Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 11/22/03. The contractual start date was in June 2012. The draft report began editorial review in April 2014 and was accepted for publication in July 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Ann S Le Couteur is one of the authors of the Autism Diagnostic Interview but receives no royalties; Elaine M McColl is a member of the NIHR Journals Library Editorial Group.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by McConachie et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 MeASURe: systematic review of tools to measure outcomes for young children with autism spectrum disorder
Introduction
Autism spectrum disorders (ASDs) are neurodevelopmental, lifelong conditions diagnosed using a set of behavioural criteria. 1 ASD is known to affect at least 1% of the child and adult population. 2–4 There is wide variation in the progress made by individuals with ASD, so that many individuals have significant lifelong needs for support. The burden and cost to the individual, family and broader society are very high, with the economic costs in the UK estimated to be £28B per year. 5
In light of increased awareness about the prevalence of ASD, and the emphasis on early identification and diagnosis, it is important that health, education and social-care services provide evidence-based interventions and early support for individuals with ASD, and their families, carers and teachers. In the past decade there has been an increase in ASD intervention research, with recent improvement in the quality of studies. 6,7 The ASD early intervention literature is largely focused on promotion of social communication skills, with less emphasis on interventions for restricted and repetitive behaviours (RRBs). It also includes interventions focused on the high rates of co-occurring behaviours and problems (e.g. sleep, faddiness about food, aggression to others, toileting difficulties). 8,9 One problem for the interpretation of research findings is the multitude of different measurement tools that have been used in collecting evidence of progress and outcomes. Furthermore, longitudinal studies highlight the variation in individual developmental pathways. 10–12 The changes in prevalence are due, in part, to earlier recognition of ASD in children in the average range of ability, with likely effects on the pattern of outcomes. 13 The literature thus presents a large set of measures, inconsistently used, of varying relevance and with variable or indeed no evidence of their psychometric properties.
What should be measured?
There are several ways to consider the question of what to measure, including what government departments need in order to measure progress and outcomes, what matters to parents and individuals with ASD, and the theoretical basis of ASD, which has implications regarding important domains to measure.
The UK Chief Medical Officer’s 2012 report focused on Child Health,14 and discussed the poor educational, health and employment outcomes for children with neurodisability. In recent years, there has been consultation about the UK National Health Service Outcomes Framework 2011/12,15 part of a strategy that aims to deliver ‘the outcomes that matter most to people’, using patient-reported outcome measures. The Kennedy report ‘Getting It Right for Children and Young People’16 highlighted the need to identify a common vision between families and professionals for what services are seeking to achieve for children. Measuring outcomes that are valued by families is central to that vision, which, in turn, will influence what services are provided and how, and potentially what services and interventions are prioritised for research evaluation. A recent National Institute for Health Research (NIHR) study has reported agreement on what are the valued outcomes of care for children with neurodisability,17 but it is not clear whether or not these would be the same if a set of core outcomes were sought specifically for children with ASD.
The aims of our MeASURe (Measurement in Autism Spectrum disorder Under Review) review are to identify the validity of tools and outcome measures used in measuring and monitoring young children with ASD, and to consider how well these reflect and measure issues of importance for patients and carers (see Appendix 1). To achieve this we have:
-
identified the tools reported in literature on quantitative research involving children of up to approximately 6 years of age with ASD (see Chapter 3)
-
conducted a detailed systematic review of the measurement properties of tools within the major domains of development and functioning (see Chapter 4)
-
synthesised evidence regarding the most robust and useful tools in these different domains (see Chapter 5)
-
identified gaps in measurement of outcomes and made research recommendations.
An important part of the strategy has been to identify what people on the autism spectrum, and parents of children with ASD, think should be measured. As these stakeholders were involved at various stages throughout the project, there is no single section on ‘patient and public involvement’ in the report. Instead, parents and people on the autism spectrum have contributed particularly to Chapters 2, 5 and 6. In Chapter 2, we address the issue of what outcomes should be measured.
Chapter 2 Development of the conceptual framework
Introduction
Within the MeASURe project, we carried out a series of consultations with stakeholders, including professionals, parents of children with ASD and people on the autism spectrum, and a scoping review of qualitative literature. The aim was to identify (1) what outcomes should be measured when monitoring the progress of young children with ASD and (2) whether there is agreement between parents and professionals about the relative importance of what to measure. The review of how to measure those outcomes in order to progress towards an agreed battery of tools is presented in later chapters. The chapter is structured to incorporate:
-
general considerations for developing a conceptual framework in ASD for the review
-
findings from scoping relevant qualitative research with families
-
consultation with people who are on the autism spectrum
-
survey consultation with professionals
-
consultation with parents
-
consultation with multiple stakeholders at a Discussion Day.
Valued outcomes
There exist recommended procedures for agreeing what should be a core set of outcomes in various fields of health care. As Williamson et al. 18 note, ‘insufficient attention has been paid to the outcomes measured in clinical trials’. Consistency and interpretation will be improved if researchers always collect and report on core outcomes. The Core Outcome Measures in Effectiveness Trials (COMET) initiative funded by the Medical Research Council Network of Hubs for Trials Methodology Research aims to develop a set of evidence-based procedures for developing a core outcome set. The suggested steps involve:
-
Step 1 Agree the scope of the area of health care.
-
Step 2 Identify existing knowledge about outcomes.
-
Step 3 Involve key stakeholders, including patients and health-care providers.
-
Step 4 Develop consensus about what to measure. Techniques for doing this in an inclusive and objective way are outlined in Williamson et al.,18 including how to determine when consensus has been achieved.
A systematic review of studies that aimed to determine which outcomes to measure in clinical trials in children concluded that in most specialties no research had been undertaken. 19
The scope for this review was determined in the Health Technology Assessment (HTA) commissioning brief (i.e. COMET step 1) and includes a potentially broader use of outcomes than only in trials. This chapter presents the work undertaken on steps 2 and 3, i.e. to identify priorities for child outcomes as valued by parents and professionals, and as explored in qualitative literature. Because of the complexity of ASD as a disorder, and the developmental context of measuring outcomes up to the age of 6 years, the MeASURe review adopted a further step of placing the findings of the consultation stages in a conceptual framework to guide the full review of tools for measurement. This framework also guided further consultation with stakeholders about the relative importance of outcomes to measure. MeASURe did not undertake a further formal process to develop consensus (step 4 above). It may be that ‘consensus’ would be hard to achieve but it would require further procedures. In principle, the choice of outcomes to focus upon depends on the specific research question being asked, and on what is important to particular groups of stakeholders.
Considerations for developing a conceptual framework in autism spectrum disorder
One important potential basis for a conceptual framework for valued outcomes for children with ASD is the International Classification of Functioning, Disability and Health for Children and Youth (ICF-CY),20 so that what is measured can be ‘mapped’ against domains of functioning (e.g. Learning, Communication, Self-Care) and participation (e.g. Relationships, Community Life).
The conceptual framework should also be influenced by an understanding of ASD. The behavioural characteristics of ASD are underpinned by genetic, brain structure and neuropsychological differences from typical development. 21 The conclusions of many studies have led to the revision of the Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (DSM-5) published in May 2013, such that the impairments in ASD are best considered within two groupings: social/communication difficulties and restricted/repetitive interests and behaviours, including hypo- or hyper-responsiveness to sensory stimuli. The aetiological underpinnings for each of these broad domains of impairments may be different, and both may be targets for interventions targeting ‘core’ features of autism.
Another aspect of complexity in the understanding of ASD is that its measurement is affected by developmental considerations, i.e. children’s profile of skills and difficulties may look very different over time, and those trajectories will also be affected by levels of ability. As an obvious example, we cannot measure children’s social ability to make and keep friendships with validity until they are of an age at which that might be expected in typical development. However, there is some recent agreement on the core early impairments that may be observed. By the age of 2 years, differences in the development of children with ASD (from typically developing children and those with developmental delay) are evident in behaviours such as fearfulness, frustration and lack of co-operation, quick mood changes, and fine and gross motor skills. 22 This knowledge has been enhanced by recent studies of the early development of baby siblings of children with autism (who have an increased chance of themselves developing ASD); for example, Zwaigenbaum et al. 23,24 reported unusual eye contact, a lack of visual attention, orientating to name, imitation, social interest and emotional affect, and heightened sensory-orientated behaviours. These combinations of deficits have consequences for development of relationships, early language and play, and, in turn, for the content and targets of early intervention.
The complexity of understanding ASD is made even greater when considering the interaction between domains of development, and how deficits in one may impact upon another; for example, visual sensory overload may lead to avoidance, which reduces opportunities for visual learning and social experience, leading to poor social skills. Furthermore, there is evidence that pragmatic skills (such as social timing in interaction) are closely associated with particular types of behavioural profiles. 25,26 Thus the conceptual framework for a review of outcome tools should consider both measurement of individual areas of functioning, which are likely to change over time, and also tools that bring together these separate areas into a more holistic assessment. It is particularly important to be able to create profiles for children with ASD, who often have difficulties in generalising learning between areas of skill and also generalising skills from one setting to another.
It is also important to detail other associated difficulties that are not unique to ASD but which, nevertheless, can play a major part in children’s development and the burden of care for families. These commonly include feeding and eating difficulties (resistance to certain food textures, faddiness about types and colours of food, etc.), behaviour and sleeping problems. Children who lack adequate nutrition and sleep are likely to be bad tempered and even more rigid in their thinking and behaviour. Furthermore, adaptive functioning may be more impaired in children with ASD than would be expected from their level of ability. Finally, as young children’s development is intimately affected by their environment, including the health, skills and resilience of parents and carers, it is important to include consideration of the impact on the family.
Although the conceptual framework developed over the process of consultation, and was informed by the separate activities described below, it is presented first for brevity and clarity (Table 1). The framework adopted was informed by discussion within the project team, and inspection of other relevant frameworks such as groupings of target symptoms/skills from interventions studies in ASD,20,27 education outcomes,28 grouping of interventions by Research Autism (http://researchautism.net/pages/autism.treatments.therapies.interventions/) and compilation of measures for children with developmental disabilities. 29 One area discussed was how to categorise quality of life, which is essentially a construct separate from the ICF-CY. The decision was made to include it in the participation domain, as it implies how an individual interacts with their environment. 30 For the MeASURe conceptual framework, there are four primary domains, with subdomains in each.
| Domains | Subdomains | Constructs of interest |
|---|---|---|
| Body Functions and Structures/Impairments | Symptom severity | Change in diagnostic category; autism severity; diagnostic scores used as measures of outcome |
| Social awareness | Joint attention skills; imitation; social attention | |
| Restricted, repetitive behaviour | Repetitive, stereotyped movements; repetitive use of objects; repetitive use of language; attention to detail; insistence on sameness | |
| Sensory processing | Hypersensitivity; hyposensitivity | |
| Language | Expressive language; receptive language; gestures | |
| Cognitive ability | IQ/developmental quotient; non-verbal ability; verbal ability/reasoning | |
| Attention | Distractibility; impulsivity; hyperactivity | |
| Emotional regulation | Happiness; irritability; distress; anxiety | |
| Physical skills | Poor co-ordination/gross motor skills; fine motor skills | |
| Physical indicators | Tics; gut/bowel symptoms; nutritional status; height and weight (growth); effectiveness of medication; adverse effects of medication; vaccination rates | |
| Activity-Level Indicators | Social communication | Frequency/quality of initiations; pragmatics |
| Social functioning | Attachment; interaction skills with other children; awareness of others’ emotions | |
| Play | Levels of play (exploratory to symbolic); organises own time/activities | |
| Behaviour | Maladaptive behaviour; tantrums/meltdowns; aggression; self-injury | |
| Habit problems | Sleep latency and waking; eating problems; toileting problems | |
| Learning | School readiness; early literacy; early numeracy | |
| Daily living skills | Feeding self using cutlery; dressing self | |
| Global measure of function | ||
| Global measure of outcome | ||
| Participation | Social relations | Sibling relationship; friendships; attending family events; attending birthday parties |
| Subjective well-being (quality of life) | Coping/resilience; self-esteem | |
| Social inclusion | Social participation; social exclusion; difficulty with attending appointments; awareness of danger | |
| Family Measures | Interaction style | Synchrony; shared attention |
| Parenting | Parent firm and fair; parent warmth to child | |
| Parent stress | Parent stress; parent coping style; parent anxiety and depression | |
| Family quality of life | Impact on family; family cohesion |
Scoping review of qualitative literature (BB, NL, CM)
Question
What child- and/or family-specific outcomes do parents of children with ASD perceive as important?
Methods
Search strategy
A systematic search was conducted (7 June 2012) using:
-
MEDLINE: 1948 to current
-
Cumulative Index to Nursing and Allied Health Literature (CINAHL): 1937 to current
-
PsycINFO: 1806 to current.
Blocks of search terms were assembled for ASD (block 1) and Qualitative Study Designs (block 2), tailored to each database (see Appendix 2).
Papers were selected if they identified themes concerning parents’ aspirations or desired outcomes for their children, experience of assessment of their children, and their priorities for intervention for, and education of, their children. Papers were excluded if (1) ASD was not outlined in the paper as a specific focus (e.g. if ‘developmental disabilities’ were the conditions of interest); (2) they did not involve parents (e.g. a paper interviewing parents and teachers would be included; a paper interviewing just teachers was excluded); (3) the focus was on parents’ views and hopes for their adult children with ASD (e.g. focus must be on parents/carers of young children); and (4) the paper was not in English.
Abstracts and titles of references retrieved by the electronic searches were screened for relevance by one reviewer only (NL); two reviewers (BB, CM) then screened these titles and abstracts, and retrieved full texts for included papers.
Data synthesis
In order to present an overview to the parent advisory groups and the research team, key findings (including illustrative quotes) and analytical frameworks from each paper were extracted and tabulated, and themes identified.
Results
Searches identified 102 relevant papers. Fourteen studies were selected as sufficiently relevant to obtain a full text of the paper. Three of these were excluded because they did not collect qualitative data on outcomes; four were excluded because they contained no data on outcomes. Seven articles remained.
It was clear from an initial inspection of these articles that the quality of data was variable and ranged in focus/topic. Three articles reported data relevant to only parent outcomes,31–33 including process outcomes. Three articles reported data relevant to child outcomes only34–36 and one reported both. 37 One study included data collected directly from children and young people with ASD,34 although original quotes from children were not presented.
The age range of children represented in these studies was 0–21 years. Just two studies31,33 focused specifically on younger children (3–6 years;31 up to 5 years33). The diagnoses represented in the studies typically relied on parental reports. Two studies35,37 focused on particular diagnostic groups (Asperger syndrome;37 ASD with no functional communication35) and others were defined in terms of use of a particular service (speech-and-language therapy;31 assessment and diagnosis;32 preschool educational intervention33).
Data collection methods included focus groups, individual face-to-face interviews and open-ended/free-text questions within postal and web-based surveys.
Although we did not appraise quality of studies formally (using any standard checklist), the quality of reporting sampling and recruitment, data collection methods and data analysis processes was extremely variable.
Given the significant limitations, in terms of quality and relevance, a ‘light touch’ data extraction was undertaken to identify outcomes and themes (see Appendix 2).
In terms of child outcomes, it was notable that some aspects deemed ‘fundamental’ by parents may not be regularly assessed (such as ‘safety’),34 and certainly not as an outcome of an early intervention trial. ‘Awareness of danger’ was added to the conceptual framework (subdomain Social inclusion) as a fundamental issue of safety. The parents’ and young people’s emphasis on participation outcomes (such as being ‘isolated from peers’ or ‘live a normal life’) may also not be reflected in what is usually measured. Constructs concerning child and parent stress, and positive mental health36,37 were supported as important to include as outcome constructs in the conceptual framework.
In addition, parents often highlighted the processes of interaction with professionals, and the utility of information from assessments. Parents expected the service to provide them with information and research literature; to involve them in decision-making processes; and to teach parents how to deliver therapies at home. 31 Braiden et al. 32 reported that parents ‘desired information relevant and applicable to their child to assist them in understanding and making sense of their own child’s presentation’. They also mentioned wanting to have positive times with their child: ‘when he is behaving well and not gearing up for a fight, he’s a very happy and pleasant child’. 37 Such parent priorities have informed the conclusions of the MeASURe project.
Consultation with people on the autism spectrum (DG, GJ)
Questions
Outcomes
What do you think it is useful for health professionals and teachers to measure in young children (up to the age of 6 years) with autism?
Process
What is the best way of assessing these skills? (observation; asking parents; testing the child; asking the child questions)
Where is the best place for observation to take place? (home; school; clinic; other)
What is it important for professionals to know about children with autism before they start to test them?
Methods
People on the autism spectrum in Birmingham and Newcastle were approached for their opinions by a person they knew well. In Birmingham, six adults were known to the University and responded by e-mail; 10 children were approached by a member of the Autism Outreach Team and were selected on the basis that they were thought able to give their views on the questions. In Newcastle, two children attending a National Autistic Society social group responded in person and, likewise, two young adults attending a social inclusion group. Responses to the questions were thus received from 12 young people aged 9–15 years, and from eight adults aged 22–43 years. Each respondent was given a shopping voucher in acknowledgement of their contribution. The verbatim responses were collated and common themes extracted.
Results
Outcomes
Responses showed that young people had a good knowledge of the areas that were likely to be affected in autism (e.g. eye contact, social skills and communication) and those likely to be measured (e.g. intellectual level). However, some of the respondents emphasised outcomes that may not usually be prioritised by professionals or researchers (the subdomains into which these suggestions fit are shown within parentheses):
-
How they respond to change in their lives (Restricted, repetitive behaviour); whether they are unhappy in a room because it might be dirty (Restricted, repetitive behaviour; Sensory processing); ability to sit still – if fidgety (Attention); whether they get angry easily (Emotional regulation); whether they like talking to people (Social functioning); how long it takes for information to stick (Learning); ability to make friends (Social relations); do they hang around with popular kids so that they are popular? (Social inclusion).
Areas that were mentioned most often by the adults as important to assess included special interests and sensory issues, and social interaction to a lesser extent. Some respondents stressed the importance of trying to understand the rationale for a young child’s repetitive actions or special interests.
Process
Many of the respondents emphasised the need to observe children, and for that observation to take place in more than one setting, as behaviour may be very different in different places. Tests (i.e. series of standard tasks) might be ‘alright’ if they are interesting, and given in manageable-length sessions. Some adults on the autism spectrum were concerned that the use of normed tests or checking against typical milestones leads to negative conclusions, because developmental trajectories of children on the autism spectrum may be atypical and strengths may be missed. Respondents suggested that those administering tests should not assume instructions are clear and have the same meaning for a child with ASD, and that testing should happen in a place where the child is comfortable.
Respondents expressed the view that people who do assessments should find out about children before assessing them. One child said: ‘Ask the child to show them what they like to do, e.g. jigsaws, lego’. They also felt that parents and support staff should be asked about special interests, motivators, sensory issues, and so on, and also about any events that have happened recently which may be affecting the child. One adult emphasised the need to be mindful of a child’s self-esteem: ‘So much of the time assessment is done in terms of measuring deficits against a supposed “normal” or “ideal” . . . I had a feeling of being ‘different’ or ‘wrong’ from approximately the age of 3 years’.
Survey of professionals working with early years children with autism spectrum disorder (GJ, JRP)
Question
What constructs are most often measured by early years professionals in monitoring children’s progress?
Methods
A survey was undertaken in autumn 2012 through the British Academy of Childhood Disability database of 240 UK Child Development Teams. Professionals were sent an electronic link to a web-based survey that took 10 minutes to complete. In parallel, education professionals received the survey via (1) ‘4 Children’, a national charity and UK Government strategic partner for early years and child care, through their database of 15,000 Early Years providers across England; (2) the database of an independent specialist centre for early years children with ASD; and (3) 150 practitioners undertaking the Birmingham University School of Education Autism Programme residential weekend.
The survey had five sections. Respondents were asked:
-
About their profession, and the setting in which they work.
-
‘Do you regularly work with children on the autism spectrum (this includes any activity that aims to improve/change an area of functioning)?’ and ‘Do you ever measure the progress or outcomes of children on the autism spectrum (i.e. more than just seeing the child once for assessment)?’. Those who indicated ‘yes’ were given access to the rest of the questions.
-
To identify all areas in which they formally measure or informally make judgements about progress or outcomes for children on the autism spectrum whom they see more than once, and who are aged ≤ 6 years. The 68 outcome constructs included were taken from the conceptual framework.
-
To indicate how frequently (on a six-point scale) they used different types of tool: standardised measures of progress or outcome (with manual and comparative age-related information); non-standardised measures (either published or created locally); informal judgements.
-
To give the three areas in which they most frequently measure progress over time, or outcome, with which of the three types of tools.
Results
The 836 respondents included 167 health professionals (paediatricians, speech-and-language therapists, clinical psychologists, occupational therapists, physiotherapists, dietitians, health visitors, social workers and educational psychologists), 353 education professionals (teachers, special educational needs co-ordinators, autism education advisors, teaching assistants, intervention practitioners), 125 nursery nurses and 191 other professionals, many of whom were childminders. Professionals worked in a variety of settings. Many health professionals worked in child development centres or hospitals but some were based mainly in educational settings. Education staff were from mainstream and specialist schools or early years settings.
Five hundred and thirty-seven professionals monitored the progress or outcome of children who were seen more than once, and were able to access the remainder of the survey.
Professionals were more likely to measure characteristics such as amount of speech (76%), social interaction (90%) and attention (79%) than life or adaptive skills (measuring for, or trying on, clothes 6%, difficulties with appointments, e.g. hairdresser, dentist 16%, use of knife and fork 29%), features related to ‘quality of life’ for the child (quality of life 21%, happiness 42%) or the family (nature of sibling relationship 18%, family quality of life 22%, impact on the family 33%).
Professionals were more likely to use their ‘own informal judgement in discussion with parents or other professionals’ than standardised measures to rate improvements (442 respondents agreed with ‘used often’, ‘most of the time’ or ‘always’ compared with 253 who checked ‘never’, ‘rarely’ or ‘sometimes’). The specific types of measures used varied very widely due to the broad range of professional respondents. However, consistently across the questions, around one-third of respondents replied that they used standardised measures, and half said that they were most likely to use parent or professional impression to gauge progress or outcome. (The standardised tools identified as used most frequently were later included in searches in Chapter 4.)
In conclusion, this survey found that professionals are most likely to measure features related to core impairment subdomains of autism, rather than aspects of daily living, family functioning, and child well-being and happiness.
Consultation with parents (DG, PG, AS le C, CM)
Question
What outcomes do parents consider as important to be assessed?
Methods
Parent advisory groups were recruited at three sites (Exeter, South London, Newcastle). In Exeter, the Peninsula Cerebra Research Unit involves families of disabled children as partners in research through a Family Faculty. 38 Parents of children with ASD were e-mailed and invited to volunteer: 12 expressed interest and seven participated in one or more meetings. In London, the Newcomen Neurodisability Team involves families of children with ASD in giving advice on an ad hoc basis; for MeASURe, 10 parents were invited by e-mail and six participated in one or more meetings. In Newcastle, parents of children with ASD aged ≤ 10 years were invited by e-mail; four participated in one or more meetings. Thus a total of 17 parents were involved in discussion meetings. Parents were given a financial acknowledgement in addition to travel expenses, to recognise their time and expertise at each attendance. Meetings were held at three points during the MeASURe project.
Early meeting To explore parents’ priorities and experiences of assessment and identify what outcomes parents saw as important, especially for monitoring their young child with ASD over time. This session involved an explanation of the aims of the project and open discussion, led by a member of the project team and a parent involvement co-ordinator.
Mid-point meeting To undertake a Q-sort of constructs emerging from the conceptual framework. Two members of the MeASURe project team (NL, GM) created ‘lay wording’ versions of the constructs. Sixty-two constructs were presented on cards in a jumbled order (i.e. not including symptom severity, physical indicators, global measure of function, global measure of outcome). The way in which the constructs had been chosen was introduced by the project team member. Through discussion within the parent group, the constructs were sorted on to a ‘forced-choice’ grid in a pyramid shape on a large piece of paper. Columns on the grid were rated for levels of importance (from ‘more’ to ‘less’ on an 11-point scale), i.e. ‘the importance of various things which could be measured when tracking the progress of children with autism aged up to 6 years, or in measuring the outcome of a specific preschool intervention’. It was stressed that none of the constructs was considered unimportant.
End-point meeting Parent groups met again to consider a summary of the findings of the literature reviews and early consultations. This included a question about the reasons for differences between what parents consider important to be measured and what professionals most often measure. The main activity was to examine five questionnaires that had been rated positively in the systematic reviews. Parents were asked to compare and contrast two questionnaires about parent stress, two questionnaires about children’s behaviour problems, and one questionnaire designed as a global measure of outcome. The issues raised were then taken by parent representatives to the MeASURe project Discussion Day on 14 February 2014 (see Chapter 2, Consultation with multiple stakeholders).
Results
Early meeting
Parents expected that professionals would focus on assessment of core features of autism, such as communication and social interaction. However, they suggested that the child’s skills should be acknowledged and more attention be paid to unusual behaviours that the child is exhibiting, as well as measuring what the child is not achieving. For parents, priority areas for measurement included habit behaviours (such as sleep, diet and food-related behaviours, sensory processing issues, toileting) and also challenging behaviours and ‘meltdowns’ (such as self-harm, hitting out, anxiety, stress, happiness, tics). Parents endorsed the importance of social communication and social functioning (interacting, playing with others, playing alone, understanding and communicating) and, furthermore, the building blocks of learning, independence and life skills (reading and academic achievements, hobbies and sport, imagination and creativity, self-care, preparing food, getting dressed, time management, vulnerability and danger). They also stated that they recognised that some activities/skills may not seem that important or be seen as relevant for this young age range but become a more significant priority later on in development and as their child progresses through school. Parents also mentioned difficulties they had with taking children to appointments for health care (vaccination, dental care, shoes, eyes and hearing). These constructs influenced the conceptual framework, and the content of the survey for professionals.
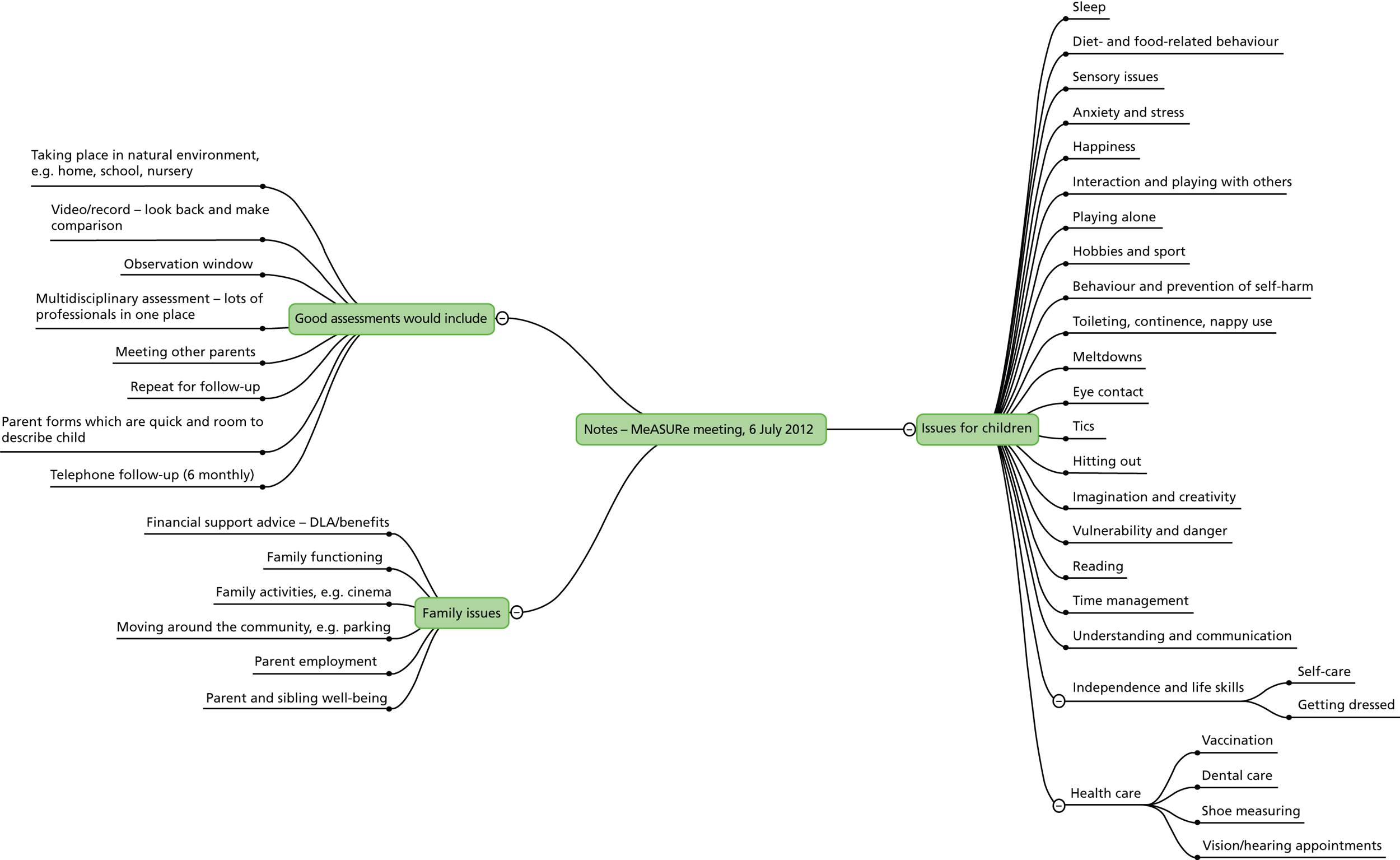
Parents also commented on aspects of the process of assessment. They recommended the use of video in relaxed environments, so that professionals may watch for changes. They stressed the value of information gathered in a range of settings (suggesting use of video to rate change over time and between different settings). Figure 1 illustrates the themes arising from one of the parent group meetings.
FIGURE 1.
Themes from Exeter parent group discussion. DLA, Disability Living Allowance.
Mid-point meetings to undertake the Q-sort
There were four groups that completed this task (two in London to accommodate parents’ availability). Taking an average of the Q-sort ratings from all sites, the items rated on average as ‘more important’ can be grouped as:
-
Body functions/impairments Hypersensitivity, anxiety, unusual fears, distress, non-verbal ability, expressive and receptive language.
-
Activity level indicators Aggression, sleep problems, school readiness.
-
Participation Happiness, self-esteem, relationships with brothers and sisters, being bullied/rejected, no awareness of danger.
-
Families Parent stress.
The highest level of consistency in rating these constructs across groups was for aggression and sleep problems. Parents rated happiness as important for all young children but one group did not agree that this could be considered an ASD-specific measurable outcome. In discussion parents mentioned that they had had to learn about autism, and so had not understood at the start of assessments of their child why skills such as ‘joint attention’ were of importance.
End-point meetings
In London it was not possible to arrange an end-point meeting; there were a number of barriers for parents’ attendance including ‘travel time’, ‘difficulties getting child care’ and ‘need to battle the new school statementing system’. In Exeter, a preliminary meeting was held to discuss with parents how to assess the strengths and weaknesses of tools used in assessment (i.e. explanations of terms such as reliability, validity and sensitivity to change).
Within the preliminary report, the ratings on importance by parents were compared with the constructs most often measured by professionals (Table 2), and parents were asked to reflect on the differences.
| Professionals: areas regularly measured | Parents: important areas to measure (rank) |
|---|---|
| 90% social interaction with children | Happiness (1) |
| 84% play skills | Anxiety, unusual fears (2) |
| 79% attention | Positive views of self (self-esteem) (3) |
| 76% amount of speech | Distress (4) |
| 75% understanding of language | Non-verbal ability (5) |
| 73% expressive communication skills | Relationships with brothers and sisters (6) |
| 72% pretend play | Parent stress (7) |
| 70% fine motor skills | Fighting, hitting others (8) |
| 68% participation in activities | Sleep problems (9) |
| 68% challenging behaviour | Being rejected by others (10) |
The only area of overlap between parents and professionals was ‘challenging behaviour’/’fighting, hitting others’. Parents in Newcastle highlighted that they believed that parents tend to focus on broader outcomes than professionals, as they see their children everyday in different environments. Anxieties and distress were emphasised; parents remarked that it is emotional needs that impact on the child’s and family’s quality of life. Parents also believe that professionals tend to be unaware of these important difficulties before a child enters the social environment of education.
The Exeter parents had a rather different way of viewing the table. They suggested that professionals measured aspects that were intermediate outcomes, which facilitate what parents rate as important. For example, they suggested that parents’ identification of ‘fighting, hitting others’, ‘distress’, ‘happiness’ and even ‘parent stress’ could be mapped from what the professionals highlighted as ‘challenging behaviour’. Similarly, when parents highlighted ‘relationships with brothers and sisters’, these benefited from adequate ‘speech’ and ‘understanding of language’. So, despite the different labels, there was general support from parents for what professionals measure, and parents had noticed their children making progress in these areas.
Consultation with multiple stakeholders
Question
What outcomes is it important to assess when monitoring the progress and outcomes for children with ASD up to the age of 6 years?
Methods
A Discussion Day was held in London on 14 February 2014. Twenty-five participants were invited: four parents of children with autism; three young people with autism, two of those with staff who support them in education; eight speech-and-language therapists, occupational therapists, paediatricians or psychologists; and two researchers working with children with autism; six MeASURe project researchers who work in health or education services also attended.
As one activity, groups of similar background carried out a further Q-sort to rate the importance of constructs, and ascertain similarities or differences between what parents, professionals and researchers consider most important. The set of 21 constructs for the parents and for the young people was drawn primarily from those reported as most often assessed by the early years professionals in the survey. The set for the professionals and the researchers included the 10 rated as most important by the parent groups, and the 10 most often measured by professionals as reported in the survey. Both sets were completed with added constructs to represent a wide span of subdomains.
We hypothesised that:
-
The young people and parents might well agree on the top 10 constructs.
-
The professionals might also agree with parents, even although what they actually measure is not in accordance.
-
The researchers might choose a different set (more based on intervention elements, symptoms and everyday function).
-
We had no expectation about parents’ views on the order of importance of what professionals tend to measure.
Results
Adverse weather conditions and train cancellations prevented several participants joining the Discussion Day, including two young people on the autism spectrum. However, four groups of four people each considered the constructs.
One young adult on the autism spectrum joined the parent group; his/her ranking showed a high level of agreement with the averaged ranking of constructs undertaken previously by parent groups (Spearman rank correlation rs = 0.618). Fine motor skills were rated higher than previously because of the experiences of the young adult as a child. ‘Friendships’ was rated higher than previously, reflecting on the precursor skills needed by the child early on that will lead later to being able to make friendships. Aspects that affect the emotional state of the child, including sensory processing, continued to be rated highly. ‘Participates in mainstream activities’ was rated low: the group thought ‘this means the ASD child has to adapt to the mainstream world rather than ‘mainstream’ adapting/understanding/respecting ASD needs’. They also gave a low rating to ‘not cooperating, throwing, spitting, won’t sit (challenging behaviour)’, as they considered it the role of adults (parents, education and care staff) to try to make the environment right for the child so his/her autism was less ‘disabling’.
The two multidisciplinary groups of health and education professionals, and the group of ASD researchers, had low agreement with the averaged ratings of the parent groups (rs = –0.268, 0.131 and –0.063, respectively). The health and education professionals commented that they measure what they can (in the setting, given the available tools) and what they traditionally have done. They emphasised as ‘important’ what they see as most urgent to try to change, such as challenging behaviour and communication skills. In contrast, although acknowledging the importance of the construct ‘positive views of self (self-esteem)’, they gave it a lower rating because of the developmental stage of children up to 6 years; researchers similarly rated self-esteem as low because of the lack of a suitable measurement tool. The researchers had rated highest ‘not cooperating, throwing, spitting, won’t sit (challenging behaviour)’ on the basis of its impact on others and on the child’s experience. Both groups of health and education professionals identified a range of additional constructs that they would consider it important to measure, including communicative competence, problems with food, functional adaptive behaviour, etc. They also mentioned the importance of identifying the skill set of support staff, and parent confidence in managing their child’s needs and behaviours.
When all groups came together, the discussion highlighted differences in perspective, in summary a ‘social’ model and a ‘medical’ model. The parents and the young adult on the autism spectrum argued that it is important to focus on what children can do, to see autism as a ‘difference’ rather than always use a ‘deficit’ model, and to focus more on how to enable children through improving their environments. Parents were encouraged that the clinicians had mentioned including assessment of the skills of care and education staff. The clinicians reflected that their approach to assessment and intervention is based on a more ‘medical’ model: early identification of specific impairments, treatment, prevention of secondary impairment, and so on. The measurement of outcomes and tools available reflect this framework, with an emphasis on problems and deficits. For the researchers, the model of intervention and outcome assessment was also primarily embedded in a ‘deficit’ model of autism, with an emphasis on treating and measuring core features of autism. Research outcomes such as helping parents manage better and understand more are seen as ‘soft outcomes’, and not given the same importance as changing children’s characteristics. A certain contradiction was pointed out between the recognition that publicly funded research must now be informed by good patient and public involvement, and yet the priority research questions, commissioning briefs and frameworks for judgement of what is good science do not necessarily value the social model of understanding a condition such as ASD.
Overall conclusions
The MeASURe project took a multifaceted approach to consultation. We aimed to identify (1) what outcomes should be measured when monitoring the progress of young children with ASD and (2) whether there is agreement between parents and people with ASD on the one hand, and professionals on the other hand, about the relative importance of what to measure. The initial stages of the review of qualitative literature, and the early parent advisory groups, added to the conceptual framework developed to guide the project. That framework of four domains and 26 subdomains appears to cover the constructs valued by various stakeholders, and enabled similarities and differences in perspective to be elicited.
We found a striking difference between the constructs rated important by parents and the constructs most frequently measured by health and education professionals. In discussion it became clear why this would be likely. Parents’ experience with their children leads them to emphasise emotional well-being as affecting the whole family. Professionals measure what they have the tools for, and acknowledge that their practice is influenced by an emphasis on the core impairments in autism and the behaviour of the individual child, rather than necessarily seeing the broader picture of how the child is affected by their environment. Thus the consultation has highlighted the need to include information from multiple sources to reflect the complementary perspectives of the different stakeholders. This greater awareness of contrasting perspectives has enriched the discussion of available tools (see Chapter 5). Furthermore, parents and young people highlighted critical points about the process of assessment and monitoring of young children with ASD which also contributed to the evidence synthesis.
Chapter 3 Systematic search of observational and intervention literature
Introduction
In preparation for the MeASURe project, an initial scoping search of published systematic reviews of intervention in ASD was conducted (in May/June 2011 by NL); this identified eight Cochrane Collaboration reviews and 13 recent journal papers. The scoping search enabled us to gather information regarding tools that are commonly used to measure outcomes, and to identify theoretically important gaps in the domains measured. This scoping search was not limited to children up to 6 years of age. Seventy-nine tools were reported in the reviews, including 23 assessing adaptive and maladaptive behaviour; 17, language/communication; 13, ability; eight, sensory; nine, ASD specific; four, impact on family; two, social interaction; one, motor skills; and two, summary scales.
Many of the reviews failed to discuss the relevance of the outcome domains, and the strengths and weakness of the included tools – those that did were relatively consistent in their recommendations for improvement. The domain most commonly cited by review authors as missing was ‘quality of life’. 39–41 Other missing outcomes included ‘school readiness’, ‘independence and daily living skills’39 and ‘behavioural outcomes’ such as sleep disturbance, self-mutilation, attention and concentration problems. 40 Also mentioned was the need for qualitative research to determine which outcomes are ‘useful and relevant to consumers, clinicians and service providers’. 41
A key limitation mentioned in the reviews concerned ASD-specific tools, developed to aid diagnostic assessment, but used to monitor change, even although not designed and validated for this purpose. 40–42 Similarly, intelligence quotient (IQ) has been used as a measure of change although designed to measure a ‘stable’ construct. 43 Two further unresolved questions are first how parents (and other stakeholders) define an important change, and, second, what magnitude of change should be considered clinically relevant (and therefore used as the target difference in intervention studies). 40–42
Several review teams commented that included studies had measured outcomes using unpublished or non-standardised measures. 8,43,44 Some reviews included studies focusing on anecdotal reports or ad hoc questionnaires created by the researchers for that specific study45 and not adequately validated.
Finally, one prominent recommendation common to all reviews was the need for a core shared battery of baseline assessment and outcome measurement tools, although the challenge of developing a single battery was recognised, because of the heterogeneity of children’s difficulties, developmental ability and trajectory of developmental change. 46 Some reviewers proposed specific key domains that they felt should be considered, including intellectual ability, developmental abilities across domains, adaptive behaviour, communication skills, severity of autism, play, social skills, challenging behaviours, rigidity and other behaviours that are characteristic of children with autism. 40,47
Review of tools in use
The purpose of this systematic review was to identify the range of tools used to date in observational and intervention evaluation studies, and relate these tools to the subdomains of the conceptual framework adopted for the MeASURe project.
Review question
What tools are in use for measuring and monitoring developmental outcomes in young children with ASD?
Search strategy
We included studies published from 1992 to coincide with the publication of the international classifications, International Classification of Diseases, 10th Edition (ICD-10) and Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition (DSM-IV). 48,49
Original searches were conducted in June and July 2012, and re-run in June and July 2013. The databases searched were:
-
Applied Social Sciences Index and Abstracts (ProQuest) 1987 to present
-
Cumulative Index of Nursing and Allied Health (CINAHL) (EBSCOhost) 1981 to present
-
The Cochrane Library [includes Database of Abstracts of Reviews of Effects, HTA, Cochrane Central Register of controlled Trials, Cochrane Database of Systematic Reviews (Ovid)] inception to present
-
Education Resources Information Center (ERIC) (ProQuest) 1966 to present
-
MEDLINE (including In-Process and Other Non-Indexed citations) (Ovid) 1946 to present
-
EMBASE (Ovid) 1988 to present
-
PsycINFO (Ovid) 1987 to present
-
Sociological Abstracts (ProQuest) 1952 to present
-
Linguistics and Language Behavior Abstracts (ProQuest) 1973 to present
-
Health Management Information Consortium (Ovid) 1979 to present
-
PapersFirst [Online Computer Library Centre (OCLC)] inception to present
-
Proceedings (OCLC) inception to present
-
Scopus, inception to present
-
Social Services Abstracts (ProQuest) 1979 to present
-
Web of Science (Science Citation Index, Social Sciences Citation Index, Arts and Humanities Citation Index and Conference Proceedings Citation Index inception to present)
-
WorldCatDissertations (OCLC) inception to present.
Additionally, grey literature was searched via Digital Education Resource Archive, Oxford Patient-Reported Outcomes Measurement database, Turning Research into Practice database, internet searches, and searching of selected websites (see Appendix 3). The National Research Register and UK Clinical Research Network were also searched for ongoing research.
A master search strategy was created and modified as needed for searching across the breadth of databases; a list of terms can be found in Appendix 3. Modifications included changes to syntax, fields searched and Medical Subject Heading/thesaurus terms. Full search strategies are available from the first author, and example search strategies for MEDLINE, ERIC and Web of Science are provided in Appendix 3. Searches were limited to English-language articles only. When possible, search filters were used to limit study types returned.
Inclusion criteria
We considered inclusion criteria based on types of studies, participants and types of measurement.
Types of studies
We included:
-
all relevant randomised and quasi-randomised trials of social, psychological and educational early interventions for children with a diagnosis of ASD
-
observational studies of children with ASD (cross-sectional and longitudinal)
-
case–control studies
-
cohort studies, including studies of baby siblings of children with autism, which provide information on tools to monitor developmental progress and follow early markers of ASD.
Types of participants
We reviewed all studies that included at least 50% of children with ASD. Child participants had a ‘best-estimate’ clinical diagnosis of an ASD, including autism, ASD, atypical autism, Asperger syndrome and pervasive developmental disorder – not otherwise specified (PDD-NOS), according to either ICD-10 or DSM-IV48,49 criteria. Use of a particular diagnostic tool such as the Autism Diagnostic Observation Schedule (ADOS) or the Autism Diagnostic Interview-Revised (ADI-R) was not required. Children with ASD and another medical condition, and children with ASD and comorbid conditions were included.
All children were aged ≤ 6 years upon entering the study.
Types of measurement included
-
Direct assessment of child ASD symptoms by trained assessor.
-
Direct assessment of developmental skills, i.e. language, cognition, play skills, fine and gross motor skills, by trained assessor.
-
Observational coding of social interaction skills.
-
Interview or self-completed (parent, teacher or other professional) questionnaire report of child ASD symptoms.
-
Interview or self-completed questionnaire report of developmental skills, i.e. language (vocabulary), adaptive skills, with/by parent, teacher or other professional.
-
Interview or self-completed (parent, teacher or other professional) questionnaire report of associated problems, including behaviour that challenges, aggression, sleeping, eating, toileting, anxiety, hyperactivity and others identified through parent consultation.
-
Idiographic measures focused on particular behaviours (e.g. goal attainment scaling, target behaviours).
-
Measures of impact on parent or family.
Types of measurement not included
-
Economic impact on home and family.
-
Experimental tasks and measures, for example barrier tasks, reaction time.
-
Biophysical measures, medical investigations.
-
Process measures, for example fidelity, adherence, parent satisfaction with intervention.
Sifting
Papers were first sifted by title and abstract (Figure 2). The decision categories were ‘potentially include’, ‘exclude’, ‘consider for Chapter 4’ (assesses the measurement properties of a tool only) or ‘unclear’. The two reviewers (NL, IPO) cross-checked sets of 20 papers at a time until they reached a high level of agreement. Regular (at least weekly) discussion of decisions was held throughout the process to maintain consistency. Then 3059 papers were examined at full text. When decisions regarding inclusion were uncertain, a third reviewer (HMcC) made the final decision.
FIGURE 2.
Flow diagram of searching and sifting. Search results up to date as of 17 July 2013 (original search and update combined). Sifting decisions up to date as of 13 August 2013. Final total for data extraction = 184 (with addition of records identified at stage 3).
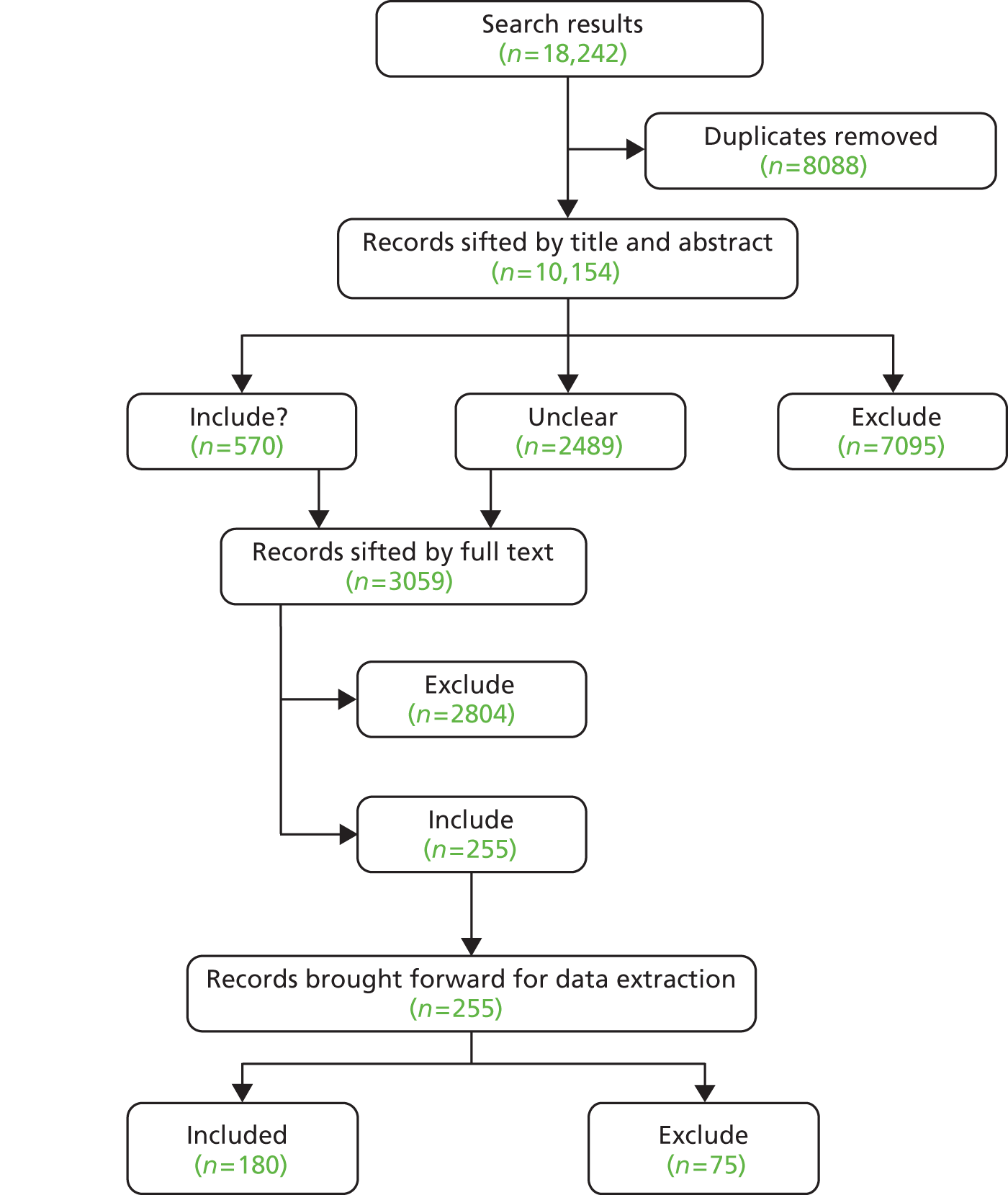
There was a further stage of sifting of records found during the search of papers about measurement properties of tools (see Chapter 4), with searches completed by 9 September 2013. Those searches revealed 118 records potentially relevant to Chapter 3. Once duplicates were removed (86), 32 additional records were sifted by full text (completed 8 December 2013): of these, 28 were excluded and four were added to the final total for data extraction.
Data extraction
A data extraction tool was created as a web-based instrument and piloted (see Appendix 4). The data extracted included study eligibility; type of study; participant characteristics; number of outcome tools (then for each tool: name, population for which designed, specific subscales, outcomes measured according to authors). Subsequently, two reviewers with expertise in ASD (JR, HMcC) reviewed each paper further and indicated which subdomains in the conceptual framework (see Table 1) were measured by each tool, including subscales.
Results
The data extracted from the 184 papers are presented in Appendix 5. All of the tools identified in the review as used to measure outcomes are presented in Table 3. In addition, there were a number of tools developed for use in particular studies; these were described as, for example, ‘Caregiver–child interaction’, ‘Coded observation of joint attention’, ‘Examiner ratings of social engagement’, ‘Naturalistic examiner–child play sample’, ‘Parent interview’, ‘Video recording of child in classroom activities’, ‘Sleep diaries’ and so on. Such tools could not be searched for in databases by name (see Chapter 4) to examine their measurement properties and so were not considered further (see Appendix 5). When tools had a generic-sounding name, information from the source reference was included in the searching. Other tools included below, but not considered further, were:
-
adaptations of tools for use in another language, or tools for which an alternative UK version exists
-
tools used only in outcome and monitoring studies published before 1995 (given different diagnostic definitions before 1994).
| Subdomains | Tools |
|---|---|
| Autism symptom severity | Autism Behavior Checklist |
| Autism Diagnostic Interview-Revised | |
| Autism Diagnostic Observation Schedule | |
| Autism Observation Scale for Infants | |
| Baby and Infant Screen for Children with aUtIsm Traits-Part 1 | |
| Behavioral Summarized Evaluation Scale (also Revised) | |
| Childhood Autism Rating Scale | |
| Gilliam Autism Rating Scale | |
| Infant Behavioral Summarized Evaluation scale | |
| Modified Checklist for Autism in Toddlers | |
| Parent Observation of Early Markers Scale | |
| Pervasive Developmental Disorders Behavior Inventory | |
| Real Life Rating Scale (Ritvo–Freeman) | |
| Social Communication Questionnaire (originally known as Autism Screening Questionnaire) | |
| Social Responsiveness Scale | |
| Childhood Autism Rating Scale – Tokyo versiona | |
| Social awareness | Communication and Symbolic Behavior Scales-Developmental Profile (Behavior Sample) |
| Early Social Communication Scales | |
| Imitation Battery | |
| Imitation Disorders Evaluation scale | |
| Motor Imitation Scale | |
| Preschool Imitation and Praxis Scale | |
| Pre-Verbal Communication Schedule | |
| Social Communication Assessment for Toddlers with Autism | |
| Social Communication Behaviour Codes | |
| Restricted, repetitive behaviour | Autism Diagnostic Interview-Revised |
| Autism Diagnostic Observation Schedule | |
| Repetitive Behavior Scale (and Revised) | |
| Sensory processing | Infant/Toddler Sensory Profile |
| Sense and Self-Regulation Checklist | |
| Sensory Profile | |
| Short Sensory Profile | |
| Autism Screening Instrument for Educational Planning | |
| Battelle Developmental Inventory-Second Edition | |
| Language | British Picture Vocabulary Scale-II |
| Clinical Evaluation of Language Fundamentals-Revised | |
| Communication and Symbolic Behavior Scales-Developmental Profile (Caregiver Questionnaire) | |
| Comprehensive Assessment of Spoken Language | |
| Expressive One-Word Picture Vocabulary Test | |
| Illinois Test of Psycholinguistic Abilities | |
| MacArthur–Bates Communicative Developmental Inventories | |
| Mullen Scales of Early Learning | |
| Pragmatics Profile | |
| Preschool Language Scales | |
| Reynell Developmental Language Scales | |
| Sequenced Inventory of Communication-Revised | |
| Test for Auditory Comprehension of Language | |
| Test of Language Development | |
| Vineland Adaptive Behavior Scales | |
| Peabody Picture Vocabulary Test-Reviseda | |
| Differential Ability Scalesa | |
| Cognitive ability | Battelle Developmental Inventory |
| Bayley Scales of Infant Development | |
| Behavior Rating Inventory of Executive Function-Preschool Version | |
| British Ability Scales | |
| Cattell Infant Intelligence | |
| Developmental Profile | |
| Griffiths Mental Developmental Scales | |
| Leiter International Performance Scale-Revised | |
| Leiter Performance Scales (Arthur adaptation) | |
| McCarthy Scales of Children’s Abilities | |
| Merrill–Palmer Scale of Mental Tests | |
| Mullen Scales of Early Learning | |
| Snijders–Oomen Non-Verbal Intelligence Test | |
| Stanford–Binet Intelligence Scale | |
| Wechsler Intelligence Scale for Children-Revised | |
| Wechsler Preschool and Primary Scale of Intelligence-Revised | |
| Differential Ability Scalesa | |
| Tanaka–Binet Intelligence Test (Japanese version of Stanford–Binet)a | |
| Kyoto Scale of Psychological Developmenta | |
| Snabbt Performance Test På Intelligence IQ IIa | |
| Attention | Behavior Assessment System for Children-Second Edition |
| Child Behavior Scale | |
| Child Behavior Checklist | |
| Connors Rating Scales-Revised | |
| Emotional regulation | Baby and Infant Screen for Children with aUtIsm Traits-Part 2 |
| Behavior Assessment System for Children-Second Edition | |
| Child Behavior Checklist | |
| Children’s Global Assessment Scale | |
| Conners Rating Scales-Revised | |
| Developmental Behaviour Checklist | |
| Emotion Regulation Checklist | |
| Infant–Toddler Social–Emotional Assessment | |
| Toddler Behavior Assessment Questionnaire | |
| Physical skills | Annett’s Pegs |
| Beery Visual–Motor Integration Test | |
| Brunet–Lezine’s Oculomotor Coordination Subtest | |
| Functional Independence Measure for Children | |
| Infant Motor Maturity and Atypicality Coding Scales | |
| Mullen Scales of Early Learning | |
| Peabody Developmental Motor Scales | |
| Vineland Adaptive Behavior Scales | |
| Physical indicators | – |
| Social communication | Autism Diagnostic Interview-Revised |
| Autism Diagnostic Observation Schedule | |
| Autism Screening Instrument for Educational Planning | |
| Communication and Symbolic Behavior Scales-Developmental Profile (Caregiver questionnaire) | |
| Early Social Communication Scales | |
| Pragmatic Profile | |
| Social Communication Assessment for Toddlers with Autism | |
| Social Communication Behavior Codes | |
| Social functioning | Autism Diagnostic Interview-Revised |
| Child Behavior Scale | |
| Nisonger Child Behavior Rating Scales | |
| Social Behavior Rating Scale | |
| Vineland Adaptive Behavior Scales | |
| Vineland Social Maturity Scale, Indian adaptationa | |
| Play | Communication and Symbolic Behavior Scales-Developmental Profile (Caregiver Questionnaire) |
| Developmental Play Assessment | |
| Structured Play Assessment | |
| Symbolic Play Test | |
| Test of Pretend Play | |
| Preschool Play Scalea | |
| Behaviour problems | Aberrant Behavior Checklist |
| Baby and Infant Screen for Children with aUtIsm Traits-Part 3 | |
| Behavior Assessment System for Children-Second Edition | |
| Behavior Screening Questionnaire | |
| Child Behavior Checklist | |
| Child Behavior Scale | |
| Conners Rating Scales-Revised | |
| Developmental Behaviour Checklist | |
| Home Situations Questionnaire-Pervasive Developmental Disorders version | |
| Nisonger Child Behavior Rating Scales | |
| Parent Target Problems (or Parent Target Behaviours) | |
| Preschool Behaviour Checklist | |
| Behavior Style Questionnaire – Chinese versiona | |
| Habit problems | Child Behavior Checklist |
| Sense and Self-Regulation Checklist | |
| Learning | Autism Screening Instrument for Educational Planning |
| Extended Basic Academic Skills Assessment System | |
| Wechsler Individualised Achievement Test | |
| Daily living skills | Functional Independence Measure for Children (WeeFIM) |
| Vineland Adaptive Behavior Scales | |
| Global measure of function | Ages and Stages Questionnaire |
| Assessment of Basic Language and Learning Skills | |
| Assessment, Evaluation and Programming System | |
| Behavior Assessment System for Children-Second Edition | |
| Brigance Diagnostic Inventory of Early Development-2 developmental profile | |
| Early Intervention Developmental Profile | |
| Early Learning Accomplishment Profile | |
| Functional and Emotional Developmental Questionnaire | |
| Learning Accomplishment Profile-Diagnostic, Third Edition | |
| Pediatric Daily Occupation Scale | |
| Preschool Developmental Profile | |
| Psychoeducational Profile-Revised | |
| Scales of Independent Behavior-Revised, Early Development Form | |
| Vineland Adaptive Behavior Scales | |
| Social Adaptive Development Quotient Scalea | |
| Global measure of outcome | Autism Treatment Evaluation Checklist |
| Behavioral Summarized Evaluation scale (and Revision) | |
| Clinical Global Impression – Improvement Scale | |
| Infant Behavioral Summarized Evaluation scale | |
| Pervasive Developmental Disorders Behavior Inventory | |
| Social relations | – |
| Subjective well-being | Kiddie–Infant Descriptive Instrument for Emotional Statesa |
| Social inclusion | School Liking and Avoidance Questionnaire |
| Teacher Rating Scale of School Adjustment | |
| Interaction style | Functional Emotional Assessment Scale |
| NICHD Early Child Care Network scales | |
| Parent stress | Autism Parenting Stress Index |
| Beck Anxiety Inventory | |
| Center for Epidemiologic Studies Depression Inventory | |
| General Health Questionnaire | |
| Hospital Anxiety and Depression Scale | |
| Parenting Sense of Competence | |
| Parenting Stress Index | |
| Positive and Negative Affect Schedule | |
| Questionnaire on Resources and Stress-Friedrich Short form | |
| Reaction to Diagnosis Interview | |
| Satisfaction with Life Scale | |
| Stress Arousal Checklist | |
| Symptom Checklist-90-Revised | |
| Family quality of life | Beach Family Quality of Life Questionnaire |
| Family Adaptability and Cohesion Evaluation Scales II | |
| Family Assessment Device-General Functioning Scale | |
| Family Assessment Measure | |
| Family Empowerment Scale | |
| Family Support Scale | |
| Kansas Inventory of Parental Perceptions | |
| McMaster Family Assessment Device | |
| Parenting Alliance Inventory |
Conclusion
There were 131 tools to be taken forward, and their names (and acronyms) were used in searches to find papers on their measurement properties (described in Chapter 4). It is apparent that, as discussed in the introduction to this chapter, the tools used in research studies to measure outcomes include many which were designed for a different purpose, such as for screening or to enable conclusions to be drawn about an ASD diagnosis in children. However, the review has adopted a pragmatic, inclusive approach to the examination of the identified tools.
The planned data extraction in this chapter was to have included information about the reliability, validity and responsiveness to change of tools as described in the intervention evaluation and observational studies. However, when this extraction was piloted, it was found that most studies simply cited the reliability and validity of tools from their source references, irrespective of whether this had been tested with samples of children with ASD. Furthermore, it was not possible to interpret the evidence on responsiveness to change without considering whether the study was adequately powered to detect change, and whether the choice of outcome tool was appropriate to the nature of the intervention. If a significant intervention effect was not shown, there were a number of possible reasons, and the properties of the tool constituted only one of those reasons. For these reasons, the decision was taken to rely on the systematic assessment of measurement properties of tools described in Chapter 4.
Chapter 4 Systematic review of measurement properties of tools
Introduction
The searches reported in Chapter 3 revealed the varied range of tools used in the 184 papers from which data were extracted. The next stage of the MeASURe project examined the measurement properties of these tools. As an introduction, we summarise the many different types of tools currently in use, involving face-to-face assessment, observation or report.
Types of measurement in use
Standardised norm-referenced assessments all have to be administered by a trained professional. They have the advantage of comparison with children of the same age but for several reasons may be misleading when used for the assessment of young children with ASD. The abilities of the children may be underestimated by lack of co-operation with standardised testing, and they may have profiles that are dissimilar to typical development.
Direct observation includes both highly structured observational procedures (such as ADOS)50 and tools used primarily to measure social interaction in naturalistic settings, especially parent–child interaction. The former are a diagnostic assessment tool conducted by a trained assessor with subsequent rating of the child’s behaviours. The latter have the advantage of providing an in-depth understanding of patterns of responsiveness, which may have long-term effects on language and other development. 51,52 However, one major disadvantage of direct observation is the limited time frame with consequent questions of validity. Further, there are almost as many different coding schedules as studies, depending on the focus of interest.
Standardised semistructured interviews have been used in the characterisation of children’s early development and current ASD characteristics (e.g. the ADI-R),53 in the broad measurement of adaptive behaviour [e.g. Vineland Adaptive Behavior Scales (VABS)]54 and to gather information on additional difficulties, such as behaviour problems, anxiety and sleep. Problems of measurement include a paucity of tools focused on behaviour, which are specifically validated for ASD (e.g. the Autism Comorbidity Interview-Present and Lifetime Version is one such tool but is validated from only 5 years of age). 55
There are very many questionnaires used in studies of children with ASD, completed by parents, teachers and clinicians. However, as with the direct observation and assessment tools, many have not been specifically validated for use in ASD and contain assumptions about patterns of typical development (e.g. standard quality-of-life measures do not ask about children’s special skills and circumscribed interests).
Search strategies
Not all tools identified in Chapter 3 could be searched for by name. There were two main reasons. First, a number of tools had been developed for a particular study (such as a coding procedure for playground behaviour or parent–child interaction, with content related to a particular intervention approach). Second, some tools were translations or adaptations of tools for use in another country, or had been used only up to 1994. Thus papers relating to 131 tools could be searched for by name. Because of its particular relevance to the review, it was decided to add the Early Years Foundation Stage Profile, identified in our consultation with professionals in Chapter 2 as being widely used in nurseries.
Original searches for stage 3 were conducted in March and April 2013, with iterative searches run in August, September and November 2013. The databases searched were:
-
ERIC (ProQuest): 1966 to present
-
MEDLINE (Ovid): 1946 to present
-
EMBASE (Ovid): 1988 to present
-
CINAHL (EBSCOhost): 1981 to present
-
PsycINFO (Ovid): 1987 to present.
In order to search for papers describing studies of the measurement properties of tools, a search filter developed by the COnsensus-based Standards for the selection of health status Measurement INstruments (COSMIN) group was applied. 56 The COSMIN filter was originally designed for use in PubMed, and was translated for use in other databases by our information specialist (SR). The translation was tested in Ovid, and discrepancies were discussed with CBT (co-investigator, and part of the team who devised COSMIN). The sensitivity of the revised filters was tested continuously through the early part of data extraction, through inspection of references for ‘marker’ papers that should have been included, until the new filters were judged satisfactory. The translation can be found in Appendix 6.
Each search consisted of four components: autism terms, age group terms, COSMIN filter and tool name. A master search strategy was created and modified as needed for searching in various databases – a list of terms can be found in Appendix 6. Tool names required basic searches in their own right to determine variant spellings, variant names and to include acronyms. For example, numerous tools include the word ‘scale’, but this might have been reported as ‘scales’, ‘scale’, ‘score’ or ‘scores’ by the authors. Some databases, notably PsycInfo, include a field for tests and measures, and this was utilised if available, as this provides a standard way of identifying a tool regardless of how an author has reported the title.
Searches were limited to English-language papers only and papers published from 1992 to present. Measurement tool-only search strategies are available in Appendix 6.
Finally, the searches in Chapter 3 had identified 128 papers which were about measurement properties of tools rather than about monitoring progress or outcomes, and so these were also included in the stage 3 sifting (see Figure 3).
Inclusion criteria
-
Study was published as a ‘full text original article’.
-
The tool measured a domain of interest (see ‘conceptual framework’, Table 1).
-
A tool identified at stage 2 (i.e. used for monitoring and/or to measure outcome in a longitudinal or intervention study with children with ASD up to 6 years old) was the focus of the study. (When a paper reported the measurement properties of a ‘new’ relevant tool this was noted but not included.)
-
The study sample overlapped with the age range 0–6 years (e.g. a sample with age range from 6 to 18 years was judged eligible; one that included 8- to 15-year-olds was ineligible).
-
The study sample included at least 50% of children with ASD. Furthermore, the study sample could be individuals who were being monitored for ASD symptoms even if they had another primary diagnosis (e.g. a paper monitoring ASD symptoms in a Fragile X population could be eligible if exploring measurement properties of a tool used as an outcome).
-
The aim of the study was the development of a measurement tool or the evaluation of one or more of its measurement properties. Note: The property ‘Hypothesis testing’ applies in COSMIN to hypothesis testing within a paper about construct validity of a tool (e.g. convergent/divergent validity against other tools; known-groups validity). Studies that tested research hypotheses about change or differences between groups as the result of an intervention, but did not set out to test the measurement properties of the tool, were excluded.
Exclusion criteria
-
Papers in which the measurement tool was tested only for its properties in diagnostic assessment or screening and not for monitoring or measuring an outcome.
-
A sample drawn only from the general population of children.
-
Sample size of < 20.
-
Studies in which the focus of the paper was not the examination of psychometric properties were not eligible (e.g. if the paper focused only on creating a subtype of ASD, or to group individuals by scores on the tool).
-
With regard to papers on translated tools, if the purpose was simply to validate the translated version then it was not eligible. If the purpose was to explore the tool’s validity in a different culture/country, and the focus was on the properties of the tool, and the findings appear relevant for use in UK then it was included.
Four reviewers (MG, JH, NL, IPO) utilised the criteria to sift 10% of articles (Figure 3) independently and to compare results, resulting in tightening of criteria. Sifting was then conducted by a single reviewer, the team having (at random) divided up assessment of titles and abstracts, selection of full-text articles and consultation of reference lists of the studies retrieved. In case of uncertainty, the paper was discussed with HMcC before making the decision regarding inclusion. As the COSMIN rating procedure (see below) involves two stages, and the second summary stage involved a different member of the team (including HMcC) in rating the content of each article, some further exclusions were made, so that the decision-making procedure was very robust.
FIGURE 3.
Flow diagram of searching and sifting. Original stage 3 search results up to date as of 9 September 2013. Sifting decisions up to date as of 24 February 2014. Final total for data extraction = 128 (with addition of records identified at stage 2).

Evaluation of methodological quality
The methodological quality of the studies of measurement properties identified was then assessed using the COSMIN checklist. 57 The checklist has 10 ‘boxes’ or subscales (Internal consistency; Reliability; Measurement error; Content validity; Structural validity; Hypotheses testing; Crosscultural validity; Criterion validity; Responsiveness; Interpretability) with standards for how each measurement property should be assessed (see Appendix 7). Each item is scored on a four-point rating scale (poor to excellent) and an overall rating for the methodological quality of each study is determined. The full tables are presented in Appendix 8.
At the same time, each reviewer extracted relevant numerical and descriptive information about the properties addressed (available from the first author). Terwee et al. 57 presented criteria for judging the adequacy of each piece of information (Table 4).
| Property | Rating | Quality criteria |
|---|---|---|
| Reliability | ||
| Internal consistency | + | Cronbach’s alpha(s) ≥ 0.70 |
| ? | Cronbach’s alpha not determined or dimensionality unknown | |
| – | Cronbach’s alpha(s) < 0.70 | |
| Reliability | + | ICC/weighted kappa ≥ 0.70 or Pearson’s r ≥ 0.80 |
| ? | Neither ICC/weighted kappa, nor Pearson’s r determined | |
| – | ICC/weighted kappa < 0.70 or Pearson’s r < 0.80 | |
| Measurement error | + | MIC > SDC OR MIC outside the LOA |
| ? | MIC not defined | |
| – | MIC ≤ SDC OR MIC equals or inside LOA | |
| Validity | ||
| Content validity | + | All items are considered to be relevant for the construct to be measured, for the target population, and for the purpose of the measurement and the questionnaire is considered to be comprehensive |
| ? | Not enough information available | |
| – | Not all items are considered to be relevant for the construct to be measured, for the target population, and for the purpose of the measurement or the questionnaire is considered not to be comprehensive | |
| Construct validity – structural validity | + | EFA: Factors should explain at least 50% of the variance; CFA: RMSEA ≤ 0.06, CFI or TLI ≥ 0.95 |
| ? | Explained variance not mentioned | |
| – | EFA: Factors explain < 50% of the variance; CFA: RMSEA > 0.06, CFI or TLI < 0.95 | |
| Hypothesis testing | + | Correlations with instruments measuring the same construct ≥ 0.50 or at least 75% of the results are in accordance with the hypotheses and correlations with related constructs are higher than with unrelated constructs |
| ? | Solely correlations determined with unrelated constructs | |
| – | Correlations with instruments measuring the same construct < 0.50 or < 75% of the results are in accordance with the hypotheses or correlations with related constructs are lower than with unrelated constructs | |
| Criterion validity | + | Convincing arguments that gold standard is ‘gold’ and correlation with gold standard ≥ 0.70 |
| ? | No convincing arguments that gold standard is ‘gold’ or doubtful design or method | |
| – | Correlation with gold standard < 0.70, despite adequate design and method | |
| Responsiveness | ||
| Responsiveness | + | Correlation with changes on instruments measuring the same construct ≥ 0.50 or at least 75% of the results are in accordance with the hypotheses or AUC ≥ 0.70 and correlations with changes in related constructs are higher than with unrelated constructs |
| ? | Solely correlations determined with unrelated constructs | |
| – | Correlations with changes on instruments measuring the same construct < 0.50 or < 75% of the results are in accordance with the hypotheses or AUC < 0.70 or correlations with changes in related constructs are lower than with unrelated constructs | |
The final step was to combine the ratings of quality of the studies with the ratings of strength of the findings (Table 5) in order to make judgements related to each measurement tool.
| Level | Rating | Criteria |
|---|---|---|
| Strong | +++ or – – – | Consistent findings in multiple studies of good methodological quality or in one study of excellent methodological quality |
| Moderate | ++ or – – | Consistent findings in multiple studies of fair methodological quality or in one study of good methodological quality |
| Limited | + or – | One study of fair methodological quality |
| Conflicting | +/– | Conflicting findings |
| Unknown | ? | Only studies of poor methodological quality |
Findings
Of the 132 tools searched by name, no papers meeting inclusion criteria were found for 75 tools, and therefore their measurement properties in use with children with ASD could not be examined further (see Appendix 8 for all tool names within subdomains). Thus the tables and summaries of findings refer to the remaining 57 tools (43%) for which evidence was obtained.
The presentation of findings is organised in terms of the subdomains of the conceptual framework for the review (see Table 1). For clarity, the first section includes tools that measure symptom severity in ASD, and then global measures of outcome (given extensive overlap between the two). Where the measurement properties of subscales of tools have been evaluated, the tools appear in several separate subdomain tables. In the tables, shaded rows indicate tools for which only poor or negative evidence was obtained. In several cases, the versions of the tools that have been evaluated in the studies have been superseded; the newer versions are referred to in Chapter 5.
The subdomains for which no tool-related evidence was found include Learning; Social relations; Subjective well-being; Social inclusion; Parent–child interaction style; Parenting; and Family quality of life. No tools for physical indicators (tics, gut/bowel symptoms, nutritional status) were included in searches. The gaps in evidence will be discussed further in Chapter 5.
Autism symptom severity
For details, see Table 6.
| Tool (number of papers) | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Test–retest | Inter-rater | Convergent/divergent validity | Known groups | Stability | Change | |||||
| Autism Behavior Checklist (3) | ++ | ? | + | |||||||
| Autism Diagnostic Interview-Revised (12) | +++ | ++ | +++ | +/– | – – | ++ | ++ | ++ | ||
| Autism Diagnostic Observation Schedule (7) | ? | ? | + | + | +++ | ++ | ++ | |||
| Autism Diagnostic Observation Schedule-Toddler Module (1) | +/– | +/– | ? | + | ||||||
| Autism Diagnostic Observation Schedule-Calibrated Severity Score (3) | +++ | + | ||||||||
| Autism Observation Scale for Infants (2) | ? | ? | ++ | |||||||
| Baby and Infant Screen for Children with aUtIsm Traits-Part 1 (3) | ++ | – – | ++ | ++ | ||||||
| Behavioral Summarized Evaluation (1990) and Behavioral Summarized Evaluation-Revised (1997) (4) | ? | + | +++ | +/– | + | + | ? | |||
| Infant Behavioral Summarized Evaluation (1) | + | ? | ||||||||
| Childhood Autism Rating Scale (10) | +++ | +++ | +++ | +/– | – – | |||||
| Gilliam Autism Rating Scale (3) | +++ | – – | – – – | – | ||||||
| Modified Checklist for Autism in Toddlers (3) | ? | ? | ? | + | ||||||
| Parent Observation of Early Markers Scale (1) | ++ | ? | – | |||||||
| Pervasive Developmental Disorders Rating Scale (2) | ++ | + | ? | |||||||
| Real Life Rating Scale (2) | ? | ? | ||||||||
| Social Communication Questionnaire (3) | ++ | ++ | ++ | + | ||||||
| Social Responsiveness Scale (5) | +++ | +/– | +/– | – – – | ++ | + | – – | |||
Autism Behavior Checklist
The Autism Behavior Checklist (AuBC)58,59 was originally constructed as a screening questionnaire completed by parents/carers. It has 57 items grouped into five subscales: Sensory; Relating; Body and object use; Language; and Social and self-help skills, and provides different profile charts for different age groups, ranging from 18 months to 35 years. Three papers60–62 considering measurement properties of the AuBC since 1992 were reviewed, of which two60,61 had very small samples. Miranda-Linné et al. 62 used AuBC with parents of 383 individuals aged 5–22 years. Using factor analysis, they found a five-factor solution that was inconsistent with the five factors suggested by the originators, explaining 80% of the variance but with good internal consistency of subscales.
Autism Diagnostic Interview-Revised
The ADI-R53,63 is a standardised semistructured investigator-based interview, which is administered by a trained clinician usually to parents/caregivers. The 1994 revision had 111 items and the 2003 published version has 93 items. Papers on measurement properties have utilised varying numbers of items; for example, Lecavalier et al. 64 considered only the algorithm items that are used in determining diagnosis. The ADI-R has good internal consistency, although the Repetitive Behaviours domain consistently shows Cronbach’s alpha coefficient to be < 0.7 in the papers examined. Several studies report that inter-rater reliability was monitored and kept at 90% agreement. Studies that formally tested inter-rater reliability reported good levels; for example, Lord et al. 65 reported kappa statistics of between 0.6 and 0.8 on individual items and 92% agreement on diagnostic cut-off.
Extensive work has been done on content validity of the ADI-R as a ‘gold standard’ diagnostic tool. One paper66 used principal components analysis to derive six clusters, but noted that the inclusion of a few specific items on to particular clusters was unexpected. The evidence concerning structural validity was somewhat contradictory; because of the large numbers of items, few papers included sufficient participants, even for reduced-item sets. The confirmatory factor analyses for two- or three-factor solutions were ‘reasonable’ [i.e. root–mean–square error of approximation (RMSEA) of ≤ 0.07],64,67,68 i.e. just above cut-off for a rating of ‘good fit’. Frazier et al. 67 indicated that factor structures fit equally well for 2- to 6-year-olds as for those aged ≥ 7 years. Other than testing level of agreement with ADOS (see Autism Diagnostic Observation Schedule, below), only one study64 explicitly addressed convergent/divergent validity, finding that the ADI-R Social domain correlated with all VABS (–0.41 to –0.45) except for motor skills. A strong indication of validity at the level of individual ADI-R items in distinguishing between children with ASD and those without (mostly non-referred) was provided by Tsuchiya et al. 69 Criterion validity was examined in the original Lord et al. 63 paper. In addition, Chawarska et al. 70 examined whether infants referred at age 14–25 months (and diagnosed 15 months later) could be classified at first assessment; 48% who later received the diagnosis of autism were classified as such, but 78% if the ADI Repetitive behaviours scale was dropped.
As a diagnostic tool, ADI-R might not be expected to be responsive to change; indeed, measurement properties papers65,71 do find general stability in meeting diagnostic cut-off after 6–8 years in each of the domains. However, Lord et al. 65 reported that classifications changed substantially more often from ages 2 to 5 years than from ages 5 to 9 years.
Autism Diagnostic Observation Schedule-Generic
The Autism Diagnostic Observation Schedule-Generic (ADOS-G)50 is a semistructured, interactive schedule designed to assess aspects of communication, social reciprocal interaction, play, and stereotyped behaviours and restricted interests. The ADOS-G consists of four modules, appropriate for children and adults of differing language levels, ranging from non-verbal to verbally fluent. The most able, verbally fluent, children may be assessed with module 3; less able children with modules 1 or 2. The social communication algorithm score is reported as the ‘total’, as repetitive behaviours may not be observed within a limited-duration play-based assessment.
Seven papers50,65,70,72–75 considering measurement properties of the ADOS-G were reviewed. The original study50 assessed internal consistency. For the social communication totals, Cronbach’s alpha coefficients were high (0.91–0.94) for modules 1–3; however, as the sample size included in each of the unidimensionality analyses was small, the study was judged poor. Three studies50,65,72 assessed inter-rater reliability. Two of these studies65,72 found kappa statistics to range from 0.60 and 0.80 on all items, and Lord et al. 65 found 92% agreement for autism/not autism. However, the lack of methodological information regarding these analyses led the study by Kamp-Becker et al. 72 to be judged as of poor methodological quality. Lord et al. 50 presented inter-rater kappa statistics for each module separately and found a mean weighted kappa statistic of 0.78 for module 1, 0.70 for module 2 and 0.65 for module 3. For the social-communication algorithm total, test–retest intraclass correlations (ICCs) ranged from 0.84 to 0.98. However, the small sample size for all reliability calculations within modules (ranging from n = 23 to n = 29) led this paper to be judged as of poor methodological quality.
Three papers50,72,73 assessed structural validity. Lord et al. 50 found almost all social and communication items loaded highly on one factor in each module, accounting for between 72% and 78% (modules 1 and 2), and 52% and 53% (modules 3 and 4) of the variance, leading to the adoption of an algorithm total of social-communication items. However, the small sample size (79 participants and 29 ratings in module 1, 55 children and 28 ratings in module 2, and 59 participants and 28 ratings in module 3) led this study to be judged to be of poor methodological quality. Kamp-Becker et al. 72 assessed structural validity and found in a three-factor solution the amount of variance explained was 47%, in the four-factor solution it was 52% and the five-factor solution explained 57% of variance. The third paper73 investigated both the original algorithm structure and the new algorithms, compatible with DSM-5. For the youngest group (≤ 6 years) they found RMSEAs of 0.057 and 0.059, respectively, for module 1 (indicating good model fit) and RMSEAs of 0.079 and 0.076, respectively, for module 3 (indicating reasonable model fit).
Two studies assessed criterion validity. Grey et al. 74 found high agreement between ADOS and a clinical diagnosis of autism [kappa (κ) = 0.73; p < 0.001] and of ASD (κ = 0.62; p < 0.001) in 209 children aged 20–55 months (120 with autism or ASD). In a study of infants aged 14–25 months, Chawarska et al. 70 found between 79% and 95% agreement between the ADOS-G module 1 diagnostic classification outcomes and clinician-assigned diagnosis of autism, although agreement with an ASD diagnosis was low. They comment that in this infant sample the ADOS tended to under-diagnose children with higher verbal and non-verbal skills.
This tool had three papers65,70,75 assessing ‘responsiveness’, or rather testing a hypothesis of stability. The first paper65 found that regression prediction of each ADOS domain score at age 9 years, by the set of three domain scores at age 2 years, showed significant continuity within the same domain (with one exception – the communication score at age 9 years – which was predicted by the ADOS Social and Repetitive domains at age 2 years, with no significant independent contribution from communication). Chawarska et al. 70 tested stability at 15 months from first assessment and found no significant diagnosis by time interactions. Ben Itzchak and Zachor75 also reported stability for 78% of their sample of 68 children, mean age 26 months, in terms of ADOS classification over 1 year; however, the lack of specific hypotheses led this paper to be judged as being of poor methodological quality.
Autism Diagnostic Observation Schedule-Toddler Module
The need for a tool that could assess children for autism at an earlier age led to development of the Autism Diagnostic Observation Schedule-Toddler Module (ADOS-T). The development paper76 involved 182 children with best estimate diagnoses of ASD, non-spectrum developmental delay or typical development, aged 12–30 months. Content validity was good; items were revised, rewritten or removed, as necessary, until all remaining items were deemed relevant. Two algorithms were developed: one for toddlers who were verbal and aged 21–30 months, and the other for younger, less-able toddlers. Internal consistency was good for the social affect scale for both groupings, and poor for RRBs. Test–retest reliability was not high (ICC = 0.6) for RRBs for the verbal toddler algorithm (and n = 8), but otherwise good (0.83–0.94). Inter-rater reliability was high, but the paper was judged to be of poor quality for this property, as the report was for the agreement of seven raters and 14 videos of assessment.
Autism Diagnostic Observation Schedule-Calibrated Severity Score
Refinement of the ADOS algorithm scores led on to the development of the ADOS-Calibrated Severity Score (ADOS-CSS). 77 The ADOS-CSS potentially allows for greater understanding of the manifestation of core autism symptom severity over time, independently of factors such as age, IQ and language level. Gotham et al. 77 tested the hypothesis that severity scores would be less related to factors such as IQ than the raw scores, and this was found. Two studies78,79 have examined the ADOS-CSS in independent samples, with somewhat mixed findings. De Bildt et al. 78 found in a large clinical Dutch sample that CSS discriminated the autism, non-autism ASD and non-spectrum classifications well, and were more comparable over various developmental groupings than the raw scores on the ADOS, especially in module 1 and somewhat less so in module 3. For module 2, the larger proportion of children with non-autism ASD relative to the Gotham sample probably contributed to differences in findings. Shumway et al. 79 examined whether or not calibrated severity scores were independent of other factors. They found that a regression model accounted for 56% of the variance in ADOS raw score, but for only 18% of the variance in calibrated severity score, i.e. independent of verbal and non-verbal developmental quotient. In addition, they found good stability of scoring after an interval of 12–24 months.
Autism Observation Scale for Infants
The Autism Observation Scale for Infants (AOSI)80 was developed to detect and monitor early signs of autism as they emerge in high-risk infants. It is an 18-item direct observational measure designed to detect and monitor putative signs of autism in infants aged 6–18 months. Data on inter-rater reliability was good, test–retest reliability less so, but the sample size was only 2081 and thus judged to be of poor methodological quality. Georgiades et al. 82 found good discrimination between high- and low-risk infants (i.e. infant siblings of children with ASD vs. no ASD).
Baby and Infant Screen for Children with aUtIsm Traits-Part 1
The Baby and Infant Screen for Children with aUtIsm Traits-Part 1 (BISCUIT-Part 183) is designed to assess symptoms of ASD in children between the ages of 17 and 37 months. It comprises 62 items scored on a three-point, Likert-type scale. Parents are asked to rate the child on each item, comparing them to a typically developing child as ‘0’ (not different; no impairment), ‘1’ (somewhat different; mild impairment) or ‘2’ (very different; severe impairment). For the factor analysis study,84 405 infants with a diagnosis of ASD were selected from a total of 1287 enrolled in a US state-funded early intervention programme for children at risk for a developmental disability. In factor analysis, a three-factor structure (socialisation, repetitive behaviour, communication) accounted for only 33% of the variance (with seven items that did not load on to any factor) but the internal consistency of the factors was good [alpha (α) = 0.93, 0.90, 0.87, respectively]. Factor scores were significantly higher than for infants without ASD. Matson et al. 85 demonstrated convergent validity of the BISCUIT-Part 1 with the Modified Checklist for Autism in Toddlers (M-CHAT) and the Personal–Social domain of the Battelle Developmental Inventory-Second Edition, and divergent validity with the Battelle Adaptive and Motor domains.
Behavioral Summarized Evaluation and Behavioral Summarized Evaluation-Revised
The Behavioral Summarized Evaluation (BSE)86 is a 20-item instrument that examines the scope and severity of behaviour problems in autistic children. Items are rated by a clinician on a five-point scale ranging from 0 (never) to 4 (continuously). A global score can be obtained by summing the 20-item scores. A revised version later added nine items. 87 Four papers considering measurement properties of the BSE were reviewed. One study88 assessed internal consistency and found that Cronbach’s alpha coefficients ranged from 0.83 to 0.90. However, the small sample size included in the unidimensionality analysis led this study to be judged as methodologically poor (20 items, 53 participants). Two studies assessed inter-rater reliability86,87 and found ICCs for the global score to range from 0.96 to 0.97. However, the small sample size (n = 29) led one of these studies87 to be judged as having poor methodological quality. The content validity was good, having been developed over several iterations in practice, with correlation of the global score or first factor with IQ and not with age. 86,87 Four studies86–88,89 assessed structural validity; however, the small sample size of two studies86,88 led them both to be judged as having poor methodological quality. Construct validity in the remaining studies was not strong overall; two main factors were found together accounting for almost 50% of the variance,86–88 with the first factor, labelled ‘autism’ or ‘interaction disorder’, relatively consistent, but the second factor very variable. Roux et al. 89 further examined the structure of the first factor and found it to account for 61% of the variance. One study88 assessed convergent validity, and found correlations between this tool and the Childhood Autism Rating Scale (CARS) to all be > 0.77. One study assessed known-groups validity87 and found all relevant hypotheses supported. This same study assessed criterion validity87 and found partial correlations between this tool and an expert clinical rating to range from 0.24 to 0.63 but the quality of the evidence was judged to be poor.
Infant Behavioral Summarized Evaluation
The Infant Behavioral Summarized Evaluation (IBSE) is an observational rating scale adapted from the BSE for the assessment of behaviours of young children having autistic disorders. The original paper90 describing the development and measurement properties of the IBSE was reviewed. Eighty-nine children aged 6–48 months, referred for clinical assessment, were included. The study assessed inter-rater reliability of the initial 33 items and found an ICC of 0.97. The same study assessed the tool’s structural validity: 59.4% of total variance was explained by a two-factor solution, with 19 items constituting the first factor labelled ‘autism’. However, the small sample size (89 participants and 31 reliable items) led this paper to be judged as having poor methodological quality.
Childhood Autism Rating Scale
The CARS91,92 is a behavioural rating scale that is widely used in the diagnosis of children with autism and pervasive developmental disorders. The CARS is a 15-item observation and parent interview measure that quantifies the severity of behaviours associated with autism. Items are rated on a scale from 1 (‘normal’) to 4 (‘severely abnormal’). Total scores ≥ 30 strongly suggest the presence of autism. In a range of small studies (see Appendix 8), internal consistency of the total score was found to be good, as it was in one large study in India. 93 However, Magyar et al. 94 conducted principal components analysis, finding four factors with only one alpha coefficient of > 0.70: social communication (0.78), social interaction (0.61), stereotypies and sensory abnormalities (0.54), and emotional regulation (0.59). At the item level, average inter-rater reliability was r = 0.71, range for the items 0.55–0.93 (only one was > 0.80). 91 However, for the total score, inter-rater reliability was reported to be good: ICC = 0.74;93 ICC = 0.73. 95 Test–retest reliability after 1 year, in children referred for ASD assessment, was high (ICC = 0.81). 93 A number of different factor solutions have been proposed. Stella et al. 96 reported five factors accounting for 64% of the variance: emotional reactivity, social communication, social orienting, odd sensory exploration, and cognitive and behavioural consistency. The four-factor structure reported by Magyar et al. 94 accounted for only 41% of the variance. Stella et al. 96 examined convergent and divergent validity of the factor scores in relation to the VABS but did not find the hypothesised pattern of correlations.
Gilliam Autism Rating Scale and Gilliam Autism Rating Scale-Second Edition
The Gilliam Autism Rating Scale (GARS) is a behavioural checklist developed for use by parents, teachers and professionals to discriminate individuals who are autistic from those with other developmental disabilities. It is intended for use with individuals aged from 3 to 22 years. The GARS has 56 items, divided into four scales; Social interaction, Communication, and Stereotyped behaviours are rated on a four-point scale of frequency, and Developmental disturbances rates early milestones on a dichotomous scale. The summary score is the Autism Quotient. South et al. 97 raised concerns about the capacity of the scale to detect autism in a sample of 119 children aged 3–10 years with strictly defined autism, finding that the mean Autism Quotient was significantly lower than the reference of 100. Lecavalier98 raised similar concerns with a broader sample aged 3–21 years. Furthermore the exploratory factor analysis (EFA) of the first three scales accounted for only 37% of the variance. Internal consistency of those three scales was good; the Developmental disturbances scale was lower, with Cronbach’s α = 0.68. However, parent–teacher inter-rater reliability was low (ICC average = 0.40). Pandolfi et al. 99 examined the GARS-Second Edition (GARS-2), a revision and normative update,100 which has very similar content in the main three scales. The EFA accounted for 34.1% of the variance and the factor model was not entirely consistent with the conceptually derived organisation of the GARS-2. A four-factor model was preferred, for which scale reliability estimates were good.
Modified Checklist for Autism in Toddlers
The M-CHAT was designed as a screening tool with 23 ‘yes/no’ items that can be given to parents by clinicians, with a focus on 18–24 months of age. It does not rely on the professional’s observation of the child, but on parents’ report of current skills and behaviours. In the original study,101 internal consistency for the whole scale (α = 0.85) and for six critical items found on discriminant function analysis (α = 0.83) was good. Snow et al. 102 reported internal consistencies of 0.80 and 0.74, respectively, in a sample of clinically referred 18- to 48-month-old children. However, both papers were judged to be of poor quality for this property, as the unidimensionality of the scale was not checked. Snow et al. 102 used the Social Communication Questionnaire (SCQ) to assess criterion validity and found a correlation of 0.77. Inada et al. 103 tested inter-rater reliability (mother–father pairs, r = 0.93) and test–retest reliability (r = 0.99) after a mean of 8 days in a Japanese translation; however, the paper had a small sample and so was judged to be poor.
Parent Observation of Early Markers Scale
The Parent Observation of Early Markers Scale (POEMS) is a new parent report instrument to monitor prospectively the behavioural development of infants at risk for ASD. 104 The target age is 1–24 months, and the development study involved 108 infants. POEMS includes 61 items that are rated on a four-point scale. Internal consistency was good at each of six age groupings. Test–retest reliability over a 1-month period was checked at 11 different age groupings and was high (with one exception); however, the evidence is of poor quality given small sample sizes. Convergent and divergent validity were established for the POEMS through correlations with domains of the Ages and Stages Questionnaire. 105 Relationships with the ASQ were stronger with the core features of ASD (social and communication problems) than with gross motor problems; however, the correlations with social and communication domains were only –0.41 and –0.45, respectively.
Pervasive Developmental Disorders Rating Scale
The Pervasive Developmental Disorders Rating Scale (PDDRS)106 is a rating scale designed to assist in the screening and diagnostic process for autistic disorder. It contains 51 items, which comprise three subscales: Arousal, Affect and Cognition. Items are rated by a parent (or teacher who has known the individual for at least 2 months) on a five-point Likert scale according to the degree of severity of the behaviour described. Two papers were evaluated. 42,107 Williams and Eaves107 reported on 456 participants with a diagnosis of ASD ranging in age from 1 to 12 years (as well as 111 adolescents and young adults). Ratings by the same teacher at a mean interval of 9.5 months, with 62.5% of the ratings having a ≥ 6-month time gap, were used to assess test–retest reliability; reliability coefficients ranged from 0.86 to 0.92 for subscales, and 0.92 for the total score. Internal consistency was also good, with subscale Cronbach’s alpha coefficients ranging from 0.75 to 0.86, and total score of 0.89. The second paper42 considered teacher ratings of 168 children aged 1–12 years. EFA found three factors, accounting for 64% of the variance, with internal consistency at least 0.80; however, because of the low sample size in relation to number of items, the evidence was judged to be poor.
Real Life Rating Scale
The Real Life Rating Scale (RLRS)108 is a behavioural rating scale used in the diagnosis of autism; in comparison with other such scales it is noted to place emphasis on disturbances in response to sensory stimuli. The 47 items of the RLRS are completed by trained assessors, for example in Sturmey et al. ,61 based on clinical assessment observations of children during a 30-minute free play period. Sturmey et al. 61 examined internal consistency; this was good for the total score (α = 0.84) but poor for the subscales, ranging from 0.42 to 0.68. However, the sample was small – 34 children and adolescents with a diagnosis of ASD – and so the evidence was judged to be poor. Similarly, Sevin et al. 109 reported on inter-rater reliability for a small sample of 24 children and adolescents. Reliability was poor for the 40 items observed, with mean agreement-level kappa = 0.31, and the highest-item kappa = 0.64 (disturbs others).
Social Communication Questionnaire
The SCQ (originally called the Autism Screening Questionnaire)110 is a 40-item questionnaire based on the ADI-R,63 which enquires about characteristic autistic behaviours. Parents are asked to indicate whether or not their child shows a particular symptom (current), and whether they did so at age 4–5 years (lifetime). Language items not suitable for non-verbal children can be omitted. Scores are out of a total of 39 or 32, depending on a child’s language level, with higher scores indicating more severe symptoms.
The factor-based and total scores evidenced good-to-excellent scale reliability using confirmatory factor analysis parameters (factor loadings and error variances) in children with Down syndrome. 111 Snow et al. 102 also found good internal consistency for total score (α = 0.81); however, for the domain scores internal consistency was not good (Reciprocal Social Interaction domain 0.70; Communication 0.47; and Restricted, Repetitive, and Stereotyped Patterns of Behaviour 0.76). Magyar et al. 111 conducted EFA, which suggested a two-factor solution accounting for 54.4% of the variance: social communication, and stereotyped behaviour and unusual interests. Some evidence of criterion validity was found; for example, Magyar et al. 111 showed agreement of the two factor scores with corresponding domains in the ADI-R.
Charman et al.,112 in a longitudinal study, aimed to compare the utility of three scales to measure developmental change in children’s profiles over time. On the SCQ (current behaviour) there was no change in 57 children with ASD (aged < 6 years at the start), whereas on the VABS-Screener version (VABS-Screener) the children gained 9 months equivalent in 11 months on the Socialisation scale, and gained 10 months on the Communication scale. Therefore, evidence suggests that the SCQ does not detect change in measurement of autism characteristics when reduction in severity might have been expected.
Social Responsiveness Scale
The Social Responsiveness Scale (SRS)113,114 is a 65-item questionnaire which takes 15–20 minutes to complete by parents, teachers or other adults who routinely observe the child in a naturalistic social setting. The item content of the two versions (36–48 months and 4–18 years) differs only on the basis of developmental appropriateness of the wording for rating the behaviours of children in the respective age groups, therefore they are considered together. Factor analyses support a one-factor solution; for example, principal components analysis revealed a primary factor explaining > 30% of the variance, with five factors accounting for 49% of the variance in total. 114 Good internal consistency115,116 has been found for the total score. However, because of poor goodness of fit (e.g. differing relevance of items across ages), Duku et al. 116 have since explored a 30-item version that correlates strongly with the 65-item scale (r = 0.94). For reliability, findings were mixed. For the 36–48 months version, Pine et al. 117 reported reasonable maternal SRS test–retest reliability (r = 0.74) measured at variable intervals (6, 24 and 42 weeks) in a mixed sample; however, Bolte et al. 115 reported r = 0.97 in an older clinical sample, including children with ASD. Agreement between parents and teachers was found to be reasonable: r = 0.78;118 ICC = 0.66,117 whereas mother–father agreement in an older clinical sample was reported to be high115 (0.97). Good convergent and divergent validity have been shown, for example, with the Child Behavior Checklist (CBCL),115,116 and Bolte et al. 115 also showed good discrimination between groups at a total and at item level. For criterion validity, correlations even with the SCQ are moderate (r = 0.58) and lower with domains of the ADI-R (e.g. r = 0.46 with the Social domain).
Global measure of outcome
For details, see Table 7.
| Tool (number of papers) | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Test–retest | Inter-rater | Convergent/divergent validity | Known groups | Stability | Change | |||||
| Autism Treatment and Evaluation Checklist (3) | ? | ++ | +/– | |||||||
| Behavioral Summarized Evaluation and Behavioral Summarized Evaluation-Revised (4) | ? | + | +++ | +/– | + | + | + | |||
| Infant Behavioral Summarized Evaluation (1) | + | ? | ||||||||
| Pervasive Developmental Disorders Behavior Inventory (2) | ++ | +/– | +++ | ++ | – | |||||
Autism Treatment and Evaluation Checklist
The Autism Treatment and Evaluation Checklist (ATEC)119 is a 77-item, one-page checklist designed to be completed by parents, teachers and/or primary caretakers of children with ASD and to measure response to treatment. Three papers considering measurement properties of the ATEC were reviewed. One study120 assessed internal consistency and found Cronbach’s alpha coefficients for the four subscales to range from 0.86 to 0.96. Owing to the small sample size (n = 22), this paper was judged to be of poor methodological quality. Two studies120,121 assessed convergent validity and found correlations between the ATEC and the British Picture Vocabulary Scale-II to range from –0.53 to –0.63, correlations with the Expressive One-Word Picture Vocabulary Test to range from –0.60 to –0.67, correlation with the VABS composite to range from –0.79 to –0.88, correlations with ADI-R total raw score to range from 0.82 to 0.88,120 and correlation with the CARS of 0.71. 121 Two studies112,120 assessed responsiveness. Charman et al. 112 found 50% of their hypotheses regarding change scores to be supported, whereas clear evidence of change was found for all subscales of the VABS-Screener (see Table 11, below). Magiati et al. 120 also found that 50% of ATEC scales changed ATEC total scores at age 4–6 years significantly predicted the extent of progress made 5–6 years later. However, there were large individual differences in ATEC score changes over time.
Pervasive Developmental Disorders Behavior Inventory
The Pervasive Developmental Disorders Behavior Inventory (PDDBI) is an informant-based questionnaire that is designed to assess responsiveness to intervention in children diagnosed with ASD. The PDDBI items are organised into six maladaptive and four adaptive scales, with parent (176 items) and teacher (144 items) versions. The subscales independently address different types of behaviours, so that each subscale can be used separately or as part of the entire inventory. This is to enable researchers to assess, more frequently, behaviours that may change over the short term (e.g. stereotypies or aggressiveness), but, less frequently, other behaviours that would be expected to change over a longer time span (e.g. non-verbal prosocial skills or expressive language skills). The PDDBI development paper122 described a comprehensive establishment of content validity from an initial large item pool and field testing. The authors then reported questionnaires completed by 311 parents of children with ASD between the ages of 1 and 17 years (mode 5 years). Alpha coefficients ranged from 0.79 to 0.97 in the parent version, and from 0.73 to 0.97 in the teacher version. Inter-rater reliability (between teachers, and between teachers and parents) was good for the verbally mediated subscales: Learning, Memory, and Receptive language; Phonological skills; and Semantic/pragmatic ability. Differences in agreement were most obvious for the Sensory/perceptual approach behaviours, Aggressiveness, and Social approach behaviours subscales. Principal components analysis of all subscales resulted in two factors together accounting for 65% of the variance. Separate factor analyses within subscales mostly found the predicted factor structure. Cohen123 found significant correlations with the ADI-R subdomain Current behaviour scores, but all were < 0.60.
Social awareness
For details, see Table 8.
| Tool (number of papers) | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Test–retest | Inter-rater | Convergent/divergent validity | Known groups | Stability | Change | |||||
| Communication and Symbolic Behavior Scales-Developmental Profile-Behavior Sample (1) | ? | |||||||||
| Early Social Communication Scales Live (1) | ? | |||||||||
| Imitation Battery (2) | ++ | ++ | ||||||||
| Imitation Disorders Evaluation scale (1) | ? | ? | ||||||||
| Motor Imitation Scale (1) | ? | |||||||||
| Preschool Imitation and Praxis Scale (2) | +++ | + | +++ | ? | ||||||
| Social Communication Assessment for Toddlers with Autism (1) | ? | ? | ? | ? | ||||||
Communication and Symbolic Behavior Scales-Developmental Profile-Behavior Sample
The Communication and Symbolic Behavior Scales-Developmental Profile (CSBS-DP)124,125 is a standardised tool for the assessment of communication and symbolic abilities of children in their second year of life. It consists of three measures: 24-item Infant–Toddler Checklist; Caregiver Questionnaire; and Behavior Sample, which is a face-to-face evaluation of the interaction between a child and parent, and clinician. Those three measures aim to assess a range of social, speech and symbolic skills. The one paper identified in stage 3126 investigated the inter-rater reliability of the CSBS-DP-Behavior Sample, and reported g coefficients ranging from 0.92 to 0.97 for the composites and total score. However, a small sample was used (20% of the data) so the evidence is judged to be poor.
Early Social Communication Scales
The Early Social Communication Scales (ESCS)127,128 measures non-verbal social communication, through rating by a trained investigator of directly observed skills in social interaction, joint attention and behaviour regulation, in children up to 30 months of age. The live scoring [Early Social Communication Scales Live (ESCS-L)] is an abbreviated version of the original ESCS coding scheme. 128 Inter-rater reliability was calculated in the one paper reviewed129 and the average percentage agreement was 88.3; however, only a proportion of the sample was used in this analysis so the evidence was judged to be poor.
Imitation Battery
The Imitation Battery (IB)130 examines imitation skills in children, including those diagnosed with ASD. Luyster et al. 129 presented a nine-item battery of manual actions, oral–facial actions and actions on objects to 164 toddlers with ASD, aged 18–34 months. Inter-rater reliability of the IB was reported as 97.2% agreement but the sample size (10%) was small. Young et al.,131 who used a 10-item battery, reported inter-rater reliability with a mean weighted kappa statistic of 0.84. This study also found, as hypothesised, lower imitation abilities in the ASD group than in typically developing children, but not in the group with other developmental delays.
Imitation Disorders Evaluation scale
The Imitation Disorders Evaluation (IDE) scale132 is a nine-item clinical scale evaluating atypical imitation in infants and young children with autism. Items are rated by a trained observer on a five-point Likert scale, ranging from 0 (behaviour never observed) to 4 (behaviour always observed). In the Malvy et al. 132 development paper, insufficient information is given on both inter-rater reliability (kappa statistics ranging between 0.4 and 1) and structural validity (72.9% of the total variance accounted for) to draw conclusions about the IDE scale measurement properties.
Motor Imitation Scale
The Motor Imitation Scale133 was developed as a structured imitation assessment for children with ASD. It includes 16 tasks, split equally between object and body imitation tasks, half of those involving meaningful and half non-meaningful actions. Items are rated by a trained investigator on a three-point scale, with a ‘0’ score when there is no imitation, ‘1’ for an emerging response and ‘2’ for exact imitation. Ingersoll and Meyer134 investigated the relationship between imitation and other social-communication skills in 27 children with autism, average age 38.7 months. After controlling for developmental level, the total imitation score was found to be significantly and positively correlated with expressive vocabulary (r = 0.36); however, the sample size used in the study was small so the evidence was judged poor.
Preschool Imitation and Praxis Scale
The Preschool Imitation and Praxis Scale (PIPS)135 is a 30-item observational scale with 10 task categories (six gestural, three procedural and one facial) assessing imitation performance in young children. In the development paper, Vanvuchelen et al. 135 reported good overall internal consistency (Cronbach’s α = 0.97) and a four-factor structure explaining 66.6% of the variance. Also they found positive and strong associations (amid r = 0.59 and 0.74) between the PIPS score and scores on language and motor measures in children with ASD. The second paper reviewed on the measurement properties of the PIPS136 demonstrated excellent inter-rater reliability for the scale (ICC = 0.986) and investigated the smallest detectable difference for the scale.
Social Communication Assessment for Toddlers with Autism
The Social Communication Assessment for Toddlers with Autism (SCATA)137 is a semistructured observational tool eliciting social communication behaviours in young children with ASD with an unfamiliar adult. Four dimensions of communicative act are scored: form, function, communicative role and complexity. Reliability was found to be excellent for the total number of communication acts (ICC = 0.93). Frequency of communication over time was stable in the study, with greater communication difficulties shown by children with more severe diagnosis. The early social communication scores were also associated with later language scores. However, the paper is judged to be of poor quality because of the small sample.
Restricted and repetitive behaviour and interests
For details, see Table 9.
| Tool (number of papers) | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Test–retest | Inter-rater | Convergent/divergent validity | Known groups | Stability | Change | |||||
| Autism Diagnostic Interview-Revised (20) | – – – | ? | ++ | +++ | +/– | +++ | + | + | ||
| Autism Diagnostic Observation Schedule (7) | ? | ? | – | + | +/– | ++ | + | ++ | ||
| Autism Diagnostic Observation Schedule-Toddler Module (1) | – | + | ? | + | ||||||
| Repetitive Behavior Scale-Revised (2) | +++ | ? | – – – | ++ | ||||||
Autism Diagnostic Interview-Revised
A total of 20 eligible papers assessed the ADI-R Restricted and Repetitive Behaviours and Interests domain. Internal consistency was assessed in five papers;63,64,68,138,139 none reached the COSMIN cut-off for internal consistency (Cronbach’s α > 0.70) with the exception of the Snow et al. 68 paper, for which Cronbach’s alpha coefficient was 0.70 for verbal children but not non-verbal children (0.61). Test–retest reliability was assessed in two papers63,140 but both were of poor quality. Inter-rater reliability was acceptable in three papers. 65,67,69 In all three papers65,67,69 the raters were trained and monitored to maintain quality and consistency of ratings. Lord et al. 63 and Moss et al. 71 also assessed inter-rater reliability but the studies were of poor methodological quality due to small sample size.
For content validity, Lord et al. 63 selected items that most closely resembled clinical descriptions and diagnostic guidelines from DSM-IV and ICD-10. By inspection of the face validity of constructs generated by factor analysis, Tadevosyan-Leyfer et al. 66 demonstrated that the ADI-R had good content validity. Thirteen papers,63,67,68,74,138,141–148 of varying quality, assessed structural validity of the Restricted and Repetitive Behaviours and Interests domain with conflicting results. Four papers68,138,141,142 provided results that supported the structural validity of the Restricted and Repetitive Behaviours and Interests domain of the ADI-R. Generally, a two-factor structure was found to be the best fit, with the factors labelled ‘insistence on sameness’ and ‘repetitive sensory and motor behaviour’. Three papers of good quality did not provide enough information to assess structural validity. 143–145 However, three good-quality papers67,146,147 and one paper,148 judged as being of excellent quality, did not support the structural validity of the ADI-R Restricted and Repetitive Behaviours and Interests domain. In Frazier et al. 67 none of the factor solutions produced acceptable model fit, as RMSEA did not reach the < 0.06 cut-off or the Tucker–Lewis fit index > 0.95 cut-off. Lecavalier et al. 146 reported a three-factor solution accounting for just 38% of the variance. Similarly, Szatmari et al. 147 reported that a two-factor solution accounted for just 36% of the variance. Finally, the excellent quality paper148 reported a two-factor solution accounting for 43% of the variance. Convergent and/or divergent validity was supported in all eight relevant papers. Both Lord et al. 63 and Grey et al. 74 showed that ASD and non-ASD groups differed significantly on RRB scores.
Responsiveness (in effect, stability) of the ADI-R was supported in two papers,65,71 both of fair methodological quality. In the Moss et al. 71 study, there was no statistically significant change in the number of participants (n = 35, average age 3.5 years) meeting autism criteria on the ADI-R at follow-up after 7 years. Lord et al. 65 also demonstrated that ADI-R ‘ever’/lifetime scores for restricted and repetitive behaviours and interests (RRBI) were higher at the age of 9 years than at 2 years, as expected, and that mean ‘current’ scores showed a marked reduction.
Autism Diagnostic Observation Schedule-Generic
Seven papers assessed one or more measurement properties of the ADOS-G in relation to RRBI. Lord et al. 50 assessed internal consistency, test–retest reliability and structural validity of modules 1–3; however, the methodological quality was poor for all assessments due to small sample sizes for each module. Inter-rater reliability did not reach the COSMIN criterion in Lord et al. 65 for modules 1 and 2.
Support for structural validity was excellent for module 1 but not for module 3, as none of the proposed models produced model fit statistics that satisfied the COSMIN criteria. 73 Kamp-Becker et al. 72 assessed the structural validity of ADOS modules 3 and 4 together, and showed that a four- and five-factor solution explained 52% and 57% of the variance, respectively. In the five-factor solution, factor 4 ‘stereotyped behaviour’ and factor 5 ‘interests and compulsions’ were relevant to the Repetitive and Restricted Behaviour domain of functioning.
Criterion validity was supported by Chawarska et al. 70 for module 1, with 91% of cases matching clinician-assigned diagnosis of autism. Grey et al. 74 provided good support for criterion validity in both modules 1 and 2 with high agreement between ADOS and clinical diagnosis (κ = 0.70; p < 0.001) and significant differences between ASD and non-ASD groups in the Repetitive and Restricted Behaviour domain.
Finally, three papers,65,70,149 all judged as of fair methodological quality, supported the responsiveness of ADOS-G. Scores in the Stereotypic Behaviours domain were shown to be stable, as expected, over a period of 15 months. 70 The ADOS-G was able to measure improvement in functioning over time in Ben Itzchak et al. 149 and change scores for ADOS-G and ADI-R gave similar findings in Lord et al. 65
Autism Diagnostic Observation Schedule-Toddler Module
The development paper76 for the ADOS-Toddler Module reported poor internal consistency for the Repetitive and Restricted Behaviours domain (Cronbach’s α = 0.50). Test–retest reliability was moderate (ICC = 0.6) for RRBs for the verbal toddler algorithm but otherwise good. Inter-rater reliability was high, but the paper76 was judged to be of poor quality for this property, as the measurement was for the agreement of seven raters and 14 videos of assessment. Luyster et al. 76 also reported that numerous drafts and pilot analyses for content validity were conducted, and items removed and added as appropriate.
Repetitive Behavior Scale-Revised
The Repetitive Behavior Scale-Revised150 is a 43-item questionnaire designed to assess problem behaviour and was revised from the original RBS to tap into some of the complex RRBs observed in people with autism. The questionnaire is completed by parents/caregivers. The items have been conceptually grouped into six subscales: (1) Stereotyped behaviour; (2) Self-injurious behaviour; (3) Compulsive behaviour; (4) Ritualistic behaviour; (5) Sameness behaviour (insisting that things stay the same); and (6) Restricted behaviour/interests.
Both Lam et al. 151 and Mirenda et al. 152 provided evidence of good internal consistency for the overall score and for all subscales. Lam et al. ’s151 assessment of test–retest reliability was judged to be poor because of a small sample size. Structural validity was not supported, although in both cases statistical tests fell just below the COSMIN cut-offs. In Lam et al.,151 47.5% of the variance was explained by a four-factor solution. Five- and six factor solutions provided a good fit to the data in Mirenda et al.,152 with RMSEA = 0.064, just missing the COSMIN cut-off of RMSEA = 0.06. Convergent validity was supported by both Mirenda et al. 152 and Lam et al. 151
Sensory processing
For details, see Table 10.
| Tool (number of papers) | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Test–retest | Inter-rater | Convergent/divergent validity | Known groups | Stability | Change | |||||
| Sense and Self-Regulation Checklist (1) | ? | – | + | + | ||||||
| Sensory Profile (1) | + | |||||||||
| Short Sensory Profile (2) | ? | + | ++ | |||||||
Sense and Self-Regulation Checklist
The Sense and Self-Regulation Checklist (SSC)153 is a 65-item caregiver questionnaire of children’s sensory and self-regulatory difficulties, rated on a four-point Likert-type scale, ranging from ‘0’ (never) to ‘3’ (often). It contains six sensory subdomains (Touch–Pain; Auditory; Visual; Taste–Smell; Hyper-reactive to non-injurious stimuli; Hyporeactive to injurious stimuli) and six self-regulatory subdomains (Sleep, Appetite–Digestion, Self-soothing, Orienting–Attending, Aggressive behaviour, Self-injurious behaviour). Only one paper153 considering measurement properties of the SSC was reviewed and used the SSC data from 265 children (including 99 children with ASD) aged < 6 years. The study153 reports good internal consistency (α = 0.87 for total) and acceptable test–retest reliability at 4 months interval (r = 0.68) and shows strong relationships between sensory and self-regulation impairment and severity of autism (however, only a subsample of 38 parents was used in the reliability study). The study showed predicted differences between children with ASD, and developmentally delayed and typically developing children, on the SSC.
Sensory Profile
The Sensory Profile (SP)154 is a caregiver questionnaire that measures a child’s sensory processing abilities. The questionnaire consists of 125 items, rated on a five-point Likert scale, ranging from almost never to almost always. The measure is divided into three main sections – Sensory Processing, Modulation, and Behavioural and Emotional Responses – and 14 sensory-processing categories. Children can also be classified as fitting into one of the four general sensory processing ‘quadrants’: sensation seeking, sensation avoiding, sensory sensitivity and low registration. The SP can be used with 3- to 10-year-olds. The reviewed paper155 reported good known-groups validity of the SP between children with autism and typically developing children in the Australian sample.
Short Sensory Profile
The Short Sensory Profile (SSP)154 is a 38-item, five-point Likert scale caregiver questionnaire intended to assess sensory processing and sensory systems. The questionnaire consists of seven factors: tactile sensitivity, taste/smell sensitivity, movement sensitivity, seeking sensation, auditory filtering, low energy levels, and visual/auditory sensitivity. Two papers156,157 looked at measurement properties of the SSP; however, in one of them,156 an adapted version of the SSP was used, with 10 additional items from the SP,154 and seven additional items from the researchers’ clinical experience. In that study,156 the information provided is not sufficient to determine the rating for internal consistency; however, it is reported that the SSP successfully classified 80.9% of the cases correctly among typically developing, learning-disabled children and those with autism. Wiggins et al. 157 found support for hypotheses that children with ASD show more sensory abnormalities than children diagnosed with developmental delays, and that sensory abnormalities are associated with stereotyped interests and behaviours as measured by ADOS.
Language
For details, see Table 11.
| Tool (number of papers) | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Test–retest | Inter-rater | Convergent/divergent validity | Known groups | Stability | Change | |||||
| Comprehensive Assessment of Spoken Language (1) | – | |||||||||
| MacArthur–Bates Communicative Development Inventories (2) | +++ | ++ | ||||||||
| Mullen Scales of Early Learning (1) | ++ | |||||||||
| Preschool Language Scale-Fourth Edition (1) | ++ | |||||||||
| Vineland Adaptive Behavior Scales (2) | + | ? | ||||||||
| Vineland Adaptive Behavior Scales-Classroom (1) | + | |||||||||
| Vineland Adaptive Behavior Scales-Screener (1) | ++ | |||||||||
Comprehensive Assessment of Spoken Language
The Comprehensive Assessment of Spoken Language (CASL)158 is a direct assessment of oral language skills in four areas: lexical/semantic, syntactic, supralinguistic and pragmatic. The subtests in the CASL can be either be administered individually or a total score can be obtained. In the Reichow et al. study,159 six specific CASL subtests were examined: Nonliteral Language, Pragmatic Judgment, Antonyms, Syntax Construction, Paragraph Comprehension and Inference. The study159 showed significant correlations between the Pragmatic Judgment and Inferences CASL subtests and the VABS Communication and Socialisation domains (r = 0.45; r = 0.62, respectively), suggesting that those two CASL subscales are not acceptable measures of language skills in individuals with ASD, as the correlation values were below COSMIN cut-offs.
MacArthur–Bates Communicative Development Inventories
The MacArthur–Bates Communicative Development Inventories (MCDI)160,161 is a parent report of children’s early language skills. It consists of two forms: ‘Words and Gestures (Infant)’ and ‘Words and Sentences’. The former is an assessment of vocabulary comprehension, vocabulary production and use of gestures in infants between 8 and 16 months. The latter measures vocabulary production, sentence complexity, grammatical development and the mean length of the child’s three longest utterances, in children between 16 and 30 months of age. Bruckner et al. 162 performed differential item functioning analysis and reported items that weakened the validity of the MCDI-Infant when scores of typically developing infants were compared with those with ASD. Luyster et al. 129 investigated associations between different measures of early language in toddlers with ASD, including both forms of MCDI. They reported high correlations between the MCDI, Mullen Scales of Early Learning (MSEL) and VABS (correlations between the MCDI receptive language scores and MSEL r = 0.52, and VABS r = 0.77; correlations between the MCDI expressive language scores and MSEL r = 0.82, and VABS r = 0.88).
Mullen Scales of Early Learning
The MSEL163 is a developmental test for young children aged 0–69 months assessing visual reception, receptive language, expressive language and fine motor skills. One study164 investigated the measurement properties of the MSEL. Burns et al. 164 found support for the hypotheses that children with developmental delays would present significantly more difficulties regarding expressive and receptive language skills than typically developing children matched for age, race and gender. Also the authors found that children with ASD were more likely to exhibit impairment in receptive language skills than children diagnosed with cerebral palsy.
Preschool Language Scale-Fourth Edition
The Preschool Language Scale-Fourth Edition (PLS-4)165 is an assessment of language skills identifying children with language disability. It can be used with children up to 7 years of age and provides a total language score, auditory comprehension and expressive communication scores. Volden et al. 166 investigated the relationship between language skills and both autism severity and adaptive communicative behaviour. The authors166 reported a small correlation with ADOS scores (r = –0.12) and a strong correlation with the Vineland Adaptive Behavior Scales-Second Edition (Vineland-II) Communication domain (r = 0.75).
Vineland Adaptive Behavior Scales
The VABS167 consist of a semistructured interview administered to the parent/carer or an adult with detailed knowledge of the functioning of the child. The ratings assess adaptive behaviour in four main domains: Communication, Daily Living Skills, Socialisation, and Motor skills (the last domain, however, is measured only for children of < 6 years of age). Also, the VABS includes a Maladaptive Behavior Scale. All of the items are rated on a three-point Likert scale, ranging from ‘0’ (seldom or never present) to ‘2’ (always present). One study168 showed that 20 children with ASD (average age 47.4 months) made significant developmental progress in the Communication Skills domain of the VABS, from baseline to year 1 and year 2; however, the small sample means that the evidence was judged to be poor. Paul et al. 169 investigated differences between 20 children with autism and 20 diagnosed with PDD-NOS, aged 4–11 years. The authors found that group differences were observed only in very specific areas, but their hypothesis was supported with regard to use of expressive language.
Vineland Adaptive Behavior Scales-Classroom version
The VABS-Classroom version (VABS-Classroom) is a 244-item questionnaire that aims to assess adaptive behaviours in a classroom environment and is usually completed by teachers. Wells et al. 170 investigated the relationship between autism severity and adaptive behaviour, including communication skills. They reported correlations between autism severity (measured by CARS) and VABS-Classroom receptive language (r = –0.27, not significant) and expressive language (r = –0.55).
Vineland Adaptive Behavior Scales-Screener version
The VABS-Screener version (VABS-Screener)171 is an adaptation of the VABS, with 45 items rated from ‘0’ (when a child does not demonstrate behaviours) to ‘2’ (when a child usually demonstrates a behaviour). Charman et al. 112 examined developmental change in children’s profiles over 11 months. The sample of 40 children gained 10 age-equivalent months in communication skills. Also paired t-tests indicated that age equivalents at time 2 were significantly higher than at time 1 for communication skills.
Cognitive ability
For details, see Table 12.
| Tool (number of papers) | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Test–retest | Inter-rater | Convergent/divergent validity | Known groups | Stability | Change | |||||
| Leiter International Performance Scale-Revised (3) | + | – | – | |||||||
| Mullen Scales of Early Learning (2) | – – | ++ | ||||||||
| Mullen Scales of Early Learning-Early Learning Composite (1) | ++ | |||||||||
| Stanford–Binet Intelligence Scales-Fifth Edition (1) | + | – | ||||||||
| Wechsler Preschool and Primary Scale of Intelligence-Revised (1) | – | |||||||||
Leiter International Performance Scale-Revised
The Leiter International Performance Scale-Revised (Leiter-R)172 was designed to assess non-verbal cognitive ability in people with a variety of language complications. It is divided into two test batteries that include 10 subscales each. The Visualisation and Reasoning battery is used to obtain a composite IQ. The Attention and Memory subscales are used to evaluate deficits in Attention or Memory domains. Three papers173–175 considering measurement properties of the Leiter-R were reviewed. The tool’s convergent validity was assessed by two studies. 173,174 The first173 found the Leiter-R to be moderately correlated with the Kaufman Brief Intelligence Test-Second Edition (r = 0.62). Tsatsanis et al. 174 found positive correlations (r ranged from 0.73 to 0.97) between the original Leiter International Performance Scale and Leiter-R IQ scores. However, the small sample size of this study (n = 26) led this paper to be judged as having poor methodological quality. One study175 assessed the tool’s known-groups validity, and found that only two of the study’s four hypotheses were supported. The tool’s criterion validity was assessed by Grondhuis and Mulick,175 who found the Leiter-R to be moderately correlated (ICC = 0.66) with the non-verbal Stanford–Binet Intelligence Scales-Fifth Edition (SB5).
Mullen Scales of Early Learning
The MSEL163 are a comprehensive measure of cognitive functioning in young children, and consist of four scales: Visual reception, Receptive language, Expressive language and Fine motor. Two papers164,176 considering measurement properties of the MSEL when used with children with ASD were reviewed. Burns et al. 164 assessed known-groups validity (their sample included 19 children with ASD) and found support for only one of the study’s two hypotheses. Bishop et al.,176 in a sample of 59 children with ASD, assessed criterion validity and found correlations between the Differential Ability Scales and the MSEL Non-verbal IQ scores to equal 0.74, and MSEL Verbal IQ scores to equal 0.83.
An Early Learning Composite of the MSEL (MSEL-Early Learning Composite) can be calculated based on scores from four scales for children aged 0–69 months. One paper82 considering the measurement properties of the MSEL-Early Learning Composite was reviewed. This study82 assessed known-groups validity and found all relevant hypotheses to be supported.
