Notes
Article history
The research reported in this issue of the journal was commissioned and funded by the HTA programme on behalf of NICE as project number 13/06/01. The protocol was agreed in June 2013. The assessment report began editorial review in December 2013 and was accepted for publication in March 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Sharma et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background and definition of the decision problem(s)
Conditions and aetiologies
Brief statement describing the health problem
People with certain clinical conditions such as atrial fibrillation or heart valve disease are at high risk of thrombosis (blood clot). Untreated, these may lead to thromboembolism affecting the brain (causing a stroke), the lungs (pulmonary embolism) or other parts of the body. Many people with these conditions are required to take lifelong blood-thinning drugs (called vitamin K antagonists) to avoid the risks associated with thrombosis. Treatment using blood-thinning drugs is termed anticoagulant therapy and it is estimated that 1.4% of the population in the UK require anticoagulant therapy. 1
Warfarin is the most common vitamin K antagonist drug given to prevent clot formation and stroke. However, serious side effects including bleeding or stroke can result from people being on the wrong dose of warfarin (over- or underdosing). Therefore, it is necessary to ensure that people taking warfarin have ongoing monitoring of their blood coaguability.
Epidemiology and prevalence
There are increasing numbers of people with atrial fibrillation, heart valve replacement or other clinical conditions requiring long-term oral anticoagulation therapy (OAT). 2 As up to 60% of people with atrial fibrillation might be undiagnosed, screening programs have the potential to increase diagnoses and associated use of OAT. 3 The prevalence of atrial fibrillation has recently been described as ‘approaching epidemic proportions’4 and it has been predicted that, by 2050, more than 5.6 million adults in the USA will be diagnosed with atrial fibrillation, compared with 2.3 million in 2001. 5 Increased use of OAT has intensified pressure upon resources, with some haematology services becoming unable to cope. 6
Atrial fibrillation
In the USA, prevalence of atrial fibrillation has been reported as 0.1% in adults < 55 years of age and 9% in those ≥ 80 years old. 5 Over 6 million people in Europe have atrial fibrillation7 and a recent Swedish study reported prevalence of 2.9% in adults > 20 years. 8 Atrial fibrillation is the most common heart arrhythmia and affects around 800,000 people in the UK, or 1.3% of the population. 9 Prevalence increases with age, being 0.5% among people aged 50–59 years and approximately 5% to 8% among people aged > 65 years. 10,11 Atrial fibrillation is more likely to affect men than women and is more common in people with other conditions, for example high blood pressure, atherosclerosis, or other heart conditions such as heart valve problems. For people with atrial fibrillation, there is a five times higher risk of stroke and a three times higher risk of congestive heart failure. 12 One-fifth of all strokes are a result of atrial fibrillation. 7 An average proportion of 47% of people with atrial fibrillation currently receive anticoagulation therapy, such as warfarin. 1
Heart valve disease
Aortic stenosis is the most common type of heart valve disease. It affects 1 in 20 adults over the age of 65 years. 13,14 Data from the UK Heart Valve Registry indicate that approximately 0.2% of the UK population has prosthetic heart valves. 15 Around 6500 adult heart valve replacements (using mechanical or biological valves) are carried out each year, of which around 5000 are aortic valve replacements. 15,16
Impact of health problem: significance for the NHS and burden of disease
The blood coaguability of people taking warfarin is monitored by the use of the international normalised ratio (INR), which is a standardised unit for measuring the time it takes for blood to clot. INR monitoring can be delivered using various options in the NHS. The options include INR monitoring managed by health-care professionals in anticoagulant clinics based in hospitals using laboratory testing or managed in primary care (with or without the use of laboratory services). The use of a personal INR testing machine at home (known as a point-of-care test) allows people to perform self-testing (when people perform the test themselves and the results of the test are managed by health-care professionals) or self-management (when people perform the test and alter the dose of anticoagulation therapy themselves according to a personalised protocol). Self-testing and self-management are together referred to as self-monitoring. Self-monitoring is considered as one of the options for INR monitoring in the NHS, but there is limited evidence on the clinical effectiveness compared with other ways of delivering services.
The use of point-of-care coagulometers for self-monitoring may avoid unnecessary visits to hospitals while allowing regular INR monitoring and timely adjustment of warfarin dosing to avoid adverse events. For people requiring monitoring of their coagulation status, this may result in better quality of life. 17
Measurement of disease
The goal of anticoagulant therapy is to establish a balance between bleeding and clotting18 and it is desirable for people on warfarin to remain within a narrow INR therapeutic range, generally between 2.0 and 3.0. 19,20 If the dose of anticoagulation therapy is too low (underanticoagulation), the risk of thromboembolism increases, while if it is too high (overanticoagulation), the risk of haemorrhage increases. Individuals’ reactions to warfarin vary according to modifiable (e.g. diet) and non-modifiable factors (e.g. age, concomitant diseases). Adequate control of INR is necessary to avoid serious complications such as stroke. Therefore, repeated and regular measurements of INR are required to allow adjustments to size and/or frequency of dosage. 21
Description of technologies under assessment
Summary of point-of-care tests
Point-of-care devices for measuring coagulation status in people receiving long-term vitamin K antagonist therapy allow both self-testing and self-management, defined as follows:
-
Self-testing: point-of-care test carried out by the patient with test results managed by their health-care provider [e.g. general practitioner (GP), nurse, specialised clinic].
-
Self-management: point-of-care test carried out by trained patient, followed by interpretation of test result and adjustment of dosage of anticoagulant according to a predefined protocol.
Self-testing and self-management are together referred to as self-monitoring for the purposes of this report.
The purpose of this assessment was to appraise the current evidence for the clinical effectiveness and cost-effectiveness of self-monitoring (self-testing and self-management) using either the CoaguChek® system (Roche Diagnostics, Basel, Switzerland), the INRatio2® PT/INR monitor, (Alere Inc., San Diego, CA, USA) or the ProTime Microcoagulation system® (International Technidyne Corporation, Nexus Dx, Edison, NJ, USA), compared with standard clinical monitoring in people with atrial fibrillation or heart valve disease for whom long-term vitamin K antagonist therapy is indicated.
All of these point-of-care devices, which are currently available for use in the NHS, are CE marked and Food and Drug Administration (FDA) approved. Point-of-care instruments work basically in the same way: a drop of capillary whole blood is obtained by a finger puncture device, applied to a test strip and inserted into a coagulometer. However, they differ in terms of methods of clot detection and general operational functions.
Summary of CoaguChek system
The CoaguChek system is a point-of-care testing device developed by Roche Diagnostics and measures prothrombin time and INR (the globally recommended unit for measuring thromboplastin time) in people on oral anticoagulation (vitamin K antagonist) therapy. A low INR indicates an increased risk of blood clots, while a high INR indicates an increased risk of bleeding events. CoaguChek S and CoaguChek XS devices are intended for patient self-monitoring. The CoaguChek XS model comprises a meter and specifically designed test strips for blood sample analysis (fresh capillary or untreated whole venous blood). The CoaguChek XS system purports to have the following advantages over the CoaguChek S: (1) the thromboplastin used in the prothrombin time test strips is a human recombinant thromboplastin, which is more sensitive and has a lower International Sensitivity Index (ISI) of 1.0 compared with 1.6; (2) test strips have onboard quality control that is automatically run with every test, rather than having to perform external quality control; (3) test strips do not have to be refrigerated; (4) a smaller blood sample can be used; and (5) the meter is smaller and lighter. The CoaguChek XS Plus model is aimed primarily at health-care professionals and possesses additional features to the XS system, including increased storage and connectivity for data management.
Summary of INRatio2 PT/INR monitor
The INRatio2 PT/INR monitor performs a modified version of the one-stage prothrombin time test using a recombinant human thromboplastin reagent. The clot formed in the reaction is detected by the change in the electrical impedance of the sample during the coagulation process. The system consists of a monitor and disposable test strips and the results for prothrombin time and INR are reported.
Summary of ProTime Microcoagulation system
The ProTime Microcoagulation system is designed for measuring prothrombin time and INR. The test is performed in a cuvette which contains the reagents. Two different cuvettes are available depending on the amount of blood that needs to be collected and tested: the standard ProTime cuvette and the ProTime3 cuvette.
Identification of important subgroups
There are a number of clinical conditions which require long-term vitamin K antagonist therapy to reduce the risk of thrombosis. These conditions include atrial fibrillation and heart valve disease.
Atrial fibrillation
Atrial fibrillation results in unorganised atrial electrical activity associated with mechanically ineffective fibrillation, that contraction which can lead to blood stagnating in parts of the atria and as a result forming a clot. This clot may then move from the heart, causing thromboembolism, most commonly in the brain where it causes stroke. People with atrial fibrillation are at a five to six times greater risk of stroke, with 12,500 strokes directly attributable to atrial fibrillation every year in the UK. Treatment with warfarin reduces the risk by 50–70%. 1,22,23
Artificial heart valves
Valve disease can affect blood flow through the heart in two ways: valve stenosis, where the valve does not open fully, and valve regurgitation (or incompetence), where the valve does not close properly, allowing blood to leak backwards. The most effective treatment for many forms of valve disease is heart valve replacement. Replacement heart valves are either artificial (mechanical), or from humans or animals (tissue). The human valve could be from the same patient (autograft) when the native pulmonary valve is used in the aortic position (part of the Ross procedure); or from another patient (heterograft). People with mechanical heart valves generally require long-term anticoagulant treatment to prevent clotting related to the valve.
Current usage in the NHS
The National Institute for Health and Care Excellence (NICE) clinical guideline on atrial fibrillation24 recommends that self-monitoring of INR should be considered for people with atrial fibrillation receiving long-term anticoagulation, if they prefer this form of testing and if the following criteria are met:
-
the patient (or a designated carer) is both physically and cognitively able to perform the self-monitoring test
-
an adequate supportive educational programme is in place to train participants and/or carers
-
the patient’s ability to self-manage is regularly reviewed
-
the equipment for self-monitoring is regularly checked via a quality control programme.
Comparators
In UK clinical practice, INR monitoring is currently managed by a range of health-care professionals, including nurses, pharmacists and GPs. INR monitoring can be carried out in primary care and secondary care. Primary care anticoagulant clinics use point-of-care tests or laboratory analysers. In the latter, blood samples are sent to a central laboratory based at a hospital (‘shared provision’). In the case of secondary care, INR monitoring can be carried out in hospital-based anticoagulant clinics using point-of-care tests or laboratory analysers.
Care pathways
The clinical population considered for the purpose of this assessment includes people with atrial fibrillation or heart valve disease for whom long-term vitamin K antagonist therapy is intended. According to the NICE clinical guideline on atrial fibrillation and the Scottish Intercollegiate Guidelines Network clinical guideline on antithrombotics,24,25 the most effective treatment considered for the treatment of atrial fibrillation is dose-adjusted warfarin, the most common vitamin K antagonist drug. Lifelong anticoagulation therapy with warfarin is also recommended in all people after artificial valve replacement. 26 Warfarin, especially if taken incorrectly, can cause severe bleeding (haemorrhages). Therefore, it is necessary to ensure that people taking warfarin have ongoing monitoring of their blood coaguability.
The routine monitoring of blood coagulation can take several configurations. The NICE anticoagulation commissioning guide1 states that UK anticoagulation therapy services can be delivered in a number of different ways, and that mixed models of provision may be required across a local health economy. This could include full service provision in primary or secondary care, shared provision, domiciliary provision or self-management.
This assessment focuses on the role of point-of-care tests (for the self-monitoring of INR by people at home) as an alternative to standard UK anticoagulation care.
Outcomes
Outcomes of interest for this review were as follows.
Clinical outcomes
-
Frequency of bleeds or blood clots.
-
Morbidity (e.g. thromboembolic and cerebrovascular events) and mortality from INR testing and vitamin K antagonist therapy.
-
Adverse events from INR testing, false test results, vitamin K antagonist therapy and sequelae.
Patient-reported outcomes
-
People‘s anxiety associated with waiting time for results and not knowing their current coagulation status and risk.
-
Acceptability of the tests.
-
Health-related quality of life.
Intermediate outcomes
-
Time and values in therapeutic range.
-
INR values.
-
Test failure rate.
-
Time to receive test result.
-
Patient compliance with testing and treatment.
-
Frequency of testing.
-
Frequency of visits to primary or secondary care clinics.
Overall aim and objectives of this assessment
The aim of this assessment was to appraise the current evidence for the clinical effectiveness and cost-effectiveness of self-monitoring (self-testing and self-management) using CoaguChek, INRatio2 PT/INR monitor and ProTime Microcoagulation system point-of-care devices, compared with standard monitoring, in people with atrial fibrillation or heart valve disease receiving long-term vitamin K antagonist therapy.
The specific objectives of this assessment were to:
-
systematically review evidence on the clinical-effectiveness of self-monitoring (self-testing and self-management) using CoaguChek, INRatio2 PT/INR monitor and ProTime Microcoagulation system point-of-care devices, compared with standard monitoring practice, in people receiving long-term vitamin K antagonist therapy
-
systematically review existing economic evaluations on self-monitoring technologies for people receiving long-term vitamin K antagonist therapy
-
develop a de novo economic model to assess the cost-effectiveness of both self-testing and self-management (using CoaguChek XS system, INRatio2 PT/INR monitor and ProTime Microcoagulation system as self-monitoring technologies) versus standard monitoring practice in people receiving long-term vitamin K antagonist therapy.
Chapter 2 Assessment of clinical effectiveness
Methods for standard systematic review of clinical effectiveness
An objective synthesis of the evidence for the clinical effectiveness of self-monitoring in people receiving long-term vitamin K antagonist therapy using either CoaguChek system, INRatio2 PT/INR monitor or ProTime Microcoagulation system compared with current standard monitoring practice has been conducted. The evidence synthesis has been carried out according to the general principles of the Centre for Reviews and Dissemination guidance for conducting reviews in health care,27 the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions28 and the indications of the NICE Diagnostics Assessment Programme Manual. 29 Preferred Reporting Items for Systematic Reviews and Meta-Analyses recommendations were followed for reporting. 30
Identification of studies
Comprehensive electronic searches were undertaken to identify relevant reports of published studies. Highly sensitive search strategies were designed using both appropriate subject headings and relevant text word terms, to retrieve randomised controlled trials (RCTs) evaluating the point-of-care tests under consideration for the self-monitoring of anticoagulation therapy. A 2007 systematic review with similar objectives to those of the current assessment was identified in The Cochrane Library. 31 As extensive literature searches had already been undertaken for the preparation of this systematic review, the literature searches for the current assessment were run in May 2013 for the period ‘2007 to date’ to identify newly published reports. All RCTs included in the Cochrane review were obtained and included for full-text assessment. Searches were restricted to publications in English. MEDLINE, MEDLINE In Process & Other Non-Indexed Citations, EMBASE, Bioscience Information Service, Science Citation Index and Cochrane Central Register of Controlled Trials (CENTRAL) were searched for primary studies, while the Cochrane Database of Systematic Reviews, the Database of Abstracts of Reviews of Effects and the Health Technology Assessment (HTA) database were searched for reports of evidence syntheses.
Reference lists of all included studies were perused in order to identify additional potentially relevant reports. The expert panel provided details of any additional potentially relevant reports.
Searches for recent conference abstracts (2011–13) were also undertaken and included the annual conferences of the American Society of Haematology, the European Haematology Association and the International Society on Thrombosis and Haemostasis, as well as the proceedings of the 12th National Conference on Anticoagulant Therapy. Ongoing studies were identified through searching Current Controlled Trials, Clinical Trials, World Health Organization, International Clinical Trials Registry and NationaI Institutes of Health Reporter. Websites of professional organisations and health technology agencies were checked to identify additional reports. Full details of the search strategies used are presented in Appendix 1.
Inclusion and exclusion criteria
The initial scoping searches performed for this assessment identified a Cochrane review31 and a few technology assessment reports21,32,33 assessing different models of managing OAT. These publications focused on several RCTs, which reported relevant clinical outcomes. In particular, the Cochrane review included both the CoaguChek S and the CoaguChek XS devices. The CoaguChek XS system is the upgraded version of CoaguChek S and uses the same technology as its precursor. Details of the performance of the two CoaguChek models compared with standard INR monitoring are provided below (see Performance of point-of-care devices).
The studies fulfilling the following criteria were included in this assessment.
Population
People with atrial fibrillation or heart valve disease for whom long-term vitamin K antagonist therapy was required.
Setting
Self-INR monitoring supervised by primary or secondary care.
Interventions
The point-of-care devices considered in this assessment were:
-
CoaguChek system
-
INRatio2 PT/INR monitor
-
ProTime Microcoagulation system.
Comparators
The comparator considered in this assessment was standard practice, which consisted of INR monitoring managed by health-care professionals. INR monitoring can be carried out in primary care, in secondary care or in a ‘shared provision’ setting:
-
Primary care: INR monitoring can be carried out in primary care anticoagulant clinics using point-of-care tests or laboratory analysers. In the latter, blood samples are sent to a central laboratory based at a hospital (shared provision).
-
Secondary care: INR monitoring can be carried out in hospital-based anticoagulant clinics using point-of-care tests or laboratory analysers.
Outcomes
The following outcomes were considered.
Clinical outcomes
-
Frequency of bleeds or blood clots.
-
Morbidity (e.g. thromboembolic and cerebrovascular events) and mortality from INR testing and vitamin K antagonist therapy.
-
Adverse events from INR testing, false test results, vitamin K antagonist therapy and sequelae.
Patient-reported outcomes
-
People’s anxiety associated with waiting time for results and not knowing their current coagulation status and risk.
-
Acceptability of the tests.
-
Health-related quality of life.
Intermediate outcomes
-
Time and INR values in therapeutic range.
-
Test failure rate.
-
Time to receive test result.
-
Patient compliance with testing and treatment.
-
Frequency of testing.
-
Frequency of visits to primary or secondary care clinics.
Study design
We identified relevant RCTs assessing the effectiveness of the CoaguChek system, the INRatio2 PT/INR monitor and the ProTime Microcoagulation system. Therefore, non-randomised studies (including observational studies) were not considered for this assessment. Systematic reviews were used as source for identifying additional relevant studies.
Studies were excluded if they did not meet the prespecified inclusion criteria, and, in particular, the following types of report were not deemed suitable for inclusion:
-
biological studies
-
reviews, editorials and opinions
-
case reports
-
non-English-language reports
-
conference abstracts published before 2012.
Data extraction strategy
Two reviewers (PS and MB) independently screened the titles and abstracts of all citations identified by the search strategies. Full-text copies of all studies deemed to be potentially relevant were obtained and assessed independently by two reviewers for inclusion (PS and MC). Any disagreements were resolved by discussion or arbitration by a third reviewer (MB).
A data extraction form was designed and piloted for the purpose of this assessment (see Appendix 2). One reviewer (PS) extracted information on study design, characteristics of participants, settings, characteristics of interventions and comparators, and relevant outcome measures. A second reviewer (MC) cross-checked the details extracted by the first reviewer. There was no disagreement between reviewers.
Assessment of risk of bias in included studies
A single reviewer (PS) assessed the risk of bias of the included studies and findings were cross-checked by a second reviewer (MC). There were a few disagreements which were resolved by consensus or arbitration by a third reviewer (MB). The reviewers were not blinded to the names of studies’ investigators, institutions and journals. Studies were not included or excluded purely on the basis of their methodological quality. The risk of bias assessment for all included RCTs was performed using the Cochrane risk of bias tool (see Appendix 3). 28 Critical assessments were made separately for all main domains: selection bias (‘random sequence generation’, ‘allocation concealment’), detection bias (‘blinding of outcome assessor’), attrition bias (‘incomplete outcome data’) and reporting bias (‘selective reporting’). The ‘blinding of participants and personnel’ was not considered relevant for this assessment due to the nature of intervention being studied (i.e. patient performing the test themselves or under supervision of health-care professionals). However, we collected information related to the blinding of outcome assessors, which was considered relevant to the assessment of risk of bias.
We judged each included study as ‘low risk of bias’, ‘high risk of bias’ or as ‘unclear risk of bias’ according to the criteria for making judgments about risk of bias described in the Cochrane Handbook for Systematic Reviews of Interventions. 28 Adequate sequence generation, allocation concealment and blinding of outcome assessor were identified as key domains for the assessment of the risk of bias of the included trials.
Data analysis
For dichotomous data (e.g. bleeding events, thromboembolic events, mortality), relative risk (RR) was calculated. For continuous data [e.g. time in therapeutic range (TTR)], weighted mean difference (WMD) was calculated. Where standard deviations (SDs) were not given, we calculated them using test statistics wherever possible. The RR and WMD effect sizes were meta-analysed as pooled summary effect sizes using the Mantel–Haenszel (M–H) method and the inverse-variance (IV) method, respectively. We also calculated 95% confidence intervals (CIs). To estimate the summary effect sizes, both fixed-effect and random-effect models were used with RR and WMD. In the absence of clinical and/or statistical heterogeneity, the fixed-effects model was selected as the model of choice, while the random-effects model was used to cross-check the robustness of the fixed-effects model. However, in the presence of either clinical or statistical heterogeneity, the random-effects model was chosen as the preferred method for pooling the effect sizes, as in this latter situation, the fixed-effects method is not considered appropriate for combining the results of included studies. 28 Heterogeneity across studies was measured by means of the chi-squared statistic and also by the I2 statistic, which describes the percentage of variability in study effects that is explained by real heterogeneity rather than chance. It is worth noting that, for bleeding and thromboembolic events, we used the total number of participants who were actually analysed as denominator in the analyses. In contrast, for mortality, we used the total number of participants randomised as denominator because participants could have died due to any causes after randomisation but before entering the self-monitoring programme.
Apart from the prespecified subgroups analysis, according to the type of anticoagulation therapy management (self-testing and self-management), we performed a post-hoc subgroup analysis according to the type of the target clinical condition (i.e. atrial fibrillation, heart valve disease and mixed clinical indication) and one according to the type of service provision for anticoagulation management (i.e. primary care, secondary care and shared provision). Where trials had multiple arms contributing to different subgroups, the control group was subdivided into two groups to avoid a unit of analysis error.
Sensitivity analyses were planned in relation to some of the study design characteristics. The methodological quality (low/high risk of bias) and the different models of the CoaguChek system were identified at protocol stage as relevant aspects to explore in sensitivity analyses. In addition to those prespecified in the protocol, we performed a sensitivity analysis by excluding the studies conducted in the UK.
Review Manager software (Review Manager 5.2, 2012, The Cochrane Collaboration, The Nordic Cochrane Centre, Copenhagen, Denmark) was used for data management and all relevant statistical analyses for this assessment. Where it proved unfeasible to perform a quantative synthesis of the results of the included studies, outcomes were tabulated and described in a narrative way.
Results
Performance of point-of-care devices
A formal evaluation of the performance of the CoaguChek, INRatio and ProTime point-of-care systems with regard to INR measurement was outside the scope of this assessment. An objective ‘true’ INR remains to be defined and usually the calculation of INR measurement is based on different assumptions. INR determined in the laboratory is regarded as the gold standard with which all other measurement methods should be compared. 34 Information on the precision and accuracy of these point-of-care devices was gathered from the available literature. Normally, the precision or reproducibility of point-of-care devices is expressed by means of the coefficient of variation (CV) of the variability, while the accuracy is the level of agreement between the result of one measurement and the true value and is expressed as correlation coefficient. 35 Table 1 summarises the performance of the target point-of-care devices according to the FDA self-test documentation and relevant published papers.
| Device | Precision | Accuracy | |||
|---|---|---|---|---|---|
| Mean (SD) INR | CV (%) | Correlation (r) | |||
| Patient | Professional | Patient | Professional | ||
| CoaguChek S36 | 2.42 (0.68) | NR | NR | NR | 0.95a |
| CoaguChek XS37 | 2.57 (0.13) | 2.52 (0.13) | 5.13 | 5.36 | 0.93 |
| INRatio 238 | 2.70 (0.153) | 2.93 (0.180) | 5.68 | 6.16 | 0.93 |
| ProTime 339 | 4.0 (0.19)b | NR | NR | NR | 0.95 |
A systematic review published by Christensen and Larsen in 201235 assessed the precision and accuracy of current available point-of-care coagulometers including CoaguChek XS, INRatio and ProTime/ProTime3. The authors found that the precision of CoaguChek XS varied from a CV of 1.4% to one of 5.9% based on data from 14 studies, while the precision of INRatio and ProTime varied from 5.4% to 8.4% based on data from six studies. The coefficient of correlation for CoaguChek XS varied from 0.81 to 0.98, while that for INRatio and ProTime varied from 0.73 to 0.95. They concluded that the precision and accuracy of point-of-care coagulometers were generally acceptable, compared with conventional laboratory-based clinical testing. The same conclusions were drawn by the Canadian Agency for Drugs and Technologies in Health report published in 2012 on point-of-care testing. 41 Similarly, the international guidelines prepared in 2005 by the International Self-Monitoring Association for oral Anticoagulation stated that ‘Point-of-care instruments have been tested in a number of different clinical settings and their accuracy and precision are considered to be more than adequate for the monitoring of OAT in both adults and children’ (p. 40). 42
CoaguChek XS versus CoaguChek S
The CoaguChek S monitor was replaced in 2006 by the XS monitor, which offers a number of new technical features such as the use of a recombinant human thromboplastin with a lower ISI and internal quality control included on the test strip. The safety and reliability of CoaguChek S and CoaguChek XS have been demonstrated in several studies in both adults and children. 43–50 A number of studies have also compared the performance of CoaguChek S with that of CoaguChek XS in relation to conventional INR measurement. Even though a good agreement between the two CoaguChek models and conventional laboratory-based results has been demonstrated, CoaguChek XS has shown more accurate and precise results than its precursor in both adults and children, especially for higher INR values (> 3.5). 34,36,51–54
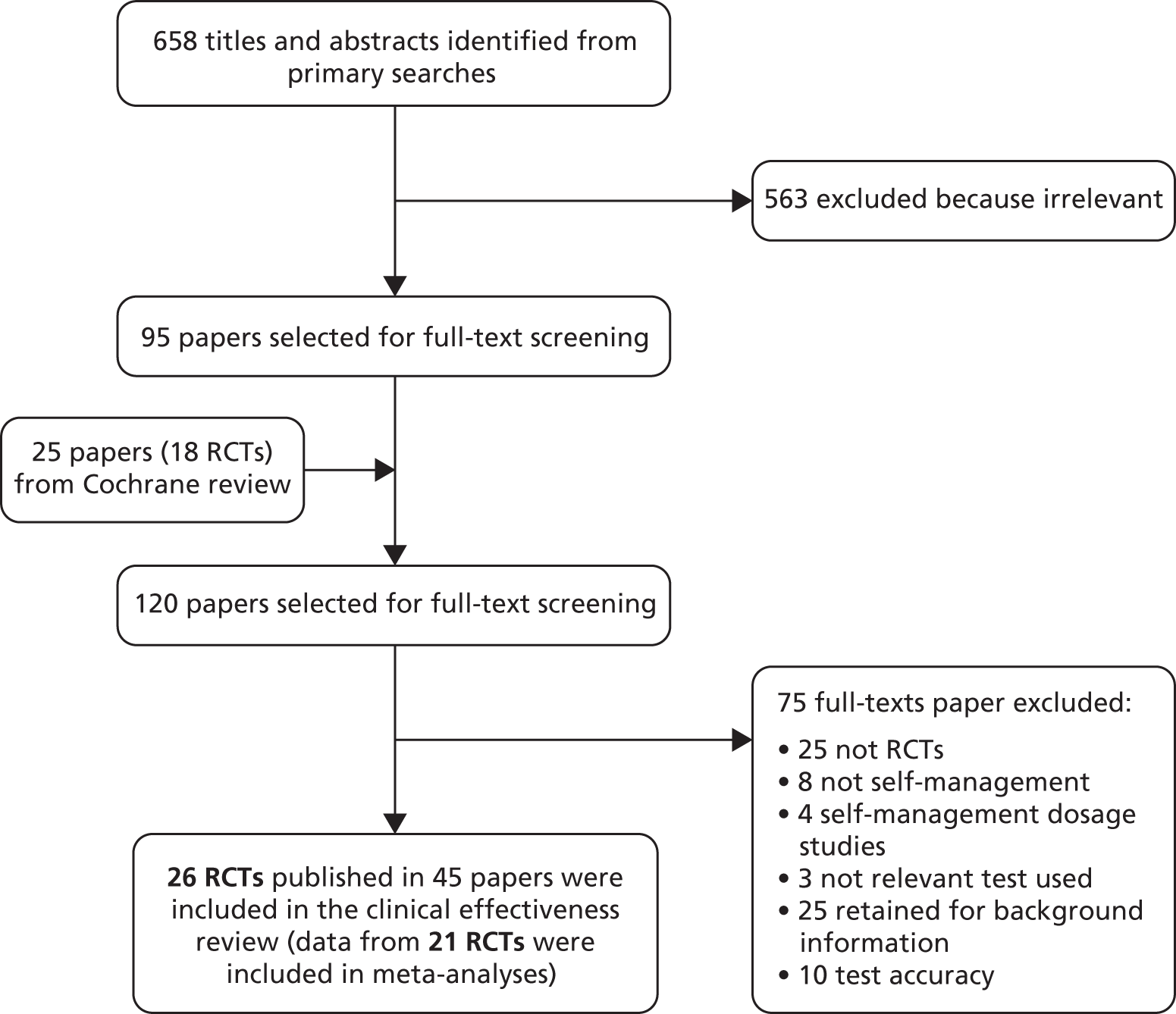
Quantity of available evidence
A total of 658 records were retrieved for the assessment of the clinical effectiveness of the point-of-care tests under investigation. After screening titles and abstracts, 563 were excluded and full-text reports of 120 potentially relevant articles were obtained for further assessment, including 25 full-text papers from the 18 trials included in the Cochrane systematic review published by Garcia-Alamino and colleagues. 31 In total, 26 RCTs (published in 45 papers) met the inclusion criteria and were included in the clinical effectiveness section of this assessment. Three of the 26 included studies were randomised crossover trials,32–34 while the remaining studies were parallel-group RCTs.
We based the primary analyses on data from 21 out of the 26 included studies relevant to the comparisons and outcomes of interest (Table 2 provides further details).
| Study ID | Comparisons | Reason for exclusion from meta-analyses | Reason for inclusion in this assessment |
|---|---|---|---|
| Bauman 201055 | Compares PSM with PST group (PST was the usual care provided in the study context) | Lack of data on SC group where people received OAT are generally managed by the primary or secondary care | Only RCT that reported acceptability outcomes on the relevant subgroup of interventions for children |
| Gardiner 200545 | Compares PST with standard care | The data collected by the participants were not used for the analysis. Instead, monthly data collected by the health-care professionals were used | Reports patient acceptability of self-testing as secondary outcome |
| Gardiner 200656 | Compares PST with PSM and then historically compares the included subgroups with the standard care they received for last 6 months before their enrolment in the study | Lack of randomised data on SC group where participants receiving OAT are usually managed by the primary or secondary care | Provide relevant data on TTR on the subgroup of interventions that were of interest |
| Hemkens 200857 | Compares PSM with standard laboratory monitoring | Do not provide data on any relevant clinical outcomes or intermediate outcomes | Reports patient satisfaction of self-management as secondary outcome |
| Rasmussen 201258 | Compares PSM with standard care | Do not provide any relevant clinical outcomes. Data provided for TTR was in median (25th to 75th percentile) which was not possible to be converted into mean (SD) | Provide data on TTR |
Of these 21 trials which provided data for statistical analyses, 15 trials were the same as those included in the Cochrane systematic review by Garcia-Alamino and colleagues31 and six were newly identified trials, published in or after 2008.
Figure 1 shows a flow diagram of the study selection process. The list of 26 included RCTs (and other linked reports) is given in Appendix 4.
FIGURE 1.
Flow diagram outlining the selection process.
Number and type of studies excluded
Appendix 5 lists the number of studies excluded after full-text assessment and the reasons for their exclusion.
Quality of research available
Figure 2 illustrates a summary of the risk of bias assessment for all included studies. The majority of trials were judged at ‘unclear’ or ‘high’ risk of bias. One trial was only reported in abstract and hence did not allow for an adequate assessment of the risk of bias. 59 Similarly, one trial was discontinued before the end of the prespecified follow-up due to difficulties in the recruitment process. 60 Overall, only four trials were assessed to have adequate sequence generation, concealed allocation and blinded outcome assessment and, therefore, were judged at low risk of bias. 55,61–63 Three of these trials used either the CoaguChek model ‘S’61,63 or the model ‘XS’62 for INR measurement, while the other trial used CoaguChek XS to measure INR in children receiving anticoagulation therapy. 55 Appendix 6 provides details of the risk of bias assessment for each individual study. Main findings of the risk of bias assessment for all included studies are described in detail below.
FIGURE 2.
Summary of risk of bias of all included studies.
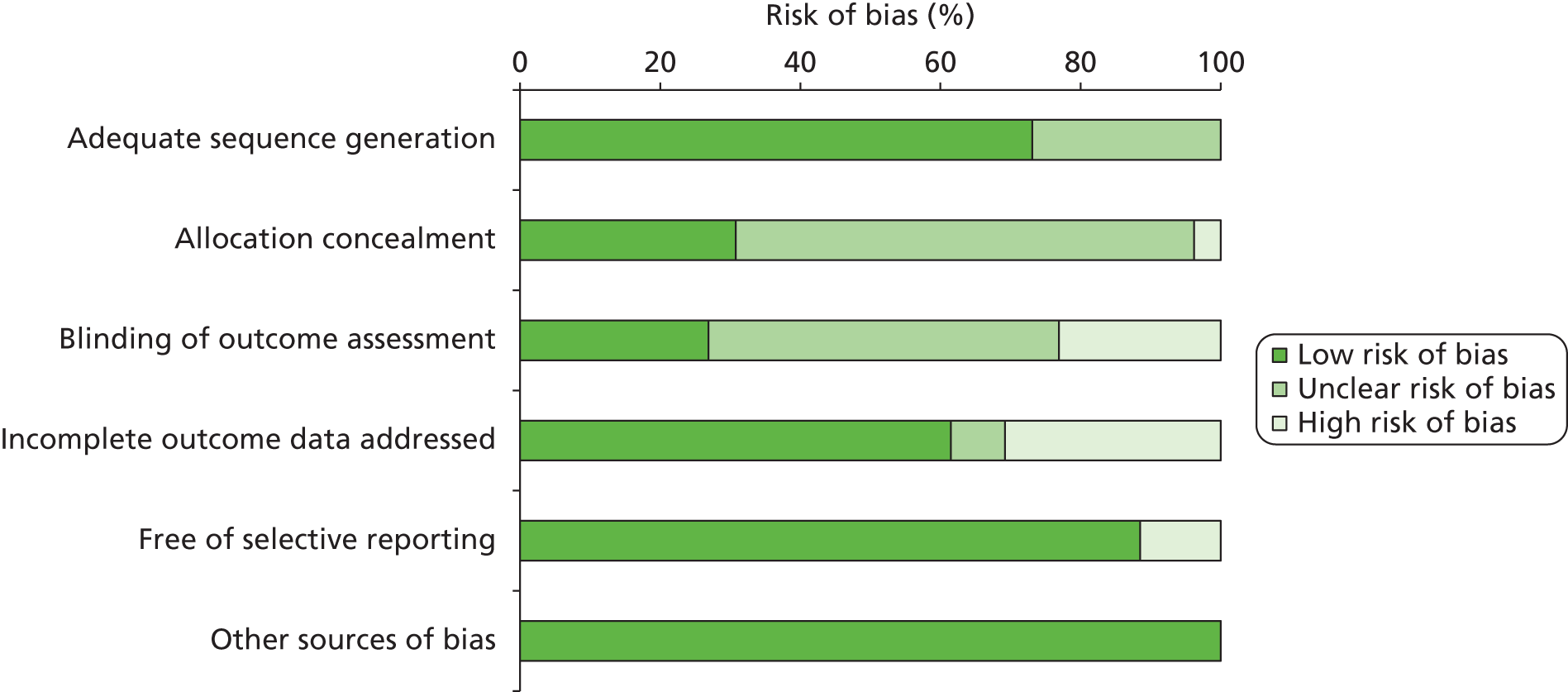
Selection bias
Of the 26 included trials, only seven trials reported adequate details on both generation of the randomisation sequence generation and concealment of allocation. 55,57,61–65 In 11 trials, the randomisation process proved to be adequate but no information was provided on the way in which participants were allocated to the study interventions. 58,60,66–74 One trial75 reported adequate details about the generation of the random sequence but failed to conceal the allocation of participants to study interventions. In contrast, another trial76 reported adequate information on allocation concealment but failed to provide details on the randomisation process. In six trials, both the randomisation process and the allocation concealment were judged as ‘unclear’ due to the lack of adequate information. 45,56,59,77–79
Attrition bias
Seventeen trials were judged to be at low risk of attrition bias. Six of them had limited missing data with similar reasons for discontinuation across intervention groups. 59,69,72,74,76,79 Seven trials relied on an intention-to-treat approach and all dropouts were fully accounted for in the statistical analyses,55,61,63–65,71,75 while the other four reported no missing data. 58,60,62,78 Eight of the 26 included trials were at high risk of attrition bias, with more than 5% dropout rate and with missing data not appropriately tackled. 45,56,57,66–68,73,77 In the Early Self-Controlled Anticoagulation Trial,70 the problem of incomplete outcome data was addressed for the first 600 participants but not for all included participants.
Performance and detection bias
Owing to the nature of the interventions being studied (use of point-of-care devices), blinding of participants or personnel was not feasible. Seven trials blinded the outcomes assessor (statistician or clinical outcome assessor). 55,58,61–63,72,77 In six trials, neither the participants nor the personnel involved in delivering the interventions were blinded. 60,65,66,71,74,75 One trial70 was described as ‘double blinded’ but no further information was given. Another trial68 reported that one of the two standard care groups studied (the untrained routine group) was blinded. In addition, this trial revealed that the nurses involved in transferring data on dosing as well as the dosing physicians were blinded. The remaining of the included trials did not provide information on blinding.
Reporting bias
With the exception of three trials,58,76,79 the outcomes reported in the trials were prespecified in the analysis section and reporting bias was not obvious in the published papers.
Other sources of biases
No other sources of biases were obvious in the included trials.
Characteristics of the included studies
Table 3 summarises the main characteristics of the 26 included RCTs. The baseline characteristics of all included trials are described below and tabulated in Appendix 7 (see Tables 31 and 32).
| Study characteristics | CoaguChek XS | CoaguChek S/CoaguChek | CoaguChek Plus | CoaguChek + INRatio | ProTime |
|---|---|---|---|---|---|
| Total no. of studies | 4 | 17 | 1 | 2 | 2 |
| Self-monitoring | |||||
| PSM | 2 | 14 | 1 | 1 | 1 |
| PST | 2 | 2 | 0 | 1 | 1 |
| PSM and PST | 0 | 1 | 0 | 0 | 0 |
| Standard care | |||||
| AC clinic | 4 | 9 | 0 | 2 | 1 |
| GP/physician | 0 | 4 | 1 | 0 | 1 |
| AC clinic or GP/physician | 0 | 4 | 0 | 0 | 0 |
| Country | |||||
| UK | 0 | 6 | 0 | 0 | 0 |
| Non-UK | 4 | 12 | 1 | 2 | 2 |
| Clinical indication | |||||
| AF only | 0 | 2 | 0 | 0 | 0 |
| AHV only | 0 | 4 | 1 | 1 | 0 |
| Mixed only (AF + AHV + others) | 4 | 12 | 0 | 1 | 2 |
| Total sample size | 414 | 3910 | 1155 | 222 | 3062 |
Study details
The majority of included trials were conducted in Europe: six trials were conducted in Germany,57,59,60,70,72,78 six in the UK,45,56,64,67,69,73 three in Denmark,58,66,75 three in the Netherlands,68,76,79 one in Ireland,62 one in Austria,63 one in France77 and one in Spain. 61 Three trials were conducted in Canada55,65,74 and one in the USA. 71 Of the 26 included trials, seven were multicentred,60,63,64,67,68,71,72 while the remaining 19 were conducted in a single centre.
The length of follow-up ranged from 14 weeks57 to more than 4 years. 63,71 Nine trials reported follow-ups ≥ 12 months. 55,61,63,64,70,71,73,78,79 One trial, which was originally supposed to run for 2 years, was discontinued prematurely due to the small number of recruited participants. 60
Nine of the included trials were funded independently by professional organisations or national/governmental agencies55,57–59,64–66,69,75 while 13 trials were fully or partly funded by industry. In the case of the remaining four trials, the source of funding was not reported. 70,76,78,79
Participants
Most of the included trials (15 out of 26) included participants with mixed indications of which atrial fibrillation, artificial heart valves (AHVs) and venous thromboembolism were the most common clinical indications,45,55–57,61–63,65,66,68,71,72,74–76 while six trials enrolled exclusively participants with AHVs59,70,73,77–79 and two trials limited inclusion to participants with atrial fibrillation. 60,69 Seven trials provided information on risk factors, comorbidity, and/or previous bleeding and thromboembolic events but did not report significant baseline differences between participants in self-monitoring and those in standard care (see Appendix 7, Table 32). 61,63,64,71,72,75,77
The mean sample size among the included trials was 337 participants (range 1639–292,271 participants). Fifteen trials performed a power analysis and a sample size calculation,58,60–66,68,69,71,72,74–76 two trials, with very small sample sizes, did not power their studies55,57 and the remaining trials did not provide information on how the sample size was determined. 45,56,59,67,70,73,77–79 The age of adult participants ranged from 16 to 91 years. 62 The only trial which assessed children reported a median age of 10 years. 55
Warfarin was the choice of vitamin K antagonist therapy in half of the included trials. 45,55,56,58,62,64–67,69,71,73,74,78 In seven trials, participants were taking phenprocoumon and/or acenocoumarol and/or fluindione57,61,63,68,72,76,77 and, in one trial, participants received either warfarin or phenprocoumon. 75 In the remaining four trials, the type of vitamin K antagonist therapy was not reported. 59,60,70,79 In nearly half of the included trials (12 out of 26), participants had been on OAT for at least 3 months before randomisation. 45,55,56,61,64,66–69,74–76 Three trials included vitamin K antagonist-naive participants for whom long-term OAT was recently indicated but who had not been on anticoagulation therapy before. 58,63,70 In the largest trial, The Home International Normalised Ratio Study (THINRS),71 randomisation was stratified according to the duration of anticoagulation but no significant differences were found between participants who had started anticoagulation therapy within the previous 3 months and those who had received anticoagulation therapy for > 3 months. In the two remaining trials, the included participants received OAT for < 3 months (1–2 months) before randomisation. 62,65
Point-of-care tests used for international normalised ratio measurement
CoaguChek system for INR monitoring was used in 22 of the 26 included trials. Nine trials used the S model,45,56,58,61,63,64,67,75,78 four used the XS model,55,62,66,74 one70 used the CoaguChek Plus model and two trials used the first model of the CoaguChek series, which was simply referred to as ‘CoaguChek’. 68,72 In six trials, it was unclear whether the CoaguChek device was the first model or its later versions. 59,60,69,73,76,79 Either the INRatio or the CoaguChek S was used for INR measurement in two trials (but results were not separated according to the type of the point-of-care device),57,77 and the ProTime system was used in other two trials. 65,71 In all six trials based in the UK, CoaguChek system (either CoaguChek or version S) was used for the INR measurement.
In 11 trials, in order to assure accuracy of the point-of-care devices being used, INR results measured directly by participants were compared with those measured in a laboratory. 45,55–58,64–67,69,77
Eight trials’ investigators who did not specify the model of the CoaguChek device (S or XS) used for INR measurement were contacted for further details. 60,68,69,72,73,76,77,79 Five of the them provided further information on the model of the CoaguChek point-of-care device. 58,68,72,77,79
Standard anticoagulant management
The type of standard care varied across trials. In 13 trials, INR was measured by professionals in anticoagulant or hospital outpatient clinics,45,57,58,61,62,64,66,68,69,71,74,76,79 by a physician or a GP in a primary care setting in six trials,59,60,65,67,70,78 and either by a physician/GP in a primary care setting or by professionals in anticoagulant/outpatient hospital clinics in five trials. 63,72,73,75,77 In two trials, comparing self-testing with self-management,55,56 self-testing within anticoagulant clinics was considered as standard care. In the majority of the included trials (17 out of 26), the anticoagulant clinic was led by a clinician (general or specialist),58–61,63,65,66,68–73,75,77–79 by a nurse in five trials, (three conducted in the UK,45,48,64 one in Canada55 and one in Germany57) and by a pharmacist in two trials, conducted in Canada74 and in Ireland. 62
International normalised ratio measurement was carried out in a laboratory in all but two trials, where CoaguChek S67 or another coagulometer75 was used instead.
Self-monitoring
The majority of the included trials (17 out of 26) compared self-management (participants performed the test and adjusted the dose of anticoagulation therapy themselves) with standard care,57–61,63–65,67,70,72–76,78,79 six assessed self-testing (participants performed the test themselves with the results managed by health-care professionals)45,62,66,69,71,77 and one evaluated both self-testing and self-management versus either trained or untrained routine care (four arms). 68 It is worth noting that for the subgroup meta-analysis according to type of OAT management, this four-arm trial contributed to two studies: one on self-testing and one on self-management. The two standard care groups (trained and untrained routine care) were initially combined to produce an overall control group and subsequently subdivided into two groups for the purpose of the subgroup analysis, which was undertaken to assess the effects of self-testing versus self-management.
The remaining two trials compared self-testing with self-management (without standard care as a comparator). 55,56 One of these two trials enrolled exclusively a population of children55 while the other provided a non-randomised comparison of participants in self-testing and self-management with those receiving standard care for a period of 6 months before study enrolment. 56 We deemed these two trials suitable for inclusion as they provide relevant outcomes for participants in both self-testing and self-management.
In 19 out of 26 included trials, participants received training and education in order to perform self-testing and self-management (see Appendix 7, Table 33). 45,55,56,61,62,64–67,69,72–77,79–81 In most of these trials (11 out of 19), the training was provided in group sessions which lasted for around 1–2 hours55,61,62,68,69,72,76,77,81 up to a maximum of 3 hours. 73,74 The training was usually administered by a single member of staff, either a nurse, a practitioner/physician45,56,61,64,69 or a pharmacist. 74 In a few trials, the training was provided by a team of professionals, such as a specialist physician together with paramedical personnel,80 a research pharmacist coupled with an haematologist62 or a physician assisted by a nurse. 63,72 In five trials, the personnel responsible for delivering the training was reported to be trained specifically on self-testing and self-management. 56,61,63,64,72
Clinical effectiveness results
Overview
This section provides evidence from 26 included trials on the clinical effectiveness of self-monitoring using CoaguChek system, INRatio2 PT/INR monitor and ProTime Microcoagulation system, compared with standard practice (see Figures 3–14; Tables 4–6; Appendix 8). For clarity, the results are reported under the broad headings of ‘clinical outcomes’, ‘intermediate outcomes’ and ‘patient-reported outcomes’. The summary effects of relevant clinical outcomes such as bleeding events, thromboembolic events and mortality have been described separately within the ‘clinical outcomes’ section. Tables 4 and 5 show the main findings of the five trials conducted in the UK and of the four trials using CoaguChek XS. The results of the sensitivity analyses for each point-of-care test are displayed in Table 6.
| Study ID | Type of SM | Type of SC | Clinical condition | Sample sizea | Bleeding events | Thromboembolic events | Mortality | TTR, % (95% CI) | Frequency of self-testing, mean (SD) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PSM/PST | SC | PSM/PST | SC | PSM/PST | SC | PSM/PST | SC | PSM/PST | SC | |||||
| Fitzmaurice 200267 | PSM | GP | Mixed | 23 | 26 | 2 | 1 | 0 | 0 | 0 | 1 | 74 (67 to 81) | 77 (67 to 86) | 1.6 weeks |
| Fitzmaurice 200564 | PSM | Hospital- or practice-based AC clinic | Mixed | 337 | 280 | 5 | 4 | 4 | 3 | 2 | 1 | b70 (68.1 to 72.4) | b68 (65.2 to 70.6) | 12.4 |
| Gardiner 200656 | PSM and PST | PST within AC was the SC | Mixed | 55/49 | – | NR | NR | NR | NR | NR | NR | PSM: 69.9 (60.8 to 76.7) PST: 71.8 (64.9 to 80.1) |
NR | |
| Khan 200469 | PST | AC clinic | AHV | 44 (40) | 41 (39) | 3 | 2 | 0 | 0 | NR | NR | c71.1 (14.5) | c70.4 (24.5) | NR |
| Sidhu 200173 | PSM | GP or AC clinic | AHV | 51 (41) | 49 (48) | 3 | 2 | 10 | 10 | 0 | 4 | 76.5 | 63.8 | NR |
| Study ID | Country | Type of SM | Type of SC | Sample sizea | Bleeding events | Thromboembolic events | Mortality | TTR, % (95% CI) | Frequency of self-testing, mean (SD) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PSM/PST | SC | PSM/PST | SC | PSM/PST | SC | PSM/PST | SC | PSM/PST | SC | |||||
| Bauman 201055 (child population) | Canada | PSM and PST | PST within AC was the SC | 14/14 | – | 0/0 | – | 0/0 | – | NR | – | b83/83.9 | – | NR |
| Christensen 201166 | Denmark | PST | AC clinic, hospital outpatient or GP | OW: 51 (46) TW: 40 (37) |
49 (40) | 0 | 0 | 0 | 0 | 0 | 0 | OW: 79.7 (79 to 80) TW: 80.2 (79.4 to 80.9) |
72.7 (71.9 to 73.4) | OW: 7.4 (2.7) TW: 4.1 (1.8) |
| Ryan 200962 | Ireland | PST | AC clinic | 72 | 60 | 0 | 1 | 2 | 1 | NR | NR | b74 (64.6–81) | b58.6 (45.6–73.1) | 4.6 (0.8) |
| Verret 201274 | Canada | PSM | AC clinic | 58 | 56 | 26 | 23 | 0 | 0 | 0 | 0 | c80 (13.5) | c75.5 (24.7) | NR |
| Outcomes | Main analyses | Sensitivity analyses | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All included trials | CoaguChek System | CoaguChek XS | ProTime | CoaguChek/INRatioa | |||||||||||
| RR (95% CI) | p-value | No. of trials | RR (95% CI) | p-value | No. of trials | RR (95% CI) | p-value | No. of trials | RR (95% CI) | p-value | No. of trials | RR (95% CI) | p-value | No. of trials | |
| Bleeding | 0.95 (0.74 to 1.21) | 0.66 | 22 | 0.90 (0.67 to 1.23) | 0.52 | 19 | 1.07 (0.70 to 1.62) | 0.77 | 3 | 1.15 (1.03 to 1.29) | 0.01 | 2 | 0.93 (0.70 to 1.23) | 0.60 | 20 |
| PSM | 0.94 (0.68 to 1.30) | 0.69 | 15 | 0.95 (0.68 to 1.32) | 0.75 | 14 | 1.09 (0.71 to 1.67) | 0.69 | 1 | 0.34 (0.01 to 8.16) | 0.50 | 1 | 0.95 (0.68 to 1.32) | 0.75 | 14 |
| PST | 1.15 (1.03 to 1.28) | 0.02 | 7 | 0.58 (0.22 to 1.47) | 0.25 | 5 | 0.28 (0.01 to 6.71) | 0.43 | 2 | 1.15 (1.03 to 1.29) | 0.01 | 1 | 0.97 (0.59 to 1.61) | 0.91 | 6 |
| Thromboembolic events | 0.58 (0.40 to 0.84) | 0.004 | 22 | 0.52 (0.38 to 0.71) | < 0.0001 | 19 | 1.67 (0.15 to 17.93) | 0.67 | 3 | 0.94 (0.48 to 1.84) | 0.86 | 2 | 0.51 (0.38 to 0.70) | < 0.0001 | 20 |
| PSM | 0.51 (0.37 to 0.69) | < 0.0001 | 15 | 0.51 (0.36 to 0.72) | 0.0001 | 14 | Not estimable | 1 | 0.20 (0.01 to 4.15) | 0.30 | 1 | 0.51 (0.36 to 0.72) | 0.0001 | 14 | |
| PST | 0.99 (0.75 to 1.31) | 0.95 | 7 | 0.71 (0.14 to 3.63) | 0.68 | 5 | 1.67 (0.15 to 17.93) | 0.67 | 2 | 1.01 (0.77 to 1.34) | 0.92 | 1 | 0.55 (0.13 to 2.31) | 0.41 | 6 |
| Mortality | 0.83 (0.63 to 1.10) | 0.20 | 13 | 0.68 (0.46 to 1.01) | 0.06 | 11 | Not estimable | Not estimable | 2 | 0.96 (0.78 to 1.19) | 0.71 | 1 | 0.69 (0.48 to 1.01) | 0.06 | 12 |
| PSM | 0.68 (0.46 to 1.01) | 0.06 | 10 | 0.68 (0.46 to 1.01) | 0.06 | 10 | Not estimable | Not estimable | 1 | Not estimable | Not estimable | Not estimable | 0.68 (0.46 to 1.01) | 0.06 | 10 |
| PST | 0.97 (0.78 to 1.19) | 0.74 | 3 | Not estimable | Not estimable | 1 | Not estimable | Not estimable | 1 | 0.96 (0.78 to 1.19) | 0.71 | 1 | 3.00 (0.48 to 1.01) | 0.50 | 2 |
| TTR | WMD 2.82 (0.44 to 5.21) | 0.02 | 11 | WMD 2.82 (–0.69 to 6.33) | 0.12 | 8 | WMD 7.18 (6.24 to 8.12) | < 0.00001 | 2 | WMD 3.83 (2.69 to 4.96) | < 0.00001 | 2 | WMD 3.21 (0.04 to 6.37) | 0.05 | 9 |
| PSM | WMD 0.47 (–1.40 to 2.34) | 0.62 | 6 | WMD 0.93 (–1.18 to 3.03) | 0.39 | 5 | WMD 4.50 (6.85 to 15.85) | 0.44 | 1 | WMD 8.60 (–7.07 to 24.27) | 0.28 | 1 | WMD 0.93 (–1.18 to 3.03) | 0.39 | 5 |
| PST | WMD 4.44 (1.71 to 7.18) | 0.001 | 5 | WMD 5.41 (1.85 to 8.97) | 0.003 | 3 | WMD 7.20 (6.25 to 8.15) | < 0.00001 | 1 | WMD 3.80 (2.69 to 4.96) | < 0.00001 | 1 | WMD 6.23 (4.10 to 8.36) | < 0.00001 | 4 |
Clinical outcomes
Bleeding
Twenty-one trials reported a total of 1472 major and minor bleeding events involving 8394 participants. 59–79 Two trials reported that there were no bleeding events and hence did not contribute to the overall effect size in the related meta-analysis. 66,75 Twenty-one trials reported 476 major bleeding events in a total of 8202 participants,59–65,67–74,77–79 while 13 trials reported 994 estimable minor bleeding events in a total of 5425 participants. 61,63,64,67,69,71–74,76,77 No statistically significant differences were observed between self-monitoring participants (self-testing and self-management) and those in standard care for any bleeding events (RR 0.95, 95% CI 0.74 to 1.21; p = 0.66) (Figure 3), major bleeding events (RR 1.02, 95% CI 0.86 to 1.22; p = 0.80) (Figure 4) and minor bleeding events (RR 0.94, 95% CI 0.65 to 1.34; p = 0.73) (Figure 5). The results were not affected by the removal of the UK-based trials (see Appendix 8) or by the removal of the trials assessing ProTime and/or INRatio (see Table 6 and Appendix 8). Similarly, sensitivity analyses restricted to CoaguChek XS trials demonstrated no differences from the all-trials results (see Table 6 and Appendix 8). A sensitivity analysis restricted to trials at low risk of bias slightly changed the estimate of effect but did not significantly impact on the findings (RR 0.59, 95% CI 0.27 to 1.30; p = 0.19) (see Appendix 8).
