Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 09/161/01. The contractual start date was in October 2010. The draft report began editorial review in November 2014 and was accepted for publication in May 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Dr Shahab has received grants and honoraria from Pfizer, a manufacturer of smoking cessation products. In the last 3 years, Professor Aveyard has received a consultancy fee for 1 day of consultancy with Pfizer, a manufacturer of smoking cessation products. Professor Coleman was paid an honorarium and travel expenses for speaking at Paris Smoking Cessation Practitioners’ Conference in January 2014. He was also reimbursed for attending two expert meetings hosted by Pierre Fabre Laboratories (PFL, France), a company that manufactures nicotine replacement therapy (2008 and 2012). Dr McRobbie has received research grants, honoraria and travel expenses from Pfizer and Johnson & Johnson, manufacturers of smoking cessation products. Dr McEwen is a trustee and board member for Action on Smoking and Health (ASH), but received no financial reimbursement for this. He has received travel funding, honorariums and consultancy payments from manufacturers of smoking cessation products (Pfizer Ltd, Novartis UK and GlaxoSmithKline Consumer Healthcare Ltd) and hospitality from North 51 that provide online and database services. He also has a shared patent on a novel nicotine device but has received no payment for, or relating to, this patent.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Dobbie et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Tobacco use is one of the leading causes of preventable death in the world. Each year an estimated 5.1 million people die from smoking and another 600,000 die from second-hand smoke exposure. 1,2 As nearly 80% of these deaths occur in low- and middle-income countries,3 tobacco causes over 90,000 deaths in the UK each year, reflecting decades of high smoking prevalence. Although smoking rates have reduced from 51% of men and 41% women in 1974 to 19% today (21.1% of men and 16.5% of women)4 they still remain high in the UK compared with countries such as Australia, Canada and Sweden. In addition, smoking rates in Britain are strongly socially patterned, with 29% of adults in routine and manual occupations smoking compared with 13% in managerial and professional groups. 4
Countries such as the UK have made concerted efforts to reduce smoking rates over several decades. Many of the policies and interventions that have been put in place form part of the Framework Convention on Tobacco Control (FCTC), the world’s first global public health treaty that was adopted by the World Health Assembly under the auspices of the World Health Organization (WHO). There are now 178 countries parties to the convention, including the UK. 5 The treaty seeks to reduce the burden of tobacco use through key supply and demand measures, which are laid out in its articles. Demand measures are highlighted in WHO’s ‘MPOWER’ report including ‘Monitoring tobacco use and prevention policies’, ‘Protecting people from tobacco smoke’, ‘Offering help to quit tobacco use’, ‘Warning about the dangers of tobacco’, ‘Enforcing bans on tobacco advertising, promotion, and sponsorship’, and ‘Raising taxes on tobacco’. 6 Guidance on ‘offering help to quit’, including the provision of services to support smokers to stop, offering counselling and effective smoking cessation medications, is contained in article 14 of the FCTC. 5 This is an important element of efforts to reduce smoking rates, as the success of unaided quit attempts is generally extremely low (around 5%). The chances of successfully stopping can be significantly raised if effective aids to quitting are made available. 7
The UK has played a significant role in developing the evidence to underpin effective interventions for smoking cessation as set out in article 14 of the FCTC. 5 This has its origins in early studies on smoking and health, to research on nicotine replacement therapy (NRT) and behavioural support, through to real-world evidence on how a national treatment service for smoking can be developed and established. To introduce this study, we set out some of this historical background here, before outlining how the current study helps to bring this evidence base up to date and should inform the design of future services.
Early research on smoking cessation in the UK
The first evidence of clear links between tobacco smoking and ill-health emerged in the 1950s when Doll and Hill published the first paper showing that smoking caused lung cancer. 8 This, and other evidence, led to the production of two important reports – one in the UK and one in the USA – on smoking and health. In the UK the Royal College of Physicians report of 1962 outlined the need for a comprehensive approach to reduce smoking rates. 9 This described a series of needed policy measures including tobacco taxes, restricting advertising and availability, education on the risks of smoking and, importantly, support for smokers wanting to quit. In the end, it would take almost 50 years for all the recommendations in Smoking and Health to be implemented, but in the meantime a range of important studies were conducted that provided better evidence on smoking as an addiction, rather than a ‘habit’, and consequently how it should be treated. 10 A number of early studies on nicotine and NRT were conducted by Professor Michael Russell and colleagues at the Addiction Research Unit at the University of London. These contributed to the licensing of the first pharmacological treatment for smoking cessation in 1981 – nicotine gum. From that period onwards a number of important research and policy developments on smoking cessation took place in the UK. Members of our team summarised these in an earlier study and we reproduce these here, outlined in Table 1. 10
| Year | Event |
|---|---|
| The 1950s | |
| 1950 | Doll and Hill paper published in the BMJ8 |
| 1951 | British doctors’ study commences |
| 1959 | First smoking dependence treatment clinic opens in Salford, Greater Manchester, UK |
| The 1960s | |
| 1962 | First RCP report, Smoking and Health9 |
| 1962 | Tobacco Practitioners Council (representing the tobacco industry) agreed to implement a code of advertising practice for cigarettes |
| 1965 | Television cigarette advertising ban |
| 1967 | Creation of Health Education Council |
| The 1970s | |
| 1970 | Mike Russell starts building a smoking research team at the Addiction Research Unit |
| 1971 | Second RCP report, Smoking and Health Now11 |
| 1971 | Voluntary agreements on advertising began |
| 1971 | Creation of ASH |
| Voluntary agreements on health warnings | |
| 1977 | Third RCP report, Smoking or Health12 |
| 1977 | Government health circular expressed need for smoking policies on all health premises |
| The 1980s | |
| 1981 | NRTs ‘blacklisted’ |
| 1983 | Fourth RCP report, Health or Smoking?13 |
| Voluntary agreements on product modification | |
| Excise duties on tobacco begin to rise significantly | |
| 1986 | British Medical Association join campaign against tobacco industry |
| The 1990s and 2000s | |
| 1991 | Illegal sales law strengthened |
| 1992 | Fifth RCP report, A Review of Your People Smoking in England14 |
| 1993 | Government commits to 3% above inflation tax increase on cigarettes |
| 1993 | Ban on oral snuff throughout European Union |
| 1997 | Government commits to 5% above inflation tax increase on cigarettes |
| 1998 | White Paper, Smoking Kills15 |
| 1998 | First English evidence-based guidelines on smoking cessation16 |
| 1999 | First smoking cessation treatment services established in the English NHS |
| 2000 | NHS smoking cessation treatment services established nationally |
| 2013 | SSSs transferred from NHS to local authorities |
NHS Stop Smoking Services
The NHS Stop Smoking Services (SSSs) were established following the publication of the 1998 White Paper, Smoking Kills. 15 Initially piloted in deprived areas of England in 1999, they were rolled-out across the UK from 2000. The services were developed on the basis of national guidance issued by the Department of Health (DH) that built on a review of the evidence of the effectiveness of smoking cessation interventions published in the journal Thorax. 16 This evidence emphasised the efficacy of intensive behavioural support (in groups or one to one) plus pharmacotherapy for smoking cessation. Services were established by primary care trusts (PCTs) and operated primarily in primary care settings delivering behavioural support and providing access to NRT and bupropion (Zyban®, GlaxoSmithKline). From 2000–4, a national evaluation of the services in England was conducted by members of our team. The evaluation found that the services were effective in supporting smokers to quit in the short term (at 4 weeks)17 and the longer term (at 1 year),18 and were reaching smokers from more deprived groups. 19 A subsequent analysis by our team also found that they were making a contribution to reducing inequalities in health caused by smoking. 20 However, since these studies were conducted, NHS SSSs have continued to evolve, attempted to adapt to meet local needs and encountered various financial and structural challenges. National developments, including the National Institute for Health and Care Excellence (NICE)’s guidance on services (published in 2008),21 have influenced what is available and smoking cessation medications have also diversified, with new NRT products and the medication varenicline (Champix®, Pfizer) providing additional options for smokers trying to stop.
One element that has changed in the past decade is the type and variety of behavioural support options available to smokers using the services. In particular, a heavier reliance on one-to-one support options in a far wider range of settings. The existing evidence base from systematic reviews of trials would suggest that there is no significant difference in outcomes for smokers receiving group or one-to-one behavioural support. In a review of 50 randomised controlled trials22 and another review of 23 studies since January 2000,23 a group format for a behavioural intervention was not found to be significantly different from an individual format; yet real-world evidence may be different from trials in this respect. Findings from our earlier studies with NHS SSSs suggest that group interventions may be more effective in practice24 but that smokers, given a choice, will choose one-to-one support. Issues of perceived preference may have led to the dominance of one-to-one support in today’s services although new forms of group counselling (such as ‘rolling groups’ where clients can join without having to wait for a new group to start) have emerged.
Another element that has evolved is who provides support to stop smoking. Before the services existed, this was primarily doctors and nurses in primary care or hospitals with a few examples of specialist clinics. Today, a wider variety of professionals are involved in delivering support. In some cases this is described as different ‘levels’ of support. We describe these levels here.
-
Level 1 practitioners are typically primary care professionals who deliver ‘brief interventions’, which usually involves opportunistic advice, discussion, awareness raising and/or referral to SSSs.
-
Level 2 practitioners (known elsewhere as community practitioners) do not work exclusively as stop smoking specialists but instead work in other health and social care roles and deliver stop smoking support as one of a number of job tasks. The majority of level 2 service provision takes place in general practitioner (GP) practices (usually delivered by nurses and health-care assistants) and pharmacies (delivered by practitioners with a variety of posts from pharmacists to pharmacy assistants). Generally one-to-one support is offered.
-
Level 3 practitioners’ sole remit is to deliver smoking cessation working as smoking cessation ‘specialists’. They offer a wider variety of behavioural support which can include: open and closed groups, one to ones, drop-in services, text and telephone support,25 and work in various locations such as community centres, GP practices and workplaces.
For clarity, throughout this report we will differentiate between level 2 and level 3 service providers by using the terms ‘level 2′ and ‘specialist’ practitioners. Data on level 1 support are not collected by the SSS and is not part of the study.
A growing proportion of clients now receive support from level 2 practitioners. Large differences have now been identified between the quit rates achieved by services in different locations, which may be partly because of the quality of behavioural support delivered by the practitioner who offers it. 26–28
The organisational context within which SSSs operate has also changed since our earlier studies. Some of these changes preceded the Evaluating Long-term Outcomes of NHS Stop Smoking Services (ELONS) study (e.g. reorganisation of PCTs in England) but possibly the most significant change occurred in April 2013, just after the fieldwork was completed, when commissioning of local SSSs moved from NHS to local authority control. This resulted in change to the funding and delivery structure of local SSSs, with some areas either reducing funding for the specialist service in favour of a greater reliance on level 2 providers or tendering out previously in-house services which has sometimes led to SSSs being run by private and voluntary sector companies. This structural change poses challenges for the services and preparation for the move also, to some extent, affected study recruitment, which is discussed further in Chapter 4.
As a result of all these changes, current research is needed to examine the longer-term efficacy of the different methods employed by NHS SSSs to deliver support to smokers trying to stop. Current evidence is also required to explore the effectiveness of services with different groups of smokers, particularly those from more disadvantaged groups. This report sets out findings from a study designed to examine these issues.
Structure of this report
This is a detailed report of a complex study with a number of different elements. Chapter 2 presents an overview of the research including aims and objectives, study design and settings. It was also describes the ethical approval and local research permissions process.
Chapters 3 and 4 present the methods and main findings of the secondary analysis element of the ELONS study respectively. Chapters 5 and 6 describe the methods and analysis (see Chapter 5) and the results and key findings (see Chapter 6) for the second (and main) part of our study. This was a prospective cohort study of smokers using the services who were followed up in the short (4 weeks post quit date) and longer term (at 1 year).
The subsequent three chapters present findings from elements that were added to the ELONS prospective study. For ease and clarity, they are presented as standalone chapters including the methods and results for each. The focus of Chapter 7 is an exploration of client satisfaction with the support received from their local SSS. Chapter 8 examines the relationship between well-being and smoking status of ELONS study participants. Chapter 9 outlines findings from a study of longer-term NRT use that was made possible by additional funding from the UK Centre for Tobacco Control Studies [now the UK Centre for Tobacco and Alcohol Studies (UKCTAS) – www.ukctas.ac.uk]. The remaining two chapters include the discussion (see Chapter 10) with conclusions presented in Chapter 11.
Chapter 2 Evaluating Long-term Outcomes of NHS Stop Smoking Services overview
This purpose of this chapter is to present an overview of the ELONS study including aims and objectives, study design, setting and the rationale for the methods used. It also describes the ethical approval and the local research permissions process.
Aim and objectives
The principal aim of the study was to explore the factors that determine longer-term abstinence from smoking following intervention by SSSs in England.
The study objectives were to:
-
examine the effectiveness of SSSs by PCT and intervention type using routine data
-
explore the reach of services by identifying what proportion of the local population set a quit date with services using routine data
-
describe the factors that determine longer-term abstinence from smoking or relapse to smoking among clients who set a quit date with services in a sample of PCTs in England
-
examine the relationship between client characteristics [in particular socioeconomic status (SES), age, gender, disability and ethnicity], adherence to treatment, intervention type received and longer-term abstinence
-
create an evidence base to guide delivery of interventions by SSSs so that these interventions will have maximal effect on smoking cessation and population health.
Overview of study design
The ELONS study was an observational study with two main stages:
-
secondary analysis of routine data collected by SSSs
-
a prospective cohort study of SSS clients with three additional elements (which are presented as standalone chapters on the report):
-
a client satisfaction survey (CSS)
-
a well-being survey
-
a study of longer-term NRT use.
-
The overall aim of the prospective element of the ELONS study was to collect long-term follow-up data at 52 weeks. A subsidiary aim was to collect detailed information about clients and the treatment they received in a consistent manner. Data were collected at three key stages: baseline (i.e. when a client registered with the SSS), 4-week follow-up and 52 weeks post quit date. The 52-week follow-up data were collected by a research company, TNS BMRB (Taylor Nelson Sofres, British Market Research Bureau), that had worked with the academic team on a previous study. 29 Table 2 describes the data collected at each time point and also summarises the data collected for the three additional elements (client satisfaction, well-being and long-term NRT). Further detail of the data collected at each stage and data collection tools can be found in Appendix 1. A flow chart depicting sample sizes and sampling frames is also available (Figure 1).
| Collection time point | Normal SSS practice | Prospective study | Client satisfaction | Well-being evaluation | Long-term NRT evaluation |
|---|---|---|---|---|---|
| Baseline (client registers with service) |
|
|
WHO-5 Well-being Index scale added to enhanced monitoring data | Clients asked by practitioner to provide two saliva samples | |
| 4 weeks post quit date |
|
Client satisfaction and well-being postal survey to all clients administered by research team | |||
| Period that client is in contact with the services |
|
|
|||
| When client leaves |
|
||||
| 12 months post quit date | TNS BMRB collect:
|
Well-being postal survey to all clients administered by research team |
|
||
FIGURE 1.
Flow diagram for the ELONS prospective study. a, n refers to quit attempts at the SSS from March/April 2012 to March 2013; b, more detail is available in Chapters 5 and 6; c, providers’ employees provide smoking cessation support rather than specialists employed directly by SSSs; d, this is an overestimate because level 2 providers who did recruit did not usually recruit for the level 2 recruitment period at each site; and e, CSS.

Definitions of smoking cessation
Smoking cessation, or ‘quitting’, was defined in the following ways for this study.
Short-term (4 weeks after quit date) self-reported quitting
In normal SSS treatment, 4 weeks after their quit date, advisors ask their clients (either in person at a session or, if they have stopped attending treatment, by telephone) whether or not they have smoked a cigarette in the last 2 weeks. Clients who indicate that they have not smoked in this period are classified as a ‘self-report’ quitter at 4 weeks.
Short-term (4 weeks after quit date) carbon monoxide-validated quitting
During treatment sessions clients are asked to breathe into a carbon monoxide (CO) monitor, which records the CO parts per million (p.p.m.). If clients reduce the number of cigarettes smoked their CO level falls. This can be motivating as it provides a visual representation of how stopping smoking reduces exposure to CO, which is a harmful chemical. If a client has not been smoking for the past 24 hours then the level usually falls below 10 p.p.m. 30 Thus, at 4 weeks if a client has self-reported that they have stopped smoking and their CO level is < 10 p.p.m. then they are said to be a CO-validated quitter at 4 weeks. In this report, we refer to CO-validated quitting and in places also as ‘biochemically validated’ quitting or abstinence. Where we state biochemical validation, we mean CO validation.
If the client refuses to take a CO test then they are classified as a self-report quitter only. In a minority of cases, clients may self-report that they have stopped smoking but their CO level will be ≥ 10 p.p.m. In this case they are said to be a ‘self-reported quitter who has been refuted by CO validation’. For this study, this small minority were classified as non-quitters in quit rate and regression analysis.
Longer-term (52 weeks after quit date) self-reported quitting
The research team (in this case TNS BMRB) contacted clients who self-reported quitting at 4 weeks by telephone 12 months after their quit date and asked if they had smoked within the last 7 days. Those that had not smoked in this period were then asked if they had smoked since their quit date. If they had smoked up to but not more than five cigarettes they were classified as achieving ‘self-reported continuous abstinence’, as consistent with the Russell standard30 (the recognised standard for smoking cessation studies and also validating cessation in clinical practice). If they had smoked more cigarettes they were classified as achieving ‘self-reported point prevalence abstinence’. For the analysis outlined here, only those achieving continuous abstinence and whose self-report was not refuted by the CO breath test were classified as 52-weeks self-report quitters.
Longer-term (52 weeks after quit date) carbon monoxide-validated quitting
All clients who had achieved point prevalence self-report abstinence were asked if a researcher could make a home visit and carry out a CO breath test. For the analysis reported here clients with a CO level of < 10 p.p.m. and who had also self-reported that they were continuously abstinent since their quit date were classified as 52 week CO-validated quitters. Biochemically (CO-validated) abstinence from smoking at 52 weeks was the primary outcome for this study.
Setting
The setting for the study was SSSs in England. For the secondary analysis, routine data from 49 services were obtained. For the prospective study, nine services were involved. These were Bristol, County Durham and Darlington, Hull and East Riding, Leicestershire County and Rutland, North and North East Lincolnshire, Northamptonshire, Oldham, Rotherham, and South East Essex. The target population was clients of these services. The health technologies that the ELONS study assessed were the treatment provided by SSSs – a combination of behavioural support and medication intended to increase the chance of a successful quit attempt. A key focus was to evaluate outcomes for smokers who received one of the five main forms of behavioural support (also called intervention types) provided by the services:
-
closed groups (scheduled group sessions of around 1–2 hours dependent on the number of clients, normally delivered once per week and facilitated by a specialist practitioner
-
open/rolling groups (drop-in groups run at a variety of times of day and in a variety of locations where clients can attend without an appointment and for as many weeks as they wish)
-
one-to-one drop-in (a clinic hosted at a regular time where clients can attend without an appointment for one-to-one support)
-
one-to-one sessions with a specialist practitioner (scheduled one-to-one sessions with a practitioner whose main role it is to help people stop smoking)
-
one-to-one sessions with a level 2 practitioner.
Ethics and local permissions
Ethical approval for the ELONS study was obtained from NHS Lothian (South East Scotland Research Ethics Committee) in June 2011. During the recruitment phase of the prospective study a total of four substantial amendments were made for alternations to the study protocol and consent process. In addition to ethical approval, we also obtained local research and development (R&D) approval for each SSS. For three SSSs, single R&D office approvals were required but for the remainder two sets of approvals were required owing to the location of the SSSs and the NHS trusts involved. All the necessary local approvals were obtained before data collection began. It was also a requirement that the research team obtain NHS research passports and, for one site, it was necessary to obtain Caldicott Guardian approval.
Public involvement
Members of the public were involved in the ELONS study in a number of ways. Within the prospective study, the public were research participants and the study was designed to provide feedback on an important public service for the benefit of future users. However, more direct forms of involvement were also included in the research.
First, the study principal investigator, Professor Bauld, serves as the public engagement lead for UKCTAS, a UK Clinical Research Collaboration Centre for Public Health Excellence that covers 13 universities (the co-investigators for the study are also UKCTAS members). In this role she convenes a panel of continuing smokers and recent quitters who meet in Bath. The original design for the ELONS study was discussed with the panel at meetings in 2010 and again in 2011, and feedback sought. Initial results were also circulated to panel members at a meeting in 2013. One of the panel members, Robert Graham, was asked to join the study steering group as a lay adviser and did so. Although he was not able to attend all steering group meetings, he maintained contact with Professor Bauld and, having used NHS SSSs himself in the past, provided very useful input.
In addition to panel contributions and Mr Graham’s involvement, we had the participant information leaflets and consent forms for the study reviewed by a patient representative. This was organised through the Primary Care Research Network (PCRN) Patient and Public Involvement Manager, and we are grateful to them for facilitating this process.
We also prepared the ELONS study newsletters for all the participating services in the prospective study. There were three of these during the study. These were intended to be available to service clients as well as staff and we sent these to each site for distribution.
Finally, tailored feedback from the study was prepared for each study site and for one site an event was held that involved a varied audience and presentations on study findings. Dissemination at a number of academic and practitioner conferences is currently under way.
Chapter 3 Secondary analysis of routine data: methods and analysis
This chapter outlines the rational, sample and analytical approach for the secondary analysis element of the ELONS study, with results presented in Chapter 4.
Rationale for secondary analysis
All SSSs in England are required to submit routine monitoring data to the Health and Social Care Information Centre. 31 These data include basic information on client characteristics and the types of treatment received. They also include self-reported smoking status at 4 weeks post quit date. These monitoring data are supplied as aggregated summary returns and so cannot be used to analyse which factors are associated with individual-level smoking cessation outcomes.
Increasingly, however, SSS outsource management of these data to private companies. The most commonly used is QuitManager (North 51, Nottingham, UK). 7,27 QuitManager provides a framework for SSSs to collect the minimum data set required by the DH, plus any additional client and service information thought to be useful locally. The research team includes the Director of the National Centre for Smoking Cessation and Training (NCSCT), who has good links with North 51 and has been able to access their data for previous research and training activities. We were therefore able to obtain QuitManager data for the ELONS study in an anonymised form. This was important as by having access to these data made it possible to examine individual-level information not available from the Health and Social Care Information Centre returns. Data were available from 49 services in England. These data were analysed to fulfil objectives 1 and 2, to examine the effectiveness and reach of services. Results from this first stage also informed the selection of SSSs for the prospective cohort study.
The secondary analysis had two aims:
-
to explore the reach of services by identifying the proportion of the local population who set a quit date with services using routine data
-
to examine the effectiveness of NHS SSSs by PCT and intervention type using routine data.
Sample
QuitManager32 is an online database for recording information on NHS SSS clients, including sociodemographic and treatment characteristics, in accordance with the DH’s standard SSS monitoring requirements. Collection of data starts at baseline (first contact with the SSS) and should be updated at each contact point. The data are collected by the stop smoking practitioner and entered onto QuitManager in ‘real time’ (via the computer software) or recorded on a paper form and entered at a later date. PCTs may elect not to ask clients questions, and clients themselves may not answer every question, leading to missing data. Within PCTs clients whose data are collected on paper forms may answer a slightly different set of questions to those whose data are entered electronically.
At 4 weeks post quit date clients are asked whether or not they have quit smoking for the past 14 days (self-report quit) and clients may also perform a CO breath test. Clients who have self-reported as quit and have CO readings of < 10 p.p.m. are said to be CO validated as quit. The DH guidelines suggest 85% of clients should be CO validated. 33
More than 60 out of the ≈ 150 English PCTs use QuitManager and 49 of these gave permission to the NCSCT for their data to be used for research purposes. Thus, data from these 49 PCTs were included in the analysis.
Data on clients who set quit dates from July to December 2010 were downloaded from QuitManager in January 2012 and data on clients with quit dates between January and June 2011 were downloaded in July 2011. In total there were 202,804 client records included in the database. Each record is a ‘treatment episode’ where the client sets a quit data and receives treatment. It is possible for clients who relapse to have more than one treatment episode in a year. 33
Measures
Outcomes
Efficacy of services: quit rates and carbon monoxide-validation rate
There were three dependent variables explored: self-report quit, CO-validated quit and CO validation. CO validation is the proportion of self-report quit who were also CO validated. We included CO-validated quit because some clients may state they have quit when they have not quit. We included self-report quit because some CO-validation rates vary so by using both of these outcomes, the results are rendered more robust.
The DH considers clients to be quitters only if self-report data are collected between 25 and 42 days after the quit date. 33 Inspection of the QuitManager database suggested that this narrow range may be underestimating the number of quitters, so all clients who self-reported as quit were included in the analysis.
As outlined above, we adhered to the Russell Standard for smoking cessation analysis by taking an intention-to-treat approach where clients with missing quit data were categorised as not quit. 30 Clients setting quit dates in December 2010 and June 2011 were therefore excluded from the analysis as they would not have reached 4 weeks post quit date (when self-report quit and CO validation occurs) when the data were downloaded. Thus, the months included were July–November 2010 and January–May 2011 (n = 19,481). Cases were also excluded from the main analysis if they were missing age (n = 201) and gender (n = 43) because too few were missing to include as a separate category. Additionally, cases were excluded if the practitioner who provided behavioural support was missing (n = 5573) because of the multilevel structure of the data. Thus, the number of cases used in the bi-variable and multilevel multivariable analysis of the efficacy of the services was 177,291.
Uptake: distribution of client groups and reach of services
In order to assess uptake we looked first at whether or not clients from all sociodemographic groups were accessing the services and which service options clients were accessing.
To understand the reach of services it is necessary to know the target population: the number of smokers in the PCT. Smoking is not asked in the UK census thus estimates have to be made from smoking rates collected by government surveys and populations that have been updated from 2001 census data. The most recent estimation of adult (≥ 16 years) smoking rates for PCTs was for 2003–5. 34 These were based on the Health Survey for England. Between 2004 and 2009 the smoking rate for Great Britain fell from 25% to 21%, thus PCT smoking rate estimates were reduced by 4% to estimate more recent smoking rates. Mid-year adult (≥ 16 years) population estimates of PCTs were available for 2010. The population multiplied by the smoking rate gave an estimate of the number of smokers in the PCT. These numbers were compared with the number of QuitManager clients aged ≥ 16 years between July 2010 and June 2011.
There were some PCTs where this formula was not suitable. First, a few PCTs started using QuitManager or gave permission for their data to be used after July 2010 so these PCTs were included only in the second data download in July 2011. For these PCTs the number of clients was doubled to provide an estimate of the annual number of clients. Second, one PCT had to a large extent merged with another and a population estimate was available only for the overall area and a smoking rate estimate for the overall estimate was calculated by taking the average of the two constituent PCTs. Third, a PCT was known to include only clients who saw practitioners through the specialist service in QuitManager. Thus it was not possible to provide an estimate of reach for this PCT. It is possible that other PCTs may not include all their clients on QuitManager. So far, however, none of the other PCTs contacted regarding the prospective study have raised this as an issue.
Predictors
The data have a multilevel structure: clients received behavioural support interventions from practitioners and practitioners are employed through SSSs. Originally each PCT had its own SSS although now some PCTs have a joint SSS so a few practitioners worked for more than one PCT, usually where both PCTs had a joint SSS.
The independent variables used cover client characteristics: age (divided into quartiles); gender (not pregnant women, pregnant woman, men); ethnicity (white, black, Asian, mixed, other, unknown); SES (eligibility for free prescriptions exempt, pays, unknown); National Statistics Socio-Economic Classification (NSSEC)35 (routine and manual occupation, intermediate occupation, managerial or professional occupation, retired or caring for the home, sick or disabled and unable to work, never worked or long-term unemployed, in prison, other); Index of Multiple Deprivation (IMD)36 (at PCT level) divided into quintiles of all English PCTs and quit attempt related characteristics [month set quit date, treatment episode number (first, second, third, fourth or more)]; medication (NRT alone, combination NRT, buproprion, varenicline, mixed medications, and other or no medication); intervention type (one to one, drop-in, open/rolling group, closed group, other); and practitioner type (specialist SSS practitioner employed by SSSs, practitioner who does cessation advice work as part of their role divided into GP, nurse, health-care practitioner, pharmacy employee, and other and unknown).
Impact: throughput and quitters per 100,000 population
Colleagues from University College London and the UK NCSCT have developed the methodology for measuring impact. Impact is calculated as ‘throughput’ (number of treated smokers per 100,000 adult population) × [percentage successfully quit at 4 weeks – 25 (if CO-verified quit or – 35 if self-report quit)]/100. The number of quitters is expressed per 100,000 of the population, not per 100,000 of the smoking population. The reason for CO-verified quit minus 25 being used in the calculation is that 25% of smokers trying to quit are estimated to be CO-verified quit at 4 weeks unaided or by use of medication alone without behavioural support. For self-reported quits minus 35 is used because of average differences between SSS self-report and CO-validated quit rates.
Owing to first to marked differences between CO-validation rates of PCTs and second to different services having a negative impact depending on whether or not the CO-validated or the self-report quit rate was used in the calculation, for this report an overall impact score was calculated. The overall impact score was the average of the CO-validated impact score and the self-report impact score.
To estimate impact on the population, unique clients were used rather than client records. The client records were aggregated so that for clients who had more than one record their age and quit status at their most recent episode at the SSS was used.
It was not possible to calculate impact for some PCTs and for others there were caveats, generally this was where there were issues in calculating uptake. Additionally, the unique patient identifier was of poor quality for four PCTs. For a further three PCTs, clients were included only in the second data download so to estimate impact the number of client records was doubled. This may be an overestimate of client records and it would be expected that some clients from the first 6 months would have revisited the services in the second 6 months so it may also be an overestimate of unique clients. Thus, these three PCTs were excluded from statistical summaries of impact data although impact data was calculated for them.
Analytic approach
The analyses were carried out using SPSS [SPSS version 19.0 (SPSS Inc., Armonk, NY, USA) and PASW version 18.0.3 (SPSS Inc., Chicago, IL, USA)]; Microsoft Excel® 2010 (Microsoft Corporation, Redmond, WA, USA); Stata (StataCorp LP, College Station, TX, USA) and MlwiN version (MLwiN, Centre for Multilevel Modelling, Bristol, UK) as follows.
See Table 3 for overall quit rates and validation rates for all clients and then for clients where their age, gender and practitioner were identified. Uptake (distribution), quit rates and CO-validation rates for subgroups of these clients with various client and quit attempt-related characteristics are presented. Chi-squared was used to assess significance.
Second, a descriptive table (see Table 4) provides further information about the PCTs. Each row represents a different PCT. It includes the number of practitioners within each PCT, the number of clients per PCT (throughout the year) and the average number of clients per practitioner (clients/practitioner) in addition to estimates of the smoking rate, population, clients aged over 16 years and reach of services of each PCT.
The analysis included a large number of predictors and three measures of SES, so in order to assess potential multicollinearity in multivariable models, the variance inflation factor (vif) and corresponding tolerance were calculated from a logistic regression using interaction expansion (part of the Stata xi suite). In this xi suite analysis, PCT was entered as a cluster variable and practitioner was entered as an explanatory variable as only one cluster variable is allowed.
Multilevel modelling (see Tables 5 and 6) allows PCT and practitioner to be treated as separate levels in the analysis – otherwise known as random effects. Thus there were three levels in the models: client (level 1), practitioner (level 2) and PCT (level 3). Other independent variables were entered as fixed effects. Practitioner types were entered as a level 2 fixed effects, IMD quintiles of the PCT entered as level 3 fixed effects and all other fixed effects were at client level. MLwiN second order penalised quasi-likelihood iterative generalised least squares (IGLS) estimation was used for the analysis.
Odds ratios (ORs) are reported for self-report quit, CO-validated quit and CO validation. Some changes were made to the predictors for the multilevel analysis. So that practitioner should completely nest within a PCT, PCTs that shared practitioners were merged. There were 63 practitioners who worked in more than one PCT. The IMD score was then recoded for the new merged PCTs so that it was the average of both PCTs taking into account the number of clients contributed by each PCT.
In preliminary analysis (not shown) MLwiN IGLS multilevel models were compared with Stata Survey Suite models. Anomalous results were explored further using SPSS crosstabulations, Stata xt and MLwiN Markov chain Monte Carlo. Full models did not converge in either Stata xt or MLwiN Markov chain Monte Carlo. However, the results that were produced tended to support IGLS results; thus only MLwiN IGLS models are presented here.
Ideally we would look at how much variance of the higher levels was explained by the fixed variables; however, when a binary outcome is modelled and there is more than one higher level, it is not possible to calculate because the level 1 variance is always constrained to be 3.29. 37 Thus the impact observed on the higher-level variances from adding a fixed-effect variable to the model may be because of the overall variance changing to allow for the addition of the variable since the level 1 variance cannot change, rather than because the new variable in the model has explained the higher-level variance. 38,39 It is not currently possible to accurately estimate how much of the change is caused by real changes in variance and how much is caused by the constrained level 1 variance (Yang M, University of Nottingham, 2012, personal communication).
The higher-level variance is shown later in the report (see Table 7). The first and second columns show higher-level variance in the CO-validated modelling. The first column displays PCT-level variance and the second column displays practitioner-level variance. The next two columns show variance for the self-report modelling and the other columns show higher-level variance for the CO-validation modelling with or without exclusions of extreme PCTs (see Table 4). The first row displays variance in null models with no fixed effects entered. The subsequent rows display variance when fixed effects are entered one at a time so there is only one fixed effect in a model. The final row displays variance for the multivariable model when all fixed effects are entered. PCTs with significantly below and above average residuals were identified.
Residuals for the PCTs were calculated and graphed using caterpillar plots.
For measures of impact by PCT, see Table 8. Each row represents a different PCT. Throughput (numbers setting a quit date per 100,000 population), CO-validated and self-report quit rates for all unique clients age 16 years or over, impact (numbers of 4-week quitters per 100,000 population) calculated using CO-validated quits only, all self-report quits and overall (average of previous two impacts) are shown and the results are also presented in a graphical format. Summary measures of unique patients, quit rates, throughput and impact, and correlations between them are provided (see Table 9).
Chapter 4 Secondary analysis of routine data: findings
As described in Chapter 3, the first part of the ELONS study involved secondary analysis of data from clients who had used SSSs in 49 of 150 PCTs in England. These PCTs’ SSSs used the QuitManager database to record and report on their routine data.
The results are ordered by topic: uptake, quitting and CO validation. Under uptake we consider client distribution of client characteristics and estimates of the percentage of each PCT’s smoking population that were using the service. Under quitting we discuss self-report quit and CO-validated quit in bivariable and multivariable multilevel models, and finally we explore the proportion of self-reported quit who were CO validated (CO validation) in bivariable and multivariable multilevel models. Please note that in addition, we have already published a paper based on this work,26 which had a particular focus on the relationship between SES and the types of behavioural support offered by the services.
Uptake
Table 3 shows which groups of clients were more or less common among service users and the service options that they were more or less likely to use.
| Client characteristics | 4-week quit rates | CO-validation rate | ||||
|---|---|---|---|---|---|---|
| n | % | Self-report quit, % (p-value) | CO-validated quit, % (p-value) | Self-report quit, n | Self-reports CO-validated, % (p-value) | |
| Total: intention-to-treat quit available (December and June starts excluded) | 182,603 | 100.0 | 44.1 | 30.7 | 89,085 | 73.9 |
| Total: intention-to-treat quit and age, gender, practitioner identifieda | 177,291 | 100.0 | 48.8 | 34.1 | 86,512 | 74.3 |
| Age quartiles (years) | ||||||
| < 30 | 44,968 | 25.4 | 39.2 | 24.9 | 17,647 | 68.2 |
| 31–42 | 47,719 | 26.9 | 49.6 | 34.4 | 23,651 | 73.6 |
| 45–53 | 40,410 | 22.8 | 50.7 | 36.2 | 20,485 | 75.8 |
| ≥ 54 | 44,194 | 24.9 | 56.0 | 41.4 | 24,729 | 78.1 |
| p-value | – | – | < 0.001 | < 0.001 | – | < 0.001 |
| Gender | ||||||
| Female (not pregnant) | 88,246 | 49.8 | 48.1 | 33.9 | 42,451 | 74.9 |
| Female (pregnant) | 5650 | 3.2 | 45.8 | 26.5 | 2585 | 62.0 |
| Male | 83,395 | 47.0 | 49.7 | 34.9 | 41,476 | 74.5 |
| p-value | – | – | < 0.001 | < 0.001 | – | < 0.001 |
| Ethnic origin | ||||||
| White | 158,377 | 89.3 | 49.3 | 34.6 | 5237 | 74.0 |
| Black, Asian, mixed, other | 12,165 | 6.9 | 43.1 | 30.9 | 78,149 | 74.6 |
| Unknown | 6749 | 3.8 | 46.3 | 28.4 | 3126 | 67.1 |
| p-value | – | – | < 0.001 | < 0.001 | – | < 0.001 |
| Occupation | ||||||
| Routine and manual | 43,741 | 24.7 | 51.7 | 36.1 | 22,621 | 74.0 |
| Intermediate | 13,376 | 7.5 | 54.2 | 36.6 | 7251 | 70.7 |
| Managerial and professional | 23,661 | 13.4 | 56.6 | 39.6 | 13,400 | 75.0 |
| Retired or home care | 32,388 | 18.3 | 54.4 | 39.7 | 17,627 | 77.5 |
| Sick or disabled and unable to work | 11,852 | 6.7 | 41.7 | 28.5 | 4943 | 73.2 |
| Never worked or long-term unemployed | 24,512 | 13.8 | 38.8 | 27.0 | 9520 | 73.6 |
| In prison | 2223 | 1.3 | 48.0 | 42.4 | 1066 | 90.0 |
| Other | 25,538 | 14.4 | 39.5 | 26.0 | 10,084 | 70.6 |
| p-value | – | – | < 0.001 | < 0.001 | 86,512 | < 0.001 |
| Prescription charges | ||||||
| Exempt | 104,304 | 58.8 | 46.2 | 33.0 | 48,194 | 75.8 |
| Pays | 56,903 | 32.1 | 54.2 | 38.1 | 30,843 | 74.5 |
| Unknown | 16,084 | 9.1 | 46.5 | 27.2 | 7475 | 63.8 |
| p-value | – | – | < 0.001 | < 0.001 | – | < 0.001 |
| Average IMD 2010 score (PCT) | ||||||
| ≤ 30 | 49,101 | 27.7 | 44.3 | 30.1 | 21,757 | 72.7 |
| 31–60 | 25,695 | 14.5 | 48.5 | 37.0 | 12,457 | 80.7 |
| 61–90 | 22,123 | 12.5 | 49.9 | 35.8 | 11,031 | 72.8 |
| 91–120 | 40,793 | 23.0 | 50.4 | 36.9 | 20,539 | 76.8 |
| ≥ 121 | 39,579 | 22.3 | 52.4 | 33.5 | 20,728 | 70.5 |
| p-value | – | – | < 0.001 | < 0.001 | – | < 0.001 |
| Month set quit date | ||||||
| July 2010 | 15,244 | 8.6 | 46.4 | 31.4 | 7066 | 72.9 |
| August 2010 | 13,892 | 7.8 | 48.0 | 32.8 | 6670 | 73.7 |
| September 2010 | 14,765 | 8.3 | 49.5 | 33.8 | 7314 | 73.6 |
| October 2010 | 15,535 | 8.8 | 49.3 | 33.7 | 7654 | 74.1 |
| November 2010 | 13,901 | 7.8 | 48.2 | 30.3 | 6694 | 69.8 |
| January 2011 | 26,924 | 15.2 | 52.9 | 38.8 | 14,242 | 76.4 |
| February 2011 | 22,565 | 12.7 | 51.4 | 36.9 | 11,595 | 75.0 |
| March 2011 | 22,490 | 12.7 | 47.8 | 33.7 | 10,740 | 73.8 |
| April 2011 | 17,221 | 9.7 | 47.4 | 33.6 | 8161 | 75.6 |
| May 2011 | 14,754 | 8.3 | 43.2 | 31.2 | 6376 | 75.5 |
| p-value | – | – | < 0.001 | < 0.001 | – | < 0.001 |
| Treatment episode | ||||||
| Episode 1 | 114,369 | 64.5 | 48.5 | 34.3 | 55,420 | 75.0 |
| Episode 2 | 36,154 | 20.4 | 49.1 | 33.5 | 17,748 | 72.7 |
| Episode 3 | 14,391 | 8.1 | 49.6 | 33.9 | 7134 | 73.6 |
| Episode 4 or more | 12,377 | 7.0 | 50.2 | 34.9 | 6210 | 74.0 |
| p-value | – | – | < 0.001 | 0.0 | – | 0.003 |
| Medication used | ||||||
| Single NRT | 40,607 | 22.9 | 37.5 | 25.4 | 15,222 | 74.0 |
| Combination NRT | 67,703 | 38.2 | 49.7 | 37.0 | 33,646 | 78.1 |
| Bupropion only | 1129 | 0.6 | 52.1 | 32.9 | 588 | 69.7 |
| Varenicline only | 45,149 | 25.5 | 60.2 | 43.0 | 27,167 | 75.8 |
| Mixed NRT/bupropion/varenicline | 4479 | 2.5 | 46.6 | 34.3 | 2085 | 76.6 |
| No medication or missing | 18,224 | 10.3 | 42.8 | 21.0 | 7804 | 52.9 |
| p-value | – | – | < 0.001 | < 0.001 | – | < 0.001 |
| Intervention type | ||||||
| One to one | 140,119 | 79.0 | 47.6 | 33.8 | 66,621 | 74.5 |
| Drop-in clinic | 24,736 | 14.0 | 50.7 | 33.3 | 12,550 | 74.8 |
| Open (rolling) group | 4780 | 2.7 | 65.5 | 52.1 | 3130 | 85.3 |
| Closed group | 2512 | 1.4 | 63.5 | 50.1 | 1595 | 80.9 |
| Other or missing | 5144 | 2.9 | 50.9 | 23.3 | 2616 | 49.8 |
| p-value | – | – | < 0.001 | < 0.001 | – | < 0.001 |
| Practitioner type | ||||||
| Specialist | 55,603 | 31.4 | 55.6 | 37.7 | 30,902 | 74.6 |
| GP | 3535 | 2.0 | 45.1 | 34.9 | 1593 | 78.7 |
| Nurse | 18,091 | 10.2 | 42.3 | 28.3 | 7660 | 69.5 |
| Health-care assistant | 7070 | 4.0 | 45.4 | 35.2 | 3206 | 80.4 |
| Pharmacy | 18,890 | 10.7 | 40.6 | 29.7 | 7670 | 76.5 |
| Other or unknown | 74,102 | 41.8 | 47.9 | 33.9 | 35,481 | 73.9 |
| p-value | – | – | < 0.001 | < 0.001 | – | < 0.001 |
| Total | 177,291 | 100.0 | < 0.001 | < 0.001 | 86,512 | < 0.001 |
Client characteristics
There were slightly more women setting quit dates than men, with 3.2% of clients pregnant at the time of data entry. Seven per cent of clients were from ethnic minorities, although 4% of client ethnicities are unknown. One-quarter of the clients were under 30 years and one-quarter were aged ≥ 54 years. A large proportion was exempt from paying prescription charges (58.8%), and for 9% this information was unavailable. The largest category of occupation in the sample was routine and manual (24.4%), with the second largest being retired or home carer (18.1%). There were over 2000 prisoners who set quit dates.
