Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 05/47/02. The contractual start date was in July 2007. The draft report began editorial review in July 2014 and was accepted for publication in May 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Carr et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
This report describes the results of the UK Rotator Cuff Surgery (UKUFF) trial assessing the clinical effectiveness and cost-effectiveness of arthroscopic compared with open rotator cuff repair for people with full-thickness rotator cuff tears. This comparison was commissioned and funded by the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) programme. The trial began in 2007 and initially also included a non-operative comparator of a rest-then-exercise programme. However, because of high crossover from the rest-then-exercise group to surgery, the trial was reconfigured in 2010 to a comparison of arthroscopic and open repair only.
Rotator cuff tear
The prevalence of shoulder complaints in the UK is estimated to be 14%, with 1–2% of adults consulting their general practitioner (GP) annually regarding new-onset shoulder pain. 1 Rotator cuff pathology, including tendonitis, calcific tendonitis and rotator cuff tears, reportedly accounts for up to 70% of shoulder pain problems. 2 Painful shoulders pose a substantial socioeconomic burden. Disability of the shoulder can impair the ability to work or perform household tasks and can result in time off work. 3,4 Shoulder problems account for 2.4% of all GP consultations in the UK and 4.5 million visits to physicians annually in the USA. 5,6 More than 300,000 surgical repairs for rotator cuff pathologies are performed annually in the USA, where the annual financial burden of shoulder pain management has been estimated to be US$3B. 7
Rotator cuff pathology is associated with progressive change in the shape of the acromion, with ‘spurs’ forming at its anteroinferior margin. Some reports suggest that these spurs narrow the subacromial space, thereby making physical contact more likely in certain positions of the arm. This is most notable in abduction and elevation of the arm and is sometimes referred to as ‘painful arc’ or impingement because pain is maximal in the mid-range of movement. This process is argued to result in inflammation of the rotator cuff tendons (particularly the supraspinatus tendon) and the overlying subacromial bursa. A conflicting theory suggests that such mechanisms are not causative and that intrinsic age-related degeneration of the tendon is the main determinant of inflammation and symptoms. 8,9
Rotator cuff tear refers to structural failure in one or more of the four muscles and tendons that form the rotator cuff. Any tear that does not extend all the way through the tendon is termed a partial-thickness tear. Asymptomatic full-thickness tears of the rotator cuff are very common in the general population. It is estimated that the overall prevalence of tears is 34% and that risk increases significantly with age. 10 Partial tears are more prevalent than full-thickness tears. 11
Conservative management
Conservative treatment may include rest, exercise, topical non-steroidal anti-inflammatory drugs (NSAIDs), oral corticosteroids, oral paracetamol, opioid analgesics, physiotherapy, activity modification, acupuncture, platelet-rich plasma injections, extracorporeal shockwave therapy, suprascapular nerve block, laser treatment, autologous blood injections, intra-articular NSAID injections, subacromial corticosteroid injections, electrical stimulation, ice and ultrasound.
A search of MEDLINE, EMBASE and The Cochrane Library up to August 2009 for treatment of shoulder pain was undertaken. 12 Harm alerts from relevant organisations, such as the US Food and Drug Administration (FDA) and the UK Medicines and Healthcare products Regulatory Agency (MHRA), were included. The review found 71 systematic reviews, randomised controlled trials (RCTs) or observational studies that met the inclusion criteria. Grading of Recommendations Assessment, Development and Evaluation (GRADE) of the quality of evidence for interventions was performed. 2 It is not known whether topical NSAIDs, oral corticosteroids, oral paracetamol or opioid analgesics improve shoulder pain, although oral NSAIDs may be effective in the short term in people with acute tendonitis/subacromial bursitis. If pain control fails, the diagnosis should be reviewed and other interventions considered. Physiotherapy may improve pain and function in people with mixed shoulder disorders compared with placebo. Platelet-rich plasma injections may improve the speed of recovery in terms of pain and function in people having open subacromial decompression for rotator cuff impingement, but further evidence is needed. Acupuncture may not improve pain or function in people with rotator cuff impingement compared with placebo or ultrasound. Extracorporeal shockwave therapy may improve pain in calcific tendonitis. There is some evidence that suprascapular nerve block, laser treatment, arthroscopic subacromial decompression and rotator cuff repair may be effective in some people with shoulder pain. There is no evidence to support the use of autologous blood injections, intra-articular NSAID injections, subacromial corticosteroid injections, electrical stimulation, ice or ultrasound. Concern exists regarding the potential longer-term damaging consequences of corticosteroid injection. 13
Role of imaging
Imaging is most useful in directing treatment in secondary care if conservative care has failed. A large proportion of the general population will demonstrate abnormalities on imaging of the rotator cuff. 14 Imaging findings need to be interpreted in the context of symptoms, disability and response to treatment. A high proportion of patients with rotator cuff pain will respond to conservative treatment. 15 The only reliable non-interventional method of determining if a rotator cuff tear has healed is use of postoperative imaging, either magnetic resonance imaging (MRI) or ultrasonography.
Surgical management
The most frequent indications for surgery are persistent and severe pain combined with functional restrictions that are resistant to conservative measures. Symptoms of pain and weakness typically disrupt daily activities and night pain affects sleep. Symptoms of a minimum of 3 months’ duration that are sufficiently severe to disrupt daily activities and rest or sleep and failure of standard conservative care (analgesics, rest and physiotherapy and cortisone injection) are usually required before surgery is considered. Surgical repair may be advised in cases of full-thickness rotator cuff tear with persistent pain and weakness after conservative treatment. A rotator cuff repair operation aims to reattach the torn tendons to the humeral bone. In general, two approaches are available for surgical repair. Open surgery involves the rotator cuff being repaired under direct vision through an incision in the skin. Arthroscopic surgery is keyhole surgery and involves the repair being performed through arthroscopic portals into the shoulder. A subacromial decompression (SAD) or acromioplasty to create space around the repaired tendon is usually performed in association with the tendon repair. Reports of the outcome of such surgery are conflicting and evidence for effectiveness is unclear. 16–18 An assessment of the treatment cost of impingement suggests that the addition of surgery, in comparison with exercise treatment alone, is not cost-effective. 19
Comparative studies of subacromial decompression and non-operative treatment options such as physiotherapy have not shown any significant difference in outcome between the two treatment modalities. 20–23 A growing number of studies have tried to assess the effectiveness of subacromial decompression against a control. Three studies of patients undergoing rotator cuff repair, including or excluding subacromial decompression in their operative treatment, did not demonstrate any difference in outcome between the groups. 24–26 A RCT of subacromial decompression plus subacromial bursectomy compared with bursectomy alone reported no significant difference in clinical outcome between the two groups. This finding suggests that removing acromial spurs might not be necessary. 27
The management of partial tears is particularly controversial and patients with such tears have commonly been treated conservatively. Favourable results have been reported following debridement of partial tears in association with subacromial decompression. 28 Higher rates of re-rupture are associated with repairs of larger tears, increased patient age and increased fatty degeneration of the cuff muscles. 29–32 Partial tears are most commonly managed without repair, but some authors advocate repair to prevent progression to full-thickness tears. The evidence supporting this approach is weak. 11 There is also uncertainty regarding the relative value of conservative care, repair surgery and debridement surgery for large and massive tears. 33–36 High failure rates of 13–68% have been reported for surgical repair of rotator cuff tears, irrespective of the surgical technique employed. 37–39 Some studies have suggested that re-rupture rates are associated with poorer outcomes. 40 Surgical decision-making in the management of rotator cuff tears was reviewed by Dunn et al. 41 They surveyed surgeons in the USA and found considerable variation in decision-making. This included the type of surgery, the surgical techniques employed and the type and duration of conservative treatment, including cortisone injections, physiotherapy, rest, analgesia and home exercises. Rates of medical visits for rotator cuff pathology in the USA were reviewed between 1996 and 2006. The volume of rotator cuff repairs had increased by 141% and the unadjusted number of arthroscopic repairs increased by 600% compared with a 34% increase in open repairs. 42 The volume of arthroscopic subacromial decompressions has also increased significantly over time. Recent figures from the USA report a 240% increase (from 30.0 to 101.9 per 100,000 people per year) in use of the procedure in New York state between 1996 and 2006. 43 This compares to a 78.3% increase in ambulatory orthopaedic surgery overall. Similar increases have recently been reported in the UK. 44 The introduction of less invasive arthroscopic techniques accounts for some of the overall increased rate of surgery, but does not explain regional variation. Patient and disease characteristics have not changed over time and there is a growing concern that this procedure is being overused. Observational studies of subacromial decompression surgery show positive results in terms of pain reduction and functional outcome, with high patient satisfaction rates. However, equally good outcomes have been noted in two studies following patients who had arthroscopic rotator cuff debridement or open rotator cuff repair in the absence of a subacromial decompression.
Rationale for the study design
The objective of the original commissioned call was to conduct a pragmatic multicentre randomised clinical trial to obtain good-quality evidence of the effectiveness and cost-effectiveness of conservative care compared with arthroscopic surgical repair compared with open surgical repair for the treatment of degenerative rotator cuff tears. Because of high crossover from the conservative arm to surgery the study was reconfigured to a comparison of the two surgical techniques only. There is conflicting evidence regarding the effectiveness of open and arthroscopic repair. 12,45–47 Proponents of arthroscopic rotator cuff surgery suggest that the procedure may have advantages over standard open techniques by causing less trauma to the deltoid muscle and overlying soft tissue. Arguably, this causes less postoperative patient discomfort together with earlier return of movement. However, the success of the repair depends partly on the ability of the surgeon to achieve a secure attachment of tendon to bone. This may be more easily and reliably achieved by open/mini-open surgery. Other potential disadvantages of the arthroscopic approach include increased technical difficulty and longer time in theatre. There is a need to compare the outcomes of the two surgical techniques.
Literature update since the call
A review updating the literature published since the original commissioned call was undertaken to inform this report and set the results in context. Only reports of RCTs were included. Quasi-RCTs, which use methods of allocating participants to a treatment that are not strictly random, for example date of birth, hospital record number or alternation, were excluded.
Types of participants
Randomised controlled trials of adults aged ≥ 18 years with a degenerative rotator cuff tear as reported in the primary studies (e.g. confirmed by physical examination, MRI, ultrasound or MRI arthrogram) were included. RCTs of adults undergoing surgery for other types of rotator cuff disease, shoulder instability, joint replacement or fractures were excluded.
Types of interventions
All randomised comparisons between a surgical procedure (e.g. open or arthroscopic) and another surgical procedure for treating rotator cuff tear were included. Randomised comparisons between a surgical procedure and a non-surgical procedure (e.g. physiotherapy, drug therapy) were also included. RCTs in which the primary aim was to compare different types of surgical technique (e.g. different suturing techniques) as part of the surgical repair of the rotator cuff were excluded.
Types of outcome measures
The primary outcome for each RCT and time point when measured, as reported by the authors, was recorded. When reported by the authors, the primary outcome was that used for the calculation of the sample size. Primary outcomes included pain, disability or function measured using shoulder-specific instruments such as the Constant score,48 American Shoulder and Elbow Surgeons (ASES) Shoulder Score49 or the Disabilities of the Arm, Shoulder and Hand (DASH) score. 50
Search methods for identification of studies
We searched Ovid MEDLINE from 2006 to March 2014 for possible reports of RCTs. The search strategy used was based on one developed by Coghlan et al. 16 for a Cochrane review of surgery for rotator cuff disease. This search strategy was modified to account for changes to the medical subject heading (MeSH) terms since the original search was conducted in 2006, the addition of free-text terms and the replacement of the original RCT filter used with the Cochrane sensitivity- and precision-maximising version RCT filter [2008 version; see http://handbook.cochrane.org/chapter_6/box_6_4_b_cochrane_hsss_2008_sensprec_pubmed.htm (accessed 23 August 2015)] (see Appendix 4 for search strategy). We also searched the World Health Organization (WHO) International Clinical Trials Registry Platform51 to identify reports of any ongoing RCTs. One author screened the titles and abstracts of all retrieved records. Full articles were then obtained for any potentially eligible studies and assessed using the predefined eligibly criteria described earlier.
Results
Description of studies
The search strategy identified 477 potentially eligible studies. Of these, eligible studies were identified as those comparing a surgical intervention with another surgical intervention and those comparing a surgical intervention with a non-surgical intervention.
Surgery compared with surgery
Six RCTs26,52–56 comparing a surgical intervention with another surgical intervention were identified (Table 1). Of these six trials, one RCT56 is ongoing, with completed recruitment but final results awaiting publication. Two other trials57,58 were identified comparing two different types of surgical intervention; however, these were excluded as the patients were not randomised.
| Study ID | Study designa | Blinding | Sample size | Participants | Intervention | Comparator | Primary outcomeb | Results |
|---|---|---|---|---|---|---|---|---|
| Included studies | ||||||||
| Abrams 201452 | RCT, single centre | Outcome assessor blinded | 114 | Full-thickness rotator cuff tear – mean age 59 years | Arthroscopic with acromioplasty repair | Arthroscopic without acromioplasty repair | ASES score at 2 years | No statistically significant difference |
| van der Zwaal 201353 | RCT, single centre | Not blinded | 100 | Small to medium rotator cuff tear – mean age 57 years | Arthroscopic repair | Mini-open repair | DASH score at 1 year | No statistically significant difference; mean difference –3.4 (95% CI –10.2 to 3.4) |
| MacDonald 201154 | RCT, multicentre | Subject and outcome assessor blinded | 86 | Full-thickness rotator cuff tear – mean age 57 years | Arthroscopic repair with acromioplasty | Arthroscopic repair without acromioplasty | Quality of life specific to rotator cuff disease (WORC) at 2 years | No statistically significant difference; mean difference –6.8 (95% CI –15.7 to 2.1) |
| Mohtadi 200855 | RCT, multicentre | Outcome assessor blinded | 73 | Full-thickness rotator cuff tear – mean age 57 years | Arthroscopic acromioplasty with mini-open repair | Open surgical repair | Rotator cuff quality-of-life score (RC-QOL) at 2 years | No statistically significant difference; p = 0.943 |
| Gartsman 200426 | RCT, single centre | Outcome assessor blinded | 93 | Full-thickness supraspinatus tear – mean age 60 years | Arthroscopic with acromioplasty repair | Arthroscopic without acromioplasty repair | ASES score at 1 year | No statistically significant difference; p = 0.363 |
| Ongoing study | ||||||||
| MacDermid 200656 | RCT, multicentre | Subject and outcome assessor blinded | 225 | Small (≤ 1 cm) to medium (1–3 cm) rotator cuff tear – age 18–75 years | Arthroscopic repair | Mini-open repair | Quality of life specific to rotator cuff disease (WORC index) within 2 years | |
| Excluded studies | ||||||||
| Cho 201257 | Quasi-RCT, single centre | Not reported | 60 | Small (< 3 cm) supraspinatus tear – mean age 56 years | Arthroscopic repair | Mini-open repair | Pain score (VAS) at 6 months | No statistically significant difference; p = 0.98 |
| Kasten 201158 | Quasi-RCT, single centre | Not reported | 34 | Supraspinatus tear – mean age 60 years | Arthroscopic repair | Mini-open repair | Pain score (VAS) at 3 months | No statistically significant difference |
Of the five completed RCTs,26,52–55 three were single-centre studies and all were relatively small, ranging from 73 to 114 participants per trial, with a mean participant age between 57 and 60 years. Four RCTs included participants with full-thickness rotator cuff tears26,52,54,55 and one included participants with small and medium rotator cuff tears. 53 The type of surgical interventions differed between trials, with one RCT comparing arthroscopic repair with mini-open repair,53 one comparing mini-open repair arthroscopic acromioplasty with open surgical repair55 and three comparing arthroscopic with acromioplasty repair with arthroscopic without acromioplasty repair. 26,52,54 The choice of primary outcome also varied across studies and included pain, disability or function measured using shoulder-specific instruments. Four26,52,54,55 of the five completed RCTs reported blinded assessment of these outcomes. Overall, no RCT showed a statistically significant difference between the two types of surgical intervention being compared.
Surgery compared with non-surgery
Three RCTs59–61 comparing a surgical intervention with a non-surgical intervention were identified, of which one61 is ongoing, having completed recruitment but with final results awaiting publication (Table 2). Of the two completed RCTs, one59 was a multicentre study and both were relatively small, ranging from 103 to 173 participants per trial, with a participant age of between 60 and 65 years. One RCT59 was a three-arm trial comparing open surgical repair, acromioplasty and physiotherapy with acromioplasty and physiotherapy and physiotherapy alone. This trial found no statistically significant difference between the interventions being compared at 1 year based on the Constant shoulder score. 48 The other RCT60 compared open surgical repair (or mini-open repair) with physiotherapy and found a statistically significant difference in favour of surgery at 1 year based on the Constant shoulder score. 48
| Study ID | Study design | Blinding | Sample size | Participants | Intervention | Comparator | Primary outcomea | Results |
|---|---|---|---|---|---|---|---|---|
| Included studies | ||||||||
| Kukkonen 201459 | RCT, multicentre | Outcome assessor blinded | 173 (180 shoulders) | Atraumatic symptomatic supraspinatus tendon tear – mean age 65 years | Open surgical repair, acromioplasty and physiotherapy | Acromioplasty and physiotherapy or physiotherapy | Constant score at 1 year | No statistically significant difference; p = 0.34 |
| Moosmayer 201060 | RCT, single centre | Outcome assessor blinded | 103 | Small (≤ 1 cm) to medium (1–3 cm) rotator cuff tear – mean age 60 years | Open surgical repair (n = 42) or mini-open repair (n = 9) | Physiotherapy | Constant score at 1 year | Statistically significant difference in favour of surgery; mean difference 13 (95% CI. 4.9 to 21.1) |
| Ongoing study | ||||||||
| Lambers Heerspink 201161 | RCT, multicentre | Not reported | 108 | Atraumatic rotator cuff tear – age 45–75 years | Open surgical repair with acromioplasty | Physiotherapy, NSAIDs (if indicated), subacromial infiltration with corticosteroids | Constant score at 1 year | |
Chapter 2 Methods
At the outset (July 2007) the UKUFF study had two complementary components [UKUFF original Research Ethics Committee (REC) reference number 07/Q1606/49]:
-
a multicentre, pragmatic RCT comparing open and arthroscopic surgical treatments with a non-operative programme of rest then exercise to assess their relative clinical effectiveness
-
an economic evaluation of the treatments to compare the cost-effectiveness of the management streams, identify the most efficient provision of future care and describe the resource impact that various policies for surgical rotator cuff repair would have on the NHS.
Eligible patients who consented to participate in the study were randomly allocated to arthroscopic surgery, open surgery or a programme of rest then exercise. Participants completed patient-reported outcome measures (PROMs) at baseline and then at 8, 12 and 24 months post randomisation. Questionnaires were also completed by telephone at 2 and 8 weeks post treatment. For those patients randomised to surgery, who had a complete repair of the rotator cuff, MRI or an ultrasound scan was also performed 12 months after their surgery.
Randomisation in the original study design was organised within three strata depending on surgeons’ stated preparedness to randomise. A detailed survey of the members of the British Elbow & Shoulder Society (BESS) was conducted in preparation for this study. This survey showed that, at the time, only around 15% of surgeons regularly undertook arthroscopic surgery. Of the surgeons who regularly performed arthroscopic surgery, only 8% indicated that they would be prepared to randomise between surgical treatments. The remainder were happy to randomise between arthroscopic surgery and the rest-then-exercise programme. The majority of surgeons indicated that they performed only open surgery. Surgeons who performed only open surgery did not appear to have equipoise for open surgery compared with arthroscopic surgery.
Reflecting this lack of individual uncertainty around certain comparisons, the trial was designed such that surgeons could randomise between:
-
stratum A – arthroscopic surgery compared with open surgery compared with rest then exercise
-
stratum B – arthroscopic surgery compared with rest then exercise
-
stratum C – open surgery compared with rest then exercise.
Reconfigured study design
A high rate of crossover (77%) of the 214 patients in the rest-then-exercise programme to surgery was observed and so the trial was adapted and reconfigured on the instruction of the funder in 2009 after consultation with the Trial Steering Committee (TSC) and the Data Monitoring Committee (DMC). Crossover did not occur at a consistent or predictable time point. The reconfigured design was a two-way parallel-group RCT of open compared with arthroscopic rotator cuff repair (UKUFF reconfigured REC reference number 10/H0402/24, April 2010). At the time of reconfiguration there were 131 participants in stratum A (n = 43, arthroscopic surgery; n = 44, open surgery; and n = 44, rest then exercise), 181 in stratum B (n = 91, arthroscopic surgery; and n = 90, rest then exercise) and 162 in stratum C (n = 82, open surgery; and n = 80, rest then exercise). The 87 patients already randomised between arthroscopic and open surgery (stratum A) were carried through to the subsequent reconfigured trial. After the reconfiguration it was calculated that a further 180 patients should be recruited and followed up for 2 years as per the original protocol, leading to a total of 267 patients treated with surgery.
During the period between 2007 and 2010, surgical opinion had changed and an increased number of surgeons were in equipoise between open and arthroscopic surgery. The UKUFF trial was reconfigured as a pragmatic multicentre study involving 20 surgeons from 16 UK centres; 15 of these surgeons had originally recruited to stratum A.
Patient and public involvement and engagement
From the outset patients were involved and engaged in the design of the trial. A patient representative (D Farrar-Hockley) was a member of the group designing the trial. He subsequently became a member of the TSC.
Interventions
Conservative care
For the original study a conservative regime of rest then exercise was developed. In view of the lack of evidence for type or dose of exercise therapy, a consensus approach was adopted with input from five physiotherapists, all with expertise and publications in shoulder physiotherapy. It was anticipated that most patients would have already undergone physiotherapy before referral to a surgeon and therefore further similar treatment would not be appropriate. In addition, there was a need for standardisation across a large geographical area and number of locations over a considerable period of time. It was decided to deliver, by post, a high-quality booklet to patients in their own home with an accompanying compact disc (CD) showing moving images. Information was given regarding rotator cuff tears and general and specific exercise options. The package included a sling, with advice to start with relative shoulder rest, using the sling if necessary, and to then start exercising. A free telephone helpline was available with physiotherapy expertise. However, because of the high crossover rate to surgery (77%), this treatment arm was discontinued in the reconfigured trial.
Surgery and surgeons
Surgery was either arthroscopic (fixation of tendon to bone using only arthroscopic techniques) or open (fixation to bone under direct vision through a surgically created opening in the deltoid muscle). The precise technique and method of fixation were not prescribed and surgeons used their preferred and usual technique. Details of the surgical technique used, including the method of repair and theatre equipment used (e.g. types of anchor), were recorded on a standard form (see Appendix 5), as well as the size of the tear, the ease of repair and the completeness of the repair. If circumstances dictated that the allocated surgical technique could not be carried out then any alternative procedure was recorded.
Participating surgeons required a ‘minimum level of expertise’ for the types of surgery undertaken. Only consultant orthopaedic shoulder surgeons with a minimum of 2 years’ experience in consultant practice could participate. Surgeons had to perform a minimum of five cases per year. The participating surgeons represented a cross-section of high-, medium- and low-volume practitioners from both general hospitals and teaching hospitals. Because of the nature of the study’s NHS setting, some patients recruited to the UKUFF study had their surgery performed by non-UKUFF surgeons. The trial accepted data from patients who were recruited by a UKUFF surgeon but who went on to have their surgery performed by a colleague of the same or similar experience and position or by a supervised senior trainee. An assessment of the surgeons’ position and experience was made by the chief investigator. NIHR local research networks provided help with patient identification, recruitment and obtaining any required data from patient notes. Patient eligibility was confirmed by the local consultant orthopaedic surgeons.
Study population
Eligible patients were those for whom care had been provided by a participating surgeon and who were deemed suitable for rotator cuff repair surgery, with the surgeon uncertain which surgical procedure was better. In addition, patients had to be aged ≥ 50 years, have symptoms from a degenerative full-thickness rotator cuff tear and be able to give informed consent.
Study registration/consent to randomise
Recruitment of patients occurred through a two-step process. A patient’s eligibility was assessed by the local consultant orthopaedic surgeon, who introduced the trial to the patient using a prompt sheet and a patient assessment form. If the patient was interested in participating, the surgeon then provided the patient with a copy of the patient information sheet (see Appendix 6), which summarised what the study involved and answered any questions the patient might have.
If the patient was willing to enter the trial then an initial consent form was signed, which allowed the patient’s details to be forwarded to the central study office in Oxford. The office then issued to the participant, by post, an invitation letter, the comprehensive patient information sheet (see Appendix 6), a consent form and a baseline questionnaire (see Appendix 7) with a prepaid return envelope. Patients were encouraged to contact the office or their surgeon if they had any further questions or concerns. Patients who had not returned their questionnaire and consent form within a week were telephoned by a member of the study team in Oxford. This contact allowed the patient to ask questions about the study and permitted the team to assess whether the patient was still willing to participate. When the full consent form and baseline questionnaire had been returned to the Oxford office the patient then officially entered the trial and was randomised to one of the surgical options. A copy of the signed consent form was returned to the patient.
Randomisation was by computer allocation using the service provided by the Centre for Healthcare Randomised Trials (CHaRT) at the Health Services Research Unit, University of Aberdeen. Allocation was minimised using surgeon, age and size of tear. After randomisation the participant was considered irrevocably part of the trial for the purpose of the research, irrespective of what occurred subsequently.
Outcomes
The primary outcome measure was the Oxford Shoulder Score (OSS)62 completed at 24 months after randomisation. The OSS is a 12-item shoulder-specific PROM that was developed, with patients, for the assessment of shoulder pain and function in the context of shoulder surgery, particularly in trials. Items refer to the past 4 weeks and each offers five ordinal response options. Originally, these were scored from 1 to 5 (5 = most severe) and then summed to produce a summary score ranging from 12 to 60. Subsequently, the recommended method of scoring was changed. 63 Under the new system, each item on the OSS is scored from 0 to 4, with 4 representing the best outcome (i.e. the opposite direction from the original method of scoring). When the 12 items are summed, this produces an overall score ranging from 0 to 48, with 48 being the best outcome. The OSS has been demonstrated to be reliable, valid, responsive and very acceptable to patients.
The primary measure of cost-effectiveness was the incremental cost per quality-adjusted life-year (QALY).
The secondary outcome measures were used to further assess functional outcome and patient health-related quality of life. These assessed a range of symptoms often experienced with rotator cuff tears, for example pain, weakness and loss of function. These included:
-
Shoulder Pain and Disability Index (SPADI)64 at 8, 12 and 24 months after randomisation. The SPADI is a self-administered questionnaire, developed by a panel of rheumatologists and a physiotherapist, to measure shoulder pain and disability in an outpatient setting. 64 It contains 13 items that assess two domains: shoulder pain (five items) and disability (eight items), all with reference to the last week. The original version scored each item on a visual analogue scale (VAS). A second version, used in this trial, replaced the VAS with a 0–10 numerical rating scale. 65 Item responses within each subscale are summed and transformed to a score out of 100. A mean is taken of the two subscales to give a total score out of 100, with a higher score indicating greater impairment or disability. The SPADI is reliable, valid and responsive. 64
-
Mental Health Inventory 5 (MHI-5)66 at 8, 12 and 24 months after randomisation. The MHI-5 is the mental health subscale of the Short Form questionnaire-36 items (SF-36) generic health status measure. 67 It contains five items that address anxiety, depression, loss of behavioural or emotional control and psychological well-being, all with reference to the past 4 weeks. Each item offers responses on a 6-point scale (ranging from ‘all of the time’ to ‘none of the time’). The total score is calculated by reversing the answers to two items (the third and fifth), summing the scores, and transforming the raw scores to a scale ranging from 0 to 100. A higher score indicates better mental health. The MHI-5 has been demonstrated to be good at detecting major depression, affective disorders generally and anxiety disorders. 66
-
European Quality of Life-5 Dimensions three levels (EQ-5D-3L)65,68 at 8, 12 and 24 months after randomisation. The EQ-5D-3L is a standardised generic instrument for use as a self-completed measure of health outcome. It provides a simple descriptive profile and a single index value for health status that can be used in the clinical and economic evaluation of health care, as well as population health surveys, and consists of five items on mobility, self-care, pain, usual activities and psychological status, with three possible answers for each item (1 = no problem, 2 = moderate problem, 3 = severe problem). The response for each item/domain is converted to a quality-of-life estimate using an algorithm (see Chapter 6 for further details) to produce an index score for each patient. Negative scores represent health states worse than death, 0 represents the state of worst health and 1.00 represents full health.
-
The OSS62 completed at 8 and 12 months after randomisation.
-
Participants’ view of the overall state of their shoulder compared with an earlier time point (‘transition item’) at 8, 12 and 24 months after randomisation. There were five possible responses to this item: ‘much better’, ‘slightly better’, ‘no change’, ‘slightly worse’ or ‘much worse’.
-
Participants’ rating of how pleased they were with their shoulder symptoms at 12 and 24 months after randomisation. There were four possible responses to this item: ‘very pleased’, ‘fairly pleased’, ‘not very pleased’ or ‘very disappointed’.
-
Surgical complications (intra- and postoperative) at 2 and 8 weeks post surgery and at 12 and 24 months after randomisation.
-
12-month postoperative imaging.
Data collection
Outcome assessment was conducted using questionnaires that participants self-completed and, as such, interviewer bias and clinical rater bias were avoided. This form of outcome measurement has consistently performed well compared to clinician-based assessments and general health status measures. All participants, including those who had withdrawn from their allocated intervention but who still wished to be involved in the study, were followed up, with analysis based on the intention-to-treat (ITT) principle.
Participants received questionnaires at the following time points:
-
baseline (see Appendix 7) – questionnaire completed before randomisation
-
2 and 8 weeks post treatment (see Appendix 8) – questionnaire completed by telephone
-
8, 12 and 24 months post randomisation (see Appendix 9) – questionnaire completed by post.
The baseline and 12 and 24 months’ post-randomisation questionnaires also incorporated a section that measured cost-effectiveness. This included questions relating to primary care consultations, other consultations, out-of-pocket costs and the work impact of the intervention received.
The study team based at the Health Services Research Unit, University of Aberdeen, contacted participants whose questionnaires had not been returned. In the first instance this was through a reminder letter by post or e-mail, depending on participant preference. If a questionnaire had still not been returned within the specified time frame, the study team telephoned the participant and addressed any administrative issues that may have arisen, such as change of address or loss of questionnaire. If any clinical issues were identified, the study team in Oxford contacted participants, if appropriate, and addressed these issues. The time period allocated to the follow-up checks depended on which outcome assessment was involved.
Magnetic resonance imaging and ultrasound scans
Postoperative imaging was performed on patients who had undergone a repair. It was not performed if a repair was either impossible to perform or when no tear was found. Both the MRI and the ultrasound scans were undertaken locally to the participant and were arranged by the study office in Oxford, at a time agreed by the trust and the participant. The scans were collected centrally. The MRI scans were reported by an independent consultant radiologist who was blinded to the type of surgery that was performed. Because of the operator-dependent nature of the ultrasound scans, an independent report on these was not valid. The report obtained from the site was used to determine the tear status. Any re-tears were not reported to the participating surgeons, so that no deviation occurred from their normal practice.
Statistical analysis of outcomes
Statistical analyses were based on all people randomised, irrespective of subsequent compliance with the randomised intervention. The principal comparison was all those allocated arthroscopic surgery compared with all those allocated open surgery. When an effect size is shown for the intervention, a negative sign on the effect size indicates that an open procedure is favoured over an arthroscopic procedure.
Reflecting the possible clustering in the data, the outcomes were compared using repeated-measures mixed models with centre as a random effect and with adjustment for minimisation variables (size of tear and age) and participant baseline values (when available) as fixed effects. Statistical significance was at the 5% level, with corresponding confidence intervals (CIs) derived. All participants remained in their allocated group for analysis (ITT).
Preplanned subgroup analyses on the primary outcome included exploration of tear size (small/medium vs. large/massive) and age (≤ 65 years vs. > 65 years); these analyses were conducted by including a subgroup by treatment interaction term in the primary outcome model described above. Conservative levels of statistical significance (p < 0.01) were sought, reflecting the exploratory nature of these subgroup analyses.
Non-response analysis
Descriptive data comparing the baseline characteristics of participants who did and did not respond at 24 months were displayed. The t-test (continuous outcomes) and chi-squared test (dichotomous outcomes) were used to estimate the statistical significance of the differences between responders and non-responders.
Sensitivity analysis: treatment received (per protocol)
Reflecting the level of non-compliance, the effect on the primary outcome of those participants who actually received an arthroscopic or open repair was estimated. In an open trial design a per-protocol analysis can have substantial selection bias. To minimise the effects of selection bias we used the instrumental variable approach as described by Nagelkerke et al. 69 The method used a two-stage least-squares approach whereby treatment randomised was regressed onto treatment received and the residuals from that model were used as an independent variable in a second model, together with the treatment received, to estimate the effects on the primary outcome measure. As with the ITT analysis, the model also adjusted for centre, minimisation variables (age, size of tear) and baseline OSS score.
Learning curve
The main analyses adjusted for centre effects and therefore adjusted for the majority of differences between centres. Learning effects may, however, be present in the trial (i.e. the surgeon’s performance improves throughout the trial). To test for these effects a covariate for each surgeon was developed that indicates the increasing surgeon experience in the trial (e.g. first patient randomised = 1; second = 2, etc.). This covariate was used in subsequent adjusted analyses to measure the size of the trend in effects over time.
Health economics methods
A cost-effectiveness analysis was performed. A simple patient cost-related questionnaire was sent out at baseline and at 12 and 24 months post randomisation to obtain information on primary care consultations, other consultations, out-of pocket costs, the work impact of the intervention received and return to work (when relevant). Although longer intervals between questionnaires may result in recall errors (in particular under-reporting of health-care use70) more frequent data collection can result in a higher proportion of missing responses, which introduces uncertainty. It has been argued that there is no optimal interval for self-reported data collection70 and as such the timing of questionnaire distribution was chosen to coincide with those for the clinical study outcomes. Unit costs came from national sources and participating hospitals. The patient questionnaire was also used to administer the European Quality of Life-5 Dimensions (EQ-5D), which was obtained at baseline. The main health economic outcome was within-trial and extrapolated QALYs, estimated using the EQ-5D. 71
Incremental cost-effectiveness was calculated as the net cost per QALY gained for arthroscopic surgery compared with open surgery. Power calculations (see following section) were based on clinical effectiveness rather than cost-effectiveness outcomes, which were estimated rather than used in hypothesis testing. Cost-effectiveness ratios and acceptability curves were calculated.
An important component of this trial was the assessment of cost. Therefore, obtaining an accurate record of procedures at each of the proposed centres was essential. To evaluate the costs of each type of surgery, information was collected from the operating theatres. Resources used, equipment costs and standard procedures for rotator cuff repairs were examined. Per-case information was also analysed. A checklist of equipment, consumables, implants, time and staff utilised during each case was completed by theatre staff. Information from theatres was collected by the Oxford office and used in a cost comparison of the arthroscopic and open surgery approaches.
Sample size
In the original UKUFF trial, with three randomised strata, the sample size was constructed to detect a difference in the OSS 24-month postoperative score of 0.38 of a standard deviation (SD) for the comparison between arthroscopic surgery and open surgery at 80% power. We did not propose any amendment to that clinically important difference in the reconfigured study. This defined difference was based on our experience of developing the OSS score and using it in a variety of settings; a 3-point score difference (0.33 of a SD) was deemed a clinically important difference. In the original UKUFF trial, the detectable difference of 0.38 was constructed by combining evidence from a direct randomised comparison with indirect (non-randomised) comparison data from the other strata. Incorporating indirect effects is a suboptimal approach to measuring effectiveness because unmeasured confounders can bias the outcomes. The proposed change in this proposal was to achieve the detectable difference of 0.38 of a SD by direct randomised comparison data only at 85% power. As described earlier, such an approach was feasible by 2010 because of the increased number of surgeons in equipoise between the arthroscopic approach and the open approach.
Attrition was expected to be low (10%), as were the effects of clustering of outcomes by surgeon [intracluster correlation (ICC) < 0.03]. 72,73 Although we did not have a direct estimate from a shoulder trial, other orthopaedic data sets available to our team support this low ICC estimate. Both of these factors required the sample size to be inflated; however, the primary analysis adjusted for baseline OSS score, which conversely allowed the sample size to be decreased by a factor of (1 – correlation squared). 74 Our previous studies showed that the correlation in the OSS score pre surgery to 6 months post surgery in patients similar to the potential trial participants was 0.57. Assuming a conservative correlation of 0.5 implied that the sample size could be reduced by 25% and still maintain the same power. Therefore, a study with a total of 267 participants would still have 85% power to detect a clinically important difference in each comparison, assuming that attrition and clustering accounted for approximately 25% of variation in the data.
Data monitoring
An independent DMC met on four occasions and did not recommend any fundamental changes to the protocol. The decision in 2009 to reconfigure the trial was made by the NIHR HTA programme. The committee did not meet after recruitment was completed.
Chapter 3 Description of the study population
This chapter describes the derivation of the populations that took part in the UKUFF study, the characteristics of the participants at presurgical assessment and the baseline characteristics of included participants.
