Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 08/44/04. The contractual start date was in September 2010. The draft report began editorial review in April 2014 and was accepted for publication in September 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Professor Hill is an advisor for Slimming World on psychological issues related to weight management.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Simpson et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Obesity: the problem
Poor diet, physical inactivity and high body mass index (BMI) have been identified as among the top 10 risk factors for the global burden of non-communicable disease. 1 Worldwide obesity has become a key public health concern, with the prevalence of obesity doubling since the 1980s. 2 Over one-quarter of adults in the UK are obese, and over 63% are either overweight or obese. 3 In 2010, 35% of men and 44% of women were at high or very high risk of health problems based on their BMI and waist circumference. 3 Obesity is associated with a reduced life expectancy of up to 14 years. 4 Obese and overweight individuals are at increased risk of developing type 2 diabetes mellitus, heart disease, osteoarthritis, depression, hypertension and certain cancers. 2 Although in some countries rates of obesity have stabilised, in others obesity rates are projected to continue increasing. 5 Despite efforts taken by many governments to tackle obesity, embracing increasingly comprehensive strategies and involving communities and key stakeholders, little progress has been made in successfully addressing ‘the obesity problem’.
The causes of obesity are complex and include biological, social, environmental and psychological influences. The Foresight report Tackling Obesities: Future Choices6 details the complex multidimensional array of influences affecting weight and concludes that tackling the obesity problem will require interventions at multiple levels of influence. Although obesity is associated with a number of potentially important genes, the effect that the genotype has on the development of obesity is strongly influenced by non-genetic factors. 7 Modern lifestyles tend to include low levels of physical activity and high levels of sedentary behaviours, resulting in reduced daily energy expenditure. Recent data, based on self-report, suggest that only 29% of women and 39% of men achieve government recommendations for physical activity in England. When this is based on objective measures, these rates are reduced to only 4% of women and 6% of men reaching government targets. 3 Many occupations have become more sedentary in nature, and easy access to different modes of transportation as well as concerns about safety negatively impact on walking and cycling. 8 Diet in developed countries has moved towards high-fat, energy-dense foods and large portions. 8 In the UK, and many other countries, the balance between energy intake and energy output has tipped in favour of weight gain.
Obesity-related illness represents a significant cost to the NHS, society and individuals. It is estimated that the NHS spends £5B per year9 treating obesity-related health problems. By 2050, if obesity continues to rise, the combined cost to the NHS and society has been estimated to be almost £50B per year. 6 In primary care, there are limited treatment options with proven effectiveness for weight management. Practice staff are often inadequately trained, and issues such as shortage of referral options, the large number of obese patients, the apparent lack of motivation of patients to change and time constraints compound the problem. 10
There is evidence that, in overweight or obese individuals, reductions in weight of 2–5 kg can lead to clinically important reductions in key cardiovascular risk factors and prevent progression to type 2 diabetes mellitus. 11–14 Evidence indicates that through various means, including lifestyle interventions and medication, this level of weight loss (and possibly more) can be achieved. 12,13,15–18 National Institute for Health and Care Excellence (NICE) guidance emphasises the importance of interventions that tackle both physical activity and diet and include behaviour change strategies. 19 Systematic reviews have shown that combining diet and physical activity is likely to be more effective than either alone. 20,21
Studies testing lifestyle interventions for weight loss have been successful in the short term; however, weight regain is common. 13,16 Weight loss interventions will ultimately be cost-effective and have a longer-term impact on health only if weight loss is maintained. Effective interventions that can help people successfully manage their weight in the longer term are therefore needed. Although there is some evidence that indicates maintenance interventions are associated with smaller weight gains than no contact, the prevention of weight regain remains a challenge. 20,22 Differences between intervention and controls tend to be small, and around one-third of weight is regained in the year following the intervention,23 with return to baseline weight within 5–6 years. 16 Helping individuals achieve long-term weight loss or maintenance has proven to be challenging. The skills and techniques used to maintain weight loss may be somewhat different to those required to lose weight. To date, research has provided limited insight into how this can be achieved;24 however, lifestyle and behavioural interventions are likely to be key to long-term weight loss.
The following two sections explore approaches to weight loss as well as weight loss maintenance (WLM). Evidence related to bariatric surgery was not considered because this group of patients are likely to require different support in terms of the strategies and psychological approaches. Bariatric surgery was also a specific exclusion criterion in the study. As there are few systematic reviews looking specifically at WLM interventions, we have included reviews that examine long-term weight loss (and, therefore, maintenance), with at least 1-year follow-up, as well as those in which the interventions being tested have a distinct focus on maintenance of weight already lost.
Weight loss interventions
A systematic review and meta-analysis of 30 randomised controlled trials (RCTs)25 of weight loss strategies, most of which included behavioural plus other approaches (13 diet alone, four diet and exercise, four exercise alone, seven meal replacement and two very low-energy diets) found that diet alone, diet and exercise, and meal replacements led to weight loss at 12 months of between 4.8% and 8%, and at 24, 36 and 48 months of between 3% and 4.3%. At 48 months, no groups regained weight to baseline levels. Only two of the studies of meal replacements went beyond a 1-year follow-up, and exercise alone did not appear to lead to successful WLM. When large weight losses were achieved using very low-energy diets, weight regain was rapid, but 5% loss could be maintained at 36 months. 25 A systematic review of six RCTs evaluating diet, exercise, or diet and exercise together indicated some advantage of combined diet and exercise interventions, which achieved a 20% greater sustained weight loss at 1 year than diet alone. 20 There is heterogeneity in the results of trials exploring type of diet and its relation to weight loss. A meta-analysis of five trials found no differences between low-carbohydrate and low-fat diets at 12 months. 26 A systematic review of 14 RCTs found that low-fat, 600 calorie deficit, or low-calorie diets were associated with weight loss at 12, 24 and 36 months. 13
Obesity medication has also been used to target long-term weight loss. A meta-analysis of 12 RCTs indicated that orlistat (Xenical®, Roche) conferred an advantage above diet alone of 3.1 kg weight loss [standard deviation (SD) 10.5 kg] at 24 months. 25 Another systematic review of 12 clinical trials found that orlistat plus dietary or lifestyle intervention resulted in a 3–10-kg loss after 12–24 months and increased the odds of attaining 5% weight loss or greater at 24 months. 27 However, the included studies suffered from high attrition rates, on average between 30% and 50%, highly selected patient populations, inadequate description of randomisation and few used intention-to-treat analyses.
Weight loss maintenance interventions
In terms of interventions specifically for WLM, there are limited data on diets suitable for WLM. However, evidence from the US Weight Control Registry indicates that those who maintain weight loss in the longer term generally follow low-fat, low-calorie diets, eat breakfast and have consistent eating patterns over weekdays and weekends. 28 A conceptual review of factors associated with WLM also found that eating breakfast and a regular meal pattern are important, as is having a healthier low-fat diet. 29
Although physical activity is important for maintenance of weight loss,30 limited evidence exists regarding the type or amount of physical activity required. A systematic review comprising 11 RCTs and 35 prospective or non-randomised studies suggested that higher levels of physical activity may be associated with WLM. 31 Secondary analyses of one well-designed trial found that individuals reporting higher levels of physical activity (275 minutes per week) were better able to maintain 10% weight loss at 24 months. 32 Another review identified that 60–90 minutes of moderate-intensity activity per day is needed to prevent weight regain. 33 The 2008 US Physical Activity Guidelines Advisory Report34 identified that the currently available evidence has a number of limitations; nevertheless, the report suggests that ‘more is better’. The studies included in the report indicated that, to prevent weight regain, individuals should walk for 60 minutes or jog for 30 minutes daily. However, many individuals find this difficult to maintain in the longer term.
A recent systematic review of trials of interventions to maintain weight loss found that behavioural interventions focusing on diet and physical activity led to an average weight difference of –1.56 kg in weight regain in intervention participants relative to controls at 12 months. 35 Orlistat plus behavioural treatment led to a –1.80 kg difference between intervention and control. 35 In addition, a review of RCTs of WLM interventions found that treatment with orlistat or sibutramine (Reductil®, Knoll Abbott) alongside a dietary intervention, caffeine or protein supplementation, physical activity, low-fat diet, ongoing contact, problem-solving therapy, or acupressure was helpful in minimising weight regain. 36 A systematic review and meta-analysis of the impact of extended care on maintenance of weight loss in the longer term found that extended care could lead to an additional maintenance of 3.2 kg at 17.6 months compared with control. 37
There is some evidence that web- or computer-based interventions may be useful for WLM,38,39 and they are likely to cost less to deliver. One review suggested that web-based interventions are about as effective as face-to-face interventions and higher website use may be associated with WLM. 40 Another recent review found that computer-based interventions were more successful for WLM than no intervention or minimal intervention. 39 When computer-based interventions were compared with in-person interventions, the weight loss was smaller and weight maintenance was of shorter duration. 39 A recent telephone- and mail-based intervention found that, at the 24-month follow-up, the odds of weight maintenance was 1.37 times greater in the guided telephone intervention than in the self-guided arm. 41 This approach is likely to be more feasible and cost-effective to deliver.
Further research is needed, as the evidence base is limited, because most trials included in reviews are of poor or moderate quality. Many trials of longer-term weight loss or WLM are inconclusive. They are heterogeneous in terms of setting, length of follow-up, type and duration of intervention, many have methodological flaws, including inadequate reporting of randomisation processes or blinding and paucity of intention-to-treat analyses, and findings are often contradictory. High levels of attrition are evident and this is probably associated with WLM failure. This makes it difficult to draw conclusions about what works in WLM. There is a need to develop and rigorously test interventions that are based on evidenced behaviour change techniques which also take contextual factors into account, that can help people with long-term weight loss or maintenance of weight loss. Although there is a lack of research evidence for interventions that can effectively support longer-term weight loss, there have been some notable successes, for example the Finnish Diabetes Prevention programme, in which participants maintained an average weight loss of 3.5 kg at 3-year follow-up. 42 Conducting trials in this area is challenging for a number of reasons: difficulties achieving blinding owing to the nature of the intervention; the difficulty of retaining participants over long-term follow-up; and the cost of running such long-term studies, which makes the production of the required evidence time-consuming and expensive.
Psychological/behavioural therapeutic approaches
Trials of interventions for long-term weight loss or maintenance of weight loss usually include some aspect of behaviour therapy or counselling as part of the intervention, alongside other elements such as dietary change. Counselling or psychotherapeutic approaches that have been successfully used for weight loss include cognitive–behavioural therapy43 and motivational interviewing (MI). 44 As well as these particular counselling approaches, many interventions have employed specific behaviour change techniques and, in many cases, the effects of these elements are not teased out. Behavioural techniques that have been specifically assessed in high-quality RCTs and shown to offer significant benefit for WLM include goal-setting,38 problem-solving,22,38 relapse prevention,38 self-monitoring22,38 and daily self-weighing. 22 Peer or social support21,22 and frequent continued professional support have also been shown to be important. 22,38
As noted above, the psychological processes, skills and strategies which are likely to be effective for WLM are potentially different from those needed to lose weight. 22,24,45,46 Research examining 5000 people on the US National Weight Control Registry suggests that the only factor those losing weight have in common is that they combined diet and exercise to do so. However, when examining the maintenance phase, a number of common factors were identified, including low-fat diet, eating breakfast, self-monitoring and high levels of physical activity. 28 Losing weight requires a negative energy balance, whereas weight maintenance requires continued energy balance. This balance needs to be sustained by behaviours that can be continued over the longer term. In reviews of factors associated with WLM, a number of issues stand out: higher levels of physical activity,32 consumption of low-calorie and low-fat foods, individual tailoring of advice, self-regulation/monitoring, social support, internal motivation and self-efficacy. 28,29
The WeIght Loss Maintenance in Adults (WILMA) trial tested an intervention that incorporated many of the evidence-based behavioural techniques described above alongside three main components: MI (incorporating action-planning and implementation intentions47,48), social support and self-monitoring. These three main elements and evidence for them will be considered briefly in Motivational interviewing, Social support and Self-monitoring. The intervention elements and theoretical approach are described in more detail in Chapter 2.
Motivational interviewing
Motivation is a key precursor for behaviour change, and ongoing motivation is important in terms of maintaining behaviour change. 49 As ongoing intervention contacts have been shown to help maintain weight loss,38 and attrition from longer-term programmes is a problem,22 motivation is likely to be important. Many people are able to lose weight by dieting and/or exercise. 45 However, sustaining these behaviours seems to be challenging and, therefore, enhancing motivation is likely to be important in terms of maintaining healthy behaviours. MI is therefore the key ingredient of the intervention. MI is defined as:
a collaborative, goal-oriented style of communication with particular attention to the language of change. It is designed to strengthen personal motivation for and commitment to a specific goal by eliciting and exploring the person’s own reasons for change within an atmosphere of acceptance and compassion. 50
The effectiveness of MI has been demonstrated in a wide range of behaviour change contexts including modification of drug use51 or alcohol consumption51 and smoking cessation. 52 Weight loss and WLM is a relatively new area for MI, and few studies have been completed. 53 MI has been shown to be effective as an adjunct to a behavioural weight control programme. 53 It can be useful in maintaining behaviour change as well as initiating change and supports participants in an ongoing, tailored way. 53,54
Brief interventions using MI have been effective in different areas of behaviour change including diet and physical activity. RCTs and systematic reviews of MI approaches have shown that it can be used successfully in interventions to change both diet and exercise. 55–59 It can also effectively be delivered by telephone, which provides a clear cost advantage over face-to-face delivery. 60,61 There is some evidence that MI can be effective when delivered in just one session62 and even when sessions are as short as 15 minutes. 57,63 One meta-analysis examining MI in different areas of disease showed a combined effect of MI on decreasing BMI by 0.72 kg/m2 (p < 0.0001) and found that longer follow-up increased the chance of an effect from 36% at 3 months to 81% at 12 months or longer. 57
A systematic review and meta-analysis identified 11 RCTs examining the effect of MI on weight loss. 64 It found that participants who received MI lost more weight than controls [weighted mean difference −1.47 kg, 95% confidence interval (CI) −2.05 kg to −0.88 kg]. The pooled effect size was 0.51. When weight loss was the primary outcome, treatment was more than 6 months and a treatment fidelity measure was used and the effect of MI on BMI increased. However, most of these studies had a follow-up period of less than 12 months. 64
No studies have tested MI as a WLM intervention, although a few have investigated longer-term WLM following an MI-based weight loss intervention. 53,54 West et al. 53 tested a weight loss intervention consisting of MI (plus a group-based weight control programme) in women with type 2 diabetes mellitus. They found that women in the MI group lost significantly more weight by the 18-month follow-up assessment than those in the control group (3.5 kg ± 6.8 kg loss in MI and 1.7 kg ± 5.7 kg in control subjects, p = 0.04). Hoy et al. 54 conducted a study with a 5-year follow-up period. They evaluated a dietary intervention with MI techniques and found that, after 1 year, body weight was lower in the intervention group and at 5 years women in the intervention group weighed significantly less than controls [6.1 lb mean weight difference between groups (p = 0.005) at 5 years].
Social support
As environmental factors can encourage or impede behaviour change and maintenance, social support has a key role. Social support may operate in a number of ways to promote healthy behaviours, for example through reinforcement, encouragement, motivation, feedback, empathy, role-modelling, increased self-efficacy, instrumental support (help), appraisal (e.g. affirmation), peer pressure for healthy behaviours or access to health information. There is evidence indicating that social support and health are related65 and that social support can promote better health behaviours when employed alongside goal-setting and self-monitoring. Ferranti et al. 66 found that social support is positively correlated with a good diet and increased physical activity. 67,68 Social support can improve WLM,69 encourage health-promoting behaviours and promote well-being. 70 Conversely, there is also evidence that unhealthy behaviours are correlated with less social support. The current NICE behaviour change draft guidance notes that, across a range of health behaviours (including diet, alcohol and physical activity), social support was present in most of the effective interventions. 71
Social support tends to be employed and theorised as one of several key elements in behaviour change interventions72 and has been identified in reviews as one contributing factor to effectiveness, alongside goal-setting and self-monitoring. 21,73 Common intervention elements thought to operate in conjunction with social support are self-efficacy,74 perceived control68,74 and social norms. 75 A trial of diet change and weight loss with the inclusion of group-based social support found that those who received social support regardless of the diet they followed lost more weight at years 1 and 2 than those who did not receive support. 76 Other studies also report that participants who received interventions which included social support lost more weight by the end of the study than did controls. 69,77 Continued professional support is also related to better WLM. 21,22,38
Self-monitoring
Self-monitoring is important for successful behaviour change. 78 In a meta-analysis of behaviour change interventions of physical activity and healthy eating, more effective interventions were shown to combine self-monitoring with at least one other technique derived from control theory (e.g. intention formation, specific goal-setting). 73 Regular self-monitoring is associated with WLM and is recommended by NICE. 19 Self-monitoring in this context consists of regular self-weighing and monitoring of diet and physical activity. 57 A systematic review found a consistent association between self-monitoring and weight loss, although the authors suggest caution as the quality of the evidence is weak. 78 One good-quality study found that daily self-weighing was associated with a decreased risk of regaining weight at the 18-month follow-up. 22 Another study exploring WLM among participants in the National Weight Control Registry found that WLM for longer than 5 years was associated with regular self-monitoring of weight. 28
The trial
The present study evaluated a 12-month, individually tailored intervention based on MI incorporating implementation intentions/action-planning, peer support and self-monitoring. The trial comprised three arms: (1) an intensive intervention arm, (2) a less intensive intervention arm and (3) a control arm. The intervention, which is described in detail in Chapter 2, was initially delivered face to face and incorporated follow-on sessions delivered by telephone as well as group-based peer support sessions. The focus of the intervention was on maintaining gains already made. It is envisaged that this intervention, if successful and cost-effective, could be rolled out to a wide variety of people who have lost weight using different methods; therefore, the participants were recruited from a variety of settings.
The original aim of the study was to evaluate the impact of a 12-month multicomponent intervention, or a less intensive version, with a control intervention on participant BMI with follow-up at 3 years from randomisation. However, set-up and recruitment challenges meant that the trial design was changed to a feasibility study. The main objectives of the feasibility study were to assess the feasibility, acceptability, compliance and delivery of a 12-month multicomponent intervention, as well as recruitment and retention, which were assessed as part of the process evaluation. The process evaluation also examined the views of participants and intervention staff. To give an indication of effect sizes for a larger trial, we evaluated the impact of the intensive or less intensive intervention on participants’ BMI (primary effectiveness outcome) at 12 months from randomisation.
We examined the effect of the intervention on physical activity, diet, health-related quality of life, binge eating, psychological well-being and health resource use. We also examined the proportion of participants maintaining their baseline weight at the 1-year follow-up (defined as having a weight at follow-up the same as or lower than their baseline weight). To assess abdominal obesity, waist circumference and waist-to-hip ratio were included as outcomes. This is important because visceral fat is independently associated with all-cause mortality79 and many of the risk factors for cardiovascular disease, including type 2 diabetes mellitus. 80 As the direct measurement of visceral fat relies on sophisticated imaging technology, most large-scale, community-based studies have relied on anthropometric measurements of the waist and hip circumference to determine abdominal obesity. Although the findings of these studies are not completely consistent, evidence suggests that a measurement of abdominal obesity (waist circumference or waist-to-hip ratio) provides explanatory information in addition to that provided by BMI. 81
We assessed mediators associated with change and hypothesised mediators include self-efficacy, social support, self-monitoring, implementation intentions, habit formation and intrinsic motivation. Analyses sought to identify the extent to which the intervention was successful at changing these mediators and the extent to which mediator change was associated with WLM (see Chapter 5). See Table 2 for a full description of mediators.
Data on key moderators were collected to examine factors associated with success in WLM. These include demographics (age, gender, socioeconomic status, ethnicity and employment status), binge eating, quality of life, source of recruitment, psychological well-being, gender and socioeconomic status. Although a number of studies have found no differential effects of gender on weight management interventions,38 some have found that the male physiological response to physical activity does impact on weight management interventions, although further work is needed. 82–84 The effects of age are also unclear, but older participants have been reported to be more successful in WLM programmes. 85 Prevalence of obesity is higher in some ethnic minority groups, and ethnicity has also been associated with better WLM in some American studies. 86,87 This may be confounded by lower socioeconomic status, which impacts on food choices resulting from environmental factors and sociocultural attitudes. 87 Finally, a cost-effectiveness evaluation was also undertaken.
Chapter 2 The WeIght Loss Maintenance in Adults trial intervention
Background
There has been a significant focus in recent years on developing behaviour change interventions with a strong theoretical foundation that are clearly described and consequently replicable. 88–92 Furthermore, there are a number of suggested frameworks and taxonomies of behaviour change techniques88,90–92 which provide a method for defining intervention components and a set of accompanying definitions that facilitate accurate description and replication of these components. Researchers have also indicated which psychological theories some of these techniques map onto, for example goal-setting and social cognitive and control theories. 88 However, there remains a significant amount of uncertainty regarding how best to match behaviour change techniques to theoretical constructs. 90 Based on these recommendations and observations, the approach taken here was to develop a well-described, theory-based intervention and to explicitly test the theorised mechanisms of effect.
Intervention components and theory
As outlined in Chapter 1, the WILMA trial intervention was based on three main components: MI (incorporating implementation intentions),47 social support and self-regulation (self-monitoring).
Motivational interviewing
Motivation is central to many theories seeking to explain behaviour change. Motivation is unlikely to be static and is a product of both internal and external factors related to the individual. 49 As highlighted in Chapter 1, motivation is likely to be critical in minimising attrition,22 which is important as sustained intervention contact is associated with better weight outcomes. 38 For this reason, MI is the key ingredient of the intervention.
Four key processes have been identified as occurring during MI counselling sessions: engaging, guiding, evoking and planning. 50 Engaging is the process whereby the counsellor develops rapport and a collaborative working alliance with the client. Guiding occurs after engagement and is the process in which the counsellor helps guide the client along a particular course in relation to change. Evoking involves prompting the client to think about and describe his or her motivations for change, and this is a key aspect of MI. Planning involves the client developing a plan in order to achieve the change that he or she desires. These processes are ongoing and may need to be revisited at different time points.
The effectiveness of MI has been demonstrated in a wide range of behaviour change contexts51,52 (see Chapter 1). MI in relation to weight loss and maintenance is a relatively new area, although MI appears to be effective as an adjunct to a behavioural weight control programme. 51 MI may facilitate maintenance of behaviour as well as behaviour change. In the context of the WILMA trial intervention, MI supports participants in an ongoing and tailored way. 53,54
Self-determination theory
Self-determination theory (SDT) provides a theoretical framework for understanding MI. 93 SDT characterises motivation as either intrinsic or extrinsic, with intrinsic motivation being linked to more sustained behaviour change. 94 According to SDT, intrinsic motivation for a behaviour is enhanced when the behaviour is associated with feelings of competence (i.e. confidence or belief that one can accomplish the behaviour), autonomy (i.e. that the behaviour is the individual’s choice) and relatedness (i.e. feeling understood and valued by significant others). MI supports feelings of competence, autonomy and relatedness and is therefore thought to help promote intrinsic motivation for behaviour change. It achieves this using a variety of techniques such as developing discrepancy, providing information, helping the client develop goals, supporting autonomy and self-efficacy, being non-directive, exploring pros and cons and avoiding blaming or judgement. 49,50 These are central to the WILMA trial intervention.
Motivational interviewing can also be said to draw on cognitive dissonance theory (CDT). 95 This states that when an individual holds conflicting cognitions it produces a state of tension or discomfort. The individual is motivated to reduce this discomfort, usually by rejecting one set of beliefs in favour of the other. MI creates cognitive dissonance by developing discrepancy, that is helping individuals see a mismatch between where they are and where they want to be.
Model of action phases
According to the model of action phases (MAP), behaviour change consists of a motivational phase, in which an individual decides to change his or her behaviour, and a volitional phase, during which the individual decides how to implement the change. 96 As such, action-planning/implementation intentions were incorporated into the MI sessions in order to target the volitional phase of behaviour change. Implementation intentions have been shown to be very effective at helping individuals achieve their goals47,97,98 and, in keeping with MAP, have been shown to be particularly useful in promoting behaviour change when combined with motivational interventions. 99,100 Implementation intentions specify a plan of when, where and how a person is going to, for example, start exercising. This is believed to result in the behaviour being elicited automatically by the relevant environmental cue rather than by a more effortful decision-making process. It also helps ensure that good opportunities to perform the target behaviour are not missed. 101 If the behaviour is repeated over time it may become increasingly automatic or habitual. Turning healthy behaviours into habits is critical if they are to be maintained over the long term as habits tend to be very resistant to change. 102 The promotion of healthy habits is therefore a key aim of the proposed intervention.
Social cognitive theory
Development of the intervention was also strongly influenced by social cognitive theory (SCT),103 which states that individuals have to believe that they possess the necessary skills to change their behaviour (self-efficacy) and also that their actions will produce certain consequences, for example improved health (outcome expectancies). Furthermore, these beliefs can be modified though observing the behaviour of others (modelling) and/or as a result of positive reinforcement.
Social support
As outlined in the previous chapter, social support can help promote healthy behaviours (e.g. through reinforcement, encouragement, motivation, feedback, empathy, role-modelling and increased self-efficacy), particularly in combination with goal-setting and self-monitoring,65 and has been identified as a component of the majority of effective behaviour change interventions. 71 Additionally, continued professional support is related to better WLM. 21,22,38
Self-monitoring
Self-monitoring is a key aspect of self-regulation and is important for successful behaviour change. 78 Regular self-monitoring is associated with both WLM22,28 and weight loss,78 and is recommended by NICE. 19 Self-monitoring allows people to track their eating, physical activity and weight, and observe links between patterns of behaviour and changes in body weight. Monitoring weight also allows individuals to identify smaller changes before these escalate and they can then take steps to prevent further weight gain.
The WeIght Loss Maintenance in Adults trial intervention model
The WILMA trial intervention model is detailed in Figure 1. The main component of the WILMA trial intervention is MI, incorporating self-monitoring and social support. The intervention utilises a number of techniques and processes central to MI, such as promoting intrinsic motivation using a collaborative and curious style (engaging, evoking), providing tailored support (guiding) and encouraging goal-setting (action-planning). Providing feedback and positive reinforcement and enabling clients to develop discrepancy between behaviours and desired outcomes are also techniques that are key to MI and the current intervention. The concept of self-monitoring was generally encouraged during MI sessions: participants were also asked to record their weight weekly and submit these weekly weights to the study team. An optional component of self-monitoring and behavioural regulation was also provided, in the form of an online and/or paper diary; these data were not collected by the study team. MI practitioners (MIPs) provided professional support and encouraged peer support; additionally the group session component described here (see Peer group support sessions) was intended to provide peer support and encourage information sharing and modelling of behaviour.
FIGURE 1.
The WILMA trial intervention model. a, MI style/technique; and b, theorised mediators.

It was hypothesised that the intervention components detailed in Figure 1 would be associated with specific variables and that these, in turn, may mediate relationships between the intervention and outcomes. Specifically, it was hypothesised that the intervention would increase intrinsic motivation, action-planning, self-efficacy, self-monitoring behaviours and boost/provide a source of social support. These variables were theorised to increase physical activity and healthy diet behaviours that would eventually become habitual, ultimately leading to successful WLM and, in some cases, further weight loss.
The components of the WILMA trial intervention and their suggested theoretical links are outlined in Table 1.
| Intervention component/outputs | Relevant theory |
|---|---|
| Promoting intrinsic motivation | SDT93 |
| Providing positive feedback/reinforcement | SDT, SCT103 |
| Developing discrepancy between current behaviours/weight and ideal behaviours/weight | CDT95 |
| Goal-setting/forming implementation intentions/action-planning | SCT (GS), MAP (II)96 |
| Self-monitoring | SCT (self-regulation) |
| Encouraging/providing social support | SCT, SDT |
| Encouraging problem-solving | SCT |
| Promoting self-efficacy | SCT, SDT |
The WeIght Loss Maintenance in Adults trial intervention
The WILMA trial comprised an individually tailored intervention based on MI, incorporating implementation intentions, social support and self-monitoring. The main part of the intervention was concentrated in the first 2 (less intensive) to 6 months (intensive), tapering down to less regular support. It was felt that this longer-term support, although not resource intensive, would be important for the effectiveness of the intervention. Previous studies that have had success with WLM have had longer-term interventions and support. 22,38,104 The trial comprised three arms: (1) an intensive intervention arm, (2) a less intensive intervention arm and (3) a control arm. We hypothesised that the intensive intervention would be effective and that the less intensive intervention would have an effect somewhere between the control and intensive intervention. This less intensive arm is important because, although some studies have emphasised the importance of long-term intervention and follow-up, it remains unclear how intensive this should be and how it is best delivered. This has important implications for cost and the feasibility of rolling out the intervention should it be successful. Effectiveness in this trial refers to maintenance of initial weight loss rather than additional weight loss, although the latter may occur for many participants.
Individual motivational interviewing sessions
Participants in the intensive intervention group had six one-to-one individually tailored MI sessions. Sessions were delivered by experienced MIPs and were delivered approximately fortnightly for 3 months, lasting around 1 hour. For the final 9 months of the intervention participants received monthly MI telephone calls lasting approximately 20 minutes. This level of monthly contact in the intensive intervention group is based on evidence from previous trials. 38 Participants in the less intensive intervention group received two face-to-face tailored MI sessions 2 weeks apart. This was based on experience from clinical practice as well as evidence from reviews and meta-analyses. 57,63 Participants also received two MI-based telephone calls at 6 and 12 months lasting around 20 minutes.
Motivational interviewing session content
Motivational interviewing practitioners were given a handbook to guide the sessions (see Appendix 1). This comprised the following information: a summary of the client group and their challenges, MI within the context of the WLM trial and intervention ‘hot topics’. Hot topics comprised self-monitoring, goal-setting and implementation intentions, habits, emotional eating and coping with relapse, diet, physical activity, barriers to maintenance, social support and self-efficacy. The purpose of this section of the handbook was to summarise, in non-expert language, the key research evidence suggesting that these components are likely to be effective for WLM. Information on each topic was provided in the following format: (1) description of the topic (‘what is it?’), (2) summary of research evidence (‘why is it important?’) and (3) suggestions on how to use the information during individual sessions in an MI-consistent (i.e. non-directive) way (‘what do I need to do?’). MIPs were also provided with summary information relating to each of these intervention hot topics on laminated sheets. This summary information covered key components of the detail provided in the practitioners’ handbook in lay language, for them to use as a reference and share with participants as required during MI sessions.
Diet and physical activity were discussed in the MI sessions in line with current government guidance. Participants were encouraged to reflect on their values, goals and current behaviour and to develop their own goals and techniques for implementing and maintaining behaviours. Participants in the intervention groups were encouraged by researchers at their baseline assessments to self-monitor by weighing themselves weekly and MIPs encouraged the concept of self-monitoring generally. Participants were able to record all self-monitoring activity, including diet, physical activity, other markers of successful maintenance (e.g. clothes fitting better), goals set at sessions and implementation intentions, in a diary provided by the study team (paper-based and brief online version); however, completion was optional. Diaries provided to participants were intended for their personal use only and were not collected by the study team for outcome assessment. However, participants were asked to record their weekly weight and send this information to the study team via the study website or by text, e-mail or telephone. MIPs kept a written record of each face-to-face and telephone session (including goal-setting and implementation intentions) using the appropriate case report form (CRF) and this information was collected by the study team. MIPs also completed a brief written summary of the session for the participant to take away.
Information on study-specific procedures [reporting serious adverse events (SAEs), lone working, actual/risk of self-harm to participants and administrative processes] was also included in the handbook.
Peer group support sessions
Professional-led peer group support sessions were planned to take place monthly, lasting 1.5 hours, for 4 months, to follow on from the face-to-face MI sessions. The group sessions were the same for both intervention arms. The number of sessions chosen was felt to provide a cost-effective method of reinforcing the main messages of the intervention as well as allowing people to share their experiences and increasing their social support. The group sessions were to be led by a facilitator with the aim of providing participants with the opportunity to share problems, techniques and tips with peers. The sessions were designed around four themes: (1) barriers to maintenance, emotional eating and coping with relapse, (2) diet, (3) physical activity and (4) intervention-related tasks and activities such as self-monitoring, goal-setting and implementation intentions, social support and habit formation. Each session was structured around a series of interactive tasks, intended to provide an opportunity to share tips and increase knowledge in these key areas. Participants were to be given a summary sheet at the end of each session to take away with them and asked to complete a brief feedback sheet aimed at gauging the extent of knowledge of topics prior to sessions and what they found most useful.
A handbook was also prepared for group facilitators (GFs) (see Appendix 2) to guide the content of sessions. Information covered the following: a summary of the study, intervention and client group, WLM issues, key intervention components (self-monitoring, goal-setting, habits, social support, self-efficacy), group facilitation skills, overview of group sessions, individual session structure and content. Information on study-specific procedures was also included.
Motivational interviewing practitioner and group facilitator training and ongoing support
Training packages were developed for both the MIPs and GFs to cover and expand on key information detailed in the handbooks. For MIPs, specific guidance was developed regarding the challenges of delivering MI in just two sessions and over the telephone. Guidance was developed in consultation with MIPs during training. Both the MIPs and GFs were given training on issues around obesity as well as diet and physical activity recommendations. We discussed with them the challenges of WLM and weight loss and how we might best support participants in this process. The GFs were additionally given training on group facilitation skills. Training was delivered face to face over 2 days by experienced MIPs and key members of the study team involved in intervention development. Training for GFs comprised a 1-day face-to-face session and was delivered by the study team. All MIPs were required to have experience of delivering individual MI in health-care settings. All GFs were required to have experience of group facilitation. The GFs were trained to deliver sessions in a MI-consistent manner and many had experience of delivering face-to-face MI counselling; however, the group sessions were not group MI sessions.
We planned to run four peer support sessions for MIPs in which they would get together in small groups to share their experiences, listen to recordings of sessions and discuss any challenges or issues in MI delivery. These sessions were designed to give WILMA trial intervention-specific support in addition to that which the MIPs arranged as part of their own supervision. We also planned to run four workshops on specific WILMA trial intervention-related topics spaced out across the intervention delivery period, to support the MIPs and discuss difficulties.
Summary
The WILMA trial intervention comprises a number of behaviour change techniques which have been shown to be effective in other domains,90 namely MI incorporating goal-setting and action-planning, self-monitoring and social support. The purpose of the current chapter and the intervention handbooks appended to this report is to describe the components and theoretical underpinnings of the WILMA trial intervention and provide sufficient detail about how it was operationalised to allow replication or modification. Chapters 5 and 8 will seek to explore and describe relationships between the behaviour change techniques used and associated intervention functions as well as outcome.
Chapter 3 Methods
As noted previously (see Chapter 1, The trial), this study was originally designed as an effectiveness trial of a multicomponent intervention, with the main outcome (BMI) assessed 3 years post randomisation. However, owing to significant problems in set-up and recruiting, the trial was closed early and is therefore reported as a feasibility study. We feel it is nonetheless important to detail the methods as originally designed (see Design through to Cost-effectiveness analysis), prior to describing changes made following conversion to a feasibility study. The changes to the trial design are described in detail in Feasibility study methods; however, the key changes were that primary outcomes were feasibility outcomes, the follow-up was shortened to 12 months and the group-based aspect of the intervention was no longer delivered because of feasibility issues.
Design
The study was a three-arm individually randomised controlled trial comprising an intensive intervention arm, a less intensive intervention arm and a control arm. The two experimental arms received a 12-month intervention based on three key elements – (1) MI, (2) self-monitoring and (3) social support – which differed only in amount of contact with the MIP. The control arm received an information pack and usual care. Follow-up was planned at 6, 12, 24 and 36 months post randomisation. The aim was to recruit 950 adults aged 18–70 years with a current or previous BMI of ≥ 30 kg/m2 who had lost a minimum 5% body weight during the previous 12 months. Ethics approval was given by the Research Ethics Committee (REC) for Wales.
Objectives
The primary objective was to evaluate the impact of the intervention on participant BMI 3 years post randomisation. Secondary objectives were to examine the effect of the intervention on waist circumference, waist-to-hip ratio, physical activity, diet, health-related quality of life, binge eating, psychological well-being and health resource use. Additionally, we planned to examine the proportion of participants maintaining their baseline weight and mediators and moderators associated with change (see Mediators and moderators). A process evaluation examined intervention delivery, participant and practitioner views, dropout, adherence and retention. A cost-effectiveness evaluation was also planned.
Participants
Participant Identification Centres selection
Participants were recruited from general practitioner (GP) practices, exercise referral schemes, a commercial weight loss programme (Slimming World) and the community. The aim was to recruit participants throughout South Wales, South West England and the East Midlands. A sample of research-active GP practices across four health boards in South Wales were approached to participate (approximately 15 practices per region in Cardiff and Vale, Cwm Taf, Aneurin Bevan and Abertawe Bro Morgannwg University Health Boards), with a view to recruiting 20–25 practices. All exercise referral and Slimming World schemes within these geographical areas, as well as within the boundaries of Derby City, Derby County and Nottingham Primary Care Trusts (PCTs), were identified and approached to act as Participant Identification Centres (PICs).
Identifying participants
Individuals were approached either face to face or via record searches from GP surgeries, exercise referral schemes and Slimming World, and provided with an information sheet and an expression of interest (EOI) form to return to the research team. Participants also self-referred from the community via poster and local media advertisements. Once an EOI form was received, two main routes for recruitment were employed.
-
Route 1: 5% weight loss achieved. Individuals able to provide independent verification of weight loss (e.g. from a referring practitioner) were invited to a baseline visit at which the researcher confirmed eligibility, provided further details about the study and took consent prior to completing assessments. Current and starting weight (i.e. pre-5% loss) were recorded on the EOI form by the referring practitioner or researcher. If it was not possible to verify weight loss, participants were referred to route 2.
-
Route 2: yet to achieve 5% weight loss. We contacted these individuals to either (1) attend a screening meeting with a researcher or (2) self-screen by providing documented evidence of starting weight and subsequent 5% loss (e.g. a printout from scales in their local chemist/supermarket, slimming club booklet, GP letter). At locally held screening appointments, participants were provided with a second information sheet outlining the screening procedure. They then consented to have their weight, height and contact details recorded and were asked to contact us once they had achieved the 5% target. If no contact was made after 2 months, potential participants were followed up by telephone at agreed time intervals. On reaching the 5% target, participants were invited to a baseline visit.
All participants referred by a GP/nurse, pharmacist, exercise referral professional or slimming club consultant were asked to confirm on the EOI form whether they had lost (route 1), or intended to lose (route 2), 5% body weight. Referring practitioners were asked to verify 5% weight loss for those approached during face-to-face consultations and who selected route 1. Participants approached by letter who returned an EOI form either sent verification directly to the research team or provided details as to how we could access verification, for example by contacting the referring practitioner. Participants approached by letter and unable to provide verification were recruited via route 2. Referring practitioners were asked to record how many patients were approached (face to face or via letter) as well as basic anonymised demographic data (age and gender).
Inclusion criteria
Adults aged 18–70 years with a current or previous BMI of ≥ 30 kg/m2 were eligible for inclusion if they had intentionally lost at least 5% body weight (by pharmacological, lifestyle and/or behavioural methods) during the previous 12 months and this weight loss had been independently verified.
Exclusion criteria
Exclusion criteria were factors rendering potential participants unable to comply with the protocol, such as previous bariatric surgery (unless fully reversed, e.g. by removal of a gastric balloon), terminal illness, poor competence in English (i.e. inability to complete study materials), living with another study participant or, in the case of women, pregnancy (note: women who became pregnant after recruitment were not excluded, but given a leaflet on exercising safely during pregnancy).
Assessment of risk
Participants’ GPs were informed of their trial participation and sent a copy of the consent form. All initial contacts with participants were in public community venues. However, some face-to-face MI sessions and/or follow-up appointments were conducted in participants’ homes. Participants’ GPs were asked to contact the study team to give an assessment of the level of risk posed to individuals undertaking home visits and a study-specific lone worker policy was developed.
Withdrawal and loss to follow-up
Participants were free to withdraw at any time; however, consent to use data already collected was assumed unless otherwise notified. The following measures were taken to maximise retention:
-
The importance of obtaining follow-up data was emphasised to participants.
-
All assessments were conducted face to face (except at 6 months which was by post) and in locations convenient to participants.
-
Newsletters and birthday cards (including a change of address form) were sent to all participants.
-
Participants in the control group were offered £50 in high-street vouchers or free 12-week attendance at a local commercial weight loss programme at the end of follow-up to minimise unequal dropout.
-
Two reminders were sent to participants requesting that they return the postal questionnaire.
-
Follow-up appointments were rearranged for those who did not attend appointments.
-
Mobile telephone numbers were obtained in order to contact participants directly for follow-up.
-
Participants were asked for their GP’s address as an alternative contact.
-
Outcomes were carefully chosen to minimise respondent burden.
-
Key questionnaires were completed by telephone when possible for non-responders to ensure a minimum data set.
-
Although we did not offer travelling expenses, participants were offered vouchers for attending follow-up outcome assessments (£10 per time point on completion of assessment) and completing and returning the questionnaire at 6 months (£5 not conditional on completion).
Interventions
Intensive intervention arm
Participants received six one-to-one individually tailored MI sessions, delivered by experienced MIPs. These sessions were delivered face to face, approximately fortnightly for 3 months, and lasted about 60 minutes. During the final 9 months of the intervention, participants received monthly MI telephone calls lasting approximately 20 minutes.
Less intensive intervention arm
Participants received two face-to-face tailored MI sessions 2 weeks apart and two MI-based telephone calls at 6 and 12 months only. All other aspects of intervention delivery were as described for the intensive intervention arm (see Chapter 2).
Peer group sessions
Participants in both the intensive and the less intensive arms had the opportunity to attend four professional-led peer group support sessions which were planned to occur monthly lasting 1.5 hours for 4 months and following on from face-to-face MI sessions (see Chapter 2). Allocation to group sessions was on a rolling basis; participants did not necessarily attend sessions in the same order.
Control arm
The control group were given an information pack also sent to participants in both intervention arms. The content of the information pack was based on useful resources for weight loss and healthy lifestyle, and advice on WLM. Participants in all arms were able to access usual care, for example attending a slimming club.
Trial procedures
Adverse events and serious adverse events
No adverse effects or SAEs were expected as recommendations for physical activity were in line with current and widely publicised UK government guidelines. However, the possibility of cardiovascular/musculoskeletal events occurring related to increased physical activity was acknowledged in the protocol and the physical activity leaflet, and the main trial information sheet stated that any increase in physical activity should be gradual. Participants were advised to contact their GP if they felt unwell as a result of increased physical activity (e.g. experiencing severe breathlessness, chest pain, fainting or dizziness). Safety reporting procedures are outlined in Appendix 3.
Risk of harm
Motivational interviewing practitioners were asked to notify the study team directly if they became concerned that a participant had caused, or was likely to cause, significant harm to him- or herself. Provision was also made to inform participants’ GPs when appropriate. MIPs were asked to inform the appropriate authorities directly if concerned that a participant had caused, or was likely to cause, harm to others.
Training
All intervention staff (MIPs and GFs) were trained as per the appropriate manual (see Chapter 2). All staff undertaking randomisation and data collection visits were trained in study-specific procedures.
Outcomes
Primary and secondary outcomes
Outcome measures were self-reported with the exception of height, weight and waist and hip measurements, which were measured by the researcher at each visit. Outcome assessors were given video training in measuring weight, height, waist and hip circumference to ensure consistency. Height was measured to the nearest 0.1 cm using a Seca 213 stadiometer (Seca, CA, USA). Weight was measured to the nearest 0.1 kg with calibrated Seca 877 weighing scales (Seca, CA, USA). Participants were weighed wearing a single layer of clothing (having removed shoes, belts, heavy items). Waist circumference was measured at the midpoint between the superior iliac crest and the lowest rib at the end of a normal expiration; hip circumference was measured at the maximal level of the maximal circumference around the buttocks with a Seca 201 measuring tape (Seca, CA, USA). A number of secondary outcomes were also assessed (Table 2): physical activity, diet, waist-to-hip ratio, health-related quality of life, health and other resource use, binge eating, psychological well-being, health-related behaviours and proportion maintaining weight loss. Maintenance of weight loss is defined as successful when the participant’s weight at the end of the trial is less than or equal to their weight at baseline. All outcomes were recorded on study-specific CRFs (see Appendix 4). For both height and hip measurements, the average across both time points was used. If a follow-up height or hip measurement was missing, then the baseline measurement alone was used.
| Outcome | Measure | Type | Time point | Modifications | Number of items |
|---|---|---|---|---|---|
| Anthropometric measures | |||||
| BMI (weight, height) | Calibrated digital scales, stadiometer | Primary | Baseline, 12-month follow-up | N/A | – |
| Waist and hip circumferences | Tape | Secondary | Baseline, 12-month follow-up | N/A | – |
| Secondary outcomes/moderators | |||||
| Physical activity | IPAQ105 | Secondary | Baseline, 12-month follow-up | Wording change to reflect UK population (‘house and yard work’ changed to ‘housework and gardening’) | Seven |
| Diet | DINE106 | Secondary | Baseline, 12-month follow-up |
|
39 |
| Health-related quality of life | EQ-5D107 | Secondary | Baseline, 6- and 12-month follow-up | None | Six |
| Proportion maintaining weight loss | Participants whose weight at 1 year is less than or equal to their weight at baseline were defined as maintainers | Secondary | 12-month follow-up | N/A | N/A |
| Alcohol and smoking status | AUDIT-C108 and HSI109 | Secondary | Baseline, 12-month follow-up | None | Three per scale |
| Health and other resource usage | Medication, health service contacts, other weight control resources used | Secondary | Baseline, 6- and 12-month follow-up | N/A | 16 |
| Binge eating | EDE-Q110 | Secondary; moderator | Baseline, 12-month follow-up | None | Six |
| Psychological well-being | GHQ-12111 | Secondary; moderator | Baseline, 12-month follow-up | None | 12 |
| Demographics | Age, gender, socioeconomic status, ethnicity, employment status | Moderators | Baseline | N/A | 10 |
| Mediators | |||||
| Social support | SSEH and SSEX112 | Mediator | Baseline, 6- and 12-month follow-up | Eating: shortened from 10 items to three on two themes – encouragement (two items) and discouragement (one item) Exercise: shortened from 10 items to three on two themes – family and friend participation (one item) and family rewards and punishments (one reward item; one punishment) |
Six |
| Self-efficacy | WEL113 | Mediator | Baseline, 6- and 12-month follow-up | None | 20 weight, 10 exercise |
| Intrinsic motivation | TSRQ diet and exercise114 | Mediator | Baseline, 6- and 12-month follow-up | None | 15 diet, 15 exercise |
| Automaticity/habits | Self-reported habit index (diet and exercise)115 | Mediator | Baseline, 12-month follow-up | None | 12 diet, 12 exercise |
| Self-monitoring/regulation | SREG116 | Mediator | Baseline, 12-month follow-up | Subset of eight questions comprising positive and negative statements selected from full SREG | Eight |
| Implementation intentions | From MI records and interviews | Mediator | All sessions | N/A | – |
Mediators and moderators
We measured a number of potential mediators and moderators associated with change. Mediators included self-efficacy, social support, self-monitoring, implementation intentions, habit formation and intrinsic motivation. Moderators included demographics, weight loss history, satisfaction with weight loss, current weight loss goals, binge eating and psychological well-being.