Stanford–Binet Intelligence Scales-Fifth Edition
The SB5177 evaluates general intellectual abilities. The full-scale IQ is derived from the Verbal and Non-verbal scales, each with five subtests bearing the same names: Fluid reasoning, Knowledge, Quantitative reasoning, Visual spatial processing and Working memory. One paper,175 considering the measurement properties of the SB5, was reviewed. Grondhuis and Mulick175 assessed known-groups validity and found that only two of the study’s four hypotheses were supported. This same study175 also assessed convergent validity and found the non-verbal SB5 to be moderately correlated (ICC = 0.66) with the Leiter-R.
Wechsler Preschool and Primary Scale of Intelligence-Revised
The Wechsler Preschool and Primary Scale of Intelligence-Revised (WPPSI-R)178,179 assesses the intelligence of children aged between 3 and 7 years. One paper180 considering the measurement properties of the WPPSI-R was reviewed. Yang et al. 180 assessed responsiveness and found R-squared for change in IQ from time 1 to time 2 was 0.50 in the total sample, and 0.37 in the ASD sample only.
Attention
For details, see Table 13.
| Tool (number of papers) | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Test–retest | Inter-rater | Convergent/divergent validity | Known groups | Stability | Change | |||||
| Behavior Assessment System for Children-Second Edition, Teacher Rating Scales (1) | ? | + | ||||||||
| Behavior Assessment System for Children-Second Edition, Parent Rating Scales (1) | ++ | |||||||||
| Child Behavior Checklist 1.5–5 (1) | – – | ++ | ||||||||
| Child Behavior Checklist 6–18 (1) | ++ | – – | ||||||||
Behavior Assessment System for Children-Second Edition
The Behavior Assessment System for Children-Second Edition (BASC-2)181 is a widely used tool for assessing behaviour and emotions in children, adolescents and young adults, ranging in age from 2 to 25 years old. The BASC-2 consists of a Structured Developmental History, an Observation System, a Parent Rating Scale, a Self-Report of Personality Scale and a Teacher Rating Scale. Two papers182,183 considering measurement properties of the BASC were reviewed. Hass et al. 182 found internal consistency of the Teacher Rating Scale only, as measured by Cronbach’s alpha, to range from 0.66 to 0.85 for the Attention problems subscale. The absence of a factor analysis, however, led this paper to be judged to be of poor methodological quality. This same paper182 assessed known-groups validity of the Teacher Rating Scale and found significant difference between groups on the Attention problems subscale. Mahan and Matson183 assessed the known-groups validity of the Parent Rating Scale only, and found support for the hypothesis that the ASD group would score higher on the Attention problems subscale.
Child Behavior Checklist 1.5–5
The CBCL 1.5–5184 is a norm-referenced measure that assesses for a wide range of emotional and behavioural disorders in children aged 1.5–5 years. It has 99 items, reported by parents on a three-point scale. Pandolfi et al. 185 found internal consistency, as measured by Cronbach’s alpha, for items relevant to Attention Problems to equal 0.68. The same study185 also found 27–52% of a typical item’s variance was attributable to the single underlying factor.
Child Behavior Checklist 6–18
The CBCL 6–18184 is a norm-referenced measure that assesses for a wide range of emotional and behavioural disorders in children aged 6–18 years. One study186 considering measurement properties of this version of the CBCL 6–18 was reviewed. Internal consistency was good, with a median scale reliability of r = 0.83 for Attention Problems. Structural validity missed the cut-off for the Attention Problems scale [RMSEA > 0.06; comparative fit index (CFI) = 0.955].
Emotional regulation
For details, see Table 14.
| Tool (number of papers) | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Test–retest | Inter-rater | Convergent/divergent validity | Known groups | Stability | Change | |||||
| Baby and Infant Screen for Children with aUtIsm Traits-Part 2 (3) | +++ | + | ? | ++ | ++ | |||||
| Behavior Assessment System for Children- Second Edition, Teacher Rating Scales (1) | ? | + | ||||||||
| Behavior Assessment System for Children- Second Edition, Parent Rating Scales (1) | +/– | |||||||||
| Brief Infant–Toddler Social and Emotional Assessment (2) | ? | + | – – | ++ | ++ | |||||
| Child Behavior Checklist 1.5–5 (1) | ++ | ++ | ||||||||
| Child Behavior Checklist 6–18 (1) | ++ | ++ | ++ | |||||||
| Children’s Global Assessment Scale (1) | + | |||||||||
| Infant–Toddler Social–Emotional Assessment (1) | ? | ++ | +++ | |||||||
Baby and Infant Screen for Children with aUtIsm Traits-Part 2
The BISCUIT-Part 2 is a 65-item parent questionnaire that was developed to assess infants and toddlers for comorbid mental health conditions reported as common in children with ASD. Internal consistency was reported as good,83,187,188 as was inter-rater reliability. 188 The sample size was rather small for an adequate assessment of structural validity. 187 The BISCUIT-Part 2 was able to distinguish between children with and without ASD in two papers. 187,188 Finally, Matson, Fodstad et al. 188 provided supportive evidence of the criterion validity of the BISCUIT-Part 2, showing that scores were correlated as expected with diagnostic categorisation made by psychologists.
Behavior Assessment System for Children-Second Edition
The BASC-2 is tool widely used for assessing behaviour and emotions in children and young people (see Attention, above). Hass et al. 182 used the Teacher Rating Scale and reported that the BASC-2 had acceptable internal consistency for children (n = 30) for the Anger control (α = 0.75), Emotional self-control (α = 0.86) and Anxiety (α = 0.88) scales. There were significant differences between ASD and matched control groups for the Anxiety (Cohen’s d = 1.23), Anger control (Cohen’s d = 1.89) and Emotional self-control scales (Cohen’s d = 1.94). A second paper183 also assessed known-groups validity of the BASC-2 using the Parent Rating Scale. ASD children scored significantly greater than typically developing children on the Depression subscale, but did not differ as expected on the anxiety and internalising composite scales.
Brief Infant–Toddler Social and Emotional Assessment
The Brief Infant–Toddler Social and Emotional Assessment (BITSEA) is a 42-item screener for parents and child-care providers, designed to identify children with social emotional/behaviour problems. The BITSEA has two scales: BITSEA/P measures emotional and behavioural problems, and BITSEA/C measures competence. Measurement properties were assessed in two papers. 189,190 Assessment of internal consistency was judged as methodologically poor in both papers. 189,190 Test–retest reliability was acceptable with 10- to 45-day test–retest ICCs of 0.87 for BITSEA/P and 0.85 for BITSEA/C. 189 Ratings by both parents were significantly correlated in both Briggs-Gowan et al. 189 (ICC = 0.68 for BITSEA/P and 0.61 for BITSEA/C) and Karabekiroglu et al. 190 (Spearman’s correlation = 0.66 for BITSEA/P and 0.63 for BITSEA/C). However, agreement did not reach the COSMIN cut-off for acceptable inter-rater agreement. Agreement between parent and child-care provider was lower than between parents. 189 Hypothesis testing showed that the BITSEA had good convergent and divergent validity, and distinguished between toddlers with and without diagnosable social and emotional problems.
Child Behavior Checklist 1.5–5
The CBCL 1.5–5 behaviour scale was assessed by one paper185 of good methodological quality. This paper185 provided evidence of good internal consistency for the Internalising Behaviour domain (Cronbach’s α > 0.70) but was just below the COSMIN cut-off for the Emotionally reactive subscale (0.67) and the Anxious/depressed subscale (0.63). Structural validity was good overall, supporting the original factor structure of the Internalising and Externalising domains. However, model fit for a one-factor model for Emotionally reactive and Anxious/depressed subscales did not reach the COSMIN cut-off of RMSEA of < 0.06 (RMSEA > 0.09 and 0.07, respectively) indicating that there may not be a single latent factor underlying these subscales.
Child Behavior Checklist 6–18
The CBCL 6–18191 was assessed with a sample of 122 ASD youth (6–18 years) in one paper186 of good methodological quality. Internal consistency was good, with a median scale reliability of r = 0.94 for anxious/depressed and 0.85 for withdrawn/depressed. Structural validity was also good for Anxious/depressed (RMSEA < 0.06; CFI = 0.995) but missed the cut-off for the Withdrawn/depressed scale (RMSEA > 0.06; CFI = 0.975). Overall, the analysis supported the original factor structure of the CBCL 6–18. Criterion validity was assessed by comparing ASD children with and without a co-occurring emotional and behavioural difficulty (EBD). Children with a co-occurring EBD scored significantly higher than those without EBDs on Anxious/depressed and Withdrawn/depressed subscales and on the Internalising domain.
Children’s Global Assessment Scale
The Children’s Global Assessment Scale (CGAS)192 is a measure of overall psychosocial functioning (including home, school, with peers and across other settings). One study193 was identified that measured responsiveness in a large sample of children attending child psychiatric outpatient services, including 1053 participants with ASD. Mean CGAS ratings improved between first visit to outpatient services and at case closure after treatment (the raters were not the clinicians involved in treatment but did have access to baseline rating when making the end-point rating). Change in CGAS ratings was significantly moderately correlated with clinician assessment of treatment response (r = 0.47).
Infant–Toddler Social–Emotional Assessment
The 169-item Infant–Toddler Social–Emotional Assessment (ITSEA)194 is a parent-completed questionnaire that assesses three broad problem domains – Externalising, Internalizing and Dysregulation – along with Competence. Visser et al. 195 failed to report statistics for scale reliability (but did report mean ICCs of 0.7) for mothers and fathers, indicating acceptable inter-rater reliability. Visser et al. 195 and Georgiades et al. 82 both demonstrated that the ITSEA could distinguish between diagnostic groups. ITSEA Internalising and Externalising domains also correlated positively with the corresponding Internalising and Externalising domains of the CBCL and the Distraction and Mood scales of the Parenting Stress Index,195 supporting convergent validity.
Physical skills
For details, see Table 15.
| Tool (number of papers) | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Test–retest | Inter-rater | Convergent/divergent validity | Known groups | Stability | Change | |||||
| Mullen Scales of Early Learning (1) | ++ | |||||||||
| Vineland Adaptive Behavior Scales (1) | ? | |||||||||
| Vineland Adaptive Behavior Scales-Screener (1) | ++ | |||||||||
Mullen Scales of Early Learning
The MSEL163 offer a developmental test for young children aged 0–69 months (see Cognitive ability, above), which includes direct assessment of fine motor skills, and in children of < 30 months gross motor skills are also examined. Burns et al. 164 found, as hypothesised, that children with developmental delays present significantly more difficulties regarding fine motor skills than typically developing children matched for age, race and gender.
Vineland Adaptive Behavior Scales
The VABS167 provide a structured interview measuring adaptive behaviour in four main domains: Communication, Daily Living Skills, Socialisation and Motor Skills. Motor Skills is measured only for children of < 6 years of age. One study168 showed that children with autism made significant developmental progress in the Motor Skills domain of the VABS, from pretest to year 1 and year 2.
Vineland Adaptive Behavior Scales-Screener version
The VABS-Screener171 is an adaptation of the VABS. Charman et al. 112 examined developmental change in children’s profiles over 11 months. The sample of 40 children gained 5.5 age-equivalent months in Motor Skills. Also paired t-tests indicated that age equivalents at time 2 were significantly higher than at time 1 for Motor Skills.
Social communication
For details, see Table 16.
| Tool (number of papers) | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Test–retest | Inter-rater | Convergent/divergent validity | Known groups | Stability | Change | |||||
| Autism Diagnostic Interview-Revised (14) | +++ | ? | ++ | +++ | +/– | – – – | +++ | – | ++ | |
| Autism Diagnostic Observation Schedule-Generic (6) | ? | + | + | + | +++ | +/– | ++ | |||
| Autism Diagnostic Observation Schedule-Toddler Module (1) | + | + | ? | + | ||||||
| Early Social Communication Scales Live (1) | ? | |||||||||
| Social Communication Assessment for Toddlers with Autism (1) | ? | ? | ||||||||
Autism Diagnostic Interview-Revised
Fourteen papers63,65–72,139,140,146,196,197 were reviewed considering measurement properties of the ADI-R in relation to Communication. Four studies63,68,139,146 assessed internal consistency, which found Cronbach’s alpha coefficient from 0.45 to 0.83 for the Communication domain. Six studies63,65,67,69,71,196 assessed inter-rater reliability of the Communication domain; 78% agreement was reported between raters by Robertson et al. 196 and kappa statistics ranging from 0.69 to 1.0. 63,65,67,69,71 The small sample size of three studies63,71,112,195 led these papers to be judged as methodologically poor. One paper140 found test–retest reliability for the Communication domain to be 0.73. However, the small sample size (n = 20) led this paper140 to be judged as being of poor methodological quality. Two studies63,66 assessed content validity and found that most items were considered relevant for the construct to be measured. Seven papers assessed structural validity providing contradictory conclusions (see Autism symptom severity, above). One paper197 found good structural validity for 28 social communication items but the paper was judged of poor quality. Three studies66,68,146 assessed convergent validity and found correlations between the ADI-R Communication domains and the VABS, the Aberrant Behavior Checklist (ABC), the Children’s Yale–Brown Obsessive Compulsive Scale, the Child’s Symptom Inventory, the Ritvo–Freeman Real Life Rating Scale, the Expressive Vocabulary Test and the Peabody Picture Vocabulary Test to range from –0.47 to 0.30. Three studies63,69,196 assessed known-groups validity and found > 75% of the study hypotheses were supported. One study70 assessed criterion validity and found the correlation between the ADI-R Communication domain and clinician impression to equal 0.49. Two studies65,71 assessed responsiveness and found that 75% of the hypotheses regarding stability in scores were supported.
Autism Diagnostic Observation Schedule-Generic
The original ADOS study50 assessed internal consistency and found Cronbach’s alpha coefficients to range from 0.74 to 0.84 for the Communication domain. Three studies50,65,72, assessed inter-rater reliability. Two of these studies65,72 found kappa statistics to range from 0.60 and 0.80 on all items. However, the lack of methodological information regarding these analyses led the study by Kamp-Becker et al. 72 to be judged as having poor methodological quality. Lord et al. 50 reported good inter-rater reliability (ICC = 0.84) and test–retest reliability (ICC = 0.73) for the Communication domain across modules. Conclusions regarding structural validity, criterion validity and for responsiveness were as described for symptom severity (see Autism symptom severity, above).
Autism Diagnostic Observation Schedule-Toddler Module
Luyster et al. 76 presented the new Toddler Module of the ADOS (see Autism symptom severity, above). Internal consistency for all groupings was high (younger and non-verbal children: α = 0.88; verbal α = 0.90) for the Social Affect score. For inter-rater reliability, ICCs for the Social Affect total were 0.84 and 0.99, respectively; however, the small sample size (n = 13) led this to be judged as being of poor methodological quality. Test–retest reliability ICCs were 0.83 and 0.94; however, there were only eight children assessed twice in the older verbal group.
Early Social Communication Scales-Live
The ESCS-Live (ESCS-L) is an abbreviated version of the original ESCS observational coding scheme,127 and is used as a measure of non-verbal social communication skills for children up to age 30 months. One study129 assessed inter-rater reliability, and found that the average inter-rater reliability for this tool was 88.33%. Yet, owing to the small sample size for assessment of this property (n = 16), the paper was judged to be of poor methodological quality.
Social Communication Assessment for Toddlers with Autism
The SCATA137 was designed to measure non-verbal communication, including early and atypical communication, in young children with ASD. Drew et al. 137 assessed inter-rater reliability and found the ICCs to range from 0.03 to 1.00, with 16 results of < 0.70 and 24 results of > 0.70. This same study135 assessed known-groups validity and found most of the results to be in accordance with the hypotheses. However, the small sample sizes (n = 17 and n = 23) led both assessments from this study135 to be judged as of poor methodological quality.
Social functioning
For details, see Table 17.
| Tool (number of papers) | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Test–retest | Inter-rater | Convergent/divergent validity | Known groups | Stability | Change | |||||
| Autism Diagnostic Interview-Revised (12) | +++ | ? | ++ | +++ | – – – | – – | +++ | – | ++ | |
| Nisonger Child Behavior Rating Form (2) | ++ | – | – | ++ | – | |||||
| Vineland Adaptive Behavior Scales (3) | – | + | ? | |||||||
| Vineland Adaptive Behavior Scales-Classroom (1) | + | |||||||||
| Vineland Adaptive Behavior Scales-Screener (1) | ++ | |||||||||
Autism Diagnostic Interview-Revised
Twelve papers63,64–71,139,140,146 considering measurement properties of the Reciprocal Social Interaction domain of the ADI-R were reviewed. Four studies 63,68,112,139,146 assessed internal consistency; Cronbach’s alpha coefficients were consistently good for Reciprocal Social Interaction, and higher than for other domains. Five studies63,65,67,69,71 assessed inter-rater reliability and reported kappa statistics to range from 0.64 to 1.0. The small sample size of two studies63,71 led these papers to be judged as being methodologically poor. One paper140 found test–retest reliability for Reciprocal Social Interaction to be 0.84. However, the small sample size (n = 20) led this paper to be judged as being of poor methodological quality. Two studies63,66 assessed content validity and found that most items were considered to be relevant for the construct to be measured. Seven papers63,64–66,69,70,71 assessed structural validity providing contradictory conclusions (see Autism symptom severity, above). Two studies64,66 assessed convergent/divergent validity. The former found ADI-R Reciprocal Social Interaction correlated with VABS scores as hypothesised, –0.41 to –0.45 (below the COSMIN criterion) and not with motor skills. Two studies63,69 assessed known-groups validity and all of the study hypotheses were supported regarding Reciprocal SociaI Interaction. One study70 assessed criterion validity and found the correlation between ADI-R Reciprocal Social Interaction and clinician impression to equal 0.46. Two studies65,71 assessed responsiveness and found that all of the hypotheses regarding stability were supported.
Nisonger Child Behavior Rating Form
The Nisonger Child Behavior Rating Form (NCBRF)198 is a rating scale designed to assess social competence and behaviour problems in children and adolescents with developmental disabilities. It has 76 items, completed by parents or teachers. Lecavalier et al. 199 assessed internal consistency and found alpha coefficients for the social competence items to range from 0.63 to 0.85 in a sample of 330 children and adolescents with ASD. Lecavalier et al. 146 assessed inter-rater reliability and report ICCs between the parent and teacher ratings to range from 0.17 to 0.23 on the social competence items. Their sample was 293 children with ASD, of whom one-third attended preschool or kindergarten. Test–retest reliability was also assessed,146 and ICCs ranged from 0.63 to 0.73 for the social competence items. One study199 assessing structural validity found RMSEA ranging from 0.000 to 0.031 for the social competence items. Lecavalier et al. 146 assessed convergent validity and found Spearman ranked correlation coefficients between Parenting Stress Index-Short Form (PSI-SF) and the social competence items of the NCBRF to range from 0.41 to 0.45.
Vineland Adaptive Behavior Scales
The VABS167 assesses four domains: Communication, Daily Living Skills, Socialisation and Motor Skills. Tyminski and Moore200 assessed test–retest reliability and found that follow-up VABS Socialisation scores were positively related to baseline VABS scores (r = 0.74). Known-groups validity was assessed by Paul et al.,169 who reported a significant difference between groups of children with autism and those with ASD in the Socialisation domain, as expected. Harris et al. 201 assessed responsiveness and found that children made significant improvements in the Socialisation domain. However, the small sample size (n = 20) led this study to be judged as being methodologically poor. One paper170 considered measurement properties of the classroom edition of the VABS. This study170 assessed convergent validity and found a correlation between Autism Severity, as measured by CARS and VABS-Classroom socialisation scale to equal –0.58. Measurement properties of the VABS-Screener171 were assessed by Charman et al. ,112 who reported that the change score for the Socialisation domain was significant, with children making 9 months’ progress in 11 months.
Play
For details, see Table 18.
| Tool (number of papers) | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Test–retest | Inter-rater | Convergent/divergent validity | Known groups | Stability | Change | |||||
| Test of Pretend Play (1) | ++ | ++ | ||||||||
Test of Pretend Play
The Test of Pretend Play (ToPP)202 is an assessment of symbolic play ability in young children (aged between 18 months and 6 years). It assesses how children substitute one object for another, and refer to an absent object, as if it was present, and attribute an imaginary property to an object. Only one study203 in our review investigated measurement properties of the ToPP. Clift et al. 203 reported a moderate positive correlation between the ToPP scores and language scores (r = 0.41), measured by FirstSTEP, a screening assessment used to identify children who may be at risk of developmental delay. The study203 showed also that the ToPP correctly classified 75.9% of the participants (children with developmental problems and/or a psychological disorder, and typically developing children).
Behaviour problems
For details, see Table 19.
| Tool (number of papers) | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Test–retest | Inter-rater | Convergent/divergent validity | Known groups | Stability | Change | |||||
| Aberrant Behavior Checklist (3) | + | – | +++ | + | + | |||||
| Baby and Infant Screen for Children with aUtIsm Traits-Part 3 (2) | +++ | – – – | ||||||||
| Behavior Assessment System for Children- Second Edition, Parent Rating Scales (2) | + | +/– | ||||||||
| Child Behavior Checklist 1.5–5 (1) | ++ | ++ | ||||||||
| Child Behavior Checklist 6–18 (1) | ++ | ++ | ++ | |||||||
| Home Situations Questionnaire-Pervasive Developmental Disorders version (2) | +++ | +++ | +++ | +++ | ||||||
| Nisonger Child Behavior Rating Form (2) | ++ | + | – | – – | + | |||||
Aberrant Behavior Checklist
The ABC204 is a 58-item caregiver report checklist designed to assess maladaptive behaviours in people with developmental disabilities. The ABC was assessed in three studies. 205–7 Internal consistency was reported as good (Cronbach’s alpha coefficients ranged from 0.68 to 0.90) by Karabekiroglu and Aman,205 whereas inter-rater reliability was reported as poor by Sigafoos et al. 206 (mean Spearman’s rank correlation coefficient between parent and teacher ratings was 0.62, range 0.50–0.83). Brinkley et al. 207 demonstrated that the ABC had good structural validity, although the irritability subscale item placement did not match the standard ABC factor structure. One note of caution here is that in the ASD sample items on self-injury clustered into one factor and the remaining items from the standard ABC irritability subscale shifted to the hyperactivity subscale. Sigafoos et al. 206 also showed that the ABC had good structural validity, with five factors that closely matched the standard ABC factor structure; however, because of the small sample size (n = 32) this paper was judged of poor methodological quality. Known-groups validity and criterion validity were shown to be acceptable by Karabekiroglu and Aman. 205 The ABC distinguished between clinical subgroups and showed significant positive correlations with related constructs measured by the CBCL and the AuBC.
Baby and Infant Screen for Children with aUtIsm Traits-Part 3
The BISCUIT-Part 383 was designed to assess challenging behaviours. Internal consistency of the BISCUIT-Part 3 was reported as good with Cronbach’s alpha coefficient of > 0.70 in two papers. 83,208 Structural validity, assessed in Matson et al. 208 was not acceptable, with EFA resulting in a three-factor solution explaining just 38.32% of the variance.
Behavior Assessment System for Children-Second Edition, Parent Rating Scales
The BASC-2, Parent Rating Scales is an omnibus instrument widely used for assessing behaviour and emotions in children and young people (see Attention, above). Hass et al. 182 showed that the BASC-2 had acceptable internal consistency for the 10-item Aggression scale and the nine-item Conduct problem scale. There were also significant large differences between children with ASD and matched control subjects on the Aggression scale (Cohen’s d = 0.58) and the Externalising problems composite scale (Cohen’s d = 0.75). Mahan and Matson183 also assessed known-groups validity of the BASC-2. ASD children scored significantly greater than typically developing children on the Conduct problems and Externalising composite scales but did not differ as expected on the Aggression subscale.
Child Behavior Checklist 1.5–5
The CBCL 1.5–5 Behaviour scale was assessed by one paper185 of good methodological quality. This paper provided evidence of good internal consistency for total problems (Cronbach’s α = 0.93) and both the Externalising Behaviour domain (Cronbach’s α = 0.90) and Aggressive behaviour subscale (Cronbach’s α = 0.80). Structural validity was also good, with acceptable model fit for a one-factor model for aggressive behaviour (RMSEA < 0.06; CFI > 0.95), indicating that there was a single latent factor underlying this subscale.
Child Behavior Checklist 6–18
The CBCL 6–18191 was assessed with a sample of ASD youth in one paper186 of good methodological quality. Internal consistency was good, with r = 0.92 for the Aggressive behaviour scale. Structural validity for the complete measure was good, and analysis supported the original two-factor structure of the CBCL 6–18 (internalising and externalising factors). Tests of unidimensionality of scales did not reach the cut-off for acceptable fit for aggressive behaviour (RMSEA = 0.10; CFI = 0.95); however, convincing arguments were provided to allow for correlated disturbances in the model for two-item pairs (destroys own things/destroys others things and disobedient at home/disobedient at school). This adjusted model demonstrated acceptable fit (RMSEA < 0.06; CFI > 0.95). Finally, criterion validity was assessed by comparing ASD children with and without a co-occurring EBD. Children with a co-occurring EBD scored significantly higher than those without EBDs on total problems. There were no significant differences between the two groups for aggressive behaviour or externalising behaviour. Given that the most commonly co-occurring EBDs were anxiety disorders, it is reasonable to assume that in this sample we would not expect to see group differences in aggressive or externalising behaviour.
Home Situations Questionnaire-Pervasive Developmental Disorders version
The Home Situations Questionnaire-Pervasive Developmental Disorders version (HSQ-PDD) is caregiver questionnaire designed to assess behavioural non-compliance in everyday situations by children with ASD. It was developed in studies of typically developing children, and was modified by Chowdhury et al. 209 and its properties assessed in a sample of 124 children with ASD, aged 4–13 years. Structural validity for a two-factor solution was a reasonable fit (RMSEA 0.06) and internal consistency good for the 25-item version thus derived (α = 0.90 for the Socially inflexible subscale and α = 0.80 for Demand-specific subscale). Known-groups validity and responsiveness (change over time) were also good for the HSQ-PDD. Responsiveness was shown related as hypothesised to change in the VABS Daily living skills scale. 210
Nisonger Child Behavior Rating Form
The NCBRF198 is a rating scale designed to assess social competence and problem behaviour in children with developmental disabilities. There are parent and teacher versions of the scale. Internal consistency of the problem behaviour scales was reported as good, with Cronbach’s alpha coefficient of > 0.70 for all subscales in both parent and teacher versions. 199 Test–retest reliability for the parent version was reported to be strong (ICC for total problem behaviour > 0.80) but the teacher version fell short of the COSMIN criterion (ICC for total problem behaviour = 0.68); however, over a 1-year time interval some change might well be expected. Agreement was low between parents and teachers on common items from the parent and teacher version of the scale, indicating that inter-rater reliability was poor. 146 Structural validity was also shown to be poor for problem behaviour with a five-factor solution accounting for 47.5% of the variance. 199 Finally, Lecavalier et al. 146 provided fair evidence for divergent and convergent validity of the NCBRF.
Habit problems
For details, see Table 20.
| Tool (number of papers) | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Test–retest | Inter-rater | Convergent/divergent validity | Known groups | Stability | Change | |||||
| Child Behavior Checklist 1.5–5 (1) | ++ | +/– | ||||||||
| Child Behavior Checklist 6–18 (1) | ++ | ++ | ++ | |||||||
| Sense and Self-Regulation Checklist (1) | ++ | + | + | |||||||
Child Behavior Checklist 1.5–5
The CBCL184 1.5–5 was originally shown to measure two higher-order factors (internalising and externalising behaviour) and seven second-order factors (emotionally reactive, anxious/depressed, somatic complaints, withdrawn, attention problems, aggressive behaviour and sleep problems). One study185 of good quality assessed the CBCL 1.5–5 in an ASD sample. Internal consistency was good for total scale and sleep problems (α > 0.80) but not acceptable for somatic complaints (α = 0.49). Structural validity was not acceptable for sleep problems (RMSEA = 0.13) but was acceptable for somatic complaints (RMSEA = 0.06), just reaching the cut-off for acceptable fit. Overall, the findings supported the original structure of the CBCL 1.5–5 but there were conflicting findings for the scales related to the Habit Problems domain.
Child Behavior Checklist 6–18
The CBCL 6–18191 was assessed with a sample of ASD youth in one paper186 of good methodological quality. Internal consistency was good, with a median scale reliability of r = 0.85 and r = 0.88 for somatic complaints. Structural validity was also strong for somatic complaints (RMSEA < 0.001; CFI = 1) and analysis supported the original factor structure of the CBCL 6–18. Criterion validity was assessed by comparing ASD children with and without a co-occurring EBD. Children with a co-occurring EBD scored significantly higher than those without EBDs on total problems and on the Somatic complaints subscale.
Sense and Self-Regulation Checklist
Silva and Schalock,211 provided an assessment of the properties of the SSC (see Sensory processing, above). Internal consistency was rated as good with Cronbach’s alpha coefficient of > 0.80 (range from 0.85 to 0.89). Although test–retest reliability overall did not reach the cut-off, the reliability coefficient was 0.83 for the Self-Regulation domain. This relates most closely to habit problems and so was considered supportive evidence of test–retest reliability. This paper211 also demonstrated that the SSC was able to distinguish between children with and without ASD.
Daily living skills
For details, see Table 21.
| Tool (number of papers) | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Test–retest | Inter-rater | Convergent/divergent validity | Known groups | Stability | Change | |||||
| Vineland Adaptive Behavior Scales (2) | – | ? | ||||||||
| Vineland Adaptive Behavior Scales-Classroom (1) | + | |||||||||
| Vineland Adaptive Behavior Scales-Screener (1) | ++ | |||||||||
Vineland Adaptive Behavior Scales
The VABS (see Language and social functioning, above) had two papers168,169 that assessed domain-level validity169 and responsiveness,168 respectively. Paul et al. 169 demonstrated that children with autism and ASD differed on Communication and Socialisation domains but not on the Daily Living Skills domain. Groups did differ on ‘phone use’, which is part of the DLS scale but was deemed to be more relevant to verbal communication than daily living skills. Hypotheses were not specifically set out in the paper and so it was rated as ‘fair’ quality. Harris et al. 168 assessed rate of change and change in developmental age. This paper168 showed that VABS was able to identify change over time but was of poor quality due to the small sample size (n < 20).
Wells et al. 170 evaluated the VABS-Classroom. The paper170 was rated as fair quality. The VABS-Classroom Daily living skills scale demonstrated convergent validity with mental age (r = 0.87) and severity of autism (r = –0.46).
Charman et al. 112 assessed responsiveness of the VABS–Screener tool in young children with ASD. This paper112 was of good methodological quality and showed that there was developmental progress from time 1 to time 2 in daily living skills as predicted.
Global measure of functioning
For details, see Table 22.
| Tool (number of papers) | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Test–retest | Inter-rater | Convergent/divergent validity | Known groups | Stability | Change | |||||
| Assessment, Evaluation, and Programming System (1) | ? | ? | ||||||||
| Behavior Assessment System for Children-Second Edition, Teacher Rating Scales (1) | ? | |||||||||
| Behavior Assessment System for Children-Second Edition, Parent Rating Scales (1) | ++ | |||||||||
| Psychoeducational Profile-Revised (5) | ? | ++ | ++ | +++ | + | ++ | ? | |||
| Psychoeducational Profile-Third Edition (2) | + | + | ? | |||||||
| Psychoeducational Profile-Third Edition, Caregiver Report (1) | ? | – | ? | |||||||
| Scales of Independent Behavior-Revised (2) | + | ? | + | |||||||
| Vineland Adaptive Behavior Scales (2) | + | ? | ||||||||
| Vineland Adaptive Behavior Scales-Classroom (1) | + | |||||||||
| Vineland Adaptive Behavior Scales-Screener (1) | ++ | |||||||||
Assessment, Evaluation, and Programming System
The Assessment, Evaluation, and Programming System212 for infants and children is a curriculum-referenced comprehensive system assessing six key developmental areas in young children: Fine Motor, Gross Motor, Cognitive, Adaptive, Social Communication and Social. Each domain has 15–54 items: 228 in total. Wang et al. 213 assessed the internal consistency of the Social domain only and found the Cronbach’s alpha coefficient to be 0.98. The same study213 assessed the tool’s responsiveness, and found significant change in the Social domain from pre-test and post test, as hypothesised. However, owing to the small sample size (n = 22), both assessments from this paper were judged to be of poor methodological quality.
Behavior Assessment System for Children-Second Edition
The BASC-2181 is a tool for assessing behaviour and emotions in children, adolescents and young adults (see Attention, above). Hass et al. 182 report internal consistency of the Teacher Rating Scale, as measured by Cronbach’s alpha, to range from 0.76 to 0.90 for the Adaptive Functioning subscales. The absence of a factor analysis, however, led this paper to be judged as being of poor methodological quality. Mahan and Matson183 assessed the known-groups validity of the Parent Rating Scale and found that all relevant hypotheses were supported.
Psychoeducational Profile-Revised
The Psychoeducational Profile-Revised (PEP-R)214 is used to assess abilities and formulate treatment programmes for children with autism and related developmental disorders. The tool consists of a Developmental scale, with a total of 153 items, and a Behavioural scale, with a total of 43 items. Four studies215–218 assessed the internal consistency of the tool’s Developmental scale and found that Cronbach’s alpha coefficients ranged from 0.81 to 0.99. Three of these studies216–218 also assessed internal consistency of the Behavioural scale and found that Cronbach’s alpha coefficients ranged from 0.74 to 0.99. However, none of these studies included a factor analysis, and therefore all assessments were judged to be of poor methodological quality. Three studies215,216,218 assessed the inter-rater reliability of the Developmental scale and found ICC values ranged from 0.84 to 0.99. Shek et al. 216 and Villa et al. 218 assessed the inter-rater reliability of the Behavioural scale and found that ICC values ranged from 0.56 to 0.88. Owing to small sample size, Alwinesh et al. 215 was judged to be of poor methodological quality. Two studies215,216 assessed the test–retest reliability of the Developmental scale and found ICC values ranging from 0.87 to 0.99. Shek et al. 216 assessed the test–retest reliability of the Behavioural scale and found ICC values ranging from 0.76 to 0.92. Steerneman et al. 217 and Heimann et al. 219 both assessed known-groups validity and, in both, the relevant hypotheses were supported. However, the small sample size led the second study219 to be judged as being of poor methodological quality. Two studies215,217 assessed the tool’s convergent validity and found correlations between the PEP-R and Snijders-Oomen Non-Verbal Intelligence Test-Revised to range from 0.90 to 0.95,217 and correlations between PEP-R and Gesell’s Developmental Schedule to range from 0.34 to 0.84. 215 Criterion validity was assessed by two studies,216,218 and found correlations between PEP-R Developmental Score and VABS to equal 0.85,218 and correlations between the PEP-R Developmental scale and Merrill–Palmer Scale of Mental Tests to equal 0.71. 216 Heimann et al. 219 assessed responsiveness and found all relevant hypotheses regarding difference in change scores to be supported. However, the small sample size (n = 20) meant that this study219 was judged to be of poor methodological quality.
Psychoeducational Profile-Third Edition
The third edition of the Psychoeducational Profile (PEP-3)220 is specifically designed for children with ASD – ranging in developmental age from 2 years to 7 years 6 months – to assess their development of communication and motor skills and the presence of maladaptive behaviours. It consists of 10 performance subtests that are combined into three composites: Communication, Motor, and Maladaptive behaviours. Fu et al. 221 tested a Chinese translation; they assessed internal consistency and found Cronbach’s alpha coefficients to range from 0.92 to 0.98. The same study221 assessed inter-rater reliability, and found ICC of the PEP-3 ranged from 0.57 to 0.94 for the performance subtests, and 0.63 to 0.89 for the composites (4 out of 13 ICCs were < 0.70). This study also assessed measurement error, and found that the standard error measurement of the PEP-3 ranged from 2.6 to 6.5 for composite scores, whereas the smallest real difference of the PEP-3 ranged from 5.8 to 12.8. Chen et al. 222 assessed responsiveness and found that composite scores and most of the subtest scores of the PEP-3 changed in raw scores and developmental ages, but were stable in percentile ranks. Owing to the absence of specific hypotheses, this study222 was judged to be of poor methodological quality.
Measurement properties of the Caregiver report of the PEP-3 were reviewed by Fu et al.,223 who assessed internal consistency and found Cronbach’s alpha coefficients to range from 0.15 to 0.85. However, as no factor analysis was conducted, this study223 was judged to be of poor methodological quality. The same study223 assessed inter-rater reliability and found the ICCs of the subtests ranged from 0.66 to 0.79, and criterion validity reporting correlation coefficients between the PEP-3-Caregiver and the VABS ranged from 0.04 to 0.82. However, the small sample size (n = 20) meant that this study was judged to be methodologically poor.
Scales of Independent Behavior-Revised
The Scales of Independent Behavior-Revised (SIB-R)224 is a comprehensive norm-referenced test used to assess adaptive behaviour. It contains 14 subscales distributed into four areas: (1) Motor Skills; (2) Social and Communication Skills; (3) Personal Living Skills; and (4) Community Living Skills. Lecavalier et al. 146 assessed internal consistency and found Cronbach’s alpha coefficients to range from 0.87 to 0.96. The same study146 also assessed known-groups validity, and found support for the hypothesis. Brown et al. 225 assessed convergent validity and found that Full Scale IQ did not positively correlate with Broad Independence, and that Verbal IQ did not positively correlate with Social Interaction, as expected. However, the small sample size (n = 25) led this study to be judged as being of poor methodological quality.
Vineland Adaptive Behavior Scales
Paul et al. 169 explored the domains and subdomains of the VABS and assessed known-groups validity, finding support for all of their relevant hypotheses. Harris et al. 168 assessed responsiveness. A series of significant differences at years 1 and 2 were presented, but, owing to the lack of specific hypotheses, it is difficult to determine if the results were as expected. Therefore, the methodological quality of the paper was judged as poor.
Wells et al. 170 examined the measurement properties of the classroom edition of the VABS and reported convergent validity between the VABS-Classroom adaptive behaviour composite and CARS (r = –0.53).
The responsiveness of the Screener version of the VABS171 was assessed. 112 The VABS-Screener age-equivalent domain scores showed clear evidence of developmental progress from times 1 to 2, although change in the composite score was not significant.
Parent stress
For details, see Table 23.
| Tool (number of papers) | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Test–retest | Inter-rater | Convergent/divergent validity | Known groups | Stability | Change | |||||
| Autism Parenting Stress Index (1) | +++ | ? | ? | ++ | ||||||
| Parenting Stress Index-Short Form (3) | +++ | +++ | + | + | ||||||
| Questionnaire on Resources and Stress-Friedrich Short Form (1) | + | ? | + | |||||||
Autism Parenting Stress Index
The Autism Parenting Stress Index (APSI)226,227 is a caregiver questionnaire designed for clinical use to identify what aspects of parenting skills would benefit from additional support, and to measure the outcome of intervention on parenting stress relative to core and comorbid symptoms of a child’s autism. The measure consists of three categories: the core social disability, difficult-to-manage behaviour and physical issues. All of the items are rated on a five-point Likert scale, ranging from ‘not stressful’ to ‘so stressful that sometimes we feel we cannot cope’. Only one study153 has examined the measurement properties of the APSI, collecting data from parents of 274 children aged < 6 years (including 109 children with ASD). Authors reported good internal consistency and 4-month test–retest reliability (however, a subsample of only 18 parents was used). The factor analysis of the APSI revealed a four-factor solution (overall parental stress scale; core autism symptoms; comorbid behaviours; comorbid physical issues); however, the explained variance is not stated. The APSI discriminated between children with ASD and those who are typically developing or have other developmental delays.
Parenting Stress Index-Short Form
The PSI-SF228 is a 36-item self-report questionnaire measuring parenting stress. It contains three subscales: Parental distress, Parent–child dysfunctional interaction, and Difficult child (the extent to which the parent considers the child to be ‘difficult’). Items are rated on a five-point Likert scale ranging from ‘strongly agree’ to ‘strongly disagree’. Three studies reported data on measurement properties of the PSI-SF. Lecavalier et al. 146 reported excellent internal consistency for the total score (Cronbach’s α = 0.93). Good internal consistency for the subscales, and support for a primary dimension for each of the PSI-SF subscales, were reported by Zaidman-Zait et al. 229 However, in Zaidman-Zait et al. 230 the three-factor model was rejected and a six-factor solution was suggested. Parenting stress was showed to be stable across time (over 1-year period) and associated with behaviour problems,146 greater severity of autism and other psychological problems. 230
Questionnaire on Resources and Stress-Friedrich Short Form
The Questionnaire on Resources and Stress-Friedrich Short Form (QRS-F)231 is a 52-item questionnaire assessing the level of stress in families of children with disabilities. It contains four subcomponents of parental perceptions of difficulties: parent and family problems (stressful aspects of the impact of the child with disability on parents and the wider family), pessimism (parents’ pessimistic beliefs about the child’s future), child characteristics (features of the child that are associated with increased demands on parents) and physical incapacity (the extent to which the child is able to perform a range of typical activities). Honey et al. 232 investigated measurement properties of the QRS-F. A total of 174 mothers and 43 fathers of a child with autism aged between 26 and 82 months completed 31 items from the QRS-F (from the child characteristics, parent and family problems and pessimism scales). The authors reported good internal consistency for the total score. Support for the expected two- or three-factor solutions for the QRS-F was not found. The study232 showed convergent validity of the QRS-F, with parents reporting more stress when raising children with more severe symptoms of autism and less stress if children were more able (as indicated by higher VABS scores).
Discussion
The detailed data extraction and appraisal using the COSMIN checklist has provided some positive evidence with regard to at least one measurement property for 41 of the tools (seven with various versions/editions) identified as being used to measure an outcome at stage 2 of the MeASURe review. Nine other tools will not be considered further, either because the quality of the evidence provided in the paper(s) was of poor quality or the only measurement property evidence suggested that the tool was weak.
Unsurprisingly, the most evidence has been gathered for tools that were developed especially for use with children with ASD. Content validity has been accepted for this review as strong, even although it may not be represented in the tables; choice of autism characteristic items was assumed to have been addressed in other publications not considered in this review, as their focus would be on measurement properties concerning screening or diagnostic accuracy. There are some recurring issues with evidence concerning test–retest reliability, as this measurement property was not assessed or because the sample sizes were small, or the evidence reviewed was found to be inconsistent.
Despite the fact that one of the main aims of the review was to assess the property of responsiveness to change, there appears a dearth of evidence about which tools may have the capacity to track children’s progress over time. In the case of tools such as the ADOS-G, designed to capture unusual quality of behaviours in order to aid diagnostic assessment, the property of stability in assessment may have been demonstrated and, in principle, this would allow detection of unexpected change. However, when a tool has been developed to measure a stable quality, the tool items may be insensitive to small changes in response to treatment. Even for the tools designed explicitly for the purpose of measuring change in response to intervention – ATEC and PDDBI – the evidence was limited. Some discussion of possible ‘newer’ tools will be included in Chapter 5.
The review also uncovered little evidence about the measurement properties of standardised assessments (e.g. of language, cognition and play) and for many questionnaires (e.g. assessing behaviour, attention and emotional regulation) when used with or about young children with ASD. Although for an individual child, the purpose of conducting an assessment may be to make comparison with patterns of typical development, this should be informed by a knowledge of what adjustments may need to be made to tools to take into account the particular ways in which children with ASD think and behave (content validity). For example, there is evidence that children with ASD on average have more expressive language than would typically be expected for their level of understanding of language. 233 Also the relative significance attributed to the observation that a young child chooses to play alone may not be the same for a child with ASD compared with their more typically developing peers.
This review has highlighted that there is relatively little information about inter-rater and test–retest reliability for questionnaire tools. Parents and teachers rating the behaviours of young children may well not agree, as they are likely to be observing the children in very different circumstances. However, the lack of test–retest reliability is concerning, and it would be appropriate for an agreed standard for an appropriate time interval between assessments to be agreed.
In our consultation with professionals (see Chapter 2), a number of tools were identified which are used in nurseries and other early years settings to monitor progress. We included in searches the Early Years Foundation Stage Profile; however, we identified no evidence about whether it has good measurement properties when used with children with ASD. The emphasis in early education tools is to record and monitor steps in building up skills, so that staff can plan learning activities for children. For this reason it would be reassuring to know whether one staff member made similar ratings to another staff member. The tools evaluated in the subdomain Global Measure of Functioning also included some that are used for individual programme planning (e.g. the AEPS, the Assessment of Basic Language and Learning Skills), again with insufficient information for their validity and appropriateness in use with young children with ASD.
We have found no evidence concerning tools that can describe and measure some of the aspects of children’s social participation and well-being (valued by parents as important, see Chapter 2). We do have evidence about some tools that measure behaviour problems and distress. We have no evidence about measures of family quality of life, but some about measuring parent stress. The issue of emphasis on measurement of ‘problems’ rather than of strengths will be returned to in Chapter 5.
Chapter 5 Evidence synthesis
Introduction
The MeASURe systematic reviews have so far (1) identified the tools used in published intervention evaluation and observational studies with children with ASD up to the age of 6 years from 1992, and (2) assessed the availability and quality of information about the measurement properties of some of these tools.
This combined systematic review process appears to be unique in the field of autism. A few groups have previously made recommendations about batteries of tools for measuring outcome in autism (e.g. consensus decision by five research teams;234 descriptive review of tools used235). These batteries have not been adopted for use consistently across research groups, and the measures considered in the first of these are not all applicable to young children (being largely focused on outcomes of medication trials for adults with autism and aggressive behaviour). Other papers review tools that have been frequently used: for example, Cunningham236 reviewed measures of social interaction in autism and made recommendations without a clear basis of evaluation. Other reviews of assessment batteries have focused on diagnosis. 237 The field of autism research, practice and policy has expended massive efforts to standardise measurement practice internationally, but with the predominant focus on improvement of assessment for diagnosis.
Recently, the US Autism Speaks Foundation has supported expert work groups to evaluate outcome measurement tools in three subdomains: Restricted interests and repetitive behaviours; Anxiety; and Social Communication behaviours. 238–240 The purpose was to identify tools that were appropriate for use in medication trials. The expert groups identified, through systematic searches, tools used in treatment trials of medication, complementary medicine or behavioural interventions from 2005 to 2012, across any age group of children and youth with ASD. Other tools known to members of the work groups were also included. The tools were rated as: appropriate, appropriate with conditions, potentially appropriate/promising, unproven or not appropriate. The definitions of each level included information on reliability, validity and sensitivity to change of the tool, use with individuals with ASD, and also aspects of burden in terms of the time and other difficulties associated with use of the tool in assessment. In each case, a small number of tools were identified as ‘appropriate with conditions’ (such as restricted age range or lack of information on sensitivity to change).
That process of evidence synthesis provides a helpful model but could not be adopted for the MeASURe project, as the US group’s aim was different and narrower. The measurement properties and appropriateness of a tool vary depending on the use to which the tool will be put. In a randomised controlled trial of early intervention in ASD, for example, it is important to identify a primary outcome that can be assessed ‘blind’ and is responsive to change. In contrast, when monitoring children’s progress in a nursery setting, properties of face validity, content validity, test–retest and inter-rater reliability, as well as burden (cost, training, time), will assume greater importance.
The approach to evidence synthesis adopted in this chapter is incremental. First, we present descriptive information on the 41 tools for which some positive evidence was found concerning their measurement properties (see Chapter 4). The information about some of these tools is amplified by points made by parents attending the advisory groups and by stakeholders who participated in the MeASURe Discussion Day (14 February 2014, described in Chapter 2). Second, we will briefly comment on other tools for which we were unable to identify evidence on measurement properties when used with young children with ASD, which may yet turn out to be ‘promising’ after further evaluation. Finally, we summarise the tools that may be, at present, the most appropriate choices, depending on the purposes of the researcher or clinician.
Methods
Descriptive information about each tool was compiled from a range of sources, including manuals, publishers’ websites, papers citing the tool, summaries of tools presented on web pages, and so on. The MeASURe project team designed the headings for the tables, to include name, source, what it is described as measuring, method/respondent, potential for blinding, number of items/time taken, subscales, required interval between repeat administrations, age range, entry criteria, whether norms or clinical cut-offs are available, population for which designed, cost/availability/languages and training required. The judgement of potential for blinding is made on the assumption that parents/caregivers will know whether a child is receiving an intervention. (However, in a medication trial, parent report may be a blind outcome.) When the tool can be completed by education or other staff, there may be potential for blinding (although it would be poor practice for parents and staff not to communicate); there may also be potential for blinding where the parent is interviewed in a standard way to provide behavioural descriptions (and the parent has been asked not to unblind the interviewer). Where sources give conflicting information, the most recent version is presented.
Discussion Day
As described in Chapter 2, 25 participants came to a Discussion Day in London on February 2014, including parents, a young adult on the autism spectrum, researchers, and health and education professionals. In addition to the Q-sort activity described in Chapter 2, participants were divided into mixed groupings and asked to evaluate tools set out on display (four sets for each grouping). The subdomains represented were symptom severity, global measure of outcome, sensory processing, cognitive ability, behaviour problems and parent stress. Two direct child assessments were shown, with videotape accompaniment. The questionnaire tools were presented in pairs to allow participants to compare and contrast. Summary information about each tool was available. Participants rated each tool for (1) the assessment experience (including questionnaire wording) and (2) how likely it would be to capture change. They were asked also to state what they liked or did not like about the tool.
Descriptions of tools
The order of the paragraphs follows the Conceptual Framework of subdomains (see Table 1). However, the 41 tools are described once only, in the subdomain table in which they are presented most fully (see Table 24). The observational and intervention evaluation studies in which they were used are listed in Appendix 5.
Autism symptom severity
For details, see Table 24.
| Name of the tool | Authors, date(s), history of revisions | What it claims to measure | Method and by whom measured/reported | No. of items and time taken | Subscales | Age range and entry criteria | Whether norms available, clinical cut-offs | Population for which designed | Cost/availability/languages | Training required |
|---|---|---|---|---|---|---|---|---|---|---|
| Autism Behavior Checklist | Krug et al. (1978,241 198058) | Assess the behaviours and symptoms of autism | Q; parents or teachers Blinding: No/potential |
57 items; 10–20 minutes Interval: NA |
Five subscales: Sensory behavior; Social relating; Body and object use; Language and communication skills; Social and adaptive skills | Children aged ≥ 3 years | NK | ASD | No publisher | NA |
| Autism Diagnostic Interview-Revised | Lord et al. (1994);63 Rutter et al. (2003)53 | Diagnosis of autism, and distinguishing autism from other developmental disorders | I; parents or caretakers interviewed by trained assessor Blinding: potential |
93 items; 90–150 minutes, including scoring Interval: NK |
Three subscales: Language/communication; Reciprocal social interactions; Restricted, repetitive, and stereotyped behaviours and interests | Children and adults with a mental age > 2.0 years | Cut-offs for ‘autism’ for communication, social interaction, and repetitive behaviour domains | ASD | Forms and manuals are available from publisher ADI-R Kit (Interview Booklets; Algorithm Forms; Manual) US$237.00 Available in Danish, Dutch, English, Finnish, French, German, Hebrew, Hungarian, Icelandic, Italian, Japanese, Korean, Norwegian, Romanian, Russian, Spanish and Swedish |
Training required before administering ADI-R DVD Training Package available (total running time 16 hours) |
| Autism Diagnostic Observation Schedule | Lord et al. (2000)50 [current version: ADOS-2 (2012)]242 | Assessment of communication, social interaction, and play or imaginative use of materials for individuals referred because of possible ASD | O; clinicians Blinding: Yes |
Module 1: 10 activities Modules 2 and 3: 14 activities Module 4: 15 activities 30–45 minutes Interval: (scores not affected by repeat administrations, ADOS-2, p. 15) |
Five subscales: Language and communication; Reciprocal social interaction; Play; Stereotyped behaviors and restricted interests; Other behaviors Algorithm: communication and reciprocal social interaction |
Toddlers to adults | Cut-offs for autism and autism spectrum (ADOS-2 includes a comparison score, i.e. the Calibrated Severity Score) | ASD | Available in Danish, Dutch, English, Finnish, French, German, Hebrew, Hungarian, Icelandic, Italian, Korean, Norwegian, Romanian, Russian, Spanish and Swedish | Training in a relevant professional discipline |
| Autism Diagnostic Observation Schedule-Toddler module | Lord et al. (2012)243 (part of ADOS-2) | Assessment of communication, social interaction, and RRBs relevant to the diagnosis of ASD in children with limited expressive language | O; clinicians Blinding: Yes |
11 activities; 45 minutes (40–60 minutes) Interval: NK |
Algorithm: Social affect and RRB | 12–30 months (who do not consistently use phrase speech), able to walk | Does not provide a cut-off score (provides ranges of concern instead) | ASD | Forms and manuals are available from publisher ADOS-2 Hand-scored Kit (manual; protocol booklets, test materials) US$1995.00 Available in Czech, Danish, Dutch, English, Finnish, French, German, Italian, Norwegian and Swedish |
Training in a relevant professional discipline; training package and courses available |
| Autism Observation Scale for Infants | Bryson et al. (2008)81 | Developed for research, a systematic method of detecting and monitoring signs of autism in high-risk infants | O; researchers Blinding: Yes |
18 items; 20 minutes Interval: NK |
NA | 6–18 months | NA because of young age | ASD | NK | An examiner who is both skilled at interacting with infants and knowledgeable about ASD For research, training required by the Canadian team |
| Baby and Infant Screen for Children with aUtIsm Traits-Part 1 | Matson et al. (2009)83 | Assessment of the core symptoms of autism in toddlers | Q; parents Blinding: No |
62 items Interval: NA |
Three subscales: Socialisation/non-verbal communication; Repetitive behaviors/restricted interest; Communication | 17–37 months | Cut-offs for probable ASD/possible ASD | ASD | Available from Disability Consultants, LLC Kit (manual, protocols, score sheets) US$325 English |
NA |
| Behavioral Summarized Evaluation (1990)86 and BSE-Revised (1997)87 | BSE: Barthelemy et al. (1990)86 BSE-R: Barthelemy et al. (1997)87 |
Enable the formalisation of behaviour observations in the different domains in which specifically autistic difficulties occur | O; Clinicians and researchers Blinding: Yes |
BSE: 20 items BSE-R: 29 items 5 minutes Interval: Once per month |
Two subscales: Interaction disorder; Modulation disorder | 1.5–12 years | A best cut-off to discriminate autistic from non-autistic children given in Barthelemy et al. (1997)87 | ASD | French (English) A copy of the BSE-R can be obtained from C Barthelemy |
A clinician who is both skilled at interacting with infants and knowledgeable about ASD |
| Behavioral Summarised Evaluation-Infant | Adrien et al. (1992)90 | Specifically related to the assessment of behaviours of young children with autistic disorders | O; clinicians Blinding: Yes |
33 items; 10–15 minutes Interval: NK |
Six subscales: Socialisation; Communication; Adaptation to environmental situations; Motility; Emotional and instinctual reactions; Attention–perception | 6–48 months | NK | ASD and developmental disorders | French and English [the English version can be found in Adrien et al. (1992)]90 | A clinician who is both skilled at interacting with infants and knowledgeable about ASD |
| Childhood Autism Rating Scale | Schopler et al. (1980, 1988)92,244 (newest version: CARS-2: Schopler and Van Bourgondien (2010)245 | Identify children with autism; distinguish them from developmentally delayed children who are not autistic; it also distinguishes mild-to-moderate from severe autism | O and Q; clinicians, teachers, parents Blinding: potential |
15 items; 10 minutes Interval: NK |
NA | Over 2 years | Cut-off scores for autism available | ASD | CARS-2 kit (manual, booklets) £148 English |
Training in a relevant professional discipline |
| Gilliam Autism Rating Scale | Gilliam (1995)246 [newest versions: GARS-2 (2006)100 and GARS-3 (2014)247] | Helps identify or diagnose autism and estimate its severity | Q; caregivers Blinding: No |
56 items; 5–10 minutes Interval: NK |
Four subscales: Stereotyped behaviors; Communication; Social interaction; Developmental disturbance (14 items each) | 3–22 years | Cut-offs discriminating children with ASD from children without autism | ASD | GARS-3 from US$35 English |
NA |
| Modified Checklist for Autism in Toddlers | Robins et al. (1999)248 [M-CHAT-R and M-CHAT-R/F (revised with follow-up, 2013, available)]249 | Identify children who may benefit from a more thorough developmental and autism evaluation | Q; to be administered to parents/guardians and interpreted by paediatric providers Blinding: Potential |
23 items | NA | 16–30 months | Cut-offs discriminating between children diagnosed with and without autism/ASD | ASD | Free online M-CHAT with instant scoring www.m-chat.org/mchat.php Available in 45 languages |
M-CHAT-R/F: First administration is parent report/questionnaire and follow-up administration is by a clinician/researcher |
| Parent Observation of Early Markers Scale | Feldman et al. (2012)104 | Screening of high-risk infants | Q; parents Blinding: No |
61 items Interval: NK |
NA | 1–24 months | Total score cut-off score for autism diagnosis available (Feldman et al. 2012104) | ASD | English | NA |
| Pervasive Developmental Disorders Rating Scale | Eaves et al. (1993);106 Eaves et al. (1987–88)250 | Identify individuals with autistic disorder | Q; parents and teachers Blinding: No/potential |
51 items Interval: NA |
Three subscales: Arousal (22 items); Affect (19 items); Cognition (10 items) | NK | NK | General/individuals with ASD | English | NA |
| Social Communication Questionnaire | Rutter et al. (2003)251 | Provides a quick and easy routine screening for ASDs | Q; parent (two forms/versions: current and lifetime) Blinding: No |
40 items, up to 10 minutes Interval: NA |
NA | Over 4 years, with a mental age of > 2 years | Cut-offs for likely ASD diagnosis | ASD | Forms and manuals are available from publisher SCQ Kit (AutoScore forms; manual) US$129.00 Available in Danish, Dutch, English, Finnish, German, Hebrew, Hungarian, Icelandic, Italian, Japanese, Korean, Norwegian, Romanian, Russian, Spanish, Swedish |
Training in a relevant professional discipline |
| Social Responsiveness Scale (SRS-2 available, 2012) | Constantino and Gruber (2005)252 | Can be used both as a screener and as an aid to clinical diagnosis | Q; parent and teacher Blinding: No/potential |
65 items; 15–20 minutes, scoring 5–10 minutes Interval: NA |
Five clinical scales: Social awareness (eight items); Social cognition (12 items); Social communication (22 items); Social motivation (11 items); Autistic mannerism (12 items) | 4–18 years (SRS-2 from 2.5 years) | Norms available | ASD | SRS-2 hand-scored Kit (manual, AutoScore forms) US$247 English |
Training in a relevant professional discipline |
The AuBC was first published in 1978 and intended for the identification of autism in groups of children with severe disabilities. The items describe specific behaviours, although some include evaluation (e.g. item 19 ‘Has special abilities in one area – seems to rule out mental retardation’). Some items were judged to apply to neurotypical development. The scoring instructions were described by the Discussion Day participants as very confusing. However, the brevity of the scale was seen as positive. The participants did not consider the items would pick up change. This tool was used in three observational and six intervention evaluation studies in the review. The evidence on measurement properties was limited.
The ADI-R has been described in the literature as a ‘gold standard’ diagnostic tool. It has therefore been used in 15 longitudinal studies in this review, but not as an outcome measure in intervention. The time commitment to training and the cost of the tool are significant; the interview takes at least 2.5 hours but parents can find this investment of time and attention positive, as it allows them to describe in detail their child’s strengths and difficulties. There is strong evidence for its measurement properties.
The ADOS was designed as a ‘partner’ diagnostic tool for the ADI-R. It was used in 14 observational studies, and 11 intervention evaluation studies in this review. However, there is considerable debate as to whether or not the ADOS can be sensitive to change, as each rating is measured on a three- or four-point scale, and the focus is on abnormalities of behaviour. A number of suggestions have been made for altered approaches to scoring253 to enhance responsiveness to change. Reliable administration and scoring of the ADOS requires specific training of assessors; there is a self-training pack but attendance at a course is advised (which can be costly) and required for research-level competence. That it can be carried out by a ‘blind’ assessor is a definite strength. The participants at the Discussion Day were all positive about the child’s experience, as ADOS focuses on the child’s actual social and play behaviour. They did consider that it would capture change, although not for short-term interventions. However, it is only a 20- to 45-minute ‘snapshot’ of behaviour in a structured setting; another potential limitation for its use as an outcome measure. The current version [Autism Diagnostic Observation Schedule-Second Edition (ADOS-2)], published in 2012, includes some small modifications to procedure and ratings, with a revised scoring algorithm, and now includes the Toddler Module. The inclusion of five age- and ability-appropriate modules is a strength in allowing conceptually linked measurement longitudinally. The creation for ADOS-2 of a calibrated comparison score is intended to allow detection of changes over time but the utility of this score is yet to be evaluated.
The AOSI was used in two observational studies in this review, having been designed for research assessment of infant siblings of children with autism. As yet the information on its measurement properties is limited.
The BSE (revised, BSE-R) was developed in Tours, France; it was used in two European observational studies in this review and has been translated into English also, although its availability is unknown. It was specifically designed for professionals to monitor the progress of children in an autism-specific treatment nursery. The evidence on measurement properties is relatively strong. The Infant BSE derives from the same clinical research group, and was used in two observational studies in this review.
The CARS combines observation of the child and interview with parents/carers to enable a clinician to rate 15 items each on a seven-point scale. The primary purpose of the tool is for diagnosis. The CARS-2 includes a version for high-functioning children, as the original was not sufficiently discriminative in making diagnosis. The evidence on reliability was strong. CARS was used in 10 observational studies and three intervention evaluation studies in this review.
The GARS is primarily a parent questionnaire. It was used in four observational and four intervention evaluation studies in this review. The evidence on measurement properties was weak. The PDDRS is similar in purpose but with a different model underlying the subscales. It was used in one observational study in this review and lacks evidence of validity.
Three early screening tools were included, each having been used in one observational study, even although the tools are not primarily designed to measure outcome. The BISCUIT-Part 1, is a recent screening questionnaire, part of a suite of three tools for children with ASD. Initial testing of measurement properties is promising but reliability is unknown. The POEMS is recently published. The M-CHAT is a well-established screening tool; it is intended to be used by clinicians with parents/caregivers, or can be completed by parents themselves. The evidence concerning measurement properties is limited for both of these tools. The M-CHAT has a newly developed version,249 which includes first a parent questionnaire and then administration by a clinician. As tools to measure outcome, these are limited by the short age range for which they were designed.
The SCQ is a screening tool for all ages, and closely related to the ADI-R. It was used on one observational study and one intervention evaluation study in this review. The measurement properties evidence is relatively strong. The wording is, in places, complex (e.g. item 32: ‘When she/he was 4 to 5, when she/he wanted something or wanted help, did she/he look at you and use gestures with sounds or words to get your attention?’); it was first developed with families who had already completed the ADI-R and so were familiar with they types of concepts included.
The SRS was developed to identify children with ASD. The original version was applicable from 4 years of age, but the Social Responsiveness Scale-Second Edition (SRS-2) includes a version for 2.5- to 4.5-year-olds. It was used in one intervention evaluation and two observational studies in this review. The measurement properties evidence is relatively strong, but the validity of the subscales is weak. At the Discussion Day, participants’ opinions were generally favourable about the wording of items, as they include positive behaviours; however, parents commented that it would be difficult to complete item 29 (‘Is regarded by other children as odd or weird’). The scale had clear instructions on how to complete it; however, a time frame of 6 months seemed too long for children in the age range up to 6 years. Participants thought that the scale would be likely to capture change. The linkage between age-related versions of the scale (into adulthood) is a strength.
Global measure of outcome
For details, see Table 25.
| Name of the tool | Authors, date(s), history of revisions | What it claims to measure | Method and by whom measured/reported | No. of items and time taken | Subscales | Age range and entry criteria | Whether norms available, clinical cut-offs | Population for which designed | Cost/availability/languages | Training required |
|---|---|---|---|---|---|---|---|---|---|---|
| Autism Treatment Evaluation Checklist | Rimland and Edelson (1999)119 | Effectiveness of various treatments | Q; parents, teachers or caretakers Can be undertaken online Blinding: No/potential |
77 items NK Interval: NA |
Four subscales: Speech/language communication (14 items); Sociability (20 items); Sensory/cognitive awareness (18 items); and Health/physical/behaviour (25 items) | NK | NA (but percentile scores are given on the website) | ASD | Free to researchers; Autism Research Institute website (www.autism.com) Languages: English, Chinese (simplified), Italian, Turkish, Portuguese, German, Spanish, Russian, Romanian, French |
NA |
| Behavioral Summarized Evaluation and BSE-Revised | (see Table 24) | |||||||||
| Infant Behavioral Summarized Evaluation | (see Table 24) | |||||||||
| Pervasive Developmental Disorders Behaviour Inventory | Cohen and Sudhalter (2003)122 | Assesses both maladaptive and adaptive behaviours, creating a behavioural profile Assess responsiveness to intervention in children with ASD |
Q; parents and teachers Blinding: no/potential |
124 items standard forms, 188 items parent-extended, 180 items teacher-extended 30–45 minutes Extended Forms scoring time: 20–30 minutes Standard Forms; scoring time: 20 minutes Interval: NK |
Domains: I. Approach/Withdrawal Problems; II. Receptive/Expressive Social Communication Abilitiesa | 2–12 years | Age norms and standardised scores available | ASD | Forms and manuals are available from the publisher PDDBI Introductory Kit (manual, rating forms, score summary sheets, profile forms) US$285.00 |
Training in an appropriate professional discipline; additional training in competent use of psychological tests |
The two additional tools considered here also cover a range of symptoms of ASD, but have specifically been designed to capture change over time or with intervention.
The ATEC is presented either as one page or can be completed (and scored) online. The evidence about its measurement properties is limited. It was used in one observational study in this review. Participants at the Discussion Day found the presentation of items crowded and the item wording too short (and some ‘unfriendly’, such as describing the child as ‘indifferent’ or ‘insensitive’). Many of the behaviours would not be the focus of intervention and therefore might be unlikely to change. They considered that a three-point rating scale might not have sufficient range to capture progress.
The parent version of the PDDBI is presented as six pages, with items scored on a four-point scale, with additional possibilities of ‘U’ (to indicate the child used to show this behaviour) or ‘?’ (don’t know). Participants at the Discussion Day found some of the language too technical and questioned the inclusion, for example, of detailed phonological skill items. Because of the large age range, some items are not appropriate for children aged < 6 years. The emphasis was on frequency, not impact of behaviours. No time frame is given for the responses. The PDDBI was used in two intervention evaluation studies in this review. The evidence on measurement properties was relatively strong but did not include responsiveness.
The Parent Interview for Autism-Clinical Version (PIA-CV)254 emerged as a ‘new tool’ from searches, but no study was found in which the tool has been used to measure change with intervention. More recently, the Autism Impact Measure (AIM) has been presented. 255 The AIM targets measurement of short-term change in core ASD symptoms, asking parents to indicate frequency and impact of 25 behaviours over a 2-week recall period. The children in the development study were aged 2–17 years. Future evidence on the sensitivity to change of the PIA-CV and the AIM will be of great interest. Furthermore, another tool targeted at the age group up to 6 years is in development, the Brief Observation of Communication Change (Lord, Columbia University, New York, personal communication, July 2013). This tool is a rating of observed behaviours by a trained investigator, with categories based on ADOS ratings, as a child interacts in play with an adult. The 16 ratings are each on a six-point scale and the important metric is the difference from one occasion to another, in order to capture change.
Social awareness
For details, see Table 26.
| Name of the tool | Authors, date(s), history of revisions | What it claims to measure | Method and by whom measured/reported | No. of items and time taken | Subscales | Age range and entry criteria | Whether norms available, clinical cut-offs | Population for which designed | Cost/availability/languages | Training required |
|---|---|---|---|---|---|---|---|---|---|---|
| Imitation Battery | Rogers et al. (2003)130 | Imitation skills in very young children, including children with ASD | O; clinicians Blinding: Yes |
Nine tasks Interval: NK |
Three categories: Manual acts; Actions on objects; Oral–facial movements | NK | NK | ASD | English Procedure and items description can be found in Rogers et al. (2003)130 |
NK |
| Preschool Imitation and Praxis Scale | Vanvuchelen (2009)256 | Investigate bodily (gestural and facial) and procedural imitation in young children | O; clinicians Blinding: Yes |
30 items; 10–20 minutes Interval: NK |
Six gestural, three procedural and one facial | 12–59 months of age | Cut-offs available | General | English and Dutch Procedure and items description can be found in Vanvuchelen et al. (2011)257 |
NK |
We now describe tools that focus on core early impairments in autism, first tools that measure aspects of social awareness. Many such tools were designed specifically for a particular study, such as coding of observed parent–child interaction (see Appendix 5). Such tools are generally related to the focus of the intervention, and information about measurement properties is restricted to reliability in that study. A number of other scales used were searched for by name but the evidence concerning measurement properties was limited or poor quality.
The two scales for which some positive evidence was found focus on imitation. The IB and the PIPS were each used in one observational study in the review. The evidence on measurement properties was relatively strong for the latter. Detailed information is presented in the papers referenced in the table.
Repetitive behaviours and interests
For details, see Table 27.
| Name of the tool | Authors, date(s), history of revisions | What it claims to measure | Method and by whom measured/reported | No. of items and time taken | Subscales | Age range and entry criteria | Whether norms available, clinical cut-offs | Population for which designed | Cost/availability/languages | Training required |
|---|---|---|---|---|---|---|---|---|---|---|
| Autism Diagnostic Interview-Revised | (see Table 24) | |||||||||
| Autism Diagnostic Observation Schedule | (see Table 24) | |||||||||
| Autism Diagnostic Observation Schedule-Toddler Module | (see Table 24) | |||||||||
| Repetitive Behavior Scale-Revised | Bodfish et al. (2000)150 [original RBS, Bodfish et al. (1999)]258 | Measure the breadth of repetitive behaviour in children, adolescents, and adults with ASDs | Q; parents or caregivers Blinding: No |
43 items; < 15 minutes Interval: NA |
Six subscales: Stereotyped behavior; Self-injurious behavior; Compulsive behavior; Routine behavior; Sameness behavior; Restricted behavior | Children and adults | NK | ASD | English | NA |
Repetitive interests and behaviours are a core feature of autism and have most often been measured with diagnostic tools in this review. However, the RBS-R was used in one intervention evaluation study. The evidence for its measurement properties is somewhat mixed, particularly structural validity, and a three-factor model may be stronger.
Sensory processing
For details, see Table 28.
| Name of the tool | Authors, date(s), history of revisions | What it claims to measure | Method and by whom measured/reported | No. of items and time taken | Subscales | Age range and entry criteria | Whether norms available, clinical cut-offs | Population for which designed | Cost/availability/languages | Training required |
|---|---|---|---|---|---|---|---|---|---|---|
| Sense and Self-Regulation Checklist | Silva, and Schalock (2012)211 | Measure of comorbid symptoms in autism | Q; parents or caregiver Blinding: No |
65 items Interval: NA |
Two domains:a Sensory, Self-regulation | Children aged < 6 years | NK | ASD | English copy available online: (www.midss.org) Available in English, Spanish and Chinese |
NA |
| Sensory Profile (also available: Infant/Toddler Sensory Profile, and the Sensory Profile School Companion) | Dunn (1999)154 | Measure a child’s sensory processing abilities and to profile the effect of sensory processing on functional performance in daily life | Q; parents or caregivers Blinding: No |
125 items Up to 25 minutes Interval: NK |
Three main subscales: Sensory processing; Modulation; and Behavioural and emotional responses Nine factors: sensory seeking; emotional reactive; low endurance/tone; oral sensory sensitivity; inattention/distractibility; poor registration; sensory sensitivity; sedentary; and fine motor/perceptual |
Most appropriate for 5–10 years, but can be used with 3- and 4-year-olds | Norms available | General | Sensory Profile Complete Kit (manual, caregiver questionnaires, short sensory profile, score sheets) US$196 Available in both English and Spanish |
Occupational therapist; other professionals with post-qualification training in sensory processing |
| Short Sensory Profile | McIntosh et al. (1999)259 (chapter 7 of The Sensory Profile: User’s Manual154) | Measures sensory modulation during daily life | Q; parents or caregivers Blinding: No |
38 items Up to 10 minutes Interval: NA |
Seven subscales: Tactile sensitivity, Taste/smell sensitivity, Movement sensitivity, Under-responsive/seeks sensation, Auditory filtering, Low energy/weak, Visual/auditory sensitivity | Most appropriate for children aged 5–10 years, but can be used with 3- and 4-year-olds | Norms available | General | (see above) Available in both English and Spanish |
NA |
The SSC is based in concepts from Chinese medicine, and was developed for use in evaluation of Qigong massage. Evidence on its measurement properties is limited. Participants in the Discussion Day noted that there is no ‘not applicable’ response option for questions (e.g. about ‘nappies’). The response scale measures frequency and not impact, without specification of a time frame. The phrasing of items was negative (e.g. ‘haircuts are difficult’).
The SP (and SSP) is a well-established clinical tool, although the review found little evidence on measurement properties in studies with children with ASD. Participants at the Discussion Day noted that the wording of items is negatively framed, the response scale captures frequency but not impact and there is no time frame. The SP was used in three observational and two intervention evaluations in the review, and the SSP in three observational studies.
Language
For details, see Table 29.
| Name of the tool | Authors, date(s), history of revisions | What it claims to measure | Method and by whom measured/reported | No. of items and time taken | Subscales | Age range and entry criteria | Whether norms available, clinical cut-offs | Population for which designed | Cost/availability/languages | Training required |
|---|---|---|---|---|---|---|---|---|---|---|
| MacArthur–Bates Communicative Development Inventories (Words and Gestures, and Words and Sentences) | Fenson et al. (1993)160 | In-depth information on the development of vocabulary, gestures, and/or grammar in children from 8 to 30 months of age | Q; parents | 20–40 minutes Interval: NA (Standardisation sample collected at monthly intervals) |
Words and gestures: major sections – phrases understood (28 items), vocabulary comprehension and production (396 words), and actions and gestures (63 items) Words and sentences: major sections – production vocabulary (680 words), grammatical complexity (37 items) |
Words and Gestures (Infant form), 8–16 months; Words and Sentences (Toddler form), 16–30 months (Either form may be used with older, developmentally delayed children) |
Norms available | General | CDI – complete kit (including user’s guide, Words and Gestures, Words and Sentences, CDI III) US$121.95 English and Spanish Versions in multiple languages available at www.sci.sdsu.edu/cdi/ |
NA |
| Mullen Scales of Early Learning | (see Table 30) | |||||||||
| Preschool Language Scale-Fourth Edition | Zimmerman et al. (2002)165 (PLS-5 available since 2011)260 | Measure young children’s receptive and expressive language | O; testing by any professional who has experience and training in assessment practices Blinding: Yes |
130 tasks (62 auditory comprehension tasks and 68 expressive comprehension tasks) 20–45 minutes Interval: NK (original standardisation sample collected at 6-monthly intervals) |
Two subscales: Auditory comprehension, and Expressive communication | Birth to 6 years 11 months | Norms available | General/children with language disorder or delay | English and Spanish PLS-4 complete kit (including manual, 15 record forms, picture manual and manipulatives set) US$438.25 |
Training in a relevant professional discipline; training in administration, scoring and interpretation of clinical assessments |
| Vineland Adaptive Behavior Scales | (see Table 34) | |||||||||
The MCDI are used extensively, and were identified in this review in seven intervention evaluation studies and seven observational studies. Parents indicate which words, from a list of vocabulary, that their child currently understands, and which the child understands and says. We did not find evidence about reliability in use with children with ASD; however, a recent study of children with autism aged 2–4 years found excellent agreement between parent and preschool teacher for the whole sample for both words produced and words understood (ICC = 0.93 and 0.77, respectively). 261 Shortened versions have been created for many languages, which could then be used in UK.
For both the direct assessments of language, the evidence for measurement properties in children with ASD was limited. The MSEL include two language scales. Both MSEL and the PLS are appropriate across the age range to 6 years. The PLS was used in nine observational studies and two intervention evaluation studies in this review.
Cognitive ability
For details, see Table 30.
| Name of the tool | Authors, date(s), history of revisions | What it claims to measure | Method and by whom measured/reported | No. of items and time taken | Subscales | Age range and entry criteria | Whether norms available, clinical cut-offs | Population for which designed | Cost/availability/languages | Training required |
|---|---|---|---|---|---|---|---|---|---|---|
| Leiter International Performance Scale-Revised | Roid et al. (1997)172 (Leiter-3 available, 2013)262 |
Measure of non-verbal intellectual functioning that consists of both perceptual and conceptual tasks designed to measure aspects of attention, cognition and memory | O; testing by clinicians, educators, researchers Blinding: Yes |
691 items; 25–40 minutes Interval: NK |
Two batteries: Visualisation and Reasoning Battery (VR) and Attention and Memory Battery (AM) | 2 years to 20 years 11 months old | Norms available | General (individuals with hearing impairments, expressive or receptive language disorders, learning disabilities, cognitive impairment, traumatic brain injury, English as a second language, attentional problems, and ASDs) | Leiter-R Psychologists Kit US$925 English |
Should be administered by a trained individual who has received supervised training and practice; it should be interpreted by someone with graduate training in psychological assessment |
| Mullen Scales of Early Learning | Mullen (1995)163 | Measure cognitive ability and motor development quickly and reliably | O; testing by any professional who has experience and training in assessment practices Blinding: Yes |
124 items; 25–35 minutes (3 years); 40–60 minutes (5 years) Interval: NK |
Five subscales: Gross motor; Visual reception; Fine motor; Expressive language; Receptive language | Birth to 68 months | Norms available | General | Mullen Scales of Early Learning – Complete Kit (record forms; test materials; manual; item administration book) US$849.65 |
Training in a relevant professional discipline; training in administration, scoring and interpretation of clinical assessments |
| Stanford–Binet Intelligence Scales-Fifth Edition | Roid (2003)177 | Intellectual and cognitive abilities | O; testing by clinicians, educators, researchers Blinding: Yes |
10 subtests, 5 minutes per subtest Interval: NK |
Two domain scores: verbal IQ and non-verbal IQ Five factors: Fluid reasoning, Knowledge, Quantitative reasoning, Visual–spatial processing, Working memory |
2–85+ years old | Norms available | General | SB-5 Complete Test Kit & Interpretive Manual £1032 English |
Training in a relevant professional discipline; training in administration, scoring and interpretation of clinical assessments |
The Leiter-R is a test of non-verbal intelligence, which may be advantageous for a range of children with neurodevelopmental impairments and limited language competence. As might be expected for a norm-referenced test, there is little specific evidence for the measurement properties of the Leiter, or the Stanford–Binet Intelligence Scales, in use with children with ASD. [We found no evidence for other such tests, such as the Bayley Scales of Infant Development (BSID) and the British Ability Scales (BAS).]
The MSEL includes five subscales, four of which make up the Early Learning Composite. The participants at the Discussion Day appreciated that the tasks have simple, developmentally appropriate materials and seem more like playing than a test. However, others found the materials ‘fiddly’ and not engaging. The participants commented that it would take a skilled administrator to avoid a child with ASD becoming anxious about getting tasks wrong (as would also be the case for any standardised test). The inclusion of Motor Skill domains was seen as an important part of the assessment, as this may be a particular area of weakness. The evidence about measurement properties in use with children with ASD did not include reliability. The MSEL was used in 32 studies included in the review, six of which were intervention evaluation studies.
The scales measuring ‘Attention’ are presented in later sections (see Behaviour problems and Global measure of functioning, below).
Emotional regulation
For details, see Table 31.
| Name of the tool | Authors, date(s), history of revisions | What it claims to measure | Method and by whom measured/reported | No. of items and time taken | Subscales | Age range and entry criteria | Whether norms available, clinical cut-offs | Population for which designed | Cost/availability/languages | Training required |
|---|---|---|---|---|---|---|---|---|---|---|
| Baby and Infant Screen for Children with aUtIsm Traits-Part 2 | Matson et al. (2009)83 | Symptoms of other emotional difficulties found to commonly occur with ASD | Q; parents or caregivers Blinding: No |
57 items Interval: NK |
Five subscales: Tantrum/conduct behavior; Inattention/impulsivity; Avoidance behavior; Anxiety/ repetitive behavior; Eating/sleep problem | 17–37 months | Cut-offs and norms available for infants with ASD, and those who have atypical development | ASD, and children with a non-ASD-related developmental delay | Available from Disability Consultants, LLC Kit (manual, protocols, score sheets) US$325 English |
NA |
| Behavior Assessment System for Children- Second Edition, Parent Rating Scales | (see Table 34) | |||||||||
| Brief Infant–Toddler Social–Emotional Assessment | Briggs-Gowan and Carter (2002)263 | Social–emotional/behavioural problems and delays in social–emotional competence | Q; parents and child-care providers Blinding: No |
42 items Up to 10 minutes Interval: NK |
Seven subscales: Internalising (eight items), Externalising (six items), Dysregulation (eight items), Competence (seven items), Social relatedness (three items), Maladaptive (three items), Atypical (four items); three additional scores | 12–36 months | Norms available | General | BITSEA Kit (manual, parent forms, childcare provider forms) US$116.00 English and Spanish |
Training in a relevant professional discipline |
| Child Behavior Checklist 1.5–5 | (see Table 33) | |||||||||
| Child Behavior Checklist 6–18 | (see Table 33) | |||||||||
| Children’s Global Assessment Scale | Shaffer et al. (1983)264 | Measure of overall severity of disturbance | S; clinicians Blinding: Yes |
One rating (the lowest overall level of psychosocial functioning of the child or adolescent during the preceding month) Interval: 1 month |
NA | 4–16 years | NA | General | The CGAS is available online: www.rcpsych.ac.uk/docs/CGAS%20tool.doc www.rcpsych.ac.uk/pdf/CGAS%20Ratings%20Guide.pdf English |
Training in a relevant professional discipline |
| Infant–Toddler Social–Emotional Assessment | Carter et al. (2003)265 | A wide array of social–emotional and behavioural problems and competencies | Q; parents Blinding: No |
166 items; 25–30 minutes Interval: NK |
Four broad domains, 17 specific subscales, and three index scoresa | 12–36 months | Norms available | General | ITSEA Kit (parent forms, child-care provider forms, and manual) US$182.60 English and Spanish |
Training in a relevant professional discipline; also requires a high level of expertise in test interpretation |
The BISCUIT-Part 2 is part of a set of three parent questionnaires. The evidence for its measurement properties was relatively strong, albeit all provided by the original research group. It was used in one observational study in this review. The remaining scales in this section are not ASD specific.
The Infant–Toddler Social–Emotional Assessment (and its Brief version) provides norms based on a national sample of children, including those who were preterm, had language delay, and children with other diagnosed disorders. The evidence for its measurement properties in children with ASD is relatively limited. The CBCL will be presented in the section on behaviour.
The CGAS is a clinician rating, giving a single summary score. As it covers a wide age range, the descriptions for each band of 10 scores do not necessarily apply to children up to the age of 6 years. Evidence of its measurement properties in ASD is lacking.
Physical skills, Social communication and Social functioning are presented under other headings.
Play
For details, see Table 32.
| Name of the tool | Authors, date(s), history of revisions | What it claims to measure | Method and by whom measured/reported | No. of items and time taken | Subscales | Age range and entry criteria | Whether norms available, clinical cut-offs | Population for which designed | Cost/availability/languages | Training required |
|---|---|---|---|---|---|---|---|---|---|---|
| Test of Pretend Play | Lewis and Boucher (1997)202 | Symbolic play, conceptual development and use of symbols | O; testing by clinicians Blinding: Yes |
Up to 45 minutes Interval: NK |
Assessing three types of symbolic play: substituting one object for another object or person; attributing an imagined property to an object or person; reference to an absent object, person or substance | 1–6 years: Non-verbal version for children up to 3 years; verbal version for children over three years |
Norms available (co-normed with the Preschool Language Scales-UK) | General | Available from Pearson English |
Training in a relevant professional discipline |
The ToPP is a direct assessment of a child’s symbolic play skills; the clinician sets up scenes with materials and observes the child’s actions. It was used in two observational studies in this review. The evidence on measurement properties when used with children with ASD is weak, with no information on reliability.
Behaviour problems
For details, see Table 33.
| Name of the tool | Authors, date(s), history of revisions | What it claims to measure | Method and by whom measured/reported | No. of items and time taken | Subscales | Age range and entry criteria | Whether norms available, clinical cut-offs | Population for which designed | Cost/availability/languages | Training required |
|---|---|---|---|---|---|---|---|---|---|---|
| Aberrant Behavior Checklist | Aman et al. (1985)266 | Originally designed to assess treatment effects in people with intellectual disabilities | Q; parents, caregivers or other individuals who know the child well Blinding: No |
58 items 10–15 minutes Interval: NA |
Five subscales: Irritability, agitation, crying (15 items); Lethargy/social withdrawal (16 items); Stereotypic behavior (seven items); Hyperactivity/non-compliance (16 items); Inappropriate speech (four items) | 6–54 years | Norms available | Individuals with mental retardation | Available in 40 languages Manual and residential and community forms/score Sheets (50) US$102 |
NA |
| Baby and Infant Screen for Children with aUtIsm Traits-Part 3 | Matson et al. (2009)83 | Challenging behaviours that are common among infants and toddlers with ASD | Q; parents or caregivers Blinding: No |
15 items Interval: NA |
Three subscales: Aggressive/disruptive behaviors; Stereotypic behaviors; Self-injurious behavior | 17–37 months | Clinical cut-off scores available for moderate impairment and severe impairment | ASD and children with a non-ASD related developmental delay | Available from Disability Consultants, LLC Kit (manual, protocols, score sheets) US$325 English |
NA |
| Behavior Assessment System for Children- Second Edition, Parent Rating Scales | (See Table 34) | |||||||||
| Child Behavior Checklist 1.5–5 | Achenbach and Rescorla (2000)184 | Specific behavioural, emotional and social problems that characterise preschool children | Q; parents, teachers Blinding: No/potential |
99 items 10–20 minutes Interval: NA |
Syndrome scales: Emotionally reactive; Anxious/depressed; Somatic complaints; Withdrawn; Sleep problems (CBCL only); Attention problems; Aggressive behavior DSM-orientated scales: Affective problems; Anxiety problems; Pervasive developmental problems; Attention deficit/hyperactivity problems; Oppositional defiant problems |
1.5–5 years | Norms available | General | Sample forms available online at www.aseba.org Ages 1.5–5 years hand-scoring starter kit (profiles, templates and manual) US$160 (computer scoring starter kit US$330) Available in nearly 100 languages |
Training in a relevant professional discipline; knowledge of the theory and methodology of standardised assessment, as well as supervised training in working with the relevant kinds of clients |
| Child Behavior Checklist 6–18 | Achenbach (2001)191 | Specific behavioural and emotional problems | Q; parents, caregivers or other individuals who know the child well Blinding: No/potential |
118 items 15 minutes Interval: NA |
Syndrome scales DSM-orientated scales |
6–18 years | Norms available | General | Sample forms available online at www.aseba.org Computer scoring starter kit US$430 English, Spanish |
(as above) |
| Home Situations Questionnaire-Pervasive Developmental Disorders version | Chowdhury et al. (2010)209 | Assessing behavioural non-compliance in children | Q; caregivers Blinding: No |
25 items Interval: NA |
Two subscales: Socially inflexible, and Demand-specific | NK (source paper sample 4–13 years) | NK | Children with pervasive developmental disorders | From authors English |
NA |
| Nisonger Child Behavior Rating Form (parent and teacher versions) | Aman et al. (1996)198 | Assessment of child and adolescent behaviour | Q; parents or teachers Blinding: No/potential |
76 items Interval: NA |
Two domains: Positive Social (10 items), subscales: Compliant/calm and Adaptive social Problem Behavior (66 items); six subscales: Conduct problem, Insecure/anxious, Hyperactive, Self-injury/stereotypic, Self-Isolated/ritualistic, and Overly sensitive |
3–16 years | NK | Children with developmental disabilities, namely those with intellectual disability and/or ASDs | Available online at: www.psychmed.osu.edu/ncbrf.htm | NA |
The CBCL has forms for children aged 1.5–5 years and 6–18 years, and this linkage across ages is a strength of the tool for longitudinal studies. The items can be scored on psychiatric scales, although this may not be as relevant for children with ASD up to the age of 6 years. It was used in three observational studies and three intervention evaluation studies in this review. Information on measurement properties is lacking in terms of reliability and sensitivity to change. The participants at the Discussion Day liked the clear instructions, with a time frame of 2 months, and the wide range of questions, including a qualitative section at the end enquiring about the best things about the child. The three-point scale may not provide sufficient range to capture change. The participants noted that the short questions do not establish the underlying reasons why a child might show the behaviours.
The following four behaviour scales have all been developed for individuals with disabilities.
The ABC only just overlaps with our target age group, and the content clearly derives from work with older individuals with intellectual impairments. It was used in four observational studies in our review, with children as young as 3 years. There is reasonably strong evidence for its measurement properties in children with ASD.
The BISCUIT-Part 3 is, by contrast, a short scale focused on infants up to 37 months of age. It was used in one observational study in our review, and the evidence for its structural validity was not strong.
The HSQ-PDD version is relatively new, and was used in one intervention evaluation study in our review. It originates from the Research Units on Pediatric Psychopharmacology Autism Network. The evidence for its measurement properties is strong, including responsiveness to change.
The NCBRF starts with 10 positive social items, before the 66 problem items. Parents are also invited to mention special circumstances that may have affected the child’s behaviour in the last month. Participants at the Discussion Day particularly appreciated that the items included some which were relevant to ASD. However, participants thought some items were poorly worded (e.g. ‘resisted provocation’), several were not relevant to children in the age range up to 6 years (including items such as ‘feels worthless or inferior’) and some items would be typical for a 3-year-old (e.g. ‘runs away from adults’). The evidence on measurement properties was mixed. This tool was used in one intervention evaluation study in the review.
Global measure of functioning
For details, see Table 34.
| Name of the tool | Authors, date(s), history of revisions | What it claims to measure | Method and by whom measured/reported | No. of items and time taken | Subscales | Age range and entry criteria | Whether norms available, clinical cut-offs | Population for which designed | Cost/availability/languages | Training required |
|---|---|---|---|---|---|---|---|---|---|---|
| Behavior Assessment System for Children- Second Edition, Parent and Teacher Rating Scales | Reynolds et al. (2004)181 | Both adaptive and problem behaviours in the community and home setting | Q; completed by: parents/caregivers, teachers, clinicians Forms: The Teacher Rating Scales (TRS), Parent Rating Scales (PRS), Student Observation System (SOS) and Structured Developmental History (SDH) Blinding: No/potential |
134–160 items (parent), 100–139 items (teacher), depending on age; 10–20 minutes Interval: NK |
Nine clinical subscales: Aggression, Anxiety, Attention problems, Atypicality, Conduct problems, Depression, Hyperactivity, Somatization, Wthdrawal; five adaptive scales: Activities of Daily Living, Functional Communication, Adaptability, Leadership, Social Skills | Ages: 2 years to 21 years, 11 months (P and T) | Norms available | General | Forms and manuals from publisher BASC-2 Starter Kit US$125.50 English, Spanish |
Professionals or paraprofessionals with formal graduate-level training or clinicians with training in psychological assessment |
| Psychoeducational Profile-Reviseda | Schopler et al. (1990)214 | The developmental level of young children with autism | O; by therapists or psychologists Blinding: Yes |
131 items, Developmental Scale; 43 items, Behavioural Scale 45–90 minutes Interval: NK |
Seven developmental subscales; four behavioural subscales | 6 months to 7 years, but can be used for up to 12 years | Norms available | Children with autism or related developmental disorders | English | The PEP-R can be administered, scored and interpreted by anyone who has experience working with and testing children |
| Psychoeducational Profile-Third Edition | Schopler et al. (2005)220 | The skills and behaviours of children with autism and communicative disabilities | O; by therapists or psychologists and Q (caregiver report, by parent/caregiver) Blinding: Yes (and no) |
45–90 minutes Interval: NK |
Three composite scores: Communication, Motor and Maladaptive behaviors 10 performance subtests: Cognitive verbal/preverbal, Expressive language, Receptive language, Fine motor, Gross motor, Visual-motor imitation, Affective expression, Social reciprocity, Characteristic motor behaviors, Characteristic verbal behaviors |
6 months to 7 years | Norms available | Children with autism and communicative disabilities | Forms and manuals from publisher STAR Program: Strategies for Teaching Based on Autism Research Level III, Complete Kit US$345 With scoring software $588.00 English |
The PEP-3 can be administered, scored and interpreted by anyone who has experience working with and testing children |
| Scales of Independent Behaviour-Revisedb | Bruininks et al. (1996)224 | Adaptive behaviour and problem behaviour | O; direct assessment by clinicians Blinding: Yes |
283 items 45–60 minutes for Full Scale; 15–20 minutes for Short Forms Interval: NK |
14 Adaptive Behaviour subscales, Eight Problem Behaviour subscales | Infants to 80+ years | Norms available | General | Forms and manuals from publisher Complete SIB-R Kit (interview book, manual, full scale, short form and early development response booklets) US$689.95 English |
Training in a relevant professional discipline |
| Vineland Adaptive Behavior Scales: Survey Form; Classroom (VABS-II, 2005 available) | Sparrow et al. (1984)167 | Personal and social sufficiency of individuals from birth to adulthood | I or Q; caregivers or teachers Blinding: potential |
297 items, (SurveyForm); 244 items, (Classroom) 20–60 minutes Interval: NK |
Five domains: Communication; Daily Living Skills; Socialisation; Motor Skills; Maladaptive Behavior | Birth to 18 years 11 months (Survey Form) 3 years to 12 years, 11 months (Classroom) |
Norms available267 (including supplementary norms for autism) | General | Vineland-II Complete Starter Kit (Survey, Expanded and Teacher Rating Forms, Manual) $420.65 English and Spanish |
Training in a relevant professional discipline |
| Vineland Adaptive Behavior Scales-Screener version | Sparrow et al. (1993)54 | Assess for research purposes the personal and social sufficiency of individuals | I; child’s primary caregiver Blinding: potential |
45 items 15–20 minutes |
Three domains: Communication, Daily Living Skills and Socialisation | Specific versions for – 2, 3–6, 6–12, 12–18 years | Norms available | Primarily developmentally disabled individuals | Forms and manuals are available from the publisher English |
Training in a relevant professional discipline; 3–4 hours of specific training required |
The BASC-2 was not developed for the assessment of individuals with disabilities. It was used in one observational study in the review. The evidence on measurement properties was restricted to discriminating between groups.
Similarly the SIB-R is for the general population (birth to old age). It was used in one intervention evaluation study in this review. The evidence on measurement properties in children with ASD is limited.
The PEP-R and PEP-3 were specifically developed for assessment of children with autism. With an emphasis on identifying learning strengths, uneven development and emerging abilities, they are primarily intended to be useful in educational programming. They were used in four intervention evaluation studies and five observational studies in this review. The evidence on measurement properties (for the PEP-R) was reasonably strong.
The VABS are very widely used in ASD research and clinical practice, and cover birth to 90 years of age. In this review it was used in 67 studies, 24 of which were intervention evaluation. However, evidence from studies specifically on measurement properties in use with children with ASD was limited. Further evidence on the VABS Screener, developed for research purposes, would be useful though the reduced number of items might well restrict responsiveness to change.
Parent stress
For details, see Table 35.
| Name of the tool | Authors, date(s), history of revisions | What it claims to measure | Method and by whom measured/reported | No. of items and time taken | Subscales | Age range and entry criteria | Whether norms available, clinical cut-offs | Population for which designed | Cost/availability/languages | Training required |
|---|---|---|---|---|---|---|---|---|---|---|
| Autism Parenting Stress Index | Silva and Schalock (2012)153 | Measure of parenting stress specific to core and comorbid symptoms of autism | Q; parents or caregivers Blinding: No |
13 items; up to 5 minutes Interval: NA |
Three categories: core autism symptoms, comorbid behaviours and comorbid physical issues | Validation done on children aged 24–72 months old | NK | ASD | Available online: www.midss.org/content/autism-parenting-stress-index-apsi English |
NA |
| Parenting Stress Index-Short Form (Third Edition) | Abidin (1995)228 (PSI-4 SF available, 2007)268 | Parenting stress across a wide range of families and children, including those with ASD | Q; parents Blinding: No |
36 items; 5 minutes Interval: NA |
Three subscales: Parental distress; Parent–child dysfunctional interaction; Difficult child | 1 month to 12 years | Norms and reference group profiles available | General | PSI Short Form Manual US$70 Questionnaire forms US$80 English, French |
NA |
| Questionnaire on Resources and Stress-Friedrich Short Form | Friedrich et al. (1983)231 | Level of stress in families of children with disabilities | Q; parents or caregivers Blinding: No |
52 items | Four factors: parent and family problems; pessimism; child characteristics; physical incapacity | To 18 years | Comparative data available | Children with disabilities | Child Psychology Portfolio269 English |
NA |
The APSI lists 13 problem behaviours or areas of concern, and asks about the degree of stress created. Parents in the MeASURe advisory groups, and at the Discussion Day, considered that many of the behaviours listed would not cause stress, and, conversely, that important areas which do cause stress, such as dealing with service providers or taking the child out into the community, were not covered. Therefore, the scale might capture change only in specific areas after intervention. The APSI was used in one intervention evaluation study in the review, by the authors. More evidence is required about its measurement properties.
The PSI has a long history and was designed to assess the level of difficulties experienced by parents of children with behavioural and emotional problems, in particular those parents who are at risk of dysfunctional parenting. The one-page Short Form has a mixture of questions about the child and about parent feelings. Participants at the Discussion Day found the questions very negatively worded and wondered whether parents would be wary of being judged. They commented that aspects such as resilience, and having a support network, were important and not included. The PSI was used in eight intervention evaluation studies and three observational studies in the review. Evidence for its measurement properties in use with parents of children with ASD is relatively strong.
The QRS-F has wide use in the field of child disability. Parents at the advisory group meetings found it negative in wording and were uncomfortable with the yes/no scoring format. They considered this would also limit measurement of change. The QRS-F had been used in four intervention evaluation studies and three observational studies in the review. Evidence on measurement properties when used with parents of children with ASD was limited.
Additional tools
There are several subdomains for which there is either a lack of tools, or a lack of evidence, about the use of such tools with young children on the autism spectrum. We will briefly consider some tools that may hold promise in future reviews, and also discuss some approaches to outcome measurement and monitoring of progress, which are overlooked by the systematic review process adopted in MeASURe.
Subdomains for which tools are lacking
In the Social awareness subdomain, evidence on measurement properties with children on the autism spectrum was limited. This is an example of when tools are likely to have been developed first with typically developing children. Examples include the ESCS270 and the CSBS-DP. 125 In the recent review of social communication scales for use in medication trials in ASD,238 both of these scales were rated ‘appropriate with conditions’ on the basis of evidence of reliability and of apparent sensitivity to change in ASD intervention studies. Nevertheless, both tools have ceiling effects, as they are appropriate up to ages equivalent to 30 months and 24 months, respectively, and both tools require detailed training and time for rating. Thus, the strategies adopted in the MeASURe review have not necessarily been overly exclusive.
A second subdomain to be discussed further is that of Habit Problems. Only two tools had been used in longitudinal or intervention studies in this review: subscales of the CBCL and the SSC. In addition, one study271 had used sleep diaries. In the process of searching for papers on measurement properties of tools identified in Chapter 3, some new tools were found for which the paper had included tools searched for by name in establishing convergent validity (see Appendix 9). For example, the Children’s Sleep Habits Questionnaire272 is designed for children aged 4–12 years, and has been reviewed by Majnemer29 for use with children with developmental disabilities. The Family Inventory of Sleep Habits for children with ASD273 focuses on the particular problems of sleep anxiety and bedtime resistance. The Brief Autism Mealtime Behavior Inventory274 is a tool recently developed specifically to assess eating problems in children with ASD. Thus future reviews should provide additional evidence regarding measurement tools in ASD for this important subdomain.
Domains of Participation and Family Measures are particularly under-represented in this review of tools. Although several Family tools had been used in studies in Chapter 3, no examination of their measurement properties in studies with children with ASD has been identified. This is a clear research gap. Similarly it would be desirable to have further exploration in ASD of tools related to social inclusion, such as the School Liking and Avoidance Questionnaire,275 which can be teacher rated or self-reported by children as young as 3 years. 276
Other approaches to measurement
The search for papers on measurement properties of tools has the effect of missing some approaches that have a legitimate place in monitoring the progress of young children with ASD. As mentioned in Chapter 4, the tool used most often in nurseries in UK is the Early Years Foundation Stage Profile. A number of other curriculum-based tools had been used in observational studies in the review. Such tools have the benefit of being closely related to programme planning for individual children. However, criterion-referenced assessment approaches are not usually examined in research for their measurement properties such as reliability and validity.
Other approaches that individualise assessment for children include ‘Target Behaviours’ and Goal Attainment Scaling. With the individuality of needs of young children with ASD, it may be particularly appropriate to adopt an idiographic approach to outcome measurement. Yet for the purposes of research, the ability to compare across individuals is required. A Target Behaviours (or target symptoms) methodology was included in the battery of tools recommended by the Research Units on Pediatric Psychopharmacology277 and used by one study278 in this review. When a specific behaviour is the target of intervention, the parent is interviewed about its nature, frequency and intensity, and a vignette description is prepared. At follow-up, the same questions are asked about the behaviour; the two vignettes are then compared and rated for degree of change on a nine-point scale by an expert panel. Thus this idiographic measure allows for ‘blind’ rating, and provides an opportunity to capture change. Inter-rater reliability across the expert panel can be assessed. Goal Attainment Scaling requires greater professional input (than Target Behaviours), including training and practice, to enable a suitable behavioural goal to be defined and scaled (with description of outcomes on a five-point scale between ‘worst expected outcome’ to ‘best expected outcome’). There are continuing debates about appropriate statistical analyses of Goal Attainment Scaling scores, such as whether accomplishment of different individual goals can be summed into a group score. Nevertheless, if the Goal Attainment Scaling scores are done by observation, the assessor can be ‘blind’. 279 These approaches to responsive measurement of relevant and individualised outcomes merit further exploration for young children with ASD.
In future, there will be a need to examine the measurement properties of biophysical tools, such as actigraphy and sleep recordings, i.e. of particular relevance to certain types of intervention, which have the apparent benefit of objectivity in measurement.
Finally, the review has not identified and evaluated tools used in economic analyses. Very little research has investigated the measurement of preference-based health-related quality-of-life outcomes in children with ASD. 280 Tools that have been examined for children with ASD include the Health Utilities Index Mark 3280 and for parents the European Quality of Life-5 Dimensions three-level version. 281 These studies indicate promising findings on the measurement properties of the tools, but further research is required to establish whether they are appropriate for use in studies of children with ASD and how they may contribute to the evaluation of the cost-effectiveness of therapies and services.
How to choose a robust outcome tool
For a researcher wishing to choose a robust outcome tool, there are a series of complex decisions to negotiate. First there is the issue of what should be the primary goal of intervention – a focus on reducing particular ASD impairments or overall severity, improving child functional outcomes or quality of life for child and/or family? Each of these goals implies different conceptual and practical considerations, and different targeted outcomes reflecting the competing priorities. The second area for consideration has to do with external validity. The dilemma here is that subjective (particularly family reported) measures are those with the greatest external validity, as it is the experience of children and families that interventions most want to improve; however, such ratings are prone to expectation and placebo effects within interventions and such evidence is downgraded in systematic review criteria (such as Grading of Recommendations, Assessment, Development and Evaluation, and The Cochrane Collaboration). A final challenge concerns ideal measurement properties. The researcher would wish to identify outcome tools that are responsive to change and also appropriate across the different settings that children experience. Aggregated measures (e.g. combining parent and teacher report with direct observation of language skills) might increase stability and reduce correlated measurement error but are controversial. Responsiveness in tools may be limited in studies involving heterogeneous samples of children by floor and ceiling effects (‘floor effects’ when children have limited capacity to change; ‘ceiling effects’ when they have already mastered the skill). Furthermore, the review of measurement properties of tools in Chapter 4 provided little evidence about measurement error or responsiveness to change.
For a clinician or educator wishing to monitor the progress of a child with ASD over time, in a nursery or other setting, there are other challenges. The tool has to have good face validity, making sense to all of those who will report on children’s behaviours, and a high level of test–retest reliability so that clear judgements can be made about whether or not observed change really represents progress. It would ideally include the whole range of outcomes (strengths and difficulties) considered important by parents and staff involved with the child, and yet not take hours to complete.
In this chapter, the synthesis of evidence has demonstrated that we know more about some tools because they have been in use for longer. This is not necessarily a strength, where the models of understanding autism or child development which informed their development has changed. For all tools identified, there are areas of evidence lacking about their measurement properties. There are also many areas, identified as important by parents of children with autism, and by practitioners and researchers, for which tools are lacking. Chapter 5 outlines recommendations for further research.
Thus, the following listing (Table 36) is not a battery of the ‘best’ tools; it is a summary of those 12 tools – identified through the MeASURe review process – that have more points in their favour than others. For inclusion in the table, the tools had positive evidence for three or more measurement properties, derived from more than one paper about its use with young children with ASD (see Chapter 4). When there was more than one similar tool within a subdomain meeting these criteria, the stronger was selected (e.g. the HSQ-PDD rather than the ABC, both tools measuring behaviour and developed in atypical populations). The level of burden (i.e. time, training, cost required) (see for example Lecavalier et al. 239) is not considered in this summary, as its relevance will vary across the circumstances and purposes of both research and clinical practice; furthermore, direct assessment tools are the most expensive in time for training, but are those for which the assessor can be ‘blind’.
| Tool name (subdomains) | Interventiona | Blindingb | Stakeholder view | Age rangec | Spreadd |
|---|---|---|---|---|---|
| Autism Diagnostic Observation Schedule (Symptom severity, Restricted/repetitive behaviour, Social communication, Social functioning) |
+ | + | + | + | + |
| Baby and Infant Screen for Children with aUtIsm Traits-Part 2 (Emotional regulation) |
– | – | NK | – | – |
| Behavioral Summarized Evaluation-Revised (Symptom severity, Global measure of outcome) |
– | + | NK | + | – |
| Child Behavior Checklist (Attention, Emotional regulation, Behaviour, Habit problems) |
+ | – | + | + | + |
| Childhood Autism Rating Scale (Symptom severity) |
+ | ? | NK | + | + |
| Home Situations Questionnaire-Pervasive Developmental Disorders version (Behaviour) |
– | – | NK | – | – |
| MacArthur–Bates Communicative Development Inventory (Language) |
+ | – | NK | – | + |
| Parenting Stress Index (Parent stress) |
+ | – | – | + | + |
| Pervasive Developmental Disorders Behavior Inventory (Global measure of outcome) |
+ | – | – | + | + |
| Preschool Imitation and Praxis Scale (Social awareness) |
– | + | NK | + | – |
| Psychoeducational Profile (Global measure of function) |
+ | + | NK | + | + |
| Social Responsiveness Scale (Symptom severity) |
+ | – | + | + | + |
Chapter 6 Conclusions and recommendations
Introduction
The MeASURe project approach had significant strengths:
-
MeASURe was delivered by a team of experts in systematic reviewing, working with health and education experts in the diagnosis, management and measurement of progress and outcomes in ASD.
-
MeASURe used a systematic and multilayered approach to searching the literature.
-
MeASURe used a validated approach to the assessment of the quality of papers concerning measurement properties of tools.
-
The MeASURe group consulted with parents of children at three stages, with young people with ASD, and engaged with UK professionals through a survey and meetings.
This combination of procedures goes beyond the approaches used by other teams and individuals making recommendations of tools to use in measuring outcome in ASD. 27,234–236,238–240
Reflections on consultation
The MeASURe project greatly benefited throughout from the involvement of parent advisory groups and individuals on the autism spectrum. To our knowledge, similar projects examining tools for outcome measurement in ASD have not included such investment in efforts for consultation and joint working with key stakeholders. Other stakeholders (health and education professionals, other researchers in ASD) were surveyed and involved in the Discussion Day.
As mentioned at the end of Chapter 2, the predominant focus of assessment tools on ‘difficulties’ rather than ‘strengths’ potentially misses some important features that would allow measurement of children’s progress in acquisition of skills and capacity to adjust to their own profile of abilities, as well as key features for planning interventions. The tasks undertaken at the Discussion Day were illuminating: several professionals commented on the experience of focusing on up to six questionnaires one after another, with about 10 minutes for each one. They felt pressured and found their mood sinking after reading so many negative descriptions of child behaviour or parent stress. Further, the professionals reflected on what they may regularly expect parents to undertake during research projects or in clinical assessments, not realising the emotional challenge that such assessments involve. As one young adult on the autism spectrum involved in the MeASURe project commented further in an e-mail:
It occurred to me quite strongly that, while we tend to think of ‘assessment’ as being essentially a descriptive, documentary process, it is to an extent also transformative . . . This led me to think about the ethical considerations regarding the use of assessment for research, because unlike in a clinical, intervention-based environment, the aspect of reciprocity and ‘what’s in it for the parents/child’ may not be quite so clear . . . I wonder whether it is considered and discussed with parents whether they consent to the possible transformative impact of taking part in assessments which . . . can be suggested to represent a pejorative deficit model of autism.
This quote reminds professionals and researchers of the essential requirement to involve parents of young children with ASD in a meaningful partnership, with full discussion of what participation in an assessment involves (benefits as well as pressures), what it can convey and how it may be used. Attention should be paid to sharing the findings of assessment in an accessible format. These are important principles to be followed by health and education professionals, and by researchers.
Ideally, questionnaire-based tools to measure outcomes in ASD would include assessment of both skills and difficulties, contain a balance of positive and negative statements, and be attractive to look at (with an adequate font size and clear instructions) – qualities that we found many tools lacked. Nowadays, many individuals may prefer to complete questionnaires online rather than on paper, allowing much greater inclusion of visual enhancements. Most tools do not have electronic versions and have not been validated for this mode of administration. Other considerations about the process of direct clinical assessments were contributed by young people on the autism spectrum. These included the need for professionals to take time to get to know the child before assessment and to make sure that practical arrangements allow the child to take part to their best capacity.
Valued outcomes not represented
The dissonance between attention to the behaviours considered in the diagnostic process in autism, and the lack of focus on valued outcomes, was very evident in the MeASURe project as touched on above and in Chapter 2. The tools that were developed primarily to aid assessment and diagnosis have influenced also what we have called ‘global measures of outcome’, i.e. they include lists of symptoms that may or may not be amenable to change, and which may or may not be related to the focus of intervention. The emphasis may arise from the orientation of some research teams whose primary aim is to ‘cure autism’. Some parents may indeed share such an aim, especially early on, around the time of the child’s diagnosis. In contrast, parents and young people on the autism spectrum consulted in the MeASURe project focused on living with autism in daily life, on reducing stress and building up skills, and on enabling environments to be more ‘autism friendly’ and thus promote participation. Bringing these different perspectives – and valued outcomes – together would be likely to benefit children with ASD and their families, and is consistent with the recommendations of the Kennedy Report. 16 Some of the additional and relevant outcomes that were considered important to measure would thus include social interaction skills (e.g. with brothers, sisters and other children) and everyday adaptive skills, recognition of co-occurring problems (e.g. sleep, eating), well-being of the child and family quality of life. The review has revealed the paucity of tools with known measurement properties in these areas.
Limitations
The aim of the MeASURe project was to identify robust tools that might be recommended for use with children with ASD up to the age of 6 years, and the procedures were designed to that end. Because of this, the chosen procedures led to some limitations of the evidence. By searching for studies which had included a sample of children with ASD (or at least consideration of autism characteristics in children with neurodevelopmental disorders) we did not assess and report the measurement properties of tools when used with other samples; very many tools are first developed with samples of typically developing children. Therefore, we are not representing the full spread of information about the quality of some of the tools considered when used for other purposes. The process adopted also disadvantages recently developed tools, for which evidence of their measurement properties will accumulate in the future.
The review did not include papers about the translation of a tool into a language other than English, except where the paper did then focus on assessment of measurement properties of the tool. Language and cultural issues can affect how tools perform. 282 Therefore, the review does not provide information on how robust a tool may be if translated for use in the UK with a child whose home language is not English. The review has not commented on how appropriate some North American tools may be (or the changes which may be required) for use in the UK. As mentioned in Chapter 5, there are important types of measurement (e.g. curriculum based, idiographic) which are also not represented in the review because of the chosen procedures.
Outcomes of MeASURe
The detailed systematic reviews and consultation processes led to production of a conceptual framework for the measurement of outcomes in studies of children with ASD up to approximately 6 years of age (see Chapter 2). We expect this framework to be of use to researchers in the field of autism, and also to practitioners when considering how to monitor the richness of potential effects of their interventions.
The fifth aim of the MeASURe project was to propose a potential battery of robust tools and outcome measures for use in research and clinical practice. It would be particularly desirable to have such a battery used across intervention studies, to enable meta-analysis. However, in the course of the project, the unbalanced nature of the evidence has meant that we have decided to list only the 12 tools with more than a minimum of positive evidence about their measurement properties (see Chapter 5). This represents the current state of evidence but given the limitations, and the scope and overlap of the tools, the list cannot constitute a ‘recommended battery’. Nevertheless, it gives guidance on some tools for which further study of measurement properties, and re-evaluation of presentation, would repay effort.
The limitations of what we know about the tools include in most instances no evidence about responsiveness to change. The COSMIN checklist did not require that a study should compare degree of change between points in time against a ‘gold standard’, which would be difficult to achieve in early autism studies when there is no such comparator; rather, it allowed for evidence to be obtained through statement of a priori directional hypotheses concerning expected change. Yet this has rarely been done to establish the measurement properties of an instrument (the development of the HSQ-PDD tool209 being an exception in the list of 12 tools). Obviously, the extent to which significant treatment effects have been found in studies using such tools as part of their evaluation could add incidental backing to the weight of positive evidence in favour of using a tool. However, given the likely effects of publication bias, and difficulties in interpretation of negative findings (whether a reflection of an ineffective intervention or of an unresponsive tool), this is not a systematic source of information.
Improvement is also required in the design and procedures of studies concerning the measurement properties of tools. In particular, the limitations in the available evidence have restricted our capacity to comment on issues such as generalisability as most studies used clinic or convenience samples, were conducted in research rather than naturalistic settings, and did not take into account appropriateness across the range of ability in children with ASD.
Nevertheless, the review has provided a searchable source of evidence for researchers, and clinicians, on the qualities of many tools used with young children with ASD. Let us take a worked example. Both parents and professionals had ‘challenging behaviour’ as an important outcome in their top 10 constructs (see Chapter 2). What can we learn about the various possible tools? In Appendix 5, we can see that 12 different approaches to the measurement of behaviour problems were found, with information about the samples of children participating in those studies, the subscales used and the outcomes measured according to the study authors. Then in Chapter 4, we can inspect Table 19 regarding Behaviour problems, where the evidence about papers reporting the measurement properties of tools is summarised. Here we find that evidence was found about only six of those tools in use with children with ASD. The detail of the findings from the individual papers can be viewed in Appendix 8. Let us say that a researcher is particularly concerned to choose a tool with positive evidence concerning structural validity in ASD. This review suggests three choices: the ABC, the CBCL and the HSQ-PDD. By inspection of Table 33 in Chapter 5, the researcher learns that the ABC was not designed for the younger end of the age range, despite having been used in studies with children with ASD as young as 3 years. The HSQ-PDD is not yet freely available, therefore the researcher might choose the CBCL 1.5–5 years, reassured that stakeholders at the Discussion Day were generally positive about the scale.
As a further example, we might consider a research team wishing to evaluate a targeted intervention focusing on improving joint attention and imitation – core impairments in young children with autism. 283,284 Skills in joint attention and imitation are fundamental to the development of language and social development. For this reason, many recent early intervention studies have focused on enhancing these skills in the context of reciprocity between a child and familiar adult (parent or teacher). 285,286 What model of outcome measurement might be appropriate for a short-term intervention focusing on joint attention and imitation? Proximal measures will include direct observation and coding of adult–child interaction (see for example Kasari et al. 287 and Kaale et al. 288). Focused measurement of joint engagement and joint attention may lend itself to standardisation in future, but could not be reviewed by MeASURe as the codes are adapted from study to study (see Appendix 5). Is there a more formal way to measure the broader subdomain of Social awareness? In Table 3, nine possible measures are listed; however, in Table 8, only two have supportive evidence on their measurement properties, and the stronger is the PIPS, included in the MeASURe list of 12 tools (see Table 36). The research team hypothesises that there will be a more distal intervention effect on Language; in Table 3, 17 measures are listed, including parent report of vocabulary and direct testing. They consult Table 11 and find limited evidence for only two direct assessments in children with ASD (the MSEL and the PLS-4). This then requires a pragmatic decision about which to choose. Parent report of vocabulary (MCDI) has greater support, and is also included in the MeASURe list of 12 tools (see Table 36). The research team expects to find a broader effect on social communication; eight tools are listed in Table 3 but only three have supportive evidence in Table 16. The ADI-R is a diagnostic interview, and so not suitable for short-term outcome measurement. The ADOS has strong properties (see Table 24) and the inclusion of the Toddler Module in ADOS-2 allows very young children to be assessed. However, it is again primarily a diagnostic tool and evidence on responsiveness to change is lacking. The Brief Observation of Social Communication Change (BOSCC), which originated as a development from the ADOS, may be an option in future having been developed explicitly for this purpose, allowing assessment blind to trial allocation (see Chapter 5). The SRS (see Table 36) would, in principle, allow parents to report on their children’s skills and difficulties, but the total score covers multiple components, and, again, this tool lacks evidence on responsiveness to change (Table 6). Thus the MeASURe review allows a research team to make an informed though difficult choice of tools to address their model of outcome measurement.
Conclusions
A number of research gaps and suggestions have been highlighted in this report. In order for a battery of robust tools and outcome measures for use with young children with ASD to become a reality, the following points would need to be taken into consideration:
-
Prior to development of new tools it would be helpful for researchers to consult approaches to evaluation of the properties of tools, such as the freely available COSMIN approach (www.cosmin.nl) or the resources provided by the Patient Reported Outcomes Measurement Group at the University of Oxford (http://phi.uhce.ox.ac.uk/home.php). This would guide the design of the development studies so that all important properties are considered.
-
Critically, stakeholders and especially parents and individuals on the autism spectrum should be included from the start of development of new tools, to discuss the purpose of the tool, its content and presentation, and the likely impact on children and parents of the tool in use. The NIHR INVOLVE (www.involve.org.uk) provides a range of resources to advise on working in partnership with service users.
-
Tools should be developed and validated particularly in areas such as quality of life (child well-being) and participation in life situations (such as social inclusion) that were highly valued by parents and people with ASD. Consideration should be given to the content of tools, so that direct assessments are attractive to young children, and questionnaires include positively worded items and strengths as well as difficulties.
-
However, there are already multiple tools available and more being developed. More is not necessarily better. There were 75 tools for which no evidence was discovered for Chapter 4. Some of these tools could be suitable for further evaluation of their measurement properties with children with ASD, as an alternative to producing brand new tools measuring the same domain. Such studies should examine face and content validity, with input from parents of young children with ASD. The study design should evaluate measurement invariance across the range of abilities in ASD and across settings.
-
The list of 44 new tools found during the Chapter 4 searches (see Appendix 9) have already been used with children with ASD, and so may also be examined further with reference to their measurement properties.
-
One urgent research priority is to establish a robust tool that can be measured ‘blind’, which captures social communication skills and is suitable across the age and ability range in children with ASD up to the age of 6 years. The BOSCC may prove to be such a tool, as mentioned in Chapter 5.
-
Measurement of RRBs is more problematic, as valid approaches to direct observation are essentially not possible after the first 1 or 2 years of life. A tool such as the ADOS does measure RRBs but only within a structured play setting, which may not elicit the behaviours that are characteristic of an individual child. Only one parent questionnaire had sufficient evidence about measurement properties to be included (see Table 9), so more development work is required on the most appropriate RRB measurement tools, which can be used across settings (such as home and nursery).
-
Questionnaire approaches to global measure of outcome have usually been hampered by covering a wide age and ability range (thus including items inappropriate for a young child) and focusing on (negatively worded) symptoms rather than skills. A new approach is needed, developed in partnership with parents and with individuals on the autism spectrum, to attempt to generate a useful and meaningful global measure of outcome and response to intervention for young children with ASD.
-
In addition to measurement of core ASD characteristics, the MeASURe project has highlighted the importance of also measuring children’s functioning in everyday life. The VABS are the most extensively used tool for global measure of function, with surprisingly little evidence available about their measurement properties in use with young children with ASD. We therefore recommend that such studies be undertaken.
-
The MeASURe project did not include all of the procedures required to establish agreement on a core outcome set for young children with autism. The COMET Network suggests various procedures (www.comet-initiative.org/resources/coreresourcepack), which enable consensus to be reached, including rounds of consultation through Delphi surveys. Using levels of agreement on which suggested outcomes are deemed ‘essential’, with feedback to consultees at each round and a final consensus meeting of stakeholders, it is possible to refine a large number of possible outcomes into a core listing. Given the foundation established in the MeASURe project, these further procedures could be followed, ideally in conjunction with international partners, in order to create a consensus core outcome set.
Research recommendations in order of priority
-
Development of a tool to measure child quality of life, with careful attention to content validation for children with ASD.
-
Assessment of the measurement properties of a newly developed tool, the BOSCC, by research group(s) in the UK, as a potential primary outcome for early intervention trials focused on improving social communication in young children with ASD.
-
Assessment of the measurement properties of tools developed for children with ASD up to the age of 6 years, which focus on problems such as anxiety and sleep.
-
Further studies of the measurement properties of the VABS in young children with ASD.
-
Assessment of the measurement properties of the UK Early Years Foundation Stage Profile for use with young children with ASD.
-
Development of a questionnaire tool appropriate for young children with ASD to measure repetitive behaviour and circumscribed interests, which can be used across settings.
-
Establishment of an agreed core set of outcomes to be measured in effectiveness trials of early intervention in ASD.
Given the rapid developments in the field of research into young children with ASD, it would be appropriate to update the review of outcome measurement within 3 years.
Acknowledgements
The MeASURe project team are very grateful to the parents of children with ASD, and the children and adults on the autism spectrum, who participated at several points in the project. They provided important insights and experiences. We are also grateful to the hundreds of health and education professionals who completed the survey of assessment practice, and especially to those who participated in the Discussion Day. We are also grateful to the Mental Health Research Network North East, which funded aspects of the public participation work.
Gillian Loomes contributed rich and clear insights from her perspective as an autism advocate. Camilla McHugh contributed to the parent advisory groups and created Figure 1. Andrew Pickles read the first draft of the report and made invaluable comments. Jane Tilbrook was the very able administrator for the project, and tireless in her battle with EndNote. We are grateful to all of these experts.
We are grateful also for the additional financial support for this project provided by the Research and Development Division of the Public Health Agency, Northern Ireland.
Contributions of authors
Helen McConachie (Professor, Clinical Psychology) led the design of the project; participated in all stages of review of the project; led aspects of consultation with stakeholders; conducted sifting and data extraction; supervised data extraction; wrote sections of the report; and finalised the report.
Jeremy R Parr (Senior Lecturer, Paediatric Neurodisability) contributed to the design of the project; participated in all stages of review of the project; led aspects of consultation with stakeholders; wrote sections of the report; created the scientific summary; and commented in detail on drafts.
