Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 12/80/01. The contractual start date was in September 2013. The draft report began editorial review in February 2014 and was accepted for publication in June 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Simmonds et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Obesity
Adiposity, or obesity, is defined as an accumulation of excess body fat to the extent that it may have an adverse effect on health. 1 Adult obesity prevalence in England has increased from approximately 16% in 1995 to approximately 26% in 2010, with the increase seemingly continuing. 1 Obesity in adults has been linked to increased mortality and morbidity. 1 A meta-analysis of 26 cohort studies reported 60,374 deaths, 17,708 deaths from coronary heart disease (CHD) and 27,099 deaths from cardiovascular disease (CVD) among 388,622 adults recruited in the studies. 2 When the normal-weight people were compared with those who were obese [using body mass index (BMI)], the risk of mortality was significantly increased for the obese group. The pooled relative risks (RRs) reported were as follows: for overall mortality, 1.20 [95% confidence interval (CI) 1.12 to 1.29] for men and 1.28 (95% CI 1.18 to 1.37) for women; for death from CHD, 1.51 (95% CI 1.36 to 1.67) for men and 1.62 (95% CI 1.46 to 1.81) for women; and for death from CVD, 1.45 (95% CI 1.33 to 1.59) for men and 1.53 (95% CI 1.38 to 1.69) for women. 2
Childhood obesity
The Health Survey for England 2012 reported that 14% of both boys and girls between the ages of 2 and 15 years were obese and that 28% of both boys and girls were classed as either overweight or obese. 3 Data for younger children have been provided by the National Child Measurement Programme (NCMP), which has been in progress for 6 years. The prevalence of obesity has been measured using BMI (using the 85th centile for overweight and 95th for obese) at two time points (aged 4/5 years and 10 years) using a cross-sectional study design. In England, in the 2012–13 school year the NCMP recorded 1,076,824 measurements in children (a participation rate of 93%). At reception (aged 4–5 years), 22.2% of children were either overweight or obese and 9.3% were obese. These figures increased in Year 6 (aged 10 years by 1 September, the start of the school year) to 33.3% of children being either overweight or obese and 18.9% being obese. 4 Data from the Health Survey for England3 show that the proportion of children aged 11–15 years in England who were obese was similar to adults (aged 16 years and over) up to 2004. Just under 15% were obese in 1995, rising to just over 25% in 2004, but, unlike the figures for adults, there has been a decrease since, with the proportion categorised as obese plateauing in 2010 at approximately 18%. In children aged 2–10 years, the proportion who were obese was lower: 10% were obese in 1995, rising to a peak of approximately 17% in 2005, followed by a decrease to just under 15% in 2010. 5 From these figures, it seems that the prevalence of overweight and obesity, and changes over time, vary for different age groups of children. It has been projected that, by 2050, the prevalence of obesity will increase in boys to over 35% of those aged 6–10 years and 23% of those aged 11–15 years, and in girls to 20% of those aged 6–10 years and 35% of those aged 11–15 years. 6 The prevalence of childhood obesity varies depending upon ethnicity. 4,7–9 It has been suggested that certain obesity metrics may misrepresent these ethnic differences. 9,10 Data on childhood obesity incidence are more limited, although US evidence suggests that incident obesity between the ages of 5 and 14 years is more likely to occur at a younger age, primarily among overweight 5-year-old children. 11
The association between childhood obesity and adult obesity and morbidity
It is generally accepted that adult obesity increases the risk of some morbidities, particularly CVD, type 2 diabetes mellitus and some types of cancer,7,12–14 and leads to a higher risk of associated mortality. 15 It may also be associated with other chronic conditions, such as rheumatological disorders, asthma, psychological illness, sleep disorders and reduced fertility. 7 However, the link between childhood obesity and adult morbidity is less clear. Recent systematic reviews have indicated that childhood obesity is associated with adult obesity16,17 and adult morbidities. 18–22 However, none of these reviews evaluated this association in terms of predictive accuracy.
A recent systematic review of 25 studies stated that all the studies consistently reported that overweight and obese children were at an increased risk of becoming overweight or obese adults, with the risk of tracking into adulthood obesity increasing as the level of overweight/obesity in childhood increased. 16 The findings from that review suggested a moderate likelihood of persistence of overweight into adulthood for children who were overweight or obese, but there were considerable variations in the predictive values across studies. Regarding the link between childhood obesity and adult morbidity, recent systematic reviews support the opinion that it is adult obesity, or the continued overweight/obesity from childhood into adulthood,1,18,20,23,24 that increases the risk of adult morbidity, rather than obesity in childhood being an independent risk factor for adult morbidities. However, there is some uncertainty and this may vary across the morbidities.
Measuring obesity
Simple measures of obesity
There are a range of simple, anthropometric, indirect measures of adiposity. 25,26 The simplest measure is weight; however, on its own this provides little useful information, as confounding variables such as a person’s height and body composition are not taken into consideration.
Body mass index is the most commonly used simple measure of obesity, and is also the only measure recommended for use in children in the UK. It is calculated by dividing weight in kilograms by height in metres squared (kg/m2). BMI increases sharply in infancy, peaking at around 9 months, and then falls to its lowest at around 6 years. 27 BMI (adjusted for age and sex) is recommended by the National Institute for Health and Care Excellence (NICE) (CG43) as a practical estimate of overweight in children and young people, but the guidance warns that the result needs to be interpreted with caution because BMI is not a direct measure of adiposity. 28 The main limitation of BMI is that it measures excess weight, rather than excess fat, which is what determines whether someone is obese or not. Therefore, those with strong bones and/or well-developed muscularity, but little fat, will have a high BMI and could be categorised as obese, as bone and muscle are more dense than fat. 29 Additionally, BMI is not consistent across the normal height range, with shorter heights producing higher BMI values. 30 BMI also does not give any indication as to the distribution of fat in the body; in adults, central adiposity is more closely associated with health risks than general adiposity,31,32 and the use of BMI and waist circumference (WC) is recommended in adults in the UK.
Simple measures other than BMI include:
-
WC A measure which gives an indication as to the distribution of excess body fat. However, in isolation it provides insufficient information regarding overall adiposity. Based on a UK reference population, 95th centile cut-off points range from 57.0 cm at age 5 years to 85.2 cm at age 16 years in boys, and from 57.2 cm at age 5 years to 75.1 cm at age 16 years in girls. 33
-
Neck circumference (NC) The use of this measure has been investigated in children, and it is thought to be reliable for identifying children with high adiposity. 34–36 Based on a US population, thresholds for obesity are suggested as 29 cm in prepubertal boys, 28 cm in prepubertal girls, 32.5 cm in pubertal boys and 31 cm in pubertal girls. 36
-
Rohrer’s Ponderal Index (Rohrer’s Index, Ponderal Index or Corpulence Index) Similar to BMI, but calculated by dividing weight in kilograms by height in metres cubed (kg/m3), rather than height in metres squared. 29 This has been compared with BMI in respect of its ability to predict percentage body fat in children and adolescents, and its long-term associations with adult obesity. 37,38
-
Benn’s Index Calculated by dividing weight in kilograms by heightp (kg/mp); p is a power index derived from the weight-to-height ratio (p = bH0/W0), making the index independent of height. 29,39 Benn’s Index is rarely used as p is neither constant nor necessarily a whole number, which means the calculations are complicated. 29 A study in boys from four countries showed that the power of p required to produce a correlation of zero between the index and height varied with age and ethnicity. For US, Japanese and Singaporean boys, the p value was < 2.8 at age 6 years, increased to < 3.5 at age 9–10 years and decreased to < 2.0 by age 16 years. For boys in the UK, p started at < 2.3, increased to < 2.6 then decreased to < 2.0. 40
-
Waist-to-height ratio (WHtR) As with the waist-to-hip ratio (WHR), WHtR is a measure of fat distribution, and primarily identifies those with abdominal obesity. A person is typically considered obese if their WC is over half their height (threshold of 0.5 across multiple countries and ethnicities). 41,42
-
WHR A measure of regional fat distribution used as a marker for intra-abdominal fat in adults. A WHR of ≥ 0.80 in females and ≥ 1.0 in males is considered to be indicative of a high risk of health problems. 43 One of the limitations with ratios using waist measurement is the potential for measurement error, as there is inconsistency in the actual site of the waist measurement.
-
Body adiposity index (BAI) This was suggested by Bergman et al. (2011)44 as reflecting the percentage body fat in adults regardless of sex or ethnicity without numerical correction, and it was therefore considered an improvement on BMI. BAI is calculated by the equation [hip circumference/(height)x] − 18, with x being a unitless power term. The correlation between BAI and percentage adiposity was highest when x was between 1.47 and 1.5, and therefore the use of 1.5 as the power term in Mexican American adults was suggested. 44 The measure has not been validated in children, and a power term for children has not been specified.
-
Skinfold thickness (SFT) A direct anthropometric measure of adiposity. Skinfold measurements are considered as good indicators as they are a direct measure of the fat layer, but the measurements are site- and sex-specific. 27 The most common sites are the subscapular and the triceps;25 other potential sites include the chest, axilla, abdomen, suprailium and thigh. 26 Scores can be presented adjusted for age and sex. There are also a large number of equations available that can be used to obtain an estimate of percentage subcutaneous fat from SFT measurements,25,26 although these may introduce biases and have not been standardised for children over the age of 6 years. 45 In adults, women with 30% or higher, and men with 25% or higher, body fat are classified as obese. 46 One of the limitations of SFT is that visceral fat (fat in the abdominal cavity) is not measured. As with waist measurements, measurement error is a particular limitation of this method. There can be considerable variability across practitioners, leading to the requirement for specific training.
-
Bioelectrical impedance analysis (BIA) This measures the opposition to the flow of an electric current applied to extremities of the body (usually the wrists or ankles; in children, foot-to-foot currents are used as this only requires the child to stand barefoot on scales), using a low-level (below the threshold of human perception; usually a single frequency of 50 kHz) alternating electrical current passing through the body. This is used to estimate total body water. As fat contains little water compared with other body tissues, impedance can be used as a proxy measure for fat-free body mass. Body fat can then be calculated from the difference between fat-free body mass and overall weight. BIA has several limitations. First, the body is a number of cylinders of different length and diameter (legs, torso, arms), rather than a single cylinder, and given that resistance decreases as the cross-section of a cylinder increases, the arms and legs contribute more to resistance than the torso. The limbs represent 50% of body weight but 90% of the body’s impedance; this means that impedance is more closely related to changes in the muscle mass of the limbs. In addition, as there is an assumption that fat-free mass is 73% water,26 factors such as dehydration, exercise, diuretics or a full bladder will affect the results. 47 Furthermore, equations based on height and weight are used to determine overall adiposity and these vary across manufacturers. The equations used by some instruments may be unknown, and results may vary across different instruments and populations. 48 Given these limitations, BIA is currently not recommended for use in the UK.
-
Fat mass index (FMI) Calculated from fat mass as determined by BIA (kg) divided by height squared. FMI plus the fat-free mass index (fat-free mass/height squared) = BMI. 49,50
-
Near-infrared interactance (NIR) A beam of infrared light is transmitted into the biceps; the light is reflected by underlying muscle and absorbed by fat, and therefore the proportion of reflected light will indicate the proportion of fat. The NIR light penetrates the tissues to a depth of 4 cm and is reflected back to the detector, which measures the optical density at wavelengths of 940 nm (optical density 1) and 950 nm (optical density 2). The underlying principle is that optical densities are linearly and inversely related to percentage body fat, and thus, the smaller the optical density, the greater the absorption of NIR light and the higher the fat composition. 26
More complex measures of obesity
Apart from SFT, the anthropometric measures listed above are indirect measures of adiposity. There are a number of more direct measures of adiposity available; these are not routinely available and need to be conducted by those who have been specifically trained, and therefore they are not useful as population measures. Such measures include:
-
Densitometry [hydrostatic weighing; underwater (hydrostatic) weighting] This method measures underwater weight. It distinguishes fat mass and fat-free mass, assuming specific densities of these two tissues, and therefore requires measurement of total body density (body mass/body volume). 51 Whereas the density of fat is relatively constant, that of fat-free mass varies according to its composition. This variability is partly explained by the process of chemical maturation that occurs before adulthood, but interindividual variability is also significant, even in healthy children.
-
Densitometry [air displacement plethysmography (ADP)] A new system that uses the displacement of air rather than water. This is thought to have better precision than hydrodensitometry in children, and is acceptable in children as young as 4 years. 52 An infant ADP has become available, allowing the measurement of body volume during the first 6 months of life. In general, densitometry is unsuitable for application as a two-component technique in patients in whom the composition of lean mass may be abnormal, such as those with excess fluid retention and undermineralisation, as these decrease the density of lean mass and lead to an overestimation of fatness. 52,53
-
Multicomponent models These models combine the results of three, four or five different measures. The three-component model divides body weight into fat, water and fat-free dry tissue, and requires measurements of body weight, body water by hydrometry and body volume by densitometry. The four-component (4-C) model further divides fat-free dry tissue into protein and mineral, and requires the measurement of bone mineral by dual-energy X-ray absorptiometry (DEXA). Its advantage is that it is the most accurate approach, with all the component measurements being acceptable. It has the disadvantage of being expensive and thus generally limited to specialist research. 51 Body volume index is a new multicomponent measure that uses BMI, WC and WHR along with other volumetric and body composition analyses. The method requires a three-dimensional full-body scanner. 54
-
DEXA DEXA51 is a three-component model, as it measures bone mineral, bone-free lean mass and fat mass. For accurate estimation of body fat, the hydration of lean body mass needs to be established; often, a constant for hydration of lean body mass (0.73 ml/g) is assumed, which is based on non-elderly, healthy, adult measurements. The use of this assumption can lead to an error in the amount of lean tissue, particularly in children, the elderly and the sick; DEXA is likely to be more reliable in healthy adults with a constant tissue hydration. 55,56 DEXA may therefore have difficulty accurately assessing body mass in infants, with increasing accuracy as body size increases. DEXA also has difficulty distinguishing between bone and non-bone lean mass in high bony areas (thorax, forearm). 55 In a review comparing DEXA with 4-C models, DEXA tended to underestimate body fat in most studies, with this underestimation usually being greater in leaner people. 57 Some studies did find DEXA overestimated body fat, and some no difference; there seemed to be differences in accuracy with different DEXA technology. 57
-
Deuterium dilution method (D2O) Deuterated water (2H2O) is currently the most accurate way of measuring total body water. The difference in secreted markers (urine, saliva) between baseline and post ingestion is used in an algorithm to calculate total body water and fat-free mass. The difference between total body mass and fat-free mass gives fat mass, allowing body composition to be worked out, but the method is most effective for total body water when used in a multi-(four-)component model with body density [underwater (hydrostatic) weighting], BIA and DEXA. The method is safe and has been validated in a wide range of populations but does have disadvantages; it is expensive, time-consuming (requiring sample collections and analyses) and rather invasive because it requires participants to ingest a dose of deuterium-enriched water. 58
Challenges when measuring obesity in children
To monitor the trend in, and to reduce the prevalence of, overweight and obesity, several initiatives have been introduced in the UK. Programmes that target obesity in general include the Department of Health’s ‘Call to Action’,59 the National Obesity Observatory60 and the International Obesity Taskforce (IOTF). 61 Programmes aimed specifically at children include the NCMP, which measures the weight and height of children in reception class (aged 4–5 years) and Year 6 (aged 10–11 years) in order to assess overweight and obesity levels within primary schools. 4 In order for such programmes to succeed, the measure of obesity needs to be accurate and simple to implement. It is therefore important to investigate whether or not BMI, the most commonly used simple measure, is the best measure for wide-ranging screening programmes, and, if not, which measure (or combination of measures) should replace it in order to ensure that children at risk of obesity-related morbidity are identified.
The assessment of childhood obesity using BMI and other anthropometric measures is more complicated than that of adults. 62 The major limitation of anthropometric measures to determine obesity in children is that most are confounded by natural, age-related physiological variations in body composition. 27,63 As a result, actual measurements are compared with reference data to determine if a child is overweight or obese. However, for BMI, the most commonly used anthropometric measure in children, there are several reference data sets available, including the centiles of the UK 1990 growth reference (UK90), IOTF thresholds and the World Health Organization (WHO) growth reference; the advantages and disadvantages of each have been summarised elsewhere. 64 This results in different thresholds being used for defining overweight and obesity across organisations and countries, which makes the comparability of data and the determination of the accuracy of these measures difficult. 65 In the UK, BMI is related to the UK90 BMI growth reference charts to determine whether or not a child is obese. For clinical purposes, overweight is defined as a BMI ≥ 91st centile and obesity as a BMI ≥ 98th centile; however, many of the data available have been collected within a research context, and for research and population monitoring purposes the 85th and 95th centiles are recommended for classifying overweight and obesity, respectively. 1 The associated standardised scores, based on UK90 reference data, are 1.04 for the 85th centile; 1.34 for the 91st centile; 1.64 for the 95th centile; and 2.0 for the 98th centile. Most of the anthropometric measures being investigated in this review will be affected by a child’s age, sex and ethnicity, and will therefore require standardisation. NC, NIR and WHtR are measures not subjected to standardisation. The fact that they are not standardised may be attributable to the lack of appropriate reference data.
A lack of requirement for standardisation for age and sex for a measure would afford that measure some advantage over anthropometric measures that do require standardisation; whether or not this would be at the cost of accuracy would need to be established.
A further challenge arises when an association needs to be made between childhood obesity and adult morbidity, as very long-term studies are required. One study followed 1000 families from Newcastle upon Tyne (UK), involving 1142 children recruited at birth in 1947; 412 were followed to the age of 50 years. 66 The study concluded that there was little tracking of obesity from childhood to adulthood, that there was no excess adult health risk from childhood or teenage overweight, and that being thin as a child offered no protection against obesity in adulthood. 66 This contrasts with the results of other studies and reviews;21,23,67,68 although this may be related to population differences owing to the age of the cohort, it may also be a result of the study being underpowered. A comparison of two British birth cohorts, one of children born in 1946 and the other of children born in 1958, showed that girls in the 1958 cohort had a higher average BMI during 7 years in childhood, and that both boys and girls in the 1958 cohort had a greater rate of increase in BMI during adulthood. 69 These studies illustrate that potential determinants and levels of adiposity in childhood differ between these birth cohorts, and are likely to differ for the present-day child population. However, the long-term relationships between childhood obesity and adult morbidity may not change as a result of these differences, and standardisation of obesity scores is thought to mitigate some of the changes observed over time.
Aims and objectives of the review
It is generally accepted that adult obesity is associated with an increased risk of morbidity (type 2 diabetes, CVD and cancer) and premature mortality in adults. However, the link between childhood obesity and adult morbidity is less clear. Recent systematic reviews have indicated that childhood obesity is associated with adult obesity16,17 and a range of adult morbidities,18–22 but none has used formal methods to estimate the accuracy (in terms of sensitivity and specificity) of childhood obesity to predict adult obesity and morbidity. In addition, these reviews have primarily been based on studies that used BMI to determine the presence and level of obesity. BMI is the most commonly used measure, but there are concerns regarding its suitability in determining obesity in children, particularly in relation to the need for standardisation. The question remains of whether or not another simple childhood measure, used either alone or in combination with BMI or some other simple measure, would be better for predicting the risk of adult obesity and (separately) adult morbidity. It is therefore important to determine the predictive accuracy of the simple measures that are available in order to inform the decision as to which should be used for screening children to identify those at risk of developing obesity and serious obesity-related morbidities as adults.
The decision problem to be addressed was, ‘What is the best simple measure, or combination of simple measures, of obesity in children for predicting the development of obesity-related health problems such as type 2 diabetes, CVD and cancer in adolescence and/or adulthood?’ Given the relationship between adult obesity and morbidity, the ability of these simple measures to predict the persistence of obesity from childhood into adolescence and adulthood was investigated. Acceptability and ease of use of the measures are also important when considering whether or not any one of these measures should be introduced as the standard method for the assessment of childhood obesity; this will also be addressed within the review.
The objective of our research was to address, through systematic reviews, the questions raised in the decision problem.
-
Is obesity in children and adolescents a risk factor for CVD, type 2 diabetes and/or cancer in adults, and do the results vary according to the simple measure of obesity employed?
-
To what degree do simple measures of obesity in children accurately predict the tracking of obesity into adolescence and adulthood?
In order to fully evaluate the predictive value of the simple measures of obesity, and therefore the relationship between the measures and subsequent adult obesity and morbidity, the relationship between the measure and classifying weight status needs to be established. Therefore, a third question was addressed:
-
How accurately do simple measures of obesity reflect actual adiposity in children?
The review investigated how accurately the simple measures diagnosed a child’s weight status (overweight or obese), rather than absolute adiposity, as this was the most relevant question.
Once the most promising measure(s) had been determined in terms of predictive accuracy, a fourth question was addressed for that measure(s):
-
How acceptable are these measures of adiposity to children and their carers, and how easy is it for health professionals to implement them?
This review has focused on differentiating between the association between childhood obesity and adult morbidity and obesity, and the ability of childhood obesity to predict adult morbidity or obesity. The analyses of association examine whether or not an increase in childhood obesity in the population as a whole will lead to increased incidence of adult morbidity and obesity. This is distinct from prediction, which examines whether or not childhood obesity could be used as a screening test for later morbidity or obesity. The focus is on whether or not individual adults who have a morbidity or are obese were obese in childhood, and, separately, whether or not obese children go on to become obese adults. This distinction is necessary because an association between childhood obesity and adult obesity or morbidity does not imply that childhood obesity is a good predictor of them. 70
In the original protocol, question 1 above was ‘Is obesity in children and adolescents an independent risk factor for CVD, type 2 diabetes and/or cancer in adults, and do the results vary according to the simple measure of obesity employed?’ The aim of this review was to assess the ability of childhood obesity specifically to predict adult morbidity such that appropriate action might be taken in childhood. Therefore, no adjustment for adult morbidity was considered. To avoid any ambiguities, the term ‘independent’ was therefore removed from the original question.
Chapter 2 Methods
The systematic reviews were conducted following the general principles recommended in Centre for Reviews and Dissemination (CRD) guidance for undertaking reviews in health care,71 and the reporting guidance of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. 72 The protocol for the systematic review is registered on PROSPERO (PROSPERO registration number: CRD42013005711).
Search strategy
Aim of the literature search
Three separate literature searches were undertaken to identify studies to answer the following questions:
-
How accurately do measures of childhood obesity predict CVD, diabetes and/or cancer in adulthood?
-
Which simple measure of obesity in children most accurately predicts the tracking of obesity into adolescence and adulthood?
-
How accurately do simple measures of obesity reflect actual adiposity in children (actual adiposity in terms of ability to correctly classify a child as normal weight, overweight or obese)?
The three search strategies were devised using a combination of indexed subject heading terms and free-text search terms appearing in the title and/or abstract of database records. Search terms were identified through discussion within the project team, by scanning background literature and ‘key articles’ already known to the project team and by browsing database thesauri. The search strategies were peer reviewed for accuracy by other information specialists based at CRD (Lisa Stirk and Melissa Harden). Once the MEDLINE search strategies were agreed and peer reviewed, they were adapted so that they could be used in the other databases. Bibliographic records were managed using EndNote XI bibliographic management software (Thomson Reuters, CA, USA).
Full details of the search strategies, dates of searches and results from all the databases and resources searched are given in Appendix 1.
Concepts of the search strategy
All three search strategies included a set of search terms for the following three concepts: ‘obesity’, ‘children’ and a collection of ‘simple anthropometric measures’ (index tests). The ‘obesity’ concept included search terms for ‘adiposity’. As BMI is the most widely used and recognised simple anthropometric measure for obesity, using this as a search term inevitably increased the sensitivity of the search strategy and the volume of literature retrieved.
The database searches were supplemented with reference checking and citation searching, as well as additional targeted searches for any gaps in the literature identified after screening of the initial set of literature search results.
The search strategy for the question on the prediction of adult morbidities was structured using the following concepts:
(Obesity OR adiposity)
AND
(Children OR adolescents)
AND
(CVD OR diabetes OR cancer)
An initial search to identify only systematic reviews was conducted, and the searches were limited to the Database of Abstracts of Reviews of Effects (DARE), the Cochrane Database of Systematic Reviews (CDSR), the Database of Promoting Health Effectiveness Reviews (DoPHER) and MEDLINE (with a methodological search filter designed to retrieve systematic reviews).
Having assessed the systematic reviews of measures for predicting morbidity in adulthood, the team was able to identify gaps in the literature and decided on the limits for the searches for primary studies. Targeted searches were conducted for the combinations of measures and morbidities shown in Table 1.
| Measures | Morbidities | Update from |
|---|---|---|
| BMI | CVD, diabetes and cancer | 2011 |
| SFT | CVD and diabetes | 2008 |
| SFT | Cancer | All dates |
| WC | CVD and diabetes | 2008 |
| WC | Cancer | All dates |
| All other measures | CVD, diabetes and cancer | All dates |
For the review question on the tracking of obesity, the search strategy was structured using the following concepts:
(Obesity OR adiposity)
AND
IT
AND
(Tracking OR Cohort studies OR longitudinal studies OR follow-up studies)
AND
(Children OR adolescents)
AND
Adults
AND
Date limit (2007–2013)
During the initial scoping searches, a systematic review about ‘tracking’ of childhood obesity into adulthood was identified [Singh et al. (2008)],16 and it was therefore decided to limit the searches to run from the date when the searches for this review were completed (2007). The final agreed search strategy was unable to identify one of the Singh review included studies, owing to the absence of any terms for ‘tracking’ or study design in the title or abstract and inadequate subject heading indexing.
The diagnostic accuracy literature searches were designed to identify studies that compared index tests with reference standards, so both concepts were combined alongside terms for ‘obesity’ and ‘children’. The diagnostic accuracy search strategy was structured using the following concepts:
(Obesity OR adiposity)
AND
(Children OR adolescents)
AND
Index tests
AND
Reference standards
NOT
Animal studies
Initially, the search for studies on the acceptability of simple measures was to be conducted for those tests previously determined to be the most promising measures in terms of predictive accuracy. However, given the lack of non-BMI studies, searches were designed to retrieve qualitative studies about the accessibility and ease of use of the following simple measures of obesity: BMI, SFT, WHR and WHtR. The searches were limited to the following databases: MEDLINE, EMBASE, PsycINFO and Cumulative Index to Nursing and Allied Health Literature (CINAHL). They were also limited by date range (2008–13).
Resources searched
The literature searches involved searching a wide range of databases. The following databases and resources were searched:
-
MEDLINE (OvidSP)
-
MEDLINE In-Process & Other Non-Indexed Citations (OvidSP)
-
PubMed (National Library of Medicine)
-
EMBASE (OvidSP)
-
PsycINFO (OvidSP)
-
CINAHL (EBSCO)
-
CDSR (Wiley Online Library)
-
Cochrane Central Register of Controlled Trials (CENTRAL) (Wiley Online Library)
-
DARE (CRD interface)
-
Health Technology Assessment (HTA) Database (CRD interface)
-
NHS Economic Evaluation Database (NHS EED) (CRD interface)
-
Science Citation Index (SCI) [ISI Web of Science (WoS)]
-
Conference Proceedings Citation Index – Science (CPCI-S) (ISI WoS)
-
Health Management Information Consortium (OvidSP)
-
Trials Register of Promoting Health Interventions [Evidence for Policy and Practice Information and Co-ordinating Centre (EPPI-Centre) interface]
-
DoPHER (EPPI-Centre interface)
-
Obesity and Sedentary Behaviour Database (EPPI-Centre interface)
-
OAIster (http://oaister.worldcat.org/)
-
OpenGrey (www.opengrey.eu/).
The following obesity-related organisation websites were searched:
-
Public Health England – Obesity Knowledge and Intelligence (previously National Obesity Observatory) (www.noo.org.uk/)
-
Association for the Study of Obesity (www.aso.org.uk/)
-
Obesity Learning Centre (www.obesitylearningcentre.org.uk/)
-
National Obesity Forum (www.nationalobesityforum.org.uk/)
-
British Dietetic Association (www.bda.uk.com/index.html)
-
Centre for Diet and Activity Research (CEDAR) (www.cedar.iph.cam.ac.uk/)
-
The Nutrition Society (www.nutritionsociety.org/)
-
International Association for the Study of Obesity (www.iaso.org/)
-
European Association for the Study of Obesity (EASO) (www.easoobesity.org/)
-
European Congress on Obesity (www.easo.org/eco2013)
-
European Childhood Obesity Group (ECOG) (www.ecog-obesity.eu/)
-
Centers for Disease Control and Prevention (CDC) Division of Nutrition, Physical Activity, and Obesity (USA) (www.cdc.gov/nccdphp/dnpao/index.html)
-
Weight-control Information Network (USA) (http://win.niddk.nih.gov/)
-
The Obesity Society (USA) (www.obesity.org/)
-
myhealthywaist.org (International Chair on Cardiometabolic Risk of Université Laval – QC, Canada) (www.myhealthywaist.org/).
Citation searches were conducted in SCI and Google Scholar. All sources proposed in the protocol are listed above.
Inclusion criteria
As systematic reviews had already been conducted for questions 1 and 2, good-quality systematic reviews that could be used as a basis for the current review were sought for these questions. Given the nature of the data required for meta-analysis, many studies included for these questions may be of cohorts recruited when influences in childhood were most likely different to those experienced by the present-day child population. However, reviews where such older cohorts are included were not excluded from the review.
Review of prediction of adult morbidities
-
Outcomes The study had to report RRs, odds ratios (ORs), hazard ratios (HRs) or summary estimates of predictive accuracy, or sufficient data from which these could be derived, for the association between childhood obesity and adult CVD, type 2 diabetes or cancer. For the purposes of this review, CVD incorporated major cardiovascular events such as cardiovascular death, myocardial infarction, stroke, heart failure, hypertension, hypercholesterolaemia and metabolic syndrome.
-
Interventions Data for the following simple measures were included: BMI, NC, WC, WHR, WHtR, BAI, Rohrer’s Ponderal Index, Benn’s Index, FMI, SFT, BIA and NIR. Studies were included for each of these measures, regardless of how the measurement was conducted (i.e. any level at which WC was measured was eligible).
-
Study design Prospective, longitudinal studies that were sufficiently powered (1000 participants) and that evaluated any one of the interventions of interest used in childhood for the prediction of a morbidity of interest in adolescence or adulthood were eligible; case–control studies and retrospective studies were excluded.
There are many other types of morbidity where evidence of an association with obesity exists, including mental health problems, respiratory conditions and musculoskeletal conditions, among others. This review considered only cardiovascular conditions, diabetes, cancer and metabolic syndrome, in order to focus on those conditions most likely to lead to mortality, where the evidence of association with obesity was strongest, and where there was most likely to be long-term evidence in cohort studies of their association with childhood obesity.
Tracking of childhood obesity into adolescence/adulthood or adolescent obesity into adulthood
-
Population Studies recruiting children and/or adolescents (up to the age of 18 years) were eligible for inclusion. Studies recruiting a mixture of adults and children/adolescents were included if the results for children/adolescents were reported separately. Studies had to recruit either population-based samples of children or overweight/obese children; studies conducted only in children who were not overweight or obese were excluded. We accepted the definition of obesity/adiposity used in the study.
-
Interventions Data for the following simple measures were sought: BMI, NC, WC, WHR, WHtR, BAI, Ponderal Index, Benn’s Index, FMI, SFT, BIA and NIR. Studies were included for each of these measures, regardless of how the measurement was conducted (i.e. any level at which WC was measured was eligible).
-
Outcomes The study had to report estimates of test accuracy, or sufficient data from which these could be derived, for the association between the weight status in childhood and/or adolescence and the incidence of obesity/overweight in adulthood. This was a change from the protocol, required as data on the association between weight status in childhood and adulthood would be insufficient to assess the predictive accuracy of childhood obesity/overweight. Studies that reported only correlations between the childhood and adult measures were also excluded.
-
Study design Prospective, longitudinal studies that evaluate any one of the interventions of interest were eligible; case–control studies and retrospective studies were excluded. Inclusion was initially restricted to studies that recruited at least 100 children; this was increased to 1000 children in studies of BMI given the volume of evidence available and so as to include only well-powered studies. As inclusion was restricted to those studies where predictive accuracy of the anthropometric measure could be established, only studies that used an acceptable reference standard in adulthood [i.e. a multicomponent model, D2O, underwater (hydrostatic) weighting, ADP or DEXA] were included. BMI was added to the list of reference standards as it is generally accepted as a suitable estimate in adults and we expected it to be the most commonly used adult measure (see Appendix 2).
The diagnostic accuracy of childhood measures of obesity
-
Population Studies recruiting children and/or adolescents (up to the age of 18 years as defined in the NICE CG43 obesity guidelines) were eligible for inclusion. Studies recruiting a mixture of adults and children/adolescents were included if the results for children/adolescents were reported separately. Studies had to recruit either a population-based sample of children or overweight/obese children; studies conducted only in children who were not overweight or obese were excluded.
-
Interventions The following simple measures were evaluated: BMI, NC, WC, WHR, WHtR, BAI, Ponderal Index, Benn’s Index, FMI, SFT, BIA and NIR.
-
Reference standard A multicomponent model that measures four or five components was considered the gold standard for assessing the accuracy of simple anthropometric measures of adiposity in children, because the precision of such a model is considered to be higher than other complex measures. The other complex measures, such as DEXA, D2O and densitometry [underwater (hydrostatic) weighting or ADP], were accepted as reference standards as they are more commonly used in research studies; these were considered imperfect reference standards.
-
Outcomes The study had to report either summary estimates of diagnostic accuracy or sufficient data from which these could be derived.
-
Study design Prospective single-gate (diagnostic cohort) studies that evaluated any one of the interventions of interest in comparison with any one of the reference standards were eligible for inclusion. For measures for which these are not available, prospective two-gate (diagnostic case–control) studies were included; these had to match cases and controls on at least age and sex, or provide estimates of sensitivity and specificity that had been adjusted for these variables.
The acceptability and ease of use of childhood measures of obesity
The original intention was to identify primary studies that undertook a robust evaluation (such as the use of questionnaires or interviews) of the acceptability and ease of the most promising measure(s) in terms of diagnostic and predictive accuracy. Given that the majority of the data identified were for BMI, this was amended to a search for studies of acceptability and ease of use for the four measures most commonly used in clinical practice: BMI, SFT, WHR and WHtR. Studies could be from the perspective of the child, parent or health professional. Studies that discussed acceptability or ease of implementation with no direct measurement were not included. Given the recent changes in distribution across the population, the emphasis placed on education and intervention for obesity and general attitudes towards obesity, the inclusion of primary studies was initially restricted to those conducted within the previous 5 years (search start date 2008). It was expected that the number of studies addressing this issue would be small. Only one study was identified that met the inclusion criteria. 73 Two further studies were identified from the searches for questions 1, 2 and 3 that were published in 200674 and 2007;75 given the paucity of evidence, the results of these are also presented.
To supplement the systematic review, a simple elicitation exercise (survey) was performed to obtain some indication of the attitudes of children, school nurses and parents to the measures being evaluated. Ethical approval from the Carnegie Faculty Committee, Leeds Metropolitan University, UK, was obtained. Overweight and obese children attending a weight management summer camp, parents of the children attending the weight management camp and school nurses were asked to complete a structured questionnaire developed specifically for the project that was suitable for the age group concerned. Opinions were elicited for the same four measures being evaluated in the systematic review of acceptability and ease of use: BMI, SFT, WHR and WHtR.
Data extraction strategy
Data extraction was conducted by one reviewer using standardised data extraction forms and independently checked by a second reviewer; separate forms were developed for the different review questions. Discrepancies were resolved by discussion, with involvement of a third reviewer when necessary. Data from multiple publications of the same study were extracted and reported as a single study, unless there was no overlap. Extraction included data on study details (e.g. author, year, country, setting, number of participants), patient characteristics (e.g. age, sex, ethnicity), details of intervention [measure used; classification and reference data used; timing of measurement; threshold used for diagnosis of overweight and obesity; variations in the method used when undertaking the measurement (e.g. equations used)], study quality and reported outcomes as specified above. For the morbidity review, where studies reported adjusted and non-adjusted outcome results, adjusted values were extracted, and where different levels of adjustments were reported [e.g. adjusting for age and sex only vs. adjusting for age, sex and socioeconomic status (SES)], results with the highest number of adjustments were generally preferred. However, results where adult weight status was not adjusted for were preferred to estimates that were adjusted for this variable. Full data extraction tables are given in Appendix 3.
Quality assessment strategy
The quality of the individual studies was assessed by one reviewer and independently checked by a second reviewer. No primary study was excluded based on the result of the quality assessment; disagreements were resolved by consensus and, if necessary, a third reviewer was consulted. The quality of included studies was assessed using standard checklists suitable for the study design: Quality Assessment of Diagnostic Accuracy Studies (QUADAS) was used for studies of diagnostic accuracy,76,77 and Quality in Prognosis Studies (QUIPS) formed the basis of the assessment of the studies of predictive value. 78,79 These tools were adapted as necessary to be review question-specific and to incorporate topic-specific quality issues; the most important of these adaptations was an assessment of measurement bias. Blinding of the assessors to index tests and reference standards was not assessed in the review of diagnostic accuracy owing to the visual clues at the time of the assessment.
The quality of the recent and relevant systematic reviews under consideration for inclusion in the current review was assessed using the criteria used by CRD for inclusion on the DARE database. Those that were included as a basis for the current review were assessed in terms of the strategy used to identify studies; the clarity of the review question and reproducibility of the inclusion criteria; the use of methods to reduce error and bias during the review process; the appropriateness of the quality assessment tool used to assess primary studies and the reporting of the results, analyses undertaken and interpretation of the results; the appropriateness of the conclusions drawn; and whether or not the patient population was representative. Primary qualitative studies were assessed using the Critical Appraisal Skills Programme Qualitative Research Checklist. 80 Full results of the quality assessments and guidance for their completion are given in Appendix 4.
Data analysis
Review of prediction of adult morbidities
The review of the association between childhood obesity and adult obesity-related morbidity, and the prediction of adult morbidities from childhood obesity status, was based on the identified cohort studies. Most cohorts were reported in multiple publications. Different publications concerning the same cohort were all included, provided they reported on different morbidities or reported results at different childhood ages.
Although studies reported many morbidity outcomes, only the following were considered in the meta-analyses:
-
diabetes (adult-onset, type 2)
-
CHD
-
stroke
-
hypertension
-
breast cancer
-
all other cancers, combined.
These were the only protocol-specified morbidities reported in at least two cohorts. Cancers were combined because a range of different cancers were reported within and across cohorts. In the narrative review we also considered hypercholesterolaemia and metabolic syndrome.
As results were reported at different ages, we grouped ages as:
-
under 7 years
-
7–11 years
-
12–18 years.
The first group represents young children who may experience adiposity rebound, where BMI declines up to around age 7 years. The other two groups represent typical UK division between primary- and secondary-level education.
Studies reported results in a variety of ways, including numbers of morbidities in different BMI categories, ORs comparing different categories of BMI, ORs between different centiles of BMI, ORs per standard deviation (SD) increase in BMI (or, equivalently, per BMI z-score unit) and across different reference populations. Given the diversity in reporting, a direct meta-analysis of results was not feasible. In order to perform a meta-analysis, all results were converted into ORs per SD of BMI (with 95% CIs), and into estimates of predictive performance in terms of sensitivity at specified obesity thresholds. The approach used for this conversion followed the methods of Morris and Wald70 for converting reported ORs into estimates of predictive performance. It requires some assumptions about the distributions of obesity in the childhood population, specifically:
-
that BMI follows a normal distribution
-
that the SD of BMI is the same in people with and without the morbidity
-
that the morbidity is rare.
It is acknowledged that the first assumption is invalid, as BMI is not normally distributed and has a positive skew, but this assumption is required for a meta-analysis to be performed, and it is applied equally to all studies, so any error applies uniformly across the analysis. The other assumptions are more reasonable in this context. Tests on simulated data suggest that, for positively skewed distributions of BMI, these assumptions may slightly overestimate ORs, but the overestimation is unlikely to exceed an absolute increase of 0.1. Using these assumptions will therefore also lead to overestimates of predictive accuracy by increasing estimates of sensitivity. The effect of the assumptions is uncertain, but tests on simulated data suggest that the area under the summary receiver operating characteristic (ROC) curve could be overestimated by up to 20%. As data in publications were presented as ORs without data on the distribution of BMI, it was not possible to transform these data to better represent a skewed distribution.
For each morbidity outcome and within each age group, a DerSimonian–Laird random-effects meta-analysis was performed to pool ORs per SD of BMI across cohorts. This produced a summary estimate of the association between childhood obesity and adult morbidity. As the SDs are specific to each cohort, these results should be interpreted as the OR per SD in a ‘typical’ population. To aid interpretation, some ORs were converted into odds per kg/m2 of BMI, based on the SD of BMI in adolescents in the UK (about 2.5 kg/m2). 81
Meta-analyses of the predictive accuracy of childhood obesity for predicting future morbidity were also performed. For each study, the sensitivities for predicting the morbidity among overweight (85th centile of BMI) and obese (95th centile) children were calculated using the methods of Morris and Wald70 described above. These sensitivities and their 95% CIs were then pooled across studies in standard DerSimonian–Laird random-effects meta-analyses to summarise the predictive sensitivity of childhood obesity to predict adult morbidity. These pooled estimates were converted into summary ROC curves. The assumption that the disease is rare means that specificity cannot be calculated in these analyses; only sensitivity at specified thresholds of BMI were presented, rather than true ROC curves. All analyses were performed using the R version 3.1 software (The R Foundation for Statistical Computing, Vienna, Austria).
No analyses of potential for publication bias were performed given both the limited number of studies in each meta-analysis and the uncertainty over the validity of such tests when reviewing predictive or prognostic outcomes.
All cohort studies in this review reported single measurements of BMI rather than repeated measurements over time. The use of single measurements may lead to regression to the mean, because children with an extreme measurement at a particular time are more likely to have a less extreme result at some later time, leading to underestimation of the association. Although regression to the mean is an acknowledged problem in measurements that change rapidly over time, such as blood pressure or blood lipids,82 it is unlikely to be a problem for BMI, which by its nature can vary little over short periods of time.
The aim of this review was to assess the ability of childhood obesity to predict adult morbidity; for this reason, no adjustment for adult morbidity was considered.
Review of tracking of obesity into adulthood
The analysis of the studies tracking obesity from childhood to adulthood was based on the diagnostic accuracy data extracted from these studies. Data were reported for tracking from childhood obesity (defined as BMI above the 95th centile) or overweight (above the 85th centile) to adult obesity (defined as BMI above the 95th centile or over 30 kg/m2) or adult overweight (above the 85th centile or over 25 kg/m2).
This allowed for four separate tracking analyses:
-
childhood obesity to later obesity
-
childhood obesity to later overweight or obesity
-
childhood overweight or obesity to later obesity
-
childhood overweight or obesity to later overweight or obesity.
Some studies reported data on only one of these comparisons, some on two and some on all four, so certain studies contributed to only some of the analyses.
Ages were split into four categories:
-
childhood (ages 7–11 years)
-
adolescence (ages 12–18 years)
-
adulthood (age 20 years and over)
-
aged over 30 years (to examine longer-term obesity tracking).
Studies reporting on obesity below age 7 years were excluded to avoid including children with adiposity rebound.
Given these ages, analyses were conducted to examine tracking:
-
from childhood to adolescence
-
from childhood to adulthood
-
from adolescence to adulthood
-
from adolescence to aged over 30 years.
Analyses were not stratified by sex as these data were too limited. Only BMI was considered as only two studies reported data on any other obesity measure (WC).
To assess the association between childhood obesity and adult obesity, the risk of being obese in adulthood given obesity status in childhood was calculated for each study from the diagnostic data. The RR of adult obesity, with its 95% CI, when comparing obese and non-obese children was calculated. These RRs were pooled in a DerSimonian–Laird random-effects meta-analysis, stratified by age group at time of obesity measurement.
The diagnostic accuracy data were synthesised in meta-analyses to estimate summary sensitivity, specificity and positive predictive values (PPVs) across the studies. As sensitivity and specificity are known to be correlated, the bivariate model was used to jointly analyse sensitivity and specificity. 83 Summary ROC curves were produced using the hierarchical summary ROC (HSROC) model,84 which is mathematically equivalent to the bivariate model. PPVs were similarly jointly modelled with negative predictive values (NPVs) using an adaptation of the bivariate model. These analyses did not correct for differences in obesity prevalence, which will lead to heterogeneity in PPVs and NPVs. The bivariate model requires full diagnostic accuracy data (i.e. numbers of true and false positives, and true and false negatives); therefore, studies that only presented summary sensitivity and specificity data were excluded. All results were presented as summary estimates with 95% CIs and HSROC curves, plotted in ROC space. The more formal 95% joint confidence regions for sensitivity and specificity were not presented for reasons of clarity.
No analyses of potential for publication bias were performed given uncertainty over the validity of such tests when reviewing predictive or prognostic outcomes.
All analyses were performed using the R software, using in-house code designed to be equivalent to the metandi library available for Stata version 13 (StataCorp LP, College Station, TX, USA).
Review of diagnostic accuracy
The review of studies of diagnostic accuracy was primarily a narrative review owing to the substantial clinical heterogeneity across the studies. The assessment of diagnostic accuracy was conducted as a supportive question to the primary reviews of predictive accuracy. As a result, data extraction was planned for those thresholds used by studies in the reviews of predictive accuracy. Given that the majority of studies in the predictive accuracy reviews evaluated BMI, using a range of commonly used cut-off points (85th centile, 95th centile, one and two SDs), these data were extracted from the diagnostic accuracy studies evaluating BMI. The other index tests of interest were rarely evaluated in the studies of predictive accuracy, and the thresholds for these tests are less well established. As a result, data were extracted for a more diverse range of cut-off points. Where a study did not report the threshold used, these data were extracted. Study details and results were tabulated.
For the analysis of BMI, inclusion was restricted to those studies that used a cut-off point of 85th centile for overweight and 95th centile for obesity and were conducted in a population representative of the UK child population. This gave us the most homogeneous data set that could be derived from the BMI studies, and we considered these to be the most informative data and those that would be the most reflective of the accuracy of BMI when used in a setting such as a school, where screening often takes place. To produce summary estimates of accuracy for BMI, HSROC curves were produced and the bivariate model fitted as described above for the tracking review using Stata version 13.
For the studies evaluating tests other than BMI, a narrative synthesis was presented, as there were fewer studies that were too heterogeneous to pool. We considered the most robust data to be from those studies that conducted direct comparisons of more than one test (two or more tests conducted in the same patients, using the same reference standard in all patients). We therefore used these studies to gain an insight into the comparative accuracy of the tests being evaluated. The results of these studies were tabulated and a narrative synthesis provided; limited numbers of studies and the range of obesity measures considered precluded any meta-analysis of these data. To aid interpretation of these data, estimates of sensitivity and specificity from studies which compared the diagnostic accuracy of BMI with some other simple obesity measure were plotted in ROC space, and diagnostic ORs (DORs) were calculated. This could only be undertaken for those studies from which 2 × 2 data could be extracted or derived; therefore, there are some test results in the tables of sensitivity and specificity that do not appear in the diagrams.
To help understand why one test may have a better predictive accuracy than another, we planned to compare the sensitivities and specificities for predictive and diagnostic accuracy of those tests evaluated in the predictive accuracy reviews. There were insufficient predictive accuracy data for non-BMI measures for this to be completed.
Review of the acceptability and ease of use of simple childhood measures of obesity
Study details and results have been summarised in tables and a narrative provided. The results of the elicitation exercise have been summarised in a narrative, with the summary results presented in tabulated form.
Chapter 3 Results
Flow of studies through the review
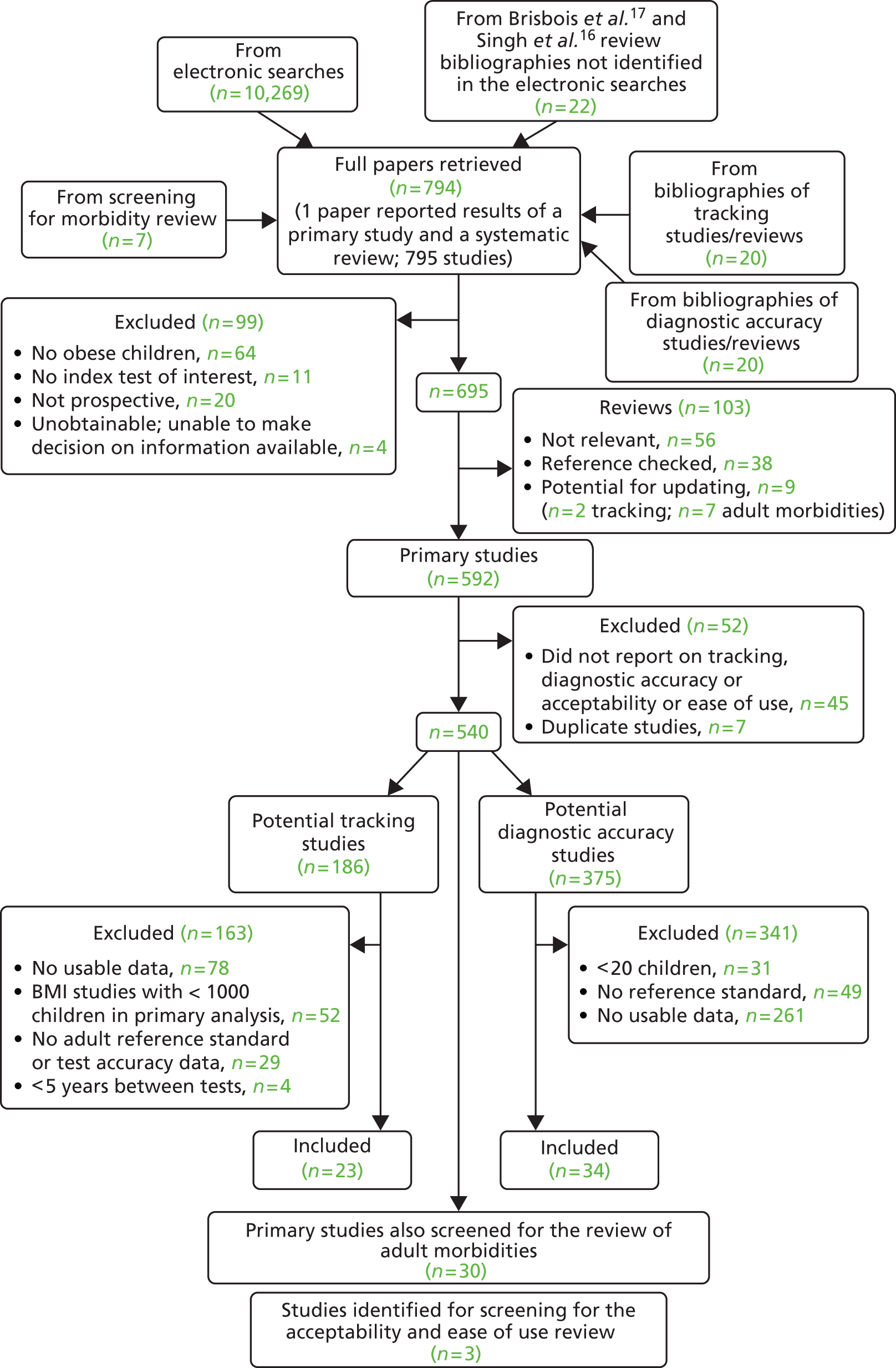
The screening process was undertaken in three stages. The initial stage was to screen for relevant systematic reviews for the morbidity review, and reviews and primary studies for the tracking and diagnostic accuracy reviews. After deduplication, there were 10,296 retrievals from the initial electronic searches, which were supplemented by the searching of bibliographies of relevant reviews, and primary diagnostic accuracy studies, which added 62 studies; seven studies were identified in the subsequent search for primary studies for the morbidity review which were also screened for inclusion in the tracking and diagnostic accuracy reviews (Figure 1).
FIGURE 1.
Flow of studies through the initial screening period of the review to identify systematic reviews for the tracking and adult morbidity reviews, and primary studies for the review of tracking and diagnostic accuracy.
Once the relevant systematic reviews were identified from the first screening stage for the morbidity review,18–22 these were used to set the parameters of the second search for primary studies. After deduplication, there were 5690 retrievals from the electronic searches, which were supplemented by the searching of bibliographies of the previous reviews of the prediction of adult morbidities, which added 52 studies. A further 30 primary studies from the initial screening stage were also considered potentially relevant and screened for the review of adult morbidities (Figure 2).
FIGURE 2.
Flow of studies through the second screening period of the review to identify primary studies of the relationship between childhood overweight and obesity and adult morbidities.

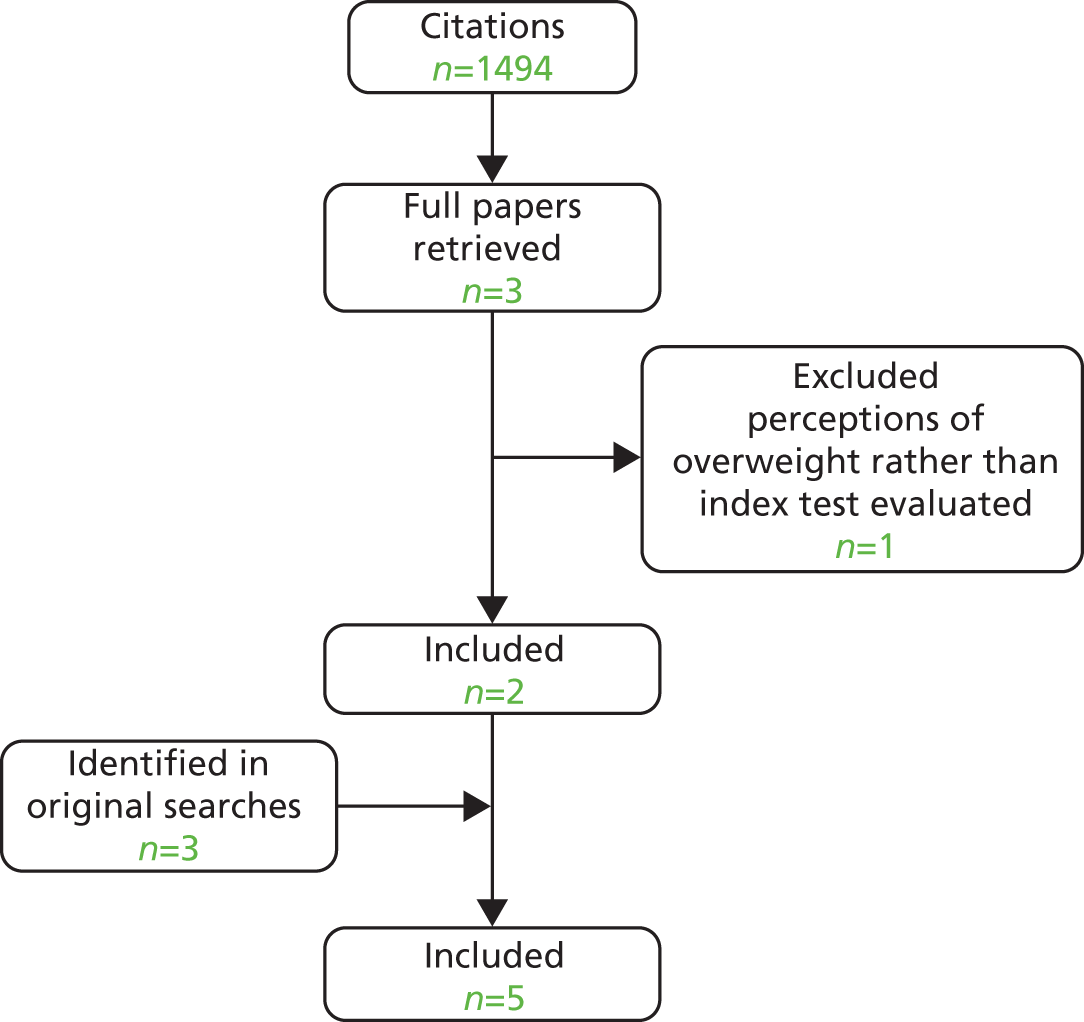
The third stage of screening was for the review of acceptability and ease of use review. From the focused searches conducted, 1494 citations were retrieved from the electronic searches; three further studies were screened that were identified during stage one of the screening process (Figure 3).
FIGURE 3.
Flow of studies through the third screening period of the review to identify primary studies of the acceptability and ease of use of four childhood measures of obesity.
Across the three searches and screening stages, 12 papers were unobtainable; for eight, the review team considered there to be sufficient information available to reliably exclude the study from the review,85–92 and for four a decision could not be made, but the study had to be excluded owing to lack of data. 93–96 Twenty studies were excluded from the review as they were linked to included studies and did not provide unique data. 97–116
After completion of the screening process, 95 studies were included in the review; 23 evaluated the tracking of obesity into adulthood,117–139 37 the association between obesity in childhood/adolescence and morbidity in adolescence/adulthood,117,118,123,129,140–172 34 diagnostic accuracy173–206 and 5 acceptability and/or ease of use. 73–75,207,208
For the review of adult morbidities, 13 reviews were identified. 18–22,209–217 One was an abstract for which there was no full paper. 210 Of the remaining 12, most evaluated only BMI. 18–22,213–215,217 Only the review by Whitlock et al. (2005)214 included studies of childhood measurements of interest other than BMI. The review reported on weight-to-height ratios and SFT and their correlation with outcomes in adulthood such as fasting insulin levels, cholesterol and blood pressure. Although the reviews by Park et al. (2011),18 Reilly et al. (2011),22 Owen et al. (2009),21 Lloyd et al. (2010)20 and Lloyd et al. (2012)19 were considered the most recent relevant, the overlap in included studies across all of the identified reviews was poor. As a result, no individual reviews were considered to be sufficiently complete. Therefore, the included studies from all of the identified reviews were screened. In addition, the bibliographies of relevant reviews that were identified by the searches but were not considered suitable for updating (mainly because they did not appear to use systematic methodology) were also searched. All potentially relevant studies were retrieved from these reviews, regardless of the age of the study.
Review of prediction of adult morbidities
Summary of the existing systematic reviews of the prediction of adult morbidities
Of the 13 reviews with potential for being updated that were identified,18–22,209–217 the reviews by Park et al. (2012),18 Reilly et al. (2011),22 Owen et al. (2009),21 Lloyd et al. (2010)20 and Lloyd et al. (2012)19 were the most recent and relevant to our review of adult morbidities. This subsection presents a brief critical summary of these five reviews.
Reilly et al. (2011)22 did not restrict their searches to any particular childhood measure of obesity, but only found studies on BMI and self-reported/recalled ‘weight status’. All other reviews included only BMI as a simple childhood measure of obesity. Most studies included in the reviews used cohort designs, although a smaller number of case–control studies were also eligible. Population eligibility criteria varied across the studies; Reilly et al. (2011)22 and Lloyd et al. (2010)20 included children from birth to age 18 years, but Park et al. (2012)18 and Lloyd et al. (2012)19 excluded children aged under 2 years. The review by Owen et al. (2009)21 reported on a significantly wider age range as it included individuals from birth up to age 30 years. The large majority of the studies were conducted in general populations from Europe (particularly Scandinavian countries and the UK) and the USA. None of the studies appeared to include specifically selected populations of children (such as children with cancer or children undergoing a weight reduction intervention). None of the reviews reported a restriction on sample size, and therefore the size of the studies varied widely, from under 100 to over 1.1 million participants.
Eligible outcomes varied across the reviews. The reviews by Park et al. (2012)18 and Reilly et al. (2011)22 had the broadest scope as they focused on both adult mortality and morbidity. Lloyd et al. (2010)20 reported outcomes relating to CVD events and CVD risk, and Owen et al. (2009)21 focused on CHD events. The review by Lloyd et al. (2012)19 was the only one to focus exclusively on metabolic syndrome and its individual components [type 2 diabetes, total cholesterol, triglycerides, high-density lipoprotein (HDL-)cholesterol, low-density lipoprotein (LDL-)cholesterol, fasting insulin, insulin resistance]. The number of individual studies included in the reviews ranged from 11 [Lloyd et al. (2012)19] to 39 [Park et al. (2012)18].
The quality of included studies was evaluated in three reviews. 18–20 However, only Lloyd et al. (201020 and 201219) reported the results of their quality assessments, which were based on the Newcastle Ottawa Scale. The key methodological limitations that they identified related to variation in type and number of adjustments made in the analyses of the primary studies, and the relatively young age of adults at follow-up in some studies. Quality relating to participant selection, comparability of study groups and measurement of outcomes was generally considered acceptable.
Only Owen et al. (2009)21 combined studies in a meta-analysis, stratified by baseline age group. All others reported the results of their included studies narratively by outcome. Lloyd et al. (201020 and 201219), Park et al. (2012)18 and Owen et al. (2009)21 also grouped studies based on whether or not they adjusted for adult BMI in their analyses.
In all reviews, a majority of studies reported a positive and statistically significant association between childhood BMI and adult morbidity. However, results varied by outcome. Both Park et al. (2012)18 and Reilly et al. (2011)22 found consistent evidence of a statistically significant positive association between childhood BMI and diabetes in adulthood. Park et al. (2012)18 reported that ORs for a one-unit increase in BMI SD score ranged from 1.22 (95% CI 1.10 to 1.36) at school entry (n = 5793) to 2.04 (95% CI 1.7 to 2.4) at 16 years of age (n = 10,683). Only 1 small study out of 10 found no association between the two variables. However, all three studies that adjusted for adult BMI found that the association was no longer significant after adjustment. In the review by Reilly et al. (2011),22 all three studies reporting diabetes outcomes found a significant increase in risk of developing the morbidity in those who were overweight or obese in childhood. Effect sizes were reported for only one study, showing significant association between overweight and obesity at age 5 years and self-reported diabetes at age 21 years (OR 2.6, 95% CI 1.3 to 5.2; n = 2639). Lloyd et al. (2012)19 found little evidence that childhood obesity is an independent risk factor for diabetes mortality, although their result was based on a single study.
Evidence of an association between childhood BMI and adult CHD was somewhat more mixed. The pooled analyses from Owen et al. (2009)21 showed that a 1-SD increase in BMI in early childhood [2–6 years (three studies)] was associated with reduced CHD risk (RR 0.94, 95% CI 0.82 to 1.07), although the association was not statistically significant. A weak positive association was found between later CHD risk and a 1-SD increase in BMI in later childhood [7 to < 18 years; RR 1.09, 95% CI 1.00 to 1.20 (seven studies)]. Both analyses showed high levels of heterogeneity. In the review by Park et al. (2012),18 10 of the 15 studies that explored the relationship between BMI in childhood and objective measures of CHD events reported that increased BMI or overweight at ages 2–25 years was associated with increased risk of CHD in later life. HRs ranged from 1.53 (95% CI not reported) for CHD mortality associated with high BMI at age 11 years to 5.43 (95% CI 2.77 to 10.62) for CHD associated with high BMI at age 17 years. One study (n = 181) found that higher BMI at ages 13–18 years was associated with increased risk of CHD morbidity and mortality in men but not in women. The remaining studies reported no association between BMI at ages 2–22 years and CHD. Reilly et al. (2011)22 and Lloyd et al (2010)20 both found that two out of three studies which examined the association between childhood BMI and CHD events reported a positive association.
Evidence of an association between childhood BMI and stroke in adulthood was mixed. Park et al. (2012)18 found that, out of nine relevant studies, only four found positive association between BMI and stroke in adulthood. Four studies (including three British studies) reported no association and one showed an inverse relationship between higher BMI at age 7 years and future stroke. Reilly et al. (2011)22 reported that two out of three studies which reported on stroke found a significant association between childhood BMI and morbidity in adulthood. Lloyd et al. (2010)20 found a pooled study from three historical cohorts and a single study which reported no significantly increased risk of CHD and stroke incidence in adults who were overweight or obese as children.
Evidence of an association between childhood BMI and the risk of developing metabolic syndrome in adulthood was limited. Lloyd et al. (2012)19 found only three studies which considered the link between the two variables. Two studies found that higher childhood BMI was associated with increased odds of developing metabolic syndrome in adulthood. The third study was the only one to adjust for adult BMI, and found that higher childhood BMI was associated with lower risk of metabolic syndrome in adult life when accounting for adult BMI.
Both Park et al. (2012)18 and Reilly et al. (2011)22 found consistent evidence of a statistically significant positive association between overweight or increased BMI in childhood and hypertension in adulthood. Park et al. (2012)18 reported ORs for overweight or increased BMI in childhood that ranged from 1.35 (95% CI 1.13 to 1.64) at age 7 years to 3.75 (95% CI 3.45 to 4.07) at ages 16–19 years in five studies. In the four studies identified by Reilly et al. (2011),22 ORs ranged from 1.46 (95% CI 1.01 to 2.12) to 5.1 (95% CI 1.4 to 18.1). On the other hand, Lloyd et al. (2010)20 found less consistent evidence that childhood obesity was an independent risk factor for hypertension.
None of the reviews reported studies focusing on hypercholesterolaemia as an outcome in adulthood. Lloyd et al. (2012)19 reported on studies focusing on LDL- and HDL-cholesterol levels. The review found little evidence to support the view that childhood obesity is an independent risk factor for higher LDL- and HDL-cholesterol levels.
Significantly less evidence was found on cancer. Park et al. (2012)18 found limited evidence that childhood BMI is associated with increased risk of colorectal and kidney cancers. Reilly et al. (2011)22 found a single study on the association between BMI and cancer, which reported a significant 30% increase (95% CI 10% to 54%) in smoking-related cancers per 1-SD increase in childhood BMI (n = 2997).
Reviews differed in their interpretation of the strength and clinical significance of the associations found. They also differed in the emphasis and importance placed on adjustments made for adult BMI. This, in addition to the fact that there was relatively little overlap across the reviews in terms of included studies, may explain why the conclusions of the reviews differed.
Reilly et al. (2011)22 concluded that there is a relatively large and highly consistent body of evidence which shows that overweight and obesity in childhood and adolescence have substantial and adverse long-term consequences for physical health. However, we feel that these conclusions were too strong; there was some variation in the size and direction of the effect estimates reported. Additionally, there were concerns about several aspects of the review methods and limited reporting of the study results. Therefore, the conclusions of Reilly et al. (2011)22 appear insufficiently cautious and may not be reliable.
The conclusions of Park et al. (2012)18 were more nuanced and more accurately reflected the evidence found. They stated that there is a consistent body of evidence for associations between childhood overweight, unadjusted for adult BMI, and cardiovascular outcomes and mortality in adulthood. They also concluded that evidence for stroke outcomes is mixed, and that there is limited evidence that childhood BMI is associated with increased risk of colorectal and kidney cancers. They also remarked that few studies have assessed the independent effects of childhood overweight on adult disease, and the results of these have been inconclusive.
Owen et al. (2009)21 concluded that higher levels of BMI may be related to increased levels of CHD risk from early childhood onwards. They stated that the control of obesity from childhood onwards may be an important priority for long-term CHD prevention, although they noted that the independent contribution of early obesity to CHD risk still needs to be established. The review by Owen et al. was the only one that conducted a meta-analysis, and the choice of methods appeared appropriate in view of the evidence found, although evidence of significant heterogeneity was reported. However, it is unclear why the authors concluded that higher BMI was associated with an increased risk of morbidity from early childhood even though they reported a weak inverse relationship with adult CHD risk in children under age 7 years. Additionally, the small magnitude of the pooled estimates in later childhood suggests that their clinical relevance may be limited in the context of adult CHD risk prediction. Therefore, the conclusions of the review may not be sufficiently cautious.
The conclusions from Lloyd et al. (2010)20 placed greater emphasis on the influence of adult BMI in the association between childhood BMI and adult morbidity than those of Owen et al. (2009)21 or Park et al. (2012). 18 The authors stated that they found little evidence to suggest that childhood obesity is an independent risk factor for CVD risk. They stated that, instead, relationships observed are dependent on the tracking of BMI from childhood to adulthood. Although the evidence found by Lloyd et al. (2010)20 appears insufficient to support the notion that childhood obesity is an independent risk factor for CVD risk, the review did not discuss the risks associated with standard adjustment for adult BMI, which may lead to overadjustment bias. 218 Additionally, the evidence presented by the review was insufficient to suggest that the relationships observed were dependent on the tracking of BMI from childhood to adulthood. Therefore, the conclusions of Lloyd et al. (2010)20 may not be reliable.
Lloyd et al. (2012)19 also concluded that there is little evidence to support the view that childhood obesity is an independent risk factor for adult blood lipid status, insulin levels, metabolic syndrome or type 2 diabetes. The conclusions reflected the evidence found, although the volume of the evidence on diabetes was significantly smaller than that reported by Park et al. (2012)18 or Reilly et al. (2011). 22
Among all five reviews, it appeared that the review by Park et al. (2012)18 was better conducted and yielded the most reliable conclusions. However, with the exception of the review by Owen et al. (2009),21 none of the reviews conducted a meta-analysis, which limited the strength of their results. Additionally, none included studies on childhood measurements other than BMI, which limits their relevance to our review questions. Some reviews addressed the issue of BMI tracking into adulthood as a potential confounder in the association between childhood BMI and adult morbidity. However, none formally evaluated the extent to which childhood measures of obesity accurately predict the tracking of obesity into adulthood. Finally, all reviews reported on the association between BMI and adult morbidities (generally expressed as ORs, RRs or HRs), but none in terms of predictive accuracy, and none used formal methods to calculate the predictive performance of childhood obesity for predicting future morbidity. This overview of recent systematic reviews highlights important gaps in the evidence for the predictive power of childhood obesity as a predictor of adult morbidity.
Quality and assessment of bias of the included primary studies for the prediction of adult morbidities
Thirty-seven studies (22 cohorts) met the inclusion criteria for the review of predictive accuracy. 117,118,123,129,140–172 The assessment of risk of bias is presented in Table 2 and the full quality assessment in Appendix 4. The most common methodological weaknesses were attrition bias and gaps in reporting about attrition rates, followed by outcomes bias (due to self-reporting of morbidities). Biases associated with selection, childhood measurements, use of confounders, reporting and analysis were low in most studies.
| Author (publication year) | Risk of selection bias | Risk of attrition bias | Risk of bias prognostic factor | Risk of bias with outcome | Risk of bias due to confounders | Risk of reporting/analysis bias |
|---|---|---|---|---|---|---|
| Ahlgren (2004)140 | Low | Unclear | Low | Low | Low | Low |
| Baker (2007)142 | Low | Unclear | Low | Low | Low | Low |
| Baker (2007)141 | Low | Low | Low | Low | Low | Low |
| Barker (2002)143 | Low | Unclear | Low | Unclear | Low | Low |
| Barker (2005)144 | Low | Low | Low | Low | Low | Low |
| Berentzen (2013)145 | Low | Low | Low | Low | Low | Low |
| Bjorge (2004)146 | Low | Low | Low | Low | Low | Low |
| Bjorge (2008)147 | Low | Low | Low | Low | Low | Low |
| Cheng (2011)117 | Low | High | Low | Low | Unclear | Low |
| Cheung (2004)118 | Low | High | Low | High | High | Low |
| De Stavola (2004)148 | Low | Low | Low | High | Low | Low |
| Engeland (2003)149 | Low | Low | Low | Low | Low | Low |
| Eriksson (2001)150 | Low | Unclear | Low | Low | Low | Low |
| Forsen (2000)151 | Low | Low | Low | Low | Low | Low |
| Forsen (2004)152 | Low | High | Low | Low | Low | Low |
| Goldhaber-Fiebert (2013)123 | Low | Unclear | Low | High | Low | Low |
| Gunnell (1998)153 | Low | High | Low | Low | Low | Low |
| Hilakivi-Clarke (2001)154 | Low | Unclear | Low | Low | Low | Low |
| Hypponen (2003)155 | Low | High | Low | High | Low | Low |
| Israeli (2007)156 | Low | Unclear | Low | Low | Low | Low |
| Janssen (2005)157 | Low | High | Low | Low | Low | Low |
| Jeffreys (2004)158 | Unclear | Low | Low | Low | Low | Unclear |
| Lawlor (2005)159 | Low | Low | Low | Low | Low | Low |
| Lawlor (2006)160 | Low | High | Low | High | Low | Low |
| Leiba (2012)161 | Low | Unclear | Low | Low | Low | Low |
| Leiba (2013)162 | Low | Unclear | Low | Low | Low | Low |
| Levi (2011)163 | Low | Unclear | Low | Low | Low | Low |
| Levi (2012)164 | Low | Unclear | Low | Low | Low | Low |
| Li (2007)165 | Low | Low | Low | Low | Low | Low |
| Magnussen (2010)166 | Unclear | High | Low | Low | Low | Low |
| Mattsson (2008)167 | Low | High | Low | Low | Low | Low |
| Merten (2010)129 | Low | High | Unclear | High | Low | Low |
| Morrison (2010)168 | Low | High | Low/uncleara | High | High | Low |
| Osmond (2007)169 | Low | Low | Low | Low | High | Low |
| Sachdev (2009)170 | Low | High | Low | Low | Low | Low |
| Schmidt (2011)171 | Low | High | Low/unclearb | Low | Low | Low |
| Tirosh (2011)172 | Low | Low | Low | Low | Low | Low |
| Total | 0 high 35 low 2 unclear |
13 high 13 low 11 unclear |
0 high 36 low 3 uncleara,b |
7 high 29 low 1 unclear |
3 high 33 low 1 unclear |
0 high 36 low 1 unclear |
Seven studies used self-reported outcome measures and were considered at high risk of outcome bias. 118,123,129,148,155,160,168 One study used drug medication use as a proxy for hypertension and risk of outcome bias was unclear. 143 Bias associated with childhood weight status measurement was high in one study, where BMI was calculated based on adolescents’ self-reporting of height and weight. 129 One study did not report sufficient information on the site of WC measurements,168 and the only study that used SFT as a childhood measurement did not report how the sum of SFTs was calculated. 171 Thirty-two studies adjusted for age and sex in their analyses, and were therefore considered at low risk of confounding bias. Two studies did not adjust for sex in their analyses;118,169 one adjusted for sex but not age;146 and one did not adjust for either sex or age. 168 One study had a high risk of reporting bias due to partial reporting of results. 158
Characteristics of studies included in the review of prediction of adult morbidities
Study characteristics for prediction of adult morbidities
The study characteristics are presented in Table 3. All 37 studies117,118,123,129,140–172 included in the prediction of adult morbidity review used BMI (calculated as kg/m2) as a childhood measurement (for details see Appendix 3). Only three studies used a childhood measurement other than BMI. Three used WC in childhood,117,168,171 and one study also measured the sum of SFTs and WHR. 171 No other simple measure of childhood obesity was investigated in relation to adult morbidity.
| Study/cohort name | Study | Country | Study dates | Setting for anthropometric measure in childhood | |
|---|---|---|---|---|---|
| Start | Finish | ||||
| Aberdeen Children of the 1950s cohort |
Lawlor (2005)159 Lawlor (2006)160 |
Scotland | 1950 | 2000 | NR |
| Boyd Orr | Gunnell (1998)153 Jeffreys (2004)158 |
England, Scotland | 1937 | 1995 | NR |
| British birth cohort 1958 | Hypponen (2003)155 Li (2007)165 |
England, Wales, Scotland | 1958 | 2000 | NR |
| MRC NSHD | De Stavola (2004)148 | UK | 1946 | 1999 | School, community |
| NCDS | Cheung (2004)118 | UK | 1958 | 2000 | NR |
| Copenhagen CSHRR (born 1930–76) |
Ahlgren (2004)140 Baker (2007)142 Baker (2007)141 Berentzen (2013)145 |
Denmark | 1930 | Up to 2011 | School |
| Young Finns Cardiovascular Risk in Young Finns (born approximately 1962–77) |
Mattsson (2008)167 Magnussen (2010)166 |
Finland | 1980 | 2001 | NR |
| Helsinki 1924 University Central Hospital (born 1924–33) |
Forsen (2000)151 Hilakivi-Clarke (2001)154 |
Finland | 1924 | Up to 1997 | School |
| Helsinki 1934 University Central Hospital, born 1934–44 |
Barker (2002)143 Barker (2005)144 Eriksson (2001)150 Forsen (2004)152 Osmond (2007)169 |
Finland | 1934 | Up to 2003 | School, outpatient clinics |
| Norway 1963–99 |
Bjorge (2004)146 Bjorge (2008)147 Engeland (2003)149 |
Norway | 1963 | Up to 2005 | School |
| Bogalusa/Young Finns Bogalusa and Cardiovascular Risk in Young Finns (pooled) |
Magnussen (2010)166 | USA and Finland | 1984 | 2007 | NR |
| NLSAH | Merten (2010)129 | USA | 1995 | 2001 | NR |
| Bogalusa Bogalusa Heart Study |
Janssen (2005)157 | USA | 1976 | 1996 | NR |
| NGHS/PFS | Morrison (2010)168 | USA | PFS: 1973 NGHS: NR |
PFS: 2003 NGHS: NR |
NR |
| NLSY79, PSID, NHANES | Goldhaber-Fiebert (2013)123 | USA | 1970 | 2008 | Community |
| ASHFS 1985 (born approximately 1970–8) |
Schmidt (2011)171 | Australia | 1985 | 2006 | School |
| Israel SPEC Medical Corps SPEC |
Israeli (2007)156 Tirosh (2011)172 |
Israel | 1976 | NR | Military medical examination centre |
| Israeli army (Born approximately 1948–89) |
Leiba (2012)161 Levi (2012)164 Levi (2011)163 Leiba (2013)162 |
Israel | 1967 | 2006 | Military service recruitment centres |
| Delhi (Born from 1969) |
Sachdev (2009)170 | India | 1969 | 2002 | NR |
| BCAMSS | Cheng (2011)117 | China | 2004 | 2010 | School |
Definitions of overweight and obesity, methods of standardisation and references used to calculate weight category varied across the studies. Details are given in Appendix 3 (see Table 49). Fifteen studies used an external reference population to define overweight/obesity status and stratify the cohort according to childhood weight status. Twenty-five studies used their own cohort as a reference population. Seven studies reported using internally and externally derived reference populations in their analyses. Of the 15 studies with external reference populations, 10 used a CDC (2000)219 reference population, four used Cole (2000),220 one used Cole (1990)221 and one used a Chinese reference population. Of the 25 studies with internal reference populations, 16 standardised BMI measurements as z-scores. Of those, most (13) calculated age- and sex-specific z-scores. Three studies calculated age-specific z-scores only and adjusted for sex in their analyses.
Studies were published between 1998 and 2013. Most studies (23 out of 36) were conducted in northern Europe. Eight studies were conducted in the UK, eight in Finland, four in Denmark and three in Norway. Six studies were from Israel, and four were conducted in the USA, one in Australia, one in China and one in India. All studies were designed as longitudinal studies except for three that used data collected as part of a tuberculosis screening programme,146,147,149 and six in the context of a military medical examination. 156,161–164,172 All childhood measurements were made directly, except for one which used recall. 129
One-third of the studies made all their childhood measurements in school. Some studies collected measurements in school as well as in the community148 or outpatient settings. In six studies, participants’ BMIs were measured in Israeli military centres. Further study characteristics are presented in Table 3.
Many of the identified cohorts were commenced between the 1920s and the 1950s, and social conditions for children have changed considerably since that time. It is not clear, therefore, whether or not the association between childhood obesity and adult morbidity from such cohorts accurately reflects the association in present-day children.
Population characteristics for prediction of adult morbidities
The population characteristics are presented in Table 4 and Appendix 3. The size of the cohorts varied widely, from 1889 to over 1.1 million individuals. Baseline age varied across the studies. Children aged between 12 and 18 years were the most often represented, followed by those aged 7–11 years and children aged 6 years or under. Twenty-eight studies measured weight status among children aged over 11 years. Twenty-three studies included children at ages 7–11 years, and seven studies included children at age 6 years or under. Most studies (23 out 36) included more than one age group. Where reported, birth year of participants ranged from 1924 to 1989.
| Study | Cohort | Number at baseline | Number at follow-up | Childhood age (years) | Adult age at final follow (years) | Male (%) |
|---|---|---|---|---|---|---|
| Ahlgren (2004)140 | Copenhagen – CSHRR | 161,063 | 117,415 | 7–14 | NR | 0 |
| Baker (2007)142 | Copenhagen – CSHRR | 276,835 | NR | 7–13 | NR | 51 |
| Baker (2007)141 | Copenhagen – CSHRR | 276,835 | NR | 7–13 | ≥ 25 | 51 |
| Barker (2002)143 | Helsinki (1934–44) | 10,519 | 8760 | 1–12 | 27–63 | 53 |
| Barker (2005)144 | Helsinki (1934–44) | 10,519 | 8760 | 0–11 | 27–64 | 53 |
| Berentzen (2013)145 | Copenhagen – CSHRR | 372,636 | 285,884 | 7–13 | 31–80 | 51 |
| Bjorge (2004)146 | Norway 1963–99 | 227,224 | 227,221 | 14–19 | 47–52 | 51 |
| Bjorge (2008)147 | Norway 1963–99 | 227,000 | 226,682 | 14–19 | Mean 52 | 51 |
| Cheng (2011)117 | Beijing – BCAMSS | 2189 | 1184 | 6–16 | 16 (SD 1.8) | 54 |
| Cheung (2004)118 | UK – NCDS | 17,000 | 12,327 | 7, 11, 16 | 42 | 52 |
| De Stavola (2004)148 | UK – MRC NSHD | 2547 | 2187 | 2–15 | 47–53 | 0 |
| Engeland (2003)149 | Norway 1963–99 | NR | 111,883 | 14–19 | Mean 41 | 0 |
| Eriksson (2001)150 | Helsinki (1934–44) | 5502 | 3544 | 0–12 | 27–63 | 100 |
| Forsen (2000)151 | Helsinki (1924–34) | NR | 7086 | 6–16 | 31–73 | 51 |
| Forsen (2004)152 | Helsinki (1934–44) | 5486 | 3003 | 0–11 | 27–64 | 0 |
| Goldhaber-Fiebert (2013)123 | USA – NLSY79/PSID/NHANES | NR | 2780 | 2–15 | 38–49 | 51 |
| Gunnell (1998)153 | England and Scotland (Boyd Orr) | NR | 2399 | 2–14 | Up to 73 | 49 |
| Hilakivi-Clarke (2001)154 | Helsinki (1924–34) | NR | 3447 | 7–15 | Minimum 38 (76% > 50) | 0 |
| Hypponen (2003)155 | Great Britain – British birth cohort | 16,751 | 10,683 | 7, 11, 16 | 41 | NR |
| Israeli (2007)156 | Israel – SPEC | 18,513 | NR | 16–19 | 26–45 | 100 |
| Janssen (2005)157 | USA – Bogalusa Heart Study | 3865 | 1709 | 4–15 | 19–38 | 44 |
| Jeffreys (2004)158 | England and Scotland (Boyd Orr) | 2997 | 2347 | 2–14 | Up to 66 | 49 |
| Lawlor (2005)159 | Aberdeen cohort | 12,150 | 11,106 | Mean 4.9 | 48–54 | NR |
| Lawlor (2006)160 | Aberdeen cohort | 12,150 | 5793 | Mean 4.9 | 46–50 | NR |
| Leiba (2012)161 | Israeli army | NR | 1,110,835 | 16–19 | Mean 35 | 100 |
| Leiba (2013)162 | Israeli army | NR | 1,110,835 | 16–19 | Mean 44 | 100 |
| Levi (2011)163 | Israeli army | NR | 1,109,864 | 16–19 | 18.7–57.3 | 100 |
| Levi (2012)164 | Israeli army | NR | 720,927 | 16–19 | 29–56 | 100 |
| Li (2007)165 | Great Britain – British birth cohort | 13,294 | 9285 | 7–16 | 45 | 52 |
| Mattsson (2008)167 | Cardiovascular Risk in Young Finns | 4320 | 2195 | 3–18 | 24–39 | 46 |
| Magnussen (2010)166 | Cardiovascular Risk in Young Finns/Bogalusa | 20,745 | 10,439 | 12–19 | 19–26 | 51.1 |
| Merten (2010)129 | USA – NLSAH | 1889 (PFS: 822; NGHS: 1067) | Up to 1058 (NGHS) | PFS: mean 12.4; NGHS: NR | PFS: 32–44; NGHS: 19 | PFS: 47; NGHS: 0 |
| Morrison (2010)168 | USA – NGHS and PFS | NR | 12,439 | 0–11 | NR | 52 |
| Osmond (2007)169 | Helsinki (1934–44) | 8181 | 1492 | 2–14 | 26–33 | 58 |
| Sachdev (2009)170 | India (Delhi) | 8498 | 2188 | 7–15 | 26–36 | 50 |
| Schmidt (2011)171 | Australia – ASHFS | NR | 37,674 | Mean 17.1 | Mean 34 | 100 |
| Tirosh (2011)172 | Israel – SPEC | 161,063 | 117,415 | Median 7.2–14.5 | NR | 0 |
Seven studies included male individuals only150,156,161–164,172 and five studies focused exclusively on females. 140,148,149,152,154 All other studies included mixed populations. Three USA-based studies included a significant proportion of black American children. 129,157,168 Two studies classed all or nearly all of their participants as Caucasian. 156,167 Four studies, which focused on the Israeli Army cohort, reported a varied range of geographical origins. 129,162–164 The remaining 27 studies did not report the ethnicity or origin of the children they included.
Seven studies reported data on baseline SES. Of those, three were part of the Israeli army cohort,161,162,164 where most individuals were classed as having ‘medium’ SES. Most individuals in the Cardiovascular Risk in Young Finns cohort were also classed as having medium SES,167 although SES definitions were not provided in these studies. Children in the remaining three studies reported a majority of individuals whose fathers were from a low SES. 151,152,158
Sixteen studies reported baseline data on the proportion of children who were overweight and/or obese according to BMI at baseline. 117,118,123,146,147,149,156–165 Definitions of overweight and obese varied across these studies. One study [Cheng et al. (2011)117] reported a high percentage of obese children at baseline (40.8%). The percentage of obese children ranged from 1% to 6.4% in other studies. 118,123,147,156,157,159,160,165 Where reported, the percentage of overweight children ranged from 6% to 18% at baseline. 118,123,146,147,156,157,159,160,165 In one study, the majority of children were overweight or obese at baseline [Cheng et al. (2011)117]. The percentage of children who were overweight or obese ranged from 3.8% to 21% in other studies. 118,123,147,149,156–165
Findings from the review of adult morbidity
Meta-analysis
The meta-analysis was based on 26 published articles representing 13 cohort studies,117,129,140–142,145,146,148–151,153–155,158–166,168,169,172 which provided data that could be converted into an OR per 1-SD increase in BMI for each morbidity. There were 32 different classifications of morbidity reported. This analysis considered only those morbidities described in Chapter 2.
Analysis of the association between childhood obesity/overweight and adult morbidity
A series of plots of the OR per SD increase in BMI for having a morbidity (with 95% CIs) are presented for each cohort and each morbidity, according to the age at which BMI was measured. Figures 4–7 present results for diabetes, CHD and cancers, as examples. A plot showing the results for all morbidities is provided in Appendix 5.
FIGURE 4.
Childhood BMI and incidence of adult diabetes. NGHS, National Growth and Health study; NLSAH, National Longitudinal Study of Adolescent Health; PFS, Princeton follow-up study; SPEC, Staff Periodic Examination Center.
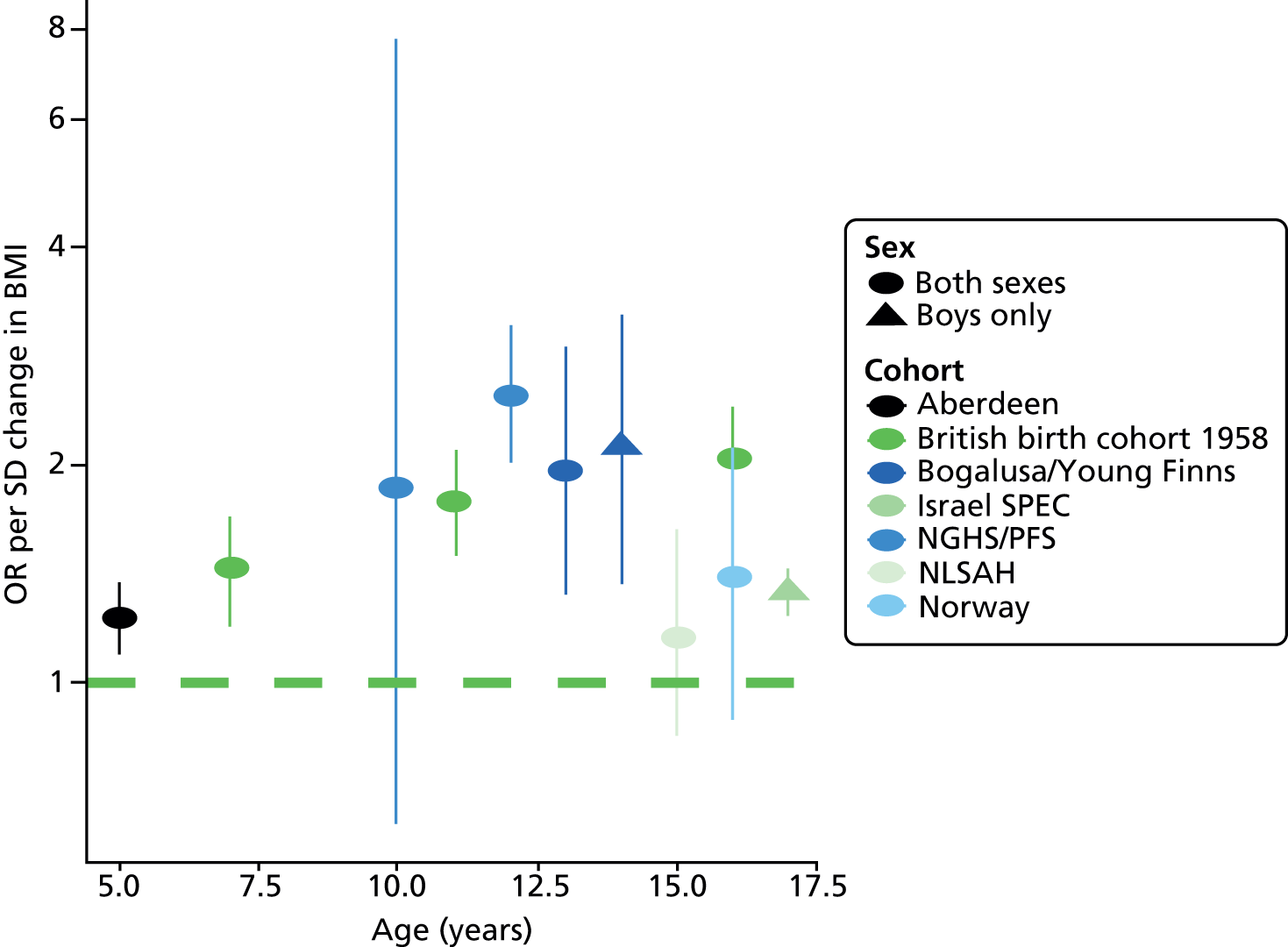
FIGURE 5.
Childhood BMI and incidence of adult CHD. SPEC, Staff Periodic Examination Center.

FIGURE 6.
Childhood BMI and incidence of adult breast cancer. MRC NSHD, Medical Research Council National Survey of Health and Development.
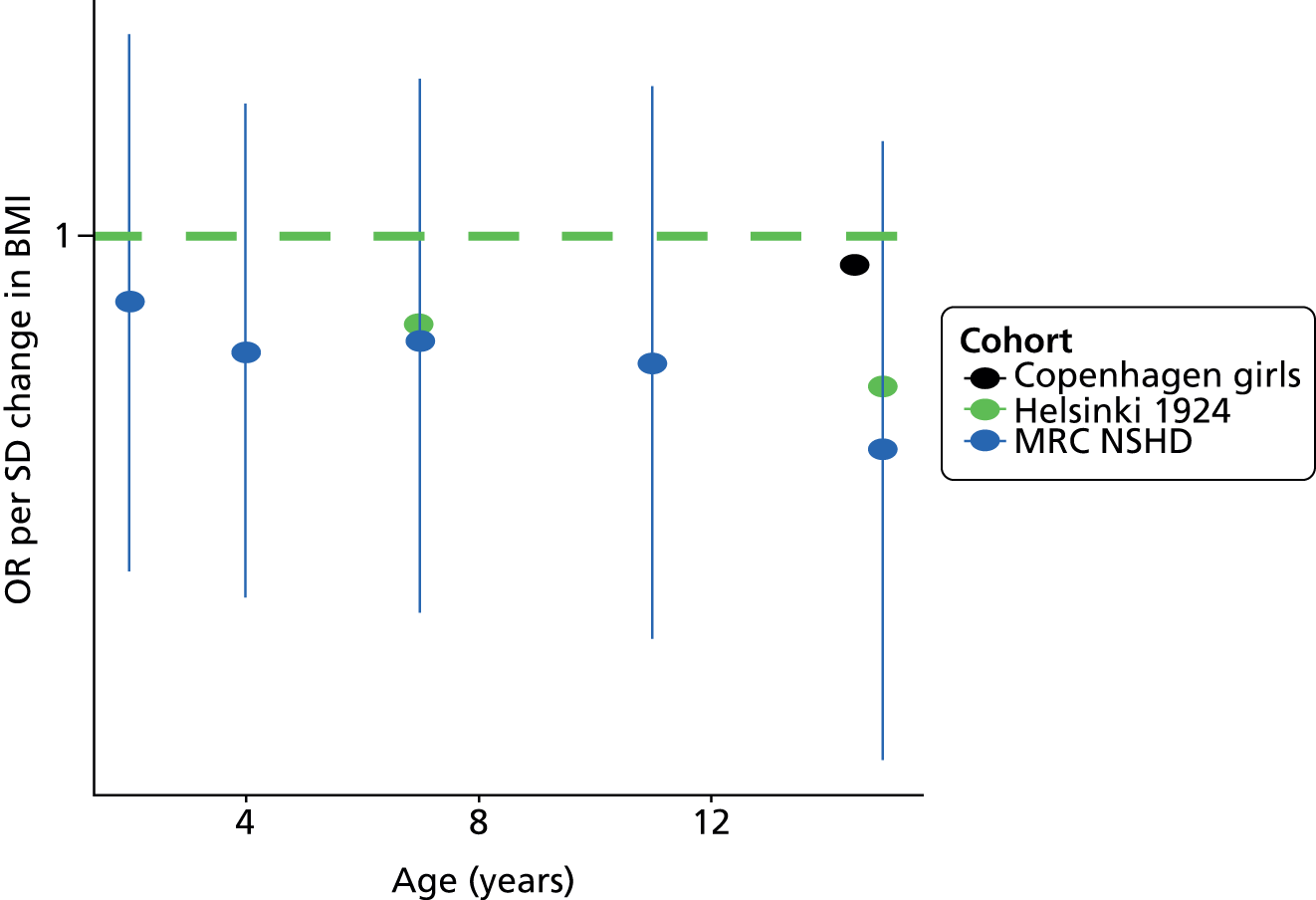
FIGURE 7.
Childhood BMI and incidence of other cancers.

Figure 4 shows the ORs for having adult diabetes, according to age. This shows that most cohorts showed a statistically significant association between childhood BMI and adult diabetes, with ORs ranging from 1.2 to 2.5 per SD BMI. Figure 5 shows the association with CHD. Results here were more varied, with two cohorts (Helsinki,150 Aberdeen159) showing no association and the others showing a modest increase in odds of CHD with increased BMI. Figure 6 shows the association of BMI with breast cancer. In this case there were no statistically significant results in any cohort. Figure 7 shows the results for other cancers. The cohort studies reported on a large number of cancers, but the general trend appears to be that higher BMI is associated with higher odds of most cancers.
The meta-analyses of ORs per SD BMI of these cohort studies are presented in forest plots, categorised by age at BMI measurement (Figures 8–13).
FIGURE 8.
Forest plot of the association between childhood BMI and diabetes. NGHS, National Growth and Health study; NLSAH, National Longitudinal Study of Adolescent Health; PFS, Princeton follow-up study; SPEC, Staff Periodic Examination Center.
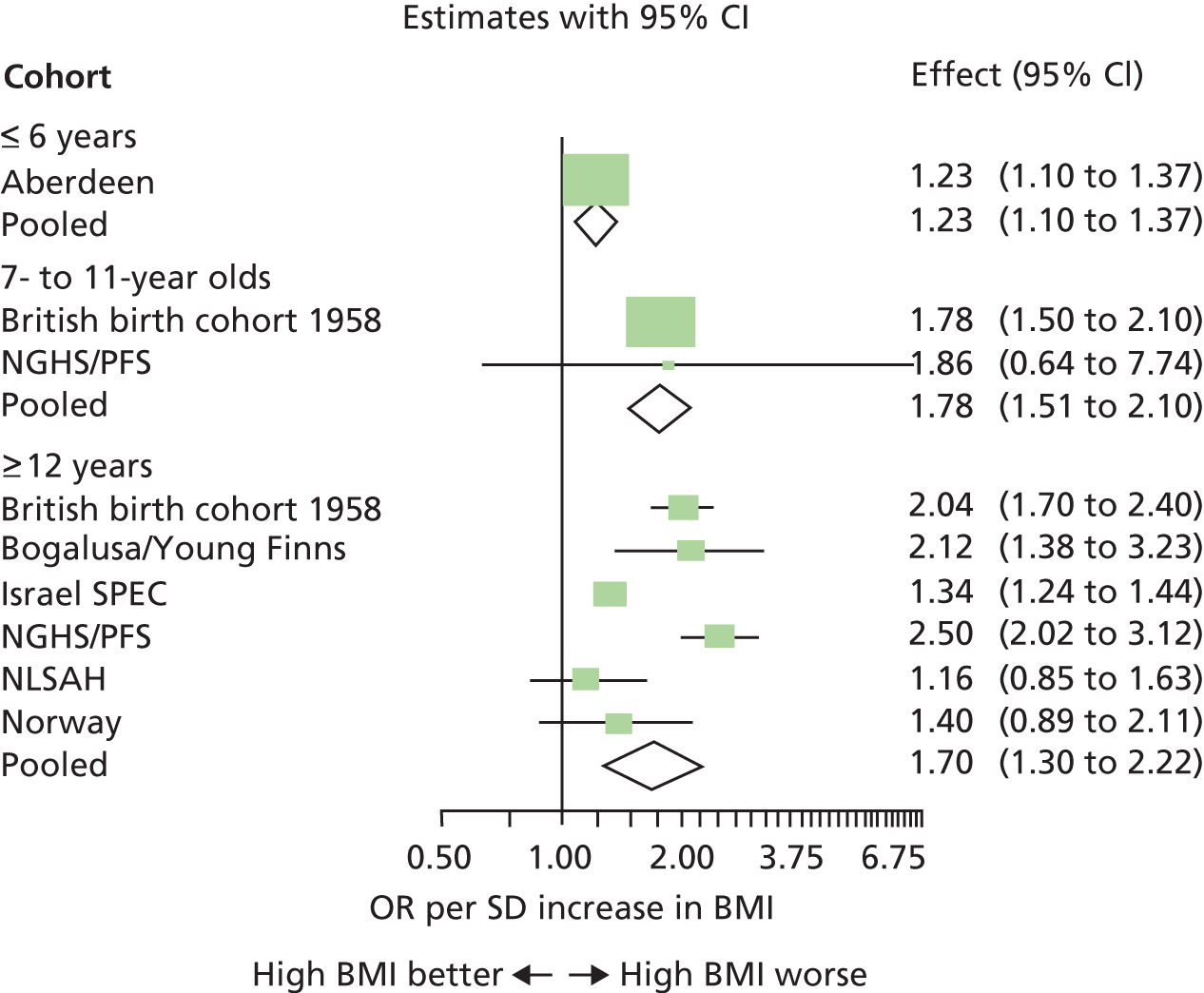
FIGURE 9.
Forest plot of the association between childhood BMI and CHD. SPEC, Staff Periodic Examination Center.