Statistical methods
Sample size
To give 90% power at the 5% significance level to detect a difference in mean BMI of 1.7 units (SD 5.5 units) between the primary contrast of the intensive intervention and control, 221 participants per group would be required. This assumes a baseline mean BMI of 32.5 kg/m2 and a mean of 34.2 kg/m2 prior to 5% weight loss. Allowing for 30% attrition,20,27,55 a total of 950 participants would be required.
Randomisation
Allocation to groups was by remote telephone randomisation, stratified by region and minimised by age, gender, ethnicity, source of recruitment (GP, exercise referral, slimming club, community), percentage weight loss and current BMI. The service was provided by the Bristol Randomised Trials Collaboration randomisation service. This used a bespoke system written in the programming language C++.
Blinding
It was not possible to blind participants to arm allocation given the complex procedural and interactive nature of the intervention. Outcome assessors were also involved in recruitment and randomisation and were therefore not blind to allocation.
Main analysis
The planned main analysis was intention to treat comparing the three groups on average BMI using a three-level linear regression model to account for clustering within MIP and groups. The main analysis was intended to examine the longest end point. A secondary analysis was planned to examine the three groups using the interim time point as the end point, with baseline BMI and previous weight loss as covariates. Both intervention groups were to be compared with the control (reduced to a one-level model if no evidence of clustering is observed). Secondary outcomes were to be analysed using linear or logistic regression or Poisson as appropriate. The analyses of BMI and weight were repeated including the self-reported weights as a sensitivity analysis. There is evidence that single-item measures are more likely to be biased than multiquestion measures. 117 We do not feel that the results for the other questionnaires are likely to be biased.
Exploratory analyses were proposed to consider the impact of demographic factors, original weight loss method and theoretical moderators on the intervention effect, using interaction terms included in main analysis models. Exploratory longitudinal analyses were proposed to explore the effect of theoretical mediators on subsequent outcomes and interactions with intervention groups. These were to be conducted in a similar manner to the primary analyses, with outcomes predicted using a hierarchical model and controlling for baseline randomisation variables and in accordance with the 1986 Baron and Kenny guidelines. 118 This analysis was used to check the postulated logic model produced by the WILMA trial team. Individuals who failed to respond would be compared with those who completed follow-up to identify potential biases. The planned sensitivity analysis assumed that those non-responders would return to weight levels prior to weight loss (i.e. not baseline, but previous BMI). A last observation carried forward assumption would not be conservative for WLM and so was not used. Self-report weight was added to objectively assessed weight to account for some loss to follow-up. A complier-average causal effect (CACE) analysis was proposed, using multilevel mixture analysis119 to focus on estimating intervention effects in the presence of non-compliance.
Subgroup and interim analysis
Primary subgroup analyses were proposed to investigate associations between WLM and age, gender, method of weight loss and weight at entry. Exploratory subgroup analyses were planned to investigate associations between WLM and smokers, binge eaters, weight-affecting medications and ethnicity.
Process evaluation
We conducted a process evaluation, the aims of which were to:
-
assess delivery of the intervention to ensure it was provided in accordance with the protocol and delivered consistently
-
establish the level of participant adherence to the intervention
-
explore participants’ views of, and satisfaction with, the intervention
-
explore MIPs’ and GFs’ experiences of delivering the intervention
-
test the logic model.
Intervention delivery
Motivational interviewing practitioners were asked to audio-record as many sessions (face to face and telephone) as possible, with a view to collecting a minimum sample of six sessions per MIP over the course of the study. A random sample of recordings from face-to-face sessions was assessed using the motivational interviewing treatment integrity (MITI) coding scale. 120 A stratified sample included sessions delivered in both intervention arms and by all MIPs. Skill in MI delivery was assessed prior to study entry (via audio-recorded mock consultations with trained actors). In order to be recruited as a practitioner, individuals were required to reach the MITI proficiency threshold (see Chapter 6). We planned to observe group sessions to assess fidelity of intervention delivery.
Participant adherence
Data on intervention delivery and exposure to the intervention were examined. Overall attendance at intervention sessions and success of telephone contact were monitored (number of contact attempts and length of calls was recorded). MI CRFs from face-to-face and telephone sessions were examined for evidence of self-regulation, goal-setting and implementation intentions and analysed descriptively. Participant self-regulation was examined by the frequency of self-weighing records/reports of self-weighing.
Participants’ views of the intervention
Semistructured telephone interviews were carried out with participants in all arms, during the intervention (at approximately 6 months) and following the end of the intervention period (see Chapter 8). Participants were purposively sampled across key factors including trial arm, gender, age, recruitment route and attendance levels. In addition to assessing general views around intervention delivery, views on efficacy, barriers and facilitators, we also examined potential mediators not examined elsewhere such as the impact of life events on adherence; environmental influences; levels and importance of social support from family and friends as well as the professional support provided as part of the intervention; impact on their wider social network; WLM challenges; intrinsic and extrinsic motivations for WLM; health value; body image; and strategies, coping mechanisms and responses to relapses (see Appendix 5). In addition, we planned to interview a small sample of participants who dropped out of the intervention to establish their reasons for discontinuing. Interviews continued until themes were saturated. Interviews were audio-recorded, transcribed and checked by the researcher.
Intervention staff’s views of the intervention
All MIPs, apart from one who took part in an interview, contributed to two focus groups designed to enable us to elicit their views of the intervention, the perceived challenges or barriers in implementing it and how they thought the intervention and training could be improved. Separate focus groups with GFs were also planned. The MIP focus groups and interview took place following recruitment closure. At this point the majority of MIPs had completed their face-to-face sessions and were mid-way through their telephone sessions. A focus group guide was developed to explore the MIPs’ experiences. This comprised 18 items and spanned four main topics (see Appendix 6). Up to three members of the research team were present during the focus groups, one of whom facilitated the session, and the interview was conducted by one member of the research team. The focus groups lasted around 2 hours, while the interview lasted 1 hour.
Qualitative analysis
All interviews and focus groups were audio-recorded and transcribed for analysis. Transcripts were checked and uploaded into QSR International NVivo10 software version 10 (QSR International, VIC, Australia) and analysed using thematic analysis. Thematic analysis is a systematic approach in which the data are initially coded and then collated into themes. 121 Themes are then analysed in more detail to map out the overall data and examine relationships between them. Finally, themes are refined to produce an overall story of participants’ views and experiences. 121,122 As outlined by Braun and Clark121 thematic analysis consists of five defining phases: (1) familiarisation, (2) initial coding, (3) creation of themes, (4) reviewing themes and (5) defining and naming themes. Our analysis followed each of these phases and is described in relation to these below. Data collection and analysis of interview data were conducted simultaneously and the analyses informed data collection in terms of changes to the interview schedule, for example adding new questions to probe particular areas of interest. Data collection continued until data saturation was reached. Analysis of the focus group data was conducted after data collection, but followed the same process.
Phase 1: familiarisation
During the familiarisation phase, a coding scheme was devised by the team to inform the coding procedures. Separate schemes were developed for the participant interview and MIP focus group (plus one interview) analysis, as they had differing aims and different questions were asked accordingly. Therefore, it was not appropriate to analyse all data across a common coding scheme. The coding schemes were developed by initially reading and rereading a few of the early transcripts. Codes were mapped out by three researchers (for the participant analysis: SS, YM and CS; for the MIP analysis: SS, YM and LC) during two face-to-face meetings (following independent coding of two interviews/focus groups) and these initial codes were pulled together into a coding scheme. Following development of the initial coding scheme, it was then applied to other interviews/focus groups independently by two coders. Each of the schemes was then further refined as new codes emerged from the data during the initial coding procedure.
Phase 2: initial coding
Following the coding scheme development, the initial coding of participant interviews was completed by CS and YM, while the focus group coding was completed by YM and LC. Transcripts were closely examined and indexed according to the coding scheme. During the coding phase, the coders had regular discussions concerning any new codes identified and sought common agreement on any further amendments needed to the scheme. This ensured consistency between coders. An analysis log was kept to record coders’ discussions and track any changes made to the coding scheme as well as to record further thoughts and developments of the analysis process. A total of 10% of the interview transcripts were double coded to ensure reliability of the coding scheme and any discrepancies discussed and resolved. Both MIP focus groups and interviews were read and reread by YM and LC in preparation for the scheme development and were therefore not double coded.
Phase 3: searching for themes
Once all transcripts were coded, codes were examined in detail and broken down further into subcodes where appropriate. Moreover, some extracts were recoded where necessary. This phase was both data driven (i.e. bottom up) and theory driven as we sought to answer specific process evaluation questions and look at mediators not measured elsewhere. Commonly expressed themes, as well as unusual cases, were identified. Relationships between codes were explored by carrying out queries to identify text common to two (or more) related codes. This analysis led to the development of overarching themes.
Phase 4: reviewing themes
The themes developed in the previous phase were reviewed by the coders, who remained in close contact to further discuss and develop their thoughts. During this phase, coders referred to the key questions identified in the process evaluation model to support the final analysis. The initial codes were examined for any instances that were inconsistent with the emerging themes. The themes were further examined across groups (arm/gender/age) to explore their differences and similarities. A thematic map was developed for both the participant interview and practitioner focus group analysis to further inform this phase.
Phase 5: defining and naming themes
During the final phase, coders examined themes in detail ensuring they accurately represented the data and captured the overall story. Themes were mapped out in order to explore broader links and relationships within the overall data and analysis. As themes were explored, a detailed narrative was written for each, which provided the structure for the final reporting of results. The qualitative findings then fed into the overall process evaluation.
Cost-effectiveness analysis
The original intention was to undertake (1) a within-trial cost–utility analysis assessing between-group differences over 3 years in total costs against differences in quality-adjusted life-years (QALYs) [derived from European Quality of Life-5 Dimensions (EQ-5D) quality-of-life data], (2) a lifetime cost–utility analysis using an economic Markov model and (3) a within-trial cost-effectiveness analysis (CEA) assessing between-group differences in total costs against differences in BMI at 3 years. All analyses were from a NHS perspective. In pursuit of this, all direct intervention costs were recorded prospectively in relevant units and valued using standard methods. 21 These included all resources used in intervention delivery (staff time, staff travel, materials, venues). All resources used in training professionals in MI skills were similarly prospectively recorded and valued. As training is a one-off investment producing a flow of benefits over time, training costs would be amortised similarly to equipment expenditures and expressed on an equivalent annual cost basis. Indirect costs would include differential use of health service resources from recruitment to end of follow-up.
Health service resource use in primary and secondary care and the community was collected for all participants at baseline and follow-up time points. Resource-use data collected at baseline, that is relating to the period prior to recruitment, would not be included in total costs but used as a covariate if shown to be different between groups. Resource-use questions related to all health service contacts and prescription medicines dispensed in the previous 3 months. The 12-month follow-up data cover resource use over a period of 6 months, based on two CRFs delivered at 6- and 12-month time points. Health service resource use would be valued using standard sources. 123 All costs relating to non-NHS weight loss/maintenance activities such as use of gyms were recorded. It was important to monitor these costs as the intervention may have substituted for some activities but these would be reported separately and not included in the cost-effectiveness ratios. Baseline BMI, age and gender might have resource implications, so all resource-use variables and costs at 12 months were to be analysed controlling for these patient-level characteristics. The analysis also involved a regression-based adjustment for any potential baseline difference in resource use and costs. 124 Analyses were planned to assess mean differential costs and resource use using tests for normality where appropriate; however, as many resource-use variables and costs are unlikely to be normally distributed, a non-parametric bootstrap method was used,125 first performing the adjustment procedure and then bootstrapping with the adjusted data. All costs are in 2012 prices.
The effectiveness measure for the cost–utility analyses was the EQ-5D107 quality-of-life instrument, administered at baseline and all follow-up time points. EQ-5D scores allow estimation of QALYs. It was planned to assess cost-effectiveness based on between-group differences in costs and QALYs, reported in the form of incremental cost–utility ratios (incremental cost/incremental QALY). This is the method of economic evaluation preferred by NICE as the resulting cost–utility estimates can be compared not only with other weight control programmes, but also with unrelated health-care interventions. Other planned analyses included a series of one-way sensitivity analyses to assess how sensitive results were to changes in assumptions used. A probabilistic sensitivity analysis would be used to assess uncertainty in the cost–utility ratio and to generate a cost-effectiveness acceptability curve showing the probability that the intervention is being cost-effective at a range of willingness-to-pay (WTP) thresholds.
It was intended to assess long-term cost-effectiveness using a decision-analytic Markov model (given uncertainty in long-term weight patterns among obese individuals). 126 The model would comprise seven health states: ‘normal’, three states reflecting increased cardiovascular disease risk [cardiovascular disease (CVD); hypertension, type 2 diabetes mellitus, hypercholesterolaemia], two states reflecting CVD risk (coronary heart disease, stroke) and a ‘death’ state. It was also our intention to model lifetime health-care costs and health effects for a hypothetical cohort of 10,000 adults in the ‘normal’ state receiving either of the interventions or standard care. The base-case assumption was that the effect of the interventions on CVD risk factors and weight loss is maintained for a period of up to 6 years, after which participants regain weight linearly for a period of 4 years, that is in 10 years’ time weight will revert to the initial weight. This assumption is in line with that used in economic evaluations of weight loss interventions127,128 and is based on observations from clinical trials. 19
We calculated mean BMI by age and gender from the trial data but, in order to assess the effect of different levels of weight loss, we planned to define two cohorts reflecting lighter and heavier trial participants. A variety of secondary sources for parameter estimates were to be used in the model. We planned to use a risk equation from the Framingham cohort study129 to estimate the risk of developing the three CVDs from ‘normal’, ‘hypertension’, ‘diabetes’ and ‘hypercholesterolaemia’ health states. We intended to use trial data on utility measures and costs of interventions in the model and to obtain costs of obesity-related complications in the UK from the published literature. 130 As a generic measure, it was considered that EQ-5D may not be sufficiently sensitive to capture differences in health-related quality of life in these essentially healthy participants. A within-trial cost-effectiveness study was therefore also planned with BMI at 3 years as the effectiveness measure.
Feasibility study methods
In September 2012, the decision was taken to close the trial to recruitment owing to the difficulties described in detail in Chapter 4. At this point we were 15 months into the trial and we had recruited 170 individuals. A closedown plan was devised to consider ethical issues and to maximise the scientific value of the trial. It was agreed with the funder that recruitment would cease immediately, but that included participants would still receive the intervention that they were randomised to and be followed up to 1 year. This meant that the whole study would finish in January 2014 and would now be considered a feasibility study. The methods for the feasibility study are similar to those described for the original trial with some key alterations. These are summarised in Table 3 followed by more detail on key components.
| Study component | Changes to design |
|---|---|
| Sample size, recruitment and retention | Sample size reduced from 950 (90% power at 5% significance level: mean BMI difference of 1.7 kg/m2) to 166a (80% power at 5% significance level: mean BMI difference of 3.5 kg/m2) |
| Incentives offered to participants for completing assessments increased from £10 to £20. Incentives (£10 vouchers) also offered to interview participants | |
| Length of follow-up | Reduced from 3 years to 1 year post randomisation |
| Intervention | Group sessions discontinued |
| Analysis of primary and secondary outcomes | Planned subgroup analyses (age, amount of weight lost, method of weight loss, satisfaction with weight loss) not undertaken; some exploratory analyses carried out (gender, binge eating, source of recruitment), but others (smoking, weight-affecting medication) dropped. Implementation intentions not included as a mediator. CACE estimated using two-stage least squares instrumental variable regression and not multilevel mixture analysis |
| Process evaluation | Group component of intervention dropped therefore GF focus group not run. Participants who withdrew from the intervention not willing to be interviewed |
| Economic evaluation | Estimation of long-term cost–utility (economic Markov modelling) not undertaken |
Objectives
The main objectives were to assess the feasibility, acceptability, compliance and delivery of a 12-month multicomponent intervention, as well as recruitment and retention. To give an indication of effect sizes for a larger trial, we evaluated the impact of the intensive or less intensive intervention on participants’ BMI (primary effectiveness outcome) at 12 months from randomisation.
Design
This was a feasibility study of a three-arm individually randomised controlled trial. The population recruited was as described in Participants. As described in the Scientific summary, the intervention changed as we stopped delivering the group element. Outcome measures used were as described in Table 2 with the exceptions noted in Table 3. After completing baseline assessments, participants were followed up at 6 months, during the intervention, by post and at the end of the intervention (approximately 12 months post randomisation, with a 3-month window to allow for any delay in receiving the intervention). A 1-year follow-up was conducted face to face in most cases, although a few were conducted by telephone with self-reported weight.
Sample size
The original sample size of 950 was based on detecting an effect size of 0.309 with 90% power at a significance level of 5%. Given that the study was now a feasibility study, the sample size was not derived statistically but based on actual recruitment at the time of closure (n = 166). This allows us to estimate a percentage of 50 (the percentage with the greatest associated variability) to within 7.6 percentage points either side for the whole sample, or to within 15.9 percentage points for percentages within each study arm (n = 38). These are the achievable precisions for estimation of the retention rate (or any other proportion). Although not primarily concerned with effectiveness, we still feel that it is informative to present power to detect differences. With our current sample size of 166 (four participants from the original 170 recruited were ineligible and randomised in error and subsequently withdrawn) and assuming 30% attrition, we have 39 in each of the three arms. We are therefore able to detect a difference in BMI of 3.537 kg/m2 at the 5% significance level with 80% power between any two arms (primary comparison between the control and intensive arms). This is a difference of about 9.75 kg between groups based on average height.
Analysis of primary and secondary outcomes
The main feasibility outcome was the proportion of participants remaining in the study for a year. A secondary feasibility outcome was the proportion of participants who adhered to the intervention in each treatment arm. Comparisons were made between those who completed the study and those who dropped out, to highlight any biases. The main effectiveness analysis was intention to treat and complete case comparing the intensive intervention arm with the control on average BMI using a three-level linear regression model to account for clustering within therapists and groups (reduced to a one-level model where there is no evidence of clustering). The main analysis examined the latest end point (12 months), controlling for individual patient characteristics (baseline BMI, age, gender, ethnicity, source of recruitment, current BMI and percentage weight loss). Both intervention groups were compared with the control. We completed augmented analyses for BMI and weight, for which self-reported follow-up weights were included with verified follow-up weights. The statistical analysis plan specified that if the primary outcome was missing for more than 10% of cases then multiple imputation would be used.
Secondary outcomes included waist circumference, waist-to-hip ratio, self-reported physical activity, proportion maintaining weight loss (defined as successful when the participant’s weight at the end of the trial is less than or equal to his or her weight at baseline), self-reported dietary intake, health-related quality of life, health service and weight control resource use, binge eating, alcohol consumption, smoking status, psychological well-being, duration of participation and dropout from the intervention. All analyses controlled for individual patient characteristics. Binary outcomes were analysed using hierarchical logistic regression and continuous outcomes (appropriately transformed if necessary). Mediation analyses were conducted on self-efficacy, social support, intrinsic motivation, habits and self-monitoring as measured at 6 months using a hierarchical model and controlling for baseline randomisation variables in accordance with Baron and Kenny guidelines. 118 Consolidated Standards of Reporting Trials – Patient Reported Outcomes guidelines are referenced for reporting patient-reported outcomes. 131 Exploratory subgroup analyses investigated WLM in binge eaters, gender and source of recruitment.
Sensitivity analyses
A sensitivity analysis was conducted assuming that non-responders returned to weight levels prior to weight loss (i.e. not baseline but previous BMI). A CACE was estimated using two-stage least squares intrumental variables regression. 119 This modelling focuses on estimating the intervention effects in the presence of non-compliance, but also incorporates adjustments for loss to follow-up. Compliance was defined as follows: for the intensive arm, attending five of the six face-to-face MI sessions; for the less intensive arm, attending both face-to-face MI sessions. Potential differences on basic demographics and the primary outcome between full responders and those providing a minimum data set were described and all models were tested for adequate fit using appropriate diagnostics.
Process evaluation methods
Minor changes to the process evaluation are listed in Table 3.
Economic evaluation
There are limitations to undertaking economic evaluations alongside a feasibility study. In particular, the change in design meant (1) the within-trial analyses would only reflect short-term (12-month) differences in costs and effects, (2) the study was less likely to have sufficient power to detect statistically significant differences in costs or effects and (3) the absence of data on longer-term WLM or costs made estimation of lifetime cost–utility through economic modelling unfeasible. Although it would not be possible to establish definitive cost–utility/effectiveness results, we nevertheless applied as far as possible the methods described in Cost-effectiveness analysis to estimate parameters and unknowns to inform future research. Specifically, (1) methods to determine costs of training and intervention delivery were unchanged; (2) methods for collecting resource use and EQ-5D data were unchanged apart from the final data collection being at 12 not 36 months; and (3) the planned estimation of long-term cost–utility was dropped.
Patient and public involvement
Kirby132 proposes that service user involvement can occur at three different levels: consultation, collaboration and user-controlled research. In the WILMA trial, user representation was at the level of collaboration. We sought to address patient and public involvement at all stages of the WILMA trial, including the design of the study and funding application as well as the subsequent running of the trial. In the research design stage we recruited a participant representative (CB) to help us to design the study and she subsequently became a co-applicant on the grant. In particular, she contributed to three things at the design stage: (1) discussions about outcome measures and follow-up, (2) recruiting potential participants and (3) intervention design. At this stage we also recruited a lay representative to the Trial Steering Committee, who helped oversee the trial and particularly advised and commented on the study materials and recruitment.
Once the study was up and running, CB attended monthly trial management group meetings and contributed to the discussions and decisions made in relation to managing the trial. In particular, she helped the team focus on the key measures that we needed, as initially the outcome assessment was overly long. She helped pilot the questionnaire with other lay people and commented on clarity, ordering of questionnaires in the booklet, etc. She also helped design the questionnaire pack and the patient information to be appealing to potential participants. She helped to ensure that the patient information was written in a clear, concise and participant-friendly way. All data collection materials were piloted with members of the public with regards acceptability and feasibility prior to being finalised. When the study ran into problems with recruitment, she helped develop the detailed recruitment strategy and, along with other team members, actually went out to try and facilitate recruitment in the community. Now that the trial is over she has been advising on possible future approaches to dissemination, for example the study website, newsletters, as well as other means and she is helping us to develop a strategy for dissemination to participants.
Chapter 4 Implementation challenges and implications for future trials
The purpose of this chapter is to describe the main challenges experienced by the WILMA trial team, in order to highlight the practical issues that could potentially impact on the successful set-up and delivery of similar pragmatic trials of complex public health interventions delivered in community (i.e. non-NHS) settings. Challenges relating to governance, recruitment and intervention delivery are summarised below.
Governance
Defining and accessing NHS costs for public health interventions
We experienced a number of issues relating to the definition of NHS costs for the WILMA trial intervention, given that there is currently no standard treatment for obesity. A great deal of regional variation in interpretation of attribution and liability of excess treatment costs (ETCs) was apparent at the time, and for this reason we experienced significant difficulties and delays in securing ETCs in England in excess of 12 months, despite the involvement of the Department of Health and the relevant Strategic Health Authorities. It is acknowledged that significant changes to guidance on attribution of NHS costs have since been implemented, as have changes to the mechanism of distribution for ETCs in England. However, there remain a number of grey areas in attribution of costs for interventions delivered by non-NHS staff, that is community public health interventions, even if it were feasible for these interventions to be delivered or commissioned by the NHS if proven to be effective. In Wales, there is a centralised budget and decision-making for primary care and public health studies, and approvals regarding ETCs were gained at the same times as research governance in all regions of Wales with no delays.
Participant Identification Centres compared with research sites
When the WILMA trial was set up, PICs were a relatively new concept in research governance and, as such, there was a degree of regional variation in terms of what constituted appropriate PIC responsibilities. Given the large number of WILMA trial sites, including non-NHS settings such as slimming clubs and exercise referral schemes, we felt it most appropriate to set up participating GP surgeries as PICs rather than full sites. In addition, general practice staff were not actively involved in any aspect of the study, other than helping to identify potential participants. However, in some English regions this model was not acceptable to participating Comprehensive Local Research Networks (CLRNs), because the costs of doing so would not be reimbursed as part of the activity-based funding model, and so a research site model was adopted for GP surgeries in England. However, we experienced significant delays in reaching this agreement, which, in addition to difficulties accessing ETCs, meant that, in England, recruitment in one region got under way only approximately 4 months prior to closing recruitment completely and not at all in three other PCTs.
Differences in infrastructure support between devolved nations at the time – specifically, the capacity of research network staff to recruit participants and undertake assessments – also had an impact on feasibility of delivery and resulted in different models of working in England and Wales and substantially different timeframes. Centralisation of systems in Wales at the time facilitated faster recruitment and set-up of PICs. However, differences in the implementation of infrastructure support between devolved nations still exist and may still present practical challenges that require a flexible approach to set-up for research teams recruiting in more than one of the devolved nations. It is in the interests of research teams looking to conduct similar trials to ensure that they are fully aware of these different approaches and systems and the impact that these are likely to have on feasibility at the study design stage.
Recruitment
Participant recruitment was open for 15 months from July 2011 to September 2012 (although in England the study was open for only 4 months of this time). By the end of the trial, we had received 1284 EOI forms from individuals who had heard about the study from various sources – the main ones being via an approach from their GP, Slimming World consultant or exercise referral practitioner. We gave each of these main sources ‘approach logs’ to keep track of and report the number of approaches made to individuals. However, these logs were poorly completed and very few were returned. As a result, data regarding sample representativeness are not presented in this report.
The EOI forms tended to capture details only of those who had received information about the study through a PIC site. Those who contacted the team to request more information in response to adverts/posters were asked how they heard about the WILMA trial, but gathering this information was less formalised and not always consistently collected. As described previously (see Chapter 3), there were two routes for entry into the study – it was always anticipated that the majority of participants would enter through route 1 with available evidence of their 5% weight loss from their GP, exercise referral or Slimming World record.
Of the 1284 who expressed an interest in the study, only 241 were initially eligible via route 1, that is were able to provide verification of a minimum 5% weight loss. For the 170 eventually recruited, 151 (88.8%) met the inclusion criterion for verifiable weight loss at the EOI stage and 19 (11.2%) were initially eligible via route 2 and subsequently met the 5% weight loss criterion. For all recruited participants, evidence mostly came in the form of slimming club record cards. It became apparent that we were attracting significantly more individuals via route 2, which was creating a substantial delay in progression through to being fully recruited into the study. The majority of route 2 individuals were either not able to lose 5% of their weight or did not maintain interest or contact with the study. We decided to revise our recruitment strategy and look at different ways of targeting those who were more likely to fall into the route 1 category.
We drafted a recruitment strategy implementation plan (Table 4) to describe and prioritise ways in which our current recruitment could be improved, expanded and monitored as well as who was to take the lead in implementing each activity. The plan was laid out according to priority and timescale, ease of implementation with the resources available and impact based on current evidence. 133,134
| Task | Priority | Actions taken |
|---|---|---|
| Section 1: PICs | ||
| Expansion of recruitment territory | High | Expand to recruit GP and exercise referral PICs in Cwm Taf. Two GPs and two exercise referral practitioners were recruited |
| Incentives | High | For exercise referral staff, a £20 high-street voucher for the best recruiter every second month. For Slimming World consultants, a £20 voucher for every five participants recruited per month. There was also a £20 voucher for the best Slimming World recruiter each month (note that GP PICs were reimbursed via NHS support costs) |
| Presenting to Slimming World | High | Attend Slimming World groups to present study to clients, 47 meetings attended. Attend Slimming World regional consultants meetings, 11 meetings attended |
| Increased Slimming World HQ involvement | High | Advert placed in Slimming World magazine and e-mail from Head of Nutrition Research at Slimming World to consultants encouraging involvement |
| Increased contact with PICs | High | Monthly telephone contact with all PICs (n = 75), PIC newsletters every second month, repeat training sessions |
| Engage with slimming club on referral from GP practices in South West England | Medium | Not implemented as study closed to recruitment before opening in South West England |
| Monitoring PICs | Medium | Monitor poor recruiters for support. Decided against closing them |
| Section 2: advertising | ||
| Study website | High | Website live |
| Poster displays | High | Posters in non-PIC GP surgeries, local gyms and classes, hospital corridors, community centres |
| Local pharmacies | High | Posters displayed in pharmacies in Tesco (n = 26) and Sainsbury’s (n = 27) in South Wales and local independent pharmacies |
| Large local employers and universities | High | 21 companies and six universities advertised study via intranet |
| Press releases | Medium | Local newspapers printed two articles. Item aired on local radio |
| Social media: Facebook® (CA, USA; www.facebook.com) and Twitter® (CA, USA; www.twitter.com) | Medium/low | Accounts live and linked to Slimming World pages and other relevant sites |
| Section 3: other | ||
| Alter emphasis to target route 1 | High | Altered posters and recruitment drive to focus on route 1 only |
| Close monitoring of recruitment rates and monthly recruitment targets | High | Figures examined weekly |
| Research network support | High | Area-specific strategies given to network staff to implement locally. CLRN nurse in Trent trained and engaged with CLRN in South West England |
| Establish links with other health professionals | High to medium | Trial Management Group members presented at dietetics meetings as well as to gym managers and fitness club managers. Specialist weight management clinic advertising study |
| Collaborate with other weight loss studies | Medium | Unsuccessful owing to lack of studies |
| Maximise use of flagging systems on practice databases | Medium | Unsuccessful owing to complexities of various practice systems |
| Manage screening process and follow-up of route 2 participants | Medium | Contact maintained with route 2 participants but emphasis that they must contact the study team with evidence of their weight loss |
| Attend and present at local health events | Low | Two events attended but little impact on recruitment |
| Section 4: actions not pursued | ||
| Use pharmacies as PICs | High | Not pursued owing to resource implications involved in training sites |
| Complete database searches for PICs | High | Not pursued owing to lack of REC approval |
| Visit PICs to problem solve | Low | Not pursued owing to lack of resource and likely low impact on recruitment rates |
| Link in with relevant patient groups | Low | Not pursued as study closed to recruitment |
| Target discussion forums/threads on the internet | Low | Not pursued as study closed to recruitment |
| Create links with other slimming groups | Low | Not pursued owing to Slimming World involvement |
| Placing adverts | Medium | Attempted to advertise on relevant internet sites but they were not appropriate/willing. Paper, TV and radio – cost proved too expensive |
| Identify a local celebrity to champion the study | Medium | Attempted but unsuccessful |
The first section of the plan focused on how we could maximise the impact/success of our PIC sites in reaching potential participants. High-priority strategies included increasing the geographical area of recruitment. We gained research governance approval from another health board in South Wales, and enlisted a further two GP practices and two exercise referral practitioners. Based on what we had learned from the way in which existing PICs approached patients, we trained staff at these new sites to approach only those who fulfilled the criteria for recruitment via route 1, thus not adding to the already substantial ‘pool’ of individuals potentially entering the study via route 2.
We examined how best to maximise Slimming World’s involvement and engagement in the study as its clients would be most likely to have lost weight and be able to provide evidence. An advert placed in both its magazine and on its website proved very successful. A large number of enquiries, and subsequently participants, heard of the study in this way. In addition, a senior member of the central Slimming World team e-mailed consultants directly, inviting them to encourage their clients to read about the study. The study team were also permitted access to various Slimming World meetings and classes. While attending classes and speaking directly to clients was useful, there were also a number of barriers, including logistical issues such as time constraints. It was found to be more effective to attend the local consultants’ meetings where between 5 and 10 consultants were present and we could speak directly about the study to a number of those who lead the classes (often several classes).
Potential participants were more likely to respond to the consultants’ backing for the study than an unfamiliar member of the study team attempting to recruit them. Advertising was also an area that was to prove effective. The use of posters and e-mail adverts was a low-cost, time-efficient and potentially far-reaching option. Our posters gave brief information about the study including eligibility criteria and contact details. They were placed in a number of local GP practices as well as pharmacies – including those based in large supermarket chains in recruiting areas. Along with adverts circulated to employees of large companies and universities in South Wales, this relatively simple approach to disseminating information to a large audience proved moderately effective.
Social media were also utilised to increase the visibility of the study; however, it became apparent that this method would not lend itself to recruitment as we had hoped. Those linking in with the study via Facebook and Twitter tended to be other weight loss organisations or health professionals (HPs) rather than potential participants.
Having worked through various alternative strategies it was apparent that linking in with a weight loss intervention or programme was a highly effective and resource-efficient way of recruiting eligible individuals. Although we did recruit significant numbers of participants via the GP route, this was significantly more resource intensive in terms of staff time and cost (note that this avenue of recruitment was also open for significantly longer). Having the backing of the Slimming World programme and being invited to approach its clients and consultants was the most direct way of targeting potentially interested and eligible individuals. Those attending exercise referral schemes were not necessarily interested in weight loss, and engagement from exercise referral staff was generally quite low. GP practices did not have the capacity to effectively screen those who might be eligible, or did not record sufficient information for verification purposes (e.g. if weight was recorded only once in a 12-month period no information about weight loss could be obtained). Practices could reach a large number of individuals but unrefined database search tools and/or a lack of information to assess eligibility meant that the majority fell into the route 2 category. GPs also made few opportunistic (i.e. face-to-face) approaches, possibly owing to lack of time during consultations and a need to focus on more acute issues requiring immediate management.
A key learning point from our experience is that careful consideration needs to be given to the viability of entry criteria at the outset. Furthermore, early piloting of the recruitment process and proposed routes (including a formal review process and associated timelines) could have identified problems earlier and ensured that resources were appropriately directed. Shifting our emphasis and resources to those who were eligible via route 1, for example, proved the more effective strategy. Mass advertising allowed us to do this without incurring significant costs or increasing workload.
Intervention delivery
The individual components of the intervention (face-to-face and telephone MI) proved feasible to deliver and compliance rates were high, particularly for the face-to-face element (see Chapter 6). However, the group sessions proved extremely challenging to deliver for logistical reasons, predominantly relating to the low recruitment, creating a challenge with establishing groups and poor uptake by recruited participants. For this reason, it was decided to remove the group component from the intervention.
Summary
The current feasibility trial highlights a number of issues important to consider at the design stage of pragmatic trials of any community-based complex intervention. First, governance issues relating to NHS (in particular excess treatment) costs and the PIC model could have a significant impact on feasibility of delivery, particularly where no standard treatment currently exists, and/or when interventions are delivered by non-NHS staff in a trial setting, even if they would ultimately be delivered or commissioned by the NHS if effective and rolled out at a later date. Second, differences in accessibility and delivery of infrastructure support between devolved nations and regional variation in England need careful consideration as early as possible, in terms of their potential impact on feasibility of recruitment and associated timelines.
There is convincing evidence that social support is an important component of successful weight loss and maintenance interventions. 21,22,38,69,76,77
However, we were not able to assess the impact of group-based peer support in this instance for the reasons described in Chapter 3, Feasibility study methods. Delivery of locally led group sessions on a rolling basis does not appear to be feasible, particularly when recruitment is lower than expected. Other, less resource-intensive and logistically challenging, approaches to providing social support that do not depend on a minimum recruitment rate should therefore be considered in future WLM studies.
For similar trials for which written verification of weight loss is a requirement for inclusion, recruitment routes linked to current or recent weight loss programmes (slimming clubs or concurrent weight loss trials) are likely to be most effective. Therefore, strategies designed to engage or maximise the involvement of such schemes as research partners are worthy of investment, particularly given that very few participants otherwise eligible for the WILMA trial who wanted to lose at least 5% body weight appeared able to do so within a 12-month period. We also identified a number of targeted advertising strategies with minimal resource implications that proved effective in this setting.
Chapter 5 Main results
Baseline
In total, 1284 EOI forms were received. These are summarised in a flow diagram (Figure 2). The greatest number of EOIs were from primary care (71.7%); however, these were least likely to translate into eligible recruits, with only 7% (n = 66) being randomised into the trial. The most common reason for ineligibility in this population was not having achieved the required 5% weight loss (or not having evidence of having achieved it). The most successful recruitment route in terms of EOIs that were translated into actual recruits was Slimming World. Clear and consistent recording of weight and, therefore, evidence of weight loss was key to this. Such clear recording should have also been available from the exercise on referral (EOR) scheme; however, there were logistical issues which made this route less successful at translating EOIs into recruits (see Chapter 4).
FIGURE 2.
Recruitment flow chart. a, 83.7% were successfully followed up at 6 months and 12 months after excluding the four ineligible subjects. FTF, face to face; SW, Slimming World; WL, weight loss.
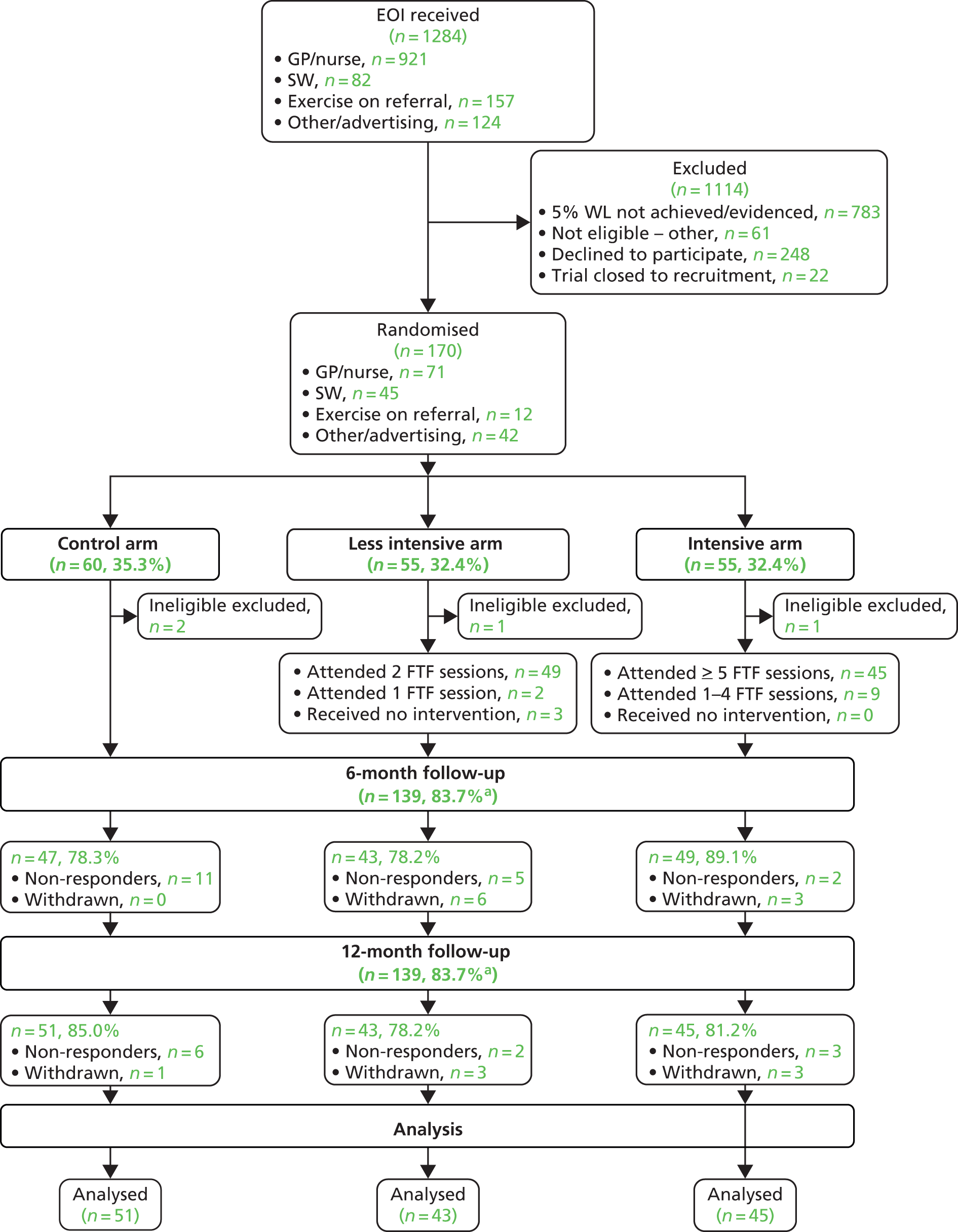
A total of 170 people were fully recruited and randomised; however, four were subsequently shown to have been inappropriate recruits and were therefore excluded. These were recruited early in the study before recruiter retraining was undertaken. The characteristics of those randomised to the three arms were broadly comparable and are given in Table 5. The majority of participants were over 30 years of age, non-smokers, female and white with an average BMI of just under 35 kg/m2.
| Demographics | Control (n = 58) | Less intensive (n = 54) | Intensive (n = 54) | Total (n = 166) |
|---|---|---|---|---|
| Age (years) | ||||
| < 30, n (%) | 6 (10.3) | 5 (9.3) | 5 (9.3) | 16 (9.6) |
| 30–59, n (%) | 36 (62.1) | 33 (61.1) | 32 (59.3) | 101 (60.8) |
| ≥ 60, n (%) | 16 (27.6) | 16 (29.6) | 17 (31.5) | 49 (29.5) |
| Gender | ||||
| Male, n (%) | 9 (15.5) | 8 (14.8) | 9 (16.7) | 26 (15.7) |
| Female, n (%) | 49 (84.5) | 46 (85.2) | 45 (83.3) | 140 (84.3) |
| BMI (kg/m2), mean (SD) | 33.3 (5.2) | 34.8 (6.2 ) | 34.4 (6.2) | 34.2 (5.9) |
| Waist-to-hip ratio, mean (SD) | 0.9 (0.1) | 0.9 (0.1) | 0.9 (0.1) | 0.9 (0.1) |
| Smoker | ||||
| No, n (%) | 52 (89.7) | 48 (88.9) | 50 (92.6) | 150 (90.4) |
| Yes, n (%) | 6 (10.3) | 6 (11.1) | 4 (7.4) | 16 (9.6) |
| AUDIT-C score, mean (SD) | 3.3 (3.0) | 3.1 (2.8) | 3.4 (2.9) | 3.3 (2.9) |
| IPAQ score, median (25–75% percentiles) | 1572.0 (0.0–2692.5) | 2088.0 (0.0–3999.0) | 1460.5(198.0–3172.5) | 1632.0 (0.0–3172.5) |
| EQ-5D health status score, mean (SD) | 82 (24) | 78 (27) | 82 (21) | 81 (24) |
| % weight lost, mean (SD) | 12.0 (7.4) | 11.4 (5.9) | 12.6 (7.0) | 12.0 (6.8) |
| Ethnicity | ||||
| White, n (%) | 53 (91.4) | 50 (92.6) | 54 (100.0) | 157 (94.6) |
| Non-white, n (%) | 5 (8.6) | 4 (7.4) | 0 (0.0) | 9 (5.4) |
| Method of recruitment | ||||
| Practices, n (%) | 21 (36.2) | 25 (46.3) | 23 (42.6) | 69 (41.6) |
| EOR, n (%) | 3 (5.2) | 3 (5.6) | 4 (7.4) | 10 (6.0) |
| Slimming World, n (%) | 18 (31.0) | 14 (25.9) | 13 (24.1) | 45 (27.1) |
| Other, n (%) | 16 (27.6) | 12 (22.2) | 14 (25.9) | 42 (25.3) |
| Comorbiditiesa | ||||
| Heart disease, n (%) | 3 (5.2) | 0 (0.0) | 2 (3.7) | 5 (3.0) |
| Diabetes mellitus, n (%) | 8 (13.8) | 9 (16.7) | 13 (24.1) | 30 (18.1) |
| Depression, n (%) | 19 (32.8) | 20 (37.0) | 21 (38.9) | 60 (36.1) |
| Stroke, n (%) | 0 (0.0) | 2 (3.7) | 0 (0.0) | 2 (1.2) |
| Arthritis, n (%) | 17 (29.3) | 13 (24.1) | 18 (33.3) | 48 (28.9) |
| Hypertension, n (%) | 26 (44.8) | 16 (29.6) | 23 (42.6) | 65 (39.2) |
| High cholesterol, n (%) | 15 (25.9) | 9 (16.7) | 14 (25.9) | 38 (22.9) |
| Asthma, n (%) | 11 (19.0) | 8 (14.8) | 10 (18.5) | 29 (17.5) |
| Chronic obstructive pulmonary disorder, n (%) | 1 (1.7) | 0 (0.0) | 1 (1.9) | 2 (1.2) |
| Back pain, n (%) | 21 (36.2) | 18 (33.3) | 20 (37.0) | 59 (35.5) |
Feasibility outcomes
The primary feasibility outcomes of the trial relate to recruitment, retention and adherence (see Chapter 3).
Recruitment
A total of 170 participants were recruited to the trial over a period of 15 months. Four participants were ineligible and randomised in error and were subsequently withdrawn. These participants were excluded from the feasibility outcomes results.
Retention
Once recruited, the vast majority of participants stayed in the study for 12 months, with only 10% (16/166) overall withdrawing, as shown in Table 6. Participants in the control group were the least likely to actively withdraw, with only one individual doing so (2%, 1/58). Participants in the less intensive arm were most likely to withdraw (17%, 9/54). The proportion of non-responders was similarly modest, at only 7% overall (11/166). Participants in the control group were the most likely to fail to respond (10%, 6/58). The combined total of 27 participants (16%, 27/166) dropping out of the study was below the 30% attrition predicted in the original sample size calculation, albeit this referred to a longer follow-up period (3 years). The overall dropout rate was 12% (7/58), 20% (11/54) and 17% (9/54) in the control arm, the less intensive arm and the intensive arm, respectively. At both the 6- and 12-month follow-up assessments, the overall retention was 83.7% (139/166) (albeit some who were present at 6 months were not at 12 months and vice versa).
| Feasibility outcome | Control (n = 58) | Less intense (n = 54) | Intense (n = 54) | Total (n = 166) |
|---|---|---|---|---|
| Withdrawals | 1 | 9 | 6 | 16 |
| Percentage (95% CI) | 2 (0 to 10) | 17 (8 to 30) | 11 (5 to 23) | 10 (6 to 15) |
| Non-responders | 6 | 2 | 3 | 11 |
| Percentage (95% CI) | 10 (4 to 22) | 4 (1 to 14) | 6 (1 to 16) | 7 (4 to 12) |
| Adherence | 49 | 45 | ||
| Percentage (95% CI) | 91 (79 to 97) | 83 (70 to 92) |
Adherence
Adherence was defined as attendance at five out of six face-to-face sessions for the intensive group and two face-to-face sessions for the less intensive group. Adherence to the intervention was excellent, with both treatment arms achieving adherence in excess of 85% in those who had not withdrawn. Detailed qualitative exploration of recruitment, retention and adherence is presented in Chapters 6–8.