FIGURE 3.
Forest plot of comparison: any bleeding events. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus; PSM, patient self-management; PST, patient self-testing.
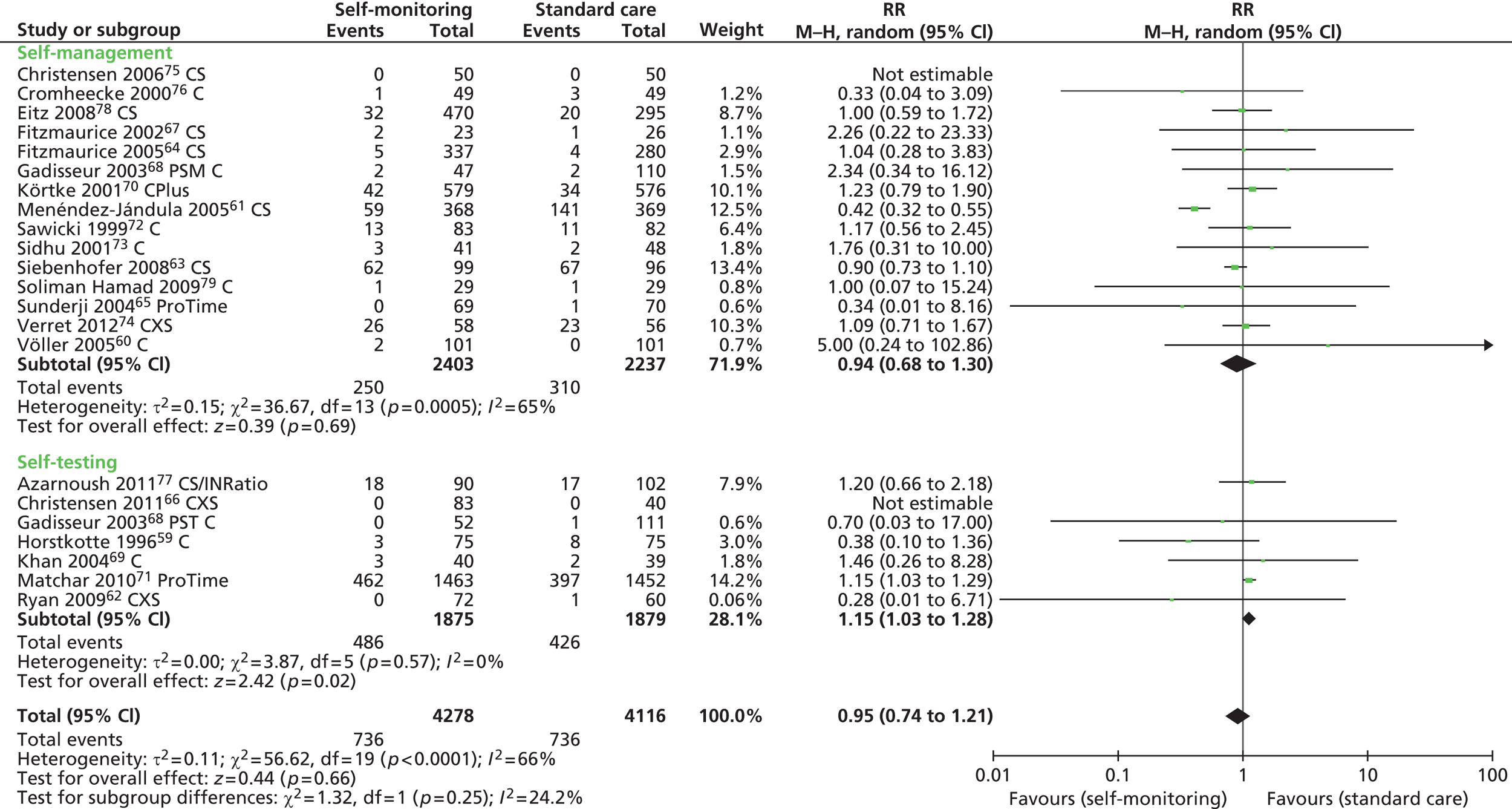
FIGURE 4.
Forest plot of comparison: major bleeding events. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus; PSM, patient self-management; PST, patient self-testing.
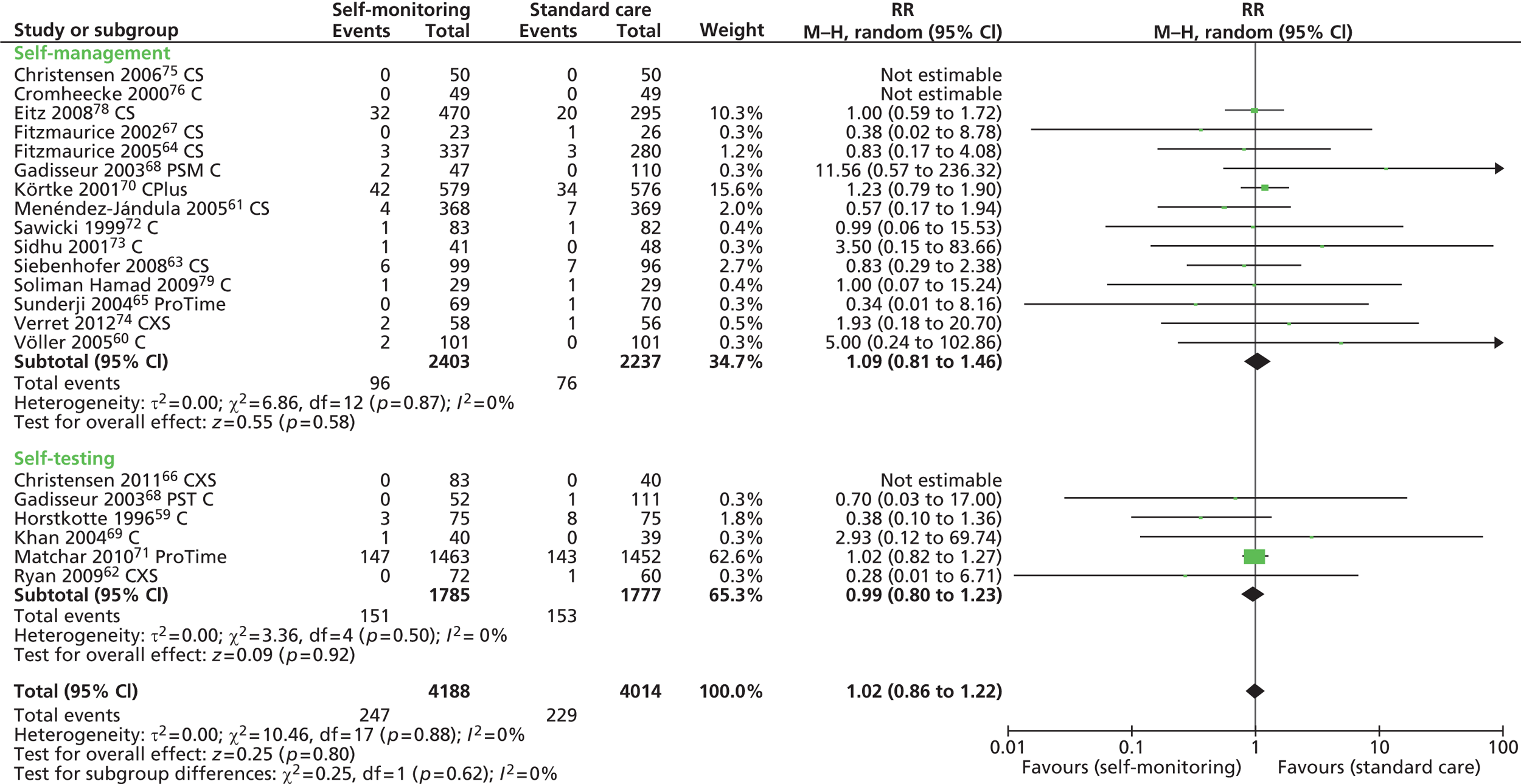
FIGURE 5.
Forest plot of comparison: minor bleeding events. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus.

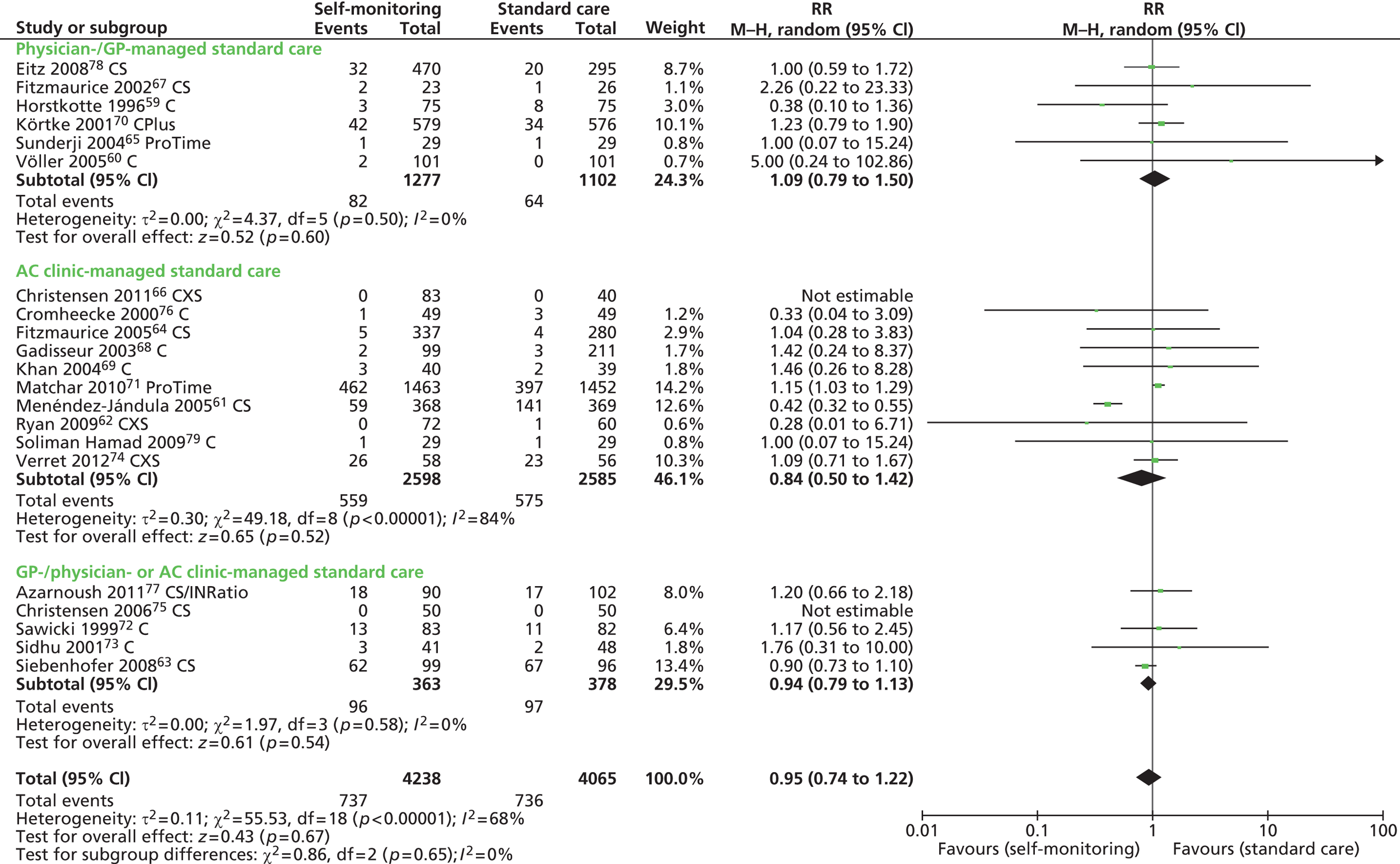
The subgroup analysis by type of anticoagulant management therapy did not show any difference between self-management and standard care for any bleeding events (RR 0.94, 95% CI 0.68 to 1.30; p = 0.69) but revealed a significant higher risk in self-testing participants than in those receiving standard care (RR 1.15, 95% CI 1.03 to 1.28; p = 0.02) (see Figure 3). When trials assessing ProTime and INRatio were removed from the analysis, a non-significant trend was observed in favour of self-testing (0.58, 95% CI 0.22 to 1.47; p = 0.25) (see Table 6 and Appendix 8). No significant differences in the risk of major bleeding were observed between self-management (RR 1.09, 95% CI 0.81 to 1.46; p = 0.58) and self-testing (RR 0.99, 95% CI 0.80 to 1.23) versus standard care (see Figure 4). When only minor bleeding events were assessed (see Figure 5), a significant increased risk was observed in self-testing participants (23%), compared with those in standard care (RR 1.23, 95% CI 1.06 to 1.42; p = 0.005), but not in those who were self-managed (RR 0.84, 95% CI 0.53 to 1.35; p = 0.47). Two trials enrolled participants with atrial fibrillation, six trials enrolled participants with AHVs and 13 trials enrolled participants with mixed indication. No statistically significant subgroup differences were found for bleeding events according to the type of clinical indication (Figure 6). Similarly, for bleeding events, no significant differences were detected when trials were grouped according to the type of control care (anticoagulant clinic care RR 0.84, 95% CI 0.50 to 1.42; p = 0.52; GP/physician RR 1.09, 95% CI 0.79 to 1.50; p = 0.60; mixed care RR 0.94, 95% CI 0.79 to 1.13; p = 0.54) (Figure 7).
FIGURE 6.
Forest plot of comparison: any bleeding events – clinical indication. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus.

FIGURE 7.
Forest plot of comparison: any bleeding events – type of standard care. AC, anticoagulant; C, CoaguChek; CS, CoaguCchek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus.
Thromboembolic events
Twenty-one trials reported 351 major and minor thromboembolic events in a total of 8394 participants. 59–79 Six of these trials did not contribute to the overall estimate of effect as they reported ‘zero’ events in both groups. 66–69,74,75 Self-monitoring (self-testing and self-management) showed a statistically significant reduction in the risk of thromboembolic events by 42% (RR 0.58, 95% CI 0.40 to 0.84; p = 0.004), compared with standard care (Figure 8). The risk reduction further increased to 48% when only major thromboembolic events were considered (RR 0.52, 95% CI 0.34 to 0.80; p = 0.003) (Figure 9). The risk of thromboembolic events significantly decreased when the analyses were restricted to non-UK trials (RR 0.50, 95% CI 0.32 to 0.76; p = 0.001); to CoaguChek trials (RR 0.52, 95% CI 0.38 to 0.71; p < 0.0001); and to trials at low risk of bias (RR 0.38, 95% CI 0.16 to 0.92; p = 0.03) (see Appendix 8).
FIGURE 8.
Forest plot of comparison: thromboembolic events. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus; PSM, patient self-management; PST, patient self-testing.
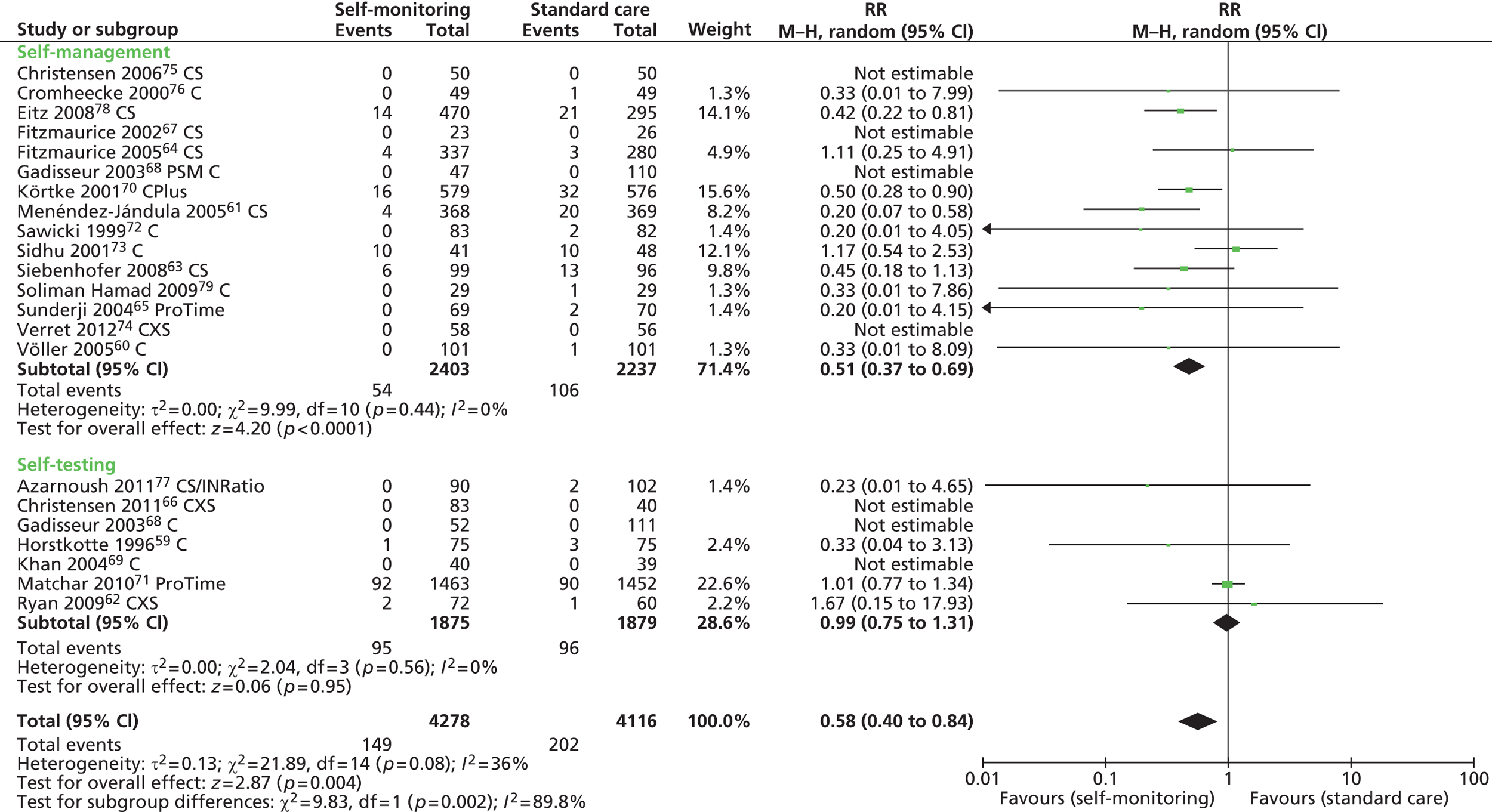
FIGURE 9.
Forest plot of comparison: major thromboembolic events. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus; PSM, patient self-management.
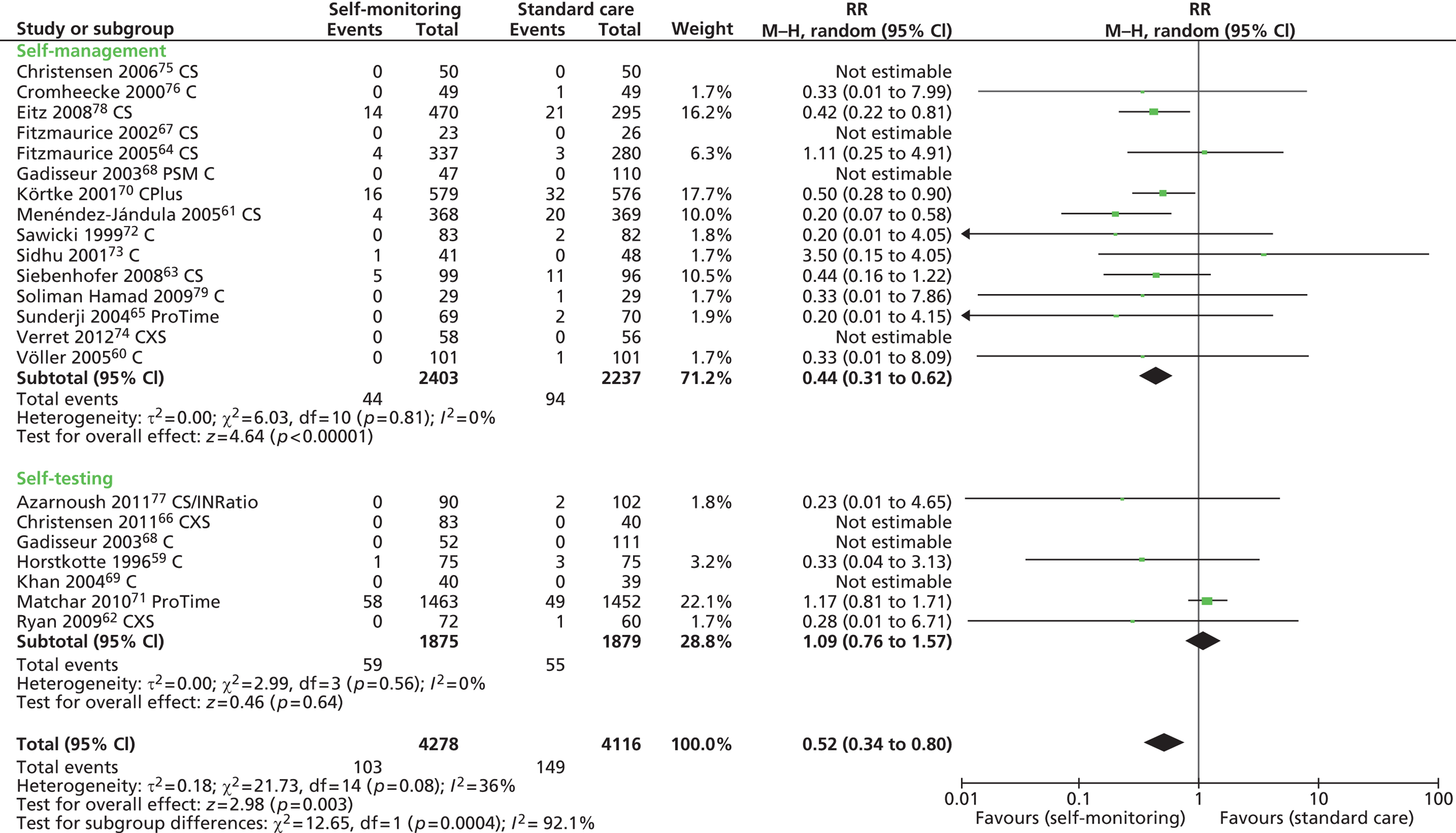
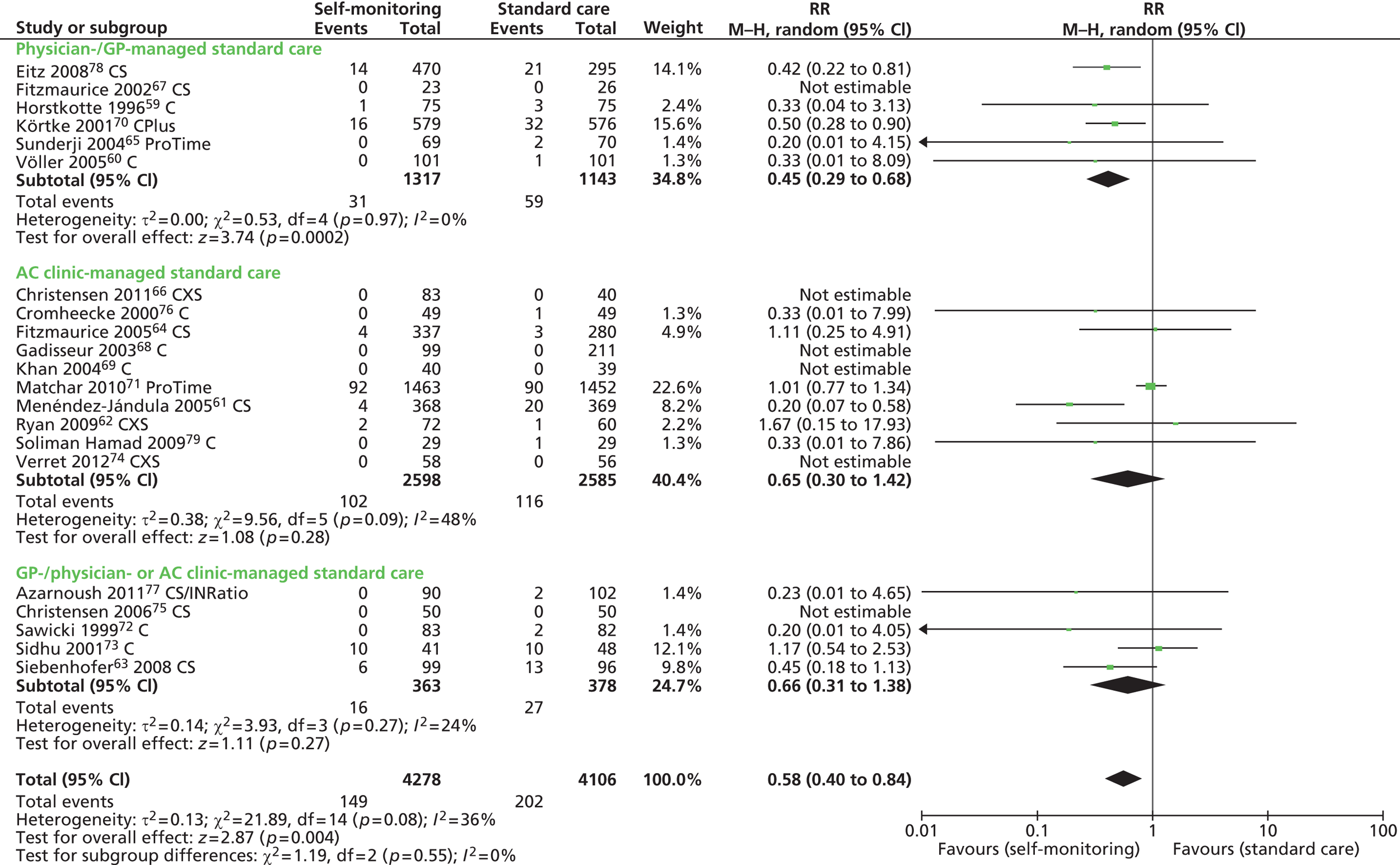
Self-management compared with standard care halved the risk of thromboembolic events (RR 0.51, 95% CI 0.37 to 0.69; p < 0.0001). In contrast, for self-testing participants59,62,71,77 no significant risk reduction was observed compared with those in standard care (RR 0.99, 95% CI 0.75 to 1.31; p = 0.95) (see Figure 8). The subgroup difference between self-management and self-testing was statistically significant (p = 0.002). When trials assessing the ProTime system were removed from the analysis, the risk reduction increased from 1% to 45% but the summary estimate of effect was not statistically different from the all-trials summary estimate (RR 0.55, 95% CI 0.13 to 2.31; p = 0.41) (see Table 6 and Appendix 8). Self-monitoring participants with AHVs showed a significant reduction in the number of thromboembolic events, compared with those in standard care (RR 0.56, 95% CI 0.38 to 0.82; p = 0.003). Among participants with mixed clinical indication (atrial fibrillation, AHVs or other conditions), the effect was larger but not statistically significant than that observed in participants receiving standard care (RR 0.57, 95% CI 0.30 to 1.09; p = 0.09) (Figure 10). The risk of thromboembolic events reduced in self-monitoring participants by 55% when routine anticoagulation control was managed by a GP or physician (RR 0.45, 95% CI 0.29 to 0.68; p = 0.0002). In contrast, even though fewer thromboembolic events were observed in participants who self-monitored their therapy than in those managed in specialised anticoagulation clinics (RR 0.65, 95% CI 0.30 to 1.42; p = 0.28) or those in mixed provision managed by either a physician/GP or a specialist (RR 0.66, 95% CI 0.31 to 1.38; p = 0.27), no significant subgroup differences were detected (Figure 11).
FIGURE 10.
Forest plot of comparison: any thromboembolic events – clinical indication. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus.

FIGURE 11.
Forest plot of comparison: any thromboembolic events – type of standard care. AC, anticoagulation; C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus.
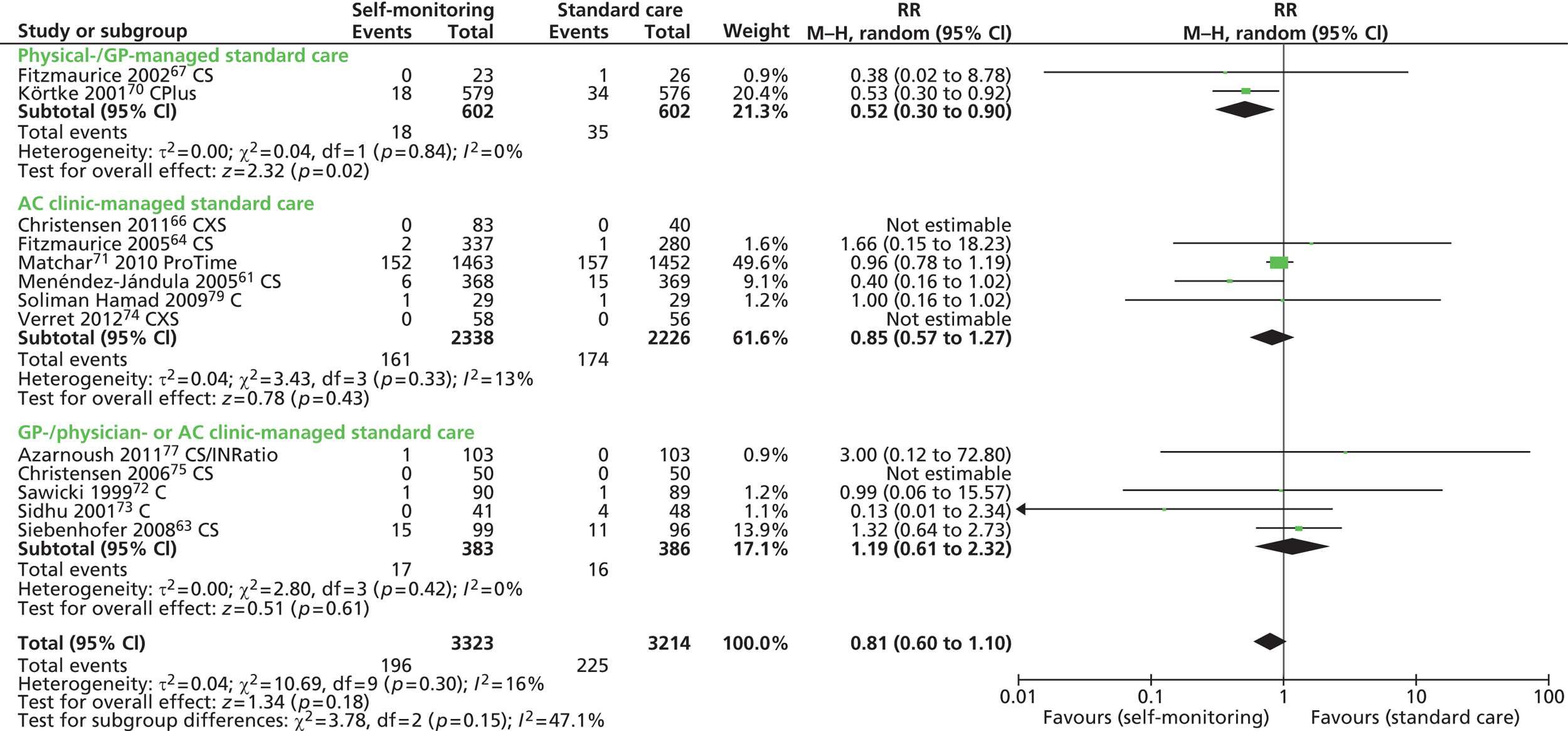
Mortality
Thirteen trials reported 422 deaths due to all-cause mortality in a total of 6537 participants. 61,63,64,66,67,70–75,77,79 Two trials with zero fatal cases did not contribute to the overall estimate of effect. 66,74 One trial of 1200 participants70 reported overall mortality data without separating the results for participants self-managed and for those receiving standard care. We contacted the corresponding author of this trial for further information but we did not receive any reply. Therefore, for mortality data, for this particular trial, we relied on the estimates published in the previous meta-analysis by Garcia-Alamino and colleagues31 and in the HTA by Connock and colleagues,21 which were based on individual patients’ data.
The risk reduction for all-cause mortality was not statistically significant different between self-monitoring (self-testing and self-management) and standard care (RR 0.83, 95% CI 0.63 to 1.10; p = 0.20) (Figure 12). The results were not affected by the removal of the UK-based trials or by the removal of trials at high or unclear risk of bias. When the analysis was restricted to trials that used the CoaguChek system, the summary estimate for self-monitoring was not different from the all-trials estimate (RR 0.68, 95% CI 0.46 to 1.01, p = 0.06) (see Table 6 and Appendix 8). Two trials reported six deaths out of a total of 932 participants, related to vitamin K antagonist therapy. 61,63
FIGURE 12.
Forest plot of comparison: mortality. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus.
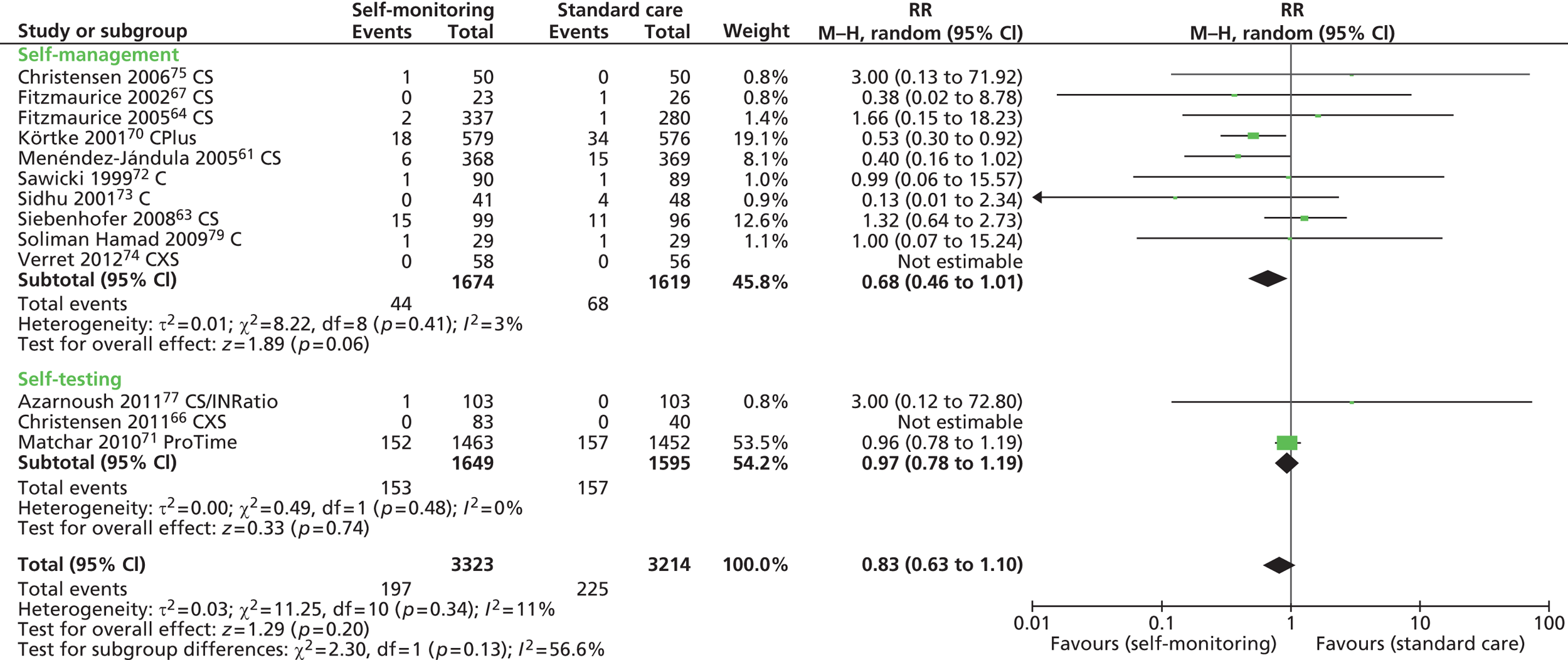
Risk of death reduced by 32% through self-management (RR 0.68, 95% CI 0.46 to 1.01; p = 0.06) but not through self-testing (RR 0.97, 95% CI 0.78 to 1.19; p = 0.74), even though the test for subgroup differences was not statistically significant (p = 0.13) (see Figure 12). Self-monitoring halved the risk of mortality in participants with AHVs (RR 0.54, 95% CI 0.32 to 0.92; p = 0.02) but not in those with mixed clinical indication for AOT (RR 0.95, 95% CI 0.78 to 1.16; p = 0.61) (Figure 13). The subgroup difference between participants with AHVs and those with mixed indication with regard to the number of deaths was statistically significant (p = 0.05). No data were available from trials that enrolled participants with atrial fibrillation. Significantly fewer deaths were recorded among participants who self-monitored their therapy than among those who were routinely managed by their GP/physician (RR 0.52, 95% CI 0.30 to 0.90; p = 0.02) (Figure 14).
FIGURE 13.
Forest plot of comparison: mortality – clinical indication. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus.

FIGURE 14.
Forest plot of comparison: mortality – type of standard care. AC, anticoagulation; C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus.
Heterogeneity among trials
A significant statistical heterogeneity was observed for any bleeding outcomes (I2 = 66%, p < 0.0001). In contrast, there was no statistically significant heterogeneity across trials for thromboembolic outcomes (I2 = 36%, p = 0.08) or for mortality (I2 = 11%, p = 0.34). The summary estimates of effect were influenced considerably by five large trials: Eitz and colleagues,78 Körtke and colleagues,70 Fitzmaurice and colleagues64 and Menéndez-Jándula and colleagues61 for self-management, and Matchar and colleagues71 for self-testing. The trial by Matchar and colleagues,71 which was the largest trial on self-testing, did not show any significant difference between self-testing and standard care with regard to the incidence of major events. Standard care was provided by means of high-quality clinic testing in this trial (a designated, trained staff responsible for participants’ visits and follow-up; the use of a standard local procedure at each site for anticoagulation management; and the performance of regular INR testing about once a month). The estimated effect of self-testing versus standard care in the subgroup analysis was dominated by this large trial, and, therefore, interpretation of this finding requires caution.
Adverse events
No other adverse events from INR testing, false test results, vitamin K antagonist therapy and sequelae were reported in the included trials.
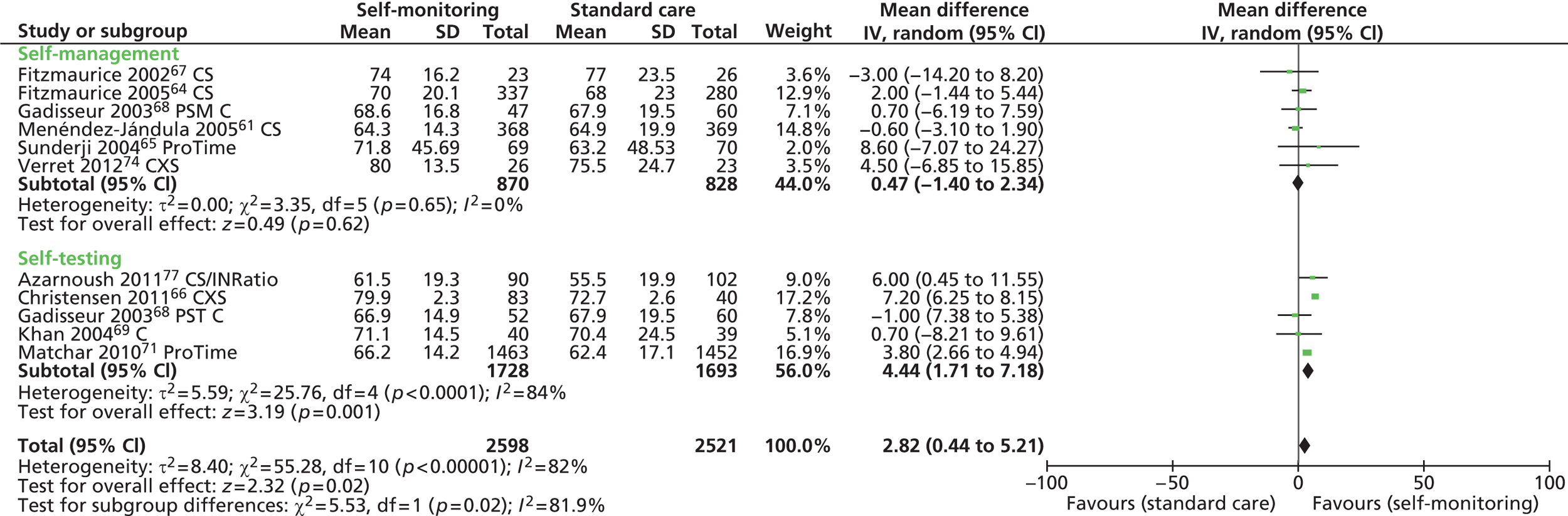
Intermediate results
Anticoagulation control: target range
Anticoagulation control can be measured as the time that INR is in the therapeutic range or as INR values in therapeutic range. Data on INR TTR were available from 18 trials. 55,56,58,60–69,71,73–75,77 However, there was variation in the measures used for reporting TTR. Seven trials comparing self-monitoring with standard care reported TTR as mean percentage;61,64,65,69,71,74,77 three as median percentage,58,62,75 five as overall percentage63,66–68,73 and one as cumulative number of days. 60 The two remaining trials, which compared patient self-management with patient self-testing, reported the TTR as mean percentage time (one trial)55 and overall percentage time (the other trial). 56 It proved impossible to convert median values into mean values due to the lack of information on the maximum or minimum value required by the conversion formula. Therefore, we were unable to pool the TTR results from the 18 trials which provided this information. The results of these trials are shown in Table 7.
| Type of point-of-care test | Study ID and country | Measure | INR TTR | INR value in target range | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| PSM/PST | Control | Difference | p-value | Measure | PSM/PST | Control | Difference | p-value | |||
| CoaguChek XS | Bauman 2010,55 Canada (children only) | Mean % (95% CI) | PSM: 83 | PST: 83.9 | 1 (–7.7 to 9.7) | NR | |||||
| Christensen 2011,66 Denmark | aOverall days % (95% CI) (SD) | PST-OW: 79.7 (79 to 80.3) (2.3) PST-TW: 80.2 (79.4 to 80.9) (2.3) |
72.7 (71.9 to 73.4) (2.6) | 7 (6 to 7.9) (73% to 80%) | < 0.001 | % of INR values (95% CI) | PST-OW: 78.3 (76.5 to 80.1) PST-TW: 80.8 (79.3 to 82.1) |
67.2 (64.1 to 70.2) | < 0.001 | ||
| Ryan 2009,62 Ireland | Median % (IQR) | 74 (64.6–81) | 58.6 (45.6–73.1) | < 0.001 | NR | ||||||
| Verret 2012,74 Canada | Mean % (SD) | 80 (13.5) | 75.5 (24.7) | 0.79 | NR | ||||||
| CoaguChek S or CoaguChek | Christensen 2006,75 Denmark | Median % (95% CI) | 78.7 (69.2 to 81.0) | 68.9 (59.3 to 78.2) | 0.14 | NR | |||||
| Cromheecke 2000,76 Netherlands | Values NR | NS | % of INR values | 55 | 49 | OR 1.2 (95% CI 1.0 to 1.6) | 0.06 | ||||
| Eitz 2008,78 Germany | NR | % of INR values | 79 | 65 | < 0.001 | ||||||
| Fitzmaurice 2002,67 UK | % (95% CI) (SD)a | 74 (67 to 81) (16.2) | 77 (67 to 86) (23.5) | NS | % of INR values (95% CI) | 66 (61 to 71) | 72 (65 to 80) | NS | |||
| Fitzmaurice 2005,64 UK | Mean % (95% CI) (SD)a | 70 (68.1 to 72.4) (20.1) | 68 (65.2 to 70.6) (23.0) | 2.4 (–1.2 to 6.0) | 0.18 | Mean % of individual (95% CI) | 70 (64.8 to 74.8) | 72 (66.3 to 77.1) | NS | ||
| Gadisseur 2003,68 Netherlands | % (95% CI) (SD)a | PSM: 68.6 (63.7 to 73.6) (16.8) PST: 66.9 (62.7 to 71.0) (14.9) |
67.9 (62.9 to 73.0) (19.5) | PST: 3.4 (–2.7 to 8.9) PSM: 5.1 (–1.1 to 11.3), p < 0.5 |
0.33 | % (95% CI) | 66.3 (61–71.5)/63.9 (59.8–68) |
61.3 (55–62.4)/58.7 | PST: + 5.2 (–1.7 to 12.1) PSM: + 7.6 (0.1 to 14), p < 0.5 |
0.14 | |
| Gardiner 2006,56 UK | % (95% CI) (SD) | PSM: 69.9 (60.8 to 76.7) (23.1) | PST: 71.8 (64.9 to 80.1) (22.1) | PSM + PST: (n = 77): 71 (64.7 to 76.4) (22.5) | 0.46 | NR | |||||
| Khan 2004,69 UK | Mean % (SD) | 71.1 (14.5) | 70.4 (24.5) | NS | NR | ||||||
| Horstkotte 1996,59 Germany | NR | % of INR values | 43.2 | 22.3 | < 0.001 | ||||||
| Menéndez-Jándula 2005,61 Spain | Mean % (SD) | 64.3 (14.3) | 64.9 (19.9) | 0.2 | Mean % of individual (SD) | 58.6 (14.3) | 55.6 (19.6) | 95% CI 0.4 to 5.4 | 0.02 | ||
| Rasmussen 2012,58 Denmark | Median (25th–75th percentile) % | 52 (33–65) | 55 (49–66) | NR | |||||||
| Sawicki 1999,72 Germany | NR | % of individual | 53 | 43.2 | 0.22 | ||||||
| Sidhu 2001,73 UK | % | 76.5 | 63.8 | < 0.0001 | NR | ||||||
| Siebenhofer 2008,63 Austria | % (IQR) 6/12 months | 70.6 (60.9–83.9)/75.4 (9.4–85.0) | 57.5 (34.2–80.3)/66.5 (47.1–81.5) | < 0.001/0.029 | NR | ||||||
| Soliman Hamad 2009,79 Netherlands | NR | Mean % per patient (SD) | 72.9 (11) | 53.9 (14) | 0.01 | ||||||
| Völler 2005,60 Germany | Mean cumulative days (SD) | 178.8 (126) | 155.9 (118.4) | NS | Mean % of INR values (SD) | 67.8 (17.6) | 58.5 (19.8) | 0.0061 | |||
| CoaguChek Plus | Körtke 2001,70 Germany | NR | % of INR values | 79.2 | 64.9 | < 0.001 | |||||
| CoaguChek/INRatio | Azarnoush 2011,77 France | Mean % (SD) | 61.5 (19.3) | 55.5 (19.9) | 0.0343 | NR | |||||
| Hemkens 2008, Germany57 | NR | NR | |||||||||
| ProTime | Matchar 2010,71 USA | Mean % (SD) | 66.2 (14.2) | 62.4 (17.1) | 3.8 (95% CI 2.7 to 5.0) | < 0.001 | NR | ||||
| Sunderji 2004,65 Canada | Mean % (SD) | 71.8 (45.69) | 63.2 (48.53) | 0.14 | NR | ||||||
Time in therapeutic range ranged from 52%58 to 80%66,74 for self-monitoring and from 55%58 to 77%67 for standard care. In all but three trials,58,61,67 TTR was higher in self-monitoring participants than in those receiving standard care and, in five of these trials, the difference between intervention groups was statistically significant. 62,66,71,73,77 Three of the UK-based trials reported no significant differences between self-monitoring and standard care. 64,67,69 Pooling of results was possible for 10 trials that provided suitable data. 61,64–69,71,74,77 No statistically significant differences were found between self-management and standard care (RR 0.47, 95% CI –1.40 to 2.34; p = 0.62). A modest but significantly higher proportion of TTR was, however, found for participants assigned to self-testing than for those in control care (WMD 4.44, 95% CI 1.71 to 7.18; p = 0.001) (Figure 15). It is worth noting that the overall estimate of effect was dominated by the largest included trial on self-testing, THINRS. 71 In two trials, one using CoaguChek XS66 and the other using ProTime,71 the WMD between self-testing and standard care for TTR was significantly higher, indicating better anticoagulation control among self-testing participants.
FIGURE 15.
Forest plot of comparison: TTR. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’.
The INR values in therapeutic range were reported in 12 trials. 59–61,64,66–68,70,72,76,78,79 There was great variation between trials in the measures used to assess INR values in therapeutic range and, therefore, the pooling of data across trials proved unfeasible. In eight trials which reported the proportion of INR measurements in the therapeutic range,59,60,66–68,70,76,78 the values ranged from 43.2%59 to 80.8%66 for self-monitoring and from 22.3%59 to 72%67 for standard care. In four trials that reported the proportion of participants in the therapeutic range instead,61,64,72,79 the values ranged from 53%72 to 72.9%79 for self-monitoring and from 43.2%79 to 72%64 for standard care. With the exception of two UK-based trials,64,67 all trials reported higher proportion of INR measurements or larger proportions of participants in therapeutic range for self-monitoring than for standard care. Significant differences between interventions were detected in six of these trials. 60,61,66,70,78,79 The INR values in therapeutic range are summarised in Table 7.
Among participants with AHVs, self-monitoring resulted in a significantly higher INR TTR73,77 or INR values in therapeutic range59,70,78,79 than standard care. In two trials that included participants with atrial fibrillation,60,69 no TTR differences were found between self-monitoring and standard care.
Test failure rate
Only one trial45 reported one instrument defect and one test strip problem in the self-testing group. No other failures were mentioned in the remaining included trials.
Time to receive test result
One trial74 reported the time for each INR monitoring (i.e. time from INR measurement to test results) and the total time spent for anticoagulant management during the 4-month follow-up period. The time spent for each INR monitoring by self-managed participants was significantly lower (mean 5.3 minutes, SD 2.6 minutes) than the time spent by participants receiving standard care (mean 158 minutes, SD 67.8 minutes; p < 0.001). During the 4-month follow-up, the total time spent for anticoagulation monitoring by participants in standard care was significantly higher (mean 614.9 minutes, SD 308.8 minutes) than the total time spent by participants who self-managed their therapy (mean 99.6 minutes, SD 46.1 minutes; p < 0.0001).
Patient compliance with testing
Gardiner and colleagues45 reported > 98% compliance with self-testing and stated that participants were conscientious in performing and recording their weekly tests. Of those who did not comply with self-testing, two had difficulties performing the test or experienced disruption due to hospitalisation and one lost the CoaguChek meter. In the trial by Khan and colleagues,69 75% (30 out of 40) of participants did not report any problems with the use of the device and expressed willingness to continue with self-monitoring. On the other hand, participants who did not comply (25%) with the testing procedure reported difficulties with the technique or problems placing the fingertip blood drop on the right position on the test strip. This resulted in the need to use multiple strips to achieve a single reading.
