Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 10/38/03. The contractual start date was in March 2012. The draft report began editorial review in June 2014 and was accepted for publication in November 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Jeremy Fairbank reports non-financial support from Integrated Shape Imaging System (ISIS) scanner during the conduct of the study. Adrian Gardner reports grants, personal fees and non-financial support from Medtronic Spine, Dublin, Ireland, and personal fees from Depuy Synthesis Spine, Leeds, UK, outside the submitted work.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Williams et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Rationale for a feasibility study
Feasibility studies are used to estimate important parameters that are needed to design a definitive trial. They are not designed to estimate the effect on the outcome of interest, and, consequently, a primary outcome is not usually defined and a typical power calculation is not normally undertaken. Instead, the sample size should be adequate to estimate the critical parameters (e.g. recruitment rate, baseline variability) to the necessary degree of precision (see www.nets.nihr.ac.uk/glossary).
The brief for the Active Treatment for Idiopathic Adolescent Scoliosis (ACTIvATeS) feasibility study stipulated that two interventions should be compared: standard NHS care and a defined package of scoliosis-specific exercise (SSE) therapy for patients with adolescent idiopathic scoliosis (AIS). The following conditions were also specified:
-
The patient group investigated should be children or adolescents, aged 10–16 years, with mild/primary AIS and a Cobb angle < 50° (i.e. conservatively managed).
-
The setting should be an outpatient clinic or community setting.
-
The control group would receive standard NHS care.
-
The acceptability and adherence of intervention should be assessed.
-
A survey of orthopaedic surgeons should be conducted to identify the available number of participants and surgeons willing to participate.
-
Training requirements of therapists should be assessed and described.
In order to achieve these specifications the ACTIvATeS study team proposed the following methods:
-
a national survey of current practice and opinion for the management of AIS
-
a systematic review of the literature regarding exercise interventions for AIS
-
development of both exercise and control interventions involving key stakeholders
-
a randomised feasibility study at multiple NHS trusts
-
a qualitative study involving patients, parents and physiotherapists.
Condition
Adolescent idiopathic scoliosis is often referred to as a structural lateral curvature of the spine, although it is actually a three-dimensional spinal deformity that results in lateral deviation, rotation and flexion/extension of the vertebrae. It is of unknown cause and occurs at or near the onset of puberty. 1 AIS is usually diagnosed by radiography using the Cobb angle (see Figure 2 for detail) and, to meet the definition, the lateral curvature must have a Cobb angle of > 10°.
In the UK, the prevalence of AIS in children aged 10–16 years is 1–3%,2,3 suggesting that there are 50,000–150,000 sufferers. 4 The effects of AIS include pain, cosmetic concerns, functional limitations, cardiorespiratory problems and possible further curve progression in adulthood. 5 About 10% of AIS patients require surgical or conservative management. 6 Current UK management includes monitoring, bracing for some and, for the most progressive and serious patients, surgery. Surgery is generally undertaken only when spinal curvature reaches a Cobb angle of > 45–50°. 7 Surgery is a very extensive procedure, with exposure of large segments of the spine and substantial fixation which, although reducing curve progression, also permanently limits mobility in the affected part of the spine. Surgery also comes with a risk of complications, which are estimated to occur in approximately 6% of patients undergoing spinal fusion for scoliosis and include pulmonary complications, wound infection and neurological damage. 8
The risk of curve progression is not completely understood but is thought to be dependent on the size of curve, stage of growth and skeletal maturity.
Existing research
Current treatments
In the UK, surveys of current surgical practice9 and advice information provided at initial diagnosis have previously been conducted;10 however, a survey of current conservative treatments provided in the NHS has not been undertaken. Currently, it is thought that the main components of conservative management of scoliosis in the UK are monitoring and a limited use of bracing.
Rationale for treatments
Braces are an intrusive and uncomfortable intervention. Two publications reported bracing protocols that lasted up to 4 years and required the brace to be worn for 23 hours per day. 11,12 The effectiveness of bracing protocols is unclear,13 although a recent trial reported by Weinstein et al. 14 suggests that there is promise of efficacy.
Exercise is a promising intervention for which there is an emerging, although low-quality, evidence base. 15,16 The rationale is to use exercises that promote spinal realignment and thus either improve or halt progression of the curvature. Exercise is, potentially, a low-cost intervention and, even if not effective in all patients, it may be of substantial benefit if the relative risk reduction in progression to curvature of > 45° or requirement for surgery was reduced in a modest proportion of those participating. It is thought that exercise should be applied as early in the disease process as possible.
Exercise therapy is not commonly provided in the UK and the USA, although it is routinely provided in parts of Europe. 17 Within continental Europe, there are various schools of exercise therapy for AIS. The Schroth method (originating in Germany), Scientific Exercises Approach to Scoliosis (SEAS; Italy), the Lyon method (France) and the DoboMed method (Poland) are among the most well-known and reported in the literature. However, there is little evidence to support the choice of one form of therapy over another or evidence of their clinical effectiveness and cost-effectiveness.
The rationale for exercise to manage AIS is that a number of underlying impairments in spinal muscular function and postural ability contribute to or accompany the development of curvature and are potentially reversible. Electromyography (EMG) of trunk muscles in AIS patients indicates disrupted patterns of muscle recruitment under static and dynamic conditions, in a broad range of postures. These asymmetries extend to the paraspinal lumbar and abdominal oblique muscles and are associated with a disparity in trunk isometric rotation strength between sides. 18–21 In keeping with differential muscle activity, there are differences in muscle fibre type distribution on the convex and the concave sides of the curve. AIS patients exhibit greater balance control problems and proprioceptive impairments. 22,23 AIS may be associated with distorted body schema, resulting in a mismatch between actual body alignment and patients’ internal bodily representation of the body. 24
Hence, to improve function and reduce or stabilise curvature, exercise programmes must include strengthening of all affected muscle groups; exercises to encourage the appropriate magnitude and timing of muscle activation; proprioceptive elements; and postural/body awareness components. These programmes will require careful tailoring to each individual. There is evidence that such approaches can remediate underlying impairments in EMG activation and strength, although effects may well be limited to curves with a Cobb angle of < 50°. 19–21,25,26
Although there is a theoretical basis for exercise in AIS, there is little robust evidence that it has a significant effect on curve progression. There are relatively few studies investigating this important outcome,15 and only one randomised controlled trial (RCT)27 had been published at the time of the application (March 2011). A small number of prospective cohort studies have attempted to evaluate the European schools of exercise including SEAS and Schroth. 15 Although these studies show a favourable outcome in support of exercises, the research is problematic for a variety of reasons. These include a lack of control group, failure to randomise, the reporting of very small statistically significant but not necessarily clinically important differences in Cobb angle, poor statistical analysis, limited descriptions of baseline characteristics of participants, and no reporting or poor adherence to treatment and the exercise programmes evaluated. 28 Clear evidence that these approaches are beneficial is lacking.
Economic considerations
There is no information on the cost-effectiveness of the various exercise approaches and whether or not they offer a viable alternative to surgery and bracing. Many patients with similar spine deformities report lower scores in physical functioning than the general population. 29 The impact of treatment of illness on health-related quality of life (HRQoL) can be measured with ‘utility’ scores that represent people’s preferences towards a particular health state. The current study used two preference-based HRQoL instruments, namely the Health Utilities Index (HUI) and the European Quality of Life-5 Dimensions (EQ-5D). These systems employ multidomain health status questionnaires completed by individuals to obtain information on self-assessed health status. Preference-based scores for those health states are then calculated using published scoring functions for the two systems. The published scoring functions are based on preferences obtained from random samples of the general population; the Canadian and UK adult populations for the Health Utilities Index Mark 2 (HUI2), the Canadian adult population for the Health Utilities Index Mark 3 (HUI3) and the UK adult population for the EQ-5D. These multiattribute preference-based instruments are significantly less resource- and time-consuming than direct utility or preference elicitation approaches, such as the standard gamble and time-trade-off approaches, which can directly measure the utility that patients attach to their health states. HUI and EQ-5D measures have been shown to be valid, reliable and responsive to changes in health status over time. 30–32
There is no evidence in the literature with respect to comparisons of the EQ-5D and the HUI in patients with AIS. One study by Adobor et al. 33 evaluated the repeatability, reliability, internal consistency and concurrent validity between the Scoliosis Research Society-22 patient questionnaire (SRS-22) and EQ-5D in AIS. Their results showed a moderate correlation between these two instruments. The authors claimed that one of the reasons for this was that the EQ-5D has been validated for use in adult populations with back pain, but not in adolescents with spine deformity (as in the ACTIvATeS study). The advantage of preference-based measures such as the HUI and EQ-5D is that they can generate health utility scores for comparative economic evaluation purposes. In addition, the HUI has been widely used in the literature to describe the self-rated health of youths and young adults. 29,34–36
Relevant evidence with regards to head-to-head comparison of the HUI and EQ-5D measures in adolescents is provided by a recent study by Oluboyede et al. ,37 which attempted to understand the practicality, validity and reliability of using these two measures for adolescents who have experienced a self-harm episode. Their results showed that the HUI had a higher rate of missing data, and adolescents had difficulties interpreting some of its questions. No missing data were observed for any questions in the EQ-5D in the population of 49 adolescents. In a study of children with meningitis38 there was evidence that, although the EQ-5D may be preferable because it has been used in many different patient populations and is the preferred measure of HRQoL in the National Institute for Health and Care Excellence (NICE) health technology assessments, the HUI classifications are more precise and discriminative. This study also indicated that both instruments would produce the same HRQoL weights or utility scores in the meningitis context.
Following structured literature searches we have found no evidence to indicate the cost of AIS in the UK. A study conducted in the USA suggested the overall national cost of AIS to be around US$1.13B (based on 2006–7 prices). 39 Earlier evidence from the World Health Organization suggests that the cost from musculoskeletal diseases in general stems mainly from hospital admissions, physician visits, nursing home services, medications and non-health-related sources. The contribution of these different health-care services to economic costs may vary by musculoskeletal disease, age and sex. Treatment of AIS is often a lengthy process and, therefore, requires considerable contributions from different providers within the health-care system.
Qualitative study
Understanding why patients and their families make the decisions they do about their health care can help us to provide the appropriate treatments. Although parents are often used in research to elicit young people’s experiences, we believed that we needed to seek information directly from the young people in order to determine the feasibility of the proposed intervention. 40 An adult may not give such a useful account of the young person’s experience. 41 This is the first qualitative study to explore the experiences of young people with AIS undergoing an exercise programme. Previous research has focused on young people’s experiences with scoliosis surgery and bracing. 42–45
Study aim
The aim of this feasibility study was to assess the feasibility of conducting a large, definitive, multicentre trial of SSE treatment for patients with AIS, in comparison with standard care. Specific objectives are listed within each of the reported sections.
Chapter 2 Systematic review update
Objective
To conduct an up-to-date systematic review of the literature evaluating the efficacy or effectiveness of SSE for patients with AIS.
This would inform the development of the interventions to be evaluated in the ACTIvATeS randomised feasibility trial and would also indicate whether or not further research is warranted at the end of the feasibility phase.
Methods
A systematic literature review published by Cochrane included publications up to 30 March 2011. 17 We have followed the methods, including the search strategy, published in the original Cochrane review to carry periodic updates of this review.
Identification of new eligible studies
We have rerun the published search strategies to identify new eligible trials and searched databases up to 12 February 2014. A further study was also identified from an e-mail alert of new research from a journal publisher (see Table 1). We attempted to source grey literature using the OpenGrey database (OpenGrey V1.0, Institut de l’Information Scientifique et Technique, Vandoeuvre-lès-Nancy, France).
Full articles of studies that seemed eligible from the abstract were examined independently by two assessors and checked for eligibility based on the original criteria for inclusion.
According to the original Cochrane review criteria, studies were eligible for the review if they were RCTs, quasi-RCTs or observational studies that included participants diagnosed with AIS (defined as at least a 10° Cobb angle) who were older than 10 years but had not reached the end of bone growth.
Studies were excluded if participants had any type of secondary scoliosis (congenital, neurological, metabolic, post-traumatic, etc.). The experimental interventions in this review included all types of SSE that are considered to be ‘specific movements performed with a therapeutic aim of reducing the deformity’. Sports, active recreational activities and generalised physiotherapy were not considered to be specific exercises for the treatment of scoliosis, and studies including these types of activities were excluded.
Control interventions included no treatment, different types of SSE, usual therapy, different doses or schedules of exercises or other non-surgical treatments. Comparison could include exercises versus no treatment; another treatment versus that treatment plus exercises; exercises versus another conservative treatment; exercises versus usual physiotherapy; and comparisons between different types of exercises or different doses/schedules of exercises.
Risk of bias assessment
After identifying eligible studies, a risk of bias assessment was carried out using the criteria published in the original review (see Table 6). This was done independently by two reviewers who then compared findings. Any differences were resolved through discussion.
Each study was then classified as at high or low risk of bias using the same criteria as the previous review. 17 A study was considered to be at low risk of bias if it fulfilled the three key criteria related to randomisation, allocation concealment and outcome assessor blinding, as well as any three of the other criteria.
Data synthesis
Data extraction was carried out independently by two assessors using a standardised form. Data were compared and any discrepancies were resolved through discussion between the two assessors.
Meta-analysis was not performed owing to lack of homogeneity between studies. The variability between exercise approaches assessed, outcome measures used and timings of follow-up was too great to allow us to combine study findings. We assessed the overall quality of evidence for each outcome using an adapted Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach as used in the original Cochrane review of exercises for AIS17 and as recommended by the Cochrane Back Review Group. 46
In accordance with the GRADE approach:
-
High-quality evidence was defined as consistent findings among at least two RCTs with low risk of bias that are generalisable to the population in question (consistency is defined as 75% or more of the studies with similar results); sufficient data, with narrow confidence intervals; no known or suspected reporting biases; further research is very unlikely to change confidence in the estimate of effect.
-
Moderate-quality evidence was defined as failure to meet one of the factors described in the high-quality definition. Further research is likely to have an important impact on confidence in the estimate of effect and may change the estimate.
-
Low-quality evidence was defined as failure to meet two of the factors described in the high-quality definition. Further research is very likely to have an important impact on confidence in the estimate of effect and is likely to change the estimate.
-
Very low-quality evidence was defined as failure to meet three of the factors described in the high-quality definition. Any estimate of effect is very uncertain.
-
No evidence was defined as complete lack of evidence from RCTs.
Results
Five new eligible studies were identified (Table 1), which, in addition to the two studies previously included in the Cochrane review,15,27 brought the total number of studies eligible for inclusion in the review to seven.
| Databases searched using search strategies from Cochrane review17 limited to March 2011 to February 2014 | Hits | Number of studies after screening of abstracts | Retrieved full articles (duplicates removed) | Eligibility after review of full article |
|---|---|---|---|---|
| MEDLINE | 302 | 1 | 8 | Eligible = 5 Ineligible = 3 |
| EMBASE | 4 | 0 | ||
| CINAHL | 392 | 3 | ||
| Cochrane | 41 | 3 | ||
| PEDro | 5 | 1 | ||
| PsycINFO | 4 | 1 | ||
| Index to Chiropractic Literature | 3 | 0 | ||
| Other sources | 1 | 1 |
With a substantial increase in the number of eligible randomised studies it was decided that the justification for inclusion of non-randomised studies provided in the original Cochrane review was no longer valid, and, therefore, we separated the synthesis and evaluation of randomised and non-randomised studies and primarily consider evidence from randomised studies in line with best Cochrane practice. 47 This resulted in two non-randomised studies15,48 being isolated for secondary evaluation.
Characteristics of included randomised studies
Characteristics of the five randomised studies and the outcomes they measured are described in Tables 2 and 3. 27,49–52 Characteristics of the two non-randomised studies are presented in Tables 4 and 5. 15,48
| Study | Number of participants at baseline/follow-up | Mean age in years (SD) | Sex, n (%) | Type of curve | Specifics of the intervention(s) | Dosage |
|---|---|---|---|---|---|---|
| Wan et al. 200527 | 80/80 | Intervention and control: 15.0 (4.0) | Intervention and control: females, 43 (54); males, 37 (46) | S-shaped scoliosis excluding C-shaped scoliosis, with mean Cobb angles of 25° (13) and 23° (11) for the control, and 26° (12) and 24° (10) for the thoracic and lumbar segments, respectively | Intervention: electrostimulation + postural training + gymnastic exercise for correcting essential S-shaped scoliosis Control: electrostimulation on the lateral body surface by therapeutic apparatus + postural training |
Gradual increase over 6 months of therapy for both groups Intervention: exercise was once daily; repeating each step 10 times up to 30 times; holding the position for 30 seconds with 30-second rests, repeated two or three times. The exercise volume and intensity was increased by attaching 0.15–0.25-kg bags on the left leg Control: first day – three times per day for 30 minutes each; second day – twice for 1 hour each; third day – once for 3 hours Afterwards treatment was increased by 1 hour every day until it reached 8 hours per day with progression to traction therapy for 30 minutes |
| Toledo et al. 201151 | 20/20 | Intervention and control: 10 (3.0) | Intervention: females, 4 (40); male, 6 (60) Control: females, 5 (50); males, 5 (50) |
Structural thoracic scoliosis excluding patients without positive tests, with mean Cobb angles of 15.0° (10.0) and 14.0° (7.0) for the intervention and control, respectively | Intervention: RPG method Control: no treatment |
Intervention: 25–30 minutes per session with 2–3-minute rests, twice per week for 12 weeks Control: no treatment |
| Diab 201249 | 76/68 | Intervention: 13.2 (1.2) Control: 14.5 (1.3) |
Intervention: females, 18 (47); males, 20 (53) Control: females, 17 (45); males, 21 (55) |
All types of curves with Cobb angle of 10–30°; Risser grade: 0, 1 or 2 and Lenke scale of 1A | Intervention: corrective exercise programme; individually adapted forward head posture correction alongside conventional stretching and strengthening exercises Control: traditional exercise treatment – stretching of concave tightened structures and strengthening of trunk muscles |
Intervention: conventional treatment three times per week + three sets of 12 repetitions of the strengthening exercises; four times per week daily, for 10 weeks Stretching cervical flexors through a chin drop in sitting; unilateral and bilateral pectoralis stretches alternating each 2-week period. Three stretching exercises held for 30 seconds each Control: conventional treatment three times per week for 10 weeks |
| Schreiber et al. 201350 | 31/31 | Intervention (Schroth + standard care): 14.4 (2.1) Control: 13.7 (1.7) |
Intervention and control: NR | All types of curves with Cobb angles of 10–45° and Risser grade of 0–5 Mean Cobb values: 32.6° (7.0) and 28.8° (10.0) for the intervention and control, respectively |
Intervention: Schroth SSE – consists of three-dimensional exercises based on sensorimotor and kinaesthetic principles, teaching patients to maintain the correct posture in daily activities in order to improve the curve, pain and self-image using endurance and strength training Control: monitoring or bracing (based on Boston brace criteria) for 6 months |
Intervention: five individual visits to learn the exercises, followed by weekly supervised group sessions of 1 hour each (tailored) 30–45 minutes of daily training using algorithm, with daily home exercises for 6 months Control: 6 months |
| Monticone et al. 201452 | 110/98 | Intervention: 12.5 (1.1) Control: 12.4 (1.1) |
Intervention: females, 39 (71); males, 16 (29) Control: females, 41 (75); males, 14 (25) |
All types of curves with Cobb angles of 10–25° and Risser grades of < 2 Mean Cobb angle values: 19.30° (3.9) and 19.20° (2.5) for the intervention and control, respectively |
Intervention: ASC, with individually adapted exercises, cognitive–behavioural strategies and ergonomic education via booklet by three experienced physiotherapists Control: general exercises aimed at spinal mobilisation |
Intervention: 60-minute outpatient workout sessions. Once per week at the institute, 30 minutes of individualised sessions twice per week at home. Mean time on treatment = 42.8 months (SD 9.09) Control: 60-minute outpatient workout sessions. Once per week at the institute, and 30 minutes of individualised sessions twice per week at home |
| Study | Follow-up | Cobb angle measures in degrees (°) | Change in trunk balance | Flexibility and muscular strength | ATR | Quality of life | Psychological issues including cosmetic issues | Back pain and disability | Global rating of change |
|---|---|---|---|---|---|---|---|---|---|
| Wan et al. 200527 | 6 months | Yes | No | No | No | No | No | No | No |
| Toledo et al. 201151 | 6 months | Yes | No | No | No | No | No | No | No |
| Diab 201249 | 10 weeks and 3 months | No | Yes | No | No | No | No | Functional rating index | No |
| Schreiber et al. 201350 | 3 months | No | No | Muscle strength: Biering-Sørensen test | No | SRS-22 total score | SRS-22 self-perceived image subscale and self-efficacy questionnaire | SRS-22 function and pain subscale | Yes |
| Monticone et al. 201452 | Skeletal maturity (mean time = 42 months) and 12 months post maturity (mean time = 52 months) | Yes | No | No | Yes | No | SRS-22 self-perceived image, mental health and satisfaction with management subscales | SRS-22 function and pain subscale | No |
| Study | Study design | Number of participants at baseline/follow-up | Mean age in years (SD) | Sex, n (%) | Type of curve | Specifics of the intervention(s) | Dosage |
|---|---|---|---|---|---|---|---|
| Negrini et al. 200815 | Prospective controlled cohort study | 74/70 | Intervention: 12.7 (2.2) Control: 12.1 (2.1) |
Intervention: females, 25 (71); males, 10 (29) Control: females, 27 (69); males, 12 (31) |
All type of curves under proven radiograph, Cobb angle > 15° or 20° and Risser grade of 0–1 or 2–3, respectively Mean Cobb angle: 15° (SD 6°) Mean ATR: 7° (SD 2°) |
Intervention: ASC and individually adapted SEAS programme Control: different exercise activities as designed by attending physiotherapist |
Intervention: 1.5 hours of quarterly (2–3 months) supervised sessions. Additionally, 40 minutes of training, twice weekly, was carried out at a nearby institute + 5 minutes of daily home exercise training for 12 months Control: 45–90 minutes of semistructured exercises (supervised and individualised sessions), two or three times per week for 12 months |
| Choi et al. 201348 | Cluster quasi-controlled trial | 44/35 | Intervention: 13.30 (0.57) Control: 13.10 (0.46) |
Intervention: females, 28 (100); males, 0 Control: females, 16 (100); males: 0 |
All type of curves within Cobb angle ranges of > 10 and < 20°s Mean Cobb angles: 14.90° (3.09) and 14.08° (1.66) for the intervention and control, respectively |
Intervention: theory of planned behaviour for posture management Control: 30 minutes of posture management behaviour using written material with photographs |
Intervention: 60 minutes per session, twice per week + five times per week of home exercise for 6 weeks. 30 minutes were allocated for strengthening attitudes, subjective norms, perceived behavioural control and behavioural intention towards posture management behaviour. The other 30 minutes were used for posture-management exercises Control: 30 minutes of daily practice of posture behavioural management for 6 weeks |
| Study | Follow-up | Cobb angle measures in degrees (°) | Change in trunk balance | Flexibility and muscular strength | ATR | Quality of life | Psychological issues including cosmetic issues | Back pain and disability | Global rating of change |
|---|---|---|---|---|---|---|---|---|---|
| Negrini et al. 200815 | 12 months | Yes | No | No | Yes | No | No | No | No |
| Choi et al. 201348 | 2 months | Yes | No | Range of movement and dynamometer measures of strength | No | No | No | No | No |
For randomised studies, samples sizes ranged from 20 participants to 110 participants, and all studies included males and females. The mean age of participants at baseline ranged from 1051 to 15 years. 27 Three studies included participants diagnosed with AIS irrespective of curve type, with the remaining two studies only including participants with specific curves: S-shaped or double curves27 and structural thoracic curves. 51
Most studies used criteria based on the Cobb angle to select patients and there was some variability here. The inclusion criteria in three studies included those patients with curves between 10° and 30°,49 those with curves from 10° to 25°52 and those with curves between 10° and 45°, respectively. 50 Two studies did not define inclusion criteria using the Cobb angle. 27,51
The mean Cobb angle of participants recruited to studies varied between approximately 15°,51 19°,52 25°27 and 30°. 50 One study did not report Cobb angles at baseline. 49
The most common lengths of follow-up were 3 months49,50 and 6 months post inclusion. 27,51 One study followed up participants to 12 months after skeletal maturity was reached (mean time to follow-up was 52 months). 52
Outcome measures varied across the studies (see Table 3). The Cobb angle was the only outcome measured in more than one study,27,51 whereas two other studies also collected additional physical measurements. 15,48 Only one study reported the Cobb angle alongside a patient-reported measure. 52 Two studies did not include the Cobb angle as an outcome. 49,50 One used postural parameters, including craniovertebral angle and spinal balance, along with a functional measure as outcomes,49 whereas the other evaluated back endurance, quality of life and self-efficacy. 50
The studies reported a variety of different approaches to exercises for scoliosis (see Table 2). No one study evaluated the same approach, although there are some similarities between the approaches used. The concept of active self-correction (ASC) underpinned the majority of the approaches,50–52 facilitated by varying degrees of assistive manual therapeutic techniques. Of the remaining studies, one included stretches of tightened structures on the concave side of the curve and strengthening of trunk muscles with and without the inclusion of exercises to correct adapted forward head posture,49 whereas the other evaluated a gymnastic-based exercise programme where participants exercised in asymmetrical postures to correct the S-shaped curve. 27
The amount of time that participants were expected to carry out exercises was variable. Although descriptions of interventions were not always clear, it appears that three studies required participants to carry out daily exercise programmes, although the amount of time spent exercising varied between approaches. 27,49,50 For example, an exercise programme based on the Schroth programme required participants to carry out 30–45 minutes of training per day. 50
Those undergoing global postural re-education attended treatment sessions twice per week. 51 Participants taking part in an ASC programme were required to attend a weekly 1-hour workout session at the institution supplemented by two 30-minute exercise sessions at home per week. 52
The duration of exercise interventions also varied between studies. These varied from 10 weeks49 and 12 weeks,51 to 6 months. 27,50 One study required participants to exercise until they reached skeletal maturity, which resulted in a mean duration of exercise intervention of 42 months. 52
Risk of bias for randomised studies
One randomised study was considered to be at low risk of bias52 and the remaining studies were considered to be at high risk of bias (Tables 6 and 7). 27,49–51
| Wan et al., 200527 | Diab, 201249 | Monticone et al., 201452 | Schreiber et al., 201350 | Toledo et al., 201151 | Trial characteristics |
|---|---|---|---|---|---|
| ? | ✓ | ✓ | ? | ? | Random sequence generation (selection bias) |
| ? | ✓ | ✓ | ? | ? | Allocation concealment |
| ✗ | ✗ | ✗ | ✗ | ✗ | Blinding (performance bias and detection bias): all outcomes – patients |
| ✗ | ✗ | ✗ | ✗ | ✗ | Blinding (performance bias and detection bias): all outcomes – providers |
| ✗ | ✗ | ✗ | ✗ | ✗ | Blinding (performance bias and detection bias): all outcomes – outcome assessors |
| ✓ | ✓ | ✓ | ✓ | ✓ | Incomplete outcome data (attrition bias): were dropouts reported and equal between groups? |
| ✓ | ✓ | ✓ | ✓ | ✓ | Incomplete outcome data (attrition bias): were all randomised participants analysed in the group to which they were allocated? |
| ✓ | ✓ | ✓ | ? | ✓ | Selective reporting (reporting bias) |
| ✓ | ✓ | ✓ | ✓ | ✓ | Group similar at baseline |
| ? | ? | ? | ? | ? | Co-interventions |
| ? | ? | ? | ✓ | ? | Adherence with interventions |
| ✓ | ✓ | ✓ | ✓ | ✓ | Similar outcome timing |
| Negrini et al., 200815 | Choi et al., 201348 | Observational study characteristics |
|---|---|---|
| ✗ | ? | Representativeness of exposed cohort |
| ✗ | ✗ | Selection of the non-exposed cohort bias (population) |
| ✓ | ✓ | Ascertainment of exposure |
| ✗ | ✓ | Comparability of cohorts on the basis of the design or analysis |
| ✓ | ✓ | Complete follow-up (attrition bias) |
| ✗ | ✗ | Independent blind assessments (detection bias) |
Allocation
The majority of studies failed to report adequate methods of random sequence generation and concealment of allocation27,50,51 and this was the main reason that studies were considered to be at high risk of bias. Explicit methods were described in Diab49 (random permuted blocks generated by independent person, sealed in opaque envelopes) and Monticone et al. 52 (random blinded treatment codes and automatic concealed assignment).
Blinding
No study blinded participants or treatment providers, which is not unreasonable owing to the nature of the interventions. However, only two studies50,52 reported the use of blinded outcome assessors, which should be possible in these types of studies and was the other reason the majority of studies were classified as being at high risk of bias.
Incomplete outcome data
Incomplete outcome data were not an apparent source of bias in any of the studies. No dropouts were reported by three studies. 50,51,56 Loss to follow-up was reported to be approximately 20% in the remaining studies with dropouts balanced across both arms. 49,52
Selective reporting
The majority of studies reported outcome data fully, as described in the methods section of each study. There was one exception to this – the study by Schreiber et al. 50 Online information about this study (see http://clinicaltrials.gov/show/NCT01610908) indicated that Cobb angle was the primary outcome, but this is not reported as an outcome in the published report. The report does stipulate that this trial is ongoing, which may account for the fact that it is not reported, but this is unclear.
Other potential sources of bias
It appears that the intervention and control groups were similar at baseline and that the timing of outcome assessment was similar for both groups in all the studies.
All studies failed to report co-interventions and so it is unclear if co-inventions may have been a source of bias. Information on adherence with exercise programmes was unreported in the majority of studies27,49,51,52 so is it unknown if adherence may have introduced bias. A high level of adherence to exercise programmes, ranging between 81% and 88%, was reported Schreiber et al. 50
Risk of bias for non-randomised studies
Both observational studies were considered to be at high risk of bias. Both studies were rated as being at high or unclear risk of bias for at least three of the six criteria (see Table 7). Both studies were considered to be at low risk of bias for ascertainment of exposure and completeness of follow-up. The self-selection process used in Negrini et al. 15 is a source of bias because it was based on participant and physician choice; however, it is reported that there were no statistically significant differences between the groups at baseline for any scoliosis parameters, which suggests that risk of bias had been minimised.