Effectiveness outcomes
Table 7 summarises the continuous outcome variables at baseline and follow-up.
| Outcome | Baseline | 12-month follow-up | ||||||
|---|---|---|---|---|---|---|---|---|
| Control, mean (SD) | Intensive, mean (SD) | Less intensive, mean (SD) | Total, mean (SD) | Control, mean (SD) | Intensive, mean (SD) | Less intensive, mean (SD) | Total, mean (SD) | |
| BMI (kg/m2) | 33.3 (5.19) | 34.4 (6.19) | 34.8 (6.20) | 34.2 (5.86) | 33.0 (5.22) | 33.3 (6.50) | 33.4 (6.03) | 33.2 (5.89) |
| BMI augmenteda (kg/m2) | N/A | 33.0 (5.39) | 33.3 (6.50) | 34.1 (6.22) | 33.5 (6.00) | |||
| Weight (kg) | 90.2 (15.41) | 92.5 (20.02) | 93.8 (17.66) | 92.1 (17.70) | 89.6 (17.21) | 90.1 (21.00) | 91.6 (17.19) | 90.4 (18.49) |
| Weight augmenteda (kg) | N/A | 90.1 (17.28) | 90.1 (21.00) | 94.3 (19.97) | 91.4 (19.34) | |||
| Waist circumference (cm) | 102.5 (11.96) | 104.3 (15.51) | 105.4 (14.10) | 104.1 (13.86) | 102.7 (14.63) | 102.8 (16.33) | 103.2 (13.56) | 102.9 (14.84) |
| Waist-to-hip ratio | 0.9 (0.08) | 0.9 (0.09) | 0.9 (0.09) | 0.9 (0.09) | 0.9 (0.10) | 0.9 (0.10) | 0.9 (0.09) | 0.9 (0.10) |
| IPAQ (MET minutes per week) | 1902 (1517) | 2805 (3412) | 2506 (2239) | 2386 (2500) | 2346 (2457) | 3017 (3343) | 3594 (4548) | 2956 (3521) |
| GHQ-12 score | 2.3 (3.52) | 1.8 (2.82) | 2.4 (3.38) | 2.2 (3.25) | 2.6 (3.81) | 2.3 (3.31) | 3.0 (3.70) | 2.6 (3.60) |
| DINE fibre score | 32.7 (10.50) | 34.7 (8.91) | 33.7 (8.64) | 33.7 (9.38) | 31.2 (8.85) | 34.0 (7.06) | 32.4 (9.79) | 32.5 (8.56) |
| DINE fat score | 14.9 (4.82) | 17.7 (5.41) | 16.7 (4.95) | 16.3 (5.11) | 17.3 (4.83) | 17.0 (3.99) | 17.5 (4.99) | 17.3 (4.56) |
| DINE healthy eating score | 17.7 (9.71) | 17.4 (9.34) | 16.3 (5.76) | 17.1 (8.34) | 14.9 (8.34) | 17.2 (7.97) | 15.9 (9.56) | 16.1 (8.57) |
| EQ-5D score | 0.8 (0.24) | 0.8 (0.21) | 0.8 (0.27) | 0.8 (0.24) | 0.8 (0.18) | 0.8 (0.18) | 0.8 (0.32) | 0.8 (0.23) |
| EDE-Q number of days binge eating | 2.4 (4.04) | 2.2 (4.92) | 2.7 (4.02) | 2.4 (4.32) | 2.5 (4.14) | 1.4 (2.61) | 4.1 (6.06) | 2.6 (4.54) |
| AUDIT-C score | 3.3 (2.95) | 3.4 (2.85) | 3.1 (2.79) | 3.3 (2.85) | 3.1 (2.78) | 3.3 (2.68) | 3.0 (2.67) | 3.1 (2.70) |
Primary effectiveness outcome
The primary effectiveness outcome was BMI (see Chapter 3). A three-level hierarchical model (with participants clustered within MIPs and groups) was proposed in the statistical analysis plan; however, the peer support groups could not be included as a third level as not enough were run. The two-level hierarchical model was fitted, but there was no evidence of clustering [intracluster correlation coefficient (ICC) < 0.000], so a linear model is reported. Each of the intervention arms was compared with the control arm. Transformations of BMI (such as square, square root and log) were investigated but did not appreciably improve model fit as measured by the adjusted R2 and so results are presented for the untransformed BMI. This is based on 129 individuals who were weighed. All results are summarised in Table 8.
| Outcome | n | Less intensivea | Intensivea | ||
|---|---|---|---|---|---|
| Mean | 95% CI | Mean | 95% CI | ||
| Primary outcome | |||||
| BMI (kg/m2) | 129 | –0.21 | –1.44 to 1.03 | –0.96 | –2.16 to 0.23 |
| BMI augmentedb (kg/m2) | 137 | –0.23 | –1.38 to 0.93 | –0.94 | –2.09 to 0.21 |
| Secondary outcomes (continuous) | |||||
| Weight (kg) | 129 | –0.70 | –4.10 to 2.70 | –2.82 | –6.09 to 0.45 |
| Weight augmentedb (kg) | 137 | –0.69 | –3.88 to 2.50 | –2.73 | –5.87 to 0.41 |
| Waist (cm)c | 129 | 0.15 | –3.34 to 3.65 | –0.84 | –4.21 to 2.59 |
| Waist-to-hip ratio | 129 | –0.001 | –0.030 to 0.027 | –0.012 | –0.039 to 0.016 |
| IPAQ MET minutes per week (transformed) | 111 | 6.33 | –5.33 to 17.98 | 0.85 | –10.61 to 12.32 |
| GHQ-12 score | Not fitted | ||||
| DINE fibre scorec | 96 | –0.60 | –4.32 to 3.12 | 0.47 | –3.20 to 4.14 |
| DINE fat scorec | 54 | –1.80 | –4.50 to 0.54 | –4.68 | –7.44 to –2.28 |
| DINE health eating scorec | 46 | –0.30 | –5.73 to 5.12 | 4.16 | –1.80 to 10.14 |
| EQ-5D score | Not fitted | ||||
| EDE-Q number of days binge eating | Not fitted | ||||
| AUDIT-C score | Not fitted | ||||
| Outcome | n | Less intensive | Intensive | ||
| OR | 95% CI | OR | 95% CI | ||
| Secondary outcomes (binary) | |||||
| Maintaining weight lost | 129 | 0.61 | 0.23 to 1.56 | 1.43 | 0.59 to 3.54 |
| Maintaining weight lost augmented | 137 | 0.69 | 0.28 to 1.71 | 1.45 | 0.61 to 3.49 |
| AUDIT-C categorised | 134 | 0.34 | 0.08 to 1.28 | 1.53 | 0.42 to 5.63 |
| GHQ-12 case ≥ 3 | 133 | 1.07 | 0.39 to 2.98 | 1.12 | 0.40 to 3.09 |
| GHQ-12 case ≥ 12 | Not fitted | ||||
| EQ-5D (< 100, 100) | 139 | 1.39 | 0.49 to 3.94 | 0.85 | 0.29 to 2.46 |
| EDE-Q recurrent | Not fitted | ||||
| EDE-Q compensatory behaviour | Not fitted | ||||
| Heaviness of smoking | Not fitted | ||||
| Sensitivity analysis assuming non-responders failed to maintain | 166 | 0.64 | 0.27 to 1.47 | 1.34 | 0.60 to 3.01 |
| Poisson regression | n | Less intensive | Intensive | ||
| Expected rate | 95% CI | Expected rate | 95% CI | ||
| EDE-Q number of days binge eating | 135 | 1.01 | 0.78 to 1.31 | 0.60 | 0.42 to 0.86 |
The analysis of the primary outcome of BMI shows that the intensive arm had a non-significant difference in BMI of –1.0 kg/m2 (95% CI –2.2 kg/m2 to 0.2 kg/m2) (i.e. mean BMI was 1 kg/m2 lower in the intensive arm than in the control group), whereas mean BMI in the less intensive arm showed a non-significant difference from the control group of –0.2 kg/m2 (95% CI –1.4 kg/m2 to 1.0 kg/m2). A difference in mean BMI of 1 kg/m2 would be considered clinically important in a fully powered RCT, but is not statistically significant in this feasibility study. However, this magnitude of difference (and the 95% CI excluding substantial weight differences in the direction of harm) does suggest that the intensive intervention is worthy of further investigation. The difference of –0.2 kg/m2 achieved by the less intensive intervention compared with the control group is unlikely to be of clinical relevance. The effect sizes associated with these results are –0.140 for the intensive arm and –0.029 for the control arm. Allowing for the inclusion of self-reported weight for missing values in BMI did not change the conclusion.
Weight
Weight measured in kilograms (kg) was formally investigated in a similar way to the primary outcome, controlling for the same covariates, but replacing baseline BMI with baseline weight. Again, no clustering was found in the hierarchical model fitted, so linear regression results are presented. Weight in the intensive treatment arm was not statistically significantly different from that in the control arm, participants in the intensive treatment arm weighing, on average, 2.8 kg less than control participants (95% CI –6.1 to 0.5 kg); participants in the less intensive arm weighed only 0.7 kg less than controls (95% CI –4.1 to 2.7 kg). The 95% CI shows that participants in the intensive arm were unlikely to be appreciably harmed by the intervention and a difference of 2.8 kg would be clinically important if shown to be a true difference. The less intensive arm is less likely to be producing an effect of clinical importance. The analysis was repeated with self-reported weight, but the results did not change appreciably.
Waist measurements
There was some indication of clustering in waist measurement, so hierarchical methods were used. The ICC was 0.040. The results show little evidence of a large effect on this outcome, with the intensive arm having an average waist measurement 0.8 cm lower than the control group (adjusted mean difference –0.8, 95% CI –4.2 to 2.6), while mean weight circumference in the less intensive arm was 0.1 cm lower than in the control group (95% CI –3.3 cm to 3.7 cm). The size of difference between groups would not be considered clinically important and there were some large and potentially implausible individual differences between baseline and follow-up waist circumference measurements (range –26.5 cm to 18 cm), which may be attributable to measurement error.
Waist-to-hip ratio
There was no evidence of a treatment effect on waist-to-hip ratio with an adjusted mean difference of –0.01 comparing the intensive with control group (95% CI –0.04 to 0.02) and an adjusted mean difference of –0.001 comparing the less intensive group with the control group (95% CI –0.03 to 0.03).
International Physical Activity Questionnaire
The International Physical Activity Questionnaire (IPAQ) follows a very skewed distribution, which is shown, split by group, in Figure 3. Transformations of the IPAQ score were investigated in our analysis. The square root performed the best (based on visual inspection of fitted versus residual plots). There was no evidence of clustering, so linear regression is reported. There was no evidence of any impact of treatment group on this outcome, with the intensive arm having a square root IPAQ score of 0.9 greater than that of the control group (95% CI –10.6 to 12.3) and the less intensive arm having a square root IPAQ score 6.3 greater than that of the control group (95% CI –5.3 to 18.0).
FIGURE 3.
Distribution of follow-up IPAQ scores between groups.
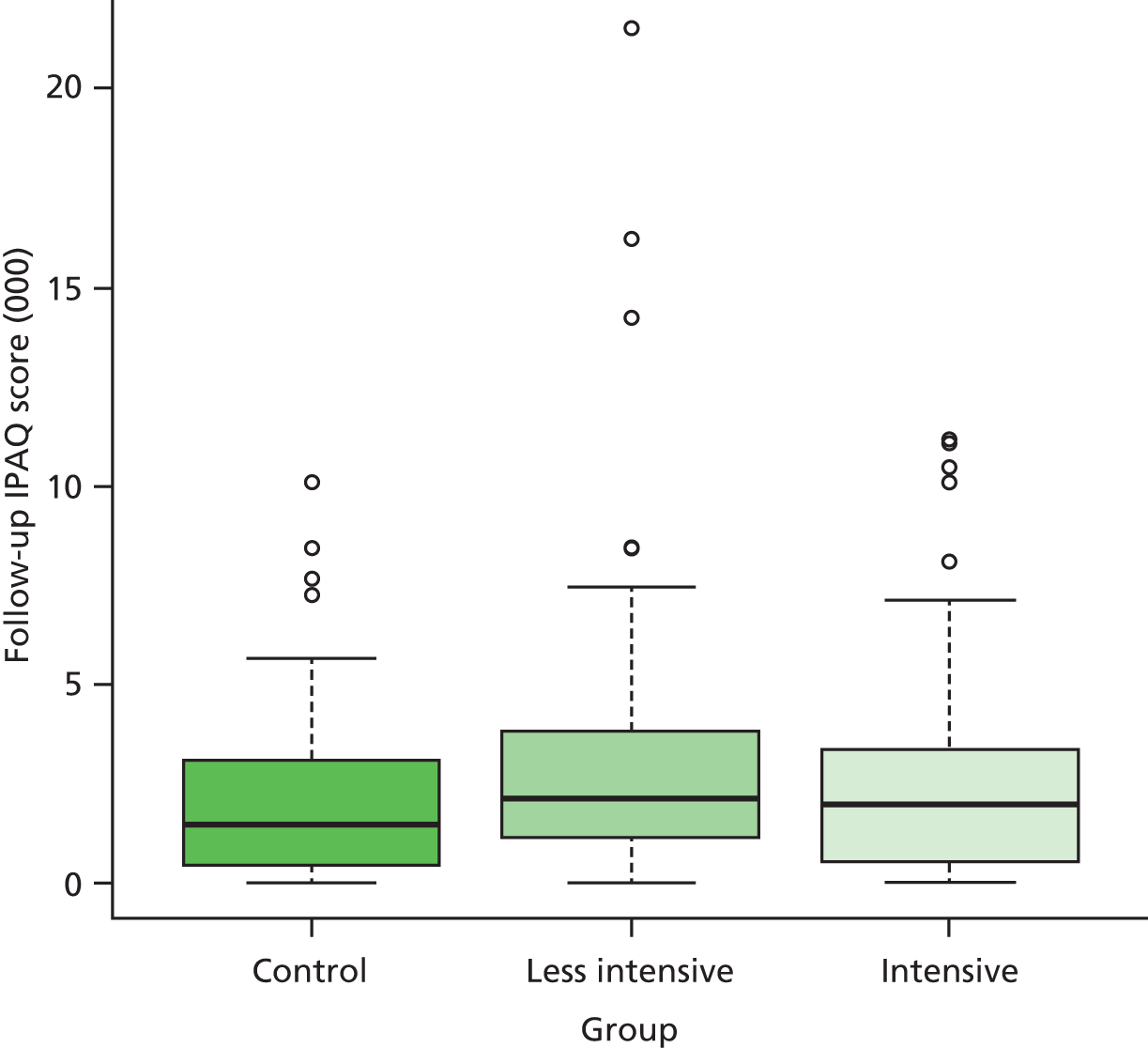
Maintaining weight lost
A binary assessment of whether or not the participants had gained weight since baseline was performed and logistic regression was used to compare groups, controlling for the same covariates used in the primary analysis. There was no evidence of clustering, so a non-hierarchical logistic regression is reported. Table 8 shows that, while mean weight in neither treatment arm was statistically significantly different to that in the control group, participants in the intensive arm had, on average, a 43% higher chance than those in the control group of maintaining weight loss (OR 1.43, 95% CI 0.6 to 3.5). In contrast, participants in the less intensive arm were, on average, 40% less successful than the control group at maintaining weight loss (OR 0.6, 95% CI 0.2 to 1.6). This analysis was repeated using self-reported weight, but the results were similar (see Table 8). The proportion of maintainers was highest in the intensive arm (56%, n = 25) and lowest in the less intensive arm (37%, n = 14) (Table 9).
| Weight status | Treatment arm | ||
|---|---|---|---|
| Control | Less intensive | Intensive | |
| Maintained weight lost? | |||
| No | 25 (54%) | 24 (63%) | 20 (44%) |
| Yes | 21 (46%) | 14 (37%) | 25 (56%) |
General Health Questionnaire: continuous score
The General Health Questionnaire – 12 items (GHQ-12) scores were not distributed normally (Figure 4). Standard transformations were investigated, but the model fit was not improved. The score was dichotomised using the standard cut-off point of 3 or more to indicate a case. There was no evidence of clustering, so non-hierarchical results are presented. The odds of scoring 3 or higher on the GHQ-12 was 12% higher for participants in the intensive arm than for those in the control arm (OR 1.12, 95% CI 0.4 to 3.09), while the less intensive arm had an odds of 7% higher than the control (OR 1.07, 95% CI 0.39 to 2.98).
FIGURE 4.
Comparison of follow-up GHQ-12 distributions between treatment arms. (a) Control group; (b) less intensive group; and (c) intensive group.
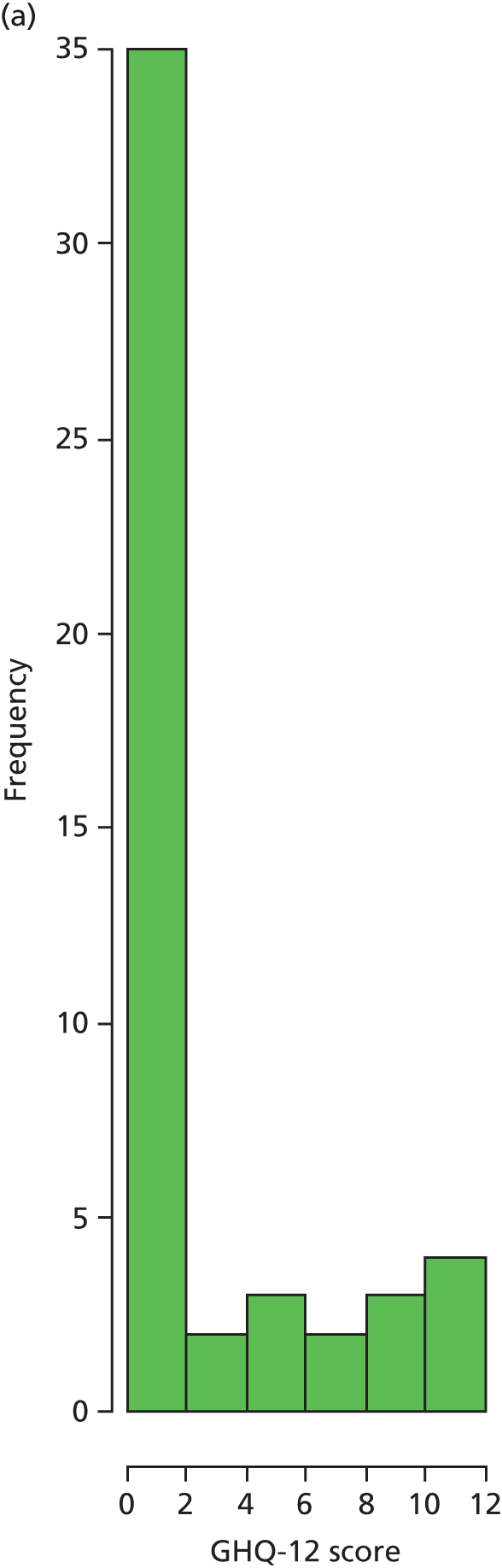


General Health Questionnaire: dichotomised
The GHQ-12 was analysed as a binary variable derived using the World Health Organization (WHO) threshold for evidence of distress (a score of 12 or more). However, in this general population sample there were very few participants who met this criterion (three individuals, Table 10) and so we were unable to fit a regression model to this variable.
| Arm | Numbers of participants meeting the WHO threshold for distress | |
|---|---|---|
| No | Yes | |
| Control | 49 (100%) | 0 (0%) |
| Less intensive | 39 (95%) | 2 (5%) |
| Intensive | 43 (98%) | 1 (2%) |
Dietary Instrument for Nutrition Education scale
We examined three scales from the Dietary Instrument for Nutrition Education (DINE): the fibre, fat and healthy eating scales.
The Dietary Instrument for Nutrition Education fibre scale
There was evidence of clustering in the DINE fibre scale scores, so the results of the hierarchical model are presented. The ICC was 0.056. Missing DINE fibre scores reduced the number of participants on which this model was run to 96. The adjusted mean difference was 0.5 greater for the intensive arm than for the control arm (95% CI –3.2 to 4.1) and 0.6 lower for the less intensive arm than for the control arm (95% CI –4.3 to 3.1). Both CIs are broadly centred about zero, representing little evidence of a treatment effect.
The Dietary Instrument for Nutrition Education fat score
There was evidence of clustering in the DINE fat score, with a very high ICC of 0.63, and so results from the hierarchical model are presented. Again, however, there were many missing values, resulting in this analysis being performed on only 54 participants. Participants in the intensive arm reported statistically significantly lower fat intake than did participants in the control group (adjusted mean difference –4.7, 95% CI –7.4 to –2.3). There is some evidence that participants in the less intensive arm also reported lower fat intake in comparison with the control group, but the difference was not statistically significantly different (adjusted mean difference –1.8, 95% CI –4.5 to 0.5).
The Dietary Instrument for Nutrition Education healthy eating score
The DINE healthy eating score is the contrast between the fat and fibre scales, so this score is affected by the missing data for dietary fat and fibre referred to above. This reduced the sample size to 46. There was clustering in evidence (the ICC was 0.097) and so the hierarchical model is reported. The intensive arm reported healthy eating scores that were, on average, 4.2 points higher than those reported by the control group (95% CI –1.8 to 10.1), while the less intensive arm reported scores 0.3 points lower than those of the control group (95% CI –5.7 to 5.1). This suggests a small potential effect of the intervention for the intensive arm only; however, the very small numbers make it hard to draw any conclusions.
European Quality of Life-5 Dimensions
The EQ-5D scores were not normally distributed (Figure 5). Standard transformations (inverse, log, square root) did not improve the fitted compared with residual plots, so a dichotomised analysis is presented (those with scores below 100, vs. those with scores of 100). There was no evidence of clustering (ICC < 0.000), so non-hierarchical results are presented. The odds of scoring 100 was 15% lower in the intensive arm than in the control arm (OR 0.85, 95% CI 0.29 to 2.46), while in the less intensive arm it was 39% greater than in the control arm (OR 1.39, 95% CI 0.49 to 3.94).
FIGURE 5.
Comparison of follow-up EQ-5D scores between treatment arms. (a) Control group; (b) less intensive group; and (c) intensive group.

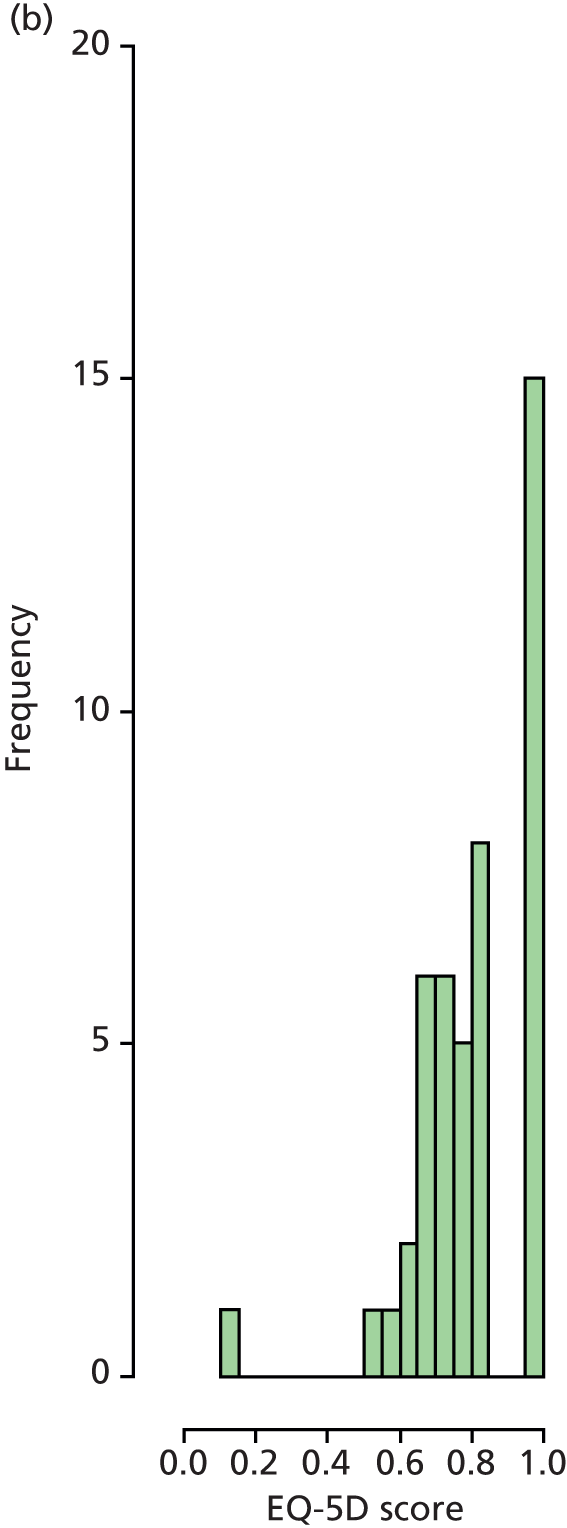
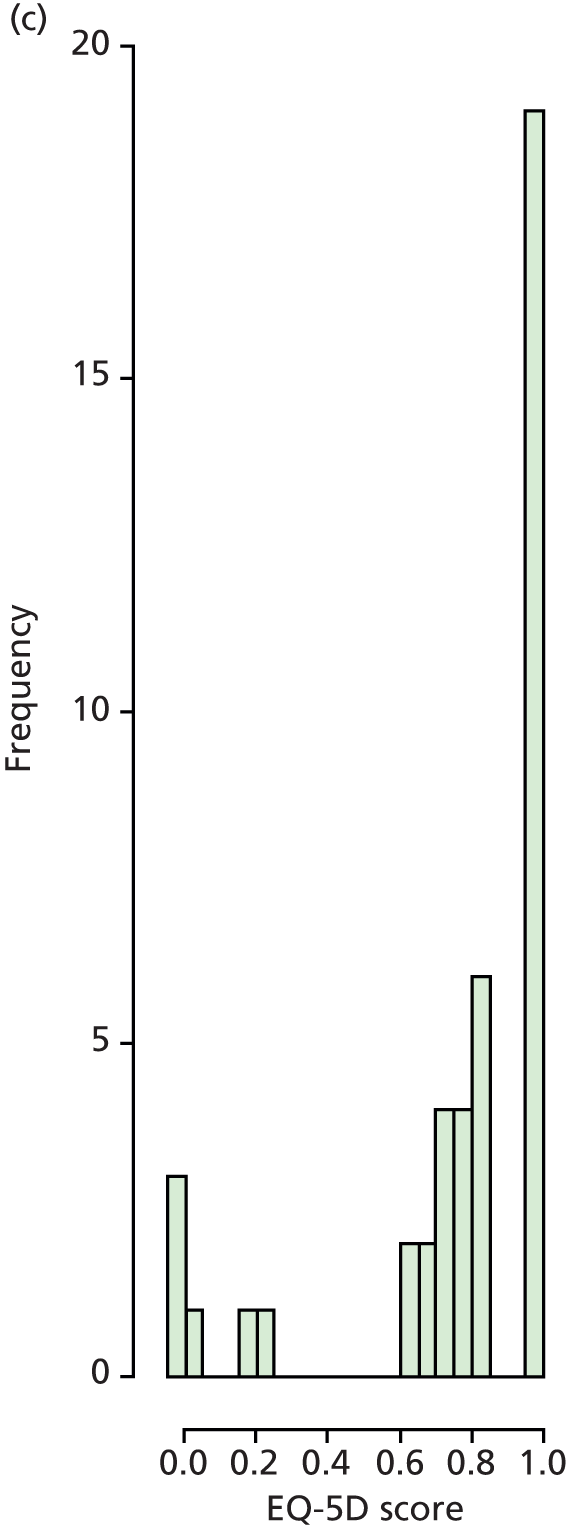
The Eating Disorder Examination Questionnaire
Three measures of binge eating [from the Eating Disorder Examination Questionnaire (EDE-Q)] were investigated: (1) a threshold for recurrent binge eating behaviour (yes/no), (2) the number of days in the last 28 days on which binge eating occurred and (3) the threshold for compensatory behaviour (yes/no). The numbers for the threshold for recurrent binge eating behaviour and for compensatory behaviour were too small for analysis and the results are therefore presented only descriptively (Tables 11 and 12).
| Follow-up recurrent binge eating behaviour | ||
|---|---|---|
| No | Yes | |
| Baseline recurrent binge eating behaviour | ||
| No | 116 (94%) | 7 (6%) |
| Yes | 6 (50%) | 6 (50%) |
| Follow-up compensatory behaviour | ||
|---|---|---|
| No | Yes | |
| Baseline compensatory behaviour | ||
| No | 126 (98%) | 3 (2%) |
| Yes | 3 (60%) | 2 (40%) |
Number of days on which binge eating occurred
The number of days on which binge eating occurred was not normally distributed (Figure 6). A zero-inflated Poisson regression was fitted to the data and showed that the mean number of days on which binge eating occurred was 40% lower in the intensive arm than in the control arm (expected rate 0.60, 95% CI 0.40 to 0.86), while in the less intensive arm this value was very similar to that in the control arm (rate 1.01, 95% CI 0.78 to 1.31).
FIGURE 6.
Comparison of the number of binge eating days at follow-up across groups. (a) Control group; (b) less intensive group; and (c) intensive group.
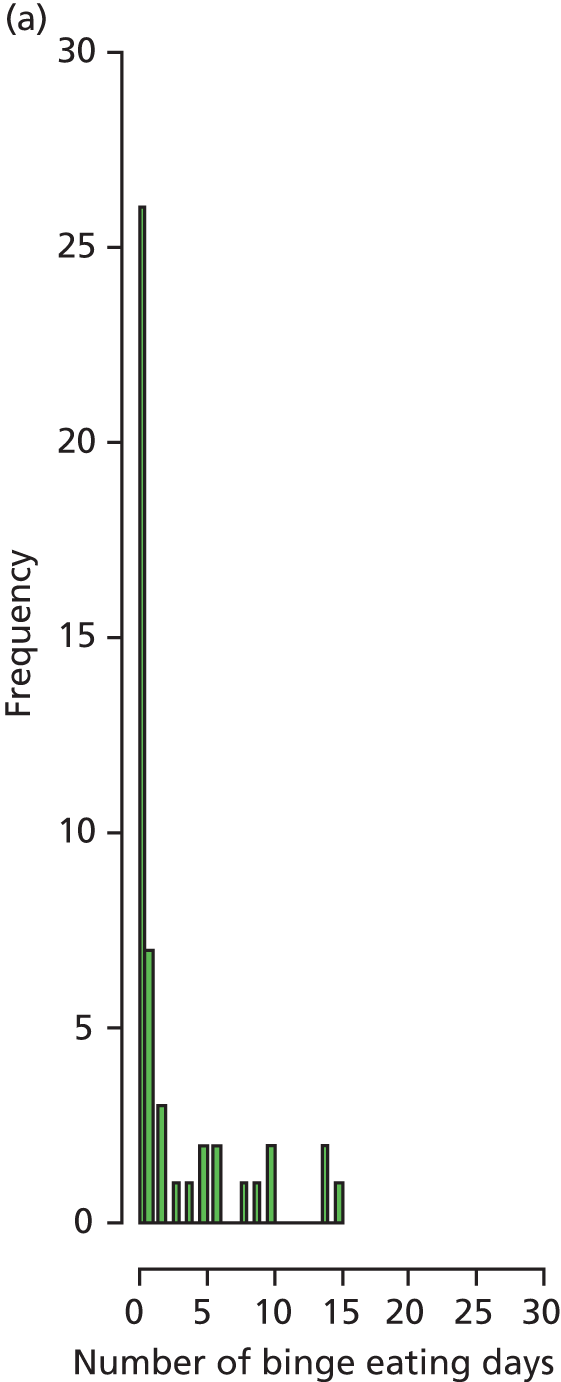

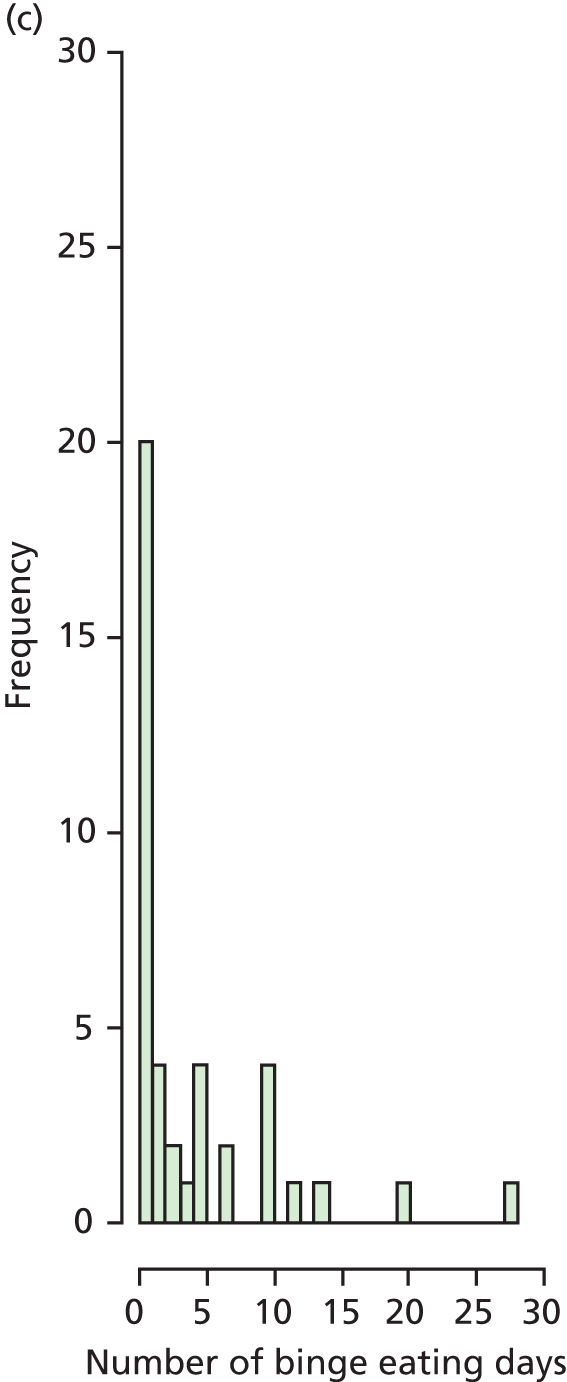
Alcohol Use Disorders Identification Test
The continuous Alcohol Use Disorders Identification Test (AUDIT-C) was highly skewed (Figure 7) and so only the AUDIT-C categorised for high-risk drinking was analysed using logistic regression. This model suggests that participants in the intensive arm were more likely to develop increasing or higher risks of drinking (OR 1.53, 95% CI 0.4 to 5.6), while those in the less intensive arm were less likely to develop increasing or higher risks of drinking (OR 0.32, 95% CI 0.1 to 1.3). However, the CIs are extremely wide for both arms, so the evidence for a treatment effect is uncertain. Table 13 shows the frequencies of categorised AUDIT-C scores at baseline and follow-up.
FIGURE 7.
Distribution of follow-up AUDIT-C scores across trial arms. (a) Control group; (b) less intensive group; and (c) intensive group.
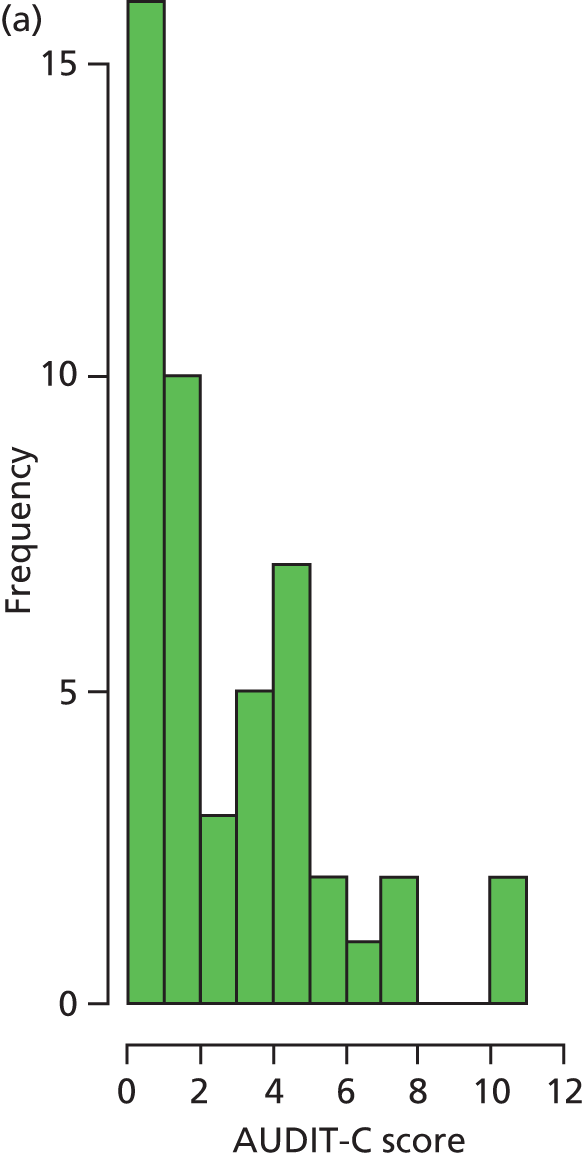

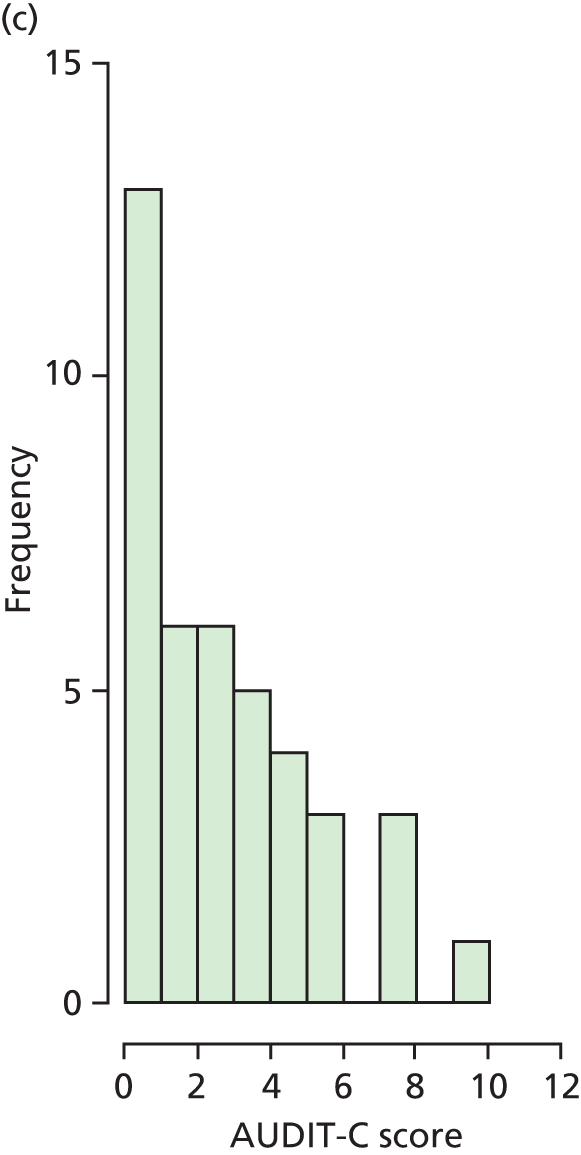
| Categorised follow-up AUDIT-C | ||
|---|---|---|
| Not increasing/higher risk of drinking | Increasing/higher risk of drinking | |
| Categorised baseline AUDIT-C | ||
| Not increasing/higher risk of drinking | 82 | 12 |
| Increasing/higher risk of drinking | 10 | 30 |
Heaviness of smoking index
The Heaviness of Smoking Index (HSI) is presented in Table 14. Very few participants changed over time so this outcome was not analysed.
| Follow-up HSI | ||
|---|---|---|
| Low addiction | Moderate addiction | |
| Baseline HSI | ||
| Low addiction | 129 | 2 |
| Moderate addiction | 2 | 2 |
Sensitivity analysis
The analysis of the proportion who maintained their weight loss was performed assuming that the 29 individuals who we were unable to follow up failed to maintain their weight loss. The results did not change dramatically, with the intensive arm having an OR of maintaining weight loss of 1.3 (95% CI 0.6 to 3.0) and the less intensive arm an OR of 0.6 (95% CI 0.3 to 1.5).
Complier-average causal effect analysis
For the purposes of this analysis, a complier will be defined as:
-
for a participant assigned to the intensive arm, attending five of the six face-to-face MI sessions
-
for a participant assigned to the less intensive arm, attending both of the face-to-face MI sessions.
Compliance with the intervention
The majority of participants (87.0%) attended the number of sessions required to be classified as a complier. Compliance was higher among those allocated to the less intensive arm (90.7%) than for those allocated to the intensive arm (83.3%), which could be expected given the lower threshold for being a complier (two sessions rather than at least five).
Missing outcome data
The majority of participants both complied with the intervention and provided follow-up BMI data (74.1% of participants in the intensive arm and 66.7% of participants in the less intensive arm; Table 15 and Figure 8). Non-compliance did not appear to be associated with dropout; in fact, in the less intensive arm more compliers dropped out than non-compliers.
| Level of compliance | BMI outcome data available | BMI outcome data not available | Total |
|---|---|---|---|
| Less intensive arm | |||
| Complied with intervention | 36 | 13 | 49 |
| Did not comply with intervention | 2 | 3 | 5 |
| Total | 38 | 16 | 54 |
| Intensive | |||
| Complied with intervention | 40 | 5 | 45 |
| Did not comply with intervention | 5 | 4 | 9 |
| Total | 45 | 9 | 54 |
FIGURE 8.
The relationship between compliance and dropout/availability of outcome data.
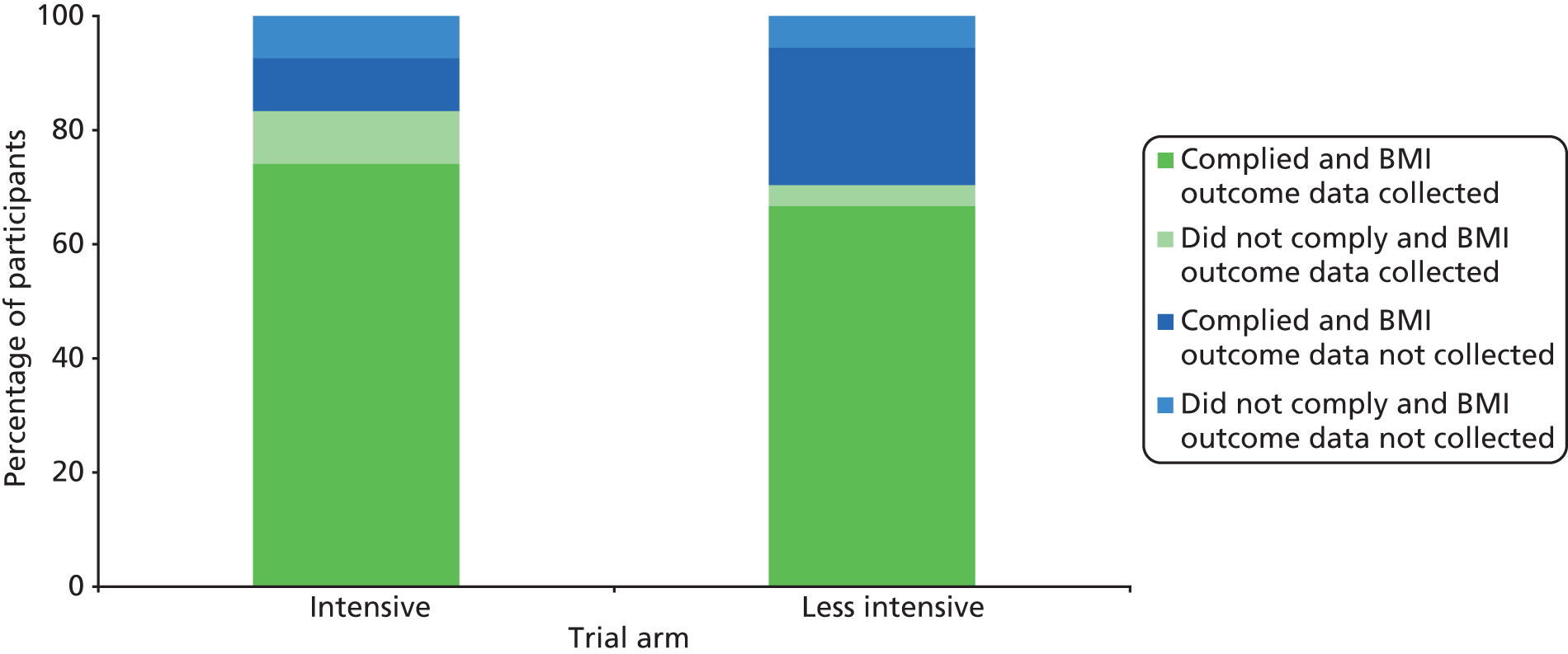
Intracluster correlation coefficients
There was no evidence of clustering of responses to the primary outcome (ICC 0.00). A small amount of clustering was observed when exploring the relationship between compliance with the intensive intervention and MIP (ICC 0.057), and there is no evidence of compliance with the less intensive intervention clustering by MIP (ICC 0.00). An ICC of 0.057 (5.7% of the total variability in compliance to the intensive intervention was related to differences between MIPs) was not particularly large. For simplicity, our CACE analyses did not take clustering into account.
Adjusting the primary analysis for compliance, we observe a larger difference in post-intervention BMI for the intensive arm, but no observable difference (to two decimal places) for the less intensive arm. This demonstrates that attending the intensive intervention reduced BMI by 1.23 kg/m2, although the 95% CI ranges from a reduction of –2.49 kg/m2 reduction to an increase of 0.03 kg/m2, so the difference was not statistically significant at the 5% level (Table 16 and Figure 9).
| Comparison | Type of analysis | Adjusted between-group mean difference in post-intervention BMIa | Lower 95% CI | Upper 95% CI | p-value |
|---|---|---|---|---|---|
| Intensive vs. control | ITT (effectiveness) | –0.96 | –2.16 | 0.23 | 0.114 |
| Intensive vs. control | CACE (efficacy) | –1.23 | –2.49 | 0.03 | 0.056 |
| Less intensive vs. control | ITT (effectiveness) | –0.21 | –1.44 | 1.03 | 0.739 |
| Less intensive vs. control | CACE (efficacy) | –0.21 | –1.40 | 0.98 | 0.733 |
FIGURE 9.