Frequency of testing
Even though the frequency of self-testing was preplanned in 18 of the included trials,45,56,59,62–69,71–77 only 10 trials eventually reported it. 59,62–68,71,76 The frequency of self-testing ranged on average (mean) from every 4.6 days62 to every 12.4 days64 (Table 8).
| Study ID | Type of OAT management | Total number in SM | Number (%) attending training | Number (%) completing and starting SM | Number (%) adherence to SM or completing SM | Planned frequency of self-testing | Actual frequency of self-testing, mean (SD) days | Clinic visit per year | QA per year |
|---|---|---|---|---|---|---|---|---|---|
| Azarnoush 201177 | PST | 103 | NR | NR | 90 (87) | Once weekly | NR | NR | NR |
| Bauman 201055 | PSM vs. PST | PSM: 14 PST: 14 |
NR | NR | PSM: 12 (86) PST: 14 (100) |
NR | NR | NR | Once |
| Christensen 200675 | PSM | 50 | 50 (100) | 48 (96) | 47 (≈ 98) | Daily for first 3 weeks then once weekly | NR | NR | Once |
| Christensen 201166 | PST: once weekly/twice weekly | 51/40 | NR | NR | 46 (90)/37 (92) | Once weekly Twice weekly |
7.4 (2.7)/4.1 (1.8) | Twice | Twice |
| Cromheecke 200076 | PSM | 50 | NR | NR | 49 (98) | Once weekly then once every 2 weeks | 8.6 | NR | NR |
| Eitz 200878 | PSM | 470 | NR | NR | NR | NR | NR | Twice | NR |
| Fitzmaurice 200267 | PSM | 30 | 27 (90) | 26 (96) | 23 (88) | Every 2 weeks | 1.6 weeks | Four visits | Four in 6 months |
| Fitzmaurice 200564 | PSM | 337 | 327 (97) | 242 (74) | 193 (80) | Every 2 weeks | 12.4 (95% CI 11.9 to 12.9) | Four visits | Four |
| Gadisseur 200368 | PSM | Total 720 | 184 (25) | 180 (98) | NR | Once weekly | NR | NR | NR |
| Gardiner 200545 | PST | 44 | 43 (98) | 39 (91) | 31 (79) | Once weekly | NR | NR | Once |
| Gardiner 200656 | PST vs. PSM | PST: 55 PSM: 49 |
NR | NR | PSM: 41 (74) PST: 36 (73) |
Every 2 weeks | NR | NR | Once |
| Hemkens 200857 | PSM | 16 | 16 (100) | NR | 14 (87) | NR | NR | Four visits in 14 weeks | NR |
| Khan 200469 | PST | 44 | NR | NR | 40 (91) | Once weekly | NR | Three visits in 24 weeks | Three in 24 weeks |
| Körtke 200170 | PSM | NR | NR | NR | NR | NR | Twice | NR | |
| Horstkotte 199659 | PSM | 75 | NR | NR | 74 (99) | Every third day | Median 3.9 (0.3) | ≈ 4 visits | NR |
| aMatchar 201071 | PST | 1465 | 1465 (100) | 1465 (100) | 1463 (> 99%) | Once weekly | 7.6 (5.4) | Four visits | NR |
| Menéndez-Jándula 200561 | PSM | 368 | 310 (84) | 300 (97) | 289 (96) | Once weekly | NR | NR | NR |
| Rasmussen 201258 | PSM | 54 | NR | NR | 54 (100) | NR | NR | NR | NR |
| Ryan 200962 | PST | 72 | NR | NR | 72 (100) | Twice weekly then every 2 weeks | 4.6 (0.8) | Three visits in 6 months | Every 2 months |
| Sawicki 199972 | PSM | 90 | NR | NR | 83 (92) | 1–2 times per week | NR | Three visits in 6 months | NR |
| Sidhu 200173 | PSM | 51 | 44 (86) | 41 (93) | 34 (83) | Once weekly | NR | No visits | NR |
| Siebenhofer 200863 | PSM | 99 | 89 (90) | 89 (90) | 83 (93) | Once weekly | Median 27 days for first 6 months and 24 days for the following 6 months | Twice | NR |
| Soliman Hamad 200979 | PSM | 29 | NR | NR | 29 (100) | NR | NR | Four visits | NR |
| Sunderji 200465 | PSM | 70 | NR | NR | 53 (76) | Once weekly for first 4 weeks, every 2 weeks for 2 months and then monthly | 9.3 | NR | Twice in 8 months |
| Verret 201274 | PSM | 58 | NR | NR | 57 (98) | Once weekly | NR | NR | |
| Völler 200560 | PSM | 101 | NR | NR | NR | NR | NR | NR | NR |
Frequency of visits to primary or secondary care clinics
Frequency of visits to clinics was reported by 12 trials. Three trials reported three visits in approximately 6 months;62,69,72 five trials reported four visits per year;59,64,67,71,79 three trials reported two visits per year;63,66,78 and the remaining trial73 reported that there were no routine clinic visits during the study period (see Table 8).
Adherence to the self-monitoring
Generally, adherence to the self-monitoring was reported to be high in the included trials. In 13 trials, > 90% of the participants completed self-monitoring,58,59,61–63,66,69,71,72,74–76,79 while in another nine trials the dropout rates ranged from 12% to 25% (see Table 8). 45,55–57,64,65,67,73,77 Few trials also provided information on the number of people who were excluded during the recruitment phase because they were incapable of performing self-monitoring. 45,56,61,67,71,73,77,80 It is worth noting that up to 50% of the participants were deemed unsuitable for inclusion. Main reasons for exclusion were old age, anxiety, lack of confidence, inadequate cognitive abilities and poor dexterity.
Patient-reported outcomes
People’s anxiety associated with waiting time for results and with not knowing their current coagulation status and related risk
The trial by Bauman and colleagues,55 which compared self-management with self-testing in children, reported that one parent (single parent of a 16-year-old male child) did not favour self-management because of the increased anxiety related to INR measurements.
Preference and acceptability of the tests
Four trials45,55,57,62 conducted a questionnaire survey to assess acceptability to participants of self-testing and self-management using point-of-care devices (Table 9). These trials reported high rates of acceptance for both self-management and self-testing (77% to 98%). 45,55,57,62 Two trials45,62 reported that 77% to 98% of participants favoured self-testing with CoaguChek S over standard care.
| Study ID | Method | Results |
|---|---|---|
| Gardiner 2005:45 PST | Participants in the self-testing group completed a patient acceptability questionnaire after 3–4 months. The acceptability questionnaire included patients’ views on ease of use of CoaguChek S, frequency of repeated tests, difficulty of getting an adequate sample, ease of the use of QC materials, confidence in the result and preference for home testing vs. hospital testing | 84% initially found it difficult to obtain an adequate sample 55% subsequently found self-testing very easy 32% found self-testing easy One patient found it difficult to use CoaguChek S 16% were still experienced difficulty in obtaining sample 87% felt confidence in CoaguChek result they obtained 77% preferred self-testing to attending the anticoagulant clinic |
| Hemkens 2008:57 PSM | Participants completed a structured questionnaire regarding the ease of use of the point-of-care device | Satisfaction with point-of-care testing: 92% rated satisfaction with INRatio high or good; 86% rated satisfaction with CoaguChek S high or good Satisfaction with self-management: 93% rated satisfaction with self-management high or good Ease of use of point-of-care: 62% preferred INRatio and 23% CoaguChek S Overall satisfaction with point-of-care: 43% preferred INRatio and 36% preferred CoaguChek S; 21% reported no difference between the two tests |
| Ryan 2009:62 PST | One hundred and seventeen participants (88.63%) completed the satisfaction survey | 99.1% found the point-of-care monitor easy to use Most participants (figure not reported) felt confident with the results they obtained All participants (100%) agreed that the CoagCare® questions and dosing instructions were clear and easy to understand 87.6% felt that they were monitored more closely by the pharmacist during the supervised PST arm of the study 94.7% felt that their INR was better controlled 98.3% preferred supervised PST over attendance in the AMS |
| Bauman 2010:55 PSM | Open-ended questionnaires (as a platform for semistructured interviews) and semistructured interviews were given. A conventional content analysis approach was taken to interpret the semistructured interviews | Except for one, all families preferred PSM. Responses to PSM by participants were:
|
Another crossover trial57 reported that 93% of participants rated their satisfaction with regard to self-monitoring (using either INRatio or CoaguChek S) as high or good. When asked about the overall relative satisfaction with the device, 43% of participants favoured INRatio, 36% favoured CoaguChek S, and 21% liked both devices equally. The trial by Bauman and colleagues,55 which assessed self-management over self-testing (usual care in this trial) in children, reported that the majority of participants (13 out of 14 participating families: 92%) opted for the use of CoaguChek XS device.
Health-related quality of life
Nine trials55,67–69,71,72,74,76,79 reported on health-related quality-of-life outcomes using one of the following measures:
-
Sawicki’s tool:68,72,74,76 a structured questionnaire containing 32 questions developed and validated by Sawicki and colleagues. 72 The questionnaire covered five treatment-related aspects: ‘general treatment satisfaction’, ‘self-efficacy’, ‘daily hassles’, ‘distress’ and ‘strained social network’. The questions were derived from the sentences formulated by the participants receiving anticoagulation describing their feelings with regard to their treatment. Each item is graded on a scale ranging from a minimum of 1 (total disagreement) to a maximum of 6 (total agreement) as self-perceived by participants. Higher scores for self-efficacy and general treatment satisfaction and lower scores for daily hassles, psychological distress and strained social network are indicative of better quality of life.
-
Short Form questionnaire-36 items (SF-36) [UK Short Form Health Survey (UKSF-36), SF-36v2]:69,79 SF-36 is a validated tool containing 36 items for the assessment of the health status and quality of life. SF-36 covered physical functioning, physical role limitation, bodily pain, general health perceptions, vitality, social functioning, emotional role limitation and mental health. UK SF-36 and the SF-36v2 questionnaire have been reported here.
-
Euroqol scores [European Quality of Life-5 Dimensions (EQ-5D)]:69 EQ-5D is a validated tool for assessing health status and quality of life.
-
Lancaster’s instrument:67,69 Lancaster’s instrument is designed to measure health beliefs specific to the use of warfarin in anticoagulant treatment.
-
Duke Anticoagulation Satisfaction Scale:71 Duke Anticoagulation Satisfaction Scale measures patient satisfaction with anticoagulation. Scores on this scale range from 25 to 225, with lower scores indicating higher satisfaction.
-
Health Utilities Index Mark 3 (HUI Mark 3):71 HUI Mark 3 is a tool to measure quality of life. Scores for the HUI Mark 3 range from −0.36 to 1.00, with a negative score indicating a state worse than being dead and a score of 1.00 indicating perfect health.
-
Schedule for Evaluation of Individual Quality of Life (SEIQoL) tool:67 SEIQoL is a semistructured interview for the assessment of quality of life.
-
KIDCLOT-PAC-QL: KIDCLOT-PAC Parent-proxy QL© (parents’ quality of life and their assessment of the child’s quality of life) and KIDCLOT-PAC Child-teen QL©. 55
Four trials reported quality of life using Sawicki’s questionnaire (Table 10). 68,72,74,76 Sawicki and colleagues72 and Verret and colleagues74 reported improvements in treatment satisfaction and self-efficacy, and reduced level of distress and daily hassles in both the self-management and the standard care groups, but the improvements were significantly greater among participants self-managed. Similarly, Cromheecke and colleagues76 showed significant improvements in treatment satisfaction and self-efficacy, and significant reductions in level of distress and daily hassles for self-management participants, compared with those in standard care. Gadisseur and colleagues68 showed increased treatment satisfaction and self-efficacy, and reduced level of distress and daily hassles among self-monitoring participants (self-testing or self-management). On the other hand, they found an increased level of distress among participants who received education but did not directly monitor their anticoagulation therapy.
| Study ID | General treatment satisfaction | Self-efficacy | Daily hassles | Distress | Strained social network | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PSM/PST | SC | p-value | PSM/PST | SC | p-value | PSM/PST | SC | p-value | PSM/PST | SC | p-value | PSM/PST | SC | p-value | |
| Mean difference (SD) between baseline and follow-up | |||||||||||||||
| Sawicki 199972 | +1.54 (1.38) | +0.24 (1.48) | < 0.001 | +0.83 (0.92) | +0.35 (0.96) | 0.003 | –0.49 (0.83) | –0.03 (0.53) | 0.01 | –0.61 (0.87) | –0.21 (0.93) | 0.008 | –0.40 (0.83) | –0.23 (0.79) | 0.19 |
| Verret 201274 | +1.3 (1.2) | +0.2 (1.1) | < 0.001 | +0.4 (1.2) | +0.3 (1.1) | 0.647 | –0.5 (0.6) | –0.2 (0.8) | < 0.024 | –0.6 (1) | –0.2 (0.8) | < 0.029 | –0.6 (0.9) | +0.1 (0.7) | < 0.001 |
| Gadisseur 200368 | +0.49/+0.19 | –0.23 | +0.32/+0.31 | +0.02 | –0.31/–0.09 | +0.23 | –0.44/+0.06 | +0.33 | –0.21/–0.02 | +0.21 | |||||
| Mean (SD) at follow-up (control group matched for age, sex and indication) | |||||||||||||||
| Cromheeceke 200076 | 4.8 (1.2) | 4.0 (1.5) | 0.015 | 5.4 (0.6) | 4.5 (1.0) | < 0.001 | 1.8 (0.5) | 2.6 (0.5) | < 0.001 | 2.5 (0.8) | 2.9 (1.1) | 0.022 | 1.7 (0.6) | 2.7 (0.9) | < 0.001 |
Two UK-based trials did not find significant differences in quality-of-life outcomes between self-management and self-testing participants, compared with those receiving standard care (Table 11). 67,69 Khan and colleagues69 reported quality-of-life data using the UK SF-36, the Euroqol scores and Lancaster’s instrument. No significant differences were observed between self-testing participants and those who received education but did not test themselves, for both the UK SF-36 parameters and the Euroqol scores. Emotional function was the only parameter that showed a significant change at 24 weeks compared with baseline (p = 0.04). Fitzmaurice and colleagues67 assessed participants’ attitude towards self-management and quality-of-life outcomes through a semistructured interview given to a random sample of 16 participants (eight in self-management and eight in standard care). Assessed themes were adapted from Lancaster’s instrument, the SEIQoL tool and a series of focus groups. Five common themes emerged from the interviews conducted on participants in self-management: knowledge and management of condition, and self-empowerment, increased anxiety and obsession with health, self-efficacy, relationship with health professionals, and societal and economic cost. The trial investigators did not find any significant difference in quality of life between participants self-managed and those in standard care. Soliman Hamad and colleagues79 measured quality of life in participants with AHVs in the Netherlands by means of the SF-36v2. Significant improvements in quality-of-life scores were observed in participants who self-managed their therapy, compared with those in standard care, with regard to the physical component summary only (see Table 11).
| Study ID | Mean (SD) at 24 weeks | ||
|---|---|---|---|
| PST | Control | p-value | |
| UK SF-36, Euroqol scores and Lancaster instrumenta | |||
| Khan 200469 | |||
| Physical functioning | 57 (29) | 53 (29) | NS |
| Physical role limitation | 45 (44) | 52 (42) | NR |
| Bodily pain | 65 (34) | 65 (31) | NS |
| General health perceptions | 53 (23) | 56 (21) | NR |
| Vitality | 53 (23) | 52 (21) | NR |
| Social functioning | 71 (32) | 72 (28) | NS |
| Emotional role limitation | 63 (42) | 63 (46) | NS |
| Mental health | 78 (18) | 76 (20) | NS |
| EQ-5D score | 0.75 (0.27) | 0.7 (0.29) | NR |
| Euroqol percentage | 67 | 66 | NR |
| Study ID | Mean % at 12 months’ follow-up | ||
| PSM | Control | p-value | |
| SF-36v2 questionnaire | |||
| Soliman Hamad 200979 | |||
| Physical functioning | 13.2 | 15.8 | NS |
| Role physical | 27.4 | 28.3 | NS |
| Bodily pain | 7.3 | –2.0 | 0.02 |
| General health | 13.4 | 9.9 | NS |
| Vitality | 25.9 | 17.6 | 0.01 |
| Social functioning | 13.3 | 10.8 | NS |
| Role emotional | 20 | 12.1 | 0.03 |
| Mental health | 14.2 | 9.2 | NS |
| Physical component summary | 20.9 | 9.8 | 0.03 |
| Mental component summary | 13.7 | 9.1 | NS |
Matchar and colleagues71 measured quality of life by means of the HUI Mark 3. They reported significant gain in health utilities at the 2-year follow up among self-testing participants who used ProTime, compared with those managed in high-quality anticoagulant clinics (p < 0.001). The same investigators71 also measured anticoagulant satisfaction using the Duke Anticoagulation Satisfaction Scale. They found that the degree of satisfaction was higher in self-testing participants than in those in standard care (p = 0.002).
Bauman and colleagues55 assessed self-management versus self-testing in children and provided quality-of-life data using the KIDCLOT-PAC Parent-proxy QL© (parents’ quality of life and their assessment of the child’s quality of life) and the KIDCLOT-PAC Child-teen QL©.
Both tools were completed pre and post intervention to assess potential changes in quality-of-life outcomes related to warfarin use. The five common themes identified from the open-ended questionnaires and the semistructured interviews were awareness, communication, relationship between parent and child, flexibility and anxiety. No significant changes in ‘tasks’ related to warfarin use were found between intervention groups.
Summary of the clinical effectiveness results
The evidence of the clinical effectiveness of self-monitoring (self-management and self-testing) of the coagulation status in people receiving vitamin K antagonist therapy compared with standard care was based on the findings of 26 RCTs. Four trials reported on CoaguChek XS (n = 414), 17 trials on CoaguChek S/CoaguChek (n = 3910), one on CoaguChek Plus (n = 1155), two on CoaguChek and INRatio (n = 222) and two on ProTime (n = 3062). No trials that exclusively assessed the clinical effectiveness of INRatio were identified by this assessment. The main results are summarised below:
-
Self-monitoring of anticoagulation therapy showed better control over thromboembolic events than standard care. No significant reductions were found in the number of bleeding events and all-cause mortality.
-
In participants with AHVs, self-monitoring almost halved the risk of thromboembolic events and all-cause mortality compared with standard care. No differences were observed between intervention groups with regard to the number of bleeding events.
-
Self-monitoring significantly reduced the risk of thromboembolic events, while self-testing did not.
-
TTR varied from 52% to 80% among self-monitoring participants and from 55% to 77% in standard care. Self-testing showed a modest but significantly higher percentage of TTR than in standard care. No significant differences were observed between self-management and standard care. UK-based trials did not find significant differences in the TTR between intervention groups.
-
77% to 93% of participants expressed a preference for self-monitoring (using CoaguChek or INRatio) over standard care.
-
Two UK-based trials did not find significant differences in quality-of-life outcomes between intervention groups.
Chapter 3 Assessment of cost-effectiveness
We assessed the cost-effectiveness of self-monitoring (self-testing and self-management) using CoaguChek system and alternative point-of-care testing devices compared with standard monitoring care in people receiving long-term vitamin K antagonist therapy.
Systematic review of existing cost-effectiveness evidence
Initial scoping searches revealed a number of previous systematic reviews of economic studies evaluating point-of-care testing devices for people receiving long-term vitamin K antagonist therapy. 21,32 Further systematic searches of MEDLINE, MEDLINE In-Process & Other Non-Indexed Citations, EMBASE, Science Citation Index, Health Management Information Consortium, NHS Economic Evaluation Database and the HTA databases were undertaken to identify any further relevant studies. The search strategies are detailed in Appendix 1.
The searches identified 12 economic evaluations of potential relevance to the scope of this assessment. All of these evaluations comparing INR self-monitoring strategies with standard care were appraised against the NICE reference case, and the methods and findings of each study are summarised briefly below in a narrative fashion and tabulated for comparison in Table 12. The studies were assessed against the NICE reference case and their relevance to the scope is shown in Table 13.
| Author | Country | Study design | Cohort | Intervention/comparators | Study perspective | Time frame | Results | Conclusion |
|---|---|---|---|---|---|---|---|---|
| Taborski 199982 | Germany | Cost–consequence analysis (incidence of thromboembolic and bleeding events) | Data collected from patients to cost treatments and complications | Usual care (monitoring by patient’s family physician or specialist) vs. PSM | Government-controlled health insurance fund (INR monitoring costs and acute treatment and rehabilitation costs for adverse events) | Not stated (results expressed as costs and complication rates per 100 patient-years) | When complication and direct costs were combined, self-management was estimated to be cost saving (DM719 per patient per year) | Self-management results in a decrease in the number of complications compared to usual care. When the costs of complications are included, PSM saves DM719.02 per patient per year |
| Lafata 200083 | USA | Cost-effectiveness/cost–utility analysis: Markov model | Hypothetical cohort of patients aged 57 years initiating long-term warfarin therapy | Usual care (14 tests per year) vs. PST (52 tests per year) vs. anticoagulation clinic testing (23 tests per year) | Health service provider and societal perspective | 5 years | From a health service provider perspective, anticoagulation clinic testing was cost saving vs. SC. Self-testing had an ICER of US$24,818 per event avoided (US$153,504 per QALY gained) vs. anticoagulation clinic testing but was cost-saving from a societal perspective | From a health service provider perspective, anticoagulation clinic testing is the most cost-effective option. However, the authors concluded that self-testing would be the most cost-effective from a societal perspective |
| Muller 200184 | Germany | Cost-effectiveness analysis (simple extrapolation model) | Hypothetical cohort of 10,000 patients | PSM vs. usual care by a family physician | Not explicitly stated (assumed German health-care payer) | 10 years | Self-management found to cost DM105,000 per life-year gained compared with usual care | Self-management led to a 30% reduction in severe complications at an acceptable cost-effectiveness ratio |
| Sola-Morales 200385 | Spain | Cost-effectiveness/minimisation analysis – Markov model | – | Usual hospital care; self-management; self-testing; use of a portable coagulometer by family physician; use of a portable coagulometer in a hospital setting | Health insurer | 5 years | Assuming equivalent clinical effects for all point-of-care strategies, hospital-based coagulometer testing was found to have the lowest cost and, therefore, be the most cost-effective option | From a previous translation, hospital-based coagulometer testing was reported as being the most efficient strategy |
| Regier 200686 | Canada | Cost–utility analysis: Bayesian Markov model | Patients receiving long-term anticoagulation for atrial fibrillation or a mechanical heart valve | PSM; physician management | Canadian health-care payer | 5 years | The ICER for self-management vs. physician-managed monitoring was C$14,129 per QALY gained | Self-management was considered cost-effective with a 95% probability of being cost-effective at a willingness to pay of C$23,800 per QALY |
| Jowett 200687 | UK | Cost–utility analysis alongside a RCT | N = 617 (337 self-management, 280 usual care). 65% male. Mean age 65 years | Self-management (CoaguChek S; 30 tests per year) vs. usual primary or secondary care clinic management (10 tests per year) | NHS and societal perspective | 1 year | The results indicated a very small non-significant increase in QALYs (0.01) associated with self-management for a cost increase of £295: ICER £32,716 per QALY gained from a health service perspective | Self-management appeared not to be cost-effective at 1 year |
| Brown 200732 | Canada | Cost–utility analysis: Markov model | Hypothetical cohort of patients on long-term warfarin therapy | Usual care (20 tests per year); anticoagulation clinic testing with CoaguChek (23 tests per year); self-testing with CoaguChek (52 tests per year); anticoagulation clinic testing with ProTime (23 tests per year) | Health-care provider and societal perspective | 5 years | Anticoagulation clinic testing with CoaguChek was cost saving vs. usual care. Self-testing had an ICER of C$57,595 from a health and social care perspective, but was cost saving from a societal perspective | From a health-care provider perspective, moving from usual care to self-testing was not considered cost-effective. From a societal perspective, it was cost saving |
| Connock 200721 | UK | Cost–utility analysis: Markov type model | Mixed cohort of patients aged 65 years | Patient self-management vs. usual primary/secondary care management | NHS and personal social services perspective | 10 years | The incremental cost per QALY gained with self-management vs. standard monitoring was £63,655. Self-management was estimated to have a 44% chance of being cost-effective at a threshold of £30,000 per QALY gained | Self-management is unlikely to be cost-effective over usual care in the UK |
| Gailly 200933 | Belgium | Cost analysis and cost-effectiveness analysis (self-management vs. lab testing with GP follow-up): decision tree | Cohort of patients on long-term anticoagulation therapy | Laboratory testing with GP follow-up; point-of-care testing by a GP; point-of-care testing by an anticoagulation clinic; PST; and self-management | Belgian health-care payer’s perspective | 10 years | Self-management was estimated to be the least costly strategy, and dominated usual care with respect to life-years gained (the other point-of-care strategies were excluded from the CEA) | Patient self-management resulted in significantly more life-years gained and was on average cost-saving compared with laboratory testing with GP follow-up |
| Medical Advisory Secretariat 200988 | Canada | Cost–utility analysis: Markov model | Patients on long-term anticoagulation therapy | Usual care (lab testing); health-care setting; point-of-care testing; self-testing; self-management | Ministry of Health and Long-Term Care | 5 years | All point-of-care testing strategies dominated lab testing (usual care). Self-testing was more costly and marginally more effective than point-of-care testing in a clinic setting. Self-management dominated both self-testing and point-of-care clinic testing | The self-management strategy was the most cost-effective strategy |
| Element of HTA | Reference case | Taborski 199982 | Lafata 200083 | Muller 200184 | Sola-Morales 200385 | Jowett 200687 | Reiger 200686 | Brown 200732 | Connock 200721 | Gailly 200933 | Medical Advisory Secretariat 200988 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Defining the decision problem | Consistent with the scope for this assessment? | No | No | No | No | Partially | No | No | Partially | No | No |
| Comparator(s) | As listed in the scope developed by NICE? | Yes | Yes | Yes | – | Yes | Yes | Yes | Yes | Yes | Yes |
| Perspective on outcomes | All direct health effects, whether for patients or, when relevant, carers | No | Yes | Yes | – | Yes | Yes | Yes | Yes | No | Yes |
| Perspective on costs | NHS and PSS | No | No | No | No | No | No | No | Yes | No | No |
| Type of economic evaluation | Cost–utility analysis with fully incremental analysis | No | Yes | No | – | Yes | Yes | Yes | Yes | No | Yes |
| Time horizon | Long enough to reflect all important differences in costs or outcomes between the technologies being compared | No | 5 years | 10 years | – | No | 5 years | 5 years | 10 years | 10 years | 5 years |
| Synthesis of evidence on health effects | Based on systematic review | No | No | No | – | No | No | Yes | No (based on trial) | No | Yes |
| Measuring and valuing health effects | Health effects should be expressed in QALYs. The EQ-5D is the preferred measure of health-related quality of life in adults | No | Yes | No | – | Yes | Yes | Yes | Yes | No | Not clear |
| Source of data for measurement of health-related quality of life | Reported directly by patients and/or carers | NA | No | NA | – | Yes | Yes | No | Yes | NA | No |
| Source of preference data for valuation of changes in health-related quality of life | Representative sample of the UK population | No | No | No | No | Yes | No | No | Yes | No | No |
| Equity considerations | An additional QALY has the same weight regardless of the other characteristics of the individuals receiving the health benefit | NA | Yes | NA | – | Yes | Yes | Yes | Yes | NA | Yes |
| Evidence on resource use and costs | Costs should relate to NHS and PSS resources and should be valued using the prices relevant to the NHS and PSS | No | No | No | No | Yes | No | No | Yes | No | No |
| Discounting | The same annual rate for both costs and health effects (currently 3.5%) | No | No | No | No | Yes | No | No | Yes | No | No |
Critique of the included studies
Taborski 199982
This German study assessed the cost-effectiveness of patient self-management versus anticoagulation clinic-based management by a family physician or specialist. The study included costs relevant to the primary cost carrier: in this case, the government-controlled health insurance fund. Information regarding the costs of self-management and clinic management, and the costs of acute treatment and rehabilitation for complications were acquired from patients and published literature. Quality of life was not considered in the analysis. When costs of complications were included in the analysis, self-management was estimated to be less costly and more effective than clinic-managed care – owing to its estimated impact on the incidence of both thromboembolic and bleeding events. However, the estimated effects of self-management on these adverse events were selected from a small number of studies reporting high baseline rates and large beneficial effects of self-management.
Lafata 200083
This study, carried out in the USA, constructed a Markov model with a 5-year time horizon to examine the cost-effectiveness of three anticoagulation management strategies: usual care with a family physician (without a point-of-care monitoring device), anticoagulation clinic testing with a point-of-care monitor, and patient self-testing with a point-of-care monitor. The self-testing strategy required participants to telephone their anticoagulation clinic for dosing instructions. For each strategy it was assumed that the time within, above and below the therapeutic range differed and that time out of the target range influenced the risk of complications. Time in range was modelled to be highest for self-testing, followed by point-of-care anticoagulation clinic testing, followed by usual care. The actual estimates were based on a number of cohort studies and clinical trials, but these did not appear to be systematically identified.
The Markov model parameter values were estimated from available literature, routine health service data, and expert opinion where necessary. The analysis was conducted for a hypothetical cohort of participants, aged 57 years, initiating long-term warfarin therapy. Both a health service provider (direct medical care costs only) and a wider societal perspective (including costs incurred by participants and their caregivers) were adopted. The patient self-testing strategy assumed the highest number of annual tests (n = 52), compared with anticoagulation clinic testing (n = 23) and usual care (n = 14). The 5-year direct health service costs (per 100 participants) were higher for the self-testing strategy ($526,014) than for usual care ($419,514) or anticoagulation clinic testing ($405,560). However, when patient and caregiver costs were included, self-testing accumulated lower 5-year costs than anticoagulation clinic testing ($622,727 vs. $645,671). From the health service provider perspective, anticoagulation clinic testing with a point-of-care monitor was considered the most favourable strategy. When patient and caregiver costs were included, self-testing dominated point-of-care anticogulation clinic testing, but remained more costly and more effective than usual care.
A number of one-way sensitivity analyses were conducted to test key parameter and structural assumptions in the model. Model findings were found to be most sensitive to assumptions regarding the frequency of yearly tests and time spent in the therapeutic range with the different strategies. Given that the setting of this study was the USA, the results cannot be generalised to the UK.
Muller 200184
This economic analysis was conducted to assess the cost-effectiveness of patient self-management compared with standard family physician-managed anticoagulation monitoring in people following a mechanical heart valve replacement. The focus was on preventing coagulation-related complications. The incidence of stroke was estimated for a hypothetical cohort of 10,000 patients from the German Experience with Low Intensity Anticoagulation (GELIA) study. 89 Data from the USA, adapted to German standards, were used to inform lifetime costs of stroke. The study assumed that self-management would reduce the incidence of severe complications by 30%, compared with family physician-managed care. The incremental cost-effectiveness ratio (ICER) was estimated to be Deutsche Mark (DM) 105,000 per life-year gained for self-management versus physician-managed care. The authors concluded that PSM may reduce the incidence of fatal strokes at an acceptable ICER.
Sola-Morales 200385
This evaluation was published in Catalan by the Catalan Agency for HTA. It was assessed partially based on a summary in a previous review21 and using a web-based translation interface to translate key passages.
The study compared several strategies including standard laboratory testing, patient self-management, patient self-testing, point-of-care monitoring by a GP and point-of-care monitoring in a hospital setting. A Markov model was constructed with a 5-year time horizon. Data to populate the model were acquired from a systematic literature review. The study assumed a higher incidence of adverse clinical outcomes for usual care than for those strategies utilising a point-of-care monitoring device. It was assumed that all strategies involving the use of a point-of-care monitor had equivalent effects. Based on these assumptions, the results indicated that, from a health insurer perspective, the use of point-of-care monitors in a hospital setting was the preferred option on grounds of cost-effectiveness. However, it was not clear what the relative cost-differences were between the monitoring strategies.
Jowett 200687
This cost–utility analysis was conducted alongside the largest UK-based RCT of patient self-management versus standard primary or secondary care INR monitoring. The follow-up period was 12 months. The analysis relied on individual patient-level cost and utility data (derived from responses to the EQ-5D), collected alongside the RCT.
The cost-effectiveness of patient self-management (average 30 tests per year with CoaguChek S) versus usual clinic management (average 10 tests per year at a combination of hospital and primary care clinics) was estimated from the perspective of the NHS and also from a wider perspective incorporating patient costs. The trial recruited 617 participants receiving long-term anticoagulation. Quality-adjusted life-years (QALYs) were derived from participant responses to the EQ-5D at baseline, 6 weeks and 6 months. Multiple imputations were used to replace missing EQ-5D data and a regression-based approach was used to estimate incremental QALYs associated with self-management.
Costs for patient self-management included training and assessment costs, device and testing strip costs, costs of any telephone calls relating to INR or device queries, and costs associated with any adverse events. Costs of standard care clinic monitoring visits were estimated for the various types of standard care on offer (from a sample of participating centres) and applied on a per-visit basis. Costs associated adverse events were taken from the NHS reference cost. Wider patient costs included out-of pocket travel costs and the value of time lost from work to attend appointments.
Based on intention to treat, the results indicated that from both the health service and the wider perspective, mean costs in the patient self-management arm were significantly higher than those in the usual care arm (+£294 and +£282.93). There was a very small, non-significant increase in QALYs in the self-management arm at 12 months (0.009, 95% CI –0.012 to 0.030).
From the health service provider perspective, the ICER for patient self-management was £32,716 per QALY gained, and an ICER of £31,437 per QALY gained was reported from a wider societal perspective. At a ceiling ratio of £20,000 per QALY gained, patient self-management had a 30% probability of being cost-effective; this probability increased to 46% when the ceiling ratio rose to £30,000 per QALY gained.
The authors concluded that, based on the general decision rules for interpreting cost-effectiveness findings in the UK, it was unlikely that self-management would be considered cost-effective compared with usual care. However, it was noted that although patient self-management incurred a higher initial cost, it could reduce the number of people attending outpatient clinics and, therefore, free up clinician time for other patients. Furthermore, the results were based on only 12 months’ follow-up of a single trial that was not powered to detect a difference in adverse events.
Regier 200686
This Canadian study assessed the cost-effectiveness of patient self-managed and family physician-managed (with laboratory testing) long-term anticoagulation therapy. A Bayesian Markov model was constructed from the perspective of a Canadian health-care payer, and analysed over a 5-year time horizon. The adopted model structure accounted for the time spent by patients within, above or below the specified INR therapeutic range, and determined patients’ risks of thromboembolic and haemorrhagic events based on this.
Model input parameter estimates were derived from a number of sources. TTR was obtained from a Canadian trial of self-management versus physician-managed warfarin therapy. Event risks for time spent in, above and below therapeutic range were derived from a prospective cohort of 2745 people with atrial fibrillation, AHVs and venous thromboembolism. Cost and utility parameters were taken from a number of different sources.
It was assumed that under the self-management strategy, people would perform 52 tests per year, while under physician-managed care, only 14 tests would be performed each year, with dosing information from the laboratory test being communicated to the patient by telephone.
The mean per-patient cost over the 5-year period was higher for the self-management strategy (C$6116) than for the physician-managed strategy (C$5127). In terms of quality of life, self-management resulted in a QALY gain at the 5 years of 0.07. This was due to a modelled reduction in both the number of thromboembolic events and the number of haemorrhagic events. The reported ICER for self-management versus physician-managed care was C$14,129 per QALY gained. The authors concluded that self-management was cost-effective for people receiving long-term anticoagulation therapy.
The methods for calculating the costs and outcomes in this study were not transparent and the time spent in the therapeutic range was derived from the results of a single clinical trial conducted in a Canadian setting. Moreover, the perspective adopted was that of a Canadian health-care payer, which makes the generalisability of these results to a UK setting difficult. In addition, the comparator in this study was physician-managed care relying on laboratory testing, rather than anticoagulation clinic-managed care using point-of-care testing. As such, the result may be less generalisable to contexts where the latter approach is used in standard practice.
Brown 200732
Another Canadian study conducted by Brown and colleagues32 adopted a decision-analytic modelling approach to assess the cost–utility of patient self-testing (52 tests per year), compared with physician-managed laboratory testing (20 tests per year) and physician-managed point-of-care testing (23 tests per year). The 5-year model presented results from both the health-care provider (estimated separately to include and exclude nursing home costs) and a wider societal perspective. The model was similar in structure to other models reported in the literature, with thromboembolic and haemorrhagic events modelled by time spent inside and outside the specified INR therapeutic range. The analysis was conducted for a hypothetical cohort of people on long-term warfarin therapy, with input parameters estimated from the published literature and a meta-analysis of studies assessing TTR. It was assumed that self-testing and physician-managed point-of-care testing were equivalent in terms of clinical effects. Cost parameters were identified from the published literature and were valued using Canadian sources.
Cumulative costs and QALYs were estimated over a 5-year period. From the health service provider perspective, the results indicated that physician-managed point-of-care testing was cost saving compared with usual care. Self-testing, on the other hand, was not found to be cost-effective in comparison with usual care (ICER $57,595 per QALY gained) and was dominated by physician-managed point-of-care testing. However, from a societal perspective self-testing was found to be cost saving over both usual laboratory testing and physician-managed point-of-care testing. A probabilistic sensitivity analysis showed that from the societal perspective, patient self-testing had a 52% probability of being cost saving compared with usual care. An important limitation of this study was that it did not assess the impact of extending the time horizon beyond 5 years, which presumably would have improved the cost-effectiveness of self-testing versus usual care (physician-managed laboratory testing).
Connock 200721
The objective of this UK-based modelling study was to assess the cost-effectiveness of patient self-management of anticoagulation therapy compared with usual care (a mixture of primary and secondary care testing). A Markov model was constructed and analysed over a 10-year time horizon, adopting a NHS and personal social services perspective. The base-case cohort was aged 65 years and was assumed to have an increased risk of death, compared with the age-/sex-matched general population.
Model input parameters were derived from a number of sources. Estimates of time spent in therapeutic range, warfarin monitoring costs and baseline health state utility (measured using the EQ-5D) were derived from a previous RCT conducted in the UK with an accompanying economic evaluation. 87 The cost of INR devices (assumed to be paid for by the NHS) were annuitised over a 3-year period, and it was assumed that where patients stopped using these for any reason within 3 years, 75% would be reused by another patient. Risks of thromboembolic, major haemorrhagic and minor haemorrhagic events were estimated from a variety of published sources by time spent in, above and below the specified INR therapeutic range. Following major events, patients could either enter a state of permanent disability with associated costs and utility decrements, or have no long-term consequences.
Following disabling events and minor haemorrhagic events, patients were modelled to be at an increased risk of death from all causes. Within the model, it was assumed that there was a non-specific 2.5% reduction in the risk of adverse events with patient self-management – mediated through patient education and empowerment rather than improved INR control. This was based on the finding that self-management was not found to have a significant impact on TTR in a pooled analysis of results from eight trials where this outcome was available. This was despite it having a significant beneficial impact on the risk of thromboembolic events and mortality (based on the pooled results from 15 trials). 21
The base-case results were presented for both a 5- and a 10-year time horizon. Over the 5-year time frame, the incremental cost per QALY for self-management was estimated to be £122,365. The cost-effectiveness of self-management improved over the longer time horizon, with the incremental cost per QALY gained being £63,655 at 10 years. Cost-effectiveness acceptability curves were generated to characterise the uncertainty surrounding the 10-year estimate. Applying a ceiling ratio of £30,000 per QALY, patient self-management was found to have only a 44% chance of being cost-effective. However, the authors also carried out a sensitivity analysis whereby the pooled estimate of effects (on major complications) from all available trials were applied, and under this scenario found the incremental cost per QALY gained to be £19,617 for self-management at 10 years. The authors concluded that patient self-management of anticoagulation therapy was unlikely to be more cost-effective than usual care in the UK, but that it might offer a cost-effective alternative for patients whose therapy could not be satisfactorily controlled in usual care.
Gailly 200933
The objective of this study was to conduct a cost-effectiveness analysis of the use of point-of-care devices for GP-managed care, anticoagulation clinic-managed care, patient self-testing and patient self-management, compared with standard laboratory testing. The analysis focused on a cohort of patients on long-term anticoagulation therapy. A decision-tree model, with a 10-year time horizon, was constructed from the perspective of a Belgian health-care provider. The models input parameters were estimated from a meta-analysis of published studies for clinical effects and Belgian health-care databases for baseline risks and resource use.
As the meta-analysis of clinical effectiveness studies only identified evidence for a significant impact of point-of-care testing on mortality for patient self-management, the cost-effectiveness analysis focused on this modality of monitoring versus usual care (GP-managed testing with analysis of the blood sample in a laboratory). Furthermore, the outcome measure was restricted to the number of life-years gained as it was reported that no reliable quality-of-life data were identified. The annual number of point-of-care tests and the number of GP consultations due to INR tests in usual care and patient self-management were varied in a sensitivity analysis.
Applying the significant beneficial effects of self-management on mortality and thromboembolic events, the results showed self-management to be the dominant strategy compared with usual care, except when 100% of the GP consultations observed in usual care were assumed to be maintained with patient self-management and when the annual number of tests with self-management increased to 52 per year. The probabilistic sensitivity analysis showed patient self-management to have a high chance of being a dominant cost-saving strategy in comparison with usual care.
Medical Advisory Secretariat 200988
This Canadian study assessed the cost–utility of health service point-of-care testing, patient self-testing and patient self-management versus standard care for patients on long-term anticoagulation therapy. A Markov decision-analytic model was developed with a 5-year time horizon, and was analysed from the perspective of the Ministry of Health and Long-Term Care. The model was analysed for a hypothetical cohort of patients, and model inputs were derived from a systematic review of effectiveness, other published literature and expert opinion. Time spent within and outside the therapeutic range was used to estimate the likelihood of patients moving from one health state to another. The results indicated that all of the evaluated point-of-care strategies were cost-effective compared with usual care, and that patient self-management appeared to be the most cost-effective strategy.
Other studies
In addition to the above published evaluations, two abstracts were identified for potential relevance. Visnansky and colleagues90 conducted a rapid HTA to explore the cost-effectiveness of patient self-testing using CoaguChek compared with standard care (laboratory testing). A Markov model was constructed and analysed for hypothetical cohorts (mean age 63 years) on long-term anticoagulation therapy for different indications, applying a lifetime horizon. The authors concluded that patient self-testing was a cost-effective (dominant) strategy compared with usual care for all diagnosis subgroups.
Schmidt and colleagues91 conducted a cost–utility analysis of patient self-management compared with standard monitoring among long-term OAT patients in an Austrian setting. A Markov model was constructed adopting a lifetime horizon with an average baseline age of 67 years. This study found that although self-management incurred higher costs initially, throughout follow-up these costs reduced due to the lower number of health-care contacts over time. Adopting a lifetime perspective, it was found that self-management was the dominant strategy based on both a cost-per-life-year and a cost-per-QALY analysis.
Summary of findings from identified studies
The above overview of existing economic evaluations illustrates that the cost-effectiveness of patient self-testing and self-management versus usual care is uncertain and largely dependent on a number of key factors.
The adopted perspective appears to have a significant impact on estimated cost-effectiveness. Existing studies have estimated costs from different perspectives, including those of health service providers, society as a whole, health-care payers and health insurance funds. When a wider societal perspective has been adopted, self-management and self-testing strategies have generally compared favourably with standard clinic-based testing, as a result of lower time costs associated with fewer health service contacts. The initial costs associated with patient self-management and self-testing also appear to be important determinants of cost-effectiveness.
Variation between the studies in terms of the estimated or assumed effects of self-monitoring (on thromboembolic and bleeding events) also helps to account for the variable findings and conclusions. The two UK-based evaluations of greatest relevance to the scope of this diagnostic assessment report (DAR)21,87 estimated or applied effect estimates consistent with small or negligible differences between self-management and usual care with respect to TTR and adverse thromboembolic and haemorrhagic events. They subsequently found there to be a low probability of patient self-management being cost-effective. Contrary to this, several studies applied large effect estimates favouring self-monitoring in terms of TTR, thromboembolic events and/or mortality, and, subsequently, found self-monitoring strategies to be cost-saving or cost-effective. 33,86,88
In relation to the scope of this assessment, the two most relevant studies are those reported by Jowett and colleagues87 and Connock and colleagues. 21 These economic evaluations were largely based on the same trial conducted in the UK. Jowett and colleagues adopted a NHS and wider societal perspective and Connock and colleagues21 adopted a health service and personal social services perspective, which was in line with the NICE reference case. Key outcomes were measured directly within the trial-based evaluation, including utility values and complications experienced. Self-testing and self-management strategies do appear to increase the costs of INR monitoring in the short run, as demonstrated by these studies and others. However, other studies have shown that these costs can be offset by future cost-saving and quality-of-life gains, depending on the relative effectiveness of self-monitoring versus usual care in reducing the incidence of mainly thromboembolic events.
The two UK-based economic evaluations suggest that for effect estimates consistent with those observed in the largest UK-based trial of patient self-management, self-monitoring of INR is unlikely to be cost-effective. However, no UK-based trials have been sufficiently powered to detect a significant difference between standard INR monitoring and patient self-monitoring in terms of major thromboembolic or haemorrhagic events. Meta-analysis of similar trials, given their rarity, provides a more powerful means of estimating the true effect of self-monitoring on these clinical outcomes. An updated meta-analysis was described and presented in Chapter 2, and included randomised evidence from a number of recent European trials where standard care is similar to that provided in the UK in terms of approach, frequency and the level of INR control achieved. Therefore, the following section describes the construction and analysis of a new economic model that builds on those described above, and which incorporates all of the available evidence on the clinical effectiveness of self-testing and self-monitoring.
Independent economic assessment
A de novo economic model was developed in TreeAge Pro (TreeAge Software, Williamstown, MA, USA). The model was designed to assess the cost-effectiveness of self-monitoring (self-testing and self-management) using alternative point-of-care devices: CoaguChek XS system, INRatio2 PT/INR monitor and ProTime Microcoagulation system. The model was structured based on the review of published models of INR self-monitoring, and previous models evaluating the cost-effectiveness of new anticoagulant drugs compared with warfarin therapy in people with atrial fibrillation. 92,93 A further unpublished economic model of INR self-monitoring was provided by Roche (the manufacturer of CoaguChek XS), and this model was also used to inform the structure of the new economic model (J Craig, York Health Economics Consortium, 2013, personal communication provided by Roche through NICE).
The model was populated using data derived from the systematic clinical effectiveness review, other focused reviews to inform key parameters (e.g. baseline risks), routine sources of cost data,94,95 and, where necessary, some study-specific cost estimates based on expert opinion. The model was built and analysed in accordance with the NICE reference case for the evaluation of diagnostic tests and devices. 29
Methods
Relevant patient population(s)
The model compared the alternative monitoring strategies for a hypothetical cohort of people with atrial fibrillation or an AHV. These two groups represent the majority of people on long-term vitamin K antagonist therapy. While self-monitoring of INR is relevant to other patient groups, including those with venous thrombotic embolism, there were insufficient data to explicitly model cost-effectiveness for all groups individually. Furthermore, the majority of studies informing the relative effects of alternative monitoring strategies were derived from trials including predominantly people with atrial fibrillation and/or an AHV. Therefore, the base-case modelling exercise was carried out for a mixed cohort consisting of people with one or other of these two conditions. In the base-case analysis, 60% of the cohort was modelled to have atrial fibrillation, with the remaining 40% having an AHV, in line with the observed proportions of patients with these conditions in self-monitoring trials.
Monitoring strategies to be evaluated
The economic model incorporated the pathways of care that individuals currently follow under standard practice in the NHS, as well as proposed new pathways for self-testing and self-management (informed by a review of current guidelines and expert opinion). Current practice was dichotomised in the model as standard monitoring in primary care and standard monitoring in secondary care. In the base-case analysis, the proportional split between standard primary and secondary care INR monitoring was taken from the manufacturer’s submission for technology appraisal 256 (TA256). 96 Based on a survey of providers in England and Wales carried out in 2011, it was estimated that 66.45% and 33.55% of warfarin monitoring appointments were managed in a primary and secondary care setting, respectively. These figures were accepted by the independent evidence review group (ERG) and appraisal committee for NICE TA256. 97
In terms of self-monitoring, the model incorporated both self-testing and self-management strategies using the alternative devices identified in the scope. However, the cost-effectiveness of self-monitoring was assessed as a whole, and it was assumed in the base-case analysis that 50% of people would self-test while 50% would self-manage. Self-testing and self-management strategies were costed separately for each device based on the assumption that self-testing people telephone in their results from all tests undertaken, while self-managing people manage their dosing independently. In reality, some self-monitoring people are likely to fall somewhere in between these two strategies, and the potential impact of this was addressed in sensitivity analysis by varying the proportional split between self-management and self-monitoring.
Framework (method of synthesis)
The alternative monitoring pathways, informed by review of previous guidance and expert opinion, were embedded in a Markov model simulating the occurrence of adverse events over time (Figure 16). The adverse events that constituted the model were ischaemic stroke (minor, non-disabling, and major, disabling or fatal), systemic embolism, minor haemorrhage and major haemorrhage [intracranial haemorrhage (ICH), including haemorrhagic stroke, gastrointestinal bleed, and others]. Systemic embolism was treated as a transient event within the model, such that people surviving this event returned to baseline levels of quality of life and did not incur ongoing costs and morbidity. Minor haemorrhage was handled in the same way. Ischaemic stroke and ICH were assigned post-event states associated with additional costs and quality-of-life decrements.
FIGURE 16.
Schematic of the model structure. AF, atrial fibrillation; HS, haemorrhagic stroke; M, Markov process.
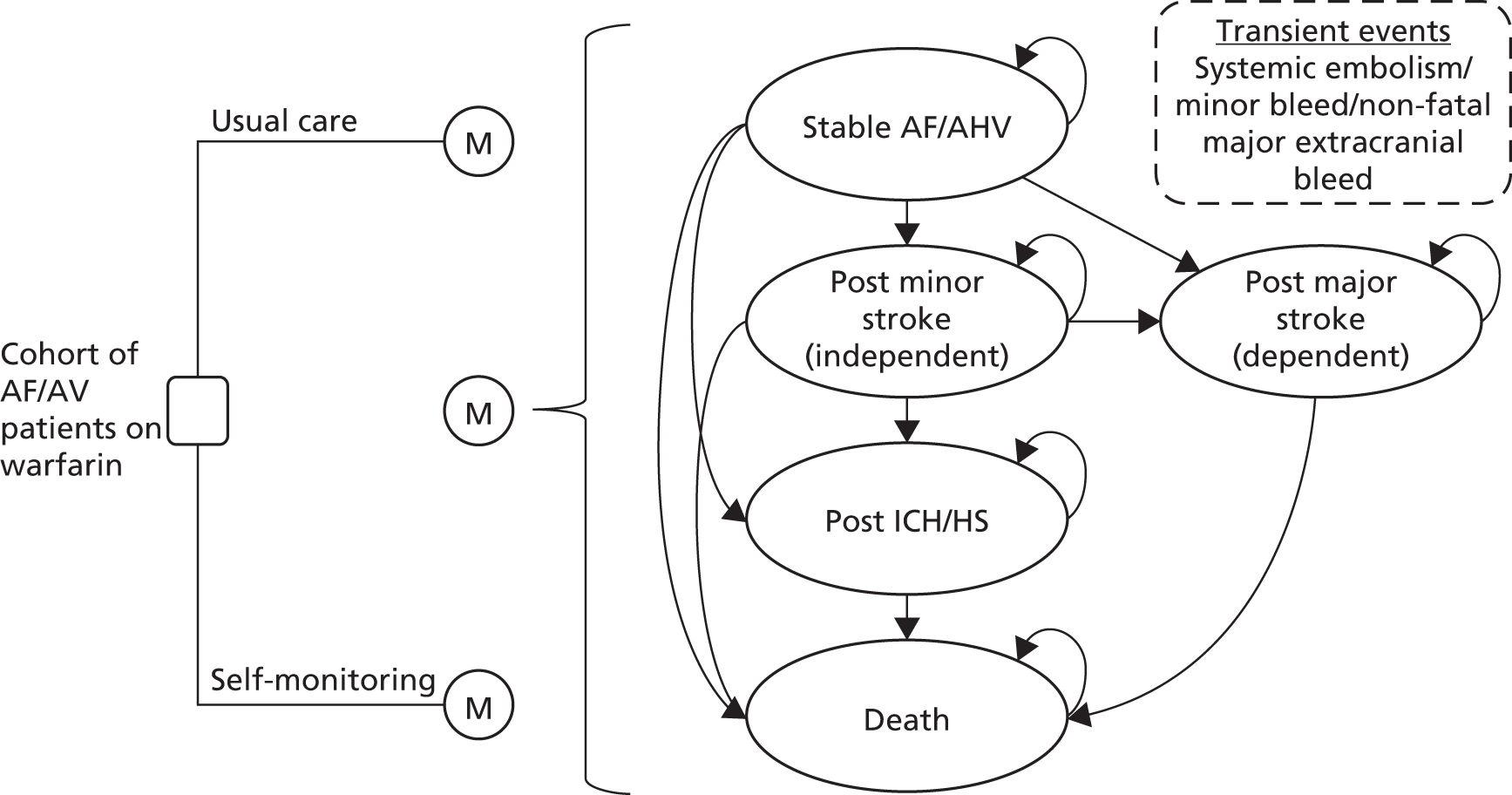
The model simulated transitions between the discrete health states, and accumulated costs and QALYs on a quarterly (3-month) cycle. Within each 3-month cycle, the simulated cohort was exposed to a risk of the aforementioned events as well as death from other causes. A constraint was applied whereby simulated people could experience only one event per cycle. A further simplifying structural assumption was applied, such that, following a major ischaemic stroke or ICH, no further events were explicitly modelled. However, all-cause mortality was inflated following these events to account for the increased risk of death.