Service type characteristics
Between 13,000 and 27,000 clients set quit dates each month. The highest numbers of clients set quit dates in January to March and the lowest numbers were in August and November. The PCTs providing client data were fairly evenly divided by disadvantage. The majority of clients (64.5%) had not used the SSS previously (treatment episode 1). Combination NRT (more than one type of NRT) was the most commonly used medication (38.2%). Less than 1% used bupropion alone. Among intervention types, one-to-one behavioural support was by far the most common (79%) whereas only 14% took part in drop-ins, 2.7% took part in open/rolling groups and 1.4% were members of closed groups. Practitioner type had a large proportion of missing values (41.8%), so it was not possible to assess how accurately the proportions of the other categories reflect the distribution of practitioner types, however, the largest category displayed was specialist practitioner at 31.4%.
Each row in Table 4 displays information about a different PCT. For each of these, the first column displays information on the number of practitioners within each PCT (ranging from 14–334). The subsequent column shows the number of clients seen in each PCT with practitioner identified and this is followed by an average of clients per practitioners for each PCT (ranging from 8–310). There was variation in the number of practitioners recorded by the PCTs (from 20–300). In some PCTs it appeared that practitioners saw over 250 clients on average whereas in others practitioners saw fewer than 10 clients each.
| Number of practitioners in QuitManager database | Clients with practitioner identified, July 2010–June 2011 | Mean clients per practitioner | Estimated PCT smoking rate (%) in 2003–5 aged ≥ 16 years (95% CI)a | Estimated population 2010 aged ≥ 16 yearsb | SSS clients aged ≥ 16 years, July 2010–June 2011c | Estimate of PCT smokers reached (%)d |
|---|---|---|---|---|---|---|
| 77 | 2876 | 37.4 | 32.1 (28.0 to 36.5) | 135,000 | 2849 | 7.5 |
| 106 | 2673 | 25.2 | 27.8 (24.1 to 31.9) | 182,100 | 2659 | 6.1 |
| 15 | 4398 | 293.2 | 24.9 (22.1 to 28.0) | 315,500 | 6132 | 9.3 |
| 22 | 5441 | 247.3 | 24.9 (22.1 to 28.0) | 278,200 | 5400 | 9.3 |
| 137 | 6635 | 48.4 | 30.3 (27.4 to 33.4) | 114,300 | 6597 | 21.9 |
| 74 | 4000 | 54.1 | 20.1 (18.6 to 21.7) | 259,300 | 4000 | 9.6 |
| 256 | 5887 | 23.0 | 24.8 (22.0 to 27.7) | 368,300 | 5868 | 7.7 |
| 121 | 2546 | 21.0 | 21.9 (19.0 to 25.2) | 251,200 | 2584 | 5.7 |
| 95 | 6236 | 65.6 | 19.6 (18.5 to 20.8) | 373,100 | 6164 | 10.6 |
| 302 | 10,038 | 33.2 | 25.0 (23.6 to 26.5) | 422,400 | 10,083 | 11.3 |
| 58 | 1662 | 28.7 | 27.9 (24.7 to 31.5) | 81,400 | 1683 | 8.6 |
| 128 | 4573 | 35.7 | 26.8 (24.3 to 29.5) | 255,200 | 4576 | 7.9 |
| 276 | 3804 | 13.8 | 25.0 (22.4 to 27.8) | 199,700 | 3769 | 9.0 |
| 44 | 7229 | 164.3 | 23.5 (22.4 to 24.5) | 599,500 | 7097 | 6.1 |
| 177 | 3113 | 17.6 | 18.6 (16.5 to 20.9) | 256,600 | 3125 | 8.3 |
| 83 | 2862 | 34.5 | 21.2 (19.1 to 23.6) | 282,000 | 2834 | 5.8 |
| 87 | 1936 | 22.3 | 14.5 (11.9 to 17.5) | 185,400 | 1965 | 10.1 |
| 102 | 3573 | 35.0 | 24.9 (22.1 to 28.0) | 215,500 | 3718 | 8.2 |
| 332e | 8203 | 24.7 | 22.9 (21.8 to 24.1) | – | – | – |
| 334e | 6293 | 18.8 | 19.8 (18.7 to 21.0) | – | – | – |
| –e | – | – | 21.4 (20.3 to 22.6) | 886,500 | 14,512 | 8.8 |
| 188 | 3689 | 19.6 | 28.2 (25.8 to 30.7) | 161,600 | 3626 | 9.3 |
| 95 | 3861 | 40.6 | 22.0 (19.4 to 24.9) | 190,100 | 3942 | 11.5 |
| 73 | 4878 | 66.8 | 40.9 (36.4 to 45.5) | 217,100 | 4824 | 6.0 |
| 131 | 3432 | 26.2 | 27.5 (22.9 to 32.6) | 163,100 | 3708 | 9.7 |
| 81 | 1154 | 14.2 | 18.8 (14.4 to 24.2) | 141,800 | 1963 | 9.4 |
| 79 | 637 | 8.1 | 21.7 (18.7 to 24.9) | 138,400 | 619 | 2.5 |
| 142 | 4993 | 35.2 | 30.1 (26.1 to 34.4) | 243,300 | 4921 | 7.8 |
| 228 | 7400 | 32.5 | 21.9 (20.8 to 22.9) | 564,000 | 7286 | 7.2 |
| 100 | 2996 | 30.0 | 26.8 (24.1 to 29.7) | 212,600 | 2985 | 6.1 |
| 280 | 10,778 | 38.5 | 23.3 (22.2 to 24.5) | 583,300 | 10,634 | 9.4 |
| 43 | 1493 | 34.7 | 24.6 (22.0 to 27.3) | 128,100 | 1487 | 5.6 |
| 123 | 3111 | 25.3 | 18.4 (16.4 to 20.6) | 173,900 | 3115 | 12.4 |
| 21 | 6518 | 310.4 | 25.9 (24.6 to 27.1) | 550,800 | 12,920f | 10.7 |
| 36 | 2215 | 61.5 | 33.5 (29.7 to 37.4) | 128,400 | 2207 | 5.8 |
| 62 | 5060 | 81.6 | 36.2 (32.1 to 40.6) | 256,600 | 4994 | 6.0 |
| 27 | 5268 | 195.1 | 29.0 (26.4 to 31.8) | 171,100 | 5203 | 12.1 |
| 89 | 1273 | 14.3 | 17.6 (15.1 to 20.3) | 211,600 | 1532 | 5.3 |
| 63 | 582 | 9.2 | 19.3 (16.1 to 23.0) | 152,900 | 573 | 2.4 |
| 130 | 5105 | 39.3 | 25.3 (22.6 to 28.1) | 205,800 | 5013 | 11.5 |
| 14 | 459 | 32.8 | 29.0 (26.1 to 32.0) | 230,900 | 1754 | 3.0 |
| 113 | 4224 | 37.4 | 21.3 (20.2 to 22.5) | 241,500 | 4163 | 10.0 |
| 21 | 603 | 28.7 | 21.1 (20.0 to 22.2) | 429,700 | 1356f | NA |
| 268 | 4155 | 15.5 | 24.5 (22.9 to 26.2) | 275,500 | 8254f | 14.6 |
| 90 | 1774 | 19.7 | 27.7 (24.2 to 31.5) | 236,500 | 1772 | 3.2 |
| 75 | 3562 | 47.5 | 25.2 (22.7 to 27.9) | 129,500 | 3501 | 12.7 |
| 113 | 2100 | 18.6 | 25.8 (23.4 to 28.4) | 203,200 | 4140f | 9.3 |
| 293 | 3937 | 13.4 | 21.3 (20.2 to 22.5) | 438,000 | 7798f | 10.3 |
| 93 | 4099 | 44.1 | 21.7 (20.3 to 23.1) | 193,000 | 4061 | 11.9 |
| 6040 | 196,511 | 32.5 (average) | – | – | – | – |
Reach of services by primary care trust
Estimated smoking rates varied from 15% to 41%. PCT populations varied from 80,000 to nearly 900,000. Most services saw between 5% and 10% of their population of smokers between July 2010 and June 2011. Note that smoking estimates were accompanied by confidence intervals (CIs) of approximately 6% thus these should be treated with caution.
Cessation
Bivariable results
The overall quit rates of the entire database (see Table 3) without exclusions for missing data in the gender, age or practitioner type variables were 44.1% (self-report) and 30.7% (CO validated). The quit rates of the sample used in the analysis were 48.8% (self-report) and 34.1% (CO validated).
The SSSs target is at least 35% for self-report and CO-validated quit. 33 Overall, the self-report quit rate comfortably passed this level and the CO-validated quit rate almost reached this level. Three PCTs did not reach the 35% target for self-report quitting. Some subgroups met this target for CO-validated quitting, they were: clients who were working or who were retired or caring for the home, prisoners, clients who paid for prescriptions, clients in PCTs who were not particularly disadvantaged or affluent, clients who set quit dates in January or February, clients who took combination NRT or just varenicline, clients who attended groups and clients whose practitioner was a specialist or a health-care assistant. Of the 49 PCTs, 28 met this target for CO-validated quitting.
Multivariable results
Multivariable modelling in Stata indicated the extent of multicollinearity. All vifs were below 2.54 for self-reported and CO-validated models so there was no significant multicollinearity in the data (concerns are raised if a vif is ≥ 10). Multilevel multivariable ORs for client variables are presented in Table 5 and ORs of quit attempt-related variables are presented in Table 6.
| Outcome | Self-report quit, OR (95% CI) (n = 177,291) | CO-verified quit, OR (95% CI) (n = 177,291) | CO validation, OR (95% CI) (n = 86,512) | CO validation, OR (95% CI) (n = 80,002) |
|---|---|---|---|---|
| Exclusions | – | – | – | Extreme PCTsa |
| Null model (constant) | 0.34 (0.27 to 0.43) | 0.13 (0.09 to 0.19) | 1.58 (0.77 to 3.25) | 1.69 (0.98 to 2.90) |
| Age (years) at quit date quartiles | ||||
| 10–30 | 1 | 1 | 1 | 1 |
| 31–42 | 1.44 (1.40 to 1.48) | 1.53 (1.48 to 1.58) | 1.29 (1.22 to 1.35) | 1.34 (1.27 to 1.41) |
| 43–53 | 1.54 (1.49 to 1.59) | 1.73 (1.67 to 1.79) | 1.48 (1.40 to 1.57) | 1.60 (1.51 to 1.69) |
| 54–100 | 2.02 (1.96 to 2.09) | 2.28 (2.20 to 2.37) | 1.69 (1.60 to 1.80) | 1.87 (1.76 to 1.99) |
| Gender | ||||
| Female (not pregnant) | 1 | 1 | 1 | 1 |
| Female (pregnant) | 1.29 (1.20 to 1.38) | 1.16 (1.07 to 1.26) | 0.93 (0.82 to 1.05) | 0.87 (0.77 to 1.00) |
| Male | 1.07 (1.04 to 1.09) | 1.04 (1.02 to 1.07) | 0.97 (0.94 to 1.01) | 0.97 (0.93 to 1.00) |
| Ethnicity | ||||
| Black, Asian, mixed, other | 1 | 1 | 1 | 1 |
| White | 1.02 (0.98 to 1.07) | 1.04 (0.99 to 1.09) | 1.05 (0.97 to 1.13) | 1.05 (0.97 to 1.14) |
| Unknown | 1.02 (0.95 to 1.09) | 0.96 (0.89 to 1.03) | 0.90 (0.80 to 1.02) | 0.89 (0.79 to 1.01) |
| NSSEC | ||||
| Routine and manual | 1 | 1 | 1 | 1 |
| Intermediate | 1.14 (1.10 to 1.19) | 1.09 (1.04 to 1.14) | 0.96 (0.89 to 1.03) | 0.96 (0.89 to 1.03) |
| Managerial and professional | 1.19 (1.15 to 1.24) | 1.14 (1.10 to 1.18) | 1.02 (0.97 to 1.08) | 1.02 (0.96 to 1.09) |
| Retired or home carer | 1.07 (1.03 to 1.11) | 1.06 (1.02 to 1.11) | 1.02 (0.96 to 1.09) | 1.02 (0.96 to 1.09) |
| Sick or disabled and unable to work | 0.70 (0.67 to 0.73) | 0.70 (0.67 to 0.74) | 0.85 (0.78 to 0.93) | 0.83 (0.76 to 0.90) |
| Always/long-term unemployed | 0.75 (0.72 to 0.78) | 0.76 (0.73 to 0.79) | 0.96 (0.90 to 1.02) | 0.94 (0.88 to 1.01) |
| In prison | 1.15 (1.00 to 1.32) | 1.98 (1.71 to 2.29) | 3.82 (2.92 to 4.98) | 4.84 (3.61 to 6.47) |
| Other | 0.84 (0.81 to 0.87) | 0.82 (0.78 to 0.85) | 0.91 (0.85 to 0.97) | 0.89 (0.83 to 0.96) |
| Prescription payment | ||||
| Exempt | 1 | 1 | 1 | 1 |
| Pays | 1.24 (1.21 to 1.27) | 1.18 (1.14 to 1.21) | 0.98 (0.93 to 1.02) | 0.97 (0.93 to 1.02) |
| Unknown | 1.08 (1.03 to 1.13) | 0.92 (0.88 to 0.97) | 0.84 (0.78 to 0.90) | 0.80 (0.74 to 0.86) |
| Average IMD score 2010 (PCT) | ||||
| Ranked 1–30 (disadvantaged) | 1 | 1 | 1 | 1 |
| Ranked 31–60 | 1.20 (0.85 to 1.69) | 1.58 (0.91 to 2.77) | 3.61 (1.14 to 11.47) | 1.67 (0.72 to 3.86) |
| Ranked 61–90 | 1.29 (0.88 to 1.89) | 1.34 (0.72 to 2.51) | 0.61 (0.17 to 2.19) | 0.60 (0.25 to 1.45) |
| Ranked 91–120 | 1.25 (0.92 to 1.70) | 1.43 (0.88 to 2.35) | 1.34 (0.49 to 3.67) | 1.19 (0.59 to 2.42) |
| Ranked ≥ 121 (affluent) | 1.36 (0.96 to 1.91) | 1.61 (0.92 to 2.81) | 1.06 (0.34 to 3.33) | 1.01 (0.45 to 2.22) |
| Outcome | Self-report quit, OR (95% CI) (n = 177,291) | CO-verified quit, OR (95% CI) (n = 177,291) | CO validation, OR (95% CI) (n = 86,512) | CO validation, OR (95% CI) (n = 80,002) |
|---|---|---|---|---|
| Exclusions | – | – | – | Extreme PCTsa |
| Quit date month | ||||
| July 2010 | 1 | 1 | 1 | 1 |
| August 2010 | 1.04 (0.99 to 1.09) | 1.04 (0.99 to 1.10) | 1.05 (0.96 to 1.15) | 1.05 (0.96 to 1.15) |
| September 2010 | 1.14 (1.08 to 1.20) | 1.11 (1.05 to 1.17) | 1.02 (0.93 to 1.11) | 1.02 (0.93 to 1.11) |
| October 2010 | 1.10 (1.05 to 1.16) | 1.08 (1.02 to 1.14) | 1.01 (0.92 to 1.09) | 1.00 (0.91 to 1.09) |
| November 2010 | 1.02 (0.97 to 1.07) | 0.88 (0.84 to 0.93) | 0.82 (0.75 to 0.89) | 0.77 (0.71 to 0.85) |
| January 2011 | 1.33 (1.27 to 1.39) | 1.34 (1.28 to 1.41) | 1.11 (1.02 to 1.19) | 1.11 (1.03 to 1.21) |
| February 2011 | 1.17 (1.12 to 1.22) | 1.19 (1.14 to 1.25) | 1.06 (0.98 to 1.15) | 1.06 (0.97 to 1.15) |
| March 2011 | 1.02 (0.98 to 1.07) | 1.04 (0.99 to 1.09) | 0.98 (0.90 to 1.06) | 0.96 (0.88 to 1.05) |
| April 2011 | 0.96 (0.91 to 1.01) | 1.02 (0.97 to 1.08) | 1.08 (0.99 to 1.17) | 1.08 (0.99 to 1.18) |
| May 2011 | 0.85 (0.81 to 0.89) | 0.97 (0.91 to 1.02) | 1.08 (0.99 to 1.19) | 1.10 (1.00 to 1.21) |
| Episode | ||||
| Episode 1 | 1 | 1 | 1 | 1 |
| Episode 2 | 0.97 (0.94 to 0.99) | 0.97 (0.94 to 0.99) | 1.00 (0.96 to 1.05) | 1.00 (0.95 to 1.05) |
| Episode 3 | 1.00 (0.96 to 1.04) | 0.98 (0.94 to 1.03) | 1.00 (0.94 to 1.07) | 0.99 (0.93 to 1.07) |
| Episode 4 or more | 1.04 (1.00 to 1.08) | 1.04 (1.00 to 1.09) | 1.05 (0.98 to 1.13) | 1.04 (0.96 to 1.13) |
| Medication | ||||
| Single NRT | 1 | 1 | 1 | 1 |
| Combination NRT | 1.88 (1.83 to 1.94) | 2.06 (2.00 to 2.13) | 1.55 (1.47 to 1.65) | 1.66 (1.56 to 1.76) |
| Bupropion only | 1.79 (1.58 to 2.03) | 1.48 (1.29 to 1.69) | 0.97 (0.79 to 1.20) | 0.96 (0.77 to 1.18) |
| Varenicline only | 2.57 (2.49 to 2.65) | 2.31 (2.24 to 2.40) | 1.31 (1.23 to 1.39) | 1.37 (1.29 to 1.45) |
| Mixed NRT/bupropion/varenicline | 1.46 (1.37 to 1.57) | 1.64 (1.53 to 1.76) | 1.46 (1.30 to 1.65) | 1.55 (1.37 to 1.76) |
| No medication or missing | 1.13 (1.08 to 1.18) | 0.80 (0.76 to 0.84) | 0.74 (0.68 to 0.80) | 0.68 (0.63 to 0.74) |
| Intervention type | ||||
| One to one | 1 | 1 | 1 | 1 |
| Drop-in clinic | 0.96 (0.91 to 1.01) | 1.02 (0.96 to 1.07) | 1.01 (0.93 to 1.10) | 0.97 (0.89 to 1.06) |
| Open (rolling) group | 1.15 (1.04 to 1.27) | 1.28 (1.15 to 1.41) | 1.39 (1.18 to 1.64) | 1.45 (1.23 to 1.73) |
| Closed group | 1.12 (1.00 to 1.26) | 1.11 (0.99 to 1.24) | 1.15 (0.96 to 1.37) | 1.16 (0.96 to 1.39) |
| Other or missing | 1.12 (1.03 to 1.21) | 0.62 (0.57 to 0.68) | 0.46 (0.40 to 0.51) | 0.41 (0.36 to 0.46) |
| SSS practitioner | ||||
| Specialist | 1 | 1 | 1 | 1 |
| GP | 0.46 (0.38 to 0.55) | 0.53 (0.42 to 0.66) | 1.15 (0.83 to 1.61) | 1.43 (0.97 to 2.10) |
| Nurse | 0.58 (0.52 to 0.64) | 0.70 (0.62 to 0.78) | 1.11 (0.95 to 1.29) | 1.19 (0.99 to 1.43) |
| Health-care assistant | 0.69 (0.60 to 0.78) | 0.86 (0.74 to 0.99) | 1.29 (1.05 to 1.58) | 1.42 (1.11 to 1.80) |
| Pharmacy | 0.67 (0.61 to 0.73) | 0.91 (0.82 to 1.02) | 1.80 (1.55 to 2.10) | 2.20 (1.84 to 2.64) |
| Other or unknown | 0.78 (0.72 to 0.84) | 0.88 (0.80 to 0.97) | 1.25 (1.10 to 1.41) | 1.34 (1.16 to 1.55) |
The results for CO-validated quit and self-report quit are mostly similar so they are discussed simultaneously with differences alluded to. Generally unknown and other classifications were associated with less chance of quitting than reference groups.
Demography
The relationship between client-related characteristics and CO-validated or self-report quits were mostly similar. As age increased so did the chances of quitting. Clients aged over 53 years were twice as likely to quit as those age 30 years or under. Men and pregnant women were more likely to quit than non-pregnant women. In the bivariable results pregnant women had the lowest quit rate. Further exploration (not shown) suggested that the change in the multivariable results was attributed to pregnant women being less likely to take medication. Ethnicity was not significantly related to quitting.
Socioeconomic status
Compared with clients with routine and manual occupations, clients with intermediate, managerial and professional occupations, the retired, home carers and prisoners were more likely to quit. Those who paid for prescriptions were more likely to quit than those who were exempt. PCT deprivation was not significantly related to quitting.
Stop Smoking Service related
September, January and February appeared to be particularly successful months for setting a quit date with a SSS. Lower chances of quitting in May and November might partly be because of late quit information not being included in the database owing to cut off points at the end of December and June. However, differences between these months and the other months were not always significant, suggesting this had a minimal effect. Clients who had used the service once before were less likely to quit than those who had never used the service before and those who had used the service four or more times were more likely to quit. Taking any medication other than single NRT increased the chances of quitting. The highest ORs were for clients who took varenicline alone. These people were more than twice as likely to self-report and CO validate as quit.
For intervention type, the highest chances of quitting were among clients who took part in open/rolling groups. Closed-group clients were significantly more likely to self-report as quit than those who undertook one-to-one counselling but the difference did not quite reach significance for CO validation. Further analysis (not shown) suggested this was caused by a number of factors such as the practitioner, SES and medication.
Among the practitioner types, clients of specialist advisers were more likely to quit than clients of other (and unspecified) practitioner types. This difference was significant for all categories except for CO validation among practitioners who held pharmacy posts. ORs were surprisingly low for GPs given bivariable results. Further analysis (not shown) suggested this was because the majority of GPs worked in one PCT (Warwickshire) where quit rates were similar to other practitioner types, but in most other PCTs, with more than 20 clients seen by GPs, GPs were achieving fewer CO-validated quits than other practitioner types.
Primary care trust and practitioner
Figure 2 is a caterpillar plot of PCT residuals for the multilevel multivariable model of self-report quit. PCT CIs that do not overlap 0.0 represent significant departures from the average. The lowest chances of self-reported quitting were found in the PCT ranked 1.
FIGURE 2.
Residual caterpillar plot of PCTs for multivariable multilevel model of self-report quits.
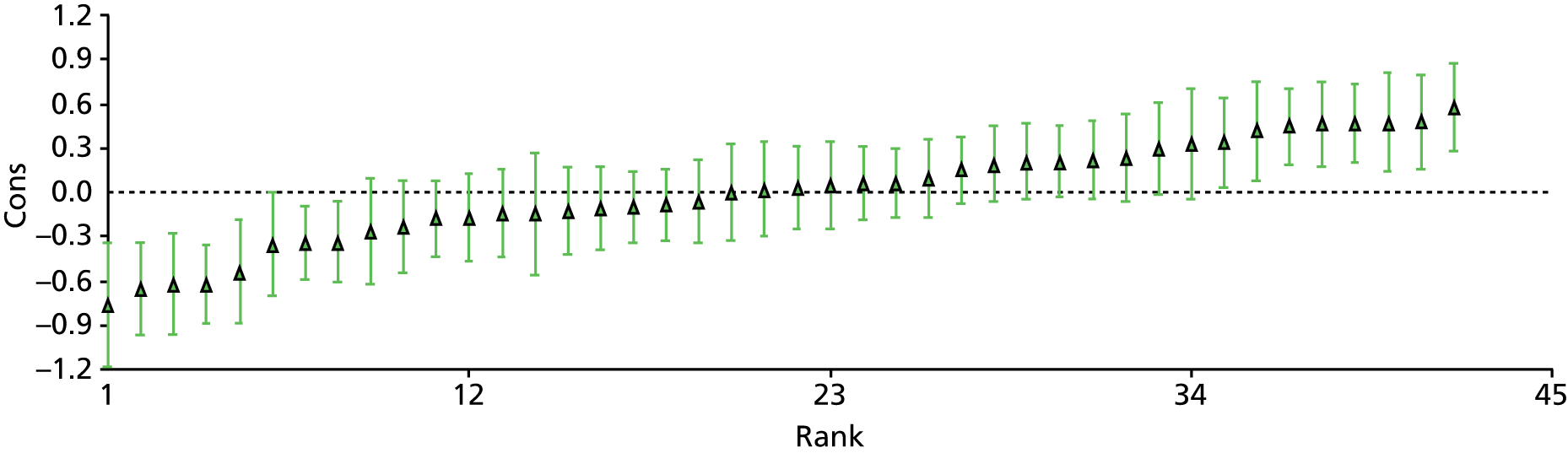
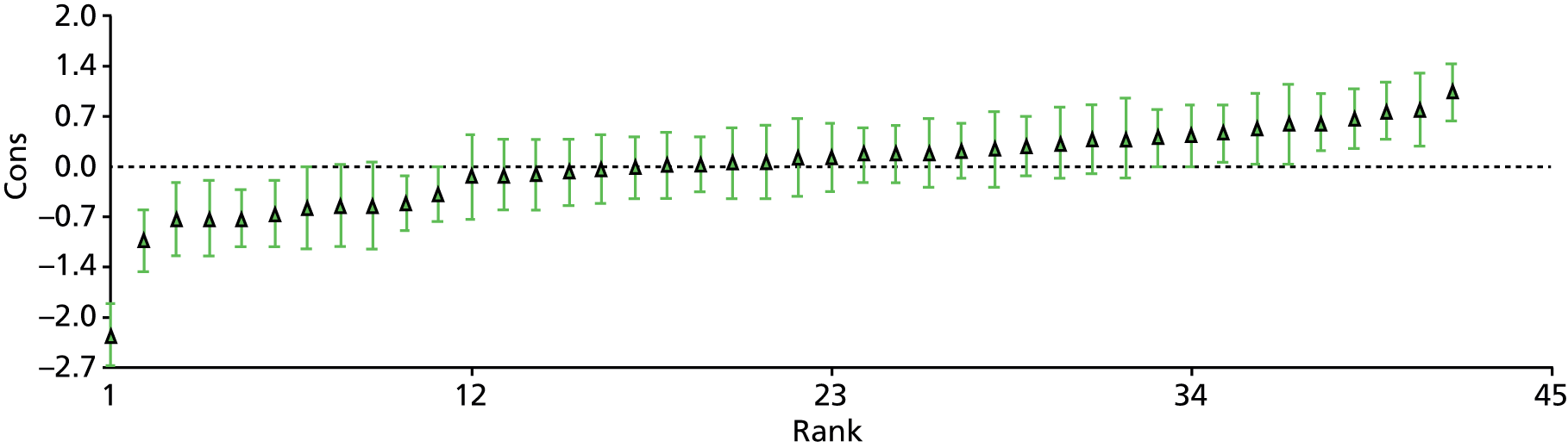
Figure 3 is a caterpillar plot of PCT residuals for CO-validated quit. PCT CIs that do not overlap 0.0 represent significant departures from the average. Further exploration (not shown) suggested that excluding clients from the lowest ranked PCT made little difference to the results.
FIGURE 3.
Residual caterpillar plot of PCTs for multivariable multilevel model of CO-validated quits.
There is little that can be said with certainty about the higher-level variance (Table 7), as it is not possible to tell how much of the change in variance between models is owing to fixed effects in the model and how much is the result of level one variance being constrained to 3.29, leading to inflated or deflated higher level variance.
| Models | CO validated | Self-report | CO validation | |||
|---|---|---|---|---|---|---|
| PCT variance (95% CI) | Practitioner variance (95% CI) | PCT variance (95% CI) | Practitioner variance (95% CI) | PCT variance (95% CI) | Practitioner variance (95% CI) | |
| No fixed effects | ||||||
| Null model (constant) | 0.36 (0.20 to 0.53) | 0.54 (0.51 to 0.58) | 0.14 (0.07 to 0.20) | 0.41 (0.38 to 0.43) | 1.83 (1.03 to 2.63) | 1.32 (1.23 to 1.42) |
| One fixed effect | ||||||
| Quit date month | 0.36 (0.20 to 0.52) | 0.54 (0.51 to 0.58) | 0.14 (0.07 to 0.20) | 0.41 (0.38 to 0.43) | 1.83 (1.02 to 2.64) | 1.33 (1.23 to 1.42) |
| Age (years) at quit date quartiles | 0.38 (0.21 to 0.55) | 0.55 (0.51 to 0.58) | 0.14 (0.08 to 0.21) | 0.40 (0.38 to 0.43) | 1.84 (1.03 to 2.65) | 1.35 (1.25 to 1.44) |
| Gender | 0.36 (0.20 to 0.53) | 0.54 (0.51 to 0.57) | 0.14 (0.07 to 0.20) | 0.41 (0.38 to 0.43) | 1.82 (1.01 to 2.63) | 1.32 (1.23 to 1.41) |
| Ethnicity | 0.37 (0.20 to 0.53) | 0.54 (0.51 to 0.57) | 0.13 (0.07 to 0.20) | 0.40 (0.38 to 0.43) | 1.83 (1.02 to 2.64) | 1.32 (1.23 to 1.42) |
| NSSEC | 0.36 (0.20 to 0.51) | 0.52 (0.49 to 0.56) | 0.12 (0.07 to 0.18) | 0.39 (0.36 to 0.41) | 1.83 (1.03 to 2.63) | 1.31 (1.22 to 1.40) |
| Prescription payment | 0.36 (0.20 to 0.52) | 0.53 (0.50 to 0.57) | 0.13 (0.07 to 0.20) | 0.40 (0.37 to 0.43) | 1.82 (1.02 to 2.63) | 1.30 (1.21 to 1.39) |
| IMD 2010 (PCT) | 0.30 (0.17 to 0.44) | 0.53 (0.49 to 0.56) | 0.11 (0.06 to 0.16) | 0.40 (0.38 to 0.43) | 1.40 (0.78 to 2.02) | 0.74 (0.68 to 0.80) |
| Episode | 0.37 (0.20 to 0.53) | 0.54 (0.51 to 0.58) | 0.14 (0.07 to 0.20) | 0.40 (0.38 to 0.43) | 1.83 (1.02 to 2.63) | 1.32 (1.23 to 1.42) |
| Medication | 0.38 (0.21 to 0.55) | 0.53 (0.50 to 0.57) | 0.15 (0.08 to 0.23) | 0.40 (0.37 to 0.43) | 1.84 (1.02 to 2.65) | 1.29 (1.19 to 1.38) |
| Intervention type | 0.35 (0.20 to 0.51) | 0.53 (0.50 to 0.56) | 0.13 (0.07 to 0.19) | 0.40 (0.37 to 0.42) | 1.80 (1.00 to 2.60) | 1.29 (1.20 to 1.38) |
| SSS practitioner | 0.37 (0.20 to 0.53) | 0.53 (0.50 to 0.57) | 0.13 (0.07 to 0.19) | 0.38 (0.35 to 0.40) | 1.91 (1.07 to 2.75) | 1.29 (1.20 to 1.38) |
| All fixed effects | ||||||
| Multivariable model | 0.34 (0.19 to 0.50) | 0.49 (0.46 to 0.52) | 0.13 (0.07 to 0.18) | 0.36 (0.33 to 0.38) | 1.47 (0.82 to 2.11) | 0.71 (0.65 to 0.76) |
| Multivariable MCMC model | 0.43 (0.22 to 0.65) | 0.53 (0.49 to 0.57) | – | – | – | – |
| Multivariable model without extreme PCTs | – | – | – | – | 0.64 (0.34 to 0.94) | 1.02 (0.94 to 1.10) |
We can safely say that there was significant variance between practitioners and between PCTs even after all fixed effects had been included for both self-report and CO-validated quit. It is probably also safe to say that there was less variance between PCTs and between practitioners for self-report quits than CO-validated quits.
Carbon monoxide validation
The CO-validation rate (self-reports that were CO validated) of the database was 73.9% and was 74.3% among clients with gender, age and practitioner identified (see Table 3). The DH has recommended that SSSs should aim to CO validate 85% of clients. 33 Client groups where CO validation of 85% was achieved were prisoners and clients enrolled in open groups. Of the 49 PCTs, 13 achieved CO-validation rates of 85% or more.
Multivariable results
Odds ratios for IMD at PCT level and multilevel variance changes suggested that some PCTs were having a disproportionate effect on the results, as an intermediate quintile was most associated with quitting (see Table 4) and including this variable in the model was associated with a major reduction in PCT-level variance (see Table 7). Two PCTs, with very high CO-validation rates and one PCT with a particularly low validation rate were consequently excluded. Both models are shown (see Table 6). Multivariable modelling in Stata provided vifs and tols. All were below 3.20, so there was no significant multicollinearity in the data.
Demography
As age increased, CO validation was more likely. Non-pregnant women were more likely to be CO validated than men and pregnant women. Ethnicity had no effect on CO-validation rates.
Socioeconomic status
Prisoners were much more likely to be CO validated than other groups, approximately four times more likely than routine and manual workers. Eligibility for paying for prescriptions and PCT deprivation (once extreme PCTs were excluded) did not significantly affect CO-validation rates.
Stop Smoking Service related
Self-report quitters who set quit dates in January were most likely to be CO validated and November quitters were least likely. Clients who took varenicline, combination NRT or a mixture of medications were more likely to be CO validated than those who took single NRT. Self-report quitters who enrolled in open groups were more likely to be CO validated. CO-validation rates were lowest among specialist practitioners. Health-care assistants, pharmacy employees and unclassified practitioners were significantly more likely to CO validate clients than specialist practitioners (see Table 6).
Primary care trust and practitioner
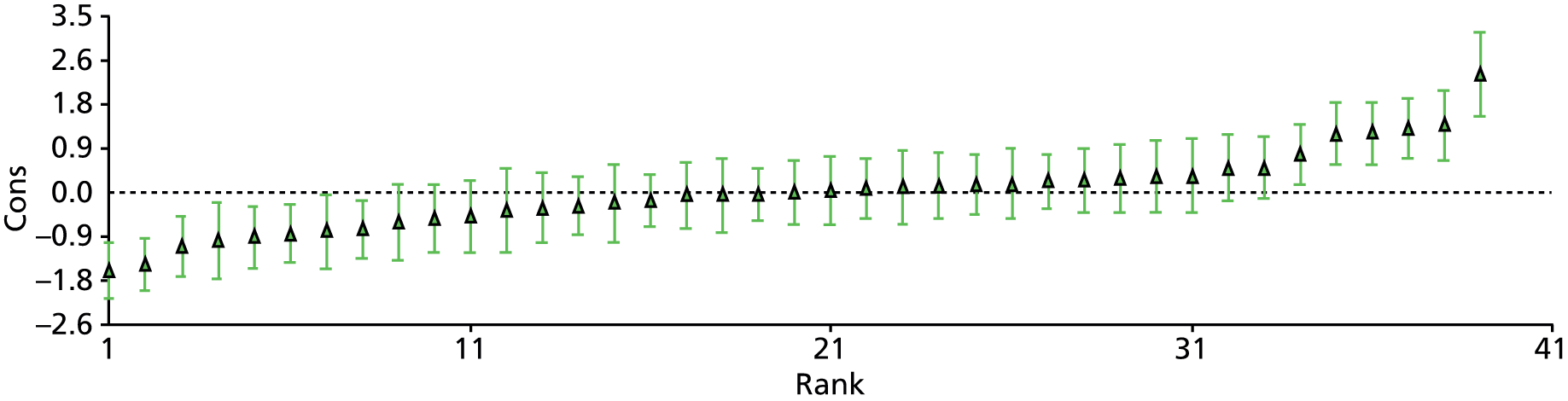
Residuals suggest (Figure 4) that, after taking other demographic- and service-related factors into account, there was significant variation in PCT validation rates.
FIGURE 4.
Caterpillar plot of residuals for multivariable multilevel model predicting CO validation (model excluding extreme PCTs).
There is little that can be said with certainty about the higher-level variance, as it is not possible to tell how much of the change in variance between models (see Table 7) is owing to fixed effects in the model and how much is the result of level one variance being constrained to 3.29 in binary outcome models.
The variance between PCTs appeared to halve when PCT deprivation was entered into the model. The fixed effects suggested that PCTs that were fairly, but not the most, disadvantaged were three times more likely to be CO validated. This suggested that idiosyncrasies were responsible rather than an effect of deprivation. When extreme PCTs were excluded the variance between PCTs halved and there was no longer significant variation between practitioners.