Recruitment to the study
Participants were recruited in 47 clinical centres, all within the UK (Table 3). Nineteen centres recruited to the randomised arthroscopic surgery and randomised open surgery comparison (referred to as the stratum A comparison). Thirteen of these centres also randomised participants to stratum A prior to reconfiguration of the study in December 2010 (see Chapter 2). Twenty centres recruited to stratum B (arthroscopic surgery vs. rest then exercise) and 18 to stratum C (open surgery vs. rest then exercise). A total of 660 participants were recruited to the study, with 317 in stratum A (n = 136, allocated to arthroscopic surgery; n = 137, allocated to open surgery; and n = 44, allocated to rest then exercise prior to reconfiguration), 181 in stratum B (n = 91, allocated to arthroscopic surgery; and n = 90, allocated to rest then exercise prior to reconfiguration) and 162 in stratum C (n = 82, allocated to open surgery; and n = 80, allocated to rest then exercise prior to reconfiguration). Table 3 shows recruitment by centre. No centre contributed more than 12% of participants to stratum A. Recruitment to the trial began on 9 November 2007 and continued until 28 February 2012, although not all centres enrolled over the total period because of the staggered introduction of centres and early closure for reconfiguration of the study (range 6 months to 39 months from first to last participant randomised in stratum A). Data were closed to follow-up on 31 December 2013.
| Centre | Stratum A, n (%) | Stratum B, n (%) | Stratum C, n (%) | Total (n = 660) | Randomised to stratum A prior to reconfiguration | Length of time randomising to stratum A | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Arthroscopic (n = 136) | Open (n = 137) | Rest then exercise (n = 44) | Arthroscopic (n = 91) | Rest then exercise (n = 90) | Open (n = 82) | Rest then exercise (n = 80) | ||||
| University Hospitals of Leicester NHS Trust | 16 (11.8) | 17 (12.4) | 4 (9.1) | 4 (4.9) | 3 (3.8) | 44 (6.67) | Yes | 3 years 0 months | ||
| Worcestershire Acute Hospitals NHS Trust | 16 (11.8) | 16 (11.7) | 4 (9.1) | 36 (5.45) | Yes | 2 years 8 months | ||||
| Gwent Healthcare NHS Trust | 13 (9.6) | 13 (9.5) | 5 (11.4) | 31 (4.70) | Yes | 3 years 3 months | ||||
| Nuffield Orthopaedic Centre | 15 (11.0) | 15 (10.9) | 18 (22.0) | 18 (22.5) | 66 (10.00) | No | 1 years 4 months | |||
| Ipswich Hospital NHS Trust | 12 (8.8) | 13 (9.5) | 4 (9.1) | 29 (4.39) | Yes | 2 years 11 months | ||||
| University Hospitals Coventry and Warwickshire NHS Trust | 8 (5.9) | 9 (6.6) | 7 (15.9) | 3 (3.7) | 4 (5.0) | 31 (4.70) | Yes | 2 years 11 months | ||
| South Tees Hospitals NHS Foundation Trust | 9 (6.6) | 8 (5.8) | 4 (9.1) | 21 (3.18) | Yes | 2 years 9 months | ||||
| Robert Jones and Agnes Hunt Orthopaedic and District Hospital NHS Foundation Trust | 7 (5.1) | 6 (4.4) | 6 (13.6) | 1 (1.1) | 1 (1.2) | 2 (2.5) | 23 (3.48) | Yes | 2 years 7 months | |
| Maidstone and Tunbridge Wells NHS Trust | 8 (5.9) | 8 (5.8) | 2 (4.5) | 18 (2.73) | Yes | 2 years 2 months | ||||
| Surrey and Sussex Healthcare NHS Trust | 8 (5.9) | 9 (6.6) | 11 (12.1) | 10 (11.1) | 38 (5.76) | No | 1 years 3 months | |||
| Dudley Group NHS Foundation Trust | 7 (5.1) | 6 (4.4) | 3 (6.8) | 16 (2.42) | Yes | 2 years 5 months | ||||
| Pennine Acute Hospitals NHS Trust | 4 (2.9) | 4 (2.9) | 2 (4.5) | 10 (1.52) | Yes | 2 years 8 months | ||||
| Swansea NHS Trust | 3 (2.2) | 5 (3.6) | 2 (4.5) | 10 (1.52) | Yes | 3 years 3 months | ||||
| University Hospital Southampton NHS Foundation Trust | 3 (2.2) | 4 (2.9) | 8 (9.8) | 8 (10.0) | 23 (3.48) | No | 0 years 2 months | |||
| North Bristol NHS Trust | 2 (1.5) | 1 (0.7) | 1 (2.3) | 4 (0.61) | Yes | 0 years 11 months | ||||
| East Lancashire Hospitals NHS Trust | 2 (1.5) | 1 (0.7) | 1 (1.1) | 4 (0.61) | No | 1 years 2 months | ||||
| Barnet and Chase Farm NHS Trust | 1 (0.7) | 1 (0.7) | 1 (1.1) | 1 (1.1) | 4 (0.61) | No | 0 years 6 months | |||
| Basingstoke and North Hampshire Hospitals NHS Trust | 1 (0.7) | 1 (0.7) | 1 (1.1) | 3 (0.45) | Yes | 1 years 1 months | ||||
| Sheffield Teaching Hospitals NHS Foundation Trust | 1 (0.7) | 1 (0.15) | No | 0 years 1 months | ||||||
| Basildon and Thurrock University Hospitals NHS Foundation Trust | 5 (6.1) | 4 (5.0) | 9 (1.36) | No | NA | |||||
| Buckinghamshire Healthcare NHS Trust | 6 (6.6) | 6 (6.7) | 12 (1.82) | No | NA | |||||
| Derby Teaching Hospitals NHS Foundation Trust | 3 (3.3) | 5 (5.6) | 8 (1.21) | No | NA | |||||
| Epsom and St Helier University Hospitals NHS Trust | 15 (16.5) | 15 (16.7) | 30 (4.55) | No | NA | |||||
| Forth Valley Acute Operating Division | 2 (2.4) | 2 (2.5) | 4 (0.61) | No | NA | |||||
| Frimley Park Hospital NHS Foundation Trust | 1 (1.1) | 1 (1.1) | 2 (0.30) | No | NA | |||||
| Guy’s and St Thomas’ NHS Foundation Trust | 1 (1.1) | 2 (2.2) | 3 (0.45) | No | NA | |||||
| Heatherwood and Wexham Park Hospitals NHS Foundation Trust | 2 (2.4) | 2 (2.5) | 4 (0.61) | No | NA | |||||
| Hereford Hospitals NHS Trust | 5 (6.1) | 4 (5.0) | 9 (1.36) | No | NA | |||||
| Lancashire Teaching Hospitals NHS Trust | 1 (1.1) | 1 (1.1) | 2 (0.30) | No | NA | |||||
| Lothian University Hospitals Division | 8 (8.8) | 9 (10.0) | 17 (2.58) | No | NA | |||||
| Mid Essex Hospital Services NHS Trust | 2 (2.4) | 1 (1.3) | 3 (0.45) | No | NA | |||||
| Mid Staffordshire General Hospitals NHS Trust | 2 (2.4) | 2 (2.5) | 4 (0.61) | No | NA | |||||
| Mid Yorkshire Hospitals NHS Trust | 5 (5.5) | 5 (5.6) | 10 (1.52) | No | NA | |||||
| Milton Keynes Hospital NHS Foundation Trust | 2 (2.4) | 1 (1.3) | 3 (0.45) | No | NA | |||||
| Norfolk and Norwich University Hospitals NHS Foundation Trust | 5 (6.1) | 6 (7.5) | 11 (1.67) | No | NA | |||||
| North Cumbria Acute Hospitals NHS Trust | 4 (4.9) | 4 (5.0) | 8 (1.21) | No | NA | |||||
| Plymouth Hospitals NHS Trust | 3 (3.7) | 3 (3.8) | 6 (0.91) | No | NA | |||||
| Queen Elizabeth Hospital NHS Trust | 1 (1.1) | 1 (0.15) | No | NA | ||||||
| Royal Berkshire NHS Foundation Trust | 5 (5.5) | 4 (4.4) | 9 (1.36) | No | NA | |||||
| Royal Devon and Exeter NHS Foundation Trust | 3 (3.7) | 3 (3.8) | 6 (0.91) | No | NA | |||||
| Royal Free Hampstead NHS Trust | 4 (4.4) | 3 (3.3) | 7 (1.06) | No | NA | |||||
| Salford Royal NHS Foundation Trust | 4 (4.4) | 4 (4.4) | 8 (1.21) | No | NA | |||||
| South Devon Healthcare NHS Foundation Trust | 8 (9.8) | 8 (10.0) | 16 (2.42) | No | NA | |||||
| St George’s Healthcare NHS Trust | 5 (5.5) | 4 (4.4) | 9 (1.36) | No | NA | |||||
| Stockport NHS Foundation Trust | 2 (2.2) | 2 (2.2) | 4 (0.61) | No | NA | |||||
| Trafford Healthcare NHS Trust | 16 (17.6) | 17 (18.9) | 33 (5.00) | No | NA | |||||
| Yeovil District Hospital NHS Foundation Trust | 5 (6.1) | 5 (6.3) | 10 (1.52) | No | NA | |||||
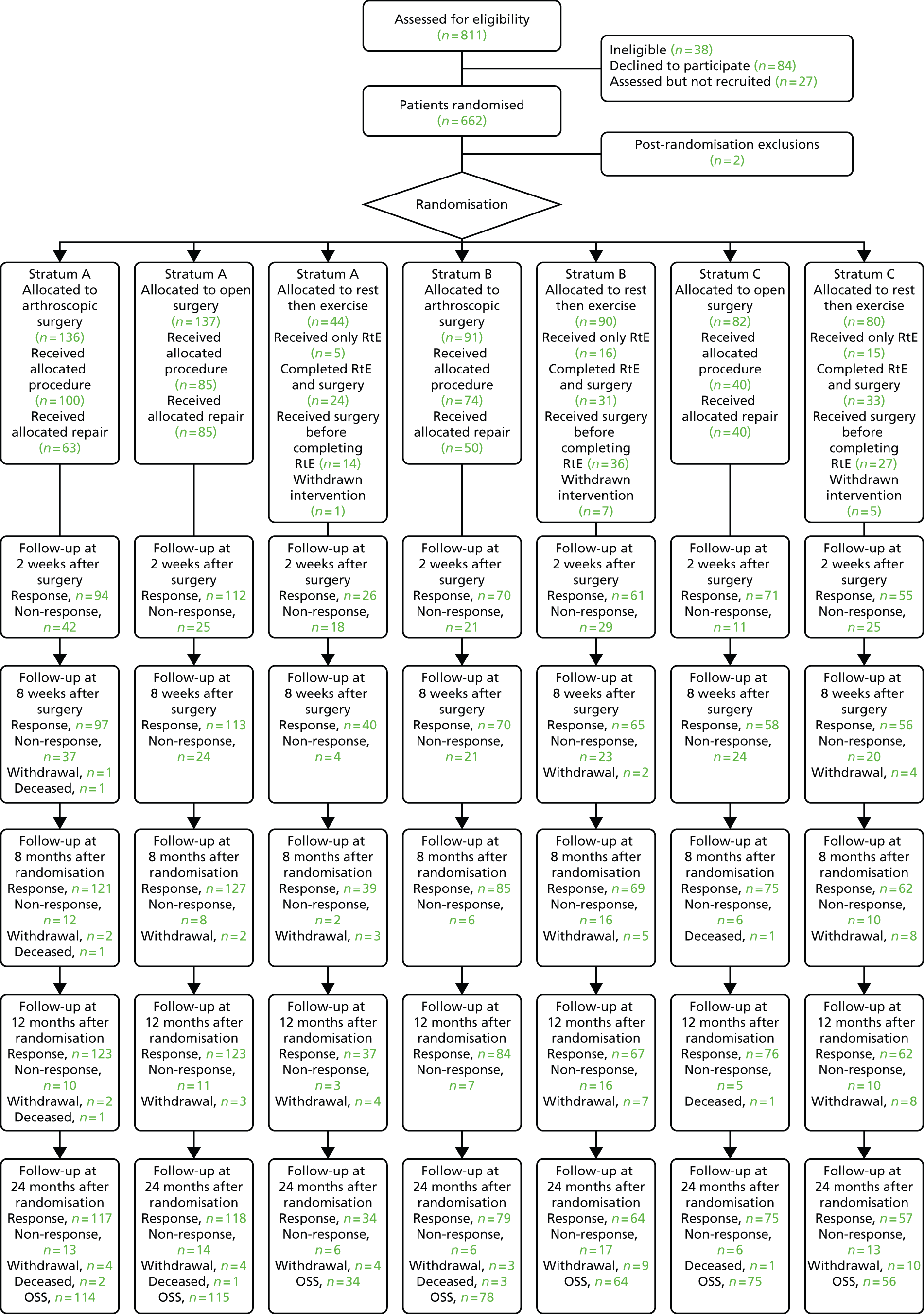
Study conduct
The derivation of the main study groups and their progress through the stages of follow-up in the trial is shown in Figure 1 This is in the form of a Consolidated Standards of Reporting Trials (CONSORT) flow diagram. In total, 811 patients were considered for trial entry and 38 (5%) of these were found not to meet one or more of the eligibility criteria. Of the 111 patients eligible for the study but not recruited, 84 declined to participate and the remaining 27 could not be randomised while the study underwent reconfiguration (because of the requirement for new research ethics and research and development approvals). Two participants were excluded post randomisation because each had received previous surgery prior to randomisation. Details of the clinical management actually received are provided in Chapter 4. The median [interquartile range (IQR)] time intervals in days between randomisation by the trial office and each subsequent follow-up are shown in Table 4; all were similar between groups, as would be expected. The 2-week and 8-week follow-ups were timed to occur at 2 weeks and 8 weeks after surgery. Table 5 illustrates the success of this strategy in the subgroup of participants who did receive a surgical procedure.
FIGURE 1.
Consolidated Standards of Reporting Trials (CONSORT) diagram. RtE, rest then exercise.
| Follow-up | Stratum A | Stratum B | Stratum C | ||||
|---|---|---|---|---|---|---|---|
| Arthroscopic (n = 136) | Open (n = 137) | Rest then exercise (n = 44) | Arthroscopic (n = 91) | Rest then exercise (n = 90) | Open (n = 82) | Rest then exercise (n = 80) | |
| 2 weeks | 99 (65–137) | 97 (65–134) | 93 (63–126) | 82 (62–108) | 99 (65–126) | 87 (60–129) | 101 (75–126) |
| 8 weeks | 135 (105–169) | 139 (102–178) | 149 (114–181) | 126 (106–152) | 134 (110–162) | 142 (107–177) | 141 (113–167) |
| 8 months | 231 (227–248) | 230 (227–236) | 232 (228–244) | 231 (227–248) | 232 (227–245) | 229 (227–239) | 234 (228–246) |
| 12 months | 374 (369–387) | 373 (369–383) | 371 (369–389) | 374 (370–383) | 375 (369–389) | 371 (368–378) | 372 (369–386) |
| 24 months | 737 (733–745) | 736 (733–745) | 740 (734–754) | 738 (734–754) | 739 (733–754) | 736 (734–752) | 736 (733–746) |
| Follow-up | Stratum A | Stratum B | Stratum C | |
|---|---|---|---|---|
| Arthroscopic (n = 100) | Open (n = 114) | Arthroscopic (n = 74) | Open (n = 68) | |
| 2 weeks | 14 (14–16) | 14 (14–15) | 14 (14–16) | 14 (14–15) |
| 8 weeks | 56 (56–59) | 56 (56–58) | 57 (56–61) | 57 (56–60) |
| 8 months | 161 (117–194) | 155 (122–188) | 169 (147–201) | 164 (122–197) |
| 12 months | 307 (258–336) | 296 (262–335) | 316 (292–342) | 306 (259–333) |
| 24 months | 656 (620–693) | 654 (622–699) | 682 (647–708) | 672 (623–712) |
The overall rates of return of follow-up questionnaires at 8, 12 and 24 months were equivalent to > 85% of the study participants allocated to surgery (see Figure 1). There were no substantive differences in response rates between the surgery groups. Seven participants are known to have died by the end of the 2-year follow-up. There was no evidence that these deaths were linked to trial participation.
Description of the groups at trial entry
Clinical assessment at baseline
Table 6 displays the results of the presurgical assessment at recruitment. Approximately two-thirds of the tears were diagnosed using ultrasound. Tears were small or medium in about 75% of the participants in strata A and C and in 58% of participants in stratum B. Within the randomised groups there were no apparent imbalances. Around 10% of participants had received no previous treatment to their shoulder. Previous treatments primarily included physiotherapy and/or cortisone injections.
| Assessment | Stratum A, n (%) | Stratum B, n (%) | Stratum C, n (%) | ||||
|---|---|---|---|---|---|---|---|
| Arthroscopic (n = 136) | Open (n = 137) | Rest then exercise (n = 44) | Arthroscopic (n = 91) | Rest then exercise (n = 90) | Open (n = 82) | Rest then exercise (n = 80) | |
| Size of tear | |||||||
| Small/medium | 103 (75.7) | 103 (75.2) | 34 (77.3) | 53 (58.2) | 52 (57.8) | 62 (75.6) | 62 (77.5) |
| Large/massive | 33 (24.3) | 34 (24.8) | 10 (22.7) | 38 (41.8) | 38 (42.2) | 20 (24.4) | 18 (22.5) |
| Method of diagnosing tear | |||||||
| MRI | 41 (30.1) | 36 (26.3) | 9 (20.5) | 20 (22.0) | 20 (22.2) | 19 (23.2) | 12 (15.0) |
| Ultrasound | 87 (64.0) | 93 (67.9) | 32 (72.7) | 64 (70.3) | 60 (66.7) | 60 (73.2) | 56 (70.0) |
| Missing | 8 (5.9) | 8 (5.8) | 3 (6.8) | 7 (7.7) | 10 (11.1) | 3 (3.7) | 12 ( 15.0) |
| Received no treatment on shoulder in the last 5 years | 15 (11.0) | 10 (7.3) | 2 (4.5) | 9 (9.9) | 9 (10.0) | 3 (3.7) | 8 (10.0) |
| Received physiotherapy on affected shoulder in the last 5 years | |||||||
| Yes | 77 (56.6) | 83 (60.6) | 28 (63.6) | 54 (59.3) | 64 (71.1) | 59 (72.0) | 49 (61.3) |
| No | 41 (30.1) | 38 (27.7) | 10 (22.7) | 22 (24.2) | 21 (23.3) | 12 (14.6) | 23 (28.8) |
| Missing | 18 (13.2) | 16 (11.7) | 6 (13.6) | 15 (16.5) | 5 (5.6) | 11 (13.4) | 8 (10.0) |
| Duration of physiotherapy (weeks) | |||||||
| ≤ 4 | 17 (22.1) | 20 (24.1) | 7 (25.0) | 10 (11.0) | 13 (20.3) | 16 (27.1) | 10 (20.4) |
| 5–12 | 24 (31.2) | 22 (26.5) | 11 (39.3) | 15 (16.5) | 18 (28.1) | 17 (28.8) | 13 (26.5) |
| > 12 | 19 (24.7) | 21 (25.3) | 8 (28.6) | 21 (23.1) | 19 (29.7) | 16 (27.1) | 13 (26.5) |
| Missing | 17 (22.1) | 20 (24.1) | 2 (7.1) | 45 (49.5) | 14 (21.9) | 10 (16.9) | 13 (26.5) |
| Received an injection in affected shoulder in the last 5 years | |||||||
| Yes | 79 (58.1) | 83 (60.6) | 30 (68.2) | 52 (57.1) | 46 (51.1) | 59 (72.0) | 53 (66.3) |
| No | 40 (29.4) | 35 (25.5) | 9 (20.5) | 25 (27.5) | 34 (37.8) | 14 (17.1) | 21 (26.3) |
| Missing | 17 (12.5) | 19 (13.9) | 5 (11.4) | 14 (15.4) | 10 (11.1) | 9 (11.0) | 6 (7.5) |
| Number of injections | |||||||
| 1 | 34 (43.0) | 35 (42.2) | 14 (46.7) | 26 (50.0) | 24 (52.2) | 25 (42.4) | 21 (39.6) |
| 2 | 21 (26.6) | 29 (34.9) | 8 (26.7) | 13 (25.0) | 10 (21.7) | 17 (28.8) | 16 (30.2) |
| 3 | 10 (12.7) | 10 (12.0) | 4 (13.3) | 9 (17.3) | 5 (10.9) | 8 (13.6) | 6 (11.3) |
| 4 | 3 (3.8) | 2 (2.4) | 1 (1.9) | 2 (4.3) | 2 (3.4) | 3 (5.7) | |
| 5 | 2 (2.5) | 1 (1.2) | 1 (3.3) | 2 (3.4) | 1 (1.9) | ||
| 6 | 1 (1.3) | 3 (3.6) | 1 (1.9) | 1 (2.2) | 1 (1.9) | ||
| 7 | 1 (1.3) | 1 (1.7) | 1 (1.9) | ||||
| 9 | 1 (1.7) | ||||||
| 10 | 1 (1.9) | ||||||
| Missing | 7 (8.9) | 3 (3.6) | 3 (10.0) | 1 (1.9) | 4 (8.7) | 3 (5.1) | 4 (7.5) |
| Received other treatment on the affected shoulder in the last 5 years | |||||||
| Yes | 18 (13.2) | 28 (20.4) | 5 (11.4) | 5 (5.5) | 2 (2.2) | 16 (19.5) | 13 (16.3) |
| No | 72 (52.9) | 61 (44.5) | 20 (45.5) | 43 (47.3) | 48 (53.3) | 36 (43.9) | 32 (40.0) |
| Missing | 46 (33.8) | 48 (35.0) | 19 (43.2) | 43 (47.3) | 40 (44.4) | 30 (36.6) | 35 (43.8) |
| Other treatment | |||||||
| Acupuncture | 2 (11.1) | 5 (17.9) | 3 (60.0) | 3 (60.0) | 5 (31.3) | 5 (38.5) | |
| Analgesics | 6 (33.3) | 13 (46.4) | 1 (20.0) | 1 (6.3) | |||
| Chiropractor | 3 (16.7) | 2 (7.1) | 1 (20.0) | 5 (31.3) | 2 (15.4) | ||
| Exercises | 2 (7.1) | 1 (50.0) | |||||
| Hydrotherapy | 2 (11.1) | ||||||
| Massage | 1 (6.3) | ||||||
| Nerve block | 1 (5.6) | ||||||
| Osteopathy | 1 (3.6) | 1 (50.0) | 1 (6.3) | 2 (15.4) | |||
| TENS | 1 (5.6) | 2 (7.1) | 1 (20.0) | 1 (6.3) | |||
| Ultrasound | 1 (3.6) | 3 (23.1) | |||||
| Missing | 3 (16.7) | 2 (7.1) | 1 (20.0) | 2 (12.5) | 1 (7.7) | ||
| Are there any problems with other shoulder? | |||||||
| No problems | 84 (61.8) | 86 (62.8) | 27 (61.4) | 49 (53.8) | 64 (71.1) | 47 (57.3) | 49 (61.3) |
| Mild problems | 32 (23.5) | 29 (21.2) | 9 (20.5) | 24 (26.4) | 11 (12.2) | 23 (28.0) | 22 (27.5) |
| Moderate problems | 11 (8.1) | 12 (8.8) | 3 (6.8) | 14 (15.4) | 11 (12.2) | 9 (11.0) | 7 (8.8) |
| Severe problems | 4 (2.9) | 5 (3.6) | 2 (4.5) | 2 (2.2) | 3 (3.3) | 1 (1.2) | |
| Missing | 5 (3.7) | 5 (3.6) | 3 (6.8) | 2 (2.2) | 1 (1.1) | 2 (2.4) | 2 (2.5) |
Participant and sociodemographic factors
Participant and sociodemographic characteristics are shown in Table 7. The average age of the participants was 63 years, 40% were female and 90% were right-handed. The mean period of time that the participants reported having the shoulder problem prior to surgery was approximately 2.5 years; however, the mean was driven by a few extreme values in each group relating to participants who had had shoulder problems for decades. The median (IQR) time that the participants had had the shoulder problem prior to recruitment was 1.2 (0.7–2.5) years. There were no substantive differences within or between strata on any of the sociodemographic factors.
| Characteristic | Stratum A, n (%) | Stratum B, n (%) | Stratum C, n (%) | ||||
|---|---|---|---|---|---|---|---|
| Arthroscopic (n = 136) | Open (n = 137) | Rest then exercise (n = 44) | Arthroscopic (n = 91) | Rest then exercise (n = 90) | Open (n = 82) | Rest then exercise (n = 80) | |
| Age (years), n, mean (SD) | 136, 62.9 (7.1) | 137, 62.9 (7.5) | 44, 62.9 (7.5) | 91, 65.7 (7.9) | 90, 64.7 (8.0) | 82, 61.9 (6.5) | 80, 61.3 (6.8) |
| Years with shoulder problem, n, mean (SD) | 136, 2.6 (5.3) | 137, 2.5 (4.1) | 43, 2.0 (2.7) | 90, 2.5 (3.4) | 87, 2.2 (3.3) | 82, 2.7 (4.7) | 79, 2.3 (2.6) |
| Sex | |||||||
| Male | 81 (59.6) | 88 (64.2) | 28 (63.6) | 53 (58.2) | 63 (70.0) | 49 (59.8) | 51 (63.8) |
| Female | 55 (40.4) | 49 (35.8) | 16 (36.4) | 36 (39.6) | 27 (30.0) | 33 (40.2) | 29 (36.3) |
| Missing | 2 (2.2) | ||||||
| Handedness | |||||||
| Right-handed | 125 (91.9) | 115 (83.9) | 40 (90.9) | 83 (91.2) | 78 (86.7) | 66 (80.5) | 66 (82.5) |
| Left-handed | 7 (5.1) | 17 (12.4) | 1 (2.3) | 8 (8.8) | 9 (10.0) | 11 (13.4) | 8 (10.0) |
| Both | 4 (2.9) | 5 (3.6) | 2 (4.5) | 3 (3.3) | 4 (4.9) | 5 (6.3) | |
| Missing | 1 (2.3) | 1 (1.2) | 1 (1.3) | ||||
| Highest qualification | |||||||
| None | 63 (46.3) | 59 (43.1) | 23 (52.3) | 39 (42.9) | 37 (41.1) | 34 (41.5) | 25 (31.3) |
| Secondary | 41 (30.1) | 49 (35.8) | 16 (36.4) | 37 (40.7) | 38 (42.2) | 33 (40.2) | 41 (51.3) |
| Higher | 32 (23.5) | 27 (19.7) | 5 (11.4) | 12 (13.2) | 12 (13.3) | 15 (18.3) | 12 (15.0) |
| Missing | 2 (1.5) | 3 (3.3) | 3 (3.3) | 2 (2.5) | |||
| Housing tenure | |||||||
| Home owner | 107 (78.7) | 119 (86.9) | 34 (77.3) | 78 (85.7) | 78 (86.7) | 69 (84.1) | 68 (85.0) |
| Private rent | 7 (5.1) | 1 (0.7) | 3 (6.8) | 3 (3.3) | 2 (2.2) | 5 (6.1) | 4 (5.0) |
| Council rent | 17 (12.5) | 9 (6.6) | 5 (11.4) | 7 (7.7) | 7 (7.8) | 5 (6.1) | 2 (2.5) |
| Other | 4 (2.9) | 8 (5.8) | 2 (4.5) | 2 (2.2) | 2 (2.2) | 3 (3.7) | 5 (6.3) |
| Missing | 1 (0.7) | 1 (1.1) | 1 (1.1) | 1 (1.3) | |||
| Lives alone | |||||||
| Yes | 23 (16.9) | 12 (8.8) | 6 (13.6) | 15 (16.5) | 19 ( 21.1) | 14 (17.1) | 12 (15.0) |
| No | 101 (74.3) | 118 (86.1) | 34 (77.3) | 74 (81.3) | 67 (74.4) | 66 (80.5) | 64 (80.0) |
| Missing | 12 (8.8) | 7 (5.1) | 4 (9.1) | 2 (2.2) | 4 (4.4) | 2 (2.4) | 4 (5.0) |
| Employment status | |||||||
| Full-time | 47 (34.6) | 58 (42.3) | 12 (27.3) | 22 (24.2) | 30 (33.3) | 28 (34.1) | 35 (43.8) |
| Part-time | 18 (13.2) | 15 (10.9) | 7 (15.9) | 13 (14.3) | 10 (11.1) | 13 (15.9) | 8 (10.0) |
| Homemaker | 4 (2.9) | 5 (3.6) | 3 (3.3) | 2 (2.4) | |||
| Retired | 59 (43.4) | 54 (39.4) | 22 (50.0) | 52 (57.1) | 45 (50.0) | 36 (43.9) | 32 (40.0) |
| Unemployed | 7 (5.1) | 4 (2.9) | 3 (6.8) | 1 (1.1) | 5 (5.6) | 3 (3.7) | 4 (5.0) |
| Missing | 1 (0.7) | 1 (0.7) | 1 (1.3) | ||||
| Type of work | |||||||
| Manual | 36 (55.4) | 41 (56.2) | 12 (63.2) | 22 (62.9) | 27 (67.5) | 24 (58.5) | 24 (55.8) |
| Non-manual | 26 (40.0) | 28 (38.4) | 6 (31.6) | 12 (34.3) | 11 (27.5) | 16 (39.0) | 15 (34.9) |
| Not sure | 3 (4.6) | 3 (4.1) | 1 (5.3) | 1 (2.9) | 1 (2.5) | 1 (2.4) | 3 (7.0) |
| Missing | 1 (1.4) | 1 (2.5) | 1 (2.3) | ||||
| Off sick or working reduced duties | |||||||
| Yes, off sick | 7 (10.8) | 6 (8.2) | 3 (15.8) | 2 (5.7) | 5 (12.5) | 3 (7.3) | 4 (9.3) |
| Yes, working reduced duties | 10 (15.4) | 7 (9.6) | 5 (26.3) | 5 (14.3) | 8 (20.0) | 9 (22.0) | 8 (18.6) |
| No | 45 (69.2) | 58 (79.5) | 11 (57.9) | 28 ( 80.0) | 27 (67.5) | 29 (70.7) | 31 (72.1) |
| Missing | 3 (4.6) | 2 (2.8) | |||||
| Would you be able to do your job or everyday activities with your arm in a sling? | |||||||
| No | 70 (51.5) | 76 (55.5) | 18 (40.9) | 51 (56.0) | 48 (53.3) | 41 (50.0) | 43 (53.8) |
| Yes, with difficulty | 62 (45.6) | 59 (43.1) | 19 (43.2) | 39 (42.9) | 35 (38.9) | 39 (47.6) | 31 (38.8) |
| Yes, no difficulty | 3 (2.2) | 1 (0.7) | 4 (9.1) | 1 (1.1) | 2 (2.2) | 5 (6.3) | |
| Missing | 1 (0.7) | 1 (0.7) | 3 (6.8) | 5 (5.6) | 2 (2.4) | 1 (1.3) | |
Health status
The health-related quality-of-life measures are shown in Table 8. The mean OSS was approximately 26 across the groups. The EQ-5D, MHI-5 and SPADI measures were broadly similar across and within the strata.
| Measure | Stratum A, n, mean (SD) | Stratum B, n, mean (SD) | Stratum C, n, mean (SD) | ||||
|---|---|---|---|---|---|---|---|
| Arthroscopic (n = 136) | Open (n = 137) | Rest then exercise (n = 44) | Arthroscopic (n = 91) | Rest then exercise (n = 90) | Open (n = 82) | Rest then exercise (n = 80) | |
| OSS | 136, 26.2 (8.1) | 137, 25.2 (7.9) | 44, 23.7 (8.3) | 91, 25.3 (8.9) | 90, 23.5 (8.0) | 82, 25.9 (8.4) | 80, 26.2 (7.9) |
| SPADI | 136, 60.9 (22.0) | 136, 61.6 (22.0) | 44, 66.9 (22.1) | 91, 60.6 (23.1) | 90, 67.8 (20.4) | 82, 60.7 (20.1) | 79, 62.3 (20.1) |
| SPADI pain | 136, 70.0 (19.5) | 137, 70.1 (20.5) | 44, 73.0 (22.0) | 91, 70.0 (21.8) | 89, 73.1 (19.4) | 82, 69.6 (19.5) | 80, 69.4 (18.2) |
| SPADI disability | 136, 55.1 (25.0) | 135, 56.4 (24.7) | 44, 63.0 (23.7) | 91, 54.7 (25.9) | 90, 64.4 (22.1) | 82, 55.2 (21.9) | 77, 57.7 (23.3) |
| MHI-5 | 136, 22.5 (4.9) | 137, 22.9 (4.5) | 44, 21.5 (5.5) | 90, 22.4 (5.1) | 90, 22.7 (4.9) | 82, 22.1 (4.7) | 80, 22.9 (4.6) |
| EQ-5D | 135, 0.548 (0.299) | 136, 0.519 (0.291) | 43, 0.448 (0.332) | 91, 0.514 (0.326) | 89, 0.503 (0.287) | 81, 0.536 (0.287) | 79, 0.538 (0.298) |
Attitudes to surgery
As expected, there was variation in participants’ attitudes to undergoing surgery in general, but the variation was not different between groups (Table 9).
| Question | Stratum A, n (%) | Stratum B, n (%) | Stratum C, n (%) | ||||
|---|---|---|---|---|---|---|---|
| Arthroscopic (n = 136) | Open (n = 137) | Rest then exercise (n = 44) | Arthroscopic (n = 91) | Rest then exercise (n = 90) | Open (n = 82) | Rest then exercise (n = 80) | |
| To what extent do you agree that doctors rely on surgery too much? | |||||||
| Strongly agree | 2 (2.2) | ||||||
| Agree | 3 (2.2) | 3 (2.2) | 3 (6.8) | 6 (6.6) | 5 (5.6) | 1 (1.2) | 5 (6.3) |
| Uncertain | 52 (38.2) | 51 (37.2) | 26 (59.1) | 40 (44.0) | 35 (38.9) | 26 (31.7) | 29 (36.3) |
| Disagree | 72 (52.9) | 76 (55.5) | 13 (29.5) | 35 (38.5) | 42 (46.7) | 52 (63.4) | 39 (48.8) |
| Strongly disagree | 7 (5.1) | 4 (2.9) | 2 (4.5) | 7 (7.7) | 7 (7.8) | 2 (2.4) | 5 (6.3) |
| Missing | 2 (1.5) | 3 (2.2) | 1 (1.1) | 1 (1.1) | 1 (1.2) | 2 (2.5) | |
| To what extent do you agree that doctors place too much trust in surgery? | |||||||
| Strongly agree | 1 (0.7) | 1 (2.3) | 2 (2.2) | ||||
| Agree | 6 (4.4) | 4 (2.9) | 9 (20.5) | 9 (9.9) | 7 (7.8) | 1 (1.2) | 8 (10.0) |
| Uncertain | 66 (48.5) | 61 (44.5) | 22 (50.0) | 47 (51.6) | 35 (38.9) | 39 (47.6) | 33 (41.3) |
| Disagree | 54 (39.7) | 62 (45.3) | 11 (25.0) | 27 (29.7) | 43 (47.8) | 36 (43.9) | 33 (41.3) |
| Strongly disagree | 9 (6.6) | 5 (3.6) | 1 (2.3) | 5 (5.5) | 4 (4.4) | 3 (3.7) | 3 (3.8) |
| Missing | 1 (0.7) | 4 (2.9) | 1 (1.1) | 1 (1.1) | 3 (3.7) | 3 (3.8) | |
| To what extent do you agree that you worry about surgery risks? | |||||||
| Strongly agree | 5 (3.7) | 5 (3.6) | 3 (6.8) | 13 (14.3) | 12 (13.3) | 2 (2.4) | 4 (5.0) |
| Agree | 58 (42.6) | 51 (37.2) | 20 (45.5) | 37 (40.7) | 35 (38.9) | 30 (36.6) | 33 (41.3) |
| Uncertain | 21 (15.4) | 18 (13.1) | 8 (18.2) | 13 (14.3) | 14 (15.6) | 22 (26.8) | 16 (20.0) |
| Disagree | 43 (31.6) | 49 (35.8) | 12 (27.3) | 23 (25.3) | 23 (25.6) | 22 (26.8) | 20 (25.0) |
| Strongly disagree | 8 (5.9) | 12 (8.8) | 1 (2.3) | (5.5) | 4 (4.4) | 3 (3.7) | 4 (5.0) |
| Missing | 1 (0.7) | 2 (1.5) | 2 (2.2) | 3 (3.7) | 3 (3.8) | ||
| To what extent do you agree that surgery should be only a last resort? | |||||||
| Strongly agree | 17 (12.5) | 19 (13.9) | 6 (13.6) | 20 (22.0) | 12 (13.3) | 11 (13.4) | 11 (13.8) |
| Agree | 75 (55.1) | 67 (48.9) | 17 (38.6) | 41 (45.1) | 48 (53.3) | 38 (46.3) | 36 (45.0) |
| Uncertain | 19 (14.0) | 24 (17.5) | 9 (20.5) | 14 (15.4) | 12 (13.3) | 16 (19.5) | 13 (16.3) |
| Disagree | 23 (16.9) | 22 (16.1) | 11 (25.0) | 9 (9.9) | 15 (16.7) | 13 (15.9) | 15 (18.8) |
| Strongly disagree | 1 (0.7) | 4 (2.9) | 1 (2.3) | 7 (7.7) | 3 (3.3) | 2 (2.4) | 2 (2.5) |
| Missing | 1 (0.7) | 1 (0.7) | 2 (2.4) | 3 (3.8) | |||
Summary
There was no evidence of any important imbalances between the groups. With a mean OSS of around 26, the population was representative of those in other shoulder studies (see Chapter 1). Most participants had undergone some form of non-surgical intervention (such as physiotherapy) before the trial and had had symptoms for over a year. In Chapter 4, the results of the randomised trial of arthroscopic compared with open surgery will be reported. A description of the findings from the rest-then-exercise programme will be provided in Chapter 5.
Chapter 4 Results: arthroscopic surgery compared with open surgery
This chapter describes the comparison between arthroscopic surgery and open surgery and includes operative characteristics and outcomes at 2 and 8 weeks post surgery as well as 8, 12 and 24 months after randomisation.
Analysis populations
Throughout the analyses presented in this chapter, the participants in the formal randomised comparison between arthroscopic surgery and open surgery (stratum A) are kept separate from those in the arthroscopic and open groups in strata B and C respectively. All 273 participants who joined the randomised arthroscopic compared with open surgery component in stratum A are referred to as the randomised ITT population; the 148 (n = 63 arthroscopic; n = 85 open) within this group who actually received a repair over the 2-year follow-up period are referred to as the per-protocol population. The non-randomised population refers to the 91 participants allocated to arthroscopic surgery from stratum B and the 82 participants allocated to open surgery in stratum C (included in this chapter for completeness and visual inspection of data). No statistical analysis is performed on the non-randomised population.
Surgical management
Randomised intention-to-treat population
Table 10 shows the types of procedure undertaken in each group. For the 136 participants randomised to receive arthroscopic surgical management, 63 (46.3%) underwent an arthroscopic repair of a tear, nine (6.6%) began as an arthroscopic procedure and converted to an open repair, 28 (20.6%) underwent an arthroscopic procedure (that did not involve a repair of a tear) and 36 (26.5%) withdrew and did not undergo any surgery. Of the arthroscopic procedures not involving a repair, a shoulder subacromial decompression was the most common procedure undertaken. Some 100 (73.5%) participants received the intended randomised arthroscopic surgical management, although only 63 (46.3%) received an arthroscopic repair.
| Surgical management | Randomised, n (%) | Non-randomised, n (%) | ||
|---|---|---|---|---|
| Arthroscopic (n = 136) | Open (n = 137) | Arthroscopic (n = 91) | Open (n = 82) | |
| Received an arthroscopic repair | 63 (46.3) | 5 (3.6) | 50 (54.9) | 2 (2.4) |
| Received a converted arthroscopic procedure | 9 (6.6) | 1 (1.1) | ||
| Received an open repair | 85 (62.0) | 40 (48.8) | ||
| Received an arthroscopic procedure | 28 (20.6) | 24 (17.5) | 23 (25.3) | 26 (31.7) |
| Details of procedure | ||||
| SAD | 20 (14.7) | 16 (11.7) | 14 (15.4) | 18 (22.0) |
| SAD and ACJ resection | 1 (0.7) | 3 (2.2) | 4 (4.4) | 6 (7.3) |
| Biceps tenotomy | 2 (1.5) | 1 (1.1) | ||
| Capsular release | 1 (0.7) | 2 (1.5) | 1 (1.2) | |
| PTT repair | 1 (0.7) | |||
| Partial repair | 1 (0.7) | |||
| Type of procedure not documented | 4 (3.0) | 1 (0.7) | 4 (4.4) | 1 (1.2) |
| Withdrawn from intervention | 36 (26.5) | 23 (16.8) | 15 (16.5) | 12 (14.6) |
| Awaiting surgery when study ended | 2 (1.5) | 2 (1.5) | 2 (2.2) | |
| Cancelled because of other surgery | 2 (1.5) | 1 (1.1) | ||
| Complete withdrawal from study | 2 (1.5) | |||
| Family commitments | 2 (1.5) | 1 (0.7) | ||
| No surgery on medical grounds | 11 (8.1) | 1 (0.7) | 3 (3.3) | 2 (2.4) |
| Patient asymptomatic | 7 (5.1) | 7 (5.1) | 2 (2.2) | 5 (6.1) |
| Patient deceased | 1 (0.7) | |||
| Patient did not want surgery | 3 (2.2) | 2 (1.5) | 3 (3.3) | 2 (2.4) |
| Patient not happy with hospital | 1 (1.1) | |||
| Patient withdrew from NHS waiting list | 4 (2.9) | 5 (3.6) | 1 (1.2) | |
| Personal reasons | 2 (2.4) | |||
| Shoulder problem improved without surgery | 1 (1.1) | |||
| Unknown | 1 (0.7) | 1 (0.7) | 2 (2.2) | |
| Work commitments | 3 (2.2) | 2 (1.5) | ||
| Surgery type missing | 2 (2.2) | 2 (2.4) | ||
Of the 137 participants randomised to receive open surgical management, 85 (62.0%) underwent an open repair of a tear and five (3.6%) an arthroscopic repair (see Table 10). Some 24 participants underwent an arthroscopic procedure and, as with the participants randomised to arthroscopic management, the most common procedure was a shoulder subacromial decompression. Twenty-three participants withdrew from any surgery. The principal reasons for participants withdrawing from surgery were related to medical conditions (primarily cardiac events) or participants being asymptomatic and not judged to be associated with either of the allocated procedures.
Non-randomised population
Similar proportions of non-randomised participants as randomised participants received the various management strategies, suggesting that the participants were broadly similar and their management was not biased by the surgeons’ preferred techniques.