Magdalena Glod (Research Assistant, Psychology) conducted sifting and data extraction; wrote sections of the report; and created tables.
Jennifer Hanratty (Research Fellow, Systematic Reviews) conducted sifting and data extraction; wrote sections of the report; and created detailed appendices and tables.
Nuala Livingstone (Research Fellow, Systematic Reviews) contributed to the design of the project; participated in all stages of review of the project; conducted the scoping review of qualitative literature; conducted sifting and data extraction; wrote sections of the report; and created tables and figures.
Inalegwu P Oono (Research Assistant, Systematic Reviews) conducted sifting and data extraction, and created tables.
Shannon Robalino (Information Specialist, Health Research) created the systematic searches and wrote sections of the report.
Gillian Baird (Professor, Paediatric Neurodisability) contributed to the design of the project and commented in detail on drafts.
Bryony Beresford (Professor, Social Policy) contributed to the design of the project; conducted the scoping review of qualitative literature; and wrote sections of the report.
Tony Charman (Professor, Clinical Psychology) contributed to the design of the project; participated in all stages of review of the project; commented in detail on drafts.
Deborah Garland (Parent, Resource Centre Manager) contributed to the design of the project; participated in all stages of review of the project; led aspects of consultation with stakeholders; and contributed to the Plain English summary.
Jonathan Green (Professor, Child and Adolescent Psychiatry) contributed to the design of the project and commented in detail on drafts.
Paul Gringras (Professor, Paediatric Neurodisability) contributed to the design of the project and led aspects of consultation with stakeholders.
Glenys Jones (Lecturer, Education) contributed to the design of the project; participated in all stages of review of the project; led aspects of consultation with stakeholders; and commented in detail on drafts.
James Law (Professor, Speech and Language Therapy) contributed to the design of the project and commented in detail on drafts.
Ann S Le Couteur (Professor, Child and Adolescent Psychiatry) contributed to the design of the project; participated in all stages of review of the project; led aspects of consultation with stakeholders; and commented in detail on drafts.
Geraldine Macdonald (Professor, Child Care Research) contributed to the design of the project; participated in all stages of review of the project; supervised data extraction; and wrote the Plain English summary.
Elaine M McColl (Professor, Health Services Research) contributed to the design of the project and commented in detail on drafts.
Christopher Morris (Senior Research Fellow, Child Health) contributed to the design of the project; participated in all stages of review of the project; led aspects of consultation with stakeholders; conducted the scoping review of qualitative literature; wrote sections of the report; contributed to the Plain English summary; and commented in detail on drafts.
Jacqueline Rodgers (Senior Lecturer, Psychology) contributed to the design of the project; participated in all stages of review of the project; supervised data extraction; and commented in detail on drafts.
Emily Simonoff (Professor, Child and Adolescent Psychiatry) contributed to the design of the project; participated in all stages of review of the project; and commented in detail on drafts.
Caroline B Terwee (Assistant Professor, Clinimetrics) contributed to the design of the project; participated in all stages of review of the project; helped to create the systematic searches; and commented in detail on drafts.
Katrina Williams (Professor, Paediatric Neurodisability) contributed to the design of the project and commented in detail on drafts.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- American Psychiatric Association (APA) . DSM-5 Development. DSM-5 Implementation and Support n.d. www.dsm5.org/Pages/Default.aspx.DSM-V (accessed 2 March 2015).
- Baird G, Simonoff E, Pickles A, Chandler S, Loucas T, Meldrum D, et al. Prevalence of the disorders of the autism spectrum in a population cohort of children in South Thames. Lancet 2006;368:210-15. http://dx.doi.org/10.1016/S0140-6736(06)69041-7.
- Baron-Cohen S, Allison C, Williams J, Matthews FE, Brayne C. Prevalence of autism-spectrum conditions: UK school-based population study. Br J Psychiatry 2009;194:500-9. http://dx.doi.org/10.1192/bjp.bp.108.059345.
- Brugha TS, McManus S, Bankart J, Scott F, Purdon S, Smith J, et al. Epidemiology of autism spectrum disorders in adults in the community in England. Arch Gen Psychiatry 2011;68:459-65. http://dx.doi.org/10.1001/archgenpsychiatry.2011.38.
- Knapp M, Romeo R, Beecham J. Economic cost of autism in the UK. Autism 2009;13:317-36. http://dx.doi.org/10.1177/1362361309104246.
- Charman T. Glass half full or half empty? Testing social communication interventions for young children with autism. J Child Psychol Psychiatry 2011;52:22-3. http://dx.doi.org/10.1111/j.1469-7610.2010.02359.x.
- Oono IP, Honey E, McConachie H. Parent-mediated early intervention for young children with autism spectrum disorders (ASD). Cochrane Database Syst Rev 2013;4. http://dx.doi.org/10.1002/ebch.1952.
- Ospina MB, Seida JK, Clark B, Karkhaneh M, Hartling L, Tjosvold L, et al. Behavioural and developmental interventions for autism spectrum disorder: a clinical systematic review. PLOS ONE 2008;3. http://dx.doi.org/10.1371/journal.pone.0003755.
- Maskey M, Warnell F, Parr JR, McConachie H. Emotional and behavioural problems in children with Autism Spectrum Disorder. J Autism Dev Disord 2012;43:851-9. http://dx.doi.org/10.1007/s10803-012-1622-9.
- Charman T, Taylor E, Cockerill H, Brown JA, Baird G. Outcome at 7 years of children diagnosed with autism at age 2: predictive validity of assessments conducted at 2 and 3 years of age and pattern of symptom change over time. J Child Psychol Psychiatry 2005;46:500-13. http://dx.doi.org/10.1111/j.1469-7610.2004.00377.x.
- Anderson DK, Lord C, Risi S, DiLavore PS, Shulman C, Thurm A, et al. Patterns of growth in verbal abilities among children with autism spectrum disorder. J Consult Clin Psychol 2007;75:594-60. http://dx.doi.org/10.1037/0022-006X.75.4.594.
- Jones EJH, Gilga T, Bedford R, Charman T, Johnson MH. Developmental pathways to autism: a review of prospective studies of infants at risk. Neurosci Biobehav Rev 2014;39:1-33. http://dx.doi.org/10.1016/j.neubiorev.2013.12.001.
- Fein D, Barton M, Eigsti I-M, Kelley E, Naigles L, Schultz R, et al. Optimal outcome in individuals with a history of autism. J Child Psychol Psychiatry 2013;54:195-20. http://dx.doi.org/10.1111/jcpp.12037.
- Annual Report of the Chief Medical Officer 2012: Our Children Deserve Better: Prevention Pays. London: DH; 2012.
- Department of Health (DH) . The NHS Outcomes Framework 2011 12 2010. www.gov.uk/government/uploads/system/uploads/attachment_data/file/213789/dh_123138.pdf (accessed 2 March 2015).
- Kennedy I. Getting it Right for Children and Young People: Overcoming Cultural Barriers in the NHS so as to Meet Their Needs. London: Department of Health; 2010.
- Morris C, Janssens A, Allard A, Thompson-Coon J, Shillling V, Tomlinson R, et al. Informing the NHS Outcomes Framework: evaluating meaningful health outcomes for children with neurodisability using multiple methods including systematic review, qualitative research, Delphi survey and consensus meeting. Health Serv Deliv Res 2014;2.
- Williamson PR, Altman DG, Blazeby JM, Clarke M, Devane D, Gargon E, et al. Developing core outcome sets for clinical trials: issues to consider. Trials 2012;13. http://dx.doi.org/10.1186/1745-6215-13-132.
- Sinha I, Smyth RL, Williamson PR. A systematic review of studies that aim to determine which outcomes to measure in clinical trials in children. PLOS Med 2008;5. http://dx.doi.org/10.1371/journal.pmed.0050096.
- International Classification of Functioning, Disability and Health for Children and Youth. Geneva: WHO; 2007.
- Lai M-C, Lombardo MV, Baron-Cohen S. Autism. Lancet 2014;383:896-910. http://dx.doi.org/10.1016/S0140-6736(13)61539-1.
- Jeans LM, Santos RM, Laxman DJ, McBride BA, Dyer WJ. Early predictors of ASD in young children using a nationally representative data set. J Early Interv 2014;35:303-31. http://dx.doi.org/10.1177/1053815114523319.
- Zwaigenbaum L, Bryson S, Rogers T, Roberts W, Brian J, Szatmari P. Behavioral manifestations of autism in the first year of life. Int J Dev Neurosci 2005;23:143-52. http://dx.doi.org/10.1016/j.ijdevneu.2004.05.001.
- Zwaigenbaum L, Bryson S, Lord C, Rogers S, Carter AS, Carver L, et al. Clinical assessment and management of toddlers with suspected autism spectrum disorder: insights from studies of high-risk infants. Pediatrics 2009;123:1383-91. http://dx.doi.org/10.1542/peds.2008-1606.
- Gilmour J, Hill B, Place M, Skuse DH. Social communication deficits in conduct disorder: a clinical and community survey. J Child Psychol Psychiatry 2004;45:967-78. http://dx.doi.org/10.1111/j.1469-7610.2004.t01-1-00289.x.
- Ketelaars MP, Cuperus J, Jansonius K, Verhoeven L. Pragmatic language impairment and associated behavioural problems. Int J Lang Commun Disord 2009;28:1-17. http://dx.doi.org/10.1080/13682820902863090.
- Bolte EE, Diehl JJ. Measurement tools and target symptoms/skills used to assess treatment response for individuals with autism spectrum disorder. J Autism Dev Disord 2013;43:2491-501. http://dx.doi.org/10.1007/s10803-013-1798-7.
- Wittemeyer K, Charman T, Cusack J, Guldberg K, Hastings R, Howlin P, et al. Educational Provision and Outcomes for People on the Autism Spectrum. London: Autism Education Trust; 2013.
- Majnemer A. Measures for Children with Developmental Disabilities: An ICF-CY Approach. London: Mac Keith Press; 2012.
- Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. J Am Med Assoc 1995;273:59-65. http://dx.doi.org/10.1001/jama.1995.03520250075037.
- Auert E, Trembath D, Arciuli J, Thomas D. Parents’ expectations, awareness, and experiences of accessing evidence-based speech-language pathology services for their children with autism. Int J Speech Lang Pathol 2012;14:109-18. http://dx.doi.org/10.3109/17549507.2011.652673.
- Braiden H, Bothwell J, Duffy J. Parents’ experience of the diagnostic process for autistic spectrum disorders. Child Care Pract 2010;16:377-89. http://dx.doi.org/10.1080/13575279.2010.498415.
- Whitaker P. Supporting families of preschool children with autism: what parents want and what helps. Autism 2002;6:411-26. http://dx.doi.org/10.1177/1362361302006004007.
- Beresford B, Tozer R, Rabiee P, Sloper P. Desired outcomes for children and adolescents with Autistic Spectrum Disorders. Child Soc 2006;21:4-16. http://dx.doi.org/10.1111/j.1099-0860.2006.00008.x.
- Serpentine EC, Tarnai B, Drager KDR, Finke EH. Decision making of parents of children with autism spectrum disorder concerning augmentative and alternative communication in Hungary. Commun Disord Q 2011;32:221-31. http://dx.doi.org/10.1177/1525740109353938.
- Mackintosh VH, GoinKochel RP, Myers BJ. ‘What do you like/dislike about the treatments you’re currently using?’: a qualitative study of parents of children with autism spectrum disorders. Focus Autism Other Dev Disabil 2012;27:51-60. http://dx.doi.org/10.1177/1088357611423542.
- Little L, Clark RR. Wonders and worries of parenting a child with Asperger syndrome and nonverbal learning disorder. MCN Am J Matern Child Nurs 2006;31:39-44. http://dx.doi.org/10.1097/00005721-200601000-00009.
- McHugh C, Bailey S, Shilling V, Morris C. Meeting the information needs of children with chronic health conditions. Phys Occup Ther Pediatr 2013;33:265-70. http://dx.doi.org/10.3109/01942638.2013.799628.
- Nye C, Brice A. Combined vitamin B6-magnesium treatment in autism spectrum disorder. Cochrane Database Syst Rev 2005;4. http://dx.doi.org/10.1002/14651858.CD003497.pub2.
- Williams K, Wheeler DM, Silove N, Hazell P. Selective serotonin reuptake inhibitors (SSRIs) for Autism Spectrum Disorders (ASD). Cochrane Database Syst Rev 2010;8. http://dx.doi.org/10.1002/14651858.CD004677.pub2.
- Wheeler D, Williams K, Seida J, Ospina M. The Cochrane Library and Autism Spectrum Disorder: an overview of reviews. Evid Based Child Health 2008;3:3-15. http://dx.doi.org/10.1002/ebch.218.
- Williams TO, Eaves RC. Factor Analysis of the Pervasive Developmental Disorders Rating Scale with teacher ratings of students with autistic disorder. Psychol Sch 2005;42:207-16. http://dx.doi.org/10.1002/pits.20051.
- Diggle TJ, McConachie HR, Randle VR. Parent-mediated early intervention for young children with Autism Spectrum Disorder. Cochrane Database Syst Rev 2003;1.
- Gold C, Wigram T, Elefant C. Music therapy for autistic spectrum disorder. Cochrane Database Syst Rev 2006;2. http://dx.doi.org/10.1002/14651858.CD004381.pub2.
- Mulloy A, Lang R, O’Reilly M, Sigafoos J, Lancioni G, Rispoli M. Gluten-free and casein-free diets in the treatment of autism spectrum disorders: a systematic review. Res Autism Spectr Disord 2010;4:328-39. http://dx.doi.org/10.1016/j.rasd.2009.10.008.
- Elchaar GM, Maisch NM, Augusto LM, Wehring HJ. Efficacy and safety of naltexone use in pediatric patients with autistic disorder. Ann Pharmacother 2006;40:1086-95. http://dx.doi.org/10.1345/aph.1G499.
- Reichow B, Wolery M. Comprehensive synthesis of early intensive behavioral interventions for young children with autism based on the UCLA young autism project model. J Autism Dev Disord 2009;39:23-41. http://dx.doi.org/10.1007/s10803-008-0596-0.
- Diagnostic and Statistical Manual of Mental Disorders. Washington: APA; 1994.
- The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research. Geneva: WHO; 1992.
- Lord C, Risi S, Lambrecht L, Cook EH, Leventhal BL, DiLavore PC, et al. The Autism Diagnostic Observation Schedule-Generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord 2000;30:205-23. http://dx.doi.org/10.1023/A:1005592401947.
- Siller M, Sigman M. The behaviors of parents of children with autism predict the subsequent development of their children’s communication. J Autism Dev Disord 2002;32:77-89. http://dx.doi.org/10.1023/A:1014884404276.
- Siller M, Sigman M. Modeling longitudinal change in the language abilities of children with autism: parent behaviors and child characteristics as predictors of change. Dev Psychol 2008;44:1691-704. http://dx.doi.org/10.1037/a0013771.
- Rutter M, Le Couteur A, Lord C. ADI-R: Autism Diagnostic Interview – Revised Manual. Los Angeles, CA: Western Psychological Services; 2003.
- Sparrow SS, Carter AS, Cicchetti DV. Vineland Screener: Overview, Reliability, Validity, Administration and Scoring. New Haven, CT: Yale University Child Study Center; 1993.
- Leyfer OT, Folstein SE, Bacalman S, Davis NO, Dinh E, Morgan J, et al. Comorbid psychiatric disorders in children with autism: interview development and rates of disorders. J Autism Dev Disord 2006;36:849-61. http://dx.doi.org/10.1007/s10803-006-0123-0.
- Terwee CB, Jansma EP, Riphagen II, de Vet HCW. Development of a methodological PubMed search filter for finding studies on measurement properties of measurement instruments. Qual Life Res 2009;18:1115-23. http://dx.doi.org/10.1007/s11136-009-9528-5.
- Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007;60:34-42. http://dx.doi.org/10.1016/j.jclinepi.2006.03.012.
- Krug D, Arick J, Almond P. Behavior checklist for identifying severely handicapped individuals with high levels of autistic behavior. J Child Psychol Psychiatry 1980;21:221-9. http://dx.doi.org/10.1111/j.1469-7610.1980.tb01797.x.
- Krug DA, Arick JR, Almond PJ. Autism Screening Instrument for Educational Planning. Examiner’s Manual. Portland, OR: ASIEP Education Company; 1980.
- Sponheim E, Spurkland I. Diagnosing childhood autism in clinical practice: an inter-rater reliability study of ICD-10, DSM-III-R, Childhood Autism Rating Scale, and Autism Behavior Checklist. Nord J Psychiatry 1996;50:5-9. http://dx.doi.org/10.3109/08039489609081381.
- Sturmey P, Matson JL, Sevin JA. Analysis of the internal consistency of three autism scales. J Autism Dev Disord 1992;22:321-8. http://dx.doi.org/10.1007/BF01058159.
- Miranda-Linné FM, Melin L. A factor analytic study of the Autism Behavior Checklist. J Autism Dev Disord 2002;32:181-8. http://dx.doi.org/10.1023/A:1015519413133.
- Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview-Revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord 1994;24:659-85. http://dx.doi.org/10.1007/BF02172145.
- Lecavalier L, Aman MG, Scahill L, McDougle CJ, McCracken JT, Vitiello B, et al. Validity of the Autism Diagnostic Interview-Revised. Am J Ment Retard 2006;111:199-215. http://dx.doi.org/10.1352/0895-8017(2006)111[199:VOTADI]2.0.CO;2.
- Lord C, Risi S, DiLavore PS, Shulman C, Thurm A, Pickles A. Autism from 2 to 9 years of age. Arch Gen Psychiatry 2006;63:694-701. http://dx.doi.org/10.1001/archpsyc.63.6.694.
- Tadevosyan-Leyfer O, Dowd M, Mankoski R, Winklosky B, Putnam S, McGrath L, et al. A principal components analysis of the Autism Diagnostic Interview-Revised. J Am Acad Child Adolesc Psychiatry 2003;42:864-72. http://dx.doi.org/10.1097/01.CHI.0000046870.56865.90.
- Frazier TW, Youngstrom EA, Kubu CS, Sinclair L, Rezai A. Exploratory and confirmatory factor analysis of the autism diagnostic interview-revised. J Autism Dev Disord 2008;38:474-80. http://dx.doi.org/10.1007/s10803-007-0415-z.
- Snow AV, Lecavalier L, Houts C. The structure of the Autism Diagnostic Interview-Revised: diagnostic and phenotypic implications. J Child Psychol Psychiatry 2009;50:734-42. http://dx.doi.org/10.1111/j.1469-7610.2008.02018.x.
- Tsuchiya KJ, Matsumoto K, Yagi A, Inada N, Kuroda M, Inokuchi E, et al. Reliability and validity of autism diagnostic interview-revised, Japanese version. J Autism Dev Disord 2013;43:643-62. http://dx.doi.org/10.1007/s10803-012-1606-9.
- Chawarska K, Klin A, Paul R, Volkmar F. Autism spectrum disorder in the second year: stability and change in syndrome expression. J Child Psychol Psychiatry 2007;48:128-38. http://dx.doi.org/10.1111/j.1469-7610.2006.01685.x.
- Moss J, Magiati I, Charman T, Howlin P. Stability of the autism diagnostic interview-revised from pre-school to elementary school age in children with autism spectrum disorders. J Autism Dev Disord 2008;38:1081-91. http://dx.doi.org/10.1007/s10803-007-0487-9.
- Kamp-Becker I, Ghahreman M, Smidt J, Remschmidt H. Dimensional structure of the autism phenotype: relations between early development and current presentation. J Autism Dev Disord 2009;39:557-71. http://dx.doi.org/10.1007/s10803-008-0656-5.
- Norris M, Lecavalier L, Edwards MC. The structure of autism symptoms as measured by the autism diagnostic observation schedule. J Autism Dev Disord 2012;42:1075-86. http://dx.doi.org/10.1007/s10803-011-1348-0.
- Gray KM, Tonge BJ, Sweeney DJ, Einfeld SL. Screening for autism in young children with developmental delay: an evaluation of the developmental behaviour checklist: early screen. J Autism Dev Disord 2008;38:1003-10. http://dx.doi.org/10.1007/s10803-007-0473-2.
- Ben Itzchak E, Zachor DA. Change in autism classification with early intervention: predictors and outcomes. Res Autism Spect Disord 2009;3:967-76. http://dx.doi.org/10.1016/j.rasd.2009.05.001.
- Luyster R, Gotham K, Guthrie W, Coffing M, Petrak R, Pierce K, et al. The autism diagnostic observation schedule – toddler module: a new module of a standardized diagnostic measure for autism spectrum disorders. J Autism Dev Disord 2009;39:1305-20. http://dx.doi.org/10.1007/s10803-009-0746-z.
- Gotham K, Pickles A, Lord C. Standardizing ADOS scores for a measure of severity in autism spectrum disorders. J Autism Dev Disord 2009;39:693-705. http://dx.doi.org/10.1007/s10803-008-0674-3.
- De Bildt A, Oosterling IJ, van Lang ND, Sytema S, Minderaa RB, van Engeland H, et al. Standardized ADOS scores: measuring severity of autism spectrum disorders in a Dutch sample. J Autism Dev Disord 2011;41:311-19. http://dx.doi.org/10.1007/s10803-010-1057-0.
- Shumway S, Farmer C, Thurm A, Joseph L, Black D, Golden C. The ADOS calibrated severity score: relationship to phenotypic variables and stability over time. Autism Res 2012;5:267-76. http://dx.doi.org/10.1002/aur.1238.
- Bryson SE, McDermott C, Rombough V, Brian J, Zwaigenbaum L. The Autism Observation Scale for Infants. New York: Basic Books; 2000.
- Bryson SE, Zwaigenbaum L, McDermott C, Rombough V, Brian J. The Autism Observation Scale for Infants: scale development and reliability data. J Autism Dev Disord 2008;38:731-8. http://dx.doi.org/10.1007/s10803-007-0440-y.
- Georgiades S, Szatmari P, Zwaigenbaum L, Bryson S, Brian J, Roberts W, et al. A prospective study of autistic-like traits in unaffected siblings of probands with autism spectrum disorder. JAMA Psychiatry 2013;70:42-8. http://dx.doi.org/10.1001/2013.jamapsychiatry.1.
- Matson JL, Wilkins J, Sevin JA, Knight C, Boisjoli JA, Sharp B. Reliability and item content of the baby and infant screen for children with aUtIsm traits (BISCUIT): Parts 1–3. Res Autism Spect Disord 2009;3:336-44. http://dx.doi.org/10.1016/j.rasd.2008.08.001.
- Matson JL, Boisjoli JA, Hess JA, Wilkins J. Factor structure and diagnostic fidelity of the Baby and Infant Screen for Children with aUtIsm Traits-Part 1 (BISCUIT-part 1). Dev Neurorehabil 2010;13:72-9. http://dx.doi.org/10.3109/17518420903213576.
- Matson JL, Wilkins J, Fodstad JC. The validity of the Baby and Infant Screen for Children with aUtIsm Traits: Part 1 (BISCUIT: Part 1). J Autism Dev Disord 2011;41:1139-46. http://dx.doi.org/10.1007/s10803-010-0973-3.
- Barthelemy C, Adrien J, Tanguay P, Garreau B, Fermanian J, Roux S, et al. The Behavioral Summarized Evaluation: validity and reliability of a scale for the assessment of autistic behaviors. J Autism Dev Disord 1990;20:189-204. http://dx.doi.org/10.1007/BF02284718.
- Barthelemy C, Roux S, Adrien JL, Hameury L, Guerin P, Garreau B. Validation of the revised behavioral summarized evaluation scale. J Autism Dev Disord 1997;27:139-53. http://dx.doi.org/10.1023/A:1025887723360.
- Oneal BJ, Reeb RN, Korte JR, Butter EJ. Assessment of home-based behavior modification programs for autistic children: reliability and validity of the behavioral summarized evaluation. J Prev Interv Community 2006;32:25-39. http://dx.doi.org/10.1300/J005v32n01_03.
- Roux S, Malvy J, Bruneau N, Garreau B, Guerin P, Sauvage D, et al. Identification of behaviour profiles with a population of autistic children using multivariate statistical methods. Eur Child Adolesc Psychiatry 1995;4:249-58. http://dx.doi.org/10.1007/BF01980489.
- Adrien JL, Barthelemy C, Perrot A, Roux S, Lenoir P, Hameury L, et al. The Infant Behavioral Summarized Evaluation (I.B.S.E.). A rating scale for the assessment of young children with autism and developmental disorders. Validity and reliability. J Autism Dev Disord 1992;22:375-94. http://dx.doi.org/10.1007/BF01048241.
- Schopler E, Reichler RJ, DeVellis RF, Daly K. Toward objective classification of childhood autism: Childhood Autism Rating Scale (CARS). J Autism Dev Disord 1980;10:91-103. http://dx.doi.org/10.1007/BF02408436.
- Schopler E, Reichler J, Renner B. The Childhood Autism Rating Scale (C.A.R.S.). Los Angeles, CA: Western Psychological Services; 1988.
- Russell PS, Daniel A, Russell S, Mammen P, Abel JS, Raj LE, et al. Diagnostic accuracy, reliability and validity of Childhood Autism Rating Scale in India. World J Pediatr 2010;6:141-7. http://dx.doi.org/10.1007/s12519-010-0029-y.
- Magyar CI, Pandolfi V. Factor structure evaluation of the childhood autism rating scale. J Autism Dev Disord 2007;37:1787-94. http://dx.doi.org/10.1007/s10803-006-0313-9.
- Darrou C, Pry R, Pernon E, Michelon C, Aussilloux C, Baghdadli A. Outcome of young children with autism: does the amount of intervention influence developmental trajectories?. Autism 2010;14:663-77. http://dx.doi.org/10.1177/1362361310374156.
- Stella J, Mundy P, Tuchman R. Social and nonsocial factors in the Childhood Autism Rating Scale. J Autism Dev Disord 1999;29:307-17. http://dx.doi.org/10.1023/A:1022111419409.
- South M, Williams BJ, McMahon WM, Owley T, Filipek PA, Shernoff E, et al. Utility of the Gilliam Autism Rating Scale in research and clinical populations. J Autism Dev Disord 2002;32:593-9. http://dx.doi.org/10.1023/A:1021211232023.
- Lecavalier L. An evaluation of the Gilliam Autism Rating Scale. J Autism Dev Disord 2005;35:795-80. http://dx.doi.org/10.1007/s10803-005-0025-6.
- Pandolfi V, Magyar CI, Dill CA. Constructs assessed by the GARS-2: factor analysis of data from the standardization sample. J Autism Dev Disord 2010;40:1118-30. http://dx.doi.org/10.1007/s10803-010-0967-1.
- Gilliam J. GARS-2: Gilliam Autism Rating Scale – Second Edition. Austin, Texas: PRO-ED; 2006.
- Robins DL, Fein D, Barton ML, Green JA. The modified checklist for autism in toddlers: an initial study investigating the early detection of autism and pervasive developmental disorders. J Autism Dev Disord 2001;31:131-44. http://dx.doi.org/10.1023/A:1010738829569.
- Snow AV, Lecavalier L. Sensitivity and specificity of the modified checklist for autism in toddlers and the social communication questionnaire in preschoolers suspected of having pervasive developmental disorders. Autism 2008;12:627-44. http://dx.doi.org/10.1177/1362361308097116.
- Inada N, Koyama T, Inokuchi E, Kuroda M, Kamio Y. Reliability and validity of the Japanese version of the Modified Checklist for autism in toddlers (M-CHAT). Res Autism Spect Disord 2011;5:330-6. http://dx.doi.org/10.1016/j.rasd.2010.04.016.
- Feldman MA, Ward RA, Savona D, Regehr K, Parker K, Hudson M, et al. Development and initial validation of a parent report measure of the Behavioral Development of Infants at Risk for Autism Spectrum Disorders. J Autism Dev Disord 2012;42:13-22. http://dx.doi.org/10.1007/s10803-011-1208-y.
- Bricker D, Squires J. The Ages and Stages Questionnaire. Baltimore, MD: Paul H Brookes; 1999.
- Eaves RC. The Pervasive Developmental Disorders Rating Scale. Opelika, AL: Small World; 1993.
- Williams TO, Eaves RC. The reliability of test scores for the Pervasive Developmental Disorders Rating Scale. Psychol Sch 2002;39:605-11. http://dx.doi.org/10.1002/pits.10059.
- Freeman BJ, Ritvo ER, Yokota A, Ritvo A. A scale for rating symptoms of patients with the syndrome of autism in real life settings. J Am Acad Child Psychiatry 1986;25:130-6. http://dx.doi.org/10.1016/S0002-7138(09)60610-5.
- Sevin JA, Matson JL, Coe DA, Fee VE, Sevin BM. A comparison and evaluation of three commonly used autism scales. J Autism Dev Disord 1991;21:417-32. http://dx.doi.org/10.1007/BF02206868.
- Berument SK, Rutter M, Lord C, Pickles A, Bailey A. E. Autism screening questionnaire: diagnostic validity. Br J Psychiatry 1999;175:444-51. http://dx.doi.org/10.1192/bjp.175.5.444.
- Magyar CI, Pandolfi V, Dill CA. An initial evaluation of the Social Communication Questionnaire for the assessment of autism spectrum disorders in children with Down syndrome. J Dev Behav Pediatr 2012;33:134-45. http://dx.doi.org/10.1097/DBP.0b013e318240d3d9.
- Charman T, Howlin P, Berry B, Prince E. Measuring developmental progress of children with autism spectrum disorder on school entry using parent report. Autism 2004;8:89-100. http://dx.doi.org/10.1177/1362361304040641.
- Constantino JN, Todd RD. Genetic structure of reciprocal social behavior. Am J Psychiatry 2000;157:2043-5. http://dx.doi.org/10.1176/appi.ajp.157.12.2043.
- Constantino JN, Gruber CP, Davis S, Hayes S, Passanante N, Przybeck T. The factor structure of autistic traits. J Child Psychol Psychiatry 2004;45:719-26. http://dx.doi.org/10.1111/j.1469-7610.2004.00266.x.
- Bolte S, Poustka F, Constantino JN. Assessing autistic traits: cross-cultural validation of the social responsiveness scale (SRS). Autism Res 2008;1:354-63. http://dx.doi.org/10.1002/aur.49.
- Duku E, Vaillancourt T, Szatmari P, Georgiades S, Zwaigenbaum L, Smith IM, et al. Investigating the measurement properties of the social responsiveness scale in preschool children with autism spectrum disorders. J Autism Dev Disord 2013;43:860-8. http://dx.doi.org/10.1007/s10803-012-1627-4.
- Pine E, Luby J, Abbacchi A, Constantino JN. Quantitative assessment of autistic symptomatology in preschoolers. Autism 2006;10:344-52. http://dx.doi.org/10.1177/1362361306064434.
- Constantino JN, Abbacchi AM, Lavesser PD, Reed H, Givens L, Chiang L, et al. Developmental course of autistic social impairment in males. Dev Psychopathol 2009;21:127-38. http://dx.doi.org/10.1017/S095457940900008X.
- Rimland B, Edelson M. The Autism Treatment Evaluation Checklist (ATEC). San Diego, CA: Autism Research Institute; 1999.
- Magiati I, Moss J, Yates R, Charman T, Howlin P. Is the Autism Treatment Evaluation Checklist a useful tool for monitoring progress in children with autism spectrum disorders?. J Intellect Disabil Res 2011;55:302-12. http://dx.doi.org/10.1111/j.1365-2788.2010.01359.x.
- Geier DA, Kern JK, Geier MR. A comparison of the Autism Treatment Evaluation Checklist (ATEC) and the Childhood Autism Rating Scale (CARS) for the quantitative evaluation of autism. J Ment Health Res Intellect Disabil 2013;6:255-67. http://dx.doi.org/10.1080/19315864.2012.681340.
- Cohen IL, Schmidt-Lackner S, Romanczyk R, Sudhalter V. The PDD Behavior Inventory: a rating scale for assessing response to intervention in children with pervasive developmental disorder. J Autism Dev Disord 2003;33:31-45. http://dx.doi.org/10.1023/A:1022226403878.
- Cohen IL. Criterion-related validity of the PDD Behavior Inventory. J Autism Dev Disord 2003;33:47-53. http://dx.doi.org/10.1023/A:1022278420716.
- Wetherby A, Prizant B, Hutchinson TA. Communicative, social/affective, and symbolic profiles of young children with autism and pervasive developmental disorders. Am J Speech Lang Pathol 1998;7:79-91. http://dx.doi.org/10.1044/1058-0360.0702.79.
- Wetherby A, Prizant B. Communication and Symbolic Behavior Scales Developmental Profile-First Normed Edition. Baltimore, MD: Paul H Brookes; 2002.
- Wetherby AM, Woods J, Allen L, Cleary J, Dickinson H, Lord C. Early indicators of autism spectrum disorders in the second year of life. J Autism Dev Disord 2004;34:473-93. http://dx.doi.org/10.1007/s10803-004-2544-y.
- Mundy P, Hogan A, Doehring P. A Preliminary Manual for the Abridged Early Social Communication Scales (ESCS). Hillsdale, NJ: Erlbaum; 1996.
- Mundy P, Delgado C, Block J, Venezia M, Hogan A, Seibert J. A Manual For The Abridged Early Social Communication Scales (ESCS). Coral Gables, FL: University of Miami, Psychology Department; 2003.
- Luyster RJ, Kadlec MB, Carter A, Tager-Flusberg H. Language assessment and development in toddlers with autism spectrum disorders. J Autism Dev Disord 2008;38:1426-38. http://dx.doi.org/10.1007/s10803-007-0510-1.
- Rogers SJ, Stackhouse T, Hepburn SL, Wehner EA. Imitation performance in toddlers with autism and those with other developmental disorders. J Child Psychol Psychiatry 2003;44:763-81. http://dx.doi.org/10.1111/1469-7610.00162.
- Young GS, Rogers SJ, Hutman T, Rozga A, Sigman M, Ozonoff S. Imitation from 12 to 24 months in autism and typical development: a longitudinal Rasch analysis. Dev Psychol 2011;47:1565-78. http://dx.doi.org/10.1037/a0025418.
- Malvy J, Roux S, Zakian A, Debuly S, Sauvage D, Barthelemy C. A brief clinical scale for the early evaluation of imitation disorders in autism. Autism 1999;3:357-69. http://dx.doi.org/10.1177/1362361399003004004.
- Stone WL, Ousley OY, Yoder PJ, Hogan KL, Hepburn SL. Nonverbal communication in two- and three-year-old children with autism. J Autism Dev Disord 1997;27:677-96. http://dx.doi.org/10.1023/A:1025854816091.
- Ingersoll B, Meyer K. Do object and gesture imitation skills represent independent dimensions in autism?. J Dev Phys Disabil 2011;23:421-31. http://dx.doi.org/10.1007/s10882-011-9237-1.
- Vanvuchelen M, Roeyers H, De Weerdt W. Development and initial validation of the Preschool Imitation and Praxis Scale (PIPS). Res Autism Spect Disord 2011;5:463-73. http://dx.doi.org/10.1016/j.rasd.2010.06.010.
- Vanvuchelen M, Vochten C. How much change is true change? The smallest detectable difference of the Preschool Imitation and Praxis Scale (PIPS) in preschoolers with intellectual disabilities of heterogeneous aetiology. Res Dev Disabil 2011;32:180-7. http://dx.doi.org/10.1016/j.ridd.2010.09.019.
- Drew A, Baird G, Taylor E, Milne E, Charman T. The Social Communication Assessment for Toddlers with Autism (SCATA): an instrument to measure the frequency, form and function of communication in toddlers with autism spectrum disorder. J Autism Dev Disord 2007;37:648-66. http://dx.doi.org/10.1007/s10803-006-0224-9.
- Cuccaro ML, Shao Y, Grubber J, Slifer M, Wolpert CM, Donnelly SL, et al. Factor analysis of restricted and repetitive behaviors in autism using the Autism Diagnostic Interview-R. Child Psychiatry Hum Dev 2003;34:3-17. http://dx.doi.org/10.1023/A:1025321707947.
- De Bildt A, Oosterling IJ, Lang ND, Kuijper S, Dekker V, Sytema S, et al. How to use the ADI-R for classifying autism spectrum disorders? Psychometric properties of criteria from the literature in 1,204 Dutch children. J Autism Dev Disord 2013;43:2280-94. http://dx.doi.org/10.1007/s10803-013-1783-1.
- Ward-King J, Cohen IL, Penning H, Holden JJ. Brief report: telephone administration of the autism diagnostic interview-revised: reliability and suitability for use in research. J Autism Dev Disord 2010;40:1285-90. http://dx.doi.org/10.1007/s10803-010-0987-x.
- Smith CJ, Lang CM, Kryzak L, Reichenberg A, Hollander E, Silverman JM. Familial associations of intense preoccupations, an empirical factor of the restricted, repetitive behaviors and interests domain of autism. J Child Psychol Psychiatry 2009;50:982-90. http://dx.doi.org/10.1111/j.1469-7610.2009.02060.x.
- Lam KS, Bodfish JW, Piven J. Evidence for three subtypes of repetitive behavior in autism that differ in familiality and association with other symptoms. J Child Psychol Psychiatry 2008;49:1193-200. http://dx.doi.org/10.1111/j.1469-7610.2008.01944.x.
- Bishop SL, Richler J, Lord C. Association Between Restricted and Repetitive Behaviors and Nonverbal IQ in Children with Autism Spectrum Disorders. Child Neuropsychol 2006;12:247-67. http://dx.doi.org/10.1080/09297040600630288.
- Richler J, Huerta M, Bishop SL, Lord C. Developmental trajectories of restricted and repetitive behaviors and interests in children with autism spectrum disorders. Dev Psychopathol 2010;22:55-69. http://dx.doi.org/10.1017/S0954579409990265.
- Shao Y, Cuccaro ML, Hauser ER, Raiford KL, Menold MM, Wolpert CM, et al. Fine mapping of autistic disorder to chromosome 15q11–q13 by use of phenotypic subtypes. Am J Hum Genet 2003;72:539-48. http://dx.doi.org/10.1086/367846.
- Lecavalier L, Leone S, Wiltz J. The impact of behaviour problems on caregiver stress in young people with autism spectrum disorders. J Intellect Disabil Res 2006;50:172-83. http://dx.doi.org/10.1111/j.1365-2788.2005.00732.x.
- Szatmari P, Georgiades S, Bryson S, Zwaigenbaum L, Roberts W, Mahoney W, et al. Investigating the structure of the restricted, repetitive behaviours and interests domain of autism. J Child Psychol Psychiatry 2006;47:582-90. http://dx.doi.org/10.1111/j.1469-7610.2005.01537.x.
- Mooney EL, Gray KM, Tonge BJ, Sweeney DJ, Taffe JR. Factor analytic study of repetitive behaviours in young children with pervasive developmental disorders. J Autism Dev Disord 2009;39:765-74. http://dx.doi.org/10.1007/s10803-008-0680-5.
- Ben Itzchak E, Lahat E, Burgin R, Zachor AD. Cognitive, behavior and intervention outcome in young children with autism. Res Dev Disabil 2008;29:447-58. http://dx.doi.org/10.1016/j.ridd.2007.08.003.
- Bodfish JW, Symons FJ, Parker DE, Lewis MH. Varieties of repetitive behavior in autism: comparisons to mental retardation. J Autism Dev Disord 2000;30:237-43. http://dx.doi.org/10.1023/A:1005596502855.
- Lam KS, Aman MG. The Repetitive Behavior Scale-Revised: independent validation in individuals with autism spectrum disorders. J Autism Dev Disord 2007;37:855-66. http://dx.doi.org/10.1007/s10803-006-0213-z.
- Mirenda P, Smith IM, Vaillancourt T, Georgiades S, Duku E, Szatmari P, et al. Validating the Repetitive Behavior Scale-revised in young children with autism spectrum disorder. J Autism Dev Disord 2010;40:1521-30. http://dx.doi.org/10.1007/s10803-010-1012-0.
- Silva LM, Schalock M. Autism Parenting Stress Index: initial psychometric evidence. J Autism Dev Disord 2012;42:566-74. http://dx.doi.org/10.1007/s10803-011-1274-1.
- Dunn W. The Sensory Profile: User’s Manual. San Antonio, TX: Psychological Corporation; 1999.
- Brown T, Leo M, Austin DW. Discriminant validity of the Sensory Profile in Australian children with autism spectrum disorder. Phys Occupat Ther Pediatr 2008;28:253-66. http://dx.doi.org/10.1080/01942630802224983.
- O’Brien J, Tsermentseli S, Cummins O, Happe F, Heaton P, Spencer J. Discriminating children with autism from children with learning difficulties with an adaptation of the Short Sensory Profile. Early Child Dev Care 2009;179:383-94. http://dx.doi.org/10.1080/03004430701567926.
- Wiggins LD, Robins DL, Bakeman R, Adamson LB. Brief report: sensory abnormalities as distinguishing symptoms of autism spectrum disorders in young children. J Autism Dev Disord 2009;39:1087-91. http://dx.doi.org/10.1007/s10803-009-0711-x.
- Carrow-Woolfolk E. Comprehensive Assessment of Spoken Language. Circle Pines, MN: American Guidance Service; 1999.
- Reichow B, Salamack S, Paul R, Volkmar FR, Klin A. Pragmatic assessment in autism spectrum disorders: a comparison of a standard measure with parent report. Commun Disord Q 2008;29:169-76. http://dx.doi.org/10.1177/1525740108318697.
- Fenson L, Dale PS, Reznick JS, Thal D, Bates E, Hartung JP, et al. The MacArthur Communicative Development Inventories: User’s Guide and Technical Manual. San Diego, CA: Singular Publishing Group; 1993.
- Fenson L, Dale P, Reznick J, Thal D, Bates E, Hartung J, et al. MacArthur Communicative Development Inventories: User’s Guide and Technical Manual. Baltimore, MD: Paul H Brookes; 2003.
- Bruckner C, Yoder P, Stone W, Saylor M. Construct validity of the MCDI-I Receptive Vocabulary scale can be improved: differential item functioning between toddlers with autism spectrum disorders and typically developing infants. J Speech Lang Hear Res 2007;50:1631-8. http://dx.doi.org/10.1044/1092-4388(2007/110).
- Mullen EM. Mullen Scales of Early Learning: AGS edition. Circle Pines, MN: American Guidance Service Inc.; 1995.
- Burns TG, King TZ, Spencer KS. Mullen scales of early learning: the utility in assessing children diagnosed with autism spectrum disorders, cerebral palsy, and epilepsy. Appl Neuropsychol Child 2013;2:33-42. http://dx.doi.org/10.1080/21622965.2012.682852.
- Zimmerman IL, Steiner VG, Pond RE. Preschool Language Scale. San Antonio, TX: The Psychological Corporation; 2002.
- Volden J, Smith IM, Szatmari P, Bryson S, Fombonne E, Mirenda P, et al. Using the preschool language scale, fourth edition to characterize language in preschoolers with autism spectrum disorders. Am J Speech Lang Pathol 2011;20:200-8. http://dx.doi.org/10.1044/1058-0360(2011/10-0035).
- Sparrow S, Balla D, Cicchetti D. Vineland Adaptive Behavior Scales: Survey Form Manual. Circle Pines, MN: American Guidance Service; 1984.
- Harris SL. The Vineland Adaptive Behavior Scales for Young Children with Autism. Austin, TX: Pro-Ed; 1995.
- Paul R, Miles S, Cicchetti D, Sparrow S, Klin A, Volkmar F, et al. Adaptive behavior in autism and Pervasive Developmental Disorder-Not Otherwise Specified: microanalysis of scores on the Vineland Adaptive Behavior Scales. J Autism Dev Disord 2004;34:223-8. http://dx.doi.org/10.1023/B:JADD.0000022612.18116.46.
- Wells K, Condillac R, Perry A, Factor DC. A comparison of three adaptive behaviour measures in relation to cognitive level and severity of autism. J Dev Disabil 2009;15:55-63.
- Sparrow SS, Carter AS, Cicchetti DV. Vineland Screener: Overview, Reliability, Validity, Administration and Scoring. New Haven, CT: Yale University Child Study Centre; 1993.
- Roid GH, Miller LJ. Leiter International Performance Scale – Revised: Examiner’s Manual. Wood Dale, IL: Stoelting; 1997.
- Scattone D, Raggio DJ, May W. Brief report: concurrent validity of the Leiter-R and KBIT-2 scales of nonverbal intelligence for children with autism and language impairments. J Autism Dev Disord 2012;42:2486-90. http://dx.doi.org/10.1007/s10803-012-1495-y.
- Tsatsanis KD, Dartnall N, Cicchetti D, Sparrow SS, Klin A, Volkmar FR. Concurrent validity and classification accuracy of the Leiter and Leiter-R in low-functioning children with autism. J Autism Dev Disord 2003;33:23-30. http://dx.doi.org/10.1023/A:1022274219808.
- Grondhuis SN, Mulick JA. Comparison of the Leiter International Performance Scale-Revised and the Stanford-Binet Intelligence Scales, 5th edition, in children with autism spectrum disorders. Am J Intellect Dev Disabil 2013;118:44-5. http://dx.doi.org/10.1352/1944-7558-118.1.44.
- Bishop SL, Guthrie W, Coffing M, Lord C. Convergent validity of the Mullen Scales of Early Learning and the Differential Ability Scales in children with autism spectrum disorders. Am J Intellect Dev Disabil 2011;116:331-43. http://dx.doi.org/10.1352/1944-7558-116.5.331.
- Roid GH. Stanford-Binet Intelligence Scales, Fifth Edition (SB:V). Itasca, IL: Riverside Publishing; 2003.
- Wechsler D. The Wechsler Preschool and Primary Scale of Intelligence–Revised. San Antonio, TX: The Psychological Corporation; 1989.
- Wechsler D. Wechsler Preschool and Primary Scale of Intelligence – Third Edition (WPPSI – III). San Antonio, TX: The Psychological Corporation; 2002.
- Yang P, Jong Y, Hsu H, Lung F. Role of assessment tests in the stability of intelligence scoring of pre-school children with uneven/delayed cognitive profile. J Intellect Disabil Res 2011;55:453-61. http://dx.doi.org/10.1111/j.1365-2788.2011.01396.x.
- Reynolds CR, Kamphaus RW. Behavior Assessment System for Children. Circle, Pines, MN: American Guidance Service; 2004.
- Hass MR, Brown RS, Brady J, Johnson DB. Validating the BASC-TRS for use with children and adolescents with an educational diagnosis of autism. Remed Spec Educ 2010;33:173-83. http://dx.doi.org/10.1177/0741932510383160.
- Mahan S, Matson JL. Children and adolescents with autism spectrum disorders compared to typically developing controls on the Behavioral Assessment System for Children, Second Edition (BASC-2). Res Autism Spect Disord 2011;5:119-25. http://dx.doi.org/10.1016/j.rasd.2010.02.007.
- Achenbach TM, Rescorla LA. Manual for the ASEBA Preschool Forms and Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth and Families; 2000.
- Pandolfi V, Magyar CI, Dill CA. Confirmatory factor analysis of the Child Behavior Checklist 1.5–5 in a sample of children with autism spectrum disorders. J Autism Dev Disord 2009;39:986-95. http://dx.doi.org/10.1007/s10803-009-0716-5.
- Pandolfi V, Magyar CI, Dill CA. An initial psychometric evaluation of the CBCL 6–18 in a sample of youth with autism spectrum disorders. Res Autism Spect Disord 2012;6:96-108. http://dx.doi.org/10.1016/j.rasd.2011.03.009.
- Matson JL, Boisjoli JA, Hess JA, Wilkins J. Comorbid psychopathology factor structure on the Baby and Infant Screen for Children with aUtIsm Traits-Part 2 (BISCUIT-Part 2). Res Autism Spect Disord 2011;5:426-32. http://dx.doi.org/10.1016/j.rasd.2010.06.005.
- Matson JL, Fodstad JC, Mahan S, Sevin JA. Cutoffs, Norms, and Patterns of Comorbid Difficulties in Children with an ASD on the Baby and Infant Screen for Children with aUtIsm Traits (BISCUIT-Part 2). Res Autism Spect Disord 2009;3:977-88. http://dx.doi.org/10.1016/j.rasd.2009.06.001.
- Briggs-Gowan MJ, Carter AS, Irwin JR, Wachtel K, Cicchetti DV. The Brief Infant-Toddler Social and Emotional Assessment: screening for social-emotional problems and delays in competence. J Pediatr Psychol 2004;29:143-55. http://dx.doi.org/10.1093/jpepsy/jsh017.
- Karabekiroglu K, Briggs-Gowan MJ, Carter AS, Rodopman-Arman A, Akbas S. The clinical validity and reliability of the Brief Infant-Toddler Social and Emotional Assessment (BITSEA). Infant Behav Dev 2010;33:503-9. http://dx.doi.org/10.1016/j.infbeh.2010.07.001.
- Achenbach TM, Rescorla LA. Manual for ASEBA School-Age Forms and Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth and Families; 2001.
- Schaffer D, Gould MS, Brasic J, Ambrosini P, Bird H, Aluwahlia S, et al. A Children’s Global Assessment Scale (CGAS). Arch Gen Psychiatry 1983;40:1228-31. http://dx.doi.org/10.1001/archpsyc.1983.01790100074010.
- Lundh A, Forsman M, Serlachius E, Lichtenstein P, Landen M. Outcomes of child psychiatric treatment. Acta Psychiatr Scand 2013;128:34-4. http://dx.doi.org/10.1111/acps.12043.
- Briggs-Gowan M, Carter AS. Preliminary acceptability and psychometrics of the Infant–Toddler Social and Emotional Assessment (ITSEA): a new adult-report questionnaire. Infant Mental Health 1998;19:422-45. http://dx.doi.org/10.1002/(SICI)1097-0355(199824)19:4<422::AID-IMHJ5>3.0.CO;2-U.
- Visser JC, Smeekens S, Rommelse N, Verkes RJ, Van der Gaag RJ, Buitelaar JK. Assessment of psychopathology in 2- to 5-year-olds: applying the infant-toddler social emotional assessment. Infant Ment Health J 2010;31:611-29. http://dx.doi.org/10.1002/imhj.20273.
- Robertson J, Tanguay P, L’Ecuyer S, Sims A, Waltrip C. Domains of social communication handicap in autism spectrum disorder. J Am Acad Child Adolesc Psychiatry 1999;38:738-45. http://dx.doi.org/10.1097/00004583-199906000-00022.
- Tanguay PE, Robertson J, Derrick A. A dimensional classification of autism spectrum disorder by social communication domains. J Am Acad Child Adolesc Psychiatry 1998;37:271-7. http://dx.doi.org/10.1097/00004583-199803000-00011.
- Aman MG, Tasse MJ, Rojahn J, Hammer D. The Nisonger CBRF: A Child Behavior Rating Form for children with developmental disabilities. Res Dev Disabil 1996;17:41-57. http://dx.doi.org/10.1016/0891-4222(95)00039-9.
- Lecavalier L, Aman MG, Hammer D, Stoica W, Mathews GL. Factor analysis of the Nisonger Child Behavior Rating Form in children with autism spectrum disorders. J Autism Dev Disord 2004;34:709-21. http://dx.doi.org/10.1007/s10803-004-5291-1.
- Tyminski RF, Moore PJ. The impact of group psychotherapy on social development in children with pervasive development disorders. Int J Group Psychother 2008;58:363-79. http://dx.doi.org/10.1521/ijgp.2008.58.3.363.
- Harris SL, Handleman JS, Belchich J, Glasberg B. The Vineland Adaptive Behavior Scales for young children with autism. Special Services in the Schools 1995;10:45-54. http://dx.doi.org/10.1300/J008v10n01_03.
- Lewis V, Boucher J. Manual of the Test of Pretend Play. London: Harcourt Brace; 1997.
- Clift S, Stagnitti K, DeMello L. A validational study of the test of pretend play using correlational and classificational analyses. Child Lang Teach Ther 1998;14:199-20. http://dx.doi.org/10.1191/026565998675895190.
- Aman MG, Singh NN. Manual for the Aberrant Behavior Checklist. East Aurora, NY: Slosson Educational Publications; 1986.
- Karabekiroglu K, Aman MG. Validity of the aberrant behavior checklist in a clinical sample of toddlers. Child Psychiatry Hum Dev 2009;40:99-110. http://dx.doi.org/10.1007/s10578-008-0108-7.
- Sigafoos J, Pittendreigh N, Pennell D. Parent and teacher ratings of challenging behaviour in young children with developmental disabilities. Br J Learn Disabil 1997;25:13-7. http://dx.doi.org/10.1111/j.1468-3156.1997.tb00003.x.
- Brinkley J, Nations L, Abramson RK, Hall A, Wright HH, Gabriels R, et al. Factor analysis of the aberrant behavior checklist in individuals with autism spectrum disorders. J Autism Dev Disord 2007;37:1949-59. http://dx.doi.org/10.1007/s10803-006-0327-3.
- Matson JL, Boisjoli J, Rojahn J, Hess J. A factor analysis of challenging behaviors assessed with the baby and infant screen for children with autism traits (Biscuit-Part 3). Res Autism Spect Disord 2009;3:714-22. http://dx.doi.org/10.1016/j.rasd.2009.01.008.
- Chowdhury M, Aman MG, Scahill L, Swiezy N, Arnold LE, Lecavalier L, et al. The Home Situations Questionnaire-PDD version: factor structure and psychometric properties. J Intellect Disabil Res 2010;54:281-91. http://dx.doi.org/10.1111/j.1365-2788.2010.01259.x.
- Arnold LE, Aman MG, Li X, Butter EJ, Humphries K, Scahill L, et al. RUPP Autism Network randomized clinical trial of parent training and medication: one year follow-up. J Am Acad Child Adolesc Psychiatry 2012;51:1173-84. http://dx.doi.org/10.1016/j.jaac.2012.08.028.
- Silva LM, Schalock M. Sense and Self-Regulation Checklist, a measure of comorbid autism symptoms: Initial psychometric evidence. Am J Occupat Ther 2012;66:177-86. http://dx.doi.org/10.5014/ajot.2012.001578.
- Bricker D. AEPS Measurement for Birth to Three Years, Volume 1. Baltimore, MD: Paul H Brookes Publishing; 1993.
- Wang H-T, Sandall SR, Davis CA, Thomas CJ. Social skills assessment in young children with autism: a comparison evaluation of the SSRS and PKBS. J Autism Dev Disord 2011;41:1487-95. http://dx.doi.org/10.1007/s10803-010-1175-8.
- Schopler E, Reichler RJ, Bashford A, Lansing M, Marcus L. Individualized assessment and treatment for autistic and developmentally disabled children. Psychoeducational profile-revised (PEP-R). Austin, TX: Pro-Ed; 1990.
- Alwinesh MT, Joseph RB, Daniel A, Abel JS, Shankar SR, Mammen P, et al. Psychometrics and utility of Psycho-Educational Profile-Revised as a developmental quotient measure among children with the dual disability of intellectual disability and autism. J Intellect Disabil 2012;16:193-20. http://dx.doi.org/10.1177/1744629512455594.
- Shek DT, Tsang SK, Lam LL, Tang FL, Cheung PM. Psychometric properties of the Chinese version of the Psycho-educational Profile-Revised (CPEP-R). J Autism Dev Disord 2005;35:37-44. http://dx.doi.org/10.1007/s10803-004-1029-3.
- Steerneman P, Muris P, Merckelbach H, Willems H. Brief report: assessment of development and abnormal behavior in children with pervasive developmental disorders: evidence for the reliability and validity of the Revised Psychoeducational Profile. J Autism Dev Disord 1997;27:177-85. http://dx.doi.org/10.1023/A:1025843908339.
- Villa S, Micheli E, Villa L, Pastore V, Crippa A, Molteni M. Further empirical data on the psychoeducational profile-revised (PEP-R): reliability and validation with the Vineland adaptive behavior scales. J Autism Dev Disord 2010;40:334-41. http://dx.doi.org/10.1007/s10803-009-0877-2.
- Heimann M, Laberg KE, Nordoen B. Imitative interaction increases social interest and elicited imitation in non-verbal children with autism. Infant Child Dev 2006;15:297-309. http://dx.doi.org/10.1002/icd.463.
- Schopler E, Lansing MD, Reichler RJ, Marcus LM. Examiner’s Manual of Psychoeducational Profile. Austin, TX: Pro-Ed Incorporation; 2005.
- Fu C-P, Hsieh C-L, Tseng M-H, Chen Y-L, Huang W-T, Wu P-C, et al. Inter-rater reliability and smallest real difference of the Chinese psychoeducational profile-third edition for children with autism spectrum disorder. Res Autism Spect Disord 2010;4:89-94. http://dx.doi.org/10.1016/j.rasd.2009.09.002.
- Chen K-L, Chiang F-M, Tseng M-H, Fu C-P, Hsieh C-L. Responsiveness of the Psychoeducational Profile-third edition for children with autism spectrum disorders. J Autism Dev Disord 2011;41:1658-64. http://dx.doi.org/10.1007/s10803-011-1201-5.
- Fu C-P, Chen K-L, Tseng M-H, Chiang F-M, Hsieh C-L. Reliability and validity of the Psychoeducational Profile-Third Edition caregiver report in children with autism spectrum disorders. Res Autism Spect Disord 2012;6:115-22. http://dx.doi.org/10.1016/j.rasd.2011.03.011.
- Bruininks R, Woodcock R, Weatherman R, Hill B. Scales of Independent Behaviour – Revised. Park Allen, TX: DLM Teaching Resources; 1996.
- Brown L, Bundy MB, Gore JS. Patterns of adaptive performance by individuals with autism spectrum disorders on the Scales of Independent Behavior-Revised (SIB-R). Int J Disabil Hum Dev 2010;9:315-18. http://dx.doi.org/10.1515/IJDHD.2010.035.
- Silva LMT, Schalock M, Ayres R, Bunse C, Budden S. Qigong massage treatment for sensory and self-regulation problems in young children with autism: a randomized controlled trial. Am J Occupat Ther 2009;63:423-32. http://dx.doi.org/10.5014/ajot.63.4.423.
- Silva L, Schalock M. Sense and Self-Regulation Checklist: initial psychometric evidence and findings. Am J Occupat Ther 2012;66:177-86. http://dx.doi.org/10.5014/ajot.2012.001578.
- Abidin RR. Parenting Stress Index: Professional Manual. Odessa, FL: Psychological Assessment Resources; 1995.
- Zaidman-Zait A, Mirenda P, Zumbo BD, Wellington S, Dua V, Kalynchuk K. An item response theory analysis of the Parenting Stress Index-Short Form with parents of children with autism spectrum disorders. J Child Psychol Psychiatry 2010;51:1269-77. http://dx.doi.org/10.1111/j.1469-7610.2010.02266.x.
- Zaidman-Zait A, Mirenda P, Zumbo BD, Georgiades S, Szatmari P, Bryson S, et al. Factor analysis of the Parenting Stress Index-Short Form form with parents of young children with autism spectrum disorders. Autism Res 2011;4:336-46. http://dx.doi.org/10.1002/aur.213.
- WN, Greenberg MT, Crnic K. A short form of the questionnaire on resources and stress. Am J Ment Defic 1983;88:41-8.
- Honey E, Hastings RP, McConachie H. Use of the Questionnaire on Resources and Stress (QRS-F) with parents of young children with autism. Autism 2005;9:246-55. http://dx.doi.org/10.1177/1362361305053256.
- Hudry K, Leadbitter K, Temple K, Slonims V, McConachie H, Aldred C, et al. Preschoolers with autism show greater impairment in receptive compared with expressive language abilities. Int J Lang Commun Disord 2010;45:681-90. http://dx.doi.org/10.3109/13682820903461493.
- Arnold LE, Aman MG, Martin A, Collier-Crespin A, Vitiello B, Tierney E, et al. Assessment in multi-site randomized clinical trials of patients with autistic disorder: the Autism RUPP Network. J Autism Dev Disord 2000;30:99-11. http://dx.doi.org/10.1023/A:1005451304303.
- Wolery M, Garfinkle AN. Measures in intervention research with young children who have autism. J Autism Dev Disord 2002;32:463-78. http://dx.doi.org/10.1023/A:1020598023809.
- Cunningham AB. Measuring change in social interaction skills of young children with autism. J Autism Dev Disord 2012;42:593-605. http://dx.doi.org/10.1007/s10803-011-1280-3.
- Ozonoff S, Goodlin-Jones L, Solomon M. Evidence-based assessment of autism spectrum disorders in children and adolescents. J Clin Child Adolesc Psychol 2005;34:523-40. http://dx.doi.org/10.1207/s15374424jccp3403_8.
- Anagnostou E, Jones N, Huerta M, Halladay AK, Wang P, Scahill L, et al. Measuring social communication behaviors as a treatment endpoint in individuals with autism spectrum disorder [published online ahead of print August 5 2014]. Autism 2014. http://dx.doi.org/10.1177/1362361314542955.
- Lecavalier L, Wood JJ, Halladay AK, Jones NE, Aman MG, Cook EH, et al. Measuring anxiety as a treatment endpoint in youth with autism spectrum disorder. J Autism Dev Disord 2013;44:1128-43. http://dx.doi.org/10.1007/s10803-013-1974-9.
- Scahill L, Aman MG, Lecavalier L, Halladay AK, Bishop SL, Bodfish JW, et al. Measuring repetitive behaviors as a treatment endpoint in youth with autism spectrum disorder. Autism 2015;9:38-52. http://dx.doi.org/10.1177/1362361313510069.
- Krug DA, Arick JR, Almond PJ. Autism Screening Instrument for Educational Planning: Background and Development. Austin, TX: University of Texas Press; 1978.
- Lord C, Rutter M, DiLavore PC, Risi S, Gotham K, Bishop SL. Autism Diagnostic Observation Schedule, Second Edition (ADOS-2) Manual (Part 1): Modules 1–4. Torrance, CA: Western Psychological Services; 2012.
- Lord C, Luyster RJ, Gotham K, Guthrie W. Autism Diagnostic Observation Schedule, Second Edition (ADOS-2) Manual (Part II) Toddler Module. Torrance, CA: Western Psychological Services; 2012.
- Schopler E, Reichler J. Toward objective classification of childhood autism: Childhood Autism Rating Scale (C.A.R.S.). J Autism Dev Disord 1980;10:91-103. http://dx.doi.org/10.1007/BF02408436.
- Schopler E, Van Bourgondien ME, Wellman GJ, Love SR. Childhood Autism Rating Scale. Los Angeles, CA: Western Psychological Services; 2010.
- Gilliam JE. Gilliam Autism Rating Scale. Austin, TX: Pro-Ed; 1995.
- Gilliam J. GARS-3: Gilliam Autism Rating Scale – Third Edition. Austin, TX: PRO-ED; 2013.
- Robins DL, Fein D, Barton ML. Modified Checklist for Autism in Toddlers (M-CHAT). 1999.
- Robins DL, Casagrande K, Barton ML, Chen CA, Dumont-Mathieu T, Fein D. Validation of the modified checklist for autism in toddlers, revised with follow-up (M-CHAT-R/F). Pediatrics 2014;133:37-45. http://dx.doi.org/10.1542/peds.2013-1813.
- Eaves RC, Hooper J. A factor analysis of psychotic behavior. J Spec Educ 1987;21:130-6.
- Rutter M, Bailey A, Lord C. Social Communication Questionnaire. Los Angeles, CA: Western Psychological Services; 2003.
- Constantino JN, Gruber CP. Social Responsiveness Scale. Los Angeles, CA: Western Psychological Services; 2005.
- Green J, Charman T, McConachie H, Aldred C, Slonims V, Howlin P, et al. Parent-mediated communication-focused treatment in children with autism (PACT): a randomised controlled trial. Lancet 2010;375:2152-60. http://dx.doi.org/10.1016/S0140-6736(10)60587-9.
- Stone WL, Coonrod EE, Pozdol SL, Turner LT. The Parent Interview for Autism-Clinical Version (PIA-CV): A measure of behavioral change for young children with autism. Autism 2003;7:9-30. http://dx.doi.org/10.1177/1362361303007001017.
- Kanne SM, Mazurek MO, Sikora D, Bellando J, Branum-Martin L, Handen B, et al. The Autism Impact Measure (AIM): initial development of a new tool for treatment outcome measurement. J Autism Dev Disord 2014;44:168-79. http://dx.doi.org/10.1007/s10803-013-1862-3.
- Vanvuchelen M. Imitation Problems in Children With Autism Spectrum Disorders. A Study of Their Nature, Clinical Significance and Utility in Diagnosis 2009.
- Vanvuchelen M, Roeyers H, De Weerdt W. Imitation assessment and its utility to the diagnosis of autism: evidence from consecutive clinical preschool referrals for suspected autism. J Autism Dev Disord 2011;41:484-96. http://dx.doi.org/10.1007/s10803-010-1074-z.
- Bodfish JW, Symons FW, Lewis MH. The Repetitive Behavior Scale. 1999.
- McIntosh DN, Miller LJ, Shyu V. Development and Validation of the Short Sensory Profile. San Antonio, TX: Psychological Corporation; 1999.
- Zimmerman IL, Steiner VG, Pond E. Preschool Language Scales – Fifth Edition (PLS-5). San Antonio, TX: Pearson; 2011.
- Nordahl-Hansen A, Kaale A, Ulvund SE. Inter-rater reliability of parent and preschool teacher ratings of language in children with autism. Res Autism Spect Disord 2013;7:1391-6. http://dx.doi.org/10.1016/j.rasd.2013.08.006.
- Roid GH, Miller LJ, Pomplun M, Koch C. Leiter-3 International Performance Scale, Third Edition. Wood Dale, IL: Stoelting Co; 2013.
- Briggs-Gowan MJ, Carter AS. Brief Infant-Toddler Social and Emotional Assessment (BITSEA) manual, version 2. New Haven, CT: Yale University; 2002.
- Shaffer D, Gould MS, Brassic J, Ambrosini P, Fisher P, Bird H, et al. A Children’s Global Assessment Scale (CGAS). Arch Gen Psychiatry 1983;40:1228-31. http://dx.doi.org/10.1001/archpsyc.1983.01790100074010.
- Carter AS, Briggs-Gowan MJ, Jones SM, Little TD. The infant-toddler social and emotional assessment ITSEA: factor structure, reliability and validity. J Abnorm Child Psychol 2003;31:495-514. http://dx.doi.org/10.1023/A:1025449031360.
- Aman MG, Singh NN, Stewart AW, Field CJ. The Aberrant Behavior Checklist: a behavior rating scale for the assessment of treatment effects. Am J Ment Defic 1985;89:485-91.
- Carter AS, Volkmar FR, Sparrow SS, Wang JJ, Lord C, Dawson G, et al. The Vineland Adaptive Behavior Scales: supplementary norms for individuals with autism. J Autism Dev Disord 1998;28:287-302. http://dx.doi.org/10.1023/A:1026056518470.
- Abidin RR. Parenting Stress Index 4th Edition Short Form (PSI-4-SF). Odessa, FL: Psychological Assessment Resources; 2012.
- Sclare I. Child Psychology Portfolio. Windsor: NFER-Nelson; 1997.
- Seibert JM, Hogan AE, Mundy PC. Assessing interactional competencies: The Early Social-Communication Scales. Infant Ment Health 1982;3:244-5. http://dx.doi.org/10.1002/1097-0355(198224)3:4<244::AID-IMHJ2280030406>3.0.CO;2-R.
- Escalona A, Field T, Singer-Strunck R, Cullen C, Hartshorn K. Improvements in the behavior of children with autism following massage therapy. Brief report. J Autism Dev Disord 2001;31:513-16. http://dx.doi.org/10.1023/A:1012273110194.
- Owens J, Nobile C, McGuinn M, Spirito A. The children’s sleep habits questionnaire: construction and validation of a sleep survey for school-aged children. Sleep 2000;23:1043-51.
- Malow BA, Crowe C, Henderson L, McGrew SG, Wang L, Song Y, et al. A sleep habits questionnaire for children with autism spectrum disorders. J Child Neurol 2009;24:19-24. http://dx.doi.org/10.1177/0883073808321044.
- Lukens CT, Linscheid TR. Development and validation of an inventory to assess mealtime behavior problems in children with autism. J Autism Dev Disord 2008;38:342-52. http://dx.doi.org/10.1007/s10803-007-0401-5.
- Ladd GW, Price JM. Predicting children’s social and school adjustment following the transition from preschool to kindergarten. Child Dev 1987;58:1168-89. http://dx.doi.org/10.2307/1130613.
- Ladd GW, Buhs ES, Seid M. Children’s initial sentiments about kindergarten: is school liking an antecedent of early classroom participation and achievement?. Merrill-Palmer Q 2000;46:255-79.
- Arnold LE, Vitiello B, McDougle CJ, Scahill L, Shah B, Gonzalez NM, et al. Parent-defined target symptoms respond to risperidone in RUPP autism study: customer approach to clinical trials. J Am Acad Child Adolesc Psychiatry 2003;42:1443-50. http://dx.doi.org/10.1097/00004583-200312000-00011.
- Bearss K, Johnson C, Handen B, Smith T, Scahill L. A pilot study of parent training in young children with autism spectrum disorder and disruptive behavior. J Autism Dev Disord 2013;43:829-40. http://dx.doi.org/10.1007/s10803-012-1624-7.
- Ruble L, McGrew JH, Toland MD. Goal attainment scaling as an outcome measure in randomized controlled trials of psychosocial interventions in autism. J Autism Dev Disord 2012;42:1974-83. http://dx.doi.org/10.1007/s10803-012-1446-7.
- Payakachat N, Tilford JM, Koyacs E, Kuhlthau K. Autism spectrum disorders: a review of measures for clinical, health services and cost-effectiveness applications. Exp Rev Pharmacoecon Outcome Res 2012;12:485-503. http://dx.doi.org/10.1586/erp.12.29.
- Khanna R, Jariwala K, Bentley JP. Psychometric properties of the EuroQol Five Dimensional Questionnaire (EQ-5D-3L) in caregivers of autistic children. Qual Life Res 2013;22:2909-20. http://dx.doi.org/10.1007/s11136-013-0423-8.
- Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health 2005;8:94-104. http://dx.doi.org/10.1111/j.1524-4733.2005.04054.x.
- Charman T. Why is joint attention a pivotal skill in autism?. Philos Trans R Soc Lond B Biol Sci 2003;358:315-24. http://dx.doi.org/10.1098/rstb.2002.1199.
- Toth K, Munson J, Meltzoff AN, Dawson G. Early predictors of communication development in young children with autism spectrum disorder: joint attention, imitation, and toy play. J Autism Dev Disord 2006;36:993-1005. http://dx.doi.org/10.1007/s10803-006-0137-7.
- White PJ, O’Reilly M, Streusand W, Levine A, Sigafoos J, Lancioni G, et al. Best practices for teaching joint attention: a systematic review of the intervention literature. Res Autism Spect Disord 2011;5:1283-95. http://dx.doi.org/10.1016/j.rasd.2011.02.003.
- Ingersoll B. Effect of a focused imitation intervention on social functioning in children with autism. J Autism Dev Disord 2012;42:1768-73. http://dx.doi.org/10.1007/s10803-011-1423-6.
- Kasari C, Gulsrud AC, Wong CS, Kwon S, Locke J. Randomized controlled caregiver mediated joint engagement intervention for toddlers with autism. J Autism Dev Disord 2010;40:1045-56. http://dx.doi.org/10.1007/s10803-010-0955-5.
- Kaale A, Smith L, Sponheim E. A randomized controlled trial of preschool-based joint attention intervention for children with autism. J Child Psychol Psychiatry 2012;53:97-105. http://dx.doi.org/10.1111/j.1469-7610.2011.02450.x.
- Bitterman A, Daley TC, Misra S, Carlson E, Markowitz J. A national sample of preschoolers with autism spectrum disorders: special education services and parent satisfaction. J Autism Dev Disord 2008;38:1509-17. http://dx.doi.org/10.1007/s10803-007-0531-9.
- Callahan K, Henson RK, Cowan AK. Social validation of evidence-based practices in autism by parents, teachers, and administrators. J Autism Dev Disord 2008;38:678-92. http://dx.doi.org/10.1007/s10803-007-0434-9.
- Pituch KA, Green VA, Didden R, Lang R, O’Reilly MF, Lancioni GE, et al. Parent reported treatment priorities for children with autism spectrum disorders. Res Autism Spect Disord 2011;5:135-43. http://dx.doi.org/10.1016/j.rasd.2010.03.003.
- Dymond SK, Gilson CL, Myran SP. Services for children with autism spectrum disorders. J Disabil Policy Stud 2007;18:133-47. http://dx.doi.org/10.1177/10442073070180030201.
- Hackett L, Shaikh S, Theodosiou L. Parental perceptions of the assessment of autistic spectrum disorders in a tier three service. Child Adolesc Ment Health 2009;14:127-32. http://dx.doi.org/10.1111/j.1475-3588.2008.00508.x.
- Read N, Schofield A. Autism: are mental health services failing children and parents?. J Fam Health Care 2010;20:120-4.
- Moore K, McConkey R, Sines D, Cassidy A. Improving diagnostic and assessment services for children with autistic spectrum disorders. Early Child Dev Care 1999;154:1-11. http://dx.doi.org/10.1080/0030443991540101.
- Bennett T, Szatmari P, Bryson S, Volden J, Zwaigenbaum L, Vaccarella L, et al. differentiating autism and Asperger syndrome on the basis of language delay or impairment. J Autism Dev Disord 2008;38:616-25. http://dx.doi.org/10.1007/s10803-007-0428-7.
- Gupta A, Singhal N. Language and learning skills and symptoms in children with autistic spectrum disorders. Asia Pac Disabil Rehabil J 2009;20:59-83.
- Jocelyn LJ, Casiro OG, Beattie D, Bow J, Kneisz J. Treatment of children with autism: a randomized controlled trial to evaluate a caregiver-based intervention program in community day-care centers. J Dev Behav Pediatr 1998;19:326-34. http://dx.doi.org/10.1097/00004703-199810000-00002.
- Silva LMT, Cignolini A, Warren R, Budden S, Skowron-Gooch A. Improvement in sensory impairment and social interaction in young children with autism following treatment with an original Qigong massage methodology. Am J Chin Med 2007;35:393-406. http://dx.doi.org/10.1142/S0192415X07004916.
- Silva LMT, Ayres R, Schalock M. Outcomes of a pilot training program in a qigong massage intervention for young children with autism. Am J Occup Ther 2008;62:538-46. http://dx.doi.org/10.5014/ajot.62.5.538.
- Silva LM, Schalock M, Gabrielsen K. Early intervention for autism with a parent-delivered ongoing massage program: a randomized controlled trial. Am J Occup Ther 2011;65:550-9. http://dx.doi.org/10.5014/ajot.2011.000661.
- Szatmari P, Bryson SE, Streiner DL, Wilson F, Archer L, Ryerse C. Two-year outcome of preschool children with autism or Asperger’s syndrome. Am J Psychiatry 2000;157:1980-7. http://dx.doi.org/10.1176/appi.ajp.157.12.1980.
- Zhang R, Jia MX, Zhang JS, Xu XJ, Shou XJ, Zhang XT, et al. Transcutaneous electrical acupoint stimulation in children with autism and its impact on plasma levels of arginine-vasopressin and oxytocin: a prospective single-blinded controlled study. Res Dev Disabil 2012;33:1136-46. http://dx.doi.org/10.1016/j.ridd.2012.02.001.
- Bennett T, Boyle M, Georgiades K, Georgiades S, Thompson A, Duku E, et al. Influence of reporting effects on the association between maternal depression and child autism spectrum disorder behaviors. J Child Psychol Psychiatry 2012;53:89-96. http://dx.doi.org/10.1111/j.1469-7610.2011.02451.x.
- Brian J, Bryson SE, Garon N, Roberts W, Smith IM, Szatmari P, et al. Clinical assessment of autism in high-risk 18-month-olds. Autism 2008;12:433-56. http://dx.doi.org/10.1177/1362361308094500.
- Hambly C, Fombonne E. The impact of bilingual environments on language development in children with autism spectrum disorders. J Autism Dev Disord 2012;42:1342-52. http://dx.doi.org/10.1007/s10803-011-1365-z.
- Honey E, McConachie H, Randle V, Shearer H, Couteur ASL. One-year change in repetitive behaviours in young children with communication disorders including autism. J Autism Dev Disord 2008;38:1439-50. http://dx.doi.org/10.1007/s10803-006-0191-1.
- Magiati I, Charman T, Howlin P. A two-year prospective follow-up study of community-based early intensive behavioural intervention and specialist nursery provision for children with autism spectrum disorders. J Child Psychol Psychiatry 2007;48:803-12. http://dx.doi.org/10.1111/j.1469-7610.2007.01756.x.
- Magiati I, Moss J, Charman T, Howlin P. Patterns of change in children with autism spectrum disorders who received community based comprehensive interventions in their pre-school years: a seven year follow-up study. Res Autism Spect Disord 2011;5:1016-27. http://dx.doi.org/10.1016/j.rasd.2010.11.007.
- Mayo J, Chlebowski C, Fein DA, Eigsti I-M. Age of first words predicts cognitive ability and adaptive skills in children with ASD. J Autism Dev Disord 2013;43:253-64. http://dx.doi.org/10.1007/s10803-012-1558-0.
- Mooney EL, Gray KM, Tonge BJ. Early features of autism: repetitive behaviours in young children. Eur Child Adolesc Psychiatry 2006;15:12-8. http://dx.doi.org/10.1007/s00787-006-0499-6.
- Munson J, Dawson G, Sterling L, Beauchaine T, Zhou A, Koehler E, et al. Evidence for latent classes of IQ in young children with autism spectrum disorder. Am J Ment Retard 2008;113:439-52. http://dx.doi.org/10.1352/2008.113:439-452.
- Ozonoff S, Iosif A-M, Baguio F, Cook IC, Hill MM, Hutman T, et al. A prospective study of the emergence of early behavioral signs of autism. J Am Acad Child Adolesc Psychiatry 2010;49:256-66.
- Pry R, Petersen A, Baghdadli A. The relationship between expressive language level and psychological development in children with autism 5 years of age. Autism 2005;9:179-89. http://dx.doi.org/10.1177/1362361305047222.
- Richler J, Bishop SL, Kleinke JR, Lord C. Restricted and repetitive behaviors in young children with autism spectrum disorders. J Autism Dev Disord 2007;37:73-85. http://dx.doi.org/10.1007/s10803-006-0332-6.
- Werner E, Dawson G, Munson J, Osterling J. Variation in early developmental course in autism and its relation with behavioral outcome at 3–4 years of age. J Autism Dev Disord 2005;35:337-50. http://dx.doi.org/10.1007/s10803-005-3301-6.
- Rogers SJ, Estes A, Lord C, Vismara L, Winter J, Fitzpatrick A, et al. Effects of a brief Early Start Denver Model (ESDM)-based parent intervention on toddlers at risk for autism spectrum disorders: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2012;51:1052-65. http://dx.doi.org/10.1016/j.jaac.2012.08.003.
- Aldred C, Green J, Adams C. A new social communication intervention for children with autism: pilot randomised controlled treatment study suggesting effectiveness. J Child Psychol Psychiatry 2004;45:1420-30. http://dx.doi.org/10.1111/j.1469-7610.2004.00338.x.
- Aldred C, Green J, Emsley R, McConachie H. Mediation of treatment effect in a communication intervention for pre-school children with autism. J Autism Dev Disord 2012;42:447-54. http://dx.doi.org/10.1007/s10803-011-1248-3.
- Ben Itzchak E, Zachor DA. Who benefits from early intervention in autism spectrum disorders?. Res Autism Spect Disord 2011;5:345-50. http://dx.doi.org/10.1016/j.rasd.2010.04.018.
- Dawson G, Rogers S, Munson J, Smith M, Winter J, Greenson J, et al. Randomized, controlled trial of an intervention for toddlers with autism: the Early Start Denver Model. Pediatrics 2010;125:e17-23. http://dx.doi.org/10.1542/peds.2009-0958.
- Gotham K, Pickles A, Lord C. Trajectories of autism severity in children using standardized ADOS scores. Pediatrics 2012;130:e1278-84. http://dx.doi.org/10.1542/peds.2011-3668.
- Hartley SLS. D. M. Sex differences in autism spectrum disorder: an examination of developmental functioning, autistic symptoms, and coexisting behavior problems in toddlers. J Autism Dev Disord 2009;39:1715-22. http://dx.doi.org/10.1007/s10803-009-0810-8.
- Landa RJK, Luther G. Long-term outcomes of toddlers with autism spectrum disorders exposed to short-term intervention. Pediatrics 2012;130:S186-90. http://dx.doi.org/10.1542/peds.2012-0900Q.
- Lerna A, Esposito D, Conson M, Russo L, Massagli A. Social-communicative effects of the Picture Exchange Communication System (PECS) in autism spectrum disorders. Int J Lang Commun Disord 2012;47:609-17. http://dx.doi.org/10.1111/j.1460-6984.2012.00172.x.
- Oosterling I, Visser J, Swinkels S, Rommelse N, Donders R, Woudenberg T, et al. Randomized controlled trial of the focus parent training for toddlers with autism: 1-year outcome. J Autism Dev Disord 2010;40:1447-58. http://dx.doi.org/10.1007/s10803-010-1004-0.
- Ray-Subramanian CE, Huai N, Weismer SE. Adaptive behavior and cognitive skills for toddlers on the autism spectrum. J Autism Dev Disord 2011;41:679-84. http://dx.doi.org/10.1007/s10803-010-1083-y.
- Ray-Subramanian CE, Ellis Weismer S. Receptive and expressive language as predictors of restricted and repetitive behaviors in young children with autism spectrum disorders. J Autism Dev Disord 2012;42:2113-20. http://dx.doi.org/10.1007/s10803-012-1463-6.
- Strauss K, Vicari S, Valeri G, D’Elia L, Arima S, Fava L. Parent inclusion in Early Intensive Behavioral Intervention: the influence of parental stress, parent treatment fidelity and parent-mediated generalization of behavior targets on child outcomes. Res Dev Disabil 2012;33:688-703. http://dx.doi.org/10.1016/j.ridd.2011.11.008.
- Sullivan M, Finelli J, Marvin A, Garrett-Mayer E, Bauman M, Landa R. Response to joint attention in toddlers at risk for autism spectrum disorder: a prospective study. J Autism Dev Disord 2007;37:37-48. http://dx.doi.org/10.1007/s10803-006-0335-3.
- Tek S, Landa RJ. Differences in autism symptoms between minority and non-minority toddlers. J Autism Dev Disord 2012;42:1967-73. http://dx.doi.org/10.1007/s10803-012-1445-8.
- Ventola P, Kleinman J, Pandey J, Wilson L, Esser E, Boorstein H, et al. Differentiating between autism spectrum disorders and other developmental disabilities in children who failed a screening instrument for ASD. J Autism Dev Disord 2007;37:425-36. http://dx.doi.org/10.1007/s10803-006-0177-z.
- Wong VCN, Kwan QK. Randomized controlled trial for early intervention for autism: a pilot study of the Autism 1–2–3 Project. J Autism Dev Disord 2010;40:677-88. http://dx.doi.org/10.1007/s10803-009-0916-z.
- Zachor D, Ben Itzchak E, Rabinovich A-L, Lahat E. Change in autism core symptoms with intervention. Res Autism Spect Disord 2006;1:304-17. http://dx.doi.org/10.1016/j.rasd.2006.12.001.
- Zachor DA, Itzchak EB. Treatment approach, autism severity and intervention outcomes in young children. Res Autism Spect Disord 2010;4:425-32. http://dx.doi.org/10.1016/j.rasd.2009.10.013.
- Fodstad JC, Matson JL, Hess J, Neal D. Social and communication behaviours in infants and toddlers with autism and pervasive developmental disorder-not otherwise specified. Dev Neurorehabil 2009;12:152-7. http://dx.doi.org/10.1080/17518420902936748.
- Receveur C, Lenoir P, DeSombre H, Roux S, Barthelemy C, Malvy J. Interaction and imitation deficits from infancy to 4 years of age in children with autism: a pilot study based on videotapes. Autism 2005;9:69-82. http://dx.doi.org/10.1177/1362361305049030.
- Maestro S, Muratori F, Cesari A, Cavallaro MC, Paziente A, Pecini C, et al. Course of autism signs in the first year of life. Psychopathology 2005;38:26-31. http://dx.doi.org/10.1159/000083967.
- Baghdadli A, Assouline B, Sonie S, Pernon E, Darrou C, Michelon C, et al. Developmental trajectories of adaptive behaviors from early childhood to adolescence in a cohort of 152 children with autism spectrum disorders. J Autism Dev Disord 2012;42:1314-25. http://dx.doi.org/10.1007/s10803-011-1357-z.
- Bopp KD, Mirenda P, Zumbo BD. Behavior predictors of language development over 2 years in children with autism spectrum disorders. J Speech Lang Hear Res 2009;52:1106-20. http://dx.doi.org/10.1044/1092-4388(2009/07-0262).
- Jonsdottir SL, Saemundsen E, Asmundsdottir G, Hjartardottir S, Asgeirsdottir BB, Smaradottir HH, et al. Follow-up of children diagnosed with pervasive developmental disorders: stability and change during the preschool years. J Autism Dev Disord 2007;37:1361-74. http://dx.doi.org/10.1007/s10803-006-0282-z.
- Malhi P, Singhi P. Follow up of children with autism spectrum disorders: stability and change in diagnosis. Indian J Pediatr 2011;78:941-5. http://dx.doi.org/10.1007/s12098-011-0370-8.
- Pajareya K, Nopmaneejumruslers K. A one-year prospective follow-up study of a DIR/Floortime parent training intervention for pre-school children with autistic spectrum disorders. J Med Assoc Thailand 2012;95:1184-93.
- Pajareya K, Nopmaneejumruslers K. A pilot randomized controlled trial of DIR/Floortime™ parent training intervention for pre-school children with autistic spectrum disorders. Autism 2011;15:563-77. http://dx.doi.org/10.1177/1362361310386502.
- Papavasiliou AS, Nikaina I, Rizou J, Alexandrou S. The effect of a psycho-educational program on CARS scores and short sensory profile in autistic children. Eur J Paediatr Neurol 2011;15:338-44. http://dx.doi.org/10.1016/j.ejpn.2011.02.004.
- Stone WL, Ousley OY, Hepburn SL, Hogan KL, Brown CS. Patterns of adaptive behavior in very young children with autism. Am J Ment Retard 1999;104:187-99. http://dx.doi.org/10.1352/0895-8017(1999)104<0187:POABIV>2.0.CO;2.
- Vorgraft Y, Farbstein I, Spiegel R, Apter A. Retrospective evaluation of an intensive method of treatment for children with pervasive developmental disorder. Autism 2007;11:413-24. http://dx.doi.org/10.1177/1362361307079605.
- Cassidy A, McConkey R, Truesdale-Kennedy M, Slevin E. Preschoolers with autism spectrum disorders: the impact on families and the supports available to them. Early Child Dev Care 2008;178:115-28. http://dx.doi.org/10.1080/03004430701491721.
- McConkey R, Truesdale-Kennedy M, Crawford H, McGreevy E, Reavey M, Cassidy A. Preschoolers with autism spectrum disorders: evaluating the impact of a home-based intervention to promote their communication. Early Child Dev Care 2010;180:299-315. http://dx.doi.org/10.1080/03004430801899187.
- Osborne LA, McHugh L, Saunders J, Reed P. Parenting stress reduces the effectiveness of early teaching interventions for autistic spectrum disorders. J Autism Dev Disord 2008;38:1092-103. http://dx.doi.org/10.1007/s10803-007-0497-7.
- Osborne LA, Reed P. The relationship between parenting stress and behavior problems of children with autistic spectrum disorders. Except Child 2009;76:54-73.
- Reed P, Osborne LA, Corness M. Brief report: relative effectiveness of different home-based behavioral approaches to early teaching intervention. J Autism Dev Disord 2007;37:1815-21. http://dx.doi.org/10.1007/s10803-006-0306-8.
- Reed P, Osborne LA, Corness M. The real-world effectiveness of early teaching interventions for children with autism spectrum disorder. Except Child 2007;73:417-33. http://dx.doi.org/10.1177/001440290707300402.
- Reed P, Osborne L. Impact of severity of autism and intervention time-input on child outcomes: comparison across several early interventions. Br J Spec Educ 2012;39:130-6. http://dx.doi.org/10.1111/j.1467-8578.2012.00549.x.
- Stahmer AC, Ingersoll B. Inclusive programming for toddlers with autism spectrum disorders: outcomes from the children’s toddler school. J Posit Behav Int 2004;6:67-82. http://dx.doi.org/10.1177/10983007040060020201.
- Eaves RC, Williams TO. Exploratory and confirmatory factor analyses of the pervasive developmental disorders rating scale for young children with autistic disorder. J Genet Psychol 2006;167:65-92. http://dx.doi.org/10.3200/GNTP.167.1.65-92.
- Eapen V, Črnčec R, Walter A. Clinical outcomes of an early intervention program for preschool children with autism spectrum disorder in a community group setting. BMC Pediatr 2013;13. http://dx.doi.org/10.1186/1471-2431-13-3.
- Remington B, Hastings RP, Kovshoff H, Degli Espinosa F, Jahr E, Brown T, et al. Early intensive behavioral intervention: outcomes for children with autism and their parents after two years. Am J Ment Retard 2007;112:418-38. http://dx.doi.org/10.1352/0895-8017(2007)112[418:EIBIOF]2.0.CO;2.
- Smith IM, Koegel RL, Koegel LK, Openden DA, Fossum KL, Bryson SE. Effectiveness of a novel community-based early intervention model for children with autistic spectrum disorder. Am J Intellect Dev Disabil 2010;115:504-23. http://dx.doi.org/10.1352/1944-7558-115.6.504.
- Takeda T, Koyama T, Kanai C, Kurita H. Clinical variables at age 2 predictive of mental retardation at age 5 in children with pervasive developmental disorder. Psychiatry Clin Neurosci 2005;59:717-22. http://dx.doi.org/10.1111/j.1440-1819.2005.01442.x.
- Casenhiser DM, Shanker SG, Stieben J. Learning through interaction in children with autism: preliminary data from a social-communication-based intervention. Autism 2013;17:220-41. http://dx.doi.org/10.1177/1362361311422052.
- Landa RJ, Holman KC, Garrett-Mayer E. Social and communication development in toddlers with early and later diagnosis of autism spectrum disorders. Arch Gen Psychiatry 2007;64:853-64. http://dx.doi.org/10.1001/archpsyc.64.7.853.
- Keen D, Couzens D, Muspratt S, Rodger S. The effects of a parent-focused intervention for children with a recent diagnosis of autism spectrum disorder on parenting stress and competence. Res Autism Spect Disord 2010;4:229-41. http://dx.doi.org/10.1016/j.rasd.2009.09.009.
- Keen D, Rodger S, Doussin K, Braithwaite M. A pilot study of the effects of a social-pragmatic intervention on the communication and symbolic play of children with autism. Autism 2007;11:63-71. http://dx.doi.org/10.1177/1362361307070901.
- Dereu M, Roeyers H, Raymaekers R, Warreyn P. Exploring individual trajectories of social communicative development in toddlers at risk for autism spectrum disorders. Res Autism Spect Disord 2012;6:1038-52. http://dx.doi.org/10.1016/j.rasd.2011.12.003.
- Goods KS, Ishijima E, Chang Y-C, Kasari C. Preschool based JASPER intervention in minimally verbal children with autism: pilot RCT. J Autism Dev Disord 2013;43:1050-6. http://dx.doi.org/10.1007/s10803-012-1644-3.
- Kalas A. Joint Attention responses of children with autism spectrum disorder to simple versus complex music. J Music Ther 2012;49:430-52. http://dx.doi.org/10.1093/jmt/49.4.430.
- Kasari C, Freeman S, Paparella T. Joint attention and symbolic play in young children with autism: a randomized controlled intervention study. J Child Psychol Psychiatry 2006;47:611-20. http://dx.doi.org/10.1111/j.1469-7610.2005.01567.x.
- Lawton K, Kasari C. Brief report: longitudinal improvements in the quality of joint attention in preschool children with autism. J Autism Dev Disord 2012;42:307-12. http://dx.doi.org/10.1007/s10803-011-1231-z.
- Paparella T, Goods KS, Freeman S, Kasari C. The emergence of nonverbal joint attention and requesting skills in young children with autism. J Commun Disord 2011;44:569-83. http://dx.doi.org/10.1016/j.jcomdis.2011.08.002.
- Roos EM, McDuffie AS, Weismer SE, Gernsbacher MA. A comparison of contexts for assessing joint attention in toddlers on the autism spectrum. Autism 2008;12:275-91. http://dx.doi.org/10.1177/1362361307089521.
- Salt J, Shemilt J, Sellars V, Boyd S, Coulson T, McCool S. The Scottish Centre for autism preschool treatment programme. II: The results of a controlled treatment outcome study. Autism 2002;6:33-46. http://dx.doi.org/10.1177/1362361302006001004.
- Wong CS. A play and joint attention intervention for teachers of young children with autism: a randomized controlled pilot study. Autism 2013;17:340-57. http://dx.doi.org/10.1177/1362361312474723.
- Yoder P, Stone WL. Randomized comparison of two communication interventions for preschoolers with autism spectrum disorders. J Consult Clin Psychol 2006;74:426-35. http://dx.doi.org/10.1037/0022-006X.74.3.426.
- Yoder PJ, Lieberman RG. Randomized test of the efficacy of picture exchange communication system on highly generalized picture exchanges in children with ASD. J Autism Dev Disord 2010;40:629-32. http://dx.doi.org/10.1007/s10803-009-0897-y.
- Ingersoll B. Brief report: pilot randomized controlled trial of reciprocal imitation training for teaching elicited and spontaneous imitation to children with autism. J Autism Dev Disord 2010;40:1154-60. http://dx.doi.org/10.1007/s10803-010-0966-2.
- Clifford SM, Dissanayake C. The early development of joint attention in infants with autistic disorder using home video observations and parental interview. J Autism Dev Disord 2008;38:791-805. http://dx.doi.org/10.1007/s10803-007-0444-7.
- Warreyn P, Roeyers H, Van Wetswinkel U, De Groote I. Temporal coordination of joint attention behavior in preschoolers with autism spectrum disorder. J Autism Dev Disord 2007;37:501-12. http://dx.doi.org/10.1007/s10803-006-0184-0.
- Colgan SE, Lanter E, McComish C, Watson LR, Crais ER, Baranek GT. Analysis of social interaction gestures in infants with autism. Child Neuropsychol 2006;12:307-19. http://dx.doi.org/10.1080/09297040600701360.
- Ingersoll B, Schreibman L, Stahmer A. Differential treatment outcomes for children with autistic spectrum disorder based on level of peer social avoidance. J Autism Dev Disord 2001;31:343-9. http://dx.doi.org/10.1023/A:1010703521704.
- Barber AB, Wetherby AM, Chambers NW. Brief report: repetitive behaviors in young children with autism spectrum disorder and developmentally similar peers: a follow up to Watt et al. J Autism Dev Disord 2012;42:2006-12. http://dx.doi.org/10.1007/s10803-011-1434-3.
- Ben-Sasson A, Cermak SA, Orsmond GI, Tager-Flusberg H, Kadlec MB, Carter AS. Sensory clusters of toddlers with autism spectrum disorders: differences in affective symptoms. J Child Psychol Psychiatry 2008;49:817-25. http://dx.doi.org/10.1111/j.1469-7610.2008.01899.x.
- Chuang IC, Tseng MH, Lu L, Shieh JY. Sensory correlates of difficult temperament characteristics in preschool children with autism. Res Autism Spect Disord 2012;6:988-95. http://dx.doi.org/10.1016/j.rasd.2012.01.002.
- Jasmin E, Couture M, McKinley P, Reid G, Fombonne E, Gisel E. Sensori-motor and daily living skills of preschool children with autism spectrum disorders. J Autism Dev Disord 2009;39:231-41. http://dx.doi.org/10.1007/s10803-008-0617-z.
- Provost B, Crowe TK, Acree K, Osbourn PL, McClain C. Sensory behaviors of preschool children with and without autism spectrum disorders. NZ J Occup Ther 2009;56:9-17.
- O’Donnell S, Deitz J, Kartin D, Nalty T, Dawson G. Sensory processing, problem behavior, adaptive behavior, and cognition in preschool children with autism spectrum disorders. Am J Occup Ther 2012;66:586-94. http://dx.doi.org/10.5014/ajot.2012.004168.
- Tomchek SD, Dunn W. Sensory processing in children with and without autism: a comparative study using the short sensory profile. Am J Occup Ther 2007;61:190-20. http://dx.doi.org/10.5014/ajot.61.2.190.
- Arick JR, Young HE, Falco RA, Loos LM, Krug DA, Gense MH, et al. Designing an outcome study to monitor the progress of students with autism spectrum disorders. Focus Autism Other Dev Disabil 2003;18:75-87. http://dx.doi.org/10.1177/108835760301800201.
- Bono MA, Daley T, Sigman M. Relations among joint attention, amount of intervention and language gain in autism. J Autism Dev Disord 2004;34:495-50. http://dx.doi.org/10.1007/s10803-004-2545-x.
- Carlsson LH, Norrelgen F, Kjellmer L, Westerlund J, Gillberg C, Fernell E. Coexisting disorders and problems in preschool children with autism spectrum disorders. Sci World J 2013;2013. http://dx.doi.org/10.1155/2013/213979.
- Miniscalco C, Franberg J, Schachinger-Lorentzon U, Gillberg C. Meaning what you say? Comprehension and word production skills in young children with autism. Res Autism Spect Disord 2012;6:204-11. http://dx.doi.org/10.1016/j.rasd.2011.05.001.
- Mitchell S, Brian J, Zwaigenbaum L, Roberts W, Szatmari P, Smith I, et al. Early language and communication development of infants later diagnosed with autism spectrum disorder. J Dev Behav Pediatr 2006;27:S69-78. http://dx.doi.org/10.1097/00004703-200604002-00004.
- Smith V, Mirenda P, Zaidman-Zait A. Predictors of expressive vocabulary growth in children with autism. J Speech Lang Hear Res 2007;50:149-60. http://dx.doi.org/10.1044/1092-4388(2007/013).
- Stone WL, Yoder PJ. Predicting spoken language level in children with autism spectrum disorders. Autism 2001;5:341-61. http://dx.doi.org/10.1177/1362361301005004002.
- Akshoomoff N. Use of the Mullen scales of early learning for the assessment of young children with autism spectrum disorders. Child Neuropsychol 2006;12:269-77. http://dx.doi.org/10.1080/09297040500473714.
- Anan RM, Warner LJ, McGillivary JE, Chong IM, Hines SJ. Group Intensive Family Training (GIFT) for preschoolers with autism spectrum disorders. Behav Interv 2008;23:165-80. http://dx.doi.org/10.1002/bin.262.
- Baker JK, Messinger DS, Lyons KK, Grantz CJ. A pilot study of maternal sensitivity in the context of emergent autism. J Autism Dev Disord 2010;40:988-99. http://dx.doi.org/10.1007/s10803-010-0948-4.
- Barbaro J, Dissanayake C. Developmental profiles of infants and toddlers with autism spectrum disorders identified prospectively in a community-based setting. J Autism Dev Disord 2012;42:1939-48. http://dx.doi.org/10.1007/s10803-012-1441-z.
- Landa RJ, Gross AL, Stuart EA, Bauman M. Latent class analysis of early developmental trajectory in baby siblings of children with autism. J Child Psychol Psychiatry 2012;53:986-96. http://dx.doi.org/10.1111/j.1469-7610.2012.02558.x.
- Lloyd M, MacDonald M, Lord C. Motor skills of toddlers with autism spectrum disorders. Autism 2013;17:133-46. http://dx.doi.org/10.1177/1362361311402230.
- Poon KK, Watson LR, Baranek GT, Poe MD. To what extent do joint attention, imitation, and object play behaviors in infancy predict later communication and intellectual functioning in ASD?. J Autism Dev Disord 2012;42:1064-74. http://dx.doi.org/10.1007/s10803-011-1349-z.
- Schertz HH, Odom SL, Baggett KM, Sideris JH. Effects of joint attention mediated learning for toddlers with autism spectrum disorders: an initial randomized controlled study. Early Child Res Q 2013;28:249-58. http://dx.doi.org/10.1016/j.ecresq.2012.06.006.
- Siller M, Hutman T, Sigman M. A parent-mediated intervention to increase responsive parental behaviors and child communication in children with ASD: A randomized clinical trial. J Autism Dev Disord 2013;43:540-55. http://dx.doi.org/10.1007/s10803-012-1584-y.
- Thurm A, Lord C, Lee L-C, Newschaffer C. Predictors of language acquisition in preschool children with autism spectrum disorders. J Autism Dev Disord 2007;37:1721-34. http://dx.doi.org/10.1007/s10803-006-0300-1.
- Roberts J, Williams K, Carter M, Evans D, Parmenter T, Silove N, et al. A randomised controlled trial of two early intervention programs for young children with autism: centre-based with parent program and home-based. Res Autism Spect Disord 2011;5:1553-66. http://dx.doi.org/10.1016/j.rasd.2011.03.001.
- Flippin M, Watson LR. Relationships between the responsiveness of fathers and mothers and the object play skills of children with autism spectrum disorders. J Early Interv 2011;33:220-34. http://dx.doi.org/10.1177/1053815111427445.
- Haebig E, McDuffie A, Weismer SE. The contribution of two categories of parent verbal responsiveness to later language for toddlers and preschoolers on the autism spectrum. Am J Speech Lang Pathol 2013;22:57-70. http://dx.doi.org/10.1044/1058-0360(2012/11-0004).
- Harris SL, Handleman JS, Gordon R, Kristoff B, Fuentes F. Changes in cognitive and language functioning of preschool children with autism. J Autism Dev Disord 1991;21:281-90. http://dx.doi.org/10.1007/BF02207325.
- Andersson GW, Gillberg C, Miniscalco C. Pre-school children with suspected autism spectrum disorders: do girls and boys have the same profiles?. Res Dev Disabil 2013;34:413-22. http://dx.doi.org/10.1016/j.ridd.2012.08.025.
- Eikeseth S, Hayward D, Gale C, Gitlesen J-P, Eldevik S. Intensity of supervision and outcome for preschool aged children receiving early and intensive behavioral interventions: a preliminary study. Res Autism Spect Disord 2009;3:67-73. http://dx.doi.org/10.1016/j.rasd.2008.04.003.
- Herring S, Gray K, Taffe J, Tonge B, Sweeney D, Einfeld S. Behaviour and emotional problems in toddlers with pervasive developmental disorders and developmental delay: Associations with parental mental health and family functioning. J Intellect Disabil Res 2006;50:874-82. http://dx.doi.org/10.1111/j.1365-2788.2006.00904.x.
- Sheinkopf SJ, Mundy P, Oller DK, Steffens M. Vocal atypicalities of preverbal autistic children. J Autism Dev Disord 2000;30:345-54. http://dx.doi.org/10.1023/A:1005531501155.
- Smith T, Groen AD, Wynn JW. Randomized trial of intensive early intervention for children with pervasive developmental disorder. Am J Ment Retard 2000;105:269-85. http://dx.doi.org/10.1352/0895-8017(2000)105<0269:RTOIEI>2.0.CO;2.
- Eldevik S, Hastings RP, Jahr E, Hughes JC. Outcomes of behavioral intervention for children with autism in mainstream pre-school settings. J Autism Dev Disord 2012;42:210-20. http://dx.doi.org/10.1007/s10803-011-1234-9.
- Eriksson MA, Westerlund J, Hedvall A, Amark P, Gillberg C, Fernell E. Medical conditions affect the outcome of early intervention in preschool children with autism spectrum disorders. Eur Child Adolesc Psychiatry 2013;22:23-3. http://dx.doi.org/10.1007/s00787-012-0312-7.
- Gabriels R, Ivers BJ, Hill DE, Agnew JA, McNeill J. Stability of adaptive behaviors in middle-school children with autism spectrum disorders. Res Autism Spect Disord 2007;1:291-303. http://dx.doi.org/10.1016/j.rasd.2006.11.004.
- Grindle CF, Hastings RP, Saville M, Hughes CJ, Huxley K, Kovshoff H, et al. Outcomes of a behavioral education model for children with autism in a mainstream school setting. Behav Modif 2012;36:298-319. http://dx.doi.org/10.1177/0145445512441199.
- Hedvall A, Fernell E, Holm A, Johnels JA, Gillberg C, Billstedt E. Sci World J 2013;2013. http://dx.doi.org/10.1155/2013/158263.
- Klintwall L, Eikeseth S. Number and controllability of reinforcers as predictors of individual outcome for children with autism receiving early and intensive behavioral intervention: a preliminary study. Res Autism Spect Disord 2012;6:493-9. http://dx.doi.org/10.1016/j.rasd.2011.07.009.
- Munson J, Dawson G, Abbott R, Faja S, Webb SJ, Friedman SD, et al. Amygdalar volume and behavioral development in autism. Arch Gen Psychiatry 2006;63:686-93. http://dx.doi.org/10.1001/archpsyc.63.6.686.
- Peters-Scheffer N, Didden R, Mulders M, Korzilius H. Low intensity behavioral treatment supplementing preschool services for young children with autism spectrum disorders and severe to mild intellectual disability. Res Dev Disabil 2010;31:1678-84. http://dx.doi.org/10.1016/j.ridd.2010.04.008.
- Restall G, Magill-Evans J. Play and preschool children with autism. Am J Occupat Ther 1994;48:113-20. http://dx.doi.org/10.5014/ajot.48.2.113.
- Rickards AL, Walstab JE, Wright-Rossi RA, Simpson J, Reddihough DS. One-year follow-up of the outcome of a randomized controlled trial of a home-based intervention programme for children with autism and developmental delay and their families. Child Care Health Dev 2009;35:593-602. http://dx.doi.org/10.1111/j.1365-2214.2009.00953.x.
- Ruble L, McDuffie A, King AS, Lorenz D. Caregiver responsiveness and social interaction behaviors of young children with autism. Topics Early Child Spec Educ 2008;28:158-70. http://dx.doi.org/10.1177/0271121408323009.
- Tonge B, Brereton A, Kiomall M, Mackinnon A, Rinehart NJ. A randomised group comparison controlled trial of ‘preschoolers with autism’: a parent education and skills training intervention for young children with autistic disorder. Autism 2014;18:166-77. http://dx.doi.org/10.1177/1362361312458186.
- VanMeter L, Fein D, Morris R, Waterhouse L, Allen D. Delay versus deviance in autistic social behavior. J Autism Dev Disord 1997;27:557-69. http://dx.doi.org/10.1023/A:1025830110640.
- Goin-Kochel RP, Myers BJ, Hendricks DR, Carr SE, Wiley SB. Early responsiveness to intensive behavioural intervention predicts outcomes among preschool children with autism. Int J Disabil Dev Educ 2007;54:151-75. http://dx.doi.org/10.1080/10349120701330404.
- Yoder P, Stone WL. A randomized comparison of the effect of two prelinguistic communication interventions on the acquisition of spoken communication in preschoolers with ASD. J Speech Lang Hear Res 2006;49:698-711. http://dx.doi.org/10.1044/1092-4388(2006/051).
- Sheinkopf SJ, Siegel B. Home-based behavioral treatment of young children with autism. J Autism Dev Disord 1998;28:15-23. http://dx.doi.org/10.1023/A:1026054701472.
- Smith T, Eikeseth S, Klevstrand M, Lovaas OI. Intensive behavioral treatment for preschoolers with severe mental retardation and pervasive developmental disorder. Am J Ment Retard 1997;102:238-49. http://dx.doi.org/10.1352/0895-8017(1997)102<0238:IBTFPW>2.0.CO;2.
- Jahromi LB, Bryce CI, Swanson J. The importance of self-regulation for the school and peer engagement of children with high-functioning autism. Res Autism Spect Disord 2013;7:235-46. http://dx.doi.org/10.1016/j.rasd.2012.08.012.
- Delmolino LM. Brief Report: use of DQ for estimating cognitive ability in young children with autism. J Autism Dev Disord 2006;36:959-63. http://dx.doi.org/10.1007/s10803-006-0133-y.
- Harris SLH. J.S. Age and IQ at intake as predictors of placement for young children with autism: a four- to six-year follow-up. J Autism Dev Disord 2000;30:137-42. http://dx.doi.org/10.1023/A:1005459606120.
- Hill-Chapman CR, Herzog TK, Maduro RS. Aligning over the child: parenting alliance mediates the association of autism spectrum disorder atypicality with parenting stress. Res Dev Disabil 2013;34:1498-504. http://dx.doi.org/10.1016/j.ridd.2013.01.004.
- Meek SE, Robinson LT, Jahromi LB. Parent-child predictors of social competence with peers in children with and without autism. Res Autism Spect Disord 2012;6:815-23. http://dx.doi.org/10.1016/j.rasd.2011.11.001.
- Taylor JL, Warren ZE. Maternal depressive symptoms following autism spectrum diagnosis. J Autism Dev Disord 2012;42:1411-18. http://dx.doi.org/10.1007/s10803-011-1375-x.
- Reed P, Osborne LA. The role of parenting stress in discrepancies between parent and teacher ratings of behavior problems in young children with autism spectrum disorder. J Autism Dev Disord 2013;43:471-7. http://dx.doi.org/10.1007/s10803-012-1594-9.
- Travers JC, Higgins K, Pierce T, Boone R, Miller S, Tandy R. Emergent literacy skills of preschool students with autism: a comparison of teacher-led and computer-assisted instruction. Educ Train Autism Dev Disabil 2011;46:326-38.
- Davis TE, Fodstad JC, Jenkins WS, Hess JA, Moree BN, Dempsey T, et al. Anxiety and avoidance in infants and toddlers with autism spectrum disorders: evidence for differing symptom severity and presentation. Res Autism Spect Disord 2010;4:305-13. http://dx.doi.org/10.1016/j.rasd.2009.10.002.
- Ozonoff S, Young GS, Goldring S, Greiss-Hess L, Herrera AM, Steele J, et al. Gross motor development, movement abnormalities, and early identification of autism. J Autism Dev Disord 2008;38:644-56. http://dx.doi.org/10.1007/s10803-007-0430-0.
- Provost B, Heimerl S, Lopez BR. Levels of gross and fine motor development in young children with autism spectrum disorder. Phys Occupat Ther Pediatr 2007;27:21-36. http://dx.doi.org/10.1080/J006v27n03_03.
- Meirsschaut M, Roeyers H, Warreyn P. The social interactive behaviour of young children with autism spectrum disorder and their mothers: is there an effect of familiarity of the interaction partner?. Autism 2011;15:43-64. http://dx.doi.org/10.1177/1362361309353911.
- Freeman S, Kasari C. Parent–child interactions in autism: characteristics of play. Autism 2013;17:147-61. http://dx.doi.org/10.1177/1362361312469269.
- Christensen L, Hutman T, Rozga A, Young GS, Ozonoff S, Rogers SJ, et al. Play and developmental outcomes in infant siblings of children with autism. J Autism Dev Disord 2010;40:946-57. http://dx.doi.org/10.1007/s10803-010-0941-y.
- Rojahn J, Matson JL, Mahan S, Fodstad JC, Knight C, Sevin JA, et al. Cutoffs, norms, and patterns of problem behaviors in children with an ASD on the Baby and Infant Screen for Children with aUtIsm Traits (BISCUIT-Part 3). Res Autism Spect Disord 2009;3:989-98. http://dx.doi.org/10.1016/j.rasd.2009.06.002.
- Robbins FR, Dunlap G. Effects of task difficulty on parent teaching skills and behavior problems of young children with autism. Am J Ment Retard 1992;96:631-43.
- Reese RM, Richman DM, Belmont JM, Morse P. Functional characteristics of disruptive behavior in developmentally disabled children with and without autism. J Autism Dev Disord 2005;35:419-28. http://dx.doi.org/10.1007/s10803-005-5032-0.
- Bryce CI, Jahromi LB. Brief report: compliance and noncompliance to parental control strategies in children with high-functioning autism and their typical peers. J Autism Dev Disord 2013;43:236-43. http://dx.doi.org/10.1007/s10803-012-1564-2.
- Brisson J, Warreyn P, Serres J, Foussier S, Adrien-Louis J. Motor anticipation failure in infants with autism: a retrospective analysis of feeding situations. Autism 2012;16:420-9. http://dx.doi.org/10.1177/1362361311423385.
- Schwartz IS, Sandall SR, McBride BJ, Boulware G-L. Project DATA (Developmentally Appropriate Treatment for Autism). An inclusive school-based approach to educating young children with autism. Topics Early Child Spec Educ 2004;24:156-68. http://dx.doi.org/10.1177/02711214040240030301.
- Virues-Ortega J, Rodriguez V, Yu CT. Prediction of treatment outcomes and longitudinal analysis in children with autism undergoing intensive behavioral intervention. Int J Clin Health Psychol 2013;13:91-100. http://dx.doi.org/10.1016/S1697-2600(13)70012-7.
- Hsieh Y-L, Lo J-L. Occupational experiences and subjective well-being of mothers of children with ASD in Taiwan. Occupat Ther Int 2013;20:45-53. http://dx.doi.org/10.1002/oti.1339.
- Ozonoff S, Cathcart K. Effectiveness of a home program intervention for young children with autism. J Autism Dev Disord 1998;28:25-32. http://dx.doi.org/10.1023/A:1026006818310.
- Trad PV, Bernstein D, Shapiro T, Hertzig M. Assessing the relationship between affective responsivity and social interaction in children with pervasive developmental disorder. J Autism Dev Disord 1993;23:361-77. http://dx.doi.org/10.1007/BF01046225.
- Davis NO, Carter AS. Parenting stress in mothers and fathers of toddlers with autism spectrum disorders: associations with child characteristics. J Autism Dev Disord 2008;38:1278-91. http://dx.doi.org/10.1007/s10803-007-0512-z.
- Tonge B, Brereton A, Kiomall M, Mackinnon A, King N, Rinehart N. Effects on parental mental health of an education and skills training program for parents of young children with autism: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2005;45:561-9. http://dx.doi.org/10.1097/01.chi.0000205701.48324.26.
- Baker-Ericzen MJ, Brookman-Frazee L, Stahmer A. Stress levels and adaptability in parents of toddlers with and without autism spectrum disorders. Res Pract Persons Severe Disabil 2005;30:194-20. http://dx.doi.org/10.2511/rpsd.30.4.194.
- Bendixen RM, Elder JH, Donaldson S, Kairalla JA, Valcante G, Ferdig RE. Effects of a father-based in-home intervention on perceived stress and family dynamics in parents of children with autism. Am J Occup Ther 2011;65:679-87. http://dx.doi.org/10.5014/ajot.2011.001271.
- Minjarez MB, Mercier EM, Williams SE, Hardan AY. Impact of pivotal response training group therapy on stress and empowerment in parents of children with autism. J Posit Behav Interv 2013;15:71-8. http://dx.doi.org/10.1177/1098300712449055.
- Wang J, Hu YJ, Wang Y, Qin XQ, Xia W, Sun CH, et al. Parenting stress in Chinese mothers of children with autism spectrum disorders. Soc Psychiatry Psychiatric Epidemiol 2013;48:575-82. http://dx.doi.org/10.1007/s00127-012-0569-7.
- Oppenheim D, Koren-Karie N, Dolev S, Yirmiya N. Maternal sensitivity mediates the link between maternal insightfulness/resolution and child–mother attachment: The case of children with Autism Spectrum Disorder. Attach Hum Dev 2012;14:567-84. http://dx.doi.org/10.1080/14616734.2012.727256.
- Wachtel K, Carter AS. Reaction to diagnosis and parenting styles among mothers of young children with ASDs. Autism 2008;12:575-94. http://dx.doi.org/10.1177/1362361308094505.
- Farmer J, Reupert A. Understanding autism and understanding my child with autism: an evaluation of a group parent education program in rural Australia. Aust J Rural Health 2013;21:20-7. http://dx.doi.org/10.1111/ajr.12004.
- Terwee CB, Mokkink LB, Knol DL, Ostelo RWJG, Bouter LM, De Vet HCW. Rating the methodological quality in systematic reviews of studies on measurement properties: a scoring system for the COSMIN checklist. Qual Life Res 2012;21:651-7. http://dx.doi.org/10.1007/s11136-011-9960-1.
- Nordin V, Gillberg C, Nyden A. The Swedish version of the Childhood Autism Rating Scale in a clinical setting. J Autism Dev Disord 1998;28:69-75. http://dx.doi.org/10.1023/A:1026067104198.
- Tachimori H, Osada H, Kurita H. Childhood Autism Rating Scale: Tokyo Version for screening pervasive developmental disorders. Psychiatry Clin Neurosci 2003;57:113-18. http://dx.doi.org/10.1046/j.1440-1819.2003.01087.x.
Appendix 1 Health Technology Assessment Commissioning Brief 11/22
Appendix 2 Scoping review of qualitative literature
Question: What child and/or family specific outcomes do parents of children with ASD perceive as important?
(Christopher Morris, Nuala Livingstone, Bryony Beresford)
Methods
Search strategy
A systematic search was conducted using MEDLINE, CINAHL and PsycINFO (via Ovid). Blocks of search terms were assembled for ASD (block 1) and Qualitative Study Designs (block 2), tailored to each database.
| Search terms | PsycINFO | ||
|---|---|---|---|
| ASD | 1 | exp Pervasive Developmental Disorders/ | 21,449 |
| 2 | exp Developmental Disabilities/ | 10,206 | |
| 3 | autis$.ab,ti. | 24,176 | |
| 4 | asperg$.ab,ti. | 2493 | |
| 5 | pdd.ab,ti. | 1192 | |
| 6 | pervasive developmental disorder$.ab,ti. | 2081 | |
| 7 | kanner$.ab,ti. | 345 | |
| 8 | 1 or 2 or 3 or 4 or 5 or 6 or 7 | 35,627 | |
| Qualitative study design | 9 | ((‘semi-structured’ or semistructured or unstructured or informal or ‘in-depth’ or indepth or ‘face-to-face’ or structured or guide) adj3 (interview* or discussion* or questionnaire*)).ab,ti. | 49,983 |
| 10 | (focus group* or qualitative or ethnograph* or fieldwork or ‘field work’ or ‘key informant’).ab,ti. | 95,482 | |
| 11 | exp Qualitative Research/ | 3248 | |
| 12 | exp Interviews/ | 9745 | |
| 13 | exp Group Discussion/ | 3127 | |
| 14 | exp Narratives/ | 10,680 | |
| 15 | (parent$ adj3 priorit$).ab,ti. | 104 | |
| 16 | (desired adj1 outcome$).ab,ti. | 849 | |
| 17 | 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 | 151,148 | |
| 18 | 8 and 17 | 1343 | |
Search results

Data extracted from included studies
|
Author: Auert
et al.
31
Title: Parents’ Expectations, Awareness, and Experiences of Accessing eVidence-based Speech–Language Pathology Services for Their Children with Autism Year: 2012 Country: USA |
|
| Child age: 3–6 years | |
| Methods: Four focus groups exploring expectations, awareness of and experiences with access to speech-and-language therapy services; 20 parents | |
| Notes: Major themes related to and use of evidence in practice in speech-and-language therapy and parents’ expectations of services No data on child outcomes Data on parent outcomes (see below) |
|
| Information/communication and feedback | The majority, for example, stated that they would like to receive regular feedback from the speech-and-language therapist regarding their children’s progress over time and more input into their children’s management: ‘. . . Most people I find don’t get the take home homework and they don’t get the “This is where we’re up to” . . . mothers need confirmation that things are happening . . . if you had a “Today I saw this and this and next week I’m gonna do X”. That’d be so helpful . . .’ |
| Expectations of service | Parents expected the service to:
|
|
Author: Beresford
et al.
34
Title: Desired Outcomes for Children and Adolescents with Autistic Spectrum Disorders Year: 2006 Country: England |
|
| Methods: Semistructured interviews with parents (n = 25) and children and young people with autistic spectrum condition (n = 5) exploring desired outcomes for children’s/young people’s lives, including maintaining current achievements and hopes and aspirations for future | |
| Notes: A hierarchy of outcomes identified (see below); aspirations within each of the ‘outcome domains’ were influenced by the child’s age, abilities and the way the features of autism were manifest Many of the long-term aspirations expressed were dependent on short- or medium-term achievements Fundamental outcomes need to be achieved if outcomes in terms of skills and abilities and ‘life-world’ are to be fully attained No quotes presented in paper but available in full project report |
|
| Fundamental |
|
| Skills and abilities |
|
| ‘Life-world’ |
|
|
Author: Braiden
et al.
32
Title: Parents’ Experience of the Diagnostic Process for Autistic Spectrum Disorders Year: 2010 Country: Northern Ireland |
|
| Child age: 5–11 years | |
| Method: Face-to-face interviews; indirect data only; interview was biographical Sample: Eleven mothers |
|
| Notes: Focus on parents’ experience of diagnosis. Speech-and-language therapy and occupational therapy identified on several occasions as valuable support and intervention for children No data on child outcomes Limited data on parent outcomes |
|
| Being informed |
|
| Understanding/parenting | Parents ‘desired information relevant and applicable to their child to assist them in understanding and making sense of their own child’s presentation’ |
|
Author: Little
et al.
37
Title: Wonders and Worries of Parenting a Child with Asperger Syndrome and Non-verbal Learning Disorder Year: 2006 Country: USA |
|
| Age: 3–21 years with Asperger syndrome and/or non-verbal learning disorder | |
| Method: Survey instrument with open-ended questions; 103 couples (each completed instrument); qualitative analysis of open-ended questions | |
| Notes: Outcome-related themes listed below: child and parent outcomes | |
| Parent outcome: positive times with child | ‘When he is behaving well and not gearing up for a fight, he’s a very happy and pleasant child, whom I can enjoy spending time with and doing things with’ |
| Concerns about adulthood | ‘Fend for (him or) herself as an adult’ ‘Lack of friends, uncontrollable temper and frustration, I just hope he will be able to grow up, get a job, raise a family, live a normal life’ ‘Loving relationships outside our family’ ‘A proper match between his abilities and living/job situation’ |
| Mental health concerns | One father reported concern that his son ‘. . . will be isolated from peers or rejected (and) will develop depression and anxiety’ Ability to manage anger and behaviour to avoid getting into trouble |
| Victimisation concerns | ‘I worry that he will unknowingly insult someone who will physically retaliate; that someone will take advantage of his social deficits and then physically harm him’ |
|
Author: Mackintosh
et al
.
36
Title: ‘What Do You Like/dislike About the Treatments You are Currently Using?’ A Qualitative Study of Parents of Children with Autism Spectrum Disorders Year: 2012 Country: USA |
|
| Child age: 2–21 years (mean = 8.3 years) | |
| Methods: ‘Web-based qualitative study’, n = 486 parents; ‘what do you like/dislike about treatments you are currently using?’ | |
| Notes: Six themes emerged and are discussed: effectiveness of treatments, relationships with professionals, access to treatments, costs, medication concerns and [parents’] stress Relevant data extracted below |
|
Effective treatments (illustrative quotes to right) identified as yielding the following outcomes:
|
‘Not “zoned out” by meds’ ‘Do not like the fact he takes regular medication but at the same time it allows him to function better‘ ‘As for behavior modifying, well we will keep on trying till we find one which works’ ‘Love the diet – makes it easier for him to learn’ ‘She is currently on Adderall. This helps her to sit still at school and focus longer. This medicine makes her aggressive at times. When she is not on it, she is silly/slap happy, goofy acting’ Occupational therapy to improve motor skills seen to improve self-esteem which ‘makes him more available to make improvements in other areas’ (including learning) ‘To find the child and bring him out’ ‘Speech therapy starting at age 2 has had a profound impact and allowed him to finally develop speech’ ‘The most effective therapy we have for him right now is OT [occupational therapy]. This is a very stress-free therapy for him, and has helped somewhat in sensory integration’ |
|
Author: Serpentine
et al.