Levels of evidence
Scoliosis-specific exercises versus no treatment or standard care
Toledo et al. 51 compared a programme of exercises based on the global postural re-education approach, with no treatment in a small group of 10-year-old participants (mean baseline Cobb angle ≈15°). Among those in the intervention arm there was a statistically significant improvement in Cobb angle (mean reduction in size of 35% compared with mean increase of 9.5% in the control group) at 12 weeks’ follow-up. Table 8 shows actual Cobb angles. No other outcomes were measured in this study.
| Study | Actual Cobb angles, degrees [mean (SD)] | Categorical outcomes, n/N (%) | ||
|---|---|---|---|---|
| Intervention | Control | Intervention | Control | |
| Wan et al., 200527 | Thoracic spine | Thoracic spine | ||
| 0 weeks: 26.0 (12.0) | 0 weeks: 25.0 (13.0) | |||
| 6 months: 10.0 (7.0)a | 6 months: 18.0 (9.0)a | |||
| Lumbar spine | Lumbar spine | |||
| 0 week: 24.0 (10.0) | 0 week: 23.0 (11.0) | |||
| 6 months: 9.0 (5.0)a | 6 months: 16.0 (8.0)a | |||
| Toledo et al., 201151 | Thoracic spine | Thoracic spine | ||
| 0 months: 15.10 (2.51) 6 months: 9.80 (2.90)a |
0 months: 14.70 (3.77) 6 months: 16.10 (3.75)a |
|||
| Diab, 201249 | ||||
| Monticone et al., 201452 | 0 months: 19.3 (3.9) | 0 months: 19.2 (2.5) | 42 months: | 42 months: |
| 42 months: 14.0 (2.4)a | 42 months: 20.9 (2.2)a | bNumber of participants whose Cobb angle changed by > 3° | bNumber of participants whose Cobb angle changed by > 3° | |
| 56 months: 14.3 (2.3)a | 56 months: 22.0 (1.6)a | Improved: 36/52 (69) | Improved: 3/51 (6) | |
| Worsened: 4/52 (8) | Worsened: 20/51 (39) | |||
| Same: 12/52 (23) | Same: 28/51 (55) | |||
| Subgroup analysis:b Age < 13 years (N = 32) |
Subgroup analysis:b Age < 13 years (N = 35) |
Subgroup analysis:b Age < 13 years |
Subgroup analysis:b Age < 13 years |
|
| 0 months: 18.9 (4.1) | 0 months: 19.3 (2.4) | Number of participants whose Cobb angle changed by > 3° | Number of participants whose Cobb angle changed by > 3° | |
| 42 months: 14.1 (2.5)a | 42 months: 20.7 (2.5)a | Improved: 22/31 (71.0) | Improved: 3/32 (9.4) | |
| 56 months: 14.2 (2.3)a | 56 months: 21.9 (1.6)a | Worsened: 3/31 (9.7) | Worsened: 10/32 (31.2) | |
| Same: 6/31 (19.3) | Same: 19/32 (59.4) | |||
| Age > 13 years | Age > 13 years | |||
| Age > 13 years (N = 23) | Age > 13 years (N = 20) | Number of participants whose Cobb angle changed by > 3° | Number of participants whose Cobb angle changed by > 3° | |
| 0 months: 19.9 (3.6) | 0 months: 19 (2.7) | Improved: 14/21 (66.7) | Improved: 0/19 (0) | |
| 42 months: 14.0 (2.4)a | 42 months: 21.4 (1.8)a | Worsened: 1/21 (4.8) | Worsened: 10/1 (31.2%) | |
| 56 months: 14.5 (2.4)a | 56 months: 22.1 (1.5)a | Same: 6/21 (19.3) | Same: 9/16 (59.4) | |
The RCT of exercises based on the Schroth method compared with standard care (monitoring or bracing) reported effect sizes at only 6-month follow-up. 50 The treatment effects reported demonstrated no effect on function and very small to small effects on pain, self-image, self-efficacy, overall SRS-22 scores and back extensor strength. The perceived mean global rating of change was greater in the intervention and was described as a moderate improvement, whereas those in the control group reported a small amount of deterioration. Cobb angle was not reported. From information available on the US Trials Register, this report includes data from only 31 out of the expected 100 study recruits, so this analysis was underpowered.
Level of evidence
There is very low-quality evidence that a SSE programme based on the global postural re-education approach improves Cobb angle compared with no treatment in the short term.
There is very low-quality evidence that a SSE programme based on the Schroth method is no different from usual care for improving function in the short term.
There is very low-quality evidence that a SSE programme based on the Schroth method results in small improvements in pain, self-image, HRQoL and back extensor strength compared with usual care in the short term.
Scoliosis-specific exercises plus other treatments versus other treatments only
One study compared the addition of an exercise programme to other treatments (traction and electrical stimulation). 27 The exercise group showed a statistically significant reduction in Cobb angle at 6-month follow-up compared with those who just received traction and electrical stimulation (mean baseline Cobb angle 23–26°). No other outcomes were measured.
Level of evidence
There is very low-quality evidence that a SSE programme added to traction and electrical stimulation improved Cobb angle compared with traction and electrical stimulation alone in the short term.
Scoliosis-specific exercises versus general exercises
The largest and best-conducted study reported that a programme of SSEs was superior to general exercises (mean baseline Cobb angle ≈19°). 52
Measurements of Cobb angle favoured the SSE group compared with general exercise on completion of the programme at skeletal maturity and 12 months later. The percentage of participants who showed improvement was higher in the SSE group than in the general exercise group, in which a greater proportion of participants either stayed the same or worsened. Stratification by age (< 13 years and ≥ 13 years) showed that the subgroup with the higher risk of progression (age < 13 years) exhibited less improvement than older participants, but differences were small and it was not reported if they had reached statistical significance or not.
A statistically significant reduction in angle of trunk rotation (ATR) was observed in the group receiving SSEs compared with those receiving general exercises following completion of training and 12 months later (Table 9).
| Study | Change in trunk balance | ATR (°) | Trunk flexibility and strength | |||
|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | Intervention | Control | |
| Diab, 201249 | Trunk inclination (mm) 0 weeks: 5.8 (0.6) 10 weeks: 4.8 (0.7)a 3 months: 5.1 (0.8)a |
Trunk inclination (mm) 0 weeks: 6.6 (0.5) 10 weeks: 6.4 (0.6)a 3 months: 6.5 (0.5)a |
||||
| Thoracic kyphosis (˚) 0 weeks: 8.9 (0.9) 10 weeks: 10.4 (1.10)a 3 months: 10.0 (1.05)a |
Thoracic kyphosis (˚) 0 weeks: 8.8 (1.5) 10 weeks: 9.0 (1.8)a 3 months: 8.9 (1.7)a |
|||||
| Lumbar lordosis (˚) 0 weeks: 18.6 (5.4) 10 weeks: 21.6 (1.8)a 3 months: 20.9 (1.9)a |
Lumbar lordosis (˚) 0 weeks: 18.1 (5.5) 10 weeks: 20.0 (1.7)a 3 months: 19.2 (1.6)a |
|||||
| Trunk imbalance (mm) 0 weeks: 22.7 (1.3) 10 weeks: 16.7 (2.7)a 3 months: 16.6 (2.3)b |
Trunk imbalance (mm) 0 weeks: 21.8 (4.3) 10 weeks: 20.0 (1.7)a 3 months: 19.2 (1.6)b |
|||||
| Lateral deviation (mm) 0 weeks: 16.8 (2.3) 10 weeks: 14.3 (2.3)a 3 months:14.7 (2.4)a |
Lateral deviation (mm) 0 weeks: 15.1 (1.8) 10 weeks: 14.5 (1.6)a 3 months: 15.5 (1.7)a |
|||||
| Pelvic torsion (˚) 0 weeks: 3.5 (1.02) 10 weeks: 2.7 (0.8)a 3 months: 2.7 (0.8)b |
Pelvic torsion (˚) 0 weeks: 2.8 (0.8) 10 weeks: 2.4 (0.5)a 3 months: 2.5 (0.5)b |
|||||
| Surface rotation (˚) 0 weeks: 7.4 (1.2) 10 weeks: 6.08 (1.6)a 3 months: 6.20 (1.5) |
Surface rotation (˚) 0 weeks: 6.7 (0.9) 10 weeks: 6.5 (1.0)a 3 months: 7.08 (0.5)a |
|||||
| Craniovertebral angle (˚) 0 weeks: 33.5 (2.5) 10 weeks: 41.2 (5.2)a 3 months: 42.1 (5.1)a |
Craniovertebral angle (˚) 0 weeks: 38.1 (2.9) 10 weeks: 38.4 (3.6) 3 months: 37.5 (4.2) |
|||||
| Schreiber et al., 201350 | 6 months Effect size (Cohen’s d) Biering-Sørensen test (back extensor strength): 0.28 |
|||||
| Monticone et al., 201452 | 0 months: 7.1 (1.4) 42 months: 3.6 (1.1)b 56 months: 3.3 (1.1)b |
0 months: 6.9 (1.3) 42 months: 6.6 (1.2)b 56 months: 6.5 (1.1)b |
||||
At baseline the SRS-22 domains had high scores in both groups. Further significant post-training improvements of > 0.75 points were achieved for all domains in the experimental group, whereas none was noted in the control group (Table 10).
| Study | Measures of pain, function or disability, mean (SD) unless otherwise stated | Quality of life, mean (SD) unless otherwise stated | Psychological measures, mean (SD) unless otherwise stated | Global rating of change, mean (SD) | ||||
|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | Intervention | Control | |||
| Diab, 201249 | Functional rating index 0 weeks: 13.9 (1.7) 10 weeks: 10.7 (0.9) 3 months: 10.0 (0.9)a |
Functional rating index 0 weeks: 16.1 (1.7) 10 weeks 11.9 (2.0) 3 months: 13.8 (1.9)a |
||||||
| Schreiber et al., 201350 | 6 months: effect size (Cohen’s d) SRS-22 function subscale: 0.00 SRS-22 pain subscale: 0.09 |
6 months: effect size (Cohen’s d) SRS-22 total score: 0.21 |
6 months: effect size (Cohen’s d) SRS-22 self-perceived image subscale: 0.09 Self-Efficacy Questionnaire: 0.18 | 6 months: 3.8 (2.2)b | 6 months: –0.3 (1.7)b | |||
| Monticone et al., 201452 | SRS-22 function subscale 0 months: 3.8 (0.5) 42 months: 4.7 (0.2)c 56 months: 4.8 (0.2)c |
SRS-22 function subscale 0 months: 3.9 (0.5) 42 months 4.0 (0.4)c 56 months: 3.9 (0.4)c |
SRS-22 self-perceived image subscale 0 months: 3.6 (0.6) 42 months: 4.4 (0.3)c 56 months: 4.6 (0.3)c |
SRS-22 self-perceived image subscale 0 months: 3.4 (0.6) 42 months: 3.7 (0.5)c 56 months: 3.6 (0.4)c |
||||
| SRS-22 mental health subscale 0 months: 3.8 (0.6) 42 months: 4.5 (0.3)c 56 months: 4.7 (0.2)c |
SRS-22 mental health subscale 0 months: 3.9 (0.6) 42 months: 3.9 (0.5)c 56 months: 3.8 (0.4)c |
|||||||
| SRS-22 pain subscale 0 months: 3.8 (0.4) 42 months: 4.6 (0.3)c 56 months: 4.7 (0.2)c |
SRS-22 pain subscale 0 months: 0.9 (0.5) 42 months: 4.3 (0.3) 56 months: 4.2 (0.4) |
SRS-22 satisfaction with management subscale 0 months: N/A 42 months: 4.8 (0.3)c 56 months: 4.9 (0.3)c |
SRS-22 satisfaction with management subscale 0 months: N/A 42 months: 4.0 (0.5)c 56 months: 4.2 (0.5)c |
|||||
Minor adverse events (AEs) of transient pain worsening were reported in each arm of the study (n = 11 in the SSE group; n = 14 in the general exercise group).
Level of evidence
There is moderate-level evidence that a long-term SSE programme improves Cobb angle, ATR and quality of life (including subscales of pain, function, mental health, self-image and satisfaction with treatment) compared with general exercise in the long term.
Traditional scoliosis exercise programme plus forward head posture correction exercises versus traditional scoliosis exercise programme only
The addition of forward head posture correction exercises to a traditional scoliosis exercise programme resulted in a statistically significant improvement in measures of trunk balance and craniovertebral angle at 10-week and 3-month follow-up compared with a traditional scoliosis exercise programme alone. 49 A statistically significant improvement in function was observed in the intervention group at 3-month follow-up compared with the control. Cobb angle was not measured.
Level of evidence
There is very low-quality evidence that the addition of forward head posture correction exercises improves trunk balance, craniovertebral angle and function compared with a traditional programme of scoliosis exercises alone in the short term.
Discussion
Five new studies were identified since the Cochrane review was published, but most of these were rated as having high risk of bias. They provide encouraging signals that exercise might be a beneficial approach, but the majority of evidence generated is of very low quality with small sample sizes (increasing the chance of false-positive findings). Follow-up was generally short term only and there are issues with generalisability. Two of the studies included participants with AIS with any type of curve, suggesting that these cohorts are generalisable to patients with AIS; however, three cohorts included only participants with small curves (mean Cobb angles < 25°). 49,50,52 Other studies had inclusion criteria that could further limit generalisability. First, in the study by Diab,49 participants were eligible if they had a Cobb angle between 10° and 30° but they also needed to have a craniovertebral angle of at least 50°. Two other studies only included participants with a specific type of curve – double curves27 or structural thoracic curves. 51
The study by Monticone et al. 52 was the only study to which the criticism of being of very low quality did not apply. This is the first study evaluating a SSE programme to be considered at low risk of bias. It also included participants with mild and moderate size curves, making it more generalisable to patients in clinical practice. This study provided moderate evidence of effectiveness of a long-term SSE programme compared with general exercises. A strength of this study is that follow-up data were collected at skeletal maturity and 12 months after, when further progression of the curve is unlikely. However, an important omission of this study was the lack of information regarding the impact of the SSEs on surgical rates and the cost-effectiveness of treatment. Cost is important because participants attended treatment, on average, for 42 months, during which time they attended a weekly physiotherapy session. It is likely that a large study is required to be definitive for these additional outcomes. Participants were also required to exercise at home twice per week for the duration of the study. Cognitive–behavioural strategies formed part of the intervention to encourage adherence with the programme but no information was provided on adherence with treatment. The SSEs evaluated in this study do seem promising, but it is questionable that such an intensive intervention would be deliverable within the NHS. Further research should investigate whether a less intensive and/or shorter programme would provide similar benefit to patients.
In addition to the studies presented, searches identified a protocol for a randomised trial53 which is due to be undertaken. This is a three-arm study evaluating general exercise advice, general exercise advice plus night-time bracing and general exercise advice plus SSEs. The SSE programme description seems broadly similar to that being tested in ACTIvATeS. The authors are aiming to recruit 45 patients in each arm. According to trial registry this research will be completed in 2019.
Conclusion
All studies that used Cobb angle as an outcome measure showed evidence of favouring the SSEs over other treatments, different types of exercises and no treatment or standard care. Generally, the level of evidence available was very low apart from one study that demonstrated a moderate level of evidence of long-term benefit from a long-term SSE programme compared with general exercise in regard to outcomes based on the Cobb angle.
Generally, there are a lack of studies evaluating patient-reported measures such as pain, disability, quality of life and psychological factors, including cosmetic issues. Evidence favouring SSEs was primarily of very low quality, apart from one study that provided moderate evidence of long-term benefit from a long-term SSE programme compared with general exercises in regard to quality of life measured by the SRS-22 and its subscales, which included pain, function, self-image, mental health and satisfaction with treatment.
No studies evaluated the cost-effectiveness of SSEs compared with other interventions or if these exercises reduced the proportion of participants requiring surgery. Further research is needed to evaluate definitively both the clinical effectiveness and cost-effectiveness of SSEs.
Chapter 3 Survey
Objectives
-
To gain an understanding of current conservative management approaches for AIS used within the NHS to allow us to standardise the control arm of the pilot RCT.
-
To estimate the number of potential participants who could take part in a definitive RCT.
-
To determine equipoise and willingness to randomise of clinicians involved in the care of patients with AIS.
-
To identify learning needs and training requirements for physiotherapists to deliver the interventions.
Design
An online questionnaire was developed by the clinical research fellows with the input of orthopaedic consultants and specialist physiotherapists at collaborating feasibility sites. Survey domains included patient population dealt with by the centre (sources and numbers of new referrals, numbers meeting the proposed inclusion and exclusion criteria), current management activities (proportions and details of surgical, bracing and therapy strategies and monitoring methods), attitudes to this research (willingness for patients to be randomised, attitudes towards conservative treatment, likely barriers to be encountered, trade-off questions), concerns and beliefs about the interventions and tips for maximising adherence. We used both closed- and open-format responses.
Ethical considerations
Approval to conduct the survey was granted by the Warwick Medical School Biological Research Ethics Committee (REC) and individual NHS trust research and development departments at each of the clinicians’ places of employment.
Informed consent
The clinician was provided with information about the survey in the contact e-mail. The clinician was deemed to have consented by completing the online survey and was informed of this in the information provided. If an individual did not wish to take part in the survey we asked them to contact the study manager stating this and did not contact them again. Approval was gained at each NHS research and development department.
Data collection
An online questionnaire was sent to orthopaedic clinicians (consultants and specialist nurses) at all NHS hospitals that manage patients with scoliosis. A list was obtained from Scoliosis Association UK (SAUK)/British Scoliosis Research Foundation, which detailed named consultants at 36 NHS trusts who managed patients with scoliosis. We then contacted physiotherapy departments to ascertain if the department was involved in managing patients with AIS and, if so, who the lead clinician was. We contacted individuals for verbal consent prior to e-mailing the survey link.
We used evidence synthesised by Edwards et al. 57 to maximise survey response. The approach e-mail was personalised, contained a brief introduction about the study and committed to providing details of results of the completed survey. If a response to the initial e-mail was not received, a telephone call was made to the clinician (or clinician’s secretary) and responses were collected over the telephone if possible.
Analysis
Questionnaire data were summarised as descriptive statistics or frequency counts for each question. Frequency counts are presented as one of three response options: (1) no or rare (< 10%) patients; (2) selected patients; or (3) most (> 90%) or all patients.
Results: survey of orthopaedic clinicians managing adolescent idiopathic scoliosis patients
Respondents
Thirty-three trusts were approached, which involved 106 individual clinicians (three of the 36 trusts were covered by clinicians working at other trusts). A response was received from 19 trusts (78%) and 39 (37%) individual clinicians. Eleven questionnaires had incomplete data, leaving 28 complete questionnaires. All respondents were consultant spinal surgeons who stated that patients with AIS were managed in their department.
Consultants who responded were generally experienced, with the majority having been managing AIS patients for at least 6 years (22/28 respondents). A similar proportion had been performing surgery for at least 6 years (21/28). Approximately half of the respondents maintained a private list of patients (17/28). The median number of consultants providing treatment in departments was 3 [interquartile range (IQR) 3–4]. Results are shown in Table 11.
| Questionnaire item | Respondent response | |||
|---|---|---|---|---|
| No or rare (< 10%) patients (n) | Selected patients (n) | Most (> 90%) or all patients (n) | No response (n) | |
| Source of referral | ||||
| Primary care | 2 | 12 | 13 | 12 |
| Secondary care | 4 | 14 | 9 | 12 |
| Self-referral | 22 | 2 | 0 | 15 |
| Other | 10 | 2 | 0 | 27 |
| Methods for monitoring progress | ||||
| Symptoms: pre pubescence | 3 | 7 | 14 | 15 |
| Symptoms: post pubescence | 2 | 6 | 14 | 17 |
| Cobb angle: pre pubescence | 1 | 1 | 22 | 15 |
| Cobb angle: post pubescence | 0 | 2 | 24 | 13 |
| Scoliometer: pre pubescence | 8 | 3 | 8 | 20 |
| Scoliometer: post pubescence | 7 | 4 | 7 | 21 |
| Visual estimation: pre pubescence | 11 | 4 | 9 | 15 |
| Visual estimation: post pubescence | 10 | 3 | 10 | 16 |
| Surface topography: pre pubescence | 11 | 3 | 6 | 19 |
| Surface topography: post pubescence | 10 | 3 | 5 | 21 |
| MRI: pre pubescence | 12 | 7 | 3 | 17 |
| MRI: post pubescence | 13 | 4 | 3 | 19 |
| Respiratory function: pre pubescence | 14 | 7 | 0 | 18 |
| Respiratory function: post pubescence | 14 | 5 | 0 | 20 |
| Other: pre pubescence | 10 | 2 | 2 | 25 |
| Other: post pubescence | 11 | 1 | 2 | 25 |
| Treatments | ||||
| Proportion having surgery: pre pubescence | 1 | 24 | 2 | 12 |
| Proportion having surgery: post pubescence | 0 | 27 | 0 | 12 |
| Proportion braced: pre pubescence | 11 | 16 | 0 | 1 |
| Proportion braced: post pubescence | 25 | 2 | 0 | 12 |
| Referrals to physiotherapy | 29 | 8 | 0 | 2 |
| Format of physiotherapy referred to | ||||
| NHS inpatient physiotherapy | 23 | 1 | 1 | 14 |
| NHS outpatient physiotherapy | 20 | 7 | 0 | 12 |
| Private inpatient physiotherapy | 25 | 0 | 0 | 14 |
| Private outpatient physiotherapy | 22 | 4 | 0 | 13 |
| Reasons for patients referral to physiotherapy | ||||
| Surgery not indicated | 17 | 6 | 0 | 16 |
| Newly diagnosed | 15 | 5 | 0 | 19 |
| For bracing management/monitoring | 16 | 5 | 1 | 17 |
| General monitoring | 0 | 0 | 0 | 0 |
| For exercise prescription | 0 | 0 | 0 | 0 |
| For education | 0 | 0 | 0 | 0 |
| If body image issues | 0 | 0 | 0 | 0 |
| Curve has a particular presentation | 0 | 0 | 0 | 0 |
| If patient is certain age | 17 | 5 | 0 | 17 |
| If patient is certain sex | 17 | 4 | 0 | 189 |
| Other | 13 | 5 | 0 | 21 |
| Beliefs about efficacy of treatments | ||||
| Proportion of patients for whom bracing is helpful: pre pubescence | 11 | 16 | 0 | 12 |
| Proportion of patients for whom bracing is helpful: post pubescence | 23 | 4 | 0 | 12 |
| Proportion of pre-pubescent patients for whom physiotherapy can limit curve progression | 25 | 1 | 0 | 13 |
| Proportion of post-pubescent patients for whom physiotherapy can limit curve progression | 25 | 1 | 0 | 13 |
| Proportion of pre-pubescent patients for whom physiotherapy can reverse curve progression | 27 | 0 | 0 | 12 |
| Proportion of post-pubescent patients for whom physiotherapy can reverse curve progression | 26 | 0 | 0 | 13 |
Patient population
Referrals were received equally from primary and secondary care. Consultants reported rarely taking self-referrals. There was a wide variation in the numbers of patients seen; the mean [standard deviation (SD)] number of new NHS patients with AIS per month was 10 [SD 6.2 (range 2–28) new NHS patients with AIS per month]. Similarly, there was a wide variation in the number of follow-up patients per month [mean 23 (SD 16, range 4–80) follow-up patients per month].
Patient management
A total of 92% (22/24) of respondents stated that most or all pre- and post-pubescent patients were monitored by Cobb angle. A total of 67% and 74% of consultants stated that respiratory function was monitored in no or rare cases in pre- and post-pubescent patients, respectively.
A majority of clinicians reported following-up pre-pubescent patients at 6-monthly intervals (74%), and post-pubescent patients at 12-monthly intervals (63%). Use of radiography mirrored this frequency of follow-up, with a majority of consultants radiographing pre-pubescent patients every 6 months (74%) and post-pubescent patients every 12 months (82%).
Most consultants stated that only selected pre- and post-pubescent patients would go on to have surgery (89% and 96% of respondents, respectively). A total of 60% of respondents said selected pre-pubescent patients were braced, whereas 93% said they either never or rarely braced post-pubescent patients. This was corroborated by reporting that 60% of consultants believed that bracing could help in selected patients, whereas 85% believed that bracing is never or rarely helpful in post-pubescent patients.
Use of physiotherapy for conservative management
A total of 78% of respondents rarely or never referred patients to NHS physiotherapy. The remainder of consultants only referred selected patients. When consultants do refer patients to physiotherapy, they report doing this mostly to NHS outpatient departments.
The majority of consultants believed that physiotherapy could not limit curve progression (65% and 73% of clinicians for pre- and post-pubescent patients, respectively). An even greater proportion of consultants believed that physiotherapy could not reverse curve progression. The remaining consultants believed it can only rarely have an effect.
Involvement in research
Approximately half of the respondents were involved in research for AIS (54%), and a majority were happy for their patients to be involved in a RCT that randomised to exercise or watchful waiting (78%).
Results: survey of physiotherapists working at NHS trusts managing adolescent idiopathic scoliosis patients
Respondents
Thirty-six trusts were approached, which involved 57 individual physiotherapists. A response was received from 28 of the 36 trusts (78%) and from 42 individual physiotherapists (74%).
Five (14%) physiotherapists reported that their trusts did not provide any physiotherapy treatment for AIS patients, despite being listed as a NHS trust that has a consultant providing care for patients with scoliosis.
Of the 37 physiotherapists who responded, eight provided pre- and post-operative care only, seven provided conservative physiotherapy management and 22 provided both.
Respondents were experienced, with the majority having at least 6 years’ experience managing AIS patients (0–5 years, n = 8; 6–10 years, n = 8; 10–15 years, n = 7; 16 + years, n = 5). The median number of physiotherapists providing treatment in departments was 3 (IQR 1–5). Results are shown in Table 12.
| Questionnaire item | Respondent response (N = 37) | |||
|---|---|---|---|---|
| No or rare (< 10%) patients (n) | Selected patients (n) | Most (> 90%) or all patients (n) | No response (n) | |
| Source of referral | ||||
| Primary care | 19 | 6 | 1 | 11 |
| Secondary care | 0 | 6 | 20 | 11 |
| Self-referral | 24 | 2 | 0 | 11 |
| Other | 26 | 0 | 0 | 11 |
| Reasons for patients referral to physiotherapy | ||||
| Surgery not indicated | 2 | 11 | 6 | 18 |
| Newly diagnosed | 7 | 8 | 3 | 19 |
| For bracing management/monitoring | 12 | 2 | 5 | 18 |
| General monitoring | 11 | 5 | 2 | 19 |
| For exercise prescription | 2 | 6 | 11 | 18 |
| For education | 7 | 6 | 6 | 18 |
| If body image issues | 10 | 6 | 3 | 18 |
| Curve has a particular presentation | 13 | 2 | 4 | 18 |
| If patient is certain age | 15 | 2 | 1 | 19 |
| If patient is certain sex | 17 | 1 | 0 | 19 |
| Other | 15 | 0 | 0 | 22 |
| Bracing | ||||
| Proportion of patients presenting to physiotherapist with brace | 16 | 7 | 3 | 11 |
| Treatments used for conservative treatments of AIS | ||||
| Joint mobilisation | 15 | 6 | 4 | 12 |
| Joint manipulation | 22 | 3 | 0 | 12 |
| Core stability exercises | 1 | 3 | 21 | 12 |
| Strengthening exercises | 2 | 3 | 20 | 12 |
| Stretching exercises | 2 | 6 | 17 | 12 |
| Postural correction exercises | 0 | 2 | 22 | 13 |
| Sensorimotor retraining (including balance/proprioception exercises) | 1 | 7 | 17 | 12 |
| Acupuncture | 22 | 3 | 0 | 12 |
| Electrotherapy | 23 | 1 | 1 | 12 |
| Education | 0 | 3 | 22 | 12 |
| Other | 16 | 5 | 2 | 14 |
| Treatment formats | ||||
| Inpatient one-to-one sessions | 16 | 2 | 1 | 18 |
| Inpatient group sessions | 19 | 0 | 0 | 18 |
| Outpatient one-to-one sessions | 0 | 2 | 17 | 18 |
| Outpatient group sessions | 15 | 3 | 1 | 18 |
| Other | 16 | 0 | 0 | 21 |
| Methods for monitoring progress | ||||
| Symptoms | 2 | 2 | 12 | 21 |
| Cobb angle | 3 | 0 | 16 | 18 |
| Scoliometer | 9 | 1 | 8 | 19 |
| Visual estimation | 5 | 5 | 7 | 20 |
| Surface topography | 12 | 3 | 2 | 20 |
| MRI | 7 | 8 | 4 | 18 |
| Respiratory function | 10 | 6 | 1 | 20 |
| Other | 14 | 0 | 1 | 22 |
| Beliefs about efficacy of treatments | ||||
| Proportion of pre-pubescent patients for whom physiotherapy can limit curve progression | 8 | 9 | 1 | 19 |
| Proportion of post-pubescent patients for whom physiotherapy can limit curve progression | 9 | 8 | 1 | 19 |
| Proportion of pre-pubescent patients for whom physiotherapy can reverse curve progression | 17 | 2 | 0 | 18 |
| Proportion of post-pubescent patients for whom physiotherapy can reverse curve progression | 18 | 1 | 0 | 18 |
| Proportion of patients for whom bracing is helpful | 1 | 10 | 5 | 21 |
Patient population
Physiotherapists reported that the most common referral source was secondary care (n = 20 for most or all patients). Only in rare cases were referrals received from primary care or self-referrals. On average, NHS departments managed three new AIS patients per month [mean 2.8 (SD 2.2) new AIS patients per month] and five follow-up patients per month [mean 5.4 (SD 5.0) follow-up patients per month]. For those departments that did provide outpatient care, a median of five (IQR 4–6) sessions were given, with respondents often specifying that this depended on individual patients. There was a wide variation in the length of time patients were kept on the caseload, ranging from a few weeks up to 4 years (or until skeletal maturity).
The reason for referral to physiotherapy was for exercise prescription. Referrals were unlikely to be received for a curve having a particular presentation (n = 12/19 said never or rarely) or for management/monitoring of bracing (n = 11/19 said no patients), and there seemed to be no discrimination of referrals owing to the age (n = 14/18 said no patients) or sex (n = 16/18 said no patients) of the patients. More than 50% of physiotherapists (16/37) reported that no or few patients were using a brace.
Patient management
In most or all cases, treatments consisted of core stability exercises, strengthening, stretching, postural correction and sensorimotor retraining. Manipulation, acupuncture and electrotherapy were never or rarely used. In most cases, conservative treatments of AIS (i.e. not pre- or post-operative physiotherapy) were provided at outpatient one-to-one appointments. Inpatient sessions or outpatient group sessions were never or rarely used.
Training
Eight (22%) physiotherapists had received training and used specialist scoliosis approaches.
Beliefs about the effectiveness of physiotherapy
Beliefs that physiotherapy and exercise can limit curve progression were mixed. Responses varied between ‘never’, ‘rarely’ and ‘in selected cases’, with no real difference for pre- and post-pubescent adolescents. Few physiotherapists believed that physiotherapy and exercise could reverse curve progression, and then only in selected patients. The most common response to the question of whether or not physiotherapists believed bracing was helpful was ‘only in selected patients’.
Involvement in research
Two physiotherapists (5%) were currently involved in research for AIS. A total of 16 (43%) respondents said they would be happy for patients to be involved in a RCT that randomised them to exercises or watchful waiting, with a number of comments about requiring consultant permission. Ten (27%) respondents were interested in their patients participating in a full trial.
Discussion
Current conservative management of AIS in the UK comprises monitoring by spinal consultants with periodic radiograph review (frequency dependent on maturity and risk of progression), with selected cases being referred for individual outpatient physiotherapy for exercise prescription. Referral for bracing occurs in a minority of selected cases.
There was a wide variation in the numbers of patients seen on a monthly basis at the different respondents’ NHS hospitals, owing to the fact that small and large centres were included in the study. An average of 10 new and 23 follow-up patients per month (equivalent to approximately 150 new and 350 follow-up patients per month from 15–20 centres) indicates that there is a sufficient pool of patients for a full-scale national trial.
A majority (78%) of the responding spinal consultants reported that they would be willing to have their patients involved in a RCT that randomised patients to either an exercise or control intervention. Interestingly, a smaller proportion of the surveyed physiotherapists reported willingness to randomise (43%), although there appeared to be a common free-text response that this would depend on the opinion of the spinal consultant in charge of the care of the patient. Physiotherapists were more optimistic about the ability of exercise to limit curve progression, with about 25% of respondents saying it could help in selected cases. Virtually all physiotherapists and consultants said that physiotherapy would reverse curve progression in no or rare cases. Overall, there appears to be favourable equipoise for the conduct of a full-scale national trial that would randomise patients to exercise or monitoring.
Evaluating training needs was limited by the necessity for a brief questionnaire to maximise response. From the findings of the survey it appears that a very small number of physiotherapists have undertaken extended training in approaches for SSEs. What is reassuring is that the average physiotherapy respondent managing patients with AIS has > 5 years’ experience working with the patient group.
The findings need to be interpreted with some caution for two reasons. First, the study is based on the reporting and opinions of consultants and physiotherapists and not on actual observed practices. Second, the response rate for the survey of orthopaedic clinicians was low at the individual level, although at a NHS trust level nearly 80% of the listed trusts were represented via the individual clinicians. Non-responders may be atypical, but the types of trusts represented varied from district generals to large university teaching hospitals.
In conclusion, NHS trusts involved in specialist management of patients with AIS are providing variable physiotherapy services.
Chapter 4 Intervention development and delivery
Objectives
-
To develop and document a best evidence intervention of SSE treatment for AIS.
-
To determine adherence to allocated treatment arm (> 60% of adolescents attended required exercise sessions).
-
To assess and finalise training requirements for the intervention.
Developing the interventions
A number of principles were taken into consideration in the development of the intervention package:
-
the need to design an intervention that was reflective of best practice
-
the need to ensure that the intervention was acceptable to the clinicians and patients (including their families)
-
the need to ensure that the intervention could be delivered within the context of the UK NHS in terms of staffing and time
-
the need to ensure that the intervention was documented to a standard that promoted consistency in delivery and that would enable replication.