FIGURE 10.
Forest plot of the association between childhood BMI and stroke.
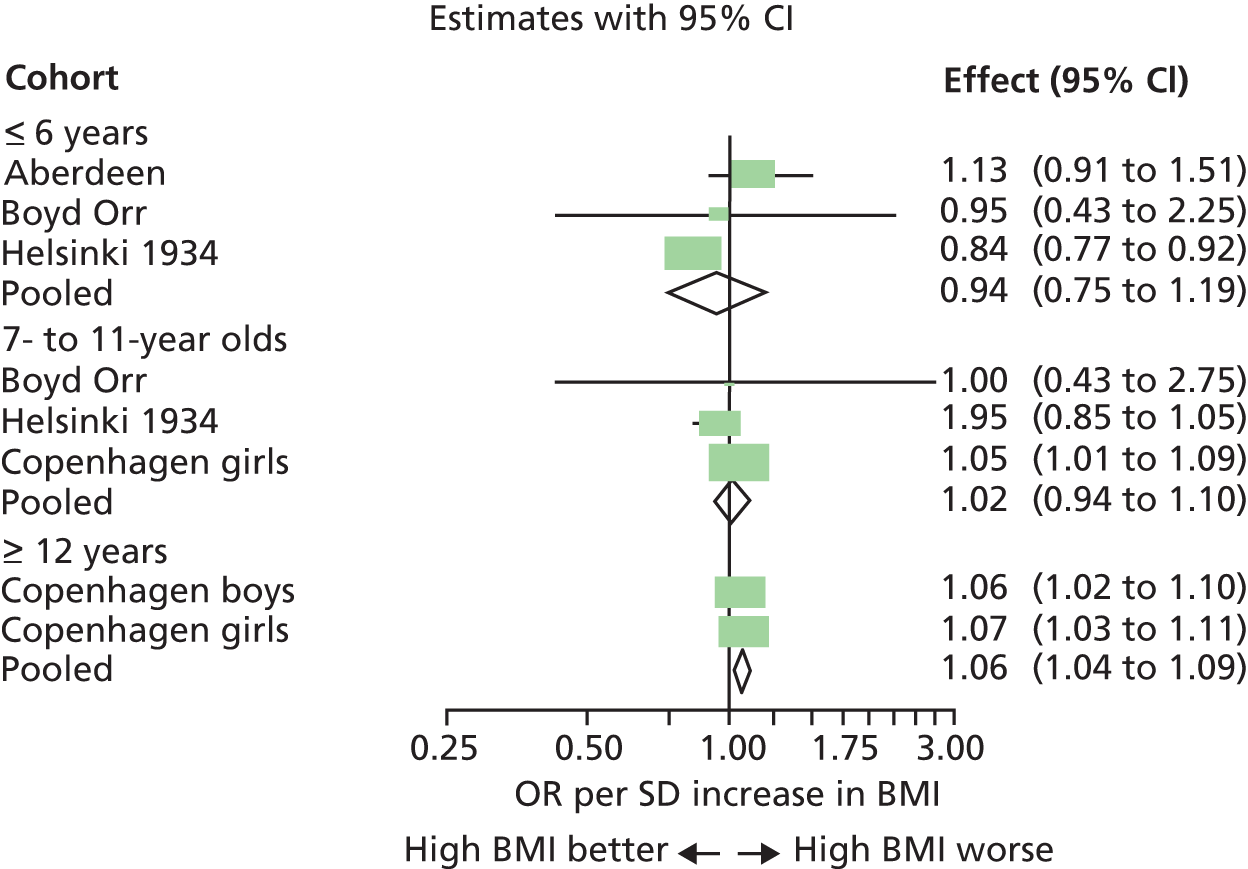
FIGURE 11.
Forest plot of the association between childhood BMI and hypertension. BCAMSS, Beijing Child and Adolescent Metabolic Syndrome study; NLSAH, National Longitudinal Study of Adolescent Health.
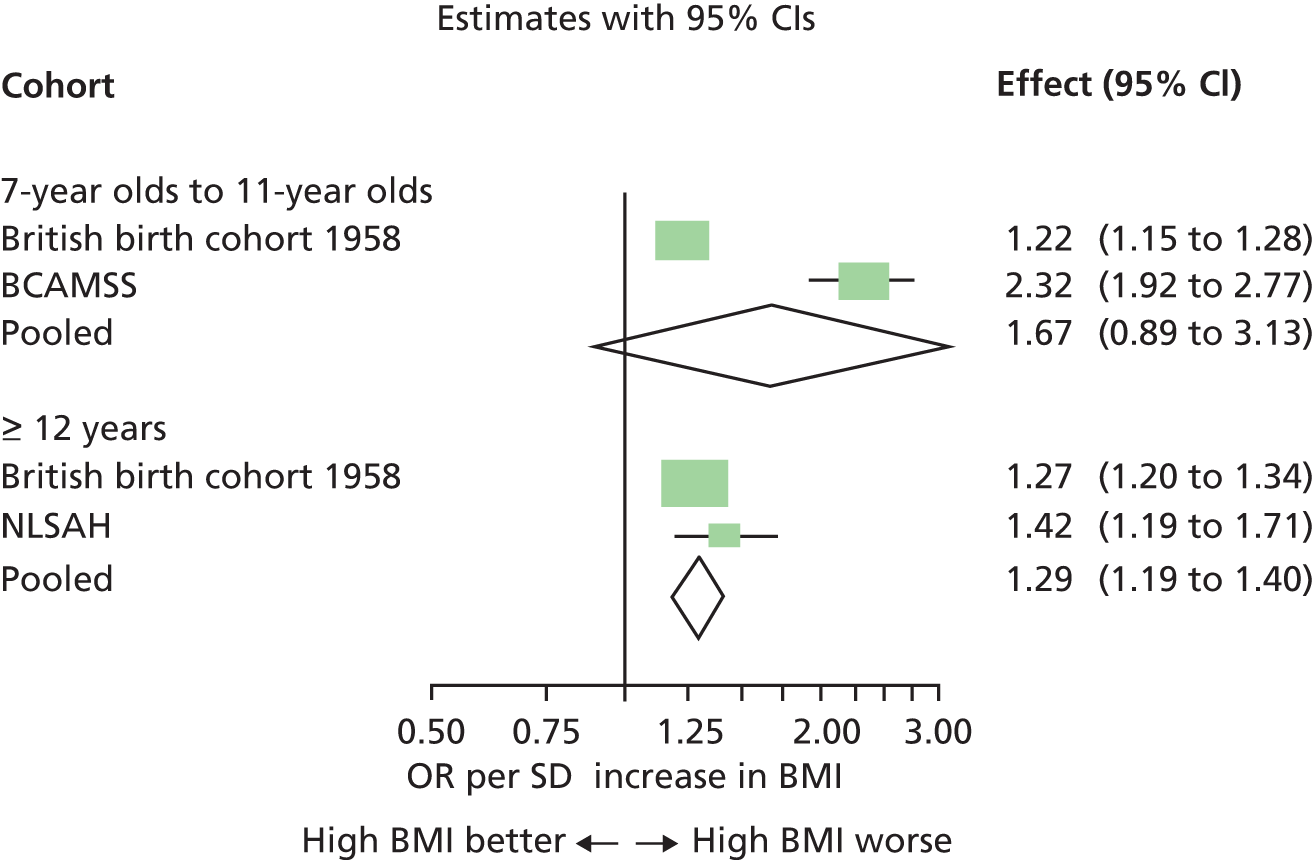
FIGURE 12.
Forest plot of the association between childhood BMI and breast cancer. MRC NSHD, Medical Research Council National Survey of Health and Development.
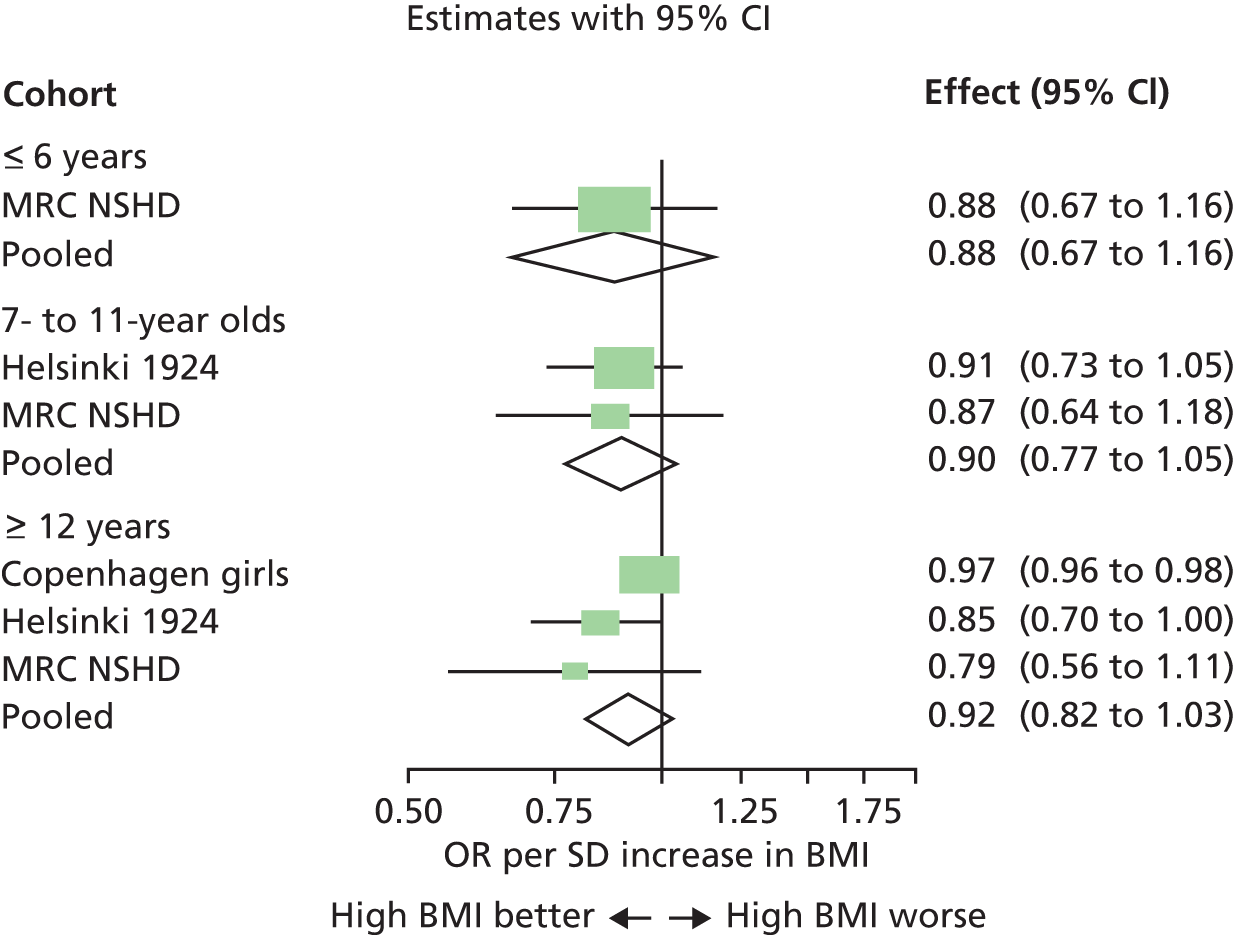
FIGURE 13.
Forest plot of the association between childhood BMI and cancers.

Figure 8 shows the results of the meta-analysis of diabetes. There is a positive association, with an OR of 1.7 for every SD increase in BMI. That is approximately equivalent to a 24% increase in odds per kg/m2 increase in BMI for an adolescent. There is no evidence that this is different in the under-twelves and over-twelves, although data for under-twelves are limited.
Figure 9 shows that there is a positive association between childhood BMI and CHD, but it is weak, with an OR per SD BMI of 1.2 in those aged over 12 years (approximately equivalent to an 8% increase in odds per kg/m2 increase in BMI for an adolescent). Again, there is no evidence that the association differs between children aged under and over 12 years, although an increasing trend with age was observed in two cohorts (see Figure 5). 142,150
Figure 10 shows the association with stroke. There is little evidence of any association between childhood BMI and stroke; the statistically significant result in those aged over 12 years is based on a single-cohort study. 142 Figure 11 shows the association with hypertension. There is some evidence that childhood BMI is positively associated with odds of adult hypertension, but the results are based on only three cohorts. 117,129,165
Figure 12 shows the relationship between childhood BMI and breast cancer. The results are not statistically significant, but the trend is negative. Figure 13 shows the association between childhood BMI and other cancers. No pooled result is presented because of the diversity of types of cancer and because more than one cancer is reported in some cohorts, but the overall trend is for a modest positive association between BMI and the odds of cancer. The results are comparatively homogeneous, with an increase in odds of around 1.2 per SD increase in BMI.
It should be noted that, because of the incorrect assumption that BMI is normally distributed, all the summary ORs presented in Figures 8–13 are likely to be overestimates.
Prediction of future morbidity from childhood body mass index
The analyses so far have examined the association between childhood BMI and adult morbidity. This section considers how well childhood BMI predicts future morbidity.
Given the normality assumptions made about the distribution of BMI described in Chapter 2, the association between BMI and morbidity can be used to estimate the predictive performance of childhood obesity for predicting future morbidity. This is because there is a simple relationship between OR per SD and the sensitivity at a specified threshold of BMI (i.e. the proportion of adults with the morbidity who were above the specified threshold of BMI in childhood). As noted in Chapter 2, this assumption is likely to result in overestimation of these sensitivities.
Results for sensitivity at the 85th centile of childhood BMI and above are presented, that is what proportion of adult morbidity occurs in children who might be considered overweight or obese, based on their BMI. Figure 14 presents the results for diabetes, and Figure 15 those for CHD. Plots for other morbidities are given in Appendix 5.
FIGURE 14.
Predicting future diabetes from childhood BMI. NGHS, National Growth and Health study; NLSAH, National Longitudinal Study of Adolescent Health; PFS, Princeton follow-up study; SPEC, Staff Periodic Examination Center.

FIGURE 15.
Predicting future CHD from childhood BMI. SPEC, Staff Periodic Examination Center.

The pattern of these two figures is identical to that seen in Figures 4 and 5, although the scales differ. The pattern of results is likewise the same for all other morbidities (see Appendix 5). These two examples show that, despite the association between obesity and later morbidity, childhood obesity is a poor predictor of morbidity. At best, around 40% of adults with diabetes were overweight or obese (above the 85th centile of BMI) as children. Only around 20% of adult CHD morbidities occurred in the most overweight 15% of children. Based on these findings, it appears that childhood BMI is not a useful predictor of future heart disease.
Summary receiver operating characteristic curves
To summarise the ability of childhood BMI to predict future morbidity, summary ROC curves are presented, based, again, on the assumptions of normally distributed BMI, and using the results from the analyses presented in the forest plots above (see Figures 4–13). As noted in Chapter 2, these summary curves probably overestimate predictive accuracy.
There are two figures: Figure 16 shows summary ROC curves for predicting morbidities for ages 7–11 years, and Figure 17 shows the ROC curves for children aged 12 years and over (these data are too sparse to present ROCs for under-sevens). Breast cancer and stroke are not included, as the analyses above found no evidence of an association between BMI and these morbidities.
FIGURE 16.
Receiver operating characteristic curves for predicting future morbidity from BMI at ages 7–11 years.
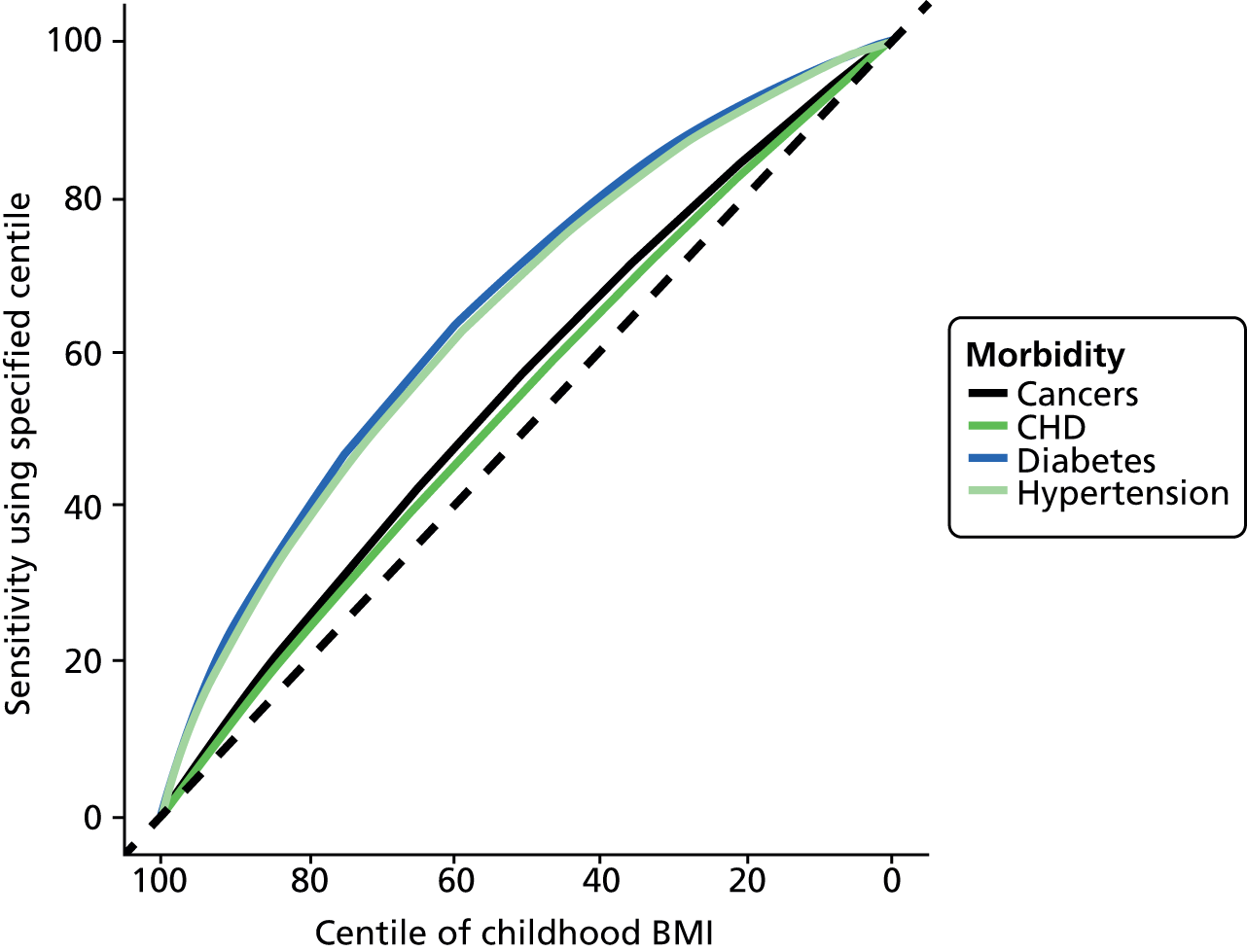
FIGURE 17.
Receiver operating characteristic curves for predicting future morbidity from BMI at ages 12 years and over.

The figures show that the power of BMI measurement to predict adult morbidities is poor. BMI cannot adequately predict future CHD or cancer (the cancer ROC curve is hidden under the CHD curve in Figure 17). Only around 20% of future CHD and cancer occurs in overweight or obese children. If we consider only obese children (above the 95th centile), then obesity cannot predict CHD or cancer; the results are no better than chance. Even for diabetes, which has the strongest association with obesity, only around 35% of adult diabetics were obese or overweight as adolescents. The ROC curve for hypertension is presented, but may not be reliable as it is based on very limited data (two cohorts). It should also be noted that, because of the assumption that BMI is normally distributed, even these poor levels of predictive accuracy may be overestimates.
Narrative review
Fourteen eligible studies reported relevant outcomes data that could not be included in the meta-analyses. 117,118,123,129,143,144,146,151,156,157,167,168,170,171 Of those, three also reported data that were included in the quantitative synthesis. 117,129,168
Thirteen studies included in the narrative review reported data on the association between childhood measurements and adult morbidity expressed in terms of RR, OR, HR or cumulative incidence. 117,123,129,143,144,146,151,156,157,166,167,170,171 Predictive accuracy data [expressed in terms of sensitivity, specificity and area under the curve (AUC)] were reported in four studies. 118,168,170,171
The evidence presented below was generally consistent with the findings presented in the meta-analyses, and provided relatively little additional evidence. However, unlike the meta-analyses, we were able to present some additional findings on simple measures of obesity other than BMI (WC, WHR, sum of SFTs), as well as the association between childhood weight status and future development of the metabolic syndrome in adults.
Association between childhood measurements and adult morbidity (13 studies)
All 13 studies used BMI as a weight status measurement in childhood. Two studies used WC in addition to BMI,117,171 and one study reported additional results for WHR and sum of SFTs. 171 The following morbidities were reported: type II diabetes (two studies),123,151 CHD (one study),144 renal cell carcinoma (one study),146 metabolic syndrome (five studies),157,166,167,170,171 hypertension (six studies),117,123,143,156,157,171 and hypercholesterolaemia (one study). 222 All studies found positive associations between childhood measurements of weight status and morbidities in adulthood.
Forsen et al. (2000)151 found a positive trend in cumulative incidence of type 2 diabetes in adulthood associated with higher BMI at 11 years in a cohort of 7806 males and females. Although statistically significant, the strength of the association was not reported. Subgroup analyses found that in women, BMI at every age from 7 to 15 years was significantly associated with risk of the disease, but not in men.
Goldhaber-Fiebert et al. (2013)123 found a weak association between BMI below age 10 years and projected diabetes in adulthood. For those who were white and above the 85th centile (CDC 2000219) at age 5 years, their model predicted that 7.9% of males would develop uncontrolled diabetes by their mid-40s, compared with an estimated 4.9% below that threshold (RR 1.6 for males). At age 15 years, the strength of the association was significantly higher. In this age group, it was estimated that 12.6% of males above the 85th centile (CDC 2000219) would develop uncontrolled diabetes by their mid-40s, whereas 2.8% of males below the threshold would develop the condition (RR 4.5 for males). RRs were not reported for females or for other ethnicity groups.
Barker et al. (2005)144 found that low BMI at age 2 years and high BMI at 11 years were both associated with higher risk of CHD events. The HRs associated with an increase in BMI of 1 SD were 0.76 (95% CI 0.66 to 0.87) for boys and 0.62 (95% CI 0.46 to 0.82) for girls at age 2 years, and 1.14 (95% CI 1.00 to 1.31) for boys and 1.35 (95% CI 1.02 to 1.78) for girls at age 11 years. Subgroup analyses stratified by BMI at ages 2 and 11 years found that the risk of developing CHD in adulthood was highest among children with a low BMI at age 2 years who had a high BMI at 11 years (HR 3.1, 95% CI 1.3 to 7.8), compared with children with a high BMI at age 2 years and a low BMI at 11 years.
There was consistent evidence of a positive association between childhood weight status and hypertension in adulthood. The odds of developing hypertension in adulthood were higher in male regular army personnel who were classed as overweight or obese according to BMI [Israeli et al. (2007)156]. Among individuals with normal baseline blood pressure, a BMI above 25 kg/m2 at ages 16.5–19 years was associated with significantly higher odds of being hypertensive at ages 26–45 years than a BMI below that threshold (OR 2.28, 95% CI 2.08 to 2.51 for a BMI of 25–30 kg/m2; OR 5.45, 95% 4.75 to 6.24 for a BMI above 30 kg/m2). Associations were higher for adolescents who were hypertensive at baseline (OR 3.1, 95% CI 2.78 to 3.46 for a BMI of 25–30 kg/m2; OR 6.45, 95% CI 5.53 to 7.53 for a BMI above 30 kg/m2).
The Chinese study by Cheng et al. (2011)117 reported higher odds of developing hypertension in adulthood among obese and overweight children measured at a mean age of approximately 11 years. Based on WC, obese children had an OR of 3.9 (95% CI 2.8 to 5.3) of being hypertensive 9 years later compared with non-obese children. When BMI was used to calculate weight status, the study also found increased odds of being hypertensive at follow-up among overweight (OR 2.6, 95% CI 1.6 to 4.2) and obese children (OR 4.9, 95% CI 3.4 to 7.0) compared with children with healthy weight status. Although associations between childhood obesity and hypertension in adulthood were reported for both WC and BMI, the comparators used for calculating ORs differed between the two measurements (obese vs. non-obese for WC, obese vs. healthy weight for BMI), limiting the comparability of the estimates of association. Additionally, the study did not assess the predictive accuracy of either of the childhood measurements. Therefore, the predictive accuracy of BMI and WC could not be compared.
Schmidt et al. (2011)171 also found a positive association between childhood WC and hypertension in adulthood. The risk of being hypertensive in adulthood was higher in girls for every 10-cm increase in WC (RR 1.6, 95% CI 1.2 to 2.1) than in boys (RR 1.2, 95% CI 1.0 to 1.4). WC measurements were not adjusted for age, although they were made in children aged from 7 to 15 years.
Barker et al. (2002)143 found a statistically significant association between high BMI from 8 to 12 years and hypertensive drug use in adulthood. At age 12 years, the study reported a statistically significant increase in the cumulative incidence of hypertension for each additional BMI point (14.2%, 95% CI 12.3% to 16.0%, for an adjusted BMI of 16 kg/m2, and 19.9%, 95% CI 18.1% to 21.7%, for an adjusted BMI of > 18 kg/m2).
Janssen et al. (2005)157 found a significant increase in the odds of developing hypertension measured with BMI at ages 5–14 years in overweight and obese children, although the relationship was statistically significant in obese children only (OR 4.39, 95% CI 1.83 to 9.72).
The model developed by Goldhaber-Fiebert et al. (2013)123 found that prevalence of hypertension in adulthood would be higher among children above the 85th centile of a US population distribution (CDC 2000219) at ages 5 and 15 years, irrespective of sex and ethnic group. However, the authors did not report whether or not these differences were statistically significant, nor did they report sufficient data to evaluate the extent to which higher childhood BMI may accurately predict hypertension among adults.
Only one study reported an association between childhood obesity and future development of hypercholesterolaemia in adulthood. Merten et al. (2010)222 found that adolescents who were obese according to BMI had higher odds of developing hypercholesterolaemia 6 years later (OR 1.81, 95% CI 1.22 to 2.75). Further results are presented in Table 5.
| Study | Age at baseline (years) | Age at follow-up (years) | n at follow-up | Outcome | Comparison | Childhood measurement | Effect size (95% Cl) | Adjustment |
|---|---|---|---|---|---|---|---|---|
| Forsen (2000)151 | 11 | 31–73 | 7806 | T2DM | NA | BMI ≤ 15.3 kg/m2 | Cumulative incidence 5.8% | Age and sex |
| BMI 15.4–15.9 kg/m2 | Cumulative incidence 6.7% | |||||||
| BMI 16.0–16.6 kg/m2 | Cumulative incidence 5.9% | |||||||
| BMI 16.7–17.4 kg/m2 | Cumulative incidence 6.7% | |||||||
| BMI > 17.4 kg/m2 | Cumulative incidence 8.4% (p-value for trend in women and both sexes < 0.001) | |||||||
| Goldhaber-Fiebert (2013)123 | 5–15 | 38–49 | 2780 | T2DM | > 85th vs. < 85th centile | BMI at 5 years | RR 1.6 (NR) | Age and sex |
| BMI at 15 years | RR 4.5 (NR) | |||||||
| Hypertension | NA | BMI (< 85th centile) | Prevalence 38.9–63.1% | |||||
| BMI (> 85th centile) | Prevalence 44.1–66.9% | |||||||
| Barker (2005)144 | 2 and 11 | 27–64 | 8760 | CHD (fatal or non-fatal) | Per 1-SD increase at 2 years | BMI | HR 0.76 (0.66 to 0.87)a | Age and sex |
| Per 1-SD increase at 11 years | HR 1.14 (1.00 to 1.31)a | |||||||
| Bjorge (2004)146 | 14–19 | 45 | 227,221 | RCC | ≥ 85th vs. 25th–74th | BMI | RR 2.64 (1.48 to 4.7) (boys) RR 1.48 (0.57 to 3.85) (girls) |
Age and sex |
| Janssen (2005)157 | 5–14 | 19–38 | 1709 | Metabolic syndrome (NCEP) | OW vs. < 85th centileb | BMI | OR 2.53 (2.26 to 5.42) | Age, sex, race, follow-up length |
| OR 4.62 (2.81 to 7.45) | ||||||||
| Hypertension | OW vs. < 85th centileb | BMI | OR 2.04 (0.7 to 5.12) | |||||
| OR 4.39 (1.83 to 9.72) | ||||||||
| Sachdev (2009)170 | 2–14 | 26–33 | 1492 | Metabolic syndrome (IDF 2009223) | Per 1-SD increase | BMI at 2 years | OR 1.2 (1.04 to 1.37) | Age and sex |
| BMI at 5 years | OR 1.19 (1.05 to 1.35) | |||||||
| BMI at 8 years | OR 1.36 (1.21 to 1.53) | |||||||
| BMI at 11 years | OR 1.63 (1.43 to 1.85) | |||||||
| BMI at 14 years | OR 1.87 (1.65 to 2.12) | |||||||
| Mattsson (2008)167 | 3–15 | 24–39 | 2195 | Metabolic syndrome (IDF 2005224) | > 80th centile (approximately 17 kg/m2) | BMI at 3–9 years | OR 3.0 (2.0 to 4.7) | Age and sex |
| > 80th centile (approximately 21.5 kg/m2) | BMI at 12–15 years | OR 2.1 (1.4 to 3.1) | ||||||
| Magnussen (2010)166 | 9–18 | 24–41 | 1755–1781 | Metabolic syndrome (IDF 2009223) | OW/O vs. non-OW/Oc | BMI | RR 2.5 (2 to 3.1) | All other metabolic syndrome components at baseline, follow-up duration, cohort |
| Schmidt (2011)171 | 7–15 | 26–36 | 2188 | Metabolic syndrome (IDF 2009223) | 4th quartile vs. 1st quartile | WC | RR 4.8 (2.5 to 9.2) (men) RR 5.8 (2.4 to 14.2) (women) |
Age, sex, follow-up |
| 4th quartile vs. 1st quartile | BMI | RR 3.0 (1.7 to 5.4) (men) RR 5.0 (2.0 to 12.3) (women) |
||||||
| 4th quartile vs. 1st quartile | WHR | RR 2.1 (1.3 to 3.6) (men) RR 4.6 (1.5 to 14.1) (women) |
||||||
| 4th quartile vs. 1st quartile | Sum SFT | RR 2.6 (1.0 to 7.2) (men) RR 11.2 (1.4 to 91.3) (women) |
||||||
| Hypertension | 10-cm increase | WC | RR 1.2 (1.0 to 1.4) (men) RR 1.6 (1.2 to 2.1) (women) |
Sex, change in WC, smoking, alcohol consumption | ||||
| Cheng (2011)117 | 10.5 | NR | 1180 | Hypertension | O vs. non-O | WCd | OR 3.9 (2.8 to 5.3) | Age and sex |
| OW vs. HW | BMId | OR 2.6 (1.6 to 4.2) | ||||||
| O vs. HW | OR 4.9 (3.4 to 7.0) | |||||||
| Barker (2002)143 | 12 | 27–63 | 8760 | Hypertension | NA | BMI (16 kg/m2) | Cumulative incidence 14.2% (12.3% to 16%) | Age only |
| BMI (17 kg/m2) | Cumulative incidence 14.2% (12.4% to 16%) | |||||||
| BMI (18 kg/m2) | Cumulative incidence 15.4% (13.5% to 17.4%) | |||||||
| BMI (> 18 kg/m2) | Cumulative incidence 19.9% (18.1% to 21.7%) | |||||||
| Israeli (2007)156 | 16.5–19 | 26–45 | 18,513 | Hypertension | OW vs. HWe | BMI (25–30 kg/m2) | OR 2.28 (2.08 to 2.51) (normal baseline tension) OR 3.1 (2.78 to 3.46) (high normal baseline tension) |
Age and sex |
| O vs. HWe | BMI (> 30 kg/m2) | OR 5.45 (4.75 to 6.24) (normal baseline tension) OR 6.45 (5.53 to 7.53) (high normal baseline tension) |
||||||
| Merten (2010)129 | 12–19 | 19–26 | 10,439 | Hypercholesterolaemia | O vs. non-Ob | BMI | OR 1.81 (1.22 to 2.75) | Sex, ethnicity, adult obesity, SES |
The definitions of metabolic syndrome differed slightly among the studies that reported this outcome. Three166,170,171 used the International Diabetes Federation (IDF) 2009 criteria,223 one167 used the IDF 2005 definition224 and one defined metabolic syndrome according to the National Cholesterol Education Program. 157 All studies reported a positive association between childhood weight status and future metabolic syndrome.
Sachdev et al. (2009)170 reported a statistically significant association between BMI at all ages from 2 to 14 years and metabolic syndrome at ages 26–33 years. The strength of the association was greater in adolescents (OR 1.87, 95% CI 1.65 to 2.12), followed by children at 11 (OR 1.63, 95% CI 1.43 to 1.85) and 8 years (OR 1.36, 95% CI 1.21 to 1.53). The strength of the association was weaker among children at 6 years or under (OR 1.19, 95% CI 1.05 to 1.35 at age 5 years; OR 1.2, 95% CI 1.04 to 1.37 at age 2 years).
Schmidt et al. (2011)171 reported the association between the risk of developing metabolic syndrome in adults and four different childhood measurements (BMI, WC, WHR and sum of SFTs) taken at ages 7–15 years. The risk of developing metabolic syndrome in adulthood was significantly higher among children within the highest quartile of the cohort than in the lowest quartile for all measurements, and the strength of the association was systematically greater in girls than in boys. The strongest associations between metabolic syndrome and childhood measurements were found with sum of SFT in girls (RR 11.2, 95% CI 1.4 to 91.3) and WC in boys (RR 4.8, 95% CI 2.5 to 9.2). The most conservative estimates were found with WHR in girls (RR 4.6, 95% CI 1.5 to 14.1), as well as in boys (RR 2.1, 95% CI 1.3 to 3.6). However, most results lacked precision (as evidenced by the wide CIs), making it difficult to compare the extent to which the strength of the associations varied across obesity measures. Additionally, the study did not report estimates of predictive accuracy for any of the childhood measurements. Therefore, the relative predictive accuracy of these childhood measures cannot be evaluated.
Magnussen et al. (2010)166 pooled data from the Young Finns Study [also reported in Mattsson et al. (2008)167] with results from the Bogalusa Heart Study on metabolic syndrome. The pooled analysis used the 91st centile as the threshold for obesity (based on Cole 2000220), and found a statistically significant association between obesity at ages 9–18 years and metabolic syndrome at ages 24–41 years (RR 2.5, 95% CI 2.0 to 3.1).
Janssen et al. (2005)157 found a statistically significant increase in the odds of developing metabolic syndrome in adulthood among overweight (OR 2.53, 95% CI 2.26 to 5.42) and obese children (OR 4.62, 95% CI 2.81 to 7.45) measured with BMI at ages 5–14 years. Similar results were reported for hypertension, although the association was statistically significant in obese children only (OR 4.39, 95% CI 1.83 to 9.72).
Mattsson et al. (2008)167 (Young Finns Study) reported a statistically significant association with metabolic syndrome in adulthood among children with a BMI above the 80th centile of the cohort and those below that threshold. Unlike the findings of Sachdev et al. (2009),170 the strength of the association tended to be greater among younger children (OR 3.0, 95% CI 2.0 to 4.7 at ages 3–9 years; OR 2.1, 95% CI 1.4 to 3.1 at ages 12–15 years).
Bjorge et al. (2004)146 found a statistically significant association between BMI above the 85th centile (CDC 2000219) and renal cell carcinoma at age 45 years in a sample of 115,267 adolescent boys (RR 2.64, 95% CI 1.48 to 4.7). However, the association was not statistically significant in 111,954 adolescent girls (RR 1.48, 95% CI 0.57 to 3.85). The fact that Bjorge et al. (2004)146 found a statistically significant association between BMI and renal cell carcinoma in adolescent boys but not in girls may be explained by a lack of power. Although the sample was large, the outcome of interest was very rare and therefore the subgroup of girls may not have been sufficiently large to show a statistically significant result.
Predicting future morbidity (four studies)
Four studies that were not included in the quantitative synthesis reported data on predictive accuracy (Table 6). 118,168,170,171 Overall, they confirmed the findings of the quantitative synthesis: obesity and overweight are poor predictors of future morbidity in adulthood.
| Study | Age at baseline (years) | Age at follow-up (years) | n at follow-up | Outcome | Comparison | Childhood measurement | Summary estimate (95% Cl) | Adjustment |
|---|---|---|---|---|---|---|---|---|
| Morrison (2010)168 | 10 | 19 | 1067 | T2DM | O vs. non-O | WC | Sensitivity: 13 Specificity: 96 PPV: 2 NPV: 99 |
None |
| BMI | Sensitivity: 13 Specificity: 96 PPV: 3 NPV: 99 |
|||||||
| Cheung (2004)118 | 7–16 years | 42 | 4047–4592 | Cancer | NA | BMI at 7 years | AUC: 0.46 (0.41 to 0.51) | Age |
| BMI at 11 years | AUC: 0.47 (0.42 to 0.513) | |||||||
| BMI at 16 years | AUC: 0.53 (0.47 to 0.58) | |||||||
| Hypertension | BMI at 7 years | AUC: 0.51 (0.48 to 0.53) | ||||||
| BMI at 11 years | AUC: 0.56 (0.53 to 0.59) | |||||||
| BMI at 16 years | AUC: 0.6 (0.57 to 0.63) | |||||||
| Diabetes | BMI at 7 years | AUC: 0.58 (0.51 to 0.66) | ||||||
| BMI at 11 years | AUC: 0.60 (0.52 to 0.67) | |||||||
| BMI at 16 years | AUC: 0.61 (0.54 to 0.68) | |||||||
| Metabolic syndrome | Cut-off: ≥ 85th centile (IOTF) | BMI at 5 years | Sensitivity: 1 Specificity: 98 |
Age, sex | ||||
| BMI at 8 years | Sensitivity: 1 Specificity: 99 |
|||||||
| BMI at 11 years | Sensitivity: 2 Specificity: 99 |
|||||||
| BMI at 14 years | Sensitivity: 7 Specificity: 97 |
|||||||
| Cut-off: ≥ 75th centile (internally derived) | BMI | Sensitivity: 50.8 Specificity: 80.0 |
||||||
| Sachdev (2009)170 | 2–14 | 26–33 | Metabolic syndrome | Cut-off: ≥ 85th centile (IOTF) | BMI at 5 years | Sensitivity: 1 Specificity: 98 |
Age, sex | |
| BMI at 8 years | Sensitivity: 1 Specificity: 99 |
|||||||
| BMI at 11 years | Sensitivity: 2 Specificity: 99 |
|||||||
| BMI at 14 years | Sensitivity: 7 Specificity: 97 |
|||||||
| Schmidt (2011)171 | 7–15 | 26–36 | 2188 | Metabolic syndrome (IDF 2009223) | 4th quartile vs. 1st quartile | Sum SFT: boys | Sensitivity: 30 (16 to 47) Specificity: 82 (77 to 86) AUC: 0.624 |
|
| Sum SFT: girls | Sensitivity: 58 (28 to 85) Specificity: 83 (79 to 87) AUC: 0.777 |
|||||||
| Sum SFT: unselected | Sensitivity: 37 (23 to 52) Specificity: 82 (79 to 85) AUC: NR |
|||||||
| 4th quartile vs. 1st quartile | WC: boys | Sensitivity: 45 (36 to 55) Specificity: 80 (77 to 82) AUC: 0.686 |
||||||
| WC: girls | Sensitivity: 49 (33 to 65) Specificity: 81 (78 to 83) AUC: 0.721 |
|||||||
| WC: unselected | Sensitivity: 46 (38 to 54) Specificity: 80 (78 to 82) AUC: NR |
|||||||
| 4th quartile vs. 1st quartile | WHR: boys | Sensitivity: 34 (25 to 43) Specificity: 79 (77 to 82) AUC: 0.612 |
||||||
| WHR: girls | Sensitivity: 33 (19 to 49) Specificity: 79 (77 to 82) AUC: 0.672 |
|||||||
| WHR: unselected | Sensitivity: 33 (26 to 41) Specificity: 79 (78 to 81) AUC: NR |
All reported weak estimates of predictive accuracy. Among the three studies that reported measures of sensitivity and specificity,166,168,170 all found that childhood BMI had high specificity but poor sensitivity when predicting adult morbidity. Of those, only one compared the predictive accuracy of more than one childhood measurement. 168 The study found that BMI and WC were equally accurate (high specificity and poor sensitivity) in predicting future morbidity among 10-year-old girls. The following outcomes were reported in adulthood: type 2 diabetes (two studies),118,168 metabolic syndrome (two studies)166,170 and hypertension (one study). 118
Cheung et al. (2004)118 reported that BMI values at ages 7, 11 and 16 years could predict self-reported history of diabetes at age 42 years. However, estimates were weak, with AUCs ranging from 0.58 to 0.61. Morrison et al. (2010)168 found that BMI and WC were equally accurate in predicting early adulthood diabetes in a relatively small sample (n = 1067) of 10-year-old obese girls. Both measurements had high specificity (96%) but low sensitivity (13%).
Cheung et al. (2004)118 reported that BMI values at ages 11 and 16 years could predict self-reported hypertension at age 42 years. However, as with diabetes, predictive estimates of adult hypertension were weak (AUC 0.56 at age 11 years and 0.60 at age 16 years). Further results are presented in Table 6.
Sachdev et al. (2009)170 found that BMI at 5, 8, 11 and 14 years had very high specificity (97–99%) but very low sensitivity (1–7%) when predicting metabolic syndrome in adulthood at ages 26–33 years. The pooled analysis from Magnussen et al. (2010)166 reported lower specificity (80%) and higher sensitivity (50.8%) for predicting adult metabolic syndrome at ages 24–41 years (CIs were not reported). The differences between the two studies may be explained by the use of different cut-off points. The pooled analysis from Magnussen et al. (2010)166 used a lower BMI cut-off point than the study by Sachdev et al. (2009)170 [internally derived 75th centile vs. IOTF 85th centile in Sachdev et al. (2009)170].
Cheung et al. (2004)118 found that BMI at ages 7, 11 and 16 years was a poor predictor of self-reported cancer at age 42 years (AUC ranging from 0.46 to 0.53).
Comparison of ‘simple’ measures of childhood obesity for prediction of adult morbidities
The evidence comparing BMI with alternative ‘simple’ measures of childhood obesity for predicting adult morbidity was very limited; the available studies are summarised in Table 7. As seen in the previous sections, only three studies evaluated relevant measures other than BMI. 117,168,171 All studies were relatively small (n = 1067 to n = 2188). All were subject to high risk of attrition bias117,168,171 and one was at high risk of bias associated with confounding factors and outcomes. 168
| Study | Age at baseline (years) | Age at follow-up (years) | Childhood measurement | n at follow-up | Outcome | Comparison | Effect size (95% CI) | Adjustment |
|---|---|---|---|---|---|---|---|---|
| Schmidt (2011)171 | 7–15 | 26–36 | WC | 2188 | Metabolic syndrome (IDF) | 4th quartile vs. 1st quartile | RR 4.8 (2.5 to 9.2) (men) RR 5.8 (2.4 to 14.2) (women) |
Age, sex, follow-up |
| BMI | 4th quartile vs. 1st quartile | RR 3.0 (1.7 to 5.4) (men) RR 5.0 (2.0 to 12.3) (women) |
||||||
| WHR | 4th quartile vs. 1st quartile | RR 2.1 (1.3 to 3.6) (men) RR 4.6 (1.5 to 14.1) (women) |
||||||
| Sum SFT | 4th quartile vs. 1st quartile | RR 2.6 (1.0 to 7.2) (men) RR 11.2 (1.4 to 91.3) (women) |
||||||
| WC | 2062 | Hypertension | 10-cm increase | RR 1.2 (1.0 to 1.4) (men) RR 1.6 (1.2 to 2.1) (women) |
Sex, change in WC, smoking, alcohol consumption | |||
| Cheng (2011)117 | 10.5 | NR | WC | 1180 | Hypertension | O vs. non-O | OR 3.9 (2.8 to 5.3) | Age, sex |
| BMI | OW vs. HW | OR 2.6 (1.6 to 4.2) | Age, sex | |||||
| O vs. HW | OR 4.9 (3.4 to 7.0) | Age, sex | ||||||
| Morrison (2010)168 | 10 | 19 | WC | 1067 | T2DM | O vs. non-O | Sensitivity: 13 Specificity: 96 PPV: 2 NPV: 99 |
None |
| BMI | O vs. non-O | Sensitivity: 13 Specificity: 96 PPV: 3 NPV: 99 |
None |
The available studies provide data only on WC, WHR and the sum of SFT measurements at more than one site (sum SFT). Accuracy data were only available for WC for predicting of diabetes. 168 Measures of association (RR, OR) between childhood measurements and adult morbidities were available for WC (for hypertension117,171 and metabolic syndrome171), and for WHR and sum SFT (metabolic syndrome only). 171
Schmidt et al. (2011)171 reported the association between the risk of developing the metabolic syndrome in adults and four different childhood measurements (BMI, WC, WHR and sum SFTs) between the ages of 7 and 15 years. As seen earlier, the association between the risk of developing the metabolic syndrome in adulthood and childhood weight status was consistently positive and statistically significant across all four childhood measures, and the strength of the associations was systematically greater in girls than in boys. However, most results lacked precision (as evidenced by the wide CIs), making it difficult to compare the strength of the associations across obesity measures.
The Chinese study by Cheng et al. (2011)117 reported higher odds of developing hypertension in adulthood among obese and overweight children measured at a mean age of approximately 11 years with both WC and BMI. Although associations between childhood obesity and hypertension in adulthood were reported for both WC and BMI, the comparators used for calculating ORs differed between the two measurements (obese vs. non-obese for WC, obese vs. healthy weight for BMI), which limits the comparability of the estimates of association. Additionally, as with Schmidt et al. (2011),171 the study did not assess the predictive accuracy of either of the childhood measurements. Therefore, their relative predictive accuracy cannot be compared.
Two studies compared the predictive accuracy of more than one childhood measure; one evaluated BMI and WC for predicting type 2 diabetes,168 and the other WC, SFT and WHR for predicting metabolic syndrome. 171 The study evaluating BMI and WC found that they were equally accurate in predicting early adult diabetes when conducted in 10-year-old girls; both had equally high specificity (96%) and poor sensitivity (13%). 168 However, the study had several limitations: the outcome of interest was collected through self-report and may have been contaminated by type 1 diabetes, follow-up duration was limited to only 9 years and the study did not report how WC was measured (including measurement site). The other study171 that categorised the most obese 25% as the ‘at-risk’ group reported poor sensitivity, which was generally below 50%, and moderate specificity; SFT appeared to be the most accurate of the three obesity measures (see Table 7).
Review of morbidities: summary of findings and conclusions
This review identified 37 cohort studies on the association between childhood weight status and adult morbidities. Of these, 26 were included in the meta-analyses. All the studies were large or very large cohort studies, most being from large national or community data sets. However, large proportions of participants were lost at final follow-up in many studies, making attrition the most common source of bias. Although most studies adjusted for key confounders such as age and sex, the observational design of the studies means that confounding bias cannot be ruled out. Studies were very diverse, with weight status measured at different ages and in different populations. Most studies tended to focus on older cohorts. Follow-up duration and age at final follow-up also varied significantly between the studies. In addition, relatively few studies were found for some outcomes. Given the range of morbidity-related outcomes that could be reported (particularly the large number of types of cancer), there is a possibility of selective reporting, where cohorts reported only outcomes showing a positive association between BMI and the outcome. These limitations should be considered when interpreting the results.
Overall, most studies reported a positive, statistically significant association between measures of childhood weight status and adult morbidity, but the findings varied by morbidity. There was consistent evidence of a statistically significant but modest association between childhood BMI and adult diabetes; there was insufficient evidence to show whether or not the association is stronger among older children. Results for CHD were more mixed, with some cohorts showing a negative association (in early childhood) or no association, and others showing a modest increase in odds of CHD with increased BMI. There is insufficient evidence to show whether or not the association differs significantly between under- and over-twelves. However, evidence from some cohorts suggests an increasing trend with age. There is little evidence of any association between obesity and stroke; the statistically significant result in the over-twelves is based on a single cohort study.
There was some consistent evidence that childhood obesity and overweight are positively associated with metabolic syndrome in adulthood. There was some very limited evidence suggesting that the strength of the associations may vary according to age and measurement tool. There was also some consistent evidence that childhood obesity and overweight are positively associated with odds of adult hypertension, although the results are based on a relatively limited number of cohorts. There was some evidence of a statistically significant positive association between BMI in adolescence and hypercholesterolaemia in early adulthood, although the evidence is based on a single cohort with limited follow-up.
The cohorts reported on a large number of cancers (although few cohorts were found for each site-specific cancer), and the general trend appears to be that obesity leads to a modest increase in risk for most cancers for which evidence was available (except for breast cancer and rectal cancer).
Despite the association between obesity and later morbidity, childhood BMI is a poor predictor of adult morbidity. At best, around 40% of adults with diabetes were overweight or obese (above the 85th centile of BMI) as children. There was some evidence from a single cohort that BMI and WC had equally high specificity and poor sensitivity when used to predict future diabetes. At most, 20% of future CHD and cancers occur in overweight or obese children. If we consider only obese children (above the 95th centile), then obesity cannot predict CHD or cancer; the results are no better than chance. Therefore, childhood BMI is not a good predictor of future heart disease or cancer.
There was some evidence that BMI has good specificity but poor sensitivity when used to predict metabolic syndrome in adults, although this finding is based on very few and small cohorts. This means that most adults who do not develop metabolic syndrome as adults were also not obese as children; however, this tells us nothing about obese children. There is some evidence from a relatively small cohort that BMI values at ages 11 and 16 years were weakly predictive of hypertension in adulthood. No evidence was found on the predictive value or association between childhood weight status and hypercholesterolaemia in adulthood.
The evidence for the predictive accuracy of simple measures other than BMI was limited, and could not be included in the meta-analyses. Only three relatively small studies used WC, and only one used WHR and measurements of SFT. Based on this evidence, the extent to which these simple measures of childhood weight status can be compared is very limited. Only one study reported predictive accuracy data on WC and BMI, and found that both had equally high specificity and low sensitivity when predicting future adult morbidity.
Overall, there was consistent evidence of positive associations between childhood measurements of weight status and morbidities in adulthood. Although higher childhood BMI tends to be associated with a higher risk of morbidity in adulthood, overall it is a poor predictor of adult morbidity. This is because the association between obesity and morbidity would need to be strong (i.e. a large RR) in order for obesity to be an effective predictor of later morbidity. 225 There is also no evidence favouring the accuracy of any of the other simple measures of childhood weight status for predicting future adult morbidity.
Review of tracking of obesity into adulthood
For the review of tracking of obesity into adulthood, five systematic reviews (across six publications) with potential for being updated were identified. 16,17,211,214,215,226 None of the reviews specifically evaluated the accuracy of simple childhood measures of obesity in predicting adult obesity. The most recent and relevant reviews were by Singh et al. (2008)16 and Brisbois et al. (2012). 17 The bibliographies of all the systematic reviews and other relevant reviews were screened for potentially relevant studies, regardless of the age of the study.
Summary of the existing systematic reviews by Singh et al. (2008) and Brisbois et al. (2012)
The systematic review by Singh et al. (2008)16 examined the evidence of the persistence of childhood overweight. The review included prospective or retrospective longitudinal studies that made at least one anthropometric measurement during youth (age ≤ 18 years) and one during adulthood (age ≥ 19 years), using BMI, SFT or WC. Eighteen studies in 25 articles were included in the review. The quality of the included studies was assessed in duplicate by the two reviewers and 52% of the articles were rated as being of high methodological quality.
All the included studies reported that overweight or obese youths were at increased risk of becoming overweight or obese adults. Four studies that stratified for different levels of youth overweight suggested that persistence of overweight was greater with increased level of overweight. It was unclear if persistence varied with sex. When only high-quality studies were included in the analysis, the risk of overweight children becoming overweight adults was at least double that for normal-weight children. Overall, the percentage of obese adolescents becoming overweight or obese adults was higher than that of obese children (24–90% based on three high-quality studies). The review concluded that there is strong evidence of moderate persistence of overweight in both overweight and obese children. A significant limitation of the review was that it was unclear how comprehensive the searches had been, and whether or not relevant studies may have been missed. Furthermore, it presented only a narrative synthesis of the results from the included studies and focused on the association between childhood and adult obesity rather than the predictive accuracy of childhood obesity. In addition, as the review’s searches had been conducted in February 2007 the list of included studies was potentially out of date. Therefore, this review was used only as a source of relevant studies for the current review.
The systematic review by Brisbois et al. (2012)17 evaluated a number of factors in children aged 5 years or under which are the most significant predictors of the development of obesity in adulthood. Studies were eligible if they included healthy individuals, performed child and adult measurements for each individual and reported quantitative results. The searching appeared adequate but the lack of overlap with Singh et al. (2008)16 raised questions over how comprehensive it had been.
The review included 24 studies, and almost all reported a significant association between childhood overweight or obesity and adult obesity. The review concluded that early childhood obesity was a probable marker of adult obesity.
The main limitations of this review were that only early childhood was considered and it was possible that studies had been missed. Furthermore, many of the studies included reported only correlation coefficients, and only a narrative synthesis of study results was conducted. Therefore, as with the review by Singh et al. (2008),16 this review was used as a source of relevant studies for the current review.
Quality and assessment of bias of the included primary studies of tracking of obesity into adulthood
In total, 23 studies were identified for the review of the tracking of childhood obesity into adulthood. These are listed in Table 8.
| Study | Risk of selection bias | Risk of attrition bias | Risk of bias associated with the prognostic factor | Risk of bias associated with outcome | Risk of bias due to confounders | Risk of reporting or analysis bias |
|---|---|---|---|---|---|---|
| Cheng (2011)117 | Low | High | Low | Low | UC | Low |
| Cheung (2004)118 | Low | High | Low | High | High | Low |
| Engeland (2004)119 | Low | Mod/UC | Mod/UC | Mod/UC | Low | Low |
| Freedman (2001)120 | Low | Low | Mod/UC | Mod/UC | Mod/UC | Low |
| Freedman (2005)122 | Low | Mod/UC | Low | Low | Low | Low |
| Freedman (2005)121 | Low | Low | Low | Low | Low | Low |
| Goldhaber-Fiebert (2013)123 | Low | Mod/UC | Mod/UC | Mod/UC | Low | Low |
| Gordon-Larsen (2004)124 | Low | Mod/UC | Low | High | Low | Low |
| Juhola (2011)125 | Low | Mod/UC | Mod/UC | Mod/UC | Low | Low |
| Juonala (2006)126 | Low | High | Mod/UC | Mod/UC | High | Low |
| Liddle (2012)127 | Low | Mod/UC | Low | High | Mod/UC | Low |
| Mamun (2005)128 | Low | Mod/UC | Low | Low | Mod/UC | Low |
| Merten (2010)129 | Low | Mod/UC | Mod/UC | Mod/UC | Mod/UC | Low |
| Nakano (2010)131 | Low | Mod/UC | Low | Low | Low | Low |
| Nakano (2010)130 | Low | Mod/UC | Low | Low | Low | Low |
| Patton (2011)132 | Low | Mod/UC | Mod/UC | Mod/UC | Low | Low |
| Power (1997)133 | Low | Mod/UC | Low | Low | Low | Low |
| Reilly (2011)134 | Low | Mod/UC | Low | Low | Mod/UC | Low |
| Starc (2011)135 | Low | Low | Low | Low | Low | Low |
| Stovitz (2010)136 | Low | Mod/UC | Low | Low | Mod/UC | Low |
| Thompson (2007)137 | Low | Mod/UC | Low | Mod/UC | Low | Low |
| Venn (2007)138 | Low | Mod/UC | Mod/UC | Mod/UC | Mod/UC | Low |
| Wang (2008)139 | Low | Low | Mod/UC | Mod/UC | Low | Low |
| All studies | All low | 16 mod/UC 3 high 4 low |
14 low 9 mod/UC |
10 mod/UC 10 low 3 high |
13 low 2 high 8 mod/UC |
All low |
The results of the quality and risk of bias assessment are summarised in Table 8 and given in full in Appendix 4. All the studies were cohort studies, and so they are already subject to greater bias than a randomised controlled trial would be. However, all the studies were large, most being from national or community data sets. The main potential source of bias arises from the lack of control in retaining participants in the cohorts; thus, although the initial cohorts were very large, many thousands of participants were not followed up at the final assessment. In itself this might not be a source of bias, but the majority of study reports did not confirm that the final cohort followed up was representative of the complete initial sample. Confounding was another significant potential source of bias in these studies. Although some presented results by age and sex, most did not, and the wide age ranges included in some studies increased the potential for age-associated effects that could not be accounted for.
Characteristics of studies included the review of tracking of obesity into adulthood
There was some overlap between a number of the studies, as they were based on the same initial cohorts. Three were based on the Bogalusa cohort in the Southern States of the USA, and two each were based on the National Child Development Study (1958 British birth cohort) (NCDS), the National Longitudinal Study of Adolescent Health (NLSAH) cohort, the Young Finns cohort, Tokushima Prefecture and the Mater-University Study of Pregnancy (MUSP) cohort in Australia (Table 9). Each study included in the review provided some unique data in terms of age of childhood assessment, adult assessment or analysis by age, sex or race. Only unique data are included in the meta-analysis and narrative synthesis.
| Cohort name | Study | Country in which study conducted | Study dates | Details of individual 'study' (paper) | |
|---|---|---|---|---|---|
| From | To | ||||
| Bogalusa | Freedman (2001)120 | USA | 1973 | 1996 | This analysis based on 2617 participants re-examined as adults (age 27 years) |
| Freedman (2005)122 | 1973 | 1994 | This analysis based on 2610 participants re-examined as adults (age 27 years) | ||
| Freedman (2005)121 | 1973 | 1996 | This analysis based on 2392 participants re-examined as adults (age 27 years) | ||
| Young Finns | Juhola (2011)125 | Finland | 1980 | 2007 | Cohort followed up in 2001 (age 30–45 years). Results presented stratified by different age at baseline, but only summary data presented |
| Juonala (2006)126 | Finland | 1980 | 2001 | Cohort followed up in 2007 (age 24–39 years). Data presented across broad age groups | |
| MUSP | Liddle (2012)127 | Australia | 1986 | NR (follow-up for 18 years) | Tracked children from age 5 to age 21 years (range 18.2–23.1 years) |
| Mamun (2005)128 | Australia | 1986–90 | 2000–4 | Tracked children from age 5 to age 14 years | |
| NCDS (1958 British birth cohort) | Power (1997)133 | UK | 1958 | 1991 | Tracked participants from age 7 to age 33 years |
| Cheung (2004)118 | UK | 1958 | 2000 | Tracked participants from age 7 to age 33 years; calculated sensitivity and specificity, etc. Compare with results from Power (1997)133 | |
| NLSAH | Gordon-Larsen (2004)124 | USA | 1996 | 2002 | Tracking of wave II participants to wave III participants, stratified by age in wave II |
| Merten (2010)129 | USA | 1995 | 2001 | Tracking of wave I participants to wave III participants | |
| Tokushima Prefecture | Nakano (2010)131 | Japan | 2001 | 2008 | Participants followed up for 7 years. Only included children who were aged 7 years at first measure [i.e. a subset of participants in Nakano (2010)130] |
| Nakano (2010)130 | Japan | 2001 | 2007 | Participants followed up for 6 years. Although whole cohort overlaps with Nakano (2010),131 the extracted data were only for a cohort aged 8 years at first measure (n = 5697) and so study does not overlap with other Nakano study | |
Study characteristics for tracking of obesity into adulthood
The study characteristics are summarised in Table 10 and presented in full in Appendix 3. The included studies were all longitudinal cohort studies in which these data were collected prospectively. They were conducted in various countries: the USA (nine studies), UK (three studies), other European countries (four studies: two in Finland, one in Norway and one in Slovenia), Australia (four studies), Japan (two studies) and China (one study). The start dates of the studies ranged from 1958 to 2008, with follow-up between 6 and 42 years; 11 of the 23 studies had follow-up of 20 years or longer.
| Cohort name | Study | Country in which study conducted | Study dates | Setting for anthropometric measure in childhood | |
|---|---|---|---|---|---|
| Start | Finish | ||||
| 1988–90 Slovenian cohort | Starc (2011)135 | Slovenia | 1997 | 2008 | School |
| ALSPAC | Reilly (2011)134 | UK | 1998/1999 | 2003/2004 | Research clinic |
| ASHFS | Venn (2007)138 | Australia | 1985 | 2005 | School |
| BCAMSS | Cheng (2011)117 | China | 2004 | 2011 | School |
| Bogalusa | Freedman (2001)120 | USA | 1973 | 1996 | School |
| Freedman (2005)122 | USA | 1973 | 1994 | School | |
| Freedman (2005)121 | USA | 1973 | 1996 | School | |
| Cardiovascular Risk in Young Finns | Juhola (2011)125 | Finland | 1980 | 2007 | NR |
| Juonala (2006)126 | Finland | 1980 | 2001 | NR | |
| CATCH | Stovitz (2010)136 | USA | 1991 | 2001 | School |
| MUSP | Liddle (2012)127 | Australia | 1986 | NR (follow-up for 18 years) | NR |
| Mamun (2005)128 | Australia | 1986–90 | 2000–4 | NR | |
| NCDS (1958 British birth cohort) | Power (1997)133 | UK | 1958 | 1991 | Community |
| Cheung (2004)118 | UK | 1958 | 2000 | Community | |
| NGHS/PFS | Thompson (2007)137 | USA | 1986 | 1997 | School |
| NHANES, NLSY79 | Goldhaber-Fiebert (2013)123 | USA | 1970 | 2008 | Community |
| NLSAH | Gordon-Larsen (2004)124 | USA | 1996 | 2002 | School |
| Merten (2010)129 | USA | 1995 | 2001 | School | |
| NLSY79 | Wang (2008)139 | USA | 1981 | 2002 | Interview/survey |
| None | Engeland (2004)119 | Norway | 1963 | 1999 | Community |
| None | Patton (2011)132 | Australia | 1992 | 2003 | School |
| Tokushima Prefecture | Nakano (2010)131 | Japan | 2001 | 2008 | School |
| Nakano (2010)130 | Japan | 2001 | 2007 | School | |
The setting for studies was not always completely clear, although not surprisingly most involved schoolchildren measured in school or the community. The childhood measures are listed in Appendix 3. In all studies, BMI was assessed in childhood (or adolescence), and in all but one study127 BMI was the only measure in childhood. In all studies, childhood BMI was routinely reported in kg/m2, and was sometimes standardised to reference data. Ten studies used IOTF61/Cole 2000220/WHO45 reference populations. Others used the CDC 2000219 reference growth charts or the UK90 reference. 221 All were extracted as equivalent to the 85th and 95th centile cut-off points in childhood to determine overweight and obesity respectively. The Bogalusa cohort used the 95th centile to define overweight. However, data at the 85th and 95th centiles were used to define overweight and obesity, in accordance with other studies. One study [Juonola et al. (2006)126] used the 80th and 90th centiles as the cut-off points for overweight and obesity; this study was included in the analyses as if it had used the 95th centile.
Skinfold thickness was the childhood measurement in only one included study127 (and was used in addition to BMI); it was measured at one site and measurements were converted to a z-score internally adjusted for age and sex. Cut-off points were generated from proportions of overweight/obese similar to Cole 2000220 BMI subgroups (BMI was also measured).
Details of the BMI measure used in adults are listed in Appendix 3. In summary, all assessments of adult weight status used the BMI cut-off points for overweight and obesity of 25 kg/m2 and 30 kg/m2. For adolescents, all studies used the cut-off points for overweight and obesity of the 85th and 95th centiles respectively, with the exception of Juonola et al. (2006),126 based on the Young Finns cohort, which used the 80th and 90th centiles respectively.
Population characteristics for tracking of obesity into adulthood
The sample sizes of the cohorts at baseline ranged from 1943 to 227,003 (Table 11; see also Appendix 3), and at follow-up from 1309 to 128,121. The age range for the baseline measurements varied across the studies, with the youngest age being 2 years and the oldest 19 years. Of the 23 studies, nine included a mix of children and adolescents at baseline, five just children and six just adolescents.
| Study | Number at baseline | Number at final follow-up | Childhood age (years) | Adult (final follow-up) age (years) | Percentage overweight or obese in childhood |
|---|---|---|---|---|---|
| Cheng (2011)117 | 2189 | 1184 | 6–16 | 12–22 | Overweight: 15.3 Obese: 40.8 |
| Cheung (2004)118 | 17,000 | 12,327; analysis on randomly selected 50% sample | 7, 11, 16 | 33 | Overweight: 10.4 Obese: 2.2 |
| Engeland (2004)119 | 227,003 | 128,121 | 14–19 | 24–54 | Overweight: 4.9 for boys and 7.3 for girls |
| Freedman (2001)120 | 9597 | 2617 | 2–17 | 18–37 | Obese: 7 |
| Freedman (2005)122 | 11,411 | 2610 | 2–17 | 18–37 | Overweight: 7 for boys and 6 for girls |
| Freedman (2005)121 | 7923 | 2392 | 5–14 | 18–37 | Overweight: ≈7 |
| Goldhaber-Fiebert (2013)123 | NR | 4884 (tracking) | 2–15 | 18 | Overweight: 9–10 for 5-year-olds; 14–15 for 15-year-olds Obese: 12–13 for 5-year-olds; 11–17 for 15-year-olds |
| Gordon-Larsen (2004)124 | 14,438 | 9795 (including total population at 13–15 years, 16–17 years and 18–20 years) | 13–20 | 19–26 | Obese: 10.9 |
| Juhola (2011)125 | 3596 | 2204 | 3–18 | 30–45 | NR |
| Juonala (2006)126 | 3596 | 2260 | 3–18 | 24–39 | Overweight: 10.5 Obese: 8.6 |
| Liddle (2012)127 | 3960 | 1755 | 5 | 18.2–23.1 | NR |
| Mamun (2005)128 | NR | 2794 | 5 | 14 | Overweight/obese: 17 |
| Merten (2010)129 | 20,745 | 10,439 | 12–19 | 22 | NR |
| Nakano (2010)130 | 22,827 | 16,245 | 8 | 14 | Overweight: 18.28 for boys and 17.09 for girls Obese: 5.94 for boys and 4.13 for girls |
| Nakano (2010)131 | 7506 | 5024 | 7 | 14 | NR |
| Patton (2011)132 | 1943 | 1520 | Mean 15 | 24 | NR |
| Power (1997)133 | 17,733 | 11,407 | 7–16 | 33 | NR |
| Reilly (2011)134 | 7759 | 5175 | 7 | 13 | Overweight: 8.1 for males and 9.6 for females Obese: 8.2 for males and 6.8 for females |
| Starc (2011)135 | 21,777 | 4833 | Mean 7 | 18 | Overweight: 13.2 for males and 13.1 for females Obese: 5.7 for males and 4.4 for females |
| Stovitz (2010)136 | 5106 | 2802 | Mean 8 | Mean 18.3 | Overweight: 14.9 Obese: 10.5 |
| Thompson (2007)137 | 1963 | 1669 | 10–16 | 21–23 | Overweight: at baseline, 7.4–8.7 for Caucasian; 17.4–18.2 for AA |
| Venn (2007)138 | 8498 | 4571 | 7–15 | 24–34 | Overweight: 8.3 for boys and 9.7 for girls Obese: 1.5 for boys and 1.4 for girls |
| Wang (2008)139 | 2513 | 1309 | 16–17 | 37–38 | Overweight: 8 Obese: 3 |
Four studies128,130,131,134 tracked weight status from childhood to adolescence, in two studies123,135 the latest follow-up age was 18 years and five studies included participants as young as 18 years in their follow-up. 117,120–122,127,136 The oldest cohorts at final follow-up included participants aged 24–54 years119 and in one case participants aged 37–38 years. 139 The cohorts generally included equal proportions of males and females; the Bogalusa cohort had a slightly lower proportion of males (43%). The ethnicity and mix of ethnicities within the cohorts varied by country. The SES of participants was reported in only four of the studies. 127,132,134,139 Of those, one reported that 47% had achieved college-level education or above,139 and the other three reported that maternal/parental education levels were post high school for 20–50%. 127,132,134 Where reported, the proportion of overweight or obese children at baseline varied considerably; overweight ranged from 5% to 18% and obesity from 2% to 17%, with generally higher rates in girls and older children.
Findings of the review of tracking of obesity into adulthood
Data extracted from the included studies, and calculated sensitivity, specificity and PPV by study, are presented in Appendix 3.
Overview of the studies of tracking of obesity into adulthood
To give an overview of these data, we present three figures showing sensitivity, specificity and PPV according to childhood age of BMI measurement and sex for each study. These plots show the diagnostic performance of using obesity in children (> 95th centile), according to age at measurement, to predict obesity in adults (aged ≥ 20 years).
Figure 18 shows that sensitivity is generally low – less than 40% – with the exception of one study [Thompson et al. (2007)137]. Most obese adults were therefore not obese in childhood. There is no obvious trend in sensitivity with age or sex. There appears to be considerable heterogeneity across studies, with sensitivities ranging from 10% to over 60% at age 16 years. Figure 19 shows that specificity is much higher and more consistent, ranging from 93% to nearly 100%. This means that nearly all non-obese adults were also not obese as children; however, this tells us nothing about the obese adults and children who are of concern. The PPV tells us what proportion of obese children go on to become obese adults. This is shown in Figure 20. The results are very heterogeneous, ranging from 40% to over 90%. The PPV depends on the prevalence of obesity, so some of this heterogeneity may be a result of varying obesity prevalence across studies.
FIGURE 18.
Sensitivity for predicting adult obesity from childhood obesity.
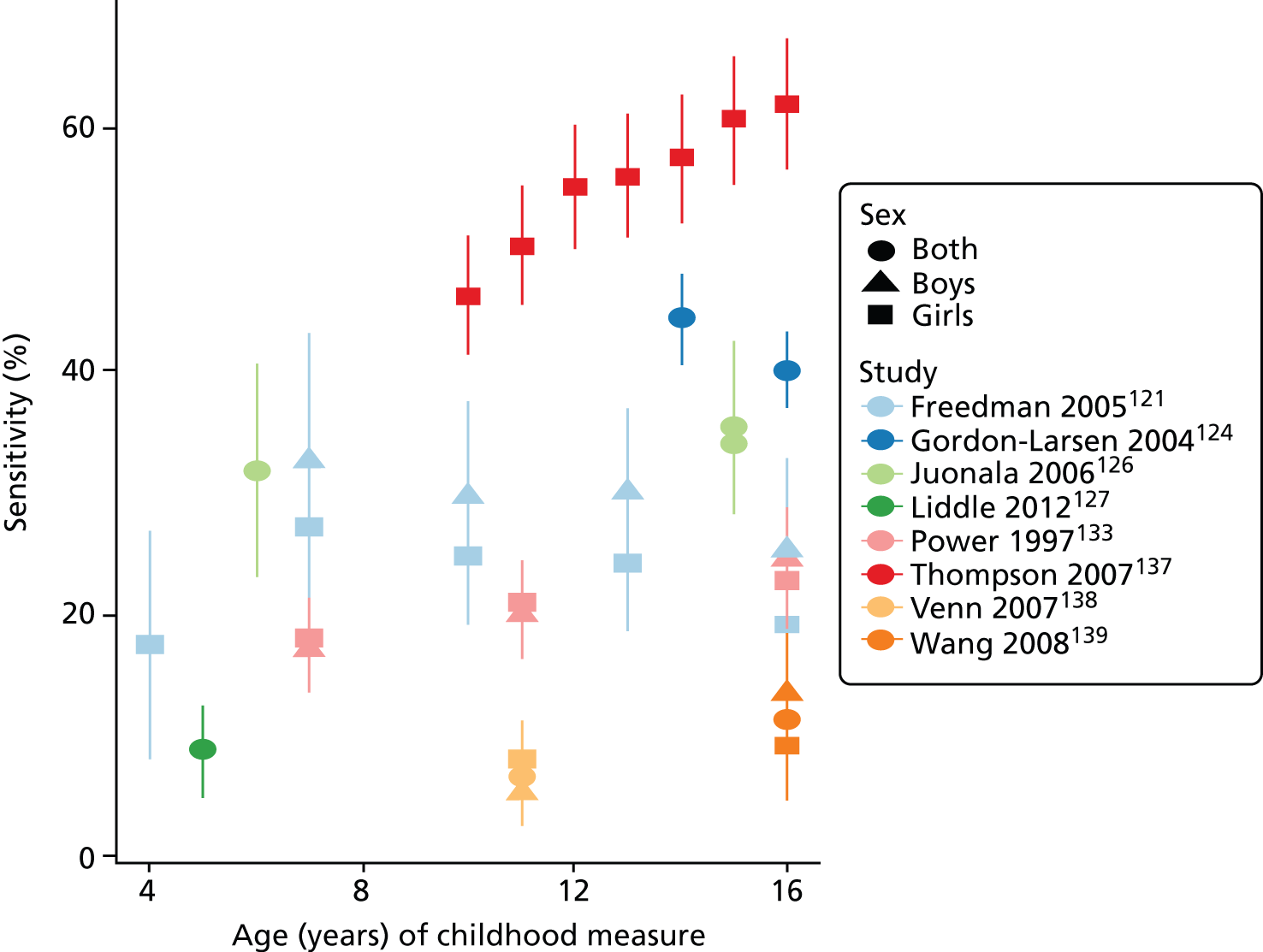
FIGURE 19.
Specificity for predicting adult obesity from childhood obesity.
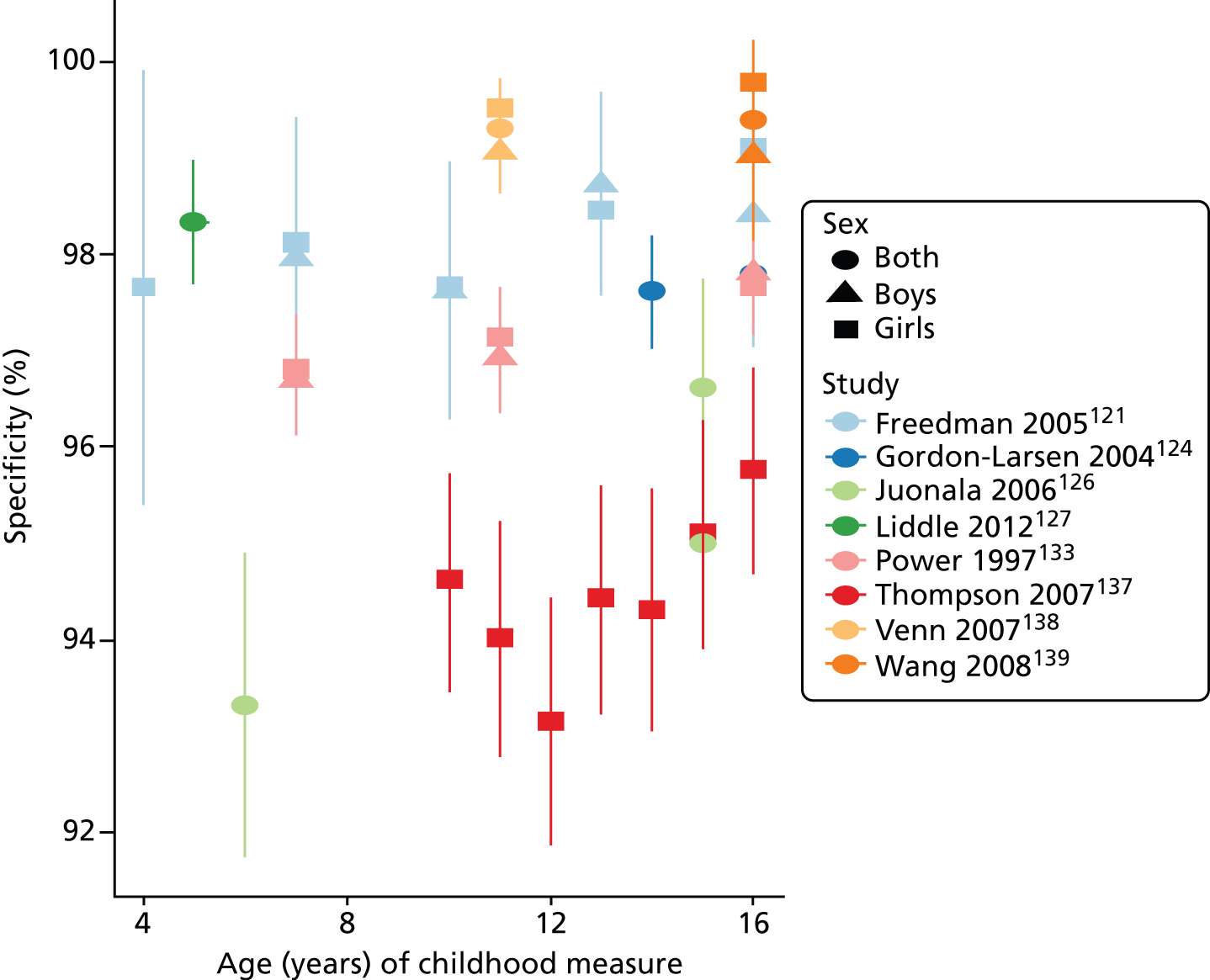
FIGURE 20.
Positive predictive value for predicting adult obesity from childhood obesity.
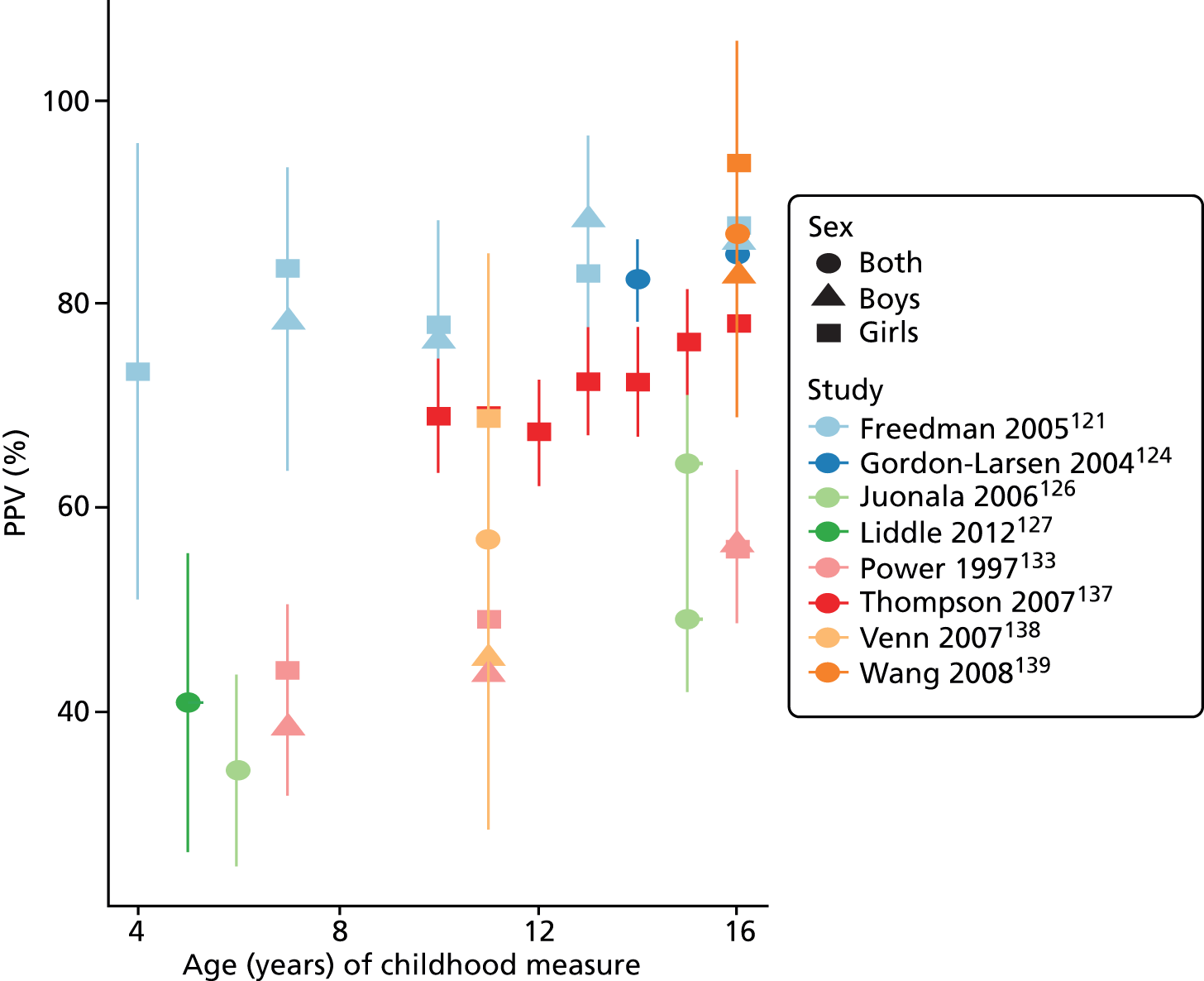
The results do suggest that obesity is moderately persistent, at least between adolescence and adulthood.
Meta-analysis of tracking of obesity into adulthood
All tracking studies that reported full diagnostic data (i.e. numbers of true and false positives, and true and false negatives) were included in the meta-analyses, except for the study by Liddle et al. (2012),127,128 which was of children aged 5 years only and therefore did not fall into the lowest age category of the meta-analysis (7–11 years); the results of this study are presented in the previous section. Different studies reported data on different comparisons between childhood and adult obesity or overweight, and at different ages. Table 12 gives a summary of which studies were included in which analyses; not all publications provided data for the meta-analysis. Studies reported tracking in a variety of ways, with some, for example, examining tracking of childhood obesity to adult obesity, some adolescent overweight to adult obesity and some childhood overweight to adolescent overweight, and therefore most meta-analyses include few studies.
| Study | Obesity categories | Age categories | ||||||
|---|---|---|---|---|---|---|---|---|
| Childhood obesity to: | Childhood overweight or obesity to: | Child to adolescent | Child to adult | Adolescent to adult | Adolescent to over 30 years | |||
| Adult obesity | Adult obesity or overweight | Adult obesity | Adult obesity or overweight | |||||
| Cheng (2011)117 | ✗ | ✗ | ✗ | ✗ | ✗ | |||
| Power (1997)133 | ✗ | ✗ | ✗ | ✗ | ✗ | |||
| Reilly (2011)134 | ✗ | ✗ | ✗ | ✗ | ✗ | |||
| Starc (2011)135 | ✗ | ✗ | ✗ | ✗ | ✗ | |||
| Venn (2007)138 | ✗ | ✗ | ✗ | ✗ | ✗ | |||
| Freedman (2005)122 | ✗ | ✗ | ✗ | ✗ | ||||
| Gordon-Larsen (2004)124 | ✗ | ✗ | ✗ | |||||
| Juonala (2006)126 | ✗ | ✗ | ✗ | ✗ | ||||
| Thompson (2007)137 | ✗ | ✗ | ✗ | |||||
| Wang (2008)139 | ✗ | ✗ | ✗ | ✗ | ||||
| Freedman (2005)121 | ✗ | ✗ | ✗ | |||||
| Patton (2011)132 | ✗ | ✗ | ✗ | |||||
| Engeland (2004)119 | ✗ | ✗ | ✗ | ✗ | ||||
| Nakano (2010)130 | ✗ | ✗ | ||||||
| Nakano (2010)131 | ✗ | ✗ | ||||||
| Stovitz (2010)136 | ✗ | ✗ | ||||||
Association between childhood weight status and adult obesity
Figure 21 shows the forest plot for the meta-analysis of RR of being obese as an adult among children who were obese. The association is strong, with obese children being more than five times more likely to be obese as adults than non-obese children. There is no apparent difference in this RR between younger and older age groups.
FIGURE 21.
Forest plot of the association between childhood obesity and adult obesity.
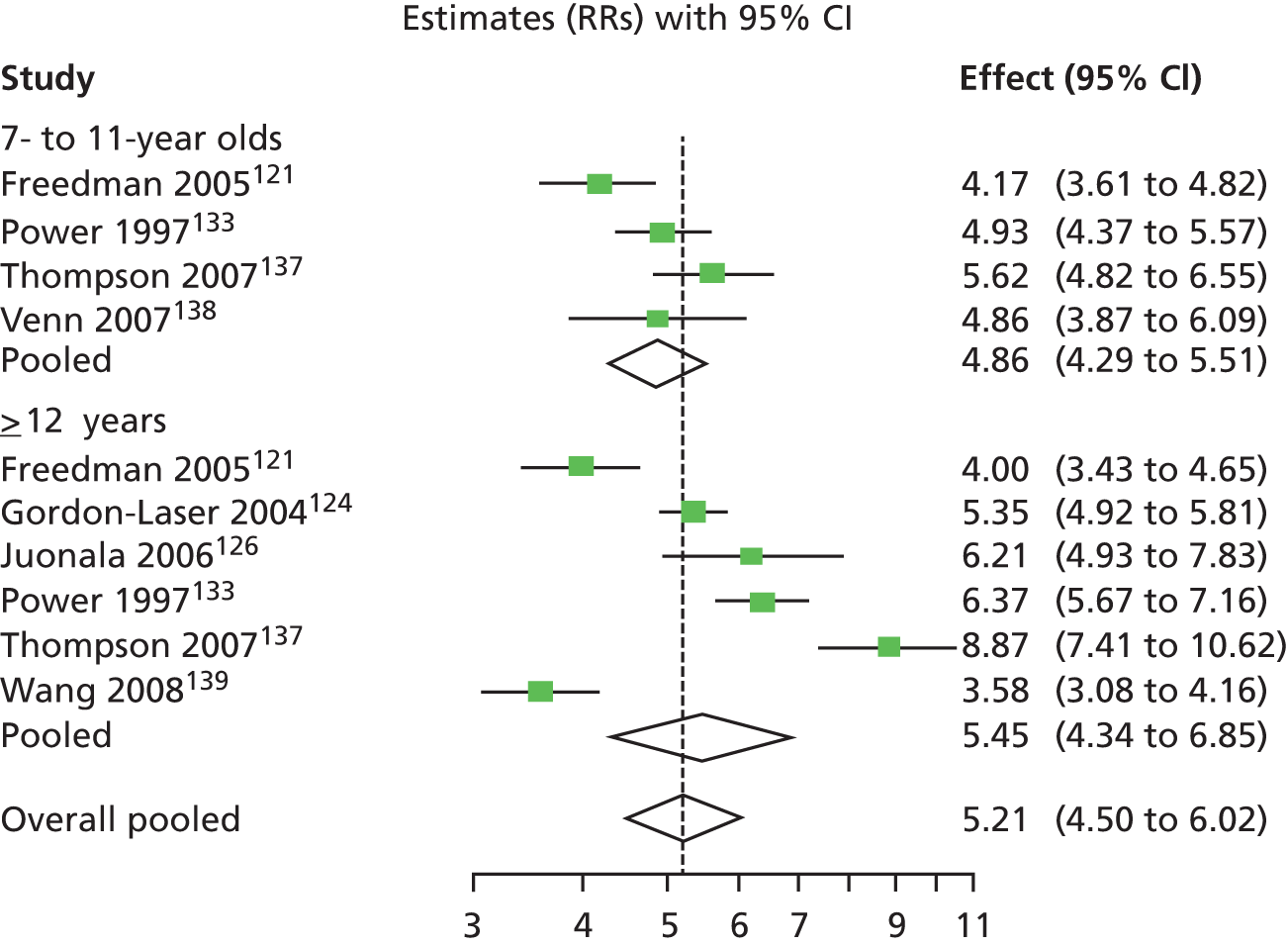
Tracking from childhood weight status to adult obesity
Figure 22 shows the results of the joint meta-analyses of sensitivity and specificity when predicting adult obesity (≥ 95th centile or > 30 kg/m2) from childhood obesity (≥ 95th centile of BMI). Four results are shown: child to adolescent (three studies), child to adult (four studies), adolescent to adult (six studies) and adolescent to over 30 years (three studies). The points show the summary sensitivities and specificities with their 95% CIs; the curves are the summary HSROC curves.
FIGURE 22.
Tracking of childhood obesity to adult obesity.
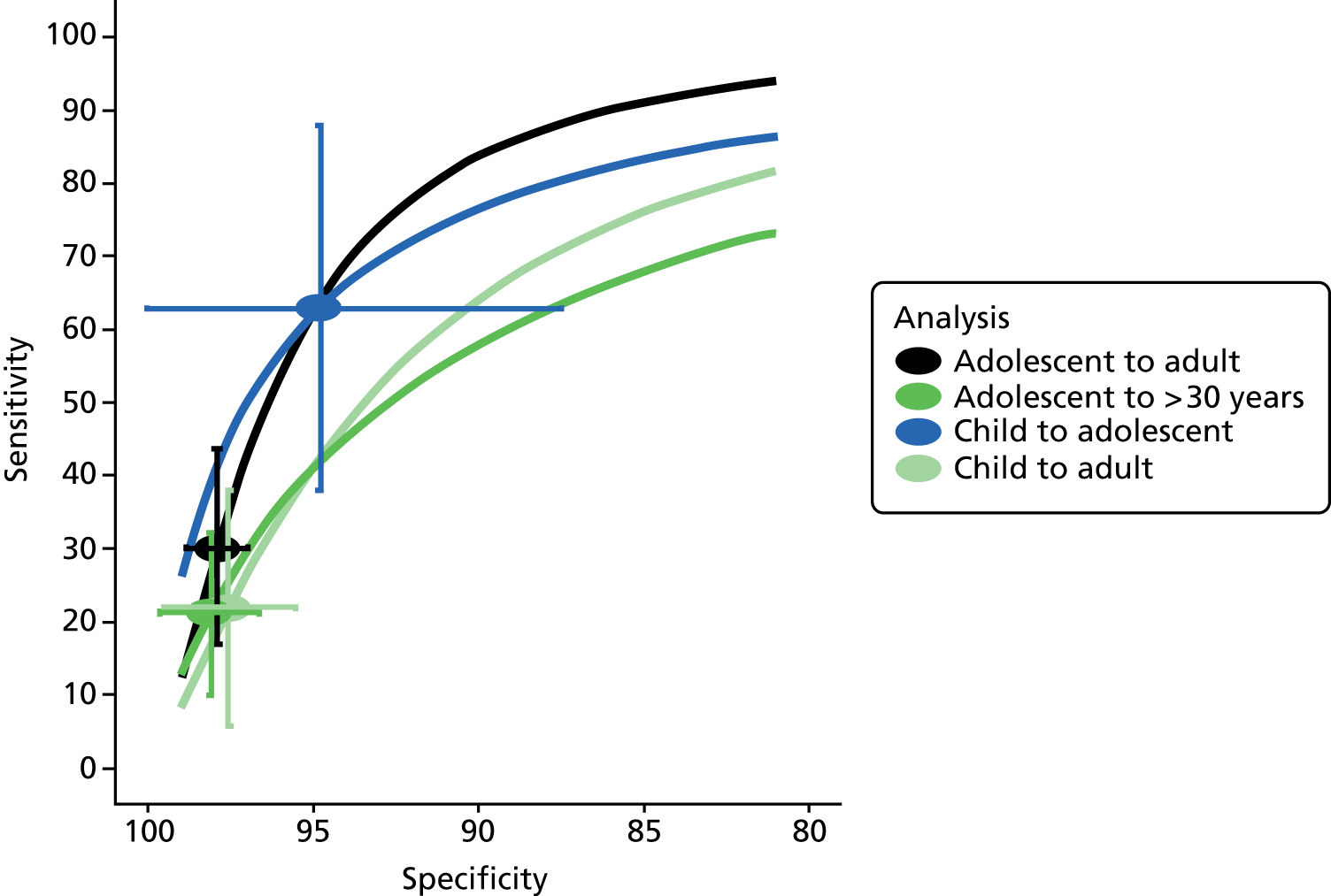
Figure 22 shows that obesity tracking is strongest over short time periods. Childhood obesity does track reasonably well to adolescent obesity; 62% of obese adolescents were obese in earlier childhood. A high specificity of 95% means that nearly all non-obese adolescents were non-obese children. For tracking into adulthood, the specificities of around 98% mean that nearly all non-obese adults were not obese in childhood or adolescence. However, by contrast, the low sensitivities mean that most obese adults were not obese as children. About 70% of obese adults were not obese in childhood or adolescence and 80% of over-thirties were not obese in adolescence.
Figure 23 shows the results for whether or not childhood obesity or overweight (≥ 85th centile of BMI) tracks to later obesity (≥ 95th centile or ≥ 30 kg/m2). Four results are shown: child to adolescent (three studies), child to adult (two studies), adolescent to adult (five studies) and adolescent to age over 30 years (three studies). The pattern of results is similar to that for childhood obesity, with low sensitivity to detect adult obesity; around 60% of obese adults were neither overweight nor obese as adolescents. Childhood overweight is, however, a good predictor of adolescent obesity; 90% of obese adolescents were overweight or obese in earlier childhood.
FIGURE 23.
Tracking of childhood overweight or obesity to adult obesity.
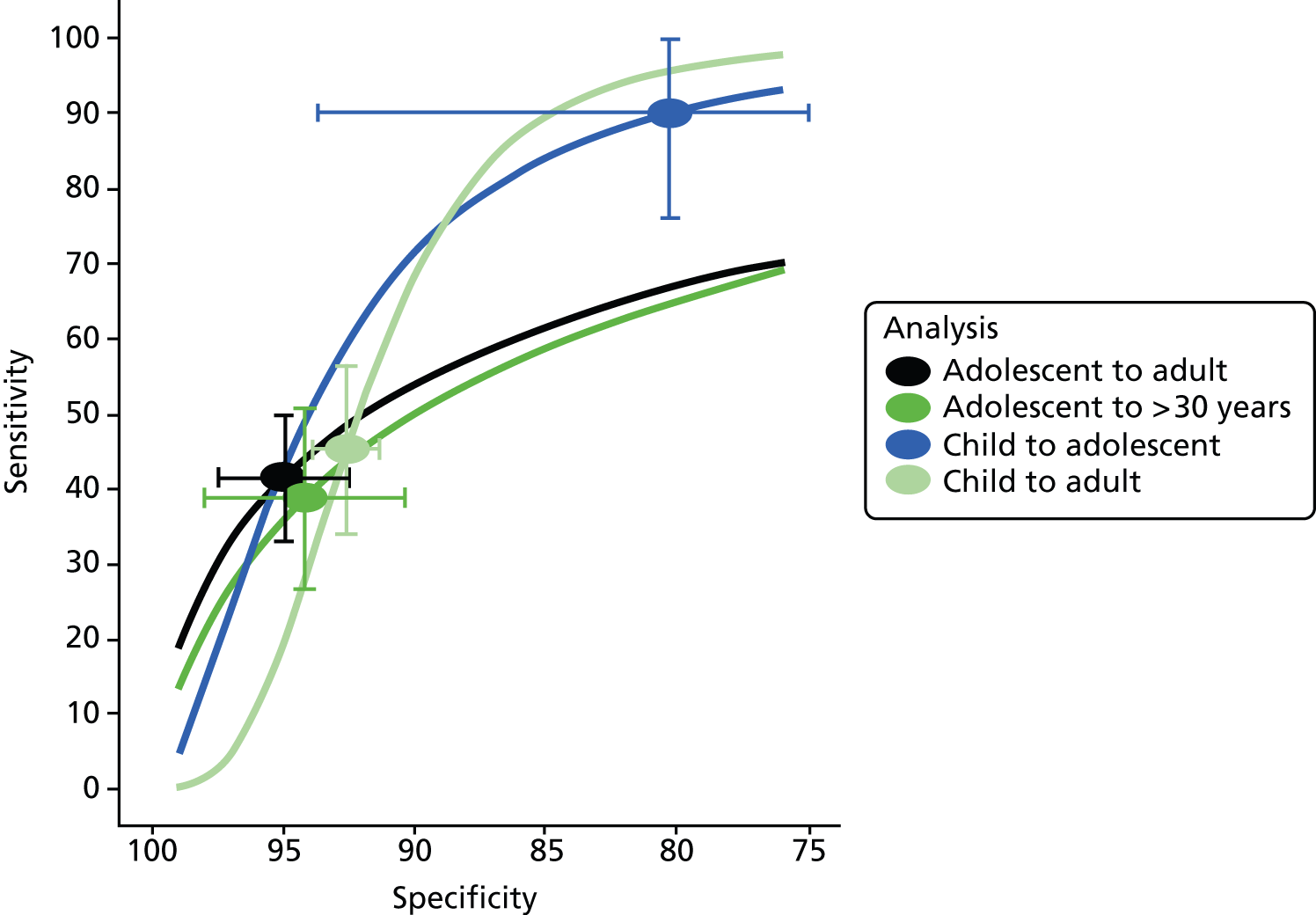
Tracking from childhood to adult overweight or obesity
Figure 24 shows the results of the joint meta-analyses examining whether or not childhood overweight or obesity (≥ 85th centile of BMI) tracks to later overweight or obesity (≥ 85th centile or > 25 kg/m2). Three results are shown: child to adolescent (six studies), child to adult (two studies) and adolescent to adult (two studies). There was only one study with data from adolescence to age over 30 years, so no analysis could be performed. We note that there were few data here for tracking into adulthood.
FIGURE 24.
Tracking of childhood overweight or obesity to adult overweight or obesity.
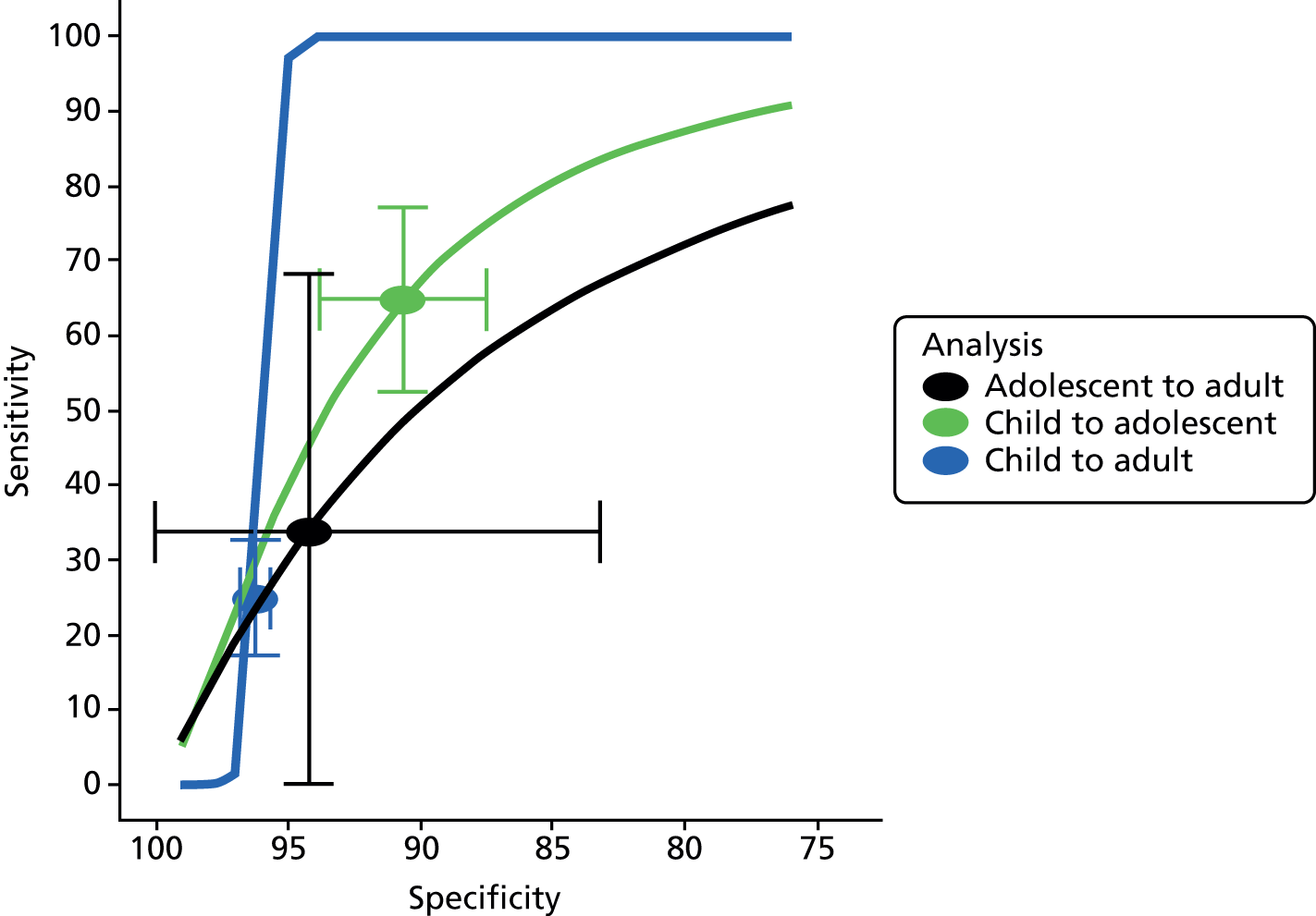
The results for childhood to adolescence suggest that 65% of obese or overweight adolescents were obese or overweight at younger ages. The limited data for tracking to adulthood suggest very low sensitivity; about three-quarters of overweight adults were not overweight in younger childhood.
Figure 25 shows how childhood obesity (excluding overweight) tracks to adult obesity or overweight. Three results are shown: child to adolescent (three studies), child to adult (three studies) and adolescent to adult (two studies). The results are broadly similar to those obtained for using childhood overweight to predict adult overweight. The results for childhood to adolescence suggest that 35% of obese or overweight adolescents were obese at younger ages. The substantial majority of overweight adults (around 90%) were not obese as children.
FIGURE 25.
Tracking of childhood obesity to adult overweight or obesity.

Positive predictive values
Meta-analyses of the PPV, which estimates the proportion of obese children who will go on to become obese adults, are presented in Figures 26 and 27. The analyses are similar to those presented above, with the same studies in each analysis as for the equivalent analyses given above.
FIGURE 26.
Positive predictive value for childhood obesity when tracking to adult obesity.

FIGURE 27.
Positive predictive value for childhood overweight and obesity when tracking to adult obesity.