35
Title: Decision Making of Parents of Children With Autism Spectrum Disorder Concerning Augmentative and Alternative Communication in Hungary Year: 2010 Country: USA but looking at parental views in Hungary |
|
| Age: 6–16 years; ASD with no functional communication | |
| Methods: A single focus group and individual interviews are referred to; methods unclear; focus of interviews was experiences of augmentative and alternative communications | |
| Notes: Six main themes emerged from the data. These included:
|
|
| Development of natural speech | ‘That his speech would develop, that he would probably start speaking, say words’ |
| Improved communication (parent to child and child to parent) | ‘We expected to be able to communicate better with our child’ |
| Improved attention | ‘That he would start using words, and that he would pay attention to such things that have not interested him before, or not for a long time’ |
| Improved behaviour | ‘I was hoping his behaviour would change, in fact that his behaviour would get better’ ‘We hoped the behaviour problems would end, finally no more tantrums’ |
| Interventions acceptable to the child | ‘We try things. If he likes it or is willing to accept it we try. If he cries or refuses we rather let it be’ |
|
Author: Whitaker
et al.
33
Title: Supporting Families of Preschool Children with Autism Year: 2002 Country: England |
| Age: Up to ∼5 years |
| Methods: Semistructured interview (no detail on what this covered) at time of leaving service (EarlyBird programme, delivered by SEN team in LA); sample size not reported; method of data analysis not reported |
Notes: Mainly focused on parents’ experiences of training, some potentially relevant issues regarding parent outcomes related to parenting/teaching skills:
|
Not qualitative research
|
Author: Bitterman
et al.
289
Title: A National Sample of Preschoolers with Autism Spectrum Disorders: Special Education Services and Parent Satisfaction Year: 2008 Country: USA |
| Child age: 3–5 years |
| Method: Telephone interview with parents (n = 3104): service use and satisfaction; teacher questionnaire. This was not a qualitative study: EXCLUDE |
|
Author: Callahan
et al.
290
Title: Social Validation of Evidence-based Practices in Autism by Parents, Teachers, and Administrators Year: 2008 Country: USA |
| Age: Not stated |
| Method: Survey to identified relative importance of elements of school-based autism programme; research instrument developed from literature review of evidence on the effectiveness of existing programmes; survey completed by parents (95), teachers (54); administrators (16) This was not a qualitative study: EXCLUDE |
|
Author: Pituch
et al.
291
Title: Parent-reported Treatment Priorities for Children with Autism Spectrum Disorders Year: 2011 Country: New Zealand |
| Age: 2–21+ years |
| Method: Online survey, fixed response, used to identify treatment priorities; 90 parents participated No qualitative data collected: EXCLUDE |
| No relevant data on outcomes |
|
Author: Dymond
et al.
292
Title: Services for Children With Autism Spectrum Disorders Year: 2007 Country: USA |
| Age: 0–22 years |
| Method: Survey of 783 parents, including some open-ended questions |
| Notes: Recommendations for improving school and community-based services for ASD No relevant data about measurement or outcomes |
|
Author: Hackett
et al.
293
Title: Parental Perceptions of the Assessment of Autistic Spectrum Disorders in a Tier Three Service Year: 2009 Country: England |
| Age: Not reported |
| Method: Parental questionnaire, self-completed or administered via a phone interview; 40 parents who had recently been through a multiagency ASD assessment |
| Notes: Service audit, focus on diagnosis and experience of that process No relevant data about measurement or outcomes |
|
Author: Read and Schofield
294
Title: Autism: Are Mental Health Services Failing Children and Parents? Year: 2010 |
| Notes: Focus on how CAMHS handles ASD No relevant data about measurement or outcomes |
|
Author: Moore
et al.
295
Title: Improving Diagnostic and Assessment Services for Children with Autistic Spectrum Disorders Year: 1999 Country: Northern Ireland |
| Age: Not reported |
| Method: Mixed-methods consultation process involving parents and professionals; concerned with diagnostic and assessment processes; no information on how qualitative elements of data collected and analysed |
| Notes: Focus on parents’ and professionals’ experiences and views to determine recommendations for services No relevant data about measurement or outcomes |
Appendix 3 Additional information on Chapter 3 search methodology
Autism-related websites searched for grey literature
Autism Education Trust: www.autismeducationtrust.org.uk/
Autism Research Centre: www.autismresearchcentre.com/
Autism Research Institute: www.autism.com/
Autism Society of America: www.autism-society.org/
Autism Speaks: www.autismspeaks.org/
Autism-Europe: www.autismeurope.org/
Interactive Autism Network: www.iancommunity.org/
Research Autism: www.researchautism.net/
UK Autism Foundation: www.ukautismfoundation.org/
List of search terms
Autism terms
ASC
ASD (NOT atrial septal defect)
Asperger*
Autis*
childhood schizophrenia
communicat*
Kanner*
language delay*
PDD
pervasive developmental disorder
speech disorder*
semantic-pragmatic disorder
PDD-NOS
exp Child Development Disorders, Pervasive/ [MeSH]
Age group terms
Child*
elementary (school)
infan*
kindergarten*
nursery
p?ediatric*
pre-school*
preschool*
primary (school)
toddler*
special needs
grammar (school)
exp child/ [MeSH]
Behaviour-related terms
Behavio?r
intervention*
non-verbal
program*
rehabilitat*
social interaction
therap*
train OR training OR trained
treatment*
verbal
Assessment-related terms
Assess*
exam*
feasib*
measur*
method*
questionnaire*
reliab*
repeat*
report*
reproducib*
self-report*
survey*
test*
valid*
score*
diagnostic*
observ*
track*
monitor*
follow-up
scale
outcome*
audit*
record*
Example search strategies
MEDLINE (Ovid)
-
(asd not atrial septal defect).ab,ti.
-
‘Asperger*’.ab,ti.
-
‘Autis*’.ab,ti.
-
childhood schizophrenia.ab,ti.
-
‘Kanner*’.ab,ti.
-
(PDD or PDD-NOS).ab,ti.
-
semantic-pragmatic disorder.ab,ti.
-
‘language delay*’.ab,ti.
-
‘speech disorder*’.ab,ti.
-
pervasive developmental disorder.ab,ti.
-
exp Child Development Disorders, Pervasive/
-
or/1-11
-
exp Child/
-
‘infan*’.ab,ti.
-
‘child*’.ab,ti.
-
‘kindergarten*’.ab,ti.
-
nursery.ab,ti.
-
‘p?ediatric*’.ab,ti.
-
(pre-school* or preschool*).ab,ti.
-
‘toddler*’.ab,ti.
-
special needs.ab,ti.
-
((primary or elementary or grammar) and school).ab,ti.
-
or/13-22
-
12 and 23
-
Behavio?r.tw.
-
‘intervention*’.tw.
-
non-verbal.tw.
-
program$4.tw.
-
‘rehabilitat*’.tw.
-
social interaction.tw.
-
‘therap*’.tw.
-
‘treatment*’.tw.
-
verbal.tw.
-
(train or training or trained).tw.
-
or/25-34
-
24 and 35
-
limit 36 to (english language and humans and yr=‘1992 -Current’)
-
‘assess*’.tw.
-
‘feasib*’.tw.
-
‘measur*’.tw.
-
‘method*’.tw.
-
‘questionnaire*’.tw.
-
‘reliab*’.tw.
-
‘repeat*’.tw.
-
‘report*’.tw.
-
‘reproducib*’.tw.
-
‘self-report*’.tw.
-
‘survey*’.tw.
-
‘valid*’.tw.
-
‘score*’.tw.
-
‘diagnostic*’.tw.
-
‘observ*’.tw.
-
‘track*’.tw.
-
‘monitor*’.tw.
-
follow-up.tw.
-
scale.tw.
-
‘outcome*’.tw.
-
‘audit*’.tw.
-
‘record*’.tw.
-
or/38-59
-
37 and 60
-
limit 61 to (english language and humans and yr=‘1992 -Current’)
-
Epidemiologic Studies/
-
62 and 63
-
cohort.ti,ab. or exp Cohort Studies/ or longitudinal.ti,ab. or prospective.ti,ab. or retrospective.ti,ab.
-
62 and 65
-
exp Clinical Trial/ or double-blind method/ or (clinical trial* or randomized controlled trial or multicenter study).pt. or exp Clinical Trials as Topic/ or ((randomi?ed adj7 trial*) or (controlled adj3 trial*) or (clinical adj2 trial*) or ((single or doubl* or tripl* or treb*) and (blind* or mask*))).ti,ab.
-
limit 67 to yr=‘1992-2012’
-
62 and 68
-
(((‘semi-structured’ or semistructured or unstructured or informal or ‘in-depth’ or indepth or ‘face-to-face’ or structured or guide) adj3 (interview* or discussion* or questionnaire*)) or (focus group* or qualitative or ethnograph* or fieldwork or ‘field work’ or ‘key informant’)).ti,ab. or interviews as topic/ or focus groups/ or narration/ or qualitative research/
-
62 and 70
-
((systematic adj3 literature) or systematic review* or meta-analy* or metaanaly* or ‘research synthesis’ or ((information or data) adj3 synthesis) or (data adj2 extract*)).ti,ab. or (cinahl or (cochrane adj3 trial*) or embase or medline or psyclit or (psycinfo not ‘psycinfo database’) or pubmed or scopus or ‘sociological abstracts’ or ‘web of science’).ab. or ‘cochrane database of systematic reviews’.jn. or ((review adj5 (rationale or evidence)).ti,ab. and review.pt.) or meta-analysis as topic/ or Meta-Analysis.pt.
-
62 and 72
-
limit 73 to yr=‘1992 -Current’
-
exp Case-Control Studies/ or Control Groups/ or Matched-Pair Analysis/ or ((case* adj5 control*) or (case adj3 comparison*) or control group*).ti,ab.
-
62 and 75
-
64 or 66 or 69 or 71 or 74 or 76
Education Resources Information Center (ProQuest)
S1 SU.EXACT(‘Pervasive Developmental Disorders’)
S2 ab(ASD OR autis* OR asperger* OR kanner*) OR ti(ASD OR autis* OR asperger* OR kanner*)
S3 ab(PDD OR PDD-NOS OR pervasive developmental disorder) OR ti(PDD OR PDD-NOS OR pervasive developmental disorder)
S4 ab(speech disorder* OR language delay*) OR ti(speech disorder* OR language delay*)
S5 ab(childhood schizophrenia OR semantic-pragmatic disorder) OR ti(childhood schizophrenia OR semantic-pragmatic disorder)
S6 S1 OR S2 OR S3 OR S4 OR S5
S7 SU.EXACT(‘Young Children’)
S8 ab(infan* OR child* OR toddler*) OR ti(infan* OR child* OR toddler*)
S9 ab(kindergarten* OR nursery OR pre-school OR preschool) OR ti(kindergarten* OR nursery OR pre-school OR preschool)
S10 ab((primary or elementary or grammar) and school) OR ti((primary or elementary or grammar) and school)
S11 ab(special needs OR pediatric* OR paediatric*) OR ti(special needs OR pediatric* OR paediatric*)
S12 s7 OR s8 OR s9 OR s10 or s11
S13 s6 and s12
S17 intervention* OR program* OR rehabilitat* OR treatment* OR therap*
S18 behaviour OR behavior
S19 non-verbal OR verbal OR social interaction
S20 train OR training OR trained
S21 s17 or s18 or s19 or s20
S22 s13 and s21
S23 assess* OR feasib* OR measur* OR method* OR questionnaire*
S24 reliab* OR repeat* OR reproducib* OR self-report* OR survey*
S25 valid* OR score* OR diagnostic* OR observ* OR track*
S26 monitor* OR follow-up OR scale OR outcome* OR audit* OR record*
S27 s23 or s24 or s25 or s26
S28 s22 and s27
S29 (s22 and s27) AND la.exact(‘ENG’) AND pd(1992-2012)
S30 (s22 and s27) AND peer(yes)
S31 (s22 and s27) AND (peer(yes) AND yr(1990-2019))
S32 (s22 and s27) AND (peer(yes) AND yr(1990-2019))
Web of Science
#1 (TI=((ASD NOT atrial septal defect) OR autis* OR asperger* OR kanner* OR PDD OR PDD-NOS OR pervasive developmental disorder OR speech disorder* OR language delay* OR childhood schizophrenia OR semantic-pragmatic disorder)) AND Language=(English) Databases=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, BKCI-S, BKCI-SSH Timespan=1992-2012 Lemmatization=On
#2 (TI=(infan* OR child* OR toddler* OR kindergarten* OR nursery OR pre-school OR preschool OR ((primary or elementary or grammar) and school) OR special needs OR pediatric* OR paediatric*)) AND Language=(English) Databases=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, BKCI-S, BKCI-SSH Timespan=1992-2012 Lemmatization=On
#3 (#1 AND #2) AND Language=(English) Databases=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, BKCI-S, BKCI-SSH Timespan=1992-2012 Lemmatization=On
#4 (TS=(intervention* OR program* OR rehabilitat* OR treatment* OR therap* OR behaviour OR behavior OR non-verbal OR verbal OR social interaction OR train OR training OR trained)) AND Language=(English) Databases=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, BKCI-S, BKCI-SSH Timespan=1992-2012 Lemmatization=On
#5 (TS=(assess* OR feasib* OR measur* OR method* OR questionnaire* OR reliab* OR repeat* OR reproducib* OR self-report* OR survey* OR valid* OR score* OR diagnostic* OR observ* OR track* OR monitor* OR follow-up OR scale OR outcome* OR audit* OR record*)) AND Language= (English) Databases=SCI-EXPANDED, SSCI, A&HCI, CPCI-S, BKCI-S, BKCI-SSH Timespan=1992-2012 Lemmatization=On
#6 #5 AND #4 AND #3 Databases=SCI-EXPANDED, SSCI, A&HCI, CPCI-S Timespan=1992-2012 Lemmatization=On
#7 (#6) AND Language=(English) Databases=SCI-EXPANDED, SSCI, A&HCI, CPCI-S Timespan=1992-2012 Lemmatization=On
Appendix 4 Stage 2: data extraction tool
Appendix 5 Tables of papers and data extracted (see Chapter 3)
Data from papers are presented in three sets of tables as follows: pp.179–272 – Tools used (paper, location, study design, study aim); pp. 273–377 – Tools used (participant description); and pp. 378–437 – Tools used (subscales, outcomes measured according to the author).
Chapter 3 Tools used (paper, location, study design, study aim)
| Symptom severity | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Autism Behavior Checklist (AuBC) | Bennett 2008296 | Canada | Longitudinal observational | To explore ‘specific language impairment’ as a predictor of children’s symptom and functional outcome |
| Gupta 2009297 | India | Cross-sectional observational | To understudy the development of language and learning skills in children with autism and compare with that of typically developing children | |
| Jocelyn 1998298 | Canada | Intervention RCT | Caregiver-based intervention programme in community day-care centres | |
| Silva 2007299 | USA | Intervention RCT | Effectiveness of qigong massage methodology, in treating sensory impairment in young children with autism | |
| Silva 2008300 | USA | Intervention RCT | Outcomes of pilot of qigong sensory training programme | |
| Silva 2009226 | USA | Intervention RCT | Improvement following a qigong massage intervention | |
| Silva 2011301 | USA | Intervention RCT | Dual parent and trainer-delivered qigong massage intervention for measures of autism, abnormal sensory responses and self-regulation | |
| Szatmari 2000302 | Canada | Longitudinal observational | Monitoring cognitive and language outcomes of groups of children with autism and Asperger syndrome | |
| Zhang 2012303 | China | Intervention quasi-experimental | TEAS was applied to children with autism to assess its therapeutic efficacy | |
| Autism Diagnostic Interview-Revised (ADI-R) | Bennett 2012304 | Canada | Longitudinal observational | Impact of maternal depression on mother’s reports of her child’s ASD behaviours |
| Ben Itzchak 2008149 | Israel | Longitudinal observational | To examine the relations between cognition and autism severity, head size and intervention outcome | |
| Brian 2008305 | Canada | Longitudinal observational | Assessment of potential behavioural markers of ASD at 18 months in a high-risk cohort of infant siblings of children with ASD | |
| Feldman 2012104 | Canada | Longitudinal observational | Development and evaluation of a new instrument: POEMS | |
| Hambly 2012306 | Canada | Cross-sectional observational | The impact of bilingual exposure on language learning in ASD | |
| Honey 2008307 | UK | Longitudinal observational | The study tests the following hypotheses:
|
|
| Magiati 2007308 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Magiati 2011309 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Mayo 2013310 | USA | Other – retrospective observational | This study examined the relationship between age of language acquisition and later functioning in children with ASD | |
| Mooney 2006311 | Australia | Cross-sectional observational | Examined whether repetitive behaviours are a feature of autism in children aged < 51 months, independent of chronological or developmental age | |
| Munson 2008312 | USA | Cross-sectional observational | Latent class analysis of IQ in ASD | |
| Ozonoff 2010313 | USA | Longitudinal observational | ‘To examine prospectively the emergence of behavioural signs of autism in the first years of life in infants at low and high risk for autism’ | |
| Pry 2005314 | France, Switzerland, Belgium and Luxembourg | Cross-sectional observational | The relationship between expressive language level and psychological development in children with autism at 5 years of age | |
| Richler 2007315 | USA | Longitudinal observational | Examination of RRBs | |
| Werner 2005316 | USA | Cross-sectional observational | Describing variations in early course of development | |
| Autism Diagnostic Observation Scale-Toddler Module (ADOS-T) | Rogers 2012317 | USA | Intervention RCT | This study was carried out to examine the efficacy of a 12-week, low-intensity (1 hour/week of therapist contact), parent-delivered intervention for toddlers at risk for ASDs aged 14–24 months and their families |
| Autism Diagnostic Observation Schedule (ADOS) | Aldred 2004318 | England | Intervention RCT | ‘Social communication intervention targeting parental communication’ |
| Aldred 2012319 | UK | Other RCT | A mediation analysis aimed at assessing the impact of targeted intervention on autism characteristics | |
| Ben Itzchak 2008149 | Israel | Longitudinal observational | To examine the relations between cognition and autism severity, head size and intervention outcome | |
| Ben Itzchak 2011320 | Israel | Intervention quasi-experimental | The study explored child and parental characteristics at baseline that may predict outcomes in adaptive skills and acquisition of cognitive gains | |
| Bennett 2012304 | Canada | Longitudinal observational | Impact of maternal depression on mother’s reports of her child’s ASD behaviours | |
| Brian 2008305 | Canada | Longitudinal observational | Assessment of potential behavioural markers of ASD at 18 months in a high-risk cohort of infant siblings of children with ASD | |
| Dawson 2010321 | USA | Intervention RCT | Efficacy of the ESDM, a comprehensive developmental behavioural intervention, for improving outcomes in ASD toddlers | |
| Gotham 2012322 | USA | Longitudinal observational | To plot longitudinal trajectories of ASD severity from early childhood to early adolescence | |
| Green 2010253 | UK | Intervention RCT | Early interventions for social communication | |
| Hartley 2009323 | USA | Cross-sectional observational | To explore developmental patterns, along gender lines, in children who have autism | |
| Landa 2012324 | USA | Intervention quasi-experimental | Comprehensive early intervention | |
| Lerna 2012325 | Italy | Intervention RCT | PECS vs. CLT | |
| Luyster 2008129 | USA | Cross-sectional observational | To systematically investigate language in toddlers with ASD and to identify early correlates of receptive and expressive language in this population | |
| Munson 2008312 | USA | Cross-sectional observational | Latent class analysis of IQ in ASD | |
| Oosterling 2010326 | The Netherlands | Intervention RCT | Intervention is ‘Focus parent training’. Home-based parent training promoting compliance, mutual enjoyment, joint attention and language development | |
| Ray-Subramanian 2011327 | USA | Cross-sectional observational | ‘Their study examined adaptive behaviour and cognitive skills for 125 toddlers on the autism spectrum using the recently updated Vineland-II and Bayley-III’ | |
| Ray-Subramanian 2012328 | USA | Longitudinal observational | This study examined whether language skills and non-verbal cognitive skills were associated with clinician-observed RRBs in children with ASD | |
| Strauss 2012329 | Italy | Intervention quasi-experimental | Influence of parent inclusion in treatment provision on child’s progress | |
| Sullivan 2007330 | USA | Longitudinal observational | To examine whether RJA was impaired as early as 14 months in children later diagnosed with ASD and whether RJA was an early marker for ASD diagnosis at outcome | |
| Tek 2012331 | USA | Cross-sectional observational | To assess whether early symptom presentation differs in toddlers with ASD from ethnic minority vs. non-minority backgrounds | |
| Ventola 2007332 | USA | Cross-sectional observational | Behavioural presentation of AD, developmental delay and developmental language disorder | |
| Werner 2005316 | USA | Cross-sectional observational | Describing variations in early course of development | |
| Wong 2010333 | China | Intervention RCT | To pilot a 2-week ‘Autism 1-2-3’ early intervention for children with autism and their parents immediately after diagnosis that targeted at (1) eye contact, (2) gesture and (3) vocalisation/words | |
| Zachor 2006334 | Israel | Intervention quasi-experimental | To compare the outcome of two centre-based interventions for autism | |
| Zachor 2010335 | Israel | Longitudinal observational | To examine the effect of the intervention approach (ABA, eclectic) on outcome in cognitive, language, and adaptive skills and on changes in autism diagnosis categories | |
| Autism Observation Scale for Infants (AOSI) | Brian 2008305 | Canada | Longitudinal observational | Assessment of potential behavioural markers of ASD at 18 months in a high-risk cohort of infant siblings of children with ASD |
| Bryson 200881 | Canada | Longitudinal observational | Putative signs of autism in infants 6–18 months | |
| Baby and Infant Screen for Children with aUtIsm Traits (BISCUIT-Part 1) | Fodstad 2009336 | USA | Longitudinal observational | To explore verbal/non-verbal and social skills in infants and toddlers with ASD |
| Behavioral Summarized Evaluation-Revised (BSE-R) | Receveur 2005337 | France | Longitudinal observational | Interaction and imitation deficits from infancy to 4 years of age in children with autism |
| Behavioral Summarized Evaluation (BSE) | Maestro 2005338 | Italy | Cross-sectional observational | Providing new criteria to describe the early course of ASD |
| Childhood Autism Rating Scale (CARS) | Baghdadli 2012339 | France | Longitudinal observational | Developmental trajectory of adaptive behaviours |
| Bopp 2009340 | Canada | Longitudinal observational | Examined the relationship between behaviour and trajectories of vocabulary and language development in young children with autism | |
| Jonsdottir 2007341 | Iceland | Longitudinal observational | The purpose of the present study was to describe stability and change of preschool children in Iceland and to contribute to the accumulation of data on outcome in autism | |
| Malhi 2011342 | India | Longitudinal observational | To assess diagnostic stability of autism diagnosis in children aged ≤ 3 years | |
| Mayo 2013310 | USA | Other – retrospective observational | This study examined the relationship between age of language acquisition and later functioning in children with ASD | |
| Pajareya 2012343 | Thailand | Intervention quasi-experimental | Determine the results of 1-year DIR/Floortime™ parent training in developmental stimulation of children with ASD | |
| Pajareya 2011344 | Thailand | Intervention RCT | RCT of DIR/Floortime intervention for autistic children | |
| Papavasiliou 2011345 | Greece | Longitudinal observational | ‘This study aimed to investigate the effect of an individually tailored psycho-educational programme for autistic children on the scores of the Childhood Autism Rating Scale (CARS) and the Short Sensory Profile (SSP)’ | |
| Pry 2005314 | France, Switzerland, Belgium and Luxembourg | Cross-sectional observational | The relationship between expressive language level and psychological development in children with autism at 5 years of age | |
| Stone 1999346 | USA | Longitudinal observational | To evaluate the reliability and stability of autism diagnosis in children aged < 3 years of age at diagnosis | |
| Ventola 2007332 | USA | Cross-sectional observational | Behavioural presentation of AD, developmental delay and developmental language disorder | |
| Vorgraft 2007347 | Israel | Cross-sectional observational | Effectiveness of the ‘Mifne Centre’ approach to PDD | |
| Zhang 2012303 | China | Intervention quasi-experimental | TEAS was applied to children with autism to assess its therapeutic efficacy | |
| Gilliam Autism Rating Scale (GARS) | Cassidy 2008348 | Northern Ireland | Cross-sectional observational | To describe the demographic characteristics of preschoolers and their families; to discover parental perceptions of the child’s difficulties; to identify the impact the child has on family life; to outline the supports available to families and those they would like to have |
| McConkey 2010349 | – | Intervention quasi-experimental | Evaluate a home-based intervention for preschool children with a confirmed diagnosis of ASD | |
| Osborne 2008350 | UK | Intervention quasi-experimental | There was great heterogeneity among the interventions delivered and so for analysis interventions were categorised into high vs. low intensity | |
| Osborne 2009351 | UK | Longitudinal observational | Evaluate relationship between child behaviour problems and parental stress | |
| Reed 2007352 | UK | Longitudinal observational | Comparing high- and low-intensity interventions (with comparison of three different types of high-intensity interventions) | |
| Reed 2007353 | UK | Longitudinal observational | Compare effectiveness of ABA, special nursery placements and portage; addressing limitations of previous studies by using the same measures at baseline and end point | |
| Reed 2012354 | UK | Intervention quasi-experimental | To explore and document the relationships between severity of autism, temporal input of the programme and the outcome effectiveness for a variety of early interventions for children on the autism spectrum. In particular, ABA, special nursery placement, an adaptation of a portage approach for individuals on the autism spectrum, and an eclectic approach developed by a local authority were chosen for study | |
| Stahmer 2004355 | USA | Intervention quasi-experimental | To analyse the outcomes for 20 young children with ASD in an inclusive programme for children aged < 3 years | |
| Infant Behavioral Summarized Evaluation (IBSE) | Adrien 199290 | France | Longitudinal observational | To observe and analyse the evolution of behavioural pathology in autistic children |
| Receveur 2005337 | France | Longitudinal observational | Interaction and imitation deficits from infancy to 4 years of age in children with autism | |
| Modified Checklist for Autism in Toddlers (M-CHAT) | Ventola 2007332 | USA | Cross-sectional observational | Behavioural presentation of AD, developmental delay and developmental language disorder |
| Parent Observation of Early Markers Scale (POEMS) | Feldman 2012104 | Canada | Longitudinal observational | Development and evaluation of a new instrument – POEMS |
| Pervasive Developmental Disorder Rating Scale (PDDRS) | Eaves 2006356 | USA | Longitudinal observational | To examine the construct validity of the PDDRS |
| Pervasive Developmental Disorders Behavior Inventory (PDDBI) | Silva 2009226 | USA | Intervention RCT | Improvement following a qigong massage intervention |
| Silva 2011301 | USA | Intervention RCT | Dual parent and trainer-delivered qigong massage intervention for measures of autism, abnormal sensory responses and self-regulation | |
| Real Life Rating Scale (Ritvo–Freeman) (RLRS) | Wong 2010333 | China | Intervention RCT | To pilot a 2-week ‘Autism 1-2-3’ early intervention for children with autism and their parents immediately after diagnosis that targeted at (1) eye contact, (2) gesture and (3) vocalisation/words |
| Social Communication Questionnaire (SCQ) | Eapen 2013357 | Australia | Longitudinal observational | Evaluation of ESDM for preschool-aged children with ASD |
| Remington 2007358 | UK | Intervention quasi-experimental | Comparison of early intensive behavioural interventions and treatment as usual | |
| Social Responsiveness Scale (SRS) | Bennett 2012304 | Canada | Longitudinal observational | Impact of maternal depression on mother’s reports of her child’s ASD behaviours |
| Hambly 2012306 | Canada | Cross-sectional observational | The impact of bilingual exposure on language learning in ASD | |
| Smith 2010359 | Canada and USA | Intervention quasi-experimental | Effect of a parent training and naturalistic one-to-one behaviour intervention using PRT on language, behaviour and ASD symptoms | |
| Childhood Autism Rating Scale (CARS) – Tokyo versiona | Takeda 2005360 | Japan | Longitudinal observational | Clinical variables at age 2 years predictive of mental retardation at age 5 years in children with PDD |
| Social awareness | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Child Behavior Rating Scale (CBRS) (Modified) | Casenhiser 2013361 | Canada | Longitudinal observational | To assess the impact of an intervention on social interaction and communication in children with ASD |
| Communication and Symbolic Behavior Scales-Developmental Profile (CSBS–DP) | Green 2010253 | UK | Intervention RCT | Early interventions for social communication |
| Landa 2007362 | USA | Longitudinal observational | To examine patterns of development from 14–24 months in children with early and later diagnosis of ASDs | |
| Sullivan 2007330 | USA | Longitudinal observational | To examine whether RJA was impaired as early as 14 months in children later diagnosed with ASD and whether RJA was an early marker for ASD diagnosis at outcome | |
| Keen 2010363 | Australia | Intervention quasi-experimental | To reduce parenting stress and increase parenting competence for families of children within 6 months of receiving an ASD diagnosis | |
| Keen 2007364 | Australia | Longitudinal observational | To investigate the effects of the Stronger Families Project on communication and symbolic behaviour of young children with autism and to explore possible correlations between post-intervention changes in children’s communication and symbolic behaviour, and child adaptive behaviour, chronological age, maternal stress and sense of parenting competence | |
| Early Social Communication Scale (ESCS) | Dereu 2012365 | Belgium | Longitudinal observational | Developmental trajectories of joint attention, imitation and pretend play impairments in autism |
| Goods 2013366 | USA | Intervention RCT | JASPER | |
| Ingersoll 2012286 | USA | Intervention RCT | Imitation intervention to improve social functioning | |
| Kaale 2012288 | Norway | Intervention RCT | To explore effectiveness of parent-mediated and specialist-mediated joint attention intervention | |
| Kalas 2012367 | USA | Cross-sectional observational | Joint attention responses to simple vs. complex music | |
| Kasari 2006368 | USA | Intervention RCT | The efficacy of targeted interventions of joint attention and symbolic play was explored | |
| Lawton 2012369 | USA | Intervention quasi-experimental | Joint attention | |
| Luyster 2008129 | USA | Cross-sectional observational | To systematically investigate language in toddlers with ASD and to identify early correlates of receptive and expressive language in this population | |
| Paparella 2011370 | USA | Longitudinal observational | Study 1: Cross-sectional study of profile of emergence of joint attention Study 2: Longitudinal study of emergence of joint attention |
|
| Remington 2007358 | UK | Intervention quasi-experimental | Comparison of early intensive behavioural interventions and treatment as usual | |
| Roos 2008371 | USA | Cross-sectional observational | Comparison of contexts for assessing joint attention in toddlers on the autism spectrum | |
| Salt 2002372 | UK | Intervention quasi-experimental | Developmentally based early intervention programme | |
| Wong 2013373 | USA | Intervention RCT | The aim of this study was to pilot test a classroom-based intervention focused on facilitating play and joint attention for young children with autism in self-contained special education classrooms | |
| Yoder 2006374 | USA | Intervention RCT | Compared the efficacy of two communication interventions (RPMT and PECS) in 36 preschoolers with ASDs | |
| Early Social Communication Scales (ESCS)-Abridged | Yoder 2010375 | USA | Intervention RCT | Effects of a social communication intervention |
| Imitation Battery (IB) | Luyster 2008129 | USA | Cross-sectional observational | To systematically investigate language in toddlers with ASD and to identify early correlates of receptive and expressive language in this population |
| Imitation Disorders Evaluation (IDE) | Receveur 2005337 | France | Longitudinal observational | Interaction and imitation deficits from infancy to 4 years of age in children with autism |
| Motor Imitation Scale (MIS) | Ingersoll 2010376 | USA | Longitudinal observational | To evaluate the effectiveness of an intervention (RIT) in young children with autism |
| Ingersoll 2012286 | USA | Intervention RCT | Imitation intervention to improve social functioning | |
| Preschool Imitation and Praxis Scale (PIPS) | Dereu 2012365 | Belgium | Longitudinal observational | Developmental trajectories of joint attention, imitation and pretend play impairments in autism |
| Pre-Verbal Communication Schedule (PVCS) | Salt 2002372 | UK | Intervention quasi-experimental | Developmentally based early intervention programme |
| Social Communication Assessment for Toddlers with Autism (SCATA) | Drew 2007137 | UK | Longitudinal observational | To describe the SCATA administration and scoring, to examine the pattern of developmental change in two samples of children with autism and PDD and to examine which aspects of early non-verbal communication are most strongly associated with later language outcomes |
| Social Communication Behavior Codes | Ozonoff 2010313 | USA | Longitudinal observational | ‘To examine prospectively the emergence of behavioural signs of autism in the first years of life in infants at low and high risk for autism’ |
| Parent interviewa | Clifford 2008377 | Australia | Cross-sectional observational | Home videos and interviews concerning four time periods: (0–5, 6–11, 12–17, 18–24 months) |
| Caregiver–child interactionb | Kasari 2006368 | USA | Intervention RCT | The efficacy of targeted interventions of joint attention and symbolic play was explored |
| Coded observation of joint attentionb | Warreyn 2007378 | Belgium | Cross-sectional observational | Joint attention in preschoolers with ASD |
| Coding of initiation of joint attentionb | Ingersoll 2012286 | USA | Intervention RCT | Imitation intervention to improve social functioning |
| Classroom Observation Measureb | Goods 2013366 | USA | Intervention RCT | JASPER |
| Examiner Ratings of Social Engagementb | Ozonoff 2010313 | USA | Longitudinal observational | ‘To examine prospectively the emergence of behavioural signs of autism in the first years of life in infants at low and high risk for autism’ |
| Naturalistic examiner–child play sampleb | Roos 2008371 | USA | Cross-sectional observational | Comparison of contexts for assessing joint attention in toddlers on the autism spectrum |
| Prelinguistic Communication Assessmentb | Stone 1997133 | USA | Cross-sectional observational | Assessing non-verbal communication on young children with autism |
| Preschool teacher–child playb | Kaale 2012288 | Norway | Intervention RCT | To explore effectiveness of parent-mediated and specialist-mediated joint attention-intervention |
| Unstructured free play with examinerb | Lerna 2012325 | Italy | Intervention RCT | PECS vs. CLT |
| Unstructured Imitation Assessmentb | Ingersoll 2012286 | USA | Intervention RCT | Imitation intervention to improve social functioning |
| Ingersoll 2010376 | USA | Longitudinal observational | To evaluate the effectiveness of an intervention (RIT) in young children with autism | |
| Video coding proceduresb | Colgan 2006379 | USA | Longitudinal observational | To examine the frequency, initiation, prompting and diversity of types of gestures used for social interaction purposes |
| Video observationb | Clifford 2008377 | Australia | Cross-sectional observational | Home videos and interviews concerning four time periods: (0–5, 6–11, 12–17, 18–24 months) |
| Video rating for expressive speechb | Baghdadli 2012339 | France | Longitudinal observational | Developmental trajectory of adaptive behaviours |
| Video recording of child in classroom activitiesb | Ingersoll 2001380 | USA | Longitudinal observational | To identify a behavioural characteristic that may affect the outcome of a particular treatment model |
| Restricted, repetitive behaviour | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Autism Diagnostic Interview-Revised (ADI-R) | Ben Itzchak 2008149 | Israel | Longitudinal observational | To examine the relations between cognition and autism severity, head size and intervention outcome |
| Bennett 2012304 | Canada | Longitudinal observational | Impact of maternal depression on mother’s reports of her child’s ASD behaviours | |
| Brian 2008305 | Canada | Longitudinal observational | Assessment of potential behavioural markers of ASD at 18 months in a high-risk cohort of infant siblings of children with ASD | |
| Feldman 2012104 | Canada | Longitudinal observational | Development and evaluation of a new instrument – POEMS | |
| Hambly 2012306 | Canada | Cross-sectional observational | The impact of bilingual exposure on language learning in ASD | |
| Honey 2008307 | UK | Longitudinal observational | The study tests the following specific hypotheses:
|
|
| Magiati 2007308 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Magiati 2011309 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Mayo 2013310 | USA | Other – retrospective observational | This study examined the relationship between age of language acquisition and later functioning in children with ASD | |
| Mooney 2006311 | Australia | Cross-sectional observational | Examined whether repetitive behaviours are a feature of autism in children aged < 51 months, independent of chronological or developmental age | |
| Munson 2008312 | USA | Cross-sectional observational | Latent class analysis of IQ in ASD | |
| Ozonoff 2010313 | USA | Longitudinal observational | ‘To examine prospectively the emergence of behavioural signs of autism in the first years of life in infants at low and high risk for autism’ | |
| Pry 2005314 | France, Switzerland, Belgium and Luxembourg | Cross-sectional observational | The relationship between expressive language level and psychological development in children with autism 5 years of age | |
| Richler 2007315 | USA | Longitudinal observational | Examination of RRBs | |
| Werner 2005316 | USA | Cross-sectional observational | Describing variations in early course of development | |
| Autism Diagnostic Observation Scale-Toddler Module (ADOS-T) | Rogers 2012317 | USA | Intervention RCT | This study was carried out to examine the efficacy of a 12-week, low-intensity (1 hour per week of therapist contact), parent-delivered intervention for toddlers at risk for ASDs aged 14–24 months and their families |
| Autism Diagnostic Observation Schedule-Generic (ADOS-G), modules 1 and 2) | Green 2010253 | UK | Intervention RCT | Early interventions for social communication |
| Autism Diagnostic Observation Schedule-Generic (ADOS-G) | Aldred 2004318 | England | Intervention RCT | ‘Social communication intervention targeting parental communication’ |
| Aldred 2012319 | UK | Other RCT | A mediation analysis aimed at assessing the impact of targeted intervention on autism characteristics | |
| Ben Itzchak 2008149 | Israel | Longitudinal observational | To examine the relations between cognition and autism severity, head size and intervention outcome | |
| Ben Itzchak 2011320 | Israel | Intervention quasi-experimental | The study explored child and parental characteristics at baseline that may predict outcomes in adaptive skills and acquisition of cognitive gains | |
| Bennett 2012304 | Canada | Longitudinal observational | Impact of maternal depression on mother’s reports of her child’s ASD behaviours | |
| Brian 2008305 | Canada | Longitudinal observational | Assessment of potential behavioural markers of ASD at 18 months in a high-risk cohort of infant siblings of children with ASD | |
| Dawson 2010321 | USA | Intervention RCT | Efficacy of the ESDM, a comprehensive developmental behavioural intervention, for improving outcomes in ASD toddlers | |
| Gotham 2012322 | USA | Longitudinal observational | To plot longitudinal trajectories of ASD severity from early childhood to early adolescence | |
| Hartley 2009323 | USA | Cross-sectional observational | To explore developmental patterns, along gender lines, in children who have autism | |
| Landa 2012324 | USA | Intervention quasi-experimental | Comprehensive early intervention | |
| Lerna 2012325 | Italy | Intervention RCT | PECS vs. CLT | |
| Luyster 2008129 | USA | Cross-sectional observational | To systematically investigate language in toddlers with ASD and to identify early correlates of receptive and expressive language in this population | |
| Munson 2008312 | USA | Cross-sectional observational | Latent class analysis of IQ in ASD | |
| Oosterling 2010326 | The Netherlands | Intervention RCT | Intervention is ‘Focus parent training’; home-based parent training promoting compliance, mutual enjoyment, joint attention and language development | |
| Ray-Subramanian 2011327 | USA | Cross-sectional observational | ‘Their study examined adaptive behaviour and cognitive skills for 125 toddlers on the autism spectrum using the recently updated Vineland-II and Bayley-III’ | |
| Ray-Subramanian 2012328 | USA | Longitudinal observational | This study examined whether language skills and non-verbal cognitive skills were associated with clinician-observed RRBs in children with ASD | |
| Strauss 2012329 | Italy | Intervention quasi-experimental | Influence of parent inclusion in treatment provision on child’s progress | |
| Sullivan 2007330 | USA | Longitudinal observational | To examine whether RJA was impaired as early as 14 months in children later diagnosed with ASD and whether RJA was an early marker for ASD diagnosis at outcome | |
| Tek 2012331 | USA | Cross-sectional observational | To assess whether early symptom presentation differs in toddlers with ASD from ethnic minority vs. non-minority backgrounds | |
| Ventola 2007332 | USA | Cross-sectional observational | Behavioural presentation of AD, developmental delay and developmental language disorder | |
| Werner 2005316 | USA | Cross-sectional observational | Describing variations in early course of development | |
| Wong 2010333 | China | Intervention RCT | To pilot a 2-week ‘Autism 1-2-3’ early intervention for children with autism and their parents immediately after diagnosis that targeted at (1) eye contact, (2) gesture and (3) vocalisation/words | |
| Zachor 2006334 | Israel | Intervention quasi-experimental | To compare the outcome of two centre-based intervention for autism | |
| Zachor 2010335 | Israel | Longitudinal observational | To examine the effect of the intervention approach (ABA, eclectic) on outcome in cognitive, language, and adaptive skills and on changes in autism diagnosis categories | |
| Repetitive Behavior Scale (RBS) | Dawson 2010321 | USA | Intervention RCT | Efficacy of the ESDM, a comprehensive developmental behavioural intervention, for improving outcomes in ASD toddlers |
| Classroom and playground behaviour observationsa | Escalona 2001271 | USA | Intervention RCT | To explore the effectiveness of massage therapy on stereotypic behaviour among children diagnosed with autism |
| Video codinga | Barber 2012381 | USA | Cross-sectional observational | Investigating RSB demonstrated by children with ASD (n = 50) and typical development (n = 50) matched on developmental age, gender and parents’ education level |
| Sensory processing | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Infant/Toddler Sensory Profile (ITSP) | Ben-Sasson 2008382 | Unclear | Cross-sectional observational | (1) What are the patterns of sensory modulation dimensions of sensory clusters of toddlers with ASDs? (2) Is there a sensory-based subgroup that has higher levels of affective symptoms? |
| Sense and Self-Regulation Checklist (SSC) | Silva 2009223 | USA | Intervention RCT | Improvement following a qigong massage intervention |
| Silva 2011301 | USA | Intervention RCT | Dual parent- and trainer-delivered qigong massage intervention for measures of autism, abnormal sensory responses and self-regulation | |
| Sensory Profile (SP) | Chuang 2012383 | Taiwan | Cross-sectional observational | To explore relationships between sensory processing and a difficult temperament characteristics in children with autism |
| Jasmin 2009384 | Canada | Cross-sectional observational | To determine the impact of sensory–motor DLS on the performance of DLS in preschool children with ASD | |
| Provost 2009385 | USA | Cross-sectional observational | Identify differences in sensory behaviours between young children with and without ASDs | |
| Silva 2007386 | USA | Intervention RCT | Effectiveness of qigong massage methodology, in treating sensory impairment in young children with autism | |
| Silva 2008300 | USA | Intervention RCT | Outcomes of pilot of qigong sensory training programme | |
| Short Sensory Profile (SSP) | O’Donnell 2012386 | USA | Cross-sectional observational | To explore sensory processing characteristics in preschool-age children with ASDs |
| Papavasiliou 2011345 | Greece | Longitudinal observational | ‘This study aimed to investigate the effect of an individually tailored psycho-educational programme for autistic children on the scores of the Childhood Autism Rating Scale (CARS) and the Short Sensory Profile (SSP)’ | |
| Tomchek 2007387 | USA | Cross-sectional observational | Differences in sensory processing between children with ASD and typically developing children |
| Language | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Autism Screening Instrument for Educational Planning (ASIEP) | Arick 2003388 | USA | Cross-sectional observational | To track programme implementation variables and outcome data for students with ASDs engaged in school or home programmes |
| Battelle Developmental Inventory (BDI) | Arick 2003388 | USA | Cross-sectional observational | To track programme implementation variables and outcome data for students with ASDs engaged in school or home programmes |
| British Picture Vocabulary Scale | Magiati 2007308 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years |
| Magiati 2011309 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Clinical Evaluation of Language Fundamentals-Revised | Bono 2004389 | USA | Longitudinal observational | Investigate the relationship between amount of intervention and language development in children with autism |
| Communication and Symbolic Behavior Scales-Developmental Profile (CSBS-DP) Caregiver Questionnaire | Tek 2012331 | USA | Cross-sectional observational | To assess whether early symptom presentation differs in toddlers with ASD from ethnic minority vs. non-minority backgrounds |
| Comprehensive Assessment of Spoken Language (CASL) | Casenhiser 2013361 | Canada | Longitudinal observational | To assess the impact of an intervention on social interaction and communication in children with ASD |
| Expressive One-Word Picture Vocabulary Test | Arick 2003388 | USA | Cross-sectional observational | To track programme implementation variables and outcome data for students with ASDs engaged in school or home programmes |
| Bopp 2009340 | Canada | Longitudinal observational | Examine the relationship between behaviour and trajectories of vocabulary and language development in young children with autism | |
| Magiati 2007308 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Magiati 2011309 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Illinois Test of Psycholinguistic Abilities | Carlsson 2013390 | Sweden | Cross-sectional observational | To analyse co-occurring disorders and problems in a representative group of 198 preschool children with ASD |
| MacArthur Communication Development Inventories (MCDI) | Aldred 2004318 | England | Intervention RCT | ‘Social communication intervention targeting parental communication’ |
| Green 2010253 | UK | Intervention RCT | Early interventions for social communication | |
| Hambly 2012306 | Canada | Cross-sectional observational | The impact of bilingual exposure on language learning in ASD | |
| Hudry 2010233 | UK | Cross-sectional observational | Recruited as part of Preschool Autism Communication Trial but this report is on baseline data for only receptive vs. expressive skills | |
| Luyster 2008129 | USA | Cross-sectional observational | To systematically investigate language in toddlers with ASD and to identify early correlates of receptive and expressive language in this population | |
| Miniscalco 2012391 | Sweden | Cross-sectional observational | To establish whether parents of young children with autism identify the same rate and type of language problems as SLPs using formal tests To describe the typical ‘language profile’ in a representative sample of toddlers with autism |
|
| Mitchell 2006392 | Canada | Longitudinal observational | Assessment at 18 and 24 months | |
| Oosterling 2010326 | The Netherlands | Intervention RCT | Intervention is ‘Focus parent training’. Home-based parent training promoting compliance, mutual enjoyment, joint attention and language development | |
| Rogers 2012317 | USA | Intervention RCT | This study was carried out to examine the efficacy of a 12-week, low-intensity (1 hour per week of therapist contact), parent-delivered intervention for toddlers at risk for ASDs aged 14–24 months and their families | |
| Salt 2002372 | UK | Intervention quasi-experimental | Developmentally based early intervention programme | |
| Smith 2007393 | Canada | Longitudinal observational | Variability and predictors of expressive vocabulary development in children with autism | |
| Smith 2010359 | Canada and USA | Intervention quasi-experimental | Effect of a parent training and naturalistic one-to-one behaviour intervention using PRT on language, behaviour and ASD symptoms | |
| Stone 2001394 | USA | Longitudinal observational | Examining factors related to development of spoken language | |
| Strauss 2012329 | Italy | Intervention quasi-experimental | Influence of parent inclusion in treatment provision on child’s progress | |
| Mullen Scales of Early Learning (MSEL) | Akshoomoff 2006395 | USA | Cross-sectional observational | Overt behaviours during cognitive assessment |
| Anan 2008396 | USA | Other – quantitative case series | To examine the efficacy of the GIFT programme, a 12-week (180 hours, delivered 3 hours each weekday) parent-training for preschoolers with ASDs | |
| Baker 2010397 | USA | Longitudinal observational | ‘Examined parent behaviour during unstructured play sessions with high- and low-risk toddlers who did or did not receive later ASD diagnoses, and investigated associations with concurrent child behaviour problems and later language growth’ | |
| Barbaro 2012398 | Australia | Longitudinal observational | To investigate the developmental profiles of children with ASDs from 12 to 24 months, who had been prospectively identified through developmental surveillance in a large community-based sample | |
| Ben Itzchak 2011320 | Israel | Intervention quasi-experimental | The study explored child and parental characteristics at baseline that may predict outcomes in adaptive skills and acquisition of cognitive gains | |
| Bishop 2011176 | USA | Cross-sectional observational | Validation of MSEL in a population of children with children with ASDs and other developmental disorders | |
| Brian 2008305 | Canada | Longitudinal observational | Assessment of potential behavioural markers of ASD at 18 months in a high-risk cohort of infant siblings of children with ASD | |
| Dawson 2010321 | USA | Intervention RCT | Efficacy of the ESDM, a comprehensive developmental behavioural intervention, for improving outcomes in ASD toddlers | |
| Dereu 2012365 | Belgium | Longitudinal observational | Developmental trajectories of joint attention, imitation and pretend play impairments in autism | |
| Eapen 2013357 | Australia | Longitudinal observational | Evaluation of ESDM for preschool-aged children with ASD | |
| Hartley 2009323 | USA | Cross-sectional observational | To explore developmental patterns, along gender lines, in children who have autism | |
| Honey 2008307 | UK | Longitudinal observational | The study tests the following specific hypotheses:
|
|
| Landa 2012399 | USA | Longitudinal observational | Developmental trajectories of siblings of ASD children | |
| Landa 2012324 | USA | Intervention quasi-experimental | Comprehensive early intervention | |
| Lloyd 2013400 | USA | Cross-sectional observational | Gross and fine motor skills of young children with ASD | |
| Luyster 2008129 | USA | Cross-sectional observational | To systematically investigate language in toddlers with ASD and to identify early correlates of receptive and expressive language in this population | |
| Mayo 2013310 | USA | Other – retrospective observational | This study examined the relationship between age of language acquisition and later functioning in children with ASD | |
| Mitchell 2006392 | Canada | Longitudinal observational | Assessment at 18 and 24 months | |
| O’Donnell 2012386 | USA | Cross-sectional observational | To explore sensory processing characteristics in preschool-age children with ASDs | |
| Ozonoff 2010313 | USA | Longitudinal observational | ‘To examine prospectively the emergence of behavioural signs of autism in the first years of life in infants at low and high risk for autism’ | |
| Poon 2012401 | USA | Longitudinal observational | ‘The current study uses retrospective video analysis (RVA) methods to investigate the longitudinal trajectories of social-communicative behaviours, as well as their associations with later developmental outcomes’ | |
| Ray-Subramanian 2012328 | USA | Longitudinal observational | This study examined whether language skills and non-verbal cognitive skills were associated with clinician-observed RRBs in children with ASD | |
| Rogers 2012317 | USA | Intervention RCT | This study was carried out to examine the efficacy of a 12-week, low-intensity (1 hour per week of therapist contact), parent-delivered intervention for toddlers at risk for ASDs aged 14–24 months and their families | |
| Schertz 2013402 | USA | Intervention RCT | The purpose of this study was to determine effects of the JAML intervention on acquisition of joint attention and other early social communication competencies for toddlers with ASDs | |
| Siller 2013403 | USA | Intervention RCT | To investigate the underlying causal mechanisms of language gain, we conducted a randomised clinical trial of an experimental intervention (FPI) that aims to enhance responsive parental communication (n = 70) | |
| Sullivan 2007330 | USA | Longitudinal observational | To examine whether RJA was impaired as early as 14 months in children later diagnosed with ASD and whether RJA was an early marker for ASD diagnosis at outcome | |
| Tek 2012331 | USA | Cross-sectional observational | To assess whether early symptom presentation differs in toddlers with ASD from ethnic minority vs. non-minority backgrounds | |
| Thurm 2007404 | USA | Longitudinal observational | Non-verbal ability, receptive communication, expressive communication and socialisation were compared as predictors of receptive and expressive language at age 5 years | |
| Toth 2006284 | USA | Longitudinal observational | This study investigated the unique contributions of joint attention, imitation, and toy play to language ability and rate of development of communication skills in young children with ASD | |
| Ventola 2007332 | USA | Cross-sectional observational | Behavioural presentation of AD, developmental delay and developmental language disorder | |
| Werner 2005316 | USA | Cross-sectional observational | Describing variations in early course of development | |
| Zachor 2010335 | Israel | Longitudinal observational | To examine the effect of the intervention approach (ABA, eclectic) on outcome in cognitive, language, and adaptive skills and on changes in autism diagnosis categories | |
| Pragmatics Profile | Roberts 2011405 | Australia | Intervention RCT | Comparison of home-based vs. centre-based early intervention programmes |
| Preschool Language Scale (PLS) | Bopp 2009340 | Canada | Longitudinal observational | Examined the relationship between behaviour and trajectories of vocabulary and language development in young children with autism |
| Casenhiser 2013361 | Canada | Longitudinal observational | To assess the impact of an intervention on social interaction and communication in children with ASD | |
| Flippin 2011406 | USA | Longitudinal observational | To investigate the concurrent relationships between the verbal and play responsiveness of 16 mothers and fathers and the object play skills of 16 children with ASDs | |
| Green 2010253 | UK | Intervention RCT | Early interventions for social communication | |
| Haebig 2013407 | USA | Longitudinal observational | Parent verbal responsiveness and language comprehension and production | |
| Harris 1991408 | USA | Longitudinal observational | To explore developmental (intellectual and language) gains made by children with autism following intervention | |
| Hudry 2010233 | UK | Cross-sectional observational | Recruited as part of Preschool Autism Communication Trial but this report is on baseline data for only receptive vs. expressive skills | |
| Mitchell 2006392 | Canada | Longitudinal observational | Assessment at 18 and 24 months | |
| Ray-Subramanian 2012328 | USA | Longitudinal observational | This study examined whether language skills and non-verbal cognitive skills were associated with clinician-observed RRBs in children with ASD | |
| Smith 2010359 | Canada and USA | Intervention quasi-experimental | Effect of a parent training and naturalistic one-to-one behaviour intervention using PRT on language, behaviour and ASD symptoms | |
| Stone 2001394 | USA | Longitudinal observational | Examining factors related to development of spoken language | |
| Reynell Developmental Language Scales | Andersson 2013409 | Sweden | Longitudinal observational | To explore gender-related differences in ASD characteristics |
| Bono 2004389 | USA | Longitudinal observational | Investigate the relationship between amount of intervention and language development in children with autism | |
| Carlsson 2013390 | Sweden | Cross-sectional observational | To analyse co-occurring disorders and problems in a representative group of 198 preschool children with ASD | |
| Eikeseth 2009410 | UK | Longitudinal observational | Effect of intensity of supervision on outcomes | |
| Goods 2013366 | USA | Intervention RCT | JASPER | |
| Herring 2006411 | Australia | Longitudinal observational | To explore the impact of developmental disorders on children and their families | |
| Miniscalco 2012391 | Sweden | Cross-sectional observational | To establish whether or not parents of young children with autism identify the same rate and type of language problems as SLPs using formal tests To describe the typical ‘language profile’ in a representative sample of toddlers with autism |
|
| Remington 2007358 | UK | Intervention quasi-experimental | Comparison of early intensive behavioural interventions and treatment as usual | |
| Roberts 2011405 | Australia | Intervention RCT | Comparison of home-based vs. centre-based early intervention programmes | |
| Sheinkopf 2000412 | USA | Cross-sectional observational | Examine both vocal and gestural communicative development in young children with autism | |
| Smith 2000413 | USA | Intervention RCT | Comparing intensive treatment group to parent training group | |
| Sequenced Inventory of Communication-Revised | Stone 2001394 | USA | Longitudinal observational | Examining factors related to development of spoken language |
| Test for Auditory Comprehension of Language | Szatmari 2000302 | Canada | Longitudinal observational | Monitoring cognitive and language outcomes of groups of children with autism and Asperger syndrome |
| Test of Language Development | Bennett 2008296 | Canada | Longitudinal observational | To explore ‘specific language impairment’ as a predictor of children’s symptom and functional outcome |
| Szatmari 2000302 | Canada | Longitudinal observational | Monitoring cognitive and language outcomes of groups of children with autism and Asperger syndrome | |
| Vineland Adaptive Behavior Scales (VABS) | Aldred 2004318 | England | Intervention RCT | ‘Social communication intervention targeting parental communication’ |
| Anan 2008396 | USA | Other – quantitative case series | To examine the efficacy of the GIFT programme, a 12-week (180 hours, delivered 3 hours each weekday) parent training for preschoolers with ASDs | |
| Andersson 2013409 | Sweden | Longitudinal observational | To explore gender-related differences in ASD characteristics | |
| Arick 2003388 | USA | Cross-sectional observational | To track programme implementation variables and outcome data for students with ASDs engaged in school or home programmes | |
| Baghdadli 2012339 | France | Longitudinal observational | Developmental trajectory of adaptive behaviours | |
| Bearss 2013278 | USA | Longitudinal observational | To assess the feasibility and efficacy of a parent training programme | |
| Ben Itzchak 2011320 | Israel | Intervention quasi-experimental | The study explored child and parental characteristics at baseline that may predict outcomes in adaptive skills and acquisition of cognitive gains | |
| Bennett 2008296 | Canada | Longitudinal observational | To explore ‘specific language impairment’ as a predictor of children’s symptom and functional outcome | |
| Carlsson 2013390 | Sweden | Cross-sectional observational | To analyse co-occurring disorders and problems in a representative group of 198 preschool children with ASD | |
| Cassidy 2008348 | Northern Ireland | Cross-sectional observational | To describe the demographic characteristics of preschoolers and their families; to discover parental perceptions of the child’s difficulties; to identify the impact the child has on family life; to outline the supports available to families and those they would like to have | |
| Dawson 2010321 | USA | Intervention RCT | Efficacy of the ESDM, a comprehensive developmental behavioural intervention, for improving outcomes in ASD toddlers | |
| Eapen 2013357 | Australia | Longitudinal observational | Evaluation of ESDM for preschool-aged children with ASD | |
| Eikeseth 2009410 | UK | Longitudinal observational | Effect of intensity of supervision on outcomes | |
| Eldevik 2012414 | UK (Wales) | Longitudinal observational | Behavioural intervention outcome for children who had autism | |
| Eriksson 2013415 | Sweden | Longitudinal observational | To explore frequency of other medical conditions in autism | |
| Gabriels 2007416 | USA | Longitudinal observational | To assess the stability of adaptive functioning in two cognitive ability groups of children with an ASD | |
| Green 2010253 | UK | Intervention RCT | Early interventions for social communication | |
| Grindle 2012417 | UK (Wales) | Intervention quasi-experimental | ABA classroom: educational intervention in a mainstream school setting | |
| Hedvall 2013418 | Sweden | Cross-sectional observational | Processing speed and adaptive function | |
| Herring 2006410 | Australia | Longitudinal observational | To explore the impact of developmental disorders on children and their families | |
| Honey 2008307 | UK | Longitudinal observational | The study tests the following specific hypotheses:
|
|
| Hudry 2010233 | UK | Cross-sectional observational | Recruited as part of Preschool Autism Communication Trial but this report is on baseline data for only receptive vs. expressive skills | |
| Jasmin 2009384 | Canada | Cross-sectional observational | To determine the impact of sensory–motor DLS on the performance of DLS in preschool children with ASD | |
| Jonsdottir 2007341 | Iceland | Longitudinal observational | The purpose of the present study was to describe stability and change of preschool children in Iceland and to contribute to the accumulation of data on outcome in autism | |
| Klintwall 2012419 | Sweden | Longitudinal observational | Number and controllability of reinforces as predictors of outcomes for autistic children receiving Early and Intense Behavioural Intervention | |
| Landa 2012324 | USA | Intervention quasi-experimental | Comprehensive early intervention | |
| Lerna 2012325 | Italy | Intervention RCT | PECS vs. CLT | |
| Lloyd 2013400 | USA | Cross-sectional observational | Gross and fine motor skills of young children with ASD | |
| Luyster 2008129 | USA | Cross-sectional observational | To systematically investigate language in toddlers with ASD and to identify early correlates of receptive and expressive language in this population | |
| Magiati 2007308 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Magiati 2011309 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Mayo 2013310 | USA | Other – retrospective observational | This study examined the relationship between age of language acquisition and later functioning in children with ASD | |
| McConkey 2010349 | – | Intervention quasi-experimental | Evaluate a home-based intervention for preschool children with a confirmed diagnosis of ASD | |
| Munson 2006420 | USA | Longitudinal observational | The relationship between amygdalar volume at age 3–4 years and outcomes at age 6 years | |
| Munson 2008312 | USA | Cross-sectional observational | Latent class analysis of IQ in ASD | |
| O’Donnell 2012386 | USA | Cross-sectional observational | To explore sensory processing characteristics in preschool-age children with ASDs | |
| Osborne 2008350 | UK | Intervention quasi-experimental | There was great heterogeneity among the interventions delivered and so for analysis interventions were categorised into high vs. low intensity | |
| Osborne 2009351 | UK | Longitudinal observational | Evaluate relationship between child behaviour problems and parental stress | |
| Peters-Scheffer 2010421 | The Netherlands | Intervention quasi-experimental | Behavioural treatment in preschool | |
| Poon 2012401 | USA | Longitudinal observational | ‘The current study uses retrospective video analysis (RVA) methods to investigate the longitudinal trajectories of social-communicative behaviours, as well as their associations with later developmental outcomes’ | |
| Pry 2005314 | France, Switzerland, Belgium and Luxembourg | Cross-sectional observational | The relationship between expressive language level and psychological development in children with autism 5 years of age | |
| Ray-Subramanian 2011327 | USA | Cross-sectional observational | ‘Their study examined adaptive behaviour and cognitive skills for 125 toddlers on the autism spectrum using the recently updated Vineland-II and Bayley-III’ | |
| Reed 2007352 | UK | Longitudinal observational | Comparing high- and low-intensity interventions (with comparison of three different types of high-intensity interventions) | |
| Reed 2007353 | UK | Longitudinal observational | Compare effectiveness of ABA, special nursery placements and portage; addressing limitations of previous studies by using the same measures at baseline and end point | |
| Reed 2012354 | UK | Intervention quasi-experimental | To explore and document the relationships between severity of autism, temporal input of the programme, and the outcome effectiveness for a variety of early interventions for children on the autism spectrum. In particular, ABA, special nursery placement, an adaptation of a portage approach for individuals on the autism spectrum, and an eclectic approach developed by a local authority were chosen for study | |
| Remington 2007358 | UK | Intervention quasi-experimental | Comparison of early intensive behavioural interventions and treatment as usual | |
| Restall 1994422 | Canada | Cross-sectional observational | How does the play of children with autism differ that of normally developing children? What are the relationships between performance and adaptive abilities? | |
| Rickards 2009423 | Australia | Intervention RCT | Does home-based programme provided over 12 months result in sustained improvement in development and behaviour? | |
| Roberts 2011405 | Australia | Intervention RCT | Comparison of home-based vs. centre-based early intervention programmes | |
| Rogers 2012317 | USA | Intervention RCT | This study was carried out to examine the efficacy of a 12-week, low-intensity (1 hour per week of therapist contact), parent-delivered intervention for toddlers at risk for ASDs aged 14–24 months and their families | |
| Ruble 2008424 | USA | Cross-sectional observational | Effect of caregiver responsiveness on child cognitive and social interactions | |
| Salt 2002372 | UK | Intervention quasi-experimental | Developmentally based early intervention programme | |
| Schertz 2013402 | USA | Intervention RCT | The purpose of this study was to determine effects of the JAML intervention on acquisition of joint attention and other early social communication competencies for toddlers with ASDs | |
| Silva 2007299 | USA | Intervention RCT | Effectiveness of qigong massage methodology, in treating sensory impairment in young children with autism | |
| Silva 2008300 | USA | Intervention RCT | Outcomes of pilot of qigong sensory training programme | |
| Smith 2000413 | USA | Intervention RCT | Comparing intensive treatment group to parent training group | |
| Smith 2010359 | Canada and USA | Intervention quasi-experimental | Effect of a parent training and naturalistic one-to-one behaviour intervention using PRT on language, behaviour and ASD symptoms | |
| Stahmer 2004355 | USA | Intervention quasi-experimental | To analyse the outcomes for 20 young children with ASD in an inclusive programme for children aged < 3 years | |
| Stone 1999346 | USA | Cross-sectional observational | Patterns of adaptive behaviour in young children with ASD | |
| Strauss 2012329 | Italy | Intervention quasi-experimental | Influence of parent inclusion in treatment provision on child’s progress | |
| Szatmari 2000302 | Canada | Longitudinal observational | Monitoring cognitive and language outcomes of groups of children with autism and Asperger syndrome | |
| Tonge 2012425 | Australia | Longitudinal observational | To determine the impact of a PEBM on the mental health and adjustment of parents with preschool children with autism | |
| Toth 2006284 | USA | Longitudinal observational | This study investigated the unique contributions of joint attention, imitation and toy play to language ability and rate of development of communication skills in young children with ASD | |
| VanMeter 1997426 | USA | Cross-sectional observational | Social, communication and DLS was examined for autistic children, compared with retarded and normal controls | |
| Ventola 2007332 | USA | Cross-sectional observational | Behavioural presentation of AD, developmental delay and developmental language disorder | |
| Werner 2005316 | USA | Cross-sectional observational | Describing variations in early course of development | |
| Zachor 2010335 | Israel | Longitudinal observational | To examine the effect of the intervention approach (ABA, eclectic) on outcome in cognitive, language, and adaptive skills and on changes in autism diagnosis categories | |
| Vineland Adaptive Behavior Scales-Classroom Edition (VABS-Classroom) | Goin-Kochel 2007427 | USA | Longitudinal observational | To assess the developmental trajectories of children with autism enrolled in ABA-based school |
| Differential Ability Scalesa | Bishop 2011176 | USA | Cross-sectional observational | Validation of MSEL in a population of children with children with ASDs and other developmental disorders |
| Ruble 2008424 | USA | Cross-sectional observational | Effect of caregiver responsiveness on child cognitive and social interactions | |
| Thurm 2007404 | USA | Longitudinal observational | Non-verbal ability, receptive communication, expressive communication and socialisation were compared as predictors of receptive and expressive language at age 5 years | |
| Peabody Picture Vocabulary Testa | Bopp 2009340 | Canada | Longitudinal observational | Examined the relationship between behaviour and trajectories of vocabulary and language development in young children with autism |
| Smith 2010359 | Canada and USA | Intervention quasi-experimental | Effect of a parent training and naturalistic one-to-one behaviour intervention using PRT on language, behaviour and ASD symptoms | |
| Szatmari 2000302 | Canada | Longitudinal observational | Monitoring cognitive and language outcomes of groups of children with autism and Asperger syndrome | |
| Processability testb | Carlsson 2013390 | Sweden | Cross-sectional observational | To analyse co-occurring disorders and problems in a representative group of 198 preschool children with ASD |
| Rating of video for expressive speechc | Baghdadli 2012339 | France | Longitudinal observational | Developmental trajectory of adaptive behaviours |
| Semi structured free-play with examinerc | Yoder 2006428 | USA | Intervention RCT | Prelinguistic communication intervention for acquisition of spoken communication |
| Video coding proceduresc | Colgan 2006379 | USA | Longitudinal observational | To examine the frequency, initiation, prompting, and diversity of types of gestures used for social interaction purposes |
| Cognitive ability | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Battelle Developmental Inventory (BDI) | Arick 2003388 | USA | Cross-sectional observational | To track programme implementation variables and outcome data for students with ASDs engaged in school or home programmes |
| Bayley Scales of Infant Development (BSID) | Ben Itzchak 2008149 | Israel | Longitudinal observational | To examine the relations between cognition and autism severity, head size and intervention outcome |
| Eikeseth 2009410 | UK | Longitudinal observational | Effect of intensity of supervision on outcomes | |
| Eldevik 2012414 | UK (Wales) | Longitudinal observational | Behavioural intervention outcome for children who had autism | |
| Grindle 2012417 | UK (Wales) | Intervention quasi-experimental | ABA classroom: educational intervention in a mainstream school setting | |
| Ingersoll 2012286 | USA | Intervention RCT | Imitation intervention to improve social functioning | |
| Jonsdottir 2007341 | Iceland | Longitudinal observational | The purpose of the present study was to describe stability and change of preschool children in Iceland and to contribute to the accumulation of data on outcome in autism | |
| Magiati 2007308 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Peters-Scheffer 2010421 | The Netherlands | Intervention quasi-experimental | Behavioural treatment in preschool | |
| Ray-Subramanian 2011327 | USA | Cross-sectional observational | ‘Their study examined adaptive behaviour and cognitive skills for 125 toddlers on the autism spectrum using the recently updated Vineland-II and Bayley-III’ | |
| Remington 2007358 | UK | Intervention quasi-experimental | Comparison of early intensive behavioural interventions and treatment as usual | |
| Rickards 2009423 | Australia | Intervention RCT | Does home-based programme provided over 12 months resulted in sustained improvement in development and behaviour? | |
| Sheinkopf 1998429 | USA | Intervention quasi-experimental | Examine the effects of intensive behaviour therapy on the intellectual functioning and symptom presentation of young children diagnosed with autism or PDD | |
| Smith 1997430 | Norway and USA | Intervention quasi-experimental | Outcomes after ‘intensive behavioural treatment’ | |
| Smith 2000413 | USA | Intervention RCT | Comparing intensive treatment group to parent training group | |
| Stahmer 2004355 | USA | Intervention quasi-experimental | To analyse the outcomes for 20 young children with ASD in an inclusive programme for children aged < 3 years | |
| Ventola 2007332 | USA | Cross-sectional observational | Behavioural presentation of AD, developmental delay and developmental language disorder | |
| Zachor 2006334 | Israel | Intervention quasi-experimental | To compare the outcome of two centre-based intervention for autism | |
| Behavior Rating Inventory of Executive Function (BRIEF)–Preschool Version | Jahromi 2013431 | USA | Longitudinal observational | The importance of self-regulation for the school and peer engagement of children with high-functioning autism |
| British Ability Scales (BAS) | Osborne 2008350 | UK | Intervention quasi-experimental | There was great heterogeneity among the interventions delivered and so for analysis interventions were categorised into high vs. low intensity |
| Osborne 2009351 | UK | Longitudinal observational | Evaluate relationship between child behaviour problems and parental stress | |
| Reed 2007352 | UK | Longitudinal observational | Comparing high- and low-intensity interventions (with comparison of three different types of high-intensity interventions) | |
| Reed 2007353 | UK | Longitudinal observational | Compare effectiveness of ABA, special nursery placements and portage; addressing limitations of previous studies by using the same measures at baseline and end point | |
| Reed 2012354 | UK | Intervention quasi-experimental | To explore and document the relationships between severity of autism, temporal input of the programme, and the outcome effectiveness for a variety of early interventions for children on the autism spectrum. In particular, ABA, special nursery placement, an adaptation of a portage approach for individuals on the autism spectrum, and an eclectic approach developed by a local authority were chosen for study | |
| Cattell Infant Intelligence | Sheinkopf 1998429 | USA | Intervention quasi-experimental | Examine the effects of intensive behaviour therapy on the intellectual functioning and symptom presentation of young children diagnosed with autism or PDD |
| Developmental Profile | Malhi 2011342 | India | Longitudinal observational | To assess diagnostic stability of autism diagnosis in children aged ≤ 3 years |
| Griffith Mental Developmental Scales | Andersson 2013409 | Sweden | Longitudinal observational | To explore gender-related differences in ASD characteristics |
| Carlsson 2013390 | Sweden | Cross-sectional observational | To analyse co-occurring disorders and problems in a representative group of 198 preschool children with ASD | |
| Hedvall 2013418 | Sweden | Cross-sectional observational | Processing speed and adaptive function | |
| Lerna 2012325 | Italy | Intervention RCT | PECS vs. CLT | |
| Strauss 2012329 | Italy | Intervention quasi-experimental | Influence of parent inclusion in treatment provision on child’s progress | |
| Leiter International Performance Scale-Revised (Leiter-R) | Gabriels 2007416 | USA | Longitudinal observational | To assess the stability of adaptive functioning in two cognitive ability groups of children with an ASD |
| Grindle 2012417 | UK (Wales) | Intervention quasi-experimental | ABA classroom: educational intervention in a mainstream school setting | |
| Leiter Performance Scales (Arthur adaptation) | Bennett 2008296 | Canada | Longitudinal observational | To explore ‘specific language impairment’ as a predictor of children’s symptom and functional outcome |
| McCarthy Scales of Children’s Abilities | Szatmari 2000302 | Canada | Longitudinal observational | Monitoring cognitive and language outcomes of groups of children with autism and Asperger syndrome |
| Merrill–Palmer Scale of Mental Tests | Eikeseth 2009410 | UK | Longitudinal observational | Effect of intensity of supervision on outcomes |
| Magiati 2007308 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Sheinkopf 1998429 | USA | Intervention quasi-experimental | Examine the effects of intensive behaviour therapy on the intellectual functioning and symptom presentation of young children diagnosed with autism or PDD | |
| Sheinkopf 2000412 | USA | Cross-sectional observational | Examine both vocal and gestural communicative development in young children with autism | |
| Smith 2000413 | USA | Intervention RCT | Comparing intensive treatment group to parent training group | |
| Merrill-Palmer-Revised | Smith 2010359 | Canada and USA | Intervention quasi-experimental | Effect of a parent training and naturalistic one-to-one behaviour intervention using PRT on language, behaviour and ASD symptoms |
| Mullen Scales of Early Learning (MSEL) | Akshoomoff 2006395 | USA | Cross-sectional observational | Overt behaviours during cognitive assessment |
| Anan 2008396 | USA | Other – quantitative case series | To examine the efficacy of the GIFT programme, a 12-week (180 hours, delivered 3 hours each weekday) parent-training for preschoolers with ASDs | |
| Baker 2010397 | USA | Longitudinal observational | ‘Examined parent behaviour during unstructured play sessions with high- and low-risk toddlers who did or did not receive later ASD diagnoses, and investigated associations with concurrent child behaviour problems and later language growth’ | |
| Barbaro 2012398 | Australia | Longitudinal observational | To investigate the developmental profiles of children with ASDs from 12 to 24 months, who had been prospectively identified through developmental surveillance in a large community-based sample | |
| Ben Itzchak 2011320 | Israel | Intervention quasi-experimental | The study explored child and parental characteristics at baseline that may predict outcomes in adaptive skills and acquisition of cognitive gains | |
| Bishop 2011176 | USA | Cross-sectional observational | Validation of MSEL in a population of children with children with ASDs and other developmental disorders | |
| Brian 2008305 | Canada | Longitudinal observational | Assessment of potential behavioural markers of ASD at 18 months in a high-risk cohort of infant siblings of children with ASD | |
| Dawson 2010321 | USA | Intervention RCT | Efficacy of the ESDM, a comprehensive developmental behavioural intervention, for improving outcomes in ASD toddlers | |
| Dereu 2012365 | Belgium | Longitudinal observational | Developmental trajectories of joint attention, imitation and pretend play impairments in autism | |
| Eapen 2013357 | Australia | Longitudinal observational | Evaluation of ESDM for preschool-aged children with ASD | |
| Hartley 2009323 | USA | Cross-sectional observational | To explore developmental patterns, along gender lines, in children who have autism | |
| Honey 2008307 | UK | Longitudinal observational | The study tests the following specific hypotheses:
|
|
| Landa 2012399 | USA | Longitudinal observational | Developmental trajectories of siblings of ASD children | |
| Landa 2012224 | USA | Intervention quasi-experimental | Comprehensive early intervention | |
| Lloyd 2013400 | USA | Cross-sectional observational | Gross and fine motor skills of young children with ASD | |
| Luyster 2008129 | USA | Cross-sectional observational | To systematically investigate language in toddlers with ASD and to identify early correlates of receptive and expressive language in this population | |
| Mayo 2013310 | USA | Other – retrospective observational | This study examined the relationship between age of language acquisition and later functioning in children with ASD | |
| Mitchell 2006392 | Canada | Longitudinal observational | Assessment at 18 and 24 months | |
| O’Donnell 2012386 | USA | Cross-sectional observational | To explore sensory processing characteristics in preschool-age children with ASDs | |
| Ozonoff 2010313 | USA | Longitudinal observational | ‘To examine prospectively the emergence of behavioural signs of autism in the first years of life in infants at low and high risk for autism’ | |
| Poon 2012401 | USA | Longitudinal observational | ‘The current study uses retrospective video analysis (RVA) methods to investigate the longitudinal trajectories of social-communicative behaviours, as well as their associations with later developmental outcomes’ | |
| Ray-Subramanian 2012328 | USA | Longitudinal observational | This study examined whether language skills and non-verbal cognitive skills were associated with clinician-observed RRBs in children with ASD | |
| Rogers 2012317 | USA | Intervention RCT | This study was carried out to examine the efficacy of a 12-week, low-intensity (1 hour per week of therapist contact), parent-delivered intervention for toddlers at risk for ASDs aged 14–24 months and their families | |
| Schertz 2013402 | USA | Intervention RCT | The purpose of this study was to determine effects of the JAML intervention on acquisition of joint attention and other early social communication competencies for toddlers with ASDs | |
| Siller 2013403 | USA | Intervention RCT | To investigate the underlying causal mechanisms of language gain, we conducted a randomised clinical trial of an experimental intervention (FPI) that aims to enhance responsive parental communication (n = 70) | |
| Sullivan 2007330 | USA | Longitudinal observational | To examine whether RJA was impaired as early as 14 months in children later diagnosed with ASD and whether RJA was an early marker for ASD diagnosis at outcome | |
| Tek 2012331 | USA | Cross-sectional observational | To assess whether early symptom presentation differs in toddlers with ASD from ethnic minority vs. non-minority backgrounds | |
| Thurm 2007404 | USA | Longitudinal observational | Non-verbal ability, receptive communication, expressive communication and socialisation were compared as predictors of receptive and expressive language at age 5 years | |
| Toth 2006284 | USA | Longitudinal observational | This study investigated the unique contributions of joint attention, imitation, and toy play to language ability and rate of development of communication skills in young children with ASD | |
| Ventola 2007332 | USA | Cross-sectional observational | Behavioural presentation of AD, developmental delay and developmental language disorder | |
| Werner 2005316 | USA | Cross-sectional observational | Describing variations in early course of development | |
| Zachor 2010335 | Israel | Longitudinal observational | To examine the effect of the intervention approach (ABA, eclectic) on outcome in cognitive, language, and adaptive skills and on changes in autism diagnosis categories | |
| Snijders Oomen Non-Verbal Intelligence Test (SON) | Peters-Scheffer 2010421 | The Netherlands | Intervention quasi-experimental | Behavioural treatment in preschool |
| Stanford–Binet Intelligence Scales | Ben Itzchak 2008149 | Israel | Longitudinal observational | To examine the relations between cognition and autism severity, head size and intervention outcome |
| Delmolino 2006432 | USA | Longitudinal observational | To assess if scores obtained by the PEP-R are reasonable estimates of cognitive ability, correlating with scores from another instrument (Stanford–Binet Intelligence Scales, 4th edn) | |
| Grindle 2012417 | UK (Wales) | Intervention quasi-experimental | ABA classroom: educational intervention in a mainstream school setting | |
| Harris 1991408 | USA | Longitudinal observational | To explore developmental (intellectual and language) gains made by children with autism following intervention | |
| Harris 2000433 | USA | Cross-sectional observational | To explore the impact of age and baseline IQ (moderators) on outcome following intervention | |
| Landa 2012224 | USA | Intervention quasi-experimental | Comprehensive early intervention | |
| Remington 2007358 | UK | Intervention quasi-experimental | Comparison of early intensive behavioural interventions and treatment as usual | |
| Smith 2000413 | USA | Intervention RCT | Comparing intensive treatment group to parent training group | |
| Szatmari 2000302 | Canada | Longitudinal observational | Monitoring cognitive and language outcomes of groups of children with autism and Asperger syndrome | |
| Zachor 2006334 | Israel | Intervention quasi-experimental | To compare the outcome of two centre-based intervention for autism | |
| Wechsler Intelligence Scale for Children | Szatmari 2000302 | Canada | Longitudinal observational | Monitoring cognitive and language outcomes of groups of children with autism and Asperger syndrome |
| Wechsler Preschool and Primary Scale of Intelligence (WPPSI) | Andersson 2013409 | Sweden | Longitudinal observational | To explore gender-related differences in ASD characteristics |
| Baghdadli 2012339 | France | Longitudinal observational | Developmental trajectory of adaptive behaviours | |
| Carlsson 2013390 | Sweden | Cross-sectional observational | To analyse co-occurring disorders and problems in a representative group of 198 preschool children with ASD | |
| Eikeseth 2009410 | UK | Longitudinal observational | Effect of intensity of supervision on outcomes | |
| Hedvall 2013418 | Sweden | Cross-sectional observational | Processing speed and adaptive function | |
| Jonsdottir 2007341 | Iceland | Longitudinal observational | The purpose of the present study was to describe stability and change of preschool children in Iceland and to contribute to the accumulation of data on outcome in autism | |
| Magiati 2007308 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Rickards 2009423 | Australia | Intervention RCT | Does home-based programme provided over 12 months resulted in sustained improvement in development and behaviour? | |
| Sheinkopf 1998429 | USA | Intervention quasi-experimental | To examine the effects of intensive behaviour therapy on the intellectual functioning and symptom presentation of young children diagnosed with autism or PDD | |
| Differential Ability Scalesa | Bishop 2011176 | USA | Cross-sectional observational | Validation of MSEL in a population of children with children with ASDs and other developmental disorders |
| Ruble 2008424 | USA | Cross-sectional observational | Effect of caregiver responsiveness on child cognitive and social interactions | |
| Thurm 2007404 | USA | Longitudinal observational | Non-verbal ability, receptive communication, expressive communication and socialisation were compared as predictors of receptive and expressive language at age 5 years | |
| Kyoto Scale of Psychological Developmenta | Takeda 2005360 | Japan | Longitudinal observational | Clinical variables at age 2 years predictive of mental retardation at age 5 years in children with PDD |
| Tanaka–Binet Intelligence Test (Japanese version of Stanford–Binet)a | Takeda 2005360 | Japan | Longitudinal observational | Clinical variables at age 2 years predictive of mental retardation at age 5 years in children with PDD |
| Snabbt Performance Test På Intelligence IQ II (SPIQ) – Swedisha | Carlsson 2013390 | Sweden | Cross-sectional observational | To analyse co-occurring disorders and problems in a representative group of 198 preschool children with ASD |
| Attention | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Behavior Assessment System for Children-Second Edition (BASC-2) | Hill-Chapman 2013434 | USA | Cross-sectional observational | Parenting stress |
| Child Behavior Scale (CBS) | Jahromi 2013431 | USA | Longitudinal observational | The importance of self-regulation for the school and peer engagement of children with high-functioning autism |
| Meek 2012435 | USA | Cross-sectional observational | To examine group differences in discrete dimensions of social competence between high-functioning autism children and their typically developing peers | |
| Child Behavior Checklist (CBCL) | Baker 2010397 | USA | Longitudinal observational | ‘Examined parent behaviour during unstructured play sessions with high- and low-risk toddlers who did or did not receive later ASD diagnoses, and investigated associations with concurrent child behaviour problems and later language growth’ |
| Hartley 2009323 | USA | Cross-sectional observational | To explore developmental patterns, along gender lines, in children who have autism | |
| Peters-Scheffer 2010421 | The Netherlands | Intervention quasi-experimental | Behavioural treatment in preschool | |
| Smith 2000413 | USA | Intervention RCT | Comparing intensive treatment group to parent training group | |
| Smith 2010359 | Canada and USA | Intervention quasi-experimental | Effect of a parent training and naturalistic one-to-one behaviour intervention using PRT on language, behaviour and ASD symptoms | |
| Taylor 2012436 | USA | Longitudinal observational | To examine the reported symptoms and correlates of depression in caregivers of young children following ASD diagnosis | |
| Child Behaviour Questionnaire-Short Form | Jahromi 2013431 | USA | Longitudinal observational | The importance of self-regulation for the school and peer engagement of children with high-functioning autism |
| Conners Rating Scales-Revised | Escalona 2001271 | USA | Intervention RCT | To explore the effectiveness of massage therapy on stereotypic behaviour among children diagnosed with autism |
| Osborne 2009351 | UK | Longitudinal observational | Evaluate relationship between child behaviour problems and parental stress | |
| Reed 2007353 | UK | Longitudinal observational | Compare effectiveness of ABA, special nursery placements and portage; addressing limitations of previous studies by using the same measures at baseline and end point | |
| Reed 2013437 | UK | Cross-sectional observational | The study assessed whether teacher and parent ratings of child behaviour problems were similar for children with ASDs | |
| Student attention – coded observationa | Travers 2011438 | USA | Cross-sectional observational | Comparing teacher- and computer-led instruction on literacy skills development |
| Emotion regulation | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Baby and Infant Screen for Children with aUtIsm Traits (BISCUIT-Part 2) | Davis 2010439 | USA | Longitudinal observational | To explore the symptoms of anxiety in very young children with ASDs |
| Behavior Assessment System for Children-Second Edition (BASC-2) | Hill-Chapman 2013434 | USA | Cross-sectional observational | Parenting stress |
| Child Behavior Checklist (CBCL) | Baker 2010397 | USA | Longitudinal observational | ‘Examined parent behaviour during unstructured play sessions with high- and low-risk toddlers who did or did not receive later ASD diagnoses, and investigated associations with concurrent child behaviour problems and later language growth’ |
| Hartley 2009323 | USA | Cross-sectional observational | To explore developmental patterns, along gender lines, in children who have autism | |
| Peters-Scheffer 2010421 | The Netherlands | Intervention quasi-experimental | Behavioural treatment in preschool | |
| Smith 2000413 | USA | Intervention RCT | Comparing intensive treatment group to parent training group | |
| Smith 2010359 | Canada and USA | Intervention quasi-experimental | Effect of a parent training and naturalistic one-to-one behaviour intervention using PRT on language, behaviour and ASD symptoms | |
| Taylor 2012436 | USA | Longitudinal observational | To examine the reported symptoms and correlates of depression in caregivers of young children following ASD diagnosis | |
| Children’s Global Assessment Scale (CGAS) | Andersson 2013409 | Sweden | Longitudinal observational | To explore gender-related differences in ASD characteristics |
| Conners Rating Scales-Revised | Escalona 2001271 | USA | Intervention RCT | To explore the effectiveness of massage therapy on stereotypic behaviour among children diagnosed with autism |
| Osborne 2009351 | UK | Longitudinal observational | To evaluate relationship between child behaviour problems and parental stress | |
| Reed 2007353 | UK | Longitudinal observational | Compare effectiveness of ABA, special nursery placements and portage; addressing limitations of previous studies by using the same measures at baseline and end point | |
| Reed 2013437 | UK | Cross-sectional observational | The study assessed whether teacher and parent ratings of child behaviour problems were similar for children with ASDs | |
| Developmental Behaviour Checklist | Herring 2006411 | Australia | Longitudinal observational | To explore the impact of developmental disorders on children and their families |
| Mooney 2006311 | Australia | Cross-sectional observational | Examined whether repetitive behaviours are a feature of autism in children aged < 51 months, independent of chronological or developmental age | |
| Remington 2007358 | UK | Intervention quasi-experimental | Comparison of early intensive behavioural interventions and treatment as usual | |
| Roberts 2011405 | Australia | Intervention RCT | Comparison of home-based vs. centre-based early intervention programmes | |
| Tonge 2012425 | Australia | Longitudinal observational | To determine the impact of a PEBM on the mental health and adjustment of parents with preschool children with autism | |
| Emotion Regulation Checklist | Jahromi 2013431 | USA | Longitudinal observational | The importance of self-regulation for the school and peer engagement of children with high-functioning autism |
| Infant–Toddler Social–Emotional Assessment (ITSEA) | Ben-Sasson 2008382 | Unclear | Cross-sectional observational |
|
| Physical skills | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Annett’s Pegs | Szatmari 2000302 | Canada | Longitudinal observational | Monitoring cognitive and language outcomes of groups of children with autism and Asperger syndrome |
| Beery Visual–Motor Integration Test | Szatmari 2000302 | Canada | Longitudinal observational | Monitoring cognitive and language outcomes of groups of children with autism and Asperger syndrome |
| Brunet–Lezine’s Oculomotor Coordination Subtest | Baghdadli 2012339 | France | Longitudinal observational | Developmental trajectory of adaptive behaviours |
| Functional Independence Measure for children (WeeFIM) | Jasmin 2009384 | Canada | Cross-sectional observational | To determine the impact of sensory–motor DLS on the performance of DLS in preschool children with ASD |
| Infant Motor Maturity and Atypicality Coding Scales | Ozonoff 2008440 | USA | Cross-sectional observational | Assessing gross motor skills in autism; abnormalities relative to developmentally matched children (DD) and TD controls |
| Mullen Scales of Early Learning (MSEL) | Akshoomoff 2006395 | USA | Cross-sectional observational | Overt behaviours during cognitive assessment |
| Anan 2008396 | USA | Other – quantitative case series | To examine the efficacy of the GIFT programme, a 12-week (180 hours, delivered 3 hours each weekday) parent-training for preschoolers with ASDs | |
| Baker 2010397 | USA | Longitudinal observational | ‘Examined parent behaviour during unstructured play sessions with high- and low-risk toddlers who did or did not receive later ASD diagnoses, and investigated associations with concurrent child behaviour problems and later language growth’ | |
| Barbaro 2012398 | Australia | Longitudinal observational | To investigate the developmental profiles of children with ASDs from 12 to 24 months, who had been prospectively identified through developmental surveillance in a large community-based sample | |
| Ben Itzchak 2011320 | Israel | Intervention quasi-experimental | The study explored child and parental characteristics at baseline that may predict outcomes in adaptive skills and acquisition of cognitive gains | |
| Bishop 2011176 | USA | Cross-sectional observational | Validation of MSEL in a population of children with children with ASDs and other developmental disorders | |
| Brian 2008305 | Canada | Longitudinal observational | Assessment of potential behavioural markers of ASD at 18 months in a high-risk cohort of infant siblings of children with ASD | |
| Dawson 2010321 | USA | Intervention RCT | Efficacy of the ESDM, a comprehensive developmental behavioural intervention, for improving outcomes in ASD toddlers | |
| Dereu 2012365 | Belgium | Longitudinal observational | Developmental trajectories of joint attention, imitation and pretend play impairments in autism | |
| Eapen 2013357 | Australia | Longitudinal observational | Evaluation of ESDM for preschool-aged children with ASD | |
| Hartley 2009323 | USA | Cross-sectional observational | To explore developmental patterns, along gender lines, in children who have autism | |
| Honey 2008307 | UK | Longitudinal observational | The study tests the following specific hypotheses:
|
|
| Landa 2012399 | USA | Longitudinal observational | Developmental trajectories of siblings of ASD children | |
| Landa 2012224 | USA | Intervention quasi-experimental | Comprehensive early intervention | |
| Lloyd 2013400 | USA | Cross-sectional observational | Gross and fine motor skills of young children with ASD | |
| Luyster 2008129 | USA | Cross-sectional observational | To systematically investigate language in toddlers with ASD and to identify early correlates of receptive and expressive language in this population | |
| Mayo 2013310 | USA | Other – retrospective observational | This study examined the relationship between age of language acquisition and later functioning in children with ASD | |
| Mitchell 2006392 | Canada | Longitudinal observational | Assessment at 18 and 24 months | |
| O’Donnell 2012386 | USA | Cross-sectional observational | To explore sensory processing characteristics in preschool-age children with ASDs | |
| Ozonoff 2010313 | USA | Longitudinal observational | ‘To examine prospectively the emergence of behavioural signs of autism in the first years of life in infants at low and high risk for autism’ | |
| Poon 2012401 | USA | Longitudinal observational | ‘The current study uses retrospective video analysis (RVA) methods to investigate the longitudinal trajectories of social-communicative behaviours, as well as their associations with later developmental outcomes’ | |
| Ray-Subramanian 2012328 | USA | Longitudinal observational | This study examined whether language skills and non-verbal cognitive skills were associated with clinician-observed RRBs in children with ASD | |
| Rogers 2012317 | USA | Intervention RCT | This study was carried out to examine the efficacy of a 12-week, low-intensity (1 hour/week of therapist contact), parent-delivered intervention for toddlers at risk for ASDs aged 14–24 months and their families | |
| Schertz 2013402 | USA | Intervention RCT | The purpose of this study was to determine effects of the JAML intervention on acquisition of joint attention and other early social communication competencies for toddlers with ASDs | |
| Siller 2013403 | USA | Intervention RCT | To investigate the underlying causal mechanisms of language gain, we conducted a randomised clinical trial of an experimental intervention (FPI) that aims to enhance responsive parental communication (n = 70) | |
| Sullivan 2007330 | USA | Longitudinal observational | To examine whether RJA was impaired as early as 14 months in children later diagnosed with ASD and whether RJA was an early marker for ASD diagnosis at outcome | |
| Tek 2012331 | USA | Cross-sectional observational | To assess whether early symptom presentation differs in toddlers with ASD from ethnic minority vs. non-minority backgrounds | |
| Thurm 2007404 | USA | Longitudinal observational | Non-verbal ability, receptive communication, expressive communication and socialisation were compared as predictors of receptive and expressive language at age 5 years | |
| Toth 2006284 | USA | Longitudinal observational | This study investigated the unique contributions of joint attention, imitation, and toy play to language ability and rate of development of communication skills in young children with ASD | |
| Ventola 2007332 | USA | Cross-sectional observational | Behavioural presentation of AD, developmental delay and developmental language disorder | |
| Werner 2005316 | USA | Cross-sectional observational | Describing variations in early course of development | |
| Zachor 2010335 | Israel | Longitudinal observational | To examine the effect of the intervention approach (ABA, eclectic) on outcome in cognitive, language, and adaptive skills and on changes in autism diagnosis categories | |
| Peabody Developmental Motor Scales | Jasmin 2009384 | Canada | Cross-sectional observational | To determine the impact of sensory–motor DLS on the performance of DLS in preschool children with ASD |
| Provost 2007441 | USA | Cross-sectional observational | Comparing the profiles of gross and fine motor skills in children with ASD and developmental delay | |
| Vineland Adaptive Behavior Scales-Classroom Edition (VABS-Classroom) | Goin-Kochel 2007427 | USA | Longitudinal observational | To assess the developmental trajectories of children with autism enrolled in ABA-based school |
| Vineland Adaptive Behavior Scales (VABS) | Aldred 2004318 | England | Intervention RCT | ‘Social communication intervention targeting parental communication’ |
| Anan 2008396 | USA | Other – quantitative case series | To examine the efficacy of the GIFT programme, a 12-week (180 hours, delivered 3 hours each weekday) parent-training for preschoolers with ASDs | |
| Andersson 2013409 | Sweden | Longitudinal observational | To explore gender-related differences in ASD characteristics | |
| Arick 2003388 | USA | Cross-sectional observational | To track programme implementation variables and outcome data for students with ASDs engaged in school or home programmes | |
| Baghdadli 2012339 | France | Longitudinal observational | Developmental trajectory of adaptive behaviours | |
| Bearss 2013278 | USA | Longitudinal observational | To assess the feasibility and efficacy of a parent training programme | |
| Ben Itzchak 2011320 | Israel | Intervention quasi-experimental | The study explored child and parental characteristics at baseline that may predict outcomes in adaptive skills and acquisition of cognitive gains | |
| Bennett 2008296 | Canada | Longitudinal observational | To explore ‘specific language impairment’ as a predictor of children’s symptom and functional outcome | |
| Carlsson 2013390 | Sweden | Cross-sectional observational | To analyse co-occurring disorders and problems in a representative group of 198 preschool children with ASD | |
| Cassidy 2008348 | Northern Ireland | Cross-sectional observational | To describe the demographic characteristics of preschoolers and their families; to discover parental perceptions of the child’s difficulties; to identify the impact the child has on family life; to outline the supports available to families and those they would like to have | |
| Dawson 2010321 | USA | Intervention RCT | Efficacy of the ESDM, a comprehensive developmental behavioural intervention, for improving outcomes in ASD toddlers | |
| Eapen 2013357 | Australia | Longitudinal observational | Evaluation of ESDM for preschool-aged children with ASD | |
| Eikeseth 2009410 | UK | Longitudinal observational | Effect of intensity of supervision on outcomes | |
| Eldevik 2012414 | UK (Wales) | Longitudinal observational | Behavioural intervention outcome for children who had autism | |
| Eriksson 2013415 | Sweden | Longitudinal observational | To explore frequency of other medical conditions in autism | |
| Gabriels 2007416 | USA | Longitudinal observational | To assess the stability of adaptive functioning in two cognitive ability groups of children with an ASD | |
| Green 2010253 | UK | Intervention RCT | Early interventions for social communication | |
| Grindle 2012417 | UK (Wales) | Intervention quasi-experimental | ABA classroom: educational intervention in a mainstream school setting | |
| Hedvall 2013418 | Sweden | Cross-sectional observational | Processing speed and adaptive function | |
| Herring 2006411 | Australia | Longitudinal observational | To explore the impact of developmental disorders on children and their families | |
| Honey 2008307 | UK | Longitudinal observational | The study tests the following specific hypotheses:
|
|
| Hudry 2010233 | UK | Cross-sectional observational | Recruited as part of Preschool Autism Communication Trial but this report is on baseline data for only receptive vs. expressive skills | |
| Jasmin 2009384 | Canada | Cross-sectional observational | To determine the impact of sensory–motor DLS on the performance of DLS in preschool children with ASD | |
| Jonsdottir 2007341 | Iceland | Longitudinal observational | The purpose of the present study was to describe stability and change of preschool children in Iceland and to contribute to the accumulation of data on outcome in autism | |
| Klintwall 2012419 | Sweden | Longitudinal observational | Number and controllability of reinforces as predictors of outcomes for autistic children receiving Early and Intense Behavioural Intervention | |
| Landa 2012224 | USA | Intervention quasi-experimental | Comprehensive early intervention | |
| Lerna 2012325 | Italy | Intervention RCT | PECS vs. CLT | |
| Lloyd 2012400 | USA | Cross-sectional observational | Gross and fine motor skills of young children with ASD | |
| Luyster 2008129 | USA | Cross-sectional observational | To systematically investigate language in toddlers with ASD and to identify early correlates of receptive and expressive language in this population | |
| Magiati 2007308 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Magiati 2011309 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Mayo 2013310 | USA | Other – retrospective observational | This study examined the relationship between age of language acquisition and later functioning in children with ASD | |
| McConkey 2010349 | – | Intervention quasi-experimental | Evaluate a home-based intervention for preschool children with a confirmed diagnosis of ASD | |
| Munson 2006420 | USA | Longitudinal observational | The relationship between amygdalar volume at age 3–4 years and outcomes at age 6 years | |
| Munson 2008312 | USA | Cross-sectional observational | Latent class analysis of IQ in ASD | |
| O’Donnell 2012386 | USA | Cross-sectional observational | To explore sensory processing characteristics in preschool-age children with ASDs | |
| Osborne 2008350 | UK | Intervention quasi-experimental | There was great heterogeneity among the interventions delivered and so for analysis interventions were categorised into high vs. low intensity | |
| Osborne 2009351 | UK | Longitudinal observational | Evaluate relationship between child behaviour problems and parental stress | |
| Peters-Scheffer 2010421 | The Netherlands | Intervention quasi-experimental | Behavioural treatment in preschool | |
| Poon 2012401 | USA | Longitudinal observational | ‘The current study uses retrospective video analysis (RVA) methods to investigate the longitudinal trajectories of social-communicative behaviours, as well as their associations with later developmental outcomes’ | |
| Pry 2005314 | France, Switzerland, Belgium and Luxembourg | Cross-sectional observational | The relationship between expressive language level and psychological development in children with autism 5 years of age | |
| Ray-Subramanian 2011327 | USA | Cross-sectional observational | ‘Their study examined adaptive behaviour and cognitive skills for 125 toddlers on the autism spectrum using the recently updated Vineland-II and Bayley-III’ | |
| Reed 2007352 | UK | Longitudinal observational | Comparing high- and low-intensity interventions (with comparison of three different types of high-intensity interventions) | |
| Reed 2007353 | UK | Longitudinal observational | Compare effectiveness of ABA, special nursery placements and portage; addressing limitations of previous studies by using the same measures at baseline and end point | |
| Reed 2012354 | UK | Intervention quasi-experimental | To explore and document the relationships between severity of autism, temporal input of the programme, and the outcome effectiveness for a variety of early interventions for children on the autism spectrum. In particular, ABA, special nursery placement, an adaptation of a portage approach for individuals on the autism spectrum, and an eclectic approach developed by a local authority were chosen for study | |
| Remington 2007358 | UK | Intervention quasi-experimental | Comparison of early intensive behavioural interventions and treatment as usual | |
| Restall 1994422 | Canada | Cross-sectional observational | How does the play of children with autism differ that of normally developing children? What are the relationships between performance and adaptive abilities? | |
| Rickards 2009423 | Australia | Intervention RCT | Does home-based programme provided over 12 months result in sustained improvement in development and behaviour? | |
| Roberts 2011405 | Australia | Intervention RCT | Comparison of home-based vs. centre-based early intervention programmes | |
| Rogers 2012317 | USA | Intervention RCT | This study was carried out to examine the efficacy of a 12-week, low-intensity (1 hour per week of therapist contact), parent-delivered intervention for toddlers at risk for ASDs aged 14–24 months and their families | |
| Ruble 2008424 | USA | Cross-sectional observational | Effect of caregiver responsiveness on child cognitive and social interactions | |
| Salt 2002372 | UK | Intervention quasi-experimental | Developmentally based early intervention programme | |
| Schertz 2013402 | USA | Intervention RCT | The purpose of this study was to determine effects of the JAML intervention on acquisition of joint attention and other early social communication competencies for toddlers with ASDs | |
| Silva 2007299 | USA | Intervention RCT | Effectiveness of qigong massage methodology, in treating sensory impairment in young children with autism | |
| Silva 2008300 | USA | Intervention RCT | Outcomes of pilot of qigong sensory training programme | |
| Smith 2000413 | USA | Intervention RCT | Comparing intensive treatment group to parent training group | |
| Smith 2010359 | Canada and USA | Intervention quasi-experimental | Effect of a parent training and naturalistic one-to-one behaviour intervention using PRT on language, behaviour and ASD symptoms | |