The effectiveness and efficacy of treatment on post-intervention BMI. Adjusted mean difference represented by the square point. Associated 95% CIs are represented by the dark bold lines. ITT, intention to treat.
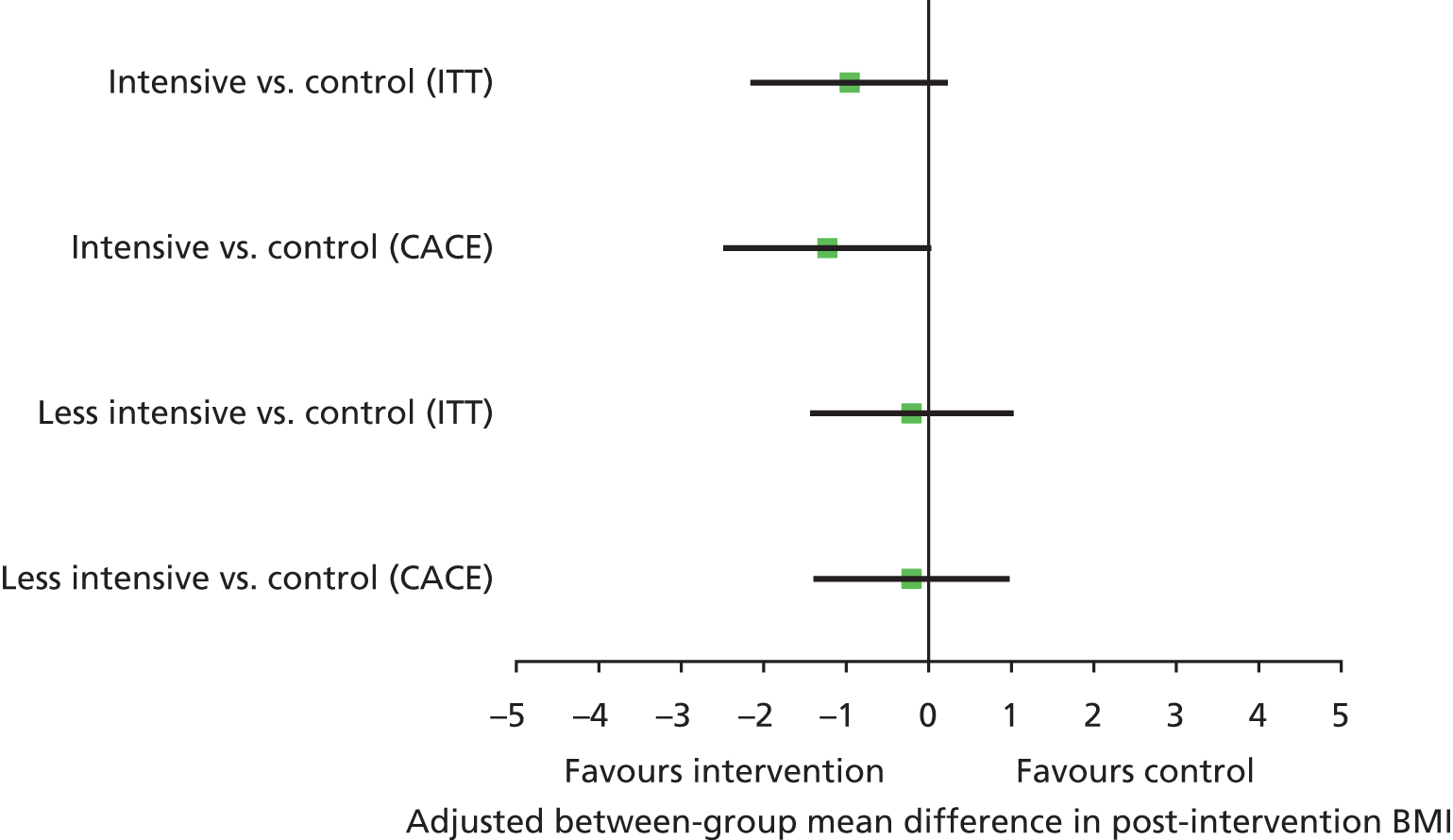
In a similar way to the BMI outcome, adjusting the analysis for compliance, we observe a larger difference in post-intervention weight and the difference was less pronounced in the less intensive arm than in the intensive arm. We found that attending the intensive intervention reduced weight by, on average, 3.69 kg, with the 95% CI ranging from a 7.08 kg reduction to a 0.31 kg reduction (p = 0.033) (Table 17 and Figure 10).
| Comparison | Type of analysis | Adjusted between-group mean difference in post-intervention weighta | Lower 95% CI | Upper 95% CI | p-value |
|---|---|---|---|---|---|
| Intensive vs. control | ITT (effectiveness) | –2.84 | –6.10 | 0.42 | 0.087 |
| Intensive vs. control | CACE (efficacy) | –3.69 | –7.08 | –0.31 | 0.033 |
| Less intensive vs. control | ITT (effectiveness) | –0.82 | –4.19 | 2.56 | 0.632 |
| Less intensive vs. control | CACE (efficacy) | –0.89 | –4.16 | 2.38 | 0.594 |
FIGURE 10.
The effectiveness and efficacy of treatment on post-intervention weight (in kg). Adjusted mean difference represented by the square point. Associated 95% CIs are represented by the dark bold lines. ITT, intention to treat.
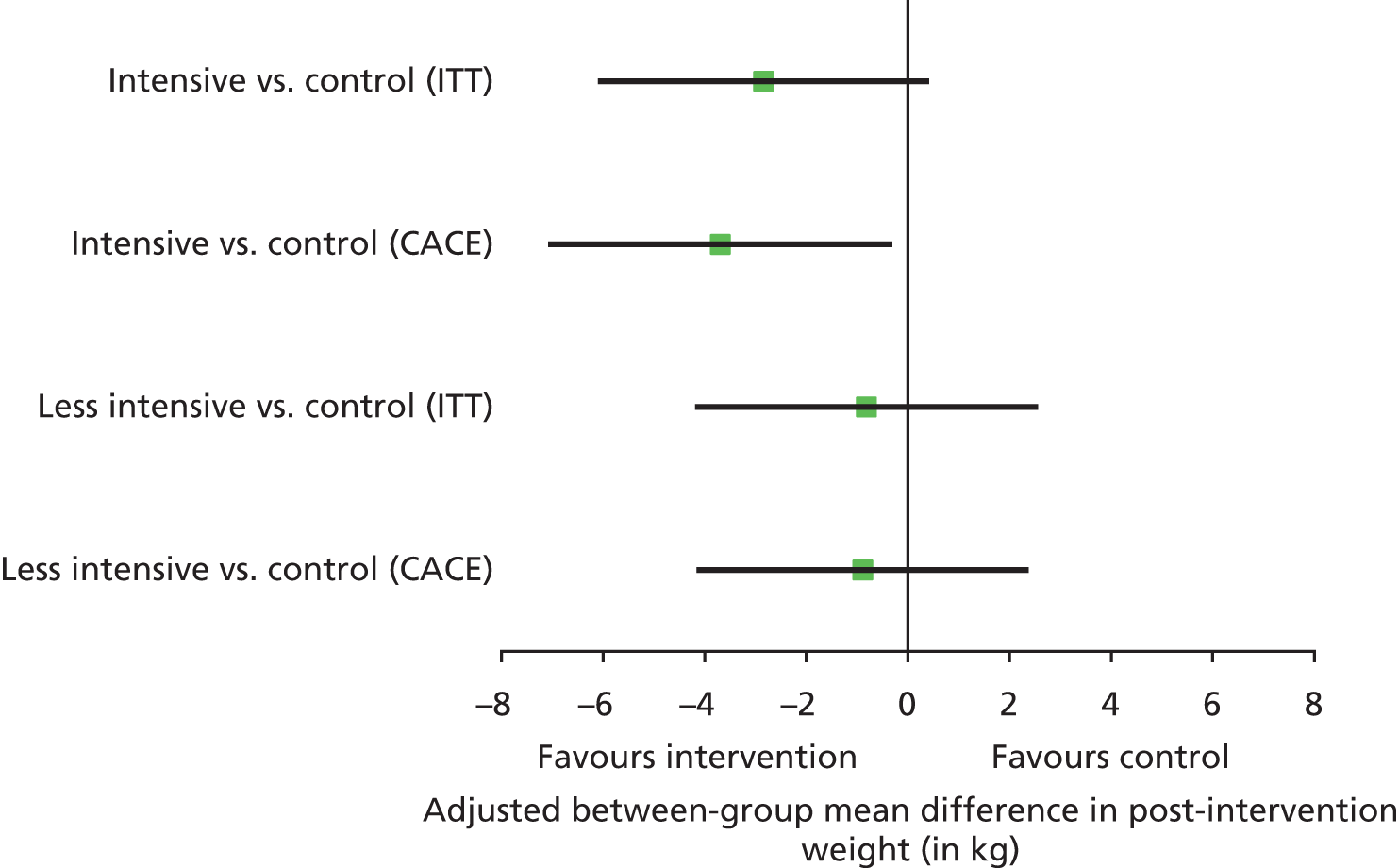
Mediation analyses
Mediation analyses were also conducted on self-efficacy, social support, intrinsic motivation, habits and self-monitoring as measured at 6 months (see Chapter 3).
It is important to note here (Figure 11) that we have assumed that there are no confounders in the relationship between the mediator(s) and the outcome. Given that mediators are measured post randomisation (by definition), it is likely that there will be some measured and unmeasured confounders that will not be taken into account in our model and, therefore, our estimates will be prone to selection bias.
FIGURE 11.
Causal-directed acyclic graph illustrating proposed mediation.
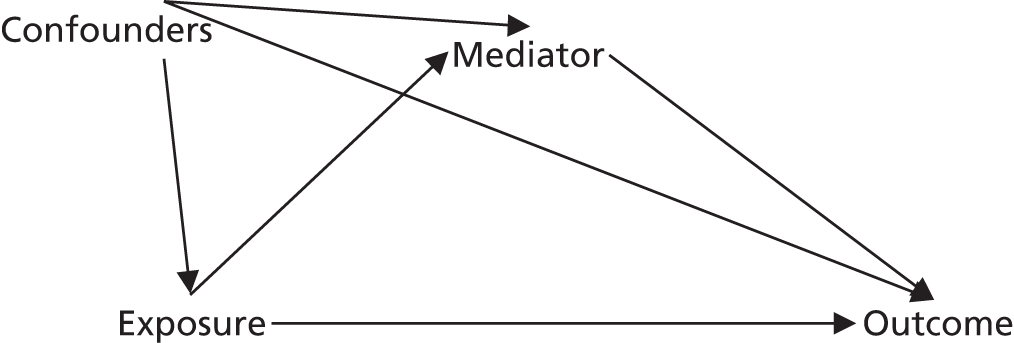
The outcome was not statistically significant at the 5% level; however, there certainly was some evidence of a treatment effect, which was made more evident by the increasing benefit obtained when the intensity of the intervention was increased (Table 18). While, strictly speaking, mediation analysis requires a significant association between exposure and outcome, mediation analyses were still conducted to explore the process/mechanisms by which the intervention may work.
| Outcomea | Number of participants | Trial arm | Estimateb | Lower 95% CI | Upper 95% CI | p-value |
|---|---|---|---|---|---|---|
| BMI | 129 | Intensive | –0.96 | –2.16 | 0.23 | 0.114 |
| Less intensive | –0.21 | –1.44 | 1.03 | 0.739 |
A linear regression model could not be fitted for two of the mediators owing to the high level of skew in the responses. None of the 10 remaining between-group comparisons for the mediators investigated was statistically significant at the 5% level and, for the majority, the 95% CIs were wide (Table 19). However, as this was a feasibility study that was not powered to detect differences on any of the above outcomes or mediators, a full mediation analysis will nevertheless be conducted to investigate whether or not the mediators may lie on the causal pathway.
| Mediatora | Brief interpretation of scale (higher scores indicate . . .) | Number of participants | Trial arm (compared with control) | Estimateb | Lower 95% CI | Upper 95% CI | p-value |
|---|---|---|---|---|---|---|---|
| WEL | Greater confidence to resist eating | 139 | Intensive | 2.33 | –9.12 | 13.78 | 0.691 |
| Less intensive | 1.90 | –9.63 | 13.44 | 0.746 | |||
| ESES | Greater confidence to exercise | 138 | Intensive | 0.19 | –0.49 | 0.88 | 0.578 |
| Less intensive | –0.03 | –0.72 | 0.66 | 0.930 | |||
| SSEH survey – sabotage domain | Greater perception that friends/family sabotage their attempts to eat healthily | 131 | Intensive | –0.04 | –1.09 | 1.00 | 0.935 |
| Less intensive | 0.33 | –0.71 | 1.38 | 0.531 | |||
| SSEH survey – encouragement domain | Greater perception that family/friends provide encouragement to eat healthily | 128 | Intensive | –0.12 | –0.77 | 0.52 | 0.706 |
| Less intensive | 0.51 | –0.14 | 1.16 | 0.126 | |||
| SSEX survey – participation domain | Greater perception that family/friends participate/involve themselves in their exercise routine | 127 | Intensive | –0.00 | –0.77 | 0.77 | 0.999 |
| Less intensive | 0.06 | –0.73 | 0.85 | 0.882 | |||
| SSEX survey – support domain | Greater perception that family/friends provide support/encouragement for their exercise routine | 123 | Intensive | 0.42 | –0.42 | 1.23 | 0.331 |
| Less intensive | 0.26 | –0.63 | 1.16 | 0.565 | |||
| SSEX survey – punishment domain | Small numbers in some cells (i.e. data were highly skewed). Unable to analyse | ||||||
| TSRD – relative autonomy | Greater autonomous regulation of their healthy eating | 139 | Intensive | –0.11 | –0.63 | 0.42 | 0.687 |
| Less intensive | –0.17 | –0.70 | 0.37 | 0.537 | |||
| TSRE – relative autonomy | Greater autonomous regulation of their motivation to exercise | 137 | Intensive | 0.41 | –0.08 | 0.90 | 0.099 |
| Less intensive | 0.04 | –0.46 | 0.54 | 0.876 | |||
| Self-monitoring regularity | Small numbers in some cells (i.e. data were highly skewed). Unable to fit a linear model | ||||||
| Self-reported habit index (diet) at 12 months | More positive habits with regards to eating healthy food | 133 | Intensive | 0.04 | –0.35 | 0.44 | 0.833 |
| Less intensive | –0.19 | –0.59 | 0.21 | 0.364 | |||
| Self-reported habit index (exercise) at 12 months | More positive habits with regards to exercising | 135 | Intensive | –0.28 | –0.89 | 0.33 | 0.366 |
| Less intensive | –0.09 | –0.70 | 0.53 | 0.781 | |||
As shown by Table 20, it was difficult to determine how much of the effect of intervention on BMI was mediated through any of the mediators. Of the 20 comparisons made, two provided a positive value for the percentage of the total effect that was via the mediator and one was zero (the remaining were negative, meaning that including the mediator in the model increased the trial arm coefficients). Table 21 provides the coefficient for the corresponding mediator from the model that regresses the trial arm, mediator and confounders onto outcome.
| Mediatora | Trial arm (compared with control) | Total effect | Direct effect (not via mediator) | Indirect effect (total – direct) | Percentage of total effect through mediator |
|---|---|---|---|---|---|
| WEL | Intensive | –0.96 | –0.87 | –0.09 | 9.38 |
| Less intensive | –0.21 | –0.25 | 0.04 | –19.05 | |
| ESES | Intensive | –0.96 | –1.13 | 0.17 | –17.71 |
| Less intensive | –0.21 | –0.37 | 0.16 | –76.19 | |
| SSEH survey – sabotage domain | Intensive | –0.96 | –0.99 | 0.03 | –3.13 |
| Less intensive | –0.21 | –0.33 | 0.12 | –57.14 | |
| SSEH survey – encouragement domain | Intensive | –0.96 | –1.19 | 0.23 | –23.96 |
| Less intensive | –0.21 | –0.56 | 0.35 | –166.67 | |
| SSEX survey – participation domain | Intensive | –0.96 | –1.07 | 0.11 | –11.46 |
| Less intensive | –0.21 | –0.65 | 0.44 | –209.52 | |
| SSEX survey – support domain | Intensive | –0.96 | –1.07 | 0.11 | –11.46 |
| Less intensive | –0.21 | –0.48 | 0.27 | –128.57 | |
| TSRD – relative autonomy | Intensive | –0.96 | –1.11 | 0.15 | –15.63 |
| Less intensive | –0.21 | –0.37 | 0.16 | –76.19 | |
| TSRE – relative autonomy | Intensive | –0.96 | –0.96 | 0.00 | 0.00 |
| Less intensive | –0.21 | –0.44 | 0.23 | –109.52 | |
| Self-reported habit index (diet) at 12 months | Intensive | –0.96 | –0.92 | –0.04 | 4.17 |
| Less intensive | –0.21 | –0.42 | 0.21 | –100.00 | |
| Self-reported habit index (exercise) at 12 months | Intensive | –0.96 | –1.02 | 0.06 | –6.25 |
| Less intensive | –0.21 | –0.25 | 0.04 | –19.05 |
| Mediatora | Coefficientb | Lower 95% CI | Upper 95% CI | p-value | Brief interpretation (as mediator increases . . .) |
|---|---|---|---|---|---|
| WEL | –0.03 | –0.05 | –0.02 | < 0.001 | BMI decreases |
| ESES | –0.28 | –0.51 | –0.05 | 0.015 | BMI decreases |
| SSEH survey – sabotage domain | 0.08 | –0.08 | 0.24 | 0.332 | |
| SSEH survey – encouragement domain | –0.09 | –0.37 | 0.20 | 0.546 | |
| SSEX survey – participation domain | –0.09 | –0.34 | 0.17 | 0.491 | |
| SSEX survey – support domain | –0.26 | –0.48 | –0.04 | 0.022 | BMI decreases |
| TSRD – relative autonomy | 0.06 | –0.28 | 0.40 | 0.732 | |
| TSRE – relative autonomy | –0.23 | –0.56 | 0.11 | 0.185 | |
| Self-reported habit index (diet) at 12 months | –0.49 | –0.85 | –0.13 | 0.007 | BMI decreases |
| Self-reported habit index (exercise) at 12 months | –0.36 | –0.61 | –0.12 | 0.004 | BMI decreases |
Table 21 demonstrates that 5 of the 10 mediators had a statistically significant association with outcome. This indicates that there was a relationship between some of the mediators and BMI, in the expected direction (increases in weight self-efficacy, exercise self-efficacy, perception that family/friends support and encourage positive exercise habits, positive habits related to healthy eating and positive habits related to exercise were associated with decreases in BMI at 12-month follow-up), but the mediation analysis was largely unable to determine the causal mechanisms behind this relationship.
Exploratory analyses
Exploratory analyses were conducted investigating binge eaters, gender and method of recruitment (Figures 12–14). Formal exploratory analyses investigated main effects and interaction terms with treatment arm. There was little evidence of effect, except for the group of binge eaters in the less intensive arm, who appear to have higher BMIs at follow-up than non-binge eaters in the less intensive arm; however, this is based on five participants only.
FIGURE 12.
Follow-up BMI (kg/m2) for binge eaters and non-binge eaters split by treatment arm.

FIGURE 13.
Follow-up BMI (kg/m2) for males and females split by treatment arm.

FIGURE 14.
Follow-up BMI (kg/m2) for participants recruited via different routes split by treatment arm. EOP, excercise on prescription.
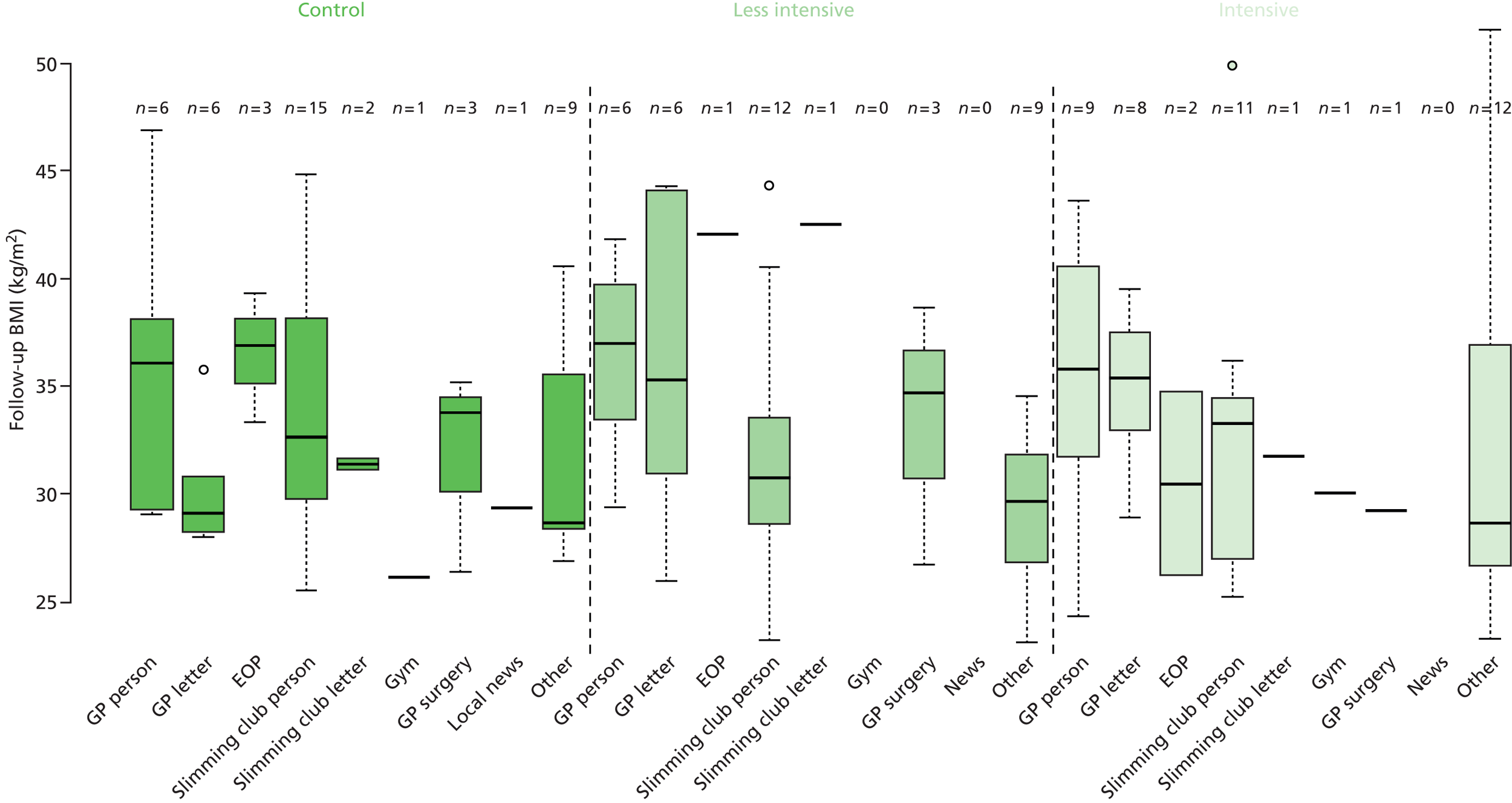
Summary
In summary, there were some promising effects of the intensive arm intervention on both BMI and weight that would be clinically important if they were shown to be true differences. There was less evidence that outcomes in the less intensive arm were different to those in the control arm. The evidence for differences between groups in secondary outcomes was less convincing, except for the DINE fat and healthy eating subscale scores and the number of days of binge eating, on which measures the intensive arm performed better than the control arm. CACE analysis revealed a slightly larger effect than the primary analysis, indicating that those who complied with the intervention had better outcomes. The mediation analysis identified five potential mediators but was not able to determine the causal mechanism behind those relationships.
Chapter 6 Process evaluation: mixed-methods results
Introduction
We conducted a process evaluation, the aims of which were to:
-
assess the delivery of the intervention to ensure it was provided in accordance with the protocol and delivered consistently
-
establish the level of participant adherence to the requirements of the intervention protocol
-
explore participants’ views of, and satisfaction with, the intervention
-
explore MIPs’ experiences of delivering the intervention
-
test the logic model.
The process evaluation utilised both quantitative and qualitative data from the practitioner-held records, the website, audio-recordings of sessions and qualitative data from individual semistructured interviews with a sample of participants and focus groups (and one interviews) with MIPs.
Method
The process evaluation was conducted in line with the framework suggested by Steckler and Linnan. 135 We developed a framework (Tables 22 and 23) to assess eight key components of process evaluation: context, reach, fidelity, exposure, recruitment, retention, contamination and theory testing. The definition of some components is clearer than others, and there is a degree of overlap between them; each is therefore defined as used in the study in the relevant sections below. Table 22 summarises the key sources of information used to explore these eight components. Each of these will be considered here, although for some more detailed methods and results are reported elsewhere and this is indicated when relevant.
| Process evaluation component | Sources of information |
|---|---|
| Context | MIP and GF demographics |
| Where MI was delivered | |
| Contextual issues explored in the focus groups and participant interviews | |
| Reach | Attendance at the intervention sessions |
| Demographics of participants compared with those not recruited | |
| Participant interviews | |
| Fidelity | MITI assessment of recorded consultations at baseline |
| MITI assessment of randomly selected recorded consultations | |
| Delivery of other intervention elements (post-session CRFs) | |
| Focus groups | |
| Exposure | Attendance at intervention sessions |
| MIP post-session CRFs | |
| Audio-recorded consultations | |
| Data from the WILMA trial website | |
| Focus groups and interviews | |
| Recruitment | Demographics of sample compared with those approached but not recruited |
| Interviews and focus groups | |
| Retention | Dropout by trial arm |
| Demographics of those dropping out compared with those remaining | |
| Focus groups | |
| Contamination | Participants asked if they shared study information |
| Participants asked about other services they utilised | |
| Theory testing | Mediation analyses using questionnaire data |
| Participant interviews |
| Process evaluation element | Outcomes | Methods | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Participant interviews | MIP focus groups | CRF data | QRF data | Session CRFs | MITI analysis | PIC log | MIP demographics | ||
| Fidelity | Quality of MI delivery | ✓ | ✓ | ||||||
| Are MIPs delivering the WLM and theory components? | ✓ | ✓ | |||||||
| Barriers to delivering the intervention | ✓ | ||||||||
| Participant’s understanding or experience of the intervention | ✓ | ✓ | |||||||
| Exposure | Participant’s satisfaction with the intervention | ✓ | ✓ | ||||||
| How much intervention exposure did participants get? | ✓ | ✓ | ✓ | ||||||
| Did participants implement the intervention? | ✓ | ✓ | ✓ | ||||||
| Reach | Did the intervention reach and influence people other people? | ✓ | |||||||
| Did the study sample represent the population of interest? | ✓ | ||||||||
| Context | MIP differences and impact on outcomes | ✓ | ✓ | ✓ | |||||
| MIP characteristics | ✓ | ||||||||
| Difficulties/issues during intervention delivery | ✓ | ||||||||
| MIPs satisfaction with intervention implementation and study procedures? | ✓ | ||||||||
| Under what circumstances or in which groups does the intervention work best? | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
| Contamination | Did control group acquire study materials from intervention participants? | ✓ | ✓ | ||||||
| Theory testing | Quantitative mediators not explored elsewhere | ✓ | ✓ | ||||||
| Qualitative mediators not explored elsewhere | ✓ | ✓ | |||||||
Context
Context includes information relating to aspects of the context in which the intervention was delivered, as well as the broader context that both the practitioner and client were operating within that may influence intervention effectiveness.
This was explored by addressing who delivered the intervention and where it was delivered. We collected the curricula vitae of MIPs and GFs in order to describe the demographics and experience of intervention staff. We also kept a record of venues used for sessions. In the qualitative work we examined issues relating to circumstances, skills, training, resources, client group and recruitment context (i.e. slimming group, EOR, primary care, community), contextual barriers to attendance and delivery of the intervention, attitudes and contextual issues relating to potential roll-out. We conducted two focus groups and one interview with intervention staff and interviewed 47 participants across the three trial arms. Interviews and focus groups were analysed using thematic analysis and further details of qualitative methods and analyses is given in Chapter 3.
In our definition of context we also include details of where participants were recruited from and what services they continued to access throughout the trial.
Reach
Reach is defined as the extent to which the target audience is reached by the intervention, as well as any ‘spillover’ effects on people not recruited, for example any impact on the family and friends of the participants.
We collected demographic data at baseline for all participants (see Chapter 5). Data on attendance at MI sessions and group sessions were collected. We also explored reach in the interviews by asking participants if they had shared any study information and whether or not receiving the intervention had any impact on family and friends such as joining in with diet or physical activities.
Fidelity
Fidelity is defined as the degree to which the MIPs and GFs delivered the intervention as intended.
We planned to improve fidelity as well as provide support for MIPs by running four workshops with specific WILMA trial-related topics and four peer group sessions, in which small groups of MIPs met up to listen to an audio-recording, share their experiences and discuss any issues that they were having. We also intended to provide feedback on four recorded sessions to prevent ‘drift’ in intervention delivery. For the recorded MI sessions we measured fidelity in two ways: using the MITI to assess delivery of MI and examination of the post-session CRFs to look at whether or not the five key WILMA trial ‘hot’ topics (diet, physical activity, self-monitoring, goal-setting and planning) were covered. The MITI rating tool comprises a number of count and score variables. ‘Global’ ratings are given for each of these: ‘evocation’, ‘collaboration’, ‘autonomy/support’, and ‘direction and empathy’. These are scored on a scale from 1 to 5. Behaviour count scores are provided for ‘giving information’, ‘MI adherent’ behaviours, ‘MI non-adherent’ behaviours, ‘closed questions’, ‘open questions’,’ simple reflections’ and ‘complex reflections’. MIPs can be rated as ‘proficient’ or ‘competent’ (the higher level).
A number of composite scores are calculable from these variables, including the ‘global spirit’ rating (which encompasses scores on evocation, collaboration, direction, empathy and ‘autonomy/support’), percentage open questions, percentage complex reflections, ratio of reflections to questions and the percentage MI adherent. There is no overall score to indicate proficiency or competence incorporating all the measures; however, the MITI guidance indicates that, in order to reach proficiency in each of the measures, a practitioner must achieve an average global spirit rating of 3.5, a reflection to question ratio of at least 1, at least 50% open questions relative to all questions, at least 40% complex reflections relative to all reflections and be 90% MI adherent. To reach competency, these values are 4, 2, 70%, 50%, 100%, respectively.
Before the study started, all MIPs were assessed to ensure that they achieved at least ‘proficiency’ in their delivery of MI according to the MITI scale. They completed a simulated counselling session with a trained actor that was audio-recorded and later assessed independently by two expert raters for proficiency or competency. In order to assess the MI delivery accurately, four raters were trained in MITI rating over 3 days by two expert trainers. The four trained team members each rated 14 MI sessions, and each rater’s scores for the 14 MI sessions were compared. The agreement level was summarised for each of the global rating scales using a Fleiss multirater kappa. 136 The behaviour counts were examined in terms of reliability (instead of agreement) using an ICC. As there are no upper limits on counts, this was explored in terms of reliability rather than agreement using an ICC. 137
During the intervention delivery period, the MIPs were asked to record all sessions, if participants consented, with a view to collecting a minimum sample of six sessions per practitioner over the course of the study. The face-to-face MI recordings were then assessed for fidelity to MI. One MIP had no recordings and two others had only one or two recordings, respectively, so it was not possible to randomly select recordings for those practitioners. Therefore, for 12 MIPs, two recordings each were randomly selected, a stratified sample included sessions delivered in both intervention arms of the trial and across all MIPs. The counselling sessions each lasted around 60 minutes, as per the MITI manual, and 20 minutes of the session was selected for coding in the MITI. If the consultation lasted 20 minutes or less, then the entire recording was used; if the consultation lasted more than 20 minutes, but less than 30 minutes, the middle 20 minutes were selected; and, if the consultation lasted over 30 minutes, a random 20-minute segment (excluding the first and last 5 minutes) was selected. We selected sessions using a random number generator in the R program, version 3.0.2 (The R Foundation for Statistical Computing, Vienna, Austria) language and workspace (with a seed set for reproducibility). A second random number was then generated to select which minute of the recording the rater should start from. For each of the 12 MIPs, two raters independently rated one individual consultation each for that practitioner. Therefore, each rater assessed 12 MI sessions independently, one for each of the MIPs for whom recordings were available. For the two practitioners who had insufficient sessions recorded to allow random selection, the three sessions available were assessed using MITI with a random start time selected.
The session CRFs (see Appendix 7) asked MIPs to rate the extent to which they discussed the different topics in each counselling session (diet, physical activity, implementation intentions or planning, goal-setting or self-monitoring) using a 10-point Likert scale. These data were summarised descriptively.
In the focus groups we explored fidelity in both telephone and face-to-face sessions. We asked MIPs whether or not they delivered the MI with fidelity, covered the hot topics and delivered anything differently or in addition to the guidance in the handbook. If there was a departure from the guidance, we asked for details and the rationale.
Exposure
Exposure is defined as the extent to which participants received and understood the different elements of the intervention and whether or not they implemented these as intended. Their satisfaction with the intervention and barriers to receipt and implementation were also considered.
There is some overlap between data analysed for exposure with those used to assess reach and fidelity. As described in Table 22, we collected data on attendance at face-to-face and telephone counselling sessions as well as group sessions and we audio-recorded counselling sessions which facilitated exploration of whether or not the intervention was actually delivered to participants.
We collected data from the online WILMA trial intervention to explore use of the website and the degree to which participants used it for self-monitoring. This was summarised descriptively. In the session CRFs we also asked MIPs to complete an exit appraisal for each participant, describing what went well and any problems experienced. These data were analysed by reading and rereading the practitioner comments and identifying initial themes, which were developed into broader themes that encapsulated the initial coding of the data. Finally, instances of these broader themes were counted.
In the focus groups we explored whether or not the MIPs delivered the different intervention components. In both the interviews and focus groups we asked if participants implemented different aspects of the intervention including goal-setting, making plans and self-monitoring using the website and the diary. We also explored participants’ satisfaction with the intervention, attendance and barriers and facilitators to attendance.
Recruitment and retention
Detailed information on methods relating to recruitment and retention can be found in Chapters 3 and 4. We also explored these issues in the focus groups and participant interviews. MIPs were asked if there were any issues related to recruitment that impacted on them and also if they had any insights into why people withdrew from the counselling and/or the study. Participants were asked why they took part in the study and about their experiences of the recruitment process. We were able to interview some participants who dropped out of the intervention but, unfortunately, not those who dropped out of the study (see Chapter 8).
Contamination
In the participant CRFs we assessed potential contamination between the intervention and control groups by asking participants if they knew anyone in the study and if they had shared intervention information with them. We also asked about details of all other services that control group participants accessed that might be similar in any way to the WILMA trial intervention, for example a slimming club that offered exercise and diet advice, goal-setting, etc. These data were analysed descriptively.
Theory testing
A final and key aspect of the process evaluation relates to theory testing. We developed a logic model (see Figure 1) that details the hypothesised processes by which the intervention brings about change. This was developed from our experiences of delivering MI in practice,50 as well as the literature describing processes within MI. We also drew on relevant theories of behaviour change (see Chapter 2). The key hypothesised mediators are self-monitoring, intrinsic motivation, self-efficacy, habits and social support, which were assessed using questionnaires (see Chapter 3). We tested the hypothesised mediators via mediation analyses (see Chapter 3, Main analysis, for methods and Chapter 5, Mediation analyses, for results). We also considered goal-setting, problem-solving and planning to be important (explored below).
The intervention theory was also examined in the qualitative data. We asked participants if they discussed the different intervention elements (e.g. self-monitoring, goal-setting, planning, problem-solving) with the MIP and which aspects of the intervention they perceived as most useful or effective and which they implemented. We asked if they weighed themselves regularly (self-monitoring) and what strategies they used, and enquired about their social support as well as other factors that influenced their success at WLM.
Results
Context
Participants were recruited from primary care, EOR, Slimming World and the community. Both the intervention and control group had access to usual care during the trial. GP surgeries at this time offered variable care for weight management, which could have included lifestyle advice, referral to a dietitian, practice nurse-led clinics, EOR and, in England, referral to Weight Watchers® (New York, NY, USA), or Slimming World in some areas. The majority of our participants who attended slimming clubs attended Slimming World or Weight Watchers, and both of these clubs provide dietary and physical activity advice and social support as well as some motivational elements. The EOR scheme involved attendance at community-based sessions of supervised exercise for 16 weeks with follow-up at 8 and 12 months and did not include any dietary counselling. Participants lost weight by a variety of means in addition to the above: weight loss medication, going to the gym or increasing physical activity, calorie counting and fitness apps.
The intervention was delivered in a community setting by 15 MIPs (24 were trained but some dropped out or never saw participants) and two GFs (22 GFs were trained in total). All were employed specifically to deliver the WILMA trial intervention (see Chapter 2) and were trained to do this. MIPs had a variety of different professional backgrounds, including dietetics, addiction and mental health. A summary of key practitioner characteristics is given in Table 24. All MIPs had experience of using MI in practice, all but three were currently using MI, all were educated to at least degree level or equivalent and all but four were female.
| MIP background | % | n |
|---|---|---|
| Nursing or health background | 67 | 10 |
| Experience of working in the field of obesity, diet or physical activity | 40 | 6 |
| MI trainer (higher-level MI qualification) | 67 | 10 |
| Currently using MI in health-related area | 80 | 12 |
| Counselling qualification | 93 | 14 |
To encourage attendance, MI sessions were delivered close to where participants lived, in a variety of settings including community centres, churches, sports centres and village halls. Many of the sessions were completed in participants’ homes.
The two GFs who delivered sessions were educated to postgraduate level and had training in MI. One was currently using MI in a health-related setting. Both had experience of facilitating groups. Group sessions were also delivered in local community venues.
In the qualitative data, participants and MIPs described contextual factors that influenced the impact of the intervention. Details of this can be found in Chapters 7 and 8.
Reach
Participant demographics are reported in Chapter 5. At baseline, all but seven participants were either overweight or obese and they represent a broad demographic spread in terms of age and social class, although men and ethnic groups were under-represented. Reach of the intervention for participants was high for the face-to-face MI sessions, the key aspect of the intervention. As attendance was high, the comparison of attenders and non-attenders was not completed. Attendance at the telephone sessions was lower (see Table 31). In terms of reach of group sessions, owing to logistical difficulties associated with organising these groups locally, poor attendance and slow recruitment, it was not feasible to run the groups as planned and this element of the intervention was dropped.
Within the qualitative data, there was evidence that participants had shared study information with family and friends and had encouraged them to change their diet and physical activity behaviours. Others described completing dietary changes and physical activity together with friends and family (see Chapter 8).
Fidelity
All MIPs assessed on the MITI before commencing the study achieved proficiency, and three achieved competence (the higher level). In terms of the peer group support sessions, some of these did take place but the data we have on these are incomplete. We ran one of the workshops a few months after the MI started being delivered, but this was not repeated. The planned feedback to MIPs on audio-recording did not happen owing to the issues we had with recruitment.
The data reported here are based on the face-to-face MI sessions. There are a number of reasons for this, including that the face-to-face sessions are the heart of the intervention, the audio-recordings are better quality, and few MIPs actually recorded telephone sessions in practice, which does not facilitate selection of a random sample. Information related to group sessions is not reported because so few sessions actually took place and the team had not started the planned session observations for the purpose of assessing fidelity.
Despite much effort to encourage MIPs to record all sessions, we did not achieve the target of six for all practitioners. The reasons included participant non-consent, practitioner resistance, technical issues and practitioner forgetfulness. For the face-to-face sessions, we received 185 recordings out of a possible 393, and for the telephone sessions we received 89 (Table 25). Eleven out of 15 MIPs recorded 50% or more of their MI sessions. It was not possible to identify exactly how many telephone sessions MIPs delivered because we had a poor return rate for the paperwork related to the telephone sessions.
| MIP | Number of face-to-face recordings | Total number of face-to-face sessions | Number of telephone recordings |
|---|---|---|---|
| 1 | 1 | 33 | 0 |
| 2 | 6 | 8 | 0 |
| 3 | 2 | 2 | 0 |
| 4 | 11 | 12 | 11 |
| 5 | 15 | 18 | 2 |
| 6 | 8 | 8 | 0 |
| 7 | 0 | 79 | 0 |
| 8 | 24 | 27 | 1 |
| 9 | 14 | 14 | 0 |
| 10 | 6 | 36 | 0 |
| 11 | 10 | 10 | 0 |
| 12 | 15 | 30 | 0 |
| 13 | 45 | 45 | 45 |
| 14 | 23 | 30 | 30 |
| 15 | 5 | 17 | 0 |
| Total | 185 | 393 | 89 |
We examined MITI ratings of the 14 MI sessions completed by the four members of the study team to explore agreement prior to assessing fidelity. In relation to the global ratings, Figure 15 shows the raw data split by interview and global rating. Global ratings are in rows and interviews in columns. Each dot represents a rating by one rater. For perfect agreement straight horizontal lines would be seen in each box (lines can be any height). For example, there is perfect agreement for direction in session 12. There appears to be more agreement for some sessions than for others (e.g. for sessions 1 or 6 than for sessions 9 or 10).
FIGURE 15.
Scores for each session for each of the global ratings. Initials on x-axis refer to the raters.

Agreement was summarised for each global rating using a Fleiss multirater kappa (Table 26). Values further away from 0 indicate better agreement. Guidance indicates that agreement of 0.21–0.40 constitutes fair agreement between raters. 138
| Global rating | Kappa |
|---|---|
| Evocation | 0.359 |
| Empathy | 0.267 |
| Direction | 0.232 |
| Collaboration | 0.315 |
| Autonomy/support | 0.192 |
| Overall | 0.282 |
In terms of the behaviour counts, as there are no upper limits, this was explored in terms of reliability rather than agreement using ICCs (Table 27). These analyses indicated high reliability overall, with less reliability for MI-adherent and complex reflection ratings.
| Behaviour count | ICC |
|---|---|
| Simple reflection | 0.507 |
| Open question | 0.827 |
| MI non-adherent | 0.760 |
| MI adherent | 0.218 |
| Giving information | 0.468 |
| Complex reflection | 0.191 |
| Closed question | 0.668 |
| Overall | 0.798 |
The agreement and reliability ratings were considered acceptable. The next step was to assess recordings for fidelity to MI. Overall there were few MIPs failing to reach proficiency in the different aspects of the sessions rated. Out of all practitioners and all measures, in only 6% of the ratings did MIPs fail to reach proficiency. For most measures practitioners reached proficiency or competence. The non-proficient ratings were roughly evenly spread between the different measures, with three practitioners not achieving proficiency in ‘global spirit’, four in ‘per cent complex reflections’, seven in ‘per cent open questions’, three in ‘reflection to question ratio’ and four in ‘per cent MI adherent’. The cut-off for per cent open questions was achieved slightly less often than the others. Table 28 shows the mean scores for each MIP based on the ratings of the four sessions. These indicate that, overall, no MIPs failed to reach proficiency on any measure and that all MIPs reached the cut-off for competent on the globals and per cent complex reflections.
| MIP | Global spirit rating | Per cent complex reflections | Per cent open questions | Reflection-to-question ratio | Per cent MI adherent |
|---|---|---|---|---|---|
| 1 | 4.8 | 66.8 | 75.5 | 2.7 | 97.8 |
| 2 | 4.6 | 74.7 | 75.0 | 2.8 | 94.5 |
| 3 | 4.1 | 65.6 | 70.8 | 2.2 | 100.0 |
| 4 | 4.2 | 57.5 | 57.4 | 2.6 | 100.0 |
| 5 | 4.6 | 69.3 | 67.9 | 1.6 | 100.0 |
| 6 | 4.5 | 67.9 | 68.4 | 2.1 | 100.0 |
| 7 | 4.3 | 56.2 | 52.4 | 4.2 | 100.0 |
| 8 | 4.5 | 71.4 | 60.2 | 1.6 | 96.5 |
| 9 | 4.3 | 69.1 | 57.8 | 1.8 | 89.3 |
| 10 | 4.6 | 59.3 | 63.4 | 1.5 | 100.0 |
| 11 | 4.8 | 58.9 | 87.9 | 5.4 | 100.0 |
| 12 | 4.2 | 59.3 | 67.3 | 1.6 | 91.8 |
| 13 | 4.9 | 83.5 | 100.0 | 3.0 | 100.0 |
| 14 | 5.0 | 62.0 | 47.0 | 1.7 | 100.0 |
For each session, practitioners were asked to rate five topics: (1) diet, (2) physical activity, (3) implementation intentions or planning, (4) goal-setting and (5) self-monitoring. This was completed using a 10-point Likert scale going from ‘did not discuss’ through ‘talked a little about’ to ‘talked in detail about’. Overall, 391 session CRFs were completed. The topics most often discussed were diet, exercise, goal-setting and planning, whereas self-monitoring was discussed least (Table 29). However, in all sessions there was some discussion of these topics. For all topics over all sessions, the mean rating was 6 or above, which indicates that coverage of each topic was somewhere between ‘talked a little about’ and ‘talked in detail about’.
| Topic | Median rating | Interquartile range |
|---|---|---|
| Goal-setting | 7 | 2 |
| Planning | 7 | 2 |
| Self-monitoring | 6 | 2 |
| Physical activity | 7 | 3 |
| Diet | 8 | 3 |
In the practitioner focus groups, we explored (1) the extent to which they delivered the intervention according to the WILMA trial manual, (2) barriers and facilitators and (3) ways in which they may have done things differently from the manual and the reasons for this. Details of the findings can be found in Chapter 7.
Exposure
Attendance at face-to-face MI sessions was very high. In the intensive group, 83% attended all six MI sessions and in the less intensive arm 91% attended both sessions. Only three participants failed to attend any sessions and, of these, two informed the study team that they wished to withdraw prior to starting the intervention (Table 30). Attendance at telephone sessions was lower (Table 31), with 72 participants (67%) receiving at least one telephone call, of whom 43% were in the less intensive group and 57% in the intensive group. Overall, 53.5% of telephone sessions that should have taken place did actually take place, and the proportion was higher in the intensive intervention arm (54%) than in the less intensive arm (51%). A number of potential explanations for this lower attendance at the telephone sessions have been identified. Within the MIP focus groups the following were acknowledged: difficulty getting hold of participants, a feeling that the telephone sessions were not as useful, difficulty delivering MI over the telephone and low MIP motivation owing to the feeling that payment for this element was inadequate. From the participant interviews, we identified disengagement with the telephone sessions, as they were perceived as less useful than the face-to-face sessions. However, it is likely that more telephone sessions were delivered than we have a record of, as the return of paperwork for these was poor.
| Number of sessions | Less-intensive arm | Intensive arm |
|---|---|---|
| 0 | 3 | 0 |
| 1 | 2 | 1 |
| 2 | 48 | 4 |
| 3 | 1a | 2 |
| 4 | N/A | 2 |
| 5 | N/A | 1 |
| 6 | N/A | 44 |
| Total | 54 | 54 |
| Number of sessions | Less-intensive arm | Intensive arm |
|---|---|---|
| 0 | 23 | 13 |
| 1 | 7 | 1 |
| 2 | 24 | 4 |
| 3 | – | 3 |
| 4 | – | 1 |
| 5 | – | 4 |
| 6 | – | 3 |
| 7 | – | 8 |
| 8 | – | 6 |
| 9 | – | 11 |
| Total | 54 | 54 |
We defined compliance to the intervention using attendance at the face-to-face sessions, as this is the core aspect of the intervention. In order to comply with the intervention, participants in the less intensive group had to attend both face-to-face sessions and those in the intensive group had to attend at least five out of six sessions. In the less intensive group, 91% complied, and in the intensive group 83% complied, according to this definition. We also explored reasons for non-compliance with the intervention in the qualitative interviews.