Figure 26 shows the PPV and NPV for predicting adult obesity from childhood obesity, classified according to age as before. This shows that obesity is moderately persistent into adulthood; just under 80% of obese adolescents were still obese as adults, although that declines to 70% when adult ages are restricted to over 30 years. Childhood obesity does not track so strongly into adolescence, however, with just over half of all children still obese as adolescents, although data were limited and therefore CIs are wide. The NPV results show that non-obesity does track into adulthood; more than 85% of non-obese children will still be non-obese in adulthood. However, this does mean that a small proportion (10–15%) of non-obese children will be obese by early adulthood.
Figure 27 shows the equivalent PPV and NPV for tracking of childhood overweight or obesity to later obesity. The pattern of results is similar, but the PPVs are smaller as many overweight children will not become obese adults. Around 66% of obese or overweight adolescents will be obese in early adulthood, dropping to around 55% by age 30 years. Only about 30% of obese or overweight children will go on to be obese in adolescence.
As both PPV and NPV depend on the prevalence of obesity, the results of these analyses should be interpreted as predictive values in a population with average obesity prevalence.
Additional information from studies that could not be included in the meta-analysis
Four studies reported data that could not be included in the meta-analyses: Goldhaber-Fiebert et al. (2013),123 Cheung et al. (2004),118 Juhola et al. (2011)125 and Liddle et al. (2012). 127 The extracted data are presented in Appendix 3. The results of these studies were broadly consistent with the findings of the meta-analyses.
The study by Goldhaber-Fiebert et al. (2013)123 could not be included in any meta-analysis, as it was not a straightforward analysis of cohort data, but included microsimulations based on combined data sets in order to estimate how well childhood obesity predicts adult obesity and to forecast the obesity-related health of future US adults. Data were sourced from the National Longitudinal Survey of Youth (NLSY79), Population Study of Income Dynamics (PSID) and National Health and Nutrition Evaluation Surveys (NHANES). The authors estimated test characteristics and predictive values of childhood BMI to identify 2-, 5-, 10- and 15-year-olds who will become obese at age 18 years (12% of 18-year-olds in the study were obese). The analysis found that screening at age 15 years would miss 9% of those who become obese adults, but screening at age 5 years would miss 50%. The predictive value of obesity screening below age 10 years was low even when maternal obesity was included as a predictor. It should be noted that the main results do not include Hispanics, owing to sample size. The authors concluded that ‘Early childhood obesity assessment adds limited information to later childhood assessment. Targeted later childhood approaches or universal strategies to prevent unhealthy weight gain should be considered’.
In the context of the present review, the results for measurement at age 15 years were not included as the distance between ages 15 and 18 years was considered too short. The results for measurements taken at ages 2, 5 and 10 years are presented in Appendix 3. The results reflect those of the meta-analysis in that childhood overweight or childhood obesity did not accurately predict obesity or overweight/obesity at age 18 years. Sensitivity did increase with increasing age of assessment in childhood, with the highest found to be the sensitivity of overweight in unselected boys at age 10 years (sensitivity 88%, 95% CI 80% to 93%) and unselected black and Hispanic children at age 10 years (sensitivity 88%, 95% CI 82% to 92%) to predict obesity. Surprisingly, the sensitivity of obesity at age 18 years to predict later obesity or overweight was lower. Specificity increased less with age, but generally the highest specificities were achieved at age 10 years (compared with younger ages); at this age, the specificity of childhood obesity for obesity and for overweight/obesity at age 18 years was 90% or more in boys, girls, black children and white children, whereas that for childhood overweight was lower, at around 80%. Thus, non-obesity in childhood accurately predicts non-obesity in adulthood. This study’s findings were consistent with the findings of the meta-analyses.
The analysis of the British birth cohort by Cheung et al. (2004)118 reported AUC data that could not be included in the meta-analysis (Table 13). These authors’ analysis of the British birth cohort data found that the AUC for the prediction of adult obesity from childhood obesity was slightly higher than that for predicting adult overweight from childhood overweight/obesity. Neither varied with sex but both increased slightly with childhood age.
| Population | Timing of first measure | Cut-off point | Total N | AUC | Upper CI | Lower CI | |
|---|---|---|---|---|---|---|---|
| Childhood obesity (age 11 years) to adult obesity (age 33 years) | Male | 7 | ROC curve BMI = 17.9 | 2174 | 0.72 | 0.68 | 0.76 |
| 11 | 2085 | 0.78 | 0.75 | 0.81 | |||
| 16 | 1903 | 0.82 | 0.78 | 0.85 | |||
| Female | 7 | ROC curve BMI = 18.3 | 2174 | 0.69 | 0.65 | 0.72 | |
| 11 | 2085 | 0.8 | 0.77 | 0.83 | |||
| 16 | 1903 | 0.83 | 0.8 | 0.86 | |||
| Childhood overweight/obesity (age 11 years) to adult overweight (age 33 years) | Male | 7 | ROC curve BMI = 17.9 | 2174 | 0.66 | 0.64 | 0.68 |
| 11 | 2085 | 0.73 | 0.71 | 0.75 | |||
| 16 | 1903 | 0.75 | 0.73 | 0.77 | |||
| Female | 7 | ROC curve BMI = 18.3 | 2174 | 0.66 | 0.63 | 0.68 | |
| 11 | 2085 | 0.75 | 0.72 | 0.77 | |||
| 16 | 1903 | 0.79 | 0.77 | 0.81 |
The sensitivities and specificities reported by Cheung et al. (2004)118 for overweight and obesity at age 11 years indicate that the sensitivity of overweight (BMI) for adult obesity was low (7.7% in boys and 6.9% in girls), as was its sensitivity for adult overweight (13.9% in boys and 23.0% in girls). The sensitivity of childhood obesity for adult obesity was higher but still low (21.9% in boys and 20.2% in girls), as was its sensitivity for adult overweight (23.3% in boys and 28.8% in girls). The specificities of overweight and obesity were high for both adult overweight and adult obesity in both boys and girls (ranging from 92.7% to 99.3%). The PPVs for childhood obesity in predicting adult obesity or overweight were low, ranging from 42% to 56%; those for childhood overweight were higher (68% to 83%). The NPVs for childhood obesity were high at around 90%, but those for childhood overweight were lower (52% to 70%).
The study by Juhola et al. (2011)125 reported summary data; these findings reflect that of the meta-analysis. Obesity across all ages of childhood (3–18 years) had very low sensitivity (15.8%) but high specificity (97.9%) for adult (age 30–45 years) obesity. This finding was not modified by age of child, but sensitivity was increased when boys (30.9%) and girls (22.9%) were analysed separately. The PPV and NPV were 61.5% and 84.7% respectively. PPV did tend to improve with increasing age, being 91.7% at age 15 years, whereas NPV remained roughly constant.
The cohort studied by Liddle et al. (2012)127 and Mamun et al. (2005)128 was followed from age 5 years and therefore was not included in the meta-analysis. Data from these studies are given in Appendix 3 and the calculated sensitivities and specificities are given in Table 14.
| Weight status categories | Sensitivity | 95% CI | Specificity | 95% CI | |||
|---|---|---|---|---|---|---|---|
| Upper | Lower | Upper | Lower | ||||
| Liddle (2012)127 MUSP cohort from age 5 years to age 21 years | |||||||
| BMI | Obesity at age 5 years to predict obesity at age 21 years | 8.7 | 4.86 | 12.53 | 98.32 | 97.68 | 98.96 |
| Obesity at age 5 years to predict overweight or obesity at age 21 years | 5.69 | 3.8 | 7.57 | 99.06 | 98.51 | 99.61 | |
| Overweight or obesity at age 5 years to predict obesity at age 21 years | 41.06 | 34.36 | 47.76 | 87.79 | 86.16 | 89.42 | |
| Overweight or obesity at age 5 years to predict overweight or obesity at age 21 years | 31.9 | 28.1 | 35.69 | 92.43 | 90.91 | 93.94 | |
| SFT | Obesity at age 5 years to predict obesity at age 21 years | 4.83 | 1.91 | 7.75 | 97.55 | 96.77 | 98.32 |
| Obesity at age 5 years to predict overweight or obesity at age 21 years | 4.48 | 2.8 | 6.17 | 98.13 | 97.35 | 98.9 | |
| Overweight or obesity at age 5 years to predict obesity at age 21 years | 30.92 | 24.62 | 37.21 | 85.66 | 83.91 | 87.4 | |
| Overweight or obesity at age 5 years to predict overweight or obesity at age 21 years | 25.86 | 22.3 | 29.43 | 88.43 | 86.6 | 90.25 | |
| Mamun (2005)128 MUSP cohort from age 5 years to age 14 years | |||||||
| BMI | Overweight or obesity at age 5 years to predict overweight or obesity at age 14 years | 42.23 | 38.57 | 45.88 | 91.73 | 90.55 | 92.91 |
The MUSP cohort of Australian children was followed from age 5 years, first to age 14 and then to age 21 years. The sensitivity and specificity of weight status, as determined using BMI at age 5 years to predict weight status at ages 14 and 21 years, are presented in Table 14. The results for the prediction of overweight at age 14 years are similar to those at age 21 years. The sensitivity of overweight or obesity at age 5 years to predict either obesity or overweight/obesity at age 21 years is low, and the sensitivity of obesity at age 5 years is particularly low. These results reflect those of the meta-analysis for older age ranges, although they might suggest that diagnosis of obesity at age 5 years does not track to adult obesity. The findings from the study by Liddle et al. (2012)127 on the predictive ability of triceps SFT reflect those for BMI, except that the sensitivity and specificity results are slightly poorer. This study does not provide evidence that SFT might be a better measure in children than BMI.
Conclusions of the tracking review
This review identified 23 studies117–139 which tracked childhood obesity or overweight into adolescence or adulthood. Of these, 20 were included in the meta-analyses. These studies were very diverse, including studies from Europe, the USA and Asia, with widely differing sample sizes. The age at which childhood assessment was carried out ranged from 7 to 18 years. Most studies included in the meta-analysis were at an unclear risk of attrition bias and confounding was considered only in terms of age and sex, if at all. BMI was measured at various ages in childhood, adolescence and adulthood, and in various populations. As a result of this diversity, very few studies were included in each specific meta-analysis, leading to considerable uncertainty in the results and wide CIs. This uncertainty should be considered when interpreting the results.
The analysis found a strong association between childhood obesity and adult obesity, with obese children being about five times more likely to be obese as adults than similar, non-obese children. This strong association is reflected in the high PPVs: just under 80% of obese adolescents go on to be obese adults. This drops to 70% when only adults over age 30 years are considered, so consequently around 30% of obese adolescents will not be obese 20 years later. Tracking of obesity from childhood to adolescence was generally good, with around 60% of obese adolescents having been obese as children, and around half of obese children still being obese in adolescence.
By contrast, most obese adults were not obese as children or adolescents: just 30% of obese adults were obese in adolescence, and around 60% of obese adults were of healthy weight during childhood and adolescence. Using childhood obesity to predict adult obesity will therefore fail to identify most adult obesity.
No data were available for tracking beyond age 40 years, but given the available data it seems that many obese children will not be obese by their forties or later (when obesity-related morbidities are most common), and most people who are obese at later ages will not have been obese in childhood.
Review of diagnostic accuracy of childhood measures of obesity
Of the 794 full papers screened, 375 were potential includes for the diagnostic accuracy review. Of these, 341 were excluded, primarily because they were correlation studies and therefore reported only associations rather than diagnostic accuracy.
Quality of the evidence for diagnostic accuracy of childhood measures of obesity
Thirty-four studies met the inclusion criteria for the review of diagnostic accuracy. 173–206 The full results of the quality assessment, along with the guidance for scoring each criterion, are given in Appendix 4. There were some duplicate papers for some cohorts, where more than one paper provided unique data. Three papers reported data from the NHANES study;101,103,180 data were extracted from the one that provided 5 × 5 data in the largest population (n = 7356) for both BMI and SFT using DEXA as the reference standard. 180 The other two NHANES papers were not extracted; one reported only PPV for BMI,103 and the other 3 × 3 tables using cut-off points < 5th, 5th–85th and > 85th internally derived centiles, so providing 2 × 2 data for overweight only, for a small subgroup of children (n = 58) with cerebral palsy and ‘reference children’ (n = 6754). 101 Three papers were identified from the Stockholm Weight Development Study. 102,192,193 One of these was a summary of the results presented in the other two papers, and was therefore excluded. 102 Data were extracted from both of the other studies; one provided data for BMI, WC and hip circumference (HC),193 and the other for a further three classification systems of BMI. 192 Two studies reported results from the Pediatric Rosetta Body Composition study. 179,190 Both studies were included in the review as one reported sensitivity and specificity for BMI of the entire population, along with SFT for boys and girls separately and for the entire population,190 and the other reported a contingency table for boys and girls separately for BMI only, from which summary measures were calculated for those subgroups. 179
All 34 studies avoided differential verification bias and incorporation bias; only one study was subject to partial verification bias, with the results of DEXA being imputed for some children. 180 Only two studies used the gold standard, a multicomponent model;175,182 the other studies used an imperfect reference standard. Of the 32 using an imperfect reference standard, three used D2O,173,204,205 one used ADP193 and four used underwater (hydrostatic) weighting,186,187,189,197 but most used the least reliable of the eligible reference standards, DEXA. 174,176–181,183–185,188,190–192,194–196,198–203,206 Brief study details are provided in Table 15.
| Study details | Population details | Tests conducted |
|---|---|---|
| Alvero-Cruz (2010)173 Esccola study Europe Study dates October–December 2006 |
n = 150 Age (years): mean 14.8 years (range 12–18 years) Sex: male 50% Ethnicity: NR Weight distribution: NR |
Index tests
|
| Bartok (2011)174 USA/Canada Study dates 2000–7 |
n = 197 at baseline; 160 at final follow-up Age: 9–15 years Sex: male 0% Ethnicity: white 100% Weight distribution: overweight 30–42% depending on age; obese 17–29% depending on age |
Index tests
|
| Bray (2002)175 USA/Canada Study dates NR |
n = 131 at baseline; 114 at final follow-up Age: mean 12.7 years (SD 0.11 years) Sex: male 53.5% Ethnicity: white 48.2%; black 51.8% Weight distribution: NR |
Index tests
|
| Dung (2006)176 Europe Study dates April 1998–September 2003 |
n = 393 Age: mean 12 years (range 0.4–18 years) Sex: male 48.6% Ethnicity: NR Weight distribution: NR |
Index tests
|
| Ellis (1999)177 USA/Canada Study dates 1994–8 |
n = 979 Age: 3–18 years Sex: male 41.5% Ethnicity: white 44.7%; black 28.9%; Hispanic 26.4% Weight distribution: NR |
Index tests
|
| Field (2003)178 USA/Canada Study dates NR |
n = 596 Age: mean 10 years (SD 2.2 years) Sex: male 39.8% Ethnicity: white 55.4%; AA 40.1%; Hispanic, Asian and other 4.5% Weight distribution: healthy weight 36.7%; overweight 12.3%; obese 51% |
Index tests
|
| Freedman (2009)179 Pediatric Rosetta Body Composition study USA/Canada Study dates 1995–2000 |
n = 1196 Age: 5–18 years Sex: male 52.3% Ethnicity: white 25%, Asian 30%, black 23%, Hispanic 14%, unclassified 8% Weight distribution: healthy weight 67%, overweight 17%, obese 16% |
Index tests
|
| Freedman (2013)180 NHANES USA/Canada Study dates 1999–2004 |
n = 7365 Age: mean 13.9 years (range 9.8–18.2 years) Sex: male 61% Ethnicity: white 61.5%, black 14.5%, Hispanic 11% Weight distribution: overweight 16.5%, obese 17.5% |
Index tests
|
| Fujita (2011)181 UK Study dates 2008–10 |
n = 466 at baseline; 422 at final follow-up Age: mean 10 years Sex: male 53.6% Ethnicity: NR Weight distribution: NR |
Index tests
|
| Fuller (2001)182 UK Study dates NR |
n = 41 at baseline; 38 in analysis Age: mean 9.4 years (SD 1.4 years) Sex: male 50% Ethnicity: NR Weight distribution: NR |
Index tests
|
| Fuller (2002)183 UK Study dates NR |
n = 41 at baseline; 37 in analysis Age: mean 9.4 years (range 8–12 years) Sex: male 48.6% Ethnicity: NR Weight distribution: 32.4% in upper tertile |
Index tests
|
| Guntsche (2010)184 Argentina Study dates 2005–7 |
n = 108 Age: mean 11 years (range 6–16 years) Sex: male 63% Ethnicity: NR Weight distribution: healthy weight 36%, overweight 13.0%, obese 50.9% |
Index tests
|
| Harrington (2013)185 USA/Canada Study dates NR |
n = 423 at baseline; 369 at final follow-up Age: 5–18 years Sex: male 46.9% Ethnicity: white 48%, black 52% Weight distribution: obese 33% |
Index tests
|
| Himes (1989)186 USA/Canada Study dates NR |
n = 316 Age: 8.4–18.99 years Sex: male 50.3% Ethnicity: NR Weight distribution: NR |
Index tests
|
| Johnston (1985)187 USA/Canada Study dates NR |
n = 235 Age: 12–17 years Sex: male 71.9% Ethnicity: white 97.4%, black 2.6% Weight distribution: obese 20.4% |
Index tests
|
| Khadgawat (2013)188 Asia Study dates NR |
n unclear at baseline; 1640 at final follow-up Age: 7–17 years Sex: male 50.3% Ethnicity: Asian 100% (presumed) Weight distribution: healthy weight 81.8%, overweight 13.8%, obese 4.5% |
Index tests
|
| Marshall (1991)189 Canadian Fitness Survey 1985 USA/Canada Study start date 1981 |
n = 600 at baseline; 540 at final follow-up Age: mean 10.9 years (range 7–14 years) Sex: male 49.3% Ethnicity: NR Weight distribution: obese 14.1% |
Index tests
|
| Mei (2006)190 Pediatric Rosetta Body Composition study USA/Canada Study dates 1995–2000 |
n = 1208 at baseline; 1196 at final follow-up Age: mean 12 years (range 5–18 years) Sex: male 52.3% Ethnicity: white 25.3%, Asian 29.9%, black 22.5%, Hispanic 20.9% Weight distribution: healthy weight 25.6%, overweight 33.9%, obese 40.5% |
Index tests
|
| Moreno (2006)191 AVENA study Europe Study dates NR |
n = 348 at baseline; 286 in analysis Age: 13–17.9 years Sex: male 40.6% Ethnicity: NR Weight distribution: NR |
Index tests
|
| Neovius (2004)192 Stockholm Weight Development Study Europe Study dates NR |
n = 481 at baseline; 474 had data available Age: mean 16.9 years (SD 0.4 years) Sex: male 42.2% Ethnicity: NR Weight distribution: NR |
Index tests
|
| Neovius (2005)193 Stockholm Weight Development Study Europe Study dates NR |
n = 481 at baseline; 474 had data available Age: mean 16.8 years (SD 0.4 years) Sex: male 42.2% Ethnicity: NR Weight distribution: NR |
Index tests
|
| Pandit (2009)194 Asia Study dates NR |
n = 566 Age: 6–17 years Sex: male 55.8% Ethnicity: NR Weight distribution: overweight 38.5% of boys and 54% of girls |
Index tests
|
| Reilly (2010)195 ALSPAC UK Study dates NR |
n = 7779 at baseline; 7722 had data available Age: mean 9.9 years (SD 0.5 years) Sex: male 49.3% Ethnicity: NR Weight distribution: overweight 25.5%, obese 13% |
Index tests
|
| Sardinha (1999)196 USA/Canada Study dates NR |
n = 328 Age: 10–15 years Sex: male 50.3% Ethnicity: white 100% Weight distribution: obese 27.3% of boys and 44.8% of girls |
Index tests
|
| Sarria (2001)197 Europe Study dates NR |
n = 175 (173 with WC measurements) Age: 7.2–16.9 years Sex: male 100% Ethnicity: NR Weight distribution: overweight 21.1% |
Index tests
|
| Sproule (2009)198 USA/Canada Study dates NR |
n = 25 (with spinal muscular atrophy) Age: mean 9.1 years (range 5–18 years) Sex: male 56% Ethnicity: NR Weight distribution: NR |
Index tests
|
| Taylor (2000)199 Australia/New Zealand Study dates NR |
n = 580 Age: mean 12.2 years (range 3.1–19.9 years) Sex: male 52.1% Ethnicity: white 100% Weight distribution: NR |
Index tests
|
| Taylor (2003)200 Australia/New Zealand Study dates NR |
n = 368 Age: mean 11.9 years (range 8.5–15.5 years) Sex: male 48.6% Ethnicity: white 100% Weight distribution: obese 25% |
Index tests
|
| Telford (2008)201 Commonwealth Institute LOOK Australia/New Zealand Study dates NR |
n = 741 Age: mean 8 years (SD 0.3 years) Sex: male 50.7% Ethnicity: NR Weight distribution: NR |
Index tests
|
| Vitolo (2007)202 Brazil Study start date 1998 |
n = 427 at baseline; 418 at final follow-up Age: mean 13.4 years (range 10–19 years) Sex: male 52.4% Ethnicity: NR Weight distribution: overweight approximately 25% |
Index tests
|
| Warner (1997)203 UK Study dates NR |
n = 143 Age: mean 13.5 years (SD 2.7 years) Sex: male 55.2% Ethnicity: NR Weight distribution: NR |
Index tests
|
| Wickramasinghe (2005)204 Australia/New Zealand Study dates NR |
n = 138 Age: mean 9.4 years (range 5–14.99 years) Sex: male 51.4% Ethnicity: white 69.6%, Asian 30.4% Weight distribution: obese 51.4% |
Index tests
|
| Wickramasinghe (2009)205 Asia Study dates September 2004–April 2005 |
n = 282 Age: mean 9.8 years (range 5–15 years) Sex: male 56% Ethnicity: NR Weight distribution: NR |
Index tests
|
| Zhang (2004)206 Asia Study dates NR |
n = 1068 at baseline; 751 at final follow-up Age: 9–14 years Sex: male 15.3% Ethnicity: Asian 100% Weight distribution: obese 28% |
Index tests
|
Eighteen studies recruited either consecutive or randomly selected children from populations representative of the UK population who would be eligible for the test in clinical practice. 173,177–181,186,189–195,201,202,205,206 One study recruited a population representative of the country in which the study was conducted. 188 Thirteen studies did not recruit a representative population, for either the country in which the study was conducted or the UK;174–176,184,185,187,196–200,203,204 these studies generally focused on specific subgroups of children. The representativeness of the population was unclear in two studies. 182,183
Most of the studies were single-gate diagnostic cohort studies undertaken specifically to determine the accuracy of a simple anthropomorphic measure (the index test). 173,175–179,181–184,186–189,193,194,196–205 Although the time lag between the index test and reference standard test was not stated, it is unlikely that this was sufficiently long for progression bias to be present. Five studies were cross-sectional, with aims beyond the determination of the diagnostic accuracy of an index test, and had either a prospective185,190,191,206 or retrospective/post-hoc180 analysis; these were also considered to have a low likelihood of progression bias. Three studies were longitudinal, and the timing of the index and reference standard tests was not specifically reported; therefore, the potential for progression bias was unclear. 174,192,195
The description of the index tests was adequate in most studies; the details provided for the reference standards were generally more poorly reported, making reproducibility of the reference standard tests more difficult. Most of the studies apparently had no uninterpretable results and no withdrawals. The number and expertise of the assessors for both the index tests and reference standards were unclear in most studies.
Owing to the poorer accuracy of DEXA compared with the other reference standards, none of the studies using DEXA was considered to be of high quality. Of the 10 studies that used a reference standard other than DEXA, eight were considered to be high quality,173,186,187,189,193,197,204,205 one did not explain withdrawals175 and another excluded withdrawals from the study. 182
Diagnostic accuracy of body mass index
A total of 30 diagnostic accuracy studies evaluated BMI. The study and population characteristics varied across these studies. In clinical practice, weight status is commonly defined using the cut-off points of 85th centile for overweight and 95th centile for obesity. In addition, the measures tend to be used in a diverse population of children. Several of the studies did not report the thresholds used, used other thresholds to define overweight and obesity or conducted the study in a population that was not representative of the UK child population. This section therefore concentrates on the 11 diagnostic accuracy studies of BMI that used the 85th centile for diagnosing overweight and the 95th centile for diagnosing obesity (regardless of the reference population used to standardise the measure for age) in unselected boys, girls or children of both sexes reflective of the UK child population (see Table 16). Results for the other studies of BMI are presented in Appendix 3, which includes the findings of all the included diagnostic accuracy studies.
The sensitivities and specificities of the 11 BMI studies are presented in Table 16. Of these, only one study was considered to be of high quality (results shown in italics in Table 16). 186 Sensitivity varied considerably across these studies, ranging from 23% to 96% for diagnosing obesity and 19% to 94% for diagnosing overweight. Specificity was less variable, ranging from 89.4% to 100% for diagnosing obesity and 82% to 100% for diagnosing overweight. Data were available as 2 × 2 contingency tables for eight studies diagnosing overweight177,179,180,188,191,192,197,203 and six studies diagnosing obesity;177,179,180,186,188,195 2 × 2 tables were not available for two studies. 181,190
| Study | Population | Age at assessment (years) | Index test details | Index test cut-off point (centile) | Reference standard | Reference standard cut-off point | Total n | Sensitivity (95% Cl), % | Specificity (95% Cl), % |
|---|---|---|---|---|---|---|---|---|---|
| Obesity | |||||||||
| Himes (1989) 186 | All children | 8.4–18.99 | NR | 85th | Underwater (hydrostatic) weighting | 90th centile | 316 | 25 (16 to 37) | 100 (98 to 100) |
| Freedman (2013)180 | All children | 8–19 | CDC | 95th | DEXA | NR | 7365 | 76 (73 to 78) | 95 (94 to 95) |
| Reilly (2010)195 | All children | Mean 9.9 | UK90 | 95th | DEXA | 90th centile | 7722 | 95 (94 to 97) | 95 (95 to 96) |
| Khadgawat (2013)188 | All children | 7–17 | IOTF | 95th | DEXA | 95th centile | 1640 | 66 (53 to 77) | 98 (97 to 99) |
| Khadgawat (2013)188 | All children | 7–17 | IOTF | 95th | DEXA | Prevalence matched to BMI | 1640 | 72 (60 to 82) | 99 (98 to 99) |
| Freedman (2009)179 | All children | 5–18 | CDC | 95th | DEXA | 95th centile | 1196 | 77 (70 to 83) | 96 (94 to 97) |
| Ellis (1999)177 | All children | 3–18 | UK90 | 95th | DEXA (adjusted for sex and ethnicity) | 95th centile | 979 | 72 (58 to 84) | 91 (89 to 93) |
| Ellis (1999)177 | All children | 3–18 | UK90 | 95th | DEXA (adjusted for sex) | 95th centile | 979 | 82 (69 to 91) | 92 (90 to 93) |
| Field (2003)178 | Unselected | Mean 10 (SD 2.2) | NR | 95th | DEXA | 90th centile | 596 | 65 (NR) | 99 (NR) |
| Mei (2006)190 | Unselected | 5–18 | CDC | 95th | DEXA | 95th centile | 1196 | 92.5 (NR) | 89.4 (NR) |
| Himes (1989) 186 | Boys | 8.4–18.99 | NR | 85th | Underwater (hydrostatic) weighting | 90th centile | 159 | 29 (11 to 51) | 99 (96 to 100) |
| Freedman (2013)180 | Boys | 8–19 | CDC | 95th | DEXA | NR | 4518 | 75 (72 to 78) | 95 (94 to 95) |
| Reilly (2010)195 | Boys | 9.9 | UK90 | 95th | DEXA | 90th centile | 3809 | 96 (94 to 98) | 95 (94 to 95) |
| Khadgawat (2013)188 | Boys | 7–17 | IOTF | 95th | DEXA | 95th centile | 825 | 85 (65 to 96) | 97 (95 to 98) |
| Khadgawat (2013)188 | Boys | 7–17 | IOTF | 95th | DEXA | Prevalence matched to BMI | 825 | 67 (52 to 80) | 98 (97 to 99) |
| Freedman (2009)179 | Boys | 5–18 | CDC | 95th | DEXA | 95th centile | 626 | 75 (65 to 83) | 95 (93 to 97) |
| Ellis (1999)177 | Boys | 3–18 | UK90 | 95th | DEXA (adjusted for sex and ethnicity) | 95th centile | 406 | 76 (53 to 92) | 91 (88 to 94) |
| Ellis (1999)177 | Boys | 3–18 | UK90 | 95th | DEXA (adjusted for sex) | 95th centile | 406 | 71 (48 to 89) | 91 (88 to 94) |
| Himes (1989) 186 | Girls | 8.4–18.99 | NR | 85th | Underwater (hydrostatic) weighting | 90th centile | 157 | 23 (10 to 40) | 100 (99 to 100) |
| Freedman (2013)180 | Girls | 8–19 | CDC | 95th | DEXA | NR | 2847 | 76 (72 to 80) | 95 (94 to 96) |
| Reilly (2010)195 | Girls | 9.9 | UK90 | 95th | DEXA | 90th centile | 3913 | 94 (91 to 96) | 96 (96 to 97) |
| Khadgawat (2013)188 | Girls | 7–17 | IOTF | 95th | DEXA | 95th centile | 815 | 54 (37 to 69) | 100 (99 to 100) |
| Khadgawat (2013)188 | Girls | 7–17 | IOTF | 95th | DEXA | Prevalence matched to BMI | 815 | 81 (61 to 93) | 99 (99 to 100) |
| Freedman (2009)179 | Girls | 5–18 | CDC | 95th | DEXA | 95th centile | 570 | 80 (70 to 88) | 97 (94 to 98) |
| Ellis (1999)177 | Girls | 3–18 | UK90 | 95th | DEXA (adjusted for sex and ethnicity) | 95th centile | 573 | 69 (49 to 85) | 91 (88 to 93) |
| Ellis (1999)177 | Girls | 3–18 | UK90 | 95th | DEXA (adjusted for sex) | 95th centile | 573 | 90 (73 to 98) | 92 (90 to 94) |
| Overweight | |||||||||
| Neovius (2004)192 | All children | Mean 16.9 (SD 0.4) | Göteborg, Sweden | 85th | ADP | 25% BF boys; 30% BF girls | 474 | 48 (40 to 57) | 95 (92 to 97) |
| Neovius (2004)192 | All children | 16.9 (SD 0.4) | WHO | 85th | ADP | 25% BF boys; 30% BF girls | 474 | 28 (20 to 36) | 99 (97 to 100) |
| Freedman (2009)179 | All children | 5–18 | CDC | 85th | DEXA | 85th centile | 1196 | 83 (79 to 87) | 92 (90 to 94) |
| Moreno (2006)191 | All children | 13–17.9 | AVENA | 85th | DEXA | 85th centile | 286 | 67 (53 to 78) | 90 (86 to 94) |
| Moreno (2006)191 | All children | 13–17.9 | IOTF | 85th | DEXA | 85th centile | 286 | 73 (60 to 84) | 88 (84 to 92) |
| Khadgawat (2013)188 | All children | 7–17 | IOTF | 85th | DEXA | 85th centile | 1640 | 72 (66 to 77) | 93 (91 to 94) |
| Khadgawat (2013)188 | All children | 7–17 | IOTF | 85th | DEXA | Prevalence matched to BMI | 1640 | 72 (67 to 77) | 94 (93 to 95) |
| Ellis (1999)177 | All children | 3–18 | UK90 | 85th | DEXA (adjusted for sex and ethnicity) | 85th centile | 979 | 92 (86 to 96) | 83 (80 to 85) |
| Ellis (1999)177 | All children | 3–18 | UK90 | 85th | DEXA (adjusted for sex) | 85th centile | 979 | 93 (87 to 96) | 83 (80 to 85) |
| Warner (1997)203 | All children | ? | SD scores | 85th/1 SD | DEXA | US 85th centile | 143 | 66 (52 to 78) | 94 (86 to 98) |
| Neovius (2004)192 | Boys | 16.9 (SD 0.4) | Göteborg, Sweden | 85th | ADP | 25% BF | 200 | 92 (NR) | 93 (NR) |
| Neovius (2004)192 | Boys | 16.9 (SD 0.4) | WHO | 85th | ADP | 25% BF | 200 | 68 (NR) | 98 (NR) |
| Freedman (2013)180 | Boys | 8–19 | CDC | 85th | DEXA | NR | 4518 | 83 (81 to 84) | 91 (90 to 92) |
| Freedman (2009)179 | Boys | 5–18 | CDC | 85th | DEXA | 85th centile | 626 | 84 (78 to 88) | 92 (89 to 95) |
| Moreno (2006)191 | Boys | 13–17.9 | AVENA | 85th | DEXA | 85th centile | 116 | 53 (28 to 77) | 88 (79 to 94) |
| Moreno (2006)191 | Boys | 13–17.9 | IOTF | 85th | DEXA | 85th centile | 116 | 71 (44 to 90) | 86 (77 to 92) |
| Khadgawat (2013)188 | Boys | 7–17 | IOTF | 85th | DEXA | 85th centile | 825 | 78 (71 to 85) | 91 (89 to 93) |
| Khadgawat (2013)188 | Boys | 7–17 | IOTF | 85th | DEXA | Prevalence matched to BMI | 825 | 77 (70 to 83) | 94 (92 to 95) |
| Ellis (1999)177 | Boys | 3–18 | UK90 | 85th | DEXA (adjusted for sex and ethnicity) | 85th centile | 406 | 92 (82 to 97) | 84 (79 to 87) |
| Ellis (1999)177 | Boys | 3–18 | UK90 | 85th | DEXA (adjusted for sex) | 85th centile | 406 | 90 (80 to 96) | 83 (79 to 87) |
| Neovius (2004)192 | Girls | 16.9 (SD 0.4) | Göteborg, Sweden | 85th | ADP | 30% BF | 274 | 39 (NR) | 97 (NR) |
| Neovius (2004)192 | Girls | 16.9 (SD 0.4) | WHO | 85th | ADP | 30% BF | 274 | 19 (NR) | 100 (NR) |
| Freedman (2013)180 | Girls | 8–19 | CDC | 85th | DEXA | ? | 2847 | 80 (77 to 82) | 90 (88 to 91) |
| Freedman (2009)179 | Girls | 5–18 | CDC | 85th | DEXA | 85th centile | 570 | 83 (77 to 88) | 92 (89 to 94) |
| Moreno (2006)191 | Girls | 13–17.9 | AVENA | 85th | DEXA | 85th centile | 170 | 79 (58 to 93) | 92 (86 to 96) |
| Moreno (2006)191 | Girls | 13–17.9 | IOTF | 85th | DEXA | 85th centile | 170 | 75 (53 to 90) | 90 (84 to 95) |
| Khadgawat (2013)188 | Girls | 7–17 | IOTF | 85th | DEXA | 85th centile | 815 | 64 (55 to 72) | 94 (92 to 96) |
| Khadgawat (2013)188 | Girls | 7–17 | IOTF | 85th | DEXA | Prevalence matched to BMI | 815 | 65 (56 to 73) | 94 (92 to 96) |
| Ellis (1999)177 | Girls | 3–18 | UK90 | 85th | DEXA (adjusted for sex and ethnicity) | 85th centile | 573 | 92 (84 to 97) | 82 (78 to 85) |
| Ellis (1999)177 | Girls | 3–18 | UK90 | 85th | DEXA (adjusted for sex) | 85th centile | 573 | 94 (87 to 98) | 83 (79 to 86) |
Using the 2 × 2 data, the pooled sensitivity, specificity, positive likelihood ratio (LR+) and negative likelihood ratio (LR−) were calculated using the HSROC model (Figure 28); analyses were conducted for boys and girls separately and combined (Table 17). Two analyses were conducted for boys and girls combined; one used the separate boy and girl subgroups,177,179,180,186,188,191,192,195,197 adding data for the one study that did not report for girls and boys separately,203 and in the other, data from the within-study boy and girl subgroups were combined to create ‘all children’ populations prior to analysis. 177,179,180,186,188,191,192,203 The former included the one study that reported results for boys only;197 this study was excluded from the latter analysis.
FIGURE 28.
Hierarchical summary ROC curves for BMI for (a) unselected boys; (b) unselected girls; (c) all children (boy and girl subgroups kept separate); and (d) all children (within-study boy and girl subgroups combined prior to analysis).
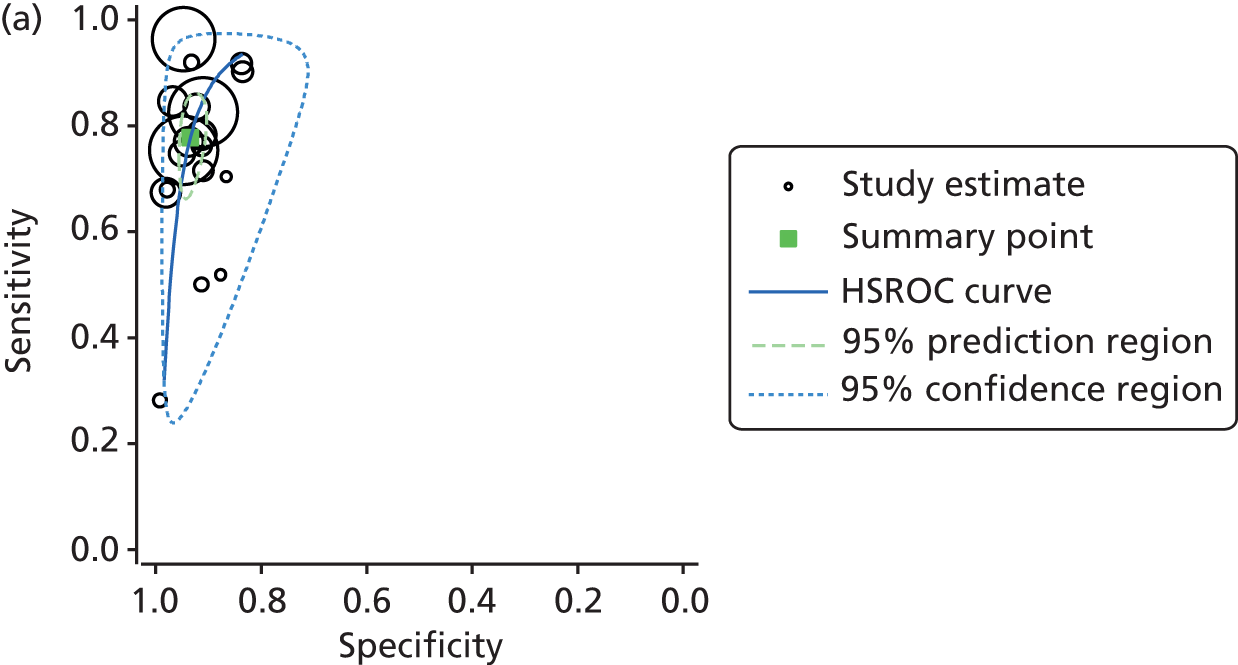
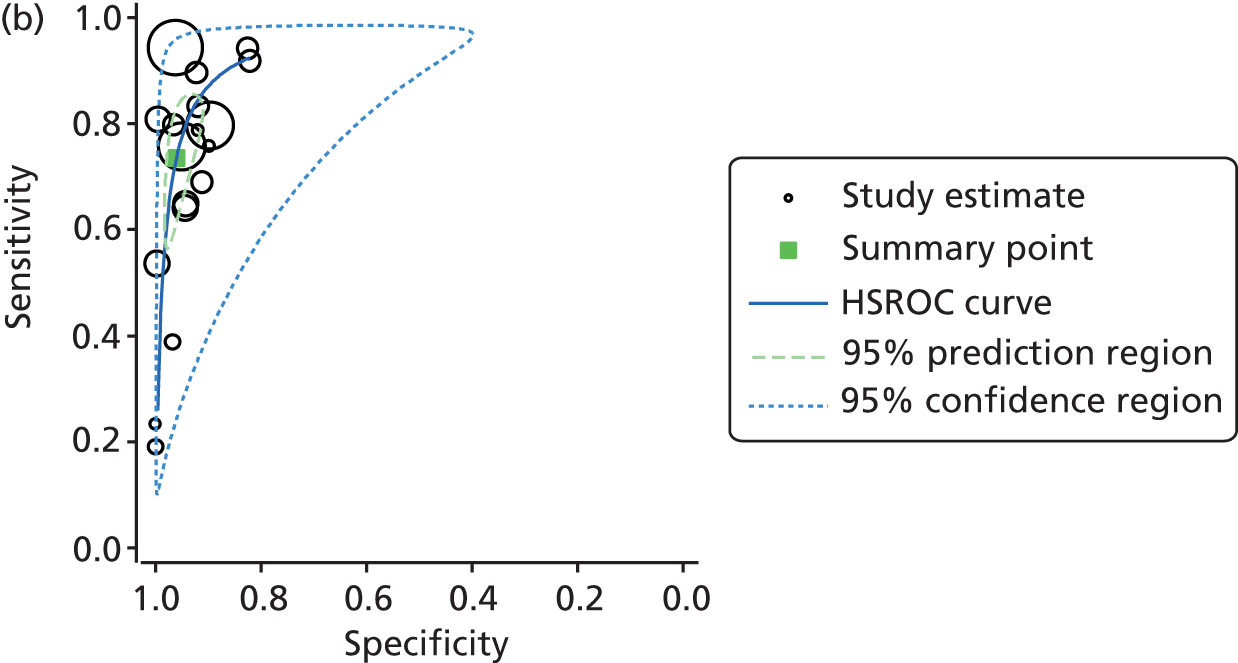
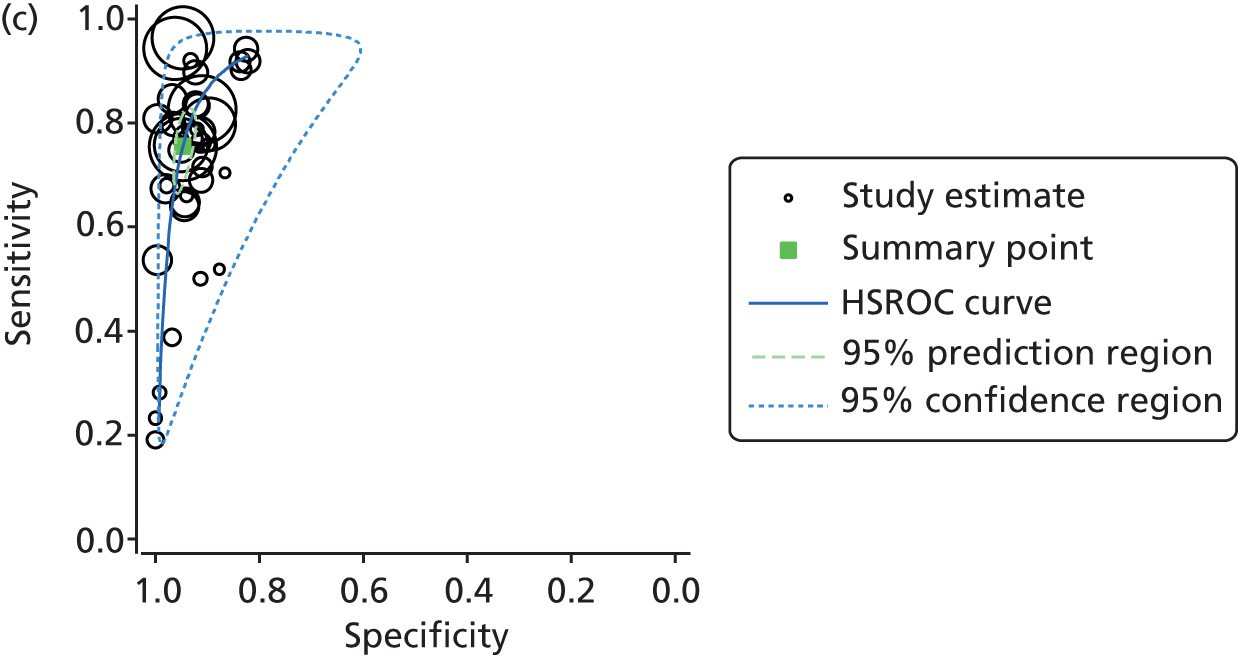
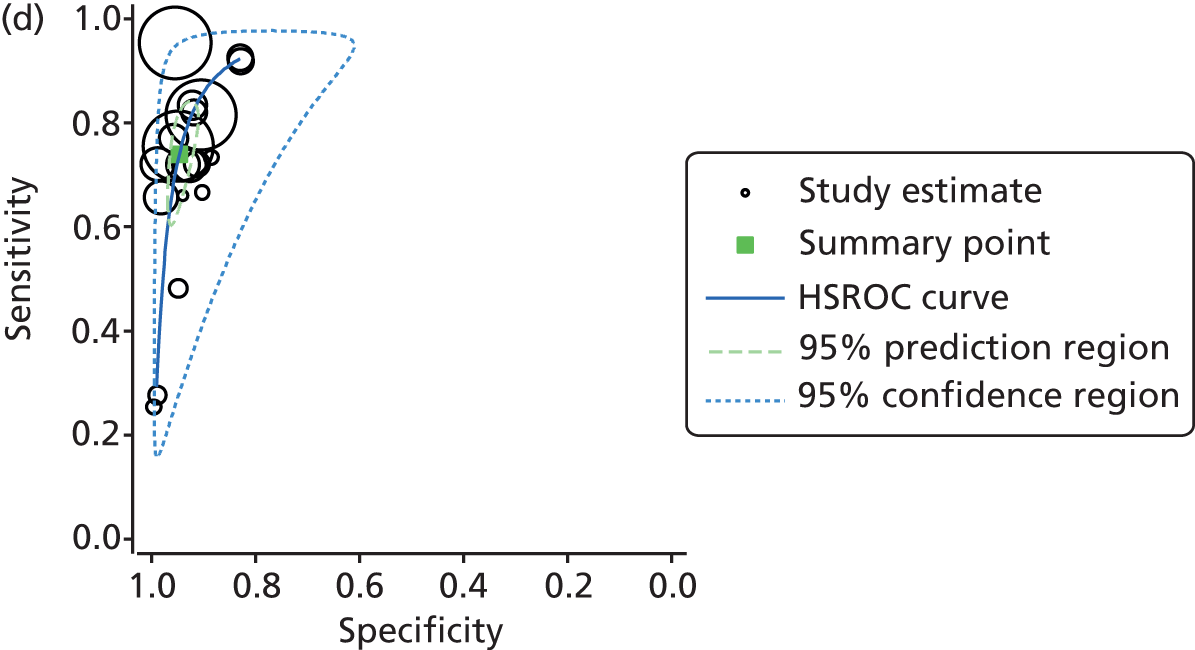
| Population | n studies/data sets | Sensitivity (95% CI), % | Specificity (95% CI), % | LR+ (95% CI) | LR− (95% CI) |
|---|---|---|---|---|---|
| Boys | 8/19 | 77.8 (69.6 to 84.2) | 93.4 (91.2 to 95.1) | 11.8 (9.05 to 15.5) | 0.238 (0.172 to 0.329) |
| Girls | 8/18 | 73.5 (61.4 to 82.8) | 96.1 (92.8 to 97.9) | 18.7 (11.07 to 31.5) | 0.276 (0.186 to 0.408) |
| Boys and girls | 10/38 | 75.5 (68.7 to 81.3) | 94.7 (92.9 to 96.1) | 14.4 (11.01 to 18.74) | 0.258 (0.201 to 0.331) |
| All children | 9/19 | 73.9 (64.2 to 81.8) | 94.7 (92.2 to 96.4) | 13.9 (10.02 to 19.24) | 0.275 (0.199 to 0.381) |
The results of these analyses (see Table 17) show that BMI has a relatively low sensitivity, but a high specificity, across the different subgroups for diagnosing overweight/obesity. With such high specificities, there are few false-positive results; therefore, BMI is better at ruling obesity in than ruling it out, hence the moderately high LR+ but poorer LR−. These summary estimates should be treated with caution, as they are based on a subset of the BMI studies, and heterogeneity was substantial (see Figure 28); there were insufficient studies to investigate the impact of this heterogeneity. The analyses also combined data from the same population using different thresholds from some studies. As a result, the uncertainty surrounding the pooled estimates (95% prediction region) is large.
Two studies provided insufficient data to derive 2 × 2 tables. Of these, one reported sensitivity of 92.5% and specificity of 89.4% for diagnosing obesity (95th centile, CDC 2000219),190 and the other reported an AUC of 0.983 (95% CI 0.968 to 0.999) for boys and 0.981 (95% CI 0.961 to 1.00) for girls for diagnosing obesity (95th centile, reference population unclear). 181
Diagnostic accuracy of skinfold thickness
Of the 34 included studies, 10175,180,182,184,186,187,189,190,196,197 evaluated SFT. Where reported, the most commonly used cut-off point was the 85th centile. Most of the studies used the measure to diagnose obesity; data for diagnosing overweight were more limited. Four studies reported the sensitivity and specificity of triceps SFT, or data to calculate these outcomes, for the diagnosis of overweight or obesity (Table 18);186,187,189,190 of these, three were considered to be high quality (results shown in italics in Table 18). 186,187,189 Sensitivity ranged from 23% to 98.5%, and specificity from 78% to 100%, across the populations and thresholds.
| Study | Population | Age at assessment (years) | Index test cut-off point (centile) | Reference standard | Reference standard cut-off point | Total n | Sensitivity (95% Cl), % | Specificity (95% Cl), % |
|---|---|---|---|---|---|---|---|---|
| Obesity | ||||||||
| Himes (1989) 186 | Boys | 8.4–18.99 | 85th | Underwater (hydrostatic) weighting | 90th centile | 159 | 24 (8 to 45) | 100 (99 to 100) |
| Himes (1989) 186 | Girls | 8.4–18.99 | 85th | Underwater (hydrostatic) weighting | 90th centile | 157 | 23 (10 to 40) | 97 (93 to 99) |
| Marshall (1991) 189 | Unselected | 7–14 | 85th | Underwater (hydrostatic) weighting | 20% BF boys; 25% BF girls | 540 | 65.8 (NR) | 94 (NR) |
| Marshall (1991) 189 | Girls | 7–14 | 85th | Underwater (hydrostatic) weighting | 25% BF | 274 | 67.7 (NR) | 93.4 (NR) |
| Marshall (1991) 189 | Boys | 7–14 | 85th | Underwater (hydrostatic) weighting | 20% BF | 266 | 64.4 (NR) | 94.6 (NR) |
| Mei (2006)190 | Unselected | 5–18 | 95th | DEXA | 95th centile | 1196 | 89.6 (NR) | 93.2 (NR) |
| Johnston (1985) 187 | Boys | 12–17 | NR | Underwater (hydrostatic) weighting | 25% BF | 169 | 48 (30 to 67) | 96 (91 to 98) |
| Johnston (1985) 187 | Girls | 12–17 | NR | Underwater (hydrostatic) weighting | 30% BF | 66 | 24 (7 to 50) | 100 (93 to 100) |
| Johnston (1985) 187 | All children | 12–17 | NR | Underwater (hydrostatic) weighting | 25% BF boys; 30% BF girls | 235 | 40 (26 to 55) | 97 (93 to 99) |
| Overweight | ||||||||
| Mei (2006)190 | Unselected | 5–18 | 85th | DEXA | 95th centile | 1196 | 98.5 (NR) | 78 (NR) |
Two studies evaluated subscapular SFT. 186,190 Sensitivity ranged from 30% to 98.5%, and specificity from 79.1% to 99% across the two studies (Table 19). Six studies evaluated sum SFT (Table 20), where more than one site was measured and an overall percentage body fat was determined. 175,180,184,186,189,197 As with the single-site SFT measurements, sensitivity varied across the six studies, but was, on the whole, higher than that for triceps and subscapular SFT individually, ranging from 57% to 98% across populations and thresholds. Most had a sensitivity of 80% or over. Specificity was more variable for the sum SFT than for the individual SFT measures, ranging from 47% to 96%, but was still reasonably high for most population and threshold combinations (see Table 20).
| Study | Population | Age at assessment (years) | Index test cut-off point (centile) | Reference standard | Reference standard cut-off point | Total n | Sensitivity (95% Cl), % | Specificity (95% Cl), % |
|---|---|---|---|---|---|---|---|---|
| Obesity | ||||||||
| Himes (1989) 186 | Boys | 8.4–18.99 | 85th | Underwater (hydrostatic) weighting | 90th | 159 | 38 (18 to 61) | 99 (97 to 100) |
| Himes (1989) 186 | Girls | 8.4–18.99 | 85th | Underwater (hydrostatic) weighting | 90th | 157 | 30 (15 to 48) | 99 (96 to 100) |
| Mei (2006)190 | Unselected | 5–18 | 95th | DEXA | 95th | 1196 | 89.6 (NR) | 94 (NR) |
| Overweight | ||||||||
| Mei (2006)190 | Unselected | 5–18 | 85th | DEXA | 95th | 1196 | 98.5 (NR) | 79.1 (NR) |
| Study | Population | Age at assessment (years) | Index test details | Index test cut-off point | Reference standard | Reference standard cut-off point | Total n | Sensitivity (95% Cl), % | Specificity (95% Cl), % |
|---|---|---|---|---|---|---|---|---|---|
| Obesity | |||||||||
| Himes (1989) 186 | Boys | 8.4–18.99 | Sum | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 159 | 57 (35 to 78) | 85 (78 to 90) |
| Himes (1989) 186 | Girls | 8.4–18.99 | Sum | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 157 | 80 (63 to 92) | 82 (75 to 88) |
| Marshall (1991) 189 | Unselected | 7–14 | Sum | 85th centile | Underwater (hydrostatic) weighting | 20% BF boys; 25% BF girls | 540 | 86.8 (NR) | 90.1 (NR) |
| Marshall (1991) 189 | Girls | 7–14 | Sum | 85th centile | Underwater (hydrostatic) weighting | 25% BF | 274 | 96.8 (NR) | 90.5 (NR) |
| Marshall (1991) 189 | Boys | 7–14 | Sum | 85th centile | Underwater (hydrostatic) weighting | 20% BF | 266 | 80 (NR) | 89.6 (NR) |
| Freedman (2013)180 | Boys | 8–19 | Sum | Elevated – prevalence matched to BMI | DEXA | NR | 4519 | 80 (77 to 83) | 96 (95 to 96) |
| Freedman (2013)180 | Girls | 8–19 | Sum | Elevated – prevalence matched to BMI | DEXA | NR | 2846 | 79 (75 to 83) | 96 (95 to 96) |
| Freedman (2013)180 | All children | 8–19 | Sum | Elevated – prevalence matched to BMI | DEXA | NR | 7365 | 80 (77 to 82) | 96 (95 to 96) |
| Overweight | |||||||||
| Sarria (2001) 197 | Girls | 7–16.9 | Sum | 85th centile | Underwater (hydrostatic) weighting | 85th centile | 175 | 58 (37 to 77) | 93 (87 to 96) |
| Freedman (2013)180 | Boys | 8–19 | Sum | Slightly elevated – prevalence matched to BMI | DEXA | NR | 4519 | 85 (83 to 87) | 92 (91 to 93) |
| Freedman (2013)180 | Girls | 8–19 | Sum | Slightly elevated – prevalence matched to BMI | DEXA | NR | 2846 | 81 (78 to 83) | 90 (89 to 92) |
| Freedman (2013)180 | All children | 8–19 | Sum | Slightly elevated – prevalence matched to BMI | DEXA | NR | 7365 | 83 (82 to 85) | 91 (91 to 92) |
| Guntsche (2010)184 | Obesity centre referrals and siblings – pubertal | 6–16 | 5-site SF Index | 1.26 | DEXA | 10 kg/m2 | 58 | 75 (NR) | 77.3 (NR) |
| Guntsche (2010)184 | Obesity centre referrals and siblings – prepubertal | 6–16 | 5-site SF Index | 1.07 | DEXA | 10 kg/m2 | 50 | 57.6 (NR) | 76.5 (NR) |
| Fat or not fat | |||||||||
| Bray (2002)175 | White and AA children | 12 | Sum Ellis | NR | 4-C model | NR | 114 | 96 (NR) | 47 (NR) |
| Bray (2002)175 | White and AA children | 12 | Sum Pennington | NR | 4-C model | NR | 114 | 94 (NR) | 82 (NR) |
| Bray (2002)175 | White and AA children | 12 | Sum Slaughter | NR | 4-C model | NR | 114 | 98 (NR) | 71 (NR) |
Diagnostic accuracy of waist circumference
Four studies reported sensitivity and specificity for WC for diagnosing obesity,181,193,195,205 and four studies for diagnosing overweight184,193,197,199 (Table 21); of these, three were considered to be of high quality (results shown in italics in Table 21). 193,197,205 As with BMI, there was substantial variation in sensitivity across the studies, ranging from 34.7% to 100% for diagnosing obesity and 53% to 90.9% for diagnosing overweight. Specificity was less variable, ranging from 81% to 100% for diagnosing obesity and 92% to 100% for diagnosing overweight.
| Study | Population | Age at assessment (years) | Index test details | Index test cut-off point | Reference standard | Reference standard cut-off point | Total n | Sensitivity (95% Cl), % | Specificity (95% Cl), % |
|---|---|---|---|---|---|---|---|---|---|
| Obesity | |||||||||
| Neovius (2005) 193 | Girls | 17 | WC smallest between ribs and iliac crest | 85th centile | ADP | 95th centile | 274 | 64 (NR) | 98 (NR) |
| Neovius (2005) 193 | Boys | 17 | WC smallest between ribs and iliac crest | 95th centile | ADP | 95th centile | 200 | 50 (NR) | 98 (NR) |
| Reilly (2010)195 | Boys | 9.9 | UK 1988 reference | 95th centile | DEXA | 90th centile | 3809 | 97 (95 to 99) | 81 (79 to 82) |
| Reilly (2010)195 | Girls | 9.9 | UK 1988 reference | 95th centile | DEXA | 90th centile | 3913 | 98 (95 to 99) | 81 (79 to 82) |
| Reilly (2010)195 | All children | 9.9 | UK 1988 reference | 95th centile | DEXA | 90th centile | 7722 | 98 (96 to 99) | 81 (80 to 82) |
| Wickramasinghe (2009) 205 | Sri Lankan boys | 5–15 | Smallest between ribs and iliac crest | 98th centile | D 2 O | 25% BF | 158 | 34.7 (NR) | 98.8 (NR) |
| Wickramasinghe (2009) 205 | Sri Lankan girls | 5–15 | WC smallest between ribs and iliac crest | 98th centile | D 2 O | 30% BF | 124 | 38.4 (NR) | 100 (NR) |
| Wickramasinghe (2009) 205 | All Sri Lankan children | 5–15 | WC smallest between ribs and iliac crest | 98th centile | D 2 O | 25% BF boys; 30% BF girls | 282 | 37 (30 to 45) | 99 (95 to 100) |
| Fujita (2011)181 | Boys | 10 | WC umbilical | 76.5 | DEXA | 95th centile | 226 | 100 (NR) | 97 (NR) |
| Fujita (2011)181 | Girls | 10 | WC umbilical | 73 | DEXA | 95th centile | 196 | 100 (NR) | 96 (NR) |
| Overweight | |||||||||
| Guntsche (2010)184 | Obesity centre referrals and siblings – prepubertal | 6–16 | Mid-point between ribs and iliac crest | 66.5 | DEXA | 10 kg/m2 | 50 | 84.8 (NR) | 100 (NR) |
| Guntsche (2010)184 | Obesity centre referrals and siblings – prepubertal | 6–16 | WC umbilical | 72 | DEXA | 10 kg/m2 | 50 | 90.9 (NR) | 100 (NR) |
| Guntsche (2010)184 | Obesity centre referrals and siblings – pubertal | 6–16 | Mid-point between ribs and iliac crest | 77 | DEXA | 10 kg/m2 | 58 | 88.9 (NR) | 95.5 (NR) |
| Guntsche (2010)184 | Obesity centre referrals and siblings – pubertal | 6–16 | WC umbilical | 85 | DEXA | 10 kg/m2 | 58 | 88.9 (NR) | 100 (NR) |
| Neovius (2005) 193 | Girls | 17 | WC smallest between ribs and iliac crest | 73.3 | ADP | 30% BF | 274 | 53 (NR) | 89 (NR) |
| Neovius (2005) 193 | Boys | 17 | WC smallest between ribs and iliac crest | 85.9 | ADP | 25% BF | 200 | 68 (NR) | 99 (NR) |
| Taylor (2000)199 | White girls | 3.1–19.8 | WC smallest between ribs and iliac crest | 80th centile | DEXA | 1 SD | 278 | 89 (77 to 96) | 94 (91 to 97) |
| Taylor (2000)199 | White boys | 3.3–19.9 | WC smallest between ribs and iliac crest | 80th centile | DEXA | 1 SD | 302 | 87 (74 to 95) | 92 (88 to 95) |
| Sarria (2001) 197 | Boys | 7–16.9 | WC smallest between ribs and iliac crest | 85th centile | Underwater (hydrostatic) weighting | 85th centile | 175 | 58 (37 to 77) | 93 (87 to 96) |
Diagnostic accuracy of waist-to-hip ratio and waist-to-height ratio
Three studies evaluated WHR184,193,199 and two evaluated WHtR. 181,184 Sensitivity for WHR across the studies was relatively poor, ranging from 0% to 78.8% across populations and thresholds; specificities were generally high, ranging from 70.6% to 100% (Table 22). Sensitivity for WHtR was high, ranging from 90.9% to 100% across populations and thresholds, with specificities also high, ranging from 95% to 100% (Table 23).
| Study | Population | Age at assessment (years) | Site of WC measurement | Index test cut-off point | Reference standard | Reference standard cut-off point | Total n | Sensitivity (95% Cl), % | Specificity (95% Cl), % |
|---|---|---|---|---|---|---|---|---|---|
| Obesity | |||||||||
| Neovius (2005) 193 | Boys | 17 | Smallest between ribs and iliac crest | 0.9 | ADP | 95th centile | 200 | 40 (NR) | 97 (NR) |
| Neovius (2005) 193 | Girls | 17 | Smallest between ribs and iliac crest | 1.02 | ADP | 95th centile | 274 | 0 (NR) | 100 (NR) |
| Overweight | |||||||||
| Neovius (2005) 193 | Girls | 17 | Smallest between ribs and iliac crest | 0.84 | ADP | 30% BF | 274 | 17 (NR) | 98 (NR) |
| Neovius (2005) 193 | Boys | 17 | Smallest between ribs and iliac crest | 0.9 | ADP | 25% BF | 200 | 24 (NR) | 98 (NR) |
| Taylor (2000)199 | White girls | 3.1–19.8 | Smallest between ribs and iliac crest | 80th centile | DEXA | 1 SD | 278 | 47 (32 to 62) | 85 (80 to 90) |
| Taylor (2000)199 | White boys | 3.3–19.9 | Smallest between ribs and iliac crest | 80th centile | DEXA | 1 SD | 302 | 46 (31 to 61) | 85 (80 to 89) |
| Guntsche (2010)184 | Obesity centre referrals and siblings – pubertal | 6–16 | Mid-point between ribs and iliac crest | 0.91 | DEXA | 10 kg/m2 | 58 | 72.2 (NR) | 90.9 (NR) |
| Guntsche (2010)184 | Obesity centre referrals and siblings – pubertal | 6–16 | Umbilical | 0.98 | DEXA | 10 kg/m2 | 58 | 77.8 (NR) | 95.5 (NR) |
| Guntsche (2010)184 | Obesity centre referrals and siblings – prepubertal | 6–16 | Mid-point between ribs and iliac crest | 0.92 | DEXA | 10 kg/m2 | 50 | 78.8 (NR) | 70.6 (NR) |
| Guntsche (2010)184 | Obesity centre referrals and siblings – prepubertal | 6–16 | Umbilical | 0.99 | DEXA | 10 kg/m2 | 50 | 66.7 (NR) | 94.1 (NR) |
| Study | Population | Age at assessment (years) | Site of WC measurement | Index test cut-off point | Reference standard | Reference standard cut-off point | Total n | Sensitivity (95% Cl), % | Specificity (95% Cl), % |
|---|---|---|---|---|---|---|---|---|---|
| Obesity | |||||||||
| Fujita (2011)181 | Boys | 10 | Umbilical | 0.519 | DEXA | 95th | 226 | 100 (NR) | 95 (NR) |
| Fujita (2011)181 | Girls | 10 | Umbilical | 0.499 | DEXA | 95th | 196 | 100 (NR) | 95 (NR) |
| Overweight | |||||||||
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – prepubertal | 6–16 | Mid-point between ribs and iliac crest | 0.49 | DEXA | 10 kg/m2 | 50 | 90.9 (NR) | 100 (NR) |
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – pubertal | 6–16 | Mid-point between ribs and iliac crest | 0.5 | DEXA | 10 kg/m2 | 58 | 97.2 (NR) | 100 (NR) |
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – pubertal | 6–16 | Umbilical | 0.54 | DEXA | 10 kg/m2 | 58 | 97.2 (NR) | 100 (NR) |
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – prepubertal | 6–16 | Umbilical | 0.54 | DEXA | 10 kg/m2 | 50 | 93.9 (NR) | 100 (NR) |
Diagnostic accuracy of bioelectrical impedance analysis
The only diagnostic accuracy study to evaluate BIA used the test to distinguish between children who were fat and those who were not, using different models to calculate the level of adiposity. 175 The study characteristics and results are presented in Table 24. No cut-off values were reported; therefore, it is unclear whether ‘fat’ means obese or overweight/obese. This study used the gold-standard 4-C model to confirm adiposity. The results are mixed across the different models. Where sensitivity is 100%, this is at the expense of specificity, which is very low (45% and 11%). Two of the models give similar sensitivities and specificities of between 80% and 90%. The Deurenberg model has the highest specificity (93%), but as expected, this is at the expense of sensitivity (65%). The choice of model would therefore depend on whether it was more important to rule in (high specificity) or rule out (high sensitivity) being fat or whether neither extreme was desirable (a closer balance between sensitivity and specificity).
| Population | Age at assessment (years) | Index test model | Index test cut-off point | Reference standard | Reference standard cut-off point | Total n | Sensitivity (95% CI), % | Specificity (95% CI), % |
|---|---|---|---|---|---|---|---|---|
| White and AA children | 12 | Deurenberg | NR | 4-C | NR | 114 | 65 (NR) | 93 (NR) |
| White and AA children | 12 | Goran | NR | 4-C | NR | 114 | 100 (NR) | 45 (NR) |
| White and AA children | 12 | Pennington | NR | 4-C | NR | 114 | 87 (NR) | 84 (NR) |
| White and AA children | 12 | Schaefer | NR | 4-C | NR | 114 | 89 (NR) | 84 (NR) |
| White and AA children | 12 | Suprasongsin | NR | 4-C | NR | 114 | 100 (NR) | 11 (NR) |
Other childhood measures
There were a small number of studies that evaluated some less common simple measures of childhood obesity: the conicity index,199 relative BMI,189 relative weight187,189 and FMI. 173 The results for FMI appeared good, with sensitivity of 100% and specificity of over 90%, but these were derived from only one study of only 150 children. 173 As with the childhood measures discussed in the previous section, specificity of these tests is generally high, with sensitivity being more variable (Table 25).
| Study | Population | Age at assessment (years) | Index test | Index test cut-off point | Reference standard | Reference standard cut-off point | Total n | Sensitivity (95% CI), % | Specificity (95% CI), % |
|---|---|---|---|---|---|---|---|---|---|
| Obesity | |||||||||
| Marshall (1991)189 | Unselected | 7–14 | Relative BMI | ≥ 120% | Underwater (hydrostatic) weighting | 20% BF boys; 25% BF girls | 540 | 71.1 (NR) | 91.6 (NR) |
| Marshall (1991)189 | Girls | 7–14 | Relative BMI | ≥ 120% | Underwater (hydrostatic) weighting | 25% BF | 274 | 74.2 (NR) | 90.5 (NR) |
| Marshall (1991)189 | Boys | 7–14 | Relative BMI | ≥ 120% | Underwater (hydrostatic) weighting | 20% BF | 266 | 68.9 (NR) | 92.8 (NR) |
| Marshall (1991)189 | Unselected | 7–14 | Relative weight | ≥ 120% | Underwater (hydrostatic) weighting | 20% BF boys; 25% BF girls | 540 | 51.6 (NR) | 95 (NR) |
| Marshall (1991)189 | Girls | 7–14 | Relative weight | ≥ 120% | Underwater (hydrostatic) weighting | 25% BF | 274 | 58.1 (NR) | 95.1 (NR) |
| Marshall (1991)189 | Boys | 7–14 | Relative weight | ≥ 120% | Underwater (hydrostatic) weighting | 20% BF | 266 | 48.9 (NR) | 95 (NR) |
| Johnston (1985)187 | Boys | 12–17 | Relative weight | NR | Underwater (hydrostatic) weighting | 25% BF | 169 | 52 (33 to 70) | 86 (79 to 92) |
| Johnston (1985)187 | Girls | 12–17 | Relative weight | NR | Underwater (hydrostatic) weighting | 30% BF | 66 | 29 (10 to 56) | 94 (83 to 99) |
| Johnston (1985)187 | All children | 12–17 | Relative weight | NR | Underwater (hydrostatic) weighting | 25% BF boys; 30% BF girls | 235 | 44 (29 to 59) | 88 (83 to 92) |
| Overweight | |||||||||
| Taylor (2000)199 | White girls | 3.1–19.8 | Conicity index | 80th centile | DEXA | 1 SD | 278 | 57 (42 to 72) | 88 (83 to 92) |
| Taylor (2000)199 | White boys | 3.3–19.9 | Conicity index | 80th centile | DEXA | 1 SD | 302 | 61 (45 to 75) | 88 (83 to 91) |
| Alvero-Cruz (2010)173 | Boys | 12–18 | FMI | 4.58 | D2O | NR | 75 | 100 (89.3 to 100) | 90.5 (77.4 to 97.3) |
| Alvero-Cruz (2010)173 | Girls | 12–18 | FMI | 7.76 | D2O | NR | 75 | 100 (66.2 to 100) | 97 (89.5 to 99.5) |
Direct comparisons of the diagnostic accuracy of simple childhood measures of obesity
The studies of diagnostic accuracy were extremely heterogeneous, assessing different populations, measurements at a range of different ages, different cut-off points for the index tests and different reference standards with different cut-off points. Several studies made direct comparisons, with each index test conducted in all study participants along with the reference standard; these are more robust when determining relative accuracy than indirect comparisons.
Diagnosing obesity
Eleven studies reported direct comparisons of childhood measures for diagnosing obesity. 178,180,181,186,187,189,190,193,195,204,205 Different reference standards were used to determine the adiposity of the children in the studies. One used ADP (Table 26),193 two used D2O (Table 27),204,205 three used underwater (hydrostatic) weighting (Table 28)186,187,189 and five used DEXA (Table 29). 178,180,181,190,195 Of the 11 studies, six were considered to be of high quality (results are shown in italics within the tables). 186,187,189,193,204,205
| Study | Population | Age at assessment (years) | Reference standard cut-off point | Total n | Sensitivity (%) | Specificity (%) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| BMI (optimal) | WHR (WC smallest between ribs and iliac crest) | WC (smallest between ribs and iliac crest) | BMI (minimising misclassifications/maximising sensitivity/specificity) | WHR (WC smallest between ribs and iliac crest) | WC (smallest between ribs and iliac crest) | |||||
| Neovius (2005) 193 | Boys | 17 | 95th centile | 200 | 40 | 40 | 50 | 98 | 97 | 98 |
| Neovius (2005) 193 | Girls | 17 | 95th centile | 274 | 86 | 0 | 64 | 98 | 100 | 98 |
| Study | Population | Age at assessment (years) | Reference standard cut-off point | Total n | Sensitivity (%) | Specificity (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BMI (IOTF) | BMI (CDC/WHO) | BMI (z-/SD scores) | WC (mid-point between ribs and iliac crest) | BMI (IOTF) | BMI (CDC/WHO) | BMI (z-/SD scores) | WC (mid-point between ribs and iliac crest) | |||||
| Wickramasinghe (2005) 204 | Sri Lankan boys | 5–14.99 | 20% BF | 27 | 0 | 12.5 | 12.5 | – | 100 | 100 | 100 | – |
| Wickramasinghe (2005) 204 | Sri Lankan girls | 5–14.99 | 30% BF | 15 | 0 | 14.3 | 14.3 | – | 100 | 100 | 100 | – |
| Wickramasinghe (2009) 205 | Sri Lankan boys | 5–15 | 25% BF | 158 | 12.5 | 19.5 | 23.6 | 34.7 | 100 | 100 | 100 | 98.8 |
| Wickramasinghe (2009) 205 | Sri Lankan girls | 5–15 | 30% BF | 124 | 0 | 16.2 | 16.2 | 38.4 | 100 | 100 | 100 | 100 |
| Wickramasinghe (2005) 204 | White boys | 5–14.99 | 20% BF | 44 | 0 | 3.5 | 6.9 | – | 100 | 100 | 93 | – |
| Wickramasinghe (2005) 204 | White girls | 5–14.99 | 30% BF | 52 | 0 | 20 | 5.2 | – | 100 | 100 | 100 | – |
| Study | Population | Age at assessment (years) | Reference standard cut-off point | Total n | Sensitivity (95% CI), % | Specificity (95% CI), % | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BMI (reference data NR) | Relative BMI | SFT (sum) | SFT (triceps) | SFT (subscapular) | Relative weight | BMI (reference data NR) | Relative BMI | SFT (sum) | SFT (triceps) | SFT (subscapular) | Relative weight | |||||
| Marshall (1991) 189 | Boys | 7–14 | 20% BF | 266 | – | 68.9 | 80 | 64.4 | – | 48.9 | – | 92.8 | 89.6 | 94.6 | – | 95 |
| Marshall (1991) 189 | Girls | 7–14 | 25% BF | 274 | – | 74.2 | 96.8 | 67.7 | – | 58.1 | – | 90.5 | 90.5 | 93.4 | – | 95.1 |
| Marshall (1991) 189 | Unselected | 7–14 | 20% BF boys; 25% BF girls | 540 | – | 71.1 | 86.8 | 65.8 | – | 51.6 | – | 91.6 | 90.1 | 94 | – | 95 |
| Johnston (1985) 187 | Boys | 12–17 | 25% BF | 169 | – | – | – | 48 (30 to 67) | – | 52 (33 to 70) | – | – | – | 96 (91 to 98) | – | 86 (79 to 92) |
| Johnston (1985) 187 | Girls | 12–17 | 30% BF | 66 | – | – | – | 24 (7 to 50) | – | 29 (10 to 56) | – | – | – | 100 (93 to 100) | – | 94 (83 to 99) |
| Himes (1989) 186 | Boys | 8.4–18.99 | 90th centile | 159 | 29 (11 to 51) | – | 57 (35 to 78) | 24 (8 to 45) | 38 (18 to 61) | – | 99 (96 to 100) | – | 85 (78 to 90) | 100 (99 to 100) | 99 (97 to 100) | – |
| Himes (1989) 186 | Girls | 8.4–18.99 | 90th centile | 157 | 23 (10 to 40) | – | 80 (63 to 92) | 23 (10 to 40) | 30 (15 to 48) | – | 100 (99 to 100) | – | 82 (75 to 88) | 97 (93 to 99) | 99 (96 to 100) | – |
| Study | Population | Age at assessment (years) | Reference standard cut-off point | Total n | Sensitivity (95% CI), % | Specificity (95% CI), % | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BMI (reference data NR) | BMI (z-/SD scores) | BMI (UK90) | BMI (CDC/WHO) | BMI (optimal) | SFT (sum) | SFT (triceps) | SFT (subscapular) | WHtR (WC umbilical) | WC (umbilical) | WC (UK 1988 reference) | BMI (reference data NR) | BMI (z-/SD scores) | BMI (UK90) | BMI (CDC/WHO) | BMI (optimal) | SFT (sum) | SFT (triceps) | SFT (subscapular) | WHtR (WC umbilical) | WC (umbilical) | WC (UK 1988 reference) | |||||
| Freedman (2013)180 | Boys | 8–19 | ? | 4518 | – | – | – | 75 (72 to 78) | – | 80 (77 to 83) | – | – | – | – | – | – | – | – | 95 (94 to 95) | – | 96 (95 to 96) | – | – | – | – | – |
| Freedman (2013)180 | Girls | 8–19 | ? | 2847 | – | – | – | 76 (72 to 80) | – | 79 (75 to 83) | – | – | – | – | – | – | – | – | 95 (94 to 96) | – | 96 (95 to 96) | – | – | – | – | – |
| Reilly (2010)195 | Boys | 9.9 | 90th centile | 3809 | – | – | 96 (94 to 98) | – | – | – | – | – | – | – | 97 (95 to 99) | – | – | 95 (94 to 95) | – | – | – | – | – | – | – | 81 (79 to 82) |
| Reilly (2010)195 | Girls | 9.9 | 90th centile | 3913 | – | – | 94 (91 to 96) | – | – | – | – | – | – | – | 98 (95 to 99) | – | – | 96 (96 to 97) | – | – | – | – | – | – | – | 81 (79 to 82) |
| Field (2003)178 | Unselected | 10 | 90th centile | 596 | 65 | 51 | – | – | – | – | – | – | – | – | – | 99 | 100 | – | – | – | – | – | – | – | – | – |
| Mei (2006)190 | Unselected | 5–18 | 95th centile | 1196 | – | – | – | 92.5 | – | – | 89.6 | 89.6 | – | – | – | – | – | – | 89.4 | – | – | 93.2 | 94 | – | – | – |
| Fujita (2011)181 | Boys | 10 | 95th centile | 226 | – | – | – | – | 100 | – | – | – | 100 | 100 | – | – | – | – | – | 96 | – | – | – | 95 | 97 | – |
| Fujita (2011)181 | Girls | 10 | 95th centile | 196 | – | – | – | – | 100 | – | – | – | 100 | 100 | – | – | – | – | – | 92 | – | – | – | 95 | 96 | – |
Where SFT was measured in the same children as BMI, sum SFT consistently had higher sensitivity than BMI with similar specificity (see Tables 28 and 29); measuring SFT at only a single location seemed to be less accurate than using the sum of several locations. When comparing the use of different BMI reference data, results were variable, with no one reference source being consistently better (see Tables 27 and 29). In studies comparing WC with BMI, the sensitivity of WC was generally better than or similar to that of BMI; specificity was similar for the two measures (see Tables 26, 27 and 29). One study showed a substantial difference between boys and girls; sensitivity was higher with BMI in girls and with WC in boys. 193 This difference was not seen in the other studies where data for boys and girls were reported separately.
The results of these studies are presented graphically, with results plotted in ROC space in Figure 29 and the DOR shown in Figure 30 for each test for which 2 × 2 tables of test performance were available.
FIGURE 29.
Results of the tests reported in the direct comparisons plotted in ROC space. RWt, relative weight.
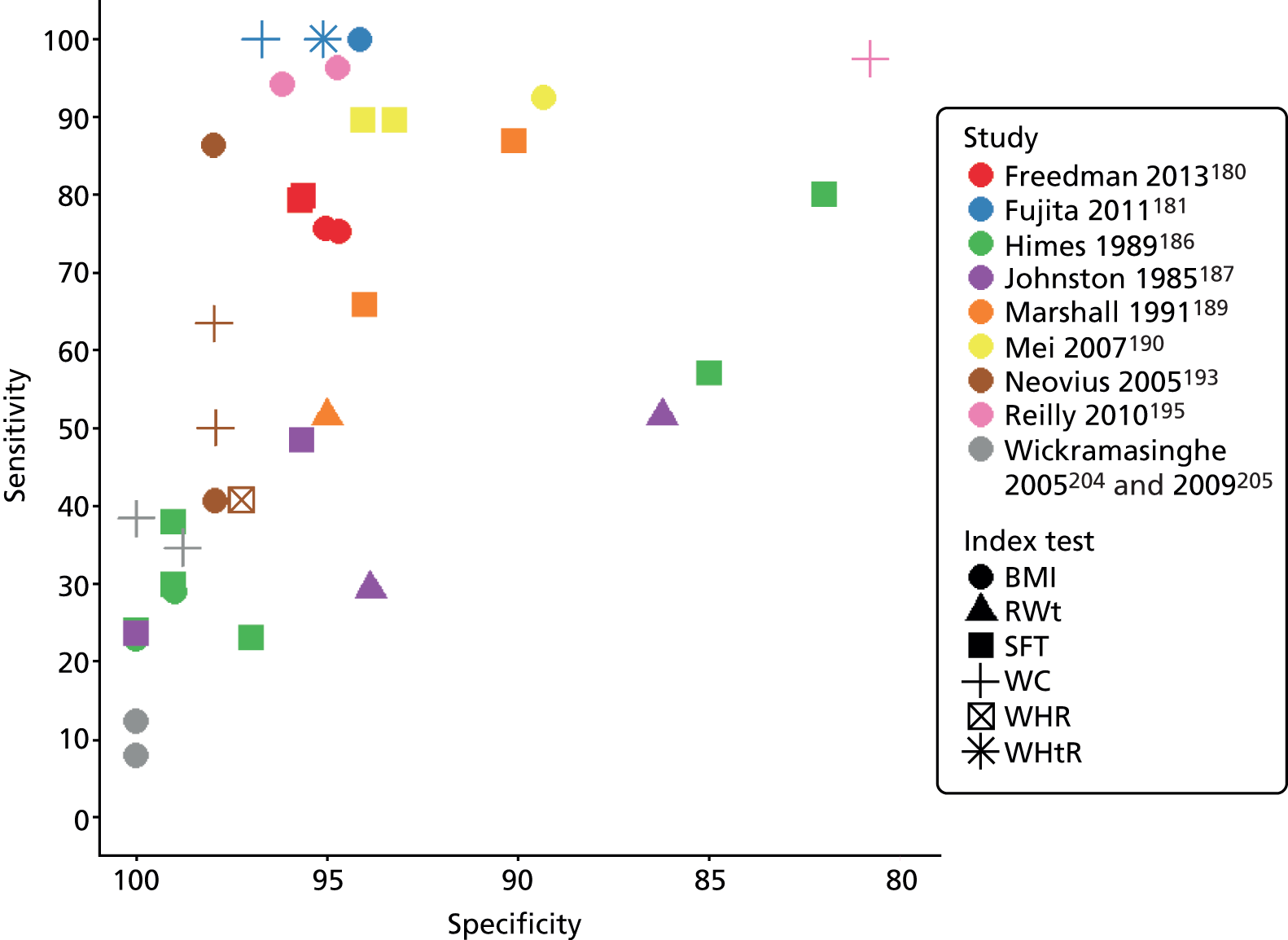
FIGURE 30.
Diagnostic OR for the tests in the studies reporting direct comparisons. RWt, relative weight.

Figure 29 demonstrates the difficulty in comparing BMI with other obesity measures, because of the trade-off between sensitivity and specificity. In the Freedman et al. (2013)180 study (in red), for example, SFT has a marginally higher sensitivity and specificity than BMI, so may be better at diagnosing obesity. Himes et al. (1989)186 (green) used several forms of SFT measurement (the green squares). These vary considerably in their sensitivity and specificity, with some having much higher sensitivity, but at a cost of reduced specificity.
The DOR provides a simpler means of comparing obesity measures, as a higher DOR indicates better diagnostic performance. As seen in Figure 30, the DORs vary enormously across studies, from 3 to nearly 4000, demonstrating the considerable heterogeneity across studies. Both Freedman et al. (2013)180 and Mei et al. (2006)190 suggest that SFT may be more accurate than BMI, but Himes et al. (1989)186 does not show that SFT is better. There is no evidence that WC, WHtR or WHR have better diagnostic performance than BMI.
Diagnosing overweight
Ten studies reported direct comparisons of childhood measures for diagnosing obesity. 173,175,180,184,191–193,197,199,202 A range of reference standards were used across the studies; one used a gold-standard 4-C model (Table 30),175 two used ADP (Table 31),192,193 one used D2O (Table 32),173 one used underwater (hydrostatic) weighting (Table 33)197 and five used DEXA (Tables 34 and 35). 180,184,191,199,202 Of the 10 studies, three were considered to be high quality (results shown in italics within the tables). 173,193,197
| Study | Population | Age at assessment (years) | Reference standard cut-off point | Total n | Sensitivity (%) | Specificity (%) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BIA Deurenberg | BIA Goran | BIA Pennington | BIA Schaefer | BIA Suprasongsin | SFT (sum Ellis) | SFT (sum Pennington) | SFT (sum Slaughter) | BIA Deurenberg | BIA Goran | BIA Pennington | BIA Schaefer | BIA Suprasongsin | SFT (sum Ellis) | SFT (sum Pennington) | SFT (sum Slaughter) | |||||
| Bray (2002)175 | White and AA children | 12 | ? | 114 | 65 | 100 | 87 | 89 | 100 | 96 | 94 | 98 | 93 | 45 | 84 | 84 | 11 | 47 | 82 | 71 |
| Study | Population | Age at assessment (years) | Reference standard cut-off point | Total n | Sensitivity (%) | Specificity (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BMI (IOTF) | BMI (CDC/WHO) | BMI (optimal) | BMI (Göteborg, Sweden) | WHR (WC smallest between ribs and iliac crest) | WC (smallest between ribs and iliac crest) | BMI (IOTF) | BMI (CDC/WHO) | BMI (optimal) | BMI (Göteborg, Sweden) | WHR (WC smallest between ribs and iliac crest) | WC (smallest between ribs and iliac crest) | |||||
| Neovius (2005) 193 | Boys | 17 | 25% BF | 200 | – | – | 72 | – | 24 | 68 | – | – | 98 | – | 98 | 99 |
| Neovius (2005) 193 | Girls | 17 | 30% BF | 274 | – | – | 65 | – | 17 | 53 | – | – | 88 | – | 98 | 89 |
| Neovius (2004)192 | Boys | 16.9 (SD 0.4) | 25% BF | 200 | 80 | 68 | 92 | 92 | – | – | 95 | 98 | 92 | 93 | – | – |
| Neovius (2004)192 | Girls | 16.9 (SD 0.4) | 30% BF | 274 | 24 | 19 | 77 | 39 | – | – | 100 | 100 | 76 | 97 | – | – |
| Study | Population | Age at assessment (years) | Reference standard cut-off point | Total n | Sensitivity (95% CI), % | Specificity (95% CI), % | ||
|---|---|---|---|---|---|---|---|---|
| BMI (reference data NR) | FMI | BMI (reference data NR) | FMI | |||||
| Alvero-Cruz (2010) 173 | Boys | 12–18 | ? | 75 | 75.8 (57.7 to 88.9) | 100 (89.3 to 100) | 83.3 (68.6 to 93) | 90.5 (77.4 to 97.3) |
| Alvero-Cruz (2010) 173 | Girls | 12–18 | ? | 75 | 88.9 (51.7 to 98.2) | 100 (66.2 to 100) | 77.3 (65.3 to 86.7) | 97 (89.5 to 99.5) |
| Study | Population | Age at assessment (years) | Reference standard cut-off point | Total n | Sensitivity (95% CI), % | Specificity (95% CI), % | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| BMI (z-/SD scores) | SFT (sum) | WC: smallest between ribs/iliac crest | BMI (z-/SD scores) | SFT (sum) | WC: smallest between ribs/iliac crest | |||||
| Sarria (2001) 197 | Boys | 7–16.9 | 85th centile | 175 | 50 (30 to 70) | 58 (37 to 77) | 58 (37 to 77) | 91 (85 to 95) | 93 (87 to 96) | 93 (87 to 96) |
| Study | Population | Age at assessment (years) | Reference standard cut-off point | Total n | Sensitivity (95% CI), % | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BMI (IOTF) | BMI (CDC/WHO) | BMI (Conde and Monteiro) | BMI (AVENA) | BMI (z-/SD scores) | SFT (sum) | WHR (WC smallest between ribs and iliac crest) | WHR (umbilical) | WHR (WC mid-point between ribs and iliac crest) | WHtR (WC umbilical) | WHtR (WC mid-point between ribs and iliac crest) | WC (smallest between ribs and iliac crest) | WC (mid-point between ribs and iliac crest) | WC (umbilical) | Conicity index | |||||
| Freedman (2013)180 | Boys | 8–19 | ? | 4518 | – | 83 (81 to 84) | – | – | – | 85 (83 to 87) | – | – | – | – | – | – | – | – | – |
| Freedman (2013)180 | Girls | 8–19 | ? | 2847 | – | 80 (77 to 82) | – | – | – | 81 (78 to 83) | – | – | – | – | – | – | – | – | – |
| Taylor (2000)199 | White girls | 3.1–19.8 | 1 SD | 278 | – | – | – | – | – | – | 47 (32 to 62) | – | – | – | – | 89 (77 to 96) | – | – | 57 (42 to 72) |
| Taylor (2000)199 | White boys | 3.3–19.9 | 1 SD | 302 | – | – | – | – | – | – | 46 (31 to 61) | – | – | – | – | 87 (74 to 95) | – | – | 61 (45 to 75) |
| Guntsche (2010)184 | Pubertal obese and siblings | 6–16 | 10 kg/m2 | 58 | – | – | – | – | 97.2 | 75 | – | 77.8 | 72.2 | 97.2 | 97.2 | – | 88.9 | 88.9 | – |
| Guntsche (2010)184 | Prepubertal obese and siblings | 6–16 | 10 kg/m2 | 50 | – | – | – | – | 96.9 | 57.6 | – | 66.7 | 78.8 | 93.9 | 90.9 | – | 84.8 | 90.9 | – |
| Vitolo (2007)202 | Boys | 10–19 | 25% BF | 219 | 79.5 | – | 84.1 | – | – | – | – | – | – | – | – | – | – | – | – |
| Vitolo (2007)202 | Boys | 10–14 | 25% BF | 128 | 84.2 | – | 84.2 | – | – | – | – | – | – | – | – | – | – | – | – |
| Vitolo (2007)202 | Boys | 15–19 | 25% BF | 91 | 50 | – | 83.3 | – | – | – | – | – | – | – | – | – | – | – | – |
| Vitolo (2007)202 | Girls | 10–19 | 30% BF | 199 | 26.6 | – | 34.5 | – | – | – | – | – | – | – | – | – | – | – | – |
| Vitolo (2007)202 | Girls | 10–14 | 30% BF | 132 | 32.6 | – | 44.2 | – | – | – | – | – | – | – | – | – | – | – | – |
| Vitolo (2007)202 | Girls | 15–19 | 30% BF | 67 | 17 | – | 18.9 | – | – | – | – | – | – | – | – | – | – | – | – |
| Moreno (2006)191 | Boys | 13–17.9 | 85th centile | 116 | 71 (44 to 90) | – | – | 53 (28 to 77) | – | – | – | – | – | – | – | – | – | – | – |
| Moreno (2006)191 | Girls | 13–17.9 | 85th centile | 170 | 75 (53 to 90) | – | – | 79 (58 to 93) | – | – | – | – | – | – | – | – | – | – | – |
| Study | Population | Age at assessment (years) | Reference standard cut-off point | Total n | Specificity (95% CI), % | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BMI (IOTF) | BMI (CDC/WHO) | BMI (Conde and Monteiro) | BMI (AVENA) | BMI (z-/SD scores) | SFT (sum) | WHR (WC smallest between ribs and iliac crest) | WHR (umbilical) | WHR (WC mid-point between ribs and iliac crest) | WHtR (WC umbilical) | WHtR (WC mid-point between ribs and iliac crest) | WC (smallest between ribs and iliac crest) | WC (mid-point between ribs and iliac crest) | WC (umbilical) | Conicity index | |||||
| Freedman (2013)180 | Boys | 8–19 | ? | 4518 | – | 91 (90 to 92) | – | – | – | 92 (91 to 93) | – | – | – | – | – | – | – | – | – |
| Freedman (2013)180 | Girls | 8–19 | ? | 2847 | – | 90 (88 to 91) | – | – | – | 90 (89 to 92) | – | – | – | – | – | – | – | – | – |
| Taylor (2000)199 | White girls | 3.1–19.8 | 1 SD | 278 | – | - | – | – | – | - | 85 (80 to 90) | – | – | – | – | 94 (91 to 97) | – | – | 88 (83 to 92) |
| Taylor (2000)199 | White boys | 3.3–19.9 | 1 SD | 302 | – | – | – | – | – | – | 85 (80 to 89) | – | – | – | – | 92 (88 to 95) | – | – | 88 (83 to 91) |
| Guntsche (2010)184 | Pubertal obese and siblings | 6–16 | 10 kg/m2 | 58 | – | – | – | – | 100 | 77.3 | – | 95.5 | 90.9 | 100 | 100 | – | 95.5 | 100 | – |
| Guntsche (2010)184 | Prepubertal obese and siblings | 6–16 | 10 kg/m2 | 50 | – | – | – | – | 100 | 76.5 | – | 94.1 | 70.6 | 100 | 100 | – | 100 | 100 | – |
| Vitolo (2007)202 | Boys | 10–19 | 25% BF | 219 | 86.9 | – | 84.6 | – | – | – | – | – | – | – | – | – | – | – | – |
| Vitolo (2007)202 | Boys | 10–14 | 25% BF | 128 | 86.7 | – | 82.2 | – | – | – | – | – | – | – | – | – | – | – | – |
| Vitolo (2007)202 | Boys | 15–19 | 25% BF | 91 | 87.1 | – | 87.1 | – | – | – | – | – | – | – | – | – | – | – | – |
| Vitolo (2007)202 | Girls | 10–19 | 30% BF | 199 | 96.7 | – | 98.3 | – | – | – | – | – | – | – | – | – | – | – | – |
| Vitolo (2007)202 | Girls | 10–14 | 30% BF | 132 | 95.7 | – | 97.8 | – | – | – | – | – | – | – | – | – | – | – | – |
| Vitolo (2007)202 | Girls | 15–19 | 30% BF | 67 | 100 | – | 100 | – | – | – | – | – | – | – | – | – | – | – | – |
| Moreno (2006)191 | Boys | 13–17.9 | 85th centile | 116 | 86 (77 to 92) | – | – | 88 (79 to 94) | – | – | – | – | – | – | – | – | – | – | – |
| Moreno (2006)191 | Girls | 13–17.9 | 85th centile | 170 | 90 (84 to 95) | – | – | 92 (86 to 96) | – | – | – | – | – | – | – | – | – | – | – |
The difference between BMI and SFT was less pronounced for diagnosing overweight than for diagnosing obesity; one study reported a higher sensitivity with BMI,184 but most reported similar accuracy (see Tables 33–35). In one study,173 FMI outperformed BMI in boys and girls for both sensitivity and specificity (see Table 32). On the whole, BIA and SFT had similar, relatively high, sensitivity. Specificity was more variable; tests with the highest sensitivities had poorer specificity. The two tests with relatively high sensitivity and specificity were BIA using the Schaefer model and sum SFT using the Pennington optimal SFT model (see Table 30). WHR seemed to perform poorly compared with BMI or WC alone (see Tables 31, 34 and 35); WHtR seemed to outperform WHR for both sensitivity and specificity, and WC alone in terms of sensitivity (see Tables 34 and 35).
The results of these studies are presented graphically, with results plotted in ROC space in Figure 31 and the DOR shown in Figure 32 for each test for which 2 × 2 tables of test performance were available.
FIGURE 31.
Results of the tests from studies of direct comparisons plotted in ROC space.

FIGURE 32.
Diagnostic OR of the tests from studies that report direct comparisons.
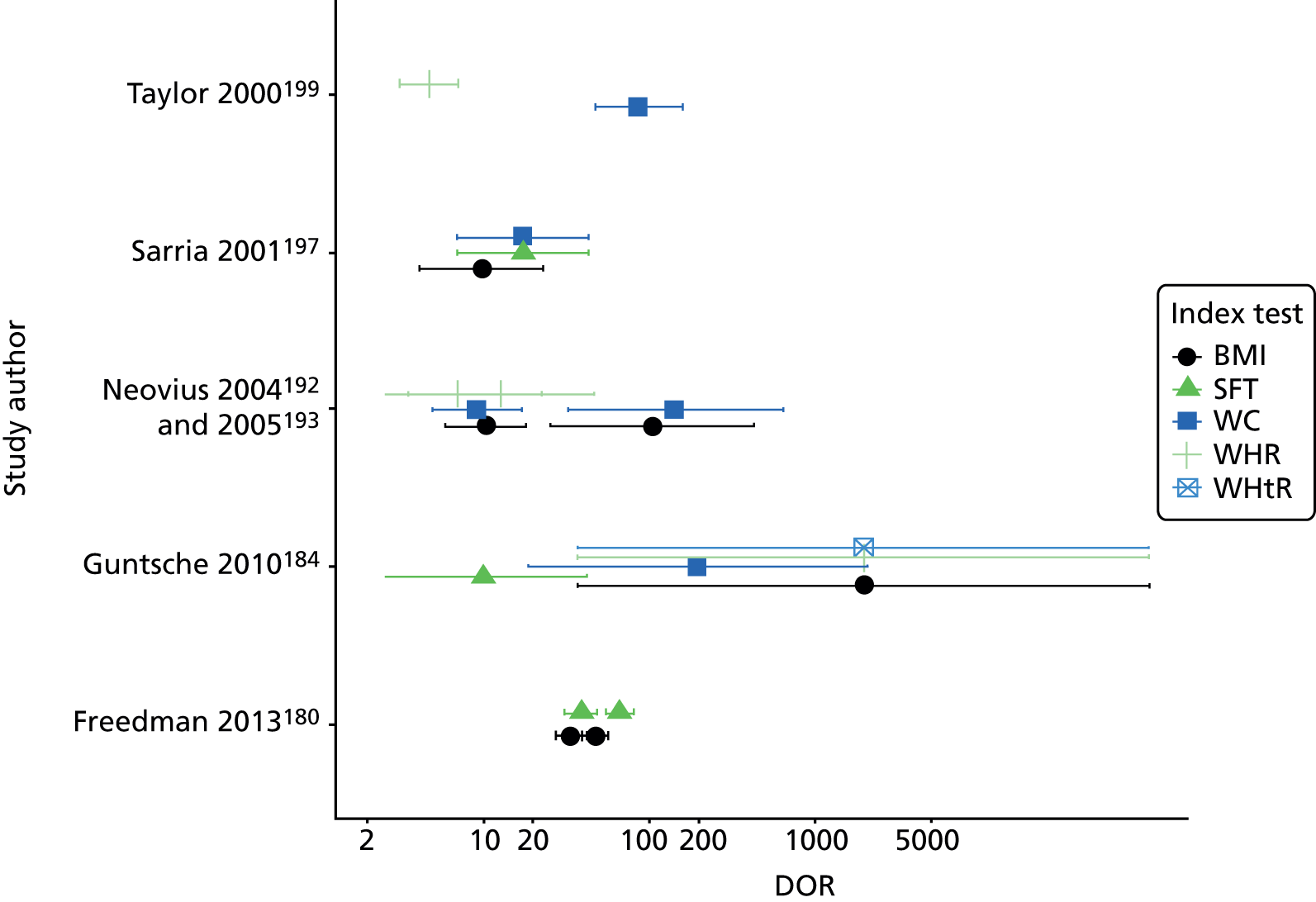
The results are similar to those seen for diagnosing obesity. From Figure 32, two studies [Freedman et al. (2013),180 Sarria et al. (2001)197] suggest that SFT may have better diagnostic performance than BMI, but results cannot be considered to be statistically significant. Neovius et al. (2004)192 found SFT to have the worst diagnostic performance of any measure. There is no evidence to suggest that any other measure can improve on BMI.
Comparisons of predictive and diagnostic accuracy
In order to understand why one childhood measure of obesity had a better predictive accuracy than another, we planned to compare the estimates of predictive accuracy from the tracking and adult morbidity reviews with estimates of diagnostic accuracy in similar studies from the diagnostic accuracy review. Unfortunately, the vast majority of data from the two predictive accuracy reviews were for BMI. Only one study in the review of tracking and two in the review of adult morbidities used a measure other than BMI: triceps SFT in the tracking review,127 and WC,117 and WC, sum SFT and WHR,171 in the studies from the adult morbidity review. There were therefore insufficient predictive accuracy data for us to make such comparisons.
Summary of the diagnostic accuracy data
In terms of diagnostic accuracy, there was little evidence to suggest that any obesity measure has better diagnostic performance than BMI. Direct comparisons suggest that sum SFT may have promise as an alternative to BMI, especially for the diagnosis of obesity. Generally, BMI has a similar level of accuracy to SFT for the diagnosis of overweight. With the limited data available, WHR seems to be a poor measure, and does not improve on BMI, with WC alone or WHtR being more promising. These relationships need to be confirmed with a full evaluation of the available diagnostic accuracy data, including searching for studies using magnetic resonance imaging (MRI) to determine abdominal fat in order to investigate the impact of the distribution of fat more fully, and contacting authors to retrieve tables of test performance for those studies where this could not be extracted or derived. Further well-designed primary studies are likely to be required for some of the measures once the full systematic review has identified the most promising diagnostic measures.
We considered a model with at least four components as the gold standard for determining actual adiposity in children; this requires the conduct of a range of tests to determine the contribution of the different components of body composition. ADP, underwater (hydrostatic) weighting, D2O and DEXA were all considered imperfect reference standards compared with four- or more-component models. Several studies have been published that have highlighted the shortcomings of these tests as reference standards, but DEXA may be a poorer reference standard than the others. 55–57,227–235 The majority of the diagnostic studies considered used DEXA as a reference standard, and we note that the diagnostic performance of all the obesity measures may be poorer if a 4-C model is used as the reference standard. Therefore, any future primary studies should ideally use a four- or more-component model to determine weight status.
Review of acceptability and ease of use of childhood measures of obesity
Children’s assessment of acceptability and ease of use
No previous studies of the opinions of children regarding simple measures of childhood obesity were identified.
The de novo study conducted as part of this review is presented here. This took the form of an elicitation exercise conducted by colleagues at Leeds Metropolitan University, during a weight management summer camp for children. A total of 72 (out of 147) children completed the questionnaire (see Appendix 3). All children who attended the summer camp were overweight or obese (> 85th centile using UK90). The characteristics of the children who completed the questionnaire are given in Table 36. As can be seen from Table 37, the vast majority of the children said that they had previously had their height and weight measured, but only 58% said they had experienced BMI being measured; this is likely to be a result of a lack of feedback of the result of the height and weight measurement, or a lack of understanding of what BMI is. The other measures were, as expected, less commonly experienced, with SFT being the least common.
| Age (years) | School year | Sex | Are you concerned about your weight? | Do you feel it is important to measure your growth? |
|---|---|---|---|---|
| Mean 12.6 Range 9–17 9: 8.3% 10: 5.6% 11: 25.0% 12: 13.9% 13: 13.9% 14: 9.7% 15: 11.1% 16: 6.9% 17: 5.6% |
Range 4–13 4: 2.8% 5: 6.9% 6: 4.2% 7: 16.7% 8: 13.9% 9: 12.5% 10: 8.3% 11: 9.7% 12: 4.2% 13: 2.8% Other: 4.2% NR: 13.9% |
Male: 51.4% Female: 48.6% |
Yes: 79.2% No: 19.4% NR: 1.4% |
Yes: 81.9% No: 16.7% NR: 1.4% |
| Measure | Yes (%) | No (%) | Don’t know (%) | NR (%) |
|---|---|---|---|---|
| Height | 91.7 | 6.9 | 1.4 | 0 |
| Weight | 93.1 | 5.6 | 1.4 | 0 |
| BMI | 58.3 | 23.6 | 16.7 | 1.4 |
| WC | 58.3 | 31.9 | 8.3 | 1.4 |
| HC | 34.7 | 48.6 | 15.3 | 1.4 |
| WHtR | 25.0 | 52.8 | 20.8 | 1.4 |
| WHR | 18.1 | 58.3 | 20.8 | 0 |
| SFT | 9.7 | 66.7 | 20.8 | 2.8 |
For the survey of children, it was considered most appropriate to obtain information on a child’s reaction to the individual components of the four measures being evaluated, as it is the conduct of these individual components that will elicit a response, good or bad, from the child. Responses to the individual components of the simple childhood measures of interest were mixed (Table 38). The vast majority of children had no problem with having their height measured, but a significant proportion had a negative reaction to being weighed [either embarrassment (39%) or a more extreme negative reaction such as anger or crying]. Of those who had experienced the measurement of WC, HC and/or SFT, similar proportions of children were embarrassed by WC and HC, although fewer were embarrassed by SFT (Table 39).
| Measure | Never had this (%) | Hurt (%) | Embarrassed (%) | Liked it/fun (%) | Did not let them do it (%) | Did not have a problem (%) | Angry (%) | Cried (%) |
|---|---|---|---|---|---|---|---|---|
| Height | 1.4 | 2.8 | 6.9 | 29.2 | 0 | 63.9 | 0 | 0 |
| Weight | 0 | 2.8 | 38.9 | 11.1 | 2.8 | 43.1 | 5.6 | 1.4 |
| WC | 37.5 | 1.4 | 19.4 | 13.9 | 2.8 | 26.4 | 1.4 | 0 |
| HC | 59.7 | 1.4 | 12.5 | 6.9 | 2.8 | 12.5 | 0 | 0 |
| SFT | 80.6 | 0 | 1.4 | 4.2 | 2.8 | 6.9 | 0 | 0 |
| Measure | Had measure (n) | Embarrassed, n (%) | Liked it/fun, n (%) | Did not have a problem, n (%) |
|---|---|---|---|---|
| WC | 45 | 14 (31) | 10 (22) | 19 (42) |
| HC | 29 | 9 (31) | 5 (17) | 9 (31) |
| SFT | 14 | 1 (7) | 3 (10) | 5 (36) |
Over 50% of children considered a weight measurement to accurately reflect their weight status, and approximately 30% thought BMI and WC did so. Similar, smaller proportions (ranging from 11% to 19% of the overall population) considered HC, WHR, WHtR and SFT to be accurate (Table 40). Of those who had actually reported experiencing the measurement of HC, WHR, WHtR and/or SFT, between 31% and 46% considered the measure to accurately reflect their weight status; the majority of the remaining children reported either not understanding the measure or never being told about it (Table 41).
| Measure | Never had this (%) | Overestimated (%) | Underestimated (%) | About right (%) | Do not understand (%) | Never been told (%) |
|---|---|---|---|---|---|---|
| Weight | 1.4 | 12.5 | 11.1 | 54.2 | 11.1 | 1.4 |
| BMI | 25.0 | 8.3 | 9.7 | 29.2 | 13.9 | 5.6 |
| WC | 30.6 | 4.2 | 5.6 | 31.9 | 12.5 | 5.6 |
| HC | 51.4 | 2.8 | 4.2 | 19.4 | 8.3 | 5.6 |
| WHtR | 55.6 | 1.4 | 5.6 | 13.9 | 6.9 | 6.9 |
| WHR | 59.7 | 1.4 | 2.8 | 13.9 | 6.9 | 5.6 |
| SFT | 66.7 | 0 | 0 | 11.1 | 8.3 | 5.6 |
| Measure | Had measure (n) | Overestimated, n (%) | Underestimated, n (%) | About right, n (%) |
|---|---|---|---|---|
| WC | 50 | 3 (6) | 4 (8) | 23 (46) |
| HC | 35 | 2 (6) | 3 (9) | 14 (40) |
| WHtR | 32 | 1 (3) | 4 (12.5) | 10 (31) |
| WHR | 29 | 1 (3) | 2 (7) | 10 (35) |
| SFT | 24 | 0 | 0 | 8 (33) |
Parents’ and caregivers’ assessment of acceptability and ease of use
Three previous studies were identified that elicited opinions about BMI from guardians (parents in two studies74,75 and mothers and grandparents in one study207). All three studies were generally considered to be of good quality; all had clearly stated aims, appropriate methodology, research designs and recruitment strategies, data that were collected and analysed appropriately, clear statements of findings, appropriate ethical considerations and the research was considered to be of value. Brief study details are given in Table 42; the full data extraction is presented in Appendix 3. None of the studies considered the relationship between researcher and participants.
| Study details | Population characteristics | Children’s details |
|---|---|---|
| Cloutier (2013)207 Country in which study conducted: USA/Canada Study dates: start October 2009, finish March 2010 |
Whose opinion?: 83% mothers; 17% grandparents Source of sample: primary care clinics; family centres; head start and child care centres Method of obtaining opinion: focus groups (n = 27); interview (n = 251) Method of recording opinions: paper questionnaire; videotapes in focus groups |
Simple childhood measure: BMI (CDC growth chart); ‘My weight ruler’ School grade of children: 2–4 Sex of children: NR Weight status of children: NR |
| Kubik (2006)74 Country in which study conducted: USA/Canada Study dates: start 2004, finish 2005 |
Whose opinion?: parents Source of sample: elementary school Method of obtaining opinion: self-administered survey Method of recording opinions: paper questionnaire |
School grade of children: kindergarten to Grade 6 Sex of children: male 54% Weight status of children: normal weight 73%; overweight/obese 27% |
| Kubik (2007)75 Country in which study conducted: USA/Canada Study dates: start 2004, finish 2005 |
Whose opinion?: parents Source of sample: elementary school Method of obtaining opinion: focus groups Method of recording opinions: videotapes |
School grade of children: kindergarten to Grade 6 Sex of children: NR Weight status of children: NR |
One study sent questionnaires to 1186 parents whose children attended school between kindergarten and Grade 6. 74 Of the 790 parents who returned questionnaires, 78% thought it was very (39%) or somewhat (39%) important for schools to screen height and weight (with parents of girls being less likely to think height/weight screening was important); 78% of parents wanted to receive results of such screening every year. Approximately 50% of the parents had received a letter informing them of their child’s BMI, of which 79% read the entire letter and 16% most of the letter; 55% of these parents did not discuss the letter with their child. Parents who worked full time were less likely to think screening was important than those who worked part time or stayed at home, and parents of older students and girls were less likely to want information than parents of younger students or boys. Most parents were either not uncomfortable (68%) or only slightly uncomfortable (12%) with their child’s BMI results; most thought their children were also either not uncomfortable (68%) or only slightly uncomfortable (15%). Parents found the results of weight/BMI measurements more helpful than information on physical activity, nutrition, screen time, health-related websites and community resources. Of the parents who expressed a concern for their child’s weight after receiving a BMI letter, 8% planned to seek medical services, 8% to make diet-related changes, 27% to increase exercise and/or sign up their child for sports and 24% to sign up to other physical activity. 74
A second study used videotaped focus groups to elicit opinions about BMI screening from 71 parents whose children attended school between kindergarten and Grade 6. 75 This may be a subset of the parents who were sent questionnaires in the larger study by Kibik et al. 74 Nearly 50% of the parents were unaware that annual health screening was done at school; however, of the parents familiar with the screening process, most were supportive of height and weight screening. Several parents queried the value of such screening when the results were not shared with them; most felt that the results of screening should be reported to the parents, and several parents thought that this would aid with the early detection of important health conditions. 75 Some parents expressed concerns about the screening process for height and weight. These included the maintenance of privacy and confidentiality, the children’s behaviour during screening – particularly the potential for teasing – and the accuracy of the results. Parents also expressed opinions as to who should be screened. Several said that screening was more important where there was a lack of health insurance or limited access to health care, and others felt that screening was less important in younger children as overweight usually resolves as children age. 75
Opinions of the 71 parents about BMI specifically were generally positive. Many parents felt that BMI was a more meaningful indicator of a child’s weight status than height and weight alone; age- and sex-adjusted BMI were considered valuable as parents felt that they could not easily calculate these themselves. Several parents thought that BMI would be a ‘wake-up call’ or ‘warning sign’ for parents of an emerging weight problem that needed attention, and others thought that children overly concerned about weight issues could be reassured if they were within the normal weight range. Most parents wanted to be notified about the BMI results, although some suggested that only parents of children with BMI values outside a healthy weight range need receive notification, to keep costs down. The preferred method of feedback to parents varied; most preferred results to be mailed directly, whereas others preferred feedback at teacher–parent conferences, parents calling the school nurse or the child bringing the information home in a sealed envelope. Few wanted the information via e-mail or the child’s report card. 75
The third study elicited opinions of caregivers (the mother or grandparent) on the ease of use of the CDC growth charts and a new presentation of BMI called ‘My Weight Ruler’. 207 The ruler was designed to simplify the presentation of results of BMI. There were two parts to this study. The first was to obtain opinions about the My Weight Ruler from 27 Hispanic and African American caregivers in order to decide descriptors for the different categories during videotaped focus groups. The Hispanic participants decided on the terms ‘underweight’, ‘healthy weight’, ‘slightly overweight’ and ‘unhealthy weight’; the African American participants decided on the terms ‘too little’, ‘just right’, ‘big’ and ‘too big’ (Figure 33). All participants of the focus groups preferred the My Weight Ruler to the CDC growth charts. 207
FIGURE 33.
The ‘My Weight Ruler’.