Operative details
Procedural details are shown in Table 11 for those participants who received any surgery. The size of tear and surgical completeness were similar between the randomised groups. In the randomised group the ease of repair, although broadly similar, was reported to be easier for the open procedure (18% of arthroscopic operations were easy vs. 36% of open repairs). Such a difference was not observed in the non-randomised groups and therefore any difference must be interpreted with caution. However, the difference may be a proxy measure that the surgeons in the randomised comparison were more comfortable with the open than the arthroscopic approach.
| Operative detail | Randomised, n (%) | Non-randomised, n (%) | ||
|---|---|---|---|---|
| Arthroscopic (n = 136) | Open (n = 137) | Arthroscopic (n = 91) | Open (n = 82) | |
| Did not receive intervention | 36 (26.5) | 23 (16.8) | 17 (18.7) | 14 (17.1) |
| Received allocated repair | 63 (46.3) | 85 (62.0) | 50 (54.9) | 40 (48.8) |
| Received allocated procedure | 100 (73.5) | 85 (62.0) | 74 (81.3) | 40 (48.8) |
| Received any surgery | 100 (73.5) | 114 (83.2) | 74 (81.3) | 68 (82.9) |
| Procedure side | ||||
| Left | 40 (40.0) | 33 (28.9) | 22 (29.7) | 27 (39.7) |
| Right | 59 (59.0) | 80 (70.2) | 51 (68.9) | 41 (60.3) |
| Missing | 1 (1.0) | 1 (0.9) | 1 (1.4) | |
| Ease of repair | ||||
| Easy | 18 (18.0) | 41 (36.0) | 13 (17.6) | 11 (16.2) |
| Moderate | 28 (28.0) | 27 (23.7) | 19 (25.7) | 14 (20.6) |
| Difficult | 17 (17.0) | 12 (10.5) | 11 (14.9) | 11 (16.2) |
| Impossible | 7 (7.0) | 9 (7.9) | 8 (10.8) | 8 (11.8) |
| Missing | 30 (30.0) | 25 (21.9) | 23 (31.1) | 24 (35.3) |
| Size of tear | ||||
| Small | 23 (23.0) | 26 (22.8) | 11 (14.9) | 7 (10.3) |
| Medium | 27 (27.0) | 36 (31.6) | 10 (13.5) | 12 (17.6) |
| Large | 13 (13.0) | 19 (16.7) | 18 (24.3) | 13 (19.1) |
| Massive | 15 (15.0) | 13 (11.4) | 18 (24.3) | 16 (23.5) |
| Not a tear | 21 (21.0) | 16 (14.0) | 15 (20.3) | 20 (29.4) |
| Missing | 1 (1.0) | 4 (3.5) | 2 (2.7) | |
| Surgical opinion of completeness of repair | ||||
| Poor | 8 (8.0) | 7 (6.1) | 4 (5.4) | 6 (8.8) |
| Good | 41 (41.0) | 46 (40.4) | 29 (39.2) | 22 (32.4) |
| Excellent | 16 (16.0) | 35 (30.7) | 9 (12.2) | 11 (16.2) |
| Missing | 35 (35.0) | 26 (22.8) | 32 (43.2) | 29 (42.6) |
| Total time in theatre (minutes), n, mean (SD) | 73, 100.3 (42.0) | 96, 87.6 (28.9) | 46, 86.8 (32.5) | 49, 85.9 (46.7) |
| Operation time (minutes), n, mean (SD) | 72, 69.4 (36.7) | 89, 57.2 (21.9) | 36, 57.3 (27.2) | 39, 63.3 (36.0) |
The operation time is also shown in Table 11. For the randomised trial, the mean operation time in minutes was statistically significantly lower in the open procedure group (–12.2, 95% CI –21.4 to –3.0; p = 0.010) as was the mean total time in minutes in theatre (–12.7, 95% CI –23.5 to –1.9; p = 0.021). In the non-randomised groups, the times were similar.
Intraoperative complications
Table 12 shows the intraoperative complications. The number of events was generally low. There were 11 (8.1%) participants with any intraoperative complication in the randomised arthroscopic group compared with nine (6.6%) in the randomised open group. The difference was not statistically significant (difference 3.1%, 95% CI –4.8% to 11.0%; p = 0.190). The event rates in the non-randomised population were similar to those in the randomised population. There were no perioperative deaths.
| Complication | Randomised, n (%) | Non-randomised, n (%) | ||
|---|---|---|---|---|
| Arthroscopic (n = 136) | Open (n = 137) | Arthroscopic (n = 91) | Open (n = 82) | |
| Intraoperative problem | ||||
| Anaesthetic | 1 (1.0) | 1 (0.9) | 1 (1.4) | 1 (1.5) |
| Equipment | 3 (3.0) | 1 (0.9) | 2 (2.7) | 2 (2.9) |
| Implant | 1 (0.9) | 1 (1.4) | 1 (1.5) | |
| Surgical | 9 (9.0) | 2 (1.8) | 4 (5.4) | 2 (2.9) |
| Other | 5 (5.0) | 6 (5.3) | 7 (9.5) | 10 (14.7) |
| Staff problems | 2 (2.9) | |||
| Any intraoperative problem | 11 (8.1) | 9 (6.6) | 14 (15.4) | 11 (13.4) |
| Did the procedure change as a result of an intraoperative problem? | ||||
| Yes | 4 (36.4) | 3 (33.3) | 9 (64.3) | 6 (54.5) |
| No | 7 (63.6) | 4 (44.4) | 4 (28.6) | 3 (27.3) |
| Unsure | 1 (7.1) | |||
| Missing | 2 (22.2) | 2 (18.2) | ||
Adverse events and deaths
Three participants in the randomised arthroscopic group and three in the randomised open group required inpatient hospitalisation as a result of taking part in the UKUFF trial. The inpatient admissions were as a result of two participants in each group requiring revision surgery and a single participant in each group having a postoperative complication. The first complication involved a participant with a deep infection, which required formal debridement and vacuum pump application. He had this surgery after 3 weeks of treatment by his GP with antibiotics. The second complication involved a participant requiring a longer stay in hospital following a continuous interscalene block in the shoulder for postoperative pain relief and some bleeding during surgery. There was a single case of revision surgery in each of the non-randomised groups. All complications and revision surgeries were managed within 17 months of randomisation.
Seven participants died while in follow-up (n = 3 randomised arthroscopic; n = 1 randomised open; n = 3 non-randomised arthroscopic; n = 1 non-randomised open). Two participants died of cancer, two were involved in road traffic accidents, one died of an unrelated and undisclosed illness and two had an unknown cause of death.
Two-week follow-up
Follow-up measures timed to occur at 2 weeks post surgery are shown in Table 13. Very few participants reported being pain free and approximately two-thirds were taking painkillers. Of those participants who were employed, about 80% were still off sick. There were no clinically important differences between or within any of the randomised or non-randomised groups.
| Question | Randomised, n (%) | Non-randomised, n (%) | ||
|---|---|---|---|---|
| Arthroscopic (n = 136) | Open (n = 137) | Arthroscopic (n = 91) | Open (n = 82) | |
| Completed follow-up forms | 94 (69.1) | 112 (81.8) | 70 (76.9) | 71 (86.6) |
| Within the last 24 hours, have you been wearing a sling at all? | ||||
| Yes | 60 (63.8) | 78 (69.6) | 44 (62.9) | 47 (66.2) |
| No | 32 (34.0) | 31 (27.7) | 26 (37.1) | 21 (29.6) |
| Missing | 2 (2.1) | 3 (2.7) | 3 (4.2) | |
| If yes, how long have you worn the sling for? | ||||
| > 12 hours | 52 (86.7) | 71 (91.0) | 39 (88.6) | 30 (63.8) |
| Between 6 and 12 hours | 4 (6.7) | 5 (6.4) | 1 (2.3) | 9 (19.1) |
| > 3 hours but < 6 hours | 4 (6.7) | 1 (1.3) | 2 (4.5) | 5 (10.6) |
| < 3 hours | 1 (1.3) | 1 (2.1) | ||
| Missing | 2 (4.5) | 2 (4.3) | ||
| Within the last 24 hours, how would you describe the worst pain from your shoulder? | ||||
| None | 6 (6.4) | 6 (5.4) | 5 (7.1) | 7 (9.9) |
| Mild | 30 (31.9) | 34 (30.4) | 25 (35.7) | 18 (25.4) |
| Moderate | 36 (38.3) | 50 (44.6) | 23 (32.9) | 33 (46.5) |
| Severe | 17 (18.1) | 19 (17.0) | 12 (17.1) | 9 (12.7) |
| Unbearable | 3 (3.2) | 1 (0.9) | 5 (7.1) | 1 (1.4) |
| Missing | 2 (2.1) | 2 (1.8) | 3 (4.2) | |
| Within the last 24 hours, how much has pain from your shoulder interfered with your usual work? | ||||
| Not at all | 17 (18.1) | 18 (16.1) | 22 (31.4) | 16 (22.5) |
| A little bit | 16 (17.0) | 10 (8.9) | 14 (20.0) | 10 (14.1) |
| Moderately | 24 (25.5) | 43 (38.4) | 11 (15.7) | 18 (25.4) |
| Greatly | 24 (25.5) | 25 (22.3) | 9 (12.9) | 17 (23.9) |
| Totally | 11 (11.7) | 13 (11.6) | 14 (20.0) | 7 (9.9) |
| Missing | 2 (2.1) | 3 (2.7) | 3 (4.2) | |
| Were you troubled by pain from your shoulder in bed last night? | ||||
| No, not at all | 25 (26.6) | 25 (22.3) | 17 (24.3) | 19 (26.8) |
| Yes, just at first | 8 (8.5) | 6 (5.4) | 4 (5.7) | 5 (7.0) |
| Yes, during some of the night | 38 (40.4) | 44 (39.3) | 32 (45.7) | 27 (38.0) |
| Yes, throughout the night | 21 (22.3) | 35 (31.3) | 17 (24.3) | 17 (23.9) |
| Missing | 2 (2.1) | 2 (1.8) | 3 (4.2) | |
| Within the last 24 hours, have you taken any painkillers because of your shoulder? | ||||
| Yes | 62 (66.0) | 76 (67.9) | 45 (64.3) | 49 (69.0) |
| No | 29 (30.9) | 34 (30.4) | 25 (35.7) | 19 (26.8) |
| Missing | 3 (3.2) | 2 (1.8) | 3 (4.2) | |
| If yes, how many painkillers have you taken in the last 24 hours? | ||||
| 1 | 29 (46.8) | 38 (50.0) | 23 (51.1) | 25 (51.0) |
| 2 | 23 (37.1) | 30 (39.5) | 16 (35.6) | 15 (30.6) |
| 3 | 7 (11.3) | 5 (6.6) | 6 (13.3) | 6 (12.2) |
| 4 | 1 (1.6) | 1 (1.3) | 2 (4.1) | |
| 5 | 1 (1.6) | 1 (1.3) | 1 (2.0) | |
| Missing | 1 (1.6) | 1 (1.3) | ||
| During the (last 2 weeks) time since the completion of surgery or rest then exercise, have you received any additional treatment on your shoulder? | ||||
| Yes | 3 (3.2) | 17 (15.2) | 8 (11.4) | 3 (4.2) |
| No | 84 (89.4) | 87 (77.7) | 59 (84.3) | 56 (78.9) |
| Missing | 7 (7.4) | 8 (7.1) | 3 (4.3) | 12 (16.9) |
| If yes, what was the additional treatment? | ||||
| Injection | 1 (12.5) | |||
| Antibiotics | 1 (5.9) | |||
| Physiotherapy | 1 (33.3) | 4 (23.5) | 4 (50.0) | 1 (33.3) |
| Wound or dressing | 5 (29.4) | 2 (25.0) | 1 (33.3) | |
| Not shoulder | 1 (33.3) | 2 (11.8) | 1 (33.3) | |
| Pain relief | 1 (33.3) | 5 (29.4) | 1 (12.5) | |
| Are you currently employed? | ||||
| Yes | 46 (48.9) | 57 (50.9) | 31 (44.3) | 38 (53.5) |
| No | 46 (48.9) | 53 (47.3) | 39 (55.7) | 30 (42.3) |
| Missing | 2 (2.1) | 2 (1.8) | 3 (4.2) | |
| Are you currently off sick or working reduced duties? | ||||
| Yes, off sick | 38 (82.6) | 44 (77.2) | 23 (74.2) | 26 (68.4) |
| Yes, working reduced duties | 3 (6.5) | 5 (8.8) | 3 (9.7) | 4 (10.5) |
| No, working usual hours or duties | 5 (10.9) | 8 (14.0) | 4 (12.9) | 6 (15.8) |
| Missing | 1 (3.2) | 2 (5.3) | ||
Eight-week follow-up
Follow-up measures timed to occur at 8 weeks post surgery are shown in Table 14. The results were similar to those at the 2-week follow-up with the exception that the percentage reporting no or mild pain improved from 35% to 50% with an apparent concomitant effect of reducing painkiller use from 66% to 55% and increasing the number of participants returning to usual work (no or a little interference) from 28% to 55%. There were no clinically important differences between or within any of the randomised or non-randomised groups.
| Question | Randomised, n (%) | Non-randomised, n (%) | ||
|---|---|---|---|---|
| Arthroscopic (n = 136) | Open (n = 137) | Arthroscopic (n = 91) | Open (n = 82) | |
| Completed follow-up forms | 97 (71.3) | 113 (82.5) | 70 (76.9) | 58 (70.7) |
| Within the last 24 hours, have you been wearing a sling at all? | ||||
| Yes | 6 (6.2) | 14 (12.4) | 6 (8.6) | 7 (12.1) |
| No | 91 (93.8) | 99 (87.6) | 64 (91.4) | 51 (87.9) |
| If yes, how long have you worn the sling for? | ||||
| > 12 hours | 1 (16.7) | 3 (21.4) | 3 (50.0) | 1 (14.3) |
| Between 6 and 12 hours | 1 (16.7) | 4 (28.6) | 1 (14.3) | |
| > 3 hours but < 6 hours | 1 (16.7) | 7 (50.0) | 1 (16.7) | 1 (14.3) |
| < 3 hours | 3 (50.0) | 2 (33.3) | 2 (28.6) | |
| Missing | 2 (28.6) | |||
| Within the last 24 hours, how would you describe the worst pain you have had from your shoulder? | ||||
| None | 11 (11.3) | 12 (10.6) | 8 (11.4) | 7 (12.1) |
| Mild | 38 (39.2) | 50 (44.2) | 22 (31.4) | 24 (41.4) |
| Moderate | 33 (34.0) | 29 (25.7) | 21 (30.0) | 20 (34.5) |
| Severe | 14 (14.4) | 20 (17.7) | 15 (21.4) | 7 (12.1) |
| Unbearable | 1 (1.0) | 1 (0.9) | 4 (5.7) | |
| Missing | 1 (0.9) | |||
| Within the last 24 hours, how much has pain from your shoulder interfered with your usual work? | ||||
| Not at all | 31 (32.0) | 26 (23.0) | 20 (28.6) | 18 (31.0) |
| A little bit | 23 (23.7) | 35 (31.0) | 20 (28.6) | 15 (25.9) |
| Moderately | 32 (33.0) | 37 (32.7) | 14 (20.0) | 18 (31.0) |
| Greatly | 9 (9.3) | 12 (10.6) | 11 (15.7) | 6 (10.3) |
| Totally | 2 (2.1) | 3 (2.7) | 5 (7.1) | 1 (1.7) |
| Were you troubled by pain from your shoulder in bed last night? | ||||
| No, not at all | 37 (38.1) | 40 (35.4) | 25 (35.7) | 23 (39.7) |
| Yes, just at first | 8 (8.2) | 9 (8.0) | 4 (5.7) | 2 (3.4) |
| Yes, during some of the night | 35 (36.1) | 38 (33.6) | 23 (32.9) | 21 (36.2) |
| Yes, throughout the night | 17 (17.5) | 26 (23.0) | 18 (25.7) | 12 (20.7) |
| Within the last 24 hours, have you taken any painkillers for your shoulder? | ||||
| Yes | 44 (45.4) | 59 (52.2) | 36 (51.4) | 32 (55.2) |
| No | 53 (54.6) | 54 (47.8) | 34 (48.6) | 26 (44.8) |
| If yes, how many painkillers have you taken? | ||||
| 1 | 25 (56.8) | 34 (57.6) | 17 (47.2) | 15 (46.9) |
| 2 | 13 (29.5) | 19 (32.2) | 9 (25.0) | 8 (25.0) |
| 3 | 4 (9.1) | 3 (5.1) | 4 (11.1) | 1 (3.1) |
| 4 | 1 (2.3) | 1 (3.1) | ||
| Missing | 1 (2.3) | 3 (5.1) | 6 (16.7) | 7 (21.9) |
| During the time (last 6 weeks) since we spoke to you last, have you had any additional treatment for your shoulder? | ||||
| Yes | 7 (7.2) | 10 (8.8) | 5 (7.1) | 7 (12.1) |
| No | 85 (87.6) | 100 (88.5) | 63 (90.0) | 49 (84.5) |
| Missing | 5 (5.2) | 3 (2.7) | 2 (2.9) | 2 (3.4) |
| If yes, what additional treatment did you receive? | ||||
| Injection | 1 (10.0) | |||
| Surgery | 1 (20.0) | |||
| Antibiotics | 2 (20.0) | 1 (14.3) | ||
| Physiotherapy | 7 (100.0) | 4 (40.0) | 2 (40.0) | 6 (85.7) |
| Wound or dressing | 1 (10.0) | |||
| Pain relief | ||||
| Hospital admission | 1 (20.0) | |||
| Surgery and antibiotics | 2 (20.0) | |||
| Injection and antibiotics | 1 (20.0) | |||
| Are you currently employed? | ||||
| Yes | 47 (48.5) | 60 (53.1) | 26 (37.1) | 26 (44.8) |
| No | 50 (51.5) | 52 (46.0) | 41 (58.6) | 28 (48.3) |
| Missing | 1 (0.9) | 3 (4.3) | 4 (6.9) | |
| Are you currently off sick or working reduced hours? | ||||
| Yes, off sick | 23 (48.9) | 29 (48.3) | 13 (50.0) | 14 (53.8) |
| Yes, working reduced duties | 9 (19.1) | 12 (20.0) | 4 (15.4) | 4 (15.4) |
| No, working usual hours/duties | 15 (31.9) | 18 (30.0) | 9 (34.6) | 8 (30.8) |
| Missing | 1 (1.7) | |||
Outcomes at 8, 12 and 24 months
Outcomes at 8, 12 and 24 months were primarily obtained from questionnaire returns. As described in Chapter 3 and reiterated here in Table 15, the return rates were similar across groups and ranged from 90% at 8 and 12 months to 86% at 24 months. There were no notable differences in baseline characteristics between those who had completed a questionnaire at 24 months and those who had not (Table 16). The only exception to this was a statistically significant difference in housing status, with 84.7% of homeowners in the responder group compared with 71.1% in the non-responder group. Given the possibility of multiple statistical testing, the difference should be interpreted with caution. As described in Chapter 2, these results confirmed that a repeated measures analysis assuming no differential loss to follow-up could be considered.
| Time point (months) | Randomised, n (%) | Non-randomised, n (%) | ||
|---|---|---|---|---|
| Arthroscopic (n = 136) | Open (n = 137) | Arthroscopic (n = 91) | Open (n = 82) | |
| 8 | 121 (89.0) | 127 (92.7) | 85 (93.4) | 75 (91.5) |
| 12 | 123 (90.4) | 123 (89.8) | 84 (92.3) | 76 (92.7) |
| 24 | 117 (86.0) | 118 (86.1) | 79 (86.8) | 75 (91.5) |
| Characteristic | Responder, n (%) | Non-responder, n (%) | p-value (two-sided) |
|---|---|---|---|
| Age (years), n, mean (SD) | 235, 62.8 (7.0) | 38, 63.1 (9.1) | 0.824 |
| Years with shoulder problem, n, mean (SD) | 235, 2.4 (4.0) | 38, 3.1 (8.0) | 0.404 |
| OSS, n, mean (SD) | 235, 25.9 (7.9) | 38, 24.0 (8.5) | 0.165 |
| SPADI, n, mean (SD) | 234, 60.3 (21.8) | 38, 67.3 (22.3) | 0.068 |
| SPADI pain, n, mean (SD) | 235, 69.3 (19.8) | 38, 74.9 (20.6) | 0.109 |
| SPADI disability, n, mean (SD) | 233, 54.7 (24.7) | 38, 62.5 (24.9) | 0.072 |
| MHI-5, n, mean (SD) | 235, 22.7 (4.7) | 38, 22.9 (4.6) | 0.771 |
| EQ-5D, n, mean (SD) | 233, 0.543 (0.290) | 38, 0.472 (0.319) | 0.170 |
| Sex | |||
| Male | 144 (61.3) | 25 (65.8) | 0.595 |
| Female | 91 (38.7) | 13 (34.2) | |
| Handedness | |||
| Right-handed | 210 (89.4) | 30 (78.9) | 0.184 |
| Left-handed | 18 (7.7) | 6 (15.8) | |
| Both | 7 (3.0) | 2 (5.3) | |
| Highest qualification | |||
| None | 101 (43.0) | 21 (55.3) | 0.207 |
| Secondary | 80 (34.0) | 10 (26.3) | |
| Higher | 53 (22.6) | 6 (15.8) | |
| Missing | 1 (0.4) | 1 (2.6) | |
| Housing tenure | |||
| Home owner | 199 (84.7) | 27 (71.1) | 0.020 |
| Private rent | 6 (2.6) | 2 (5.3) | |
| Council rent | 19 (8.1) | 7 (18.4) | |
| Other | 11 (4.7) | 1 (2.6) | |
| Missing | 1 (2.6) | ||
| Lives alone | |||
| Yes | 27 (11.5) | 8 (21.1) | 0.253 |
| No | 191 (81.3) | 28 (73.7) | |
| Missing | 17 (7.2) | 2 (5.3) | |
| Employment status | |||
| Full-time | 89 (37.9) | 16 (42.1) | 0.567 |
| Part-time | 31 (13.2) | 2 (5.3) | |
| Homemaker | 8 (3.4) | 1 (2.6) | |
| Retired | 97 (41.3) | 16 (42.1) | |
| Unemployed | 8 (3.4) | 3 (7.9) | |
| Missing | 2 (0.9) | ||
| Type of work | |||
| Manual | 67 (55.8) | 10 (55.6) | 0.474 |
| Non-manual | 48 (40.0) | 6 (33.3) | |
| Not sure | 4 (3.3) | 2 (11.1) | |
| Missing | 1 (0.8) | ||
| Off sick or working reduced duties | |||
| Yes, off sick | 13 (10.8) | 0.096 | |
| Yes, reduced duties | 12 (10.0) | 5 (27.8) | |
| No, working usual hours | 91 (75.8) | 12 (66.7) | |
| Missing | 4 (3.3) | 1 (5.6) | |
| Able to do job | |||
| No | 127 (54.0) | 19 (50.0) | 0.443 |
| Yes, but with difficulty | 104 (44.3) | 17 (44.7) | |
| Yes, with no difficulty | 3 (1.3) | 1 (2.6) | |
| Missing | 1 (0.4) | 1 (2.6) | |
Health status
Health status measures at 8, 12 and 24 months are shown in Table 17. Full details of the statistical testing of the health status measures can be found in the following sections.
| Measure | Randomised, n, mean (SD) | Effect size | 95% CI | p-value | Non-randomised, n, mean (SD) | ||
|---|---|---|---|---|---|---|---|
| Arthroscopic | Open | Arthroscopic | Open | ||||
| OSS | |||||||
| Baseline | 129, 26.3 (8.2) | 131, 25.0 (8.0) | 91, 25.3 (8.9) | 82, 25.9 (8.4) | |||
| 8 months | 121, 36.1 (9.2) | 127, 37.0 (8.6) | –1.27 | –3.21 to 0.67 | 0.200 | 85, 37.2 (9.7) | 75, 37.4 (9.2) |
| 12 months | 122, 38.3 (9.5) | 122, 39.6 (8.5) | –1.60 | –3.55 to 0.35 | 0.108 | 83, 37.4 (10.3) | 75, 40.6 (6.8) |
| 24 months (primary outcome) | 114, 41.7 (7.9) | 115, 41.5 (7.9) | –0.76 | –2.75 to 1.22 | 0.452 | 78, 41.3 (7.7) | 75, 41.3 (7.3) |
| SPADI | |||||||
| Baseline | 128, 60.4 (22.1) | 130, 61.8 (21.7) | 91, 60.6 (23.1) | 82, 60.7 (20.1) | |||
| 8 months | 117, 31.8 (26.6) | 124, 31.7 (27.8) | 1.02 | –4.73 to 6.77 | 0.728 | 82, 28.7 (24.9) | 73, 27.8 (23.3) |
| 12 months | 119, 24.2 (26.3) | 120, 23.4 (26.4) | 1.83 | –3.93 to 7.59 | 0.533 | 80, 23.9 (25.8) | 74, 18.6 (20.2) |
| 24 months | 115, 16.1 (21.7) | 118, 17.5 (23.7) | 0.50 | –5.30 to 6.30 | 0.866 | 75, 16.6 (21.8) | 71, 17.3 (22.9) |
| SPADI pain | |||||||
| Baseline | 128, 69.2 (19.6) | 130, 70.5 (20.4) | 91, 70.0 (21.8) | 82, 69.6 (19.5) | |||
| 8 months | 118, 36.7 (27.7) | 126, 35.4 (28.9) | 2.00 | –4.26 to 8.26 | 0.532 | 84, 32.9 (27.8) | 72, 31.7 (24.9) |
| 12 months | 119, 28.1 (27.8) | 119, 25.9 (27.1) | 2.91 | –3.39 to 9.21 | 0.365 | 80, 26.2 (27.0) | 75, 23.1 (23.8) |
| 24 months | 114, 18.7 (23.1) | 118, 20.1 (26.1) | 0.92 | –5.42 to 7.26 | 0.777 | 75, 18.0 (22.8) | 71, 20.3 (24.5) |
| SPADI disability | |||||||
| Baseline | 128, 54.9 (25.1) | 130, 56.5 (24.4) | 91, 54.7 (25.9) | 82, 55.2 (21.9) | |||
| 8 months | 117, 28.7 (26.9) | 124, 29.3 (28.1) | 0.41 | –5.26 to 6.07 | 0.889 | 82, 26.3 (24.4) | 74, 26.2 (24.9) |
| 12 months | 119, 21.8 (26.3) | 120, 21.7 (26.9) | 1.12 | –4.57 to 6.80 | 0.700 | 80, 22.4 (26.9) | 74, 16.2 (19.5) |
| 24 months | 116, 14.8 (22.5) | 118, 15.8 (22.8) | 0.36 | –5.35 to 6.07 | 0.902 | 76, 16.3 (22.7) | 72, 15.5 (22.5) |
| MHI-5 | |||||||
| Baseline | 128, 22.4 (4.9) | 130, 22.9 (4.5) | 90, 22.4 (5.1) | 82, 22.1 (4.7) | |||
| 8 months | 118, 23.8 (4.9) | 124, 23.8 (4.4) | 0.32 | –0.61 to 1.26 | 0.500 | 81, 23.8 (4.6) | 74, 24.0 (4.1) |
| 12 months | 118, 23.5 (5.0) | 119, 23.6 (4.6) | 0.13 | –0.81 to 1.07 | 0.783 | 78, 24.4 (4.6) | 73, 24.2 (3.8) |
| 24 months | 116, 24.4 (4.0) | 118, 24.3 (4.5) | 0.22 | –0.72 to 1.17 | 0.648 | 76, 23.8 (4.9) | 71, 24.2 (4.2) |
| EQ-5D | |||||||
| Baseline | 129, 0.551 (0.297) | 131, 0.518 (0.293) | 91, 0.514 (0.326) | 81, 0.536 (0.287) | |||
| 8 months | 120, 0.680 (0.300) | 124, 0.700 (0.257) | –0.032 | –0.092 to 0.028 | 0.296 | 79, 0.709 (0.244) | 74, 0.711 (0.194) |
| 12 months | 119, 0.727 (0.278) | 118, 0.711 (0.300) | 0.011 | –0.050 to 0.071 | 0.724 | 80, 0.696 (0.293) | 71, 0.761 (0.192) |
| 24 months | 116, 0.760 (0.235) | 118, 0.778 (0.219) | –0.043 | –0.104 to 0.017 | 0.163 | 79, 0.760 (0.262) | 74, 0.753 (0.258) |
Oxford Shoulder Score
Figure 2 graphically displays the OSS over the course of the follow-up period for the randomised and non-randomised groups. All groups followed a similar pattern. The OSS increased markedly from baseline (mean 25.7) to 8 months (mean 36.5) and continued to increase thereafter (at a much slower rate) to 24 months (mean 41.5).
FIGURE 2.
Means and 95% CIs for the OSS across time for the ITT and non-randomised groups.

European Quality of Life-5 Dimensions
Figure 3 displays the EQ-5D score over the follow-up period. The pattern is similar to that seen for the OSS.
FIGURE 3.
Means and 95% CIs for the EQ-5D across time for the ITT and non-randomised groups.

Shoulder Pain and Disability Index
The SPADI overall score, together with the pain and disability subscales (Figures 4–6), followed a similar pattern to that for the OSS (note that a lower SPADI score is a better outcome), with a large improvement from baseline at 8 months followed by a smaller rate of improvement thereafter. All randomised and non-randomised groups followed a similar pattern.
FIGURE 4.
Means and 95% CIs for the SPADI overall score across time for the ITT and non-randomised groups.
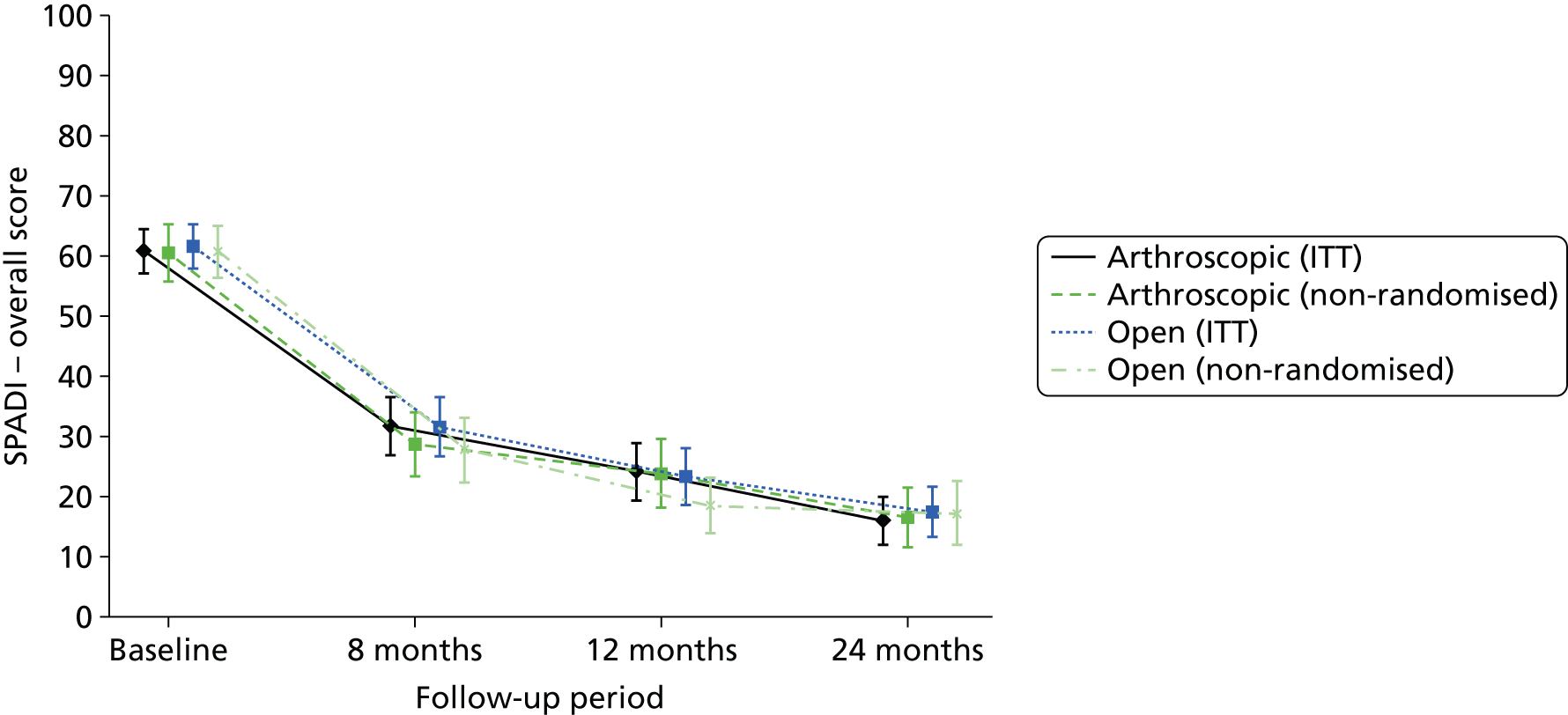
FIGURE 5.
Means and 95% CIs for the SPADI disability subscale score across time for the ITT and non-randomised groups.
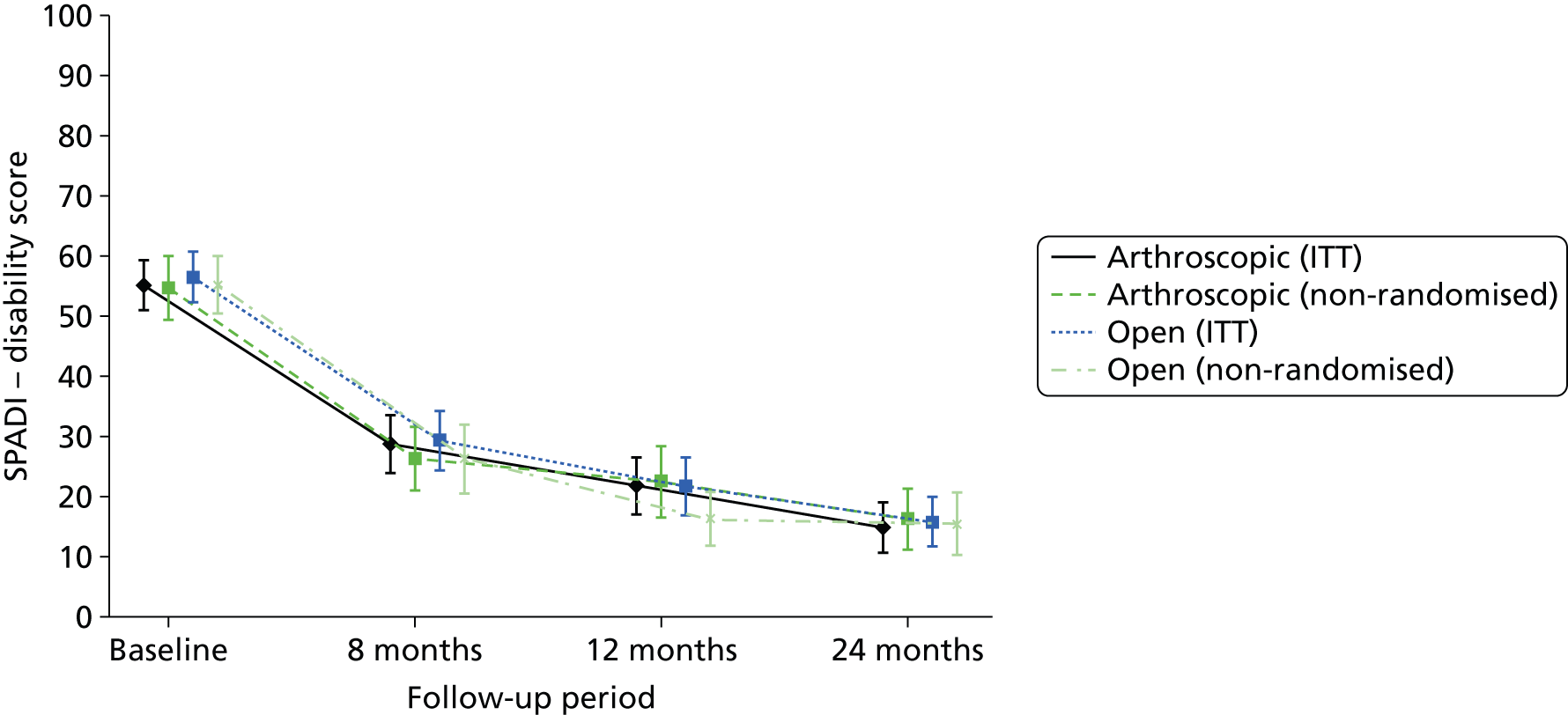
FIGURE 6.
Means and 95% CIs for the SPADI pain subscale score across time for the ITT and non-randomised groups.
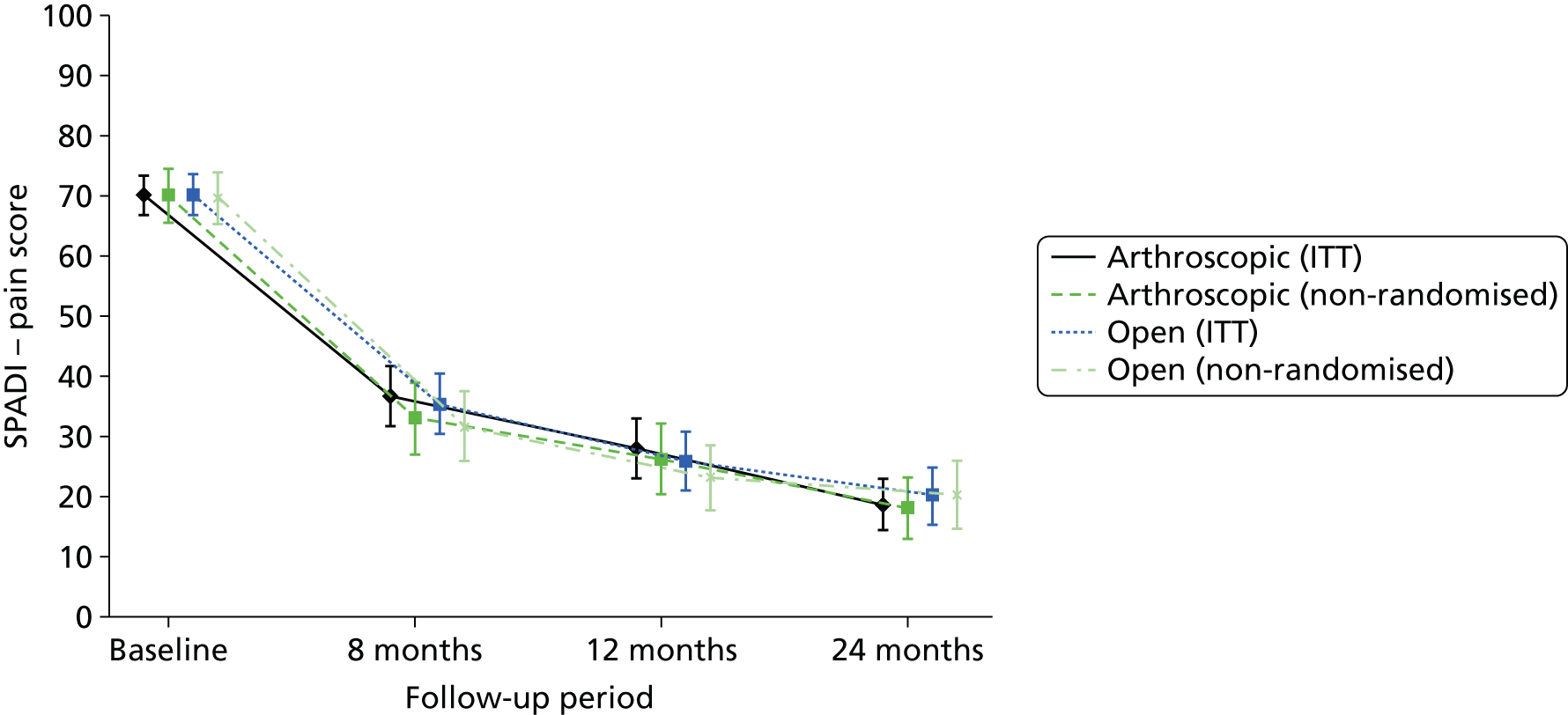
Mental Health Inventory
The MHI-5 scores showed very little change across time from baseline (Figure 7).
FIGURE 7.
Means and 95% CIs for the MHI-5 score across time for the ITT and non-randomised groups.