Only six group sessions were actually run for a total of 15 participants. Participants were asked to attend four sessions, but only two attended four sessions and most attended two or fewer. The total number of attendances for all 15 participants was 10 in the intensive group and 18 in the less intensive group. We interviewed three participants who actually received the group intervention, two attended two sessions and one attended a single session. Further information on their views of the group sessions can be found in Chapter 8.
In terms of participants actually implementing the intervention elements, we asked if they regularly self-monitored their weight at baseline. In response, 90% in the control, 83% in the less-intensive and 87% in the intensive arms indicated they did. At follow-up, this was lower in all arms: 71% in the intensive, 63% in the less intensive and 68% in the control group indicated they weighed themselves at least once a week. This indicated that participants in all three arms of the trial were regularly self-monitoring their weight.
With regards to use of the online WILMA trial website, 78 (71%) participants logged onto the system. The highest number of logins by a single individual was 51; however, the majority of participants who logged in did so 10 times or fewer (51%). The median number of logins was 26 (range 1–51). With regards to self-monitoring of weight, 75 used the weight-logging facility at least once; however, most participants did this 10 times or fewer (52%). The online diary was used less often; 33 used it at least once to record diet and physical activity and the median number of entries was nine (range 1–49). Thirty-three participants in the study chose to send their weight to the study team via text message. Eight people did this only once and the median number of times that weight was sent by text message was five (range 1–37).
As well as self-monitoring, we gained insights into whether or not participants were implementing the other intervention elements (i.e. diet, physical activity, planning and goal-setting) from the qualitative interviews and the session CRFs. At the end of each counselling session the practitioners noted discussion in five key areas in the CRFs. These data are reported in the previous section, Fidelity. The final session CRF included a summary of how successful the MIP felt the sessions had been, challenges and barriers, and what had worked well. A summary of the key themes can be found in Table 32. In the majority of cases MIPs felt that participants had found the sessions useful. The most common themes were that the sessions increased motivation and provided an opportunity for reflection, feedback and support as well as to be listened to in a non-judgemental way. Issues relating to participants’ mental and physical health were considered barriers to behaviour change; other barriers are listed in Table 32.
| Theme | How often reported over all MI sessions? |
|---|---|
| Worked well | |
| Increased, reinforced/focused on motivation | 41 |
| Greater self-awareness/self-knowledge/insight | 10 |
| Helped clarify thoughts and feeling about weight and weight loss/renew focus on weight and importance of weight loss/helped with ambivalence | 15 |
| Space to talk/being listened to | 19 |
| Appreciated positive feedback/support | 10 |
| Client engaged well/worked hard | 11 |
| WILMA trial intervention components: self-monitoring, increased self-efficacy, client feeling better equipped to deal with lapses/setbacks; focusing on planning/implementation intentions, setting and reviewing goals and problem-solving (knowing MIP will review progress, recognising barriers, keeping goals realistic) | 45 |
| MI techniques/counselling techniques: elicit–provide–elicit (n = 2), importance and confidence (n = 6), challenging self-defeating thoughts (n = 3), looking at discrepancies (n = 1), empathic listening (n = 1), addressing mood (n = 1) and agenda setting (n = 2) | 16 |
| The future (preferred future and planning for the future, aims in life, challenges ahead, focus on improving health) | 13 |
| Reflective space/opportunities for reflection/reflecting on what worked well in the past/what is different this time | 27 |
| Therapeutic alliance (good rapport) | 11 |
| Recognising/reinforcing how well participant has done/focus on the positive and what has been achieved/affirmation, improved self esteem | 17 |
| Understanding links between emotions, thoughts and behaviours/underlying issues causing the behaviours/relationship with food/emotional eating | 8 |
| Lifestyle changes in diet and physical activity/increased awareness of diet/advice on diet and physical activity helpful, hearing some else’s experience | 14 |
| Challenges | |
| Physical problems making it hard to implement diet or physical activity strategies, e.g. diabetes mellitus or joint problems | 16 |
| Challenging not being able to explore other issues (e.g. mental health) owing to time restrictions | 4 |
| Difficult family/life circumstances/stresses | 6 |
| Low mood/depression/emotional eating/other psychological issues often leading to poor control of eating and yo-yoing weight | 13 |
| Clients’ lifestyle (travelling a lot, eating out) | 4 |
| Maintaining motivation | 8 |
| Condensing work into only two sessions (often not enough for people) | 5 |
| Lack of social support | 4 |
| Client time pressures/work pressures difficult to find the time | 11 |
| Low self-esteem/low confidence/ambivalence | 7 |
| Other barriers: keeping focus, telephone sessions problematic, weather, relationship with food, not enthusiastic about exercise, lack of money for healthy food and activity, difficult to achieve goals | 11 |
The interview and focus group data indicated that participants were setting goals and making plans in relation to diet and physical activity as well as regularly self-monitoring their behaviour (see Chapters 7 and 8).
Recruitment and retention
Data on recruitment are reported in Chapter 5. In the interviews we asked participants why they took part and reasons included wanting to learn how to maintain their weight, helping keep them focused on their goals, having an interest in MI and receiving long-term support or supporting research.
We assessed overall study retention by intervention or control and compared those dropping out with those remaining in the trial in terms of demographics (see Chapter 5). When participants withdrew from the study, they usually did not give a reason, but those who did cited the following: family illness, time, life events, working away, mental health issues, travel problems and privacy issues related to venues. Two participants felt that they were not getting anything out of the study and another felt that being in the study made her anxious. We also asked the MIPs why people dropped out: they had limited insight as to reasons for dropout, but reported life events and not wanting to complete the telephone MI (see Chapter 8).
Contamination
Thirty participants indicated that they knew someone else in the trial, but only 11 (10%) in the intervention arms said that they had shared study information with them (five in the intensive arm, six in the less intensive arm). Only two people in the control group said that the people they knew in the study had shared information with them. The information shared included the food diary, motivational tips and information on diet, portion size and food labelling. Only one control participant reported using this information. We suggest the impact of contamination via this route is likely to be minimal.
Access to services at which the content might overlap with the WILMA trial intervention was checked, for example slimming clubs, health clubs, gyms, swimming pools and exercise classes. We found that, at 6 months, 63% of the controls, 67% of the less intensive group and 58% of the intensive group had paid for these types of services in the previous 3 months. At 12 months, these figures were 65%, 71% and 49%, respectively. Attendance at these services was high among all groups but in the intensive group was noticeably lower at 12 months; it could be that the MI was substituting somewhat for these other services. Although these types of services can offer some elements that overlap with the WILMA trial intervention, including social support, advice on diet and physical activity, goal-setting and monitoring, they lack the key aspect of MI. As these services were frequently accessed across all arms, we feel that this is unlikely to constitute a significant source of bias.
Theory testing
We tested the hypothesised mediators via mediation analyses, the results of which are reported in Chapter 5. The mechanism of effect of the intervention was also explored in the participant interviews and focus groups (see Chapters 7 and 8).
Summary
The MI aspect of the intervention was successfully delivered in a community setting with trained MIPs to a group of mostly overweight or obese individuals who had a spread of different demographic characteristics. Attendance was high at the face-to-face MI sessions and overall compliance was high. There were issues with delivery of the intervention over the telephone, which included both MIPs’ and participants’ concerns with this medium of delivery. The intervention was delivered with good fidelity and participants seemed to have implemented many of the intervention components. The group-based part of the intervention was less successful, and the reasons for this have been outlined above. Recruitment was problematic as outlined in Chapter 4; however, the retention rate was high at 12 months and, as there seemed to be no systematic differences between those dropping out and those remaining in the study, it is unlikely this has biased the results. It is also unlikely that contamination was an issue, as few participants in the intervention groups indicated they had shared information with the controls.
Chapter 7 Process evaluation: focus group results
Overview
One of the aims of the study was to explore what the MIPs’ views of the WILMA trial intervention were and to understand their experiences of delivering it. Two focus groups with 11 MIPs and one interview were conducted. The MIP focus groups and interview took place following recruitment closure. At this point the majority of MIPs had completed their face-to-face sessions and were mid-way through their telephone sessions. Further details of participating MIPs’ characteristics can be found in Chapter 6. Three MIPs were unable to attend. A focus group guide was developed to explore the MIPs experiences. This comprised 18 items and spanned four main topics (see Appendix 6). The focus groups lasted approximately 2 hours, while the interview lasted 1 hour. All were audio-recorded and transcribed for analysis. Further details of the methods and analysis can be found in Chapter 3. Figure 16 shows a schematic overview of the analysis and Table 33 shows an overview of the key themes from the focus groups.
FIGURE 16.
Schematic overview of focus group analysis.

| Overarching themes | Subthemes |
|---|---|
| WILMA trial intervention training and development | Perceptions and experiences of training |
| Timing of training | |
| Intervention delivery | Delivering within a set structure |
| Intervention content | |
| Participation, attendance and logistics | |
| Impact on participants and MI for WLM | |
| Future intervention implementation | Training improvements |
| Intervention-specific improvements | |
| Study process improvements | |
| Implementation in a real-world context |
WeIght Loss Maintenance in Adults trial intervention: training and development
Perceptions and experiences of training
The MIPs were trained to deliver the intervention (see Chapter 2). Many said that they enjoyed the training and found it useful. They felt that it was set at an appropriate level and contributed to their personal development, as they had a chance to learn new skills and assess their current skills. Moreover, they appreciated the opportunity to enhance their telephone counselling skills. As part of the training, MIPs were given guidance on delivering telephone counselling and brief (i.e. two sessions) MI. MIPs found this helpful as it differed from their normal practice.
The guidance on, if you had an intensive or less intensive participant (. . .), it gave me a really good idea of what was expected of me. Cos, I come from the weight loss field, where I’m not restricted on the number of appointments. Suddenly I was having to do things within a certain time frame, so it really helped me to know where I was gonna go.
MIP4
The WILMA trial intervention incorporated hot topics into the MI session (see Chapter 2). The MIPs felt that the training helped them understand how to bring these things together and allowed them to practise delivering the intervention before they saw their first participants. During training, an actor was used to portray a potential participant, MIPs did not feel that this reflected the reality of their clients and did not prepare them for the realities of working with WLM clients.
I think what was difficult was that the training didn’t necessarily prepare me for the reality. I think that all of the different elements that were covered in the training were certainly things that I used at various points, but actually, there were things that came up in the reality of working with the clients, that I think could only have come up through experience.
MIP3
As part of their training, and during the intervention, the MITI coding scale was used to assess MIPs’ MI skills (see Chapter 6). This form of assessment was new to many MIPs. They felt that it was useful and liked receiving feedback in this format. The feedback built their confidence in their MI skills and supported their professional development.
I’ve been sort of hankering for someone to do that for a long time for me, so to have the opportunity to do that was brilliant, and then to get the feedback and really specific feedback as well was fantastic.
MIP4
Some MIPs felt that the length of training was appropriate and equipped them with sufficient knowledge to deliver the intervention.
It equipped me enough to do all of the things that I needed to do for it. I didn’t feel as if I went out there from the training and thought ‘I don’t know what I’m going to do now, I don’t know where to start’.
MIP4
However, some felt that there was too much focus on MI skills and not enough on the weight management aspect of the intervention. Many outlined their inexperience of working with clients dealing with weight loss or maintenance.
MIPs were given a study handbook that outlined the intervention and MI aspects, issues relating to weight loss and maintenance as well as study procedures (see Chapter 2). However, many predominantly used the manual to consult on process issues rather than the intervention. More specifically, they referred to it when completing paperwork or answering participants’ study-specific questions. It was described as being overcomplicated and could have been simplified.
I found it useful if a client would ask me a direct question (. . .) about the programme, what was going on. Umm, but I didn’t find that I needed it actually in the sessions as it were.
MIP10
Timing of training
Motivational interviewing practitioner training was delivered early on and helped engage them in the study. However, owing to research governance issues, there was a 10-month delay between MIPs receiving training and seeing participants. This left them feeling less energised when the time came to deliver the intervention. A refresher session was organised; however, this took place after around half of MIPs had begun delivering the intervention.
At the end of the training I felt (. . .) energised. (. . .) I certainly felt excited, you know about working on the project and then there was a big gap.
MIP3
Intervention delivery
Delivering within a set structure
Motivational interviewing practitioners were required to deliver the intervention through both face-to-face and telephone sessions (see Chapter 2). They were specifically asked about their experience of delivering the telephone element, as this was a new experience for many. One MIP described the challenge of having to juggle many different things during a telephone counselling session.
I didn’t realise how tricky this could be; listening, processing and then trying to keep it in my angle. Whilst at the same time I (. . .) was thinking ‘Ok, I’m interested in finding out where, what’s going on with the exercise from our last calls’. So, you know; review last goals, listen, MI, talk and then new goals. So for me that was, yeah . . . and this was my first experience of real telephone counselling.
MIP10
The MIPs showed a preference for the face-to-face sessions and described this style of delivery as more beneficial. It allowed for more personal interaction with the client and they considered it important for building relationships. One MIP said they found it difficult to maintain ongoing relationship over the telephone and, moreover, MIPs explained that face-to-face delivery allowed them to use non-verbal cues, which were seen as vital for counselling. Despite the drawbacks of telephone counselling, MIPs were in agreement that it can be useful under certain circumstances and that this delivery method was better than providing no counselling. One MIP explained that the focus of the telephone sessions was different to that of face to face, in that they saw this as an opportunity for participants to check in rather than deliver the full intervention. Telephone sessions were seen as useful to support participants in reviewing their goals and giving them a timeframe to achieve these.
I spoke to a man last week, he’s just come back from Australia (. . .) and he’s put on some weight, and he’s, ‘Right, now, by the time you phone me again, this is what I’m going to do’.
MIP4
One of the MIPs was required to deliver two participants’ face-to-face sessions via telephone because the participants struggled to make a face-to-face meeting. Despite acknowledging the aforementioned difficulties, this MIP felt that the 1-hour duration meant that she did not experience the same difficulties in maintaining an ongoing relationship as when delivering the standard 20-minute telephone sessions.
I’m puzzled that the 20-minute phone calls didn’t work in the same way
oh right
because when I did the face-to-face, 1-hour slots on the phone
Yeah
. . . it worked like clockwork you know, people were there, they’d pick up we’d set a schedule, we’d set a time. Something about the phone calls, the 20 minute phone calls em just felt like, like an add on.
Many MIPs found it challenging to work within a set structure and deliver according to the schedule. Some MIPs described experiences whereby they struggled to fill their 1-hour sessions, as participants did not engage fully. In these circumstances MIPs found themselves talking to participants about their wider support needs and even, in some instances, cutting sessions short. The number of sessions participants received depended on which intervention arm they were in. Many MIPs discussed the challenges of delivering a pre-set number of sessions. They expressed frustration with the design as they felt that, in some instances, participants would have benefited more from being in a different intervention arm to the one they were in.
Often it’s not matched. So there’s people that I’ve got (. . .) two phone calls over a year that really could do with one a month. (. . .) You know and it’s really hard, when you’ve got people who’ve got nine that don’t need them.
MIP4
The MIPs commonly expressed difficulty in delivering the less intensive intervention, as they were required to be as concise as possible. They felt they did not have time to discuss the root of participants’ weight management issues and support their needs fully.
In a way your first session is really sort of listening most of it and trying to give them that sort of opportunity to get it all out, and then the second session would be a lot about sort of really giving them as much tools and information (. . .) ready for them to sort of go and do what they can. (. . .) You’d work (. . .) different with somebody with two than you would with six (. . .)
So was it, so more sort of focused in a way then?
Yeah
Can I use the word rushed!? (. . .) I’m used to working on the beginning and an ending. So I felt like I’m doing a beginning and then next time I see you I’m doing an ending. So it felt like, there’s the beginning quickly saying your bit. And it’s almost like ‘come on, come on’. And just as the client starts to feel safe and give you stuff and you’re working, it’s like ‘OK thanks a lot I’ll speak to you in a couple of weeks’.
Frequency of telephone sessions differed between intervention arms. For the less intensive group, the two telephone sessions were delivered 6 months apart. This gap was regarded as too long and had an impact on the MIP/participant relationship as well as the MIPs’ confidence in delivering the intervention.
The telephone counselling, after the two sessions, was in 6 months. (. . .) So that was a long time in a way of touching base. So we felt as if it was too short.
MIP15
A further difficulty MIPs described included the timelines that the intervention needed to be delivered in. As a result MIPs explained the differences between their usual practice and working within a research framework.
I didn’t stay on time track as closely as I should have…and then I remember I used to get these e-mails back to say (. . .) ‘you’ve kind of missed your deadline’. I got a fright because I didn’t actually realise there were deadlines, but of course there were and they described them in the handbook.
MIP3
Intervention content
Motivational interviewing practitioners were provided with a set of hot topics to address during MI sessions (see Chapter 2). When asked what they thought of these topics and how they used them, MIPs said that they occurred naturally throughout their sessions and were at the heart of supporting participants’ weight management goals. Moreover, MIPs explained that they did not find themselves making a conscious effort to address these owing to their natural occurrence.
I covered them but not . . . I didn’t sort of consciously work with them. I didn’t sort of, you know, take them out and say ‘right, today we’re going to talk about such and such.’. . . em but we certainly did dip into that because those are things that you know just came up quite naturally in the conversation.
MIP3
However, when they were used, topics provided MIPs with a routine that ensured that all required aspects were covered.
You do talk about (. . .) exercise, checking about the diet you know, the self-monitoring. (. . .) There was almost a process, wasn’t there?
MIP7
Motivational interviewing practitioners explained that they often structured sessions by revisiting participants’ goals and progress since their previous session rather than using the topics specifically, stating that this felt more natural and fitted with their usual practice.
We’d always end the sessions with some kind of plan in moving forward (. . .) and then we’d always start the next session with some kind of ‘how they’d been getting on since last time’ and revisiting em those (. . .) goals that they’d set for themselves.
MIP3
Despite mostly positive feedback, a few MIPs commented on the fact that the information given on some of the topics was too simplistic, for example on binge eating. One MIP raised the difficulty of addressing complex topics like this within the time available to deliver the intervention.
Participation, attendance and logistics
Participant attendance during the trial was excellent. Only on a few occasions were MIPs able to reflect on participants’ reasons for non-attendance. This was mostly because of personal circumstances, a lack of interest in telephone counselling and disappointment with their allocation to the less intensive group, in which they felt they would not receive enough of the intervention to make it worth their while.
I had two who withdrew at that stage [phone sessions] as well. (. . .) One just said (. . .) she’d been thinking about it and she didn’t want to speak on the phone, she just wasn’t comfortable with it. And the other person said that (. . .) there was too much pressure. (. . .) I don’t think that was the real reason, I don’t know what it was. But you know, two great sessions, really useful and then, just not interested in the phone.
MIP8
The MIPs felt that it was important to build good rapport and relationships with clients to maintain engagement and outlined that those they found difficult to engage from the start were the ones who subsequently withdrew. Although MIPs did not experience low attendance, logistical issues preventing them from delivering sessions were more common. The most widely discussed difficulty was making contact with participants to arrange appointments, particularly for telephone sessions.
The MIPs commonly expressed the feeling that the routine of daily life conflicted with participants’ engagement with the study, which was a contributing factor in the difficulties of scheduling sessions.
It is tricky to book a phone call and agree a phone call. (. . .) Life happens, so clients are just not there at that particular time or they’ve got to cancel for whatever reason, so that can be quite tricky.
MIP10
Moreover, one MIP described a participant’s unwillingness to book sessions too far in advance. Although sympathetic, MIPs felt having to constantly chase participants to arrange appointments became an effort that was very time-consuming and carried a cost implication.
In terms of engaging participants, MIPs described surprise at their reasons for volunteering for the study. Many participants told MIPs they were taking part to support the project and help the MIPs, rather than for their own benefit, which created an extra barrier for MIPs during delivery.
I think one of the things that happened with some clients, [is that they] seemed to have been recruited feeling that they were doing [us] a favour, taking part in a trial. So rather than what they were getting out of it, they were here to offer something.
MIP6 (general agreement from the group)
A further point of discussion was that of venue choice for the sessions, which yielded a mixed response. Some MIPs chose to use local venues such as community and leisure centres recommended by the WILMA trial team, whereas others chose to travel to participants’ homes. Although some MIPs provided participants with the choice of home or local venues, others steered away from visiting participants’ homes as they felt that they were full of distractions.
Motivational interviewing practitioners who chose to see participants in their homes commented that this supported engagement and attendance levels, as it was innately more difficult for participants not to attend.
I ended up seeing nearly all of mine at home. Which, obviously you’ve got a captive audience then, and you know, I don’t think I had any cancellations.
MIP7
The MIPs who used the suggested venues expressed mixed views. They commented on the unsuitability of many of them, particularly for counselling purposes.
I think working in sort of like community centres and leisure centres wasn’t really working, I mean, my first client I saw in a basement. (. . .) I mean she was a young girl, I felt really safe, but you know when you’re thinking, this is not right you know, there’s no fire exit, there’s no window. (. . .) This person could have an emotional breakdown and where do I go from here?
MIP15
However, some MIPs preferred using these as they felt that it was more appropriate to meet in a neutral environment. Moreover, once familiar with the booking process, they felt it worked well.
Impact on participants and motivational interviewing for weight loss maintenance
The MIPs reported receiving positive feedback from participants with regards to their experience of the intervention and described witnessing participants’ positive development throughout sessions. In particular, MIPs commented on participants’ increased self-awareness and confidence in their achievements. They described how sessions gave participants the opportunity to speak openly and be listened to. MIPs emphasised the importance of listening to participants, and it was apparent that, to them, giving participants the opportunity to speak to someone was the most important element of the intervention. However, MIPs felt that, although the aim was to deliver MI, the key techniques that participants benefited from and supported them in their goal achievement were good listening and reflection skills.
It’s a lot about the being with the person and the listening and letting them hear back, you know. The skills of reflective listening I think comes up again and again you know, letting them hear back the type of things that they’ve been saying and linking everything together and seeing realisation.
MIP4
While MIPs discussed the participants’ individual goals and achievements, many agreed that what participants gained as a whole from participation was a realisation and understanding of their achievements. In particular, MIPs discussed participants’ realisation that it was OK to maintain their weight and shift their focus from wanting to keep losing weight, as maintaining was an achievement in its own right.
Actually happiness to recognise that; actually maintaining weight was OK. Because I think that takes a bit of a mind shift. (. . .) A lot of people have been on losing weight, actually just not gaining weight, was a real (. . .) that really shifted them, the not gaining weight and just keeping, weight, weight constant was actually could potentially be a goal within itself.
MIP1
A key question for the research team was whether or not MI worked within a WLM population. MIPs’ responses were mixed in this regard. Some described having witnessed the positive impact of using MI with these participants. Others described participants for whom the intervention did not seem to work as they kept coming back looking for a ‘magic bullet’.
I think (. . .) she was one of the ones that expected me to go in and tell her something new that she hadn’t heard, but actually it’s, it’s what she knew anyway, it’s about moderating your diet and regular movement basically and you know, increasing your exercise. So you know, I think she was a bit disappointed thinking that I, I was going to go there with something she’d never heard of before.
MIP7
Motivational interviewing practitioners agreed that the success of using MI was reliant on the participant. If participants were already motivated and engaged, then pure MI worked really well, but this was not the case for those not at this stage. Participant engagement and a good relationship with their practitioners were seen as key for progression.
So, what I felt made a good session was when people would come thinking ‘ooh maybe I could try that, what do you think about that?’ (. . .) They were kind of really engaged in working with you. They weren’t all like that.
MIP5
A number of MIPs said that they were unsure whether or not they delivered pure MI and that they tended to use MI as part of their overall delivery method.
I never do pure MI, so this is very different for me because I’m, I’m a CBT [cognitive–behavioural therapy] therapist so I use MI as part of my whole intervention. So yeah, very different to do a whole 50 minutes of MI. I’m not convinced still that I did. [Laughs.]
MIP6
Future intervention implementation
Training improvements
One of the most common suggestions for training improvement was to increase the number of training sessions, including a refresher session at a later date. This would have allowed more focus on study-related elements to ensure that MIPs knew what data to provide to the study team. Furthermore, it would have enabled MIPs to receive feedback after seeing participants and facilitated discussion of day-to-day issues.
[It] would have been good to have another sort of days training to see how we were all doing and to tweak the things that maybe we were struggling with, but it felt as if we didn’t get that far.
MIP15
Although MIPs were originally due to receive continual feedback through regular MITI assessments, this did not occur owing to recruitment and other challenges. However, MIPs felt that further assessment and feedback on their skills during the intervention would have been valuable. This would have allowed them to reflect on their development and delivery.
Rather than like the first one, which was a judgement call as in ‘yay or nay’, I would have wanted that to be rolled in to a kind of coaching/supervision.
MIP11
A further suggestion was to have an additional training day for the telephone sessions. MIPs proposed that a ‘role play telephone session’ would have been beneficial, allowing them to practise delivering this element and adapt their practice to working with participants in the absence of non-verbal cues.
Intervention-specific improvements
In order to gain a better understanding of the strengths and weaknesses of the intervention, MIPs were asked what they thought should be changed. MIPs recognised that participants’ needs varied dramatically, and this was particularly influenced by the stage of their weight management journey (weight loss vs. WLM). Owing to this large variation, MIPs felt that it was challenging to design an intervention that would fit all people. They reiterated the struggles they had whereby some participants in the less intensive arm needed more sessions, while some of those allocated to the intensive arm did not need six face-to-face sessions. MIPs expressed the difficulty in getting at the root of participants’ problems within the set number of sessions. In some cases they felt that even six sessions were not enough.
You could be touching on what’s a much, much bigger issue which you could, you can never really address it in six sessions. It’s still there and that bigger issue will come back and in a way be a problem again in the future. But whether you can extend that and talk about just the dieting, it wouldn’t really address that bigger issue.
MIP8
They suggested that a more tailored approach is needed, in which each participant’s needs are assessed and then the participant is allocated to the most appropriate arm. However, MIPs did acknowledge the difficulty of embedding this design within a randomised trial.
Just some degree of matching, and I know that’s really hard to do in terms of a design. But I do feel that actually, (. . .) in terms of it being a realistic study, in the real world you wouldn’t deliver it [makes ‘rigid’ sounds to indicate that a rigid approach to delivery cannot always be used and there needs to be some flexibility].
MIP9
It was additionally suggested that two sessions of face-to-face contact as a minimum was not sufficient. One MIP suggested using three sessions as the less intensive intervention because this would provide a better structure, consisting of a beginning, middle and end, which would allow for some progress to be made during the intervention. MIPs also outlined the difficulties of maintaining ongoing relationships when faced with large gaps between delivery time points. Although there were mixed views on the value of telephone sessions, it was suggested that increasing their duration to 1 hour might improve them.
The one [participant] I mentioned, I think that would have been enough two sessions and to go to, to telephone would have been fine, but if the telephone had (. . .) the same length of period of involvement, but it’s done by phone and not face to face.
MIP8
The MIPs expressed the need for better clinical support for the duration of the project. They outlined how this would have further supported their delivery through the exchange of ideas and ongoing support. It was suggested that experts in MI for weight loss or WLM could have been recruited to the core study team and delivered the intervention to all participants. This would have allowed for a smoother delivery and increased the robustness and fidelity of the intervention as practitioner variation would have been reduced.
I kind of felt that I needed somebody there who’d actually tried it, you know who’d really tried it with these people, who’d sort of given it a go, who’d come back and sort of worked through some of the MI principles and said look you’re going to come across this, you’re going to come across that, you know this is how we, we envisage this working you know.
MIP3
Study process improvements
Some MIPs outlined improvements required to support them in their delivery. This was focused on having easier to use paperwork and more training on how to do this and how to use the equipment they were provided with. It was suggested that some pre-study piloting work could have been done on completing the study paperwork and session recordings.
Implementation in a real-world context
The MIPs spent some time discussing how an intervention such as WILMA could work in practice. This included discussions around wider contextual factors as well as the practical elements of implementing it within the NHS. More specifically, they were aware of the impact that environmental factors could have on participants’ motivation and success in WLM. They felt that it was particularly important to recognise that counselling may work for some but not others owing to wider environmental factors.
One factor that MIPs felt impacted on people’s abilities to engage with weight management more generally was financial circumstances, which could act as a barrier or facilitator to engage with support services and activity classes. They suggested that this could have an adverse effect on the individual’s motivation and engagement.
One MIP felt that it would be difficult to sustain an intervention such as WILMA on its own as further and more in-depth psychological interventions were needed to really make a difference. However, it was recognised that the issue of obesity is complex and that addressing it effectively is challenging. MIPs suggested that, in order to see real change, obesity needs to be tackled on a broader scale. An example of this was described by one MIP in relation to food banks, at which people are being taught about food to allow them to make healthier choices.
When thinking how weight management interventions might work within the NHS, MIPs recognised that much had changed in recent years. It was highlighted that it will always be difficult to increase session numbers within the NHS, despite the potential benefits.
It used to be we had one appointment with people and never see them again, there was no follow-up. Then it was ‘oh you can have two or three appointment’s’ and then it was like ‘it’s five now’. And actually because my boss was so flexible, she knows that there is huge benefit to be had by having more and more time with these people. So I’m actually spending up to 12 to 14, maybe more than that, months with people. (. . .) It’s something that I think the NHS will always want to restrict us to five appointments but with weight management I just don’t think that’s possible.
MIP14
However, it was suggested that with current NHS restructuring and increased financial autonomy within health boards/Clinical Commissioning Groups there may be some scope to allow for individual decisions to be made to support such interventions taking place.
Summary
Despite experiencing some challenges while delivering the MI sessions, MIPs were overwhelmingly positive about the intervention and they described the encouraging impact it had on participants. MIPs repeatedly highlighted the importance of an ongoing supportive relationship with clients. This allowed them to build good rapport and delve much deeper into participants’ weight management issues. Furthermore, it allowed for a supportive environment in which participants could feel safe to speak openly. In terms of the practical aspects of the intervention, MIPs were particularly favourable towards face-to-face delivery; however, they felt restricted by the low number of sessions for the less intensive group and described challenges of working in this way. Furthermore, the large time gap between telephone sessions for the less intensive group was also regarded as problematic.
In terms of improvements, MIPs highlighted the importance of incorporating a further training session at a later date. Furthermore, some logistical issues were discussed, particularly around the required study paperwork and session recordings. MIPs recognised the difficulties of successfully implementing the intervention in the ‘real world’ as contextual and environmental factors are important influences on people’s weight management. They also acknowledged the resource restrictions inherent in working within the NHS. However, they were positive about the importance of implementing such an intervention to address obesity as part of a broader strategy.
Chapter 8 Process evaluation: interview results
Overview
The participant interviews were designed to address some of the issues raised in the process evaluation (see Chapter 6), specifically issues pertaining to context, reach, exposure, recruitment and the psychological theory underpinning the intervention (see Figure 1 and Table 22). The interviews also explored participants’ views and satisfaction with the intervention as well as their experiences of weight loss and WLM.
Semistructured telephone interviews were carried out at 6 (mid-intervention) and 12 (post intervention) months. An interview schedule (see Appendix 5) was developed and regularly reviewed and amended. The interviews lasted between 45 and 60 minutes and were audio-recorded, transcribed and analysed using thematic analysis. There were two parts to the analyses: first, a study-specific analysis (e.g. participants’ views and satisfaction with the intervention) and, second, a more general analysis exploring mediators of weight management that explored the data in relation to the underlying theory of the intervention. Further details of the methods are given in Chapter 3.
Results
Forty-seven participants were interviewed. Details of their characteristics are given in Table 34.
| Characteristic | Control | Brief | Intensive | Total |
|---|---|---|---|---|
| Time of interview | ||||
| 6 months | 0 | 7 | 8 | 15 |
| 12 months | 7 | 11 | 14 | 32 |
| Gender | ||||
| Female | 4 | 17 | 15 | 36 |
| Male | 3 | 1 | 7 | 11 |
| Age (years) | ||||
| ≤ 40 | 1 | 4 | 4 | 9 |
| 41–59 | 2 | 8 | 11 | 21 |
| ≥ 60 | 4 | 6 | 7 | 17 |
| Recruitment source | ||||
| Slimming World | 2 | 4 | 6 | 12 |
| GP | 2 | 7 | 5 | 14 |
| EOR | 0 | 0 | 1 | 1 |
| Other (usually advert or poster) | 3 | 7 | 10 | 20 |
| Attendance level | ||||
| Attended no face-to-face sessions | N/A | 0 | 0 | 0 |
| Attended two or fewer in the intensive or one in the less intensive | N/A | 1 | 1 | 2 |
| Attended three or more in the intensive and both sessions in the less intensive | N/A | 17 | 21 | 38 |
| Total sample | 7 | 18 | 22 | 47 |
Quotes from participants will be identified according to identification number, group [intensive, less intensive or control (Int/LessInt/Cont)], gender (M/F) and time since randomisation (6mnth/12mnth). A summary of key themes identified in the participant interviews can be seen in Table 35.
| Overarching themes | Subthemes |
|---|---|
| Context | Initial motivation, weight loss history |
| Perceptions and satisfaction with the intervention | Counselling sessions |
| Length and frequency of sessions | |
| Telephone sessions | |
| Session content | |
| Group sessions | |
| Online WILMA trial intervention | |
| Information sharing and impact of family/friends | |
| Mediators of weight management | Ongoing motivation |
| Support | |
| Professional | |
| Peer | |
| Family and friends | |
| Positive reinforcement | |
| A sense of achievement | |
| Health benefits | |
| Control | |
| Routine/habit formation | |
| Barriers to maintaining motivation | |
| Cultural attitudes | |
| Life events | |
| Adapting to weight loss |
Context
Initial motivation
The most commonly reported reason for participants’ weight loss was desired improved health. This was either preventative, triggered by serious health events in family members, or a response to their own long-term health issues such as diabetes mellitus, high cholesterol and arthritis. Other participants had been advised to lose weight either prior to or following surgery.
Poor self-image was also reported as a motivation for weight loss, commonly triggered by upcoming social events, such as weddings and holidays, and involved a desire to find better-fitting clothes and avoid embarrassing situations (e.g. requiring a seat belt extension on a plane). Weight loss was also perceived as facilitating a more active role in family social life, such as playing with children or grandchildren. For some participants, a sudden realisation of weight gain prompted their weight loss, which was described by one participant as ‘having a light bulb moment’ (0073-LessInt-F-12mnth). However, for many this was linked to an awareness of increasing age, particularly when reaching significant milestones, and the health concerns that come with ageing.
Weight loss history
Prior to entering the study, many participants had lost a substantial amount of weight, often significantly more than the required 5% eligibility threshold. Reports of lifelong struggles with weight gain were common, resulting in experiences of yo-yoing, a repeated cycle of weight loss and regain.
Participants described using many different weight loss techniques including diet change, physical activity or professional support. Diet strategies included calorie counting, reducing sugar or fat intake, decreasing portion size and making healthier choices, along with various diets such as Slim Fast® (Unilever, NJ, USA). More specifically, participants reported skipping breakfast, eating little but often and having small portions during the day and a large portion for dinner. Physical activity was discussed less often than diet, with the most commonly mentioned strategy being walking. Some participants had sought professional support from their GP or a dietitian.
Perceptions and satisfaction with the intervention
The counselling sessions
The majority of participants in both intervention arms identified the counselling sessions as the best component of the study. The support provided by practitioners was in line with the professional support described in the Mediators of weight management section, with an emphasis on the psychological benefits of having a non-judgemental and impartial listener.
What was particularly good about it was the non-judgemental element of it.
0358-Int-M-12mnth
Participants felt that the practitioner was caring and concerned for their well-being and that they could tell them anything.
Well the best was that somebody was interested in, you know, your well-being and health.
0634-Int-F-12mnth
Participants recognised the psychological expertise provided by practitioners, which was perceived to be a valuable resource.
I thought they were very helpful because I know that is what I really need more of. Because as I say, a lot of my problems are psychological, and to talk to somebody who can help you on that score I think is one of the most important things of any study to do with anybody that’s obese or big built.
0080-LessInt-F-6mnth
The counselling sessions provided a level of insight and understanding that was not gained from other sources of support such as friends or family.
There were a couple of things that, in talking to her, that I got to realise about those patterns of eating, about how I think about food and how I handle both the weight loss and the weight maintenance, so for me those sessions were really, really helpful.
0073-LessInt-F-12mnth
In addition, participants expressed an understanding of the counselling methods in that it drew them to a deeper level of understanding through the use of questioning and probing, and encouraged them to find their own solutions, giving participants greater control (described as a mediator of weight management below).
He was very good about not telling me things but asking me things, and asking me to formulate my own plan if you like, of how to maintain or lose more.
0647-LessInt-F-12mnth
Reports of increased awareness and understanding were more frequently offered by those in the intensive group, so promoting awareness and insight likely took time as the therapeutic relationships developed. It was also dependent on whether or not individuals were able to talk freely.
In the beginning I found it really hard, because you, you know, you’ve got to spill your guts, cos you’ve got to find out why you do what you do and it was really, really hard to do that.
0341-Int-F-12mnth
However, some acknowledged that it just gave them an opportunity to ‘off load’ (0079-Int-F-6mnth) and to have dedicated time to talk about their weight management issues and they valued the individual attention that counselling provided.
When you go [to] the Slimming World group you get a very short amount of time and you have to make an effort to speak to somebody on your own, whereas having that allotted time to yourself, it really helps you to talk through and explore particular issues of mine I might not have brought up in the group.
1801-Int-F-6mnth
Participants reported a perception of accountability on seeing the MIP, which provided additional motivation.
. . . that would give me motivation before he [the practitioner] came because if I lose a couple more pounds before he comes or he’s going to be phoning this day so I better stick to it this week now, you know like that, like a check-up type of thing.
2703-LessInt-F-6mnth
However, just being part of the study gave some participants more focus on their weight management with a level of accountability inherent in the study measurements, which were, for some, the most useful aspect of the study.
As is described in the Mediators of weight management section, an important element of support is encouragement and positive reinforcement, and both of these needs were fulfilled by the MIPs.
He gave me quite a lot of help with motivation, you know, encouragement just to keep going.
0349-LessInt-F-12mnth
The encouragement, positive reinforcement and support provided in the counselling sessions boosted participants’ confidence and increased their self-efficacy.
I think motivation interview made me feel quite strong in my decisions . . . it made me feel even stronger in what I was doing was the right thing for me.
0645-LessInt-F-12mnth
Negative views of the counselling sessions
A minority of the sample did not find the counselling sessions helpful. These tended to be either males or younger women. Some men expected the practitioner to be controlling and to drive and motivate them by setting targets, in the mode of a personal trainer.
He was very good for telling you if you were doing well, and ‘you’re doing really well and keep it going’ kind of thing, but he didn’t actually say ‘right lets set the target’. It was you set the target.
0076-Int-M-6mnth
Another dissatisfaction expressed was an expectation for more novel information with the complaint that they had not learnt anything new. When asked about the worst aspects of the study, several participants mentioned the location of the counselling sessions and travel difficulties. Conversely, participants did value practitioners making the effort to see them in their own homes.
Length and frequency of sessions
Views on the number and frequency of sessions varied. More people in the intensive group expressed satisfaction with the number of sessions, although there were still a number in the less intensive group who thought they had sufficient sessions. There was a consistent view that the number of sessions should be based on the circumstances or characteristics of the individual, or vary at different stages of the weight management journey.
Some people might only need three, some people might need more, it depends how quickly you can identify what your problem is and get it out and then start working your way through it.
0341-Int-F-12mnth
What I think would be better is if somebody said like ‘well, if you hit crisis and if you get yourself into trouble then you can reaccess this service’. Because I, there would be no point in me having six/eight sessions if in the first few sessions I felt refocused and remotivated.
0645-LessInt-F-12mnth
Views on the frequency of sessions also varied. Some felt monthly sessions would allow for more time to work on their goals compared with every 2 weeks, whereas others felt they needed more regular support. It was also recognised that people attending a weight loss group get weekly support whereas those without this type of support might need counselling more frequently, again reflecting the view that it was dependent on individuals’ circumstances.
The need for long-term support was also expressed by participants in the intensive group and one woman tentatively suggested that length of support was more important than frequency of sessions.
Maybe once a month was enough, but maybe for a longer period of time? (. . .) There’s a lot of people who have lost their weight, you know, they reach goal and they stop going to class [Slimming World] and then 6 months later they’re back, and they’re back where they were because they’ve put it all back on.
0649-Int-F-12mnth
Telephone sessions
The majority of participants preferred the face-to-face to telephone sessions because of the availability of non-verbal cues. It was suggested that the client could be less than truthful or at least hide things from the practitioner over the telephone.
It’s completely different being on the telephone. I suppose when you’re face to face with somebody they can read your body language and you can read their body language, so in a way there isn’t any hiding.
0079-Int-F-6mnth
It was also felt that compared with telephone calls, face-to-face sessions outside the home environment had fewer competing distractions. However, one participant preferred the telephone sessions as she was more distracted at face-to-face sessions, thinking about competing demands on her time. The acceptability of telephone sessions also depended on participants’ expectations and the stage of their counselling. In-depth or very personal discussions were less acceptable over the telephone.
I really wasn’t keen on doing it over the phone, (. . .) that was so intensely personal to me, that I just felt it was impersonal doing it on the phone.
0645-LessInt-F-12mnth
The fact that the telephone sessions were shorter was also not conducive to more in-depth discussion. Alternatively, if viewed as a progress ‘check-in’ they gave a further opportunity for accountability (described in the Mediators of weight management section).
You did look forward to the next one, just to have a check-in . . . [laugh] . . . Because you’ve got used to the contact and having to be responsible to somebody.
0341-Int-F-12mnth
Acceptability of the telephone sessions was also increased if the participant had previously met the MIP in the face-to-face sessions.
If it had been without having met her I’m not sure that would have been as useful (. . .) but carrying on a conversation with someone that you know quite well has been absolutely fine.
0361-Int-F-12mnth
Content of the counselling sessions
The MIPs were advised to address certain issues such as goal-setting, self-monitoring, encouraging social support as well as advice on diet and physical activity. Goal-setting appeared to be addressed with most participants, with varying success.
Most of the goals that we tried to set were exercise related (. . .) and they didn’t work, and then I fail, because I failed on those. That’s very demotivating.
0649-Int-F-12mnth
Participants did not recall self-monitoring being discussed routinely in the counselling sessions, possibly because this was a strategy participants used prior to entering the study. Some discussed frequency of self-monitoring as those who were struggling with weight management found it demotivating to weigh themselves too frequently. Coping with relapse was reported to be a major topic of the counselling sessions, including discussion of planning for occasions that were likely to be difficult.
But certainly the sort of the thing that I most discussed with [practitioner] was the bit about don’t beat yourself up about it all the time and, sort of accept the positives (. . .) about you know your weight loss and things.
2101-LessInt-F-6mnth
Group sessions
Few participants had attended the group sessions before they were terminated. For those who did attend, some participants found them helpful, whereas others did not.
I only had three sessions with, you know, the group, but anything like that, that gets you speaking to other people is always going to be helpful.
0051-LessInt-F-6mnth
No I didn’t find really anything that they had to say useful because it, there was quite a lot of negativity (. . .) about losing weight and it seemed to me that they weren’t looking for a solution as much as someone waving a magic wand.
0060-LessInt-F-12mnth
Those who did not find the groups helpful emphasised the importance of the motivations and attitudes of group members and the facilitation skills of the group leader. This was recognised particularly by those who reported bad experiences in other weight management groups.
There was variation in the response to cancellation of the group sessions. Some participants were very disappointed and others were disappointed but felt they got peer support through commercial weight loss groups. A minority did not feel comfortable taking part in a group or were unsure how they would feel in a group situation. A few participants pointed out that those taking part in the WILMA trial would have lost their weight using various strategies and so there might have been a good opportunity for exchange of information.
WeIght Loss Maintenance in Adults online
Participants already using an alternative website tended not to make full use of the WILMA trial website, although many recorded their weekly weight as requested. There were aspects of commercial websites that participants were using that they preferred, for example they could enter half pounds, they could backdate their weight and there was more information.
However, they did acknowledge the usefulness of the website for anyone who did not use an alternative, as they felt it gave them an opportunity to monitor their progress and increased motivation by having the accountability of entering their weight on a weekly basis. The ability to enter additional comments to explain weight loss/gain was felt to be a useful monitoring tool.
You couldn’t think ‘oh well, I won’t bother being careful this week’ but it’s because I knew I had to go on that site more or less every week and put my weight in so, it kept me on the straight and narrow. (. . .) When I’d weighed myself if I’d put on a couple of pounds I’d put a comment about why I thought I’d put it on (. . .) and you know it was handy to actually look back and see.
2706-Int-F-6mnth
A few participants said they did not use the website frequently because of lack of time or because they forgot to use it. Others used it for a short time and then lost motivation and discontinued.
Suggestions for improvements to the website included provision of recipes and food facts, and opportunities to interact with other participants in an anonymised way. One woman had difficulties reading the font and another felt that it was a bit bland but, overall, participants felt that it was well presented.
Information sharing and impact on family and friends
The risk of contamination between groups through sharing of specific study information seemed to be low. Some participants merely disclosed that they were taking part in the study to other participants, while others reported sharing no information at all. Some information was shared with family, friends and colleagues, including information on healthy eating, portion size, food labelling, physical activity strategies, self-monitoring, coping with barriers and relapse, and the importance of looking at the bigger picture rather than short-term weight loss. It was difficult in many cases to distinguish the impact of taking part in the study on family and friends from the impact of weight management more generally. However, positive impacts on family and friends included a healthier diet and in some cases unintentional weight loss owing to the change in diet.
Family, friends and colleagues were often motivated to lose weight when they saw the participants’ success, and relaying study information to family members was reported to have had a direct impact on their weight management.
My partner’s lost 6 stone.
And do you think that that’s related to what you’ve been taking part in?
Absolutely, no question, yeah.
And how do you think you’ve influenced that?
I suppose talking to him about the motivation interviewing and making aware of that. But I suppose it’s just that kind of interdependent support really.