The second part of the study involved 251 caregivers who completed a questionnaire which asked them to interpret two plots on the My Weight Ruler and the CDC BMI growth chart. One plot was equivalent to the 50th centile and the other to the 97th centile. Of the 251 participants, 92% had previously seen a CDC BMI growth chart; none had seen the My Weight Ruler.
More respondents correctly classified both plotted measurements on the My Weight Ruler (92%) than on the CDC growth chart (37%); significantly more participants provided incorrect answers to both measurements on the CDC growth chart (32%) than on the My Weight Ruler (1%); and significantly more responded ‘I don’t know’ to the CDC growth chart (12% compared with 0.5%). Those who correctly interpreted the CDC BMI growth chart plots were more likely to have a higher level of education and higher household incomes; there were no significant trends for level of education, household income, ethnicity or first language for the My Weight Ruler. The need to take action when the result was at the 97th centile was understood by 61% of participants on the My Weight Ruler compared with 1% on the CDC growth chart. Overall, 79% of participants preferred the My Weight Ruler and 17% preferred the CDC BMI growth chart. 207
Leeds Metropolitan University’s de novo study of overweight or obese children attending summer camp
To supplement the information identified for the systematic review, the parents of the children attending the obesity management summer camp reported in Children’s assessment of acceptability and ease of use were also asked to give their opinion about simple measures of childhood obesity. Sixty-four parents completed a questionnaire. The opinions of the parents can only be generalised to those with an overweight or obese child, owing to the setting in which the survey was undertaken. The characteristics of the parents who completed the questionnaire are given in Table 43.
| Parents | Children | |||
|---|---|---|---|---|
| Age (years) | Sex (%) | Concerned about child’s weight? (%) | Age (years) | Sex (%) |
| Mean 40.7 Range 20–69 |
Male: 17.2 Female: 79.7 NR: 3.1 |
Yes: 89.1 No: 4.7 NR: 3.1 Sort of/slightly: 3.1 |
Mean 12 Range 9–17 |
Male: 40.6 Female: 59.4 |
Most of the parents said that their child had experienced height and weight measurements (Table 44). A proportion of these did not believe that their children had experienced their BMI being calculated, possibly as a consequence of the result not being fed back to them. Nearly 50% were aware that their children had had their WC measured, although, again, far fewer said that their children had experienced the composite measures that utilise WC. Only a small proportion of parents/caregivers were aware that their child had experienced SFT measurements, and one parent said that their child had undergone a measurement of muscle mass, although how this was measured is uncertain (see Table 44). When considering the usefulness of a measure, responses were generally positive, although the value of HC and SFT was uncertain for a large proportion of parents (Table 45). Nearly all of the parents were happy for their children to undergo any of the measures (see Table 45), although a large proportion considered the measurement of weight to be embarrassing for their child (Table 46).
| Measure | Yes (%) | No (%) | Don’t know (%) | NR (%) |
|---|---|---|---|---|
| Height | 87.5 | 3.1 | 7.8 | 1.6 |
| Weight | 92.2 | 3.1 | 3.1 | 1.6 |
| BMI | 67.2 | 15.6 | 15.6 | 1.6 |
| WC | 48.4 | 26.6 | 23.4 | 1.6 |
| HC | 26.6 | 40.6 | 31.3 | 1.6 |
| WHtR | 25.0 | 40.6 | 32.8 | 1.6 |
| WHR | 23.4 | 43.8 | 31.3 | 1.6 |
| SFT | 14.1 | 45.3 | 34.4 | 6.3 |
| Muscle mass | 1.6 | 0 | 0 | 0 |
| Do you think the measure is useful? | |||||
|---|---|---|---|---|---|
| Measure | Yes (%) | No (%) | Don’t know (%) | NR (%) | What is it? (%) |
| Height | 85.9 | 1.6 | 10.9 | 1.6 | 0 |
| Weight | 89.1 | 0 | 7.8 | 3.1 | 0 |
| WC | 73.4 | 1.6 | 21.9 | 3.1 | 0 |
| HC | 57.8 | 1.6 | 35.9 | 3.1 | 1.6 |
| SFT | 48.4 | 4.7 | 40.6 | 4.7 | 1.6 |
| Are you happy for your child to have the measure? | |||||
| Measure | Yes (%) | No (%) | Don’t know (%) | NR (%) | What is it? (%) |
| Height | 98.4 | 0 | 1.6 | 0 | 0 |
| Weight | 98.4 | 0 | 1.6 | 0 | 0 |
| WC | 98.4 | 0 | 1.6 | 0 | 0 |
| HC | 96.9 | 0 | 3.1 | 0 | 0 |
| SFT | 96.9 | 0 | 3.1 | 0 | 0 |
| Measure | Not had measure (%) | I don’t know (%) | Physical pain (%) | Embarrassed (%) | Fun/liked it (%) | Opted out (%) | Didn’t have a problem (%) | Anger (%) | Crying (%) | Other (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Height | 3.1 | 17.2 | 0 | 1.6 | 12.5 | 0 | 60.9 | 0 | 0 | 0 |
| Weight | 1.6 | 15.6 | 0 | 31.3 | 6.3 | 0 | 29.7 | 3.1 | 9.4 | 3.1 |
| WC | 23.4 | 26.6 | 0 | 7.8 | 6.3 | 0 | 25.0 | 1.6 | 0 | 0 |
| HC | 42.2 | 25.0 | 0 | 3.1 | 3.1 | 0 | 17.2 | 0 | 0 | 0 |
| SFT | 46.9 | 26.6 | 0 | 0 | 3.1 | 0 | 10.9 | 0 | 0 | 0 |
The measure that parents considered most useful was a child’s weight, with BMI and WC considered to be useful by over 40% of parents. Parents were less certain about the usefulness of HC, WHtR, WHR and SFT; most were either unfamiliar with the measure, or had not had the results fed back to them in order to form an opinion (Table 47).
| Measure | Child had not had measure (%) | Agreed that measure was accurate (%) | Measure overestimated child’s weight (%) | Measure underestimated child’s weight (%) | Didn’t understand the information (%) | Didn’t receive any information (%) |
|---|---|---|---|---|---|---|
| Weight | 4.7 | 68.8 | 7.8 | 1.6 | 0 | 10.9 |
| BMI | 12.5 | 46.9 | 12.5 | 1.6 | 0 | 20.3 |
| WC | 25.0 | 40.6 | 1.6 | 0 | 1.6 | 20.3 |
| HC | 45.3 | 17.2 | 3.1 | 0 | 4.7 | 17.2 |
| WHtR | 48.4 | 17.2 | 1.6 | 0 | 4.7 | 17.2 |
| WHR | 50.0 | 12.5 | 3.1 | 0 | 4.7 | 17.2 |
| SFT | 54.7 | 9.4 | 3.1 | 0 | 6.3 | 15.6 |
Health professionals’ assessment of acceptability and ease of use
Two previous studies were identified that elicited opinions about BMI from health-care professionals, one of school nurses73 and the other of family doctors and paediatricians. 208 Both of the studies were generally considered to be of good quality; both had clear aims and appropriate methodology, research designs and recruitment strategies, findings were clearly stated and the research was considered to be of value. One study had data that were collected and analysed appropriately; the other was only an abstract, and therefore data relating to analysis were limited. Neither study considered the relationship between researcher and participants or stated that ethical approval was gained. Brief study details are given in Table 48; the full data extraction is given in Appendix 3.
| Study details | Population characteristics | Children’s details |
|---|---|---|
| Hendershot (2008)73 Country in which study conducted: USA Study dates: NR |
Whose opinion?: school nurses Source of sample: National Association of School Nurses database Method of obtaining opinion: electronic survey Method of recording opinions: electronic/online |
School grade of children: NR Sex of children: NR Weight status of children: NR |
| Woolford (2008)208 Country in which study conducted: USA/Canada Study dates: start 2006, finish 2006 |
Whose opinion?: GPs, paediatricians Source of sample: American Medical Association Masterfile Method of obtaining opinion: self-administered survey (12-item Likert scales and multiple-choice questions) Method of recording opinions: paper questionnaire |
School grade of children: preschool (age 2–5 years) Sex of children: NR Weight status of children: NR |
The study of school nurses was an online survey. 73 Of the 2629 school nurses who completed the survey (97% of whom were female), 67% said that BMI should be measured in school, with 62% believing that BMI results should be sent home to parents. Most respondents stated that school nurses should be designing programmes to help overweight children (81%), that BMI helped create awareness of a problem (73%) and that BMI provided evidence to change policies to reduce obesity levels (72%). There were some concerns expressed over the use of BMI, with 31% believing that measuring BMI could be psychologically or socially damaging to the child. 73 A number of barriers to the use of BMI were highlighted, the most common of which was inadequate school resources (57.6%). Other barriers included inadequate or inappropriate parental responses (55.2%) and insufficient time for the measure (42%). Most of the school nurses were confident or very confident in measuring height and weight (94%), calculating BMI (74%) and helping parents interpret BMI results (93%). Over 50% of nurses agreed or strongly agreed that tracking BMI would help administrators to address the childhood overweight/obesity issue. 73
The study of family doctors and paediatricians took the form of a questionnaire aimed at eliciting opinions on the use of BMI in preschool children aged 2–5 years; 267 completed the survey. 208 Of the 267 respondents, 37% generally did not use BMI charts for children between 2 and 5 years old; 24% did generally use BMI charts for this age group and 39% endorsed the use of BMI charts for selected 2- to 5-year-olds. Of the 39% who used BMI charts for selected children, 87% indicated that this was for children who appear overweight from height and weight curves, 72% for children who appear overweight by visual inspection and 68% for children who have crossed upwards between weight centiles. 208 Barriers to the use of BMI included the time taken to calculate and plot BMI (65% of all respondents; 75% of those who did not use BMI or who used it selectively); the time and complexity of explaining the findings to parents (70% of all respondents; 76% of those who did not use BMI or who used it selectively); and parental familiarity with height and weight curves (57% of all respondents; 59% of those who did not use BMI or who used it selectively). Physicians who did not use BMI charts were more likely to report these as major barriers than physicians who did use BMI charts generally or selectively. Colour-coded charts were considered by 60%, and the inclusion of management recommendations on BMI charts by 61%, as strong influences in increasing the likelihood of using BMI charts at preschool well-child visits; 35% considered that computerised calculation and plotting of results would also improve use. Recommendations for addressing obesity were workshops at national and regional medical conferences (47%), online websites (45%) and DVD training (43%); 30% said they would participate in a 2-day behaviour management course, with paediatricians significantly more likely than family physicians to endorse this option (38% vs. 17%). Just 5% indicated that they probably would not participate in any training activities related to behaviour management skills to address obesity. 208
In order to supplement the information identified in the systematic review, we attempted to elicit the opinions of school nurses on the simple childhood measures most commonly used during screening in schools. We have no responses from school nurses to report.
Summary of acceptability and ease of use
The evidence identified from the systematic searches was limited. Three studies elicited opinions about BMI from parents/grandparents, one from school nurses and one from family doctors and paediatricians; no studies were identified that elicited the opinions of children on BMI or any other measure. The opinion of parents regarding the usefulness of BMI was generally positive; on the whole, parents considered height and weight screening useful and wanted to be made aware of the results of the screening of their children, although probably in a more user-friendly format than CDC growth charts, which were evaluated in one of the studies. School nurses were also generally positive about the usefulness of BMI, and most agreed with parents that the results of screening should be fed back to the child’s parent. The usefulness of measuring BMI in preschool children was less well accepted among doctors; however, it was considered by many to be useful for selected children aged 2–5 years who appear overweight from height and weight curves or visual inspection, or who have crossed upwards between weight centiles.
From the elicitation exercise, it seems that parents are generally unfamiliar with measurements such as WHR, WHtR and SFT, and therefore their potential accuracy and usefulness. This highlights the need to increase parents’ awareness of these measures if they are to be introduced as screening tools for school-aged children. The children who completed a questionnaire were most familiar with measurements of height and weight. Although most did not seem to have a problem with their height being measured, a large proportion were embarrassed by, or had other adverse reactions to, being weighed. This was, however, a small sample of children who were attending a weight management summer camp, and may not be representative of a more diverse population of children. Of those who experienced WC, HC and SFT measurements, a large proportion were also embarrassed when WC and HC were measured.
Chapter 4 Discussion
Summary of findings
This review sought to answer the question ‘What is the best simple measure, or combination of simple measures, of obesity in children for predicting the development of obesity-related health problems in adulthood?’ To answer this question, the review focused on four areas: the prediction of adult morbidity from childhood obesity; the tracking of obesity from childhood into adolescence and adulthood; the diagnosis of obesity in childhood; and the acceptability and ease of use of obesity measures. The review identified 37 studies on the prediction of adult morbidities, 23 studies on the tracking of obesity into adolescence and adulthood, 34 relevant diagnostic accuracy studies and five studies on acceptability, along with the elicitation exercise performed as part of the review.
Prediction of adult obesity-related morbidities
Thirteen existing systematic reviews were identified, of which four were judged to be of direct relevance to this review. These reviews generally concluded that there was a positive association between childhood BMI and adult obesity-related morbidities, with high BMI leading to greater incidence of diabetes, CHD and hypertension. One review found that the association between childhood obesity and morbidity was a consequence of obese children becoming obese adults and that childhood obesity was not an independent predictor of morbidity once adult obesity had been accounted for. 18
A total of 37 studies representing 22 distinct cohorts met the inclusion criteria for this review. Of these, 26 studies (13 cohorts) were included in meta-analyses. All studies included BMI. Three measured WC, and one used WHR and sum SFT. No evidence was found for other simple childhood measures.
In general, elevated childhood BMI was found to be modestly associated with an increased risk of adult morbidity. The association between a 1-SD increase in BMI and adult diabetes had an OR of 1.7 (95% CI 1.30 to 2.22), approximately equivalent to a 24% increase in risk per BMI unit in an adolescent. The association between a 1-SD increase in BMI and adult CHD had an OR of 1.2 (95% CI 1.20 to 1.31), approximately equivalent to obese children having an odds of CHD 44% higher than normal-weight children. There was no convincing evidence of an association between childhood obesity and stroke. Across a range of cancers, there was evidence that childhood obesity was associated with a higher risk of cancer in adulthood. Increases in odds were generally around 20% per SD of BMI. However, there was no evidence of an association between childhood BMI and breast cancer.
Despite the positive association between childhood BMI and morbidities, childhood BMI was not found to be a good predictor of adult disease. Given the associations identified, only 40% of adult diabetes and only 20% of CHD and cancers would occur in overweight or obese children (above the 85th centile for BMI). Hence, the majority of adult morbidity occurs in people who were of normal weight as children. This poor predictive accuracy is a consequence of the comparatively small magnitude of the association between childhood BMI and morbidities. As noted above, a large association would be required for BMI to be a useful predictor of adult morbidity.
In the narrative review, childhood obesity was found to be associated with adult metabolic syndrome, and there was some very limited evidence that BMI had poor sensitivity to predict adult metabolic syndrome. The existence and nature of metabolic syndrome remains controversial, with no standard definition. Most definitions of metabolic syndrome include obesity measurement, so the strong association between childhood BMI and metabolic syndrome may be a consequence of tracking of obesity into adulthood. Evidence on the association between childhood BMI and hypertension and hypercholesterolaemia was very limited. The number of studies was too small to draw conclusions about the effect of variables such as age and sex on adult morbidity.
Evidence was too limited to draw any firm conclusions about other childhood measures of obesity.
The studies included in the review tended to focus on older cohorts of children, who were born before the modern obesity epidemic in most cases. Earlier obesity onset and more extreme forms of childhood obesity are more common in contemporary populations than in the recent past. 236 This should be considered when interpreting the findings of this review.
Tracking of childhood obesity into adulthood
Two directly relevant systematic reviews of the tracking of overweight/obesity into adulthood had already been conducted prior to our review. Both reviews looked at correlations or associations between childhood and adult weight status. One of these reviews16 found that there was strong evidence of moderate persistence of overweight in both overweight and obese children, and that this association was possibly stronger for adolescent than for childhood overweight or obesity. The other, which focused on early childhood, found that childhood obesity (at age 5 years or earlier) was a probable marker of adult obesity. 17
From existing systematic reviews and searches for primary studies, a total of 23 studies from 16 cohorts met the inclusion criteria for this review. Only one study evaluated a childhood measure other than BMI (SFT). The association between childhood obesity (≥ 95th centile) and obesity in adults (age ≥ 20 years) was strong, with obese children being more than five times more likely to be obese as adults than non-obese children (pooled RR 5.21, 95% CI 4.50 to 6.02). There was no apparent difference in this RR between younger and older age groups.
Obesity tracked moderately well from childhood into adolescence; around half of obese children were still obese in adolescence. Obesity tracked well from adolescence to adulthood; about 80% of obese adolescents were still obese in adulthood and 70% were still obese after age 30 years. No data were available for tracking beyond the age of 40 years.
Body mass index was less effective at identifying those who would be obese in adulthood; 70% of obese adults were not obese as children or in adolescence, and 80% of obese people aged over 30 years were not obese in adolescence, so childhood BMI has poor sensitivity to detect adult obesity. Analyses of the tracking of childhood overweight (≥ 85th centile) to adult obesity or overweight gave broadly similar results.
Four studies reported data that could not be included in the meta-analyses; the results of these studies were broadly consistent with the findings of the meta-analyses. There were insufficient data on any simple measure other than BMI to suggest that any might improve the ability of childhood obesity to predict adult obesity.
Diagnostic accuracy of simple measures for childhood obesity
Thirty-four studies met the inclusion criteria for the review of diagnostic accuracy, of which 30 assessed the diagnostic accuracy of BMI, 10 of SFT, seven of WC, four of WHR, two of WHtR, one of BIA and five of other childhood measures of obesity. Sixteen studies reported direct comparisons of two or more childhood measures. Most of the studies used DEXA, which is the least reliable of the eligible reference standards. Of the 34 studies, only eight were considered to be high quality.
Overall, the sensitivity of BMI for diagnosing both obesity and overweight varied considerably; specificity was less variable. The most homogeneous subset of studies evaluating BMI were meta-analysed, that is those using the cut-off points most commonly used in clinical practice (85th centile for overweight and 95th centile for obesity), in a population of children representative of the UK child population who would receive the measure in practice. The resulting pooled sensitivity was approximately 74% (95% CI 64.2% to 81.8%) and pooled specificity was approximately 95% (95% CI 92.2% to 96.4%) for diagnosing overweight or obesity.
Data on other measures of obesity were more limited, with insufficient numbers of studies that were sufficiently homogeneous to undertake a meta-analysis. The most commonly evaluated non-BMI test was SFT. Sensitivity ranged from 23% to 98.5% and specificity from 78% to 100% across the populations and thresholds for triceps SFT (four studies). Sensitivity ranged from 30% to 98.5% and specificity from 79.1% to 99% for subscapular SFT (two studies). Sensitivity ranged from 57% to 98% and specificity from 47% to 96% for sum SFT (six studies). Several studies evaluated WC, either alone or in association with HC or height. Across populations and thresholds, sensitivity ranged from 34.7% to 100% and specificity from 81% to 100% for WC alone, sensitivity from 0% to 78.8% and specificity from 70.6% to 100% for WHR, and sensitivity from 90.9% to 100% and specificity from 95% to 100% for WHtR.
Using the studies reporting direct comparisons, there was little evidence to suggest that any measure that reported 2 × 2 tables of test performance to allow plotting into ROC would have substantially better diagnostic performance than BMI. FMI was evaluated alongside BMI in one study and looks promising, but would require further research. Sum SFT also shows potential as an alternative or supplementary measure to BMI. Of the measures that incorporate a WC measurement, it seems that WHtR was more accurate than WC alone or WHR, although WHtR was evaluated in fewer studies.
Acceptability and ease of use of simple measures for childhood obesity
Five studies were identified for the review of acceptability and ease of use, all eliciting opinions about BMI. None of the studies elicited the opinions of children; three elicited the opinions of caregivers/guardians, and two those of health professionals (one of school nurses and one of family doctors and paediatricians). The opinion of parents regarding the usefulness of BMI was generally positive. Most parents considered height and weight screening useful and wanted to be made aware of the results for their children, although in a more user-friendly format than CDC growth charts. School nurses were also generally positive about the usefulness of BMI, and most agreed with parents that the results of screening should be fed back to the child’s parent. The usefulness of measuring BMI in preschool children was less well accepted among doctors; however, it was considered by many to be useful for selected children aged 2–5 years who appear overweight from height and weight curves or visual inspection, or who have crossed upwards between weight centiles.
An elicitation exercise was conducted to obtain the views of children, parents/guardians and school nurses on four of the measures of childhood obesity: BMI, SFT, WHR and WHtR. The 72 children questioned, who were attending a weight management summer camp, were most familiar with height and weight measurement. Although most did not seem to have a problem with their height being measured, a large proportion were embarrassed by, or had other adverse reactions to, being weighed. Of those who experienced measurements of WC, HC and SFT, a large proportion were also embarrassed when WC and HC were measured. The 71 parents/caregivers questioned were generally unfamiliar with measures of WHR, WHtR and SFT, and therefore their potential accuracy and usefulness. Many felt that BMI was a more meaningful indicator of a child’s weight status than height and weight alone; age- and sex-adjusted BMI were considered valuable as parents/caregivers felt that they could not easily calculate these themselves. We had no data to report from school nurses.
Strengths and limitations of the review
Strengths
This review was conducted according to the PRISMA guidelines and provided a comprehensive analysis of the link between childhood obesity and adult obesity and morbidity by considering the four review areas described above. For each subreview, extensive searching was undertaken to identify published and unpublished studies, so that all relevant, appropriately powered studies were included.
Most previous systematic reviews in this field have been narrative reviews; this is the first review to combine results across studies in meta-analyses. In addition, unlike previous systematic reviews, this review has focused on the accuracy of childhood obesity to predict adult obesity or morbidity, rather than on estimating correlations or associations between test results and outcomes, and has used meta-analysis to calculate estimates of predictive accuracy for the ability of childhood obesity/overweight to predict adult morbidities and obesity/overweight. This is particularly important as an association between obesity and adult morbidity or obesity does not imply that childhood obesity will be a useful predictor of adult morbidity or obesity. In general, the association between a risk factor (such as obesity) and a subsequent medical condition has to be substantial before the risk factor can usefully be used to predict the future incidence of the condition. 70,237
The results of this review complement the findings of previous reviews rather than superseding them.
Limitations
Despite a large number of studies being identified for the morbidity and tracking review questions, the number from which the necessary data could be obtained was small. Furthermore, the limited reporting of most studies and the diversity in the reporting of morbidities, assessments of BMI and ages at which obesity was measured further reduced the number of studies that could be combined in any particular meta-analysis. This meant that most results have a high degree of uncertainty, with wide CIs, and it also limited the ability of the analyses to test for the impact of important confounders such as age and sex.
The diversity of reporting across studies also meant that most meta-analyses required a number of assumptions to be made to permit analysis. This was particularly the case for the prediction of morbidities, especially the assumption of normality for BMI, which is acknowledged to be inaccurate. Without individual patient data, there was no way for us to transform the BMI to meet the assumption of a normal distribution. This will have limited the reliability of the pooled estimate, and so the results should be taken as indicating general trends rather than providing precise estimates of association or predictive accuracy.
The number of studies of the prediction of adult morbidities or adult obesity that used a childhood measure of weight status other than BMI was surprisingly low: only four studies. This greatly hampered the review’s ability to address the original review question.
The cohort studies of the association between childhood obesity and adult morbidities included in the review were, of necessity, long-term studies, with recruitment often occurring in the 1960s or earlier. As this was before the rise in general obesity, it is unclear whether or not the findings from this part of the review apply to present-day children, among whom obesity is more prevalent.
Very few studies compared simple measures of obesity with our ‘gold standard’ measurement tool. In addition, several studies included in the review of diagnostic tools used internally derived, distribution-based cut-off points rather than set thresholds of adiposity. This limited the extent to which our third objective (to answer the question ‘how accurately do simple measures of obesity reflect actual adiposity in children?’) could be addressed.
Our review on the acceptability of simple measures of childhood obesity identified gaps in the evidence regarding the views of children, parents and health professionals. The elicitation exercise did contribute to filling some of these gaps. However, we acknowledge that this primary study only included a small, self-selected sample of children and parents, and did not include the views of health-care professionals. Therefore, the applicability of its findings to the broader population of children, parents and health professionals is unclear.
Chapter 5 Conclusions
In general, the review found that childhood obesity (when measured using BMI) was associated with moderately increased risks of adult obesity-related morbidity, but the increase in risk was not large enough for childhood BMI to be a good predictor of the incidence of adult morbidities; the majority of adult obesity-related morbidity occurs in adults who were of healthy weight in childhood.
Owing to lack of data, the review was unable to determine whether or not other simple measures of obesity might improve the prediction of adult morbidities.
The review of tracking studies found that obese children, and particularly obese adolescents, are likely to become obese adults. This is because childhood obesity (again when measured using BMI) is strongly associated with adult obesity. This strong association was matched by a strong persistence of childhood obesity into adulthood. However, childhood BMI is not a good predictor of the incidence of adult obesity or overweight; most obese adults were not obese in childhood, so overall adult obesity is not primarily determined by childhood obesity.
No information was available on tracking of obesity into later adulthood, when most obesity-related morbidities are likely to occur.
The usefulness of BMI as a screening tool therefore depends upon the objectives of screening. It may be useful for identifying a group of obese or overweight children who may benefit from intervention, but does not identify all children who will go on to be obese or to develop obesity-related morbidities in adulthood.
Body mass index was found to be reasonably good at diagnosing obesity during childhood, with around 75% of genuinely adipose children being classified as obese using BMI, and around 95% of non-obese children also being correctly classified. This result was, however, based mostly on studies using DEXA, which is not generally regarded as a gold standard for diagnosing obesity.
There is a lack of evidence to help determine whether or not any simple measure is better or worse than BMI for assessing childhood weight status, either for diagnosing obesity in childhood or for predicting adult obesity or obesity-related morbidities. If a simple childhood measure of obesity is to be introduced as a screening tool, its usefulness will depend upon the objectives of screening. If the objective is to identify a group of children who will benefit from intervention, then screening would be useful, as long as there are efficacious interventions available. If, however, the objective is to identify all children who will go on to become obese adults, then screening in childhood using one of these measures is unlikely to be useful.
When considering the acceptability and ease of use of the childhood measures of obesity, the opinion of parents and nurses on the usefulness of BMI was generally positive; however, its usefulness in preschool children was less well accepted among doctors, although it was considered useful for selected young children. From the elicitation exercise, the acceptability to children and their carers of BMI or other common simple measures was generally good, although adverse reactions were not uncommon when children had their weight measured. Parents were unfamiliar with measurements such as WHR, WHtR and SFT and therefore their potential usefulness, highlighting the need to increase the awareness of these measures if they are to be introduced as screening tools for school-aged children.
Implications for practice
This review has found evidence that childhood obesity (when measured using BMI) is strongly associated with increased adult obesity, but more weakly associated with increased adult obesity-related morbidity. Childhood overweight and obesity is therefore a genuine public health problem, and reducing the overall prevalence of obesity and overweight in childhood should reduce obesity and morbidities in later life.
Most obese children (when measured using BMI) will still be obese in early adulthood, so BMI is useful for identifying that group of children at higher risk of adult obesity. Whether or not this obesity persists into later adulthood (> 30 years) is uncertain.
However, most obese adults were of healthy weight in childhood, and the substantial majority of obesity-related morbidities occur in adults who were of healthy weight in childhood. Using BMI to identify obese children as being at risk of later obesity or morbidity, and targeting weight-reduction interventions specifically at these obese children, is therefore unlikely to have a meaningful impact on reducing the overall morbidity or obesity burden in adulthood.
This review suggests that, given the modest size of the association between childhood obesity and later morbidity, it may not be appropriate to categorise obese children as being at ‘high risk’ of later adult morbidity.
The evidence on measures of obesity other than BMI was too limited to draw any conclusions regarding whether such measures are better or worse than BMI when used to assess childhood obesity.
Issues around applicability may be considered alongside the question of parental interpretation of simple measures of overweight and obesity. There is evidence to suggest that some parents may not perceive their child as being overweight or at higher risk of health problems in later life. 238,239 Reasons for these misperceptions may be considered when communicating with parents of overweight and obese children. 239
Further research
There is limited evidence of the accuracy of childhood measures of obesity to predict adult obesity and morbidity. This suggests the following areas for future research:
-
To seek to review and analyse the individual-level raw data from the identified cohort studies. This could greatly enhance understanding of the association between childhood BMI and adult obesity and obesity-related morbidity, by avoiding the limitations found when using published results and reducing the need for making inaccurate assumptions in the analyses. It may also allow for examination of other simple measures, such as WC or WHtR, that may have been recorded but not reported in publications.
-
A high research priority is to determine which childhood measure is the most accurate for diagnosing childhood obesity. A full assessment is required of the diagnostic accuracy of childhood measures of obesity, at a range of ages from 2 to 18 years, particularly of studies using MRI as the reference standard. Primary diagnostic accuracy studies may need to be undertaken for those childhood measures for which data are sparse or missing completely. Any future diagnostic accuracy studies of other simple childhood measures should include BMI as a comparator and use at least a 4-C model as the reference standard, as this is the gold standard.
-
Primary predictive accuracy studies of measures other than BMI may be appropriate once it is clear that the required data are currently unavailable, and when the most accurate simple childhood measure for diagnosing childhood obesity has been determined, as such studies would be time-consuming and expensive.
-
Cohort studies to assess tracking of obesity and incidence of obesity-related morbidities should be undertaken to investigate the effect of contemporary childhood obesity on long-term obesity and morbidity. This could be achieved through appropriate maintenance and analysis of NHS records.
-
Any future assessment of simple measures of obesity should consider assessment of acceptability and ease of use of these measures.
Acknowledgements
We would like to thank members of our advisory group, Professor Charlotte Wright and Dr Jason Halford, for their advice, comments and suggestions throughout the conduct of the review. We would also like to thank Professor Christine Power for her advice during the protocol development stage of the project. Thanks too to Dr Leah Li for providing us with the full text of her manuscript which we were unable to locate, and to Dr David Freeman for providing us with unpublished 5 × 5 data.
Contribution of authors
Mark Simmonds contributed to the protocol development. Performed the statistical analyses in the morbidity and tracking reviews and performed some analyses for the diagnostic review; performed the data extraction for the morbidity review; wrote the sections of the report relating to the morbidity and tracking analyses, and the discussion; contributed generally to the writing of the report.
Jane Burch contributed to the protocol development. Performed the study selection for all four review questions, and the data extraction, validity assessment and most of the analyses for the diagnostic accuracy and acceptability and ease of use reviews; wrote the sections of the report relating to the diagnostic accuracy and acceptability and ease of use reviews, and the introduction; contributed generally to the writing of the report.
Alexis Llewellyn contributed to the protocol development. Performed the study selection, data extraction and validity assessment of the morbidity review; wrote sections of the report for the morbidity review; contributed generally to the writing of the report.
Claire Griffiths contributed to the protocol development. Was responsible for the conduct of the elicitation exercise, and provided comments on drafts of the report.
Huiqin Yang contributed to the protocol development. Performed the study selection and data extraction for the tracking and diagnostic accuracy reviews.
Christopher Owen contributed to the protocol development. Provided the team with advice throughout the project and commented on drafts of the report.
Steven Duffy contributed to the protocol development. Information specialist responsible for developing the search strategies, conducting a range of searches to locate studies and writing the methodological sections relating to the search.
Nerys Woolacott contributed to the protocol development. Took overall managerial responsibility for the project, contributed to all aspects of the project and provided comments on drafts of the report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Obesity. Department of Health; n.d.
- McGee DL. Diverse Populations Collaboration. Body mass index and mortality: a meta-analysis based on person-level data from twenty-six observational studies. Ann Epidemiol 2005;15:87-9. http://dx.doi.org/10.1016/j.annepidem.2004.05.012.
- Health Survey for England – 2012 [NS]. London: Health and Social Care Information Centre; 2012.
- National Child Measurement Programme: England, 2011–12, School Year. NHS Information Centre for Health and Social Care; 2012.
- National Statistics Health Survey for England – 2011, Health, Social Care and Lifestyles [NS]. London: Health and Social Care Information Centre; 2012.
- Butland B, Jebb S, Kopelman P, McPherson K, Thomas S, Mardell J, et al. Foresight. Tackling Obesities: Future Choices. Project Report. London: Government Office for Science; 2007.
- Swanton K. Healthy Weight, Healthy Lives: A Toolkit for Developing Local Strategies. London: Department of Health National Heart Forum; 2008.
- Nightingale CM, Rudnicka AR, Owen CG, Cook DG, Whincup PH. Patterns of body size and adiposity among UK children of South Asian, black African-Caribbean and white European origin: Child Heart And health Study in England (CHASE Study). Int J Epidemiol 2011;40:33-44. http://dx.doi.org/10.1093/ije/dyq180.
- El-Sayed AM, Scarborough P, Galea S. Ethnic inequalities in obesity among children and adults in the UK: a systematic review of the literature. Obes Rev 2011;12:e516-34. http://dx.doi.org/10.1111/j.1467-789X.2010.00829.x.
- Nightingale CM, Rudnicka AR, Owen CG, Donin AS, Newton SL, Furness CA, et al. Are ethnic and gender specific equations needed to derive fat free mass from bioelectrical impedance in children of South Asian, black African-Caribbean and white European origin? Results of the assessment of body composition in children study. PLOS One 2013;8. http://dx.doi.org/10.1371/journal.pone.0076426.
- Cunningham SA, Kramer MR, Narayan KMV. Incidence of childhood obesity in the United States. N Engl J Med 2014;370:403-11. http://dx.doi.org/10.1056/NEJMoa1309753.
- Vucenik I, Stains JP. Obesity and cancer risk: evidence, mechanisms, and recommendations. Ann N Y Acad Sci 2012;1271:37-43. http://dx.doi.org/10.1111/j.1749-6632.2012.06750.x.
- Shields M, Tremblay MS, Connor Gorber S, Janssen I. Abdominal obesity and cardiovascular disease risk factors within body mass index categories. Health Rep 2012;23:7-15.
- Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev 2012;13:275-86. http://dx.doi.org/10.1111/j.1467-789X.2011.00952.x.
- Prospective Studies Collaboration . Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 2009;373:1083-96. http://dx.doi.org/10.1016/S0140-6736(09)60318-4.
- Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev 2008;9:474-88. http://dx.doi.org/10.1111/j.1467-789X.2008.00475.x.
- Brisbois TD, Farmer AP, McCargar LJ. Early markers of adult obesity: a review. Obes Rev 2012;13:347-67. http://dx.doi.org/10.1111/j.1467-789X.2011.00965.x.
- Park MH, Falconer C, Viner RM, Kinra S. The impact of childhood obesity on morbidity and mortality in adulthood: a systematic review. Obes Rev 2012;13:985-1000. http://dx.doi.org/10.1111/j.1467-789X.2012.01015.x.
- Lloyd LJ, Langley-Evans SC, McMullen S. Childhood obesity and risk of the adult metabolic syndrome: a systematic review. Int J Obes (Lond) 2012;36:1-11. http://dx.doi.org/10.1038/ijo.2011.186.
- Lloyd LJ, Langley-Evans SC, McMullen S. Childhood obesity and adult cardiovascular disease risk: a systematic review. Int J Obes (Lond) 2010;34:18-2. http://dx.doi.org/10.1038/ijo.2009.61.
- Owen CG, Whincup PH, Orfei L, Chou QA, Rudnicka AR, Wathern AK, et al. Is body mass index before middle age related to coronary heart disease risk in later life? Evidence from observational studies. Int J Obes (Lond) 2009;33:866-77. http://dx.doi.org/10.1038/ijo.2009.102.
- Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes (Lond) 2011;35:891-8. http://dx.doi.org/10.1038/ijo.2010.222.
- Power C, Lake JK, Cole TJ. Measurement and long-term health risks of child and adolescent fatness. Int J Obes (Lond) 1997;21:507-26. http://dx.doi.org/10.1038/sj.ijo.0800454.
- Lawlor DA, Benfield L, Logue J, Tilling K, Howe LD, Fraser A, et al. Association between general and central adiposity in childhood, and change in these, with cardiovascular risk factors in adolescence: prospective cohort study. BMJ 2010;341. http://dx.doi.org/10.1136/bmj.c6224.
- Al-Sindi AM. Methods of measuring obesity, with special emphasis on children adolescents. Bahrain Med Bull 2000;22:98-102.
- Cornier MA, Després JP, Davis N, Grossniklaus DA, Klein S, Lamarche B, et al. Assessing adiposity: a scientific statement from the American Heart Association. Circulation 2011;124:1996-2019. http://dx.doi.org/10.1161/CIR.0b013e318233bc6a.
- Livingstone B. Epidemiology of childhood obesity in Europe. Eur J Pediatr 2000;59:14-3. http://dx.doi.org/10.1007/PL00014363.
- Obesity Guidance on the Prevention, Identification, Assessment and Management of Overweight and Obesity in Adults and Children. NICE Clinical Guideline 43. London: National Institute for Health and Care Excellence; 2006.
- Sweeting HN. Measurement and definitions of obesity in childhood and adolescence: a field guide for the uninitiated. Nutr J 2007;6. http://dx.doi.org/10.1186/1475-2891-6-32.
- Trefethen N. BMI (Body Mass Index): Calculate Your ‘New BMI’ 2013. http://people.maths.ox.ac.uk/trefethen/bmi.html (accessed 29 August 2013).
- Coutinho T, Goel K, Corrêa de Sá D, Carter RE, Hodge DO, Kragelund C, et al. Combining body mass index with measures of central obesity in the assessment of mortality in subjects with coronary disease: role of ‘normal weight central obesity’. J Am Coll Cardiol 2013;61:553-60. http://dx.doi.org/10.1016/j.jacc.2012.10.035.
- Wang Y, Rimm EB, Stampfer MJ, Willett WC, Hu FB. Comparison of abdominal adiposity and overall obesity in predicting risk of type 2 diabetes among men. Am J Clin Nutr 2005;81:555-63.
- McCarthy HD, Jarrett KV, Crawley HF. The development of waist circumference percentiles in British children aged 5.0–16.9 y. Eur J Clin Nutr 2001;55:902-7. http://dx.doi.org/10.1038/sj.ejcn.1601240.
- Nafiu OO, Burke C, Lee J, Voepel-Lewis T, Malviya S, Tremper KK. Neck circumference as a screening measure for identifying children with high body mass index. Pediatrics 2010;126:E306-10. http://dx.doi.org/10.1542/peds.2010-0242.
- LaBerge RC, Vaccani JP, Gow RM, Gaboury I, Hoey L, Katz SL. Inter- and intra-rater reliability of neck circumference measurements in children. Pediatr Pulmonol 2009;44:64-9. http://dx.doi.org/10.1002/ppul.20944.
- Hatipoglu N, Mazicioglu MM, Kurtoglu S, Kendirci M. Neck circumference: an additional tool of screening overweight and obesity in childhood. Eur J Pediatr 2010;169:733-9. http://dx.doi.org/10.1007/s00431-009-1104-z.
- Mei ZG, Grummer-Strawn LM, Pietrobelli A, Goulding A, Goran MI, Dietz WH. Validity of body mass index compared with other body-composition screening indexes for the assessment of body fatness in children and adolescents. Am J Clin Nutr 2002;75:978-85.
- Valdez R, Greenlund KJ, Wattigney WA, Bao W, Berenson GS. Use of weight-for-height indices in children to predict adult overweight: the Bogalusa Heart Study. Int J Obes Relat Metab Disord 1996;20:715-21.
- Flegal KM. Ratio of actual to predicted weight as an alternative to a power-type weight-height index (Benn index). Am J Clin Nutr 1990;51:540-7.
- Franklin MF. Comparison of weight and height relations in boys from 4 countries. Am J Clin Nutr 1999;70:157S-62S.
- Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr Res Rev 2010;23:247-69. http://dx.doi.org/10.1017/S0954422410000144.
- Ashwell M, Lejeune S, McPherson K. Ratio of waist circumference to height may be better indicator of need for weight management. BMJ 1996;312. http://dx.doi.org/10.1136/bmj.312.7027.377.
- Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation (WHO Technical Report Series 894). Geneva: World Health Organization; 2000.
- Bergman RN, Stefanovski D, Buchanan TA, Sumner AE, Reynolds JC, Sebring NG, et al. A better index of body adiposity. Obesity 2011;19:1083-9. http://dx.doi.org/10.1038/oby.2011.38.
- WHO Child Growth Standards. Head Circumference-For-Age, Arm Circumference-For-Age, Triceps Skinfold-For-Age and Subscapular Skinfold-For-Age: Methods and Development. Geneva: World Health Organization; 2007.
- Williams DP, Going SB, Lohman TG, Harsha DW, Srinivasan SR, Webber LS, et al. Body fatness and risk for elevated blood-pressure, total cholesterol, and serum–lipoprotein ratios in children and adolescents. Am J Public Health 1992;82:358-63. http://dx.doi.org/10.2105/AJPH.82.3.358.
- Formula for Life . Bioelectrical Impedance – BIA 2006. www.formulamedical.com/formula%20for%20life/measurement&diaries/BIA.htm (accessed 26 March 2013).
- Nichols J, Going S, Loftin M, Stewart D, Nowicki E, Pickrel J. Comparison of two bioelectrical impedance analysis instruments for determining body composition in adolescent girls. Int J Body Compos Res 2006;4:153-60.
- Eto C, Komiya S, Nakao T, Kikkawa K. Validity of the BMI and fat mass index as an indicator of obesity in children aged 3–5 years. J Physiol Anthropol Appl Human Sci 2004;23:25-30. http://dx.doi.org/10.2114/jpa.23.25.
- Freedman DS, Sherry B. The validity of BMI as an indicator of body fatness and risk among children. Pediatrics 2009;124:23-34. http://dx.doi.org/10.1542/peds.2008-3586E.
- Wells JC, Fewtrell MS. Measuring body composition. Arch Dis Child 2006;91:612-17. http://dx.doi.org/10.1136/adc.2005.085522.
- Urlando A, Dempster P, Aitkens S. A new air displacement plethysmograph for the measurement of body composition in infants. Pediatr Res 2003;53:486-92. http://dx.doi.org/10.1203/01.PDR.0000049669.74793.E3.
- Ginde SR, Geliebter A, Rubiano F, Silva AM, Wang J, Heshka S, et al. Air displacement plethysmography: validation in overweight and obese subjects. Obes Res 2005;13:1232-7. http://dx.doi.org/10.1038/oby.2005.146.
- Blueberry Health . Bespoke Software for Body Volume Index (BVI) 3D Body Scanner n.d. www.blueberry-health.co.uk/BodyVolumeIndexBVI.aspx (accessed 14 March 2013).
- Roubenoff R, Kehayias JJ, Dawson-Hughes B, Heymsfield SB. Use of dual-energy X-ray absorptiometry in body-composition studies: not yet a ‘gold standard’. Am J Clin Nutr 1993;58:589-91.
- Fuller NJ, Wells JCK, Elia M. Evaluation of a model for total body protein mass based on dual-energy X-ray absorptiometry: comparison with a reference four-component model. Br J Nutr 2001;86:45-52. http://dx.doi.org/10.1079/BJN2001387.
- Toombs RJ, Ducher G, Shepherd JA, De Souza MJ. The impact of recent technological advances on the trueness and precision of DXA to assess body composition. Obesity (Silver Spring) 2012;20:30-9. http://dx.doi.org/10.1038/oby.2011.211.
- Introduction to Body Composition Assessment Using the Deuterium Dilution Technique with Analysis of Urine Samples by Isotope Ratio Mass Spectrometry. IAEA Human Health Series No.13. Vienna: International Atomic Energy Agency; 2010.
- Healthy Lives, Healthy People: A Call to Action on Obesity in England. London: Department of Health; 2011.
- National Obesity Observatory . The National Obesity Observatory (NOO) n.d. www.noo.org.uk (accessed 14 March 2013).
- International Obesity Taskforce . International Obesity Taskforce (IOTF) n.d. www.iaso.org/iotf (accessed 14 March 2013).
- Griffiths C. Understanding Childhood Obesity in Leeds: From a Cross Sectional and Longitudinal Perspective. Leeds: Leeds Metropolitan University; 2012.
- Kipping RR, Jago R, Lawlor DA. Obesity in children. Part 1: Epidemiology, measurement, risk factors, and screening. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a1824.
- Consideration of Issues Around the Use of BMI Centile Thresholds for Defining Underweight, Overweight and Obesity in Children Aged 2–18 Years in the UK. London: Scientific Advisory Committee on Nutrition, Royal College of Paediatrics and Child Health; 2012.
- Reilly JJ. Assessment of childhood obesity: national reference data or international approach?. Obes Res 2002;10:838-40. http://dx.doi.org/10.1038/oby.2002.113.
- Wright CM, Parker L, Lamont D, Craft AW. Implications of childhood obesity for adult health: findings from thousand families cohort study. BMJ 2001;323:1280-4. http://dx.doi.org/10.1136/bmj.323.7324.1280.
- Singh R, Gupta SK. Childhood body mass index: a predictor of adult coronary heart disease?. Natl Med J India 2008;21:79-80.
- Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med 2011;365:1876-85. http://dx.doi.org/10.1056/NEJMoa1010112.
- Li L, Hardy R, Kuh D, Lo Conte R, Power C. Child-to-adult body mass index and height trajectories: a comparison of 2 British birth cohorts. Am J Epidemiol 2008;168:1008-15. http://dx.doi.org/10.1093/aje/kwn227.
- Wald NJ, Morris JK. Assessing risk factors as potential screening tests: a simple assessment tool. Arch Intern Med 2011;171:286-91. http://dx.doi.org/10.1001/archinternmed.2010.378.
- Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care. York: Centre for Reviews and Dissemination, University of York; 2009.
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b2535.
- Hendershot CH. Elementary school nurses’ perceptions and practices regarding body mass index measurement in school children. Diss Abstr Int B 2008;69. http://dx.doi.org/10.1177/1059840508323094.
- Kubik MY, Fulkerson JA, Story M, Rieland G. Parents of elementary school students weigh in on height, weight, and body mass index screening at school. J Sch Health 2006;76:496-501. http://dx.doi.org/10.1111/j.1746-1561.2006.00147.x.
- Kubik MY, Story M, Rieland G. Developing school-based BMI screening and parent notification programs: findings from focus groups with parents of elementary school students. Health Educ Behav 2007;34:622-33. http://dx.doi.org/10.1177/1090198105285373.
- Whiting PF, Weswood ME, Rutjes AW, Reitsma JB, Bossuyt PN, Kleijnen J. Evaluation of QUADAS, a tool for the quality assessment of diagnostic accuracy studies. BMC Med Res Methodol 2006;6. http://dx.doi.org/10.1186/1471-2288-6-9.
- School of Social and Community Medicine, University of Bristol . QUADAS-2 2011. www.bris.ac.uk/quadas/quadas-2/ (accessed 22 March 2013).
- Hayden JA, Côté P, Bombardier C. Evaluation of the quality of prognosis studies in systematic reviews. Ann Int Med 2006;144:427-37. http://dx.doi.org/10.7326/0003-4819-144-6-200603210-00010.
- Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Int Med 2013;158:280-6. http://dx.doi.org/10.7326/0003-4819-158-4-201302190-00009.
- Critical Appraisal Skills Programme (CASP) . CASP Qualitative Research Checklist 2013. www.casp-uk.net/wp-content/uploads/2011/11/CASP-Qualitative-Research-Checklist-31.05.13.pdf (accessed 6 June 2013).
- Prentice AM. Body mass index standards for children. BMJ 1998;317:1402-3. http://dx.doi.org/10.1136/bmj.317.7170.1401.
- Freedman DS, Wang YC, Dietz WH, Xu JH, Srinivasan SR, Berenson GS. Changes and variability in high levels of low-density lipoprotein cholesterol among children. Pediatrics 2010;126:266-73. http://dx.doi.org/10.1542/peds.2009-3454.
- Reitsma JB, Glas AS, Rutjes AW, Scholten RJPM, Bossuyt PN, Zwinderman AH. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol 2005;58:982-90. http://dx.doi.org/10.1016/j.jclinepi.2005.02.022.
- Rutter CM, Gatsonis CA. A hierarchical regression approach to meta-analysis of diagnostic test accuracy evaluations. Stat Med 2001;20:2865-84. http://dx.doi.org/10.1002/sim.942.
- Barba G, Casullo C, Dello Russo M, Russo P, Nappo A, Lauria F, et al. Gender-related differences in the relationships between blood pressure, age, and body size in prepubertal children. Am J Hypertens 2008;21:1007-10. http://dx.doi.org/10.1038/ajh.2008.228.
- Fagherazzi G, Guillas G, Boutron-Ruault MC, Clavel-Chapelon F, Mesrine S. Body shape throughout life and the risk for breast cancer at adulthood in the French E3N cohort. Eur J Cancer Prev 2013;22:29-37. http://dx.doi.org/10.1097/CEJ.0b013e328355ec04.
- Juonala M, Viikari JS, Raitakari OT. Main findings from the prospective Cardiovascular Risk in Young Finns Study. Curr Opin Lipidol 2013;24:57-64. http://dx.doi.org/10.1097/MOL.0b013e32835a7ed4.
- Gigante DP, Victora CG, Horta BL, Lima RC. Undernutrition in early life and body composition of adolescent males from a birth cohort study. Br J Nutr 2007;97:949-54. http://dx.doi.org/10.1017/S0007114507433025.
- Piechaczek H. Assessment of total body fat by anthropometric and densitometric methods. Mat Prace Antrop 1975;89:3-48.
- Rowe DA, Dubose KD, Donnelly JE, Mahar MT. Agreement between skinfold-predicted percent fat and percent fat from whole-body bioelectrical impedance analysis in children and adolescents. Int J Pediatr Obes 2006;1:168-75. http://dx.doi.org/10.1080/17477160600881296.
- Williams S, Davie G, Lam F. Predicting BMI in young adults from childhood data using two approaches to modelling adiposity rebound. Int J Obes Relat Metab Disord 1999;23:348-54. http://dx.doi.org/10.1038/sj.ijo.0800824.
- Zack PM, Harlan WR, Leaverton PE, Cornoni-Huntley J. A longitudinal study of body fatness in childhood and adolescence. J Pediatr 1979;95:126-30. http://dx.doi.org/10.1016/S0022-3476(79)80105-5.
- Bandini LG, Dietz WH. Assessment of body fatness in childhood obesity: evaluation of laboratory and anthropometric techniques. J Am Diet Assoc 1987;87:1344-8.
- Fisberg M. Metabolic Complications of Obesity in Children and Adolescents 2004:47-52.
- Reilly JJ, Dorosty AR, Emmett PM. Identification of the obese child: adequacy of the body mass index for clinical practice and epidemiology. Int J Obes (Lond) 2000;24:1623-7. http://dx.doi.org/10.1038/sj.ijo.0801436.
- Zheng XF, Tang QY, Tao YX, Lu W, Cai W. Clinical value of methods for analyzing the abdominal fat levels of obese children and adolescents. Obe Metab 2010;6:105-10.
- Addo OY, Pereira MA, Himes JH. Is skinfold thickness as good as DXA when measuring adiposity contributions to insulin resistance in adolescents?. Am J Hum Biol 2012;24:806-11. http://dx.doi.org/10.1002/ajhb.22321.
- Freedman DS, Khan LK, Mei ZG, Dietz WH, Srinivasan SR, Berenson GS. Relation of childhood height to obesity among adults: the Bogalusa Heart Study. Pediatrics 2002;109. http://dx.doi.org/10.1542/peds.109.2.e23.
- Freedman DS, Dietz WH, Tang R, Mensah GA, Bond MG, Urbina EM, et al. The relation of obesity throughout life to carotid intima–media thickness in adulthood: the Bogalusa Heart Study. Int J Obes (Lond) 2004;28:159-66. http://dx.doi.org/10.1038/sj.ijo.0802515.
- Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. Inter-relationships among childhood BMI, childhood height, and adult obesity: the Bogalusa Heart Study. Int J Obes (Lond) 2004;28:10-6. http://dx.doi.org/10.1038/sj.ijo.0802544.
- Kuperminc MN, Gurka MJ, Bennis JA, Busby MG, Grossberg RI, Henderson RC, et al. Anthropometric measures: poor predictors of body fat in children with moderate to severe cerebral palsy. Dev Med Child Neurol 2010;52:824-30. http://dx.doi.org/10.1111/j.1469-8749.2010.03694.x.
- Neovius M. Diagnostic Tests for Adiposity and Metabolic Risk Factors in Adolescence: Results from the Stockholm Weight Development Study (SWEDES). Stockholm: Karolinska Institute; 2005.
- Weber DR, Moore RH, Leonard MB, Zemel BS. Fat and lean BMI reference curves in children and adolescents and their utility in identifying excess adiposity compared with BMI and percentage body fat. Am J Clin Nutr 2013;98:49-56. http://dx.doi.org/10.3945/ajcn.112.053611.
- Andersen LG, Angquist L, Eriksson JG, Forsen T, Gamborg M, Osmond C, et al. Birth weight, childhood body mass index and risk of coronary heart disease in adults: combined historical cohort studies. PLoS One 2010;5. http://dx.doi.org/10.1371/journal.pone.0014126.
- Baker JL, Olsen LW, Sorensen TIA. Excess BMI among 267,456 Danish school children is associated with adult coronary heart disease. Obesity 2006;14.
- Baker JL, Olsen LW, Sorensen TIA. Excess BMI among 267,456 Danish school children is associated with stroke in adulthood. Obesity 2006;14.
- Baker JL, Olsen LW, Sorensen TIA. Excess BMI and excess growth during childhood are associated with adult coronary heart disease (CHD). Int J Obes (Lond) 2007;31.
- Baker JL, Olsen LW, Sørensen TIA. Birth weight and childhood BMI among 191,163 Danish schoolchildren and the risk of stroke in adulthood. Int J Obes (Lond) 2007;32.
- Cheng H, Yan YK, Mi J. Association between obesity in childhood and hypertension incidence: a prospective cohort study. J Hypertens 2011;29. http://dx.doi.org/10.1097/01.hjh.0000408125.13482.a7.
- Eriksson JG, Forsen T, Tuomilehto J, Winter PD, Osmond C, Barker DJ. Catch-up growth in childhood and death from coronary heart disease: longitudinal study. BMJ 1999;318:427-31. http://dx.doi.org/10.1136/bmj.318.7181.427.
- Ford CA, Nonnemaker JM, Wirth KE. The influence of adolescent body mass index, physical activity, and tobacco use on blood pressure and cholesterol in young adulthood. J Adolesc Health 2008;43:576-83. http://dx.doi.org/10.1016/j.jadohealth.2008.06.010.
- Landsvig Berentzen T, Gamborg M, Holst C, Sorensen TI, Baker JL. Childhood body size and the risk of liver cancer in adulthood. Obes Facts 2012;5.
- Li L, Pinot de Moira A, Power C. Predicting cardiovascular disease risk factors in midadulthood from childhood body mass index: utility of different cutoffs for childhood body mass index. Am J Clin Nutr 2011;93:1204-11. http://dx.doi.org/10.3945/ajcn.110.001222.
- Power C, Thomas C. Changes in BMI, duration of overweight and obesity, and glucose metabolism: 45 years of follow-up of a birth cohort. Diabetes Care 2011;34:1986-91. http://dx.doi.org/10.2337/dc10-1482.
- Tirosh A, Shai I, Afek A, Dubnov-Raz G, Ayalon N, Gordon B, et al. Dynamics of body mass index from adolescence to adulthood and risk of diabetes versus coronary heart disease. Diabetes 2011;60. http://dx.doi.org/10.1056/NEJMoa1006992.
- Yan Y, Cheng H, Duan J, Er Y, Mi J. Association between obesity in childhood and hypertension incidence: a prospective cohort study. Int J Cardiol 2011;152. http://dx.doi.org/10.1016/j.ijcard.2011.08.668.
- Cheng H, Yan YK, Duan JL, Er YL, Mi J. Association between obesity in childhood and hypertension incidence: a prospective cohort study. Chung Hua Yu Fang I Hsueh Tsa Chih 2011;45:696-701. http://dx.doi.org/10.1097/01.hjh.0000408125.13482.a7.
- Cheung YB, Machin D, Karlberg J, Khoo KS. A longitudinal study of pediatric body mass index values predicted health in middle age. J Clin Epidemiol 2004;57:1316-22. http://dx.doi.org/10.1016/j.jclinepi.2004.04.010.
- Engeland A, Bjørge T, Tverdal A, Søgaard AJ. Obesity in adolescence and adulthood and the risk of adult mortality. Epidemiology 2004;15:79-85. http://dx.doi.org/10.1097/01.ede.0000100148.40711.59.
- Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa Heart Study. Pediatrics 2001;108:712-18. http://dx.doi.org/10.1542/peds.108.3.712.
- Freedman DS, Khan AK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. Racial differences in tracking of childhood BMI to adulthood. Obes Res 2005;13:928-35. http://dx.doi.org/10.1038/oby.2005.107.
- Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. The relation of childhood BMI to adult adiposity: the Bogalusa Heart Study. Pediatrics 2005;115:22-7.
- Goldhaber-Fiebert JD, Rubinfeld RE, Bhattacharya J, Robinson TN, Wise PH. The utility of childhood and adolescent obesity assessment in relation to adult health. Med Decis Making 2013;33:163-75. http://dx.doi.org/10.1177/0272989X12447240.
- Gordon-Larsen P, Adair LS, Nelson MC, Popkin BM. Five-year obesity incidence in the transition period between adolescence and adulthood: the National Longitudinal Study of Adolescent Health. Am J Clin Nutr 2004;80:569-75.
- Juhola J, Magnussen CG, Viikari JS, Kahonen M, Hutri-Kahonen N, Jula A, et al. Tracking of serum lipid levels, blood pressure, and body mass index from childhood to adulthood: the Cardiovascular Risk in Young Finns Study. J Pediatr 2011;159:584-90. http://dx.doi.org/10.1016/j.jpeds.2011.03.021.
- Juonala M, Raitakari M, Viikari JSA, Raitakari OT. Obesity in youth is not an independent predictor of carotid IMT in adulthood. The Cardiovascular Risk in Young Finns Study. Atherosclerosis 2006;185:388-93. http://dx.doi.org/10.1016/j.atherosclerosis.2005.06.016.
- Liddle K, O’Callaghan M, Mamun A, Najman J, Williams G. Comparison of body mass index and triceps skinfold at 5 years and young adult body mass index, waist circumference and blood pressure. J Paediatr Child Health 2012;48:424-9. http://dx.doi.org/10.1111/j.1440-1754.2011.02247.x.
- Mamun AA, Lawlor DA, O’Callaghan MJ, Williams GM, Najman JM. Effect of body mass index changes between ages 5 and 14 on blood pressure at age 14: findings from a birth cohort study. Hypertension 2005;45:1083-7. http://dx.doi.org/10.1161/01.HYP.0000166720.18319.51.
- Merten MJ. Weight status continuity and change from adolescence to young adulthood: examining disease and health risk conditions. Obesity (Silver Spring) 2010;18:1423-8. http://dx.doi.org/10.1038/oby.2009.365.
- Nakano T, Sei M, Ewis AAA, Munakata H, Onishi C, Nakahori Y. Tracking overweight and obesity in Japanese children; a six years longitudinal study. J Med Invest 2010;57:114-23. http://dx.doi.org/10.2152/jmi.57.114.
- Nakano T, Sei M, Ewis AA, Munakata H, Onishi C, Nakahori Y. Weight and height growth velocities of Japanese boys and girls between age 7 and 14 years: a critical window for early adolescent overweight risk. J Med Invest 2010;57:124-32. http://dx.doi.org/10.2152/jmi.57.124.
- Patton GC, Coffey C, Carlin JB, Sawyer SM, Williams J, Olsson CA, et al. Overweight and obesity between adolescence and young adulthood: a 10-year prospective cohort study. J Adolesc Health 2011;48:275-80. http://dx.doi.org/10.1016/j.jadohealth.2010.06.019.
- Power C, Lake JK, Cole TJ. Body mass index and height from childhood to adulthood in the 1958 British birth cohort. Am J Clin Nutr 1997;66:1094-101.
- Reilly JJ, Bonataki M, Leary SD, Wells JC, Davey-Smith G, Emmett P, et al. Progression from childhood overweight to adolescent obesity in a large contemporary cohort. Int J Pediatr Obes 2011;6:e138-43. http://dx.doi.org/10.3109/17477166.2010.497538.
- Starc G, Strel J. Tracking excess weight and obesity from childhood to young adulthood: a 12-year prospective cohort study in Slovenia. Public Health Nutr 2011;14:49-55. http://dx.doi.org/10.1017/S1368980010000741.
- Stovitz SD, Hannan PJ, Lytle LA, Demerath EW, Pereira MA, Himes JH. Child height and the risk of young-adult obesity. Am J Prev Med 2010;38:74-7. http://dx.doi.org/10.1016/j.amepre.2009.09.033.
- Thompson DR, Obarzanek E, Franko DL, Barton BA, Morrison J, Biro FM, et al. Childhood overweight and cardiovascular disease risk factors: the National Heart, Lung, and Blood Institute Growth and Health Study. J Pediatr 2007;150:18-25. http://dx.doi.org/10.1016/j.jpeds.2006.09.039.
- Venn AJ, Thomson RJ, Schmidt MD, Cleland VJ, Curry BA, Gennat HC, et al. Overweight and obesity from childhood to adulthood: a follow-up of participants in the 1985 Australian Schools Health and Fitness Survey. Med J Aust 2007;186:458-60.
- Wang LY, Chyen D, Lee S, Lowry R. The association between body mass index in adolescence and obesity in adulthood. J Adolesc Health 2008;42:512-18. http://dx.doi.org/10.1016/j.jadohealth.2007.10.010.
- Ahlgren M, Melbye M, Wohlfahrt J, Sorensen TI. Growth patterns and the risk of breast cancer in women. Int J Gynecol Cancer 2006;16:569-75. http://dx.doi.org/10.1111/j.1525-1438.2006.00698.x.
- Baker JL, Olsen LW, Sorensen TI. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med 2007;357:2329-37. http://dx.doi.org/10.1056/NEJMoa072515.
- Baker JL, Olsen LW, Sorensen TIA. Excess BMI in childhood is associated with stroke in adulthood. Int J Obes (Lond) 2007;31.
- Barker DJP, Forsen T, Eriksson JG, Osmond C. Growth and living conditions in childhood and hypertension in adult life: a longitudinal study. J Hypertens 2002;20:1951-6. http://dx.doi.org/10.1097/00004872-200210000-00013.
- Barker DJ, Osmond C, Forsén TJ, Kajantie E, Eriksson JG. Trajectories of growth among children who have coronary events as adults. N Engl J Med 2005;353:1802-9. http://dx.doi.org/10.1056/NEJMoa044160.
- Berentzen TL, Gamborg M, Holst C, Sørensen TI, Baker JL. Body mass index in childhood and adult risk of primary liver cancer. J Hepatol 2014;60:325-30. http://dx.doi.org/10.1016/j.jhep.2013.09.015.
- Bjorge T, Tretli S, Engeland A. Relation of height and body mass index to renal cell carcinoma in two million Norwegian men and women. Am J Epidemiol 2004;160:1168-76. http://dx.doi.org/10.1093/aje/kwh345.
- Bjorge T, Engeland A, Tverdal A, Smith GD. Body mass index in adolescence in relation to cause-specific mortality: a follow-up of 230,000 Norwegian adolescents. Am J Epidemiol 2008;168:30-7. http://dx.doi.org/10.1093/aje/kwn096.
- De Stavola BL, dos Santos Silva I, McCormack V, Hardy RJ, Kuh DJ, Wadsworth MEJ. Childhood growth and breast cancer. Am J Epidemiol 2004;159:671-82. http://dx.doi.org/10.1093/aje/kwh097.
- Engeland A, Tretli S, Bjorge T. Height, body mass index, and ovarian cancer: a follow-up of 1.1 million Norwegian women. J Natl Cancer Inst 2003;95:1244-8. http://dx.doi.org/10.1093/jnci/djg010.
- Eriksson JG, Forsen T, Tuomilehto J, Osmond C, Barker DJ. Early growth and coronary heart disease in later life: longitudinal study. BMJ 2001;322:949-53. http://dx.doi.org/10.1136/bmj.322.7292.949.
- Forsen T, Eriksson J, Tuomilehto J, Reunanen A, Osmond C, Barker D. The fetal and childhood growth of persons who develop type 2 diabetes. Ann Int Med 2000;133:176-82. http://dx.doi.org/10.7326/0003-4819-133-3-200008010-00008.
- Forsen T, Osmond C, Eriksson JG, Barker DJ. Growth of girls who later develop coronary heart disease. Heart 2004;90:20-4. http://dx.doi.org/10.1136/heart.90.1.20.
- Gunnell DJ, Frankel SJ, Nanchahal K, Peters TJ, Davey Smith G. Childhood obesity and adult cardiovascular mortality: a 57-year follow-up study based on the Boyd Orr cohort. Am J Clin Nutr 1998;67:1111-18.
- Hilakivi-Clarke L, Forsén T, Eriksson JG, Luoto R, Tuomilehto J, Osmond C, et al. Tallness and overweight during childhood have opposing effects on breast cancer risk. Br J Cancer 2001;85:1680-4. http://dx.doi.org/10.1054/bjoc.2001.2109.
- Hypponen E, Power C, Smith GD. Prenatal growth, BMI, and risk of type 2 diabetes by early midlife. Diabetes Care 2003;26:2512-17. http://dx.doi.org/10.2337/diacare.26.9.2512.
- Israeli E, Korzets ZE, Tekes-Manova D, Tirosh A, Schochat T, Bernheim J, et al. Blood-pressure categories in adolescence predict development of hypertension in accordance with the European guidelines. Am J Hypertens 2007;20:705-9. http://dx.doi.org/10.1016/j.amjhyper.2007.01.020.
- Janssen I, Katzmarzyk PT, Srinivasan SR, Chen W, Malina RM, Bouchard C, et al. Utility of childhood BMI in the prediction of adulthood disease; comparison of national and international references. Obes Res 2005;13:1106-15. http://dx.doi.org/10.1038/oby.2005.129.
- Jeffreys M, Smith GD, Martin RM, Frankel S, Gunnell D. Childhood body mass index and later cancer risk: a 50-year follow-up of the Boyd Orr study. Int J Cancer 2004;112:348-51. http://dx.doi.org/10.1002/ijc.20423.
- Lawlor DA, Leon DA. Association of body mass index and obesity measured in early childhood with risk of coronary heart disease and stroke in middle age: findings from the Aberdeen children of the 1950s prospective cohort study. Circulation 2005;111:1891-6. http://dx.doi.org/10.1161/01.CIR.0000161798.45728.4D.
- Lawlor DA, Davey Smith G, Clark H, Leon DA. The associations of birthweight, gestational age and childhood BMI with type 2 diabetes: findings from the Aberdeen Children of the 1950s cohort. Diabetologia 2006;49:2614-17. http://dx.doi.org/10.1007/s00125-006-0408-z.
- Leiba A, Kark JD, Afek A, Levi Z, Barchana M, Tzur D, et al. Overweight in adolescence is related to increased risk of future urothelial cancer. Obesity 2012;20:2445-50. http://dx.doi.org/10.1038/oby.2012.83.
- Leiba A, Kark JD, Afek A, Derazne E, Barchana M, Tzur D, et al. Adolescent obesity and paternal country of origin predict renal cell carcinoma: a cohort study of 1.1 million 16 to 19-year-old males. J Urol 2013;189:25-9. http://dx.doi.org/10.1016/j.juro.2012.08.184.
- Levi Z, Kark JD, Barchana M, Liphshitz I, Zavdi O, Tzur D, et al. Measured body mass index in adolescence and the incidence of colorectal cancer in a cohort of 1.1 million males. Cancer Epidemiol Biomarkers Prev 2011;20:2524-31. http://dx.doi.org/10.1158/1055-9965.EPI-11-0531.
- Levi Z, Kark JD, Afek A, Derazne E, Tzur D, Furman M, et al. Measured body mass index in adolescence and the incidence of pancreatic cancer in a cohort of 720,000 Jewish men. Cancer Causes Control 2012;23:371-8. http://dx.doi.org/10.1007/s10552-011-9886-5.
- Li L, Law C, Power C. Body mass index throughout the life-course and blood pressure in mid-adult life: a birth cohort study. J Hypertens 2007;25:1215-23. http://dx.doi.org/10.1097/HJH.0b013e3280f3c01a.
- Magnussen CG, Koskinen J, Chen W, Thomson R, Schmidt MD, Srinivasan SR, et al. Pediatric metabolic syndrome predicts adulthood metabolic syndrome, subclinical atherosclerosis, and type 2 diabetes mellitus but is no better than body mass index alone: the Bogalusa Heart Study and the Cardiovascular Risk in Young Finns Study. Circulation 2010;122:1604-11. http://dx.doi.org/10.1161/CIRCULATIONAHA.110.940809.
- Mattsson N, Ronnemaa T, Juonala M, Viikari JS, Raitakari OT. Childhood predictors of the metabolic syndrome in adulthood. The Cardiovascular Risk in Young Finns Study. Ann Med 2008;40:542-52. http://dx.doi.org/10.1080/07853890802307709.
- Morrison JA, Glueck CJ, Horn PS, Wang P. Childhood predictors of adult type 2 diabetes at 9- and 26-year follow-ups. Arch Pediatr Adolesc Med 2010;164:53-60. http://dx.doi.org/10.1001/archpediatrics.2009.228.
- Osmond C, Kajantie E, Forsen TJ, Eriksson JG, Barker DJ. Infant growth and stroke in adult life: the Helsinki birth cohort study. Stroke 2007;38:264-70. http://dx.doi.org/10.1161/01.STR.0000254471.72186.03.
- Sachdev HP, Osmond C, Fall CH, Lakshmy R, Ramji S, Dey Biswas SK, et al. Predicting adult metabolic syndrome from childhood body mass index: follow-up of the New Delhi birth cohort. Arch Dis Child 2009;94:768-74. http://dx.doi.org/10.1136/adc.2008.140905.
- Schmidt MD, Dwyer T, Magnussen CG, Venn AJ. Predictive associations between alternative measures of childhood adiposity and adult cardio-metabolic health. Int J Obes (Lond) 2011;35:38-45. http://dx.doi.org/10.1038/ijo.2010.205.
- Tirosh A, Shai I, Afek A, Dubnov-Raz G, Ayalon N, Gordon B, et al. Adolescent BMI trajectory and risk of diabetes versus coronary disease. N Engl J Med 2011;364:1315-25. http://dx.doi.org/10.1056/NEJMoa1006992.
- Alvero-Cruz JR, Alvarez Carnero E, Fernandez-Garcia JC, Barrera Exposito J, Carrillo de Albornoz Gil M, Sardinha LB. Validity of body mass index and fat mass index as indicators of overweight status in Spanish adolescents: Esccola Study. Med Clin (Barc) 2010;135:8-14. http://dx.doi.org/10.1016/j.medcli.2010.01.017.
- Bartok CJ, Marini ME, Birch LL. High body mass index percentile accurately reflects excess adiposity in white girls. J Am Diet Assoc 2011;111:437-41. http://dx.doi.org/10.1016/j.jada.2010.11.015.
- Bray GA, DeLany JP, Volaufova J, Harsha DW, Champagne C. Prediction of body fat in 12-y-old African American and white children: evaluation of methods. Am J Clin Nutr 2002;76:980-90.
- Dung NQ, Fusch G, Armbrust S, Jochum F, Karaolis-Danckert N, Fusch C, et al. Body Composition and Nutritional Status in Neonates and Sick Children as Accessed by Dual Energy X-Ray Absorptiometry, Bioelectrical Impedance Analysis and Anthropometric Methods. Impact of Nutrition on Postnatal Growth. Greifswald: Ernst-Moritz-Arndt-Universität Greifswald; 2006.
- Ellis KJ, Abrams SA, Wong WW. Monitoring childhood obesity: assessment of the weight/height index. Am J Epidemiol 1999;150:939-46. http://dx.doi.org/10.1093/oxfordjournals.aje.a010102.
- Field AE, Laird N, Steinberg E, Fallon E, Semega-Janneh M, Yanovski JA. Which metric of relative weight best captures body fatness in children?. Obes Res 2003;11:1345-52. http://dx.doi.org/10.1038/oby.2003.182.
- Freedman DS, Wang J, Thornton JC, Mei Z, Sopher AB, Pierson RN, et al. Classification of body fatness by body mass index-for-age categories among children. Arch Pediatr Adolesc Med 2009;163:805-11. http://dx.doi.org/10.1001/archpediatrics.2009.104.
- Freedman DS, Ogden CL, Blanck HM, Borrud LG, Dietz WH. The abilities of body mass index and skinfold thicknesses to identify children with low or elevated levels of dual-energy X-ray absorptiometry-determined body fatness. J Pediatr 2013;163:160-6. http://dx.doi.org/10.1016/j.jpeds.2012.12.093.
- Fujita Y, Kouda K, Nakamura H, Iki M. Cut-off values of body mass index, waist circumference, and waist-to-height ratio to identify excess abdominal fat: population-based screening of Japanese school children. J Epidemiol 2011;21:191-6. http://dx.doi.org/10.2188/jea.JE20100116.
- Fuller NJ, Dewit O, Wells JCK. The potential of near infra-red interactance for predicting body composition in children. Eur J Clin Nutr 2001;55:967-72. http://dx.doi.org/10.1038/sj.ejcn.1601253.
- Fuller NJ, Fewtrell MS, Dewit O, Elia M, Wells JC. Segmental bioelectrical impedance analysis in children aged 8–12 y: 2. The assessment of regional body composition and muscle mass. Int J Obes Relat Metab Disord 2002;26:692-700. http://dx.doi.org/10.1038/sj.ijo.0801989.
- Guntsche Z, Guntsche EM, Saravi FD, Gonzalez LM, Lopez Avellaneda C, Ayub E, et al. Umbilical waist-to-height ratio and trunk fat mass index (DXA) as markers of central adiposity and insulin resistance in Argentinean children with a family history of metabolic syndrome. J Pediatr Endocrinol 2010;23:245-56. http://dx.doi.org/10.1515/JPEM.2010.23.3.245.
- Harrington DM, Staiano AE, Broyles ST, Gupta AK, Katzmarzyk PT. BMI percentiles for the identification of abdominal obesity and metabolic risk in children and adolescents: evidence in support of the CDC 95th percentile. Eur J Clin Nutr 2013;67:218-22. http://dx.doi.org/10.1038/ejcn.2012.203.
- Himes JH, Bouchard C. Validity of anthropometry in classifying youths as obese. Int J Obes (Lond) 1989;13:183-93.
- Johnston FE. Validity of triceps skinfold and relative weight as measures of adolescent obesity. J Adolesc Health Care 1985;6:185-90. http://dx.doi.org/10.1016/S0197-0070(85)80015-2.
- Khadgawat R, Marwaha RK, Tandon N, Mehan N, Upadhyay AD, Sastry A, et al. Reference intervals of percentage body fat in apparently healthy North-Indian school children and adolescents. Indian Pediatr 2013;50:859-66. http://dx.doi.org/10.1007/s13312-013-0237-3.
- Marshall JD, Hazlett CB, Spady DW, Conger PR, Quinney HA. Validity of convenient indicators of obesity. Hum Biol 1991;63:137-53.
- Mei Z, Grummer-Strawn LM, Wang J, Thornton JC, Freedman DS, Pierson RN, et al. Do skinfold measurements provide additional information to body mass index in the assessment of body fatness among children and adolescents?. Pediatrics 2007;119:e1306-13. http://dx.doi.org/10.1542/peds.2006-2546.
- Moreno LA, Blay MG, Rodriguez G, Blay VA, Mesana MI, Olivares JL, et al. Screening performances of the International Obesity Task Force body mass index cut-off values in adolescents. J Am Coll Nutr 2006;25:403-8. http://dx.doi.org/10.1080/07315724.2006.10719552.
- Neovius MG, Linne YM, Barkeling BS, Rossner SO. Sensitivity and specificity of classification systems for fatness in adolescents. Am J Clin Nutr 2004;80:597-603.
- Neovius M, Linne Y, Rossner S. BMI, waist-circumference and waist-hip-ratio as diagnostic tests for fatness in adolescents. Int J Obes (Lond) 2005;29:163-9. http://dx.doi.org/10.1038/sj.ijo.0802867.
- Pandit D, Chiplonkar S, Khadilkar A, Khadilkar V, Ekbote V. Body fat percentages by dual-energy X-ray absorptiometry corresponding to body mass index cutoffs for overweight and obesity in Indian children. Clin Med Pediatr 2009;3:55-61.
- Reilly JJ, Dorosty AR, Ghomizadeh NM, Sherriff A, Wells JC, Ness AR. Comparison of waist circumference percentiles versus body mass index percentiles for diagnosis of obesity in a large cohort of children. Int J Pediatr Obes 2010;5:151-6. http://dx.doi.org/10.3109/17477160903159440.
- Sardinha LB, Going SB, Teixeira PJ, Lohman TG. Receiver operating characteristic analysis of body mass index, triceps skinfold thickness, and arm girth for obesity screening in children and adolescents. Am J Clin Nutr 1999;70:1090-5.
- Sarria A, Moreno LA, Garcia-Llop LA, Fleta J, Morellon MP, Bueno M. Body mass index, triceps skinfold and waist circumference in screening for adiposity in male children and adolescents. Acta Paediatr 2001;90:387-92. http://dx.doi.org/10.1080/080352501750126195.
- Sproule DM, Montes J, Montgomery M, Battista V, Koenigsberger D, Shen W, et al. Increased fat mass and high incidence of overweight despite low body mass index in patients with spinal muscular atrophy. Neuromuscul Disord 2009;19:391-6. http://dx.doi.org/10.1016/j.nmd.2009.03.009.
- Taylor RW, Jones IE, Williams SM, Goulding A. Evaluation of waist circumference, waist-to-hip ratio, and the conicity index as screening tools for high trunk fat mass, as measured by dual-energy X-ray absorptiometry, in children aged 3–19 y. Am J Clin Nutr 2000;72:490-5.
- Taylor RW, Falorni A, Jones IE, Goulding A. Identifying adolescents with high percentage body fat: a comparison of BMI cutoffs using age and stage of pubertal development compared with BMI cutoffs using age alone. Eur J Clin Nutr 2003;57:764-9. http://dx.doi.org/10.1038/sj.ejcn.1601608.
- Telford RD, Cunningham RB, Daly RM, Reynolds GJ, Lafferty AR, Gravenmaker KJ, et al. Discordance of international adiposity classifications in Australian boys and girls – the LOOK study. Ann Hum Biol 2008;35:334-41. http://dx.doi.org/10.1080/03014460802014625.
- Vitolo MR, Campagnolo PD, Barros ME, Gama CM, Ancona Lopez F. Evaluation of two classifications for overweight among Brazilian adolescents. Rev Saude Publica 2007;41:653-6. http://dx.doi.org/10.1590/S0034-89102007000400021.
- Warner JT, Cowan FJ, Dunstan FD, Gregory JW. The validity of body mass index for the assessment of adiposity in children with disease states. Ann Hum Biol 1997;24:209-15. http://dx.doi.org/10.1080/03014469700004942.
- Wickramasinghe VP, Cleghorn GJ, Edmiston KA, Murphy AJ, Abbott RA, Davies PS. Validity of BMI as a measure of obesity in Australian white Caucasian and Australian Sri Lankan children. Ann Hum Biol 2005;32:60-71. http://dx.doi.org/10.1080/03014460400027805.
- Wickramasinghe VP, Lamabadusuriya SP, Cleghorn GJ, Davies PS. Validity of currently used cutoff values of body mass index as a measure of obesity in Sri Lankan children. Ceylon Med J 2009;54:114-19. http://dx.doi.org/10.4038/cmj.v54i4.1451.
- Zhang Q, Du WJ, Hu XQ, Liu AL, Pan H, Ma GS. The relation between body mass index and percentage body fat among Chinese adolescent living in urban Beijing. Chung Hua Liu Hsing Ping Hsueh Tsa Chih 2004;25:113-16.
- Cloutier MM, Lucuara-Revelo P, Wakefield DB, Gorin AA. My Weight Ruler: a simple and effective tool to enhance parental understanding of child weight status. Prev Med 2013;57:550-4. http://dx.doi.org/10.1016/j.ypmed.2013.07.014.
- Woolford SJ, Clark SJ, Strecher VJ, Gebremariam A, Davis MM. Physicians’ perspectives on increasing the use of BMI charts for young children. Clin Pediatr 2008;47:573-7. http://dx.doi.org/10.1177/0009922808314905.
- Robinson WR, Poole C, Godley PA. Systematic review of prostate cancer’s association with body size in childhood and young adulthood. Cancer Causes Control 2008;19:793-80. http://dx.doi.org/10.1007/s10552-008-9142-9.
- Yazdanpanahi Z, Hajifoghaha M, Nematollahi A. Metabolic syndrom: birth weight and childhood obesity. Arch Dis Child 2012;97:A486-7. http://dx.doi.org/10.1136/archdischild-2012-302724.1722.
- Adami F, Vasconcelos Fde A. Childhood and adolescent obesity and adult mortality: a systematic review of cohort studies. Cad Saude Publica 2008;24:558-68. http://dx.doi.org/10.1590/S0102-311X2008001600008.
- Ruiz JR, Castro-Pinero J, Artero EG, Ortega FB, Sjostrom M, Suni J, et al. Predictive validity of health-related fitness in youth: a systematic review. Br J Sports Med 2009;43:909-23. http://dx.doi.org/10.1136/bjsm.2008.056499.
- Sakurai Y. Duration of obesity and risk of non-insulin-dependent diabetes mellitus. Biomed Pharmacother 2000;54:80-4. http://dx.doi.org/10.1016/S0753-3322(00)88856-3.
- Whitlock EP, Williams SB, Gold R, Smith PR, Shipman SA. Screening and interventions for childhood overweight: a summary of evidence for the US preventive services task force. Pediatrics 2005;116:E125-44. http://dx.doi.org/10.1542/peds.2005-0242.
- Whitlock EP, Williams SB, Gold R, Smith P, Shipman S. Screening and Interventions for Childhood Overweight. Rockville, MD: Agency for Healthcare Research and Quality; 2005.
- Nadeau KJ, Maahs DM, Daniels SR, Eckel RH. Childhood obesity and cardiovascular disease: links and prevention strategies. Nat Rev Cardiol 2011;8:513-25. http://dx.doi.org/10.1038/nrcardio.2011.86.
- Reilly JJ, Methven E, McDowell ZC, Hacking B, Alexander D, Stewart L, et al. Health consequences of obesity. Arch Dis Child 2003;88:748-52. http://dx.doi.org/10.1136/adc.88.9.748.
- Schisterman EF, Cole SR, Platt RW. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology 2009;20:488-95. http://dx.doi.org/10.1097/EDE.0b013e3181a819a1.
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11 2002;246:1-190.
- Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000;320:1240-3. http://dx.doi.org/10.1136/bmj.320.7244.1240.
- Cole TJ, Freeman JV, Preece MA. Body-mass index reference curves for the UK, 1990. Arch Dis Child 1995;73:25-9. http://dx.doi.org/10.1136/adc.73.1.25.
- Nonnemaker JM, Morgan-Lopez AA, Pais JM, Finkelstein EA. Youth BMI trajectories: evidence from the NLSY97. Obesity 2009;17:1274-80. http://dx.doi.org/10.1038/oby.2009.5.
- Alberti K, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009;120:1640-5. http://dx.doi.org/10.1161/CIRCULATIONAHA.109.192644.
- Ezzahir N, Alberti C, Deghmoun S, Zaccaria I, Czernichow P, Lévy-Marchal C, et al. Time course of catch-up in adiposity influences adult anthropometry in individuals who were born small for gestational age. Pediatr Res 2005;58:243-7. http://dx.doi.org/10.1203/01.PDR.0000169980.35179.89.
- Wald NJ, Hackshaw AK, Frost CD. When can a risk factor be used as a worthwhile screening test?. BMJ 1999;319:1562-5. http://dx.doi.org/10.1136/bmj.319.7224.1562.
- Bayer O, Kruger H, von Kries R, Toschke AM. Factors associated with tracking of BMI: a meta-regression analysis on BMI tracking. Obesity 2011;19:1069-76. http://dx.doi.org/10.1038/oby.2010.250.
- Gately PJ, Radley D, Cooke CB, Carroll S, Oldroyd B, Truscott JG, et al. Comparison of body composition methods in overweight and obese children. J Appl Physiol 2003;95:2039-46. http://dx.doi.org/10.1152/japplphysiol.00377.2003.
- Crook TA, Armbya N, Cleves MA, Badger TM, Andres A. Air displacement plethysmography, dual-energy X-ray absorptiometry, and total body water to evaluate body composition in preschool-age children. J Acad Nutr Diet 2012;112:1993-8. http://dx.doi.org/10.1016/j.jand.2012.08.020.
- Shypailo RJ, Butte NF, Ellis KJ. DXA: can it be used as a criterion reference for body fat measurements in children?. Obesity 2008;16:457-62. http://dx.doi.org/10.1038/oby.2007.81.
- Wells JC, Haroun D, Williams JE, Wilson C, Darch T, Viner RM, et al. Evaluation of DXA against the four-component model of body composition in obese children and adolescents aged 5–21 years. Int J Obes (Lond) 2010;34:649-55. http://dx.doi.org/10.1038/ijo.2009.249.
- Lockner DW, Heyward VH, Baumgartner RN, Jenkins KA. Comparison of air-displacement plethysmography, hydrodensitometry, and dual X-ray absorptiometry for assessing body composition of children 10 to 18 years of age. Ann N Y Acad Sci 2000;904:72-8. http://dx.doi.org/10.1111/j.1749-6632.2000.tb06423.x.
- Plank LD. Dual-energy X-ray absorptiometry and body composition. Curr Opin Clin Nutr Metab Care 2005;8:305-9. http://dx.doi.org/10.1097/01.mco.0000165010.31826.3d.
- Radley D, Gately PJ, Cooke CB, Carroll S, Oldroyd B, Truscott JG. Percentage fat in overweight and obese children: comparison of DXA and air displacement plethysmography. Obes Res 2005;13:75-8. http://dx.doi.org/10.1038/oby.2005.10.
- Silva AM, Fields AF, Sardinha LB. A PRISMA-driven systematic review of predictive equations for assessing fat and fat-free mass in healthy children and adolescents using multicomponent molecular models as the reference method. Br J Nutr 2013;2013.
- Scafoglieri A, Provyn S, Wallace J, Louis O, Tresignie J, Bautmans I, et al. Whole body composition by hologic QDR 4500/A DXA: system reliability versus user accuracy and precision. Applications and Experiences of Quality Control 2011:45-62. www.intechopen.com (accessed March 2014).
- Lee JM, Pilli S, Gerbremariam A, Keirns CC, Davis MM, Vilan S, et al. Getting heavier younger: trajectories of obesity over the life course. Int J Obes (Lond) 2010;34:614-23. http://dx.doi.org/10.1038/ijo.2009.235.
- Wald NJ, Simmonds M, Morris JK. Screening for future cardiovascular disease using age alone compared with multiple risk factors and age. PLOS One 2011;6. http://dx.doi.org/10.1371/journal.pone.0018742.
- West DS, Raczynski JM, Phillips MM, Bursac Z, Gauss CH, Montgomery BEE. Parental recognition of overweight in school-age children. Obesity 2008;16:630-6. http://dx.doi.org/10.1038/oby.2007.108.
- Syrad H, Falconer C, Cooke L, Saxena SK, Kessel AS, Viner R, et al. ‘Health and happiness is more important than weight’: a qualitative investigation of the views of parents receiving written feedback on their child’s weight as part of the National Child Measurement Programme. J Hum Nutr Diet 2015;28:47-55. http://dx.doi.org/10.1111/jhn.12217.
Appendix 1 Literature searches
Review of adult morbidities: search for systematic reviews
Cochrane Database of Systematic Reviews (Wiley Online Library)
2013: Issue 6/12. Searched 11 June 2013. Retrieved four records.
#1 Medical subject heading (MeSH) descriptor: [Obesity] explode all trees (6452)
#2 MeSH descriptor: [Overweight] this term only (1072)
#3 MeSH descriptor: [Weight Gain] this term only (1416)
#4 MeSH descriptor: [Weight Loss] this term only (2918)
#5 obes*:ti,ab,kw (9909)
#6 (overweight or (over next weight)):ti,ab,kw (3234)
#7 ((weight next gain) or (weight next loss)):ti,ab,kw (9014)
#8 #1 or #2 or #3 or #4 or #5 or #6 or #7 (15,983)
#9 MeSH descriptor: [Adiposity] explode all trees (203)
#10 MeSH descriptor: [Body Composition] explode all trees (2773)
#11 MeSH descriptor: [Body Weight] explode all trees (14,255)
#12 (adiposity or adipose):ti,ab,kw (2114)
#13 (body near/2 (composition or fat or weight)):ti,ab,kw (18,126)
#14 fatness:ti,ab,kw (86)
#15 #8 or #9 or #10 or #11 or #12 or #13 or #14 (30,161)
#16 MeSH descriptor: [Child] explode all trees (64)
#17 MeSH descriptor: [Infant] explode all trees (12,099)
#18 MeSH descriptor: [Adolescent] this term only (69,925)
#19 MeSH descriptor: [Young Adult] this term only (112)
#20 (child* or infant* or pediat* or paediat* or schoolchild* or (school next age*) or schoolage*):ti,ab,kw (83,102)
#21 (adolescen* or juvenile* or youth* or teenage* or youngster*):ti,ab,kw (83,300)
#22 (girl or girls or boy or boys or kid or kids):ti,ab,kw (3932)
#23 ((young next people) or (young next person) or (young next persons) or (young next adult*)):ti,ab,kw (21,801)
#24 #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 (149,550)
#25 MeSH descriptor: [Body Mass Index] this term only (5044)
#26 MeSH descriptor: [Skinfold Thickness] this term only (269)
#27 MeSH descriptor: [Waist Circumference] this term only (261)
#28 MeSH descriptor: [Waist-Hip Ratio] this term only (158)
#29 MeSH descriptor: [Electric Impedance] this term only (313)
#30 ((“body mass” near/3 (index* or indices)) or bmi or quetelet*):ti,ab,kw (11,870)
#31 ((“fat mass” near/3 (index* or indices)) or fmi):ti,ab,kw (49)
#32 ((“fat free mass” near/3 (index* or indices)) or fmi):ti,ab,kw (35)
#33 (“body adipos*” near/3 (index* or indices)):ti,ab,kw (1)
#34 (“body fat” near/2 percentage*):ti,ab,kw (328)
#35 ((“skin fold” or skinfold) near/3 (thickness* or test* or measure*)):ti,ab,kw (590)
#36 ((waist or hip or neck) near/3 circumference*):ti,ab,kw (1244)
#37 ((waist-to-hip or waist-hip or “waist to hip” or “waist hip”) near/3 ratio*):ti,ab,kw (542)
#38 ((waist-to-height or waist-height or “waist to height” or “waist height”) near/3 ratio*):ti,ab,kw (16)
#39 (((bioelectric* or electric*) near/3 (impedance or resistance)) or bia):ti,ab,kw (598)
#40 (“near infrared interactance” or NIR):ti,ab,kw (49)
#41 ((benn* or rohrer* or ponderal or corpulence) near/3 (index* or indices)):ti,ab,kw (32)
#42 (“sagittal abdominal diameter*” or “supine abdominal diameter*”):ti,ab,kw (8)
#43 #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 (13,412)
#44 #15 and #24 and #43 (2163)
#45 MeSH descriptor: [Cardiovascular Diseases] explode all trees (68,582)
#46 ((cardiovascular or cardio or vascular or peripheral) near/3 (disease* or disorder* or failure*)):ti,ab,kw (11,739)
#47 ((heart or cardiac or myocardial) near/3 (disease* or disorder* or failure* or attack* or arrest*)):ti,ab,kw (19,972)
#48 (coronary near/3 (disease* or disorder* or failure* or attack* or arrest* or syndrome*)):ti,ab,kw (14,665)
#49 (circulatory near/3 (disease* or disorder* or failure*)):ti,ab,kw (139)
#50 CVD or CHD:ti,ab,kw (2049)
#51 (myocardial near/3 (infarc* or disease* or disorder* or failure* or attack* or arrest*)):ti,ab,kw (13,949)
#52 (ami or mi):ti,ab,kw (3681)
#53 (angina* or “atrial fibril*”):ti,ab,kw (11,114)
#54 MeSH descriptor: [Stroke] explode all trees (4414)
#55 (stroke* or poststroke*):ti,ab,kw (18,467)
#56 (cerebrovascular or (cerebral next vascular)):ti,ab,kw (4312)
#57 ((brain* or cerebral* or lacunar) near/3 (accident* or infarc*)):ti,ab,kw (2049)
#58 (apoplexy or CVA):ti,ab,kw (305)
#59 MeSH descriptor: [Hypertension] this term only (12,874)
#60 MeSH descriptor: [Blood Pressure] explode all trees (21,914)
#61 (hypertens* or (blood next pressure*) or bloodpressure* or diastolic or systolic):ti,ab,kw (55,771)
#62 MeSH descriptor: [Cholesterol] this term only (5091)
#63 MeSH descriptor: [Hypercholesterolemia] this term only (2311)
#64 (cholesterol or hypercholesterol?emia* or hypercholester?emia*):ti,ab,kw (16,019)
#65 #45 or #46 or #47 or #48 or #49 or #50 or #51 or #52 or #53 or #54 or #55 or #56 or #57 or #58 or #59 or #60 or #61 or #62 or #63 or #64 (134,104)
#66 MeSH descriptor: [Diabetes Mellitus, Type 2] explode all trees (7712)
#67 (diabetes near/2 “type 2”):ti,ab,kw (9307)
#68 (diabetes near/2 “type II”):ti,ab,kw (599)
#69 (diabetes near/2 (“non insulin” or noninsulin)):ti,ab,kw (1744)
#70 (NIDDM or T2DM):ti,ab,kw (1353)
#71 MeSH descriptor: [Metabolic Syndrome X] explode all trees (689)
#72 ((metabolic or dysmetabolic or reaven or insulin resistance) near/2 syndrome*):ti,ab,kw (1211)
#73 #66 or #67 or #68 or #69 or #70 or #71 or #72 (11,163)
#74 MeSH descriptor: [Neoplasms] explode all trees (46,049)
#75 (cancer* or neoplas* oncolog* or malignan* or tumo?r* or carcinoma* or adenocarcinoma*):ti,ab,kw (62,530)
#76 #74 or #75 (74,856)
#77 #65 or #73 or #76 (210,175)
#78 #44 and #77 (712)
Database of Abstracts of Reviews of Effects (Centre for Reviews and Dissemination public interface)
7 June 2013. Searched 11 June 2013. Retrieved 56 records.
-
MeSH DESCRIPTOR Obesity EXPLODE ALL TREES (685)
-
MeSH DESCRIPTOR Overweight EXPLODE ALL TREES (698)
-
MeSH DESCRIPTOR Weight Gain EXPLODE ALL TREES (108)
-
MeSH DESCRIPTOR Weight Loss EXPLODE ALL TREES (310)
-
(obes* or overweight or “over weight” or “weight gain” or “weight loss”) (1772)
-
MeSH DESCRIPTOR Adiposity EXPLODE ALL TREES (11)
-
MeSH DESCRIPTOR Body Composition EXPLODE ALL TREES (72)
-
MeSH DESCRIPTOR Body Weight EXPLODE ALL TREES (1005)
-
(adiposity or adipose or fatness) (70)
-
((body NEAR2 (composition or fat or weight))) (723)
-
(#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10) (2222)
-
MeSH DESCRIPTOR Body Mass Index EXPLODE ALL TREES (220)
-
MeSH DESCRIPTOR Skinfold Thickness EXPLODE ALL TREES (4)
-
MeSH DESCRIPTOR Waist Circumference EXPLODE ALL TREES (14)
-
MeSH DESCRIPTOR Waist-Hip Ratio EXPLODE ALL TREES (0)
-
MeSH DESCRIPTOR Electric Impedance EXPLODE ALL TREES (14)
-
(((“body mass” NEAR3 (index* or indices)) or bmi or quetelet*)) (927)
-
(((“fat mass” NEAR3 (index* or indices)) or fmi)) (5)
-
(((“fat free mass” NEAR3 (index* or indices)) or ffmi)) (0)
-
((“body adipos*” NEAR3 (index* or indices))) (1)
-
((“body fat” NEAR2 percentage*)) (9)
-
(((“skin fold” or skinfold) NEAR3 (thickness* or test* or measure*))) (48)
-
(((waist or hip or neck) NEAR3 circumference*)) (66)
-
(((waist-to-hip or waist-hip) NEAR3 ratio*)) (22)
-
(((waist-to-height or waist-height) NEAR3 ratio*)) (2)
-
((((bioelectric* or electric*) NEAR3 (impedance or resistance)) or bia)) (28)
-
(((benn* or rohrer* or ponderal or corpulence) NEAR3 (index* or indices))) (6)
-
((“infrared interactance” or NIR)) (7)
-
((“sagittal abdominal diameter*” or “supine abdominal diameter*”)) (0)
-
(#12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29) (983)
-
MeSH DESCRIPTOR Child EXPLODE ALL TREES (3665)
-
MeSH DESCRIPTOR Infant EXPLODE ALL TREES (2258)
-
MeSH DESCRIPTOR Adolescent EXPLODE ALL TREES (3456)
-
MeSH DESCRIPTOR Young Adult EXPLODE ALL TREES (1124)
-
((child* or infant* or pediat* or paediat* or schoolchild* or “school age*” or schoolage*)) (9033)
-
((adolescen* or juvenile* or youth* or teenage* or youngster*)) (4300)
-
((girl or girls or boy or boys or kid or kids)) (278)
-
((“young people” or “young person” or “young persons” or “young adult*”)) (1492)
-
(#31 or #32 or #33 or #34 or #35 or #36 or #37 or #38) (11,234)
-
MeSH DESCRIPTOR Cardiovascular Diseases EXPLODE ALL TREES (7964)
-
(((cardiovascular or cardio or vascular or peripheral) NEAR3 (disease* or disorder* or failure*))) (1837)
-
(((heart or cardiac or myocardial) NEAR3 (disease* or disorder* or failure* or attack* or arrest*)) ) (2805)
-
((coronary NEAR3 (disease* or disorder* or failure* or attack* or arrest* or syndrome*)) ) (1970)
-
((circulatory NEAR3 (disease* or disorder* or failure*)) ) (4)
-
(CVD or CHD ) (351)
-
((myocardial NEAR3 (infarc* or disease* or disorder* or failure* or attack* or arrest*)) ) (2211)
-
( (ami or mi) ) (838)
-
((angina* or “atrial fibril*”) ) (1288)
-
MeSH DESCRIPTOR Stroke EXPLODE ALL TREES (909)
-
(stroke* or poststroke*) (2514)
-
(cerebrovascular or “cerebral vascular”) (479)
-
(((brain* or cerebral* or lacunar) NEAR3 (accident* or infarc*)) ) (94)
-
((apoplexy or CVA) ) (31)
-
MeSH DESCRIPTOR Hypertension EXPLODE ALL TREES (687)
-
MeSH DESCRIPTOR Blood Pressure EXPLODE ALL TREES (384)
-
((hypertens* or “blood pressure*” or bloodpressure* or diastolic or systolic) ) (2854)
-
MeSH DESCRIPTOR Cholesterol EXPLODE ALL TREES (301)
-
MeSH DESCRIPTOR Hypercholesterolemia EXPLODE ALL TREES (149)
-
((cholesterol or hypercholesterol?emia* or hypercholester?emia*)) (962)
-
MeSH DESCRIPTOR Diabetes Mellitus, Type 2 EXPLODE ALL TREES (0)
-
((diabetes NEAR2 “type 2”) or (diabetes NEAR2 “type II”) or (diabetes NEAR2 (“non insulin” or noninsulin)) or NIDDM or T2DM ) (890)
-
MeSH DESCRIPTOR Metabolic Syndrome X EXPLODE ALL TREES (34)
-
(((metabolic or dysmetabolic or reaven or insulin resistance) NEAR2 syndrome*) ) (88)
-
MeSH DESCRIPTOR Neoplasms EXPLODE ALL TREES (8227)
-
((cancer* or neoplas* or oncolog* or malignan* or tumo?r* or carcinoma* or adenocarcinoma*) ) (9628)
-
#40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47 OR #48 OR #49 OR #50 OR #51 OR #52 OR #53 OR #54 OR #55 OR #56 OR #57 OR #58 OR #59 OR #60 OR #61 OR #62 OR #63 OR #64 OR #65 (22,000)
-
#11 AND #30 AND #39 AND #66 (66)
-
* IN DARE (31,884)
-
#67 AND #68 (56)
Database of Abstracts of Reviews of Effects (Centre for Reviews and Dissemination internal administration database)
7 June 2013. Searched 11 June 2013. Retrieved 149 records.
| Search term | Number retrieved | |
|---|---|---|
| #1 | MeSH DESCRIPTOR Obesity | 333 |
| #2 | MeSH DESCRIPTOR Overweight | 69 |
| #3 | MeSH DESCRIPTOR Weight Gain | 97 |
| #4 | obes* or overweight or over weight or weight gain or weight loss | 10,755 |
| #5 | MeSH DESCRIPTOR Adiposity | 10 |
| #6 | MeSH DESCRIPTOR Body Composition | 51 |
| #7 | MeSH DESCRIPTOR Body Weight | 118 |
| #8 | adiposity or adipose or fatness | 646 |
| #9 | (body NEAR2 composition) | 438 |
| #10 | (body NEAR2 fat) or (body NEAR2 weight) | 1634 |
| #11 | #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 | 11,151 |
| #12 | MeSH DESCRIPTOR Body Mass Index | 126 |
| #13 | MeSH DESCRIPTOR Skinfold Thickness | 3 |
| #14 | MeSH DESCRIPTOR Waist Circumference | 13 |
| #15 | MeSH DESCRIPTOR Waist-Hip Ratio | 2 |
| #16 | MeSH DESCRIPTOR Electric Impedance | 3 |
| #17 | (body mass NEAR3 index*) or (body mass NEAR3 indices) or bmi or quetelet*“fat mass index*” or “fat free mass index*” or adiposity index* | 2306 |
| #18 | fat mass index* or fat free mass index* or adiposity index* | 2 |
| #19 | body fat NEAR3 percentage* | 16 |
| #20 | skinfold or skin fold | 62 |
| #21 | waist circumference or hip circumference or neck circumference | 222 |
| #22 | waist-to-hip or waist-hip | 112 |
| #23 | waist-to-height or waist-height | 10 |
| #24 | bioelectric* impedance or bioelectric* resistance or electric* impedance or electric* resistance | 51 |
| #25 | (benn* or rohrer* or ponderal or corpulence) and (index* or indices) | 209 |
| #26 | infrared interactance or NIR or sagittal abdominal diameter* or supine abdominal diameter* | 26 |
| #27 | #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 | 2655 |
| #28 | MeSH DESCRIPTOR Child | 1756 |
| #29 | MeSH DESCRIPTOR Infant | 582 |
| #30 | MeSH DESCRIPTOR Adolescent | 1525 |
| #31 | MeSH DESCRIPTOR Young Adult | 441 |
| #32 | child* or infant* or pediat* or paediat* or schoolchild* or school age* or schoolage* | 27,579 |
| #33 | adolescen* or juvenile* or youth* or teenage* or youngster* | 9836 |
| #34 | girl or girls or boy or boys or kid or kids | 929 |
| #35 | young people or young person or young persons or young adult* | 2092 |
| #36 | #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 | 31,535 |
| #37 | MeSH DESCRIPTOR Cardiovascular Diseases | 471 |
| #38 | cardiovascular NEAR3 disease* | 5050 |
| #39 | cardiovascular disease* or cardiovascular disorder* or cardiovascular failure* | 4981 |
| #40 | cardio disease* or cardio disorder* or cardio failure* | 5046 |
| #41 | vascular disease* or vascular disorder* or vascular failure* | 1097 |
| #42 | peripheral disease* or peripheral disorder* or peripheral failure* | 7 |
| #43 | heart disease* or heart disorder* or heart failure* or heart attack* or heart arrest* | 6301 |
| #44 | cardiac disease* or cardiac disorder* or cardiac failure* or cardiac attack* or cardiac arrest* | 939 |
| #45 | myocardial disease* or myocardial disorder* or myocardial failure* or myocardial attack* or myocardial arrest* | 14 |
| #46 | coronary disease* or coronary disorder* or coronary failure* or coronary attack* or coronary arrest* or coronary syndrome* | 2251 |
| #47 | ami or mi or angina* or atrial fibril* | 5266 |
| #48 | MeSH DESCRIPTOR Stroke | 554 |
| #49 | stroke* or poststroke* or cerebrovascular or cerebral vascular | 7127 |
| #50 | (brain* or cerebral* or lacunar) NEAR3 (accident* or infarc*) | 315 |
| #51 | MeSH DESCRIPTOR Hypertension | 357 |
| #52 | MeSH DESCRIPTOR Blood Pressure | 270 |
| #53 | hypertens* or blood pressure* or bloodpressure* or diastolic or systolic | 8581 |
| #54 | MeSH DESCRIPTOR Cholesterol | 95 |
| #55 | MeSH DESCRIPTOR Hypercholesterolemia | 66 |
| #56 | cholesterol or hypercholesterol?emia* or hypercholester?emia* | 2501 |
| #57 | MeSH DESCRIPTOR Diabetes Mellitus, Type 2 | 424 |
| #58 | (diabetes NEAR2 “type 2”) or (diabetes NEAR2 “type II”) or (diabetes NEAR2 (“non insulin” or noninsulin)) or NIDDM or T2DM | 1314 |
| #59 | MeSH DESCRIPTOR Metabolic Syndrome X | 26 |
| #60 | (metabolic or dysmetabolic or reaven or insulin resistance) NEAR2 syndrome* | 895 |
| #61 | MeSH DESCRIPTOR Neoplasms | 584 |
| #62 | cancer* or neoplas* or oncolog* or malignan* or tumo?r* or carcinoma* or adenocarcinoma* | 31,338 |
| #63 | #37 OR #38 OR #39 OR #40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47 OR #48 OR #49 OR #50 OR #51 OR #52 OR #53 OR #54 OR #55 OR #56 OR #57 OR #58 OR #59 OR #60 OR #61 OR #62 | 55,949 |
| #64 | #11 AND #27 AND #36 AND #63 | 149 |
MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations (OvidSP)
1946–2013, May week 5. Searched 11 June 2013. Retrieved 687 records in MEDLINE and 27 records in MEDLINE In-Process & Other Non-Indexed Citations.
-
review.ab. (636,359)
-
review.pt. (1,830,463)
-
meta-analysis as topic/ (13,280)
-
meta-analysis.ab. (34,787)
-
meta-analysis.pt. (42,681)
-
meta-analysis.ti. (23,835)
-
or/1-6 (2,076,188)
-
(letter or editorial or comment).pt. (1,197,336)
-
animals/ not humans/ (3,811,795)
-
7 not (8 or 9) (1,910,614)
-
exp Obesity/ (133,014)
-
Overweight/ (10,556)
-
Weight Gain/ (21,776)
-
Weight Loss/ (22,903)
-
obes$.ti,ab. (152,384)
-
(overweight or over weight).ti,ab. (32,167)
-
(weight gain or weight loss).ti,ab. (82,180)
-
or/11-17 (267,262)
-
Adiposity/ or Adipose Tissue/ (63,489)
-
exp Body Composition/ (35,563)
-
Body Weight/ (159,038)
-
(adiposity or adipose).ti,ab. (56,647)
-
(body adj2 (composition or fat or weight)).ti,ab. (168,451)
-
fatness.ti,ab. (2834)
-
or/18-24 (541,557)
-
exp child/ (1,510,589)
-
exp Infant/ (916,662)