| Stahmer 2004355 | USA | Intervention quasi-experimental | To analyse the outcomes for 20 young children with ASD in an inclusive programme for children aged < 3 years | |
| Stone 1999346 | USA | Cross-sectional observational | Patterns of adaptive behaviour in young children with ASD | |
| Strauss 2012329 | Italy | Intervention quasi-experimental | Influence of parent inclusion in treatment provision on child’s progress | |
| Szatmari 2000302 | Canada | Longitudinal observational | Monitoring cognitive and language outcomes of groups of children with autism and Asperger syndrome | |
| Tonge 2012425 | Australia | Longitudinal observational | To determine the impact of a PEBM on the mental health and adjustment of parents with preschool children with autism | |
| Toth 2006284 | USA | Longitudinal observational | This study investigated the unique contributions of joint attention, imitation, and toy play to language ability and rate of development of communication skills in young children with ASD | |
| VanMeter 1997426 | USA | Cross-sectional observational | Social, communication and DLS was examined for autistic children, compared with retarded and normal controls | |
| Ventola 2007332 | USA | Cross-sectional observational | Behavioural presentation of AD, developmental delay and developmental language disorder | |
| Werner 2005316 | USA | Cross-sectional observational | Describing variations in early course of development | |
| Zachor 2010335 | Israel | Longitudinal observational | To examine the effect of the intervention approach (ABA, eclectic) on outcome in cognitive, language, and adaptive skills and on changes in autism diagnosis categories |
| Social communication | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Autism Diagnostic Interview-Revised (ADI-R) | Ben Itzchak 2008149 | Israel | Longitudinal observational | To examine the relations between cognition and autism severity, head size and intervention outcome |
| Bennett 2012304 | Canada | Longitudinal observational | Impact of maternal depression on mother’s reports of her child’s ASD behaviours | |
| Brian 2008305 | Canada | Longitudinal observational | Assessment of potential behavioural markers of ASD at 18 months in a high-risk cohort of infant siblings of children with ASD | |
| Feldman 2012104 | Canada | Longitudinal observational | Development and evaluation of a new instrument – POEMS | |
| Hambly 2012306 | Canada | Cross-sectional observational | The impact of bilingual exposure on language learning in ASD | |
| Honey 2008307 | UK | Longitudinal observational | The study tests the following specific hypotheses:
|
|
| Magiati 2007308 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Magiati 2011309 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Mayo 2013310 | USA | Other – retrospective observational | This study examined the relationship between age of language acquisition and later functioning in children with ASD | |
| Mooney 2006311 | Australia | Cross-sectional observational | Examined whether repetitive behaviours are a feature of autism in children aged < 51 months, independent of chronological or developmental age | |
| Munson 2008312 | USA | Cross-sectional observational | Latent class analysis of IQ in ASD | |
| Ozonoff 2010313 | USA | Longitudinal observational | ‘To examine prospectively the emergence of behavioural signs of autism in the first years of life in infants at low and high risk for autism’ | |
| Pry 2005314 | France, Switzerland, Belgium and Luxembourg | Cross-sectional observational | The relationship between expressive language level and psychological development in children with autism 5 years of age | |
| Richler 2007315 | USA | Longitudinal observational | Examination of RRBs | |
| Werner 2005316 | USA | Cross-sectional observational | Describing variations in early course of development | |
| Autism Diagnostic Observation Scale-Toddler Module (ADOS-T) | Rogers 2012317 | USA | Intervention RCT | This study was carried out to examine the efficacy of a 12-week, low-intensity (1 hour per week of therapist contact), parent-delivered intervention for toddlers at risk for ASDs aged 14–24 months and their families |
| Autism Diagnostic Observation Schedule (ADOS) | Aldred 2004318 | England | Intervention RCT | ‘Social communication intervention targeting parental communication’ |
| Aldred 2012319 | UK | Other RCT | A mediation analysis aimed at assessing the impact of targeted intervention on autism characteristics | |
| Ben Itzchak 2008149 | Israel | Longitudinal observational | To examine the relations between cognition and autism severity, head size and intervention outcome | |
| Ben Itzchak 2011320 | Israel | Intervention quasi-experimental | The study explored child and parental characteristics at baseline that may predict outcomes in adaptive skills and acquisition of cognitive gains | |
| Bennett 2012304 | Canada | Longitudinal observational | Impact of maternal depression on mother’s reports of her child’s ASD behaviours | |
| Brian 2008305 | Canada | Longitudinal observational | Assessment of potential behavioural markers of ASD at 18 months in a high-risk cohort of infant siblings of children with ASD | |
| Dawson 2010321 | USA | Intervention RCT | Efficacy of the ESDM, a comprehensive developmental behavioural intervention, for improving outcomes in ASD toddlers | |
| Gotham 2012322 | USA | Longitudinal observational | To plot longitudinal trajectories of ASD severity from early childhood to early adolescence | |
| Green 2010253 | UK | Intervention RCT | Early interventions for social communication | |
| Hartley 2009323 | USA | Cross-sectional observational | To explore developmental patterns, along gender lines, in children who have autism | |
| Landa 2012224 | USA | Intervention quasi-experimental | Comprehensive early intervention | |
| Lerna 2012325 | Italy | Intervention RCT | PECS vs. CLT | |
| Luyster 2008129 | USA | Cross-sectional observational | To systematically investigate language in toddlers with ASD and to identify early correlates of receptive and expressive language in this population | |
| Munson 2008312 | USA | Cross-sectional observational | Latent class analysis of IQ in ASD | |
| Oosterling 2010326 | The Netherlands | Intervention RCT | Intervention is ‘Focus parent training’. Home-based parent training promoting compliance, mutual enjoyment, joint attention and language development | |
| Ray-Subramanian 2011327 | USA | Cross-sectional observational | ‘Their study examined adaptive behaviour and cognitive skills for 125 toddlers on the autism spectrum using the recently updated Vineland-II and Bayley-III’ | |
| Ray-Subramanian 2012328 | USA | Longitudinal observational | This study examined whether language skills and non-verbal cognitive skills were associated with clinician-observed RRBs in children with ASD | |
| Strauss 2012329 | Italy | Intervention quasi-experimental | Influence of parent inclusion in treatment provision on child’s progress | |
| Sullivan 2007330 | USA | Longitudinal observational | To examine whether RJA was impaired as early as 14 months in children later diagnosed with ASD and whether RJA was an early marker for ASD diagnosis at outcome | |
| Tek 2012331 | USA | Cross-sectional observational | To assess whether early symptom presentation differs in toddlers with ASD from ethnic minority vs. non-minority backgrounds | |
| Ventola 2007332 | USA | Cross-sectional observational | Behavioural presentation of AD, developmental delay and developmental language disorder | |
| Werner 2005316 | USA | Cross-sectional observational | Describing variations in early course of development | |
| Wong 2010333 | China | Intervention RCT | To pilot a 2-week ‘Autism 1-2-3’ early intervention for children with autism and their parents immediately after diagnosis that targeted at (1) eye contact, (2) gesture and (3) vocalisation/words | |
| Zachor 2006334 | Israel | Intervention quasi-experimental | To compare the outcome of two centre-based intervention for autism | |
| Zachor 2010335 | Israel | Longitudinal observational | To examine the effect of the intervention approach (ABA, eclectic) on outcome in cognitive, language, and adaptive skills and on changes in autism diagnosis categories | |
| Autism Screening Instrument for Educational Planning (ASIEP) | Arick 2003388 | USA | Cross-sectional observational | To track programme implementation variables and outcome data for students with ASDs engaged in school or home programmes |
| Communication and Symbolic Behavior Scales-Developmental Profile (CSBS-DP) Caregiver Questionnaire | Tek 2012331 | USA | Cross-sectional observational | To assess whether early symptom presentation differs in toddlers with ASD from ethnic minority vs. non-minority backgrounds |
| Early Social Communication Scale (ESCS) | Dereu 2012365 | Belgium | Longitudinal observational | Developmental trajectories of joint attention, imitation and pretend play impairments in autism |
| Goods 2013366 | USA | Intervention RCT | JASPER | |
| Ingersoll 2012286 | USA | Intervention RCT | Imitation intervention to improve social functioning | |
| Kaale 2012294 | Norway | Intervention RCT | To explore effectiveness of parent-mediated and specialist-mediated joint attention-intervention | |
| Kalas 2012367 | USA | Cross-sectional observational | Joint attention responses to simple vs. complex music | |
| Kasari 2006368 | USA | Intervention RCT | The efficacy of targeted interventions of joint attention and symbolic play was explored | |
| Lawton 2012369 | USA | Intervention quasi-experimental | Joint attention | |
| Luyster 2008129 | USA | Cross-sectional observational | To systematically investigate language in toddlers with ASD and to identify early correlates of receptive and expressive language in this population | |
| Paparella 2011370 | USA | Longitudinal observational | Study 1: Cross-sectional study of profile of emergence of joint attention Study 2: Longitudinal study of emergence of joint attention |
|
| Remington 2007358 | UK | Intervention quasi-experimental | Comparison of early intensive behavioural interventions and treatment as usual | |
| Roos 2008371 | USA | Cross-sectional observational | Comparison of contexts for assessing joint attention in toddlers on the autism spectrum | |
| Wong 2013373 | USA | Intervention RCT | The aim of this study was to pilot test a classroom-based intervention focused on facilitating play and joint attention for young children with autism in self-contained special education classrooms. | |
| Yoder 2006374 | USA | Intervention RCT | Compared the efficacy of two communication interventions (RPMT and PECS) in 36 preschoolers with ASDs | |
| Salt 2002372 | UK | Intervention quasi-experimental | Developmentally based early intervention programme | |
| Early Social Communication Scales (ESCS)-Abridged | Yoder 2010375 | USA | Intervention RCT | Effects of a social communication intervention |
| Pragmatics Profile | Roberts 2011405 | Australia | Intervention RCT | Comparison of home-based vs. centre-based early intervention programmes |
| Social Communication Assessment for Toddlers with Autism (SCATA) | Drew 2007137 | UK | Longitudinal observational | To describe the SCATA administration and scoring, to examine the pattern of developmental change in two samples of children with autism and PDD and to examine which aspects of early non-verbal communication are most strongly associated with later language outcomes |
| Social Communication Behavior Codes | Ozonoff 2010313 | USA | Longitudinal observational | ‘To examine prospectively the emergence of behavioural signs of autism in the first years of life in infants at low and high risk for autism’ |
| Vineland Adaptive Behavior Scales-Classroom Edition (VABS-Classroom) | Goin-Kochel 2007427 | USA | Longitudinal observational | To assess the developmental trajectories of children with autism enrolled in ABA-based school |
| Vineland Adaptive Behavior Scales (VABS) | Aldred 2004318 | England | Intervention RCT | ‘Social communication intervention targeting parental communication’ |
| Anan 2008396 | USA | Other – quantitative case series | To examine the efficacy of the GIFT programme, a 12-week (180 hours, delivered 3 hours each weekday) parent-training for preschoolers with ASDs | |
| Andersson 2013409 | Sweden | Longitudinal observational | To explore gender-related differences in ASD characteristics | |
| Arick 2003388 | USA | Cross-sectional observational | To track programme implementation variables and outcome data for students with ASDs engaged in school or home programmes | |
| Baghdadli 2012339 | France | Longitudinal observational | Developmental trajectory of adaptive behaviours | |
| Bearss 2013278 | USA | Longitudinal observational | To assess the feasibility and efficacy of a parent training programme | |
| Bennett 2008296 | Canada | Longitudinal observational | To explore ‘specific language impairment’ as a predictor of children’s symptom and functional outcome | |
| Carlsson 2013390 | Sweden | Cross-sectional observational | To analyse co-occurring disorders and problems in a representative group of 198 preschool children with ASD | |
| Cassidy 2008348 | Northern Ireland | Cross-sectional observational | To describe the demographic characteristics of preschoolers and their families; to discover parental perceptions of the child’s difficulties; to identify the impact the child has on family life; to outline the supports available to families and those they would like to have | |
| Dawson 2010321 | USA | Intervention RCT | Efficacy of the ESDM, a comprehensive developmental behavioural intervention, for improving outcomes in ASD toddlers | |
| Eikeseth 2009410 | UK | Longitudinal observational | Effect of intensity of supervision on outcomes | |
| Eldevik 2012414 | UK (Wales) | Longitudinal observational | Behavioural intervention outcome for children who had autism | |
| Eriksson 2013415 | Sweden | Longitudinal observational | To explore frequency of other medical conditions in autism | |
| Gabriels 2007416 | USA | Longitudinal observational | To assess the stability of adaptive functioning in two cognitive ability groups of children with an ASD | |
| Green 2010253 | UK | Intervention RCT | Early interventions for social communication | |
| Grindle 2012417 | UK (Wales) | Intervention quasi-experimental | ABA classroom: educational intervention in a mainstream school setting | |
| Hedvall 2013418 | Sweden | Cross-sectional observational | Processing speed and adaptive function | |
| Herring 2006411 | Australia | Longitudinal observational | To explore the impact of developmental disorders on children and their families | |
| Honey 2008307 | UK | Longitudinal observational | The study tests the following specific hypotheses:
|
|
| Hudry 2010233 | UK | Cross-sectional observational | Recruited as part of Preschool Autism Communication Trial but this report is on baseline data for only receptive vs. expressive skills | |
| Ben Itzchak 2011320 | Israel | Intervention quasi-experimental | The study explored child and parental characteristics at baseline that may predict outcomes in adaptive skills and acquisition of cognitive gains | |
| Jasmin 2009384 | Canada | Cross-sectional observational | To determine the impact of sensory–motor DLS on the performance of DLS in preschool children with ASD | |
| Jonsdottir 2007341 | Iceland | Longitudinal observational | The purpose of the present study was to describe stability and change of preschool children in Iceland and to contribute to the accumulation of data on outcome in autism | |
| Klintwall 2012419 | Sweden | Longitudinal observational | Number and controllability of reinforces as predictors of outcomes for autistic children receiving early and intense behavioural intervention | |
| Landa 2012224 | USA | Intervention quasi-experimental | Comprehensive early intervention | |
| Lerna 2012325 | Italy | Intervention RCT | PECS vs. CLT | |
| Lloyd 2013400 | USA | Cross-sectional observational | Gross and fine motor skills of young children with ASD | |
| Luyster 2008129 | USA | Cross-sectional observational | To systematically investigate language in toddlers with ASD and to identify early correlates of receptive and expressive language in this population | |
| Magiati 2007308 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Magiati 2011309 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Mayo 2013310 | USA | Other – retrospective observational | This study examined the relationship between age of language acquisition and later functioning in children with ASD | |
| McConkey 2010349 | – | Intervention quasi-experimental | Evaluate a home-based intervention for preschool children with a confirmed diagnosis of ASD | |
| Munson 2006420 | USA | Longitudinal observational | The relationship between amygdalar volume at age 3–4 years and outcomes at age 6 years | |
| Munson 2008312 | USA | Cross-sectional observational | Latent class analysis of IQ in ASD | |
| O’Donnell 2012386 | USA | Cross-sectional observational | To explore sensory processing characteristics in preschool-age children with ASDs | |
| Eapen 2013357 | Australia | Longitudinal observational | Evaluation of ESDM for preschool-aged children with ASD | |
| Osborne 2008350 | UK | Intervention quasi-experimental | There was great heterogeneity among the interventions delivered and so for analysis interventions were categorised into high vs. low intensity | |
| Osborne 2009351 | UK | Longitudinal observational | Evaluate relationship between child behaviour problems and parental stress | |
| Peters-Scheffer 2010421 | The Netherlands | Intervention quasi-experimental | Behavioural treatment in preschool | |
| Poon 2012401 | USA | Longitudinal observational | ‘The current study uses retrospective video analysis (RVA) methods to investigate the longitudinal trajectories of social-communicative behaviours, as well as their associations with later developmental outcomes’ | |
| Pry 2005314 | France, Switzerland, Belgium and Luxembourg | Cross-sectional observational | The relationship between expressive language level and psychological development in children with autism 5 years of age | |
| Ray-Subramanian 2011327 | USA | Cross-sectional observational | ‘Their study examined adaptive behaviour and cognitive skills for 125 toddlers on the autism spectrum using the recently updated Vineland-II and Bayley-III’ | |
| Reed 2007352 | UK | Longitudinal observational | Comparing high- and low-intensity interventions (with comparison of three different types of high-intensity interventions) | |
| Reed 2007353 | UK | Longitudinal observational | Compare effectiveness of ABA, special nursery placements and portage; addressing limitations of previous studies by using the same measures at baseline and end point | |
| Reed 2012354 | UK | Intervention quasi-experimental | To explore and document the relationships between severity of autism, temporal input of the programme, and the outcome effectiveness for a variety of early interventions for children on the autism spectrum. In particular, ABA, special nursery placement, an adaptation of a portage approach for individuals on the autism spectrum, and an eclectic approach developed by a local authority were chosen for study | |
| Remington 2007358 | UK | Intervention quasi-experimental | Comparison of early intensive behavioural interventions and treatment as usual | |
| Restall 1994422 | Canada | Cross-sectional observational | How does the play of children with autism differ that of normally developing children? What are the relationships between performance and adaptive abilities? | |
| Rickards 2009423 | Australia | Intervention RCT | Does home-based programme provided over 12 months result in sustained improvement in development and behaviour? | |
| Roberts 2011405 | Australia | Intervention RCT | Comparison of home-based vs. centre-based early intervention programmes | |
| Rogers 2012317 | USA | Intervention RCT | This study was carried out to examine the efficacy of a 12-week, low-intensity (1 hour per week of therapist contact), parent-delivered intervention for toddlers at risk for ASDs aged 14–24 months and their families | |
| Ruble 2008424 | USA | Cross-sectional observational | Effect of caregiver responsiveness on child cognitive and social interactions | |
| Salt 2002372 | UK | Intervention quasi-experimental | Developmentally based early intervention programme | |
| Schertz 2013402 | USA | Intervention RCT | The purpose of this study was to determine effects of the JAML intervention on acquisition of joint attention and other early social communication competencies for toddlers with ASDs | |
| Silva 2007299 | USA | Intervention RCT | Effectiveness of qigong massage methodology, in treating sensory impairment in young children with autism | |
| Silva 2008300 | USA | Intervention RCT | Outcomes of pilot of qigong sensory training programme | |
| Smith 2000413 | USA | Intervention RCT | Comparing intensive treatment group to parent training group | |
| Smith 2010359 | Canada and USA | Intervention quasi-experimental | Effect of a parent training and naturalistic one-to-one behaviour intervention using PRT on language, behaviour and ASD symptoms | |
| Stahmer 2004355 | USA | Intervention quasi-experimental | To analyse the outcomes for 20 young children with ASD in an inclusive programme for children aged < 3 years | |
| Stone 1999346 | USA | Cross-sectional observational | Patterns of adaptive behaviour in young children with ASD | |
| Strauss 2012329 | Italy | Intervention quasi-experimental | Influence of parent inclusion in treatment provision on child’s progress | |
| Szatmari 2000302 | Canada | Longitudinal observational | Monitoring cognitive and language outcomes of groups of children with autism and Asperger syndrome | |
| Tonge 2012425 | Australia | Longitudinal observational | To determine the impact of a PEBM on the mental health and adjustment of parents with preschool children with autism | |
| Toth 2006284 | USA | Longitudinal observational | This study investigated the unique contributions of joint attention, imitation, and toy play to language ability and rate of development of communication skills in young children with ASD | |
| VanMeter 1997426 | USA | Cross-sectional observational | Social, communication and DLS was examined for autistic children, compared with retarded and normal controls | |
| Ventola 2007332 | USA | Cross-sectional observational | Behavioural presentation of AD, developmental delay and developmental language disorder | |
| Werner 2005316 | USA | Cross-sectional observational | Describing variations in early course of development | |
| Zachor 2010335 | Israel | Longitudinal observational | To examine the effect of the intervention approach (ABA, eclectic) on outcome in cognitive, language, and adaptive skills and on changes in autism diagnosis categories | |
| Parent Surveya | Arick 2003388 | USA | Cross-sectional observational | To track programme implementation variables and outcome data for students with ASDs engaged in school or home programmes |
| Caregiver–child interactionb | Kasari 2006368 | USA | Intervention RCT | The efficacy of targeted interventions of joint attention and symbolic play was explored |
| Classroom and playground behaviour observationsb | Escalona 2001271 | USA | Intervention RCT | To explore the effectiveness of massage therapy on stereotypic behaviour among children diagnosed with autism |
| Coding of initiation of joint attentionb | Ingersoll 2012286 | USA | Intervention RCT | Imitation intervention to improve social functioning |
| Examiner ratings of social engagementb | Ozonoff 2010313 | USA | Longitudinal observational | ‘To examine prospectively the emergence of behavioural signs of autism in the first years of life in infants at low and high risk for autism’ |
| Parent–child interactionb | Green 2010253 | UK | Intervention RCT | Early interventions for social communication |
| Parent–Child Interaction measureb | Aldred 2012319 | UK | Other – a RCT | A mediation analysis aimed at assessing the impact of targeted intervention on autism characteristics |
| Preschool teacher–child playb | Kaale 2012294 | Norway | Intervention RCT | To explore effectiveness of parent-mediated and specialist-mediated joint attention-intervention |
| Unstructured free play with examinerb | Lerna 2012325 | Italy | Intervention RCT | PECS vs. CLT |
| Video coding proceduresb | Colgan 2006379 | USA | Longitudinal observational | To examine the frequency, initiation, prompting and diversity of types of gestures used for social interaction purposes |
| Video recording of child in classroom activitiesb | Ingersoll 2001380 | USA | Longitudinal observational | To identify a behavioural characteristic that may affect the outcome of a particular treatment model |
| Social functioning | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Autism Diagnostic Interview-Revised (ADI-R) | Ben Itzchak 2008149 | Israel | Longitudinal observational | To examine the relations between cognition and autism severity, head size and intervention outcome |
| Bennett 2012304 | Canada | Longitudinal observational | Impact of maternal depression on mother’s reports of her child’s ASD behaviours | |
| Brian 2008305 | Canada | Longitudinal observational | Assessment of potential behavioural markers of ASD at 18 months in a high-risk cohort of infant siblings of children with ASD | |
| Feldman 2012104 | Canada | Longitudinal observational | Development and evaluation of a new instrument – POEMS | |
| Hambly 2012306 | Canada | Cross-sectional observational | The impact of bilingual exposure on language learning in ASD | |
| Honey 2008307 | UK | Longitudinal observational | The study tests the following specific hypotheses:
|
|
| Magiati 2007308 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Magiati 2011309 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Mayo 2013310 | USA | Other – retrospective observational | This study examined the relationship between age of language acquisition and later functioning in children with ASD | |
| Mooney 2006311 | Australia | Cross-sectional observational | Examined whether repetitive behaviours are a feature of autism in children aged < 51 months, independent of chronological or developmental age | |
| Munson 2008312 | USA | Cross-sectional observational | Latent class analysis of IQ in ASD | |
| Ozonoff 2010313 | USA | Longitudinal observational | ‘To examine prospectively the emergence of behavioural signs of autism in the first years of life in infants at low and high risk for autism’ | |
| Pry 2005314 | France, Switzerland, Belgium and Luxembourg | Cross-sectional observational | The relationship between expressive language level and psychological development in children with autism 5 years of age | |
| Richler 2007315 | USA | Longitudinal observational | Examination of RRBs | |
| Werner 2005316 | USA | Cross-sectional observational | Describing variations in early course of development | |
| Child Behavior Scale (CBS) | Jahromi 2013431 | USA | Longitudinal observational | The importance of self-regulation for the school and peer engagement of children with high-functioning autism |
| Meek 2012435 | USA | Cross-sectional observational | To examine group differences in discrete dimensions of social competence between high-functioning autism children and their typically developing peers | |
| Nisonger Child Behavior Rating Scales | Remington 2007358 | UK | Intervention quasi-experimental | Comparison of early intensive behavioural interventions and treatment as usual |
| Social Behavior Rating Scale | Vorgraft 2007347 | Israel | Cross-sectional observational | Effectiveness of the ‘Mifne Centre’ approach to PDD |
| Vineland Adaptive Behavior Scales-Classroom Edition (VABS-Classroom) | Goin-Kochel 2007427 | USA | Longitudinal observational | To assess the developmental trajectories of children with autism enrolled in ABA-based school |
| Vineland Adaptive Behavior Scales (VABS) | Aldred 2004318 | England | Intervention RCT | ‘Social communication intervention targeting parental communication’ |
| Anan 2008396 | USA | Other – quantitative case series | To examine the efficacy of the GIFT programme, a 12-week (180 hours, delivered 3 hours each weekday) parent-training for preschoolers with ASDs | |
| Andersson 2013409 | Sweden | Longitudinal observational | To explore gender-related differences in ASD characteristics | |
| Arick 2003388 | USA | Cross-sectional observational | To track programme implementation variables and outcome data for students with ASDs engaged in school or home programmes | |
| Baghdadli 2012339 | France | Longitudinal observational | Developmental trajectory of adaptive behaviours | |
| Bearss 2013278 | USA | Longitudinal observational | To assess the feasibility and efficacy of a parent training programme | |
| Bennett 2008296 | Canada | Longitudinal observational | To explore ‘specific language impairment’ as a predictor of children’s symptom and functional outcome | |
| Carlsson 2013390 | Sweden | Cross-sectional observational | To analyse co-occurring disorders and problems in a representative group of 198 preschool children with ASD | |
| Cassidy 2008348 | Northern Ireland | Cross-sectional observational | To describe the demographic characteristics of preschoolers and their families; to discover parental perceptions of the child’s difficulties; to identify the impact the child has on family life; to outline the supports available to families and those they would like to have | |
| Dawson 2010321 | USA | Intervention RCT | Efficacy of the ESDM, a comprehensive developmental behavioural intervention, for improving outcomes in ASD toddlers | |
| Eikeseth 2009410 | UK | Longitudinal observational | Effect of intensity of supervision on outcomes | |
| Eldevik 2012414 | UK (Wales) | Longitudinal observational | Behavioural intervention outcome for children who had autism | |
| Eriksson 2013415 | Sweden | Longitudinal observational | To explore frequency of other medical conditions in autism | |
| Gabriels 2007416 | USA | Longitudinal observational | To assess the stability of adaptive functioning in two cognitive ability groups of children with an ASD | |
| Green 2010253 | UK | Intervention RCT | Early interventions for social communication | |
| Grindle 2012417 | UK (Wales) | Intervention quasi-experimental | ABA classroom: educational intervention in a mainstream school setting | |
| Hedvall 2013418 | Sweden | Cross-sectional observational | Processing speed and adaptive function | |
| Herring 2006411 | Australia | Longitudinal observational | To explore the impact of developmental disorders on children and their families | |
| Honey 2008307 | UK | Longitudinal observational | The study tests the following specific hypotheses:
|
|
| Hudry 2010233 | UK | Cross-sectional observational | Recruited as part of Preschool Autism Communication Trial but this report is on baseline data for only receptive vs. expressive skills | |
| Ben Itzchak 2011320 | Israel | Intervention quasi-experimental | The study explored child and parental characteristics at baseline that may predict outcomes in adaptive skills and acquisition of cognitive gains | |
| Jasmin 2009384 | Canada | Cross-sectional observational | To determine the impact of sensory–motor DLS on the performance of DLS in preschool children with ASD | |
| Jonsdottir 2007341 | Iceland | Longitudinal observational | The purpose of the present study was to describe stability and change of preschool children in Iceland and to contribute to the accumulation of data on outcome in autism | |
| Klintwall 2012419 | Sweden | Longitudinal observational | Number and controllability of reinforces as predictors of outcomes for autistic children receiving early and intense behavioural intervention | |
| Landa 2012224 | USA | Intervention quasi-experimental | Comprehensive early intervention | |
| Lerna 2012325 | Italy | Intervention RCT | PECS vs. CLT | |
| Lloyd 2013400 | USA | Cross-sectional observational | Gross and fine motor skills of young children with ASD | |
| Luyster 2008129 | USA | Cross-sectional observational | To systematically investigate language in toddlers with ASD and to identify early correlates of receptive and expressive language in this population | |
| Magiati 2007308 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Magiati 2011309 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Mayo 2013310 | USA | Other – retrospective observational | This study examined the relationship between age of language acquisition and later functioning in children with ASD | |
| McConkey 2010349 | – | Intervention quasi-experimental | Evaluate a home-based intervention for preschool children with a confirmed diagnosis of ASD | |
| Munson 2006420 | USA | Longitudinal observational | The relationship between amygdalar volume at age 3–4 years and outcomes at age 6 years | |
| Munson 2008312 | USA | Cross-sectional observational | Latent class analysis of IQ in ASD | |
| O’Donnell 2012386 | USA | Cross-sectional observational | To explore sensory processing characteristics in preschool-age children with ASDs | |
| Eapen 2013357 | Australia | Longitudinal observational | Evaluation of ESDM for preschool-aged children with ASD | |
| Osborne 2008350 | UK | Intervention quasi-experimental | There was great heterogeneity among the interventions delivered and so for analysis interventions were categorised into high vs. low intensity | |
| Osborne 2009351 | UK | Longitudinal observational | Evaluate relationship between child behaviour problems and parental stress | |
| Peters-Scheffer 2010421 | The Netherlands | Intervention quasi-experimental | Behavioural treatment in preschool | |
| Poon 2012401 | USA | Longitudinal observational | ‘The current study uses retrospective video analysis (RVA) methods to investigate the longitudinal trajectories of social-communicative behaviours, as well as their associations with later developmental outcomes’ | |
| Pry 2005314 | France, Switzerland, Belgium and Luxembourg | Cross-sectional observational | The relationship between expressive language level and psychological development in children with autism 5 years of age | |
| Ray-Subramanian 2011327 | USA | Cross-sectional observational | ‘Their study examined adaptive behaviour and cognitive skills for 125 toddlers on the autism spectrum using the recently updated Vineland-II and Bayley-III’ | |
| Reed 2007352 | UK | Longitudinal observational | Comparing high- and low-intensity interventions (with comparison of three different types of high-intensity interventions) | |
| Reed 2007353 | UK | Longitudinal observational | Compare effectiveness of ABA, special nursery placements and portage; addressing limitations of previous studies by using the same measures at baseline and end point | |
| Reed 2012354 | UK | Intervention quasi-experimental | To explore and document the relationships between severity of autism, temporal input of the programme and the outcome effectiveness for a variety of early interventions for children on the autism spectrum. In particular, ABA, special nursery placement, an adaptation of a portage approach for individuals on the autism spectrum, and an eclectic approach developed by a local authority were chosen for study | |
| Remington 2007358 | UK | Intervention quasi-experimental | Comparison of early intensive behavioural interventions and treatment as usual | |
| Restall 1994422 | Canada | Cross-sectional observational | How does the play of children with autism differ that of normally developing children? What are the relationships between performance and adaptive abilities? | |
| Rickards 2009423 | Australia | Intervention RCT | Does home-based programme provided over 12 months result in sustained improvement in development and behaviour? | |
| Roberts 2011405 | Australia | Intervention RCT | Comparison of home-based vs. centre-based early intervention programmes | |
| Rogers 2012317 | USA | Intervention RCT | This study was carried out to examine the efficacy of a 12-week, low-intensity (1 hour per week of therapist contact), parent-delivered intervention for toddlers at risk for ASDs aged 14–24 months and their families | |
| Ruble 2008424 | USA | Cross-sectional observational | Effect of caregiver responsiveness on child cognitive and social interactions | |
| Salt 2002372 | UK | Intervention quasi-experimental | Developmentally based early intervention programme | |
| Schertz 2013402 | USA | Intervention RCT | The purpose of this study was to determine effects of the JAML intervention on acquisition of joint attention and other early social communication competencies for toddlers with ASDs | |
| Silva 2007299 | USA | Intervention RCT | Effectiveness of qigong massage methodology, in treating sensory impairment in young children with autism | |
| Silva 2008300 | USA | Intervention RCT | Outcomes of pilot of qigong sensory training programme | |
| Smith 2000413 | USA | Intervention RCT | Comparing intensive treatment group to parent training group | |
| Smith 2010359 | Canada and USA | Intervention quasi-experimental | Effect of a parent training and naturalistic one-to-one behaviour intervention using PRT on language, behaviour and ASD symptoms | |
| Stahmer 2004355 | USA | Intervention quasi-experimental | To analyse the outcomes for 20 young children with ASD in an inclusive programme for children aged < 3 years | |
| Stone 1999346 | USA | Cross-sectional observational | Patterns of adaptive behaviour in young children with ASD | |
| Strauss 2012329 | Italy | Intervention quasi-experimental | Influence of parent inclusion in treatment provision on child’s progress | |
| Szatmari 2000302 | Canada | Longitudinal observational | Monitoring cognitive and language outcomes of groups of children with autism and Asperger syndrome | |
| Tonge 2012425 | Australia | Longitudinal observational | To determine the impact of a PEBM on the mental health and adjustment of parents with preschool children with autism | |
| Toth 2006284 | USA | Longitudinal observational | This study investigated the unique contributions of joint attention, imitation, and toy play to language ability and rate of development of communication skills in young children with ASD | |
| VanMeter 1997426 | USA | Cross-sectional observational | Social, communication and DLS was examined for autistic children, compared with retarded and normal controls | |
| Ventola 2007332 | USA | Cross-sectional observational | Behavioural presentation of AD, developmental delay and developmental language disorder | |
| Werner 2005316 | USA | Cross-sectional observational | Describing variations in early course of development | |
| Zachor 2010335 | Israel | Longitudinal observational | To examine the effect of the intervention approach (ABA, eclectic) on outcome in cognitive, language, and adaptive skills and on changes in autism diagnosis categories | |
| Vineland Social Maturity Scale, Indian adaptationa | Malhi 2011342 | India | Longitudinal observational | To assess diagnostic stability of autism diagnosis in children aged ≤ 3 years |
| Parent Surveyb | Arick 2003388 | USA | Cross-sectional observational | To track programme implementation variables and outcome data for students with ASDs engaged in school or home programmes |
| Classroom and playground behaviour observationsc | Escalona 2001271 | USA | Intervention RCT | To explore the effectiveness of massage therapy on stereotypic behaviour among children diagnosed with autism |
| Coded observation of social behaviourc | Meirsschaut 2011442 | Belgium | Cross-sectional observational | Assessment of ASD vs. TD mother–child dyads and mothers–unfamiliar child dyad interactions |
| Video recording of child in classroom activitiesc | Ingersoll 2001380 | USA | Longitudinal observational | To identify a behavioural characteristic that may affect the outcome of a particular treatment model |
| Play | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Autism Diagnostic Observation Scale-Toddler Module (ADOS-T) | Rogers 2012317 | USA | Intervention RCT | This study was carried out to examine the efficacy of a 12-week, low-intensity (1 hour per week of therapist contact), parent-delivered intervention for toddlers at risk for ASDs aged 14–24 months and their families |
| Autism Diagnostic Observation Schedule (ADOS) | Aldred 2004318 | England | Intervention RCT | ‘Social communication intervention targeting parental communication’ |
| Aldred 2012319 | UK | Other RCT | A mediation analysis aimed at assessing the impact of targeted intervention on autism characteristics | |
| Ben Itzchak 2008149 | Israel | Longitudinal observational | To examine the relations between cognition and autism severity, head size and intervention outcome | |
| Ben Itzchak 2011320 | Israel | Intervention quasi-experimental | The study explored child and parental characteristics at baseline that may predict outcomes in adaptive skills and acquisition of cognitive gains | |
| Bennett 2012304 | Canada | Longitudinal observational | Impact of maternal depression on mother’s reports of her child’s ASD behaviours | |
| Brian 2008305 | Canada | Longitudinal observational | Assessment of potential behavioural markers of ASD at 18 months in a high-risk cohort of infant siblings of children with ASD | |
| Dawson 2010321 | USA | Intervention RCT | Efficacy of the ESDM, a comprehensive developmental behavioural intervention, for improving outcomes in ASD toddlers | |
| Gotham 2012322 | USA | Longitudinal observational | To plot longitudinal trajectories of ASD severity from early childhood to early adolescence | |
| Green 2010253 | UK | Intervention RCT | Early interventions for social communication | |
| Hartley 2009323 | USA | Cross-sectional observational | To explore developmental patterns, along gender lines, in children who have autism | |
| Landa 2012224 | USA | Intervention quasi-experimental | Comprehensive early intervention | |
| Lerna 2012325 | Italy | Intervention RCT | PECS vs. CLT | |
| Luyster 2008129 | USA | Cross-sectional observational | To systematically investigate language in toddlers with ASD and to identify early correlates of receptive and expressive language in this population | |
| Oosterling 2010326 | The Netherlands | Intervention RCT | Intervention is ‘Focus parent training’. Home-based parent training promoting compliance, mutual enjoyment, joint attention and language development | |
| Ray-Subramanian 2011327 | USA | Cross-sectional observational | ‘Their study examined adaptive behaviour and cognitive skills for 125 toddlers on the autism spectrum using the recently updated Vineland-II and Bayley-III’ | |
| Ray-Subramanian 2012328 | USA | Longitudinal observational | This study examined whether or not language skills and non-verbal cognitive skills were associated with clinician-observed RRBs in children with ASD | |
| Strauss 2012329 | Italy | Intervention quasi-experimental | Influence of parent inclusion in treatment provision on child’s progress | |
| Sullivan 2007330 | USA | Longitudinal observational | To examine whether RJA was impaired as early as 14 months in children later diagnosed with ASD and whether RJA was an early marker for ASD diagnosis at outcome | |
| Autism Diagnostic Observation Schedule (ADOS) | Werner 2005316 | USA | Cross-sectional observational | Describing variations in early course of development |
| Wong 2010333 | China | Intervention RCT | To pilot a 2-week ‘Autism 1-2-3’ early intervention for children with autism and their parents immediately after diagnosis that targeted at (1) eye contact, (2) gesture and (3) vocalisation/words | |
| Zachor 2006334 | Israel | Intervention quasi-experimental | To compare the outcome of two centre-based intervention for autism | |
| Zachor 2010335 | Israel | Longitudinal observational | To examine the effect of the intervention approach (ABA, eclectic) on outcome in cognitive, language, and adaptive skills and on changes in autism diagnosis categories | |
| Autism Diagnostic Observation Schedule-Generic (ADOS-G) | Munson 2008312 | USA | Cross-sectional observational | Latent class analysis of IQ in ASD |
| Tek 2012331 | USA | Cross-sectional observational | To assess whether early symptom presentation differs in toddlers with ASD from ethnic minority vs. non-minority backgrounds | |
| Ventola 2007332 | USA | Cross-sectional observational | Behavioural presentation of AD, developmental delay and developmental language disorder | |
| Communication and Symbolic Behavior Scales Developmental Profile Caregiver Questionnaire | Tek 2012331 | USA | Cross-sectional observational | To assess whether early symptom presentation differs in toddlers with ASD from ethnic minority vs. non-minority backgrounds |
| Developmental Play Assessment (DPA), Instrument Sequence of Categories | Freeman 2013443 | USA | Cross-sectional observational | Parent–child play |
| Structured Play Assessment | Freeman 2013443 | USA | Cross-sectional observational | Parent–child play |
| Goods 2013366 | USA | Intervention RCT | JASPER | |
| Kasari 2006368 | USA | Intervention RCT | The efficacy of targeted interventions of joint attention and symbolic play was explored | |
| Symbolic Play Test | Wong 2010333 | China | Intervention RCT | To pilot a 2-week ‘Autism 1-2-3’ early intervention for children with autism and their parents immediately after diagnosis that targeted at (1) eye contact, (2) gesture and (3) vocalisation/words |
| Salt 2002372 | UK | Intervention quasi-experimental | Developmentally based early intervention programme | |
| Magiati 2007308 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Test of Pretend Play (ToPP) | Magiati 2007308 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years |
| Dereu 2012365 | Belgium | Longitudinal observational | Developmental trajectories of joint attention, imitation and pretend play impairments in autism | |
| Preschool Play Scalea | Restall 1994422 | Canada | Cross-sectional observational | How does the play of children with autism differ that of normally developing children? What are the relationships between performance and adaptive abilities? |
| Caregiver–child interactionb | Kasari 2006368 | USA | Intervention RCT | The efficacy of targeted interventions of joint attention and symbolic play was explored |
| Coded observation of social behaviourb | Meirsschaut 2011442 | Belgium | Cross-sectional observational | Assessment of ASD vs. TD mother–child dyads and mothers–unfamiliar child dyad interactions |
| Coding of videosb | Flippin 2011406 | USA | Longitudinal observational | To investigate the concurrent relationships between the verbal and play responsiveness of 16 mothers and fathers and the object play skills of 16 children with ASDs |
| Free play assessmentb | Christensen 2010444 | USA | Cross-sectional observational | Assessing the relationship between play behaviours at 18 months and developmental outcomes in infant siblings of autistic children |
| Parent–child free playb | Freeman 2013443 | USA | Cross-sectional observational | Parent–child play |
| Behaviour | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Aberrant Behavior Checklist (ABC) | Baghdadli 2012339 | France | Longitudinal observational | Developmental trajectory of adaptive behaviours |
| Bearss 2013278 | USA | Longitudinal observational | To assess the feasibility and efficacy of a parent training programme | |
| O’Donnell 2012386 | USA | Cross-sectional observational | To explore sensory processing characteristics in preschool-age children with ASDs | |
| Werner 2005316 | USA | Cross-sectional observational | Describing variations in early course of development | |
| Baby and Infant Screen for Children with aUtIsm Traits (BISCUIT-Part 3) | Rojahn 2009445 | USA | Cross-sectional observational | Frequency and patterns of various challenging behaviours were evaluated |
| Behaviour Assessment System for Children-Second Edition (BASC-2) | Hill-Chapman 2013434 | USA | Cross-sectional observational | Parenting stress |
| Behavior Screening Questionnaire | Rickards 2009423 | Australia | Intervention RCT | Does home-based programme provided over 12 months result in sustained improvement in development and behaviour? |
| Child Behavior Checklist (CBCL) | Baker 2010397 | USA | Longitudinal observational | ‘Examined parent behaviour during unstructured play sessions with high- and low-risk toddlers who did or did not receive later ASD diagnoses, and investigated associations with concurrent child behaviour problems and later language growth’ |
| Hartley 2009323 | USA | Cross-sectional observational | To explore developmental patterns, along gender lines, in children who have autism | |
| Peters-Scheffer 2010421 | The Netherlands | Intervention quasi-experimental | Behavioural treatment in preschool | |
| Smith 2000413 | USA | Intervention RCT | Comparing intensive treatment group to parent training group | |
| Smith 2010359 | Canada and USA | Intervention quasi-experimental | Effect of a parent training and naturalistic one-to-one behaviour intervention using PRT on language, behaviour and ASD symptoms | |
| Taylor 2012436 | USA | Longitudinal observational | To examine the reported symptoms and correlates of depression in caregivers of young children following ASD diagnosis | |
| Child Behavior Scale (CBS) | Jahromi 2013431 | USA | Longitudinal observational | The importance of self-regulation for the school and peer engagement of children with high-functioning autism |
| Meek 2012435 | USA | Cross-sectional observational | To examine group differences in discrete dimensions of social competence between high-functioning autism children and their typically developing peers | |
| Conners Rating Scales-Revised | Escalona 2001271 | USA | Intervention RCT | To explore the effectiveness of massage therapy on stereotypic behaviour among children diagnosed with autism |
| Osborne 2009351 | UK | Longitudinal observational | Evaluate relationship between child behaviour problems and parental stress | |
| Reed 2007353 | UK | Longitudinal observational | Compare effectiveness of ABA, special nursery placements and portage; addressing limitations of previous studies by using the same measures at baseline and end point | |
| Reed 2013437 | UK | Cross-sectional observational | The study assessed whether teacher and parent ratings of child behaviour problems were similar for children with ASDs | |
| Developmental Behaviour Checklist | Herring 2006411 | Australia | Longitudinal observational | To explore the impact of developmental disorders on children and their families |
| Mooney 2006311 | Australia | Cross-sectional observational | Examined whether repetitive behaviours are a feature of autism in children aged < 51 months, independent of chronological or developmental age | |
| Remington 2007358 | UK | Intervention quasi-experimental | Comparison of early intensive behavioural interventions and treatment as usual | |
| Roberts 2011405 | Australia | Intervention RCT | Comparison of home-based vs. centre-based early intervention programmes | |
| Tonge 2012425 | Australia | Longitudinal observational | To determine the impact of a PEBM on the mental health and adjustment of parents with preschool children with autism | |
| Home Situations Questionnaire (HSQ) | Bearss 2013278 | USA | Longitudinal observational | To assess the feasibility and efficacy of a parent training programme |
| Nisonger Child Behavior Rating Scales | Remington 2007358 | UK | Intervention quasi-experimental | Comparison of early intensive behavioural interventions and treatment as usual |
| Parent Target Problems | Bearss 2013278 | USA | Longitudinal observational | To assess the feasibility and efficacy of a parent training programme |
| Pre-School Behavior Checklist | Rickards 2009423 | Australia | Intervention RCT | Does home-based programme provided over 12 months resulted in sustained improvement in development and behaviour? |
| Behaviour Style Questionnaire – Chinese versiona | Chuang 2012383 | Taiwan | Cross-sectional observational | To explore relationships between sensory processing and a difficult temperament characteristics in children with autism |
| Coded observation of child behaviour problemsb | Robbins 1992446 | USA | Longitudinal observational | Investigating the effects of task difficulty on child behaviour problems |
| Functional behaviour assessment interviewc | Reese 2005447 | USA | Cross-sectional observational | ‘Examining the functions of disruptive behaviour in young children with autism compared with developmentally delayed children without autism matched for sex, developmental age, and chronological age‘ |
| Parent surveyc | Arick 2003388 | USA | Cross-sectional observational | To track programme implementation variables and outcome data for students with ASDs engaged in school or home programmes |
| Video coding procedures (for children and parents)d | Bryce 2013448 | USA | Longitudinal observational | To examine children’s compliance and non-compliance behaviours in response to parental control strategies |
| Habit problems | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Child Behavior Checklist (CBCL) | Smith 2000413 | USA | Intervention RCT | Comparing intensive treatment group to parent training group |
| Baker 2010397 | USA | Longitudinal observational | ‘Examined parent behaviour during unstructured play sessions with high- and low-risk toddlers who did or did not receive later ASD diagnoses, and investigated associations with concurrent child behaviour problems and later language growth’ | |
| Peters-Scheffer 2010421 | The Netherlands | Intervention quasi-experimental | Behavioural treatment in preschool | |
| Smith 2010359 | Canada and USA | Intervention quasi-experimental | Effect of a parent training and naturalistic one-to-one behaviour intervention using PRT on language, behaviour and ASD symptoms | |
| Taylor 2012436 | USA | Longitudinal observational | To examine the reported symptoms and correlates of depression in caregivers of young children following ASD diagnosis | |
| Hartley 2009323 | USA | Cross-sectional observational | To explore developmental patterns, along gender lines, in children who have autism | |
| Sense and Self-Regulation Checklist (SSC) | Silva 2009226 | USA | Intervention RCT | Improvement following a qigong massage intervention |
| Silva 2011301 | USA | Intervention RCT | Dual parent and trainer-delivered qigong massage intervention for measures of autism, abnormal sensory responses and self-regulation | |
| Sleep diariesa | Escalona 2001271 | USA | Intervention RCT | To explore the effectiveness of massage therapy on stereotypic behaviour among children diagnosed with autism |
| Learning | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Autism Screening Instrument for Educational Planning (ASIEP) | Arick 2003388 | USA | Cross-sectional observational | To track programme implementation variables and outcome data for students with ASDs engaged in school or home programmes |
| Extended Basic Academic Skills Assessment System | Arick 2003388 | USA | Cross-sectional observational | To track programme implementation variables and outcome data for students with ASDs engaged in school or home programmes |
| Wechsler Individualised Achievement Test | Smith 2000413 | USA | Intervention RCT | Comparing intensive treatment group to parent training group |
| Student Learning Profilea | Arick 2003388 | USA | Cross-sectional observational | To track programme implementation variables and outcome data for students with ASDs engaged in school or home programmes |
| Classroom Observation Formb | Arick 2003388 | USA | Cross-sectional observational | To track programme implementation variables and outcome data for students with ASDs engaged in school or home programmes |
| Daily living skills | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Functional Independence Measure for children (WeeFIM) | Jasmin 2009384 | Canada | Cross-sectional observational | To determine the impact of sensory–motor DLS on the performance of DLS in preschool children with ASD |
| Vineland Adaptive Behavior Scales-Classroom Edition (VABS-Classroom) | Goin-Kochel 2007427 | USA | Longitudinal observational | To assess the developmental trajectories of children with autism enrolled in ABA-based school |
| Vineland Adaptive Behavior Scales (VABS) | Aldred 2004318 | England | Intervention RCT | ‘Social communication intervention targeting parental communication’ |
| Anan 2008396 | USA | Other – quantitative case series | To examine the efficacy of the GIFT programme, a 12-week (180 hours, delivered 3 hours each weekday) parent-training for preschoolers with ASDs | |
| Andersson 2013409 | Sweden | Longitudinal observational | To explore gender-related differences in ASD characteristics | |
| Arick 2003388 | USA | Cross-sectional observational | To track programme implementation variables and outcome data for students with ASDs engaged in school or home programmes | |
| Baghdadli 2012339 | France | Longitudinal observational | Developmental trajectory of adaptive behaviours | |
| Bearss 2013278 | USA | Longitudinal observational | To assess the feasibility and efficacy of a parent training programme | |
| Ben Itzchak 2011320 | Israel | Intervention quasi-experimental | The study explored child and parental characteristics at baseline that may predict outcomes in adaptive skills and acquisition of cognitive gains | |
| Bennett 2008296 | Canada | Longitudinal observational | To explore ‘specific language impairment’ as a predictor of children’s symptom and functional outcome | |
| Carlsson 2013390 | Sweden | Cross-sectional observational | To analyse co-occurring disorders and problems in a representative group of 198 preschool children with ASD | |
| Cassidy 2008348 | Northern Ireland | Cross-sectional observational | To describe the demographic characteristics of preschoolers and their families; to discover parental perceptions of the child’s difficulties; to identify the impact the child has on family life; to outline the supports available to families and those they would like to have | |
| Dawson 2010321 | USA | Intervention RCT | Efficacy of the ESDM, a comprehensive developmental behavioural intervention, for improving outcomes in ASD toddlers | |
| Eapen 2013357 | Australia | Longitudinal observational | Evaluation of ESDM for preschool-aged children with ASD | |
| Eikeseth 2009410 | UK | Longitudinal observational | Effect of intensity of supervision on outcomes | |
| Eldevik 2012414 | UK (Wales) | Longitudinal observational | Behavioural intervention outcome for children who had autism | |
| Eriksson 2013415 | Sweden | Longitudinal observational | To explore frequency of other medical conditions in autism | |
| Gabriels 2007416 | USA | Longitudinal observational | To assess the stability of adaptive functioning in two cognitive ability groups of children with an ASD | |
| Green 2010253 | UK | Intervention RCT | Early interventions for social communication | |
| Grindle 2012417 | UK (Wales) | Intervention quasi-experimental | ABA classroom: educational intervention in a mainstream school setting | |
| Hedvall 2013418 | Sweden | Cross-sectional observational | Processing speed and adaptive function | |
| Herring 2006411 | Australia | Longitudinal observational | To explore the impact of developmental disorders on children and their families | |
| Honey 2008307 | UK | Longitudinal observational | The study tests the following specific hypotheses:
|
|
| Hudry 2010233 | UK | Cross-sectional observational | Recruited as part of Preschool Autism Communication Trial but this report is on baseline data for only receptive vs. expressive skills | |
| Jasmin 2009384 | Canada | Cross-sectional observational | To determine the impact of sensory–motor DLS on the performance of DLS in preschool children with ASD | |
| Jonsdottir 2007341 | Iceland | Longitudinal observational | The purpose of the present study was to describe stability and change of preschool children in Iceland and to contribute to the accumulation of data on outcome in autism | |
| Klintwall 2012419 | Sweden | Longitudinal observational | Number and controllability of reinforces as predictors of outcomes for autistic children receiving early and intense behavioural intervention | |
| Landa 2012224 | USA | Intervention quasi-experimental | Comprehensive early intervention | |
| Lerna 2012325 | Italy | Intervention RCT | PECS vs. CLT | |
| Lloyd 2013400 | USA | Cross-sectional observational | Gross and fine motor skills of young children with ASD | |
| Luyster 2008129 | USA | Cross-sectional observational | To systematically investigate language in toddlers with ASD and to identify early correlates of receptive and expressive language in this population | |
| Magiati 2007308 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Magiati 2011309 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Mayo 2013310 | USA | Other – retrospective observational | This study examined the relationship between age of language acquisition and later functioning in children with ASD | |
| McConkey 2010349 | – | Intervention quasi-experimental | Evaluate a home-based intervention for preschool children with a confirmed diagnosis of ASD | |
| Munson 2006420 | USA | Longitudinal observational | The relationship between amygdalar volume at age 3–4 years and outcomes at age 6 years | |
| Munson 2008312 | USA | Cross-sectional observational | Latent class analysis of IQ in ASD | |
| O’Donnell 2012386 | USA | Cross-sectional observational | To explore sensory processing characteristics in preschool-age children with ASDs | |
| Osborne 2008350 | UK | Intervention quasi-experimental | There was great heterogeneity among the interventions delivered and so for analysis interventions were categorised into high vs. low intensity | |
| Osborne 2009351 | UK | Longitudinal observational | Evaluate relationship between child behaviour problems and parental stress | |
| Peters-Scheffer 2010421 | The Netherlands | Intervention quasi-experimental | Behavioural treatment in preschool | |
| Poon 2012401 | USA | Longitudinal observational | ‘The current study uses retrospective video analysis (RVA) methods to investigate the longitudinal trajectories of social-communicative behaviours, as well as their associations with later developmental outcomes’ | |
| Pry 2005314 | France, Switzerland, Belgium and Luxembourg | Cross-sectional observational | The relationship between expressive language level and psychological development in children with autism 5 years of age | |
| Ray-Subramanian 2011327 | USA | Cross-sectional observational | ‘Their study examined adaptive behaviour and cognitive skills for 125 toddlers on the autism spectrum using the recently updated Vineland-II and Bayley-III’ | |
| Reed 2007352 | UK | Longitudinal observational | Comparing high- and low-intensity interventions (with comparison of three different types of high-intensity interventions) | |
| Reed 2007353 | UK | Longitudinal observational | Compare effectiveness of ABA, special nursery placements and portage; addressing limitations of previous studies by using the same measures at baseline and end point | |
| Reed 2012354 | UK | Intervention quasi-experimental | To explore and document the relationships between severity of autism, temporal input of the programme, and the outcome effectiveness for a variety of early interventions for children on the autism spectrum. In particular, ABA, special nursery placement, an adaptation of a portage approach for individuals on the autism spectrum and an eclectic approach developed by a local authority were chosen for study | |
| Remington 2007358 | UK | Intervention quasi-experimental | Comparison of early intensive behavioural interventions and treatment as usual | |
| Restall 1994422 | Canada | Cross-sectional observational | How does the play of children with autism differ that of normally developing children? What are the relationships between performance and adaptive abilities? | |
| Rickards 2009423 | Australia | Intervention RCT | Does home-based programme provided over 12 months result in sustained improvement in development and behaviour? | |
| Roberts 2011405 | Australia | Intervention RCT | Comparison of home-based vs. centre-based early intervention programmes | |
| Rogers 2012317 | USA | Intervention RCT | This study was carried out to examine the efficacy of a 12-week, low-intensity (1 hour per week of therapist contact), parent-delivered intervention for toddlers at risk for ASDs aged 14–24 months and their families | |
| Ruble 2008424 | USA | Cross-sectional observational | Effect of caregiver responsiveness on child cognitive and social interactions | |
| Salt 2002372 | UK | Intervention quasi-experimental | Developmentally based early intervention programme | |
| Schertz 2013402 | USA | Intervention RCT | The purpose of this study was to determine effects of the JAML intervention on acquisition of joint attention and other early social communication competencies for toddlers with ASDs | |
| Silva 2007299 | USA | Intervention RCT | Effectiveness of qigong massage methodology, in treating sensory impairment in young children with autism | |
| Silva 2008300 | USA | Intervention RCT | Outcomes of pilot of qigong sensory training programme | |
| Smith 2000413 | USA | Intervention RCT | Comparing intensive treatment group to parent training group | |
| Smith 2010359 | Canada and USA | Intervention quasi-experimental | Effect of a parent training and naturalistic one-to-one behaviour intervention using PRT on language, behaviour and ASD symptoms | |
| Stahmer 2004355 | USA | Intervention quasi-experimental | To analyse the outcomes for 20 young children with ASD in an inclusive programme for children aged < 3 years | |
| Stone 1999346 | USA | Cross-sectional observational | Patterns of adaptive behaviour in young children with ASD | |
| Strauss 2012329 | Italy | Intervention quasi-experimental | Influence of parent inclusion in treatment provision on child’s progress | |
| Szatmari 2000302 | Canada | Longitudinal observational | Monitoring cognitive and language outcomes of groups of children with autism and Asperger syndrome | |
| Tonge 2012425 | Australia | Longitudinal observational | To determine the impact of a PEBM on the mental health and adjustment of parents with preschool children with autism | |
| Toth 2006284 | USA | Longitudinal observational | This study investigated the unique contributions of joint attention, imitation, and toy play to language ability and rate of development of communication skills in young children with ASD | |
| VanMeter 1997426 | USA | Cross-sectional observational | Social, communication and DLS was examined for autistic children, compared with retarded and normal controls | |
| Ventola 2007332 | USA | Cross-sectional observational | Behavioural presentation of AD, developmental delay and developmental language disorder | |
| Werner 2005316 | USA | Cross-sectional observational | Describing variations in early course of development | |
| Zachor 2010335 | Israel | Longitudinal observational | To examine the effect of the intervention approach (ABA, eclectic) on outcome in cognitive, language, and adaptive skills and on changes in autism diagnosis categories | |
| Video coding of feeding behavioura | Brisson 2012449 | France and Belgium | Cross-sectional observational | Motor anticipation failure in feeding situations |
| Global measure of function | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Ages and Stages Questionnaire (ASQ) | Feldman 2012104 | Canada | Longitudinal observational | Development and evaluation of a new instrument – POEMS |
| Assessment of Basic Language and Learning Skills (ABLLS) | Goin-Kochel 2007427 | USA | Longitudinal observational | To assess the developmental trajectories of children with autism enrolled in ABA-based school |
| Grindle 2012417 | UK (Wales) | Intervention quasi-experimental | ABA classroom: educational intervention in a mainstream school setting | |
| Gupta 2009303 | India | Cross-sectional observational | To understudy the development of language and learning skills in children with autism and compare with that of typically developing children | |
| Assessment, Evaluation and Programming System (AEPS) | Schwartz 2004450 | USA | Longitudinal observational | Effect of Project DATA school programme |
| Behaviour Assessment System for Children-Second Edition (BASC-2) | Hill-Chapman 2013434 | USA | Cross-sectional observational | Parenting stress |
| Brigance Diagnostic Inventory of Early Development | Travers 2011438 | USA | Cross-sectional observational | Comparing teacher- and computer-led instruction on literacy skills development |
| Developmental Profile | Malhi 2011342 | India | Longitudinal observational | To assess diagnostic stability of autism diagnosis in children aged ≤ 3 years |
| Early Development Interview | Werner 2005316 | USA | Cross-sectional observational | Describing variations in early course of development |
| Early Intervention Developmental Profile (EIDP) | Jocelyn 1998298 | Canada | Intervention RCT | Caregiver-based intervention programme in community day care centres |
| Early Learning Accomplishment Profile (E-LAP) | Virues-Ortega 2013451 | Spain | Longitudinal observational | This article describes growth patterns of motor, cognitive, verbal, DLS and social skills in a sample of children with ASD admitted into a home-based IBI programme managed by trained behaviour analysts and delivering 20–40 weekly hours of intervention |
| Functional and Emotional Developmental Questionnaire | Pajareya 2012343 | Thailand | Intervention quasi-experimental | Determine the results of 1-year DIR/Floortime parent training in developmental stimulation of children with ASD |
| Pajareya 2011344 | Thailand | Intervention RCT | RCT of DIR/Floortime intervention for autistic children | |
| Learning Accomplishment Profile-Diagnostic, Third Edition, (LAP-D) | Virues-Ortega 2013451 | Spain | Longitudinal observational | This article describes growth patterns of motor, cognitive, verbal, DLS and social skills in a sample of children with ASD admitted into a home-based IBI programme managed by trained behaviour analysts and delivering 20–40 weekly hours of intervention |
| Paediatric Daily Occupation Scale | Hsieh 2013452 | Taiwan | Cross-sectional observational | Well-being of mothers of children with ASD in Taiwan |
| Preschool Developmental Profile (PSDP) | Jocelyn 1998298 | Canada | Intervention RCT | Caregiver-based intervention programme in community day care centres |
| Psychoeducational Profile-Revised (PEP-R) | Delmolino 2006432 | USA | Longitudinal observational | To assess if scores obtained by the PEP-R are reasonable estimates of cognitive ability, correlating with scores from another instrument (Stanford–Binet Intelligence Scales, 4th edn) |
| Herring 2006411 | Australia | Longitudinal observational | To explore the impact of developmental disorders on children and their families | |
| McConkey 2010349 | – | Intervention quasi-experimental | Evaluate a home-based intervention for preschool children with a confirmed diagnosis of ASD | |
| Osborne 2008350 | UK | Intervention quasi-experimental | There was great heterogeneity among the interventions delivered and so for analysis interventions were categorised into high vs. low intensity | |
| Ozonoff 1998453 | USA | Intervention quasi-experimental | Evaluate the effectiveness of a TEACCH-based home programme intervention | |
| Reed 2007352 | UK | Longitudinal observational | Comparing high- and low-intensity interventions (with comparison of three different types of high-intensity interventions) | |
| Reed 2007353 | UK | Longitudinal observational | Compare effectiveness of ABA, special nursery placements and portage; addressing limitations of previous studies by using the same measures at baseline and end point | |
| Reed 2012354 | UK | Intervention quasi-experimental | To explore and document the relationships between severity of autism, temporal input of the programme, and the outcome effectiveness for a variety of early interventions for children on the autism spectrum. In particular, ABA, special nursery placement, an adaptation of a portage approach for individuals on the autism spectrum, and an eclectic approach developed by a local authority were chosen for study | |
| Tonge 2012425 | Australia | Longitudinal observational | To determine the impact of a PEBM on the mental health and adjustment of parents with preschool children with autism | |
| Scales of Independent Behavior Revised-early development form (SIB-R) | Keen 2010363 | Australia | Intervention quasi-experimental | To reduce parenting stress and increase parenting competence for families of children within 6 months of receiving an ASD diagnosis |
| Vineland Adaptive Behavior Scales-Classroom Edition (VABS-Classroom) | Goin-Kochel 2007427 | USA | Longitudinal observational | To assess the developmental trajectories of children with autism enrolled in ABA-based school |
| Vineland Adaptive Behavior Scales (VABS) | Aldred 2004318 | England | Intervention RCT | ‘Social communication intervention targeting parental communication’ |
| Anan 2008396 | USA | Other – quantitative case series | To examine the efficacy of the GIFT programme, a 12-week (180 hours, delivered 3 hours each weekday) parent-training for preschoolers with ASDs | |
| Andersson 2013409 | Sweden | Longitudinal observational | To explore gender-related differences in ASD characteristics | |
| Arick 2003388 | USA | Cross-sectional observational | To track programme implementation variables and outcome data for students with ASDs engaged in school or home programmes | |
| Baghdadli 2012339 | France | Longitudinal observational | Developmental trajectory of adaptive behaviours | |
| Bearss 2013278 | USA | Longitudinal observational | To assess the feasibility and efficacy of a parent training programme | |
| Ben Itzchak 2011320 | Israel | Intervention quasi-experimental | The study explored child and parental characteristics at baseline that may predict outcomes in adaptive skills and acquisition of cognitive gains | |
| Bennett 2008296 | Canada | Longitudinal observational | To explore ‘specific language impairment’ as a predictor of children’s symptom and functional outcome | |
| Carlsson 2013390 | Sweden | Cross-sectional observational | To analyse co-occurring disorders and problems in a representative group of 198 preschool children with ASD | |
| Cassidy 2008348 | Northern Ireland | Cross-sectional observational | To:
|
|
| Dawson 2010321 | USA | Intervention RCT | Efficacy of the ESDM, a comprehensive developmental behavioural intervention, for improving outcomes in ASD toddlers | |
| Eapen 2013357 | Australia | Longitudinal observational | Evaluation of ESDM for preschool-aged children with ASD | |
| Eikeseth 2009410 | UK | Longitudinal observational | Effect of intensity of supervision on outcomes | |
| Eldevik 2012414 | UK (Wales) | Longitudinal observational | Behavioural intervention outcome for children who had autism | |
| Eriksson 2013415 | Sweden | Longitudinal observational | To explore frequency of other medical conditions in autism | |
| Gabriels 2007416 | USA | Longitudinal observational | To assess the stability of adaptive functioning in two cognitive ability groups of children with an ASD | |
| Green 2010253 | UK | Intervention RCT | Early interventions for social communication | |
| Grindle 2012417 | UK (Wales) | Intervention quasi-experimental | ABA classroom: educational intervention in a mainstream school setting | |
| Hedvall 2013418 | Sweden | Cross-sectional observational | Processing speed and adaptive function | |
| Herring 2006411 | Australia | Longitudinal observational | To explore the impact of developmental disorders on children and their families | |
| Honey 2008307 | UK | Longitudinal observational | The study tests the following specific hypotheses:
|
|
| Hudry 2010233 | UK | Cross-sectional observational | Recruited as part of Preschool Autism Communication Trial but this report is on baseline data for only receptive vs. expressive skills | |
| Jasmin 2009384 | Canada | Cross-sectional observational | To determine the impact of sensory–motor DLS on the performance of DLS in preschool children with ASD | |
| Jonsdottir 2007341 | Iceland | Longitudinal observational | The purpose of the present study was to describe stability and change of preschool children in Iceland and to contribute to the accumulation of data on outcome in autism | |
| Klintwall 2012419 | Sweden | Longitudinal observational | Number and controllability of reinforces as predictors of outcomes for autistic children receiving early and intense behavioural intervention | |
| Landa 2012224 | USA | Intervention quasi-experimental | Comprehensive early intervention | |
| Lerna 2012325 | Italy | Intervention RCT | PECS vs. CLT | |
| Lloyd 2013400 | USA | Cross-sectional observational | Gross and fine motor skills of young children with ASD | |
| Luyster 2008129 | USA | Cross-sectional observational | To systematically investigate language in toddlers with ASD and to identify early correlates of receptive and expressive language in this population | |
| Magiati 2007308 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Magiati 2011309 | UK | Longitudinal observational | To provide data on long-term outcome for children with ASD who have received intensive, comprehensive interventions in their preschool years | |
| Mayo 2013310 | USA | Other – retrospective observational | This study examined the relationship between age of language acquisition and later functioning in children with ASD | |
| McConkey 2010349 | – | Intervention quasi-experimental | Evaluate a home-based intervention for preschool children with a confirmed diagnosis of ASD | |
| Munson 2006420 | USA | Longitudinal observational | The relationship between amygdalar volume at age 3–4 years and outcomes at age 6 years | |
| Munson 2008312 | USA | Cross-sectional observational | Latent class analysis of IQ in ASD | |
| O’Donnell 2012386 | USA | Cross-sectional observational | To explore sensory processing characteristics in preschool-age children with ASDs | |
| Osborne 2008350 | UK | Intervention quasi-experimental | There was great heterogeneity among the interventions delivered and so for analysis interventions were categorised into high vs. low intensity | |
| Osborne 2009351 | UK | Longitudinal observational | Evaluate relationship between child behaviour problems and parental stress | |
| Peters-Scheffer 2010421 | The Netherlands | Intervention quasi-experimental | Behavioural treatment in preschool | |
| Poon 2012401 | USA | Longitudinal observational | ‘The current study uses retrospective video analysis (RVA) methods to investigate the longitudinal trajectories of social-communicative behaviours, as well as their associations with later developmental outcomes’ | |
| Pry 2005314 | France, Switzerland, Belgium and Luxembourg | Cross-sectional observational | The relationship between expressive language level and psychological development in children with autism 5 years of age | |
| Ray-Subramanian 2011327 | USA | Cross-sectional observational | ‘Their study examined adaptive behaviour and cognitive skills for 125 toddlers on the autism spectrum using the recently updated Vineland-II and Bayley-III’ | |
| Reed 2007352 | UK | Longitudinal observational | Comparing high- and low-intensity interventions (with comparison of three different types of high-intensity interventions) | |
| Reed 2007353 | UK | Longitudinal observational | Compare effectiveness of ABA, special nursery placements and portage; addressing limitations of previous studies by using the same measures at baseline and end point | |
| Reed 2012354 | UK | Intervention quasi-experimental | To explore and document the relationships between severity of autism, temporal input of the programme, and the outcome effectiveness for a variety of early interventions for children on the autism spectrum. In particular, ABA, special nursery placement, an adaptation of a portage approach for individuals on the autism spectrum, and an eclectic approach developed by a local authority were chosen for study | |
| Remington 2007358 | UK | Intervention quasi-experimental | Comparison of early intensive behavioural interventions and treatment as usual | |
| Restall 1994422 | Canada | Cross-sectional observational | How does the play of children with autism differ that of normally developing children? What are the relationships between performance and adaptive abilities? | |
| Rickards 2009423 | Australia | Intervention RCT | Does home-based programme provided over 12 months result in sustained improvement in development and behaviour? | |
| Roberts 2011405 | Australia | Intervention RCT | Comparison of home-based vs. centre-based early intervention programmes | |
| Rogers 2012317 | USA | Intervention RCT | This study was carried out to examine the efficacy of a 12-week, low-intensity (1 hour per week of therapist contact), parent-delivered intervention for toddlers at risk for ASDs aged 14–24 months and their families | |
| Ruble 2008424 | USA | Cross-sectional observational | Effect of caregiver responsiveness on child cognitive and social interactions | |
| Salt 2002372 | UK | Intervention quasi-experimental | Developmentally based early intervention programme | |
| Schertz 2013402 | USA | Intervention RCT | The purpose of this study was to determine effects of the JAML intervention on acquisition of joint attention and other early social communication competencies for toddlers with ASDs | |
| Silva 2007299 | USA | Intervention RCT | Effectiveness of qigong massage methodology, in treating sensory impairment in young children with autism | |
| Silva 2008300 | USA | Intervention RCT | Outcomes of pilot of qigong sensory training programme | |
| Smith 2000413 | USA | Intervention RCT | Comparing intensive treatment group to parent training group | |
| Smith 2010359 | Canada and USA | Intervention quasi-experimental | Effect of a parent training and naturalistic one-to-one behaviour intervention using PRT on language, behaviour and ASD symptoms | |
| Stahmer 2004355 | USA | Intervention quasi-experimental | To analyse the outcomes for 20 young children with ASD in an inclusive programme for children aged < 3 years | |
| Stone 1999346 | USA | Cross-sectional observational | Patterns of adaptive behaviour in young children with ASD | |
| Strauss 2012329 | Italy | Intervention quasi-experimental | Influence of parent inclusion in treatment provision on child’s progress | |
| Szatmari 2000302 | Canada | Longitudinal observational | Monitoring cognitive and language outcomes of groups of children with autism and Asperger syndrome | |
| Tonge 2012425 | Australia | Longitudinal observational | To determine the impact of a PEBM on the mental health and adjustment of parents with preschool children with autism | |
| Toth 2006284 | USA | Longitudinal observational | This study investigated the unique contributions of joint attention, imitation, and toy play to language ability and rate of development of communication skills in young children with ASD | |
| VanMeter 1997426 | USA | Cross-sectional observational | Social, communication and DLS was examined for autistic children, compared with retarded and normal controls | |
| Ventola 2007332 | USA | Cross-sectional observational | Behavioural presentation of AD, developmental delay and developmental language disorder | |
| Werner 2005316 | USA | Cross-sectional observational | Describing variations in early course of development | |
| Zachor 2010335 | Israel | Longitudinal observational | To examine the effect of the intervention approach (ABA, eclectic) on outcome in cognitive, language, and adaptive skills and on changes in autism diagnosis categories | |
| Social Adaptive Development Quotient Scale (ADQ)a | Zhang 2012303 | China | Intervention quasi-experimental | TEAS was applied to children with autism to assess its therapeutic efficacy |
| Global measure of outcome | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Autism Treatment Evaluation Checklist (ATEC) | Goin-Kochel 2007427 | USA | Longitudinal observational | To assess the developmental trajectories of children with autism enrolled in ABA-based school |
| Behavioral Summarized Evaluation Scale-Revised (BSE-R) | Receveur 2005337 | France | Longitudinal observational | Interaction and imitation deficits from infancy to 4 years of age in children with autism |
| Maestro 2005338 | Italy | Cross-sectional observational | Providing new criteria to describe the early course of ASD | |
| Clinical Global Impression – Improvement Scale | Bearss 2013278 | USA | Longitudinal observational | To assess the feasibility and efficacy of a parent training programme |
| Oosterling 2010326 | The Netherlands | Intervention RCT | Intervention is ‘Focus parent training’. Home-based parent training promoting compliance, mutual enjoyment, joint attention and language development | |
| Infant Behavioral Summarized Evaluation (IBSE) | Adrien 199290 | France | Longitudinal observational | To observe and analyse the evolution of behavioural pathology in autistic children |
| Receveur 2005337 | France | Longitudinal observational | Interaction and imitation deficits from infancy to 4 years of age in children with autism | |
| Pervasive Developmental Disorders Behavior Inventory (PDDBI) | Silva 2009226 | USA | Intervention RCT | Improvement following a qigong massage intervention |
| Silva 2011301 | USA | Intervention RCT | Dual parent and trainer-delivered qigong massage intervention for measures of autism, abnormal sensory responses and self-regulation |
| Subjective well-being | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Kiddie-Infant Descriptive Instrument for Emotional States (KIDIES)a | Trad 1993454 | USA | Cross-sectional observational | To determine whether the KIDIES tool could detect individual differences in responsivity among the PDD subjects, ’to ascertain the KIDIES’ sensitivity in identifying group differences between PDD subjects and control children with other developmental disorders |
| Social inclusion | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| School Liking and Avoidance Questionnaire | Jahromi 2013431 | USA | Longitudinal observational | The importance of self-regulation for the school and peer engagement of children with high-functioning autism |
| Teacher Rating Scale of School Adjustment | Jahromi 2013431 | USA | Longitudinal observational | The importance of self-regulation for the school and peer engagement of children with high-functioning autism |
| Interaction style | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Functional Emotional Assessment Scale | Pajareya 2012343 | Thailand | Intervention quasi-experimental | Determine the results of 1-year DIR/Floortime parent training in developmental stimulation of children with ASD |
| Pajareya 2011344 | Thailand | Intervention RCT | RCT of DIR/Floortime intervention for autistic children | |
| NICHD Early Child Care Network scales | Baker 2010397 | USA | Longitudinal observational | ‘Examined parent behaviour during unstructured play sessions with high- and low-risk toddlers who did or did not receive later ASD diagnoses, and investigated associations with concurrent child behaviour problems and later language growth’ |
| Coded observation of social behavioura | Meirsschaut 2011442 | Belgium | Cross-sectional observational | Assessment of ASD vs. TD mother–child dyads and mothers–unfamiliar child dyad interactions |
| Coding of videosa | Flippin 2011406 | USA | Longitudinal observational | To investigate the concurrent relationships between the verbal and play responsiveness of 16 mothers and fathers and the object play skills of 16 children with ASDs |
| Parental skills – video ratingsa | Oosterling 2010326 | The Netherlands | Intervention RCT | Intervention is ‘Focus parent training’. Home-based parent training promoting compliance, mutual enjoyment, joint attention and language development |
| Parent–child free playa | Freeman 2013443 | USA | Cross-sectional observational | Parent–child play |
| Parent–child interactiona | Green 2010253 | UK | Intervention RCT | Early interventions for social communication |
| Parent–Child Interaction measurea | Aldred 2012319 | UK | Other – a RCT | A mediation analysis aimed at assessing the impact of targeted intervention on autism characteristics |
| Preschool teacher–child playa | Kaale 2012294 | Norway | Intervention RCT | To explore effectiveness of parent-mediated and specialist-mediated joint attention-intervention |
| Social Interaction Rating Scalea | Ruble 2008424 | USA | Cross-sectional observational | Effect of caregiver responsiveness on child cognitive and social interactions |
| Parent stress | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Autism Parenting Stress Index (APSI) | Silva 2011301 | USA | Intervention RCT | Dual parent and trainer-delivered qigong massage intervention for measures of autism, abnormal sensory responses and self-regulation |
| Beck Anxiety Inventory | Davis 2008455 | USA | Longitudinal observational | To explore the associations between child behaviour and parenting stress |
| Center for Epidemiologic Studies Depression Inventory | Davis 2008455 | USA | Longitudinal observational | To explore the associations between child behaviour and parenting stress |
| Taylor 2012436 | USA | Longitudinal observational | To examine the reported symptoms and correlates of depression in caregivers of young children following ASD diagnosis | |
| General Health Questionnaire (GHQ) | Herring 2006411 | Australia | Longitudinal observational | To explore the impact of developmental disorders on children and their families |
| McConkey 2010349 | – | Intervention quasi-experimental | Evaluate a home-based intervention for preschool children with a confirmed diagnosis of ASD | |
| Tonge 2005456 | Australia | Intervention RCT | To determine the impact of a PEBM on the mental health and adjustment of parents with preschool children with autism | |
| Hospital Anxiety and Depression Scale (HADS) | Remington 2007358 | UK | Intervention quasi-experimental | Comparison of early intensive behavioural interventions and treatment as usual |
| Parenting Stress Index-Short Form (PSI-SF) | Strauss 2012329 | Italy | Intervention quasi-experimental | Influence of parent inclusion in treatment provision on child’s progress |
| Parenting Sense of Competence (PSOC) | Keen 2007364 | Australia | Longitudinal observational | To investigate the effects of the Stronger Families Project on communication and symbolic behaviour of young children with autism and to explore possible correlations between post-intervention changes in children’s communication and symbolic behaviour, and child adaptive behaviour, chronological age, maternal stress and sense of parenting competence |
| Keen 2010363 | Australia | Intervention quasi-experimental | To reduce parenting stress and increase parenting competence for families of children within 6 months of receiving an ASD diagnosis | |
| Parenting Stress Index (PSI) | Aldred 2004318 | England | Intervention RCT | ‘Social communication intervention targeting parental communication’ |
| Baker-Ericzen 2005457 | USA | Intervention quasi-experimental | Examine parental stress before and after involvement in an inclusive toddler programme | |
| Keen 2010363 | Australia | Intervention quasi-experimental | To reduce parenting stress and increase parenting competence for families of children within 6 months of receiving an ASD diagnosis | |
| Roberts 2011405 | Australia | Intervention RCT | Comparison of home-based vs. centre-based early intervention programmes | |
| Salt 2002372 | UK | Intervention quasi-experimental | Developmentally based early intervention programme | |
| Parenting Stress Index-Short Form (PSI-SF) | Bendixen 2011458 | USA | Intervention quasi-experimental | To explore parental differences pre–post an interdisciplinary in-home training programme |
| Davis 2008455 | USA | Longitudinal observational | To explore the associations between child behaviour and parenting stress | |
| Hill-Chapman 2013434 | USA | Cross-sectional observational | Parenting stress | |
| Minjarez 2013459 | USA | Intervention quasi-experimental | To evaluate whether participating in a PRT group therapy programme for parents of children with autism influenced related aspects of parents’ lives, namely, their levels of stress and empowerment | |
| Wang 2013460 | China | Cross-sectional observational | The aim of the current study was to further the knowledge about stress experienced by Chinese mothers of children with ASD by examining maternal parenting stress in Heilongjiang province of China | |
| Wong 2010333 | China | Intervention RCT | To pilot a 2-week ‘Autism 1-2-3’ early intervention for children with autism and their parents immediately after diagnosis that targeted at (1) eye contact, (2) gesture and (3) vocalisation/words | |
| Positive and Negative Affect Scale (PANAS) | Hsieh 2013452 | Taiwan | Cross-sectional observational | Well-being of mothers of children with ASD in Taiwan |
| Questionnaire on Resources and Stress | Cassidy 2008348 | Northern Ireland | Cross-sectional observational | To describe the demographic characteristics of preschoolers and their families; to discover parental perceptions of the child’s difficulties; to identify the impact the child has on family life; to outline the supports available to families and those they would like to have |
| McConkey 2010349 | – | Intervention quasi-experimental | Evaluate a home-based intervention for preschool children with a confirmed diagnosis of ASD | |
| Osborne 2008350 | UK | Intervention quasi-experimental | There was great heterogeneity among the interventions delivered and so for analysis interventions were categorised into high vs. low intensity | |
| Osborne 2009351 | UK | Longitudinal observational | Evaluate relationship between child behaviour problems and parental stress | |
| Remington 2007358 | UK | Intervention quasi-experimental | Comparison of early intensive behavioural interventions and treatment as usual | |
| Rickards 2009423 | Australia | Intervention RCT | Does home-based programme provided over 12 months resulted in sustained improvement in development and behaviour? | |
| Questionnaire on Resources and Stress-Short Form | Reed 2013437 | UK | Cross-sectional observational | The study assessed whether teacher and parent ratings of child behaviour problems were similar for children with ASDs |
| Reaction to Diagnosis Interview | Oppenheim 2012461 | Israel | Cross-sectional observational | This study examined the hypothesis that maternal sensitivity mediates the association between maternal insightfulness/resolution and child attachment in a sample of preschool age boys with ASDs |
| Wachtel 2008462 | USA | Longitudinal observational | Examined the relationship between a mother’s acceptance of and sense of resolution regarding her child’s diagnosis of an ASD and maternal interaction style, controlling for child competence, autism symptoms and maternal depression | |
| Satisfaction with Life Scale | Hsieh 2013452 | Taiwan | Cross-sectional observational | Well-being of mothers of children with ASD in Taiwan |
| Stress Arousal Checklist | Jocelyn 1998298 | Canada | Intervention RCT | Caregiver-based intervention programme in community day care centres |
| Symptom Checklist-90-Revised (SCL-90) | Bennett 2012304 | Canada | Longitudinal observational | Impact of maternal depression on mother’s reports of her child’s ASD behaviours |
| Daily occupational experiencea | Hsieh 2013452 | Taiwan | Cross-sectional observational | Well-being of mothers of children with ASD in Taiwan |
| Parent–Child Interaction Rating Scalesa | Wachtel 2008462 | USA | Longitudinal observational | Examined the relationship between a mother’s acceptance of and sense of resolution regarding her child’s diagnosis of an ASD and maternal interaction style, controlling for child competence, autism symptoms and maternal depression |
| Parenting stress thermometera | Tonge 2005456 | Australia | Intervention RCT | To determine the impact of a PEBM on the mental health and adjustment of parents with preschool children with autism |
| Self-constructed questionnairea | Farmer 2013463 | Australia | Longitudinal observational | To parent’s knowledge and understanding of autism, improve their confidence in managing their child and decrease parental anxiety |
| Stress thermometera | Herring 2006411 | Australia | Longitudinal observational | To explore the impact of developmental disorders on children and their families |
| Family quality of life | Paper | Location | Study design | Study aim |
|---|---|---|---|---|
| Beach Family Quality of Life Questionnaire | Roberts 2011405 | Australia | Intervention RCT | Comparison of home-based vs. centre-based early intervention programmes |
| Family Adaptability and Cohesion Evaluation Scales | Bendixen 2011458 | USA | Intervention quasi-experimental | To explore parental differences pre–post an interdisciplinary in-home training programme |
| Family Assessment Device | Herring 2006411 | Australia | Longitudinal observational | To explore the impact of developmental disorders on children and their families |
| Tonge 2005456 | Australia | Intervention RCT | To determine the impact of a PEBM on the mental health and adjustment of parents with preschool children with autism | |
| Family Assessment Measure | Jocelyn 1998298 | Canada | Intervention RCT | Caregiver-based intervention programme in community day care centres |
| Family Empowerment Scale | Minjarez 2013459 | USA | Intervention quasi-experimental | To evaluate whether participating in a PRT group therapy programme for parents of children with autism influenced related aspects of parents’ lives, namely, their levels of stress and empowerment |
| Rickards 2009423 | Australia | Intervention RCT | Does home-based programme provided over 12 months result in sustained improvement in development and behaviour? | |
| Family Support Scale | Rickards 2009423 | Australia | Intervention RCT | Does home-based programme provided over 12 months result in sustained improvement in development and behaviour? |
| Kansas Inventory of Parental Perceptions | Remington 2007358 | UK | Intervention quasi-experimental | Comparison of early intensive behavioural interventions and treatment as usual |
| Parenting Alliance Inventory | Hill-Chapman 2013434 | USA | Cross-sectional observational | Parenting stress |
| Familial Resources Indexa | Baghdadli 2012339 | France | Longitudinal observational | Developmental trajectory of adaptive behaviours |
| TRE-ADD Autism Quiz (TAQ)a | Jocelyn 1998298 | Canada | Intervention RCT | Caregiver-based intervention programme in community day care centres |
| Family Satisfaction Questionnairea | Smith 2000413 | USA | Intervention RCT | Comparing intensive treatment group to parent training group |
Chapter 3 Tools used (participant description)
| Symptom severity | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Autism Behavior Checklist (AuBC) | Bennett 2008296 | Children aged between 4 and 6 years | 64 | 64 | 100 | – | – | 4–6 | Years | 57 | 7 | Asperger syndrome, high-functioning autism |
| Gupta 2009303 | Children had a mean age of 4.8 years at start of the study and were diagnosed of autism based on DSM-IV-TR criteria | 40 | 20 | 50 | 4.16 | 0.86 | – | Years | 12 | 8 | Autism | |
| Jocelyn 1998298 | 24- to 72-month-old children who met DSM III-R criteria | 35 | 35 | 100 | 43.2 | 9.1 | – | Months | 27 | 8 | Autism, PDD-NOS | |
| Silva 2007299 | 3–6 years old with DSM-IV diagnosis of ASD | 15 | 15 | 100 | 4.83 | – | 3–6 | Years | 13 | 2 | AD | |
| Silva 2008300 | 3–6 years old with DSM-IV diagnosis of ASD | 26 | 26 | 100 | 56.3 | 12.5 | – | Months | 21 | 5 | Autism | |
| Silva 2009226 | 3–6 years old with DSM-IV diagnosis of ASD | 46 | 46 | 100 | 59.2 | – | – | Months | 37 | 9 | Autism | |
| Silva 2011301 | 3–6 years old with clinical diagnosis of ASD | 47 | 47 | 100 | 4.83 | – | 3–6 | Years | 33 | 14 | Autism | |
| Szatmari 2000302 | 4–6 years old (upon entering study) diagnosed by ADI | 134 | 68 | 51 | 66.8 | – | – | Months | 59 | 7 | Autism, Asperger syndrome | |
| Zhang 2012303 | 76 children with ASD (mean age 4.09, SD 1.66) | 96 | 96 | 100 | 4.37 | 1.6 | – | Years | 68 | 8 | Autistic | |
| Autism Diagnostic Interview-Revised (ADI-R) | Bennett 2012304 | Children with ASD aged 2–4 years old | 214 | 178 | 83 | – | – | 2–4 | Years | 181 | 33 | AD, Asperger syndrome, PDD-NOS |
| Ben Itzchak 2008149 | Children aged 19–35 months with autism diagnosis based on DSM-IV criteria | 81 | 44 | 54 | – | – | 16–35 | Months | 43 | 1 | Autism | |
| Brian 2008305 | Children had no diagnosis of ASD but were followed up to 36 months at which point some were diagnosed with ASD | 228 | 35 | 15 | – | – | 6–12 | Months | NR | NR | Autism, Asperger syndrome, PDD-NOS | |
| Feldman 2012104 | Children who aged between 1 and 24 months who were ‘at risk’ for autism (they had a sibling with a diagnosis of ASD, Asperger syndrome or PDD-NOS) | 108 (parents) | 108 | 100 | 8 | 5 | – | Months | 74 | 34 | AD, PDD-NOS, Asperger syndrome and high-functioning autism | |
| Hambly 2012306 | Children with ASDs from bilingual and monolingual homes | 75 | 75 | 100 | – | – | 36–78 | Months | 60 | 15 | Autism, ASD, Asperger syndrome, PDD-NOS | |
| Honey 2008307 | 24–48 months diagnosed by ICD-10 criteria | 104 | 79 | 76 | 37.05 | 6.08 | 24–48 | Months | 65 | 14 | ASD | |
| Magiati 2007308 | Children aged between 22 and 54 months who met Autism Diagnostic Interview-Revised criteria for autism/ASD diagnosis | 44 | 44 | 100 | – | – | 22–54 | Months | 39 | 5 | Autism, ASD | |
| Magiati 2011309 | Mean age of 3.4 years at start of the study | 44 | 44 | 100 | 38.9 | 7.1 | 27–55 | Months | 39 | 5 | Autism, ASD | |
| Mayo 2013310 | 45–72 months with DSM-IV-TR criteria | 119 | 119 | 100 | 52.22 | 6.09 | 45–72 | Months | 99 | 20 | AD, PDD-NOS | |
| Mooney 2006311 | 22–51 months with DSM-IV diagnosis of ASD | 55 | 40 | 73 | 36.95 | 7.26 | 22–51 | Months | 34 | 6 | AD | |
| Munson 2008312 | 24–66 months with ADI or ADOS diagnosis of ASD | 456 | 456 | 100 | 43.4 | 8.7 | 24–66 | Months | 370 | 86 | Autism, ASD | |
| Ozonoff 2010313 | Assessed between 6 and 36 months, diagnosed using ADOS | 50 | 25 | 50 | – | – | 6 | Months | 19 | 6 | AD, PDD-NOS | |
| Pry 2005314 | 21 months to 7 years with ICD-10 diagnosis of ASD | 222 | 222 | 100 | 5 | 1.75 | 1.75–7 | Years | 180 | 42 | Infantile autism | |
| Richler 2007315 | Up to 3 years old, with ‘clinical’ diagnosis of ASD | 279 | 192 | 69 | – | – | 0–37 | Months | 162 | 30 | Autism, PDD-NOS | |
| Werner 2005316 | 12–57 months with DSM-IV diagnosis of ASD | 145 | 72 | 50 | 43.5 | 4.3 | – | Months | 60 | 12 | AD, PDD-NOS | |
| Autism Diagnostic Observation Scale-Toddler Module (ADOS-T) | Rogers 2012317 | 14–24 months with ASD | 98 | 98 | 100 | 21 | – | – | Months | 76 | 22 | ASD |
| Autism Diagnostic Observation Schedule (ADOS) | Aldred 2004318 | 2 years to 5 years 11 months with ADI diagnosis | 28 | 28 | 100 | – | – | 24–71 | Months | 25 | 3 | AD or ‘classical autism’ |
| Aldred 2012319 | Children aged 2–5 years assessed using ADOS and ADI-R | 28 | 28 | 100 | – | – | 2–5 | Years | 25 | 3 | Autism | |
| Ben Itzchak 2008149 | Children aged 19–35 months with autism diagnosis based on DSM-IV criteria | 81 | 44 | 54 | – | – | 16–35 | Months | 43 | 1 | Autism | |
| Ben Itzchak 2011320 | Children aged 15–35 months were included in the study | 78 | 78 | 100 | – | – | 15–35 | Months | 71 | 7 | Autism | |
| Bennett 2012304 | Children with ASD aged 2–4 years old | 214 | 178 | 83 | – | – | 2–4 | Years | 181 | 33 | AD, Asperger syndrome, PDD-NOS | |
| Brian 2008305 | Children had no diagnosis of ASD but were followed up to 36 months at which point some were diagnosed of ASD | 228 | 35 | 15 | – | – | 6–12 | Months | NR | NR | Autism, Asperger syndrome, PDD-NOS | |
| Dawson 2010321 | 18–30 months, diagnosed by ADOS, ADI and DSM-IV | 48 | 48 | 100 | – | – | 18–30 | Months | 37 | 11 | AD, PDD-NOS | |
| Gotham 2012322 | Best-estimate clinical diagnosis of ASD at one or more time points | 345 | 345 | 100 | 3.3 | 1.4 | – | Years | 282 | 63 | Autism, PDD-NOS | |
| Green 2010253 | 24–60 months, ADOS or ADI diagnosed | 152 | 152 | 100 | 45 | – | 24–60 | Months | 138 | 14 | Core autism | |
| Hartley 2009323 | Children aged 1.5–3.9 years based on DSM-IV-TR criteria and ADOS-G classification | 499 | 199 | 40 | – | – | 18–47 | Months | 157 | 42 | AD, PDD-NOS | |
| Landa 2012224 | 22-to 33-month-old children with ASD or autism | 48 | 48 | 100 | 27 | 2.8 | 22–33 | Months | 39 | 9 | ASD | |
| Lerna 2012325 | 18–60 months old with diagnosis of autism and little or no functional language | 18 | 18 | 100 | – | – | 18–60 | Months | 17 | 1 | Autism | |
| Luyster 2008129 | Participants were aged 18–33 months and met ADI-R criteria for ASD diagnosis | 164 | 164 | 100 | – | – | 18–33 | Months | 129 | 35 | ASD | |
| Munson 2008312 | 24–66 months with ADI or ADOS diagnosis of ASD | 456 | 456 | 100 | 43.4 | 8.7 | 24–66 | Months | 370 | 86 | Autism, ASD | |
| Oosterling 2010326 | 12–42 months old with ‘clinical’ diagnosis of ASD | 80 | 80 | 100 | 34.8 | – | – | Months | 62 | 18 | Autism, PDD-NOS | |
| Ray-Subramanian 2011327 | 23–39 months with DSM-IV or ICD-10 diagnosis of ASD | 125 | 125 | 100 | 31 | 4.1 | 23–39 | Months | 108 | 17 | Autism, AD, PDD-NOS | |
| Ray-Subramanian 2012328 | 2–3 years with DSM-IV diagnosis | 115 | 115 | 100 | 31 | 4.1 | – | Months | 97 | 18 | Autism, AD, PDD-NOS | |
| Strauss 2012329 | 26–81 months with DSM-IV diagnosis of ASD | 44 | 44 | 100 | – | – | 26–81 | Months | 41 | 3 | Autism, PDD-NOS | |
| Sullivan 2007330 | Tested at 14–24 months and 30–36 months, and who met DSM-IV criteria for diagnosis | 51 | 16 | 31 | – | – | 14–36 | Months | 14 | 2 | Autism, PDD-NOS | |
| Tek 2012331 | 16–38 months with ADOS diagnosis | 84 | 84 | 100 | 27 | – | 16–38 | Months | NR | NR | ASD | |
| Ventola 2007332 | 16–32 months old with M-CHAT diagnosis of ASD | 195 | 195 | 100 | – | – | 16–32 | Months | 152 | 43 | ASD | |
| Werner 2005316 | 12–57 months with DSM-IV diagnosis of ASD | 145 | 72 | 50 | 43.5 | 4.3 | – | Months | 60 | 12 | AD, PDD-NOS | |
| Wong 2010333 | 17–36 months children diagnosed by DSM-IV, ADI and ADOS | 17 | 17 | 100 | – | – | 17–36 | Months | 16 | 1 | – | |
| Zachor 2006334 | Participants were aged 23–33 months and met DSM-IV criteria for autism diagnosis | 39 | 39 | 100 | – | – | 23–33 | Months | 37 | 2 | Autism | |
| Zachor 2010335 | 15- to 35-month-old children who met DSM-IV criteria | 71 | 71 | 100 | 25.55 | 4.25 | 15–35 | Months | 71 | 7 | Autism | |
| Autism Observation Scale for Infants (AOSI) | Brian 2008305 | Children had no diagnosis of ASD but were followed up to 36 months at which point some were diagnosed of ASD | 228 | 35 | 15 | – | – | 6–12 | Months | NR | NR | Autism, Asperger syndrome, PDD-NOS |
| Bryson 200881 | Infant siblings of children with ASD or autism | 34 | 34 | 100 | 6.7 | – | 6.1–18.9 | Months | 19 | 15 | Autism, ASD, Asperger syndrome, PDD-NOS | |
| Baby and Infant Screen for Children with aUtIsm Traits (BISCUIT-Part 1) | Fodstad 2009342 | Children were aged 17–37 months and met the criteria for ASD or PDD-NOS based on DSMI-V-TR | 886 | 886 | 100 | 26.53 | 5.02 | 17–37 | Months | 618 | 268 | Autism, PDD-NOS |
| Behavioral Summarized Evaluation Scale-Revised (BSE-R) | Receveur 2005337 | Observed from 10 months old to 4 years old – met DSM-IV criteria for ASD | 18 | 18 | 100 | 58 | 3.2 | 10–59 | Months | 13 | 5 | AD |
| Behavioral Summarized Evaluation (BSE) | Maestro 2005338 | Videos of first year of life observed, all met DSM-IV criteria for ASD | 40 | 40 | 100 | – | – | 0–1 | Years | 32 | 8 | AD, PDD-NOS |
| Childhood Autism Rating Scale (CARS) | Baghdadli 2012339 | Age < 7 years, ICD-10 diagnosis of autism | 280 | 280 | 100 | 4.9 | 1.3 | – | Months | 230 | 50 | Childhood autism, atypical autism |
| Bopp 2009340 | Children were aged 1–6 years at start of the study | 69 | 69 | 100 | – | – | 1–6 | Years | 58 | 11 | Autism, PDD-NOS | |
| Jonsdottir 2007341 | Mean age was 41.43 months; diagnosis was based on ICD-10 criteria | 41 | 41 | 100 | 41.43 | 9.06 | 22–59 | Months | 34 | 7 | Childhood autism | |
| Malhi 2011342 | Children were ≤ 3 years at start of the study and had an ASD diagnosis based on DSM-IV criteria | 77 | 77 | 100 | – | – | 0–3 | Years | 64 | 13 | AD, PDD-NOS | |
| Mayo 2013310 | 45–72 months with DSM-IV-TR criteria | 119 | 119 | 100 | 52.22 | 6.09 | 45–72 | Months | 99 | 20 | AD, PDD-NOS | |
| Pajareya 2012343 | 2–6 years old with ASD | 34 | 34 | 100 | 4.23 | 1.16 | 2–6 | Years | 30 | 4 | Autism, PDD-NOS | |
| Pajareya 2011344 | 24–72 months old with DSM-IV diagnosis for ASD | 32 | 32 | 100 | 54.05 | – | 24–72 | Months | 28 | 4 | Autism, PDD-NOS | |
| Papavasiliou 2011350 | 3–5 years (at start of study) with DSM-IV diagnosis of ASD | 40 | 40 | 100 | 3.9 | – | 3–5 | Years | 36 | 4 | ASD | |
| Pry 2005314 | 21 months to 7 years with ICD-10 diagnosis of ASD | 222 | 222 | 100 | 5 | 1.75 | 1.75–7 | Years | 180 | 42 | Infantile autism | |
| Stone 1999346 | Children who met DSM-IV criteria for autism and were aged 31.4 months (SD = 3.4 months) at start of the study | 37 | 37 | 100 | 31.4 | 3.4 | – | Months | 29 | 8 | Autism, PDD-NOS | |
| Ventola 2007332 | 16–32 months old with M-CHAT diagnosis of ASD | 195 | 195 | 100 | – | – | 16–32 | Months | 152 | 43 | ASD | |
| Vorgraft 2007347 | 38–49 month old children with DSM-IV diagnosis of PDD-NOS | 23 | 23 | 100 | 42.8 | – | 38–49 | Months | 15 | 8 | Autism, PDD-NOS | |
| Zhang 2012303 | 76 children with ASD (mean age 4.09, SD 1.66) | 96 | 96 | 100 | 4.37 | 1.6 | – | Years | 68 | 8 | Autistic | |
| Gilliam Autism Rating Scale (GARS) | Cassidy 2008348 | Parents of children aged < 5 years with ICD-10 diagnosis of ASD | 104 | 104 | 100 | – | – | 2–4 | Years | 95 | 9 | ASD |
| McConkey 2010349 | Children with ASD diagnosis (criteria not given, it was only stated as ‘confirmed diagnosis of ASD from a specialist clinic’) who had a mean age of 2.8 years at start of the study | 62 (families) | 61 | 98 | – | – | < 4 | Years | 55 | 6 | Autism | |
| Osborne 2008350 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | – | – | 2.6–4.0 | Years | 59 | 6 | ASD | |
| Osborne 2009351 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | 3.4 | 0.75 | 2.6–4.0 | Years | 59 | 6 | ASD | |
| Reed 2007352 | 2 years 6 months to 4 years old diagnosed with ASD | 27 | 27 | 100 | – | – | 2.5–4.0 | Years | 27 | 0 | ASD | |
| Reed 2007353 | 2 years 6 months to 4 years old with ‘paediatrician’ diagnosis of ASD | 53 | 53 | 100 | – | – | 2.5–4.0 | Years | Unclear | Unclear | ASD | |
| Reed 2012354 | 2.5–4 years with GARS diagnosis of ASD | 66 | 66 | 100 | 40.2 | 5.6 | – | Months | 59 | 7 | AD, PDD-NOS | |
| Stahmer 2004355 | 0–3 years with DSM-IV diagnosis | 20 | 20 | 100 | 28.6 | – | 22–32 | Months | 16 | 4 | AD, PDD-NOS | |
| Infant Behavioral Summarized Evaluation (IBSE) | Adrien 199290 | 0–2 years, DSM-III-R criteria | 24 | 12 | 50 | – | – | 0–2 | Years | 10 | 2 | Autism |
| Receveur 2005337 | Observed from 10 months old to 4 years old – met DSM-IV criteria for ASD | 18 | 18 | 100 | 58 | 3.2 | 10–59 | Months | 13 | 5 | AD | |
| Modified Checklist for Autism in Toddlers (M-CHAT) | Ventola 2007332 | 16–32 months old with M-CHAT diagnosis of ASD | 195 | 195 | 100 | – | – | 16–32 | Months | 152 | 43 | ASD |
| Parent Observation of Early Markers Scale (POEMS) | Feldman 2012104 | Children who aged between 1 and 24 months who were ‘at risk’ for autism (they had a sibling with a diagnosis of ASD, Asperger syndrome or PDD-NOS) | 108 (parents) | 108 | 100 | 8 | 5 | – | Months | 74 | 34 | AD, PDD-NOS, Asperger syndrome and high-functioning autism |
| Pervasive Developmental Disorder Rating Scale (PDDRS) | Eaves 2006356 | Details of how diagnosis was made not stated. Children were aged 1–6 years | 199 | 199 | 100 | – | – | 1.8–3.9 | Years | 157 | 42 | AD |
| Pervasive Developmental Disorders Behavior Inventory (PDDBI) | Silva 2009226 | 3–6 years with DSM-IV diagnosis of ASD | 46 | 46 | 100 | 59.2 | – | – | Months | 37 | 9 | Autism |
| Silva 2011301 | 3–6 years old with clinical diagnosis of ASD | 47 | 47 | 100 | 4.83 | – | 3–6 | Years | 33 | 14 | Autism | |
| Real Life Rating Scale (Ritvo–Freeman) (RLRS) | Wong 2010333 | 17–36 months children diagnosed by DSM-IV, ADI and ADOS | 17 | 17 | 100 | – | – | 17–36 | Months | 16 | 1 | – |
| Social Communication Questionnaire (SCQ) | Eapen 2013357 | Mean age of 49.6 months | 26 | 26 | 100 | 49.6 | 6.08 | 36–58 | Months | 21 | 5 | AD |
| Remington 2007358 | 30–42 months of age with ADI diagnosis of ASD | 44 | 44 | 100 | 37 | 4.2 | 30–42 | Months | NR | NR | Autism or suspected autism | |
| Social Responsiveness Scale (SRS) | Bennett 2012304 | Children with ASD aged 2–4 years old | 214 | 178 | 83 | – | – | 2–4 | Years | 181 | 33 | AD, Asperger syndrome, PDD-NOS |
| Hambly 2012306 | Children with ASDs from bilingual and monolingual homes | 75 | 75 | 100 | – | – | 36–78 | Months | 60 | 15 | Autism, ASD, Asperger syndrome, PDD-NOS | |
| Smith 2010359 | All < 6 years with ADOS/ADI/DSM-IV diagnosis of ASD | 53 | 53 | 100 | 50.1 | 10 | – | Months | 47 | 6 | Autism | |
| Childhood Autism Rating Scale (CARS) – Tokyo versiona | Takeda 2005360 | 23–35 months with DSM-IV criteria | 57 | 57 | 100 | 31.4 | 3.3 | 23–35 | Months | 45 | 12 | AD, PDD-NOS, Asperger |
| Social awareness | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Child Behaviour Rating Scale (CBRS) (Modified) | Casenhiser 2013361 | Children aged 2–4 years 11 months who met ADI-R criteria | 51 | 51 | 100 | – | – | 2.0–4.9 | Years | NR | NR | ASD |