Participants’ increased physical activity motivated other family members to be more active and produced subtle changes in family attitudes and lifestyle.
We’ll say to the boys, ‘what would you want to do?’ [as a reward] And probably before it would’ve been ‘eat something’, and now it’s well ‘can we go out on our bikes’.
0045-Int-F-6mnths
A greater awareness of good nutrition also became part of family culture.
She’s [daughter] a lovely tall, slim 5-year-old, and I, something clicked in my head and I’m going ‘hang on a minute, I wasn’t fat as a child, I was slim. She’s going to get addicted to sugar’ (. . .) and so Monday to Thursday – no chocolate, she can have a yogurt or an apple or a banana or grapes, whatever we’ve got home, after school. Because it was always a chocolate and can I have crisps, and it was all that kind of, salt/sugar.
0364-LessInt-F-12mnth
Mediators of weight management
The central category in this analysis (i.e. the category that was related to most other categories) was ‘ongoing motivation’, which is also key in WLM. A model is presented in Figure 17 of the relationships found between the conceptual categories organising the data and ‘ongoing motivation’, the central category. Each of these categories will now be discussed in turn.
FIGURE 17.
Model of mediators identified in participant interviews.
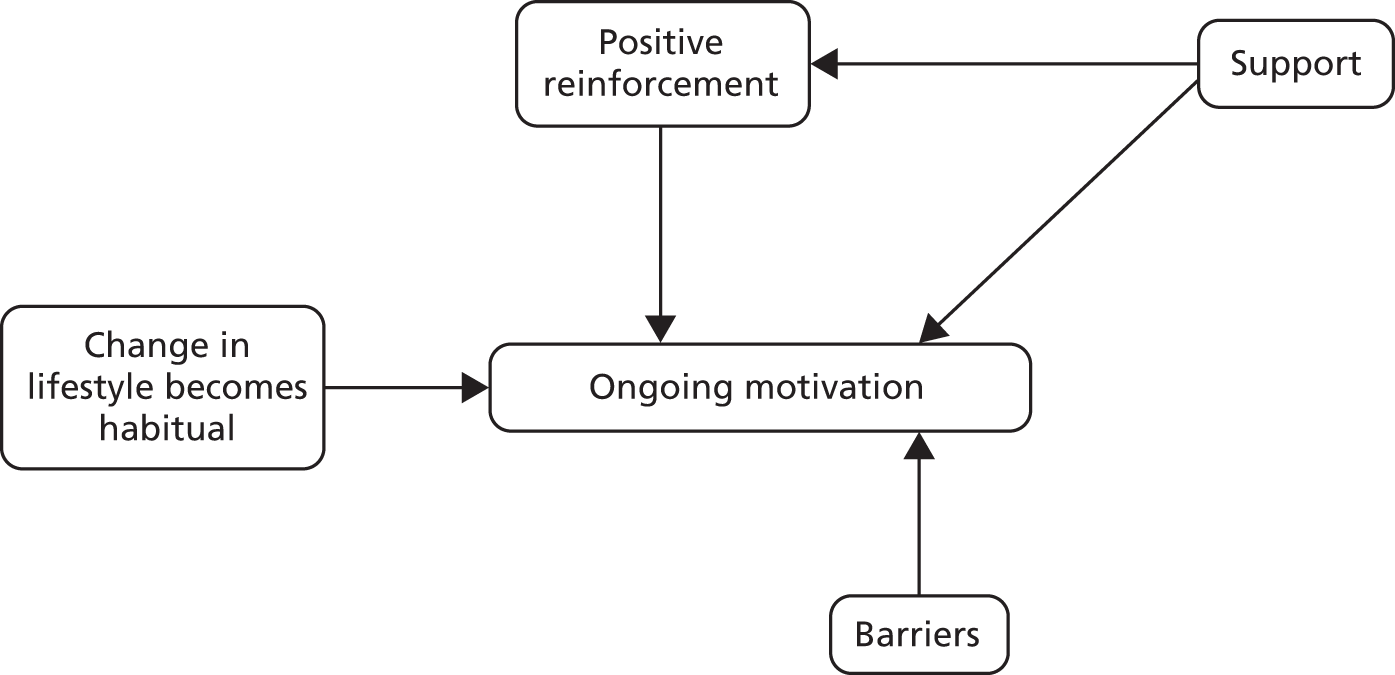
Ongoing motivation
Ongoing motivation was strongly influenced, both positively and negatively, by the type of support provided by others. Support fulfilled a number of different needs, one of which was positive reinforcement. This also had a direct link to motivation, independent of the support of others (e.g. by self-satisfaction or self-fulfilment). Other influences on motivation were ‘changes in lifestyle’ and ‘barriers’ to success (e.g. negative life events and cultural attitudes to food).
Support
Support was felt to be important for maintaining motivation, with a view expressed that they could not lose weight ‘on their own’. Support came from three different sources: professionals (including the MIPs), peer weight losers, and family and/or friends. Some aspects of support were provided by any or all of these three groups and some were particular to a certain group.
Professional support
Professional support was provided through the WILMA study (see Chapter 2), weight management groups such as Slimming World, and from GPs and dietitians. What participants sought from professionals was someone to listen to their issues in a caring, empathic and non-judgemental way, with psychological support being an important component and, as described in Perceptions and satisfaction with the intervention, the WILMA trial MIPs fulfilled these needs. Straightforward information giving was felt to be insufficient.
I didn’t find that the GP, although they’re sympathetic and they know exactly what to do, what to say; but I know what to do as well, and as far as eating and activity is concerned, but I think they need to be a lot more rigorous in their approach really and, it wasn’t enough for me anyway.
0647-LessInt-F-12mnth
It also gave them reassurance they were not on their own.
You felt like, ‘Christ I’m not actually on my own’.
0068-LessInt-F-6mnth
What was different from other types of support was the objectivity; having an independent and non-judgemental confidante with whom they could talk honestly about topics they would not address with a family member or friend. A good professional relationship facilitated motivation by instilling in participants a feeling of ‘wanting to please’, that is by being successful in their weight management. This was related to a need for ‘accountability’ whereby they were accountable to an independent party for progress. One participant expressed this as needing the ‘external discipline’. This was most often provided in the current sample via weight loss groups, but could take place elsewhere, for example entering weekly weight on the website, attending the GP surgery for weigh-ins. However, there could be negative effects resulting in a minicycle of ‘yo-yoing’, in which participants would eat badly for a few days after their ‘weigh-in’ but then try and claw back their transgressions immediately prior to the next ‘weigh-in’.
Peer support
Peer support was also important. This provided a more immediate source of support on a more frequent basis than that provided by professionals. In addition to weekly meetings, members of slimming groups reported telephoning, texting and e-mailing other members when they needed specific encouragement or advice, thus helping prevent relapses.
Everybody that wants to shares phone numbers [does], so there’s always support from someone . . . somewhere, by some means. So it’s, you know, even if it’s (. . .) ‘I’m shopping I want to buy this cream cake somebody stop me’, and generally somebody does.
0053-Cont-F-12mnth
Again, it alleviated feelings of isolation but was distinct from other types of support because of the shared experience. It also provided a yardstick against which they could measure their own progress. When people were unsuccessful, it was reassuring that others also experienced set-backs and when people were successful, it provided a role model which had the potential to increase self-efficacy, particularly in an environment that reinforced achievements. Experiencing success and achieving consistent weight loss appeared to be a crucial element for maintaining motivation. Peer comparisons could also be viewed in a competitive light, particularly by male participants.
. . . with a bit of competition, when there’s like eight or ten of you in the class and I want to do the best and it’s a good, good stimulus.
0076-Int-M-6mnth
The caring and supportive environment engendered in a cohesive weight loss group provided a sense of community that went beyond the immediate issue of weight. Members provided support to each other for life events generally, which could indirectly impact on their weight management. Participants were intrinsically motivated to attend the groups because they enjoyed the meetings on a social level and often made friends, but recognised the dual effects of having an activity they enjoyed that had a positive impact on their weight management. Friendships, however, were frequently focused on their weight management support and were not extended into other areas of their life.
Support from family and friends
Weight management provided fewer challenges if family and friends took an active part in helping promote a change in lifestyle. The most helpful scenario was when both husband and wife undertook a weight management programme together, or when a mother or sister started weight loss at the same time. Practically, the logistics of catering for a healthier eating regime was more manageable when the whole family ate the same meals, allowing the change in diet to become integrated into their lifestyle.
My husband, you know, will eat the same food as I do. My son actually has taken on board some of the healthier things that I’ve tried in the past, things like dry roast potatoes (. . .) and it’s part of their lives now.
0060-LessInt-F-12mnth
If all the family did not eat healthy food, the participant found it difficult to resist temptation. Additional difficulties were faced if family members lacked understanding of the weight management process.
The first week I lost weight he bought me a big bag of Maltesers[®, Mars Inc., VA, USA] to say ‘oh well done you’ve done really well this week’, and I was like ‘what are you doing, why are you doing this?’
0045-Int-F-6mnth
On the whole, families were supportive and provided encouragement, positive reinforcement and practical help. Friends were, perhaps, less helpful although some did go out of their way to accommodate the participant’s diet. However, participants did experience situations where friends and/or family would try to persuade them to eat high-calorie foods. Whether or not participants succumbed to persuasion depended on the individual, the context and how they were feeling at the time. One woman pointed out that the responses of friends would be different if she refused to eat something because she wanted to lose weight rather than if she said she was diabetic.
If she’d went ‘oh, [name] is dieting’ they would have gone ‘oh go on, one won’t hurt’, but because it’s medical [diabetes] they went ‘oh that’s fine then’.
0075-LessInt-F-6mnth
Positive reinforcement
A sense of achievement
As well as the positive reinforcement received from others, there was also positive reinforcement from a sense of achievement. In this regard, achieving a weight loss at the weekly slimming group ‘weigh-in’ was crucial in maintaining motivation and conversely seeing a gain in weight was demotivating. One woman likened a weekly weight loss to a pay day.
Every week going to a slimming group and losing weight, that was my sense of achievement for the week, and it was like it had all paid off, it’s all been worth it, it’s almost like a payday.
0045-Int-F-6mnth
A lack of this sense of achievement was blamed for failure to be able to maintain weight losses as the praise given to weight losers is in excess of that given to maintainers.
It sounds like its attention seeking but it’s not, it’s just, you don’t feel like you’re achieving anything anymore, you don’t sort of get any praise for losing a pound or losing two pound (. . .) and psychologically it was harder.
0045-Int-F-6mnth
Health benefits
Improvements in health acted as a positive reinforcement. For some it was the relief of pain in joints from losing weight and increasing exercise, and for others it was just an increased sense of well-being when a healthy diet was maintained.
You do notice when you, after a day or two of eating poorly, you wake up and you feel sluggish or you have a headache and you just don’t feel very good, because when you eat well you feel good.
0355-LessInt-F-6mnth
Others maintained motivation by reminding themselves of the potential negative health effects of being overweight, which was often reinforced by events like stroke or heart attack in family members.
Control
Having a feeling of being ‘in control’ was closely linked to diet and successful weight loss and was empowering for individuals and positively reinforcing in itself.
But I’m quite happy also not to eat tons and tons of food, in fact I’m much better when I’m in control, I feel happier more you know psychologically, I benefit from it all, I feel wonderful when I’m in control.
2101-LessInt-F-6mnth
Some viewed eating and weight as one thing that they could control, in the face of other more uncontrollable factors in their life, such as losing a job.
The converse of control in relation to food was likened to an addiction, and a loss of control could result in a bingeing experience. However, being too rigid about diet and continually feeling deprived meant that control was very difficult to maintain, so that failure and loss of motivation was more likely.
One of the things that I did when I was eating carefully was to hold a sense of, I don’t know how to express it, ‘I’m not allowed that, I’m depriving myself of that’(. . .) so that when I would remove that restriction (. . .) I would then have a kind of ‘I can do anything I like. I can have another chocolate bar. I can have another biscuit’.
0058-Cont-F-12mnth
Control could be maintained by taking a more flexible approach to diet.
Yes that’s right and cutting it [a cake] in sort of proper sizes you know instead of going and thinking ‘oh blow it’ and coming back and going into ‘sod it’ mode and just think you know . . . I’ll finish the whole lot (. . .) I don’t do that. We might open a bottle of wine between the two of us, but it could take us 2 or 3 days to finish it.
0051-LessInt-F-6mnth
In a WLM phase, continual self-monitoring gave that sense of control.
You know, it’s a lot easier to lose 2 pound than it is 2 stone, and as long as I keep it in short bites then, I can control it a lot easier.
0651-Cont-M-12mnth
Routine/habit formation
To maintain motivation it was important for some participants to establish a routine with their diet and/or exercise.
I do have to motivate myself, but I also know if I get out of a routine it all collapses.
0062-Int-F-12mnth
Any change of diet and exercise required, in the first instance, conscious effort to maintain, and as the participant above (0062-Int-F-12mnth) reported, any disruption to their routine resulted in abandonment of their healthy lifestyle. It was recognised the changes need to become automatic, requiring little or no conscious effort, and to become so ingrained that it would be difficult not to do those activities.
On the other hand there are now a couple of ideas and a couple of habits that are so ingrained that it’s more difficult to not to do them things like the portion control and like the exercise.
0073-LessInt-F-12mnth
In this way, the need for conscious and effortful ongoing motivation diminished over time and new habits developed.
Barriers to maintaining motivation
Cultural attitudes
Food was viewed as an integral part of peoples’ pleasure in life, particularly at times of celebration such as holidays, birthdays and Christmas.
Yes, keeping your motivation going is really hard because there are things that happen. For a start there’s things get in the way, like birthdays, Christmas, holidays.
0068-LessInt-F-6mnth
Within this context it was felt to be socially unacceptable to refuse food offered. Some participants went along with social expectations and ate whatever they were given, while others tried to choose the healthiest option available. Because of the strong link between food and enjoyment, friends could resent participants who chose healthy options.
I’ve got it sussed what I eat and basically one of the friends in the group turned round and said ‘oh don’t whinge about the food you’re eating now, we’re here to enjoy ourselves’ (. . .) because I decided not to have a set menu and just eat the healthiest option on the menu (. . .) they made me feel rotten and it just spoilt the whole thing for me.
0645-LessInt-F-12mnth
Many attitudes to both food and exercise were reported to stem from childhood.
I think as a child, and I had two brothers and they were quite sporty, my father used to take them to the rugby as children, take them to rugby clubs to play (. . .) and, they were encouraged to be very sporty and I don’t recall as a girl, I remember staying at home with my mum. (. . .) And I don’t recall ever being encouraged to be sporty.
0355-LessInt-F-6mnth
Female participants reported having an issue with emotional eating, which was less common in males. This was linked to family attitudes because food was a cultural response to both positive and negative events, as well as being used in a nurturing and caring context.
If I’m upset or depressed or unhappy, I eat. And if I’m happy, we all have a good meal, you know so whatever it is, it revolves around food! (. . .) And it seems that way with my whole family.
0355-LessInt-F-6mnth
Other beliefs, passed on through families, such as ‘you should never feel hungry’ or ‘always eat everything on your plate’ also made managing weight challenging.
I was taught and conditioned, not to leave anything on my plate and I still find that difficult.
0638-Cont-M-12mnth
Some individuals were labelled as ‘big’ or ‘big boned’, which served to lower self-efficacy by convincing them that being ‘big’ was natural for them.
[I] think it was probably experience in like growing up and you know my Nan being big (. . .) and always being told by people ‘oh you’re big boned’, and ‘you’re big built’. And, as a child, you know, puppy fat and you’re a chubby baby, and I think you just always think you’re a big person so you can’t possibly maintain this.
0045-Int-F-6mnth
Environmental context is also important here, as participants found that the availability of healthy foods was often limited in shops and restaurants.
Life events
Negative life events could create the stress necessary to trigger comfort eating, or could result in periods of depression making it difficult to focus the emotional energy required for weight management.
Even though I wanted to do it, it’s just stuff going on in my life and I couldn’t bring myself to be dieting on top of it.
0043-Int-F-12mnth
Significant changes in life circumstances, such as retirement could either help or hinder weight management. Pregnancy and childbirth figured consistently as a life event that had negative impacts on weight management. However, life events did not necessarily lead to negative impacts on weight management if participants accepted that food was not a necessary coping mechanism.
I’ve made a huge step forward and I think ‘What is eating going to do? . . . What problem will that solve?’ And I think it’s just a realisation that food is not the answer.
2103-Int-F-12mnth
Adapting to weight loss
For those who were successful there could be challenges in coming to terms with a changed self-image and also the physical results of extreme weight loss, that is excess skin, which was felt to be more unattractive than fat.
. . . so I’ve got I want to say flabby bits (. . .) and I’m more ugly than seeing a fat person and I know that sounds bizarre but without being awful when I was big all those bits were filled out with fat. Now I’m skinny they jiggle about.
0068-LessInt-F-6mnth
Summary
Participants were generally positive about the intervention and the counselling sessions. Counselling provided support not received from other sources and participants particularly valued the psychological input. The MIPs provided encouragement and positive reinforcement, which helped boost confidence and increase self-efficacy. Face-to-face sessions were preferred over telephone sessions, although telephone sessions were felt to have their place as an opportunity to ‘check in’ with practitioners. Views on the number and frequency of counselling varied but it was felt that this should be based on individual needs.
In terms of the underlying theory, the central category in this analysis was ‘ongoing motivation’ which is crucial for WLM. This was facilitated by support from three sources: professionals, peers, and family and friends. Professional support (as given by the study practitioners) needed to be independent, non-judgemental and empathic. Peer support provided more frequent and immediate support from those with shared concerns. Support from family and friends was crucial in facilitating changes in lifestyle, in relation to both diet and exercise.
Positive reinforcement was provided by professionals, peers, and family and friends but was also acquired through a sense of achievement. Continuing success was crucial in maintaining motivation. Weight maintenance did not elicit the same levels of positive reinforcement, which made maintenance difficult. Positive reinforcement also occurred with regards to the health benefits experienced. A sense of control was also perceived as reinforcing and empowering with loss of control sometimes resulting in bingeing. In a maintenance situation, self-monitoring provided a sense of control. Participants felt that it was important for changes in lifestyle to become routine and habitual in order to be maintained. Barriers to weight management included cultural attitudes, environmental context, life events and difficulties adapting to weight loss.
Chapter 9 Economic evaluation results
Training costs
Motivational interviewing practitioners
A total of 24 MIPs were trained through attendance at one of three seminars. Following the seminars, 20 MIPs were assessed using the MITI scale. Simulated counselling sessions were conducted between each MIP and an actor. Finally, 15 MIPs attended supervision workshops (see Chapter 2). The total costs incurred in all aspects of MIP training are shown in Table 36. Individual seminar costs varied owing to actors only being trained once and not being used in seminar 3 (other than for the MITI assessment), which was completed in a shorter time as fewer MIPs were trained and the seminar did not include the evening engagement element. Administrative costs of setting up the training seminars were not recorded. Unit costs are given in Appendix 8.
| Aspects of MIP training | Number of units | Unit cost | Cost (£) |
|---|---|---|---|
| Seminar 1 (18.5 hours) | |||
| Venue and refreshments | Amount paid | 2233 | |
| Materials | Various | 62 | |
| MIPs | 12 × 18.5 | Variousa | 6105 |
| Trainers | 4 × 18.5 | Variousa | 2741 |
| Actors training | 4 | Fee | 800 |
| Actors’ performance | 6 | Fee | 1800 |
| Travel expenses (all) | Claims | 171 | |
| Seminar 2 (18.5 hours) | |||
| Venue and refreshments | Amount paid | 1941 | |
| Materials | Various | 30 | |
| MIPs | 8 × 18.5 | Variousa | 3280 |
| Trainers | 6 × 18.5 | Variousa | 3935 |
| Actors’ performance | 4 | Fee | 1200 |
| Travel expenses (all) | Claim | 255 | |
| Overnight accommodation | 6 | 3 × 2 nights | 595 |
| Seminar 3 (8.5 hours) | |||
| Venue and refreshments | Amount paid | 100 | |
| Materials | Various | 20 | |
| MIPs | 4 × 8.5 | Variousa | 634 |
| Trainersb | 4 × 8.5 | Variousa | 1007 |
| Travel expenses | Claim | 0 | |
| MITI individual assessment session 1 | |||
| Venue | Amount paid | 0 | |
| MIPsc | 16 × 1 | Variousa | 391 |
| Actors | 2 | Fee | 574 |
| Assessorsd | 0.5 × 16 | Variousa | 255 |
| Travel expenses (all) | Claim | 0 | |
| MITI individual assessment session 2 | |||
| Venue | Amount paid | 150 | |
| MIPsc | 4 × 1 | Variousa | 98 |
| Actors | 1 | Fee | 144 |
| Assessorsd | 4 × 0.5 | Variousa | 64 |
| Travel expenses (all) | Claim | 182 | |
| MITI individual assessment session 3e | |||
| Venue | Amount paid | 0 | |
| MIPsc | 2 × 1 | Variousa | 49 |
| Actors | 1 | WILMA trial team member | 19 |
| Assessorsd | 2 × 0.5 | Variousa | 32 |
| Travel expenses (all) | Claim | 0 | |
| Supervision meeting (2 hours) | |||
| Venue | Amount paid | 0 | |
| MIPsc | 15 × 2 | Variousa | 733 |
| Trainersd | 4 × 2 | Variousa | 255 |
| Total MIP training costs (£) | 29,855 | ||
| Mean cost per MIP trained (£) | 1244 | ||
Group facilitators
A total of 22 GFs were trained by attending one of three seminars, which ranged from 6.26 hours to 8 hours (see Chapter 2). The costs incurred in GF training are shown in Table 37. Unit costs are given in Appendix 8.
| Number of units | Unit cost | Cost (£) | |
|---|---|---|---|
| Seminar 1 (8 hours) | |||
| Venue and refreshments | Amount paid | 103 | |
| Materials | Various | 259 | |
| GFs | 5 × 8 | Variousa | 826 |
| Trainers | 3 × 8 | Variousa | 760 |
| Travel expenses (all) | Claims | 10 | |
| Seminar 2 (8 hours) | |||
| Venue and refreshments | Amount paid to venue | 206 | |
| Materials | Various | 49 | |
| GFs | 10 × 8 | Variousa | 1839 |
| Trainers | 3 × 8 | Variousa | 760 |
| Travel expenses (all) | Claims | 436 | |
| Overnight accommodation | 4 | 4 × 1 night | 228 |
| Seminar 3 (6.25 hours) | |||
| Venue and refreshments | Amount paid | 140 | |
| Materials | Various | 34 | |
| GFs | 7 × 6.25 | Variousa | 794 |
| Trainers | 2 × 6.25 | Variousa | 311 |
| Travel expenses (all) | Claims | 16 | |
| Total GF training costs (£) | 6771 | ||
| Mean cost per GF trained | 308 | ||
Apportioning training costs across participants receiving the WeIght Loss Maintenance in Adults interventions
The total cost of training the 24 MIPs (£29,855) and the 22 GFs (£6771) was £36,626. As this investment can produce a flow of benefit over time, these costs have been amortised at 3.5% assuming a 5-year training life. The annuitised annual cost of training is £8111.
This can be expressed on a per participant basis. Assuming that all participants receive all intended face-to-face sessions, that each MIP and GF can deliver the intensive intervention to a maximum of 165 participants or the less-intensive intervention to 500 participants per year, the cost per participant attributable to training is £49 for intensive and £16 for less intensive intervention, respectively. The above estimate is based on an assumed maximum of 25 intensive sessions per week per MIP (191 participants per year) conservatively reduced by 15% to 165 participants per year.
As explained in Chapter 3 the group sessions were shown to be unfeasible and it is recommended they be excluded from the WILMA trial intervention. Without GF training, total WILMA trial training costs are £29,855 (£6611 annuitised) or £40 per intensive participant and £13 per less intensive participant.
Given the magnitude of these costs per participant, no sensitivity analyses on training costs have been performed as they are unlikely to have any effect on overall cost differences between the three arms of the trial.
Costs of delivering the interventions
According to the WILMA trial protocol, the intensive group were to receive six face-to-face sessions, nine telephone interviews and four group sessions. The less intensive group were to receive two face-to-face sessions, two telephone interviews and four group sessions (see Chapter 2). All individualised elements were delivered by MIPs and group sessions were delivered by GFs.
In the event, following the change to feasibility study, only six group sessions had been delivered to a total of 15 participants (four intensive, 11 less intensive) and the sessions lasted 1.5 hours. On the same unit cost basis as for face-to-face sessions (see Table 39) the cost of delivering a group session was £105 per session or £630 for the six sessions.
Participants attended between one and four sessions as shown in Table 38. The total number of attendances by the intensive group was 10 and by the less intensive group was 18 (see Table 38). Dividing the total cost of delivering all sessions (£620) by the total number attending (28) produces a cost per attendance of £22.14.
| Number of sessions attended | Intensive group | Less intensive group |
|---|---|---|
| 1 | 1 × 1 | 6 × 1 |
| 2 | 1 × 2 | 4 × 2 |
| 3 | 1 × 3 | 0 × 3 |
| 4 | 1 × 4 | 1 × 4 |
| Total | 10 | 18 |
For face-to-face sessions, MIP time was valued at £70 per hour including travel,123 which is the unit cost for a 1-hour home visit by a community nurse on a salary of £32,600. This was considered appropriate as the face-to-face sessions were 1 hour, involved the MIP travelling and the median salary of the MIPs in the study was £31,248. This figure understates the £90 per face-to-face session that was paid to MIPs and included travel and time taken to write notes. The effect of varying this unit is shown in Sensitivity analyses.
The total costs of delivering the WILMA trial interventions are shown in Table 39.
| Intervention delivery elements | Intensive group (n = 54) | Intensive group cost (£) | Less intensive group (n = 54) | Less intensive group cost (£) |
|---|---|---|---|---|
| Face-to-face sessionsa | 275 sessions @ 1 hour | 19,250 | 92 sessions @ 1 hour | 6440 |
| Cost of hiring the venue per session | 275 sessions @ £10 | 2750 | 92 sessions @ £10 | 920 |
| Telephone sessions (value of time)b | 255 sessions @ 20 minutes | 2077 | 55 sessions @ 20 minutes | 448 |
| Telephone (cost) | 5100 minutes @ 14 ppm | 714 | 1100 minutes @ 14 ppm | 154 |
| Group sessions (cost per attendance) | Four sessions @ £22.14 | 89 | 11 sessions @ £22.14 | 244 |
| Total cost | 24,880 | 8206 | ||
| Cost per participant (excluding training) | 460.74 | 151.96 | ||
| Total cost per participant including training | @ £49 | 509.74 | @ £16 | 167.96 |
On the above basis, the total cost per person receiving the WILMA trial intensive intervention was £510 and £168 for those receiving the less-intensive intervention.
Sensitivity analyses
Table 40 below shows the effect of varying the base-case unit costs as follows:
-
Face-to-face session unit cost at fee paid to MIPs in the study (£90/hour).
-
Face-to-face session unit costs reduced by 15% (£59.50/hour) on basis that lowest salary for an MIP in the study was 15% below median used in base case.
-
Telephone sessions valued at median MIP unit costs (£19.84) rather than mean as unit costs for some MIPs were significantly above mean.
-
Group sessions at £17.50 per attendance. While, in theory, group sessions could be given to up to 10–15 participants, in practice, this would be unlikely to exceed six given the logistics involved. With full attendance, cost per session would fall to £105 divided by six group sessions = £17.50.
-
The cost of GF training and GF delivery removed as feasibility study showed group sessions to be impractical and should not form part of the WILMA trial intervention.
| Sessions and cost elements | Intensive group (n = 54) | Intensive group cost (£) | Less intensive group (n = 54) | Less intensive group cost (£) |
|---|---|---|---|---|
| Face-to-face sessions at amount paid to MIPs | ||||
| Sessions | 275 sessions @ 1 hour | 24,750 | 92 sessions @ 1 hour | 8280 |
| Total cost (including all other elements) | 30,380 | 10,046 | ||
| Cost per participant (including training) | 611.59 | 202.04 | ||
| Face-to-face sessions at 15% of base case | ||||
| Sessions | 275 sessions @ 1 hour | 16,362 | 92 sessions @ 1 hour | 5474 |
| Total cost (including all other elements) | 21,992 | 7240 | ||
| Cost per participant (including training) | 456.26 | 150.07 | ||
| Telephone sessions at median MIP unit cost | ||||
| Telephone sessions (value of time) @ median | 255 sessions @ 20 minutes | 1686 | 55 sessions @ 20 minutes | 364 |
| Total cost (including all other elements) | 24,489 | 8122 | ||
| Cost per participant (including training) | 502.50 | 166.41 | ||
| Group sessions assuming full attendance | ||||
| Group sessions | Four sessions @ £17.50 | 70 | 11 sessions @ £17.50 | 193 |
| Total cost (including all other elements) | 24,861 | 8155 | ||
| Cost per participant (including training) | 509.39 | 167.02 | ||
| No group sessions | ||||
| Group sessions | 0 | 0 | 0 | 0 |
| Total cost (including all other elements) | 24,791 | 7961 | ||
| Cost per participant (excluding training) | 459.09 | 147.43 | ||
| Cost per participant including training | @ 40 | 499.09 | @ 13 | 160.43 |
Using fees paid to MIPs increased total costs by 20% for both groups. Reducing them by 15% has reduced total costs by 10% for intensive and 11% for less intensive groups, respectively. The effect of using median rather than mean MIP unit costs is small. Although the costs of group sessions would be considerable if participants attended as per protocol, the fact that so few group sessions were delivered within the study means that the effect on total costs of removing GF training and the delivery of group sessions is small.
No participants received the full interventions per protocol. The costs reported here are as they were incurred. Although the WILMA trial was only a feasibility study, all outcomes reported here relate to effects of the interventions as received by study participants. Thus, although they cannot be related to any of the outcomes, Table 41 indicates what it might cost to deliver the complete intensive intervention to 54 participants and the complete less intensive intervention to 54 participants assuming full participation and excluding GF training and group sessions.
| Intervention delivery elements | Intensive group (n = 54) | Intensive group cost (£) | Less intensive group (n = 54) | Less intensive group cost (£) |
|---|---|---|---|---|
| Face-to-face sessions | 330 sessions @ 1 hour | 23,100 | 110 sessions @ 1 hour | 7700 |
| Cost of hiring the venue per session | 330 sessions @ £10 | 3330 | 110 sessions @ £10 | 1100 |
| Telephone sessions (value of time) | 495 sessions @ 20 minutes | 4033 | 110 sessions @ 20 minutes | 896 |
| Telephone (cost) | 9900 minutes @ 14 ppm | 1386 | 2200 minutes @ 14 ppm | 308 |
| Total cost | 31,849 | 10,004 | ||
| Cost per participant (excluding training) | 589.80 | 185.26 | ||
| Total cost per participant including apportioned training | @ £40 | 629.80 | @ £13 | 198.26 |
NHS resource use
Complete-case analysis of NHS resource use by the three groups and associated costs at baseline and 12-month follow-up are shown in Tables 42 and 43, respectively. Unit costs are shown in Appendix 8. Baseline resource-use data are historic and are not included in the 12-month resource-use and cost figures. At baseline, participants in the less intensive group were (historically) higher users of NHS resources. The mean cost of resource use in the 3 months preceding baseline in the less intensive group was more than double that in the control group (£137 and £58, respectively).
Costs at 12-month follow-up are reported in Table 42. ‘Other services’ refers to weight control services paid for by study participants. These data were collected to monitor whether or not the WILMA trial interventions might have been substituting for private sector weight control services. They are not included in the CEA in Table 43. The results show that, although the control group and less intensive groups spent roughly the same on non-NHS WLM services at baseline [mean (SD): control = £79 (£86), less intensive = £69 (£89)], expenditure after 12 months of follow-up was much lower for the controls than for the less intensive group [mean (SD): control = £81 (£62), less intensive = £121 (£126)].
| Services | Control (n = 43) | Less intensive (n = 39) | Intensive (n = 44) | |||
|---|---|---|---|---|---|---|
| Baseline | 12 months | Baseline | 12 months | Baseline | 12 months | |
| GP surgery visit | 0.81 (0.85) | 2.30 (2.60) | 2.08 (4.50) | 2.28 (2.16) | 0.75 (0.92) | 1.68 (1.79) |
| Nurse surgery visit | 0.63 (0.87) | 1.12 (1.92) | 0.51 (1.43) | 0.89 (1.31) | 0.52 (0.85) | 0.75 (1.14) |
| Other HP surgery visit | 0.05 (0.31) | 1.09 (2.77) | 0.28 (0.76) | 0.41 (1.14) | 0.11 (0.49) | 1.41 (3.38) |
| GP home visit | 0 | 0.07 (0.34) | 0 | 0 | 0.05 (0.21) | 0 |
| Nurse home visit | 0 | 0 | 0 | 0.15 (0.96) | 0 | 0 |
| Other HP home visit | 0 | 0.30 (1.49) | 0 | 0.15 (0.67) | 0 | 0.02 (0.15) |
| A&E visit | 0.05 (0.21) | 0.28 (0.98) | 0.03 (0.16) | 0.21 (0.50) | 0.05 (0.21) | 0.07 (0.25) |
| Hospitalisations (number) | 0 | 0.07 (0.26) | 0.03 (0.16) | 0.05 (0.22) | 0.02 (0.15) | 0.11 (0.39) |
| Inpatient days | 0 | 0.09 (0.37) | 0.08 (0.48) | 0.28 (1.23) | 0.02 (0.15) | 0.16 (0.68) |
| Services | Control (n = 43) | Less intensive (n = 39) | Intensive (n = 44) | |||
|---|---|---|---|---|---|---|
| Baseline | 12 months | Baseline | 12 months | Baseline | 12 months | |
| GP surgery visit | 35.00 (36.60) | 99.00 (111.63) | 89.31 (193.41) | 98.13 (93.04) | 32.25 (39.48) | 72.32 (76.90) |
| Nurse surgery visit | 8.60 (11.95) | 15.28 (26.25) | 7.02 (19.58) | 12.29 (17.98) | 7.16 (11.62) | 10.26 (15.66) |
| Other HPs surgery visit | 0 | 4.65 (16.30) | 1.22 (5.81) | 0 | 1.16 (7.69) | 5.80 (26.14) |
| GP home visit | 0 | 7.67 (37.15) | 0 | 0 | 5.00 (23.18) | 0 |
| Nurse home visit | 0 | 0 | 0 | 2.94 (18.36) | 0 | 0 |
| Other HP home visit | 0 | 0 | 0 | 0 | 0 | 0 |
| A&E visit | 1.91 (8.74) | 11.44 (40.34) | 1.05 (6.56) | 8.41 (19.23) | 1.86 (8.64) | 2.79 (10.45) |
| Hospitalisations | 0 | 20.33 (80.02) | 16.81 (105.01) | 66.07 (289.34) | 4.97 (32.95) | 35.56 (153.20) |
| Medicines | 12.63 (16.77) | 19.16 (26.77) | 21.35 (35.29) | 40.46 (56.14) | 20.01 (37.09) | 36.27 (56.69) |
| Other services | 79.00 (86.46) | 80.84 (62.10) | 69.27 (89.44) | 120.87 (126.11) | 63.75 (94.37) | 79.39 (96.14) |
| Intervention cost (per participant) | 167.96 | 509.74 | ||||
| Total NHS costa | 58.13 (55.36) | 177.55 (174.48) | 136.77 (243.85) | 396.25 (359.15) | 72.41 (85.55) | 672.75 (233.57) |
Unadjusted mean differences in NHS resource use and costs are shown columns 2 and 5, respectively, in Table 44. Bootstrapped mean differences of the same variables adjusted for age, gender, baseline BMI and the baseline value are shown in columns 3 and 6. Bias-corrected bootstrapped 95% CIs are shown in columns 4 and 7. Total NHS costs excluding intervention costs are higher for the less intensive group and lower for the intensive group – both compared with control – but neither difference is statistically significant. When intervention costs are included, total NHS costs are statistically significantly higher for both intervention groups than controls.
| Services | Control vs. less intensive | Control vs. intensive | ||||
|---|---|---|---|---|---|---|
| Unadjusted mean difference (less intensive – control) | Bootstrapped differencea | Bootstrapped 95% CIb | Unadjusted mean difference (intensive – control) | Bootstrapped differencea | Bootstrapped 95% CIb | |
| Resource quantities | ||||||
| GP visit | –0.02 | –0.41 | –1.55 to 0.65 | –0.62 | –0.69 | –1.71 to 0.26 |
| Nurse visit | –0.22 | –0.14 | –0.97 to 0.62 | –0.37 | –0.32 | –1.10 to 0.36 |
| Other HP visit | –0.68 | –0.89 | –2.05 to 0.14 | 0.32 | 0.24 | –1.04 to 1.63 |
| A&E visit | –0.07 | –0.07 | –0.54 to 0.23 | –0.21 | –0.22 | –0.65 to 0.05 |
| Hospitalisation (number) | –0.02 | –0.03 | –0.15 to 0.08 | 0.04 | 0.04 | –0.14 to 0.20 |
| Inpatient days | 0.19 | 0.16 | –0.17 to 0.55 | 0.07 | 0.05 | –0.15 to 0.30 |
| Resource costs (£) | ||||||
| GP visit | –0.87 | –17.82 | –66.80 to 25.88 | –26.68 | –29.77 | –72.95 to 10.04 |
| Nurse visit | –2.99 | –1.92 | –12.54 to 8.00 | –5.01 | –4.43 | –14.67 to 4.35 |
| A&E visit | –3.03 | –3.02 | –21.27 to 9.40 | –8.65 | –9.12 | –26.74 to 2.46 |
| Hospitalisation | 45.73 | 38.75 | –36.97 to 134.89 | 15.22 | 11.76 | –33.07 to 66.37 |
| Medicines | 21.30 | 10.76 | –0.21 to 22.00 | 17.11 | 7.45 | –1.89 to 16.68 |
| Other services | 40.03 | 38.61 | –0.60 to 75.07 | –1.45 | 1.24 | –31.63 to 34.93 |
| Total NHS costs (excludes intervention) | 50.75 | 15.87 | –89.31 to 140.19 | –14.54 | –25.99 | –108.62 to 63.37 |
| Total NHS Cost | 215.95 | 183.84 | 80.59 to 306.72 | 486.82 | 483.75 | 400.96 to 568.19 |
Health effects and cost–utility analysis
Mean EQ-5D scores are shown in Table 45. The control group had slightly higher scores at baseline and this was maintained at both follow-up points.
| Measure | Control (n = 43) | Less intensive (n = 39) | Intensive (n = 41) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | 6 months | 12 months | Baseline | 6 months | 12 months | Baseline | 6 months | 12 months | |
| EQ-5D | 0.836 (0.18) | 0.862 (0.17) | 0.816 (0.18) | 0.776 (0.29) | 0.749 (0.32) | 0.751 (0.32) | 0.796 (0.21) | 0.806 (0.22) | 0.813 (0.18) |
Bootstrapped between-group differences in mean QALYs, adjusted for age, gender, baseline BMI and baseline EQ-5D are shown in Table 46. The adjusted differences between intervention groups and controls are small and not statistically significant.
| Measure | Less intensive minus controls | Intensive minus controls | ||||
|---|---|---|---|---|---|---|
| Unadjusted mean difference | Bootstrapped difference | Bootstrapped 95% CIa | Unadjusted mean difference | Bootstrapped difference | Bootstrapped 95% CIa | |
| QALY | –0.087 | –0.032b | –0.080 to 0.014b | –0.039 | 0.001b | –0.036 to 0.041b |
Difference in costs and QALYs are shown in Table 47. The less intensive intervention is less effective and more costly, meaning that it is dominated by the control, with a negative incremental cost-effectiveness ratio (ICER) which falls in the north-west quadrant of the cost-effectiveness plane (see Figure 18). The intensive intervention is marginally more effective than control but more costly, producing an ICER of £483,750. These results are subject to considerable uncertainty because the differences in QALYs (see Table 46) are not statistically significant.
| Measure | Less intensive minus control | Intensive minus control |
|---|---|---|
| Difference in QALYs | –0.032 (less effective) | 0.001 (more effective) |
| Difference in costs | (More costly) £183.84 | (More costly) £483.75 |
| Cost-effectiveness | Dominated by control | ICER = £483,750 |
One-way sensitivity analyses
Two one-way sensitivity analyses on cost-effectiveness were undertaken to reflect two of the sensitivity analyses on costs, that is:
Sensitivity analysis 1: changing face-to-face session unit costs to reflect the amount paid to MIPs increased intervention costs from £509.74 to £662.59 (intensive) and from £167.96 to £186.04 (less intensive).
Sensitivity analysis 2: changing face-to-face session unit costs to reflect the salary of the lowest paid MIP decreased intervention costs from £509.74 to £459.09 (intensive) and from £167.96 to £160.43 (less intensive).
Hospitalisation is a high-cost item and, as no data were collected regarding the reasons for hospitalisation, a third sensitivity analysis was undertaken.
Sensitivity analysis 3: intervention costs as in baseline analysis but hospitalisation costs removed from NHS costs.
Results of the sensitivity analyses are given in Table 48. In all cases the less intensive intervention remained dominated by controls and ICERs for intensive intervention all remained high.
| Measure | Less intensive minus control | Intensive minus control |
|---|---|---|
| Difference in QALYs | –0.032 (less effective) | 0.001 (more effective) |
| Difference in costs: sensitivity analysis 1 | (More costly) £201.91 | (More costly) £636.60 |
| Cost–utility | Dominated by control | ICER = £636,600 |
| Difference in costs: sensitivity analysis 2 | (More costly) £176.30 | (More costly) £433.10 |
| Cost–utility | Dominated by control | ICER = £433,100 |
| Difference in costs: sensitivity analysis 3 | (More costly) £145.67 | (More costly) £472.49 |
| Cost–utility | Dominated by control | ICER = £472,490 |
Probabilistic sensitivity analysis
A probabilistic sensitivity analysis was carried out using a non-parametric bootstrap method, which allows both costs and QALYs to be varied from their joint distribution. The scatterplot in Figure 18 shows the uncertainty surrounding the cost–utility of intensive versus control based on 5000 bootstrapped resamples. All points represent higher costs for the intensive intervention compared with controls, and most show reduced QALYs.
FIGURE 18.
Cost-effectiveness plane for intensive intervention compared with control: adjusted QALYs and costs.

Figure 18 shows the probability of the intensive intervention being cost-effective, that is having an ICER below a range of WTP thresholds. The adjusted curve (Figure 19) shows only about a 9% probability that intensive intervention is cost-effective at a WTP threshold of £20,000 per additional QALY, which is the lower threshold used by NICE.
FIGURE 19.
Cost-effectiveness acceptability curve for control compared with intensive: unadjusted and adjusted QALYs and costs.
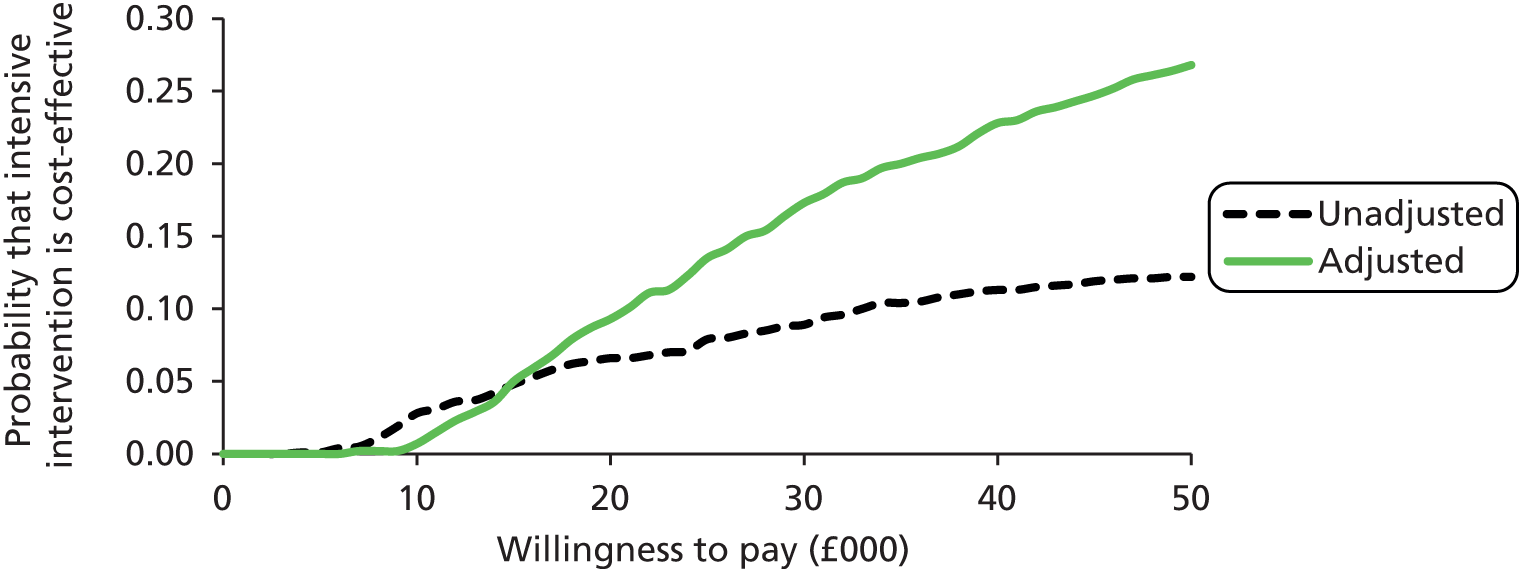
Body mass index effects and cost-effectiveness analysis
Bootstrapped differences between groups in mean BMI scores, adjusted for age, gender and baseline BMI are shown in Table 49.
| Measure | Less intensive minus controls | Intensive minus controls | ||||
|---|---|---|---|---|---|---|
| Unadjusted mean difference | Bootstrapped difference | Bootstrapped 95% CIa | Unadjusted mean difference | Bootstrapped difference | Bootstrapped 95% CIa | |
| BMI | 0.75 | –0.24b | –1.57 to 1.09b | 0.83 | –1.17b | –2.47 to 0.11b |
The negative adjusted differences suggest that both intervention groups show decreased BMI compared with controls at 12 months’ follow-up, but the differences are small and not statistically significant.
A CEA assessing costs against the primary outcome of the study (BMI) was also undertaken. The results are shown in Table 50. In the cost–utility analysis above, higher QALYs reflect greater health gain. A positive effect is thus shown when the difference in QALYs is in favour of an intervention over its comparator. In the case of BMI, however, higher values reflect worse outcomes. In order to produce an ICER in which, as by convention, a positive denominator reflects a positive effect, the figures in Table 50 are those for control minus intervention.
| Measure | Control minus less intensive | Control minus intensive |
|---|---|---|
| Difference in BMI | 0.24 (more effective) | 1.17 (more effective) |
| Difference in costs | (More costly) £183.84 | (More costly) £483.75 |
| ICER | £766.00 per unit of BMI reduction | £413.46 per unit of BMI reduction |
These results show both interventions to be more effective than controls, with the intensive intervention being more effective than the less intensive intervention. Both interventions were more costly, producing positive ICERs of £766 and £413 per unit reduction in BMI for the less intensive and intensive interventions, respectively. There was much uncertainty around these results because differences in BMI did not approach the traditional level of significance (see Table 49). These point estimates fall on the north-east quadrant of the cost-effectiveness plane.