Symptoms
A comparison of current shoulder problems with baseline levels is given in Table 18. In response to a transition item concerning change in their shoulder problems at 8 months, 77% of participants reported that shoulder problems were much or slightly better, increasing to 85% at 24 months. When asked how pleased they were with their shoulder symptoms, on average 77% of participants were either very or fairly pleased at 8 months, increasing to 83% by 24 months. All groups responded in a similar manner.
| Question | Randomised, n (%) | OR | 95% CI | p-value | Non-randomised, n (%) | ||
|---|---|---|---|---|---|---|---|
| Arthroscopic (n = 136) | Open (n = 137) | Arthroscopic (n = 91) | Open (n = 82) | ||||
| How are the problems related to your shoulder now compared with 8 months ago? | |||||||
| Much better | 63 (52.1) | 76 (59.8) | 0.80 | 0.41 to 1.58 | 0.522 | 55 (64.7) | 47 (62.7) |
| Slightly better | 30 (24.8) | 22 (17.3) | 14 (16.5) | 17 (22.7) | |||
| No change | 18 (14.9) | 11 (8.7) | 7 (8.2) | 1 (1.3) | |||
| Slightly worse | 3 (2.5) | 6 (4.7) | 4 (4.7) | 4 (5.3) | |||
| Much worse | 4 (3.3) | 4 (3.1) | 3 (3.5) | 2 (2.7) | |||
| Missing | 3 (2.5) | 8 (6.3) | 2 (2.4) | 4 (5.3) | |||
| How are the problems related to your shoulder now compared with a year ago? | |||||||
| Much better | 72 (58.5) | 85 (69.1) | 0.57 | 0.31 to 1.03 | 0.061 | 51 (60.7) | 56 (73.7) |
| Slightly better | 20 (16.3) | 18 (14.6) | 19 (22.6) | 11 (14.5) | |||
| No change | 12 (9.8) | 4 (3.3) | 4 (4.8) | 6 (7.9) | |||
| Slightly worse | 9 (7.3) | 5 (4.1) | 1 (1.2) | 1 (1.3) | |||
| Much worse | 4 (3.3) | 7 (5.7) | 3 (3.6) | 1 (1.3) | |||
| Missing | 6 (4.9) | 4 (3.3) | 6 (7.1) | 1 (1.3) | |||
| How are the problems related to your shoulder now compared with 2 years ago? | |||||||
| Much better | 83 (70.9) | 81 (68.6) | 0.97 | 0.43 to 2.18 | 0.939 | 61 (77.2) | 49 (65.3) |
| Slightly better | 16 (13.7) | 20 (16.9) | 6 (7.6) | 14 (18.7) | |||
| No change | 6 (5.1) | 6 (5.1) | 6 (7.6) | 4 (5.3) | |||
| Slightly worse | 5 (4.3) | 4 (3.4) | 3 (3.8) | 3 (4.0) | |||
| Much worse | 3 (2.6) | 4 (3.4) | 0 (0.0) | 2 (2.7) | |||
| Missing | 4 (3.4) | 3 (2.5) | 3 (3.8) | 3 (4.0) | |||
| How pleased are you with your shoulder symptoms at 8 months? | |||||||
| Very pleased | 45 (37.2) | 51 (40.2) | 1.11 | 0.57 to 2.16 | 0.769 | 44 (51.8) | 37 (49.3) |
| Fairly pleased | 51 (42.1) | 45 (35.4) | 26 (30.6) | 27 (36.0) | |||
| Not very pleased | 17 (14.0) | 18 (14.2) | 6 (7.1) | 5 (6.7) | |||
| Very disappointed | 4 (3.3) | 4 (3.1) | 7 (8.2) | 1 (1.3) | |||
| Missing | 4 (3.3) | 9 (7.1) | 2 (2.4) | 5 (6.7) | |||
| How pleased are you with your shoulder symptoms at 12 months? | |||||||
| Very pleased | 59 (48.0) | 57 (46.3) | 0.57 | 0.31 to 1.05 | 0.071 | 42 (50.0) | 45 (59.2) |
| Fairly pleased | 33 (26.8) | 47 (38.2) | 27 (32.1) | 20 (26.3) | |||
| Not very pleased | 16 (13.0) | 8 (6.5) | 8 (9.5) | 6 (7.9) | |||
| Very disappointed | 7 (5.7) | 7 (5.7) | 2 (2.4) | 4 (5.3) | |||
| Missing | 8 (6.5) | 4 (3.3) | 5 (6.0) | 1 (1.3) | |||
| How pleased are you with your shoulder symptoms at 24 months? | |||||||
| Very pleased | 73 (62.4) | 64 (54.2) | 1.37 | 0.73 to 2.60 | 0.330 | 47 (59.5) | 42 (56.0) |
| Fairly pleased | 26 (22.2) | 33 (28.0) | 21 (26.6) | 19 (25.3) | |||
| Not very pleased | 7 (6.0) | 13 (11.0) | 7 (8.9) | 7 (9.3) | |||
| Very disappointed | 6 (5.1) | 4 (3.4) | 1 (1.3) | 4 (5.3) | |||
| Missing | 5 (4.3) | 4 (3.4) | 3 (3.8) | 3 (4.0) | |||
Employment information
Table 19 shows participant employment status at 8, 12 and 24 months. There was no substantial change in employment status from 8 to 24 months.
| Employment status | Randomised, n (%) | Non-randomised, n (%) | ||
|---|---|---|---|---|
| Arthroscopic (n = 136) | Open (n = 137) | Arthroscopic (n = 91) | Open (n = 82) | |
| Employed at 8 months | ||||
| Yes | 51 (42.1) | 54 (42.5) | 29 (34.1) | 33 (44.0) |
| No | 67 (55.4) | 63 (49.6) | 54 (63.5) | 38 (50.7) |
| Missing | 3 (2.5) | 10 (7.9) | 2 (2.4) | 4 (5.3) |
| Employed at 12 months | ||||
| Yes | 50 (40.7) | 49 (39.8) | 23 (27.4) | 32 (42.1) |
| No | 68 (55.3) | 70 (56.9) | 56 (66.7) | 43 (56.6) |
| Missing | 5 (4.1) | 4 (3.3) | 5 (6.0) | 1 (1.3) |
| Employed at 24 months | ||||
| Yes | 42 (35.9) | 42 (35.6) | 22 (27.8) | 31 (41.3) |
| No | 71 (60.7) | 72 (61.0) | 54 (68.4) | 41 (54.7) |
| Missing | 4 (3.4) | 4 (3.4) | 3 (3.8) | 3 (4.0) |
| If you are employed, are you off sick or working reduced duties because of your shoulder at 8 months? | ||||
| Yes, off sick | 10 (8.3) | 7 (5.5) | 5 (5.9) | 2 (2.7) |
| Yes, working reduced hours | 4 (3.3) | 8 (6.3) | 4 (4.7) | 7 (9.3) |
| No, working usual hours/duties | 36 (29.8) | 36 (28.3) | 19 (22.4) | 23 (30.7) |
| Missing | 71 (58.7) | 76 (59.8) | 57 (67.1) | 43 (57.3) |
| Are you currently out of work, off sick or working reduced duties because of your shoulder at 12 months? | ||||
| Yes | 12 (9.8) | 10 (8.1) | 5 (6.0) | 9 (11.8) |
| No | 93 (75.6) | 93 (75.6) | 63 (75.0) | 59 (77.6) |
| Missing | 18 (14.6) | 20 (16.3) | 16 (19.0) | 8 (10.5) |
| Are you currently out of work, off sick or working reduced duties because of your shoulder at 24 months? | ||||
| Yes | 8 (6.8) | 6 (5.1) | 4 (5.1) | 5 (6.7) |
| No | 99 (84.6) | 94 (79.7) | 65 (82.3) | 60 (80.0) |
| Missing | 10 (8.5) | 18 (15.3) | 10 (12.7) | 10 (13.3) |
Magnetic resonance imaging findings at 12 months post surgery
The findings of those participants undergoing an MRI at 12 months post surgery are displayed in Table 20. Of the 136 participants randomised to receive arthroscopic repair, 69 (51%) had an MRI scan at 12 months. For the 137 participants randomised to receive open repair, 83 (61%) had an MRI. The primary reasons for not receiving were that the patient did not have a tear at initial surgery, it was impossible to repair or the patient received a revision surgery prior to 12 months.
| Measure | Randomised, n (%) | Non-randomised, n (%) | ||
|---|---|---|---|---|
| Arthroscopic (n = 136) | Open (n = 137) | Arthroscopic (n = 91) | Open (n = 82) | |
| MRI scans received, n | 69 | 83 | 41 | 40 |
| Result of MRI scan | ||||
| Re-tear | 32 (46.4) | 32 (38.6) | 15 (36.6) | 14 (35.0) |
| No tear | 32 (46.4) | 47 (56.6) | 23 (56.1) | 24 (60.0) |
| Inconclusive | 1 (1.4) | 1 (1.2) | ||
| Missing | 4 (5.8) | 3 (3.6) | 3 (7.3) | 2 (5.0) |
| Size of tear if MRI scan shows a re-tear | ||||
| Partial | 2 (6.3) | 1 (3.1) | 1 (6.7) | |
| Small | 9 (28.1) | 10 (31.3) | 1 (6.7) | 4 (28.6) |
| Medium | 5 (15.6) | 9 (28.1) | 6 (40.0) | 5 (35.7) |
| Large | 5 (15.6) | 3 (9.4) | 2 (13.3) | 2 (14.3) |
| Massive | 8 (25.0) | 7 (21.9) | 4 (26.7) | 3 (21.4) |
| Missing | 3 (9.4) | 2 (6.3) | 1 (6.7) | |
| OSS at 24 months, n, mean (SD) | ||||
| Re-tear | 30, 41.8 (8.8) | 29, 40.8 (7.6) | 15, 38.8 (5.8) | 13, 39.8 (7.2) |
| No tear | 30, 44.5 (4.1) | 47, 43.6 (5.8) | 22, 43.9 (4.2) | 20, 44.3 (4.5) |
| Impossible to repair | 7, 37.3 (6.1) | 8, 35.1 (9.7) | 6, 37.0 (9.8) | 8, 32.4 (9.8) |
The rate of re-tear was similar across the randomised groups (46.4% vs. 38.6% for arthroscopic and open surgery respectively) (relative effect: OR 1.52, 95% CI 0.84 to 2.75; absolute risk difference 9.5%, 95% CI –6.9% to 25.8%; p = 0.256).
The OSS demonstrated a consistent pattern within each group, with the impossible-to-repair participants having the worst OSS, participants with a re-tear having a slightly better OSS and participants with no tear having the most improved OSS (see Table 20).
Per-protocol population
For completeness, data on the per-protocol population are included in Appendix 1. These data are from the 63 participants who were randomised to an arthroscopic procedure and who actually received an arthroscopic repair and the 85 participants who were randomised to an open procedure and who received an open repair. Similarly, the data reported also include the 50 arthroscopic repairs and the 40 open repairs in the non-randomised group.
Recognising that caution must be used when interpreting the per-protocol group, we nevertheless note that the lack of important differences between the arthroscopic and the open ITT groups was also observed in the per-protocol data. The similarity is illustrated visually in Figures 8 and 9, where the OSS and EQ-5D scores, respectively, are contrasted between the ITT population and the per-protocol population.
FIGURE 8.
Means and 95% CIs for the OSS across time for the ITT and per-protocol groups.

FIGURE 9.
Means and 95% CIs for the EQ-5D across time for the ITT and per-protocol groups.
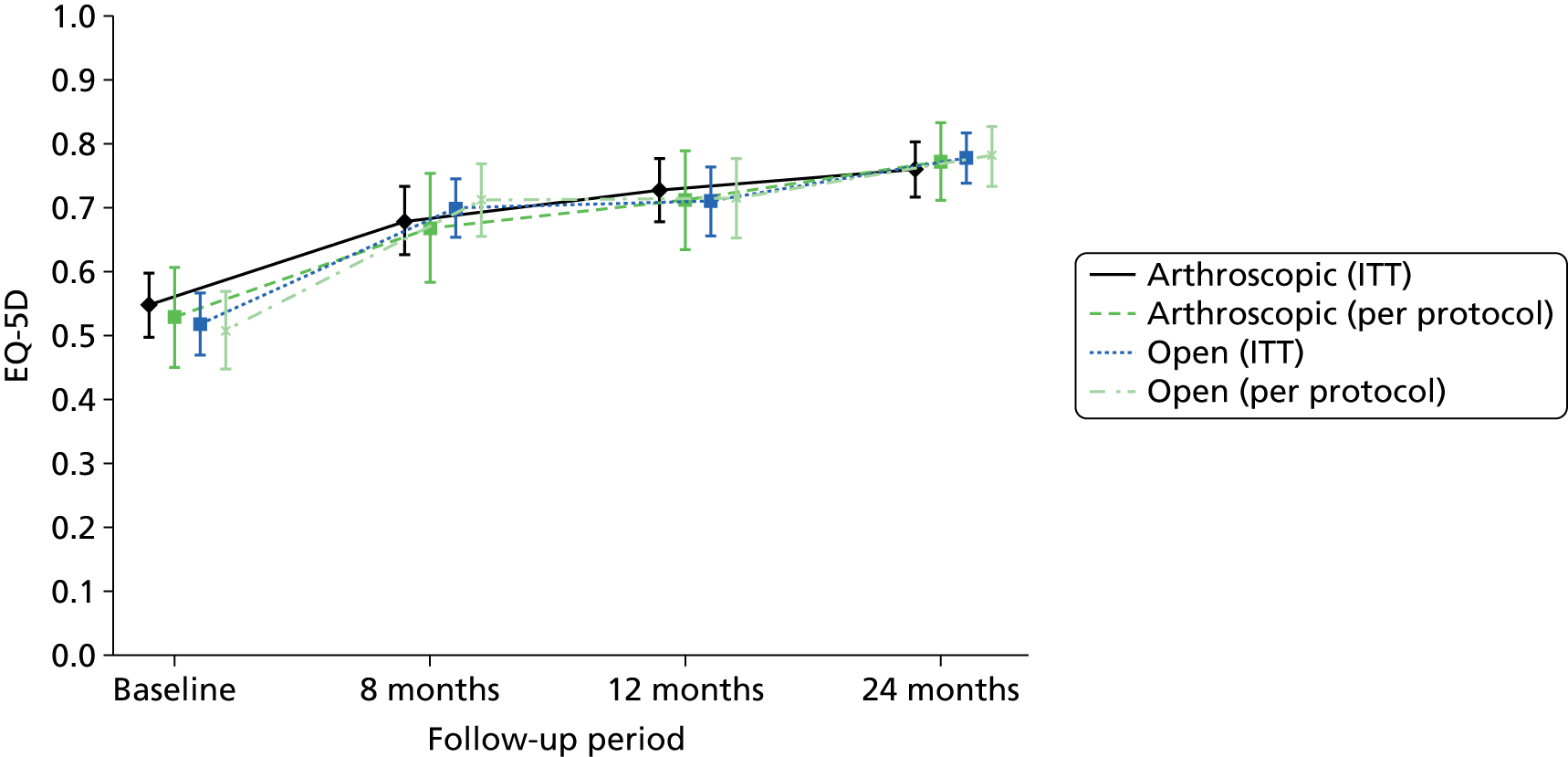
Statistical between-group analysis
Primary outcome
The pre-chosen primary outcome was the OSS score at 24 months’ follow-up, for which the effect sizes and 95% CIs are shown in Table 17. Under ITT analysis there was no evidence of a difference between those randomised to receive an arthroscopic procedure and those randomised to receive an open procedure (difference –0.76, 95% CI –2.75 to 1.22; p = 0.452). The 95% CI was also small enough to exclude the prespecified clinically important difference of 3 points.
To test the sensitivity of the primary outcome to the actual procedure received we also performed a per-protocol analysis of the 24-month OSS using the instrumental variable approach described in Chapter 2. A similar result to that of the ITT analysis was produced, although the CIs were much wider, as expected (difference –0.46, 95% CI –5.30 to 4.39; p = 0.854). We are therefore confident that there was no evidence of important differences between surgical treatments.
Secondary outcomes
The secondary outcomes were the health status measures (EQ-5D, SPADI and MHI-5), the change in symptom measures (transition items regarding shoulder problems and shoulder symptoms) and satisfaction ratings (‘How pleased are you with your shoulder symptoms?’) at 8, 12 and 24 months, the OSS at 8 and 12 months and MRI-diagnosed re-tears at 12 months post surgery. Analyses of these outcomes are shown in Tables 17 and 18.
Health status
There was no evidence of any differences between the randomised groups for any of the health status measures at all follow-up times (see Table 17).
Change in symptoms and satisfaction
There was no evidence of any differences between the randomised groups for either of the symptom transition or satisfaction measures at all follow-up times (see Table 18). For example, at 24 months, when asked how pleased they were with their shoulder symptoms, 84.6% of participants in the arthroscopic group and 82.4% in the open group were either very or fairly pleased (OR 1.37, 95% CI 0.73 to 2.60; p = 0.330).
Magnetic resonance imaging findings
The rate of re-tear was similar across the randomised groups, at 46.4% in the arthroscopic repair group and 38.6% in the open surgery group (difference 9.5%, 95% CI –6.9% to 25.8%; p = 0.256).
Subgroup analysis
Two preplanned subgroup analyses on the primary outcome (OSS at 24 months) were conducted: size of tear at baseline assessment (small or medium vs. large or massive) and age at recruitment (< 65 years vs. ≥ 65 years). Figure 10 displays the means and 95% CIs for the differences in OSS score at 24 months in the subgroups. There was no evidence that any of the subgroups was statistically significantly different at the 1% level (p = 0.843 for tear size and p = 0.024 for age).
FIGURE 10.
Prespecified subgroup analysis of the OSS at 24 months (size of tear; age of patient).

Learning curve
The statistical model for investigating any trend in OSS at 24 months as surgeon experience increased during the trial did not demonstrate any significant learning effect (trend in OSS +0.04 per procedure, 95% CI –0.21 to 0.29; p = 0.744).
Chapter 5 Rest then exercise
In total, 214 patients were randomised to rest then exercise before the reconfiguration of the trial, with 44 randomised within stratum A (arthroscopic surgery vs. open surgery vs. rest then exercise), 90 within stratum B (arthroscopic surgery vs. rest then exercise) and 80 within stratum C (open surgery vs. rest then exercise). Data from these participants are presented in this chapter. Reflecting the observational status of these data, no statistical analysis or formal interpretation of the data is presented.
Description of the rest-then-exercise group at trial entry
All baseline data collected on these patients were presented in Chapter 3. We replicate a subset of the baseline data here to illustrate that participants randomised to rest then exercise across the three strata displayed broadly similar characteristics and beliefs at baseline (Tables 21 and 22, respectively).
| Characteristic | Stratum A (n = 44), n (%) | Stratum B (n = 90), n (%) | Stratum C (n = 80), n (%) |
|---|---|---|---|
| Age (years) | 44, 62.9 (7.5) | 90, 64.7 (8.0) | 80, 61.3 (6.8) |
| Years with shoulder problem | 43, 2.0 (2.7) | 87, 2.2 (3.3) | 79, 2.3 (2.6) |
| Sex | |||
| Male | 28 (63.6) | 63 (70.0) | 51 (63.8) |
| Female | 16 (36.4) | 27 (30.0) | 29 (36.3) |
| Handedness | |||
| Right-handed | 40 (90.9) | 78 (86.7) | 66 (82.5) |
| Left-handed | 1 (2.3) | 9 (10.0) | 8 (10.0) |
| Both | 2 (4.5) | 3 (3.3) | 5 (6.3) |
| Missing | 1 (2.3) | 1 (1.3) | |
| Highest qualification | |||
| None | 23 (52.3) | 37 (41.1) | 25 (31.3) |
| Secondary | 16 (36.4) | 38 (42.2) | 41 (51.3) |
| Higher | 5 (11.4) | 12 (13.3) | 12 (15.0) |
| Missing | 3 (3.3) | 2 (2.5) | |
| Housing tenure | |||
| Home owner | 34 (77.3) | 78 (86.7) | 68 (85.0) |
| Private rent | 3 (6.8) | 2 (2.2) | 4 (5.0) |
| Council rent | 5 (11.4) | 7 (7.8) | 2 (2.5) |
| Other | 2 (4.5) | 2 (2.2) | 5 (6.3) |
| Missing | 1 (1.1) | 1 (1.3) | |
| Lives alone | |||
| Yes | 6 (13.6) | 19 (21.1) | 12 (15.0) |
| No | 34 (77.3) | 67 (74.4) | 64 (80.0) |
| Missing | 4 (9.1) | 4 (4.4) | 4 (5.0) |
| Employment status | |||
| Full-time | 12 (27.3) | 30 (33.3) | 35 (43.8) |
| Part-time | 7 (15.9) | 10 (11.1) | 8 (10.0) |
| Homemaker | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Retired | 22 (50.0) | 45 (50.0) | 32 (40.0) |
| Unemployed | 3 (6.8) | 5 (5.6) | 4 (5.0) |
| Missing | 1 (1.3) | ||
| Type of work | |||
| Manual | 12 (63.2) | 27 (67.5) | 24 (55.8) |
| Non-manual | 6 (31.6) | 11 (27.5) | 15 (34.9) |
| Not sure | 1 (5.3) | 1 (2.5) | 3 (7.0) |
| Missing | 1 (2.5) | 1 (2.3) | |
| Off sick or working reduced duties | |||
| Yes, off sick | 3 (15.8) | 5 (12.5) | 4 (9.3) |
| Yes, working reduced duties | 5 (26.3) | 8 (20.0) | 8 (18.6) |
| No, working usual duties | 11 (57.9) | 27 (67.5) | 31 (72.1) |
| Would you be able to do your job or everyday activities with arm in a sling? | |||
| No | 18 (40.9) | 48 (53.3) | 43 (53.8) |
| Yes, with difficulty | 19 (43.2) | 35 (38.9) | 31 (38.8) |
| Yes, no difficulty | 4 (9.1) | 2 (2.2) | 5 (6.3) |
| Missing | 3 (6.8) | 5 (5.6) | 1 (1.3) |
| Attitude | Stratum A (n = 44), n (%) | Stratum B (n = 90), n (%) | Stratum C (n = 80), n (%) |
|---|---|---|---|
| Doctors rely on surgery too much | |||
| Agree | 3 (6.8) | 5 (5.6) | 5 (6.3) |
| Uncertain | 26 (59.1) | 35 (38.9) | 29 (36.3) |
| Disagree | 13 (29.5) | 42 (46.7) | 39 (48.8) |
| Strongly disagree | 2 (4.5) | 7 (7.8) | 5 (6.3) |
| Missing | 1 (1.1) | 2 (2.5) | |
| Doctors place too much trust in surgery | |||
| Strongly agree | 1 (2.3) | ||
| Agree | 9 (20.5) | 7 (7.8) | 8 (10.0) |
| Uncertain | 22 (50.0) | 35 (38.9) | 33 (41.3) |
| Disagree | 11 (25.0) | 43 (47.8) | 33 (41.3) |
| Strongly disagree | 1 (2.3) | 4 (4.4) | 3 (3.8) |
| Missing | 1 (1.1) | 3 (3.8) | |
| Worry about surgery risks | |||
| Strongly agree | 3 (6.8) | 12 (13.3) | 4 (5.0) |
| Agree | 20 (45.5) | 35 (38.9) | 33 (41.3) |
| Uncertain | 8 (18.2) | 14 (15.6) | 16 (20.0) |
| Disagree | 12 (27.3) | 23 (25.6) | 20 (25.0) |
| Strongly disagree | 1 (2.3) | 4 (4.4) | 4 (5.0) |
| Missing | 2 (2.2) | 3 (3.8) | |
| Surgery should be only a last resort | |||
| Strongly agree | 6 (13.6) | 12 (13.3) | 11 (13.8) |
| Agree | 17 (38.6) | 48 (53.3) | 36 (45.0) |
| Uncertain | 9 (20.5) | 12 (13.3) | 13 (16.3) |
| Disagree | 11 (25.0) | 15 (16.7) | 15 (18.8) |
| Strongly disagree | 1 (2.3) | 3 (3.3) | 2 (2.5) |
| Missing | 3 (3.8) | ||
Outcomes in those allocated to rest then exercise
Outcomes of all those allocated to rest then exercise (i.e. by ITT) are presented in Table 23. As with the full trial data presented in previous chapters, these data show that participants demonstrated substantial improvements in quality of life from baseline to final follow-up at 2 years.
| Measure | Stratum A (n = 44), n, mean (SD) | Stratum B (n = 90), n, mean (SD) | Stratum C (n = 80), n, mean (SD) |
|---|---|---|---|
| OSS | |||
| Baseline | 44, 23.7 (8.3) | 90, 23.5 (8.0) | 80, 26.2 (7.9) |
| 8 months | 39, 37.6 (7.0) | 69, 34.8 (9.7) | 68, 37.1 (8.8) |
| 12 months | 37, 39.3 (7.4) | 65, 38.7 (8.9) | 62, 40.1 (9.0) |
| 24 months | 34, 41.1 (7.5) | 64, 39.2 (10.8) | 56, 41.9 (8.2) |
| SPADI pain | |||
| Baseline | 44, 73.0 (22.0) | 89, 73.1 (19.4) | 80, 69.4 (18.2) |
| 8 months | 39, 33.3 (24.5) | 68, 37.4 (28.1) | 64, 30.0 (26.1) |
| 12 months | 35, 26.3 (27.1) | 61, 24.3 (26.6) | 58, 22.0 (25.2) |
| 24 months | 33, 19.1 (23.4) | 62, 22.9 (30.1) | 54, 16.4 (23.8) |
| SPADI disability | |||
| Baseline | 44, 63.0 (23.7) | 90, 64.4 (22.1) | 77, 57.7 (23.3) |
| 8 months | 38, 26.6 (23.5) | 66, 33.3 (27.9) | 65, 26.3 (25.3) |
| 12 months | 35, 21.8 (22.7) | 60, 20.7 (24.7) | 57, 20.0 (26.8) |
| 24 months | 32, 16.2 (22.4) | 62, 20.0 (27.6) | 54, 13.2 (22.3) |
| SPADI | |||
| Baseline | 44, 66.9 (22.1) | 90, 67.8 (20.4) | 79, 62.3 (20.1) |
| 8 months | 38, 29.2 (23.4) | 67, 34.9 (27.5) | 64, 27.7 (25.0) |
| 12 months | 35, 23.5 (23.9) | 61, 22.5 (25.2) | 57, 21.1 (26.3) |
| 24 months | 32, 17.1 (22.5) | 62, 21.1 (28.2) | 54, 14.7 (22.5) |
| MHI-5 | |||
| Baseline | 44, 21.5 (5.5) | 90, 22.7 (4.9) | 80, 22.9 (4.6) |
| 8 months | 37, 24.5 (4.3) | 68, 23.8 (4.8) | 64, 23.8 (4.8) |
| 12 months | 35, 22.9 (4.8) | 62, 23.8 (5.4) | 58, 24.2 (4.6) |
| 24 months | 33, 24.1 (3.8) | 62, 24.6 (4.6) | 54, 25.3 (4.0) |
| EQ-5D | |||
| Baseline | 43, 0.448 (0.332) | 89, 0.503 (0.287) | 79, 0.538 (0.298) |
| 8 months | 36, 0.740 (0.143) | 68, 0.691 (0.272) | 67, 0.722 (0.232) |
| 12 months | 35, 0.703 (0.262) | 63, 0.750 (0.257) | 61, 0.778 (0.257) |
| 24 months | 34, 0.797 (0.153) | 63, 0.736 (0.291) | 57, 0.780 (0.304) |
Outcomes in those allocated to rest then exercise but who did not complete the 10-week course before progressing to surgery
In total, 77 (36%) of the 214 participants initially randomised to rest then exercise progressed to surgery before completion of the 10-week rest-then-exercise course. Outcomes at each time point in this specific subgroup of participants are presented in Table 24.
| Measure | Stratum A (n = 14), n, mean (SD) | Stratum B (n = 36), n, mean (SD) | Stratum C (n = 27), n, mean (SD) |
|---|---|---|---|
| OSS | |||
| Baseline | 14, 24.5 (8.8) | 36, 23.3 (8.2) | 27, 26.3 (8.3) |
| 8 months | 14, 39.4 (5.7) | 26, 35.8 (9.7) | 27, 39.4 (8.5) |
| 12 months | 13, 40.0 (8.1) | 26, 39.3 (8.1) | 25, 41.3 (9.3) |
| 24 months | 12, 40.7 (8.0) | 25, 39.4 (10.7) | 22, 42.1 (9.8) |
| SPADI pain | |||
| Baseline | 14, 70.0 (23.7) | 35, 74.7 (19.8) | 27, 72.1 (16.6) |
| 8 months | 14, 28.7 (22.1) | 26, 36.0 (29.3) | 27, 22.4 (23.6) |
| 12 months | 13, 20.2 (24.6) | 25, 19.3 (21.4) | 24, 17.2 (24.6) |
| 24 months | 11, 16.4 (23.8) | 24, 25.9 (31.8) | 22, 16.2 (29.4) |
| SPADI disability | |||
| Baseline | 14, 60.4 (27.3) | 36, 65.0 (21.9) | 25, 58.4 (22.9) |
| 8 months | 14, 26.4 (21.5) | 25, 28.8 (27.5) | 27, 20.1 (25.6) |
| 12 months | 13, 19.7 (22.7) | 25, 14.7 (18.8) | 25, 17.3 (26.5) |
| 24 months | 11, 16.9 (24.1) | 24, 19.5 (26.8) | 22, 13.6 (26.9) |
| SPADI | |||
| Baseline | 14, 64.1 (25.3) | 36, 23.3 (8.2) | 27, 26.3 (8.3) |
| 8 months | 14, 27.3 (21.2) | 26, 30.9 (27.7) | 27, 21.0 (24.4) |
| 12 months | 13, 19.9 (22.8) | 25, 16.5 (19.5) | 25, 18.3 (26.9) |
| 24 months | 11, 16.7 (23.7) | 24, 22.0 (28.4) | 22, 14.6 (27.6) |
| MHI-5 | |||
| Baseline | 14, 23.3 (3.9) | 36, 23.3 (4.4) | 27, 23.0 (5.5) |
| 8 months | 14, 24.7 (3.3) | 26, 24.1 (4.5) | 26, 23.7 (5.2) |
| 12 months | 13, 23.1 (5.2) | 26, 24.3 (4.1) | 25, 23.6 (5.5) |
| 24 months | 11, 23.7 (4.2) | 24, 24.5 (3.8) | 22, 24.7 (5.2) |
| EQ-5D | |||
| Baseline | 14, 0.460 (0.343) | 36, 0.476 (0.289) | 26, 0.525 (0.306) |
| 8 months | 13, 0.817 (0.138) | 26, 0.735 (0.198) | 26, 0.765 (0.239) |
| 12 months | 12, 0.813 (0.138) | 26, 0.754 (0.241) | 25, 0.785 (0.300) |
| 24 months | 12, 0.777 (0.171) | 25, 0.714 (0.311) | 22, 0.812 (0.289) |
Outcomes in those allocated to rest then exercise who completed the full 10-week course but still progressed to have surgery
In total, 88 (41%) of those allocated to rest then exercise completed the full 10-week course but despite this progressed to surgery. Outcomes at each time point in this specific subgroup of participants are presented in Table 25.
| Measure | Stratum A (n = 24), n, mean (SD) | Stratum B (n = 31), n, mean (SD) | Stratum C (n = 33), n, mean (SD) |
|---|---|---|---|
| OSS | |||
| Baseline | 24, 21.6 (7.6) | 31, 22.6 (7.0) | 33, 24.8 (7.6) |
| 8 months | 20, 35.6 (8.1) | 27, 34.6 (9.6) | 30, 35.0 (9.5) |
| 12 months | 19, 38.3 (7.4) | 24, 39.8 (8.3) | 27, 39.6 (8.4) |
| 24 months | 18, 42.1 (6.8) | 24, 41.8 (10.8) | 25, 42.1 (7.8) |
| SPADI pain | |||
| Baseline | 24, 78.8 (20.2) | 31, 74.6 (14.4) | 33, 69.9 (18.0) |
| 8 months | 20, 39.2 (27.0) | 27, 36.4 (25.5) | 29, 37.1 (27.3) |
| 12 months | 18, 32.3 (30.8) | 22, 22.0 (26.6) | 25, 23.4 (25.0) |
| 24 months | 18, 20.4 (25.6) | 24, 12.4 (25.1) | 23, 15.3 (21.3) |
| SPADI disability | |||
| Baseline | 24, 69.2 (20.2) | 31, 68.3 (18.2) | 32, 59.4 (23.0) |
| 8 months | 19, 31.7 (25.9) | 27, 34.5 (28.3) | 29, 32.2 (24.4) |
| 12 months | 18, 25.0 (24.7) | 22, 20.7 (26.2) | 24, 20.8 (27.6) |
| 24 months | 18, 15.9 (23.2) | 24, 13.9 (27.4) | 23, 11.8 (20.0) |
| SPADI | |||
| Baseline | 24, 73.0 (19.1) | 31, 70.8 (16.3) | 33, 63.1 (20.2) |
| 8 months | 19, 34.7 (26.2) | 27, 35.2 (26.8) | 29, 34.0 (24.6) |
| 12 months | 18, 27.8 (26.8) | 22, 21.2 (26.1) | 24, 22.2 (26.2) |
| 24 months | 18, 17.6 (23.8) | 24, 13.3 (26.2) | 23, 13.7 (20.2) |
| MHI-5 | |||
| Baseline | 24, 20.1 (6.4) | 31, 22.6 (4.9) | 33, 22.8 (4.0) |
| 8 months | 18, 24.1 (5.2) | 27, 24.9 (3.8) | 29, 23.5 (4.7) |
| 12 months | 18, 22.8 (4.7) | 22, 24.6 (5.6) | 24, 24.8 (3.5) |
| 24 months | 18, 24.8 (3.4) | 24, 26.3 (3.7) | 23, 25.2 (2.9) |
| EQ-5D | |||
| Baseline | 23, 0.386 (0.323) | 30, 0.532 (0.242) | 33, 0.518 (0.304) |
| 8 months | 19, 0.669 (0.116) | 27, 0.726 (0.225) | 29, 0.657 (0.250) |
| 12 months | 18, 0.603 (0.306) | 24, 0.812 (0.165) | 27, 0.780 (0.209) |
| 24 months | 18, 0.811 (0.141) | 23, 0.808 (0.258) | 26, 0.717 (0.354) |
Outcomes in those allocated to rest then exercise who completed the full 10-week course and did not proceed to surgery
In total, 36 (17%) of those allocated to rest then exercise completed the full 10-week course and had no surgical intervention. Outcomes at each time point in this specific subgroup of participants are presented in Table 26. A further 14 rest-then-exercise patients withdrew from the study over the course of the study.
| Measure | Stratum A (n = 5), n, mean (SD) | Stratum B (n = 16), n, mean (SD) | Stratum C (n = 15), n, mean (SD) |
|---|---|---|---|
| OSS | |||
| Baseline | 5, 32.0 (6.4) | 16, 25.3 (8.4) | 15, 27.7 (7.7) |
| 8 months | 5, 40.8 (3.4) | 15, 35.0 (9.4) | 11, 37.4 (6.5) |
| 12 months | 5, 41.2 (5.8) | 14, 37.8 (9.2) | 10, 38.4 (10.1) |
| 24 months | 4, 37.5 (9.6) | 14, 36.5 (8.5) | 9, 40.9 (5.2) |
| SPADI | |||
| Baseline | 5, 54.8 (19.2) | 16, 69.9 (25.5) | 15, 64.7 (21.5) |
| 8 months | 5, 22.4 (15.3) | 14, 38.4 (30.0) | 8, 30.0 (25.8) |
| 12 months | 4, 19.5 (10.0) | 13, 32.5 (29.2) | 9, 30.7 (27.5) |
| 24 months | 4, 20.6 (13.9) | 13, 31.4 (27.5) | 9, 20.0 (15.2) |
| SPADI disability | |||
| Baseline | 5, 42.8 (21.9) | 16, 59.9 (25.2) | 15, 54.3 (26.4) |
| 8 months | 5, 7.9 (5.9) | 13, 35.5 (26.1) | 9, 26.3 (25.7) |
| 12 months | 4, 14.1 (12.0) | 12, 27.3 (24.1) | 8, 26.1 (27.8) |
| 24 months | 3, 15.0 (17.4) | 13, 28.1 (25.6) | 9, 15.6 (16.7) |
| SPADI | |||
| Baseline | 5, 47.4 (18.4) | 16, 63.8 (24.7) | 15, 58.3 (23.4) |
| 8 months | 5, 13.5 (7.2) | 13, 37.9 (26.9) | 8, 27.7 (26.0) |
| 12 months | 4, 16.2 (11.1) | 13, 30.9 (25.3) | 8, 26.5 (27.2) |
| 24 months | 3, 15.6 (15.6) | 13, 29.3 (25.9) | 9, 17.3 (15.1) |
| MHI-5 | |||
| Baseline | 5, 23.8 (3.3) | 16, 22.2 (4.8) | 15, 22.5 (4.4) |
| 8 months | 5, 25.8 (3.3) | 14, 21.0 (6.4) | 9, 25.4 (3.8) |
| 12 months | 4, 22.6 (5.1) | 13, 22.0 (6.9) | 9, 24.0 (4.4) |
| 24 months | 4, 22.0 (4.7) | 13, 21.9 (6.2) | 9, 26.8 (2.6) |
| EQ-5D | |||
| Baseline | 5, 0.655 (0.335) | 16, 0.469 (0.345) | 15, 0.603 (0.271) |
| 8 months | 4, 0.829 (0.115) | 14, 0.548 (0.419) | 12, 0.782 (0.116) |
| 12 months | 5, 0.800 (0.199) | 12, 0.636 (0.392) | 9, 0.755 (0.289) |
| 24 months | 4, 0.790 (0.187) | 14, 0.674 (0.305) | 9, 0.883 (0.094) |
Chapter 6 Health economics
Methods: overview
The health economic analyses evaluate the total resource use and costs of rotator cuff repair and quality of life over the follow-up period of the trial. The primary economic outcome is additional cost per QALY gained of arthroscopic repair compared with open repair over a time horizon of 24 months, by ITT analysis. This outcome was assessed using patients allocated to arthroscopic and open repair in stratum A only, although cost and quality-of-life outcomes from stratum B (arthroscopic repair only) and stratum C (open repair only) are also reported. Lifetime extrapolation was not conducted for this analysis.
All analyses were conducted from the perspective of the NHS. Cost components included all initial and subsequent inpatient episodes and outpatient hospital visits, as well as GP, nurse and physiotherapist visits during follow-up.
Resource-use data collection
Resource-use for initial surgery
Individual patient data on time in theatre and number and type of bone anchors used were collected using a data collection form completed by health-care staff at the time of surgery. Additional equipment use during surgery was incorporated as a fixed cost of consumables. Further details of the assumed costs are given in Tables 27 and 28. The number of nights in hospital immediately following initial surgery was calculated for each patient as the difference between the date of surgery and the discharge date reported on the patient questionnaire at 2 weeks (or at 8 weeks if not reported at 2 weeks).
| Cost category | Unit cost (GB£ 2012/13) | Source and description |
|---|---|---|
| Rest-then-exercise programme | ||
| Cost of rest-then-exercise programme materials | 44.56 | Based on actual printing costs for main trial booklets and rest-then-exercise intervention booklets, cost of envelopes for sending materials to patients, cost of a sling and set-up costs for a Freephone number |
| Surgery costs (all patients)a | ||
| Cost per minute in theatre | 16.43 | Mean cost per minute in orthopaedic operating theatre. Average over 15 NHS boards in Scotland, year end March 2013. Information Services Division Scotland release 17 December 201375 |
| Cost per anchor | ||
| Open repair | 103.67/105.34 | Manufacturers’ list prices with a price discount applied. Costs presented are the average anchor cost for patients receiving each type of surgery (stratum A/all patients). The undiscounted list prices for the anchors ranged from £141 to £262. The illustrative average anchor cost here is based on the mean total anchor cost divided by the mean number of anchors (using imputed data) |
| Arthroscopic repair | 107.43/107.31 | |
| Other procedures | 98.52/102.96 | |
| Additional fixed surgical costs | ||
| Average cost per suture | 7.14 | Average of manufacturers’ list prices (discountedb) for each suture type recorded on theatre forms |
| Drapesc | 16.41 | Manufacturers’ list prices (discountedb) for shoulder arthroscopy drape and video camera drape |
| Fluid management system 1-day tubingc | 20.30 | Manufacturers’ list prices, discountedb |
| 90° suction electroded | 90.00 | Hospital cost obtained (£90 discounted price provided by manufacturerb) |
| 5.5 mm full radius resectore | 57.51 | Manufacturers’ list prices, discountedb |
| 4.0 mm oval burre | 57.51 | Manufacturers’ list prices, discountedb |
| Monopolar diathermy ESU pencilf | 1.93 | Manufacturers’ list prices, discountedb |
| Arthroscopic suture needleg | 157.14 | Cost obtained from supplier to the Nuffield Orthopaedic Centre, discountedb |
| Post-surgery and follow-up costsa | ||
| Cost per inpatient bed-day | 378.93 | Elective inpatient excess bed-day from 2012–13 NHS reference costs (‘The main schedule’, ‘El_XS’ tab).76 Weighted average of all shoulder and upper-arm procedures for non-trauma, ‘Trauma and Orthopaedics’ |
| Surgery during follow-up | ||
| Repair (open) | 1977.68 | All calculated from the average cost for each type of procedure within the trial (cost of time in theatre, anchors and fixed equipment). The cost of nights in hospital relating to surgery during follow-up was incorporated separately |
| Repair (arthroscopic) | 2192.80 | |
| Repair (unknown type) | 2085.24 | |
| Reverse shoulder replacement | 3722.11 | Elective inpatient excess bed-day from 2012–13 NHS reference costs (‘The main schedule’, ‘El_XS’ tab).76 Weighted average inpatient cost for major shoulder and upper-arm procedures with/without CC, non-trauma, ‘Trauma and Orthopaedics’ |
| Washout procedure | 337.48 | Elective inpatient excess bed-day from 2012–13 NHS reference costs (‘The main schedule’, ‘El_XS’ tab).76 Weighted average of minor and intermediate shoulder and upper arm procedures for non-trauma, ‘Trauma and Orthopaedics’ |
| Cost per appointment with GP | 37.00 | Consultation lasting 11.7 minutes, including direct care staff costs, excluding qualification costs. From Unit Costs of Health and Social Care 2013, Table 10.8b77 |
| Cost per appointment with nurse | 11.34 | Based on a 15.5-minute face-to-face consultation. From Unit Costs of Health and Social Care 2013, Table 10.677 |
| Cost per session with physiotherapist | 43.69 | Weighted average of NHS own costs for hospital- and community-based appointments. From 2012–13 NHS reference costs (‘The main schedule’, ‘NCL’ and ‘CHSAHP’ tabs)76 |
| Outpatient visits (shoulder) | 162.08 | Weighted average outpatient cost for major, intermediate and minor outpatient procedures. From 2012–13 NHS reference costs (OPROC tab)76 |
| Procedure details | n (%)a | Fixed procedure costs (GB£, discountedb) |
|---|---|---|
| Open repair | ||
| Fully-open | 84 (44) | 39.96 |
| Mini-open (with arthroscopic SAD) | 105 (55) | 244.97 |
| Weighted average | 153.98 | |
| Arthroscopic repair | 190 (100) | 319.64 |
| Other procedures | ||
| Biceps tenotomy | 4 (3) | 126.71 |
| Capsular release | 5 (4) | 126.71 |
| Partial-thickness tear (open) | 1 (1) | 38.64 |
| SAD ± ACJ excision (arthroscopic) | 112 (81) | 241.72 |
| Impossible to repair/no other procedure | 6 (4) | 36.71 |
| Weighted average | 222.29 | |
Resource use during follow-up
Information on health-care resource use after discharge was collected using patient questionnaires that were administered to all patients at 12 and 24 months, with responses in both questionnaires covering the 12 months prior to form completion. Data collected included the number of visits to a GP, nurse or physiotherapist/occupational therapist, the number of hospital outpatient and inpatient admissions and the number of nights in hospital; data were also collected on employment status, as reported in Chapter 4. Resource-use data were also available from a questionnaire administered at 8 months; however, the 12-month questionnaire also covered the 8-month follow-up period and so the 8-month responses were not used in the resource-use analysis (but they were used in the quality-of-life analysis; see later in this chapter).