Baseline risks for the modelled events were derived from the observed event rates in cohorts of people being managed under current standard models of care. RRs of these events resulting from improved/reduced INR control, conferred by self-monitoring, were derived from the meta-analysis of RCTs of self-monitoring versus standard practice. Appropriate costs and quality-of-life weights were attached to modelled events and health states, allowing cumulative health and social care costs and QALYs to be modelled over time. Further details of the event risks, transitions, costs and quality-of-life weights applied in the model are provided in the following sections.
Modelled baseline risks for people with atrial fibrillation
Previous economic models relied on a variety of sources to inform the underlying baseline risks of adverse events, ranging from single-centre trials to data pooled from a number of trials. The unpublished model provided by Roche made use of event rates reported by TTR,98–100 based on data from the control arms of large multinational trials comparing new anticoagulant drugs with standard treatment with warfarin for people with atrial fibrillation.
The Randomised Evaluation of Long-term Anticoagulation Therapy (RE-LY) trial of dabigatran etexilate versus warfarin provides a detailed source of event-rate data by centre-level quartiles of mean TTR. 99,101 The advantage of these data is that they allow underlying risks to be modelled by the level of anticoagulation control achieved, but there is a question surrounding their generalisability to the atrial fibrillation population on warfarin therapy in the UK. However, a previous study assessed the representativeness of the RE-LY clinical trial population to real-world atrial fibrillation patients in the UK,102 and found that the majority of patients in the UK (65–74%) would have met the inclusion criteria. Furthermore, to assess the generalisability of the annual risks of stroke derived from RE-LY data, these were compared with those derived from a large cohort study of atrial fibrillation patients on warfarin in the UK. Gallagher and colleagues103 analysed longitudinal data from the General Practice Research Database on 27,458 warfarin users with atrial fibrillation, and provided a Kaplan–Meier plot of the probability of being stroke free by different levels of TTR. Points on these plots were extracted using DigitizeIt software (DigitizeIt, Braunschweig, Germany: www.digitizeit.de), and used to estimate the annual risks of stroke by TTR groupings.
These stroke risks were found to be very similar to those for people in the corresponding TTR quartiles of the RE-LY trial control arm. Therefore, the control arm of the RE-LY trial was considered to be an appropriate source for estimating baseline risks by level of TTR in the economic model. The study by Gallagher and colleagues103 also estimated a mean TTR (INR 2–3) of 63% for the UK cohort of people with atrial fibrillation on warfarin, and so the baseline risks in the model were set to those observed in RE-LY trial centres that achieved a mean TTR between 57.1% and 65.5%.
The analysis of RE-LY trial data by TTR quartiles99 provided estimated annual event rates for non-haemorrhagic stroke and systemic embolism, major haemorrhage (including intracranial bleed, haemorrhagic stroke and major gastrointestinal bleeds) and minor haemorrhage. These rates were entered in the model, where they were converted into annual risks (Table 14). Following further adjustment, where appropriate, with RRs, the annual risks were converted into quarterly risks using the following equation:
| Event | Annual risk by INR control (TTR) | |||
|---|---|---|---|---|
| < 57.1% | 57.1–65.5% | 65.6–72.6% | > 72.6% | |
| Non-haemorrhagic stroke and systemic embolism | 0.0162 | 0.0162 | 0.0110 | 0.0097 |
| Major bleeding | 0.0353 | 0.0405 | 0.0334 | 0.0306 |
| Minor bleeding (inferred) | 0.1174 | 0.1323 | 0.1375 | 0.1387 |
The events were modelled within each cycle of the model, and were further disaggregated based on the observed numbers of different types of event observed within each composite outcome in the RE-LY trial99,101 (Table 15).
| Composite event | Proportional disaggregation | Distributional form | Source |
|---|---|---|---|
| Non-haemorrhagic stroke and systemic embolism | Beta | ||
| Non-haemorrhagic stroke | 0.909 | (α = 14; β = 140) | Connolly 2009101 |
| SE | 0.091 | Connolly 2009101 | |
| Major bleeding | Dirichlet | ||
| Intracranial bleed/haemorrhagic stroke | 0.178 | α = 89 | Connolly 2009101 |
| Other major bleed | 0.426 | α = 183 | Connolly 2009101 |
| Gastrointestinal bleed | 0.396 | α = 147 | Connolly 2009101 |
| Non-haemorrhagic stroke | Beta | ||
| Non-disabling (Rankin score 0–2) | 0.369 | (α = 69; β = 118) | Connolly 2009101 |
| Disabling or fatal (Rankin score 3–6) | 0.631 | Connolly 2009101 | |
| Intracranial bleed/haemorrhagic stroke | Beta | ||
| Fatal by 30 days | 0.388 | (α = 36.8; β = 58.1) | NICE TA25696 |
| Non-CNS major bleed | Omitted from PSA | ||
| Proportion fatal | 0.0155 | NICE TA25696 | |
| Disabling or fatal stroke (Rankin score 3–6) | Beta | ||
| Fatal in hospital | 0.06 | (α = 11; β = 177) | Hylek 2003104 |
| Fatal by 30 days post discharge | 0.159 | (α = 29; β = 151) | Hylek 2003104 |
| Non-disabling stroke | Beta | ||
| Fatal by 30 days post discharge | 0.01 | (α = 2; β = 176) | Hylek 2003104 |
| Systemic embolism | Omitted from PSA | ||
| Fatal | 0.004 | NICE TA249105 |
Further adjustments were applied to the risk of stroke in atrial fibrillation patients, to reflect the importance of age as a risk factor. For this purpose, the same approach as used in the model for NICE TA256 (rivaroxaban for the prevention of stroke and systemic embolism in people with atrial fibrillation) was applied. 96 RRs of stroke by age, compared with a 70- to 74-year-old cohort (the average age of participants in RE-LY trial), were derived from a Framingham-based risk score calculator for patients with atrial fibrillation,106 and applied to adjust the risk of stroke and systemic embolism by 5-year age bands. 96 A similar approach was also used to inflate the risk of bleeding with increasing age, using data from Hobbs and colleagues. 107
Death following stroke was estimated by applying case fatality rates to these modelled events. Death following stroke utilised the same approach as used in the model of dabigatran versus warfarin for NICE TA249. 105 Based on Hylek,104 the hospital case fatality rate was first applied, followed by the reported 30-day mortality by severity of stroke (Rankin score 0–2; 3–5) post discharge (see Table 15).
Modelled baseline risks for people with an artificial heart valve
Less extensive data were identified describing the baseline risk of adverse events for people with AHVs by level of INR control. Previous economic models have tended to use overall event risks for mixed cohorts rather than explicit event risks for individual patient groups included in the modelled cohort. However, the model provided by Roche used a dichotomised cohort with event risks estimated separately for people with atrial fibrillation and an AHV. This approach is useful for modelling subgroups and cohorts with varying proportions of people with the two conditions. Therefore, the same general approach was adopted.
As per the model provided by Roche (J Craig, York Health Economics Consortium, 2013, personal communication provided by Roche through NICE), a recent meta-analysis of individual patient-level data from 11 RCTs of self-monitoring versus standard care provided the source of event data. 108 Heneghan and colleagues108 presented a subgroup analysis where they presented the estimated pooled hazard ratio and number needed to treat to prevent one major thromboembolic event (ischaemic stroke and systemic embolism) and one major haemorrhagic event by year of follow-up (up to 5 years) based on 2243 people with an AHV. The formula used by Heneghan and colleagues108 to estimate the number needed to treat was:
Sc(t) is the survival probability in the control group (standard monitoring) at time t, Sc(t)h is the corresponding survival probability in the active treatment group (self-monitoring), and h is the hazard ratio. The 5-year probability of experiencing a thromboembolic (0.089) and major haemorrhagic event (0.169) in the control group were back calculated for people with an AHV, and converted into annual probabilities (Table 16). These were incorporated in the model for subsequent adjustment and conversion into quarterly probabilities for use as baseline risks.
| Event | Annual risk | Distributional form |
|---|---|---|
| Non-haemorrhagic stroke and systemic embolism | 0.0185 | Beta (α = 19.2; β = 1020.8) |
| Major bleed | 0.0363 | Beta (α = 37.3; 977.7) |
| Minor bleed (assumed) | 0.1323 | See Table 14 |
A focused search was undertaken to identify alternative sources of data to inform the baseline risk of thromboembolic events in people with an AHV. A previous meta-analysis estimated a pooled annual linearised risk of 1.6% for people with a mechanical aortic valve. A further large Canadian series (including 1622 people with a mechanical heart valve) estimated linearised embolic stroke risks of 1.4% and 2.3% per year for people with an artificial aortic and a mitral valve, respectively. 109 These figures are generally consistent with the baseline estimates used in the model. However, a smaller series from a single centre in the south-west of England reported a lower rate of 1.15% per patient-year based on 2 years’ follow-up of 567 people with a Sorin Bileaflet third-generation prosthesis. 110 The impact of applying this lower baseline risk was assessed through sensitivity analysis.
In the absence of more detailed data for people with an AHV, the same proportional splits used to disaggregate thromboembolic and major haemorrhagic events for people with atrial fibrillation were applied (see Table 15). Furthermore, as data on minor bleeds were not available from Heneghan and colleagues108 for people with an AHV, the same baseline risk applied for people with atrial fibrillation was adopted. This was justified on the grounds of the two groups of people facing similar risks of a major bleed (0.405 and 0.363).
Further adjustments to baseline risks
Within the model, a number of simplifying structural assumptions were made. Following the occurrence of a major disabling ischaemic stroke or an ICH/haemorrhagic stroke, no further events were modelled. However, the risk of age-/sex-specific all-cause mortality was inflated following these events using RRs estimated by Sundberg and colleagues. 111 Deaths from other causes following minor stroke were also inflated in the model to account for the observed increased risk of death from all causes following this event. 111,112
The background risk of death from other causes also was increased for the atrial fibrillation and AHV cohorts using standardised mortality ratios reported by Friberg and colleagues113 and Kvidal and colleagues114 (Table 17).
| Parameter | Value | SEM | Distributional form | Source |
|---|---|---|---|---|
| SMR: death from all causes for AF patients | 1.30 | 0.082 | Normal | Friberg 2007113 |
| RR: death post minor stroke | 2.33a | 0.276 | Normal | Sundberg 2003111 |
| RR: death post disabling stroke | 4.11 | 0.486 | Normal | Sundberg 2003111 |
| SMR: death from all causes for AHV patients | Kvidal 2000114 | |||
| ≤ 50 years | 4.56 | 0.861 | Normal | |
| 51–60 years | 2.66 | 0.276 | Normal | |
| 61–70 years | 1.80 | 0.111 | Normal | |
| ≥ 71 years | 1.02 | 0.071 | Normal |
Baseline rates of death from all and other causes were modelled by age and sex based on interim life tables. For other cause mortality, deaths due to stroke, systemic embolism and ICH were removed. 116,117
Incorporation of relative treatment effects
Pooled estimates of RR derived from the meta-analysis of RCTs of self-monitoring versus standard practice were used to adjust the baseline risks of events in the model (Table 18). Given the limitations of the available data, it was not possible to accurately estimate the relative clinical effectiveness of using the alternative self-monitoring devices. Therefore, in the first instance, equivalent effects were assumed on the basis of several studies showing reasonable correlation between the instruments in terms of precision and accuracy. However, it is worth noting that the majority of the clinical effectiveness evidence relates to CoaguChek S, with only one trial included in the systematic review using the INRatio2 PT/INR monitor (although not exclusively), and two trials using the ProTime Microcoagulation system (exclusively).
| Event/monitoring strategy | RR | 95% CI | Distributional form |
|---|---|---|---|
| Any thromboembolic event | |||
| Self-management | 0.51 | 0.37 to 0.69 | Log-normal |
| Self-testing | 0.99 | 0.75 to 1.31 | Log-normal |
| Self-monitoring (overall) | 0.58 | 0.40 to 0.84 | Log-normal |
| Major bleed | |||
| Self-management | 1.09 | 0.81 to 1.46 | Log-normal |
| Self-testing | 0.99 | 0.8 to 1.23 | Log-normal |
| Self-monitoring (overall) | 1.02 | 0.86 to 1.22 | Log-normal |
| Minor bleed | |||
| Self-management | 0.84 | 0.53 to 1.35 | Log-normal |
| Self-testing | 1.23 | 1.06 to 1.42 | Log-normal |
| Self-monitoring (overall) | 0.94 | 0.65 to 1.34 | Log-normal |
For the base-case analysis, relative effects were entered separately for the different types of event (any thromboembolic event, major bleed and minor bleed) by type of self-monitoring strategy (self-management and self-testing) (see Table 18). While not all effects were significant, the point estimates were applied in the model with appropriate distributions assigned to reflect the uncertainty surrounding them. These RRs, which represent pooled estimates obtained from trials with follow-up periods varying between 3 and 24 months, were assumed to apply directly to the 12-month risk of an event. Therefore, they were used to adjust the estimated annual baseline risk of events in the model, from which constant 3-month transition probabilities were derived, assuming constant proportional hazards over time. The RRs were applied only to people continuing on self-monitoring in the model.
Resource use estimation
Data on the resource use and costs associated with the alternative monitoring strategies were informed by published literature, existing guidance, expert opinion, manufacturers’ and suppliers’ prices, and other routine sources of unit cost data. 94,95 As noted above, certain costs were informed by expert opinion where suitable data from other sources were not available.
Costs of standard care
Resource use associated with standard monitoring was informed by a number of sources. The model provided by Roche used estimates of monitoring costs (under standard primary and secondary care) based on previous estimates calculated by the independent ERG for NICE technology appraisal TA249, Dabigatran etixilate for the prevention of stroke and systemic embolism in atrial fibrillation. 118 These estimates of monitoring costs in standard care, which were later applied in the NICE costing template for dabigatran,119 were derived by the ERG based on previous estimates used in the NICE costing report for clinical guideline CG36 on atrial fibrillation. 24 This report summarised the estimated annual resource use required for monitoring people in primary care, assuming 20 monitoring visits per year. These measures of resource use, per visit, are summarised in Table 19.
| Resource | Unit costs (2011–12), £ | Cost per patient per visit (2011–12), £ | Source/assumptions |
|---|---|---|---|
| Primary care | |||
| Reagents | 2.80 | 2.80 | Roche (assumes point-of-care testing) |
| Lancet | 0.04 | 0.04 | Roche |
| Nursing time (15 minutes) | 35.00 (per hour) | 8.75 | PSSRU, 201295 |
| Administration time (15 minutes) | Accounted for in allocated costs for nursing time | – | PSSRU, 201295 |
| Office consumables per clinic | 2.52 | 0.21 | CG36, costing report, inflated to 2011–12 prices, assumes 12 patients per clinic24,119 |
| Use of shared equipment (equivalent annual cost) | 171.65 | 0.29 | Roche (CoaguChek XS Plus, annuitised over 5 years, assuming 600 uses per year) |
| Total variable cost per patient monitoring visit | 11.76 | ||
| Total variable cost per year, assuming 20 visits | 235.20 | ||
| Total variable cost per year, assuming 12 visits | 141.12 | ||
| Cost per quartera | 35.28 | ||
| Secondary care | |||
| NHS anticoagulation services | 23 (per visit) | 23 | NHS reference costs, 2012 (anticoagulation services)94 |
| Assumed variable cost component (0.6667) | 15.33 (per visit) | 5.33 | TA249 ERG report, 201193,118 |
| Total variable cost per patient monitoring visit | 15.33 | ||
| Total variable cost per year, assuming 20 visits | 306.94 | ||
| Total variable cost per year, assuming 12 visitsa | 184.16 | ||
| Cost per quartera | 46.04 | ||
An alternative source of standard monitoring costs per visit was identified from the largest UK-based RCT of self-monitoring. 64 Jowett and colleagues carried out the economic analysis alongside the Self-Management of Anticoagulation, a Randomised Trial (SMART), where people in the control arm received a mix of standard primary and secondary care monitoring. 87 A unit cost per visit (accounting for staff time, equipment, consumables and overheads) was estimated for each care setting from a sample of NHS providers. The resultant cost estimates (per visit) for different types of standard care are presented in Table 20, inflated to 2011–12 prices.
| Care setting | Cost per visit (2002–3), £ | Inflation factor | Cost per visit (2011–12), £ | Annual costs (assuming 20 visits per year), £ |
|---|---|---|---|---|
| Hospital clinic | 6.35 | 1.337 | 8.49 | 169.79 |
| GP blood sample, hospital analysis and dosing | 9.38 | 1.337 | 12.54 | 250.81 |
| GP blood sample and dosing, hospital analysis | 10.69 | 1.337 | 14.29 | 285.83 |
| Practice based near patient testing clinic | 14.16 | 1.337 | 18.93 | 378.62 |
| Pharmacist-led practice clinic | 17.66 | 1.337 | 23.61 | 472.20 |
| MLSO-led practice clinic | 11.62 | 1.337 | 15.54 | 310.70 |
Updated unit costs have been applied to provide a total cost per patient monitoring visit in 2011–12 GBP. When calculating the variable cost per patient associated with monitoring in a secondary care setting, the ERG in their report on dabigatran etexelate assumed that 33% of secondary care monitoring costs would be fixed and not influenced by changes in the number of people being monitored. This assumption was based on the observed proportional split between fixed and variable costs in the bottom-up calculation of the total cost of INR monitoring in primary care. 24 This same assumption was applied in our updated estimates.
When updating the unit costs for practice nurse time in primary care, we used an estimate per hour that incorporates allocated overhead costs (including management and administration) and use of practice space. Some of these allocated costs were not included in previous variable cost estimates for monitoring in primary care. It was considered appropriate to include them here to capture the opportunity cost associated with use of primary care facilities for INR monitoring. 120 However, as the allocated costs account for administration, additional administration time per patient visit was not costed separately as it was in previous estimates. 24,93,118
Given the slightly different approach to updating the unit costs for standard monitoring services, our cost estimates based on 20 monitoring visits (£235.20 and £306.94 for primary and secondary care monitoring, respectively) differ somewhat from those used in the NICE costing template for dabigatran (£220.90 and £303.43, respectively, for monitoring in primary and secondary care in 2009–10 prices) and also from those applied in the model provided by Roche (£231.33 and £317.90, respectively, for primary and secondary care monitoring in 2012–13 prices).
For primary care monitoring, these unit costs are somewhat higher than those presented in Table 19. However, the cost estimate for monitoring in a secondary care (hospital clinic) is substantially lower. Furthermore, while the proportional mix of standard care service use was not reported in the study by Jowett and colleagues,87 a total mean standard care monitoring cost of only £89.89 (£120.18 in 2011–12 prices) was reported at 12 months. The actual annual monitoring frequency observed in the control arm of the SMART trial was 37.9 days. 64
This suggests that an annual number of only ≈ 10 monitoring visits per year was required to achieve the level of control reported for the standard-care arm of this pragmatic UK-based RCT.
The assumption of 20 visits being the average number of monitoring visits required for people on long-term vitamin K antagonist therapy comes from the NICE costing report for the clinical guideline on the management of atrial fibrillation. 24,119 This was estimated based on the ratio of second to first attendances at anticoagulation clinics (≈ 19 from reported activity in the 2004–5 NHS reference costs) and a previous study by Jones and colleagues,121 which reported a median frequency of INR testing of 16 days for people receiving warfarin (equating to ≈ 22 tests per year). A repeat of the calculation based on reference costs activity data for 2011–12 yielded a ratio of only 9.5. However, this lower value may merely reflect a trend for more people to be followed up in primary care following initiation of therapy.
Given the uncertainty surrounding the average number of monitoring visits for people under standard primary and secondary care, the DAR specialist committee members were consulted on this parameter. Opinion on the frequency of monitoring suggested that 10–12 visits would be required on average in primary and secondary care, but that the number of visits would be highly variable across participants. It was also noted by one member that more monitoring visits may be required for people managed in secondary care, as it tends to be the people with poorer control who are managed in this setting. A further question was raised about the nursing time requirements for routine monitoring visits used in the previous cost estimates informing TA249 (15 minutes of band 5 nurse time per patient visit). One source suggested that 10 minutes would suffice for this.
Based on consideration of the all of the above evidence, it was assumed in the base-case analysis that, on average, 12 monitoring visits would be required per year for people under standard primary and secondary care monitoring. To retain consistency with previous analyses used to inform NICE guidance, we applied the unit costs per visit based on the figures in Table 19.
The impact of altering the number of standard care monitoring visits per year was also assessed through sensitivity analysis. We also conducted sensitivity analyses where the updated unit costs in Table 20 were applied to cost monitoring visits, and where we assumed only 10 minutes of nurse time per standard care monitoring visit.
Finally, given the reliance of some people on NHS transport for attending secondary care monitoring visits, a cost of transport was applied for a percentage of people modelled to receive this form of monitoring. The percentage of 8.55% was taken from a previous survey of patient pathways used to inform the manufacturer’s model for NICE TA25696 and the return transport cost was taken from the NHS reference costs (£30.96). 94
Costs of self-monitoring
An average testing frequency of 35 tests per year (every 10.42 days) was assumed for self-monitoring in the base-case analysis. This number was chosen to be consistent with the trials from which the relative effect estimates for self-monitoring were obtained. In a recent meta-analysis of patient-level data,108 11 of the self-monitoring trials included in our review reported the mean increase in the number of tests performed with self-monitoring versus control. There was an average of 24 additional tests by 12 months for people with atrial fibrillation and 22 additional tests for people with an AHV. The average of these two values was added to the estimated 12 tests per year for standard care, to give an estimate of 35 tests per year for self-monitoring. The impact of altering the difference in testing frequency between standard care and self-monitoring, through the 95% CIs reported by Heneghan and colleagues (13–30 per year), was assessed through sensitivity analysis. 108 Furthermore, we assessed scenarios where self-monitoring was not used to increase the frequency of monitoring as a means to improve INR control, but simply used to replace primary and secondary care testing. Under this scenario, we assumed no relative effects of self-monitoring on outcomes. The sections below provide further details on the cost of self-monitoring, with a summary of cost elements provided in Table 21.
| Self-monitoring unit cost | CoaguChek XS (£) | ProTime (£) | INRatio2 (£) | |||
|---|---|---|---|---|---|---|
| Device cost | 299 | 884 | 275 | |||
| Equivalent quarterly cost for use | 16.56 | 48.95 | 15.23 | |||
| Test strips (per unit) | 2.81 | 4.96 | 2.75 | |||
| Lancets (£ per unit) | 0.04 | 0.10 | 0.05 | |||
| Self-monitoring costs | Primary care (£) | Secondary care (£) | ||||
| CoaguChek XS | ProTime | INRatio2 | CoaguChek XS | ProTime | INRatio2 | |
| Training | ||||||
| Self-testing | 90 | 90 | 90 | 170 | 170 | 170 |
| Self-management | 180 | 180 | 180 | 340 | 340 | 340 |
| Annual self-testing costs | ||||||
| Test strips and lancets (× 35) | 99.62 | 177.24 | 98.00 | 99.62 | 177.24 | 98.00 |
| External quality control twice a year (two strips + two lancets) | 5.69 | 10.13 | 5.60 | 5.69 | 10.13 | 5.60 |
| Routine clinic assessment twice per year | 22.50 | 22.50 | 22.50 | 42.50 | 42.50 | 42.50 |
| Telephone calls (5 minutes of nurse time × 35 per year) | 102.08 | 102.08 | 102.08 | 102.08 | 102.08 | 102.08 |
| Cost per year based on 35 tests | 229.90 | 311.95 | 228.18 | 249.90 | 331.95 | 248.18 |
| Cost per quartera | 57.47 | 77.99 | 57.05 | 62.47 | 82.99 | 62.05 |
| Annual self-management costs | ||||||
| Test strips and lancets (× 35) | 99.62 | 177.24 | 98.00 | 99.62 | 177.24 | 98.00 |
| External quality control twice a year (two strips + two lancets) | 5.69 | 10.13 | 5.60 | 5.69 | 10.13 | 5.60 |
| Routine clinic assessment twice per year | 22.50 | 22.50 | 22.50 | 42.50 | 42.50 | 42.50 |
| Cost per year based on 35 tests | 127.81 | 209.87 | 126.10 | 147.81 | 229.87 | 146.10 |
| Cost per quartera | 31.95 | 52.47 | 31.53 | 36.95 | 57.47 | 36.53 |
Equipment
Self-monitoring device costs were obtained from the manufacturers. However, no up-to-date cost could be obtained for ProTime Microcoagulation System. The UK distributor of this device [International Technidyne Corporation (ITC), NJ, USA] was contacted for information, but stated that the device was not marketed for patient self-monitoring in the UK, and that the device was being superseded by the ProTime InRhythm™ System, ELITech (Berkhamsled, Herts, UK), which is being marketed in the UK for professional use only. For completeness, a self-monitoring strategy using the ProTime Microcoagulation System was included in the economic model, by applying a NHS list price from 2008. 122 Finally, a new promotional price (of £195) was provided for INRatio2. The impact of using this price was assessed in a sensitivity analysis.
Device costs were treated in the same way that capital investments are normally dealt with in economic evaluation. It was assumed that the NHS would pay for these and loan them out to patients. As such, they were annuitised over their expected use life to provide an equivalent annual/quarterly cost of use. While these devices have a potentially long life span based on the advice of manufacturers, their costs were annuitised over a 5-year period in the base-case analysis to account for the potential for loss and accidental damage.
There was also a degree of uncertainty about the suitability of the devices for reuse following discontinuation of self-monitoring by participants. In the base-case analysis, the same assumption that was used in a previous UK-based economic modelling study21 was applied, i.e. three-quarters of devices are reused by another patient in situations where a patient discontinues self-monitoring (see Training, for details on assumptions about discontinuation).
Consumables
The cost of test strips were provided by the manufacturers, and it was assumed in the base-case analysis that the annual cost of test strips would be equal to the number of tests performed annually multiplied by the cost per strip (i.e. that there would be no wastage). It was further assumed that two more test strips would be used annually to cross-check each device against a quality assured clinic-based machine. This was modelled to take place during biannual assessments for self-monitoring participants (see Biannual routine assessments).
NHS staff time
The staff time input required to oversee self-monitoring relied on expert opinion. People who are self-monitoring can require varying degrees of input from clinical staff to check readings and respond to queries. In the base case, it was assumed that all self-testing people would call in each and every test result on a dedicated telephone line, and that a nurse would later check and enter each patient’s result, and then telephone the patient back with instructions to either maintain or alter their warfarin dose. This was assumed to incur 5 minutes of band 5 nurse time per patient (based on the opinion of the specialist advisory committee), which was valued using nationally available unit costs. 95 It was assumed that self-managing people would not require any further support from nursing staff other than biannual routine assessments (see next section).
Biannual routine assessments
It was assumed that quality control of self-monitoring devices would take place at biannual clinic appointments, at the local anticoagulant clinic or practice from where self-monitoring was initiated. It was assumed that this would involve checking the patient’s instrument against an externally validated one, and that it would incur 15 minutes of direct face-to-face contact time with a practice nurse (£45 per hour) or hospital clinic nurse (£85 per hour). 95 In line with the base-case assumption that 34% of people are monitored in secondary care under standard practice, it was assumed that 34% of self-monitoring people would return to this setting for routine assessments, while the remainder would return to primary care clinics.
Training
Based on existing literature,123 as well as consultation with members of expert advisory committee, it was assumed that self-testing people would require 2 hours of one-to-one training, while those progressing to self-management would receive 4 hours of one-to-one training prior to initiation. These assumptions are consistent with those applied in the model that was provided by Roche (J Craig, York Health Economics Consortium, 2013, personal communication provided by Roche through NICE) and the literature on training requirements from RCTs of self-monitoring. Training time was costed using hourly unit costs for direct patient contact time (£45 per hour for practice nurse time and £85 per hour for hospital clinic nurse time).
The RCT literature64 and the expert advisory committee were also consulted with respect to training success rates and ongoing adherence to self-monitoring. In light of this, we incorporated a training failure rate of 15% – the mid-point between 5%, suggested by members of the expert advisory committee, and 24%, a pragmatic UK-trial-based estimate64 – and assumed that these people would incur the cost of training but return to standard care without incurring the cost of a monitoring device.
In addition to including a training failure rate in the model, it was considered unrealistic to assume that 100% of participants would continue to self-monitor after initiation. Therefore, we incorporated a discontinuation rate of 10% by 12 months in the model, based on consideration of the views of the expert advisory committee (≈ 5%) and a rate of 14% reported in the largest UK-based trial. 64 Beyond 12 months, it was assumed that self-monitoring people would continue to do so unless they experienced a fatal or disabling adverse event.
Warfarin costs
In line with previous evaluations, it was assumed that the quantity and cost of vitamin K antagonist drugs would not vary significantly between self-monitoring and standard monitoring. Therefore, these costs were excluded from the model.
Costs of adverse events
The cost of minor bleed was based on the NHS reference cost for VB07Z: Accident and emergency services, category 2 with category 2 treatment (weighted average). A major non-intracranial bleed was taken as the weighted average reference cost for the Healthcare Resource Group (HRG) codes related to non-elective admissions for gastro-intestinal bleeds (Table 22).
For the cost of a systemic embolism, a weighted average of the reference costs for non-elective admissions relating to the HRG for non-surgical peripheral vascular disease (QZ17A, QZ17B, QZ17C) was applied.
The initial cost of a minor stroke was taken as the weighted average of the 2011–12 non-elective reference costs for the HRG codes AA22A and AA22B (non-transient stroke or cerebrovascular accident, nervous system infections or encephalopathy, with and without complications and comorbidities). This equates to a cost of £3082.
For major stroke, the cost used in the rivaroxaban submission was also updated, whereby the initial treatment cost was taken as the weighted average of AA22A and AA22B (£3082), with the addition of 10.97 additional bed-days costed using the weighted average excess bed-day cost (£236.16 per day) for AA22A and AA22B. The excess bed-days were estimated by subtracting the length of stay accounted for in the reference costs for AA22A and AA22B – up to 24.43 days94 – from the average length of stay in hospital for people suffering a major stroke (34.4 days based on Saka and colleagues124). In addition, 14 days’ rehabilitation was added at a cost per day of £313.41 – based on the HRG VC04Z (rehabilitation for stroke) – to estimate the total cost of a major stroke to 3 months (£10,061). This estimate is lower than that used in the model for NICE TA256 (updated cost of £13,547), as excess bed-day costs were applied only to days above the costing trim-point for AA22A and AA22B, rather than days above the average length of stay for these codes. This is conservative in favour of standard care.
The costs associated with adverse events were adapted from those used in the model informing NICE TA256; rivaroxaban for the prevention of stroke and systemic embolism in people with atrial fibrillation. 96 These cost estimates were based largely on NHS reference costs, and were considered appropriate by the independent ERG in their critique of the manufacturer’s submission. 97 These costs were updated for the current analysis using the National Schedules of NHS Reference Cost, 2011–12,94 where possible, or were otherwise inflated from previously reported 2009–10 prices using the Hospital and Community Health Services (HCHS) pay and prices index. 95 These costs are presented in Table 22.
| Health states/events | Cost element | Unit costs, £ | Cost source | Assumptions/description | Total cost, £ |
|---|---|---|---|---|---|
| Transient events | |||||
| Minor bleed | Acute treatment | 134 | National schedule of reference costs 2011–1294 | VB07Z: accident and emergency services. Category 2 with category 2 treatment (weighted average) | 134 |
| Major bleed (non-intracranial) | Acute treatment | 975 | Cost of a gastrointestinal bleeding treatment episode. Weighted average of codes: FZ38D, FZ38E, FZ38F, FZ43A, FZ43B, FZ43C | 975 | |
| Systemic embolism | Acute treatment | 1639 | Cost of non-surgical peripheral vascular disease. Weighted average of codes: QZ17A, QZ17B, QZ17C | 1639 | |
| Permanent events | |||||
| Minor stroke | Acute treatment | 3082 | National schedule of reference costs 2011–1294 | AA22Z: non-transient stroke OR cerebrovascular accident, nervous system infections or encephalopathy | 3082 |
| Post minor stroke (Rankin score 0–2) | Follow-on care costs per quarter | 219 | Wardlaw 2006,125 NICE clinical guideline CG92126 | Annual cost of stroke care per year following an index event, inflated to 2011–12 prices and quartered | 303 |
| Major stroke | Acute treatment | 3082 | National schedule of reference costs 2011–12: non elective inpatient94 | AA22Z: non-transient stroke OR cerebrovascular accident, nervous system infections or encephalopathy – with 10.97 excess bed-days | 10,061 |
| Acute treatment cost per excess bed-day | 236 | ||||
| Rehabilitation (cost per day) – 14 days | 313 | National schedule of reference costs 2011–1294 | VC04Z: rehabilitation for stroke (weighted average) | ||
| Post major stroke (Rankin score 3–5) | Follow-on care costs per quarter | 2823 | Wardlaw 2006,125 NICE clinical guideline CG92126 | Annual cost of stroke care per year following an index event, inflated to 2011–12 prices and quartered | 3906 |
| Intracranial bleed | Acute treatment | 2250 | National Schedule of Reference Costs 2011–1294 | AA23Z: haemorrhagic cerebrovascular disorders (weighted average) | 6638 |
| Rehabilitation (cost per day) – 14 days | 313 | VC04Z: rehabilitation for stroke (weighted average) | |||
| Post intracranial bleed/HS | Follow-on care (costs per quarter) | 2576 | NICE clinical guideline CG92126 | Assumed weighted average of quarterly costs following ischaemic stroke (assumes 38% of patients dependent, and 62% independent) | 2576 |
Further costs were applied on a quarterly basis in the years following ischaemic stroke. These costs were adapted from those applied in NICE clinical guideline CG92, which were initially based on costs reported by Wardlaw and colleagues125 of £11,292 per year for disabling stroke and £876 per year for non-disabling stroke (2001–2) prices. These costs were inflated to 2011–12 values using the HCHS pay and prices index. 95
For the acute treatment costs associated with an intracranial bleed, a weighted average of the non-elective reference costs for HRG AA23Z (haemorrhagic cerebrovascular disorders) was applied. In addition, the same rehabilitation costs as applied following major ischaemic stroke were applied following ICH, and the following quarterly health and social care costs were taken as the weighted average of those following minor (0.369) and major (0.631) ischaemic stroke. The cost of minor bleed was based on the NHS reference cost for VB07Z: accident and emergency services, category 2 with category 2 treatment (weighted average). A major non-intracranial bleed was taken as the weighted average reference cost for the HRG codes related to non-elective admissions for gastrointestinal bleeds (see Table 22).
Health measurement and valuation
Time spent in different states of the model was adjusted using utility weights reflecting the desirability of those states on a scale where 0 is equal to death and 1 is equal to full health. With the model structure similar to that of the model used to inform NICE TA256 (rivaroxaban for the prevention of stroke and systemic embolism in people with atrial fibrillation), a number of the utility values used in this previous model were applied (acute major and minor stroke, acute major haemorrhage and ICH). These values were considered appropriate by the independent ERG for NICE TA25697 and accepted by the appraisal committee. However, the utility values applied to the states ‘post minor’ and ‘post major stroke’ in TA256, were derived from a Norwegian study where values were elicited directly from participants and the general population. 127 Alternative values were identified for these states based on the EQ-5D responses of stroke people in the UK. Dorman and colleagues128 used the EQ-5D to measure the health status of 867 people enrolled in the International Stroke Trial. 129 The reported values of 0.31 for dependent health states and 0.71 for independent health states were considered more consistent with the NICE reference case than the directly elicited Norwegian values (0.482 and 0.719, respectively) used in TA256. Further, it was assumed that for people experiencing an ICH or a haemorrhagic stroke, the proportion of people returning to independent living would match that observed for ischaemic stroke, and that the same utilities for minor and major ischaemic stroke would apply to dependent and independent states following ICH. This approach was used as it was noted that the value used in the rivaroxaban submission92,96 was higher than the age-specific UK EQ-5D population norm for people ≥ 75 years of age. Finally, the baseline utility value for people with atrial fibrillation or mechanical heart valve who were stable was taken as the baseline EQ-5D value of patients enrolled in the SMART trial (0.738). 87
This value was applied to 65- to 70-year-old people. The difference between the UK EQ-5D population norm for 65- to 70-year-olds and the utility estimate from the SMART trial (0.042) was used to estimate age-specific baseline utilities in the model. The resultant utility values applied to events and health states are provided in Table 23.
| State/event | Utility value/decrement | Source | Description |
|---|---|---|---|
| Stable AF/AHV | |||
| < 25 years | 0.898 | Kind 1999130 | EQ-5D, UK population norm adjusted for AF/AHV |
| 25–34 years | 0.888 | Kind 1999130 | EQ-5D, UK population norm adjusted for AF/AHV |
| 35–44 years | 0.868 | Kind 1999130 | EQ-5D, UK population norm adjusted for AF/AHV |
| 45–54 years | 0.808 | Kind 1999130 | EQ-5D, UK population norm adjusted for AF/AHV |
| 55–64 years | 0.758 | Kind 1999130 | EQ-5D, UK population norm adjusted for AF/AHV |
| 65–74 years | 0.738 | Jowett 200687 | EQ-5D values for people with AF |
| ≥ 75 years | 0.688 | Kind 1999130 | EQ-5D, UK population norm adjusted for AF/AHV |
| Minor stroke | 0.641 | Robinson 2001131 | Standard gamble, UK people |
| Post minor stroke | 0.71 | Dorman 2000128 | EQ-5D, UK stroke people |
| Major stroke | 0.189 | Robinson 2001131 | Standard gamble, UK people |
| Post major stroke | 0.31 | Dorman 2000128 | EQ-5D, UK stroke people |
| Systemic embolism (decrement) | –0.119 | Sullivan 2006132 | Based on EQ-5D scores from a US cohort |
| Minor bleed | 0.7757 | Sullivan 2006132 | As above |
| > 75 years | 0.7257 | As above, adjusted for consistency with UK population norms | |
| Major bleed (decrement) | –0.1814 | Sullivan 2006132 | As above |
| Post IC bleed | 0.461 | Assumption | Weighted average of post minor and post major stroke utilities |
Utilities associated with acute events were applied for the 3-month period following the event. For post-event states with associated ongoing morbidity, the appropriate health state utilities were applied for all subsequent cycles spent in these states. Half-cycle corrections were applied, by assuming that people experienced events on average at the mid-point of the cycle. Thus, a patient starting off in the well state and experiencing a major stroke in a given cycle of the model would accrue 6 weeks at the utility value for well and 6 weeks at the utility value for major stroke.
Time horizon, and discounting of costs and benefits
Both costs and benefits (QALYs) were discounted at 3.5% per annum, in line with the NICE reference case. 29 The model was initially analysed over a 10-year period, but the impact of adopting longer time horizons (including the patient’s lifetime) was explored in sensitivity analyses. It was anticipated that a 10-year time horizon would be sufficient to demonstrate the main health and cost impact of any identified differences in adverse event rates between the alternative monitoring strategies, while avoiding the uncertainty surrounding assumptions about event rates far into the future.
Analysis
The results of the model are presented in terms of a cost–utility analysis (i.e. costs for and number of QALYs generated by each monitoring strategy). Each strategy was compared incrementally with its next less costly, non-dominated comparator, to estimate its incremental cost per QALY gained. In addition, given the uncertainty surrounding the relative effectiveness of the alternative self-monitoring devices, self-monitoring using each device was also compared incrementally with the standard care monitoring strategy (mixed primary and secondary care monitoring).
Further analyses were undertaken to assess cost-effectiveness by age, indication for anticoagulation therapy (atrial fibrillation, AHV), the standard care comparator (primary care monitoring, secondary care monitoring), and the active intervention (self-monitoring, self-management). The impact of altering key parameter values and assumptions was also assessed through extensive sensitivity analysis.
Given the computational burden of running the model probabilistically for each scenario assessed, results of main analyses and sensitivity analyses are presented based on deterministic runs of the model using the point estimates for input parameters. To characterise the joint uncertainty surrounding point estimates of incremental costs and effects, probabilistic sensitivity analysis was also undertaken. 133 Each parameter was assigned an appropriate distribution as indicated in the preceding parameter tables. The model was then run iteratively 1000 times, with a value drawn randomly for each input parameter from its assigned distribution for each run. The estimated mean cost and effects for each strategy, based on these 1000 iterations, are presented for comparison with the deterministic results. The results of the probabilistic analysis are also presented in the form of incremental cost-effectiveness scatterplots and cost-effectiveness acceptability curves – for self-monitoring using each device compared with standard practice. As no direct evidence for the relative clinical effectiveness of the alternative monitoring devices could be identified, the strategies have not been compared simultaneously in the probabilistic analysis. Parameters excluded from the probabilistic analysis were self-monitoring training costs; in-hospital fatal stroke costs; post-stroke costs; the proportion of the cohort with atrial fibrillation; the proportion male; the proportional split between primary and secondary standard care monitoring; discontinuation rates; and unit costs of devices, consumables and staff time.
Results
Base-case analysis
This section presents the results of the base-case analysis. The following assumptions were applied:
-
66.45% of standard care monitoring occurs in primary care with practice nurses. 96
-
60% of the cohort have atrial fibrillation, 40% have an AHV. 108
-
Average age of the cohort is 65 years, and 55% are male. 108
-
50% of self-monitoring people self-test, 50% self-manage (assumption).
-
The increase in the number of tests performed per year with self-monitoring is 23. 108
-
Relative treatment effects are estimated and applied separately for self-testing and self-management (see Table 10).
-
15% of participants do not commence self-monitoring following training (see Training).
-
10% of participants discontinue self-monitoring within a year of commencing (see Training).
-
Self-monitoring device costs are annuitised over 5 years (see Equipment).
-
75% of devices are reused by another patient when a patient discontinues self-monitoring (see Equipment).
Figure 17 indicates the modelled proportion of the cohort (under standard monitoring care) experiencing a stroke, thromboembolic event, major bleeding event, and death by time in years. Figure 18 presents the same outcomes under the self-monitoring strategy. Applying the base-case assumptions, the results indicate that over a 10-year period, the introduction of self-monitoring would reduce the proportion of people suffering a thromboembolic event by 2.5%, while slightly increasing the proportion suffering a major haemorrhagic event by 1.4% (Table 24).
FIGURE 17.
Modelled cumulative probability of a first thromboembolic and major haemorrhagic event, and death from all causes (standard-care cohort).

FIGURE 18.
Modelled cumulative probability of a first thromboembolic and major haemorrhagic event, and death from all causes (self-monitoring cohort).
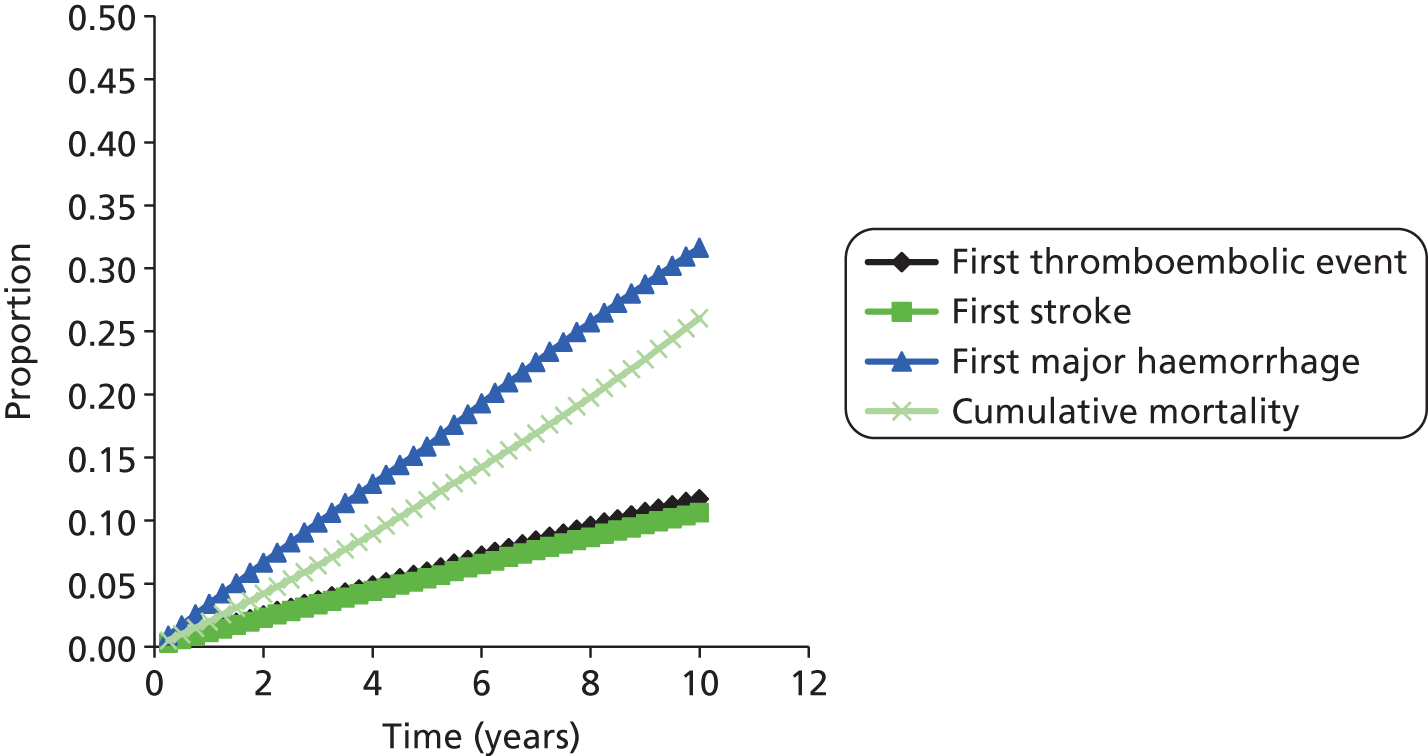
| Strategy | Mean costs, £ | Cumulative monitoring/device costs, £ | First thromboembolic event, % | First major bleed, % | Mean QALYs |
|---|---|---|---|---|---|
| Standard monitoring | 7324 | 1269 | 14.2 | 30.2 | 5.479 |
| Self-monitoring: INRatio2 | 7295 | 1908 | 11.7 | 31.6 | 5.507 |
| Self-monitoring: CoaguChek XS | 7333 | 1944 | 11.7 | 31.6 | 5.507 |
| Self-monitoring: ProTime | 8609 | 3192 | 11.7 | 31.6 | 5.507 |
While the predicted monitoring costs are higher with self-monitoring (see Table 24), the total health and social care costs are similar and in some cases lower, and the QALY gains are greater. Thus, under the base-case scenario, the self-monitoring strategies compare favourably with standard care, except for with ProTime, where the incremental cost per QALY gained is £47,640 (Table 25, Figure 19). Furthermore, due to the lower cost of the INRatio2 device and testing strips, coupled with the assumption of equivalent clinical effectiveness of the alternative self-monitoring devices, INRatio2 dominates CoaguChek XS. However, it should be noted that no direct evidence of clinical effectiveness was identified exclusively for INRatio2 from the systematic review.
| Strategy | Mean costs | Incremental costs | Mean QALYs | Incremental QALYs | ICERa | ICER vs. SC |
|---|---|---|---|---|---|---|
| Self-monitoring: INRatio2 | £7295 | £0 | 5.507 | 0 | – | Dominant |
| Standard monitoring | £7324 | £29 | 5.479 | –0.027 | Dominated | – |
| Self-monitoring: CoaguChek XS | £7333 | £37 | 5.507 | 0 | Dominated | £319 |
| Self-monitoring: ProTime | £8609 | £1314 | 5.507 | 0 | Dominated | £47,604 |
FIGURE 19.
Cost-effectiveness frontier (base case).
