0 (–10.0 to –1.0) | –22 | 4 | |
| Total score 12 months | CCBT | 30 | 4.10 (5.36) | 2.0 (0.0 to 6.0) | 0 | 20 |
| CCBT + MCBT | 29 | 6.21 (6.04) | 5.0 (1.0 to 9.0) | 0 | 22 | |
| CCBT + MCI | 33 | 3.45 (4.83) | 1.0 (0.0 to 5.0) | 0 | 18 | |
| Total score baseline | CCBT | 30 | 8.10 (6.72) | 5.5 (4.0 to 9.0) | 1 | 24 |
| CCBT + MCBT | 29 | 12.52 (8.17) | 12.0 (7.0 to 19.0) | 0 | 26 | |
| CCBT + MCI | 33 | 9.09 (7.15) | 8.0 (2.0 to 14.0) | 0 | 23 | |
| Questionnaire | Treatment | n | Mean (SD) | Median (IQR) | Minimum | Maximum |
|---|---|---|---|---|---|---|
| CAS-t | ||||||
| Total score difference baseline–12 months | CCBT | 9 | –2.22 (4.99) | –1.0 (–3.0 to 2.0) | –11 | 3 |
| CCBT + MCBT | 10 | 0.40 (4.14) | –0.5 (–3.0 to 2.0) | –4 | 8 | |
| CCBT + MCI | 12 | –1.75 (4.05) | –2.0 (–5.0 to 1.5) | –7 | 5 | |
| Total score 12 months | CCBT | 9 | 5.00 (4.92) | 2.0 (2.0 to 8.0) | 0 | 14 |
| CCBT + MCBT | 10 | 4.60 (3.41) | 4.5 (2.0 to 7.0) | 0 | 10 | |
| CCBT + MCI | 12 | 5.25 (2.93) | 6.0 (3.5 to 7.5) | 0 | 9 | |
| Total score baseline | CCBT | 9 | 7.22 (3.63) | 6.0 (5.0 to 10.0) | 3 | 13 |
| CCBT + MCBT | 10 | 4.20 (2.90) | 3.5 (3.0 to 6.0) | 0 | 10 | |
| CCBT + MCI | 12 | 7.00 (4.29) | 6.5 (4.5 to 10.0) | 1 | 16 | |
| SCAS-t | ||||||
| Total score difference baseline–12 months | CCBT | 4 | –8.25 (3.77) | –8.0 (–11.0 to –5.5) | –13 | –4 |
| CCBT + MCBT | 4 | 4.25 (23.13) | 2.0 (–12.5 to 21.0) | –21 | 34 | |
| CCBT + MCI | 5 | –13.20 (16.30) | –15.0 (–20.0 to 2.0) | –36 | 3 | |
| Total score 12 months | CCBT | 4 | 13.00 (12.70) | 7.0 (6.0 to 20.0) | 6 | 32 |
| CCBT + MCBT | 4 | 22.00 (11.92) | 18.5 (14.0 to 30.0) | 12 | 39 | |
| CCBT + MCI | 5 | 8.80 (3.90) | 10.0 (7.0 to 11.0) | 3 | 13 | |
| Total score baseline | CCBT | 4 | 21.25 (12.66) | 18.0 (12.5 to 30.0) | 10 | 39 |
| CCBT + MCBT | 4 | 17.75 (16.82) | 12.0 (6.5 to 29.0) | 5 | 42 | |
| CCBT + MCI | 5 | 22.00 (14.25) | 25.0 (10.0 to 31.0) | 5 | 39 | |
| SDQ-t conduct subscale | ||||||
| Total score difference baseline–12 months | CCBT | 9 | –0.11 (1.17) | 0.0 (–1.0 to 0.0) | –2 | 2 |
| CCBT + MCBT | 11 | –0.27 (1.49) | 0.0 (–1.0 to 0.0) | –4 | 2 | |
| CCBT + MCI | 12 | 0.58 (1.62) | 0.0 (–0.5 to 1.5) | –1 | 4 | |
| Total score 12 months | CCBT | 9 | 1.22 (1.92) | 0.0 (0.0 to 1.0) | 0 | 5 |
| CCBT + MCBT | 11 | 0.36 (0.67) | 0.0 (0.0 to 1.0) | 0 | 2 | |
| CCBT + MCI | 12 | 1.33 (1.78) | 0.5 (0.0 to 2.5) | 0 | 5 | |
| Total score baseline | CCBT | 9 | 1.33 (1.58) | 1.0 (0.0 to 2.0) | 0 | 5 |
| CCBT + MCBT | 11 | 0.64 (1.29) | 0.0 (0.0 to 1.0) | 0 | 4 | |
| CCBT + MCI | 12 | 0.75 (1.48) | 0.0 (0.0 to 1.0) | 0 | 5 | |
List of abbreviations
- A&E
- accident and emergency
- ADIS-C/P
- Anxiety Disorder Interview Schedule for DSM-IV – child and parent report
- ADIS-IV
- Anxiety Disorder Interview Schedule for DSM-IV
- CAIS
- Child Anxiety Impact Scale
- CAIS-c
- Child Anxiety Impact Scale – child report
- CAIS-p
- Child Anxiety Impact Scale – parent report
- CAMHS
- Child and Adolescent Mental Health Services
- CAS-t
- Child Adjustment to School – teacher report
- CBT
- cognitive–behavioural therapy
- CCBT
- child cognitive–behavioural therapy
- CEAC
- cost-effectiveness acceptability curve
- CGI-I
- Clinical Global Impression – Improvement
- CI
- confidence interval
- CSR
- clinical severity rating
- CUA
- cost–utility analysis
- DASS-21
- Depression Anxiety Stress Scale
- DSM-IV
- Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition
- EQ-5D
- European Quality of Life-5 Dimensions
- FH
- family health
- GAD
- generalised anxiety disorder
- HCHS
- Hospital and Community Health Service
- ICC
- intraclass correlation
- ICER
- incremental cost-effectiveness ratio
- ITT
- intention to treat
- MCBT
- maternal cognitive–behavioural therapy
- MCI
- mother–child interaction
- NDC
- non-directive counselling
- NICE
- National Institute for Health and Care Excellence
- NMB
- net monetary benefit
- OLS
- ordinary least squares
- PD
- panic disorder
- PP
- per protocol
- PSWQ
- Penn State Worry Questionnaire
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- RPI
- Retail Price Index
- RR
- risk ratio
- SAD
- separation anxiety disorder
- SCAS
- Spence Child Anxiety Scale
- SCAS-c
- Spence Child Anxiety Scale – child report
- SCAS-p
- Spence Child Anxiety Scale – parent report
- SCAS-t
- Spence Child Anxiety Scale – teacher report
- SD
- standard deviation
- SDQ
- Strengths and Difficulties Questionnaire
- SDQ-c
- Strengths and Difficulties Questionnaire – child report
- SDQ-p
- Strengths and Difficulties Questionnaire – parent report
- SDQ-t
- Strengths and Difficulties Questionnaire – teacher report
- SES
- socioeconomic status
- SIAS
- Social Interaction Anxiety Scale
- SMFQ
- Short Mood and Feelings Questionnaire
- SMFQ-c
- Short Mood and Feelings Questionnaire – child report
- SMFQ-p
- Short Mood and Feelings Questionnaire – parent report
- SPS
- Social Phobia Scale
- TSC
- Trial Steering Committee