-
Adolescent/ (1,568,189)
-
Young Adult/ (310,115)
-
(child$ or infant$ or pediat$ or paediat$ or schoolchild$ or school age$ or schoolage$).ti,ab. (1,205,015)
-
(adolescen$ or juvenile$ or youth$ or teenage$ or youngster$).ti,ab. (236,539)
-
(girl or girls or boy or boys or kid or kids).ti,ab. (155,309)
-
(young people or young person or young persons or young adult$).ti,ab. (67,202)
-
or/26-33 (3,198,543)
-
body mass index/ (75,019)
-
Skinfold Thickness/ (5476)
-
Waist Circumference/ (3842)
-
Waist-Hip Ratio/ (2713)
-
Electric Impedance/ (11,165)
-
((body mass adj3 (index$ or indices)) or bmi or quetelet$).ti,ab. (113,321)
-
((fat mass adj3 (index$ or indices)) or fmi).ti,ab. (823)
-
((fat free mass adj3 (index$ or indices)) or ffmi).ti,ab. (343)
-
(body adipos$ adj3 (index$ or indices)).ti,ab. (35)
-
(body fat adj2 percentage$).ti,ab. (3469)
-
((skin fold or skinfold) adj3 (thickness$ or test$ or measure$ or ratio$)).ti,ab. (4808)
-
((waist or hip or neck) adj3 circumference$).ti,ab. (13,184)
-
((waist-to-hip or waist-hip) adj3 (ratio$ or test$ or measure$)).ti,ab. (6364)
-
((waist-to-height or waist-height) adj3 (ratio$ or test$ or measure$)).ti,ab. (522)
-
(((bioelectric$ or electric$) adj3 (impedance or resistance)) or bia).ti,ab. (10,288)
-
(near infrared interactance or NIR).ti,ab. (4634)
-
((benn$ or rohrer$ or ponderal or corpulence) adj3 (index$ or indices)).ti,ab. (999)
-
(sagittal abdominal diameter$ or supine abdominal diameter$).ti,ab. (108)
-
or/35-52 (168,981)
-
exp Cardiovascular Diseases/ (1,817,863)
-
((cardiovascular or cardio or vascular or peripheral) adj3 (disease$ or disorder$ or failure$)).ti,ab. (145,737)
-
((heart or cardiac or myocardial) adj3 (disease$ or disorder$ or failure$ or attack$ or arrest$)).ti,ab. (257,933)
-
(coronary adj3 (disease$ or disorder$ or failure$ or attack$ or arrest$ or syndrome$)).ti,ab. (116,718)
-
(CVD or CHD).ti,ab. (28,240)
-
(myocardial adj3 (infarc$ or disease$ or disorder$ or failure$ or attack$ or arrest$)).ti,ab. (141,002)
-
(ami or mi).ti,ab. (37,701)
-
(circulatory adj3 (disease$ or disorder$)).ti,ab. (4164)
-
angina$.ti,ab. (43,678)
-
atrial fibril$.ti,ab. (33,386)
-
exp Stroke/ (79,531)
-
(stroke$ or poststroke$).ti,ab. (132,480)
-
(cerebrovascular or cerebral vascular).ti,ab. (38,448)
-
((brain$ or cerebral$ or lacunar) adj3 (accident$ or infarc$)).ti,ab. (19,623)
-
apoplexy.ti,ab. (2150)
-
CVA.ti,ab. (1653)
-
Hypertension/ (187,947)
-
exp Blood Pressure/ (243,419)
-
hypertens$.ti,ab. (294,407)
-
(blood pressure$ or bloodpressure$).ti,ab. (209,312)
-
(diastolic or systolic).ti,ab. (143,044)
-
Cholesterol/ (102,941)
-
Hypercholesterolemia/ (21,568)
-
cholesterol.ti,ab. (166,494)
-
(hypercholesterol?emia$ or hypercholester?emia$).ti,ab. (21,597)
-
or/54-78 (2,328,244)
-
Diabetes Mellitus, Type 2/ (81,449)
-
(diabetes adj2 type 2).ti,ab. (56,501)
-
(diabetes adj2 type II).ti,ab. (5757)
-
(diabetes adj2 (non insulin or noninsulin)).ti,ab. (9422)
-
(NIDDM or T2DM).ti,ab. (11,346)
-
Metabolic Syndrome X/ (17,954)
-
((metabolic or dysmetabolic or reaven or insulin resistance) adj2 syndrome$).ti,ab. (25,583)
-
or/80-86 (122,953)
-
exp Neoplasms/ (2,503,418)
-
cancer$.ti,ab. (983,533)
-
(neoplas$ or oncolog$ or malignan$ or tumo?r$ or carcinoma$ or adenocarcinoma$).ti,ab. (1,593,573)
-
or/88-90 (2,907,785)
-
79 or 87 or 91 (5,088,112)
-
10 and 25 and 34 and 53 and 92 (687)
PubMed (National Library of Medicine)
1946–11 June 2013. Searched 11 June 2013. Retrieved 174 records.
#51 Search (#1 AND #10 AND #16 AND #29 AND #50) (174)
#50 Search (#41 or #46 or #49) (5,156,219)
#49 Search (#47 or #48) (2,973,617)
#48 Search cancer*[tiab] or neoplas*[tiab] or oncolog*[tiab] or malignan*[tiab] or tumour*[tiab] or tumor*[tiab] or carcinoma* [tiab] or adenocarcinoma*[tiab] (2,088,303)
#47 Search “Neoplasms”[Mesh] (2,448,239)
#46 Search (#42 or #43 or #44 or #45) (105,866)
#45 Search metabolic syndrome*[tiab] or dysmetabolic syndrome*[tiab] or reaven syndrome*[tiab] or insulin resistance syndrome*[tiab] (26,957)
#44 Search “Metabolic Syndrome X”[Mesh] (16,908)
#43 Search diabetes type 2[tiab] or diabetes type II[tiab] or diabetes non insulin[tiab] or diabetes noninsulin[tiab] or NIDDM [tiab] or T2DM[tiab] (12,728)
#42 Search “Diabetes Mellitus, Type 2”[Mesh] (77,427)
#41 Search (#30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40) (2,333,774)
#40 Search cholesterol[tiab] or hypercholesterolaemia*[tiab] or hypercholesteraemia*[tiab] or hypercholesterolemia*[tiab] or hypercholesteremia*[tiab] (183,386)
#39 Search “Cholesterol”[Mesh] or “Hypercholesterolemia”[Mesh] (141,654)
#38 Search hypertens*[tiab] or blood pressure*[tiab] or bloodpressure*[tiab] or diastolic[tiab] or systolic[tiab] (503,837)
#37 Search “Hypertension”[Mesh] or “Blood Pressure”[Mesh] (386,155)
#36 Search stroke*[tiab] or poststroke*[tiab] or cerebrovascular[tiab] or cerebral vascular[tiab] or brain* accident*[tiab] or cerebral* accident*[tiab] or lacunar accident*[tiab] or cerebral infarc*[tiab] or brain* infarc*[tiab] or cerebral* infarc*[tiab] or lacunar infarc*[tiab] or apoplexy[tiab] or CVA[tiab] (44,293)
#35 Search “Stroke”[Mesh] (76,757)
#34 Search CVD[tiab] or CHD[tiab] or ami[tiab] or mi[tiab] or angina*[tiab] or atrial fibril*[tiab] (144,210)
#33 Search coronary disease*[tiab] or coronary disorder*[tiab] or coronary failure*[tiab] or coronary attack*[tiab] or coronary arrest*[tiab] or coronary syndrome*[tiab] (53,502)
#32 Search heart disease*[tiab] or cardiac disease*[tiab] or myocardial disease*[tiab] or heart disorder*[tiab] or cardiac disorder*[tiab] or myocardial disorder*[tiab] or heart failure*[tiab] or cardiac failure*[tiab] or myocardial failure*[tiab] or heart failure*[tiab] or cardiac failure*[tiab] or myocardial failure*[tiab] or heart attack*[tiab] or cardiac attack*[tiab] or myocardial attack*[tiab] or heart attack*[tiab] or cardiac attack*[tiab] or myocardial attack*[tiab] or heart arrest*[tiab] or cardiac arrest*[tiab] or myocardial arrest*[tiab] or heart arrest*[tiab] or cardiac arrest*[tiab] or myocardial arrest*[tiab] (252,579)
#31 Search cardiovascular disease*[tiab] or cardio disease*[tiab] or vascular disease*[tiab] or peripheral disease*[tiab] or cardiovascular disorder*[tiab] or cardio disorder*[tiab] or vascular disorder*[tiab] or peripheral disorder*[tiab] or cardiovascular failure*[tiab] or cardio failure*[tiab] or vascular failure*[tiab] or peripheral failure*[tiab] (272,760)
#30 Search “Cardiovascular Diseases”[Mesh] (1,788,644)
#29 Search (#17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28) (168,726)
#28 Search “bioelectric impedance”[tiab] or “bioelectrical impedance”[tiab] or “electric impedance”[tiab] or “electrical impedance”[tiab] or “bioelectric resistance”[tiab] or “bioelectrical resistance”[tiab] or “electric resistance”[tiab] or “electrical resistance”[tiab] or bia[tiab] (10,600)
#27 Search “waist-to-height ratio”[tiab] or “waist-to-height ratios”[tiab] or “waist-height ratio”[tiab] or “waist-height ratios”[tiab] (600)
#26 Search “waist-to-hip ratio”[tiab] or “waist-to-hip ratios”[tiab] or “waist-hip ratio”[tiab] or “waist-hip ratios”[tiab] (6377)
#25 Search “waist circumference”[tiab] or “hip circumference”[tiab] or “neck circumference”[tiab] (13,577)
#24 Search (“skinfold thickness”[tiab] or “skinfold test”[tiab] or “skinfold tests”[tiab] or “skinfold measure”[tiab] or “skinfold measurement”[tiab] or “skinfold measures”[tiab] or “skinfold measurements”[tiab]) (3357)
#23 Search (“skin fold thickness”[tiab] or “skin fold test”[tiab] or “skin fold tests”[tiab] or “skin fold measure”[tiab] or “skin fold measurement”[tiab] or “skin fold measures”[tiab] or “skin fold measurements”[tiab]) (658)
#22 Search ((“body fat percentage”[tiab] or “body fat percentages”[tiab])) (1222)
#21 Search “body adiposity index”[tiab] or “body adiposity indices”[tiab] or “body adiposie index”[tiab] or “body adipose indices”[tiab] (47)
#20 Search (“fat free mass index”[tiab] or “fat free mass indices”[tiab] or ffmi[tiab]) (248)
#19 Search “fat mass index”[tiab] or “fat mass indices”[tiab] or fmi[tiab] (434)
#18 Search (“body mass index”[tiab] or “body mass indices”[tiab] or bmi[tiab] or quetelet*[tiab]) (119,706)
#17 Search ((((“Body Mass Index”[Mesh]) OR “Skinfold Thickness”[Mesh]) OR “Waist Circumference”[Mesh]) OR “Waist-Hip Ratio”[Mesh]) OR “Electric Impedance”[Mesh] (86,627)
#16 Search (#11 OR #12 OR #13 OR #14 OR #15) (3,221,920)
#15 Search “young people”[tiab] or “young person”[tiab] or “young persons”[tiab] or young adult*[tiab] (69,376)
#14 Search girl[tiab] or girls[tiab] or boy[tiab] or boys[tiab] or kid[tiab] or kids[tiab] (163,334)
#13 Search adolescen*[tiab] or juvenile*[tiab] or youth*[tiab] or teenage*[tiab] or youngster*[tiab] (248,889)
#12 Search child*[tiab] or infant*[tiab] or pediat*[tiab] or paediat*[tiab] or schoolchild*[tiab] or school age*[tiab] or schoolage*[tiab] (1,254,419)
#11 Search (((“Child”[Mesh]) OR “Infant”[Mesh]) OR “Adolescent”[Mesh]) OR “Young Adult”[Mesh] (2,849,606)
#10 Search (#7 OR #8 OR #9) (583,003)
#9 Search adiposity[tiab] or adipose[tiab] or “body composition”[tiab] or “body fat”[tiab] or “body weight”[tiab] or fatness[tiab] (216,116)
#8 Search (((“Adiposity”[Mesh]) OR “Adipose Tissue”[Mesh]) OR “Body Composition”[Mesh]) OR “Body Weight”[Mesh] (386,174)
#7 Search (#2 OR #3 OR #4 OR #5 OR #6) (281,116)
#6 Search “weight gain”[tiab] or “weight loss”[tiab] (86,556)
#5 Search overweight[tiab] or “over weight*”[tiab] (34,320)
#4 Search obes*[tiab] (160,601)
#3 Search ((“Overweight”[Mesh]) OR “Weight Gain”[Mesh]) OR “Weight Loss”[Mesh] (160,439)
#2 Search “Obesity”[Mesh] (127,351)
#1 Search ((systematic review [ti] OR meta-analysis [pt] OR meta-analysis [ti] OR systematic literature review [ti] OR (systematic review [tiab] AND review [pt]) OR consensus development conference [pt] OR practice guideline [pt] OR cochrane database syst rev [ta] OR acp journal club [ta] OR health technol assess [ta] OR evid rep technol assess summ [ta] OR drug class reviews [ti]) OR (clinical guideline [tw] AND management [tw]) OR ((evidence based[ti] OR evidence-based medicine [mh] OR best practice* [ti] OR evidence synthesis [tiab]) AND (review [pt] OR diseases category[mh] OR behavior and behavior mechanisms [mh] OR therapeutics [mh] OR evaluation studies[pt] OR validation studies[pt] OR guideline [pt] OR pmcbook)) OR ((systematic [tw] OR systematically [tw] OR critical [tiab] OR (study selection [tw]) OR (predetermined [tw] OR inclusion [tw] AND criteri* [tw]) OR exclusion criteri* [tw] OR main outcome measures [tw] OR standard of care [tw] OR standards of care [tw]) AND (survey [tiab] OR surveys [tiab] OR overview* [tw] OR review [tiab] OR reviews [tiab] OR search* [tw] OR handsearch [tw] OR analysis [tiab] OR critique [tiab] OR appraisal [tw] OR (reduction [tw]AND (risk [mh] OR risk [tw]) AND (death OR recurrence))) AND (literature [tiab] OR articles [tiab] OR publications [tiab] OR publication [tiab] OR bibliography [tiab] OR bibliographies [tiab] OR published [tiab] OR unpublished [tw] OR citation [tw] OR citations [tw] OR database [tiab] OR internet [tiab] OR textbooks [tiab] OR references [tw] OR scales [tw] OR papers [tw] OR datasets [tw] OR trials [tiab] OR meta-analy* [tw] OR (clinical [tiab] AND studies [tiab]) OR treatment outcome [mh] OR treatment outcome [tw] OR pmcbook)) NOT (letter [pt] OR newspaper article [pt] OR comment [pt])) (206,739)
Database of Promoting Health Effectiveness Reviews (Evidence for Policy and Practice Information and Co-ordinating Centre)
12 June 2013. Searched 12 June 2013. Retrieved 13 records.
-
Freetext: “obes*” OR overweight OR “over weight” OR “weight gain” OR “weight loss” (429)
-
Freetext: adiposity OR adipose OR fatness OR “body composition” or “body fat” or “body weight” (93)
-
1 OR 2 (348)
-
Freetext: “body mass index*” OR “body mass indices” OR bmi OR quetelet* (85)
-
Freetext: “fat mass” NEAR “index*” OR “fat mass” NEAR “indices*” OR fmi (1)
-
Freetext: “fat free mass” NEAR “index*” OR “fat free mass” NEAR “indices*” OR ffmi (0)
-
Freetext: “body adipos*” NEAR “index*” OR “body adipos*” NEAR “indices*” (1)
-
Freetext: “body fat” NEAR “percentage*” (11)
-
Freetext: “skin fold” or skinfold (10)
-
Freetext: “waist” NEAR “circumference*” OR “hip” NEAR “circumference*” OR “neck” NEAR “circumference*” (6)
-
Freetext: “waist-to-hip” OR “waist-hip” OR “waist-to-height” OR “waist-height” (4)
-
Freetext: “bioelectric*” NEAR “impedance” OR “electric*” NEAR “impedance” OR “bioelectric*” NEAR “resistance” OR “electric*” NEAR “resistance” (2)
-
Freetext: “benn*” NEAR “index*” OR “rohrer*” NEAR “index*” OR “ponderal” NEAR “index*” OR “corpulence” NEAR “index*” OR “benn*” NEAR “indices*” OR “rohrer*” NEAR “indices*” OR “ponderal” NEAR “indices*” OR “corpulence” NEAR “indices*” (2)
-
Freetext: “infrared interactance” OR NIR OR “sagittal abdominal diameter*” OR “supine abdominal diameter*” (0)
-
4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 (87)
-
Freetext: cardiovascular OR cardio OR vascular OR peripheral OR heart OR cardiac OR myocardial OR coronary OR circulatory OR CVD OR CHD OR AMI OR MI OR “angina*” OR atrial (239)
-
Freetext: “stroke*” OR “poststroke*” OR cerebrovascular OR “cerebral vascular” (21)
-
Freetext: “brain*” NEAR “accident*” OR “cerebral*” NEAR “accident*” OR “lacunar” NEAR “accident*” OR “brain*” NEAR “infarc*” OR “cerebral*” NEAR “infarc*” OR “lacunar” NEAR “infarc*” OR apoplexy OR CVA (1)
-
Freetext: “hypertens*” OR “blood pressure*” OR “bloodpressure*” OR diastolic OR systolic (114)
-
Freetext: cholesterol OR “hypercholesterolemia*” OR “hypercholesterolaemia*” OR “hypercholesteremia*” OR “hypercholesteraemia*” (58)
-
Freetext: diabetes OR NIDDM OR “T2DM” (113)
-
Freetext: “metabolic” NEAR “syndrome*”OR “dysmetabolic” NEAR “syndrome*”OR “reaven” NEAR “syndrome*”OR “insulin resistance” NEAR “syndrome*” (9)
-
Freetext: “cancer*” OR “neoplas*” OR “oncolog*” OR “malignan*” OR “tumor*” OR “tumour*” OR “carcinoma*” OR “adenocarcinoma*” (180)
-
16 OR 17 OR 18 OR 19 OR 20 OR 21 OR 22 OR 23 (501)
-
3 AND 15 AND 24 (40)
-
Freetext: “child*” OR “infant*” OR “pediat*” OR “paediat*” OR “schoolchild*” OR “school age*” OR “schoolage*” OR “adolescen*” OR “juvenile*” OR “youth*” OR “teenage*” OR “youngster*” OR girl OR girls OR boy OR boys OR kid OR kids OR “young people” OR “young person” OR “young persons” OR “young adult*” (1249)
-
25 AND 26 (13)
Internet sites searched
Organisation websites were browsed (publications and/or research) and searched. Searches were conducted in June 2013.
Public Health England – Obesity Knowledge and Intelligence (previously National Obesity Observatory) (www.noo.org.uk/)
Association for the Study of Obesity (www.aso.org.uk/)
Obesity Learning Centre (www.obesitylearningcentre.org.uk/)
National Obesity Forum (www.nationalobesityforum.org.uk/)
British Dietetic Association (www.bda.uk.com/index.html)
CEDAR (www.cedar.iph.cam.ac.uk/)
The Nutrition Society (www.nutritionsociety.org/)
International Association for the Study of Obesity (www.iaso.org/)
EASO (www.easoobesity.org/)
European Congress on Obesity (www.easo.org/eco2013)
ECOG (www.ecog-obesity.eu/)
CDC Division of Nutrition, Physical Activity, and Obesity (USA) (www.cdc.gov/nccdphp/dnpao/index.html)
Weight-control Information Network (USA) (http://win.niddk.nih.gov/)
The Obesity Society (USA) (www.obesity.org/)
myhealthywaist.org (International Chair on Cardiometabolic Risk of Université Laval – Quebec, Canada) (www.myhealthywaist.org/)
Citation searches: Web of Science and Google Scholar
1. Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obesity Reviews 2008 9(5):474-88.
WoS: 210 records (database updated 12 June 2013; searched 13 June 2013)
Google Scholar: 391 records (13 June 2013)
2. Falaschetti E, Hingorani AD, Jones A, Charakida M, Finer N, Whincup P, Lawlor DA, Davey Smith G, Sattar N, Deanfield JE. Adiposity and cardiovascular risk factors in a large contemporary population of pre-pubertal children. European Heart Journal 2010;31(24):3063-72.
WoS: 18 records (database updated 19 June 2013; searched 21 June 2013)
Google Scholar: 30 records (21 June 2013)
3. Okorodudu DO, Jumean MF, Montori VM, Romero-Corral A, Somers VK, Erwin PJ, Lopez-Jimenez F. Diagnostic performance of body mass index to identify obesity as defined by body adiposity: a systematic review and meta-analysis. International Journal of Obesity 2010;34(5):791-9.
WoS: 52 records (database updated 19 June 2013; searched 21 June 2013)
Google Scholar: 99 records (21 June 2013)
4. Nimptsch K, Giovannucci E, Willett WC, Fuchs CS, Wei EK, Wu K. Body fatness during childhood and adolescence, adult height, and risk of colorectal adenoma in women. Cancer Prevention Research (Philadelphia, PA) 2011;4(10):1710-8.
WoS: 3 records (database updated 21 June 2013; searched 24 June 2013)
Google Scholar: 5 records (24 June 2013)
5. Cameron AJ, Magliano DJ, Söderberg S. A systematic review of the impact of including both waist and hip circumference in risk models for cardiovascular diseases, diabetes and mortality. Obesity Reviews 2013;14(1):86-94.
WoS: 0 records (database updated 21 June 2013; searched 24 June 2013)
Google Scholar: 1 record (24 June 2013)
6. Clarke WR, Lauer RM. Does childhood obesity track into adulthood? Critical Reviews in Food Science and Nutrition 1993;33(4-5):423-30.
WoS: 110 records (database updated 21 June 2013; searched 24 June 2013)
Google Scholar: 152 records (24 June 2013)
7. Liddle K, O’Callaghan M, Mamun A, Najman J, Williams G. Comparison of body mass index and triceps skinfold at 5 years and young adult body mass index, waist circumference and blood pressure. Journal of Paediatrics and Child Health 2012;48(5):424-9.
WoS: 0 records (database updated 21 June 2013; searched 24 June 2013)
Google Scholar: 0 records (24 June 2013)
8. Freedman DS, Ogden CL, Blanck HM, Borrud LG, Dietz WH. The Abilities of Body Mass Index and Skinfold Thicknesses to Identify Children with Low or Elevated Levels of Dual-Energy X-Ray Absorptiometry-Determined Body Fatness. Journal of Pediatrics 2013 Feb 11. pii: S0022-3476(13)00005-X. [Epub ahead of print].
WoS: 0 records (database updated 21 June 2013; searched 24 June 2013)
Google Scholar: 1 record (24 June 2013)
9. Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. New England Journal of Medicine 2010;11;362(6):485-93.
WoS: 180 records (database updated 21 June 2013; searched 24 June 2013)
Google Scholar: 344 records (24 June 2013)
10. Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. Journal of Pediatrics 2007;150(1):12-17.e2.
WoS: 30 records (database updated 21 June 2013; searched 25 June 2013)
Google Scholar: 491 records (25 June 2013)
11. Conway JM, Norris KH, Bodwell CE. A new approach for the estimation of body composition: infrared interactance. American Journal of Clinical Nutrition 1984;40(6):1123-30.
WoS: 221 records (database updated 21 June 2013; searched 25 June 2013)
Google Scholar: 306 records (25 June 2013)
12. Freedman DS, Kahn HS, Mei Z, Grummer-Strawn LM, Dietz WH, Srinivasan SR, Berenson GS. Relation of body mass index and waist-to-height ratio to cardiovascular disease risk factors in children and adolescents: the Bogalusa Heart Study. American Journal of Clinical Nutrition 2007;86(1):33-40.
WoS: 81 records (database updated 21 June 2013; searched 26 June 2013)
Google Scholar: 161 records (26 June 2013)
13. Goldhaber-Fiebert JD, Rubinfeld RE, Bhattacharya J, Robinson TN, Wise PH. The utility of childhood and adolescent obesity assessment in relation to adult health. Medical Decision Making 2013;33(2):163-75.
WoS: 1 record (database updated 21 June 2013; searched 26 June 2013)
Google Scholar: 2 records (26 June 2013)
14. Gunnell DJ, Frankel SJ, Nanchahal K, Peters TJ, Davey Smith G. Childhood obesity and adult cardiovascular mortality: a 57-y follow-up study based on the Boyd Orr cohort. American Journal of Clinical Nutrition 1998;67(6):1111-8.
WoS: 232 records (database updated 21 June 2013; searched 26 June 2013)
Google Scholar: 453 records (26 June 2013)
15. Fayter D, Nixon J, Hartley S, Rithalia A, Butler G, Rudolf M, Glasziou P, Bland M, Stirk L, Westwood M. A systematic review of the routine monitoring of growth in children of primary school age to identify growth-related conditions. Health Technology Assessment 2007;11(22):1-163.
WoS: 8 records (database updated 26 June 2013; searched 27 June 2013)
Google Scholar: 23 records (27 June 2013)
16. Juonala M, Magnussen CG, Berenson GS, Venn A, Burns TL, Sabin MA, Srinivasan SR, Daniels SR, Davis PH, Chen W, Sun C, Cheung M, Viikari JS, Dwyer T, Raitakari OT. Childhood adiposity, adult adiposity, and cardiovascular risk factors. New England Journal of Medicine 2011;365(20):1876-85.
WoS: 73 records (database updated 26 June 2013; searched 27 June 2013)
Google Scholar: 136 records (27 June 2013)
17. Lazarus R, Baur L, Webb K, Blyth F. Body mass index in screening for adiposity in children and adolescents: systematic evaluation using receiver operating characteristic curves. American Journal of Clinical Nutrition 1996;63(4):500-6.
WoS: 77 records (database updated 26 June 2013; searched 27 June 2013)
Google Scholar: 154 records (27 June 2013)
18. Li L, Law C, Power C. Body mass index throughout the life-course and blood pressure in mid-adult life: a birth cohort study. Journal of Hypertension 2007;25(6):1215-23.
WoS: 32 records (database updated 26 June 2013; searched 27 June 2013)
Google Scholar: 42 records (27 June 2013)
19. Li L, Hardy R, Kuh D, Lo Conte R, Power C. Child-to-adult body mass index and height trajectories: a comparison of 2 British birth cohorts. American Journal of Epidemiology 2008;168(9):1008-15.
WoS: 17 records (database updated 26 June 2013; searched 27 June 2013)
Google Scholar: 23 records (27 June 2013)
20. Lloyd LJ, Langley-Evans SC, McMullen S. Childhood obesity and adult cardiovascular disease risk: a systematic review. International Journal of Obesity (London) 2010;34(1):18-28.
WoS: 22 records (database updated 26 June 2013; searched 27 June 2013)
Google Scholar: 55 records (27 June 2013)
21. Lloyd LJ, Langley-Evans SC, McMullen S. Childhood obesity and risk of the adult metabolic syndrome: a systematic review. Journal of Obesity (London) 2012;36(1):1-11.
WoS: 10 records (database updated 26 June 2013; searched 27 June 2013)
Google Scholar: 21 records (27 June 2013)
22. Mei Z, Grummer-Strawn LM, Pietrobelli A, Goulding A, Goran MI, Dietz WH. Validity of body mass index compared with other body-composition screening indexes for the assessment of body fatness in children and adolescents. American Journal of Clinical Nutrition 2002;75(6):978-85.
WoS: 240 records (database updated 26 June 2013; searched 27 June 2013)
Google Scholar: 541 records (27 June 2013)
23. Nichols J, Going S, Loftin M, Stewart D, Nowicki E, Pickrel J. Comparison of two bioelectrical impedance analysis instruments for determining body composition in adolescent girls. International Journal of Body Composition Research 2006;4(4):153-160.
WoS: 6 records (database updated 26 June 2013; searched 27 June 2013)
Google Scholar: 11 records (27 June 2013)
24. Nooyens AC, Koppes LL, Visscher TL, Twisk JW, Kemper HC, Schuit AJ, van Mechelen W, Seidell JC. Adolescent skinfold thickness is a better predictor of high body fatness in adults than is body mass index: the Amsterdam Growth and Health Longitudinal Study. American Journal of Clinical Nutrition 2007;85(6):1533-9.
WoS: 33 records (database updated 26 June 2013; searched 27 June 2013)
Google Scholar: 49 records (27 June 2013)
25. Park MH, Falconer C, Viner RM, Kinra S. The impact of childhood obesity on morbidity and mortality in adulthood: a systematic review. Obesity Reviews 2012;13(11):985-1000.
WoS: 7 records (database updated 26 June 2013; searched 27 June 2013)
Google Scholar: 20 records (27 June 2013)
26. Power C, Lake JK, Cole TJ. Measurement and long-term health risks of child and adolescent fatness. International Journal of Obesity and Related Metabolic Disorders 1997;21(7):507-26.
WoS: 354 records (database updated 26 June 2013; searched 28 June 2013)
Google Scholar: 619 records (28 June 2013)
27. Power C, Thomas C. Changes in BMI, duration of overweight and obesity, and glucose metabolism: 45 years of follow-up of a birth cohort. Diabetes Care 2011;34(9):1986-91.
WoS: 8 records (database updated 26 June 2013; searched 28 June 2013)
Google Scholar: 13 records (28 June 2013)
28. Reilly JJ, Kelly J, Wilson DC. Accuracy of simple clinical and epidemiological definitions of childhood obesity: systematic review and evidence appraisal. Obesity Reviews 2010;11(9):645-55.
WoS: 20 records (database updated 26 June 2013; searched 28 June 2013)
Google Scholar: 35 records (28 June 2013)
29. Sardinha LB, Going SB, Teixeira PJ, Lohman TG. Receiver operating characteristic analysis of body mass index, triceps skinfold thickness, and arm girth for obesity screening in children and adolescents. American Journal of Clinical Nutrition 1999;70(6):1090-5.
WoS: 93 records (database updated 26 June 2013; searched 28 June 2013)
Google Scholar: 197 records (28 June 2013)
30. Serdula MK, Ivery D, Coates RJ, Freedman DS, Williamson DF, Byers T. Do obese children become obese adults? A review of the literature. Preventive Medicine 1993;22(2):167-77.
WoS: 706 records (database updated 26 June 2013; searched 28 June 2013)
Google Scholar: 1367 records (28 June 2013)
31. Thomas C, Hyppönen E, Power C. Obesity and type 2 diabetes risk in midadult life: the role of childhood adversity. Pediatrics 2008 May;121(5):e1240-9.
WoS: 57 records (database updated 26 June 2013; searched 28 June 2013)
Google Scholar: 95 records (28 June 2013)
32. Wright CM, Parker L, Lamont D, Craft AW. Implications of childhood obesity for adult health: findings from thousand families cohort study. BMJ 2001;323(7324):1280-4.
WoS: 155 records (database updated 26 June 2013; searched 28 June 2013)
Google Scholar: 298 records (28 June 2013)
Review of adult morbidities: search for additional primary studies
MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations (OvidSP)
1946–2013, September week 4. Searched 4 October 2013. Retrieved 2484 records in MEDLINE and 301 records in MEDLINE In-Process & Other Non-Indexed Citations.
-
exp *Obesity/ (99,951)
-
*Overweight/ (7376)
-
*Adiposity/ (2824)
-
obes$.ti,ab. (164,847)
-
(overweight or over weight).ti,ab. (35,402)
-
adiposity.ti,ab. (13,484)
-
or/1-6 (196,646)
-
exp child/ or exp Infant/ or Adolescent/ (2,882,142)
-
(child$ or infant$ or pediat$ or paediat$ or schoolchild$ or school age$ or schoolage$).ti,ab. (1,253,562)
-
(adolescen$ or juvenile$ or youth$ or teenage$ or youngster$).ti,ab. (250,426)
-
(girl or girls or boy or boys or kid or kids).ti,ab. (161,260)
-
or/8-11 (3,152,555)
-
*body mass index/ (12,267)
-
((body mass adj3 (index$ or indices)) or bmi or quetelet$).ti,ab. (123,839)
-
13 or 14 (125,030)
-
*Skinfold Thickness/ (866)
-
*Waist Circumference/ (1108)
-
((skin fold or skinfold) adj3 (thickness$ or test$ or measure$ or ratio$)).ti,ab. (5000)
-
(waist adj3 circumference$).ti,ab. (14,012)
-
or/16-19 (18,848)
-
*Waist-Hip Ratio/ or *Electric Impedance/ (2810)
-
((fat mass adj3 (index$ or indices)) or fmi).ti,ab. (915)
-
((fat free mass adj3 (index$ or indices)) or ffmi).ti,ab. (370)
-
(body adipos$ adj3 (index$ or indices)).ti,ab. (41)
-
((hip or neck) adj3 circumference$).ti,ab. (3136)
-
((waist-to-hip or waist-hip) adj3 (ratio$ or test$ or measure$)).ti,ab. (6774)
-
((waist-to-height or waist-height) adj3 (ratio$ or test$ or measure$)).ti,ab. (601)
-
(((bioelectric$ or electric$) adj3 (impedance or resistance)) or bia).ti,ab. (11,001)
-
(near infrared interactance or NIR).ti,ab. (5084)
-
((benn$ or rohrer$ or ponderal or corpulence) adj3 (index$ or indices)).ti,ab. (1030)
-
(sagittal abdominal diameter$ or supine abdominal diameter$).ti,ab. (120)
-
or/21-31 (27,437)
-
exp *Cardiovascular Diseases/ (1,575,263)
-
exp *Stroke/ (63,420)
-
*Hypertension/ (139,094)
-
*Hypercholesterolemia/ or *Dyslipidemias/ (17,458)
-
((cardiovascular or cardio or vascular or peripheral) adj3 (disease$ or disorder$ or failure$)).ti,ab. (156,163)
-
((heart or cardiac or myocardial) adj3 (disease$ or disorder$ or failure$ or attack$ or arrest$)).ti,ab. (270,179)
-
(coronary adj3 (disease$ or disorder$ or failure$ or attack$ or arrest$ or syndrome$)).ti,ab. (121,849)
-
(CVD or CHD or IHD).ti,ab. (34,257)
-
(myocardial adj3 (infarc$ or disease$ or disorder$ or failure$ or attack$ or arrest$)).ti,ab. (146,283)
-
(ami or mi).ti,ab. (39,951)
-
(circulatory adj3 (disease$ or disorder$)).ti,ab. (4271)
-
angina$.ti,ab. (44,684)
-
atrial fibril$.ti,ab. (35,395)
-
(stroke$ or poststroke$).ti,ab. (141,434)
-
(cerebrovascular or cerebral vascular).ti,ab. (40,112)
-
((brain$ or cerebral$ or lacunar) adj3 (accident$ or infarc$)).ti,ab. (20,320)
-
hypertens$.ti,ab. (306,843)
-
high blood pressure.ti,ab. (10,087)
-
high cholesterol.ti,ab. (4917)
-
(hypercholesterol?emia$ or hypercholester?emia$).ti,ab. (22,466)
-
(dyslipid?emia$ or dyslipoprotein?emias$).ti,ab. (17,481)
-
or/33-53 (1,910,195)
-
*Diabetes Mellitus, Type 2/ (69,067)
-
*Metabolic Syndrome X/ (15,189)
-
(diabetes adj2 type 2).ti,ab. (61,812)
-
(diabetes adj2 type II).ti,ab. (6078)
-
(diabetes adj2 (non insulin or noninsulin)).ti,ab. (9514)
-
(NIDDM or T2DM or T2D).ti,ab. (14,261)
-
((metabolic or dysmetabolic or reaven or insulin resistance) adj2 syndrome$).ti,ab. (27,945)
-
or/55-61 (121,005)
-
exp *Neoplasms/ (2,243,426)
-
cancer$.ti,ab. (1,054,643)
-
(neoplas$ or oncolog$ or malignan$ or tumo?r$ or carcinoma$ or adenocarcinoma$).ti,ab. (1,673,022)
-
or/63-65 (2,819,554)
-
exp Animals/ not Humans/ (4,058,478)
-
(comment or editorial or letter).pt. (1,245,317)
-
67 or 68 (5,253,117)
-
7 and 12 and 15 and (54 or 62 or 66) (5576)
-
70 not 69 (5547)
-
(2011$ or 2012$ or 2013$).ed,dc,ep. (2,547,833)
-
71 and 72 (1862)
-
7 and 12 and 20 and (54 or 62) (1542)
-
74 not 69 (1538)
-
(2008$ or 2009$ or 2010$ or 2011$ or 2012$ or 2013$).ed,dc,ep. (5,017,455)
-
75 and 76 (1076)
-
7 and 12 and 20 and 66 (128)
-
78 not 69 (128)
-
7 and 12 and 32 and (54 or 62 or 66) (817)
-
80 not 69 (812)
-
73 or 77 or 79 or 81 (2980)
NB: After removal of duplicate records, the final total was 2484.
EMBASE (OvidSP)
1974–2013, week 39. Searched 4 October 2013. Retrieved 3405 records.
-
exp *obesity/ (154,266)
-
obes$.ti,ab. (229,244)
-
(overweight or over weight).ti,ab. (50,550)
-
adiposity.ti,ab. (17,157)
-
or/1-4 (282,623)
-
child/ or preschool child/ or infant/ or adolescent/ (2,386,317)
-
(child$ or infant$ or pediat$ or paediat$ or schoolchild$ or school age$ or schoolage$).ti,ab. (1,602,771)
-
(adolescen$ or juvenile$ or youth$ or teenage$ or youngster$).ti,ab. (320,105)
-
(girl or girls or boy or boys or kid or kids).ti,ab. (215,455)
-
or/6-9 (3,051,058)
-
*body mass/ (13,758)
-
((body mass adj3 (index$ or indices)) or bmi or quetelet$).ti,ab. (191,016)
-
11 or 12 (192,700)
-
*skinfold thickness/ (877)
-
*waist circumference/ (1514)
-
((skin fold or skinfold) adj3 (thickness$ or test$ or measure$ or ratio$)).ti,ab. (6057)
-
(waist adj3 circumference$).ti,ab. (21,661)
-
or/14-17 (27,483)
-
*waist hip ratio/ or *waist to height ratio/ or *weight height ratio/ or *neck circumference/ (543)
-
((fat mass adj3 (index$ or indices)) or fmi).ti,ab. (1254)
-
((fat free mass adj3 (index$ or indices)) or ffmi).ti,ab. (537)
-
(body adipos$ adj3 (index$ or indices)).ti,ab. (83)
-
((hip or neck) adj3 circumference$).ti,ab. (4655)
-
((waist-to-hip or waist-hip) adj3 (ratio$ or test$ or measure$)).ti,ab. (9084)
-
((waist-to-height or waist-height) adj3 (ratio$ or test$ or measure$)).ti,ab. (929)
-
(((bioelectric$ or electric$) adj3 (impedance or resistance)) or bia).ti,ab. (14,541)
-
(near infrared interactance or NIR).ti,ab. (6862)
-
((benn$ or rohrer$ or ponderal or corpulence) adj3 (index$ or indices)).ti,ab. (1246)
-
(sagittal abdominal diameter$ or supine abdominal diameter$).ti,ab. (146)
-
or/19-29 (35,697)
-
exp *cardiovascular disease/ (2,055,464)
-
exp *cerebrovascular accident/ (31,720)
-
*hypertension/ (187,647)
-
*hypercholesterolemia/ or *dyslipidemia/ (26,658)
-
((cardiovascular or cardio or vascular or peripheral) adj3 (disease$ or disorder$ or failure$)).ti,ab. (213,224)
-
((heart or cardiac or myocardial) adj3 (disease$ or disorder$ or failure$ or attack$ or arrest$)).ti,ab. (376,201)
-
(coronary adj3 (disease$ or disorder$ or failure$ or attack$ or arrest$ or syndrome$)).ti,ab. (171,524)
-
(CVD or CHD or IHD).ti,ab. (49,922)
-
(myocardial adj3 (infarc$ or disease$ or disorder$ or failure$ or attack$ or arrest$)).ti,ab. (198,567)
-
(ami or mi).ti,ab. (62,188)
-
(circulatory adj3 (disease$ or disorder$)).ti,ab. (5203)
-
angina$.ti,ab. (60,695)
-
atrial fibril$.ti,ab. (57,424)
-
(stroke$ or poststroke$).ti,ab. (205,519)
-
(cerebrovascular or cerebral vascular).ti,ab. (55,507)
-
((brain$ or cerebral$ or lacunar) adj3 (accident$ or infarc$)).ti,ab. (29,059)
-
hypertens$.ti,ab. (426,356)
-
high blood pressure.ti,ab. (14,098)
-
high cholesterol.ti,ab. (6446)
-
(hypercholesterol?emia$ or hypercholester?emia$).ti,ab. (30,335)
-
(dyslipid?emia$ or dyslipoprotein?emias$).ti,ab. (27,695)
-
or/31-51 (2,547,699)
-
*non insulin dependent diabetes mellitus/ (81,799)
-
*metabolic syndrome X/ (23,897)
-
(diabetes adj2 type 2).ti,ab. (90,512)
-
(diabetes adj2 (non insulin or noninsulin)).ti,ab. (11,127)
-
(NIDDM or T2DM or T2D).ti,ab. (22,350)
-
((metabolic or dysmetabolic or reaven or insulin resistance) adj2 syndrome$).ti,ab. (43,565)
-
or/53-58 (165,434)
-
exp *neoplasm/ (2,652,219)
-
cancer$.ti,ab. (1,389,393)
-
(neoplas$ or oncolog$ or malignan$ or carcinoma$ or adenocarcinoma$).ti,ab. (1,302,882)
-
or/60-62 (3,268,818)
-
(editorial or letter or note).pt. (1,885,479)
-
5 and 10 and 13 and (52 or 59 or 63) (6295)
-
65 not 64 (6277)
-
(2011$ or 2012$ or 2013$).em. (3,692,841)
-
66 and 67 (2498)
-
5 and 10 and 18 and (52 or 59) (1997)
-
69 not 64 (1992)
-
(2008$ or 2009$ or 2010$ or 2011$ or 2012$ or 2013$).em. (6,973,364)
-
70 and 71 (1525)
-
5 and 10 and 18 and 63 (76)
-
73 not 64 (76)
-
5 and 10 and 30 and (52 or 59 or 63) (845)
-
75 not 64 (843)
-
68 or 72 or 74 or 76 (3802)
-
limit 77 to human (3405)
Science Citation Index (Web of Science)
1900–1 October 2013. Searched 4 October 2013. Retrieved 3025 records.
| Search term | Number retrieved | |
|---|---|---|
| # 32 | #25 or #26 or #29 or #31 Databases=SCI-EXPANDED Timespan=All years |
3025 |
| # 31 | #30 not #23 Databases=SCI-EXPANDED Timespan=All years |
882 |
| # 30 | #1 and #2 and #5 and (#16 or #21 or #22) Databases=SCI-EXPANDED Timespan=All years |
898 |
| # 29 | #28 not #23 Databases=SCI-EXPANDED Timespan=All years |
73 |
| # 28 | #1 and #2 and #4 and #22 Databases=SCI-EXPANDED Timespan=All years |
75 |
| # 27 | #26 not #23 Databases=SCI-EXPANDED Timespan=2008-2013 |
1165 |
| # 26 | #1 and #2 and #4 and (#16 or #21) Databases=SCI-EXPANDED Timespan=All years |
1623 |
| # 25 | #24 not #23 Databases=SCI-EXPANDED Timespan=2011-2013 |
1809 |
| # 24 | #1 and #2 and #3 and (#16 or #21 or #22) Databases=SCI-EXPANDED Timespan=All years |
5340 |
| # 23 | (TS=(rat or rats or mouse or mice or murine or hamster or hamsters or animal or animals or dogs or dog or pig or pigs or cats or bovine or cow or sheep or ovine or porcine or monkey)) Databases=SCI-EXPANDED Timespan=All years |
3,694,533 |
| # 22 | (TS=(cancer* or neoplas* or oncolog* or malignan* or carcinoma* or adenocarcinoma*)) Databases=SCI-EXPANDED Timespan=All years |
1,773,464 |
| # 21 | (#17 or #18 or #19 or #20) Databases=SCI-EXPANDED Timespan=All years |
128,589 |
| # 20 | TS=((metabolic or dysmetabolic or reaven or “insulin resistance”) NEAR/2 syndrome*)) Databases=SCI-EXPANDED Timespan=All years |
48,002 |
| # 19 | TS=(NIDDM or T2DM or T2D)) Databases=SCI-EXPANDED Timespan=All years |
18,476 |
| # 18 | TS=(diabetes NEAR/2 (“non insulin” or noninsulin))) Databases=SCI-EXPANDED Timespan=All years |
8853 |
| # 17 | TS=(diabetes NEAR/2 “type 2”) or TS=(diabetes NEAR/2 “type II”)) Databases=SCI-EXPANDED Timespan=All years |
76,238 |
| # 16 | (#6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15) Databases=SCI-EXPANDED Timespan=All years | 1,067,535 |
| # 15 | (TS=(hypertens* or “high blood pressure” or “high cholesterol” or hypercholesterol?emia* or hypercholester?emia* or dyslipid?emia* or dyslipoprotein?emia*)) Databases=SCI-EXPANDED Timespan=All years |
329,965 |
| # 14 | (TS=((brain* or cerebral* or lacunar) NEAR/3 (accident* or infarc*))) Databases=SCI-EXPANDED Timespan=All years |
21,191 |
| # 13 | (TS=(stroke* or poststroke* or cerebrovascular)) Databases=SCI-EXPANDED Timespan=All years |
183,819 |
| # 12 | (TS=(angina* or “atrial fibril*”)) Databases=SCI-EXPANDED Timespan=All years |
84,084 |
| # 11 | (TS=(circulatory NEAR/3 (disease* or disorder*))) Databases=SCI-EXPANDED Timespan=All years |
1415 |
| # 10 | (TS=(myocardial NEAR/3 (infarc* or disease* or disorder* or failure* or attack* or arrest*))) Databases=SCI-EXPANDED Timespan=All years |
196,005 |
| # 9 | (TS=(CVD or CHD or IHD)) Databases=SCI-EXPANDED Timespan=All years |
52,225 |
| # 8 | (TS=(coronary NEAR/3 (disease* or disorder* or failure* or attack* or arrest* or syndrome*))) Databases=SCI-EXPANDED Timespan=All years |
183,720 |
| # 7 | (TS=((heart or cardiac or myocardial) NEAR/3 (disease* or disorder* or failure* or attack* or arrest*))) Databases=SCI-EXPANDED Timespan=All years |
336,341 |
| # 6 | (TS=((cardiovascular or peripheral) NEAR/3 (disease* or disorder* or failure*))) Databases=SCI-EXPANDED Timespan=All years |
147,514 |
| # 5 | (TS=((“fat mass” NEAR/3 (index* or indices)) or fmi) or TS=((“fat free mass” NEAR/3 (index* or indices)) or ffmi) or TS=(“body adiposity” NEAR/3 (index* or indices)) or TS=(“body fat” NEAR/2 percentage*) or TS=((hip or neck) NEAR/3 circumference*) or TS=((waist-to-hip or waist-hip) NEAR/3 ratio*) or TS=((waist-to-height or waist-height) NEAR/3 ratio*) or TS=(((bioelectric* or electric*) NEAR/3 (impedance or resistance)) or bia) or TS=(“near infrared interactance” or NIR) or TS=((benn* or rohrer* or ponderal or corpulence) NEAR/3 (index* or indices)) or TS=(sagittal abdominal diameter* or supine abdominal diameter*)) Databases=SCI-EXPANDED Timespan=All years |
58,595 |
| # 4 | (TS=((“skin fold” or skinfold) NEAR/3 (thickness* or test* or measure*)) or TS=(waist NEAR/3 circumference*)) Databases=SCI-EXPANDED Timespan=All years |
16,378 |
| # 3 | (TS=((“body mass” NEAR/3 (index* or indices)) or bmi or quetelet*)) Databases=SCI-EXPANDED Timespan=All years |
116,916 |
| # 2 | (TS=(child* or infant* or pediat* or paediat* or schoolchild* or “school age” or “school aged” or schoolage* or adolescen* or juvenile* or youth* or teenage* or youngster* or girl or girls or boy or boys or kid or kids or “young people” or “young person” or “young persons” or “young adult” or “young adults”)) AND Language=(English) Databases=SCI-EXPANDED Timespan=All years |
1,281,780 |
| # 1 | (TS=(obes* or overweight or “over weight” or adiposity)) Databases=SCI-EXPANDED Timespan=All years |
206,204 |
The Cochrane Library: Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, Database of Abstracts of Reviews of Effects, Health Technology Assessment and NHS Economic Evaluation Database (Wiley Online Library)
2013: CDSR Issue 10/12, CENTRAL Issue 10/12, DARE Issue 3/4, HTA Issue 3/4 and NHS EED Issue 3/4. Searched 4 October 2013. Retrieved 2 records in CDSR, 125 records in CENTRAL, 1 record in DARE, 0 records in HTA and 0 records in NHS EED.
#1 MeSH descriptor: [Obesity] explode all trees (6646)
#2 MeSH descriptor: [Overweight] explode all trees (7151)
#3 MeSH descriptor: [Adiposity] explode all trees (213)
#4 (obes* or overweight or (over next weight) or adiposity):ti,ab,kw (11,502)
#5 #1 or #2 or #3 or #4 (11,529)
#6 MeSH descriptor: [Child] explode all trees (122)
#7 MeSH descriptor: [Infant] explode all trees (12,348)
#8 MeSH descriptor: [Adolescent] explode all trees (70,756)
#9 child* or infant* or pediat* or paediat* or schoolchild* or (school next age*) or schoolage*:ti,ab,kw (84,824)
#10 adolescen* or juvenile* or youth$ or teenage* or youngster*:ti,ab,kw (84,511)
#11 girl or girls or boy or boys or kid or kids:ti,ab,kw (3991)
#12 #6 or #7 or #8 or #9 or #10 or #11 (141,741)
#13 MeSH descriptor: [Cardiovascular Diseases] explode all trees (69,868)
#14 MeSH descriptor: [Stroke] explode all trees (4580)
#15 MeSH descriptor: [Hypertension] this term only (13,068)
#16 MeSH descriptor: [Hypercholesterolemia] this term only (2328)
#17 MeSH descriptor: [Dyslipidemias] explode all trees (4660)
#18 ((cardiovascular or vascular or peripheral) near/3 (disease* or disorder* or failure*)):ti,ab,kw (12,157)
#19 ((heart or cardiac or myocardial) near/3 (disease* or disorder* or failure* or attack* or arrest*)):ti,ab,kw (20,649)
#20 (coronary near/3 (disease* or disorder* or failure* or attack* or arrest* or syndrome*)):ti,ab,kw (15,079)
#21 CVD or CHD or IHD:ti,ab,kw (2325)
#22 (myocardial near/3 (infarc* or disease* or disorder* or failure* or attack* or arrest*)):ti,ab,kw (14,322)
#23 circulatory near/3 (disease* or disorder*):ti,ab,kw (100)
#24 angina* or (atrial next fibril*):ti,ab,kw (11,477)
#25 stroke* or poststroke* or cerebrovascular:ti,ab,kw (22,044)
#26 ((brain* or cerebral* or lacunar) near/3 (accident* or infarc*)):ti,ab,kw (2104)
#27 hypertens* or (high next blood next pressure) or (high next cholesterol):ti,ab,kw (28,550)
#28 hypercholesterol?emia* or hypercholester?emia* or dyslipid?emia* or dyslipoprotein?emia*:ti,ab,kw (790)
#29 #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 (113,868)
#30 MeSH descriptor: [Diabetes Mellitus, Type 2] this term only (7914)
#31 MeSH descriptor: [Metabolic Syndrome X] explode all trees (717)
#32 diabetes near/2 (type next 2):ti,ab,kw (9705)
#33 diabetes near/2 (type next II):ti,ab,kw (610)
#34 (diabetes near/2 (“non insulin” or noninsulin)):ti,ab,kw (1755)
#35 NIDDM or T2DM or T2D:ti,ab,kw (1468)
#36 ((metabolic or dysmetabolic or reaven or “insulin resistance”) near/2 syndrome*):ti,ab,kw (1376)
#37 #30 or #31 or #32 or #33 or #34 or #35 or #36 (11,742)
#38 MeSH descriptor: [Neoplasms] explode all trees (47,634)
#39 cancer* or neoplas* or oncolog* or malignan* or carcinoma* or adenocarcinoma*:ti,ab,kw (73,437)
#40 (#38 or #39) (78,770)
#41 MeSH descriptor: [Body Mass Index] explode all trees (5177)
#42 ((“body mass” near/3 (index* or indices)) or bmi or quetelet*):ti,ab,kw (12,162)
#43 #41 or #42 (12,162)
#44 #5 and #12 and #43 and (#29 or #37 or #40) from 2011 to 2013 (65)
#45 MeSH descriptor: [Skinfold Thickness] this term only (272)
#46 MeSH descriptor: [Waist Circumference] this term only (278)
#47 ((“skin fold” or skinfold) near/3 (thickness* or test* or measure*)):ti,ab,kw (595)
#48 (waist near/3 circumference*):ti,ab,kw (1260)
#49 #45 or #46 or #47 or #48 (1804)
#50 #5 and #12 and #49 (266)
#51 #50 and (#29 or #37) from 2008 to 2010 (20)
#52 #50 and #40 from 1900 to 2010 (2)
#53 MeSH descriptor: [Waist-Hip Ratio] explode all trees (163)
#54 MeSH descriptor: [Electric Impedance] this term only (318)
#55 ((“fat mass” near/3 (index* or indices)) or fmi):ti,ab,kw (52)
#56 ((“fat free mass” near/3 (index* or indices)) or ffmi):ti,ab,kw (28)
#57 (“body adipos*” near/3 (index* or indices)):ti,ab,kw (2)
#58 (“body fat” near/2 percentage*):ti,ab,kw (336)
#59 ((hip or neck) near/3 circumference*):ti,ab,kw (239)
#60 ((waist-to-hip or waist-hip) near/3 ratio*):ti,ab,kw (549)
#61 ((waist-to-height or waist-height) near/3 ratio*):ti,ab,kw (18)
#62 (((bioelectric* or electric*) near/3 (impedance or resistance)) or bia):ti,ab,kw (606)
#63 (“near infrared interactance” or NIR):ti,ab,kw (52)
#64 ((benn* or rohrer* or ponderal or corpulence) near/3 (index* or indices)):ti,ab,kw (32)
#65 (“sagittal abdominal diameter*” or “supine abdominal diameter*”):ti,ab,kw (8)
#66 #53 or #54 or #55 or #56 or #57 or #58 or #59 or #60 or #61 or #62 or #63 or #64 or #65 (1709)
#67 #5 and #12 and #66 and (#29 or #37 or #40) (49)
#68 #44 or #51 or #52 or #67 (127)
Review of tracking of obesity into adulthood
Searches were limited by entry date 2007–13; Singh (ENL #454) tracking systematic review searches were completed in February 2007.
MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations (OvidSP)
1946–2013, June week 1. Searched 17 June 2013. Retrieved 2677 records in MEDLINE and 126 records in MEDLINE In-Process & Other Non-Indexed Citations.
-
exp Obesity/ (133,174)
-
Overweight/ (10,590)
-
Weight Gain/ (21,800)
-
Weight Loss/ (22,928)
-
obes$.ti,ab. (152,595)
-
(overweight or over weight).ti,ab. (32,221)
-
(weight gain or weight loss).ti,ab. (82,269)
-
or/1-7 (267,570)
-
Adiposity/ or Adipose Tissue/ (63,551)
-
exp Body Composition/ (35,621)
-
Body Weight/ (159,105)
-
(adiposity or adipose).ti,ab. (56,741)
-
(body adj2 (composition or fat)).ti,ab. (37,403)
-
fatness.ti,ab. (2835)
-
or/8-14 (468,298)
-
body mass index/ (75,120)
-
Skinfold Thickness/ (5477)
-
Waist Circumference/ (3853)
-
Waist-Hip Ratio/ (2715)
-
Electric Impedance/ (11,187)
-
((body mass adj3 (index$ or indices)) or bmi or quetelet$).ti,ab. (113,508)
-
((fat mass adj3 (index$ or indices)) or fmi).ti,ab. (824)
-
((fat free mass adj3 (index$ or indices)) or ffmi).ti,ab. (345)
-
(body adipos$ adj3 (index$ or indices)).ti,ab. (35)
-
(body fat adj2 percentage$).ti,ab. (3478)
-
((skin fold or skinfold) adj3 (thickness$ or test$ or measure$ or ratio$)).ti,ab. (4810)
-
((waist or hip or neck) adj3 circumference$).ti,ab. (13,212)
-
((waist-to-hip or waist-hip) adj3 (ratio$ or test$ or measure$)).ti,ab. (6373)
-
((waist-to-height or waist-height) adj3 (ratio$ or test$ or measure$)).ti,ab. (523)
-
(((bioelectric$ or electric$) adj3 (impedance or resistance)) or bia).ti,ab. (10,305)
-
(near infrared interactance or NIR).ti,ab. (4648)
-
((benn$ or rohrer$ or ponderal or corpulence) adj3 (index$ or indices)).ti,ab. (1001)
-
(sagittal abdominal diameter$ or supine abdominal diameter$).ti,ab. (108)
-
or/16-33 (169,256)
-
track$.ti,ab. (65,784)
-
traject$.ti,ab. (26,434)
-
(persistence or persistent$).ti,ab. (199,631)
-
(observ$ adj3 (repeat$ or regular$ or continu$ or frequent$ or period$ or recurr$ or perenn$ or prolong$ or perpetu$ or long term)).ti,ab. (72,559)
-
(monitor$ adj3 (repeat$ or regular$ or continu$ or frequent$ or period$ or recurr$ or perenn$ or prolong$ or perpetu$ or long term)).ti,ab. (34,703)
-
(surveil$ adj3 (repeat$ or regular$ or continu$ or frequent$ or period$ or recurr$ or perenn$ or prolong$ or perpetu$ or long term)).ti,ab. (6320)
-
(measure$ adj3 (repeat$ or regular$ or continu$ or frequent$ or period$ or recurr$ or perenn$ or prolong$ or perpetu$ or long term)).ti,ab. (58,971)
-
((annual$ or regular$ or recurr$) adj3 (interview$ or questionnaire$)).ti,ab. (1252)
-
(lifespan or life span or lifecourse or life course).ti,ab. (32,271)
-
or/35-43 (482,887)
-
*Cohort Studies/ (916)
-
*Longitudinal Studies/ (1144)
-
((cohort or panel) adj1 (study or studies or analy$)).ti,ab. (82,658)
-
(longitudinal adj1 (study or studies or survey or surveys or analy$ or pattern$ or data)).ti,ab. (50,985)
-
*Follow-up Studies/ (497)
-
(follow up adj1 (study or studies or survey or surveys or analy$ or data)).ti,ab. (50,500)
-
or/44-50 (646,777)
-
exp child/ (1,511,291)
-
exp Infant/ (917,072)
-
Adolescent/ (1,569,130)
-
Young Adult/ (311,210)
-
(child$ or infant$ or pediat$ or paediat$ or schoolchild$ or school age$ or schoolage$).ti,ab. (1,205,816)
-
(adolescen$ or juvenile$ or youth$ or teenage$ or youngster$).ti,ab. (236,753)
-
(girl or girls or boy or boys or kid or kids).ti,ab. (155,425)
-
(young people or young person or young persons or young adult$).ti,ab. (67,269)
-
or/52-59 (3,200,696)
-
exp Adult/ (5,408,792)
-
(adult$ or midadult$ or middle age$ or later life).ti,ab. (765,494)
-
61 or 62 (5,769,283)
-
15 and 34 and 51 and 60 and 63 (2818)
-
(relation$ or association$ or predict$ or risk or risks or mortality).ti,ab. (3,350,562)
-
(obes$ or overweight or weight status or BMI or body mass index).ti,ab. (231,751)
-
(adult$ or middle-age$ or men or women or later life).ti,ab. (1,444,222)
-
(((relation$ or association$ or predict$ or risk or risks or mortality) adj5 (obes$ or overweight or weight status or BMI or body mass index) adj6 (adult$ or middle-age$ or men or women or later life))).ti,ab. [65 adj5 66 adj6 67] (3566)
-
68 and 60 (1519)
-
64 or 69 (4012)
-
(2007$ or 2008$ or 2009$ or 2010$ or 2011$ or 2012$ or 2013$).ed,dc,ep. (5,166,979)
-
70 and 71 (2677)
PubMed (National Library of Medicine)
1946–17 June 2013. Searched 17 June 2013. Retrieved 2195 records.
#52 (#50 AND #51) (2195)
#51 2007:2013[edat] (5,408,518)
#50 (#46 OR #49) (3413)
#49 (#48 AND #42) (788)
#48 ((relation*[TI] or association*[TI] or predict*[TI] or risk[TI] or risks[TI] or mortality[TI]) AND (obes*[TI] or overweight[TI] or “weight status”[TI] or BMI[TI] or “body mass index”[TI]) AND (adult*[TI] or middle-age*[TI] or men[TI] or women[TI] or “later life”[TI])) (2583) [Title only]
#47 (relation*[TIAB] or association*[TIAB] or predict*[TIAB] or risk[TIAB] or risks[TIAB] or mortality[TIAB]) AND (obes*[TIAB] or overweight[TIAB] or “weight status”[TIAB] or BMI[TIAB] or “body mass index”[TIAB]) AND (adult*[TIAB] or middle-age*[TIAB] or men[TIAB] or women[TIAB] or “later life”[tiab]) (59,518) [without adjacency this line is too sensitive]
#46 (#8 AND #24 AND #36 AND #42 AND #45) (2790)
#45 (#43 OR #44) (5,643,266)
#44 adult*[tiab] or midadult*[tiab] or middle age*[tiab] or later life[tiab] (785,580)
#43 “Adult”[Mesh] (5,240,400)
#42 (#37 OR #38 OR #39 OR #40 OR #41) (3,207,673)
#41 (“young people”[tiab] or “young person”[tiab] or “young persons”[tiab] or young adult*[tiab]) (68,922)
#40 girl[tiab] or girls[tiab] or boy[tiab] or boys[tiab] or kid[tiab] or kids[tiab] (162,454)
#39 adolescen*[tiab] or juvenile*[tiab] or youth*[tiab] or teenage*[tiab] or youngster*[tiab] (247,200)
#38 child*[tiab] or infant*[tiab] or pediat*[tiab] or paediat*[tiab] or schoolchild*[tiab] or school age*[tiab] or schoolage*[tiab] (1,248,537)
#37 (((“Child”[Mesh]) OR “Infant”[Mesh]) OR “Adolescent”[Mesh]) OR “Young Adult”[Mesh] (2,838,299)
#36 (#25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35) (660,605)
#35 “follow up study”[tiab] or “follow up studies”[tiab] or “follow up survey”[tiab] or “follow up surveys”[tiab] or follow up analy*[tiab] or follow up pattern*[tiab] or “follow up data”[tiab] (50,170)
#34 “longitudinal study”[tiab] or “longitudinal studies”[tiab] or “longitudinal survey”[tiab] or “longitudinal surveys”[tiab] or longitudinal analy*[tiab] or longitudinal pattern*[tiab] or “longitudinal data”[tiab] (51,648)
#33 “cohort study”[tiab] or “cohort studies”[tiab] or cohort analy*[tiab] or “panel study”[tiab] or “panel studies”[tiab] or panel analy*[tiab] (79,961)
#32 ((“Cohort Studies”[Majr]) OR “Longitudinal Studies”[Majr]) OR “Follow-Up Studies”[Majr] (2993)
#31 measure* repeat*[tiab] or measure* regular*[tiab] or measure* continu*[tiab] or measure* frequent*[tiab] or measure* period*[tiab] or measure* recurr*[tiab] or measure* perenn*[tiab] or measure* prolong*[tiab] or measure* perpetu*[tiab] or measure* long term[tiab] (78,057)
#30 annual* interview*[tiab] or annual* questionnaire*[tiab] or regular* interview*[tiab] or regular* questionnaire*[tiab] or recurr* interview*[tiab] or recurr* questionnaire*[tiab] (8822)
#29 lifespan[tiab] or “life span”[tiab] or lifecourse[tiab] or “life course”[tiab] (32,727)
#28 surveil* repeat*[tiab] or surveil* regular*[tiab] or surveil* continu*[tiab] or surveil* frequent*[tiab] or surveil* period*[tiab] or surveil* recurr*[tiab] or surveil* perenn*[tiab] or surveil* prolong*[tiab] or surveil* perpetu*[tiab] or surveil* long term[tiab] (6687)
#27 (monito* repeat*[tiab] or monito* regular*[tiab] or monito* continu*[tiab] or monito* frequent*[tiab] or monito* period*[tiab] or monito* recurr*[tiab] or monito* perenn*[tiab] or monito* prolong*[tiab] or monito* perpetu*[tiab] or monito* long term[tiab]) (29,418)
#26 observ* repeat*[tiab] or observ* regular*[tiab] or observ* continu*[tiab] or observ* frequent*[tiab] or observ* period*[tiab] or observ* recurr*[tiab] or observ* perenn*[tiab] or observ* prolong*[tiab] or observ* perpetu*[tiab] or observ* long term[tiab] (85,510)
#25 track*[tiab] or traject*[tiab] or persistence[tiab] or persistent*[tiab] (302,985)
#24 (#9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23) (174,219)
#23 (sagittal abdominal diameter*[tiab] or supine abdominal diameter*[tiab]) (114)
#22 benn* index[tiab] or benn* indices[tiab] or rohrer* index[tiab] or rohrer* indices[tiab] or “ponderal index”[tiab] or “ponderal indices”[tiab] or “corpulence index”[tiab] or “corpulance indices”[tiab] (973)
#21 ((((“Body Mass Index”[Mesh]) OR “Skinfold Thickness”[Mesh]) OR “Waist Circumference”[Mesh]) OR “Waist-Hip Ratio”[Mesh]) OR “Electric Impedance”[Mesh] (85,824)
#20 (“body mass index”[tiab] or “body mass indices”[tiab] or bmi[tiab] or quetelet*[tiab]) (118,394)
#19 “fat mass index”[tiab] or “fat mass indices”[tiab] or fmi[tiab] (430)
#18 (“fat free mass index”[tiab] or “fat free mass indices”[tiab] or ffmi[tiab]) (244)
#17 “body adiposity index”[tiab] or “body adiposity indices”[tiab] or “body adiposie index”[tiab] or “body adipose indices”[tiab] (43)
#16 (“body fat percentage”[tiab] or “body fat percentages”[tiab]) (1203)
#15 (“skin fold thickness”[tiab] or “skin fold test”[tiab] or “skin fold tests”[tiab] or “skin fold measure”[tiab] or “skin fold measurement”[tiab] or “skin fold measures”[tiab] or “skin fold measurements”[tiab]) (658)
#14 (“skinfold thickness”[tiab] or “skinfold test”[tiab] or “skinfold tests”[tiab] or “skinfold measure”[tiab] or “skinfold measurement”[tiab] or “skinfold measures”[tiab] or “skinfold measurements”[tiab]) (3340)
#13 “waist circumference”[tiab] or “hip circumference”[tiab] or “neck circumference”[tiab] (13,399)
#12 “waist-to-hip ratio”[tiab] or “waist-to-hip ratios”[tiab] or “waist-hip ratio”[tiab] or “waist-hip ratios”[tiab] (6338)
#11 “waist-to-height ratio”[tiab] or “waist-to-height ratios”[tiab] or “waist-height ratio”[tiab] or “waist-height ratios”[tiab] (587)
#10 “bioelectric impedance”[tiab] or “bioelectrical impedance”[tiab] or “electric impedance”[tiab] or “electrical impedance”[tiab] or “bioelectric resistance”[tiab] or “bioelectrical resistance”[tiab] or “electric resistance”[tiab] or “electrical resistance”[tiab] or bia[tiab] (10,533)
#9 (“near infrared interactance”[tiab] or NIR[tiab]) (6556)
#8 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7) (579,710)
#7 adiposity[tiab] or adipose[tiab] or “body composition”[tiab] or “body fat”[tiab] or “body weight”[tiab] or fatness[tiab] (214,862)
#6 (((“Adiposity”[Mesh]) OR “Adipose Tissue”[Mesh]) OR “Body Composition”[Mesh]) OR “Body Weight”[Mesh] (384,283)
#5 “weight gain”[tiab] or “weight loss”[tiab] (85,952)
#4 overweight[tiab] or “over weight*”[tiab] (33,914)
#3 obes*[tiab] (159,094)
#2 ((“Overweight”[Mesh]) OR “Weight Gain”[Mesh]) OR “Weight Loss”[Mesh] (159,224)
#1 “Obesity”[Mesh] (126,355)
EMBASE (OvidSP)
1974–2013, week 24. Searched 17 June 2013. Retrieved 2287 records.
-
exp obesity/ (263,295)
-
weight gain/ (58,597)
-
weight reduction/ (85,394)
-
obes$.ti,ab. (214,390)
-
(overweight or over weight).ti,ab. (46,472)
-
(weight gain or weight loss).ti,ab. (112,861)
-
or/1-6 (442,794)
-
exp body composition/ (58,550)
-
body weight/ (180,005)
-
(adiposity or adipose).ti,ab. (73,719)
-
(body adj2 (composition or fat or weight)).ti,ab. (214,677)
-
fatness.ti,ab. (3315)
-
or/7-12 (717,815)
-
body mass/ (160,301)
-
skinfold thickness/ (7828)
-
waist circumference/ (18,940)
-
waist hip ratio/ (5962)
-
waist to height ratio/ (171)
-
weight height ratio/ (10)
-
neck circumference/ (152)
-
((body mass adj3 (index$ or indices)) or bmi or quetelet$).ti,ab. (176,160)
-
((fat mass adj3 (index$ or indices)) or fmi).ti,ab. (1125)
-
((fat free mass adj3 (index$ or indices)) or ffmi).ti,ab. (494)
-
(body adipos$ adj3 (index$ or indices)).ti,ab. (60)
-
(body fat adj2 percentage$).ti,ab. (4433)
-
((skin fold or skinfold) adj3 (thickness$ or test$ or measure$)).ti,ab. (5749)
-
((waist or hip or neck) adj3 circumference$).ti,ab. (20,813)
-
((waist-to-hip or waist-hip) adj3 ratio$).ti,ab. (8313)
-
((waist-to-height or waist-height) adj3 ratio$).ti,ab. (783)
-
(((bioelectric$ or electric$) adj3 (impedance or resistance)) or bia).ti,ab. (13,714)
-
(near infrared interactance or NIR).ti,ab. (6331)
-
((benn$ or rohrer$ or ponderal or corpulence) adj3 (index$ or indices)).ti,ab. (1205)
-
(sagittal abdominal diameter$ or supine abdominal diameter$).ti,ab. (138)
-
or/14-33 (259,277)
-
track$.ti,ab. (87,589)
-
traject$.ti,ab. (32,963)
-
(persistence or persistent$).ti,ab. (256,530)
-
(observ$ adj3 (repeat$ or regular$ or continu$ or frequent$ or period$ or recurr$ or perenn$ or prolong$ or perpetu$ or long term)).ti,ab. (97,714)
-
(monitor$ adj3 (repeat$ or regular$ or continu$ or frequent$ or period$ or recurr$ or perenn$ or prolong$ or perpetu$ or long term)).ti,ab. (48,403)
-
(surveil$ adj3 (repeat$ or regular$ or continu$ or frequent$ or period$ or recurr$ or perenn$ or prolong$ or perpetu$ or long term)).ti,ab. (8671)
-
(measure$ adj3 (repeat$ or regular$ or continu$ or frequent$ or period$ or recurr$ or perenn$ or prolong$ or perpetu$ or long term)).ti,ab. (79,155)
-
((annual$ or regular$ or recurr$) adj3 (interview$ or questionnaire$)).ti,ab. (1580)
-
(lifespan or life span or lifecourse or life course).ti,ab. (38,855)
-
or/35-43 (630,994)
-
*cohort analysis/ (4457)
-
*longitudinal study/ (2201)
-
*follow up/ (12,602)
-
((cohort or panel) adj1 (study or studies or analy$)).ti,ab. (109,818)
-
(longitudinal adj1 (study or studies or survey or surveys or analy$ or pattern$ or data)).ti,ab. (62,065)
-
(follow up adj1 (study or studies or survey or surveys or analy$ or data)).ti,ab. (66,939)
-
or/44-50 (852,107)
-
child/ (1,267,520)
-
preschool child/ (500,626)
-
infant/ (522,480)
-
adolescent/ (1,241,285)
-
(child$ or infant$ or pediat$ or paediat$ or schoolchild$ or school age$ or schoolage$).ti,ab. (1,546,923)
-
(adolescen$ or juvenile$ or youth$ or teenage$ or youngster$).ti,ab. (305,377)
-
(girl or girls or boy or boys or kid or kids).ti,ab. (207,250)
-
(young people or young person or young persons or young adult$).ti,ab. (86,569)
-
or/52-58 (2,954,917)
-
adult/ or middle aged/ (4,773,254)
-
(adult$ or midadult$ or middle age$ or later life).ti,ab. (962,049)
-
61 or 62 (5,296,190)
-
13 and 34 and 51 and 60 and 63 (2511)
-
(relation$ or association$ or predict$ or risk or risks or mortality).ti,ab. (4,479,904)
-
(obes$ or overweight or weight status or BMI or body mass index).ti,ab. (336,578)
-
(adult$ or middle-age$ or men or women or later life).ti,ab. (1,840,835)
-
((relation$ or association$ or predict$ or risk or risks or mortality) adj4 (obes$ or overweight or weight status or BMI or body mass index) adj5 (adult$ or middle-age$ or men or women or later life)) [65 adj4 66 adj5 67].ti,ab. (4263)
-
60 and 68 (1181)
-
64 or 69 (3419)
-
(2007$ or 2008$ or 2009$ or 2010$ or 2011$ or 2012$ or 2013$).em. (7,043,444)
-
70 and 71 (2287)
PsycINFO (OvidSP)
1806–2013, June week 2. Searched 17 June 2013. Retrieved 806 records.
-
obesity/ (13,943)
-
overweight/ (2266)
-
weight gain/ or weight loss/ (3366)
-
obes$.ti,ab. (20,620)
-
(overweight or over weight).ti,ab. (7922)
-
(weight gain or weight loss).ti,ab. (12,721)
-
or/1-6 (32,261)
-
body weight/ (9833)
-
(adiposity or adipose).ti,ab. (1914)
-
(body adj2 (composition or fat or weight)).ti,ab. (13,243)
-
fatness.ti,ab. (462)
-
or/7-11 (43,208)
-
body mass index/ (2147)
-
((body mass adj3 (index$ or indices)) or bmi or quetelet$).ti,ab. (13,066)
-
((fat mass adj3 (index$ or indices)) or fmi).ti,ab. (87)
-
((fat free mass adj3 (index$ or indices)) or ffmi).ti,ab. (23)
-
(body adipos$ adj3 (index$ or indices)).ti,ab. (0)
-
(body fat adj2 percentage$).ti,ab. (315)
-
((skin fold or skinfold) adj3 (thickness$ or test$ or measure$)).ti,ab. (256)
-
((waist or hip or neck) adj3 circumference$).ti,ab. (1288)
-
((waist-to-hip or waist-hip) adj3 ratio$).ti,ab. (508)
-
((waist-to-height or waist-height) adj3 ratio$).ti,ab. (44)
-
(((bioelectric$ or electric$) adj3 (impedance or resistance)) or bia).ti,ab. (456)
-
(near infrared interactance or NIR).ti,ab. (38)
-
((benn$ or rohrer$ or ponderal or corpulence) adj3 (index$ or indices)).ti,ab. (79)
-
(sagittal abdominal diameter$ or supine abdominal diameter$).ti,ab. (7)
-
or/13-26 (14,533)
-
(track$ or traject$ or persistence or persistent$).ti,ab. (69,027)
-
((observ$ or monitor$ or surveil$ or measure$) adj3 (repeat$ or regular$ or continu$ or frequent$ or period$ or recurr$ or perenn$ or prolong$ or perpetu$ or long term)).ti,ab. (26,566)
-
((annual$ or regular$ or recurr$) adj3 (interview$ or questionnaire$)).ti,ab. (603)
-
(lifespan or life span or lifecourse or life course).ti,ab. (15,357)
-
or/28-31 (109,073)
-
cohort analysis/ (971)
-
exp *longitudinal studies/ (2561)
-
*followup studies/ (1496)
-
((cohort or panel) adj1 (study or studies or analy$)).ti,ab. (11,031)
-
(longitudinal adj1 (study or studies or survey or surveys or analy$ or pattern$ or data)).ti,ab. (36,916)
-
(follow up adj1 (study or studies or survey or surveys or analy$ or data)).ti,ab. (13,649)
-
or/32-38 (164,950)
-
(adolescence 13 17 yrs or childhood birth 12 yrs or preschool age 2 5 yrs or school age 6 12 yrs).ag. (567,131)
-
(child$ or infant$ or pediat$ or paediat$ or schoolchild$ or school age$ or schoolage$).ti,ab. (537,261)
-
(adolescen$ or juvenile$ or youth$ or teenage$ or youngster$).ti,ab. (207,480)
-
(girl or girls or boy or boys or kid or kids).ti,ab. (77,464)
-
(young people or young person or young persons or young adult$).ti,ab. (41,916)
-
or/40-44 (853,904)
-
(adulthood 18 yrs older or middle age 40 64 yrs or thirties 30 39 yrs or young adulthood 18 29 yrs).ag. (1,223,100)
-
(adult$ or midadult$ or middle age$ or later life).ti,ab. (285,272)
-
46 or 47 (1,336,121)
-
12 and 27 and 39 and 45 and 48 (360)
-
(relation$ or association$ or predict$ or risk or risks or mortality).ti,ab. (1,068,050)
-
(obes$ or overweight or weight status or BMI or body mass index).ti,ab. (30,601)
-
(adult$ or middle-age$ or men or women or later life).ti,ab. (482,086)
-
((relation$ or association$ or predict$ or risk or risks or mortality) adj5 (obes$ or overweight or weight status or BMI or body mass index) adj6 (adult$ or middle-age$ or men or women or later life)).ti,ab. [50 adj5 51 adj6 52] (798)
-
49 or 53 (1106)
-
(2007$ or 2008$ or 2009$ or 2010$ or 2011$ or 2012$ or 2013$).dp. (1,005,336)
-
54 and 55 (806)
Cumulative Index to Nursing and Allied Health Literature (EBSCOhost)
1981–7 June 2013. Searched 17 June 2013. Retrieved 1156 records.
| Search term | Number retrieved | |
|---|---|---|
| S59 | S57 AND S58 | 1156 |
| S58 | EM 2007 OR EM 2008 OR EM 2009 OR EM 2010 OR EM 2011 OR EM 2012 OR EM 2013 | 1,536,421 |
| S57 | S52 OR S56 | 1791 |
| S56 | S53 N5 S54 N6 S55 | 1342 |
| S55 | TI (adult* or middle-age* or men or women or “later life”) or AB (adult* or middle-age* or men or women or “later life”) | 239,088 |
| S54 | TI (obes* or overweight or “weight status” or BMI or “body mass index”) or AB (obes* or overweight or “weight status” or BMI or “body mass index”) | 40,211 |
| S53 | TI (relation* or association* or predict* or risk or risks or mortality) or AB (relation* or association* or predict* or risk or risks or mortality) | 449,134 |
| S52 | S10 AND S29 AND S42 AND S48 AND S51 | 555 |
| S51 | S49 OR S50 | 583,307 |
| S50 | TI (adult* or midadult* or “middle age*” or “later life”) or AB (adult* or midadult* or “middle age*” or “later life”) | 108,318 |
| S49 | (ZG “adult: 19-44 years”) or (ZG “middle aged: 45-64 years”) | 533,351 |
| S48 | S43 OR S44 OR S45 OR S46 OR S47 | 413,550 |
| S47 | TI (“young people” or “young person” or “young persons” or “young adult*”) or AB (“young people” or “young person” or “young persons” or “young adult*”) | 14,989 |
| S46 | TI (girl or girls or boy or boys or kid or kids) or AB (girl or girls or boy or boys or kid or kids) | 20,952 |
| S45 | TI (adolescen* or juvenile* or youth* or teenage* or youngster*) or AB (adolescen* or juvenile* or youth* or teenage* or youngster*) | 56,605 |
| S44 | TI (child* or infant* or pediat* or paediat* or schoolchild* or “school age*” or schoolage*) or AB (child* or infant* or pediat* or paediat* or schoolchild* or “school age*” or schoolage*) | 213,504 |
| S43 | (ZG “adolescent: 13-18 years”) or (ZG “child, preschool: 2-5 years”) or (ZG “child: 6-12 years”) | 320,940 |
| S42 | S37 OR S38 OR S39 OR S40 OR S41 | 94,591 |
| S41 | TI (“follow up” N2 stud* or “follow up” N2 survey* or “follow up” N2 analy* or “follow up” data) or AB (“follow up” N2 stud* or “follow up” N2 survey* or “follow up” N2 analy* or “follow up” data) | 10,078 |
| S40 | TI (longitudinal N2 stud* or longitudinal N2 survey* or longitudinal N2 analy* or longitudinal N2 pattern* or longitudinal N2 data) or AB (longitudinal N2 stud* or longitudinal N2 survey* or longitudinal N2 analy* or longitudinal N2 pattern* or longitudinal N2 data) | 14,785 |
| S39 | TI (cohort N2 stud* or cohort N2 analy* or panel N2 stud* or panel N2 analy*) or AB (cohort N2 stud* or cohort N2 analy* or panel N2 stud* or panel N2 analy*) | 22,482 |
| S38 | (MM “Prospective Studies+”) | 433 |
| S37 | S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 | 54,403 |
| S36 | TI (lifespan or “life span” or lifecourse or “life course”) or AB (lifespan or “life span” or lifecourse or “life course”) | 3428 |
| S35 | TI (annual* N3 interview* or annual* N3 questionnaire* or regular* N3 interview* or regular* N3 questionnaire* or recurr* N3 interview* or recurr* N3 questionnaire*) or AB (annual* N3 interview* or annual* N3 questionnaire* or regular* N3 interview* or regular* N3 questionnaire* or recurr* N3 interview* or recurr* N3 questionnaire*) | 393 |
| S34 | TI (measure* N3 repeat* or measure* N3 regular* or measure* N3 continu* or measure* N3 frequent* or measure* N3 period* or measure* N3 recurr* or measure* N3 perenn* or measure* N3 prolong* or measure* N3 perpetu* or measure* N3 “long term”) or AB (measure* N3 repeat* or measure* N3 regular* or measure* N3 continu* or measure* N3 frequent* or measure* N3 period* or measure* N3 recurr* or measure* N3 perenn* or measure* N3 prolong* or measure* N3 perpetu* or measure* N3 “long term”) | 12,762 |
| S33 | TI (surveil* N3 repeat* or surveil* N3 regular* or surveil* N3 continu* or surveil* N3 frequent* or surveil* N3 period* or surveil* N3 recurr* or surveil* N3 perenn* or surveil* N3 prolong* or surveil* N3 perpetu* or surveil* N3 “long term”) or AB (surveil* N3 repeat* or surveil* N3 regular* or surveil* N3 continu* or surveil* N3 frequent* or surveil* N3 period* or surveil* N3 recurr* or surveil* N3 perenn* or surveil* N3 prolong* or surveil* N3 perpetu* or surveil* N3 “long term”) | 805 |
| S32 | TI (monitor* N3 repeat* or monitor* N3 regular* or monitor* N3 continu* or monitor* N3 frequent* or monitor* N3 period* or monitor* N3 recurr* or monitor* N3 perenn* or monitor* N3 prolong* or monitor* N3 perpetu* or monitor* N3 “long term”) or AB (monitor* N3 repeat* or monitor* N3 regular* or monitor* N3 continu* or monitor* N3 frequent* or monitor* N3 period* or monitor* N3 recurr* or monitor* N3 perenn* or monitor* N3 prolong* or monitor* N3 perpetu* or monitor* N3 “long term”) | 4382 |
| S31 | TI (observ* N3 repeat* or observ* N3 regular* or observ* N3 continu* or observ* N3 frequent* or observ* N3 period* or observ* N3 recurr* or observ* N3 perenn* or observ* N3 prolong* or observ* N3 perpetu* or observ* N3 “long term”) or AB (observ* N3 repeat* or observ* N3 regular* or observ* N3 continu* or observ* N3 frequent* or observ* N3 period* or observ* N3 recurr* or observ* N3 perenn* or observ* N3 prolong* or observ* N3 perpetu* or observ* N3 “long term”) | 4657 |
| S30 | TI (track* or traject* or persistence or persistent*) or AB (track* or traject* or persistence or persistent*) | 29,753 |
| S29 | S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 | 40,956 |
| S28 | TI (“sagittal abdominal diameter*” or “supine abdominal diameter*”) or AB (“sagittal abdominal diameter*” or “supine abdominal diameter*”) | 21 |
| S27 | TI (benn* N3 index* or benn* N3 indices or rohrer* N3 index* or rohrer* N3 indices* or ponderal N3 index* or ponderal N3 indices or corpulence N3 index* or corpulence N3 indices) or AB (benn* N3 index* or benn* N3 indices or rohrer* N3 index* or rohrer* N3 indices* or ponderal N3 index* or ponderal N3 indices or corpulence N3 index* or corpulence N3 indices) | 79 |
| S26 | TI (“near infrared interactance” or NIR) or AB (“near infrared interactance” or NIR) | 57 |
| S25 | TI (bioelectric* N3 impedance or electric* N3 impedance or bioelectric* N3 resistance or electric* N3 resistance or bia) or AB (bioelectric* N3 impedance or electric* N3 impedance or bioelectric* N3 resistance or electric* N3 resistance or bia) | 883 |
| S24 | TI (waist-to-height N3 ratio* or waist-height N3 ratio*) or AB (waist-to-height N3 ratio* or waist-height N3 ratio*) | 98 |
| S23 | TI (waist-to-hip N3 ratio* or waist-hip N3 ratio*) or AB (waist-to-hip N3 ratio* or waist-hip N3 ratio*) | 855 |
| S22 | TI (waist N3 circumference* or hip N3 circumference* or neck N3 circumference*) or AB (waist N3 circumference* or hip N3 circumference* or neck N3 circumference*) | 2383 |
| S21 | TI (“skin fold” N3 thickness* or skinfold N3 thickness* or “skin fold” N3 test* or skinfold N3 test* or “skin fold” N3 measure* or skinfold N3 measure*) or AB (“skin fold” N3 thickness* or skinfold N3 thickness* or “skin fold” N3 test* or skinfold N3 test* or “skin fold” N3 measure* or skinfold N3 measure*) | 712 |
| S20 | TI (“body fat” N3 percentage*) or AB (“body fat” N3 percentage*) | 783 |
| S19 | TI (“body adipos*” N3 index* or “body adipos*” N3 indices) or AB (“body adipos*” N3 index* or “body adipos*” N3 indices) | 9 |
| S18 | TI (“fat free mass” N3 index* or “fat free mass” N3 indices or ffmi) or AB (“fat free mass” N3 index* or “fat free mass” N3 indices or ffmi) | 78 |
| S17 | TI (“fat mass” N3 index* or “fat mass” N3 indices or fmi) or AB (“fat mass” N3 index* or “fat mass” N3 indices or fmi) | 144 |
| S16 | TI (“body mass” N3 index* or “body mass” N3 indices or bmi or quetelet*) or AB (“body mass” N3 index* or “body mass” N3 indices or bmi or quetelet*) | 19,190 |
| S15 | (MH “Electric Impedance”) | 1562 |
| S14 | (MH “Waist-Hip Ratio”) | 1252 |
| S13 | (MH “Waist Circumference”) | 275 |
| S12 | (MH “Skinfold Thickness”) | 2268 |
| S11 | (MH “Body Mass Index”) | 28,392 |
| S10 | S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 | 71,298 |
| S9 | TI (body N2 composition or body N2 fat or body N2 weight) or AB (body N2 composition or body N2 fat or body N2 weight) | 13,891 |
| S8 | TI (adiposity or adipose or fatness) or AB (adiposity or adipose or fatness) | 3867 |
| S7 | (MH “Body Weight”) | 8959 |
| S6 | (MH “Body Composition”) | 7940 |
| S5 | (MH “Adipose Tissue”) | 4511 |
| S4 | TI (“weight gain” or “weight loss”) or AB (“weight gain” or “weight loss”) | 11,296 |
| S3 | TI (obes* or overweight or “over weight”) or AB (obes* or overweight or “over weight”) | 27,898 |
| S2 | (MH “Weight Gain”) OR (MH “Weight Loss”) | 12,531 |
| S1 | (MH “Obesity+”) | 32,334 |
The Cochrane Library: Cochrane Database of Systematic Reviews and Cochrane Central Register of Controlled Trials (Wiley Online Library)
2013: CDSR Issue 6/12, CENTRAL Issue 5/12. Searched 17 June 2013. Retrieved 4 records in CDSR and 281 records in CENTRAL.
#1 MeSH descriptor: [Obesity] explode all trees (6452)
#2 MeSH descriptor: [Overweight] this term only (1072)
#3 MeSH descriptor: [Weight Gain] this term only (1416)
#4 MeSH descriptor: [Weight Loss] this term only (2918)
#5 (obes* or overweight or (over next weight)):ti,ab,kw (10,756)
#6 ((weight next gain) or (weight next loss)):ti,ab,kw (9014)
#7 MeSH descriptor: [Adiposity] this term only (203)
#8 MeSH descriptor: [Body Composition] explode all trees (2773)
#9 MeSH descriptor: [Body Weight] this term only (5538)
#10 (adiposity or adipose or fatness):ti,ab,kw (2168)
#11 (body near/2 (composition or fat or weight)):ti,ab,kw (18,126)
#12 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 (29,278)
#13 MeSH descriptor: [Body Mass Index] this term only (5044)
#14 MeSH descriptor: [Skinfold Thickness] this term only (269)
#15 MeSH descriptor: [Waist Circumference] this term only (261)
#16 MeSH descriptor: [Waist-Hip Ratio] this term only (158)
#17 MeSH descriptor: [Electric Impedance] this term only (313)
#18 ((“body mass” near/3 (index* or indices)) or bmi or quetelet*):ti,ab,kw (11,870)
#19 ((“fat mass” near/3 (index* or indices)) or fmi):ti,ab,kw (49)
#20 ((“fat free mass” near/3 (index* or indices)) or ffmi):ti,ab,kw (28)
#21 (“body adipos*” near/3 (index* or indices)):ti,ab,kw (1)
#22 (“body fat” near/2 percentage*):ti,ab,kw (328)
#23 ((“skin fold” or skinfold) near/3 (thickness* or test* or measure*)):ti,ab,kw (590)
#24 ((waist or hip or neck) near/3 circumference*):ti,ab,kw (1244)
#25 ((waist-to-hip or waist-hip) near/3 ratio*):ti,ab,kw (542)
#26 ((waist-to-height or waist-height) near/3 ratio*):ti,ab,kw (16)
#27 (((bioelectric* or electric*) near/3 (impedance or resistance)) or bia):ti,ab,kw (598)
#28 (“near infrared interactance” or NIR):ti,ab,kw (49)
#29 ((benn* or rohrer* or ponderal or corpulence) near/3 (index* or indices)):ti,ab,kw (32)
#30 (“sagittal abdominal diameter*” or “supine abdominal diameter*”):ti,ab,kw (8)
#31 #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 (13,412)
#32 track* or traject* or persistence or persistent*:ti,ab,kw (11,683)
#33 (observ* or monitor* or surveil* or measure*) near/3 (repeat* or regular* or continu* or frequent* or period* or recurr* or perenn* or prolong* or perpetu* or “long term”):ti,ab,kw (17,771)
#34 (annual* or regular* or recurr*) near/3 (interview* or questionnaire*):ti,ab,kw (348)
#35 lifespan or “life span” or lifecourse or “life course”:ti,ab,kw (286)
#36 MeSH descriptor: [Cohort Studies] this term only (5618)
#37 MeSH descriptor: [Longitudinal Studies] this term only (3807)
#38 MeSH descriptor: [Follow-Up Studies] this term only (38,849)
#39 (cohort or panel) near/1 (study or studies or analy*):ti,ab,kw (7541)
#40 longitudinal near/1 (study or studies or survey or surveys or analy* or pattern* or data):ti,ab,kw (5152)
#41 (followup or follow-up or “follow up”) near/1 (study or studies or survey or surveys or analy* or pattern* or data):ti,ab,kw (42,804)
#42 #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 (78,737)
#43 MeSH descriptor: [Child] explode all trees (64)
#44 MeSH descriptor: [Infant] explode all trees (12,099)
#45 MeSH descriptor: [Adolescent] explode all trees (69,924)
#46 MeSH descriptor: [Young Adult] this term only (112)
#47 child* or infant* or pediat* or paediat* or schoolchild* or “school age*” or schoolage*:ti,ab,kw (83,100)
#48 adolescen* or juvenile* or youth* or teenage* or youngster*:ti,ab,kw (83,300)
#49 girl or girls or boy or boys or kid or kids:ti,ab,kw (3932)
#50 “young people” or “young person” or “young persons” or “young adult*”:ti,ab,kw (21,570)
#51 #43 or #44 or #45 or #46 or #47 or #48 or #49 or #50 (149,377)
#52 MeSH descriptor: [Adult] explode all trees (863)
#53 adult* or midadult* or (middle next age*) or “later life”:ti,ab,kw (356,717)
#54 #52 or #53 (357,080)
#55 #12 and #31 and #42 and #51 and #54 (235)
#56 ((relation* or association* or predict* or risk or risks or mortality) near/5 (obes* or overweight or weight status or BMI or body mass index) near/6 (adult* or middle-age* or men or women or later life)):ti,ab,kw (264)
#57 #55 or #56 from 2007 (292)
Centre for Reviews and Dissemination databases: Database of Abstracts of Reviews of Effects, Health Technology Assessment and NHS Economic Evaluation Database (Centre for Reviews and Dissemination interface)
17 June 2013. Searched 17 June 2013. Retrieved 26 records in DARE, 2 records in HTA and 9 records in NHS EED.
-
MeSH DESCRIPTOR Obesity EXPLODE ALL TREES (685)
-
MeSH DESCRIPTOR Overweight EXPLODE ALL TREES (698)
-
MeSH DESCRIPTOR Weight Gain EXPLODE ALL TREES (108)
-
MeSH DESCRIPTOR Weight Loss EXPLODE ALL TREES (309)
-
(obes* or overweight or “over weight” or “weight gain” or “weight loss”) (1773)
-
MeSH DESCRIPTOR Adiposity EXPLODE ALL TREES (11)
-
MeSH DESCRIPTOR Body Composition EXPLODE ALL TREES (72)
-
MeSH DESCRIPTOR Body Weight EXPLODE ALL TREES (1005)
-
(adiposity or adipose or fatness) (70)
-
((body NEAR2 (composition or fat or weight))) (723)
-
(#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10) (2223)
-
MeSH DESCRIPTOR Body Mass Index EXPLODE ALL TREES (221)
-
MeSH DESCRIPTOR Skinfold Thickness EXPLODE ALL TREES (4)
-
MeSH DESCRIPTOR Waist Circumference EXPLODE ALL TREES (14)
-
MeSH DESCRIPTOR Waist-Hip Ratio EXPLODE ALL TREES (0)
-
MeSH DESCRIPTOR Electric Impedance EXPLODE ALL TREES (14)
-
(((“body mass” NEAR3 (index* or indices)) or bmi or quetelet*)) (930)
-
(((“fat mass” NEAR3 (index* or indices)) or fmi)) (5)
-
(((“fat free mass” NEAR3 (index* or indices)) or ffmi)) (0)
-
((“body adipos*” NEAR3 (index* or indices))) (1)
-
((“body fat” NEAR2 percentage*)) (9)
-
(((“skin fold” or skinfold) NEAR3 (thickness* or test* or measure*))) (48)
-
(((waist or hip or neck) NEAR3 circumference*)) (66)
-
(((waist-to-hip or waist-hip) NEAR3 ratio*)) (22)
-
(((waist-to-height or waist-height) NEAR3 ratio*)) (2)
-
((((bioelectric* or electric*) NEAR3 (impedance or resistance)) or bia)) (28)
-
(((benn* or rohrer* or ponderal or corpulence) NEAR3 (index* or indices))) (6)
-
((“infrared interactance” or NIR)) (7)
-
((“sagittal abdominal diameter*” or “supine abdominal diameter*”)) (0)
-
(#12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29) (986)
-
(track* or traject* or persistence or persistent*) (17,333)
-
((observ* or monitor* or surveil* or measure*) near3 (repeat* or regular* or continu* or frequent* or period* or recurr* or perenn* or prolong* or perpetu* or “long term”)) (602)
-
((annual* or regular* or recurr*) near3 (interview* or questionnaire*)) (6)
-
(lifespan or “life span” or lifecourse or “life course”) (108)
-
MeSH DESCRIPTOR Cohort Studies (1111)
-
MeSH DESCRIPTOR Longitudinal Studies (129)
-
MeSH DESCRIPTOR Follow-Up Studies EXPLODE ALL TREES (0)
-
((cohort or panel) near2 (study or studies or analy*)) (3956)
-
(longitudinal near2 (study or studies or survey or surveys or analy* or pattern* or data)) (421)
-
((“follow up” or followup) near2 (study or studies or survey or surveys or analy* or pattern* or data)) (3166)
-
#31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37 OR #38 OR #39 OR #40 (23,434)
-
MeSH DESCRIPTOR Child EXPLODE ALL TREES (3678)
-
MeSH DESCRIPTOR Infant EXPLODE ALL TREES (2265)
-
(MeSH DESCRIPTOR Adolescent EXPLODE ALL TREES) (3457)
-
(MeSH DESCRIPTOR Young Adult EXPLODE ALL TREES) (1125)
-
(((child* or infant* or pediat* or paediat* or schoolchild* or “school age*” or schoolage*))) (9055)
-
(((adolescen* or juvenile* or youth* or teenage* or youngster*))) (4302)
-
(((girl or girls or boy or boys or kid or kids))) (278)
-
(((“young people” or “young person” or “young persons” or “young adult*”)) ) (1494)
-
#42 OR #43 OR #44 OR #45 OR #46 OR #47 OR #48 OR #49 (11,257)
-
MeSH DESCRIPTOR Adult EXPLODE ALL TREES (13,312)
-
(adult* or midadult* or “middle age*” or “later life”) (16,889)
-
#51 OR #52 (18,319)
-
#11 AND #30 AND #41 AND #50 AND #53 (40)
-
(((relation* or association* or predict* or risk or risks or mortality) near5 (obes* or overweight or weight status or BMI or body mass index) near6 (adult* or middle-age* or men or women or later life))) (15)
-
#54 OR #55 (52)
-
(* FROM 2007 TO 2013) (34,534)
-
#56 AND #57 (37)
Science Citation Index (Web of Science)
1900–14 June 2013. Searched 17 June 2013. Retrieved 1829 records.
| Search term | Number retrieved | |
|---|---|---|
| # 19 | #17 not #18 Databases=SCI-EXPANDED |
1829 |
| # 18 | TS=(rat or rats or mouse or mice or murine or hamster or hamsters or animal or animals or dogs or dog or pig or pigs or cats or bovine or cow or sheep or ovine or porcine or monkey) Databases=SCI-EXPANDED |
3,803,559 |
| # 17 | #15 AND #16 Databases=SCI-EXPANDED |
1894 |
| # 16 | PY=(2007-2013) Databases=SCI-EXPANDED |
10,274,844 |
| # 15 | #13 OR #14 Databases=SCI-EXPANDED |
2927 |
| # 14 | TS=((relation* or association* or predict* or risk or risks or mortality) NEAR/3 (obes* or overweight or “weight status” or BMI or “body mass index”) NEAR/4 (adult* or middle-age* or men or women or “later life”)) AND TS=(child* or infant* or pediat* or paediat* or schoolchild* or “school age” or “school aged” or schoolage* or adolescen* or juvenile* or youth* or teenage* or youngster* or girl or girls or boy or boys or kid or kids or “young people” or “young person” or “young persons” or “young adult” or “young adults”) Databases=SCI-EXPANDED |
1383 |
| # 13 | #1 AND #6 AND #10 AND #11 AND #12 Databases=SCI-EXPANDED |
1873 |
| # 12 | TS=(adult* or midadult* or “middle age*” or “later life”) Databases=SCI-EXPANDED |
803,294 |
| # 11 | TS=(child* or infant* or pediat* or paediat* or schoolchild* or “school age” or “school aged” or schoolage* or adolescen* or juvenile* or youth* or teenage* or youngster* or girl or girls or boy or boys or kid or kids or “young people” or “young person” or “young persons” or “young adult” or “young adults”) Databases=SCI-EXPANDED |
1,339,321 |
| # 10 | #7 OR #8 OR #9 Databases=SCI-EXPANDED |
913,241 |
| # 9 | TS=((cohort or panel) NEAR/1 (study or studies or analy*)) or TS=((longitudinal or “follow up” or followup) NEAR/1 (study or studies or survey or surveys or analy* or pattern* or data)) Databases=SCI-EXPANDED |
188,765 |
| # 8 | TS=((annual* or regular* or recur*) NEAR/3 (interview* or questionnaire*)) or TS=(lifespan or “life span” or lifecourse or “life course”) Databases=SCI-EXPANDED |
41,054 |
| # 7 | TS=( track* or traject* or persistence or persistent*) or TS=((observ* or monitor* or surveil* or measure*) NEAR/3 (repeat* or regular* or continu* or frequent* or period* or recur* or perenn* or prolong* or perpetu* or “long term”)) Databases=SCI-EXPANDED |
703,711 |
| # 6 | #2 OR #3 OR #4 OR #5 Databases=SCI-EXPANDED |
169,737 |
| # 5 | TS=(((bioelectric* or electric*) NEAR/3 (impedance or resistance)) or bia) or TS=(“near infrared interactance” or NIR) or TS=((benn* or rohrer* or ponderal or corpulence) NEAR/3 (index* or indices)) or TS=(sagittal abdominal diameter* or supine abdominal diameter*) Databases=SCI-EXPANDED |
48,466 |
| # 4 | TS=((waist or hip or neck) NEAR/3 circumference*) or TS=((waist-to-hip or waist-hip) NEAR/3 ratio*) or TS=((waist-to-height or waist-height) NEAR/3 ratio*) Databases=SCI-EXPANDED |
17,338 |
| # 3 | TS=(“body adiposity” NEAR/3 (index* or indices)) or TS=(“body fat” NEAR/2 percentage*) or TS=((“skin fold” or skinfold) NEAR/3 (thickness* or test* or measure*)) Databases=SCI-EXPANDED |
6792 |
| # 2 | TS=((“body mass” NEAR/3 (index* or indices)) or bmi or quetelet*) or TS=((“fat mass” NEAR/3 (index* or indices)) or fmi) or TS=((“fat free mass” NEAR/3 (index* or indices)) or ffmi) Databases=SCI-EXPANDED |
115,482 |
| # 1 | TS=(obes* or overweight or “over weight” or “weight gain” or “weight loss” or adiposity or adipose or fatness) or TS=(body NEAR/2 (composition or fat or weight)) Databases=SCI-EXPANDED |
453,027 |
Conference Proceedings Citation Index – Science (Web of Science)
1990–14 June 2013. Searched 17 June 2013. Retrieved 152 records.
| Search term | Number retrieved | |
|---|---|---|
| # 15 | #13 OR #14 Databases=CPCI-S |
152 |
| # 14 | TS=((relation* or association* or predict* or risk or risks or mortality) NEAR/3 (obes* or overweight or “weight status” or BMI or “body mass index”) NEAR/4 (adult* or middle-age* or men or women or “later life”)) AND TS=(child* or infant* or pediat* or paediat* or schoolchild* or “school age” or “school aged” or schoolage* or adolescen* or juvenile* or youth* or teenage* or youngster* or girl or girls or boy or boys or kid or kids or “young people” or “young person” or “young persons” or “young adult” or “young adults”) Databases=CPCI-S |
91 |
| # 13 | #1 AND #6 AND #10 AND #11 AND #12 Databases=CPCI-S |
69 |
| # 12 | TS=(adult* or midadult* or “middle age*” or “later life”) Databases=CPCI-S |
66,704 |
| # 11 | TS=(child* or infant* or pediat* or paediat* or schoolchild* or “school age” or “school aged” or schoolage* or adolescen* or juvenile* or youth* or teenage* or youngster* or girl or girls or boy or boys or kid or kids or “young people” or “young person” or “young persons” or “young adult” or “young adults”) Databases=CPCI-S |
134,639 |
| # 10 | #7 OR #8 OR #9 Databases=CPCI-S |
220,083 |
| # 9 | TS=((cohort or panel) NEAR/1 (study or studies or analy*)) or TS=((longitudinal or “follow up” or followup) NEAR/1 (study or studies or survey or surveys or analy* or pattern* or data)) Databases=CPCI-S |
19,090 |
| # 8 | TS=((annual* or regular* or recur*) NEAR/3 (interview* or questionnaire*)) or TS=(lifespan or “life span” or lifecourse or “life course”) Databases=CPCI-S |
4413 |
| # 7 | TS=(track* or traject* or persistence or persistent*) or TS=((observ* or monitor* or surveil* or measure*) NEAR/3 (repeat* or regular* or continu* or frequent* or period* or recur* or perenn* or prolong* or perpetu* or “long term”)) Databases=CPCI-S |
198,195 |
| # 6 | #2 OR #3 OR #4 OR #5 Databases=CPCI-S |
23,836 |
| # 5 | TS=(((bioelectric* or electric*) NEAR/3 (impedance or resistance)) or bia) or TS=(“near infrared interactance” or NIR) or TS=((benn* or rohrer* or ponderal or corpulence) NEAR/3 (index* or indices)) or TS=(sagittal abdominal diameter* or supine abdominal diameter*) Databases=CPCI-S |
14,260 |
| # 4 | TS=((waist or hip or neck) NEAR/3 circumference*) or TS=((waist-to-hip or waist-hip) NEAR/3 ratio*) or TS=((waist-to-height or waist-height) NEAR/3 ratio*) Databases=CPCI-S |
886 |
| # 3 | TS=(“body adiposity” NEAR/3 (index* or indices)) or TS=(“body fat” NEAR/2 percentage*) or TS=((“skin fold” or skinfold) NEAR/3 (thickness* or test* or measure*)) Databases=CPCI-S |
351 |
| # 2 | TS=((“body mass” NEAR/3 (index* or indices)) or bmi or quetelet*) or TS=((“fat mass” NEAR/3 (index* or indices)) or fmi) or TS=((“fat free mass” NEAR/3 (index* or indices)) or ffmi) Databases=CPCI-S |
9083 |
| # 1 | TS=(obes* or overweight or “over weight” or “weight gain” or “weight loss” or adiposity or adipose or fatness) or TS=(body NEAR/2 (composition or fat or weight)) Databases=CPCI-S |
48,448 |
Health Management Information Consortium (OvidSP)
1979–March 2013. Searched 17 June 2013. Retrieved 52 records.
-
exp Obesity/ (2727)
-
(obes$ or overweight or over weight or weight gain or weight loss).ti,ab. (3514)
-
exp Body weight/ (842)
-
(adiposity or adipose or (body adj2 (composition or fat or weight)) or fatness).ti,ab. (621)
-
or/1-4 (4574)
-
exp body mass index/ (496)
-
weight size ratios/ (72)
-
((body mass adj3 (index$ or indices)) or bmi or quetelet$).ti,ab. (1674)
-
((fat mass adj3 (index$ or indices)) or fmi).ti,ab. (10)
-
((fat free mass adj3 (index$ or indices)) or ffmi).ti,ab. (4)
-
(body adipos$ adj3 (index$ or indices)).ti,ab. (0)
-
(body fat adj2 percentage$).ti,ab. (31)
-
((skin fold or skinfold) adj3 (thickness$ or test$ or measure$)).ti,ab. (32)
-
((waist or hip or neck) adj3 circumference$).ti,ab. (222)
-
((waist-to-hip or waist-hip) adj3 ratio$).ti,ab. (72)
-
((waist-to-height or waist-height) adj3 ratio$).ti,ab. (10)
-
(((bioelectric$ or electric$) adj3 (impedance or resistance)) or bia).ti,ab. (15)
-
(near infrared interactance or NIR).ti,ab. (1)
-
((benn$ or rohrer$ or ponderal or corpulence) adj3 (index$ or indices)).ti,ab. (5)
-
(sagittal abdominal diameter$ or supine abdominal diameter$).ti,ab. (2)
-
or/6-20 (1881)
-
(track$ or traject$ or persistence or persistent$).ti,ab. (2602)
-
((observ$ or monitor$ or surveil$ or measure$) adj3 (repeat$ or regular$ or continu$ or frequent$ or period$ or recurr$ or perenn$ or prolong$ or perpetu$ or long term)).ti,ab. (1287)
-
((annual$ or regular$ or recurr$) adj3 (interview$ or questionnaire$)).ti,ab. (56)
-
(lifespan or life span or lifecourse or life course).ti,ab. (456)
-
cohort studies/ (757)
-
longitudinal studies/ (457)
-
((cohort or panel) adj1 (study or studies or analy$)).ti,ab. (2763)
-
(longitudinal adj1 (study or studies or survey or surveys or analy$ or pattern$ or data)).ti,ab. (1552)
-
(follow up adj1 (study or studies or survey or surveys or analy$ or data)).ti,ab. (835)
-
or/22-30 (9166)
-
exp Children/ or exp Older children/ or exp Pre school children/ (17,728)
-
exp Infants/ (1520)
-
exp Young people/ (9377)
-
exp Young adults/ (281)
-
(child$ or infant$ or pediat$ or paediat$ or schoolchild$ or school age$ or schoolage$).ti,ab. (29,945)
-
(adolescen$ or juvenile$ or youth$ or teenage$ or youngster$).ti,ab. (6446)
-
(girl or girls or boy or boys or kid or kids).ti,ab. (1508)
-
(young people or young person or young persons or young adult$).ti,ab. (5502)
-
or/32-39 (40,506)
-
adults/ or middle aged people/ (2555)
-
(adult$ or midadult$ or middle age$ or later life).ti,ab. (12,127)
-
41 or 42 (12,746)
-
5 and 21 and 31 and 40 and 43 (67)
-
(2007$ or 2008$ or 2009$ or 2010$ or 2011$ or 2012$ or 2013$).dp,yr. (68,585)
-
44 and 45 (52)
Trials Register of Promoting Health Interventions (Evidence for Policy and Practice Information and Co-ordinating Centre)
18 June 2013. Searched 18 June 2013. Retrieved 14 records (post-2007).
-
Freetext: “obes*” OR overweight OR “over weight” OR “weight gain” OR “weight loss” (862)
-
Freetext: adiposity OR adipose OR fatness OR “body composition” or “body fat” or “body weight” (280)
-
1 OR 2 (918)
-
Freetext: “track*” OR “traject*” OR persistence OR “persistent*” (101)
-
Freetext: “cohort study” OR “cohort studies” OR “longitudinal study” OR “longitudinal studies” OR “follow up study” OR “follow up studies” (129)
-
4 OR 5 (223)
-
3 AND 6 (27)
Obesity and Sedentary Behaviour Database (Evidence for Policy and Practice Information and Co-ordinating Centre)
18 June 2013. Searched 18 June 2013. Retrieved 13 records (post-2007).
-
Freetext: “track*” OR “traject*” OR persistence OR “persistent*” (9)
-
Freetext: “cohort study” OR “cohort studies” OR “longitudinal study” OR “longitudinal studies” OR “follow up study” OR “follow up studies” (27)
-
1 OR 2 (32)
OAIster (http://oaister.worldcat.org/)
Searched 18 June 2013. Retrieved 79 records.
kw:(obes* OR overweight OR “weight gain” OR adiposity) kw:(“body mass index*” OR bmi OR quetelet* OR “fat mass index*” OR “fat free mass index*” OR “body adiposity index*” OR “body fat percentage” OR “skin fold” OR skinfold OR “waist circumference*” OR “hip circumference*” OR “neck circumference*” OR “waist-to-hip” OR “waist-hip” OR “waist-to-height” OR “waist-height” OR “bioelectric* impedance” OR “electric* impedance” OR “benn* index*” OR “rohrer* index*” OR “ponderal index*” OR “corpulence index*” OR “sagittal abdominal diameter*” OR “supine abdominal diameter*”) AND (track* OR traject* OR persistence OR persistent* OR “cohort study” OR “cohort studies” OR “longitudinal study” OR “longitudinal studies” OR “follow up study” OR “follow up studies”) kw:(child* OR infant* OR pediat* OR paediat* OR schoolchild* OR “school age*” OR schoolage* OR adolescen* OR juvenile* OR youth* OR teenage* OR youngster* OR “young people” OR “young person” OR “young persons” OR “young adult*”) AND (adult* OR “middle age*”)' > '2007..2013' limited to Libraries Worldwide
OpenGrey (www.opengrey.eu/)
Searched 18 June 2013. Retrieved 0 records.
(obes* OR overweight OR “weight gain” OR adiposity) AND (track* OR traject* OR persistence OR persistent* OR “cohort study” OR “cohort studies” OR “longitudinal study” OR “longitudinal studies” OR “follow up study” OR “follow up studies”)
Review of the diagnostic accuracy of childhood measures of obesity
MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations (OvidSP)
1946–2013, May week 5. Searched 10 June 2013. Retrieved 2412 records in MEDLINE and 50 records in MEDLINE In-Process & Other Non-Indexed Citations.
-
exp Obesity/ (133,014)
-
Overweight/ (10,556)
-
Weight Gain/ (21,776)
-
Weight Loss/ (22,903)
-
obes$.ti,ab. (152,384)
-
(overweight or over weight).ti,ab. (32,167)
-
(weight gain or weight loss).ti,ab. (82,180)
-
or/1-7 (267,262)
-
Adiposity/ or Adipose Tissue/ (63,489)
-
exp Body Composition/ (35,563)
-
Body Weight/ (159,038)
-
(adiposity or adipose).ti,ab. (56,647)
-
(body adj2 (composition or fat or weight)).ti,ab. (168,451)
-
fatness.ti,ab. (2834)
-
or/8-14 (541,557)
-
Body Mass Index/ (75,019)
-
Skinfold Thickness/ (5476)
-
Waist Circumference/ (3842)
-
Waist-Hip Ratio/ (2713)
-
Electric Impedance/ (11,165)
-
((body mass adj3 (index$ or indices)) or bmi or quetelet$).ti,ab. (113,321)
-
((fat mass adj3 (index$ or indices)) or fmi).ti,ab. (823)
-
((fat free mass adj3 (index$ or indices)) or ffmi).ti,ab. (343)
-
(body adipos$ adj3 (index$ or indices)).ti,ab. (35)
-
(body fat adj2 percentage$).ti,ab. (3469)
-
((skin fold or skinfold) adj3 (thickness$ or test$ or measure$)).ti,ab. (4708)
-
((waist or hip or neck) adj3 circumference$).ti,ab. (13,184)
-
((waist-to-hip or waist-hip) adj3 ratio$).ti,ab. (6212)
-
((waist-to-height or waist-height) adj3 ratio$).ti,ab. (514)
-
(((bioelectric$ or electric$) adj3 (impedance or resistance)) or bia).ti,ab. (10,288)
-
(near infrared interactance or NIR).ti,ab. (4634)
-
((benn$ or rohrer$ or ponderal or corpulence) adj3 (index$ or indices)).ti,ab. (999)
-
(sagittal abdominal diameter$ or supine abdominal diameter$).ti,ab. (108)
-
or/16-33 (168,960)
-
exp Densitometry/ (28,031)
-
exp Plethysmography/ (18,381)
-
Neutron Activation Analysis/ (1682)
-
(body volume adj3 (index$ or indices)).ti,ab. (1)
-
(densitometr$ or hydrodensitometr$).ti,ab. (13,282)
-
((hydrostatic or underwater or water) adj3 (weighing or analys$ or measure$)).ti,ab. (12,322)
-
(absorptiometry or DXA or DEXA).ti,ab. (18,761)
-
((water or air) adj3 displacement).ti,ab. (999)
-
(air displacement plethysmograph$ or pea pod or peapod or infant body composition system$ or bodpod or bod pod).ti,ab. (319)
-
(neutron$ adj3 activat$).ti,ab. (2611)
-
((multicomponent$ or multi component$ or multimodal$ or multi modal$ or composit$) adj3 model$).ti,ab. (2039)
-
(deuterium adj3 dilut$).ti,ab. (452)
-
or/35-46 (80,449)
-
exp child/ (1,510,589)
-
exp Infant/ (916,662)
-
Adolescent/ (1,568,189)
-
Young Adult/ (310,115)
-
(child$ or infant$ or pediat$ or paediat$ or schoolchild$ or school age$ or schoolage$).ti,ab. (1,205,015)
-
(adolescen$ or juvenile$ or youth$ or teenage$ or youngster$).ti,ab. (236,539)
-
(girl or girls or boy or boys or kid or kids).ti,ab. (155,309)
-
(young people or young person or young persons or young adult$).ti,ab. (67,202)
-
or/48-55 (3,198,543)
-
15 and 34 and 47 and 56 (2417)
-
exp Animals/ not Humans/ (3,903,550)
-
57 not 58 (2412)
PubMed (National Library of Medicine)
1946–10 June 2013. Searched 10 June 2013. Retrieved 2116 records.
#45 (#43 NOT #44) (2116)
#44 (animals [mh] NOT humans [mh]) (3,786,976)
#43 (#9 AND #25 AND #36 AND #42) (2120)
#42 ((#37 OR #38 OR #39 OR #40 OR #41)) (3,204,504)
#41 “young people”[tiab] or “young person”[tiab] or “young persons”[tiab] or young adult*[tiab] (68,815)
#40 girl[tiab] or girls[tiab] or boy[tiab] or boys[tiab] or kid[tiab] or kids[tiab] (162,265)
#39 adolescen*[tiab] or juvenile*[tiab] or youth*[tiab] or teenage*[tiab] or youngster*[tiab] (246,765)
#38 child*[tiab] or infant*[tiab] or pediat*[tiab] or paediat*[tiab] or schoolchild*[tiab] or school age*[tiab] or schoolage*[tiab] (1,247,217)
#37 (((“Child”[Mesh]) OR “Infant”[Mesh]) OR “Adolescent”[Mesh]) OR “Young Adult”[Mesh] (2,835,930)
#36 ((#26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35)) (70,730)
#35 Search deuterium dilut*[tiab] (255)
#34 (“multicomponent model”[tiab] or “multicomponent models”[tiab] or “multi component model”[tiab] or “multi component models”[tiab] or “multimodal model”[tiab] or “multimodal models”[tiab] or “multi modal model”[tiab] or “multi modal models”[tiab] or “composite model”[tiab] or “composite models”[tiab]) (422)
#33 neutron* activat*[tiab] (3609)
#32 air displacement plethysmograph*[tiab] or “pea pod”[tiab] or peapod[tiab] or infant body composition system*[tiab] or bodpod[tiab] or “bod pod”[tiab] (385)
#31 water displacement[tiab] or air displacement[tiab] (815)
#30 absorptiometry[tiab] or DXA[tiab] or DEXA[tiab] (19,261)
#29 (hydrostatic weighing[tiab] or hydrostatic analys*[tiab] or hydrostatic measure*[tiab] or underwater weighing[tiab] or underwater analys*[tiab] or underwater measure*[tiab] or water weighing[tiab] or water analys*[tiab] or water measure*[tiab]) (3067)
#28 densitometr*[tiab] or hydrodensitometr*[tiab] (13,428)
#27 “body volume index”[TIAB] or “body volume indices”[tiab] (0)
#26 ((“Densitometry”[Mesh]) OR “Plethysmography”[Mesh]) OR “Neutron Activation Analysis”[Mesh] (46,668)
#25 ((#10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24)) (173,811)
#24 (sagittal abdominal diameter*[tiab] or supine abdominal diameter*[tiab]) (114)
#23 benn* index[tiab] or benn* indices[tiab] or rohrer* index[tiab] or rohrer* indices[tiab] or “ponderal index”[tiab] or “ponderal indices”[tiab] or “corpulence index”[tiab] or “corpulance indices”[tiab] (972)
#22 (“near infrared interactance”[tiab] or NIR[tiab]) (6538)
#21 “bioelectric impedance”[tiab] or “bioelectrical impedance”[tiab] or “electric impedance”[tiab] or “electrical impedance”[tiab] or “bioelectric resistance”[tiab] or “bioelectrical resistance”[tiab] or “electric resistance”[tiab] or “electrical resistance”[tiab] or bia[tiab] (10,514)
#20 “waist-to-height ratio”[tiab] or “waist-to-height ratios”[tiab] or “waist-height ratio”[tiab] or “waist-height ratios”[tiab] (584)
#19 “waist-to-hip ratio”[tiab] or “waist-to-hip ratios”[tiab] or “waist-hip ratio”[tiab] or “waist-hip ratios”[tiab] (6331)
#18 “waist circumference”[tiab] or “hip circumference”[tiab] or “neck circumference”[tiab] (13,353)
#17 (“skinfold thickness”[tiab] or “skinfold test”[tiab] or “skinfold tests”[tiab] or “skinfold measure”[tiab] or “skinfold measurement”[tiab] or “skinfold measures”[tiab] or “skinfold measurements”[tiab]) (3335)
#16 (“skin fold thickness”[tiab] or “skin fold test”[tiab] or “skin fold tests”[tiab] or “skin fold measure”[tiab] or “skin fold measurement”[tiab] or “skin fold measures”[tiab] or “skin fold measurements”[tiab]) (658)
#15 (“body fat percentage”[tiab] or “body fat percentages”[tiab]) (1198)
#14 “body adiposity index”[tiab] or “body adiposity indices”[tiab] or “body adiposie index”[tiab] or “body adipose indices”[tiab] (43)
#13 (“fat free mass index”[tiab] or “fat free mass indices”[tiab] or ffmi[tiab]) (244)
#12 “fat mass index”[tiab] or “fat mass indices”[tiab] or fmi[tiab] (430)
#11 (“body mass index”[tiab] or “body mass indices”[tiab] or bmi[tiab] or quetelet*[tiab]) (118,076)
#10 ((((“Body Mass Index”[Mesh]) OR “Skinfold Thickness”[Mesh]) OR “Waist Circumference”[Mesh]) OR “Waist-Hip Ratio”[Mesh]) OR “Electric Impedance”[Mesh] (85,640)
#9 (#6 OR #7 OR #8) (578,940)
#8 adiposity[tiab] or adipose[tiab] or “body composition”[tiab] or “body fat”[tiab] or “body weight”[tiab] or fatness[tiab] (214,556)
#7 (((“Adiposity”[Mesh]) OR “Adipose Tissue”[Mesh]) OR “Body Composition”[Mesh]) OR “Body Weight”[Mesh] (383,871)
#6 ((#1 OR #2 OR #3 OR #4 OR #5)) (278,389)
#5 “weight gain”[tiab] or “weight loss”[tiab] (85,808)
#4 overweight[tiab] or “over weight*”[tiab] (33,801)
#3 obes*[tiab] (158,729)
#2 ((“Overweight”[Mesh]) OR “Weight Gain”[Mesh]) OR “Weight Loss”[Mesh] (158,971)
#1 “Obesity”[Mesh] (126,162)
EMBASE (OvidSP)
1974–2013, week 23. Searched 10 June 2013. Retrieved 2274 records.
-
exp obesity/ (262,617)
-
weight gain/ (58,401)
-
weight reduction/ (85,101)
-
obes$.ti,ab. (213,837)
-
(overweight or over weight).ti,ab. (46,324)
-
(weight gain or weight loss).ti,ab. (112,520)
-
or/1-6 (441,658)
-
exp body composition/ (58,421)
-
body weight/ (179,655)
-
(adiposity or adipose).ti,ab. (73,593)
-
(body adj2 (composition or fat or weight)).ti,ab. (214,271)
-
fatness.ti,ab. (3314)
-
or/7-12 (716,288)
-
body mass/ (159,745)
-
skinfold thickness/ (7810)
-
waist circumference/ (18,862)
-
waist hip ratio/ (5940)
-
waist to height ratio/ (166)
-
weight height ratio/ (10)
-
neck circumference/ (143)
-
((body mass adj3 (index$ or indices)) or bmi or quetelet$).ti,ab. (175,493)
-
((fat mass adj3 (index$ or indices)) or fmi).ti,ab. (1119)
-
((fat free mass adj3 (index$ or indices)) or ffmi).ti,ab. (491)
-
(body adipos$ adj3 (index$ or indices)).ti,ab. (60)
-
(body fat adj2 percentage$).ti,ab. (4420)
-
((skin fold or skinfold) adj3 (thickness$ or test$ or measure$)).ti,ab. (5741)
-
((waist or hip or neck) adj3 circumference$).ti,ab. (20,733)
-
((waist-to-hip or waist-hip) adj3 ratio$).ti,ab. (8299)
-
((waist-to-height or waist-height) adj3 ratio$).ti,ab. (778)
-
(((bioelectric$ or electric$) adj3 (impedance or resistance)) or bia).ti,ab. (13,679)
-
(near infrared interactance or NIR).ti,ab. (6312)
-
((benn$ or rohrer$ or ponderal or corpulence) adj3 (index$ or indices)).ti,ab. (1205)
-
(sagittal abdominal diameter$ or supine abdominal diameter$).ti,ab. (136)
-
or/14-33 (258,369)
-
densitometry/ (16,109)
-
exp plethysmograph/ (451)
-
neutron activation analysis/ (5326)
-
(body volume adj3 (index$ or indices)).ti,ab. (6)
-
(densitometr$ or hydrodensitometr$).ti,ab. (17,847)
-
((hydrostatic or underwater or water) adj3 (weighing or analys$ or measure$)).ti,ab. (17,975)
-
(absorptiometry or DXA or DEXA).ti,ab. (25,906)
-
((water or air) adj3 displacement).ti,ab. (1325)
-
(air displacement plethysmograph$ or pea pod or peapod or infant body composition system$ or bodpod or bod pod).ti,ab. (511)
-
(neutron$ adj3 activat$).ti,ab. (5851)
-
((multicomponent$ or multi component$ or multimodal$ or multi modal$ or composit$) adj3 model$).ti,ab. (2750)
-
(deuterium adj3 dilut$).ti,ab. (529)
-
or/35-46 (78,881)
-
child/ (1,266,225)
-
preschool child/ (500,023)
-
infant/ (522,108)
-
adolescent/ (1,240,231)
-
(child$ or infant$ or pediat$ or paediat$ or schoolchild$ or school age$ or schoolage$).ti,ab. (1,545,191)
-
(adolescen$ or juvenile$ or youth$ or teenage$ or youngster$).ti,ab. (304,919)
-
(girl or girls or boy or boys or kid or kids).ti,ab. (206,972)
-
(young people or young person or young persons or young adult$).ti,ab. (86,424)
-
or/48-55 (2,993,496)
-
13 and 34 and 47 and 56 (2274)
PsycINFO (OvidSP)
1806–2013, June week 1. Searched 11 June 2013. Retrieved 133 records.
-
obesity/ (13,925)
-
overweight/ (2263)
-
weight gain/ or weight loss/ (3364)
-
obes$.ti,ab. (20,582)
-
(overweight or over weight).ti,ab. (7911)
-
(weight gain or weight loss).ti,ab. (12,709)
-
or/1-6 (32,209)
-
body weight/ (9825)
-
(adiposity or adipose).ti,ab. (1912)
-
(body adj2 (composition or fat or weight)).ti,ab. (13,234)
-
fatness.ti,ab. (462)
-
or/7-11 (43,149)
-
body mass index/ (2140)
-
((body mass adj3 (index$ or indices)) or bmi or quetelet$).ti,ab. (13,043)
-
((fat mass adj3 (index$ or indices)) or fmi).ti,ab. (87)
-
((fat free mass adj3 (index$ or indices)) or ffmi).ti,ab. (23)
-
(body adipos$ adj3 (index$ or indices)).ti,ab. (0)
-
(body fat adj2 percentage$).ti,ab. (315)
-
((skin fold or skinfold) adj3 (thickness$ or test$ or measure$)).ti,ab. (256)
-
((waist or hip or neck) adj3 circumference$).ti,ab. (1284)
-
((waist-to-hip or waist-hip) adj3 ratio$).ti,ab. (507)
-
((waist-to-height or waist-height) adj3 ratio$).ti,ab. (43)
-
(((bioelectric$ or electric$) adj3 (impedance or resistance)) or bia).ti,ab. (455)
-
(near infrared interactance or NIR).ti,ab. (37)
-
((benn$ or rohrer$ or ponderal or corpulence) adj3 (index$ or indices)).ti,ab. (79)
-
(sagittal abdominal diameter$ or supine abdominal diameter$).ti,ab. (7)
-
or/13-26 (14,507)
-
plethysmography/ (133)
-
(body volume adj3 (index$ or indices)).ti,ab. (0)
-
(densitometr$ or hydrodensitometr$).ti,ab. (210)
-
((hydrostatic or underwater or water) adj3 (weighing or analys$ or measure$)).ti,ab. (516)
-
(absorptiometry or DXA or DEXA).ti,ab. (513)
-
((water or air) adj3 displacement).ti,ab. (34)
-
(air displacement plethysmograph$ or pea pod or peapod or infant body composition system$ or bodpod or bod pod).ti,ab. (18)
-
(neutron$ adj3 activat$).ti,ab. (13)
-
((multicomponent$ or multi component$ or multimodal$ or multi modal$ or composit$) adj3 model$).ti,ab. (678)
-
(deuterium adj3 dilut$).ti,ab. (14)
-
or/28-37 (2084)
-
(adolescence 13 17 yrs or childhood birth 12 yrs or preschool age 2 5 yrs or school age 6 12 yrs or young adulthood 18 29 yrs).ag. (778,079)
-
(child$ or infant$ or pediat$ or paediat$ or schoolchild$ or school age$ or schoolage$).ti,ab. (536,641)
-
(adolescen$ or juvenile$ or youth$ or teenage$ or youngster$).ti,ab. (207,223)
-
(girl or girls or boy or boys or kid or kids).ti,ab. (77,393)
-
(young people or young person or young persons or young adult$).ti,ab. (41,848)
-
or/39-43 (1,040,736)
-
12 and 27 and 38 and 44 (133)
Cumulative Index to Nursing and Allied Health Literature (EBSCOhost)