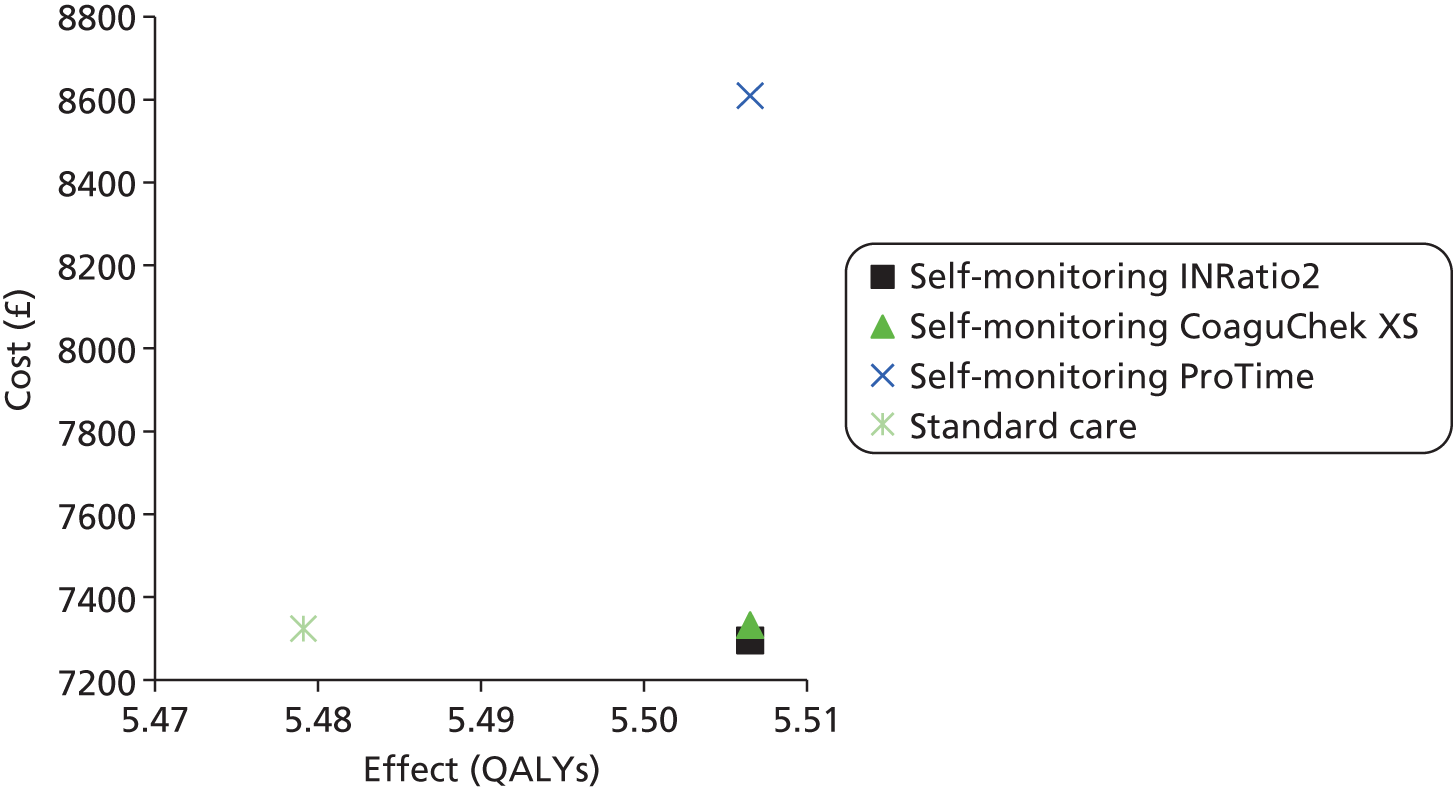
Incremental analysis of alternative scenarios
Table 26 shows the results of further scenario analyses. For exclusive self-testing and self-management versus mixed primary/secondary care standard monitoring, and for mixed self-monitoring versus exclusive primary and secondary care clinic testing. Exclusive self-management with INRatio2 and CoaguChek XS was cost saving under the base-case assumptions, whereas self-testing was not cost-effective. The results also showed the mixed self-monitoring strategy (50% self-testing, 50% self-management) to be cost saving with CoaguChek XS and INRatio2 in comparison with exclusive secondary care testing. When applying the pooled RR for adverse events (derived from all self-monitoring studies) to both self-testing and self-managing participants, the cost savings and QALY gains associated with self-monitoring increased (see Table 26, scenario 5). This is because under this scenario self-testing becomes independently more effective. The same pattern of results was identified when self-monitoring was compared with exclusive secondary care anticoagulation clinic testing (see Table 26, scenario 6) using the point estimates of RRs derived only from trials making this comparison (see Figures 6 and 14). Finally, scenario 7 (see Table 26) shows the results when restricting the comparison to CoaguChek XS versus standard monitoring, using the pooled point estimates of RR derived only from trials of CoaguChek versus standard practice.
| Strategy | Mean costs | Incremental costs | Mean QALYs | Incremental QALYs | ICERa | ICER vs. SC |
|---|---|---|---|---|---|---|
| Base case (100% self-management vs. standard care) | ||||||
| Self-monitoring: INRatio2 | £6370 | – | 5.534 | – | – | Dominant |
| Self-monitoring: CoaguChek XS | £6407 | £37 | 5.534 | 0 | Dominated | Dominant |
| Standard monitoring | £7324 | £954 | 5.479 | –0.054 | Dominated | – |
| Self-monitoring: ProTime | £7691 | £1321 | 5.534 | 0 | Dominated | £6797 |
| Base case (100% self-testing vs. standard care) | ||||||
| Standard monitoring | £7324 | – | 5.479 | – | – | – |
| Self-monitoring: INRatio2 | £8221 | £897 | 5.479 | 0 | £2,699,665 | £2,699,665 |
| Self-monitoring: CoaguChek XS | £8258 | £37 | 5.479 | 0 | Dominated | £2,811,298 |
| Self-monitoring: ProTime | £9528 | £1306 | 5.479 | 0 | Dominated | £6,631,414 |
| Base case (100% primary care) | ||||||
| Standard monitoring | £7132 | – | 5.479 | – | – | – |
| Self-monitoring: INRatio2 | £7208 | £75 | 5.507 | 0.027 | £2749 | £2749 |
| Self-monitoring: CoaguChek XS | £7245 | £37 | 5.507 | 0 | Dominated | £4108 |
| Self-monitoring: ProTime | £8522 | £1314 | 5.507 | 0 | Dominated | £50,689 |
| Base case (100% secondary care) | ||||||
| Self-monitoring: INRatio2 | £7469 | – | 5.507 | – | – | Dominant |
| Self-monitoring: CoaguChek XS | £7506 | £37 | 5.507 | 0 | Dominated | Dominant |
| Standard monitoring | £7704 | £235 | 5.479 | –0.027 | Dominated | – |
| Self-monitoring: ProTime | £8783 | £1314 | 5.507 | 0 | Dominated | £39,963 |
| Self-monitoring (50–50 split between self-testing and self-management) vs. standard care, but applying pooled RR estimates for all self-monitoring as a whole | ||||||
| Self-monitoring: INRatio2 | £6753 | – | 5.530 | – | – | Dominant |
| Self-monitoring: CoaguChek XS | £6790 | £37 | 5.530 | 0 | Dominated | Dominant |
| Standard monitoring | £7324 | £571 | 5.479 | –0.051 | Dominated | – |
| Self-monitoring: ProTime | £8073 | £1321 | 5.530 | 0 | Dominated | £14,690 |
| Self-monitoring (50–50 split between self-testing and self-management) vs. secondary care anticoagulation clinic testing, applying pooled RR estimates from RCTs where this represented the comparator (see Chapter 2, Figures 6 and 11) | ||||||
| Self-monitoring: INRatio2 | £7064 | – | 5.532 | – | – | Dominant |
| Self-monitoring: CoaguChek XS | £7102 | £37 | 5.532 | 0 | Dominated | Dominant |
| Standard monitoring | £7704 | £639 | 5.479 | –0.053 | Dominated | – |
| Self-monitoring: ProTime | £8386 | £1321 | 5.532 | 0 | Dominated | £12,872 |
| Self-monitoring with CoaguChek (50–50 split between self-testing and self-management) vs. standard care, applying pooled RR estimates trials including only CoaguChek (see Chapter 2, Table 6) | ||||||
| Self-monitoring: CoaguChek XS | £7019 | – | 5.531 | – | – | – |
| Standard monitoring | £7324 | £305 | 5.479 | –0.052 | Dominated | Dominated |
Table 27 presents the results of alternative non-base-case scenarios, assessing the impact of using self-monitoring not to increase the number of tests performed annually, but to replace standard monitoring tests (average 12 per year). For these analyses it was assumed that no difference in clinical effectiveness exists between self-management, self-testing and standard care. Under most of these scenarios, standard monitoring was found to be less costly than self-monitoring. However, self-testing and self-management with INRatio2 and CoaguChek XS remained cost saving in comparison with exclusive secondary care anticoagulation clinic monitoring.
| Strategy | Mean costs | Incremental costs | Mean QALYs | Incremental QALYs | ICERa | ICER vs. SC |
|---|---|---|---|---|---|---|
| Self-monitoring (50% self-test, 50% self-manage) with no increase in number of tests performed, compared with standard care (66% primary care, 34% secondary care) | ||||||
| Standard monitoring | £7324 | – | 5.479 | – | – | – |
| Self-monitoring: INRatio2 | £7423 | £99 | 5.479 | 0 | Dominated | Dominated |
| Self-monitoring: CoaguChek XS | £7457 | £34 | 5.479 | 0 | Dominated | Dominated |
| Self-monitoring: ProTime | £8435 | £978 | 5.479 | 0 | Dominated | Dominated |
| 100% self-test with no increase in the number of tests performed, compared with standard care (66% primary care, 34% secondary care) | ||||||
| Standard monitoring | £7324 | – | 5.479 | – | – | – |
| Self-monitoring: INRatio2 | £7463 | £139 | 5.479 | 0 | Dominated | Dominated |
| Self-monitoring: CoaguChek XS | £7498 | £34 | 5.479 | 0 | Dominated | Dominated |
| Self-monitoring: ProTime | £8475 | £978 | 5.479 | 0 | Dominated | Dominated |
| 100% self-manage with no increase in number of tests performed, compared with standard care (66% primary care, 34% secondary care) | ||||||
| Standard monitoring | £7324 | – | 5.479 | – | – | – |
| Self-monitoring: INRatio2 | £7383 | £59 | 5.479 | 0 | Dominated | Dominated |
| Self-monitoring: CoaguChek XS | £7417 | £34 | 5.479 | 0 | Dominated | Dominated |
| Self-monitoring: ProTime | £8395 | £978 | 5.479 | 0 | Dominated | Dominated |
| 100% self-test with no increase in number of tests performed, compared with standard care (compared with standard monitoring in secondary care) | ||||||
| Self-monitoring: INRatio2 | £7638 | – | 5.479 | – | – | Dominant |
| Self-monitoring: CoaguChek XS | £7672 | £34 | 5.479 | 0 | Dominated | Dominant |
| Standard monitoring | £7704 | £66 | 5.479 | 0 | Dominated | – |
| Self-monitoring: ProTime | £8650 | £1012 | 5.479 | 0 | Dominated | Dominated |
| 100% self-manage with no increase in number of tests performed, compared with standard care (compared with standard monitoring in secondary care) | ||||||
| Self-monitoring: INRatio2 | £7557 | – | 5.489 | – | – | Dominant |
| Self-monitoring: CoaguChek XS | £7592 | £34 | 5.489 | 0 | Dominated | Dominant |
| Standard monitoring | £7704 | £146 | 5.489 | 0 | Dominated | – |
| Self-monitoring: ProTime | £8570 | £1012 | 5.489 | 0 | Dominated | Dominated |
Differential results for subgroups
Table 28 presents the results for self-monitoring versus standard care by indication (atrial fibrillation and AHVs) and cohort age. Compared with standard monitoring, self-monitoring in a 65-year-old cohort with atrial fibrillation was estimated to cost £2574 and £4160 per QALY gained with INRatio2 and CoaguChek XS, respectively. Self-monitoring with ProTime was estimated to cost £58,584 per QALY gained. For a 65-year-old AHV cohort, self-monitoring with INRatio2 and CoaguChek XS was found to be more effective and less costly (dominant) than standard monitoring.
| Strategy | Mean costs | Incremental costs | Mean QALYs | Incremental QALYs | ICERa | ICER vs. SC |
|---|---|---|---|---|---|---|
| Atrial fibrillation cohort (aged 65 years) | ||||||
| Standard monitoring | £6951 | – | 5.533 | – | – | – |
| Self-monitoring: INRatio2 | £7012 | £61 | 5.557 | 0.024 | £2574 | £2574 |
| Self-monitoring: CoaguChek XS | £7049 | £37 | 5.557 | 0 | Dominated | £4160 |
| Self-monitoring: ProTime | £8335 | £1323 | 5.557 | 0 | Dominated | £58,584 |
| Mechanical heart valve cohort (aged 65 years) | ||||||
| Self-monitoring: INRatio2 | £7721 | – | 5.431 | – | – | Dominant |
| Self-monitoring: CoaguChek XS | £7758 | £37 | 5.431 | 0 | Dominated | Dominant |
| Standard monitoring | £7884 | £163 | 5.398 | –0.033 | Dominated | – |
| Self-monitoring: ProTime | £9020 | £1300 | 5.431 | 0 | Dominated | £34,449 |
| Atrial fibrillation cohort with TTR 65.6–72.6% (aged 65 years) | ||||||
| Standard monitoring | £5522 | – | 5.608 | – | – | – |
| Self-monitoring: INRatio2 | £5780 | £257 | 5.623 | 0.016 | £16,409 | £16,409 |
| Self-monitoring: CoaguChek XS | £5817 | £38 | 5.623 | 0 | Dominated | £18,817 |
| Self-monitoring: ProTime | £7117 | £1337 | 5.623 | 0 | Dominated | £101,677 |
| Atrial fibrillation cohort with TTR > 72.6% (aged 65 years) | ||||||
| Standard monitoring | £5090 | – | 5.631 | – | – | – |
| Self-monitoring: INRatio2 | £5401 | £310 | 5.645 | 0.014 | £22,768 | £22,768 |
| Self-monitoring: CoaguChek XS | £5438 | £38 | 5.645 | 0 | Dominated | £25,548 |
| Self-monitoring: ProTime | £6743 | £1342 | 5.645 | 0 | Dominated | £121,280 |
| Mixed cohort (aged 55 years) | ||||||
| Standard monitoring | £6956 | – | 5.945 | – | – | – |
| Self-monitoring: INRatio2 | £7050 | £94 | 5.965 | 0.02 | £4592 | £4592 |
| Self-monitoring: CoaguChek XS | £7088 | £38 | 5.965 | 0 | Dominated | £6465 |
| Self-monitoring: ProTime | £8411 | £1361 | 5.965 | 0 | Dominated | £71,262 |
| Mixed cohort (aged 75 years) | ||||||
| Standard monitoring | £6560 | – | 4.452 | – | – | – |
| Self-monitoring: INRatio2 | £6563 | £4 | 4.484 | 0.032 | £116 | £116 |
| Self-monitoring: CoaguChek XS | £6598 | £35 | 4.484 | 0 | Dominated | £1209 |
| Self-monitoring: ProTime | £7771 | £1208 | 4.484 | 0 | Dominated | £37,776 |
| Mixed cohort (aged 85 years) | ||||||
| Standard monitoring | £3705 | – | 3.008 | – | – | – |
| Self-monitoring: INRatio2 | £3922 | £218 | 3.037 | 0.029 | £7485 | £7485 |
| Self-monitoring: CoaguChek XS | £3952 | £29 | 3.037 | 0 | £0 | £8491 |
| Self-monitoring: ProTime | £4874 | £951 | 3.037 | 0 | £0 | £40,169 |
A further analysis was carried out for the atrial fibrillation cohort using the baseline risks observed for participants with better INR control in standard care, assuming a constant RR reduction for thromboembolic events associated with self-monitoring. As the INR TTR increased in the control group, and the baseline risk of thromboembolic events consequently dropped, the cost-effectiveness of self-monitoring also decreased. However, the ICERs for CoaguChek XS and INRatio2 rose above £20,000 per QALY only when the baseline TTR was set at > 72.6%.
While cost-effectiveness was found to decrease slightly in a younger mixed cohort (due to the lower baseline risk of thromboembolic events), the ICERs for CoaguChek XS and INRatio2 remained below £20,000 per QALY gained. Self-monitoring was found to be most cost-effective in a 75-year-old cohort.
Further analysis of uncertainty (sensitivity analysis)
Deterministic sensitivity analysis was undertaken to test the robustness of the model, based findings to various parameter and structural assumptions (Table 29). The findings were found to be most sensitive to the baseline risk of thromboembolic events and the effectiveness of self-monitoring for preventing these events (see Table 29, scenarios 14–16). Applying a baseline risk of 1.15% coupled with the upper 95% confidence limit of the RR estimate for self-management (0.69), the ICERs for the mixed self-monitoring strategies rose above £30,000 per QALY gained (see Table 29, scenario 17). The same was found when the lower baseline risk (1.15%) was coupled with the upper confidence limit for the RR (for thromboembolic events) associated with self-monitoring as a whole (0.84 applied for self-testing and self-management). One hundred per cent self-management remained cost saving under the former combined scenario but not the latter.
| Strategy | Mean costs | Incremental costs | Mean QALYs | Incremental QALYs | ICERa | ICER vs. SC |
|---|---|---|---|---|---|---|
| Assume 10 minutes of nurse time per standard primary care monitoring visit, rather than 15 minutes | ||||||
| Standard monitoring | £7146 | – | 5.479 | – | – | – |
| Self-monitoring: INRatio2 | £7249 | £103 | 5.507 | 0.027 | £3,760 | £3760 |
| Self-monitoring: CoaguChek XS | £7287 | £37 | 5.507 | 0 | Dominated | £5119 |
| Self-monitoring: ProTime | £8563 | £1314 | 5.507 | 0 | Dominated | £51,699 |
| Unit costs of standard care as per Jowett and colleagues87 | ||||||
| Self-monitoring: INRatio2 | £7333 | – | 5.507 | – | – | Dominant |
| Self-monitoring: CoaguChek XS | £7370 | £37 | 5.507 | 0 | Dominated | Dominant |
| Standard monitoring | £7468 | £136 | 5.479 | –0.027 | Dominated | – |
| Self-monitoring: ProTime | £8647 | £1314 | 5.507 | 0 | Dominated | £43,640 |
| 10 standard care visits per year (with no change in the baseline risk of adverse events) | ||||||
| Standard monitoring | £7112 | – | 5.479 | – | – | – |
| Self-monitoring: INRatio2 | £7241 | £128 | 5.507 | 0.027 | £4676 | £4676 |
| Self-monitoring: CoaguChek XS | £7278 | £37 | 5.507 | 0 | Dominated | £6035 |
| Self-monitoring: ProTime | £8555 | £1314 | 5.507 | 0 | Dominated | £52,616 |
| 20 standard care visits per year (with no increase in baseline risk adverse events) | ||||||
| Self-monitoring: INRatio2 | £7514 | – | 5.507 | – | – | Dominant |
| Self-monitoring: CoaguChek XS | £7551 | £37 | 5.507 | 0 | Dominated | Dominant |
| Standard monitoring | £8170 | £656 | 5.479 | –0.027 | Dominated | – |
| Self-monitoring: ProTime | £8828 | £1314 | 5.507 | 0 | Dominated | £24,365 |
| Self-monitoring training failure rate 24% and subsequent discontinuation rate 14% | ||||||
| Standard monitoring | £7324 | – | 5.479 | – | – | – |
| Self-monitoring: INRatio2 | £7328 | £4 | 5.503 | 0.023 | £190 | £190 |
| Self-monitoring: CoaguChek XS | £7361 | £32 | 5.503 | 0 | Dominated | £1563 |
| Self-monitoring: ProTime | £8459 | £1131 | 5.503 | 0 | Dominated | £48,488 |
| 26 self-monitoring tests per year with the same relative effects | ||||||
| Self-monitoring: INRatio2 | £7079 | – | 5.507 | – | – | Dominant |
| Self-monitoring: CoaguChek XS | £7115 | £36 | 5.507 | 0 | Dominated | Dominant |
| Standard monitoring | £7324 | £245 | 5.479 | –0.027 | Dominated | – |
| Self-monitoring: ProTime | £8277 | £1198 | 5.507 | 0 | Dominated | £35,287 |
| 52 self-monitoring tests per year with the same relative effects | ||||||
| Standard monitoring | £7324 | – | 5.479 | – | – | – |
| Self-monitoring: INRatio2 | £7704 | £380 | 5.507 | 0.027 | £13,879 | £13,879 |
| Self-monitoring: CoaguChek XS | £7744 | £39 | 5.507 | 0 | Dominated | £15,309 |
| Self-monitoring: ProTime | £9237 | £1533 | 5.507 | 0 | Dominated | £69,814 |
| Reduce the increased number of tests with self-monitoring by 50% (+12) and halve the relative effect sizes | ||||||
| Standard monitoring | £7324 | – | 5.479 | – | – | – |
| Self-monitoring: INRatio2 | £7353 | £29 | 5.494 | 0.015 | £1,990 | £1990 |
| Self-monitoring: CoaguChek XS | £7389 | £36 | 5.494 | 0 | Dominated | £4440 |
| Self-monitoring: ProTime | £8522 | £1169 | 5.494 | 0 | Dominated | £81,724 |
| Higher acute costs for major stroke, based on the application of excess bed-day costs for each day over the mean HRG length of stay | ||||||
| Self-monitoring: INRatio2 | £7478 | – | 5.507 | – | – | Dominant |
| Self-monitoring: CoaguChek XS | £7515 | £37 | 5.507 | 0 | Dominated | Dominant |
| Standard monitoring | £7547 | £69 | 5.479 | –0.027 | Dominated | – |
| Self-monitoring: ProTime | £8792 | £1314 | 5.507 | 0 | Dominated | £46,101 |
| Cost-effectiveness over a 20-year time horizon | ||||||
| Self-monitoring: INRatio2 | £13,002 | – | 7.711 | – | – | Dominant |
| Self-monitoring: CoaguChek XS | £13,055 | £53 | 7.711 | 0 | Dominated | Dominant |
| Standard monitoring | £13,417 | £415 | 7.635 | –0.076 | Dominated | – |
| Self-monitoring: ProTime | £14,892 | £1890 | 7.711 | 0 | Dominated | £19,407 |
| Cost-effectiveness over a 30-year time horizon | ||||||
| Self-monitoring: INRatio2 | £13,877 | – | 8.156 | – | – | Dominant |
| Self-monitoring: CoaguChek XS | £13,934 | £57 | 8.156 | 0 | Dominated | Dominant |
| Standard monitoring | £14,300 | £424 | 8.054 | –0.102 | Dominated | – |
| Self-monitoring: ProTime | £15,910 | £2034 | 8.156 | 0 | Dominated | £15,784 |
| 60% of self-monitoring patients self-test, 40% self-manage | ||||||
| Standard monitoring | £7324 | – | 5.479 | – | – | – |
| Self-monitoring: INRatio2 | £7480 | £157 | 5.501 | 0.022 | £7166 | £7116 |
| Self-monitoring: CoaguChek XS | £7518 | £37 | 5.501 | 0 | Dominated | £8808 |
| Self-monitoring: ProTime | £8793 | £1312 | 5.501 | 0 | Dominated | £66,792 |
| 40% of self-monitoring patients self-test, 60% self-manage | ||||||
| Self-monitoring: INRatio2 | £7110 | – | 5.512 | – | – | Dominant |
| Self-monitoring: CoaguChek XS | £7147 | £37 | 5.512 | 0 | Dominated | Dominant |
| Standard monitoring | £7324 | £214 | 5.479 | –0.033 | Dominated | – |
| Self-monitoring: ProTime | £8426 | £1315 | 5.512 | 0 | Dominated | £33,383 |
| Baseline risk of thromboembolic events set at 1.15% | ||||||
| Standard monitoring | £5999 | – | 5.537 | – | – | – |
| Self-monitoring: INRatio2 | £6214 | £215 | 5.554 | 0.017 | £12,729 | £12,729 |
| Self-monitoring: CoaguChek XS | £6252 | £37 | 5.554 | 0 | Dominated | £14,944 |
| Self-monitoring: ProTime | £7538 | £1323 | 5.554 | 0 | Dominated | £91,005 |
| RR for thromboembolic events associated with self-management = 0.69 (self-testing 0.99 as per base case) | ||||||
| Standard monitoring | £7324 | – | 5.479 | – | – | – |
| Self-monitoring: INRatio2 | £7564 | £240 | 5.495 | 0.016 | £15,318 | £15,318 |
| Self-monitoring: CoaguChek XS | £7601 | £37 | 5.495 | 0 | Dominated | £17,688 |
| Self-monitoring: ProTime | £8875 | £1311 | 5.495 | 0 | Dominated | £98,856 |
| RR for thromboembolic events associated with self-monitoring = 0.84 for self-testing and self-management | ||||||
| Standard monitoring | £7324 | – | 5.479 | – | – | – |
| Self-monitoring: INRatio2 | £7552 | £228 | 5.495 | 0.016 | £13,964 | £13,964 |
| Self-monitoring: CoaguChek XS | £7589 | £37 | 5.495 | 0 | Dominated | £16,241 |
| Self-monitoring: ProTime | £8863 | £1311 | 5.495 | 0 | Dominated | £94,228 |
| Baseline risk of thromboembolic events 1.15%, RR associated with self-management 0.69 | ||||||
| Standard monitoring | £5999 | – | 5.537 | – | – | – |
| Self-monitoring: INRatio2 | £6397 | £398 | 5.546 | 0.009 | £44,308 | £44,308 |
| Self-monitoring: CoaguChek XS | £6434 | £37 | 5.546 | 0 | Dominated | £48,478 |
| Self-monitoring: ProTime | £7718 | £1321 | 5.546 | 0 | Dominated | £191,567 |
| Baseline risk of thromboembolic events 1.15%, RR associated with self-management and self-testing 0.84 | ||||||
| Standard monitoring | £5999 | – | 5.537 | – | – | – |
| Self-monitoring: INRatio2 | £6388 | £389 | 5.546 | 0.009 | £41,225 | £41,225 |
| Self-monitoring: CoaguChek XS | £6425 | £37 | 5.546 | 0 | Dominated | £45,193 |
| Self-monitoring: ProTime | £7709 | £1321 | 5.546 | 0 | Dominated | £181,371 |
| Mechanical heart valve cohort (approximation for children aged 10 years) | ||||||
| Self-monitoring: INRatio2 | £7897 | – | 7.324 | – | – | Dominant |
| Self-monitoring: CoaguChek XS | £7936 | £39 | 7.324 | 0 | Dominated | Dominant |
| Standard monitoring | £7946 | £49 | 7.291 | –0.033 | Dominated | – |
| Self-monitoring: ProTime | £9296 | £1399 | 7.324 | 0 | Dominated | £40,906 |
| Self-monitoring device costs annuitised over 3 years | ||||||
| Standard monitoring | £7324 | – | 5.479 | – | – | – |
| Self-monitoring: INRatio2 | £7526 | £202 | 5.507 | 0.027 | £7387 | £7387 |
| Self-monitoring: CoaguChek XS | £7584 | £57 | 5.507 | 0 | Dominated | £9480 |
| Self-monitoring: ProTime | £9352 | £1826 | 5.507 | 0 | Dominated | £74,001 |
| 50% of devices are reused following patients discontinuing self-monitoring | ||||||
| Self-monitoring: INRatio2 | £7301 | – | 5.507 | – | – | Dominant |
| Standard monitoring | £7324 | £23 | 5.479 | –0.027 | Dominated | – |
| Self-monitoring: CoaguChek XS | £7338 | £38 | 5.507 | 0 | Dominated | £533 |
| Self-monitoring: ProTime | £8626 | £1326 | 5.507 | 0 | Dominated | £48,234 |
| Lower cost of £195 applied for the INRatio2 PT/INR monitor | ||||||
| Self-monitoring: INRatio2 | £7185 | – | 5.507 | – | – | Dominant |
| Standard monitoring | £7324 | £139 | 5.479 | –0.027 | Dominated | – |
| Self-monitoring: CoaguChek XS | £7333 | £147 | 5.507 | 0 | Dominated | £319 |
| Self-monitoring: ProTime | £8609 | £1424 | 5.507 | 0 | Dominated | £47,604 |
The cost-effectiveness of self-monitoring improved further when the modelled time horizon was extended to 20 and 30 years, with both CoaguChek XS and INRatio2 dominating standard primary/secondary care-based monitoring. The incremental cost per QALY gained for self-monitoring with CoaguChek XS and INRatio2 also remained below £20,000 when higher training failure and discontinuation rates were applied, and when higher self-monitoring testing frequencies were applied (with no change in effects). The cost-effectiveness findings were also robust to the number of tests performed annually in standard primary/secondary care-based clinic monitoring.
A final sensitivity analysis was conducted to approximate the cost-effectiveness of self-monitoring for a cohort of children with an AHV on long-term vitamin K antagonist therapy. For this analysis, the cohort age was set to 10 years, the baseline risk of thromboembolic events was reduced to 1.4%, and the annual risk of all-cause mortality following a stroke was set at 14.5. 134 Under this scenario, the ICERs for self-monitoring with CoaguChek XS and INRatio2 remained favourable. However, it should be noted that no good data were identified to appropriately adjust the risk of death from all causes in children with an AHV, and therefore the standardised mortality ratio estimated for an 18- to 55-year-old cohort of AHV participants was applied.
Probabilistic sensitivity analysis of the base case
Table 30 presents the mean costs and effects, and mean incremental cost-effectiveness results, for the four strategies based on 1000 probabilistic simulations. Compared with the deterministic analysis presented in Table 25, the results are very similar.
| Strategy | Mean costs | Incremental costs | Mean QALYs | Incremental QALYs | ICERa | ICER vs. SC |
|---|---|---|---|---|---|---|
| Self-monitoring: INRatio2 | £7290 | – | 5.507 | – | – | Dominant |
| Standard monitoring | £7312 | £22 | 5.479 | –0.028 | Dominated | – |
| Self-monitoring: CoaguChek XS | £7327 | £37 | 5.507 | 0 | Dominated | £533 |
| Self-monitoring: ProTime | £8603 | £1313 | 5.507 | 0 | Dominated | £46,632 |
Figure 20 shows the scatterplot of the estimated mean incremental costs and effects of self-monitoring with CoaguChek XS compared with standard monitoring, derived from 1000 probabilistic iterations of the model. Approximately 50% of the points lie below zero on the cost axis and above zero on the effect axis, indicating a 50% chance of the self-monitoring strategy (50% self-testing, 50% self-managing) dominating standard care monitoring. The acceptability curve (Figure 21) indicates an 80% chance of self-monitoring with CoaguChek XS being cost-effective compared with standard monitoring at a willingness-to-pay threshold of £20,000 per QALY gained.
FIGURE 20.
Incremental cost-effectiveness scatterplot: self-monitoring with CoaguChek XS vs. standard monitoring.
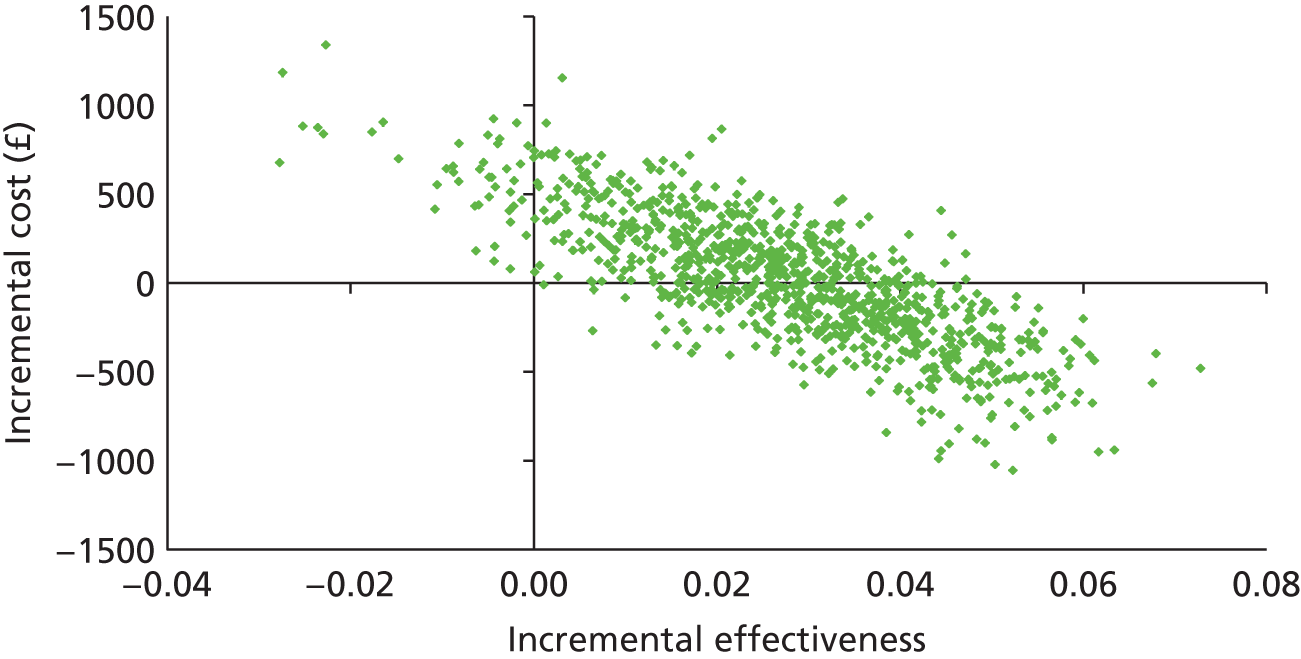
FIGURE 21.
Cost-effectiveness acceptability curves: self-monitoring with CoaguChek XS vs. standard care. WTP, wllingness to pay.

Figures 22 and 23 show the corresponding incremental cost and effect scatterplot, and acceptability curve for self-monitoring with INRatio2 versus standard care. This analysis assumes equivalent effects for INRatio2 compared with CoaguChek XS. Self-monitoring with INRatio2 was estimated to have an 81% chance of being cost-effective at a threshold of £20,000 per QALY gained under these assumptions. However, it should be noted that no direct RCT evidence was identified for the effect of INRatio2 on long-term adverse outcomes, with the majority of RCT evidence relating to versions of CoaguChek.
FIGURE 22.
Incremental cost-effectiveness scatterplot: self-monitoring with INRatio2 vs. standard monitoring.
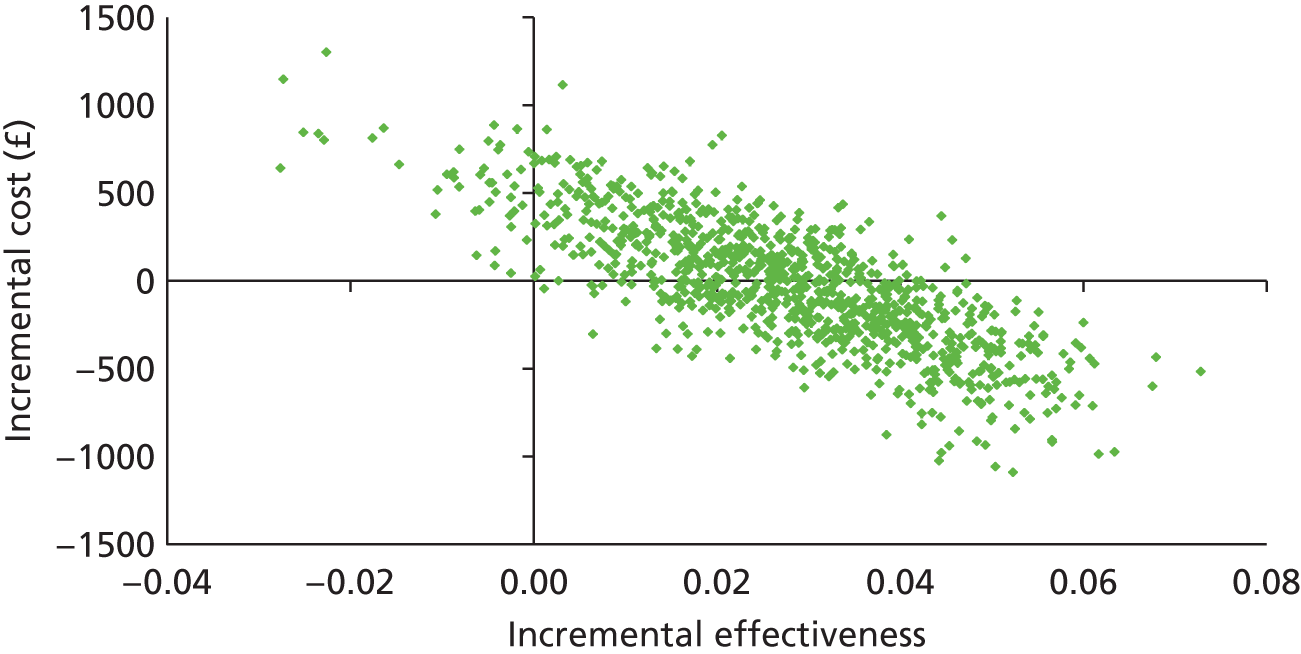
FIGURE 23.
Cost-effectiveness acceptability curves: self-monitoring with INRatio2 vs. standard care.
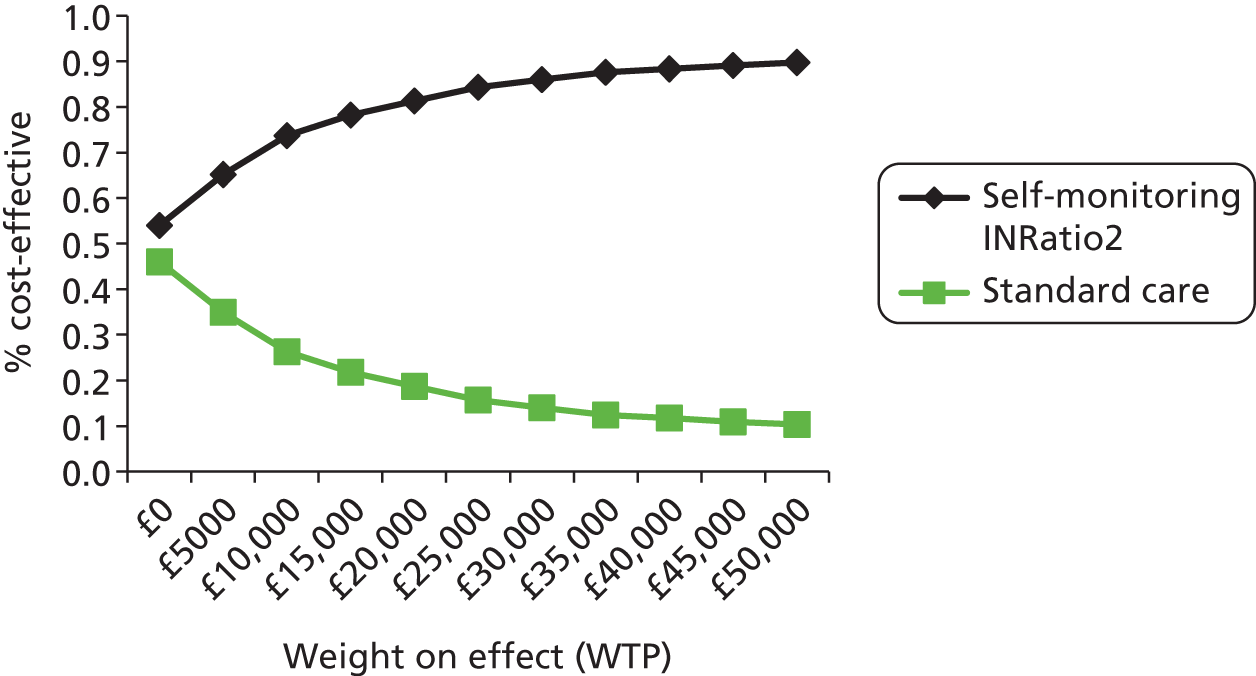
Figures 24 and 25 summarise the results of the probabilistic analysis for self-monitoring with ProTime versus standard monitoring. Owing to the higher cost of the device, this strategy was found to have a lower chance of being cost-effective in than standard practice.
FIGURE 24.
Incremental cost-effectiveness scatterplot: self-monitoring with ProTime vs. standard monitoring.
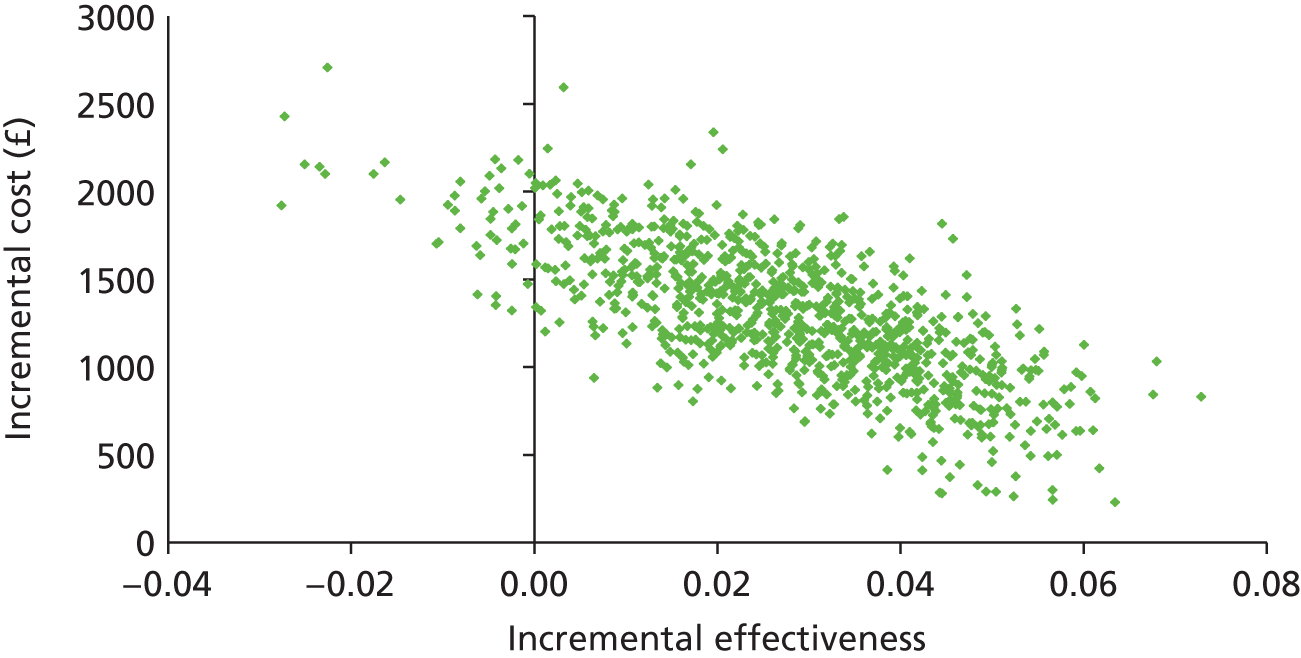
FIGURE 25.
Cost-effectiveness acceptability curves: self-monitoring with ProTime vs. standard care.

Finally, Figures 26 and 27 summarise the uncertainty surrounding the cost-effectiveness of self-monitoring with CoaguChek XS versus secondary care anticoagulation clinic testing (applying RR distributions based on the pooled estimates from trials making this comparison) and mixed (primary/secondary care) standard monitoring (using RRs derived from trials using only CoaguChek).
FIGURE 26.
Cost-effectiveness acceptability curves: self-monitoring with CoaguChek XS vs. standard monitoring (based on pooled RR estimates from CoaguChek studies only).
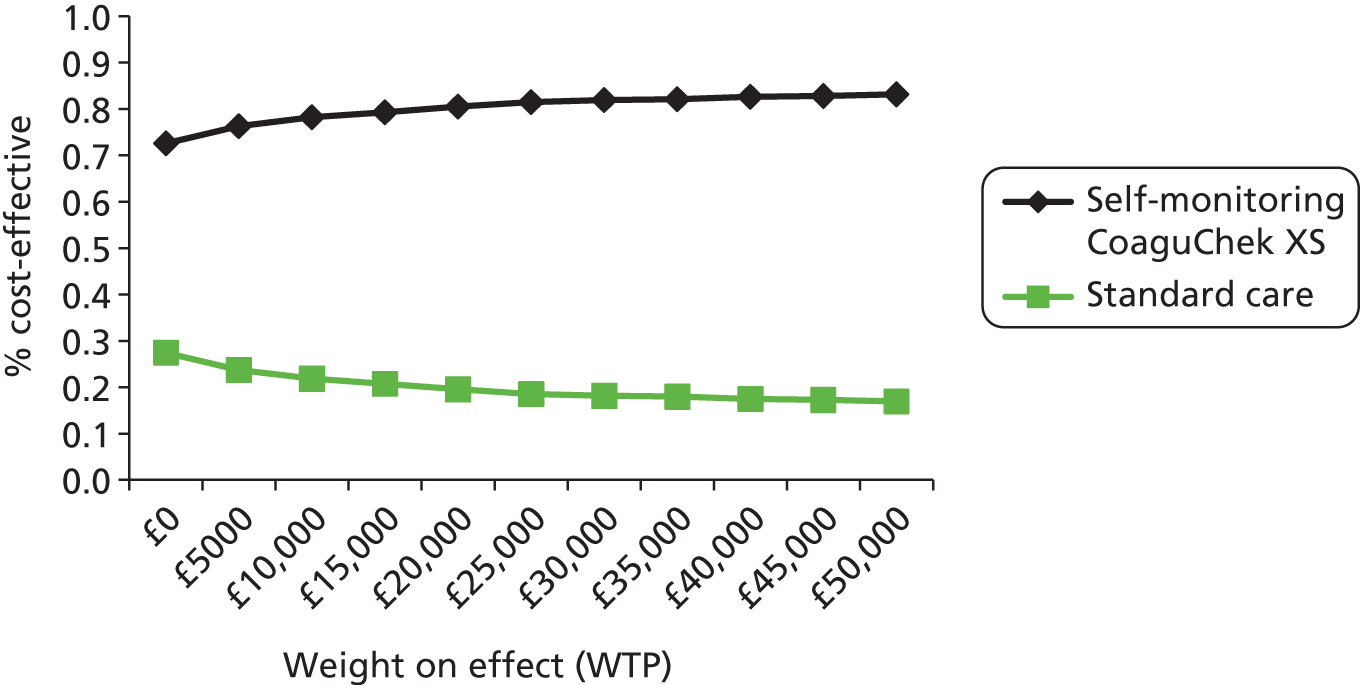
FIGURE 27.
Cost-effectiveness acceptability curves: self-monitoring with CoaguChek XS vs. secondary care anticoagulation clinic monitoring (applying RRs for self-monitoring vs. specialised anticoagulation clinic testing).
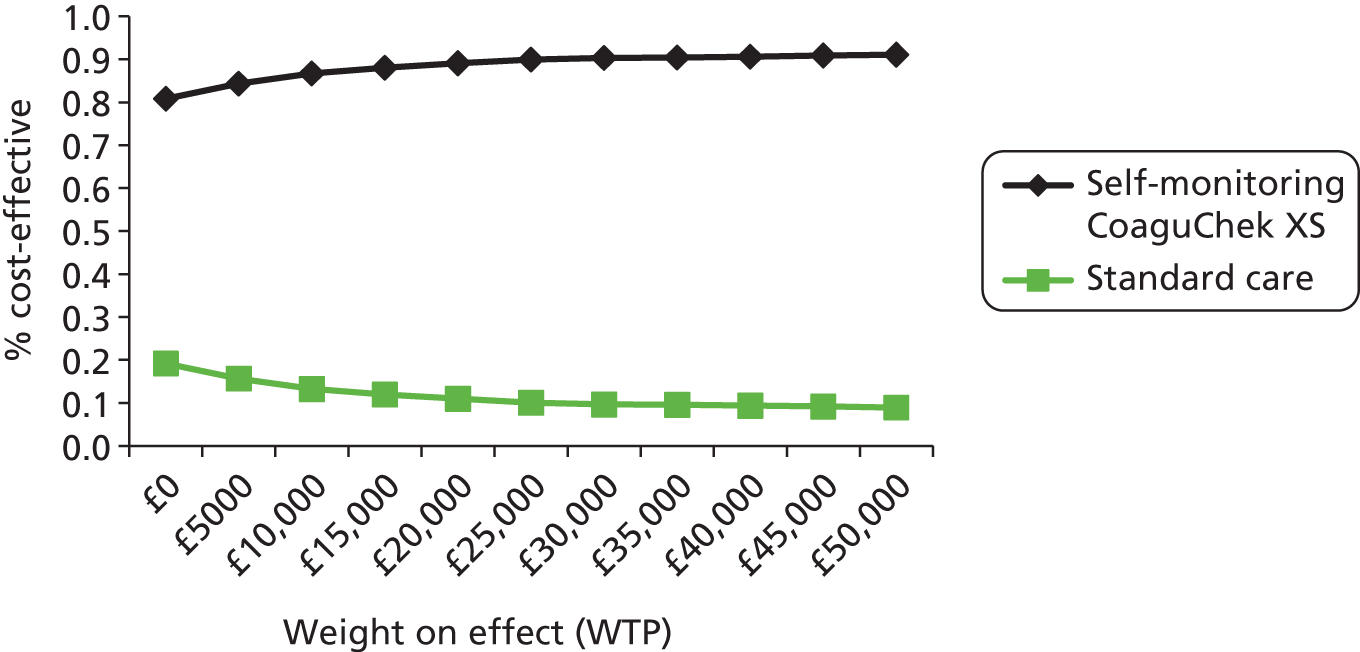
Summary
Self-monitoring, and in particular self-management, of anticoagulation status appears cost-effective when pooled estimates of clinical effectiveness are applied. However, if self-monitoring does not result in significant reductions in thromboembolic events, it is unlikely to be cost-effective from the NHS and personal social services perspective at the frequency of testing observed in RCTs.
We are most confident in the applicability of the base-case cost-effectiveness findings to self-monitoring strategies using CoaguChek XS. The majority of clinical effectiveness evidence relates to a previous version of CoaguChek (CoaguChek S), to which the current version (CoaguChek XS) has been shown to have very similar or slightly superior performance in terms of accuracy and precision (see Independent economic assessment). While INRatio and ProTime have been shown to have acceptable performance in relation to laboratory testing, very few studies have directly compared CoaguChek XS with the INRatio2 PT/INR monitor and/or ProTime Microcoagulation system. Further studies are needed to assess relative diagnostic and clinical performance.
The main findings and uncertainties are discussed further in Chapter 4.
Chapter 4 Discussion
Statement of principal findings
Clinical effectiveness
This assessment is based on 26 RCTs evaluating the use of point-of-care devices for the self-monitoring (self-testing and self-management) of people receiving AOT. The results of this assessment indicate that:
-
Self-monitoring (self-testing or self-management) of anticoagulation therapy leads to significantly fewer thromboembolic events than standard primary care or anticoagulation control in specialised clinics (RR 0.58, 95% CI 0.40 to 0.84; p = 0.004).
-
There is no evidence of a difference in bleeding events (RR 0.95, 95% CI 0.74 to 1.21; p = 0.66).
-
Self-monitoring almost halved the risk of thromboembolic events in people with AHVs.
-
A statistically significantly greater reduction in thromboembolic events was observed among self-managed people than among those in self-testing.
-
Among people who self-monitored their therapy, there was a trend towards fewer thromboembolic events when compared with those who were managed by their GPs or physicians than those managed in specialised anticoagulation clinic. The subgroup analysis was not, however, statistically significant.
-
Self-monitoring significantly reduced the risk of mortality among people with AHVs but not among those with mixed clinical indication. There was lower all-cause mortality through self-management but not through self-testing. In particular, significantly fewer deaths were observed among people who self-managed their AOT than those who received primary standard care (control care by a GP or a physician).
-
Compared with standard care, self-monitoring (self-testing and self-management) did not demonstrate a significant reduction in the number of major and minor bleeding events.
-
In the majority of included trials (23 out of 26), the INR TTR was higher in self-monitoring people than in people receiving standard anticoagulation control, and in five of these trials there was a statistically significant difference between intervention groups.
-
The overall percentage of participants who completed self-monitoring was fairly high (at least 80%), and in the few trials that collected participant views, participants expressed high satisfaction and willingness to continue with the intervention at home.
-
Six of the trials were conducted in the UK and there was no evidence that the UK trial populations were importantly different from the rest of the included studies.
-
The majority of the trials (22 out of 26) investigated the use of the CoaguChek system, the results are, therefore, more robust for CoaguChek than for ProTime and INRatio.
-
Four of the 22 trials investigating the CoaguChek system used the CoaguChek XS system. There was insufficient evidence to determine whether or not the CoaguChek XS outcomes differed from those for previous versions of CoaguChek systems.
-
A brief overview of diagnostic performance of the various CoaguChek systems demonstrated that across several studies INR results were more accurate in adults and children when comparing CoaguChek XS with other CoaguChek models. We are of the opinion that this provides evidence that the clinical outcomes can be compared across different versions of the CoaguChek system.
Comparison with other studies
Our findings are in line with those of previously published systematic reviews on self-monitoring using point-of-care devices for the management of anticoagulation therapy, which found that self-monitoring was associated with a significantly lower incidence of thromboembolic events21,31,33,88,108,135–137 and deaths. 21,31,33,135–138
The results of the subgroup analyses according to the type of control care (for thromboembolic events and mortality) may be considered broadly in line with the current published evidence, which suggests that people managed by their GPs or physicians in primary care settings have poorer anticoagulation control than those managed in specialised anticoagulation clinics. 65,139
Cost-effectiveness
The base-case model assessed the impact on costs and outcomes of using self-monitoring to increase the number of INR tests performed annually (by 23), so as to improve INR control and prevent adverse outcomes. The primary findings are detailed below.
-
While self-monitoring (50% self-testing, 50% self-management) is likely to increase the INR monitoring cost compared with mixed primary/secondary care standard monitoring, it is likely to be cost-effective as a result of its impact on the incidence of thromboembolic events. This finding assumes that the pooled relative effects of self-testing and self-management, obtained from the meta-analysis of all RCTs, are applicable to the UK setting.
-
Underlying this general observation is the finding that the pooled effect estimate for self-testing on thromboembolic events is small and non-significant (RR 0.99), while the effect estimate for self-management is large (RR 0.51) and significant. Thus, within the base-case model, self-management alone is highly cost-effective (or dominant), while self-testing is not cost-effective.
-
In an alternative specification, the overall pooled effect estimates obtained from all self-testing and self-management trials were applied to both the self-testing and self-management strategies in the model. Under this scenario, both self-testing and self-management, with CoaguChek XS or INRatio2, were found to be dominant or highly cost-effective compared with standard monitoring.
-
Two key parameters underpinning the above findings are the baseline risk of thromboembolic events, and the relative effect of self-monitoring on these events. The model findings were robust to individual changes in these parameters through feasible ranges. However, when the lower baseline risk of thromboembolic events was combined with the upper confidence limit for the RR for associated self-management (RR 0.69), the ICERs for self-monitoring as a whole rose above £30,000 per QALY. The same was found when the lower baseline risk of thromboembolic events was coupled with the upper confidence limit of the pooled RR for self-monitoring as whole (RR 0.89). It should be noted, however, that self-management on its own remained cost saving under the former combined scenario.
-
Further uncertainty relates to the applicability of the pooled effect estimates to the UK setting. The few identified UK-based trials of self-monitoring versus standard practice did not demonstrate significant effects on thromboembolic or bleeding events. Applying these effect estimates, self-monitoring would not be cost-effective at the self-monitoring testing frequency observed in RCTs.
-
Alternative scenarios assessed the potential for self-monitoring to be cost-effective if used to replace clinic-based testing without increasing the frequency of testing. Under these scenarios, it was assumed that there would be no effect on the number of thromboembolic or bleeding events and a cost-minimisation approach was adopted. This showed that when holding all other base-case parameters constant, self-monitoring (50% self-testing, 50% self-managing) was more costly than standard primary care monitoring, but less costly than standard secondary care monitoring. These findings were, however, sensitive to the unit costs applied to standard care monitoring visits. Applying the alternative standard monitoring unit costs estimated by Jowett and colleagues,87 the opposite was observed, with self-monitoring dominating secondary care monitoring but being dominated by primary care monitoring.
Comparison with other economic evaluations
The findings of the model are generally consistent with those of previous evaluations, depending on the assumptions and input values applied. In line with previous models that have assumed or applied significant reductions in thromoembolic events with self-management,33,82,84,86,88 our model suggests that self-monitoring is likely to be cost-effective under this scenario.
Our model also produces findings that are generally consistent with the previous UK-based economic evaluations, in that self-monitoring (under base assumptions) will increase the monitoring costs to the NHS. However, our base case differs from previous UK evaluations in that the pooled relative effects for self-management and self-testing, compared with standard care, were applied. This results in significant future cost savings and quality-of-life gains from a significant reduction in the number of thromboembolic events. This in turn translates into more favourable estimates of cost-effectiveness. Further differences between the current analysis and the previous UK-based model include the application of higher standard secondary care monitoring costs, lower self-monitoring device costs (in line with current prices), and higher acute treatment costs for stroke and major bleeding events. Our analyses suggest that the cost-effectiveness of self-monitoring is robust to variations in these parameters when pooled clinical effect estimates are applied.
Uncertainties from the assessment
Clinical effectiveness
Although our assessment has been conducted according to current standards and recommendations, and is the most up-to-date review undertaken, we need to acknowledge some potential limitations and uncertainties. The areas of uncertainty were:
-
The included trials varied considerably in terms of clinical indications for anticoagulation therapy, type of control care, reporting structure for the time and/or values in therapeutic range, type and structure of the pre-intervention training and education programme, length of follow-up and methodological study quality. While the meta-analysis results demonstrated low statistical heterogeneity (which makes it statistically reasonable to combine the studies), there remains uncertainty around the fact that clinical heterogeneity could have over- or underestimated the effects.
-
Quantifying the impact of the potential risk of bias in the estimates was not possible. Only four trials55,61–63 were judged at low risk of bias. In some trials, outcomes were not assessed blinded, allocation of participants to intervention groups was not concealed, statistical analyses were not conducted according to an intention-to-treat principle, or many methodological details were lacking.