Information on use of medications provided by the health-care system (mostly painkillers) was obtained from the 2-week and 8-week post-surgery questionnaires. It was assumed that the dosages reported on the questionnaires were the daily doses taken throughout the time period covered by the questionnaire responses (2 weeks for the 2-week questionnaire, 6 weeks for the 8-week questionnaire).
Data on surgical procedures during follow-up (e.g. revision repair surgery, washout for infection), along with nights spent in hospital relating to the procedures, were obtained from the 8-, 12-, and 24-month questionnaires.
Unit costs and application to resource use
Cost of initial treatment
Costs relating to surgical procedures were based on time in theatre, anchors used and nights spent in hospital after the procedure. Time in theatre was obtained from a surgery data collection form and a unit cost per minute in theatre was obtained using a national average figure for orthopaedic surgery theatres reported by the Information Services Division in Scotland. 75 List prices for the anchors used in the trial (identified by brand and product name from the surgery data collection form) were obtained from the various manufacturers and a 30% price discount was applied to these costs based on the assumption that the amount paid by the hospital would be less than the list price. The unit cost used for nights in hospital following surgery was the cost of an orthopaedic inpatient bed-day, obtained from NHS reference costs. 76
Additional fixed equipment costs
In addition to patient-specific time in theatre and number of anchors, a fixed cost for consumables was included in the cost of initial surgery, under the assumption that the same set of single-use consumables would be used for each procedure (but varying by procedure type). This cost incorporated single-use items such as drapes, tubing and surgical devices, including bone shavers and needle passers. The surgical items used were assumed to be the same for each patient receiving a certain type of procedure (open repair, arthroscopic repair and so on). Further information on these items is given Table 27, with the total fixed costs given in Table 28. Other surgery-related resource-use items, such as theatre running costs, staffing, machinery and reusable equipment, were incorporated in the running costs per minute in theatre given in Table 27, which was applied using time in theatre for each patient.
Cost of revision surgery
Individual patient data on time in theatre and number of anchors were not available for revision surgery. Therefore, patients returning for a revision repair procedure were assumed to accrue a cost equal to the total procedure cost observed for the initial procedure (for the reported revision procedure type). Information on the total number of nights spent in hospital during follow-up was reported separately on the follow-up form and was assumed to include nights spent in hospital during the revision procedure.
Costs for non-repair procedures during follow-up (e.g. washout for infection, shoulder replacement) were obtained from NHS reference costs,76 as detailed in Table 27.
Unit costs for other health-care resource use were obtained from national sources,76,77 as summarised in Table 27.
Costs for the rest-then-exercise arm
Costs for the rest-then-exercise intervention were applied for all patients who had been allocated to the intervention (and therefore were sent the materials), regardless of their subsequent treatment.
The rest-then-exercise intervention consisted of an A4 colour booklet with information on rotator cuff tears and a management strategy of relative rest and then subsequent exercises. This was delivered by post with a sling and an accompanying CD showing moving images of the exercises. A Freephone number giving access to a shoulder physiotherapist was provided. Information on the costs of preparing, printing and distributing the booklet and CD was obtained from the trial co-ordinators in Oxford.
Application of unit costs
Unit costs were multiplied by resource use to obtain a total cost for each resource-use component and a total cost for each patient was obtained by summing all components. No further costs were accrued for patients who had died.
A discount rate of 3.5% per annum was applied to all costs accrued after 12 months, in line with standard guidelines for economic evaluations. 78 Costs are reported in UK pounds and the cost year is 2012–13.
Quality of life
Quality of life was measured at baseline and 8, 12 and 24 months using the five domains of the EQ-5D-3L questionnaire,68,71 with patients reporting levels of mobility, self-care, usual activities, pain/discomfort and anxiety/depression using a 3-point scale. (For a summary of the proportion of responses at each level of each domain for each time point of follow-up, see Table 38.) The responses for the domains were converted to quality-of-life valuations using the Stata command ‘eq5d’ (Stata/SE version 12; StataCorp LP, College Station, TX, USA), which uses a value set based on the preferences of a large sample of the UK population to produce a EQ-5D index score for each patient at each time point. The possible range for the index scores when using the UK value set runs from –0.594 to 1, with a higher index indicating a better quality of life and an index of zero representing quality of life equivalent to death. An EQ-5D index score of zero was assumed for patients who had died.
The EQ-5D index scores were used to estimate the total QALYs for each patient between the 8-, 12- and 24-month follow-up points, as well as the total QALYs at 24 months. QALYs were calculated from the area under the curve after linear interpolation of the EQ-5D index score between time points. A discount rate was applied to QALYs after 12 months, at a rate of 3.5% per annum. 78
Dealing with missing data
Table 29 shows the number of complete cases (individuals with complete data for all resource-use, cost and QALY outcome variables) at each follow-up point by treatment arm. Missing data were handled using multiple imputation methods. Imputation via chained equations (with the ‘mi impute chained’ command in Stata) was used to impute the missing values in the original data set, based on all other variables included in the imputation model, to produce a specified number of complete data sets. Three imputation models were constructed for (1) resource-use parameters (number of health-care visits and number of nights in hospital), (2) reported out-of-pocket costs (medications, transportation, private health care, lost earnings) and (3) the five EQ-5D-3L domains at each follow-up point. Thirty data sets were produced for this analysis to align with the greatest level of missingness among the imputed variables. The data sets were then combined using the ‘mi estimate’ command in Stata, which applies Rubin’s rules when combining estimates from multiple imputed data sets to account for variation both within and between data sets. Imputation was conducted separately for initial hospitalisation, follow-up resource-use/costs and quality-of-life data. All imputation models included variables for patient characteristics (age, sex, size of tear, duration of shoulder problems at baseline) and indicators for centre and treatment allocation. For quality of life each domain of the EQ-5D-3L was imputed (rather than the index score directly) and baseline EQ-5D-3L domains were also included in the imputation model.
| Follow-up point | n (%) with complete data for all outcome variables | ||
|---|---|---|---|
| Stratum A (n = 317) | Stratum B (n = 181) | Stratum C (n = 162) | |
| At dischargea | 199 (63) | 94 (52) | 92 (57) |
| 12 monthsb | 113 (36) | 40 (22) | 46 (28) |
| 24 monthsc | 104 (33) | 36 (20) | 42 (26) |
Incremental analysis
Under conventional decision rules, specifically those used by the National Institute for Health and Care Excellence (NICE), the cost-effectiveness of a technology is assessed using the incremental cost-effectiveness ratio (ICER), which is based on the additional cost per QALY gained compared with the current best practice. The guidance for methods of economic evaluation produced by NICE78 states that a technology with an ICER below £20,000 per QALY gained is likely to be deemed cost-effective. Technologies with ICERs above £30,000 are unlikely to be considered cost-effective unless additional justification is provided. In addition, the likelihood of a technology being accepted as cost-effective decreases as the ICER increases from £20,000 to £30,000.
Incremental cost-effectiveness ratio
The incremental analysis is presented in terms of the total additional cost per QALY gained for arthroscopic repair compared with open repair (referred to as the ICER throughout). The ICER was calculated as the difference in total costs at 24 months divided by the difference in QALYs for arthroscopic repair compared with open repair.
Analysis of uncertainty
Uncertainty around the ICER was characterised using 1000 non-parametric bootstrap replicates of the mean total cost and effect differences (adjusted for covariates for certain analyses, as detailed in the results section) between the arthroscopic repair group and the open repair group in the data. The 30 multiple imputed data sets were merged to produce one data set prior to bootstrapping.
Results
This section presents the results of the economic analysis. Resource use during initial surgery (implants, theatre time) and the follow-up period (appointments with health-care professionals, hospital visits and so on) is presented, along with the associated costs up to 24 months after surgery. Results were adjusted for covariates when specified [EQ-5D score at baseline (for QALY outcomes only), age, tear size, centre]. All results are based on imputed data unless ‘original data’ is specified.
Four analyses are presented for the economic outcomes:
-
ITT, no adjustment for covariates – base case
-
ITT, adjusting for covariates
-
per protocol (only those patients receiving the allocated treatment), no adjustment for covariates
-
per protocol (only those patients receiving the allocated treatment), adjusting for covariates.
Covariates for age, tear size and centre were included when calculating mean cost and effect differences for analyses (b) and (d). Effect differences for analyses (b) and (d) were also adjusted for EQ-5D index score at baseline.
Resource-use results
Resource-use results for initial surgery and during follow-up are presented in Tables 30–32. There were no significant differences between the arthroscopic repair group and the open repair group for any of the resource-use categories for the base-case ITT analysis, apart from outpatient visits, for which there were 0.7 (95% CI –1.5 to 0.0) fewer visits between surgery and the 12-month follow-up for the arthroscopic repair group (see Table 31). When adjusting for covariates this difference became non-significant.
| Resource use | Stratum A | Stratum B | Stratum C | |||
|---|---|---|---|---|---|---|
| Arthroscopic, mean (SE) | Open, mean (SE) | Arthroscopic vs. open mean difference (95% CI;a p-value) (base case, no covariate adjustment) | Arthroscopic vs. open mean difference (95% CI;a p-value) (adjusting for age, tear size, centre) | Arthroscopic, mean (SE) | Open, mean (SE) | |
| Results for all patients (ITT) | (n = 136) | (n = 137) | (n = 91) | (n = 82) | ||
| Time in theatre (minutes) | 71.0 (4.9) | 71.1 (3.6) | –0.2 (–12.1 to 11.8; 0.981) | 6.8 (–1.3 to 14.9; 0.102) | 75.1 (5.0) | 73.9 (6.1) |
| Anchor quantity | 1.2 (0.1) | 1.4 (0.1) | –0.2 (–0.5 to 0.2; 0.352) | 0.0 (–0.3 to 0.3; 0.889) | 1.4 (0.2) | 1.5 (0.2) |
| Nights in hospital | 0.5 (0.1) | 0.7 (0.1) | –0.1 (–0.4 to 0.2; 0.399) | –0.1 (–0.4 to 0.2; 0.578) | 0.4 (0.1) | 1.0 (0.1) |
| Results for patients treated per protocol | (n = 63) | (n = 85) | (n = 50) | (n = 40) | ||
| Time in theatre (minutes) | 104.3 (4.8) | 86.5 (3.4) | 17.8 (6.4 to 29.2; 0.003) | 14.1 (4.0 to 24.3; 0.007) | 98.5 (5.0) | 101.2 (8.9) |
| Anchor quantity | 1.8 (0.1) | 1.8 (0.1) | 0.0 (–0.4 to –0.4; 0.954) | 0.1 (–0.3 to 0.4; 0.589) | 1.9 (0.2) | 2.3 (0.2) |
| Nights in hospital | 0.6 (0.1) | 0.9 (0.1) | –0.2 (–0.6 to 0.1; 0.179) | –0.3 (–0.6 to 0.1; 0.176) | 0.4 (0.1) | 1.3 (0.2) |
| Resource use | Stratum A | Stratum B | Stratum C | |||
|---|---|---|---|---|---|---|
| Arthroscopic (n = 136), mean (SE) | Open (n = 137), mean (SE) | Arthroscopic vs. open mean difference (95% CI;a p-value) (base case, no covariate adjustment) | Arthroscopic vs. open mean difference (95% CI;a p-value) (adjusting for age, tear size, centre) | Arthroscopic (n = 50), mean (SE) | Open (n = 40), mean (SE) | |
| Revision surgery between surgery and 12 months | 0 (–) | 0.0 (0.0) | –0.01 (–0.02 to 0.01; 0.320) | –0.01 (–0.02 to 0.01; 0.339) | 0.01 (0.01) | 0 (–) |
| GP visits between surgery and 12 months | 1.1 (0.2) | 1.2 (0.2) | –0.1 (–0.6 to 0.5; 0.831) | 0.0 (–0.6 to 0.5; 0.948) | 0.9 (0.2) | 1.0 (0.2) |
| Nurse visits between surgery and 12 months | 0.3 (0.1) | 0.5 (0.1) | –0.2 (–0.5 to 0.1; 0.256) | –0.2 (–0.5 to 0.2; 0.354) | 0.4 (0.2) | 0.4 (0.1) |
| Physiotherapist visits between surgery and 12 months | 6.1 (0.6) | 6.3 (0.5) | –0.2 (–1.7 to 1.4; 0.818) | 0.3 (–1.1 to 1.7; 0.685) | 5.4 (0.7) | 5.4 (0.8) |
| Inpatient visits between surgery and 12 months | 0.3 (0.1) | 0.4 (0.1) | –0.1 (–0.5 to 0.2; 0.418) | –0.1 (–0.5 to 0.2; 0.485) | 0.3 (0.2) | 0.4 (0.1) |
| Outpatient visits between surgery and 12 months | 1.6 (0.2) | 2.3 (0.3) | –0.7 (–1.5 to 0.0; 0.045) | –0.6 (–1.3 to 0.2; 0.134) | 1.9 (0.4) | 1.9 (0.3) |
| Revision surgery between 12 and 24 months | 0.01 (0.01) | 0.02 (0.01) | –0.01 (–0.04 to 0.02; 0.659) | 0.00 (–0.04 to 0.03; 0.768) | 0.01 (0.01) | 0 (–) |
| GP visits between 12 and 24 months | 0.4 (0.1) | 0.4 (0.1) | 0.1 (–0.2 to 0.4; 0.597) | 0.1 (–0.2 to 0.4; 0.600) | 0.6 (0.2) | 0.5 (0.1) |
| Nurse visits between 12 and 24 months | 0.1 (0.1) | 0.1 (0.0) | 0.0 (–0.1 to 0.2; 0.750) | 0.0 (–0.1 to 0.1; 0.819) | 0.1 (0.1) | 0.1 (0.0) |
| Physiotherapist visits between 12 and 24 months | 1.2 (0.5) | 0.5 (0.2) | 0.7 (–0.3 to 1.7; 0.196) | 0.7 (–0.3 to 1.7; 0.160) | 1.0 (0.4) | 0.9 (0.3) |
| Inpatient visits between 12 and 24 months | 0.03 (0.02) | 0.00 (0.00) | 0.03 (–0.02 to 0.08) | 0.03 (–0.02 to 0.08) | 0.01 (0.01) | 0.00 (0.00) |
| Outpatient visits between 12 and 24 months | 0.4 (0.1) | 0.2 (0.1) | 0.2 (–0.1 to 0.5; 0.282) | 0.2 (–0.1 to 0.5; 0.212) | 0.3 (0.1) | 0.3 (0.1) |
| Resource use | Stratum A | Stratum B | Stratum C | |||
|---|---|---|---|---|---|---|
| Arthroscopic (n = 63), mean (SE) | Open (n = 85), mean (SE) | Arthroscopic vs. open mean difference (95% CI;a p-value) (base case, no covariate adjustment) | Arthroscopic vs. open mean difference (95% CI;a p-value) (adjusting for age, tear size, centre) | Arthroscopic (n = 50), mean (SE) | Open (n = 40), mean (SE) | |
| Revision surgery between surgery and 12 months | 0 (–) | 0.01 (0.01) | –0.01 (–0.04 to 0.02; 0.391) | –0.01 (–0.04 to 0.01; 0.327) | 0.02 (0.02) | 0 (–) |
| GP visits between surgery and 12 months | 1.0 (0.2) | 1.4 (0.2) | –0.3 (–1.0 to 0.4; 0.356) | –0.2 (–0.9 to 0.5; 0.567) | 0.8 (0.3) | 1.1 (0.4) |
| Nurse visits between surgery and 12 months | 0.5 (0.2) | 0.8 (0.2) | –0.3 (–0.9 to 0.3; 0.308) | –0.4 (–1.0 to 0.3; 0.251) | 0.5 (0.2) | 0.4 (0.2) |
| Physiotherapist visits between surgery and 12 months | 7.7 (0.8) | 8.0 (0.7) | –0.3 (–2.2 to 1.8; 0.800) | 0.4 (–1.7 to 2.4; 0.728) | 6.3 (0.9) | 6.8 (1.1) |
| Inpatient visits between surgery and 12 months | 0.5 (0.2) | 0.6 (0.2) | –0.2 (–0.7 to 0.4; 0.596) | –0.3 (–0.9 to 0.3; 0.373) | 0.2 (0.2) | 0.4 (0.1) |
| Outpatient visits between surgery and 12 months | 1.9 (0.3) | 2.9 (0.5) | –1.0 (–2.2 to 0.2; 0.111) | –0.7 (–1.9 to 0.6; 0.283) | 1.6 (0.4) | 2.2 (0.5) |
| Revision surgery between 12 and 24 months | 0.03 (0.02) | 0.04 (0.02) | 0.00 (–0.06 to 0.06; 0.907) | –0.01 (–0.08 to 0.06; 0.777) | 0.02 (0.02) | 0 (–) |
| GP visits between 12 and 24 months | 0.4 (0.2) | 0.4 (0.2) | 0.0 (–0.5 to 0.4; 0.936) | 0.1 (–0.5 to 0.5; 0.981) | 0.5 (0.3) | 0.6 (0.2) |
| Nurse visits between 12 and 24 months | 0.0 (0.0) | 0.1 (0.1) | –0.1 (–0.2 to 0.1; 0.369) | –0.1 (–0.2 to 0.1; 0.388) | 0.1 (0.1) | 0.1 (0.1) |
| Physiotherapist visits between 12 and 24 months | 1.9 (1.0) | 0.7 (0.3) | 1.3 (–0.5 to 3.0; 0.165) | 1.4 (–0.4 to 3.2; 0.116) | 1.0 (0.5) | 0.9 (0.4) |
| Inpatient visits between 12 and 24 months | 0 (–) | 0 (–) | NA | NA | 0.02 (0.02) | 0.00 (0.00) |
| Outpatient visits between 12 and 24 months | 0.5 (0.3) | 0.3 (0.1) | 0.2 (–0.3 to 0.7; 0.488) | 0.2 (–0.2 to 0.7; 0.334) | 0.3 (0.2) | 0.4 (0.2) |
For the per-protocol analysis there was a significant difference in theatre time between patients receiving an arthroscopic repair and patients receiving an open repair, at a mean of 17.8 (95% CI 6.4 to 29.2) minutes longer for arthroscopic repair when not adjusting for covariates and 14.1 (95% CI 4.0 to 24.3) minutes longer for arthroscopic repair when adjusting for covariates (see Table 30). However, none of the other resource-use categories for either initial surgery or follow-up were significantly different between the two treatment groups (see Tables 30 and 32).
Cost results
Intention-to-treat analysis
Cost outcomes for initial surgery for the base-case ITT analysis are presented in Table 33. For the ITT analysis the difference in total initial procedure-related costs between treatment groups was not significant at the p = 0.05 level, whether adjusting for covariates or not.
| Cost item | Stratum A (£) | Stratum B (£) | Stratum C (£) | |||
|---|---|---|---|---|---|---|
| Arthroscopic, mean (SE) | Open, mean (SE) | Arthroscopic vs. open mean difference (95% CI;a p-value) (base case, no covariate adjustment) | Arthroscopic vs. open mean difference (95% CI;a p-value) (adjusting for age, tear size, centre) | Arthroscopic, mean (SE) | Open, mean (SE) | |
| Results for all patients (ITT analysis) | (n = 136) | (n = 137) | (n = 91) | (n = 82) | ||
| Theatre time | 1166 (80) | 1169 (60) | –2 (–199 to 194; 0.981) | 111 (–22 to 244; 0.102) | 1233 (83) | 1214 (100) |
| Anchor costs | 127 (14) | 147 (14) | –20 (–56 to 17; 0.288) | –1 (–29 to 28; 0.959) | 145 (18) | 158 (22) |
| Equipment costs | 202 (12) | 145 (7) | 58 (31 to 84; 0.000) | 77 (56 to 97; 0.000) | 237 (13) | 164 (9) |
| Total cost of surgery | 1497 (96) | 1460 (71) | 36 (–200 to 271; 0.766) | 187 (35 to 339; 0.016) | 1615 (102) | 1536 (115) |
| Nights in hospital | 206 (46) | 255 (36) | –49 (–165 to 66; 0.399) | –32 (–147 to 82; 0.578) | 144 (38) | 365 (54) |
| Total procedure-related costs | 1701 (115) | 1715 (86) | –14 (–297 to 270; 0.924) | 155 (–45 to 354; 0.129) | 1760 (113) | 1900 (142) |
| Results for patients treated per protocol | (n = 63) | (n = 85) | (n = 50) | (n = 40) | ||
| Theatre time | 1714 (78) | 1422 (56) | 292 (105 to 479; 0.003) | 232 (66 to 399; 0.007) | 1619 (82) | 1663 (146) |
| Anchor costs | 198 (14) | 193 (15) | 5 (–36 to 47; 0.799) | 12 (–24 to 49; 0.507) | 201 (17) | 245 (22) |
| Equipment costs | 320 (–) | 154 (–) | 166 (–) | 166 (–) | 320 (–) | 154 (–) |
| Total cost of surgery | 2231 (83) | 1768 (63) | 463 (260 to 666; 0.000) | 410 (232 to 589; 0.000) | 2139 (89) | 2062 (152) |
| Nights in hospital | 231 (48) | 323 (46) | –92 (–227 to 43; 0.179) | –96 (–235 to 44; 0.176) | 166 (51) | 477 (77) |
| Total procedure-related costs | 2462 (90) | 2091 (75) | 371 (135 to 607; 0.002) | 315 (93 to 536; 0.006) | 2306 (102) | 2539 (180) |
The difference in total cost of surgery alone (excluding the cost of nights in hospital after the procedure) was non-significant without covariate adjustment in the base case but significant when adjusted for covariates, at a mean of £187 (95% CI £35 to £339) more costly for the arthroscopic repair group than the open repair group. Additional equipment costs were significantly more costly for arthroscopic repair, being £58 (95% CI £31 to £84) more costly for arthroscopic repair without covariate adjustment and £77 (95% CI £56 to £97) more costly for arthroscopic repair with covariate adjustment.
Follow-up costs to 24 months for the base-case ITT analysis are presented in Table 34. The only resource-use category that had a significance cost difference between groups was outpatient visits, which were £121 (95% CI £2 to £240) less costly between surgery and 12 months’ follow-up for the arthroscopic group than for the open repair group (without adjustment for covariates). When adjusting for covariates this difference became non-significant. There were no significant differences in mean cost between the arthroscopic repair group and the open repair group for any other component resource-use category, nor were there any significant differences in total follow-up costs at 12 months or 24 months. The total time-discounted mean cost difference between arthroscopic repair and open repair at 24 months for the unadjusted base-case ITT analysis was negative at –£132 (95% CI –£589 to £324), suggesting that arthroscopic repair is less costly overall. The difference was positive after adjusting for covariates (£105, 95% CI –£255 to £466), suggesting that arthroscopic repair is more costly overall, although both results were non-significant.
| Cost item | Stratum A (£) | Stratum B (£) | Stratum C (£) | |||
|---|---|---|---|---|---|---|
| Arthroscopic (n = 136), mean (SE) | Open (n = 137), mean (SE) | Arthroscopic vs. open mean difference (95% CI;a p-value) (base case, no covariate adjustment) | Arthroscopic vs. open mean difference (95% CI;a p-value) (adjusting for age, tear size, centre) | Arthroscopic (n = 91), mean (SE) | Open (n = 82), mean (SE) | |
| Revision surgery between surgery and 12 months | 0 (–) | 2 (2) | –2 (–7 to 2; 0.320) | –2 (–7 to 3; 0.339) | 41 (41) | 0 (–) |
| GP visits between surgery and 12 months | 40 (7) | 43 (6) | –2 (–22 to 18; 0.831) | –1 (–21 to 19; 0.948) | 34 (8) | 38 (9) |
| Nurse visits between surgery and 12 months | 4 (1) | 6 (2) | –2 (–6 to 2; 0.256) | –2 (–6 to 2; 0.354) | 5 (2) | 5 (1) |
| Physiotherapist visits between surgery and 12 months | 267 (24) | 275 (24) | –8 (–75 to 59; 0.818) | 13 (–49 to 74; 0.685) | 234 (31) | 235 (33) |
| Inpatient visits between surgery and 12 months | 119 (37) | 170 (51) | –52 (–178 to 74; 0.418) | –45 (–173 to 83; 0.485) | 113 (64) | 169 (46) |
| Outpatient visits between surgery and 12 months | 259 (31) | 380 (52) | –121 (–240 to -2; 0.045) | –92 (–213 to 29; 0.134) | 312 (64) | 306 (49) |
| Medication costs between surgery and 12 months | 6 (1) | 4 (1) | 1 (–2 to 5; 0.386) | 2 (–2 to 5; 0.336) | 7 (2) | 6 (3) |
| Cost after surgery to 12-month follow-up | 694 (66) | 881 (93) | –187 (–413 to 40; 0.106) | –128 (–350 to 94; 0.256) | 745 (138) | 758 (93) |
| Total cost up to 12 months | 2395 (149) | 2596 (142) | –200 (–607 to 207; 0.333) | 26 (–283 to 337; 0.867) | 2055 (182) | 2659 (194) |
| Revision surgery between 12 and 24 months | 30 (21) | 31 (22) | –1 (–60 to 59; 0.986) | 4 (–58 to 66; 0.899) | 0 (–) | 0 (–) |
| GP visits between 12 and 24 months | 17 (5) | 13 (4) | 3 (–9 to 15; 0.597) | 3 (–9 to 16; 0.600) | 23 (7) | 19 (5) |
| Nurse visits between 12 and 24 months | 1 (1) | 1 (0) | 0 (–1 to 2; 0.750) | 0 (–1 to 2; 0.819) | 1 (1) | 1 (0) |
| Physiotherapist visits between 12 and 24 months | 51 (21) | 23 (8) | 29 (–15 to 72; 0.196) | 31 (–12 to 75; 0.160) | 44 (17) | 38 (12) |
| Inpatient visits between 12 and 24 months | 12 (9) | 0 (–) | 11 (–6 to 29; 0.209) | 12 (–6 to 30; 0.198) | 4 (4) | 1 (10) |
| Outpatient visits between 12 and 24 months | 67 (23) | 39 (12) | 27 (–23 to 77; 0.282) | 31 (–18 to 80; 0.212) | 54 (24) | 44 (18) |
| Total cost from 12 to 24 months | 177 (59) | 107 (30) | 70 (–59 to 200; 0.268) | 82 (–49 to 212; 0.219) | 127 (40) | 103 (28) |
| Total cost over 24 months | 2573 (177) | 2703 (150) | –130 (–589 to 329; 0.578) | 108 (–255 to 471; 0.558) | 2632 (195) | 2762 (201) |
| Total cost over 24 months (discounted) | 2567 (176) | 2699 (149) | –132 (–589 to 324; 0.569) | 105 (–255 to 466; 0.565) | 2628 (194) | 2758 (201) |
Per-protocol analysis
For the per-protocol analysis there was a significant difference in the total initial procedure-related cost between the arthroscopic repair group and the open repair group, at £371 (95% CI £135 to £607) more costly for arthroscopic repair with no covariate adjustment and £315 (95% CI £93 to £536) more costly for arthroscopic repair with covariate adjustment (see Table 33).
The total cost of surgery alone (excluding nights in hospital) was also significantly different between the two groups, at £463 (95% CI £260 to £666) more costly for arthroscopic repair without covariate adjustment and £410 (95% CI £232 to £589) more costly for arthroscopic repair with covariate adjustment. This difference was largely driven by the longer theatre time for the arthroscopic repair group. The cost of theatre time was significantly different between the two treatment groups, in line with the resource-use outcomes for time in theatre. Theatre time was £292 (95% CI £105 to £479) more costly for arthroscopic repair without covariate adjustment and £232 (95% CI £66 to £399) more costly for arthroscopic repair with covariate adjustment.
Follow-up costs to 24 months for the per-protocol analysis are presented in Table 35. There were no significant differences between the two treatment groups for any of the cost components. The mean total cost at 24 months was greater for arthroscopic repair by £222 (95% CI –£328 to £773) without covariate adjustment and by £207 (95% CI –£341 to £754) with covariate adjustment, suggesting that arthroscopic repair is more costly over the follow-up period, although again neither outcome was significant.
| Cost item | Stratum A (£) | Stratum B (£) | Stratum C (£) | |||
|---|---|---|---|---|---|---|
| Arthroscopic (n = 63), mean (SE) | Open (n = 85), mean (SE) | Arthroscopic vs. open mean difference (95% CI;a p-value) (base case, no covariate adjustment) | Arthroscopic vs. open mean difference (95% CI;a p-value) (adjusting for age, tear size, centre) | Arthroscopic (n = 50), mean (SE) | Open (n = 40), mean (SE) | |
| Revision surgery between surgery and 12 months | 0 (–) | 4 (4) | –4 (–13 to 5; 0.391) | –5 (–15 to 5; 0.327) | 74 (74) | 0 (–) |
| GP visits between surgery and 12 months | 38 (9) | 50 (9) | –12 (–37 to 13; 0.356) | –8 (–35 to 19; 0.567) | 30 (10) | 39 (14) |
| Nurse visits between surgery and 12 months | 5 (2) | 9 (2) | –3 (–10 to 3; 0.308) | –4 (–11 to 3; 0.245) | 6 (3) | 4 (2) |
| Physiotherapist visits between surgery and 12 months | 337 (33) | 348 (29) | –11 (–99 to 76; 0.800) | 16 (–73 to 105; 0.728) | 273 (40) | 296 (48) |
| Inpatient visits between surgery and 12 months | 181 (74) | 240 (78) | –59 (–278 to 160; 0.596) | –103 (–333 to 126; 0.373) | 84 (62) | 164 (57) |
| Outpatient visits between surgery and 12 months | 313 (54) | 469 (74) | –157 (–350 to 37; 0.111) | –111 (–315 to 93; 0.283) | 263 (64) | 358 (77) |
| Medication costs between surgery and 12 months | 7 (2) | 5 (1) | 1 (–3 to 6; 0.529) | 1 (–3 to 5; 0.662) | 6 (2) | 8 (4) |
| Cost after surgery to 12 month follow-up | 881 (109) | 1126 (131) | –245 (–599 to 109; 0.174) | –215 (–583 to 154; 0.251) | 736 (164) | 869 (135) |
| Total cost over 12 months | 3343 (141) | 3217 (159) | 126 (–316 to 569; 0.573) | 100 (–340 to 540; 0.653) | 3042 (208) | 3408 (258) |
| Revision surgery between 12 and 24 months | 65 (46) | 50 (35) | 16 (–96 to 127; 0.782) | 9 (–114 to 132; 0.882) | 0 (–) | 0 (–) |
| GP visits between 12 and 24 months | 15 (6) | 15 (6) | –1 (–17 to 16; 0.936) | 0 (–18 to 18; 0.981) | 19 (10) | 23 (8) |
| Nurse visits between 12 and 24 months | 0 (–) | 1 (1) | –1 (–2 to 1; 0.369) | –1 (–2 to 1; 0.388) | 1 (1) | 1 (1) |
| Physiotherapist visits between 12 and 24 months | 84 (43) | 29 (12) | 55 (–23 to 132; 0.165) | 63 (–16 to 142; 0.116) | 44 (22) | 39 (16) |
| Inpatient visits between 12 and 24 months | 0 (–) | 0 (–) | NA | NA | 8 (8) | 1 (2) |
| Outpatient visits between 12 and 24 months | 82 (44) | 53 (17) | 30 (–55 to 115; 0.488) | 39 (–40 to 118; 0.334) | 54 (29) | 63 (33) |
| Total cost from 12 to 24 months | 247 (119) | 148 (46) | 99 (–128 to 327; 0.391) | 110 (–126 to 347; 0.357) | 126 (50) | 127 (48) |
| Total cost over 24 months | 3590 (226) | 3365 (171) | 226 (–330 to 781; 0.423) | 210 (–342 to 763; 0.452) | 3168 (229) | 3534 (269) |
| Total cost over 24 months (discounted) | 3582 (223) | 3360 (171) | 222 (–328 to 773; 0.426) | 207 (–341 to 754; 0.456) | 3164 (228) | 3530 (268) |
Quality-of-life results
Table 36 presents a summary of the mean EQ-5D index score at each follow-up point (8, 12 and 24 months). The proportions of responses at each level of the five domains at each time point are presented in Tables 37–40 for the non-imputed data and in Tables 41–44 for the imputed data. QALYs from baseline to 24 months’ follow-up are presented in Table 45.