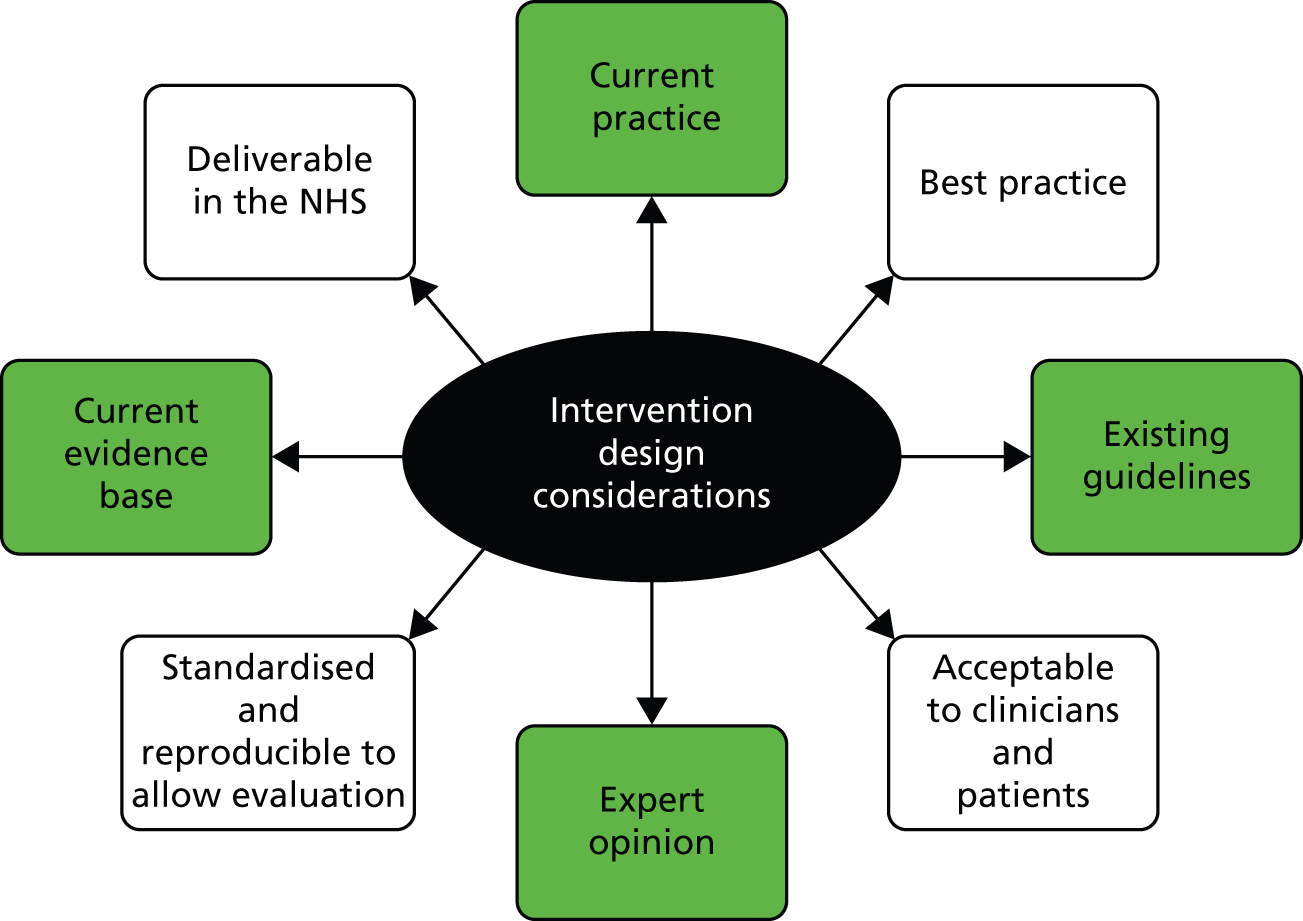
This was achieved by a triangulation of methods, including the survey of current practice, a review of existing guidelines, evidence from the literature and expert opinion (Figure 1), and following guidance on developing complex interventions. 58
FIGURE 1.
Intervention design methods and considerations.
Current practice
Current practice regarding conservative treatment for AIS was assessed as part of a nation-wide survey of orthopaedic consultants and specialist physiotherapists (see Chapter 3 for more details). The results indicate that the main components of conservative management of scoliosis in the UK are ‘watchful waiting’ and, in a minority of cases, bracing. Although some NHS trusts offer other services, including referral to physiotherapy for advice and/or exercises, these are not routinely offered within the NHS in the UK, and survey responses suggest that only a small percentage of patients are referred to physiotherapy. The majority of consultants at these centres rarely or never refer patients to physiotherapy for conservative management of AIS.
Once diagnosed with AIS, patients generally will come under the care of a specialist spinal consultant. Depending on the size of the curve and prognosis regarding potential progression, a monitoring plan will be instituted to maintain regular evaluation of the spinal deformity. Typically, this will occur every 6 or 12 months and will involve some form of imaging, although the timing will alter depending on prognosis and the speed of any changes. For 90% of patients with AIS, monitoring is the only ‘treatment’ they will receive.
Clinical guidelines
We searched for but did not find UK guidelines concerning conservative management of AIS. The Society on Scoliosis Orthopaedic and Rehabilitation Treatment, an international group dedicated to scoliosis treatment and research, has produced a series of papers detailing the results of consensus exercises using Delphi techniques. They state the aims of conservative management to be stopping curve progression; preventing pulmonary dysfunction; treating any pain; and improving appearance via postural correction. 59 A series of recommendations regarding conservative treatment were also made. These include:
-
SSE programmes should be used and should include education, postural self-correction and integration of postural correction into activities of daily living (ADLs).
-
Exercise programmes should be individualised according to patients’ needs and curve type.
-
SSEs should be performed regularly.
No specific recommendations were provided regarding the type of exercises or their exact frequency or delivery method.
Evidence base
The majority of the studies included in the systematic review update described in Chapter 2 were not published when the ACTIvATeS trial intervention was developed. At that time, the evidence base for the effectiveness of exercise in AIS consisted of the Cochrane review published in August 2012,17 which included publication of studies up to 30 March 2011. This review included two studies (154 participants): the RCT by Wan et al. 27 and the prospective controlled cohort study by Negrini et al. 15
In order to ensure that we had the most up-to-date information, we reran the search strategies used in the original March 2011 review. This yielded one new study,51 a RCT of Global Posture Re-education evaluated with 20 patients. All of these were considered to be at high risk of bias in the latest update. The basic exercise approach was broadly similar in two of the studies. However, the exercise intervention used by Wan et al. 27 differs greatly from the consensus within Europe where exercises are used routinely as treatment for AIS (see Table 2 for further intervention details).
The Controlled Trials Register (International Standard Randomised Controlled Trial Number Register) was also searched for any current trials investigating exercises as treatment for AIS, but no further trials were identified at that time.
Expert opinion
A crucial part of the development of the intervention was the advice received by clinicians. Most notably, a consensus meeting was held with 17 specialist physiotherapists from across England to gain further understanding of normal practice within typical NHS clinics and to assist in the design of the exercise intervention. Invitations were made through professional forums (interactive Chartered Society of Physiotherapy), links with large NHS centres and private providers (Scoliosis SOS Clinic, London, UK).
It needed to be feasible to perform the SSE intervention within NHS outpatient clinics, taking into account normal appointment duration and commonly available rehabilitation materials. A list of exercises described in the literature, along with others proposed by various therapists, were examined in detail and decisions made as to which of these were the most important. A consensus was reached through voting on inclusion of individual exercises. The results of this were used to guide the design of the programme used in the feasibility study. Discussions as to what the control intervention should consist of were facilitated by the study team. Feedback regarding the design of the online tools and paperwork associated with the trial were also provided by patients and clinicians.
Control intervention
At the beginning of the study we understood that current standard practice for the patient group being investigated consisted of advice, monitoring under the care of a specialist spinal consultant and, in a small proportion of patients, bracing. This was confirmed in the survey of current practice.
We anticipated that participants randomised to the control arm would receive one or two sessions with a physiotherapist, which would encompass musculoskeletal assessment, information and advice regarding their condition and support groups (e.g. SAUK), and, if relevant, information about brace use and care.
A study assessing the education needs of patients with AIS found that patients with scoliosis want to know about the following topics:60
-
What is scoliosis and what causes it?
-
Will it get better?
-
What are the treatment options and what happens now?
-
Will I need an operation?
-
How will it affect me later in life?
Consultants who also took part in this research suggested that the most frequently asked questions by patients were about:
-
the causes or aetiology of scoliosis
-
the natural history of scoliosis
-
the clinical presentation of scoliosis
-
the type of management, including benefits and risks
-
websites and special-interest groups to contact for more information.
Consultants emphasised the need for:
-
evidenced-based information
-
patients’ anxiety and the emotional aspect of living with AIS to be addressed
-
clear information about the natural history of AIS to be provided
-
ways for patients to contact other patients with AIS who have/have not had surgery to be provided.
Therefore, the advice session with the participant and their family included:
-
a description of AIS and its causes
-
current treatment approaches: monitoring, bracing and surgery
-
self-help tips, as outlined in the NHS Choices ‘Self-help’ information page
-
talking to others
-
exercising: advice about general exercise and being active
-
reassurance
-
-
sources of information, for example SAUK website61
-
brace care (if appropriate).
The design of the control intervention was consistent with standard best practice in the UK, as evidenced by our clinician survey and by discussions with a number of experienced therapists. The needs of the trial required a control intervention that would appeal to patients so that they would be happy to take part, while at the same time not containing any of the ‘active’ ingredients of the exercise intervention.
It was anticipated that a single session would be sufficient for delivery of the control intervention. However, depending on the needs of the patient, a further session was also available if required.
The control intervention can be summarised as follows:
-
between 1 and 2 sessions with a physiotherapist
-
brief assessment, including story of diagnosis, educational needs, worries or concerns of family, current activity levels, any symptoms related to AIS
-
education about condition, ‘self-help’ advice and information about support groups and other resources
-
scoliosis information pack
-
advice about bracing if required.
Participants continued to attend for orthopaedic review as per standard practice at their centre.
Exercise intervention
The overall aims of the exercise intervention were based on the European guidelines for the management of AIS. 59,62 Broadly, they were to avoid surgery and/or bracing where possible. The specific objectives of the exercise intervention were:
-
to achieve ASC of spinal deformity
-
to address a restricted range of movement that may prevent ASC
-
to achieve maintenance of the self-corrected position during movement, including integration in activities of daily living
-
to improve sensorimotor integration and balance reactions while maintaining the corrected position
-
to provide education and support for the participant and family
-
to promote strategies to encourage adherence to the exercise programme.
The primary objective was to teach the patient to be able to self-correct their spine (ASC) to minimise the deformity as much as possible. Maintenance of this correction and integrating it into ADLs was also a vital component of the programme. Secondary objectives included addressing any range of motion (ROM), strength or sensorimotor deficits that may contribute to the condition.
Originally, we proposed to utilise the exercises proposed by Wan et al. ,27 supplemented by some of the SEAS techniques, as they have the greatest theoretical and research evidence to support their use. However, given that the programme used by Wan et al. 27 was designed for a specific curve type, and that the authors’ approach was very different from that used in the majority of other studies, the decision was made to base the ACTIvATeS exercise programme on the SEAS approach. This uses concepts broadly in line with most other European schools of SSE.
Participants were asked to carry out exercise primarily as a daily home exercise programme with initial physiotherapy assessment and regular therapy review sessions (between six and nine sessions over 6 months) to provide support, encourage adherence and allow monitoring and progression of the exercises. Although some clinicians, particularly those following the European schools of thought, advocate prolonged inpatient exercise programmes, recent evidence suggests that such intensive programmes that disrupt normal schooling and socialisation are not necessary. 63 The intervention was delivered by UK-registered physiotherapists with expertise in scoliosis and/or musculoskeletal paediatrics. All physiotherapists were NHS employees who treated trial participants alongside their normal caseload. In all centres, therapists delivered both the usual-care components and the exercise programme to participants.
Content of the exercise intervention
Each participant was assessed by their physiotherapist and given an individualised exercise programme based on the presenting spinal deformity. The first step of the exercise programme was to teach the participant to correct their posture (ASC to reduce the spinal deformity). Participants were also given additional exercises that progressively challenged their ability to maintain the corrected posture by altering position, adding load or resistance, adding movement or distractions and incorporating it into activities of daily living. Exercises to address any secondary impairments (e.g. balance, ROM, strength) were also included to be used where required.
Alongside the exercise programme and adherence strategies, the physiotherapist also provided education, advice and support for the participant and family, similar to that provided in the control intervention. All treatments provided during each session were recorded in a detailed log.
Adherence
Adherence is defined as how closely a patient’s behaviour is aligned with a prescriber’s recommendations. 64 Adherence with any exercise programme is vital to ensure that there is sufficient dosage received in order to effect a change. Unfortunately, patient adherence with home treatment programmes is typically low. Reasons for this include a lack of understanding of how home treatment may directly benefit patients personally; patients’ lack of confidence in their own ability; intrusion into normal life; and various other barriers (both real and imagined). This may be compounded by the age of patients with AIS (i.e. adolescents).
Many of the approaches in Europe provide extensive supervised sessions. However, it is not feasible within the UK NHS to provide supervision for the duration and frequency reported in the literature (e.g. 5 days/week for 4 weeks65). We aimed to maximise adherence to the prescribed exercise regimen by integrating evidence-based adherence strategies66,67 into the exercise programme to counter these factors, utilising behavioural methods and techniques including exercise contracts, an online exercise diary and an online chat forum (see Appendices 4 and 5). 68 The behavioural strategies have been successful in other areas of health intervention for adolescents. Exercise diaries are effective in improving adherence to home exercise programmes, particularly if the participant is aware that the diary is being monitored by a health professional. 69
The online forum was designed as a means by which the participants in the exercise intervention arm could communicate with each other and discuss issues both related and unrelated to AIS as well as their involvement in the ACTIvATeS study. Participants could also use the forum to ask questions of the physiotherapists. The forum was moderated by the central study team.
The online exercise diary was part of the same website as the forum. It consisted of a calendar and a series of drop-down menus from which physiotherapists could select exercises for the home exercise programme. Each exercise was represented by a photograph or a video and came with pre-loaded instructions, which could be modified. Participants were then able to access the online diary at home and check-off exercises when they had performed them.
Summary of scoliosis-specific exercise programme intervention
The programme involved between six and nine appointments spread over 6 months and was designed following a review of the available literature and a professional consensus meeting of specialist UK physiotherapists. We added a number of additional elements designed to increase long-term effectiveness, including standardised progression and specific adherence strategies. The programme included components to address all the aims described earlier in this section. An individualised programme could be created by selecting and progressing each exercise according to each participant’s capabilities.
The programme was performed at home as well as in the clinic in order to stimulate psychomotor or muscular adaptation. 70 The experimental intervention can be summarised as follows:
-
SSE programme involving between six and nine contact sessions with the physiotherapist spread over 6 months
-
information and advice to patients about their condition and self-management
-
an emphasis on teaching the participant to be able to achieve ASC of spinal deformity
-
a menu of exercises aiming to:
-
achieve maintenance of the self-corrected position during movement including integration into ADLs
-
address secondary factors including restricted range of movement, strength, sensorimotor and balance deficits that may inhibit ASC
-
-
a home exercise plan with exercises being performed daily
-
a standardised protocol for progression and regression of exercise difficulty
-
strategies to improve programme adherence
-
participants continued to attend for orthopaedic review as per standard practice at their centre.
Therapist training
In order to standardise the treatment provided, therapists attended two training sessions, including a practical demonstration and treatment simulation with a patient with AIS, where they were instructed in how to treat participants in accordance with to the trial protocol. Therapists were provided with treatment manuals that comprehensively described the rationale for the study, intervention protocols, including a session-by-session guide, and required research processes. None of the proposed interventions was beyond the scope of normal therapy practice.
Quality assurance
A clinical research fellow ensured adherence to study protocols at all sites. Periodic observations of treatment appointments for all physiotherapists were carried out. Treatment logs and notes were audited and observations of control and experimental arm intervention sessions were made.
Piloting the interventions
Two physiotherapists at two separate trusts who were experienced in providing conservative treatments for patients with AIS agreed to pilot the exercise intervention within their current caseload prior to commencing the randomised feasibility study. Issues with computer access and administrative procedures were addressed. The content of the exercise intervention was reported to be acceptable with no major changes required.
Delivery of the interventions within the randomised feasibility study
Attendance and treatment logs
Physiotherapists were asked to complete treatment for all participants within 6 months of randomisation in order to gauge short-term effects. Fifty-eight participants took part in the randomised pilot feasibility study. Treatment for participants in the exercise arm was completed, on average, within 6 months of randomisation at two sites and within 9 months of randomisation at a further site (Table 13). Final figures for this will not be known until those participants still receiving treatment have completed the course.
| Centre | Days since randomisation, median (IQR, n) | |||||
|---|---|---|---|---|---|---|
| Advice and education | Exercise programme | |||||
| First Rx | Last Rx | Number of sessions | First Rx | Last Rx | Number of sessions | |
| ROH | 23.5 (22.0, 10) | 23.5 (22.0, 10) | 1.0 (0, 10) | 27.0 (10.0, 5) | 153.0 (48.0, 5) | 7.5 (5.3, 5) |
| NOC | 15.5 (2.5, 10) | 15.5 (2.8, 10) | 1.0 (0, 10) | 14.0 (7.8, 8) | 106.0 (81.5, 8) | 3.5 (2.3, 8) |
| FRE | 42.0 (6.0, 5) | 42.0 (6.0, 5) | 1.0 (0, 5) | 43.0 (24.0, 3) | 260.0 (28.5, 3) | 7 (1.5, 3) |
| JCH | 16.5 (14.8, 4) | 16.5 (14.8, 4) | 1.0 (0, 4) | – | – | – |
| Total | 19.0 (23.0, 29) | 22.0 (25.0, 29) | 1.0 (0, 29) | 22.0 (20.8, 16) | 155.0 (83.5, 16) | 5 (3.8, 16) |
Table 14 presents attendance rates for the different treatment arms by centre. Table 15 details how many sessions were attended by the participants in each arm.
| Centre | Advice and education (maximum two sessions) | Exercise programme (maximum nine sessions) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| FRE (n = 5) | NOC (n = 10) | ROH (n = 10) | JCH (n = 4) | Total (N = 29) | FRE (n = 6) | NOC (n = 10) | ROH (n = 10) | JCH (n = 3) | Total (N = 29) | |
| Median number of sessions (IQR) | 1 (0) | 1 (0) | 1 (0) | 1 (0) | 1 (0) | 7 (1.5) | 3.5 (2.25) | 7.5 (5.25) | – | 5 (3.8) |
| Failed to attend any appointment | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 (20%) | 0 | 2 (6.9%) |
| Attended for assessment only | 5 | 9 | 10 | 4 | 28 | 0 | 0 | 0 | 0 | 0 |
| Partial completion of treatment | 0 | 0 | 0 | 0 | 0 | 1 (16.7%) | 8 (80%) | 1 (10%) | 0 | 10 (34.5%) |
| Completed treatmenta | 5 | 10 | 10 | 4 | 29 | 2 (33.3%) | 0 | 4 (40%) | 0 | 6 (20.7%) |
| Withdrew from treatmentb | 0 | 0 | 0 | 0 | 0 | 0 | 2 (20%) | 1 (10%) | 0 | 3 (10.3%) |
| Treatment ongoing | 0 | 0 | 0 | 0 | 0 | 3 (50%) | 2 (20%) | 2 (20%) | 3 (100%) | 10 (34.5%) |
| Unclassified | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 (10%) | 0 | 1 (3.4%) |
| Arm | Number of sessions attended by participants | Total | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unclassified | Treatment not yet complete | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
| Advice and education, n (%) | 0 | 0 | 0 | 28 (97) | 1 (3) | 29 (100) | |||||||
| Exercise programme, n (%) | 1 (3) | 10 (34) | 2 (7) | 0 (0) | 2 (7) | 3 (10) | 1 (3) | 4 (14) | 1 (3) | 1 (3) | 1 (3) | 3 (10) | 29 (100) |
All 29 control arm participants had completed their treatment by report date, with only one having more than one session (two sessions in total). None of the control participants declined further treatment or failed to attend.
Of the 29 exercise arm participants, 16 had either partially or fully completed treatment by report date (including three who declined further treatment), 10 were still receiving treatment, two had not responded to attempts to book an initial session and one remained unclassified.
Three out of the four NHS trusts were able to commit to up to nine sessions over a 6-month period within their current NHS resources. One trust was unable to manage between six and nine sessions for exercise programme participants, owing to limited resources. This was reflected in the median number of treatment sessions for the exercise arm participants, which was seven or higher at the two trusts with participants who had completed treatment sessions but only 3.5 at the trust with resource issues.
It is expected that the overall median number of sessions (currently five) will increase to above the pre-defined minimum threshold of six sessions once the fourth site completes treatment of their exercise arm participants.
All sites were asked to hold the initial treatment session within 4 weeks of randomisation, and, ideally, within 2 weeks. Three of the four sites were successful in complying with this request (see Table 13). At two of the four sites, patients attended the initial treatment session at a median time of approximately 2 weeks from randomisation date. At one trust, the initial treatment session occurred at a median time of between 3 and 4 weeks. Participants were seen initially at a median time of 6 weeks at the remaining site. There was no difference between arms for time to initial attendance.
Table 16 details the content of each treatment session as recorded by the physiotherapists on the treatment logs for each participant. Very high figures for provision of the different information categories were recorded for both the control and exercise arms. The low figures for brace information (provided to just over 50% of participants) reflect the low number of participants being braced. The core component of the exercise programme (ASC) was provided to 94% (15/16) of exercise arm participants, with high figures for stabilising, balance and abdominal (core) strengthening exercises. In terms of treatment contamination, one control participant had a previous exercise programme reviewed and progressed when she attended her trial assessment and advice session.
| Type of treatment | Participants included in treatment, n (%) | |
|---|---|---|
| Advice and education (maximum two sessions, n = 29 participants) (total number of sessions = 30) | Exercise programme (maximum nine sessions, n = 16 participants) (total number of sessions = 85) | |
| Assessed spinal deformity | 28 (97) | 16 (100) |
| Assessed function | 29 (100) | 15 (94) |
| Assessed impairment | 26 (90) | 14 (88) |
| Information: AIS | 29 (100) | 16 (100) |
| Information: current treatment | 29 (100) | 16 (100) |
| Information: self-help | 29 (100) | 16 (100) |
| Information: other | 29 (100) | 16 (100) |
| Information: brace | 16 (55) | 9 (56) |
| Provide information pack | 29 (100) | 15 (94) |
| Online tools | 0 | 11 (69) |
| Spinal awareness | 0 | 11 (69) |
| Exercise: ASC | 0 | 15 (94) |
| Exercise: stability | 0 | 13 (81) |
| Exercise: balance | 0 | 15 (94) |
| Exercise: core | 0 | 12 (75) |
| Exercise: spinal ROM | 0 | 8 (50) |
| Exercise: upper limb ROM | 0 | 9 (56) |
| Exercise: lower limb ROM | 0 | 7 (44) |
| Review diary | 0 | 15 (94) |
| Progress exercise | 0 | 15 (94) |
| Exercise action plan | 0 | 14 (88) |
| Follow-up appointment | 1 (3) | 16 (100) |
| GP letter | 28 (97) | 16 (100) |
| Other treatment | 7 (24) | 0 (0) |
Use of the online exercise diary
At baseline, the vast majority (98%) of participants had daily access to the internet in their home, suggesting that there would not be an issue with accessing the online exercise diary.
Of the 18 participants who had completed the treatment process, 14 had used the online exercise diary (Table 17). Three participants reported problems with access to the online facilities owing to incompatibility issues with some internet browsers. Solutions to these problems were provided, although these participants in general either did not use the diary or reported low usage rates.
| Participant | Exercise days seta | Exercise days completed | % |
|---|---|---|---|
| Treatment completer 1 | 209 | 150 | 72 |
| Treatment completer 2 | 279 | 214 | 77 |
| Treatment completer 3 | 97 | 97 | 100 |
| Treatment completer 4 | 122 | 122 | 100 |
| Treatment completer 5 | 335 | 97 | 29 |
| Treatment completer 6 | 51 | 51 | 100 |
| Partial treatment completer 1 | 84 | 18 | 21 |
| Partial treatment completer 2 | 1164 | 281 | 24 |
| Partial treatment completer 3 | 903 | 138 | 15 |
| Partial treatment completer 4 | 480 | 206 | 43 |
| Partial treatment completer 5 | 899 | 845 | 94 |
| Partial treatment completer 6 | 671 | 125 | 19 |
| Partial treatment completer 7 | 223 | 4 | 2 |
| Partial treatment completer 8 | 280 | 0 | 0 |
| Partial treatment completer 9 | 58 | 0 | 0 |
| Partial treatment completer 10 | 583 | 124 | 21 |
| Treatment non-attender 1 | 0 | 0 | 0 |
| Treatment non-attender 2 | 0 | 0 | 0 |
| Total | 6438 | 2472 | 27 |
There was wide variation in the number of exercises prescribed, and, therefore, the number of exercise days counted for the 16 participants who were partial or full treatment completers (range 51–1164 exercise days counted). The six participants who completed treatment sessions (attended between six and nine sessions) completed, on average, 80% of the prescribed exercises.
The 10 participants who partially completed treatment sessions (attended < 6 sessions) completed, on average, 24% of the prescribed exercises.
Use of the online forum
Only four of the exercise programme participants used the online forum, providing seven posts. Attempts were made to increase activity with various challenges and information requests but this had little impact. Feedback from the qualitative study indicated that participants were reluctant to use the forum owing to the presence of other adults and also because of the availability of other social media sites.
Therapists’ ratings of adherence and ability to correct curve
After the last treatment session physiotherapists were asked the following:
Overall, how well do you think the participant completed the programme according to what was agreed? (On a scale of 1 to 7, where 1 = not at all and 7 = completely.) Physiotherapists’ mean (SD) rating of adherence was 5.6 (SD 1.4).
Feedback on control intervention
We asked all of the participants of the control intervention to provide written feedback on their experience of the trial intervention and to return this to the study team in a pre-paid envelope. We asked the participants and their parents, ‘How do you feel about the treatment that you received as part of the trial?’ and ‘How do you feel about the treatment that your child received as part of the trial?’, respectively.
We received five forms from the 29 participants who had completed their treatment. All recorded favourable comments about the control intervention, although some indicated that they would have preferred to have had the exercise intervention if they could have chosen.
Discussion
We have developed and manualised a best-evidence intervention of SSE treatment for AIS. Feedback from therapists was captured in the qualitative study and is described in Chapter 7.
As would be expected, adherence to allocated treatment arms was variable. All control arm participants attended at least (and usually) one session as per the protocol. Participants of the exercise programme arm varied in their adherence. Data from 16 participants suggest that 38% of these participants had attended the minimum requirement of six sessions, although for eight of these participants the trust providing treatments was unable to provide the minimum six sessions. For the remaining eight participants, 75% (6/8) attended a minimum of six sessions, indicating a promising adherence rate where resources were available.
Use of the online exercise diary appeared to mirror adherence to face-to-face sessions, such that those participants who completed at least six treatment sessions completed, on average, 80% of exercises prescribed, whereas the partial treatment completers only performed 24% of prescribed exercises.
Chapter 5 Patient and public involvement
Patient and public involvement (PPI) – the development of an active partnership between patients and/or members of the public and researchers71 – is now recognised as an increasingly important and integral part of the research process. Patients and members of the public are able to offer researchers unique perspectives, skills and experiences that may prove invaluable to the research but that would otherwise be unavailable. Patients living with a specific illness or condition, for example, may have very different views and priorities to researchers about what will improve their quality of life. We believed the recommendations made following this feasibility study would have a greater focus and relevance for patients with AIS and their families if PPI representatives were consulted throughout the study. 72
We are conscious that sourcing and appraising quality and impact of PPI research relies on good-quality reporting and have, therefore, utilised the Guidance for Reporting Involvement of Patients and Public (GRIPP) checklist for guidance. 73
Objective
To gain user input in all relevant stages of the treatment and protocol design.
Sourcing patient and public involvement
Links with patients and the public for this study were made in a number of ways, including by means of the national patient charity SAUK, consultant spinal clinics and informal individual contact. This resulted in three patients with AIS and their families providing consultation at multiple points in the research. Consultation was provided in a number of formats, such as face-to-face meetings, telephone or e-mail. Mechanisms for involvement in project work do not necessarily allow for all voices to be heard, and, therefore, we were very conscious of ensuring that children would feel able to contribute. We did not provide training for roles but ensured that clear explanations for the reasons for seeking PPI and expectations of input were given. We offered funding for time and travel costs where appropriate.
Patient and public involvement activity
When we contacted PPI representatives we sought information about a number of areas we felt were crucial to assessing and improving feasibility of a study evaluating the effectiveness of SSEs.
First, we sought information about issues surrounding participation, that is, the approach, patient information, the consent process and documents, and the burden of clinical assessments. Second, we sought views on the interventions and associated documentation (online and hard copies). Third, we asked about outcome measures and the means by which they were collected.
A family provided input into the design of the participant information sheets; initial draft documents were sent to a family who had three children of different ages with AIS and they provided detailed suggestions on ways to improve the information sheets. This family also attended the physiotherapy training day, at which they provided feedback on the exercise programme and online materials, and contributed to general discussions about the arrangements for the study. Further comments on the exercise programme were provided from another young person with AIS and her mother, who also assisted with the development of the online materials, including modelling for photographs and videos of the exercises.
Prior to commencing the full qualitative study, a young person and their parents were consulted and their feedback received on the interview schedule, the consent process and the opportunity to interview patients and parents separately. A pilot interview was conducted with this family. They also reviewed the questionnaires to be used in the study.
A representative from SAUK sat on the Independent Monitoring Committee.
Results/impact of patient and public involvement
With regard to participation in a trial, PPI feedback was very positive, and parties were very keen to hear about the research. Our suggestion to seek consent/agreement from both patients and their families was validated and PPI representatives helped us to make minor modifications to the consent forms.
We made significant changes to the child’s version of the patient information sheet with the help of PPI representatives and were commended for the resulting document by the ethics committee. Following a suggestion from at least one PPI representative, we provided all three variations of the patient information sheets as a pack to ensure patients and parents had a choice of materials to read.
Following demonstration of the online materials, we received suggestions on how we could improve content and layout for the online exercise diary and the online forum, which resulted in changes being made. One PPI representative patient and parent assisted by modelling for photographs and videos of exercise performance for the online exercise diary.
We made minor wording changes to questionnaires and improvements to the online exercise diary following PPI feedback.
Discussion
Through involvement of patient and public representatives, we have refined the processes and documentation for approaching patients and their families for a study, providing and documenting physiotherapy treatments and measuring intervention outcomes.
We were aiming for a collaborative approach to the PPI for this study, but it was more consultative in nature. We found it difficult to maintain involvement with PPI representatives owing to their other commitments, which were mostly based around schooling. This was a challenge not limited to the PPI aspects of the study.
For a main study we would recommend taking further time and resources to recruit a larger number and more diverse sample of PPI representatives to ensure a continuous source of collaboration. We also suggest that we should engage more closely with SAUK to utilise their infrastructure of membership and regional meetings to raise awareness of the study and the opportunity of contribution.
We are unaware of any previous research studies on AIS incorporating PPI representation so this feasibility study should be viewed as the very start.
Chapter 6 Randomised feasibility study
Objectives
-
To determine the rate of recruitment and if the pre-specified recruitment rate could be achieved.
-
To determine the acceptability and uptake of randomisation.
-
To determine data quality and completeness.
-
To estimate the SD of a sample recruited from a generalisable selection of secondary care settings.
-
To evaluate the feasibility of the ISIS-2 (Integrated Shape Imaging System 2, Oxford Metrics Group, Oxford, UK) outcome measurement.
-
To estimate the cost of providing treatment, control and training.
Methods
Design
A multicentre randomised feasibility study.