Impact
In general, the services had a positive impact over and above what would be expected from quitting spontaneously or with medication only. When the impact was calculated using all self-report quitters, two services were estimated to have a negative impact as did six services when only CO-validated quitters were included. However, only one service was judged to have a negative impact when both CO-validated quitting and all self-report quitting were taken into account. At the other end of the scale, two PCTs were estimated to have independently added over 400 ex-smokers per 100,000 population between mid-2010 and mid-2011 (Table 8).
| Unique clients aged ≥ 16 years | Clients per 100,000 PCT populationa | ||||||
|---|---|---|---|---|---|---|---|
| Throughput | Impact (4-week quitters) calculated | ||||||
| n | Client records unique clients (%) | CO-validated quit (%)b | Self-report quit (%)b | From CO-validated quit | From self-report quit | Overall (average self-report and CO validated) | |
| 2658 | 93.3 | 39.5 | 47.9 | 1969 | 285 | 254 | 270 |
| 2496 | 93.9 | 49.6 | 53.2 | 1371 | 337 | 249 | 293 |
| 5565 | 90.8 | 38.8 | 46.2 | 1764 | 243 | 198 | 220 |
| 4776 | 88.4 | 31.7 | 42.0 | 1717 | 115 | 120 | 118 |
| 5718 | 86.7 | 5.8 | 36.3 | 5003 | – | – | – |
| 3556 | 88.9 | 23.1 | 49.6 | 1371 | –26 | 200 | 87 |
| 5429 | 92.5 | 35.3 | 46.4 | 1474 | 152 | 168 | 160 |
| 2463 | 95.3 | 36.8 | 44.6 | 980 | 116 | 94 | 105 |
| 5555 | 90.1 | 25.3 | 47.0 | 1489 | 4 | 179 | 92 |
| 9618 | 95.4 | 42.9 | 53.1 | 2277 | 408 | 412 | 410 |
| 1611 | 95.7 | 41.3 | 50.5 | 1979 | 323 | 307 | 315 |
| 4010 | 87.6 | 38.1 | 48.9 | 1571 | 206 | 218 | 212 |
| 3453 | 91.6 | 40.8 | 61.4 | 1729 | 273 | 456 | 365 |
| 6748 | 95.1 | 45.7 | 57.3 | 1126 | 233 | 251 | 242 |
| 2657 | 85.0 | 36.7 | 55.1 | 1035 | 121 | 208 | 165 |
| 2655 | 93.7 | 45.3 | 64.8 | 941 | 191 | 281 | 236 |
| 2991 | 95.2 | 31.3 | 37.5 | 1667 | 105 | 42 | 73 |
| 1822 | 92.7 | 35.4 | 42.1 | 983 | 102 | 70 | 86 |
| 3433 | 92.3 | 40.0 | 45.5 | 1593 | 239 | 167 | 203 |
| 7197 | 87.8 | 27.2 | 55.7 | – | – | – | – |
| 5620 | 89.1 | 28.1 | 55.1 | – | – | – | – |
| 12,817 | 88.3 | 27.7 | 55.4 | 1446 | 38 | 295 | 167 |
| 3324 | 91.7 | 20.1 | 45.6 | 2057 | –101 | 218 | 59 |
| 3374 | 85.6 | 23.9 | 45.7 | 1775 | –20 | 190 | 85 |
| 4409 | 91.4 | 41.5 | 60.8 | 2031 | 335 | 524 | 430 |
| 3395 | 91.6 | 24.3 | 39.5 | 2082 | –15 | 94 | 40 |
| 1892 | 96.4 | 15.2 | 52.3 | 1334 | –131 | 231 | 50 |
| 580 | 93.7 | 53.3 | 64.9 | 419 | 119 | 125 | 122 |
| 4403 | 89.5 | 37.0 | 44.2 | 1810 | 217 | 166 | 192 |
| 6842 | 93.9 | 44.8 | 61.7 | 1213 | 240 | 324 | 282 |
| 2828 | 94.7 | 34.7 | 41.8 | 1330 | 129 | 90 | 110 |
| 9679 | 91.0 | 41.4 | 55.6 | 1659 | 272 | 342 | 307 |
| 1407 | 94.6 | 52.1 | 60.8 | 1098 | 298 | 283 | 291 |
| 2826 | 90.7 | 35.2 | 48.3 | 1625 | 166 | 216 | 191 |
| 2071 | 93.8 | 56.9 | 64.1 | 1613 | 515 | 469 | 492 |
| 4533 | 90.8 | 28.4 | 53.1 | 1767 | 60 | 320 | 190 |
| 4626 | 88.9 | 26.8 | 41.1 | 2704 | 49 | 165 | 107 |
| 1487 | 97.1 | 34.6 | 54.4 | 703 | 67 | 136 | 102 |
| 549 | 95.8 | 45.3 | 58.9 | 359 | 73 | 86 | 79 |
| 4474 | 89.2 | 40.2 | 56.1 | 2174 | 330 | 459 | 395 |
| 1422 | 81.1 | 31.0 | 33.2 | 616 | 37 | –11 | 13 |
| 1296c | 95.6 | 47.3 | 65.8 | – | – | – | – |
| 7880c | 95.5 | 28.2 | 46.7 | 2860 | 92 | 335 | 213 |
| 1683c | 95.0 | 18.0 | 26.4 | 712 | –50 | –61 | –56 |
| 3974c | 96.0 | 38.7 | 45.4 | 1956 | 268 | 203 | 236 |
| 7646c | 98.1 | 39.6 | 49.9 | 1746 | 255 | 260 | 257 |
| 3676 | 90.5 | 26.3 | 41.1 | 1905 | 25 | 116 | 70 |
To represent quit rates, throughput and impact on the same graph (Figure 5), different scales were used. Thus, a point of 100 on the y-axis represents 100 extra ex-smokers per 100,000 population (impact), 1000 clients setting quit dates per 100,000 population (throughput) or a quit rate of 10%. The graph suggests that impact is more strongly related to quit rates than throughput. Two London PCTs displayed high quit rates but low throughput whereas three others displayed particularly high throughput but low CO-validated quit rates.
FIGURE 5.
Impact, throughput and quit rates by PCT.
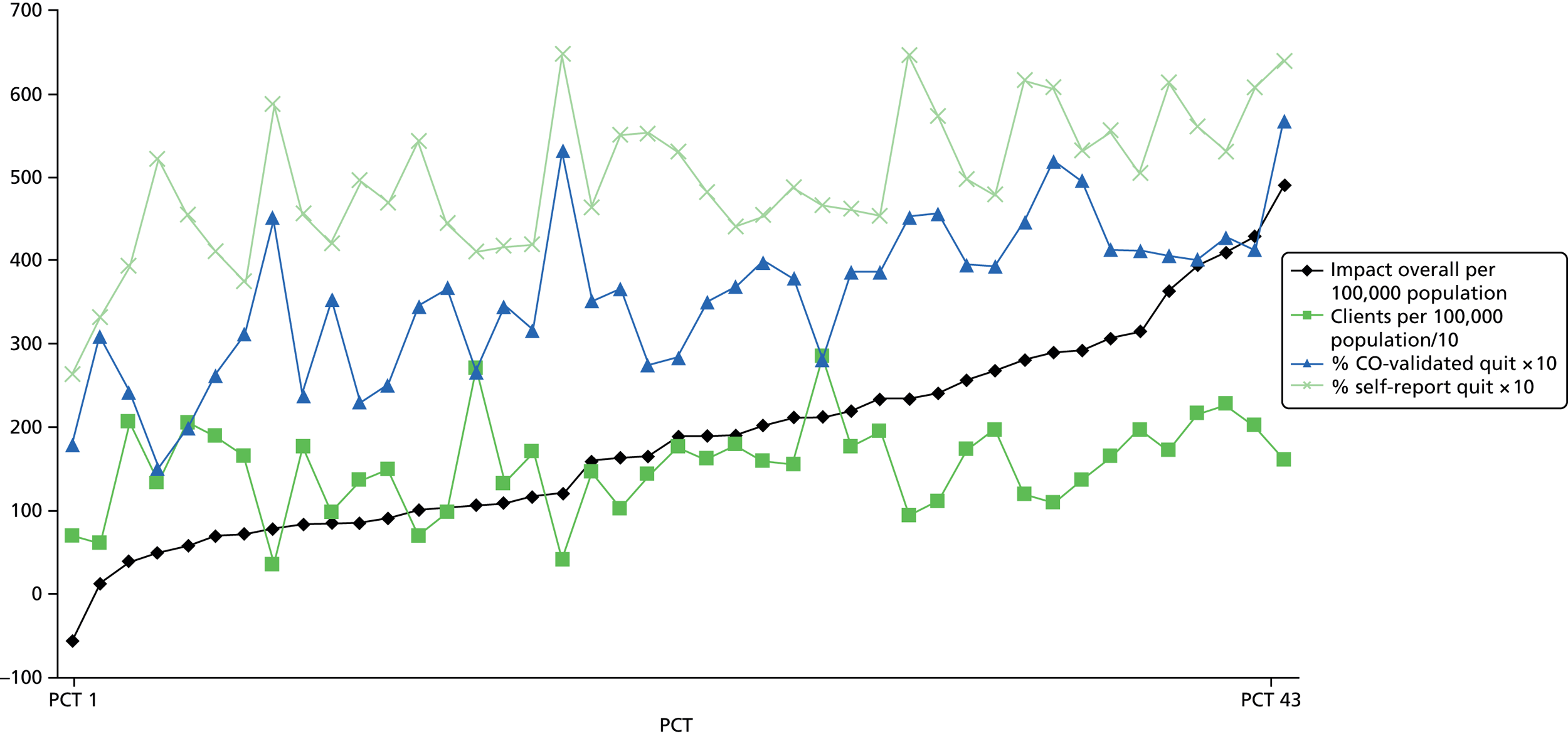
Summary statistics for unique clients (as opposed to client records) and impact in general were also calculated. There were 171,830 unique clients (note that unique clients could not be identified for three PCTs) and 157,479 clients where quit rates could be calculated (i.e. did not quit in December or June). The CO-validated quit rate of unique clients was 34.4%, the self-report quit rate was 49.8% and the CO-validation rate for clients who self-reported as quit was 73.3%. There were 169,909 unique clients aged ≥ 16 years altogether. The CO-validated quit rate for these clients was 34.5% and the self-report quit rate was 50.0%.
Impact rate summaries and correlations between impact rates throughput and quit rates were calculated for 40 PCTs for adults aged ≥ 16 years. The distribution of client records and unique clients among the PCTs were skewed, and quit rates and impact measures were normally distributed.
The median number of client records per PCT was 3713 (interquartile range 2101–5136) and the median number of unique clients was 3385 (interquartile range 2169–4603). There were 92.0% (interquartile range 89.7–94.7) of client records that referred to unique clients.
The mean quit rates for unique clients aged ≥ 16 years in the PCTs used for calculations were 36% (CO validated) and 50% (self-report) (Table 9). On average 1487 unique clients set a quit date per 100,000 population and 184 ex smokers per 100,000 population were added. If only CO-validated quits were taken into account there were 152 extra ex-smokers and if all self-report quits were included there were 216 extra ex-smokers.
| Measure | Mean (SD) | Correlation with throughput | Correlation with CO-validated impact | Correlation with self-report impact | Correlation with overall impact | ||||
|---|---|---|---|---|---|---|---|---|---|
| r | p-value | r | p-value | r | p-value | r | p-value | ||
| CO-validated quit | 35.9% (9.7%) | –0.204 | 0.207 | 0.845 | < 0.001 | 0.439 | 0.005 | 0.716 | < 0.001 |
| Self-report quit | 50.0% (8.9%) | –0.133 | 0.414 | 0.505 | 0.001 | 0.735 | < 0.001 | 0.675 | < 0.001 |
| Throughput | 1487 (521) | – | – | – | – | ||||
| Impact (CO validated) | 152 (144) | 0.218 | 0.177 | 1 | – | 0.657 | < 0.001 | 0.919 | < 0.001 |
| Impact (self-report) | 216 (131) | 0.450 | 0.004 | – | – | 1 | – | 0.901 | < 0.001 |
| Impact overall | 184 (125) | 0.361 | 0.022 | – | – | – | – | 1 | – |
Overall, impact was significantly positively associated with CO-validated quitting, self-report quitting and impact, taking into account either only CO-validated quits or taking into account all self-report quits. Throughput was not significantly associated with quitting or impact, taking into account CO-validated quits but it was significantly associated with impact taking into account all self-reported quits and overall impact. Thus, PCTs with a better throughput did have a higher increase in the number of self-reported smokers in the population but such PCTs were not CO validating sufficiently to be sure that the number of ex-smokers is increasing with a higher number of clients.
Impact and quitting
Two PCTs with particularly low CO-validated quit rates were reaching the highest proportion of smokers in their local area. It is therefore possible that these PCTs were focusing on reach at the expense of achieving quits. This was corroborated by the impact analysis.
The PCTs with the highest impact were generally those with high quit-rates and vice versa.
Socioeconomic status
Results presented in the published multivariable analysis26 showed that affluent smokers were more likely to be abstinent from smoking at 4 weeks post quit date than disadvantaged smokers as measured by either eligibility for free prescriptions or by occupational group (as measured by the NSSEC), for example adjusted odds ratio (aOR) 1.38 (95% CI 1.35 to 1.42) for clients who paid for prescriptions compared with those eligible for free prescriptions. In total, almost 80% of the service clients received one-to-one counselling but open group forms of behavioural therapy were more successful [main effect aOR 1.26 (95% CI 1.12 to 1.41)] except among some of the most disadvantaged clients (prisons and long-term unemployed). Closed groups were little deployed and they were not significantly more successful than one-to-one behavioural therapy after controls. Practitioner type did make a difference for some clients, with all but the most affluent less likely to be successful if they had been treated by a nurse compared with other types of practitioners, including smoking cessation specialists [main effect aOR 0.73 (95% CI 0.65 to 0.83)]. More details are found in the published paper. 26
Summary of key points
-
The estimated number of clients treated by SSSs from mid-2010 to mid-2011 was 5–10% of their smoking population.
-
The self-reported and CO-validated quit rates were 49% and 34% respectively at 4 weeks post quit date.
-
Smokers attempting to stop with NRT and minimal behavioural support have previously been estimated to have quit rates of 25% (for CO-validated quits) and 35% (for self-reported quits) at 4 weeks, so SSS interventions need to show rates higher than these and they should aim for rates of at least 50% for self-report and at least 35% for CO validated. 33,42
-
The lower CO-validation rate was likely to be the result of the CO-validation rate of self-report quits being below recommended levels (74% compared with the recommended 85%). 33 This was, however, slightly better than that reported for all PCTs in 2009/10 (69%). 33
-
The self-reported quit rate for all English SSSs from April 2010 to March 2011 was also 49%, with 70% of these CO validated43 compared with 74% in the current sample. Overall, 787,527 people set a quit date43 compared with the 202,084 client records in the QuitManager database used here. Thus, the North 51 PCTs that allowed their data for research purposes comprised roughly one-quarter of the total and have similar self-report quit and CO-validation rates. It must be noted that the self-report quit rate used was not as narrow as the DH quit rate regarding time of data collection but was more stringent in that it was an intention-to-treat analysis.
-
Highest quit rates were found among older people, men and clients with higher SES. January was the month with the highest number of quit dates set and the most successful quitters.
-
Affluent smokers were more likely to be abstinent from smoking at 4 weeks post quit date than disadvantaged smokers.
-
Varenicline and combination NRT were both used frequently and increased the chances of quitting compared with a single NRT product.
-
The majority (79%) of clients received one-to-one behavioural support. This type of support was significantly less successful than open rolling groups [aOR open groups 1.28 (95% CI 1.15 to 1.41) compared with one to one].
-
Clients who saw specialist practitioners had higher quit rates than those who saw other types of practitioners.
-
As a result of SSS treatment, the estimated number of ex-smokers per 100,000 population was 184 from mid-2010 to mid-2011.
Chapter 5 Prospective study: methods and analysis
This chapter describes the methods used in the prospective study element of the ELONS study, including the rationale, recruitment, sample and approach to data analysis. A particular focus of this chapter is recruitment challenges faced during this part of the research and strategies implemented by the research team to address these.
Rationale for the second element: prospective cohort study
Stop Smoking Services in England are not required to routinely collect data on longer-term cessation outcomes. Only outcomes 4 weeks after a client’s quit date are collected and reported. Furthermore, the routine data collected by SSSs are limited in scope, and the quality and quantity of data collected varies between service providers. Consequently, there was a need for a prospective cohort study to collect long-term (12-month) follow-up data and more detailed and consistent information on client and service characteristics. Data from the prospective study were used to fulfil study objectives 3, 4 and 5 of the ELONS study, to explore the relationship between client characteristics, treatment characteristics and longer-term abstinence from smoking.
Recruitment
Stop Smoking Service clients were eligible to be recruited to the ELONS study if they were aged 16 years or over and were not pregnant. In order to compare behavioural support types, initial power calculations suggested that we needed data from quit attempts made by 5000 individuals, with at least 370 quit attempts within each behavioural support type with 90% power and an average quit rate of 15%. This quit rate was based on the previous evaluation of long-term outcomes of the English services. 18
Recruitment to the ELONS study was a multistage process:
-
Secondary analysis of QuitManager data was conducted (see Chapter 3 and 4). The PCTs became the sampling frame of services. To achieve statistical power we initially approached services on the basis that they offered clients a range of behavioural support types. In order for our PCTs to be representative we also approached services with a range of short-term (4 week) quit rates and geographies (urban and rural areas, affluent and disadvantaged areas, and include areas from most regions of England).
-
Once services were identified within this sampling frame, a member of the research team made contact with the service commissioner and service manager to invite them to take part in the study.
-
After the service manager had agreed to participate, the research team obtained permission from the local PCT R&D department, and service support costs used to reimburse SSSs for staff time spent on the ELONS study were negotiated.
-
While this process was under way, the team liaised with services to decide whether to include only specialists or additionally include level 2 providers.
-
If it was decided that level 2 providers could be included, they needed to be approached individually (as each is a separate contractor, i.e. a pharmacy) to determine if they would take part.
-
Once participation of a service (and if relevant its linked level 2 practitioners) was confirmed, a study briefing was delivered to smoking cessation practitioners to enable them to recruit clients to the ELONS study.
-
After these elements were in place, stop smoking advisors recruited clients to the study. Inclusion criteria were all clients who were over 16 years old, were not pregnant and had set a quit date.
The recruitment process was aided considerably by the involvement of the PCRN staff, who helped us make initial contact with SSS managers and colleagues in R&D, promoted the study to level 2 providers, finalised service support costs and delivered study briefings. Two service managers (Northamptonshire and Rotherham) did not want their practitioners to be burdened with recruitment to the ELONS study or collecting the extra monitoring data. In these sites, PCRN-funded staff recruited clients, and collected client and treatment characteristics on paper forms. However, as PCRNs are organised by area and each have their own budget, the level of support available did vary across the nine ELONS study sites.
Recruitment challenges
Recruitment was a particular challenge for the prospective study. The initial hurdle was that the data collected in QuitManager did not consistently differentiate between behavioural support types. The main ambiguity was between one-to-one specialist practitioner support and level 2 support and, to a lesser extent, between one to one and drop-in. To overcome this, to some extent, the likely behavioural support range was checked with site managers when they were first contacted.
The second hurdle was securing the participation of SSSs as study sites. If services agreed to take part, this would involve SSS practitioners consenting clients to the study and collecting additional client and treatment data. This could be perceived as onerous in the context of limited appointment times and with local targets to meet. In addition, when we approached SSSs they were preparing for their busiest time of the year (post Christmas/New Year and No Smoking Day on 14 March. Moreover, local service funding was contracting in the face of NHS reforms and the move of public health from the NHS to Local Authorities in England (see Chapter 1). This led to some staff being made redundant or having their employment grade changed. Despite this, only three PCTs that the research team approached declined to participate in the study. The main reasons for declining were that they perceived available service support costs to be inadequate, it was an onerous consent process and there were factors related to service reorganisation.
Eight services were initially recruited to the study. From the numbers of clients attending these services recorded in the data set used for secondary analysis, it was thought that the target of 5000 participants (as set out in the original study proposal) would be achievable. However, the process of site recruitment took longer than expected (it was common for this process to take months rather than weeks): site managers needed to engage with colleagues and senior staff to explain what participation would involve before they could agree to take part; R&D permissions, liaison with local PCRN and service support cost calculation also were needed before a site could be confirmed as taking part and start recruitment. As a result of this, client recruitment started later than planned, after the busy New Year period had ended. In addition, the recruitment start date was staggered by site.
The third recruitment challenge was engaging with level 2 providers. As discussed previously, SSSs are delivered via specialist providers (their remit is purely smoking cessation) and level 2 providers such as GP practices, pharmacies and dentists (also called community providers) whose staff deliver smoking cessation in conjunction with their other responsibilities. Level 2 provision has grown over the past decade44 and thus it was important to involve these providers as well as specialists. Level 2 providers have different management arrangements to the specialist service, so each level 2 provider needed to be contacted separately. We therefore had to implement a recruitment strategy, which is summarised below (note there was some deviation between sites depending on the extent of SSS management commitment to the study, PCRN involvement and service support costs):
-
we identified which sites had level 2 service provision
-
we agreed with SSS managers whether or not we could approach their level 2 providers
-
where permission was granted, we publicised the study and letters were sent to all level 2 providers (via the SSS) to describe the evaluation and invite them to opt in by completing an ‘expression of interest form’ and returning in a reply paid envelope
-
to increase the number of providers, telephone calls were made by the research team and PCRN staff to practice managers and pharmacy managers/pharmacists from GP practices and pharmacies who had been active in the previous 6 months
-
a news article was added to the newsfeed page of QuitManager for each site, with instructions on how to register interest as a recruitment site
-
the research team and PCRN staff briefed the level 2 providers through lunchtime and early evening briefing events (with refreshment and buffet to encourage attendance) or individual face-to-face and telephone briefings for those who were unable to attend events.
Six sites recruited level 2 service providers. The number of individual providers recruited varied between 4 and 23.
The fourth challenge was obtaining informed consent. In order to secure PCRN help and to be able to reimburse SSSs for their time using service support costs, we asked the NHS Ethics Committee to classify the ELONS study as a research study rather than an audit or evaluation. This classification differed from that taken in ethical review processes for our previous national study of SSSs, conducted between 2001 and 2004. 18 In the earlier study, the National Institute for Health Research (NIHR) and PCRNs, etc., did not exist, there were no service support costs available and ethical requirements were arguably not as onerous. At that time we were permitted to merely add consent to take part in the research as a single question on existing service data collection sheets, but not for this study. For the ELONS study, the Research Ethics Committee required a consent form for each client with a section relating to each element of the study. Clients were asked to consent to each part. This procedure and the length of the consent form was undoubtedly a barrier to participation and SSSs reported that it resulted in serious time implications, which was the fifth recruitment barrier.
One of our study sites served as a within-study pilot and we tried out our recruitment methods there. This was Country Durham and Darlington, where we were able to estimate that the process of recruiting a client, seeking informed consent, asking the additional monitoring questions and collecting saliva samples added an additional 10–15 minutes to the appointment. This meant that the ELONS study added additional time to each consultation, which affected the number of people that the service could see. From a service manager perspective, this was of concern because they had local targets to meet (in terms of the number of clients they see and successful ‘quits’ at 4-week follow-up) with ongoing funding dependent on these targets being met. Some sites found this easier to manage than others, depending on how they delivered their service. Situations where there were particular problems included:
-
Groups where the consent process and collection of baseline data had to be done for all group members. With limited staff, this could take up the majority of a session.
-
One-to-one sessions where slots were doubled/triple booked because of a high did-not-attend rate in order to keep service busy. This meant the additional time required to recruit clients to the ELONS study was limited.
A sixth recruitment challenge was ‘buy-in’ from both the SSS practitioner and clients. The ELONS study mostly relied on practitioners to recruit clients and some were more confident and committed to this than others. This is an issue in any research study that recruits in routine practice. Some practitioners were genuinely interested in, and could see the value of, research and so made extra efforts to encourage their clients to consent to participate. Others were not so enthusiastic, or had more limited time. Client ‘buy-in’ was also an important issue for recruitment. Some practitioners, particularly pharmacy employees, reported that clients simply did not want to take part. Practitioner feedback suggests that the main reasons were that clients did not have time to go through the recruitment process (particularly for working people who scheduled appointments) or did not want to be contacted for follow-up (often older people).
A further challenge was failure to set quit dates. In the previous English longer-term evaluation,18 clients were included in a study only if they ‘set a quit date’ (i.e. gave the SSS a particular day when they were going to attempt to stop smoking). In some of the services, clients were recruited to the study when they registered with the SSS, which was sometimes before they set a quit date. Some of these clients never did set a quit date. Comparing the QuitManager prospective study extracts with the saliva samples database for the long-term NRT use study revealed further clients who had been initially recruited to the ELONS study (as they had provided saliva samples) but had been dropped from QuitManager owing to lack of progress with their quit attempt.
The last challenge was footfall. Several sites reported a general decrease in the number of people using their service during the study period. Analysis of the number of quit dates set over the recruitment period for the ELONS study (March 2012–March 2013) suggests that this was a reality. The number of quit dates set in SSSs in England for 2011/12 was 816,444 and in 2012/13 this has decreased by 11% to 724,247. 31 The decline continued after recruitment was completed, and much or at least some of this has been attributed to more smokers using electronic cigarettes (e-cigarettes) for cutting down or quitting rather than more established methods.
Strategies to address recruitment challenges
By late July 2012 it became clear that the client recruitment rate was considerably below the level that was expected from the previous English long-term evaluation, where up to 80% of clients in the two study areas had been recruited. 18 Various strategies were implemented to improve recruitment:
-
We negotiated further assistance from the PCRN/Clinical Research Unit and we were able to boost the number of level 2 providers.
-
A substantial amendment was submitted to the ethics committee requesting to simplify the consent form from six points, each of which the client was asked to initial, to three tick boxes. This request was approved (we initially asked for a move away from written to verbal consent which was rejected).
-
In order to support and motivate sites, we encouraged practitioners who were recruiting well to share their approach with their peers who were performing less well. We also supplied fortnightly updates to site leads with a breakdown of recruits by practitioner name so that they could monitor performance and discuss with staff when appropriate. Practitioners were sent a newsletter and either a mug or a pen with the ELONS study logo to both thank them and act as a reminder to keep recruiting.
-
A further two sites were approached to take part in the ELONS study. One of these, Hull and East Riding, agreed to take part.
-
Clients who had agreed to be recruited to the ELONS study but where there was no record of quit date set were included in the analysis.
-
We postponed the end of recruitment from the end of November 2013 to the end of January 2014 where sites were willing.
Sample
Despite efforts to boost recruitment, the challenges described above meant that our initial target baseline sample of 5000 (as set out in our original research proposal) was too ambitious. Therefore, in consultation with the chairperson of the NIHR Health Technology Assessment (HTA) Board and statistical practitioner we revised our sample size calculation to a more realistic target sample of 3000, which allowed us to maintain a sufficient level of power to detect meaningful effect sizes between the intervention groups (90% to 80% power).
The NIHR HTA agreed the revised sample size of 3000 and the study was also granted a 7-month extension to allow us to successfully recruit this number of participants.
The measures taken and the timing of measures are presented in Chapter 2 and Table 2.
Prospective study analysis
For the prospective study, seven stages of analysis were undertaken. These were:
-
preliminary analysis of short-term quit rates using unweighted data
-
comparison with the ‘all cases’ data set to develop weights
-
short- and longer-term unweighted and weighted quit rates
-
multivariable and multilevel logistic regression modelling of CO-validated abstinence at 4 weeks
-
multivariable logistic regression modelling of CO-validated abstinence at 52 weeks
-
adherence to treatment
-
comparison of longer-term quit rates with those in other evaluations.
Preliminary analysis of short-term quit rates using unweighted data
We present tables of 4-week quit rates for variables grouped into 10 key themes: location; demography; SES; health and well-being; smoking behaviour; support; behavioural support type; medication; introduction to the service; and finally, data collection variables. We also created crosstabulations of relationships between each variable and location, behavioural support type and sociodemographic characteristics, and results from these are referred to where relevant. These figures are not tabulated in this report, as they are very detailed, but are available on request.
Unless it is stated otherwise ‘quitting’ refers to CO-validated abstinence at 4 weeks. We have taken a finding to be significant at the traditional p < 0.05 level. Sometimes the chi-squared test result was invalid owing to low numbers of expected cases in cells, in which case significance was recorded as p = not available. For contingency (2 × 2) tables we could have used Fisher’s exact test but in practice most variables we used generated tables greater than 2 × 2.
Weighting
As the requirements for detailed consent (along with the other pressures on services outlined above) meant that it was not possible to recruit a high proportion of clients, weighting was undertaken to correct for non-response so that the quit rates would take into account any differences in important variables such as demographics between the ELONS study sample and the population. In order to create the weights, the ELONS study research team requested a QuitManager extract of all quit attempts (with quit dates) that took place at the nine study sites from March 2012 to March 2013 (the months where any ELONS study client set a quit date). All nine SSS managers gave permission for the data from their service to be made available. The database included the majority of the routine data that was collected by the sites but without identifying information. This database is referred to as ‘all cases’ in the remainder of the report.
The ‘all cases’ database was used to develop weights in order to calculate quit rates generalisable to the nine services that took part in the ELONS study. The weights were trimmed rim weights, which were provided by TNS BMRB. Rim weights are created using an iterative algorithm to ensure that the weight is the best fit to the proportions of various characteristics in the population. Trimming reduces the size of overly large weights so that they cannot go above a particular value. The weights were created using these variables: behavioural support type, age, gender and SES (measured by NSSEC). Note that the ‘other/unclear’ group of behavioural support in the ELONS study was too small for weighting so quit attempts in this group were redistributed to either the nearest group or the group of which they were most likely to be a member (three quit attempts to GP practice service and the remainder to one-to-one specialist). We also intended to weight for location (study site) but there were large differences in proportions recruited by location, which led to instability in the weighting and so the decision was made to exclude this, with behavioural support used to explain some of the differences by location. As an alternative, quit rates were calculated taking into account clustering by location.
Short- and longer-term weighted quit rates: variable definitions
Short- (4 week) and longer-term (52 week) raw and weighted CO-validated quit rates are presented for the variables that were significant predictors of 4-week quitting. Clients lost to follow-up were coded as still smoking, consistent with conducting an intention-to-treat analysis as set out in the Russell Standard. 30 The same rim weights were used for the 12-month quit rates as the 4-week quit rates to allow our estimates to be generalisable to the nine services that took part in the ELONS study.
Data were collected from all nine study sites. The behavioural support types used in the analysis were specialist closed groups, open groups, drop-ins and one-to-one sessions; GP practice, pharmacy service and other/unknown. Seasonality effects were analysed through the time of year that a quit attempt started. Quit attempts that started during the main summer holiday period, the post-summer holiday ‘back to school’ period and the New Year were differentiated from those starting at other times of year.
Demographic variables included age, gender and ethnicity. Age at first contact was included in the analysis as data were available for all respondents. Ethnicity was categorised as white British, other white, Asian (including mixed white and Asian) and other.
Socioeconomic status was measured through a count of the number of indicators of disadvantage. The indicators of disadvantage were routine and manual occupation/unemployed/permanently sick; no educational qualifications or highest qualification is General Certificate of Secondary Education or equivalent; eligible for free prescriptions; housing is rented and single parent (see Table 11) for details of these indicators. The variable was dichotomised into 0 to 1 indicators compared with two or more indicators.
Medication was operationalised by whether or not clients had taken varenicline at week 1. Combination NRT (using more than one NRT product concurrently) was not included because it was not associated with quitting in preliminary analysis. This is further discussed in Chapter 6, Adherence to treatment. This may be because one of the more successful sites and the only user of open groups used very little combination NRT. We could not explore this further because of multicollinearity between site and medication. Varenicline at week 1 was measured because abstinence from smoking was strongly associated with higher numbers of records of smoking medication and clients who had more records had more opportunity to change medication (see Chapter 6, Adherence to treatment).
For the element assessing well-being, following standard practice the WHO-5 Well-being Index45 items were converted to a percentage. Thus, a score of 0 indicates the lowest well-being and a score of 100 represents the highest well-being.
Initial analysis of dependence showed that high daily consumption of cigarettes and smoking within 5 minutes of waking were associated with low quit rates. However, the highest quit rates were associated with quitting between 6 and 60 minutes after waking (47–49% in preliminary analysis); quit rates of clients who smoked over 60 minutes after waking had quit rates similar to clients who smoked within 5 minutes of waking (42% and 41% respectively). Furthermore there was not a linear relationship between cigarettes smoked per day and quitting. Thus the Heaviness of Smoking Index was of only borderline significance in preliminary analysis and had a non-linear relationship with quitting. Thus concerns arose that the true importance of being dependent might be missed if the Heaviness of Smoking Index was used to represent dependence in the analysis, so instead a dichotomous variable was used: clients who smoked > 30 cigarettes per day or who smoked within 5 minutes of waking were coded as dependent and contrasted with all other clients.
Clients who were very or extremely determined to quit were differentiated from other clients. Clients who stated that their spouse or partner was supporting them during their quit attempt were also differentiated from other clients, as were clients who indicated that a half, a few or none of their friends and family smoked.
Multivariable predictors of quitting at 4 weeks in the prospective study
Multilevel logistic regression was conducted using MLwiN version 2.29. The dependent variable was CO-validated abstinence at 4 weeks. Weighting is not recommended in multilevel modelling, including variables where differential recruitment has occurred is preferred. 46 Thus all final models using prospective study data needed to include behavioural support types and locations.
Fixed effects
The fixed-effects variables are described in Short- and longer-term weighted quit rates: variable definitions.
Four other fixed effects were tested because preliminary bivariable analysis (see Chapter 6) suggested they might be of importance but were excluded from the final model:
-
Marital status (non-significant in multivariable analysis).
-
Practitioner had the ELONS study clients who did not set a quit date (non-significant in multi-variable analysis).
-
Saliva collected (non-significant in multivariable analysis).
-
Serious previous quit attempt with or without quitting aids (clients who had made a quit attempt in the last 12 months but had not used aids were less likely to quit than both those who had not made a quit attempt and those who had made a quit attempt with quitting aids. Owing to the non-intuitive results and the desire for simplicity, this variable was excluded).
Random effects
There were potentially five levels:
-
client quit attempt
-
client – only 22 clients were recruited to the ELONS study twice, so the client level was not included
-
practitioner
-
service provider – the models failed to run because of conflicts with practitioner and location
-
location – there was no significant level 2 variance as there were only nine locations, so location was included as a fixed effect.
Thus in the final models two levels were included: the first level was client quit attempt and the second level was practitioner. There were 234 practitioners in the prospective study and the median number of clients recruited was four.
Modelling
Modelling occurred in three stages. First, all fixed effects were entered into the model individually, second, all fixed effects were entered into the model simultaneously, and third, all fixed effects were entered into the model.
The model was then tested for multicollinearity by comparing the size of the CI when each variable was added individually with the CI when each variable was added simultaneously. 46 If the standard error increased by 50% or more multicollinearity was deemed to be present. 46 This did not occur.
Multivariable logistic regression modelling of carbon monoxide-validated cessation at 52 weeks
Initial multilevel modelling revealed that there was consistently no evidence of variance between practitioners (i.e. the practitioner made no difference to the chances of long-term quitting), so single level logistic regression modelling was undertaken using SPSS. All significant fixed effects at 4 weeks (analysis 2) were entered into the model and a backwards-stepwise method was used to eliminate non-significant variables. However, the a priori variables, behavioural support, location, time of year and sociodemographic variables, (with the exception of ethnicity) were kept in the model irrespective of statistical significance. Variables that did not reach statistical significance in the 4-week multivariate analyses (marital status, medical conditions, how introduced to the service) were then added to the model; however, none of these reached statistical significance in the multivariable model. Multicollinearity was tested by comparing the standard error in models with each variable added individually and simultaneously. If the standard error increased by 50% or more multicollinearity was present. This did not occur.
Adherence to treatment
Adherence – or continuing to attend SSSs – could not be included in multilevel modelling. This was owing to issues with direction of causality: it is not clear whether failure to adhere reduces the chances of quitting or whether clients relapse and then stop attending sessions and taking medication.
There were two measures of adherence collected in the prospective study: number of behavioural support sessions attended and number of occasions that medication was recorded. Sample distributions and weighted quit rates at 4 and 52 weeks were calculated for adherence, adherence and medication, and medication taken on any occasion and on the first occasion. Medication types included ‘single NRT’ (one form of NRT recorded), ‘combination NRT’ and varenicline. The other/mixed medication category included bupropion or clients who had taken more than one of the aforementioned medication types.
In an attempt to overcome issues with direction of causality we have followed work by Shiffman and colleagues47,48 and we have considered adherence prior to a person being abstinent. Thus we have analysed whether or not adherence was associated with 52-week quitting only in those who attained 4 weeks abstinence; we have assessed their attendance prior to 4 weeks using weighted means.
Comparing longer-term outcomes with those in other evaluations
Quit rates and follow-up rates in the ELONS study were compared with previous evaluations of SSSs in the UK. This type of comparison is not normally attempted or appropriate for observational studies, but was included here as the studies in question were conducted by the same research team and employed an almost identical research design. The previous studies were of two English services in 2002 (the ‘national evaluation’ in England described in the introduction to this report)17–19 and of pharmacy and group-based services in Glasgow in 2007. Raw data rather than weighted data are presented. This is because none of the three data sets include data from all SSSs in England – all collected data from a small number of locations. In addition, weights for the final percentage (CO-validated quit rate of those successfully followed-up) could not be calculated because not all clients were included in the denominator. Thus the only meaningful comparison is between the raw data from all three studies.
Chapter 6 Prospective study findings
This chapter presents findings from the prospective cohort study. Findings from the additional elements of the prospective cohort study (CSS, well-being and longer-term NRT) are presented in Chapters 7–9.
Sections of this chapter describe findings from the different stages of analysis conducted in the prospective study including:
-
analysis of short-term outcomes using unweighted data
-
comparing the ELONS study and the ‘all cases’ data sets
-
short- and longer-term quit rates
-
adjusted ORs from logistic regression of quitting in the short and long term
-
adherence with treatment
-
comparison of longer-term quit rates with those in other evaluations.
Analysis of short-term outcomes using unweighted data
This section describes the characteristics of the ELONS study clients, the types of support they received from services and how these were associated with stopping smoking in the short term (4 weeks after their quit date). Note: this material represents an early stage of work, using unweighted data, in order to inform further refining of the variables and multivariable analysis. Thus, these are not the main findings of our study.
Data were available from 3075 clients; there were, however, six participants that were excluded from this preliminary analysis because they were pregnant, leaving 3069 cases. Overall, at 4 weeks post quit date just over a half of study participants reported that they had quit smoking (56.6%). Most of these clients had their report of abstinence confirmed by CO validation – the 4-week CO-validated quit rate was 44%.
Note that chi-squared tests test only the significance of the greatest difference between categories: they cannot differentiate intermediate categories. For several variables, particularly those that were collected only for the ELONS study clients, it was the other/unknown category that was the least likely to quit. This was because clients who did not complete the ELONS study monitoring form often were those also who failed to engage properly with the service and many did not set a quit date. For these variables we therefore do not know whether or not the categories of interest differ significantly at this stage but we can assess if quit rates are in the expected direction.
Demographic characteristics
As Table 10 shows, short-term quit rates varied between clients with different characteristics.
| Demographic variables | n (N = 3069) | % | Self-report quit (%) | CO-validated quit (%) |
|---|---|---|---|---|
| Age (years) | ||||
| 16–24 | 330 | 10.8 | 41.2 | 24.9 |
| 25–34 | 676 | 22.0 | 53.4 | 38.2 |
| 35–44 | 760 | 24.8 | 55.5 | 41.8 |
| 45–54 | 631 | 20.6 | 59.0 | 47.5 |
| 55–64 | 458 | 14.9 | 65.3 | 57.2 |
| 65–85 | 214 | 7.0 | 69.2 | 60.8 |
| p-value | – | – | < 0.001 | < 0.001 |
| Gender | ||||
| Male | 1355 | 44.2 | 58.5 | 44.9 |
| Female | 1714 | 55.9 | 55.1 | 43.3 |
| p-value | – | – | = 0.60 | = 0.408 |
| Ethnicity | ||||
| White British | 2877 | 93.7 | 56.7 | 44.1 |
| Other white | 70 | 2.3 | 61.4 | 48.6 |
| Asian (including mixed white and Asian) | 64 | 2.1 | 46.9 | 26.6 |
| Black (including mixed white and black) | 24 | 0.8 | 54.2 | 41.7 |
| Other/unknown | 34 | 1.1 | 64.7 | 58.8 |
| p-value | – | – | = 0.393 | < 0.001 |
| Marital status | ||||
| Separated/divorced | 369 | 12.0 | 57.5 | 46.1 |
| Single (including widowed) | 684 | 22.3 | 50.4 | 36.8 |
| Married/living with partner | 1443 | 47.0 | 61.5 | 48.1 |
| Other/unknown | 573 | 18.7 | 51.3 | 40.8 |
| p-value | – | – | < 0.001 | < 0.001 |
Age
Smokers recruited in the study were from all age groups, but primarily 25–54 years (68%). The older a client, the more likely they were to stop smoking at 4 weeks (69% of 65- to 85-year-olds compared with 41% of 16- to 24-year-olds; p < 0.001). In addition, more of the older clients had their self-report of abstinence validated by CO breath test. For example, 41% of 16- to 24-year-olds reported that they had quit but only 25% were validated with a CO test, a gap of 16%. In contrast, the gap between self-report and CO-validated quits at 4 weeks was just 8% for clients aged 65–85 years (69% and 61% respectively).
Gender
Around a half of both males and females self-reported as quit at 4 weeks (58% and 55% respectively; p = 0.06) but there was no significant gender difference at 52 weeks.
Ethnicity
Most (94%) of the recruited population were white British, 2% were ‘other white’ ethnicities or Asian (including mixed Asian and white). About 1% were either black (or mixed black and white) or ‘other/unknown’. Clients in this final category were significantly more likely to quit than Asians (59% compared with 27%; p < 0.001) although the numbers are very small. There was no difference in self-reported quit rates possibly because of the gap between self-report and CO-validated quit rates for Asians. The majority of Asian clients (80%) were men.
Marital status
Clients who reported that they were married were more likely to have stopped smoking at 4 weeks (p < 0.001).