| Time point | Stratum A | Stratum B | Stratum C | ||||
|---|---|---|---|---|---|---|---|
| Arthroscopic, mean (SE) | Open, mean (SE) | Arthroscopic vs. open mean difference (95% CI;a p-value) (base case, no covariate adjustment) | Arthroscopic vs. open mean difference (95% CI;a p-value) (adjusting for baseline EQ-5D index) | Arthroscopic vs. open mean difference (95% CI;a p-value) (adjusting for baseline EQ-5D index, age, tear size, centre) | Arthroscopic, mean (SE) | Open, mean (SE) | |
| Results for all patients (ITT) | (n = 136) | (n = 137) | (n = 91) | (n = 82) | |||
| Baseline | 0.55 (0.03) | 0.52 (0.02) | 0.03 (–0.04 to 0.10; 0.352) | NA | 0.03 (–0.04 to 0.11; 0.336)b | 0.51 (0.03) | 0.54 (0.03) |
| 8 months | 0.68 (0.03) | 0.69 (0.02) | –0.01 (–0.08 to 0.05; 0.691) | –0.03 (–0.09 to 0.04; 0.391) | –0.03 (–0.09 to 0.04; 0.392) | 0.69 (0.03) | 0.70 (0.02) |
| 12 months | 0.72 (0.02) | 0.71 (0.03) | 0.01 (–0.06 to 0.08; 0.852) | –0.01 (–0.07 to 0.06; 0.878) | –0.01 (–0.08 to 0.06; 0.788) | 0.70 (0.03) | 0.73 (0.03) |
| 24 months | 0.74 (0.02) | 0.76 (0.02) | –0.03 (–0.09 to 0.03; 0.389) | –0.04 (–0.09 to 0.02; 0.218) | –0.04 (–0.10 to 0.02; 0. 232) | 0.72 (0.03) | 0.74 (0.03) |
| Results for patients (per protocol) | (n = 63) | (n = 85) | (n = 50) | (n = 40) | |||
| Baseline | 0.53 (0.04) | 0.50 (0.03) | 0.03 (–0.07 to 0.13; 0.579) | NA | 0.02 (–0.08 to 0.12; 0.663)b | 0.51 (0.05) | 0.47 (0.05) |
| 8 months | 0.67 (0.04) | 0.70 (0.03) | –0.03 (–0.13 to 0.06; 0.519) | –0.04 (–0.13 to 0.04; 0.326) | –0.03 (–0.12 to 0.06; 0.494) | 0.72 (0.03) | 0.65 (0.04) |
| 12 months | 0.71 (0.04) | 0.72 (0.03) | –0.00 (–0.10 to 0.09; 0.952) | –0.01 (–0.10 to 0.08; 0.786) | –0.03 (–0.11 to 0.06; 0.569) | 0.76 (0.03) | 0.71 (0.04) |
| 24 months | 0.74 (0.03) | 0.78 (0.02) | –0.04 (–0.12 to 0.04; 0.353) | –0.05 (–0.12 to 0.03; 0.256) | –0.05 (–0.13 to 0.03; 0.188) | 0.74 (0.04) | 0.75 (0.04) |
| Level | Mobility | Self-care | Activity | Pain | Anxiety |
|---|---|---|---|---|---|
| Baseline | |||||
| 1 | 505 (77) | 358 (54) | 90 (14) | 16 (2) | 427 (65) |
| 2 | 152 (23) | 299 (45) | 519 (79) | 474 (72) | 207 (31) |
| 3 | – | 2 (0) | 51 (8) | 169 (26) | 25 (4) |
| Missing | 3 (0) | 1 (0) | – | 1 (0) | 1 (0) |
| 8 months | |||||
| 1 | 437 (66) | 413 (63) | 241 (37) | 142 (22) | 412 (63) |
| 2 | 141 (21) | 158 (24) | 309 (47) | 399 (61) | 151 (23) |
| 3 | – | 5 (1) | 27 (4) | 35 (5) | 12 (2) |
| Missing | 80 (12) | 82 (12) | 81 (12) | 82 (12) | 83 (13) |
| 12 months | |||||
| 1 | 414 (63) | 443 (67) | 290 (44) | 194 (29) | 408 (62) |
| 2 | 145 (22) | 112 (17) | 247 (38) | 323 (49) | 137 (21) |
| 3 | 1 (0) | 3 (0) | 24 (4) | 42 (6) | 12 (2) |
| Missing | 98 (15) | 100 (15) | 97 (15) | 99 (15) | 101 (15) |
| 24 months | |||||
| 1 | 387 (59) | 449 (69) | 308 (47) | 232 (36) | 414 (63) |
| 2 | 155 (24) | 90 (14) | 219 (34) | 283 (43) | 119 (18) |
| 3 | – | 4 (1) | 16 (2) | 28 (4) | 9 (1) |
| Missing | 111 (17) | 110 (17) | 110 (17) | 110 (17) | 111 (17) |
| Level | Mobility | Self-care | Activity | Pain | Anxiety |
|---|---|---|---|---|---|
| Baseline | |||||
| 1 | 244 (77) | 176 (56) | 45 (14) | 9 (3) | 209 (66) |
| 2 | 72 (23) | 139 (44) | 252 (80) | 223 (70) | 95 (30) |
| 3 | – | 2 (1) | 20 (6) | 84 (27) | 12 (4) |
| Missing | 1 (0) | – | – | 1 (0) | 1 (0) |
| 8 months | |||||
| 1 | 216 (68) | 210 (66) | 115 (36) | 72 (23) | 194 (61) |
| 2 | 68 (22) | 67 (21) | 155 (49) | 193 (61) | 81 (26) |
| 3 | – | 5 (2) | 15 (5) | 19 (6) | 8 (3) |
| Missing | 32 (10) | 34 (11) | 31 (10) | 32 (10) | 33 (10) |
| 12 months | |||||
| 1 | 202 (64) | 220 (70) | 137 (43) | 95 (30) | 202 (64) |
| 2 | 75 (24) | 55 (17) | 129 (41) | 161 (51) | 70 (22) |
| 3 | 1 (0) | 3 (1) | 14 (4) | 24 (8) | 6 (2) |
| Missing | 38 (12) | 38 (12) | 36 (11) | 36 (11) | 38 (12) |
| 24 months | |||||
| 1 | 191 (61) | 224 (71) | 151 (48) | 107 (34) | 203 (65) |
| 2 | 77 (25) | 42 (13) | 112 (36) | 153 (49) | 61 (19) |
| 3 | – | 2 (1) | 5 (2) | 8 (3) | 4 (1) |
| Missing | 46 (15) | 46 (15) | 46 (15) | 46 (15) | 46 (15) |
| Level | Mobility | Self-care | Activity | Pain | Anxiety |
|---|---|---|---|---|---|
| Baseline | |||||
| 1 | 132 (73) | 91 (50) | 25 (14) | 5 (3) | 110 (61) |
| 2 | 48 (27) | 90 (50) | 141 (78) | 127 (70) | 65 (36) |
| 3 | – | – | 15 (8) | 49 (27) | 6 (3) |
| Missing | 1 (1) | – | – | – | – |
| 8 months | |||||
| 1 | 111 (61) | 101 (56) | 73 (40) | 36 (20) | 110 (61) |
| 2 | 39 (22) | 49 (27) | 71 (39) | 101 (56) | 37 (20) |
| 3 | – | – | 4 (2) | 12 (7) | 3 (2) |
| Missing | 31 (17) | 31 (17) | 33 (18) | 32 (18) | 31 (17) |
| 12 months | |||||
| 1 | 105 (58) | 112 (62) | 70 (39) | 49 (27) | 103 (57) |
| 2 | 42 (23) | 34 (19) | 73 (40) | 83 (46) | 38 (21) |
| 3 | – | – | 4 (2) | 13 (7) | 4 (2) |
| Missing | 34 (19) | 35 (19) | 34 (19) | 36 (20) | 36 (20) |
| 24 months | |||||
| 1 | 100 (56) | 116 (65) | 80 (45) | 62 (35) | 108 (61) |
| 2 | 42 (24) | 26 (15) | 56 (31) | 71 (40) | 33 (19) |
| 3 | – | 1 (1) | 7 (4) | 10 (6) | 2 (1) |
| Missing | 36 (20) | 35 (20) | 35 (20) | 35 (20) | 35 (20) |
| Level | Mobility | Self-care | Activity | Pain | Anxiety |
|---|---|---|---|---|---|
| Baseline | |||||
| 1 | 129 (80) | 91 (56) | 20 (12) | 2 (1) | 108 (67) |
| 2 | 32 (20) | 70 (43) | 126 (78) | 124 (77) | 47 (29) |
| 3 | – | – | 16 (10) | 36 (22) | 7 (4) |
| Missing | 1 (1) | 1 (1) | – | – | – |
| 8 months | |||||
| 1 | 110 (68) | 102 (63) | 53 (33) | 34 (21) | 108 (67) |
| 2 | 34 (21) | 42 (26) | 83 (52) | 105 (65) | 33 (21) |
| 3 | – | – | 8 (5) | 4 (2) | 1 (1) |
| Missing | 17 (11) | 17 (11) | 17 (11) | 18 (11) | 19 (12) |
| 12 months | |||||
| 1 | 107 (66) | 111 (69) | 83 (52) | 50 (31) | 103 (64) |
| 2 | 28 (17) | 23 (14) | 45 (28) | 79 (49) | 29 (18) |
| 3 | – | – | 6 (4) | 5 (3) | 2 (1) |
| Missing | 26 (16) | 27 (17) | 27 (17) | 27 (17) | 27 (17) |
| 24 months | |||||
| 1 | 96 (60) | 109 (68) | 77 (48) | 63 (39) | 103 (64) |
| 2 | 36 (22) | 22 (14) | 51 (32) | 59 (37) | 25 (16) |
| 3 | – | 1 (1) | 4 (2) | 10 (6) | 3 (2) |
| Missing | 29 (18) | 29 (18) | 29 (18) | 29 (18) | 30 (19) |
| Level | Mobility | Self-care | Activity | Pain | Anxiety |
|---|---|---|---|---|---|
| Baseline | |||||
| 1 | 76.9 (1.6) | 54.3 (1.9) | 13.6 (1.3) | 2.4 (0.6) | 64.8 (1.9) |
| 2 | 23.1 (1.6) | 45.4 (1.9) | 78.6 (1.6) | 71.9 (1.8) | 31.4 (1.8) |
| 3 | |||||
| Missing | – | 0.3 (0.2) | 7.7 (1.0) | 25.6 (1.7) | 3.8 (0.7) |
| 8 months | |||||
| 1 | 75.3 (1.8) | 71.2 (1.9) | 41.4 (2.0) | 24.4 (1.8) | 71.2 (1.9) |
| 2 | 24.7 (1.8) | 27.9 (1.9) | 53.8 (2.1) | 69.4 (1.9) | 26.6 (1.8) |
| 3 | |||||
| Missing | – | 1.0 (0.4) | 4.9 (0.9) | 6.2 (1.0) | 2.2 (0.6) |
| 12 months | |||||
| 1 | 73.5 (1.8) | 78.7 (1.7) | 51.2 (2.1) | 34.3 (2.0) | 73.1 (1.8) |
| 2 | 26.2 (1.9) | 20.7 (1.7) | 44.3 (2.1) | 57.7 (2.1) | 24.6 (1.8) |
| 3 | 0.3 (0.3) | 0.6 (0.4) | 4.5 (0.9) | 8.0 (1.1) | 2.3 (0.6) |
| Missing | 73.5 (1.8) | 78.7 (1.7) | 51.2 (2.1) | 34.3 (2.0) | 73.1 (1.8) |
| 24 months | |||||
| 1 | 69.9 (1.9) | 81.7 (1.7) | 55.8 (2.0) | 42.6 (2.1) | 75.5 (1.8) |
| 2 | 30.1 (1.9) | 17.5 (1.6) | 41.0 (2.0) | 51.9 (2.2) | 22.6 (1.8) |
| 3 | – | 0.8 (0.4) | 3.2 (0.8) | 5.5 (1.0) | 1.9 (0.6) |
| Missing | 69.9 (1.9) | 81.7 (1.7) | 55.8 (2.0) | 42.6 (2.1) | 75.5 (1.8) |
| Level | Mobility | Self-care | Activity | Pain | Anxiety |
|---|---|---|---|---|---|
| Baseline | |||||
| 1 | 77.2 (2.4) | 55.5 (28.0) | 14.2 (2.0) | 2.8 (0.9) | 66.2 (2.7) |
| 2 | 22.8 (2.4) | 43.8 (2.8) | 79.5 (2.3) | 70.6 (2.6) | 30.0 (2.6) |
| 3 | – | 0.6 (0.4) | 6.3 (1.4) | 26.6 (2.5) | 3.8 (1.1) |
| 8 months | |||||
| 1 | 75.8 (2.5) | 73.9 (2.6) | 40.2 (2.9) | 25.1 (2.6) | 68.6 (2.7) |
| 2 | 24.2 (2.5) | 24.4 (2.6) | 54.5 (3.0) | 68.3 (2.7) | 28.6 (2.7) |
| 3 | – | 1.6 (0.7) | 5.3 (1.3) | 6.6 (1.5) | 2.8 (0.9) |
| 12 months | |||||
| 1 | 72.3 (2.7) | 78.5 (2.5) | 48.9 (2.9) | 33.8 (2.8) | 72.6 (2.6) |
| 2 | 27.2 (2.7) | 20.5 (2.4) | 45.9 (2.9) | 57.3 (2.9) | 25.1 (25.7) |
| 3 | 0.5 (0.4) | 1.1 (0.6) | 5.2 (1.3) | 8.9 (1.7) | 2.3 (0.9) |
| 24 months | |||||
| 1 | 69.6 (2.8) | 82.0 (2.3) | 55.5 (3.0) | 39.7 (2.9) | 74.7 (2.6) |
| 2 | 30 4 (2.8) | 17.1 (2.3) | 42.2 (3.0) | 56.4 (3.0) | 23.5 (2.5) |
| 3 | – | 1.0 (0.6) | 2.3 (0.9) | 3.9 (1.2) | 1.7 (0.8) |
| Level | Mobility | Self-care | Activity | Pain | Anxiety |
|---|---|---|---|---|---|
| Baseline | |||||
| 1 | 73.4 (3.3) | 50.3 (3.7) | 13.8 (2.6) | 2.8 (1.2) | 60.8 (3.6) |
| 2 | 26.6 (3.3) | 49.7 (3.7) | 77.9 (3.1) | 70.2 (3.4) | 35.9 (3.6) |
| 3 | – | – | 8.3 (2.1) | 27.1 (3.3) | 3.3 (1.3) |
| 8 months | |||||
| 1 | 73.7 (3.5) | 67.2 (2.2) | 47.6 (3.9) | 23.7 (3.3) | 72.1 (3.5) |
| 2 | 26.3 (3.5) | 32.3 (2.4) | 49.0 (4.0) | 68.1 (3.8) | 25.7 (3.4) |
| 3 | – | 0.5 (0.7) | 3.4 (1.6) | 8.2 (2.3) | 2.2 (1.2) |
| 12 months | |||||
| 1 | 71.7 (2.5) | 76.9 (1.9) | 47.7 (4.2) | 33.2 (3.8) | 71.2 (3.6) |
| 2 | 28.1 (2.6) | 23.0 (2.0) | 49.1 (4.2) | 57.6 (4.0) | 26.1 (3.4) |
| 3 | 0.1 (0.5) | 0.1 (0.4) | 3.2 (1.5) | 9.2 (2.3) | 2.8 (1.3) |
| 24 months | |||||
| 1 | 68.5 (3.8) | 80.9 (3.2) | 55.1 (4.1) | 43.4 (4.1) | 74.7 (3.5) |
| 2 | 31.5 (2.8) | 18.4 (3.1) | 40.2 (4.2) | 49.8 (4.2) | 23.5 (3.4) |
| 3 | – | 0.7 (0.7) | 4.7 (1.7) | 6.7 (2.0) | 1.8 (1.2) |
| Level | Mobility | Self-care | Activity | Pain | Anxiety |
|---|---|---|---|---|---|
| Baseline | |||||
| 1 | 80.1 (3.2) | 56.5 (3.9) | 12.3 (2.6) | 1.2 (0.9) | 66.7 (3.7) |
| 2 | 19.9 (3.2) | 43.5 (3.9) | 77.8 (3.3) | 76.5 (3.3) | 29.0 (3.6) |
| 3 | – | – | 9.9 (2.4) | 22.2 (3.3) | 4.3 (1.6) |
| 8 months | |||||
| 1 | 76.0 (3.6) | 70.2 (2.1) | 36.6 (4.0) | 23.6 (3.6) | 75.3 (3.6) |
| 2 | 24.0 (3.6) | 29.7 (2.0) | 57.8 (4.0) | 73.1 (3.8) | 23.8 (3.5) |
| 3 | – | 0.1 (0.5) | 5.5 (1.9) | 3.3 (1.6) | 0.9 (0.8) |
| 12 months | |||||
| 1 | 78.0 (2.1) | 81.1 (1.7) | 59.6 (4.1) | 36.5 (4.1) | 76.2 (3.6) |
| 2 | 21.9 (2.1) | 18.8 (1.6) | 35.7 (4.1) | 58.6 (4.2) | 22.1 (3.5) |
| 3 | 0.0 (0.3) | 0.2 (0.7) | 4.6 (1.8) | 4.9 (1.9) | 1.7 (1.2) |
| 24 months | |||||
| 1 | 72.0 (3.7) | 81.9 (3.4) | 57.3 (4.1) | 47.4 (4.2) | 78.0 (3.5) |
| 2 | 28.0 (3.7) | 17.3 (3.3) | 39.5 (4.1) | 45.5 (4.2) | 19.9 (3.4) |
| 3 | – | 0.8 (0.8) | 3.1 (1.5) | 7.1 (2.1) | 2.2 (1.3) |
| Time point | Stratum A | Stratum B | Stratum C | ||||
|---|---|---|---|---|---|---|---|
| Arthroscopic, mean (SE) | Open, mean (SE) | Arthroscopic vs. open mean difference (95% CI;a p-value) (base case, no covariate adjustment) | Arthroscopic vs. open mean difference (95% CI;a p-value) (adjusting for baseline EQ-5D index) | Arthroscopic vs. open mean difference (95% CI;a p-value) (adjusting for baseline EQ-5D index, age, tear size, centre) | Arthroscopic, mean (SE) | Open, mean (SE) | |
| Results for all patients (ITT) | (n = 136) | (n = 137) | (n = 91) | (n = 82) | |||
| QALYs from baseline to 8 months | 0.41 (0.01) | 0.40 (0.01) | 0.01 (–0.03 to 0.05; 0.740) | –0.01 (–0.03 to 0.01; 0.391) | –0.01 (–0.03 to 0.01; 0.392) | 0.40 (0.02) | 0.41 (0.02) |
| QALYs from 8 months to 12 months | 0.23 (0.01) | 0.23 (0.01) | –0.00 (–0.02 to 0.02; 0.911) | –0.01 (–0.02 to 0.13; 0.575) | –0.01 (–0.03 to 0.01; 0.529) | 0.23 (0.01) | 0.24 (0.01) |
| QALYs from 12 months to 24 months | 0.73 (0.02) | 0.74 (0.02) | –0.01 (–0.07 to 0.05; 0.734) | –0.02 (–0.07 to 0.03; 0.449) | –0.02 (–0.08 to 0.03; 0.414) | 0.71 (0.03) | 0.74 (0.03) |
| Total QALYs over 24 months | 1.37 (0.04) | 1.37 (0.04) | 0.00 (–0.11 to 0.10; 0.931) | –0.04 (–0.12 to 0.05; 0.423) | –0.04 (–0.12 to 0.05; 0.392) | 1.34 (0.05) | 1.39 (0.04) |
| Total QALYs over 24 months (time discounted) | 1.34 (0.04) | 1.35 (0.04) | 0.00 (–0.11 to 0.10; 0.935) | –0.03 (–0.12 to 0.05; 0.423) | –0.04 (–0.12 to 0.05; 0.392) | 1.32 (0.05) | 1.36 (0.04) |
| Results for patients (per protocol) | (n = 63) | (n = 85) | (n = 50) | (n = 40) | |||
| QALYs from baseline to 8 months | 0.40 (0.02) | 0.40 (0.02) | 0.00 (–0.06 to 0.05; 0.964) | –0.01 (–0.04 to 0.01; 0.326) | –0.01 (–0.04 to 0.02; 0.494) | 0.41 (0.02) | 0.38 (0.02) |
| QALYs from 8 months to 12 months | 0.23 (0.01) | 0.24 (0.01) | –0.01 (–0.03 to 0.02; 0.697) | –0.01 (–0.04 to 0.02; 0.484) | –0.01 (–0.03 to 0.02; 0.473) | 0.25 (0.01) | 0.23 (0.01) |
| QALYs from 12 months to 24 months | 0.73 (0.03) | 0.75 (0.03) | –0.02 (–0.10 to 0.06; 0.612) | –0.03 (–0.10 to 0.05; 0.449) | –0.04 (–0.11 to 0.03; 0.291) | 0.75 (0.03) | 0.73 (0.04) |
| Total QALYs over 24 months | 1.36 (0.06) | 1.39 (0.04) | –0.03 (–0.18 to 0.12; 0.713) | –0.05 (–0.17 to 0.07; 0.386) | –0.06 (–0.17 to 0.06; 0.318) | 1.41 (0.05) | 1.33 (0.07) |
| Total QALYs over 24 months (time discounted) | 1.34 (0.06) | 1.36 (0.04) | –0.03 (–0.17 to 0.12; 0.715) | –0.05 (–0.17 to 0.07; 0.385) | –0.06 (–0.17 to 0.06; 0.319) | 1.38 (0.05) | 1.31 (0.07) |
Intention-to-treat analysis
For the base-case ITT analysis, there were no significant differences in total QALYs between the arthroscopic repair group and the open repair group at 8, 12 or 24 months. The mean difference in total QALYs between the groups at 24 months with time discounting was negative, both without (0.00, 95% CI –0.11 to 0.10) and with (–0.04, 95% CI –0.12 to 0.05) adjustment for covariates, suggesting worse outcomes for the arthroscopic repair group, although both values were non-significant.
Per-protocol analysis
There were no significant differences between the two groups in the per-protocol analysis for any of the quality-of-life outcomes. Again, the mean difference in total QALYs between the groups was negative for both the unadjusted analysis (–0.03, 95% CI –0.17 to 0.12) and the adjusted analysis (–0.06, 95% CI –0.17 to 0.06), suggesting that arthroscopic repair may be less effective, although again both results were non-significant.
Incremental cost-effectiveness results
The incremental cost-effectiveness results are presented in Table 46 for the ITT and per-protocol analyses, with and without covariate adjustment. To illustrate the uncertainty around the point estimate for the ICER, Figures 11–14 show 1000 bootstrapped cost and effect differences as a scatter plot on the cost-effectiveness plane.
| Analysis | Total costs over 24 months (discounted) (£)a | Total QALYs over 24 months (discounted)a | ICER (quadrant) (£)b | Probability (%) that arthroscopic repair is | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Arthroscopic, mean (SE) | Open, mean (SE) | Mean difference (95% CI) | Arthroscopic, mean (SE) | Open, mean (SE) | Mean difference (95% CI) | More effective | Less costly | Dominant | Dominated | Cost-effective at £20,000 per QALY gained | ||
| (A) Base case: ITT, no adjustment for covariates | 2567 (176) | 2699 (149) | –132 (–589 to 324; 0.569) | 1.34 (0.04) | 1.35 (0.04) | 0.00 (–0.11 to 0.10; 0.935) | 30,001 (SW) | 47.5 | 74.4 | 37.5 | 15.6 | 53.7 |
| (B) ITT, adjusted for covariatesc | 2567 (176) | 2699 (149) | 105 (–255 to 466; 0.565) | 1.34 (0.04) | 1.35 (0.04) | –0.04 (–0.12 to 0.05; 0.392) | Dominated (–2845; NW) | 23.0 | 26.6 | 9.4 | 59.8 | 20.9 |
| (C) Per protocol, no adjustment for covariates | 3582 (223) | 3360 (171) | 222 (–328 to 773; 0.426) | 1.34 (0.06) | 1.36 (0.04) | –0.03 (–0.17 to 0.12; 0.715) | Dominated (–8272; NW) | 36.5 | 19.2 | 9.9 | 55.1 | 30.0 |
| (D) Per protocol, adjusted for covariatesc | 3582 (223) | 3360 (171) | 207 (–341 to 754; 0.456) | 1.34 (0.06) | 1.36 (0.04) | –0.06 (–0.17 to 0.06; 0.319) | Dominated (–3628; NW) | 21.2 | 24.3 | 8.5 | 63.0 | 18.8 |
FIGURE 11.
Cost-effectiveness plane, analysis A (base case: ITT, unadjusted).

FIGURE 12.
Cost-effectiveness plane, analysis B (ITT, adjusted).
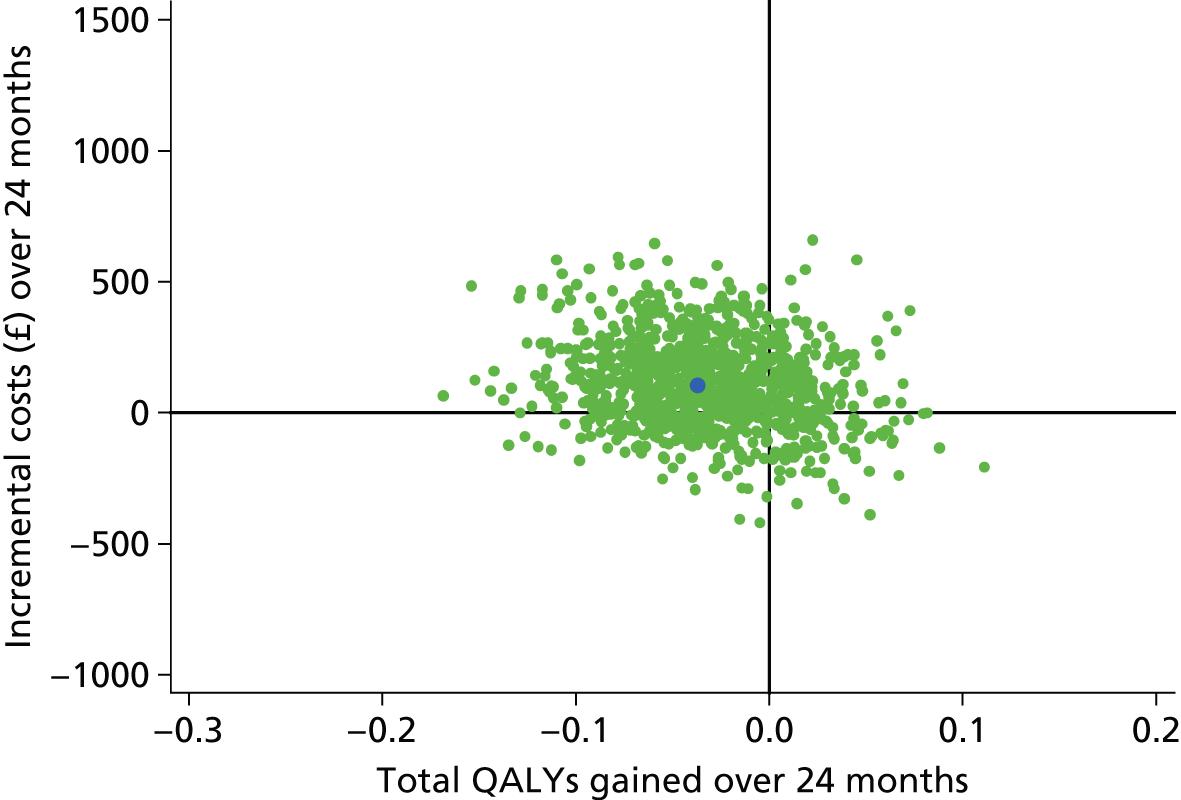
FIGURE 13.
Cost-effectiveness plane, analysis C (per protocol, unadjusted).
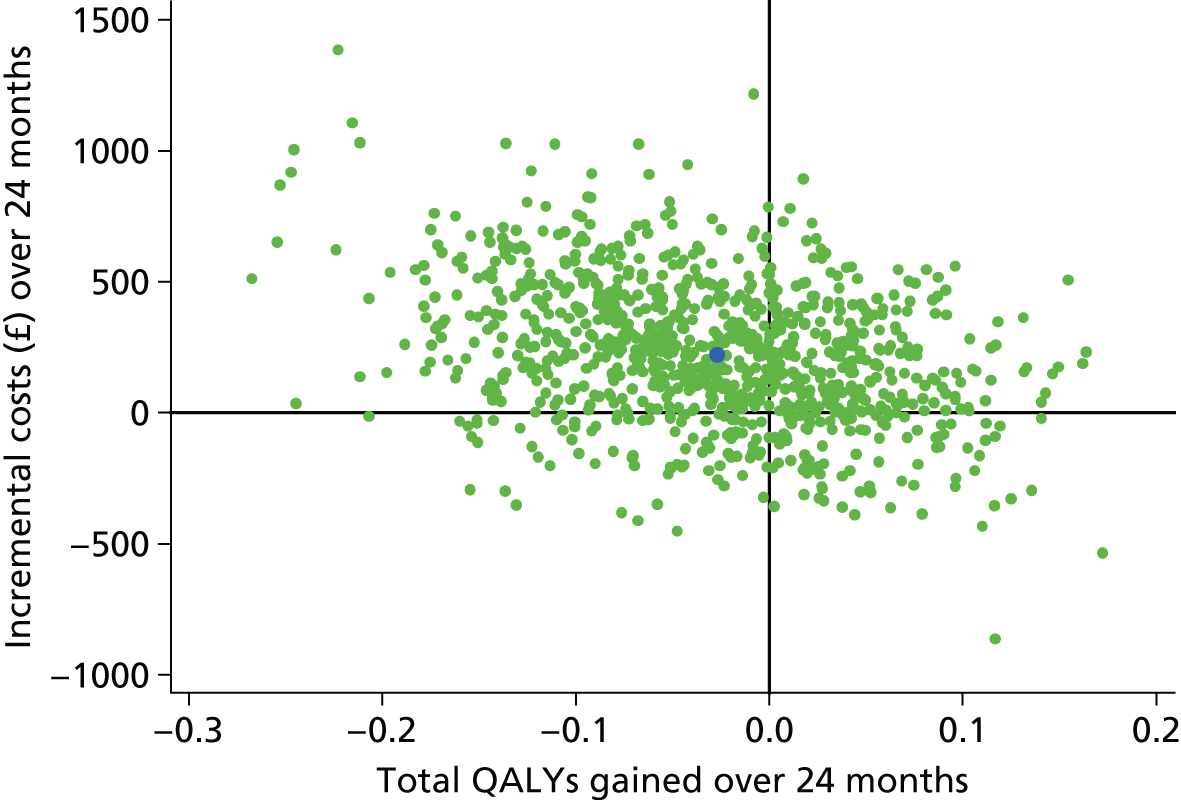
FIGURE 14.
Cost-effectiveness plane, analysis D (per protocol, adjusted).

When considering only the point estimate of the ICER, negative ICERs resulting from negative cost and positive effect differences (in the south-east quadrant of the cost-effectiveness plane) are indistinguishable from negative ICERs resulting from positive cost and negative effect differences (in the north-west quadrant); this is also the case for positive ICERs (north-east and south-west quadrants). As the uncertainty around the ICER for each of the four analyses (A–D) spans all four quadrants of the cost-effectiveness plane (more/less costly and more/less effective), CIs cannot be produced by taking the 25th and 975th value of the ranked bootstrapped ICER estimates. Instead, the graphs in Figures 15–18 show cost-effectiveness acceptability curves, which plot the probability that arthroscopic repair is cost-effective compared with open repair at different levels of willingness to pay for health gains, ranging from £0 to £100,000 per QALY.
FIGURE 15.
Cost-effectiveness acceptability curve, analysis A (base case: ITT, unadjusted). Dotted lines represent 95% CIs.

FIGURE 16.
Cost-effectiveness acceptability curve, analysis B (ITT, adjusted). Dotted lines represent 95% CIs.

FIGURE 17.
Cost-effectiveness acceptability curve, analysis C (per protocol, unadjusted). Dotted lines represent 95% CIs.
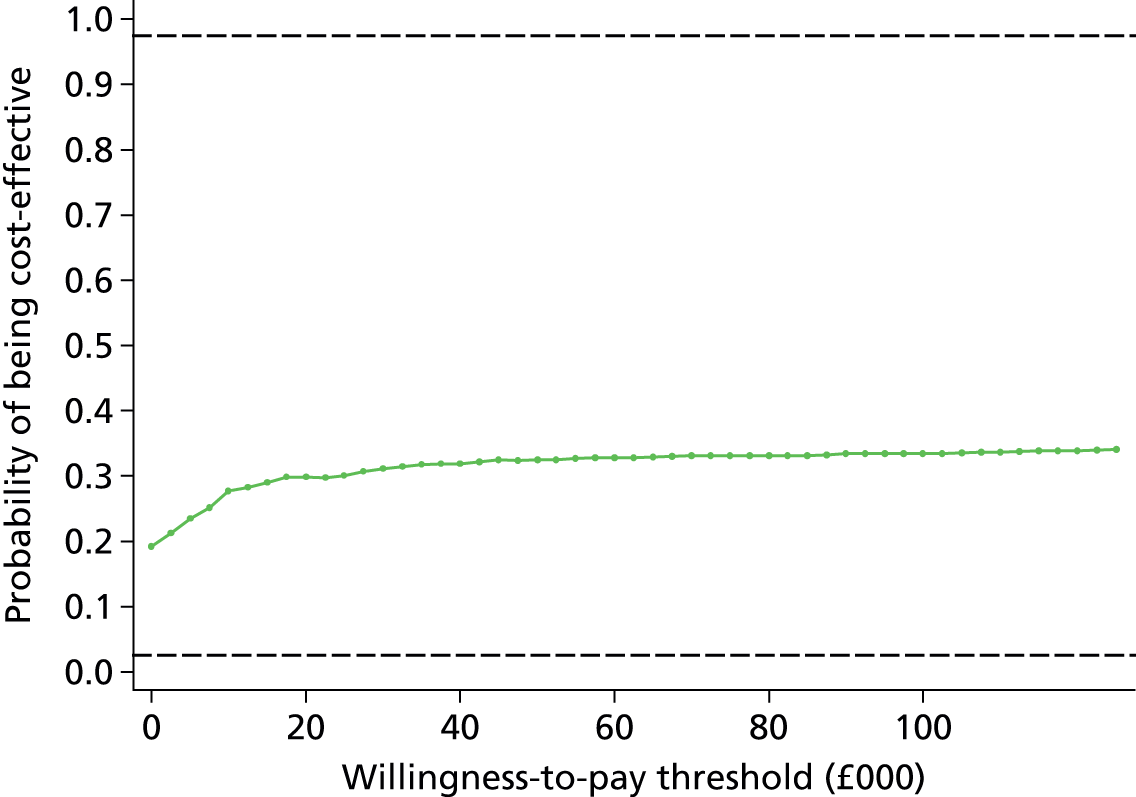
FIGURE 18.
Cost-effectiveness acceptability curve, analysis D (per protocol, adjusted). Dotted lines represent 95% CIs.

The uncertainty around the ICER is also presented in Table 46 in terms of the probability that arthroscopic repair is more effective, less costly, dominant (more effective and less costly), dominated (less effective and more costly) and cost-effective at a willingness to pay of £20,000 per QALY compared with open repair.
Intention-to-treat analysis
For the base-case ITT analysis without adjustment for covariates, arthroscopic repair was less costly but less effective than open repair, resulting in a point estimate for the ICER of £30,001. This value represents the additional cost per QALY gained for open repair compared with arthroscopic repair. The probability of arthroscopic repair being less costly than open repair was 74% and the probability of arthroscopic repair being more effective than open repair was 48%.
When adjusting for covariates the probability of arthroscopic repair being more effective than open repair decreased to 23% and the probability of it being less costly decreased to 27%. The probability that arthroscopic repair was dominated by open repair in this analysis was 60%, compared with 16% in the unadjusted analysis. The probability of arthroscopic repair being cost-effective compared with open repair at a willingness to pay of £20,000 per QALY gained was 54% in the unadjusted analysis and 21% in the adjusted analysis.
Per-protocol analysis
In the per-protocol analysis, the point estimate for the ICER suggested that arthroscopic repair was both more costly and less effective in both the unadjusted and the adjusted analyses, meaning that it was dominated by open repair. Using the uncertainty results from the bootstrap replicates, the probability that arthroscopic repair is dominated by (more costly and less effective than) open repair was 55% in the unadjusted analysis and 63% in the adjusted analysis and the probability that arthroscopic repair is cost-effective compared with open repair at a willingness to pay of £20,000 per QALY gained was 30% in the unadjusted analysis and 19% in the adjusted analysis.
Conclusion
For the ITT analysis there were no significant differences in mean costs between the arthroscopic repair group and the open repair group for any of the component resource-use categories, nor for the total follow-up costs at 12 months or 24 months. For the per-protocol analysis there was a significant difference in total initial procedure-related costs between the arthroscopic repair group and the open repair group, with arthroscopic repair being more costly by £371 (95% CI £135 to £607) with no covariate adjustment and £315 (95% CI £93 to £536) with covariate adjustment. The total cost of surgery alone (excluding nights in hospital) was also significantly different between the two groups, at £463 (95% CI £260 to £660) more costly for arthroscopic repair without covariate adjustment and £410 (95% CI £232 to £589) more costly for arthroscopic repair with covariate adjustment. Total QALYs accrued at 2 years averaged 1.34 (SE 0.04) in the arthroscopic group and 1.35 (SE 0.04) in the open repair group. The overall treatment cost at 2 years was £2567 (SE £176) for arthroscopic surgery and £2699 (SE £149) for open surgery, according to ITT analysis. This difference was not statistically significant.
For quality-of-life outcomes there was no statistically significant difference between the arthroscopic repair group and the open repair group, either for the ITT analysis or for the per-protocol analysis. The difference remained non-significant after adjusting for covariates.
In terms of incremental cost-effectiveness, arthroscopic repair was less costly but less effective than open repair in the ITT analysis, resulting in a point estimate for the ICER of £30,001 (without adjustment for covariates). The probability of arthroscopic repair being less costly than open repair was 74% and the probability of it being more effective than open repair was 48%. When adjusting for covariates, the probability of arthroscopic repair being more effective than open repair decreased to 23% and the probability of it being less costly decreased to 27%. For both the unadjusted and adjusted per-protocol analyses the point estimate for the ICER suggested that arthroscopic repair was both more costly and less effective, meaning that it was dominated by open repair.
Chapter 7 Discussion
The results of this RCT involving patients aged > 50 years with a symptomatic degenerative rotator cuff tear indicate that there are no significant differences in effectiveness, health-care costs or cost-effectiveness between arthroscopic repair and open repair. Both surgical techniques resulted in a significant improvement in the primary outcome, change in OSS between baseline and 2 years, and in all of the prespecified secondary outcome measures, which included the SPADI, the EQ-5D and the MHI-5. At 2 and 8 weeks post surgery an assessment was also carried out of analgesic use, return to activities and return to work. Patients improved from a baseline OSS of 25.7 to 41.5 at 24 months. All groups followed a similar pattern.
Response rates during follow-up
The protocol specified follow-up at times equivalent to 2 and 8 weeks after surgery. The success of this approach can be assessed in Table 5. Data were also collected through self-completed postal questionnaires, backed up by postal and telephone reminders and occasional completion of the questionnaire over the telephone. The standard rule in most trials is to time follow-up from randomisation. This was not appropriate for the early outcomes in this trial because of the variable time between randomisation and surgery. This variability occurred because of differences in NHS waiting times between centres. The overall response rates for the post-randomisation postal questionnaires were 408 out of 446 (91.5%) at 8 months, 406 out of 446 (91.0%) at 12 months and 389 out of 446 (87.2%) at 24 months. Response analysis showed that responders at 24 months had similar characteristics to non-responders.
Telephone questionnaires at 2 and 8 weeks post surgery
At 2 and 8 weeks there were no differences between groups for reported pain, levels of painkiller use or return to work. At 2 weeks, 131 out of 446 (29.4%) had no or mild pain, 232 out of 446 (52.0%) were taking painkillers and 80% of those in work were off sick. At 8 weeks 161 out of 446 (36.1%) had no or mild pain, 171 out of 446 (38.3%) were taking painkillers and 45% of those in work were off sick. These findings are broadly in line with advice given to patients before surgery.
Postal questionnaires at 8, 12 and 24 months
At 8 months, 77% of participants reported that their symptoms were much or slightly better; this had improved to 85% at 24 months, with no differences found between the groups. Operation time and time in theatre were both significantly lower (by approximately 12 minutes) in the open surgery group than in the arthroscopic group. The difference, however, was not observed in the non-randomised group. It may be the case that surgeons, when performing their preferred procedure, can undertake the procedures equally efficiently. One reason why we continued to follow-up the stratum B and stratum C participants after the rest-then-exercise arm was discontinued (see Rest-then-exercise programme) was to gather more information on surgical outcomes of the arthroscopic and open procedures. To that end we obtained data on another 142 surgical procedures from the non-randomised arms. Taken at face value it would appear that the procedures had a similar rate of complications and were safe.
Health economics
Follow-up at 24 months revealed no significant differences in costs or QALYs between arthroscopic and open treatment of rotator cuff tears (for either the ITT or the per-protocol analysis). There was no significant difference in time in theatre between arthroscopic and open surgery in the base-case ITT analysis using multiple imputed data (see Table 30). The cost of surgery and the total overall procedure costs were significantly more for arthroscopic repair than for open repair in the per-protocol analysis but not in the ITT analysis (see Table 33). There was no significant difference in QALYs accruing to each group at 24 months, with a mean of 1.34 and 1.35 QALYs per patient for arthroscopic repair and open repair, respectively, in the base-case ITT analysis (see Table 45). There was also no significant different between the groups when the results were analysed per protocol. As a result, the incremental cost-effectiveness of arthroscopic repair compared with open repair is subject to a great deal of uncertainty. The probability that arthroscopic repair is cost-effective compared with open repair when the willingness to pay for health benefits is set at £20,000 per QALY was 54% in the base case (when not adjusting results for covariates) and only 21% when incorporating covariate adjustment (see Table 46).
Complications
The number of patients suffering significant complications was very low and less than the rate described by Moosmayer et al. ,60 but similar to that described by Kukkonen et al. 59 The infection rate in this study was 0.7% and the rate of revision surgery was 1.5%.
Cuff repair integrity at 12 months
During surgery, 72 out of 356 participants (20.2%) randomised to surgery and who underwent surgery were found not to have a tear (see Table 11). This rate of false-positive reporting of tears potentially indicates the relatively inaccurate diagnostic work-up of the participants. The majority (68%) of tears were diagnosed by ultrasound and the remainder by MRI (see Table 6). A Cochrane systematic review of the use of MRI, MRI arthrography and ultrasound for assessing rotator cuff tears in people for whom shoulder surgery is being considered analysed 20 studies. 79 For full-thickness tears they reported a sensitivity and specificity of 94% (95% CI 85% to 98%) and 93% (95% CI 83% to 97%), respectively, for MRI and 92% (95% CI 82% to 96%) and 93% (95% CI 81% to 97%), respectively, for ultrasound. These results do not seem to be reflected in the real-world setting of the NHS. At baseline, 321 out of 446 tears (72.0%) were classified as small/medium and 125 out of 446 tears (28.0%) were classified as large/massive, whereas at surgery 152 out of 330 tears (46.1%) were judged by the surgeon to be small/medium, 125 out of 330 tears (37.9%) were judged by the surgeon to be large/massive and 72 out of 356 participants (20.2%) were judged to have no tear (see Table 11). It is possible that tears had changed in size between the preoperative scan and surgery; however, it is more likely that these differences reflect inaccuracies in the interpretation of preoperative imaging. The operative findings should be used as the standard. 79
In the randomised comparison, the mean difference in OSS at 2 years between healed tears and re-tears was 3 OSS points. The mean difference in OSS at 2 years between retears and unrepairable tears was also 3 OSS points. Healed repairs therefore fared best and unrepairable tears worst (see Table 20). A healed repair resulted in the greatest improvement in OSS. In the randomised group the OSS improved from 26.3 (SD 8.2) at baseline to 44.5 (SD 4.1) for the arthroscopic group and from 25.0 (SD 8.0) at baseline to 43.6 (SD 5.8) for the open group. The next best results were for the repaired tears that re-tore, which improved to 41.8 (SD 8.8) for the arthroscopic group and 40.8 (SD 7.6) for the open group. The worst results were seen for tears that were impossible to repair, which improved to 37.3 (SD 6.1) for the arthroscopic group and 35.1 (SD 9.7) for the open group. The results were similar for the non-randomised preference groups.
This improvement may be a result of the subacromial decompression surgery and tissue debridement that was invariably performed in these cases. Alternative reasons for the treatment effect include a period of rest after surgery, physiotherapy after surgery, spontaneous resolution or a placebo effect. It is clear that patients’ symptoms can improve even after a protracted course, with 22 out of 81 participants (27.2%) who withdrew from the trial while on the waiting list for surgery also reporting resolution of symptoms (see Table 10).
Comparison with other randomised clinical trials
A Cochrane review of treatment for rotator cuff tears was published in 2008 in which no clear evidence in support of any particular intervention was reported. 16 A systematic review was conducted in May 2014 (see Chapter 1) and found one trial53 of arthroscopic repair compared with mini-open repair in 100 patients published since the UKUFF trial started. Patients were followed for 1 year using the DASH questionnaire, with no treatment difference found for small and medium tears. 53 We found two further trials of surgery compared with conservative care published since the trial began. In the single-centre trial of small and medium tears by Moosmayer et al. ,60 the surgical group had better outcomes at 1 year. This study reported a full-thickness re-tear rate of 8% and a partial-thickness re-tear rate of 12%. In this study 14 out of 103 (13.6%) patients had previously received glucocorticoid injections, 49 out of 103 (47.6%) had received physiotherapy and the mean duration of symptoms was 9 and 12 months in the two groups, respectively. It would appear that, in this trial, patients were being advised to have surgery after a much shorter duration of symptoms and after a less comprehensive course of conservative therapies than is the case in the UK. In the Kukkonen et al. 59 study of small and medium tears the duration of symptoms was similar to that in this study at 26–28 months. Only 103 out of 167 (61.7%) had previously received conservative treatment in the form of cortisone injections. The waiting list for surgery in this Finnish study was < 4 weeks. There was no postoperative imaging and so repair integrity could not be assessed.
Strengths and weaknesses
This study was carried out in a large number of centres in the UK with wide geographical representation. Despite the length of time that has elapsed since the trial began, uncertainty still exists in the global surgical community regarding surgery for rotator cuff tear and the results of this trial are likely to influence care in the UK and globally.
Previous studies comparing surgery with conservative care have treated patients at an earlier stage with a shorter duration of symptoms and less, or no, previous experience of conservative care programmes, particularly physiotherapy and glucocorticoid injections. One reason why the original study design failed was that a high proportion of patients had already received and failed to respond to physiotherapy treatment (91.5%) and so it is not surprising that they were reluctant to pursue a further programme of conservative care.