| Communication and Symbolic Behavior Scales-Developmental Profile (CSBS–DP) | Green 2010253 | 24–60 months, ADOS or ADI diagnosed | 152 | 152 | 100 | 45 | – | 24–60 | Months | 138 | 14 | Core autism |
| Landa 2007368 | Assessed between 14–36 months of age, 30/107 sibling subsequently diagnosed with ASD using DSM-IV criteria | 125 | 30 | 24 | – | – | 6–36 | Months | 30 | 25 | Autism, PDD-NOS | |
| Sullivan 2007330 | Tested at 14–24 months and 30–36 months who met DSM-IV criteria for diagnosis | 51 | 16 | 31 | – | – | 14–36 | Months | 14 | 2 | Autism, PDD-NOS | |
| Keen 2010363 | Children aged 2–4 years who met the DSM-IV criteria for ASD diagnosis | 39 | 39 | 100 | – | – | 2–4 | Years | 34 | 5 | ASD | |
| Keen 2007364 | Diagnosis of autism was based on DSM-IV criteria | 16 | 16 | 100 | – | – | 2–4 | Years | 14 | 2 | Autism | |
| Early Social Communication Scale (ESCS) | Dereu 2012365 | Children aged 2–4 years; ADOS was used for diagnosis | 17 | 9 | 53 | – | – | 17–39 | Months | 6 | 3 | ASD |
| Goods 2013366 | 36- to 60-month-old children with autism (ADOS assessment) | 15 | 15 | 100 | 51.9 | – | – | Months | NR | NR | Autism | |
| Ingersoll 2012286 | 27 children between 27 and 47 months old who met DSM-IV-TR criteria | 29 | 29 | 100 | 37.9 | – | 22–47 | Months | 24 | 5 | AD | |
| Kaale 2012294 | Children aged 29–60 months who had a diagnosis of autistic disorder based on ICD-10 criteria | 61 | 61 | 100 | – | – | 24–60 | Months | 48 | 13 | Autism | |
| Kalas 2012367 | 4- to 6-year-old children with ASD | 30 | 30 | 100 | – | – | 4–6 | Years | 28 | 2 | ASD | |
| Kasari 2006368 | Children were aged 3–4 years and had a diagnosis of autism based on ADI-R and ADOS criteria | 58 | 58 | 100 | – | – | 3–4 | Years | 46 | 12 | Autism | |
| Lawton 2012369 | Preschool age children who had a diagnosis of autism, validated by ADI-R | 52 | 52 | 100 | 43.05 | 6.86 | – | Months | 40 | 12 | Autism | |
| Luyster 2008129 | Participants were aged 18–33 months and met ADI-R criteria for ASD diagnosis | 164 | 164 | 100 | – | – | 18–33 | Months | 129 | 35 | ASD | |
| Paparella 2011370 | 20–72 months old with ADI diagnosis of ASD | 83 | 50 | 60 | 53.6 | – | 36–72 | Months | 42 | 8 | Autism | |
| Remington 2007358 | 30–42 months of age with ADI diagnosis of ASD | 44 | 44 | 100 | 37 | 4.2 | 30–42 | Months | NR | NR | Autism or suspected autism | |
| Roos 2008371 | 30–38 months with ADOS diagnosis of ASD | 20 | 20 | 100 | 33.2 | – | 30–38 | Months | 16 | 4 | ASD | |
| Salt 2002372 | Preschool children in Scotland, (mean 42.36 months) with ICD-10 diagnosis of ASD | 17 | 17 | 100 | 40.015 | – | – | Months | 14 | 3 | Childhood autism | |
| Wong 2013373 | 3–6 years with CARS diagnosis | 33 | 33 | 100 | 56.79 | – | – | Months | 29 | 4 | Autism | |
| Yoder 2006374 | 1.9–4.5 years with ADOS diagnosis of ASD | 36 | 36 | 100 | 2.9 | – | – | Years | 31 | 5 | Autism, PDD-NOS | |
| Early Social Communication Scales (ESCS)-Abridged | Yoder 2010375 | 18–60 months with ADOS diagnosis of ASD | 36 | 36 | 100 | 2.9 | – | – | Years | NR | NR | Autism, PDD-NOS |
| Imitation Battery (IB) | Luyster 2008129 | Participants were aged 18–33 months and met ADI-R criteria for ASD diagnosis | 164 | 164 | 100 | – | – | 18–33 | Months | 129 | 35 | ASD |
| Imitation Disorders Evaluation (IDE) scale | Receveur 2005337 | Observed from 10 months old to 4 years old – met DSM-IV criteria for ASD | 18 | 18 | 100 | 58 | 3.2 | 10–59 | Months | 13 | 5 | AD |
| Motor Imitation Scale (MIS) | Ingersoll 2010376 | Participants were aged 27–47 months and met DSM-IV-TR criteria for autism diagnosis | 22 | 22 | 100 | – | – | 27–47 | Months | 19 | 3 | Autism |
| Ingersoll 2012286 | 27 children between 27 and 47 months old who met DSM-IV-TR criteria | 29 | 29 | 100 | 37.9 | – | 22–47 | Months | 24 | 5 | AD | |
| Preschool Imitation and Praxis Scale (PIPS) | Dereu 2012365 | Children aged 2–4 years; ADOS was used for diagnosis | 17 | 9 | 53 | – | – | 17–39 | Months | 6 | 3 | ASD |
| Pre-Verbal Communication Schedule (PVCS) | Salt 2002372 | Preschool children in Scotland, (mean 42.36 months) with ICD-10 diagnosis of ASD | 17 | 17 | 100 | 40.015 | – | – | Months | 14 | 3 | Childhood autism |
| Social Communication Assessment for Toddlers with Autism (SCATA) | Drew 2007137 | Children aged between 21–43 months with a diagnosis of autism or PDD based on ICD-10 criteria | 46 | 46 | 100 | 25 | 5.6, NR | 18–44, NR | Months | 39 | 7 | Autism, PDD-NOS |
| Social Communication Behavior Codes | Ozonoff 2010313 | Assessed between 6 and 36 months, diagnosed using ADOS | 50 | 25 | 50 | – | – | 6 | Months | 19 | 6 | AD, PDD-NOS |
| Parent interviewa | Clifford 2008377 | 3–5 years with DSM-IV criteria | 63 | 36 | 57 | 51.05 | – | – | Months | 33 | 3 | AD |
| Caregiver–child interactionb | Kasari 2006368 | Children were aged 3–4 years and had a diagnosis of autism based on ADI-R and ADOS criteria | 58 | 58 | 100 | – | – | 3–4 | Years | 46 | 12 | Autism |
| Coded observation of joint attentionb | Warreyn 2007384 | 1.83–5.5 years with DSM-IV diagnosis of ASD | 36 | 18 | 50 | 4.01 | 0.86 | 2.17–5.5 | Years | 15 | 3 | AD, PDD-NOS |
| Coding of initiation of joint attentionb | Ingersoll 2012286 | 27 children between 27 and 47 months old who met DSM-IV-TR criteria | 29 | 29 | 100 | 37.9 | – | 22–47 | Months | 24 | 5 | AD |
| Classroom Observation Measureb | Goods 2013366 | 36- to 60-month-old children with autism (ADOS assessment) | 15 | 15 | 100 | 51.9 | – | – | Months | NR | NR | Autism |
| Examiner Ratings of Social Engagementb | Ozonoff 2010313 | Assessed between 6 and 36 months, diagnosed using ADOS | 50 | 25 | 50 | – | – | 6 | Months | 19 | 6 | AD, PDD-NOS |
| Naturalistic examiner– child play sampleb | Roos 2008371 | 30–38 months with ADOS diagnosis of ASD | 20 | 20 | 100 | 33.2 | – | 30–38 | Months | 16 | 4 | ASD |
| Pre-linguistic Communication Assessmentb | Stone 1997135 | 25–39 months with DSM-III or DSM-IV diagnosis of ASD | 28 | 14 | 50 | 32.8 | 3.5 | 27–38 | Months | NR | NR | Autism |
| Preschool teacher–child playb | Kaale 2012294 | Children aged 29–60 months who had a diagnosis of autistic disorder based on ICD-10 criteria | 61 | 61 | 100 | – | – | 24–60 | Months | 48 | 13 | Autism |
| Unstructured free play with examinerb | Lerna 2012325 | 18–60 months old with diagnosis of autism and little or no functional language | 18 | 18 | 100 | – | – | 18–60 | Months | 17 | 1 | Autism |
| Unstructured Imitation Assessmentb | Ingersoll 2012286 | 27 children between 27 and 47 months old who met DSM-IV-TR criteria | 29 | 29 | 100 | 37.9 | – | 22–47 | Months | 24 | 5 | AD |
| Ingersoll 2010376 | Participants were aged 27–47 months and met DSM-IV-TR criteria for autism diagnosis | 22 | 22 | 100 | – | – | 27–47 | Months | 19 | 3 | Autism | |
| Video coding proceduresb | Colgan 2006379 | Children aged 8–12 months with diagnosis of autism based on DSM-III-R or DSM-IV criteria | 35 | 21 | 60 | – | – | 0–2 | Years | 17 | 4 | AD |
| Video observationb | Clifford 2008377 | 3–5 years with DSM-IV criteria | 63 | 36 | 57 | 51.05 | – | – | Months | 33 | 3 | AD |
| Video rating for expressive speechb | Baghdadli 2012339 | Age < 7 years, ICD-10 diagnosis of autism | 280 | 280 | 100 | 4.9 | 1.3 | – | Months | 230 | 50 | Childhood autism, atypical autism |
| Video recording of child in classroom activitiesb | Ingersoll 2001380 | Children ages 26–41 months who met DSM-IV criteria for ASD | 9 | 6 | 67 | – | – | 26–41 | Months | NR | NR | Autism, PDD-NOS |
| Restricted, repetitive behaviour | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Autism Diagnostic Interview (ADI) | Ben Itzchak 2008149 | Children aged 19–35 months with autism diagnosis based on DSM-IV criteria | 81 | 44 | 54 | – | – | 16–35 | Months | 43 | 1 | Autism |
| Autism Diagnostic Interview-Revised (ADI-R) | Bennett 2012304 | Children with ASD aged 2–4 years old | 214 | 178 | 83 | – | – | 2–4 | Years | 181 | 33 | AD, Asperger syndrome, PDD-NOS |
| Brian 2008305 | Children had no diagnosis of ASD but were followed up to 36 months at which point some were diagnosed of ASD | 228 | 35 | 15 | – | – | 6–12 | Months | NR | NR | Autism, Asperger syndrome, PDD-NOS | |
| Feldman 2012104 | Children who aged between 1 and 24 months who were ‘at risk’ for autism (they had a sibling with a diagnosis of ASD, Asperger syndrome or PDD-NOS) | 108 (parents) | 108 | 100 | 8 | 5 | – | Months | 74 | 34 | AD, PDD-NOS, Asperger syndrome and high-functioning autism | |
| Autism Diagnostic Interview-Revised (ADI-R) | Hambly 2012306 | Children with ASDs from bilingual and monolingual homes | 75 | 75 | 100 | – | – | 36–78 | Months | 60 | 15 | Autism, ASD, Asperger syndrome, PDD-NOS |
| Autism Diagnostic Interview (ADI) | Honey 2008307 | 24–48 months diagnosed by ICD-10 criteria | 104 | 79 | 76 | 37.05 | 6.08 | 24–48 | Months | 65 | 14 | ASD |
| Autism Diagnostic Interview-Revised (ADI-R) | Magiati 2007308 | Children aged between 22 and 54 months who met ADI-R criteria for autism/ASD diagnosis | 44 | 44 | 100 | – | – | 22–54 | Months | 39 | 5 | Autism, ASD |
| Magiati 2011309 | Mean age of 3.4 years at start of the study | 44 | 44 | 100 | 38.9 | 7.1 | 27–55 | Months | 39 | 5 | Autism, ASD | |
| Mayo 2013310 | 45–72 months with DSM-IV-TR criteria | 119 | 119 | 100 | 52.22 | 6.09 | 45–72 | Months | 99 | 20 | AD, PDD-NOS | |
| Mooney 2006311 | 22–51 months with DSM-IV diagnosis of ASD | 55 | 40 | 73 | 36.95 | 7.26 | 22–51 | Months | 34 | 6 | AD | |
| Munson 2008312 | 24–66 months with ADI or ADOS diagnosis of ASD | 456 | 456 | 100 | 43.4 | 8.7 | 24–66 | Months | 370 | 86 | Autism, ASD | |
| Ozonoff 2010313 | Assessed between 6 and 36 months, diagnosed using ADOS | 50 | 25 | 50 | – | – | 6 | Months | 19 | 6 | AD, PDD-NOS | |
| Autism Diagnostic Interview (ADI) | Pry 2005314 | 21 months to 7 years with ICD-10 diagnosis of ASD | 222 | 222 | 100 | 5 | 1.75 | 1.75–7 | Years | 180 | 42 | Infantile autism |
| ADI-R (ADI-R) | Richler 2007315 | Up to 3 years old, with ‘clinical’ diagnosis of ASD | 279 | 192 | 69 | – | – | 0–37 | Months | 162 | 30 | Autism, PDD-NOS |
| Autism Diagnostic Interview (ADI) | Werner 2005316 | 12–57 months with DSM-IV diagnosis of ASD | 145 | 72 | 50 | 43.5 | 4.3 | – | Months | 60 | 12 | AD, PDD-NOS |
| Autism Diagnostic Observation Scale-Toddler Module (ADOS-T) | Rogers 2012317 | 14–24 months with ASD | 98 | 98 | 100 | 21 | – | – | Months | 76 | 22 | ASD |
| Autism Diagnostic Observation Schedule-Generic (ADOS-G) – Modules 1 and 2) | Green 2010253 | 24–60 months, ADOS or ADI diagnosed | 152 | 152 | 100 | 45 | – | 24–60 | Months | 138 | 14 | Core autism |
| Aldred 2004318 | 2 years to 5 years 11 months with ADI diagnosis | 28 | 28 | 100 | – | – | 24–71 | Months | 25 | 3 | AD or ‘classical autism’ | |
| Aldred 2012319 | Children aged 2–5 years assessed using ADOS and ADI-R | 28 | 28 | 100 | – | – | 2–5 | Years | 25 | 3 | Autism | |
| Ben Itzchak 2008149 | Children aged 19–35 months with autism diagnosis based on DSM-IV criteria | 81 | 44 | 54 | – | – | 16–35 | Months | 43 | 1 | Autism | |
| Ben Itzchak 2011320 | Children aged 15–35 months were included in the study | 78 | 78 | 100 | – | – | 15–35 | Months | 71 | 7 | Autism | |
| Bennett 2012304 | Children with ASD aged 2–4 years old | 214 | 178 | 83 | – | – | 2–4 | Years | 181 | 33 | AD, Asperger syndrome, PDD-NOS | |
| Brian 2008305 | Children had no diagnosis of ASD but were followed up to 36 months at which point some were diagnosed of ASD | 228 | 35 | 15 | – | – | 6–12 | Months | NR | NR | Autism, Asperger syndrome, PDD-NOS | |
| Dawson 2010321 | 18–30 months, diagnosed by ADOS, ADI and DSM-IV | 48 | 48 | 100 | – | – | 18–30 | Months | 37 | 11 | AD, PDD-NOS | |
| Gotham 2012322 | Best-estimate clinical diagnosis of ASD at one or more time points | 345 | 345 | 100 | 3.3 | 1.4 | – | Years | 282 | 63 | Autism, PDD-NOS | |
| Hartley 2009323 | Children aged 1.5–3.9 years based on DSM-IV-TR criteria and ADOS-G classification | 499 | 199 | 40 | – | – | 18–47 | Months | 157 | 42 | AD, PDD-NOS | |
| Landa 2012224 | 22- to 33-month-old children with ASD or autism | 48 | 48 | 100 | 27 | 2.8 | 22–33 | Months | 39 | 9 | ASD | |
| Lerna 2012325 | 18–60 months old with diagnosis of autism and little or no functional language | 18 | 18 | 100 | – | – | 18–60 | Months | 17 | 1 | Autism | |
| Luyster 2008129 | Participants were aged 18–33 months and met ADI-R criteria for ASD diagnosis | 164 | 164 | 100 | – | – | 18–33 | Months | 129 | 35 | ASD | |
| Munson 2008312 | 24–66 months with ADI or ADOS diagnosis of ASD | 456 | 456 | 100 | 43.4 | 8.7 | 24–66 | Months | 370 | 86 | Autism, ASD | |
| Oosterling 2010326 | 12–42 months old with ‘clinical’ diagnosis of ASD | 80 | 80 | 100 | 34.8 | – | – | Months | 62 | 18 | Autism, PDD-NOS | |
| Ray-Subramanian 2011327 | 23–39 months with DSM-IV or ICD-10 diagnosis of ASD | 125 | 125 | 100 | 31 | 4.1 | 23–39 | Months | 108 | 17 | Autism, AD, PDD-NOS | |
| Ray-Subramanian 2012328 | 2–3 years with DSM-IV diagnosis | 115 | 115 | 100 | 31 | 4.1 | – | Months | 97 | 18 | Autism, AD, PDD-NOS | |
| Strauss 2012329 | 26–81 months with DSM-IV diagnosis of ASD | 44 | 44 | 100 | – | – | 26–81 | Months | 41 | 3 | Autism, PDD-NOS | |
| Sullivan 2007330 | Tested at 14–24 months and 30–36 months who met DSM-IV criteria for diagnosis | 51 | 16 | 31 | – | – | 14–36 | Months | 14 | 2 | Autism, PDD-NOS | |
| Tek 2012331 | 16–38 months with ADOS diagnosis | 84 | 84 | 100 | 27 | – | 16–38 | Months | NR | NR | ASD | |
| Ventola 2007332 | 16–32 months old with M-CHAT diagnosis of ASD | 195 | 195 | 100 | – | – | 16–32 | Months | 152 | 43 | ASD | |
| Werner 2005316 | 12–57 months with DSM-IV diagnosis of ASD | 145 | 72 | 50 | 43.5 | 4.3 | – | Months | 60 | 12 | AD, PDD-NOS | |
| Wong 2010333 | 17–36 months children diagnosed by DSM-IV, ADI and ADOS | 17 | 17 | 100 | – | – | 17–36 | Months | 16 | 1 | – | |
| Zachor 2006334 | Participants were aged 23–33 months and met DSM-IV criteria for autism diagnosis | 39 | 39 | 100 | – | – | 23–33 | Months | 37 | 2 | Autism | |
| Zachor 2010335 | 15- to 35-month-old children who met DSM-IV criteria | 71 | 71 | 100 | 25.55 | 4.25 | 15–35 | Months | 71 | 7 | Autism | |
| Repetitive Behavior Scale (RBS) | Dawson 2010321 | 18–30 months, diagnosed by ADOS, ADI and DSM-IV | 48 | 48 | 100 | – | – | 18–32 | Months | 37 | 11 | AD, PDD-NOS |
| Classroom and playground behaviour observationsa | Escalona 2001271 | Children were aged 3–6 years based on DSM III – R | 20 | 20 | 100 | 5.2 | 1.8 | 3–6 | Years | 12 | 8 | Autism |
| Video codinga | Barber 2012381 | 18–24 months ASD | 100 | 50 | 50 | – | – | 18–24 | Months | 43 | 7 | AD, PDD-NOS |
| Sensory processing | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Infant/Toddler Sensory Profile (ITSP) | Ben-Sasson 2008382 | 18–33 months old children, diagnosed by ADOS and ADI | 170 | 170 | 100 | 28 | 4 | 18–33 | Months | 133 | 37 | AD, PDD-NOS |
| Sense and Self-Regulation Checklist (SSC) | Silva 2009226 | 3–6 years with DSM-IV diagnosis of ASD | 46 | 46 | 100 | 59.2 | – | – | Months | 37 | 9 | Autism |
| Sense and Self-Regulation Checklist (SSC) | Silva 2011301 | 3–6 years old with clinical diagnosis of ASD | 47 | 47 | 100 | 4.83 | – | 3–6 | Years | 33 | 14 | Autism |
| Sensory Profile (SP) | Chuang 2012383 | Children were aged 48–84 months and had DSM-IV-TR diagnosis of autism | 111 | 67 | 60 | – | – | 48–84 | Months | 57 | 10 | Autism |
| Jasmin 2009384 | Children aged 3–4 years who had a diagnosis of ASD based on DSM-IV criteria | 35 | 35 | 100 | – | – | 3–4 | Years | 32 | 3 | Autistic, PDD-NOS, Asperger syndrome | |
| Provost 2009385 | 3–5 years with DSM-IV criteria of ASD | 50 | 25 | 50 | – | – | 3.0–5.9 | Years | 19 | 6 | AD, PDD-NOS | |
| Silva 2007299 | 3–6 years old with DSM-IV diagnosis of ASD | 15 | 15 | 100 | 4.83 | – | 3–6 | Years | 13 | 2 | AD | |
| Silva 2008300 | 3–6 years old with DSM-IV diagnosis of ASD | 26 | 26 | 100 | 56.3 | 12.5 | – | Months | 21 | 5 | Autism | |
| Short Sensory Profile (SSP) | O’Donnell 2012386 | 3–4 years old with DSM-IV diagnosis of ASD | 42 | 42 | 100 | 45.5 | – | 36–59 | Months | NR | NR | Autism, PDD-NOS |
| Papavasiliou 2011345 | 3–5 years (at start of study) with DSM-IV diagnosis of ASD | 40 | 40 | 100 | 3.9 | – | 3–5 | Years | 36 | 4 | ASD | |
| Tomchek 2007387 | 3–6 years with DSM-IV criteria for ASD | 562 | 281 | 50 | 51.58 | 10.3 | – | Months | 235 | 46 | Autism, PDD-NOS, Asperger syndrome |
| Language | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Autism Screening Instrument for Educational Planning (ASIEP) | Arick 2003388 | Children between the ages of 2 and 6 years (at baseline) who have been said to have a diagnosis of autism; details of criteria used not provided | 67 | 67 | 100 | – | – | 2–6 | Years | NR | NR | ASD |
| Battelle Developmental Inventory (BDI) | Arick 2003388 | Children between the ages of 2 and 6 years (at baseline) who have been said to have a diagnosis of autism; details of criteria used not provided | 67 | 67 | 100 | – | – | 2–6 | Years | NR | NR | ASD |
| British Picture Vocabulary Scale | Magiati 2007308 | Children aged between 22 and 54 months who met ADI-R criteria for autism/ASD diagnosis | 44 | 44 | 100 | – | – | 22–54 | Months | 39 | 5 | Autism, ASD |
| Magiati 2011309 | Mean age of 3.4 years at start of the study | 44 | 44 | 100 | 38.9 | 7.1 | 27–55 | Months | 39 | 5 | Autism, ASD | |
| Clinical Evaluation of Language Fundamentals-Revised | Bono 2004389 | 31–64 months with DSM-IV diagnosis of ASD | 29 | 29 | 100 | 46.68 | 9.64 | 31–64 | Months | 22 | 7 | AD |
| Communication and Symbolic Behavior Scales-Developmental Profile (CSBS-DP) (Caregiver Questionnaire) | Tek 2012331 | 16–38 months with ADOS diagnosis | 84 | 84 | 100 | 27 | – | 16–38 | Months | NR | NR | ASD |
| Comprehensive Assessment of Spoken Language (CASL) | Casenhiser 2013361 | Children aged 2–4 years 11 months who met ADI-R criteria | 51 | 51 | 100 | – | – | 2.0–4.9 | Years | NR | NR | ASD |
| Expressive One-Word Picture Vocabulary Test | Arick 2003388 | Children between the ages of 2 and 6 years (at baseline) who have been said to have a diagnosis of autism; details of criteria used not provided | 67 | 67 | 100 | – | – | 2–6 | Years | NR | NR | ASD |
| Bopp 2009340 | Children were aged 1–6 years at start of the study | 69 | 69 | 100 | – | – | 1–6 | Years | 58 | 11 | Autism, PDD-NOS | |
| Magiati 2007308 | Children aged between 22 and 54 months who met ADI-R criteria for autism/ASD diagnosis | 44 | 44 | 100 | – | – | 22–54 | Months | 39 | 5 | Autism, ASD | |
| Magiati 2011309 | Mean age of 3.4 years at start of the study | 44 | 44 | 100 | 38.9 | 7.1 | 27–55 | Months | 39 | 5 | Autism, ASD | |
| Illinois Test of Psycholinguistic Abilities | Carlsson 2013390 | Children aged from 4.5 to 6.5 years who were assessed to have autism based on DSM-IV criteria | 198 | 119 | 60 | – | – | 4.5–6.5 | Years | NR | NR | Autistic-like condition, Asperger syndrome, autistic traits |
| MacArthur–Bates Communicative Development Inventories (MCDI) | Aldred 2004318 | 2 years to 5 years 11 months with ADI diagnosis | 28 | 28 | 100 | – | – | 24–71 | Months | 25 | 3 | AD or ‘classical autism’ |
| Green 2010253 | 24–60 months, ADOS or ADI diagnosed | 152 | 152 | 100 | 45 | – | 24–60 | Months | 138 | 14 | Core autism | |
| Hambly 2012306 | Children with ASDs from bilingual and monolingual homes | 75 | 75 | 100 | – | – | 36–78 | Months | 60 | 15 | Autism, ASD, Asperger syndrome, PDD-NOS | |
| Hudry 2010233 | 24- to 59-month-old children with ADOS-G diagnosis | 152 | 152 | 100 | 44.83 | 7.98 | 24–59 | Months | 138 | 14 | Core autism | |
| Luyster 2008129 | Participants were aged 18–33 months and met ADI-R criteria for ASD diagnosis | 164 | 164 | 100 | – | – | 18–33 | Months | 129 | 35 | ASD | |
| Miniscalco 2012391 | 20–47 months with DSM-IV diagnosis of ASD | 31 | 31 | 100 | 36 | – | 20–47 | Months | 27 | 4 | Autistic disorder | |
| Mitchell 2006392 | ‘At risk’ children with a sibling with ‘clinical’ diagnosis of ASD – 11–15 months at first assessment | 146 | 15 | 10 | – | – | 11–15 | Months | 10 | 5 | ASD | |
| Oosterling 2010326 | 12–42 months old with ‘clinical’ diagnosis of ASD | 80 | 80 | 100 | 34.8 | – | – | Months | 62 | 18 | Autism, PDD-NOS | |
| Rogers 2012317 | 14–24 months with ASD | 98 | 98 | 100 | 21 | – | – | Months | 76 | 22 | ASD | |
| Salt 2002372 | Preschool children in Scotland, (mean 42.36 months) with ICD-10 diagnosis of ASD | 17 | 17 | 100 | 40.015 | – | – | Months | 14 | 3 | Childhood autism | |
| Smith 2007393 | 20–71 months old with DSM-IV diagnosis of ASD | 35 | 35 | 100 | 45.59 | 9.89 | 20.5–67.6 | Months | 28 | 7 | Autism | |
| Smith 2010359 | All < 6 years with ADOS/ADI/DSM-IV diagnosis of ASD | 53 | 53 | 100 | 50.1 | 10 | – | Months | 47 | 6 | Autism | |
| Stone 2001394 | Assessed at 2 years and 4 years, met DSM-III or DSM-IV criteria for ASD | 35 | 35 | 100 | 57.9 | 4.5 | 50–67 | Months | 28 | 8 | Autism, PDD-NOS | |
| Strauss 2012329 | 26–81 months with DSM-IV diagnosis of ASD | 44 | 44 | 100 | – | – | 26–81 | Months | 41 | 3 | Autism, PDD-NOS | |
| Mullen Scales of Early Learning (MSEL) | Akshoomoff 2006395 | 16–43 months with ADI-R and ADOS diagnosis of ASD | 42 | 22 | 52 | – | – | 16–43 | Months | 17 | 5 | Autism, ASD |
| Anan 2008396 | 25- to 68-month-old children who met the diagnosis of ASD based on DSM-IV criteria | 72 | 72 | 100 | – | – | 25–68 | Months | 61 | 11 | AD, PDD-NOS | |
| Baker 2010397 | 33 ‘at-risk’ children, entered study between ages of 2–18 months, assessed at 18, 24, 30 and 36 months. [24 of the 33 children had a sibling with ASD or PDD (DSM-IV diagnosed)] | 33 | 12 | 36 | 18 | – | – | Months | NR | NR | ASD | |
| Barbaro 2012398 | 12- to 22-month children with AD, ASD or DD/language delay | 154 | 125 | 81 | – | – | 12–27 | Months | 100 | 25 | AD, ASD | |
| Ben Itzchak 2011320 | Children aged 15–35 months were included in the study | 78 | 78 | 100 | – | – | 15–35 | Months | 71 | 7 | Autism | |
| Bishop 2011176 | Children were aged between 2 years and 5 years 11 months | 72 | 53 | 74 | – | – | 1–68 | Months | 44 | 9 | Not given | |
| Brian 2008305 | Children had no diagnosis of ASD but were followed up to 36 months at which point some were diagnosed of ASD | 228 | 35 | 15 | – | – | 6–12 | Months | NR | NR | Autism, Asperger syndrome, PDD-NOS | |
| Dawson 2010321 | 18–30 months, diagnosed by ADOS, ADI and DSM-IV | 48 | 48 | 100 | – | – | 18–31 | Months | 37 | 11 | AD, PDD-NOS | |
| Dereu 2012365 | Children aged 2–4 years; ADOS was used for diagnosis | 17 | 9 | 53 | – | – | 17–39 | Months | 6 | 3 | ASD | |
| Eapen 2013357 | Mean age of 49.6 months | 26 | 26 | 100 | 49.6 | 6.08 | 36–58 | Months | 21 | 5 | AD | |
| Hartley 2009323 | Children aged 1.5–3.9 years based on DSM-IV-TR criteria and ADOS-G classification | 499 | 199 | 40 | – | – | 18–49 | Months | 157 | 42 | AD, PDD-NOS | |
| Honey 2008307 | 24–48 months diagnosed by ICD-10 criteria | 104 | 79 | 76 | 37.05 | 6.08 | 24–48 | Months | 65 | 14 | ASD | |
| Landa 2012399 | Assessed at aged 6–36 months – 52/197 subsequently diagnosed ASD by ADOS | 204 | 52 | 25 | 6 | – | – | Months | 43 | 9 | ASD | |
| Landa 2012224 | 22- to 33-month-old children with ASD or autism | 48 | 48 | 100 | 27 | 2.8 | 22–33 | Months | 39 | 9 | ASD | |
| Lloyd 2013400 | 12- to 36-month-old children with ASD | 162 | 162 | 100 | – | – | 12–36 | Months | 140 | 22 | ASD | |
| Luyster 2008129 | Participants were aged 18–33 months and met ADI-R criteria for ASD diagnosis | 164 | 164 | 100 | – | – | 18–33 | Months | 129 | 35 | ASD | |
| Mayo 2013310 | 45–72 months with DSM-IV-TR criteria | 119 | 119 | 100 | 52.22 | 6.09 | 45–72 | Months | 99 | 20 | AD, PDD-NOS | |
| Mitchell 2006392 | ‘At risk’ children with a sibling with ‘clinical’ diagnosis of ASD – 11–15 months at first assessment | 146 | 15 | 10 | – | – | 11–15 | Months | 10 | 5 | ASD | |
| O’Donnell 2012386 | 3–4 years old with DSM-IV diagnosis of ASD | 42 | 42 | 100 | 45.5 | – | 36–59 | Months | NR | NR | Autism, PDD-NOS | |
| Ozonoff 2010313 | Assessed between 6 and 36 months, diagnosed using ADOS | 50 | 25 | 50 | – | – | 6 | Months | 19 | 6 | AD, PDD-NOS | |
| Poon 2012401 | 9–12 months (upon entering study) with ADOS, ADI or CARS diagnosis of ASD | 29 | 29 | 100 | 4.46 | 1.49 | – | Months | 24 | 5 | AD, PDD-NOS, Asperger syndrome | |
| Ray-Subramanian 2012328 | 2–3 years with DSM-IV diagnosis | 115 | 115 | 100 | 31 | 4.1 | – | Months | 97 | 18 | Autism, AD, PDD-NOS | |
| Rogers 2012317 | 14–24 months with ASD | 98 | 98 | 100 | 21 | – | – | Months | 76 | 22 | ASD | |
| Schertz 2013402 | Mean age 24.6 and 27.5 months with ADOS diagnosis | 23 | 23 | 100 | 26.05 | – | – | Months | NR | NR | ASD | |
| Siller 2013403 | 32–82 months with ADI-R and ADOS-G diagnosis | 70 | 70 | 100 | – | – | 32–82 | Months | 64 | 6 | AD | |
| Sullivan 2007330 | Tested at 14–24 months and 30–36 months who met DSM-IV criteria for diagnosis | 51 | 16 | 31 | – | – | 14–36 | Months | 14 | 2 | Autism, PDD-NOS | |
| Tek 2012331 | 16–38 months with ADOS diagnosis | 84 | 84 | 100 | 27 | – | 16–38 | Months | NR | NR | ASD | |
| Thurm 2007404 | 2–3 years and 4–5 years | 118 | 83 | 70 | 29.98 | 4.28 | – | Months | 71 | 12 | Autism, PDD-NOS | |
| Toth 2006284 | 34–52 months with ADI-diagnosis of ASD | 60 | 60 | 100 | 43.6 | 4.3 | 34–52 | Months | 51 | 9 | AD, PDD-NOS | |
| Ventola 2007332 | 16–32 months old with M-CHAT diagnosis of ASD | 195 | 195 | 100 | – | – | 16–32 | Months | 152 | 43 | ASD | |
| Werner 2005316 | 12–57 months with DSM-IV diagnosis of ASD | 145 | 72 | 50 | 43.5 | 4.3 | – | Months | 60 | 12 | AD, PDD-NOS | |
| Zachor 2010335 | 15- to 35-month-old children who met DSM-IV criteria | 71 | 71 | 100 | 25.55 | 4.25 | 15–35 | Months | 71 | 7 | Autism | |
| Pragmatics Profile | Roberts 2011405 | 2.2–5 years with DSM-IV diagnosis of ASD | 95 | 95 | 100 | – | – | 26.3–60.3 | Months | 86 | 9 | AD, ASD |
| Preschool Language Scale | Bopp 2009340 | Children were aged 1–6 years at start of the study | 69 | 69 | 100 | – | – | 1–6 | Years | 58 | 11 | Autism, PDD-NOS |
| Casenhiser 2013361 | Children aged 2–4 years 11 months who met ADI-R criteria | 51 | 51 | 100 | – | – | 2.0–4.9 | Years | NR | NR | ASD | |
| Flippin 2011406 | Children aged 40–69 months with autism diagnosis based on ADOS | 16 | 16 | 100 | 53.3 | 9.6 | 40–69 | Months | 12 | 4 | ASD | |
| Green 2010253 | 24–60 months, ADOS or ADI diagnosed | 152 | 152 | 100 | 45 | – | 24–60 | Months | 138 | 14 | Core autism | |
| Haebig 2013407 | 24–39 months old children with ASD | 40 | 40 | 100 | 31.15 | 4.37 | 24–39 | Months | 33 | 7 | Autism, ASD | |
| Harris 1991408 | Preschool children with a diagnosis of autism based on DSM-III and DSM-III-R criteria | 46 | 25 | 54 | 53.245 | – | 40–67 | Months | 21 | 4 | Autism | |
| Hudry 2010233 | 24- to 59-month-old children with ADOS-G diagnosis | 152 | 152 | 100 | 44.83 | 7.98 | 24–59 | Months | 138 | 14 | Core autism | |
| Mitchell 2006392 | ‘At risk’ children with a sibling with ‘clinical’ diagnosis of ASD – 11–15 months at first assessment | 146 | 15 | 10 | – | – | 11–15 | Months | 10 | 5 | ASD | |
| Ray-Subramanian 2012328 | 2–3 years with DSM-IV diagnosis | 115 | 115 | 100 | 31 | 4.1 | – | Months | 97 | 18 | Autism, AD, PDD-NOS | |
| Smith 2010359 | All < 6 years with ADOS/ADI/DSM-IV diagnosis of ASD | 53 | 53 | 100 | 50.1 | 10 | – | Months | 47 | 6 | Autism | |
| Stone 2001394 | Assessed at 2 years and 4 years, met DSM-III or DSM-IV criteria for ASD | 35 | 35 | 100 | 57.9 | 4.5 | 50–67 | Months | 28 | 8 | Autism, PDD-NOS | |
| Reynell Developmental Language Scales | Andersson 2013409 | Children aged 1.8–3.9 years who met DSM-IV criteria | 40 | 37 | 93 | – | – | 1.8–3.9 | Years | 18 | 19 | AD, ASD, atypical autism, Asperger syndrome |
| Bono 2004389 | 31–64 months with DSM-IV diagnosis of ASD | 29 | 29 | 100 | 46.68 | 9.64 | 31–64 | Months | 22 | 7 | AD | |
| Carlsson 2013390 | Children aged from 4.5 to 6.5 years who were assessed to have autism based on DSM-IV criteria | 198 | 119 | 60 | – | – | 4.5–6.5 | Years | NR | NR | Autistic-like condition, Asperger syndrome, autistic traits | |
| Eikeseth 2009410 | 24–42 months with ICD-10 diagnosis of ASD | 23 | 23 | 100 | 34.9 | 5.7 | 28–42 | Months | 17 | 6 | Autism | |
| Goods 2013366 | 36- to 60-month-old children with autism (ADOS assessment) | 15 | 15 | 100 | 51.9 | – | – | Months | NR | NR | Autism | |
| Herring 2006411 | Children were aged between 20 and 51 months who met the DSM-IV criteria for diagnosis | 123 | 84 | 68 | 37.75 | 7.07 | – | Months | 75 | 9 | AD, PDD-NOS | |
| Miniscalco 2012391 | 20–47 months with DSM-IV diagnosis of ASD | 31 | 31 | 100 | 36 | – | 20–47 | Months | 27 | 4 | Autistic disorder | |
| Remington 2007358 | 30–42 months of age with ADI diagnosis of ASD | 44 | 44 | 100 | 37 | 4.2 | 30–42 | Months | NR | NR | Autism or suspected autism | |
| Roberts 2011405 | 2.2–5 years with DSM-IV diagnosis of ASD | 95 | 95 | 100 | – | – | 26.3–60.3 | Months | 86 | 9 | AD, ASD | |
| Sheinkopf 2000412 | Mean age ranged from 36.09 months (SD = 11.23) to 44.07 months (SD = 8.35) with CARS diagnosis of ASD | 26 | 15 | 58 | 36.09 | – | – | Months | 22 | 4 | Autism | |
| Smith 2000413 | 18–42 months with ‘clinical’ diagnosis of ASD | 28 | 28 | 100 | 35.92 | – | – | Months | 23 | 5 | Autism, PDD-NOS | |
| Sequenced Inventory of Communication-Revised | Stone 2001394 | Assessed at 2 years and 4 years, met DSM-III or DSM-IV criteria for ASD | 35 | 35 | 100 | 57.9 | 4.5 | 50–67 | Months | 28 | 8 | Autism, PDD-NOS |
| Test for Auditory Comprehension of Language | Szatmari 2000302 | 4- to 6-year-old children (upon entering study) diagnosed by ADI | 134 | 68 | 51 | 66.8 | – | – | Months | 59 | 7 | Autism, Asperger syndrome |
| Test of Language Development | Bennett 2008296 | Children aged between 4–6 years | 64 | 64 | 100 | – | – | 4–6 | Years | 57 | 7 | Asperger syndrome, high-functioning autism |
| Szatmari 2000302 | 4- to 6-year-old children (upon entering study) diagnosed by ADI | 134 | 68 | 51 | 66.8 | – | – | Months | 59 | 7 | Autism, Asperger syndrome | |
| Vineland Adaptive Behavior Scales (VABS) | Aldred 2004318 | 2–5, 11 years with ADI diagnosis | 28 | 28 | 100 | – | – | 24–71 | Months | 25 | 3 | AD or ‘classical autism’ |
| Anan 2008396 | 25- to 68- month-old children who met the diagnosis of ASD based on DSM-IV criteria | 72 | 72 | 100 | – | – | 25–68 | Months | 61 | 11 | AD, PDD-NOS | |
| Andersson 2013409 | Children aged 1.8–3.9 years who met DSM-IV criteria | 40 | 37 | 93 | – | – | 1.8–3.9 | Years | 18 | 19 | AD, ASD, atypical autism, Asperger syndrome | |
| Arick 2003388 | Children between the ages of 2 and 6 years (at baseline) who have been said to have a diagnosis of autism; details of criteria used not provided | 67 | 67 | 100 | – | – | 2–6 | Years | NR | NR | ASD | |
| Baghdadli 2012339 | Age < 7 years, ICD-10 diagnosis of autism | 280 | 280 | 100 | 4.9 | 1.3 | – | Months | 230 | 50 | Childhood autism, atypical autism | |
| Bearss 2013278 | Children were aged between 3 years and 6 years 11 months, and assessed to have autism based on ADOS and clinical observation | 16 | 16 | 100 | – | – | 3–6 | Years | 16 | 0 | AD, PDD-NOS | |
| Ben Itzchak 2011320 | Children aged 15–35 months were included in the study | 78 | 78 | 100 | – | – | 15–35 | Months | 71 | 7 | Autism | |
| Bennett 2008296 | Children aged between 4 and 6 years | 64 | 64 | 100 | – | – | 4–6 | Years | 57 | 7 | Asperger syndrome, high-functioning autism | |
| Carlsson 2013390 | Children aged from 4.5 to 6.5 years who were assessed to have autism based on DSM-IV criteria | 198 | 119 | 60 | – | – | 4.5–6.5 | Years | NR | NR | Autistic-like condition, Asperger syndrome, autistic traits | |
| Cassidy 2008348 | Parents of children aged < 5 years with ICD-10 diagnosis of ASD | 104 | 104 | 100 | – | – | 2–4 | Years | 95 | 9 | ASD | |
| Dawson 2010321 | 18–30 months, diagnosed by ADOS, ADI and DSM-IV | 48 | 48 | 100 | – | – | 18–33 | Months | 37 | 11 | AD, PDD-NOS | |
| Eapen 2013357 | Mean age of 49.6 months | 26 | 26 | 100 | 49.6 | 6.08 | 36–58 | Months | 21 | 5 | AD | |
| Eikeseth 2009410 | 24–42 months with ICD-10 diagnosis of ASD | 23 | 23 | 100 | 34.9 | 5.7 | 28–42 | Months | 17 | 6 | Autism | |
| Eldevik 2012414 | Children aged 2–6 who had autism diagnosis based on ICD-10 criteria and ADI-R | 43 | 43 | 100 | 4.26 | 1.48 | 1–6 | Years | 33 | 10 | Autism, PDD-NOS, Asperger syndrome | |
| Eriksson 2013415 | Children aged 20–54 months. Criteria not stated | 208 | 208 | 100 | – | – | 20–54 | Months | 176 | 32 | ASD | |
| Gabriels 2007416 | Children had a mean age of 31 months and had a clinical diagnosis of autistic disorder or PDD-NOS based on DSM-IV criteria | 14 | 14 | 100 | 31 | – | – | Months | 10 | 4 | AD, PDD-NOS | |
| Green 2010253 | 24–60 months, ADOS or ADI diagnosed | 152 | 152 | 100 | 45 | – | 24–60 | Months | 138 | 14 | Core autism | |
| Grindle 2012417 | 3- to 7-year-old children with autism | 29 | 29 | 100 | – | – | 43–72 | Months | 25 | 4 | Autism | |
| Hedvall 2013418 | 3.6- to 6.6-year-old children with ASD | 190 | 168 | 88 | 55 | 0.8 | 42–76 | Months | 147 | 21 | AD, PDD-NOS, Asperger syndrome | |
| Herring 2006411 | Children were aged between 20 and 51 months who met the DSM-IV criteria for diagnosis | 123 | 84 | 68 | 37.75 | 7.07 | – | Months | 75 | 9 | AD, PDD-NOS | |
| Honey 2008307 | 24–48 months diagnosed by ICD-10 criteria | 104 | 79 | 76 | 37.05 | 6.08 | 24–48 | Months | 65 | 14 | ASD | |
| Hudry 2010233 | 24- to 59-month-old children with ADOS-G diagnosis | 152 | 152 | 100 | 44.83 | 7.98 | 24–59 | Months | 138 | 14 | Core autism | |
| Jasmin 2009384 | Children aged 3–4 years who had a diagnosis of ASD based on DSM-IV criteria | 35 | 35 | 100 | – | – | 3–4 | Years | 32 | 3 | Autistic, PDD-NOS, Asperger syndrome | |
| Jonsdottir 2007341 | Mean age was 41.43 months; diagnosis was based on ICD-10 criteria | 41 | 41 | 100 | 41.43 | 9.06 | 22–59 | Months | 34 | 7 | Childhood autism | |
| Klintwall 2012419 | 2 years and 3 months to 4 years and 11 months, with clinical diagnosis by paediatrician | 21 | 21 | 100 | 3.6 | – | 2.25–4.9 | Years | 16 | 5 | Autism | |
| Landa 2012224 | 22- to 33-month-old children with ASD or autism | 48 | 48 | 100 | 27 | 2.8 | 22–33 | Months | 39 | 9 | ASD | |
| Lerna 2012325 | 18–60 months old with diagnosis of autism and little or no functional language | 18 | 18 | 100 | – | – | 18–60 | Months | 17 | 1 | Autism | |
| Lloyd 2013400 | 12- to 36-month-old children with ASD | 162 | 162 | 100 | – | – | 12–37 | Months | 140 | 22 | ASD | |
| Luyster 2008129 | Participants were aged 18–33 months and met ADI-R criteria for ASD diagnosis | 164 | 164 | 100 | – | – | 18–33 | Months | 129 | 35 | ASD | |
| Magiati 2007308 | Children aged between 22 and 54 months who met ADI-R criteria for autism/ASD diagnosis | 44 | 44 | 100 | – | – | 22–54 | Months | 39 | 5 | Autism, ASD | |
| Magiati 2011309 | Mean age of 3.4 years at start of the study | 44 | 44 | 100 | 38.9 | 7.1 | 27–55 | Months | 39 | 5 | Autism, ASD | |
| Mayo 2013310 | 45–72 months with DSM-IV-TR criteria | 119 | 119 | 100 | 52.22 | 6.09 | 45–72 | Months | 99 | 20 | AD, PDD-NOS | |
| McConkey 2010349 | Children with ASD diagnosis (criteria not given, it was only stated as ‘confirmed diagnosis of ASD from a specialist clinic’) who had a mean age of 2.8 years at start of the study | 62 (families) | 61 | 98 | – | – | < 4 | Years | 55 | 6 | Autism | |
| Munson 2006420 | 38–54 months with DSM-IV diagnosis of ASD | 45 | 45 | 100 | 47.4 | 4.2 | 38–54 | Months | 38 | 7 | AD, PDD-NOS | |
| Munson 2008312 | 24–66 months with ADI or ADOS diagnosis of ASD | 456 | 456 | 100 | 43.4 | 8.7 | 24–66 | Months | 370 | 86 | Autism, ASD | |
| O’Donnell 2012386 | 3–4 years old with DSM-IV diagnosis of ASD | 42 | 42 | 100 | 45.5 | – | 36–59 | Months | NR | NR | Autism, PDD-NOS | |
| Osborne 2008350 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | – | – | 2.6–4.0 | Years | 59 | 6 | ASD | |
| Osborne 2009351 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | 3.4 | 0.75 | 2.6–4.0 | Years | 59 | 6 | ASD | |
| Peters-Scheffer 2010421 | 3- to 6-year-old children with DSM-IV diagnosis of AD or PDD-NOS | 34 | 34 | 100 | 53.5 | 5.52 | 42–62 | Months | NR | NR | AD, PDD-NOS | |
| Poon 2012401 | 9–12 months (upon entering study) with ADOS, ADI or CARS diagnosis of ASD | 29 | 29 | 100 | 4.46 | 1.49 | – | Months | 24 | 5 | AD, PDD-NOS, Asperger syndrome | |
| Pry 2005314 | 21 months to 7 years with ICD-10 diagnosis of ASD | 222 | 222 | 100 | 5 | 1.75 | 1.75–7 | Years | 180 | 42 | Infantile autism | |
| Ray-Subramanian 2011327 | 23–39 months with DSM-IV or ICD-10 diagnosis of ASD | 125 | 125 | 100 | 31 | 4.1 | 23–39 | Months | 108 | 17 | Autism, AD, PDD-NOS | |
| Reed 2007352 | 2 years 6 months to 4 years old diagnosed with ASD | 27 | 27 | 100 | – | – | 2.6–4.0 | Years | 27 | 0 | ASD | |
| Reed 2007353 | 2 years 6 months to 4 years old with ‘paediatrician’ diagnosis of ASD | 53 | 53 | 100 | – | – | 2.6–4.0 | Years | Unclear | Unclear | ASD | |
| Reed 2012354 | 2.5–4 years with GARS diagnosis of ASD | 66 | 66 | 100 | 40.2 | 5.6 | – | Months | 59 | 7 | AD, PDD-NOS | |
| Remington 2007358 | 30–42 months of age with ADI diagnosis of ASD | 44 | 44 | 100 | 37 | 4.2 | 30–42 | Months | NR | NR | Autism or suspected autism | |
| Restall 1994422 | 3–6 years with DSM-III diagnosis of ASD | 18 | 9 | 50 | 64.76 | 6.4 | – | Months | 8 | 1 | Autism | |
| Rickards 2009423 | 3–5 years, 35/59 diagnosed ASD by DSM-IV criteria | 54 | 54 | 100 | 69.65 | – | – | Months | 43 | 11 | ASD | |
| Roberts 2011405 | 2.2–5 years with DSM-IV diagnosis of ASD | 95 | 95 | 100 | – | – | 26.3–60.3 | Months | 86 | 9 | AD, ASD | |
| Rogers 2012317 | 14–24 months with ASD | 98 | 98 | 100 | 21 | – | – | Months | 76 | 22 | ASD | |
| Ruble 2008424 | 40–71 months with DSM-IV diagnosis of ASD | 35 | 35 | 100 | 55.9 | – | 40.9–70.9 | Months | 30 | 5 | Autism | |
| Salt 2002372 | Preschool children in Scotland, (mean 42.36 months) with ICD-10 diagnosis of ASD | 17 | 17 | 100 | 40.015 | – | – | Months | 14 | 3 | Childhood autism | |
| Schertz 2013402 | Mean age 24.6 and 27.5 months with ADOS diagnosis | 23 | 23 | 100 | 26.05 | – | – | Months | NR | NR | ASD | |
| Silva 2007299 | 3–6 years old with DSM-IV diagnosis of ASD | 15 | 15 | 100 | 4.83 | – | 3–6 | Years | 13 | 2 | AD | |
| Silva 2008300 | 3–6 years old with DSM-IV diagnosis of ASD | 26 | 26 | 100 | 56.3 | 12.5 | – | Months | 21 | 5 | Autism | |
| Smith 2000413 | 18–42 months with ‘clinical’ diagnosis of ASD | 28 | 28 | 100 | 35.92 | – | – | Months | 23 | 5 | Autism, PDD-NOS | |
| Smith 2010359 | All < 6 years with ADOS/ADI/DSM-IV diagnosis of ASD | 53 | 53 | 100 | 50.1 | 10 | – | Months | 47 | 6 | Autism | |
| Stahmer 2004355 | 0–3 years with DSM-IV diagnosis | 20 | 20 | 100 | 29.6 | – | 22–33 | Months | 16 | 4 | AD, PDD-NOS | |
| Stone 1999346 | 23–35 months with DSM-III or DSM-IV diagnosis of ASD | 60 | 30 | 50 | 31.3 | 3.3 | 23–35 | Months | 25 | 5 | Autism | |
| Strauss 2012329 | 26–81 months with DSM-IV diagnosis of ASD | 44 | 44 | 100 | – | – | 26–81 | Months | 41 | 3 | Autism, PDD-NOS | |
| Szatmari 2000302 | 4- to 6-year-old children (upon entering study) diagnosed by ADI | 134 | 68 | 51 | 66.8 | – | – | Months | 59 | 7 | Autism, Asperger syndrome | |
| Tonge 2012425 | Children were aged 2.5–5 years and diagnosis was made using a combination of medical reviews, ADI-R and CARS | 107 | 107 | 100 | – | – | 2.5–5.0 | Years | 90 | 17 | AD | |
| Toth 2006284 | 34–52 months with ADI-diagnosis of ASD | 60 | 60 | 100 | 43.6 | 4.3 | 34–52 | Months | 51 | 9 | AD, PDD-NOS | |
| VanMeter 1997426 | Mean ages ranged from 2.9 (SD = 0.77) years to 5.7 (SD = 1.31) years meeting DSM-III criteria for ASD | 143 | 57 | 40 | – | – | 5.2–6.0 | Years | 54 | 3 | AD | |
| Ventola 2007332 | 16–32 months old with M-CHAT diagnosis of ASD | 195 | 195 | 100 | – | – | 16–32 | Months | 152 | 43 | ASD | |
| Werner 2005316 | 12–57 months with DSM-IV diagnosis of ASD | 145 | 72 | 50 | 43.5 | 4.3 | – | Months | 60 | 12 | AD, PDD-NOS | |
| Zachor 2010335 | 15- to 35-month-old children who met DSM-IV criteria | 71 | 71 | 100 | 25.55 | 4.25 | 15–35 | Months | 71 | 7 | Autism | |
| Vineland Adaptive Behavior Scales-Classroom version (VABS-Classroom) | Goin-Kochel 2007427 | Children were aged between 29.6–61.4 months; diagnosis was based on ADOS criteria | 29 | 29 | 100 | 45.7 | 9.6 | 29.6–61.4 | Months | 27 | 2 | Autism, PDD-NOS |
| Differential Ability Scalesa | Bishop 2011176 | Children were aged between 2 years and 5 years 11 months | 72 | 53 | 74 | – | – | 1–68 | Months | 44 | 9 | Not given |
| Ruble 2008424 | 40–71 months with DSM-IV diagnosis of ASD | 35 | 35 | 100 | 55.9 | – | 40.9–70.9 | Months | 30 | 5 | Autism | |
| Thurm 2007404 | 2–3 years and 4–5 years | 118 | 83 | 70 | 29.98 | 4.28 | – | Months | 71 | 12 | Autism, PDD-NOS | |
| Peabody Picture Vocabulary Testa | Bopp 2009340 | Children were aged 1–6 years at start of the study | 69 | 69 | 100 | – | – | 1–6 | Years | 58 | 11 | Autism, PDD-NOS |
| Smith 2010359 | All < 6 years with ADOS/ADI/DSM-IV diagnosis of ASD | 53 | 53 | 100 | 50.1 | 10 | – | Months | 47 | 6 | Autism | |
| Szatmari 2000302 | 4- to 6-year-old children (upon entering study) diagnosed by ADI | 134 | 68 | 51 | 66.8 | – | – | Months | 59 | 7 | Autism, Asperger syndrome | |
| Processability testb | Carlsson 2013390 | Children aged from 4.5 to 6.5 years who were assessed to have autism based on DSM-IV criteria | 198 | 119 | 60 | – | – | 4.5–6.5 | Years | NR | NR | Autistic-like condition, Asperger syndrome, autistic traits |
| Rating of video for expressive speechc | Baghdadli 2012339 | Age < 7 years, ICD-10 diagnosis of autism | 280 | 280 | 100 | 4.9 | 1.3 | – | Months | 230 | 50 | Childhood autism, atypical autism |
| Semistructured free play with examinerc | Yoder 2006428 | 21–54 months old with ADOS diagnosis of ASD | 36 | 36 | 100 | 33.6 | 8.4 | 21–54 | Months | NR | NR | Autism, PDD-NOS |
| Video coding proceduresc | Colgan 2006379 | Children aged 8–12 months with diagnosis of autism based on DSM-III-R or DSM-IV criteria | 35 | 21 | 60 | – | – | 0–2 | Years | 17 | 4 | AD |
| Cognitive ability | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Battelle Developmental Inventory (BDI) | Arick 2003388 | Children between the ages of 2 and 6 years (at baseline) who have been said to have a diagnosis of autism; details of criteria used not provided | 67 | 67 | 100 | – | – | 2–6 | Years | NR | NR | ASD |
| Bayley Scales of Infant Development (BSID) | Ben Itzchak 2008149 | Children aged 19–35 months with autism diagnosis based on DSM-IV criteria | 81 | 44 | 54 | – | – | 16–35 | Months | 43 | 1 | Autism |
| Eikeseth 2009410 | 24–42 months with ICD-10 diagnosis of ASD | 23 | 23 | 100 | 34.9 | 5.7 | 28–42 | Months | 17 | 6 | Autism | |
| Eldevik 2012414 | Children aged 2–6 who had autism diagnosis based on ICD-10 criteria and ADI-R | 43 | 43 | 100 | – | – | 1–6 | Years | 33 | 10 | Autism, PDD-NOS, Asperger | |
| Grindle 2012417 | 3- to 7-year-old children with autism | 29 | 29 | 100 | – | – | 43–72 | Months | 25 | 4 | Autism | |
| Ingersoll 2012286 | 27 children between 27 and 47 months old who met DSM-IV-TR criteria | 29 | 29 | 100 | 37.9 | – | 22–47 | Months | 24 | 5 | AD | |
| Jonsdottir 2007341 | Mean age was 41.43 months; diagnosis was based on ICD-10 criteria | 41 | 41 | 100 | 41.43 | 9.06 | 22–59 | Months | 34 | 7 | Childhood autism | |
| Magiati 2007308 | Children aged between 22 and 54 months who met ADI-R criteria for autism/ASD diagnosis | 44 | 44 | 100 | – | – | 22–54 | Months | 39 | 5 | Autism, ASD | |
| Peters-Scheffer 2010421 | 3- to 6-year-old children with DSM-IV diagnosis of AD or PDD-NOS | 34 | 34 | 100 | 53.5 | 5.52 | 42–62 | Months | NR | NR | AD, PDD-NOS | |
| Ray-Subramanian 2011327 | 23–39 months with DSM-IV or ICD-10 diagnosis of ASD | 125 | 125 | 100 | 31 | 4.1 | 23–39 | Months | 108 | 17 | Autism, AD, PDD-NOS | |
| Remington 2007358 | 30–42 months of age with ADI diagnosis of ASD | 44 | 44 | 100 | 37 | 4.2 | 30–42 | Months | NR | NR | Autism or suspected autism | |
| Rickards 2009423 | 3–5 years, 35/59 diagnosed ASD by DSM-IV criteria | 54 | 54 | 100 | 69.65 | – | – | Months | 43 | 11 | ASD | |
| Sheinkopf 1998429 | 23–47 months with DSM-III diagnosis of ASD | 22 | 22 | 100 | – | – | 23–47 | Months | NR | NR | Autism, PDD-NOS | |
| Smith 1997430 | Up to 46 months at intake, within DSM-III diagnosis of ASD | 21 | 21 | 100 | 37 | – | – | Months | 19 | 2 | PDD-NOS | |
| Smith 2000413 | 18–42 months with ‘clinical’ diagnosis of ASD | 28 | 28 | 100 | 35.92 | – | – | Months | 23 | 5 | Autism, PDD-NOS | |
| Stahmer 2004355 | 0–3 years with DSM-IV diagnosis | 20 | 20 | 100 | 27.6 | – | 22–31 | Months | 16 | 4 | AD, PDD-NOS | |
| Ventola 2007332 | 16–32 months old with M-CHAT diagnosis of ASD | 195 | 195 | 100 | – | – | 16–32 | Months | 152 | 43 | ASD | |
| Zachor 2006334 | Participants were aged 23–33 months and met DSM-IV criteria for autism diagnosis | 39 | 39 | 100 | – | – | 23–33 | Months | 37 | 2 | Autism | |
| Behavior Rating Inventory of Executive Function (BRIEF)-Preschool Version | Jahromi 2013431 | 20 TD and 20 children with high-functioning autism | 40 | 20 | 50 | 58.95 | 11.5 | – | Months | 36 | 4 | High-functioning autism |
| British Ability Scale (BAS) | Osborne 2008350 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | – | – | 2.6–4.0 | Years | 59 | 6 | ASD |
| Osborne 2009351 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | 3.4 | 0.75 | 2.6–4.0 | Years | 59 | 6 | ASD | |
| Reed 2007352 | 2 years 6 months to 4 years old diagnosed with ASD | 27 | 27 | 100 | – | – | 2.5–4.0 | Years | 27 | 0 | ASD | |
| Reed 2007353 | 2 years 6 months to 4 years old with ‘paediatrician’ diagnosis of ASD | 53 | 53 | 100 | – | – | 2.5–4.0 | Years | Unclear | Unclear | ASD | |
| Reed 2012354 | 2.5–4 years with GARS diagnosis of ASD | 66 | 66 | 100 | 40.2 | 5.6 | – | Months | 59 | 7 | AD, PDD-NOS | |
| Cattell Infant Intelligence | Sheinkopf 1998429 | 23–47 months with DSM-III diagnosis of ASD | 22 | 22 | 100 | – | – | 23–47 | Months | NR | NR | Autism, PDD-NOS |
| Developmental Profile | Malhi 2011342 | Children were ≤ 3 years at start of the study and had an ASD diagnosis based on DSM-IV criteria | 77 | 77 | 100 | – | – | 0–3 | Years | 64 | 13 | AD, PDD-NOS |
| Griffiths Mental Developmental Scales | Andersson 2013409 | Children aged 1.8–3.9 years who met DSM-IV criteria | 40 | 37 | 93 | – | – | 1.8–3.9 | Years | 18 | 19 | AD, ASD, atypical autism, Asperger syndrome |
| Carlsson 2013390 | Children aged from 4.5 to 6.5 years who were assessed to have autism based on DSM-IV criteria | 198 | 119 | 60 | – | – | 4.5–6.5 | Years | NR | NR | Autistic-like condition, Asperger syndrome, autistic traits | |
| Hedvall 2013418 | 3.6- to 6.6-year-old children with ASD | 190 | 168 | 88 | 55 | 0.8 | 42–76 | Months | 147 | 21 | AD, PDD-NOS, Asperger syndrome | |
| Lerna 2012325 | 18–60 months old with diagnosis of autism and little or no functional language | 18 | 18 | 100 | – | – | 18–60 | Months | 17 | 1 | Autism | |
| Strauss 2012329 | 26–81 months with DSM-IV diagnosis of ASD | 44 | 44 | 100 | – | – | 26–81 | Months | 41 | 3 | Autism, PDD-NOS | |
| Leiter International Performance Scale-Revised (Leiter-R) | Gabriels 2007416 | Children had a mean age of 31 months and had a clinical diagnosis of autistic disorder or PDD-NOS based on DSM-IV criteria | 14 | 14 | 100 | 31 | – | – | Months | 10 | 4 | AD, PDD-NOS |
| Grindle 2012417 | 3- to 7-year-old children with autism | 29 | 29 | 100 | – | – | 43–72 | Months | 25 | 4 | Autism | |
| Leiter Performance Scales (Arthur adaptation) | Bennett 2008296 | Children aged between 4 and 6 years | 64 | 64 | 100 | – | – | 4–6 | Years | 57 | 7 | Asperger syndrome, high-functioning autism |
| McCarthy Scales of Children’s Abilities | Szatmari 2000302 | 4- to 6-year-old children (upon entering study) diagnosed by ADI | 134 | 68 | 51 | 66.8 | – | – | Months | 59 | 7 | Autism, Asperger syndrome |
| Merrill–Palmer Scale of Mental Tests | Eikeseth 2009410 | 24–42 months with ICD-10 diagnosis of ASD | 23 | 23 | 100 | 34.9 | 5.7 | 28–42 | Months | 17 | 6 | Autism |
| Magiati 2007308 | Children aged between 22 and 54 months who met ADI-R criteria for autism/ASD diagnosis | 44 | 44 | 100 | – | – | 22–54 | Months | 39 | 5 | Autism, ASD | |
| Sheinkopf 1998429 | 23–47 months with DSM-III diagnosis of ASD | 22 | 22 | 100 | – | – | 23–47 | Months | NR | NR | Autism, PDD-NOS | |
| Sheinkopf 2000412 | Mean age ranged from 36.09 months (SD = 11.23) to 44.07 months (SD = 8.35) with CARS diagnosis of ASD | 26 | 15 | 58 | 36.09 | – | – | Months | 22 | 4 | Autism | |
| Smith 2000413 | 18–42 months with ‘clinical’ diagnosis of ASD | 28 | 28 | 100 | 35.92 | – | – | Months | 23 | 5 | Autism, PDD-NOS | |
| Smith 2010359 | All < 6 years with ADOS/ADI/DSM-IV diagnosis of ASD | 53 | 53 | 100 | 50.1 | 10 | – | Months | 47 | 6 | Autism | |
| Mullen Scales of Early Learning (MSEL) | Akshoomoff 2006395 | 16–43 months with ADI-R and ADOS diagnosis of ASD | 42 | 22 | 52 | – | – | 16–43 | Months | 17 | 5 | Autism, ASD |
| Anan 2008396 | 25- to 68-month-old children who met the diagnosis of ASD based on DSM-IV criteria | 72 | 72 | 100 | – | – | 25–68 | Months | 61 | 11 | AD, PDD-NOS | |
| Baker 2010397 | 33 ‘at-risk’ children, entered study between ages of 2–18 months, assessed at 18, 24, 30 and 36 months. [24 of the 33 children had a sibling with ASD or PDD (DSM-IV diagnosed)] | 33 | 12 | 36 | 18 | – | – | Months | NR | NR | ASD | |
| Barbaro 2012398 | 12- to 22-month children with AD, ASD or DD/language delay | 154 | 125 | 81 | – | – | 12–27 | Months | 100 | 25 | AD, ASD | |
| Ben Itzchak 2011320 | Children aged 15–35 months were included in the study | 78 | 78 | 100 | – | – | 15–35 | Months | 71 | 7 | Autism | |
| Bishop 2011176 | Children were aged between 2 years to 5 years 11 months | 72 | 53 | 74 | – | – | 1–68 | Months | 44 | 9 | Not given | |
| Brian 2008305 | Children had no diagnosis of ASD but were followed up to 36 months at which point some were diagnosed of ASD | 228 | 35 | 15 | – | – | 6–12 | Months | NR | NR | Autism, Asperger syndrome, PDD-NOS | |
| Dawson 2010321 | 18–30 months, diagnosed by ADOS, ADI and DSM-IV | 48 | 48 | 100 | – | – | 18–31 | Months | 37 | 11 | AD, PDD-NOS | |
| Dereu 2012365 | Children aged 2–4 years; ADOS was used for diagnosis | 17 | 9 | 53 | – | – | 17–39 | Months | 6 | 3 | ASD | |
| Eapen 2013357 | Mean age of 49.6 months | 26 | 26 | 100 | 49.6 | 6.08 | 36–58 | Months | 21 | 5 | AD | |
| Hartley 2009323 | Children aged 1.5 to 3.9 years based on DSM-IV TR criteria and ADOS-G classification | 499 | 199 | 40 | – | – | 18–49 | Months | 157 | 42 | AD, PDD-NOS | |
| Honey 2008307 | 24–48 months diagnosed by ICD-10 criteria | 104 | 79 | 76 | 37.05 | 6.08 | 24–48 | Months | 65 | 14 | ASD | |
| Landa 2012399 | Assessed at aged 6–36 months – 52/197 subsequently diagnosed ASD by ADOS | 204 | 52 | 25 | 6 | – | – | Months | 43 | 9 | ASD | |
| Landa 2012224 | 22- to 33-month-old children with ASD or autism | 48 | 48 | 100 | 27 | 2.8 | 22–33 | Months | 39 | 9 | ASD | |
| Lloyd 2013400 | 12- to 36-month-old children with ASD | 162 | 162 | 100 | – | – | 12–36 | Months | 140 | 22 | ASD | |
| Luyster 2008129 | Participants were aged 18–33 months and met ADI-R criteria for ASD diagnosis | 164 | 164 | 100 | – | – | 18–33 | Months | 129 | 35 | ASD | |
| Mayo 2013310 | 45–72 months with DSM-IV-TR criteria | 119 | 119 | 100 | 52.22 | 6.09 | 45–72 | Months | 99 | 20 | AD, PDD-NOS | |
| Mitchell 2006392 | ‘At risk’ children with a sibling with ‘clinical’ diagnosis of ASD – 11–15 months at first assessment | 146 | 15 | 10 | – | – | 11–15 | Months | 10 | 5 | ASD | |
| O’Donnell 2012386 | 3–4 years old with DSM-IV diagnosis of ASD | 42 | 42 | 100 | 45.5 | – | 36–59 | Months | NR | NR | Autism, PDD-NOS | |
| Ozonoff 2010313 | Assessed between 6 and 36 months, diagnosed using ADOS | 50 | 25 | 50 | – | – | 6 | Months | 19 | 6 | AD, PDD-NOS | |
| Poon 2012401 | 9–12 months (upon entering study) with ADOS, ADI or CARS diagnosis of ASD | 29 | 29 | 100 | 4.46 | 1.49 | – | Months | 24 | 5 | AD, PDD-NOS, Asperger syndrome | |
| Ray-Subramanian 2012328 | 2–3 years with DSM-IV diagnosis | 115 | 115 | 100 | 31 | 4.1 | – | Months | 97 | 18 | Autism, AD, PDD-NOS | |
| Rogers 2012317 | 14–24 months with ASD | 98 | 98 | 100 | 21 | – | – | Months | 76 | 22 | ASD | |
| Schertz 2013402 | Mean age 24.6 and 27.5 months with ADOS diagnosis | 23 | 23 | 100 | 26.05 | – | – | Months | NR | NR | ASD | |
| Siller 2013403 | 32–82 months with ADI-R and ADOS-G diagnosis | 70 | 70 | 100 | – | – | 32–82 | Months | 64 | 6 | AD | |
| Sullivan 2007330 | Tested at 14–24 months and 30–36 months who met DSM-IV criteria for diagnosis | 51 | 16 | 31 | – | – | 14–36 | Months | 14 | 2 | Autism, PDD-NOS | |
| Tek 2012331 | 16–38 months with ADOS diagnosis | 84 | 84 | 100 | 27 | – | 16–38 | Months | NR | NR | ASD | |
| Thurm 2007404 | 2–3 years and 4–5 years | 118 | 83 | 70 | 29.98 | 4.28 | – | Months | 71 | 12 | Autism, PDD-NOS | |
| Toth 2006284 | 34–52 months with ADI-diagnosis of ASD | 60 | 60 | 100 | 43.6 | 4.3 | 34–52 | Months | 51 | 9 | AD, PDD-NOS | |
| Ventola 2007332 | 16–32 months old with M-CHAT diagnosis of ASD | 195 | 195 | 100 | – | – | 16–32 | Months | 152 | 43 | ASD | |
| Werner 2005316 | 12–57 months with DSM-IV diagnosis of ASD | 145 | 72 | 50 | 43.5 | 4.3 | – | Months | 60 | 12 | AD, PDD-NOS | |
| Zachor 2010335 | 15- to 35-month-old children who met DSM-IV criteria | 71 | 71 | 100 | 25.55 | 4.25 | 15–35 | Months | 71 | 7 | Autism | |
| Snijders–Oomen Non-Verbal Intelligence Test (SON) | Peters-Scheffer 2010421 | 3- to 6-year-old children with DSM-IV diagnosis of AD or PDD-NOS | 34 | 34 | 100 | 53.5 | 5.52 | 42–62 | Months | NR | NR | AD, PDD-NOS |
| Stanford–Binet Intelligence Scales | Ben Itzchak 2008149 | Children aged 19–35 months with autism diagnosis based on DSM-IV criteria | 81 | 44 | 54 | – | – | 16–35 | Months | 43 | 1 | Autism |
| Delmolino 2006432 | Mean age was 44 months (range = 37–60 months). Diagnosis were made prior to inclusion in the study and confirmed using ADOS and ADI-R | 27 | 27 | 100 | – | – | 3–6 | Years | 23 | 4 | Autism, PDD-NOS | |
| Grindle 2012417 | 3- to 7-year-old children with autism | 29 | 29 | 100 | – | – | 43–72 | Months | 25 | 4 | Autism | |
| Harris 1991408 | Preschool children with a diagnosis of autism based on DSM-III and DSM-III-R criteria | 46 | 25 | 54 | 53.245 | – | 40–67 | Months | 21 | 4 | Autism | |
| Harris 2000433 | Children between the age of 31 and 65 months who had a diagnosis of autistic disorder based on DSM-III-R criteria | 27 | 27 | 100 | – | – | 31–65 | Months | 25 | 2 | AD | |
| Landa 2012224 | 22- to 33-month-old children with ASD or autism | 48 | 48 | 100 | 27 | 2.8 | 22–33 | Months | 39 | 9 | ASD | |
| Remington 2007358 | 30–42 months of age with ADI diagnosis of ASD | 44 | 44 | 100 | 37 | 4.2 | 30–42 | Months | NR | NR | Autism or suspected autism | |
| Smith 2000413 | 18–42 months with ‘clinical’ diagnosis of ASD | 28 | 28 | 100 | 35.92 | – | – | Months | 23 | 5 | Autism, PDD-NOS | |
| Szatmari 2000302 | 4- to 6-year-old children (upon entering study) diagnosed by ADI | 134 | 68 | 51 | 66.8 | – | – | Months | 59 | 7 | Autism, Asperger syndrome | |
| Zachor 2006334 | Participants were aged 23–33 months and met DSM-IV criteria for autism diagnosis | 39 | 39 | 100 | – | – | 23–33 | Months | 37 | 2 | Autism | |
| Wechsler Intelligence Scale for Children | Szatmari 2000302 | 4- to 6-year-old children (upon entering study) diagnosed by ADI | 134 | 68 | 51 | 66.8 | – | – | Months | 59 | 7 | Autism, Asperger syndrome |
| Wechsler Preschool and Primary Scale of Intelligence (WPPSI) | Andersson 2013409 | Children aged 1.8–3.9 years who met DSM-IV criteria | 40 | 37 | 93 | – | – | 1.8–3.9 | Years | 18 | 19 | AD, ASD, atypical autism, Asperger syndrome |
| Baghdadli 2012339 | Age < 7 years, ICD-10 diagnosis of autism | 280 | 280 | 100 | 4.9 | 1.3 | – | Months | 230 | 50 | Childhood autism, atypical autism | |
| Baghdadli 2012339 | Age < 7 years, ICD-10 diagnosis of autism | 280 | 280 | 100 | 4.9 | 1.3 | – | Months | 230 | 50 | Childhood autism, atypical autism | |
| Carlsson 2013390 | Children aged from 4.5 to 6.5 years who were assessed to have autism based on DSM-IV criteria | 198 | 119 | 60 | – | – | 4.5–6.5 | Years | NR | NR | Autistic-like condition, Asperger syndrome, autistic traits | |
| Eikeseth 2009410 | 24–42 months with ICD-10 diagnosis of ASD | 23 | 23 | 100 | 34.9 | 5.7 | 28–42 | Months | 17 | 6 | Autism | |
| Hedvall 2013418 | 3.6- to 6.6-year-old children with ASD | 190 | 168 | 88 | 55 | 0.8 | 42–76 | Months | 147 | 21 | AD, PDD-NOS, Asperger syndrome | |
| Jonsdottir 2007341 | Mean age was 41.43 months; diagnosis was based on ICD-10 criteria | 41 | 41 | 100 | 41.43 | 9.06 | 22–59 | Months | 34 | 7 | Childhood autism | |
| Magiati 2007308 | Children aged between 22 and 54 months who met ADI-R criteria for autism/ASD diagnosis | 44 | 44 | 100 | – | – | 22–54 | Months | 39 | 5 | Autism, ASD | |
| Rickards 2009423 | 3–5 years, 35/59 diagnosed ASD by DSM-IV criteria | 54 | 54 | 100 | 69.65 | – | – | Months | 43 | 11 | ASD | |
| Sheinkopf 1998429 | 23–47 months with DSM-III diagnosis of ASD | 22 | 22 | 100 | – | – | 23–47 | Months | NR | NR | Autism, PDD-NOS | |
| Differential Ability Scalesa | Bishop 2011176 | Children were aged between 2 years to 5 years 11 months | 72 | 53 | 74 | – | – | 1–68 | Months | 44 | 9 | Not given |
| Ruble 2008424 | 40–71 months with DSM-IV diagnosis of ASD | 35 | 35 | 100 | 55.9 | – | 40.9–70.9 | Months | 30 | 5 | Autism | |
| Thurm 2007404 | 2–3 years and 4–5 years | 118 | 83 | 70 | 29.98 | 4.28 | – | Months | 71 | 12 | Autism, PDD-NOS | |
| Kyoto scale of psychological developmenta | Takeda 2005360 | 23–35 months with DSM-IV criteria | 57 | 57 | 100 | 31.4 | 3.3 | 23–35 | Months | 45 | 12 | AD, PDD-NOS, Asperger syndrome |
| Tanaka-Binet intelligence test (Japanese version of Stanford–Binet)a | Takeda 2005360 | 23–35 months with DSM-IV criteria | 57 | 57 | 100 | 31.4 | 3.3 | 23–35 | Months | 45 | 12 | AD, PDD-NOS, Asperger syndrome |
| Snabbt Performance test Pa Intelligence IQ II (SPIQ) – Swedisha | Carlsson 2013390 | Children aged from 4.5 to 6.5 years who were assessed to have autism based on DSM-IV criteria | 198 | 119 | 60 | – | – | 4.5–6.5 | Years | NR | NR | Autistic-like condition, Asperger syndrome, autistic traits |
| Attention | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Behavior Assessment System for Children-Second Edition (BASC-2) | Hill-Chapman 2013434 | Parents of children with ASD | 56 (parents) | 56 | 100 | 3.98 | 1.31 | – | Years | N/A | N/A | AD, PDD-NOS, Asperger syndrome |
| Child Behavior Scale (CBS) | Jahromi 2013431 | 20 TD and 20 children with high-functioning autism | 40 | 20 | 50 | 58.95 | 11.5 | – | Months | 36 | 4 | High-functioning autism |
| Meek 2012435 | 2.75–6.5 years with ADI diagnosis of ASD | 40 | 20 | 50 | 58.95 | 11.5 | – | Months | 36 | 4 | Autism | |
| Child Behavior Checklist (CBCL) Effortful control Conners Rating Scales-Revised |
Baker 2010397 | 33 ‘at-risk’ children, entered study between ages of 2–18 months, assessed at 18, 24, 30 and 36 months. [24 of the 33 children had a sibling with ASD or PDD (DSM-IV diagnosed)] | 33 | 12 | 36 | 18 | – | – | Months | NR | NR | ASD |
| Hartley 2009323 | Children aged 1.5 to 3.9 years based on DSM-IV-TR criteria and ADOS-G classification | 499 | 199 | 40 | – | – | 18–48 | Months | 157 | 42 | AD, PDD-NOS | |
| Peters-Scheffer 2010421 | 3- to 6-year-old children with DSM-IV diagnosis of AD or PDD-NOS | 34 | 34 | 100 | 53.5 | 5.52 | 42–62 | Months | NR | NR | AD, PDD-NOS | |
| Smith 2000413 | 18–42 months with ‘clinical’ diagnosis of ASD | 28 | 28 | 100 | 35.92 | – | – | Months | 23 | 5 | Autism, PDD-NOS | |
| Smith 2010359 | All < 6 years with ADOS/ADI/DSM-IV diagnosis of ASD | 53 | 53 | 100 | 50.1 | 10 | – | Months | 47 | 6 | Autism | |
| Taylor 2012436 | Mothers of ASD children aged mean 3.72 years (SD = 1.82) and 4.18 (SD = 2.65) at diagnosis | 75 (mothers) | 75 | 100 | 3.72 | 18.2 | – | Months | NR | NR | ASD | |
| Jahromi 2013431 | 20 TD and 20 children with high-functioning autism | 40 | 20 | 50 | 58.95 | 11.5 | – | Months | 36 | 4 | High-functioning autism | |
| Escalona 2001271 | Children were aged 3–6 years based on DSM III – R | 20 | 20 | 100 | 5.2 | 1.8 | 3–6 | Years | 12 | 8 | Autism | |
| Osborne 2009351 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | 3.4 | 0.75 | 2.6–4.0 | Years | 59 | 6 | ASD | |
| Reed 2007353 | 2 years 6 months to 4 years old with ‘paediatrician’ diagnosis of ASD | 53 | 53 | 100 | – | – | 2.5–4.0 | Years | NR | NR | ASD | |
| Reed 2013437 | – | 52 | 52 | 100 | 44.4 | 7.9 | 36.77 | Months | 46 | 6 | Childhood autism, PDD-NOS | |
| Student attention – coded observationa | Travers 2011438 | 3–6 years meeting a ‘state educational definition of Autism’ | 17 | 17 | 100 | – | – | 3–6 | Years | NR | NR | Autism |
| Emotion regulation | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baby and Infant Screen for Children with aUtIsm Traits (BISCUIT-Part 2) | Davis 2010439 | Toddlers (17–37 months) with a diagnosis of AD | 513 | 313 | 61 | 27.09 | 5.02 | 17–37 | Months | 371 | 142 | AD, PDD-NOS |
| Behavior Assessment System for Children-Second Edition (BASC-2) | Hill-Chapman 2013434 | Parents of children with ASD | 56 (parents) | 56 | 100 | 3.98 | 1.31 | – | Years | N/A | N/A | AD, PDD-NOS, Asperger syndrome |
| Child Behavior Checklist (CBCL) | Baker 2010397 | 33 ‘at-risk’ children, entered study between ages of 2–18 months, assessed at 18, 24, 30 and 36 months. [24 of the 33 children had a sibling with ASD or PDD (DSM-IV diagnosed)] | 33 | 12 | 36 | 18 | – | – | Months | NR | NR | ASD |
| Hartley 2009323 | Children aged 1.5–3.9 years based on DSM-IV-TR criteria and ADOS-G classification | 499 | 199 | 40 | – | – | 18–48 | Months | 157 | 42 | AD, PDD-NOS | |
| Peters-Scheffer 2010421 | 3- to 6-year-old children with DSM-IV diagnosis of AD or PDD-NOS | 34 | 34 | 100 | 53.5 | 5.52 | 42–62 | Months | NR | NR | AD, PDD-NOS | |
| Smith 2000413 | 18–42 months with ‘clinical’ diagnosis of ASD | 28 | 28 | 100 | 35.92 | – | – | Months | 23 | 5 | Autism, PDD-NOS | |
| Smith 2010359 | All < 6 years with ADOS/ADI/DSM-IV diagnosis of ASD | 53 | 53 | 100 | 50.1 | 10 | – | Months | 47 | 6 | Autism | |
| Taylor 2012436 | Mothers of ASD children aged mean 3.72 years (SD = 1.82) and 4.18 (SD = 2.65) at diagnosis | 75 (mothers) | 75 | 100 | 3.72 | 18.2 | – | Months | NR | NR | ASD | |
| Children’s Global Assessment Scale (CGAS) | Andersson 2013409 | Children aged 1.8 to 3.9 years who met DSM-IV criteria | 40 | 37 | 93 | – | – | 1.8–3.9 | Years | 18 | 19 | AD, ASD, atypical autism, Asperger syndrome |
| Conners Rating Scales-Revised | Escalona 2001271 | Children were aged 3–6 years based on DSM-III-R | 20 | 20 | 100 | 5.2 | 1.8 | 3–6 | Years | 12 | 8 | Autism |
| Osborne 2009351 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | 3.4 | 0.75 | 2.6–4.0 | Years | 59 | 6 | ASD | |
| Reed 2007353 | 2 years 6 months to 4 years old with ‘paediatrician’ diagnosis of ASD | 53 | 53 | 100 | – | – | 2.5–4.0 | Years | NR | NR | ASD | |
| Reed 2013437 | – | 52 | 52 | 100 | 44.4 | 7.9 | 36.77 | Months | 46 | 6 | Childhood autism, PDD-NOS | |
| Developmental Behaviour Checklist | Herring 2006411 | Children were aged between 20 and 51 months who met the DSM-IV criteria for diagnosis | 123 | 84 | 68 | 37.75 | 7.07 | – | Months | 75 | 9 | AD, PDD-NOS |
| Mooney 2006311 | 22–51 months with DSM-IV diagnosis of ASD | 55 | 40 | 73 | 36.95 | 7.26 | 22–51 | Months | 34 | 6 | AD | |
| Remington 2007358 | 30–42 months of age with ADI diagnosis of ASD | 44 | 44 | 100 | 37 | 4.2 | 30–42 | Months | NR | NR | Autism or suspected autism | |
| Roberts 2011405 | 2.2–5 years with DSM-IV diagnosis of ASD | 95 | 95 | 100 | – | – | 26.3–60.3 | Months | 86 | 9 | AD, ASD | |
| Tonge 2012425 | Children were aged 2.5–5 years and diagnosis was made using a combination of medical reviews, ADI-R and CARS | 107 | 107 | 100 | – | – | 2.5–5.0 | Years | 90 | 17 | AD | |
| Emotion Regulation Checklist | Jahromi 2013431 | 20 TD and 20 children with high-functioning autism | 40 | 20 | 50 | 58.95 | 11.5 | – | Months | 36 | 4 | High-functioning autism |
| Infant–Toddler Social–Emotional Assessment (ITSEA) | Ben-Sasson 2008382 | 18–33 months old children, diagnosed by ADOS and ADI | 170 | 170 | 100 | 28 | 4 | 18–33 | Months | 133 | 37 | AD, PDD-NOS |
| Physical skills | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Annett’s Pegs | Szatmari 2000302 | 4- to 6-year-old children (upon entering study) diagnosed by ADI | 134 | 68 | 51 | 66.8 | – | – | Months | 59 | 7 | Autism, Asperger syndrome |
| Beery Visual–Motor Integration Test | Szatmari 2000302 | 4- to 6-year-old children (upon entering study) diagnosed by ADI | 134 | 68 | 51 | 66.8 | – | – | Months | 59 | 7 | Autism, Asperger syndrome |
| Brunet–Lezine’s Oculomotor Coordination Subtest | Baghdadli 2012339 | Age < 7 years, ICD-10 diagnosis of autism | 280 | 280 | 100 | 4.9 | 1.3 | – | Months | 230 | 50 | Childhood autism, atypical autism |
| Functional Independence Measure for Children (WeeFIM) | Jasmin 2009384 | Children aged 3–4 years who had a diagnosis of ASD based on DSM-IV criteria | 35 | 35 | 100 | – | – | 3–4 | Years | 32 | 3 | Autistic, PDD-NOS, Asperger syndrome |
| Infant Motor Maturity and Atypicality Coding Scales | Ozonoff 2008440 | 16–61 months with DSM-IV diagnosis of ASD | 103 | 54 | 52 | – | – | 26–61 | Months | 48 | 6 | AD, PDD-NOS |
| Mullen Scales of Early Learning (MSEL) | Akshoomoff 2006395 | 16–43 months with ADI-R and ADOS diagnosis of ASD | 42 | 22 | 52 | – | – | 16–43 | Months | 17 | 5 | Autism, ASD |
| Anan 2008396 | 25- to 68-month-old children who met the diagnosis of ASD based on DSM-IV criteria | 72 | 72 | 100 | – | – | 25–68 | Months | 61 | 11 | AD, PDD-NOS | |
| Baker 2010397 | 33 ‘at-risk’ children, entered study between ages of 2–18 months, assessed at 18, 24, 30 and 36 months. [24 of the 33 children had a sibling with ASD or PDD (DSM-IV diagnosed)] | 33 | 12 | 36 | 18 | – | – | Months | NR | NR | ASD | |
| Barbaro 2012398 | 12- to 22-month children with AD, ASD or DD/language delay | 154 | 125 | 81 | – | – | 12–27 | Months | 100 | 25 | AD, ASD | |
| Ben Itzchak 2011320 | Children aged 15–35 months were included in the study | 78 | 78 | 100 | – | – | 15–35 | Months | 71 | 7 | Autism | |
| Bishop 2011176 | Children were aged between 2 years to 5 years 11 months | 72 | 53 | 74 | – | – | 1–68 | Months | 44 | 9 | Not given | |
| Brian 2008305 | Children had no diagnosis of ASD but were followed up to 36 months at which point some were diagnosed of ASD | 228 | 35 | 15 | – | – | 6–12 | Months | NR | NR | Autism, Asperger syndrome, PDD-NOS | |
| Dawson 2010321 | 18–30 months, diagnosed by ADOS, ADI and DSM-IV | 48 | 48 | 100 | – | – | 18–31 | Months | 37 | 11 | AD, PDD-NOS | |
| Dereu 2012365 | Children aged 2–4 years; ADOS was used for diagnosis | 17 | 9 | 53 | – | – | 17–39 | Months | 6 | 3 | ASD | |
| Eapen 2013357 | Mean age of 49.6 months | 26 | 26 | 100 | 49.6 | 6.08 | 36–58 | Months | 21 | 5 | AD | |
| Hartley 2009323 | Children aged 1.5 to 3.9 years based on DSM-IV-TR criteria and ADOS-G classification | 499 | 199 | 40 | – | – | 18–49 | Months | 157 | 42 | AD, PDD-NOS | |
| Honey 2008307 | 24–48 months diagnosed by ICD-10 criteria | 104 | 79 | 76 | 37.05 | 6.08 | 24–48 | Months | 65 | 14 | ASD | |
| Landa 2012399 | Assessed at aged 6–36 months – 52/197 subsequently diagnosed ASD by ADOS | 204 | 52 | 25 | 6 | – | – | Months | 43 | 9 | ASD | |
| Landa 2012224 | 22- to 33-month-old children with ASD or autism | 48 | 48 | 100 | 27 | 2.8 | 22–33 | Months | 39 | 9 | ASD | |
| Lloyd 2013400 | 12- to 36-month-old children with ASD | 162 | 162 | 100 | – | – | 12–36 | Months | 140 | 22 | ASD | |
| Luyster 2008129 | Participants were aged 18–33 months and met ADI-R criteria for ASD diagnosis | 164 | 164 | 100 | – | – | 18–33 | Months | 129 | 35 | ASD | |
| Mayo 2013310 | 45–72 months with DSM-IV-TR criteria | 119 | 119 | 100 | 52.22 | 6.09 | 45–72 | Months | 99 | 20 | AD, PDD-NOS | |
| Mitchell 2006392 | ‘At risk’ children with a sibling with ‘clinical’ diagnosis of ASD – 11–15 months at first assessment | 146 | 15 | 10 | – | – | 11–15 | Months | 10 | 5 | ASD | |
| O’Donnell 2012386 | 3–4 years old with DSM-IV diagnosis of ASD | 42 | 42 | 100 | 45.5 | – | 36–59 | Months | NR | NR | Autism, PDD-NOS | |
| Ozonoff 2010313 | Assessed between 6 and 36 months, diagnosed using ADOS | 50 | 25 | 50 | – | – | 6 | Months | 19 | 6 | AD, PDD-NOS | |
| Poon 2012401 | 9–12 months (upon entering study) with ADOS, ADI or CARS diagnosis of ASD | 29 | 29 | 100 | 4.46 | 1.49 | – | Months | 24 | 5 | AD, PDD-NOS, Asperger syndrome | |
| Ray-Subramanian 2012328 | 2–3 years with DSM-IV diagnosis | 115 | 115 | 100 | 31 | 4.1 | – | Months | 97 | 18 | Autism, AD, PDD-NOS | |
| Rogers 2012317 | 14–24 months with ASD | 98 | 98 | 100 | 21 | – | – | Months | 76 | 22 | ASD | |
| Schertz 2013402 | Mean age 24.6 and 27.5 months with ADOS diagnosis | 23 | 23 | 100 | 26.05 | – | – | Months | NR | NR | ASD | |
| Siller 2013403 | 32–82 months with ADI-R and ADOS-G diagnosis | 70 | 70 | 100 | – | – | 32–82 | Months | 64 | 6 | AD | |
| Sullivan 2007330 | Tested at 14–24 months and 30–36 months who met DSM-IV criteria for diagnosis | 51 | 16 | 31 | – | – | 14–36 | Months | 14 | 2 | Autism, PDD-NOS | |
| Tek 2012331 | 16–38 months with ADOS diagnosis | 84 | 84 | 100 | 27 | – | 16–38 | Months | NR | NR | ASD | |
| Thurm 2007404 | 2–3 years and 4–5 years | 118 | 83 | 70 | 29.98 | 4.28 | – | Months | 71 | 12 | Autism, PDD-NOS | |
| Toth 2006284 | 34–52 months with ADI-diagnosis of ASD | 60 | 60 | 100 | 43.6 | 4.3 | 34–52 | Months | 51 | 9 | AD, PDD-NOS | |
| Ventola 2007332 | 16–32 months old with M-CHAT diagnosis of ASD | 195 | 195 | 100 | – | – | 16–32 | Months | 152 | 43 | ASD | |
| Werner 2005316 | 12–57 months with DSM-IV diagnosis of ASD | 145 | 72 | 50 | 43.5 | 4.3 | – | Months | 60 | 12 | AD, PDD-NOS | |
| Zachor 2010335 | 15- to 35-month-old children who met DSM-IV criteria | 71 | 71 | 100 | 25.55 | 4.25 | 15–35 | Months | 71 | 7 | Autism | |
| Peabody Developmental Motor Scales | Jasmin 2009384 | Children aged 3–4 years who had a diagnosis of ASD based on DSM-IV criteria | 35 | 35 | 100 | – | – | 3–4 | Years | 32 | 3 | Autistic, PDD-NOS, Asperger syndrome |
| Provost 2007441 | 21 to 41 month olds with DSM-IV diagnosis of ASD | 38 | 19 | 50 | 30.1 | 4.5 | 21–41 | Months | 15 | 4 | Autism, PDD-NOS | |
| Vineland Adaptive Behavior Scales-Classroom version (VABS-Classroom) | Goin-Kochel 2007427 | Children were aged between 29.6–61.4 months; diagnosis was based on ADOS criteria | 29 | 29 | 100 | 45.7 | 9.6 | 29.6–61.4 | Months | 27 | 2 | Autism, PDD-NOS |
| Vineland Adaptive Behavior Scales (VABS) | Aldred 2004318 | 2 years to 5 years 11 months with ADI diagnosis | 28 | 28 | 100 | – | – | 24–71 | Months | 25 | 3 | AD or ‘classical autism’ |
| Anan 2008396 | 25 to 68 months old children who met the diagnosis of ASD based on DSM-IV criteria | 72 | 72 | 100 | – | – | 25–68 | Months | 61 | 11 | AD, PDD-NOS | |
| Andersson 2013409 | Children aged 1.8 to 3.9 years who met DSM-IV criteria | 40 | 37 | 93 | – | – | 1.8–3.9 | Years | 18 | 19 | AD, ASD, atypical autism, Asperger syndrome | |
| Arick 2003388 | Children between the ages of 2 and 6 years (at baseline) who have been said to have a diagnosis of autism; details of criteria used not provided | 67 | 67 | 100 | – | – | 2–6 | Years | NR | NR | ASD | |
| Baghdadli 2012339 | Age < 7 years, ICD-10 diagnosis of autism | 280 | 280 | 100 | 4.9 | 1.3 | – | Months | 230 | 50 | Childhood autism, atypical autism | |
| Bearss 2013278 | Children were aged between 3 years and 6 years 11 months, and assessed to have autism based on ADOS and clinical observation | 16 | 16 | 100 | – | – | 3–6 | Years | 16 | 0 | AD, PDD-NOS | |
| Ben Itzchak 2011320 | Children aged 15–35 months were included in the study | 78 | 78 | 100 | – | – | 15–35 | Months | 71 | 7 | Autism | |
| Bennett 2008296 | Children aged between 4 and 6 years | 64 | 64 | 100 | – | – | 4–6 | Years | 57 | 7 | Asperger syndrome, high-functioning autism | |
| Carlsson 2013390 | Children aged from 4.5 to 6.5 years who were assessed to have autism based on DSM-IV criteria | 198 | 119 | 60 | – | – | 4.5–6.5 | Years | NR | NR | Autistic-like condition, Asperger syndrome, autistic traits | |
| Cassidy 2008348 | Parents of children aged < 5 years with ICD-10 diagnosis of ASD | 104 | 104 | 100 | – | – | 2–4 | Years | 95 | 9 | ASD | |
| Dawson 2010321 | 18–30 months, diagnosed by ADOS, ADI and DSM-IV | 48 | 48 | 100 | – | – | 18–33 | Months | 37 | 11 | AD, PDD-NOS | |
| Eapen 2013357 | Mean age of 49.6 months | 26 | 26 | 100 | 49.6 | 6.08 | 36–58 | Months | 21 | 5 | AD | |
| Eikeseth 2009410 | 24–42 months with ICD-10 diagnosis of ASD | 23 | 23 | 100 | 34.9 | 5.7 | 28–42 | Months | 17 | 6 | Autism | |
| Eldevik 2012414 | Children aged 2 to 6 who had autism diagnosis based on ICD-10 criteria and ADI-R | 43 | 43 | 100 | 4.26 | 1.48 | 1–6 | Years | 33 | 10 | Autism, PDD-NOS, Asperger | |
| Eriksson 2013415 | Children aged 20–54 months. Criteria not stated | 208 | 208 | 100 | – | – | 20–54 | Months | 176 | 32 | ASD | |
| Gabriels 2007416 | Children had a mean age of 31 months and had a clinical diagnosis of autistic disorder or PDD-NOS based on DSM-IV criteria | 14 | 14 | 100 | 31 | – | – | Months | 10 | 4 | AD, PDD-NOS | |
| Green 2010253 | 24–60 months, ADOS or ADI diagnosed | 152 | 152 | 100 | 45 | – | 24–60 | Months | 138 | 14 | Core autism | |
| Grindle 2012417 | 3- to 7-year-old children with autism | 29 | 29 | 100 | – | – | 43–72 | Months | 25 | 4 | Autism | |
| Hedvall 2013418 | 3.6- to 6.6-year-old children with ASD | 190 | 168 | 88 | 55 | 0.8 | 42–76 | Months | 147 | 21 | AD, PDD-NOS, Asperger syndrome | |
| Herring 2006411 | Children were aged between 20 and 51 months who met the DSM-IV criteria for diagnosis | 123 | 84 | 68 | 37.75 | 7.07 | – | Months | 75 | 9 | AD, PDD-NOS | |
| Honey 2008307 | 24–48 months diagnosed by ICD-10 criteria | 104 | 79 | 76 | 37.05 | 6.08 | 24–48 | Months | 65 | 14 | ASD | |
| Hudry 2010233 | 24- to 59-month-old children with ADOS-G diagnosis | 152 | 152 | 100 | 44.83 | 7.98 | 24–59 | Months | 138 | 14 | Core autism | |
| Jasmin 2009384 | Children aged 3–4 years who had a diagnosis of ASD based on DSM-IV criteria | 35 | 35 | 100 | – | – | 3–4 | Years | 32 | 3 | Autistic, PDD-NOS, Asperger syndrome | |
| Jonsdottir 2007341 | Mean age was 41.43 months; diagnosis was based on ICD-10 criteria | 41 | 41 | 100 | 41.43 | 9.06 | 22–59 | Months | 34 | 7 | Childhood autism | |
| Klintwall 2012419 | 2 years and 3 months to 4 years and 11 months, with clinical diagnosis by paediatrician | 21 | 21 | 100 | 3.6 | – | 2.25–4.9 | Years | 16 | 5 | Autism | |
| Landa 2012224 | 22- to 33-month-old children with ASD or autism | 48 | 48 | 100 | 27 | 2.8 | 22–33 | Months | 39 | 9 | ASD | |
| Vineland Adaptive Behavior Scales-Second Edition (Vineland-II) | Lerna 2012325 | 18–60 months old with diagnosis of autism and little or no functional language | 18 | 18 | 100 | – | – | 18–60 | Months | 17 | 1 | Autism |
| Vineland Adaptive Behavior Scales (VABS) | Lloyd 2013400 | 12- to 36-month-old children with ASD | 162 | 162 | 100 | – | – | 12–37 | Months | 140 | 22 | ASD |
| Vineland Adaptive Behavior Scales-Expanded Form | Luyster 2008129 | Participants were aged 18–33 months and met ADI-R criteria for ASD diagnosis | 164 | 164 | 100 | – | – | 18–33 | Months | 129 | 35 | ASD |
| Vineland Adaptive Behavior Scales (VABS) | Magiati 2007308 | Children aged between 22 and 54 months who met ADI-R criteria for autism/ASD diagnosis | 44 | 44 | 100 | – | – | 22–54 | Months | 39 | 5 | Autism, ASD |
| Magiati 2011309 | Mean age of 3.4 years at start of the study | 44 | 44 | 100 | 38.9 | 7.1 | 27–55 | Months | 39 | 5 | Autism, ASD | |
| Mayo 2013310 | 45–72 months with DSM-IV-TR criteria | 119 | 119 | 100 | 52.22 | 6.09 | 45–72 | Months | 99 | 20 | AD, PDD-NOS | |
| McConkey 2010349 | Children with ASD diagnosis (criteria not given, it was only stated as ‘confirmed diagnosis of ASD from a specialist clinic’) who had a mean age of 2.8 years at start of the study | 62 (families) | 61 | 98 | – | – | < 4 | Years | 55 | 6 | Autism | |
| Munson 2006420 | 38–54 months with DSM-IV diagnosis of ASD | 45 | 45 | 100 | 47.4 | 4.2 | 38–54 | Months | 38 | 7 | AD, PDD-NOS | |
| Munson 2008312 | 24–66 months with ADI or ADOS diagnosis of ASD | 456 | 456 | 100 | 43.4 | 8.7 | 24–66 | Months | 370 | 86 | Autism, ASD | |
| O’Donnell 2012386 | 3–4 years old with DSM-IV diagnosis of ASD | 42 | 42 | 100 | 45.5 | – | 36–59 | Months | NR | NR | Autism, PDD-NOS | |
| Osborne 2008350 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | – | – | 2.6–4.0 | Years | 59 | 6 | ASD | |
| Osborne 2009351 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | 3.4 | 0.75 | 2.6–4.0 | Years | 59 | 6 | ASD | |
| Peters-Scheffer 2010421 | 3- to 6-year-old children with DSM-IV diagnosis of AD or PDD-NOS | 34 | 34 | 100 | 53.5 | 5.52 | 42–62 | Months | NR | NR | AD, PDD-NOS | |
| Poon 2012401 | 9–12 months (upon entering study) with ADOS, ADI or CARS diagnosis of ASD | 29 | 29 | 100 | 4.46 | 1.49 | – | Months | 24 | 5 | AD, PDD-NOS, Asperger syndrome | |
| Pry 2005314 | 21 months to 7 years with ICD-10 diagnosis of ASD | 222 | 222 | 100 | 5 | 1.75 | 1.75–7 | Years | 180 | 42 | Infantile autism | |
| Ray-Subramanian 2011327 | 23–39 months with DSM-IV or ICD-10 diagnosis of ASD | 125 | 125 | 100 | 31 | 4.1 | 23–39 | Months | 108 | 17 | Autism, AD, PDD-NOS | |
| Reed 2007352 | 2 years 6 months to 4 years old diagnosed with ASD | 27 | 27 | 100 | – | – | 2.5–4.0 | Years | 27 | 0 | ASD | |
| Reed 2007353 | 2 years 6 months to 4 years old with ‘paediatrician’ diagnosis of ASD | 53 | 53 | 100 | – | – | 2.5–4.0 | Years | Unclear | Unclear | ASD | |
| Reed 2012354 | 2.5–4 years with GARS diagnosis of ASD | 66 | 66 | 100 | 40.2 | 5.6 | – | Months | 59 | 7 | AD, PDD-NOS | |
| Remington 2007358 | 30–42 months of age with ADI diagnosis of ASD | 44 | 44 | 100 | 37 | 4.2 | 30–42 | Months | NR | NR | Autism or suspected autism | |
| Restall 1994422 | 3–6 years with DSM-III diagnosis of ASD | 18 | 9 | 50 | 64.76 | 6.4 | – | Months | 8 | 1 | Autism | |
| Rickards 2009423 | 3–5 years, 35/59 diagnosed ASD by DSM-IV criteria | 54 | 54 | 100 | 69.65 | – | – | Months | 43 | 11 | ASD | |
| Roberts 2011405 | 2.2–5 years with DSM-IV diagnosis of ASD | 95 | 95 | 100 | – | – | 26.3–60.3 | Months | 86 | 9 | AD, ASD | |
| Rogers 2012317 | 14–24 months with ASD | 98 | 98 | 100 | 21 | – | – | Months | 76 | 22 | ASD | |
| Ruble 2008424 | 40–71 months with DSM-IV diagnosis of ASD | 35 | 35 | 100 | 55.9 | – | 40.9–70.9 | Months | 30 | 5 | Autism | |
| Salt 2002372 | Preschool children in Scotland, (mean 42.36 months) with ICD-10 diagnosis of ASD | 17 | 17 | 100 | 40.015 | – | – | Months | 14 | 3 | Childhood autism | |
| Schertz 2013402 | Mean age 24.6 and 27.5 months with ADOS diagnosis | 23 | 23 | 100 | 26.05 | – | – | Months | NR | NR | ASD | |
| Silva 2007299 | 3–6 years old with DSM-IV diagnosis of ASD | 15 | 15 | 100 | 4.83 | – | 3–6 | Years | 13 | 2 | AD | |
| Silva 2008300 | 3–6 years old with DSM-IV diagnosis of ASD | 26 | 26 | 100 | 56.3 | 12.5 | – | Months | 21 | 5 | Autism | |
| Smith 2000413 | 18–42 months with ‘clinical’ diagnosis of ASD | 28 | 28 | 100 | 35.92 | – | – | Months | 23 | 5 | Autism, PDD-NOS | |
| Smith 2010359 | All < 6 years with ADOS/ADI/DSM-IV diagnosis of ASD | 53 | 53 | 100 | 50.1 | 10 | – | Months | 47 | 6 | Autism | |
| Stahmer 2004355 | 0–3 years with DSM-IV diagnosis | 20 | 20 | 100 | 29.6 | – | 22–33 | Months | 16 | 4 | AD, PDD-NOS | |
| Stone 1999346 | 23–35 months with DSM-III or DSM-IV diagnosis of ASD | 60 | 30 | 50 | 31.3 | 3.3 | 23–35 | Months | 25 | 5 | Autism | |
| Strauss 2012329 | 26–81 months with DSM-IV diagnosis of ASD | 44 | 44 | 100 | – | – | 26–81 | Months | 41 | 3 | Autism, PDD-NOS | |
| Szatmari 2000302 | 4- to 6-year-old children (upon entering study) diagnosed by ADI | 134 | 68 | 51 | 66.8 | – | – | Months | 59 | 7 | Autism, Asperger syndrome | |
| Tonge 2012425 | Children were aged 2.5–5 years and diagnosis was made using a combination of medical reviews, ADI-R and CARS | 107 | 107 | 100 | – | – | 2.5–5.0 | Years | 90 | 17 | AD | |
| Toth 2006284 | 34–52 months with ADI-diagnosis of ASD | 60 | 60 | 100 | 43.6 | 4.3 | 34–52 | Months | 51 | 9 | AD, PDD-NOS | |
| VanMeter 1997426 | Mean ages ranged from 2.9 (SD = 0.77) to 5.7 (SD = 1.31) years meeting DSM-III criteria for ASD | 143 | 57 | 40 | – | – | 5.2–6.0 | Years | 54 | 3 | AD | |
| Ventola 2007332 | 16–32 months old with M-CHAT diagnosis of ASD | 195 | 195 | 100 | – | – | 16–32 | Months | 152 | 43 | ASD | |
| Werner 2005316 | 12–57 months with DSM-IV diagnosis of ASD | 145 | 72 | 50 | 43.5 | 4.3 | – | Months | 60 | 12 | AD, PDD-NOS | |
| Zachor 2010335 | 15- to 35-month-old children who met DSM-IV criteria | 71 | 71 | 100 | 25.55 | 4.25 | 15–35 | Months | 71 | 7 | Autism |
| Social communication | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Autism Diagnostic Interview (ADI) | Ben Itzchak 2008149 | Children aged 19–35 months with autism diagnosis based on DSM-IV criteria | 81 | 44 | 54 | – | – | 16–35 | Months | 43 | 1 | Autism |
| Autism Diagnostic Interview-Revised (ADI-R) | Bennett 2012304 | Children with ASD aged 2–4 years old | 214 | 178 | 83 | – | – | 2–4 | Years | 181 | 33 | AD, Asperger syndrome, PDD-NOS |
| Brian 2008305 | Children had no diagnosis of ASD but were followed up to 36 months at which point some were diagnosed of ASD | 228 | 35 | 15 | – | – | 6–12 | Months | NR | NR | Autism, Asperger syndrome, PDD-NOS | |
| Feldman 2012104 | Children who aged between 1 and 24 months who were ‘at risk’ for autism (they had a sibling with a diagnosis of ASD, Asperger syndrome or PDD-NOS) | 108 (parents) | 108 | 100 | 8 | 5 | – | Months | 74 | 34 | AD, PDD-NOS, Asperger syndrome and high-functioning autism | |
| Hambly 2012306 | Children with ASDs from bilingual and monolingual homes | 75 | 75 | 100 | – | – | 36–78 | Months | 60 | 15 | Autism, ASD, Asperger syndrome, PDD-NOS | |
| Honey 2008307 | 24–48 months diagnosed by ICD-10 criteria | 104 | 79 | 76 | 37.05 | 6.08 | 24–48 | Months | 65 | 14 | ASD | |
| Magiati 2007308 | Children aged between 22 and 54 months who met ADI-R criteria for autism/ASD diagnosis | 44 | 44 | 100 | – | – | 22–54 | Months | 39 | 5 | Autism, ASD | |
| Magiati 2011309 | Mean age of 3.4 years at start of the study | 44 | 44 | 100 | 38.9 | 7.1 | 27–55 | Months | 39 | 5 | Autism, ASD | |
| Mayo 2013310 | 45–72 months with DSM-IV-TR criteria | 119 | 119 | 100 | 52.22 | 6.09 | 45–72 | Months | 99 | 20 | AD, PDD-NOS | |
| Mooney 2006311 | 22–51 months with DSM-IV diagnosis of ASD | 55 | 40 | 73 | 36.95 | 7.26 | 22–51 | Months | 34 | 6 | AD | |
| Munson 2008312 | 24–66 months with ADI or ADOS diagnosis of ASD | 456 | 456 | 100 | 43.4 | 8.7 | 24–66 | Months | 370 | 86 | Autism, ASD | |
| Ozonoff 2010313 | Assessed between 6 and 36 months, diagnosed using ADOS | 50 | 25 | 50 | – | – | 6 | Months | 19 | 6 | AD, PDD-NOS | |
| Autism Diagnostic Interview (ADI) | Pry 2005314 | 21 months to 7 years with ICD-10 diagnosis of ASD | 222 | 222 | 100 | 5 | 1.75 | 1.75–7.0 | Years | 180 | 42 | Infantile autism |
| Autism Diagnostic Interview-Revised (ADI-R) | Richler 2007315 | Up to 3 years old, with ‘clinical’ diagnosis of ASD | 279 | 192 | 69 | – | – | 0–37 | Months | 162 | 30 | Autism, PDD-NOS |
| Autism Diagnostic Interview (ADI) | Werner 2005316 | 12–57 months with DSM-IV diagnosis of ASD | 145 | 72 | 50 | 43.5 | 4.3 | – | Months | 60 | 12 | AD, PDD-NOS |
| Autism Diagnostic Observation Scale-Toddler Module (ADOS-T) | Rogers 2012317 | 14–24 months with ASD | 98 | 98 | 100 | 21 | – | – | Months | 76 | 22 | ASD |
| Autism Diagnostic Observation Schedule (ADOS) | Aldred 2004318 | 2 years to 5 years 11 months with ADI diagnosis | 28 | 28 | 100 | – | – | 24–71 | Months | 25 | 3 | AD or ‘classical autism’ |
| Aldred 2012319 | Children aged 2–5 years assessed using ADOS and ADI-R | 28 | 28 | 100 | – | – | 2–5 | Years | 25 | 3 | Autism | |
| Ben Itzchak 2008149 | Children aged 19–35 months with autism diagnosis based on DSM-IV criteria | 81 | 44 | 54 | – | – | 16–35 | Months | 43 | 1 | Autism | |
| Ben Itzchak 2011320 | Children aged 15–35 months were included in the study | 78 | 78 | 100 | – | – | 15–35 | Months | 71 | 7 | Autism | |
| Bennett 2012304 | Children with ASD aged 2–4 years old | 214 | 178 | 83 | – | – | 2–4 | Years | 181 | 33 | AD, Asperger syndrome, PDD-NOS | |
| Brian 2008305 | Children had no diagnosis of ASD but were followed up to 36 months at which point some were diagnosed of ASD | 228 | 35 | 15 | – | – | 6–12 | Months | NR | NR | Autism, Asperger syndrome, PDD-NOS | |
| Dawson 2010321 | 18–30 months, diagnosed by ADOS, ADI and DSM-IV | 48 | 48 | 100 | – | – | 18–30 | Months | 37 | 11 | AD, PDD-NOS | |
| Gotham 2012322 | Best-estimate clinical diagnosis of ASD at one or more time points | 345 | 345 | 100 | 3.3 | 1.4 | – | Years | 282 | 63 | Autism, PDD-NOS | |
| Autism Diagnostic Observation Schedule-Generic (ADOS-G) | Green 2010253 | 24–60 months, ADOS or ADI diagnosed | 152 | 152 | 100 | 45 | – | 24–60 | Months | 138 | 14 | Core autism |
| Hartley 2009323 | Children aged 1.5–3.9 years based on DSM-IV-TR criteria and ADOS-G classification | 499 | 199 | 40 | – | – | 18–47 | Months | 157 | 42 | AD, PDD-NOS | |
| Autism Diagnostic Observation Schedule (ADOS) | Landa 2012224 | 22- to 33-month-old children with ASD or autism | 48 | 48 | 100 | 27 | 2.8 | 22–33 | Months | 39 | 9 | ASD |
| Lerna 2012325 | 18–60 months old with diagnosis of autism and little or no functional language | 18 | 18 | 100 | – | – | 18–60 | Months | 17 | 1 | Autism | |
| Luyster 2008129 | Participants were aged 18–33 months and met ADI-R criteria for ASD diagnosis | 164 | 164 | 100 | – | – | 18–33 | Months | 129 | 35 | ASD | |
| Autism Diagnostic Observation Schedule-Generic (ADOS-G) | Munson 2008312 | 24–66 months with ADI or ADOS diagnosis of ASD | 456 | 456 | 100 | 43.4 | 8.7 | 24–66 | Months | 370 | 86 | Autism, ASD |
| Oosterling 2010326 | 12–42 months old with ‘clinical’ diagnosis of ASD | 80 | 80 | 100 | 34.8 | – | – | Months | 62 | 18 | Autism, PDD-NOS | |
| Ray-Subramanian 2011327 | 23–39 months with DSM-IV or ICD-10 diagnosis of ASD | 125 | 125 | 100 | 31 | 4.1 | 23–39 | Months | 108 | 17 | Autism, AD, PDD-NOS | |
| Ray-Subramanian 2012328 | 2–3 years with DSM-IV diagnosis | 115 | 115 | 100 | 31 | 4.1 | – | Months | 97 | 18 | Autism, AD, PDD-NOS | |
| Strauss 2012329 | 26–81 months with DSM-IV diagnosis of ASD | 44 | 44 | 100 | – | – | 26–81 | Months | 41 | 3 | Autism, PDD-NOS | |
| Sullivan 2007330 | Tested at 14–24 months and 30–36 months who met DSM-IV criteria for diagnosis | 51 | 16 | 31 | – | – | 14–36 | Months | 14 | 2 | Autism, PDD-NOS | |
| Tek 2012331 | 16–38 months with ADOS diagnosis | 84 | 84 | 100 | 27 | – | 16–38 | Months | NR | NR | ASD | |
| Ventola 2007332 | 16–32 months old with M-CHAT diagnosis of ASD | 195 | 195 | 100 | – | – | 16–32 | Months | 152 | 43 | ASD | |
| Autism Diagnostic Observation Schedule (ADOS) | Werner 2005316 | 12–57 months with DSM-IV diagnosis of ASD | 145 | 72 | 50 | 43.5 | 4.3 | – | Months | 60 | 12 | AD, PDD-NOS |
| Wong 2010333 | 17–36 months children diagnosed by DSM-IV, ADI and ADOS | 17 | 17 | 100 | – | – | 17–36 | Months | 16 | 1 | – | |
| Zachor 2006335 | Participants were aged 23–33 months and met DSM-IV criteria for autism diagnosis | 39 | 39 | 100 | – | – | 23–33 | Months | 37 | 2 | Autism | |
| Zachor 2010335 | 15- to 35-month-old children who met DSM-IV criteria | 71 | 71 | 100 | 25.55 | 4.25 | 15–35 | Months | 71 | 7 | Autism | |
| Autism Screening Instrument for Educational Planning (ASIEP) | Arick 2003388 | Children between the ages of 2 and 6 years (at baseline) who have been said to have a diagnosis of autism; details of criteria used not provided | 67 | 67 | 100 | – | – | 2–6 | Years | NR | NR | ASD |
| Communication and Symbolic Behavior Scales-Developmental Profile (Caregiver Questionnaire) (CSBS-DP-CQ); (Wetherby and Prizant 2002) | Tek 2012331 | 16–38 months with ADOS diagnosis | 84 | 84 | 100 | 27 | – | 16–38 | Months | NR | NR | ASD |
| Early Social Communication Scale (ESCS) | Dereu 2012365 | Children aged 2–4 years; ADOS was used for diagnosis | 17 | 9 | 53 | – | – | 17–39 | Months | 6 | 3 | ASD |
| Goods 2013366 | 36- to 60-month-old children with autism (ADOS assessment) | 15 | 15 | 100 | 51.9 | – | – | Months | NR | NR | Autism | |
| Ingersoll 2012286 | 27 children between 27 and 47 months old who met DSM-IV-TR criteria | 29 | 29 | 100 | 37.9 | – | 22–47 | Months | 24 | 5 | AD | |
| Kaale 2012294 | Children aged 29–60 months who had a diagnosis of autistic disorder based on ICD-10 criteria | 61 | 61 | 100 | – | – | 24–60 | Months | 48 | 13 | Autism | |
| Kalas 2012367 | 4- to 6-year-old children with ASD | 30 | 30 | 100 | – | – | 4–6 | Years | 28 | 2 | ASD | |
| Kasari 2006368 | Children were aged 3 to 4 years and had a diagnosis of autism based on ADI-R and ADOS criteria | 58 | 58 | 100 | – | – | 3–4 | Years | 46 | 12 | Autism | |
| Lawton 2012369 | Preschool age children who had a diagnosis of autism, validated by ADI-R | 52 | 52 | 100 | 43.05 | 6.86 | – | Months | 40 | 12 | Autism | |
| Luyster 2008129 | Participants were aged 18–33 months and met ADI-R criteria for ASD diagnosis | 164 | 164 | 100 | – | – | 18–33 | Months | 129 | 35 | ASD | |
| Paparella 2011370 | 20–72 months old with ADI diagnosis of ASD | 83 | 50 | 60 | 53.6 | – | 36–72 | Months | 42 | 8 | Autism | |
| Remington 2007358 | 30–42 months of age with ADI diagnosis of ASD | 44 | 44 | 100 | 37 | 4.2 | 30–42 | Months | NR | NR | Autism or suspected autism | |
| Roos 2008371 | 30–38 months with ADOS diagnosis of ASD | 20 | 20 | 100 | 33.2 | – | 30–38 | Months | 16 | 4 | ASD | |
| Wong 2013373 | 3–6 years with CARS diagnosis | 33 | 33 | 100 | 56.79 | – | – | Months | 29 | 4 | Autism | |
| Yoder 2006374 | 1.9–4.5 years with ADOS diagnosis of ASD | 36 | 36 | 100 | 2.9 | – | – | Years | 31 | 5 | Autism, PDD-NOS | |
| Salt 2002372 | Preschool children in Scotland, (mean 42.36 months) with ICD-10 diagnosis of ASD | 17 | 17 | 100 | 40.015 | – | – | Months | 14 | 3 | Childhood autism | |
| Early Social Communication Scales (ESCS)-Abridged | Yoder 2010375 | 18–60 months with ADOS diagnosis of ASD | 36 | 36 | 100 | 2.9 | – | – | Years | NR | NR | Autism, PDD-NOS |
| Pragmatics Profile | Roberts 2011405 | 2.2–5 years with DSM-IV diagnosis of ASD | 95 | 95 | 100 | – | – | 26.3–60.3 | Months | 86 | 9 | AD, ASD |
| Social Communication Assessment for Toddlers with Autism (SCATA) | Drew 2007137 | Children aged between 21 to 43 months with a diagnosis of autism or PDD based on ICD-10 criteria | 46 | 46 | 100 | 25 | 5.6, NR | 18–44, NR | Months | 39 | 7 | Autism, PDD-NOS |
| Social Communication Behavior Codes | Ozonoff 2010313 | Assessed between 6 and 36 months, diagnosed using ADOS | 50 | 25 | 50 | – | – | 6 | Months | 19 | 6 | AD, PDD-NOS |
| Vineland Adaptive Behavior Scales-Classroom version (VABS-Classroom) | Goin-Kochel 2007427 | Children were aged between 29.6–61.4 months; diagnosis was based on ADOS criteria | 29 | 29 | 100 | 45.7 | 9.6 | 29.6–61.4 | Months | 27 | 2 | Autism, PDD-NOS |
| Vineland Adaptive Behavior Scales (VABS) | Aldred 2004318 | 2 years to 5 years 11 months with ADI diagnosis | 28 | 28 | 100 | – | – | 24–71 | Months | 25 | 3 | AD or ‘classical autism’ |
| Anan 2008396 | 25 to 68 months old children who met the diagnosis of ASD based on DSM-IV criteria | 72 | 72 | 100 | – | – | 25–68 | Months | 61 | 11 | AD, PDD-NOS | |
| Andersson 2013409 | Children aged 1.8 to 3.9 years who met DSM-IV criteria | 40 | 37 | 93 | – | – | 1.8–3.9 | Years | 18 | 19 | AD, ASD, atypical autism, Asperger syndrome | |
| Arick 2003388 | Children between the ages of 2 and 6 years (at baseline) who have been said to have a diagnosis of autism; details of criteria used not provided | 67 | 67 | 100 | – | – | 2–6 | Years | NR | NR | ASD | |
| Baghdadli 2012339 | Age < 7 years, ICD-10 diagnosis of autism | 280 | 280 | 100 | 4.9 | 1.3 | – | Months | 230 | 50 | Childhood autism, atypical autism | |
| Bearss 2013278 | Children were aged between 3 years and 6 years 11 months, and assessed to have autism based on ADOS and clinical observation | 16 | 16 | 100 | – | – | 3–6 | Years | 16 | 0 | AD, PDD-NOS | |
| Bennett 2008296 | Children aged between 4 and 6 years | 64 | 64 | 100 | – | – | 4–6 | Years | 57 | 7 | Asperger syndrome, high-functioning autism | |
| Carlsson 2013390 | Children aged from 4.5 to 6.5 years who were assessed to have autism based on DSM-IV criteria | 198 | 119 | 60 | – | – | 4.5–6.5 | Years | NR | NR | Autistic-like condition, Asperger syndrome, autistic traits | |
| Cassidy 2008348 | Parents of children aged < 5 years with ICD-10 diagnosis of ASD | 104 | 104 | 100 | – | – | 2–4 | Years | 95 | 9 | ASD | |
| Dawson 2010321 | 18–30 months, diagnosed by ADOS, ADI and DSM-IV | 48 | 48 | 100 | – | – | 18–33 | Months | 37 | 11 | AD, PDD-NOS | |
| Eikeseth 2009410 | 24–42 months with ICD-10 diagnosis of ASD | 23 | 23 | 100 | 34.9 | 5.7 | 28–42 | Months | 17 | 6 | Autism | |
| Eldevik 2012414 | Children aged 2 to 6 who had autism diagnosis based on ICD-10 criteria and ADI-R | 43 | 43 | 100 | 4.26 | 1.48 | 1–6 | Years | 33 | 10 | Autism, PDD-NOS, Asperger syndrome | |
| Eriksson 2013415 | Children aged 20–54 months. Criteria not stated | 208 | 208 | 100 | – | – | 20–54 | Months | 176 | 32 | ASD | |
| Gabriels 2007416 | Children had a mean age of 31 months and had a clinical diagnosis of autistic disorder or PDD-NOS based on DSM-IV criteria | 14 | 14 | 100 | 31 | – | – | Months | 10 | 4 | AD, PDD-NOS | |
| Green 2010253 | 24–60 months, ADOS or ADI diagnosed | 152 | 152 | 100 | 45 | – | 24–60 | Months | 138 | 14 | Core autism | |
| Grindle 2012417 | 3- to 7-year-old children with autism | 29 | 29 | 100 | – | – | 43–72 | Months | 25 | 4 | Autism | |
| Hedvall 2013418 | 3.6- to 6.6-year-old children with ASD | 190 | 168 | 88 | 55 | 0.8 | 42–76 | Months | 147 | 21 | AD, PDD-NOS, Asperger syndrome | |
| Herring 2006411 | Children were aged between 20 and 51 months who met the DSM-IV criteria for diagnosis | 123 | 84 | 68 | 37.75 | 7.07 | – | Months | 75 | 9 | AD, PDD-NOS | |
| Honey 2008307 | 24–48 months diagnosed by ICD-10 criteria | 104 | 79 | 76 | 37.05 | 6.08 | 24–48 | Months | 65 | 14 | ASD | |
| Hudry 2010233 | 24- to 59-month-old children with ADOS-G diagnosis | 152 | 152 | 100 | 44.83 | 7.98 | 24–59 | Months | 138 | 14 | Core autism | |
| Ben Itzchak 2011320 | Children aged 15–35 months were included in the study | 78 | 78 | 100 | – | – | 15–35 | Months | 71 | 7 | Autism | |
| Jasmin 2009384 | Children aged 3–4 years who had a diagnosis of ASD based on DSM-IV criteria | 35 | 35 | 100 | – | – | 3–4 | Years | 32 | 3 | Autistic, PDD-NOS, Asperger syndrome | |
| Jonsdottir 2007341 | Mean age was 41.43 months; diagnosis was based on ICD-10 criteria | 41 | 41 | 100 | 41.43 | 9.06 | 22–59 | Months | 34 | 7 | Childhood autism | |
| Klintwall 2012419 | 2 years and 3 months to 4 years and 11 months, with clinical diagnosis by paediatrician | 21 | 21 | 100 | 3.6 | – | 2.25–4.9 | Years | 16 | 5 | Autism | |
| Landa 2012224 | 22- to 33-month-old children with ASD or autism | 48 | 48 | 100 | 27 | 2.8 | 22–33 | Months | 39 | 9 | ASD | |
| Lerna 2012325 | 18–60 months old with diagnosis of autism and little or no functional language | 18 | 18 | 100 | – | – | 18–60 | Months | 17 | 1 | Autism | |
| Lloyd 2013400 | 12- to 36-month-old children with ASD | 162 | 162 | 100 | – | – | 12–37 | Months | 140 | 22 | ASD | |
| Luyster 2008129 | Participants were aged 18–33 months and met ADI-R criteria for ASD diagnosis | 164 | 164 | 100 | – | – | 18–33 | Months | 129 | 35 | ASD | |
| Magiati 2007308 | Children aged between 22 and 54 months who met ADI-R criteria for autism/ASD diagnosis | 44 | 44 | 100 | – | – | 22–54 | Months | 39 | 5 | Autism, ASD | |
| Magiati 2011309 | Mean age of 3.4 years at start of the study | 44 | 44 | 100 | 38.9 | 7.1 | 27–55 | Months | 39 | 5 | Autism, ASD | |
| Mayo 2013310 | 45–72 months with DSM-IV-TR criteria | 119 | 119 | 100 | 52.22 | 6.09 | 45–72 | Months | 99 | 20 | AD, PDD-NOS | |
| McConkey 2010349 | Children with ASD diagnosis (criteria not given, it was only stated as ‘confirmed diagnosis of ASD from a specialist clinic’) who had a mean age of 2.8 years at start of the study | 62 (families) | 61 | 98 | – | – | < 4 | Years | 55 | 6 | Autism | |
| Munson 2006420 | 38–54 months with DSM-IV diagnosis of ASD | 45 | 45 | 100 | 47.4 | 4.2 | 38–54 | Months | 38 | 7 | AD, PDD-NOS | |
| Munson 2008312 | 24–66 months with ADI or ADOS diagnosis of ASD | 456 | 456 | 100 | 43.4 | 8.7 | 24–66 | Months | 370 | 86 | Autism, ASD | |
| O’Donnell 2012386 | 3–4 years old with DSM-IV diagnosis of ASD | 42 | 42 | 100 | 45.5 | – | 36–59 | Months | NR | NR | Autism, PDD-NOS | |
| Eapen 2013357 | Mean age of 49.6 months | 26 | 26 | 100 | 49.6 | 6.08 | 36–58 | Months | 21 | 5 | AD | |
| Osborne 2008350 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | – | – | 2.6–4 | Years | 59 | 6 | ASD | |
| Osborne 2009351 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | 3.4 | 0.75 | 2.6–4.0 | Years | 59 | 6 | ASD | |
| Peters-Scheffer 2010421 | 3- to 6-year-old children with DSM-IV diagnosis of AD or PDD-NOS | 34 | 34 | 100 | 53.5 | 5.52 | 42–62 | Months | NR | NR | AD, PDD-NOS | |
| Poon 2012401 | 9–12 months (upon entering study) with ADOS, ADI or CARS diagnosis of ASD | 29 | 29 | 100 | 4.46 | 1.49 | – | Months | 24 | 5 | AD, PDD-NOS, Asperger syndrome | |
| Pry 2005314 | 21 months to 7 years with ICD-10 diagnosis of ASD | 222 | 222 | 100 | 5 | 1.75 | 1.75–7 | Years | 180 | 42 | Infantile autism | |
| Ray-Subramanian 2011327 | 23–39 months with DSM-IV or ICD-10 diagnosis of ASD | 125 | 125 | 100 | 31 | 4.1 | 23–39 | Months | 108 | 17 | Autism, AD, PDD-NOS | |
| Reed 2007352 | 2 years 6 months to 4 years old diagnosed with ASD | 27 | 27 | 100 | – | – | 2.5–4.0 | Years | 27 | 0 | ASD | |
| Reed 2007353 | 2 years 6 months to 4 years old with ‘paediatrician’ diagnosis of ASD | 53 | 53 | 100 | – | – | 2.5–4.0 | Years | Unclear | Unclear | ASD | |
| Reed 2012354 | 2.5–4 years with GARS diagnosis of ASD | 66 | 66 | 100 | 40.2 | 5.6 | – | Months | 59 | 7 | AD, PDD-NOS | |
| Remington 2007358 | 30–42 months of age with ADI diagnosis of ASD | 44 | 44 | 100 | 37 | 4.2 | 30–42 | Months | NR | NR | Autism or suspected autism | |
| Restall 1994422 | 3–6 years with DSM-III diagnosis of ASD | 18 | 9 | 50 | 64.76 | 6.4 | – | Months | 8 | 1 | Autism | |
| Rickards 2009423 | 3–5 years, 35/59 diagnosed ASD by DSM-IV criteria | 54 | 54 | 100 | 69.65 | – | – | Months | 43 | 11 | ASD | |
| Roberts 2011405 | 2.2–5 years with DSM-IV diagnosis of ASD | 95 | 95 | 100 | – | – | 26.3–60.3 | Months | 86 | 9 | AD, ASD | |
| Rogers 2012317 | 14–24 months with ASD | 98 | 98 | 100 | 21 | – | – | Months | 76 | 22 | ASD | |
| Ruble 2008424 | 40–71 months with DSM-IV diagnosis of ASD | 35 | 35 | 100 | 55.9 | – | 40.9–70.9 | Months | 30 | 5 | Autism | |
| Salt 2002372 | Preschool children in Scotland, (mean 42.36 months) with ICD-10 diagnosis of ASD | 17 | 17 | 100 | 40.015 | – | – | Months | 14 | 3 | Childhood autism | |
| Schertz 2013402 | Mean age 24.6 and 27.5 months with ADOS diagnosis | 23 | 23 | 100 | 26.05 | – | – | Months | NR | NR | ASD | |
| Silva 2007299 | 3–6 years old with DSM-IV diagnosis of ASD | 15 | 15 | 100 | 4.83 | – | 3–6 | Years | 13 | 2 | AD | |
| Silva 2008300 | 3–6 years old with DSM-IV diagnosis of ASD | 26 | 26 | 100 | 56.3 | 12.5 | – | Months | 21 | 5 | Autism | |
| Smith 2000413 | 18–42 months with ‘clinical’ diagnosis of ASD | 28 | 28 | 100 | 35.92 | – | – | Months | 23 | 5 | Autism, PDD-NOS | |
| Smith 2010359 | All < 6 years with ADOS/ADI/DSM-IV diagnosis of ASD | 53 | 53 | 100 | 50.1 | 10 | – | Months | 47 | 6 | Autism | |
| Stahmer 2004355 | 0–3 years with DSM-IV diagnosis | 20 | 20 | 100 | 29.6 | – | 22–33 | Months | 16 | 4 | AD, PDD-NOS | |
| Stone 1999346 | 23–35 months with DSM-III or DSM-IV diagnosis of ASD | 60 | 30 | 50 | 31.3 | 3.3 | 23–35 | Months | 25 | 5 | Autism | |
| Strauss 2012329 | 26–81 months with DSM-IV diagnosis of ASD | 44 | 44 | 100 | – | – | 26–81 | Months | 41 | 3 | Autism, PDD-NOS | |
| Szatmari 2000302 | 4- to 6-year-old children (upon entering study) diagnosed by ADI | 134 | 68 | 51 | 66.8 | – | – | Months | 59 | 7 | Autism, Asperger syndrome | |
| Tonge 2012425 | Children were aged 2.5–5 years and diagnosis was made using a combination of medical reviews, ADI-R and CARS | 107 | 107 | 100 | – | – | 2.5–5.0 | Years | 90 | 17 | AD | |
| Toth 2006284 | 34–52 months with ADI-diagnosis of ASD | 60 | 60 | 100 | 43.6 | 4.3 | 34–52 | Months | 51 | 9 | AD, PDD-NOS | |
| VanMeter 1997426 | Mean ages ranged from 2.9 (SD = 0.77) to 5.7 (SD = 1.31) years meeting DSM-III criteria for ASD | 143 | 57 | 40 | – | – | 5.2–6.0 | Years | 54 | 3 | AD | |
| Ventola 2007332 | 16–32 months old with M-CHAT diagnosis of ASD | 195 | 195 | 100 | – | – | 16–32 | Months | 152 | 43 | ASD | |
| Werner 2005316 | 12–57 months with DSM-IV diagnosis of ASD | 145 | 72 | 50 | 43.5 | 4.3 | – | Months | 60 | 12 | AD, PDD-NOS | |
| Zachor 2010335 | 15- to 35-month-old children who met DSM-IV criteria | 71 | 71 | 100 | 25.55 | 4.25 | 15–35 | Months | 71 | 7 | Autism | |
| Parent Surveya | Arick 2003388 | Children between the ages of 2 and 6 years (at baseline) who have been said to have a diagnosis of autism; details of criteria used not provided | 67 | 67 | 100 | – | – | 2–6 | Years | NR | NR | ASD |
| Caregiver–child interactionb | Kasari 2006368 | Children were aged 3 to 4 years and had a diagnosis of autism based on ADI-R and ADOS criteria | 58 | 58 | 100 | – | – | 3–4 | Years | 46 | 12 | Autism |
| Classroom and playground behaviour observationsb | Escalona 2001271 | Children were aged 3 to 6 years based on DSM III – R | 20 | 20 | 100 | 5.2 | 1.8 | 3–6 | Years | 12 | 8 | Autism |
| Coding of initiation of joint attentionb | Ingersoll 2012286 | 27 children between 27 and 47 months old who met DSM-IV-TR criteria | 29 | 29 | 100 | 37.9 | – | 22–47 | Months | 24 | 5 | AD |
| Examiner Ratings of Social Engagementb | Ozonoff 2010313 | Assessed between 6 and 36 months, diagnosed using ADOS | 50 | 25 | 50 | – | – | 6 | Months | 19 | 6 | AD, PDD-NOS |
| Parent–child interactionb | Green 2010253 | 24–60 months, ADOS or ADI diagnosed | 152 | 152 | 100 | 45 | – | 24–60 | Months | 138 | 14 | Core autism |
| Parent–child interactionb | Aldred 2012319 | Children aged 2–5 years assessed using ADOS and ADI-R | 28 | 28 | 100 | – | – | 2–5 | Years | 25 | 3 | Autism |
| Preschool teacher–child playb | Kaale 2012294 | Children aged 29–60 months who had a diagnosis of autistic disorder based on ICD-10 criteria | 61 | 61 | 100 | – | – | 24–60 | Months | 48 | 13 | Autism |
| Unstructured free play with examinerb | Lerna 2012325 | 18–60 months old with diagnosis of autism and little or no functional language | 18 | 18 | 100 | – | – | 18–60 | Months | 17 | 1 | Autism |
| Video coding proceduresb | Colgan 2006379 | Children aged 8–12 months with diagnosis of autism based on DSM-III-R or DSM-IV criteria | 35 | 21 | 60 | – | – | 0–2 | Years | 17 | 4 | AD |
| Video recording of child in classroom activitiesb | Ingersoll 2001380 | Children ages 26 to 41 months who met DSM-IV criteria for ASD | 9 | 6 | 67 | – | – | 26–41 | Months | NR | NR | Autism, PDD-NOS |
| Social functioning | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Autism Diagnostic Interview (ADI) | Ben Itzchak 2008149 | Children aged 19–35 months with autism diagnosis based on DSM-IV criteria | 81 | 44 | 54 | – | – | 16–35 | Months | 43 | 1 | Autism |
| Autism Diagnostic Interview-Revised (ADI-R) | Bennett 2012304 | Children with ASD aged 2–4 years old | 214 | 178 | 83 | – | – | 2–4 | Years | 181 | 33 | AD, Asperger syndrome, PDD-NOS |
| Brian 2008305 | Children had no diagnosis of ASD but were followed up to 36 months at which point some were diagnosed of ASD | 228 | 35 | 15 | – | – | 6–12 | Months | NR | NR | Autism, Asperger syndrome, PDD-NOS | |
| Feldman 2012104 | Children who aged between 1 and 24 months who were ‘at risk’ for autism (they had a sibling with a diagnosis of ASD, Asperger syndrome or PDD-NOS) | 108 (parents) | 108 | 100 | 8 | 5 | – | Months | 74 | 34 | AD, PDD-NOS, Asperger syndrome and high-functioning autism | |
| Hambly 2012306 | Children with ASDs from bilingual and monolingual homes | 75 | 75 | 100 | – | – | 36–78 | Months | 60 | 15 | Autism, ASD, Asperger syndrome, PDD-NOS | |
| Autism Diagnostic Interview (ADI) | Honey 2008307 | 24–48 months diagnosed by ICD-10 criteria | 104 | 79 | 76 | 37.05 | 6.08 | 24–48 | Months | 65 | 14 | ASD |
| Autism Diagnostic Interview-Revised (ADI-R) | Magiati 2007308 | Children aged between 22 and 54 months who met ADI-R criteria for autism/ASD diagnosis | 44 | 44 | 100 | – | – | 22–54 | Months | 39 | 5 | Autism, ASD |
| Magiati 2011309 | Mean age of 3.4 years at start of the study | 44 | 44 | 100 | 38.9 | 7.1 | 27–55 | Months | 39 | 5 | Autism, ASD | |
| Mayo 2013310 | 45–72 months with DSM-IV-TR criteria | 119 | 119 | 100 | 52.22 | 6.09 | 45–72 | Months | 99 | 20 | AD, PDD-NOS | |
| Mooney 2006311 | 22–51 months with DSM-IV diagnosis of ASD | 55 | 40 | 73 | 36.95 | 7.26 | 22–51 | Months | 34 | 6 | AD | |
| Munson 2008312 | 24–66 months with ADI or ADOS diagnosis of ASD | 456 | 456 | 100 | 43.4 | 8.7 | 24–66 | Months | 370 | 86 | Autism, ASD | |
| Ozonoff 2010313 | Assessed between 6 and 36 months, diagnosed using ADOS | 50 | 25 | 50 | – | – | 6 | Months | 19 | 6 | AD, PDD-NOS | |
| Autism Diagnostic Interview (ADI) | Pry 2005314 | 21 months to 7 years with ICD-10 diagnosis of ASD | 222 | 222 | 100 | 5 | 1.75 | 1.75–7 | Years | 180 | 42 | Infantile autism |
| Autism Diagnostic Interview-Revised (ADI-R) | Richler 2007315 | Up to 3 years old, with ‘clinical’ diagnosis of ASD | 279 | 192 | 69 | – | – | 0–37 | Months | 162 | 30 | Autism, PDD-NOS |
| Autism Diagnostic Interview (ADI) | Werner 2005316 | 12–57 months with DSM-IV diagnosis of ASD | 145 | 72 | 50 | 43.5 | 4.3 | – | Months | 60 | 12 | AD, PDD-NOS |
| Child Behavior Scale (CBS) | Jahromi 2013431 | 20 TD and 20 children with high-functioning autism | 40 | 20 | 50 | 58.95 | 11.5 | – | Months | 36 | 4 | High-functioning autism |
| Meek 2012435 | 2.75–6.5 years with ADI diagnosis of ASD | 40 | 20 | 50 | 58.95 | 11.5 | – | Months | 36 | 4 | Autism | |
| Nisonger Child Behavior Rating Scales | Remington 2007358 | 30–42 months of age with ADI diagnosis of ASD | 44 | 44 | 100 | 37 | 4.2 | 30–42 | Months | NR | NR | Autism or suspected autism |
| Social Behavior Rating Scale | Vorgraft 2007347 | 38–49-month-old children with DSM-IV diagnosis of PDD-NOS | 23 | 23 | 100 | 42.8 | – | 38–19 | Months | 15 | 8 | Autism, PDD-NOS |
| Vineland Adaptive Behavior Scales-Classroom version (VABS-Classroom) | Goin-Kochel 2007427 | Children were aged between 29.6–61.4 months; diagnosis was based on ADOS criteria | 29 | 29 | 100 | 45.7 | 9.6 | 29.6–61.4 | Months | 27 | 2 | Autism, PDD-NOS |
| Vineland Adaptive Behavior Scales (VABS) | Aldred 2004318 | 2 years to 5 years 11 months with ADI diagnosis | 28 | 28 | 100 | – | – | 24–71 | Months | 25 | 3 | AD or ‘classical autism’ |
| Anan 2008396 | 25 to 68 months old children who met the diagnosis of ASD based on DSM-IV criteria | 72 | 72 | 100 | – | – | 25–68 | Months | 61 | 11 | AD, PDD-NOS | |
| Andersson 2013409 | Children aged 1.8 to 3.9 years who met DSM-IV criteria | 40 | 37 | 93 | – | – | 1.8–3.9 | Years | 18 | 19 | AD, ASD, atypical autism, Asperger syndrome | |
| Arick 2003388 | Children between the ages of 2 and 6 years (at baseline) who have been said to have a diagnosis of autism; details of criteria used not provided | 67 | 67 | 100 | – | – | 2–6 | Years | NR | NR | ASD | |
| Baghdadli 2012339 | Age < 7 years, ICD-10 diagnosis of autism | 280 | 280 | 100 | 4.9 | 1.3 | – | Months | 230 | 50 | Childhood autism, atypical autism | |
| Bearss 2013278 | Children were aged between 3 years and 6 years 11 months, and assessed to have autism based on ADOS and clinical observation | 16 | 16 | 100 | – | – | 3–6 | Years | 16 | 0 | AD, PDD-NOS | |
| Bennett 2008296 | Children aged between 4 and 6 years | 64 | 64 | 100 | – | – | 4–6 | Years | 57 | 7 | Asperger syndrome, high-functioning autism | |
| Carlsson 2013390 | Children aged from 4.5 to 6.5 years who were assessed to have autism based on DSM-IV criteria | 198 | 119 | 60 | – | – | 4.5–6.5 | Years | NR | NR | Autistic-like condition, Asperger syndrome, autistic traits | |
| Cassidy 2008348 | Parents of children aged < 5 years with ICD-10 diagnosis of ASD | 104 | 104 | 100 | – | – | 2–4 | Years | 95 | 9 | ASD | |
| Dawson 2010321 | 18–30 months, diagnosed by ADOS, ADI and DSM-IV | 48 | 48 | 100 | – | – | 18–33 | Months | 37 | 11 | AD, PDD-NOS | |
| Eikeseth 2009410 | 24–42 months with ICD-10 diagnosis of ASD | 23 | 23 | 100 | 34.9 | 5.7 | 28–42 | Months | 17 | 6 | Autism | |
| Eldevik 2012414 | Children aged 2 to 6 who had autism diagnosis based on ICD-10 criteria and ADI-R | 43 | 43 | 100 | 4.26 | 1.48 | 1–6 | Years | 33 | 10 | Autism, PDD-NOS, Asperger | |
| Eriksson 2013415 | Children aged 20–54 months. Criteria not stated | 208 | 208 | 100 | – | – | 20–54 | Months | 176 | 32 | ASD | |
| Gabriels 2007416 | Children had a mean age of 31 months and had a clinical diagnosis of autistic disorder or PDD-NOS based on DSM-IV criteria | 14 | 14 | 100 | 31 | – | – | Months | 10 | 4 | AD, PDD-NOS | |
| Green 2010253 | 24–60 months, ADOS or ADI diagnosed | 152 | 152 | 100 | 45 | – | 24–60 | Months | 138 | 14 | Core autism | |
| Grindle 2012417 | 3- to 7-year-old children with autism | 29 | 29 | 100 | – | – | 43–72 | Months | 25 | 4 | Autism | |
| Hedvall 2013418 | 3.6- to 6.6-year-old children with ASD | 190 | 168 | 88 | 55 | 0.8 | 42–76 | Months | 147 | 21 | AD, PDD-NOS, Asperger syndrome | |
| Herring 2006411 | Children were aged between 20 and 51 months who met the DSM-IV criteria for diagnosis | 123 | 84 | 68 | 37.75 | 7.07 | – | Months | 75 | 9 | AD, PDD-NOS | |
| Honey 2008307 | 24–48 months diagnosed by ICD-10 criteria | 104 | 79 | 76 | 37.05 | 6.08 | 24–48 | Months | 65 | 14 | ASD | |
| Hudry 2010233 | 24- to 59-month-old children with ADOS-G diagnosis | 152 | 152 | 100 | 44.83 | 7.98 | 24–59 | Months | 138 | 14 | Core autism | |
| Ben Itzchak 2011320 | Children aged 15–35 months were included in the study | 78 | 78 | 100 | – | – | 15–35 | Months | 71 | 7 | Autism | |
| Jasmin 2009384 | Children aged 3–4 years who had a diagnosis of ASD based on DSM-IV criteria | 35 | 35 | 100 | – | – | 3–4 | Years | 32 | 3 | Autistic, PDD-NOS, Asperger syndrome | |
| Jonsdottir 2007341 | Mean age was 41.43 months; diagnosis was based on ICD-10 criteria | 41 | 41 | 100 | 41.43 | 9.06 | 22–59 | Months | 34 | 7 | Childhood autism | |
| Klintwall 2012419 | 2 years and 3 months to 4 years and 11 months, with clinical diagnosis by paediatrician | 21 | 21 | 100 | 3.6 | – | 2.25–4.9 | Years | 16 | 5 | Autism | |
| Landa 2012224 | 22- to 33-month-old children with ASD or autism | 48 | 48 | 100 | 27 | 2.8 | 22–33 | Months | 39 | 9 | ASD | |
| Lerna 2012325 | 18–60 months old with diagnosis of autism and little or no functional language | 18 | 18 | 100 | – | – | 18–60 | Months | 17 | 1 | Autism | |
| Lloyd 2013400 | 12- to 36-month-old children with ASD | 162 | 162 | 100 | – | – | 12–37 | Months | 140 | 22 | ASD | |
| Luyster 2008129 | Participants were aged 18–33 months and met ADI-R criteria for ASD diagnosis | 164 | 164 | 100 | – | – | 18–33 | Months | 129 | 35 | ASD | |
| Magiati 2007308 | Children aged between 22 and 54 months who met ADI-R criteria for autism/ASD diagnosis | 44 | 44 | 100 | – | – | 22–54 | Months | 39 | 5 | Autism, ASD | |
| Magiati 2011309 | Mean age of 3.4 years at start of the study | 44 | 44 | 100 | 38.9 | 7.1 | 27–55 | Months | 39 | 5 | Autism, ASD | |
| Mayo 2013310 | 45–72 months with DSM-IV-TR criteria | 119 | 119 | 100 | 52.22 | 6.09 | 45–72 | Months | 99 | 20 | AD, PDD-NOS | |
| McConkey 2010349 | Children with ASD diagnosis (criteria not given, it was only stated as ‘confirmed diagnosis of ASD from a specialist clinic’) who had a mean age of 2.8 years at start of the study | 62 (families) | 61 | 98 | – | – | < 4 | Years | 55 | 6 | Autism | |
| Munson 2006420 | 38–54 months with DSM-IV diagnosis of ASD | 45 | 45 | 100 | 47.4 | 4.2 | 38–54 | Months | 38 | 7 | AD, PDD-NOS | |
| Munson 2008312 | 24–66 months with ADI or ADOS diagnosis of ASD | 456 | 456 | 100 | 43.4 | 8.7 | 24–66 | Months | 370 | 86 | Autism, ASD | |
| O’Donnell 2012386 | 3–4 years old with DSM-IV diagnosis of ASD | 42 | 42 | 100 | 45.5 | – | 36–59 | Months | NR | NR | Autism, PDD-NOS | |
| Eapen 2013357 | Mean age of 49.6 months | 26 | 26 | 100 | 49.6 | 6.08 | 36–58 | Months | 21 | 5 | AD | |
| Osborne 2008350 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | – | – | 2.6–4.0 | Years | 59 | 6 | ASD | |
| Osborne 2009351 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | 3.4 | 0.75 | 2.6–4.0 | Years | 59 | 6 | ASD | |
| Peters-Scheffer 2010421 | 3- to 6-year-old children with DSM-IV diagnosis of AD or PDD-NOS | 34 | 34 | 100 | 53.5 | 5.52 | 42–62 | Months | NR | NR | AD, PDD-NOS | |
| Poon 2012401 | 9–12 months (upon entering study) with ADOS, ADI or CARS diagnosis of ASD | 29 | 29 | 100 | 4.46 | 1.49 | – | Months | 24 | 5 | AD, PDD-NOS, Asperger syndrome | |
| Pry 2005314 | 21 months to 7 years with ICD-10 diagnosis of ASD | 222 | 222 | 100 | 5 | 1.75 | 1.75–7.00 | Years | 180 | 42 | Infantile autism | |
| Ray-Subramanian 2011327 | 23–39 months with DSM-IV or ICD-10 diagnosis of ASD | 125 | 125 | 100 | 31 | 4.1 | 23–39 | Months | 108 | 17 | Autism, AD, PDD-NOS | |
| Reed 2007352 | 2 years 6 months to 4 years old diagnosed with ASD | 27 | 27 | 100 | – | – | 2.5–4.0 | Years | 27 | 0 | ASD | |
| Reed 2007353 | 2 years 6 months to 4 years old with ‘paediatrician’ diagnosis of ASD | 53 | 53 | 100 | – | – | 2.5–4.0 | Years | Unclear | Unclear | ASD | |
| Reed 2012354 | 2.5–4 years with GARS diagnosis of ASD | 66 | 66 | 100 | 40.2 | 5.6 | – | Months | 59 | 7 | AD, PDD-NOS | |