-
All included trials enrolled highly selected samples of people requiring anticoagulation therapy, and so it was uncertain whether or not there was strong external validity (i.e. applicability of the study results to the entire population of eligible participants). To be enrolled in the trials, participants needed to demonstrate adequate cognitive and physical abilities, as well as dexterity and confidence in using the point-of-care device. In some of the included trials,61,64,67,68 a considerable proportion of eligible participants (up to 50%) ultimately were not considered suitable for inclusion.
-
The frequency of testing was not consistently reported in the included studies. This hampered the possibility to conduct further analyses with regard to different monitoring strategies. The frequency of INR testing in the trials was generally weekly for self-monitoring participants and monthly in standard care. It was unclear what the optimal frequency might be, especially at long-term follow up where there was little evidence.
-
There remains some uncertainty on the applicability of the pooled results to the UK population. In our view, the greatest uncertainty relates to the applicability of the standard-care comparators in the trials and not to the participants in the trial.
-
The majority of the trials included participants with mixed clinical indications for anticoagulation therapy, which made it challenging to extrapolate the results to specific clinical populations. In particular, only limited data were available for people with atrial fibrillation and, consequently, no reliable conclusions could be drawn in relation to this patient population.
-
The majority of trials investigated the use of the CoaguChek system (22 out of 26) for the self-monitoring of anticoagulation therapy and it proved unfeasible to conduct reliable comparisons according to the type of point-of-care device. While the CoaguChek device has the most robust evidence, ProTime and, particularly, INRatio do not. Given the broadly similar performance of all the devices compared with the gold-standard laboratory test, we are of the opinion that it is not unreasonable to consider pooled estimates of effect across all studies and devices. However, this is an assumption that currently has no direct comparative evidence available and so a degree of caution is necessary.
-
The subgroup analysis according to the type of anticoagulation therapy management (self-management vs. self-testing) was limited due to the results being dominated by the largest trial published so far, THINRS,71 which enrolled 2922 people and assessed patient self-testing using the ProTime device versus routine clinical care. The trial results showed similar rates of main clinical outcomes between intervention groups with the exception of a small but significant improvement in the percentage of time in target range for self-testing people. It is worth pointing out that this trial had a highly specialised routine care and the longest follow-up period (mean 3 years). It is probable that the quality of the standard care in this trial exceeds current routine care for anticoagulation monitoring and the lack of significant differences between self-testing and routine monitoring could be explained by the rigorous criteria used to ensure high-standard care.
Cost-effectiveness
The model developed for this assessment has built upon previous models developed to assess the cost-effectiveness of INR self-monitoring strategies and new pharmaceuticals compared with warfarin therapy under standard INR monitoring arrangements. Where possible, the input parameter values used have previously been reviewed for NICE submissions by independent ERGs and accepted by appraisal committees. A further strength of the model comes through the dichotomisation of indication for warfarin use (atrial fibrillation/AHVs), mode of standard-care monitoring (primary/secondary care) and mode of self-monitoring (self-testing/self-management). This allowed assessment of cost-effectiveness by subgroups based on these indicators. Nevertheless, the main uncertainties are given below:
-
A weakness of the modelling relates to the uncertainty surrounding the pooled clinical effectiveness estimates (for self-testing and self-management) and, in particular, their applicability to the NHS setting.
-
A further weakness relates to the structural assumptions required to estimate cost-effectiveness in younger cohorts, i.e. those below the average age of cohorts used to inform the baseline risks of events and standardised mortality ratios associated with the clinical indications and adverse events. To reflect the importance of age as a risk factor for thromboembolic events, RRs by 5-year age bands were taken from a previous atrial fibrillation model92,96,97 and applied. Given a lack of similar evidence relating to people with a mechanical heart valve, the same RRs were also applied to this subgroup in the model. While this is not ideal, the model results were found to be robust to a range of alternative baseline risks when applied in isolation.
-
Owing to data limitations, very young cohorts were not formally included in subgroup analyses for the economic modelling. A sensitivity analysis was conducted to approximate the results for a cohort of children, but the estimates of baseline risk and self-monitoring effects were not well informed.
-
It should finally be noted that the perspective of the cost-effectiveness analysis was that of the NHS and personal social services. Therefore, our modelling does not capture any wider benefits or cost savings to patients and their families, such as a reduction in time spent travelling to and waiting in clinics.
Implications for research
Trials investigating the longer-term outcomes of self-management versus usual care are needed, and direct comparisons of the various point-of-care coagulometers ought to be incorporated into any future evaluation. The technology related to point-of-care testing devices is constantly changing and future research needs to target larger cohorts of people with different clinical indications requiring long-term anticoagulation therapy who may benefit from the use of these new generations of devices.
Acknowledgements
The authors would like to thank the investigators who kindly provided additional trials details, the NICE Assessment Subgroup specialist members (Dianna Oxley, Dianne Kitchen, Niall O’Keeffe, Peter Birtles, Peter MacCallum, Rishabh Prasad and Sue Rhodes) for their assistance with some queries related to the interventions and their use in clinical practice, Charles Boachie for statistical support and Lara Kemp for secretarial support. The Health Services Research Unit and Health Economics Research Unit, Institute of Applied Health Sciences, University of Aberdeen, are both core-funded by the Chief Scientist Office of the Scottish Government Health Directorates.
The views expressed in this report are those of the authors and not necessarily those of the Chief Scientist Office of the Scottish Government Health Directorates or of the NIHR HTA Programme. Any errors are the responsibility of the authors.
Contributions of authors
Pawana Sharma and Moira Cruickshank (Research Fellows) screened the search results, assessed full-text studies for inclusion, and undertook data extraction and quality assessment with assistance from Miriam Brazzelli (Senior Research Fellow).
Pawana Sharma reviewed the evidence on the clinical effectiveness of the target interventions.
Graham Scotland (Senior Health Economist) developed the economic model and conducted the economic evaluation.
Emma Tassie (Research Assistant) reviewed the evidence on the cost-effectiveness of the target interventions and contributed to the economic evaluation under the supervision of Graham Scotland.
Cynthia Fraser developed and ran the literature searches and provided information support to the appraisal.
Chris Burton and Bernard Croal provided expert advice on the clinical aspects of this appraisal.
Craig R Ramsay jointly co-ordinated the appraisal and commented on an early draft of this report.
Miriam Brazzelli oversaw and co-ordinated all aspects of this appraisal.
All authors commented on the final report.
Publication
Sharma P, Scotland G, Cruickshank M, Tassie E, Fraser C, Burton C, et al. Is self-monitoring an effective option for people receiving long-term vitamin K antagonist therapy? A systematic review and economic evaluation. BMJ Open 2015;5:e007758.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- National Insititute for Health and Care Excellence . Anticoagulation Therapy Service Commissioning Guide 2010. www.nice.org.uk/usingguidance/commissioningguides/anticoagulationtherapyservice/anticoagulationtherapyservice.jsp (accessed October 2013).
- Cayley J. Self-monitoring and self-management of anticoagulation therapy. Am Fam Physician 2011;84:266-8.
- Rose PE. Audit of anticoagulant therapy. J Clin Pathol 1996;49:5-9. http://dx.doi.org/10.1136/jcp.49.1.5.
- Ahmad Y, Lip GY, Lane DA. Recent developments in understanding epidemiology and risk determinants of atrial fibrillation as a cause of stroke. Can J Cardiol 2013;29:S4-13. http://dx.doi.org/10.1016/j.cjca.2013.03.009.
- Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 2001;285:2370-5. http://dx.doi.org/10.1001/jama.285.18.2370.
- Tamayo AE, Vergara-Mitxeltorena I, Uranga Saez del BE, Ostiza-Irigoyen A, Garcia-Carro A, Lopez-Fernandez I, et al. Oral anticoagulation and self-management: analysis of the factors that determine the feasibility of using self-testing and self-management in primary care. BMC Cardiovas Disord 2013;13. http://dx.doi.org/10.1186/1471-2261-13-59.
- Camm AJ, Kirchhof P, Lip GY, Schotten U, . European Association for Cardio-Thoracic Surgery . Guidelines for the management of atrial fibrillation: the task force for the management of atrial fibrillation of the European Society of Cardiology (ESC). Eur Heart J 2010;31:2369-429. http://dx.doi.org/10.1093/eurheartj/ehq278.
- Friberg L, Bergfeldt L. Atrial fibrillation prevalence revisited. J Intern Med 2013;274:461-8. http://dx.doi.org/10.1111/joim.12114.
- DeWilde S, Carey IM, Emmas C, Richards N, Cook DG. Trends in the prevalence of diagnosed atrial fibrillation, its treatment with anticoagulation and predictors of such treatment in UK primary care. Heart 2006;92:1064-70. http://dx.doi.org/10.1136/hrt.2005.069492.
- Kannel WB, Wolf PA, Benjamin EJ, Levy D. Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimates. Am J Cardiol 1998;82:2N-9N. http://dx.doi.org/10.1016/S0002-9149(98)00583-9.
- Sudlow M, Thomson R, Thwaites B, Rodgers H, Kenny RA. Prevalence of atrial fibrillation and eligibility for anticoagulants in the community. Lancet 1998;352:1167-71. http://dx.doi.org/10.1016/S0140-6736(98)01401-9.
- Dunning J, Nagendran M, Alfieri OR, Elia S, Kappetein AP, Lockowandt U, et al. Guideline for the surgical treatment of atrial fibrillation. Eur J Cardiothorac Surg 2013;44:777-91. http://dx.doi.org/10.1093/ejcts/ezt413.
- British Heart Foundation . Heart Valve Disease 2013. www.bhf.org.uk/heart-health/conditions/heart-valve-disease.aspx (accessed October 2013).
- Patient.co.uk . Aortic Stenosis 2013. www.patient.co.uk/health/aortic-stenosis (accessed October 2013).
- NHS Health and Social Care Information Centre . UK Heart Valve Registry 2010. http://docdat.ic.nhs.uk/DatabaseList.aspx (accessed October 2013).
- NHS Choices . Aortic Valve Replacement 2013. www.nhs.uk/conditions/Aorticvalvereplacement/Pages/Whatisitpage.aspx (accessed October 2013).
- Jones S, Monagle P, Manias E, Bruce AA, Newall F. Quality of life assessment in children commencing home INR self-testing. Thromb Res 2013;132:37-43. http://dx.doi.org/10.1016/j.thromres.2013.05.011.
- Pollack CV. Managing bleeding in anticoagulated patients in the emergency care setting. J Emerg Med 2013;45:467-77. http://dx.doi.org/10.1016/j.jemermed.2013.03.016.
- Fuster V, Ryden LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, et al. ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation. Circulation 2006;8:651-745.
- You JJ, Singer DE, Howard PA, Lane DA, Eckman MH, Fang MC, et al. Antithrombotic therapy for atrial fibrillation: antithrombotic therapy and prevention of thrombosis, 9th edn. American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012;141:e531S-75S.
- Connock M, Stevens C, Fry-Smith A, Jowett S, Fitzmaurice D, Moore D, et al. Clinical effectiveness and cost-effectiveness of different models of managing long-term oral anticoagulation therapy: a systematic review and economic modelling. Health Technol Assess 2007;11. http://dx.doi.org/10.3310/hta11380.
- British Heart Foundation . Atrial Fibrillation 2013. www.bhf.org.uk/heart-health/conditions/atrial-fibrillation.aspx (accessed October 2013).
- NHS Improvement . Atrial Fibrillation 2013. www.improvement.nhs.uk/heart/HeartImprovementHome/AtrialFibrillation/tabid/128/Default.aspx (accessed October 2013).
- Atrial Fibrillation. London: National Insititute for Health and Care Excellence; 2006.
- Health Improvement Scotland . SIGN 129 Antithrombotics: Indications and Management 2012. www.sign.ac.uk/pdf/SIGN129.pdf (accessed October 2013).
- Vahanian A, Baumgartner H, Bax J, Butchart E, Dion R, Filippatos G, et al. Guidelines on the management of valvular heart disease: the task force on the management of valvular heart disease of the European Society of Cardiology. Eur Heart J 2007;28:230-68.
- Systematic Reviews: CRD’s Guidance for Undertaking Systematic Reviews in Health Care. University of York: Centre for Reviews and Dissemination; 2009.
- Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration; 2011.
- National Institute for Health and Care Excellence . NICE Diagnostic Assessment Programme Manual 2011. www.nice.org.uk/media/A0B/97/DAPManualFINAL.pdf (accessed October 2013).
- Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group . Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006-12. http://dx.doi.org/10.1016/j.jclinepi.2009.06.005.
- Garcia-Alamino JM, Ward AM, Alonso-Coello P, Perera R, Bankhead C, Fitzmaurice D, et al. Self-monitoring and self-management of oral anticoagulation. Cochrane Database Syst Rev 2010;4. http://dx.doi.org/10.1002/14651858.CD003839.pub2.
- Brown A, Wells P, Jaffey J, McGahan L, Poon MC, Cimon K, et al. Point-of-Care Monitoring Devices for Long-Term Oral Anticoagulation Therapy: Clinical and Cost-Effectiveness. Ottawa, ON: Canadian Agency for Drugs and Technologies in Health; 2007.
- Gailly J, Gerkens S, van den Bruel A, Devriese S, Obyn C. Use of Point-of-Care Devices in Patients with Oral Anticoagulation: A Health Technology Assessment. Brussels: Belgian Health Care Knowledge Centre; 2009.
- Christensen TD, Larsen TB, Jensen C, Maegaard M, Sorensen B. International normalised ratio (INR) measured on the CoaguChek S and XS compared with the laboratory for determination of precision and accuracy. Thromb Haemostast 2009;101:563-9.
- Christensen TD, Larsen TB. Precision and accuracy of point-of-care testing coagulometers used for self-testing and self-management of oral anticoagulation therapy. J Thromb Haemostas 2012;10:251-60. http://dx.doi.org/10.1111/j.1538-7836.2011.04568.x.
- Sobieraj-Teague M, Daniel D, Farrelly B, Coghlan D, Gallus A. Accuracy and clinical usefulness of the CoaguChek S and XS Point of Care devices when starting warfarin in a hospital outreach setting. Thromb Res 2009;123:909-13. http://dx.doi.org/10.1016/j.thromres.2008.10.006.
- CoaguChek® XS System (Patient Self-Testing): Substantial Equivalence Determination Decision Summary 510(k)062925. Silver Spring, MD: US Food and Drug Administration Agency; 2007.
- Alere INRatio®2 PT/INR Home Monitoring System: Substantial Equivalence Determination Decision Summary 510(k)110212. Silver Spring, MD: US Food and Drug Administration Agency; 2012.
- ProTime Microcoagulation System: Substantial Equivalence Determination Decision Summary 510(k)010599. Silver Spring, MD: US Food and Drug Administration Agency; 2001.
- Patient Self-Testing Using the Roche Coaguchek S. London: Medicines and Healthcare products Regulatory Agency; 2004.
- Point-of-Care Testing: A Review of Systematic Reviews on Testing Accuracy and Cost-Effectiveness. Ottawa, ON: Canadian Agency for Drugs and Technologies in Health; 2012.
- Ansell J, Jacobson A, Levy J, Voller H, Hasenkam JM. International Self-Monitoring Association for Oral Anticoagulation . Guidelines for implementation of patient self-testing and patient self-management of oral anticoagulation. International consensus guidelines prepared by International Self-Monitoring Association for Oral Anticoagulation. Int J Cardiol 2005;99:37-45. http://dx.doi.org/10.1016/j.ijcard.2003.11.008.
- Bauman ME, Black KL, Massicotte MP, Bauman ML, Kuhle S, Howlett-Clyne S, et al. Accuracy of the CoaguChek XS for point-of-care international normalized ratio (INR) measurement in children requiring warfarin. Thromb Haemostas 2008;99:1097-103. http://dx.doi.org/10.1160/TH07-10-0634.
- Bereznicki LR, Jackson SL, Peterson GM, Jeffrey EC, Marsden KA, Jupe DM. Accuracy and clinical utility of the CoaguChek XS portable international normalised ratio monitor in a pilot study of warfarin home-monitoring. J Clin Pathol 2007;60:311-14. http://dx.doi.org/10.1136/jcp.2006.037820.
- Gardiner C, Williams K, Mackie IJ, Machin SJ, Cohen H. Patient self-testing is a reliable and acceptable alternative to laboratory INR monitoring. Br J Haematol 2005;128:242-7. http://dx.doi.org/10.1111/j.1365-2141.2004.05300.x.
- Havrda DE, Hawk TL, Marvin CM. Accuracy and precision of the CoaguChek S versus laboratory INRs in a clinic. Ann Pharmacother 2002;36:769-75. http://dx.doi.org/10.1345/aph.1A310.
- Hentrich DP, Fritschi J, Muller PR, Wuillemin WA. INR comparison between the CoaguChek S and a standard laboratory method among patients with self-management of oral anticoagulation. Thromb Res 2007;119:489-95. http://dx.doi.org/10.1016/j.thromres.2006.04.003.
- Jackson SL, Bereznicki LR, Peterson GM, Marsden KA, Jupe DM, Vial JH, et al. Accuracy and clinical usefulness of the near-patient testing CoaguChek S international normalised ratio monitor in rural medical practice. Aust J Rural Health 2004;12:137-42. http://dx.doi.org/10.1111/j.1440-1854.2004.00585.x.
- Kitchen S, Kitchen D, Jennings I, Woods T, Walker I. External quality assessment of CoaguChek point-of-care testing prothrombin time/international ratio monitors. Am J Clin Pathol 2008;129:825-6.
- Moon JR, Jeong SI, Huh J, Lee HJ, Park PW, Kang IS. Accuracy of CoaguChek XS for point-of-care antithrombotic monitoring in children with heart disease. Ann Clin Lab Sci 2010;40:247-51.
- Braun S, Watzke H, Hasenkam JM, Schwab M, Wolf T, Dovifat C, et al. Performance evaluation of the new CoaguChek XS system compared with the established CoaguChek system by patients experienced in INR-self management. Thromb Haemostas 2007;97:310-14.
- Paioni P, Kroiss S, Kagi E, Bergstrasser E, Fasnacht M, Bauersfeld U, et al. Self-monitoring of oral anticoagulation therapy in children. Acta Haematol 2009;122:58-63. http://dx.doi.org/10.1159/000243726.
- Williams VK, Griffiths AB. Acceptability of CoaguChek S and CoaguChek XS generated international normalised ratios against a laboratory standard in a paediatric setting. Pathology 2007;39:575-9. http://dx.doi.org/10.1080/00313020701684797.
- Ryan F, O’Shea S, Ortel TL, Byrne S. The reliability of point-of-care (POC) prothrombin time testing: a comparison of CoaguChek XS(R) INR measurements with hospital laboratory monitoring. Blood 2007;110.
- Bauman ME, Black K, Bauman ML, Bruce AA, Kuhle S, Bajzar L, et al. EMPoWarMENT: Edmonton pediatric warfarin self-management pilot study in children with primarily cardiac disease. Thromb Res 2010;126:e110-15. http://dx.doi.org/10.1016/j.thromres.2010.05.024.
- Gardiner C, Williams K, Longair I, Mackie IJ, Machin SJ, Cohen H. A randomised control trial of patient self-management of oral anticoagulation compared with patient self-testing. Br J Haematol 2006;132:598-603. http://dx.doi.org/10.1111/j.1365-2141.2005.05899.x.
- Hemkens LG, Hilden KM, Hartschen S, Kaiser T, Didjurgeit U, Hansen R, et al. A randomized trial comparing INR monitoring devices in patients with anticoagulation self-management: evaluation of a novel error-grid approach. J Thromb Thrombolysis 2008;26:22-30. http://dx.doi.org/10.1007/s11239-007-0070-4.
- Rasmussen RS, Corell P, Madsen P, Overgaard K. Effects of computer-assisted oral anticoagulant therapy. Thrombosis J 2012;10. http://dx.doi.org/10.1186/1477-9560-10-17.
- Horstkotte D, Piper C, Wiemer M, Schulte H.D. Improvement of prognosis by home prothrombin estimation In patients with life-long anticoagulant therapy. Eur Heart J 1996;17.
- Völler H, Glatz J, Taborski U, Bernardo A, Dovifat C, Heidinger K. Self-management of oral anticoagulation in nonvalvular atrial fibrillation (SMAAF study). Zeitschrift für Kardiologie 2005;94:182-6. http://dx.doi.org/10.1007/s00392-005-0199-0.
- Menéndez-Jándula JB, Souto JC, Oliver A, Montserrat I, Quintana M, Gich I, et al. Comparing self-management of oral anticoagulant therapy with clinic management: a randomized trial. Ann Intern Med 2005;142:1-10. http://dx.doi.org/10.7326/0003-4819-142-1-200501040-00006.
- Ryan F, Byrne S, O’Shea S. Randomized controlled trial of supervised patient self-testing of warfarin therapy using an internet-based expert system. J Thromb Haemost 2009;7:1284-90. http://dx.doi.org/10.1111/j.1538-7836.2009.03497.x.
- Siebenhofer A, Rakovac I, Kleespies C, Piso B, Didjurgeit U. SPOG 6 . Self-management of oral anticoagulation reduces major outcomes in the elderly. A randomized controlled trial. Thromb Haemost 2008;100:1089-98.
- Fitzmaurice DA, Murray ET, McCahon D, Holder R, Raftery JP, Hussain S, et al. Self management of oral anticoagulation: randomised trial. BMJ 2005;331. http://dx.doi.org/10.1136/bmj.38618.580903.AE.
- Sunderji R, Gin K, Shalansky K, Carter C, Chambers K, Davies C, et al. A randomized trial of patient self-managed versus physician-managed oral anticoagulation. Can J Cardiol 2004;20:1117-23.
- Christensen TD. Self-management of oral anticoagulation therapy – methodological and clinical aspects. Dan Med Bull 2011;58.
- Fitzmaurice DA, Murray ET, Gee KM, Allan TF, Hobbs FD. A randomised controlled trial of patient self management of oral anticoagulation treatment compared with primary care management. J Clin Pathol 2002;55:845-9. http://dx.doi.org/10.1136/jcp.55.11.845.
- Gadisseur AP, Breukink-Engbers WG, Meer FJ, Besselaar AM, Sturk A, Rosendaal FR. Comparison of the quality of oral anticoagulant therapy through patient self-management and management by specialized anticoagulation clinics in the Netherlands: a randomized clinical trial. Arch Intern Med 2003;163:2639-46. http://dx.doi.org/10.1001/archinte.163.21.2639.
- Khan TI, Kamali F, Kesteven P, Avery P, Wynne H. The value of education and self-monitoring in the management of warfarin therapy in older patients with unstable control of anticoagulation. Br J Haematol 2004;126:557-64. http://dx.doi.org/10.1111/j.1365-2141.2004.05074.x.
- Körtke H, Minami K, Breymann T, Seifert D, Baraktaris A, Wagner O, et al. INR self-management after mechanical heart valve replacement: ESCAT (Early Self-Controlled Anticoagulation Trial). Z Kardiol 2001;90:VI/118-24. http://dx.doi.org/10.1007/s003920170019.
- Matchar DB, Jacobson A, Dolor R, Edson R, Uyeda L, Phibbs CS, et al. Effect of home testing of international normalized ratio on clinical events. N Engl J Med 2010;363:1608-20. http://dx.doi.org/10.1056/NEJMoa1002617.
- Sawicki PT. A structured teaching and self-management program for patients receiving oral anticoagulation: a randomized controlled trial. Working Group for the Study of Patient Self-Management of Oral Anticoagulation. JAMA 1999;281:145-50. http://dx.doi.org/10.1001/jama.281.2.145.
- Sidhu P, O’Kane HO. Self-managed anticoagulation: results from a two-year prospective randomized trial with heart valve patients. Ann Thorac Surg 2001;72:1523-7. http://dx.doi.org/10.1016/S0003-4975(01)03049-1.
- Verret L, Couturier J, Rozon A, Saudrais-Janecek S, St-Onge A, Nguyen A, et al. Impact of a pharmacist-led warfarin self-management program on quality of life and anticoagulation control: a randomized trial. Pharmacotherapy 2012;32:871-9. http://dx.doi.org/10.1002/j.1875-9114.2012.01116.
- Christensen TD, Maegaard M, Sorensen HT, Hjortdal VE, Hasenkam JM. Self-management versus conventional management of oral anticoagulant therapy: a randomized, controlled trial. Eur J Intern Med 2006;17:260-6. http://dx.doi.org/10.1016/j.ejim.2005.11.021.
- Cromheecke ME, Levi M, Colly LP, Mol BJ, Prins MH, Hutten BA, et al. Oral anticoagulation self-management and management by a specialist anticoagulation clinic: a randomised cross-over comparison. Lancet 2000;356:97-102. http://dx.doi.org/10.1016/S0140-6736(00)02470-3.
- Azarnoush K, Camilleri L, Aublet-Cuvelier B, Geoffroy E, Dauphin C, Dubray C, et al. Results of the first randomised French study evaluating self-testing of the International Normalized Ratio. J Heart Valve Dis 2011;20:518-25.
- Eitz T, Schenk S, Fritzsche D, Bairaktaris A, Wagner O, Koertke H, et al. International normalized ratio self-management lowers the risk of thromboembolic events after prosthetic heart valve replacement. Ann Thorac Surg 2008;85:949-54. http://dx.doi.org/10.1016/j.athoracsur.2007.08.071.
- Soliman Hamad MA, van Eekelen E, van Agt T, van Straten AH. Self-management program improves anticoagulation control and quality of life: a prospective randomized study. Eur J Cardiothorac Surg 2009;35:265-9. http://dx.doi.org/10.1016/j.ejcts.2008.10.020.
- Gadisseur AP, Kaptein AA, Breukink-Engbers WG, Meer FJ, Rosendaal FR. Patient self-management of oral anticoagulant care vs. management by specialized anticoagulation clinics: positive effects on quality of life. J Thrombo Haemostas 2004;2:584-91. http://dx.doi.org/10.1111/j.1538-7836.2004.00659.x.
- Siebenhofer A, Rakovac I, Kleespies C, Piso B, Didjurgeit U. Self-management of oral anticoagulation in the elderly: rationale, design, baselines and oral anticoagulation control after one year of follow-up. A randomized controlled trial. Thromb Haemost 2007;97:408-16.
- Taborski U, Wittstamm FJ, Bernardo A. Cost-effectiveness of self-managed anticoagulant therapy in Germany. Semin Thromb Hemost 1999;25:103-7. http://dx.doi.org/10.1055/s-2007-996432.
- Lafata JE, Martin SA, Kaatz S, Ward RE. The cost-effectiveness of different management strategies for patients on chronic warfarin therapy. J Gen Intern Med 2000;15:31-7. http://dx.doi.org/10.1046/j.1525-1497.2000.01239.x.
- Muller E, Bergemann R. GELIA Study Group . Economic analysis of bleeding and thromboembolic sequelae after heart valve replacement (GELIA 7). Eur Heart J Suppl 2001;3:Q65-9. http://dx.doi.org/10.1016/S1520-765X(01)90046-X.
- Sola-Morales O. Portable Coagulometers: Revision of the Scientific Evidence and Economic Assessment of Their Use in Self-Control of Oral Anticoagulant Treatment. Barcelona: Catalan Agency for Health Technology Assessment and Research (CAHTA); 2003.
- Regier DA, Sunderji R, Lynd LD, Gin K, Marra CA. Cost-effectiveness of self-managed versus physician-managed oral anticoagulation therapy. CMAJ 2006;174:1847-52. http://dx.doi.org/10.1503/cmaj.051104.
- Jowett S, Bryan S, Murray E, McCahon D, Raftery J, Hobbs FD, et al. Patient self-management of anticoagulation therapy: a trial-based cost-effectiveness analysis. Br J Haematol 2006;134:632-9. http://dx.doi.org/10.1111/j.1365-2141.2006.06243.x.
- Point-of-Care International Normalized Ratio (INR) Monitoring Devices for Patients on Long-term Oral Anticoagulation Therapy. Toronto, ON: Medical Advisory Secretariat Ministry of Health and Long-Term Care; 2009.
- Horstkotte D, Bergemann R, Althaus U, Babin-Ebell J, Chares M, Dahm M, et al. German experience with low intensity anticoagulation (GELIA): protocol of a multi-centre randomzsed, prospective study with the St. Jude Medical valve. J Heart Valve Dis 1993;2:411-19.
- Visnansky M, Mesaros S. Patient self-testing of oral anticoagulation therapy by CoaguChek® XS system. Rapid health technology assessment in Slovak health care environment. Value Health 2011;14:A257-8. http://dx.doi.org/10.1016/j.jval.2011.08.146.
- Schmidt LJ, Habacher W, Koenig C, Beck P. PCV44 Cost-utility associated with different monitoring strategies among patients receiving long-term oral anticoagulation therapy in Austria. Value Health 2011;14. http://dx.doi.org/10.1016/j.jval.2011.08.765.
- Rivaroxaban for the Prevention of Stroke and Systemic Embolism in People with Atrial Fibrillation. London: National Insititute for Health and Care Excellence; 2012.
- Dabigatran Etexilate for the Prevention of Stroke and Systemic Embolism in Atrial Fibrillation. London: National Insititute for Health and Care Excellence; 2012.
- NHS Reference Costs 2011–12. London: Department of Health; 2012.
- Curtis L. Unit Costs of Health and Social Care 2012. Canterbury: Personal Social Services Research Unit; 2012.
- Bayer PLC. Single Technology Appraisal (STA) of Rivaroxaban (Xarelto®). London: National Institute for Health and Care Excellence; 2011.
- Edwards S, Hamilton V, Nherera L, Trevor N, Barton S. Rivaroxaban for the Prevention of Stroke and Systemic Embolism in People with Atrial Fibrillation. National Insititute for Health and Care Excellence; 2011.
- ROCKET AF Study Investigators . Rivaroxaban-Once daily, oral, direct factor Xa inhibition Compared with vitamin K antagonism for prevention of stroke and Embolism Trial in Atrial Fibrillation: rationale and design of the ROCKET AF study. Am Heart J 2010;159:340-7. http://dx.doi.org/10.1016/j.ahj.2009.11.025.
- Wallentin L, Yusuf S, Ezekowitz MD, Alings M, Flather M, Franzosi MG, et al. Efficacy and safety of dabigatran compared with warfarin at different levels of international normalised ratio control for stroke prevention in atrial fibrillation: an analysis of the RE-LY trial. Lancet 2010;376:975-83. http://dx.doi.org/10.1016/S0140-6736(10)61194-4.
- Wallentin L, Lopes RD, Hanna M, Thomas L, Hellkamp A, Nepal S, et al. Efficacy and safety of apixaban compared with warfarin at different levels of predicted international normalized ratio control for stroke prevention in atrial fibrillation. Circulation 2013;127:2166-76. http://dx.doi.org/10.1161/CIRCULATIONAHA.112.142158.
- Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009;361:1139-51. http://dx.doi.org/10.1056/NEJMoa0905561.
- Lee S, Monz BU, Clemens A, Brueckmann M, Lip GYH. Representativeness of the dabigatran, apixaban and rivaroxaban clinical trial populations to real-world atrial fibrillation patients in the United Kingdom: a cross-sectional analysis using the General Practice Research Database. BMJ Open 2012;2. http://dx.doi.org/10.1136/bmjopen-2012-001768.
- Gallagher AM, Setakis E, Plumb JM, Clemens A, van Staa TP. Risks of stroke and mortality associated with suboptimal anticoagulation in atrial fibrillation patients. Thromb Haemost 2011;106:968-77. http://dx.doi.org/10.1160/TH11-05-0353.
- Hylek EM, Go AS, Chang Y, Jensvold NG, Henault LE, Selby JV, et al. Effect of intensity of oral anticoagulation on stroke severity and mortality in atrial fibrillation. N Engl J Med 2003;349:1019-26. http://dx.doi.org/10.1056/NEJMoa022913.
- Atrial Fibrillation – Dabigatran Etexilate: Boehringer Ingelheim Submission. London: National Insititute for Health and Care Excellence; 2011.
- Wang TJ, Massaro JM, Levy D, Vasan RS, Wolf PA, D’Agostino RB, et al. A risk score for predicting stroke or death in individuals with new-onset atrial fibrillation in the community: the Framingham Heart Study. JAMA 2003;290:1049-56. http://dx.doi.org/10.1001/jama.290.8.1049.
- Hobbs FD, Fitzmaurice DA, Mant J, Murray E, Jowett S, Bryan S, et al. A randomised controlled trial and cost-effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in people aged 65 and over. The SAFE study. Health Technol Assess 2005;9. http://dx.doi.org/10.3310/hta9400.
- Heneghan C, Ward A, Perera R, Bankhead C, Fuller A, Stevens R, et al. Self-monitoring of oral anticoagulation: systematic review and meta-analysis of individual patient data. Lancet 2012;379:322-34. http://dx.doi.org/10.1016/S0140-6736(11)61294-4.
- Ruel M, Masters RG, Rubens FD, Bedard PJ, Pipe AL, Goldstein WG, et al. Late incidence and determinants of stroke after aortic and mitral valve replacement. Ann Thorac Surg 2004;78:77-83. http://dx.doi.org/10.1016/j.athoracsur.2003.12.058.
- Ascione R, Culliford L, Rogers CA, Wild J, Narajan P, Angelini GD. Mechanical heart valves in septuagenarians. J Card Surg 2008;23:8-16. http://dx.doi.org/10.1111/j.1540-8191.2007.00504.x.
- Sundberg G, Bagust A, Terent A. A model for costs of stroke services. Health Policy 2003;63:81-94. http://dx.doi.org/10.1016/S0168-8510(02)00055-6.
- Bronnum-Hansen H, Davidsen M, Thorvaldsen P. Danish MONICA Study Group . Long-term survival and causes of death after stroke. Stroke 2001;32:2131-6. http://dx.doi.org/10.1161/hs0901.094253.
- Friberg L, Hammar N, Pettersson H, Rosenqvist M. Increased mortality in paroxysmal atrial fibrillation: report from the Stockholm Cohort-Study of Atrial Fibrillation (SCAF). Eur Heart J 2007;28:2346-53. http://dx.doi.org/10.1093/eurheartj/ehm308.
- Kvidal P, Bergstrom R, Horte LG, Stahle E. Observed and relative survival after aortic valve replacement. J Am Coll Cardiol 2000;35:747-56. http://dx.doi.org/10.1016/S0735-1097(99)00584-7.
- Slot KB, Berge E, Dorman P, Lewis S, Dennis M, Sandercock P, et al. Impact of functional status at six months on long term survival in patients with ischaemic stroke: prospective cohort studies. BMJ 2008;336:376-9. http://dx.doi.org/10.1136/bmj.39456.688333.BE.
- Deaths Registered in England and Wales, 2011. London: Office for National Statistics; 2012.
- Interim Life Tables, England and Wales, 2009–2011. London: Office for National Statistics; 2013.
- Spackman E, Burch J, Faria R, Corbacho B, Fox D, Woolacott N. Dabigatran Etexilate for the Prevention of Stroke and Systemic Embolism in Atrial Fibrillation: Evidence Review Group Report. London: National Insititute for Health and Care Excellence; 2011.
- TA249 Atrial Fibrillation – Dabigatran Etexilate: Costing Template. London: National Institute for Health and Care Excellence; 2012.
- Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the Economic Evaluation of Health Care Programmes. Oxford: Oxford University Press; 2005.
- Jones M, McEwan P, Morgan CL, Peters JR, Goodfellow J, Currie CJ. Evaluation of the pattern of treatment, level of anticoagulation control, and outcome of treatment with warfarin in patients with non-valvar atrial fibrillation: a record linkage study in a large British population. Heart 2005;91:472-7. http://dx.doi.org/10.1136/hrt.2004.042465.
- Point of Care Coagulometers for Monitoring Oral Anticoagulation: Buyers’ Guide. NHS Purchasing and Supply Agency Centre for Evidence-based Purchasing; 2008.
- Murray E, Fitzmaurice D, McCahon D, Fuller C, Sandhur H. Training for patients in a randomised controlled trial of self management of warfarin treatment. BMJ 2004;328:437-8. http://dx.doi.org/10.1136/bmj.328.7437.437.
- Saka O, McGuire A, Wolfe C. Cost of stroke in the United Kingdom. Age Ageing 2009;38:27-32. http://dx.doi.org/10.1093/ageing/afn281.
- Wardlaw JM, Chappell FM, Stevenson M, De NE, Thomas S, Gillard J, et al. Accurate, practical and cost-effective assessment of carotid stenosis in the UK. Health Technol Assess 2006;10. http://dx.doi.org/10.3310/hta10300.
- Venous Thromboembolism – Reducing the Risk. London: National Insititute for Health and Care Excellence; 2010.
- Hallan S, Asberg A, Indredavik B, Wideroe TE. Quality of life after cerebrovascular stroke: a systematic study of patients’ preferences for different functional outcomes. J Intern Med 1999;246:309-16. http://dx.doi.org/10.1046/j.1365-2796.1999.00531.x.
- Dorman P, Dennis M, Sandercock P. Are the modified ‘simple questions’ a valid and reliable measure of health related quality of life after stroke? United Kingdom Collaborators in the International Stroke Trial. J Neurol Neurosurg Psychiatry 2000;69:487-93. http://dx.doi.org/10.1136/jnnp.69.4.487.
- International Stroke Trial Collaborative Group . The International Stroke Trial (IST): a randomised trial of aspirin, subcutaneous heparin, both, or neither among 19435 patients with acute ischaemic stroke. Lancet 1997;349:1569-81. http://dx.doi.org/10.1016/S0140-6736(97)04011-7.
- Kind P, Hardman G, Macran S. UK Population Norms for EQ-5D. University of York: Centre for Health Economics; 1999.
- Robinson A, Thomson R, Parkin D, Sudlow M, Eccles M. How patients with atrial fibrillation value different health outcomes: a standard gamble study. J Health Serv Res Policy 2001;6:92-8. http://dx.doi.org/10.1258/1355819011927288.
- Sullivan PW, Arant TW, Ellis SL, Ulrich H. The cost-effectiveness of anticoagulation management services for patients with atrial fibrillation and at high risk of stroke in the US. Pharmacoeconomics 2006;24:1021-33. http://dx.doi.org/10.2165/00019053-200624100-00009.
- Briggs A, Sculpher M, Claxton K. Decision Modelling for Health Economic Evaluation. Oxford: Oxford University Press; 2006.
- Marini C, Totaro R, Carolei A. Long-term prognosis of cerebral ischemia in young adults. National Research Council Study Group on stroke in the young. Stroke 1999;30:2320-5. http://dx.doi.org/10.1161/01.STR.30.11.2320.
- Wells PS, Brown A, Jaffey J, McGahan L, Poon MC, Cimon K. Safety and effectiveness of point-of-care monitoring devices in patients on oral anticoagulant therapy: a meta-analysis. Open Medicine 2007;1:E131-46.
- Bloomfield HE, Krause A, Greer N, Taylor BC, MacDonald R, Rutks I, et al. Meta-analysis: effect of patient self-testing and self-management of long-term anticoagulation on major clinical outcomes. Ann Intern Med 2011;154:472-82. http://dx.doi.org/10.7326/0003-4819-154-7-201104050-00005.
- Heneghan C, Alonso-Coello P, Garcia-Alamino JM, Perera R, Meats E, Glasziou P. Self-monitoring of oral anticoagulation: a systematic review and meta-analysis. Lancet 2006;367:404-11. http://dx.doi.org/10.1016/S0140-6736(06)68139-7.
- Christensen TD, Johnsen SP, Hjortdal VE, Hasenkam JM. Self-management of oral anticoagulant therapy: a systematic review and meta-analysis. Int J Cardiol 2007;118:54-61. http://dx.doi.org/10.1016/j.ijcard.2006.06.018.
- van WC, Jennings A, Oake N, Fergusson D, Forster AJ. Effect of study setting on anticoagulation control: a systematic review and metaregression. Chest 2006;129:1155-66. http://dx.doi.org/10.1378/chest.129.5.1155.
- Dauphin C, Legault B, Jaffeux P, Motreff P, Azarnoush K, Joly H, et al. Comparison of INR stability between self-monitoring and standard laboratory method: preliminary results of a prospective study in 67 mechanical heart valve patients. Arch Cardiovasc Dis 2008;101:753-61. http://dx.doi.org/10.1016/j.acvd.2008.10.007.
- Bauman ME, Conroy S, Massicotte MP. Point-of-care INR measurement in children requiring warfarin: what has been evaluated and future directions. Pediatr Health 2008;2:651-9. http://dx.doi.org/10.2217/17455111.2.5.651.
- Christensen TD, Maegaard M, Sorensen HT, Hjortdal VE, Hasenkam JM. Self- versus conventional management of oral anticoagulant therapy: effects on INR variability and coumarin dose in a randomized controlled trial. Am J Cardiovasc Drug 2007;7:191-7. http://dx.doi.org/10.2165/00129784-200707030-00005.
- Koertke H, Zittermann A, Mommertz S, El AM, Litmathe J, Koerfer R. The bad oeynhausen concept of INR self-management. J Thromb Thrombolysis 2005;19:25-31. http://dx.doi.org/10.1007/s11239-005-0937-1.
- Fitzmaurice DA, Hobbs FD, Murray ET, Holder RL, Allan TF, Rose PE. Oral anticoagulation management in primary care with the use of computerized decision support and near-patient testing: a randomized, controlled trial. Arch Intern Med 2000;160:2343-8. http://dx.doi.org/10.1001/archinte.160.15.2343.
- McCahon D, Fitzmaurice DA, Murray ET, Fuller CJ, Hobbs RF, Allan TF, et al. SMART: Self-Management of Anticoagulation, a Randomised Trial [ISRCTN19313375]. BMC Fam Pract 2003;4. http://dx.doi.org/10.1186/1471-2296-4-11.
- Horstkotte D, Piper C, Wiemer M. Optimal frequency of patient monitoring and intensity of oral anticoagulation therapy in valvular heart disease. J Thromb Thrombolysis 1998;5:19-24. http://dx.doi.org/10.1023/A:1013228718768.
- Koertke H, Minami K, Bairaktaris A, Wagner O, Koerfer R. INR self-management following mechanical heart valve replacement. J Thromb Thrombolysis 2000;9:S41-5. http://dx.doi.org/10.1023/A:1018712520472.
- Koertke H, Zittermann A, Wagner O, Koerfer R. Self-management of oral anticoagulation therapy improves long-term survival in patients with mechanical heart valve replacement. Ann Thorac Surg 2007;83:24-9. http://dx.doi.org/10.1016/j.athoracsur.2006.08.036.
- Körtke H, Körfer R. International normalized ratio self-management after mechanical heart valve replacement: is an early start advantageous?. Ann Thorac Surg 2001;72:44-8. http://dx.doi.org/10.1016/S0003-4975(01)02656-X.
- Matchar DB, Jacobson AK, Edson RG, Lavori PW, Ansell JE, Ezekowitz MD, et al. The impact of patient self-testing of prothrombin time for managing anticoagulation: rationale and design of VA cooperative study #481 – The Home INR Study (THINRS). J Thromb Thrombolysis 2005;19:163-72. http://dx.doi.org/10.1007/s11239-005-1452-0.
- Matchar DB, Dolor R, Jacobson A, Love S, Edson R, Uyeda L. More frequent self-testing of prothrombin time results in improved time in target range. Circulation 2012;126.
- Ryan F, O’Shea S, Byrne S. The ‘carry-over’ effects of patient self-testing: positive effects on usual care management by an anticoagulation management service. Thromb Res 2010;126:e345-8. http://dx.doi.org/10.1016/j.thromres.2010.08.001.
- Sawicki PT, Glaser B, Kleespies C, Stubbe J, Schmitz N, Kaiser T, et al. Long-term results of patients’ self-management of oral anticoagulation. J Clin Basic Cardiol 2003;6:59-62.
- Sunderji R, Campbell L, Shalansky K, Fung A, Carter C, Gin K. Outpatient self-management of warfarin therapy: a pilot study. Pharmacotherapy 1999;19:787-93. http://dx.doi.org/10.1592/phco.19.9.787.31546.
- Voller H, Glatz J, Taborski U, Bernardo A, Dovifat C, Burkard G, et al. Background and evaluation plan of a study on self-management of anticoagulation in patients with non-valvular atrial fibrillation (SMAAF Study). Z Kardiol 2000;89:284-8.
Appendix 1 Search strategies
Point-of-care tests for coagulation self-monitoring: clinical effectiveness
EMBASE
Searched: 1980 to week 22 2013.
Ovid MEDLINE(R)
Searched: 1946 to week 5 May 2013.
Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations
Searched: 5 June 2013.
OVID Multifile searched
Searched: 5 June 2013.
URL: https://shibboleth.ovid.com/
Search strategy
-
exp 4-Hydroxycoumarins/ use mesz
-
exp coumarin anticoagulant/ use emez
-
antivitamin k/ use emez
-
warfarin.tw
-
vitamin k antagonist$.tw.
-
*anticoagulants/ad use mesz
-
*anticoagulant agent/ad use emez
-
Prothrombin Time/
-
prothrombin time.tw.
-
or/1-9
-
Self Administration/ use mesz
-
Self Care/
-
Self-monitoring/ use emez or Home Monitoring/ use emez
-
point-of-care systems/
-
poc.tw
-
point-of-care.tw.
-
(((patient$ or self) adj1 (monitor$ or manag$ or measur$)) or (self adj1 test$)).tw.
-
or/11-17
-
10 and 18
-
coaguche?k$.tw,dv
-
INRatio$.tw,dv
-
(ProTime$ or pro time$).tw,dv
-
coagulometer$.tw.
-
or/19-23
-
randomized controlled trial.pt.
-
controlled clinical trial.pt.
-
exp clinical trial/ use emez
-
randomization/ use emez
-
randomi?ed.ab.
-
drug therapy.fs.
-
randomly.ab.
-
trial.ab.
-
groups.ab.
-
or/25-33
-
exp animals/ not humans/
-
34 not 35
-
19 and 36
-
limit 37 to yr="2007 -Current"
-
(coaguche?k$ or INRatio$ or ProTime$ or pro time$).tw,dv.
-
38 or 39
-
limit 40 to english language
-
41 not conference abstract.pt
-
41 and conference abstract.pt. and ("2012" or "2013").yr.
-
42 or 43
-
remove duplicates from 44
Science Citation Index
Searched: 1970 to 5 June 2013.
BIOSIS
Searched: 1956 to 5 June 2013.
Conference Proceedings Citation Index – Science
Searched: 2012 to 5 June 2013.
ISI Web of Knowledge
Searched: 5 June 2013.
Search strategy
# 1 TS=anticoagulant*
# 2 TS=vitamin k antagonist*
# 3 TS=warfarin
# 4 TS=prothrombin time
# 5 #1 or #2 or #3 or #4
# 6 TS= ((patient* or self) N1 (monitor* or manag* or measur*))
# 7 TS=(self N1 test*)
# 8 TS=poc
# 9 TS=point-of-care
# 10 #9 or #8 OR #7 OR #6
# 11 #10 AND #5
# 12 TS=(CoaguChek* OR CoaguChek*)
# 13 TS=(INRatio* OR ProTime*)
# 14 #13 OR #12 OR #11
# 15 (#14) AND Language=(English) AND Document Types=(Article) Timespan=2007-2013
# 16 (#14) AND Language=(English) AND Document Types=(Meeting Abstract) Timespan=2012-201
# 17 #16 OR #15 Timespan=2007-2013
The Cochrane Library, Issue 4, 2013 (Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, Database of Abstracts of Review of Effects, HTA database)
Searched: May 2013.
URL: www3.interscience.wiley.com/
Search strategy
#1 MeSH descriptor: [4-Hydroxycoumarins] explode all trees
#2 warfarin or vitamin k antagonist*:ti,ab,kw
#3 MeSH descriptor: [Anticoagulants] this term only and with qualifiers: [Administration & dosage - AD]
#4 international normali?ed ratio?:ti,ab,kw
#5 #1 or #2 or #3 or #4
#6 MeSH descriptor: [Self Administration] explode all trees
#7 MeSH descriptor: [Self Care] explode all trees
#8 MeSH descriptor: [Point-of-Care Systems] this term only
#9 poc:ti,ab,kw
#10 (patient near/3 (monitor or manage or measure)):ti,ab,kw
#11 (self near/3 (manage or monitor or measure)):ti,ab,kw
#12 #6 or #7 or #8 or #9 or #10 or #11
#13 #5 and #12
#14 CoaguChek or INRatio or ProTime or coagulometer
#15 #13 or #14
HTA/Database of Abstracts Reviews of Effects, Centre for Reviews and Dissemination
Searched: May 2013.
Search strategy
-
MeSH DESCRIPTOR 4-Hydroxycoumarins EXPLODE ALL TREES
-
(warfarin) OR (vitamin k antagonist*)
-
MeSH DESCRIPTOR anticoagulants EXPLODE ALL TREES WITH QUALIFIER AD
-
#1 OR #2 OR #3
-
MeSH DESCRIPTOR self administration
-
MeSH DESCRIPTOR self care
-
MeSH DESCRIPTOR Point-of-Care Systems
-
(poc) OR (self NEAR3 (monitor* or manag* or measur*)) OR (patient* NEAR3 (monitor* or manag* or measur*))
-
#5 OR #6 OR #7 OR #8
-
#4 AND #9
Additional conference proceedings
ASH 2012, 54th ASH Annual Meeting and Exposition, Atlanta, GA, 8–11 December 2012.
EHA 2012, 17th Congress, Amsterdam, 14–17 June 2012.
ISTH 2011, XXIII Congress of the International Society on Thrombosis and Haemostasis 57th Annual SSC Meeting, ICC Kyoto, Kyoto, Japan, 23–28 July 2011.
Proceedings of the 12th National Conference on Anticoagulant Therapy, Phoenix, Arizona, 9–11 May 2013.
Search strategy
CoaguChek OR INRatio OR ProTime OR ((“point-of-care” or self) AND anticoagulant OR warfarin))
Searched: International Clinical Trials Registry Platform (ICTRP)
Date of search: June 2013.
World Health Organization
Searched: 5 June 2013.
Search strategy
CoaguChek OR INRatio OR ProTime OR ((“point-of-care” or self) AND
anticoagulant OR warfarin))
Point-of-care tests for coagulation self-monitoring: acceptability
EMBASE
Searched: 1980 to week 23 2013.
Ovid MEDLINE(R)
Searched: 1946 to week 5 May 2013.
Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations
Searched: 7 June 2013.
OVID Multifile
Searched: 5 June 2013.
URL: https://shibboleth.ovid.com/
Search strategy
-
exp 4-Hydroxycoumarins/ use mesz
-
exp coumarin anticoagulant/ use emez
-
antivitamin k/ use emez
-
warfarin.tw
-
vitamin k antagonist$.tw.
-
*anticoagulants/ad use mesz
-
*anticoagulant agent/ad use emez
-
Prothrombin Time/
-
prothrombin time.tw.
-
or/1-9
-
Self Administration/ use mesz
-
Self Care/
-
Self-monitoring/ use emez or Home Monitoring/ use emez
-
point-of-care systems/
-
poc.tw.
-
point-of-care.tw.
-
(((patient$ or self) adj1 (monitor$ or manag$ or measur$)) or (self adj1 test$)).tw.
-
or/11-17 (197928)
-
10 and 18 (2639)
-
exp patient acceptance of health care/ use mesz
-
exp patient attitude/ use emez
-
consumer satisfaction/ use mesz
-
(patient? adj3 (compliance or participat$ or accept$ or refus$)).tw.
-
(patient? adj2 (attitude? or prefer$ or perception? or satisfaction)).tw.
-
qualitative research/
-
questionnaires/
-
(qualitative or interview$ or focus group? or questionnaire$ or survey$).tw.
-
(ethno$ or grounded or thematic or interpretive or narrative).tw.
-
or/20-28
-
19 and 29
-
remove duplicates from 30
Point-of-care tests for coagulation self-monitoring: cost-effectiveness
EMBASE
Searched: 1980 to week 22 2013.
Ovid MEDLINE(R)
Searched: 1946 to week 5 May 2013.
Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations
Searched: 5 June 2013.
OVID Multifile
URL: https://shibboleth.ovid.com/
Search strategy
-
exp 4-Hydroxycoumarins/ use mesz
-
exp coumarin anticoagulant/ use emez
-
antivitamin k/ use emez
-
warfarin.tw.
-
vitamin k antagonist$.tw.
-
*anticoagulants/ad use mesz
-
*anticoagulant agent/ad use emez
-
Prothrombin Time/
-
prothrombin time.tw.
-
or/1-9
-
Self Administration/ use mesz
-
Self Care/
-
Self-monitoring/ use emez or Home Monitoring/ use emez
-
point-of-care systems/
-
poc.tw.
-
point-of-care.tw.
-
(((patient$ or self) adj1 (monitor$ or manag$ or measur$)) or (self adj1 test$)).tw
-
or/11-17
-
10 and 18
-
coaguche?k.tw.
-
INRatio.tw.
-
ProTime.tw.
-
coagulometer$.tw
-
or/19-23
-
exp “costs and cost analysis”/ use mesz
-
exp economic evaluation/ use emez
-
economics/
-
health economics/ use emez
-
exp economics,hospital/ use mesz
-
exp economics,medical/ use mesz
-
economics,pharmaceutical/ use mesz
-
exp budgets/
-
exp models, economic/ use mesz
-
exp decision theory/
-
monte carlo method/
-
markov chains/
-
exp technology assessment, biomedical/
-
cost$.ti.