Testing surgical interventions against non-operative treatments in a randomised trial is often challenging. This is particularly the case for chronic conditions with indolent onset that cause pain and reduce quality of life. If patients are recruited at the conventional stage of the treatment pathway they will invariably have already received conservative care (as was the case with this study). We involved patients during both the design and the conduct of the trial. The consistent feedback was that patients would be reluctant to try more conventional conservative care. For this reason experienced physiotherapy leaders within BESS designed the rest-then-exercise programme as a novel conservative programme that could be delivered to patients across the UK. An important consideration was the wide variation in conservative care programmes across the UK and the absence of standardisation of physiotherapy treatments. The rest-then-exercise programme was designed so that it could be delivered remotely and in the same way to all patients. We did consider the option of bringing surgery forward in the treatment pathway to try and recruit patients who had not yet received physiotherapy but this was not supported by either our patient representatives or our independent surgical advisers.
A second reason for crossover was that patients in the non-operative arm were put on the waiting list for surgery at the time of randomisation. At the time the trial was commissioned and designed NHS waiting lists for this type of surgery were > 12 months on average. This design was proposed in an attempt to improve recruitment by not disadvantaging patients randomised to the conservative arm who subsequently needed surgery in the belief that with 12 months on the waiting list the conservative programme could be evaluated fairly. Feedback from patient representatives during the study design process was that patients would not agree to participate in the rest-then-exercise programme if they were not also put on the NHS waiting list. During the course of the trial the introduction of waiting list targets reduced waiting times in the NHS and this adversely affected the trial.
The rate of withdrawal from the planned surgery was 81 out 446 (18.2%) for the surgical groups. We believe that this is likely to be a real NHS phenomenon. The reasons for withdrawal were not different between the groups and included the patient becoming asymptomatic and the development of other medical conditions that prevented surgery taking place (see Table 10). It is important to note that the levels of withdrawal were equal in all groups, including the non-randomised groups.
The reasons why patients did not receive a surgical repair were because no tear was found (scan false positive) or because the tear was impossible to repair. The relative inaccuracy of preoperative scanning in a real-world NHS setting compared with the accuracy reported in the literature is worthy of further investigation.
We have considered these issues further in the design of the CSAW (Can Shoulder Arthroscopy Work) trial [see https://clinicaltrials.gov/ct2/show/NCT01623011 (accessed 25 August 2015)], which has also been led from Oxford with the same chief investigator. This trial uses the same network of shoulder surgeons and centres and compares arthroscopic subacromial decompression with placebo surgery and active monitoring in patients with subacromial shoulder pain but no rotator cuff tear. It has successfully completed recruitment of 300 patients without any significant crossover between the randomised groups. Various factors have contributed to the success of this trial compared with the UKUFF trial. First, the trial works within accepted patient pathways and does not attempt to offer to patients treatments that have already been tried and which have failed to result in improvement, nor does it offer surgical treatment too early; all patients in the CSAW trial had a minimum duration of symptoms and had received well-delivered conservative care. In the CSAW trial 30 surgeons were involved in recruiting participants, all of whom were provided with instruction in recruiting before the trial and feedback from site visits during the trial. This feedback included the recording of patient consultations with advice about how individual surgeons might improve recruitment.
Patient and public involvement and engagement
Patients were involved in the interpretation of the trial findings and in the preparation of the monograph through patient representation on the TSC. The results were discussed with patient groups associated with BESS and with priority-setting forums, including the James Lind Alliance.
Generalisability of the results
We designed the trial with the aim of making the management policies as similar as possible to normal NHS care. In the first configuration the trial involved 47 centres and then, after the rest-then-exercise programme was closed, 19 centres. The centres were widely dispersed across the UK and included teaching hospitals and district general hospitals. Recruitment was performed by surgeons and surgeons chose the specific aspects of the procedure once a patient had been allocated to either arthroscopic repair or open repair. There was no requirement for extra tests or hospital visits and simple entry criteria identified people eligible for the study. The results should therefore be easily generalisable to standard NHS care. No single centre recruited > 10% of the total patients, which significantly enhances the generalisability of the results. All participating surgeons had been trained in the techniques, had undergone at least 2 years of independent practice as a consultant surgeon and undertook a minimum of five rotator cuff repair operations per annum.
Rest-then-exercise programme
The rest-then-exercise programme was designed by a group of leading shoulder physiotherapists representing the physiotherapy section of BESS. All members of the group had considerable experience in the non-operative management of patients with shoulder pain and with rotator cuff tears in particular. The programme was designed to be delivered remotely using an information booklet and CD, with access to physiotherapy guidance on a free telephone line. The same programme was provided to patients recruited to all 47 centres participating in the trial. All patients were provided with a sling, which they were advised to wear for up to 4 weeks with the aim of reducing pain levels to, or below, 4/10 on a VAS. In addition to information regarding rotator cuff tears (e.g. lack of correlation between pain and structure), a variety of exercises were detailed with advice to perform them for a further 6–12 weeks.
As described in the approved grant application and required by the ethics committee, patients in the rest-then-exercise arm were put on the NHS waiting list to prevent disadvantaging them should the rest-then-exercise programme fail to adequately resolve their symptoms. When the trial was designed NHS waiting lists were around 12 months, giving more than sufficient time to determine whether the conservative programme was effective. During the course of the study additional funding was made available to the NHS and waiting lists shortened to an average of 2–4 months, which may have played a part in the problems encountered with the rest-then-exercise programme.
Because of the reconfiguration of the trial, data from participants allocated to the rest-then-exercise arm of the original UKUFF study no longer contribute to the formal comparisons being reported within this monograph. However, it is important to record the details of all patients randomised across the totality of the study for completeness and transparency of reporting (but also in accordance with the expectation provided to participants as part of the consent process).
The outcomes of those allocated to rest then exercise were presented in Table 23. In total, 77 of the 214 participants (36%) did not complete the 10-week course of treatment and progressed to surgery (see Table 24), 88 (41%) completed the course before progressing to surgery (see Table 25) and 36 (17%) completed the full course and did not have surgery (see Table 26). A further 14 patients withdrew. As this component of the trial was stopped, no formal comparisons can be or have been made. All patients appeared to improve but it is not possible to determine why improvements were made. The number of patients previously having received non-operative care (including physiotherapy and cortisone injections) was high [604/660 (91.5%)]. In total, 401 out of 660 (60.8%) had received a cortisone injection in the last 5 years, 414 out of 660 (62.7%) had received physiotherapy and 87 out of 660 (13.2%) had received any other treatment. Of those randomised to rest then exercise, 141 out of 214 (65.9%) had received physiotherapy, 129 out of 214 (60.3%) had received a cortisone injection and 20 out of 214 (9.3%) had received some other treatment, such as acupuncture. Only 19 out of 214 (8.9%) patients randomised to rest then exercise [56/660 (8.5%) of the total trial participants] had not received treatment prior to randomisation. The mean duration of symptoms at baseline is shown in Table 7 and ranged from 2.0 to 2.7 years across the groups, with no significant differences between them.
Data across all subgroups show that participants’ assessments of their disease-specific and generic quality-of-life scores improved markedly from baseline to final outcomes. However, because of the sizeable rates of surgical intervention in this cohort of participants, it is difficult to dissect the specific gains that could be attributed to the rest-then-exercise programme and to surgery.
Chapter 8 Conclusion
In patients aged > 50 years with a degenerative rotator cuff tear there were no significant differences in the primary outcome (OSS) and all other prespecified secondary outcomes between open repair and arthroscopic repair at 2 years. Rotator cuff surgery resulted in a significant improvement in symptoms (OSS 25.7/48 at baseline to 41.5/48 at 2 years). Improvement occurred despite the relatively small number of patients who underwent a rotator cuff repair. Patients who had an unrepairable tear at surgery and those in whom the repair subsequently re-tore also improved from baseline.
In total, 1.34 (SE 0.04) QALYs accrued at 2 years in the arthroscopic repair group and 1.35 (SE 0.04) QALYs accrued at 2 years in the open repair group, whereas the overall treatment cost at 2 years was £2567 (SE £176) for arthroscopic surgery and £2699 (SE £149) for open surgery, according to ITT analysis; neither cost nor QALY differences were statistically significant.
The incidence of complications and serious adverse events was low, with only 0.7% of deep infections and 1.5% of revision repair operations.
Only 162 out of 273 (59%) patients randomised to surgery underwent a rotator cuff repair. In total, 59 out of 273 (22%) patients withdrew while on the waiting list. The most common reasons for this were improvement in symptoms and the development of another medical condition. A total of 52 out of 273 (19%) patients underwent subacromial decompression and no rotator cuff repair. The most common reasons for this were that no tear was found or that the tear was impossible to repair. The best outcome was seen in patients in whom the repair had healed; strategies to improve tendon healing are likely to improve outcomes for all tear sizes and ages. This was followed by a repair that subsequently re-tore. The worst outcome was seen in patients whose tear was unrepairable at surgery. Re-tears were found in 93 out of 233 (40%) patients who underwent repair surgery, with no difference between the open and arthroscopic groups. Re-tears occurred after repairs to all tear sizes and the risk of re-tear was not influenced by age. Previous studies have been small and either single-centre or in a small number of centres and have not had the same generalisability as this trial.
It proved impossible to test a rest-then-exercise programme in the context of a pragmatic trial in the 47 centres during routine NHS care. In total, 91.5% of patients randomised had previously received conservative care and the mean duration of symptoms was 2.5 years.
Implications for health care
Clinical
-
Suitably selected patients can benefit equally well from either open or arthroscopic rotator cuff repair with a low risk of complications.
-
In the subset of patients for whom repair was possible the greatest benefit is seen in patients in whom the rotator cuff repair is successful and remains intact.
-
A significant improvement was seen in all randomised and non-randomised groups, including in those in whom a repair was not possible or in whom there was a postoperative re-tear, suggesting that there are other treatment effects.
-
No evidence of an effect of age or tear size on outcome was found.
Health economics
-
There is no significant cost difference at 2 years between open and arthroscopic rotator cuff repair.
-
Per protocol the costs of arthroscopic surgery are significantly greater than the costs of open surgery. This is largely because of the longer operating time for arthroscopic surgery.
Recommendations for future research
Clinical
-
There is a case to continue follow-up of the patients who underwent surgery and who had a repair that healed, who had a repair that re-tore, who had a tear that was impossible to repair or who had no tear. There is early evidence at 2 years’ follow-up that these groups have different outcomes. This unique study cohort provides the opportunity to determine the longer-term consequences of rotator cuff tear and repair.
-
There is a need to explore the basis of the treatment effect seen with a RCT of rotator cuff repair compared with placebo surgery.
Health economics
-
With enforced restrictions on surgical training time there is also a need to understand both the costs and the time required for surgeons to learn arthroscopy and open surgery, including the volume of cases that needs to be performed to maintain skills. If the time required for training and maintaining either arthroscopic or open skills differs then this will have cost implications for surgical training programmes and workforce planning.
-
There is a need to evaluate cost-effectiveness over a longer period than 24 months using further follow-up data from this study and elsewhere on the longer-term consequences of rotator cuff tear and repair.
Acknowledgements
Independent members of the Trial Steering Committee were as follows: Professor Jane Blazeby (Chair), Ms Jo Gibson, Mr David Stanley, Dr Andrew Cook, Major General Dair Farrar-Hockley (patient and public representative) and Professor Jeremy Fairbank.
Members of the independent Data Monitoring Committee were as follows: Professor Roger Emery (Chair), Dr Jeremy Lewis and Dr Richard Morris.
The authors wish to thank the following researchers for their contribution and assistance throughout the trial: John Norrie and Jonathan Cook for their methodology expertise during the early phases of the study; Alison McDonald, Suzanne Breeman, Julie Murdoch, Loretta Davies, Vandana Ayyar-Gupta and Joy Eldridge for their management of the trial at different stages; Gladys McPherson for database and programming management; Graeme MacLennan, David Jenkins and Ted Bassinga for statistical support; and Kim Wheway and Bridget Watkins for the research nurse support that they offered at the Oxford site and within the central study office.
Administration support has been provided throughout the study in Oxford from Claire Pumfrey and in Aberdeen from Margaret MacNeil, Diana Collins and Lindsay Grant. Help with completion of follow-up data collection was provided by Christine Dallas and Lynn Swan.
Members of the UKUFF study group responsible for recruitment in the clinical centres were as follows.
| Middlesborough: South Tees Hospitals NHS Foundation Trust | Professor A Rangan, Mr B Hanusch and Mr L Micklewright |
| Gwent: Aneurin Bevan University Health Board | Mr R Kulkarni and Mr M Williams |
| Worcester: Worcestershire Acute Hospitals NHS Trust | Mr D Robinson, Mrs J Thrush and Ms R Morris |
| Leicester: University Hospitals of Leicester NHS Trust | Miss A Armstrong, Mr R Pandey, Mr A Modi, Ms EJ Alderton and Ms M Attwal |
| Maidstone: Maidstone and Tunbridge Wells NHS Trust | Mr H Jahnich |
| Surrey and Sussex: Surrey and Sussex Healthcare NHS Trust | Mr TP Selvan, Ms S Allen and Ms A Shears |
| Ipswich: Ipswich Hospital NHS Trust | Mr C Roberts, Ms J Gascoigne and Ms C Tricker |
| Dudley: Dudley Group of Hospitals NHS Trust | Mr MS Butt and Ms E Cooke |
| Barnet: Barnet and Chase Farm NHS Trust | Mr D Rossouw and Ms J Monteath |
| Burnley: East Lancashire Hospitals NHS Trust | Mr H Marynissen and Ms H Peel |
| Oldham: Pennine Acute Hospitals NHS Trust | Mr L Jacobs, Ms L Lock and Mr RM Seagger |
| Oswestry: Robert Jones and Agnes Hunt Orthopaedic and District Hospital | Mr C Kelly and Ms L Sharp |
| Swansea: Abertawe Bro Morgannwg University Health Board | Mr M Pritchard, Mr C Hoddinott and Ms L Quinn |
| Coventry: University Hospitals Coventry and Warwickshire NHS Trust | Mr S Drew, Ms C Richmond, Ms K Dennison and Ms H Richmond |
| Basingstoke: Basingstoke and North Hampshire Hospitals NHS Trust | Mr N Rossiter and Mrs M Wright |
| Sheffield: Sheffield Teaching Hospitals NHS Foundation Trust | Mr D Stanley and Ms C Faulkner |
| Southampton: University Hospital Southampton NHS Foundation Trust | Mr A Cole and Mr C Hand |
Contribution of authors
Andrew J Carr (Nuffield Professor of Orthopaedics, Head of Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences, University of Oxford) was the principal grant applicant and contributed to the development of the trial protocol and the preparation of the report and was responsible overall for the conduct of the trial.
Cushla D Cooper (Trial Co-ordinator, Oxford) contributed to the development of the trial protocol and was responsible for the daily management and conduct of the trial throughout and contributed to the preparation of the report.
Marion K Campbell (Grant Holder, Director of Health Services Research Unit, University of Aberdeen) contributed to the grant application and the trial design, commented on all aspects of the conduct of the trial and contributed to the preparation of the report.
Jonathan L Rees (Grant Holder, Consultant Orthopaedic Surgeon) contributed to the grant application and the trial design and the preparation of the report.
Jane Moser (Grant Holder, Consultant Shoulder Physiotherapist) contributed to the grant application and the trial design, led the development of the non-operative comparator and contributed to the preparation of the report.
David J Beard (Grant Holder, Professor of Musculoskeletal Sciences), contributed to the grant application and the trial design and the preparation of the report.
Ray Fitzpatrick (Grant Holder, Professor of Public Health) contributed to the grant application and the trial design and the preparation of the report.
Alastair Gray (Grant Holder, Professor of Health Economics) was responsible for the economic evaluation section of the grant application and protocol and contributed to the preparation of the report.
Jill Dawson (Grant Holder, Senior Research Scientist and University Research Lecturer) contributed to the grant application and the trial design and the preparation of the report.
Jacqueline Murphy (Research Fellow, Health Economics) conducted the analysis of the economic models for the report and contributed to the preparation of the report.
Hanne Bruhn (Trial Manager, Aberdeen) was responsible for the oversight of data collection and contributed to the preparation of the final report.
David Cooper (Statistician) conducted the statistical analysis and data cleaning and contributed to the preparation of the report.
Craig R Ramsay (Grant Holder, Professor of Health Technology Assessment) contributed to the grant application and the trial design, oversaw the statistical analysis and contributed to the preparation of the report.
Publications
Carr AJ, Cooper CD. The UKUFF trial and the NIHR comprehensive local research networks. Shoulder Elbow 2009;2:63–4.
Judge A, Murphy RJ, Maxwell R, Arden NK, Carr AJ. Temporal trends and geographical variation in the use of subacromial decompression and rotator cuff repair of the shoulder in England. Bone Joint J 2014;1:70–4.
Data-sharing statement
Data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Urwin M, Symmons D, Allison T, Brammah T, Busby H, Roxby M, et al. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis 1998;557:649-55. http://dx.doi.org/10.1136/ard.57.11.649.
- Mitchell C, Adebajo A, Hay E, Carr A. Shoulder pain: diagnosis and management in primary care. BMJ 2005;331:1124-8. http://dx.doi.org/10.1136/bmj.331.7525.1124.
- Harkness EF, Macfarlane GJ, Nahit ES, Silman AJ, McBeth J. Mechanical and psychosocial factors predict new onset shoulder pain: a prospective cohort study of newly employed workers. Occup Environ Med 2003;60:850-7. http://dx.doi.org/10.1136/oem.60.11.850.
- van der Windt DAWM, Thomas E, Pope D, de Winter AF, Macfarlane G, Bouter L, et al. Occupational risk factors for shoulder pain: a systematic review. Occup Environ Med 2000;57:215-21. http://dx.doi.org/10.1136/oem.57.7.433.
- Linsell L, Dawson J, Zondervan K, Rose P, Randall T, Fitzpatrick R, et al. Prevalence and incidence of adults consulting for shoulder conditions in UK primary care; patterns of diagnosis and referral. Rheumatology 2006;45:215-21. http://dx.doi.org/10.1093/rheumatology/kei139.
- Oh LS, Wolf BR, Hall MP, Levy BA, Marx RG. Indications for rotator cuff repair: a systematic review. Clin Orthop Relat Res 2007;455:52-63. http://dx.doi.org/10.1097/BLO.0b013e31802fc175.
- van der Windt DA, Koes BW, Boeke AJ, Devillé W, De Jong BA, Bouter LM. Shoulder disorders in general practice: prognostic indicators of outcome. Br J Gen Pract 1996;46:519-23.
- Neer CS. Anterior acromioplasty for the chronic impingement syndrome in the shoulder. J Bone Joint Surg Am 2005;87. http://dx.doi.org/10.2106/JBJS.8706.cl.
- Lewis JS. Rotator cuff tendinopathy/subacromial impingement syndrome: is it time for a new method of assessment?. Br J Sports Med 2009;43:259-64. http://dx.doi.org/10.1136/bjsm.2008.052183.
- Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Br 1995;77:10-5.
- Cordasco FA, Backer M, Craig EV, Klein D, Warren RF. The partial-thickness rotator cuff tear: is acromioplasty without repair sufficient?. Am J Sports Med 2002;30:257-60.
- Murphy RJ, Carr AJ. Shoulder pain. BMJ Clin Evid 2010;2010.
- Dean BJF, Lostis E, Oakley T, Rombach I, Morrey ME, Carr AJ. The risks and benefits of glucocorticoid treatment for tendinopathy: a systematic review of the effects of local glucocorticoid on tendon. Semin Arthritis Rheum 2014;43:570-6. http://dx.doi.org/10.1016/j.semarthrit.2013.08.006.
- Oag H, Daines M, Nichols A, Kiran A, Arden N, Carr AJ. Relationship of rotator cuff tears, shoulder pain and functional loss in a normal population. Bone Joint Surg Br 2012;94–B.
- Cummins CA, Sasso LM, Nicholson D. Impingement syndrome: temporal outcomes of nonoperative treatment. J Shoulder Elbow Surg 2009;18:172-7. http://dx.doi.org/10.1016/j.jse.2008.09.005.
- Coghlan JA, Buchbinder R, Green S, Johnston RV, Bell SN. Surgery for rotator cuff disease. Cochrane Database Syst Rev 2008;1. http://dx.doi.org/10.1002/14651858.cd005619.pub2.
- Dorrestijn O, Stevens M, Winters JC, van der Meer K, Diercks RL. Conservative or surgical treatment for subacromial impingement syndrome? A systematic review. J Shoulder Elbow Surg 2009;18:652-60. http://dx.doi.org/10.1016/j.jse.2009.01.010.
- Holmgren T, Björnsson Hallgren H, Oberg B, Adolfsson L, Johansson K. Effect of specific exercise strategy on need for surgery in patients with subacromial impingement syndrome: randomised controlled study. BMJ 2012;344. http://dx.doi.org/10.1136/bmj.e787.
- Ketola S, Lehtinen J, Arnala I, Nissinen M, Westenius H, Sintonen H, et al. Does arthroscopic acromioplasty provide any additional value in the treatment of shoulder impingement syndrome?. J Bone Joint Surg Br 2009;91:1326-34. http://dx.doi.org/10.1302/0301-620X.91B10.22094.
- Ellman H, Kay S. Arthroscopic subacromial decompression for chronic impingement. Two- to five-year results. J Bone Joint Surg Br 1991;73:395-8.
- Patel VR, Singh D, Calvert PT, Bayley JI. J Shoulder Elbow Surg 1999;8:231-7. http://dx.doi.org/10.1016/S1058-2746(99)90134-9.
- Olsewski JM, Depew AD. Arthroscopic subacromial decompression and rotator cuff debridement for stage II and stage III impingement. Arthroscopy 1994;10:61-8. http://dx.doi.org/10.1016/S0749-8063(05)80294-4.
- Chin PYK, Sperling JW, Cofield RH, Stuart MJ, Crownhart BS. Anterior acromioplasty for the shoulder impingement syndrome: long-term outcome. J Shoulder Elbow Surg 2007;16:697-700. http://dx.doi.org/10.1016/j.jse.2007.02.116.
- Goldberg BA, Lippitt SB, Matsen FAI. Improvement in comfort and function after cuff repair without acromioplasty. Clin Orthop Relat Res 2001;390:42-50. http://dx.doi.org/10.1097/00003086-200109000-00017.
- Rockwood C, Williams G, Burkhead W. Debridement of degenerative, irreparable lesions of the rotator cuff. J Bone Joint Surg Am 1995;77:857-66.
- Gartsman GM, O’Connor DP. Arthroscopic rotator cuff repair with and without arthroscopic subacromial decompression: a prospective, randomised study of one-year outcomes. J Shoulder Elbow Surg 2004;13:424-6. http://dx.doi.org/10.1016/j.jse.2004.02.006.
- Henkus HE, de Witte PB, Nelissen RG, Brand R, van Arkel ER. Bursectomy compared with acromioplasty in the management of subacromial impingement syndrome: a prospective randomised study. J Bone Joint Surg Br 2009;91:504-10. http://dx.doi.org/10.1302/0301-620X.91B4.21442.
- Snyder SJ, Pachelli AF, Del Pizzo W, Friedman MJ, Ferkel RD, Pattee G. Partial thickness rotator cuff tears: results of arthroscopic treatment. Arthroscopy 1991;7:1-7. http://dx.doi.org/10.1016/0749-8063(91)90070-E.
- Goutallier D, Postel JM, Gleyze P, Leguilloux P, Van Driessche S. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg 2003;12:550-4. http://dx.doi.org/10.1016/S1058-2746(03)00211-8.
- Matthews TJW, Hand GC, Rees JL, Athanasou NA, Carr AJ. Pathology of the torn rotator cuff tendon: reduction in potential for repair as tear size increases. J Bone Joint Surg Br 2006;88:489-95. http://dx.doi.org/10.1302/0301-620X.88B4.16845.
- Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am 2007;89:953-60. http://dx.doi.org/10.2106/JBJS.F.00512.
- Jost B, Pfirrmann CWA, Gerber C. Clinical outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am 2000;82:304-14.
- Ogilvie-Harris DJ, Demaziere A. Arthroscopic debridement versus open repair for rotator cuff tears. A prospective cohort study. J Bone Joint Surg Br 1993;75:416-20.
- Melillo AS, Savoie FH, Field LD. Massive rotator cuff tears: debridement versus repair. Orthop Clin North Am 1997;28:117-24. http://dx.doi.org/10.1016/S0030-5898(05)70269-8.
- Motycka T, Lehner A, Landsiedl F. Comparison of debridement versus suture in large rotator cuff tears: long-term study of 64 shoulders. Arch Orthop Trauma Surg 2004;124:654-8. http://dx.doi.org/10.1007/s00402-004-0737-7.
- Ainsworth R, Lewis JS. Exercise therapy for the conservative management of full thickness tears of the rotator cuff: a systematic review. Br J Sports Med 2007;41:200-10. http://dx.doi.org/10.1136/bjsm.2006.032524.
- Harryman DT, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA. Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am 1991;73:982-9.
- Bishop J, Klepps S, Lo IK, Bird J, Gladstone JN, Flatow EL. Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study. J Shoulder Elbow Surg 2006;15:290-9. http://dx.doi.org/10.1016/j.jse.2005.09.017.
- Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal?. J Bone Joint Surg Am 2005;87:1229-40. http://dx.doi.org/10.2106/JBJS.D.02035.
- Fehringer EV, Sun J, VanOeveren LS, Keller BK, Matsen FA. Full-thickness rotator cuff tear prevalence and correlation with function and co-morbidities in patients sixty-five years and older. J Shoulder Elbow Surg 2008;17:881-5. http://dx.doi.org/10.1016/j.jse.2008.05.039.
- Dunn WR, Schackman BR, Walsh C, Lyman S, Jones EC, Warren RF, et al. Variation in orthopaedic surgeons’ perceptions about the indications for rotator cuff surgery. J Bone Joint Surg Am 2005;87:1978-84. http://dx.doi.org/10.2106/JBJS.D.02944.
- Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL. National trends in rotator cuff repair. J Bone Joint Surg Br 2012;94:227-33. http://dx.doi.org/10.2106/JBJS.J.00739.
- Vitale MA, Arons RR, Hurwitz S, Ahmad CS, Levine WN. The rising incidence of acromioplasty. J Bone Joint Surg Br 2010;92:1842-50. http://dx.doi.org/10.2106/JBJS.I.01003.
- Judge A, Murphy RJ, Maxwell R, Arden NK, Carr AJ. Temporal trends and geographical variation in the use of subacromial decompression and rotator cuff repair of the shoulder in England. Bone Joint J 2014;96:70-4. http://dx.doi.org/10.1302/0301-620X.96B1.32556.
- Chaudhury S, Gwilym SE, Moser J, Carr AJ. Surgical options for patients with shoulder pain. Nat Rev Rheumatol 2010;6:217-26. http://dx.doi.org/10.1038/nrrheum.2010.25.
- Weber SC. Arthroscopic debridement and acromioplasty versus mini-open repair in the treatment of significant partial-thickness rotator cuff tears. Arthroscopy 1999;15:126-31. http://dx.doi.org/10.1053/ar.1999.v15.0150121.
- Youm T, Murray DH, Kubiak EN, Rokito AS, Zuckerman JD. Arthroscopic versus mini-open rotator cuff repair: a comparison of clinical outcomes and patient satisfaction. J Shoulder Elbow Surg 2005;14:455-9. http://dx.doi.org/10.1016/j.jse.2005.02.002.
- Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 1987;214:160-4. http://dx.doi.org/10.1097/00003086-198701000-00023.
- Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg 2002;11:587-94. http://dx.doi.org/10.1067/mse.2002.127096.
- Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (Disabilities of the Arm, Shoulder and Hand). The Upper Extremity Collaborative Group (UECG). Am J Ind Med 1996;29:602-8. http://dx.doi.org/10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L.
- World Health Organization . International Clinical Trials Registry Platform (ICTRP) n.d. www.who.int/ictrp/search/en/ (accessed 20 June 2014).
- Abrams GD, Gupta AK, Hussey KE, Tetteh ES, Karas V, Bach BR, et al. Arthroscopic repair of full-thickness rotator cuff tears with and without acromioplasty: randomised prospective trial with 2-year follow-up. Am J Sports Med 2014;14:1296-303. http://dx.doi.org/10.1177/0363546514529091.
- van der Zwaal P, Thomassen BJ, Nieuwenhuijse MJ, Lindenburg R, Swen JW, van Arkel ER. Clinical outcome in all-arthroscopic versus mini-open rotator cuff repair in small to medium-sized tears: a randomised controlled trial in 100 patients with 1-year follow-up. Arthroscopy 2013;29:266-73. http://dx.doi.org/10.1016/j.arthro.2012.08.022.
- MacDonald P, McRae S, Leiter J, Mascarenhas R, Lapner P. Arthroscopic rotator cuff repair with and without acromioplasty in the treatment of full-thickness rotator cuff tears: a multicenter, randomised controlled trial. J Bone Joint Surg Am 2011;93:1953-60. http://dx.doi.org/10.2106/JBJS.K.00488.
- Mohtadi NG, Hollinshead RM, Sasyniuk TM, Fletcher JA, Chan DS, Li FX. A randomised clinical trial comparing open to arthroscopic acromioplasty with mini-open rotator cuff repair for full-thickness rotator cuff tears: disease-specific quality of life outcome at an average 2-year follow-up. Am J Sports Med 2008;36:1043-51. http://dx.doi.org/10.1177/0363546508314409.
- MacDermid JC, Holtby R, Razmjou H, Bryant D. All-arthroscopic versus mini-open repair of small or moderate-sized rotator cuff tears: a protocol for a randomised trial (NCT00128076). BMC Musculoskelet Disord 2006;7. http://dx.doi.org/10.1186/1471-2474-7-25.
- Cho CH, Song KS, Jung GH, Lee YK, Shin HK. Early postoperative outcomes between arthroscopic and mini-open repair for rotator cuff tears. Orthopedics 2012;35:e1347-52. http://dx.doi.org/10.3928/01477447-20120822-20.
- Kasten P, Keil C, Grieser T, Raiss P, Streich N, Loew M. Prospective randomised comparison of arthroscopic versus mini-open rotator cuff repair of the supraspinatus tendon. Int Orthop 2011;35:1663-70. http://dx.doi.org/10.1007/s00264-011-1262-2.
- Kukkonen J, Joukainen A, Lehtinen J, Mattila KT, Tuominen EK, Kauko T, et al. Treatment of non-traumatic rotator cuff tears: a randomised controlled trial with one-year clinical results. Bone Joint J 2014;96:75-81. http://dx.doi.org/10.1302/0301-620X.96B1.32168.
- Moosmayer S, Lund G, Seljom U, Svege I, Hennig T, Tariq R, et al. Comparison between surgery and physiotherapy in the treatment of small and medium-sized tears of the rotator cuff: a randomised controlled study of 103 patients with one-year follow-up. J Bone Joint Surg Br 2010;92:83-91. http://dx.doi.org/10.1302/0301-620X.92B1.22609.
- Lambers Heerspink FO, Hoogeslag RA, Diercks RL, van Eerden PJM, van den Akker-Sceek I, van Raay JJ. Clinical and radiological outcome of conservative vs. surgical treatment of atraumatic degenerative rotator cuff rupture: design of a randomised controlled trial. BMC Musculoskelet Disord 2011;12. http://dx.doi.org/10.1186/1471-2474-12-25.
- Dawson J, Fitzpatrick R, Carr A. Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br 1996;78:593-600.
- Dawson J, Rogers K, Fitzpatrick R, Carr A. The Oxford Shoulder Score revisited. Arch Orthop Trauma Surg 2009;129:119-23. http://dx.doi.org/10.1007/s00402-007-0549-7.
- Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y. Development of a shoulder pain and disability index. Arthritis Care Res 1991;4:143-9. http://dx.doi.org/10.1002/art.1790040403.
- Williams JWJ, Holleman DRJ, Simel DL. Measuring shoulder function with the Shoulder Pain and Disability Index. J Rheumatol 1995;22:727-32.
- Berwick DM, Murphy JM, Goldman PA, Ware JE, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Arch Orthop Trauma Surg 1991;29:169-76. http://dx.doi.org/10.1097/00005650-199102000-00008.
- Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care 1992;30:473-81. http://dx.doi.org/10.1097/00005650-199206000-00002.
- EuroQol Group . EuroQol – a new facility for the measurement of health-related quality of life. Health Policy n.d.;16:199-208. http://dx.doi.org/10.1016/0168-8510(90)90421-9.
- Nagelkerke N, Fidler V, Bersen R, Borgdorff M. Estimating treatment effects in randomized clinical trials in the presence of non-compliance. Stat Med 2000;19:1849-64. http://dx.doi.org/10.1002/1097-0258(20000730)19:14<1849::AID-SIM506>3.0.CO;2-1.
- Clarke PM1, Fiebig DG, Gerdtham UG. Optimal recall length in survey design. J Health Econ 2008;27:1275-84. http://dx.doi.org/10.1016/j.jhealeco.2008.05.012.
- Brooks R. EuroQol: the current state of play. Health Policy 1996;37:53-72. http://dx.doi.org/10.1016/0168-8510(96)00822-6.
- Campbell M, Grimshaw J, Steen N. Sample size calculations for cluster randomised trials. Changing Professional Practice in Europe Group (EU BIOMED II Concerted Action). J Health Serv Res Policy 2000;5:12-6.
- Hoyle RA. Statistical Strategies For Small Sample Research. London: Sage Publications; 1999.
- Goldstein H. Multilevel Statistical Models. London: Arnold; 1996.
- Information Services Division (ISD) Scotland . Cost Book Table R142X_2013 n.d. www.isdscotland.org/Health-Topics/Finance/Costs/File-Listings-2013.asp (accessed 20 August 2015).
- Department of Health . National Schedule of Reference Costs 2012 to 2013 – NHS Trusts and NHS Foundation Trusts n.d. www.gov.uk/government/publications/nhs-reference-costs-2012-to-2013 (accessed 24 August 2015).
- Curtis L. Unit Costs of Health Social Care 2013. Canterbury: Personal Social Services Research Unit, University of Kent; 2013.
- Guide to the Methods of Technology Appraisal 2013. London: NICE; 2013.
- Lenza M, Buchbinder R, Takwoingi Y, Johnston RV, Hanchard NCA, Faloppa F. Magnetic resonance imaging, magnetic resonance arthrography and ultrasonography for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered. Cochrane Database Syst Rev 2013;9. http://dx.doi.org/10.1002/14651858.cd009020.pub2.