Socioeconomic status
Baseline data collection included a range of questions about SES; these are described below and presented in Table 11.
| SES | n (N = 3069) | % | Self-report quit (%) | CO-validated quit (%) |
|---|---|---|---|---|
| NSSEC | ||||
| Routine and manual | 941 | 30.7 | 59.4 | 46.3 |
| Intermediate | 284 | 9.3 | 58.5 | 44.0 |
| Managerial/professional | 434 | 14.1 | 65.4 | 51.2 |
| Retired | 344 | 11.2 | 69.2 | 59.0 |
| Home carer | 197 | 6.4 | 46.2 | 35.5 |
| Sick/disabled and unable to work | 220 | 7.2 | 50.0 | 36.8 |
| Never worked/long-term unemployed | 443 | 14.4 | 46.5 | 35.2 |
| Full-time student | 102 | 3.3 | 41.2 | 23.5 |
| Other/unknown | 104 | 3.4 | 40.4 | 31.7 |
| p-value | – | – | < 0.001 | < 0.001 |
| NSSEC (four category) | ||||
| Routine and manual | 941 | 30.7 | 59.4 | 46.3 |
| Managerial/professional and intermediate | 718 | 23.4 | 62.7 | 48.3 |
| Sick/disabled and never worked/long term | 663 | 21.6 | 47.7 | 35.8 |
| Other/unknown | 747 | 24.3 | 55.3 | 44.2 |
| p-value | – | – | < 0.001 | < 0.001 |
| Education | ||||
| None | 602 | 19.6 | 56.6 | 46.2 |
| GCSE or equivalent | 855 | 27.9 | 56.8 | 44.2 |
| Apprenticeship/vocational | 148 | 4.8 | 60.8 | 48.0 |
| A-level or equivalent | 316 | 10.3 | 60.8 | 44.6 |
| Degree or equivalent | 290 | 9.5 | 62.8 | 46.2 |
| Other/unknown | 858 | 28.0 | 52.1 | 40.6 |
| p-value | – | – | = 0.011 | = 0.231 |
| Eligibility for free prescriptions | ||||
| Eligible for free prescriptions | 1437 | 46.8 | 48.6 | 37.2 |
| Pays | 1081 | 35.2 | 63.6 | 48.0 |
| Outside 19–59 years age group/unknown | 551 | 18.0 | 63.9 | 53.9 |
| p-value | – | – | < 0.001 | < 0.001 |
| Housing tenure | ||||
| Private renting | 742 | 24.2 | 51.8 | 37.3 |
| Social/council renting | 753 | 24.5 | 49.1 | 39.0 |
| Buying on a mortgage | 789 | 25.7 | 65.3 | 51.7 |
| Own outright | 468 | 15.3 | 69.9 | 57.9 |
| Other/unknown | 317 | 10.3 | 44.8 | 31.6 |
| p-value | – | – | < 0.001 | < 0.001 |
| Household type | ||||
| Lone parenta | 232 | 7.6 | 48.3 | 38.4 |
| ≥ 2 adults and children | 912 | 29.7 | 57.6 | 41.7 |
| No children in household | 1839 | 59.9 | 58.2 | 46.7 |
| Other/unknown | 86 | 2.8 | 36.0 | 26.7 |
| p-value | – | – | < 0.001 | < 0.001 |
Occupation
Around one-third of clients (31%) reported working in routine and manual occupations, with other types of occupational group fairly evenly distributed. The best 4-week outcomes were found in the managerial/professional and retired groups (65% and 69% self-report compared with 51% and 59% CO validated, respectively). There was a significant difference between retired and other/unknown SES. Outcomes for full-time students were among the poorest and also had the largest gap between self-report and CO-validated quits (41% compared with 23%). This is not surprising considering that the majority of students will be under 24 years and similar outcomes were found when looking at 4-week outcome by age; 16- to 24-year-olds had the poorest outcomes. Only 20% of clients with professional, managerial and intermediate occupations reported having degrees, which seems low. In the general population, 30% women and 20% men have a degree. 49
Education
Highest educational qualification was an extra question added for the ELONS study, not required in routine monitoring. It was particularly poorly answered by most sites, with 28% missing overall. From the data available, there was no relationship between reported education and CO-validated quitting, although there was a relationship in the expected direction for self-report [i.e. better outcomes for clients with a degree than those with no qualifications (63% compared with 57%)] (p = 0.011).
Eligibility for free prescriptions
Clients who reported paying for prescriptions were more likely to have better 4-week outcomes than those who did not (64% compared with 49% self-report outcomes) but those whose eligibility was unknown or were outside the 19–59 years age range where eligibility reflects SES were most likely to quit (p < 0.001).
Housing tenure
Short-term quit rates were higher among homeowners compared with those reporting living in rented accommodation. Those buying outright were most likely to quit, which is likely to reflect age and those whose tenure was unknown were least likely, which is likely to reflect lack of engagement with the services (p <0 .001).
Lone parents
Of the sample, 80% stated that they were lone parents. Overall, lone parents had very low quit rates (36%). Of these lone parents, 16% were men (p < 0.001).
Health and well-being
A number of medical conditions can affect which stop smoking medications are appropriate for clients and, probably for this reason, data on health issues were well recorded by practitioners who completed monitoring forms with clients. Some key results are described here and presented in Table 12.
| Health and well-being variables | n (N = 3069) | % | Self-report quit (%) | CO-validated quit (%) |
|---|---|---|---|---|
| Any medical condition | ||||
| Has one or more medical condition(s) | 1725 | 56.2 | 57.3 | 45.3 |
| Has no medical condition | 1344 | 43.8 | 55.8 | 42.3 |
| p-value | – | – | = 0.414 | = 0.089 |
| Mental health condition(s)a | ||||
| Has mental health condition | 486 | 15.8 | 50.8 | 38.9 |
| Does not have mental health condition | 2583 | 84.2 | 57.7 | 45.0 |
| p-value | – | – | = 0.005 | = 0.014 |
| Heart/blood/circulation condition | ||||
| Has heart/blood/circulation condition(s) | 532 | 17.3 | 61.3 | 51.1 |
| Does not have heart/blood/circulation condition(s) | 2537 | 82.7 | 55.7 | 42.5 |
| p-value | – | – | = 0.017 | < 0.001 |
| All lung and respiratory illnessb | ||||
| Has lung and respiratory illness | 648 | 21.1 | 53.7 | 43.1 |
| Does not have any lung and respiratory illness | 2421 | 78.9 | 57.4 | 44.2 |
| p-value | – | – | = 0.090 | = 0.590 |
| Other conditionc | ||||
| Has other condition | 354 | 11.5 | 60.2 | 47.2 |
| Does not have any other condition | 2715 | 88.5 | 56.2 | 43.7 |
| p-value | – | – | = 0.153 | = 0.199 |
| Medical conditions limiting | ||||
| Severely limiting | 202 | 6.6 | 57.9 | 43.6 |
| Moderately limiting | 562 | 18.3 | 56.9 | 47.3 |
| No limiting effects | 961 | 31.3 | 57.3 | 44.5 |
| No medical condition | 1344 | 43.8 | 55.8 | 42.3 |
| p-value | – | – | = 0.867 | = 0.230 |
| Self-assessment of health | ||||
| Not good | 658 | 21.4 | 51.1 | 38.8 |
| Fairly good | 1325 | 43.2 | 56.5 | 44.6 |
| Good | 1003 | 32.7 | 61.9 | 47.4 |
| Unknown | 83 | 2.7 | 39.8 | 35.0 |
| p-value | – | – | < 0.001 | = 0.002 |
| WHO-5 Well-being Index | ||||
| Concerning level of well-being | 1646 | 53.6 | 55.1 | 41.9 |
| Good level of well-being | 1325 | 43.2 | 59.9 | 47.3 |
| Missing | 98 | 3.2 | 37.8 | 34.7 |
| p-value | – | – | < 0.001 | = 0.002 |
Medical conditions
Having a medical condition was not related to abstinence at 4 weeks and neither was having a more severe medical condition. This may be because the type of medical condition was important: clients who had a mental health condition were less likely to quit than those without (39% compared with 45%; p = 0.014) whereas clients with a heart, blood or circulation condition were more likely to quit than those without (51% compared with 43%; p < 0.001). There was no relationship for respiratory conditions or other medical conditions. Heart, blood and circulation conditions were 25 times more prevalent in the oldest age group than in the youngest age group (49% compared with 2%; p < 0.001). Mental health conditions were about twice as common among clients claiming sickness or unemployment benefits as among clients overall (29% compared with 15%; p < 0.001). Mental health conditions were about twice as prevalent in the 45–54 years age group as in the youngest and oldest age group (20% compared with 10% and 12% respectively; p = 0.003).
Self-assessed health and well-being
The ELONS study participants were also asked about their own perceptions of health and well-being. Interestingly, clients who chose not answer these questions had the lowest chances of stopping smoking. Thus we cannot tell from the chi-squared tests whether or not there were significant differences in quitting by self-assessed health or well-being.
Around two-fifths of people aged 45 years and younger assessed their health as good before age 45 years, compared with one-quarter of people aged 46 years and above (p < 0.001).
Over a half of the sample (54%) had a concerning level of well-being. A concerning level of well-being was more common in people who had a mental health condition (71% vs. 53%; p < 0.001). Clients receiving group-based treatment were more likely to have good levels of well-being than those receiving one-to-one treatment (51–55% vs. 41–44%; p < 0.001). Highest levels of well-being (about a half reporting good well-being) were found in the two youngest age groups. Lowest levels of good well-being (35%) were found in the 45–54 years age groups, who were also more likely than other age groups to have a mental health condition (p < 0.001). Well-being was similar among clients with professional/managerial/intermediate occupations and clients with routine and manual occupations (49% to 50%) but poorer among clients claiming sickness or unemployment benefits (35%; p < 0.001).
Smoking behaviour
Questions on smoking behaviour were centred on assessing nicotine dependence and motivation to stop smoking. The pattern of responses is shown in Table 13.
| Smoking behaviour variables | n (N = 3069) | % | Self-report quit (%) | CO-validated quit (%) |
|---|---|---|---|---|
| HSI tobacco dependence score | ||||
| 0 – little or no dependence | 144 | 4.7 | 67.4 | 49.3 |
| 1 – lower dependence | 194 | 6.3 | 60.8 | 43.3 |
| 2 | 363 | 11.8 | 60.3 | 44.6 |
| 3 | 834 | 27.2 | 61.4 | 48. |
| 4 | 839 | 27.3 | 53.3 | 41.8 |
| 5 | 487 | 15.9 | 51.3 | 42.7 |
| 6 – higher dependence | 179 | 5.8 | 46.4 | 36.9 |
| Missing | 29 | 0.9 | – | – |
| p-value | – | – | < 0.001 | = 0.049 |
| Smoking after waking | ||||
| ≤ 5 minutes | 1334 | 43.5 | 52.0 | 41.0 |
| 6–30 minutes | 1158 | 37.7 | 59.8 | 47.1 |
| 31–60 minutes | 290 | 9.4 | 62.4 | 48.6 |
| > 60 minutes | 268 | 8.7 | 60.8 | 42.2 |
| Missing | 19 | 0.6 | – | – |
| p-value | – | – | < 0.001 | = 0.007 |
| Cigarettes smoked per day | ||||
| ≤ 10 | 498 | 16.2 | 65.3 | 48.0 |
| 11–20 | 1634 | 53.2 | 56.6 | 43.4 |
| 21–30 | 695 | 22.7 | 54.7 | 45.5 |
| ≥ 31 | 230 | 7.5 | 44.8 | 35.7 |
| Other/unknown | 12 | 0.4 | 41.7 | 33.3 |
| p-value | – | – | < 0.001 | = 0.025 |
| Number of years smoked | ||||
| < 10 | 472 | 15.4 | 49.4 | 35.4 |
| 11–20 | 873 | 28.5 | 52.6 | 38.8 |
| 21–30 | 699 | 22.8 | 57.7 | 45.1 |
| 31–40 | 566 | 18.4 | 61.3 | 50.5 |
| > 40 | 438 | 14.3 | 66.9 | 58.0 |
| Missing | 21 | 0.7 | 14.3 | 14.3 |
| p-value | – | – | < 0.001 | < 0.001 |
| How determined to quita | ||||
| Not at all or quite determined | 263 | 8.6 | 43.4 | 30.0 |
| Very determined | 1183 | 38.6 | 54.5 | 42.4 |
| Extremely determined | 1557 | 50.7 | 61.7 | 48.6 |
| Unknown | 66 | 2.2 | 27.3 | 19.7 |
| p-value | – | – | < 0.001 | < 0.001 |
Smoking dependence
Of those who smoked ≤ 10 cigarettes per day, 65% reported that they were abstinent at 4 weeks in comparison with just 45% of those who smoked ≥ 31 cigarettes per day. There was not a linear relationship for the intermediate categories. Clients who smoked within 5 minutes of waking were least likely to quit by 4 weeks (41% compared with 42–49%; p < 0.001). However, the relationship was not linear. There were better outcomes for those who smoked the longest; 67% of those smoked for ≥ 40 years had quit, in comparison with just 49% of those who smoked for ≤ 10 years (p < 0.001). This variable is, however, strongly correlated with age and older people are more likely to be successful in stopping smoking. The sick/unemployed (p < 0.001), males (p = 0.002) and middle-age groups (p < 0.001) reported higher nicotine dependency than other groups.
Motivation
Over half (51%) of clients were extremely determined to quit and they had the highest quit rates, with 62% self-reported abstinence at 4 weeks. There were no SES or gender differences in determination to quit. As outlined above, clients in midlife were most dependent on tobacco (4–9% had the highest dependency score compared with 3% in the oldest and youngest age groups; p < 0.001) but were also the most determined to quit (50–54% compared with 44–47%; p = not available).
Support for the quit attempt
Participants were also asked about sources of support to stop smoking other than SSS staff, and about previous experience of smoking cessation. This included support from friends and family, work colleagues, number of previous quit attempts and previous use of pharmacotherapy. Results are summarised here and further detail is available in Table 14.
| Support variables | n (N = 3069) | % | Self-report quit (%) | CO-validated quit (%) |
|---|---|---|---|---|
| Smokers in the home | ||||
| Other smokers at home | 1266 | 41.3 | 55.1 | 42.5 |
| No one else smokes at home | 1619 | 52.8 | 58.5 | 45.4 |
| Missing | 184 | 6.0 | 50.5 | 41.9 |
| p-value | – | – | = 0.045 | = 0.247 |
| Friends and family smokers | ||||
| All smoke | 104 | 3.4 | 45.2 | 29.8 |
| Most smoke | 577 | 18.8 | 50.8 | 36.4 |
| About half smoke | 611 | 19.9 | 54.3 | 42.6 |
| A few smoke | 1424 | 46.4 | 60.9 | 48.0 |
| None smoke | 259 | 8.4 | 64.9 | 52.5 |
| Not applicable or missing | 94 | 3.1 | 33.0 | 30.9 |
| p-value | – | – | < 0.001 | < 0.001 |
| Work or study smokers | ||||
| All smoke | 60 | 2.0 | 46.7 | 25.0 |
| Most smoke | 300 | 9.8 | 55.0 | 42.7 |
| About half smoke | 396 | 12.9 | 60.4 | 45.2 |
| A few smoke | 926 | 30.2 | 60.0 | 45.9 |
| None smoke | 324 | 10.6 | 62.0 | 48.8 |
| Not applicable or missing | 1063 | 34.6 | 51.7 | 41.9 |
| p-value | – | – | < 0.001 | = 0.008 |
| Access to support | ||||
| Supporter available | 2669 | 87.0 | 54.7 | 44.6 |
| No one supporting | 322 | 10.5 | 58.5 | 42.9 |
| Missing | 78 | 2.5 | 34.6 | 26.9 |
| p-value | – | – | < 0.001 | = 0.007 |
| Family support | ||||
| Family supporting attempt | 1185 | 38.6 | 55.4 | 41.9 |
| No family support | 1806 | 58.9 | 58.4 | 46.1 |
| Missing | 78 | 2.5 | 34.6 | 26.9 |
| p-value | – | – | < 0.001 | < 0.001 |
| Friend support | ||||
| Friend supporting attempt | 561 | 18.3 | 54.9 | 41.5 |
| No friend support | 2430 | 79.2 | 57.7 | 45.1 |
| Missing | 78 | 2.5 | 34.6 | 26.9 |
| p-value | – | – | (< 0.001) | (= 0.003) |
| Spouse support | ||||
| Spouse supporting attempt | 1556 | 50.7 | 61.1 | 48.3 |
| No spousal support | 1435 | 46.8 | 53.0 | 40.3 |
| Missing | 78 | 2.5 | 34.6 | 26.9 |
| p-value | – | – | < 0.001 | < 0.001 |
| Colleague support | ||||
| Work colleague support attempt | 200 | 6.5 | 60.5 | 46.0 |
| No work support | 2791 | 90.9 | 57.0 | 44.3 |
| Missing | 78 | 2.5 | 34.6 | 26.9 |
| p-value | – | – | < 0.001 | = 0.008 |
| Number of previous attempts | ||||
| Serious previous quit attempt in the last year | 1253 | 40.8 | 57.2 | 44.0 |
| No serious quit attempt in last year | 1755 | 57.2 | 57.3 | 44.7 |
| Unknown | 61 | 2.0 | 24.6 | 24.6 |
| p-value | – | – | < 0.001 | = 0.008 |
| SSS attendance | ||||
| Attended SSS in LPA | 394 | 12.8 | 56.9 | 44.4 |
| Did not attend SSS in LPA | 859 | 28.0 | 57.4 | 43.8 |
| Missing | 1816 | 59.2 | 56.2 | 44.0 |
| p-value | – | – | = 0.846 | = 0.977 |
| Varenicline use | ||||
| Used varenicline in LPA | 347 | 11.3 | 62.5 | 48.1 |
| Did not use varenicline | 906 | 29.5 | 55.2 | 42.4 |
| Missing | 1816 | 59.2 | 56.2 | 44.0 |
| p-value | – | – | = 0.055 | = 0.187 |
| Previous use of over-the-counter NRT | ||||
| Used NRT over the counter in LPA | 281 | 9.2 | 59.8 | 44.8 |
| Did not use NRT bought over the counter | 972 | 31.7 | 56.5 | 43.7 |
| Missing | 1816 | 59.2 | 56.2 | 44.0 |
| p-value | – | – | = 0.530 | = 0.946 |
| Previous use of prescribed NRT | ||||
| Used NRT prescribed by GP in LPA | 232 | 7.6 | 57.8 | 46.1 |
| Did not use NRT prescribed by GP | 1021 | 33.3 | 57.1 | 43.5 |
| Missing | 1816 | 59.2 | 56.2 | 44.0 |
| p-value | – | – | = 0.846 | = 0.766 |
| Bupropion use | ||||
| Used bupropion in LPA | 17 | 0.6 | 64.7 | 58.8 |
| Did not use bupropion | 1236 | 40.3 | 57.1 | 43.8 |
| Missing | 1816 | 59.2 | 56.2 | 44.0 |
| p-value | – | – | = 0.706 | = 0.462 |
| Use of smoking helpline | ||||
| Used smoking helpline in LPA | 11 | 0.4 | 72.7 | 54.6 |
| Did not use smoking helpline | 1242 | 40.5 | 57.1 | 43.9 |
| Missing | 1816 | 59.2 | 56.2 | 44.0 |
| p-value | – | – | = 0.500 | = 0.777 |
| Use of support | ||||
| Used nothing in LPA | 208 | 6.8 | 45.2 | 33.2 |
| Used some form of support | 1045 | 34.1 | 59.6 | 46.1 |
| Missing | 1816 | 59.2 | 56.2 | 44.0 |
| p-value | – | – | = 0.001 | = 0.003 |
Social support
The best outcomes were found in clients who were not surrounded by smokers: 30% of clients who reported that all their friends and family were CO validated as quit at 4 weeks compared with 53% who reported that none of their friends or family members smoked (p < 0.001).
There was very little difference in quit rates between the 87% who had sources of support to stop and the 11% who did not. Clients who did not provide information about this type of support were less likely to quit – 27% compared with 43–45% (p = 0.007). Quit rates were slightly higher for clients who had a spouse/partner or work colleagues supporting their quit attempt and slightly lower for clients who had family or friends supporting their quit attempt. It was not possible to tell whether or not these differences were significant because those who did not provide any information about support were much less likely to quit.
Female participants were more likely than male participants to have other smokers in the home (43% vs. 39%; p = 0.007) and not to have support from a spouse/partner (53% vs. 41%; p < 0.001).
Previous serious quit attempt in the last year
Clients who did not answer questions about their previous quit attempt were less likely to quit (25%) but there was little difference between clients who had and had not made a quit attempt (44–45%). Those who had used some sort of support in their previous quit attempt (e.g. varenicline or the SSS) were significantly more likely to quit than those who had not (33% vs. 46%; p = 0.003).
Behavioural support
Behavioural support describes the format of counselling that participants received from the SSS (e.g. closed groups, open groups, drop-in and one to one) (Table 15).
| Behavioural support type variables | n (N = 3069) | % | Self-report quit (%) | CO-validated quit (%) |
|---|---|---|---|---|
| Practitioner level | ||||
| Level 2 | 379 | 12.4 | 48.0 | 38.7 |
| Specialist | 2679 | 87.3 | 58.0 | 45.2 |
| Missing | 11 | 0.4 | – | – |
| p-value | – | – | < 0.001 | = 0.001 |
| Support type | ||||
| Closed-group specialist | 102 | 3.3 | 52.9 | 43.1 |
| Open-group specialist | 550 | 17.9 | 61.6 | 53.0 |
| Drop-in specialist | 887 | 28.9 | 52.1 | 39.4 |
| One-to-one specialist | 1131 | 36.9 | 61.4 | 46.3 |
| GP practice service | 270 | 8.8 | 48.9 | 35.9 |
| Pharmacy service | 97 | 3.2 | 45.4 | 38.1 |
| Other or unclear | 32 | 1.0 | 40.6 | 21.9 |
| p-value | – | – | < 0.001 | < 0.001 |
| Intervention type | ||||
| Closed group | 102 | 3.3 | 52.9 | 43.1 |
| Open (rolling) group | 550 | 17.9 | 61.6 | 53.1 |
| Drop-in clinic | 887 | 28.9 | 52.1 | 39.4 |
| One-to-one support (any provider) | 1517 | 49.4 | 57.8 | 43.6 |
| Other | 10 | 0.3 | 50.0 | 20.0 |
| Missing | 3 | 0.1 | – | – |
| p-value | – | – | = 0.009 | < 0.001 |
| Practitioner type | ||||
| Specialist | 2679 | 87.3 | 58.0 | 45.2 |
| Health-care assistanta | 134 | 4.4 | 57.5 | 38.8 |
| Practice nurse | 120 | 3.9 | 40.0 | 32.5 |
| Assistant (pharmacy) | 35 | 1.1 | 40.0 | 28.6 |
| Dispenser/technician | 37 | 1.2 | 37.8 | 35.1 |
| Pharmacist/manager | 25 | 0.8 | 64.0 | 56.0 |
| Other | 27 | 0.9 | 48.2 | 40.7 |
| Missing | 12 | 0.4 | – | – |
| p-value | – | – | < 0.001 | = 0.0003 |
| Intervention setting | ||||
| Pharmacy | 121 | 3.9 | 45.5 | 37.2 |
| GP practiceb | 1592 | 51.9 | 57.7 | 43.8 |
| Community-oriented building | 634 | 20.7 | 59.0 | 47.2 |
| Well-being centre (e.g. healthy living centre) | 67 | 2.2 | 50.8 | 37.3 |
| Workplace or education | 161 | 5.3 | 59.6 | 49.1 |
| Children’s centre | 92 | 3.0 | 60.9 | 51.1 |
| Sports and leisure | 88 | 2.9 | 59.1 | 48.9 |
| Dedicated SSS shop or stall | 110 | 3.6 | 42.7 | 27.3 |
| Other | 204 | 6.7 | 52.0 | 41.7 |
| p-value | – | – | = 0.007 | = 0.003 |
| Sessions | ||||
| One session | 449 | 14.6 | 19.8 | 14.7 |
| Two sessions | 331 | 10.8 | 15.7 | 4.5 |
| Three sessions | 348 | 11.3 | 25.3 | 15.8 |
| Four sessions | 336 | 11.0 | 47.3 | 28.9 |
| Five sessions | 374 | 12.2 | 70.3 | 55.4 |
| Six sessions | 360 | 11.7 | 83.6 | 65.3 |
| Seven or eight sessions | 467 | 15.2 | 88.9 | 76.0 |
| Nine or more sessions | 374 | 12.2 | 97.3 | 84.5 |
| Unknown | 30 | 1.0 | 23.3 | 13.3 |
| p-value | – | – | < 0.001 | < 0.001 |
At the basic level, using the unweighted data, key findings (see Table 15) included:
-
more than 40% of clients who received three of the four ‘specialist’ type of behavioural support (closed group, open group, and one to one) were CO validated as quit
-
fewer than 40% of clients who received behavioural support in a GP practice or pharmacy setting, or who attended a specialist drop-in were CO validated as quit
-
open-group clients were the most likely to be CO validated as quit (53%; p < 0.001) but the self-report quit rates of one-to-one clients and open-group clients were similar (approximately 60%).
What might explain these patterns? There are a number of potential confounders:
-
Pharmacy clients were less likely to be prescribed varenicline (20% of pharmacy clients were prescribed varenicline compared with ≥ 40% for the other behavioural support types; p < 0.001).
-
Older clients were more likely to attend GP practices than other clients (12% of 65- to 85-year-olds received GP practice services compared with 6% of 16- to 17-year-olds), whereas younger clients were more likely to attend pharmacy services (5% of 16- to 17-year-olds received pharmacy services compared with 2% of 65- to 85-year-olds; p = 0.026).
-
Drop-in clients were likely to have a lower SES. Drop-in groups had the highest percentage of sick/unemployed clients (25% of drop-in clients were sick/unemployed compared with ≤ 24% of clients participating in other behavioural support types), clients eligible for free prescriptions (54% drop-in clients were eligible compared with ≤ 52% of clients in other behavioural support types; p < 0.001) and social rent (28% of drop-in clients were social renters compared with ≤ 25% of clients in other behavioural support types; p < 0.001).
-
Medication was more likely to be recorded on three or more occasions by specialists (46% of clients who received specialist support has medication recorded compared with 36% of clients who received GP or pharmacy services; p < 0.001).
-
Group clients had higher levels of well-being (51–55% of group clients had higher well-being scores compared with 41–45% of clients who received other behavioural support types; p < 0.001).
-
Clients of level 2 providers were less determined to quit (43% of clients who attended level 2 providers were extremely determined compared with 52% of specialist clients; p = 0.003) and were less likely to have a heart/blood/circulation condition (2% of level 2 clients compared with 8% of specialist clients; p = 0.002).
However, specialists were more likely to see clients with some characteristics associated with lower quit rates:
-
mental health condition (16% of specialist clients compared with 12% of level 2 clients; p = 0.041)
-
permanently sick/unemployed (23% of specialist clients compared with 14% of level 2 clients; p < 0.001)
-
high dependency on tobacco (6% of specialist clients compared with 5% of level 2 clients scored highest on dependence and 5% of specialist clients compared with 6% of level 2 clients scored lowest on the dependence scale (p = 0.007)
-
higher proportion of smokers among friends and family (23% compared with 16% all or most of friends and family smoke; p = 0.031).
Practitioner type
Clients were supported to stop by a range of types of practitioner working in for a number of different service providers (see Table 15).
-
Most clients (87%) were seen by a specialist practitioner.
-
About 8% of clients were seen by practice nurses and health-care assistants based in GP practices. Only two-thirds of people seen in a GP practice by a health-care practitioner who claimed to be quit were actually validated to be so.
-
About 3% of clients were seen by pharmacy practitioners.
-
Pharmacy practitioners had the most extreme quit rates (i.e. the highest and lowest), but altogether pharmacy practitioners recruited only 97 clients so subgroups are very small.
-
Clients who saw pharmacy assistants were least likely to be CO validated as quit, and clients who saw pharmacy managers or pharmacists were most likely to have a CO-validated quit compared with all other practitioner types (p = 0.0003).
-
-
One per cent of clients were seen by other types of practitioners. Most of these were GP practice staff who worked in roles such as administration and receptionists and/or those who worked in a general well-being improvement field such as health trainers and people working in healthy living centres. There were a few clients who were seen by dental practice staff.
Intervention setting
Clients were treated in a wide range of venues (see Table 15). Over a half of the ELONS study participants were seen in GP practices (52%) and one-fifth (21%) in a community-oriented building such as a community centre. Clients who attended sessions in a children’s centre were most likely quit (51%) and those who attended a dedicated SSS shop or stall were least likely to quit (27%; p =0 .003). However, this might reflect who was recruited from these settings:
-
Sick/unemployed people made up a higher proportion of clients seen at a dedicated SSS shop/stall (33% of a dedicated SSS shop/stall clients were sick/unemployed compared with ≤ 28% at other locations; p < 0.001).
-
A higher proportion of dedicated SSS shop/stall clients were in the youngest age group than was true for all other settings except for well-being centres (18% dedicated SSS shop/stall clients and 19% well-being centre clients compared with ≤ 11% at other locations; p < 0.001).
Session attendance
The more sessions a client attended, the better the 4-week outcome (97% of clients who attended at least nine sessions reported a quit at 4 weeks compared with just 16% of clients who attended two sessions; p < 0.001) (see Table 15). However, it should be noted that 11 of the 23 level 2 providers in site 1 used paper forms and these had to be returned to the specialist service after the 4-week quit outcome was recorded, which meant that not all sessions may have been recorded. In contrast, practitioners who entered data electronically at source could record up to 12 sessions. However, these paper-based providers recruited only 87 clients.
Medication
Practitioners recorded which smoking cessation medication their clients were taking to help them quit – this would normally happen during their behavioural support session. The derived variables from this information focused on frequency and type (Table 16).
| Medication variables | n (N = 3069) | % | Self-report quit (%) | CO-validated quit (%) |
|---|---|---|---|---|
| Medication (frequency of recording) | ||||
| No occasions | 93 | 3.0 | 24.7 | 17.2 |
| 1 occasion | 998 | 32.5 | 32.9 | 21.8 |
| 2 occasions | 616 | 20.1 | 46.8 | 32.1 |
| 3 occasions | 540 | 17.6 | 70.0 | 56.5 |
| 4 occasions | 471 | 15.4 | 88.5 | 74.5 |
| 5–10 occasions | 338 | 11.0 | 89.9 | 77.5 |
| Missing | 13 | 0.4 | – | – |
| p-value | – | – | < 0.001 | < 0.001 |
| Medication (frequency truncated) | ||||
| No occasions | 93 | 3.0 | 24.7 | 17.2 |
| 1 or 2 occasions | 1614 | 52.6 | 38.2 | 25.8 |
| 3–10 occasions | 1349 | 44.0 | 81.5 | 68.1 |
| Missing | 13 | 0.4 | – | – |
| p-value | – | – | < 0.001 | < 0.001 |
| Medication and occasions | ||||
| Single NRT only 1–2 occasions | 407 | 13.3 | 37.6 | 26.8 |
| Single NRT only 3 or more occasions | 189 | 6.2 | 81.5 | 73.5 |
| Combination NRT only 1–2 occasions | 448 | 14.6 | 30.1 | 15.9 |
| Combination NRT only 3 or more occasions | 125 | 4.0 | 79.2 | 67.2 |
| Varenicline only 1–2 occasions | 614 | 20.0 | 42.8 | 31.9 |
| Varenicline only 3 or more occasions | 699 | 22.8 | 85.3 | 69.4 |
| Other/mixed medication 1–2 occasions | 145 | 4.7 | 44.8 | 27.6 |
| Other/mixed medication 3 or more occasions | 336 | 11.0 | 74.4 | 62.5 |
| No medication recorded | 93 | 3.0 | 24.7 | 17.2 |
| Missing | 13 | 0.4 | – | – |
| p-value | – | – | < 0.001 | < 0.001 |
| Medication (type only) | ||||
| Single NRT only | 596 | 19.4 | 51.5 | 41.6 |
| Combination NRT only | 573 | 18.7 | 40.8 | 27.1 |
| Varenicline only | 1313 | 42.8 | 65.4 | 51.9 |
| Other/mixed medication | 481 | 15.7 | 65.5 | 52.0 |
| No medication recorded | 93 | 3.0 | 24.7 | 17.2 |
| Missing | 13 | 0.4 | – | – |
| p-value | – | – | < 0.001 | < 0.001 |
| Varenicline use | ||||
| Took varenicline | 1445 | 47.1 | 64.3 | 50.7 |
| Did not take varenicline | 1611 | 52.5 | 50.2 | 38.3 |
| Missing | 13 | 0.4 | – | – |
| p-value | – | – | < 0.001 | < 0.001 |
| Bupropion use | ||||
| Took bupropion | 32 | 1.0 | 53.1 | 31.3 |
| Did not take bupropion | 3024 | 98.5 | 56.9 | 44.3 |
| Missing | 13 | 0.4 | – | – |
| p-value | – | – | < 0.001 | = 0.002 |
| NRT combination use | ||||
| NRT combination | 962 | 31.4 | 52.1 | 38.8 |
| Did not take NRT combination | 2092 | 68.2 | 59.1 | 46.7 |
| Missing | 15 | 0.5 | – | – |
| p-value | – | – | < 0.001 | < 0.001 |
| NRT single use | ||||
| NRT single | 1003 | 32.7 | 58.7 | 47.2 |
| Did not take NRT single | 2051 | 66.8 | 56.0 | 42.8 |
| Missing | 15 | 32.7 | – | – |
| p-value | – | – | < 0.168 | < 0.024 |
| NRT patch use | ||||
| Used NRT patch | 1321 | 43.0 | 52.7 | 41.2 |
| Did not use NRT patch | 1735 | 56.5 | 60.1 | 46.5 |
| Missing | 13 | 0.4 | – | – |
| p-value | – | – | < 0.001 | < 0.001 |
| Lozenge use | ||||
| Took lozenge | 390 | 12.7 | 55.4 | 40.3 |
| Did not take Lozenge | 2666 | 86.9 | 57.1 | 44.8 |
| Missing | 13 | 0.4 | – | – |
| p-value | – | – | < 0.001 | < 0.001 |
| Gum use | ||||
| Took gum | 222 | 7.2 | 59.0 | 43.7 |
| Did not use gum | 2834 | 92.3 | 56.7 | 44.1 |
| Missing | 13 | 0.4 | – | – |
| p-value | – | – | < 0.001 | = 0.006 |
| Inhaler use | ||||
| Used inhaler | 545 | 17.8 | 48.4 | 36.9 |
| Did not use an inhalator | 2511 | 81.8 | 58.7 | 45.8 |
| Missing | 13 | 0.4 | – | – |
| p-value | – | – | < 0.001 | < 0.001 |
| Spray use | ||||
| Used spray | 303 | 9.9 | 50.5 | 35.3 |
| Did not use mouth/nasal spray | 2753 | 89.7 | 57.6 | 45.2 |
| Missing | 13 | 0.4 | – | – |
| p-value | – | – | < 0.001 | < 0.001 |
| Minitab | ||||
| Used Minitab | 30 | 1.0 | 53.3 | 40.0 |
| Did not use Minitab | 3026 | 98.6 | 56.9 | 44.2 |
| Missing | 13 | 0.4 | – | – |
| p-value | – | – | < 0.001 | = 0.005 |
Frequency
There was a lot of variation in number of days between sessions; bearing this in mind the following key points emerged from the data:
-
the more occasions that medication was recorded as being taken, the more likely clients were to quit [68% who had medication recorded on three or more occasions quit compared with 26% who took medication on one or two occasions and 17% where medication was not recorded (p < 0.001)]
-
younger people took medication on fewer occasions. Only 30% took medication on three or more occasions compared with 44% or more in the other age groups (p < 0.001).
Medication type
People who used combination NRT (taking two or more forms of NRT in the same week and never single NRT) were no more likely to quit than those using a single form of NRT. In fact, a much lower proportion were likely to achieve abstinence at 4 weeks (27% quit compared with 42% of people who took single NRT). Combination NRT varied between 66% and 3% between study sites (p < 0.001).
Varenicline was the most common type of medication (43% used at least once). Varenicline use also varied by study site (p < 0.001) and by NSSEC (33% sick/unemployed clients compared with 53% clients with routine and manual occupations and 51% clients with professional, managerial and intermediate occupations; p < 0.001). Only 1% took bupropion.
Type and frequency
Single NRT and combination NRT tended to be recorded on one or two occasions. Varenicline and other/mixed medication were more likely to be recorded on three or more occasions. Quit rates were approximately 32% or below if medications were recorded only on one or two occasions but were over 60% if they were noted on three or more occasions (p < 0.001). There were marked variations in medication type and frequency by study site.
Accessing services
At baseline, participants were asked questions about how they had accessed the service (Table 17).
| Accessing services | n (N = 3069) | % | Self-report quit (%) | CO-validated quit (%) |
|---|---|---|---|---|
| Introduction to the SSS | ||||
| Marketing | 154 | 5.0 | 52.6 | 42.9 |
| Friends and family | 317 | 10.3 | 53.6 | 38.9 |
| GP practice | 568 | 18.5 | 58.8 | 45.8 |
| Other organisations | 211 | 6.9 | 47.9 | 38.9 |
| Unknown | 202 | 6.6 | 54.5 | 42.1 |
| Previous quit attempt with services | 1617 | 52.7 | 58.3 | 45.4 |
| p-value | – | – | = 0.035 | = 0.150 |
| Mention of Stopober | ||||
| Mentioned Stoptober | 81 | 2.6 | 48.2 | 44.4 |
| No mention of Stoptober | 2988 | 97.4 | 56.9 | 44.0 |
| p-value | – | – | < 0.001 | = 0.933 |
Over half already knew of their SSS because they had made a previous quit attempt (53%). Only 5% of clients had heard about the service through marketing.
Men were more likely to be introduced by referral from a GP practice (21% compared with 17% of women; p < 0.001). The youngest age groups were most likely to be introduced through friends and family (22% compared with 11% or below for the other age groups; p < 0.001). ’Stoptober’ (a government-supported campaign to encourage smokers to quit for at least the month of October) was mentioned as a route into the service for 81 clients.
The quit rates were similar regardless of the route by which people got to the service.
Some data collection issues to consider
The way in which data are collected has the potential to influence the smoking cessation outcomes reported. Here we highlight this so that the prospective study results can be better understood. Four methodological issues are described: first, the time of year that the client set their quit date; second, clients not setting a quit date; third, the numbers of clients who were recruited to the ELONS study who had more than one quit attempt with the SSS; and fourth, whether or not clients provided a saliva sample at baseline (for analysis of long-term NRT use).
Clients in the ELONS study set quit dates between March 2012 and March 2013, as shown in Table 18. These were clustered, however, with most being set between July and November 2012. This reflects the staggered start and end of data collection for each site. There were 150 clients who did not set a quit date from only three of the nine sites. These locations collected monitoring information before clients were required to set a quit date and so needed to ask for consent to the ELONS study before they knew whether or not clients were going to get as far as actually setting a quit date. These clients were not excluded in the analysis – they form part of the prospective study data set.
| Data collection variables | n (N = 3069) | % | Self-report quit (%) | CO-validated quit (%) |
|---|---|---|---|---|
| Month quit date set | ||||
| March 2012 | 2 | 0.1 | 0.0 | 0.0 |
| April 2012 | 24 | 0.8 | 70.8 | 62.5 |
| May 2012 | 53 | 1.7 | 43.4 | 30.2 |
| June 2012 | 137 | 4.5 | 57.7 | 47.5 |
| July 2012 | 429 | 14.0 | 54.8 | 44.8 |
| August 2012 | 505 | 16.5 | 53.5 | 42.0 |
| September 2012 | 497 | 16.2 | 61.4 | 48.1 |
| October 2012 | 589 | 19.2 | 63.8 | 50.1 |
| November 2012 | 343 | 11.2 | 60.6 | 43.2 |
| December 2012 | 152 | 5.0 | 63.2 | 44.1 |
| January 2013 | 144 | 4.7 | 66.0 | 53.5 |
| February 2013 | 41 | 1.3 | 80.5 | 58.5 |
| March 2013 | 3 | 0.1 | 33.3 | 0.0 |
| Missing quit date | 150 | 4.9 | 0.00 | 0.0 |
| p-value | – | – | < 0.001 | < 0.001 |
| Saliva collection | ||||
| Saliva collected | 1874 | 61.1 | 54.5 | 41.5 |
| Saliva not collected | 1195 | 38.9 | 60.0 | 48.0 |
| p-value | – | – | = 0.003 | < 0.001 |
There were 22 clients, from five of the nine sites, who were recruited twice to the ELONS study. This means they had more than one quit attempt with the service during the study period – they were ‘repeat’ attenders (this is not shown in Table 18).
Two-thirds of clients gave a saliva sample, as Table 18 illustrates. These clients were significantly less likely to quit at 4 weeks. Younger clients were more likely to give a saliva sample (68% compared with 55% and 57% for the two oldest age groups).
Comparing the ELONS study and ‘all cases’ data sets
The final ELONS study sample consisted of 3057 SSS clients, once pregnant clients and clients whose advisor was unclear had been excluded. For the reasons described in Chapter 5, these participants represented a small proportion of those who accessed SSSs in the study areas during the recruitment period. The sample is therefore not representative of all service clients in those areas. This is important as the ELONS study was designed to try and draw some overall conclusions about the longer-term effectiveness of the support to stop smoking offered by services in England. As a first stage in the analysis, therefore, we conducted comparisons between the ELONS study data and that available for all service clients, drawn from the routine (QuitManager) data available for each site.
The ‘all cases’ database contained quit attempts with quit dates that took place at the nine study sites from March 2012 to March 2013 (the months where any ELONS study client set a quit date; n = 71,800). Quit attempts where the client was pregnant, under the age of 16 years or were a prisoner who attended the specialist service were excluded because these clients were not recruited to the ELONS study (n = 65,972). Additionally, to be consistent with the final ELONS study sample, quit attempts where the practitioner was unknown were also excluded (n = 65,937). Thus, 5% of qualifying quit attempts that were made in the nine study sites were included in the ELONS study. However, because the recruitment period for each site was variable, if we just look at periods when the specialists and level 2 providers were actually recruiting, 9% of quit attempts were included in the ELONS study. Recruitment rates were higher for the specialist service (14%) than the level 2 providers (2%) at least partly because not all level 2 providers took part and those that did recruited for different periods.