Settings
Four centres were selected from 35 NHS trust hospitals specialising in scoliosis management and surgery. The 35 trusts were those listed by SAUK/British Scoliosis Research Foundation as having clinicians actively managing and performing surgery for patients with scoliosis. We originally planned to run the randomised study in three of these NHS trusts. The sites were chosen to represent a range of the types of hospital likely to be eligible to recruit for a main study to ensure we got a representative estimate of recruitment rate and baseline variability. Some of the three sites we had worked with before, others we had not worked with previously. Some sites had not participated in research previously and had no specialist physiotherapy service. Sites were of a median size for scoliosis centres listed by SAUK/British Scoliosis Research Foundation. As a result of delays in obtaining governance approvals, we added an additional site to ensure that we reached our sample size target. The fourth NHS trust was chosen based on collaborations with researchers and clinicians that had evolved in the early stages of developing the study as well as on the availability of an ISIS system at the centre.
Participants
Inclusion criteria:
-
10- to 16-year-olds with AIS
-
mild to moderate AIS, defined by a Cobb angle of between 10° and 50° (measured radiographically).
Exclusion criteria:
-
individuals who had had previous surgery or were on a waiting list for spinal surgery within the next 6 months
-
individuals with non-idiopathic scoliosis, for example congenital malformations, syringomyelia, neurofibromatosis, spina bifida, polio or cerebral palsy.
Other treatments including bracing and previous physiotherapy were not exclusion criteria.
Interventions
The control intervention consisted of one or two sessions of education and advice delivered by a physiotherapist. This was compared with an experimental intervention consisting of between six and nine sessions of education, advice and a programme of SSEs delivered by a physiotherapist, supported by a daily home exercise programme. Full details of the interventions and their development are provided in Chapter 4.
Procedures
Randomised feasibility study procedures are summarised in a flow chart in Appendix 1.
Screening and recruitment
Participants were recruited directly from spinal deformity or scoliosis clinics. Patients with AIS were approached to participate in the feasibility study by clinicians supported by research clinicians (nurses or physiotherapists).
The screening and recruitment systems were tailored to individual sites, so, in some sites, research clinicians would be present in clinic and discuss the study with patients and, at others, clinicians would perform the screening and pass details to the research clinicians to contact patients and families at a later date. We also piloted an additional recruitment strategy at the fourth site, whereby a specialist nurse approached patients who appeared to be potentially eligible according to hospital records and were due to attend a new patient or review clinic appointment in the next 3 months. They were then booked in for a designated clinic appointment if they were interested in participating in the study.
Screening logs were recorded at two stages: (1) screening was performed in spinal clinics; and (2) subsequent screening was performed on the telephone by research clinicians. These logs were returned to the central study team at the end of each month of activity.
Patients were invited to a research clinic assessment where a trained research clinician rechecked eligibility, responded to any questions about the study and, if appropriate, took written informed consent, assessed and randomised the patient.
Informed consent
We followed the Medical Research Council guidance on seeking consent from children to participate in research. 74 Where a child was assessed as having the capacity to consent to take part in the study we sought his or her consent. In addition, we sought agreement from parents to allow their children to participate. Where a child was judged not to have the capacity to consent to participate, consent was obtained from his or her parent provided agreement was also obtained from the child. Thus, in all patients we had agreement (either consent or assent) from both the child and the parent. Researchers responsible for obtaining consent were provided with training in seeking consent from children and assessing capacity to consent.
We developed three versions of patient information sheets to provide potential participants and parents with information about the possible risks and benefits of taking part in the trial: one for younger children unlikely to have capacity to consent; one for older children likely to have capacity to consent; and one for parents. All three patient information sheets were provided as a pack to ensure that patients and their parents had a choice of materials to read. They were developed with the help of patients and parents.
Baseline assessment
Baseline assessments were conducted by research clinicians who had received training in the measurement protocol. The assessment consisted of self-report questionnaires and physical measurements to capture characteristics, as shown in Table 18.
| Type and method of measure | Measurement (units/scale) | Time points taken |
|---|---|---|
| Primary outcomes | ||
| Spine curvature | Primary Cobb angle from radiograph (°) | Baseline and 6 months |
| Characteristics | ||
| Age, sex, ethnic group | Self-report questionnaire | Baseline |
| Height, weight, body mass index | Standing and seated height (m) Weight (kg) |
Baseline and 6 months |
| Pubescent status | Onset of puberty and age of occurrence | Baseline |
| Skeletal maturity | Risser classification (0–5) from radiograph Pre or post menarche |
Baseline and 6 months |
| Treatments received | Current bracing status Previous exercise treatments received |
Baseline and 6 months |
| Secondary outcomes | ||
| Disease-specific function | SRS-2275 | Baseline and 6 months |
| Participant perceived spinal deformity | SAQ76 | Baseline and 6 months |
| Generic function | PODCI77 | Baseline and 6 months |
| HRQoL | EQ-5D HUI |
Baseline and 6 months |
| Coronal and sagittal curve balance | Coronal and sagittal balance calculated from radiographs | Baseline and 6 months |
| Topographical spinal deformity | ISIS-2 system measurements | Baseline and 6 months |
| Treatment preference | Control or experimental intervention (with the awareness these were randomly allocated) | Baseline |
| Global perceived change in scoliosis | Seven categories ranging from vastly improved to vastly worsened | 6 months |
| Perceived benefit or harm from study treatments | Five categories ranging from substantial benefit to substantial harm | 6 months |
| Treatment satisfaction | Seven categories ranging from extremely satisfied to extremely dissatisfied | 6 months |
| Exercise performance | Participant-reported frequency Online exercise diary output |
6 months |
| Brace wearing status | Currently wearing brace (Y/N) | Baseline and 6 months |
| Progression to surgery | Listed for or received surgery | 6 months |
| Resource use for economic analysis | 6 months | |
| AEs | AEs or SAEs | During treatment and 6 months |
We anticipated that the primary outcome measure for a main study would be progression/stabilisation of curvature quantified by Cobb angle. This is measured using standing posteroanterior radiographs of the full spine and assessing the lateral curvature of the spine. To do this, the most tilted vertebra above and below the apex of the curve is identified. The angle between intersecting lines drawn perpendicular to the top of the top vertebra and the bottom of the bottom vertebra is the Cobb angle (Figure 2).
FIGURE 2.
Measurement of Cobb angle.
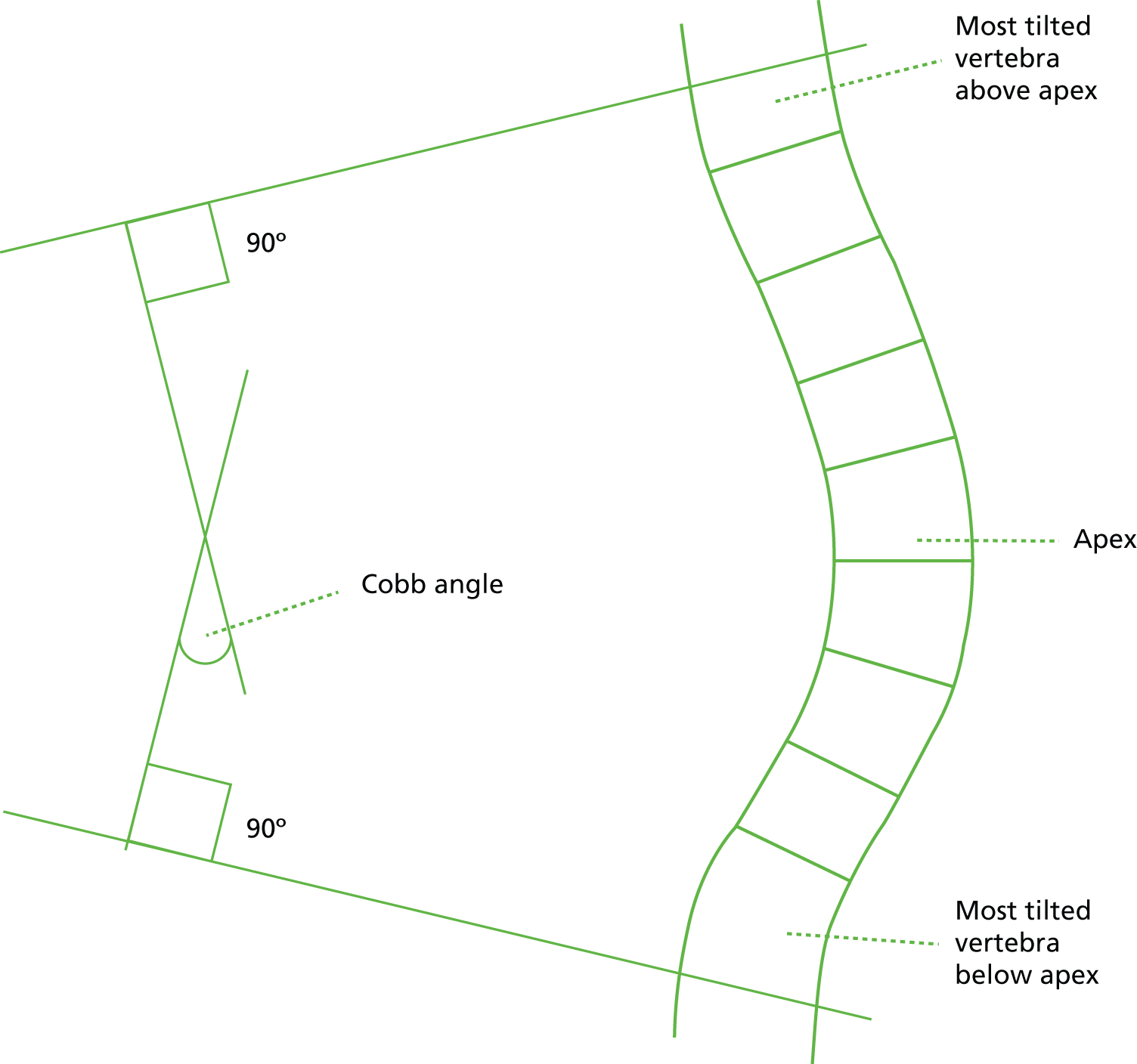
Other measures that we collected from radiograph were the Risser classification and coronal and sagittal spinal balance. Risser classification divides the steps of ossification and fusion of the iliac apophysis into six stages (0–5), where stage 0 describes no apophyseal ossification and stage 5 represents complete ossification and fusion. This provides an indication of skeletal maturity, which in turn helps to predict growth potential and velocity and, therefore, likelihood of curve progression. 78 Risser classification is probably the most widely used indicator of skeletal maturity, although correct classification relies on a sufficient radiograph of visualisation of the entire pelvis.
Coronal balance was evaluated by measuring the horizontal distances between two lines in millimetres (mm); one vertical plumb line is drawn downwards through the centre of the C7 vertebral body and another vertical line is drawn upwards from the centre of the S1 vertebral body. The spine was considered to be balanced when the difference between these two lines was < 40 mm. 79 Sagittal balance was evaluated by measuring the distance between a vertical line drawn up from the posterosuperior aspect of the S1 vertebral body and the plumb line down from the centre of the T1 vertebral body. Sagittal balance can be divided as negative or neutral/positive. 79
Details and timings of most recent radiographic images were obtained from patient records. Cobb angles, spinal balance distances and Risser grades were calculated/recorded by spinal consultants at individual centres.
Some NHS trusts have invested in topographical measurement equipment that allows for assessment of a representation of the Cobb angle and rib hump by means of a digital photographic image rather than exposure to X-rays. The ISIS-2 system was developed as a low-cost method to reduce the dependence on serial radiography and to reduce radiation exposure when monitoring spinal deformity. 80 The system produces a version of the Cobb angle (although this is known to not correlate completely with radiographic versions) and volumetric asymmetry. One of the study objectives was to evaluate the feasibility of using the ISIS-2 topographical measurement system in all centres in the main study.
Disease-specific quality of life was measured using the SRS-22, the most widely used patient-reported outcome measure, which contains 22 questions covering five domains (function/activity, pain, self-perceived image, mental health and satisfaction). It has been demonstrated to be valid, reliable and responsive to change, with a minimally clinically important difference of 13 points out of 100 for the sum score. 81
Patient-perceived spinal deformity was measured using the Spinal Appearance Questionnaire (SAQ). In its refined format, it has two domains – appearance (10 items) and satisfaction (4 items) – and has been shown to be valid and reliable,82 although a minimally clinically important difference has yet to be derived.
A generic orthopaedic function measure was also collected in the form of the Pediatric Outcomes Data Collection Instrument (PODCI). This covers eight domains (upper extremity function, transfers and mobility, physical function and sports, comfort, happiness, satisfaction with symptoms, expectations of treatment and global functioning) on an overall scale of 0–100, with 100 being the highest level of function. It has been shown to have good psychometric properties. 77,83
Randomisation
Randomisation was carried out on an individual basis using the Warwick Clinical Trials Unit telephone randomisation service. Randomisation was stratified by centre and age (10- to 13-year-olds vs. 14- to 16-year-olds) to control for any local differences in case mix between sites. Allocation was concealed from the research clinicians involved in outcome measurement. Maintenance of blinding was assessed by asking research clinicians whether or not they had been unblinded at the 6-month follow-up point.
Treatment organisation
Following the baseline research clinic appointment, participants were informed that the physiotherapy department would contact them within 2 weeks to arrange their initial appointment. Allocation was emailed directly to physiotherapists who informed the participant of their allocation at this initial appointment. Physiotherapists maintained a log of treatments provided at each session. If participants did not wish to continue treatment, physiotherapists would clarify if they also wished to withdraw from the feasibility study entirely. This information was passed to the central study team.
Follow-up assessment
Outcome measures were taken at 6 months post randomisation during face-to-face research clinic appointments, as detailed in Table 18. If participants were unable to attend these clinic appointments, we attempted to obtain core data via postal or telephone questionnaire.
Sample size requirements
We sized the pilot study in order to estimate the baseline variance in the outcome measures, which will be one of the most important drivers of a sample size estimate for a definitive trial. A minimum of 30 participants are needed to estimate the variance of parameters underlying the sample size estimate. 84 We chose a target of 50 because this allows for better estimation of recruitment rates at each of the centres.
By aiming to recruit 50 participants from three centres over the course of 12 months, we were pre-specifying an average recruitment rate of 1.4 participants per centre per month. In our original proposal we anticipated that at least 400 patients would be required for a definitive trial. If this pre-specified rate was achieved for 15–20 sites, it would require between 16 months and 20 months to complete, which is an acceptable time frame.
Clinical reporting/analysis
Pilot RCT data are summarised and reported in accordance with Consolidated Standards of Reporting Trials (CONSORT) guidelines for RCTs where possible. 85 The purpose of the statistical analysis was not to make comparisons between groups but to compare against the progression criteria we set. We report the number of participants approached, the numbers meeting the eligibility criteria, the numbers agreeing to randomisation, the numbers attending the trial treatment sessions, the overall proportion of people who attended 60% of the sessions and use of the online exercise diary. Completion of measures is recorded alongside descriptive data. Only an observed data set has been used, as imputation was not appropriate.
Withdrawals from treatment, withdrawals from the trial, AEs and serious adverse events (SAEs) are reported.
Health economics reporting/analysis
The study collected data on the use of services within the health-care system and other sectors of the economy, as well as on broader costs to society, in an attempt to capture relevant components that comprise the overall cost of treating AIS. Key items included data completeness and the costs of the control and experimental interventions.
Data were collected from information gathered via the study participant questionnaires completed by participants, their parents and research physiotherapists at baseline and 6 months post randomisation. Questionnaires captured the frequency of use of community-based health and social care services, number and duration of admissions to inpatient wards, number of diagnostic tests, use of outpatient services (classified as orthopaedic/spinal, paediatric, physiotherapy, orthotics/bracing), medication use and equipment provided, indirect costs borne by parents and carers as a result of attending hospital visits, as well as direct non-medical costs (including travel expenses), attributable to the child’s health state. The parent-completed questionnaires recorded employment status, weekly working hours, self-reported annual income and work-days lost as a result of the child’s health state.
To measure effectiveness, two multiattribute utility measures were piloted in the study, the EuroQol EQ-5D-3L questionnaire and the HUI, at baseline and 6 months.
The practicalities and difficulties associated with an assessment of the cost to providers, individuals and, more broadly, to society entailed by the introduction of the exercise intervention, along with the identification of appropriate sources of unit cost data, were addressed. A NHS and Personal Social Services perspective was adopted for the costing component of the feasibility study. 86
Data on consumable use were taken from the study records. Similarly, physiotherapist training time, length of treatment sessions and programming input were obtained using primary research methods.
Valuation of resource-use cost data
The unit costs for resources used for the implementation of the exercise programme were mainly obtained from the ACTIvATeS feasibility study records, apart from the unit costs of physiotherapists’ time, which were obtained from the Personal Social Services Research Unit’s Unit Costs of Health and Social Care 2013 cost compendium87 (Table 19; see also Tables 39–41). Unit costs for the broader resources used by adolescents during the study were obtained from a range of primary and secondary sources (see Table 1). Estimation of unit costs used followed recent guidelines on costing health and social care services as part of health economic evaluations. Unit costs for hospital- and community-based health and social care services were derived from the NHS Reference Costs (2012–13) (Department of Health 2013)88 and the Personal Social Services Research Unit’s Unit Costs of Health and Social Care 2013 cost compendium. 87 A list of all medications used was collated, and costs for individual preparations related to idiopathic scoliosis were identified for inclusion in a prospective trial-based economic evaluation. This list included musculoskeletal drugs, central nervous system drugs, endocrine system drugs, skin drugs, ear drugs, nose and oropharynx drugs, obstetrics drugs, gynaecology and urinary tract disorder drugs, and nutrition and blood agents. The drug prescription costs were obtained from the Health and Social Care Information Centre Prescription Cost Analysis database. 87 All unit costs were expressed in GBP (£) and valued at 2012–13 prices.
| Resource item | Unit | Mean cost (£ per unit) | Sources |
|---|---|---|---|
| GP | Session | 45.00 | PSSRU |
| GP | Home visit | 292.00 | PSSRU |
| GP | Telephone call | 27.00 | PSSRU |
| District nurse | Hour | 48.00 | PSSRU |
| Physiotherapist | Hour | 34.00 | PSSRU |
| Occupational therapist | Hour | 44.00 | PSSRU |
| Orthotist | Hour | 34.00 | Assume same as physiotherapist based on salaries |
| Social worker | Hour | 57.00 | PSSRU |
| Inpatient stay | Day | 137.06 | Reference cost: Elective FZ49E |
| Orthopaedic/spinal clinic | Session | 131.00 | Reference cost: 214 |
| Paediatrics department | Session | 187.00 | Reference cost: 420 |
| Emergency department | Session | 117.00 | Reference cost: 180 |
| Physiotherapist department | Session | 42.00 | Reference cost: 650 |
| Orthotics/bracing department | Session | 131.00 | Reference cost: 214 |
| Radiography | Test | 5.00 | Assumption |
| CT scan | Test | 92.00 | Reference cost: RA08B-RA09B |
| MRI scan | Test | 145.00 | Reference cost: RA01B-RA02B |
| Blood tests | Test | 3.00 | Reference cost: DAPS05 |
Calculation of health utilities
The EQ-5D is the generic, multiattribute, preference-based measure preferred by NICE for broader cost-effectiveness comparative purposes. The EQ-5D consists of two principal measurement components. The first is a descriptive system, which defines HRQoL in terms of five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Responses to each of these dimensions are divided into three ordinal levels – first, no problems; second, some or moderate problems; and third, severe or extreme problems – generating a total of 243 possible health states. Utility scores can be produced from the responses to the descriptive system using a UK-specific tariff,89 calculated from a time-trade-off study of 3336 people from the UK general population, taking values between –0.594 and 1.0. The second measurement component of the EQ-5D, the vertical visual analogue scale (VAS), which ranges from 100 (best imaginable health state) to 0 (worst imaginable health state), was also included in ACTIvATeS.
The HUI is a family of generic health profiles and preference-based systems for the purposes of measuring health status, reporting HRQoL and producing utility scores. The HUI 15-item questionnaire for usual health status assessment completed by adolescents in the study covers both the HUI2 and the HUI3 health status classification systems. The HUI2 and HUI3 health status classification systems are complementary. Together they provide descriptive measures of ability or disability for health-state attributes and descriptions of comprehensive health status. Utility scores have interval-scale measurement properties. The multiattribute scales of overall HRQoL are defined such that the score for dead = 0.00 and the score for perfect health = 1.00. Both HUI2 and HUI3 allow for negative scores of HRQoL that represent health states considered worse than dead. The lowest possible HRQoL scores are –0.03 for HUI2 and –0.36 for HUI3. 30,90,91
Ethical approval and monitoring
Ethics committee approval
Approval to conduct the feasibility study was granted by the East of England – Cambridge South REC (reference number 12/EE/0331) and by the Research and Development department of each participating trust.
Independent monitoring committee
The Independent Monitoring Committee was independent of the study and tasked with monitoring ethics, safety and data integrity. Membership of the Independent Monitoring Committee is detailed in the Acknowledgements section.
Study management group
A study management group was responsible for the day-to-day management of the trial, consisting of the study lead, research fellows, study co-ordinator, statistician and health economist. This group met on a monthly basis.
Quality assurance
A clinical research fellow ensured adherence to study protocols at all sites. Periodic observations of research clinic appointments for all research clinicians were carried out. At baseline research clinic appointments, checks were made of the consent process and research assessments.
Results
Sites and therapists
Four centres recruited patients for the study:
-
Frenchay Hospital, Bristol, UK
-
Royal Orthopaedic Hospital, Birmingham, UK
-
Nuffield Orthopaedic Centre, Oxford, UK
-
James Cook Hospital, Middlesbrough, UK.
Seven physiotherapists delivered interventions. These senior physiotherapists had a range of experience in treating scoliosis (9–40 years qualified, Agenda for Change bands 6–8a), with a minority having taken specialist training in prescribing SSEs.
Screening of patients
Screening and recruitment took place between December 2012 and October 2013. Clinic screening data are summarised in Table 20, and subsequent telephone screening is summarised in Table 21. There are some missing data at case or item level (age).
| Clinic screening | FRE | ROH | NOC | JCH | Overall | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 10- to 13-year-olds | 14- to 16-year-olds | Total | 10- to 13-year-olds | 14- to 16-year-olds | Total | 10- to 13-year-olds | 14- to 16-year-olds | Total | 10- to 13-year-olds | 14- to 16-year-olds | Total | 10- to 13-year-olds | 14- to 16-year-olds | Total | |
| Patients screened, n | 337 | 807 | 476 | 12 | 1632 | ||||||||||
| Eligible patients, n (%) | 5 (22) | 18 (78) | 27 (8) | 15 (27) | 40 (73) | 55 (7) | 28 (33) | 57 (67) | 85 (18) | 0 | 10 | 10 (83) | 48 (28) | 125 (72) | 177 (11) |
| Willing to be contacted, n (%) | 4 | 15 | 22 (81) | 9 (60) | 27 (68) | 36 (65) | 16 (57) | 31 (54) | 69 (81) | 0 | 8 | 8 (80) | 29 (60) | 81 (65) | 135 (76) |
| Not willing to be contacted, n (%) | 1 | 1 | 3 | 0 (0) | 4 (10) | 4 (7) | 1 | 7 | 9 (11) | 0 | 2 | 2 | 2 (4) | 14 (11) | 18 (10) |
| Reason: not happy to be randomised, n (%) | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 (11) | 0 | 0 | 0 | 0 (0) | 2 (14) | 2 (11) |
| Reason: does not have time for study, n (%) | 1 | 0 | 1 | 0 | 2 | 2 | 1 | 4 | 6 (67) | 0 | 2 | 2 | 2 (100) | 8 (57) | 11 (61) |
| Reason: other, n (%) | 0 | 1 | 2 | 0 | 1 | 1 | 0 | 3 | 4 (44) | 0 | 0 | 0 | 0 | 5 (36) | 7 (39) |
| Willingness not ticked, n (%) | 0 | 2 | 2 | 7 (40) | 11 (28) | 18 (33) | 4 | 2 | 6 | 0 | 0 | 0 | 11 (23) | 15 (12) | 26 (14) |
| Ineligible patients, n (%) | 309 (92) | 714 (88) | 381 (80) | 2 | 2 | 0 | 2 | 1406 (86) | |||||||
| Eligibility unknown, n (%) | 1 | 38 (5) | 4 (< 1) | 0 | 0 | 0 | 0 | 43 (3) | |||||||
| Telephone screening | FRE | ROH | NOC | JCH | Overall | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 10- to 13-year-olds | 14- to 16-year-olds | Total | 10- to 13-year-olds | 14- to 16-year-olds | Total | 10- to 13-year-olds | 14- to 16-year-olds | Total | 10- to 13-year-olds | 14- to 16-year-olds | Total | 10- to 13-year-olds | 14- to 16-year-olds | Total | |
| Patients to be contacted, n (%) | 3 | 14 | 28 | 13 | 38 | 51 | 11 | 26 | 61 | 8 | 8 | 27 (24) | 86 (76) | 148 | |
| Patients successfully contacted, n (%) | 3 | 10 | 15 | 7 | 19 | 26 | 8 | 18 | 34 | 7 | 7 | 18 (67) | 54 (63) | 82 (55) | |
| Eligible after telephone call, n (%) | 3 | 9 | 14 | 7 | 18 | 25 | 8 | 17 | 31 | 7 | 7 | 18 (100) | 51 (94) | 77 (93) | |
| Willing to arrange research clinic, n (%) | 3 | 8 | 13 | 5 | 12 | 17 | 6 | 7 | 17 | 7 | 7 | 14 (78) | 34 (67) | 54 (70) | |
| Not willing to arrange research clinic, n (%) | 0 | 0 | 0 | 2 | 6 | 8 | 2 | 7 | 9 | 0 | 0 | 4 (22) | 13 (25) | 17 (22) | |
| Reason: not happy to be randomised, n | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | |
| Reason: does not have time for study, n | 0 | 0 | 0 | 0 | 5 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 5 | |
| Reason: not willing to travel for study, n | 0 | 0 | 0 | 1 | 2 | 3 | 1 | 2 | 3 | 0 | 0 | 2 | 4 | 6 | |
| Reason: other, n | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 1 | 4 | ||
| Not eligible after telephone call, n (%) | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 2 | 3 (4) | |
| Unable to contact, n (%) | 4 | 8 | 13 | 6 | 12 | 18 | 2 | 5 | 15 | 1 | 1 | 12 (44) | 26 (30) | 47 (31) | |
Screening logs recorded 1632 patients being screened in the spinal clinics of the four centres. Of these, 177 (11%) patients were eligible. The range of proportions of eligible patients between the centres varied from 7% to 83%, although the upper range is somewhat artificial as a result of the strategic screening that was conducted at the James Cook Hospital, Middlesbrough. Of those who were eligible to participate, 25% were 10- to 13-year-olds and 75% were 14- to 16-year-olds.
The main reason for ineligibility was that the patient did not have a diagnosis of AIS (≈60% of patients). Overall, 76% (n = 135, between-centre range 65–81%) of eligible patients were willing to be contacted by the research team. Of the 18 patients not willing to consider participation, the main reason given was lack of time (n = 11, 61% of patients). No patients gave the reason of not being willing to travel for study.
Of the 148 patients logged to be contacted by telephone (note that missing data mean that this figure is different from the 135 recorded in the clinic screening data), just over half (n = 82, 55%) were successfully contacted and the vast majority of these were still eligible (n = 77, 93%). The 25%/75% split between the age categories persisted. A total of 54 patients are recorded as having a clinic appointment arranged, highlighting the issue of some missing data (as we have records of 60 attending clinics and 58 patients being randomised; see Figure 5).
Seventeen patients were not willing to arrange a research clinic appointment, with the reasons stated varying from not having time to commit to the study (n = 5), not being willing to travel (bearing in mind that some of the patients travel a long way to the specialist centres; n = 6) and other miscellaneous reasons (n = 4). One participant gave the reason of not being willing to be randomised. There were no major differences between older and younger age categories in terms of willingness to be contacted and willingness to arrange a research clinic if successfully contacted. A slightly higher proportion of 10- to 13-year-olds were unable to be contacted [n = 12 (44%), compared with n = 26 (30%) for 14- to 16-year-olds].
Recruitment of participants
Sixty patients were booked for a research clinic appointment between January and October 2013. Of these, one patient was unwilling to be involved in the study and one had been placed on a surgical list between agreeing to attend and the research clinic appointment. Therefore, 58 patients consented and were recruited to the study.
The original timetable detailed the start of recruitment as September 2012 but delays were experienced with contracting and governance approvals, so that the first screening began in December 2012. (Governance approvals took between 5 months and 6 months to obtain.) Figure 3 illustrates the expected and observed overall recruitment of participants by month. Figure 4 illustrates recruitment by individual sites by month.
FIGURE 3.
Cumulative monthly overall recruitment.
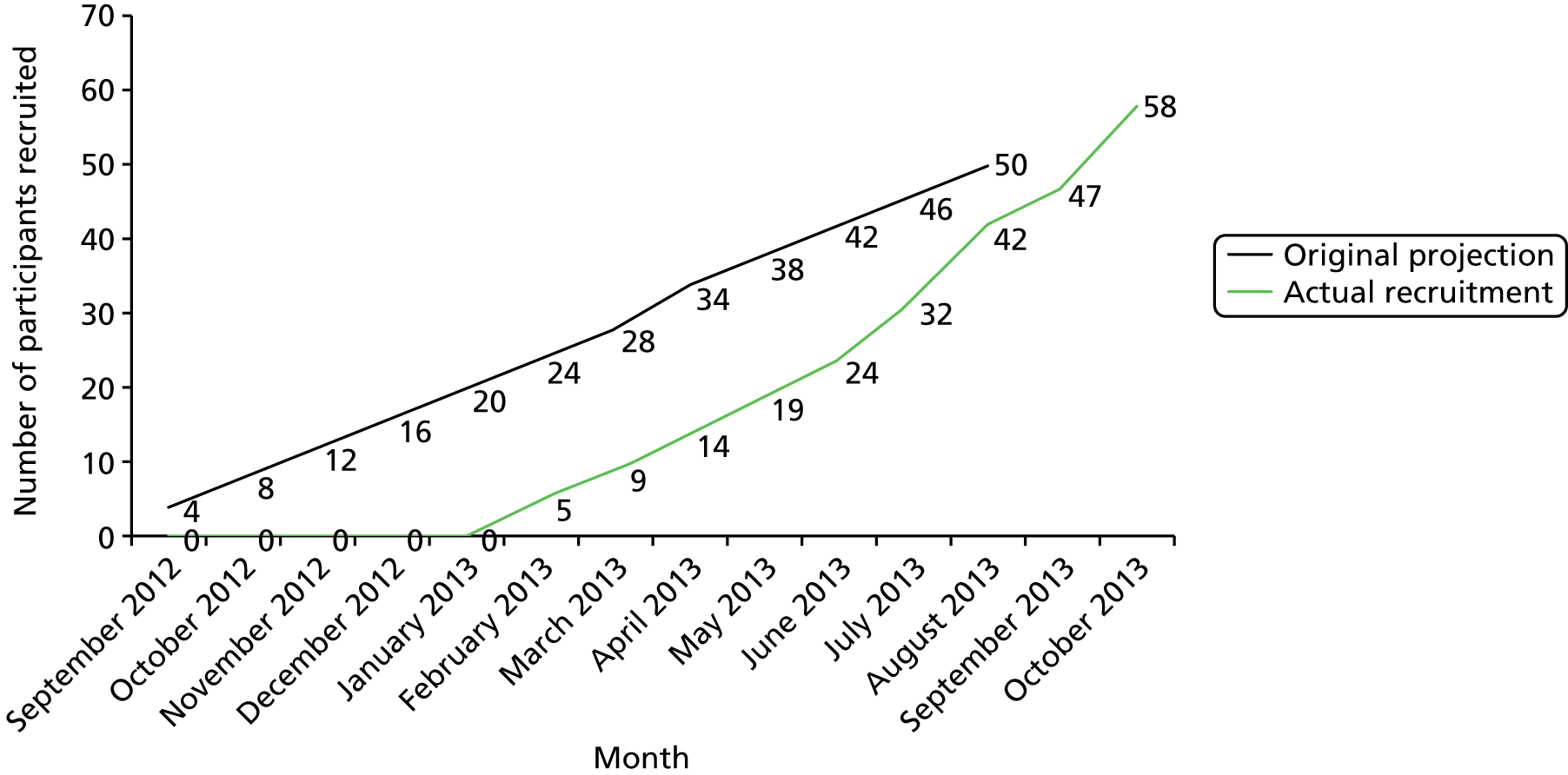
FIGURE 4.