Probabilistic sensitivity analysis
A probabilistic sensitivity analysis was carried out using a non-parametric bootstrap method as in the cost–utility analysis (see Health effects and cost–utility analysis). The scatterplot in Figure 20 shows the joint uncertainty of costs and effects (BMI) for the intensive intervention, based on 5000 bootstrapped resamples. All replications show higher costs for the intensive intervention than for controls, with approximately 95% showing increased effect (lower BMI).
FIGURE 20.
Cost-effectiveness plane for control vs. intensive: adjusted BMI and costs.
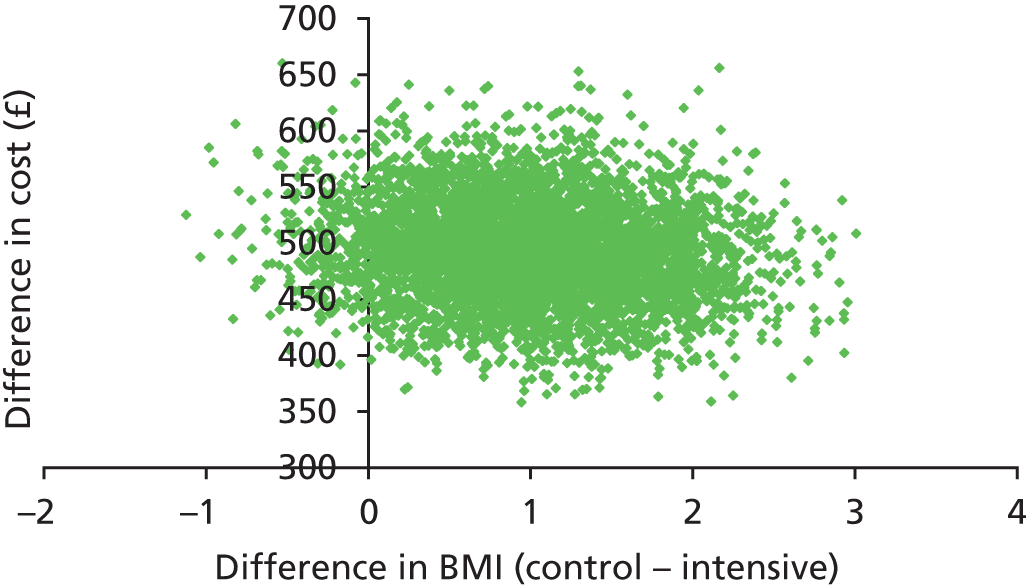
The curve in Figure 19 shows the probability of the ICER for the intensive intervention being below the NICE WTP threshold of £20,000 per extra QALY. To repeat the exercise here would require us to predict how much the NHS would be willing to pay for a 1-kg/m2 reduction in BMI. That figure would be only a fraction of the identified WTP threshold for an extra QALY but, in the absence of any guidance on what that figure might be, no attempt has been made here to produce a cost-effectiveness acceptability curve with respect to BMI.
Summary
It would be inappropriate to conclude that the WILMA trial interventions are not cost-effective on the basis of the data collected in this feasibility study. Apart from the issue of the reduced sample size, the early termination of the study and the change to a feasibility trial meant that no participants received the full intervention as described in the protocol. Moreover, and perhaps more importantly, the WILMA trial is about WLM, which suggests that a much longer follow-up period (as in the initial trial) is needed to establish the effect to which weight loss is maintained in the longer term.
Chapter 10 Discussion and conclusions
Summary of main findings
This study assessed the acceptability and feasibility of a theory-based intervention at two levels of intensity for WLM in participants who had initially lost at least 5% of their body weight. We also explored the impact of the intervention on BMI and a number of other secondary outcomes at 12 months’ follow-up and assessed mediators associated with change including self-efficacy, social support, self-monitoring and action-planning (including implementation intentions), habit formation and intrinsic motivation (see Chapter 5). Finally, process and cost-effectiveness evaluations were also conducted.
The trial recruited 166 eligible people and follow-up rates were excellent, 84% at 6 months and 12 months. There were no systematic differences between those dropping out and those remaining in the study. Adherence to face-to-face MI was also high, 87% overall, 83% and 91% in the intensive and less intensive group, respectively. MI sessions delivered by telephone were less successful for a variety of reasons, including the logistics of arranging them and practitioner and participant concerns with this medium of delivery. The key feasibility issues related to the difficulty of delivering the group-based support sessions and also recruitment into the trial.
The three arms were broadly similar in terms of key demographics and comorbidities. More women than men were recruited, which presents a problem for future studies attempting to generalise their results to the male population. The between-group difference in mean BMI at 12 months, controlling for baseline variables, indicated that although not statistically significant, the intensive arm had a difference in BMI relative to the control group, which would be considered clinically important, that is lower by 1 kg/m2. 11–14 This also excluded a potentially harmful effect (worse BMI than controls). The difference between the less intensive arm and controls would not be considered clinically relevant, but it was in the same direction as the intensive arm, giving some plausibility to a potential dose–response effect as was a priori predicted. The same pattern was seen with weight, with a non-significant difference between both intervention arms and control. The potential size of the effect for the intensive intervention is relatively large and likely to be clinically meaningful. 11–14 To explore the potential efficacy of the interventions, CACE analyses were conducted and indicated, after adjusting the primary analysis for compliance, that average BMI was 1.23 points lower in the intensive arm than in the control group, but this difference was not statistically significant. When using weight as the outcome, the intensive intervention led to a statistically significant lower average weight (3.7 kg).
Waist circumference showed the same pattern of slightly lower values in both intervention groups relative to controls. The proportion of weight maintainers (i.e. those whose 1-year follow-up weight was the same as or lower than their weight at baseline) was not significantly different between the intensive (56%) and control arms (46%), but a smaller proportion of the less intensive group maintained or lost weight (37%). However, the formal analysis of maintenance in this group revealed a wide CI around the odds ratio, which was nearly symmetrical at about 1 (95% CI 0.23 to 1.56), which indicates a very small effect if one exists at all. There was evidence of a statistically significant reduction in the number of days of binge eating in the intensive group (60% less than control). For the other secondary outcomes (IPAQ, GHQ-12, DINE fibre, EQ-5D, AUDIT-C, HSI), there was no evidence of any difference between groups. On the DINE questionnaire there was evidence that participants in the intensive arm reduced fat intake statistically significantly more than controls. There is some evidence that participants in the less intensive arm may have reduced fat intake more than controls, on average, but the difference was not statistically significant. In the case of the DINE healthy eating score, there was some evidence of an effect of the intervention in the intensive arm (non-significant). However, there were a considerable number of missing data for DINE and this finding may, therefore, be subject to bias.
Interpretation of the mediation analyses results is limited by the small sample size, the absence of a statistically significant effect of the intervention on the primary outcome and the absence of any statistically significant between-group differences in the analyses of mediators. When exploring how much of the effect of the intervention on BMI is mediated by any mediator, two variables – weight self-efficacy and diet habit index – showed positive effects. Five of the 10 mediators had a statistically significant association with outcome, which indicates that there is a relationship between some of the mediators and BMI, in the expected direction (increases in weight self-efficacy, exercise self-efficacy, perception that family/friends support and encourage positive exercise habits, positive habits related to healthy eating and positive habits related to exercise are associated with decreases in BMI at the 12-month follow-up), but the mediation analysis is largely unable to determine the potential causal mechanisms behind this relationship. The intervention does not appear to have influenced these mediators; however, the analyses are likely to be underpowered.
The process evaluation sought to assess the delivery of the intervention, adherence, participants’ views of the intervention, MIPs’ experiences of delivering the intervention, as well as testing the logic model. The process evaluation framework assessed eight key components: context, reach, fidelity, exposure, recruitment, retention, contamination and theory testing (see Chapter 6). The intervention was successfully delivered in the community by trained practitioners. There was good adherence, although there were some issues with the MI delivery by telephone. Use of the website for self-monitoring was also not as high as anticipated. The face-to-face MI was delivered with good fidelity, and participants seem to have implemented at least some intervention components. There did not appear to be any issues with contamination, as few participants in the intervention group indicated they had shared information with the controls.
The MIPs were very positive about the intervention (see Chapter 7); however, they felt that two sessions was not enough for some participants while six sessions was too many for others and the MIPs would have preferred the number of sessions to be based on ‘need’ rather than chance (i.e. randomisation) as in the study. Future studies could look to accommodate this in their design, whereby the intervention arm could receive MI that is tailored by the MIP up to perhaps six sessions maximum and the data are analysed to explore dose and its relationship to outcome. They also suggested that three sessions might be better for the less intensive intervention, that the time delay between telephone sessions in the less intensive group should be shortened and that face-to-face delivery was preferable to telephone delivery. MIPs felt that participants benefited from the supportive ongoing relationship, which allowed people space to open up about their weight management issues as well as develop goals and plans to achieve them. They were very positive about implementing such an intervention in ‘the real world’; however, they cautioned that wider social and environmental factors might mitigate the effect of such a brief intervention.
The interviews indicated that participants were satisfied with the intervention. They appreciated the counselling as it facilitated discussion of their weight issues in a safe, caring and non-judgemental environment. They valued the psychological expertise of the practitioners as well as the support and reinforcement, and some liked the accountability provided in seeing the MIP and felt it increased their motivation. Participants said that sessions gave them increased insight and understanding that was different from their other sources of support as well as encouragement to find their own solutions which helped boost their feelings of control in relation to weight management.
More participants in the intensive arm (than in the less intensive arm) were happy with the number of sessions and, like the MIPs, participants felt that the number of sessions should be based on the circumstances of the individual (see Chapter 8). The higher overall dropout in the less intensive arm could be interpreted as a lack of acceptability of the less intensive intervention. They also said that long-term support or contact was important for maintenance. Most preferred the face-to-face to the telephone sessions, as some did not like talking about personal or in-depth issues over the telephone; however, the telephone sessions were felt to be useful for ‘checking in’. Participants’ use of the WILMA trial website was relatively limited and this was owing to lack of time and motivation as well as their previous or ongoing use of a commercially available alternative such as Slimming World. This type of self-monitoring via either the WILMA trial website or commercial websites was used by most participants and was a popular monitoring resource. However, use of the website tended to decline over time, which could be because either motivation declined or diet and exercise strategies became more habitual.
Some participants said that they had shared information with family and friends, and some reported a positive impact on the behaviour of family or friends. This took the form of unintentional weight losses, uptake of healthier lifestyles and greater awareness of healthy diet and exercise strategies. However, it was difficult to directly attribute the intervention itself to these changes. Reasons for not finding the sessions useful included that they were not directive enough and did not include any new information. Most participants did not get the opportunity to take part in the group sessions, but it was generally felt these would have been an important aspect of the intervention.
The qualitative data provided insights into the mediators of intervention effect. The most important was ongoing motivation, which was strongly influenced positively and negatively by the support of others including family, friends, peers and professionals. The idea of positive reinforcement, which could come from direct reinforcement from peers or family as well as just maintaining or losing weight, was also important. In this regard, self-monitoring in the form of regular self-weighing was seen as useful. Routine and habit formation were described as crucial to longer-term maintenance of healthy behaviours. Participants described a number of barriers to managing their weight, which included enviromental influences, cultural attitudes around food and eating, and significant life events.
The economic evaluation identified the total cost per person of receiving the intensive and less intensive interventions, including apportioned costs of training the MIPs and GFs, to be £510 and £168, respectively (see Chapter 9). Subsequent use of NHS resources was reduced in the intensive group compared with controls and increased for the less intensive group, but neither difference was statistically significant. The addition of intervention costs meant that total NHS costs were statistically significantly higher in both groups than in controls.
The cost–utility analysis indicated a small QALY gain for the intensive group (0.001) and a small QALY loss (0.032) for the less intensive group compared with controls, but neither difference was statistically significant. As total NHS costs for both intervention groups were higher than for controls, the less intensive intervention was dominated (i.e. not cost-effective) and the intensive intervention produced a positive ICER of £483,750 per additional QALY gained. Probabilistic sensitivity analysis showed the intensive intervention to have only a 9% probability of being cost-effective at the current lower NICE WTP threshold of £20,000 per extra QALY gained. The CEAs using adjusted BMI as the outcome indicated that both interventions were more effective than control, with the intensive intervention being the more effective although neither difference was statistically significant. As total NHS costs for both intervention groups were higher, both produced positive ICERs (£414 intensive, £766 less intensive) per kg/m2 reduction in BMI.
Strengths and limitations
This feasibility trial has a number of strengths. It is the first trial of an intervention for WLM for adults in the UK and, as far as we are aware, it is one of only three trials evaluating an intervention for WLM for adults who had already lost weight before entering the study. Most other RCTs have included a weight loss element in their design. It was conducted rigorously, assessed a range of relevant outcomes and included a CEA. We combined both quantitative and qualitative methods, which provided important insights. We achieved excellent retention rates at 12 months, and excellent adherence to the key face-to-face MI element of the intervention. The study recruited a diverse range of participants from different geographical areas in Wales and a few from the East Midlands.
We were able to conduct in-depth interviews with a large sample of participants that generated rich data on their views of the intervention as well as their general weight management experiences. We also sought the views of those delivering the intervention. Both of these are important in terms of the design of any future trial as well as potential roll-out. We developed a logic model and theory of the intervention, which was tested using both the qualitative data and mediation analyses. The measurement of mediators is rarely completed in intervention research. 91,92 We developed a detailed process evaluation framework and were careful to assess intervention fidelity. The intervention itself was delivered with good fidelity. There also did not appear to be any problems with contamination between study arms. The intervention is safe, as the single SAE reported was related to a pre-existing condition and not to the intervention.
We involved patient representatives at all stages of the trial and this has benefited not only the trial but also the other team members. The involvement of a patient representative early on in the development work proved invaluable and led to the decision to involve her as a co-applicant. Our experience with user involvement throughout the study has been very positive and we feel that it led to an enhanced study design as well as assisting us during the running of the trial. Feedback from our user representative indicated a number of pointers for future patient and public involvement. In terms of positive aspects of her experience, she felt that the team made her feel that her contribution was important and this made it easier to engage with the study and the team. She felt listened to and was asked for her opinion on all aspects of the study. When asked to review documents she felt she was never rushed and that her comments or suggestions were listened to, acted on or acknowledged and, if not instigated, the reasons were explained. She felt that her own experience of yo-yo dieting and weight control problems gave her a unique and valuable perspective on the study. In terms of areas for improvement, she suggested a more formal induction into the trials unit and the research process would be useful, as well as at the beginning a more formal introduction to the members of the trial management team and their areas of expertise. She also suggested that it would have been helpful to have more information on MI and the different behaviour change models.
The original study was an adequately powered, pragmatic RCT which aimed to evaluate the impact of the intervention on BMI at 3 years’ follow-up. However, a number of issues impacted negatively on the trial, including governance and challenges related to accessing NHS costs as well as issues related to verification of 5% weight loss. We received 1284 EOIs from individuals who had heard about the study, but the majority of those were unable to provide independent evidence of 5% weight loss. Despite a comprehensive recruitment strategy, we were unable to recruit an adequate number of participants in a reasonable timescale. The governance and NHS costs issues impacted directly on our ability to recruit as we were delayed in opening the study in England by around 12 months.
Because of these difficulties, the study became a feasibility trial with a shortened follow-up of 12 months. Thus, the trial was underpowered to demonstrate effectiveness or cost-effectiveness and we are limited in our ability to draw conclusions from the quantitative analyses. For a future study, based on the results observed in this study (i.e. assuming a difference in BMI between the intensive intervention and control groups of 1 kg/m2, a SD of 6.5 and a correlation between baseline and follow-up BMI of 0.88) and assuming we test at the 5% significance level and require 90% power, we need 201 per group for analysis. Assuming 30% attrition (over 3 years) we would need 576 in total. If the effect were halved in size over 3 years (to a difference in BMI of 0.5 kg/m2) we would require 2292 in total for analysis. If it increased by 50% (a difference in BMI of 1.5 kg/m2) we would require 258 in total for analysis.
The shortened follow-up did not facilitate exploration of longer-term maintenance of weight loss. We were unable to test the full intervention owing to issues with running the groups, which was partly due to slow recruitment rates. There were also some issues with delivery of the telephone MI. We were unable to recruit many men or those from lower socioeconomic groups or of ethnicities other than white British. There are therefore potential limitations to the generalisability of the results. Despite recruiting from a wide range of sources, it is likely that we recruited a non-representative group of participants. Most of the outcome measures used in the study were self-reported, and there are limitations of self-report measures, including recall bias and under-reporting139–141 as well as social desirability effects. 142,143 These effects are likely to be strong in these behaviours. 144,145 It is also likely that some of these measures, particularly diet and physical activity as well as some of the mediators, were not sufficiently sensitive to detect small but potentially important changes in behaviour.
Owing to uncertainty about continuation of the study, some of the 6-month follow-up interviews were delayed and were completed quite a while after the face-to-face elements of the intervention were delivered. However, they were all completed within 4–9 months of the last face-to-face MI session. This may have had an impact on the participants’ ability to remember the different aspects of the intervention. As is usual in pragmatic trials, it was not possible to blind participants to treatment arm or those completing follow-up.
Although participants had used a range of strategies for their initial weight loss, there was a predominance of people who had attended weight loss groups, probably partly because of our recruitment strategies. This may have impacted on the effect of the intervention since there was overlap in approaches and aims, although those attending weight loss groups were distributed roughly evenly between control and intervention arms. This also made it difficult to attribute weight management activities and attitudes exclusively to the intervention, particularly as some participants relied on Slimming World for maintenance as well as weight loss. There was a predominance of female participants although there was evidence that men also benefited from the intervention. There did appear to be some differences in attitudes and needs between men and women, which needs further exploration. Few participants were in a purely ‘maintenance’ stage, with many still attempting to lose weight, and, consequently, this may have impacted on the WLM intervention.
Interpretation and comparison with previous studies
The key feasibility issue of slow recruitment is perhaps unsurprising, as issues with recruitment are common in RCTs. 146 A HTA monograph exploring this issue that examined 114 funded trials found that only 31% successfully recruited to target and 45% achieved less than 80% of the original sample size. 147 The authors also noted that it is more to difficult to recruit to target in non-drug trials. Additionally, it is likely that the rather complicated inclusion criteria, in particular the requirement of written verification of weight loss, compounded the issues we experienced with recruitment. Most of the 1284 people who expressed an interest in taking part in the trial were unable to provide written verification. We devoted a significant amount of resource to identifying potential participants with 5% weight loss from primary care and EOR, with limited success relative to effort (although primary care did provide 39% of recruits). This was primarily because records kept by GPs and EOR practitioners were not sufficient for our verification requirements. GPs often record weight but lack systematic monitoring, with the result that a 5% loss within a 12-month period is often not recorded in an easily searchable manner. Therefore, when written verification of weight loss is an entry requirement, recruitment routes linked to current or recent weight loss programmes (slimming clubs or concurrent weight loss trials) are likely to be most effective, although this may limit generalisability. In addition, delays in obtaining treatment and service support costs (particularly in England), as well as governance delays, were related to our recruitment problems. Although the landscape has changed considerably since this trial, consideration should still be given to these issues as well as to obtaining infrastructure support and how this might vary between the devolved nations.
Our reduced sample size and thus reduced power means that we are able to draw only limited conclusions about the impact of the intervention on BMI. This sample size is, however, considerably larger than many trials of WLM interventions. 148–152 In a systematic review of WLM following at least 1 month of intervention and then 1 year of no intervention, the sample sizes of the 12 included studies152 (with 22 intervention groups)153–169 ranged from 44170 to 241,171–173 with only three studies having a larger sample size than the present study. There are no studies of MI for WLM; however, in a review of studies using MI as an intervention for weight loss, only one-third of the 12 included studies had a larger sample size than the current study and the range was 22–599. 64
Our retention rate for the trial is excellent and compares favourably with other trials of complex behavioural interventions for weight loss or WLM, in which dropout rates can be high even at 1 year. A systematic review of long-term weight loss interventions found an average dropout of 29% at 1 year. 25 In the MI review for weight loss,64 two-thirds of included studies had a higher dropout than the current study with a range of 8–35%; only one study had a longer follow-up than this study (18 months). 53
With regard to the elements considered in the process evaluation, the intervention was delivered with good fidelity. There was evidence that practitioners covered the topics required by the WILMA study. The participants appeared to receive the intervention as intended because understanding of the purpose and methods of the counselling sessions was demonstrated. However, a couple of men had unfulfilled expectations of the sessions, anticipating a much more directive approach. In terms of adherence to the intervention, we had excellent adherence to the key face-to-face MI, at 87% overall. This compares favourably with adherence in other counselling-type interventions. 53,59,174 However, we did have an issue with the group-based aspect of the intervention. Delivery of local group sessions on a rolling basis did not appear to be feasible, although the low recruitment rates had an impact on the ability to run these as planned. Other, less resource-intensive and less logistically challenging, approaches to providing social support that do not depend on a minimum recruitment rate should be considered in the design of any future trial. Telephone MI sessions were also not as successful as the face-to-face MI. There were a number of reasons for this, some of which could be addressed in future studies, including more training for delivering MI over the telephone, better reimbursement for MIPs to account for time taken in arranging these sessions, longer sessions and possibly sessions closer together, particularly for those in the less intensive arm. However, it was difficult to gauge the adherence rate because of poor return of paperwork. It is likely that more of these were completed than we have records for and participants in many cases found this contact useful. Evidence also indicates the importance of ongoing contact for WLM. 38,175,176
For a feasibility study, both the qualitative and quantitative results look encouraging. As expected, there are few statistically significant results owing to the analyses being underpowered; however, there are promising mean differences and CIs on important outcomes. The intensive arm has a consistently larger treatment effect and generally in the direction of benefit, representing a clear signal that the intensive treatment potentially leads to improvements on a wide range of health-related outcomes. This leads us to suggest that any future trial should consider comparing only the intensive intervention with a control. Although weight loss in neither treatment arm was statistically significantly different to that in the control group, the odds of maintaining weight loss was 43% higher in the intensive arm than in the control group. According to CACE analyses, the average weight loss was 3.69 kg lower in the intensive arm relative to the control group. In the case of BMI, average BMI was 1.23 kg/m2 lower in the intensive arm relative to the control group. This compares well with other trials, and this degree of difference is likely to be clinically significant in this group of individuals, many of whom are probably at increased risk of cardiovascular disease. Several studies indicate that loss of 2–5 kg weight can lead to reductions in cardiovascular risk factors. 11–14,177 In a trial of MI delivered in five sessions in primary care, the mean difference in BMI between the intervention and control groups was 0.36 kg/m2 at 12 months (from end of intervention) and 0.1 kg/m2 at 6 months. 178 A recent systematic review of trials of behavioural interventions (focusing on diet and physical activity) to help individuals maintain weight loss found an average weight difference of –1.56 kg in weight regain relative to controls at the 12-month follow-up. 35 If the findings in this study were true differences, then this compares favourably with other trials. The Barte et al. 152 systematic review of 12 studies found that the percentage of initial weight loss that was maintained after 1 year’s unsupervised follow-up ranged from 25% to 88% and the average was 54%. Four of these studies had an intervention period of 3 months or less, so were similar in length of follow-up to this study. This percentage maintenance has also been found in other systematic reviews20,149 that have reported 50% maintenance at 1 year post intervention.
With regard to the other secondary outcomes, there are few indications of an effect from the intervention, with the exception of the DINE fat and healthy eating scores and the number of days of binge eating. However, there are issues with the sensitivity of the measures to detect an effect, and measuring physical activity and diet accurately are particularly problematic. 179,180
With regards to the theory testing and the mediation analyses, we are limited in what conclusions can be drawn from the analyses because they are underpowered. There does appear to be a relationship between a number of the mediators and outcomes, but we cannot say whether or not changes in these are influenced by the intervention. In terms of studies using mediation analyses to look at the impact of MI, the evidence base is limited; however, there is mixed evidence of the impact of MI on self-efficacy. 181–184 An impact of MI on self-monitoring was found in one study53 while another that explored the link between MI and motivation found that MI is related to increased autonomous motivation. 183 One study found that an intervention using the core principles of MI led to improved planning as it generated more detailed action plans and longer duration of physical activity than the control. 99 One other study has noted the importance of some of these mediators in WLM, including self-efficacy and intrinsic motivation. 185 A recent systematic review looking at mechanisms of MI within health behaviours found that MI ‘spirit’ and motivation were the most promising mechanisms of MI but concluded that there is a dearth of research exploring this issue, and more studies need to be completed. 184
Another potential concern with the assessment of mediators is that the measurement tools we used may not have been sufficiently sensitive to detect a change. In addition, the timing of the measurement of the mediators could be important. If assessment does not occur at the critical time, then this could affect our ability to detect the impact of the intervention on these mediators and, thus, on outcome. We had originally planned a 6-month time point for assessment of mediators as we estimated this would be after all the face-to-face sessions would have been delivered and, therefore, participants would have had a full dose of intervention to influence these mediators. In the majority of cases this did happen, and 39 out of 54 participants in the intensive arm received five or six sessions of MI before their 6-month assessment.
There is some support in the qualitative data for the theoretical underpinning of the intervention and thus the different elements of the logic model. Ongoing motivation was seen as central; however, other aspects, such as self-monitoring, self-efficacy, habit formation and social support, were all seen as important by participants. Ongoing motivation was strongly influenced positively and negatively by the support of others including family, friends, peers and professionals. Participants reflected on the MIPs’ skills in MI of providing an empathic, non-judgemental environment in which they allowed individuals to control and direct their own plans for weight management. Professional support that was caring, objective and non-judgemental and provided psychological support was thought to be important. A good professional relationship helped with motivation because participants wanted to please their practitioner; it also provided the checking in or accountability elements that participants found useful.
Social support was discussed in detail by participants and was seen as key for WLM. Peer support was considered important because it provides accessible, regular opportunities for support, reduces isolation and provides opportunities for reinforcement, encouragement, feedback, role-modelling, instrumental support and comparison as well as learning from each other. Peer support is distinct from other support because of the shared experience, and it also provides opportunities to improve self-efficacy, which is integral to the psychological theories underpinning the intervention. Support from family and friends was also deemed important, particularly if these individuals were committed to maintaining a healthy lifestyle. If they were not, then often this led to temptation; for example, some family and friends deliberately tempted participants or, less directly, had a negative influence by bringing unhealthy foods into the house. Positive reinforcement was a crucial aspect of support and could come from direct reinforcement from peers or family. It also appeared to work independently to facilitate self-efficacy and maintain motivation, particularly the reinforcement acquired through continued weight loss or maintenance. Improvements in health also acted as a positive reinforcer.
Control was seen as important, and participants indicated that feelings of control were reinforcing and were important in relation to motivation. Conversely, loss of control could lead to bingeing and thus demotivation and feelings of failure; however, if the diet was too rigid and participants felt deprived, then failure was more likely. Participants suggested that control could be retained by taking a more flexible approach to their diet. Self-monitoring was seen as important to both weight loss and maintenance, in the form of regular weighing. Self-monitoring was described as helping people to feel in control. This was something that the majority of participants were carrying out prior to entering the study and was recognised by many as an important tool. The importance of control and not feeling deprived has been noted in other research. 185,186
Routine and habit formation were described as important to longer-term maintenance of healthy behaviours, and the development of ‘good habits’ in relation to WLM was also part of the theory underlying the WILMA trial intervention. Those who failed to develop healthy lifestyle habits continued to struggle with their weight management. There is evidence from the psychological literature about the importance of developing healthy habits, which are not effortful to maintain, and enhance maintenance of behaviour changes. 187–189
The analyses also revealed some of the potential barriers faced by weight loss maintainers, including environmental and cultural barriers and the important role that food has within our society. The issues identified by participants make maintaining weight loss particularly challenging as so much of our lives revolve around food. There are inherent tensions in dealing with food, which is simultaneously a source of pleasure but is also at the heart of participants’ struggles. It is not a behaviour that we can stop doing: we need to eat to live. Our environment presents a number of challenges, including the ready availability of high-fat unhealthy food relative to healthier options, which can make weight management difficult. Other people can help or hinder weight management through various direct and more subtle routes, as noted earlier.
There are few qualitative studies exploring WLM; however, those that have been completed have described many similar findings to the present study. Studies have indicated the importance of realistic goal-setting, use of routines, self-monitoring, avoiding deprivation and effective coping skills. 186,190 Another study emphasised the importance of support during maintenance, problem-solving skills and motivation. 191 Evidence from the qualitative literature on MI indicates that participants found monitoring to be useful when losing weight. They felt that being accountable to someone was helpful, especially when they struggled with self-monitoring, and they also mentioned increased motivation to change and an increased feeling of personal control. 192 A Swedish study193 found that WLM was seen as a ‘tightrope walk’ and the strategies that participants found useful in this regard were finding things to enjoy about WLM, such as nice foods and focusing on well-being rather than body weight; routine was seen as important, as was the support of significant others. Participants described the importance of being in control, and this included using self-monitoring. 193 In another study, the respondents described the presence of saboteurs as well as the lack of positive reinforcement during the maintenance stage as a particular challenge. 194
Although the cost-effectiveness results suggest that the interventions may not be cost-effective, we must again bear in mind that this feasibility study had a reduced sample size and was therefore underpowered to fully explore these issues. Moreover, the trial is about WLM, and a much longer follow-up period is needed to establish whether or not weight loss is maintained in the long term and thus whether or not the intervention is cost-effective at meeting its intended aim.
The main cost-effectiveness study focused on QALY gains based on EQ-5D scores. Although there is evidence to suggest that higher BMI is associated with lower EQ-5D scores,195 obesity is largely considered a health problem because of its association with raised risk factors for conditions including type 2 diabetes mellitus and cardiovascular disease. Therefore, success in terms of reduced BMI ought to produce long-term health gains in terms of reductions in the incidence and severity of these conditions and consequent reductions in health service treatment costs. An original aim of the WILMA study was therefore to estimate lifetime costs and QALYs via economic modelling using trial-based data on BMI, EQ-5D and costs. This was dropped when the WILMA trial became a feasibility study.
The overall benefits of the interventions are nevertheless likely to be observed over a far longer time period, while the intervention costs are more short term and weighted to the early stages. The short-term nature of this analysis is therefore likely to be a lower bound for the potential cost-effectiveness of these interventions. Few trials of WLM or long-term weight loss have looked at cost-effectiveness. A HTA monograph suggests that there is some evidence that weight loss management interventions may be cost-effective; however, the authors suggest caution owing to methodological limitations of the two included studies. 196
Generalisability
In terms of the participants recruited, we were unable to recruit many men or those of ethnic groups other than white British. Fewer men than women generally engage with weight loss research197,198 and recruiting different ethnicities into trials has proven difficult. 198,199 One qualitative study found that men want weight loss programmes that include individual-level feedback and involve others with whom they identify. 200 It is likely that in order to engage men and non-white ethnic group in trials, interventions may have to be specifically targeted. 201 A recent trial of recruiting men into a group-based intervention delivered at football grounds was successful in helping men lose weight. 202 In terms of increasing the representation of non-white ethnic groups in trials, suggestions have included training recruiters in greater cultural sensitivity, employing advocacy workers and using outreach approaches. 199
Although we did manage to recruit from diverse sources, we are likely to have recruited a fairly motivated group of participants. This is often an issue where research study participants are not necessarily representative of the general population. Therefore, the intervention is tested out in a tightly controlled trial with motivated participants and the subsequent roll-out in the ‘real world’ is much less effective. However, if this were delivered in practice it is likely that those participating would also be fairly motivated, having already lost a significant proportion of their body weight. Given the challenges we faced with recruitment, any future trial will need to consider carefully how best to recruit participants who have already lost weight. We did consider an initial weight loss intervention followed by the maintenance intervention and follow-up; however, we felt this would limit the generalisability of the findings.
Conclusions
Recruitment into the trial was much lower than originally anticipated, and this was caused by problems with obtaining independent verification of 5% weight loss as well as delays in opening the trial in England because of issues with research governance and infrastructure support leading to the study becoming a feasibility trial. We tried many different approaches to improve recruitment, but these two issues were key to the recruitment challenges we faced. For any future trial, consideration of different approaches to verification would be prudent as well as to infrastructure support and governance issues. The trial tested an intervention based on MI to support individuals who had previously lost at least 5% of their body weight. As a feasibility study the results look very promising; however, we are limited in what can be concluded from the quantitative, mediation and CEAs owing to the reduced sample size as well as the shortened follow-up. As expected, there are few statistically significant results, but there are encouraging mean differences and CI on important outcomes. The intensive arm seems to consistently have the biggest treatment effect and generally in the direction of benefit. Data from the qualitative work also suggest that increased awareness and understanding were more frequently described in the intensive group, so it is likely that developing insight took time as the therapeutic relationship developed.
We included a less intensive arm as we thought that this might be more feasible to deliver within the NHS. However, the impact of this brief intervention does not look encouraging and the results look very similar to the control group, which is in keeping with the available evidence. A systematic review of MI as an intervention across a range of health behaviours found an effect in 87% of studies with more than five encounters, compared with only 40% with one session of MI. 57 Two large studies of successful long-term weight loss indicate that intensive and, therefore, costly interventions may be necessary to help people lose weight over a longer-term period and maintain their weight loss. The Finnish Diabetes Prevention Study42 and the Look AHEAD study203 found positive results at 3 and 8 years, respectively. In the Look AHEAD trial, the intervention consisted of both group and individual sessions up to the 6 months time point, the participants attended group sessions for the first 3 weeks of each month then on the fourth week they had an individual sessions instead. In months 7–12, they had monthly individual sessions but group sessions were only delivered twice per month. The average weight loss was 8.5% in the intervention group. In years 2–8, the focus was on maintenance, but individuals still received monthly face-to-face sessions, monthly telephone calls and monthly group sessions for 8 years. The average weight loss from baseline at 8 years was 4.7% relative to 2.1% in the controls. This trial is the largest and longest evaluation of a lifestyle intervention. A few trials have found less intensive interventions effective for WLM at shorter follow-up; however, these are few and far between and are still not ‘light touch’ as they still involve quite a lot of contact. 41,204 This and other evidence indicates that trying to identify brief interventions as a ‘quick fix’ for the problem may not be appropriate. Brief interventions should be recommended in the NHS only when they have proven efficacy, and at present there is a dearth of evidence for WLM interventions, intensive or otherwise. Obesity should be viewed as a chronic condition for which longer-term support, and probably quite intensive support, is needed.
Weight loss maintenance is extremely challenging; individuals faced with their own motivational struggles are also confronted with an obesogenic environment, which does not facilitate making healthy choices. Their efforts can also be undermined by friends and family as well as by the central role food has in our lives and society. This intervention may help some individuals with their WLM, but it can only be part of a broader strategy to support healthy choices. The House of Lords Scientific and Technology Committee Report on Behaviour Change205 highlighted that no single approach is likely to be effective in tackling priority health behaviours and that complex interventions addressing multiple levels of behavioural determinants are likely to be needed to bring about sustained change. 205
One observation we have from the work completed here is that there is scope for confusion in defining successful WLM. This has also been noted by Stevens et al. ,206 who have pointed to a range of definitions of WLM. Successful long-term weight loss has been described as losing at least 5% for at least 1 year. 207 Patterns of weight loss and regain are complex, and most individuals tend to regain some weight over time, even in successful interventions. Stevens et al. 206 point out that most definitions of WLM allow for some regain of weight. RCTs tend to focus on the differences in weight regain as an outcome rather than maintenance. Long-term weight loss and WLM are terms that are sometimes used interchangeably, and systematic reviews often include studies of long-term weight loss, that is maintenance following a weight loss intervention, as well as those specifically testing WLM interventions. We have defined successful WLM as being successful when the participant does not exceed their pre-weight loss weight at the end of the trial. This includes both those who simply maintained as well as those who lost more weight.
There is also confusion over whether or not interventions for initial weight loss, which then lead to long-term weight loss, are suitable to support WLM. In addition, although strategies for WLM have been proposed as different from those for weight loss, this may not be the case. A recent systematic review concluded that, in order to achieve WLM, the strategies that had led to the initial weight loss had to be continued over the longer term. 208 It is likely that this may at least be partly true, although clearly there will have to be some adjustment to behaviours used for initial weight loss or participants would continue to lose weight. Evidence from the National Weight Control Registry29 indicates that for successful weight maintainers, using approaches such as dietary restrictions, physical activity and self-monitoring are important in WLM. Psychological theories of behaviour change often do not clearly differentiate between initiation of a behaviour change and maintenance.
A minority of our participants were actually in the ‘maintenance stage’, in which they were consolidating and reflecting on how to maintain the weight loss that they had already achieved. Most (92% at baseline and 76% at follow-up, split roughly equally between arms) were seeking to lose further weight. Although this intervention was designed to help individuals with WLM, many participants wished to continue their weight loss and were supported in this. While we sought to help participants maintain weight loss, the idea that people hit their target weight and then adopt maintenance behaviours was not what emerged from the qualitative work. Participants reported that it was an ongoing process, and the battle was never won – they still had to put the work in to prevent weight regain; however, if they could get to the stage at which their weight fluctuated around a certain point, which could be managed, then this could be considered maintenance. Patterns of weight loss and gain are complex, and future interventions need to consider that many participants will still be planning further weight loss.
Weight loss maintenance research is still relatively undeveloped. There is a need for the enhancement of theory which will help inform the development of interventions to be tested in rigorously designed RCTs with cost-effectiveness assessed.
Implications for health care
Obesity is a significant contributor to diseases such as cardiovascular disease, diabetes mellitus and cancer. Treating obesity and the consequences of it represents a significant and growing cost to the NHS and society. The causes of obesity are multifold and complex209 and, therefore, our response to it will have to be multifaceted, including individual-level approaches and wider public health approaches. Interventions will have to tackle multiple levels of influence.
There is good evidence that lifestyle interventions can promote weight loss;18,25,176 however, long-term maintenance of weight loss is a challenge. This intervention may provide one approach to tackling this issue. The development of healthy habits is crucial for WLM, and weight loss can be maintained only by behaviours that fit with individual lifestyles, motivations and preferences. MI looks like a promising psychological approach for WLM; however, significant resources are required to deliver this level of intervention, including training and support for those delivering MI in practice, including regular supervision. This intervention could be rolled out in a primary care setting by trained health-care staff and may prove cost-effective to deliver in a larger trial with longer follow-up. It is possible that the intervention could have a wider impact on health as those who are successful weight maintainers may influence others in their social circle, as we found in the present study. In addition, individuals’ own experience of MI and their enhanced motivation might influence them in relation to other health behaviours, for example smoking.
Obesity is one of the key public health challenges of our time. Costs to the NHS and society have been estimated at £49.9B by 2050 if the trends in obesity remain unchecked. 209 There is a need for interventions to support individuals with WLM. The stakes are high with potentially large health benefits and cost savings to the NHS and society as a whole.
Recommendations for future research
This work has identified a number of key areas for future research in WLM.
There is a need for well-designed RCTs, which include cost-effectiveness evaluations, testing interventions to support individuals with WLM, as many studies to date have had significant methodological limitations. We also need more research to help improve our understanding of the cost-effectiveness of WLM over different time periods.
-
Based on the findings of this feasibility study, an intervention focusing on MI and self-monitoring looks promising for helping people who have already lost weight to maintain their weight loss. We therefore recommend that a fully powered RCT of the intensive intervention compared with control be conducted. This would enable a proper evaluation of this intervention using dose–response curves to explore what level of MI is needed to produce a clinically significant effect and trial-based data would facilitate the use of economic modelling. The intervention and trial design would be informed by the findings of this feasibility study. Given the likely importance of social support for behaviour initiation and maintenance, an additional component would seek to facilitate effective social support, as originally proposed; however, alternative ways of providing this would be considered including utilising new technologies to mobilise social support.
-
Our qualitative data suggest that ongoing support is likely to be important, as does other work in this area. 210 However, research is required on intervention intensity and effectiveness in terms of both total contact time as well as number of contacts required and over what time period. Given the resource issues with providing ongoing contact, further work needs to be completed on delivering interventions by telephone, internet, smartphones, etc. With regard to the challenges we experienced in running the groups, these methods could also be explored to deliver the social support element of the intervention.
-
Further development of psychological theory in relation to both maintenance and interventions is required. 211 Presently, most theories do not address ‘maintenance of behaviours’ directly, and most seem to assume that the psychological processes needed for initial behaviour change are, in essence, the same as for maintenance. The majority of interventions tested are not based on psychological theory, and few measure psychological determinants or behavioural outcomes. There is a clear need for better description of theory and the behavioural components of interventions. In order to build and test theories and to identify potentially useful behavioural techniques, behavioural outcomes and theorised mechanisms of the effect of interventions should be measured. Based on current evidence, a number of potential approaches are likely to be important in WLM, including habit formation, intrinsic motivation and social support. 21,28,29,69,74,185 More exploration of how to encourage or support these is needed. MI may be a useful strategy for improving intrinsic motivation.
-
Given that our sample included few men and people from ethnic minorities, thereby limiting the generalisability of our results, further research needs to be completed on interventions that are targeted specifically at men and ethnic minorities as well as more effort to recruit these groups into trials.
-
In our qualitative data and our other work, we identified that defining WLM and understanding the associated processes is complex. Future research needs to look at transitions from weight loss to maintenance and to unpick people’s experiences of ‘maintenance’ and the processes needed to maintain.
-
Finally, there is limited evidence on the type of diet or amount or type of exercise required for WLM and more work needs to be completed.
Acknowledgements
We would like to acknowledge Professor Steve Rollnick for his contributions to the design of the study and also to the development of the intervention and the training of the MIPs.
We would like to thank Rhys Thomas for his help with administering the study and for his artwork, and Naomi Southern for her help with administration. We would also like to thank Carolyn Blake for her invaluable input in her role as patient representative on the trial.
We would like to acknowledge National Institute for Social Care and Health Research Clinical Research Centre staff in Wales and network staff in England for their help with recruitment and follow-up. We are also grateful to the GP practices, Slimming World and the EOR schemes that helped us to recruit the participants. We would also like to thank the MIPs and GFs who helped us to deliver the study intervention and we would like to thank all those who kindly gave up their time to participate in the trial.
Finally, we would also like to thank the members of our Trial Steering Committee [Dr Jim McCambridge (chairperson), Dr Margaret Cupples, Dr Ruth Pickering, Professor Janice Thompson and Nicola Rossiter] for their help and guidance.
Contributions of authors
Dr Sharon A Simpson (Senior Research Fellow, psychology) led the design of the trial and the intervention as well as the implementation of the study. She led the writing of the report.
Dr Rachel McNamara (Research Fellow, psychology) contributed to study and intervention design. She also managed the trial and led the writing of several chapters.
Dr Christine Shaw (Reader, qualitative methods) was key to the design of the trial and the intervention. She also led the qualitative components of the study and contributed to drafting and revising the report.
Dr Mark Kelson (Research Fellow, statistics) contributed to study design and led the quantitative analyses and contributed to drafting and revising the report.
Yvonne Moriarty (Research Assistant, qualitative methods) conducted the qualitative interviews, led the analyses of the focus groups and contributed to the analyses of the interviews. She also contributed to drafting and revising the report.
Elizabeth Randell (Research Associate, psychology) was involved in analysing and interpreting the data as well as drafting and revising the report.
Professor David Cohen (Professor, health economics) led the health economics analyses and contributed to drafting and revising the report.
Dr M Fasihul Alam (Senior Research Fellow, health economics) conducted the health economics analyses and contributed to drafting and revising the report.
Lauren Copeland (PhD student, psychology) was involved in the analyses of the focus groups as well as revising the report.
Donna Duncan (Deputy Head of Nutrition and Dietetics) was involved in the design of the trial and contributed to revising the report.
Aude Espinasse (Research Assistant, data management) was the data manager and contributed to interpretation of the results. She also contributed to revising the report.
David Gillespie (Research Associate, statistics) conducted some of the quantitative analyses and contributed to drafting and revising the report.
Professor Andy Hill (Professor, medical psychology) was involved in the design of the trial and contributed to revising the report.
Dr Eleri Owen-Jones (Research Associate, trial management) was involved in the design of the trial and contributed to revising the report.
Dr Katy Tapper (Senior Lecturer, psychology) was involved in the design of the trial and contributed to revising the report.
Julia Townson (Research Fellow, trial management) was involved in the design of the trial and contributed to drafting and revising the report.
Dr Simon Williams (Principal Lecturer, exercise science) was involved in the design of the trial and contributed to revising the report.
Professor Kerry Hood (Professor, statistics) oversaw the quantitative analyses and was involved in the design of the trial and contributed to drafting and revising the report.
All authors approved the final version of the report.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2013;380:2224-60. http://dx.doi.org/10.1016/S0140-6736(12)61766-8.
- WHO . Obesity and Overweight. Factsheet No. 311 2014. www.who.int/mediacentre/factsheets/fs311/en/ (accessed 27 August 2014).
- The NHS Information Centre for Health and Social Care . Statistics on Obesity, Physical Activity and Diet: England 2012 n.d. www.hscic.gov.uk/catalogue/PUB05131/obesphys-acti-diet-eng-2012-rep.pdf (accessed 15 March 2013).
- Jebb S. Tackling the Weight of the Nation. London: MRC Human Nutrition Research; 2004.
- Organisation for Economic Co-operation and Development (OECD) . Obesity Update 2012 2012. www.oecd.org/health/49716427.pdf (accessed 30 August 2013).
- Foresight . Tackling Obesities: Future Choices – Project Report 2007. www.bis.gov.uk/assets/foresight/docs/obesity/17.pdf (accessed 30 August 2013).
- Temelkova-Kurktschiev T, Stefanov T. Lifestyle and genetics in obesity and type 2 diabetes. Exp Clin Endocrinol Diabetes 2012;120:1-6. http://dx.doi.org/10.1055/s-0031-1285832.
- Wilding J. Are the causes of obesity primarily environmental? Yes. BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e5843.
- Department of Health . Reducing Obesity and Improving Diet n.d. www.gov.uk/government/policies/reducing-obesity-and-improving-diet (accessed 28 August 2014).
- Goldie C, Brown J. Managing obesity in primary care. Nurs Times 2012;108:14-6.
- Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001;344:1343-50. http://dx.doi.org/10.1056/NEJM200105033441801.
- Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393-40. http://dx.doi.org/10.1056/NEJMoa012512.
- Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, et al. Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement. Health Technol Assess 2004;8. http://dx.doi.org/10.3310/hta8210.