| Remington 2007358 | 30–42 months of age with ADI diagnosis of ASD | 44 | 44 | 100 | 37 | 4.2 | 30–42 | Months | NR | NR | Autism or suspected autism | |
| Restall 1994422 | 3–6 years with DSM-III diagnosis of ASD | 18 | 9 | 50 | 64.76 | 6.4 | – | Months | 8 | 1 | Autism | |
| Rickards 2009423 | 3–5 years, 35/59 diagnosed ASD by DSM-IV criteria | 54 | 54 | 100 | 69.65 | – | – | Months | 43 | 11 | ASD | |
| Roberts 2011405 | 2.2–5 years with DSM-IV diagnosis of ASD | 95 | 95 | 100 | – | – | 26.3–60.3 | Months | 86 | 9 | AD, ASD | |
| Rogers 2012317 | 14–24 months with ASD | 98 | 98 | 100 | 21 | – | – | Months | 76 | 22 | ASD | |
| Ruble 2008424 | 40–71 months with DSM-IV diagnosis of ASD | 35 | 35 | 100 | 55.9 | – | 40.9–70.9 | Months | 30 | 5 | Autism | |
| Salt 2002372 | Preschool children in Scotland, (mean 42.36 months) with ICD-10 diagnosis of ASD | 17 | 17 | 100 | 40.015 | – | – | Months | 14 | 3 | Childhood autism | |
| Schertz 2013402 | Mean age 24.6 and 27.5 months with ADOS diagnosis | 23 | 23 | 100 | 26.05 | – | – | Months | NR | NR | ASD | |
| Silva 2007299 | 3–6 years old with DSM-IV diagnosis of ASD | 15 | 15 | 100 | 4.83 | – | 3–6 | Years | 13 | 2 | AD | |
| Silva 2008300 | 3–6 years old with DSM-IV diagnosis of ASD | 26 | 26 | 100 | 56.3 | 12.5 | – | Months | 21 | 5 | Autism | |
| Smith 2000413 | 18–42 months with ‘clinical’ diagnosis of ASD | 28 | 28 | 100 | 35.92 | – | – | Months | 23 | 5 | Autism, PDD-NOS | |
| Smith 2010359 | All < 6 years with ADOS/ADI/DSM-IV diagnosis of ASD | 53 | 53 | 100 | 50.1 | 10 | – | Months | 47 | 6 | Autism | |
| Stahmer 2004355 | 0–3 years with DSM-IV diagnosis | 20 | 20 | 100 | 29.6 | – | 22–33 | Months | 16 | 4 | AD, PDD-NOS | |
| Stone 1999346 | 23–35 months with DSM-III or DSM-IV diagnosis of ASD | 60 | 30 | 50 | 31.3 | 3.3 | 23–35 | Months | 25 | 5 | Autism | |
| Strauss 2012329 | 26–81 months with DSM-IV diagnosis of ASD | 44 | 44 | 100 | – | – | 26–81 | Months | 41 | 3 | Autism, PDD-NOS | |
| Szatmari 2000302 | 4- to 6-year-old children (upon entering study) diagnosed by ADI | 134 | 68 | 51 | 66.8 | – | – | Months | 59 | 7 | Autism, Asperger syndrome | |
| Tonge 2012425 | Children were aged 2.5–5 years and diagnosis was made using a combination of medical reviews, ADI-R and CARS | 107 | 107 | 100 | – | – | 2.5–5.0 | Years | 90 | 17 | AD | |
| Toth 2006284 | 34–52 months with ADI-diagnosis of ASD | 60 | 60 | 100 | 43.6 | 4.3 | 34–52 | Months | 51 | 9 | AD, PDD-NOS | |
| VanMeter 1997426 | Mean ages ranged from 2.9 (SD = 0.77) to 5.7 (SD = 1.31) years meeting DSM-III criteria for ASD | 143 | 57 | 40 | – | – | 5.2–6.0 | Years | 54 | 3 | AD | |
| Ventola 2007332 | 16–32 months old with M-CHAT diagnosis of ASD | 195 | 195 | 100 | – | – | 16–32 | Months | 152 | 43 | ASD | |
| Werner 2005316 | 12–57 months with DSM-IV diagnosis of ASD | 145 | 72 | 50 | 43.5 | 4.3 | – | Months | 60 | 12 | AD, PDD-NOS | |
| Zachor 2010335 | 15- to 35-month-old children who met DSM-IV criteria | 71 | 71 | 100 | 25.55 | 4.25 | 15–35 | Months | 71 | 7 | Autism | |
| Vineland Social Maturity Scale, Indian adaptationa | Malhi 2011342 | Children were ≤ 3 years at start of the study and had an ASD diagnosis based on DSM-IV criteria | 77 | 77 | 100 | – | – | 0–3 | Years | 64 | 13 | AD, PDD-NOS |
| Parent Surveyb | Arick 2003388 | Children between the ages of 2 and 6 years (at baseline) who have been said to have a diagnosis of autism; details of criteria used not provided | 67 | 67 | 100 | – | – | 2–6 | Years | NR | NR | ASD |
| Classroom and playground behaviour observationsc | Escalona 2001271 | Children were aged 3 to 6 years based on DSM III – R | 20 | 20 | 100 | 5.2 | 1.8 | 3–6 | Years | 12 | 8 | Autism |
| Coded observation of social behaviourc | Meirsschaut 2011442 | 21–56 months meeting ADOS criteria for ASD | 42 | 21 | 50 | 36.94 | – | 21–56 | Months | 18 | 3 | Autism, ASD |
| Video recording of child in classroom activitiesc | Ingersoll 2001380 | Children ages 26 to 41 months who met DSM-IV criteria for ASD | 9 | 6 | 67 | – | – | 26–41 | Months | NR | NR | Autism, PDD-NOS |
| Play | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Autism Diagnostic Observation Scale-Toddler Module (ADOS-T) | Rogers 2012317 | 14–24 months with ASD | 98 | 98 | 100 | 21 | – | – | Months | 76 | 22 | ASD |
| Autism Diagnostic Observation Schedule (ADOS) | Aldred 2004318 | 2 years to 5 years 11 months with ADI diagnosis | 28 | 28 | 100 | – | – | 24–71 | Months | 25 | 3 | AD or ‘classical autism’ |
| Aldred 2012319 | Children aged 2–5 years assessed using ADOS and ADI-R | 28 | 28 | 100 | – | – | 2–5 | Years | 25 | 3 | Autism | |
| Ben Itzchak 2008149 | Children aged 19–35 months with autism diagnosis based on DSM-IV criteria | 81 | 44 | 54 | – | – | 16–35 | Months | 43 | 1 | Autism | |
| Ben Itzchak 2011320 | Children aged 15–35 months were included in the study | 78 | 78 | 100 | – | – | 15–35 | Months | 71 | 7 | Autism | |
| Bennett 2012304 | Children with ASD aged 2–4 years old | 214 | 178 | 83 | – | – | 2–4 | Years | 181 | 33 | AD, Asperger syndrome, PDD-NOS | |
| Brian 2008305 | Children had no diagnosis of ASD but were followed up to 36 months at which point some were diagnosed of ASD | 228 | 35 | 15 | – | – | 6–12 | Months | NR | NR | Autism, Asperger syndrome, PDD-NOS | |
| Dawson 2010321 | 18–30 months, diagnosed by ADOS, ADI and DSM-IV | 48 | 48 | 100 | – | – | 18–30 | Months | 37 | 11 | AD, PDD-NOS | |
| Gotham 2012322 | Best-estimate clinical diagnosis of ASD at one or more time points | 345 | 345 | 100 | 3.3 | 1.4 | – | Years | 282 | 63 | Autism, PDD-NOS | |
| Autism Diagnostic Observation Schedule-Generic (ADOS-G) | Green 2010253 | 24–60 months, ADOS or ADI diagnosed | 152 | 152 | 100 | 45 | – | 24–60 | Months | 138 | 14 | Core autism |
| Hartley 2009323 | Children aged 1.5 to 3.9 years based on DSM-IV-TR criteria and ADOS-G classification | 499 | 199 | 40 | – | – | 18–47 | Months | 157 | 42 | AD, PDD-NOS | |
| Autism Diagnostic Observation Schedule (ADOS) | Landa 2012224 | 22- to 33-month-old children with ASD or autism | 48 | 48 | 100 | 27 | 2.8 | 22–33 | Months | 39 | 9 | ASD |
| Lerna 2012325 | 18–60 months old with diagnosis of autism and little or no functional language | 18 | 18 | 100 | – | – | 18–60 | Months | 17 | 1 | Autism | |
| Luyster 2008129 | Participants were aged 18–33 months and met ADI-R criteria for ASD diagnosis | 164 | 164 | 100 | – | – | 18–33 | Months | 129 | 35 | ASD | |
| Autism Diagnostic Observation Schedule-Generic (ADOS-G) | Munson 2008312 | 24–66 months with ADI or ADOS diagnosis of ASD | 456 | 456 | 100 | 43.4 | 8.7 | 24–66 | Months | 370 | 86 | Autism, ASD |
| Autism Diagnostic Observation Schedule (ADOS) | Oosterling 2010326 | 12–42 months old with ‘clinical’ diagnosis of ASD | 80 | 80 | 100 | 34.8 | – | – | Months | 62 | 18 | Autism, PDD-NOS |
| Ray-Subramanian 2011327 | 23–39 months with DSM-IV or ICD-10 diagnosis of ASD | 125 | 125 | 100 | 31 | 4.1 | 23–39 | Months | 108 | 17 | Autism, AD, PDD-NOS | |
| Ray-Subramanian 2012328 | 2–3 years with DSM-IV diagnosis | 115 | 115 | 100 | 31 | 4.1 | – | Months | 97 | 18 | Autism, AD, PDD-NOS | |
| Strauss 2012329 | 26–81 months with DSM-IV diagnosis of ASD | 44 | 44 | 100 | – | – | 26–81 | Months | 41 | 3 | Autism, PDD-NOS | |
| Sullivan 2007330 | Tested at 14–24 months and 30–36 months who met DSM-IV criteria for diagnosis | 51 | 16 | 31 | – | – | 14–36 | Months | 14 | 2 | Autism, PDD-NOS | |
| Autism Diagnostic Observation Schedule-Generic (ADOS-G) | Tek 2012331 | 16–38 months with ADOS diagnosis | 84 | 84 | 100 | 27 | – | 16–38 | Months | NR | NR | ASD |
| Ventola 2007332 | 16–32 months old with M-CHAT diagnosis of ASD | 195 | 195 | 100 | – | – | 16–32 | Months | 152 | 43 | ASD | |
| Autism Diagnostic Observation Schedule (ADOS) | Werner 2005316 | 12–57 months with DSM-IV diagnosis of ASD | 145 | 72 | 50 | 43.5 | 4.3 | – | Months | 60 | 12 | AD, PDD-NOS |
| Wong 2010333 | 17–36 months children diagnosed by DSM-IV, ADI and ADOS | 17 | 17 | 100 | – | – | 17–36 | Months | 16 | 1 | – | |
| Zachor 2006334 | Participants were aged 23–33 months and met DSM-IV criteria for autism diagnosis | 39 | 39 | 100 | – | – | 23–33 | Months | 37 | 2 | Autism | |
| Zachor 2010335 | 15- to 35-month-old children who met DSM-IV criteria | 71 | 71 | 100 | 25.55 | 4.25 | 15–35 | Months | 71 | 7 | Autism | |
| Communication and Symbolic Behavior Scales-Developmental Profile (Caregiver Questionnaire) (CSBS-DP CQ; Wetherby and Prizant 2002127) | Tek 2012331 | 16–38 months with ADOS diagnosis | 84 | 84 | 100 | 27 | – | 16–38 | Months | NR | NR | ASD |
| Developmental Play Assessment (DPA) – Instrument Sequence of Categories | Freeman 2013443 | 18- to 55-month-old children, 50 met DSM-IV criteria | 32 (parent–child dyads) | 16 | 50 | 49.5 | 11.8 | – | Months | 12 | 4 | Autism |
| Structured Play Assessment | Freeman 2013443 | 18- to 55-month-old children, 50 met DSM-IV criteria | 32 (parent–child dyads) | 16 | 50 | 49.5 | 11.8 | – | Months | 12 | 4 | Autism |
| Goods 2013366 | 36- to 60-month-old children with autism (ADOS assessment) | 15 | 15 | 100 | 51.9 | – | – | Months | NR | NR | Autism | |
| Kasari 2006368 | Children were aged 3 to 4 years and had a diagnosis of autism based on ADI-R and ADOS criteria | 58 | 58 | 100 | – | – | 3–4 | Years | 46 | 12 | Autism | |
| Symbolic Play Test | Wong 2010333 | 17–36 months children diagnosed by DSM-IV, ADI and ADOS | 17 | 17 | 100 | – | – | 17–36 | Months | 16 | 1 | – |
| Salt 2002372 | Preschool children in Scotland, (mean 42.36 months) with ICD-10 diagnosis of ASD | 17 | 17 | 100 | 40.02 | – | – | Months | 14 | 3 | Childhood autism | |
| Magiati 2007308 | Children aged between 22 and 54 months who met ADI-R criteria for autism/ASD diagnosis | 44 | 44 | 100 | – | – | 22–54 | Months | 39 | 5 | Autism, ASD | |
| Test of Pretend Play (ToPP) | Magiati 2007308 | Children aged between 22 and 54 months who met ADI-R criteria for autism/ASD diagnosis | 44 | 44 | 100 | – | – | 22–54 | Months | 39 | 5 | Autism, ASD |
| Dereu 2012365 | Children aged 2–4 years; ADOS was used for diagnosis | 17 | 9 | 53 | – | – | 17–39 | Months | 6 | 3 | ASD | |
| Preschool Play Scalea | Restall 1994422 | 3–6 years with DSM-III diagnosis of ASD | 18 | 9 | 50 | 64.76 | 6.4 | – | Months | 8 | 1 | Autism |
| Caregiver–child interactionb | Kasari 2006368 | Children were aged 3 to 4 years and had a diagnosis of autism based on ADI-R and ADOS criteria | 58 | 58 | 100 | – | – | 3–4 | Years | 46 | 12 | Autism |
| Coded observation of social behaviourb | Meirsschaut 2011442 | 21–56 months meeting ADOS criteria for ASD | 42 | 21 | 50 | 36.94 | – | 21–56 | Months | 18 | 3 | Autism, ASD |
| Coding of videosb | Flippin 2011406 | Children aged 40–69 months with autism diagnosis based on ADOS | 16 | 16 | 100 | 53.3 | 9.6 | 40–69 | Months | 12 | 4 | ASD |
| Free play assessmentb | Christensen 2010444 | 18 months upon entering – 17/77 subsequently diagnosed as ASD using ADOS | 77 | 17 | 22 | 33.95 | 4.69 | 18–40 | Months | 14 | 3 | ASD |
| Parent–child free playb | Freeman 2013443 | 18- to 55-month-old children, 50 met DSM-IV criteria | 32 (parent–child dyads) | 16 | 50 | 49.5 | 11.8 | – | Months | 12 | 4 | Autism |
| Behaviour | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aberrant Behavior Checklist (ABC) | Baghdadli 2012339 | Age < 7 years, ICD-10 diagnosis of autism | 280 | 280 | 100 | 4.9 | 1.3 | – | Months | 230 | 50 | Childhood autism, atypical autism |
| Bearss 2013278 | Children were aged between 3 years and 6 years 11 months, and assessed to have autism based on ADOS and clinical observation | 16 | 16 | 100 | – | – | 3–6 | Years | 16 | 0 | AD, PDD-NOS | |
| O’Donnell 2012386 | 3–4 years old with DSM-IV diagnosis of ASD | 42 | 42 | 100 | 45.5 | – | 36–59 | Months | NR | NR | Autism, PDD-NOS | |
| Werner 2005316 | 12–57 months with DSM-IV diagnosis of ASD | 145 | 72 | 50 | 43.5 | 4.3 | – | Months | 60 | 12 | AD, PDD-NOS | |
| Baby and Infant Screen for Children with aUtIsm Traits (BISCUIT-Part 3) | Rojahn 2009445 | 17–37 months with DSM-IV diagnosis of ASD | 762 | 312 | 41 | 27.29 | 4.73 | 17–37 | Months | 227 | 85 | Autism, PDD-NOS |
| Behavior Assessment System for Children-Second Edition (BASC-2) | Hill-Chapman 2013434 | Parents of children with ASD | 56 (parents) | 56 | 100 | 3.98 | 1.31 | – | Years | N/A | N/A | AD, PDD-NOS, Asperger syndrome |
| Behavior Screening Questionnaire | Rickards 2009423 | 3–5 years, 35/59 diagnosed ASD by DSM-IV criteria | 54 | 54 | 100 | 69.65 | – | – | Months | 43 | 11 | ASD |
| Child Behavior Checklist (CBCL) | Baker 2010397 | 33 ‘at-risk’ children, entered study between ages of 2–18 months, assessed at 18, 24, 30 and 36 months. [24 of the 33 children had a sibling with ASD or PDD (DSM-IV diagnosed)] | 33 | 12 | 36 | 18 | – | – | Months | NR | NR | ASD |
| Hartley 2009323 | Children aged 1.5 to 3.9 years based on DSM-IV-TR criteria and ADOS-G classification | 499 | 199 | 40 | – | – | 18–48 | Months | 157 | 42 | AD, PDD-NOS | |
| Peters-Scheffer 2010421 | 3- to 6-year-old children with DSM-IV diagnosis of AD or PDD-NOS | 34 | 34 | 100 | 53.5 | 5.52 | 42–62 | Months | NR | NR | AD, PDD-NOS | |
| Smith 2000413 | 18–42 months with ‘clinical’ diagnosis of ASD | 28 | 28 | 100 | 35.92 | – | – | Months | 23 | 5 | Autism, PDD-NOS | |
| Smith 2010359 | All < 6 years with ADOS/ADI/DSM-IV diagnosis of ASD | 53 | 53 | 100 | 50.1 | 10 | – | Months | 47 | 6 | Autism | |
| Taylor 2012436 | Mothers of ASD children aged mean 3.72 years (SD = 1.82) and 4.18 (SD = 2.65) at diagnosis | 75 (mothers) | 75 | 100 | 3.72 | 18.2 | – | Months | NR | NR | ASD | |
| Child Behavior Scale (CBS) | Jahromi 2013431 | 20 TD and 20 children with high-functioning autism | 40 | 20 | 50 | 58.95 | 11.5 | – | Months | 36 | 4 | High-functioning autism |
| Meek 2012435 | 2.75–6.5 years with ADI diagnosis of ASD | 40 | 20 | 50 | 58.95 | 11.5 | – | Months | 36 | 4 | Autism | |
| Conners Rating Scales-Revised | Escalona 2001271 | Children were aged 3 to 6 years based on DSM-III-R | 20 | 20 | 100 | 5.2 | 1.8 | 3–6 | Years | 12 | 8 | Autism |
| Osborne 2009351 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | 3.4 | 0.75 | 2.6–4.0 | Years | 59 | 6 | ASD | |
| Reed 2007353 | 2 years 6 months to 4 years old with ‘paediatrician’ diagnosis of ASD | 53 | 53 | 100 | – | – | 2.5–4.0 | Years | NR | NR | ASD | |
| Reed 2013437 | – | 52 | 52 | 100 | 44.4 | 7.9 | 36.77 | Months | 46 | 6 | Childhood autism, PDD-NOS | |
| Developmental Behaviour Checklist | Herring 2006411 | Children were aged between 20 and 51 months who met the DSM-IV criteria for diagnosis | 123 | 84 | 68 | 37.75 | 7.07 | – | Months | 75 | 9 | AD, PDD-NOS |
| Mooney 2006311 | 22–51 months with DSM-IV diagnosis of ASD | 55 | 40 | 73 | 36.95 | 7.26 | 22–51 | Months | 34 | 6 | AD | |
| Remington 2007358 | 30–42 months of age with ADI diagnosis of ASD | 44 | 44 | 100 | 37 | 4.2 | 30–42 | Months | NR | NR | Autism or suspected autism | |
| Roberts 2011405 | 2.2–5 years with DSM-IV diagnosis of ASD | 95 | 95 | 100 | – | – | 26.3–60.3 | Months | 86 | 9 | AD, ASD | |
| Tonge 2012425 | Children were aged 2.5–5 years and diagnosis was made using a combination of medical reviews, ADI-R and CARS | 107 | 107 | 100 | – | – | 2.5–5.0 | Years | 90 | 17 | AD | |
| Home Situations Questionnaire (HSQ) | Bearss 2013278 | Children were aged between 3 years and 6 years 11 months, and assessed to have autism based on ADOS and clinical observation | 16 | 16 | 100 | – | – | 3–6 | Years | 16 | 0 | AD, PDD-NOS |
| Nisonger Child Behavior Rating Scales | Remington 2007358 | 30–42 months of age with ADI diagnosis of ASD | 44 | 44 | 100 | 37 | 4.2 | 30–42 | Months | NR | NR | Autism or suspected autism |
| Parent Target Problems | Bearss 2013278 | Children were aged between 3 years and 6 years 11 months, and assessed to have autism based on ADOS and clinical observation | 16 | 16 | 100 | – | – | 3–6 | Years | 16 | 0 | AD, PDD-NOS |
| Pre-School Behavior Checklist | Rickards 2009423 | 3–5 years, 35/59 diagnosed ASD by DSM-IV criteria | 54 | 54 | 100 | 69.65 | – | – | Months | 43 | 11 | ASD |
| Behaviour Style Questionnaire – Chinese version (Xu 1979)a | Chuang 2012383 | Children were aged 48–84 months and had DSM-IV-TR diagnosis of autism | 111 | 67 | 60 | – | – | 48–84 | Months | 57 | 10 | Autism |
| Coded Observation of Child Behaviour problemsb | Robbins 1992446 | 24–60 months upon entry, diagnosed by ‘outside agency’ | 15 | 15 | 100 | – | – | 24–60 | Months | 14 | 1 | Autism or autism characteristics |
| Functional Behaviour Assessment Interview (O’Neill et al. 1997)c | Reese 2005447 | 24–60 months with DSM-IV criteria of ASD | 46 | 23 | 50 | 45.1 | 13.8 | 24–60 | Months | 17 | 6 | Autism |
| Parent Surveyc | Arick 2003388 | Children between the ages of 2 and 6 years (at baseline) who have been said to have a diagnosis of autism; details of criteria used not provided | 67 | 67 | 100 | – | – | 2–6 | Years | NR | NR | ASD |
| Video coding procedures (for children and parents)d | Bryce 2013448 | 58.95 months (SD = 11.50), ADI-R was used to confirm diagnosis | 40 | 20 | 50 | 58.95 | 11.5 | – | Months | NR | NR | Autism |
| Habit problems | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Child Behavior Checklist (CBCL) | Smith 2000413 | 18–42 months with ‘clinical’ diagnosis of ASD | 28 | 28 | 100 | 35.92 | – | – | Months | 23 | 5 | Autism, PDD-NOS |
| Baker 2010397 | 33 ‘at-risk’ children, entered study between ages of 2–18 months, assessed at 18, 24, 30 and 36 months. [24 of the 33 children had a sibling with ASD or PDD (DSM-IV diagnosed)] | 33 | 12 | 36 | 18 | – | – | Months | NR | NR | ASD | |
| Peters-Scheffer 2010421 | 3- to 6-year-old children with DSM-IV diagnosis of AD or PDD-NOS | 34 | 34 | 100 | 53.5 | 5.52 | 42–62 | Months | NR | NR | AD, PDD-NOS | |
| Smith 2010359 | All < 6 years with ADOS/ADI/DSM-IV diagnosis of ASD | 53 | 53 | 100 | 50.1 | 10 | – | Months | 47 | 6 | Autism | |
| Taylor 2012436 | Mothers of ASD children aged mean 3.72 years (SD = 1.82) and 4.18 (SD = 2.65) at diagnosis | 75 (mothers) | 75 | 100 | 3.72 | 18.2 | – | Months | NR | NR | ASD | |
| Hartley 2009323 | Children aged 1.5 to 3.9 years based on DSM-IV-TR criteria and ADOS-G classification | 499 | 199 | 40 | – | – | 18–48 | Months | 157 | 42 | AD, PDD-NOS | |
| Sense and Self-Regulation Checklist (SSC) | Silva 2009226 | 3–6 years with DSM-IV diagnosis of ASD | 46 | 46 | 100 | 59.2 | – | – | Months | 37 | 9 | Autism |
| Silva 2011301 | 3–6 years old with clinical diagnosis of ASD | 47 | 47 | 100 | 4.83 | – | 3–6 | Years | 33 | 14 | Autism | |
| Sleep diariesa | Escalona 2001271 | Children were aged 3–6 years based on DSM-III-R | 20 | 20 | 100 | 5.2 | 1.8 | 3–6 | Years | 12 | 8 | Autism |
| Learning | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Autism Screening Instrument for Educational Planning (ASIEP) | Arick 2003388 | Children between the ages of 2 and 6 years (at baseline) who have been said to have a diagnosis of autism; details of criteria used not provided | 67 | 67 | 100 | – | – | 2–6 | Years | NR | NR | ASD |
| Extended Basic Academic Skills Assessment System | Arick 2003388 | Children between the ages of 2 and 6 years (at baseline) who have been said to have a diagnosis of autism; details of criteria used not provided | 67 | 67 | 100 | – | – | 2–6 | Years | NR | NR | ASD |
| Wechsler Individualised Achievement Test | Smith 2000413 | 18–42 months with ‘clinical’ diagnosis of ASD | 28 | 28 | 100 | 35.92 | – | – | Months | 23 | 5 | Autism, PDD-NOS |
| Student Learning Profilea | Arick 2003388 | Children between the ages of 2 and 6 years (at baseline) who have been said to have a diagnosis of autism; details of criteria used not provided | 67 | 67 | 100 | – | – | 2–6 | Years | NR | NR | ASD |
| Classroom Observation Formb | Arick 2003388 | Children between the ages of 2 and 6 years (at baseline) who have been said to have a diagnosis of autism; details of criteria used not provided | 67 | 67 | 100 | – | – | 2–6 | Years | NR | NR | ASD |
| Daily living skills | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Functional Independence Measure for Children (WeeFIM) | Jasmin 2009384 | Children aged 3–4 years who had a diagnosis of ASD based on DSM-IV criteria | 35 | 35 | 100 | – | – | 3–4 | Years | 32 | 3 | Autistic, PDD-NOS, Asperger syndrome |
| Vineland Adaptive Behavior Scales-Classroom version (VABS-Classroom) | Goin-Kochel 2007427 | Children were aged between 29.6–61.4 months; diagnosis was based on ADOS criteria | 29 | 29 | 100 | 45.7 | 9.6 | 29.6–61.4 | Months | 27 | 2 | Autism, PDD-NOS |
| Vineland Adaptive Behavior Scales (VABS) | Aldred 2004318 | 2 years to 5 years 11 months with ADI diagnosis | 28 | 28 | 100 | – | – | 24–71 | Months | 25 | 3 | AD or ‘classical autism’ |
| Anan 2008396 | 25 to 68 months old children who met the diagnosis of ASD based on DSM-IV criteria | 72 | 72 | 100 | – | – | 25–68 | Months | 61 | 11 | AD, PDD-NOS | |
| Andersson 2013409 | Children aged 1.8 to 3.9 years who met DSM-IV criteria | 40 | 37 | 93 | – | – | 1.8–3.9 | Years | 18 | 19 | AD, ASD, atypical autism, Asperger syndrome | |
| Arick 2003388 | Children between the ages of 2 and 6 years (at baseline) who have been said to have a diagnosis of autism; details of criteria used not provided | 67 | 67 | 100 | – | – | 2–6 | Years | NR | NR | ASD | |
| Baghdadli 2012339 | Age < 7 years, ICD-10 diagnosis of autism | 280 | 280 | 100 | 4.9 | 1.3 | – | Months | 230 | 50 | Childhood autism, atypical autism | |
| Bearss 2013278 | Children were aged between 3 years and 6 years 11 months, and assessed to have autism based on ADOS and clinical observation | 16 | 16 | 100 | – | – | 3–6 | Years | 16 | 0 | AD, PDD-NOS | |
| Ben Itzchak 2011320 | Children aged 15–35 months were included in the study | 78 | 78 | 100 | – | – | 15–35 | Months | 71 | 7 | Autism | |
| Bennett 2008296 | Children aged between 4 and 6 years | 64 | 64 | 100 | – | – | 4–6 | Years | 57 | 7 | Asperger syndrome, high-functioning autism | |
| Carlsson 2013390 | Children aged from 4.5 to 6.5 years who were assessed to have autism based on DSM-IV criteria | 198 | 119 | 60 | – | – | 4.5–6.5 | Years | NR | NR | Autistic-like condition, Asperger syndrome, autistic traits | |
| Cassidy 2008348 | Parents of children aged < 5 years with ICD-10 diagnosis of ASD | 104 | 104 | 100 | – | – | 2–4 | Years | 95 | 9 | ASD | |
| Dawson 2010321 | 18–30 months, diagnosed by ADOS, ADI and DSM-IV | 48 | 48 | 100 | – | – | 18–33 | Months | 37 | 11 | AD, PDD-NOS | |
| Eapen 2013357 | Mean age of 49.6 months | 26 | 26 | 100 | 49.6 | 6.08 | 36–58 | Months | 21 | 5 | AD | |
| Eikeseth 2009410 | 24–42 months with ICD-10 diagnosis of ASD | 23 | 23 | 100 | 34.9 | 5.7 | 28–42 | Months | 17 | 6 | Autism | |
| Eldevik 2012414 | Children aged 2 to 6 who had autism diagnosis based on ICD-10 criteria and ADI-R | 43 | 43 | 100 | 4.26 | 1.48 | 1–6 | Years | 33 | 10 | Autism, PDD-NOS, Asperger | |
| Eriksson 2013415 | Children aged 20–54 months. Criteria not stated | 208 | 208 | 100 | – | – | 20–54 | Months | 176 | 32 | ASD | |
| Gabriels 2007416 | Children had a mean age of 31 months and had a clinical diagnosis of autistic disorder or PDD-NOS based on DSM-IV criteria | 14 | 14 | 100 | 31 | – | – | Months | 10 | 4 | AD, PDD-NOS | |
| Green 2010253 | 24–60 months, ADOS or ADI diagnosed | 152 | 152 | 100 | 45 | – | 24–60 | Months | 138 | 14 | Core autism | |
| Grindle 2012417 | 3- to 7-year-old children with autism | 29 | 29 | 100 | – | – | 43–72 | Months | 25 | 4 | Autism | |
| Hedvall 2013418 | 3.6- to 6.6-year-old children with ASD | 190 | 168 | 88 | 55 | 0.8 | 42–76 | Months | 147 | 21 | AD, PDD-NOS, Asperger syndrome | |
| Herring 2006411 | Children were aged between 20 and 51 months who met the DSM-IV criteria for diagnosis | 123 | 84 | 68 | 37.75 | 7.07 | – | Months | 75 | 9 | AD, PDD-NOS | |
| Honey 2008307 | 24–48 months diagnosed by ICD-10 criteria | 104 | 79 | 76 | 37.05 | 6.08 | 24–48 | Months | 65 | 14 | ASD | |
| Hudry 2010233 | 24- to 59-month-old children with ADOS-G diagnosis | 152 | 152 | 100 | 44.83 | 7.98 | 24–59 | Months | 138 | 14 | Core autism | |
| Jasmin 2009384 | Children aged 3–4 years who had a diagnosis of ASD based on DSM-IV criteria | 35 | 35 | 100 | – | – | 3–4 | Years | 32 | 3 | Autistic, PDD-NOS, Asperger syndrome | |
| Jonsdottir 2007341 | Mean age was 41.43 months; diagnosis was based on ICD-10 criteria | 41 | 41 | 100 | 41.43 | 9.06 | 22–59 | Months | 34 | 7 | Childhood autism | |
| Klintwall 2012419 | 2 years and 3 months to 4 years and 11 months, with clinical diagnosis by paediatrician | 21 | 21 | 100 | 3.6 | – | 2.25–4.9 | Years | 16 | 5 | Autism | |
| Landa 2012224 | 22- to 33-month-old children with ASD or autism | 48 | 48 | 100 | 27 | 2.8 | 22–33 | Months | 39 | 9 | ASD | |
| Lerna 2012325 | 18–60 months old with diagnosis of autism and little or no functional language | 18 | 18 | 100 | – | – | 18–60 | Months | 17 | 1 | Autism | |
| Lloyd 2013400 | 12- to 36-month-old children with ASD | 162 | 162 | 100 | – | – | 12–37 | Months | 140 | 22 | ASD | |
| Luyster 2008129 | Participants were aged 18–33 months and met ADI-R criteria for ASD diagnosis | 164 | 164 | 100 | – | – | 18–33 | Months | 129 | 35 | ASD | |
| Magiati 2007308 | Children aged between 22 and 54 months who met ADI-R criteria for autism/ASD diagnosis | 44 | 44 | 100 | – | – | 22–54 | Months | 39 | 5 | Autism, ASD | |
| Magiati 2011309 | Mean age of 3.4 years at start of the study | 44 | 44 | 100 | 38.9 | 7.1 | 27–55 | Months | 39 | 5 | Autism, ASD | |
| Mayo 2013310 | 45–72 months with DSM-IV-TR criteria | 119 | 119 | 100 | 52.22 | 6.09 | 45–72 | Months | 99 | 20 | AD, PDD-NOS | |
| McConkey 2010349 | Children with ASD diagnosis (criteria not given, it was only stated as ‘confirmed diagnosis of ASD from a specialist clinic’) who had a mean age of 2.8 years at start of the study | 62 (families) | 61 | 98 | – | – | < 4 | Years | 55 | 6 | Autism | |
| Munson 2006420 | 38–54 months with DSM-IV diagnosis of ASD | 45 | 45 | 100 | 47.4 | 4.2 | 38–54 | Months | 38 | 7 | AD, PDD-NOS | |
| Munson 2008312 | 24–66 months with ADI or ADOS diagnosis of ASD | 456 | 456 | 100 | 43.4 | 8.7 | 24–66 | Months | 370 | 86 | Autism, ASD | |
| O’Donnell 2012386 | 3–4 years old with DSM-IV diagnosis of ASD | 42 | 42 | 100 | 45.5 | – | 36–59 | Months | NR | NR | Autism, PDD-NOS | |
| Osborne 2008350 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | – | – | 2.6–4.0 | Years | 59 | 6 | ASD | |
| Osborne 2009351 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | 3.4 | 0.75 | 2.6–4.0 | Years | 59 | 6 | ASD | |
| Peters-Scheffer 2010421 | 3- to 6-year-old children with DSM-IV diagnosis of AD or PDD-NOS | 34 | 34 | 100 | 53.5 | 5.52 | 42–62 | Months | NR | NR | AD, PDD-NOS | |
| Poon 2012401 | 9–12 months (upon entering study) with ADOS, ADI or CARS diagnosis of ASD | 29 | 29 | 100 | 4.46 | 1.49 | – | Months | 24 | 5 | AD, PDD-NOS, Asperger syndrome | |
| Pry 2005314 | 21 months to 7 years with ICD-10 diagnosis of ASD | 222 | 222 | 100 | 5 | 1.75 | 1.75–7 | Years | 180 | 42 | Infantile autism | |
| Ray-Subramanian 2011327 | 23–39 months with DSM-IV or ICD-10 diagnosis of ASD | 125 | 125 | 100 | 31 | 4.1 | 23–39 | Months | 108 | 17 | Autism, AD, PDD-NOS | |
| Reed 2007352 | 2 years 6 months to 4 years old diagnosed with ASD | 27 | 27 | 100 | – | – | 2.5–4.0 | Years | 27 | 0 | ASD | |
| Reed 2007353 | 2 years 6 months to 4 years old with ‘paediatrician’ diagnosis of ASD | 53 | 53 | 100 | – | – | 2.5–4.0 | Years | Unclear | Unclear | ASD | |
| Reed 2012354 | 2.5–4 years with GARS diagnosis of ASD | 66 | 66 | 100 | 40.2 | 5.6 | – | Months | 59 | 7 | AD, PDD-NOS | |
| Remington 2007358 | 30–42 months of age with ADI diagnosis of ASD | 44 | 44 | 100 | 37 | 4.2 | 30–42 | Months | NR | NR | Autism or suspected autism | |
| Restall 1994422 | 3–6 years with DSM-III diagnosis of ASD | 18 | 9 | 50 | 64.76 | 6.4 | – | Months | 8 | 1 | Autism | |
| Rickards 2009423 | 3–5 years, 35/59 diagnosed ASD by DSM-IV criteria | 54 | 54 | 100 | 69.65 | – | – | Months | 43 | 11 | ASD | |
| Roberts 2011405 | 2.2–5 years with DSM-IV diagnosis of ASD | 95 | 95 | 100 | – | – | 26.3–60.3 | Months | 86 | 9 | AD, ASD | |
| Rogers 2012317 | 14–24 months with ASD | 98 | 98 | 100 | 21 | – | – | Months | 76 | 22 | ASD | |
| Ruble 2008424 | 40–71 months with DSM-IV diagnosis of ASD | 35 | 35 | 100 | 55.9 | – | 40.9–70.9 | Months | 30 | 5 | Autism | |
| Salt 2002372 | Preschool children in Scotland, (mean 42.36 months) with ICD-10 diagnosis of ASD | 17 | 17 | 100 | 40.02 | – | – | Months | 14 | 3 | Childhood autism | |
| Schertz 2013402 | Mean age 24.6 and 27.5 months with ADOS diagnosis | 23 | 23 | 100 | 26.05 | – | – | Months | NR | NR | ASD | |
| Silva 2007299 | 3–6 years old with DSM-IV diagnosis of ASD | 15 | 15 | 100 | 4.83 | – | 3–6 | Years | 13 | 2 | AD | |
| Silva 2008300 | 3–6 years old with DSM-IV diagnosis of ASD | 26 | 26 | 100 | 56.3 | 12.5 | – | Months | 21 | 5 | Autism | |
| Smith 2000413 | 18–42 months with ‘clinical’ diagnosis of ASD | 28 | 28 | 100 | 35.92 | – | – | Months | 23 | 5 | Autism, PDD-NOS | |
| Smith 2010359 | All < 6 years with ADOS/ADI/DSM-IV diagnosis of ASD | 53 | 53 | 100 | 50.1 | 10 | – | Months | 47 | 6 | Autism | |
| Stahmer 2004355 | 0–3 years with DSM-IV diagnosis | 20 | 20 | 100 | 29.6 | – | 22–33 | Months | 16 | 4 | AD, PDD-NOS | |
| Stone 1999346 | 23–35 months with DSM-III or DSM-IV diagnosis of ASD | 60 | 30 | 50 | 31.3 | 3.3 | 23–35 | Months | 25 | 5 | Autism | |
| Strauss 2012329 | 26–81 months with DSM-IV diagnosis of ASD | 44 | 44 | 100 | – | – | 26–81 | Months | 41 | 3 | Autism, PDD-NOS | |
| Szatmari 2000302 | 4- to 6-year-old children (upon entering study) diagnosed by ADI | 134 | 68 | 51 | 66.8 | – | – | Months | 59 | 7 | Autism, Asperger syndrome | |
| Tonge 2012425 | Children were aged 2.5–5 years and diagnosis was made using a combination of medical reviews, ADI-R and CARS | 107 | 107 | 100 | – | – | 2.5–5.0 | Years | 90 | 17 | AD | |
| Toth 2006284 | 34–52 months with ADI-diagnosis of ASD | 60 | 60 | 100 | 43.6 | 4.3 | 34–52 | Months | 51 | 9 | AD, PDD-NOS | |
| VanMeter 1997426 | Mean ages ranged from 2.9 (SD = 0.77) to 5.7 (SD = 1.31) years meeting DSM-III criteria for ASD | 143 | 57 | 40 | – | – | 5.2–6.0 | Years | 54 | 3 | AD | |
| Ventola 2007332 | 16–32 months old with M-CHAT diagnosis of ASD | 195 | 195 | 100 | – | – | 16–32 | Months | 152 | 43 | ASD | |
| Werner 2005316 | 12–57 months with DSM-IV diagnosis of ASD | 145 | 72 | 50 | 43.5 | 4.3 | – | Months | 60 | 12 | AD, PDD-NOS | |
| Zachor 2010335 | 15- to 35-month-old children who met DSM-IV criteria | 71 | 71 | 100 | 25.55 | 4.25 | 15–35 | Months | 71 | 7 | Autism | |
| Video coding of feeding behavioura | Brisson 2012449 | 3- to 6-month-old children later diagnosed with an ASD | 27 | 13 | 48 | – | – | 3–6 | Months | 13+ | NR | AD, ASD |
| Global measure of function | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ages and Stages Questionnaire (ASQ) | Feldman 2012104 | Children who aged between 1 and 24 months who were ‘at risk’ for autism (they had a sibling with a diagnosis of ASD, Asperger syndrome or PDD-NOS) | 108 (parents) | 108 | 100 | 8 | 5 | – | Months | 74 | 34 | AD, PDD-NOS, Asperger syndrome and high-functioning autism |
| Assessment of Basic Language and Learning Skills (ABLLS) | Goin-Kochel 2007427 | Children were aged between 29.6–61.4 months; diagnosis was based on ADOS criteria | 29 | 29 | 100 | 45.7 | 9.6 | 29.6–61.4 | Months | 27 | 2 | Autism, PDD-NOS |
| Grindle 2012417 | 3- to 7-year-old children with autism | 29 | 29 | 100 | – | – | 43–72 | Months | 25 | 4 | Autism | |
| Gupta 2009303 | Children had a mean age of 4.8 years at start of the study and were diagnosed of autism based on DSM-IV-TR criteria | 40 | 20 | 50 | 4.16 | 0.86 | – | Years | 12 | 8 | Autism | |
| Assessment, Evaluation and Programming System (AEPS) | Schwartz 2004450 | 3–6 years old with CARS diagnosis of ASD | 48 | 48 | 100 | – | – | 3–6 | Years | 37 | 11 | Autism, PDD-NOS |
| Behavior Assessment System for Children-Second Edition (BASC-2) | Hill-Chapman 2013434 | Parents of children with ASD | 56 (parents) | 56 | 100 | 3.98 | 1.31 | – | Years | N/A | N/A | AD, PDD-NOS, Asperger syndrome |
| Brigance Diagnostic Inventory of Early Development | Travers 2011438 | 3–6 years meeting a ‘state educational definition of Autism’ | 17 | 17 | 100 | – | – | 3–6 | Years | NR | NR | Autism |
| Developmental Profile | Malhi 2011342 | Children were ≤ 3 years at start of the study and had an ASD diagnosis based on DSM-IV criteria | 77 | 77 | 100 | – | – | 0–3 | Years | 64 | 13 | AD, PDD-NOS |
| Early Development Interview | Werner 2005316 | 12–57 months with DSM-IV diagnosis of ASD | 145 | 72 | 50 | 43.5 | 4.3 | – | Months | 60 | 12 | AD, PDD-NOS |
| Early Intervention Developmental Profile (EIDP) | Jocelyn 1998298 | 24- to 72-month-old children who met DSM-III-R criteria | 35 | 35 | 100 | 43.2 | 9.1 | – | Months | 27 | 8 | Autism, PDD-NOS |
| Early Learning Accomplishment Profile (E-LAP) | Virues-Ortega 2013451 | Mean age 51.91 (SD = 27.31) with DSM-IV diagnosis | 24 | 24 | 100 | 51.91 | 27.3 | – | Months | 21 | 3 | ASD |
| Functional Emotional Developmental Questionnaire | Pajareya 2012343 | 2–6 years old with ASD | 34 | 34 | 100 | 4.23 | 1.16 | 2–6 | Years | 30 | 4 | Autism, PDD-NOS |
| Pajareya 2011344 | 24–72 months old with DSM-IV diagnosis for ASD | 32 | 32 | 100 | 54.05 | – | 24–72 | Months | 28 | 4 | Autism, PDD-NOS | |
| Learning Accomplishment Profile-Diagnostic, Third Edition (LAP-D) | Virues-Ortega 2013451 | Mean age 51.91 (SD = 27.31) with DSM-IV diagnosis | 24 | 24 | 100 | 51.91 | 27.3 | – | Months | 21 | 3 | ASD |
| Paediatric Daily Occupation Scale | Hsieh 2013452 | Parents of children with ASD | 40 | 40 | 100 | 5 | 0.9 | 2.5–6.0 | Years | 35 | 5 | Autism, PDD-NOS, Asperger |
| Preschool Developmental Profile (PSDP) | Jocelyn 1998298 | 24- to 72-month-old children who met DSM-III-R criteria | 35 | 35 | 100 | 43.2 | 9.1 | – | Months | 27 | 8 | Autism, PDD-NOS |
| Psychoeducational Profile-Revised (PEP-R) | Delmolino 2006432 | Mean age was 44 months (range = 37 to 60 months). Diagnosis was made prior to inclusion in the study and confirmed using ADOS and ADI-R | 27 | 27 | 100 | – | – | 3–6 | Years | 23 | 4 | Autism, PDD-NOS |
| Herring 2006411 | Children were aged between 20 and 51 months who met the DSM-IV criteria for diagnosis | 123 | 84 | 68 | 37.75 | 7.07 | – | Months | 75 | 9 | AD, PDD-NOS | |
| McConkey 2010349 | Children with ASD diagnosis (criteria not given, it was only stated as ‘confirmed diagnosis of ASD from a specialist clinic’) who had a mean age of 2.8 years at start of the study | 62 (families) | 61 | 98 | – | – | < 4 | Years | 55 | 6 | Autism | |
| Osborne 2008350 | 2.6–4.0 years old with GARS diagnosis of ASD | 65 | 65 | 100 | – | – | 2.6–4.0 | Years | 59 | 6 | ASD | |
| Ozonoff 1998453 | 31–69 months diagnosed by CARS | 22 | 11 | 50 | 53.3 | 12.3 | 31–69 | Months | 9 | 2 | Autism | |
| Reed 2007352 | 2 years 6 months to 4 years old diagnosed with ASD | 27 | 27 | 100 | – | – | 2.5–4.0 | Years | 27 | 0 | ASD | |
| Reed 2007353 | 2 years 6 months to 4 years old with ‘paediatrician’ diagnosis of ASD | 53 | 53 | 100 | – | – | 2.5–4.0 | Years | Unclear | Unclear | ASD | |
| Reed 2012354 | 2.5–4 years with GARS diagnosis of ASD | 66 | 66 | 100 | 40.2 | 5.6 | – | Months | 59 | 7 | AD, PDD-NOS | |
| Tonge 2012425 | Children were aged 2.5–5 years and diagnosis was made using a combination of medical reviews, ADI-R and CARS | 107 | 107 | 100 | – | – | 2.5–5.0 | Years | 90 | 17 | AD | |
| Scales of Independent Behavior-Revised (SIB-R) | Keen 2010363 | Children aged 2–4 years who met the DSM-IV criteria for ASD diagnosis | 39 | 39 | 100 | – | – | 2–4 | Years | 34 | 5 | ASD |
| Vineland Adaptive Behavior Scales-Classroom version (VABS-Classroom) | Goin-Kochel 2007427 | Children were aged between 29.6–61.4 months; diagnosis was based on ADOS criteria | 29 | 29 | 100 | 45.7 | 9.6 | 29.6–61.4 | Months | 27 | 2 | Autism, PDD-NOS |
| Vineland Adaptive Behavior Scales (VABS) | Aldred 2004318 | 2 years to 5 years 11 months with ADI diagnosis | 28 | 28 | 100 | – | – | 24–71 | Months | 25 | 3 | AD or ‘classical autism’ |
| Anan 2008396 | 25 to 68 months old children who met the diagnosis of ASD based on DSM-IV criteria | 72 | 72 | 100 | – | – | 25–68 | Months | 61 | 11 | AD, PDD-NOS | |
| Andersson 2013409 | Children aged 1.8 to 3.9 years who met DSM-IV criteria | 40 | 37 | 93 | – | – | 1.8–3.9 | Years | 18 | 19 | AD, ASD, atypical autism, Asperger syndrome | |
| Arick 2003388 | Children between the ages of 2 and 6 years (at baseline) who have been said to have a diagnosis of autism; details of criteria used not provided | 67 | 67 | 100 | – | – | 2–6 | Years | NR | NR | ASD | |
| Baghdadli 2012339 | Age < 7 years, ICD-10 diagnosis of autism | 280 | 280 | 100 | 4.9 | 1.3 | – | Months | 230 | 50 | Childhood autism, atypical autism | |
| Bearss 2013278 | Children were aged between 3 years and 6 years 11 months, and assessed to have autism based on ADOS and clinical observation | 16 | 16 | 100 | – | – | 3–6 | Years | 16 | 0 | AD, PDD-NOS | |
| Ben Itzchak 2011320 | Children aged 15–35 months were included in the study | 78 | 78 | 100 | – | – | 15–35 | Months | 71 | 7 | Autism | |
| Bennett 2008296 | Children aged between 4 and 6 years | 64 | 64 | 100 | – | – | 4–6 | Years | 57 | 7 | Asperger syndrome, high-functioning autism | |
| Carlsson 2013390 | Children aged from 4.5 to 6.5 years who were assessed to have autism based on DSM-IV criteria | 198 | 119 | 60 | – | – | 4.5–6.5 | Years | NR | NR | Autistic-like condition, Asperger syndrome, autistic traits | |
| Cassidy 2008348 | Parents of children aged < 5 years with ICD-10 diagnosis of ASD | 104 | 104 | 100 | – | – | 2–4 | Years | 95 | 9 | ASD | |
| Dawson 2010321 | 18–30 months, diagnosed by ADOS, ADI and DSM-IV | 48 | 48 | 100 | – | – | 18–33 | Months | 37 | 11 | AD, PDD-NOS | |
| Eapen 2013357 | Mean age of 49.6 months | 26 | 26 | 100 | 49.6 | 6.08 | 36–58 | Months | 21 | 5 | AD | |
| Eikeseth 2009410 | 24–42 months with ICD-10 diagnosis of ASD | 23 | 23 | 100 | 34.9 | 5.7 | 28–42 | Months | 17 | 6 | Autism | |
| Eldevik 2012414 | Children aged 2 to 6 who had autism diagnosis based on ICD-10 criteria and ADI-R | 43 | 43 | 100 | 4.26 | 1.48 | 1–6 | Years | 33 | 10 | Autism, PDD-NOS, Asperger | |
| Eriksson 2013415 | Children aged 20–54 months. Criteria not stated | 208 | 208 | 100 | – | – | 20–54 | Months | 176 | 32 | ASD | |
| Gabriels 2007416 | Children had a mean age of 31 months and had a clinical diagnosis of autistic disorder or PDD-NOS based on DSM-IV criteria | 14 | 14 | 100 | 31 | – | – | Months | 10 | 4 | AD, PDD-NOS | |
| Green 2010253 | 24–60 months, ADOS or ADI diagnosed | 152 | 152 | 100 | 45 | – | 24–60 | Months | 138 | 14 | Core autism | |
| Grindle 2012417 | 3- to 7-year-old children with autism | 29 | 29 | 100 | – | – | 43–72 | Months | 25 | 4 | Autism | |
| Hedvall 2013418 | 3.6- to 6.6-year-old children with ASD | 190 | 168 | 88 | 55 | 0.8 | 42–76 | Months | 147 | 21 | AD, PDD-NOS, Asperger syndrome | |
| Herring 2006411 | Children were aged between 20 and 51 months who met the DSM-IV criteria for diagnosis | 123 | 84 | 68 | 37.75 | 7.07 | – | Months | 75 | 9 | AD, PDD-NOS | |
| Honey 2008307 | 24–48 months diagnosed by ICD-10 criteria | 104 | 79 | 76 | 37.05 | 6.08 | 24–48 | Months | 65 | 14 | ASD | |
| Hudry 2010233 | 24- to 59-month-old children with ADOS-G diagnosis | 152 | 152 | 100 | 44.83 | 7.98 | 24–59 | Months | 138 | 14 | Core autism | |
| Jasmin 2009384 | Children aged 3–4 years who had a diagnosis of ASD based on DSM-IV criteria | 35 | 35 | 100 | – | – | 3–4 | Years | 32 | 3 | Autistic, PDD-NOS, Asperger syndrome | |
| Jonsdottir 2007341 | Mean age was 41.43 months; diagnosis was based on ICD-10 criteria | 41 | 41 | 100 | 41.43 | 9.06 | 22–59 | Months | 34 | 7 | Childhood autism | |
| Klintwall 2012419 | 2 years and 3 months to 4 years and 11 months, with clinical diagnosis by paediatrician | 21 | 21 | 100 | 3.6 | – | 2.25–4.9 | Years | 16 | 5 | Autism | |
| Landa 2012224 | 22- to 33-month-old children with ASD or autism | 48 | 48 | 100 | 27 | 2.8 | 22–33 | Months | 39 | 9 | ASD | |
| Lerna 2012325 | 18–60 months old with diagnosis of autism and little or no functional language | 18 | 18 | 100 | – | – | 18–60 | Months | 17 | 1 | Autism | |
| Lloyd 2013400 | 12- to 36-month-old children with ASD | 162 | 162 | 100 | – | – | 12–37 | Months | 140 | 22 | ASD | |
| Luyster 2008129 | Participants were aged 18–33 months and met ADI-R criteria for ASD diagnosis | 164 | 164 | 100 | – | – | 18–33 | Months | 129 | 35 | ASD | |
| Magiati 2007308 | Children aged between 22 and 54 months who met ADI-R criteria for autism/ASD diagnosis | 44 | 44 | 100 | – | – | 22–54 | Months | 39 | 5 | Autism, ASD | |
| Magiati 2011309 | Mean age of 3.4 years at start of the study | 44 | 44 | 100 | 38.9 | 7.1 | 27–55 | Months | 39 | 5 | Autism, ASD | |
| Mayo 2013310 | 45–72 months with DSM-IV-TR criteria | 119 | 119 | 100 | 52.22 | 6.09 | 45–72 | Months | 99 | 20 | AD, PDD-NOS | |
| McConkey 2010349 | Children with ASD diagnosis (criteria not given, it was only stated as ‘confirmed diagnosis of ASD from a specialist clinic’) who had a mean age of 2.8 years at start of the study | 62 (families) | 61 | 98 | – | – | < 4 | Years | 55 | 6 | Autism | |
| Munson 2006420 | 38–54 months with DSM-IV diagnosis of ASD | 45 | 45 | 100 | 47.4 | 4.2 | 38–54 | Months | 38 | 7 | AD, PDD-NOS | |
| Munson 2008312 | 24–66 months with ADI or ADOS diagnosis of ASD | 456 | 456 | 100 | 43.4 | 8.7 | 24–66 | Months | 370 | 86 | Autism, ASD | |
| O’Donnell 2012386 | 3–4 years old with DSM-IV diagnosis of ASD | 42 | 42 | 100 | 45.5 | – | 36–59 | Months | NR | NR | Autism, PDD-NOS | |
| Osborne 2008350 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | – | – | 2.6–4.0 | Years | 59 | 6 | ASD | |
| Osborne 2009351 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | 3.4 | 0.75 | 2.6–4.0 | Years | 59 | 6 | ASD | |
| Peters-Scheffer 2010421 | 3- to 6-year-old children with DSM-IV diagnosis of AD or PDD-NOS | 34 | 34 | 100 | 53.5 | 5.52 | 42–62 | Months | NR | NR | AD, PDD-NOS | |
| Poon 2012401 | 9–12 months (upon entering study) with ADOS, ADI or CARS diagnosis of ASD | 29 | 29 | 100 | 4.46 | 1.49 | – | Months | 24 | 5 | AD, PDD-NOS, Asperger syndrome | |
| Pry 2005314 | 21 months to 7 years with ICD-10 diagnosis of ASD | 222 | 222 | 100 | 5 | 1.75 | 1.75–7 | Years | 180 | 42 | Infantile autism | |
| Ray-Subramanian 2011327 | 23–39 months with DSM-IV or ICD-10 diagnosis of ASD | 125 | 125 | 100 | 31 | 4.1 | 23–39 | Months | 108 | 17 | Autism, AD, PDD-NOS | |
| Reed 2007352 | 2 years 6 months to 4 years old diagnosed with ASD | 27 | 27 | 100 | – | – | 2.5–4.0 | Years | 27 | 0 | ASD | |
| Reed 2007353 | 2 years 6 months to 4 years old with ‘paediatrician’ diagnosis of ASD | 53 | 53 | 100 | – | – | 2.5–4.0 | Years | Unclear | Unclear | ASD | |
| Reed 2012354 | 2.5–4 years with GARS diagnosis of ASD | 66 | 66 | 100 | 40.2 | 5.6 | – | Months | 59 | 7 | AD, PDD-NOS | |
| Remington 2007358 | 30–42 months of age with ADI diagnosis of ASD | 44 | 44 | 100 | 37 | 4.2 | 30–42 | Months | NR | NR | Autism or suspected autism | |
| Restall 1994422 | 3–6 years with DSM-III diagnosis of ASD | 18 | 9 | 50 | 64.76 | 6.4 | – | Months | 8 | 1 | Autism | |
| Rickards 2009423 | 3–5 years, 35/59 diagnosed ASD by DSM-IV criteria | 54 | 54 | 100 | 69.65 | – | – | Months | 43 | 11 | ASD | |
| Roberts 2011405 | 2.2–5 years with DSM-IV diagnosis of ASD | 95 | 95 | 100 | – | – | 26.3–60.3 | Months | 86 | 9 | AD, ASD | |
| Rogers 2012317 | 14–24 months with ASD | 98 | 98 | 100 | 21 | – | – | Months | 76 | 22 | ASD | |
| Ruble 2008424 | 40–71 months with DSM-IV diagnosis of ASD | 35 | 35 | 100 | 55.9 | – | 40.9–70.9 | Months | 30 | 5 | Autism | |
| Salt 2002372 | Preschool children in Scotland, (mean 42.36 months) with ICD-10 diagnosis of ASD | 17 | 17 | 100 | 40.02 | – | – | Months | 14 | 3 | Childhood autism | |
| Schertz 2013402 | Mean age 24.6 and 27.5 months with ADOS diagnosis | 23 | 23 | 100 | 26.05 | – | – | Months | NR | NR | ASD | |
| Silva 2007299 | 3–6 years old with DSM-IV diagnosis of ASD | 15 | 15 | 100 | 4.83 | – | 3–6 | Years | 13 | 2 | AD | |
| Silva 2008300 | 3–6 years old with DSM-IV diagnosis of ASD | 26 | 26 | 100 | 56.3 | 12.5 | – | Months | 21 | 5 | Autism | |
| Smith 2000413 | 18–42 months with ‘clinical’ diagnosis of ASD | 28 | 28 | 100 | 35.92 | – | – | Months | 23 | 5 | Autism, PDD-NOS | |
| Smith 2010359 | All < 6 years with ADOS/ADI/DSM-IV diagnosis of ASD | 53 | 53 | 100 | 50.1 | 10 | – | Months | 47 | 6 | Autism | |
| Stahmer 2004355 | 0–3 years with DSM-IV diagnosis | 20 | 20 | 100 | 29.6 | – | 22–33 | Months | 16 | 4 | AD, PDD-NOS | |
| Stone 1999346 | 23–35 months with DSM-III or DSM-IV diagnosis of ASD | 60 | 30 | 50 | 31.3 | 3.3 | 23–35 | Months | 25 | 5 | Autism | |
| Strauss 2012329 | 26–81 months with DSM-IV diagnosis of ASD | 44 | 44 | 100 | – | – | 26–81 | Months | 41 | 3 | Autism, PDD-NOS | |
| Szatmari 2000302 | 4- to 6-year-old children (upon entering study) diagnosed by ADI | 134 | 68 | 51 | 66.8 | – | – | Months | 59 | 7 | Autism, Asperger syndrome | |
| Tonge 2012425 | Children were aged 2.5–5 years and diagnosis was made using a combination of medical reviews, ADI-R and CARS | 107 | 107 | 100 | – | – | 2.5–5.0 | Years | 90 | 17 | AD | |
| Toth 2006284 | 34–52 months with ADI-diagnosis of ASD | 60 | 60 | 100 | 43.6 | 4.3 | 34–52 | Months | 51 | 9 | AD, PDD-NOS | |
| VanMeter 1997426 | Mean ages ranged from 2.9 (SD = 0.77) to 5.7 (SD = 1.31) years meeting DSM-III criteria for ASD | 143 | 57 | 40 | – | – | 5.2–6.0 | Years | 54 | 3 | AD | |
| Ventola 2007332 | 16–32 months old with M-CHAT diagnosis of ASD | 195 | 195 | 100 | – | – | 16–32 | Months | 152 | 43 | ASD | |
| Werner 2005316 | 12–57 months with DSM-IV diagnosis of ASD | 145 | 72 | 50 | 43.5 | 4.3 | – | Months | 60 | 12 | AD, PDD-NOS | |
| Zachor 2010335 | 15- to 35-month-old children who met DSM-IV criteria | 71 | 71 | 100 | 25.55 | 4.25 | 15–35 | Months | 71 | 7 | Autism | |
| Social Adaptive Development Quotient Scale (ADQ)a | Zhang 2012303 | 76 children with ASD (mean age 4.09, SD 1.66) | 96 | 96 | 100 | 4.37 | 1.6 | – | Years | 68 | 8 | Autistic |
| Global measure of outcome | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Autism Treatment Evaluation Checklist (ATEC) | Goin-Kochel 2007427 | Children were aged between 29.6–61.4 months; diagnosis was based on ADOS criteria | 29 | 29 | 100 | 45.7 | 9.6 | 29.6–61.4 | Months | 27 | 2 | Autism, PDD-NOS |
| Behavioral Summarized Evaluation-Revised (BSE-R) | Receveur 2005337 | Observed from 10 months old to 4 years old – met DSM-IV criteria for ASD | 18 | 18 | 100 | 58 | 3.2 | 10–59 | Months | 13 | 5 | AD |
| Behavioral Summarized Evaluation (BSE) | Maestro 2005338 | Videos of first year of life observed, all met DSM-IV criteria for ASD | 40 | 40 | 100 | – | – | 0–1 | Years | 32 | 8 | AD, PDD-NOS |
| Clinical Global Impression Improvement Scale | Bearss 2013278 | Children were aged between 3 years and 6 years 11 months, and assessed to have autism based on ADOS and clinical observation | 16 | 16 | 100 | – | – | 3–6 | Years | 16 | 0 | AD, PDD-NOS |
| Oosterling 2010326 | 12–42 months old with ‘clinical’ diagnosis of ASD | 80 | 80 | 100 | 34.8 | – | – | Months | 62 | 18 | Autism, PDD-NOS | |
| Infant Behavioral Summarized Evaluation (IBSE) | Adrien 199290 | 0–2 years, DSM-III-R criteria | 24 | 12 | 50 | – | – | 0–2 | Years | 10 | 2 | Autism |
| Receveur 2005337 | Observed from 10 months old to 4 years old – met DSM-IV criteria for ASD | 18 | 18 | 100 | 58 | 3.2 | 10–59 | Months | 13 | 5 | AD | |
| Pervasive Developmental Disorders Behavior Inventory (PDDBI) | Silva 2009226 | 3–6 years with DSM-IV diagnosis of ASD | 46 | 46 | 100 | 59.2 | – | – | Months | 37 | 9 | Autism |
| Silva 2011301 | 3–6 years old with clinical diagnosis of ASD | 47 | 47 | 100 | 4.83 | – | 3–6 | Years | 33 | 14 | Autism |
| Subjective well-being | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kiddie–Infant Descriptive Instrument for Emotional States (KIDIES)a | Trad 1993454 | 24–55 months with DSM-III diagnosis of ASD | 47 | 26 | 55 | 39 | – | 24–55 | Months | NR | NR | AD, PDD-NOS |
| Social inclusion | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| School Liking and Avoidance Questionnaire | Jahromi 2013431 | 20 TD and 20 children with high-functioning autism | 40 | 20 | 50 | 58.95 | 11.5 | – | Months | 36 | 4 | High-functioning autism |
| Teacher Rating Scale of School Adjustment | Jahromi 2013431 | 20 TD and 20 children with high-functioning autism | 40 | 20 | 50 | 58.95 | 11.5 | – | Months | 36 | 4 | High-functioning autism |
| Interaction style | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Functional Emotional Assessment Scale | Pajareya 2012343 | 2–6 years old with ASD | 34 | 34 | 100 | 4.23 | 1.16 | 2–6 | Years | 30 | 4 | Autism, PDD-NOS |
| Pajareya 2011344 | 24–72 months old with DSM-IV diagnosis for ASD | 32 | 32 | 100 | 54.05 | – | 24–72 | Months | 28 | 4 | Autism, PDD-NOS | |
| NICHD Early Child Care Network scales | Baker 2010397 | 33 ‘at-risk’ children, entered study between ages of 2–18 months, assessed at 18, 24, 30 and 36 months. | 33 | 12 | 36 | 18 | – | – | Months | NR | NR | ASD |
| Coded observation of social behavioura | Meirsschaut 2011442 | 21–56 months meeting ADOS criteria for ASD | 42 | 21 | 50 | 36.94 | – | 21–56 | Months | 18 | 3 | Autism, ASD |
| Coding of videosa | Flippin 2011406 | Children aged 40–69 months with autism diagnosis based on ADOS | 16 | 16 | 100 | 53.3 | 9.6 | 40–69 | Months | 12 | 4 | ASD |
| Parental skills – video ratingsa | Oosterling 2010326 | 12–42 months old with ‘clinical’ diagnosis of ASD | 80 | 80 | 100 | 34.8 | – | – | Months | 62 | 18 | Autism, PDD-NOS |
| Parent–child free playa | Freeman 2013443 | 18- to 55-month-old children, 50 met DSM-IV criteria | 32 (parent–child dyads) | 16 | 50 | 49.5 | 11.8 | – | Months | 12 | 4 | Autism |
| Parent–child interactiona | Green 2010253 | 24–60 months, ADOS or ADI diagnosed | 152 | 152 | 100 | 45 | – | 24–60 | Months | 138 | 14 | Core autism |
| Parent–Child Interaction measurea | Aldred 2012319 | Children aged 2–5 years assessed using ADOS and ADI-R | 28 | 28 | 100 | – | – | 2–5 | Years | 25 | 3 | Autism |
| Preschool teacher–child playa | Kaale 2012294 | Children aged 29–60 months who had a diagnosis of autistic disorder based on ICD-10 criteria | 61 | 61 | 100 | – | – | 24–60 | Months | 48 | 13 | Autism |
| Social Interaction Rating Scalea | Ruble 2008424 | 40–71 months with DSM-IV diagnosis of ASD | 35 | 35 | 100 | 55.9 | – | 40.9–70.9 | Months | 30 | 5 | Autism |
| Parent stress | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Autism Parenting Stress Index (PSI) (APSI) | Silva 2011301 | 3–6 years old with clinical diagnosis of ASD | 47 | 47 | 100 | 4.83 | – | 3–6 | Years | 33 | 14 | Autism |
| Beck Anxiety Inventory | Davis 2008455 | Children had a mean age of 26.9 months | 54 (parents) | 54 | 100 | 26.9 | 4.2 | – | Months | 40 | 14 | Autism, PDD-NOS |
| Center for Epidemiologic Studies Depression Inventory | Davis 2008455 | Children had a mean age of 26.9 months | 54 (parents) | 54 | 100 | 26.9 | 4.2 | – | Months | 40 | 14 | Autism, PDD-NOS |
| Center for Epidemiologic Studies Depression Inventory | Taylor 2012436 | Mothers of ASD children aged mean 3.72 years (SD = 1.82) and 4.18 (SD = 2.65) at diagnosis | 75 (mothers) | 75 | 100 | 3.72 | 18.2 | – | Months | NR | NR | ASD |
| General Health Questionnaire (GHQ) | Herring 2006411 | Children were aged between 20 and 51 months who met the DSM-IV criteria for diagnosis | 123 | 84 | 68 | 37.75 | 7.07 | – | Months | 75 | 9 | AD, PDD-NOS |
| McConkey 2010349 | Children with ASD diagnosis (criteria not given, it was only stated as ‘confirmed diagnosis of ASD from a specialist clinic’) who had a mean age of 2.8 years at start of the study | 62 (families) | 61 | 98 | – | – | < 4 | Years | 55 | 6 | Autism | |
| Tonge 2005456 | Parents of children 2.5−5 years old with DSM-IV diagnosis of ASD | 105 (parents) | 103 | 100 | – | – | 23–70 | Months | 87 | 16 | AD | |
| Hospital Anxiety and Depression Scale (HADS) | Remington 2007358 | 30–42 months of age with ADI diagnosis of ASD | 44 | 44 | 100 | 37 | 4.2 | 30–42 | Months | NR | NR | Autism or suspected autism |
| Parenting Stress Index-Short Form (PSI-SF) | Strauss 2012329 | 26–81 months with DSM-IV diagnosis of ASD | 44 | 44 | 100 | – | – | 26–81 | Months | 41 | 3 | Autism, PDD-NOS |
| Parenting Sense of Competence (PSOC) | Keen 2007364 | Diagnosis of autism was based on DSM-IV criteria | 16 | 16 | 100 | – | – | 2–4 | Years | 14 | 2 | Autism |
| Keen 2010363 | Children aged 2–4 years who met the DSM-IV criteria for ASD diagnosis | 39 | 39 | 100 | – | – | 2–4 | Years | 34 | 5 | ASD | |
| Parenting Stress Index (PSI) | Aldred 2004318 | 2 years to 5 years 11 months with ADI diagnosis | 28 | 28 | 100 | – | – | 24–71 | Months | 25 | 3 | AD or ‘classical autism’ |
| Baker-Ericzen 2005457 | Parents of toddlers (mean age 28.35 months) with ASD | 60 (parents) | 37 (parents) | 62 | 28.35 | 5.2 | – | Months | 29 | 8 | ASD | |
| Keen 2010363 | Children aged 2–4 years who met the DSM-IV criteria for ASD diagnosis | 39 | 39 | 100 | – | – | 2–4 | Years | 34 | 5 | ASD | |
| Roberts 2011405 | 2.2–5 years with DSM-IV diagnosis of ASD | 95 | 95 | 100 | – | – | 26.3–60.3 | Months | 86 | 9 | AD, ASD | |
| Salt 2002372 | Preschool children in Scotland, (mean 42.36 months) with ICD-10 diagnosis of ASD | 17 | 17 | 100 | 40.02 | – | – | Months | 14 | 3 | Childhood autism | |
| Parenting Stress Index-Short Form (PSI-SF) | Bendixen 2011458 | Children had a mean age of 4.41 years (SD = 1.36, range = 3–8 years) | 19 | 19 | 100 | 4.41 | 1.36 | 3–8 | Years | 18 | 1 | AD |
| Davis 2008455 | Children had a mean age of 26.9 months | 54 (parents) | 54 | 100 | 26.9 | 4.2 | – | Months | 40 | 14 | Autism, PDD-NOS | |
| Hill-Chapman 2013434 | Parents of children with ASD | 56 | 56 | 100 | 3.98 | 1.31 | – | Years | N/A | N/A | AD, PDD-NOS, Asperger syndrome | |
| Minjarez 2013459 | 2–6 years, with DSM-IV-TR criteria | 17 | 17 | 100 | 3.11 | 1.1 | 2.5–6.7 | Years | 17 | 0 | AD, PDD-NOS | |
| Wang 2013460 | Mothers of children [mean (SD) = 5.15 years (1.72)] with DSM-IV diagnosis | 150 | 150 | 100 | 5.15 | 1.72 | – | Years | 124 | 26 | Autism, PDD-NOS, Asperger | |
| Wong 2010333 | 17–36 months children diagnosed by DSM-IV, ADI and ADOS | 17 | 17 | 100 | – | – | 17–36 | Months | 16 | 1 | – | |
| Positive and Negative Affect Scale (PANAS) | Hsieh 2013452 | Parents of children with ASD | 40 | 40 | 100 | 5 | 0.9 | 2.5–6.0 | Years | 35 | 5 | Autism, PDD-NOS, Asperger |
| Questionnaire on Resources and Stress-Friedrich Short Form (QRS-F) | Cassidy 2008348 | Parents of children aged < 5 years with ICD-10 diagnosis of ASD | 104 | 104 | 100 | – | – | 2–4 | Years | 95 | 9 | ASD |
| McConkey 2010349 | Children with ASD diagnosis (criteria not given, it was only stated as ‘confirmed diagnosis of ASD from a specialist clinic’) who had a mean age of 2.8 years at start of the study | 62 (families) | 61 | 98 | – | – | < 4 | Years | 55 | 6 | Autism | |
| Osborne 2008350 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | – | – | 2.6–4 | Years | 59 | 6 | ASD | |
| Osborne 2009351 | 2.6–4 years old with GARS diagnosis of ASD | 65 | 65 | 100 | 3.4 | 0.75 | 2.6–4.0 | Years | 59 | 6 | ASD | |
| Remington 2007358 | 30–42 months of age with ADI diagnosis of ASD | 44 | 44 | 100 | 37 | 4.2 | 30–42 | Months | NR | NR | Autism or suspected autism | |
| Rickards 2009423 | 3–5 years, 35/59 diagnosed ASD by DSM-IV criteria | 54 | 54 | 100 | 69.65 | – | – | Months | 43 | 11 | ASD | |
| Questionnaire on Resources and Stress-Friedrich Short Form (QRS-F) | Reed 2013437 | 0 | 52 | 52 | 100 | 44.4 | 7.9 | 36.77 | Months | 46 | 6 | Childhood autism, PDD-NOS |
| Reaction to Diagnosis Interview | Oppenheim 2012461 | 45 boys and their mothers | 45 | 45 | 100 | 49.35 | 9.56 | 32–69 | Months | 45 | 0 | AD, PDD-NOS |
| Wachtel 2008462 | Mothers of ASD children, aged 18–33 months, diagnosed by ADOS and ADI | 63 | 63 | 100 | 32 | 7.1 | 20–50 | Months | 48 | 15 | ASD | |
| Satisfaction with Life Scale | Hsieh 2013452 | Parents of children with ASD | 40 | 40 | 100 | 5 | 0.9 | 2.5–6.0 | Years | 35 | 5 | Autism, PDD-NOS, Asperger |
| Stress Arousal Checklist | Jocelyn 1998298 | 24- to 72-month-old children who met DSM-III-R criteria | 35 | 35 | 100 | 43.2 | 9.1 | – | Months | 27 | 8 | Autism, PDD-NOS |
| Symptom Checklist-90-Revised (SCL-90) | Bennett 2012304 | Children with ASD aged 2–4 years old | 214 | 178 | 83 | – | – | 2–4 | Years | 181 | 33 | AD, Asperger syndrome, PDD-NOS |
| Daily occupational experiencea | Hsieh 2013452 | Parents of children with ASD | 40 | 40 | 100 | 5 | 0.9 | 2.5–6.0 | Years | 35 | 5 | Autism, PDD-NOS, Asperger |
| Parent–child Interaction Rating Scalesa | Wachtel 2008462 | Mothers of ASD children, aged 18–33 months, diagnosed by ADOS and ADI | 63 | 63 | 100 | 32 | 7.1 | 20–50 | Months | 48 | 15 | ASD |
| Parenting stress thermometera | Tonge 2005456 | Parents of children 2.5−5 years old with DSM-IV diagnosis of ASD | 105 (parents) | 103 | 100 | – | – | 23–70 | Months | 87 | 16 | AD |
| Self-constructed questionnairea | Farmer 2013463 | Children aged 2–6 years; criteria for diagnosis not stated | 102 | 102 | 100 | – | – | 2–6 | Years | 37 | 65 | Autism |
| Stress thermometera | Herring 2006411 | Children were aged between 20 and 51 months who met the DSM-IV criteria for diagnosis | 123 | 84 | 68 | 37.75 | 7.07 | – | Months | 75 | 9 | AD, PDD-NOS |
| Family quality of life | Paper | Participant description | n | n with ASD | % ASD | Mean age | Age SD | Age range | Years/months | M | F | Diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beach Family Quality of Life Questionnaire | Roberts 2011405 | 2.2–5 years with DSM-IV diagnosis of ASD | 95 | 95 | 100 | – | – | 26.3–60.3 | Months | 86 | 9 | AD, ASD |
| Family Adaptability and Cohesion Evaluation Scales | Bendixen 2011458 | Children had a mean age of 4.41 years (SD = 1.36, range = 3–8 years) | 19 | 19 | 100 | 4.41 | 1.36 | 3–8 | Years | 18 | 1 | AD |
| Family Assessment Device | Herring 2006411 | Children were aged between 20 and 51 months who met the DSM-IV criteria for diagnosis | 123 | 84 | 68 | 37.75 | 7.07 | – | Months | 75 | 9 | AD, PDD-NOS |
| Tonge 2005456 | Parents of children aged 2.5–5 years old with DSM-IV diagnosis of ASD | 105 (parents) | 103 | 100 | – | – | 23–70 | Months | 87 | 16 | AD | |
| Family Assessment Measure (Skinner et al. 1983) | Jocelyn 1998298 | 24- to 72-month-old children who met DSM-III-R criteria | 35 | 35 | 100 | 43.2 | 9.1 | – | Months | 27 | 8 | Autism, PDD-NOS |
| Family Empowerment Scale | Minjarez 2013459 | 2–6 years with DSM-IV-TR criteria | 17 | 17 | 100 | 3.11 | 1.1 | 2.5–6.7 | Years | 17 | 0 | AD, PDD-NOS |
| Rickards 2009423 | 3–5 years, 35/59 diagnosed ASD by DSM-IV criteria | 54 | 54 | 100 | 69.65 | – | – | Months | 43 | 11 | ASD | |
| Family Support Scale | Rickards 2009423 | 3–5 years, 35/59 diagnosed ASD by DSM-IV criteria | 54 | 54 | 100 | 69.65 | – | – | Months | 43 | 11 | ASD |
| Kansas Inventory of Parental Perceptions | Remington 2007358 | 30–42 months of age with ADI diagnosis of ASD | 44 | 44 | 100 | 37 | 4.2 | 30–42 | Months | NR | NR | Autism or suspected autism |
| Parenting Alliance Inventory | Hill-Chapman 2013434 | Parents of children with ASD | 56 | 56 | 100 | 3.98 | 1.31 | – | Years | N/A | N/A | AD, PDD-NOS, Asperger syndrome |
| Familial Resources Indexa | Baghdadli 2012339 | Age < 7 years, ICD-10 diagnosis of autism | 280 | 280 | 100 | 4.9 | 1.3 | – | Months | 230 | 50 | Childhood autism, atypical autism |
| TRE-ADD Autism Quiz (TAQ)a | Jocelyn 1998298 | 24- to 72-month-old children who met DSM-III-R criteria | 35 | 35 | 1 | 43.2 | 9.1 | – | Months | 27 | 8 | Autism, PDD-NOS |
| Family Satisfaction Questionnairea | Smith 2000413 | 18–42 months with ‘clinical’ diagnosis of ASD | 28 | 28 | 100 | 35.92 | – | – | Months | 23 | 5 | Autism, PDD-NOS |
Chapter 3 Tools used (subscales, outcomes measured)
| Symptom severity | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Autism Behavior Checklist (AuBC) | Bennett 2008296 | – | Clinical diagnosis at different time points |
| Gupta 2009303 | Total, sensory, relating, body/object use, language/social, self-help behaviours | Sensory, relating, body/object use, language/social, self-help | |
| Jocelyn 1998298 | Sensory, relating, body/object use, language/social, self-help behaviours | – | |
| Silva 2007299 | – | ‘Non-adaptive behaviours’ | |
| Silva 2008300 | – | ‘Autistic behaviour’ | |
| Silva 2009300 | – | ‘Autistic behaviour’ | |
| Silva 2011301 | – | ‘Autistic behaviour’ | |
| Szatmari 2000302 | – | ‘Pervasive developmental disorder symptoms’ | |
| Zhang 2012303 | – | Typical autistic behaviours | |
| Autism Diagnostic Interview-Revised (ADI-R) | Bennett 2012304 | Non-verbal items were used so that results could be compared between verbal and non-verbal children | – |
| Ben Itzchak 2008149 | – | Autism severity | |
| Brian 2008305 | – | – | |
| Feldman 2012104 | – | – | |
| Hambly 2012306 | Items on language (#42, 46, 29, 30, 9, 10) | Sociocommunicative levels, ages of early language milestones | |
| Honey 2008307 | Repetitive behaviour algorithm items | ‘Repetitive behaviour’ | |
| Magiati 2007308 | – | Autism severity and diagnosis confirmation | |
| Magiati 2011309 | Total score | Autism severity | |
| Mayo 2013310 | – | Communication, social development and play, and the presence of repetitive or restricted behaviours | |
| Mooney 2006311 | – | ‘Repetitive behaviours’ | |
| Munson 2008312 | Social relatedness, communication, repetitive, restricted behaviours | ‘Autism severity’ | |
| Ozonoff 2010313 | – | ‘Parent recall of symptom onset and possible regression’ | |
| Pry 2005314 | – | ‘Expressive language level’ | |
| Richler 2007315 | Restricted and repetitive behaviours items | ‘Restricted and repetitive behaviours’ | |
| Werner 2005316 | Social, communication, repetitive | ‘Developmental outcomes’ | |
| Autism Diagnostic Observation Scale-Toddler Module (ADOS-T) | Rogers 2012317 | Social affect, restricted, repetitive behaviours | ‘Social and communicative behaviours, as well as repetitive behaviours diagnostic of autism’ |
| Autism Diagnostic Observation Schedule (ADOS) | Aldred 2004318 | Reciprocal social interaction, communication, stereotyped and restricted behaviours | ‘Interaction, communication, repetitive behaviours and play’ |
| Aldred 2012319 | Total social communication algorithm score | Social communication | |
| Ben Itzchak 2008149 | Language and communication, reciprocal social interaction, play, and stereotyped behaviour and restricted interests | Social and communicative functioning | |
| Ben Itzchak 2011320 | ADOS standardised measure of severity | Autism severity, diagnostic algorithm | |
| Bennett 2012304 | – | Social and communication behaviours | |
| Brian 2008305 | Module 1 | – | |
| Dawson 2010321 | Social relatedness, communication, play, repetitive behaviours | ‘Autism symptoms’ | |
| Gotham 2012322 | – | Symptom severity | |
| Green 2010253 | Communication, social | ‘Severity of the symptoms of autism’ | |
| Hartley 2009323 | Communication, social interaction, restricted behaviours | ASD symptoms | |
| Landa 2012224 | – | Symptom severity | |
| Lerna 2012325 | Communication, reciprocal social interaction | Social communicative abilities | |
| Luyster 2008129 | Play | – | |
| Munson 2008312 | Communication, social | ‘Autism severity’ | |
| Oosterling 2010326 | Level of non-echoed language, joint attention, social affect | Language development, early precursors of social communication | |
| Ray-Subramanian 2011327 | – | ‘Social communication skills and behaviours characteristic of autism’ | |
| Ray-Subramanian 2012328 | Calibrated ADOS severity scores, composite RRB variable | RRB | |
| Strauss 2012329 | Communication, social | ‘Severity of autism symptoms’ | |
| Sullivan 2007330 | Response to joint attention item | ‘Response to joint attention’ | |
| Tek 2012331 | Communication, reciprocal social interaction | Assessment for ASD | |
| Ventola 2007332 | Communication, social | ‘Communication, social interactions and relatedness, play, and imagination’ | |
| Werner 2005316 | Communication, social | ‘Developmental outcomes’ | |
| Wong 2010333 | Language and communication, reciprocal social interaction | ‘Assessing Autism Spectrum Disorder’ | |
| Zachor 2006334 | Language and communication, reciprocal social interaction | Language and communication and reciprocal social interaction | |
| Zachor 2010335 | – | ‘Autism severity’ | |
| Autism Observation Scale for Infants (AOSI) | Brian 2008305 | – | ‘Putative signs of autism in infants aged 6 to 18 months’ |
| Bryson 200881 | – | – | |
| Baby and Infant Screen for Children with aUtIsm Traits (BISCUIT-Part 1) | Fodstad 2009342 | – | ASD symptoms |
| Behavioral Summarized Evaluation (BSE)-Revised | Receveur 2005337 | – | ‘Interaction disorders’ |
| Behavioral Summarized Evaluation (BSE) | Maestro 2005344 | – | ‘Severity of behavioural problems’ |
| Childhood autism Rating Scale (CARS) | Baghdadli 2012339 | – | Symptom severity |
| Bopp 2009340 | – | Autism severity | |
| Jonsdottir 2007341 | – | Behaviour | |
| Malhi 2011342 | – | Severity of autism symptom | |
| Mayo 2013310 | – | Presence and severity of symptoms of ASD | |
| Pajareya 2012343 | – | Degree of autistic symptoms | |
| Pajareya 2011344 | – | ‘Degree of autistic symptoms’ | |
| Papavasiliou 2011345 | – | ‘Severity of autistic behaviour’ | |
| Pry 2005314 | – | ‘Severity of autistic symptoms’ | |
| Stone 1999346 | – | Autism characteristics | |
| Ventola 2007332 | – | ‘Presence and severity of pervasive developmental disorders’ | |
| Vorgraft 2007347 | – | ‘Interactive behaviour . . . degree of autism’ | |
| Zhang 2012303 | – | ‘Behaviours that are generally affected by severe autism’ | |
| Gilliam Autism Rating Scale (GARS) | Cassidy 2008348 | Stereotyped behaviors, communication, social interaction, developmental disturbances | ‘Features of autism’ |
| McConkey 2010349 | – | Autism features such as stereotyped behaviours, communication, social interaction and developmental disturbances | |
| Osborne 2008350 | Stereotyped behaviors, communication, social interaction, developmental disturbances | ‘Behaviours symptomatic of autism’ | |
| Osborne 2009351 | Stereotyped behaviors, communication, social interaction, developmental disturbances | ‘Autism severity’ | |
| Reed 2007352 | Stereotyped behaviors, communication, social interaction, developmental disturbances | ‘Autism severity’ | |
| Reed 2007353 | Stereotyped behaviors, communication, social interaction, developmental disturbance | ‘Autism severity’ | |
| Reed 2012354 | Stereotyped behaviors, communication, social interaction, developmental disturbances | Severity of autism | |
| Stahmer 2004355 | – | Severity of autistic symptoms | |
| Infant Behavioral Summarized Evaluation (IBSE) | Adrien 199290 | – | General autism characteristics |
| Receveur 2005337 | – | ‘Early signs of autism’ and ‘behavioural evaluation’ | |
| Modified Checklist for Autism in Toddlers (M-CHAT) | Ventola 2007 | – | ‘Joint attention, interest in other children, responding to name, and imitation’ |
| Parent Observation of Early Markers Scale (POEMS) | Feldman 2012104 | – | Social and communicative development, restricted interests, ritualistic, repetitive non-functional behaviours |
| Pervasive Developmental Disorder Rating Scale (PDDRS) | Eaves 2006356 | Arousal, affect, cognition | The construct of autism through three scales |
| Pervasive Developmental Disorders Behavior Inventory (PDDBI) | Silva 2009226 | Receptive/expressive social communication abilities composite, approach/withdrawal problems composite, sensory | ‘Social and language abilities and maladaptive behaviour’ |
| Silva 2011301 | Sensory, maladaptive behaviour, social/language/communication abilities | ‘Social and language abilities and maladaptive behaviour’ | |
| Real Life Rating Scale (Ritvo–Freeman) (RLRS) | Wong 2010333 | Sensory motor behaviour, social relationship to people, affectual reaction, sensory response, language | ‘Parents’ perception of their children’s social and communication behaviour’ |
| Social Communication Questionnaire (SCQ) | Eapen 2013357 | – | Communication behaviours |
| Remington 2007358 | – | ‘Autism symptoms’ | |
| Social Responsiveness Scale (SRS) | Bennett 2012304 | – | ASD symptoms or behaviours |
| Hambly 2012306 | – | Severity of autism symptoms within children’s natural environments (Constantino 2002) | |
| Smith 2010359 | – | ‘Autism symptoms’ | |
| Childhood autism rating scale-Tokyo versiona | Takeda 2005360 | – | ‘Autistic symptoms’ |
| Social awareness | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Child Behaviour Rating Scale (CBRS) (Modified) | Casenhiser 2013361 | – | Child behaviour |
| Communication and Symbolic Behavior Scales-Developmental Profile (CSBS-DP) | Green 2010253 | Social composite | ‘Child social communication’ |
| Landa 2007368 | Gaze shifts, shared positive affect, response to joint attention bids, initiation of joint attention, initiation of behaviour regulation, inventory of gestures, consonants in syllables, words and word combinations, action schema inventory, action schema sequences, action schema towards others | ‘Communicative, social affective, and symbolic abilities’ | |
| Sullivan 2007330 | Gaze-point following variable | ‘Response to joint attention . . . look and point trial’ | |
| Keen 2010363 | – | Social communication, speech and symbolic behaviour | |
| Keen 2007364 | Social, speech, symbolic | Social, speech and symbolic abilities | |
| Early Social Communication Scale (ESCS) | Dereu 2012365 | – | Initiating joint attention, responding to joint attention |
| Goods 2013366 | Spontaneous requesting gestures | Spontaneous requesting gestures | |
| Ingersoll 2012286 | – | Social interaction | |
| Kaale 2012294 | – | Joint attention | |
| Kalas 2012367 | – | Responses to bids for joint attention | |
| Kasari 2006368 | – | Social communication | |
| Lawton 2012369 | – | Joint attention, social interaction, symbolic play and behaviour regulation | |
| Luyster 2008129 | Initiating joint attention, responding to joint attention | – | |
| Paparella 2011370 | – | ‘Initiations and responses of joint attention behaviours’ | |
| Remington 2007358 | Initiating joint attention, responding to joint attention | ‘Non-verbal social communication’ | |
| Roos 2008371 | Initiating joint attention, responding to joint attention | ‘Joint attention’ | |
| Salt 2002372 | Joint attention, requesting, social interaction | ‘Non-verbal social communication’ | |
| Wong 2013373 | – | Non-verbal initiations and responses to joint attention, behaviour regulation or requesting behaviours, and social interactions | |
| Yoder 2006374 | Communication | – | |
| Early Social Communication Scales (ESCS)-Abridged | Yoder 2010375 | – | ‘Number of picture exchanges at post treatment assessment’ |
| Imitation Battery (IB) | Luyster 2008129 | – | – |
| Imitation Disorders Evaluation (IDE) | Receveur 2005337 | – | ‘Deficient and atypical imitation’ |
| Motor Imitation Scale (MIS) | Ingersoll 2010376 | – | Ability of child to imitate in a structured and elicited context |
| Ingersoll 2012286 | – | Imitation | |
| Preschool Imitation and Praxis Scale (PIPS) | Dereu 2012365 | Subscales for bodily imitation and procedural imitation were used | Motor imitation abilities |
| Pre-Verbal Communication Schedule (PVCS) | Salt 2002372 | Motor imitation subscale, social imitation subscale | ‘Imitation’ |
| Social Communication Assessment for Toddlers with Autism (SCATA) | Drew 2007137 | – | Social communication (contexts: free play, turn-taking, activated musical toys, bubbles, specific prompts) |
| Social Communication Behavior Codes | Ozonoff 2010313 | Gaze to faces, gaze to objects, smiles, non-verbal vocalisations, single word verbalisations, phrase verbalisations | ‘Social communication behaviour’ |
| Parent interviewa | Clifford 2008377 | Gaze, affect, joint attention, requesting | ‘Parent’s perception of their child’s early behaviours’ |
| Caregiver–child interactionb | Kasari 2006368 | – | Functional play acts, play levels, joint attention skills, joint engagement |
| Coded observation of joint attentionb | Warreyn 2007384 | Initiating requesting, following declarative, initiating declarative | ‘Joint attention’ |
| Coding of initiation of joint attentionb | Ingersoll 2012286 | – | Initiation of joint attention |
| Classroom observation measure (Wong and Kasari 2012)b | Goods 2013366 | – | Engagement states, spontaneous communicative gesture |
| Examiners Ratings of Social Engagementb | Ozonoff 2010313 | Frequency of eye contact, frequency of shared affect, overall social responsiveness | ‘Social engagement’ |
| Naturalistic examiner–child play sampleb | Roos 2008371 | Initiating joint attention, responding to joint attention | ‘Joint attention’ |
| Prelinguistic Communication Assessmentb | Stone 1997135 | – | ‘Non-verbal communication’ |
| Preschool teacher–child playb | Kaale 2012294 | – | Joint attention and joint engagement |
| Unstructured free play with examinerb | Lerna 2012325 | – | Co-operative play, joint attention, requests labelling |
| Unstructured Imitation Assessmentb | Ingersoll 2012286 | – | Imitation |
| Ingersoll 2010376 | – | Child’s ability to imitate in a spontaneous, social-interactive context | |
| Video coding proceduresb | Colgan 2006379 | – | Communicative gestures |
| Video observationb | Clifford 2008377 | Gaze, affect, joint attention, requesting | ‘Early social deficits’ |
| Video rating for expressive speechb | Baghdadli 2012339 | – | Expressive speech |
| Video recording of child in classroom activitesb | Ingersoll 2001380 | Language, peer social avoidance | Peer social avoidance behaviour, language |
| Restricted, repetitive behaviour | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Ben Itzchak 2008149 | – | Autism severity | |
| Autism Diagnostic Interview-Revised (ADI-R) | Bennett 2012304 | Non verbal items were used so that results could be compared between verbal and non-verbal children | – |
| Brian 2008305 | – | – | |
| Feldman 2012104 | – | – | |
| Hambly 2012306 | Items on language (#42, 46, 29, 30, 9, 10) | Sociocommunicative levels, ages of early language milestones | |
| Honey 2008307 | Repetitive behaviour algorithm items | ‘Repetitive behaviour’ | |
| Magiati 2007308 | – | Autism severity and diagnosis confirmation | |
| Magiati 2011309 | Total score | Autism severity | |
| Mayo 2013310 | – | Communication, social development and play, and the presence of repetitive or restricted behaviours | |
| Mooney 2006311 | – | ‘Repetitive behaviours’ | |
| Munson 2008312 | Social relatedness, communication, repetitive, restricted behaviours | ‘Autism severity’ | |
| Ozonoff 2010313 | – | ‘Parent recall of symptom onset and possible regression’ | |
| Pry 2005314 | – | ‘Expressive language level’ | |
| Richler 2007315 | RRB items | ‘Restricted and repetitive behaviours’ | |
| Werner 2005316 | Social, communication, repetitive | ‘Developmental outcomes’ | |
| Autism Diagnostic Observation Scale-Toddler Module (ADOS-T) | Rogers 2012317 | Social affect, restricted, repetitive behaviours | ‘Social and communicative behaviours, as well as repetitive behaviours diagnostic of autism’ |
| Autism Diagnostic Observation Schedule-Generic (ADOS-G) – Modules 1 and 2) | Green 2010253 | Communication, social | ‘Severity of the symptoms of autism’ |
| Autism Diagnostic Observation Schedule-Generic (ADOS-G) | Aldred 2004318 | Reciprocal social interaction, communication, stereotyped and restricted behaviours | ‘Interaction, communication, repetitive behaviours and play’ |
| Aldred 2012319 | Total social communication algorithm score | Social communication | |
| Ben Itzchak 2008149 | Language and communication, reciprocal social interaction, play, and stereotyped behaviour and restricted interests | Social and communicative functioning | |
| Ben Itzchak 2011320 | ADOS standardised measure of severity | Autism severity, diagnostic algorithm | |
| Bennett 2012304 | – | Social and communication behaviours | |
| Brian 2008305 | Module 1 | – | |
| Dawson 2010321 | Social relatedness, communication, play, repetitive behaviours | ‘Autism symptoms’ | |
| Gotham 2012322 | – | Symptom severity | |
| Hartley 2009323 | Communication, social interaction, restricted behaviours | ASD symptoms | |
| Landa 2012224 | – | Symptom severity | |
| Lerna 2012325 | Communication, reciprocal social interaction | Social communicative abilities | |
| Luyster 2008129 | Play | – | |
| Munson 2008312 | Communication, social | ‘Autism severity’ | |
| Oosterling 2010326 | Level of non-echoed language, joint attention, social affect | Language development, early precursors of social communication | |
| Ray-Subramanian 2011327 | – | ‘Social communication skills and Behaviours characteristic of autism’ | |
| Ray-Subramanian 2012328 | Calibrated ADOS severity scores, composite RRB variable | RRB | |
| Strauss 2012329 | Communication, social | ‘Severity of autism symptoms’ | |
| Sullivan 2007330 | Response to joint attention item | ‘Response to joint attention’ | |
| Tek 2012331 | Communication, reciprocal social interaction | Assessment for ASD | |
| Ventola 2007332 | Communication, social | ‘Communication, social interactions and relatedness, play, and imagination’ | |
| Werner 2005316 | Communication, social | ‘Developmental outcomes’ | |
| Wong 2010333 | Language and communication, reciprocal social interaction | ‘Assessing autism spectrum disorder’ | |
| Zachor 2006334 | Language and communication, reciprocal social interaction | Language and communication and reciprocal social interaction | |
| Zachor 2010335 | – | ‘Autism severity’ | |
| Repetitive Behavior Scale (RBS) | Dawson 2010321 | – | ‘Severity of repetitive behaviours’ |
| Classroom and playground behaviour observationsa | Escalona 2001271 | – | Positive response to touch, on-task behaviour, stereotypical behaviour, social relatedness to the teacher |
| Video codinga | Barber 2012381 | – | Repetitive and stereotyped behaviours (RSB) |
| Sensory processing | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Infant/Toddler Sensory Profile (ITSP) | Ben-Sasson 2008382 | Low registration (sensory under responsivity), sensation seeking, sensory sensitivity, sensation avoiding, sensory over responding (sum of sensitivity and avoiding) | ‘Sensory processing behaviours in daily experiences’ |
| Sense and Self-Regulation Checklist (SSC) | Silva 2009226 | – | ‘Parent questionnaire (on) changes in sensory impairment, appetite, digestion, and sleep’ |
| Silva 2011301 | Sense, self-regulation | ‘Sensory and self-regulatory symptoms commonly reported by parents’ | |
| Sensory Profile (SP) | Chuang 2012383 | – | Sensory events |
| Jasmin 2009384 | – | Sensory processing, modulation, behavioural and emotional responses | |
| Provost 2009385 | Sensory processing area, modulation area, behavioural and emotional responses area | ‘Sensory behaviours’ | |
| Silva 2007299 | Sensory processing section, modulation section, behaviour and emotional responses, sensory factor scale | ‘Children’s responses to commonly occurring sensory experiences’ | |
| Silva 2008300 | Sensory processing, modulation, behaviour and emotional responses | ‘Child’s sensory processing abilities’ | |
| Short Sensory Profile (SSP) | O’Donnell 2012386 | Tactile sensitivity, taste/smell sensitivity, movement sensitivity, under-responsive/seeks sensation, auditory filtering, low energy/weak, visual/auditory sensitivity | ‘Sensory processing difficulties and associated behaviours’ |
| Papavasiliou 2011345 | – | ‘Children’s response capability to sensory and behavioural/emotional stimuli and daily performance’ | |
| Tomchek 2007387 | – | ‘Atypical sensory processing’ |
| Language | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Autism Screening Instrument for Educational Planning (ASIEP) | Arick 2003388 | Autism behavior checklist, sample of vocal behavior, social interaction assessment, educational assessment | Educational progress |
| Battelle Developmental Inventory (BDI) | Arick 2003388 | – | Conceptual skills and abilities |
| British Picture Vocabulary Scale | Magiati 2007308 | – | Receptive and expressive language |
| Magiati 2011309 | – | Language comprehension | |
| Clinical Evaluation of Language Fundamentals-Revised | Bono 2004389 | – | ‘Language abilities’ |
| Communication and Symbolic Behavior Scales-Developmental Profile (Caregiver Questionnaire) CSBS-DP (CQ) | Tek 2012331 | CSBS-DP CQ Words, CSBS-DP CQ Understanding Words, CSBS-DP CQ Social Composite | Language and social development |
| Comprehensive Assessment of Spoken Language (CASL) | Casenhiser 2013361 | – | Language – receptive and expressive |
| Expressive One-Word Picture Vocabulary Test | Arick 2003388 | – | English vocabulary |
| Bopp 2009340 | – | Expressive vocabulary | |
| Magiati 2007308 | – | Receptive and expressive language | |
| Magiati 2011309 | – | Expressive language | |
| Illinois Test of Psycholinguistic Abilities | Carlsson 2013390 | – | Language – expressive and receptive |
| MacArthur–Bates Communicative Development Inventories (MCDI) | Aldred 2004318 | Language comprehension, expressive language | ‘Understanding and expression of words and gestures’ |
| Green 2010253 | – | ‘Child language and social communication’ | |
| Hambly 2012306 | Words and sentences | Vocabulary | |
| Hudry 2010233 | Receptive (words understood), expressive (words understood and said) | ‘Receptive and expressive language skills’ | |
| Luyster 2008129 | Expressive, receptive, gestures | Early language abilities | |
| Miniscalco 2012391 | Early words, handling and gestures | ‘Expressive and comprehension skills’ and ‘development of early communicative gestures’ | |
| Mitchell 2006392 | Phrases understood, vocabulary comprehension, vocabulary production, early gestures, late gestures | ‘Assessment of language development’ | |
| Oosterling 2010326 | Language, gestures | Language development, early precursors of social communication | |
| Rogers 2012317 | Phrases understood, vocabulary comprehension, vocabulary production, total gestures | Expressive words, gestures and receptive vocabulary | |
| Salt 2002372 | Words understood, words produced | ‘Receptive and expressive language’ | |
| Smith 2007393 | – | ‘Prelinguistic and early language development’ | |
| Smith 2010359 | – | ‘Language/communication’ | |
| Stone 2001394 | – | ‘Expressive language’ | |
| Strauss 2012329 | Comprehension, production | ‘Vocabulary comprehension and vocabulary production’ | |
| Mullen Scales of Early Learning (MSEL) | Akshoomoff 2006395 | Visual reception, fine motor, receptive language, expressive language | ‘Cognitive Ability . . . separate scores for verbal and non-verbal skills’ |
| Anan 2008396 | Visual reception, fine motor, receptive language, expressive language | Cognitive functioning | |
| Baker 2010397 | Expressive language, receptive language | ‘Language ability’ | |
| Barbaro 2012398 | Visual perception, fine motor, receptive language, expressive language | Developmental status | |
| Ben Itzchak 2011320 | Visual reception, fine motor, expressive language, language comprehension | Cognitive abilities | |
| Bishop 2011176 | Non-verbal, verbal | Intellectual development (non-verbal and verbal IQ) | |
| Brian 2008305 | Composite (visual reception, receptive, expressive, fine motor) | Cognitive ability | |
| Dawson 2010321 | Fine motor, receptive language, expressive language, visual problem-solving | ‘Fine motor, visual reception, expressive language, and receptive language’ | |
| Dereu 2012365 | Age equivalents | General development | |
| Eapen 2013357 | – | Early development | |
| Hartley 2009323 | Visual reception, fine motor, receptive language, expressive language | Cognitive development | |
| Honey 2008307 | Receptive language, expressive language | ‘Children’s abilities’ | |
| Landa 2012399 | Gross motor, fine motor, visual reception, receptive language, expressive language | ‘Development’ | |
| Landa 2012224 | – | IQ | |
| Lloyd 2013400 | Gross motor, fine motor, visual reception, receptive language, expressive language | IQ, gross and fine motor skills | |
| Luyster 2008129 | Receptive language, expressive language, visual reception, fine motor skill | Language ability | |
| Mayo 2013310 | Gross motor, fine motor, visual reception, receptive language, expressive language | Cognitive development | |
| Mitchell 2006392 | – | ‘Expressive and receptive language skills’ | |
| O’Donnell 2012386 | Visual reception, receptive language, expressive language, fine motor | ‘Cognitive functioning’ | |
| Ozonoff 2010313 | Fine motor, receptive language, expressive language, visual problem solving | ‘Cognitive functioning’ | |
| Poon 2012401 | – | ‘Intellectual abilities’ | |
| Ray-Subramanian 2012328 | Visual reception raw scores | Non-verbal cognition | |
| Rogers 2012317 | Receptive language, expressive language, visual reception, fine motor skill | An overall index of ability | |
| Schertz 2013402 | Receptive language, expressive language | Cognitive functioning | |
| Siller 2013403 | Expressive language | Non-verbal cognitive and language abilities | |
| Sullivan 2007330 | Gross motor, fine motor, visual reception, receptive language, expressive language | ‘Overall cognitive development’ | |
| Tek 2012331 | Visual reception, expressive language, receptive language, fine motor, gross motor | Comprehensive assessment of development | |
| Thurm 2007404 | Receptive language organisation, expressive language organisation | ‘Language ability’ | |
| Toth 2006284 | Receptive language, expressive language | ‘Receptive and expressive language’ | |
| Ventola 2007332 | Fine motor, receptive language, expressive language, visual problem solving | ‘Ability’ | |
| Werner 2005316 | Composite IQ, verbal IQ | ‘Developmental outcomes’ | |
| Zachor 2010335 | Visual reception, fine motor, expressive language, receptive language | ‘Non-verbal cognitive measure . . . and verbal measure’ | |
| Pragmatics Profile | Roberts 2011405 | – | ‘Communication’ |
| Preschool Language Scale (PLS) | Bopp 2009340 | Auditory comprehension, expressive communication | Language skills |
| Casenhiser 2013361 | – | Language – receptive and expressive | |
| Flippin 2011406 | Auditory comprehension, expressive communication | Language skills | |
| Green 2010253 | – | ‘Child language and social communication’ | |
| Haebig 2013407 | – | Receptive and expressive communication | |
| Harris 1991408 | – | Language development | |
| Hudry 2010233 | Receptive language, expressive language | ‘Receptive and expressive language skills’ | |
| Mitchell 2006392 | – | ‘Expressive and receptive language skills’ | |
| Ray-Subramanian 2012328 | Auditory comprehension, expressive communication | Understanding of language, ability to communicate | |
| Smith 2010359 | Receptive language, expressive language | ‘Language/communication’ | |
| Stone 2001394 | – | ‘Language comprehension’ | |
| Reynell Developmental Language Scales | Andersson 2013409 | – | Language comprehension |
| Bono 2004389 | Comprehension, expression | ‘Language abilities’ | |
| Carlsson 2013390 | – | Language – receptive and expressive | |
| Eikeseth 2009410 | – | ‘Language functioning’ | |
| Goods 2013366 | Verbal comprehension, expressive language | Verbal comprehension, expressive language | |
| Herring 2006411 | – | Language ability | |
| Miniscalco 2012391 | Comprehension, language production | ‘Combined comprehension and language production test’ | |
| Remington 2007358 | – | ‘Language’ | |
| Roberts 2011405 | – | ‘Communication’ | |
| Sheinkopf 2000412 | – | ‘Expressive language ability’ | |
| Smith 2000413 | Comprehension, expressive language | ‘Language functioning’ | |
| Sequenced Inventory of Communication-Revised | Stone 2001394 | – | ‘Receptive and expressive language’ |
| Test for Auditory Comprehension of Language | Szatmari 2000302 | Grammatic morphemes subtest | ‘Child’s understanding of grammatic structures’ |
| Test of Language Development | Bennett 2008296 | Grammatic completion, grammatic understanding | Grammatical comprehension and usage |
| Szatmari 2000302 | Grammatic understanding subtest, grammatic completion subtests | ‘Grammatic comprehension and usage’ | |
| Vineland Adaptive Behavior Scales (VABS) | Aldred 2004318 | Communication, DLS, socialisation | ‘Communication, daily living skills, and socialisation’ |
| Anan 2008396 | Communication, DLS, socialisation, motor skills | Adaptive functioning | |
| Andersson 2013409 | – | Adaptive skills | |
| Arick 2003388 | – | Adaptive behaviour | |
| Baghdadli 2012339 | Communication, DLS, socialisation | Adaptive behaviours | |
| Bearss 2013278 | – | Communication, DLS, socialisation, motor skills | |
| Ben Itzchak 2011320 | Communication, DLS, socialisation, motor skills | Adaptive skills | |
| Bennett 2008296 | Social, communication, DLS | Personal and social sufficiency | |
| Carlsson 2013390 | Motor Skills domain | Motor function | |
| Cassidy 2008348 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Dawson 2010321 | Communication, DLS, socialisation, motor skills | ‘Social, communication, motor, and daily living skills’ | |
| Eapen 2013357 | – | Communication – expressive and receptive, DLS, socialisation, motor skills | |
| Eikeseth 2009410 | – | ‘Adaptive behaviours’ | |
| Eldevik 2012414 | Adaptive behaviour composite, communication, daily living, socialisation | Adaptive behaviour | |
| Eriksson 2013415 | – | Adaptive skills | |
| Gabriels 2007416 | Communication, DLS, socialisation, motor skills, adaptive behaviour composite | Adaptive behaviour skills | |
| Green 2010253 | – | ‘Adaptive functioning in school beyond the family’ | |
| Grindle 2012417 | – | Adaptive skills, socialisation, communication, DLS, motor skills | |
| Hedvall 2013418 | Communication, DLS, socialisation, motor skills | – | |
| Herring 2006411 | Derived Adaptive Behaviour Composite (ABC) standard score | Adaptive behaviour | |
| Honey 2008307 | Communication, socialisation | ‘Children’s abilities’ | |
| Hudry 2010233 | Receptive language, expressive language | ‘Receptive and expressive language skills’ | |
| Jasmin 2009384 | DLS | DLS | |
| Jonsdottir 2007341 | Composite | Adaptive behaviour in communication, DLS, socialisation and motor skills | |
| Klintwall 2012419 | – | ‘Treatment gains . . . treatment outcomes’ | |
| Landa 2012224 | Communication domain standard score | Communication skills | |
| Lerna 2012325 | – | Child communication, social abilities | |
| Lloyd 2013400 | Communication, DLS, socialisation, motor skills | Communication, DLS, social skills, motor development | |
| Luyster 2008129 | Motor, communication | Children’s personal and social sufficiency in communication (receptive, expressive, written), DLS (personal, domestic, community), socialisation (interpersonal relationships, play and leisure, time, coping skills), and motor skills (gross, fine) | |
| Magiati 2007308 | Communication, DLS, socialisation | Adaptive behaviour | |
| Magiati 2011309 | Communication, DLS, socialisation, composite | Adaptive behaviour | |
| Mayo 2013310 | Communication, DLS, socialisation, motor skills | Adaptive functioning | |
| McConkey 2010349 | Communication, DLS, socialisation, motor skills | Communication, DLS, socialisation and motor skills | |
| Munson 2006420 | Socialisation, communication | ‘Socialisation and communication skills’ | |
| Munson 2008312 | Social, communication, DLS, motor skills | ‘Adaptive behaviours’ | |
| O’Donnell 2012386 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Osborne 2008350 | Communication, DLS, socialisation, motor skills | ‘Day-to-day adaptive functioning’ | |
| Osborne 2009351 | Communication, DLS, socialisation, motor skills | ‘Adaptive behavioural functioning’ | |
| Peters-Scheffer 2010421 | Communication, DLS, socialisation | ‘Adaptive behaviour’ | |
| Poon 2012401 | Communication | ‘Communication’ | |
| Pry 2005314 | Communication, DLS, socialisation | ‘Child’s knowledge about the social norms, conventions, and scripts that govern social life at all levels’ | |
| Ray-Subramanian 2011327 | Communication, DLS, socialisation, motor skills | ‘Adaptive skills’ | |
| Reed 2007352 | Communication, DLS, socialisation, motor skills | ‘Adaptive functioning’ | |
| Reed 2007353 | Communication, DLS, socialisation, motor skills | ‘Adaptive functioning’ | |
| Reed 2012354 | Communication, DLS, socialisation, motor skills | Day-to-day adaptive behaviour | |
| Vineland Adaptive Behavior Scales (VABS) | Remington 2007358 | Socialisation, communication, DLS, motor skills | ‘Adaptive skills’ |
| Restall 1994422 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Rickards 2009423 | – | ‘Communication, daily living skills, socialisation and motor skills’ | |
| Roberts 2011405 | – | ‘Communication and social skills’ | |
| Rogers 2012317 | Communication, DLS, socialisation, motor skills | Adaptive behaviour | |
| Ruble 2008424 | Socialisation, communication | ‘Adaptive functioning’ | |
| Salt 2002372 | Communication, DLS, socialisation, motor skills | ‘Communication, daily living skills, socialisation and motor skills’ | |
| Schertz 2013402 | Communication | Adaptive behaviour | |
| Silva 2007299 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Silva 2008300 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Smith 2000413 | Communication, DLS, socialisation | ‘Adaptive functioning’ | |
| Smith 2010359 | Communication, DLS, socialisation, motor skills | ‘Language/communication’, ‘adaptive behaviour’ | |
| Stahmer 2004355 | Communication, DLS, socialisation, motor skills | Child adaptive functioning | |
| Stone 1999346 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Strauss 2012329 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour functioning’ | |
| Szatmari 2000302 | Socialisation, communication | ‘Social skills’ and ‘language’ | |
| Tonge 2012425 | – | Adaptive behaviour | |
| Toth 2006284 | Communication | ‘Communication skills’ | |
| VanMeter 1997426 | Communication, DLS, socialisation | ‘Social, communication, and daily living skills’ | |
| Ventola 2007332 | Socialisation, communication, DLS, motor skills | ‘Adaptive functioning’ | |
| Werner 2005316 | Communication, DLS, socialisation, motor skills | ‘Developmental outcomes’ | |
| Zachor 2010335 | Communication, DLS, socialisation, motor skills | ‘Adaptive functioning’ | |
| Vineland Adaptive Behavior Scales-Classroom version (VABS-Classroom) | Goin-Kochel 2007427 | Communication, DLS, socialisation, motor skills | Communication skills, DLS, socialisation skills, motor skills |
| Differential Ability Scalesa | Bishop 2011176 | Non-verbal IQ, Verbal IQ | – |
| Ruble 2008424 | – | ‘Cognitive functioning’ | |
| Thurm 2007404 | Verbal comprehension subtest, naming vocabulary subtest | ‘Receptive language’ | |
| Peabody Picture Vocabulary Testa | Bopp 2009340 | – | Receptive vocabulary skills |
| Smith 2010359 | – | ‘Language/communication’, ‘adaptive behaviour’ | |
| Szatmari 2000302 | – | ‘Single word comprehension’ | |
| Processability testb | Carlsson 2013390 | – | Language (grammar screening) |
| Rating of video for expressive speechc | Baghdadli 2012339 | – | Expressive speech |
| Semistructured free play with examinerc | Yoder 2006428 | Non-imitative spoken communication acts, different non-imitative words | ‘Spoken communication’ |
| Video coding proceduresc | Colgan 2006379 | – | Communicative gestures |
| Cognitive ability | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Battelle Developmental Inventory (BDI) | Arick 2003388 | – | Conceptual skills and abilities |
| Ben Itzchak 2008149 | – | Cognitive ability | |
| Eikeseth 2009410 | – | ‘Intellectual functioning’ | |
| Eldevik 2012414 | – | Intellectual functioning | |
| Grindle 2012417 | – | IQ | |
| Ingersoll 2012286 | The Social–Emotional Scale | Social and emotional development | |
| Jonsdottir 2007341 | – | Developmental level | |
| Magiati 2007308 | – | Cognitive ability and mental age | |
| Peters-Scheffer 2010421 | – | ‘Developmental age and mental development index’ | |
| Ray-Subramanian 2011327 | Cognitive scale | ‘Cognitive skills’ | |
| Remington 2007358 | – | ‘Intellectual functioning’ | |
| Rickards 2009423 | Mental development index (MDI), behaviour rating scale | ‘Cognition’, ‘behaviour’ | |
| Sheinkopf 1998429 | – | ‘Cognitive measure’ | |
| Smith 1997430 | Mental development quotient | IQ | |
| Smith 2000413 | – | ‘Intellectual functioning’ | |
| Stahmer 2004355 | Mental development quotient | Change in child intellectual functioning’ | |
| Ventola 2007332 | – | ‘Mental and psychomotor development’ | |
| Zachor 2006334 | – | Mental Developmental Index | |
| Behavior Rating Inventory of Executive Function (BRIEF)-Preschool Version | Jahromi 2013431 | Inhibitory Self-Control Index | Executive function |
| British Ability Scale (BAS) | Osborne 2008350 | Verbal comprehension, early number concepts, picture matching, naming vocabulary | ‘Cognitive abilities’ |
| Osborne 2009351 | Verbal comprehension, early number concepts, picture matching, naming vocabulary | ‘Intellectual functioning’ | |
| Reed 2007352 | Verbal comprehension, early number concepts, picture matching, naming vocabulary | ‘Cognitive ability’ | |
| Reed 2007353 | Verbal comprehension, early number concepts, picture matching, naming vocabulary | ‘Cognitive ability . . . educational achievement’ | |
| Reed 2012354 | Early Years Battery, verbal comprehension, early number concepts, picture matching, naming vocabulary | Educational achievement | |
| Cattell Infant Intelligence | Sheinkopf 1998429 | – | ‘Cognitive measure’ |
| Developmental Profile | Malhi 2011342 | Academic | Developmental assessment; developmental quotient was derived from the academic subscale |
| Griffiths Mental Developmental Scales | Andersson 2013409 | – | Developmental quotient |
| Carlsson 2013390 | – | Cognitive/intellectual function | |
| Hedvall 2013418 | – | Intelligence/mental age | |
| Lerna 2012325 | Language subscale, personal–social | Receptive language, expressive language, activities of daily living, level of independence, interaction with other children | |
| Strauss 2012329 | – | ‘Mental developmental state’ | |
| Leiter International Performance Scale-Revised (Leiter-R) | Gabriels 2007416 | Figure ground, form completion, sequential order, repeated patterns | Intelligence levels |
| Grindle 2012417 | – | IQ | |
| Leiter Performance Scales (Arthur adaptation) | Bennett 2008296 | – | Non-verbal problem solving or IQ |
| McCarthy Scales of Children’s Abilities | Szatmari 2000302 | Oral vocabulary section | ‘Child’s language fluency’ |
| Merrill–Palmer Scale of Mental Tests | Eikeseth 2009410 | – | ‘Visual spatial IQ’ |
| Magiati 2007308 | – | Cognitive ability/mental age | |
| Sheinkopf 1998429 | – | ‘Cognitive measure’ | |
| Sheinkopf 2000412 | – | ‘Cognitive developmental level . . . emphasis on nonverbal skills’ | |
| Smith 2000413 | – | ‘Intellectual functioning’ | |
| Merrill-Palmer-Revised | Smith 2010359 | Receptive language subscale, cognition, fine motor | ‘Language/communication’, ‘cognitive ability’ |
| Mullen Scales of Early Learning (MSEL) | Akshoomoff 2006395 | Visual reception, fine motor, receptive language, expressive language | ‘Cognitive ability . . . separate scores for verbal and non-verbal skills’ |
| Anan 2008396 | Visual reception, fine motor, receptive language, expressive language | Cognitive functioning | |
| Baker 2010397 | Expressive language, receptive language | ‘Language ability’ | |
| Barbaro 2012398 | Visual perception, fine motor, receptive language, expressive language | Developmental status | |
| Ben Itzchak 2011320 | Visual reception, fine motor, expressive language, language comprehension | Cognitive abilities | |
| Bishop 2011176 | Non-verbal, verbal | Intellectual development (non-verbal and verbal IQ) | |
| Brian 2008305 | Composite (visual reception, receptive, expressive, fine motor) | Cognitive ability | |
| Dawson 2010321 | Fine motor, receptive language, expressive language, visual problem solving | ‘Fine motor, visual reception, expressive language, and receptive language’ | |
| Dereu 2012365 | Age equivalents | General development | |
| Eapen 2013357 | – | Early development | |
| Hartley 2009323 | Visual reception, fine motor, receptive language, expressive language | Cognitive development | |
| Honey 2008307 | Receptive language, expressive language | ‘Children’s abilities’ | |
| Landa 2012399 | Gross motor, fine motor, visual reception, receptive language, expressive language | ‘Development’ | |
| Landa 2012224 | – | IQ | |
| Lloyd 2013400 | Gross motor, fine motor, visual reception, receptive language, expressive language | IQ, gross and fine motor skills | |
| Luyster 2008129 | Receptive language, expressive language, visual reception, fine motor skill | Language ability | |
| Mayo 2013310 | Gross motor, fine motor, visual reception, receptive language, expressive language | Cognitive development | |
| Mitchell 2006392 | – | ‘Expressive and receptive language skills’ | |
| O’Donnell 2012386 | Visual reception, receptive language, expressive language, fine motor | ‘Cognitive functioning’ | |
| Ozonoff 2010313 | Fine motor, receptive language, expressive language, visual problem solving | ‘Cognitive functioning’ | |
| Poon 2012401 | – | ‘Intellectual abilities’ | |
| Ray-Subramanian 2012328 | Visual reception raw scores | Non-verbal cognition | |
| Rogers 2012317 | Receptive language, expressive language, visual reception, fine motor skill | An overall index of ability | |
| Schertz 2013402 | Receptive language, expressive language | Cognitive functioning | |
| Siller 2013403 | Expressive language | Non-verbal cognitive and language abilities | |
| Sullivan 2007330 | Gross motor, fine motor, visual reception, receptive language, expressive language | ‘Overall cognitive development’ | |
| Tek 2012331 | Visual reception, expressive language, receptive language, fine motor, gross motor | Comprehensive assessment of development | |
| Thurm 2007404 | Receptive language organisation, expressive language organisation | ‘Language ability’ | |
| Toth 2006284 | Receptive language, expressive language | ‘Receptive and expressive language’ | |
| Ventola 2007332 | Fine motor, receptive language, expressive language, visual problem solving | ‘Ability’ | |
| Werner 2005316 | Composite IQ, verbal IQ | ‘Developmental outcomes’ | |
| Zachor 2010335 | Visual reception, fine motor, expressive language, receptive language | ‘Non-verbal cognitive measure . . . and verbal measure’ | |
| Snijders–Oomen Non-Verbal Intelligence Test (SON) | Peters-Scheffer 2010421 | – | ‘Non-verbal intelligence’ |
| Ben Itzchak 2008149 | – | Cognitive ability – verbal reasoning, quantitative reasoning, abstract/visual reasoning and short-term memory skills | |
| Stanford–Binet Intelligence Scales | Delmolino 2006432 | Verbal reasoning, abstract visual reasoning, quantitative reasoning, short term memory | Cognitive development, general development |
| Grindle 2012417 | – | IQ | |
| Harris 1991408 | – | IQ | |
| Harris 2000433 | – | IQ | |
| Landa 2012224 | – | IQ | |
| Remington 2007358 | – | ‘Intellectual functioning’ | |
| Smith 2000413 | – | ‘Intellectual functioning’ | |
| Szatmari 2000302 | Pattern analysis subtest | ‘Non-verbal problem-solving skills’ | |
| Zachor 2006334 | – | Cognitive ability – verbal reasoning, quantitative reasoning, abstract/visual reasoning and short-term memory skills | |
| Wechsler Intelligence Scale for Children | Szatmari 2000 | Block design subtest | ‘Visual-analytic skills’ |
| Wechsler Preschool and Primary Scale of Intelligence (WPPSI) | Andersson 2013409 | – | Intelligence (verbal and performance) |
| Baghdadli 2012339 | Block design | Psychological development, object-related cognition functioning: perceptual organisation and/or simultaneous information processing | |
| Baghdadli 2012339 | Block design | Psychological development, object-related cognition functioning: perceptual organisation and/or simultaneous information processing | |
| Carlsson 2013390 | – | Intellectual/cognitive function | |
| Eikeseth 2009410 | – | ‘Intellectual functioning’ | |
| Hedvall 2013418 | Full-scale IQ, verbal IQ, performance IQ, processing speed quotient, general language composite | – | |
| Jonsdottir 2007341 | – | Developmental progress | |
| Magiati 2007308 | – | Cognitive ability and mental age | |
| Rickards 2009423 | – | ‘Cognition’ | |
| Sheinkopf 1998429 | – | ‘Cognitive measure’ | |
| Differential Ability Scalesa | Bishop 2011176 | Non-verbal IQ, verbal IQ | – |
| Ruble 2008424 | – | ‘Cognitive functioning’ | |
| Thurm 2007404 | Verbal comprehension subtest, naming vocabulary subtest | ‘Receptive language’ | |
| Kyoto scale of psychological developmenta | Takeda 2005360 | Posture–movement subtest, cognition–adaptation subtest, language–sociability subtest | ‘Development’ |
| Tanaka–Binet intelligence test (Japanese version of Stanford–Binet)a | Takeda 2005360 | – | ‘Intelligence’ |
| Snabbt Performance Test På Intelligence IQ II (SPIQ) – Swedisha | Carlsson 2013390 | – | Language – expressive and receptive |
| Attention | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Behavior Assessment System for Children-Second Edition (BASC-2) | Hill-Chapman 2013434 | – | Atypicality of symptoms |
| Child Behavior Scale (CBS) | Jahromi 2013431 | Prosocial behaviours | Prosocial peer engagement |
| Meek 2012435 | Prosocial behaviours, asocial, exclusion, aggressive behaviours, hyperactive–distractible behaviours, anxious–fearful behaviours, social competence composite | ‘Social competence with peers’ | |
| Child Behavior Checklist (CBCL) | Baker 2010397 | N/A | ‘Child behaviour problems’ |
| Hartley 2009323 | – | Emotionally reactive, anxious/depressed, somatic complaints, sleep problems, attention problems, aggressive behaviour | |
| Peters-Scheffer 2010421 | Behavioural problem scale | ‘Emotional and behavioural problems’ | |
| Smith 2000413 | Social withdrawal, somatisation, anxiety/depression, social problems, thought problems, attention problems, delinquency, aggression | ‘Socioeconomic functioning’ | |
| Smith 2010359 | Total problems, internalising problems, externalising problems, aggressive behavioural | ‘Behavioural problems’ | |
| Taylor 2012436 | Internalising problems, externalising problems, total problems composite | ‘Internalising and externalising behaviours in children’ | |
| Child Behaviour Questionnaire–Short Form | Jahromi 2013431 | Inhibitory control, attentional focusing, low-intensity pleasure, perceptual sensitivity | Jahromi 2013431 |
| Conners Rating Scales-Revised | Escalona 2001271 | ADHD index, restless–impulsive behaviour, emotional index, the global index, inattentiveness | – |
| Osborne 2009351 | Oppositional behaviour, cognitive problems, hyperactivity, ADHD index | ‘Behavioural problems, hyperactivity and attention deficit disorder’ | |
| Reed 2007353 | Oppositional behaviour, cognitive problems, hyperactivity, ADHD index | ‘Behavioural difficulties’ | |
| Reed 2013437 | Oppositional behaviour, cognitive problems, hyperactivity, the ADHD index | Behavioural problems, hyperactivity and attention deficit disorder | |
| Student attention – coded observationa | Travers 2011438 | Attention to task, undesirable behaviour | ‘Student attention’ |
| Emotion regulation | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Baby and Infant Screen for Children with aUtIsm Traits (BISCUIT-Part 2) | Davis 2010439 | Avoidance behaviour, anxiety/repetitive behaviour | Psychopathology comorbid with ASD |
| Behavior Assessment System for Children-Second Edition (BASC-2) | Hill-Chapman 2013434 | – | Atypicality of symptoms |
| Child Behavior Checklist (CBCL) | Baker 2010397 | N/A | ‘Child behaviour problems’ |
| Hartley 2009323 | – | Emotionally reactive, anxious/depressed, somatic complaints, sleep problems, attention problems, aggressive behaviour | |
| Peters-Scheffer 2010421 | Behavioural problem scale | ‘Emotional and behavioural problems’ | |
| Smith 2000413 | Social withdrawal, somatisation, anxiety/depression, social problems, thought problems, attention problems, delinquency, aggression | ‘Socioeconomic functioning’ | |
| Smith 2010359 | Total problems, internalising problems, externalising problems, aggressive behavioural | ‘Behavioural problems’ | |
| Taylor 2012436 | Internalising problems, externalising problems, total problems composite | ‘Internalising and externalising behaviours in children’ | |
| Children’s Global Assessment Scale (CGAS) | Andersson 2013409 | – | General social and psychiatric functioning |
| Conners Rating Scales-Revised | Escalona 2001271 | ADHD index, restless–impulsive behaviour, emotional index, the global index, inattentiveness | – |
| Osborne 2009351 | Oppositional behaviour, cognitive problems, hyperactivity, ADHD index | ‘Behavioural problems, hyperactivity and attention deficit disorder’ | |
| Reed 2007353 | Oppositional behaviour, cognitive problems, hyperactivity, ADHD index | ‘Behavioural difficulties’ | |
| Reed 2013437 | Oppositional behaviour, cognitive problems, hyperactivity, the ADHD index | Behavioural problems, hyperactivity and attention deficit disorder | |
| Developmental Behaviour Checklist | Herring 2006411 | – | Child behavioural and emotional problems |
| Mooney 2006311 | – | ‘Repetitive behaviour’ | |
| Remington 2007358 | – | ‘Child behaviour’ | |
| Roberts 2011405 | – | ‘Adaptive functioning and psychopathology’ | |
| Tonge 2012425 | – | Severity of autism | |
| Emotion Regulation Checklist | Jahromi 2013431 | Negativity/lability, emotion regulation | Emotion regulation |
| Infant–Toddler Social–Emotional Assessment (ITSEA) | Ben-Sasson 2008382 | Negative emotionality, depression/withdrawal, general anxiety, separation distress, inhibition to novelty | ‘Social–emotional and behavioural problems and competencies’ |
| Physical skills | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Annett’s Pegs | Szatmari 2000302 | – | ‘Motor dexterity’ |
| Beery Visual–Motor Integration Test | Szatmari 2000302 | – | ‘Visual-motor integration’ |
| Brunet–Lezine’s Oculomotor Coordination Subtest | Baghdadli 2012339 | Oculomotor co-ordination subtest | Psychological development, object related cognition functioning, person related cognition functioning |
| Functional Independence Measure for Children (WeeFIM) | Jasmin 2009384 | – | DLS |
| Infant Motor Maturity and Atypicality Coding Scales | Ozonoff 2008440 | Walk, crawl, sit, roll, prone, supine abnormalities | ‘Motor maturity, protective responses, and movement abnormalities’ |
| Mullen Scales of Early Learning (MSEL) | Akshoomoff 2006395 | Visual reception, fine motor, receptive language, expressive language | ‘Cognitive ability . . . separate scores for verbal and non-verbal skills’ |
| Anan 2008396 | Visual reception, fine motor, receptive language, expressive language | Cognitive functioning | |
| Baker 2010397 | Expressive language, receptive language | ‘Language ability’ | |
| Barbaro 2012398 | Visual perception, fine motor, receptive language, expressive language | Developmental status | |
| Ben Itzchak 2011320 | Visual reception, fine motor, expressive language, language comprehension | Cognitive abilities | |
| Bishop 2011176 | Non-verbal, verbal | Intellectual development (non-verbal and verbal IQ) | |
| Brian 2008305 | Composite (visual reception, receptive, expressive, fine motor) | Cognitive ability | |
| Dawson 2010321 | Fine motor, receptive language, expressive language, visual problem solving | ‘Fine motor, visual reception, expressive language, and receptive language’ | |
| Dereu 2012365 | Age equivalents | General development | |
| Eapen 2013357 | – | Early development | |
| Hartley 2009323 | Visual reception, fine motor, receptive language, expressive language | Cognitive development | |
| Honey 2008307 | Receptive language, expressive language | ‘Children’s abilities’ | |
| Landa 2012399 | Gross motor, fine motor, visual reception, receptive language, expressive language | ‘Development’ | |
| Landa 2012224 | – | IQ | |
| Lloyd 2013400 | Gross motor, fine motor, visual reception, receptive language, expressive language | IQ, gross and fine motor skills | |
| Luyster 2008129 | Receptive language, expressive language, visual reception, fine motor skill | Language ability | |
| Mayo 2013310 | Gross motor, fine motor, visual reception, receptive language, expressive language | Cognitive development | |
| Mitchell 2006392 | – | ‘Expressive and receptive language skills’ | |
| O’Donnell 2012386 | Visual reception, receptive language, expressive language, fine motor | ‘Cognitive functioning’ | |
| Ozonoff 2010313 | Fine motor, receptive language, expressive language, visual problem-solving | ‘Cognitive functioning’ | |
| Poon 2012401 | – | ‘Intellectual abilities’ | |
| Ray-Subramanian 2012328 | Visual reception raw scores | Non-verbal cognition | |
| Rogers 2012317 | Receptive language, expressive language, visual reception, fine motor skill | An overall index of ability | |
| Schertz 2013402 | Receptive language, expressive language | Cognitive functioning | |
| Siller 2013403 | Expressive language | Non-verbal cognitive and language abilities | |
| Sullivan 2007330 | Gross motor, fine motor, visual reception, receptive language, expressive language | ‘Overall cognitive development’ | |
| Tek 2012331 | Visual reception, expressive language, receptive language, fine motor, gross motor | Comprehensive assessment of development | |
| Thurm 2007404 | Receptive language organisation, expressive language organisation | ‘Language ability’ | |
| Toth 2006284 | Receptive language, expressive language | ‘Receptive and expressive language’ | |
| Ventola 2007332 | Fine motor, receptive language, expressive language, visual problem solving | ‘Ability’ | |
| Werner 2005316 | Composite IQ, verbal IQ | ‘Developmental outcomes’ | |
| Zachor 2010335 | Visual reception, fine motor, expressive language, receptive language | ‘Non-verbal cognitive measure . . . and verbal measure’ | |