Cumulative monthly recruitment by individual sites. FRE, Frenchay Hospital, Bristol, UK; JCH, James Cook Hospital, Middlesbrough, UK; NOC, Nuffield Orthopaedic Centre, Oxford, UK; ROH, Royal Orthopaedic Hospital, Birmingham, UK.

Table 22 displays projected and actual recruitment by centre. The mean projected recruitment rate per centre per month was 1.4 (50/36), whereas the actual recruitment rate per centre per month was 1.8 (58/33).
| Type of recruitment | FRE | ROH | NOC | JCH | Total |
|---|---|---|---|---|---|
| Expected centre months of recruitment, n | 12 | 12 | 12 | 2 | 36 |
| Actual centre months of recruitment, n | 10 | 11 | 10 | 2 | 33 |
| Expected recruitment, n | 17 | 17 | 17 | < 10 | 50 |
| Actual recruitment, n | 11 | 20 | 20 | 7 | 58 |
Randomisation
Participants were randomised in equal proportion to the advice and education and exercise programme arms (n = 29 in each). Table 23 demonstrates that randomisation was well balanced at each centre.
| Centre | Treatment A, n (%) | Treatment B, n (%) | Total, N |
|---|---|---|---|
| FRE | 5 (45) | 6 (55) | 11 |
| ROH | 10 (50) | 10 (50) | 20 |
| NOC | 10 (50) | 10 (50) | 20 |
| JCH | 4 (57) | 3 (43) | 7 |
| Total | 29 | 29 | 58 |
Figure 5 presents the CONSORT flow diagram for the pilot RCT.
FIGURE 5.
The CONSORT flow diagram.
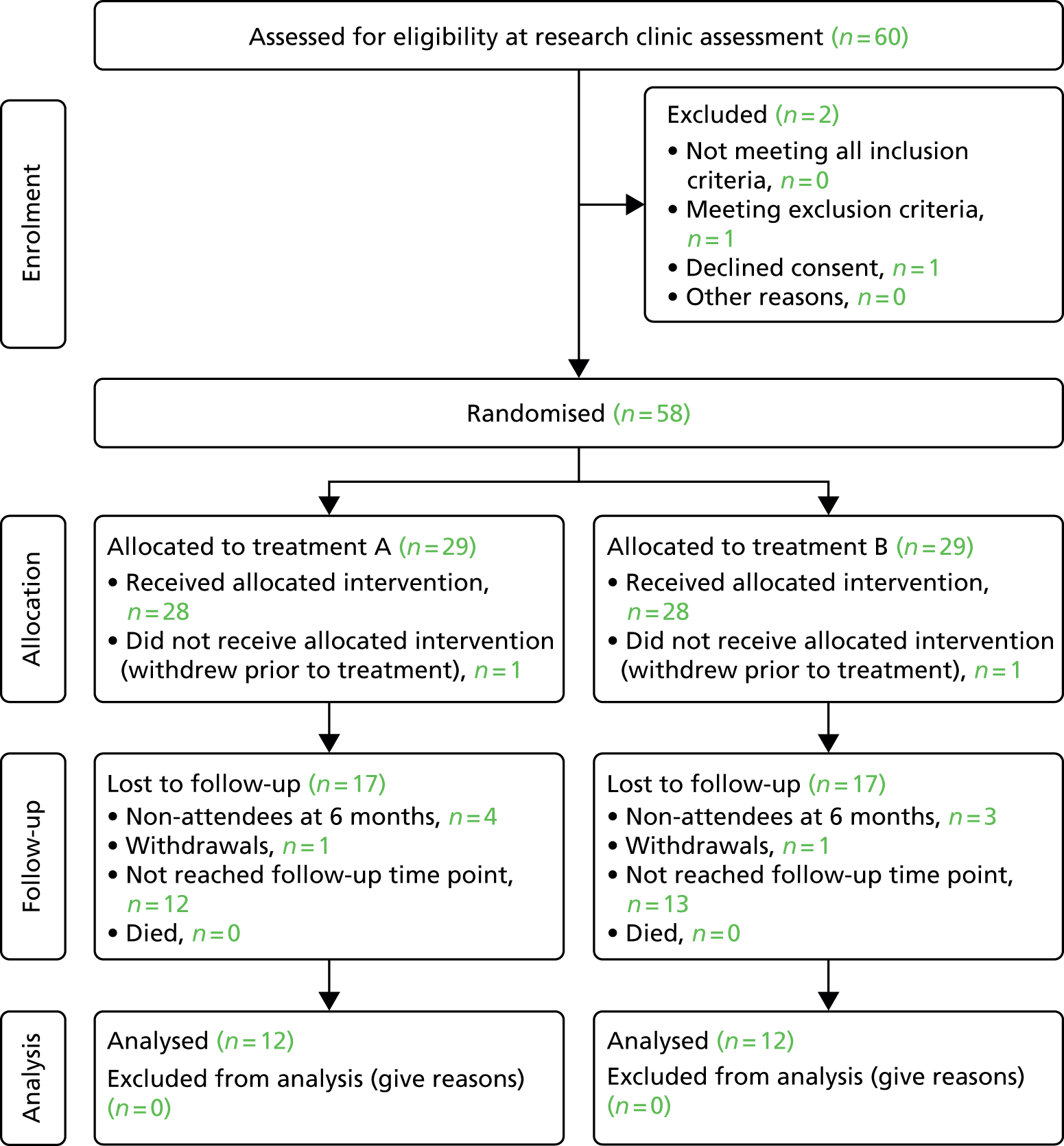
Baseline data
Baseline characteristics
Baseline data are presented in Tables 24–29. The cohort was predominantly white females in their mid-teens, who were post-pubescent. Risser gradings reflect this, with almost half (47%) of participants with an available grading showing skeletal maturity (grade 4 or 5). It should be noted that there was a considerable number of missing data for Risser gradings; reasons were mainly to do with having an insufficient radiograph.
The majority of the cohort was diagnosed with AIS within the past year. A minority of patients were regularly wearing a brace (17%). Approximately half of the participants had received previous treatments for their AIS; most commonly this was physiotherapy (26%). Only one participant recalled participating in a SSE programme.
| Demographics | Treatment A (N = 29 unless stated) | Treatment B (N = 29 unless stated) | Total |
|---|---|---|---|
| Age (years), n | |||
| Mean (SD) | 13.9 (1.66) | 13.9 (1.79) | 13.9 (1.71) |
| Median (range) | 14.0 (6) | 14.0 (6) | 14.0 (6) |
| Sex, n (%) | |||
| Male | 5 (17) | 5 (17) | 10 (17) |
| Female | 24 (83) | 24 (83) | 48 (83) |
| Ethnic group, n (%) | |||
| Mixed | 0 (0) | 0 (0) | 0 (0) |
| White | 23 (79.3) | 28 (96.6) | 51 (87.9) |
| Indian | 0 (0) | 0 (0) | 0 (0) |
| Pakistani | 0 (0) | 0 (0) | 0 (0) |
| Bangladeshi | 0 (0) | 0 (0) | 0 (0) |
| Black or black British | 3 (10.3) | 0 (0) | 3 (5.17) |
| Chinese | 1(3.45) | 0 (0) | 1 (1.72) |
| Other ethnic group | 1 (3.45) | 1 (3.45) | 2 (3.45) |
| Missing | 1 (3.45) | 0 (0) | 1 (1.72) |
| Age diagnosed with scoliosis (years), n | |||
| Mean (SD) | 12.6 (2.79) | 11.3 (3.70) | 11.9 (3.32) |
| Median (range) | 12.5 (14) | 12 (14) | 12 (15) |
| Missing | 1 | 0 | 1 |
| Physical measures | |||
| Standing height (m), mean (SD) | 1.64 (0.11) | 1.61 (0.11) | 1.62 (0.11) |
| Seated height (m), mean (SD) | 0.78 (0.07) | 0.77 (0.23) | 0.78 (0.17) |
| Weight (kg), mean (SD) | 54.0 (12.9) | 51.7 (11.3) | 52.8 (12.0) |
| Body mass index, mean (SD) | 19.8 (3.3) | 19.9 (5.0) | 19.9 (4.2) |
| Pubescence status | |||
| Onset of puberty, n (%) | |||
| Yes | 23 (79) | 23 (79.3) | 46 (79.3) |
| No | 5 (17) | 6 (20.7) | 11 (17.2) |
| Missing | 2 (6.90) | 0 (0) | 2 (3.45) |
| Age of onset of puberty (years), n | |||
| Mean, n (SD) | 12.4 (1.26) | 12.6 (0.92) | 12.5 (1.09) |
| Median, n (range) | 13 (6) | 13 (3) | 13 (6) |
| Missing | 9 | 8 | 17 |
| Skeletal maturity | |||
| Risser classification, n (%) | |||
| 0 | 2 (7) | 5 (17) | 7 (12) |
| 1 | 1 (3) | 2 (7) | 3 (5) |
| 2 | 2 (7) | 0 (0) | 2 (3) |
| 3 | 2 (7) | 5 (17) | 7 (12) |
| 4 | 7 (24) | 4 (14) | 11 (19) |
| 5 | 4 (14) | 2 (7) | 6 (10) |
| Missing | 11 (38) | 11 (38) | 22 (38) |
| Treatments received | |||
| Do you currently wear a brace? | |||
| Yes | 6 (21) | 4 (14) | 10 (17) |
| No | 22 (76) | 24 (83) | 46 (79) |
| Missing | 1 (3) | 1 (3) | 2 (3) |
| Previous exercise treatments | |||
| No | 13 (45) | 15 (52) | 28 (48) |
| Yes: physiotherapy | 6 (21) | 9 (31) | 15 (26) |
| Yes: SSEs | 1 (3) | 0 (0) | 1 (2) |
| Yes: Pilates | 1 (3) | 0 (0) | 1 (2) |
| Yes: other | 7 (24) | 4 (14) | 11 (19) |
| Missing | 1 (3) | 1 (3) | 2 (3) |
| Computer and internet access | |||
| Yes: daily at home | 28 (97) | 29 (100) | 57 (98) |
| Missing | 1 (3) | 0 (0) | 1 (2) |
Table 25 presents baseline characteristics of participants at each centre.
| Demographics | Centre 1 | Centre 2 | Centre 3 | Centre 4 |
|---|---|---|---|---|
| Age, years | ||||
| Mean (SD) | 13.9 (1.33) | 13.3 (2.11) | 14.9 (1.07) | 13.9 (1.71) |
| Median (range) | 14.0 (4) | 13.5 (6) | 15.0 (3) | 14.0 (6) |
| Sex, n (%) | ||||
| Male | 5 (25) | 3 (15) | 0 (0) | 2 (18) |
| Female | 15 (75) | 17 (85) | 7 (100) | 9 (82) |
| Ethnic group, n (%) | ||||
| Mixed | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| White | 16 (80) | 18 (90) | 7 (100) | 11 (100) |
| Indian | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Pakistani | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Bangladeshi | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Black or black British | 2 (10) | 1 (5) | 0 (0) | 0 (0) |
| Chinese | 1 (5) | 0 (0) | 0 (0) | 0 (0) |
| Other ethnic group | 0 (0) | 1 (5) | 0 (0) | 0 (0) |
| Missing | 1 (5) | 0 (0) | 0 (0) | 0 (0) |
| Age diagnosed with scoliosis (years), n | ||||
| Mean (SD) | 11.9 (4.16) | 11.0 (3.08) | 13.0 (1.63) | 13.0 (2.69) |
| Median (range) | 13 (15) | 12 (13) | 13 (5) | 13 (9) |
| Missing (%) | 1 (5) | 0 (0) | 0 (0) | 0 (0) |
| Onset of puberty, n (%) | ||||
| Yes | 16 (80) | 13 (65) | 7 (100) | 10 (91) |
| No | 3 (15) | 6 (30) | 0 (0) | 1 (9) |
| Missing | 1 (5) | 1 (5) | 0 (0) | 0 (0) |
| Age of onset of puberty (years), n | ||||
| Mean (SD) | 12.4 (0.76) | 12.4 (1.31) | 12.1 (1.07) | 13.3 (1.11) |
| Median (range) | 13 (2) | 12.5 (5) | 12.0 (3) | 13.0 (3) |
| Missing | 6 (30) | 8 (40) | 0 (0) | 4 (36) |
| Currently wearing a brace, n (%) | ||||
| Yes | 2 (10) | 6 (30) | 3 (43) | 0 (0) |
| No | 18 (90) | 13 (65) | 3 (43) | 0 (0) |
| Missing | 1 (5) | 1 (5) | 0 (0) | 0 (0) |
| Computer and internet access, n (%) | ||||
| Yes: daily at home | 19 (95) | 20 (100) | 7 (100) | 11 (100) |
| Missing | 1 (5) | 0 (0) | 0 (0) | 0 (0) |
Baseline curve data including primary outcome
For the primary outcome measure of the largest Cobb angle, the mean and median scores of the largest Cobb angle were similar at around 35° (Table 26). The scores ranged from 14° to 50°. There was an approximate 50/50 split between single and double curves. There were similar numbers of thoracic and thoracolumbar curves and a minority of lumbar curves. There were, on average, small coronal and sagittal imbalances in the participants’ curves which would be classified as balanced according to Glassman et al. 79
| Baseline primary outcome | Treatment A (n = 29 unless stated) | Treatment B (n = 29 unless stated) | Total |
|---|---|---|---|
| Cobb angle of largest curve (°) | |||
| Mean (SD) | 34.3 (10.1) | 33.8 (10.1) | 34.0 (10.0) |
| Median (IQR) | 35.5 (15.0) | 34.0 (16.0) | 34.0 (14.0) |
| Missing | 1 | 0 | 1 |
| Curve type, n (%) | |||
| Single | 12 (41) | 18 (62) | 30 (52) |
| Double | 15 (52) | 11 (38) | 26 (45) |
| Triple | 1 (3) | 0 | 1 (2) |
| Missing | 1 (3) | 0 | 1 (2) |
| Area of curve, n (%) | |||
| Thoracic | 10 (34) | 11 (38) | 21 (36) |
| Thoracolumbar | 15 (52) | 11 (38) | 26 (45) |
| Lumbar | 3 (10) | 7 (24) | 10 (17) |
| Missing | 1 (3) | 0 (0) | 1 (2) |
| Coronal balance (cm) | |||
| Mean (SD) | 1.8 (1.2) | 1.9 (1.3) | 1.7 (1.3) |
| Median (IQR) | 1.5 (1.8) | 1.6 (1.7) | |
| Sagittal balance (cm) | |||
| Mean (SD) | 3.2 (2.8) | 4.4 (2.9) | 3.8 (2.9) |
| Median (IQR) | 2.7 (4.1) | 3.8 (5.2) | |
| ISIS scan present, n (%) | 12 (41) | 15 (52) | 27 (47) |
| Sagittal curve, n | |||
| Mean (SD) | 20.6 (8.5) | 27.4 (10.4) | 24.4 (10.1) |
| Median (IQR) | 19 (12) | 28 (16) | 24 (18) |
We received data from sites for ISIS scans of 23 participants. Reasons for not receiving scan data were either that the scan was not taken (as this was not part of routine data collection) or that the ISIS scanner was not available for use. For the data that were collected, the sagittal curve reading was approximately 10° less than the radiographically derived Cobb angle.
Baseline scores for secondary outcome measures
Secondary outcomes are presented in Table 27. The SRS-22 scores were lower than previous cohorts of non-surgical patients of a similar age and curve size79 (indicating greater problems with function, pain, self-image, mental health and treatment satisfaction) but almost identical between the groups. A similar finding was made for the SAQ scores, which were relatively well matched between the groups and appear higher (indicating lower self-image) than a similar cohort of non-surgical patients. 86 The PODCI scores were similar to a cohort of 102 AIS patients in the USA. 81
| Baseline secondary outcome | Treatment A (n = 29 unless stated) | Treatment B (n = 29 unless stated) | Total |
|---|---|---|---|
| SRS-22 total (5, best, to 1, worst) | |||
| N | 29 | 29 | 58 |
| Mean | 2.60 | 2.61 | 2.60 |
| SD | 0.333 | 0.305 | 0.316 |
| Median | 2.525 | 2.5 | 2.5 |
| Range | 1.2 | 1.2 | 1.25 |
| Missing | 1 | 0 | 1 |
| SAQ-14 total (14, best, to 70, worst) | |||
| N | 29 | 29 | 58 |
| Mean | 32.8 | 37.8 | 35.3 |
| SD | 8.35 | 9.73 | 9.35 |
| Median | 34 | 37.5 | 36 |
| Range | 31 | 35 | 40 |
| Missing | 2 | 1 | 3 |
| PODCI: global function score | |||
| N | 29 | 29 | 58 |
| Mean | 89.6 | 90.0 | 89.8 |
| SD | 8.3 | 9.8 | 9.0 |
| Median | 91 | 92 | 91 |
| Range | 26 | 42 | 42 |
| Missing | 1 | 0 | 1 |
Table 28 presents treatment preferences of patients and parents by arm (this was collected before randomisation). This shows that a majority of patients (69%) were happy to receive either treatment but, of the remaining patients, most would have preferred a course of SSEs if they could have chosen (28%). A greater number of parents had a preference for their child to receive the course of SSEs (55%). There were no great differences in preferences between the arms.
| Preference of patients and parents | Treatment arm, n (%) | ||
|---|---|---|---|
| Treatment A | Treatment B | Total | |
| Patients | |||
| Patient would prefer physiotherapy advice and education session | 1 (3.7) | 1 (3.7) | 2 (3.7) |
| Patient would prefer a course of SSE | 9 (33.3) | 6 (22.2) | 15 (27.8) |
| Patient equally happy to receive either treatment | 17 (63.0) | 20 (74.1) | 37 (68.5) |
| Total | 27 (50) | 27 (50) | 54 (100) |
| Missing | 2 | 2 | 4 |
| Parents | |||
| Parent would prefer physiotherapy advice and education session | 1 (3.8) | 3 (11.1) | 4 (8) |
| Parent would prefer a course of SSE | 14 (53.8) | 15 (55.6) | 29 (55) |
| Parent equally happy to receive either treatment | 11 (42.3) | 9 (33.3) | 20 (37) |
| Total | 26 (49.1) | 27 (50.9) | 53 (100) |
| Missing | 3 | 2 | 5 |
Baseline health economic measures
A total of 57 adolescents completed the HUI as part of the baseline questionnaire, 28 in the usual-care arm of the feasibility study and 29 in the exercise programme. For this cohort HUI, EQ-5D and EQ-5D VAS scores are all approximately 0.8, or 80%, of the maximum score (Table 29) for both treatment arms.
| Baseline scores for health-related quality of life | Treatment A (n = 29 unless stated) | Treatment B (n = 29 unless stated) | Total |
|---|---|---|---|
| EQ-5D utility score | |||
| N | 28 | 29 | 57 |
| Mean | 0.799 | 0.776 | 0.787 |
| SD | 0.193 | 0.244 | 0.219 |
| Median | 0.796 | 0.796 | 0.796 |
| Range | 0.97 | 0.85 | 0.972 |
| Missing | 0 | 0 | 0 |
| EQ-5D VAS score | |||
| N | 28 | 29 | 57 |
| Mean | 79.54 | 75.83 | 77.65 |
| SD | 17.49 | 20.79 | 19.165 |
| Median | 84 | 84 | 85 |
| Range | 65 | 78 | 80 |
| Missing | 0 | 0 | 0 |
| HUI | |||
| HUI2_Canada, mean (SE) | 0.82 (0.23) | 0.88 (0.11) | 0.85 (0.02) |
| HUI2_UK, mean (SE) | 0.80 (0.16) | 0.79 (0.13) | 0.81 (0.02) |
| HUI3_Canada, mean (SE) | 0.79 (0.19) | 0.80 (0.19) | 0.80 (0.03) |
| Missing | 1 | 0 | 1 |
Follow-up data
Attrition
Up to 7 February 2014, 33 participants were due to be followed up at 6 months. Of these participants, nine were lost to follow-up (seven non-responders and two withdrawals) (Table 30). The response rate at Royal Orthopaedic Hospital was lower than at the other two active sites at the time of database freezing for this report. This low response rate was a temporary problem attributable to staffing issues and response has now improved to be in line with other sites. This provided data for 24 participants (closed case response rate = 73%). The response rates were similar between the two treatment arms (Table 31). The reasons for withdrawals are shown in Table 32.
| Response | Centre | Total | |||
|---|---|---|---|---|---|
| FRE | ROH | NOC | JCH | ||
| Questionnaire due, n | 8 | 11 | 14 | 0 (0) | 33 |
| Questionnaire received, n (%) | 8 (100) | 5 (45) | 11 (78) | 0 (0) | 24 (73) |
| Non-responder, n (%) | 0 (0) | 5 (45) | 2 (14) | 0 (0) | 7 (21) |
| Withdrawal, n (%) | 0 (0) | 1 (10) | 1 (8) | 0(0) | 2 (6) |
| Response | Treatment arm | Total | |
|---|---|---|---|
| Treatment A | Treatment B | ||
| Questionnaire due, n | 17 | 16 | 33 |
| Questionnaire received, n (%) | 12 (71) | 12 (75) | 24 (73) |
| Non-responder, n (%) | 4 (24) | 3 (19) | 7 (21) |
| Withdrawal, n (%) | 1 (5) | 1 (6) | 2 (6) |
| Treatment arm | Reason for withdrawal |
|---|---|
| Treatment A | No benefit from being in trial |
| Treatment B | Too much schoolwork, unable to commit to trial |
There were no major differences between those retained and lost to follow-up in terms of sex, age and key clinical characteristics (Table 33).
| Baseline characteristic | Responders | Non-responders |
|---|---|---|
| Age (years) | ||
| Mean (SD) | 13.9 (1.7) | 13.8 (1.5) |
| Median (range) | 14.0 (6) | 14 (4) |
| Sex, n (%) | ||
| Male | 10 (17) | 2 (22) |
| Female | 48 (83) | 7 (78) |
| Ethnic group, n (%) | ||
| White | 51 (88) | 8 (89) |
| Black or black British | 3 (5) | 1 (11) |
| Chinese | 1 (2) | 0 (0) |
| Other ethnic group | 2 (3) | 0 (0) |
| Missing | 1 (2) | 0 (0) |
| Cobb angle of largest curve (°) | ||
| Mean (SD) | 34.0 (10.0) | 32.9 (10.0) |
| Median (IQR) | 34.0 (14.0) | 34.0 (12.3) |
| Missing | 1 | 0 |
| Curve type, n (%) | ||
| Single | 30 (52) | 3 (33) |
| Double | 26 (45) | 5 (56) |
| Triple | 1 (2) | 0 (0) |
| Missing | 1 (2) | 1 (11) |
Missing data
Table 34 presents missing items or patients for key measurements or questionnaires.
| Missing items | Baseline (N = 29) | 6 months (N = 12) | ||
|---|---|---|---|---|
| Treatment A, n (%) | Treatment B, n (%) | Treatment A, n (%) | Treatment B, n (%) | |
| Age | 0 (0) | 0 (0) | N/A | N/A |
| Sex | 0 (0) | 0 (0) | N/A | N/A |
| Ethnicity | 1 (3) | 0 (0) | N/A | N/A |
| Brace wearing status | 0 (0) | 1 (3) | 0 (0) | 0 (0) |
| Risser classification | 11 (38) | 11 (38) | 6 (50) | 8 (66) |
| Cobb angle | 1 (3) | 0 (0) | 1 (8) | 1 (8) |
| Curve type | 1 (3) | 0 (0) | 1 (8) | 1 (8) |
| Area of curve | 25 (86) | 23 (79) | ||
| Curve balance: coronal | 2 (7) | 1 (3) | 3 (25) | 3 (25) |
| Curve balance: sagittal | 7 (24) | 9 (31) | 7 (58) | 6 (50) |
| SRS-22 function domain: 1–3 missing items (out of 22)a | 0 (0) | 0 (0) | 1 (8) | 0 (0) |
| SRS-22 function domain: > 3 missing items | 1 (3) | 0 (0) | 5 (42) | 4 (33) |
| SRS-22 pain domain: 1–3 missing items (out of 22) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| SRS-22 pain domain: > 3 missing items | 1 (3) | 0 (0) | 6 (50) | 4 (33) |
| SRS-22 self-image domain: 1–3 missing items (out of 22) | 0 (0) | 0 (0) | 1 (8) | 0 (0) |
| SRS-22 self-image domain: > 3 missing items | 1 (3) | 0 (0) | 5 (42) | 4 (33) |
| SRS-22 mental health domain: 1–3 missing items (out of 22) | 0 (0) | 0 (0) | 1 (8) | 0 (0) |
| SRS-22 mental health domain: > 3 missing items | 1 (3) | 0 (0) | 5 (42) | 4 (33) |
| SRS-22 satisfaction/dissatisfaction with management items: any missing items (/2) | 0 (0) | 2 (7) | 1 (8) | 0 (0) |
| SAQ: 1–2 items missing from appearance domain (questions 1–10)b | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| SAQ: > 2 items missing from appearance domain (questions 1–10) | 2 (7) | 0 (0) | 5 (42) | 4 (33) |
| SAQ: 1 item missing from expectations domain (questions 11–14) | 0 (0) | 1 (3) | 0 (0) | 0 (0) |
| SAQ: > 1 item missing from expectations domain (questions 11–14) | 1 (3) | 0 (0) | 5 (42) | 4 (33) |
| PODCI (case level) | 1 (3) | 0 (0) | 0 (0) | 0 (0) |
| EQ-5D (case level)c | 1 (3) | 0 (0) | 0 (0) | 0 (0) |
| HUI (case level)c | 1 (3) | 0 (0) | 0 (0) | 0 (0) |
Adverse events
Serious adverse events were classified through discussions with local principal investigators and the trial lead. As much information as possible was requested from the participant when a potential AE was noted, particularly with regards to the likelihood of the cause being trial treatment. No SAEs were deemed both unexpected and related to the trial involvement, and, therefore, no SAEs were communicated to the Multicentre Research Ethics Committee. The description, category and likelihood of relatedness of SAEs are summarised in Table 35.
| Treatment arm | SAE | Likelihood of relatedness to trial procedure |
|---|---|---|
| Treatment A | ||
| Treatment B |
|
|
Clinical outcomes
Clinical outcomes are presented in Table 36.
| Six-month curve and imaging data | Total (n = 24 unless stateda) |
|---|---|
| Cobb angle of largest curve (°) | |
| Mean (SD) | 35.4 (9.5) |
| Median (range) | 35 (34) |
| Missing | 2 |
| Curve type, n (%) | |
| Single | 16 (67) |
| Double | 6 (25) |
| Missing | 2 (8) |
| Area of curve, n (%) | |
| Thoracic | 10 (42) |
| Thoracolumbar | 7 (29) |
| Lumbar | 6 (25) |
| Missing | 1 (4) |
| Coronal balance (cm) | |
| Mean (SD) | 2.0 (1.3) |
| Median (range) | 2.1 (4.5) |
| Sagittal balance (cm) | |
| Mean (SD) | 3.0 (2.1) |
| Median (range) | 2.5 (7.8) |
| Risser grade (skeletal maturity), n (%) | |
| 0 | 0 (0) |
| 1 | 0 (0) |
| 2 | 1 (4) |
| 3 | 3 (13) |
| 4 | 2 (8) |
| 5 | 4 (17) |
| Missing | 14 (58) |
| ISIS scan, n (%) | |
| Present | 11 (46) |
| Sagittal curve, n | |
| Mean (SD) | 30.5 (11.2) |
| Median (IQR) | 32 (14) |
Six-month curve data including primary outcome
Cobb angle had changed very little between baseline and the 6-month follow-up (a 1° increase on average).
Six-month scores for secondary outcome measures
Secondary outcomes are presented in Table 37. SRS-22 scores increased by approximately 6 points in both groups combined, indicating a reduction in problems with function, pain, self-image, mental health and treatment satisfaction. The SAQ and the PODCI scores remained much the same. No changes in brace-wearing status were observed during the 6-month follow-up period, and only one participant was listed for surgery. No patient reported perceived harm as a result of the study treatments.
| Six-month scores for secondary outcomes | Total |
|---|---|
| SRS-22 total | |
| N | 24 |
| Mean | 8.78 |
| 95% CI | 6.01 to 11.5 |
| SD | 1.41 |
| Median | 8.80 |
| Range | 5.64 |
| Missing | 0 |
| SAQ-14 total | |
| N | 24 |
| Mean | 34.5 |
| 95% CI | 15.2 to 53.8 |
| SD | 9.86 |
| Median | 33.5 |
| Range | 38 |
| Missing | 0 |
| PODCI | |
| N | 24 |
| Mean | 90.0 |
| SD | 9.8 |
| Median | 94 |
| Range | 38 |
| Missing | 0 |
| Change to brace-wearing status, n | |
| Yes | 0 |
| Missing | 0 |
| Had surgery | |
| N (%) | 0 (0) |
| Put on waiting list for surgery | |
| N (%) | 1 |
| Participant perceived change in scoliosis, n (%) | |
| Vastly improved | 0 (0) |
| Much improved | 2 (8.33) |
| Slightly improved | 0 (0.0) |
| No change | 13 (54.2) |
| Slightly worsened | 6 (25.0) |
| Much worsened | 1 (4.17) |
| Vastly worsened | 0 (0.0) |
| Missing | 2 (8.33) |
| Participant perceived benefit or harm from the study treatments, n (%) | |
| Substantial benefit | 5 (20.8) |
| Moderate benefit | 6 (25) |
| No benefit or harm | 9 (37.5) |
| Moderate harm | 0 (0.0) |
| Substantial harm | 0 (0.0) |
| Missing | 4 (16.7) |
Participants’ rating of treatment satisfaction
A majority of participants were satisfied with the treatments provided as part of the ACTIvATeS pilot trial (16/24) (Table 38). Three participants reported being extremely or very dissatisfied, although these reports did not necessarily correspond to their reports of benefit from treatments (reporting either substantial or moderate benefit) or overall change (moderate to much improved).
| Treatment satisfaction | Total, n (%) |
|---|---|
| How satisfied were you with the advice or treatment that you received as part of the ACTIvATeS trial? | |
| Extremely dissatisfied | 1 (4.17) |
| Very dissatisfied | 2 (8.33) |
| Somewhat dissatisfied | 1 (4.17) |
| Neither satisfied nor dissatisfied | 4 (16.7) |
| Somewhat satisfied | 8 (33.3) |
| Very satisfied | 6 (25.0) |
| Extremely satisfied | 2 (8.33) |
| Missing | 0 (0.00) |
Allocation concealment
Research clinicians were asked to record at the 6-month follow-up whether or not they had been unblinded and the reasons for this. For 8 out of the 24 participants (33%) followed up at 6 months, the research clinicians reported being unblinded. Reasons for this included being told by parent (n = 3), told by participant (n = 2) and implied by participant (n = 2).