1981–7 June 2013. Searched 11 June 2013. Retrieved 551 records.
| Search term | Number retrieved | |
|---|---|---|
| S49 | S10 AND S29 AND S42 AND S48 | 551 |
| S48 | S43 OR S44 OR S45 OR S46 OR S47 | 412,874 |
| S47 | TI (“young people” or “young person” or “young persons” or “young adult*”) or AB (“young people” or “young person” or “young persons” or “young adult*”) | 14,961 |
| S46 | TI (girl or girls or boy or boys or kid or kids) or AB (girl or girls or boy or boys or kid or kids) | 20,926 |
| S45 | TI (adolescen* or juvenile* or youth* or teenage* or youngster*) or AB (adolescen* or juvenile* or youth* or teenage* or youngster*) | 56,494 |
| S44 | TI (child* or infant* or pediat* or paediat* or schoolchild* or “school age*” or schoolage*) or AB (child* or infant* or pediat* or paediat* or schoolchild* or “school age*” or schoolage*) | 213,146 |
| S43 | (ZG “adolescent: 13-18 years”) or (ZG “child, preschool: 2-5 years”) or (ZG “child: 6-12 years”) | 320,453 |
| S42 | S30 OR S31 OR S32 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 | 6568 |
| S41 | TI (deuterium N3 dilut*) or AB (deuterium N3 dilut*) | 72 |
| S40 | TI (multicomponent* N3 model* or “multi component*” N3 model* or multimodal* N3 model* or “multi modal* N3 model or composit* N3 model*) or AB (multicomponent* N3 model* or “multi component*” N3 model* or multimodal* N3 model* or “multi modal* N3 model or composit* N3 model*) | 24 |
| S39 | TI (neutron* N3 activat*) or AB (neutron* N3 activat*) | 32 |
| S38 | TI (“air displacement plethysmograph*” or “pea pod” or peapod or “infant body composition system*” or bodpod or “bod pod”) or AB (“air displacement plethysmograph*” or “pea pod” or peapod or “infant body composition system*” or bodpod or “bod pod”) | 93 |
| S37 | TI (water N3 displacement or air N3 displacement) or AB (water N3 displacement or air N3 displacement) | 147 |
| S36 | TI (absorptiometry or DXA or DEXA) or AB (absorptiometry or DXA or DEXA) | 2237 |
| S35 | TI (hydrostatic N3 weighing or hydrostatic N3 analys* or hydrostatic N3 measure* or underwater N3 weighing or underwater N3 analys* or underwater N3 measure* or water N3 weighing or water N3 analys* or water N3 measure*) or AB (hydrostatic N3 weighing or hydrostatic N3 analys* or hydrostatic N3 measure* or underwater N3 weighing or underwater N3 analys* or underwater N3 measure* or water N3 weighing or water N3 analys* or water N3 measure*) | 732 |
| S34 | TI (densitometr* or hydrodensitometr*) or AB (densitometr* or hydrodensitometr*) | 520 |
| S33 | TI (“body volume” N3 index* or “body volume” N3 indices) or AB (“body volume” N3 index* or “body volume” N3 indices) | 178 |
| S32 | TI (“body volume” N3 index* or “body volume” N3 indices) or AB (“body volume” N3 index* or “body volume” N3 indices) [CINAHL SmartText Searching – ignored] | 0 |
| S31 | (MH “Plethysmography+”) | 1090 |
| S30 | (MH “Densitometry+”) | 3881 |
| S29 | S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 | 40,846 |
| S28 | TI (“sagittal abdominal diameter*” or “supine abdominal diameter*”) or AB (“sagittal abdominal diameter*” or “supine abdominal diameter*”) | 21 |
| S27 | TI (benn* N3 index* or benn* N3 indices or rohrer* N3 index* or rohrer* N3 indices* or ponderal N3 index* or ponderal N3 indices or corpulence N3 index* or corpulence N3 indices) or AB (benn* N3 index* or benn* N3 indices or rohrer* N3 index* or rohrer* N3 indices* or ponderal N3 index* or ponderal N3 indices or corpulence N3 index* or corpulence N3 indices) | 79 |
| S26 | TI (“near infrared interactance” or NIR) or AB (“near infrared interactance” or NIR) | 57 |
| S25 | TI (bioelectric* N3 impedance or electric* N3 impedance or bioelectric* N3 resistance or electric* N3 resistance or bia) or AB (bioelectric* N3 impedance or electric* N3 impedance or bioelectric* N3 resistance or electric* N3 resistance or bia) | 882 |
| S24 | TI (waist-to-height N3 ratio* or waist-height N3 ratio*) or AB (waist-to-height N3 ratio* or waist-height N3 ratio*) | 97 |
| S23 | TI (waist-to-hip N3 ratio* or waist-hip N3 ratio*) or AB (waist-to-hip N3 ratio* or waist-hip N3 ratio*) | 853 |
| S22 | TI (waist N3 circumference* or hip N3 circumference* or neck N3 circumference*) or AB (waist N3 circumference* or hip N3 circumference* or neck N3 circumference*) | 2378 |
| S21 | TI (“skin fold” N3 thickness* or skinfold N3 thickness* or “skin fold” N3 test* or skinfold N3 test* or “skin fold” N3 measure* or skinfold N3 measure*) or AB (“skin fold” N3 thickness* or skinfold N3 thickness* or “skin fold” N3 test* or skinfold N3 test* or “skin fold” N3 measure* or skinfold N3 measure*) | 712 |
| S20 | TI (“body fat” N3 percentage*) or AB (“body fat” N3 percentage*) | 783 |
| S19 | TI (“body adipos*” N3 index* or “body adipos*” N3 indices) or AB (“body adipos*” N3 index* or “body adipos*” N3 indices) | 9 |
| S18 | TI (“fat free mass” N3 index* or “fat free mass” N3 indices or ffmi) or AB (“fat free mass” N3 index* or “fat free mass” N3 indices or ffmi) | 78 |
| S17 | TI (“fat mass” N3 index* or “fat mass” N3 indices or fmi) or AB (“fat mass” N3 index* or “fat mass” N3 indices or fmi) | 144 |
| S16 | TI (“body mass” N3 index* or “body mass” N3 indices or bmi or quetelet*) or AB (“body mass” N3 index* or “body mass” N3 indices or bmi or quetelet*) | 19,132 |
| S15 | (MH “Electric Impedance”) | 1560 |
| S14 | (MH “Waist-Hip Ratio”) | 1251 |
| S13 | (MH “Waist Circumference”) | 271 |
| S12 | (MH “Skinfold Thickness”) | 2268 |
| S11 | (MH “Body Mass Index”) | 28,324 |
| S10 | S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 | 71,129 |
| S9 | TI (body N2 composition or body N2 fat or body N2 weight) or AB (body N2 composition or body N2 fat or body N2 weight) | 13,869 |
| S8 | TI (adiposity or adipose or fatness) or AB (adiposity or adipose or fatness) | 3860 |
| S7 | (MH “Body Weight”) | 8937 |
| S6 | (MH “Body Composition”) | 7934 |
| S5 | (MH “Adipose Tissue”) | 4507 |
| S4 | TI (“weight gain” or “weight loss”) or AB (“weight gain” or “weight loss”) | 11,268 |
| S3 | TI (obes* or overweight or “over weight”) or AB (obes* or overweight or “over weight”) | 27,804 |
| S2 | (MH “Weight Gain”) OR (MH “Weight Loss”) | 12,508 |
| S1 | (MH “Obesity+”) | 32,251 |
The Cochrane Library: Cochrane Database of Systematic Reviews and Cochrane Central Register of Controlled Trials (Wiley Online Library)
2013: CDSR Issue 5/12, CENTRAL Issue 5/12. Searched 11 June 2013. Retrieved 0 records in CDSR and 169 records in CENTRAL.
#1 MeSH descriptor: [Obesity] explode all trees (6452)
#2 MeSH descriptor: [Overweight] this term only (1072)
#3 MeSH descriptor: [Weight Gain] this term only (1416)
#4 MeSH descriptor: [Weight Loss] this term only (2918)
#5 (obes* or overweight or (over next weight)):ti,ab,kw (10,756)
#6 ((weight next gain) or (weight next loss)):ti,ab,kw (9014)
#7 MeSH descriptor: [Adiposity] this term only (203)
#8 MeSH descriptor: [Body Composition] explode all trees (2773)
#9 MeSH descriptor: [Body Weight] this term only (5538)
#10 (adiposity or adipose or fatness):ti,ab,kw (2168)
#11 (body near/2 (composition or fat or weight)):ti,ab,kw (18,126)
#12 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 (29,278)
#13 MeSH descriptor: [Body Mass Index] this term only (5044)
#14 MeSH descriptor: [Skinfold Thickness] this term only (269)
#15 MeSH descriptor: [Waist Circumference] this term only (261)
#16 MeSH descriptor: [Waist-Hip Ratio] this term only (158)
#17 MeSH descriptor: [Electric Impedance] this term only (313)
#18 ((“body mass” near/3 (index* or indices)) or bmi or quetelet*):ti,ab,kw (11,870)
#19 ((“fat mass” near/3 (index* or indices)) or fmi):ti,ab,kw (49)
#20 ((“fat free mass” near/3 (index* or indices)) or ffmi):ti,ab,kw (28)
#21 (“body adipos*” near/3 (index* or indices)):ti,ab,kw (1)
#22 (“body fat” near/2 percentage*):ti,ab,kw (328)
#23 ((“skin fold” or skinfold) near/3 (thickness* or test* or measure*)):ti,ab,kw (590)
#24 ((waist or hip or neck) near/3 circumference*):ti,ab,kw (1244)
#25 ((waist-to-hip or waist-hip) near/3 ratio*):ti,ab,kw (542)
#26 ((waist-to-height or waist-height) near/3 ratio*):ti,ab,kw (16)
#27 (((bioelectric* or electric*) near/3 (impedance or resistance)) or bia):ti,ab,kw (598)
#28 (“near infrared interactance” or NIR):ti,ab,kw (49)
#29 ((benn* or rohrer* or ponderal or corpulence) near/3 (index* or indices)):ti,ab,kw (32)
#30 (“sagittal abdominal diameter*” or “supine abdominal diameter*”):ti,ab,kw (8)
#31 #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 (13,412)
#32 MeSH descriptor: [Densitometry] explode all trees (1365)
#33 MeSH descriptor: [Plethysmography] explode all trees (948)
#34 MeSH descriptor: [Neutron Activation Analysis] this term only (15)
#35 (“body volume” near/3 (index* or indices)):ti,ab,kw (0)
#36 (densitometr* or hydrodensitometr*):ti,ab,kw (610)
#37 ((hydrostatic or underwater or water) near/3 (weighing or analys* or measure*)):ti,ab,kw (517)
#38 absorptiometry or DXA or DEXA:ti,ab,kw (2626)
#39 ((water or air) near/3 displacement):ti,ab,kw (62)
#40 (“air displacement plethysmograph*” or “pea pod” or peapod or “infant body composition system*” or bodpod or “bod pod”):ti,ab,kw (18)
#41 (neutron* near/3 activat*):ti,ab,kw (58)
#42 ((multicomponent* or “multi component*” or multimodal* or “multi modal*” or composit*) near/3 model*):ti,ab,kw (44)
#43 (deuterium near/3 dilut*):ti,ab,kw (31)
#44 #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 (4645)
#45 MeSH descriptor: [Child] explode all trees (64)
#46 MeSH descriptor: [Infant] explode all trees (12,099)
#47 MeSH descriptor: [Adolescent] this term only (69,925)
#48 MeSH descriptor: [Young Adult] this term only (112)
#49 (child* or infant* or pediat* or paediat* or schoolchild* or “school age*” or schoolage*):ti,ab,kw (83,100)
#50 (adolescen* or juvenile* or youth* or teenage* or youngster*):ti,ab,kw (83,300)
#51 (girl or girls or boy or boys or kid or kids):ti,ab,kw (3932)
#52 (“young people” or “young person” or “young persons” or “young adult*”):ti,ab,kw (21,570)
#53 #45 or #46 or #47 or #48 or #49 or #50 or #51 or #52 (149,377)
#54 #12 and #31 and #44 and #53 (170)
Centre for Reviews and Dissemination databases: Database of Abstracts of Reviews of Effects, Health Technology Assessment and NHS Economic Evaluation Database (Centre for Reviews and Dissemination interface)
10 June 2013. Searched 11 June 2013. Retrieved 8 records in DARE, 1 record in HTA and 0 records in NHS EED.
-
MeSH DESCRIPTOR Obesity EXPLODE ALL TREES (685)
-
MeSH DESCRIPTOR Overweight EXPLODE ALL TREES (698)
-
MeSH DESCRIPTOR Weight Gain EXPLODE ALL TREES (108)
-
MeSH DESCRIPTOR Weight Loss EXPLODE ALL TREES (310)
-
(obes* or overweight or “over weight” or “weight gain” or “weight loss”) (1772)
-
MeSH DESCRIPTOR Adiposity EXPLODE ALL TREES (11)
-
MeSH DESCRIPTOR Body Composition EXPLODE ALL TREES (72)
-
MeSH DESCRIPTOR Body Weight EXPLODE ALL TREES (1005)
-
(adiposity or adipose or fatness) (70)
-
((body NEAR2 (composition or fat or weight))) (723)
-
(#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10) (2222)
-
MeSH DESCRIPTOR Body Mass Index EXPLODE ALL TREES (220)
-
MeSH DESCRIPTOR Skinfold Thickness EXPLODE ALL TREES (4)
-
MeSH DESCRIPTOR Waist Circumference EXPLODE ALL TREES (14)
-
MeSH DESCRIPTOR Waist-Hip Ratio EXPLODE ALL TREES (0)
-
MeSH DESCRIPTOR Electric Impedance EXPLODE ALL TREES (14)
-
(((“body mass” NEAR3 (index* or indices)) or bmi or quetelet*)) (927)
-
(((“fat mass” NEAR3 (index* or indices)) or fmi)) (5)
-
(((“fat free mass” NEAR3 (index* or indices)) or ffmi)) (0)
-
((“body adipos*” NEAR3 (index* or indices))) (1)
-
((“body fat” NEAR2 percentage*)) (9)
-
(((“skin fold” or skinfold) NEAR3 (thickness* or test* or measure*))) (48)
-
(((waist or hip or neck) NEAR3 circumference*)) (66)
-
(((waist-to-hip or waist-hip) NEAR3 ratio*)) (22)
-
(((waist-to-height or waist-height) NEAR3 ratio*)) (2)
-
((((bioelectric* or electric*) NEAR3 (impedance or resistance)) or bia)) (28)
-
(((benn* or rohrer* or ponderal or corpulence) NEAR3 (index* or indices))) (6)
-
((“infrared interactance” or NIR)) (7)
-
((“sagittal abdominal diameter*” or “supine abdominal diameter*”)) (0)
-
(#12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29) (983)
-
MeSH DESCRIPTOR Densitometry EXPLODE ALL TREES (81)
-
MeSH DESCRIPTOR Plethysmography EXPLODE ALL TREES (21)
-
MeSH DESCRIPTOR Neutron Activation Analysis EXPLODE ALL TREES (0)
-
((“body volume” NEAR3 (index* or indices))) (0)
-
((densitometr* or hydrodensitometr*)) (61)
-
(((hydrostatic or underwater or water) NEAR3 (weighing or analys* or measure*))) (16)
-
(absorptiometry or DXA or DEXA) (137)
-
(((water or air) NEAR3 displacement)) (7)
-
((“air displacement plethysmograph*” or “pea pod” or peapod or “infant body composition system*” or bodpod or “bod pod”)) (4)
-
((neutron* NEAR3 activat*)) (0)
-
(((multicomponent* or “multi component*” or multimodal* or “multi modal*” or composit*) NEAR3 model*)) (1)
-
((deuterium NEAR3 dilut*)) (1)
-
(#31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42) (196)
-
MeSH DESCRIPTOR Child EXPLODE ALL TREES (3665)
-
MeSH DESCRIPTOR Infant EXPLODE ALL TREES (2258)
-
MeSH DESCRIPTOR Adolescent EXPLODE ALL TREES (3456)
-
MeSH DESCRIPTOR Young Adult EXPLODE ALL TREES (1124)
-
((child* or infant* or pediat* or paediat* or schoolchild* or “school age*” or schoolage*)) (9033)
-
((adolescen* or juvenile* or youth* or teenage* or youngster*)) (4300)
-
((girl or girls or boy or boys or kid or kids)) (278)
-
((“young people” or “young person” or “young persons” or “young adult*”)) (1492)
-
(#44 or #45 or #46 or #47 or #48 or #49 or #50 or #51) (11,234)
-
#11 AND #30 AND #43 AND #52 (9)
Science Citation Index (Web of Science)
1900–7 June 2013. Searched 11 June 2013. Retrieved 1666 records.
| Search term | Number retrieved | |
|---|---|---|
| # 13 | #11 NOT #12 Databases=SCI-EXPANDED Timespan=All years |
1666 |
| # 12 | TS=(rat or rats or mouse or mice or murine or hamster or hamsters or animal or animals or dogs or dog or pig or pigs or cats or bovine or cow or sheep or ovine or porcine or monkey) Databases=SCI-EXPANDED Timespan=All years |
3,774,018 |
| # 11 | #1 AND #6 AND #9 AND #10 Databases=SCI-EXPANDED Timespan=All years |
1721 |
| # 10 | TS=(child* or infant* or pediat* or paediat* or schoolchild* or “school age” or “school aged” or schoolage* or adolescen* or juvenile* or youth* or teenage* or youngster* or girl or girls or boy or boys or kid or kids or “young people” or “young person” or “young persons” or “young adult” or “young adults”) Databases=SCI-EXPANDED Timespan=All years |
1,337,616 |
| # 9 | #7 OR #8 Databases=SCI-EXPANDED Timespan=All years |
134,636 |
| # 8 | TS=((water or air) NEAR/3 displacement) or TS=(“air displacement plethysmography” or “pea pod” or peapod or “infant body composition system” or bodpod or “bod pod”) or TS=(neutron* NEAR/3 activat*) or TS=((multicomponent* or “multi component” or multimodal* or “multi modal” or composit*) NEAR/3 model*) or TS=(deuterium NEAR/3 dilut*) Databases=SCI-EXPANDED Timespan=All years |
40,070 |
| # 7 | TS=(“body volume” NEAR/3 (index* or indices)) or TS=(densitometr* or hydrodensitometr*) or TS=((hydrostatic or underwater or water) NEAR/3 (weighing or analys* or measure*)) or TS=(absorptiometry or DXA or DEXA) Databases=SCI-EXPANDED Timespan=All years |
95,866 |
| # 6 | #2 OR #3 OR #4 OR #5 Databases=SCI-EXPANDED Timespan=All years |
169,334 |
| # 5 | TS=(((bioelectric* or electric*) NEAR/3 (impedance or resistance)) or bia) or TS=(“near infrared interactance” or NIR) or TS=((benn* or rohrer* or ponderal or corpulence) NEAR/3 (index* or indices)) or TS=(sagittal abdominal diameter* or supine abdominal diameter*) Databases=SCI-EXPANDED Timespan=All years |
48,378 |
| # 4 | TS=((waist or hip or neck) NEAR/3 circumference*) or TS=((waist-to-hip or waist-hip) NEAR/3 ratio*) or TS=((waist-to-height or waist-height) NEAR/3 ratio*) Databases=SCI-EXPANDED Timespan=All years |
17,295 |
| # 3 | TS=(“body adiposity” NEAR/3 (index* or indices)) or TS=(“body fat” NEAR/2 percentage*) or TS=((“skin fold” or skinfold) NEAR/3 (thickness* or test* or measure*)) Databases=SCI-EXPANDED Timespan=All years |
6781 |
| # 2 | TS=((“body mass” NEAR/3 (index* or indices)) or bmi or quetelet*) or TS=((“fat mass” NEAR/3 (index* or indices)) or fmi) or TS=((“fat free mass” NEAR/3 (index* or indices)) or ffmi) Databases=SCI-EXPANDED Timespan=All years |
115,175 |
| # 1 | TS=(obes* or overweight or “over weight” or “weight gain” or “weight loss” or adiposity or adipose or fatness) or TS=(body NEAR/2 (composition or fat or weight)) Databases=SCI-EXPANDED Timespan=All years |
452,263 |
Conference Proceedings Citation Index – Science (Web of Science)
1990–7 June 2013. Searched 11 June 2013. Retrieved 80 records.
| Search term | Number retrieved | |
|---|---|---|
| # 11 | #1 AND #6 AND #9 AND #10 Databases=CPCI-S Timespan=All years |
80 |
| # 10 | TS=(child* or infant* or pediat* or paediat* or schoolchild* or “school age” or “school aged” or schoolage* or adolescen* or juvenile* or youth* or teenage* or youngster* or girl or girls or boy or boys or kid or kids or “young people” or “young person” or “young persons” or “young adult” or “young adults”) Databases=CPCI-S Timespan=All years |
134,449 |
| # 9 | #7 OR #8 Databases=CPCI-S Timespan=All years |
26,397 |
| # 8 | TS=((water or air) NEAR/3 displacement) or TS=(“air displacement plethysmography” or “pea pod” or peapod or “infant body composition system” or bodpod or “bod pod”) or TS=(neutron* NEAR/3 activat*) or TS=((multicomponent* or “multi component” or multimodal* or “multi modal” or composit*) NEAR/3 model*) or TS=(deuterium NEAR/3 dilut*) Databases=CPCI-S Timespan=All years |
10,641 |
| # 7 | TS=(“body volume” NEAR/3 (index* or indices)) or TS=(densitometr* or hydrodensitometr*) or TS=((hydrostatic or underwater or water) NEAR/3 (weighing or analys* or measure*)) or TS=(absorptiometry or DXA or DEXA) Databases=CPCI-S Timespan=All years |
15,925 |
| # 6 | #2 OR #3 OR #4 OR #5 Databases=CPCI-S Timespan=All years |
23,800 |
| # 5 | TS=(((bioelectric* or electric*) NEAR/3 (impedance or resistance)) or bia) or TS=(“near infrared interactance” or NIR) or TS=((benn* or rohrer* or ponderal or corpulence) NEAR/3 (index* or indices)) or TS=(sagittal abdominal diameter* or supine abdominal diameter*) Databases=CPCI-S Timespan=All years |
14,242 |
| # 4 | TS=((waist or hip or neck) NEAR/3 circumference*) or TS=((waist-to-hip or waist-hip) NEAR/3 ratio*) or TS=((waist-to-height or waist-height) NEAR/3 ratio*) Databases=CPCI-S Timespan=All years |
886 |
| # 3 | TS=(“body adiposity” NEAR/3 (index* or indices)) or TS=(“body fat” NEAR/2 percentage*) or TS=((“skin fold” or skinfold) NEAR/3 (thickness* or test* or measure*)) Databases=CPCI-S Timespan=All years |
351 |
| # 2 | TS=((“body mass” NEAR/3 (index* or indices)) or bmi or quetelet*) or TS=((“fat mass” NEAR/3 (index* or indices)) or fmi) or TS=((“fat free mass” NEAR/3 (index* or indices)) or ffmi) Databases=CPCI-S Timespan=All years |
9065 |
| # 1 | TS=(obes* or overweight or “over weight” or “weight gain” or “weight loss” or adiposity or adipose or fatness) or TS=(body NEAR/2 (composition or fat or weight)) Databases=CPCI-S Timespan=All years |
48,407 |
Health Management Information Consortium (OvidSP)
1979–March 2013. Searched 11 June 2013. Retrieved 13 records.
-
exp Obesity/ (2727)
-
(obes$ or overweight or over weight or weight gain or weight loss).ti,ab. (3514)
-
exp Body weight/ (842)
-
(adiposity or adipose or (body adj2 (composition or fat or weight)) or fatness).ti,ab. (621)
-
or/1-4 (4574)
-
exp body mass index/ (496)
-
weight size ratios/ (72)
-
((body mass adj3 (index$ or indices)) or bmi or quetelet$).ti,ab. (1674)
-
((fat mass adj3 (index$ or indices)) or fmi).ti,ab. (10)
-
((fat free mass adj3 (index$ or indices)) or ffmi).ti,ab. (4)
-
(body adipos$ adj3 (index$ or indices)).ti,ab. (0)
-
(body fat adj2 percentage$).ti,ab. (31)
-
((skin fold or skinfold) adj3 (thickness$ or test$ or measure$)).ti,ab. (32)
-
((waist or hip or neck) adj3 circumference$).ti,ab. (222)
-
((waist-to-hip or waist-hip) adj3 ratio$).ti,ab. (72)
-
((waist-to-height or waist-height) adj3 ratio$).ti,ab. (10)
-
(((bioelectric$ or electric$) adj3 (impedance or resistance)) or bia).ti,ab. (15)
-
(near infrared interactance or NIR).ti,ab. (1)
-
((benn$ or rohrer$ or ponderal or corpulence) adj3 (index$ or indices)).ti,ab. (5)
-
(sagittal abdominal diameter$ or supine abdominal diameter$).ti,ab. (2)
-
or/6-20 (1881)
-
(body volume adj3 (index$ or indices)).ti,ab. (0)
-
(densitometr$ or hydrodensitometr$).ti,ab. (19)
-
((hydrostatic or underwater or water) adj3 (weighing or analys$ or measure$)).ti,ab. (22)
-
(absorptiometry or DXA or DEXA).ti,ab. (55)
-
((water or air) adj3 displacement).ti,ab. (2)
-
(air displacement plethysmograph$ or pea pod or peapod or infant body composition system$ or bodpod or bod pod).ti,ab. (3)
-
(neutron$ adj3 activat$).ti,ab. (6)
-
((multicomponent$ or multi component$ or multimodal$ or multi modal$ or composit$) adj3 model$).ti,ab. (9)
-
(deuterium adj3 dilut$).ti,ab. (1)
-
or/22-30 (110)
-
exp Children/ or exp Older children/ or exp Pre school children/ (17,728)
-
exp Infants/ (1520)
-
exp Young people/ (9377)
-
exp Young adults/ (281)
-
(child$ or infant$ or pediat$ or paediat$ or schoolchild$ or school age$ or schoolage$).ti,ab. (29,945)
-
(adolescen$ or juvenile$ or youth$ or teenage$ or youngster$).ti,ab. (6446)
-
(girl or girls or boy or boys or kid or kids).ti,ab. (1508)
-
(young people or young person or young persons or young adult$).ti,ab. (5502)
-
or/32-39 (40,506)
-
5 and 21 and 31 and 40 (13)
Trials Register of Promoting Health Interventions (Evidence for Policy and Practice Information and Co-ordinating Centre)
12 June 2013. Searched 12 June 2013. Retrieved 22 records.
1 Freetext: “obes*” OR overweight OR “over weight” OR “weight gain” OR “weight loss” (862)
2 Freetext: adiposity OR adipose OR fatness OR “body composition” or “body fat” or “body weight” (280)
3 1 OR 2 (918)
4 Freetext: “body mass index*” OR “body mass indices” OR bmi OR quetelet* (459)
5 Freetext: “fat mass” NEAR “index*” OR “fat mass” NEAR “indices*” OR fmi (4)
6 Freetext: “fat free mass” NEAR “index*” OR “fat free mass” NEAR “indices*” OR ffmi (3)
7 Freetext: “fat free mass” NEAR “index*” OR “fat free mass” NEAR “indices*” OR ffmi (3)
8 Freetext: “body adipos*” NEAR “index*” OR “body adipos*” NEAR “indices*” (0)
9 Freetext: “body fat” NEAR “percentage*” (29)
10 Freetext: “skin fold” or skinfold (38)
11 Freetext: “waist” NEAR “circumference*” OR “hip” NEAR “circumference*” OR “neck” NEAR “circumference*” (119)
12 Freetext: “waist-to-hip” OR “waist-hip” OR “waist-to-height” OR “waist-height” (36)
13 Freetext: “bioelectric*” NEAR “impedance” OR “electric*” NEAR “impedance” OR “bioelectric*” NEAR “resistance” OR “electric*” NEAR “resistance” (7)
14 Freetext: “benn*” NEAR “index*” OR “rohrer*” NEAR “index*” OR “ponderal” NEAR “index*” OR “corpulence” NEAR “index*” OR “benn*” NEAR “indices*” OR “rohrer*” NEAR “indices*” OR “ponderal” NEAR “indices*” OR “corpulence” NEAR “indices*” (0)
15 Freetext: “infrared interactance” OR NIR OR “sagittal abdominal diameter*” OR “supine abdominal diameter*” (2)
16 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 (520)
17 Freetext: “body volume” NEAR “index*” OR “body volume” NEAR “indices” (0)
18 Freetext: “densitometr*” OR “hydrodensitometr*” (2)
19 Freetext: “hydrostatic” NEAR “weighing” OR “underwater” NEAR “weighing” OR “water” NEAR “weighing” OR “hydrostatic” NEAR “analys*” OR “underwater” NEAR “analys*” OR “water” NEAR “analys*” OR “hydrostatic” NEAR “measure*” OR “underwater” NEAR “measure*” OR “water” NEAR “measure*” (42)
20 Freetext: absorptiometry OR “DXA” OR “DEXA” (22)
21 Freetext: “water” NEAR “displacement” OR “air” NEAR “displacement” (0)
22 Freetext: “plethysmograph*” OR “pea pod” OR “peapod” OR “infant body composition system*” OR bodpod OR “bod pod” (0)
23 Freetext: “multicomponent*” NEAR “model*”OR “multi component*” NEAR “model*”OR “multimodal*” NEAR “model*“OR “multi modal*” NEAR “model*”OR “composit*” NEAR “model*” (46)
24 Freetext: “deuterium” NEAR “dilut*” (0)
25 17 OR 18 OR 19 OR 23 OR 24 OR 25 OR 26 OR 27 (108)
26 Freetext: “child*” OR “infant*” OR “pediat*” OR “paediat*” OR “schoolchild*” OR “school age*” OR “schoolage*” OR “adolescen*” OR “juvenile*” OR “youth*” OR “teenage*” OR “youngster*” OR girl OR girls OR boy OR boys OR kid OR kids OR “young people” OR “young person” OR “young persons” OR “young adult*” (2789)
27 3 AND 16 AND 28 AND 29 (22)
Obesity and Sedentary Behaviour Database (Evidence for Policy and Practice Information and Co-ordinating Centre)
12 June 2013. Searched 12 June 2013. Retrieved 5 records.
-
Freetext: “body mass index*” OR “body mass indices” OR bmi OR quetelet* (226)
-
Freetext: “fat mass” NEAR “index*” OR “fat mass” NEAR “indices*” OR fmi (6)
-
Freetext: “fat free mass” NEAR “index*” OR “fat free mass” NEAR “indices*” OR ffmi (3)
-
Freetext: “body adipos*” NEAR “index*” OR “body adipos*” NEAR “indices*” (0)
-
Freetext: “body fat” NEAR “percentage*” (20)
-
Freetext: “skin fold” or skinfold (17)
-
Freetext: “waist” NEAR “circumference*” OR “hip” NEAR “circumference*” OR “neck” NEAR “circumference*” (22)
-
Freetext: “waist-to-hip” OR “waist-hip” OR “waist-to-height” OR “waist-height” (3)
-
Freetext: “bioelectric*” NEAR “impedance” OR “electric*” NEAR “impedance” OR “bioelectric*” NEAR “resistance” OR “electric*” NEAR “resistance” (9)
-
Freetext: “benn*” NEAR “index*” OR “rohrer*” NEAR “index*” OR “ponderal” NEAR “index*” OR “corpulence” NEAR “index*” OR “benn*” NEAR “indices*” OR “rohrer*” NEAR “indices*” OR “ponderal” NEAR “indices*” OR “corpulence” NEAR “indices*” (0)
-
Freetext: “infrared interactance” OR NIR OR “sagittal abdominal diameter*” OR “supine abdominal diameter*” (0)
-
1 OR 2 OR 3 OR 4 OR 5 OR 7 OR 8 OR 9 OR 10 OR 11 (236)
-
Freetext: “body volume” NEAR “index*” OR “body volume” NEAR “indices” (0)
-
Freetext: “densitometr*” OR “hydrodensitometr*” (0)
-
Freetext: “hydrostatic” NEAR “weighing” OR “underwater” NEAR “weighing” OR “water” NEAR “weighing” OR “hydrostatic” NEAR “analys*” OR “underwater” NEAR “analys*” OR “water” NEAR “analys*” OR “hydrostatic” NEAR “measure*” OR “underwater” NEAR “measure*” OR “water” NEAR “measure*” (3)
-
Freetext: absorptiometry OR “DXA” OR “DEXA” (10)
-
Freetext: “water” NEAR “displacement” OR “air” NEAR “displacement” (1)
-
Freetext: “plethysmograph*” OR “pea pod” OR “peapod” OR “infant body composition system*” OR bodpod (0)
-
Freetext: “multicomponent*” NEAR “model*”OR “multi component*” NEAR “model*”OR “multimodal*” NEAR “model*”OR “multi modal*” NEAR “model*”OR “composit*” NEAR “model*” (3)
-
Freetext: “deuterium” NEAR “dilut*” (0)
-
13 OR 14 OR 15 OR 17 OR 18 OR 19 OR 20 (6)
-
12 AND 21 (5)
OAIster (http://oaister.worldcat.org/)
Searched 12 June 2013. Retrieved 92 records.
Search results for 'kw:(obes* OR overweight OR “weight gain” OR adiposity) kw:(“body mass index*” OR bmi OR quetelet* OR “fat mass index*” OR “fat free mass index*” OR “body adiposity index*” OR “body fat percentage” OR “skin fold” OR skinfold OR “waist circumference*” OR “hip circumference*” OR “neck circumference*” OR “waist-to-hip” OR “waist-hip” OR “waist-to-height” OR “waist-height” OR “bioelectric* impedance” OR “electric* impedance” OR “benn* index*” OR “rohrer* index*” OR “ponderal index*” OR “corpulence index*” OR “sagittal abdominal diameter*” OR “supine abdominal diameter*”) AND (“body volume index*” OR densitometr* OR hydrodensitometr* OR hydrostatic OR “water weighing” OR “water analys*” OR “water measure*” OR absorptiometry OR DXA OR DEXA OR “water displacement” OR “air displacement” OR plethysmograph* OR “pea pod” OR peapod OR bodpod OR “neutron* activat*” OR “multicomponent* model*” OR “multimodal* model*” OR “deuterium dilute*”) kw:(child* OR infant* OR pediat* OR paediat* OR schoolchild* OR “school age*” OR schoolage* OR adolescen* OR juvenile* OR youth* OR teenage* OR youngster* OR “young people” OR “young person” OR “young persons” OR “young adult*”)' limited to Libraries Worldwide.
OpenGrey (www.opengrey.eu/)
Searched 12 June 2013. Retrieved 0 records.
(obes* OR overweight OR “weight gain” OR adiposity) AND (“body volume index*” OR densitometr* OR hydrodensitometr* OR hydrostatic OR “water weighing” OR “water analys*” OR “water measure*” OR absorptiometry OR DXA OR DEXA OR “water displacement” OR “air displacement” OR plethysmograph* OR “pea pod” OR peapod OR bodpod OR “neutron* activat*” OR “multicomponent* model*” OR “multimodal* model*” OR “deuterium dilute*”).
Review of the acceptability and ease of use of childhood measures of obesity
MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations (OvidSP)
1946–2013, November week 3. Searched 29 November 2013. Retrieved 1786 records in MEDLINE and 160 records in MEDLINE In-Process & Other Non-Indexed Citations.
-
exp *Obesity/ (100,481)
-
*Overweight/ (7451)
-
*Adiposity/ (2859)
-
obes$.ti,ab. (165,769)
-
(overweight or over weight).ti,ab. (35,631)
-
adiposity.ti,ab. (13,580)
-
or/1-6 (197,718)
-
exp child/ or exp Infant/ or Adolescent/ (2,890,432)
-
(child$ or infant$ or pediat$ or paediat$ or schoolchild$ or school age$ or schoolage$).ti,ab. (1,257,816)
-
(adolescen$ or juvenile$ or youth$ or teenage$ or youngster$).ti,ab. (251,350)
-
(girl or girls or boy or boys or kid or kids).ti,ab. (161,848)
-
or/8-11 (3,161,861)
-
*body mass index/ (12,360)
-
((body mass adj3 (index$ or indices)) or bmi or quetelet$).ti,ab. (124,654)
-
*Skinfold Thickness/ (869)
-
((skin fold or skinfold) adj3 (thickness$ or test$ or measure$ or ratio$)).ti,ab. (5012)
-
*Waist-Hip Ratio/ (559)
-
((waist-to-hip or waist-hip) adj3 (ratio$ or test$ or measure$)).ti,ab. (6800)
-
((waist-to-height or waist-height) adj3 (ratio$ or test$ or measure$)).ti,ab. (612)
-
or/13-19 (130,736)
-
exp *qualitative research/ (1460)
-
exp *Interviews as Topic/ (4502)
-
exp *questionnaires/ (31,966)
-
qualitative.ti. (19,194)
-
(qualitative adj2 (research or design or analy$ or study or studies)).ab. (31,413)
-
((semi structured or semistructured or “in depth” or indepth or “face to face” or structured) adj3 (interview$ or questionnaire$)).ti,ab. (57,395)
-
focus group$.ti,ab. (20,402)
-
(survey or surveys).ti,ab. (350,023)
-
or/21-28 (469,146)
-
7 and 12 and 20 and 29 (2990)
-
limit 30 to yr=“2008 -Current” (1786)
EMBASE (OvidSP)
1974–2013, week 47. Searched 29 November 2013. Retrieved 1817 records.
-
exp *obesity/ (155,014)
-
obes$.ti,ab. (230,793)
-
(overweight or over weight).ti,ab. (50,932)
-
adiposity.ti,ab. (17,286)
-
or/1-4 (284,389)
-
child/ or preschool child/ or infant/ or adolescent/ (2,393,076)
-
(child$ or infant$ or pediat$ or paediat$ or schoolchild$ or school age$ or schoolage$).ti,ab. (1,609,328)
-
(adolescen$ or juvenile$ or youth$ or teenage$ or youngster$).ti,ab. (321,701)
-
(girl or girls or boy or boys or kid or kids).ti,ab. (216,205)
-
or/6-9 (3,060,352)
-
*body mass/ (13,857)
-
*skinfold thickness/ (878)
-
*waist hip ratio/ (435)
-
*waist to height ratio/ (73)
-
((body mass adj3 (index$ or indices)) or bmi or quetelet$).ti,ab. (192,624)
-
((skin fold or skinfold) adj3 (thickness$ or test$ or measure$ or ratio$)).ti,ab. (6078)
-
((waist-to-hip or waist-hip) adj3 (ratio$ or test$ or measure$)).ti,ab. (9123)
-
((waist-to-height or waist-height) adj3 (ratio$ or test$ or measure$)).ti,ab. (943)
-
or/11-18 (200,267)
-
*qualitative research/ (1999)
-
exp *interview/ (4976)
-
exp *questionnaire/ (21,687)
-
qualitative.ti. (23,346)
-
(qualitative adj2 (research or design or analy$ or study or studies)).ab. (39,253)
-
((semi structured or semistructured or “in depth” or indepth or “face to face” or structured) adj3 (interview$ or questionnaire$)).ti,ab. (73,258)
-
focus group$.ti,ab. (24,951)
-
(survey or surveys).ti,ab. (439,960)
-
or/20-27 (577,107)
-
5 and 10 and 19 and 28 (3065)
-
limit 29 to yr=“2008 -Current” (1981)
-
limit 30 to human (1817)
PsycINFO (OvidSP)
1806–2013, November week 4. Searched 29 November 2013. Retrieved 407 records.
-
obesity/ (14,582)
-
overweight/ (2395)
-
obes$.ti,ab. (21,761)
-
(overweight or over weight).ti,ab. (8389)
-
(adiposity or adipose).ti,ab. (2017)
-
or/1-5 (26,356)
-
(adolescence 13 17 yrs or childhood birth 12 yrs or preschool age 2 5 yrs or school age 6 12 yrs).ag. (580,191)
-
(child$ or infant$ or pediat$ or paediat$ or schoolchild$ or school age$ or schoolage$).ti,ab. (548,894)
-
(adolescen$ or juvenile$ or youth$ or teenage$ or youngster$).ti,ab. (213,993)
-
(girl or girls or boy or boys or kid or kids).ti,ab. (79,108)
-
or/7-10 (857,627)
-
body mass index/ (2341)
-
((body mass adj3 (index$ or indices)) or bmi or quetelet$).ti,ab. (13,959)
-
((skin fold or skinfold) adj3 (thickness$ or test$ or measure$)).ti,ab. (266)
-
((waist-to-hip or waist-hip) adj3 ratio$).ti,ab. (536)
-
((waist-to-height or waist-height) adj3 ratio$).ti,ab. (49)
-
or/12-16 (14,433)
-
qualitative research/ (3954)
-
surveys/ (5716)
-
Interviews/ (6289)
-
questionnaires/ (13,293)
-
qualitative.ti. (12,856)
-
(qualitative adj2 (research or design or analy$ or study or studies)).ab. (39,640)
-
((semi structured or semistructured or “in depth” or indepth or “face to face” or structured) adj3 (interview$ or questionnaire$)).ti,ab. (54,779)
-
focus group$.ti,ab. (18,305)
-
(survey or surveys).ti,ab. (167,456)
-
or/18-26 (277,935)
-
6 and 11 and 17 and 27 (580)
-
limit 28 to (human and yr=“2008 -Current”) (407)
Cumulative Index to Nursing and Allied Health Literature (EBSCOhost)
1981–25 November 2013. Searched 29 November 2013. Retrieved 1087 records.
| Search term | Number retrieved | |
|---|---|---|
| S32 | S30 AND S31 | 1087 |
| S31 | EM 2008 OR EM 2009 OR EM 2010 OR EM 2011 OR EM 2012 OR EM 2013 | 2,101,609 |
| S30 | S4 AND S9 AND S17 AND S29 | 1436 |
| S29 | S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 | 237,317 |
| S28 | TI (survey or surveys) or AB (survey or surveys) | 101,965 |
| S27 | TI (“focus group*”) or AB (“focus group*”) | 13,696 |
| S26 | TI (“semi structured” N3 questionnaire* or semistructured N3 questionnaire* or “in depth” N3 questionnaire* or indepth N3 questionnaire* or “face to face” N3 questionnaire* or structured N3 questionnaire*) or AB (“semi structured” N3 questionnaire* or semistructured N3 questionnaire* or “in depth” N3 questionnaire* or indepth N3 questionnaire* or “face to face” N3 questionnaire* or structured N3 questionnaire*) | 4055 |
| S25 | TI (“semi structured” N3 interview* or semistructured N3 interview* or “in depth” N3 interview* or indepth N3 interview* or “face to face” N3 interview* or structured N3 interview*) or AB (“semi structured” N3 interview* or semistructured N3 interview* or “in depth” N3 interview* or indepth N3 interview* or “face to face” N3 interview* or structured N3 interview*) | 26,782 |
| S24 | AB (qualitative N2 research or qualitative N2 design or qualitative N2 analy* or qualitative N2 study or qualitative N2 studies) | 25,762 |
| S23 | TI (qualitative) | 11,199 |
| S22 | (MH “Surveys”) | 80,428 |
| S21 | (MH “Focus Groups”) | 23,633 |
| S20 | (MH “Structured Questionnaires”) | 3621 |
| S19 | (MH “Structured Interview”) | 7582 |
| S18 | (MH “Qualitative Studies”) | 54,848 |
| S17 | S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 | 55,290 |
| S16 | TI (waist-to-height N3 ratio* or waist-height N3 ratio*) or AB (waist-to-height N3 ratio* or waist-height N3 ratio*) | 152 |
| S15 | TI (waist-to-hip N3 ratio* or waist-hip N3 ratio*) or AB (waist-to-hip N3 ratio* or waist-hip N3 ratio*) | 1080 |
| S14 | TI (“skin fold” N3 thickness* or skinfold N3 thickness* or “skin fold” N3 test* or skinfold N3 test* or “skin fold” N3 measure* or skinfold N3 measure*) or AB (“skin fold” N3 thickness* or skinfold N3 thickness* or “skin fold” N3 test* or skinfold N3 test* or “skin fold” N3 measure* or skinfold N3 measure*) | 831 |
| S13 | TI (“body mass” N3 index* or “body mass” N3 indices or bmi or quetelet*) or AB (“body mass” N3 index* or “body mass” N3 indices or bmi or quetelet*) | 25,156 |
| S12 | (MH “Waist-Hip Ratio”) | 1862 |
| S11 | (MH “Skinfold Thickness”) | 2693 |
| S10 | (MH “Body Mass Index”) | 41,875 |
| S9 | S5 OR S6 OR S7 OR S8 | 583,162 |
| S8 | TI (girl or girls or boy or boys or kid or kids) or AB (girl or girls or boy or boys or kid or kids) | 27,490 |
| S7 | TI (adolescen* or juvenile* or youth* or teenage* or youngster*) or AB (adolescen* or juvenile* or youth* or teenage* or youngster*) | 78,940 |
| S6 | TI (child* or infant* or pediat* or paediat* or schoolchild* or “school age*” or schoolage*) or AB (child* or infant* or pediat* or paediat* or schoolchild* or “school age*” or schoolage*) | 288,578 |
| S5 | (ZG “adolescent: 13-18 years”) or (ZG “child, preschool: 2-5 years”) or (ZG “child: 6-12 years”) | 464,855 |
| S4 | S1 or S2 or S3 | 60,863 |
| S3 | TI (adiposity) or AB (adiposity) | 2421 |
| S2 | TI (obes* or overweight or “over weight”) or AB (obes* or overweight or “over weight”) | 40,025 |
| S1 | (MH “Obesity”) | 47,606 |
Appendix 2 Protocol changes
Review of adult morbidities
Minimum study size of 1000.
Review of tracking of obesity into adulthood
Need for test accuracy data:
-
reference standard in adulthood
-
measures of effect.
Originally modelling and the tracking of obesity, regardless of measurement, increases data and reduces uncertainty in model. As no model studies report RR OR of obesity in adulthood, or use same simple measure as in childhood, do not give accuracy data – no evidence for accuracy in adulthood. Therefore these studies have been identified for future modelling but have not informed the review of predictive accuracy. Need reference standard and data from which accuracy estimates can be derived.
Review of the diagnostic accuracy of obesity measures in childhood
No protocol changes.
Review of the acceptability and ease of use of childhood measures of obesity
No protocol changes.
Appendix 3 Data extraction tables
Review of adult morbidities
| Study | Childhood measurement | Reference data |
|---|---|---|
| Ahlgren (2004)140 | BMI | Internally derived BMI at 14 years divided into median of each quintile |
| Baker (2007)142 | BMI | Internally derived age- and sex-specific z-scores based on health examinations performed between 1955 and 1960 |
| Baker (2007)141 | BMI | Internally derived age- and sex-specific z-scores based on health examinations performed between 1955 and 1960 |
| Barker (2002)143 | BMI | Internally derived age- and sex-specific z-scores based on piecewise linear function, backtransformed into corresponding BMI values |
| Barker (2005)144 | BMI | Internally derived age- and sex-specific z-scores backtransformed into corresponding BMI values |
| Berentzen (2013)145 | BMI | Internally derived |
| Bjorge (2004)146 | BMI | Externala |
| Bjorge (2008)147 | BMI | Externala |
| Cheng (2011)117 | BMI, WC | External CDC 2000219 (age 6 years) and Chinese government standard |
| Cheung (2004)118 | BMI |
|
| De Stavola (2004)148 | BMI | Internally derived age- and sex-specific z-scores |
| Engeland (2003)149 | BMI | Externala |
| Eriksson (2001)150 | BMI | Internally derived age- and sex-specific z-scores based on piecewise linear function. z-scores were backtransformed into corresponding BMI values |
| Forsen (2000)151 | BMI | Internally derived age- and sex-specific z-scores based on piecewise linear function. z-scores were backtransformed into corresponding BMI values |
| Forsen (2004)152 | BMI | Internally derived age- and sex-specific z-scores based on piecewise linear function. z-scores were backtransformed into corresponding BMI values |
| Goldhaber-Fiebert (2013)123 | BMI | Externala |
| Gunnell (1998)153 | BMI |
|
| Hilakivi-Clarke (2001)154 | BMI | Internally derived age- and sex-specific z-scores based on piecewise linear function. z-scores were backtransformed into corresponding BMI values |
| Hypponen (2003)155 | BMI | Internally derived age- and sex-specific z-score |
| Israeli (2007)156 | BMI | Internal, using adult WHO cut-off points (O: ≥ 30 kg/m2; OW: 25.0–29.9 kg/m2) |
| Janssen (2005)157 | BMI | Externala,b |
| Jeffreys (2004)158 | BMI | Internally derived sex-specific z-scores (adjusted for sex in analyses) |
| Lawlor (2005)159 | BMI |
|
| Lawlor (2006)160 | BMI | Internally derived sex- and age-specific z-scores |
| Leiba (2012)161 | BMI | Externala |
| Leiba (2013)162 | BMI | Internally derived BMI quintiles and 2.5 BMI unit increments |
| Levi (2011)163 | BMI | Internally derived (main and secondary analyses) using 85th centile cut-off point and by BMI quintiles |
| Levi (2012)164 | BMI | Internally derived (main and secondary analyses) using 85th centile cut-off point and by BMI quintiles |
| Li (2007)165 | BMI | Externalb |
| Mattsson (2008)167 | BMI | Internally derived age- and sex-specific 80th centile (approximately 17 kg/m2 in children, 21.5 kg/m2 in adolescents) |
| Magnussen (2010)166 | BMI | Externalb |
| Merten (2010)129 | BMI | Externala |
| Morrison (2010)168 | BMI, WCd | Internally derived using 95th centile cut-off point (for both BMI and WC) |
| Osmond (2007)169 | BMI | Internally derived age-specific z-scores (adjusted for sex in analyses) |
| Sachdev (2009)170 | BMI |
|
| Schmidt (2011)171 | BMI, WC, WHR, sum of SFTe | Internally derived quartiles for BMI, WC, SFT (equation NR) |
| Tirosh (2011)172 | BMI |
|
| Study | Cohort | Number at baseline | Number at follow-up | Childhood age (years) | Adult age at final follow-up (years) | Male (%) | Ethnicity (%) | SES (%) | Weight distribution (%) |
|---|---|---|---|---|---|---|---|---|---|
| Ahlgren (2004)140 | Copenhagen | 161,063 | 117,415 | 7–14 | NR | 0 | NR | NR | NR |
| Baker (2007)142 | Copenhagen | 276,835 | NR | 7–13 | NR | 51 | NR | NR | NR |
| Baker (2007)141 | Copenhagen | 276,835 | NR | 7–13 | ≥ 25 | 51 | NR | NR | NR |
| Barker (2002)143 | Helsinki 1934 | 10,519 | 8760 | 1–12 | 27–63 | 53 | NR | NR | NR |
| Barker (2005)144 | Helsinki 1934 | 10,519 | 8760 | 0–11 | 27–64 | 53 | NR | NR | NR |
| Berentzen (2013)145 | Copenhagen | 372,636 | 285,884 | 7–13 | 31–80 | 51 | NR | NR | NR |
| Bjorge (2004)146 | Norway | 227,224 | 227,221 | 14–19 | 47–52 | 51 | NR | NR | OW:a 6 |
| Bjorge (2008)147 | Norway | 227,000 | 226,682 | 14–19 | Mean 52 | 51 | NR | NR | OW:a 6 O:a 1 |
| Cheng (2011)117 | BCAMSS | 2189 | 1184 | 6–16 | Mean 16 (SD 1.8) | 54 | Asian (Chinese) 100 | Urban ‘more affluent’: 80 | OW:b 15.3 O:b 40.8 |
| Cheung (2004)118 | NCDS | 17,000 | 12,327 | 7, 11, 16 | 42 | 52 | NR | NR | OW:c 10.4 (7 years) to 11.4 (16 years) O:c 2.2 (7 years) to 1.4 (16 years) |
| De Stavola (2004)148 | MRC NSHD | 2547 | 2187 | 2–15 | 47–53 | 0 | NR | NR | NR |
| Engeland (2003)149 | Norway | NR | 111,883 | 14–19 | Mean 41 | 0 | NR | NR | Low (< 25th centile): 16 Medium (25th–74th centile): 65 High (75th–84th centile): 11 Very high (≥ 85th centile):a 8 |
| Eriksson (2001)150 | Helsinki 1934 | 5502 | 3544 | 0–12 | 27–63 | 100 | NR | NR | NR |
| Forsen (2004)152 | Helsinki 1934 | 5486 | 3003 | 0–11 | 27–64 | 0 | NR | Low: 68 Medium: 21 High: 11 |
NR |
| Forsen (2000)151 | Helsinki 1924 | NR | 7086 | 6–16 | 31–73 | 51 | NR | Low: 88 High: 4 NR: 8 |
NR |
| Goldhaber-Fiebert (2013)123 | NLSY79/PSID/NHANES | NR | 2780 | 2–15 | 38–49 | 51 | NR | NR | OW:a 9–10 for 5-year-olds; 14–15 for 15-year-olds O:a 12–13 for 5-year-olds; 11–17 for 15-year-olds |
| Gunnell (1998)153 | Boyd Orr | NR | 2399 | 2–14 | Up to 73 | 49 | NR | NR | NR |
| Hilakivi-Clarke (2001)154 | Helsinki 1924 | NR | 3447 | 7 and 15 | Minimum 38 (76% > 50 years) | 0 | NR | NR | NR |
| Hypponen (2003)155 | British birth cohort | 16,751 | 10,683 | 7, 11, 16 | 41 | NR | NR | NR | NR |
| Israeli (2007)156 | Israel SPEC | 18,513 | NR | 16–19 | 26–45 | 100 | NR; nearly all Caucasian | NR | OW:d 7.4 O:d 1.1 |
| Janssen (2005)157 | Bogalusa | 3865 | 1709 | 4–15 | 19–38 | 44 | White: 66 Black: 34 |
NR | HW:a 83.7 OW:a 9.9 O:a 6.4 OW or O:a 16.3 |
| Jeffreys (2004)158 | Boyd Orr | 2997 | 2347 | 2–14 | Up to 66 | 49 | NR | Low: 67 | NR |
| Lawlor (2005)159 | Aberdeen | 12,150 | 11,106 | Mean 4.9 | 48–54 | NR | NR | NR | OW:c 18 O:c 3 |
| Lawlor (2006)160 | Aberdeen | 12,150 | 5793 | Mean 4.9 | 46–50 | NR | NR | NR | OW:c 18 O:c 3 |
| Leiba (2012)161 | Israeli army | NR | 1,110,835 | 16–19 | Mean 35 | 100 | Origin: Europe 41.5; Asia 26.7; Africa 26.3; Israel 5.2 | Low: 27 Medium: 51.3 High: 21.7 |
OW or O:a 12.1 |
| Leiba (2013)162 | Israeli army | NR | 1,110,835 | 16–19 | Mean 44 | 100 | Origin: Europe 41.5; Asia 26.7; Africa 26.3; Israel 5.2 | Low: 27 Medium: 51.3 High: 21.7 |
OW or O:a 12.1 |
| Levi (2011)163 | Israeli army | NR | 1,109,864 | 16–19 | 19–57 | 100 | Origin: Europe 41.5; Asia 26.7; Africa 26.3; Israel 5.2 | NR | OW or O:a 12.5 |
| Levi (2012)164 | Israeli army | NR | 720,927 | 16–19 | 29–56 | 100 | Origin: Europe 41.5; Asia 26.7; Africa 26.3; Israel 5.2 | Low: 28.6 Medium: 48.9 High: 21.6 |
O or OW:a 10 |
| Li (2007)165 | British birth cohort 1958 | 13,294 | 9285 | 7–16 | 45 | 52 | NR | NR | OW:a 8 O:a 2 OW or O:a 10 |
| Mattsson (2008)167 | Young Finns | 4320 | 2195 | 3–18 | 24–39 | 46 | Caucasian 100 | Low: 3.4–13.1 Medium 73.7–86.6 High: 9–17.2 |
NR |
| Magnussen (2010)166 | Young Finns/Bogalusa | 20,745 | 10,439 | 12–19 | 19–26 | 51.1 | White: 55 Asian: 6 Black: 22 Hispanic: 16 Native American: ≈ 1 |
NR | NR |
| Merten (2010)129 | NLSAH | 1889 (PFS 822; NGHS 1067) | Up to 1058 (NGHS) | PFS: mean 12.4 NGHS: NR |
PFS: 32–44 NGHS: 19 |
PFS: 47 NGHS: 0 |
White: 72 Black: 28 |
NR | NR |
| Morrison (2010)168 | NGHS/PFS | NR | 12,439 | 0–11 | NR | 52 | NR | NR | NR |
| Osmond (2007)169 | Helsinki 1934 | 8181 | 1492 | 2–14 | 26–33 | 58 | NR (presumably Asian) | NR | NR |
| Sachdev (2009)170 | Delhi | 8498 | 2188 | 7–15 | 26–36 | 50 | NR | NR | NR |
| Schmidt (2011)171 | ASHFS | NR | 37,674 | Mean 17.1 | Mean 34 | 100 | NR | NR | NR; range from 15 to 36 kg/m2 |
| Tirosh (2011)172 | Israel – SPEC | 161,063 | 117,415 | Median 7.2 to 14.5 | NR | 0 | NR | NR | NR |
Review of tracking of obesity into adulthood
| Study | Country in which study conducted | Study/cohort name | Study dates | Study design | Setting for anthropometric measure in childhood | |
|---|---|---|---|---|---|---|
| Start | Finish | |||||
| Cheng (2011)117 | China | BCAMSS | 2004 | 2010 | Longitudinal | School |
| Cheung (2004)118 | UK | NCDS (1958 British birth cohort) | 1958 | 2000 | Longitudinal | Community |
| Engeland (2004)119 | Norway | None | 1963 | 1999 | Longitudinal | Community |
| Freedman (2001)120 | USA/Canada | Bogalusa | 1973 | 1996 | Longitudinal | School children |
| Freedman (2005)122 | USA/Canada | Bogalusa | 1973 | 1994 | Longitudinal | School children |
| Freedman (2005)121 | USA/Canada | Bogalusa | 1973 | 1996 | Longitudinal | School children |
| Gordon-Larsen (2004)124 | USA/Canada | NLSAH | 1996 | 2002 | Longitudinal | School |
| Goldhaber-Fiebert (2013)123 | USA/Canada | NHANES/NLSY79 | 1970 | 2008 | Longitudinal | Community |
| Juhola (2011)125 | Finland | Cardiovascular Risk in Young Finns | 1980 | 2007 | Longitudinal | NR |
| Juonala (2006)126 | Finland | Cardiovascular Risk in Young Finns | 1980 | 2001 | Longitudinal | NR |
| Liddle (2012)127 | Australia/New Zealand | MUSP | 1986 | NR (follow-up for 18 years) | Longitudinal | NR |
| Mamun (2005)128 | Australia/New Zealand | MUSP | 1986–90 | 2000–4 | Longitudinal | NR |
| Merten (2010)129 | USA/Canada | NLSAH | 1995 | 2001 | Longitudinal | School |
| Nakanio (2010)131 | Japan | Tokushima Prefecture | 2001 | 2008 | Longitudinal | School |
| Nakano (2010)130 | Japan | Tokushima Prefecture | 2001 | 2007 | Longitudinal | School |
| Patton (2011)132 | Australia/New Zealand | None | 1992 | 2003 | Longitudinal | School |
| Power (1997)133 | UK | NCDS (1958 British birth cohort) | 1958 | 1991 | Longitudinal | Community |
| Reilly (2011)134 | UK | ALSPAC | 1998/1999 | 2003/2004 | Longitudinal | Research clinic |
| Starc (2011)135 | Slovenia | 1988–90 Slovenian cohort | 1997 | 2008 | Longitudinal | School |
| Stovitz (2010)136 | USA/Canada | CATCH | 1991 | 2001 | Longitudinal | School |
| Thompson (2007)137 | USA/Canada | NGHS/PFS | 1986 | 1997 | Longitudinal | School |
| Venn (2007)138 | Australia/New Zealand | ASHFS | 1985 | 2005 | Longitudinal | School |
| Wang (2008)139 | USA/Canada | NLSY79 | 1981 | 2002 | Longitudinal | Self-reported; data collected by interview/survey |
| Study | Childhood measure | Reference data/standardisation |
|---|---|---|
| Cheng (2011)117 | BMI | CDC 2000219 > 85th centile (OW)/> 95th centile (O) |
| WC | ‘Chinese reference population’ | |
| Cheung (2004)118 | BMI (kg/m2) | IOTF/Cole/WHO BMI 25 kg/m2 (OW)/30 kg/m2 (O), ROC derived |
| Engeland (2004)119 | BMI (kg/m2) | CDC 2000219 > 85th centile (OW)/> 95th centile (O) (≥ 85th centile very high weight) |
| Freedman (2001)120 | BMI (kg/m2) | The authors used cut-off points < 50th, 50th–74th, 75th–84th, 85th–94th and ≥ 95th centiles. The cut-off point of ≥ 95th centile was defined as OW in the paper, but extracted as O for the review |
| Freedman (2005)122 | BMI (kg/m2) | Children: BMI ≥ 95th centile OW |
| Freedman (2005)121 | BMI (kg/m2) | > 85th–94th centile at risk of OW, > 95th centile OW |
| Goldhaber-Fiebert (2013)123 | BMI (kg/m2) | CDC 2000219 > 85th centile (OW)/> 95th centile (O) |
| Gordon-Larsen (2004)124 | BMI (kg/m2) | IOTF/Cole/WHO BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Juhola (2011)125 | BMI (kg/m2) | IOTF/Cole/WHO BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Juonala (2006)126 | BMI (kg/m2) | BMI 80th–90th centile (OW)/90th centile (O) |
| Liddle (2012)127 | BMI | IOTF/Cole: > 17.42 kg/m2 OW/O for boys and > 17.15 kg/m2 OW/O for girls |
| SFT | One site measured; measurements were converted to a z-score internally adjusted for age and sex. Cut-off points generated proportions of OW/O similar to Cole 2000 BMI subgroups | |
| Mamun (2005)128 | BMI (kg/m2) | IOTF/Cole/WHO BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Merten (2010)129 | BMI (kg/m2) | CDC 2000219 > 95th centile O |
| Nakano (2010)130 | BMI (kg/m2) | IOTF/Cole/WHO BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Nakano (2010)131 | BMI (kg/m2) | IOTF/Cole/WHO BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Patton (2011)132 | BMI (kg/m2) | IOTF/Cole/WHO BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Power (1997)133 | BMI (kg/m2) | UK90 > 91st centile (OW)/≥ 98th centile (O); 95th centile used also |
| Reilly (2011)134 | BMI (kg/m2) | UK90 > 85th centile (OW)/> 95th centile (O) |
| Starc (2011)135 | BMI (kg/m2) | IOTF/Cole/WHO BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Stovitz (2010)136 | BMI (kg/m2) | CDC 2000 reference growth charts BMI > 85th centile (OW)/> 95th centile (O) |
| Thompson (2007)137 | BMI (kg/m2) | CDC 2000219 > 85th centile (OW)/> 95th centile (O). The authors used CDC 95th centile to define OW, but it was extracted as O in this review |
| Venn 2007 138 | BMI (kg/m2) | IOTF/Cole/WHO BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Wang (2008)139 | BMI (kg/m2) | CDC 2000 revised growth chart > 85th centile (OW)/> 95th centile (O) |
| Study | Reference data/standardisation |
|---|---|
| Cheng (2011)117 | CDC 2000219 > 85th centile (OW)/> 95th centile (O) |
| Cheung (2004)118 | IOTF/Cole/WHO adult BMI 25 kg/m2 (OW)/30 kg/m2 (O); cut-off points derived from ROC curves |
| Engeland (2004)119 | IOTF/Cole/WHO adult BMI 25 kg/m2 (OW)/30 kg/m2 (O); the authors used additional intermediate cut-off points |
| Freedman (2001)120 | IOTF/Cole/WHO adult BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Freedman (2005)122 | IOTF/Cole/WHO adult BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Freedman (2005)121 | IOTF/Cole/WHO adult BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Goldhaber-Fiebert (2013)123 | CDC 2000219 > 85th centile (OW)/> 95th centile (O) |
| Gordon-Larsen (2004)124 | IOTF/Cole/WHO adult BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Juhola (2011)125 | IOTF/Cole/WHO adult BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Juonala (2006)126 | IOTF/Cole/WHO adult BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Liddle (2012)127 | IOTF/Cole/WHO adult BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Mamun (2005)128 | IOTF/Cole/WHO adult BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Merten (2010)129 | IOTF/Cole/WHO adult BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Nakano (2010)130 | IOTF (Cole 2000220) children cut-off points |
| Nakano (2010)131 | IOTF/Cole/WHO adult BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Patton (2011)132 | IOTF/Cole/WHO adult BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Power (1997)133 | IOTF/Cole/WHO adult BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Reilly (2011)134 | > 85th centile (OW)/> 95th centile (O) |
| Starc (2011)135 | IOTF/Cole/WHO adult BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Stovitz (2010)136 | IOTF/Cole/WHO adult BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Thompson (2007)137 | IOTF/Cole/WHO adult BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Venn (2007)138 | IOTF/Cole/WHO adult BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Wang (2008)139 | IOTF/Cole/WHO adult BMI 25 kg/m2 (OW)/30 kg/m2 (O) |
| Study | Total n at baseline | Total n at final follow-up | Childhood age (years) | Adult (final follow-up) age (years) | Male (%) | Ethnicity (%) | Weight distribution (%) | SES (%) |
|---|---|---|---|---|---|---|---|---|
| Cheng (2011)117 | 2189 | 1184 | 6–16 | Mean 16 (SD 1.8) | 54 | Asian (Chinese) | OW: 15.3 O: 40.8 |
Urban ‘more affluent’ |
| Cheung (2004)118 | 17,000 | 12,327; analysis on randomly selected 50% sample | 7, 11, 16 | 33 for tracking, 42 for morbidities | 52 (at 7 years) | NR | OW: 10.4 (7 years) to 11.4 (16 years) (whole cohort at baseline) O: 2.2 (7 years) to 1.4 (16 years) (whole cohort at baseline) |
NR |
| Engeland (2004)119 | 227,003 | 128,121 | Mean 17 (range 14–19) | Range 24–54 | NR | NR | OW: 4.9 for boys and 7.3 for girls (OW ≥ 85th centile) |
NR |
| Freedman (2001)120 | 9597 | 2617 | Mean 10 (SD 3), range 2–17 | Mean 27 (SD 5), range 18–37 | 43 | Black: 32 | O: 7 Note: the authors defined ≥ 95th centile as OW but extracted as O here |
NR |
| Freedman (2005)122 | 11,411 | 2610 | Mean 10.0 (SD 3), range 2–17 | Mean 27.5 (range 18–37) | 42.7 | Black: 32 | OW: 7 for boys and 6 for girls | NR |
| Freedman (2005)121 | 7923 | 2392 | Mean 9.7 (range 5–14) | Range 18–37 | 44.9 | Black: 36 | OW: ≈ 7 | NR |
| Goldhaber-Fiebert (2013)123 | NR | 4884 (tracking), 2780 (morbidities) | 2–15 | 18 years (for tracking), 38–49 (for morbidities) | 51 | NR | OW: 9–10 for 5-year-olds, 14–15 for 15-year-olds O: 12–13 for 5-year-olds, 11–17 for 15-year-olds |
NR |
| Gordon-Larsen (2004)124 | 14,438 | 9795 (including total population at 13–15 years, 16–17 years and 18–20 years) | Mean 16.0 (95% CI 15.8 to 16.2), range 13–20 | Mean 21.4 (range 19–26) | 49 | White: 55.9 Asian: 7.5 Black: 20.5 Hispanic: 16.2 (all of whole cohort) |
O: 10.9 (95% CI 9.8 to 12.1) | NR |
| Juhola (2011)125 | 3596 | 2204 | Range 3–18 | 30–45 | 45.1 | NR | NR | NR |
| Juonala (2006)126 | 3596 | 2260 | Range 3–18 | 24–39 | NR | NR | HW/lean: 51 (BMI < 50th centile) OW: 10.5 (BMI 80th–90th centile) O: 8.6 (BMI > 90th centile) |
NR |
| Liddle (2012)127 | 3960 | 1755 | 5 | Mean 20.5 (range 18.2–23.1) | 50 | 98% European descent | NR | NR Maternal education: did not complete secondary school 15%; completed secondary school 64.9%; post-high school 20.1% |
| Mamun (2005)128 | NR | 2794 | 5 | 14 | NR | NR | OW: 17 (OW or O) | NR |
| Merten (2010)129 | 20,745 | 10,439 | Mean 15 (range 12–19) | 22 | 51.1 | White: 55 Asian: 6 Black: 22 Hispanic: 16 Native American: ≈ 1 |
NR | NR |
| Nakano (2010)130 | 22,827 | 16,245 | 8 | 14 | 51.9 | NR | OW: 18.28 for boys and 17.09 for girls O: 5.94 for boys and 4.13 for girls |
NR |
| Nakano (2010)131 | 7506 | 5024 | 7 | 14 | 51.8 | NR | NR | NR |
| Patton (2011)132 | 1943 | 1520 | Mean age 14.9 and 15.5 for two entry points at 1992 and 1993 | 24 | 46 | NR | NR | NR Parental education: one-third had incomplete schooling; one-third completed schooling; half had university degree |
| Power (1997)133 | 17,733 (n = 13,296 at first assessment at age 7 years) |
11,407 | 7–16 | 33 | 51.7 | NR | NR | NR |
| Reilly (2011)134 | 7759 | 5175 | 7 | 13 | 49.4 | NR | HW: 83.6 OW: 8.1 for male and 9.6 for female O: 8.2 for male and 6.8 for female |
By maternal educational attainment: no qualification, 10.4 for males and 10.9 for females; degree qualification, 17.4 for males and 18.4 for females |
| Starc (2011)135 | 21,777 | 4833 | 7.7 (SD 0.3) | 18 | 48.2 | NR | HW: males 81.1, females 82.5 OW: males 13.2, females 13.1 O: males 5.7, females 4.4 |
NR |
| Stovitz (2010)136 | 5106 | 2802 | 8.7 (SD 0.45) | 18.3 (SD 0.5) | 48.8 | White: 74 Black: 12 Hispanic: 10 Other: 4 |
HW: 74.6 OW: 14.9 OW or O: 25.4 O: 10.5 |
NR |
| Thompson (2007)137 | 1963 | 1669 (at age 16 years) | 10–16 | 21–23 | 0 | White: 49 Black: 51 |
OW: at baseline, 7.4–8.7 for Caucasian; 17.4–18.2 for AA (the authors used CDC 95th centile to define OW, but it was extracted as O in the review) Note: the baseline measurements (visit 1) involved girls at age 9 or 10 years |
NR |
| Venn (2007)138 | 8498 | 4571 | 7–15 | 24–34 | 48 (of adults) | NR | OW: boys 8.3, girls 9.7 O: boys 1.5, girls 1.4 |
NR |
| Wang (2008)139 | 2513 | 1309 | 16–17 | 37–38 | 52 | White: 52 Black: 28 Hispanic: 20 |
HW: 89 OW: 8 O: 3 |
NR The authors reported that 47% of the study sample had educational attainment of college or above |
| Author | Population | Obesity measure | Childhood | Adult | Numbers | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age at measure (years) | Definition/cut-off point | Age at measure (years) | Definition/cut-off point | Bad to bad | Bad to good | Good to bad | Bad to bad | |||||
| Good | Bad | Good | Bad | |||||||||
| Nakano131 | Boys and girls | BMI | 7 | ≤ 85th centile | > 85th centile | 14 | ≤ 85th centile | > 85th centile | 458 | 363 | 356 | 3847 |
| Nakano131 | Boys | BMI | 7 | ≤ 85th centile | > 85th centile | 14 | ≤ 85th centile | > 85th centile | 259 | 188 | 192 | 1962 |
| Nakano131 | Girls | BMI | 7 | ≤ 85th centile | > 85th centile | 14 | ≤ 85th centile | > 85th centile | 199 | 175 | 164 | 1885 |
| Gordon-Larsen124 | Boys and girls | BMI | 13–15 | ≤ 95th centile | > 95th centile | 19–26 | < 30 kg/m2 | ≥ 30 kg/m2 | 289 | 62 | 364 | 2537 |
| Gordon-Larsen124 | Boys and girls | BMI | 16–17 | ≤ 95th centile | > 95th centile | 19–26 | < 30 kg/m2 | ≥ 30 kg/m2 | 395 | 71 | 592 | 3142 |
| Gordon-Larsen124 | Boys and girls | BMI | 13–15 | ≤ 85th centile | > 85th centile | 19–26 | < 30 kg/m2 | ≥ 30 kg/m2 | 322 | 91 | 315 | 2521 |
| Gordon-Larsen124 | Boys and girls | BMI | 16–17 | ≤ 85th centile | > 85th centile | 19–26 | < 30 kg/m2 | ≥ 30 kg/m2 | 412 | 84 | 533 | 3176 |
| Stovitz136 | Boys and girls | BMI | 8.7 (SD 0.45) | ≤ 85th centile | > 85th centile | Mean 18.3 (SD 0.5) | ≤ 85th centile | > 85th centile | 566 | 146 | 431 | 1659 |
| Thompson137 | Girls | BMI | 10 | ≤ 95th centile | > 95th centile | 21–23 | < 30 kg/m2 | ≥ 30 kg/m2 | 187 | 84 | 218 | 1474 |
| Thompson137 | Girls | BMI | 11 | ≤ 95th centile | > 95th centile | 21–23 | < 30 kg/m2 | ≥ 30 kg/m2 | 195 | 88 | 193 | 1381 |
| Thompson137 | Girls | BMI | 12 | ≤ 95th centile | > 95th centile | 21–23 | < 30 kg/m2 | ≥ 30 kg/m2 | 211 | 102 | 172 | 1389 |
| Thompson137 | Girls | BMI | 13 | ≤ 95th centile | > 95th centile | 21–23 | < 30 kg/m2 | ≥ 30 kg/m2 | 209 | 80 | 164 | 1354 |
| Thompson137 | Girls | BMI | 14 | ≤ 95th centile | > 95th centile | 21–23 | < 30 kg/m2 | ≥ 30 kg/m2 | 196 | 75 | 145 | 1241 |
| Thompson137 | Girls | BMI | 15 | ≤ 95th centile | > 95th centile | 21–23 | < 30 kg/m2 | ≥ 30 kg/m2 | 202 | 63 | 131 | 1221 |
| Thompson137 | Girls | BMI | 16 | ≤ 95th centile | > 95th centile | 21–23 | < 30 kg/m2 | ≥ 30 kg/m2 | 202 | 57 | 124 | 1286 |
| Mamun128 | Boys and girls | BMI | 5 | ≤ 85th centile | > 85th centile | 14 | ≤ 85th centile | > 85th centile | 296 | 173 | 405 | 1920 |
| Nakano130 | Boys | BMI | 8 | ≤ 85th centile | > 85th centile | 14 | ≤ 85th centile | > 85th centile | 336 | 209 | 155 | 2282 |
| Nakano130 | Girls | BMI | 8 | ≤ 85th centile | > 85th centile | 14 | ≤ 85th centile | > 85th centile | 232 | 232 | 170 | 2081 |
| Nakano130 | Boys | BMI | 8 | ≤ 95th centile | > 95th centile | 14 | ≤ 95th centile | > 95th centile | 63 | 114 | 45 | 2760 |
| Nakano130 | Girls | BMI | 8 | ≤ 95th centile | > 95th centile | 14 | ≤ 95th centile | > 95th centile | 35 | 77 | 25 | 2578 |
| Merten129 | Boys and girls | BMI | 12–19 | ≤ 95th centile | > 95th centile | 19–26 | ≤ 95th centile | > 95th centile | 1081 | 294 | 1579 | 7485 |
| Author | Population | Obesity measure | Childhood | Adulthood | Numbers | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age at measure (years) | Definition/cut-off point | Age at measure (years) | Definition/cut-off point | ||||||||||||||||
| HW | OW | O | HW | OW | O | O to O | O to OW | O to HW | OW to O | OW to OW | OW to HW | HW to O | HW to OW | HW to HW | |||||
| Freedman120 | Boys and girls | BMI | 2–17 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 18–37 | < 25 kg/m2 | 25–29 kg/m2 | 30 kg/m2 | 144 | 30 | 12 | 129 | 84 | 40 | 308 | 555 | 1315 |
| Liddle127 | Boys and girls | BMI | 5 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 18.2–23.1 | < 25 kg/m2 | 25–29 kg/m2 | 30 kg/m2 | 18 | 15 | 11 | 67 | 85 | 78 | 122 | 273 | 1086 |
| Liddle127 | Boys and girls | Triceps SFT | 5 | NR | NR | NR | 18.2–23.1 | < 25 kg/m2 | 25–29 kg/m2 | 30 kg/m2 | 10 | 16 | 22 | 54 | 70 | 114 | 143 | 287 | 1039 |
| Reilly134 | Boys and girls | BMI | 7 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 13 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 281 | 68 | 41 | 152 | 167 | 140 | 206 | 446 | 3674 |
| Reilly134 | Boys | BMI | 7 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 13 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 158 | 34 | 19 | 78 | 62 | 68 | 103 | 222 | 1816 |
| Reilly134 | Girls | BMI | 7 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 13 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 123 | 34 | 22 | 74 | 105 | 72 | 103 | 224 | 1858 |
| Freedman121 | Boys and girls | BMI | 5–14 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 18–37 | < 25 kg/m2 | 25–29 kg/m2 | 30 kg/m2 | 128 | 29 | 16 | 112 | 81 | 32 | 279 | 505 | 1210 |
| Freedman121 | Boys/blacks | BMI | 5–14 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 18–37 | < 25 kg/m2 | 25–29 kg/m2 | 30 kg/m2 | 23 | 2 | 3 | 9 | 10 | 5 | 42 | 73 | 216 |
| Freedman121 | Boys/whites | BMI | 5–14 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 18–37 | < 25 kg/m2 | 25–29 kg/m2 | 30 kg/m2 | 39 | 10 | 6 | 33 | 30 | 7 | 70 | 196 | 300 |
| Freedman121 | Girls/blacks | BMI | 5–14 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 18–37 | < 25 kg/m2 | 25–29 kg/m2 | 30 kg/m2 | 32 | 4 | 2 | 35 | 14 | 6 | 72 | 111 | 201 |
| Freedman121 | Girls/whites | BMI | 5–14 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 18–37 | < 25 kg/m2 | 25–29 kg/m2 | 30 kg/m2 | 34 | 13 | 5 | 35 | 27 | 14 | 94 | 126 | 493 |
| Starc135 | Boys | BMI | 7 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 18 | NR | NR | 30 kg/m2 | 24 | 70 | 27 | 20 | 128 | 131 | 15 | 281 | 1416 |
| Starc135 | Boys | BMI | 11 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 18 | NR | NR | 30 kg/m2 | 23 | 50 | 14 | 23 | 181 | 154 | 3 | 196 | 1272 |
| Starc135 | Girls | BMI | 7 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 18 | NR | NR | 30 kg/m2 | 17 | 45 | 38 | 13 | 88 | 195 | 6 | 118 | 1747 |
| Starc135 | Girls | BMI | 11 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 18 | NR | NR | 30 kg/m2 | 16 | 24 | 9 | 13 | 118 | 196 | 2 | 83 | 1601 |
| Venn138 | Boys and girls | BMI | 7–15 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 24–34 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 37 | 19 | 9 | 174 | 152 | 88 | 354 | 1194 | 2544 |
| Venn138 | Boys | BMI | 7–15 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 24–34 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 15 | 15 | 3 | 77 | 78 | 29 | 196 | 797 | 998 |
| Venn138 | Girls | BMI | 7–15 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 24–34 | ≤ 84th centile | 85th–94th centile | ≥ 95th centile | 22 | 4 | 6 | 97 | 74 | 59 | 158 | 397 | 1546 |
| Cheng117 | Boys and girls | BMI | 6–16 | NR | NR | NR | 12–22 | NR | NR | NR | 309 | 136 | 38 | 33 | 85 | 63 | 10 | 57 | 452 |
| Author | Population | Obesity measure | Childhood | Adulthood | Numbers | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age at measure (years) | Definition/cut-off point (centile) | Age at measure (years) | Definition/cut-off (kg/m2) | ||||||||||||
| Good | Bad | HW | OW | O | Bad to O | Bad to OW | Bad to HW | Good to O | Good to OW | Good to HW | |||||
| Power133 | Boys | BMI | 7 | ≤ 95th | > 95th | 33 | < 25 | 25–29 | 30 | 81 | 87 | 43 | 396 | 1759 | 2039 |
| Power133 | Boys | BMI | 11 | ≤ 95th | > 95th | 33 | < 25 | 25–29 | 30 | 91 | 83 | 34 | 365 | 1673 | 1999 |
| Power133 | Boys | BMI | 16 | ≤ 95th | > 95th | 33 | < 25 | 25–29 | 30 | 98 | 64 | 12 | 303 | 1510 | 1871 |
| Power133 | Girls | BMI | 7 | ≤ 95th | > 95th | 33 | < 25 | 25–29 | 30 | 98 | 59 | 66 | 446 | 1042 | 2776 |
| Power133 | Girls | BMI | 11 | ≤ 95th | > 95th | 33 | < 25 | 25–29 | 30 | 107 | 71 | 40 | 408 | 998 | 2763 |
| Power133 | Girls | BMI | 16 | ≤ 95th | > 95th | 33 | < 25 | 25–29 | 30 | 104 | 62 | 20 | 354 | 929 | 2492 |
| Engeland119 | Boys | BMI | 14–19 | ≤ 85th | > 85th | 24–54 | < 25 | 25–29 | 30 | 1500 | 1316 | 190 | 3833 | 26,265 | 28,418 |
| Engeland119 | Girls | BMI | 14–19 | ≤ 85th | > 85th | 24–54 | < 25 | 25–29 | 30 | 1830 | 1867 | 1185 | 3438 | 14,784 | 43,495 |
| Author | Population | Obesity measure | Childhood | Adulthood | Numbers | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age at measure (years) | Definition/cut-off point (centile) | Age at measure (years) | Definition/cut-off point | ||||||||||||
| HW | OW | O | Good (kg/m2) | Bad (kg/m2) | O to bad | O to good | OW to bad | OW to good | HW to bad | HW to good | |||||
| Freedman122 | Boys | BMI | 2–5 | < 85th | 85th–95th | > 95th | Mean 27.5 (range 18–37) | < 30 | > 30 | NR | NR | 13 | 1 | 23 | 114 |
| Freedman122 | Boys | BMI | 6–8 | < 85th | 85th–95th | > 95th | Mean 27.5 (range 18–37) | < 30 | > 30 | 25 | 7 | 15 | 18 | 37 | 316 |
| Freedman122 | Boys | BMI | 9–11 | < 85th | 85th–95th | > 95th | Mean 27.5 (range 18–37) | < 30 | > 30 | 39 | 12 | 34 | 31 | 59 | 461 |
| Freedman122 | Boys | BMI | 12–14 | < 85th | 85th–95th | > 95th | Mean 27.5 (range 18–37) | < 30 | > 30 | 52 | 7 | 45 | 49 | 76 | 492 |
| Freedman122 | Boys | BMI | 15–17 | < 85th | 85th–95th | > 95th | Mean 27.5 (range 18–37) | < 30 | > 30 | 31 | 5 | 30 | 21 | 62 | 290 |
| Freedman122 | Girls | BMI | 2–5 | < 85th | 85th–95th | > 95th | Mean 27.5 (range 18–37) | < 30 | > 30 | 11 | 4 | 11 | 10 | 41 | 157 |
| Freedman122 | Girls | BMI | 6–8 | < 85th | 85th–95th | > 95th | Mean 27.5 (range 18–37) | < 30 | > 30 | 45 | 9 | 34 | 23 | 87 | 449 |
| Freedman122 | Girls | BMI | 9–11 | < 85th | 85th–95th | > 95th | Mean 27.5 (range 18–37) | < 30 | > 30 | 56 | 16 | 63 | 39 | 107 | 626 |
| Freedman122 | Girls | BMI | 12–14 | < 85th | 85th–95th | > 95th | Mean 27.5 (range 18–37) | < 30 | > 30 | 53 | 11 | 70 | 45 | 96 | 658 |
| Freedman122 | Girls | BMI | 15–17 | < 85th | 85th–95th | > 95th | Mean 27.5 (range 18–37) | < 30 | > 30 | 28 | 4 | 41 | 18 | 77 | 428 |
| Wang139 | Boys and girls | BMI | 16–17 | < 85th | 85th–95th | > 95th | 37–38 | < 30 | > 30 | 39 | 6 | 69 | 32 | 237 | 926 |
| Wang139 | Boys | BMI | 16–17 | < 85th | 85th–95th | > 95th | 37–38 | < 30 | > 30 | 24 | 5 | 33 | 20 | 123 | 479 |
| Wang139 | Girls | BMI | 16–17 | < 85th | 85th–95th | > 95th | 37–38 | < 30 | > 30 | 15 | 1 | 36 | 12 | 114 | 447 |
| Patton132 | Boys and girls | BMI | 14.9–17.4 | < 85th | 85th–95th | > 95th | 24 | < 25 | > 25 | 89 | 10 | 228 | 159 | 163 | 871 |
| Patton132 | Boys | BMI | 14.9–17.4 | < 85th | 85th–95th | > 95th | 24 | < 25 | > 25 | 34 | 2 | 130 | 52 | 105 | 373 |
| Patton132 | Girls | BMI | 14.9 – 17.4 | < 85th | 85th–95th | > 95th | 24 | < 25 | > 25 | 55 | 8 | 98 | 107 | 58 | 498 |
| Patton132 | Boys and girls | BMI | 14.9–17.4 | < 85th | 85th–95th | > 95th | 24 | < 25 | > 25 | 48 | 51 | 38 | 349 | 12 | 1022 |
| Patton132 | Boys | BMI | 14.9–17.4 | < 85th | 85th–95th | > 95th | 24 | < 25 | > 25 | 18 | 18 | 20 | 162 | 5 | 473 |
| Patton132 | Girls | BMI | 14.9–17.4 | < 85th | 85th–95th | > 95th | 24 | < 25 | > 25 | ||||||
| Juonala126 | Boys and girls | BMI | 3–9 | < 85th | 85th–95th | > 95th | 24–39 | < 30 | > 30 | 34 | 65 | 23 | 89 | 50 | 820 |
| Juonala126 | Boys and girls | BMI | 12–18 | < 85th | 85th–95th | > 95th | 24–39 | < 30 | > 30 | 61 | 34 | 34 | 91 | 78 | 881 |
| Juonala126 | Boys and girls | BMI | 3–18 | < 85th | 85th–95th | > 95th | 24–39 | < 30 | > 30 | 95 | 99 | 57 | 180 | 128 | 1701 |
| Author | Sex | Age in childhood (years) | Age in adulthood/adolescence (years) | Sensitivity | Specificity | PPV | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | 95% CI (lower limit) | 95% CI (upper limit) | Estimate | 95% CI (lower limit) | 95% CI (upper limit) | Estimate | 95% CI (lower limit) | 95% CI (upper limit) | ||||
| Gordon-Larsen (2004)124 | Both | 13–15 | 19–26 | 44.3 | 6.2 | 82.4 | 97.6 | 91.7 | 100 | 82.3 | 42.4 | 100 |
| Gordon-Larsen (2004)124 | Both | 16–17 | 19–26 | 40 | 9.4 | 70.6 | 97.8 | 92.7 | 100 | 84.8 | 52.2 | 100 |
| Thompson (2007)137 | Girls | 10 | 21–23 | 46.2 | 0 | 94.8 | 94.6 | 83.4 | 100 | 69 | 13.9 | 100 |
| Thompson (2007)137 | Girls | 11 | 21–23 | 50.3 | 0.5 | 100 | 94 | 81.9 | 100 | 68.9 | 15 | 100 |
| Thompson (2007)137 | Girls | 12 | 21–23 | 55.1 | 5.3 | 100 | 93.2 | 80.4 | 100 | 67.4 | 15.5 | 100 |
| Thompson (2007)137 | Girls | 13 | 21–23 | 56 | 5.6 | 100 | 94.4 | 82.5 | 100 | 72.3 | 20.7 | 100 |
| Thompson (2007)137 | Girls | 14 | 21–23 | 57.5 | 5 | 100 | 94.3 | 81.8 | 100 | 72.3 | 19 | 100 |
| Thompson (2007)137 | Girls | 15 | 21–23 | 60.7 | 8.2 | 100 | 95.1 | 83.3 | 100 | 76.2 | 24.9 | 100 |
| Thompson (2007)137 | Girls | 16 | 21–23 | 62 | 9.3 | 100 | 95.8 | 85.1 | 100 | 78 | 27.5 | 100 |
| Nakano (2010)130 | Boys | 8 | 14 | 58.3 | 0 | 100 | 96 | 88.8 | 100 | 35.6 | 0 | 100 |
| Nakano (2010)130 | Girls | 8 | 14 | 58.3 | 0 | 100 | 97.1 | 90.7 | 100 | 31.3 | 0 | 100 |
| Liddle (2012)127 | Both | 5 | 18–23 | 8.7 | 0 | 47.1 | 98.3 | 91.9 | 100 | 40.9 | 0 | 100 |
| Reilly (2011)134 | Both | 7 | 13 | 44 | 5.5 | 82.5 | 97.6 | 93.1 | 100 | 72.1 | 27.6 | 100 |
| Reilly (2011)134 | Boys | 7 | 13 | 46.6 | 0 | 99.7 | 97.6 | 91.2 | 100 | 74.9 | 16.4 | 100 |
| Reilly (2011)134 | Girls | 7 | 13 | 41 | 0 | 96.7 | 97.6 | 91.4 | 100 | 68.7 | 0.8 | 100 |
| Starc (2011)135 | Boys | 7 | 18 | 40.7 | 0 | 100 | 95.3 | 86.1 | 100 | 19.8 | 0 | 90.8 |
| Starc (2011)135 | Boys | 11 | 18 | 46.9 | 0 | 100 | 96.6 | 88.4 | 100 | 26.4 | 0 | 100 |
| Starc (2011)135 | Girls | 7 | 18 | 47.2 | 0 | 100 | 96.3 | 88.5 | 100 | 17 | 0 | 90.6 |
| Starc (2011)135 | Girls | 11 | 18 | 51.6 | 0 | 100 | 98.4 | 92.9 | 100 | 32.7 | 0 | 100 |
| Venn (2007)138 | Both | 7–15 | 24–34 | 6.5 | 0 | 26.8 | 99.3 | 96.7 | 100 | 56.9 | 0 | 100 |
| Venn (2007)138 | Boys | 7–15 | 24–34 | 5.2 | 0 | 30.8 | 99.1 | 94.9 | 100 | 45.5 | 0 | 100 |
| Venn (2007)138 | Girls | 7–15 | 24–34 | 7.9 | 0 | 39.7 | 99.5 | 96.5 | 100 | 68.8 | 0 | 100 |
| Cheng (2011)117 | Both | 7–16 | 12–22 | 87.8 | 53.6 | 100 | 79.1 | 51.5 | 100 | 64 | 21.2 | 100 |
| Power (1997)133 | Boys | 7 | 33 | 17 | 0 | 50.7 | 96.7 | 91.1 | 100 | 38.4 | 0 | 100 |
| Power (1997)133 | Boys | 11 | 33 | 20 | 0 | 56.7 | 96.9 | 91.4 | 100 | 43.8 | 0 | 100 |
| Power (1997)133 | Boys | 16 | 33 | 24.4 | 0 | 66.4 | 97.8 | 92.9 | 100 | 56.3 | 0 | 100 |
| Power (1997)133 | Girls | 7 | 33 | 18 | 0 | 50.3 | 96.8 | 91.3 | 100 | 43.9 | 0 | 100 |
| Power (1997)133 | Girls | 11 | 33 | 20.8 | 0 | 55.9 | 97.1 | 91.8 | 100 | 49.1 | 0 | 100 |
| Power (1997)133 | Girls | 16 | 33 | 22.7 | 0 | 61.1 | 97.7 | 92.7 | 100 | 55.9 | 0 | 100 |
| Freedman (2005)121 | Boys | 6–8 | 27 | 32.5 | 0 | 100 | 97.9 | 82.7 | 100 | 78.1 | 0 | 100 |
| Freedman (2005)121 | Boys | 9–11 | 27 | 29.5 | 0 | 100 | 97.6 | 84.2 | 100 | 76.5 | 0 | 100 |
| Freedman (2005)121 | Boys | 12–14 | 27 | 30.1 | 0 | 98.5 | 98.7 | 89.2 | 100 | 88.1 | 5.5 | 100 |
| Freedman (2005)121 | Boys | 15–17 | 27 | 25.2 | 0 | 100 | 98.4 | 84.6 | 100 | 86.1 | 0 | 100 |
| Freedman (2005)121 | Girls | 2–5 | 27 | 17.5 | 0 | 100 | 97.7 | 75.2 | 100 | 73.3 | 0 | 100 |
| Freedman (2005)121 | Girls | 6–8 | 27 | 27.1 | 0 | 94.7 | 98.1 | 85.9 | 100 | 83.3 | 0 | 100 |
| Freedman (2005)121 | Girls | 9–11 | 27 | 24.8 | 0 | 81.1 | 97.7 | 86.4 | 100 | 77.8 | 0 | 100 |
| Freedman (2005)121 | Girls | 12–14 | 27 | 24.2 | 0 | 80.9 | 98.5 | 89.6 | 100 | 82.8 | 0 | 100 |
| Freedman (2005)121 | Girls | 15–17 | 27 | 19.2 | 0 | 83.1 | 99.1 | 90.4 | 100 | 87.5 | 0 | 100 |
| Wang (2008)139 | Both | 16–17 | 27 | 11.3 | 0 | 44.7 | 99.4 | 94.5 | 100 | 86.7 | 0 | 100 |
| Wang (2008)139 | Boys | 16–17 | 37–38 | 13.3 | 0 | 62.9 | 99 | 90.3 | 100 | 82.8 | 0 | 100 |
| Wang (2008)139 | Girls | 16–17 | 37–38 | 9.1 | 0 | 53 | 99.8 | 95.7 | 100 | 93.8 | 0 | 100 |
| Juonala (2006)126 | Both | 3–9 | 24–39 | 31.8 | 0 | 100 | 93.3 | 77.6 | 100 | 34.3 | 0 | 100 |
| Juonala (2006)126 | Both | 12–18 | 24–39 | 35.3 | 0 | 100 | 96.6 | 85.4 | 100 | 64.2 | 0 | 100 |
| Juonala (2006)126 | Both | 3–18 | 24–39 | 33.9 | 0 | 89.3 | 95 | 85.4 | 100 | 49 | 0 | 100 |
| Author | Sex | Age in childhood (years) | Age in adulthood/adolescence (years) | Sensitivity | Specificity | PPV | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | 95% CI (lower limit) | 95% CI (upper limit) | Estimate | 95% CI (lower limit) | 95% CI (upper limit) | Estimate | 95% CI (lower limit) | 95% CI (upper limit) | ||||
| Liddle (2012)127 | Both | 5 | 18–23 | 5.7 | 0 | 24.6 | 99.1 | 93.7 | 100 | 75 | 0 | 100 |
| Reilly (2011)134 | Both | 7 | 13 | 26.4 | 2.6 | 50.2 | 98.9 | 95.6 | 100 | 89.5 | 59.1 | 100 |
| Reilly (2011)134 | Boys | 7 | 13 | 29.2 | 0 | 64 | 99 | 94.5 | 100 | 91 | 52.4 | 100 |
| Reilly (2011)134 | Girls | 7 | 13 | 23.7 | 0 | 56.1 | 98.9 | 94.3 | 100 | 87.7 | 39.6 | 100 |
| Freedman (2005)122 | Both | 5–14 | 18–37 | 13.8 | 0 | 33.9 | 98.7 | 92.4 | 100 | 90.8 | 47.7 | 100 |
| Starc (2011)135 | Boys | 7 | 18 | 17.5 | 0 | 49.6 | 98.3 | 91.9 | 100 | 77.7 | 3.5 | 100 |
| Starc (2011)135 | Boys | 11 | 18 | 15.3 | 0 | 47.6 | 99 | 93.9 | 100 | 83.9 | 6.7 | 100 |
| Starc (2011)135 | Girls | 7 | 18 | 21.6 | 0 | 69.2 | 98.1 | 92.1 | 100 | 62 | 0 | 100 |
| Starc (2011)135 | Girls | 11 | 18 | 15.6 | 0 | 60 | 99.5 | 96.2 | 100 | 81.6 | 0 | 100 |
| Venn (2007)138 | Both | 7–15 | 24–34 | 2.9 | 0 | 10.4 | 99.7 | 97.6 | 100 | 86.2 | 2.4 | 100 |
| Venn (2007)138 | Boys | 7–15 | 24–34 | 2.5 | 0 | 11.4 | 99.7 | 96.4 | 100 | 90.9 | 0 | 100 |
| Venn (2007)138 | Girls | 7–15 | 24–34 | 3.5 | 0 | 16.6 | 99.6 | 96.5 | 100 | 81.3 | 0 | 100 |
| Cheng (2011)117 | Both | 7–16 | 12–22 | 70.6 | 35 | 100 | 93.1 | 72 | 100 | 92.1 | 68 | 100 |
| Power (1997)133 | Boys | 7 | 33 | 7.2 | 0 | 17.7 | 97.9 | 91.7 | 100 | 79.6 | 25.2 | 100 |
| Power (1997)133 | Boys | 11 | 33 | 7.9 | 0 | 19.1 | 98.3 | 92.7 | 100 | 83.7 | 33.5 | 100 |
| Power (1997)133 | Boys | 16 | 33 | 8.2 | 0 | 20.3 | 99.4 | 95.9 | 100 | 93.1 | 55.4 | 100 |
| Power (1997)133 | Girls | 7 | 33 | 9.5 | 0 | 23.7 | 97.7 | 92.2 | 100 | 70.4 | 10.5 | 100 |
| Power (1997)133 | Girls | 11 | 33 | 11.2 | 0 | 26.7 | 98.6 | 94.3 | 100 | 81.7 | 30.4 | 100 |
| Power (1997)133 | Girls | 16 | 33 | 11.5 | 0 | 27.9 | 99.2 | 95.7 | 100 | 89.2 | 44.6 | 100 |
| Patton (2011)132 | Both | 15–17 | 24 | 18.5 | 0 | 53.2 | 99 | 93 | 100 | 89.9 | 30.5 | 100 |
| Patton (2011)132 | Boys | 15–17 | 24 | 12.6 | 0 | 52.3 | 99.5 | 92.8 | 100 | 94.4 | 19.3 | 100 |
| Patton (2011)132 | Girls | 15–17 | 24 | 26.1 | 0 | 85.4 | 98.7 | 89.7 | 100 | 87.3 | 5.1 | 100 |
| Patton (2011)132 | Both | 15–17 | 24 | 49 | 0 | 100 | 96.4 | 86.7 | 100 | 48.5 | 0 | 100 |
| Patton (2011)132 | Boys | 15–17 | 24 | 41.9 | 0 | 100 | 97.2 | 84.5 | 100 | 50 | 0 | 100 |
| Author | Sex | Age in childhood (years) | Age in adulthood/adolescence (years) | Sensitivity | Specificity | PPV | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | 95% CI (lower limit) | 95% CI (upper limit) | Estimate | 95% CI (lower limit) | 95% CI (upper limit) | Estimate | 95% CI (lower limit) | 95% CI (upper limit) | ||||
| Gordon-Larsen (2004)124 | Both | 13–15 | 19–26 | 50.5 | 11.7 | 89.3 | 96.5 | 89.5 | 100 | 78 | 38 | 100 |
| Gordon-Larsen (2004)124 | Both | 16–17 | 19–26 | 43.6 | 12 | 75.2 | 97.4 | 91.9 | 100 | 83.1 | 50.1 | 100 |
| Liddle (2012)127 | Both | 5 | 18–23 | 41.1 | 0 | 100 | 87.8 | 71.5 | 100 | 31 | 0 | 85.8 |
| Reilly (2011)134 | Both | 7 | 13 | 67.8 | 31.6 | 100 | 90.8 | 82.4 | 99.2 | 51 | 17.4 | 84.6 |
| Reilly (2011)134 | Boys | 7 | 13 | 69.6 | 20.6 | 100 | 91.8 | 80.4 | 100 | 56.3 | 8.8 | 100 |
| Reilly (2011)134 | Girls | 7 | 13 | 65.7 | 12 | 100 | 89.9 | 77.6 | 100 | 45.8 | 0 | 92.9 |
| Starc (2011)135 | Boys | 7 | 18 | 74.6 | 0 | 100 | 82.7 | 66.3 | 99.1 | 11 | 0 | 41.7 |
| Starc (2011)135 | Boys | 11 | 18 | 93.9 | 26.9 | 100 | 78.6 | 60 | 97.2 | 10.3 | 0 | 38.5 |
| Starc (2011)135 | Girls | 7 | 18 | 83.3 | 0 | 100 | 83.6 | 68.2 | 99 | 7.6 | 0 | 33.7 |
| Starc (2011)135 | Girls | 11 | 18 | 93.5 | 6.7 | 100 | 82.9 | 66.5 | 99.3 | 7.7 | 0 | 34.6 |
| Venn (2007)138 | Both | 7–15 | 24–34 | 37.3 | 0 | 77.2 | 93.3 | 85.6 | 100 | 44.1 | 0 | 88.6 |
| Venn (2007)138 | Boys | 7–15 | 24–34 | 31.9 | 0 | 85.7 | 93.5 | 82.5 | 100 | 42.4 | 0 | 100 |
| Venn (2007)138 | Girls | 7–15 | 24–34 | 43 | 0 | 100 | 93.1 | 82.2 | 100 | 45.4 | 0 | 100 |
| Cheng (2011)117 | Both | 7–16 | 12–22 | 97.2 | 80 | 100 | 61.3 | 28.2 | 94.4 | 51.5 | 13.5 | 89.5 |
| Engeland (2004)119 | Boys | 14–19 | 24–54 | 28.1 | 16 | 40.2 | 97.3 | 96 | 98.6 | 49.9 | 32 | 67.8 |
| Engeland (2004)119 | Girls | 14–19 | 24–54 | 34.7 | 21.8 | 47.6 | 95 | 93.3 | 96.7 | 37.5 | 23.9 | 51.1 |
| Freedman (2005)121 | Boys | 2–5 | 27 | 36.1 | 0 | 100 | 99.1 | 81.8 | 100 | 92.9 | 0 | 100 |
| Freedman (2005)121 | Boys | 6–8 | 27 | 51.9 | 0 | 100 | 92.7 | 65.1 | 100 | 61.5 | 0 | 100 |
| Freedman (2005)121 | Boys | 9–11 | 27 | 55.3 | 0 | 100 | 91.5 | 67.2 | 100 | 62.9 | 0 | 100 |
| Freedman (2005)121 | Boys | 12–14 | 27 | 56.1 | 0 | 100 | 89.8 | 64.5 | 100 | 63.4 | 0 | 100 |
| Freedman (2005)121 | Boys | 15–17 | 27 | 49.6 | 0 | 100 | 91.8 | 61.5 | 100 | 70.1 | 0 | 100 |
| Freedman (2005)121 | Girls | 2–5 | 27 | 34.9 | 0 | 100 | 91.8 | 50.7 | 100 | 61.1 | 0 | 100 |
| Freedman (2005)121 | Girls | 6–8 | 27 | 47.6 | 0 | 100 | 93.3 | 71 | 100 | 71.2 | 0 | 100 |
| Freedman (2005)121 | Girls | 9–11 | 27 | 52.7 | 0 | 100 | 91.9 | 71.4 | 100 | 68.4 | 0 | 100 |
| Freedman (2005)121 | Girls | 12–14 | 27 | 56.2 | 0 | 100 | 92.2 | 72.5 | 100 | 68.7 | 0.8 | 100 |
| Freedman (2005)121 | Girls | 15–17 | 27 | 47.3 | 0 | 100 | 95.1 | 75.2 | 100 | 75.8 | 0 | 100 |
| Wang (2008)139 | Both | 16–17 | 37–38 | 31.3 | 0 | 80.2 | 96.1 | 83.9 | 100 | 74 | 2.8 | 100 |
| Wang (2008)139 | Boys | 16–17 | 37–38 | 31.7 | 0 | 99.7 | 95 | 76 | 100 | 69.5 | 0 | 100 |
| Wang (2008)139 | Girls | 16–17 | 37–38 | 30.9 | 0 | 100 | 97.2 | 82.1 | 100 | 79.7 | 0 | 100 |
| Juonala (2006)126 | Both | 3–9 | 24–39 | 53.3 | 0 | 100 | 84.2 | 61.3 | 100 | 27 | 0 | 86.9 |
| Juonala (2006)126 | Both | 12–18 | 24–39 | 54.9 | 0 | 100 | 87.6 | 67.2 | 100 | 43.2 | 0 | 100 |
| Juonala (2006)126 | Both | 12–18 | 24–39 | 54.3 | 0 | 100 | 85.9 | 70.6 | 100 | 35.3 | 0 | 80.4 |
| Author | Sex | Age in childhood (years) | Age in adulthood/adolescence (years) | Sensitivity | Specificity | PPV | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | 95% CI (lower limit) | 95% CI (upper limit) | Estimate | 95% CI (lower limit) | 95% CI (upper limit) | Estimate | 95% CI (lower limit) | 95% CI (upper limit) | ||||
| Nakano (2010)131 | Both | 7 | 14 | 56.3 | 22.2 | 90.4 | 91.4 | 82.9 | 99.9 | 55.8 | 21.8 | 89.8 |
| Nakano (2010)131 | Boys | 7 | 14 | 57.4 | 11.8 | 100 | 91.3 | 79.4 | 100 | 57.9 | 12.1 | 100 |
| Nakano (2010)131 | Girls | 7 | 14 | 54.8 | 3.6 | 100 | 91.5 | 79.5 | 100 | 53.2 | 2.6 | 100 |
| Stovitz (2010)136 | Both | 9 | 18 | 56.8 | 26.1 | 87.5 | 91.9 | 79.3 | 100 | 79.5 | 49.8 | 100 |
| Nakano (2010)130 | Boys | 8 | 14 | 68.4 | 27.3 | 100 | 91.6 | 80.7 | 100 | 61.7 | 20.9 | 100 |
| Nakano (2010)130 | Girls | 8 | 14 | 57.7 | 9.4 | 100 | 90 | 77.8 | 100 | 50 | 4.5 | 95.5 |
| Liddle (2012)127 | Both | 5 | 18–23 | 31.9 | 0 | 69.8 | 92.4 | 77.2 | 100 | 67.5 | 12 | 100 |
| Reilly (2011)134 | Both | 7 | 13 | 50.6 | 23.6 | 77.6 | 95.3 | 88.6 | 100 | 78.7 | 51.2 | 100 |
| Reilly (2011)134 | Boys | 7 | 13 | 50.5 | 12.3 | 88.7 | 95.4 | 86 | 100 | 79.2 | 40.3 | 100 |
| Reilly (2011)134 | Girls | 7 | 13 | 50.7 | 12.6 | 88.8 | 95.2 | 85.7 | 100 | 78.1 | 39 | 100 |
| Freedman (2005)122 | Both | 5–14 | 18–37 | 30.9 | 4 | 57.8 | 96.2 | 85.6 | 100 | 87.9 | 55.9 | 100 |
| Starc (2011)135 | Boys | 7 | 18 | 45 | 3 | 87 | 90 | 75.2 | 100 | 60.5 | 12.6 | 100 |
| Starc (2011)135 | Boys | 11 | 18 | 58.2 | 13.9 | 100 | 88.3 | 71.7 | 100 | 62.2 | 17.1 | 100 |
| Starc (2011)135 | Girls | 7 | 18 | 56.8 | 0 | 100 | 88.2 | 74 | 100 | 41.2 | 0 | 89.7 |
| Starc (2011)135 | Girls | 11 | 18 | 66.8 | 9.1 | 100 | 88.6 | 73.9 | 100 | 45.5 | 0 | 95.8 |
| Venn (2007)138 | Both | 7–15 | 24–34 | 19.8 | 2 | 37.6 | 96.3 | 89.1 | 100 | 79.7 | 43.7 | 100 |
| Venn (2007)138 | Boys | 7–15 | 24–34 | 15.7 | 0 | 36.5 | 96.9 | 86.3 | 100 | 85.3 | 38.2 | 100 |
| Venn (2007)138 | Girls | 7–15 | 24–34 | 26.2 | 0 | 57.6 | 96 | 86.4 | 100 | 75.2 | 22.9 | 100 |
| Cheng (2011)117 | Both | 7–16 | 12–22 | 89.4 | 65.4 | 100 | 81.7 | 49.5 | 100 | 84.8 | 57.5 | 100 |
| Engeland (2004)119 | Boys | 14–19 | 24–54 | 8.6 | 5.6 | 11.6 | 99.3 | 98.3 | 100 | 93.7 | 85 | 100 |
| Engeland (2004)119 | Girls | 14–19 | 24–54 | 16.9 | 11.9 | 21.9 | 97.3 | 95.8 | 98.8 | 75.7 | 63.7 | 87.7 |
| Patton (2011)132 | Both | 15–17 | 24 | 66 | 23.6 | 100 | 83.8 | 61.4 | 100 | 65.2 | 22.9 | 100 |
| Patton (2011)132 | Boys | 15–17 | 24 | 61 | 2.7 | 100 | 87.4 | 55.9 | 100 | 75.2 | 17.9 | 100 |
| Patton (2011)132 | Girls | 15–17 | 24 | 72.5 | 12.3 | 100 | 81.2 | 50.3 | 100 | 57.1 | 0 | 100 |
| Patton (2011)132 | Both | 15–17 | 24 | 87.8 | 23 | 100 | 71.9 | 48.5 | 95.3 | 17.7 | 0 | 51.6 |
| Patton (2011)132 | Boys | 15–17 | 24 | 88.4 | 0 | 100 | 72.4 | 38.1 | 100 | 17.4 | 0 | 67.7 |
| Population | Measure | Timing of first measure (age in years) | Cut-off point (centile) | Cut-off point (kg/m2) | Children positive (%) | Total n | Sensitivity | 95% CI (upper limit) | 95% CI (lower limit) | Specificity | 95% CI (upper limit) | 95% CI (lower limit) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Boys | BMI | 2 | > 85th | ≥ 30 | 34 | 663 | 51 | 62 | 40 | 68 | 72 | 64 |
| Boys | BMI | 5 | > 85th | ≥ 30 | 21 | 838 | 48 | 57 | 40 | 83 | 86 | 81 |
| Boys | BMI | 10 | > 85th | ≥ 30 | 30 | 1105 | 88 | 93 | 80 | 77 | 79 | 74 |
| Girls | BMI | 2 | > 85th | ≥ 30 | 31 | 675 | 44 | 55 | 33 | 70 | 74 | 66 |
| Girls | BMI | 5 | > 85th | ≥ 30 | 23 | 766 | 52 | 62 | 41 | 81 | 83 | 77 |
| Girls | BMI | 10 | > 85th | ≥ 30 | 32 | 1128 | 84 | 89 | 76 | 75 | 78 | 73 |
| Boys | BMI | 2 | > 95th | ≥ 30 | 24 | 663 | 37 | 49 | 27 | 78 | 81 | 75 |
| Boys | BMI | 5 | > 95th | ≥ 30 | 12 | 838 | 33 | 42 | 26 | 92 | 94 | 90 |
| Boys | BMI | 10 | > 95th | ≥ 30 | 15 | 1105 | 64 | 72 | 55 | 90 | 92 | 88 |
| Girls | BMI | 2 | > 95th | ≥ 30 | 20 | 675 | 31 | 42 | 22 | 81 | 84 | 78 |
| Girls | BMI | 5 | > 95th | ≥ 30 | 13 | 766 | 38 | 48 | 28 | 90 | 92 | 87 |
| Girls | BMI | 10 | > 95th | ≥ 30 | 14 | 1128 | 57 | 65 | 48 | 92 | 93 | 90 |
| Boys | BMI | 2 | > 85th | ≥ 25 | 34 | 663 | 42 | 49 | 36 | 70 | 74 | 65 |
| Boys | BMI | 5 | > 85th | ≥ 25 | 21 | 838 | 34 | 39 | 29 | 85 | 88 | 82 |
| Boys | BMI | 10 | > 85th | ≥ 25 | 30 | 1105 | 64 | 68 | 58 | 86 | 88 | 83 |
| Girls | BMI | 2 | > 85th | ≥ 25 | 31 | 675 | 38 | 45 | 32 | 71 | 75 | 67 |
| Girls | BMI | 5 | > 85th | ≥ 25 | 23 | 766 | 40 | 46 | 34 | 85 | 87 | 81 |
| Girls | BMI | 10 | > 85th | ≥ 25 | 32 | 1128 | 64 | 69 | 59 | 83 | 85 | 80 |
| Boys | BMI | 2 | > 95th | ≥ 25 | 24 | 663 | 31 | 38 | 26 | 80 | 84 | 76 |
| Boys | BMI | 5 | > 95th | ≥ 25 | 12 | 838 | 21 | 26 | 17 | 93 | 95 | 90 |
| Boys | BMI | 10 | > 95th | ≥ 25 | 15 | 1105 | 37 | 42 | 32 | 95 | 96 | 93 |
| Girls | BMI | 2 | > 95th | ≥ 25 | 20 | 675 | 24 | 30 | 18 | 81 | 84 | 77 |
| Girls | BMI | 5 | > 95th | ≥ 25 | 13 | 766 | 25 | 31 | 20 | 92 | 94 | 89 |
| Girls | BMI | 10 | > 95th | ≥ 25 | 14 | 1128 | 36 | 41 | 31 | 96 | 97 | 94 |
| White children | BMI | 2 | > 85th | ≥ 30 | 29 | 659 | 31 | 45 | 20 | 72 | 75 | 68 |
| White children | BMI | 5 | > 85th | ≥ 30 | 20 | 750 | 49 | 59 | 39 | 83 | 86 | 80 |
| White children | BMI | 10 | > 85th | ≥ 30 | 26 | 1018 | 81 | 88 | 71 | 79 | 81 | 76 |
| Black and Hispanic children | BMI | 2 | > 85th | ≥ 30 | 37 | 679 | 54 | 63 | 45 | 66 | 70 | 62 |
| Black and Hispanic children | BMI | 5 | > 85th | ≥ 30 | 24 | 854 | 50 | 59 | 42 | 81 | 84 | 78 |
| Black and Hispanic children | BMI | 10 | > 85th | ≥ 30 | 35 | 1215 | 88 | 92 | 82 | 74 | 76 | 71 |
| White children | BMI | 2 | > 95th | ≥ 30 | 18 | 659 | 19 | 32 | 10 | 82 | 85 | 78 |
| White children | BMI | 5 | > 95th | ≥ 30 | 11 | 750 | 33 | 43 | 24 | 92 | 94 | 90 |
| White children | BMI | 10 | > 95th | ≥ 30 | 11 | 1018 | 55 | 66 | 44 | 93 | 95 | 91 |
| Black and Hispanic children | BMI | 2 | > 95th | ≥ 30 | 25 | 679 | 41 | 51 | 32 | 77 | 81 | 74 |
| Black and Hispanic children | BMI | 5 | > 95th | ≥ 30 | 14 | 854 | 37 | 46 | 29 | 90 | 92 | 87 |
| Black and Hispanic children | BMI | 10 | > 95th | ≥ 30 | 18 | 1215 | 62 | 69 | 55 | 89 | 91 | 87 |
| White children | BMI | 2 | > 85th | ≥ 25 | 29 | 659 | 33 | 40 | 26 | 73 | 77 | 69 |
| White children | BMI | 5 | > 85th | ≥ 25 | 20 | 750 | 37 | 43 | 30 | 86 | 89 | 83 |
| White children | BMI | 10 | > 85th | ≥ 25 | 26 | 1018 | 59 | 65 | 53 | 85 | 88 | 83 |
| Black and Hispanic children | BMI | 2 | > 85th | ≥ 25 | 37 | 679 | 45 | 51 | 39 | 68 | 72 | 63 |
| Black and Hispanic children | BMI | 5 | > 85th | ≥ 25 | 24 | 854 | 36 | 42 | 31 | 84 | 87 | 80 |
| Black and Hispanic children | BMI | 10 | > 85th | ≥ 25 | 35 | 1215 | 67 | 71 | 62 | 83 | 86 | 80 |
| White children | BMI | 2 | > 95th | ≥ 25 | 18 | 659 | 20 | 27 | 14 | 82 | 85 | 78 |
| White children | BMI | 5 | > 95th | ≥ 25 | 11 | 750 | 22 | 28 | 17 | 93 | 95 | 91 |
| White children | BMI | 10 | > 95th | ≥ 25 | 11 | 1018 | 32 | 38 | 26 | 96 | 98 | 95 |
| Black and Hispanic children | BMI | 2 | > 95th | ≥ 25 | 25 | 679 | 33 | 39 | 27 | 79 | 83 | 75 |
| Black and Hispanic children | BMI | 5 | > 95th | ≥ 25 | 14 | 854 | 24 | 29 | 19 | 92 | 94 | 89 |
| Black and Hispanic children | BMI | 10 | > 95th | ≥ 25 | 18 | 1215 | 39 | 44 | 34 | 94 | 96 | 92 |
| Population | First measure | Timing of first measure (age in years) | Cut-off point (kg/m2) | Second measure | Timing of second measure (age in years) | Cut-off point (kg/m2) | Comparison | Total n | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Random 50% – male | BMI | 11 | International BMI = 25.6 | BMI | 33 | 30 | O vs. OW/HW | 2135 | 7.7 | 99.3 | 56.3 | 89.8 |
| Random 50% – male | BMI | 11 | ROC curve BMI = 17.9 | BMI | 33 | 30 | O vs. OW/HW | 2135 | 71.7 | 72.4 | 24.1 | 95.4 |
| Random 50% – male | BMI | 11 | 95th centile BMI = 22.3 | BMI | 33 | 30 | O vs. OW/HW | 2135 | 21.9 | 97.2 | 49 | 91 |
| Random 50% – female | BMI | 11 | International BMI = 26.1 | BMI | 33 | 30 | O vs. OW/HW | 2096 | 6.9 | 99.1 | 51.5 | 88.9 |
| Random 50% – female | BMI | 11 | ROC curve BMI = 18.3 | BMI | 33 | 30 | O vs. OW/HW | 2096 | 75.7 | 69.7 | 25 | 95.6 |
| Random 50% – female | BMI | 11 | 95th centile BMI = 23.2 | BMI | 33 | 30 | O vs. OW/HW | 2096 | 20.2 | 96.3 | 42 | 90 |
| Random 50% – male | BMI | 11 | International BMI = 20.9 | BMI | 33 | 25 | O/OW vs. HW | 2135 | 13.9 | 97.1 | 83.4 | 52.2 |
| Random 50% – male | BMI | 11 | ROC curve BMI = 17.0 | BMI | 33 | 25 | O/OW vs. HW | 2135 | 65.6 | 68.6 | 68.4 | 65.8 |
| Random 50% – male | BMI | 11 | 85th centile BMI = 19.5 | BMI | 33 | 25 | O/OW vs. HW | 2135 | 23.3 | 94 | 80.1 | 54.2 |
| Random 50% – female | BMI | 11 | International BMI = 21.2 | BMI | 33 | 25 | O/OW vs. HW | 2096 | 23 | 95 | 71.3 | 69.5 |
| Random 50% – female | BMI | 11 | ROC curve BMI = 17.5 | BMI | 33 | 25 | O/OW vs. HW | 2096 | 69.8 | 63.6 | 50.9 | 79.6 |
| Random 50% – female | BMI | 11 | 85th centile BMI = 20.5 | BMI | 33 | 25 | O/OW vs. HW | 2096 | 28.8 | 92.7 | 68 | 70.6 |
| Population | First measure | Timing of first measure (age in years) | Cut-off point (kg/m2) | Second measure | Timing of second measure (age in years) | Cut-off point (kg/m2) | Comparison | Total n | AUC | 95% CI (upper limit) | 95% CI (lower limit) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Random 50% – male | BMI | 7 | ROC curve BMI = 17.9 | BMI | 33 | 30 | O vs. OW/HW | 2174 | 0.72 | 0.68 | 0.76 |
| Random 50% – male | BMI | 11 | ROC curve BMI = 17.9 | BMI | 33 | 30 | O vs. OW/HW | 2085 | 0.78 | 0.75 | 0.81 |
| Random 50% – male | BMI | 16 | ROC curve BMI = 17.9 | BMI | 33 | 30 | O vs. OW/HW | 1903 | 0.82 | 0.78 | 0.85 |
| Random 50% – female | BMI | 7 | ROC curve BMI = 18.3 | BMI | 33 | 30 | O vs. OW/HW | 2174 | 0.69 | 0.65 | 0.72 |
| Random 50% – female | BMI | 11 | ROC curve BMI = 18.3 | BMI | 33 | 30 | O vs. OW/HW | 2085 | 0.8 | 0.77 | 0.83 |
| Random 50% – female | BMI | 16 | ROC curve BMI = 18.3 | BMI | 33 | 30 | O vs. OW/HW | 1903 | 0.83 | 0.8 | 0.86 |
| Random 50% – male | BMI | 7 | ROC curve BMI = 17.9 | BMI | 33 | 25 | O/OW vs. HW | 2174 | 0.66 | 0.64 | 0.68 |
| Random 50% – male | BMI | 11 | ROC curve BMI = 17.9 | BMI | 33 | 25 | O/OW vs. HW | 2085 | 0.73 | 0.71 | 0.75 |
| Random 50% – male | BMI | 16 | ROC curve BMI = 17.9 | BMI | 33 | 25 | O/OW vs. HW | 1903 | 0.75 | 0.73 | 0.77 |
| Random 50% – female | BMI | 7 | ROC curve BMI = 18.3 | BMI | 33 | 25 | O/OW vs. HW | 2174 | 0.66 | 0.63 | 0.68 |
| Random 50% – female | BMI | 11 | ROC curve BMI = 18.3 | BMI | 33 | 25 | O/OW vs. HW | 2085 | 0.75 | 0.72 | 0.77 |
| Random 50% – female | BMI | 16 | ROC curve BMI = 18.3 | BMI | 33 | 25 | O/OW vs. HW | 1903 | 0.79 | 0.77 | 0.81 |
| Population | First measure | Timing of first measure (age in years) | Cut-off point (first measure) | Second measure | Timing of second measure (age in years) | Cut-off point (second measure) | Total n | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Boys and girls | BMI | 3 | O: 95th centile | BMI | 30–45 | O: 30 kg/m2 | 314 | 14.6 | 96.7 | 40 | 88.3 |
| Boys and girls | BMI | 6 | O: 95th centile | BMI | 30–45 | O: 30 kg/m2 | 342 | 11.1 | 96.6 | 33.3 | 87.8 |
| Boys and girls | BMI | 9 | O: 95th centile | BMI | 30–45 | O: 30 kg/m2 | 360 | 15.9 | 97.6 | 58.8 | 84.6 |
| Boys and girls | BMI | 12 | O: 95th centile | BMI | 30–45 | O: 30 kg/m2 | 399 | 16.3 | 97.8 | 66.7 | 81 |
| Boys and girls | BMI | 15 | O: 95th centile | BMI | 30–45 | O: 30 kg/m2 | 395 | 18 | 99.7 | 91.7 | 87 |
| Boys and girls | BMI | 18 | O: 95th centile | BMI | 30–45 | O: 30 kg/m2 | 344 | 16.9 | 98.9 | 81.3 | 80.5 |
| Boys and girls | BMI | 3–18 | O: 95th centile | BMI | 30–45 | O: 30 kg/m2 | 2154 | 15.8 | 97.9 | 61.5 | 84.7 |
| Boys | BMI | 3 | IOTF cut-off points | BMI | 30–45 | O: 30 kg/m2 | 153 | 18.2 | 99.2 | 80 | 87.8 |
| Boys | BMI | 6 | IOTF cut-off points | BMI | 30–45 | O: 30 kg/m2 | 142 | 25 | 94.3 | 25 | 88.5 |
| Boys | BMI | 9 | IOTF cut-off points | BMI | 30–45 | O: 30 kg/m2 | 172 | 30 | 92.3 | 45 | 86.2 |
| Boys | BMI | 12 | IOTF cut-off points | BMI | 30–45 | O: 30 kg/m2 | 171 | 38.2 | 97.1 | 76.5 | 86.4 |
| Boys | BMI | 15 | IOTF cut-off points | BMI | 30–45 | O: 30 kg/m2 | 182 | 31.4 | 98.6 | 84.6 | 85.8 |
| Boys | BMI | 18 | IOTF cut-off points | BMI | 30–45 | O: 30 kg/m2 | 155 | 35 | 95.7 | 73.7 | 80.9 |
| Boys | BMI | 3–18 | IOTF cut-off points | BMI | 30–45 | O: 30 kg/m2 | 975 | 30.9 | 96.2 | 65.1 | 85.9 |
| Girls | BMI | 3 | IOTF cut-off points | BMI | 30–45 | O: 30 kg/m2 | 161 | 5.3 | 96.5 | 16.7 | 88.4 |
| Girls | BMI | 6 | IOTF cut-off points | BMI | 30–45 | O: 30 kg/m2 | 200 | 36 | 91.1 | 37.5 | 90.9 |
| Girls | BMI | 9 | IOTF cut-off points | BMI | 30–45 | O: 30 kg/m2 | 188 | 30.3 | 93.6 | 50 | 86.3 |
| Girls | BMI | 12 | IOTF cut-off points | BMI | 30–45 | O: 30 kg/m2 | 228 | 19.2 | 94.3 | 50 | 79.8 |
| Girls | BMI | 15 | IOTF cut-off points | BMI | 30–45 | O: 30 kg/m2 | 213 | 23.1 | 99.5 | 85.7 | 90.3 |
| Girls | BMI | 18 | IOTF cut-off points | BMI | 30–45 | O: 30 kg/m2 | 189 | 21.6 | 98 | 72.7 | 90.3 |
| Girls | BMI | 3–18 | IOTF cut-off points | BMI | 30–45 | O: 30 kg/m2 | 1179 | 22.9 | 95.5 | 50 | 86.4 |
Review of the diagnostic accuracy of obesity measures in childhood
| Author | Population | Age at assessment (years) | Index test details | Index test cut-off point | Reference standard | Reference standard cut-off point | Total n | Sensitivity (95% CI), % | Specificity (95% CI), % |
|---|---|---|---|---|---|---|---|---|---|
| BMI | |||||||||
| Bartok (2011)174 | White girls | 11 | CDC | 82nd centile | DEXA | 95th centile | 172 | 95 (NR) | 83 (NR) |
| Bartok (2011)174 | White girls | 13 | CDC | 82nd centile | DEXA | 95th centile | 151 | 93 (NR) | 88 (NR) |
| Bartok (2011)174 | White girls | 9 | CDC | 85th centile | DEXA | 95th centile | 173 | 90 (NR) | 94 (NR) |
| Bartok (2011)174 | White girls | 15 | CDC | 85th centile | DEXA | 95th centile | 160 | 96 (NR) | 95 (NR) |
| Himes (1989)186 | Boys | 8.4–18.99 | ? | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 159 | 29 (11 to 51) | 99 (96 to 100) |
| Himes (1989)186 | Girls | 8.4–18.99 | ? | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 157 | 23 (10 to 40) | 100 (99 to 100) |
| Himes (1989)186 | All children | 8.4–18.99 | ? | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 316 | 25 (16 to 37) | 100 (98 to 100)a |
| Sproule (2009)198 | Spinal muscular atrophy | 5–18 | CDC | 85th centile | DEXA | 95th centile | 25 | 80 (NR) | 95 (NR) |
| Harrington (2013)185 | White girls | 5–18 | Optimal | 89th centile | DEXA | ? | 83 | 100 (NR) | 90 (NR) |
| Harrington (2013)185 | White boys | 5–18 | Optimal | 94th centile | DEXA | ? | 94 | 100 (NR) | 97 (NR) |
| Field (2003)178 | Unselected | 10 (SD 2.2) | ? | 95th centile | DEXA | 90th centile | 596 | 65 (NR) | 99 (NR) |
| Mei (2006)190 | Unselected | 5–18 | CDC | 95th centile | DEXA | 95th centile | 1196 | 92.5 (NR) | 89.4 (NR) |
| Freedman (2013)180 | Boys | 8–19 | CDC | 95th centile | DEXA | ? | 4518 | 75 (72 to 78)b | 95 (94 to 95)b |
| Freedman (2013)180 | Girls | 8–19 | CDC | 95th centile | DEXA | ? | 2847 | 76 (72 to 80)b | 95 (94 to 96)b |
| Freedman (2013)180 | All children | 8–19 | CDC | 95th centile | DEXA | ? | 7365 | 76 (73 to 78) | 95 (94 to 95)a |
| Reilly (2010)195 | Boys | 9.9 | UK90 | 95th centile | DEXA | 90th centile | 3809 | 96 (94 to 98)b | 95 (94 to 95)b |
| Reilly (2010)195 | Girls | 9.9 | UK90 | 95th centile | DEXA | 90th centile | 3913 | 94 (91 to 96)b | 96 (96 to 97)b |
| Reilly (2010)195 | All children | 9.9 | UK90 | 95th centile | DEXA | 90th centile | 7722 | 95 (94 to 97) | 95 (95 to 96)a |
| Khadgawat (2013)188 | Boys | 7–17 | IOTF | 95th centile | DEXA | 95th centile | 825 | 85 (65 to 96)b | 97 (95 to 98)b |
| Khadgawat (2013)188 | Girls | 7–17 | IOTF | 95th centile | DEXA | 95th centile | 815 | 54 (37 to 69)b | 100 (99 to 100)b |
| Khadgawat (2013)188 | All children | 7–17 | IOTF | 95th centile | DEXA | 95th centile | 1640 | 66 (53 to 77) | 98 (97 to 99)a |
| Khadgawat (2013)188 | Boys | 7–17 | IOTF | 95th centile | DEXA | Prevalence matched to BMI | 825 | 67 (52 to 80)b | 98 (97 to 99)b |
| Khadgawat (2013)188 | Girls | 7–17 | IOTF | 95th centile | DEXA | Prevalence matched to BMI | 815 | 81 (61 to 93)b | 99 (99 to 100)b |
| Khadgawat (2013)188 | All children | 7–17 | IOTF | 95th centile | DEXA | Prevalence matched to BMI | 1640 | 72 (60 to 82) | 99 (98 to 99)a |
| Freedman (2009)179 | Boys | 5–18 | CDC | 95th centile | DEXA | 95th centile | 626 | 75 (65 to 83)b | 95 (93 to 97)b |
| Freedman (2009)179 | Girls | 5–18 | CDC | 95th centile | DEXA | 95th centile | 570 | 80 (70 to 88)b | 97 (94 to 98)b |
| Freedman (2009)179 | All children | 5–18 | CDC | 95th centile | DEXA | 95th centile | 1196 | 77 (70 to 83) | 96 (94 to 97)a |
| Ellis (1999)177 | Boys | 3–18 | UK90 | 95th centile | DEXA (adjusted for sex and ethnicity) | 95th centile | 406 | 76 (53 to 92)b | 91 (88 to 94)b |
| Ellis (1999)177 | Girls | 3–18 | UK90 | 95th centile | DEXA (adjusted for sex and ethnicity) | 95th centile | 573 | 69 (49 to 85)b | 91 (88 to 93)b |
| Ellis (1999)177 | All children | 3–18 | UK90 | 95th centile | DEXA (adjusted for sex and ethnicity) | 95th centile | 979 | 72 (58 to 84) | 91 (89 to 93)a |
| Ellis (1999)177 | Boys | 3–18 | UK90 | 95th centile | DEXA (adjusted for sex) | 95th centile | 406 | 71 (48 to 89)b | 91 (88 to 94)b |
| Ellis (1999)177 | Girls | 3–18 | UK90 | 95th centile | DEXA (adjusted for sex) | 95th centile | 573 | 90 (73 to 98)b | 92 (90 to 94)b |
| Ellis (1999)177 | All children | 3–18 | UK90 | 95th centile | DEXA (adjusted for sex) | 95th centile | 979 | 82 (69 to 91) | 92 (90 to 93)a |
| Wickramasinghe (2005)204 | White boys | 5–14.99 | CDC | 95th centile | D2O | 20% BF | 44 | 3.5 (NR) | 100 (NR) |
| Wickramasinghe (2005)204 | White girls | 5–14.99 | CDC | 95th centile | D2O | 30% BF | 52 | 20 (NR) | 100 (NR) |
| Wickramasinghe (2005)204 | White children | 5–14.99 | CDC | 95th centile | D2O | Boys 20% BF; girls 30% BF | 96 | 6 (1 to 17) | 98 (89 to 100)a |
| Wickramasinghe (2005)204 | Sri Lankan boys | 5–14.99 | CDC | 95th centile | D2O | 20% BF | 27 | 12.5 (NR) | 100 (NR) |
| Wickramasinghe (2005)204 | Sri Lankan girls | 5–14.99 | CDC | 95th centile | D2O | 30% BF | 15 | 14.3 (NR) | 100 (NR) |
| Wickramasinghe (2005)204 | All Sri Lankan children | 5–14.99 | CDC | 95th centile | D2O | Boys 20% BF; girls 30% BF | 42 | 13 (3 to 34) | 100 (82 to 100)a |
| Wickramasinghe (2009)205 | Sri Lankan boys | 5–15 | CDC | 95th centile | D2O | 25% BF | 158 | 19.5 (NR) | 100 (NR) |
| Wickramasinghe (2009)205 | Sri Lankan girls | 5–15 | CDC | 95th centile | D2O | 30% BF | 124 | 16.2 (NR) | 100 (NR) |
| Wickramasinghe (2009)205 | All Sri Lankan children | 5–15 | CDC | 95th centile | D2O | Boys 25% BF; girls 30% BF | 282 | 18 (12 to 24) | 100 (97 to 100)a |
| Sproule (2009)198 | Spinal muscular atrophy | 5–18 | CDC | 95th centile | DEXA | 95th centile | 25 | 40 (NR) | 100 (NR) |
| Wickramasinghe (2009)205 | Sri Lankan boys | 5–15 | IOTF | 95th centile | D2O | 25% BF | 158 | 12.5 (NR) | 100 (NR) |
| Wickramasinghe (2009)205 | Sri Lankan girls | 5–15 | IOTF | 95th centile | D2O | 30% BF | 124 | 8 (NR) | 100 (NR) |
| Wickramasinghe (2009)205 | All Sri Lankan children | 5–15 | IOTF | 95th centile | D2O | Boys 25% BF; girls 30% BF | 282 | 10 (6 to 15) | 100 (97 to 100)a |
| Field (2003)178 | Unselected | 10 (SD 2.2) | SD | 2 | DEXA | 90th centile | 596 | 51 (NR) | 100 (NR) |
| Wickramasinghe (2005)204 | White boys | 5–14.99 | SD | 2 | D2O | 20% BF | 44 | 6.9 (NR) | 93 (NR) |
| Wickramasinghe (2005)204 | Sri Lankan boys | 5–14.99 | SD | 2 | D2O | 20% BF | 27 | 12.5 (NR) | 100 (NR) |
| Wickramasinghe (2005)204 | White girls | 5–14.99 | SD | 2 | D2O | 30% BF | 52 | 5.2 (NR) | 100 (NR) |
| Wickramasinghe (2005)204 | Sri Lankan girls | 5–14.99 | SD | 2 | D2O | 30% BF | 15 | 14.3 (NR) | 100 (NR) |
| Wickramasinghe (2009)205 | Sri Lankan boys | 5–15 | SD | 2 | D2O | 25% BF | 158 | 23.6 (NR) | 100 (NR) |
| Wickramasinghe (2009)205 | Sri Lankan girls | 5–15 | SD | 2 | D2O | 30% BF | 124 | 16.2 (NR) | 100 (NR) |
| Taylor (2003)200 | Boys | 8.5–15.5 | Optimal z-score (adjusted for age) | ? | DEXA | 25% BF | 179 | 85.7 (NR) | 89.2 (NR) |
| Taylor (2003)200 | Girls | 8.5–15.5 | Optimal z-score (adjusted for age) | ? | DEXA | 35% BF | 189 | 86 (NR) | 96.6 (NR) |
| Taylor (2003)200 | Boys | 8.5–15.5 | Optimal z-score (adjusted for age and pubertal status) | ? | DEXA | 25% BF | 179 | 89.8 (NR) | 92.3 (NR) |
| Taylor (2003)200 | Girls | 8.5–15.5 | Optimal z-score (adjusted for age and pubertal status) | ? | DEXA | 35% BF | 189 | 88.4 (NR) | 92.5 (NR) |
| Harrington (2013)185 | Unselected | 5–18 | Optimal | 96th centile | DEXA | ? | 369 | 90 (NR) | 89 (NR) |
| Sproule (2009)198 | Spinal muscular atrophy | 5–18 | CDC | 97th centile | DEXA | 95th centile | 25 | 40 (NR) | 100 (NR) |
| Harrington (2013)185 | AA boys | 5–18 | Optimal | 97th centile | DEXA | ? | 79 | 100 (NR) | 98 (NR) |
| Harrington (2013)185 | AA girls | 5–18 | Optimal | 98th centile | DEXA | ? | 113 | 93 (NR) | 93 (NR) |
| Fujita (2011)181 | Girls | 10 | Optimal | 19.6 | DEXA | 95th centile | 196 | 100 (NR) | 92 (NR) |
| Fujita (2011)181 | Boys | 10 | Optimal | 20.8 | DEXA | 95th centile | 226 | 100 (NR) | 96 (NR) |
| Telford (2008)201 | Boys | 8 | IOTF | 21.6 | DEXA | Mueller | 375 | 87.5 (NR) | 95.6 (NR) |
| Telford (2008)201 | Girls | 8 | IOTF | 21.6 | DEXA | Mueller | 366 | 78.1 (NR) | 97.6 (NR) |
| Telford (2008)201 | All children | 8 | IOTF | 21.6 | DEXA | Mueller | 741 | 80 (64 to 91) | 97 (95 to 98)a |
| Telford (2008)201 | Boys | 8 | IOTF | 21.6 | DEXA | McCarthy | 375 | 26.1 (NR) | 100 (NR) |
| Telford (2008)201 | Girls | 8 | IOTF | 21.6 | DEXA | McCarthy | 366 | 25.4 (NR) | 100 (NR) |
| Telford (2008)201 | All children | 8 | IOTF | 21.6 | DEXA | McCarthy | 741 | 26 (20 to 32) | 100 (99 to 100)a |
| Neovius (2005)193 | Girls | 17 | Optimal | 26.5 | ADP | 95th centile | 274 | 86 (NR) | 98 (NR) |
| Neovius (2005)193 | Boys | 17 | Optimal | 29.2 | ADP | 95th centile | 200 | 40 (NR) | 98 (NR) |
| Zhang (2004)206 | City/suburb-residing girls | 13.5 | IOTF | 30 | DEXA | 35% BF | 414 | 100 (69 to 100)b | 69 (64 to 73)b |
| Zhang (2004)206 | Rural-residing girls | 10.1 | IOTF | 30 | DEXA | 35% BF | 165 | 100 (48 to 100)b | 81 (74 to 86)b |
| Zhang (2004)206 | City/suburb-residing boys | 13.7 | IOTF | 30 | DEXA | 25% BF | 172 | 100 (59 to 100)b | 82 (75 to 87)b |
| Wickramasinghe (2005)204 | White boys | 5–14.99 | IOTF | 30 | D2O | 20% BF | 44 | 0 (NR) | 100 (NR) |
| Wickramasinghe (2005)204 | Sri Lankan boys | 5–14.99 | IOTF | 30 | D2O | 20% BF | 27 | 0 (NR) | 100 (NR) |
| Wickramasinghe (2005)204 | White girls | 5–14.99 | IOTF | 30 | D2O | 30% BF | 52 | 0 (NR) | 100 (NR) |
| Wickramasinghe (2005)204 | Sri Lankan girls | 5–14.99 | IOTF | 30 | D2O | 30% BF | 15 | 0 (NR) | 100 (NR) |
| Relative BMI | |||||||||
| Marshall (1991)189 | Unselected | 7–14 | – | ≥ 120% | Underwater (hydrostatic) weighting | Boys 20% BF; girls 25% BF | 540 | 71.1 (NR) | 91.6 (NR) |
| Marshall (1991)189 | Girls | 7–14 | – | ≥ 120% | Underwater (hydrostatic) weighting | 25% BF | 274 | 74.2 (NR) | 90.5 (NR) |
| Marshall (1991)189 | Boys | 7–14 | – | ≥ 120% | Underwater (hydrostatic) weighting | 20% BF | 266 | 68.9 (NR) | 92.8 (NR) |
| Relative weight | |||||||||
| Marshall (1991)189 | Unselected | 7–14 | – | ≥ 120% | Underwater (hydrostatic) weighting | Boys 20% BF; girls 25% BF | 540 | 51.6 (NR) | 95 (NR) |
| Marshall (1991)189 | Girls | 7–14 | – | ≥ 120% | Underwater (hydrostatic) weighting | 25% BF | 274 | 58.1 (NR) | 95.1 (NR) |
| Marshall (1991)189 | Boys | 7–14 | – | ≥ 120% | Underwater (hydrostatic) weighting | 20% BF | 266 | 48.9 (NR) | 95 (NR) |
| Johnston (1985)187 | Boys | 12–17 | – | ? | Underwater (hydrostatic) weighting | 25% BF | 169 | 52 (33 to 70)b | 86 (79 to 92)b |
| Johnston (1985)187 | Girls | 12–17 | – | ? | Underwater (hydrostatic) weighting | 30% BF | 66 | 29 (10 to 56)b | 94 (83 to 99)b |
| Himes (1989)186 | Boys | 8.4–18.99 | Subscapular | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 159 | 38 (18 to 61) | 99 (97 to 100) |
| Himes (1989)186 | Girls | 8.4–18.99 | Subscapular | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 157 | 30 (15 to 48) | 99 (96 to 100) |
| Himes (1989)186 | Boys | 8.4–18.99 | Sum SFT | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 159 | 57 (35 to 78) | 85 (78 to 90) |
| Himes (1989)186 | Girls | 8.4–18.99 | Sum | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 157 | 80 (63 to 92) | 82 (75 to 88) |
| Himes (1989)186 | Boys | 8.4–18.99 | Triceps | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 159 | 24 (8 to 45) | 100 (99 to 100) |
| Himes (1989)186 | Girls | 8.4–18.99 | Triceps | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 157 | 23 (10 to 40) | 97 (93 to 99) |
| Marshall (1991)189 | Unselected | 7–14 | Sum | 85th centile | Underwater (hydrostatic) weighting | Boys 20% BF; girls 25% BF | 540 | 86.8 (NR) | 90.1 (NR) |
| Marshall (1991)189 | Girls | 7–14 | Sum | 85th centile | Underwater (hydrostatic) weighting | 25% BF | 274 | 96.8 (NR) | 90.5 (NR) |
| Marshall (1991)189 | Boys | 7–14 | Sum | 85th centile | Underwater (hydrostatic) weighting | 20% BF | 266 | 80 (NR) | 89.6 (NR) |
| Marshall (1991)189 | Unselected | 7–14 | Triceps | 85th centile | Underwater (hydrostatic) weighting | Boys 20% BF; girls 25% BF | 540 | 65.8 (NR) | 94 (NR) |
| Marshall (1991)189 | Girls | 7–14 | Triceps | 85th centile | Underwater (hydrostatic) weighting | 25% BF | 274 | 67.7 (NR) | 93.4 (NR) |