The ‘all cases’ database was used to develop weights in order to calculate quit rates generalisable to the nine services that took part in the ELONS prospective study. The frequencies of the variables included and response rates are provided in Table 19. The response rate was the number of ELONS study clients divided by the number of all cases clients multiplied by 100.
| Variables | ‘All cases’, n | ELONS, n | Response rate (%) |
|---|---|---|---|
| Behavioural support | |||
| Closed-group specialist | 541 | 102 | 18.9 |
| Open-group specialist | 2159 | 550 | 25.5 |
| Drop-in specialist | 11,308 | 887 | 7.8 |
| One-to-one specialist | 21,796 | 1131 | 5.2 |
| Level 2 GP practice | 16,412 | 269 | 1.6 |
| Level 2 pharmacy | 9821 | 97 | 1.0 |
| Other or unclear | 3900 | 21 | 0.5 |
| Gender | |||
| Female | 34,955 | 1710 | 4.9 |
| Male | 30,982 | 1347 | 4.3 |
| Age group (years) | |||
| 16–24 | 7120 | 327 | 4.6 |
| 25–34 | 13,226 | 673 | 5.1 |
| 35–44 | 15,338 | 758 | 4.9 |
| 45–54 | 13,851 | 629 | 4.5 |
| 55–64 | 9933 | 456 | 4.6 |
| ≥ 65 | 6469 | 214 | 3.3 |
| NSSEC | |||
| Routine and manual occupations | 18,201 | 939 | 5.2 |
| Managerial/professional and intermediate occupations | 14,098 | 716 | 5.1 |
| Sick/disabled and never worked/long-term unemployed | 14,932 | 660 | 4.4 |
| Other/unknown | 18,706 | 742 | 4.0 |
| Total | 65,937 | 3057 | 4.6 |
Clustering by service also had to be taken into account when producing final quit rates. This was because different locations offered different behavioural support types and some sites we were not able to recruit clients accessing some behavioural support types. The overall profiles of the ELONS study clients behavioural support types, however, strongly reflected ‘all cases’ behavioural support types. This is illustrated in Figure 6, which compares the behavioural support in each site the ‘all cases’ data set with the behavioural support types of clients recruited to the ELONS prospective study.
FIGURE 6.
Distribution of behavioural support by location in the routine monitoring data and clients recruited to the prospective study.

Short- and longer-term quit rates
The main results for the ELONS study are the short- and longer-term cessation rates achieved by participants in the prospective study. The CO-validated raw quit rate at 4 weeks was 44.1% but after weighting this reduced marginally to 41.2% (95% CI 34.9% to 47.9%). The raw quit rate in the longer term, at 1 year, was 9.3% but after weighting this reduced marginally to 7.7% (95% CI 6.6% to 9.0%). The weighted results are shown in Table 20. These also include the proportion of people who had relapsed to smoking at 4 and 52 weeks post quit date, and also those lost to follow-up. Participants who were lost to follow-up (22.6% at 4 weeks and 45.2% at 52 weeks) were assumed to be smoking, consistent with an intention-to-treat analysis.
| Short- and longer-term weighted quit status | Weighted (%) (95% CI) |
|---|---|
| Short-term quit status (4 weeks) | |
| CO validated | 41.3 (34.9 to 48.0) |
| Self-report not CO validated | 12.2 (8.3 to 17.5) |
| Relapsed (including quit refuted by CO validation) | 23.9 (15.8 to 34.5) |
| Lost to follow-up | 22.6 (15.1 to 32.4) |
| Longer-term quit status (52 weeks) | |
| CO validated | 7.7 (6.6 to 9.0) |
| Self-report not CO validated | 5.6 (5.1 to 6.1) |
| Relapsed at 4 or 52 weeks (including quit refuted by CO validation) | 41.6 (31.0 to 53.0) |
| Lost to follow-up at 4 or 52 weeks | 45.2 (34.6 to 56.2) |
We also examined differences in short- and longer-term cessation outcomes by key variables of interest, including client and service characteristics (Table 21). Quit rates in the short and longer term did vary between groups of clients with particular characteristics, and the type of support provided by the SSSs.
| Key variables | n | % | 4 weeks (95% CI) | 52 weeks (95% CI) |
|---|---|---|---|---|
| Behavioural support | ||||
| Closed-group specialist | 102 | 3.3 | 42.9 (28.6 to 58.6) | 13.8 (8.7 to 21.3) |
| Open-group specialist | 550 | 18.0 | 53.1 (36.4 to 69.1) | 11.6 (6.5 to 20.1) |
| Drop-in specialist | 887 | 29.0 | 39.6 (24.3 to 57.2) | 7.6 (5.1 to 11.0) |
| One-to-one specialist | 1131 | 37.0 | 46.1 (39.5 to 52.8) | 10.2 (7.6 to 13.7) |
| GP practice service | 269 | 8.8 | 36.1 (26.2 to 47.3) | 5.1 (2.9 to 8.8) |
| Pharmacy service | 97 | 3.2 | 38.2 (18.7 to 62.5) | 5.2 (1.5 to 15.8) |
| Other or unclear | 21 | 0.7 | NA | NA |
| Behavioural support (truncated) | ||||
| Group specialist | 652 | 21.3 | – | 12.1 (10.5 to 13.8) |
| Drop-in specialist | 887 | 29.0 | – | 7.6 (5.1 to 11.0) |
| One-to-one specialist | 1131 | 37.0 | – | 10.2 (7.6 to 13.7) |
| GP practice or pharmacy service | 366 | 12.0 | – | 5.1 (2.8 to 9.3) |
| Other or unknown | 21 | 0.7 | – | NA |
| Time of year of quit attempt | ||||
| Other months | 767 | 25.1 | 39.4 (33.6 to 45.5) | 7.0 (5.2 to 9.4) |
| Summer – July and August | 970 | 31.7 | 38.0 (31.4 to 45.0) | 6.3 (4.4 to 8.9) |
| Back to school – September and October | 1128 | 36.9 | 46.2 (37.8 to 54.8) | 8.7 (6.4 to 11.7) |
| New Year – January and February | 192 | 6.3 | 37.8 (24.5 to 53.3) | 13.1 (5.1 to 29.6) |
| Age (years) (weighted mean) a | ||||
| Not quit mean | – | – | 41.1 (40.1 to 42.0) | 43.3 (42.5 to 44.1) |
| Quit mean | – | – | 47.2 (46.0 to 48.3) | 46.8 (44.4 to 49.2) |
| Gender | ||||
| Female | 1710 | 55.9 | 40.1 (35.3 to 45.1) | 7.2 (6.0 to 8.5) |
| Male | 1347 | 44.1 | 42.5 (33.4 to 52.2) | 8.4 (6.8 to 10.2) |
| Ethnicity | ||||
| White British | 2866 | 93.8 | 41.6 (35.7 to 47.8) | 7.4 (6.1 to 9.0) |
| Other white | 69 | 2.3 | 39.9 (18.2 to 66.3) | 11.5 (4.5 to 26.0) |
| Asian (including mixed white and Asian) | 64 | 2.1 | 25.1 (13.9 to 41.0) | 3.6 (1.3 to 9.5) |
| Other and unknown | 58 | 1.9 | 40.3 (17.5 to 68.3) | 21.6 (7.0 to 50.1) |
| SES | ||||
| 0–1 indicators of low SES | 1123 | 36.7 | 48.4 (38.5 to 58.4) | 10.3 (8.4 to 12.7) |
| 2–5 indicators of low SES | 1934 | 63.3 | 37.1 (30.2 to 44.6) | 6.2 (5.0 to 7.7) |
| WHO-5 Well-being Index (weighted mean) a | ||||
| Not quit mean | – | – | 51.6 (50.0 to 53.2) | 52.7 (51.4 to 53.9) |
| Quit mean | – | – | 55.5 (53.8 to 57.1) | 59.3 (56.5 to 62.1) |
| Medication in week 1 | ||||
| Varenicline not recorded | 1661 | 54.3 | 37.0 (31.7 to 42.7) | 6.2 (4.9 to 7.7) |
| Took varenicline | 1396 | 45.7 | 47.4 (39.1 to 55.8) | 10.0 (7.2 to 13.8) |
| Dependence | ||||
| Other | 1681 | 55.0 | 45.4 (40.3 to 50.6) | 9.8 (7.7 to 12.4) |
| Highly dependent | 1376 | 45.0 | 35.7 (26.1 to 46.6) | 4.9 (2.9 to 8.2) |
| Determination to quit | ||||
| Other | 328 | 10.7 | 26.6 (20.9 to 33.2) | 5.9 (4.3 to 8.0) |
| Very/extremely determined | 2729 | 89.3 | 43.0 (36.0 to 50.4) | 8.0 (6.7 to 9.5) |
| Support from spouse partner | ||||
| Other | 1507 | 49.3 | 38.5 (32.3 to 45.1) | 6.2 (4.5 to 8.5) |
| Support from spouse/partner | 1550 | 50.7 | 43.9 (37.0 to 51.0) | 9.2 (7.4 to 11.3) |
| Friends and family | ||||
| Other | 771 | 25.2 | 33.3 (27.5 to 39.7) | 3.4 (2.6 to 4.4) |
| Half or fewer smoke | 2286 | 74.8 | 43.7 (36.9 to 50.8) | 9.1 (7.5 to 10.9) |
| Total | 3057 | 100.0 | 41.2 (34.9 to 47.9) | 7.7 (6.6 to 9.0) |
Client characteristics and abstinence
In the short term, at 4 weeks, quit rates were higher among older people and clients with higher levels of well-being. There were no significant gender, socioeconomic or ethnic differences. Differences in medication, dependence on tobacco, social network and support from a spouse or partner did not reach significance for short-term quit rates. However, quit rates were higher among those who were more determined to quit.
In the longer term, at 52 weeks, quit rates were higher among older people [mean age of quitters 46.8 years (95% CI 44.4 to 49.2 years) compared with a mean age of 43.3 years (95% CI 42.5 to 44.1 years) for non-quitters]. Less-disadvantaged people had a quit rate of 10.3% (95% CI 8.4% to 12.7%) compared with a quit rate of 6.2% (95% CI 5.0% to 7.7%) among more-disadvantaged people. Clients with higher levels of well-being when they began their quit attempt were more likely to quit than those with lower well-being [mean well-being score was 59.3 out of 100 (95% CI 56.5 to 62.1) compared with 52.7 out of 100 (95% CI 51.4 to 53.9) for non-quitters]. There were no significant gender or ethnic differences. Likewise, at 52 weeks, differences in medication, dependence on tobacco, determination to quit and support from a spouse or partner did not quite reach significance. Quit rates were higher among those whose social network was less populated with smokers, 9.1% (95% CI 7.5% to 10.9%) compared with 3.4% (95% CI 2.6% to 4.4%).
Service characteristics, timing and abstinence
In the initial analysis, we differentiated six forms of behavioural support offered by services. These were closed and open specialist groups, specialist drop-ins, one-to-one specialist and behavioural support provided by GP practice employees and pharmacy employees. CIs overlapped for all forms of support but there were only about 100 clients who received closed group support or pharmacy service support leading to very wide CIs. Initially, the sample design was powered so that the smallest group size was 100 and the next group size was 500. Furthermore, the power calculations were based on a quit rate of 15% rather than 8%. Thus, CI overlap could be because of lack of power because both closed groups and pharmacies consisted only of about 100 clients. As Table 21 shows, quit rates for both forms of group support were similar and were higher than other forms of support, and quit rates for non-specialist services were similar and lower than other forms of support groups. Thus some behavioural support groups were merged for the 52-week analysis. Clients who received group support had significantly higher quit rates, 12.1% (95% CI 10.5% to 13.8%) compared with clients who received support from a GP practice or pharmacy service, 5.1% (95% CI 2.8% to 9.3%). Clients who received one-to-one or drop-in specialist support quit rates were intermediate, 10.2% (95% CI 7.6% to 13.7%) and 7.6% (95% CI 5.1% to 11.0%), respectively. At 52 weeks, there were no significant seasonality effects.
Multivariable predictors of abstinence in the short term
Multivariable logistic regression was undertaken in order to better understand which characteristics of clients and services were most closely related to abstinence from smoking after taking other factors into account at 4 and 52 weeks. These results are shown in Table 22.
| Key variables | n (N = 3057) | % | 4 weeks (95% CI) | 52 weeks (95% CI) |
|---|---|---|---|---|
| Behavioural support | ||||
| Closed-group specialist | 102 | 3.3 | 0.9 (0.6 to 1.5) | N/A |
| Open-group specialist | 550 | 18.0 | 1.5 (1.0 to 2.2) | N/A |
| Drop-in specialist | 887 | 29.0 | 0.7 (0.6 to 0.9) | N/A |
| One-to-one specialist | 1131 | 37.0 | 1 | N/A |
| GP practice service | 269 | 8.8 | 0.8 (0.5 to 1.3) | N/A |
| Pharmacy service | 97 | 3.2 | 0.9 (0.6 to 1.6) | N/A |
| Other or unclear | 21 | 0.7 | 0.6 (0.2 to 1.7) | N/A |
| Behavioural support (truncated) | ||||
| Group specialist | 652 | 21.3 | N/A | 3.4 (1.7 to 6.7) |
| Drop-in specialist | 887 | 29.0 | N/A | 1.7 (0.9 to 3.5) |
| One-to-one specialist | 1131 | 37.0 | N/A | 2.3 (1.2 to 4.6) |
| GP practice or pharmacy service | 366 | 12.0 | N/A | 1 |
| Other or unknown | 21 | 0.7 | N/A | 2.3 (0.5 to 11.6) |
| Time of year of quit attempt | ||||
| Other months | 767 | 25.1 | 1 | 1.2 (0.8 to 1.7) |
| Summer – July and August | 970 | 31.7 | 1.2 (1.0 to 1.5) | 1 |
| Back to school – September and October | 1128 | 36.9 | 1.4 (1.1 to 1.7) | 1.2 (0.9 to 1.6) |
| New Year – January and February | 192 | 6.3 | 1.5 (1.1 to 2.2) | 1.7 (1.0 to 2.9) |
| Age (in years) | – | – | 1.032 (1.026 to 1.039) | 1.011 (1.002 to 1.020) |
| Gender | ||||
| Female | 1710 | 55.9 | 1 | 1 |
| Male | 1347 | 44.1 | 1.1 (0.9 to 1.3) | 1.2 (0.9 to 1.5) |
| Ethnicity | ||||
| White British | 2866 | 93.8 | 1.3 (0.7 to 2.4) | Did not enter |
| Other white | 69 | 2.3 | 2.5 (1.1 to 5.5) | Did not enter |
| Asian (including mixed white and Asian) | 64 | 2.1 | 1 | Did not enter |
| Other and unknown | 58 | 1.9 | 2.4 (1.1 to 5.6) | Did not enter |
| SES | ||||
| 0–1 indicators of low SES | 1123 | 36.7 | 1.3 (1.1 to 1.6) | 1.4 (1.1 to 1.9) |
| 2–5 indicators of low SES | 1934 | 63.3 | 1 | 1 |
| WHO-5 Well-being Index (weighted mean) | – | – | 1.004 (1.000 to 1.007) | 1.007 (1.001 to 1.013) |
| Medication in week 1 | ||||
| Varenicline not recorded | 1661 | 54.3 | 1 | 1 |
| Took varenicline | 1396 | 45.7 | 1.6 (1.4 to 1.9) | 1.7 (1.3 to 2.3) |
| Dependence | ||||
| Other | 1681 | 55.0 | 1.3 (1.1 to 1.5) | 1.5 (1.1 to 1.9) |
| Highly dependent | 1376 | 45.0 | 1 | 1 |
| Determination to quit | ||||
| Other | 328 | 10.7 | 1 | Did not enter |
| Very/extremely determined | 2729 | 89.3 | 2.3 (1.7 to 3.0) | Did not enter |
| Support from spouse partner | ||||
| Other | 1507 | 49.3 | 1 | 1.0 |
| Support from spouse/partner | 1550 | 50.7 | 1.3 (1.1 to 1.5) | 1.4 (1.0 to 1.8) |
| Friends and family | ||||
| Other | 771 | 25.2 | 1 | 1.0 |
| Half or fewer smoke | 2286 | 74.8 | 1.2 (1.0 to 1.5) | 2.0 (1.4 to 2.9) |
| Practitioner | – | – | Variance = 0.140 (SE = 0.049) | No variance identified |
Looking first at the 4-week predictors, shown in Table 22, clients who attended open groups had the highest ORs of quitting in the short term, at 4 weeks, aOR 1.5 (95% CI 1.0 to 2.2). Clients who attended open groups were significantly more likely to quit than clients who attended specialist one-to-one sessions. Cessation at 4 weeks was associated with: attending services in the New Year, aOR 1.5 (95% CI 1.1 to 2.2); older age, aOR 1.032 (95% CI 1.026 to 1.039); affluence, aOR 1.3 (95% CI 1.1 to 1.6); white (non-British) compared with Asian, aOR 2.5 (95% CI 1.1 to 5.5); lower dependence on tobacco, aOR 1.3 (95% CI 1.1 to 1.5); determination to quit, aOR 2.3 (95% CI 1.7 to 3.0); taking varenicline, aOR 1.6 (95% CI 1.4 to 1.9); higher levels of well-being, aOR 1.004 (95% CI 1.000 to 1.007); support from a spouse or partner, aOR 1.3 (95% CI 1.1 to 1.5); or low levels of smoking among friends and family, aOR 1.2 (95% CI 1.0 to 1.5). The difference between men and women was not significant.
Multivariable predictors of abstinence in the longer term
A number of factors contributed to whether or not SSS clients maintained abstinence from smoking in the longer term. Compared with clients who received support from either a GP practice or pharmacy service, the odds of quitting were three times higher for those who received group support, aOR 3.4 (95% CI 1.7 to 6.7) and the odds of quitting were twice as high for clients who received support on a one-to-one basis from a specialist adviser, aOR 2.3 (95% CI 1.2 to 4.6).
For every year of age, clients were more likely to quit, aOR 1.011 (95% CI 1.002 to 1.020). There was no evidence that men were more likely to maintain abstinence than women. Clients whose quit attempt began in the New Year were more likely to quit than those who started during the summer holiday period, aOR 1.7 (95% CI 1.0 to 2.9). More-affluent clients were more likely to have stopped smoking at 1 year, aOR 1.4 (95% CI 1.1 to 1.9) than less-affluent clients.
Clients who had higher levels of well-being were more likely to be abstinent from smoking at 1 year. Thus for every increase of 1 on the well-being scale (range 0–100), clients were more likely to be non-smokers, aOR 1.007 (95% CI 1.0003 to 1.013). Clients who were less dependent on tobacco were significantly more likely to quit, aOR 1.5 (95% CI 1.1 to 1.9). Clients whose quit attempt was supported by a spouse or partner were significantly more likely to be abstinent at 1 year, aOR 1.4 (95% CI 1.0 to 1.8). Clients whose social network included fewer smokers were more likely to quit, aOR 2.0 (95% CI 1.4 to 2.9). Starting a quit attempt taking varenicline was also associated with abstinence in the longer term, aOR 1.7 (95% CI 1.3 to 2.3). Ethnicity and determination to quit were eliminated from the model by the backwards-stepwise procedure.
Adherence to treatment
It is likely that an important determinant of successful quit attempts is the extent to which service clients continue to attend sessions and also use stop smoking medication. One general term we can apply to describe these two issues (attendance and medication use) is ‘adherence’. Owing to concerns about reverse causality we could not include adherence in multilevel modelling. Instead, we tried to examine this issue in some depth. The two measures of adherence collected were number of sessions of behavioural support and number of occasions that medication was recorded.
As Table 23 shows, drop-off among the ELONS study clients from attending sessions was steady: a little over 10% of the sample did not return following each session. In addition, about half the sample were recorded as only taking medication on one occasion.
| Adherence measures | n (N = 3057) | % | Weighted quit at 4 weeks (%) (95% CI) | Weighted quit at 52 weeks (%) (95% CI) |
|---|---|---|---|---|
| Number of sessions | ||||
| 1 | 447 | 14.6 | 9.2 (2.3 to 30.0) | 3.4 (0.8 to 13.3) |
| 2 | 331 | 10.8 | 5.4 (1.5 to 17.4) | 1.9 (0.8 to 4.2) |
| 3 | 348 | 11.4 | 21.8 (12.8 to 34.6) | 5.7 (2.8 to 11.4) |
| 4 | 336 | 11.0 | 42.2 (26.6 to 59.4) | 7.2 (3.6 to 13.6) |
| 5 | 374 | 12.2 | 58.0 (47.3 to 67.9) | 9.2 (4.7 to 17.0) |
| 6 | 360 | 11.8 | 68.1 (53.3 to 80.0) | 10.6 (6.4 to 17.0) |
| 7 or 8 | 467 | 15.3 | 78.3 (69.4 to 85.2) | 13.1 (8.5 to 19.7) |
| 9 or more | 374 | 12.2 | 84.0 (74.7 to 90.3) | 16.1 (10.8 to 23.3) |
| Unknown | 20 | 0.7 | 15.8 (1.3 to 72.7) | 0.0 (0.0 to 0.0) |
| Occasions medication recorded (full) | ||||
| No occasions or none recorded | 101 | 3.3 | 11.1 (4.5 to 24.9) | 5.0 (0.7 to 26.9) |
| 1 occasion | 991 | 32.4 | 13.2 (7.7 to 21.8) | 4.6 (3.0 to 7.2) |
| 2 occasions | 616 | 22.0 | 30.1 (22.0 to 39.6) | 7.3 (5.2 to 10.2) |
| 3 occasions | 540 | 17.7 | 57.4 (49.5 to 64.9) | 8.9 (4.9 to 15.6) |
| 4 occasions | 471 | 15.4 | 76.7 (66.3 to 84.7) | 9.4 (5.9 to 14.8) |
| 5–10 occasions | 338 | 11.1 | 80.7 (66.9 to 89.7) | 14.1 (9.4 to 20.7) |
| Occasions medication recorded (short) | ||||
| No occasions or none recorded | 101 | 3.3 | 11.1 (4.5 to 24.9) | 5.0 (0.7 to 26.9) |
| 1 or 2 occasions | 1607 | 52.6 | 20.0 (14.5 to 26.9) | 5.7 (4.2 to 7.7) |
| 3 or more occasions | 1349 | 44.1 | 70.0 (63.9 to 75.5) | 10.4 (8.3 to 12.9) |
Adherence was much more strongly associated with cessation at 4 weeks than 52 weeks. This provides some evidence that reverse causality does exist: clients who had not quit at 4 weeks did not continue to attend sessions after 4 weeks. At 52 weeks differences were smaller but still significant for both number of sessions and medication taken.
Adherence to medication was explored further by taking into consideration the type of medication taken (Table 24). The majority of clients who took either only single NRT or only combination NRT were recorded only taking medication on one or two occasions. Similar proportions were recorded taking varenicline on one or two occasions and three or more occasions. Thus those who took varenicline were more likely to adhere to taking their medication.
| Medication and adherence | n (N = 3057) | % | Weighted quit at 4 weeks (%) (95% CI) | Weighed quit at 52 weeks (%) (95% CI) |
|---|---|---|---|---|
| Single NRT only one or two occasions | 407 | 13.3 | 23.4 (14.3 to 35.9) | 7.5 (4.6 to 11.7) |
| Single NRT only three or more occasions | 189 | 6.2 | 84.3 (67.4 to 93.3) | 4.0 (2.0 to 7.9) |
| Combination NRT only one or two occasions | 444 | 14.5 | 13.0 (8.6 to 19.3) | 4.8 (2.8 to 7.9) |
| Combination NRT only three or more occasions | 125 | 4.1 | 64.6 (52.5 to 75.0) | 9.0 (3.6 to 20.7) |
| Varenicline only one or two occasions | 611 | 20.0 | 22.6 (13.1 to 36.3) | 5.4 (2.7 to 10.5) |
| Varenicline only three or more occasions | 699 | 22.9 | 70.3 (65.6 to 74.6) | 14.1 (10.9 to 18.1) |
| Other/mixed medication only one or two occasions | 145 | 4.7 | 23.9 (15.5 to 34.9) | 5.4 (3.0 to 9.4) |
| Other/mixed medication only three or more occasions | 336 | 11.0 | 63.1 (57.4 to 68.4) | 8.1 (5.0 to 12.6) |
| No medication recorded | 101 | 3.3 | 11.1 (4.5 to 24.9) | 5.0 (0.7 to 26.9) |
The 4-week quit rates of clients who took all types of medication for three or more occasions were significantly higher than those who took medication on one or two occasions. Differences are marked: fewer than one-quarter of clients quit if medication was recorded only once or twice, whereas approximately two-thirds or more of clients quit if they took medication three or more times (irrespective of medication type).
Number of occasions on which NRT was recorded did not have a significant impact on quit rates but clients who took varenicline on three or more occasions were significantly more likely to quit than clients who took varenicline on one or two occasions. Quit rates of clients who took varenicline on three or more occasions were also significantly higher than the quit rates of clients who took combination NRT on one to two occasions or clients who took single NRT on three or more occasions.
If we consider what type of medication clients took at any point (Table 25), two-fifths of clients took varenicline and one-fifth took either only single or combination NRT. Clients who at any point took more than one form of NRT on one occasion (thus combination NRT) were significantly less likely to quit at 4 weeks. This is not consistent with evidence on the effectiveness of combination NRT and raises some questions about the recording of combination therapy use in the study. There were no significant differences at 52 weeks.
| Medication and time point | n (N = 3057) | % | Weighed quit at 4 weeks (%) (95% CI) | Weighed quit at 52 weeks (%) (95% CI) |
|---|---|---|---|---|
| Medication at any point | ||||
| Single NRT only | 596 | 19.5 | 43.8 (38.0 to 49.8) | 6.3 (4.2 to 9.4) |
| Combination NRT only | 569 | 18.6 | 25.1 (20.3 to 30.6) | 5.8 (3.8 to 8.6) |
| Varenicline only | 1310 | 42.9 | 48.1 (40.0 to 56.4) | 10.1 (7.2 to 14.0) |
| Other/mixed medication | 481 | 15.7 | 49.7 (40.8 to 58.7) | 7.1 (5.1 to 10.0) |
| No medication recorded | 101 | 3.3 | 11.1 (4.5 to 24.9) | 5.0 (0.7 to 26.9) |
| Medication at week 1 | ||||
| Single NRT only | 652 | 21.3 | 44.6 (39.0 to 50.3) | 5.9 (4.1 to 8.4) |
| Combination NRT only | 864 | 28.3 | 34.7 (27.3 to 42.8) | 6.5 (4.8 to 8.7) |
| Varenicline only | 1396 | 45.7 | 47.5 (39.1 to 56.0) | 10.0 (7.2 to 13.8) |
| Other/mixed/none recorded | 145 | 4.7 | 17.8 (10.8 to 28.1) | 5.2 (1.5 to 16.2) |
Clients who adhered to medication protocols (i.e. took medication for several weeks) have more chances to change medication. Thus, we also looked at medication recorded in week 1 because then there was no chance of dropping out through failure to quit. There were no significant differences in quitting detected at 4 or 52 weeks.
Adherence among clients who were carbon monoxide-validated as quit at 4 weeks
In further analysis we investigated whether or not the number of sessions that clients who quit at 4 weeks attended was associated with cessation at 52 weeks. Given that SSS clients normally attend and have medication recorded once a week, we looked at whether or not clients attended up to four sessions or had medication recorded up to four times. These results are shown in Table 26.
| Adherence measures | n | Weighted CO-validated 52-week quit (%) (95% CI) |
|---|---|---|
| Sessions attended | ||
| One | 65 | 21.0 (13.1 to 32.0) |
| Two | 15 | 19.9 (10.8 to 33.8) |
| Three | 55 | 16.3 (9.6 to 26.3) |
| Four or more | 1210 | 15.4 (12.4 to 18.9) |
| Sessions unknown or not 4-week CO-validated quit | 1712 | 2.1 (1.4 to 3.2) |
| Total | 3057 | – |
| Occasions medication recorded | ||
| No occasions | 16 | 44.5 (6.2 to 90.6) |
| One occasion | 217 | 22.3 (14.6 to 32.6) |
| Two occasions | 198 | 20.5 (11.9 to 32.8) |
| Three occasions | 305 | 13.6 (7.6 to 23.1) |
| Four or more occasions | 613 | 13.3 (10.0 to 17.5) |
| Not 4-week CO-validated quit | 1708 | 2.1 (1.4 to 3.2) |
| Total | 3057 | – |
| Single NRT only | ||
| One occasion | 55 | 27.3 (7.9 to 62.0) |
| Two occasions | 54 | 25.1 (9.6 to 51.4) |
| Three occasions | 46 | 6.2 (1.3 to 25.3) |
| Four or more occasions | 93 | 4.3 (1.4 to 12.5) |
| Total | 248 | – |
| Combination NRT only | ||
| One occasion | 39 | 20.2 (9.7 to 37.3) |
| Two occasions | 31 | 33.3 (17.7 to 53.8) |
| Three occasions | 42 | 12.0 (2.1 to 46.6) |
| Four or more occasions | 42 | 15.9 (4.5 to 43.2) |
| Total | 154 | – |
| Varenicline only | ||
| One occasion | 120 | 20.6 (13.5 to 30.2) |
| Two occasions | 76 | 14.6 (5.5 to 33.6) |
| Three occasions | 150 | 19.5 (9.6 to 35.4) |
| Four or more occasions | 335 | 17.0 (12.6 to 22.5) |
| Total | 681 | – |
| Total | 3057 | 7.7 (6.6 to 9.0) |
These results suggest that adherence has no discernible effect on quitting as CIs overlap. Note that the vast majority of clients who quit at 4 weeks did attend for four sessions.
Comparisons between the ELONS study and other studies
How do the short- and longer-term results from the ELONS study compare with previous studies? Some limited comparisons can be made, although these come with a range of caveats (discussed further in Chapter 10) owing to the observational nature of the data. There are two previous pieces of research conducted by members of our team that employed very similar approaches. The first of these was the previous ‘national evaluation’ of SSSs in England that was conducted between 2001 and 2004,17,18 already mentioned in Chapter 1. This involved two areas of England – Nottingham and North Cumbria. The second study was conducted in Glasgow between 2005 and 2007 and compared a pharmacy-based SSS with another service providing closed-group behavioural support. 28 Both reported abstinence rates at 1 year.
As Table 27 shows, the previous English evaluation in Nottingham and North Cumbria had a higher CO-validated quit rate at 52 weeks (14.6%) than the ELONS study and a lower lost to follow-up rate (37.5%). The difference in lost to follow-up occurred at all stages (4-week follow-up, 52-week telephone and 52-week validation) but was highest for the 52-week telephone interview. The Glasgow evaluation had a lower CO-validated quit rate. This was primarily because of a much higher loss to follow-up at 4 weeks. These comparisons are discussed in more detail in Chapter 10.
| Quit rates and follow-up rates | Nottingham/North Cumbria 2002, n (%) (N = 2069) | Glasgow 2007, n (%) (N = 1785) | ELONSa 2012/13, n (%) (N = 3057) |
|---|---|---|---|
| 4-week follow-up | |||
| 1. CO-validated quit | 1129 (54.6) | 401 (22.5) | 1349 (44.1) |
| 2. Self-report not CO validated | 139 (6.7) | 151 (8.5) | 380 (12.4) |
| 3. Self-report refuted by CO validation | 4 (0.2) | 16 (0.9) | 6 (0.2) |
| 4. Non-quitters | 388 (18.8) | 259 (14.5) | 676 (22.1) |
| 5. Lost to follow-up | 409 (19.8) | 958b (53.7) | 646 (21.1) |
| Total 4-week self-report (excluding refuted by CO test) | 1268 (61.3) | 552 (70.3) | 1729 (56.5) |
| 52-weeks follow-up (Russell Standard): | |||
| 1. CO-validated quit (0–5 cigarettes since quit date) | 303 (14.6) | 64 (3.6) | 285 (9.3) |
| 2. Self-report not CO validated | 65 (3.1) | 63 (3.5) | 165 (5.4) |
| 3. Self-report refuted by CO validation | 8 (0.4) | 1 (0.1) | 18 (0.6) |
| 4. Non-quitters at 52 weeks | 525 (25.4) | 264 (14.8) | 583 (19.1) |
| 5. Non-quitters at 4 weeks | 392 (18.9) | 259 (14.5) | 676 (22.1) |
| 6. Lost to follow-up at 52 weeks | 367 (17.7) | 179 (10.0) | 684 (22.4) |
| 7. Lost to follow-up at 4 weeks | 409 (19.8) | 955 (53.5) | 646 (21.1) |
| Total 52-week self-report (excluding refuted by CO test) | 368 (17.7) | 127 (7.1) | 450 (14.7) |
| Alternative self-report quit rates at 52 weeksc | |||
| Point prevalenced | NA | 131 (7.3) | 558 (18.3) |
| Continuous abstinence (not a puffe) | 377 (18.2) | 108 (6.1) | 390 (12.8) |
| Alternative CO-validated quit rates at 52 weeks | |||
| Point prevalenced | NA | NA | 348 (11.4) |
| Continuous abstinence (not a puffe) | 303 (14.6) | 62 (3.5) | 260 (8.5) |
| Total eligible for follow-up at 52 weeks (all 4-week self-report) | 1272 (61.5) | 568 (31.8) | 1735 (56.7) |
| Total successfully followed up at 52 weeks | 901 (43.5) | 392 (22.0) | 1051 (34.4) |
| Total eligible for CO validation at Russell Standard | 376 (18.2) | 128 (7.2) | 475 (15.5) |
| Total given CO test | 311 (15.0) | 65 (3.6) | 310 (10.1) |
| CO-validated quit rate of those successfully followed up | 34.5% | 16.1% | 27.1% |
Summary of key points
-
The prospective study collected data from over 3000 SSS clients at 4 and 52 weeks after their quit date. Only a small proportion (9%) of all service clients in the nine study areas were recruited. To correct for this, weights were applied, drawing on an ‘all cases’ database created from routine data in the study areas.
-
Recruitment rates were higher for the specialist service (14%) than the level 2 providers (2%) at least partly because not all level 2 providers took part and those that did recruited for different periods.
-
In terms of smoking cessation in the short term, the raw quit rate at 4 weeks was 44.1%. With weighting this reduced marginally to 41.2%. In comparison, the quit rate for England from April 2012 to March 2013 was 37%. 31
-
For smoking cessation in the longer term, the raw quit rate at 1 year was 9.3% but after weighting this reduced to 7.7%.
-
Predictors of smoking abstinence at 4 weeks were:
-
attending an open group
-
attending SSS in the New Year
-
being older
-
being more affluent
-
having a lower dependence on tobacco
-
being determined to quit
-
having a higher well-being score
-
having support from a spouse or partner
-
having a social network not populated with smokers.
-
-
Predictors of abstinence at 52 weeks were largely similar and included:
-
attending group behavioural support or receiving one-to-one support from a specialist practitioner
-
taking varenicline
-
attending SSS in the New Year
-
being older
-
being more affluent
-
having a lower dependence on tobacco
-
having a higher well-being score
-
having support from a spouse or partner
-
having a social network not populated with smokers.
-
-
Taking stop smoking medication and attending support sessions (described here as ‘adherence’) was significantly associated with smoking cessation – more so at 4 weeks than at 1 year.
-
Limited comparisons with previous evaluations of SSSs in England are possible. Quit rates for 4 and 52 weeks from the ELONS prospective study were lower than those identified in the previous national evaluation in England, but higher than a recent study in Glasgow that examined closed-group and pharmacy-based services.
Chapter 7 Client satisfaction survey
All clients who participated in the prospective cohort (regardless of the outcome of their quit attempt) were sent a CSS to give feedback on the service they received. This chapter presents the rationale for adding the CSS to the prospective studies, the recruitment approach, sample analysis and results. Results are presented in two sections. Section one groups findings under six headings: client characteristics; thoughts of the SSS overall; making initial contact with SSS; appointment times and venues; service received; and medication. In order to assess whether or not levels of satisfaction have an influence on abstinence from smoking, section two compares CSS findings with three key variables from the ELONS prospective study data set: CO-validated quitting, location and behavioural support type.
Rationale
A questionnaire to measure client satisfaction with SSSs was developed by members of the research team in 2008 as part of the DH’s ‘gold standard’ monitoring and evaluation guidance for SSSs. 50 The questions were designed to assess the overall level of client satisfaction with SSSs, with additional questions to look at specific elements of the service, for example, appointment times, convenience of venue, type of support received, willingness to recommend the service to others and smoking status. A copy of the questionnaire is appended (see Appendix 1).
Stop Smoking Services are under no obligation to use a CSS, which means that there was no consistency of use among the nine ELONS study sites. Some administered the survey but had no resource to analyse or make use of the findings to improve their service; others asked some questions but not all. Thus, despite not being directly relevant to research objectives, the research team thought that by offering to administer, analyse and write up the CSS and feed findings back to sites, this might encourage sign-up from the selected SSSs. This, in turn, would boost the study sample and contribute to answering the research objectives. In addition, the CSS generated useful data, highlighting the value of the service provided to smokers trying to quit.
Recruitment, sample and analysis
The research team posted a self-complete questionnaire to all clients 4-weeks after their quit date was set (regardless of the outcome of their quit attempt). To encourage response, two reminder mailings were sent and a prize draw of £200 of high street vouchers was offered.
There were 1006 questionnaires received and the final data set had 996 cases (one was removed because of missing data and nine discarded because they had been completed twice). This means that one-third (33%) of the ELONS study participants completed this survey. Questionnaire data were entered into Excel and then transferred to SPSS (version 19.0) for analysis. Respondents were also given the opportunity to write additional comments about the service they received. These have been analysed thematically and placed in the relevant sections, with quotes to illustrate where relevant. As a result of missing data, the number of clients responding to each question will vary.
Findings
Client characteristics
Table 28 presents sample characteristics of clients who completed a CSS in comparison with the main ELONS study sample. Of the respondents who completed a CSS, 71% were CO validated as abstinent from smoking 4 weeks after their quit date. In the overall ELONS study sample, the proportion of clients who had a CO-validated quit was a lot lower (44%). Clients who were successful in their quit attempt were more likely to complete the survey and this should be remembered when reviewing the findings.
| CSS sample characteristics | Recruited to ELONS | Responded to CSS | ||
|---|---|---|---|---|
| n (N = 3069) | % | n (N = 996) | % | |
| Smoking status | ||||
| CO-validated quit | 1350 | 44.0 | 711 | 71.4 |
| Self-report quit | 1737 | 56.6 | 831 | 83.4 |
| Smoking | 1332 | 43.4 | 165 | 16.6 |
| Gender | ||||
| Male | 1355 | 44.2 | 558 | 56.0 |
| Female | 1714 | 55.8 | 438 | 44.0 |
| Age group (years) | ||||
| 16–24 | 330 | 10.8 | 66 | 6.6 |
| 25–34 | 676 | 22.0 | 149 | 15.0 |
| 35–44 | 760 | 24.8 | 198 | 19.9 |
| 45–54 | 631 | 20.6 | 236 | 23.7 |
| 55–64 | 458 | 14.9 | 221 | 22.2 |
| 65–85 | 214 | 7.0 | 126 | 12.7 |
| Ethnicity | ||||
| White British | 2877 | 93.7 | 937 | 94.1 |
| Other white | 70 | 2.3 | 22 | 2.2 |
| Asian (including mixed white and Asian) | 64 | 2.1 | 9 | 0.9 |
| Black (including mixed white and black) | 24 | 0.8 | 11 | 1.1 |
| Other/unknown | 34 | 1.1 | 17 | 1.7 |
| SES | ||||
| Professional managerial | 718 | 23.4 | 243 | 24.4 |
| Routine and manual | 941 | 30.7 | 258 | 25.9 |
| Unemployed/permanently sick | 663 | 21.6 | 194 | 19.5 |
| Other | 747 | 24.3 | 301 | 30.2 |
| Behavioural support type | ||||
| Closed group | 102 | 3.3 | 32 | 3.2 |
| Open group | 550 | 17.9 | 207 | 20.8 |
| Drop-in | 887 | 28.9 | 255 | 25.6 |
| One-to-one specialist | 1131 | 36.9 | 389 | 39.1 |
| GP practice | 270 | 8.8 | 79 | 7.9 |
| Pharmacy | 97 | 3.2 | 25 | 2.5 |
| Other or unclear | 32 | 1.0 | 9 | 0.9 |
Overall opinions
Clients were asked for their overall opinion of the SSS, with 87% saying they were either very satisfied or satisfied.
In open-ended responses, clients described the service they had attended as: ‘supportive’; ‘encouraging’; ‘very good’; ‘excellent’; ‘friendly’; ‘welcoming’; ‘reassuring’; ‘good advice’; ‘well-informed’; ‘enthusiastic’; ‘helpful’; and ‘understanding’.
Satisfaction with the support received was also high; 87% of respondents were either very satisfied or satisfied with the support they received. In addition, nearly all respondents (96%) said that they would recommend the SSS to other smokers who want to stop smoking. As one respondent wrote:
I would have struggled to stop smoking without the help of the service. I would definitely recommend anyone wishing to stop smoking to use this service.
A further 94% would return to a SSS should they start smoking again and 86% felt that they would be welcomed back:
I hope to never use the service again but would not hesitate to if the requirement came about again.
Perhaps not surprisingly, positive feedback was more likely among ‘quitters’ (i.e. respondents who had a successful quit attempt at 4 weeks) than ‘non-quitters’. This is examined further in this chapter.