Health economics outcomes
Analysis of costs
The costs of consumables and training and computer programming for the exercise intervention are provided in Tables 39 and 40, respectively.
| Resource item | Unit | Cost per unit (£) | Quantity per participant | |
|---|---|---|---|---|
| Usual care | Exercise programme | |||
| Home exercise guide A4 | Item | 0.18 | 0 | 1 |
| Ball | Item | 16.50 | 0 | 1 |
| Balance mat | Item | 18 | 0 | 1 |
| Cardboard folder | Item | 1.85 | 1 | 1 |
| Resource item | Unit | Source |
|---|---|---|
| Training for exercise programme | ||
| Total physiotherapist hours spent on training, including computer training (hours) | 8 | Study records |
| Number of physiotherapists | 6 | Study records |
| Mean training time per physiotherapist (hours) | 1.33 | Study records |
| Physiotherapist cost per hour | 36 | PSSRU estimate |
| Patient attending at least one session | 16 | Study records |
| Total cost of training for trial (including computer training and exercise manual) | 288 | Study records |
| Cost per participant attending at least one session | 18 | Estimate |
| Treatment sessions | ||
| First session (minutes) | 60 | Estimate |
| Second session (minutes) | 30 | Estimate |
| Third session (minutes) | 30 | Estimate |
| Fourth session (minutes) | 30 | Estimate |
| Fifth session (minutes) | 30 | Estimate |
| Sixth session (minutes) | 30 | Estimate |
| Seventh session (minutes) | 30 | Estimate |
| Eighth session (minutes) | 30 | Estimate |
| Ninth session (minutes) | 30 | Estimate |
| Programming | ||
| Number of programmers | 1 | Study records |
| Programmer cost per hour (grade 6) (£) | 17.68 | University of Warwick records |
| Total cost of programming (including creation, maintenance and electronic diary) (£) | 5537.73 | Estimate |
| Cost per participant in exercise arm (£) | 190.96 | Estimate |
The costs of delivering each of the interventions are provided in Table 41.
| Type of cost | Usual care | Exercise programme |
|---|---|---|
| Therapist training (per patients attending at least one session) | £0.00 | £18 |
| Consumables | £1.85 | £36.53 |
| Electronic diaries | £0.00 | £190.96 |
| Cost of therapist time | ||
| Session 1 | £36 | £36 |
| Sessions 2–9 | £18 | £18 |
| Cost by number of sessions attended | ||
| No sessions | £0.00 | £0.00 |
| One session | £37.85 | £281.49 |
| Two sessions | £55.85 | £299.49 |
| Three sessions | – | £317.49 |
| Four sessions | – | £335.49 |
| Five sessions | – | £353.49 |
| Six sessions | – | £371.49 |
| Seven sessions | – | £389.49 |
| Eight sessions | – | £407.49 |
| Nine sessions | – | £425.49 |
In terms of broader resource consequences, diagnostic tests (Table 42) represented the least costly resource category in both study arms, whereas paediatric outpatient visits to outpatient departments represented the most costly resource category (£240.42 and £261.8 for the usual-care and exercise programme groups, respectively). Table 43 presents the direct non-medical costs borne by adolescents’ parents as captured by travel costs (taxi fares, bus fares, etc.), as well as valuations of days of work lost as a result of a child’s health, represented by income losses. There were no missing data for the resources use questions owing to the face-to-face nature of data collection.
| Resource category | Usual care: mean (SE)a | Exercise programme: mean (SE) |
|---|---|---|
| NHS and social care costs from randomisation to 6 months, £ | ||
| Community and social care | ||
| GP, surgery visit | 77.14 (9.93) | 60 (8.46) |
| GP, home visit | 0 | 0 |
| GP, telephone/e-mail | 27 (0) | 27 (0) |
| District nurse | 96 (48) | 96 (0) |
| Physiotherapist | 34 (0) | 139.78 (29.14) |
| Occupational therapist | 0 | 0 |
| Orthotist | 40.8 (6.8) | 51 (17) |
| Social worker | 171 (0) | 0 |
| Outpatient attendance | ||
| Orthopaedic/spinal clinic | 172.92 (16.43) | 169.81 (18.25) |
| Paediatrics department | 240.42 (53.43) | 261.8 (45.81) |
| Emergency department | 175.5 (58.5) | 117.0 (0) |
| Physiotherapist department | 77 (20.05) | 141.75 (37.17) |
| Orthotics/bracing department | 152.83 (21.83) | 183.4 (32.09) |
| Diagnostic tests | ||
| Radiographs | 5.58 (0.32) | 5.38 (0.27) |
| CT scan | 0 | 92 (0) |
| MRI scan | 145 (0) | 145 (0) |
| Blood tests | 3 (0) | 3 (0) |
| Medication | ||
| Medication | 9.35 (3.60) | 18.68 (13.18) |
| Resource | Usual care, mean (SE) | Exercise programme, mean (SE) |
|---|---|---|
| Non-NHS costs from randomisation to 6 months, £ | ||
| Total travel (parents) | 22.18 (4.06) | 36.12 (5.42) |
| Income loss | 74.54 (28.75) | 32.86 (19.27) |
At 6 months, the mean EQ-5D scores showed a slight improvement in participants’ HRQoL. At 6 months the mean HUI scores also show a slight improvement in participants’ quality of life (Table 44).
| Outcome | Total |
|---|---|
| EQ-5D score (today) | |
| N | 24 |
| Mean | 0.805 |
| SD | 0.177 |
| Median | 0.796 |
| Range | 0.772 |
| Missing | 0 |
| EQ-5D VAS score | |
| N | 24 |
| Mean | 76.25 |
| SD | 17.526 |
| Median | 80 |
| Range | 70 |
| Missing | 0 |
| HUI | |
| HUI2_Canada, mean (SE) | 0.82 (0.03) |
| HUI2_UK, mean (SE) | 0.83 (0.03) |
| HUI3_Canada, mean (SE) | 0.83 (0.05) |
| Missing | 1 |
Quality assurance
We conducted a quality assurance visit for each research clinician and physiotherapist at each of the four sites to ensure research and treatment protocols were being adhered to. All visits were graded as satisfactory.
Discussion
Recruitment
Our first aim was to determine the rate of recruitment and if pre-specified recruitment rate could be achieved. Once delays with governance approvals had been addressed, the recruitment rate exceeded the original target at three of the four sites and, overall, equated to almost two patients per centre per month on average. Recruiting to a trial that randomises patients to either a control group of advice and active monitoring or a programme of SSEs is feasible.
The 58 participants recruited to this feasibility study will undergo a 12-month follow-up as part of a Doctor of Philosophy (PhD) project carried out by one of the ACTIvATeS team. Should the modifications to the trial methods and interventions be minor, these participants could be retained for analysis as part of a main trial (we have ethical approval to follow them up annually should this be the case). The first participant was due to have their 12-month follow-up in February 2014 and, therefore, their data would expire in February 2015.
Randomisation and interventions
The second objective was to determine the acceptability of randomisation and the compliance to allocated treatment arm (60%). Randomisation was equally distributed between the arms, well balanced at each of the centres, and characteristics of participants in each arm were similar, indicating that the procedure worked well. All participants of the control intervention attended at least one session, indicating that the process of blinding the participants to allocation until the initial physiotherapy appointment worked well. Maintaining blinding for outcome assessors is always challenging when participants are unblinded. Implementing a formalised reminder system to participants prior to follow-up would reduce the incidence of this for a main study.
Adherence to attending treatment sessions and performing home exercises in the exercise programme arm of the study was more variable, although where physiotherapists had the resources to provide at least six individualised sessions a majority of patients attended. Some considerations should be given to whether or not adherence could be increased through small alterations in the format of the intervention; for example, participants may benefit from telephone follow-up contact. Data from the treatment logs and quality assurance visits suggest good adherence by the physiotherapists with the treatment protocols of each arm.
This study has been conducted at a time when there is potential for conservative clinical practice to change more rapidly than normal following the robust bracing study reported by Weinstein et al. in 2013. 14 This may result in an increase in the number of patients offered bracing as a conservative treatment, which may impact on the effect or the ability to estimate the effect of SSE interventions. There were no changes in bracing status for any of the participants who had completed follow-up at the time of freezing the database for purposes of reporting. Currently, we maintain the recommendation given prior to conducting the study that sensitivity analyses should be undertaken to investigate the effect of bracing on results of effectiveness of SSE.
Data collection
We aimed to determine data quality and completeness from the feasibility study. Data quality and completeness were generally very good, most likely as a result of the face-to-face data collection in research clinics. From the quality assurance visits, evidence suggested that the training in obtaining consent and data collection for research clinicians was sufficient to conduct the baseline and follow-up evaluation with accuracy and precision.
The one area where there was substantial incomplete data was for some of the radiography measures, particularly the Risser grading. Generating and implementing a clear imaging protocol would reduce this occurrence for a main study.
Estimating variability of sample for main trial sample size calculation
We aimed to estimate the SD of a sample recruited from a generalisable selection of secondary care settings. For this cohort of 58 patients, the baseline SD for the Cobb angle was 10°. This was lower than the SD we anticipated from the previous literature and stated in our original application of 15°, providing the possibility that the estimated sample size could be reduced. However, to measure our secondary outcomes and conduct an economic analysis it is likely that our original estimate of 400–500 participants is still accurate.
Feasibility of using the ISIS-2 system as outcome measure
We stated that we would explore the feasibility of using the ISIS-2 measurement system in the main trial owing to its advantage of reducing exposure to radiation. Discussing the validity of the measurements with clinical experts and the ISIS-2 creators highlighted that the measurements generated by the system are not directly analogous to the radiographic Cobb angle and hence clinicians and researchers do not place as much confidence or emphasis in this measure.
There were also difficulties with capturing these data; at times the system was not working or staff were unavailable to run the system. Furthermore, the four sites involved in the feasibility study constitute the majority of centres that have the ISIS-2 system currently in place. If this were to be used as an outcome measure for a main trial it would be necessary to purchase approximately 20 units, which would incur at least an additional £150,000.
We suggest that the ISIS-2 system is not worth investing in further for the purposes of a main study, but we would see it as a beneficial secondary outcome at sites where an ISIS-2 system is already in place and being used as part of routine clinical monitoring.
Health economics and the cost of the interventions
The current feasibility study has shown that is it possible to collect the data necessary for a full cost-effectiveness analysis of the ACTIvATeS exercise intervention compared with usual care. There were no practical issues in accessing information to collect and evaluate the elements of the exercise programme per se. Similarly, participant inputs on use of health and social care services and broader service use, and measurement of preference-based HRQoL outcomes, were accessible through the participant questionnaires. It is a requirement for both clinical effectiveness and cost-effectiveness analyses that follow-up be of sufficient length to capture skeletal maturity and potential avoidance of future surgery to evaluate potential offset costs of the exercise intervention.
Study limitations
Imprecision is inherent in data from small samples and, therefore, it is inappropriate for the data generated from this feasibility study to be used to carry out inferential statistical comparisons. This feasibility study was not conducted to evaluate efficacy or safety definitively, although we have proposed that it could be an indicator for safety. To date, there is no evidence of harm occurring as a result of the trial interventions.
We have delivered a report of a study evaluating the feasibility of conducting a definitive RCT of SSEs for idiopathic scoliosis. Some uncertainty remains in some of the conclusions, as only half of the cohort have completed the short-term follow-up. Data collection is ongoing. This is particularly important for assessing progression rates to surgery as set out in the original protocol.
Completing a feasibility study successfully is not a guarantee of main trial success. Despite having worked with some of the sites in previous research projects, considerable time and effort were required for the governance approval, set-up and maintenance of the four pilot sites and this may be more difficult with the research-naive and new sites that would be required for a large multicentre main trial.
Chapter 7 Qualitative study
Objective
To explore factors that influenced the acceptability and perception of the trial and interventions, issues influencing exercise adherence and appropriateness of the chosen outcome measurement to participants of the exercise programme.
Sampling
When they had completed their treatment programme, the physiotherapist invited participants of the exercise programme arm and their parents/carers to an interview with a qualitative researcher (FT) about their experience of the trial. If they were interested in being interviewed (as indicated on their initial consent form), the physiotherapist passed their contact details on to FT so that she could arrange a convenient time for an in-depth interview. We planned to try to interview at least one boy and his parents. The physiotherapists delivering the treatments were also invited to take part in an interview after they had delivered the exercise intervention for at least two participants.
Data collection
We developed an interview schedule in collaboration with relevant stakeholders (children, parents, health-care professionals). However, the schedule was used as a guide, and interviews remained semistructured to allow the flexibility to follow leads opened by participants. This is a useful approach in research where the aim is to explore personal meanings. 92,93 FT did not interview patients or their parents when they had just been informed of their diagnosis, as this might cause undue distress. Participants were given the choice to be interviewed at hospital or in their own home. They were encouraged to discuss any area they felt was relevant to their experience of the trial. Interviews were audio-recorded, transcribed and analysed prior to the completion of the next interview. Kirk94 emphasises the importance of making children feel an important part of the research, talking to and interviewing children with respect and empathy, ensuring that interviewers are aware of non-verbal cues that children may use to indicate that they wish to terminate an interview, and inviting children to comment on their transcript. We adopted this guidance.
Analysis
The study used the methods of interpretive phenomenological analysis. 95 Analyses of qualitative data for interpretive phenomenological analysis involve coding the narrative data and then grouping coded data into conceptual categories or themes with shared meanings. This is done through an iterative process of constant comparison which allows the researcher to interpret similarities and differences throughout the narrative data, codes and themes. FT used NVivo 9 Software for Qualitative Analysis (QSR International, Warrington, UK) to assist coding and organising of the data. FT coded the data and developed conceptual categories, which she presented to three members of the research team (SL, EW and MW) for discussion. This discussion did not aim to reach consensus regarding final categories but to introduce other perspectives and thus contribute to the collaborative rigour of the study. 96 We indicate whether or not the words are spoken by a patient, parent or physiotherapist. For ethical reasons, owing to the small size of the sample, we have chosen not to identify individual participants’ quotations in order to retain their anonymity.
Results
Participants
Sixteen people involved in the randomised feasibility trial, from the three original pilot sites (Oxford, Birmingham and Bristol), were interviewed by FT:
-
Six girls (age range 10–16 years), three of whom had significant pain before the trial (one had no improvement in pain). Table 45 presents baseline characteristics for qualitative and overall cohorts. The qualitative study cohort was of similar age. All were female, all were white, and all were similar in terms of sexual maturity but at lower risk of curve progression (from Risser grading, although the large number of missing data introduce considerable uncertainty) and with smaller curves. They had similar scores on the SRS-22 questionnaire (disability) and SAQ (self-image).
-
Six parents; two interviews were with mothers on their own and two interviews were with mother and father together.
-
Four physiotherapists (two experienced in providing the exercise intervention for patients with AIS and two with more limited experience).
| Baseline characteristics | Qualitative study cohort | Pilot RCT cohort |
|---|---|---|
| Demographics | ||
| Age (years) | ||
| Mean (SD) | 14.3 (2.25) | 13.9 (1.71) |
| Median (range) | 15.0 (6) | 14.0 (6) |
| Sex, n (%) | ||
| Male | 0 (0) | 10 (17) |
| Female | 6 (100) | 48 (83) |
| Ethnic group, n (%) | ||
| Mixed | 0 (0) | 0 (0) |
| White | 6 (100) | 51 (87.9) |
| Indian | 0 (0) | 0 (0) |
| Pakistani | 0 (0) | 0 (0) |
| Bangladeshi | 0 (0) | 0 (0) |
| Black or black British | 0 (0) | 3 (5.17) |
| Chinese | 0 (0) | 1 (1.72) |
| Other ethnic group | 0 (0) | 2 (3.45) |
| Missing | 0 (0) | 1 (1.72) |
| Age diagnosed with scoliosis (years) | ||
| Mean (SD) | 12.8 (3.06) | 11.9 (3.32) |
| Median (range) | 14 (8) | 12 (15) |
| Missing | 0 | 1 |
| Pubescence status | ||
| Onset of puberty, n (%) | ||
| Yes | 5 (83) | 46 (79) |
| No | 1 (17) | 10 (17) |
| Missing | 0 (0) | 2 (4) |
| Skeletal maturity | ||
| Risser classification, n (%) | ||
| 0 | 0 (0) | 7 (12) |
| 1 | 0 (0) | 3 (5) |
| 2 | 0 (0) | 2 (3) |
| 3 | 1 (17) | 7 (12) |
| 4 | 1 (17) | 11 (19) |
| 5 | 0 (0) | 6 (10) |
| Missing | 4 (68) | 22 (38) |
| Treatments received | ||
| Currently wearing a brace, n (%) | ||
| Yes | 1 (17) | 10 (17) |
| No | 5 (83) | 46 (79) |
| Missing | 0 (0) | 2 (3) |
| Curve characteristics | ||
| Cobb angle of largest curve (º) | ||
| Mean (SD) | 26.2 (11.8) | 34.0 (10.0) |
| Median (range) | 28 (34) | 34.0 (14.0) |
| Missing | 0 | 1 |
| Curve type, n (%) | ||
| Single | 4 (66.7) | 30 (52) |
| Double | 2 (33.3) | 26 (45) |
| Triple | 0 (0) | 1 (2) |
| Missing | 0 (0) | 1 (2) |
| Participant-reported measures | ||
| SRS-22 total (5, best, to 1, worst) | ||
| N | 6 | 58 |
| Mean | 2.58 | 2.60 |
| SD | 0.375 | 0.316 |
| Median | 2.45 | 2.5 |
| Range | 1 | 1.25 |
| Missing | 0 | 1 |
| SAQ-14 total (14, best, to 70, worst) | ||
| N | 6 | 58 |
| Mean | 33.7 | 35.3 |
| SD | 9.46 | 9.35 |
| Median | 35.5 | 36 |
| Range | 23 | 40 |
| Missing | 0 | 3 |
Interview duration ranged from 35 minutes to 2 hours.
This section reports findings from the nested qualitative study relevant to a future trial. Findings are organised into:
-
outcomes
-
being in the ACTIvATeS trial
-
trial components
-
additional themes impacting on a future trial (experience of health care, specific worries, unmet information needs).
Outcomes
This section relates to trial outcomes:
-
Motivations for being in the trial (desired outcomes).
-
What are the important outcomes from AIS interventions (relevant outcomes)?
-
Positive outcomes from the trial (actual outcomes).
Families’ motivations for being in the trial
The physiotherapists describe families’ motivations for participating in the trial as an opportunity to access treatment that was not usually available in order to:
-
control the curve and, thus, prevent surgery (one experienced physiotherapist)
-
improve cosmetic appearance
-
control pain.
Physiotherapists who did not routinely provide an exercise programme for AIS did not know what the outcomes would be, and, at the outset, were somewhat sceptical of positive outcomes. There was a sense that preventing curve progression, rather than reversing ‘the curve’, was the aim of an intervention, with a view to preventing future surgery (in line with trial aims).
What did you get a sense that their main aim of being involved?
Get rid of the scoliosis, but of course they can’t do that . . . certainly to keep it under control; for it not to get worse certainly . . . our treatment is always to control things, it can’t be to get rid of what is there because it’s a structure. It’s to control it and to control pain.
However, a cosmetic improvement (modifying posture, rather than correcting the curve) was described as an important and modifiable outcome by the physiotherapists.
Families’ motivations for being in the trial were broader than those indicated by the physiotherapists and included such reasons as, for example, it is better to do something than nothing, learning to manage a long-term chronic condition, and helping others with scoliosis in the future. The children’s and parents’ motivations are listed in Table 46. Only one girl described her motivation as being ‘make me straighter’.
| Parents’ motivations | Children’s motivations |
|---|---|
| At least we are doing something/might as well give it a go | Proactive approach: more than nothing |
| To help others | To help others |
| Will get good advice | Learn about scoliosis |
| It will be interesting | Interested and excited |
| It must do some good or they would not do it | Be monitored more |
| Help posture and how she looksa | Make me straighter (one girl) |
| Learning to manage for the long term | Slow down curvea |
| To get rid of paina |
What are the important outcomes from adolescent idiopathic scoliosis interventions?
Physiotherapists describe important outcomes as:
-
prevention of curve getting worse
-
positive habitual change in curve
-
reduced pain
-
improved body image
-
better appearance
-
fitness
-
prevention of physical limitations as a result of AIS
-
avoidance of or delay in surgery (until a time that is not crucial to education)
-
patient and parent satisfaction
-
gaining correct knowledge of AIS
-
feeling better/how they feel about themselves
-
happiness with new posture
-
have you gained from coming to see a physiotherapist (global assessment of gain made by the child or family)?
Physiotherapists recognised the complexity of measuring outcomes for AIS interventions; ‘It’s just hard to capture what you actually want to capture’. They recognised that outcome measurement should focus subjectively on what the patient wants to achieve.
I think if you can stop the curve getting worse and improve self-image, self-confidence, pain and core strength I think that’s all positive. It’s like your day-to-day function and almost psychological kind of things.
Physiotherapist
However, they also realised that there was a need to pay important attention to the ‘mechanistic’ (or ‘bony’) outcomes as well as the subjective ones. For example, even if the individual’s self-esteem and confidence has improved as a result of intervention, it would not be considered a good outcome if the curve had progressed and the child went on to have surgery.
What outcomes are you looking at actually being able to achieve?
I think parent and patient satisfaction and them achieving their goals, I’m pretty confident that’s going to be quite high. I really don’t know what to expect with the actual outcome on the scoliosis . . . it should be more focused on what the patient wants to achieve but I think with scoliosis if [the intervention] is not working and [the curve] is progressing then it’s slightly different isn’t it. They might say I’m not bothered by [the curve] but the reality might be that the curve is progressing and it’s getting worse and it’s not a good outcome. It’s a tricky one.
With a patient a good outcome for them is to feel better and for them to be happy with their new posture, or whatever their goal was. From a surgeon’s point of view the outcome is looking at the actual Cobb angles and X-rays and position of the spine so I think it’s both of those are important.
Physiotherapists also recognised the difficulty of measuring relevant outcomes, for example, improvements in core strength or habitual change in curve.
The ability to hold themselves let’s say in a more aligned way unthinkingly . . . that is the crux of it . . . the proof of it, is that it becomes a positive habitual change. Conscious change is irrelevant so focussed attention has to convert to an unconscious behaviour . . . to the extent where it convinces us that their body position is better physically and its sustained unconsciously we may have confidence when they walk away from the department they actually do that in real life.
Physiotherapist
Physiotherapists also discussed the need to be able to describe and record curve type as a potential confounding factor. In short, some curve types might be less responsive to treatment depending on:
-
flexibility
-
amenability to conscious correction
-
balanced or single curve
-
curve magnitude.
Important outcomes described by children and their parents are shown in Table 47. Both children and their parents described how the intervention would not necessarily change the curve itself; however, stopping it getting worse was important.
Did you think doing the exercises would have any impact on the scoliosis?
No, not on her bones, on the degrees or anything on her spine. I knew it would be purely muscular and posture . . . I think knowing that it couldn’t cure (is the wrong word) but help her but might help because she did used to come home and say my back is very painful, and she can’t swallow tablets so that is a nightmare, so I thought at least if it helps that part it is a positive.
| Parent: important outcomes | Child: important outcomes |
|---|---|
| Pain reduction | Pain reduction |
| Stop it getting worse | Stop it getting worse |
| Aesthetic improvement (not ‘ bony bits’) | Am I happy with the way I look? |
| Physiotherapist’s subjective assessment of improvement in posture | To improve posture (e.g. contours) |
| Personal goal achievement | To get spine straighter (for one child) |
| Learning how to help themselves |
Positive outcomes from trial
Physiotherapists describe the following positive outcome for patients following intervention:
-
reduced pain (two out of three of those with pain)
-
improved posture
-
sense of confidence
-
a feeling of control from taking a positive rather than passive approach to AIS.
Physiotherapists describe the sense of control that the intervention brings. The girls were now doing something positive to help themselves, rather than ‘waiting’ passively for what may or may not occur. This gave the girls a sense of responsibility and control over their condition. Physiotherapists also described improvements in posture and the effects of this irrespective of possible improvement in the curve. This could give a sense of confidence for the future.
She was just really, really pleased with it and she actually went out in a vest top last week. For me that was really lovely.
Physiotherapist
Physiotherapists also described how the intervention provided a ‘tool for the bottom drawer’; in other words, a useful tool that the girls may not use now but that will be available if needed in the future.
The positive outcomes from taking part in the trial described by children and their parents are shown in Table 48.
| Parent: positive outcomes | Child: positive outcomes |
|---|---|
| ‘A growth point for my child’ (described below) | Becoming more informed |
| Helped pain | Helps pain |
| Posture | Effect on posture and awareness of posture |
| Improved curve (not assessed on radiograph) | Improved curve (not assessed on radiograph) |
| Tool for future |
Two of the three girls with pain noticed a marked improvement in pain, suggesting another modifiable factor.
If I stop doing the exercises then I am in a lot more pain and then I will start doing them again. It becomes easier. The exercises themselves they don’t really get any easier they just, when I am not doing them I am getting a lot of pain.
Girl whose pain levels had not improved significantly
I certainly noticed a big improvement; that she doesn’t get the pain any more. She was complaining about it every day and I’ve really noticed she hasn’t mentioned it any more so it’s obviously done some good.
Mother
Awareness of posture and the ability to change posture was marked as an important positive outcome by parents and children, thus indicating a potential modifiable outcome that is important to families.
I think I have a much better understanding of my curve and how it affects me . . . I didn’t really realise how I kind of stood . . . before I had the physio it was more like one of my hips jutted out more. I think the whole giving me more awareness; we had quite a lot of work which taught me a new position to stand in and looking in the mirror and seeing my curve and how it affected my body. I thought that was helpful because now I just stand in that position, like normally, which is a big improvement.
Girl
She knows that if she doesn’t want her shoulder to be lower than the other, she doesn’t want her hip to stick out as far that she can correct that herself slightly. She had her prom earlier this year and she was having photographs taken for that, so she would have corrected herself so that her shoulders were even for the photos.
Mother
Parents described the intervention as providing a tool for the future, specifically to help to control pain, to enable my child to adjust her posture and to encourage her to become more physically active in order to achieve positive health as an adult.
I think before, if you’ve never been into a gym you’re scared about gym stuff aren’t you, but now she’s done a few things in the gym and she knows what she’s doing . . . and actually she doesn’t have to have somebody showing her what to do.
Mother
The girls had been given the choice to be involved in the trials and this was described as marking a ‘growth point’ or ‘educational experience’ for the children, giving them a sense of control over a chronic condition:
Being involved has been a ‘growth point’ for her.
In what way do you mean?
First it has made a connection with something that she has learnt in school about research methods. Also she has seen herself in a different role; she has got satisfaction from feeling in a small way that she has contributed to something that will be helpful . . . You could call it an educational experience. I am not saying that I would want my daughters to have this; if I could change it I would, but ‘how have I personally coped with this?’ – When living, what you make of things and the choices you make in relation to your situation shape you. Anyone with an illness, probably the last thing you want is to get involved in a project; why would you want any additional workload? But your choices shape what you become. It has been an education.
One mother suggested that it would be useful to include information on healthy eating and living in the study information pack in order to focus on the ‘normal’ adolescent rather than on controlling an illness.
Being in the trial
This section focuses on relevant experiences of being in the trial for physiotherapist, parent and child.
Physiotherapists’ experiences
Randomising to non-intervention group
Physiotherapists described the issues for randomising the non-intervention group. At sites where exercise intervention had not been routinely used, physiotherapists did not have concerns about allocating participants to the non-intervention group. This was because the patients would still receive a level of treatment that was above routine care, so the physiotherapists perceived no conflict related to duty of care.
We’ve never provided an exercise alternative for the milder scoliosis. From our point of view, even when they come in and they get all that advice and an information pack, that is still more than they would get normally anyway so we can still see that as a positive.
Physiotherapist
In addition, these physiotherapists did not have an intuitive sense about who would do particularly well from intervention and, thus, did not face the issue of allocating patients into an arm that they considered ‘inappropriate’ (‘that’s the whole point of the trial’). However, they did describe the issue of having to deal with the disappointment of families that were allocated to the non-intervention arm, who had ‘pinned their hopes’ on exercise. They described how this disappointment might have an impact on trial outcomes (i.e. inflate the positive outcomes for the intervention group). One family was so unhappy about it that they went back to the consultant in order to be referred for physiotherapy after the trial.
It sort of puts a dampener on the whole session really because they then don’t really want to be here because they wanted something different. A lot of them know a lot of information without telling them anyway. They don’t necessarily feel like they’ve gained a lot from driving an hour and a half to get here to do that.
Physiotherapist
It depends how it’s marketed. If it was still marketed as we’ve got a lot of information, we’ve got a lot of education we could give to you which could be beneficial, then yes they might [turn up] but the risk is that obviously we won’t. If they wanted the exercise, then yes, they might not turn up.
Physiotherapist
Physiotherapists suggest that it would be useful for families to know which group they had been allocated to before they come back, even though this might mean that some families choose not to come back.
Physiotherapists suggested that it would be helpful for families to know before they arrived for the advice session. Perhaps produce a DVD with the relevant advice and information as an option if they do not want to come in once they have been allocated to the non-intervention group.
One physiotherapist, who routinely provided an exercise intervention for AIS, highlights ‘duty of care’ as a potential issue: ‘In short if the health professional thinks that the exercise intervention would benefit a particular patient, they have a duty of care to provide it; the person is a patient prior to being a research subjects’. This issue focuses on clinical equipoise.
If a consultant’s patient is coming into a trial in the context of a referral to physiotherapy [as a patient], the physiotherapist has a duty of care . . . If I had someone presented to me in the advice group, and I said that in my opinion that patient has a right to [and will benefit from] physiotherapy input . . . that patient should be pulled out of the trial.
Physiotherapist
The need for a flexible exercise protocol
Physiotherapists described the challenges of:
-
organising appointments to fit around school time
-
fitting the trial and its administration around their routine and ongoing working day.
All physiotherapists had made great efforts ‘above and beyond the call of duty’ to make the trial work and they discussed the need to consider this additional workload when planning the main trial.
We all work pretty flexible hours . . . we’re tending to do them on days when they’re requesting them at 4 o’clock or 4.30pm. We just see them at the end of our normal working day and that’s how we’ve been fitting them in.
Physiotherapist
Physiotherapists described how these constraints of fitting in appointments made a flexible trial protocol necessary; school and other commitments could make it difficult for families to attend a lot of appointments. Although physiotherapists understood the importance of a fixed exercise protocol for trial rigour, flexibility of protocol was also linked to the need for professional autonomy.
I don’t think you can look at trials in quite the same way as you can look at [routine] treatment sessions. I wouldn’t normally see the patients as frequently as I have seen them for the trial . . . a lot of them were happy to come [for the trial] but actually it was a distance for them . . . [they might not] have as much flexibility . . . if they weren’t trying to comply with what they felt was expected from them from the trial.
Physiotherapist
Do we need a specialist to provide the intervention?
Delivering the intervention was seen as a skill that would be transferable to non-specialists.
There is nothing I do that I couldn’t share and transpose to any of the physiotherapist that I work with here. It’s not rocket science, it’s common sense, it’s just being able to relate to people really.
Physiotherapist
However, another consideration raised by the physiotherapists was the level of specialism necessary to provide a successful trial intervention and the potential impact of non-specialism on trial outcomes. For example, families’ expectations of seeing a therapist with expertise in scoliosis within a specialist service might have an impact.
It can be challenging because their expectation has been cranked up . . . whereas to be referred to a standard though competent local centre may have a different impact, and how will those impacts play out in terms of the outcomes?
Physiotherapist
There are also the additional benefits of working closely with surgeons who make daily decisions about the need for surgical intervention.
Training needs for non-specialist physiotherapists
Physiotherapists new to the exercise intervention described it as a ‘bit daunting at first’ and expressed the need for skills development. They described the following transferable skills that they have learnt from being part of the trial:
-
learning a new body of exercises for posture correction
-
learning exercises that are transferable to other conditions
-
learning new transferable techniques (e.g. mirrors for posture correction)
-
learning how to recognise accurately spinal curves
-
becoming more aware of people’s feelings and more able to discuss this
-
learning about health research: ‘its common sense not a mystery’.
Physiotherapists also described the following issues related to training needs for the trial.
Realising that ‘the patient is the family’
Physiotherapists describe AIS as something that affects the entire family, and, thus, the need to develop skills that include the whole family is important. For example, the ability to discuss a person’s feelings is crucial.
I would be disappointed if my child was seeing a physiotherapist who . . . isn’t thinking about my child’s life in term of education and impacts on how my child feels about themselves. I’d have an expectation of an expert physiotherapist to be incorporating that in their thinking.
Physiotherapist
No matter how many families you meet you always learn something from each family . . . whatever family you always take something away from the family. And you know it’s a great privilege to be allowed to be in contact with somebody’s family because they do obviously open up to you to tell you things . . . You are always learning something that may apply to another family.
Physiotherapist
Needing to provide accurate information about adolescent idiopathic scoliosis
Physiotherapists describe the need to provide correct information to families, thus highlighting a training need for the less specialist physiotherapist.
If you haven’t got experience it’s going to be knowing what sort of questions to expect from parents and the children about scoliosis, so it’s just about having some background knowledge really about the condition because people do want to know.