| Marshall (1991)189 | Boys | 7–14 | Triceps | 85th centile | Underwater (hydrostatic) weighting | 20% BF | 266 | 64.4 (NR) | 94.6 (NR) |
| Mei (2006)190 | Unselected | 5–18 | Triceps | 95th centile | DEXA | 95th centile | 1196 | 89.6 (NR) | 93.2 (NR) |
| Mei (2006)190 | Unselected | 5–18 | Subscapular | 95th centile | DEXA | 95th centile | 1196 | 89.6 (NR) | 94 (NR) |
| Freedman (2013)180 | Boys | 8–19 | Sum | Elevated: prevalence matched to BMI | DEXA | ? | 4519 | 80 (77 to 83)b | 96 (95 to 96)b |
| Freedman (2013)180 | Girls | 8–19 | Sum | Elevated: prevalence matched to BMI | DEXA | ? | 2846 | 79 (75 to 83)b | 96 (95 to 96)b |
| Freedman (2013)180 | All children | 8–19 | Sum | Elevated: prevalence matched to BMI | DEXA | ? | 7365 | 80 (77 to 82) | 96 (95 to 96)a |
| Johnston (1985)187 | Boys | 12–17 | Triceps | ? | Underwater (hydrostatic) weighting | 25% BF | 169 | 48 (30 to 67)b | 96 (91 to 98)b |
| Johnston (1985)187 | Girls | 12–17 | Triceps | ? | Underwater (hydrostatic) weighting | 30% BF | 66 | 24 (7 to 50)b | 100 (93 to 100)b |
| Johnston (1985)187 | All children | 12–17 | Triceps | ? | Underwater (hydrostatic) weighting | Boys 25% BF; girls 30% BF | 235 | 40 (26 to 55) | 97 (93 to 99)a |
| WC | |||||||||
| Neovius (2005)193 | Girls | 17 | WC smallest between ribs and iliac crest | 85th centile | ADP | 95th centile | 274 | 64 (NR) | 98 (NR) |
| Neovius (2005)193 | Boys | 17 | WC smallest between ribs and iliac crest | 95th centile | ADP | 95th centile | 200 | 50 (NR) | 98 (NR) |
| Reilly (2010)195 | Boys | 9.9 | UK 1988 reference | 95th centile | DEXA | 90th centile | 3809 | 97 (95 to 99)b | 81 (79 to 82)b |
| Reilly (2010)195 | Girls | 9.9 | UK 1988 reference | 95th centile | DEXA | 90th centile | 3913 | 98 (95 to 99)b | 81 (79 to 82)b |
| Wickramasinghe (2009)205 | Sri Lankan boys | 5–15 | WC smallest between ribs and iliac crest | 98th centile | D2O | 25% BF | 158 | 34.7 (NR) | 98.8 (NR) |
| Wickramasinghe (2009)205 | Sri Lankan girls | 5–15 | WC smallest between ribs and iliac crest | 98th centile | D2O | 30% BF | 124 | 38.4 (NR) | 100 (NR) |
| Wickramasinghe (2009)205 | Sri Lankan girls | 5–15 | WC smallest between ribs and iliac crest | 98th centile | D2O | Boys 25% BF; girls 30% BF | 282 | 37 (30 to 45) | 99 (95 to 100)a |
| Fujita (2011)181 | Boys | 10 | WC umbilical | 76.5 | DEXA | 95th centile | 226 | 100 (NR) | 97 (NR) |
| Fujita (2011)181 | Girls | 10 | WC umbilical | 73 | DEXA | 95th centile | 196 | 100 (NR) | 96 (NR) |
| WHR | |||||||||
| Neovius (2005)193 | Boys | 17 | WC smallest between ribs and iliac crest | 0.9 | ADP | 95th centile | 200 | 40 (NR) | 97 (NR) |
| Neovius (2005)193 | Girls | 17 | WC smallest between ribs and iliac crest | 1.02 | ADP | 95th centile | 274 | 0 (NR) | 100 (NR) |
| WHtR | |||||||||
| Fujita (2011)181 | Boys | 10 | WC umbilical | 0.519 | DEXA | 95th centile | 226 | 100 (NR) | 95 (NR) |
| Fujita (2011)181 | Girls | 10 | WC umbilical | 0.499 | DEXA | 95th centile | 196 | 100 (NR) | 95 (NR) |
| Author | Population | Age at assessment (years) | Index test details | Index test cut-off point | Reference standard | Reference standard cut-off point | Total n | Sensitivity (95% CI), % | Specificity (95% CI), % |
|---|---|---|---|---|---|---|---|---|---|
| BMI | |||||||||
| Bartok (2011)174 | White girls | 9 | CDC | 73rd centile | DEXA | 85th centile | 173 | 92 (NR) | 91 (NR) |
| Bartok (2011)174 | White girls | 13 | CDC | 77th centile | DEXA | 85th centile | 151 | 91 (NR) | 89 (NR) |
| Bartok (2011)174 | White girls | 15 | CDC | 78th centile | DEXA | 85th centile | 160 | 69 (NR) | 94 (NR) |
| Bartok (2011)174 | White girls | 11 | CDC | 81st centile | DEXA | 85th centile | 172 | 85 (NR) | 96 (NR) |
| Neovius (2004)192 | Boys | 16.9 (SD 0.4) | Göteborg, Sweden | 85th centile | ADP | 25% BF | 200 | 92 (NR) | 93 (NR) |
| Neovius (2004)192 | Girls | 16.9 (SD 0.4) | Göteborg, Sweden | 85th centile | ADP | 30% BF | 274 | 39 (NR) | 97 (NR) |
| Neovius (2004)192 | All children | 16.9 (SD 0.4) | Göteborg, Sweden | 85th centile | ADP | Boys 25% BF; girls 30% BF | 474 | 48 (40 to 57) | 95 (92 to 97)a |
| Neovius (2004)192 | Boys | 16.9 (SD 0.4) | WHO | 85th centile | ADP | 25% BF | 200 | 68 (NR) | 98 (NR) |
| Neovius (2004)192 | Girls | 16.9 (SD 0.4) | WHO | 85th centile | ADP | 30% BF | 274 | 19 (NR) | 100 (NR) |
| Neovius (2004)192 | All children | 16.9 (SD 0.4) | WHO | 85th centile | ADP | Boys 25% BF; girls 30% BF | 474 | 28 (20 to 36) | 99 (97 to 100)a |
| Sproule (2009)198 | Spinal muscular atrophy | 5–18 | CDC | 85th centile | DEXA | 85th centile | 25 | 50 (NR) | 100 (NR) |
| Freedman (2013)180 | Boys | 8–19 | CDC | 85th centile | DEXA | ? | 4518 | 83 (81 to 84)b | 91 (90 to 92)b |
| Freedman (2013)180 | Girls | 8–19 | CDC | 85th centile | DEXA | ? | 2847 | 80 (77 to 82)b | 90 (88 to 91)b |
| Freedman (2009)179 | Boys | 5–18 | CDC | 85th centile | DEXA | 85th centile | 626 | 84 (78 to 88)b | 92 (89 to 95)b |
| Freedman (2009)179 | Girls | 5–18 | CDC | 85th centile | DEXA | 85th centile | 570 | 83 (77 to 88)b | 92 (89 to 94)b |
| Freedman (2009)179 | All children | 5–18 | CDC | 85th centile | DEXA | 85th centile | 1196 | 83 (79 to 87) | 92 (90 to 94)a |
| Moreno (2006)191 | Boys | 13–17.9 | AVENA | 85th centile | DEXA | 85th centile | 116 | 53 (28 to 77) | 88 (79 to 94) |
| Moreno (2006)191 | Girls | 13–17.9 | AVENA | 85th centile | DEXA | 85th centile | 170 | 79 (58 to 93) | 92 (86 to 96) |
| Moreno (2006)191 | All children | 13–17.9 | AVENA | 85th centile | DEXA | 85th centile | 286 | 67 (53 to 78) | 90 (86 to 94)a |
| Moreno (2006)191 | Boys | 13–17.9 | IOTF | 85th centile | DEXA | 85th centile | 116 | 71 (44 to 90) | 86 (77 to 92) |
| Moreno (2006)191 | Girls | 13–17.9 | IOTF | 85th centile | DEXA | 85th centile | 170 | 75 (53 to 90) | 90 (84 to 95) |
| Moreno (2006)191 | All children | 13–17.9 | IOTF | 85th centile | DEXA | 85th centile | 286 | 73 (60 to 84) | 88 (84 to 92)a |
| Khadgawat (2013)188 | Boys | 7–17 | IOTF | 85th centile | DEXA | 85th centile | 825 | 78 (71 to 85)b | 91 (89 to 93)b |
| Khadgawat (2013)188 | Girls | 7–17 | IOTF | 85th centile | DEXA | 85th centile | 815 | 64 (55 to 72)b | 94 (92 to 96)b |
| Khadgawat (2013)188 | All children | 7–17 | IOTF | 85th centile | DEXA | 85th centile | 1640 | 72 (66 to 77) | 93 (91 to 94)a |
| Khadgawat (2013)188 | Boys | 7–17 | IOTF | 85th centile | DEXA | Prevalence matched to BMI | 825 | 77 (70 to 83)b | 94 (92 to 95)b |
| Khadgawat (2013)188 | Girls | 7–17 | IOTF | 85th centile | DEXA | Prevalence matched to BMI | 815 | 65 (56 to 73)b | 94 (92 to 96)b |
| Khadgawat (2013)188 | All children | 7–17 | IOTF | 85th centile | DEXA | Prevalence matched to BMI | 1640 | 72 (67 to 77) | 94 (93 to 95)a |
| Ellis (1999)177 | Boys | 3–18 | UK90 | 85th centile | DEXA (adjusted for sex and ethnicity) | 85th centile | 406 | 92 (82 to 97)b | 84 (79 to 87)b |
| Ellis (1999)177 | Girls | 3–18 | UK90 | 85th centile | DEXA (adjusted for sex and ethnicity) | 85th centile | 573 | 92 (84 to 97)b | 82 (78 to 85)b |
| Ellis (1999)177 | All children | 3–18 | UK90 | 85th centile | DEXA (adjusted for sex and ethnicity) | 85th centile | 979 | 92 (86 to 96) | 83 (80 to 85)a |
| Ellis (1999)177 | Boys | 3–18 | UK90 | 85th centile | DEXA (adjusted for sex) | 85th centile | 406 | 90 (80 to 96)b | 83 (79 to 87)b |
| Ellis (1999)177 | Girls | 3–18 | UK90 | 85th centile | DEXA (adjusted for sex) | 85th centile | 573 | 94 (87 to 98)b | 83 (79 to 86)b |
| Ellis (1999)177 | All children | 3–18 | UK90 | 85th centile | DEXA (adjusted for sex) | 85th centile | 979 | 93 (87 to 96) | 83 (80 to 85)a |
| Sarria (2001)197 | Boys | 7–16.9 | z-scores | 85th centile | Underwater (hydrostatic) weighting | 85th centile | 175 | 50 (30 to 70) | 91 (85 to 95) |
| Warner (1997)203 | All children | ? | SD scores | 85th centile/1 | DEXA | US 85th centile | 143 | 66 (52 to 78) | 94 (86 to 98) |
| Warner (1997)203 | Cancer survivors | 12 (SD 3.7) | SD scores | 85th centile/1 | DEXA | US 85th centile | 43 | 68 (47 to 85) | 88 (62 to 98) |
| Warner (1997)203 | Growth hormone-deficient | 15.7 (SD 1.2) | SD scores | 85th centile/1 | DEXA | US 85th centile | 27 | 70 (35 to 93) | 94 (71 to 100) |
| Warner (1997)203 | Inflammatory bowel disease | 14.3 (SD 2.8) | SD scores | 85th centile/1 | DEXA | US 85th centile | 33 | 55 (23 to 83) | 96 (77 to 100) |
| Warner (1997)203 | Healthy | 11.8 (SD 3.1) | SD scores | 85th centile/1 | DEXA | US 85th centile | 40 | 67 (35 to 90) | 96 (81 to 100) |
| Pandit (2009)194 | Boys | 6–17 | CDC z-/SD score | 1 | DEXA | 85th centile | 316 | 77 (NR) | 97 (NR) |
| Pandit (2009)194 | Girls | 6–17 | CDC z-/SD score | 1 | DEXA | 85th centile | 250 | 83 (NR) | 97 (NR) |
| Pandit (2009)194 | All children | 6–17 | CDC z-/SD score | 1 | DEXA | 85th centile | 566 | 66 (59 to 72) | 98 (96 to 99)a |
| Dung (2006)176 | Boys referred for hospital treatment | 11.9 | German reference | 90th centile | DEXA | 90th centile | 191 | 87 (79 to 93)b | 92 (85 to 97)b |
| Dung (2006)176 | Girls referred for hospital treatment | 12.1 | German reference | 90th centile | DEXA | 90th centile | 202 | 82 (73 to 89)b | 96 (90 to 99)b |
| Dung (2006)176 | All children referred for hospital treatment | 12.1 | German reference | 90th centile | DEXA | 90th centile | 393 | 85 (79 to 90) | 94 (90 to 97)a |
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – pubertal | 6–16 | SD scores | 1.99 | DEXA | 10 kg/m2 | 58 | 97.2 (NR) | 100 (NR) |
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – prepubertal | 6–16 | SD scores | 2.13 | DEXA | 10 kg/m2 | 50 | 96.9 (NR) | 100 (NR) |
| Sproule (2009)198 | Spinal muscular atrophy | 5–18 | CDC | 95th centile | DEXA | 85th centile | 25 | 20 (NR) | 100 (NR) |
| Sproule (2009)198 | Spinal muscular atrophy | 5–18 | CDC | 97th centile | DEXA | 85th centile | 25 | 20 (NR) | 100 (NR) |
| Telford (2008)201 | Boys | 8 | IOTF | 18.4 | DEXA | Mueller | 375 | 78.5 (NR) | 91 (NR) |
| Telford (2008)201 | Girls | 8 | IOTF | 18.4 | DEXA | Mueller | 366 | 85.5 (NR) | 89.3 (NR) |
| Telford (2008)201 | All children | 8 | IOTF | 18.4 | DEXA | Mueller | 741 | 82 (75 to 88) | 90 (87 to 92)a |
| Telford (2008)201 | Boys | 8 | IOTF | 18.4 | DEXA | McCarthy | 375 | 58.6 (NR) | 100 (NR) |
| Telford (2008)201 | Girls | 8 | IOTF | 18.4 | DEXA | McCarthy | 366 | 49.2 (NR) | 97 (NR) |
| Telford (2008)201 | All children | 8 | IOTF | 18.4 | DEXA | McCarthy | 741 | 54 (49 to 59) | 99 (97 to 100)a |
| Alvero-Cruz (2010)173 | Boys | 12–18 | ? | 23.07 | D2O | ? | 75 | 75.8 (57.7 to 88.9) | 83.3 (68.6 to 93) |
| Alvero-Cruz (2010)173 | Girls | 12–18 | ? | 23.18 | D2O | ? | 75 | 88.9 (51.7 to 98.2) | 77.3 (65.3 to 86.7) |
| Vitolo (2007)202 | Boys | 10–19 | Conde and Monteiro | 25 | DEXA | 25% BF | 219 | 84.1 (NR) | 84.6 (NR) |
| Vitolo (2007)202 | Boys | 10–14 | Conde and Monteiro | 25 | DEXA | 25% BF | 128 | 84.2 (NR) | 82.2 (NR) |
| Vitolo (2007)202 | Boys | 15–19 | Conde and Monteiro | 25 | DEXA | 25% BF | 91 | 83.3 (NR) | 87.1 (NR) |
| Vitolo (2007)202 | Girls | 10–19 | Conde and Monteiro | 25 | DEXA | 30% BF | 199 | 34.5 (NR) | 98.3 (NR) |
| Vitolo (2007)202 | Girls | 10–14 | Conde and Monteiro | 25 | DEXA | 30% BF | 132 | 44.2 (NR) | 97.8 (NR) |
| Vitolo (2007)202 | Boys | 10–19 | Conde and Monteiro | 25 | DEXA | Boys 25% BF; girls 30% BF | 418 | 46 (39 to 54) | 88 (83 to 92)a |
| Vitolo (2007)202 | All children | 10–19 | IOTF | 25 | DEXA | Boys 25% BF; girls 30% BF | 418 | 39 (32 to 47) | 89 (85 to 93)a |
| Vitolo (2007)202 | All children | 15–19 | Conde and Monteiro | 25 | DEXA | 30% BF | 67 | 18.9 (NR) | 100 (NR) |
| Vitolo (2007)202 | Boys | 10–19 | IOTF | 25 | DEXA | 25% BF | 219 | 79.5 (NR) | 86.9 (NR) |
| Vitolo (2007)202 | Boys | 10–14 | IOTF | 25 | DEXA | 25% BF | 128 | 84.2 (NR) | 86.7 (NR) |
| Vitolo (2007)202 | Boys | 15–19 | IOTF | 25 | DEXA | 25% BF | 91 | 50 (NR) | 87.1 (NR) |
| Vitolo (2007)202 | Girls | 10–19 | IOTF | 25 | DEXA | 30% BF | 199 | 26.6 (NR) | 96.7 (NR) |
| Vitolo (2007)202 | Girls | 10–14 | IOTF | 25 | DEXA | 30% BF | 132 | 32.6 (NR) | 95.7 (NR) |
| Vitolo (2007)202 | Girls | 15–19 | IOTF | 25 | DEXA | 30% BF | 67 | 17 (NR) | 100 (NR) |
| Neovius (2004)192 | Boys | 16.9 (SD 0.4) | IOTF | 25 | ADP | 25% BF | 200 | 80 (NR) | 95 (NR) |
| Neovius (2004)192 | Girls | 16.9 (SD 0.4) | IOTF | 25 | ADP | 30% BF | 274 | 24 (NR) | 100 (NR) |
| Neovius (2004)192 | All children | 16.9 (SD 0.4) | IOTF | 25 | ADP | Boys 25% BF; girls 30% BF | 474 | 34 (26 to 42) | 97 (95 to 99)a |
| Neovius (2004)192 | Boys | 17 | Optimal | 25.2 | ADP | 25% BF | 200 | 72 (NR) | 98 (NR) |
| Neovius (2004)192 | Girls | 17 | Optimal | 22.2 | ADP | 30% BF | 274 | 65 (NR) | 88 (NR) |
| Neovius (2004)192 | Boys | 16.9 (SD 0.4) | Optimal | ? | ADP | 25% BF | 200 | 92 (NR) | 92 (NR) |
| Neovius (2004)192 | Girls | 16.9 (SD 0.4) | Optimal | ? | ADP | 30% BF | 274 | 77 (NR) | 76 (NR) |
| Neovius (2004)192 | All children | 16.9 (SD 0.4) | Optimal | ? | ADP | Boys 25% BF; girls 30% BF | 474 | 79 (72 to 86) | 84 (80 to 88)a |
| Conicity index | |||||||||
| Taylor (2000)199 | White girls | 3.1–19.8 | 80th centile | DEXA | 1 SD | 278 | 57 (42 to 72) | 88 (83 to 92) | |
| Taylor (2000)199 | White boys | 3.3–19.9 | 80th centile | DEXA | 1 SD | 302 | 61 (45 to 75) | 88 (83 to 91) | |
| FMI | |||||||||
| Alvero-Cruz (2010)173 | Boys | 12–18 | 4.58 | D2O | ? | 75 | 100 (89.3 to 100) | 90.5 (77.4 to 97.3) | |
| Alvero-Cruz (2010)173 | Girls | 12–18 | 7.76 | D2O | ? | 75 | 100 (66.2 to 100) | 97 (89.5 to 99.5) | |
| SFT | |||||||||
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – pubertal | 6–16 | Index | 1.26 | DEXA | 10 kg/m2 | 58 | 75 (NR) | 77.3 (NR) |
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – prepubertal | 6–16 | Index | 1.07 | DEXA | 10 kg/m2 | 50 | 57.6 (NR) | 76.5 (NR) |
| Mei (2006)190 | Unselected | 5–18 | Subscapular | 85th centile | DEXA | 95th centile | 1196 | 98.5 (NR) | 79.1 (NR) |
| Mei (2006)190 | Unselected | 5–18 | Triceps | 85th centile | DEXA | 95th centile | 1196 | 98.5 (NR) | 78 (NR) |
| Sarria (2001)197 | Girls | 7–16.9 | Sum | 85th centile | Underwater (hydrostatic) weighting | 85th centile | 175 | 58 (37 to 77) | 93 (87 to 96) |
| Freedman (2013)180 | Boys | 8–19 | Sum | Elevated/slightly elevated – prevalence matched to BMI | DEXA | ? | 4519 | 85 (83 to 87)b | 92 (91 to 93)b |
| Freedman (2013)180 | Girls | 8–19 | Sum | Elevated/slightly elevated – prevalence matched to BMI | DEXA | ? | 2846 | 81 (78 to 83)b | 90 (89 to 92)b |
| Freedman (2013)180 | All children | 8–19 | Sum | Elevated/slightly elevated – prevalence matched to BMI | DEXA | ? | 7365 | 83 (82 to 85) | 91 (91 to 92)a |
| WC | |||||||||
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – prepubertal | 6–16 | Mid-point between ribs and iliac crest | 66.5 | DEXA | 10 kg/m2 | 50 | 84.8 (NR) | 100 (NR) |
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – prepubertal | 6–16 | Umbilical | 72 | DEXA | 10 kg/m2 | 50 | 90.9 (NR) | 100 (NR) |
| Neovius (2005)193 | Girls | 17 | Smallest between ribs and iliac crest | 73.3 | ADP | 30% BF | 274 | 53 (NR) | 89 (NR) |
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – pubertal | 6–16 | Mid-point between ribs and iliac crest | 77 | DEXA | 10 kg/m2 | 58 | 88.9 (NR) | 95.5 (NR) |
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – pubertal | 6–16 | Umbilical | 85 | DEXA | 10 kg/m2 | 58 | 88.9 (NR) | 100 (NR) |
| Neovius (2005)193 | Boys | 17 | Smallest between ribs and iliac crest | 85.9 | ADP | 25% BF | 200 | 68 (NR) | 99 (NR) |
| Taylor (2000)199 | White girls | 3.1–19.8 | Smallest between ribs and iliac crest | 80th centile | DEXA | 1 SD | 278 | 89 (77 to 96) | 94 (91 to 97) |
| Taylor (2000)199 | White boys | 3.3–19.9 | Smallest between ribs and iliac crest | 80th centile | DEXA | 1 SD | 302 | 87 (74 to 95) | 92 (88 to 95) |
| Sarria (2001)197 | Boys | 7–16.9 | Smallest between ribs and iliac crest | 85th centile | Underwater (hydrostatic) weighting | 85th centile | 175 | 58 (37 to 77) | 93 (87 to 96) |
| WHR | |||||||||
| Neovius (2005)193 | Girls | 17 | WC smallest between ribs and iliac crest | 0.84 | ADP | 30% BF | 274 | 17 (NR) | 98 (NR) |
| Neovius (2005)193 | Boys | 17 | WC smallest between ribs and iliac crest | 0.9 | ADP | 25% BF | 200 | 24 (NR) | 98 (NR) |
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – pubertal | 6–16 | WC mid-point between ribs and iliac crest | 0.91 | DEXA | 10 kg/m2 | 58 | 72.2 (NR) | 90.9 (NR) |
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – prepubertal | 6–16 | WC mid-point between ribs and iliac crest | 0.92 | DEXA | 10 kg/m2 | 50 | 78.8 (NR) | 70.6 (NR) |
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – pubertal | 6–16 | WC umbilical | 0.98 | DEXA | 10 kg/m2 | 58 | 77.8 (NR) | 95.5 (NR) |
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – prepubertal | 6–16 | WC umbilical | 0.99 | DEXA | 10 kg/m2 | 50 | 66.7 (NR) | 94.1 (NR) |
| Taylor (2000)199 | White girls | 3.1–19.8 | WC smallest between ribs and iliac crest | 80th centile | DEXA | 1 SD | 278 | 47 (32 to 62) | 85 (80 to 90) |
| Taylor (2000)199 | White boys | 3.3–19.9 | WC smallest between ribs and iliac crest | 80th centile | DEXA | 1 SD | 302 | 46 (31 to 61) | 85 (80 to 89) |
| WHtR | |||||||||
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – prepubertal | 6–16 | WC mid-point between ribs and iliac crest | 0.49 | DEXA | 10 kg/m2 | 50 | 90.9 (NR) | 100 (NR) |
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – pubertal | 6–16 | WC mid-point between ribs and iliac crest | 0.5 | DEXA | 10 kg/m2 | 58 | 97.2 (NR) | 100 (NR) |
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – pubertal | 6–16 | WC umbilical | 0.54 | DEXA | 10 kg/m2 | 58 | 97.2 (NR) | 100 (NR) |
| Guntsche (2010)184 | Children referred to an obesity centre and their siblings – prepubertal | 6–16 | WC umbilical | 0.54 | DEXA | 10 kg/m2 | 50 | 93.9 (NR) | 100 (NR) |
| Author | Population | Age at assessment (years) | Index test details | Index test cut-off point | Reference standard | Reference standard cut-off point | Total n | Sensitivity (95% CI) | Specificity (95% CI) |
|---|---|---|---|---|---|---|---|---|---|
| SFT | |||||||||
| Bray (2002)175 | White and AA children | 12 | Sum Ellis | ? | 4-C | ? | 114 | 96 (NR) | 47 (NR) |
| Bray (2002)175 | White and AA children | 12 | Sum Pennington | ? | 4-C | ? | 114 | 94 (NR) | 82 (NR) |
| Bray (2002)175 | White and AA children | 12 | Sum Slaughter | ? | 4-C | ? | 114 | 98 (NR) | 71 (NR) |
| BIA | |||||||||
| Bray (2002)175 | White and AA children | 12 | Deurenberg | ? | 4-C | ? | 114 | 65 (NR) | 93 (NR) |
| Bray (2002)175 | White and AA children | 12 | Goran | ? | 4-C | ? | 114 | 100 (NR) | 45 (NR) |
| Bray (2002)175 | White and AA children | 12 | Pennington | ? | 4-C | ? | 114 | 87 (NR) | 84 (NR) |
| Bray (2002)175 | White and AA children | 12 | Schaefer | ? | 4-C | ? | 114 | 89 (NR) | 84 (NR) |
| Bray (2002)175 | White and AA children | 12 | Suprasongsin | ? | 4-C | ? | 114 | 100 (NR) | 11 (NR) |
| Study | Population | Age at assessment (years) | Index test | Index test cut-off point | Reference standard | Reference standard cut-off point | 1 to 1 | 1 to 2/3 | 2/3 to 1 | 2/3 to 2/3 | Sensitivity | Specificity |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fuller (2002)183 | Unselected | 8–12 | BIA | ? | DEXA | ? | 9 | 3 | 3 | 22 | 75.0 | 88.0 |
| Fuller (2001)182 | Unselected | 8–12 | NIR OD 940 | ? | 4-C | ? | 9 | 4 | 4 | 21 | 69.2 | 84.0 |
| Fuller (2001)182 | Unselected | 8–12 | NIR OD 950 | ? | 4-C | ? | 9 | 4 | 4 | 21 | 69.2 | 84.0 |
| Fuller (2001)182 | Unselected | 8–12 | SFT | ? | 4-C | ? | 8 | 5 | 5 | 20 | 61.5 | 80.0 |
| Study | Population | Age at assessment (years) | Index test | Index test cut-off point | Reference standard | Reference standard cut-off point | 1/2 to 1/2 | 1/2 to 3 | 3 to 1/2 | 3 to 3 | Sensitivity | Specificity |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fuller (2002)183 | Unselected | 8–12 | BIA | ? | DEXA | ? | 24 | 1 | 1 | 11 | 96.0 | 91.7 |
| Fuller (2001)182 | Unselected | 8–12 | NIR OD 940 | ? | 4-C | ? | 21 | 4 | 4 | 9 | 84.0 | 69.2 |
| Fuller (2001)182 | Unselected | 8–12 | NIR OD 950 | ? | 4-C | ? | 24 | 1 | 1 | 12 | 96.0 | 92.3 |
| Fuller (2001)182 | Unselected | 8–12 | SFT | ? | 4-C | ? | 24 | 1 | 1 | 12 | 96.0 | 92.3 |
| Study | Population | Age at assessment (years) | Index test details | Index test cut-off point | Reference standard | Reference standard cut-off point | Total n | LR+ | LR– |
|---|---|---|---|---|---|---|---|---|---|
| BMI | |||||||||
| Bartok (2011)174 | White girls | 11 | CDC | 82nd centile | DEXA | 95th centile | 172 | 5.59 | 0.060a |
| Bartok (2011)174 | White girls | 13 | CDC | 82nd centile | DEXA | 95th centile | 151 | 7.75 | 0.080a |
| Himes (1989)186 | Boys | 8.4–18.99 | ? | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 159 | 29.00 | 0.717a |
| Himes (1989)186 | Girls | 8.4–18.99 | ? | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 157 | Infinite | 0.770a |
| Himes (1989)186 | Girls | 8.4–18.99 | ? | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 316 | Infinite | 0.750a,b |
| Bartok (2011)174 | White girls | 9 | CDC | 85th centile | DEXA | 95th centile | 173 | 15.00 | 0.106a |
| Bartok (2011)174 | White girls | 15 | CDC | 85th centile | DEXA | 95th centile | 160 | 19.20 | 0.042a |
| Sproule (2009)198 | Spinal muscular atrophy | 5–18 | CDC | 85th centile | DEXA | 95th centile | 25 | 16.00 | 0.211a |
| Harrington (2013)185 | White girls | 5–18 | Optimal | 89th centile | DEXA | ? | 83 | 10.00 | 0.000a |
| Harrington (2013)185 | White boys | 5–18 | Optimal | 94th centile | DEXA | ? | 94 | 33.33 | 0.000a |
| Sproule (2009)198 | Spinal muscular atrophy | 5–18 | CDC | 95th centile | DEXA | 95th centile | 25 | Infinite | 0.600a |
| Mei (2006)190 | Unselected | 5–18 | CDC | 95th centile | DEXA | 95th centile | 1196 | 8.73 | 0.084a |
| Freedman (2013)180 | Boys | 8–19 | CDC | 95th centile | DEXA | ? | 4518 | 15.00 | 0.263a |
| Freedman (2009)179 | Healthy unselected boys | 5–18 | CDC | 95th centile | DEXA | 95th centile | 626 | 15.00 | 0.263a |
| Wickramasinghe (2005)204 | White boys | 5–14.99 | CDC | 95th centile | D2O | 20% BF | 44 | Infinite | 0.965a |
| Wickramasinghe (2005)204 | Sri Lankan boys | 5–14.99 | CDC | 95th centile | D2O | 20% BF | 27 | Infinite | 0.875a |
| Wickramasinghe (2009)205 | Sri Lankan boys | 5–15 | CDC | 95th centile | D2O | 25% BF | 158 | Infinite | 0.805a |
| Wickramasinghe (2009)205 | Sri Lankan girls | 5–15 | CDC | 95th centile | D2O | 30% BF | 124 | Infinite | 0.838a |
| Wickramasinghe (2009)205 | All Sri Lankan children | 5–15 | CDC | 95th centile | D2O | Boys 25% BF; girls 30% BF | 282 | Infinite | 0.820a,b |
| Freedman (2013)180 | Girls | 8–19 | CDC | 95th centile | DEXA | ? | 2847 | 15.20 | 0.253a |
| Freedman (2013)180 | All children | 8–19 | CDC | 95th centile | DEXA | ? | 7365 | 15.20 | 0.253a,b |
| Freedman (2009)179 | Girls | 5–18 | CDC | 95th centile | DEXA | 95th centile | 570 | 26.67 | 0.206a |
| Freedman (2009)179 | Girls | 5–18 | CDC | 95th centile | DEXA | 95th centile | 1196 | 19.25 | 0.240a,b |
| Wickramasinghe (2005)204 | White girls | 5–14.99 | CDC | 95th centile | D2O | 30% BF | 52 | Infinite | 0.800a |
| Wickramasinghe (2005)204 | Sri Lankan girls | 5–14.99 | CDC | 95th centile | D2O | 30% BF | 15 | Infinite | 0.857a |
| Khadgawat (2013)188 | Boys | 7–17 | IOTF | 95th centile | DEXA | 95th centile | 825 | 28.33 | 0.155a |
| Khadgawat (2013)188 | Boys | 7–17 | IOTF | 95th centile | DEXA | Prevalence matched to BMI | 825 | 33.50 | 0.337a |
| Wickramasinghe (2009)205 | Sri Lankan boys | 5–15 | IOTF | 95th centile | D2O | 25% BF | 158 | Infinite | 0.875a |
| Wickramasinghe (2009)205 | Sri Lankan girls | 5–15 | IOTF | 95th centile | D2O | 30% BF | 124 | Infinite | 0.920a |
| Wickramasinghe (2009)205 | All Sri Lankan children | 5–15 | IOTF | 95th centile | D2O | Boys 25% BF; girls 30% BF | 282 | Infinite | 0.900a,b |
| Khadgawat (2013)188 | Girls | 7–17 | IOTF | 95th centile | DEXA | 95th centile | 815 | Infinite | 0.460a |
| Khadgawat (2013)188 | Girls | 7–17 | IOTF | 95th centile | DEXA | 95th centile | 1640 | 33.00 | 0.347a,b |
| Khadgawat (2013)188 | Girls | 7–17 | IOTF | 95th centile | DEXA | Prevalence matched to BMI | 815 | 81.00 | 0.192a |
| Khadgawat (2013)188 | Girls | 7–17 | IOTF | 95th centile | DEXA | Prevalence matched to BMI | 1640 | 72.00 | 0.283a,b |
| Ellis (1999)177 | Boys | 3–18 | UK90 | 95th centile | DEXA (adjusted for sex and ethnicity) | 95th centile | 406 | 8.44 | 0.264a |
| Ellis (1999)177 | Boys | 3–18 | UK90 | 95th centile | DEXA (adjusted for sex) | 95th centile | 406 | 7.89 | 0.319a |
| Reilly (2010)195 | Boys | 9.9 | UK90 | 95th centile | DEXA | 90th centile | 3809 | 19.20 | 0.042a |
| Ellis (1999)177 | Girls | 3–18 | UK90 | 95th centile | DEXA (adjusted for sex and ethnicity) | 95th centile | 573 | 7.67 | 0.341a |
| Ellis (1999)177 | Girls | 3–18 | UK90 | 95th centile | DEXA (adjusted for sex) | 95th centile | 573 | 11.25 | 0.109a |
| Ellis (1999)177 | All children | 3–18 | UK90 | 95th centile | DEXA (adjusted for sex and ethnicity) | 95th centile | 979 | 8.00 | 0.308a,b |
| Ellis (1999)177 | All children | 3–18 | UK90 | 95th centile | DEXA (adjusted for sex) | 95th centile | 979 | 10.25 | 0.196a,b |
| Reilly (2010)195 | Girls | 9.9 | UK90 | 95th centile | DEXA | 90th centile | 3913 | 23.50 | 0.063a |
| Reilly (2010)195 | Girls | 9.9 | UK90 | 95th centile | DEXA | 90th centile | 7722 | 19.00 | 0.053a,b |
| Field (2003)178 | Unselected | 10 (SD 2.2) | ? | 95th centile | DEXA | 90th centile | 596 | 65.00 | 0.354a |
| Field (2003)178 | Unselected | 10 (SD 2.2) | SD score | 2 | DEXA | 90th centile | 596 | Infinite | 0.490a |
| Wickramasinghe (2005)204 | White boys | 5–14.99 | SD score | 2 | D2O | 20% BF | 44 | 0.99 | 1.001a |
| Wickramasinghe (2005)204 | Sri Lankan boys | 5–14.99 | SD score | 2 | D2O | 20% BF | 27 | Infinite | 0.875a |
| Wickramasinghe (2009)205 | Sri Lankan boys | 5–15 | SD score | 2 | D2O | 25% BF | 158 | Infinite | 0.764a |
| Wickramasinghe (2005)204 | White girls | 5–14.99 | SD score | 2 | D2O | 30% BF | 52 | Infinite | 0.948a |
| Wickramasinghe (2009)205 | Sri Lankan girls | 5–15 | SD score | 2 | D2O | 30% BF | 124 | Infinite | 0.838a |
| Wickramasinghe (2005)204 | Sri Lankan girls | 5–14.99 | SD score | 2 | D2O | 30% BF | 15 | Infinite | 0.857a |
| Wickramasinghe (2009)205 | All Sri Lankan children | 5–15 | SD score | 2 | D2O | Boys 25% BF; girls 30% BF | 282 | Infinite | 0.810a,b |
| Wickramasinghe (2009)204 | All Sri Lankan children | 5–14.99 | SD score | 2 | D2O | Boys 20% BF; girls 30% BF | 42 | Infinite | 0.870a,b |
| Wickramasinghe (2009)204 | White children | 5–14.99 | SD score | 2 | D2O | Boys 20% BF; girls 30% BF | 96 | 3.00 | 0.959a,b |
| Taylor (2003)200 | Boys | 8.5–15.5 | Optimal z-score (adjusted for age) | ? | DEXA | 25% BF | 179 | 7.94 | 0.160a |
| Taylor (2003)200 | Boys | 8.5–15.5 | Optimal z-score (adjusted for age and pubertal status) | ? | DEXA | 25% BF | 179 | 11.66 | 0.111a |
| Taylor (2003)200 | Girls | 8.5–15.5 | Optimal z-score (adjusted for age) | ? | DEXA | 35% BF | 189 | 25.29 | 0.145a |
| Taylor (2003)200 | Girls | 8.5–15.5 | Optimal z-score (adjusted for age and pubertal status) | ? | DEXA | 35% BF | 189 | 11.79 | 0.125a |
| Harrington (2013)185 | Unselected | 5–18 | Optimal | 96th centile | DEXA | ? | 369 | 8.18 | 0.112a |
| Sproule (2009)198 | Spinal muscular atrophy | 5–18 | CDC | 97th centile | DEXA | 95th centile | 25 | Infinite | 0.600a |
| Harrington (2013)185 | AA boys | 5–18 | Optimal | 97 | DEXA | ? | 79 | 50.00 | 0.000a |
| Harrington (2013)185 | AA girls | 5–18 | Optimal | 98 | DEXA | ? | 113 | 13.29 | 0.075a |
| Fujita (2011)181 | Girls | 10 | Optimal | 19.6 | DEXA | 95th centile | 196 | 12.50 | 0.000a |
| Fujita (2011)181 | Boys | 10 | Optimal | 20.8 | DEXA | 95th centile | 226 | 25.00 | 0.000a |
| Telford (2008)201 | Boys | 8 | IOTF | 21.6 | DEXA | Mueller | 375 | 19.89 | 0.131a |
| Telford (2008)201 | Boys | 8 | IOTF | 21.6 | DEXA | McCarthy | 375 | Infinite | 0.739a |
| Telford (2008)201 | Girls | 8 | IOTF | 21.6 | DEXA | Mueller | 366 | 32.54 | 0.224a |
| Telford (2008)201 | Girls | 8 | IOTF | 21.6 | DEXA | McCarthy | 366 | Infinite | 0.746a |
| Telford (2008)201 | All children | 8 | IOTF | 21.6 | DEXA | McCarthy | 741 | Infinite | 0.740a,b |
| Telford (2008)201 | All children | 8 | IOTF | 21.6 | DEXA | Mueller | 741 | 26.67 | 0.206a,b |
| Neovius (2005)193 | Girls | 17 | Optimal | 26.5 | ADP | 95th centile | 274 | 37.10 | 0.200 |
| Neovius (2005)193 | Boys | 17 | Optimal | 29.2 | ADP | 95th centile | 200 | 25.30 | 0.600 |
| Wickramasinghe (2005)204 | White boys | 5–14.99 | IOTF | 30 | D2O | 20% BF | 44 | Infinite | 1.000a |
| Wickramasinghe (2005)204 | Sri Lankan boys | 5–14.99 | IOTF | 30 | D2O | 20% BF | 27 | Infinite | 1.000a |
| Wickramasinghe (2005)204 | White girls | 5–14.99 | IOTF | 30 | D2O | 30% BF | 52 | Infinite | 1.000a |
| Wickramasinghe (2005)204 | Sri Lankan girls | 5–14.99 | IOTF | 30 | D2O | 30% BF | 15 | Infinite | 1.000a |
| Wickramasinghe (2005)204 | White children | 5–14.99 | IOTF | 30 | D2O | Boys 20% BF; girls 30% BF | 96 | Infinite | 1.000 |
| Wickramasinghe (2005)204 | All Sri Lankan children | 5–14.99 | IOTF | 30 | D2O | Boys 20% BF; girls 30% BF | 42 | Infinite | 0.990 |
| Zhang (2004)206 | City-/suburb-residing boys | 13.7 | IOTF | 30 | DEXA | 25% BF | 172 | 5.56 | 0.000a |
| Zhang (2004)206 | City-/suburb-residing girls | 13.5 | IOTF | 30 | DEXA | 35% BF | 414 | 3.23 | 0.000a |
| Zhang (2004)206 | Rural-residing girls | 10.1 | IOTF | 30 | DEXA | 35% BF | 165 | 5.26 | 0.000a |
| Relative BMI | |||||||||
| Marshall (1991)189 | Unselected | 7–14 | – | ≥ 120% | Underwater (hydrostatic) weighting | Boys 20% BF; girls 25% BF | 540 | 8.46 | 0.316a |
| Marshall (1991)189 | Girls | 7–14 | – | ≥ 120% | Underwater (hydrostatic) weighting | 25% BF | 274 | 7.81 | 0.285a |
| Marshall (1991)189 | Boys | 7–14 | – | ≥ 120% | Underwater (hydrostatic) weighting | 20% BF | 266 | 9.57 | 0.335a |
| Relative weight | |||||||||
| Johnston (1985)187 | Boys | 12–17 | – | ? | Underwater (hydrostatic) weighting | 25% BF | 169 | 3.71 | 0.558a |
| Johnston (1985)187 | Girls | 12–17 | – | ? | Underwater (hydrostatic) weighting | 30% BF | 66 | 4.83 | 0.755a |
| Marshall (1991)189 | Unselected | 7–14 | – | ≥ 120% | Underwater (hydrostatic) weighting | Boys 20% BF; girls 25% BF | 540 | 10.32 | 0.509a |
| Marshall (1991)189 | Girls | 7–14 | – | ≥ 120% | Underwater (hydrostatic) weighting | 25% BF | 274 | 11.86 | 0.441a |
| Marshall (1991)189 | Boys | 7–14 | – | ≥ 120% | Underwater (hydrostatic) weighting | 20% BF | 266 | 9.78 | 0.538a |
| SFT | |||||||||
| Himes (1989)186 | Boys | 8.4–18.99 | Subscapular | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 159 | 38.00 | 0.626a |
| Himes (1989)186 | Girls | 8.4–18.99 | Subscapular | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 157 | 30.00 | 0.707a |
| Himes (1989)186 | Boys | 8.4–18.99 | Sum | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 159 | 3.80 | 0.506a |
| Himes (1989)186 | Girls | 8.4–18.99 | Sum | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 157 | 4.44 | 0.244a |
| Himes (1989)186 | Boys | 8.4–18.99 | Triceps | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 159 | Infinite | 0.760a |
| Himes (1989)186 | Girls | 8.4–18.99 | Triceps | 85th centile | Underwater (hydrostatic) weighting | 90th centile | 157 | 7.67 | 0.794a |
| Marshall (1991)189 | Unselected | 7–14 | Sum | 85th centile | Underwater (hydrostatic) weighting | Boys 20% BF; girls 25% BF | 540 | 8.77 | 0.147a |
| Marshall (1991)189 | Girls | 7–14 | Sum | 85th centile | Underwater (hydrostatic) weighting | 25% BF | 274 | 10.19 | 0.035a |
| Marshall (1991)189 | Boys | 7–14 | Sum | 85th centile | Underwater (hydrostatic) weighting | 20% BF | 266 | 7.69 | 0.223a |
| Marshall (1991)189 | Boys | 7–14 | Triceps | 85th centile | Underwater (hydrostatic) weighting | 20% BF | 266 | 11.93 | 0.376a |
| Marshall (1991)189 | Unselected | 7–14 | Triceps | 85th centile | Underwater (hydrostatic) weighting | Boys 20% BF; girls 25% BF | 540 | 10.97 | 0.364a |
| Marshall (1991)189 | Girls | 7–14 | Triceps | 85th centile | Underwater (hydrostatic) weighting | 25% BF | 274 | 10.26 | 0.346a |
| Mei (2006)190 | Unselected | 5–18 | Subscapular | 95th centile | DEXA | 95th centile | 1196 | 14.93 | 0.111a |
| Mei (2006)190 | Unselected | 5–18 | Triceps | 95th centile | DEXA | 95th centile | 1196 | 13.18 | 0.112a |
| Freedman (2013)180 | Boys | 8–19 | Sum | Elevated – prevalence matched to BMI | DEXA | ? | 4519 | 20.00 | 0.208a |
| Freedman (2013)180 | Girls | 8–19 | Sum | Elevated – prevalence matched to BMI | DEXA | ? | 2846 | 19.75 | 0.219a |
| Johnston (1985)187 | Boys | 12–17 | Triceps | ? | Underwater (hydrostatic) weighting | 25% BF | 169 | 12.00 | 0.542a |
| Johnston (1985)187 | Girls | 12–17 | Triceps | ? | Underwater (hydrostatic) weighting | 30% BF | 66 | Infinite | 0.760a |
| Johnston (1985)187 | All children | 12–17 | Triceps | ? | Underwater (hydrostatic) weighting | Boys 25% BF; girls 30% BF | 235 | 13.33 | 0.619a,b |
| Freedman (2013)180 | All children | 8–19 | Sum | Elevated – prevalence matched to BMI | DEXA | ? | 7365 | 20.00 | 0.208a,b |
| WC | |||||||||
| Neovius (2005)193 | Boys | 17 | Smallest between ribs and iliac crest | 95 | ADP | 95th centile | 200 | 23.80 | 0.500 |
| Neovius (2005)193 | Girls | 17 | Smallest between ribs and iliac crest | 85 | ADP | 95th centile | 274 | 27.90 | 0.400 |
| Reilly (2010)195 | Boys | 9.9 | UK 1988 reference | 95th centile | DEXA | 90th centile | 3809 | 5.11 | 0.037a |
| Reilly (2010)195 | Girls | 9.9 | UK 1988 reference | 95th centile | DEXA | 90th centile | 3913 | 5.16 | 0.025a |
| Wickramasinghe (2009)205 | Sri Lankan boys | 5–15 | Smallest between ribs and iliac crest | 98th centile | D2O | 25% BF | 158 | 28.92 | 0.661a |
| Wickramasinghe (2009)205 | Sri Lankan girls | 5–15 | Smallest between ribs and iliac crest | 98th centile | D2O | 30% BF | 124 | Infinite | 0.616a |
| Wickramasinghe (2009)205 | All Sri Lankan children | 5–15 | Smallest between ribs and iliac crest | 98th centile | D2O | Boys 25% BF; girls 30% BF | 282 | 37.00 | 0.636a,b |
| Fujita (2011)181 | Boys | 10 | Umbilical | 76.5 | DEXA | 95th centile | 226 | 33.33 | 0.000a |
| Fujita (2011)181 | Girls | 10 | Umbilical | 73 | DEXA | 95th centile | 196 | 25.00 | 0.000a |
| WHR | |||||||||
| Neovius (2005)193 | Boys | 17 | WC smallest between ribs and iliac crest | 0.9 | ADP | 95th centile | 200 | 15.20 | 0.600 |
| Neovius (2005)193 | Girls | 17 | WC smallest between ribs and iliac crest | 1.02 | ADP | 95th centile | 274 | Infinite | 1.000 |
| WHtR | |||||||||
| Fujita (2011)181 | Boys | 10 | WC umbilical | 0.519 | DEXA | 95th centile | 226 | 20.00 | 0.000a |
| Fujita (2011)181 | Girls | 10 | WC umbilical | 0.499 | DEXA | 95th centile | 196 | 20.00 | 0.000a |
| Study | Population | Age at assessment (years) | Index test details | Index test cut-off point | Reference standard | Reference standard cut-off point | Total n | LR+ | LR− |
|---|---|---|---|---|---|---|---|---|---|
| BMI | |||||||||
| Bartok (2011)174 | White girls | 9 | CDC | 73rd centile | DEXA | 85th centile | 173 | 10.22 | 0.088a |
| Bartok (2011)174 | White girls | 13 | CDC | 77th centile | DEXA | 85th centile | 151 | 8.27 | 0.101a |
| Bartok (2011)174 | White girls | 15 | CDC | 78th centile | DEXA | 85th centile | 160 | 11.50 | 0.330a |
| Bartok (2011)174 | White girls | 11 | CDC | 81st centile | DEXA | 85th centile | 172 | 21.25 | 0.156a |
| Neovius (2004)192 | Boys | 16.9 (SD 0.4) | WHO | 85th centile | ADP | 25% BF | 200 | 34.00 | 0.327a |
| Neovius (2004)192 | Boys | 16.9 (SD 0.4) | Göteborg, Sweden | 85th centile | ADP | 25% BF | 200 | 13.14 | 0.086a |
| Neovius (2004)192 | Girls | 16.9 (SD 0.4) | WHO | 85th centile | ADP | 30% BF | 274 | Infinite | 0.810a |
| Neovius (2004)192 | Girls | 16.9 (SD 0.4) | Göteborg, Sweden | 85th centile | ADP | 30% BF | 274 | 13.00 | 0.629a |
| Neovius (2004)192 | All children | 16.9 (SD 0.4) | Göteborg, Sweden | 85th centile | ADP | Boys 25% BF; girls 30% BF | 474 | 9.60 | 0.547a,b |
| Neovius (2004)192 | All children | 16.9 (SD 0.4) | WHO | 85th centile | ADP | Boys 25% BF; girls 30% BF | 474 | 28.00 | 0.727a,b |
| Freedman (2009)179 | Boys | 5–18 | CDC | 85th centile | DEXA | 85th centile | 626 | 10.50 | 0.174a |
| Freedman (2009)179 | Girls | 5–18 | CDC | 85th centile | DEXA | 85th centile | 570 | 10.38 | 0.185a |
| Freedman (2009)179 | All children | 5–18 | CDC | 85th centile | DEXA | 85th centile | 1196 | 10.38 | 0.185a,b |
| Khadgawat (2013)188 | Boys | 7–17 | IOTF | 85th centile | DEXA | 85th centile | 825 | 8.67 | 0.242a |
| Khadgawat (2013)188 | Girls | 7–17 | IOTF | 85th centile | DEXA | 85th centile | 815 | 10.67 | 0.383a |
| Khadgawat (2013)188 | All children | 7–17 | IOTF | 85th centile | DEXA | 85th centile | 1640 | 10.29 | 0.301a,b |
| Khadgawat (2013)188 | Boys | 7–17 | IOTF | 85th centile | DEXA | Prevalence matched to BMI | 825 | 12.83 | 0.245a |
| Khadgawat (2013)188 | Girls | 7–17 | IOTF | 85th centile | DEXA | Prevalence matched to BMI | 815 | 10.83 | 0.372a |
| Khadgawat (2013)188 | All children | 7–17 | IOTF | 85th centile | DEXA | Prevalence matched to BMI | 1640 | 12.00 | 0.298a,b |
| Freedman (2013)180 | Boys | 8–19 | CDC | 85th centile | DEXA | ? | 4518 | 9.22 | 0.187a |
| Freedman (2013)180 | Girls | 8–19 | CDC | 85th centile | DEXA | ? | 2847 | 8.00 | 0.222a |
| Freedman (2013)180 | All children | 8–19 | CDC | 85th centile | DEXA | ? | 7365 | 8.10 | 0.211a,b |
| Ellis (1999)177 | Boys | 3–18 | UK90 | 85th centile | DEXA (adjusted for sex and ethnicity) | 85th centile | 406 | 5.75 | 0.095a |
| Ellis (1999)177 | Girls | 3–18 | UK90 | 85th centile | DEXA (adjusted for sex and ethnicity) | 85th centile | 573 | 5.11 | 0.098a |
| Ellis (1999)177 | Boys | 3–18 | UK90 | 85th centile | DEXA (adjusted for sex) | 85th centile | 406 | 5.29 | 0.120a |
| Ellis (1999)177 | Girls | 3–18 | UK90 | 85th centile | DEXA (adjusted for sex) | 85th centile | 573 | 5.53 | 0.072a |
| Ellis (1999)177 | All children | 3–18 | UK90 | 85th centile | DEXA (adjusted for sex and ethnicity) | 85th centile | 979 | 5.41 | 0.096a,b |
| Ellis (1999)177 | All children | 3–18 | UK90 | 85th centile | DEXA (adjusted for sex) | 85th centile | 979 | 5.47 | 0.084a,b |
| Moreno (2006)191 | Boys | 13–17.9 | IOTF | 85th centile | DEXA | 85th centile | 116 | 5.07 | 0.337a |
| Moreno (2006)191 | Girls | 13–17.9 | IOTF | 85th centile | DEXA | 85th centile | 170 | 7.50 | 0.278a |
| Moreno (2006)191 | Boys | 13–17.9 | AVENA | 85th centile | DEXA | 85th centile | 116 | 4.42 | 0.534a |
| Moreno (2006)191 | Girls | 13–17.9 | AVENA | 85th centile | DEXA | 85th centile | 170 | 9.88 | 0.228a |
| Moreno (2006)191 | All children | 13–17.9 | IOTF | 85th centile | DEXA | 85th centile | 286 | 6.08 | 0.307a,b |
| Moreno (2006)191 | All children | 13–17.9 | AVENA | 85th centile | DEXA | 85th centile | 286 | 6.70 | 0.367a,b |
| Sproule (2009)198 | Spinal muscular atrophy | 5–18 | CDC | 85th centile | DEXA | 85th centile | 25 | Infinite | 0.500a |
| Sarria (2001)197 | Healthy unselected boys | 7–16.9 | z-score | 85th centile | Underwater (hydrostatic) weighting | 85th centile | 175 | 5.56 | 0.549a |
| Warner (1997)203 | All children | ? | SD score | 85th centile/1 SD | DEXA | US 85th centile | 143 | 11.00 | 0.362a |
| Warner (1997)203 | Cancer survivors | 12 (SD 3.7) | SD score | 85th centile/1 SD | DEXA | US 85th centile | 43 | 5.67 | 0.364a |
| Warner (1997)203 | Growth hormone-deficient | 15.7 (SD 1.2) | SD score | 85th centile/1 SD | DEXA | US 85th centile | 27 | 11.67 | 0.319a |
| Warner (1997)203 | Inflammatory bowel disease | 14.3 (SD 2.8) | SD score | 85th centile/1 SD | DEXA | US 85th centile | 33 | 13.75 | 0.469a |
| Warner (1997)203 | Healthy | 11.8 (SD 3.1) | SD score | 85th centile/1 SD | DEXA | US 85th centile | 40 | 16.75 | 0.344a |
| Pandit (2009)194 | Boys | 6–17 | CDC z-/SD score | 1 | DEXA | 85th centile | 316 | 25.67 | 0.237a |
| Pandit (2009)194 | Girls | 6–17 | CDC z-/SD score | 1 | DEXA | 85th centile | 250 | 27.67 | 0.175a |
| Pandit (2009)194 | All children | 6–17 | CDC z-/SD score | 1 | DEXA | 85th centile | 566 | 33.00 | 0.347a,b |
| Dung (2006)176 | Boys referred for hospital treatment | 11.9 | German reference | 90th centile | DEXA | 90th centile | 191 | 10.88 | 0.141a |
| Dung (2006)176 | Girls referred for hospital treatment | 12.1 | German reference | 90th centile | DEXA | 90th centile | 202 | 20.50 | 0.188a |
| Dung (2006)176 | All children referred for hospital treatment | 12.1 | German reference | 90th centile | DEXA | 90th centile | 393 | 14.17 | 0.160a,b |
| Sproule (2009)198 | Spinal muscular atrophy | 5–18 | CDC | 95th centile | DEXA | 85th centile | 25 | Infinite | 0.800a |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – pubertal | 6–16 | SD scores | 1.99 | DEXA | 10 kg/m2 | 58 | Infinite | 0.028a |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – prepubertal | 6–16 | SD scores | 2.13 | DEXA | 10 kg/m2 | 50 | Infinite | 0.031a |
| Sproule (2009)198 | Spinal muscular atrophy | 5–18 | CDC | 97th centile | DEXA | 85th centile | 25 | Infinite | 0.800a |
| Telford (2008)201 | Boys | 8 | IOTF | 18.4 | DEXA | Mueller | 375 | 8.72 | 0.236a |
| Telford (2008)201 | Boys | 8 | IOTF | 18.4 | DEXA | McCarthy | 375 | Infinite | 0.414a |
| Telford (2008)201 | Girls | 8 | IOTF | 18.4 | DEXA | Mueller | 366 | 7.99 | 0.162a |
| Telford (2008)201 | Girls | 8 | IOTF | 18.4 | DEXA | McCarthy | 366 | 16.40 | 0.524a |
| Telford (2008)201 | All children | 8 | IOTF | 18.4 | DEXA | Mueller | 741 | 8.20 | 0.200a,b |
| Telford (2008)201 | All children | 8 | IOTF | 18.4 | DEXA | McCarthy | 741 | 54.00 | 0.465a,b |
| Neovius (2005)193 | Girls | 17 | Optimal | 22.2 | ADP | 30% BF | 274 | 5.40 | 0.400 |
| Alvero-Cruz (2010)173 | Boys | 12–18 | ? | 23.07 | D2O | ? | 75 | 4.55 | 0.290 |
| Alvero-Cruz (2010)173 | Girls | 12–18 | ? | 23.18 | D2O | ? | 75 | 3.91 | 0.140 |
| Neovius (2004)192 | Boys | 16.9 (SD 0.4) | IOTF | 25 | ADP | 25% BF | 200 | 16.00 | 0.211a |
| Neovius (2004)192 | Girls | 16.9 (SD 0.4) | IOTF | 25 | ADP | 30% BF | 274 | Infinite | 0.760a |
| Neovius (2004)192 | All children | 16.9 (SD 0.4) | IOTF | 25 | ADP | Boys 25% BF; girls 30% BF | 474 | 11.33 | 0.680a,b |
| Vitolo (2007)202 | Boys | 10–19 | IOTF | 25 | DEXA | 25% BF | 219 | 6.07 | 0.236a |
| Vitolo (2007)202 | Boys | 10–19 | IOTF | 25 | DEXA | 25% BF | 219 | 5.46 | 0.188a |
| Vitolo (2007)202 | Boys | 10–14 | IOTF | 25 | DEXA | 25% BF | 128 | 6.33 | 0.182a |
| Vitolo (2007)202 | Boys | 10–14 | Conde and Monteiro | 25 | DEXA | 25% BF | 128 | 4.73 | 0.192a |
| Vitolo (2007)202 | Boys | 15–19 | IOTF | 25 | DEXA | 25% BF | 91 | 3.88 | 0.574a |
| Vitolo (2007)202 | Boys | 15–19 | Conde and Monteiro | 25 | DEXA | 25% BF | 91 | 6.46 | 0.192a |
| Vitolo (2007)202 | Girls | 10–19 | IOTF | 25 | DEXA | 30% BF | 199 | 8.06 | 0.759a |
| Vitolo (2007)202 | Girls | 10–19 | Conde and Monteiro | 25 | DEXA | 30% BF | 199 | 20.29 | 0.666a |
| Vitolo (2007)202 | Girls | 10–14 | IOTF | 25 | DEXA | 30% BF | 132 | 7.58 | 0.704a |
| Vitolo (2007)202 | Girls | 10–14 | Conde and Monteiro | 25 | DEXA | 30% BF | 132 | 20.09 | 0.571a |
| Vitolo (2007)202 | Girls | 15–19 | IOTF | 25 | DEXA | 30% BF | 67 | Infinite | 0.830a |
| Vitolo (2007)202 | Girls | 15–19 | Conde and Monteiro | 25 | DEXA | 30% BF | 67 | Infinite | 0.811a |
| Vitolo (2007)202 | All children | 10–19 | Conde and Monteiro | 25 | DEXA | Boys 25% BF; girls 30% BF | 418 | 3.83 | 0.614a,b |
| Vitolo (2007)202 | All children | 10–19 | IOTF | 25 | DEXA | Boys 25% BF; girls 30% BF | 418 | 3.55 | 0.685a,b |
| Neovius (2005)193 | Boys | 17 | Optimal | 25.2 | ADP | 25% BF | 200 | 31.50 | 0.300 |
| Neovius (2004)192 | Boys | 16.9 (SD 0.4) | Optimal | ? | ADP | 25% BF | 200 | 12.00 | 0.090 |
| Neovius (2004)192 | Girls | 16.9 (SD 0.4) | Optimal | ? | ADP | 30% BF | 274 | 3.00 | 0.300 |
| Neovius (2004)192 | Boys | 16.9 (SD 0.4) | Optimal | ? | ADP | 25% BF | 200 | 11.50 | 0.087a |
| Neovius (2004)192 | Girls | 16.9 (SD 0.4) | Optimal | ? | ADP | 30% BF | 274 | 3.21 | 0.303a |
| Neovius (2004)192 | All children | 16.9 (SD 0.4) | Optimal | ? | ADP | Boys 25% BF; girls 30% BF | 474 | 4.94 | 0.250a,b |
| Conicity index | |||||||||
| Taylor (2000)199 | White girls | 3.1–19.8 | – | 80th centile | DEXA | 1 SD | 278 | 4.70 | 0.480 |
| Taylor (2000)199 | White boys | 3.3–19.9 | – | 80th centile | DEXA | 1 SD | 302 | 4.90 | 0.450 |
| FMI | |||||||||
| Alvero-Cruz (2010)173 | Boys | 12–18 | – | 4.58 | D2O | ? | 75 | 10.50 | 0.000 |
| Alvero-Cruz (2010)173 | Girls | 12–18 | – | 7.76 | D2O | ? | 75 | 33.00 | 0.000 |
| SFT | |||||||||
| Guntsche (2010)184 | Children referred to obesity centre and siblings – pubertal | 6–16 | SF index | 1.26 | DEXA | 10 kg/m2 | 58 | 3.30 | 0.323a |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – prepubertal | 6–16 | SF index | 1.07 | DEXA | 10 kg/m2 | 50 | 2.45 | 0.554a |
| Mei (2006)190 | Unselected | 5–18 | Subscapular | 85th centile | DEXA | 95th centile | 1196 | 4.71 | 0.019a |
| Mei (2006)190 | Unselected | 5–18 | Triceps | 85th centile | DEXA | 95th centile | 1196 | 4.48 | 0.019a |
| Sarria (2001)197 | Boys | 7–16.9 | Sum | 85th centile | Underwater (hydrostatic) weighting | 85th centile | 175 | 8.29 | 0.452a |
| Freedman (2013)180 | Boys | 8–19 | Sum | Elevated/slightly elevated – prevalence matched to BMI | DEXA | ? | 4519 | 10.63 | 0.163a |
| Freedman (2013)180 | Girls | 8–19 | Sum | Elevated/slightly elevated – prevalence matched to BMI | DEXA | ? | 2846 | 8.10 | 0.211a |
| Freedman (2013)180 | All children | 8–19 | Sum | Elevated/slightly elevated – prevalence matched to BMI | DEXA | ? | 7365 | 9.22 | 0.187a,b |
| WC | |||||||||
| Neovius (2005)193 | Boys | 17 | Smallest between ribs and iliac crest | 85.9 | ADP | 25% BF | 200 | 59.50 | 0.300 |
| Neovius (2005)193 | Girls | 17 | Smallest between ribs and iliac crest | 73.3 | ADP | 30% BF | 274 | 4.90 | 0.500 |
| Taylor (2000)199 | White girls | 3.1–19.8 | Smallest between ribs and iliac crest | 80th centile | DEXA | 1 SD | 278 | 15.90 | 0.110 |
| Taylor (2000)199 | White boys | 3.3–19.9 | Smallest between ribs and iliac crest | 80th centile | DEXA | 1 SD | 302 | 11.10 | 0.140 |
| Sarria (2001)197 | Boys | 7–16.9 | Smallest between ribs and iliac crest | 85th centile | Underwater (hydrostatic) weighting | 85th centile | 175 | 8.29 | 0.452a |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – pubertal | 6–16 | Umbilical | 85 | DEXA | 10 kg/m2 | 58 | Infinite | 0.111a |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – prepubertal | 6–16 | Umbilical | 72 | DEXA | 10 kg/m2 | 50 | Infinite | 0.091a |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – pubertal | 6–16 | Mid-point between ribs and iliac crest | 77 | DEXA | 10 kg/m2 | 58 | 19.76 | 0.116a |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – prepubertal | 6–16 | Mid-point between ribs and iliac crest | 66.5 | DEXA | 10 kg/m2 | 50 | Infinite | 0.152a |
| WHR | |||||||||
| Neovius (2005)193 | Boys | 17 | WC smallest between ribs and iliac crest | 0.9 | ADP | 25% BF | 200 | 14.00 | 0.800 |
| Neovius (2005)193 | Girls | 17 | WC smallest between ribs and iliac crest | 0.84 | ADP | 30% BF | 274 | 9.10 | 0.800 |
| Taylor (2000)199 | White girls | 3.1–19.8 | WC smallest between ribs and iliac crest | 80th centile | DEXA | 1 SD | 278 | 3.20 | 0.620 |
| Taylor (2000)199 | White boys | 3.3–19.9 | WC smallest between ribs and iliac crest | 80th centile | DEXA | 1 SD | 302 | 3.00 | 0.640 |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – pubertal | 6–16 | WC umbilical | 0.98 | DEXA | 10 kg/m2 | 58 | 17.29 | 0.232a |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – prepubertal | 6–16 | WC umbilical | 0.99 | DEXA | 10 kg/m2 | 50 | 11.31 | 0.354a |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – pubertal | 6–16 | WC mid-point between ribs and iliac crest | 0.91 | DEXA | 10 kg/m2 | 58 | 7.93 | 0.306a |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – prepubertal | 6–16 | WC mid-point between ribs and iliac crest | 0.92 | DEXA | 10 kg/m2 | 50 | 2.68 | 0.300a |
| WHtR | |||||||||
| Guntsche (2010)184 | Children referred to obesity centre and siblings – pubertal | 6–16 | WC umbilical | 0.54 | DEXA | 10 kg/m2 | 58 | Infinite | 0.028a |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – prepubertal | 6–16 | WC umbilical | 0.54 | DEXA | 10 kg/m2 | 50 | Infinite | 0.061a |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – pubertal | 6–16 | WC mid-point between ribs and iliac crest | 0.5 | DEXA | 10 kg/m2 | 58 | Infinite | 0.028a |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – prepubertal | 6–16 | WC mid-point between ribs and iliac crest | 0.49 | DEXA | 10 kg/m2 | 50 | Infinite | 0.091a |
| Author | Population | Age at assessment (years) | Index test details | Index test cut-off point | Reference standard | Reference standard cut-off point | Total n | LR+ | LR− |
|---|---|---|---|---|---|---|---|---|---|
| SFT | |||||||||
| Bray (2002)175 | White and AA children | 12 | Sum Ellis | ? | 4-C | ? | 114 | 1.8 | 0.1a |
| Bray (2002)175 | White and AA children | 12 | Sum Pennington | ? | 4-C | ? | 114 | 5.2 | 0.1a |
| Bray (2002)175 | White and AA children | 12 | Sum Slaughter | ? | 4-C | ? | 114 | 3.4 | 0.0a |
| BIA | |||||||||
| Bray (2002)175 | White and AA children | 12 | Deurenberg | ? | 4-C | ? | 114 | 9.3 | 0.4a |
| Bray (2002)175 | White and AA children | 12 | Goran | ? | 4-C | ? | 114 | 1.8 | 0.0a |
| Bray (2002)175 | White and AA children | 12 | Pennington | ? | 4-C | ? | 114 | 5.4 | 0.2a |
| Bray (2002)175 | White and AA children | 12 | Schaefer | ? | 4-C | ? | 114 | 5.6 | 0.1a |
| Bray (2002)175 | White and AA children | 12 | Suprasongsin | ? | 4-C | ? | 114 | 1.1 | 0.0a |
| Study | Population | Age at assessment (years) | Index test | Index test cut-off point | Reference standard | Reference standard cut-off point | Total n | LR+ | LR− |
|---|---|---|---|---|---|---|---|---|---|
| Fuller (2002)183 | Unselected | 8–12 | BIA | ? | DEXA | ? | 37 | 6.3 | 0.3a |
| Fuller (2001)182 | Unselected | 8–12 | NIR OD 940 | ? | 4-C | ? | 38 | 4.3 | 0.4a |
| Fuller (2001)182 | Unselected | 8–12 | NIR OD 950 | ? | 4-C | ? | 38 | 4.3 | 0.4a |
| Fuller (2001)182 | Unselected | 8–12 | SFT | ? | 4-C | ? | 38 | 3.1 | 0.5a |
| Study | Population | Age at assessment (years) | Index test | Index test cut-off point | Reference standard | Reference standard cut-off point | Total n | LR+ | LR− |
|---|---|---|---|---|---|---|---|---|---|
| Fuller (2002)183 | Unselected | 8–12 | BIA | ? | DEXA | ? | 37 | 11.5 | 0.0 |
| Fuller (2001)182 | Unselected | 8–12 | NIR OD 940 | ? | 4-C | ? | 38 | 2.7 | 0.2 |
| Fuller (2001)182 | Unselected | 8–12 | NIR OD 950 | ? | 4-C | ? | 38 | 12.5 | 0.0 |
| Fuller (2001)182 | Unselected | 8–12 | SFT | ? | 4-C | ? | 38 | 12.5 | 0.0 |
| Author | Population | Age at assessment (years) | Index test details | Index test cut-off point | Reference standard | Reference standard cut-off point | Prevalence (%) | Total n | AUC (95% CI) |
|---|---|---|---|---|---|---|---|---|---|
| BMI | |||||||||
| Neovius (2005)193 | Boys | 17 | Optimal | 29.2 | ADP | 95th centile | ? | 200 | 0.97 (0.94 to 1) |
| Neovius (2005)193 | Girls | 17 | Optimal | 26.5 | ADP | 95th centile | ? | 274 | 0.99 (0.97 to 1) |
| Bartok (2011)174 | White girls | 9 | CDC | 85th centile | DEXA | 95th centile | 29 | 173 | 0.93 (NR) |
| Bartok (2011)174 | White girls | 11 | CDC | 82nd centile | DEXA | 95th centile | 24 | 172 | 0.95 (NR) |
| Bartok (2011)174 | White girls | 13 | CDC | 82nd centile | DEXA | 95th centile | 20 | 151 | 0.94 (NR) |
| Bartok (2011)174 | White girls | 15 | CDC | 85th centile | DEXA | 95th centile | 17 | 160 | 0.98 (NR) |
| Taylor (2003)200 | Boys | 8.5–15.5 | Optimal z-score (adjusted for age) | ? | DEXA | 25% BF | ? | 179 | 0.95 (0.92 to 0.98) |
| Taylor (2003)200 | Boys | 8.5–15.5 | Optimal z-score (adjusted for age and pubertal status) | ? | DEXA | 25% BF | ? | 179 | 0.96 (0.94 to 0.99) |
| Taylor (2003)200 | Girls | 8.5–15.5 | Optimal z-score (adjusted for age) | ? | DEXA | 35% BF | ? | 189 | 0.98 (0.96 to 0.99) |
| Taylor (2003)200 | Girls | 8.5–15.5 | Optimal z-score (adjusted for age and pubertal status) | ? | DEXA | 35% BF | ? | 189 | 0.96 (0.93 to 0.99) |
| Sardinha (1999)196 | Girls | 10–11 | ? | ? | DEXA | 30% BF | ? | 54 | 0.95 (0.85 to 0.99) |
| Sardinha (1999)196 | Girls | 12–13 | ? | ? | DEXA | 30% BF | ? | 60 | 0.89 (0.79 to 0.96) |
| Sardinha (1999)196 | Girls | 14–15 | ? | ? | DEXA | 30% BF | ? | 49 | 0.9 (0.78 to 0.98) |
| Sardinha (1999)196 | Boys | 10–11 | ? | ? | DEXA | 25% BF | ? | 55 | 0.97 (0.88 to 0.99) |
| Sardinha (1999)196 | Boys | 12–13 | ? | ? | DEXA | 25% BF | ? | 52 | 0.86 (0.73 to 0.94) |
| Sardinha (1999)196 | Boys | 14–15 | ? | ? | DEXA | 25% BF | ? | 58 | 0.61 (0.47 to 0.72) |
| Mei (2006)190 | 5–11 years | 5–18 | CDC | 95th centile | DEXA | 95th centile | ? | 572 | 0.966 (SE 0.022) |
| Mei (2006)190 | 12–18 years | 5–18 | CDC | 95th centile | DEXA | 95th centile | ? | 624 | 0.97 (SE 0.021) |
| Mei (2006)190 | Boys | 5–18 | CDC | 95th centile | DEXA | 95th centile | ? | 626 | 0.958 (SE 0.025) |
| Mei (2006)190 | Girls | 5–18 | CDC | 95th centile | DEXA | 95th centile | ? | 570 | 0.977 (SE 0.018) |
| Mei (2006)190 | White | 5–18 | CDC | 95th centile | DEXA | 95th centile | ? | 303 | 0.992 (SE 0.017) |
| Mei (2006)190 | Black | 5–18 | CDC | 95th centile | DEXA | 95th centile | ? | 269 | 0.972 (SE 0.025) |
| Mei (2006)190 | Hispanic | 5–18 | CDC | 95th centile | DEXA | 95th centile | ? | 250 | 0.947 (SE 0.034) |
| Mei (2006)190 | Asian | 5–18 | CDC | 95th centile | DEXA | 95th centile | ? | 358 | 0.937 (SE 0.056) |
| Fujita (2011)181 | Boys | 10 | ? | 95th centile | DEXA | 95th centile | ? | 226 | 0.98 (0.97 to 0.99) |
| Fujita (2011)181 | Girls | 10 | ? | 95th centile | DEXA | 95th centile | ? | 196 | 0.98 (0.961 to 1) |
| Harrington (2013)185 | Unselected | 5–18 | Optimal | 96th centile | DEXA | ? | 33.1 | 369 | 0.97 (0.95 to 0.98) |
| Harrington (2013)185 | White boys | 5–18 | Optimal | 94th centile | DEXA | ? | 26.6 | 94 | 0.98 (0.96 to 1) |
| Harrington (2013)185 | AA boys | 5–18 | Optimal | 97th centile | DEXA | ? | 32.9 | 79 | 0.99 (0.99 to 1) |
| Harrington (2013)185 | White girls | 5–18 | Optimal | 89th centile | DEXA | ? | 20.5 | 83 | 0.98 (0.96 to 1) |
| Harrington (2013)185 | AA girls | 5–18 | Optimal | 98th centile | DEXA | ? | 47.8 | 113 | 0.98 (0.96 to 1) |
| SFT | |||||||||
| Mei (2006)190 | Unselected | 5–11 | Subscapular | 95th centile | DEXA | 95th centile | ? | 572 | 0.952 (SE 0.026) |
| Mei (2006)190 | Unselected | 12–18 | Subscapular | 95th centile | DEXA | 95th centile | ? | 624 | 0.962 (SE 0.024) |
| Mei (2006)190 | Boys | 5–18 | Subscapular | 95th centile | DEXA | 95th centile | ? | 626 | 0.947 (SE 0.027) |
| Mei (2006)190 | Girls | 5–18 | Subscapular | 95th centile | DEXA | 95th centile | ? | 570 | 0.967 (SE 0.022) |
| Mei (2006)190 | White | 5–18 | Subscapular | 95th centile | DEXA | 95th centile | ? | 303 | 0.986 (SE 0.023) |
| Mei (2006)190 | Black | 5–18 | Subscapular | 95th centile | DEXA | 95th centile | ? | 269 | 0.969 (SE 0.026) |
| Mei (2006)190 | Hispanic | 5–18 | Subscapular | 95th centile | DEXA | 95th centile | ? | 250 | 0.924 (SE 0.04) |
| Mei (2006)190 | Asian | 5–18 | Subscapular | 95th centile | DEXA | 95th centile | ? | 358 | 0.922 (SE 0.062) |
| Sardinha (1999)196 | Girls | 10–11 | Triceps | ? | DEXA | 30% BF | ? | 54 | 0.96 (0.87 to 0.99) |
| Sardinha (1999)196 | Girls | 12–13 | Triceps | ? | DEXA | 30% BF | ? | 60 | 0.94 (0.85 to 0.98) |
| Sardinha (1999)196 | Girls | 14–15 | Triceps | ? | DEXA | 30% BF | ? | 49 | 0.95 (0.84 to 0.99) |
| Sardinha (1999)196 | Boys | 10–11 | Triceps | ? | DEXA | 25% BF | ? | 55 | 0.98 (0.91 to 0.99) |
| Sardinha (1999)196 | Boys | 12–13 | Triceps | ? | DEXA | 25% BF | ? | 52 | 0.94 (0.84 to 0.98) |
| Sardinha (1999)196 | Boys | 14–15 | Triceps | ? | DEXA | 25% BF | ? | 58 | 0.86 (0.74 to 0.93) |
| Mei (2006)190 | Unselected | 5–11 | Triceps | 95th centile | DEXA | 95th centile | ? | 572 | 0.958 (SE 0.024) |
| Mei (2006)190 | Unselected | 12–18 | Triceps | 95th centile | DEXA | 95th centile | ? | 624 | 0.955 (SE 0.026) |
| Mei (2006)190 | Boys | 5–18 | Triceps | 95th centile | DEXA | 95th centile | ? | 626 | 0.96 (SE 0.024) |
| Mei (2006)190 | Girls | 5–18 | Triceps | 95th centile | DEXA | 95th centile | ? | 570 | 0.954 (SE 0.025) |
| Mei (2006)190 | White | 5–18 | Triceps | 95th centile | DEXA | 95th centile | ? | 303 | 0.975 (SE 0.03) |
| Mei (2006)190 | Black | 5–18 | Triceps | 95th centile | DEXA | 95th centile | ? | 269 | 0.969 (SE 0.026) |
| Mei (2006)190 | Hispanic | 5–18 | Triceps | 95th centile | DEXA | 95th centile | ? | 250 | 0.947 (SE 0.034) |
| Mei (2006)190 | Asian | 5–18 | Triceps | 95th centile | DEXA | 95th centile | ? | 358 | 0.922 (SE 0.062) |
| WC | |||||||||
| Fujita (2011)181 | Boys | 10 | Umbilical | 95th centile | DEXA | 95th centile | ? | 226 | 0.987 (0.974 to 1) |
| Fujita (2011)181 | Girls | 10 | Umbilical | 95th centile | DEXA | 95th centile | ? | 196 | 0.986 (0.971 to 1) |
| Neovius (2005)193 | Boys | 17 | Smallest between ribs and iliac crest | 95th centile | ADP | 95th centile | ? | 200 | 0.96 (0.92 to 1) |
| Neovius (2005)193 | Girls | 17 | Smallest between ribs and iliac crest | 85th centile | ADP | 95th centile | ? | 274 | 0.95 (0.92 to 0.99) |
| WHR | |||||||||
| Neovius (2005)193 | Boys | 17 | WC smallest between ribs and iliac crest | 0.9 | ADP | 95th centile | ? | 200 | 0.8 (0.66 to 094) |
| Neovius (2005)193 | Girls | 17 | WC smallest between ribs and iliac crest | 1.02 | ADP | 95th centile | ? | 274 | 0.65 (0.49 to 0.8) |
| WHtR | |||||||||
| Fujita (2011)181 | Boys | 10 | WC smallest between ribs and iliac crest | 95th centile | DEXA | 95th centile | ? | 226 | 0.981 (0.964 to 0.998) |
| Fujita (2011)181 | Girls | 10 | WC smallest between ribs and iliac crest | 95th centile | DEXA | 95th centile | ? | 196 | 0.992 (0.981 to 1) |
| Author | Population | Age at assessment (years) | Index test details | Index test cut-off point | Reference standard | Reference standard cut-off point | Prevalence (%) | Total n | AUC (95% CI) |
|---|---|---|---|---|---|---|---|---|---|
| BMI | |||||||||
| Neovius (2004)192 | Boys | 16.9 (SD 0.4) | Optimal | ADP | 25% BF | 12.7 | 200 | 0.97 (0.94 to 1) | |
| Neovius (2004)192 | Girls | 16.9 (SD 0.4) | Optimal | ADP | 30% BF | 42.5 | 274 | 0.84 (0.8 to 0.89) | |
| Neovius (2005)193 | Boys | 17 | Optimal | 25.2 | ADP | 25% BF | ? | 200 | 0.97 (0.94 to 1) |
| Neovius (2005)193 | Girls | 17 | Optimal | 22.2 | ADP | 30% BF | ? | 274 | 0.84 (0.8 to 0.89) |
| Alvero-Cruz (2010)173 | Boys | 12–18 | ? | 23.07 | D2O | ? | ? | 75 | 0.842 (0.740 to 0.916) |
| Alvero-Cruz (2010)173 | Girls | 12–18 | ? | 23.18 | D2O | ? | ? | 75 | 0.828 (0.724 to 0.906) |
| Bartok (2011)174 | White girls | 9 | CDC | 73rd centile | DEXA | 85th centile | 42 | 173 | 0.96 (NR) |
| Bartok (2011)174 | White girls | 11 | CDC | 81st centile | DEXA | 85th centile | 41 | 172 | 0.95 (NR) |
| Bartok (2011)174 | White girls | 13 | CDC | 77th centile | DEXA | 85th centile | 30 | 151 | 0.94 (NR) |
| Bartok (2011)174 | White girls | 15 | CDC | 78th centile | DEXA | 85th centile | 33 | 160 | 0.88 (NR) |
| Mei (2006)190 | 5–11 years | 5–11 | CDC | 85th centile | DEXA | 85th centile | ? | 572 | 0.952 (SE 0.015) |
| Mei (2006)190 | 12–18 years | 12–18 | CDC | 85th centile | DEXA | 85th centile | ? | 624 | 0.954 (SE 0.016) |
| Mei (2006)190 | Boys | 5–18 | CDC | 85th centile | DEXA | 85th centile | ? | 626 | 0.946 (SE 0.016) |
| Mei (2006)190 | Girls | 5–18 | CDC | 85th centile | DEXA | 85th centile | ? | 570 | 0.96 (SE 0.014) |
| Mei (2006)190 | White | 5–18 | CDC | 85th centile | DEXA | 85th centile | ? | 303 | 0.969 (SE 0.02) |
| Mei (2006)190 | Black | 5–18 | CDC | 85th centile | DEXA | 85th centile | ? | 269 | 0.972 (SE 0.016) |
| Mei (2006)190 | Hispanic | 5–18 | CDC | 85th centile | DEXA | 85th centile | ? | 250 | 0.956 (SE 0.02) |
| Mei (2006)190 | Asian | 5–18 | CDC | 85th centile | DEXA | 85th centile | ? | 358 | 0.915 (SE 0.029) |
| Pandit (2009)194 | Boys | 6–17 | CDC z-/SD score | 1 | DEXA | 85th centile | ? | 316 | 0.919 (0.882 to 0.956) |
| Pandit (2009)194 | Girls | 6–17 | CDC z-/SD score | 1 | DEXA | 85th centile | ? | 250 | 0.961 (0.939 to 0.983) |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – pubertal | 6–16 | SD scores | 1.99 | DEXA | 10 kg/m2 | ? | 58 | 0.99 (NR) |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – prepubertal | 6–16 | SD scores | 2.13 | DEXA | 10 kg/m2 | ? | 50 | 0.99 (NR) |
| Conicity index and trunk fat mass | |||||||||
| Taylor (2000)199 | White girls | 3.1–19.8 | 80th centile | DEXA | 1 SD | ? | 278 | 0.8 (0.72 to 0.86) | |
| Taylor (2000)199 | White boys | 3.3–19.9 | 80th centile | DEXA | 1 SD | ? | 302 | 0.81 (0.74 to 0.88) | |
| FMI | |||||||||
| Alvero-Cruz (2010)173 | Boys | 12–18 | 4.58 | D2O | ? | ? | 75 | 0.988 (0.93 to 0.998) | |
| Alvero-Cruz (2010)173 | Girls | 12–18 | 7.76 | D2O | ? | ? | 75 | 0.996 (0.943 to 1) | |
| SFT | |||||||||
| Guntsche (2010)184 | Children referred to obesity centre and siblings – pubertal | 6–16 | SF index | 1.26 | DEXA | 10 kg/m2 | ? | 58 | 0.835 (NR) |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – prepubertal | 6–16 | SF index | 1.07 | DEXA | 10 kg/m2 | ? | 50 | 0.649 (NR) |
| Mei (2006)190 | Unselected | 5–11 | Subscapular | 85th centile | DEXA | 85th centile | ? | 572 | 0.961 (SE 0.014) |
| Mei (2006)190 | Unselected | 12–18 | Subscapular | 85th centile | DEXA | 85th centile | ? | 624 | 0.947 (SE 0.016) |
| Mei (2006)190 | Boys | 5–18 | Subscapular | 85th centile | DEXA | 85th centile | ? | 626 | 0.949 (SE 0.016) |
| Mei (2006)190 | Girls | 5–18 | Subscapular | 85th centile | DEXA | 85th centile | ? | 570 | 0.959 (SE 0.015) |
| Mei (2006)190 | White | 5–18 | Subscapular | 85th centile | DEXA | 85th centile | ? | 303 | 0.966 (SE 0.021) |
| Mei (2006)190 | Black | 5–18 | Subscapular | 85th centile | DEXA | 85th centile | ? | 269 | 0.975 (SE 0.015) |
| Mei (2006)190 | Hispanic | 5–18 | Subscapular | 85th centile | DEXA | 85th centile | ? | 250 | 0.956 (SE 0.021) |
| Mei (2006)190 | Asian | 5–18 | Subscapular | 85th centile | DEXA | 85th centile | ? | 358 | 0.935 (SE 0.026) |
| Mei (2006)190 | Unselected | 5–11 | Triceps | 85th centile | DEXA | 85th centile | ? | 572 | 0.951 (SE 0.015) |
| Mei (2006)190 | Unselected | 12–18 | Triceps | 85th centile | DEXA | 85th centile | ? | 624 | 0.952 (SE 0.016) |
| Mei (2006)190 | Boys | 5–18 | Triceps | 85th centile | DEXA | 85th centile | ? | 626 | 0.954 (SE 0.015) |
| Mei (2006)190 | Girls | 5–18 | Triceps | 85th centile | DEXA | 85th centile | ? | 570 | 0.95 (SE 0.016) |
| Mei (2006)190 | White | 5–18 | Triceps | 85th centile | DEXA | 85th centile | ? | 303 | 0.968 (SE 0.021) |
| Mei (2006)190 | Black | 5–18 | Triceps | 85th centile | DEXA | 85th centile | ? | 269 | 0.973 (SE 0.016) |
| Mei (2006)190 | Hispanic | 5–18 | Triceps | 85th centile | DEXA | 85th centile | ? | 250 | 0.942 (SE 0.023) |
| Mei (2006)190 | Asian | 5–18 | Triceps | 85th centile | DEXA | 85th centile | ? | 358 | 0.923 (SE 0.028) |
| WC | |||||||||
| Guntsche (2010)184 | Children referred to obesity centre and siblings – pubertal | 6–16 | WC umbilical | 85 | DEXA | 10 kg/m2 | ? | 58 | 0.98 (NR) |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – prepubertal | 6–16 | WC umbilical | 72 | DEXA | 10 kg/m2 | ? | 50 | 0.972 (NR) |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – pubertal | 6–16 | WC mid-point between ribs and iliac crest | 77 | DEXA | 10 kg/m2 | ? | 58 | 0.962 (NR) |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – prepubertal | 6–16 | WC mid-point between ribs and iliac crest | 66.5 | DEXA | 10 kg/m2 | ? | 50 | 0.967 (NR) |
| Neovius (2005)193 | Boys | 17 | WC smallest between ribs and iliac crest | 85.9 | ADP | 25% BF | ? | 200 | 0.94 (0.89 to 1) |
| Neovius (2005)193 | Girls | 17 | WC smallest between ribs and iliac crest | 73.3 | ADP | 30% BF | ? | 274 | 0.81 (0.75 to 0.86) |
| WC and trunk fat mass | |||||||||
| Taylor (2000)199 | White girls | 3.1–19.8 | WC smallest between ribs and iliac crest | 80th centile | DEXA | 1 SD | ? | 278 | 0.97 (0.95 to 0.99) |
| Taylor (2000)199 | White boys | 3.3–19.9 | WC smallest between ribs and iliac crest | 80th centile | DEXA | 1 SD | ? | 302 | 0.97 (0.95 to 0.99) |
| WHR | |||||||||
| Neovius (2005)193 | Boys | 17 | WC smallest between ribs and iliac crest | 0.9 | ADP | 25% BF | ? | 200 | 0.79 (0.69 to 0.89) |
| Neovius (2005)193 | Girls | 17 | WC smallest between ribs and iliac crest | 0.84 | ADP | 30% BF | ? | 274 | 0.63 (0.56 to 0.7) |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – pubertal | 6–16 | WC umbilical | 0.98 | DEXA | 10 kg/m2 | ? | 58 | 0.915 (NR) |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – prepubertal | 6–16 | WC umbilical | 0.99 | DEXA | 10 kg/m2 | ? | 50 | 0.838 (NR) |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – pubertal | 6–16 | WC mid-point between ribs and iliac crest | 0.91 | DEXA | 10 kg/m2 | ? | 58 | 0.842 (NR) |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – prepubertal | 6–16 | WC mid-point between ribs and iliac crest | 0.92 | DEXA | 10 kg/m2 | ? | 50 | 0.736 (NR) |
| WHR and trunk fat mass | |||||||||
| Taylor (2000)199 | White girls | 3.1–19.8 | WC smallest between ribs and iliac crest | 80th centile | DEXA | 1 SD | ? | 278 | 0.73 (0.64 to 0.81) |
| Taylor (2000)199 | White boys | 3.3–19.9 | WC smallest between ribs and iliac crest | 80th centile | DEXA | 1 SD | ? | 302 | 0.71 (0.62 to 0.8) |
| WHtR | |||||||||
| Guntsche (2010)184 | Children referred to obesity centre and siblings – pubertal | 6–16 | WC umbilical | 0.54 | DEXA | 10 kg/m2 | ? | 58 | 0.99 (NR) |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – prepubertal | 6–16 | WC umbilical | 0.54 | DEXA | 10 kg/m2 | ? | 50 | 0.98 (NR) |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – pubertal | 6–16 | WC mid-point between ribs and iliac crest | 0.5 | DEXA | 10 kg/m2 | ? | 58 | 0.99 (NR) |
| Guntsche (2010)184 | Children referred to obesity centre and siblings – prepubertal | 6–16 | WC mid-point between ribs and iliac crest | 0.49 | DEXA | 10 kg/m2 | ? | 50 | 0.97 (NR) |
Review of the acceptability and ease of use of childhood measures of obesity
| Study details | Population characteristics | Children’s details | Results |
|---|---|---|---|
| Cloutier (2013)207 Language of publication: English Data source: full paper Country in which study conducted: USA/Canada Study/cohort name: none Study dates: start October 2009, finish March 2010 Study design: qualitative Analysis: prospective Setting for use of anthropometric measure: community GP clinic/primary care, outpatient/specialist clinic |
Total n = 278 Number invited for interview = 259 Response rate 97% Whose opinion?: caregivers (83% mothers, 17% grandparents) Source of sample:
Sex: NR Ethnicity (%):
SES (%):
|
Simple childhood measure: BMI (CDC growth chart), My Weight Ruler School grade of children: 2–4 Ethnicity of children: NR Sex of children: NR Weight status of children: NR |
Participants in both the African American and Hispanic focus groups (n = 27) overwhelmingly preferred the My Weight Ruler 92% of the interviewed participants (n = 251) had previously seen a CDC BMI growth chart; none had seen the My Weight Ruler More respondents correctly classified two plotted measurements (one corresponding to the 50% centile and the other to the 97% centile) on the My Weight Ruler than on the CDC growth chart (92% vs. 37%) Significantly more participants provided incorrect answers to both plotted measurements on the CDC growth chart than on the My Weight Ruler (32% vs. 1%) Significantly more participants responded ‘I don’t know’ to both of the CDC growth chart plots than to the My Weight Ruler (12% vs. 0.5%) Caregivers with higher education and higher household incomes were more likely to correctly identify the CDC BMI growth chart plots There were no significant trends between the number of correct identifications and level of education, household income, ethnicity or first language for the My Weight Ruler 61% of participants understood the health risk and the need to take action associated with plots in the 97th centile on the My Weight Ruler, compared to 1% of participants using the CDC growth chart 79% of participants preferred the My Weight Ruler as the tool to educate them on their children’s weight status during well-child visits; 17% preferred the CDC BMI growth chart |
| Hendershot (2008)73 Language of publication: English Data source: abstract Country in which study conducted: other European Study/cohort name: none Study dates: NR Study design: cross-sectional Analysis: prospective Setting for use of anthropometric measure: school |
Total n = 2629 completed questionnaires Number approached/invited = 6288 Response rate 42% Whose opinion?: school nurses Source of sample: National Association of School Nurses Database Method of obtaining opinions: electronic survey Method of recording opinions: electronic/online Age: NR Sex: male 3% Ethnicity (%):
Duration of obesity: NR SES: NR |
Simple childhood measure: BMI School grade of children: NR Ethnicity of children: NR Sex of children: NR Weight status of children: NR |
67%: BMI should be measured in school 62%: BMI results should be sent home 81%: nurses should be designing programmes to help overweight children 31%: measuring BMI was psychologically or socially damaging to the child 73%: BMI helped create awareness of the problem 72%: measuring BMI provided evidence to change policies to reduce obesity levels Largest barrier to measuring BMI: 57.6% – inadequate school resources; 55.2% – inadequate or inappropriate parental responses; 42% – not enough time to measure BMI 94%: confident or very confident in measuring height and weight 74%: confident or very confident in calculating BMI 93%: confident or very confident in helping parents to interpret BMI results School nurses with a mandate measured BMI for a year or more at a significantly higher rate than those without a mandate (77.9% vs. 21.3%) and had a higher rate of seriously considering measuring BMI (95.2% vs. 70.3%) > 50% of nurses agreed or strongly agreed that tracking BMI would help administrators to address the childhood overweight/obesity issue |
| Kubik (2006)74 Language of publication: English Data source: full paper Country in which study conducted: USA/Canada Study/cohort name: none Study dates: start 2004, finish 2005 Study design: cross-sectional Analysis: prospective Setting for use of anthropometric measure: school |
Total n = 790 completed questionnaires Number approached/invited = 1133 (plus 53 not deliverable) Response rate 70% Whose opinion?: parents Source of sample: elementary school Method of obtaining opinions: self-administered survey Method of recording opinions: paper questionnaire Age: NR Sex: male 54.3% Ethnicity: NR Weight distribution: NR Duration of obesity: NR SES: low 21% |
Simple childhood measure: BMI School grade of children:
Weight status of children (%):
|
78%: very (39%) or somewhat (39%) important for schools to include height/weight as part of annual student health screening 78%: wanted to receive information on their child’s height, weight and BMI every year Parents of girls were less likely to think height/weight screening was important than parents of boys Parents who worked full time were less likely to think screening was important than those who worked part time or stayed at home There were no differences by treatment condition, child’s weight status or other sociodemographic characteristics Parents of older students and girls were less likely to want information than parents of younger students or boys Approximately 50% of parents received a BMI letter; 79% read all, and 16% most, of the letter 55% of the parents chose not to discuss the letter with their child; 68% thought their child did not feel uncomfortable and 15% thought they felt slightly uncomfortable The information in the letter made 68% of parents feel not uncomfortable at all and 12% only slightly The information parents shared most often with their child was weight/BMI, followed by nutrition, physical activity and screen time In descending order, parents found the following information helpful: weight/BMI, physical activity, nutrition, screen time, health-related websites and community resources Of the parents who received the BMI letter and expressed a weight concern for their child, 8% planned to seek medical services, 8% to make diet-related changes, 27% to increase exercise and/or sign up their child for sports and 24% to sign up to other physical activity |
| Kubik (2007)75 Language of publication: English Data source: full paper Country in which study conducted: USA/Canada Study/cohort name: none Study dates: start 2004, finish 2005 Study design: cross-sectional Analysis: prospective Setting for use of anthropometric measure: school |
Total n = 71 Number approached/invited NR Response rate NR Whose opinion?: parents Source of sample: elementary school Method of obtaining opinion: focus groups Method of recording opinions: videotapes Age (years): mean 39 (range 27–49) Sex: male 10% Ethnicity (%):
Duration of obesity: NR SES: low 17% |
Simple childhood measure details: BMI Which measure(s)?: BMI School grade of children:
Sex of children: NR Weight status of children: NR |
General opinions about health screening:
|
| Woolford (2008)208 Language of publication: English Data source: full paper Country in which study conducted: USA/Canada Study/cohort name: none Study dates: start 2006, finish 2006 Study design: qualitative Analysis: prospective Setting for use of anthropometric measure: GP clinic/primary care |
Total n = 267 in analysis Number approached/invited = 600 Response rate 52% (after 21 were excluded; 50% of original sample) Whose opinion?:
Method of obtaining opinions: self-administered survey (12-item Likert scales and multiple-choice questions) Method of recording opinions: paper questionnaire Age: maximum 69 years Sex: NR Ethnicity: NR Weight distribution: NR Duration of obesity: NR SES: NR |
Simple childhood measure details: BMI Which measure(s)?: BMI School grade of children: preschool (ages 2 to 5 years) Ethnicity of children: NR Sex of children: NR Weight status of children: NR |
37% of physicians generally did not use BMI charts for patients who are between the ages of 2 and 5 years; 24% indicated that they generally used BMI charts for this age group, and the remaining 39% endorsed the use of BMI charts for selected patients who are at the age of 2–5 years Among physicians reporting the use of BMI charts for selected patients, 87% indicated that they use BMI charts for children who appear overweight from height and weight curves, 72% for children who appear overweight by visual inspection and 68% for children who have crossed upwards between weight centiles The time to calculate and plot BMI were perceived as a barrier (major and small) by 65% of all respondents and 75% of respondents who did not use and who used it selectively Time and complexity of explaining the findings to parents was a barrier for 70% of all respondents and 76% of respondents who did not use and who used the BMI charts selectively Parental familiarity with height and weight curves was a barrier for 57% of all respondents and 59% of respondents who did not use and who used the BMI charts selectively Physicians who did not use BMI charts were more likely to report all measured factors as major barriers than physicians who did use BMI charts generally or selectively Colour-coded charts and the inclusion of management recommendations on BMI charts were considered strong influences on the likelihood of using BMI charts more frequently at preschool well-child visits, in 60% and 61%, respectively Computerised calculation and plotting was endorsed by 35% of all respondents as a strong influence on use 47% of respondents endorsed workshops at national and regional medical conferences, 45% endorsed online websites and 43% endorsed DVD training for addressing obesity. Online training was endorsed more often by recent graduates 30% of all respondents indicated that they would participate in a 2-day behaviour management course; paediatricians were significantly more likely than family physicians to endorse this option (38% vs. 17%) 5% of respondents indicated that they probably would not participate in any training activities related to behaviour management skills to address obesity |
Appendix 4 Quality assessment tables
Review of adult morbidities
| Study | Representative population? | Follow-up sufficiently complete? | Analysed sample representative of whole sample? | Valid prognostic factor used? | Prognostic factor measured appropriately? | Prognostic factor measured consistently across sample? | Was a valid outcome measure used? | Outcome measured appropriately? | Outcome measured consistently across sample? | Confounders described? | Confounders measured appropriately? | At least age and sex adjusted for? | Data presented and analysed appropriately? | Selective reporting of outcomes? |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ahlgren (2004)140 | Yes Municipality of Copenhagen |
Yes 73% |
UC | Yes | UC | UC | Yes | Yes Registry data |
Yes | Yes | Yes | Yes | Yes | UC |
| Baker (2007)142 | Yes Public and private schools in Copenhagen |
UC | UC | Yes | UC | UC | Yes | Yes | Yes Registry data |
Yes | Yes | Yes | Yes | UC |
| Baker (2007)141 | Yes Public and private schools in Copenhagen |
Yes 88% in register |
UC | Yes | UC | UC | Yes | Yes Registry data |
Yes Registry data |
Yes | Yes | Yes | Yes | UC |
| Barker (2002)143 | Yes | Yes 83% follow-up (8760/10,519) |
UC | Yes | UC | UC | Yes | No Hypertensive medication use (may exclude undiagnosed and include false positive) |
Yes Hypertensive drug prescription |
Yes | Yes | Yes | Yes | UC |
| Barker (2005)144 | Yes | Yes | Yes | Yes | UC | UC | Yes | Yes | UC | Yes | Yes | Yes | Yes | UC |
| Berentzen (2013)145 | Yes Copenhagen school health records |
Yes 77% at follow-up |
UC | Yes | Yes | UC | Yes | Yes National registry |
UC | Yes | Yes | Yes | Yes | UC |
| Bjorge (2004)146 | Yes | Yes | Yes | Yes | Yes Trained staff |
Yes | Yes | Yes Histology |
Yes Histology for all |
Yes | Yes | Yes | Yes | UC |
| Bjorge (2008)147 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes Registry data |
Yes | Yes | Yes | Yes | Yes | UC |
| Cheng (2011)117 | Yes Typical of city-dwelling Chinese |
No Only 54.1% followed up |
No Statistically significantly higher weight, BMI and blood pressure in those followed up than in whole sample |
Yes | Yes for BMI No for WC |
Yes Trained personnel |
Yes BMI for tracking; hypertension for morbidities |
Yes | Yes Trained personnel |
Yes Age, sex, rural/urban |
Yes | Yes Age, sex, rural/urban |
Yes | UC |
| Cheung (2004)118 | Yes | No ∼ 50% of initial cohort for analyses |
UC | Yes | Yes | Yes Medical personnel |
No Definitions for any of the morbidities |
No Self-report |
Yes | Yes | Yes | No Age only |
Yes | UC |
| De Stavola (2004)148 | Yes Or selected because fewer (1/4) fathers were manual workers |
Yes 86% at follow-up |
Yes | Yes | UC | UC | Yes | No Self-report |
Yes | Yes | Yes | Yes By age for women only |
Yes Imputation method OK |
UC |
| Engeland (2003)149 | Yes | Yes Large proportion (exact numbers NR) |
Yes | Yes | Yes Trained staff |
Yes Trained staff |
Yes | Yes 98% measured histologically |
Yes 98% measured histologically |
Yes | Yes | Yes | Yes | UC |
| Eriksson (2001)150 | Yes | No 64% at follow-up |
UC | Yes | UC | Yes Welfare clinics and school |
Yes | Yes | Yes | Yes Age and birth weight |
Yes | Yes | Yes | UC |
| Forsen (2000)151 | Yes | Yes | Yes | Yes | UC | UC | Yes Diabetes requiring medication |
Yes | Yes | Yes | Yes | Yes | Yes | UC |
| Forsen (2004)152 | Yes | No 55% |
UC | Yes | UC | UC | Yes | Yes | Yes | Yes | Yes | Yes | Yes | UC |
| Goldhaber-Fiebert (2013)123 | Yes | UC | UC | Yes | UC | UC | Yes | No Self-reported for morbidities |
UC | Yes | Yes | Yes | Yes | No |
| Gunnell (1998)153 | Yes No evidence of significant difference between eligible participants and non-participants |
UC Insufficient reporting |
No. Differences in sex and age between follow-up and complete cohort |
Yes | Yes | UC | Yes | Yes | Yes | Yes | Yes | Yes | Yes | UC |
| Hilakivi-Clarke (2001)154 | Yes | UC | UC | Yes | UC | UC | Yes | Yes | Yes | Yes | Yes | Yes | Yes | UC |
| Hypponen (2003)155 | Yes | No 64% at follow-up |
UC | Yes | UC | UC | Yes | No Self-report |
Yes Self-report |
Yes | Yes | Yes | Yes | UC |
| Israeli (2007)156 | Yes Military career service personnel (likely more athletic than average?) |
UC | UC | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | UC |
| Janssen (2005)157 | Yes Note: semi-rural, biracial with high proportion of black participants (35%) |
No 44% at follow-up |
UC | Yes | Yes | UC | Yes | Yes | Yes | Yes Age, race, sex, follow-up length |
UC | Yes | Yes | UC |
| Jeffreys (2004)158 | UC Underprivileged and working class over-represented? |
Yes 78% |
UC | Yes | Yes | Yes | Yes | Yes Registry data or death certificate |
Yes | Yes | Yes | Yes | Yes | UC Site-specific cancer results NR |
| Lawlor (2005)159 | Yes | Yes | UC | Yes | Yes | Yes | Yes | UC | UC | Yes | Yes | Yes | Yes | UC |
| Lawlor (2006)160 | Yes | No 52% attrition |
UC | Yes | UC | UC | No Self-report |
UC | UC | Yes | Yes | Yes | Yes | UC |
| Leiba (2012)161 | Yes | UC | UC | Yes | UC | UC | Yes | Yes Histology |
Yes Histology |
Yes | Yes | Yes | Yes | UC |
| Leiba (2013)162 | Yes | UC | UC | Yes | Yes Medical examination |
UC | Yes | Yes Most appear to have been measured histologically |
Yes Most classified according to standard coding |
Yes | Yes | Yes | Yes | UC |
| Levi (2011)163 | Yes Males only, military recruitment centre |
UC Loss to follow-up NR |
UC | Yes | Yes | Yes | Yes | Yes | Yes Histology |
Yes | Yes | Yes | Yes | UC |
| Levi (2012)164 | Yes Male only |
UC Loss to follow-up NR |
UC | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | UC |
| Li (2007)165 | Yes | No 70% |
Yes | Yes | Yes | Yes ‘Standard protocols’ |
Yes | Yes | Yes | Yes | Yes | Yes | Yes | UC |
| Magnussen (2010)166 | UC Characteristics of large proportion of eligible non-participants in Bogalusa unknown |
No 89% attrition in Bogalusa |
UC | Yes | UC | UC | Yes | Yes Two nurses using standard tool |
Yes | Yes | Yes | Yes | Yes | UC |
| Mattsson (2008)167 | Yes Although only 46% male |
No 51% at follow-up |
UC | Yes | UC | UC | Yes, IDF definition | Yes | Yes | Yes | Yes | Yes | Yes | UC |
| Merten (2010)129 | Yes | No (50% at follow-up) |
UC | Yes | No Self-reporting data |
No Self-reporting data |
Yes | No Self-reported |
No Self-reported |
Yes | UC | Yes | Yes | UC for morbidity |
| Morrison (2010)168 | Yes Note: large proportion of black participants NGHS: girls only |
No PFS: 53% of eligible at 22–30 years follow-up; NGHS: 80.2% at 9 years |
UC only some covariates were reported to be similar between baseline and follow-up (some only after adjustments) | Yes | UC NGHS: UC how WC was measured | Yes | Yes | No No gold standard for distinguishing between type 2 and type 1 diabetes, and appears partially self-reported |
No Collected differently across cohorts |
Yes | Yes | No | Yes | UC |
| Osmond (2007)169 | Yes | Yes National registry data used |
Yes | Yes | Yes | Yes | Yes | UC | UC | Yes | Yes | No Adjusted for sex |
Yes | UC |
| Sachdev (2009)170 | Yes | No 18% at follow-up UC. High proportion of boys |
UC | Yes | Yes Trained personnel |
Yes Trained personnel |
Yes IOTF criteria |
Yes | Yes | Yes | Yes | Yes | Yes | UC |
| Schmidt (2011)171 | Yes | No 26% of baseline group |
No Follow-up group had lower BMI and were more likely to have lived in a higher SES area in childhood (p ≤ 0.01) |
Yes | Yes Or WC, BMI and waist-to-hip UC for sum of SFT |
Yes | Yes | Yes | Yes | Yes | Yes | Yes Adjusted for sex and change in WC |
Yes | UC |
| Tirosh (2011)172 | Yes Military career service personnel (likely more athletic than average?) |
Yes | Yes | Yes | UC | UC | Yes | Yes | Yes | Yes | Yes | Yes | Yes | UC |
Review of tracking of obesity into adulthood
| Study | Representative population? | Follow-up sufficiently complete? | Analysed sample representative of whole sample? | Valid prognostic factor used? | Prognostic factor measured appropriately? | Prognostic factor measured consistently across sample? | Was a valid outcome measure used? | Outcome measured appropriately? | Outcome measured consistently across sample? | Confounders described? | Confounders measured appropriately? | At least age and sex adjusted for? | Data presented and analysed appropriately? | Selective reporting of outcomes? |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cheng (2011)117 | Yes Typical of city dwelling Chinese |
No Only 54.1% followed up |
No Statistically significantly higher weight, BMI and blood pressure in those followed up than whole sample |
Yes | Yes for BMI, no for WC | Yes Trained personnel |
Yes BMI for tracking; hypertension for morbidities |
Yes | Yes Trained personnel |
Yes Age, sex, rural/urban |
Yes | Yes Age, sex, rural/urban |
Yes | Unclear |
| Cheung (2004)118 | Yes | No Approximately 50% of initial cohort not available for analyses |
Unclear | Yes | Yes | Yes Medical personnel |
No Definitions NR for any of the morbidities |
No Self-report |
Yes | Yes | Yes | Yes For tracking; no for morbidity: age only |
Yes | Unclear |
| Engeland (2004)119 | Yes | No | Unclear | Yes | Yes | Unclear | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | No |
| Freedman (2001)120 | Yes | No | Yes | Yes | Yes | Unclear | Yes | Yes | Unclear | Yes | Unclear | Unclear The authors reported that they adjusted race and sex, but was unclear if they also adjusted age |
Yes | No |
| Freedman (2005)122 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| Freedman (2005)121 | Yes | No | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| Goldhaber-Fiebert (2013)123 | Yes | Unclear | Unclear | Yes | Unclear | Unclear | Yes | No Self-reported for morbidities; unclear for tracking |
Unclear | Yes | Yes | Yes | Yes | No |
| Gordon-Larsen (2004)124 | Yes | No | Unclear | Yes | Yes | Yes | Yes | Yes | No Self-reported data were used for a large number of respondents who refused measurements. 71 weighed in excess of the scale capacity. |
Yes | Yes | Yes But not the data we extracted |
Yes | No |
| Juhola (2011) 125 | Yes | No 61.3% |
Unclear | Yes | Unclear | Unclear | Yes | Unclear | Unclear | Yes | Yes | Yes | Yes | No |
| Juonala (2006)126 | Yes | No | No There were more males than females in the dropouts. The people in the dropouts were older than participants |
Yes | Yes | Unclear It was unclear whether or not the measurement was performed consistently across the sample |
Yes | Yes | Unclear The authors did not state whether or not the measurement was performed consistently across sample |
No | Unclear | No | Yes | No |
| Liddle (2012)127 | Yes | No | No Those who lost to follow-up were younger, less well educated and have lower family income |
Yes | Yes | Yes | Yes | No Some self-report |
No Objective and subjective methods |
Yes | Yes | No | Yes | No |
| Mamun (2005)128 | Yes | No | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes The studies described age- or sex- adjusted values for other outcomes but not for tracking data |
Yes | No Tracking data were not stratified by age/sex |
Yes | No |
| Merten (2010)129 | Yes | No | Unclear | Yes | No Self-reporting data |
No Self-reporting data |
Yes | No Self-reported |
No Self-reported |
No | No | No | Yes | No For tracking; unclear for morbidity |
| Nakano (2010)130 | Yes | No | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| Nakano (2010) 131 | Yes | No | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| Patton (2011)132 | Yes | No | Unclear | Yes | Yes | No Self-reported data were used for those who had left school in the later teenage waves |
Yes | No Self-reported data were used in the adult phase |
No Self-reported data were used |
Yes | Yes | Yes | Yes | No |
| Power (1997)133 | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| Reilly (2011)134 | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes | No |
| Starc (2010)135 | Yes | No | Yes The authors reported that the mean values and SDs of the population sample and the subsample analysed were very similar |
Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| Stovitz (2010)136 | Yes | No | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | No |
| Thompson (2007)137 | Yes | Yes | Unclear | Yes | Yes | Yes | Yes | No Self-reporting data |
No Self-reporting data |
Yes Age, race |
Yes | Yes Only girls included |
Yes | No |
| Venn 2007 138 | Yes | No | Yes | Yes | Yes | Unclear | Yes | Yes | No It appears that some self-reported outcome data were included |
Yes | Yes | No | Yes | No |
| Wang (2008)139 | Yes | No | Yes | Yes | No Self-reported data |
No Self-reported data |
Yes | No Self-reported data |
No Self-reported data |
Yes | Yes | Yes | Yes | No |
| Study | Risk of selection bias | Risk of attrition bias | Risk of bias associated with the prognostic factor | Risk of bias associated with outcome | Risk of bias due to confounders | Risk of reporting or analysis bias |
|---|---|---|---|---|---|---|
| All studies | All low | Most unclear, 3 high, 4 low | 14 low, rest unclear | 10 moderate/unclear, 10 low, 3 high | 13 low, 2 high, 8 moderate/unclear | All low |
| Cheng (2011) 117 | Low | High | Low | Low | Moderate/unclear | Low |
| Cheung (2004)118 | Low | High | Low | High | High | Low |
| Engeland (2004)119 | Low | Moderate/unclear | Moderate/unclear | Moderate/unclear | Low | Low |
| Freedman (2001)120 | Low | Low | Moderate/unclear | Moderate/unclear | Moderate/unclear | Low |
| Freedman (2005)122 | Low | Moderate/unclear | Low | Low | Low | Low |
| Freedman (2005)121 | Low | Low | Low | Low | Low | Low |
| Goldhaber-Fiebert (2013)123 | Low | Moderate/unclear | Moderate/unclear | Moderate/unclear | Low | Low |
| Gordon-Larsen (2004)124 | Low | Moderate/unclear | Low | High | Low | Low |
| Juhola (2011) 125 | Low | Moderate/unclear | Moderate/unclear | Moderate/unclear | Low | Low |
| Juonala (2006)126 | Low | High | Moderate | Moderate/unclear | High | Low |
| Liddle (2012)127 | Low | Moderate/unclear | Low | High | Moderate/unclear | Low |
| Mamun (2005)128 | Low | Moderate/unclear | Low | Low | Moderate/unclear | Low |
| Merten (2010)129 | Low | Moderate/unclear | Moderate/unclear | Moderate/unclear | Moderate/unclear | Low |
| Nakano (2010) 131 | Low | Moderate/unclear | Low | Low | Low | Low |
| Nakano (2010)130 | Low | Moderate/unclear | Low | Low | Low | Low |
| Patton (2011)132 | Low | Moderate/unclear | Moderate/unclear | Moderate/unclear | Low | Low |
| Power (1997)133 | Low | Moderate/unclear | Low | Low | Low | Low |
| Reilly (2011)134 | Low | Moderate/unclear | Low | Low | Moderate/unclear | Low |
| Starc (2010)135 | Low | Low | Low | Low | Low | Low |
| Stovitz (2010)136 | Low | Moderate/unclear | Low | Low | Moderate/unclear | Low |
| Thompson (2007)137 | Low | Moderate/unclear | Low | Moderate/unclear | Low | Low |
| Venn (2007)138 | Low | Moderate/unclear | Moderate/unclear | Moderate/unclear | Moderate/unclear | Low |
| Wang (2008)139 | Low | Low | Moderate/unclear | Moderate/unclear | Low | Low |
Review of the diagnostic accuracy of childhood measures of obesity
| Short title | 1. Representative population | 2. Progression bias | 3. Partial verification bias | 4. Differential verification bias | 5. Incorporation bias | 6. Description of selection criteria | 7. Appropriateness of RS | 8. Description of index text | 9. Used validated index text | 10. Description of RS | 11. Uninterpretable/intermediate results reported | 12. Withdrawals explained | 13. Measurement bias | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 13a. Training/experience Index test personnel | 13b. Number of index text assessors | 13c. Training/experience RS test personnel | 13d. Number of RS assessors | |||||||||||||
| Alvero-Cruz (2010)173 | Yes | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Inadequate | Yes | Inadequate | Apparently none | None | UC | UC | UC | UC |
| Bartok (2011)174 | No | UC | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | No | UC | UC | UC | UC |
| Bray (2002)175 | No | Probably avoided | Avoided | Avoided | Avoided | Adequate | Gold standard | Inadequate | Yes | Inadequate | Apparently none | Noa | UC | UC | UC | UC |
| Dung (2006)176 | No | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | None | UC | UC | UC | UC |
| Ellis (1999)177 | Yes | Probably avoided | Avoided | Avoided | Avoided | Inadequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | None | Yesb | Multib | UC | UC |
| Field (2003)178 | Yes | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | None | UC | UC | UC | UC |
| Freedman (2009)179 | Yes | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Inadequate | Yes | Nonec | UC | UC | UC | UC |
| Freedman (2013)180 | Yes | Probably avoided | Presentd | Avoided | Avoided | Adequate | Imperfect | Adequate for BMI Inadequate for SFT | Yes | Inadequate | Yes | Noe | UC | UC | UC | UC |
| Fujita (2011)181 | Yes | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | Yes | UC | UC | UC | UC |
| Fuller (2001)182 | UC | Probably avoided | Avoided | Avoided | Avoided | Inadequate | Gold standard | Adequate | Yes | Adequate | Completer analysis | Yes | UC | UC | UC | UC |
| Fuller (2002)183 | UC | Probably avoided | Avoided | Avoided | Avoided | Inadequate | Imperfect | Adequate | Yes | Inadequate | Completer analysis | Yes | UC | UC | UC | UC |
| Guntsche (2010)184 | No | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Inadequate | Yes | Inadequate | Apparently none | None | UC | UC | UC | UC |
| Harrington (2013)185 | Nof | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | Yes | UC | UC | UC | UC |
| Himes (1989)186 | Yes | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Inadequate | Yes | Inadequate | Apparently none | None | UC | UC | UC | UC |
| Johnston (1985)187 | No | Probably avoided | Avoided | Avoided | Avoided | Inadequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | None | UC | UC | UC | UC |
| Khadgawat (2013)188 | Yesg | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | Yes | UC | UC | UC | UC |
| Marshall (1991)189 | Yes | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | Yes | UC | UC | UC | UC |
| Mei (2007)190 | Yes | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | Yes | Yesh | 2 | UC | UC |
| Moreno (2006)191 | Yes | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | Yes | UC | UC | Yesh | 1 |
| Neovius (2004)192 | Yes | UC | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | Yes | UC | UC | UC | UC |
| Neovius (2005)193 | Yes | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Inadequate | Yes | Inadequate | Apparently none | Yes | UC | UC | UC | UC |
| Pandit (2009)194 | Yes | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | None | UC | UC | UC | 1 |
| Reilly (2010)195 | Yes | UC | Avoided | Avoided | Avoided | Adequate | Imperfect | Inadequatei | Yes | Inadequate | Apparently none | Yes | UC | UC | UC | UC |
| Sardinha (1999)196 | No | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Inadequate | Yes | Inadequate | Apparently none | None | Yesh | UC | UC | 1 |
| Sarria (2001)197 | No | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Adequate | Yes | Yes | UC | UC | UC | UC |
| Sproule (2009)198 | No | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | None | UC | UC | UC | UC |
| Taylor (2000)199 | Noj | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | None | UC | UC | UC | UC |
| Taylor (2003)200 | Noj | Probably avoided | Avoided | Avoided | Avoided | Inadequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | None | UC | UC | Yesh | 2 |
| Telford (2008)201 | Yes | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | None | UC | UC | UC | UC |
| Vitolo (2007)202 | Yes | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | Yes | UC | UC | UC | UC |
| Warner (1997)203 | No | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | None | UC | UC | UC | UC |
| Wickramasinghe (2005)204 | No | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Adequate | Apparently none | None | UC | UC | UC | UC |
| Wickramasinghe (2009)205 | Yes | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | None | UC | UC | UC | UC |
| Zhang (2004)206 | Yes | Probably avoided | Avoided | Avoided | Avoided | Adequate | Imperfect | Adequate | Yes | Inadequate | Apparently none | No | Yes | UC | UC | UC |
Yes: unselected children, or children randomly selected from a representative population, recruited prospectively.
No: all other patient spectra including a retrospectively selected patient population.
Unclear: insufficient details were provided to make a judgement on whether or not the patient spectrum was representative.
Was the study subject to progression bias?Avoided: the index test and reference standard were conducted within days or weeks of each other; therefore, progression bias was avoided.
Probably avoided: there was not specific information regarding the timing of the index test and reference standard, but the description of the study design makes progression bias unlikely.
Not avoided: there was a substantial delay between the index test and reference standard during which weight status could have changed.
Unclear: there was insufficient information to determine whether or not progression bias was present or absent.
Was the study subject to partial verification bias?Avoided: all children had their adiposity determined using a reference standard and partial verification bias was avoided.
Not avoided: some children did not have their adiposity determined using a reference standard.
Unclear: there was insufficient information to determine whether or not all children had their adiposity determined using a reference standard.
Was the study subject to differential verification bias?Avoided: all children had the same reference standard and differential verification bias was avoided.
Not avoided: children underwent different reference standards.
Unclear: there was insufficient information to determine whether or not all children had the same reference standard.
Was the study subject to incorporation bias?Avoided: the index test was independent of the reference standard and incorporation bias was avoided.
Not avoided: the results of the index test formed part of the reference standard.
Unclear: there was insufficient information to determine whether or not the index test was independent of the reference standard.
Was the description of the selection criteria adequately described to allow replication?Adequate: sufficient details were reported.
Inadequate: insufficient details were reported.
Was the reference standard used appropriate?Gold standard: a four or more component model was used.
Imperfect: underwater (hydrostatic) weighting, D2O, ADP or DEXA alone was used.
Was the description of the conduct of the index test adequate to allow replication?Adequate: sufficient details were reported.
Inadequate: insufficient details were reported.
Was the index test used a validated measure?Yes: the index test used was validated and used recognised cut-off points and reference data.
No: the index test used was not validated.
Unclear: insufficient details were reported to determine whether or not the index test used was validated.
Was the description of the conduct of the reference standard adequate to allow replication?Adequate: sufficient details were reported.
Inadequate: insufficient details were reported.
Were uninterpretable/intermediate results reported?None: there were no uninterpretable results.
Apparently none: given the data in the analysis, it seems that there were no uninterpretable results or they were accounted for but details not provided.
Yes: uninterpretable results occurred and these were reported and accounted for in the analysis.
Completer analysis: uninterpretable results occurred and only those with interpretable results were included in the analysis.
Unclear: it was not clear whether or not there were any uninterpretable/intermediate test results.
Were withdrawals from the study reported/explained?None: there were no withdrawals.
Yes: withdrawals occurred, but these were explained.
No: there appeared to be patients who were recruited who were not accounted for.
Unclear: it was not clear whether or not any withdrawals occurred.
Did the study avoid measurement bias:Yes: the study used a single, appropriately trained individual for the conduct of all childhood measures of obesity.
No: the study used multiple assessors, or inadequately trained individual(s).
Unclear: insufficient details were reported on the number and/or experience of assessors.
Review of the acceptability and ease of use of simple childhood measures of obesity
| Study | 1. Clear statement of aims? | 2. Appropriate methodology? | 3. Appropriate research design? | 4. Appropriate recruitment strategy? | 5. Data collected appropriately? | 6. Relationship between researcher and participants considered? | 7. Ethical considerations considered? | 8. Rigorous data analysis? | 9. Clear statement of findings? | 10. Research of value? |
|---|---|---|---|---|---|---|---|---|---|---|
| Cloutier (2013)207 | Yes | Yes | Yes | No | Yes | No | Yes | Yes | Yes | Yes |
| Hendershot (2008)73 | Yes | Yes | Yes | Yes | Yes | UC | NA | UC | Yes | Yes |
| Kubik (2006)74 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Kubik (2007)75 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Woolford (2008)208 | Yes | Yes | Yes | Yes | Yes | No | NA | Yes | Yes | Yes |
Yes: the aims of the study were clearly stated and relevant.
No: the aims of the study were not clearly stated and/or were not relevant.
2. Qualitative methodology appropriate?Yes: the study was seeking to interpret subjective experiences of participants, making qualitative methodology the correct methodology to use.
No: the study was not seeking to interpret subjective experiences of participants.
3. Appropriate research design?Yes: a prospective cohort of children, parents/guardians and/or health professionals.
No: any other study design.
Unclear: insufficient details of the study methodology were reported.
4. Appropriate recruitment strategyYes: unselected consecutive participants, or randomly selected participants, from a population of children, parents/guardians and/or health professionals representative of those who will (whose children will) undergo the test(s) for which opinions were being sought in clinical practice.
No: non-consecutive or random selection, or selection from a population not representative of those who will undergo the test(s) for which opinions were being sought in clinical practice.
Unclear: insufficient details of recruitment were reported.
5. Data collected appropriately?Yes: focus groups or structured interviews or questionnaires were used to elicit opinions.
No: other methods of elicitation.
Unclear: insufficient details of the method of elicitation of opinions were reported.
6. Relationship between researcher and participants considered?Yes: the relationship between the researcher and participants, and the researcher’s responses to events during the study, were discussed.
No: the relationship between the researcher and participants was not discussed.
7. Ethical considerations considered?Yes: ethical considerations were discussed, or ethical approval obtained.
No: ethical considerations were neither discussed nor was ethical approval obtained.
Not applicable: the study was conducted in adults for whom ethical approval was not required, and ethical considerations were thought to be relevant.
8. Rigorous data analysis?Yes: the methods used to evaluate findings was rigorous, although simple in some cases.
No: the methods used to evaluate findings was not rigorous, or insufficient data were presented to support the findings.
Unclear: insufficient details were reported as to how the synthesis was conducted.
9. Clear statement of findings?Yes: the findings were explicitly stated.
No: the findings were not explicitly stated.
10. Research of value?Yes: the value of the research was considered by the study authors, recommendations were reported and the research was considered to be of value by the review team.
No: the value of the research was either not considered by the study authors, or recommendations were not reported, and/or the research was considered to be of value by the review team.
Unclear: the value of the research was not discussed by the study authors and was unclear to the review team.
Appendix 5 Review of adult morbidities: additional results from the meta-analyses
FIGURE 34.
Odds ratios for all adult morbidities. BCAMSS, Beijing Child and Adolescent Metabolic Syndrome study; MRC NSHD, Medical Research Council National Survey of Health and Development; NGHS, National Growth and Health study; PFS, Princeton follow-up study; SPEC, Staff Periodic Examination Center.