Making initial contact with Stop Smoking Service
Respondent feedback on making initial contact and arranging an appointment with the SSS was also extremely positive (Table 29). The majority of respondents (94%) said it was easy to contact the SSS and the majority (88%) were given an appointment date or told how long they would need to wait to receive one. Three-fifths (60%) waited 5 or fewer days for their first appointment (22% were seen straight or away or within 24 hours) and the majority (92.5%) felt the time they waited was acceptable. One-third (31%) were contacted by the SSS before their first appointment to encourage and motivate them to attend (it should be noted that in some service clients are seen straight away so this question was not relevant to some participants).
| Initial contact with SSSs | Responded to CSS | |
|---|---|---|
| n (N = 940–988) | % | |
| Easy to contact SSS | ||
| Yes | 926 | 93.7 |
| No | 29 | 2.9 |
| Unsure | 33 | 3.3 |
| Given appointment date | ||
| Yes | 852 | 87.6 |
| No | 95 | 9.8 |
| Unsure | 26 | 2.7 |
| How long for appointment date (days) | ||
| 0–5 | 568 | 60.4 |
| 6–10 | 281 | 29.9 |
| ≥ 10 | 91 | 9.7 |
| Length of time acceptable | ||
| Yes | 902 | 92.5 |
| No | 31 | 3.2 |
| Unsure | 42 | 4.3 |
| Contact from SSS before appointment | ||
| Yes | 303 | 31.2 |
| No | 553 | 56.9 |
| Unsure | 116 | 11.9 |
Appointment times and venue
Appointment times and venues were rated very highly with 95% of respondents reporting that appointment times were convenient, and a further 97% stating that the venue was also convenient (Table 30). Child care costs were irrelevant for 83% of the sample. Three respondents said that they were offered support with child care costs. Two-fifths (41.5%) were given the choice of whether they would like an individual or group appointment.
| Appointment times and venues | Responded to CSS | |
|---|---|---|
| n (N = 972–996) | % | |
| Time convenient | ||
| Yes | 936 | 95.2 |
| No | 23 | 2.3 |
| Unsure | 24 | 2.4 |
| Place convenient | ||
| Yes | 955 | 97.0 |
| No | 18 | 1.8 |
| Unsure | 12 | 1.2 |
| Child care support | ||
| Yes | 3 | 0.3 |
| No | 157 | 15.8 |
| Unsure | 7 | 0.7 |
| Not applicable/did not answer | 829 | 83.2 |
| Able to choose group or one to one | ||
| Yes | 403 | 41.5 |
| No | 460 | 47.3 |
| Unsure | 109 | 11.2 |
Similar findings were evident from the open-ended comments, with an appreciation of the flexible consultation approach and the different type of behavioural support on offer:
As working full time was unable to attend weekly appointments – staff arranged telephone consultations which was great otherwise would most probably have stopped going.
I liked the idea of walk in centre, every Wednesday, just for smokers and the one to one appointments which I had every week with the same person. To me it was better than a group session.
However, there were suggestions for improvement, which mainly centred on having more flexible appointment times, a wider choice of behavioural support, a longer treatment period, more telephone contact to maintain morale and introducing a diet class to address potential weight gain after smoking cessation.
There are no evening appointments at my local clinic, which makes things difficult for those who work full time.
I would have preferred individual appointments to group therapy.
I feel that instead of having to attend for just 4 weeks it should be rolled out to at least 8. From past experience I feel 4 weeks is too quick.
Maybe a text or phone call between appointment time, i.e. 2 weeks is a long time to leave someone without encouragement. I liked the way my smoking service only encourages a full quit.
Maybe introduce a dieting class, i.e. dieting support. I think many people especially woman don’t want, or find it hard to quit smoking because they put on too much weight.
Service received
Respondents were either satisfied or very satisfied with support from SSS staff (89%). Nine out of 10 (90%) rated the information and advice they received as very helpful or helpful and a further 82% found the written advice helpful/very helpful. Finally, 86% found having their CO checked at every visit helpful or very helpful. This was also the view from the open-ended comments; however, there were some important comments about practitioners. As we have already seen, in the main, practitioners were highly praised and appreciated but there were some comments that suggested that practitioner/client rapport was inadequate in some way. The same applied to continuity of practitioners, that is, not seeing the same practitioner at each visit and being able to make contact. Both the ELONS study secondary analysis and prospective data sets revealed that the individual practitioner had a significant influence, at least on short-term quit rates.
A couple of us had not fully stopped smoking, whereas most had. The attitude displayed by one nurse seemed patronising and dismissive. It needed to be more constructive. It put me off going back and without the support which was otherwise good I failed to stop.
[Name of practitioner] was the best person for the job, she was dead easy to talk to about anything but the woman who took over from her made me feel really unsettled in a telephone consultation therefore never went back!!!
It would be helpful to see the same person every week. Sometimes I saw different people and had to keep introducing myself and explaining how long I’d given up etc.
Medication
Respondents indicated that the information given about different types of stop smoking medication was helpful (94%) and 92% reported that it was easy to obtain their medication of choice [with a half (49.8%) via GP prescription] (Table 31).
| Medication | Responded to CSS | |
|---|---|---|
| n (N = 974–993) | % | |
| Medication information helpful | ||
| Yes | 929 | 93.9 |
| No | 20 | 2.0 |
| Unsure | 40 | 4.0 |
| Source of medicationa | ||
| GP prescription | 485 | 49.8 |
| Chemist (bought myself) | 27 | 2.8 |
| Chemist (with a voucher) | 132 | 13.6 |
| Chemist (with service letter or prescription) | 174 | 17.9 |
| SSS | 198 | 20.3 |
| Ease of accessing medication | ||
| Yes | 897 | 91.8 |
| No | 54 | 5.5 |
| Unsure | 26 | 2.7 |
However, analysis of open-ended comments highlighted two areas for consideration: a lack of information on the side effects of medication and difficulty obtaining medication.
Side effects of varenicline need to be highlighted – include info on all possible side effects.
Explain more about how stopping smoking will affect your immunity to illness. I have never had so many colds/flu infections/virus infections as this in my life since I stopped smoking.
Chemist don’t carry enough stock! Most weeks I have to wait for some. Normally next day + costs of travel again.
It would be better if stop smoking staff could give out medication as I had to make three trips with letters, prescriptions etc. to finally get medication 5 days later.
Client satisfaction survey findings and the ELONS prospective study data set
Satisfaction levels by three key variables from the ELONS study data set (CO-validated quitting, location and behavioural support type) are explored in this section. CO-validated abstinence from smoking (in the short term) was chosen in order to explore whether or not any of the satisfaction variables might point to facilitators for cessation. Location was chosen because some issues with satisfaction may be study site specific and so may be relevant for only some sites. Finally, behavioural support was chosen as one of the aims of the ELONS study in order to assess the effectiveness of various forms of behavioural support and establish whether or not the support that clients receive affects their satisfaction.
Some sites and behavioural support categories did not support analysis owing to insufficient respondent numbers and were merged into ‘other’ categories. Note that different sites offered different forms of behavioural support and recruitment was higher for some support types than others. The percentage of respondents from each location for each support type is tabulated (Table 32). Nearly two-thirds (63%) of GP practice respondents were from site 1 and 96% of open-group respondents were from site 6.
| Behavioural support group | Site 1, % (n = 94) | Site 2, % (n = 245) | Site 4, % (n = 136) | Site 6, % (n = 245) | Site 8, % (n = 156) | Other sites, % (n = 117) | Total, % | Total, n (N = 996) |
|---|---|---|---|---|---|---|---|---|
| Open group | 3.9 | – | – | 96.1 | – | – | 100.0 | 207 |
| Drop-in | – | 39.6 | 22.0 | – | 22.0 | 16.5 | 100.0 | 255 |
| One-to-one specialist | 3.6 | 33.7 | 18.5 | 9.3 | 24.2 | 10.8 | 100.0 | 389 |
| GP practice | 63.3 | 15.2 | 2.5 | 5.1 | – | 13.9 | 100.0 | 79 |
| Other supporta | 33.3 | 1.5 | 9.1 | 9.1 | 13.6 | 33.3 | 100.0 | 66 |
| Percentage of clients from each site | 9.4 | 24.6 | 13.7 | 24.6 | 16.0 | 11.7 | 100.0 | – |
Response categories for the 5-point Likert scales were merged to enable analysis. Chi-squared tests were conducted between CO-validated quitting and all the satisfaction variables. If there was a significant difference between quitters and non-quitters (p < 0.05) then chi-squared tests were conducted for location and behavioural support types. Results are presented where p < 0.05.
Overall satisfaction and supportiveness of staff
Those who were CO validated as having stopped smoking were slightly more likely to be very satisfied with the services overall (64% vs. 51%) and less likely to state they were satisfied or unsure, unsatisfied and very unsatisfied (Table 33). A similar pattern emerged for satisfaction with staff supportiveness. Of the quitters, 68% were very satisfied with staff supportiveness versus 54% of non-quitters. The highest level of satisfaction with supportiveness was among respondents who attended open groups (70% very satisfied).
| Behavioural support type | Very satisfied (%) | Satisfied (%) | Unsure, unsatisfied, very unsatisfied (%) |
|---|---|---|---|
| Quitting (p = 0.001) | |||
| Not CO validated as quit | 51.1 | 33.3 | 15.6 |
| Quit (CO validated) | 64.4 | 23.8 | 11.8 |
| Total | 60.6 | 26.5 | 12.9 |
| Quitting (p < 0.001) | |||
| Not CO validated as quit | 54.1 | 31.4 | 14.5 |
| Quit (CO validated) | 67.5 | 23.0 | 9.5 |
| Total | 63.7 | 25.4 | 10.9 |
| Behavioural support (p = 0.014) | |||
| Open group | 70.0 | 24.2 | 5.8 |
| Drop-in | 62.5 | 29.2 | 8.3 |
| One-to-one specialist | 64.0 | 22.0 | 14.0 |
| GP practice | 58.2 | 27.8 | 13.9 |
| Other support | 53.0 | 31.8 | 15.2 |
| Total | 63.7 | 25.4 | 10.9 |
Returning to the services
The majority of respondents (those who were abstinent from smoking and those who had not stopped or relapsed by 4 weeks) said they would return to the SSS if they needed help with another quit attempt (Table 34). There was a small but significant difference: 96% of quitters said they would return compared with 89% of non-quitters.
| Client views | Yes (%) | No or unsure (%) |
|---|---|---|
| Return to SSS | ||
| Quitting (p < 0.001) | ||
| Not CO validated as quit | 89.3 | 10.7 |
| Quit (CO validated) | 96.3 | 3.7 |
| Total | 94.3 | 5.7 |
| Welcomed back to SSS | ||
| Quitting (p < 0.001) | ||
| Not CO validated as quit | 79.2 | 20.8 |
| Quit (CO validated) | 88.2 | 11.8 |
| Total | 85.6 | 14.4 |
| Behavioural support (p = 0.011) | ||
| Open group | 92.2 | 7.8 |
| Drop-in | 87.3 | 12.7 |
| One-to-one specialist | 82.9 | 17.1 |
| GP practice | 81.0 | 19.0 |
| Other support | 80.3 | 19.7 |
| Total | 85.6 | 14.4 |
| Whether or not given written information | ||
| Quitting (p = 0.017) | ||
| Not CO validated as quit | 89.8 | 10.2 |
| Quit (CO validated) | 94.3 | 5.7 |
| Total | 93.0 | 7.0 |
| Location (p < 0.001) | ||
| Site1 | 90.3 | 9.7 |
| Site 2 | 92.1 | 7.9 |
| Site 4 | 87.2 | 12.8 |
| Site 6 | 99.2 | 0.8 |
| Site 8 | 91.1 | 8.9 |
| Other sites | 93.2 | 6.8 |
| Total | 93.0 | 7.0 |
| Medication information helpful | ||
| Quitting (p < 0.001) | ||
| Not CO validated as quit | 88.7 | 11.3 |
| Quit (CO validated) | 96.0 | 4.0 |
| Total | 93.9 | 6.1 |
| Location (p < 0.001) | ||
| Site1 | 83.9 | 16.1 |
| Site 2 | 94.3 | 5.7 |
| Site 4 | 92.5 | 7.5 |
| Site 6 | 96.3 | 3.7 |
| Site 8 | 93.7 | 6.3 |
| Other sites | 98.3 | 1.7 |
| Total | 93.9 | 6.1 |
| Whether or not given CO test each session (p = 0.011) | ||
| Not CO validated as quit | 90.8 | 9.2 |
| Quit (CO validated) | 95.3 | 4.7 |
| Total | 94.0 | 6.0 |
Although the majority of respondent’s thought they would be welcomed back, quitters were slightly more likely to say they would be welcomed (88% vs. 79%). This may reflect differences in behavioural support as it was only among respondents who had attended open groups where over 90% believed they would be welcomed back.
Information provided
The majority of respondents were given written information, however, those who had stopped smoking by 4 weeks were slightly more likely to report that they had been given written information (94% vs. 90%). There was a significant difference between locations but even the site with the lowest provision achieved 87% clients being given written information.
Of those who had stopped smoking, 96% found information about medication helpful compared with 89% of those who had not. Helpfulness of information about medication was lower in site 1 (84%) than other sites (or site groups) analysed where over 90% agreed that information about medication was helpful. Comments about medication from site 1, which came from respondents who attended a variety of behavioural support types, included reports that side effect issues were not covered, they were encouraged to take medication when they did not want it and that their choice of medication was not easily available:
I’d like to see that mild smokers are taken just as seriously as heavy smokers, in the sense that the whole course of patches should be offered not only an inhaler, I did manage to get some but only with protest.
Carbon monoxide validation at each session
Carbon monoxide-validated quitters were slightly more likely to state that they had a CO-validation test at each session than those quit but not CO validated (95% vs. 91%). Among those who had taken a CO-validated test at each session (see Table 34), quitters were more likely to say it was very helpful than non-quitters (73% vs. 63%). There was a significant difference between location, with respondents from site 6 reporting highest levels of helpfulness (81%) and site 1 respondents were least likely to say that the CO-validation test was very helpful (57%). This may reflect the behavioural support type: 87% of open-group clients said that a CO test during each session was very helpful, compared with 59% of GP practice clients. Site 8 was chosen for the study because of its low CO-validation rate. Clients in site 8 were most likely to say that they were unsure about CO validation or they found it unhelpful or very unhelpful (13% compared with an average of 9% in all other sites).
Summary of key points
-
A consistent pattern emerged that suggests that smokers who accessed SSSs, in the ELONS study areas and responded to the survey, had a very positive experience, for both quitters and non-quitters. The vast majority who replied to the questionnaire indicated that they would recommend the service to others and return should the need arise.
-
There were several examples of good practice, when SSSs offered more than they are required to do by the DH (e.g. contacting clients before their first appointment to encourage them to attend and offering child care and a choice of behavioural support options).
-
Additional comments highlighted the importance of practitioner/client rapport, and multilevel modelling of the ELONS study secondary analysis and prospective study data sets suggests that this is an important factor in a successful quit attempt, at least in the short term.
-
Despite quantitative findings suggesting that medication was easy to acquire, additional comments pointed to a more complex picture where the process of obtaining medication was overcomplicated and time-consuming for some respondents.
-
Suggested improvements centred on evening appointment times, having a choice of group or one-to-one support and a longer period of support.
-
Analysis of client satisfaction between quitters and non-quitters, SSS location and behavioural support types revealed some small but significant differences:
-
Quitters were more likely to be satisfied with staff supportiveness and happier to return to the services if needed, with the information provided and CO validation.
-
Open-group clients were happier about staff supportiveness, returning to the service and CO testing. GP practice clients were least comfortable with CO testing. It must be noted that open-group clients were mostly recruited from a single site.
-
-
Finally, despite an encouraging response rate (response to self-completion postal surveys are generally low, even with repeated reminders) clients who were motivated to complete the survey were also more likely to have had a successful quit attempt. This means the views of those who did not quit are under-represented.
Chapter 8 Well-being study
Well-being can improve after smoking cessation, but smokers often have concerns about stopping because they believe smoking itself brings benefits, such as reduced stress levels. 51 The ELONS study provided an opportunity to examine changes in well-being before and after stopping smoking to add to our understanding of this issue.
Rationale
Additional information on the health and well-being of the ELONS prospective study participants was collected for a number of reasons. First, it has been argued that the ultimate aim of health care is to improve quality of life. 52 It would, therefore, be expected that a health intervention, such as a smoking cessation programme, would improve well-being,53–55 but previous research has highlighted some unintended consequences. 52,56 In addition, as well as being a desired outcome of a health interventions, well-being may also be a predictor of successful smoking cessation. 55–59 No studies that we could identify had examined changes in well-being among clients of NHS SSSs and thus we decided to include a focus on this in the current study.
Recruitment
As part of the baseline monitoring data collection for the prospective study, clients were asked additional questions about their health and well-being. In addition, all clients, regardless of their smoking status, were sent postal questionnaires at 4 and 52 weeks post quit date, which included questions on well-being (see Appendix 1).
Measures
Medical conditions variables
Health was operationalised as the presence or absence of medical conditions. Practitioners collected detailed information on medical conditions for two reasons. First, SSSs provide medication to support smoking cessation and other medications need to be understood to make sure the medication is appropriate. Second, we wished to consider medical conditions because there is an association between many medical conditions and smoking. For the ELONS study, each service was required to ask about a list of medical conditions for consistency. Medical conditions reported by clients were amalgamated into the following for analysis: any medical condition; heart, blood and circulatory conditions; lung and respiratory conditions; mental health conditions; client had a condition but none of the above conditions were present; and a limiting medical condition (in conjunction with the limiting illness variable).
Well-being variables
Well-being data were chiefly collected through the WHO-5 Well-being Index45 (Box 1). The WHO-5 Well-being Index has been used in studies on diabetes, suicide, substance abuse, obesity and depression. In a sample of over 3000 clients who received health trainer services in the West Midlands,60 the WHO-5 Well-being Index score improved by 37.5% (from a score of 44.1 to a score of 60.7) after receiving the service.
I have felt cheerful and in good spirits.
I have felt calm and relaxed.
I have felt active and vigorous.
I woke up feeling fresh and rested.
My daily life has been filled with things that interest me.
Response scaleAll of the time = 5.
Most of the time = 4.
More than half the time = 3.
Less than half the time = 2.
Some of the time = 1.
At no time = 0.
The five items that make up this scale were asked at three time points: baseline, as an extension to the client satisfaction postal survey, at 4 weeks and a further postal survey sent to all the ELONS study participants at 52 weeks.
A score for the WHO-5 Well-being Index is derived by summing the responses to the five constituent items and multiplying by four, which provides a continuous variable with a potential range of 0 to 100. The range and skew were calculated. A dichotomised variable can also be derived: a concerning level (as opposed to a good level) of well-being occurs where the overall well-being score is under 13 or any individual item score is 0 or 1.
Additional questions on well-being were asked in the 4-week and 52-week postal surveys, including a ‘components of well-being’ scale modified from the validated psychosocial benefits from home scale61–63 to apply to smoking cessation clients. The components, measuring protection, control, prestige and response to change, are theoretically related to ontological security but also implicitly assume that well-being is affected by outside, and therefore modifiable, sources rather than fixed personality traits. Thus the ten items are intended to measure psychosocial feelings, which may connect well-being to external factors (Table 35). These items were included in both postal surveys.
| Concept | Items |
|---|---|
| Protection | I can deal with stress; I feel safe |
| Control | I feel in control; I can do what I want, when I want |
| Prestige | Most people would like a life like mine; I feel I’m doing well in life |
| Response to change | My life has a sense of routine; I worry about things going wrong (reversed); I enjoy a challenge; I’m frightened of change (reversed) |
Socioeconomic status
An alternative measure of SES was used in the analysis described here because of possible contamination between the prospective study measure of SES, and health and well-being with the inclusion of permanently sick and eligibility for free prescriptions. Here, a three-category variable was used: low SES [(unemployed or basic education or social renting) and no high SES conditions, n = 1179] mid SES (mixed or no indicators of low or high SES, n = 1480) and high SES (owns home and either has a professional/managerial occupation or has tertiary education and no low SES conditions, n = 300).
Analysis
The analysis for this element of the ELONS study was intended to be exploratory. The following questions were examined:
-
What was the level of response to the well-being questions?
This analysis was undertaken in order to see whether or not the WHO-5 Well-being Index scale was acceptable to respondents and whether or not the samples of respondents who answered the well-being questions were adequate for analysis.
-
Did health and well-being at baseline predict quitting at 4 weeks and 52 weeks?
This analysis was undertaken in order to consider first, whether or not well-being and smoking cessation were significantly associated, and second, which health and well-being variables should be included in the final model of factors predicting quitting reported on elsewhere in this report.
-
How did well-being change over time among quitters and non-quitters?
This analysis was undertaken in order to explore whether or not findings of a systematic review50 (that well-being improves after cessation) were replicated among the ELONS study clients or whether or not attending the smoking cessation services had unintended adverse consequences for well-being.
-
Which clients had the highest well-being at baseline, 4 weeks and 52 weeks?
This analysis was undertaken to explore first, the stability of the concept of well-being over time (for instance, if the same factors constantly associated with well-being), second, which factors are associated with well-being, and third, which psychosocial factors may link external factors to well-being.
What was the level of response to the well-being questions?
The number of clients who responded to the well-being questions at baseline and in the 4- and 52-week surveys were as follows: 2959 clients responded at baseline only, 953 responded at 4 weeks only, 939 at baseline and 4 weeks, 479 at 52 weeks only, 471 at baseline and 52 weeks, 325 at all three points and 77 had no well-being score at any point (see Table 45 for more details about the responses). Response rates were low at 4 and 52 weeks, as was expected from a postal survey, but were adequate to proceed with analysis given that there was good representation from all demographic groups (see Table 46) and convergence was achieved in multivariable modelling.
Did health and well-being at baseline predict quitting?
The aim of this analysis was to establish whether or not clients’ levels of well-being at the start of their quit attempt was related to quitting or if more traditional measures of medical conditions were preferable.
Outcomes of logistic regression analyses were 4-week and 52-week CO-validated quitting. For 4-week quitting, practitioner was added as a level two variable. For 52-week quitting, there was no evidence of variance between practitioners consistently, so single-level modelling was used. Each medical condition and well-being variable was analysed separately. Other fixed-effect variables included in the models were location, behavioural support type, month quit attempt started, age, gender, ethnicity, SES, whether or not they had taken varenicline, dependence on tobacco and determination to quit (4 weeks only), supportive spouse or partner, and friends and family smoking status.
How did well-being change over time among quitters and non-quitters?
The aim of this analysis was to explore whether or not quitting smoking was associated with changes in well-being.
Initially the distribution of the continuous well-being score was examined in order to establish whether parametric or non-parametric statistics should be used in this analysis.
Mean well-being of quitters and non-quitters
Weighted means were calculated, using the same weights as the prospective study analysis, overall and by 4- and 52-week CO-validated quitting. Means were calculated for clients who had data at different combinations of time points (e.g. baseline and 4 weeks or baseline and 52 weeks). The sample size was kept constant by adding dummy data (e.g. the mean) to clients who did not have a well-being score at 4 weeks or 52 weeks, and an indicator variable was created to distinguish between clients with real data (as they had answered the questions) and clients with dummy data. The weighted means (excluding clients with dummy data) were tabulated and drawn on a line graph (see Figure 7 and Table 37).
Which clients had the highest well-being at baseline, 4 and 52 weeks?
In this analysis the aim was to explore associations with well-being in order to understand how high levels of well-being may be achieved. This may be helpful because clients with higher well-being are more likely to be able to successfully quit smoking long term.
There was no evidence of variance between practitioners at baseline, so single-level models were used for modelling well-being at baseline; however, practitioner was included a random effect at the second level for 4 weeks and 52 weeks. Modelling occurred in two stages. In the first stage, variables that had been used in the prospective study analysis were included in addition to well-being. Non-significant variables (with the exception of a priori variables: location, behavioural support, quit attempt start date, age, gender and SES) were excluded from the model. For modelling of well-being collected in the 4-week and 52-week postal surveys there was then a second stage where ontological security variables were added as continuous variables. Non-significant optional variables were removed and multicollinearity was checked.
Which ontological security variables explained why other variables were associated with quitting?
Each ontological security variable that was significant in the final model was added individually to the stage one model and the changes in coefficients of other independent variables were noted. This final analysis was undertaken only for well-being measured at 4 weeks because of the smaller response to the postal survey at 52 weeks.
Findings
Did health and well-being at baseline predict quitting?
The analysis presented below suggests that well-being at baseline was a predictor of abstinence from smoking in the short and longer term, but medical conditions were not.
Logistic regression modelling was used to examine whether or not health and well-being at baseline predicted quitting at 4 weeks and 52 weeks once other factors had been taken into account (Table 36). This analysis suggested that none of the medical conditions variables predicted either short- or long-term quitting. Well-being analysed as a continuous variable did predict abstinence but not as a dichotomous variable.
| Health or well-being scale | CO-validated quit at 4 weeks (95% CI) | CO-validated quit at 52 weeks (95% CI) |
|---|---|---|
| Medical conditions | ||
| Any | 0.92 (0.78 to 1.08) | 0.85 (0.65 to 1.12) |
| Heart, blood, circulation | 1.01 (0.81 to 1.26) | 0.81 (0.56 to 1.16) |
| Respiratory | 0.88 (0.72 to 1.07) | 0.86 (0.62 to 1.19) |
| Mental health | 0.91 (0.73 to 1.13) | 0.75 (0.50 to 1.12) |
| Other condition but none of above | 0.97 (0.76 to 1.24) | 1.12 (0.77 to 1.63) |
| Severely limiting (vs. no condition) | 0.77 (0.55 to 1.09) | 0.59 (0.32 to 1.11) |
| WHO-5 Well-being Index | ||
| Continuous: 1% increase in well-being | 1.004 (1.00004 to 1.007) | 1.007 (1.0013 to 1.014) |
| Dichotomy: good vs. concerning level of well-being | 1.11 (0.94 to 1.31) | 1.10 (0.85 to 1.43) |
How did well-being change over time among quitters and non-quitters?
Well-being at baseline approximately followed a normal distribution. Skew was below ± 0.8 and could be disregarded so parametric statistics could be used. The range of well-being scores was between 0 and 100 and so could be viewed as a percentage.
The weighted well-being mean of the sample was 53.15 (95% CI 51.96 to 54.34) (Table 37). Clients who did not manage to quit for 4 weeks had lower well-being at baseline than those who quit (Figure 7). In addition, the mean well-being at baseline of 52-week quitters was higher than those who did not manage to quit for 52 weeks. CIs did not overlap for 4-week quitters and non-quitters, and CIs of clients who did manage to quit for 52 weeks did not overlap with those who did not manage to quit for 52 weeks, 4 weeks and the sample overall. This indicates that there were significant differences between these client groups.
| Follow-up and quit status | Baseline (95% CI) | 4 weeks (95% CI) | 52 weeks (95% CI) |
|---|---|---|---|
| 4 weeks | |||
| Total | 53.15 (51.96 to 54.34) | 57.29 (55.25 to 59.32) | – |
| Not quit | 51.48 (49.83 to 53.13) | 51.82 (47.98 to 55.66) | – |
| Quit | 55.48 (53.80 to 57.16) | 59.93 (57.60 to 62.26) | – |
| Responded to WHO-5 scale questions at 4 weeks if answered baseline and 4 weeks | |||
| Total | 54.90 (52.96 to 56.84) | 57.43 (55.39 to 59.48) | – |
| Not quit | 49.90 (46.41 to 53.40) | 52.08 (48.22 to 55.94) | – |
| Quit | 57.30 (55.01 to 59.58) | 59.99 (57.65 to 62.34) | – |
| 52 weeks | |||
| Total | 53.15 (51.96 to 54.34) | 57.29 (55.25 to 59.32) | 52.76 (49.91 to 55.62) |
| Not quit | 52.62 (51.36 to 53.88) | 56.40 (54.11 to 58.69) | 49.01 (45.72 to 52.31) |
| Quit | 59.31 (56.47 to 62.14) | 61.80 (57.82 to 65.77) | 65.29 (61.29 to 69.28) |
| Responded to WHO-5 scale questions at 52 weeks if answered baseline and 52 weeks | |||
| Total | 51.63 (48.96 to 54.31) | – | 53.10 (50.26 to 55.93) |
| Not quit | 49.47 (46.24 to 52.70) | – | 49.34 (46.05 to 52.63) |
| Quit | 58.64 (54.64 to 62.64) | – | 65.29 (61.29 to 69.28) |
| Responded to WHO-5 scale questions at 52 weeks if answered all three points | |||
| Total | 53.60 (50.54 to 56.67) | 57.43 (55.39 to 59.48) | 55.42 (52.31 to 58.52) |
| Not quit | 51.02 (47.13 to 54.90) | 54.18 (50.41 to 57.96) | 52.19 (48.48 to 55.90) |
| Quit | 60.20 (56.12 to 64.27) | 61.28 (57.33 to 65.24) | 63.64 (58.81 to 68.47) |
FIGURE 7.
Well-being over time by smoking status.

Confidence intervals for weighted means of well-being for non-quitters over the three time points overlapped when clients provided data at three time points. CIs for non-quitters also overlapped for both time points if the clients provided data at any two time points. The well-being scores of quitters consistently increased over time but CIs of the first time points overlapped with those of later time points. However, CIs for quitters and non-quitters at each time point did not overlap. This is an indication that quitters had significantly higher well-being than non-quitters.
Which clients had the highest well-being at baseline, 4 and 52 weeks?
A summary of variables that were associated with well-being at each time point is presented in Table 38. Full models with all coefficients are presented in Appendix 2 (see Tables 46 and 47).
| Variables | Baseline | 4 weeks | 52 weeks | ||
|---|---|---|---|---|---|
| Model 1 | Model 1a (OS excluded) | Model 2b (OS included) | Model 1a (OS excluded) | Model 2b (OS included) | |
| Quit smoking | – | Quit at 4 weeks | Quit at 4 weeks | Quit at 52 weeks | Quit at 52 weeks |
| Age | Age (U-shaped) | Age (U-shaped) | Age 25–34 years | Age (U-shaped) | – |
| Ethnicity | Ethnicity (Asian) | Ethnicity (Asian) | Ethnicity (Asian) | – | – |
| Dependence | Low dependence | Low dependence | – | Low dependence | – |
| Mental health | No mental health problems | No mental health problems | – | No mental health problems | – |
| Heart, blood, circulation or respiratory conditions | No heart, blood or circulation condition, no respiratory, no other condition | – | No heart, blood or circulation conditions | No respiratory conditions | – |
| Support | Spouse/partner support | Spouse/partner support | – | – | – |
| Determination | More determined to quit | – | – | – | – |
| Medication | Taking varenicline | – | – | – | – |
| OS answers | – | – | I enjoy a challenge; I feel I’m doing well in life; I feel in control; I can deal with stress; Most people would like a life like mine | – | I enjoy a challenge; I feel I’m doing well in life; I feel in control; I can do what I want, when I want; I feel safe; I worry about things going wrong (reversed); My life has a sense of routine |
Factors associated with higher well-being at baseline
At baseline, multivariable modelling suggested that the factor with the strongest association with well-being was absence of a mental health condition. Thus, clients without a mental health condition had well-being scores nearly 10 points higher than those with a condition (see Tables 38 and 46 for more details). Other factors with significant associations with well-being at baseline were high SES, with the most affluent clients having well-being scores that were 4 points higher than the most disadvantaged clients. Support from spouse or partner, determination to quit, lower dependence on tobacco, taking varenicline and the absence of a physical medical condition (such as not having heart, blood or circulatory problems) were all significantly associated with well-being at baseline. Age had a U-shaped relationship with well-being, where well-being was poorest in those aged 45–54 years compared with clients aged 16–24 years and 65–85 years. Asian clients had significantly higher well-being than non-British white clients, although numbers of these clients were very small.
Factors associated with higher well-being at 4 weeks
Well-being scores at 4 weeks were associated with: successful cessation; age; Asian ethnicity (compared with non-British whites); absence of heart, blood and circulatory diseases; and five ontological security items (I enjoy a challenge; I feel I’m doing well in life; I feel in control; I can deal with stress; and most people would like a life like mine) (see Tables 38 and 47 for more details). If ontological security items were not entered, then dependence on tobacco (low dependence), no mental health issues, and spouse and partner support were significantly associated with well-being (see Appendix 2, Table 47).
As the inclusion of the ontological security items caused attrition in the coefficients of other variables, this was explored further by adding each ontological security variable separately (Tables 39 and 40). Attrition in the well-being coefficients of the youngest and oldest clients, the highest SES groups and those who had a spouse/partner supporting their quit attempt was particularly marked when the item ‘I’m doing well in life’ was added to the model. Attrition in the well-being scores of clients with an absence of mental health conditions was particularly marked when the item ‘I feel in control’ was added to the model. Feeling in control partly attenuated the relationship between well-being and quitting but the association still remained significant.
| Variable | Model 1 | Add OS1a | Add OS2b | Add OS5c | Add OS6d | Add OS9e |
|---|---|---|---|---|---|---|
| Age group (years) | ||||||
| 16–24 (95% CI) | 9.05 (3.28 to 14.82) | 6.58 (1.07 to 12.09) | 8.77 (3.54 to 14.00) | 7.16 (1.77 to 12.55) | 6.24 (1.23 to 11.25) | 5.73 (0.75 to 10.71) |
| 25–34 (95% CI) | 6.66 (2.34 to 10.97) | 4.40 (0.27 to 8.53) | 6.98 (3.07 to 10.89) | 6.23 (2.21 to 10.24) | 4.11 (0.35 to 7.86) | 5.10 (1.38 to 8.82) |
| 35–44 (95% CI) | 3.48 (–0.50 to 7.46) | 2.98 (–0.81 to 6.77) | 1.82 (–1.80 to 5.44) | 4.14 (0.43 to 7.86) | 2.08 (–1.38 to 5.53) | 3.47 (0.03 to 6.90) |
| 45–54 | 0 | 0 | 0 | 0 | 0 | 0 |
| 55–64 (95% CI) | 2.27 (–1.61 to 6.15) | 2.54 (–1.15 to 6.22) | 1.72 (–1.79 to 5.24) | 0.93 (–2.69 to 4.55) | 1.37 (–2.00 to 4.73) | 1.25 (–2.09 to 4.59) |
| 65–85 (95% CI) | 5.44 (0.66 to 10.23) | 6.95 (2.39 to 11.51) | 4.36 (0.02 to 8.69) | 3.31 (–1.16 to 7.79) | 3.49 (–0.67 to 7.64) | 3.06 (–1.07 to 7.19) |
| Gender | ||||||
| Male (95% CI) | 0.58 (–2.16 to 3.32) | –0.36 (–2.98 to 2.25) | –0.74 (–3.23 to 1.75) | 0.84 (–1.71 to 3.39) | –0.34 (–2.72 to 2.04) | 1.74 (–0.63 to 4.10) |
| Female | 0 | 0 | 0 | 0 | 0 | 0 |
| SES | ||||||
| Low SES | 0 | 0 | 0 | 0 | 0 | 0 |
| Mid SES (95% CI) | 1.39 (–1.63 to 4.41) | 0.74 (–2.13 to 3.62) | –0.39 (–3.14 to 2.36) | –0.72 (–3.55 to 2.12) | –0.21 (–2.84 to 2.41) | –1.85 (–4.47 to 0.78) |
| High SES (95% CI) | 4.04 (–0.50 to 8.58) | 2.62 (–1.71 to 6.94) | 1.12 (–3.01 to 5.25) | 0.26 (–4.01 to 4.54) | 2.11 (–1.83 to 6.05) | –1.40 (–5.35 to 2.55) |
| Practitioner variance (standard error) | 0.9 (4.4) | 0.8 (3.9) | 2.7 (4.2) | 2.2 (4.3) | 0.0 (0.0) | 1.8 (3.6) |
| Client-level unexplained error (standard error) | 415.6 (19.5) | 376 (17.6) | 339.7 (16.0) | 359.8 (16.9) | 313.4 (14.4) | 307.3 (14.4) |
| –2log likelihood | 8453.0 | 8357.4 | 8265.4 | 8319.0 | 8181.9 | 8168.5 |
| Variable | Model 1 | Add OS1a | Add OS2b | Add OS5c | Add OS6d | Add OS9e |
|---|---|---|---|---|---|---|
| Smoking dependence | ||||||
| Not recorded as dependent (95% CI) | 3.31 (0.55 to 6.07) | 2.54 (–0.09 to 5.17) | 0.66 (–1.86 to 3.19) | 2.96 (0.39 to 5.54) | 1.50 (–0.90 to 3.91) | 1.30 (–1.08 to 3.69) |
| Dependent | 0 | 0 | 0 | 0 | 0 | 0 |
| Quit attempt supported by spouse/partner | ||||||
| Supported (95% CI) | 4.83 (2.14 to 7.53) | 4.24 (1.67 to 6.80) | 3.92 (1.48 to 6.37) | 2.24 (–0.31 to 4.79) | 3.59 (1.25 to 5.93) | 1.34 (–1.02 to 3.69) |
| Other | 0 | 0 | 0 | 0 | 0 | 0 |
| Mental health condition | ||||||
| Yes | 0 | 0 | 0 | 0 | 0 | 0 |
| Not recorded (95% CI) | 10.77 (7.05 to 14.49) | 8.56 (5.00 to 12.12) | 5.05 (1.59 to 8.51) | 7.79 (4.29 to 11.29) | 4.85 (1.56 to 8.14) | 6.71 (3.48 to 9.95) |
| CO-validated quit rate | ||||||
| Quit at 4 weeks (95% CI) | 6.11 (3.05 to 9.17) | 5.87 (2.96 to 8.77) | 4.78 (2.00 to 7.56) | 5.26 (2.40 to 8.11) | 3.25 (0.58 to 5.92) | 3.62 (0.97 to 6.27) |
| Not quit at 4 weeks | 0 | 0 | 0 | 0 | 0 | 0 |
Factors associated with higher well-being at 52 weeks
At 1 year after the quit date, only the ontological security items [I enjoy a challenge, I can do what I want when I want, I feel in control, I feel safe, I worry about things going wrong (reversed), I feel I’m doing well in life, My life has a sense of routine] and being abstinent from smoking at 52 weeks were associated with well-being (see Tables 38 and 47). However, if the ontological security items were not entered into the model, well-being was associated with cessation at 52 weeks and also the following variables collected at baseline: age, low dependence and not having either a lung/respiratory or a mental health condition (see Table 47).
Summary of key points
-
The WHO-5 Well-being Index was integrated successfully into routine questions asked of service clients at baseline. This suggests services could ask about well-being if useful for monitoring purposes.
-
Clients who arrived at the SSS and who had higher levels of well-being at the start of their quit attempt were significantly more likely to be non-smokers at 4 weeks and 52 weeks.
-
In addition, well-being among those who stopped smoking remained higher than that of continuing smokers at all measurement points. There was a linear rise in the levels of well-being among quitters, however, the CIs of quitters’ well-being at baseline, 4 weeks and 52 weeks overlapped.
-
The most consistent factors associated with well-being at baseline, 4 weeks and 52 weeks were: not having a diagnosed mental health condition; low dependence on tobacco; and young or older age.
-
Clients aged 45 to 54 years had lower well-being scores than younger and older clients at all three time points, although differences were not always significant.
-
Clients who had higher levels of well-being were consistently more likely to agree that they enjoyed a challenge, were doing well in life and felt more in control than other clients. A mediator of the association between dependence on tobacco and well-being appeared to be not being able to cope with stress.
Chapter 9 Longer-term nicotine replacement therapy study
This chapter presents findings from the additional research on longer-term NRT use that was added to the ELONS study after the prospective study had commenced. This work was made possible by additional funding from the UK Centre for Tobacco Control Studies to Lion Shahab at University College London, who collaborated with the ELONS study team and drew on additional advice from Professor Ann McNeill of King’s College London.
Like previous chapters it begins by describing the value that this adds to the ELONS study. Next is a description of the method, sample and analytical approach, followed by the findings and a summary of key points.
Rationale and study aims
There is good evidence from both population studies and clinical trials that the provision of NRT to smokers who cut down their cigarette consumption results in more sustained decreases in cigarette consumption and improves their chances of stopping smoking completely. 64,65 Cutting down with NRT is associated with both increased motivation to stop and improved quit rates64,66 and does not increase overall nicotine intake. 67 Trials have also shown that extended use of NRT by ex-smokers may result in better long-term abstinence rates. 68,69 For this reason, NRT in the UK is licensed for smoking reduction, that is, dual use, and available to smokers who cannot or are unwilling to stop smoking completely, as a long-term harm reduction measure70 NRT licensing is also being changed to allow its use for harm reduction purposes among ex-smokers. 71
Harm reduction refers to the reduced psychological or physiological harm from substance use without complete cessation. 66 In the case of tobacco use, harm reduction may refer to the partial substitution of cigarettes with non-combustible forms such as NRT to reduce cigarette consumption or for temporary abstinence. However, harm reduction may also constitute the complete and permanent substitution of cigarettes with less harmful products, switching smokers from combustible to non-combustible nicotine delivery devices, including NRT. 72
The reason for focusing on NRT is that the burning of tobacco causes the most harm and not nicotine per se. 73 Nonetheless, there is considerable worry among potential users74 and SSS staff75 regarding the safety of long-term NRT use.