Physiotherapist
It’s the information I think because that is always the key. And if someone comes that you recognise [that they have received] information that is incorrect that is the most important thing . . . I think a lot of people want to know how likely the scoliosis is likely to progress and that sort of thing and at what stage would they then be looking at other treatment options so like bracing and surgery and that kind of thing. I think that’s one of the most common questions I get asked, that sort of thing, the progression.
Physiotherapist
Needing to bounce ideas around
Physiotherapists describe the need to ‘bounce ideas off’ someone else (preferably someone with more experience) as an important way of learning, as well as usefulness of being watched and discussing ideas. They discuss a system of mentoring as a way of learning, particularly for curve assessment.
[Physiotherapists] need to have access to somebody if they have got problems, if they have got questions . . . for people that are less familiar there may need to be some sort of monitoring; they may need to be seen every so often just so that, I suppose like a mentoring . . . I think there needs to be a mentoring system, let’s put it like that, not a monitoring system.
Physiotherapist
Physiotherapists described it as useful to watch, discuss and learn from working with each other.
Can you think of any particular example of a patient that you discussed?
I think the one that I just wanted to chat about with the others was the first patient I had in the trial (on the exercise group); when I was coming towards the end of it – it was ‘where’s the end point?’ . . . so I had a good chat with the others about what they would have done with this patient, and what level they were at . . . to just try and decide really when you were at that end point.
Getting stuck in and learning on the job
Although physiotherapists described the pre-trial demonstrations conducted on ‘real patients’ as extremely important, they highlight that, ultimately, the best way to learn is to do it ‘for real’ and discuss it with others (‘this is how physiotherapists learn’):
It probably would have been beneficial to see a few more but I think some of it you just have to get stuck in and go for it because that’s how you get used to it.
Physiotherapist
I think that the training needs to be as much patient contact as possible because I think that’s how most physios tend to learn best, it’s hands-on and doing things and getting a chance to do that, and maybe then do it on your own, and then discuss it with other people who have got more experience of it . . . in my experience that’s how a lot of physios tend to learn.
Physiotherapist
What comes after the feasibility study?
Finally, physiotherapists describe an interest in knowing the outcomes of the feasibility study and where it is going next. They also describe the potential impact on AIS service provision for the host physiotherapy service (irrespective of an ongoing trial). In short, because physiotherapists have learnt skills and developed an interest for this additional service, this is likely to boost referrals and thus have a possible cost implication for the host NHS trust.
Families’ experiences
It has been a positive experience
The children and their parents described positive experiences of being in the trial and said that they would not change the trial in any particular ways. They described a positive relationship with the physiotherapists that was both interesting and fun. Physiotherapists and trial staff seemed genuinely interested in the families and treated the child as the central focus of care.
Two specific points were highlighted:
-
the importance of the appropriate timing for recruitment (i.e. being given time to think, particularly if you have just been given your diagnosis)
-
families wanted to know the outcomes of the feasibility study, perhaps demonstrating a lack of understanding of feasibility study objectives.
One father suggested that it would be useful to let participant families know about the positive experiences of participating in the trial by using the authentic words of participants as a way of boosting recruitment:
I am just thinking about perhaps some sort of . . . recommendations from people who have been part of it and gone, ‘I thought this and actually it was all right and this happened and that was fine’ you know to get some of the people who have been part of it to give a little comment.
Father
Although this highlights the possible added value for families of participating in a trial, there may be ethical issues to consider surrounding the potential for coercion if we were to use this type of information in trial information letters.
What if I had been in the non-trial group?
When asked what they would have done if they had been allocated to the non-exercise group, children and parents described how they would have been extremely disappointed (mother: she ‘would have been gutted’). Although some participants realised the need for a non-intervention group, they could not see the point of being in that group; exercises at least ‘give you a fighting chance’ even if you are not certain about the real outcomes.
Parents describe the following options that they would have taken if their child had been allocated to the non-exercise group:
-
would have tried other treatments (yoga, Pilates, spinal touch)
-
would have requested child to be put forward for the main trial when it was launched
-
would have sought second opinion (not because we doubted opinion but because we wanted to do something) – ‘if you sit back and do nothing then you don’t know’.
I would be a bit, I wouldn’t say like annoyed but I would be a bit disappointed as I would prefer to be in that one, you have more of a chance of something changing. I wouldn’t have minded too much if I could get this.
Girl
Trying to fit treatment in around school
Both children and their parents describe the importance and difficulty of fitting the appointments around school, as well as a feeling that health reception staff did not fully understand the issue.
’Cos you had a couple of strange conversations and you felt sometimes that the people on the end of the phone couldn’t quite understand why you needed to come in after school.
Girl
That is a bit stiff if you have got an appointment . . . and you do have to miss school, but you were doing your GCSEs [General Certificate of Secondary Education] . . . because you were part of the research stuff and in a more voluntary capacity . . . and I think that that message hadn’t got through [to hospital staff].
Mother
However, although families described the impact on their time in terms of travel, time off work and school, they were still prepared to do this in order to see a ‘specialist’.
Trial components
This section describes physiotherapists’, children’s and parents’ perceptions of the outcome measurement (questionnaire and physical testing) and trial components (diary, study information pack, goal-setting, patient forum, exercises, contracts).
Questionnaires and physical tests
Parents described the questionnaire assessment as arduous and a bit repetitive but understood that it was necessary for the trial (mother: ‘you need to check you are solid across the board’). Parents described physical tests as a bit of a mystery, although interesting, and would have liked a short explanation of their purpose. However, they realised that knowing their purpose might have some effect on the trial results.
For one child who wore a brace it was difficult to answer questions about body image as they were uncertain whether it referred to the effect of AIS or the brace.
For one child who wore a brace it was difficult to answer questions about body image as they were uncertain whether it referred to the effect of AIS or the brace.
None of the children objected to filling in the questionnaires, despite them ‘going on a bit’. One girl described herself as ‘freaked out’ by the pictures illustrating more severe curve types. Children described a keen interest in the physical tests and generally viewed them as a positive experience.
Online diary
Physiotherapists described the usefulness of being able to upload exercises onto the online diary. Although they might not find the time to check the exercises daily, they saw it as an incentive to adherence. One physiotherapist questioned the usefulness of the diary in terms of adherence, as children were able to tick retrospectively to indicate that they had done the exercises. One of the experienced physiotherapists described the limitations of using the set of available exercises and need to write more detailed individualised descriptions about each exercise.
Although parents thought that it was useful for the physiotherapist to check on their child’s exercise adherence, they also thought that the diary could be a bit of a ‘faff’ in terms of ease of computer access. Some found that they had installed an incompatible browser or that the computer was being used by someone else. A paper copy of the exercises was, therefore, still invaluable for remembering the exercises and recording adherence. Children found the online diary useful as a reminder, particularly the videos. They confirmed that a paper copy could be a useful backup. Children suggested that YouTube (www.youtube.com, LLC, San Bruno, CA, USA) would make access easier.
Physiotherapists and parents found it useful to video exercises on the child’s or parent’s mobile telephone.
Information pack
Parents described the information pack as a comprehensive resource for information on scoliosis. In addition to the information included in the information pack, children and parents described how they would like to find out about other people’s experiences of having scoliosis and the options available, thus highlighting a potential unmet information need. They described how they had found it difficult to find this type of experiential knowledge (see additional themes in Unmet information needs).
Goal-setting
Physiotherapists describe the challenges of setting goals for children who are fit and well and who have no pain or physical limitations. The child may describe their aim as simply being ‘stopping it getting worse’:
. . . They’re not particularly bothered about their back, they’re not in any pain, and you tend to end up finding they say they want to stop it getting worse.
Physiotherapist
Although goals were described as a useful way of giving children a sense of control, given that children with AIS are generally not restricted functionally, physiotherapists described the challenge of setting goals:
I think as physios we’re used to people coming in and pain being their primary problem and this is completely different. It’s nice in that way . . . to be treating someone who . . . you’re trying to make them better
Is that something that you’ve had to learn about for this trial?
I think more so for this trial, yes. Generally with the day-to-day patients that we normally see they’ve got a problem that you’re treating them for; they’ve got pain, they’ve got a decreased range of movement, all those kinds of things, so their goals are a little bit different, and in a lot of ways easier to set, rather than a patient who has come in and is functioning quite happily.
Parents and children did not remember much about goal-setting. Children described possible goals as being getting rid of pain, improving posture and preventing the curve getting worse. One child described goal-setting as useful because ‘I could see what I needed to focus on rather than just that I have bad back pain’.
Patient forum
Physiotherapists and parents felt that the forum was not utilised by children because it was monitored by adults. Although parents felt it was a good idea, even when the child did use it, they did not continue to: ‘it felt like it was the adults rather than the kids chatting to each other’. Families also mentioned that there were alternative sites available for ‘social networking’ about AIS (e.g. Instagram; see https://instagram.com), and that technical difficulties could be a disincentive when other more accessible options were available.
Although children agreed that talking to others with AIS would be useful, they did not use the forum. They also described how it felt more like an interaction with adults. Although children described that finding out about other people’s experiences of AIS was useful, they accessed other social networking sites for this.
I guess it would be kind of interesting, also a good thing to be able to find out if you have something in common for people with a similar thing. I don’t know many people with the same condition, sometimes I feel a bit lonely.
Girl
When I was looking originally it seemed to be that it was all the physios and the research staff and everything and it wasn’t so much the kids . . . and I think my daughter went on once and said she requested some information but she got replies from the adults and I think once it was just the adults she lost interest.
Mother
One child suggested that it would be good to get a text or e-mail if someone had posted something on the forum to flag up a new message.
I think it was quite difficult to use it because you never knew if anyone had posted anything on it. So you have to go on and check it and obviously people aren’t really going to do that, I think it would be useful if there was an option of like if someone posted something and you get an e-mail about it.
Girl
Exercises
Physiotherapists describe the complexity of the posture correction exercises and felt that the child needed to grasp the ‘concept’ in order to do the exercises correctly. They felt that this might make the exercises inaccessible to some children. They also described the need for motivation and commitment to do the exercises and felt that this motivation might waver if there was not the incentive of being part of a trial.
I think it is quite an in-depth programme of exercises so I think they do need a certain level of understanding . . . It happens with any exercise that you give out, especially if you are trying to train someone’s core strength. It’s quite technical with anyone . . . and some people just, for whatever reason, find it harder than others . . . Some of them will just pick it up very naturally and very easily and others just struggle with it a little bit more.
Physiotherapist
You don’t need to be a ‘straight A’. . . some children seem to have, it’s more about a developing sense of self-awareness. . . I think it’s more a problem around self-attention or self-awareness, than actually any kind of academic or even emotional intelligence.
Physiotherapist
In contrast, parents described how the children just got on with the exercises and that some seemed to enjoy them.
My daughter will come bounding through the door and she can’t wait to show [her father] the new set of exercises, she absolutely can’t wait and he’s very positive about it. And 9 times out of 10 he does the whole ball-throwing exercise with her because they get a lot out of that.
Mother
Children sometimes needed a gentle reminder to do their exercises or even another pair of hands. One mother described how there was nowhere for her daughter to do exercises privately and this made it difficult. The children described the need to adjust their busy school routine to fit in the exercises, and noted that ‘someone checking up on me’ (parent or physiotherapist) was an incentive to keep going. The children did not describe the exercises as difficult to grasp.
Exercises and stretches were described as tools for the future. Some children and parents said that after the trial they were likely to carry on exercises on an ‘as-necessary’ basis; for example, to help when the back is painful.
Text reminders to exercise would be useful.
Contracts
Physiotherapists described how they were not sure if signing a contract made any difference to adherence. In some patients, this might make children and their parents take it more seriously, and in other patients it would make no difference. The mother of the youngest girl (aged 10 years) said that her daughter enjoyed the ‘grown-up’ aspect of signing a contract and that it had made her take it very seriously. Children did not remember the details of signing contracts, although agreed it might be useful for making people think about what was involved.
Additional themes impacting on success of interventions for adolescent idiopathic scoliosis
The findings highlighted several areas with a potential impact on the success of interventions for AIS and on recruitment into a larger trial:
-
experience of health-care services
-
specific concerns related to AIS
-
information needs and accessing information about AIS.
Experience of health-care services
Children and their parents describe mostly positive and friendly experiences of health care. In particular, they appreciated the child being the focus of consultation, rather than the health-care professional directing attention towards the parent. For some parents, the diagnosis of AIS came as a relief (e.g. it is not a tumour).
For parents, any negative experiences of health care focused around a ‘cursory attitude’ of a specialist (although ‘I know he is a good doctor’). They describe the negative experience of decompartmentalising patient; ‘I have done my bit’ and ‘now it’s not my problem’. Parents stressed the need for a holistic approach and good communication, particularly when children are the patients.
A specialist in anything is going to become a little bit, not blasé but a little bit more distant perhaps from the patient because you are looking from a true clinical point of view which is natural.
Father
[The surgeon] was very cursory particularly when he was dealing with a child which might have helped get my daughter a bit more upset than she was . . . with an adult it’s not so bad, because there is not an emotional involvement . . . but as a child you want somebody interested in you rather than . . . only being worried about the angles, saying ‘don’t worry about it everything is fine, off you go’.
Father
Parents and children also describe potential issues related to privacy. These included not only undressing in front of people (including other family members) but also being talked about by others and being asked questions about their bodies (e.g. their menstrual cycle).
Do I want someone to talk about my body, and do I want to think about it that much and what they are going to do to me, and does it mean more scans and more people prodding me and . . . my daughter was saying ‘I’ve got to wear this funny t-shirt’ . . . and doing all that at that age when they are supersensitive about all of those things.
Mother
[That surgeon] was brilliant because he gave her a gown he left the room. [The other surgeon] just said to her ‘take your top off’ . . . she is 16 and I’m her Dad and that wasn’t good, she wasn’t given a gown or anything to put on for him . . . we are making him sound like an ogre (which he wasn’t) . . . when you have seen a couple of thousand people over the years you maybe lose sight of that initial, well we need to think about this for a moment before saying anything like, ‘take your top off’.
Father
For the children, ‘bad experiences’ included frustration about the process of accessing a specialist, feeling dismissed if treatment was not indicated and being left with a feeling of not knowing what is going to happen now (‘my curve is not bad enough for surgery so what is going to happen next?’):
I went to my GP. He told me I would need surgery or a back brace so I had prepared myself to have one of those, and then I got told I didn’t need it as it wasn’t bad enough, so I said ‘Oh all right’ . . . he didn’t tell me what options I had to help it, he just said I don’t need surgery, I don’t need a back brace, but he didn’t say anything else to particularly help it. So I think it would be good if doctors did that. But yeah he didn’t really give me much information on scoliosis or anything. He just was like, ‘OK we will send you for an X-ray’, and that was it really.
Girl
Specific worries related to adolescent idiopathic scoliosis
Physiotherapists describe parents’ worries as including: ‘will my child feel like everyone else ‘visually’ and will there be any psychological impact?’; ‘is it going to get worse?’; ‘will she need surgery?’; ‘will this have any impact on her education?’; and ‘is this my fault?’. In contrast to this, physiotherapists describe the children as ‘taking it in their stride’ and being able to do everything that other children do (they are not ill). Parents and children worried about their pain; for one girl (out of three girls with pain) this affected her ability to do normal things. In contrast, physiotherapists did not describe pain as a significant feature of AIS. Children’s and parents’ worries are listed in Table 49.
| Parents’ worries | Children’s worries |
|---|---|
| My child is in pain | Pain gets me down |
| What effect will it have on possible career choices? | What will happen in the future? |
| What will other kids say? | I am conscious of my body and want to look straighter |
| Will it get worse so that she needs surgery? | Worry about needing surgery but some ambivalence (if it works I will be straight/will not have pain) |
| Will other family members get it (sibling, grandchild)? | |
| Childbirth | |
| She does not let on how she feels | |
| Will she continue to have pain and what will be the effects of this? |
Parents’ worries focus on the future and the unknown. They want to know more about what the odds are. They describe ‘watchful waiting’ as a place of anxiety and worry highlighting the uncertainty for the future; will this curve get worse?
From sitting in the waiting room and thinking we’re really lucky that my daughter is the way that she is and then I could always come and think ‘oh God that her mind so I’ve never mentioned it to her but I wonder if she’s thinking along the same lines.
Mother
They describe the ‘sheer panic’ of potential surgery and balancing the need for surgery versus the disadvantages (for example, surgical risks and interference on education at a crucial time). Parents also describe their shock regarding the severity of the curve; ‘how did I not notice sooner?’; ‘how did I let it get this far?’; ‘is it something I did?’; ‘I could kick myself for not doing something sooner’; ‘I am her parent and can do nothing to make it right’.
The first X-ray was a big shock. I think because my daughter had come out, she can be quite a joker, and she said ‘my spine is really bent’ . . . and when we went in it was. And the doctor said ‘you have actually got two curves and its more severe than I first thought’ and he clicked it up on screen and it was a shock to see . . . The X-ray for me was a real wake-up call.
Father
When she was 3 months I had to have a lumbar puncture so I was thinking was it the lumbar puncture? When I was carrying her . . . I was thinking maybe it was because (I was quite small at the time) she didn’t have enough space to grow . . . So there was a fair bit of guilt . . . the logical side of my brain knows that that is absolute nonsense . . . but I think there were times when I did torture myself.
Mother
For a parent it’s frustrating because actually you want to press a magic button and do something and you want to take them for treatment and let them get better but it’s not going to be the case . . . it’s that old cliché isn’t it the only thing you want for your children is good health.
Mother
However, parents also describe AIS as having no major impact on the way that the girls lead their lives; ‘they just get on with it’. Some parents described how it was mum and dad who were worrying and had to ‘take strength’ from the child’s strength (with the proviso that the child may not actually be letting you know how she really feels). Suspicious that the child might ‘not be letting on’, parents attempted to put a positive spin on the situation so as not to worry them.
Show us to take our cues from the children. Take strength from how children approach it. They have been amazingly laid back. What difference has it [scoliosis] made? It has had precious little effect. It would be different if they had pain or obvious deformity; we are lucky.
Father
Children without pain describe AIS as ‘not a big deal’ and ‘pretty common’; ‘I just get on with it’. Often they described how they had not even noticed it. However, pain could have a significant impact (one girl).
I kind of have to be fussy about what I need and what I don’t need, I can’t stand up for too long, always having to change positions always lying forward or back always having to straighten myself.
Girl
It sometimes it frustrates me that I am always in a lot of pain and sometimes I feel like I need special needs and I don’t want to be treated that way I want to be treated like everyone else . . . sometimes it can be pretty depressing.
Girl
Unmet information needs
Families described the need to find out about AIS following a diagnosis, but stressed caution when ‘Googling’ [Google Inc., Mountain View, CA, USA (mother: ‘I made the mistake of Googling it’)]. When asked, they did not remember accessing the SAUK website (www.sauk.org.uk). Parents talked things through with friends and colleagues and also accessed the internet for information.
I made the mistake of googling on the internet and it was the worst thing I could have done really; and I would just advise anyone else not to do it because you see the most extreme patients and I scared the absolute life out of myself . . . I googled ‘spinal braces’ which again they were like these things out of Hannibal Lecter, it was just the scariest contraptions. And yes I think that was a big mistake.
Mother
The parents highlight an unmet information need – ‘I want to find out about what this has been like for other people rather than the worst case scenarios’:
I think just genuine input from the child and the parent . . . It would be useful to have quoted word from actual parents who have shared this experience, or recordings (now we have the technology to do that kind of thing), two or three line statements would be heartening, especially early on to provide some sort of reassurance. For example, ‘your child will probably be worrying less about it than you will’. Knowing what the experience of others is like is useful. Actual words of other real parents . . . Authentic words of others; not propaganda. You would recognise the truth in statements of that kind; not advertising blurb; recognising yourself in the situation.
Father
Children found information about AIS from books, newspaper and magazine articles, Google (www.google.com) and social networking. They also talked to other children that they meet with scoliosis on an ad hoc basis. They described the need to compare their experience with ‘like-others’. Although they might avoid looking at pictures of surgery, they said it was nice to share experiences.
I think some experiences of young people who have it would be useful. Maybe a bit about knowing that other people have it as well and yet they probably have the same worries about it as you have and a kind of thing about people who are worried about the surgery or it is stopping them doing stuff or cosmetic reasons so that they get a sense other people are going through the same things.
Girl
I guess it would be kind of interesting, also a good thing to be able to find out if you have something in common for people with a similar thing. I don’t know many people with the same condition, sometimes I feel a bit lonely.
Girl
Discussion
The exercise intervention
The overall feedback from all participants about the exercise intervention was that it was acceptable. Some physiotherapists expressed concerns over the complexity of the exercises but this was not reflected in the experiences of the patients who appeared to cope well with the programme. No indication was given by the young people or parents that it was too onerous or difficult to perform but, instead, feedback suggested that they enjoyed doing the exercises and benefited from them. Elements of the intervention designed to increase adherence with the programme, including the online diary, goal-setting and contract, were generally viewed in a positive light. One suggestion was made to include text messages to remind participants to do their exercises. The one element of the online resources that was not utilised was the forum, and participants gave examples of other places they had sought peer support, which suggests it was not needed.
Recommendations for a future trial
-
Discontinue the online forum.
-
Consider the inclusion of other reminders to exercise, such as text messaging.
Need for an active approach
The findings support the usefulness of a more active approach to the management of chronic conditions in adolescents. ‘Feeling in control’ was an important outcome described by all participants. Physiotherapists described the difficulties of negotiating the disappointment of families who were allocated to the non-intervention arm, which they regarded as not ‘giving you a chance to improve’. This could potentially threaten the validity of treatment outcomes if those in the comparison groups perform worse on the outcome measures because they do not consider that they are ‘doing something’ (resentful demoralisation). Participants describe how they would try other interventions rather than ‘do nothing’ in the comparator arm. We did not interview patients in the non-exercise group and should consider what people in this group are doing beyond ‘watchful waiting’.
Recommendations for a future trial
-
Repackage the control intervention to frame it more positively so that allocation to the control arm is not viewed in a negative light and the chances of resentful demoralisation are reduced. This could be, for example, a healthy lifestyle intervention, which includes a more structured approach to the delivery of information about AIS alongside education about good health behaviours, and support to perform regular exercise (e.g. based on the World Health Organization guidelines). This would make the control intervention more ‘active’ and in essence, result in the comparison of two active interventions. This approach has been taken in prostate cancer research where ‘watchful waiting’ was considered to be an unacceptable treatment approach by potential participants and resulted in a very low uptake of recruitment to the study. It was reframed as ‘active monitoring’ to reflect the regular tests and review appointments that it entailed.
-
There is also a need to ensure that recruitment staff and treating clinicians convey an attitude of true clinical equipoise and do not suggest, even subconsciously, that one treatment is superior to the other.
Modifiable outcomes: ‘bony curve’ or ‘posture’
The findings also raise queries about the participants’ (both physiotherapists’ and families’) expected modifiable outcomes of the trial. Participants make a distinction between:
-
‘bony curve’, which they perceive as not modifiable (with the exception of one family)
-
aesthetic or ‘postural’ changes, which are modifiable and important.
This is further complicated by the difficulty of actually measuring:
-
changes in the ‘bony curve’
-
habitual changes in postural change
-
consciously controlled changes in posture (e.g. when having radiography, a person can adapt their posture).
Recommendations for a future trial
-
Currently the primary outcome for a future study is the Cobb angle. Although this remains an important measure, as it is a major factor when surgeons make decisions about surgery, it is apparent from the interviews that other outcomes are also important. We have collected a range of secondary outcome measures that appear to capture information broadly about these other outcomes including appearance and pain. These measures should be included in a future study.
Trial procedures
The participants and their parents were generally happy with taking part in physical measurements and completing questionnaires. There were some suggestions that the questionnaires were long and repetitive, and one participant who wore a brace was unsure if the questionnaires were related to her curve or her brace.
Recommendations for a future trial
-
Reduce the length of the questionnaire. This is one of the aims of the feasibility study and all the outcome measures included in the questionnaire will be reviewed.
-
Wording of the questionnaires should be reviewed to ensure that questions are clear about whether they are referring to a participant’s curve or brace.
Fitting service around families
All participants discuss the fundamental difficulties of fitting treatments around the commitments of school, often at a crucial time at school.
Recommendations for a future trial
-
Service provision based on patients’ needs should be considered when setting up the main trial.
Unmet information need
The findings suggest that hearing other people’s stories and experiences about their scoliosis would be a useful adjunct to improve the experience of families with AIS.
Recommendations for a future trial
-
Further consideration of the information needs of families is important for a future trial.
Training to support positive outcomes
The findings suggest possible areas for further training to support a future trial:
-
‘The family is the patient’: physiotherapists recognised the importance of a holistic approach to the family, for example the ability to empower families to face worries about the future and the impact of scoliosis on school and life. They recognised that working with adolescents required skills in this area that they had developed during the trial.
-
Accurate information about scoliosis. Physiotherapists and families focused on the importance of accurate information about scoliosis. Families in particular wanted to know more about the potential paths so that they could prepare for them (e.g. what are the odds of needing surgery?).
-
Physiotherapists discussed the importance of mentoring and learning ‘on the job’ as part of training. Those inexperienced in providing exercises for AIS developed skills ‘on the job’.
-
Physiotherapists could find it challenging to set goals for patients who had no pain or functional limitation.
-
Issues related to research: equipoise and standardisation of treatment protocols.
Recommendations for a future trial
-
Training for any future trial should address the points outlined above.
Limitations
From the comparisons of characteristics of the qualitative participants to the whole cohort, it is apparent that there are important differences. We cannot know what the experience was for boys and for patients from ethnic minority groups. There was limited exploration of the experiences of the participants of the control group through written feedback. These should be explored in a further qualitative study.
Chapter 8 Overall conclusions
From our up-to-date systematic review of the literature, a definitive trial evaluating clinical effectiveness and cost-effectiveness of SSEs for AIS in the NHS is still warranted, particularly to investigate cost-effectiveness. Previous or ongoing studies are mostly small, with short-term follow-up, and are at high risk of bias.
According to our UK survey, there is sufficient willingness from orthopaedic clinicians at a sufficient number of specialist centres to provide a full sample for a definitive trial. This is in tandem with evidence that patients with AIS and their parents are willing to consent to randomisation, treatments and follow-up.
Providing an experimental intervention of a SSE programme involving six sessions with a physiotherapist is currently deliverable within most NHS outpatient settings and highly acceptable to patients and their families. Use of an online exercise diary to support a home exercise plan is viable; computer and internet access was not an issue. Adherence to daily exercise appears to be linked to adherence to attending therapy sessions, with further emphasis required to maximise adherence to the exercise programme. There does not appear to be a requirement for an online forum with pre-existing media already playing a part for patients to communicate with one another. We have a manualised intervention ready for use. Some further refinement of the control intervention is required.
One-and-a-half days’ training is required for physiotherapists to deliver the interventions, with the addition of further within-service training/coaching by more experienced physiotherapists. We were able to deliver high-quality adherence to the intervention protocol with this level of training. There is a requirement to ensure good training on research, equipoise and evidence (or lack of) for SSEs to ensure that clinicians are balanced in their approach to patient intervention for the trial.
The number of outcome measures should be reduced as anticipated at the start of this feasibility study. This reduced burden and a system to collect core outcomes where necessary should enable longer-term loss to follow-up rates to be minimised to within acceptable levels. A radiographic protocol should be implemented with a single rater assessment of curve types (single or double and an assessment of whether or not curves are structural) and sizes and ensuring that Risser grading is possible using full-length film.
We recommend a move to a labelling of idiopathic scoliosis rather than AIS to avoid uncertainty around the exact stage at which the scoliosis has developed.
Progression criteria to full trial
In the original detailed project description we specified the following progression criteria:
-
Demonstrate that assumptions underlying sample size were correct (these were a SD of 15° for primary Cobb angle, 30% loss to follow-up, 20% control group progress to surgery).
-
SD of baseline primary Cobb angle is 9.9°, loss to follow-up at 6 months on current records is 20%, progression to surgery is difficult to predict from current pilot data owing to short-term follow-up.
-
-
Demonstrate that there are sufficient numbers of centres to finalise the recruitment strategy for a main trial.
-
Following a national survey of specialist centres, of those that responded (n = 19 NHS trusts) nearly 80% said that they would be willing to have their patients involved in a RCT that randomised patients to either an exercise or control intervention. Individual consultants reported seeing, on average, 10 new AIS patients per month (range 2–30 patients per month) and 23 follow-up AIS patients per month (range 8–80 patients per month). Assuming 10% of patients are eligible, willing and randomised this would equate to approximately 30–40 patients per month from 15 sites, and a recruitment of 400 patients would take 12 months.
-
-
Pilot an intervention that delivers sufficient dosage within current NHS resources and with > 60% of patients attending all necessary sessions and evidence of performing home exercises.
-
Three out of the four trusts were able to commit to up to nine sessions within their current NHS resources. One trust was unable to manage between six and nine sessions for exercise programme participants during the pilot study owing to limited resources; however, they expressed willingness to provide the sessions should excess treatment costs be supplied. Where the full nine sessions were available, 75% of participants attended the number of sessions deemed necessary by the physiotherapist and there was evidence that 83% of these performed regular home exercises.
-
Acknowledgements
We wish to thank and acknowledge the respondents of the survey of current practice, the participants of the intervention refinement day and the patients and parents who participated in the randomised feasibility study and embedded interview study. We wish to thank the PPI representatives who provided input throughout the study. We wish to thank SAUK for their support of the study and for the provision of information leaflets for use in the randomised feasibility study.
We also wish to thank and acknowledge physiotherapists Steve Bunce, North Bristol NHS Trust, and Anne Richards, Nuffield Orthopaedic Centre, Oxford University Hospitals NHS Trust, for their time and expertise in developing and facilitating training for the physiotherapy interventions.
We developed this report in association with the NIHR Collaboration for Leadership in Applied Health Research & Care (CLAHRC) Oxford, UK, and the NIHR Oxford Musculoskeletal Biomedical Research Unit (SEL, EMW and MAW). The NIHR CLAHRC Oxford acknowledges funding from NIHR. The views and opinions expressed therein are those of the authors and do not necessarily represent those of the Health Technology Assessment programme, NIHR, the NHS or the UK Department of Health.
Contributions of authors
Mark A Williams: study lead, study design, development of interventions, supervision, writing and reviewing the report.
Peter J Heine: development of interventions, quality assurance of interventions, study management, writing and reviewing the report.
Esther M Williamson: qualitative study design and conduct, development of interventions, writing and reviewing the report.
Francine Toye: qualitative study design and conduct, writing and reviewing the report.
Melina Dritsaki: designing and conducting economic analysis, writing and reviewing the report.
Stavros Petrou: study conception and design of economic analysis, supervision, writing and reviewing the report.
Richard Crossman (statistician): conducting statistical analysis, writing and reviewing the report.
Ranjit Lall: study conception and design, of statistical analysis, writing and reviewing the report.
Karen L Barker: study conception and design, development of interventions, writing and reviewing the report.
Jeremy Fairbank: study conception and design, study supervision, writing and reviewing the report.
Ian Harding: study conception and design, study supervision, writing and reviewing the report.
Adrian Gardner: study conception and design, study supervision, writing and reviewing the report.
Anne-Marie Slowther: study conception and design, study supervision, writing and reviewing the report.
Neil Coulson: study conception and design, study supervision, writing and reviewing the report.
Sarah E Lamb: chief investigator, led funding application, study conception and design, development of interventions, supervision, writing and reviewing the report.
ACTIvATeS pilot sites
Frenchay Hospital, North Bristol NHS Trust, Bristol, UK.
Nuffield Orthopaedic Centre, Oxford University Hospitals NHS Trust, Oxford, UK.
Royal Orthopaedic Hospital, Royal Orthopaedic Hospital NHS Foundation Trust, Birmingham, UK.
James Cook University Hospital, South Tees Hospitals NHS Foundation Trust, Middlesbrough, UK.
ACTIvATeS research clinicians
Wendy Bertram (Frenchay Hospital, Bristol, UK).
Tamsin Hughes (Nuffield Orthopaedic Centre, Oxford, UK).
Catherine Minns-Lowe (Nuffield Orthopaedic Centre, Oxford, UK).
Laura Bird (Royal Orthopaedic Hospital, Birmingham, UK).
Melony Hayes (Royal Orthopaedic Hospital, Birmingham, UK).