| Peabody Developmental Motor Scales | Jasmin 2009384 | – | Gross and fine motor skills |
| Provost 2007441 | Reflexes, stationary, locomotion, object manipulation, grasping, visual motor integration | ‘Gross motor and fine motor development’ | |
| Vineland Adaptive Behavior Scales-Classroom version (VABS-Classroom) | Goin-Kochel 2007427 | Communication, DLS, socialisation, motor skills | Communication skills, DLS, socialisation skills, motor skills |
| Vineland Adaptive Behavior Scales (VABS) | Aldred 2004318 | Communication, DLS, socialisation | ‘Communication, daily living skills, and socialisation’ |
| Anan 2008396 | Communication, DLS, socialisation, motor skills | Adaptive functioning | |
| Andersson 2013409 | – | Adaptive skills | |
| Arick 2003388 | – | Adaptive behaviour | |
| Baghdadli 2012339 | Communication, DLS, socialisation | Adaptive behaviours | |
| Bearss 2013278 | – | Communication, DLS, socialisation, motor skills | |
| Ben Itzchak 2011320 | Communication, DLS, socialisation, motor skills | Adaptive skills | |
| Bennett 2008296 | Social, communication, DLS | Personal and social sufficiency | |
| Carlsson 2013390 | Motor skills domain | Motor function | |
| Cassidy 2008348 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Dawson 2010321 | Communication, DLS, socialisation, motor skills | ‘Social, communication, motor, and daily living skills’ | |
| Eapen 2013357 | – | Communication – expressive and receptive, DLS, socialisation, motor skills | |
| Eikeseth 2009410 | – | ‘Adaptive behaviours’ | |
| Eldevik 2012414 | Adaptive behaviour composite, communication, daily living, socialisation | Adaptive behaviour | |
| Eriksson 2013415 | – | Adaptive skills | |
| Gabriels 2007416 | Communication, DLS, socialisation, motor skills, adaptive behaviour composite | Adaptive behaviour skills | |
| Green 2010253 | – | ‘Adaptive functioning in school beyond the family’ | |
| Grindle 2012417 | – | Adaptive skills, socialisation, communication, DLS, motor skills | |
| Hedvall 2013418 | Communication, DLS, socialisation, motor skills | – | |
| Herring 2006411 | Derived Adaptive Behaviour Composite (ABC) standard score | Adaptive behaviour | |
| Honey 2008307 | Communication, socialisation | ‘Children’s abilities’ | |
| Hudry 2010233 | Receptive language, expressive language | ‘Receptive and expressive language skills’ | |
| Jasmin 2009384 | DLS | DLS | |
| Jonsdottir 2007341 | Composite | Adaptive behaviour in communication, DLS, socialisation and motor skills | |
| Klintwall 2012419 | – | ‘Treatment gains . . . treatment outcomes’ | |
| Landa 2012224 | Communication domain standard score | Communication skills | |
| Lerna 2012325 | – | Child communication, social abilities | |
| Lloyd 2013400 | Communication, DLS, socialisation, motor skills | Communication, DLS, social skills, motor development | |
| Luyster 2008129 | Motor, communication | Children’s personal and social sufficiency in communication (receptive, expressive, written), DLS (personal, domestic, community), socialisation (interpersonal relationships, play and leisure, time, coping skills) and motor skills (gross, fine) | |
| Magiati 2007308 | Communication, DLS, socialisation | Adaptive behaviour | |
| Magiati 2011309 | Communication, DLS, socialisation, composite | Adaptive behaviour | |
| Mayo 2013310 | Communication, DLS, socialisation, motor skills | Adaptive functioning | |
| McConkey 2010349 | Communication, DLS, socialisation, motor skills | Communication, DLS, socialisation and motor skills | |
| Munson 2006420 | Socialisation, communication | ‘Socialisation and communication skills’ | |
| Munson 2008312 | Social, communication, DLS, motor skills | ‘Adaptive behaviours’ | |
| O’Donnell 2012386 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Osborne 2008350 | Communication, DLS, socialisation, motor skills | ‘Day-to-day adaptive functioning’ | |
| Osborne 2009351 | Communication, DLS, socialisation, motor skills | ‘Adaptive behavioural functioning’ | |
| Peters-Scheffer 2010421 | Communication, DLS, socialisation | ‘Adaptive behaviour’ | |
| Poon 2012401 | Communication | ‘Communication’ | |
| Pry 2005314 | Communication, DLS, socialisation | ‘Child’s knowledge about the social norms, conventions, and scripts that govern social life at all levels’ | |
| Ray-Subramanian 2011327 | Communication, DLS, socialisation, motor skills | ‘Adaptive skills’ | |
| Reed 2007352 | Communication, DLS, socialisation, motor skills | ‘Adaptive functioning’ | |
| Reed 2007353 | Communication, DLS, socialisation, motor skills | ‘Adaptive functioning’ | |
| Reed 2012354 | Communication, DLS, socialisation, motor skills | Day-to-day adaptive behaviour | |
| Remington 2007358 | Socialisation, communication, DLS, motor skills | ‘Adaptive skills’ | |
| Restall 1994422 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Rickards 2009423 | – | ‘Communication, daily living skills, socialisation and motor skills’ | |
| Roberts 2011405 | – | ‘Communication and social skills’ | |
| Rogers 2012317 | Communication, DLS, socialisation, motor skills | Adaptive behaviour | |
| Ruble 2008424 | Socialisation, communication | ‘Adaptive functioning’ | |
| Salt 2002372 | Communication, DLS, socialisation, motor skills | ‘Communication, daily living skills, socialisation and motor skills’ | |
| Schertz 2013402 | Communication | Adaptive behaviour | |
| Silva 2007299 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Silva 2008300 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Smith 2000413 | Communication, DLS, socialisation | ‘Adaptive functioning’ | |
| Smith 2010359 | Communication, DLS, socialisation, motor skills | ‘Language/communication’, ‘adaptive behaviour’ | |
| Stahmer 2004355 | Communication, DLS, socialisation, motor skills | Child adaptive functioning | |
| Stone 1999346 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Strauss 2012329 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour functioning’ | |
| Szatmari 2000302 | Socialisation, communication | ‘Social skills’ and ‘language’ | |
| Tonge 2012425 | – | Adaptive behaviour | |
| Toth 2006284 | Communication | ‘Communication skills’ | |
| VanMeter 1997426 | Communication, DLS, socialisation | ‘Social, communication, and daily living skills’ | |
| Ventola 2007332 | Socialisation, communication, DLS, motor skills | ‘Adaptive functioning’ | |
| Werner 2005316 | Communication, DLS, socialisation, motor skills | ‘Developmental outcomes’ | |
| Zachor 2010335 | Communication, DLS, socialisation, motor skills | ‘Adaptive functioning’ |
| Social communication | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Autism Diagnostic Interview (ADI) | Ben Itzchak2008149 | – | Autism severity |
| Autism Diagnostic Interview-Revised (ADI-R) | Bennett 2012304 | Non verbal items were used so that results could be compared between verbal and non-verbal children | – |
| Brian 2008305 | – | – | |
| Feldman 2012104 | – | – | |
| Hambly 2012306 | Items on language (#42, 46, 29, 30, 9, 10) | Sociocommunicative levels, ages of early language milestones | |
| Honey 2008307 | Repetitive behaviour algorithm items | ‘Repetitive behaviour’ | |
| Magiati 2007308 | – | Autism severity and diagnosis confirmation | |
| Magiati 2011309 | Total score | Autism severity | |
| Mayo 2013310 | – | Communication, social development and play, and the presence of repetitive or restricted behaviours | |
| Mooney 2006311 | – | ‘Repetitive behaviours’ | |
| Munson 2008312 | Social relatedness, communication, repetitive, restricted behaviours | ‘Autism severity’ | |
| Ozonoff 2010313 | – | ‘Parent recall of symptom onset and possible regression’ | |
| Pry 2005314 | – | ‘Expressive language level’ | |
| Richler 2007315 | RRB items | ‘Restricted and repetitive behaviours’ | |
| Werner 2005316 | Social, communication, repetitive | ‘Developmental outcomes’ | |
| Autism Diagnostic Observation Scale-Toddler Module (ADOS-T) | Rogers 2012317 | Social affect, restricted, repetitive behaviours | ‘Social and communicative behaviours, as well as repetitive behaviours diagnostic of autism’ |
| Aldred 2004318 | Reciprocal social interaction, communication, stereotyped and restricted behaviours | ‘Interaction, communication, repetitive behaviours and play’ | |
| Aldred 2012319 | Total social communication algorithm score | Social communication | |
| Ben Itzchak 2008149 | Language and communication, reciprocal social interaction, play, and stereotyped behaviour and restricted interests | Social and communicative functioning | |
| Ben Itzchak 2011320 | ADOS standardised measure of severity | Autism severity, diagnostic algorithm | |
| Autism Diagnostic Observation Schedule (ADOS) | Bennett 2012304 | – | Social and communication behaviours |
| Brian 2008305 | Module 1 | – | |
| Dawson 2010321 | Social relatedness, communication, play, repetitive behaviours | ‘Autism symptoms’ | |
| Gotham 2012322 | – | Symptom severity | |
| Green 2010253 | Communication, social | ‘Severity of the symptoms of autism’ | |
| Hartley 2009323 | Communication, social interaction, restricted behaviours | ASD symptoms | |
| Landa 2012224 | – | Symptom severity | |
| Lerna 2012325 | Communication, reciprocal social interaction | Social communicative abilities | |
| Luyster 2008129 | Play | – | |
| Munson 2008312 | Communication, social | ‘Autism severity’ | |
| Oosterling 2010326 | Level of non-echoed language, joint attention, social affect | Language development, early precursors of social communication | |
| Ray-Subramanian 2011327 | – | ‘Social communication skills and behaviours characteristic of autism’ | |
| Ray-Subramanian 2012328 | Calibrated ADOS severity scores, composite RRB variable | RRB | |
| Strauss 2012329 | Communication, social | ‘Severity of autism symptoms’ | |
| Sullivan 2007330 | Response to joint attention item | ‘Response to joint attention’ | |
| Tek 2012331 | Communication, reciprocal social interaction | Assessment for ASD | |
| Ventola 2007332 | Communication, social | ‘Communication, social interactions and relatedness, play, and imagination’ | |
| Werner 2005316 | Communication, social | ‘Developmental outcomes’ | |
| Wong 2010333 | Language and communication, reciprocal social interaction | ‘Assessing autism spectrum disorder’ | |
| Zachor 2006334 | Language and communication, reciprocal social interaction | Language and communication and reciprocal social interaction | |
| Zachor 2010335 | – | ‘Autism severity’ | |
| Autism Screening Instrument for Educational Planning (ASIEP) | Arick 2003388 | Autism Behavior Checklist, Sample of Vocal Behaviour, Social Interaction Assessment, Educational Assessment | Educational progress |
| Communication and Symbolic Behavior Scales-Developmental Profile (Caregiver Questionnaire) (CSBS-DP-CQ); Wetherby and Prizant 2002125) | Tek 2012331 | CSBS-DP-CQ Words, CSBS-DP-CQ Understanding Words, CSBS-DP-CQ Social Composite | Language and social development |
| Early Social Communication Scale (ESCS) | Dereu 2012365 | – | Initiating joint attention, responding to joint attention |
| Goods 2013366 | Spontaneous requesting gestures | Spontaneous requesting gestures | |
| Ingersoll 2012286 | – | Social interaction | |
| Kaale 2012294 | – | Joint attention | |
| Kalas 2012367 | – | Responses to bids for joint attention | |
| Kasari 2006368 | – | Social communication | |
| Lawton 2012369 | – | Joint attention, social interaction, symbolic play and behaviour regulation | |
| Luyster 2008129 | Initiating joint attention, responding to joint attention | – | |
| Paparella 2011370 | – | ‘Initiations and responses of Joint Attention behaviours’ | |
| Remington 2007358 | Initiating joint attention, responding to joint attention | ‘Non-verbal social communication’ | |
| Roos 2008371 | Initiating joint attention, responding to joint attention | ‘Joint attention’ | |
| Wong 2013373 | – | Non-verbal initiations and responses to joint attention, behaviour regulation or requesting behaviours, and social interactions | |
| Yoder 2006374 | Communication | – | |
| Joint attention, requesting, social interaction | ‘Non-verbal social communication’ | ||
| Early Social Communication Scales (ESCS)-Abridged | Yoder 2010375 | – | ‘Number of picture exchanges at post treatment assessment’ |
| Pragmatics Profile | Roberts 2011405 | – | ‘Communication’ |
| Social Communication Assessment for Toddlers with Autism (SCATA) | Drew 2007137 | – | Social communication (contexts: free play, turn-taking, activated musical toys, bubbles, specific prompts) |
| Social Communication Behavior Codes | Ozonoff 2010313 | Gaze to faces, gaze to objects, smiles, non-verbal vocalisations, single word verbalisations, phrase verbalisations | ‘Social communication behaviour’ |
| Vineland Adaptive Behavior Scales-Classroom version (VABS-Classroom) | Goin-Kochel 2007427 | Communication, DLS, socialisation, motor skills | Communication skills, DLS, socialisation skills, motor skills |
| Vineland Adaptive Behavior Scales (VABS) | Aldred 2004318 | Communication, DLS, socialisation | ‘Communication, daily living skills, and socialisation’ |
| Anan 2008396 | Communication, DLS, socialisation, motor skills | Adaptive functioning | |
| Andersson 2013409 | – | Adaptive skills | |
| Arick 2003388 | – | Adaptive behaviour | |
| Baghdadli 2012339 | Communication, DLS, socialisation | Adaptive behaviours | |
| Bearss 2013278 | – | Communication, DLS, socialisation, motor skills | |
| Bennett 2008296 | Social, communication, DLS | Personal and social sufficiency | |
| Carlsson 2013390 | Motor skills domain | Motor function | |
| Cassidy 2008348 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Dawson 2010321 | Communication, DLS, socialisation, motor skills | ‘Social, communication, motor, and daily living skills’ | |
| Eikeseth 2009410 | – | ‘Adaptive behaviours’ | |
| Eldevik 2012414 | Adaptive behaviour composite, communication, DLS, socialisation | Adaptive behaviour | |
| Eriksson 2013415 | – | Adaptive skills | |
| Gabriels 2007416 | Communication, DLS, socialisation, motor skills, adaptive behaviour composite | Adaptive behaviour skills | |
| Green 2010253 | – | ‘Adaptive functioning in school beyond the family’ | |
| Grindle 2012417 | – | Adaptive skills, socialisation, communication, DLS, motor skills | |
| Hedvall 2013418 | Communication, DLS, socialisation, motor skills | – | |
| Herring 2006411 | Derived Adaptive Behaviour Composite (ABC) standard score | Adaptive behaviour | |
| Honey 2008307 | Communication, socialisation | ‘Children’s abilities’ | |
| Hudry 2010233 | Receptive language, expressive language | ‘Receptive and expressive language skills’ | |
| Ben Itzchak 2011320 | Communication, DLS, socialisation, motor skills | Adaptive skills | |
| Jasmin 2009384 | DLS | DLS | |
| Jonsdottir 2007341 | Composite | Adaptive behaviour in communication, DLS, socialisation, and motor skills | |
| Klintwall 2012419 | – | ‘Treatment gains . . . treatment outcomes’ | |
| Landa 2012224 | Communication domain standard score | Communication skills | |
| Lerna 2012325 | – | Child communication, social abilities | |
| Lloyd 2013400 | Communication, DLS, socialisation, motor skills | Communication, DLS, social skills, motor development | |
| Luyster 2008129 | Motor, communication | Children’s personal and social sufficiency in communication (receptive, expressive, written), DLS (personal, domestic, community), socialisation (interpersonal relationships, play and leisure, time, coping skills) and motor skills (gross, fine) | |
| Magiati 2007308 | Communication, DLS, socialisation | Adaptive behaviour | |
| Magiati 2011309 | Communication, DLS, socialisation, composite | Adaptive behaviour | |
| Mayo 2013310 | Communication, DLS, socialisation, motor skills | Adaptive functioning | |
| McConkey 2010349 | Communication, DLS, socialisation, motor skills | Communication, DLS, socialisation and motor skills | |
| Munson 2006420 | Socialisation, communication | ‘Socialisation and communication skills’ | |
| Munson 2008312 | Social, communication, DLS, motor skills | ‘Adaptive behaviours’ | |
| O’Donnell 2012386 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Eapen 2013357 | – | Communication – expressive and receptive, DLS, socialisation, motor skills | |
| Osborne 2008350 | Communication, DLS, socialisation, motor skills | ‘Day-to-day adaptive functioning’ | |
| Osborne 2009351 | Communication, DLS, socialisation, motor skills | ‘Adaptive behavioural functioning’ | |
| Peters-Scheffer 2010421 | Communication, DLS, socialisation | ‘Adaptive behaviour’ | |
| Poon 2012401 | Communication | ‘Communication’ | |
| Pry 2005314 | Communication, DLS, socialisation | ‘Child’s knowledge about the social norms, conventions, and scripts that govern social life at all levels’ | |
| Ray-Subramanian 2011327 | Communication, DLS, socialisation, motor skills | ‘Adaptive skills’ | |
| Reed 2007352 | Communication, DLS, socialisation, motor skills | ‘Adaptive functioning’ | |
| Reed 2007353 | Communication, DLS, socialisation, motor skills | ‘Adaptive functioning’ | |
| Reed 2012354 | Communication, DLS, socialisation, motor skills | Day-to-day adaptive behaviour | |
| Remington 2007358 | Socialisation, communication, DLS, motor skills | ‘Adaptive skills’ | |
| Restall 1994422 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Rickards 2009423 | – | ‘Communication, daily living skills, socialisation and motor skills’ | |
| Roberts 2011405 | – | ‘Communication and social skills’ | |
| Rogers 2012317 | Communication, DLS, socialisation, motor skills | Adaptive behaviour | |
| Ruble 2008424 | Socialisation, communication | ‘Adaptive functioning’ | |
| Salt 2002372 | Communication, DLS, socialisation, motor skills | ‘Communication, daily living skills, socialisation and motor skills’ | |
| Schertz 2013402 | Communication | Adaptive behaviour | |
| Silva 2007299 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Silva 2008300 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Smith 2000413 | Communication, DLS, socialisation | ‘Adaptive functioning’ | |
| Smith 2010359 | Communication, DLS, socialisation, motor skills | ‘Language/communication’, ‘adaptive behaviour’ | |
| Stahmer 2004355 | Communication, DLS, socialisation, motor skills | Child adaptive functioning | |
| Stone 1999346 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Strauss 2012329 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour functioning’ | |
| Vineland Adaptive Behavior Scales (VABS) | Szatmari 2000302 | Socialisation, communication | ‘Social skills’ and ‘language’ |
| Tonge 2012425 | – | Adaptive behaviour | |
| Toth 2006284 | Communication | ‘Communication skills’ | |
| VanMeter 1997426 | Communication, DLS, socialisation | ‘Social, communication, and daily living skills’ | |
| Ventola 2007332 | Socialisation, communication, DLS, motor skills | ‘Adaptive functioning’ | |
| Werner 2005316 | Communication, DLS, socialisation, motor skills | ‘Developmental outcomes’ | |
| Zachor 2010335 | Communication, DLS, socialisation, motor skills | ‘Adaptive functioning’ | |
| Parent Surveya | Arick 2003388 | – | Communication, social interaction, behaviour, parents’ satisfaction |
| Caregiver–child interactionb | Kasari 2006368 | – | Functional play acts, play levels, joint attention skills, joint engagement |
| Classroom and playground behaviour observationsb | Escalona 2001271 | – | Positive response to touch, on-task behaviour, stereotypical behaviour, social relatedness to the teacher |
| Coding of initiation of joint attentionb | Ingersoll 2012286 | – | Initiation of joint attention |
| Examiner Ratings of Social Engagementb | Ozonoff 2010313 | Frequency of eye contact, frequency of shared affect, overall social responsiveness | ‘Social engagement’ |
| Parent–child interactionb | Green 2010253 | Parent synchrony, child initiations, mutual shared attention | Parent–child interaction during naturalistic play |
| Parent–Child Interaction measureb | Aldred 2012319 | – | Aldred 2012319 |
| Preschool teacher–child playb | Kaale 2012294 | – | Joint attention and joint engagement |
| Unstructured free play with examinerb | Lerna 2012325 | – | Co-operative play, joint attention, requests labelling |
| Video coding proceduresb | Colgan 2006379 | – | Communicative gestures |
| Video recording of child in classroom activitiesb | Ingersoll 2001380 | Language, peer social avoidance | Peer social avoidance behaviour, language |
| Social functioning | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Autism Diagnostic Interview (ADI) | Ben Itzchak 2008149 | – | Autism severity |
| Autism Diagnostic Interview-Revised (ADI-R) | Bennett 2012304 | Non-verbal items were used so that results could be compared between verbal and non-verbal children | – |
| Brian 2008305 | – | – | |
| Feldman 2012104 | – | – | |
| Hambly 2012306 | Items on language (#42, 46, 29, 30, 9, 10) | Sociocommunicative levels, ages of early language milestones | |
| Autism Diagnostic Interview (ADI) | Honey 2008307 | Repetitive behaviour algorithm items | ‘Repetitive behaviour’ |
| Autism Diagnostic Interview-Revised (ADI-R) | Magiati 2007308 | – | Autism severity and diagnosis confirmation |
| Magiati 2011309 | Total score | Autism severity | |
| Mayo 2013310 | – | Communication, social development and play, and the presence of repetitive or restricted behaviours | |
| Mooney 2006311 | – | ‘Repetitive behaviours’ | |
| Munson 2008312 | Social relatedness, communication, repetitive, restricted behaviours | ‘Autism severity’ | |
| Ozonoff 2010313 | – | ‘Parent recall of symptom onset and possible regression’ | |
| Autism Diagnostic Interview (ADI) | Pry 2005314 | – | ‘Expressive language level’ |
| Autism Diagnostic Interview-Revised (ADI-R) | Richler 2007315 | RRB | ‘Restricted and repetitive behaviours’ |
| Autism Diagnostic Interview (ADI) | Werner 2005316 | Social, communication, repetitive | ‘Developmental outcomes’ |
| Child Behavior Scale (CBS) | Jahromi 2013431 | Prosocial behaviours | Prosocial peer engagement |
| Meek 2012435 | Prosocial behaviours, asocial, exclusion, aggressive behaviours, hyperactive–distractible behaviours, anxious–fearful behaviours, social competence composite | ‘Social competence with peers’ | |
| Nisonger Child Behavior Rating Scales | Remington 2007358 | Positive Social Subscale | ‘Child behaviour’ |
| Social Behavior Rating Scale | Vorgraft 2007347 | – | ‘Children’s social interactive behaviour’ |
| Vineland Adaptive Behavior Scales-Classroom version (VABS-Classroom) | Goin-Kochel 2007427 | Communication, DLS, socialisation, motor skills | Communication skills, DLS, socialisation skills, motor skills |
| Vineland Adaptive Behavior Scales (VABS) | Aldred 2004318 | Communication, DLS, socialisation | ‘Communication, daily living skills, and socialisation’ |
| Anan 2008396 | Communication, DLS, socialisation, motor skills | Adaptive functioning | |
| Andersson 2013409 | – | Adaptive skills | |
| Arick 2003388 | – | Adaptive behaviour | |
| Baghdadli 2012339 | Communication, DLS, socialisation | Adaptive behaviours | |
| Bearss 2013278 | – | Communication, DLS, socialisation, motor skills | |
| Bennett 2008296 | Social, communication, DLS | Personal and social sufficiency | |
| Carlsson 2013390 | Motor Skills domain | Motor function | |
| Cassidy 2008348 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Dawson 2010321 | Communication, DLS, socialisation, motor skills | ‘Social, communication, motor, and daily living skills’ | |
| Eikeseth 2009410 | – | ‘Adaptive behaviours’ | |
| Eldevik 2012414 | Adaptive behaviour composite, communication, daily living, socialisation | Adaptive behaviour | |
| Eriksson 2013415 | – | Adaptive skills | |
| Gabriels 2007416 | Communication, DLS, socialisation, motor skills, adaptive behaviour composite | Adaptive behaviour skills | |
| Green 2010253 | – | ‘Adaptive functioning in school beyond the family’ | |
| Grindle 2012417 | – | Adaptive skills, socialisation, communication, DLS, motor skills | |
| Hedvall 2013418 | Communication, DLS, socialisation, motor skills | – | |
| Herring 2006411 | Derived Adaptive Behaviour Composite (ABC) standard score | Adaptive behaviour | |
| Honey 2008307 | Communication, socialisation | ‘Children’s abilities’ | |
| Hudry 2010233 | Receptive language, expressive language | ‘Receptive and expressive language skills’ | |
| Ben Itzchak 2011320 | Communication, DLS, socialisation, motor skills | Adaptive skills | |
| Jasmin 2009384 | DLS | DLS | |
| Jonsdottir 2007341 | Composite | Adaptive behaviour in communication, DLS, socialisation and motor skills | |
| Klintwall 2012427 | – | ‘Treatment gains . . . treatment outcomes’ | |
| Landa 2012224 | Communication domain standard score | Communication skills | |
| Lerna 2012325 | – | Child communication, social abilities | |
| Lloyd 2013400 | Communication, DLS, socialisation, motor skills | Communication, DLS, social skills, motor development | |
| Luyster 2008129 | Motor, communication | Children’s personal and social sufficiency in communication (receptive, expressive, written), DLS (personal, domestic, community), socialisation (interpersonal relationships, play and leisure, time, coping skills) and motor skills (gross, fine) | |
| Magiati 2007308 | Communication, DLS, socialisation | Adaptive behaviour | |
| Magiati 2011309 | Communication, DLS, socialisation, composite | Adaptive behaviour | |
| Mayo 2013310 | Communication, DLS, socialisation, motor skills | Adaptive functioning | |
| McConkey 2010349 | Communication, DLS, socialisation, motor skills | Communication, DLS, socialisation and motor skills | |
| Munson 2006420 | Socialisation, communication | ‘Socialisation and communication skills’ | |
| Munson 2008312 | Social, communication, DLS, motor skills | ‘Adaptive behaviours’ | |
| O’Donnell 2012386 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Eapen 2013357 | – | Communication – expressive and receptive, DLS, socialisation, motor skills | |
| Osborne 2008350 | Communication, DLS, socialisation, motor skills | ‘Day-to-day adaptive functioning’ | |
| Osborne 2009351 | Communication, DLS, socialisation, motor skills | ‘Adaptive behavioural functioning’ | |
| Peters-Scheffer 2010421 | Communication, DLS, socialisation | ‘Adaptive behaviour’ | |
| Poon 2012401 | Communication | ‘Communication’ | |
| Pry 2005314 | Communication, DLS, socialisation | ‘Child’s knowledge about the social norms, conventions, and scripts that govern social life at all levels’ | |
| Ray-Subramanian 2011327 | Communication, DLS, socialisation, motor skills | ‘Adaptive skills’ | |
| Reed 2007352 | Communication, DLS, socialisation, motor skills | ‘Adaptive functioning’ | |
| Reed 2007353 | Communication, DLS, socialisation, motor skills | ‘Adaptive functioning’ | |
| Reed 2012354 | Communication, DLS, socialisation, motor skills | Day-to-day adaptive behaviour | |
| Remington 2007358 | Socialisation, communication, DLS, motor skills | ‘Adaptive skills’ | |
| Restall 1994422 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Rickards 2009423 | – | ‘Communication, daily living skills, socialisation and motor skills’ | |
| Roberts 2011405 | – | ‘Communication and social skills’ | |
| Rogers 2012317 | Communication, DLS, socialisation, motor skills | Adaptive behaviour | |
| Ruble 2008424 | Socialisation, communication | ‘Adaptive functioning’ | |
| Salt 2002372 | Communication, DLS, socialisation, motor skills | ‘Communication, daily living skills, socialisation and motor skills’ | |
| Schertz 2013402 | Communication | Adaptive behaviour | |
| Silva 2007299 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Silva 2008300 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Smith 2000413 | Communication, DLS, socialisation | ‘Adaptive functioning’ | |
| Smith 2010359 | Communication, DLS, socialisation, motor skills | ‘Language/communication’, ‘adaptive behaviour’ | |
| Stahmer 2004355 | Communication, DLS, socialisation, motor skills | Child adaptive functioning | |
| Stone 1999346 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Strauss 2012329 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour functioning’ | |
| Szatmari 2000302 | Socialisation, communication | ‘Social skills’ and ‘language’ | |
| Tonge 2012425 | – | Adaptive behaviour | |
| Toth 2006284 | Communication | ‘Communication skills’ | |
| VanMeter 1997426 | Communication, DLS, socialisation | ‘Social, communication, and daily living skills’ | |
| Ventola 2007332 | Socialisation, communication, DLS, motor skills | ‘Adaptive functioning’ | |
| Werner 2005316 | Communication, DLS, socialisation, motor skills | ‘Developmental outcomes’ | |
| Zachor 2010335 | Communication, DLS, socialisation, motor skills | ‘Adaptive functioning’ | |
| Vineland Social Maturity Scale, Indian adaptationa | Malhi 2011342 | – | Adaptive behaviour |
| Parent Surveyb | Arick 2003388 | – | Communication, social interaction, behaviour, parents’ satisfaction |
| Classroom and playground behaviour observationsc | Escalona 2001271 | – | Positive response to touch, on-task behaviour, stereotypical behaviour, social relatedness to the teacher |
| Coded observation of social behaviourc | Meirsschaut 2011442 | Child’s level of play, mother’s play-stimulation, child’s social initiatives, child responses, mother’s social initiatives, mother’s responses | ‘Social behaviour’ |
| Video recording of child in classroom activitiesc | Ingersoll 2001380 | Language, peer social avoidance | Peer social avoidance behaviour, language |
| Play | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Autism Diagnostic Observation Scale-Toddler Module (ADOS-T) | Rogers 2012317 | Social affect, restricted, repetitive behaviours | ‘Social and communicative behaviours, as well as repetitive behaviours diagnostic of autism’ |
| Autism Diagnostic Observation Schedule (ADOS) | Aldred 2004318 | Reciprocal social interaction, communication, stereotyped and restricted behaviours | ‘Interaction, communication, repetitive behaviours and play’ |
| Aldred 2012319 | Total social communication algorithm score | Social communication | |
| Ben Itzchak 2008149 | Language and communication, reciprocal social interaction, play, and stereotyped behaviour and restricted interests | Social and communicative functioning | |
| Ben Itzchak 2011320 | ADOS standardised measure of severity | Autism severity, diagnostic algorithm | |
| Bennett 2012304 | – | Social and communication behaviours | |
| Brian 2008305 | Module 1 | – | |
| Dawson 2010321 | Social relatedness, communication, play, repetitive behaviours | ‘Autism symptoms’ | |
| Gotham 2012322 | – | Symptom severity | |
| Autism Diagnostic Observation Schedule-Generic (ADOS-G) | Green 2010253 | Communication, social | ‘Severity of the symptoms of autism’ |
| Hartley 2009323 | Communication, social interaction, restricted behaviours | ASD symptoms | |
| Autism Diagnostic Observation Schedule (ADOS) | Landa 2012224 | – | Symptom severity |
| Lerna 2012325 | Communication, reciprocal social interaction | Social communicative abilities | |
| Luyster 2008129 | Play | – | |
| Autism Diagnostic Observation Schedule-Generic (ADOS-G) | Munson 2008312 | Communication, social | ‘Autism severity’ |
| Autism Diagnostic Observation Schedule (ADOS) | Oosterling 2010326 | Level of non-echoed language, joint attention, social affect | Language development, EARLY precursors of social communication |
| Ray-Subramanian 2011327 | – | ‘Social communication skills and behaviours characteristic of autism’ | |
| Ray-Subramanian 2012328 | Calibrated ADOS severity scores, composite RRB variable | RRB | |
| Strauss 2012329 | Communication, social | ‘Severity of autism symptoms’ | |
| Sullivan 2007330 | Response to joint attention item | ‘Response to joint attention’ | |
| Autism Diagnostic Observation Schedule-Generic (ADOS-G) | Tek 2012331 | Communication, reciprocal social interaction | Assessment for ASD |
| Ventola 2007332 | Communication, social | ‘Communication, social interactions and relatedness, play, and imagination’ | |
| Autism Diagnostic Observation Schedule (ADOS) | Werner 2005316 | Communication, social | ‘Developmental outcomes’ |
| Wong 2010333 | Language and communication, reciprocal social interaction | ‘Assessing autism spectrum disorder’ | |
| Zachor 2006334 | Language and communication, reciprocal social interaction | Language and communication and reciprocal social interaction | |
| Zachor 2010335 | – | ‘Autism severity’ | |
| Communication and Symbolic Behavior Scales-Developmental Profile (Caregiver Questionnaire) (CSBS-DP-CQ); Wetherby and Prizant 2002125) | Tek 2012331 | CSBS-DP-CQ Words, CSBS-DP-CQ Understanding Words, CSBS-DP-CQ Social Composite | Language and social development |
| Developmental Play Assessment (DPA) - Instrument Sequence of Categories | Freeman 2013443 | Play acts, play schemes, level of play | – |
| Freeman 2013443 | – | Level of play, type of play behaviour, frequency of play behaviours | |
| Goods 2013366 | – | Play | |
| Kasari 2006368 | – | Functional play (the number of different novel, child initiated, functional play acts), symbolic play types, play level | |
| Symbolic Play Test | Wong 2010333 | – | ‘Language potential of preverbal children’ |
| Salt 2002372 | – | ‘Functional play’ | |
| Magiati 2007308 | – | Symbolic play | |
| Test of Pretend Play (ToPP) | Magiati 2007308 | – | Symbolic play |
| Dereu 2012365 | – | Functional and symbolic play development | |
| Preschool Play Scalea | Restall 1994422 | Space management, material management, imitation, participation | ‘Play performance’ |
| Caregiver–child interactionb | Kasari 2006368 | – | Functional play acts, play levels, joint attention skills, joint engagement |
| Coded observation of social behaviourb | Meirsschaut 2011442 | Child’s level of play, mother’s play stimulation, child’s social initiatives, child responses, mother’s social initiatives, mother’s responses | ‘Social behaviour’ |
| Coding of videosb | Flippin 2011406 | Parent play responsiveness, parent verbal responsiveness, child object play (exploratory, relational, functional, symbolic) | Object play skills, parent responsiveness |
| Free play assessmentb | Christensen 2010444 | Total functional play, object directed functional play, self-directed functional play, other directed functional play, symbolic play, functional repeated play, non-functional repeated play, total play acts | ‘Play behaviours’ |
| Parent–child free playb | Freeman 2013443 | – | Play acts, play schemes |
| Behaviour | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Aberrant Behavior Checklist (ABC) | Baghdadli 2012339 | – | Self-injurious behaviours (SIB) |
| Bearss 2013278 | Irritability (tantrums, aggression and self-injury), social withdrawal, stereotypes, hyperactivity, inappropriate speech | Irritability, social withdrawal, stereotypes, hyperactivity, inappropriate speech | |
| O’Donnell 2012386 | Irritability, agitation, crying, lethargy, social withdrawal, stereotypic behaviour, hyperactivity, non-compliance, inappropriate speech | ‘Challenging behaviours’ | |
| Werner 2005316 | Lethargy/withdrawal, stereotypic behaviour, hyperactivity, compliance, inappropriate speech | ‘Developmental outcomes’ | |
| Baby and Infant Screen for Children with aUtIsm Traits (BISCUIT-Part 3) | Rojahn 2009445 | – | ‘Challenging behaviours in toddlers’ |
| Behavior Assessment System for Children-Second Edition (BASC-2) | Hill-Chapman 2013434 | – | Atypicality of symptoms |
| Behavior Screening Questionnaire | Rickards 2009423 | – | ‘Behaviour’ |
| Child Behavior Checklist (CBCL) | Baker 2010397 | N/A | ‘Child behaviour problems’ |
| Hartley 2009323 | – | Emotionally reactive, anxious/depressed, somatic complaints, sleep problems, attention problems, aggressive behaviour | |
| Peters-Scheffer 2010421 | Behavioural problem scale | ‘Emotional and behavioural problems’ | |
| Smith 2000413 | Social withdrawal, somatisation, anxiety/depression, social problems, thought problems, attention problems, delinquency, aggression | ‘Socioeconomic functioning’ | |
| Smith 2010359 | Total problems, internalising problems, externalising problems, aggressive behavioural | ‘Behavioural problems’ | |
| Taylor 2012436 | Internalising problems, externalising problems, total problems composite | ‘Internalising and externalising behaviours in children’ | |
| Child Behavior Scale (CBS) | Jahromi 2013431 | Prosocial behaviours | Prosocial peer engagement |
| Meek 2012435 | Prosocial behaviours, asocial, exclusion, aggressive behaviours, hyperactive–distractible behaviours, anxious–fearful behaviours, social competence composite | ‘Social competence with peers’ | |
| Conners Rating Scales-Revised | Escalona 2001271 | ADHD Index, restless–impulsive behaviour, emotional index, the global index, inattentiveness | – |
| Osborne 2009351 | Oppositional behaviour, cognitive problems, hyperactivity, ADHD index | ‘Behavioural problems, hyperactivity and attention deficit disorder’ | |
| Reed 2007353 | Oppositional behaviour, cognitive problems, hyperactivity, ADHD index | ‘Behavioural difficulties’ | |
| Reed 2013437 | Oppositional behaviour, cognitive problems, hyperactivity, ADHD index | Behavioural problems, ADHD | |
| Developmental Behaviour Checklist | Herring 2006411 | – | Child behavioural and emotional problems |
| Mooney 2006311 | – | ‘Repetitive behaviour’ | |
| Remington 2007358 | – | ‘Child behaviour’ | |
| Roberts 2011405 | – | ‘Adaptive functioning and psychopathology’ | |
| Tonge 2012425 | – | Severity of autism | |
| Home Situations Questionnaire (HSQ) | Bearss 2013278 | – | Non-compliance in children |
| Nisonger Child Behavior Rating Scales | Remington 2007358 | Positive Social Subscale | ‘Child behaviour’ |
| Parent Target Problems | Bearss 2013278 | – | Most pressing or important child needs |
| Pre-School Behavior Checklist | Rickards 2009423 | – | ‘Behaviour’ |
| Behaviour Style Questionnaire–Chinese version (Xu 1979)a | Chuang 2012383 | – | Children’s temperament |
| Coded observation of child behaviour problemsb | Robbins 1992446 | – | ‘Child behaviour problems’ |
| Functional behaviour assessment interview (O’Neill et al. 1997)c | Reese 2005447 | Gain attention, escape demand, gain item | ‘Disruptive behaviours’ |
| Parent Surveyc | Arick 2003388 | – | Communication, social interaction, behaviour, parents’ satisfaction |
| Video coding procedures (for children and parents)d | Bryce 2013448 | – | – |
| Habit problems | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Child Behavior Checklist (CBCL) | Smith 2000413 | Social withdrawal, somatisation, anxiety/depression, social problems, thought problems, attention problems, delinquency, aggression | ‘Socioeconomic functioning’ |
| Baker 2010397 | – | ‘Child behaviour problems’ | |
| Peters-Scheffer 2010421 | Behavioural problem scale | ‘Emotional and behavioural problems’ | |
| Smith 2010359 | Total problems, internalising problems, externalising problems, aggressive behavioural | ‘Behavioural problems’ | |
| Taylor 2012436 | Internalising problems, externalising problems, total problems composite | ‘Internalising and externalising behaviours in children’ | |
| Hartley 2009323 | – | Emotionally reactive, anxious/depressed, somatic complaints, sleep problems, attention problems, aggressive behaviour | |
| Sense and Self-Regulation Checklist (SSC) | Silva 2009226 | – | ‘Parent questionnaire (on) changes in sensory impairment, appetite, digestion, and sleep’ |
| Silva 2011301 | Sense, self-regulation | ‘Sensory and self-regulatory symptoms commonly reported by parents’ | |
| Sleep Diariesa | Escalona 2001271 | – | Amount of fussing, restlessness, crying, self-stimulating behaviour, number of times the child left the bed |
| Learning | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Autism Screening Instrument for Educational Planning (ASIEP) | Arick 2003388 | Autism Behavior Checklist, sample of vocal behaviour, social interaction assessment, educational assessment | Educational progress |
| Extended Basic Academic Skills Assessment System | Arick 2003388 | – | Educational progress in reading, writing and maths |
| Wechsler Individualised Achievement Test | Smith 2000413 | – | ‘Academic achievement’ |
| Student Learning Profilea | Arick 2003388 | Expressive language, receptive language, daily routines, pre-academics, play behaviour, social interaction behaviour | Progress on written curriculum-based programmes; how the participants requested wants or needs |
| Classroom Observation Formb | Arick 2003388 | – | Child’s involvement level in classroom activities |
| Daily living skills | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Functional Independence Measure for Children (WeeFIM) | Jasmin 2009384 | – | DLS |
| Vineland Adaptive Behavior Scales-Classroom version (VABS-Classroom) | Goin-Kochel 2007427 | Communication, DLS, socialisation, motor skills | Communication skills, DLS, socialisation skills, motor skills |
| Vineland Adaptive Behavior Scales (VABS) | Aldred 2004318 | Communication, DLS, socialisation | ‘Communication, daily living skills, and socialisation’ |
| Anan 2008396 | Communication, DLS, socialisation, motor skills | Adaptive functioning | |
| Andersson 2013409 | – | Adaptive skills | |
| Arick 2003388 | – | Adaptive behaviour | |
| Baghdadli 2012339 | Communication, DLS, socialisation | Adaptive behaviours | |
| Bearss 2013278 | – | Communication, DLS, socialisation, motor skills | |
| Ben Itzchak 2011320 | Communication, DLS, socialisation, motor skills | Adaptive skills | |
| Bennett 2008296 | Social, communication, DLS | Personal and social sufficiency | |
| Carlsson 2013390 | Motor skills domain | Motor function | |
| Cassidy 2008348 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Dawson 2010321 | Communication, DLS, socialisation, motor skills | ‘Social, communication, motor, and daily living skills’ | |
| Eapen 2013357 | – | Communication – expressive and receptive, DLS, socialisation, motor skills | |
| Eikeseth 2009410 | – | ‘Adaptive behaviours’ | |
| Eldevik 2012414 | Adaptive behaviour composite, communication, daily living, socialisation | Adaptive behaviour | |
| Eriksson 2013415 | – | Adaptive skills | |
| Gabriels 2007416 | Communication, DLS, socialisation, motor skills, adaptive behaviour composite | Adaptive behaviour skills | |
| Green 2010253 | – | ‘Adaptive functioning in school beyond the family’ | |
| Grindle 2012417 | – | Adaptive skills, socialisation, communication, DLS, motor skills | |
| Hedvall 2013418 | Communication, DLS, socialisation, motor skills | – | |
| Herring 2006411 | Derived Adaptive Behaviour Composite (ABC) standard score | Adaptive behaviour | |
| Honey 2008307 | Communication, socialisation | ‘Children’s abilities’ | |
| Hudry 2010233 | Receptive language, expressive language | ‘Receptive and expressive language skills’ | |
| Jasmin 2009384 | DLS | DLS | |
| Jonsdottir 2007341 | Composite | Adaptive behaviour in communication, DLS, socialisation and motor skills | |
| Klintwall 2012427 | – | ‘Treatment gains . . . treatment outcomes’ | |
| Landa 2012224 | Communication domain standard score | Communication skills | |
| Lerna 2012325 | – | Child communication, social abilities | |
| Lloyd 2013400 | Communication, DLS, socialisation, motor skills | Communication, DLS, social skills, motor development | |
| Luyster 2008129 | Motor, communication | Children’s personal and social sufficiency in communication (receptive, expressive, written), DLS (personal, domestic, community), socialisation (interpersonal relationships, play and leisure, time, coping skills) and motor skills (gross, fine) | |
| Magiati 2007308 | Communication, DLS, socialisation | Adaptive behaviour | |
| Magiati 2011309 | Communication, DLS, socialisation, composite | Adaptive behaviour | |
| Mayo 2013310 | Communication, DLS, socialisation, motor skills | Adaptive functioning | |
| McConkey 2010349 | Communication, DLS, socialisation, motor skills | Communication, DLS, socialisation and motor skills | |
| Munson 2006420 | Socialisation, communication | ‘Socialisation and communication skills’ | |
| Munson 2008312 | Social, communication, DLS, motor skills | ‘Adaptive behaviours’ | |
| O’Donnell 2012386 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Osborne 2008350 | Communication, DLS, socialisation, motor skills | ‘Day-to-day adaptive functioning’ | |
| Osborne 2009351 | Communication, DLS, socialisation, motor skills | ‘Adaptive behavioural functioning’ | |
| Peters-Scheffer 2010421 | Communication, DLS, socialisation | ‘Adaptive behaviour’ | |
| Poon 2012401 | Communication | ‘Communication’ | |
| Pry 2005314 | Communication, DLS, socialisation | ‘Child’s knowledge about the social norms, conventions, and scripts that govern social life at all levels’ | |
| Ray-Subramanian 2011327 | Communication, DLS, socialisation, motor skills | ‘Adaptive skills’ | |
| Reed 2007352 | Communication, DLS, socialisation, motor skills | ‘Adaptive functioning’ | |
| Reed 2007353 | Communication, DLS, socialisation, motor skills | ‘Adaptive functioning’ | |
| Reed 2012354 | Communication, DLS, socialisation, motor skills | Day-to-day adaptive behaviour | |
| Remington 2007358 | Socialisation, communication, DLS, motor skills | ‘Adaptive skills’ | |
| Restall 1994422 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Rickards 2009423 | – | ‘Communication, daily living skills, socialisation and motor skills’ | |
| Roberts 2011405 | – | ‘Communication and social skills’ | |
| Rogers 2012317 | Communication, DLS, socialisation, motor skills | Adaptive behaviour | |
| Ruble 2008424 | Socialisation, communication | ‘Adaptive functioning’ | |
| Salt 2002372 | Communication, DLS, socialisation, motor skills | ‘Communication, daily living skills, socialisation and motor skills’ | |
| Schertz 2013402 | Communication | Adaptive behaviour | |
| Silva 2007299 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Silva 2008300 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Smith 2000413 | Communication, DLS, socialisation | ‘Adaptive functioning’ | |
| Smith 2010359 | Communication, DLS, socialisation, motor skills | ‘Language/communication’, ‘adaptive behaviour’ | |
| Stahmer 2004355 | Communication, DLS, socialisation, motor skills | Child adaptive functioning | |
| Stone 1999346 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Strauss 2012329 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour functioning’ | |
| Szatmari 2000302 | Socialisation, communication | ‘Social skills’ and ‘language’ | |
| Tonge 2012425 | – | Adaptive behaviour | |
| Toth 2006284 | Communication | ‘Communication skills’ | |
| VanMeter 1997426 | Communication, DLS, socialisation | ‘Social, communication, and daily living skills’ | |
| Ventola 2007332 | Socialisation, communication, DLS, motor skills | ‘Adaptive functioning’ | |
| Werner 2005316 | Communication, DLS, socialisation, motor skills | ‘Developmental outcomes’ | |
| Zachor 2010335 | Communication, DLS, socialisation motor skills | ‘Adaptive functioning’ | |
| Video coding of feeding behavioura | Brisson 2012449 | – | – |
| Global measure of function | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Ages and Stages Questionnaire (ASQ) | Feldman 2012104 | Communication, gross motor, fine motor, problem solving, personal–social, overall | Infant development |
| Assessment of Basic Language and Learning Skills (ABLLS) | Goin-Kochel 2007427 | Language, social, academic, self-help, motor, composite | Language, social/play, academics, self-help and motor skills |
| Grindle 2012417 | – | Learning skills, language, social skills and play, academic, self-help, motor-skills | |
| Gupta 2009303 | – | Language and learning skills | |
| Assessment, Evaluation and Programming System (AEPS) | Schwartz 2004450 | Adaptive, cognitive, social communication, gross motor, fine motor | ‘Developmental progress’ |
| Behavior Assessment System for Children-Second Edition (BASC-2) | Hill-Chapman 2013434 | – | Atypicality of symptoms |
| Brigance Diagnostic Inventory of Early Development | Travers 2011438 | Alphabet Recognition Assessments | ‘Alphabet Recognition’ |
| Developmental Profile | Malhi 2011342 | Academic | Developmental assessment. Developmental quotient was derived from the academic subscale |
| Early Development Interview | Werner 2005316 | – | ‘Early Developmental Course’ |
| Early Intervention Developmental Profile (EIDP) | Jocelyn 1998298 | Cognition, language, perceptual/fine motor, gross motor, social–emotional, self-care | – |
| Early Learning Accomplishment Profile (E-LAP) | Virues-Ortega 2013451 | – | Fine and gross motor, cognitive, language, self-care and social skills |
| Functional Emotional Developmental Questionnaire | Pajareya 2012343 | – | Developmental rating of the children |
| Pajareya 2011344 | – | ‘Developmental rating’ and ‘fundamental development’ | |
| Learning Accomplishment Profile-Diagnostic, Third Edition (LAP-D) | Virues-Ortega 2013451 | – | Fine and gross motor, cognitive, language, self-care and social skills |
| Paediatric Daily Occupation Scale | Hsieh 2013452 | – | Occupational performance |
| Preschool Developmental Profile (PSDP) | Jocelyn 1998298 | Cognition, language, perceptual/fine motor, gross motor, social/emotional, self-care | – |
| Psychoeducational Profile-Revised (PEP-R) | Delmolino 2006432 | Imitation, perception, eye–hand integration, fine motor, gross motor, cognitive verbal, cognitive performance | Cognitive development, general development |
| Herring 2006411 | – | Developmental age | |
| McConkey 2010349 | Imitation, perception, fine motor skills, gross motor skills, eye–hand co-ordination, non-verbal conceptual ability, verbal conceptual ability | Learning style, strengths and deficits | |
| Osborne 2008350 | Imitation, perception, fine motor skills, gross motor skills, eye–hand co-ordination, non-verbal conceptual ability, verbal conceptual ability | ‘Typical strengths and characteristic weaknesses of children with ASD’ | |
| Ozonoff 1998453 | Imitation, perception, fine motor skills, gross motor skills, eye–hand co-ordination, non-verbal conceptual ability, verbal conceptual ability | ‘Typical strengths and the characteristic weaknesses of children with autism’ | |
| Reed 2007352 | Imitation, perception, fine motor skills, gross motor skills, eye–hand co-ordination, non-verbal conceptual ability, verbal conceptual ability | ‘Developmental functioning’ | |
| Reed 2007353 | Imitation, perception, fine motor skills, gross motor skills, eye–hand co-ordination, non-verbal conceptual ability, verbal conceptual ability | ‘Developmental functioning’ | |
| Reed 2012354 | Imitation, perception, fine motor skills, gross motor skills, eye–hand co-ordination, non-verbal conceptual ability, verbal conceptual ability | Typical strengths and weaknesses of children on the autism spectrum | |
| Tonge 2012425 | – | Cognitive development | |
| Scales of Independent Behavior-Revised (SIB-R) | Keen 2010363 | – | Adaptive and maladaptive behaviour: internalising behaviour, externalising behaviour and asocial behaviour |
| Vineland Adaptive Behavior Scales-Classroom version (VABS-Classroom) | Goin-Kochel 2007427 | Communication, DLS, socialisation, motor skills | Communication skills, DLS, socialisation skills, motor skills |
| Vineland Adaptive Behavior Scales (VABS) | Aldred 2004318 | Communication, DLS, socialisation | ‘Communication, daily living skills, and socialisation’ |
| Anan 2008396 | Communication, DLS, socialisation, motor skills | Adaptive functioning | |
| Andersson 2013409 | – | Adaptive skills | |
| Arick 2003388 | – | Adaptive behaviour | |
| Baghdadli 2012339 | Communication, DLS, socialisation | Adaptive behaviours | |
| Bearss 2013278 | – | Communication, DLS, socialisation, motor skills | |
| Ben Itzchak 2011320 | Communication, DLS, socialisation, motor skills | Adaptive skills | |
| Bennett 2008296 | Social, communication, DLS | Personal and social sufficiency | |
| Carlsson 2013390 | Motor skills domain | Motor function | |
| Cassidy 2008348 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Dawson 2010321 | Communication, DLS, socialisation, motor skills | ‘Social, communication, motor, and daily living skills’ | |
| Eapen 2013357 | – | Communication – expressive and receptive, DLS, socialisation, motor skills | |
| Eikeseth 2009410 | – | ‘Adaptive behaviours’ | |
| Eldevik 2012414 | Adaptive behaviour composite, communication, daily living, socialisation | Adaptive behaviour | |
| Eriksson 2013415 | – | Adaptive skills | |
| Gabriels 2007416 | Communication, DLS, socialisation, motor skills, adaptive behaviour composite | Adaptive behaviour skills | |
| Green 2010253 | – | ‘Adaptive functioning in school beyond the family’ | |
| Grindle 2012417 | – | Adaptive skills, socialisation, communication, DLS, motor skills | |
| Hedvall 2013418 | Communication, DLS, socialisation, motor skills | – | |
| Herring 2006411 | Derived Adaptive Behaviour Composite (ABC) standard score | Adaptive behaviour | |
| Honey 2008307 | Communication, socialisation | ‘Children’s abilities’ | |
| Hudry 2010233 | Receptive language, expressive language | ‘Receptive and expressive language skills’ | |
| Jasmin 2009384 | DLS | DLS | |
| Jonsdottir 2007341 | Composite | Adaptive behaviour in communication, DLS, socialisation, and motor skills | |
| Klintwall 2012427 | – | ‘Treatment gains . . . treatment outcomes’ | |
| Landa 2012224 | Communication domain standard score | Communication skills | |
| Lerna 2012325 | – | Child communication, social abilities | |
| Lloyd 2013400 | Communication, DLS, socialisation, motor skills | Communication, DLS, social skills, motor development | |
| Luyster 2008129 | Motor, communication | Children’s personal and social sufficiency in communication (receptive, expressive, written), DLS (personal, domestic, community), socialisation (interpersonal relationships, play and leisure, time, coping skills), and motor skills (gross, fine) | |
| Magiati 2007308 | Communication, DLS, socialisation | Adaptive behaviour | |
| Magiati 2011309 | Communication, DLS, socialisation, composite | Adaptive behaviour | |
| Mayo 2013310 | Communication, DLS, socialisation, motor skills | Adaptive functioning | |
| McConkey 2010349 | Communication, DLS, socialisation, motor skills | Communication, DLS, socialisation and motor skills. | |
| Munson 2006420 | Socialisation, communication | ‘Socialisation and communication skills’ | |
| Munson 2008312 | Social, communication, DLS, motor skills | ‘Adaptive behaviours’ | |
| O’Donnell 2012386 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Osborne 2008350 | Communication, DLS, socialisation, motor skills | ‘Day-to-day adaptive functioning’ | |
| Osborne 2009351 | Communication, DLS, socialisation, motor skills | ‘Adaptive behavioural functioning’ | |
| Peters-Scheffer 2010421 | Communication, DLS, socialisation | ‘Adaptive behaviour’ | |
| Poon 2012401 | Communication | ‘Communication’ | |
| Pry 2005314 | Communication, DLS, socialisation | ‘Child’s knowledge about the social norms, conventions, and scripts that govern social life at all levels’ | |
| Ray-Subramanian 2011327 | Communication, DLS, socialisation, motor skills | ‘Adaptive skills’ | |
| Reed 2007352 | Communication, DLS, socialisation, motor skills | ‘Adaptive functioning’ | |
| Reed 2007353 | Communication, DLS, socialisation, motor skills | ‘Adaptive functioning’ | |
| Reed 2012354 | Communication, DLS, socialisation, motor skills | Day-to-day adaptive behaviour | |
| Remington 2007358 | Socialisation, communication, DLS, motor skills | ‘Adaptive skills’ | |
| Restall 1994422 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Rickards 2009423 | – | ‘Communication, daily living skills, socialisation and motor skills’ | |
| Roberts 2011405 | – | ‘Communication and social skills’ | |
| Rogers 2012317 | Communication, DLS, socialisation, motor skills | Adaptive behaviour | |
| Ruble 2008424 | Socialisation, communication | ‘Adaptive functioning’ | |
| Salt 2002372 | Communication, DLS, socialisation, motor skills | ‘Communication, daily living skills, socialisation and motor skills’ | |
| Schertz 2013402 | Communication | Adaptive behaviour | |
| Silva 2007299 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Silva 2008300 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Smith 2000413 | Communication, DLS, socialisation | ‘Adaptive functioning’ | |
| Smith 2010359 | Communication, DLS, socialisation, motor skills | ‘Language/communication’, ‘adaptive behaviour’ | |
| Stahmer 2004355 | Communication, DLS, socialisation, motor skills | Child adaptive functioning | |
| Stone 1999346 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour’ | |
| Strauss 2012329 | Communication, DLS, socialisation, motor skills | ‘Adaptive behaviour functioning’ | |
| Szatmari 2000302 | Socialisation, communication | ‘Social skills’ and ‘language’ | |
| Tonge 2012425 | – | Adaptive behaviour | |
| Toth 2006284 | Communication | ‘Communication skills’ | |
| VanMeter 1997426 | Communication, DLS, socialisation | ‘Social, communication, and daily living skills’ | |
| Ventola 2007332 | Socialisation, communication, DLS, motor skills | ‘Adaptive functioning’ | |
| Werner 2005316 | Communication, DLS, socialisation, motor skills | ‘Developmental outcomes’ | |
| Zachor 2010335 | Communication, DLS, socialisation, motor skills | ‘Adaptive functioning’ | |
| Social Adaptive Development Quotient Scale (ADQ)a | Zhang 2012303 | – | ‘Motor, daily life, language development, personal orientation, social responsibility, time and space, labour skills, and economic activity’ |
| Global measure of outcome | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Autism Treatment Evaluation Checklist (ATEC) | Goin-Kochel 2007427 | Speech/language/communication, sociability, sensory/cognitive awareness, health/physical/behaviour, composite | Speech/language/communication, sociability, health/physical/behaviour, sensory/cognitive awareness |
| Behavioral Summarized Evaluation-Revised (BSE-R) | Receveur 2005337 | – | ‘Interaction disorders’ |
| Behavioral Summarized Evaluation (BSE) | Maestro 2005338 | – | ‘Severity of behavioural problems’ |
| Clinical Global Impression –Improvement Scale | Bearss 2013278 | – | Overall improvement |
| Oosterling 2010326 | – | ‘General improvement’ | |
| Infant Behavioral Summarized Evaluation (IBSE) | Adrien 199290 | – | General autism characteristics |
| Receveur 2005337 | – | ‘Early signs of autism’ and ‘behavioural evaluation’ | |
| Pervasive Developmental Disorders Behavior Inventory (PDDBI) | Silva 2009226 | Receptive/expressive social communication abilities composite, approach/withdrawal problems composite, sensory | ‘Social and language abilities and maladaptive behaviour’ |
| Silva 2011301 | Sensory, maladaptive behaviour, social/language/communication abilities | ‘Social and language abilities and maladaptive behaviour’ |
| Subjective well-being | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Kiddie–Infant Descriptive Instrument for Emotional States (KIDIES)a | Trad 1993454 | Happiness, attention to persons, attention to things | ‘Affective and behavioural dimensions’ |
| Social Inclusion | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| School Liking and Avoidance Questionnaire | Jahromi 2013431 | – | School engagement |
| Teacher Rating Scale of School Adjustment | Jahromi 2013431 | – | Behavioural school engagement |
| Interaction Style | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Functional Emotional Assessment Scale | Pajareya 2012343 | – | Changes in children’s functional development |
| Pajareya 2011344 | – | ‘Changes in children’s functional development’ | |
| NICHD Early Child Care Network scales | Baker 2010397 | Parenting subscale | ‘Maternal sensitivity’ |
| Coded observation of social behavioura | Meirsschaut 2011442 | Child’s level of play, mother’s play stimulation, child’s social initiatives, child responses, mother’s social initiatives, mother’s responses | ‘Social behaviour’ |
| Coding of videosa | Flippin 2011406 | Parent play responsiveness, parent verbal responsiveness, child object play (exploratory, relational, functional, symbolic) | Object play skills, parent responsiveness |
| Parental skills – video ratingsa | Oosterling 2010326 | Supportive presence, respect for the child’s autonomy, effective structure and limit setting, quality of instructions, non-hostility | ‘Quality of parental skills in their interaction with their child’ |
| Parent–child free playa | Freeman 2013443 | – | Play acts, play schemes |
| Parent–child interactiona | Green 2010253 | Parent synchrony, child initiations, mutual shared attention | Parent–child interaction during naturalistic play |
| Parent–Child Interaction measurea | Aldred 2012319 | – | Parent–child interaction |
| Preschool teacher–child playa | Kaale 2012294 | – | Joint attention and joint engagement |
| Social Interaction Rating Scalea | Ruble 2008424 | Contingency, directiveness, initiation towards the child, movement with the child, affect, maintenance of interaction with the child | ‘Parent interaction’ |
| Parent stress | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Autism Parenting Stress Index (PSI) (APSI) | Silva 2011301 | – | ‘Parent stress’ |
| Beck Anxiety Inventory | Davis 2008455 | – | Anxiety in parents |
| Center for Epidemiologic Studies Depression Inventory | Davis 2008455 | – | – |
| Taylor 2012436 | – | ‘Caregiver depressive symptoms’ | |
| General Health Questionnaire (GHQ) | Herring 2006411 | – | Parental mental health |
| McConkey 2010349 | Somatic, anxiety | Parents’ psychiatric morbidity | |
| Tonge 2005456 | Somatic symptoms, anxiety and insomnia, social dysfunction, severe depression | ‘Parental mental health’ | |
| Hospital Anxiety and Depression Scale (HADS) | Remington 2007358 | Depression, anxiety | ‘Parental mental health’ |
| Parenting Stress Index-Short Form (PSI-SF) | Strauss 2012329 | Parent distress, dysfunctional parent–child interaction, child difficulty | ‘Parental stress’ |
| Parenting Sense of Competence (PSOC) | Keen 2007364 | – | Parental satisfaction and efficacy |
| Keen 2010363 | – | Parental satisfaction and efficacy | |
| Parenting Stress Index (PSI) | Aldred 2004318 | Parent distress, dysfunctional parent–child interaction, child difficulty | ‘(Parent) total stress’ |
| Baker-Ericzen 2005457 | Child domain, parent domain | Parent stress | |
| Keen 2010363 | – | Stress resulting from parental perceptions of the child’s contribution to the parent–child relationship (child stress), the impact of the parental role on the parent with respect to psychological well-being, health, marital and other relationships (parental stress) | |
| Roberts 2011405 | – | ‘Stress’ | |
| Salt 2002372 | Parent distress, dysfunctional parent–child interaction, child difficulty | ‘Total stress’ | |
| Parenting Stress Index-Short Form (PSI-SF) | Bendixen 2011458 | – | Parent stress |
| Davis 2008455 | – | Parent stress | |
| Hill-Chapman 2013434 | – | Levels of stress in parent–child relationship | |
| Minjarez 2013459 | Parent distress, dysfunctional parent–child interaction, child difficulty | Parent stress | |
| Wang 2013460 | Parent distress, dysfunctional parent–child interaction, child difficulty | Parenting stress | |
| Wong 2010333 | Parent distress, dysfunctional parent–child interaction, child difficulty | ‘Parent stress’ | |
| Positive and Negative Affect Scale (PANAS) | Hsieh 2013452 | Positive affect, negative affect | – |
| Questionnaire on Resources and Stress-Friedrich Short Form (QRS-F) | Cassidy 2008348 | Parent and family problems, pessimism | ‘Parent stress’ |
| McConkey 2010349 | – | Impact of a developmentally delayed or ‘mentally retarded child’ on the family | |
| Osborne 2008350 | Parent and family problems, pessimism, child characteristics, physical incapacity | ‘Parent stress’ | |
| Osborne 2009351 | Parent and family problems, pessimism, child characteristics, physical incapacity | ‘Parenting stress’ | |
| Remington 2007358 | Parent and family problems subscale | ‘Parental stress’ | |
| Rickards 2009423 | – | ‘Adaptation and coping in families caring for a child with a disability’ | |
| Questionnaire on Resources and Stress-Friedrich Short Form (QRS-F) | Reed 2013437 | Parent and family problems, pessimism, child characteristics, physical incapacity | Parental perceptions of the impact of a developmentally delayed, or chronically ill, child on other family members |
| Reaction to Diagnosis Interview | Oppenheim 2012461 | – | – |
| Wachtel 2008462 | – | ‘Reactions, beliefs, and memories of the diagnostic experience’ | |
| Satisfaction with Life Scale | Hsieh 2013452 | – | Subjective well-being |
| Stress Arousal Checklist | Jocelyn 1998298 | – | Stress, arousal |
| Symptom Checklist-90-Revised (SCL-90) | Bennett 2012304 | Depression, interpersonal sensitivity, somatisation | Maternal depression |
| Daily occupational experiencea | Hsieh 2013452 | Productive, restoration, pleasure | Productive, restoration and pleasure experiences in daily occupations |
| Parent–child Interaction Rating Scalesa | Wachtel 2008462 | – | ‘Parent–child interaction’ |
| Parenting stress thermometera | Tonge 2005456 | – | ‘General level of stress’ |
| Self-constructed questionnairea | Farmer 2013463 | – | Parent knowledge of autism, parents understanding of autism, parents confidence in managing autistic child |
| Stress thermometera | Herring 2006411 | – | Parenting stress |
| Family quality of life | Paper | Subscales used | Outcome(s) measured according to the author |
|---|---|---|---|
| Beach Family Quality of Life Questionnaire | Roberts 2011405 | – | ‘Quality of life’ |
| Family Adaptability and Cohesion Evaluation Scales | Bendixen 2011458 | Cohesion, adaptability | Family cohesion, family adaptability, perceived and ideal family functioning |
| Family Assessment Device | Herring 2006411 | – | Family functioning |
| Tonge 2005456 | – | ‘General family function’ | |
| Family Assessment Measure (Skinner et al. 1983) | Jocelyn 1998298 | – | Task accomplishment, role performance, communication, affective expression, affective involvement, control |
| Family Empowerment Scale | Minjarez 2013459 | Family empowerment, service empowerment, community/political empowerment | Level of empowerment and the way in which it is expressed |
| Rickards 2009423 | – | ‘Family, service and community level empowerment’ | |
| Family Support Scale | Rickards 2009423 | – | ‘Social support’ |
| Kansas Inventory of Parental Perceptions | Remington 2007358 | Positive contributions subscale | ‘Parent perceptions’ |
| Parenting Alliance Inventory | Hill-Chapman 2013434 | – | Self-focused parenting alliance, child-focused parenting alliance |
| Familial Resources Indexa | Baghdadli 2012339 | – | Family functioning and coping behaviours |
| TRE-ADD Autism Quiz (TAQ)a | Jocelyn 1998298 | – | Knowledge about autism |
| Family Satisfaction Questionnairea | Smith 2000413 | – | ‘Parent evaluation’ |
Appendix 6 Additional information on Chapter 4 search methodology
COnsensus-based Standards for the selection of health status Measurement INstruments translation (for Ovid)
instrumentation.sh. OR methods.sh. OR Validation Studies.pt. OR Comparative Study.pt. OR psychometrics/ OR psychometr*.ab,ti. OR clinimetr*.tw. OR clinometr*.tw. OR ‘Outcome Assessment (Health Care)’/ OR outcome assessment.ab,ti. OR outcome measure*.tw. OR observer variation/ OR observer variation.ab,ti. OR Health Status Indicators/ OR reproducibility of results/ OR reproducib*.ab,ti. OR discriminant analysis/ OR reliab*.ab,ti. OR unreliab*.ab,ti. OR valid*.ab,ti. OR coefficient.ab,ti. OR homogeneity.ab,ti. OR homogeneous.ab,ti. OR internal consistency.ab,ti. OR (cronbach*.ab,ti. AND (alpha.ab,ti. OR alphas.ab,ti.)) OR (item.ab,ti. AND (correlation*.ab,ti. OR selection*.ab,ti. OR reduction*.ab,ti.)) OR agreement.ab,ti. OR precision.ab,ti. OR imprecision.ab,ti. OR precise values.ab,ti. OR test-retest.ab,ti. OR (test.ab,ti. AND retest.ab,ti.) OR (reliab*.ab,ti. AND (test.ab,ti. OR retest.ab,ti.)) OR stability.ab,ti. OR interrater.ab,ti. OR inter-rater.ab,ti. OR intrarater.ab,ti. OR intra-rater.ab,ti. OR intertester.ab,ti. OR inter-tester.ab,ti. OR intratester.ab,ti. OR intra-tester.ab,ti. OR interobserver.ab,ti. OR inter-observer.ab,ti. OR intraobserver.ab,ti. OR intraobserver.ab,ti. OR intertechnician.ab,ti. OR inter-technician.ab,ti. OR intratechnician.ab,ti. OR intra-technician.ab,ti. OR interexaminer.ab,ti. OR inter-examiner.ab,ti. OR intraexaminer.ab,ti. OR intra-examiner.ab,ti. OR interassay.ab,ti. OR inter-assay.ab,ti. OR intraassay.ab,ti. OR intra-assay.ab,ti. OR interindividual.ab,ti. OR inter-individual.ab,ti. OR intraindividual.ab,ti. OR intra-individual.ab,ti. OR interparticipant.ab,ti. OR inter-articipant.ab,ti. OR intraparticipant.ab,ti. OR intra-participant.ab,ti. OR kappa.ab,ti. OR kappa’s.ab,ti. OR kappas.ab,ti. OR repeatab*.ab,ti. OR ((replicab*.ab,ti. OR repeated.ab,ti.) AND (measure.ab,ti. OR measures.ab,ti. OR findings.ab,ti. OR result.ab,ti. OR results.ab,ti. OR test.ab,ti. OR tests.ab,ti.)) OR generaliza*.ab,ti. OR generalisa*.ab,ti. OR concordance.ab,ti. OR (intraclass.ab,ti. AND correlation*.ab,ti.) OR discriminative.ab,ti. OR known group.ab,ti. OR factor analysis.ab,ti. OR factor analyses.ab,ti. OR dimension*.ab,ti. OR subscale*.ab,ti. OR (multitrait.ab,ti. AND scaling.ab,ti. AND (analysis.ab,ti. OR analyses.ab,ti.)) OR item discriminant.ab,ti. OR interscale correlation*.ab,ti. OR error.ab,ti. OR errors.ab,ti. OR individual variability.ab,ti. OR (variability.ab,ti. AND (analysis.ab,ti. OR values.ab,ti.)) OR (uncertainty.ab,ti. AND (measurement.ab,ti. OR measuring.ab,ti.)) OR standard error of measurement.ab,ti. OR sensitiv*.ab,ti. OR responsive*.ab,ti. OR ((minimal.ab,ti. OR minimally.ab,ti. OR clinical.ab,ti. OR clinically.ab,ti.) AND (important.ab,ti. OR significant.ab,ti. OR detectable.ab,ti.) AND (change.ab,ti. OR difference.ab,ti.)) OR (small*.ab,ti. AND (real.ab,ti. OR detectable.ab,ti.) AND (change.ab,ti. OR difference.ab,ti.)) OR meaningful change.ab,ti. OR ceiling effect.ab,ti. OR floor effect.ab,ti. OR Item response model.ab,ti. OR IRT.ab,ti. OR Rasch.ab,ti. OR Differential item functioning.ab,ti. OR DIF.ab,ti. OR computer adaptive testing.ab,ti. OR item bank.ab,ti. OR cross-cultural equivalence.ab,ti.
Search terms
Autism terms
Asd (not atrial septal defect)
Asperg*
Autis*
childhood schizophrenia
Kanner*
(PDD or PDD-NOS)
semantic-pragmatic disorder
pervasive developmental disorder?
exp Child Development Disorders, Pervasive/
Age group
Child*
infan*
kindergarten*
p?ediatric*
nursery
toddler*
(pre-school* or preschool*)
special needs
((primary or elementary or grammar) and school)
Measurement tool strategies
Sensory processing tools
(Infant Toddler Sensory Profile or Infant?Toddler Sensory Profile).ti,ab.
(Pervasive Developmental Disorders Behavio?r Inventory or pddbi or pdd Behavio?r Inventory).ti,ab.
(Sense and Self-Regulation Checklist).ti,ab.
((Sensory Profile or Short Sensory Profile or SSP) adj5 dunn).ti,ab.
or/1-4
Attention
(Achenbach Child Behavio?r Checklist or (Achenbach adj2 CBCL)).ti,ab.
Child Behavio?r Scale.ti,ab.
(Conner* Rating Scales adj2 revised).ti,ab.
Achenbach Child Behavio?r Check?list.ti,ab.
or/1-4
Emotional regulation tools
Conner* Parent Rating Scale.ti,ab.
(CPRS-R or (cprs* adj5 (autis* or asperger*))).ti,ab.
(DBC-P adj5 (autis* or asperger*)).ti,ab.
Developmental Behavio?r Checklist Primary Carer Version.ti,ab.
(Infant Toddler Social adj2 Emotional Assessment).ti,ab.
bitsea.ti,ab.
Toddler Behavio?r Assessment Questionnaire.ti,ab.
TBAQ.ti,ab.
or/1-8
Physical skills
Peg Moving Task.ab,ti.
annett? peg?.ti,ab.
(Assessment, Evaluation adj3 Programming System).ti,ab.
aeps test.ti,ab.
(Assessment, Evaluation adj3 Program?ing System).ti,ab.
Beery Visual-Motor Integration Test.ti,ab.
beery vmi.ti,ab.
(vmi adj3 test).ti,ab.
(Infant Motor Maturity adj3 Atypicality Coding Scales).ti,ab.
IMMACS.ti,ab.
Infant Motor Maturity.ti,ab.
Atypicality Coding Scales.ti,ab.
Mullen Scales of Early Learning.ti,ab.
msel.ti,ab.
Peabody Developmental Motor Scales.ti,ab.
pdms-2.ti,ab.
Psycho-educational Profile.ti,ab.
Psycho-educational Profile-revised.ti,ab.
(pep-r adj10 (autis* or asperg*)).ti,ab.
(Ages adj3 Stages Questionnaire).ti,ab.
ASQs.ti,ab.
Vineland Adaptive Behavio?r Scales.ti,ab.
vineland-ii.ti,ab.
VABS-II.ti,ab.
VABS2.ti,ab.
or/1-25
Play
Structured Play Assessment.ti,ab.
Symbolic Play Test.ti,ab.
Test of Pretend Play.ti,ab.
or/1-3
Social communications
Autism Screening Instrument for Educational Planning.ti,ab.
(ASIEP-2 or ASIEP-3).ti,ab.
ASIEP?.ti,ab.
Early Social Communication Scales-Abridged.ti,ab.
Early Social Communication Scales Abridged.ti,ab.
Ritvo-Freeman Real Life Rating Scale.ti,ab.
(RLRS adj10 freeman).ti,ab.
Real Life Rating Scale.ti,ab.
Social Communication Behavio?r Codes.ti,ab.
Social Communication Behavior Codes.ti,ab.
or/1-10
Social functioning
ABLLS-R.ti,ab,tm.
(Assessment of basic Language adj2 Learning Skills).ti,ab,tm.
Pervasive Developmental Disorder? Behavio?r* Inventory.ti,ab,tm.
pdd behavio?r* inventory.ti,ab,tm.
Social Behavio?r* Rating Scale?.ti,ab,tm.
(ssrs adj10 (autis* or asperg*)).ti,ab.
Student Learning Profile.ti,ab,tm.
(vineland Adaptive Behavio?r* Scale? adj5 interview).ti,ab,tm.
(vineland Adaptive Behavio?r Scales adj5 (interview edition or survey form)).ti,ab,tm.
1or/1-9
Play
Structured Play Assessment.ti,ab,tm.
Symbolic Play Test?.ti,ab,tm.
Test? of Pretend Play.ti,ab,tm.
or/1-3
Behaviour
Behavio?r* Screening Questionnaire.ti,ab,tm.
(bsq adj10 (autis* or asperg* or screen*)).ti,ab.
bsq.tm.
Functional Behavio?r* Assessment Interview*.ti,ab,tm.
(Pre?school Behavio?r* Checklist* or Pre?school Behavio?r* Check list*).ti,ab,tm.
(pbcl adj10 (autis* or asperg* or asd)).ti,ab.
pbcl.tm.
Scale? of independent behavio?r* revised-early development form.ti,ab,tm.
Scale? of independent behavio?r* revised.ti,ab,tm.
SIB-R.ti,ab,tm.
(Scale* of independent behavio?r* adj2 revised).ti,ab,tm.
or/1-11
Habit problems
Brigance Diagnostic Inventory of Early Development.ti,ab.
Brigance Diagnostic Inventory of Early Development*.ti,ab,tm.
brigance diagnostic.ti,ab,tm.
or/1-3
Learning
Extended Basic Academic Skill? Assessment System.ti,ab,tm.
basic academic skill? assessment system.ti,ab,tm.
Wechsler Individuali* Achievement Test?.ti,ab,tm.
WIAT-II.ti,ab,tm.
or/1-4
Daily living skills
Functional Emotional Assessment Scale?.ti,ab,tm.
Functional Emotional Assessment Score?.ti,ab,tm.
Functional Independence Measure for children.ti,ab,tm.
Peabody Picture Vocabulary Test?.ti,ab,tm.
(FEAS or FIMC).tm. or PPVT*.ti,ab,tm.
or/1-4
Global measure of function
Autis* treatment Evaluation Checklist.ti,ab,tm.
Autis* treatment Evaluation Check list.ti,ab,tm.
ATEC.tm. or (atec adj10 (autis* or asperg* or asd)).ti,ab.
Clinical Global Impression Improvement scale?.ti,ab,tm.
nical Global Impression Improvement score?
CGI-I.tm. or (cgi-i adj10 (autis* or asperg* or asd)).ti,ab.
Functional Emotional Development* Questionnaire.ti,ab,tm.
fedq.tm. or (fedq adj10 (autis* or asperg* or asd)).ti,ab.
or/1-7
Parent stress
‘Autism Parent* Stress Index’.ab,ti,tm.
apsi.tm.
(apsi adj10 (autis* or asperg* or asd)).ti,ab,tm.
General Health Questionnaire.ti,ab,tm.
ghq.tm. or (ghq adj10 (autis* or asperg* or asd)).ti,ab.
Parent* Stress Index.ti,ab,tm.
(Hospital Anxiety adj2 Depression Scale?).ti,ab,tm.
(Hospital Anxiety adj2 Depression Score?).ti,ab,tm.
HADS.tm. or (hads adj10 (autis* or asperg* or asd)).ti,ab.
(Questionnaire on Resources adj2 Stress).ti,ab,tm.
QRS-F.tm,ti,ab.
Symptom Checklist-90-Revised.ti,ab,tm.
Symptom Check list-90-Revised.ti,ab,tm.
SCL-90-R.ti,ab,tm.
beck anxiety inventory.ti,ab,tm.
bai.tm. or (bai adj10 (autis* or asperg* or asd)).ti,ab.
beck anxiety scale?.ti,ab,tm.
ck anxiety score?.ti,ab,tm.
Cent* for Epidemiologic Studies Depression Inventory.ti,ab,tm.
CES-D.tm. or (ces-d adj10 (autis* or asperg* or asd)).ti,ab.
Cent* for Epidemiologic Studies Depression scale?.ti,ab,tm.
Cent* for Epidemiologic Studies Depression score?.ti,ab,tm.
or/1-19
Family quality of life
(Family Adaptability adj2 Cohesion Evaluation Scale? ii).ti,ab,tm.
faces.tm. or (faces adj10 (autis* or asperg* or asd)).ti,ab.
facesii.tm. or (facesii adj10 (autis* or asperg* or asd)).ti,ab.
Family Assessment Device General Functioning Scale?.ti,ab,tm.
fad.tm. or (fad adj10 (autis* or asperg* or asd)).ti,ab.
Family Empowerment Scale?.ti,ab,tm.
Kansas Inventory of Parent* Perception?.ti,ab,tm.
McMaster Family Assessment Device?.ti,ab,tm.
Beach Family Quality of Life Questionnaire.ti,ab,tm.
Beach Centre Family Quality of Life Scale?.ti,ab,tm.
Beach Cent* Family Quality of Life Scale?.ti,ab,tm.
kipp.tm. or (kipp adj10 (autis* or asperg* or asd)).ti,ab.
fes.tm. or (fes adj10 (autis* or asperg* or asd)).ti,ab.
or/1-13
Language
Battelle Development* Inventory.ti,ab,tm.
bdi-2.ti,ab,tm.
British Picture Vocabulary Scale?.ti,ab,tm.
British Picture Vocabulary Score?.ti,ab,tm.
bpvs*.ti,ab,tm.
Expressive One-Word Picture Vocabulary Test?.ti,ab,tm.
eowpvt*.ti,ab,tm.
MacArthur Communicati* Development* Inventory.ti,ab,tm.
MacArthur Communicati* Development* scale?.ti,ab,tm.
MacArthur Communicati* Development* score?.ti,ab,tm.
Macarthur CDI.ti,ab,tm.
(cdi adj10 (autis* or asperg* or asd)).ti,ab.
McCarthy Scale? of Children* Abilit*.ti,ab,tm.
McCarthy Score? of Children* Abilit*.ti,ab,tm.
msca.tm. or (msca adj10 (autis* or asperg* or asd)).ti,ab.
Merrill-Palmer-Revised.ti,ab,tm.
m-p-r.tm. or (m-p-r adj10 (autis* or asperg* or asd)).ti,ab.
Pre?school Language Scale?.ti,ab,tm.
Pre?school Language Score?.ti,ab,tm.
Reynell Developmental Language Scale?.ti,ab,tm.
Reynell Developmental Language Score?.ti,ab,tm.
(NRDLS or RDLS).tm. or ((nrdls or rdls) adj10 (austis* or asperg* or asd)).ti,ab.
Sequenced Inventory of Communication Revised.ti,ab,tm.
Sequenced Inventory of Communication.ti,ab,tm.
sicd-r.ti,ab,tm.
Test? for Auditory Comprehension of Language.ti,ab,tm.
tacl*.tm. or (tacl* adj10 (autis* or asperg* or asd)).ti,ab.
Test? of Language Development.ti,ab,tm.
TOLD.tm. or (told adj10 (autis* or asperg* or asd)).ti,ab.
Pragmatic? Profile?.ti,ab,tm.
or/1-30
Cognitive abilities
Arthur* Adaptation of the Leiter* international Performance scale?.ti,ab,tm.
AALIPS.ti,ab,tm.
Arthur* Adaptation of the Leiter* international Performance score?.ti,ab,tm.
Bayley Scale? of Infant Development.ti,ab,tm.
BSID*.tm. or (bsid* adj10 (autis* or asperg* or asd)).ti,ab.
British Abilit* Scale?.ti,ab,tm.
British Abilit* Score?.ti,ab,tm.
Cattell Infant Intelligence.ti,ab,tm.
CIIS.tm. or (ciis adj10 (autis* or asperg* or asd)).ti,ab.
Development* Profile?.ti,ab,tm.
(Development* Profile? adj10 ahern).ti,ab,tm.
Griffith? Mental Development* Scale?.ti,ab,tm.
Griffith? Mental Development* Score?.ti,ab,tm.
GMDS*.tm. or (gmds* adj10 (autis* or asperg* or asd)).ti,ab.
Cattell? Infant Intelligence.ti,ab,tm.
Bayley? Scale? of Infant Development.ti,ab,tm.
(Leiter? International Performance Scale? Revised Visuali?ation adj2 reasoning Battery).ti,ab,tm.
Arthur? Adaptation of the Leiter? international Performance scale?.ti,ab,tm.
LEITER-R.ti,ab,tm.
Merrill Palmer Scale? of Mental Test?.ti,ab,tm.
Merrill Palmer Scale? of Mental score?.ti,ab,tm.
Merrill Palmer Scale? of Mental scale?.ti,ab,tm.
Snijder? Oomen? Non?verbal Intelligence Test?.ti,ab,tm.
SON-test?.ti,ab,tm.
son-r.ti,ab,tm.
Stanford Binet? Intelligence Scale?.ti,ab,tm.
Stanford Binet? Intelligence Score?.ti,ab,tm.
sb5.tm. or (sb5 adj10 (autis* or asperg* or asd)).ti,ab.
Wechsler? Intelligence Scale? for Children Revised.ti,ab,tm.
(Wechsler? Pre?school adj2 Primary Scale? of Intelligence Revised).ti,ab,tm.
Wechsler? Intelligence Score? for Children Revised.ti,ab,tm.
(Wechsler? Pre?school adj2 Primary Score? of Intelligence Revised).ti,ab,tm.
WPPSI.ti,ab,tm.
or/1-33
Iterative search: August 2013
((Behavio?r* Assessment System? adj2 Children) or BASC or BASC-2 or BASC2).ti,ab,tm.
(Home Situation? Questionnaire or HSQ).ti,ab,tm.
(Target adj1 (Problem* or Symptom* or Behavio?r*)).ti,ab,tm.
Behavio?r* Rating? Inventor* of Executive Function* Pre?school.ti,ab,tm.
BRIEF-P.ti,ab,tm.
(Children* Global Assessment* adj1 (Scale* or score*)).ti,ab,tm.
cgas.ti,ab,tm.
Emotion* Regulation Check?list*.ti,ab,tm.
ERC.ti,ab,tm.
Or/1-9
Parent* Alliance Inventor*.ti,ab,tm.
(PAI adj10 (autis* or asperg* or asd)).ti,ab,tm.
famil* assessment* measur*.ti,ab,tm.
(FAM adj10 (autis* or asperg* or asd)).ti,ab,tm.
(Famil* Support Scale* or Famil* Support score*).ti,ab,tm.
((P?ediatric Daily Occupation* Scale*) or (P?ediatric Daily Occupation* score*)).ti,ab,tm.
Pdos adj10 (autis* or asperg* or asd).ti,ab,tm.
(Pre?school Development* Profile* or (PSDP adj10 (autis* or asperg* or asd)).ti,ab,tm.
(Early Intervention* Development* Profile* or EIDP).ti,ab,tm.
((Early Learning Accomplishment* Profile*) or ((E-LAP or ELAP) adj10 (autis* or asperg* or asd))).ti,ab,tm.
(Learning Accomplishment* Profile?-Diagnostic* or Learning Accomplishment* Profile? Diagnostic* or ((LAP-D or LAPD) adj10 (autis* or asperg* or asd))) .ti,ab,tm.
Or/11-21
Clinical Evaluation of Language* Fundamental?-Revised.ti,ab,tm.
CELF-R.ti,ab,tm.
Comprehensive Assessment? of Spoken Language?.ti,ab,tm.
casl.ti,ab,tm.
Illinois test? of psycholinguistic abilit*.ti,ab,tm.
ITPA.ti,ab,tm.
((Positive adj1 Negative Affect? Scale?) or (Positive adj1 Negative Affect Score?)).ti,ab,tm.
((Positive-Negative Affect? Scale?) or (Positive-Negative Affect? Score?)).ti,ab,tm.
PANAS.ti,ab,tm.
(Satisfaction with Life Scale? or Satisfaction with Life Score?).ti,ab,tm.
Reaction? to Diagnosis Interview?.ti,ab,tm.
(rdi adj10 (autis* or asperg* or asd)).ti,ab,tm.
Brunet Lezine* oculomotor coordination subtest.ti,ab,tm.
(Brunet Lezine* Test* or Brunet-Lezine* Test*).ti,ab,tm.
oculomotor coordination subtest.ti,ab,tm.
Development* Play Assessment?.ti,ab,tm.
((Pre?school Imitation adj1 Praxis Scale?) or (Pre?school Imitation adj1 Praxis Score?)).ti,ab,tm.
(School Liking adj1 Avoidance Questionnaire).ti,ab,tm.
(Teacher? Rating Scale? of School Adjustment? or Teacher? Rating Score? of School Adjustment?).ti,ab,tm.
TRSSA.ti,ab,tm.
(stress-arousal adj1 (checklist or check-list or check list)).ti,ab,tm.
(stress?arousal adj1 (checklist or check-list or check list)).ti,ab,tm.
(stress arousal adj1 (checklist or check-list or check list)).ti,ab,tm.
(Goal attainment scal* or Goal attainment scor*).ti,ab,tm.
(GAS adj10 (autis* or asperg* or asd)).ti,ab,tm.
Parent* Interview* for Autism clinical version.ti,ab,tm.
pia-cv.ti,ab,tm.
Early Years Foundation Stage Profile?.ti,ab,tm.
EYFSP.ti,ab,tm.
Social Cognitive Evaluation Battery.ti,ab,tm.
Sceb.ti,ab,tm.
(Pervasive Development* Disorder? Behavio?r Inventory or pddbi or pdd Behavio?r Inventory).ti,ab,tm.
Clinical Global Impression? Improvement?.ti,ab,tm.
Clinical Global Impression-Improvement.ti,ab,tm.
Cgi-i.ti,ab,tm.
(Autis* treatment Evaluation adj1 (Checklist or check-list or check list)).ti,ab,tm.
Atec.ti,ab,tm.
Or/46-60
10 or 22 or 60
Iterative search: September 2013
Child Behavio?r Questionnaire.ti,ab.
Child Behavio?r Questionnaire.ti,ab,tm.
Child* Behavio?r* Questionnaire short form.ti,ab,tm.
Child* Behavio?r* Questionnaire-Short Form.ti,ab,tm.
(cbqsf or cbq-sf).ti,ab,tm.
cbq.ti,ab,tm.
Maternal Behavio?r* Rat* Scale*.ti,ab,tm.
Maternal Behavio?r* Rat* Score*.ti,ab,tm.
Child* Behavio?r* Rat* Scale*.ti,ab,tm.
Child* Behavio?r* Rat* Score*.ti,ab,tm.
Mbrs or cbrs.ti,ab,tm.
Appendix 7 COSMIN checklist with four-point scale
Appendix 8 Tables of papers and data extracted (see Chapter 4)
| Symptom severity (change in diagnostic category, autism severity, diagnostic scores used as measures of outcome) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Stability | Stability | Change | ||||||
| Autism Behavior Checklist | Miranda-Linne 200262 | Good+ | Fair+ | ||||||||
| Sponheim 199660 | Poor? | ||||||||||
| Sturmey 199261 | Poor? | ||||||||||
| Autism Diagnostic Interview-Revised | Chawarska 200770 | Fair+ | |||||||||
| De Bildt 2013139 | Fair+ | ||||||||||
| Frazier 200867 | Fair+ | Good– | |||||||||
| Kamp-Becker 200972 | Poor– | ||||||||||
| Lecavalier 2006146 | Good+ | Good– | Good– | ||||||||
| Lord 199463 | Poor+ | Poor+ | Excellent+ | Good+ | |||||||
| Lord 200665 | Fair+ | Fair+ | |||||||||
| Moss 200871 | Poor+ | Fair+ | |||||||||
| Snow 200968 | Fair+ | Fair+ | |||||||||
| Tadevosyan-Leyfer 200366 | Good? | Poor? | Good– | ||||||||
| Tsuchiya 201369 | Good+ | Good+ | |||||||||
| Ward-King 2010140 | Poor+ | ||||||||||
| Autism Diagnostic Observation Schedule-Calibrated Severity Score | De Bildt 201178 | Fair+ | |||||||||
| Gotham 200977 | Good+ | ||||||||||
| Shumway 201279 | Good+ | Fair+ | |||||||||
| Autism Diagnostic Observation Schedule-Generic | Chawarska 200770 | Fair+/– | Fair+ | ||||||||
| Ben Itzchak 200975 | Poor+ | ||||||||||
| Grey 200874 | Good+ | ||||||||||
| Kamp-Becker 200972 | Poor+ | Good+ | |||||||||
| Lord 2000 (module 1)50 | Poor+ | Poor+ | Poor+ | ||||||||
| Lord 2000 (module 2)50 | Poor+ | Poor+ | Poor+ | ||||||||
| Lord 200050 | Poor+ | Poor+ | Poor+ | ||||||||
| Lord 200665 | Fair+ | Fair+ | |||||||||
| Norris 2012 (module 1)73 | Excellent+ | ||||||||||
| Norris 2012 (module 3)73 | Excellent– | ||||||||||
| Autism Diagnostic Observation Schedule-Toddler Module | Luyster 200976 | Fair+/– | Fair+/– | Poor+ | Fair+ | ||||||
| Autism Observation Scale for Infants | Bryson 200881 | Poor? | Poor+ | ||||||||
| Georgiades 201382 | Good+ | ||||||||||
| Baby and Infant Screen for Children with aUtIsm Traits-Part 1 (BISCUIT-Part 1) | Matson 200983 | Poor+ | |||||||||
| Matson 201084 | Good+ | Good– | Good+ | ||||||||
| Matson 201185 | Good+ | ||||||||||
| Behavioral Summarized Evaluation | Barthelemy 199086 | Fair+ | Excellent+ | Poor+ | |||||||
| Oneal 200688 | Poor+ | Poor– | Fair+ | ||||||||
| Behavioral Summarized Evaluation Scale-Revised | Barthelemy 199787 | Poor+ | Fair+ | Fair+ | Poor? | ||||||
| Roux 199589 | Excellent+ | ||||||||||
| Childhood Autism Rating Scale | Darrou 201095 | Good+ | |||||||||
| Magyar 200794 | Excellent+ | Excellent– | |||||||||
| Nordin 1998465 | Poor+ | Good– | |||||||||
| Russell 201093 | Excellent+ | Excellent+ | Excellent+ | ||||||||
| Schopler 1980244 | Poor+ | Good– | |||||||||
| Sevin 1991109 | Poor– | ||||||||||
| Sponheim 199660 | Poor? | ||||||||||
| Stella 199996 | Good+ | Good– | |||||||||
| Sturmey 199261 | Poor+ | ||||||||||
| Tachimori 2003466 | Poor+ | ||||||||||
| Gilliam Autism Rating Scale | Lecavalier 200598 | Good+ | Good– | Good– | |||||||
| South 200297 | Fair– | ||||||||||
| Gilliam Autism Rating Scale-Second Edition | Pandolfi 201099 | Good+ | Fair– | ||||||||
| Infant Behavioral Summarized Evaluation | Adrien 199290 | Fair+ | Poor+ | ||||||||
| Modified Checklist for Autism in Toddlers | Inada 2011103 | Poor+ | Poor– | ||||||||
| Robins 2001101 | Poor+ | ||||||||||
| Snow 2008102 | Poor+ | Fair+ | |||||||||
| Parent Observation of Early Markers Scale | Feldman 2012104 | Good+ | Poor+ | Good– | |||||||
| Pervasive Developmental Disorders Behavior Inventory | Cohen 2003122 | Good+ | Good+/– | Excellent+ | Good+ | ||||||
| Cohen 2003123 | Fair– | ||||||||||
| Pervasive Developmental Disorders Rating Scale | Williams 2002107 | Good+ | Fair+ | ||||||||
| Williams 200542 | Poor+ | Poor+ | |||||||||
| Real Life Rating Scale | Sevin 1991109 | Poor– | |||||||||
| Sturmey 199261 | Poor– | ||||||||||
| Social Communication Questionnaire | Charman 2004112 | Good+ | |||||||||
| Magyar 2012111 | Good+ | Good+ | Good+ | ||||||||
| Snow 2008102 | Poor? | Fair+ | |||||||||
| Social Responsiveness Scale | Pine 2006117 | Fair– | Fair– | Poor– | |||||||
| Bolte 2008115 | Good+ | Fair+ | Fair+ | Good– | Fair+ | Good– | |||||
| Constantino 2004114 | Good– | ||||||||||
| Constantino 2009118 | Fair– | Poor? | |||||||||
| Duku 2013116 | Good+ | Poor– | Excellent– | Good+ | |||||||
| Pre-Verbal Communication Schedule | N/A | ||||||||||
| Social Communication Behaviour Codes | N/A | ||||||||||
| Social awareness (joint attention skills, imitation, social attention) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Communication and Symbolic Behavior Scales-Developmental Profile-Behavior Sample | Wetherby 2004126 | Poor? | |||||||||
| Early Social Communication Scales Live | Luyster 2008129 | Poor? | |||||||||
| Imitation Battery | Luyster 2008129 | Poor? | |||||||||
| Young 2011131 | Good+ | Good+ | |||||||||
| Imitation Disorders Evaluation scale | Malvy 1999132 | Poor? | Poor+ | ||||||||
| Motor Imitation Scale | Ingersoll 2011134 | Poor+ | |||||||||
| Preschool Imitation and Praxis Scale | Vanvuchelen 2011135 | Excellent+ | Excellent+ | Poor+ | |||||||
| Vanvuchelen 2011136 | Fair+ | ||||||||||
| Social Communication Assessment for Toddlers with Autism | Drew 2007137 | Poor+ | Poor+ | Poor+ | Poor+ | ||||||
| Restricted, repetitive behaviour (repetitive, stereotyped movements; repetitive use of objects; attention to detail; insistence on sameness) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Autism Diagnostic Interview-Revised | Bishop 2006143 | Good? | Fair+ | ||||||||
| Cuccaro 2003138 | Excellent– | Excellent+ | Fair+ | ||||||||
| De Bildt 2013139 | Good– | ||||||||||
| Frazier 200867 | Fair+ | Good– | |||||||||
| Grey 200874 | Good+ | ||||||||||
| Kamp-Becker 200972 | Poor– | Fair+ | |||||||||
| Lam 2008142 | Fair+ | Fair+ | |||||||||
| Lecavalier 200664 | Good– | Good– | Good+ | ||||||||
| Lord 199463 | Poor– | Poor+ | Poor+ | Excellent+ | Good+ | ||||||
| Lord 200665 | Fair+ | Fair+ | |||||||||
| Mooney 2009148 | Excellent– | ||||||||||
| Moss 200871 | Poor+ | Fair+ | |||||||||
| Richler 2010144 | Good? | ||||||||||
| Shao 2003145 | Good? | ||||||||||
| Smith 2009141 | Excellent+ | ||||||||||
| Snow 200968 | Excellent– | Excellent+ | Fair+ | ||||||||
| Szatmari 2006147 | Good– | ||||||||||
| Tadevosyan-Leyfer 200366 | Good? | Poor– | Good+ | ||||||||
| Tsuchiya 201369 | Good+ | Good+ | |||||||||
| Ward-King 2010140 | Poor+ | ||||||||||
| Autism Diagnostic Observation Schedule-Generic | Chawarska 200770 | Fair+ | Fair+ | ||||||||
| Grey 2008 (modules 1 and 2)74 | Good+ | ||||||||||
| Ben Itzchak 200975 | Fair+ | ||||||||||
| Kamp-Becker 200972 | Poor? | Good+ | |||||||||
| Lord 2000 (modules 1–3)50 | Poor– | Poor– | Poor+ | ||||||||
| Lord 200665 | Fair– | Fair+ | |||||||||
| Norris 2012 (modules 1 and 3)73 | Excellent+ (modules 1 and 3) | ||||||||||
| Autism Diagnostic Observation Schedule-Toddler Module | Luyster 200976 | Fair– | Fair? | Poor+ | Fair+ | ||||||
| Repetitive Behavior Scale-Revised | Lam 2007151 | Excellent+ | Poor– | Excellent– | Fair+ | ||||||
| Mirenda 2010152 | Excellent+ | Excellent– | Fair+ | ||||||||
| Sensory processing (hypersensitivity or hyposensitivity) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Sense and Self-Regulation Checklist | Silva 2012153 | Poor+ | Fair– | Fair+ | Fair+ | ||||||
| Sensory Profile | Brown 2008155 | Fair+ | |||||||||
| Short Sensory Profile | O’Brien 2009156 | Poor+ | Fair+ | ||||||||
| Wiggins 2009157 | Fair+ | Fair+ | |||||||||
| Infant/Toddler Sensory Profile | N/A | ||||||||||
| Language (expressive language, receptive language, gestures) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Comprehensive Assessment of Spoken Language | Reichow 2008159 | Fair– | |||||||||
| MacArthur–Bates Communicative Development Inventories | Bruckner 2007162 | Excellent+ | Fair+ | ||||||||
| Luyster 2008129 | Fair+ | ||||||||||
| Mullen Scales of Early Learning | Burns 2013164 | Good+ | |||||||||
| Preschool Language Scale-Fourth Edition | Volden 2011166 | Good+ | |||||||||
| Vineland Adaptive Behavior Scales | Harris 1995168 | Poor+ | |||||||||
| Paul 2004169 | Fair+ | ||||||||||
| Vineland Adaptive Behavior Scales-Classroom version | Wells 2009170 | Fair+ | |||||||||
| Vineland Adaptive Behavior Scales-Screener version | Charman 2004112 | Poor+ | |||||||||
| Autism Screening Instrument for Educational Planning (ASIEP and ASIEP-2) | N/A | ||||||||||
| Battelle Developmental Inventory | N/A | ||||||||||
| British Picture Vocabulary Scale | N/A | ||||||||||
| Clinical Evaluation of Language Fundamentals-Revised | N/A | ||||||||||
| Expressive One-Word Picture Vocabulary Test | N/A | ||||||||||
| Illinois Test of Psycholinguistic Abilities | N/A | ||||||||||
| Pragmatics Profile | N/A | ||||||||||
| Reynell Developmental Language Scales | N/A | ||||||||||
| Sequenced Inventory of Communication | N/A | ||||||||||
| Test for Auditory Comprehension of Language | N/A | ||||||||||
| Test of Language Development | N/A | ||||||||||
| Cognitive ability (IQ/developmental quotient, non-verbal ability, verbal ability/reasoning) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Leiter International Performance Scale-Revised | Grondhuis 2013175 | Fair– | Fair– | ||||||||
| Scattone 2012173 | Fair+ | ||||||||||
| Tsatsanis 2003174 | Poor+ | ||||||||||
| Mullen Scales of Early Learning-Early Learning Composite | Georgiades 201382 | Good+ | |||||||||
| Mullen Scales of Early Learning | Bishop 2011176 | Good+ | |||||||||
| Burns 2013164 | Good– | ||||||||||
| Stanford–Binet Intelligence Scales-Fifth Edition | Grondhuis 2013175 | Fair+ | Fair– | ||||||||
| Wechsler Preschool and Primary Scale of Intelligence-Revised | Yang 2011180 | Fair– | |||||||||
| Battelle Developmental Inventory | N/A | ||||||||||
| Bayley Scales of Infant Development | N/A | ||||||||||
| Behaviour Rating Inventory of Executive Function (BRIEF)-Preschool Version | N/A | ||||||||||
| British Ability Scales | N/A | ||||||||||
| Cattell Infant Intelligence | N/A | ||||||||||
| Developmental Profile | N/A | ||||||||||
| Griffiths Mental Developmental Scales | N/A | ||||||||||
| Leiter Performance Scales-Arthur adaptation | N/A | ||||||||||
| McCarthy Scales of Children’s Abilities | N/A | ||||||||||
| Merrill–Palmer Scale of Mental Tests | N/A | ||||||||||
| Snijders Oomen Non-verbal Intelligence Test | N/A | ||||||||||
| Wechsler Intelligence Scale for Children-Revised | N/A | ||||||||||
| Attention (distractibility, impulsivity, hyperactivity) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Behavior Assessment System for Children-Parent Rating Scales, Second Edition | Hass 2010182 | Poor+ | |||||||||
| Mahan 2011183 | Good+ | ||||||||||
| Child Behavior Checklist 1.5–5 | Pandolfi 2009185 | Good– | Good+ | ||||||||
| Child Behavior Checklist 6–18 | Pandolfi 2012186 | Poor+ | |||||||||
| Child Behavior Scale | N/A | ||||||||||
| Conners Rating Scales-Revised | N/A | ||||||||||
| Emotional regulation (irritability, distress, anxiety) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Baby and Infant Screen for Children with aUtIsm Traits-Part 2 | Matson 2009188 | Good+ | Fair+ | Fair+ | Good+ | ||||||
| Matson 200983 | Poor+ | ||||||||||
| Matson 2011187 | Excellent+ | Poor– | Fair+ | ||||||||
| Behavior Assessment System for Children-Second Edition | Hass 2010182 | Fair+ | Fair+ | ||||||||
| Mahan 2011183 | Good– | ||||||||||
| Brief Infant-Toddler Social and Emotional Assessment | Karabekiroglu 2010190 | Poor– | Fair+ | Fair– | Fair+ | Fair+ | |||||
| Briggs-Gowan 2004189 | Poor– | Fair– | Good+ | ||||||||
| Child Behavior Checklist 1.5–5 | Pandolfi 2009185 | Good+ | Good+ | ||||||||
| Child Behavior Checklist 6–18 | Pandolfi 2012186 | Good+ | Good+ | Good+ | |||||||
| Children’s Global Assessment Scale | Lundh 2013193 | Fair+ | |||||||||
| Infant–Toddler Social–Emotional Assessment | Georgiades 201382 | Good+ | |||||||||
| Visser 2010195 | Poor? | Good+ | Good+ | ||||||||
| Conners Rating Scales and Revised | N/A | ||||||||||
| Developmental Behaviour Checklist | N/A | ||||||||||
| Emotion Regulation Checklist | N/A | ||||||||||
| Toddler Behaviour Assessment Questionnaire | N/A | ||||||||||
| Physical skills (poor co-ordination/gross motor skills, fine motor skills) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Mullen Scales of Early Learning | Burns 2013164 | Good+ | |||||||||
| Vineland Adaptive Behavior Scales | Harris 1995168 | Poor+ | |||||||||
| Vineland Adaptive Behavior Scales-Screener | Charman 2004112 | Poor+ | |||||||||
| Beery Visual-Motor Integration Test | N/A | ||||||||||
| Brunet-Lezine’s oculomotor co-ordination subtest | N/A | ||||||||||
| Functional Independence Measure for children (WeeFIM) | N/A | ||||||||||
| Infant Motor Maturity and Atypicality Coding Scales | N/A | ||||||||||
| Peabody Developmental Motor Scales | N/A | ||||||||||
| Social communication (frequency/quality of initiations, pragmatics) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Autism Diagnostic Interview-Revised | Chawarska 200770 | Fair– | |||||||||
| De Bildt 2013139 | Good+ | ||||||||||
| Frazier 200867 | Fair+ | Good– | |||||||||
| Kamp-Becker 200972 | Poor– | ||||||||||
| Lecavalier 200664 | Good+ | Good– | Good– | ||||||||
| Lord 199463 | Poor– | Poor+ | Excellent+ | Good+ | |||||||
| Lord 200665 | Fair+ | Fair+ | |||||||||
| Moss 200871 | Poor+ | Fair+ | |||||||||
| Robertson 1999196 | Poor+ | Poor+ | Good+ | ||||||||
| Snow 200968 | Fair+ | Fair– | |||||||||
| Tadevosyan-Leyfer 200366 | Good+ | Poor– | Good– | ||||||||
| Tanguay 1998197 | Poor+ | ||||||||||
| Tsuchiya 201369 | Good+ | Good+ | |||||||||
| Ward-King 2010140 | Poor+ | ||||||||||
| Autism Diagnostic Observation Schedule-Generic | Chawarska 200770 | Poor+ | Poor– | ||||||||
| Ben Itzchak 200975 | Poor+ | ||||||||||
| Kamp-Becker 200972 | Poor+ | Good+ | |||||||||
| Lord 2000 (module 1)50 | Poor+ | Poor+ | Poor+ | ||||||||
| Lord 2000 (module 2)50 | Poor+ | Poor+ | Poor+ | ||||||||
| Lord 2000 (module 3)50 | Poor+ | Poor– | Poor+ | ||||||||
| Lord 2006 (ADOS)65 | Fair– | Fair+ | |||||||||
| Norris 2012 (module 1)73 | Excellent– | ||||||||||
| Norris 2012 (module 3)73 | Excellent– | ||||||||||
| Autism Diagnostic Observation Schedule-Toddler Module | Luyster 200976 | Fair+ | Fair+ | Poor+ | Fair+ | ||||||
| Early Social Communication Scales Live | Luyster 2008129 | Poor+ | |||||||||
| Social Communication Assessment for Toddlers with Autism | Drew 2007137 | Poor+ | Poor+ | ||||||||
| Vineland Adaptive Behavior Scales | Harris 1995168 | Poor+ | |||||||||
| Paul 2004169 | Fair+ | ||||||||||
| Vineland Adaptive Behavior Scales-Classroom version | Wells 2009170 | Fair– | |||||||||
| Vineland Adaptive Behavior Scales-Screener version | Charman 2004112 | Poor+ | |||||||||
| Autism Screening Instrument for Educational Planning (ASIEP and ASIEP 2) | N/A | ||||||||||
| Child Behavior Scale | N/A | ||||||||||
| Pragmatics Profile | N/A | ||||||||||
| Social Communication Behaviour Codes | N/A | ||||||||||
| Social functioning (attachment, interaction skills with other children, awareness of others’ emotions) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Autism Diagnostic Interview-Revised | Chawarska 200770 | Fair– | |||||||||
| De Bildt 2013139 | Good+ | ||||||||||
| Frazier 200867 | Fair+ | Good– | |||||||||
| Kamp-Becker 200972 | Poor– | ||||||||||
| Lecavalier 200664 | Good+ | Good– | Good– | ||||||||
| Lord 199463 | Poor+ | Poor+ | Excellent+ | Good+ | |||||||
| Lord 200665 | Fair+ | Fair+ | |||||||||
| Moss 200871 | Poor+ | Fair+ | |||||||||
| Snow 200968 | Fair+ | Fair– | |||||||||
| Tadevosyan-Leyfer 200366 | Good+ | Poor– | Good– | ||||||||
| Tsuchiya 201369 | Good+ | Good+ | |||||||||
| Ward-King 2010140 | Poor+ | ||||||||||
| Nisonger Child Behavior Rating Form | Lecavalier 2004199 | Fair+ | Fair+ | ||||||||
| Lecavalier 2006146 | Fair– | Fair– | Fair– | ||||||||
| Vineland Adaptive Behavior Scales | Harris 1995168 | Poor+ | |||||||||
| Paul 2004169 | Fair+ | ||||||||||
| Tyminski 2008200 | Fair– | ||||||||||
| Vineland Adaptive Behavior Scales-Classroom version | Wells 2009170 | Fair+ | |||||||||
| Vineland Adaptive Behavior Scales-Screener version | Charman 2004112 | Poor+ | |||||||||
| Social Behaviour Rating Scale | N/A | ||||||||||
| Play (levels of play: exploratory to symbolic, organises own time/activities) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Test of Pretend Play | Clift 1998203 | Good+ | Good+ | ||||||||
| Developmental Play Assessment | N/A | ||||||||||
| Structured Play Assessment | N/A | ||||||||||
| Symbolic Play Test | N/A | ||||||||||
| Behaviour (maladaptive behaviour, tantrums/meltdowns, aggression, self-injury) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Aberrant Behavior Checklist | Brinkley 2007207 | Excellent+ | |||||||||
| Karabekiroglu 2009205 | Fair+ | Fair+ | Fair+ | ||||||||
| Sigafoos 1997206 | Fair– | Poor+ | |||||||||
| Baby and Infant Screen for Children with aUtIsm Traits-Part 3 (BISCUIT-Part 3) | Matson 200983 | Good+ | |||||||||
| Matson 2009208 | Excellent+ | Excellent– | |||||||||
| Behavior Assessment System for Children-Parent Rating Scales, Second Edition | Hass 2010182 | Fair+ | Fair+ | ||||||||
| Mahan 2011183 | Good– | ||||||||||
| Child Behavior Checklist 1.5–5 | Pandolfi 2009185 | Good+ | Good+ | ||||||||
| Child Behavior Checklist 6–18 | Pandolfi 2012186 | Good+ | Good+ | Good+ | |||||||
| Home Situations Questionnaire-Pervasive Developmental Disorders version | Chowdhury 2010212 | Excellent+ | Excellent+ | Excellent+ | Excellent+ | ||||||
| Arnold 2012210 | Good+ | ||||||||||
| Nisonger Child Behavior Rating Form | Lecavalier 2004199 | Good+ | Good– | ||||||||
| Lecavalier 2006146 | Fair+ | Fair– | Fair+ | ||||||||
| Behavior Screening Questionnaire | N/A | ||||||||||
| Child Behavior Scale | N/A | ||||||||||
| Conners Rating Scales-Revised | N/A | ||||||||||
| Developmental Behaviour Checklist | N/A | ||||||||||
| Parent Target Problems or Parent Target Behaviours | N/A | ||||||||||
| Preschool Behaviour Checklist | N/A | ||||||||||
| Habit problems [sleep latency and waking, (including actigraphy), eating problems, toileting problems] | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Child Behavior Checklist 1.5–5 | Pandolfi 2009185 | Good+ | Good+/– | ||||||||
| Child Behavior Checklist 6–18 | Pandolfi 2012186 | Good+ | Good+ | Good+ | |||||||
| Sense and Self-Regulation Checklist | Silva 2012153 | Good+ | Fair+ | Fair+ | |||||||
| Learning (school readiness, early literacy, early numeracy) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Autism Screening Instrument for Educational Planning (ASIEP and ASIEP 2) | N/A | ||||||||||
| Extended Basic Academic Skills Assessment System | N/A | ||||||||||
| Wechsler Individualised Achievement Test | N/A | ||||||||||
| Daily living skills (feeding self-using cutlery, dressing self) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Vineland Adaptive Behavior Scales | Harris 1995168 | Poor+ | |||||||||
| Paul 2004169 | Fair– | ||||||||||
| Vineland Adaptive Behavior Scales-Classroom version | Wells 2009170 | Fair+ | |||||||||
| Vineland Adaptive Behavior Scales-Screener version | Charman 2004112 | Good+ | |||||||||
| Functional Independence Measure for children | N/A | ||||||||||
| Global measure of function | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Assessment, Evaluation, and Programming System | Wang 2011213 | Poor+ | Poor+ | ||||||||
| Behavior Assessment System for Children-Parent Rating Scales, Second Edition | Hass 2010182 | Poor+ | |||||||||
| Mahan 2011183 | Good+ | ||||||||||
| Psychoeducational Profile-Revised | Alwinesh 2012215 | Poor+ | Good+ | Poor+ | Excellent+ | ||||||
| Heimann 2006219 | Poor+ | Poor+ | |||||||||
| Shek 2005216 | Poor+ | Fair+ | Fair+ | Fair+ | |||||||
| Steerneman 1997217 | Poor+ | Fair+ | Fair+ | ||||||||
| Villa 2010218 | Poor+ | Fair+ | Good+ | ||||||||
| Psychoeducational Profile-Third Edition | Chen 2011222 | Poor– | |||||||||
| Fu 2010221 | Fair+ | Fair+ | |||||||||
| Psychoeducational Profile-Third Edition, Caregiver Report | Fu 2012223 | Poor– | Fair– | Poor– | |||||||
| Scales of Independent Behavior-Revised | Brown 2010225 | Poor– | |||||||||
| Lecavalier 2006146 | Fair+ | Fair+ | |||||||||
| Vineland Adaptive Behavior Scales | Harris 1995168 | Poor? | |||||||||
| Paul 2004169 | Fair+ | ||||||||||
| Tyminski 2008200 | Fair– | ||||||||||
| Vineland Adaptive Behavior Scales-Classroom version | Wells 2009170 | Fair+ | |||||||||
| Vineland Adaptive Behavior Scales-Screener version | Charman 2004112 | Poor+ | |||||||||
| Ages and Stages Questionnaire | N/A | ||||||||||
| Assessment of Basic Language and Learning Skills | N/A | ||||||||||
| Brigance Diagnostic Inventory of Early Development | N/A | ||||||||||
| Developmental Profile | N/A | ||||||||||
| Early Development Interview | N/A | ||||||||||
| Early Intervention Developmental Profile | N/A | ||||||||||
| Early Learning Accomplishment Profile | N/A | ||||||||||
| Functional Emotional Developmental Questionnaire | N/A | ||||||||||
| Learning Accomplishment Profile-Diagnostic, Third Edition | N/A | ||||||||||
| Paediatric Daily Occupation Scale | N/A | ||||||||||
| Preschool Developmental Profile | N/A | ||||||||||
| Global measure of outcome | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Autism Treatment and Evaluation Checklist | Charman 2004112 | Poor– | |||||||||
| Geier 2013121 | Good+ | ||||||||||
| Magiati 2011309 | Poor+ | Poor+ | Poor+ | ||||||||
| Behavioral Summarized Evaluation | Barthelemy 199086 | Fair+ | Excellent– | Poor– | |||||||
| Oneal 200688 | Poor+ | Poor– | Fair+ | ||||||||
| Revised Behavioral Summarized Evaluation Scale | Barthelemy 199787 | Poor+ | Fair– | Fair+ | Poor– | ||||||
| Roux 199589 | Excellent+ | ||||||||||
| PDD Behavior Inventory | Cohen 2003123 | Good+ | Good– | Excellent+ | Good+ | ||||||
| Cohen 2003123 | Fair– | ||||||||||
| Infant Behavioral Summarized Evaluation | Adrien 199290 | Fair+ | Poor+ | ||||||||
| Clinical Global Impression – Improvement Scale | N/A | ||||||||||
| Social inclusion (social participation, social exclusion, difficulty with attending appointments, awareness of danger) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| School Liking and Avoidance Questionnaire | N/A | ||||||||||
| Teacher Rating Scale of School Adjustment | N/A | ||||||||||
| Interaction style (synchrony, shared attention) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Functional Emotional Assessment Scale | N/A | ||||||||||
| NICHD Early Child Care Network scales | N/A | ||||||||||
| Parent stress (parent stress, parent coping style, parent anxiety and depression) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Autism Parenting Stress Index | Silva 2012153 | Excellent+ | Poor+ | Poor? | Good+ | ||||||
| Parenting Stress Index-Short Form | Lecavalier 2006146 | Fair+ | Fair+ | Fair+ | |||||||
| Zaidman-Zait 2010229 | Poor+ | Poor? | |||||||||
| Zaidman-Zait 2011230 | Excellent+ | Excellent+ | Poor– | ||||||||
| Questionnaire on Resources and Stress | Honey 2005232 | Fair+ | Poor? | Fair+ | |||||||
| Beck Anxiety Inventory | N/A | ||||||||||
| Center for Epidemiologic Studies Depression Inventory | N/A | ||||||||||
| General Health Questionnaire | N/A | ||||||||||
| Hospital Anxiety and Depression Scale | N/A | ||||||||||
| Parenting Sense of Competence | N/A | ||||||||||
| Positive and Negative Affect Scale | N/A | ||||||||||
| Reaction to Diagnosis Interview | N/A | ||||||||||
| Satisfaction with Life Scale | N/A | ||||||||||
| Stress Arousal Checklist | N/A | ||||||||||
| Symptom Checklist-90-Revised | N/A | ||||||||||
| Family quality of life (impact on family, family cohesion) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurement tool | Report ID | Internal consistency | Reliability | Content validity | Structural validity | Hypothesis testing | Criterion validity | Responsiveness | |||
| Test–retest | Inter-rater | Convergent/divergent | Known groups | Stability | Change | ||||||
| Beach Family Quality of Life Questionnaire | N/A | ||||||||||
| Family Adaptability and Cohesion Evaluation Scales | N/A | ||||||||||
| Family Assessment Device-General Functioning Scale | N/A | ||||||||||
| Family Assessment Measure | N/A | ||||||||||
| Family Empowerment Scale | N/A | ||||||||||
| Family Support Scale | N/A | ||||||||||
| Kansas Inventory of Parental Perceptions | N/A | ||||||||||
| McMaster Family Assessment Device | N/A | ||||||||||
| Parenting Alliance Inventory | N/A | ||||||||||
Appendix 9 List of new tools encountered
‘New’ tools meet the criteria for stage 3 (i.e. included in a paper about measurement properties with children with ASD) but were not found in stage 2 (i.e. not yet used as outcome measurement tools with ASD children up to 6 years old in observational or intervention evaluation studies).
Name of new tool
Autism Spectrum Disorder Observation for Children (ASD-OC).
Autism Spectrum Disorder-Diagnostic for Children (ASD-DC).
Autism Spectrum Disorders-Comorbidity for Children (ASD-CC).
Behavioral Assessment of Social Interactions in Young Children (BASYC).
Behaviour Function Inventory (BFI).
Bender Visual-Motor Gestalt Test-Second Edition (BG-II).
Brief Autism Mealtime Behavior Inventory (BAMBI).
Caregiver Strain Questionnaire (CGSQ).
Carey Temperament Scales.
Children’s Global Assessment Scale – Developmental Disabilities Modification (DD-CGAS).
Children’s Communication Checklist (CCC).
Children’s Scale of Hostility and Aggression: Reactive/Proactive (C-SHARP).
Children’s Sleep Habits Questionnaire (CSHQ).
Children’s Social Behavior Questionnaire (CSBQ).
Children’s Yale-Brown Obsessive Compulsive Scales (CYBOCS).
Child’s Challenging Behaviour Scale (CCBS).
Classroom Observation Schedule to Measure Intentional Communication (COSMIC).
Developmental, diagnostic and dimensional interview (3Di) – shortened form.
Family Inventory of Sleep Habits.
Happe’s Strange Stories.
Health Utilities Index (HUI) 3.
Manchester Inventory for Playground Observation (MIPO).
Modified Simonds & Parraga Sleep Questionnaire (MSPSQ).
Modified-Classroom Observation Schedule to Measure Intentional Communication (M-COSMIC).
Motivation Assessment Scale (MAS).
Multi-dimensional Scale for Pervasive Developmental Disorder and attention-deficit/hyperactivity disorder (MSPA).
Parent Interview for Autism-Clinical Version (PIA-CV).
Perceptions of Children’s Theory of Mind Measure (Experimental version; PCToMM-E).
Quality of Well-Being Self-Administered (QWB-SA) scale.
Repetitive and Restricted Behaviour Scale (RRB Scale).
Repetitive Behaviour Questionnaire (RBQ).
Responsive Augmentative and Alternative Communication Style (RAACS) scale Version 2.
Sensory Experiences Questionnaire.
Social and Communication Disorders Checklist (SCDC).
Social Cognitive Evaluation Battery (SCEB).
Social Orienting Continuum and Response Scale (SOC-RS).
Social Vulnerability Scale (SVS).
Social-Communication Assessment Tool (S-CAT).
Standardized Observational Analogue Procedure (SOAP).
Test of Pragmatic Language (TOPL).
Theory of Mind Inventory (ToMI).
Theory-of-Mind (ToM) Storybooks.
Wing Subgroups Questionnaire.
Yale–Brown Obsessive–Compulsive Scale (Y-BOCS).
List of abbreviations
- ABC
- Aberrant Behavior Checklist
- ADI-R
- Autism Diagnostic Interview-Revised
- ADOS
- Autism Diagnostic Observation Schedule
- ADOS-G
- Autism Diagnostic Observation Schedule-Generic
- AOSI
- Autism Observation Scale for Infants
- APSI
- Autism Parenting Stress Index
- ASD
- autism spectrum disorder
- ATEC
- Autism Treatment and Evaluation Checklist
- AuBC
- Autism Behavior Checklist
- BASC-2
- Behavior Assessment System for Children-Second Edition
- BISCUIT
- Baby and Infant Screen for Children with aUtIsm Traits
- BITSEA
- Brief Infant – Toddler Social and Emotional Assessment
- BSE
- Behavioral Summarized Evaluation
- BOSCC
- Brief Observation of Social Communication Change
- CARS
- Childhood Autism Rating Scale
- CASL
- Comprehensive Assessment of Spoken Language
- CBCL
- Child Behavior Checklist
- CFI
- comparative fit index
- CGAS
- Children’s Global Assessment Scale
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- COMET
- Core Outcome Measures in Effectiveness Trials
- COSMIN
- COnsensus-based Standards for the selection of health status Measurement INstruments
- CSBS-DP
- Communication and Symbolic Behavior Scales-Developmental Profile
- DSM-5
- Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition
- DSM-IV
- Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition
- EBD
- emotional and behavioural difficulty
- EFA
- exploratory factor analysis
- ERIC
- Education Resources Information Center
- ESCS
- Early Social Communication Scales
- GARS
- Gilliam Autism Rating Scale
- HSQ-PDD
- Home Situations Questionnaire-Pervasive Developmental Disorders version
- HTA
- Health Technology Assessment
- IB
- Imitation Battery
- ICC
- intraclass correlation
- ICD-10
- International Classification of Diseases, 10th Edition
- ICF-CY
- International Classification of Functioning, Disability and Health for Children and Youth
- IQ
- intelligence quotient
- M-CHAT
- Modified Checklist for Autism in Toddlers
- MCDI
- MacArthur–Bates Communicative Development Inventories
- MeASURe
- Measurement in Autism Spectrum disorder Under Review
- MSEL
- Mullen Scales of Early Learning
- NCBRF
- Nisonger Child Behavior Rating Form
- NIHR
- National Institute for Health Research
- OCLC
- Online Computer Library Centre
- PDDBI
- Pervasive Developmental Disorders Behavior Inventory
- PDD-NOS
- pervasive developmental disorder – not otherwise specified
- PDDRS
- Pervasive Developmental Disorders Rating Scale
- PEP-3
- Psychoeducational Profile-Third Edition
- PEP-R
- Psychoeducational Profile-Revised
- PIPS
- Preschool Imitation and Praxis Scale
- PLS-4
- Preschool Language Scale-Fourth Edition
- POEMS
- Parent Observation of Early Markers Scale
- PSI-SF
- Parenting Stress Index-Short Form
- QRS-F
- Questionnaire on Resources and Stress-Friedrich Short Form
- RBS
- Repetitive Behavior Scale
- RLRS
- Real Life Rating Scale
- RRB
- restricted and repetitive behaviour
- RRBI
- restricted and repetitive behaviours and interests
- SB5
- Standard – Binet Intelligence Scales-Fifth Edition
- SCATA
- Social Communication Assessment for Toddlers with Autism
- SCQ
- Social Communication Questionnaire
- SIB-R
- Scales of Independent Behavior-Revised
- SP
- Sensory Profile
- SRS
- Social Responsiveness Scale
- SSC
- Sense and Self-Regulation Checklist
- SSP
- Short Sensory Profile
- ToPP
- Test of Pretend Play
- VABS
- Vineland Adaptive Behavior Scales