There is little research in this topic, and the studies that have looked at this issue suggest that long-term NRT use is safe and any associated health risks are small,76 certainly compared with continued smoking. 77,78 Yet, surprisingly few data exist on the impact of long-term NRT use in terms of health outcomes in the general population. Most data come from clinical trials, which have samples that tend to differ in important ways from general population samples79 and in which NRT is provided free together with behavioural support, which may affect normal usage patterns. By contrast, most NRT in the UK is used without advice and bought over the counter,80 and in many other countries (unlike in the UK) it is rarely provided for free on prescription. 81 Consequently, there is a need for further research in the area of harm reduction (as recently indicated by NICE)82 as investigating this issue will allow more precise quantification of the likely benefits or harms of substituting cigarettes with NRT among current and ex-smokers.
To help add to research to this topic, this addition to the ELONS study aimed to:
-
examine the prevalence of long-term NRT use among current smokers and ex-smokers
-
explore the impact of long-term NRT use on biomarkers of nicotine exposure and stress among current smokers and ex-smokers.
Methods and sample
All clients recruited to the ELONS study were asked by practitioners to provide two saliva samples at baseline and (if they received a home visit and had provided samples at baseline) an additional two saliva samples at 52 week follow up. The saliva samples were collected to measure two biomarkers of interest: cotinine, the primary metabolite of nicotine as a biomarker of exposure; and alpha-amylase, a digestive enzyme and indicator of autonomic nervous system activation that correlates with acute and chronic stress as a biomarker of risk/potential harm. 83
In order to maximise recruitment to the main ELONS study, clients were able to consent to participate even if they did not want to provide saliva samples. In addition, saliva sample collection at baseline was not conducted with some community practitioners (level 2 practitioners) who were not willing or able to conduct this element. For these two reasons, not all the ELONS study participants took part in the additional research on long-term NRT use. This addition to the prospective study also included a randomly selected sample of clients who were not abstinent at the 4-week follow-up who were also sent a saliva kit through the post at 12-months follow-up and asked to return samples in a reply paid envelope. This was done in order to obtain a comparable sample of smokers. The saliva kit contained two Salivettes®, a letter from the project lead asking for help and detailed instructions on how to collect their own sample as well as a £10 Marks and Spencer voucher.
This request to provide a saliva sample resulted in 1875 useable saliva samples for analysis (which represents 61% of the ELONS study participants). At 12-month follow-up, salvia samples were obtained from 169 of a potential 320 participants (i.e. those who took part in the follow-up telephone interview, were abstinent from smoking and had given a saliva sample at baseline). In addition a random sample (n = 392) of participants who had given a saliva sample at baseline and were known to have relapsed at 4-week follow-up were contacted at 12-month follow-up and asked to provide a saliva sample. This resulted in saliva samples from 89 participations.
Analysis
Data were analysed with IBM SPSS Statistics 20.0.0. Comparisons were made between those who did and did not respond to the follow-up phone call and questionnaire, and between those who did and did not provide a saliva sample at baseline and at follow-up. Differences were assessed with chi-squared tests and independent t-tests for categorical and continuous variables, respectively.
Owing to the typically positively skewed distribution of cotinine and alpha-amylase values, and a relatively small sample size, non-parametric Kruskal–Wallis tests were used to compare differences between smokers and quitters with and without NRT use. As we were concerned about the potential of confounders, we conducted a sensitivity analysis to assess the impact of these on the results. We used a generalised linear model, which enabled adjustment for potential confounders with a gamma distribution and a log link (all 0 values were replaced with 0.001) to account for the non-normal distribution.
Given the longitudinal study design, where participants were essentially their own control, we conducted an analysis to see how levels of biomarkers changed over time as this would tell us about the influence of using NRT or stopping smoking on these health indices. For the mixed-design analysis (looking at change across time), generalised linear models with a normal distribution and identity link were run using the change score in biomarkers to determine the impact of NRT use and smoking status on these biomarkers over time. Statistical significance was set at the standard level (p < 0.05), and the Bonferroni correction was applied in post-hoc analyses. Prevalence estimates are weighted where indicated (see Chapter 5, Weighting for further information) but, unless otherwise stated, all data are unweighted.
Please note that given the complexity of study design, respondents were treated in the analysis according to their last status, that is, relapsers at 4 weeks who had stopped smoking by the 12-month follow-up were counted as quitters, and self-reported quitters at 12-months who failed CO assessment were counted as relapsers and analysed accordingly.
Findings
Findings are divided into two sections:
-
prevalence of longer-term NRT use
-
impact of longer-term NRT use.
Prevalence of longer-term nicotine replacement therapy use among current smokers and ex-smokers
A total of 1047 participants (34.4% of the whole sample) provided information on long-term NRT use and therefore form the analytic sample for the prevalence analysis. As shown in Table 41, those who were lost at follow-up were younger, had smoked for a shorter period of time, were less likely to have a medical condition and were less likely to be white or cohabiting.
| Baseline characteristics | Follow-up at 12 months | |
|---|---|---|
| Responded (N = 1047) | Did not respond (N = 681) | |
| Sociodemographic/health characteristics | ||
| Age (years), mean (SD) | 46.4 (14.0) | 41.1 (13.7)*** |
| Female, % (n) | 55.0 (576) | 53.6 (365) |
| White, % (n) | 97.2 (1018) | 94.7 (645)** |
| Cohabiting, % (n) | 53.4 (559) | 47.3 (322)* |
| Routine/manual occupation, % (n) | 30.9 (323) | 34.5 (235) |
| Degree or equivalent, % (n) | 10.6 (111) | 10.4 (71) |
| Medical condition, % (n) | 59.5 (622) | 52.9 (360)** |
| Smoking characteristics | ||
| HSI, mean (SD) | 3.28 (1.45) | 3.22 (1.46) |
| Smoking length < 10 years, % (n) | 10.9 (114) | 17.4 (118)*** |
| Quit attempt last 12 months, % (n) | 41.7 (434) | 41.0 (275) |
| SSS treatment characteristics | ||
| Intervention type, % (n) | ||
| Closed group | 3.2 (34) | 2.9 (20) |
| Open (rolling) group | 20.8 (218) | 17.6 (120) |
| Drop-in clinic | 26.5 (277) | 27.2 (185) |
| One-to-one support | 49.2 (515) | 51.9 (353) |
| Other | 0.3 (3) | 0.3 (2) |
| Medication, % (n) | ||
| Single NRT | 17.4 (182) | 17.9 (122) |
| Combination NRT | 12.2 (128) | 15.1 (103) |
| Varenicline | 50.2 (526) | 48.5 (330) |
| Other | 19.0 (199) | 17.0 (116) |
| None | 1.1 (12) | 1.5 (10) |
Of clients followed up, 61.5% (95% CI 58.4% to 64.6%, n = 583) claimed that they had used NRT during their initial quit attempt. (Note: all prevalence estimates in this section are weighted but n numbers are unweighted.) However, this estimate is likely to include over-the-counter use, as this number is substantially higher than the number of participants recorded as using NRT by the services as shown in Table 41 (34.4%, 95% CI 31.4% to 37.4%; n = 310). Figure 8 provides a breakdown of clients’ length of use of NRT as a function of smoking status at follow-up and type of NRT used long term. As can be seen, most clients who started on NRT used it for at least 8 weeks and more than one in five (21.5%, 95% CI 18.3% to 25.0%, n = 137) used it for longer than the standard 3 months. However, long-term use was relatively rare with fewer than 1 in 10 participants still using non-combustible nicotine products at 12-months follow-up (8.4%, 95% CI 6.4% to 11.0%; n = 50). Prevalence of NRT use was even lower when excluding participants who used e-cigarettes only (6.0%, 4.3% to 8.3%; n = 35) and use of e-cigarettes was also relatively uncommon (2.9%, 1.8% to 4.7%; n = 18). However, it should be noted that these data include smokers and non-smokers, and most people had relapsed.
FIGURE 8.
Prevalence of (a) length of NRT use following quit date; and (b) product type used long term. a, Continuing users at follow-up (this includes e-cigarettes and provides base for Figure 8b). b, No use of nicotine nasal spray.
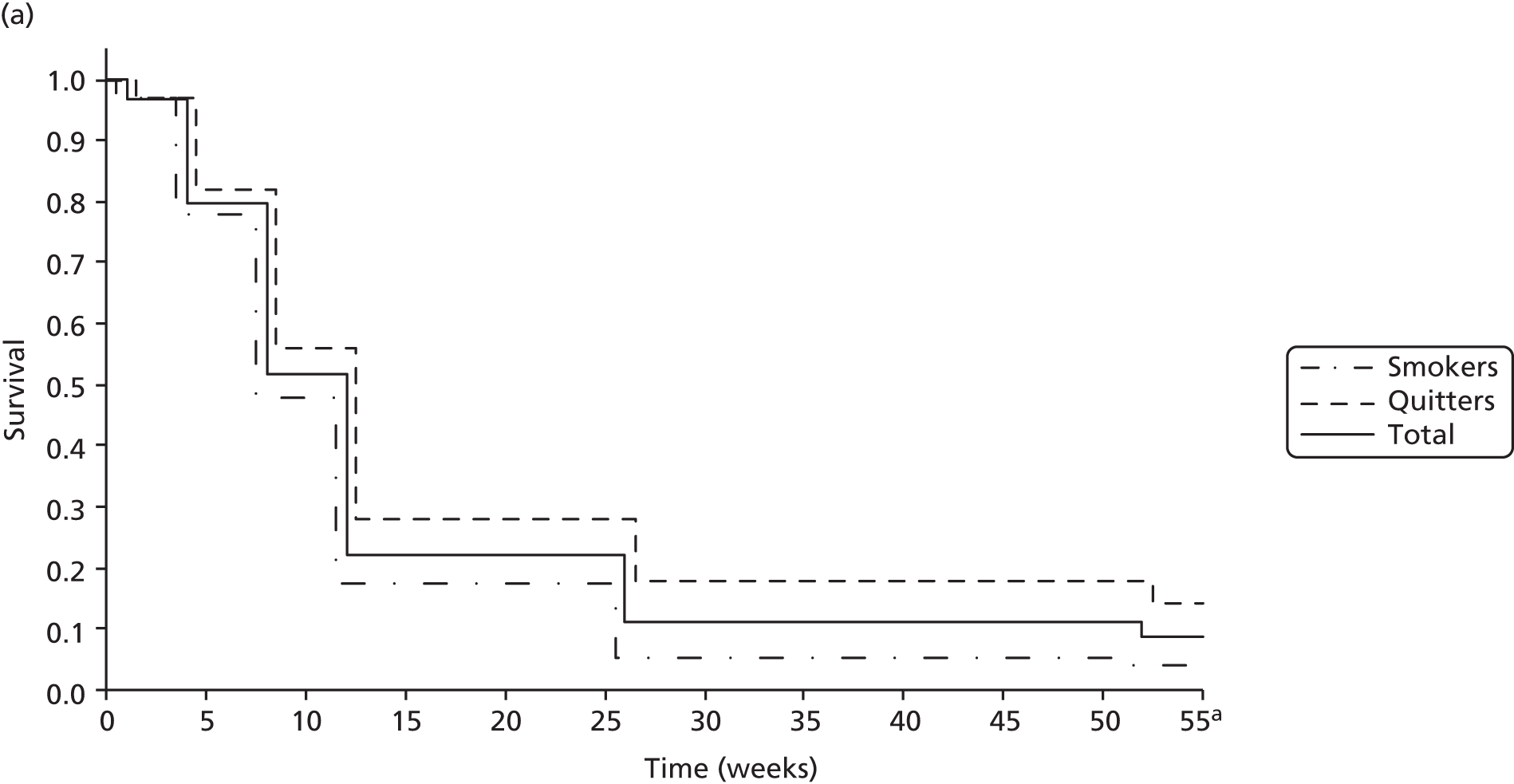

Generally, there were few differences between those clients who had relapsed between the 4-week and 12-month follow-up and those who had remained abstinent in terms of their NRT use (see Figure 8a). However, long-term ex-smokers were much more likely still be using non-combustible nicotine products at 12-month follow-up than relapsers (OR 4.25, 95% CI 2.15 to 8.40); concurrent use among relapsers stood at 3.7% (95% CI 2.0% to 6.5%, n = 12) compared with 14.0% (95% CI 10.3% to 18.7%, n = 38) among continuous abstainers. The difference between ex- and current smokers was attenuated but remained significant when excluding those who used e-cigarettes only (OR 2.91, 95% CI 1.38 to 6.11) with 3.5% (95% CI 1.9% to 6.3%, n = 10) of relapsers and 9.5% (95% CI 6.4% to 13.8%, n = 25) of abstainers still using NRT.
Figure 8b provides a breakdown of the prevalence of products used as well as the incidence of multiple use. Overall, e-cigarettes were the most popular product followed by the nicotine lozenge, patch and gum. Microtab (Nicorette®, McNeil) and nasal spray were the least popular products. Around 20% of clients were using multiple products. Owing to the small numbers involved (only 50 clients used products long term), there was insufficient power to detect meaningful differences between those who had remained abstinent and those who had relapsed. However, the use of the nicotine patch appeared particularly prevalent among current smokers, while the use of e-cigarettes, gum and the inhaler was more common among ex-smokers.
Impact of longer-term nicotine replacement therapy use on biomarkers of nicotine exposure and stress among current smokers and ex-smokers
A total of 258 participants (8.5% of the whole sample) provide baseline and follow-up saliva samples and therefore formed the analytic sample for the biomarker analysis. Table 42 shows the characteristics of those who did or did not provide saliva samples at baseline or follow-up. As can be seen, those providing samples at baseline were younger, more likely to be male and non-white, and slightly less likely to be cohabiting. There were also some differences in the treatment sought (they were less likely to have used varenicline or gone to a drop-in clinic) but there were few differences in terms of smoking characteristics. At follow-up, those who provided a saliva sample were older and more likely to be cohabiting. Again, there were some treatment differences (they were less likely to have used a drop-in clinic but more likely to have used varenicline). Clients for whom a follow-up sample was available had lower baseline levels of dependence (likely reflecting the lower response rate among those who smoked at 4 weeks compared with those who had stopped at 4 weeks).
| Baseline characteristics | Baseline | Follow-up at 12 months | ||
|---|---|---|---|---|
| Sample available (n = 1875) | No sample available (n = 1170) | Sample available (n = 258) | No sample available (n = 454) | |
| Sociodemographic/health characteristics | ||||
| Age, mean (SD) | 41.7 (14.1) | 43.7 (14.1)*** | 45.7 (13.4) | 42.2 (14.6)** |
| Female, % (n) | 52.7 (989) | 60.9 (713)*** | 51.6 (133) | 48.7 (221) |
| White, % (n) | 95.0 (1782) | 97.5 (1141)*** | 96.5 (249) | 93.8 (426) |
| Cohabiting, % (n) | 45.4 (852) | 49.5 (579)* | 53.9 (139) | 44.9 (204)* |
| Routine/manual occupation, % (n) | 30.6 (573) | 31.1 (364) | 25.2 (65) | 30.6 (139) |
| Degree or equivalent, % (n) | 8.9 (167) | 10.5 (123) | 10.5 (27) | 9.3 (42) |
| Medical condition, % (n) | 55.5 (1041) | 57.3 (670) | 57.4 (148) | 58.4 (265) |
| Smoking characteristics | ||||
| HSI, mean (SD) | 3.39 (1.46) | 3.37 (1.43) | 3.19 (1.54) | 3.51 (1.41)** |
| Smoking length < 10 years, % (n) | 16.6 (308) | 13.6 (159)* | 9.3 (24) | 14.3 (65) |
| Quit attempt last 12 months, % (n) | 41.3 (752) | 41.6 (485) | 38.1 (98) | 38.4 (172) |
| SSS treatment characteristics | ||||
| Intervention type, % (n) | – | *** | – | * |
| Closed group | 4.5 (84) | 1.5 (18) | 6.6 (17) | 4.6 (21) |
| Open (rolling) group | 19.0 (357) | 16.2 (189) | 21.3 (55) | 13.9 (63) |
| Drop-in clinic | 25.4 (476) | 35.2 (411) | 24.4 (63) | 30.4 (138) |
| One-to-one support | 50.8 (952) | 46.8 (547) | 47.7 (123) | 50.7 (230) |
| Other | 0.3 (6) | 0.3 (4) | 0 (0) | 0.4 (2) |
| Medication, % (n) | – | *** | – | ** |
| Single NRT | 17.3 (323) | 23.0 (269) | 17.4 (45) | 15.2 (69) |
| Combination NRT | 21.4 (400) | 14.2 (166) | 16.3 (42) | 27.3 (124) |
| Varenicline | 41.4 (774) | 45.7 (534) | 48.4 (125) | 37.4 (170) |
| Other | 16.9 (316) | 14.4 (165) | 16.3 (42) | 19.2 (87) |
| None | 2.9 (55) | 3.0 (35) | 1.6 (4) | 0.9 (4) |
Table 43 provides an overview of available viable cotinine and alpha-amylase saliva samples as function of smoking status and NRT use. Unfortunately, some samples provided insufficient saliva or were contaminated and, therefore, cotinine and/or alpha-amylase levels could not be determined (5.7%). In addition, a number of participants (18.1%) provided only one rather than two saliva samples at either baseline or follow-up, which meant not all analytes could be assessed. However, in each of the relevant subgroups at least 50% of the analytic sample had a complete set of data on all analytes, and at least 67% and 58% had both baseline and follow-up data on cotinine and alpha-amylase, respectively.
| Biomarker results availability | Smokers | Quitters | ||
|---|---|---|---|---|
| NRT use (n = 18) | No NRT use (n = 73) | NRT use (n = 12)a | No NRT use (n = 153) | |
| Baseline assessment | ||||
| Cotinine sample, % (n) | 94.4 (17) | 93.2 (68) | 91.7 (11) | 95.4 (146) |
| Alpha-amylase sample, % (n) | 66.7 (12) | 61.6 (45) | 75.0 (9) | 71.2 (109) |
| Follow-up assessment | ||||
| Cotinine samples, % (n) | 88.9 (16) | 94.5 (69) | 75.0 (9) | 97.4 (149) |
| Alpha-amylase samples, % (n) | 72.2 (13) | 58.9 (43) | 75.0 (9) | 72.5 (111) |
| All assessments | ||||
| Cotinine samples, % (n) | 83.3 (15) | 89.0 (65) | 66.7 (8) | 92.8 (142) |
| Alpha-amylase samples, % (n) | 61.1 (11) | 57.5 (42) | 75.0 (9) | 67.3 (103) |
| All samples, % (n) | 61.1 (11) | 53.4 (39) | 58.3 (7) | 66.0 (101) |
As can be seen in Table 44, there were some differences in baseline cotinine levels between groups (p = 0.025). Those who had stopped smoking at follow-up and were still using NRT had higher levels than other groups. However, these overall differences in baseline cotinine became barely significant when adjusting for potential confounders (age, gender, ethnicity, occupation, any medical condition and nicotine dependence; p = 0.245) and after taking into account multiple comparisons, quitters who used NRT at follow-up, did not differ from any other group. In addition to older age (p = 0.011), dependence as measured by the Heaviness of Smoking Index was the only other significant predictor (p < 0.001). There were no differences as a function of NRT use and smoking status at follow-up in baseline levels of alpha-amylase (p = 0.956). This was confirmed in adjusted analysis (p = 0.185), which showed that older age (p = 0.001), being non-white (p = 0.021) and having any medical condition (p = 0.002) were associated with higher alpha-amylase activity at baseline.
| Biomarker results | Smokers | Quitters | ||
|---|---|---|---|---|
| NRT use (n = 18) | No NRT use (n = 73) | NRT use (n = 12) | No NRT use (n = 153) | |
| Baseline assessment | ||||
| Cotinine (ng/ml), mean (SEM) | 280.2 (36.7) | 320.1 (22.0) | 414.3 (90.4) | 270.1 (13.7) |
| Alpha-amylase (U/ml), mean (SEM) | 75.6 (41.2) | 32.6 (4.4) | 32.8 (7.4) | 34.9 (3.2) |
| Follow-up assessment | ||||
| Cotinine (ng/ml), mean (SEM) | 280.6 (36.6)a | 333.1 (22.3)a | 324.4 (102.5) | 45.8 (9.7)b,c,d |
| Alpha-amylase (U/ml), mean (SEM) | 48.3 (17.7) | 39.4 (5.7) | 42.6 (17.7) | 43.7 (4.2) |
There was a clear difference between groups in follow-up cotinine levels (p < 0.001), confirmed in adjusted analysis (p < 0.001). Non-NRT users who were abstinent had significantly lower cotinine values than smokers with (p = 0.017) or without concurrent NRT use (p < 0.001) but not compared with quitters who used NRT (p = 0.232). Baseline nicotine dependence was the only other significant predictor (p < 0.001). Yet, even among CO-validated non-smokers at follow-up who indicated that they did not use NRT, over one in five had cotinine values above the usual cut-off level, suggesting either a high rate of deception in this group or undeclared use of other nicotine-containing products. No differences were apparent in alpha-amylase levels at follow-up (p = 0.684), confirmed in adjusted analysis (p = 0.734). Only lower dependence at baseline had an association with greater follow-up alpha-amylase activity (p = 0.004) but none of the other covariates or factors were associated.
Changes in biomarkers from baseline to follow-up were analysed in those with complete data (Figure 9). For cotinine values, greater dependence at baseline was associated with an increase in cotinine levels (p = 0.047). In addition, over and above an expected main effect of smoking status (p < 0.001), there was a significant NRT use by smoking status interaction (p = 0.021). This can be seen clearly in Figure 9a. Compared with current smokers, there was a significant reduction in cotinine values only among quitters who did not use NRT or put differently, smoking status did not have an impact on cotinine values among those who used NRT but did among those who did not. By contrast, there was no discernible impact of either smoking status or NRT use on alpha-amylase activity (see Figure 9b). However, there was a marginal effect of dependence (p = 0.062) and ethnicity (p = 0.052) on changes in alpha-amylase activity. Both lower baseline nicotine dependence and non-white ethnicity were associated with an increase in alpha-amylase activity across time.
FIGURE 9.
Change in (a) cotinine levels; and (b) alpha-amylase activity from baseline to follow-up as a function of NRT use and smoking status at follow-up. a, Plotted on log-2 scale.


Summary of key points
-
Just over one-third of the ELONS prospective study participants provided information on longer-term NRT use (n = 1047) and were included in this addition to the main ELONS study.
-
Of clients followed up at 12 months, 61.5% reported that they had used NRT during their initial quit attempt. However, this is likely to include over-the-counter use, as this number is substantially higher than the number of participants recorded as using NRT by the services (34.4%).
-
Most clients who started on NRT used it for at least 8 weeks and more than one in five (21.5%) used it for longer than the standard 3 months.
-
Long-term use was relatively rare, with fewer than 1 in 10 participants still using non-combustible nicotine products at 12 months’ follow-up (8.4%).
-
Within this category of non-combustible nicotine products were e-cigarettes. Few participants reported their use at 1 year, just 2.9%, although these data include smokers and non-smokers and most people had relapsed by 1 year post quit date. However, e-cigarettes were the most popular single product at 1 year (used more commonly than the gum, lozenge or patch).
-
Long-term ex-smokers had much higher odds of still using non-combustible nicotine products at 12-month follow-up than those who relapsed. Concurrent use among relapsers was 3.7%, compared with 14.0% of continuous abstainers. This difference remained significant even after removing those who used e-cigarettes only.
-
In terms of the biomarker analysis, 258 participants (8.5% of the whole ELONS study sample) provided baseline and follow-up saliva samples and were included. Greater levels of cotinine (a metabolite of nicotine) were associated with greater self-reported dependence. As expected, within-group analysis showed that smokers who had stopped had significantly lower cotinine levels at follow-up than those who had relapsed to smoking at follow-up. However, this was the case only for ex-smokers who did not use NRT. Cotinine levels for smokers who had stopped at follow-up but who used NRT long term had not changed from baseline to follow-up and neither did cotinine levels for those who had relapsed to smoking (irrespective of NRT use). There were no differences as a function of NRT use and smoking status at follow-up in baseline levels of alpha-amylase, a biomarker of stress.
Chapter 10 Discussion
The UK remains one of very few countries in the world that offers free at the point of use treatment services for people seeking support to stop smoking. 10 These services form an important part of a wider network of policies aimed to reduce smoking rates, including policies such as tobacco taxation, mass media campaigns, bans on advertising and Smokefree laws. 15 The ELONS study was designed to provide up-to-date evidence on the effectiveness of these SSSs, building on earlier research. As routine data collected by the services report on only short-term outcomes and are limited in detail, this study was also intended to examine longer-term outcomes and explore the factors that influence quit rates.
The findings raise a number of issues. Here we reflect on the results, focusing on key themes:
-
short- and longer-term cessation rates in context
-
the influence of client characteristics
-
the influence of service characteristics
-
satisfaction with services
-
well-being
-
longer-term use of NRT
-
limitations
-
future research.
Short- and longer-term cessation rates in context
This study examined smoking cessation in the short term (at 4 weeks) in two ways: through an analysis of routine data and through the prospective study. Our prospective study results were broadly comparable with those from routinely collected data from services. Among 3000 smokers attending SSSs in nine areas of England, we found that just over 4 in 10 (41.2%) were biochemically validated as abstinent from smoking at 4 weeks post quit date. Our secondary analysis of routine data from 49 of 150 services in England found 4-week quit rates of 48% when self-reported data were included, falling to 34% when biochemical validation had occurred. This same analysis found that services were reaching up to 10% of smokers in their area in the year from July 2010, with the majority coming from more-deprived areas. NICE guidance previously recommended that services aim to reach at least 5% of their smoking population in a year. 21 These results provided suggest that (a) routine data provide a useful and not inaccurate indicator of short-term smoking cessation outcomes and (b) services are continuing to effectively reach smokers and support them to stop.
In the longer term, we found that fewer than 8% of smokers were still abstinent from smoking 1 year after setting a quit date with their local service. Outcomes were influenced by characteristics of clients and there was also a clear link with service characteristics such as the type of behavioural support received, and the background and training of the smoking cessation practitioner.
Cessation rates identified in this study were lower at both 4 and 52 weeks than in our previous research conducted over a decade ago as part of a ‘national’ evaluation of the services in England shortly after they were established. 17,18 At face value it might be assumed that service standards had slipped in the intervening period, but our view is that this is too simplistic an explanation. Our earlier work was conducted with just two (albeit large) services that performed better than the national average based on comparisons with routine data. The ELONS study purposively selected nine services that offered different types of interventions in a range of settings, some of which reported quit rates higher than the national average while others reported lower rates. In addition, the configuration of services has changed in the last decade and there is clearly a greater reliance on community practitioners (such as pharmacists and practice nurses) with lower short-term quit rates delivering support rather than specialist smoking cessation staff. Others have argued that the smoking population itself may have changed84,85 and that remaining smokers are more nicotine dependent and find it harder to stop. Research design differences between the studies may also explain some of the difference.
Despite rates of abstinence from smoking being lower in the ELONS study than in some previous studies with service clients, they remain significantly higher than in untreated populations. Previous research with ‘self-quitters’ not participating in a smoking treatment programme has estimated abstinence rates at 25% at 4 weeks,42 which is considerably lower than the overall 4-week quit rate (41%) and the lowest 95% CI boundary (36%). At 1 year, abstinence rates with self-quitters are approximately 3%,86 considerably lower than the 8% found here. Thus the behavioural support and stop smoking medication provided by the services makes a significant difference and improves outcomes for individual smokers. The ELONS study is consistent with previous studies in demonstrating this. 7,17
The ELONS study only assessed smoking status up to 1 year after an initial quit attempt, yet it is possible to extrapolate our results to estimate the number of life-long non-smokers achieved.
The study took place during the financial year 2012–13. In that year, routine data returns from all SSSs in England showed that 724,247 quit dates were set. 87 Applying the ELONS study results (8% quit at 1 year), 55,767 would have been CO validated as abstinent at 1 year. The best estimates of the relapse rate to smoking after 1 year are 35%. 88 This would leave 36,249 lifelong abstinent quitters. This is a substantial figure and is one indicator of the ongoing value of the life-saving treatment that the services provide.
The influence of client characteristics
Consistent with other studies, we found that smoking cessation outcomes varied significantly between different groups of people who accessed SSSs. At 1 year, for example, a number of client characteristics were associated with either maintaining abstinence of having relapsed to smoking. As other studies have found, the odds of maintaining a quit attempt increased with age. 89,90 This may be caused by a range of factors including learning from previous quit attempts, contact with health services, personal circumstances (such as the death of loved ones owing to smoking-related disease) or for some, additional time to commit to focusing on getting the most from the support on offer. Individuals with higher levels of well-being when they began their quit attempt were more likely to be successful in the longer term, as were those who had fewer smokers in their social network – neither of these findings are surprising but being aware of these factors may be useful for practitioners treating smokers.
Although some predictors of relapse to smoking identified in previous studies did not quite reach significance here (e.g. level of dependence on smoking, lower levels of determination to quit), others did, including deprivation. More disadvantaged clients were less likely to remain abstinent from smoking at 1 year, as our previous work and that of others has shown. 18,91,92 Thus, although SSSs are able to reach significant numbers of smokers living in disadvantaged areas,19 these smokers face additional barriers to quitting. This poses challenges for service delivery, and requires time and resources to ensure particularly effective forms of support (including medication) are delivered to those who need it most.
The influence of service characteristics
Client characteristics cannot be easily modified, but service characteristics can, and our findings show that some interventions are more effective than others. We found that smokers supported to quit with specialist services (including group behavioural support and one-to-one support from a specialist) were more likely to have stopped smoking in the longer term. This is consistent with other studies24,44,93 and reflects the training and expertise that specialist practitioners have, and also that they see more smokers than part-time (level 2) practitioners and are therefore more likely to maintain standards of knowledge and practice. Time and resource pressures in settings such as GP practices and pharmacies may also contribute to poorer outcomes for clients of non-specialists. 94,95
Important differences in outcomes between forms of behavioural support were also identified. Clients attending open groups achieved the highest quit rates and maintained the highest ORs compared with other forms of behavioural support, even after controls. These results reflect those of our previously published paper26 on the success of open groups.
In addition, we found that drop-ins (i.e. where people can simply drop-in to see a SSS practitioner without an appointment) did not result in as positive cessation outcomes as other types of support types. Potential reasons for this lower performance might include less client motivation contact (especially if demand is high) or drop-ins being selected by smokers who were less likely to quit, or that practitioners have limited capacity to plan and deliver effective behavioural support within this setting.
One of the objectives of this study was to provide guidance on interventions that will have maximal benefits. From the secondary analysis it would appear that the services that had the highest impact focused on quit rates rather than throughput. The results from the prospective study suggest that services will be particularly effective in terms of achieving long-term cessation if they provide groups or one-to-one support by specialist practitioners.
Satisfaction with services
Feedback from patients or clients is important to inform service development. In our satisfaction survey of SSS clients, we found that those who responded had a positive experience, and this was true both for those who were successful in stopping smoking and those who were not. The vast majority of participants who replied to the questionnaire indicated that they would recommend the service to others and return should the need arise. In addition, we found several examples of good practice where SSSs have offered more than they are required to do by national service standards. 96 This included, for example, contacting clients before their first appointment to encourage them to attend and offering child care and a choice of behavioural support options.
Additional comments highlighted the importance of practitioner/client rapport. In addition, despite many clients finding stop smoking medication easy to acquire, additional comments pointed to a more complex picture where the process of obtaining medication was overcomplicated and time-consuming for some respondents. Suggested improvements to the SSS centred on evening appointment times, having a choice of group or one-to-one support and a longer period of support.
Analysis of client satisfaction between quitters and non-quitters, SSS location and behavioural support types revealed some small but significant differences. Those who had stopped smoking were more likely to be satisfied with staff supportiveness and happier to return to the services if needed, with the information provided and CO validation. Open-group clients were also more positive about staff supportiveness, returning to the service and CO testing. GP practice clients were least comfortable with CO testing.
Despite an encouraging response rate (response to self-completion postal surveys are generally low, even with repeated reminders) clients who were motivated to complete the survey were also more likely to have had a successful quit attempt. This means the views of those who did not quit are under-represented.
Well-being
As outlined earlier in the report, we included a modest exploratory study of well-being and smoking cessation within the ELONS prospective study. Positive well-being at baseline significantly predicted abstinence from smoking 1 year later. Although few other studies have looked at positive well-being, research has found that psychological distress and mental health conditions can reduce the chances of successfully stopping smoking. 57,97,98 Smokers in these previous studies have reported experiencing more negative moods shortly after quitting that may be related to relapse. 98
In our analysis we did not find that levels of well-being changed significantly over time, unlike a previous systematic review. 50 Those who stopped smoking did tend to have higher well-being than non-quitters at all time points. This suggests that the level of well-being at baseline is important as a predictor of who may quit smoking, and that this difference is maintained.
Clients who managed to stop smoking in the ELONS study and who completed the well-being survey were more likely to agree that they felt in control. Feelings of control have not received much attention in the context of smoking cessation, although perceived control has been found to positively influence intention to quit smoking. 99 In addition, having financial difficulties, which could signify feelings of a lack of control, has been associated with fewer quit attempts and less success in the quit attempts that did take place. 100
Clients who were more dependent on tobacco at baseline had lower well-being at all three time measurement points. This was possibly mediated by being unable to cope with stress. Other studies have found that stress is associated with higher levels of smoking. 101,102 Neurologically, this may be related to higher levels of cortisol and adrenocorticotrophic hormone as a response to stress. 103 However, despite smokers stating that they smoke to cope with stress, higher levels of stress have been found among smokers,104 which then declines with smoking cessation. 105 Thus, smoking tobacco (rather than stopping) appears to be associated with heightened feelings of stress. This is an important message for services to communicate to clients.
Well-being was low among many smokers approaching the SSS, and well-being is a predictor of smoking cessation success. This raises the issue of whether or not it could be helpful to train practitioners in techniques such as cognitive–behavioural therapy, or alternatively employ practitioners already qualified with cognitive–behavioural therapy, in order to address feelings of stress and insufficient control.
Longer-term use of nicotine replacements therapy
We found that over one in five NHS SSS clients who achieved short-term abstinence reported continuing to use NRT beyond the standard treatment length of 3 months. However, complete substitution of cigarettes with non-combustible nicotine products long term was less common, at just below 10%. In our previous ‘national’ evaluation of SSSs in England, conducted in Nottingham and North Cumbria in 2002, self-reported longer-term NRT use at 1 year was just 5%. 106 This means that more people may now be using cleaner forms of nicotine longer term, with 6% of our sample reporting using NRT at 1 year and 2.9% using e-cigarettes at 1 year post quit date. Recent policy and licensing changes in favour of harm reduction70,82 may have offered some reassurance in this regard, although it is worth noting that the reported rate of longer-term e-cigarette usage in the ELONS study is low compared with the estimates of one in five smokers or recent ex-smokers using e-cigarettes in the general population. 107
Concurrent long-term use of NRT among SSS clients in the study who have relapsed to smoking, reflecting partial substitution, was much lower, at less than 4%. This is in agreement with similar figures from the general population suggesting that longer-term NRT use among smokers is rare. 108 Indeed, concurrent NRT use among smokers, either for temporary abstinence or for cutting down, has remained relatively stable since 2002109 and mostly reflects short-term use. 108
This study provides some rare insights in the exposure to nicotine associated with single use or long-term dual use of NRT as well as its impact on a biological indicator of stress, alpha-amylase. Clinical trials suggest that permanent replacement of cigarettes with NRT among ex-smokers can result in 40% of baseline levels of nicotine being substituted by nicotine-replacement products. 110,111 Although the cross-sectional analysis did not detect a significant increase in cotinine levels among ex-smokers using NRT compared with those not using NRT, the within-group analysis suggests that virtually all baseline nicotine may be replaced by NRT among long-term ex-smokers. This finding is against a background of excluding participants from analysis based on CO verification of their smoking status and concurrent use of other nicotine delivery devices, that is, e-cigarettes. Moreover, confirming previous research,67,112 the concurrent use of NRT among smokers did not appear to increase their nicotine intake. These findings reflect that smokers are very adept at titrating nicotine levels, with some nicotine otherwise obtained from cigarettes being replaced by nicotine from NRT. 113 However, our results indicate this may also apply to ex-smokers, which is consistent with a strong genetic component in nicotine intake,114 but at odds with clinical studies showing that nicotine substitution from NRT tapers off over time. 110 The fact that long-term use among ex-smokers did not result in a decrease in cotinine levels, however, does not mean that long-term use maintains addiction to nicotine. Although we controlled for baseline characteristics, the study design cannot exclude reverse causation, that is, the fact that particular individuals who happen to have a high sensitivity to nicotine intake, use NRT for longer.
Although it is unlikely that a substantially increased nicotine intake from NRT would be harmful,115,116 it clearly is a concern for some people and a potential barrier to effective use of nicotine products. 74 Our results do not suggest that NRT use leads to an increased intake compared with continued smoking. Moreover, there was no evidence that use of NRT (either concurrently or among ex-smokers) was associated with an increase in a biomarker of stress response, alpha-amylase, used as a proxy here to signal potential harm. The somewhat paradoxical finding that greater activity in alpha-amylase at follow-up and an increase in alpha-amylase activity across time were both associated with lower nicotine dependence is likely because tobacco smoke has been shown to acutely inhibit alpha-amylase activity. 117 Given that lower nicotine dependence was associated with lower exposure to tobacco smoke, as measured by cotinine levels, and smaller increases in cotinine levels from baseline, the inhibitory action of tobacco smoke on alpha-amylase in this group of users was therefore likely to be smaller. Altogether, these findings suggest that long-term NRT use is safe and not associated with increased health risks, certainly compared with continued smoking. 78
Limitations
Each element of the ELONS study had a number of limitations. For example, in the secondary analysis our estimates of the reach of the services were based on estimates of both the number of smokers and the population in the PCT. We also assumed that smoking declined uniformly by 4% in all PCTs between 2003 and 2005, and also in 2009, when it is likely that the smoking rate declined more in PCTs with an affluent population and less in PCTs with a more disadvantaged population. 118 For all but the impact analysis we assumed that each client in the database was unique when we estimated that 8% of clients used the SSS more than once during the year. However, the consistency of our estimates between PCTs (the majority between 5% and 12%) and the consistency of quit rates calculated for unique clients and client records gives support to the technique used.
Other limitations pertain to the use of routine monitoring data with pre-set variables: SES was measured using NSSEC, IMD and free prescriptions. NSSEC is complicated to classify and may not reflect SES for clients who are not the chief income earner of the household. IMD was included at PCT level, which is large geographically and may explain the lack of significant results. Eligibility for free prescriptions can be for medical or age reasons in addition to low income. In the analysis all ethnic minorities were compared with white people. Ethnicity was not disaggregated further because of small numbers.
The secondary analysis includes only data from PCTs who agreed to their QuitManager data set being used for research purposes. North 51 is based in Nottingham, which may be the reason for a concentration of PCTs in central England. Nevertheless there are PCTs included in all regions of England from County Durham and Darlington in the North East to Bristol in the South West. Comparison with 2010/11 data for all English PCTs found similar rates of self-report quit and CO validation. Furthermore, the self-reported quit rate for all English SSSs from April 2010 to March 2011 was also 49%, and 70% were CO validated43 compared with 74% in the secondary analysis sample suggesting that the sample were representative of the whole.
Some of the limitations of the secondary analysis were ameliorated by the prospective study. These include, for example, only short-term follow-up data collected for routine monitoring, which may be of lower quality, and inconsistently collected data on levels of tobacco dependence and social support, which could not be used in the analysis. Data on the practitioner type was also poorly collected, perhaps partly because the DH does not publish it.
However, the prospective study also had limitations, the most substantial being recruitment. Reasons for this are discussed in detail in Chapter 5, but were partly because of the cumbersome consent process to the study required by ethical review and the need for all aspects to be classified as research (rather than service evaluation) to be eligible to become a NIHR portfolio study and access service support costs. This type of consent process would be expected and appropriate in a trial or study of a new intervention, but it is problematic in an observational study of an existing service. Far simpler questions and a simpler process (such as those we have been permitted to use in earlier studies with NHS SSSs) could still have protected client confidentiality.
In addition, policy and service changes also affected recruitment, as described in Chapter 5. The result was that we recruited only a small proportion of eligible service clients in each study area. To overcome the low response rate we have used weighting and multivariable analysis. However, CIs of quit rates for many behavioural support types were wide and it may be that some non-significant differences are a consequence of the study being underpowered.
Owing to selection of the PCTs for the secondary analysis and the prospective study being limited to services that used Quit Manager software, this could raise issues of validity – specifically representativeness. If we redid, in particular the prospective study, with completely different areas, we might have obtained slightly different results. This is an important caveat. That said, we did try as much as possible to recruit areas in varying parts of the country that offered a range of types of interventions as outlined in Chapter 5. However, it is should be remembered that the 4-week quit rate for the prospective study was 41.2%, which is remarkably similar to the quit rate for England from April 2012 to March 2013 (37%)31 given the impact profile of the PCTs that enrolled in the study (see Chapter 4). Moreover, the ELONS prospective study sample differed little in terms of demographic characteristics to all the clients that attended the nine services. This should go some way to allay concerns about representativeness.