-
(cost$ adj2 (effective$ or utilit$ or benefit$ or minimis$)).ab.
-
economics model$.tw.
-
(economic$ or pharmacoeconomic$).tw.
-
(price or prices or pricing).tw.
-
(value adj1 money).tw
-
markov$.tw.
-
monte carlo.tw.
-
(decision$ adj2 (tree? or analy$ or model$)).tw.
-
or/25-46
-
24 and 47
-
remove duplicates from 48
Health Management Information Consortium
Searched: 1979 to March 2013.
URL: https://auth.athensams.net/
Search strategy
-
anticoagulant agent/
-
warfarin.tw.
-
vitamin k antagonist$.tw.
-
prothrombin time.tw.
-
or/1-4
-
Self Care/
-
self management/
-
(((patient$ or self) adj1 (monitor$ or manag$ or measur$)) or (self adj1 test$)).tw.
-
point-of-care.tw.)
-
poc.tw.
-
or/6-10
-
5 and 11
-
(coaguche?k$ or INRatio$ or ProTime$ or pro time$).tw.
-
12 or 13
NHS Economic Evaluation Database
Searched: May 2013.
Centre for Reviews and Dissemination
Searched: May 2013.
URL: http://nhscrd.york.ac.uk/welcome.htm
Search strategy
-
MeSH DESCRIPTOR 4-Hydroxycoumarins EXPLODE ALL TREES
-
(warfarin) OR (vitamin k antagonist*)
-
MeSH DESCRIPTOR anticoagulants EXPLODE ALL TREES WITH QUALIFIER AD
-
#1 OR #2 OR #3
-
MeSH DESCRIPTOR self administration
-
MeSH DESCRIPTOR self care
-
MeSH DESCRIPTOR Point-of-Care Systems
-
(poc) OR (self NEAR3 (monitor* or manag* or measur*)) OR (patient* NEAR3 (monitor* or manag* or measur*))
-
#5 OR #6 OR #7 OR #8
-
#4 AND #9
RePEc (Research Papers in Economics)
Searched: June 2013.
URL: http://repec.org/
anticoagulation | anticoagulants | warfarin | “vitamin k antagonist”|prothrombin
self management | self-monitoring | self-testing|prothrombin
Point-of-care tests for coagulation self-monitoring: quality of life
EMBASE
Searched: 1980 to week 22 2013.
Ovid MEDLINE(R)
Searched: 1946 to week 5 May 2013.
Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations
Searched: 5 June 2013.
Ovid Multifile
URL: https://shibboleth.ovid.com/
Search strategy
-
exp 4-Hydroxycoumarins/ use mesz
-
exp coumarin anticoagulant/ use emez
-
antivitamin k/ use emez
-
warfarin.tw.
-
vitamin k antagonist$.tw.
-
*anticoagulants/ad use mesz
-
*anticoagulant agent/ad use emez
-
Prothrombin Time/
-
prothrombin time.tw.
-
or/1-9
-
Self Administration/ use mesz
-
Self Care/
-
Self-monitoring/ use emez or Home Monitoring/ use emez
-
point-of-care systems/
-
poc.tw.
-
point-of-care.tw.
-
(((patient$ or self) adj1 (monitor$ or manag$ or measur$)) or (self adj1 test$)).tw.
-
or/11-17
-
10 and 18
-
coaguche?k.tw.
-
INRatio.tw.
-
ProTime.tw
-
coagulometer$.tw.
-
or/19-23
-
quality of life/
-
quality adjusted life year/
-
“Value of Life”/ use mesz
-
health status indicators/ use mesz
-
health status/ use emez
-
sickness impact profile/ use mesz
-
disability evaluation/ use mesz
-
disability/ use emez
-
activities of daily living/ use mesz
-
exp daily life activity/ use emez
-
cost utility analysis/ use emez
-
rating scale/
-
questionnaires/
-
(quality adj1 life).tw.
-
quality adjusted life.tw.
-
disability adjusted life.tw.
-
(qaly? or qald? or qale? or qtime? or daly?).tw.
-
(euroqol or euro qol or eq5d or eq 5d).tw.
-
(hql or hqol or h qol or hrqol or hr qol).tw.
-
(hye or hyes).tw
-
health$ year$ equivalent$.tw.
-
(hui or hui1 or hui2 or hui3).tw.
-
(health adj3 (utilit$ or disutili$)).tw.
-
(health adj3 (state or status)).tw.
-
(sf36 or sf 36 or short form 36 or shortform 36).tw.
-
(sf6 or sf 6 or short form 6 or shortform 6).tw.
-
(sf12 or sf 12 or short form 12 or shortform 12).tw.
-
(sf16 or sf 16 or short form 16 or shortform 16).tw.
-
(sf20 or sf 20 or short form 20 or shortform 20).tw.
-
willingness to pay.tw
-
standard gamble.tw.
-
trade off.tw.
-
conjoint analys?s.tw.
-
discrete choice.tw.
-
or/25-58
-
(case report or editorial or letter).pt.
-
case report/
-
(24 and 59) not (60 or 61)
CEA Registry June 2013
URL: https://research.tufts-nemc.org/cear4/default.asp
Search strategy
Oral anticoagulation
Websites consulted
Agency for Healthcare Research and Quality: www.ahrq.gov/
American Heart Association: www.americanheart.org/
Alere: www.alereINRatio.com/
Belgian Health Care Knowledge Centre: https://kce.fgov.be/
Canadian Agency for Drugs and Technologies in Health: www.cadth.ca/
CoaguChek System: www.CoaguChek.com/uk/
European Society of Cardiology: www.escardio.org/
French National Authority for Health: www.has-sante.fr/
Health Information & Quality Authority: www.hiqa.ie/
Institute for Clinical and Economic Review: www.icer-review.org/
Institute for Quality and Efficiency in Health Care: www.iqwig.de/
International Society of Thrombosis and Haemostasis: www.med.unc.edu/welcome.htm
International Technidyne Corporation: www.itcmed.com/
Medicines and Healthcare Products Regulatory Agency: www.mhra.gov.uk/
Medical Services Advisory Committee, Australia: www.msac.gov.au/
National Institute for Health and Care Excellence: www.nice.org.uk/
NHS Quality Improvement Scotland: www.healthcareimprovementscotland.org/
US Food and Drug Administration: www.fda.gov/default.htm
Appendix 2 Data extraction form
CoaguChek, INRatio and ProTime microcoagulation system for self-monitoring in people taking long-term vitamin K antagonists: data extraction form
Appendix 3 Quality assessment
The Cochrane Collaboration’s tool for assessing risk of bias
| Domain | Support for judgement | Review authors’ judgement |
|---|---|---|
| Selection bias | ||
| Random sequence generation | Describe the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether or not it should produce comparable groups | Selection bias (biased allocation to interventions) due to inadequate generation of a randomised sequence |
| Allocation concealment | Describe the method used to conceal the allocation sequence in sufficient detail to determine whether or not intervention allocations could have been foreseen in advance of, or during, enrolment | Selection bias (biased allocation to interventions) due to inadequate concealment of allocations prior to assignment |
| Performance bias | ||
| Blinding of participants and personnel Assessments should be made for each main outcome (or class of outcomes) | Describe all measures used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. Provide any information relating to whether or not the intended blinding was effective | Performance bias due to knowledge of the allocated interventions by participants and personnel during the study |
| Detection bias | ||
| Blinding of outcome assessment Assessments should be made for each main outcome (or class of outcomes) | Describe all measures used, if any, to blind outcome assessors from knowledge of which intervention a participant received. Provide any information relating to whether or not the intended blinding was effective | Detection bias due to knowledge of the allocated interventions by outcome assessors |
| Attrition bias | ||
| Incomplete outcome data Assessments should be made for each main outcome (or class of outcomes) | Describe the completeness of outcome data for each main outcome, including attrition and exclusions from the analysis. State whether or not attrition and exclusions were reported, the numbers in each intervention group (compared with total randomised participants), reasons for attrition/exclusions where reported, and any reinclusions in analyses performed by the review authors | Attrition bias due to amount, nature or handling of incomplete outcome data |
| Reporting bias | ||
| Selective reporting | State how the possibility of selective outcome reporting was examined by the review authors, and what was found | Reporting bias due to selective outcome reporting |
| Other bias | ||
| Other sources of bias | State any important concerns about bias not addressed in the other domains in the toolIf particular questions/entries were pre-specified in the review’s protocol, responses should be provided for each question/entry | Bias due to problems not covered elsewhere in the table |
Appendix 4 List of included randomised controlled trials and linked reports
Azarnoush 2011
Primary study
Azarnoush K, Camilleri L, Aublet-Cuvelier B, Geoffroy E, Dauphin C, Dubray C, et al. Results of the first randomized French study evaluating self-testing of the International Normalized Ratio. J Heart Valve Dis 2011;20:518–20.
Secondary study
Dauphin C, Legault B, Jaffeux P, Motreff P, Azarnoush K, Joly H, et al. Comparison of INR stability between self-monitoring and standard laboratory method: preliminary results of a prospective study in 67 mechanical heart valve patients. Arch Cardiovasc Dis 2008;101:753–61.
Bauman 2010
Primary study
Bauman ME, Black K, Bauman ML, Bruce AA, Kuhle S, Bajzar L, et al. EMPoWarMENT: Edmonton pediatric warfarin self-management pilot study in children with primarily cardiac disease. Thromb Res 2010;126:e110–15.
Secondary study
Bauman ME, Conroy S, Massicotte MP. Point-of-care INR measurement in children requiring warfarin: what has been evaluated and future directions. Pediat Health 2008;2:651–9.
Christensen 2011
Christensen H, Lauterlein JJ, Sorensen PD, Petersen ER, Madsen JS, Brandslund I. Home management of oral anticoagulation via telemedicine versus conventional hospital-based treatment. Telemedicine J E-Health 2011;17:169–76.
Christensen 2006
Primary study
Christensen TD, Maegaard M, Sorensen HT, Hjortdal VE, Hasenkam JM. Self-management versus conventional management of oral anticoagulant therapy: a randomized, controlled trial. Eur J Intern Med 2006;17:260–6.
Secondary study
Christensen TD, Maegaard M, Sorensen HT, Hjortdal VE, Hasenkam JM. Self-versus conventional management of oral anticoagulant therapy: effects on INR variability and coumarin dose in a randomized controlled trial. Am J Cardiovasc Drugs 2007;7:191–7.
Cromheecke 2000
Cromheecke ME, Levi M, Colly LP, Mol BJ, Prins MH, Hutten BA, et al. Oral anticoagulation self-management and management by a specialist anticoagulation clinic: a randomised cross-over comparison. Lancet 2000;356:97–102.
Eitz 2008
Primary study
Eitz T, Schenk S, Fritzsche D, Bairaktaris A, Wagner O, Koertke H, et al. International normalized ratio self-management lowers the risk of thromboembolic events after prosthetic heart valve replacement. Ann Thorac Surg 2008;85:949–54.
Secondary study
Koertke H, Zittermann A, Mommertz S, El AM, Litmathe J, Koerfer R. The Bad Oeynhausen concept of INR self-management. J Thromb Thrombolysis 2005;19:25–31.
Fitzmaurice 2002
Primary study
Fitzmaurice DA, Murray ET, Gee KM, Allan TF, Hobbs FD. A randomised controlled trial of patient self management of oral anticoagulation treatment compared with primary care management. J Clin Pathol 2002;55:845–9.
Secondary study
Fitzmaurice DA, Hobbs FD, Murray ET, Holder RL, Allan TF, Rose PE. Oral anticoagulation management in primary care with the use of computerized decision support and near-patient testing: a randomized, controlled trial. Arch Intern Med 2000;160:2343–8.
Fitzmaurice 2005
Primary study
Fitzmaurice DA, Murray ET, McCahon D, Holder R, Raftery JP, Hussain S, et al. Self management of oral anticoagulation: randomised trial. BMJ 2005;331:1057.
Secondary studies
Murray E, Fitzmaurice D, McCahon D, Fuller C, Sandhur H. Training for patients in a randomised controlled trial of self management of warfarin treatment. BMJ 2004;328:437–8.
McCahon D, Fitzmaurice DA, Murray ET, Fuller CJ, Hobbs RF, Allan TF, et al. SMART: self-management of anticoagulation, a randomised trial. BMC Fam Pract 2003;4:11.
Gadisseur 2003
Primary study
Gadisseur AP, Breukink-Engbers WG, Meer FJ, Besselaar AM, Sturk A, Rosendaal FR. Comparison of the quality of oral anticoagulant therapy through patient self-management and management by specialized anticoagulation clinics in the Netherlands: a randomized clinical trial. Arch Intern Med 2003;163:2639–46.
Secondary study
Gadisseur AP, Kaptein AA, Breukink-Engbers WG, Meer FJ, Rosendaal FR. Patient self-management of oral anticoagulant care vs. management by specialized anticoagulation clinics: positive effects on quality of life. J Thromb Haemost 2004;2:584–91.
Gardiner 2006
Gardiner C, Williams K, Longair I, Mackie IJ, Machin SJ, Cohen H. A randomised control trial of patient self-management of oral anticoagulation compared with patient self-testing. Br J Haematol 2006;132:598–603.
Gardiner 2005
Gardiner C, Williams K, Mackie IJ, Machin SJ, Cohen H. Patient self-testing is a reliable and acceptable alternative to laboratory INR monitoring. Br J Haematol 2005;128:242–7.
Hemkens 2008
Hemkens LG, Hilden KM, Hartschen S, Kaiser T, Didjurgeit U, Hansen R, et al. A randomized trial comparing INR monitoring devices in patients with anticoagulation self-management: evaluation of a novel error-grid approach. J Thromb Thrombolysis 2008;26:22–30.
Horstkotte 1996
Primary study
Horstkotte D, Piper C, Wiemer M, Schulte H.D. Improvement of prognosis by home prothrombin estimation In patients with life-long anticoagulant therapy. Euro Heart J 1996;17:230.
Secondary study
Horstkotte D, Piper C, Wiemer M. Optimal frequency of patient monitoring and intensity of oral anticoagulation therapy in valvular heart disease. J Thromb Thrombolysis 1998;5:19–24.
Khan 2004
Khan TI, Kamali F, Kesteven P, Avery P, Wynne H. The value of education and self-monitoring in the management of warfarin therapy in older patients with unstable control of anticoagulation. Br J Haematol 2004;126:557–64.
Koertke 2001
Primary study
Körtke H, Minami k, Breymann T, Seifert D, Baraktaris A, Wagner O, et al. INR self-management after mechanical heart valve replacement. Z Kardiol 2001;9(Suppl. 6):VI/118–24.
Secondary studies
Koertke H, Minami K, Bairaktaris A, Wagner O, Koerfer R. INR self-management following mechanical heart valve replacement. J Thromb Thrombolysis 2000;9(Suppl. 1):S41–5.
Körtke H, Körfer R. International normalized ratio self-management after mechanical heart valve replacement: is an early start advantageous? Ann Thorac Surg 2001;72:44–8.
Koertke H, Zittermann A, Wagner O, Koerfer R. Self-management of oral anticoagulatin therapy improves long-term survival in patients with mechanical heart valve replacement. Ann Thorac Surg 2007;83:24–9.
Matchar 2010
Primary study
Matchar DB, Jacobson A, Dolor R, Edson R, Uyeda L, Phibbs CS, et al. Effect of home testing of international normalized ratio on clinical events. N Engl J Med 2010;363:1608–20.
Secondary studies
Matchar DB, Dolor R, Jacobson A, Love S, Edson R, Uyeda L. More frequent self-testing of prothrombin time results in improved time in target range. Circulation 2012;126(Suppl. 1):A10606.
Matchar DB, Jacobson AK, Edson RG, Lavori PW, Ansell JE, Ezekowitz MD, et al. The impact of patient self-testing of prothrombin time for managing anticoagulation: rationale and design of VA cooperative study #481 – The Home INR Study (THINRS). J Thromb Thrombolysis 2005;19:163–72.
Menendez-Jandula 2005
Menéndez JB, Souto JC, Oliver A, Montserrat I, Quintana M, Gich I, et al. Comparing self-management of oral anticoagulant therapy with clinic management: a randomized trial. Ann Intern Med 2005;142:1–10.
Rasmussen 2012
Rasmussen RS, Corell P, Madsen P, Overgaard K. Effects of computer-assisted oral anticoagulant therapy. Thrombosis J 2012;10:17.
Ryan 2009
Primary study
Ryan F, Byrne S, O’Shea S. Randomized controlled trial of supervised patient self-testing of warfarin therapy using an internet-based expert system. J Thromb Haemostasis 2009;7:1284–90.
Secondary study
Ryan F, O’Shea S, Byrne S. The ‘carry-over’ effects of patient self-testing: positive effects on usual care management by an anticoagulation management service. Thromb Res 2010;126:e345–8.
Sawicki 1999
Primary study
Sawicki PT. A structured teaching and self-management program for patients receiving oral anticoagulation: a randomized controlled trial. Working Group for the Study of Patient Self-Management of Oral Anticoagulation. JAMA 1999;281:145–50.
Secondary study
Sawicki PT, Glaser B, Kleespies C, Stubbe J, Schmitz N, Kaiser T, et al. Long-term results of patients’ self-management of oral anticoagulation. J Clin Basic Cardiol 2003;6:2003.
Sidhu 2001
Sidhu P, O’Kane HO. Self-managed anticoagulation: results from a two-year prospective randomized trial with heart valve patients. Ann Thorac Surg 2001;72:1523–7.
Siebenhofer 2008
Primary study
Siebenhofer A, Rakovac I, Kleespies C, Piso B, Didjurgeit U, SPOG 6. Self-management of oral anticoagulation reduces major outcomes in the elderly. A randomized controlled trial. Thromb Haemost 2008;100:1089–98.
Secondary study
Siebenhofer A, Rakovac I, Kleespies C, Piso B, Didjurgeit U. Self-management of oral anticoagulation in the elderly: rationale, design, baselines and oral anticoagulation control after one year of follow up. A randomized controlled trial. Thromb Haemost 2007;97:408–16.
Soliman Hamad 2009
Soliman Hamad MA, van Eekelen E, van Agt T, van Straten AH. Self-management program improves anticoagulation control and quality of life: a prospective randomized study. Eur J Cardiothorac Surg 2009;35:265–9.
Sunderji 2004
Primary study
Sunderji R, Gin K, Shalansky K, Carter C, Chambers K, Davies C, et al. A randomized trial of patient self-managed versus physician-managed oral anticoagulation. Can J Cardiol 2004;20:1117–23.
Secondary study
Sunderji R, Campbell L, Shalansky K, Fung A, Carter C, Gin K. Outpatient self-management of warfarin therapy: a pilot study. Pharmacotherapy 1999;19:787–93.
Verret 2012
Verret L, Couturier J, Rozon A, Saudrais-Janecek S, St-Onge A, Nguyen A, et al. Impact of a pharmacist-led warfarin self-management program on quality of life and anticoagulation control: a randomized trial. Pharmacotherapy 2012;32:871–9.
Völler 2005
Primary Study
Völler H, Glatz J, Taborski U, Bernardo A, Dovifat C, Heidinger K. Self-management of oral anticoagulation in nonvalvular atrial fibrillation (SMAAF study). Z Kardiol 2005;94:182–6.
Secondary study
Völler H, Glatz J, Taborski U, Bernard A, Dovifat C, Burkard G, et al. Background and evaluation plan of a study on self-management of anticoagulation in patients with non-valvular atrial fibrillation (SMAAF Study). Z Kardiol 2000;89:284–8.
Appendix 5 List of excluded studies with reasons for exclusion
Study design not a randomised controlled trial (n = 25)
Adedeji-Zakari S, Anthony VP, Honeywell M. The CoaguChek S system. U.S. Pharmacist 2007;32.
Ansell JE. Empowering patients to monitor and manage oral anticoagulation therapy. J Am Med Assoc 1999;281:182–3.
Ansell JE. Is self-management of oral anticoagulation a feasible and safe option? Nat Clin Pract Cardiovasc Med 2005;2:240–1.
Arellano-Rodrigo E. Home monitoring of warfarin effects. N Engl J Med 2011;364:378–9.
Bevan H, Giles M, Heads J, Parker V, Walters J. Point-of-care INR testing in cardiac wards. Aust Nurs J 2007;15:31.
Biss T, Avery PJ, Walsh PM, Kamali F. Warfarin treatment outcomes in children monitored at home with a point-of-care device. Thromb Haemost 2011;105:1103–5.
Coleman B, Patterson D, Long M, Farrell J. Setting quality standards for a community pharmacist-led anticoagulant clinic. Pharm J 2003;270:308–11.
Deom A, Reber G, Tsakiris DA, Hannes FM, Plesch W. Evaluation of the CoaguChek XS Plus system in a Swiss community setting. Thromb Haemost 2009;101:988–90.
Ferretti G, Giannarelli D, Carlini P, Felici A, Ciccarese M, Mandala M, et al. Self-monitoring versus standard monitoring of oral anticoagulation. Thromb Res 2007;119:389–90.
Fitzmaurice DA, Machin SJ. Recommendations for patients undertaking self management of oral anticoagulation. BMJ 2001;323:985–9.
Ford PW, Close A. Management of warfarin in atrial fibrillation. Med J Aust 2007;187:371.
Heidinger KS, Bernardo A, Taborski U, Muller-Berghaus G. Clinical outcome of self-management of oral anticoagulation in patients with atrial fibrillation or deep-vein thrombosis. Thromb Res 2000;98:287–93.
Herijgers P, Verhamme P. Improving the quality of anticoagulant therapy in patients with mechanical heart valves: what are we waiting for? Eur Heart J 2007;28:2424–6.
Kitchen S, Kitchen D, Jennings I, Woods T, Walker I. External quality assessment of CoaguChek point-of-care testing prothrombin time/international ratio monitors. Am J Clin Pathol 2008;129:825–6.
Kitchen S, Kitchen D, Jennings I, Woods T, Walker I. Quality assessment of CoaguChek point-of-care international normalized ratio monitors: a note of caution. Clin Chem 2007;53:1555–6.
Lippi G, Franchini M. Home monitoring of warfarin effects. N Engl J Med 2011;364:378–9.
Martin M. Home and community anticoagulation by GPs and patients. Br J Cardiol 1999;6:144–6.
Pluddemann A, Thompson M, Wolstenholme J, Price CP, Heneghan C. Point-of-care INR coagulometers for self-management of oral anticoagulation: primary care diagnostic technology update. Br J Gen Pract 2012;62:e798–800.
Rodgers G. Patient self-management of oral anticoagulation. Clin Adv Hematol Oncol 2005;3:94–5.
Stafford L, Peterson GM, Bereznicki LR, Jackson SL. A role for pharmacists in community-based post-discharge warfarin management: protocol for the ‘the role of community pharmacy in post hospital management of patients initiated on warfarin’ study. BMC Health Serv Res 2011;11:16.
Taborski U, Voller H, Kortke H, Blunt J, Wegscheider K. Self management of oral anticoagulation with the INRatio System: accuracy and reliability following a two-day structured training program. Lab Med 2004;35:303–7.
Thompson JL, Sundt TM, Sarano ME, Santrach PJ, Schaff HV. In-patient International Normalized Ratio self-testing instruction after mechanical heart valve implantation. Ann Thorac Surg 2008;85:46–50.
Williams MS. Long-term anticoagulation and home monitoring. Drug Benefit Trends 2000;12:15.
Williams VK, Griffiths ABM. Re: Acceptability of CoaguChek S and CoaguChek XS generated international normalised ratios against a laboratory standard in a paediatric setting: authors’ reply. Pathology 2008;40:438–9.
Zimmerman CR. The role of point-of-care anticoagulation monitoring in arterial and venous thromboembolic disorders. J Thromb Thrombolysis 2000;9:187–98.
Not self-management (n = 8)
Claes N, Buntinx F, Vijgen J, Arnout J, Vermylen J, Fieuws S, et al. The Belgian Improvement Study on Oral Anticoagulation Therapy: a randomized clinical trial. Eur Heart J 2005;26:2159–65.
Fitzmaurice DA, Hobbs FD, Murray ET, Bradley CP, Holder R. Evaluation of computerized decision support for oral anticoagulation management based in primary care. Br J Gen Pract 1996;46:533–5.
Jackson SL, Peterson GM, Vial JH, Jupe DM. Improving the outcomes of anticoagulation: an evaluation of home follow-up of warfarin initiation. J Intern Med 2004;256:137–44.
Lalonde L, Martineau J, Blais N, Montigny M, Ginsberg J, Fournier M, et al. Is long-term pharmacist-managed anticoagulation service efficient? A pragmatic randomized controlled trial. Am Heart J 2008;156:148–54.
Laurence C, Gialamas A, Yelland L, Bubner T, Ryan P, Willson K, et al. A pragmatic cluster randomised controlled trial to evaluate the safety, clinical effectiveness, cost-effectiveness and satisfaction with point-of-care testing in a general practice setting – rationale, design and baseline characteristics. Trials 2008;9:50.
Shiach CR, Campbell B, Poller L, Keown M, Chauhan N. Reliability of point-of-care prothrombin time testing in a community clinic: a randomized crossover comparison with hospital laboratory testing. Br J Haematol 2002;119:370–5.
Wilson SJ, Wells PS, Kovacs MJ, Lewis GM, Martin J, Burton E, et al. Comparing the quality of oral anticoagulant management by anticoagulation clinics and by family physicians: a randomized controlled trial. CMAJ 2003;169:293–8.
Woods K, Douketis JD, Schnurr T, Kinnon K, Powers P, Crowther MA. Patient preferences for capillary vs. venous INR determination in an anticoagulation clinic: a randomized controlled trial. Thromb Res 2004;114:161–5.
Self-management dosage studies (n = 4)
Koertke H, Zittermann A, Wagner O, Ennker J, Saggau W, Sack FU, et al. Efficacy and safety of very low-dose self-management of oral anticoagulation in patients with mechanical heart valve replacement. Ann Thorac Surg 2010;90:1487–93.
Kortke H, Secer S. Telemedical based thrombosis service of patients with mechanical heart valve replacement. Vasa 2012;41(Suppl. 82):25.
Koertke H, Minami K, Boethig D, Breymann T, Seifert D, Wagner O, et al. INR self-management permits lower anticoagulation levels after mechanical heart valve replacement. Circulation 2003;108(Suppl. 1):II75–8.
Koertke H, Zittermann A, Tenderich G, Wagner O, El-Arousy M, Krian A, et al. Low-dose oral anticoagulation in patients with mechanical heart valve prostheses: final report from the early self-management anticoagulation trial II. Eur Heart J 2007;28:2479–84
Excluded tests (n = 3)
Beyth RJ, Quinn L, Landefeld CS. A multicomponent intervention to prevent major bleeding complications in older patients receiving warfarin. A randomised, controlled trial. Ann Intern Med 2000;133:687–95.
Grunau BE, Wiens MO, Harder KK. Patient self-management of warfarin therapy: pragmatic feasibility study in Canadian primary care. Can Fam Physician 2011;57:e292–8.
White RH, McCurdy SA, Marensdorff H, Woodruff DE, Leftgoff L. Home prothrombin time monitoring after the initiation of warfarin therapy. A randomised, prospective study. Ann Intern Med 1989;111:730–7.
Background information (n = 25)
Bloomfield HE, Krause A, Greer N, Taylor BC, MacDonald R, Rutks I, et al. Meta-analysis: effect of patient self-testing and self-management of long-term anticoagulation on major clinical outcomes. Ann Intern Med 2011;154:472–82.
Bussey HI. Transforming oral anticoagulation by combining international normalised ratio (INR) self-testing and online automated management. J Thromb Thrombolysis 2011;31:265–74.
Cayley J. Self-monitoring and self-management of anticoagulation therapy. Am Fam Physician 2011;84:266–8.
Christensen TD, Larsen TB. Precision and accuracy of point-of-care testing coagulometers used for self-testing and self-management of oral anticoagulation therapy. J Thromb Haemost 2012;10:251–60.
Christensen TD, Johnsen SP, Hjortdal VE, Hasenkam JM. Self-management of oral anticoagulant therapy: a systematic review and meta-analysis. Int J Cardiol 2007;118:54–61.
Christensen TD. Self-management of oral anticoagulation therapy--methodological and clinical aspects. Dan Med Bull 2011;58:B4284.
Connock M, Stevens C, Fry-Smith A, Jowett S, Fitzmaurice D, Moore D, et al. Clinical effectiveness and cost-effectiveness of different models of managing long-term oral anticoagulation therapy: a systematic review and economic modelling. Health Technol Assess 2007;11(38).
Dolan G, Smith LA, Collins S, Plumb JM. Effect of setting, monitoring intensity and patient experience on anticoagulation control: a systematic review and meta-analysis of the literature. Curr Med Res Opin 2008;24:1459–72.
Dolor RJ, Ruybalid RL, Uyeda L, Edson RG, Phibbs C, Vertrees, JE et al. An evaluation of patient self-testing competency of prothrombin time for managing anticoagulation: pre-randomisation results of VA Cooperative Study #481 – The Home INR Study (THINRS). J Thromb Thrombolysis 2010;30:263–75.
Garcia-Alamino JM, Ward AM, Alonso-Coello P, Perera R, Bankhead C, Fitzmaurice D, et al. Self-monitoring and self-management of oral anticoagulation. Cochrane Database Syst Rev 2010;4:CD003839.
Health Q. Point-of-care international normalized ratio (INR) monitoring devices for patients on long-term oral anticoagulation therapy: an evidence-based analysis. Ontario Health Technol Assess Series 2009;9:1–114.
Heneghan C, Ward A, Perera R, Self-Monitoring Triallist collaboration, Bankhead C, Fuller A, et al. Self-monitoring of oral anticoagulation: systematic review and meta-analysis of individual patient data. Lancet 2012; 379:322–34. [Erratum published in. Lancet 2012;379:1102.]
Holbrook A, Schulman S, Witt DM, Vandvik PO, Fish J, Kovacs MJ, et al. Evidence-based management of anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012;141:e152S–84S.
Jennings I, Walker ID, Kitchen S, Kitchen D, Woods TA, Keeling D, et al. Management of patients receiving oral anticoagulants using computer dosing software--does everyone agree? Data from a UK NEQAS (blood coagulation) exercise. Int J Lab Haematol 2012;34:70–80.
Mazor KM, Baril J, Dugan E, Spencer F, Burgwinkle P, Gurwitz JH. Patient education about anticoagulant medication: is narrative evidence or statistical evidence more effective? Patient Educ Couns 2007;69:145–57.
Murray ET, Jennings I, Kitchen D, Kitchen S, Fitzmaurice DA. Quality assurance for oral anticoagulation self-management: a cluster randomized trial. J Thromb Haemost 2008;6:464–9.
Newall F, Bauman M. Point-of-care antithrombotic monitoring in children. Thromb Res 2006;118:113–21.
Nieuwlaat R, Barker L, Kim YK, Haynes RB, Eikelboom JW, Yusuf S, et al. Underuse of evidence-based warfarin dosing methods for atrial fibrillation patients. Thromb Res 2010;125:e128–31.
Perera R, Heneghan C, Fitzmaurice D, Self M. Individual patient meta-analysis of self-monitoring of an oral anticoagulation protocol. J Heart Valve Dis 2008;17:233–8.
Shermock KM, Streiff MB, Pinto BL, Kraus P, Pronovost PJ. Novel analysis of clinically relevant diagnostic errors in point-of-care devices. J Thromb Haemost 2011;9:1769–75.
Spinler SA, Nutescu EA, Smythe MA, Wittkowsky AK. Anticoagulation monitoring part 1: warfarin parenteral direct thrombin inhibitors. Ann Pharmacother 2005;39:1049–55.
Stigendal L, Andre U. Workshop: Patient self-management: update of ongoing studies in Sweden. J Thromb Thrombolysis 1998;5:S63–4.
Völler H, Dovifat C, Glatz J, Kortke H, Taborski U, Wegscheider K. Self management of oral anticoagulation with the IN Ratio system: impact of a structured teaching program on patient’s knowledge of medical background and procedures. Eur J Cardiovasc Prev Rehabil 2004;11:442–7.
Wilds D, Murray M, Shakespeare A, Reaney M, von M. Patient-reported treatment satisfaction measures for long-term anticoagulant therapy. Expert Rev Pharmacoeconomics Outcomes Res 2008;8:291–9.
Xu Z, Wang Z, Ou J, Xu Y, Yang S, Zhang X. Two monitoring methods of oral anticoagulant therapy in patients with mechanical heart valve prothesis: a meta-analysis. J Thromb Thrombolysis 2012;33:38–47.
Accuracy of CoaguChek XS versus S (n = 10)
Braun S, Watzke H, Hasenkam JM, Schwab M, Wolf T, Dovifat C, et al. Performance evaluation of the new CoaguChek XS system compared with the established CoaguChek system by patients experienced in INR-self management. Thromb Haemost 2007;97:310–14.
Christensen TD, Larsen TB, Jensen C, Maegaard M, Sorensen B. International normalised ratio (INR) measured on the CoaguChek S and XS compared with the laboratory for determination of precision and accuracy. Thromb Haemost 2009;101:563–9.
Karon BS, McBane RD, Chaudhry R, Beyer LK, Santrach PJ. Accuracy of capillary whole blood international normalized ratio on the CoaguChek S, CoaguChek XS, and i-STAT 1 point-of-care analyzers. Am J Clin Pathol 2008;130:88–92.
Kong MC, Lim TG, Ng HJ, Chan YH, Lee LH. Feasibility, cost-effectiveness and patients’ acceptance of point-of-care INR testing in a hospital-based anticoagulation clinic. Ann Hematol 2008;87:905–10.
Paioni P, Kroiss S, Kagi E, Bergstrasser E, Fasnacht M, Bauersfeld U, et al. Self-monitoring of oral anticoagulation therapy in children. Acta Haematol 2009;122:58–63.
Poller L. Precision and accuracy of CoaguChek S and XS monitors: the need for external quality assessment. Thrombo Haemost 2009;101:419–21.
Reverdin S, Schnetzler B, Gagneux G, Gavignet C, Boehlen F, De Moerloose P. Implementation of an INR self-testing and self-management programme in common ambulatory private practice: our experience with 90 patients. Swiss Med Wkly 2011;141:w13199.
Ryan F, O’Shea S, Byrne S. The reliability of point-of-care prothrombin time testing. A comparison of CoaguChek S and XS INR measurements with hospital laboratory monitoring. Int J Lab Hematol 2010;32:e26–33.
Sobieraj-Teague M, Daniel D, Farrelly B, Coghlan D, Gallus A. Accuracy and clinical usefulness of the CoaguChek S and XS Point-of-care devices when starting warfarin in a hospital outreach setting. Thromb Res 2009;123:909–13.
Williams VK, Griffiths AB. Acceptability of CoaguChek S and CoaguChek XS generated international normalised ratios against a laboratory standard in a paediatric setting. Pathology 2007;39:575–9.
Appendix 6 Quality assessment results for the individual included studies
| Study ID | aAdequate sequence generation | aAllocation concealment | aBlinding of outcome assessment | Incomplete outcome data addressed | Free of selective reporting | Other sources of bias | Dropout rates, % | ITT performed | Overall judgement | |
|---|---|---|---|---|---|---|---|---|---|---|
| SM | SC | |||||||||
| CoaguChek XS | ||||||||||
| Bauman 201055 | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB | 14 | 0 | Yes | Low RoB |
| Christensen 201166 | Low RoB | Unclear RoB | High RoB | High RoB | Low RoB | Low RoB | 9 | 18 | NR | High RoB |
| Ryan 200962 | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB | 0 | 0 | NR | Low RoB |
| Verret 201274 | Low RoB | Unclear RoB | High RoB | Low RoB | Low RoB | Low RoB | ≈2 | 0 | NR | High RoB |
| CoaguChek S or CoaguChek | ||||||||||
| Christensen 200675 | Low RoB | High RoB | High RoB | Low RoB | Low RoB | Low RoB | 2 | 2 | Yes | High RoB |
| Cromheecke 200076 | Unclear RoB | Low RoB | Unclear RoB | Low RoB | High RoB | Low RoB | 2 | 0 | NR | Unclear RoB |
| Eitz 200878 | Unclear RoB | Unclear RoB | Unclear RoB | Low RoB | Low RoB | Low RoB | 0 | 0 | NR | Unclear RoB |
| Fitzmaurice 200267 | Low RoB | Unclear RoB | Unclear RoB | High RoB | Low RoB | Low RoB | 23.3 | 0 | NR | Unclear RoB |
| Fitzmaurice 200564 | Low RoB | Low RoB | Unclear RoB | Low RoB | Low RoB | Low RoB | 41.5 | 10 | Yes | Unclear RoB |
| Gadisseur 200368 | Low RoB | Unclear RoB | Unclear RoB | High RoB | Low RoB | Low RoB | 13.6 | NR | Unclear RoB | |
| Gardiner 200545 | Unclear RoB | Unclear RoB | Unclear RoB | High RoB | Low RoB | Low RoB | 31.8 | 2.5 | NR | Unclear RoB |
| Gardiner 200656 | Unclear RoB | Unclear RoB | Unclear RoB | High RoB | Low RoB | Low RoB | PSM 25.5,PST 26.5 | – | NR | Unclear RoB |
| Horstkotte 199659 | Unclear RoB | Unclear RoB | Unclear RoB | Low RoB | Low RoB | Low RoB | NR | NR | NR | Unclear RoB |
| Khan 200469 | Low RoB | Unclear RoB | Unclear RoB | Low RoB | Low RoB | Low RoB | 9.1 | 4.9 | NR | Unclear RoB |
| Menéndez-Jándula 200561 | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB | 21.5 | 2.4 | Yes | Low RoB |
| Rasmussen 201258 | Low RoB | Unclear RoB | Low RoB | Unclear RoB | High RoB | Low RoB | NR | NR | NR | Unclear RoB |
| Sawicki 199972 | Low RoB | Unclear RoB | Low RoB | Low RoB | Low RoB | Low RoB | 7.8 | 7.8 | Yes | Unclear RoB |
| Sidhu 200173 | Low RoB | Unclear RoB | Unclear RoB | High RoB | Low RoB | Low RoB | 31.4 | 2 | NR | Unclear RoB |
| Siebenhofer 200863 | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB | 16 | 23 | Yes | Low RoB |
| Soliman Hamad 200979 | Unclear RoB | Unclear RoB | Unclear RoB | Low RoB | High RoB | Low RoB | 6.4 | NR | Unclear RoB | |
| Völler 200560 | Low RoB | Unclear RoB | High RoB | Low RoB | Low RoB | Low RoB | NR | NR | Yes | High RoB |
| CoaguChek Plus | ||||||||||
| Körtke 200170 | Low RoB | Unclear RoB | Unclear RoB | Unclear RoB | Low RoB | Low RoB | NR | NR | NR | Unclear RoB |
| ProTime | ||||||||||
| Matchar 201071 | Low RoB | Unclear RoB | High RoB | Low RoB | Low RoB | Low RoB | < 1 | < 1 | Yes | High RoB |
| Sunderji 200465 | Low RoB | Low RoB | High RoB | Low RoB | Low RoB | Low RoB | 24.6 | 4.3 | Yes | High RoB |
| CoaguChek/INRatio | ||||||||||
| Azarnoush 201177 | Unclear RoB | Unclear RoB | Low RoB | High RoB | Low RoB | Low RoB | 13 | 1 | NR | Unclear RoB |
| Hemkens 200857 | Low RoB | Low RoB | Unclear RoB | High RoB | Low RoB | Low RoB | 12 | NR | Unclear RoB | |
Appendix 7 Descriptive details of the individual included studies (Tables 31–33; these include characteristics, risk factors, training and education)
| Study ID | Geographical location | Study duration (months) | Sample size, n | Mean age (years) (range) SM/SC | INR range | SM | Point-of-care test | SC | INR measured | Clinical indication | Vitamin K antagonist used | Funding | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PSM/PST | SC | AF, % | AHV, % | VTE, % | Other, % | |||||||||||
| Azarnoush 201177,140 | France | 49 weeksa | 103 | 103 | 55.1/57.5 | 2–3.5 | PST | CoaguChek S and INRatio | AC clinic/GP | Lab analysis | 100 | Fluindione, acenocoumarol | Partly industry | |||
| Bauman 201055,141 | Canada | 12 | 14/14 | – | c10 (1–19) | 2–3.5 | PSM | CoaguChek XS | PST within specialised AC clinic was the usual care | CoaguChek XS | 50 | 50 | Warfarin | Non-industry | ||
| Christensen 200675,142 | Denmark | 6 | 50 | 50 | NR (adult) | 2.5 | PSM | CoaguChek S | Hospital outpatient 6%, highly specialised AC (1%)/or GP (93%) | Coagulometer or lab measurement | 24 | 35 | 8 | 33 | Warfarin, phenprocoumon | Non-industry |
| Christensen 201166 | Denmark | ≈10a | 91 | 49 | 62.5 (21–86)/66.0 (49–82) | 2– ≥ 3 | PST | CoaguChek XS | AC clinic | Lab analysis | 54 | 13.4 | 17 | 25.6 | Warfarin | Non-industry |
| Cromheecke 200076 | Netherlands | 6 | 50 | 50 | 42 (22–71) | 2– ≥ 3 | PSM | CoaguChek | Thrombosis service | Lab analysis | 46 | 30 | 24 | Acenocoumarol, phenprocoumon | NR | |
| Eitz 200878,143 | Germany | 24 | 470 | 295 | 56.4/62.4 | 2.5–4.5 | PSM | CoaguChek S | GP | Lab analysis | 100 | Warfarin | NR | |||
| Fitzmaurice 200267,144 | UK | 6 | 23 | 26 | 63/69 | NR | PSM | CoaguChek S | GP | CoaguChek S | 55 | NR | NR | NR | Warfarin | Partly industry |
| Fitzmaurice 200564,123,145 | UK | 12 | 337 | 280 | 65 (18–87) | 3.5 | PSM | CoaguChek S | Hospital- or practice-based AC clinics | NR | NR | NR | NR | Warfarin | Non-industry | |
| Gadisseur 200368,80 | Netherlands | 24.4 weeksa | 47/52 | 221 | 54.35 (24–75)/59 (21–75) | 2.5–4 | PST and PSM | CoaguChek | AC clinic | Lab analysis | 21.2 | 19.1 | 20.3 | 39.4 | Acenocoumarol, phenprocoumon | Partly industry |
| Gardiner 200545 | UK | 6 | 44 | 40 | 57.9 (26–83)/58.4 (31–75) | 2–4 | PST | CoaguChek S | AC clinic | Lab analysis | 27.4 | 30 | 28.6 | 14 | Warfarin | Partly industry |
| Gardiner 200656 | UK | 6 | 55/49 | – | 59.0 (30–85)/60.9 (22–88) | 2–3.5 | PSM | CoaguChek S | PST | CoaguChek S | 40.4 | 23.1 | 19.2 | 17.3 | Warfarin | Partly industry |
| Hemkens 200857 | Germany | 14 weeks | 16 | 65.8 | NR | PSM | CoaguChek S and INRatio | AC clinic | Lab analysis | 38 | 31 | 31.3 | Phenprocoumon | Non-industry | ||
| Horstkotte 199659,146 | Germany | 40,607 patient-days | 75 | 75 | NR | 3–4.5 | PSM | CoaguChek | Private physician | NR | 100 | NR | Non-industry | |||
| Khan 200469 | UK | 6 | 44 | 41 | c71(65–91)/75(65–87) | 2–3 | PST | CoaguChek | AC clinic | Lab analysis | 100 | Warfarin | Non-industry | |||
| Körtke 200170,147–149 | Germany | 24 | 579 | 576 | 62.5 | 2.5–4.5 | PSM | CoaguChek Plus | Family practitioner | NR | 100 | NR | NR | |||
| Matchar 201071,150,151 | USAa | 36a (24–57) | 1465 | 1457 | 66.6 (23–89)/67.4 (33–99) | NR | PST | ProTime microcoagulation | High-quality clinic testing | Lab analysis | 76.5 | 23.4 | 0.1 | Warfarin | Partly industry | |
| Menéndez-Jándula 200561 | Spain | 11.8b (0.3–16.9) | 368 | 369 | 64.5/65.5 | 2– ≥ 3 | PSM | CoaguChek S | AC clinic | Lab analysis | 50.3 | 37.15 | 12.5 | Acenocoumarol | Partly industry | |
| Rasmussen 201258 | Denmark | 28a weeks | 37 | 17 | c68–70/69 | NR | PSM | CoaguChek S | Specialist clinic | Lab analysis | NR | NR | NR | NR | Warfarin | Non-industry |
| Ryan 200962,152 | Ireland | 6 | 72 | 60 | 58.7 (16–91) | 2– ≥ 3 | PST | CoaguChek XS | AC service | Lab analysis | 32.6 | 37.1 | 22 | 8.3 | Warfarin | Partly industry |
| Sawicki 199972,153 | Germany | 6 | 90 | 89 | 55.0 | NR | PSM | CoaguChek | Hospital outpatient or family practitioner | Lab analysis or by the physician | 5 | 84.4 | Phenprocoumon | Industry | ||
| Sidhu 200173 | UK | 24 | 51 | 49 | 61 (32–85) | 2.5–3 | PSM (51) | CoaguChek | GP or AC clinic (49) | Lab analysis | 100 | Warfarin | Industry | |||
| Siebenhofer 200863,81 | Austria | ≈36a | 99 | 96 | 69/69 | 2– ≥ 3 | PSM | CoaguChek S | GP or specialised AC clinic | NR | 45.6 | 16.4 | 28.7 | 9.2 | Phenprocoumon, acenocoumarol | Industry |
| Soliman Hamad 200979 | Netherlands | 12 | 29 | 29 | 56.3/55.7 | 2.5–4.5 | PSM | CoaguChek | Dutch Thrombosis Service | Lab analysis | 100 | NR | NR | |||
| Sunderji 200465,154 | Canada | 8 | 70 | 70 | 57.6 (20–79)/62.3 (24–85) | 2–3.5 | PSM | ProTime Microcoagulation | GP | NR | 34 | 59 | 5 | 2 | Warfarin | Non-industry |
| Verret 201274 | Canada | 4 | 58 | 56 | 58.4/57.0 | 2–3.5 | PSM | CoaguChek XS | AC clinic | NR | 51 | 42 | 7 | Warfarin | Partly industry | |
| Völler 200560,155 | Germany | ≈5a | 101 | 101 | 64.3 (9.2) | 2–3 | PSM | CoaguChek | Family doctor | Lab analysis | 100 | NR | Partly industry | |||
| Study ID | Risk factors/comorbidity | History of previous complications | ||||||
|---|---|---|---|---|---|---|---|---|
| SM | RC | p-value | SM | RC | p-value | |||
| Azarnoush 201177 | Systemic HT, % | 40 | 38 | NS | ||||
| Diabetes, % | 9 | 14 | NS | |||||
| CABG, % | 15 | 20 | NS | |||||
| EuroSCORE, mean (SD) | 4.2 (2.1) | 4.7 (2.0) | NS | |||||
| LVEF at 3 months, mean (SD) | 60 (8.3) | 58 (9.5) | NS | |||||
| LVEF at 6 months, mean (SD) | 61 (6.9) | 61 (7.9) | NS | |||||
| Christensen 200675 | Major thromboembolic events | 2 | 8 | NR | ||||
| Major bleeding | 10 | 8 | NR | |||||
| Fitzmaurice 200564 | HT, % | 42.43 | 48.57 | NS | ||||
| Hyperlipidaemia, % | 24.92 | 21.78 | NS | |||||
| Matchar 201071 | DM, % | 32.22 | 33.97 | 0.31 | ||||
| HT, % | 71.06 | 69.32 | 0.31 | |||||
| Previous stroke, % | 9.28 | 9.61 | 0.76 | |||||
| CHADS2 score for AF without AHV, % | 0.42 | |||||||
| 0 | 11.5 | 9.79 | ||||||
| 1 | 29 | 29 | ||||||
| 2 | 29.38 | 31.79 | ||||||
| 3 | 17.88 | 18.52 | ||||||
| 4 | 8.62 | 7.3 | ||||||
| 5 | 3.05 | 3.2 | ||||||
| 6 | < 1 | < 1 | ||||||
| Mean CHADS2 score | 1.94 | 1.95 | ||||||
| Menendez-Jandula 200561 | Arterial HT, % | 48.6 | 42.80 | NS | Severe bleeding, % | 11.10 | 9.8 | NS |
| DM, % | 15.40 | 13.60 | NS | Thromboembolic events, % | 13.50 | 7.90 | NS | |
| Gastric ulcer, % | 17.80 | 15.70 | NS | |||||
| Cancer, % | 9.20 | 8.70 | NS | |||||
| Liver disease, % | 9.70 | 8.40 | NS | |||||
| Sawicki 199972 | Minor bleeding, % | 11.11 | 11.23 | NR | ||||
| Major bleeding, % | 1.11 | 1.12 | NR | |||||
| Siebenhofer 200863 | Cardiovascular disease other than AF or AHV, % | 78 | 84 | 0.24 | Thromboembolic events, % | 45 | 49 | 0.624 |
| HT, % | 43 | 49 | 0.439 | Severe bleeding, % | 4 | 6 | 0.484 | |
| DM, % | 23 | 25 | 0.773 | |||||
| Pulmonary disease, % | 13 | 12 | 0.895 | |||||
| GI tract disease, % | 12 | 11 | 0.886 | |||||
| Cancer, % | 7 | 8 | 0.741 | |||||
| Study ID | Country | Type of OAT management | Care provider | Training | ||
|---|---|---|---|---|---|---|
| Training provider | Time spent | Training description | ||||
| Azarnoush 201177,140 | France | PST | Cardiologist and or GP | NR | NR | Group session; 3–6 additional practical sessions |
| Bauman 201055,141 | Canada | PSM vs. PST | Nurse practitioner or physician within VPat | NR | 1 hour | Group session |
| Christensen 200675,142 | Denmark | PSM | Physician | NR | Daily for 3 weeks | NR |
| Christensen 201166 | Denmark | PST | Attending AC clinic doctor | Training on point-of-care test by biomedical laboratory scientists | 2 hours | NR |
| Cromheecke 200076 | Netherlands | PSM | NR | NR | 2 hours per session | Two group sessions; 4–6 per group |
| Eitz 200878,143 | Germany | PSM | GP (SC); staff at outpatient clinic (SM) | NR | NR | NR |
| Fitzmaurice 200267,144 | UK | PSM | Nurse led, GP | Research staff, practice staff | 1–2 hours per session | Two sessions |
| Fitzmaurice 200564,123,145 | UK | PSM | Anticoagulant nurse at practice-based clinics | Trained AC nurse | Two sessions | |
| Gadisseur 200368,80 | Netherlands | PSM | Physician, nurse | Specialised teams including physician and paramedical personnel | 90 to 120 minutes per session | Three group sessions: 4–5 per group |
| Gardiner 200545 | UK | PST | Nurse practitioner (SC); clinic staffs (SM) | Trained nurse practitioner | Two sessions | |
| Gardiner 200656 | UK | PST vs. PSM | Clinic staffs (SM) | Trained and experienced nurse | Two sessions | |
| Hemkens 200857 | Germany | PSM | Nurse | Skilled teaching nurse | NR | Four weekly sessions |
| Khan 200469 | UK | PST | Study researchers (SM); clinic staffs (SC) | Clinic doctor | 2 hours | Group session; 2–3 per group |
| Körtke 200170,147–149 | Germany | PSM | Family practitioner | NR | NR | NR |
| Horstkotte 199659,146 | Germany | PSM | Private physician | NR | NR | NR |
| Matchar 201071,150,151 | USA | PST | Trained clinic staff | NR | NR | NR |
| Menéndez-Jándula 200561 | Spain | PSM | Haematologists, trained nurse, physician | Trained nurse | 2 hours per session | Two group sessions |
| Rasmussen 201258 | Denmark | PSM | Physician | NR | NR | NR |
| Ryan 200962,152 | Ireland | PST | Clinic pharmacist or doctor | Research pharmacists and haematologist | 90 minutes | 1–3 per group |
| Sawicki 199972,153 | Germany | PSM | Family practitioner or clinic staff at outpatient clinic | Trained nurse and physician (2 days’ training) | 60 to 90 minutes per group | Three group sessions; 3–6 per group |
| Sidhu 200173 | UK | PSM | Family physician or AC clinic staff | NR | 3 hours per session | Two group sessions; 2–5 per group |
| Siebenhofer 200863,81 | Austria | PSM | GP or specialised AC clinic staff | Trained nurse and physician (2 days’ training) | 90 to 120 minutes per group | Four group sessions; 3–6 per group |
| Soliman Hamad 200979 | Netherlands | PSM | Physician | NR | At least 1 week | NR |
| Sunderji 200465,154 | Canada | PSM | Physician (SC); clinical pharmacist (SM) | Probably study pharmacist | First session 2–3 hours; second session 1–2 hours | Two sessions |
| Verret 201274 | Canada | PSM | Pharmacist (SM) | Pharmacist | First session 3 hours; second session 2 hours | 23 sessions held; 1–9 per group |
| Völler 200560,155 | Germany | PSM | Family physician or specialist physician | NR | NR | NR |
Appendix 8 Sensitivity analysis results (Table 34, Figures 28–47)
| Outcomes | All included studies, RR (95% CI) | Non-UK trials, RR (95% CI) | UK trials, RR (95% CI) | Trials at low risk of bias, RR (95% CI) |
|---|---|---|---|---|
| Any bleeding | 0.95 (0.74 to 1.21); p = 0.66 | 0.91 (0.70 to 1.20); p = 0.51 | 1.40 (0.61 to 3.23); p = 0.43 | 0.72 (0.41 to 1.26); p = 0.25 |
| PSM | 0.94 (0.68 to 1.30); p = 0.69 | 0.90 (0.63 to 1.28); p = 0.56 | 1.38 (0.53 to 3.59); p = 0.50 | 0.74 (0.42 to 1.32); p = 0.31 |
| PST | 1.15 (1.03 to 1.28); p = 0.02 | 1.14 (1.02 to 1.28); p = 0.02 | 1.46 (0.26 to 8.28); p = 0.67 | 0.28 (0.01 to 6.71); p = 0.43 |
| Thromboembolic events | 0.58 (0.40 to 0.84); p = 0.004 | 0.50 (0.32 to 0.76); p = 0.001 | 1.16 (0.58 to 2.29); p = 0.68 | 0.42 (0.22 to 0.77); p = 0.006 |
| PSM | 0.51 (0.37 to 0.69); p < 0.00001 | 0.40 (0.28 to 0.58); p < 0.00001 | 1.16 (0.58 to 2.29); p = 0.68 | 0.38 (0.20 to 0.69); p = 0.002 |
| PST | 0.99 (0.75 to 1.31); p = 0.95 | 0.99 (0.75 to 1.31); p = 0.95 | Not estimable | 1.67 (0.15 to 17.93); p = 0.67 |
| Mortality | 0.83 (0.63 to 1.10); p = 0.20 | 0.83 (0.60 to 1.15); p = 0.26 | 0.52 (0.11 to 2.58); p = 0.43 | 0.85 (0.40 to 1.81); p = 0.68 |
| PSM | 0.68 (0.46 to 1.01); p = 0.06 | 0.71 (0.43 to 1.16); p = 0.17 | 0.52 (0.11 to 2.58); p = 0.43 | 0.85 (0.40 to 1.81); p = 0.68 |
| PST | 0.97 (0.78 to 1.19); p = 0.74 | 0.97 (0.78 to 1.19); p = 0.74 | Not estimable | Not estimable |
FIGURE 28.