Glossary
- D2O
- Deuterium dilution method.
- Sum SFT
- The sum of skinfold thickness measurements at more than one site.
- UK90
- The British 1990 growth reference.
List of abbreviations
- 4-C
- four-component
- ADP
- air displacement plethysmography
- AUC
- area under the curve
- BAI
- body adiposity index
- BIA
- bioelectrical impedance analysis
- BMI
- body mass index
- CDC
- Centers for Disease Control and Prevention
- CDSR
- Cochrane Database of Systematic Reviews
- CEDAR
- Centre for Diet and Activity Research
- CENTRAL
- Cochrane Central Register of Controlled Trials
- CHD
- coronary heart disease
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CPCI-S
- Conference Proceedings Citation Index – Science
- CRD
- Centre for Reviews and Dissemination
- CVD
- cardiovascular disease
- DARE
- Database of Abstracts of Reviews of Effects
- DEXA
- dual-energy X-ray absorptiometry
- DoPHER
- Database of Promoting Health Effectiveness Reviews
- DOR
- diagnostic odds ratio
- EASO
- European Association for the Study of Obesity
- ECOG
- European Childhood Obesity Group
- EPPI-Centre
- Evidence for Policy and Practice Information and Co-ordinating Centre
- FMI
- fat mass index
- HC
- hip circumference
- HDL
- high-density lipoprotein
- HR
- hazard ratio
- HSROC
- hierarchical summary receiver operating characteristic
- HTA
- Health Technology Assessment
- IDF
- International Diabetes Federation
- IOTF
- International Obesity Taskforce
- LDL
- low-density lipoprotein
- LR−
- negative likelihood ratio
- LR+
- positive likelihood ratio
- MeSH
- medical subject heading
- MRI
- magnetic resonance imaging
- MUSP
- Mater-University Study of Pregnancy
- NC
- neck circumference
- NCDS
- National Child Development Study
- NCMP
- National Child Measurement Programme
- NHANES
- National Health and Nutrition Evaluation Surveys
- NHS EED
- NHS Economic Evaluation Database
- NICE
- National Institute for Health and Care Excellence
- NIR
- near-infrared interactance
- NLSAH
- National Longitudinal Study of Adolescent Health
- NLSY79
- National Longitudinal Survey of Youth
- NPV
- negative predictive value
- OR
- odds ratio
- PPV
- positive predictive value
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PSID
- Population Study of Income Dynamics
- ROC
- receiver operating characteristic
- RR
- relative risk
- SCI
- Science Citation Index
- SD
- standard deviation
- SES
- socioeconomic status
- SFT
- skinfold thickness
- WC
- waist circumference
- WHO
- World Health Organization
- WHR
- waist-to-hip ratio
- WHtR
- waist-to-height ratio
- WoS
- Web of Science