Cheryl Honeyman (James Cook Hospital, Middlesbrough, UK).
ACTIvATeS physiotherapists
Steve Bunce (Frenchay Hospital, Bristol, UK).
Anne Richards (Nuffield Orthopaedic Centre, Oxford, UK).
Laura Billing (Royal Orthopaedic Hospital, Birmingham, UK).
Emma Cockbain (Royal Orthopaedic Hospital, Birmingham, UK).
Hannah Walker (Royal Orthopaedic Hospital, Birmingham, UK).
Amanda Trees (James Cook Hospital, Middlesbrough, UK).
Independent Monitoring Committee
Chairperson: Mrs Sally Kerry, Reader in Medical Statistics, Bart’s and The London School of Medicine and Dentistry, London, UK.
Independent member: Dr Alison Rushton, Senior Lecturer in Physiotherapy, University of Birmingham, Birmingham, UK.
Independent member: Mr Jayesh Trivedi, Chief Deformity Surgeon, Alder Hey Children’s NHS Foundation Trust, Liverpool, UK.
Independent member and user representative: Dr Stephanie Clark, Chairperson, Scoliosis Association (UK), London, UK.
Study statistician: Dr Ranjit Lall, Principal Research Fellow Statistician, Warwick Clinical Trials Unit, University of Warwick, Coventry, UK.
Study member/chief investigator: Professor Sarah Lamb, Oxford Clinical Trials Research Unit, University of Oxford, Oxford, UK.
Study member/co-applicant: Dr Mark Williams, Study Lead, Oxford Clinical Trials Research Unit, University of Oxford, Oxford, UK.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Lonstein JE. Scoliosis: surgical versus nonsurgical treatment. Clin Orthop Relat Res 2006;443:248-59. http://dx.doi.org/10.1097/01.blo.0000198725.54891.73.
- Parent S, Newton PO, Wenger DR. Adolescent idiopathic scoliosis: etiology, anatomy, natural history, and bracing. Instr Course Lect 2005;54:529-36.
- Kesling KL, Reinker KA. Scoliosis in twins. A meta-analysis of the literature and report of six cases. Spine 1997;22:2009-14.
- Mid 2009 Population Estimates: Great Britain; Estimated Resident Population By Single Year of Age and Sex. London: Office for National Statistics; 2009.
- Weinstein SL, Dolan LA, Spratt KF, Peterson KK, Spoonamore MJ, Ponseti IV. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA 2003;289:559-67. http://dx.doi.org/10.1001/jama.289.5.559.
- Scoliosis Association UK . Late Onset (Adolescent) Idiopathic Scoliosis 2010. www.sauk.org.uk/uploads/Late%20onset%20idiopathic%20scoliosis.pdf.
- Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA. Adolescent idiopathic scoliosis. Lancet 2008;371:1527-37. http://dx.doi.org/10.1016/S0140-6736(08)60658-3.
- Coe JD, Arlet V, Donaldson W, Berven S, Hanson DS, Mudiyam R, et al. Complications in spinal fusion for adolescent idiopathic scoliosis in the new millennium. A report of the Scoliosis Research Society Morbidity and Mortality Committee. Spine 2006;31:345-9. http://dx.doi.org/10.1097/01.brs.0000197188.76369.13.
- Michael AL, Loughenbury PR, Rao AS, Dunsmuir RA, Millner PA. A survey of current controversies in scoliosis surgery in the United Kingdom. Spine 2012;37:1573-8. http://dx.doi.org/10.1097/BRS.0b013e31825409f4.
- Bettany-Saltikov J, Martin D, Wellburn S, Van Schaik P. Information provided to patients with adolescent idiopathic scoliosis (AIS) at the first point of diagnosis in the hospital clinic: a survey of UK NHS scoliosis consultants. Scoliosis 2012;7. http://dx.doi.org/10.1186/1748-7161-7-S1-O36.
- Wong MS, Cheng JC, Lam TP, Ng BK, Sin SW, Lee-Shum SL, et al. The effect of rigid versus flexible spinal orthosis on the clinical efficacy and acceptance of the patients with adolescent idiopathic scoliosis. Spine 2008;33:1360-5. http://dx.doi.org/10.1097/BRS.0b013e31817329d9.
- Nachemson AL, Peterson LE. Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis. A prospective, controlled study based on data from the Brace Study of the Scoliosis Research Society. J Bone Joint Surg Am 1995;77:815-22.
- Negrini S, Minozzi S, Bettany-Saltikov J, Zaina F, Chockalingam N, Grivas TB, et al. Braces for idiopathic scoliosis in adolescents. Spine 2010;35:1285-93. http://dx.doi.org/10.1002/14651858.cd006850.pub2.
- Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 2013;369:1512-21. http://dx.doi.org/10.1056/NEJMoa1307337.
- Negrini S, Fusco C, Minozzi S, Atanasio S, Zaina F, Romano M. Exercises reduce the progression rate of adolescent idiopathic scoliosis: results of a comprehensive systematic review of the literature. Disabil Rehabil 2008;30:772-85. http://dx.doi.org/10.1080/09638280801889568.
- Fusco C, Zaina F, Atanasio S, Romano M, Negrini A, Negrini S. Physical exercises in the treatment of adolescent idiopathic scoliosis: an updated systematic review. Physiother Theory Pract 2011;27:80-114. http://dx.doi.org/10.3109/09593985.2010.533342.
- Romano M, Minozzi S, Bettany-Saltikov J, Zaina F, Chockalingam N, Kotwicki T, et al. Exercises for adolescent idiopathic scoliosis. Cochrane Database Syst Rev 2012;8. http://dx.doi.org/10.1002/14651858.cd007837.pub2.
- Avikainen VJ, Rezasoltani A, Kauhanen HA. Asymmetry of paraspinal EMG-time characteristics in idiopathic scoliosis. J Spinal Disord 1999;12:61-7. http://dx.doi.org/10.1097/00002517-199902000-00010.
- Mooney V, Gulick J, Pozos R. A preliminary report on the effect of measured strength training in adolescent idiopathic scoliosis. J Spinal Disord 2000;13:102-7. http://dx.doi.org/10.1097/00002517-200004000-00002.
- McIntire KL, Asher MA, Burton DC, Liu W. Trunk rotational strength asymmetry in adolescents with idiopathic scoliosis: an observational study. Scoliosis 2007;2. http://dx.doi.org/10.1186/1748-7161-2-9.
- McIntire KL, Asher MA, Burton DC, Liu W. Treatment of adolescent idiopathic scoliosis with quantified trunk rotational strength training: a pilot study. J Spinal Disord Tech 2008;21:349-58. http://dx.doi.org/10.1097/BSD.0b013e318145b7e9.
- Simoneau M, Mercier P, Blouin J, Allard P, Teasdale N. Altered sensory-weighting mechanisms is observed in adolescents with idiopathic scoliosis. BMC Neurosci 2006;7. http://dx.doi.org/10.1186/1471-2202-7-68.
- Bruyneel AV, Chavet P, Bollini G, Ebermeyer E, Mesure S. Idiopathic scoliosis and balance organisation in seated position on a seesaw. Eur Spine J 2010;19:739-46. http://dx.doi.org/10.1007/s00586-010-1325-x.
- Smania N, Picelli A, Romano M, Negrini S. Neurophysiological basis of rehabilitation of adolescent idiopathic scoliosis. Disabil Rehabil 2008;30:763-71. http://dx.doi.org/10.1080/17483100801921311.
- Weiss HR. Imbalance of electromyographic activity and physical rehabilitation of patients with idiopathic scoliosis. Eur Spine J 1993;1:240-3. http://dx.doi.org/10.1007/BF00298367.
- Schmid AB, Dyer L, Böni T, Held U, Brunner F. Paraspinal muscle activity during symmetrical and asymmetrical weight training in idiopathic scoliosis. J Sport Rehabil 2010;19:315-27.
- Wan L, Wang G, Bian R. Results of exercise therapy in treatment of essentially S-shaped scoliosis: evaluation of Cobb angle in breast and lumbar segment through a follow-up of half a year. Chin J Clin Rehabil 2005;9:82-4.
- Mordecai SC, Dabke HV. Efficacy of exercise therapy for the treatment of adolescent idiopathic scoliosis: a review of the literature. Eur Spine J 2012;21:382-9. http://dx.doi.org/10.1007/s00586-011-2063-4.
- Young NL, Sheridan K, Burke TA, Mukherjee S, McCormick A. Health outcomes among youths and adults with spina bifida. J Pediatr 2013;162:993-8. http://dx.doi.org/10.1016/j.jpeds.2012.10.042.
- Furlong WJ, Feeny DH, Torrance GW, Barr RD. The Health Utilities Index (HUI) system for assessing health-related quality of life in clinical studies. Ann Med 2001;33:375-84. http://dx.doi.org/10.3109/07853890109002092.
- Barr R, Pai M, Weitzman S, Feeny D, Furlong W, Rosenbaum P, et al. A multiattribute approach to health-status measurement and clinical management illustrated by an application to brain tumors in childhood. Int J Oncol 1994;4:639-48. http://dx.doi.org/10.3892/ijo.4.3.639.
- Blanchard C, Feeny D, Mahon JL, Bourne R, Rorabeck C, Stitt L, et al. Is the Health Utilities Index responsive in total hip arthroplasty patients?. J Clin Epidemiol 2003;56:1046-54. http://dx.doi.org/10.1016/S0895-4356(03)00203-8.
- Adobor RD, Rimeslåtten S, Keller A, Brox JI. Repeatability, reliability, and concurrent validity of the scoliosis research society-22 questionnaire and EuroQol in patients with adolescent idiopathic scoliosis. Spine 2010;35:206-9. http://dx.doi.org/10.1097/BRS.0b013e3181b43bdf.
- Rodrigues KE, Machado ST, Ferreira MA, Martins TF, Viana MB, Oliveira BM. Health-related quality of life among teenagers during cancer treatment in a developing country: patients’ and proxies’ reports. Paediatr Haematol Oncol 2013;30:307-16. http://dx.doi.org/10.3109/08880018.2013.775617.
- Davison SN, Jhangri GS, Feeny DH. Comparing the Health Utilities Index Mark 3 (HUI3) with the Short Form-36 preference-based SF-6D in chronic kidney disease. Value Health 2009;12:340-5. http://dx.doi.org/10.1111/j.1524-4733.2008.00433.x.
- Petrou S, Johnson S, Wolke D, Hollis C, Kochhar P, Marlow N. Economic costs and preference-based health-related quality of life outcomes associated with childhood psychiatric disorders. Br J Psychiatry 2010;197:395-404. http://dx.doi.org/10.1192/bjp.bp.110.081307.
- Oluboyede Y, Tubeuf S, McCabe C. Measuring health outcomes of adolescents: report from a pilot study. Eur J Health Econ 2013;14:11-9. http://dx.doi.org/10.1007/s10198-011-0340-0.
- Oostenbrink R, A Moll H, Essink-Bot M-L. The EQ-5D and the Health Utilities Index for permanent sequelae after meningitis: a head-to-head comparison. J Clin Epidemiol 2002;55:791-9. http://dx.doi.org/10.1016/S0895-4356(02)00448-1.
- Studin M. Chiropractic vs. medical management of scoliosis: let’s look at the numbers. Dynamic Chiropractic 2012;30.
- Mahon A, Glendinning C, Clarke K, Craig G. Researching children: methods and ethics. Child Soc 1996;10:145-54. http://dx.doi.org/10.1002/(SICI)1099-0860(199606)10:2<145::AID-CHI19>3.0.CO;2-H.
- Beresford B. Personal Accounts: Involving Disabled Children in Research. New York, NY: Social Policy Research Unit; 1997.
- Bull J, Grogan S. Children having spinal surgery to correct scoliosis: a qualitative study of parents’ experiences. J Health Psychol 2010;15:299-30. http://dx.doi.org/10.1177/1359105309351607.
- Macculloch R, Nyhof-Young J, Nicholas D, Donaldson S, Wright JG. Development of an online information and support resource for adolescent idiopathic scoliosis patients considering surgery: perspectives of health care providers. Scoliosis 2010;5. http://dx.doi.org/10.1186/1748-7161-5-13.
- Macculloch R, Donaldson S, Nicholas D, Nyhof-Young J, Hetherington R, Lupea D, et al. Towards an understanding of the information and support needs of surgical adolescent idiopathic scoliosis patients: a qualitative analysis. Scoliosis 2009;4. http://dx.doi.org/10.1186/1748-7161-4-12.
- Sapountzi-Krepia D, Psychogiou M, Peterson D, Zafiri V, Iordanopoulou E, Michailidou F, et al. The experience of brace treatment in children/adolescents with scoliosis. Scoliosis 2006;1. http://dx.doi.org/10.1186/1748-7161-1-8.
- Furlan AD, Pennick V, Bombardier C, van Tulder M. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine 2009;34:1929-41. http://dx.doi.org/10.1097/BRS.0b013e3181b1c99f.
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Cochrane; 2008.
- Choi J, Kim HS, Kim GS, Lee H, Jeon H-S, Chung K-M. Posture management program based on theory of planned behaviour for adolescents with mild idiopathic scoliosis. Asian Nurs Res 2013;7:120-7. http://dx.doi.org/10.1016/j.anr.2013.07.001.
- Diab AA. The role of forward head correction in management of adolescent idiopathic scoliotic patients: a randomised controlled trial. Clin Rehabil 2012;26:1123-32. http://dx.doi.org/10.1177/0269215512447085.
- Schreiber S, Parent EC, Hedden DM, Moreau M, Hill D, Watkins EM. The effects of a 6-month Schroth intervention for adolescent idiopathic scoliosis (AIS): preliminary analysis of an ongoing randomized controlled trial. Scoliosis 2013;8. http://dx.doi.org/10.1186/1748-7161-8-S2-O44.
- Toledo PCV, Mello DBd, Araújo ME, Daoud R, Dantas EHM. Global Posture Reeducation effects in students with scoliosis. Fisioterapia E Pesquisa 2011;18:329-34.
- Monticone M, Ambrosini E, Cazzaniga D, Rocca B, Ferrante S. Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis. Results of a randomised controlled trial. Eur Spine J 2014;23:1204-14. http://dx.doi.org/10.1007/s00586-014-3241-y.
- Abbott A, Möller H, Gerdhem P. CONTRAIS: CONservative TReatment for Adolescent Idiopathic Scoliosis: a randomised controlled trial protocol. BMC Musculoskelet Disord 2013;14. http://dx.doi.org/10.1186/1471-2474-14-261.
- Lee M, Hwang J, Seo B, Im G, Jeon N, Yang H, et al. The effects of the core muscle release technique on scoliosis. J Phys Ther Sci 2013;25:445-8. http://dx.doi.org/10.1589/jpts.25.445.
- Pugacheva N. Corrective exercises in multimodality therapy of idiopathic scoliosis in children – analysis of six weeks efficiency – pilot study. Stud Health Technol Inform 2012;176:365-71.
- Wang SF, Teng CC, Lin KH. Measurement of cervical range of motion pattern during cyclic neck movement by an ultrasound-based motion system. Manual Ther 2005;10:68-72. http://dx.doi.org/10.1016/j.math.2004.08.009.
- Edwards PJ, Roberts I, Clarke MJ, Diguiseppi C, Wentz R, Kwan I, et al. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev 2009;3. http://dx.doi.org/10.1002/14651858.mr000008.pub4.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337.
- Negrini S, Aulisa AG, Aulisa L, Circo AB, de Mauroy JC, Durmala J, et al. 2011 SOSORT guidelines: Orthopaedic and Rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis 2012;7. http://dx.doi.org/10.1186/1748-7161-7-3.
- Bettany-Saltikov J, Wellburn S, Watson P, Arai L, Robinson E, Hamilton S. An Evaluation of the Information Needs of People with Adolescent Idiopathic Scoliosis at the Point of First Diagnosis at the Hospital Clinic: Final Report. Middlesbrough: Teesside University; 2011.
- Scoliosis Association UK . Scoliosis Association UK Webpage n.d. www.sauk.org.uk/2014 (accessed 23 March 2014).
- Weiss H-R, Negrini S, Rigo M, Kotwicki T, Hawes MC, Grivas TB, et al. Indications for conservative management of scoliosis (guidelines). Scoliosis 2006;1. http://dx.doi.org/10.1186/1748-7161-1-5.
- Weiss HR, Goodall D. Is in-patient scoliosis rehabilitation clinically effective: a systematic PubMed review. Scoliosis 2009;4. http://dx.doi.org/10.1186/1748-7161-4-S2-O32.
- Horne R, Weinman J, Barber N, Elliott R, Morgan M, Cribb A, et al. Concordance, Adherence and Compliance in Medicine Taking: Report for the National Co-ordinating Centre for NHS Service Delivery and Organisation R & D (NCCSDO). London: NCCSDO; 2005.
- Rigo M, Quera-Salvá G, Villagrasa M, Ferrer M, Casas A, Corbella C, et al. Scoliosis intensive out-patient rehabilitation based on Schroth method. Stud Health Technol Informat 2008;135:208-27.
- Rejeski W, Craven T, Ettinger WJ, McFarlane M, Shumaker S. Self-efficacy and pain in disability with osteoarthritis of the knee. J Gerontol B Psychol Sci Soc Sci 1996;51:P24-9. http://dx.doi.org/10.1093/geronb/51B.1.P24.
- Orbell S, Sheeran P. ‘Inclined abstainers’: a problem for predicting health-related behaviour. Br J Soc Psychol 1998;37:151-65. http://dx.doi.org/10.1111/j.2044-8309.1998.tb01162.x.
- Sheeran P, Trafimow D, Armitage CJ. Predicting behaviour from perceived behavioural control: tests of the accuracy assumption of the theory of planned behaviour. Br J Soc Psychol 2003;42:393-410. http://dx.doi.org/10.1348/014466603322438224.
- Moseley GL. Do training diaries affect and reflect adherence to home programs?. Arthritis Rheum 2006;55:662-4. http://dx.doi.org/10.1002/art.22086.
- Vliet Vlieland T. Rehabilitation of people with rheumatoid arthritis. Best Pract Res Clin Rheumatol 2003;17:847-61. http://dx.doi.org/10.1016/S1521-6942(03)00043-3.
- Patient and Public Involvement in Health and Social Care Research: A Handbook for Researchers by Research Design Service. London: Research Design Service London; 2014.
- Patient and Public Involvement Policy. London: NICE; 2013.
- Staniszewska S, Brett J, Mockford C, Barber R. The GRIPP checklist: strengthening the quality of patient and public involvement reporting in research. Int J Technol Assess Health Care 2011;27:391-9. http://dx.doi.org/10.1017/S0266462311000481.
- MRC Ethics Guide: Medical Research Involving Children. London: Medical Research Council; 2004.
- Asher M, Min Lai S, Burton D, Manna B. The reliability and concurrent validity of the scoliosis research society-22 patient questionnaire for idiopathic scoliosis. Spine 2003;28:63-9. http://dx.doi.org/10.1097/00007632-200301010-00015.
- Sanders JO, Harrast JJ, Kuklo TR, Polly DW, Bridwell KH, Diab M, et al. The Spinal Appearance Questionnaire: results of reliability, validity, and responsiveness testing in patients with idiopathic scoliosis. Spine 2007;32:2719-22. http://dx.doi.org/10.1097/BRS.0b013e31815a5959.
- Lerman JA, Sullivan E, Haynes RJ. The Pediatric Outcomes Data Collection Instrument (PODCI) and functional assessment in patients with adolescent or juvenile idiopathic scoliosis and congenital scoliosis or kyphosis. Spine 2002;27:2052-7. http://dx.doi.org/10.1097/00007632-200209150-00016.
- Hacquebord JH, Leopold SS. In brief: the Risser classification: a classic tool for the clinician treating adolescent idiopathic scoliosis. Clin Orthop Relat Res 2012;470:2335-8. http://dx.doi.org/10.1007/s11999-012-2371-y.
- Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine 2005;30:682-8. http://dx.doi.org/10.1097/01.brs.0000155425.04536.f7.
- Berryman F, Pynsent P, Fairbank J, Disney S. A new system for measuring three-dimensional back shape in scoliosis. Eur Spine J 2008;17:663-72. http://dx.doi.org/10.1007/s00586-007-0581-x.
- Bago J, Perez-Grueso FJ, Les E, Hernandez P, Pellise F. Minimal important differences of the SRS-22 Patient Questionnaire following surgical treatment of idiopathic scoliosis. Eur Spine J 2009;18:1898-904. http://dx.doi.org/10.1007/s00586-009-1066-x.
- Carreon LY, Sanders JO, Polly DW, Sucato DJ, Parent S, Roy-Beaudry M, et al. Spinal appearance questionnaire: factor analysis, scoring, reliability, and validity testing. Spine 2011;36:E1240-4. http://dx.doi.org/10.1097/BRS.0b013e318204f987.
- Daltroy LH, Liang MH, Fossel AH, Goldberg MJ. The POSNA pediatric musculoskeletal functional health questionnaire: report on reliability, validity, and sensitivity to change. Pediatric Outcomes Instrument Development Group. Pediatric Orthopaedic Society of North America. J Pediatr Orthop 1998;18:561-71. http://dx.doi.org/10.1097/00004694-199809000-00001.
- Lancaster G, Dodd S, Williamson P. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract 2004;10:307-12. http://dx.doi.org/10.1111/j. 2002.384.doc.x.
- Schulz KF, Altman DG, Moher D, Group C. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340. http://dx.doi.org/10.1136/bmj.c332.
- Guide to The Methods of Technology Appraisal. London: NICE; 2013.
- Curtis L. Unit Costs of Health and Social Care 2011. Canterbury: PSSRU, University of Kent; 2011.
- NHS Reference Costs 2013. London: Department of Health; 2013.
- Dolan P, Gudex C, Kind P, Williams A. A Social Tariff for EuroQol. York: Publications Unit, Centre for Health Economics, University of York; 1996.
- Torrance GW, Feeny DH, Furlong WJ, Barr RD, Zhang Y, Wang Q. Multiattribute utility function for a comprehensive health status classification system: Health Utilities Index Mark 2. Med Care 1996;34:702-22. http://dx.doi.org/10.1097/00005650-199607000-00004.
- Feeny D, Furlong W, Torrance GW, Goldsmith CH, Zhu Z, DePauw S, et al. Multiattribute and single-attribute utility functions for the health utilities index mark 3 system. Med Care 2002;40:113-28. http://dx.doi.org/10.1097/00005650-200202000-00006.
- Fontana A, Frey JH, Denzin NK, Lincoln YS. Handbook of Qualitative Research. Thousand Oaks, CA: Sage Publications; 2000.
- Smith JA, Smith JA, Harre R, van Langenhove L. Rethinking Methods in Psychology. London: Sage Publications; 1995.
- Kirk S. Methodological and ethical issues in conducting qualitative research with children and young people: a literature review. Int J Nurs Stud 2007;44:1250-60. http://dx.doi.org/10.1016/j.ijnurstu.2006.08.015.
- Smith JA, Flowers P, Larkin M. Interpretative Phenomenological Analysis: Theory, Method and Research. London: Sage Publications; 2009.
- Toye F, Seers K, Allcock N, Briggs M, Carr E, Andrews J, et al. ‘Trying to pin down jelly’ – exploring intuitive processes in quality assessment for meta-ethnography. BMC Med Res Methodol 2013;13. http://dx.doi.org/10.1186/1471-2288-13-46.
Appendix 1 Flow chart of pilot study procedures
FIGURE 6.
Flow chart of pilot study procedures. CLRN, Comprehensive Local Research Network; PIS, patient information sheet; WCTU, Warwick Clinical Trials Unit.
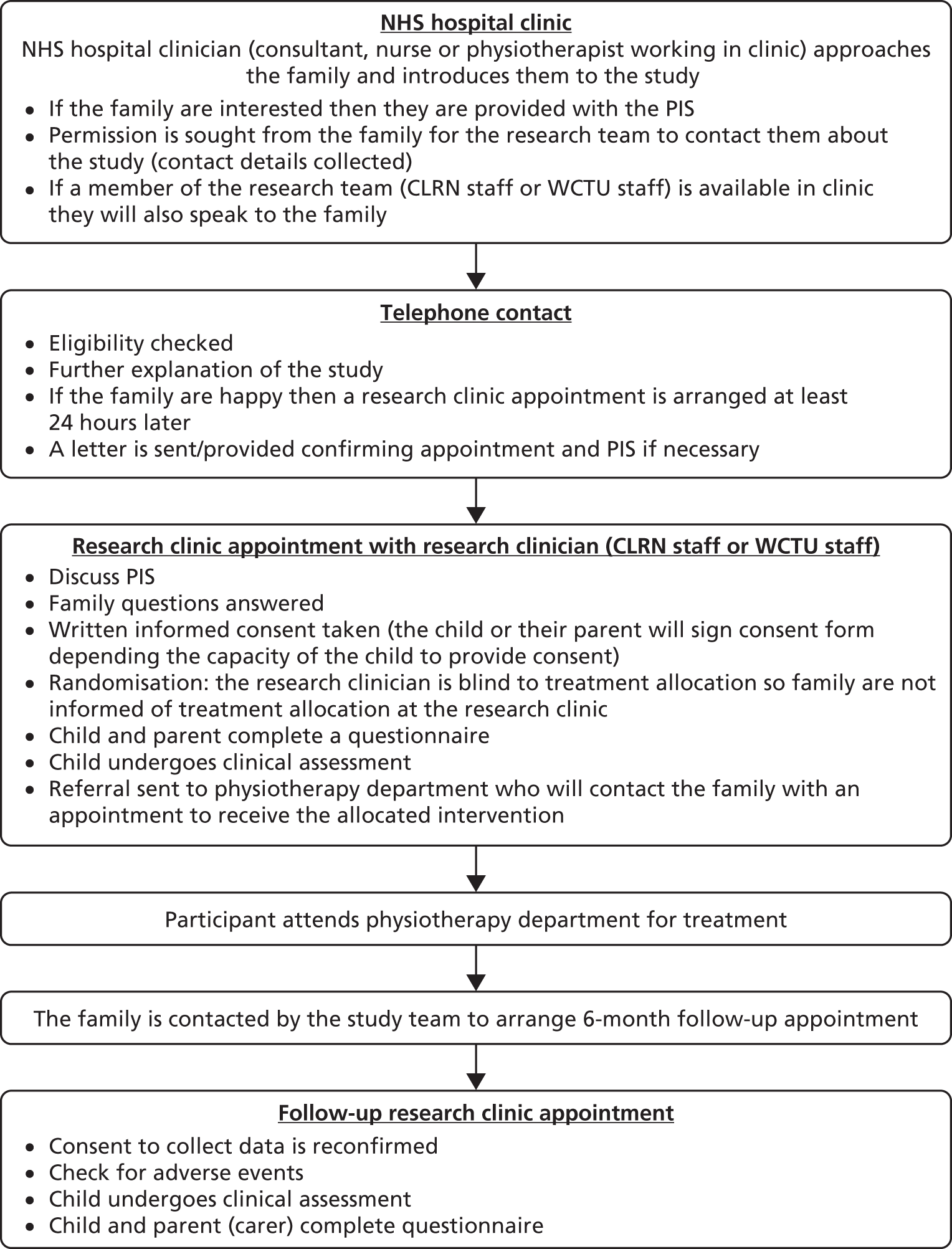
Appendix 2 Baseline case report/record forms
Appendix 3 Six-month case report/record forms
Appendix 4 Screenshot of interactive online exercise calendar

Appendix 5 Screenshot of online forum
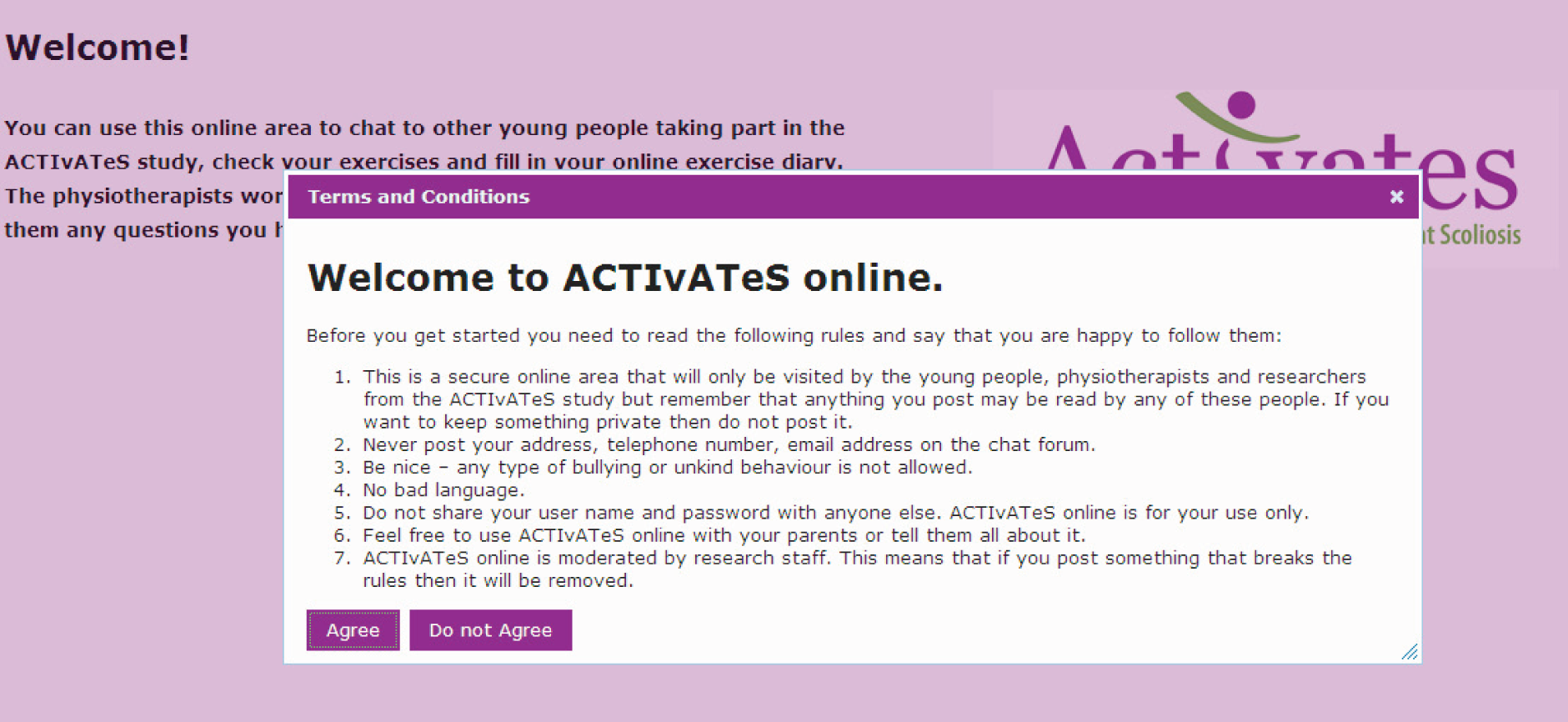
List of abbreviations
- ACTIvATeS
- Active Treatment for Idiopathic Adolescent Scoliosis
- ADL
- activity of daily living
- AE
- adverse event
- AIS
- adolescent idiopathic scoliosis
- ASC
- active self-correction
- ATR
- angle of trunk rotation
- CONSORT
- Consolidated Standards of Reporting Trials
- EMG
- electromyography
- EQ-5D
- European Quality of Life-5 Dimensions
- GRADE
- Grading of Recommendations Assessment, Development and Evaluation
- HRQoL
- health-related quality of life
- HUI
- Health Utilities Index
- HUI2
- Health Utilities Index Mark 2
- HUI3
- Health Utilities Index Mark 3
- IQR
- interquartile range
- ISIS-2
- Integrated Shape Imaging System 2
- NICE
- National Institute for Health and Care Excellence
- PODCI
- Pediatric Outcomes Data Collection Instrument
- PPI
- patient and public involvement
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- ROM
- range of motion
- SAE
- serious adverse event
- SAQ
- spinal appearance questionnaire
- SAUK
- Scoliosis Association UK
- SD
- standard deviation
- SEAS
- Scientific Exercises Approach to Scoliosis
- SRS-22
- Scoliosis Research Society-22 questionnaire
- SSE
- scoliosis-specific exercise
- VAS
- visual analogue scale