Appendix 1 Per-protocol data tables
| Assessment | Stratum A, n (%) | Stratum B, n (%) | Stratum C, n (%) | |
|---|---|---|---|---|
| Arthroscopic (n = 63) | Open (n = 85) | Arthroscopic (n = 50) | Open (n = 40) | |
| Size of tear | ||||
| Small/medium | 49 (77.8) | 66 (77.6) | 23 (46.0) | 28 (70.0) |
| Large/massive | 14 (22.2) | 19 (22.4) | 27 (54.0) | 12 (30.0) |
| Method of diagnosing tear | ||||
| MRI | 18 (28.6) | 22 (25.9) | 9 (18.0) | 11 (27.5) |
| Ultrasound | 43 (68.3) | 56 (65.9) | 36 (72.0) | 27 (67.5) |
| Missing | 2 (3.2) | 7 (8.2) | 5 (10.0) | 2 (5.0) |
| Received physiotherapy on affected shoulder in the last 5 years | ||||
| Yes | 35 (55.6) | 54 (63.5) | 34 (68.0) | 29 (72.5) |
| No | 19 (30.2) | 24 (28.2) | 11 (22.0) | 4 (10.0) |
| Missing | 9 (14.3) | 7 (8.2) | 5 (10.0) | 7 (17.5) |
| Duration of physiotherapy (weeks) | ||||
| ≤ 4 | 8 (22.9) | 11 (20.4) | 3 (8.8) | 7 (24.1) |
| 5–12 | 12 (34.3) | 14 (25.9) | 11 (32.4) | 10 (34.5) |
| > 12 | 5 (14.3) | 17 (31.5) | 14 (41.2) | 7 (24.1) |
| Missing | 10 (28.6) | 12 (22.2) | 6 (17.6) | 5 (17.2) |
| Received an injection in affected shoulder in the last 5 years | ||||
| Yes | 35 (55.6) | 52 (61.2) | 31 (62.0) | 26 (65.0) |
| No | 23 (36.5) | 22 (25.9) | 13 (26.0) | 7 (17.5) |
| Missing | 5 (7.9) | 11 (12.9) | 6 (12.0) | 7 (17.5) |
| Number of injections | ||||
| 1 | 14 (40.0) | 20 (38.5) | 13 (41.9) | 11 (42.3) |
| 2 | 10 (28.6) | 17 (32.7) | 10 (32.3) | 7 (26.9) |
| 3 | 1 (2.9) | 8 (15.4) | 6 (19.4) | 7 (26.9) |
| 4 | 2 (5.7) | 1 (1.9) | ||
| 5 | 2 (5.7) | 1 (1.9) | ||
| 6 | 1 (2.9) | 2 (3.8) | ||
| 7 | ||||
| 9 | 1 (3.8) | |||
| 10 | 1 (3.2) | |||
| Missing | 5 (14.3) | 3 (5.8) | 1 (3.2) | |
| Received other treatment on the affected shoulder in the last 5 years | ||||
| Yes | 7 (11.1) | 19 (22.4) | 2 (4.0) | 7 (17.5) |
| No | 33 (52.4) | 41 (48.2) | 28 (56.0) | 15 (37.5) |
| Missing | 23 (36.5) | 25 (29.4) | 20 (40.0) | 18 (45.0) |
| Other treatment | ||||
| Acupuncture | 1 (14.3) | 3 (15.8) | 1 (50.0) | 3 (42.9) |
| Analgesics | 2 (28.6) | 9 (47.4) | 1 (14.3) | |
| Chiropractor | 1 (14.3) | 2 (10.5) | 1 (14.3) | |
| Exercises | 1 (5.3) | |||
| Massage | 1 (14.3) | |||
| Osteopathy | 1 (5.3) | 1 (14.3) | ||
| TENS | 1 (14.3) | |||
| Ultrasound | 1 (5.3) | |||
| Missing | 2 (28.6) | 2 (10.5) | 1 (50.0) | |
| Received no previous treatment on shoulder in the last 5 years | 9 (14.3) | 5 (5.9) | 6 (12.0) | 2 (5.0) |
| Are there any problems with patient’s other shoulder? | ||||
| No problems | 41 (65.1) | 51 (60.0) | 27 (54.0) | 23 (57.5) |
| Mild problems | 12 (19.0) | 21 (24.7) | 14 (28.0) | 10 (25.0) |
| Moderate problems | 6 (9.5) | 7 (8.2) | 7 (14.0) | 6 (15.0) |
| Severe problems | 2 (3.2) | 3 (3.5) | 1 (2.0) | 1 (2.5) |
| Missing | 2 (3.2) | 3 (3.5) | 1 (2.0) | |
| Characteristic | Stratum A, n (%) | Stratum B, n (%) | Stratum C, n (%) | |
|---|---|---|---|---|
| Arthroscopic (n = 63) | Open (n = 85) | Arthroscopic (n = 50) | Open (n = 40) | |
| Age (years), n, mean (SD) | 63, 61.7 (6.5) | 85, 62.2 (7.3) | 50, 65.3 (6.7) | 40, 61.1 (6.2) |
| Years with shoulder problem, n, mean (SD) | 63, 2.8 (4.6) | 85, 2.6 (4.9) | 49, 2.5 (3.3) | 40, 3.3 (6.3) |
| OSS, n, mean (SD) | 63, 25.6 (8.4) | 85, 24.6 (7.8) | 50, 25.5 (8.5) | 40, 24.8 (7.7) |
| SPADI, n, mean (SD) | 63, 63.7 (22.7) | 85, 62.8 (21.6) | 50, 61.5 (22.9) | 40, 64.6 (17.7) |
| SPADI pain, n, mean (SD) | 63, 71.2 (19.9) | 85, 71.7 (19.6) | 50, 72.1 (21.4) | 40, 74.6 (17.1) |
| SPADI disability, n, mean (SD) | 63, 59.0 (25.8) | 84, 57.4 (24.8) | 50, 54.9 (26.2) | 40, 58.4 (20.1) |
| MHI-5, n, mean (SD) | 63, 21.9 (5.0) | 85, 22.8 (4.5) | 49, 22.9 (5.1) | 40, 22.3 (4.7) |
| EQ-5D, n, mean (SD) | 62, 0.529 (0.315) | 84, 0.509 (0.285) | 50, 0.505 (0.320) | 39, 0.472 (0.306) |
| Sex | ||||
| Male | 36 (57.1) | 55 (64.7) | 33 (66.0) | 26 (65.0) |
| Female | 27 (42.9) | 30 (35.3) | 16 (32.0) | 14 (35.0) |
| Missing | 1 (2.0) | |||
| Highest qualification | ||||
| None | 26 (41.3) | 34 (40.0) | 22 (44.0) | 20 (50.0) |
| Secondary | 21 (33.3) | 33 (38.8) | 21 (42.0) | 9 (22.5) |
| Higher | 16 (25.4) | 17 (20.0) | 5 (10.0) | 11 (27.5) |
| Missing | 1 (1.2) | 2 (4.0) | ||
| Housing tenure | ||||
| Home owner | 49 (77.8) | 76 (89.4) | 46 (92.0) | 35 (87.5) |
| Private rent | 4 (6.3) | 1 (2.5) | ||
| Council rent | 7 (11.1) | 3 (3.5) | 4 (8.0) | 3 (7.5) |
| Other | 3 (4.8) | 6 (7.1) | 1 (2.5) | |
| Lives alone | ||||
| Yes | 13 (20.6) | 6 (7.1) | 7 (14.0) | 5 (12.5) |
| No | 46 (73.0) | 73 (85.9) | 42 (84.0) | 34 (85.0) |
| Missing | 4 (6.3) | 6 (7.1) | 1 (2.0) | 1 (2.5) |
| Employment status | ||||
| Full-time | 22 (34.9) | 36 (42.4) | 15 (30.0) | 17 (42.5) |
| Part-time | 10 (15.9) | 12 (14.1) | 10 (20.0) | 6 (15.0) |
| Homemaker | 2 (3.2) | 4 (4.7) | 1 (2.5) | |
| Retired | 26 (41.3) | 29 (34.1) | 25 (50.0) | 15 (37.5) |
| Unemployed | 3 (4.8) | 3 (3.5) | 1 (2.5) | |
| Missing | 1 (1.2) | |||
| Type of work | ||||
| Manual | 17 (53.1) | 30 (62.5) | 17 (68.0) | 14 (60.9) |
| Non-manual | 13 (40.6) | 15 (31.3) | 8 (32.0) | 9 (39.1) |
| Not sure | 2 (6.3) | 2 (4.2) | ||
| Missing | 1 (2.1) | |||
| Off sick or working reduced duties | ||||
| Yes, off sick | 2 (6.3) | 6 (12.5) | 2 (8.0) | 1 (4.3) |
| Yes, working reduced duties | 6 (18.8) | 5 (10.4) | 5 (20.0) | 5 (21.7) |
| No, working usual duties | 22 (68.8) | 36 (75.0) | 18 (72.0) | 17 (73.9) |
| Missing | 2 (6.3) | 1 (2.1) | ||
| Handedness | ||||
| Right-handed | 57 (90.5) | 76 (89.4) | 48 (96.0) | 33 (82.5) |
| Left-handed | 3 (4.8) | 6 (7.1) | 2 (4.0) | 5 (12.5) |
| Both | 3 (4.8) | 3 (3.5) | 2 (5.0) | |
| Would you be able to do your job or everyday activities with arm in a sling? | ||||
| No | 38 (60.3) | 55 (64.7) | 29 (58.0) | 21 (52.5) |
| Yes, with difficulty | 25 (39.7) | 30 (35.3) | 21 (42.0) | 19 (47.5) |
| Operative detail | Stratum A, n (%) | Stratum B, n (%) | Stratum C, n (%) | |
|---|---|---|---|---|
| Arthroscopic (n = 63) | Open (n = 85) | Arthroscopic (n = 50) | Open (n = 40) | |
| Procedure side | ||||
| Left | 26 (41.3) | 26 (30.6) | 11 (22.0) | 12 (30.0) |
| Right | 37 (58.7) | 59 (69.4) | 39 (78.0) | 28 (70.0) |
| Missing | ||||
| Ease of repair | ||||
| Easy | 18 (28.6) | 39 (45.9) | 12 (24.0) | 11 (27.5) |
| Moderate | 28 (44.4) | 25 (29.4) | 19 (38.0) | 12 (30.0) |
| Difficult | 12 (19.0) | 12 (14.1) | 11 (22.0) | 11 (27.5) |
| Impossible | 2 (2.4) | 1 (2.0) | 2 (5.0) | |
| Missing | 5 (7.9) | 7 (8.2) | 7 (14.0) | 4 (10.0) |
| Size of tear | ||||
| Small | 22 (34.9) | 25 (29.4) | 11 (22.0) | 6 (15.0) |
| Medium | 25 (39.7) | 32 (37.6) | 10 (20.0) | 11 (27.5) |
| Large | 10 (15.9) | 18 (21.2) | 16 (32.0) | 13 (32.5) |
| Massive | 5 (7.9) | 9 (10.6) | 13 (26.0) | 10 (25.0) |
| Missing | 1 (1.6) | 1 (1.2) | ||
| Surgical opinion of completeness of repair | ||||
| Poor | 6 (9.5) | 6 (7.1) | 4 (8.0) | 5 (12.5) |
| Good | 37 (58.7) | 42 (49.4) | 29 (58.0) | 20 (50.0) |
| Excellent | 16 (25.4) | 33 (38.8) | 9 (18.0) | 11 (27.5) |
| Missing | 4 (6.3) | 4 (4.7) | 8 (16.0) | 4 (10.0) |
| Total minutes in theatre, n, mean (SD) | 48, 107.5 (33.3) | 74, 87.8 (30.1) | 32, 99.2 (25.8) | 30, 99.9 (52.6) |
| Operation time, n, mean (SD) | 48, 76.4 (30.5) | 72, 58.1 (22.8) | 24, 70.4 (23.5) | 25, 75.4 (38.3) |
| Complication | Stratum A, n (%) | Stratum B, n (%) | Stratum C, n (%) | |
|---|---|---|---|---|
| Arthroscopic (n = 63) | Open (n = 85) | Arthroscopic (n = 50) | Open (n = 40) | |
| Intraoperative problem | ||||
| Anaesthetic | 1 (1.2) | |||
| Equipment | 3 (4.8) | 1 (1.2) | 2 (4.0) | |
| Implant | 1 (1.2) | 1 (2.0) | ||
| Surgical | 5 (7.9) | 1 (1.2) | 3 (6.0) | |
| Other | 2 (3.2) | 4 (4.7) | 3 (6.0) | 2 (5.0) |
| Staff problems | 2 (5.0) | |||
| Any intraoperative problems | 7 (11.1) | 6 (7.1) | 2 (4.0) | 7 (14.0) |
| Did the procedure change as a result of an intraoperative problem? | ||||
| Yes | 2 (28.6) | |||
| No | 7 (100.0) | 4 (66.7) | 4 (57.1) | 2 (100.0) |
| Unsure | 1 (14.3) | |||
| Missing | 2 (33.3) | |||
| Question | Stratum A, n (%) | Stratum B, n (%) | Stratum C, n (%) | |
|---|---|---|---|---|
| Arthroscopic (n = 63) | Open (n = 85) | Arthroscopic (n = 50) | Open (n = 40) | |
| Completed follow-up forms | 56 (88.9) | 77 (90.6) | 42 (84.0) | 36 (90.0) |
| Within the last 24 hours, have you been wearing a sling at all? | ||||
| Yes | 49 (87.5) | 64 (83.1) | 40 (95.2) | 32 (88.9) |
| No | 6 (10.7) | 12 (15.6) | 2 (4.8) | 4 (11.1) |
| Missing | 1 (1.8) | 1 (1.3) | ||
| If yes, how long have you worn the sling for? | ||||
| > 12 hours | 45 (91.8) | 61 (95.3) | 36 (90.0) | 23 (71.9) |
| > 6 hours but < 12 hours | 3 (6.1) | 2 (3.1) | 1 (2.5) | 6 (18.8) |
| > 3 hours but < 6 hours | 1 (2.0) | 1 (2.5) | 1 (3.1) | |
| < 3 hours | 1 (1.6) | |||
| Missing | 2 (5.0) | 2 (6.3) | ||
| Within the last 24 hours, how would you describe the worst pain from your shoulder? | ||||
| None | 4 (7.1) | 3 (3.9) | 2 (4.8) | 2 (5.6) |
| Mild | 16 (28.6) | 19 (24.7) | 13 (31.0) | 12 (33.3) |
| Moderate | 22 (39.3) | 38 (49.4) | 17 (40.5) | 17 (47.2) |
| Severe | 11 (19.6) | 15 (19.5) | 8 (19.0) | 5 (13.9) |
| Unbearable | 2 (3.6) | 1 (1.3) | 2 (4.8) | |
| Missing | 1 (1.8) | 1 (1.3) | ||
| Within the last 24 hours, how much has pain from your shoulder interfered with your usual work? | ||||
| Not at all | 9 (16.1) | 7 (9.1) | 9 (21.4) | 7 (19.4) |
| A little bit | 6 (10.7) | 8 (10.4) | 7 (16.7) | 6 (16.7) |
| Moderately | 14 (25.0) | 26 (33.8) | 7 (16.7) | 7 (19.4) |
| Greatly | 16 (28.6) | 22 (28.6) | 7 (16.7) | 11 (30.6) |
| Totally | 10 (17.9) | 13 (16.9) | 12 (28.6) | 5 (13.9) |
| Missing | 1 (1.8) | 1 (1.3) | ||
| Were you troubled by pain from your shoulder in bed last night? | ||||
| No, not at all | 14 (25.0) | 13 (16.9) | 8 (19.0) | 10 (27.8) |
| Yes, just at first | 5 (8.9) | 5 (6.5) | 4 (9.5) | |
| Yes, during some of the night | 25 (44.6) | 28 (36.4) | 19 (45.2) | 14 (38.9) |
| Yes, throughout the night | 11 (19.6) | 30 (39.0) | 11 (26.2) | 12 (33.3) |
| Missing | 1 (1.8) | 1 (1.3) | ||
| Within the last 24 hours, have you taken any painkillers because of your shoulder? | ||||
| Yes | 40 (71.4) | 56 (72.7) | 31 (73.8) | 28 (77.8) |
| No | 15 (26.8) | 20 (26.0) | 11 (26.2) | 8 (22.2) |
| Missing | 1 (1.8) | 1 (1.3) | ||
| If yes, how many painkillers have you taken in the last 24 hours? | ||||
| 1 | 18 (45.0) | 25 (44.6) | 15 (48.4) | 14 (50.0) |
| 2 | 15 (37.5) | 25 (44.6) | 11 (35.5) | 8 (28.6) |
| 3 | 5 (12.5) | 3 (5.4) | 5 (16.1) | 3 (10.7) |
| 4 | 1 (1.8) | 2 (7.1) | ||
| 5 | 1 (2.5) | 1 (1.8) | 1 (3.6) | |
| Missing | 1 (2.5) | 1 (1.8) | ||
| During the (last 2 weeks) time since the completion of surgery or rest then exercise, have you received any additional treatment on your shoulder? | ||||
| Yes | 3 (5.4) | 14 (18.2) | 5 (11.9) | 2 (5.6) |
| No | 50 (89.3) | 60 (77.9) | 36 (85.7) | 32 (88.9) |
| Missing | 3 (5.4) | 3 (3.9) | 1 (2.4) | 2 (5.6) |
| If yes, what was the additional treatment? | ||||
| Injection | ||||
| Antibiotics | 1 (7.1) | |||
| Physiotherapy | 1 (33.3) | 2 (14.3) | 2 (40.0) | 1 (50.0) |
| Wound or dressing | 5 (35.7) | 2 (40.0) | ||
| Not for shoulder problem | 1 (33.3) | 1 (7.1) | 1 (50.0) | |
| Pain relief | 1 (33.3) | 5 (35.7) | 1 (20.0) | |
| Are you currently employed? | ||||
| Yes | 28 (50.0) | 40 (51.9) | 22 (52.4) | 24 (66.7) |
| No | 27 (48.2) | 36 (46.8) | 20 (47.6) | 12 (33.3) |
| Missing | 1 (1.8) | 1 (1.3) | ||
| If employed, are you currently off sick or working reduced duties because of your shoulder? | ||||
| Yes, off sick | 24 (85.7) | 36 (90.0) | 18 (81.8) | 19 (79.2) |
| Yes, working reduced duties | 3 (10.7) | 2 (5.0) | 3 (13.6) | 4 (16.7) |
| No, working usual hours/duties | 1 (3.6) | 2 (5.0) | 1 (4.5) | |
| Missing | 1 (4.2) | |||
| Question | Stratum A, n (%) | Stratum B, n (%) | Stratum C, n (%) | |
|---|---|---|---|---|
| Arthroscopic (n = 63) | Open (n = 85) | Arthroscopic (n = 50) | Open (n = 40) | |
| Completed follow-up forms | 55 (87.3) | 78 (91.8) | 41 (82.0) | 32 (80.0) |
| Within the last 24 hours, have you been wearing a sling at all? | ||||
| Yes | 5 (9.1) | 13 (16.7) | 5 (12.2) | 6 (18.8) |
| No | 50 (90.9) | 65 (83.3) | 36 (87.8) | 26 (81.3) |
| If yes, how long have you worn the sling for? | ||||
| > 12 hours | 1 (20.0) | 3 (23.1) | 2 (40.0) | 1 (16.7) |
| > 6 hours but < 12 hours | 4 (30.8) | 1 (16.7) | ||
| > 3 hours but < 6 hours | 1 (20.0) | 6 (46.2) | 1 (20.0) | 1 (16.7) |
| < 3 hours | 3 (60.0) | 2 (40.0) | 1 (16.7) | |
| Missing | 2 (33.3) | |||
| Within the last 24 hours, how would you describe the worst pain you have had from your shoulder? | ||||
| None | 4 (7.3) | 6 (7.7) | 3 (7.3) | 3 (9.4) |
| Mild | 26 (47.3) | 38 (48.7) | 13 (31.7) | 12 (37.5) |
| Moderate | 18 (32.7) | 19 (24.4) | 16 (39.0) | 11 (34.4) |
| Severe | 7 (12.7) | 14 (17.9) | 9 (22.0) | 6 (18.8) |
| Unbearable | 1 (1.3) | |||
| Within the last 24 hours, how much has pain from your shoulder interfered with your usual work? | ||||
| Not at all | 16 (29.1) | 13 (16.7) | 8 (19.5) | 7 (21.9) |
| A little bit | 15 (27.3) | 23 (29.5) | 14 (34.1) | 10 (31.3) |
| Moderately | 17 (30.9) | 27 (34.6) | 11 (26.8) | 9 (28.1) |
| Greatly | 5 (9.1) | 12 (15.4) | 6 (14.6) | 5 (15.6) |
| Totally | 2 (3.6) | 3 (3.8) | 2 (4.9) | 1 (3.1) |
| Were you troubled by pain from your shoulder in bed last night? | ||||
| No, not at all | 24 (43.6) | 25 (32.1) | 14 (34.1) | 10 (31.3) |
| Yes, just at first | 3 (5.5) | 5 (6.4) | 4 (9.8) | 1 (3.1) |
| Yes, during some of the night | 19 (34.5) | 27 (34.6) | 16 (39.0) | 13 (40.6) |
| Yes, throughout the night | 9 (16.4) | 21 (26.9) | 7 (17.1) | 8 (25.0) |
| Within the last 24 hours, have you taken any painkillers for your shoulder? | ||||
| Yes | 28 (50.9) | 44 (56.4) | 23 (56.1) | 20 (62.5) |
| No | 27 (49.1) | 34 (43.6) | 18 (43.9) | 12 (37.5) |
| If yes, how many painkillers have you taken? | ||||
| 1 | 19 (67.9) | 26 (59.1) | 12 (52.2) | 8 (40.0) |
| 2 | 7 (25.0) | 15 (34.1) | 6 (26.1) | 4 (20.0) |
| 3 | 1 (3.6) | 3 (6.8) | 2 (8.7) | 1 (5.0) |
| 4 | 1 (3.6) | 1 (5.0) | ||
| Missing | 3 (13.0) | 6 (30.0) | ||
| During the time (last 6 weeks) since we spoke to you last, have you had any additional treatment for your shoulder? | ||||
| Yes | 5 (9.1) | 8 (10.3) | 3 (7.3) | 5 (15.6) |
| No | 47 (85.5) | 69 (88.5) | 38 (92.7) | 27 (84.4) |
| Missing | 3 (5.5) | 1 (1.3) | ||
| If yes, what additional treatment did you receive? | ||||
| Injection | 1 (12.5) | |||
| Antibiotics | 2 (25.0) | 1 (20.0) | ||
| Physiotherapy | 5 (100.0) | 2 (25.0) | 2 (66.7) | 4 (80.0) |
| Wound or dressing | 1 (12.5) | |||
| Hospital admission | 1 (33.3) | |||
| Surgery and antibiotics | 2 (25.0) | |||
| Are you currently employed? | ||||
| Yes | 28 (50.9) | 42 (53.8) | 17 (41.5) | 18 (56.3) |
| No | 27 (49.1) | 35 (44.9) | 22 (53.7) | 13 (40.6) |
| Missing | 1 (1.3) | 2 (4.9) | 1 (3.1) | |
| If yes, are you currently off sick or working reduced hours because of your shoulder? | ||||
| Yes, off sick | 13 (46.4) | 23 (54.8) | 11 (64.7) | 11 (61.1) |
| Yes, working reduced duties | 7 (25.0) | 10 (23.8) | 4 (23.5) | 3 (16.7) |
| No, working usual hours/duties | 8 (28.6) | 8 (19.0) | 2 (11.8) | 4 (22.2) |
| Missing | 1 (2.4) | |||
| Question | Stratum A, n (%) | Stratum B, n (%) | Stratum C, n (%) | |
|---|---|---|---|---|
| Arthroscopic (n = 63) | Open (n = 85) | Arthroscopic (n = 50) | Open (n = 40) | |
| 8-month follow-up forms completed | 60 (95.2) | 82 (96.5) | 50 (100.0) | 38 (95.0) |
| 12-month follow-up forms completed | 62 (98.4) | 83 (97.7) | 47 (94.0) | 38 (95.0) |
| 24-month follow-up forms completed | 58 (92.1) | 81 (95.3) | 45 (90.0) | 36 (90.0) |
| How are the problems related to your shoulder now compared with 8 months ago? | ||||
| Much better | 40 (66.7) | 55 (67.1) | 34 (68.0) | 23 (60.5) |
| Slightly better | 12 (20.0) | 11 (13.4) | 11 (22.0) | 6 (15.8) |
| No change | 3 (5.0) | 5 (6.1) | 1 (2.0) | 1 (2.6) |
| Slightly worse | 3 (5.0) | 4 (4.9) | 2 (4.0) | 4 (10.5) |
| Much worse | 2 (3.3) | 2 (2.4) | 1 (2.0) | 2 (5.3) |
| Missing | 5 (6.1) | 1 (2.0) | 2 (5.3) | |
| How are the problems related to your shoulder now compared with a year ago? | ||||
| Much better | 43 (69.4) | 61 (73.5) | 34 (72.3) | 30 (78.9) |
| Slightly better | 10 (16.1) | 16 (19.3) | 9 (19.1) | 4 (10.5) |
| No change | 1 (1.6) | 2 (5.3) | ||
| Slightly worse | 3 (4.8) | 1 (1.2) | 1 (2.1) | |
| Much worse | 2 (3.2) | 5 (6.0) | 1 (2.6) | |
| Missing | 3 (4.8) | 3 (6.4) | 1 (2.6) | |
| How are the problems related to your shoulder now compared with 2 years ago? | ||||
| Much better | 48 (82.8) | 58 (71.6) | 39 (86.7) | 25 (69.4) |
| Slightly better | 5 (8.6) | 16 (19.8) | 2 (4.4) | 5 (13.9) |
| No change | 1 (1.7) | 1 (1.2) | 1 (2.2) | 2 (5.6) |
| Slightly worse | 2 (3.4) | 2 (2.5) | 1 (2.2) | 2 (5.6) |
| Much worse | 1 (1.7) | 2 (2.5) | ||
| Missing | 1 (1.7) | 2 (2.5) | 2 (4.4) | 2 (5.6) |
| How pleased are you with your shoulder symptoms at 8 months? | ||||
| Very pleased | 29 (48.3) | 37 (45.1) | 28 (56.0) | 21 (55.3) |
| Fairly pleased | 24 (40.0) | 32 (39.0) | 17 (34.0) | 12 (31.6) |
| Not very pleased | 6 (10.0) | 5 (6.1) | 2 (4.0) | 2 (5.3) |
| Very disappointed | 1 (1.7) | 3 (3.7) | 2 (4.0) | 1 (2.6) |
| Missing | 5 (6.1) | 1 (2.0) | 2 (5.3) | |
| How pleased are you with your shoulder symptoms at 12 months? | ||||
| Very pleased | 33 (53.2) | 42 (50.6) | 26 (55.3) | 26 (68.4) |
| Fairly pleased | 18 (29.0) | 33 (39.8) | 18 (38.3) | 9 (23.7) |
| Not very pleased | 6 (9.7) | 3 (3.6) | 1 (2.1) | |
| Very disappointed | 2 (3.2) | 5 (6.0) | 2 (5.3) | |
| Missing | 3 (4.8) | 2 (4.3) | 1 (2.6) | |
| How pleased are you with your shoulder symptoms at 24 months? | ||||
| Very pleased | 44 (75.9) | 46 (56.8) | 27 (60.0) | 25 (69.4) |
| Fairly pleased | 9 (15.5) | 23 (28.4) | 13 (28.9) | 6 (16.7) |
| Not very pleased | 1 (1.7) | 6 (7.4) | 3 (6.7) | 1 (2.8) |
| Very disappointed | 3 (5.2) | 3 (3.7) | 2 (5.6) | |
| Missing | 1 (1.7) | 3 (3.7) | 2 (4.4) | 2 (5.6) |
| Employment status | Stratum A, n (%) | Stratum B, n (%) | Stratum C, n (%) | |
|---|---|---|---|---|
| Arthroscopic (n = 63) | Open (n = 85) | Arthroscopic (n = 50) | Open (n = 40) | |
| Employed at 8 months | ||||
| Yes | 27 (45.0) | 38 (46.3) | 21 (42.0) | 20 (52.6) |
| No | 33 (55.0) | 37 (45.1) | 28 (56.0) | 16 (42.1) |
| Missing | 7 (8.5) | 1 (2.0) | 2 (5.3) | |
| Employed at 12 months | ||||
| Yes | 29 (46.8) | 34 (41.0) | 16 (34.0) | 20 (52.6) |
| No | 31 (50.0) | 48 (57.8) | 29 (61.7) | 17 (44.7) |
| Missing | 2 (3.2) | 1 (1.2) | 2 (4.3) | 1 (2.6) |
| Employed at 24 months | ||||
| Yes | 25 (43.1) | 30 (37.0) | 16 (35.6) | 19 (52.8) |
| No | 32 (55.2) | 48 (59.3) | 27 (60.0) | 15 (41.7) |
| Missing | 1 (1.7) | 3 (3.7) | 2 (4.4) | 2 (5.6) |
| If you are employed, are you off sick or working reduced duties because of your shoulder at 8 months? | ||||
| Yes, off sick | 7 (11.7) | 6 (7.3) | 4 (8.0) | 1 (2.6) |
| Yes, working reduced hours | 1 (1.7) | 6 (7.3) | 3 (6.0) | 4 (10.5) |
| No, working usual hours/duties | 18 (30.0) | 24 (29.3) | 14 (28.0) | 14 (36.8) |
| Missing | 34 (56.7) | 46 (56.1) | 29 (58.0) | 19 (50.0) |
| Are you currently out of work, off sick or working reduced duties because of your shoulder at 12 months? | ||||
| Yes | 6 (9.7) | 8 (9.6) | 3 (6.4) | 3 (7.9) |
| No | 44 (71.0) | 64 (77.1) | 37 (78.7) | 29 (76.3) |
| Missing | 12 (19.4) | 11 (13.3) | 7 (14.9) | 6 (15.8) |
| Are you currently out of work, off sick or working reduced duties because of your shoulder at 24 months? | ||||
| Yes, off sick | 4 (6.9) | 4 (4.9) | 2 (4.4) | 2 (5.6) |
| No, working usual hours/duties | 48 (82.8) | 64 (79.0) | 38 (84.4) | 28 (77.8) |
| Missing | 6 (10.3) | 13 (16.0) | 5 (11.1) | 6 (16.7) |
| Measure | Stratum A, n, mean (SD) | Stratum B, n, mean (SD) | Stratum C, n, mean (SD) | |
|---|---|---|---|---|
| Arthroscopic (n = 63) | Open (n = 85) | Arthroscopic (n = 50) | Open (n = 40) | |
| OSS | ||||
| Baseline | 63, 25.6 (8.4) | 85, 24.6 (7.8) | 50, 25.5 (8.5) | 40, 24.8 (7.7) |
| 8 months | 60, 35.9 (10.3) | 81, 37.1 (8.4) | 50, 37.6 (8.3) | 38, 35.5 (10.6) |
| 12 months | 61, 38.6 (9.9) | 82, 40.3 (8.2) | 46, 40.0 (5.9) | 38, 41.1 (6.9) |
| 24 months (primary outcome) | 57, 42.9 (7.1) | 79, 42.0 (7.5) | 45, 41.9 (5.9) | 36, 42.7 (5.9) |
| SPADI | ||||
| Baseline | 63, 63.7 (22.7) | 85, 62.8 (21.6) | 50, 61.5 (22.9) | 40, 64.6 (17.7) |
| 8 months | 59, 30.4 (28.2) | 80, 30.1 (27.4) | 49, 28.6 (23.2) | 36, 31.7 (26.1) |
| 12 months | 93, 23.1 (26.1) | 83, 22.4 (25.5) | 65, 21.5 (22.8) | 37, 18.8 (21.6) |
| 24 months | 91, 15.2 (21.3) | 81, 16.9 (22.7) | 61, 13.8 (17.5) | 34, 15.0 (22.2) |
| SPADI pain | ||||
| Baseline | 63, 71.2 (19.9) | 85, 71.7 (19.6) | 50, 72.1 (21.4) | 40, 74.6 (17.1) |
| 8 months | 60, 34.0 (27.9) | 81, 32.8 (27.6) | 50, 31.4 (24.8) | 36, 35.9 (27.7) |
| 12 months | 61, 24.3 (26.8) | 82, 24.4 (26.4) | 46, 21.6 (17.3) | 37, 21.9 (24.6) |
| 24 months | 57, 13.4 (18.0) | 81, 18.7 (24.4) | 42, 15.6 (15.3) | 34, 16.9 (23.4) |
| SPADI disability | ||||
| Baseline | 63, 59.0 (25.8) | 84, 57.4 (24.8) | 50, 54.9 (26.2) | 40, 58.4 (20.1) |
| 8 months | 59, 28.2 (29.0) | 80, 28.2 (27.9) | 49, 26.5 (23.1) | 37, 31.0 (28.3) |
| 12 months | 61, 21.0 (26.7) | 83, 21.0 (26.0) | 46, 16.9 (17.8) | 37, 16.7 (20.3) |
| 24 months | 58, 11.5 (20.7) | 81, 15.7 (22.4) | 43, 14.1 (19.0) | 34, 13.7 (22.2) |
| MHI-5 | ||||
| Baseline | 63, 21.9 (5.0) | 85, 22.8 (4.5) | 49, 22.9 (5.1) | 40, 22.3 (4.7) |
| 8 months | 60, 23.5 (4.9) | 81, 23.9 (4.4) | 48, 24.1 (4.5) | 38, 24.1 (4.1) |
| 12 months | 60, 23.3 (5.0) | 82, 23.3 (4.9) | 45, 25.0 (4.3) | 37, 24.4 (3.9) |
| 24 months | 58, 24.7 (3.7) | 81, 24.6 (4.6) | 43, 23.9 (5.0) | 34, 24.1 (4.9) |
| EQ-5D | ||||
| Baseline | 62, 0.529 (0.315) | 84, 0.509 (0.285) | 50, 0.505 (0.320) | 39, 0.472 (0.306) |
| 8 months | 59, 0.669 (0.332) | 80, 0.713 (0.258) | 45, 0.717 (0.233) | 37, 0.668 (0.236) |
| 12 months | 61, 0.712 (0.308) | 81, 0.715 (0.288) | 45, 0.767 (0.212) | 35, 0.748 (0.181) |
| 24 months | 57, 0.773 (0.236) | 81, 0.782 (0.218) | 45, 0.771 (0.223) | 36, 0.788 (0.222) |
| Measure | Stratum A, n (%) | Stratum B, n (%) | Stratum C, n (%) | |
|---|---|---|---|---|
| Arthroscopic (n = 63) | Open (n = 85) | Arthroscopic (n = 50) | Open (n = 40) | |
| MRI scans received | 60 | 79 | 39 | 36 |
| Result of MRI scan | ||||
| Re-tear | 29 (48.3) | 30 (38.0) | 14 (35.9) | 13 (36.1) |
| No tear | 28 (46.7) | 46 (58.2) | 22 (56.4) | 21 (58.3) |
| Inconclusive | 1 (1.7) | 1 (1.3) | ||
| Missing | 2 (3.3) | 2 (2.5) | 3 (7.7) | 2 (5.6) |
| Size of tear if MRI scan shows a re-tear | ||||
| Partial | 2 (6.9) | 1 (3.3) | 1 (7.1) | |
| Small | 8 (27.6) | 9 (30.0) | 1 (7.1) | 3 (23.1) |
| Medium | 5 (17.2) | 8 (26.7) | 6 (42.9) | 5 (38.5) |
| Large | 5 (17.2) | 3 (10.0) | 2 (14.3) | 2 (15.4) |
| Massive | 7 (24.1) | 7 (23.3) | 3 (21.4) | 3 (23.1) |
| Missing | 2 (6.9) | 2 (6.7) | 1 (7.1) | |
Appendix 2 Health economics complete case analysis
| Outcome | Stratum A | Stratum B | Stratum C | |||
|---|---|---|---|---|---|---|
| Arthroscopic (n = 136), mean (SE) | Open (n = 137), mean (SE) | Arthroscopic vs. open mean difference (95% CI; p-value) (no covariate adjustment) | Arthroscopic vs. open mean difference (95% CI; p-value) (adjusting for age, size of tear, centre) | Arthroscopic (n = 91), mean (SE) | Open (n = 82), mean (SE) | |
| Theatre time (minutes) | (n = 109), 67.2 (5.6) | (n = 119), 70.7 (4.0) | (n = 228) –3.5 (–16.8 to 9.9; 0.608) | (n = 163) 12.1 (3.3 to 20.9; 0.007) | (n = 63), 65.1 (5.8) | (n = 61), 69.0 (6.9) |
| Anchor quantity | (n = 109), 1.3 (0.1) | (n = 110), 1.4 (0.1) | (n = 219) –0.1 (–0.5 to 0.2; 0.553) | (n = 156) 0.1 (–0.3 to 0.4; 0.647) | (n = 70), 1.4 (0.1) | (n = 58), 1.6 (0.2) |
| Nights in hospital | (n = 119), 0.5 (0.1) | (n = 129), 0.7 (0.1) | (n = 248) –0.2 (–0.4 to 0.1; 0.281) | (n = 180) –0.1 (–0.5 to 0.3; 0.589) | (n = 73), 0.3 (0.1) | (n = 72), 1.0 (0.1) |
| Outcome | Stratum A (£) | Stratum B (£) | Stratum C (£) | |||
|---|---|---|---|---|---|---|
| Arthroscopic (n = 136), mean (SE) | Open (n = 137), mean (SE) | Arthroscopic vs. open mean difference (95% CI; p-value) (no covariate adjustment) | Arthroscopic vs. open mean difference (95% CI; p-value) (adjusting for age, size of tear, centre) | Arthroscopic (n = 91), mean (SE) | Open (n = 82), mean (SE) | |
| Theatre time | (n = 109), 1104 (92) | (n = 119), 1161 (65) | (n = 228) –57 (–277 to 162; 0.608) | (n = 228) 113 (–19 to 245; 0.093) | (n = 63), 1070 (96) | (n = 61), 1133 (114) |
| Anchor costs | (n = 109), 134 (13) | (n = 110), 147 (13) | (n = 219) –13 (–50 to 24; 0.493) | (n = 219) 1 (–25 to 27; 0.939) | (n = 70), 148 (16) | (n = 58), 170 (21) |
| Equipment costs | (n = 136), 202 (12) | (n = 137), 145 (7) | (n = 273) 58 (31 to 84; 0.000) | (n = 273) 77 (56 to 98; 0.000) | (n = 91), 237 (13) | (n = 82), 164 (9) |
| Total cost of surgery | (n = 91), 1395 (134) | (n = 100), 1381 (90) | (n = 191) 14 (–299 to 327; 0.930) | (n = 191) 250 (112 to 387; 0.000) | (n = 52), 1422 (143) | (n = 47), 1445 (167) |
| Nights in hospital | (n = 119), 191 (40) | (n = 129), 250 (37) | (n = 248) –59 (–166 to 48; 0.281) | (n = 248) –37 (–142 to 68; 0.485) | (n = 73), 109 (22) | (n = 72), 368 (51) |
| Total procedure-related costs | (n = 85), 1522 (160) | (n = 94), 1606 (114) | (n = 179) –83 (–465 to 298; 0.666) | (n = 179) 225 (56 to 395; 0.010) | (n = 46), 1487 (168) | (n = 43), 1674 (208) |
| Cost after surgery to 12-month follow-up | (n = 72), 771 (75) | (n = 95), 971 (107) | (n = 167) –200 (–46 to 75; 0.153) | (n = 167) –155 (–431 to 122; 0.271) | (n = 46), 494 (70) | (n = 45), 764 (118) |
| Total costs up to 12 months | (n = 45), 2852 (249) | (n = 64), 2915 (193) | (n = 109) –63 (–680 to 554; 0.840) | (n = 109) 231 (–216 to 679; 0.307) | (n = 24), 2182 (293) | (n = 23), 2526 (410) |
| Total cost from 12 to 24 months | (n = 115), 175 (66) | (n = 117), 116 (34) | (n = 232) 59 (–87 to 205; 0.429) | (n = 232) 61 (–87 to 209; 0.418) | (n = 76), 119 (33) | (n = 70), 95 (28) |
| Total cost over 24 months | (n = 40), 2975 (264) | (n = 61), 3080 (209) | (n = 101) –105 (–770 to 561; 0.756) | (n = 101) 10 (–502 to 523; 0.968) | (n = 22), 2368 (298) | (n = 21), 2714 (462) |
| Total cost over 24 months (discounted) | (n = 40), 2974 (264) | (n = 61), 3076 (208) | (n = 101) –102 (–766 to 562; 0.760) | (n = 101) 13 (–498 to 524; 0.959) | (n = 22), 2362 (297) | (n = 21), 2710 (461) |
| Outcome | Stratum A | Stratum B | Stratum C | ||||
|---|---|---|---|---|---|---|---|
| Arthroscopic (n = 136), mean (SD) | Open (n = 137), mean (SD) | Arthroscopic vs. open mean difference (95% CI; p-value) (no covariate adjustment) | Arthroscopic vs. open mean difference (95% CI; p-value) (adjusting for baseline EQ-5D, index) | Arthroscopic vs. open mean difference (95% CI; p-value) (adjusting for baseline EQ-5D, index, age, tear size, centre) | Arthroscopic (n = 91), mean (SD) | Open (n = 82), mean (SD) | |
| QALYs from baseline to 8 months | (n = 120), 0.41 (0.02) | (n = 123), 0.40 (0.01) | (n = 243) 0.00 (–0.04 to 0.04; 0.884) | (n = 243) –0.01 (–0.03 to 0.01; 0.211) | (n = 243) –0.01 (–0.04 to 0.01; 0.188) | (n = 79), 0.41 (0.02) | (n = 74), 0.41 (0.02) |
| QALYs from 8 months to 12 months | (n = 112), 0.23 (0.01) | (n = 113), 0.24 (0.01) | (n = 225) –0.01 (–0.03 to 0.02; 0.671) | (n = 224) –0.01 (–0.03 to 0.01; 0.328) | (n = 224) –0.01 (–0.03 to 0.01; 0.444) | (n = 70), 0.24 (0.01) | (n = 68), 0.24 (0.01) |
| QALYs from 12 months to 24 months | (n = 111), 0.74 (0.02) | (n = 111), 0.74 (0.02) | (n = 222) 0.00 (–0.06 to 0.07, 0.948) | (n = 221) –0.01 (–0.07 to 0.05; 0.754) | (n = 221) –0.01 (–0.07 to 0.06; 0.864) | (n = 74), 0.73 (0.03) | (n = 69), 0.75 (0.03) |
| Total QALYs over 24 months | (n = 106), 1.41 (0.04) | (n = 106), 1.40 (0.04) | (n = 212) 0.01 (–0.11 to 0.13; 0.867) | (n = 212) –0.02 (–0.12 to 0.07; 0.631) | (n = 212) –0.01 (–0.11 to 0.10; 0.896) | (n = 66), 1.43 (0.05) | (n = 64), 0.42 (0.05) |
| Total QALYs over 24 months (time discounted) | (n = 106), 1.38 (0.04) | (n = 106), 1.37 (0.04) | (n = 212) 0.01 (–0.11 to 0.13; 0.865) | (n = 212) –0.02 (–0.12 to 0.07; 0.630) | (n = 212) –0.01 (–0.11 to 0.09; 0.894) | (n = 66), 1.40 (0.05) | (n = 64), 1.39 (0.04) |
Appendix 3 Trial protocol
Appendix 4 Search terms used in the literature review
MEDLINE (OVID platform): 1946 to March Week 4 2014
Using the Cochrane sensitivity- and precision-maximising version RCT filter (2008 version).
-
exp Shoulder/
-
shoulder$.tw.
-
exp Shoulder Joint/
-
exp Shoulder Pain/
-
exp Rotator Cuff/
-
rotator cuff$.tw.
-
exp Acromion/
-
acromion$.tw.
-
exp Scapula/
-
musculotendinous cuff$.tw.
-
(degenerative adj tear$).ti,ab.
-
or/1-11
-
exp Joints/
-
exp Tendons/
-
exp Tendinopathy/
-
exp Bursitis/
-
exp Calcinosis/
-
exp Calcium/
-
exp Joint Diseases/
-
or/13-19
-
12 and 20
-
exp Shoulder Impingement Syndrome/
-
subacromial impingement.tw.
-
((shoulder$ or rotator cuff or scapula or subacromial or acromion) adj5 (joint$ or tendon$ or bursitis or calcinosis or calcium or impinge$)).tw.
-
or/21-24
-
exp General Surgery/
-
surg$.tw.
-
su.fs.
-
exp Decompression, Surgical/
-
decompress$.tw.
-
bursectom$.tw.
-
acromioplast$.tw.
-
(calcium adj remov$).tw.
-
exp Debridement/
-
debrid$.tw.
-
exp Arthroscopy/
-
arthroscop$.tw.
-
Orthopedics/
-
(open adj procedure$).ti,ab.
-
(open adj technique$).ti,ab.
-
mini-open.ti,ab.
-
or/26-41
-
25 and 42
-
Randomised controlled trial.pt.
-
controlled clinical trial.pt.
-
Randomised.ab.
-
placebo.ab.
-
clinical trials as topic.sh.
-
randomly.ab.
-
trial.ti.
-
or/44-50
-
exp animals/ not humans.sh.
-
51 not 52
-
43 and 53
-
Limit 54 to yr=”2006-2014”
Appendix 5 Operation record
Appendix 6 Patient information sheet
Appendix 7 Baseline questionnaire
Appendix 8 Two- and 8-week telephone assessments
Appendix 9 Eight-, 12- and 24-month questionnaires
Appendix 10 Rest-then-exercise programme
Appendix 11 Original trial protocol
List of abbreviations
- ASES
- American Shoulder and Elbow Surgeons
- BESS
- British Elbow & Shoulder Society
- CD
- compact disc
- CI
- confidence interval
- CSAW
- Can Shoulder Arthroscopy Work
- DASH
- Disabilities of the Arm, Shoulder and Hand
- DMC
- Data Monitoring Committee
- EQ-5D
- European Quality of Life-5 Dimensions
- EQ-5D-3L
- European Quality of Life-5 Dimensions three levels
- GP
- general practitioner
- HTA
- Health Technology Assessment
- ICC
- intracluster correlation
- ICER
- incremental cost-effectiveness ratio
- IQR
- interquartile range
- ITT
- intention to treat
- MHI-5
- Mental Health Inventory 5
- MRI
- magnetic resonance imaging
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NSAID
- non-steroidal anti-inflammatory drug
- OSS
- Oxford Shoulder Score
- PROM
- patient-reported outcome measure
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- SAD
- subacromial decompression
- SD
- standard deviation
- SPADI
- Shoulder Pain and Disability Index
- TSC
- Trial Steering Committee
- UKUFF
- UK Rotator Cuff Surgery
- VAS
- visual analogue scale