- Espeland M, Pi-Sunyer X, Blackburn G, Brancati FL, Bray GA, Bright R, et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes – one-year results of the Look AHEAD trial. Diabetes Care 2007;30:1374-83. http://dx.doi.org/10.2337/dc07-0048.
- Tuomilehto J, Lindstrom J. The major diabetes prevention trials. Curr Diab Rep 2003;3:115-22. http://dx.doi.org/10.1007/s11892-003-0034-9.
- Dansinger ML, Tatsioni A, Wong JB, Chung M, Balk EM. Meta-analysis: the effect of dietary counseling for weight loss. Ann Intern Med 2007;147:41-50. http://dx.doi.org/10.7326/0003-4819-147-1-200707030-00007.
- Jebb SA, Ahern AL, Olson AD, Aston LM, Holzapfel C, Stoll J, et al. Primary care referral to a commercial provider for weight loss treatment versus standard care: a randomised controlled trial. Lancet 2011;378:1485-92. http://dx.doi.org/10.1016/S0140-6736(11)61344-5.
- Jolly K, Lewis A, Beach J, Denley J, Adab P, Deeks JJ, et al. Comparison of range of commercial or primary care led weight reduction programmes with minimal intervention control for weight loss in obesity: lighten Up randomised controlled trial. BMJ 2011;343:1-16. http://dx.doi.org/10.1136/bmj.d6500.
- NICE . Obesity: Guidance on the Prevention, Identification, Assessment and Management of Overweight and Obesity in Adults and Children 2006 n.d. www.nice.org.uk/guidance/cg43/evidence/cg43-obesity-full-guideline-section-1-introduction-methods-and-recommendations2 (accessed 1 May 2013).
- Curioni CC, Lourenco PM. Long-term weight loss after diet and exercise: a systematic review. Int J Obes 2005;29:1168-74. http://dx.doi.org/10.1038/sj.ijo.0803015.
- Greaves CJ, Sheppard KE, Abraham C, Hardeman W, Roden M, Evans PH, et al. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health 2011;11:1-12. http://dx.doi.org/10.1186/1471-2458-11-119.
- Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL. A self-regulation program for maintenance of weight loss. N Engl J Med 2006;355:1563-71. http://dx.doi.org/10.1056/NEJMoa061883.
- Wadden TA, Brownell KD, Foster GD. Obesity: responding to the global epidemic. J Consult Clin Psychol 2002;70:510-25. http://dx.doi.org/10.1037/0022-006X.70.3.510.
- Cooper Z, Fairburn CG. A new cognitive behavioural approach to the treatment of obesity. Behav Res Ther 2001;39:499-511. http://dx.doi.org/10.1016/S0005-7967(00)00065-6.
- Franz MJ, VanWormer JJ, Crain AL, Boucher JL, Histon T, Caplan W, et al. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc 2007;107:1755-67. http://dx.doi.org/10.1016/j.jada.2007.07.017.
- Nordmann AJ, Nordmann A, Briel M, Keller U, Yancy WS, Brehm BJ, et al. Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: a meta-analysis of randomized controlled trials. Arch Intern Med 2006;166:285-93. http://dx.doi.org/10.1001/archinte.166.3.285.
- Douketis JD, Macie C, Thabane L, Williamson DF. Systematic review of long-term weight loss studies in obese adults: clinical significance and applicability to clinical practice. Int J Obes 2005;29:1153-67. http://dx.doi.org/10.1038/sj.ijo.0802982.
- Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr 2005;82:222S-5S.
- Elfhag K, Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev 2005;6:67-85. http://dx.doi.org/10.1111/j.1467-789X.2005.00170.x.
- Jakicic JM, Davis KK. Obesity and physical activity. Psychiatr Clin North Am 2011;34:829-40. http://dx.doi.org/10.1016/j.psc.2011.08.009.
- Fogelholm M, Kukkonen-Harjula K. Does physical activity prevent weight gain – a systematic review. Obes Rev 2000;1:95-111. http://dx.doi.org/10.1046/j.1467-789x.2000.00016.x.
- Jakicic JM, Marcus BH, Lang W, Janney C. Effect of exercise on 24-month weight loss maintenance in overweight women. Arch Intern Med 2008;168:1550-9. http://dx.doi.org/10.1001/archinte.168.14.1550.
- Saris WH, Blair SN, van Baak MA, Eaton SB, Davies PS, Di Pietro L, et al. How much physical activity is enough to prevent unhealthy weight gain? Outcome of the IASO 1st Stock Conference and consensus statement. Obes Rev 2003;4:101-14. http://dx.doi.org/10.1046/j.1467-789X.2003.00101.x.
- Physical Activity Guidelines Advisory Committee Report, 2008. Washington, DC: US Department of Health and Human Services; 2008.
- Dombrowski SU, Knittle K, Avenell A, Araujo-Soares V, Sniehotta FF. Long term maintenance of weight loss with non-surgical interventions in obese adults: systematic review and meta-analyses of randomised controlled trials. BMJ 2014;348. http://dx.doi.org/10.1136/bmj.g2646.
- Turk MW, Yang K, Hravnak M, Sereika SM, Ewing LJ, Burke LE. Randomized clinical trials of weight loss maintenance: a review. J Cardiovasc Nurs 2009;24:58-80. http://dx.doi.org/10.1097/01.JCN.0000317471.58048.32.
- Middleton KM, Patidar SM, Perri MG. The impact of extended care on the long-term maintenance of weight loss: a systematic review and meta-analysis. Obes Rev 2012;13:509-17. http://dx.doi.org/10.1111/j.1467-789X.2011.00972.x.
- Svetkey LP, Stevens VJ, Brantley PJ, Appel LJ, Hollis JF, Loria CM, et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. JAMA 2008;299:1139-48. http://dx.doi.org/10.1001/jama.299.10.1139.
- Wieland LS, Falzon L, Sciamanna CN, Trudeau KJ, Brodney S, Schwartz JE, et al. Interactive computer-based interventions for weight loss or weight maintenance in overweight or obese people. Cochrane Database Syst Rev 2012;8. http://dx.doi.org/10.1002/14651858.CD007675.pub2.
- Neve M, Morgan PJ, Jones PR, Collins CE. Effectiveness of web-based interventions in achieving weight loss and weight loss maintenance in overweight and obese adults: a systematic review with meta-analysis. Obes Rev 2010;11:306-21. http://dx.doi.org/10.1111/j.1467-789X.2009.00646.x.
- Sherwood NE, Crain AL, Martinson BC, Anderson CP, Hayes MG, Anderson JD, et al. Enhancing long-term weight loss maintenance: 2 year results from the Keep It Off randomized controlled trial. Prev Med 2013;56:171-7. http://dx.doi.org/10.1016/j.ypmed.2012.12.014.
- Lindstrom J, Louheranta A, Mannelin M, Rastas M, Salminen V, Eriksson J, et al. The Finnish Diabetes Prevention Study (DPS): lifestyle intervention and 3-year results on diet and physical activity. Diabetes Care 2003;26:3230-6. http://dx.doi.org/10.2337/diacare.26.12.3230.
- Rodriguez-Hernandez H, Morales-Amaya UA, Rosales-Valdez R, Rivera-Hinojosa F, Rodriguez-Moran M, Guerrero-Romero F. Adding cognitive behavioural treatment to either low-carbohydrate or low-fat diets: differential short-term effects. Br J Nutr 2009;102:1847-53. http://dx.doi.org/10.1017/S0007114509991231.
- Greaves CJ, Middlebrooke A, O’Loughlin L, Holland S, Piper J, Steele A, et al. Motivational interviewing for modifying diabetes risk: a randomised controlled trial. Br J Gen Pract 2008;58:535-40. http://dx.doi.org/10.3399/bjgp08X319648.
- Hill JO, Thompson H, Wyatt H. Weight maintenance: what’s missing?. J Am Diet Assoc 2005;105:S63-6. http://dx.doi.org/10.1016/j.jada.2005.02.016.
- Sciamanna CN, Kiernan M, Rolls BJ, Boan J, Stuckey H, Kephart D, et al. Practices associated with weight loss versus weight-loss maintenance results of a national survey. Am J Prev Med 2011;41:159-66. http://dx.doi.org/10.1016/j.amepre.2011.04.009.
- Gollwitzer PM, Sheeran P. Implementation intentions and goal achievement: a meta-analysis of effects and processes. Adv Exp Soc Psychol 2006;38:69-119. http://dx.doi.org/10.1016/S0065-2601(06)38002-1.
- Gollwitzer PM. Goal achievement: the role of intentions. Eur Rev Soc Psychol 1993;4:141-85. http://dx.doi.org/10.1080/14792779343000059.
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. New York, NY: Guildford Press; 2002.
- Miller WR, Rollnick S. Motivational Interviewing, Third Edition: Helping People Change. London: Guilford Press; 2012.
- Smedslund G, Berg RC, Hammerstrøm KT, Steiro A, Leiknes KA, Dahl HM, et al. Motivational interviewing for substance abuse. Cochrane Database Syst Rev 2011;5. http://dx.doi.org/10.1002/14651858.CD008063.pub2.
- Hettema JE, Hendricks PS. Motivational interviewing for smoking cessation: a meta-analytic review. J Consult Clin Psychol 2010;78:868-84. http://dx.doi.org/10.1037/a0021498.
- West DS, DiLillo V, Bursac Z, Gore SA, Greene PG. Motivational interviewing improves weight loss in women with type 2 diabetes. Diabetes Care 2007;30:1081-7. http://dx.doi.org/10.2337/dc06-1966.
- Hoy MK, Winters BL, Chlebowski RT, Papoutsakis C, Shapiro A, Lubin MP, et al. Implementing a low-fat eating plan in the women’s intervention nutrition study. J Am Diet Assoc 2009;109:688-96. http://dx.doi.org/10.1016/j.jada.2008.12.016.
- Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. J Consult Clin Psychol 2003;71:843-61. http://dx.doi.org/10.1037/0022-006X.71.5.843.
- Hettema J, Steele J, Miller WR. Motivational interviewing. Ann Rev Clin Psychol 2005;1:91-111. http://dx.doi.org/10.1146/annurev.clinpsy.1.102803.143833.
- Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract 2005;55:305-12.
- Carels RA, Darby L, Cacciapaglia HM, Konrad K, Coit C, Harper J, et al. Using motivational interviewing as a supplement to obesity treatment: A stepped-care approach. Health Psychol 2007;26:369-74. http://dx.doi.org/10.1037/0278-6133.26.3.369.
- Hardcastle S, Taylor A, Bailey M, Castle R. A randomised controlled trial on the effectiveness of a primary health care based counselling intervention on physical activity, diet and CHD risk factors. Patient Educ Couns 2008;70:31-9. http://dx.doi.org/10.1016/j.pec.2007.09.014.
- Resnicow K, Jackson A, Blissett D, Wang T, McCarty F, Rahotep S, et al. Results of the healthy body healthy spirit trial. Health Psychol 2005;24:339-48. http://dx.doi.org/10.1037/0278-6133.24.4.339.
- Resnicow K, Jackson A, Wang T, De AK, McCarty F, Dudley WN, et al. A motivational interviewing intervention to increase fruit and vegetable intake through Black churches: results of the eat for life trial. Am J Public Health 2001;91:1686-93. http://dx.doi.org/10.2105/AJPH.91.10.1686.
- McCambridge J, Strang J. Deterioration over time in effect of motivational interviewing in reducing drug consumption and related risk among young people. Addiction 2005;100:470-8. http://dx.doi.org/10.1111/j.1360-0443.2005.01013.x.
- Britt E, Hudson SM, Blampied NM. Motivational interviewing in health settings: a review. Patient Educ Couns 2004;53:147-55. http://dx.doi.org/10.1016/S0738-3991(03)00141-1.
- Armstrong MJ, Mottershead TA, Ronksley PE, Sigal RJ, Campbell TS, Hemmelgarn BR. Motivational interviewing to improve weight loss in overweight and/or obese patients: a systematic review and meta-analysis of randomized controlled trials. Obes Rev 2011;12:709-23. http://dx.doi.org/10.1111/j.1467-789X.2011.00892.x.
- Nieminen T, Prättälä R, Martelin T, Härkänen T, Hyyppä MT, Alanen E, et al. Social capital, health behaviours and health: a population-based associational study. BMC Public Health 2013;13:1-11. http://dx.doi.org/10.1186/1471-2458-13-613.
- Ferranti EP, Dunbar SB, Higgins M, Dai J, Ziegler TR, Frediani JK, et al. Psychosocial factors associated with diet quality in a working adult population. Res Nurs Health 2013;36:242-56. http://dx.doi.org/10.1002/nur.21532.
- Aggarwal B, Liao M, Mosca L. Predictors of physical activity at 1-year in a randomized controlled trial of family members of patients with cardiovascular disease. J Cardiovasc Nurs 2010;25:444-9. http://dx.doi.org/10.1097/JCN.0b013e3181defd3e.
- Molloy GJ, Dixon D, Hamer M, Sniehotta FF. Social support and regular physical activity: does planning mediate this link?. Br J Health Psychol 2010;15:859-70. http://dx.doi.org/10.1348/135910710X490406.
- Wing RR, Jeffery RW. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. J Consult Clin Psychol 1999;67:132-8. http://dx.doi.org/10.1037/0022-006X.67.1.132.
- Strine TW, Chapman DP, Balluz LS, Moriarty DG, Mokdad AH. The associations between life satisfaction and health-related quality of life, chronic illness, and health behaviors among US community-dwelling adults. J Community Health 2008;33:40-5. http://dx.doi.org/10.1007/s10900-007-9066-4.
- NICE . Behaviour Change: Individual Approaches 2014. www.nice.org.uk/guidance/ph49/resources/guidance-behaviour-change-individual-approaches-pdf (accessed 9 March 2015).
- O’Connell KA. Theories used in nursing research on smoking cessation. Ann Rev Nurs Res 2009;27:33-62. http://dx.doi.org/10.1891/0739-6686.27.33.
- Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol 2009;28:690-701. http://dx.doi.org/10.1037/a0016136.
- Lim YM, Sung MH, Joo KS. Factors affecting health-promoting behaviors of community-dwelling Korean older women. J Gerontol Nurs 2010;36:42-5. http://dx.doi.org/10.3928/00989134-20100504-05.
- Priebe CS, Spink KS. When in Rome: descriptive norms and physical activity. Psychol Sport Exerc 2011;12:93-8. http://dx.doi.org/10.1016/j.psychsport.2010.09.001.
- Turner-McGrievy GM, Barnard ND, Scialli AR. A two-year randomized weight loss trial comparing a vegan diet to a more moderate low-fat diet. Obesity 2007;15:2276-81. http://dx.doi.org/10.1038/oby.2007.270.
- Depue JD, Clark MM, Ruggiero L, Medeiros ML, Pera V. Maintenance of weight-loss – a needs assessment. Obes Res 1995;3:241-8. http://dx.doi.org/10.1002/j.1550-8528.1995.tb00144.x.
- Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc 2011;111:92-102. http://dx.doi.org/10.1016/j.jada.2010.10.008.
- Kuk JL, Katzmarzyk PT, Nichaman MZ, Church TS, Blair SN, Ross R. Visceral fat is an independent predictor of all-cause mortality in men. Obesity 2006;14:336-41. http://dx.doi.org/10.1038/oby.2006.43.
- Despres JP, Arsenault BJ, Cote M, Cartier A, Lemieux I. Abdominal obesity: the cholesterol of the 21st century?. Can J Cardiol 2008;24:7D-12D. http://dx.doi.org/10.1016/S0828-282X(08)71043-2.
- Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr 2004;79:379-84.
- Ballor DL, Keesey RE. A meta-analysis of the factors affecting exercise-induced changes in body mass, fat mass and fat-free mass in males and females. Int J Obes 1991;15:717-26.
- Donnelly JE, Hill JO, Jacobsen DJ, Potteiger J, Sullivan DK, Johnson SL, et al. Effects of a 16-month randomized controlled exercise trial on body weight and composition in young, overweight men and women: the Midwest Exercise Trial. Arch Intern Med 2003;163:1343-50. http://dx.doi.org/10.1001/archinte.163.11.1343.
- Donnelly JE, Smith BK. Is exercise effective for weight loss with ad libitum diet? Energy balance, compensation, and gender differences. Exerc Sport Sci Rev 2005;33:169-74. http://dx.doi.org/10.1097/00003677-200510000-00004.
- Svetkey LP, Clark JM, Funk K, Corsino L, Batch BC, Hollis JF, et al. Greater weight loss with increasing age in the weight loss maintenance trial. Obesity 2014;22:39-44. http://dx.doi.org/10.1002/oby.20506.
- Hollis JF, Gullion CM, Stevens VJ, Brantley PJ, Appel LJ, Ard JD, et al. Weight loss during the intensive intervention phase of the weight-loss maintenance trial. Am J Prev Med 2008;35:118-26. http://dx.doi.org/10.1016/j.amepre.2008.04.013.
- Tussing-Humphreys LM, Fitzgibbon ML, Kong A, Odoms-Young A. Weight loss maintenance in African American women: a systematic review of the behavioral lifestyle intervention literature. J Obes 2013;2013. http://dx.doi.org/10.1155/2013/437369.
- Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol 2008;27:379-87. http://dx.doi.org/10.1037/0278-6133.27.3.379.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337. http://dx.doi.org/10.1136/bmj.a1655.
- Michie S, Ashford S, Sniehotta FF, Dombrowski SU, Bishop A, French DP. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health 2011;26:1479-98. http://dx.doi.org/10.1080/08870446.2010.540664.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6. http://dx.doi.org/10.1186/1748-5908-6-42.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95. http://dx.doi.org/10.1007/s12160-013-9486-6.
- Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000;55:68-7. http://dx.doi.org/10.1037/0003-066X.55.1.68.
- Silva MN, Markland D, Minderico CS, Vieira PN, Castro MM, Coutinho SR, et al. A randomized controlled trial to evaluate self-determination theory for exercise adherence and weight control: rationale and intervention description. BMC Public Health 2008;8:1-13. http://dx.doi.org/10.1186/1471-2458-8-234.
- Festinger L. Theory of Cognitive Dissonance. Evanston, IL: Row Petersen; 1957.
- Heckhausen H. Motivation and Action. Berlin: Springer-Verlag; 1991.
- Adriaanse MA, Vinkers CDW, De Ridder DTD, Hox JJ, De Wit JBF. Do implementation intentions help to eat a healthy diet? A systematic review and meta-analysis of the empirical evidence. Appetite 2011;56:183-93. http://dx.doi.org/10.1016/j.appet.2010.10.012.
- Williams S, French D. What are the most effective intervention techniques for changing physical activity self-efficacy and physical activity behaviour – and are they the same?. Health Educ Res 2011;26:308-22. http://dx.doi.org/10.1093/her/cyr005.
- Ziegelmann JP, Lippke S, Schwarzer R. Adoption and maintenance of physical activity: planning interventions in young, middle-aged, and older adults. Psychol Health 2006;21:145-63. http://dx.doi.org/10.1080/1476832050018891.
- Prestwich A, Ayres K, Lawton R. Crossing two types of implementation intentions with a protection motivation intervention for the reduction of saturated fat intake: a randomized trial. Social Sci Med 2008;67:1550-8. http://dx.doi.org/10.1016/j.socscimed.2008.07.019.
- Webb TL, Sheeran P. How do implementation intentions promote goal attainment? A test of component processes. J Exp Soc Psychol 2007;43:295-302. http://dx.doi.org/10.1016/j.jesp.2006.02.001.
- Neal DT, Wood W, Wu MJ, Kurlander D. The pull of the past: when do habits persist despite conflict with motives?. Pers Soc Psychol Bull 2011;37:1428-37. http://dx.doi.org/10.1177/0146167211419863.
- Bandura A. Human Agency in Social Cognitive Theory. Am Psychol 1989;44:1175-84. http://dx.doi.org/10.1037/0003-066X.44.9.1175.
- Perri MG, Limacher MC, Durning PE, Janicke DM, Lutes LD, Bobroff LB, et al. Extended-care programs for weight management in rural communities: the treatment of obesity in underserved rural settings (TOURS) randomized trial. Arch Intern Med 2008;168:2347-54. http://dx.doi.org/10.1001/archinte.168.21.2347.
- Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;35:1381-95. http://dx.doi.org/10.1249/01.MSS.0000078924.61453.FB.
- Roe L, Strong C, Whiteside C, Neil A, Mant D. Dietary intervention in primary care: validity of the DINE method for diet assessment. Fam Pract 1994;11:375-81. http://dx.doi.org/10.1093/fampra/11.4.375.
- Brooks R. EuroQol: the current state of play. Health Policy 1996;37:53-72. http://dx.doi.org/10.1016/0168-8510(96)00822-6.
- Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res 2007;31:1208-17. http://dx.doi.org/10.1111/j.1530-0277.2007.00403.x.
- Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self reported time to the first cigarette of the day and number of cigarettes smoked per day. Br J Addict 1989;84:791-800. http://dx.doi.org/10.1111/j.1360-0443.1989.tb03059.x.
- Fairburn CG, Beglin SJ. Assessment of eating disorders: interview or self-report questionnaire?. Int J Eat Disord 1994;16:363-70.
- Goldberg DP, Williams P. A User’s Guide to the General Health Questionnaire. Basingstoke: NFER Nelson; 1988.
- Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med 1987;16:825-36. http://dx.doi.org/10.1016/0091-7435(87)90022-3.
- Clark MM, Abrams DB, Niaura RS, Eaton CA, Rossi JS. Self-efficacy in weight management. J Consult Clin Psychol 1991;59:739-44. http://dx.doi.org/10.1037/0022-006X.59.5.739.
- Williams GC, Grow VM, Freedman ZR, Ryan RM, Deci EL. Motivational predictors of weight loss and weight-loss maintenance. J Pers Soc Psychol 1996;70:115-26. http://dx.doi.org/10.1037/0022-3514.70.1.115.
- Verplanken B, Orbell S. Reflections on past behavior: a self-report index of habit strength. J Appl Soc Psychol 2003;33:1313-30. http://dx.doi.org/10.1111/j.1559-1816.2003.tb01951.x.
- Carey KB, Neal DJ, Collins SE. A psychometric analysis of the self-regulation questionnaire. Addict Behav 2004;29:253-60. http://dx.doi.org/10.1016/j.addbeh.2003.08.001.
- Hood K, Robling M, Ingledew D, Gillespie D, Greene G, Ivins R, et al. Mode of data elicitation, acquisition and response to surveys: a systematic review. Health Technol Assess 2012;16. http://dx.doi.org/10.3310/hta16270.
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986;51:1173-82. http://dx.doi.org/10.1037/0022-3514.51.6.1173.
- Jo B, Asparouhov T, Muthen BO. Intention-to-treat analysis in cluster randomized trials with noncompliance. Stat Med 2008;27:5565-77. http://dx.doi.org/10.1002/sim.3370.
- Moyers TB, Martin T, Manuel JK, Hendrickson SML, Miller WR. Assessing competence in the use of motivational interviewing. J Subst Abuse Treat 2005;28:19-26. http://dx.doi.org/10.1016/j.jsat.2004.11.001.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77-101. http://dx.doi.org/10.1191/1478088706qp063oa.
- Pope C, Mays N. Qualitative Research in Health Care. London: BMJ Books; 2006.
- Curtis L. Unit Costs of Health and Social Care 2013. Kent: University of Kent; 2013.
- van Asselt ADI, van Mastrigt GAPG, Dirksen CD, Arntz A, Severens JL, Kessels AGH. How to deal with cost differences at baseline. Pharmacoeconomics 2009;27:519-28. http://dx.doi.org/10.2165/00019053-200927060-00007.
- Briggs AH, Wonderling DE, Mooney CZ. Pulling cost-effectiveness analysis up by its bootstraps: a non-parametric approach to confidence interval estimation. Health Econ 1997;6:327-40. http://dx.doi.org/10.1002/(SICI)1099-1050(199707)6:4<327::AID-HEC282>3.0.CO;2-W.
- McGuire MT, Wing RR, Hill JO. The prevalence of weight loss maintenance among American adults. Int J Obes Relat Metab Disord 1999;23:1314-19. http://dx.doi.org/10.1038/sj.ijo.0801075.
- Maetzel A, Ruof J, Covington M, Wolf A. Economic evaluation of orlistat in overweight and obese patients with type 2 diabetes mellitus. Pharmacoeconomics 2003;21:501-12. http://dx.doi.org/10.2165/00019053-200321070-00005.
- Hertzman P. The cost-effectiveness of orlistat in a 1-year weight-management programme for treating overweight and obese patients in Sweden: a treatment responder approach. Pharmacoeconomics 2005;23:1007-20. http://dx.doi.org/10.2165/00019053-200523100-00004.
- Anderson KM, Odell PM, Wilson PW, Kannel WB. Cardiovascular disease risk profiles. Am Heart J 1991;121:293-8. http://dx.doi.org/10.1016/0002-8703(91)90861-B.
- Ara R, Blake L, Gray L, Hernandez M, Crowther M, Dunkely A, et al. What is the clinical effectiveness and cost-effectiveness of using drugs in treating obese patients in primary care? A systematic review. Health Technol Assess 2012;16. http://dx.doi.org/10.3310/hta16050.
- Calvert M, Blazeby J, Altman DG, Revicki DA, Moher D, Brundage MD, et al. Reporting of patient-reported outcomes in randomized trials: the CONSORT PRO extension. JAMA 2013;309:814-22. http://dx.doi.org/10.1001/jama.2013.879.
- Kirby P. A Guide to Actively Involving Young People in Research: For Researchers, Research Commissioners and Managers. Eastleigh: INVOLVE; 2004.
- Treweek S, Mitchell E, Pitkethly M, Cook J, Kjeldstrøm M, Taskila T, et al. Strategies to improve recruitment to randomised controlled trials. Cochrane Database Syst Rev 2010;1. http://dx.doi.org/10.1002/14651858.MR000013.pub4.
- Treweek S, Lockhart P, Pitkethly M, Cook JA, Kjeldstrøm M, Johansen M, et al. Methods to improve recruitment to randomised controlled trials: Cochrane systematic review and meta-analysis. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2012-002360.
- Steckler A, Linnan L. Process Evaluation for Public Health Interventions and Research. San Francisco, CA: John Wiley & Sons; 2002.
- Fleiss J. Measuring nominal scale agreement among many raters. Psychol Bull 1971;76:378-82. http://dx.doi.org/10.1037/h0031619.
- Bartko J. The intraclass correlation coefficient as a measure of reliability. Psychol Rep 1966;19:3-11. http://dx.doi.org/10.2466/pr0.1966.19.1.3.
- Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med 2005;37:360-3.
- Hill RJ, Davies PS. The validity of self-reported energy intake as determined using the doubly labelled water technique. Br J Nutr 2001;85:415-30. http://dx.doi.org/10.1079/BJN2000281.
- Subar AF, Thompson FE, Kipnis V, Midthune D, Hurwitz P, McNutt S, et al. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires: the Eating at America’s Table Study. Am J Epidemiol 2001;154:1089-99. http://dx.doi.org/10.1093/aje/154.12.1089.
- Prince S, Adamo K, Hamel M, Hardt J, Gorber S, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act 2008;5:1-24. http://dx.doi.org/10.1186/1479-5868-5-56.
- Hebert JR, Ma Y, Clemow L, Ockene IS, Saperia G, Stanek EJ, et al. Gender differences in social desirability and social approval bias in dietary self-report. Am J Epidemiol 1997;146:1046-55. http://dx.doi.org/10.1093/oxfordjournals.aje.a009233.
- Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport 2000;71:S1-14. http://dx.doi.org/10.1080/02701367.2000.11082780.
- Adams SA, Matthews CE, Ebbeling CB, Moore CG, Cunningham JE, Fulton J, et al. The effect of social desirability and social approval on self-reports of physical activity. Am J Epidemiol 2005;161:389-98. http://dx.doi.org/10.1093/aje/kwi054.
- Miller TM, Abdel-Maksoud MF, Crane LA, Marcus AC, Byers TE. Effects of social approval bias on self-reported fruit and vegetable consumption: a randomized controlled trial. Nutr J 2008;7. http://dx.doi.org/10.1186/1475-2891-7-18.
- Gates S, Brocklehurst P, Campbell M, Elbourne D. Recruitment to multicentre trials. BJOG 2004;111:3-5. http://dx.doi.org/10.1111/j.1471-0528.2004.00011.x.
- Campbell MK, Snowdon C, Francis D, Elbourne D, McDonald AM, Knight R, et al. Recruitment to randomised trials: strategies for trial enrollment and participation study. The STEPS study. Health Technol Assess 2007;11. http://dx.doi.org/10.3310/hta11480.
- Leermakers EA, Perri MG, Shigaki CL, Fuller PR. Effects of exercise-focused versus weight-focused maintenance programs on the management of obesity. Addict Behav 1999;24:219-27. http://dx.doi.org/10.1016/S0306-4603(98)00090-2.
- Anderson JW, Konz EC, Frederich RC, Wood CL. Long-term weight-loss maintenance: a meta-analysis of US studies. Am J Clin Nutr 2001;74:579-84.
- Kukkonen-Harjula KT, Borg PT, Nenonen AM, Fogelholm MG. Effects of a weight maintenance program with or without exercise on the metabolic syndrome: a randomized trial in obese men. Prev Med 2005;41:784-90. http://dx.doi.org/10.1016/j.ypmed.2005.07.008.
- Keranen AM, Savolainen MJ, Reponen AH, Kujari ML, Lindeman SM, Bloigu RS, et al. The effect of eating behavior on weight loss and maintenance during a lifestyle intervention. Prev Med 2009;49:32-8. http://dx.doi.org/10.1016/j.ypmed.2009.04.011.
- Barte JC, Ter Bogt NC, Bogers RP, Teixeira PJ, Blissmer B, Mori TA, et al. Maintenance of weight loss after lifestyle interventions for overweight and obesity, a systematic review. Obes Rev 2010;11:899-906. http://dx.doi.org/10.1111/j.1467-789X.2010.00740.x.
- Cussler EC, Teixeira PJ, Going SB, Houtkooper LB, Metcalfe LL, Blew RM, et al. Maintenance of weight loss in overweight middle-aged women through the Internet. Obesity 2008;16:1052-60. http://dx.doi.org/10.1038/oby.2008.19.
- Teixeira PJ, Going SB, Houtkooper LB, Cussler EC, Martin CJ, Metcalfe LL, et al. Weight loss readiness in middle-aged women: psychosocial predictors of success for behavioral weight reduction. J Behav Med 2002;25:499-523. http://dx.doi.org/10.1023/A:1020687832448.
- Fogelholm M, Kukkonen-Harjula K, Nenonen A, Pasanen M. Effects of walking training on weight maintenance after a very-low-energy diet in premenopausal obese women: a randomized controlled trial. Arch Intern Med 2000;160:2177-84. http://dx.doi.org/10.1001/archinte.160.14.2177.
- Fogelholm M, Kukkonen-Harjula K, Oja P. Eating control and physical activity as determinants of short-term weight maintenance after a very-low-calorie diet among obese women. Int J Obes Relat Metab Disord 1999;23:203-10. http://dx.doi.org/10.1038/sj.ijo.0800825.
- Jeffery RW, Wing RR. Long-term effects of interventions for weight loss using food provision and monetary incentives. J Consult Clin Psychol 1995;63:793-6. http://dx.doi.org/10.1037/0022-006X.63.5.793.
- Jeffery RW, Wing RR, Thorson C, Burton LR, Raether C, Harvey J, et al. Strengthening behavioral interventions for weight loss: a randomized trial of food provision and monetary incentives. J Consult Clin Psychol 1993;61:1038-45. http://dx.doi.org/10.1037/0022-006X.61.6.1038.
- Borg P, Kukkonen-Harjula K, Fogelholm M, Pasanen M. Effects of walking or resistance training on weight loss maintenance in obese, middle-aged men: a randomized trial. Int J Obes Relat Metab Disord 2002;26:676-83. http://dx.doi.org/10.1038/sj.ijo.0801962.
- Ramirez EM, Rosen JC. A comparison of weight control and weight control plus body image therapy for obese men and women. J Consult Clin Psychol 2001;69:440-6. http://dx.doi.org/10.1037/0022-006X.69.3.440.
- Rapoport L, Clark M, Wardle J. Evaluation of a modified cognitive–behavioural programme for weight management. Int J Obes Relat Metab Disord 2000;24:1726-37. http://dx.doi.org/10.1038/sj.ijo.0801465.
- Riebe D, Blissmer B, Greene G, Caldwell M, Ruggiero L, Stillwell KM, et al. Long-term maintenance of exercise and healthy eating behaviors in overweight adults. Prev Med 2005;40:769-78. http://dx.doi.org/10.1016/j.ypmed.2004.09.023.
- Riebe D, Greene GW, Ruggiero L, Stillwell KM, Blissmer B, Nigg CR, et al. Evaluation of a healthy-lifestyle approach to weight management. Prev Med 2003;36:45-54. http://dx.doi.org/10.1006/pmed.2002.1126.
- Blissmer B, Riebe D, Dye G, Ruggiero L, Greene G, Caldwell M. Health-related quality of life following a clinical weight loss intervention among overweight and obese adults: intervention and 24 month follow-up effects. Health Qual Life Outcomes 2006;4. http://dx.doi.org/10.1186/1477-7525-4-43.
- Foreyt JP, Goodrick GK, Reeves RS, Raynaud AS, Darnell L, Brown AH, et al. Response of free-living adults to behavioral treatment of obesity: attrition and compliance to exercise. Behav Ther 1993;24:659-69. http://dx.doi.org/10.1016/S0005-7894(05)80324-7.
- Skender ML, Goodrick GK, Del Junco DJ, Reeves RS, Darnell L, Gotto AM, et al. Comparison of 2-year weight loss trends in behavioral treatments of obesity: diet, exercise, and combination interventions. J Am Diet Assoc 1996;96:342-6. http://dx.doi.org/10.1016/S0002-8223(96)00096-X.
- Stahre L, Tarnell B, Hakanson CE, Hallstrom T. A randomized controlled trial of two weight-reducing short-term group treatment programs for obesity with an 18-month follow-up. Int J Behav Med 2007;14:48-55. http://dx.doi.org/10.1007/BF02999227.
- Wadden TA, Vogt RA, Andersen RE, Bartlett SJ, Foster GD, Kuehnel RH, et al. Exercise in the treatment of obesity: effects of four interventions on body composition, resting energy expenditure, appetite, and mood. J Consult Clin Psychol 1997;65:269-77. http://dx.doi.org/10.1037/0022-006X.65.2.269.
- Wadden TA, Vogt RA, Foster GD, Anderson DA. Exercise and the maintenance of weight loss: 1-year follow-up of a controlled clinical trial. J Consult Clin Psychol 1998;66:429-33. http://dx.doi.org/10.1037/0022-006X.66.2.429.
- Carels RA, Darby L, Cacciapaglia HM, Douglass OM, Harper J, Kaplar ME, et al. Applying a stepped-care approach to the treatment of obesity. J Psychosom Res 2005;59:375-83. http://dx.doi.org/10.1016/j.jpsychores.2005.06.060.
- Burke V, Beilin LJ, Cutt HE, Mansour J, Williams A, Mori TA. A lifestyle program for treated hypertensives improved health-related behaviors and cardiovascular risk factors, a randomized controlled trial. J Clin Epidemiol 2007;60:133-41. http://dx.doi.org/10.1016/j.jclinepi.2006.05.012.
- Burke V, Beilin LJ, Cutt HE, Mansour J, Wilson A, Mori TA. Effects of a lifestyle programme on ambulatory blood pressure and drug dosage in treated hypertensive patients: a randomized controlled trial. J Hypertens 2005;23:1241-9. http://dx.doi.org/10.1097/01.hjh.0000170388.61579.4f.
- Burke V, Mansour J, Beilin LJ, Mori TA. Long-term follow-up of participants in a health promotion program for treated hyper-tensives (ADAPT). Nutr Metab Cardiovasc Dis 2008;18:198-206. http://dx.doi.org/10.1016/j.numecd.2006.10.004.
- Cooper Z, Doll HA, Hawker DM, Byrne S, Bonner G, Eeley E, et al. Testing a new cognitive behavioural treatment for obesity: a randomized controlled trial with three-year follow-up. Behav Res Ther 2010;48:706-13. http://dx.doi.org/10.1016/j.brat.2010.03.008.
- The Management of Obesity and Overweight: An Analysis of Reviews of Diet, Physical Activity and Behavioural Approaches. HDA: London; 2003.
- Simpson SA, Shaw C, McNamara R. What is the most effective way to maintain weight loss in adults. BMJ 2011;343. http://dx.doi.org/10.1136/bmj.d8042.
- Hamman RF, Wing RR, Edelstein SL, Lachin JM, Bray GA, Delahanty L, et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care 2006;29:2102-7. http://dx.doi.org/10.2337/dc06-0560.
- Hardcastle SJ, Taylor AH, Bailey MP, Harley RA, Hagger MS. Effectiveness of a motivational interviewing intervention on weight loss, physical activity and cardiovascular disease risk factors: a randomised controlled trial with a 12-month post-intervention follow-up. Int J Behav Nutr Phys Act 2013;10. http://dx.doi.org/10.1186/1479-5868-10-40.
- Shephard RJ. Limits to the measurement of habitual physical activity by questionnaires. Br J Sport Med 2003;37:197-206. http://dx.doi.org/10.1136/bjsm.37.3.197.
- Olafsdottir AS, Thorsdottir I, Gunnarsdottir I, Thorgeirsdottir H, Steingrimsdottir L. Comparison of women’s diet assessed by FFQs and 24-hour recalls with and without underreporters: associations with biomarkers. Ann Nutr Metab 2006;50:450-60. http://dx.doi.org/10.1159/000094781.
- Channon SJ, Huws-Thomas MV, Rollnick S, Hood K, Cannings-John RL, Rogers C, et al. A multicenter randomized controlled trial of motivational interviewing in teenagers with diabetes. Diabetes Care 2007;30:1390-5. http://dx.doi.org/10.2337/dc06-2260.
- Bennett JA, Young HM, Nail LM, Winters-Stone K, Hanson G. A telephone-only motivational intervention to increase physical activity in rural adults: a randomized controlled trial. Nurs Res 2008;57:24-32. http://dx.doi.org/10.1097/01.NNR.0000280661.34502.c1.
- Shaikh AR, Vinokur AD, Yaroch AL, Williams GC, Resnicow K. Direct and mediated effects of two theoretically based interventions to increase consumption of fruits and vegetables in the Healthy Body Healthy Spirit trial. Health Educ Behav 2011;38:492-501. http://dx.doi.org/10.1177/1090198110384468.
- Copeland L, McNamara R, Kelson M, Simpson S. Mechanisms of change within motivational interviewing in relation to health behaviour; a systematic review. Patient Education &Amp; Counselling 2015;98:401-11. http://dx.doi.org/10.1016/j.pec.2014.11.022.
- Teixeira PJ, Silva MN, Coutinho SR, Palmeira AL, Mata J, Vieira PN, et al. Mediators of weight loss and weight loss maintenance in middle-aged women. Obesity 2010;18:725-35. http://dx.doi.org/10.1038/oby.2009.281.
- McKee H, Ntoumanis N, Smith B. Weight maintenance: self-regulatory factors underpinning success and failure. Psychol Health 2013;28:1207-23. http://dx.doi.org/10.1080/08870446.2013.799162.
- Lally P, Chipperfield A, Wardle J. Healthy habits: efficacy of simple advice on weight control based on a habit-formation model. Int J Obesity 2008;32:700-7. http://dx.doi.org/10.1038/sj.ijo.0803771.
- Rothman AJ, Sheeran P, Wood W. Reflective and automatic processes in the initiation and maintenance of dietary change. Ann Behav Med 2009;38:S4-17. http://dx.doi.org/10.1007/s12160-009-9118-3.
- Lally P, Van Jaarsveld CHM, Potts HWW, Wardle J. How are habits formed: modelling habit formation in the real world. Eur J Soc Psychol 2010;40:998-1009. http://dx.doi.org/10.1002/ejsp.674.
- Chambers JA, Swanson V. Stories of weight management: factors associated with successful and unsuccessful weight maintenance. Br J Health Psychol 2012;17:223-43. http://dx.doi.org/10.1111/j.2044-8287.2011.02030.x.
- Reyes NR, Oliver TL, Klotz AA, Lagrotte CA, Vander Veur SS, Virus A, et al. Similarities and differences between weight loss maintainers and regainers: a qualitative analysis. J Acad Nutr Diet 2012;112:499-505. http://dx.doi.org/10.1016/j.jand.2011.11.014.
- Hardcastle S, Hagger MS. ‘You Can’t Do It on Your Own’: experiences of a motivational interviewing intervention on physical activity and dietary behaviour. Psychol Sport Exerc 2011;12:314-23. http://dx.doi.org/10.1016/j.psychsport.2011.01.001.
- Lindvall K, Larsson C, Weinehall L, Emmelin M. Weight maintenance as a tight rope walk – a grounded theory study. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-51.
- Hindle L, Carpenter C. An exploration of the experiences and perceptions of people who have maintained weight loss. J Hum Nutr Diet 2011;24:342-50. http://dx.doi.org/10.1111/j.1365-277X.2011.01156.x.
- Sach TH, Barton GR, Doherty M, Muir KR, Jenkinson C, Avery AJ. The relationship between body mass index and health-related quality of life: comparing the EQ-5D, EuroQol VAS and SF-6D. Int J Obesity 2007;31:189-96. http://dx.doi.org/10.1038/sj.ijo.0803365.
- Loveman E, Frampton GK, Shepherd J, Picot J, Cooper K, Bryant J, et al. The clinical effectiveness and cost-effectiveness of long-term weight management schemes for adults: a systematic review. Health Technol Assess 2011;15. http://dx.doi.org/10.3310/hta15020.
- Morgan PJ, Warren JM, Lubans DR, Collins CE, Callister R. Engaging men in weight loss: experiences of men who participated in the male only SHED-IT pilot study. Obes Res Clin Pract 2011;5:e169-266. http://dx.doi.org/10.1016/j.orcp.2011.03.002.
- Pagoto SL, Schneider KL, Oleski JL, Luciani JM, Bodenlos JS, Whited MC. Male inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity 2012;20:1234-9. http://dx.doi.org/10.1038/oby.2011.140.
- Hussain-Gambles M, Atkin K, Leese B. Why ethnic minority groups are under-represented in clinical trials: a review of the literature. Health Soc Care Community 2004;12:382-8. http://dx.doi.org/10.1111/j.1365-2524.2004.00507.x.
- Sabinsky MS, Toft U, Raben A, Holm L. Overweight men’s motivations and perceived barriers towards weight loss. Eur J Clin Nutr 2007;61:526-31.
- Morgan PJ, Callister R, Collins CE, Plotnikoff RC, Young MD, Berry N, et al. The SHED-IT community trial: a randomized controlled trial of internet- and paper-based weight loss programs tailored for overweight and obese men. Ann Behav Med 2013;45:139-52. http://dx.doi.org/10.1007/s12160-012-9424-z.
- Hunt K, Wyke S, Gray CM, Anderson AS, Brady A, Bunn C, et al. A gender-sensitised weight loss and healthy living programme for overweight and obese men delivered by Scottish Premier League football clubs (FFIT): a pragmatic randomised controlled trial. Lancet 2014;383:1211-21. http://dx.doi.org/10.1016/S0140-6736(13)62420-4.
- Look Ahead Research Group . Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity 2014;22:5-13. http://dx.doi.org/10.1002/oby.20662.
- Mehring M, Haag M, Linde K, Wagenpfeil S, Frensch F, Blome J, et al. Effects of a general practice guided web-based weight reduction program--results of a cluster-randomized controlled trial. BMC Fam Pract 2013;14. http://dx.doi.org/10.1186/1471-2296-14-76.
- Behaviour Change. London: UK Parliament; 2011.
- Stevens J, Truesdale KP, McClain JE, Cai J. The definition of weight maintenance. Int J Obes 2006;30:391-9. http://dx.doi.org/10.1038/sj.ijo.0803175.
- Weighing the Options: Criteria for Evaluating Weight Management Programs. Washington, DC: Government Printing Office; 1995.
- Ramage S, Farmer A, Apps Eccles K, McCargar L. Healthy strategies for successful weight loss and weight maintenance: a systematic review. Appl Physiol Nutr Metab 2014;39:1-20. http://dx.doi.org/10.1139/apnm-2013-0026.
- Butland B, Jebb S, Kopelman P, McPherson K, Thomas S, J. M, . Foresight. Tackling Obesities: Future Choices – Modelling Future Trends in Obesity & Their Impact on Health. London: The Stationery Office; 2007.
- Butryn ML, Webb V, Wadden TA. Behavioral treatment of obesity. Psychiatr Clin North Am 2011;34:841-59. http://dx.doi.org/10.1016/j.psc.2011.08.006.
- Sniehotta FF, Simpson SA, Greaves CJ. Weight loss maintenance: an agenda for health psychology. Br J Health Psychol 2014;19:459-64. http://dx.doi.org/10.1111/bjhp.12107.
Appendix 1 Motivational interviewing practitioners’ handbook
Appendix 2 Group facilitators’ handbook
Appendix 3 Safety reporting procedure
Appendix 4 Participant questionnaires and case report forms (example versions)
Appendix 5 Qualitative interviews topic guides
Appendix 6 Focus group interview schedule
Appendix 7 Motivational interviewing case report forms
Appendix 8 Unit costs
Appendix 9 Summary of protocol changes
List of abbreviations
- AUDIT-C
- Alcohol Use Disorders Identification Test
- BMI
- body mass index
- CACE
- complier-average causal effect
- CDT
- cognitive dissonance theory
- CEA
- cost-effectiveness analysis
- CI
- confidence interval
- CLRN
- Comprehensive Local Research Network
- CRF
- case report form
- CVD
- cardiovascular disease
- DINE
- Dietary Instrument for Nutrition Education
- EDE-Q
- Eating Disorder Examination Questionnaire
- EOI
- expression of interest
- EOR
- exercise on referral
- EQ-5D
- European Quality of Life-5 Dimensions
- ETC
- excess treatment cost
- GF
- group facilitator
- GHQ-12
- General Health Questionnaire – 12 items
- GP
- general practitioner
- HP
- health professional
- HSI
- Heaviness of Smoking Index
- ICC
- intracluster correlation coefficient
- ICER
- incremental cost-effectiveness ratio
- IPAQ
- International Physical Activity Questionnaire
- MAP
- model of action phases
- MI
- motivational interviewing
- MIP
- motivational interviewing practitioner
- MITI
- motivational interviewing treatment integrity
- NICE
- National Institute for Health and Care Excellence
- OR
- odds ratio
- PCT
- primary care trust
- PIC
- Participant Identification Centre
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- SAE
- serious adverse event
- SCT
- social cognitive theory
- SD
- standard deviation
- SDT
- self-determination theory
- WHO
- World Health Organization
- WILMA
- WeIght Loss Maintenance in Adults
- WLM
- weight loss maintenance
- WTP
- willingness to pay