Forest plot of comparison: any bleeding – sensitivity analysis restricted to CoaguChek system trials. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus; PSM, patient self-management; PST, patient self-testing.
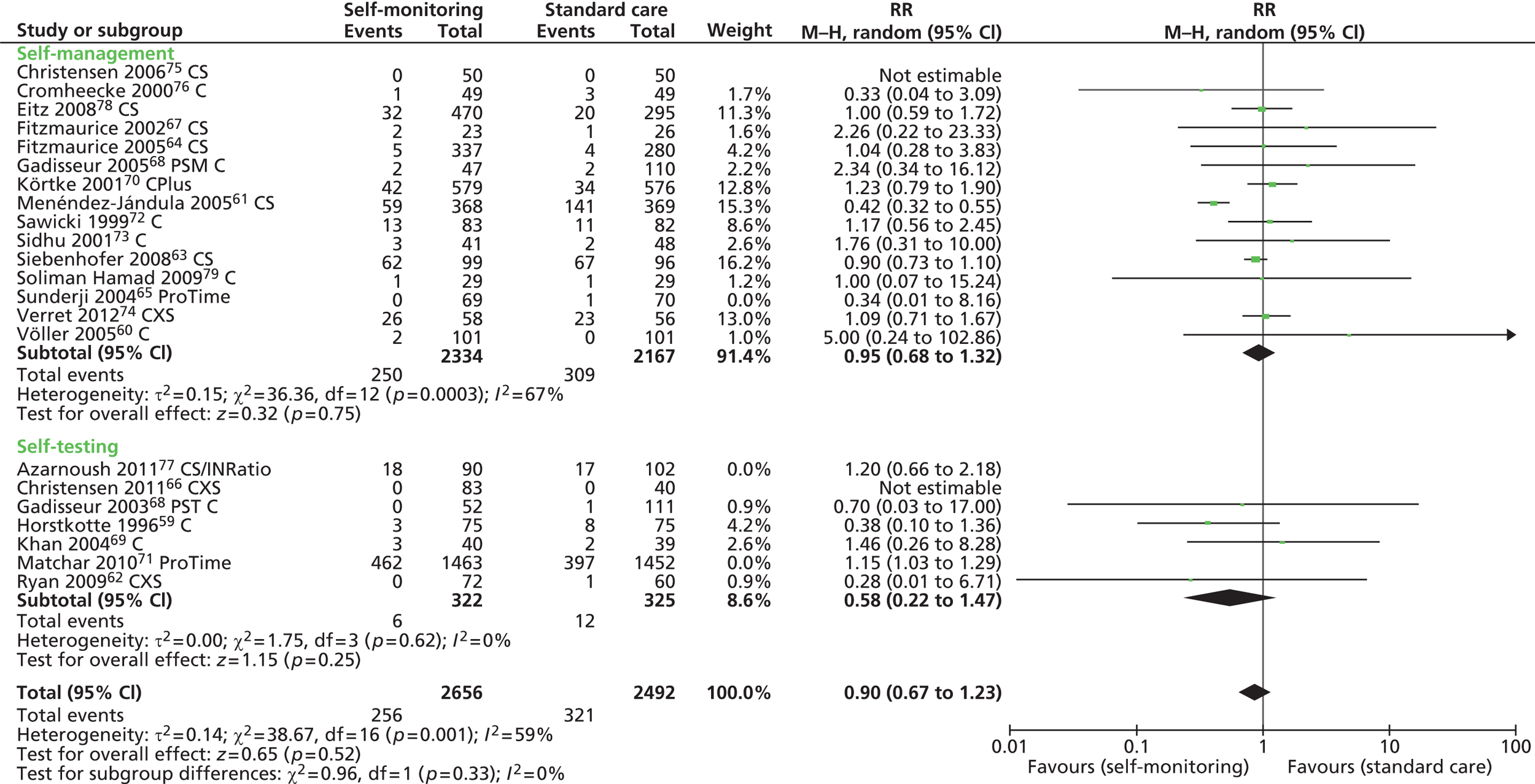
FIGURE 29.
Forest plot of comparison: any bleeding – sensitivity analysis restricted to CoaguChek XS trials. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus; PSM, patient self-management; PST, patient self-testing.
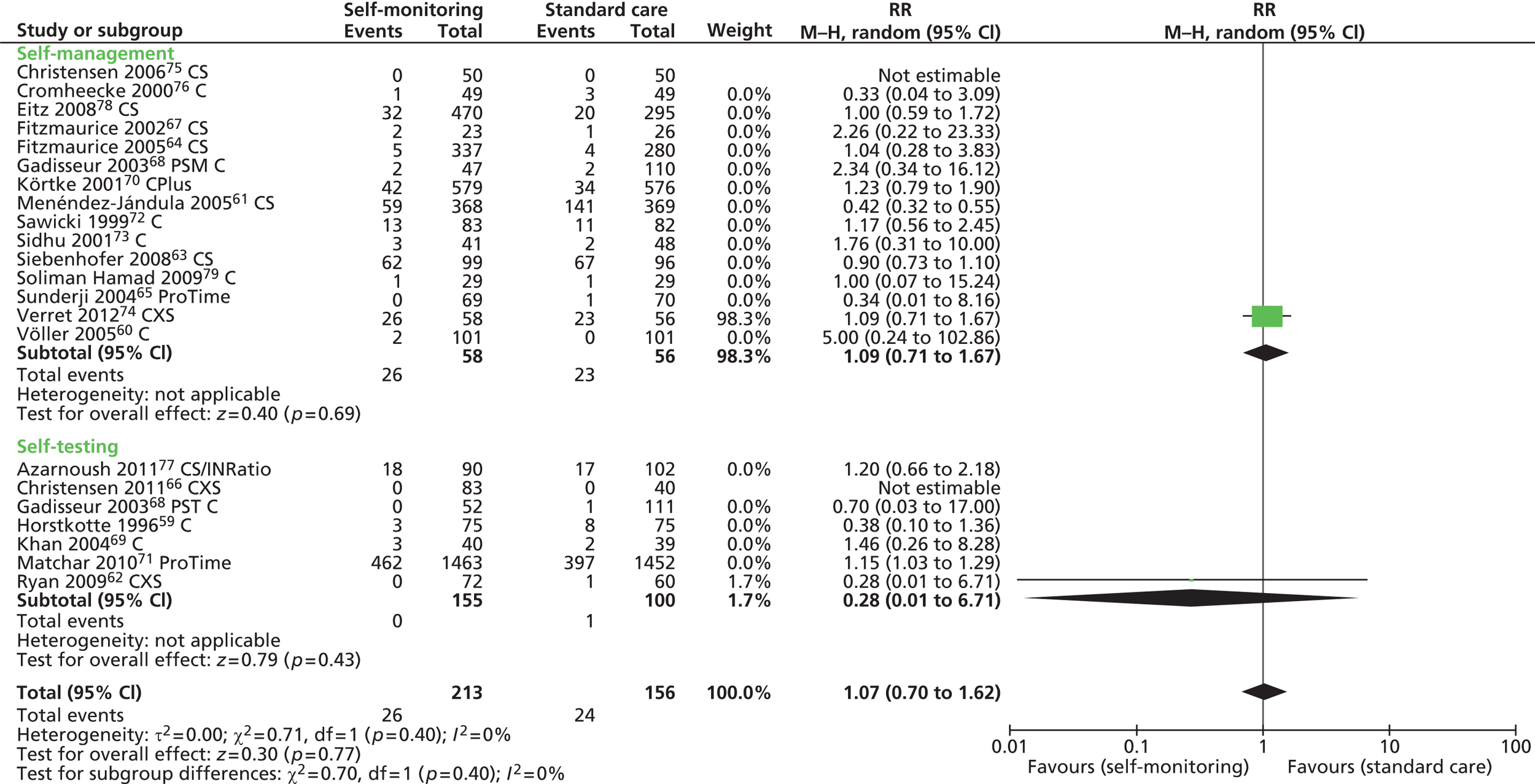
FIGURE 30.
Forest plot of comparison: any bleeding – sensitivity analysis restricted to ProTime trials. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus; PSM, patient self-management; PST, patient self-testing.

FIGURE 31.
Forest plot of comparison: any bleeding – sensitivity analysis restricted to CoaguChek and INRatio trials. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus; PSM, patient self-management; PST, patient self-testing.
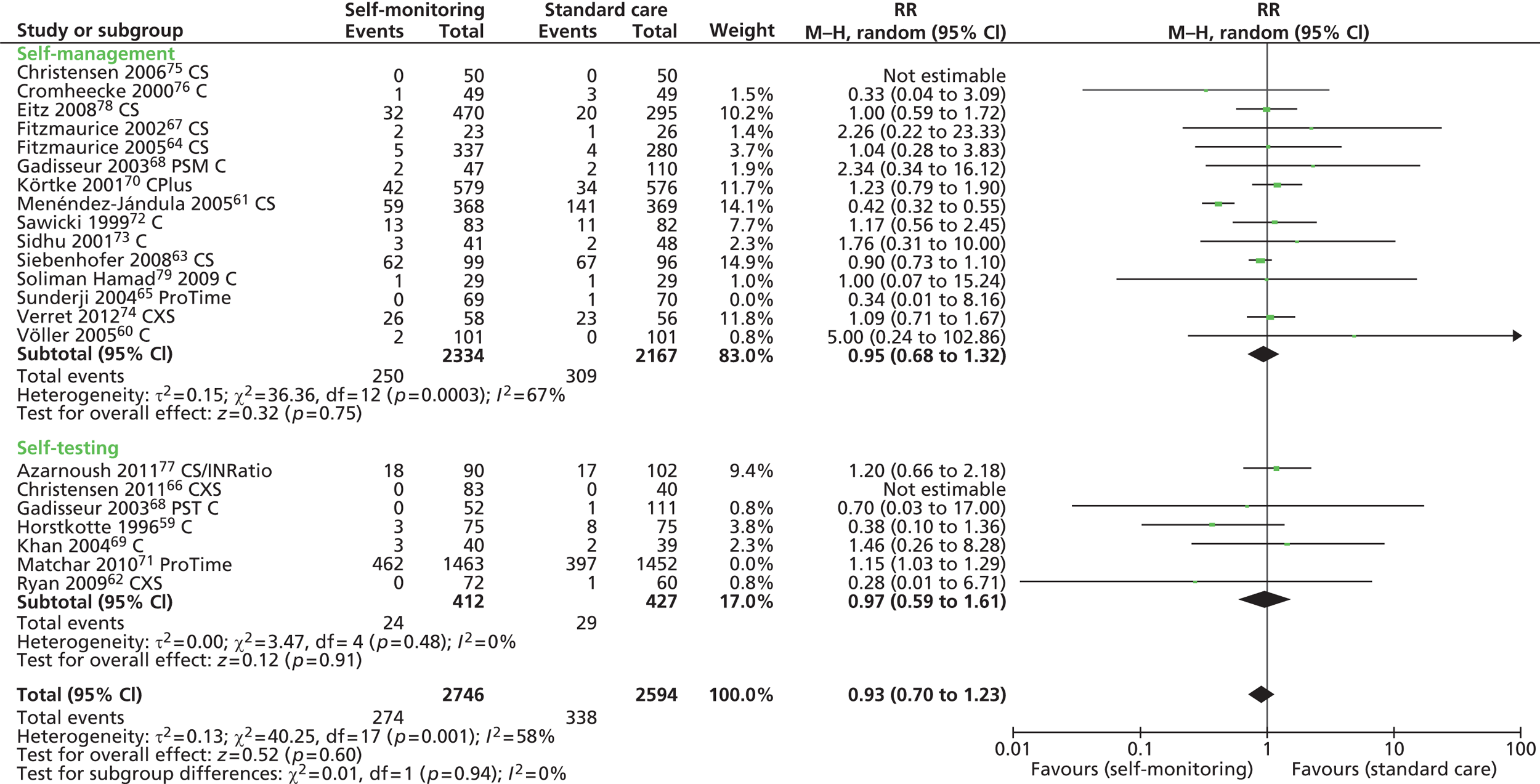
FIGURE 32.
Forest plot of comparison: thromboembolic events – sensitivity analysis restricted to CoaguChek system trials. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus; PSM, patient self-management.
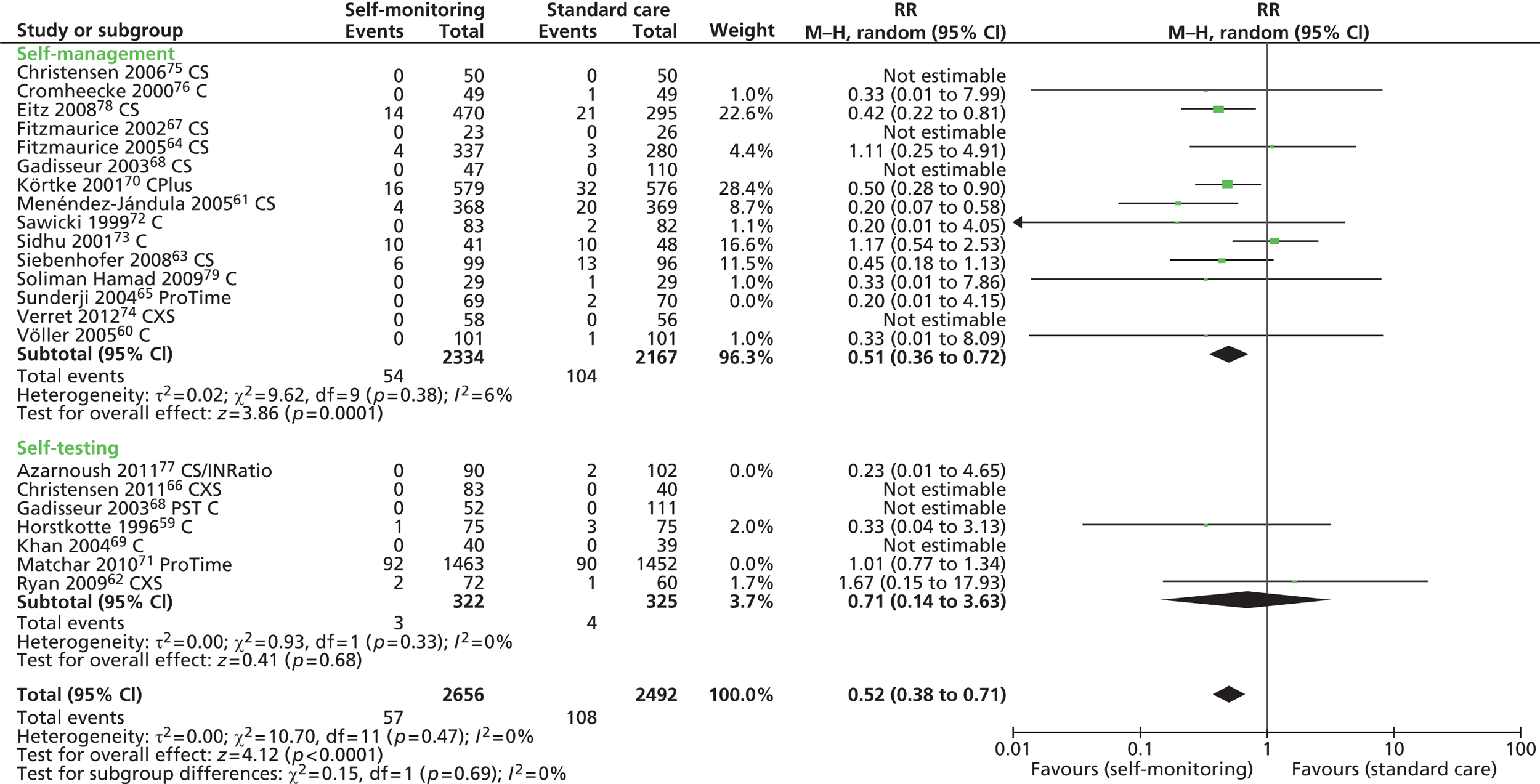
FIGURE 33.
Forest plot of comparison: thromboembolic events – sensitivity analysis restricted to CoaguChek XS trials. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus; PSM, patient self-management; PST, patient self-testing.
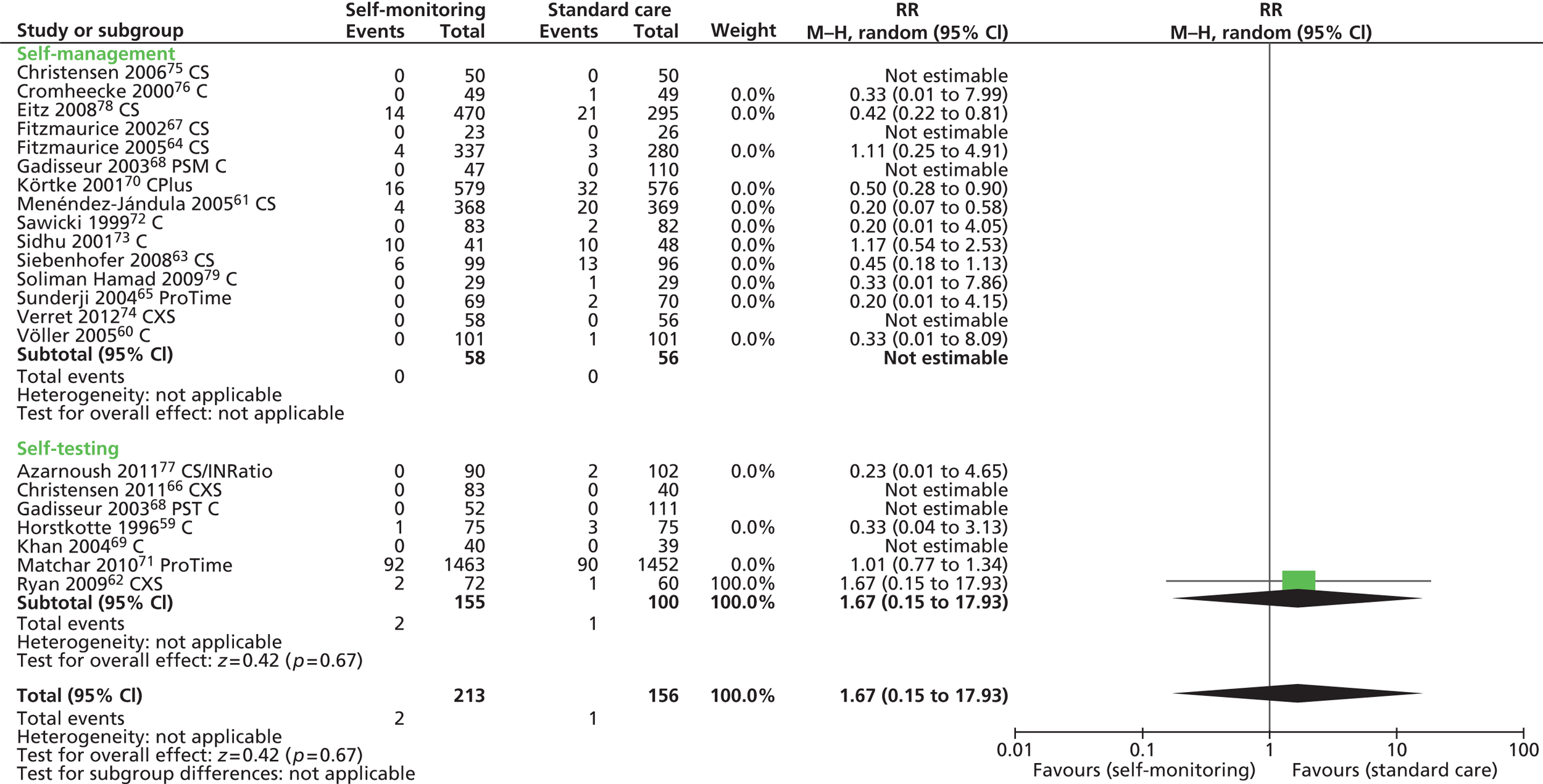
FIGURE 34.
Forest plot of comparison: thromboembolic events – sensitivity analysis restricted to ProTime trials. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus; PSM, patient self-management; PST, patient self-testing.
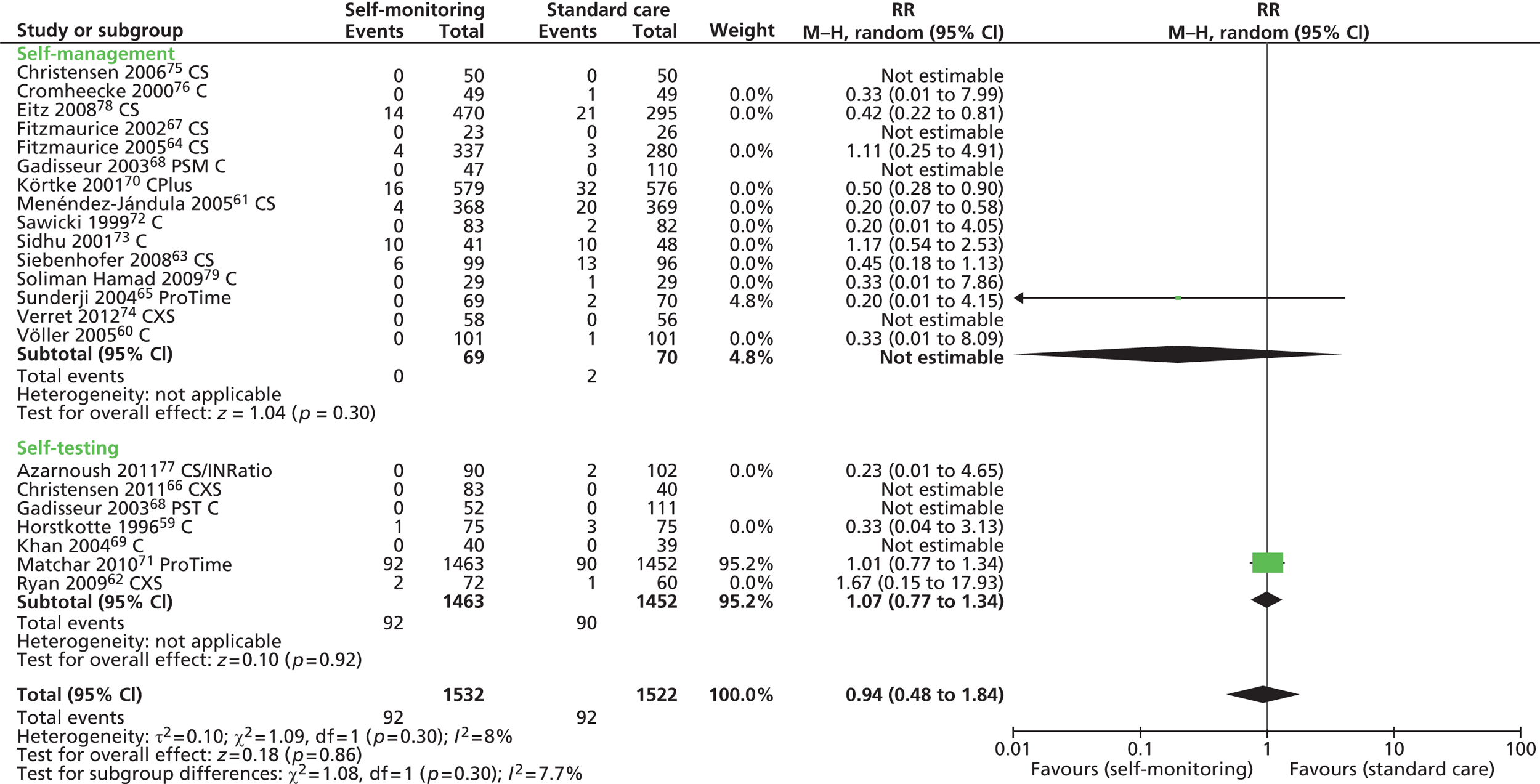
FIGURE 35.
Forest plot of comparison: thromboembolic events – sensitivity analysis restricted to CoaguChek and INRatio trials. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus; PSM, patient self-management; PST, patient self-testing.

FIGURE 36.
Forest plot of comparison: mortality – sensitivity analysis restricted to CoaguChek system. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus.
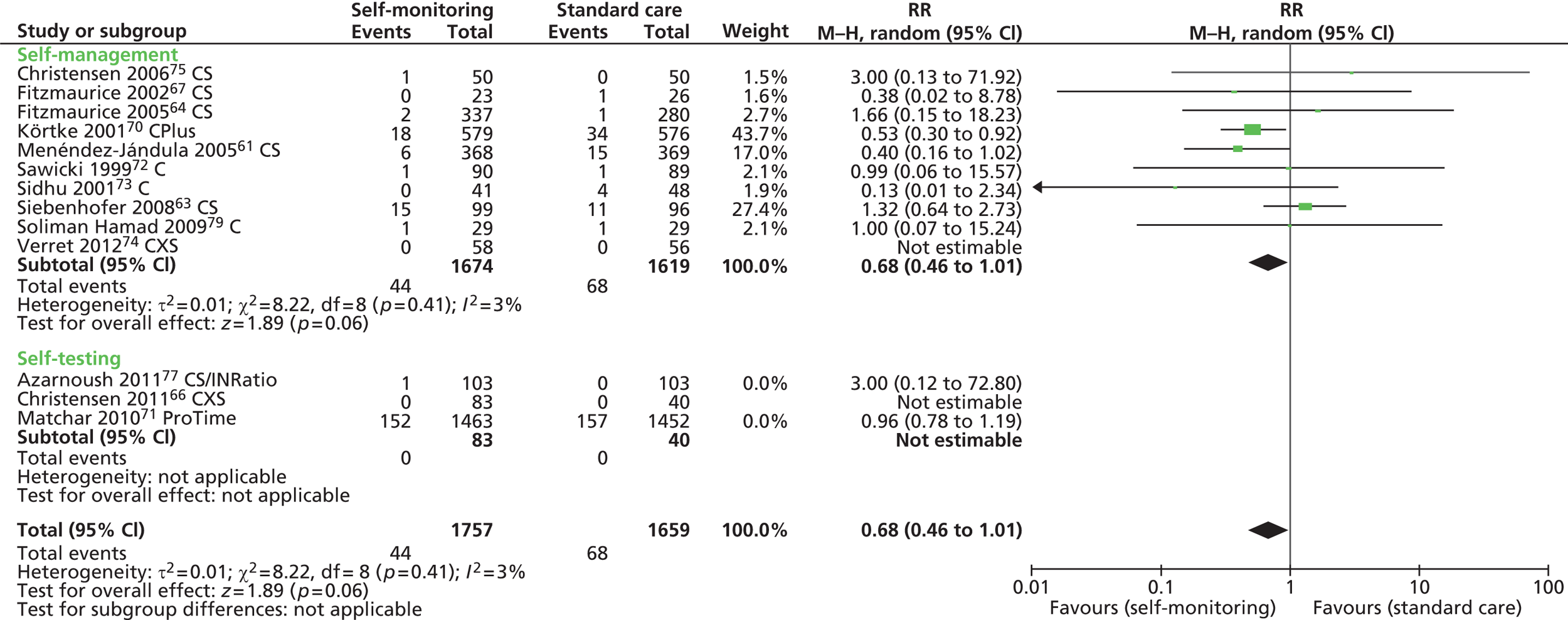
FIGURE 37.
Forest plot of comparison: mortality – sensitivity analysis restricted to ProTime. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus.

FIGURE 38.
Forest plot of comparison: mortality – sensitivity analysis restricted to CoaguChek and INRatio. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus.
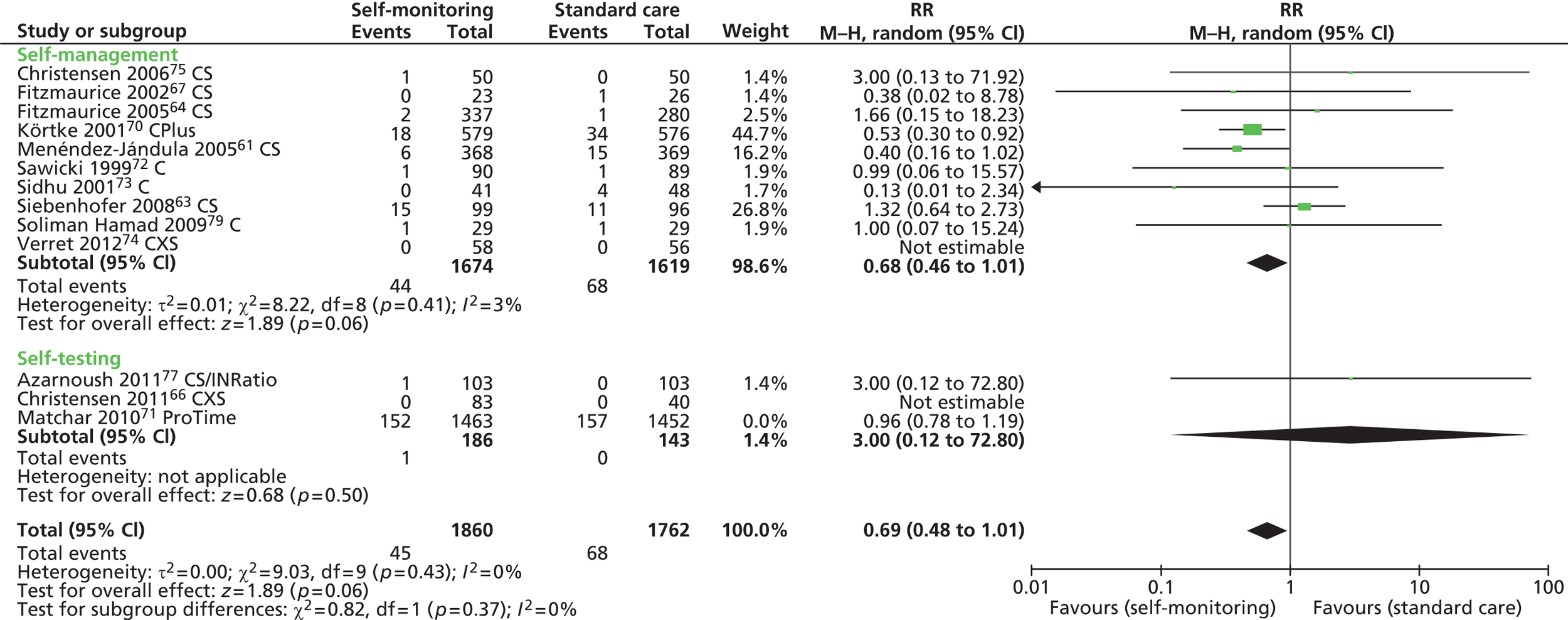
FIGURE 39.
Forest plot of comparison: any bleeding – sensitivity analysis restricted to non-UK trials. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus; PSM, patient self-management; PST, patient self-testing.
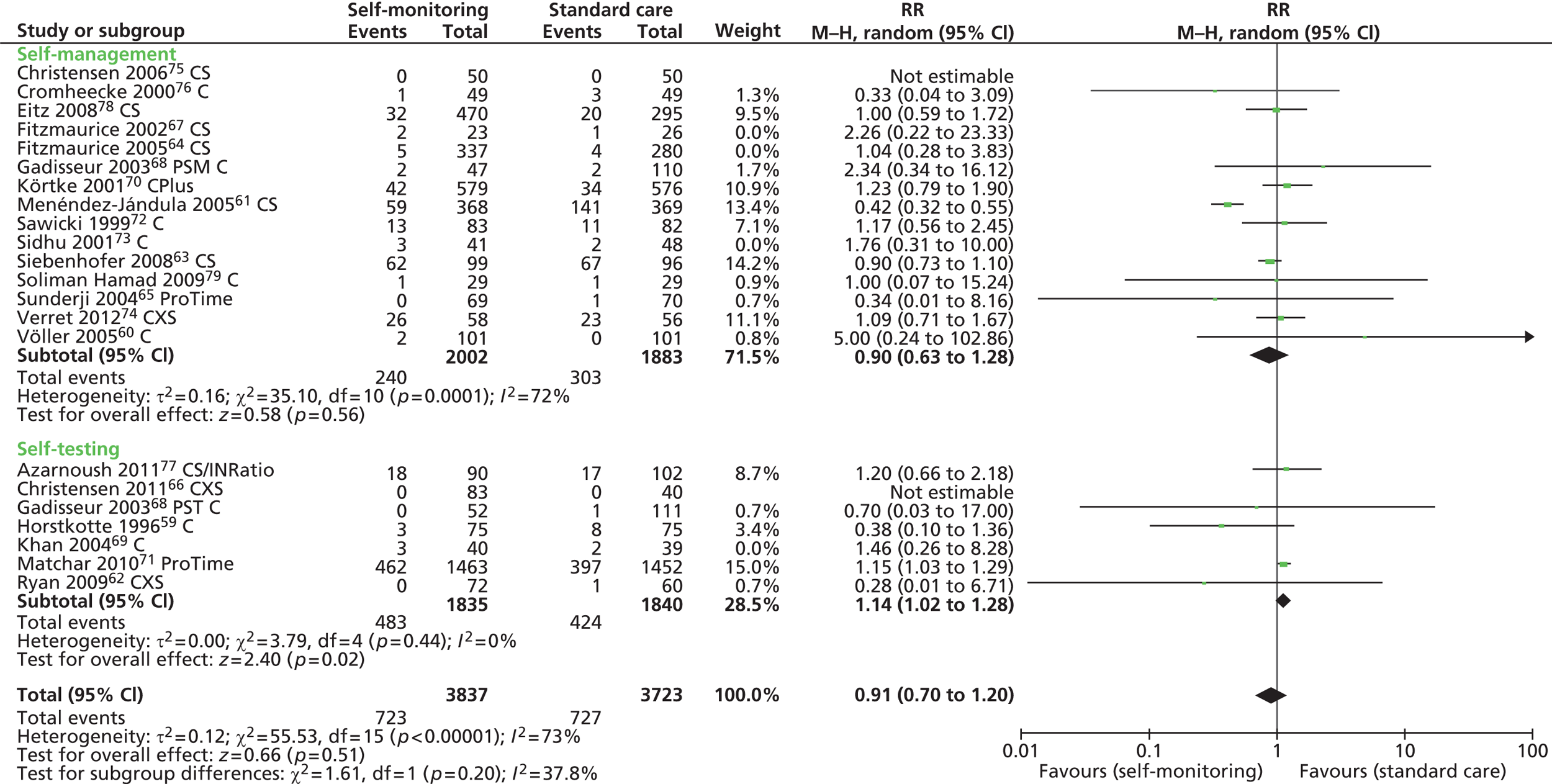
FIGURE 40.
Forest plot of comparison: any bleeding – sensitivity analysis restricted to UK trials. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus; PSM, patient self-management; PST, patient self-testing.

FIGURE 41.
Forest plot of comparison: thromboembolic events – sensitivity analysis restricted to non-UK trials. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus; PSM, patient self-management; PST, patient self-testing.
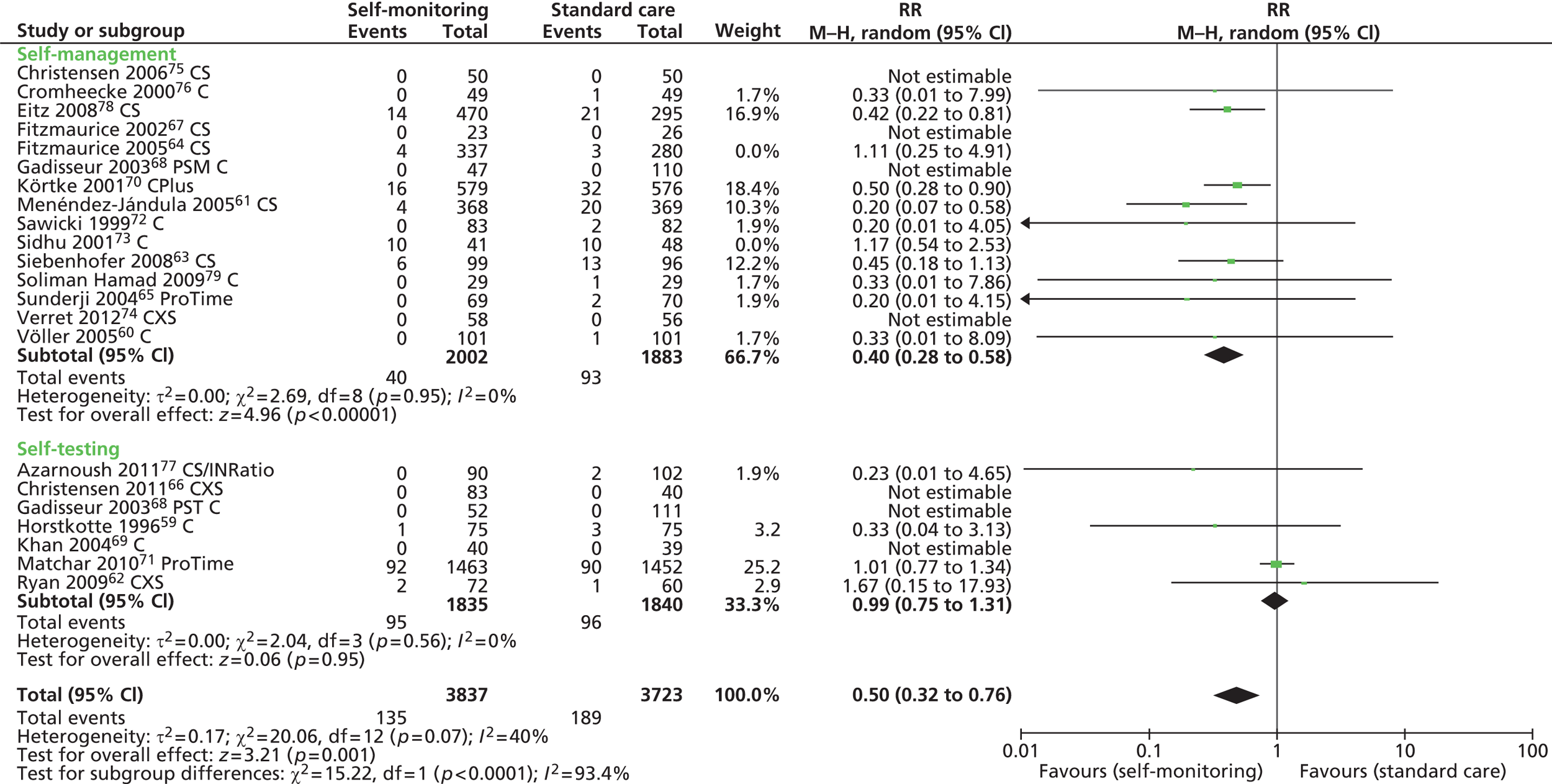
FIGURE 42.
Forest plot of comparison: thromboembolic events – sensitivity analysis restricted to UK trials. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus; PSM, patient self-management; PST, patient self-testing.

FIGURE 43.
Forest plot of comparison: mortality – sensitivity analysis restricted to non-UK trials. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus.
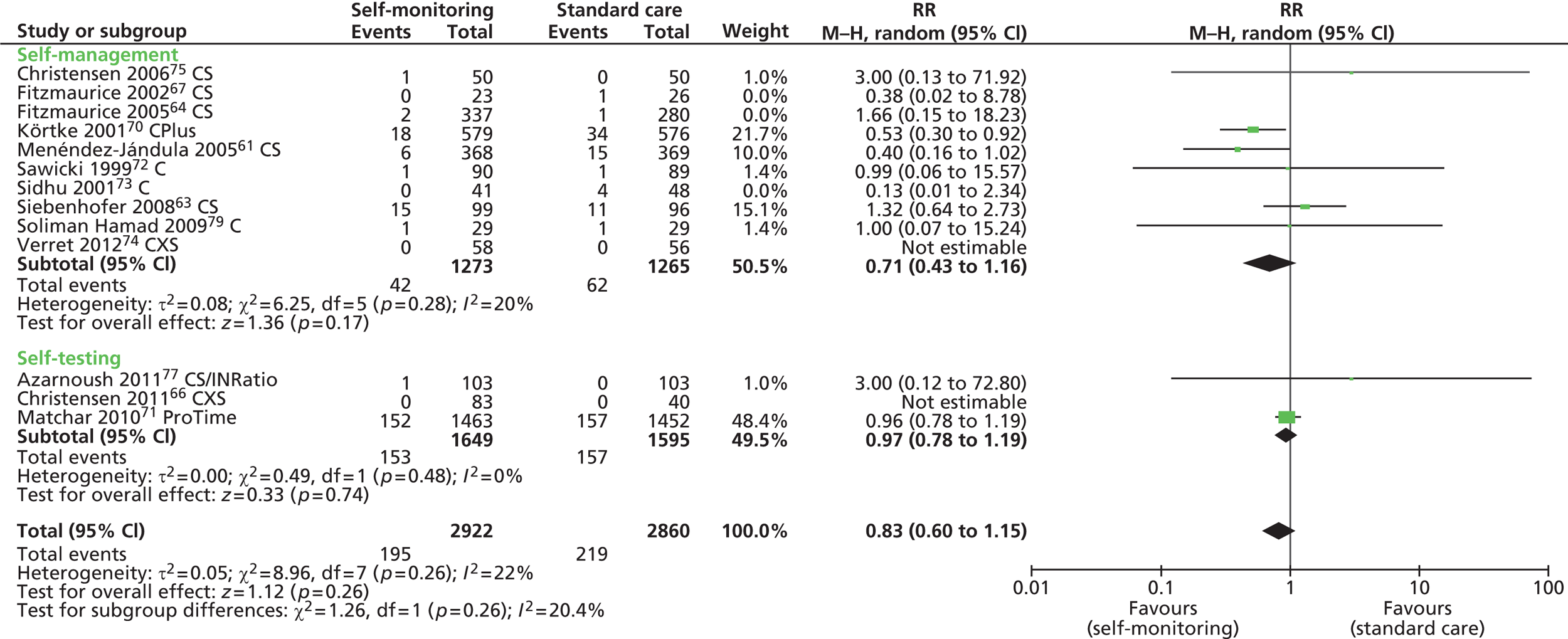
FIGURE 44.
Forest plot of comparison: mortality – sensitivity analysis restricted to UK trials. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus.

FIGURE 45.
Forest plot of comparison: any bleeding – sensitivity analysis restricted to low risk of bias trials. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus; PSM, patient self-management; PST, patient self-testing.
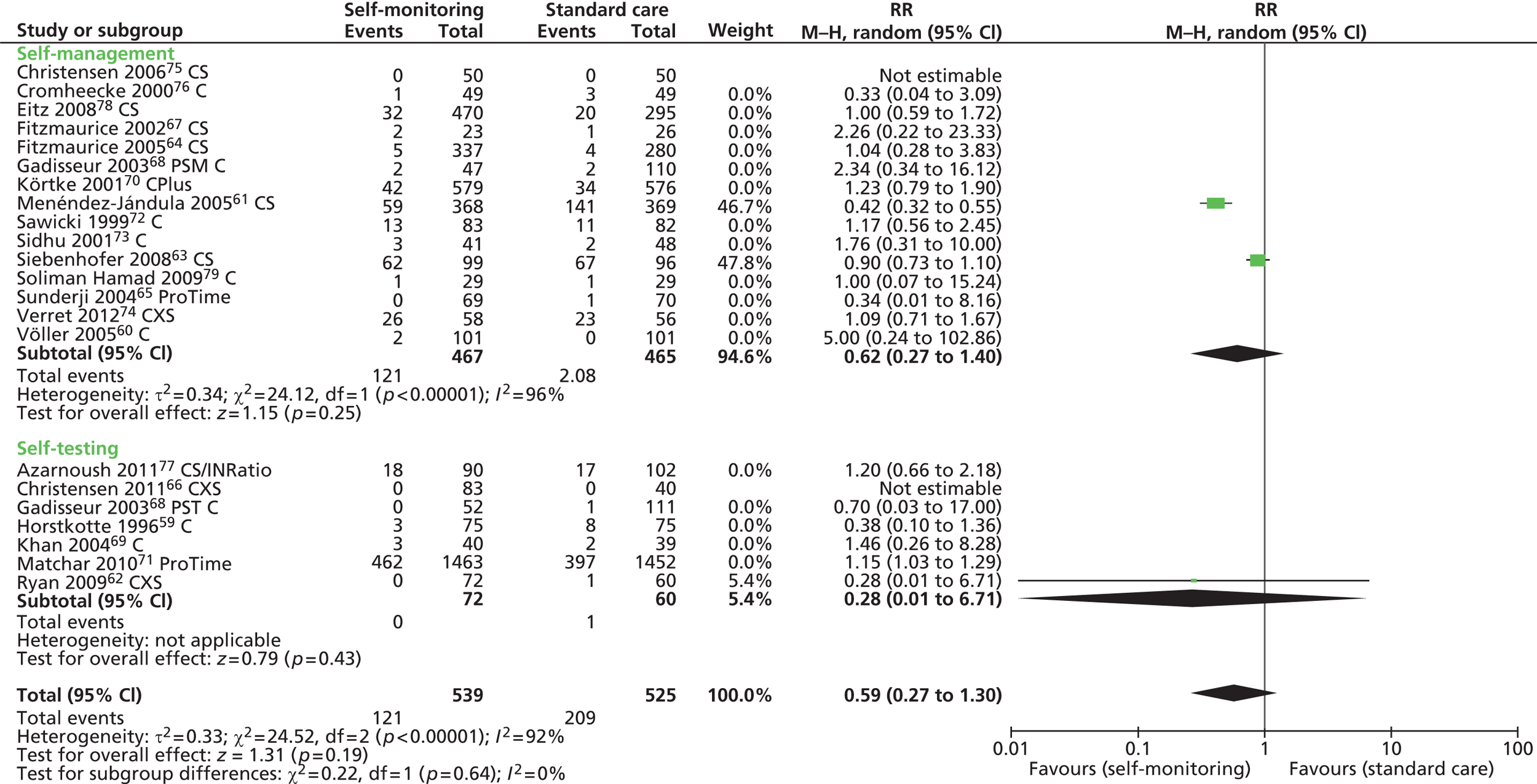
FIGURE 46.
Forest plot of comparison: thromboembolic events – sensitivity analysis restricted to low risk of bias trials. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus; PSM, patient self-management; PST, patient self-testing.
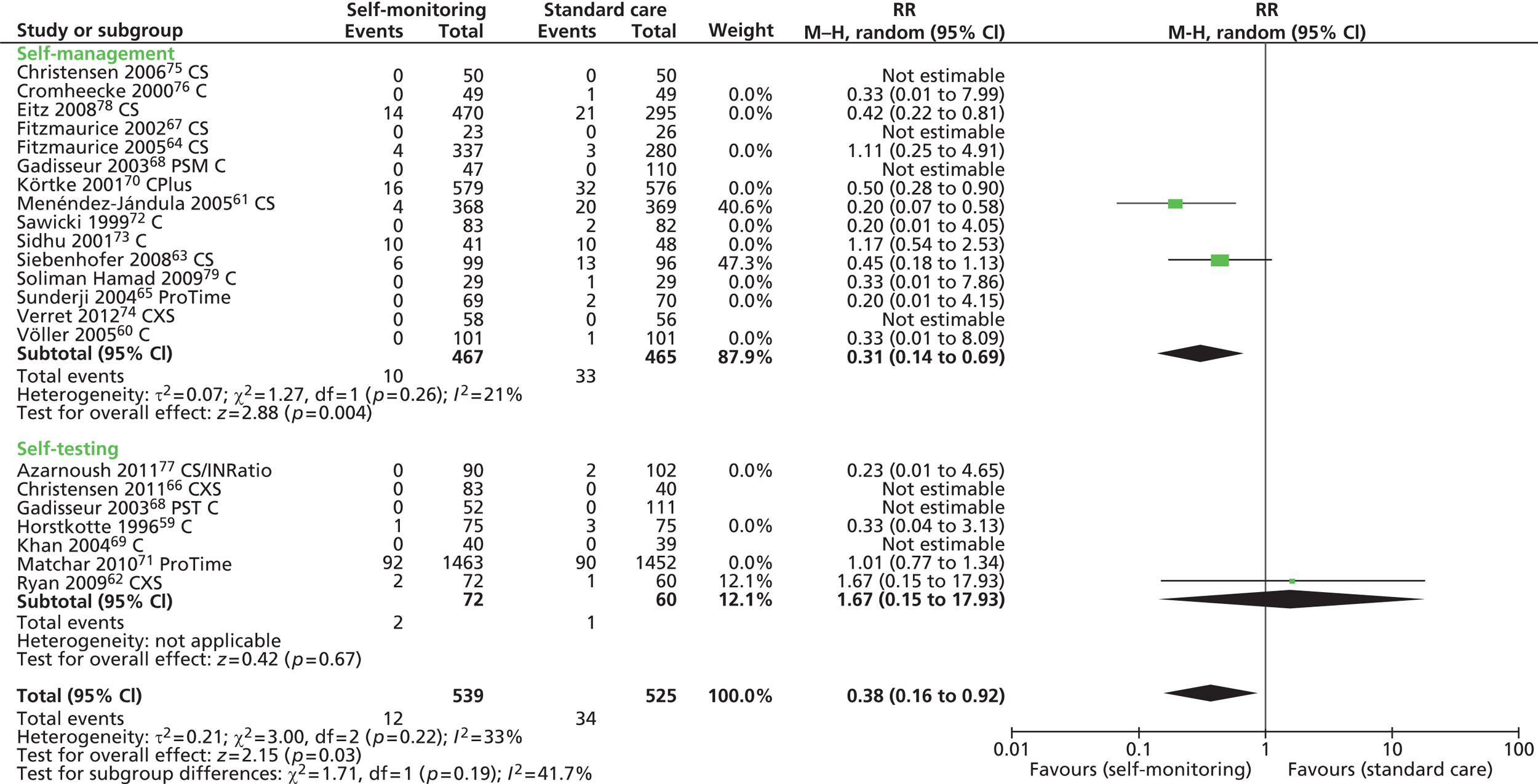
FIGURE 47.
Forest plot of comparison: mortality – sensitivity analysis restricted to low risk of bias trials. C, CoaguChek; CS, CoaguChek ‘S’; CXS, CoaguChek ‘XS’; CPlus, CoaguChek Plus.

List of abbreviations
- AHV
- artificial heart valve
- CI
- confidence interval
- CV
- coefficient of variation
- DAR
- diagnostic assessment report
- EQ-5D
- European Quality of Life-5 Dimensions
- ERG
- evidence review group
- FDA
- Food and Drug Administration
- GP
- general practitioner
- HCHS
- Hospital and Community Health Services
- HRG
- Healthcare Resource Group
- HTA
- Health Technology Assessment
- HUI
- Health Utilities Index
- ICER
- incremental cost-effectiveness ratio
- ICH
- intracranial haemorrhage
- INR
- international normalised ratio
- ISI
- International Sensitivity Index
- IV
- inverse variance
- M–H
- Mantel–Haenszel
- NICE
- National Institute for Health and Care Excellence
- OAT
- oral anticoagulation therapy
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- RE-LY
- Randomised Evaluation of Long-term Anticoagulation Therapy
- RR
- relative risk
- SD
- standard deviation
- SEIQoL
- Schedule for Evaluation of Individual Quality of Life
- SF-36
- Short Form questionnaire-36 items
- THINRS
- The Home International Normalised Ratio Study
- TTR
- time in therapeutic range
- WMD
- weighted mean difference