There are data collection issues common to both the secondary analysis and the prospective study that focus on issues of definition of interventions that were beyond our control. In brief, we were dependent on local understandings of what formed different behavioural support types for example, and different settings for delivery and practitioner categories. In the 4-week analysis in the prospective study we were also dependent on local data collection being accurate and timely, which we suspect it was not in all cases. Busy practitioners do not always collect the best data, for a variety of reasons. This may explain some of the differences between the 4-week results that go against the findings of previous studies,7,17 in particular our findings around combination NRT not being as effective as other medication forms. This finding was not carried through into the 52-week results, where we saw results that were more consistent with previous research.
We treated group clients as independent, whereas the chances of a group member quitting may depend to some extent on the other group members and the culture of the group. The effect of a group is very difficult to take into account especially for open groups where members change and the number of sessions attended may vary markedly. 119–121
The well-being and client satisfaction elements of the ELONS study also had limitations. At baseline, the WHO-5 items were included in routine monitoring questions administered by practitioners so almost all participants had well-being data at this stage. At follow-up the well-being questions were included in postal surveys sent to clients’ home addresses, as was the satisfaction questionnaire. As with most postal surveys, the response rate was low and caution is therefore required in interpreting the results. For the well-being element in particular, it is also the case that the analysis reported was largely exploratory and any conclusions can only be tentative.
The longer-term NRT element added to the ELONS study also had a number of limitations. Despite an initial large sample size, dropout across the main study was inevitably substantial, resulting in relatively few clients with complete baseline and follow-up data on biomarkers. In addition, the baseline sample differed from the sample followed up. However, differences were relatively modest and therefore unlikely to have substantially biased findings. In addition, weighting was used in the assessment of long-term NRT use prevalence, which should account for differential dropout. Although clients self-selected into groups rather than being experimentally assigned, this reflects real-world use of NRT. Moreover, the study design allowed clients to be their own control, thus further reducing confounding. Assessment was carried out with established, ecologically valid measures and smoking status verified.
Future research
The study raises a number of issues for future research. First, a significant gap in the research relates to the use of e-cigarettes. When the ELONS study was commissioned in 2010/11, e-cigarette use was still relatively rare, but has grown significantly since then. Although we asked about e-cigarette use in the longer-term NRT study, we did not address it elsewhere. Recent monitoring data and reports from service managers indicate that the ‘rise’ of e-cigarettes has coincided with a significant drop in SSS client numbers, particularly in the period since the ELONS study was conducted. Future research should examine this issue, and also look at effective ways to combine e-cigarette use with the support provided by services. Useful pilots and some ongoing research in England are already under way, but more is needed.
In addition, previous research has shown that effective behavioural support delivered by trained practitioners roughly doubles smokers’ chances of successfully stopping. 122,123 However, there was great variety in the type and, in all likelihood, the quality of the behavioural support provided to the ELONS study participants. This study did not set out to capture factors that affect the quality of behavioural support such as the training status of practitioners (whether NCSCT certified or not), the presence, perception and use of treatment protocols, and the amount of support and supervision available to individual practitioners. This is both a limitation of the ELONS study and an issue to be explored in more detail in further research. Within that, a priority should be to explore in more detail what factors influence the success of a rolling-group model of behavioural support when compared with other options.
For the well-being element, no formal tests for differences between well-being scores over time or between quitters and non-quitters were undertaken. In further analysis, regression models or propensity scores could be used to test relationships more precisely. Alternatively a qualitative approach to well-being may yield insights. For example, interviews or a diary over the quit attempt may aid understanding of how and when well-being changes occur and their relationship to failure or success of the quit attempt. Slightly broader research may also be helpful in this area, examining issues such as insecurities in housing,124 relationships125 and income,100 which may impact on the success of quit attempts. While these wider contributors to poorer well-being are difficult to tackle, helping to create resilience in smokers who face multiple life challenges may help them to move away from tobacco, which will yield mental as well as physical health benefits for them in the longer term.
We began to explore longer-term use of nicotine-containing products in this study but there is a sizeable research agenda on this topic that is still to be explored. In particular, further research would benefit from measuring a wider array of biomarkers of smoking-related harm, such as lung function tests or carcinogen metabolites to confirm our preliminary results.
Although there are some obvious and clear conclusions from this evidence base (such as behavioural support type and client demographic characteristics) that can guide service delivery, there are some questions that are more difficult to answer – for example, why do some services find it easier to meet targets than others? It is likely that a process evaluation collating qualitative evidence from individual poorly performing services and services with excellent performance would provide further insights into this important area. Additionally, despite non-quitters appearing to be highly satisfied with the services, the low response rate to the CSS calls for more qualitative research among clients who drop out and relapse to understand how the service can support these groups.
Finally, there is a need for ongoing research on NHS SSSs that is useful to inform policy, including determining the factors that contribute to the ongoing development and sustainability of the services. This is useful not only in a UK context but to inform work in other countries to establish or improve the provision of services to support smokers to stop using tobacco.
Chapter 11 Conclusions
This detailed observational study of smoking treatment services in England has yielded a number of findings that allow us to draw conclusions about the factors that influence outcomes for clients, as well as describe effectiveness in the short and longer term.
In terms of smoking cessation in the short term, the findings of the ELONS study are broadly comparable with those from routinely collected data from services. From our prospective study of just over 3000 smokers attending SSSs in nine areas of England, we found that just over 4 in 10 (41.2%) were biochemically validated as abstinent from smoking at 4 weeks post quit date. The secondary analysis of routine data from 49 of 150 services in England found 4-week quit rates of 48% when self-reported data were included, falling to 34% when biochemical validation had occurred. This same analysis found that services were reaching up to 10% of smokers in their area in the year from July 2010, with the majority coming from more deprived areas. NICE guidance previously recommended that services aim to reach at least 5% of their smoking population in a year. 21 These results provide a useful indicator that (a) routine data provide a helpful and not inaccurate indicator of short-term smoking cessation outcomes and (b) services are continuing to effectively reach smokers and support them to stop.
No routine data exist on longer-term cessation at 1 year and it is some time since a study in England has looked at this issue. We found that just fewer than 8% of smokers were still abstinent from smoking 1 year after setting a quit date with their local service. If these results are applied to all of England, then we estimate that in the year 2012–13 the services supported 36,249 clients to become non-smokers for the remainder of their lives, which is a significant number.
A range of factors, including many linked to the characteristics of clients, but also service characteristics, influenced smoking cessation outcomes in the prospective study. For example, smokers supported to quit with the specialist service were more likely to stop smoking in the longer term. In addition, the ELONS study builds on previous research that shows that longer-term outcomes are influenced by the type of behavioural support a smoker receives – rolling groups resulted in better outcomes than other forms of behavioural support.
Three additional elements were added to the ELONS study that were more exploratory in nature. These focused on client satisfaction, well-being and longer-term NRT use. Overall, we found that those who responded to the satisfaction survey were positive about the support they received and would recommend SSSs to others. We found that assessment of well-being using a standard set of questions could be included in routine monitoring and that smokers who had higher levels of well-being when they first started attending services were more likely to be non-smokers at 4 weeks and 1 year later. Assessing well-being may therefore help give advisers an indication of who may need more support during their quit attempt. It may also provide an opportunity to help clients make links with other local services or networks who could assist them in improving other aspects of their lives that may be responsible for lower levels of well-being.
The longer-term NRT study found that use of NRT while smoking did not appear to increase overall nicotine intake. Its long-term use among former SSS clients who remained abstinent was not uncommon compared with concurrent use among smokers. Long-term use of NRT did not appear to have a detrimental effect on the chronic stress response among smokers or ex-smokers and did not increase exposure to nicotine among smokers. In contrast, it was associated with continuing high cotinine levels among ex-smokers. This analysis provides some reassurance about longer-term nicotine use when not delivered through tobacco. It builds on earlier research indicating that long-term NRT use is not associated with increased health risks as assessed here, and is certainly safer than continued smoking.
Acknowledgements
The study would not have been possible without the input of a number of colleagues from a range of different organisations.
We are grateful to the service managers, practitioners, administration staff and clients from the nine SSSs who took part in the prospective study element of the ELONS study. In addition, we would also like to thank:
-
The study steering group, chaired by Professor Ann McNeill, for their advice and support. Members included Amanda Amos, Darcy Brown, Robbie Graham, David Hardy, Peter Hayjek, Justine Hill and Robert West.
-
Dr Leonie Brose, who helped facilitate access to QuitManager data, provided very helpful input to the secondary analysis element of the ELONS study, helped source CO monitors and helped deliver an interviewer briefing for the 52-week follow-up.
-
The staff from the local PRCNs and Clinical Research Networks, who assisted with recruitment, data collections and service support costs.
-
Lisa Austin from the University of Bath who assisted with advice on approaches to ideas to boost recruitment.
-
Local R&D leads who helped facilitate the research permission processed for each area.
-
Alex Bailey and Joyce Clearly from NHS Lothian who assisted with National Research Ethics Service applications, queries and amendments.
-
Staff from North 51 who led data extraction from QuitManager.
-
Staff from TNS BMRB, lead by Sarah Simms, who conducted the 52-week follow-up for the prospective study.
-
Our NIHR, HTA project managers (Kate Fenton and Sandy Wilkins) for their support and assistance.
For the NRT study, we would like to acknowledge the administrative support of Claire Mimnagh and Madiha Sajid, technical support by ABS Labs and Salimetrics, and input in the write-up from the University College London Tobacco and Alcohol Research Group.
We would also like to thank colleagues who helped deliver the project and prepare the final report: Carol Anne Greenan for managing the administration of the study, Maureen Kennedy for data entry, Emily Greenan and Alice Greenan for helping to prepare the CSS for distribution and Aileen Paton for formatting the final report.
Contributions of authors
Fiona Dobbie (Research Fellow) was the project manager responsible for delivering the study. She also drafted and edited chapters of the final report, contributed to outputs from the study and delivered presentations at national conferences and to local SSSs.
Rosemary Hiscock (Research Fellow) was the lead analyst for the study, selected sites for the prospective study, drafted and edited chapters of the final report, wrote first drafts of journal articles and presented findings at national conferences.
Jo Leonardi-Bee (Associate Professor, Faculty of Medicine and Health Sciences) was the project statistician and offered advice to the lead analyst (Rosemary Hiscock). She also assisted with the design and delivery of the study, and commented on all outputs including the final report.
Susan Murray (Research Fellow) was the data manager, conducted analysis for the study, and contributed to study outputs and presented findings at a national conference.
Lion Shahab (Lecturer in Health Psychology) lead the NRT study, and assisted with the design and delivery of the study. He drafted and edited Chapter 9 of the final report.
Paul Aveyard (Professor of Behavioural Medicine), Tim Coleman (Professor of Primary Care), Andy McEwen (Executive Director, NCSCT) and Hayden McRobbie (Professor of Public Health Interventions) played a key role in all elements of the original design of the study. They advised on aspects of delivery as relevant to their areas of expertise and contributed to all study outputs, including providing detailed feedback on the final report and draft articles.
Richard Purves (Research Fellow) assisted with the organisation and analysis of the prospective study and contributed to study outputs.
Linda Bauld (Professor of Health Policy) was the principal investigator with overall responsibility for the design, co-ordination and delivery of the study. Along with the co-investigators, she designed the study. She drafted and edited chapters of the final report and contributed to all outputs from the study. She has also led the dissemination of results to date at national and international conferences, and to practitioner audiences.
Publications
Hiscock R, Murray S, Brose LS, McEwen A, Bee JL, Dobbie F, et al. Behavioural therapy for smoking cessation: the effectiveness of different intervention types for disadvantaged and affluent smokers. Addict Behav 2013;38:2787–96.
Hiscock R, Dobbie F, Bauld L. Smoking cessation and socioeconomic status; an update of existing evidence from a national evaluation of English Stop Smoking Services. Biomed Res Int 2015.
Data sharing statement
Data sharing requests should be directed to the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLOS Med 2006;3. http://dx.doi.org/10.1371/journal.pmed.0030442.
- Oberg M, Jaakkola MS, Woodward A, Peruga A, Prüss-Ustün A. Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. Lancet 2011;377:139-46. http://dx.doi.org/10.1016/S0140-6736(10)61388-8.
- Eriksen M, Mackay J, Ross H. The Tobacco Atlas: Fourth Edition. Atlanta, GA: American Cancer Society and World Lung Society; 2012.
- Office for National Statistics . Integrated Household Survey: January to December 2013, Smoking Prevalence 2014. www.ons.gov.uk/ons/rel/integrated-household-survey/integrated-household-survey/january-to-december-2013/stb-intergrated-household.html (accessed 2 October 2014).
- World Health Organization . Framework Convention on Tobacco Control 2005. http://whqlibdoc.who.int/publications/2003/9241591013.pdf (accessed 2 October 2014).
- WHO Report on the Global Tobacco Epidemic: Enforcing Bans on Tobacco Advertising, Promotion, and Sponsorship. Geneva: WHO; 2013.
- Brose LS, West R, Mcdermott MS, Fidler JA, Croghan E, McEwen A. What makes for an effective stop-smoking service?. Thorax 2011;66:924-6. http://dx.doi.org/10.1136/thoraxjnl-2011-200251.
- Doll R, Hill A. Smoking and carcinoma of the lung; preliminary report. Br Med J 1950;2:739-48. http://dx.doi.org/10.1136/bmj.2.4682.739.
- Smoking and Health. London: Pitman Publishing; 1962.
- McNeill A, Raw M, Whybrow J, Bailey P. A national strategy for smoking cessation treatment in England. Addiction 2005;100:1-11. http://dx.doi.org/10.1111/j.1360-0443.2005.01022.x.
- Smoking and Health Now: A New Report and Summary on Smoking and its Effects on Health, from the Royal College of Physicians of London. London: Pitman Medical and Scientific Publishing Company; 1971.
- Smoking or Health: The Third Report from the Royal College of Physicians of London. London: Pitman Medical and Scientific Publishing Company; 1977.
- Health or Smoking? Follow-up Report from the Royal College of Physicians of London. London: Pitman Medical and Scientific Publishing Company; 1983.
- Amos A, Angus K, Fidler J, Hastings G. A Review of Your People Smoking in England. York: Public Health Research Consortium; 2009.
- Smoking Kills: A White Paper on Tobacco. London: The Stationery Office; 1998.
- Raw M, McNeill A, West R. Smoking cessation guidelines for health professionals: a guide to effective smoking cessation interventions for the health care system. Thorax 1998;53:S1-19. http://dx.doi.org/10.1136/thx.53.2008.S1.
- Judge K, Bauld L, Chesterman J, Ferguson J. The English smoking treatment services: short-term outcomes. Addiction 2005;100:46-58. http://dx.doi.org/10.1111/j.1360-0443.2005.01027.x.
- Ferguson J, Bauld L, Chesterman J, Judge K. The English smoking treatment services: one-year outcomes. Addiction 2005;100:59-6. http://dx.doi.org/10.1111/j.1360-0443.2005.01028.x.
- Chesterman J, Judge K, Bauld L, Ferguson J. How effective are the English smoking treatment services in reaching disadvantaged smokers?. Addiction 2005;100:36-45. http://dx.doi.org/10.1111/j.1360-0443.2005.01026.x.
- Bauld L, Judge K, Platt S. Assessing the impact of smoking cessation services on reducing health inequalities in England: observational study. Tob Control 2007;16:400-4. http://dx.doi.org/10.1136/tc.2007.021626.
- Smoking Cessation Services, NICE Public Health Guidance 10. Manchester: NICE; 2008.
- Mottillo S, Filion KB, Belisle P, Joseph L, Gervais A, O’Loughlin J, et al. Behavioural interventions for smoking cessation: a meta-analysis of randomized controlled trials. Eur Heart J 2009;30:718-30. http://dx.doi.org/10.1093/eurheartj/ehn552.
- Lemmen V, Oenema A, Knut I, Brug J. Effectiveness of smoking cessation interventions among adults: a systematic review of reviews. Eur J Cancer Prev 2008;17:535-44. http://dx.doi.org/10.1097/CEJ.0b013e3282f75e48.
- McEwen A, West R, McRobbie H. Effectiveness of specialist group treatment for smoking cessation vs. one-to-one treatment in primary care. Addict Behav 2006;31:1650-60. http://dx.doi.org/10.1016/j.addbeh.2005.12.014.
- Local Stop Smoking Services: Service and Delivery Guidance 2014. London: NCSCT; 2014.
- Hiscock R, Murray S, Brose LS, McEwen A, Bee JL, Dobbie F, et al. Behavioural therapy for smoking cessation: the effectiveness of different intervention types for disadvantaged and affluent smokers. Addict Behav 2013;38:2787-96. http://dx.doi.org/10.1016/j.addbeh.2013.07.010.
- Brose LS, McEwen A, West R. Does it matter who you see to help you stop smoking? Short-term quit rates across specialist stop smoking practitioners in England. Addiction 2012;107:2029-36. http://dx.doi.org/10.1111/j.1360-0443.2012.03935.x.
- Bauld L, Briggs A, Boyd K, Chesterman J, Ferguson J, Judge K. Comparing Models of Smoking Treatment in Glasgow: Final Report. Glasgow: Glasgow Centre for Population Health; 2009.
- Ferguson J, Docherty G, Bauld L, Lewis S, Lorgelly P, Boyd Ka, et al. Effect of offering different levels of support and free nicotine replacement therapy via an English national telephone quitline: randomised controlled trial. BMJ 2012;344. http://dx.doi.org/10.1136/bmj.e1696.
- West R. Assessing Smoking Cessation Performance in NHS Stop Smoking Services: The Russell Standard (Clinical). Version 2 n.d. www.ncsct.co.uk/usr/pub/assessing-smoking-cessation-performance-in-nhs-stop-smoking-services-the-russell-standard-clinical.pdf (accessed 25 August 2015).
- Health and Social Care Information Centre . Statistics on NHS Stop Smoking Services, England – April 2012 to March 2013 2013. www.hscic.gov.uk/searchcatalogue?productid=12938&q=title%3a%22Statistics±on±NHS±Stop±Smoking±Services±-±England%22&sort=Relevance&size=10&page=1#top (accessed 20 January 2014).
- QuitManager: The Stop Smoking Database. Nottingham; 2010.
- NHS Stop Smoking Services – Service and Monitoring Guidance 2011/12. London: Department of Health; 2011.
- NHS Information Centre . Model Based Estimates of Smoking (Adults) 2008. www.ic.nhs.uk/statistics-and-data-collections/population-and-geography/neighbourhood-statistics/neighbourhood-statistics:-model-based-estimates-of-healthy-lifestyle-behaviours-at-pco-level-2003-05 (accessed 19 February 2012).
- Office for National Statistics . The National Statistics Socio-Economic Classification (NS-SEC) 2008. www.ons.gov.uk/about-statistics/classifications/current/ns-sec/index.html (accessed 25 July 2010).
- Department of Communities and Local Government . English Indices of Deprivation – Consultation 2010. www.communities.gov.uk/documents/localgovernment/pdf/1524728.pdf (accessed 26 October 2010).
- Rasbash J, Steele F, Browne W, Goldstein H. A User’s Guide to MLwiN, v2.10. Bristol: University of Bristol, Centre for Multilevel Modelling; 2009.
- Aveyard P, Markham WA, Lancashire E, Bullock A, Macarthur C, Cheng KK, et al. The influence of school culture on smoking among pupils. Soc Sci Med 2004;58:1767-80. http://dx.doi.org/10.1016/S0277-9536(03)00396-4.
- Fielding A. Scaling for residual variance components of ordered category responses in generalised linear mixed multilevel models. Qual Quant 2004;3:425-33. http://dx.doi.org/10.1023/B:QUQU.0000043118.19835.6c.
- Office for National Statistics . Mid-2010 Population Estimates for Primary Care Organisations in England by Broad Age and Sex 2011. www.statistics.gov.uk/hub/population/population-change/population-estimates/index.html (accessed 19 February 2012).
- Office for National Statistics . Smoking and Drinking Among Adults, 2009: A Report on the 2009 General Lifestyle Survey 2011. www.ons.gov.uk/ons/rel/ghs/general-lifestyle-survey/2009-report/index.html (accessed 23 December 2011).
- West R, May S, West M, Croghan E, McEwen A. Performance of English stop smoking services in first 10 years: analysis of service monitoring data. BMJ 2013;347. http://dx.doi.org/10.1136/bmj.f4921.
- NHS Information Centre . Statistics on NHS Stop Smoking Services: England, April 2010 – March 2011 2011. www.ic.nhs.uk/webfiles/publications/003_Health_Lifestyles/NHS%20Stop%20Smoking%20Services%20201011/SSS_2010_11.pdf (accessed 27 February 2011).
- McDermott MS, Beard E, Brose LS, West R, McEwen A. Factors associated with differences in quit rates between ‘specialist’ and ‘community’ stop-smoking practitioners in the English stop-smoking services. Nicotine Tob Res 2013;15:1239-47. http://dx.doi.org/10.1093/ntr/nts262.
- Psychiactric Research Unit at the Medical Health Centre North Zealand . WHO-Five Well-Being Index (WHO-5) 2013. www.who-5.org/ (accessed 2 December 2013).
- Salmond C. Fitting Complex Models Using Health Survey Data 2006 2006. www.otago.ac.nz/wellington/otago020178.pdf (accessed 25 August 2015).
- Shiffman S. Use of more nicotine lozenges leads to better success in quitting smoking. Addiction 2007;102:809-14. http://dx.doi.org/10.1111/j.1360-0443.2007.01791.x.
- Shiffman S, Ferguson SG, Sembower MA, Sweeney CT, Gitchell JG. Relationship between adherence to daily nicotine patch use and treatment efficacy: secondary analysis of a 10 week randomized, double-blind, placebo-controlled clinical trial simulating over-the-counter use in adult smokers. Clin Ther 2008;30:1852-8. http://dx.doi.org/10.1016/j.clinthera.2008.09.016.
- Higher Education Careers Services Unit . What Proportion of the Population Has a Degree-Level Qualification? 2013. http://ww2.prospects.ac.uk/cms/ShowPage/Home_page/Labour_market_information/Labour_market_FAQs/What_proportion_of_the_population_has_a_degree_level_qualification_/p!eXepbmk (accessed 25 August 2015).
- May S, McEwen A, Arnoldi H, Bauld L, Ferguson J, Stead M. How to examine client satisfaction with stop smoking services: a pilot study in the NHS. J Smok Cessat 2009;4:52-8. http://dx.doi.org/10.1375/jsc.4.1.52.
- Taylor G, McNeill A, Girling A, Farley A, Lindson-Hawley N, Aveyard P. Change in mental health after smoking cessation: systematic review and meta-analysis. BMJ 2014;348. http://dx.doi.org/10.1136/bmj.g1151.
- Glasgow RE. RE-AIMing research for application: ways to improve evidence for family medicine. J Am Board Famil Med 2006;19:11-9. http://dx.doi.org/10.3122/jabfm.19.1.11.
- Stewart A, King A, Killen J, Ritter P. Does smoking cessation improve health-related quality-of-life?. Ann Behav Med 1995;17:331-8. http://dx.doi.org/10.1007/BF02888598.
- Hays JT, Croghan IT, Baker CL, Cappelleri JC, Bushmakin AG. Changes in health-related quality of life with smoking cessation treatment. Eur J Public Health 2012;22:224-9. http://dx.doi.org/10.1093/eurpub/ckq137.
- Piper M, Kenford S, Fiore M, Baker T. Smoking cessation and quality of life: changes in life satisfaction over 3 years following a quit attempt. Ann Behav Med 2012;43:262-70. http://dx.doi.org/10.1007/s12160-011-9329-2.
- Caponnetto P, Polosa R. Common predictors of smoking cessation in clinical practice. Respir Med 2008;102:1182-92. http://dx.doi.org/10.1016/j.rmed.2008.02.017.
- Seguire M, Chalmers K. Addressing the ‘costs of quitting’ smoking: a health promotion issue for adolescent girls in Canada. Health Promot Int 2000;15:227-35. http://dx.doi.org/10.1093/heapro/15.3.227.
- Lawrence D, Mitrou F, Zubrick SR. Non-specific psychological distress, smoking status and smoking cessation: United States National Health Interview Survey 2005. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-256.
- van der Deen F, Carter K, Wilson N, Collings S. The association between failed quit attempts and increased levels of psychological distress in smokers in a large New Zealand cohort. BMC Public Health 2011;11. http://dx.doi.org/10.1186/1471-2458-11-598.
- Lister G. Value for Money of Health Trainer Services: Final Report 2010. www.building-leadership-for-health.org.uk/app/download/3834447/HTSAssessmenr+2014 (accessed 6 February 2012).
- Kearns A, Hiscock R, Ellaway A, Macintyre S. Beyond four walls. The psycho-social benefits of home: evidence from West Central Scotland. Hous Stud 2000;15:387-410. http://dx.doi.org/10.1080/02673030050009249.
- Hiscock R, Macintyre S, Ellaway A, Kearns A. Residents and residence: factors predicting the health disadvantage of social renters compared to owner-occupiers. J Soc Issues 2003;59:527-46. http://dx.doi.org/10.1111/1540-4560.00076.
- Kearns A, Whitley E, Mason P, Petticrew M, Hoy C. Material and meaningful homes: mental health impacts and psychosocial benefits of rehousing to new dwellings. Int J Equity Health 2011;56:597-60. http://dx.doi.org/10.1007/s00038-011-0275-3.
- Wang D, Connock M, Barton P, Fry-Smith A, Aveyard P, Moore D. Cut down to quit with nicotine replacement therapies in smoking cessation: a systematic review of effectiveness and economic analysis. Health Technol Assess 2008;12. http://dx.doi.org/10.3310/hta12020.
- Moore D, Aveyard P, Connock M, Wang D, Fry-Smith A, Barton P. Effectiveness and safety of nicotine replacement therapy assisted reduction to stop smoking: systematic review and meta-analysis. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.b1024.
- Beard E, McNeill A, Aveyard P, Fidler J, Michie S, West R. Association between use of nicotine replacement therapy for harm reduction and smoking cessation: a prospective study of English smokers. Tob Control 2011;22:118-22. http://dx.doi.org/10.1136/tobaccocontrol-2011-050007.
- Beard E, Fidler J, West R. Is use of nicotine replacement therapy while continuing to smoke associated with increased nicotine intake? Evidence from a population sample. Psychopharmacology 2011;218:609-10. http://dx.doi.org/10.1007/s00213-011-2359-4.
- Schnoll RA, Patterson F, Wileyto EP, Heitjan DF, Shields AE, Asch DA, et al. Effectiveness of extended-duration transdermal nicotine therapy: a randomized trial. Ann Intern Med 2010;152:144-51. http://dx.doi.org/10.7326/0003-4819-152-3-201002020-00005.
- Joseph AM, Fu SS, Lindgren B, Rothman AJ, Kodl M, Lando H, et al. Chronic disease management for tobacco dependence: a randomized, controlled trial. Arch Intern Med 2011;171:1894-900. http://dx.doi.org/10.1001/archinternmed.2011.500.
- MHRA Public Assessment Report: The Use of Nicotine Replacement Therapy to Reduce Harm in Smokers. London: MHRA; 2010.
- Fucito LM, Bars MP, Forray A, Rojewski AM, Shiffman S, Selby P, et al. Addressing the evidence for FDA nicotine replacement therapy label changes: a policy statement of the Association for the Treatment of Tobacco Use and Dependence and the Society for Research on Nicotine and Tobacco. Nicotine Tob Res 2014;16:909-14. http://dx.doi.org/10.1093/ntr/ntu087.
- Le Houezec J, McNeill A, Britton J. Tobacco, nicotine and harm reduction. Drug Alcohol Rev 2011;30:119-23. http://dx.doi.org/10.1111/j.1465-3362.2010.00264.x.
- Stratton S, Shetty P, Wallace R, Bondurant S. Clearing the Smoke: Addressing the Science Base for Tobacco Harm Reduction. Washington, DC: National Academy Press; 2001.
- Black A, Beard E, Brown J, Fidler J, West R. Beliefs about the harms of long-term use of nicotine replacement therapy: perceptions of smokers in England. Addiction 2012;107:2037-42. http://dx.doi.org/10.1111/j.1360-0443.2012.03955.x.
- Beard E, McDermott M, McEwen A, West R. Beliefs of stop smoking practitioners in United Kingdom on the use of nicotine replacement therapy for smoking reduction. Nicotine Tob Res 2012;14:639-47. http://dx.doi.org/10.1093/ntr/ntr260.
- Eliasson B, Taskinen MR, Smith U. Long-term use of nicotine gum is associated with hyperinsulinemia and insulin resistance. Circulation 1996;94:878-81. http://dx.doi.org/10.1161/01.CIR.94.5.878.
- Murray RP, Connett JE, Zapawa LM. Does nicotine replacement therapy cause cancer? Evidence from the Lung Health Study. Nicotine Tob Res 2009;11:1076-82. http://dx.doi.org/10.1093/ntr/ntp104.
- Sims TH, Fiore MC. Pharmacotherapy for treating tobacco dependence: what is the ideal duration of therapy?. CNS Drugs 2002;16:653-62. http://dx.doi.org/10.2165/00023210-200216100-00001.
- Le Strat Y, Rehm J, Le FB. How generalisable to community samples are clinical trial results for treatment of nicotine dependence: a comparison of common eligibility criteria with respondents of a large representative general population survey. Tob Control 2011;20:338-43. http://dx.doi.org/10.1136/tc.2010.038703.
- Shiffman S, Sweeney CT. Ten years after the Rx-to-OTC switch of nicotine replacement therapy: what have we learned about the benefits and risks of non-prescription availability?. Health Policy 2008;86:17-26. http://dx.doi.org/10.1016/j.healthpol.2007.08.006.
- Shahab L, Cummings KM, Hammond D, Borland R, West R, McNeill A. The impact of changing nicotine replacement therapy licensing laws in the United Kingdom: findings from the International Tobacco Control Four Country Survey. Addiction 2009;104:1420-7. http://dx.doi.org/10.1111/j.1360-0443.2009.02641.x.
- National Institute for Health and Care Excellence . Tobacco – Harm Reduction 2013. http://publications.nice.org.uk/tobacco-harm-reduction-approaches-to-smoking-ph45 (accessed 26 August 2015).
- Soo-Quee Koh D, Choon-Huat Koh G. The use of salivary biomarkers in occupational and environmental medicine. Occup Environ Med 2007;64:202-10. http://dx.doi.org/10.1136/oem.2006.026567.
- Jarvis MJ, Wardle J, Waller J, Owen L. Prevalence of hardcore smoking in England, and associated attitudes and beliefs: cross sectional study. BMJ 2003;326. http://dx.doi.org/10.1136/bmj.326.7398.1061.
- MacIntosh H, Coleman T. Characteristics and prevalence of hardcore smokers attending UK general practitioners. BMC Fam Pract 2006;7. http://dx.doi.org/10.1186/1471-2296-7-24.
- Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction 2004;99:29-38. http://dx.doi.org/10.1111/j.1360-0443.2004.00540.x.
- Health and Social Care Information Centre . NHS Stop Smoking Services Annual Return 2013–2014 2014. www.hscic.gov.uk/stopsmoking (accessed 20 January 2014).
- Stapleton JA, West R. A direct method and ICER tables for the estimation of the cost-effectiveness of smoking cessation interventions in general populations: application to a new cytisine trial and other examples. Nicotine Tob Res 2012;14:463-71. http://dx.doi.org/10.1093/ntr/ntr236.
- Hymowitz N, Cummings KM, Hyland A, Lynn WR, Pechacek TF, Hartwell TD. Predictors of smoking cessation in a cohort of adult smokers followed for five years. Tob Control 1997;6. http://dx.doi.org/10.1136/tc.6.suppl_2.S57.
- Osler M, Prescott E. Psychosocial, behavioural, and health determinants of successful smoking cessation: a longitudinal study of Danish adults. Tob Control 1998;7:262-7. http://dx.doi.org/10.1136/tc.7.3.262.
- Hiscock R, Judge K, Bauld L. Social inequalities in quitting: what factors mediate the relationship between socioeconomic position and smoking cessation?. J Public Health 2010;33:39-47. http://dx.doi.org/10.1093/pubmed/fdq097.
- Hiscock R, Bauld L, Amos A, Fidler J, Munafo M. Socio-economic status and smoking: a review. Ann N Y Acad Sci 2011;1248:107-23. http://dx.doi.org/10.1111/j.1749-6632.2011.06202.x.
- Bauld L, Ferguson J, McEwen A, Hiscock R. Evaluation of a drop-in rolling-group model of support to stop smoking. Addiction 2012;107:1687-95. http://dx.doi.org/10.1111/j.1360-0443.2012.03861.x.
- Bhardwa S. Primary Care Funding Slipping 2014 2014. www.independentnurse.co.uk/cgi-bin/go.pl/library/articlehtml.cgi?uid=104073;type=News (accessed 10 July 2014).
- Tumilty D, Gilmore G. Improving Quality in Stop Smoking Services n.d.
- Department of Health . Stop Smoking Service: Monitoring and Guidance Update 2012. www.gov.uk/government/publications/stop-smoking-service-monitoring-and-guidance-update-published (accessed 20 January 2014).
- Leung J, Gartner C, Dobson A, Lucke J, Hall W. Psychological distress is associated with tobacco smoking and quitting behaviour in the Australian population: evidence from National Cross-Sectional Surveys. Aust N Z J Psychiatry 2011;45:170-8. http://dx.doi.org/10.3109/00048674.2010.534070.
- Mendelsohn C. Smoking and depression: a review. Aust Fam Physician 2012;41.
- Curtis B. Understanding tailored Internet smoking cessation messages: a reasoned action approach. Ann Am Acad Pol Soc Sci 2012;640:136-49. http://dx.doi.org/10.1177/0002716211423642.
- Caleyachetty A, Lewis S, McNeill A, Leonardi-Bee J. Struggling to make ends meet: exploring pathways to understand why smokers in financial difficulties are less likely to quit successfully. Eur J Public Health 2012;22:41-8. http://dx.doi.org/10.1093/eurpub/ckr199.
- Ng DM, Jeffery RW. Relationships between perceived stress and health behaviors in a sample of working adults. Health Psychol 2003;22:638-42. http://dx.doi.org/10.1037/0278-6133.22.6.638.
- Todd M. Daily processes in stress and smoking: effects of negative events, nicotine dependence, and gender. Psychol Addict Behav 2004;18:31-9. http://dx.doi.org/10.1037/0893-164X.18.1.31.
- McKee SA, Sinha R, Weinberger AH, Sofuoglu M, Harrison EL, Lavery M, et al. Stress decreases the ability to resist smoking and potentiates smoking intensity and reward. J Psychopharmacol 2011;25:490-502. http://dx.doi.org/10.1177/0269881110376694.
- Parrott AC. Does cigarette smoking cause stress?. Am Psychol 1999;54:817-20. http://dx.doi.org/10.1037/0003-066X.54.10.817.
- Hajek P, Taylor T, McRobbie H. The effect of stopping smoking on perceived stress levels. Addiction 2010;105:1466-71. http://dx.doi.org/10.1111/j.1360-0443.2010.02979.x.
- Hajek P, McRobbie H, Gillison F. Dependence potential of nicotine replacement treatments: effects of product type, patient characteristics, and cost to user. Prev Med 2007;44:230-4. http://dx.doi.org/10.1016/j.ypmed.2006.10.005.
- Brown J, West R, Beard E, Michie S, Shahab L, McNeil A. Prevalence and characteristics of e-cigarette users in Great Britain: Findings from a general population survey of smokers. Addict Behav 2014;39:1120-5. http://dx.doi.org/10.1016/j.addbeh.2014.03.009.
- Silla K, Beard E, Shahab L. Characterization of long-term users of nicotine replacement therapy: evidence from a national survey. Nicotine Tob Res 2014;16:1050-5. http://dx.doi.org/10.1093/ntr/ntu019.
- West R, DiMarino ME, Gitchell J, McNeill A. Impact of UK policy initiatives on use of medicines to aid smoking cessation. Tob Control 2005;14:166-71. http://dx.doi.org/10.1136/tc.2004.008649.
- Tonnesen P, Paoletti P, Gustavsson G, Russell MA, Saracci R, Gulsvik A, et al. Higher dosage nicotine patches increase one-year smoking cessation rates: results from the European CEASE trial. Collaborative European Anti-Smoking Evaluation. European Respiratory Society. Eur Respir J 1999;13:238-46. http://dx.doi.org/10.1034/j.1399-3003.1999.13b04.x.
- Wennike P, Danielsson T, Landfeldt B, Westin A, Tonnesen P. Smoking reduction promotes smoking cessation: results from a double blind, randomized, placebo-controlled trial of nicotine gum with 2-year follow-up. Addiction 2003;98:1395-402. http://dx.doi.org/10.1046/j.1360-0443.2003.00489.x.
- Fidler JA, Stapleton JA, West R. Variation in saliva cotinine as a function of self-reported attempts to reduce cigarette consumption. Psychopharmacology 2011;217:587-93. http://dx.doi.org/10.1007/s00213-011-2317-1.
- Fagerstrom KO, Tejding R, Westin A, Lunell E. Aiding reduction of smoking with nicotine replacement medications: hope for the recalcitrant smoker?. Tob Control 1997;6:311-16.
- Malaiyandi V, Sellers EM, Tyndale RF. Implications of CYP2A6 genetic variation for smoking behaviors and nicotine dependence. Clin Pharmacol Ther 2005;77:145-58. http://dx.doi.org/10.1016/j.clpt.2004.10.011.
- Benowitz NL, Gourlay SG. J Am Coll Cardiol 1997;29:1422-31. http://dx.doi.org/10.1016/S0735-1097(97)00079-X.
- Benowitz NL, Jacob P III, Jones RT, Rosenberg J. Interindividual variability in the metabolism and cardiovascular effects of nicotine in man. J Pharmacol Exp Ther 1982;221:368-72.
- Rohleder N, Nater UM. Determinants of salivary alpha-amylase in humans and methodological considerations. Psychoneuroendocrinology 2009;34:469-85. http://dx.doi.org/10.1016/j.psyneuen.2008.12.004.
- Amos A, Bauld L, Clifford D, Fidler J, Hill S, Hiscock R, et al. Tobacco Control, Inequalities in Health and Action at a Local Level. York: Public Health Research Consortium; 2011.
- Bauer DJ, Sterba SK, Hallfors DD. Evaluating group-based interventions when control participants are ungrouped. Multivariate Behav Res 2008;43:210-36. http://dx.doi.org/10.1080/00273170802034810.
- Morgan-Lopez AA, Saavedra LM, Hien DA, Fals-Stewart W. Estimating statistical power for open-enrollment group treatment trials. J Subst Abuse Treat 2011;40:3-17. http://dx.doi.org/10.1016/j.jsat.2010.07.010.
- Paddock SM, Hunter SB, Watkins KE, McCaffrey DF. Analysis of rolling group therapy data using conditionally autoregressive priors. Ann Appl Stat 2011;5:605-27. http://dx.doi.org/10.1214/10-AOAS434.
- Stead LF, Lancaster T. Group behaviour therapy programmes for smoking cessation. Cochrane Database Syst Rev 2005;2.
- Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. Cochrane Database Syst Rev 2005;2. http://dx.doi.org/10.1002/14651858.cd001292.pub2.
- Harvey TBJ. Housing renewal and mental health: a case study. J Ment Health 2001;10:571-83. http://dx.doi.org/10.1080/09638230120041335.
- Smith PM, Spadoni MM, Proper VM. Abuse and smoking cessation in clinical practice. J Clin Nurs 2014;23:361-6. http://dx.doi.org/10.1111/j.1365-2702.2012.04219.x.
Appendix 1 Data collection instruments
Appendix 2 Supplementary tables from well-being study
The main aims of the ELONS prospective study were to determine the proportion of SSS clients who remained abstinent from smoking 12 months after setting a quit date, and which clients were most likely to have stopped. A novel aspect of the ELONS study was that data on well-being was also collected from participants, not something normally done by the services. Well-being at baseline was a predictor of both short- and long-term quitting (see Chapters 6 and 8). Data on well-being were also collected through postal surveys at 4 weeks and 12 months post quit date (or since first contact for the 150 clients who did not set a quit date) in order to explore whether or not well-being changed over the course of a quit attempt and which client and service characteristics were associated with well-being at different time points. The main results of this analysis are presented in Chapter 8. This Appendix contains three tables that provide extra information supporting the findings presented in Chapter 8.
Table 45 presents information on clients’ levels of response to the main measure of well-being used in the study (whether or not it was possible to calculate a score for the WHO-5 Well-being Index) in the postal surveys compared with the ELONS prospective study sample at baseline and all clients who set a quit date with the services when clients in each service were being recruited to the ELONS study.
| Variables | All cases | ELONS | 4-week postal survey | 52-week postal survey | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Age (years) | ||||||||
| 16–24 | 7120 | 11 | 327 | 10.7 | 65 | 6.8 | 28 | 5.8 |
| 25–34 | 13,226 | 20 | 673 | 22.0 | 147 | 15.4 | 47 | 9.8 |
| 35–44 | 15,338 | 23 | 758 | 24.8 | 194 | 20.4 | 97 | 20.3 |
| 45–54 | 13,851 | 21 | 629 | 20.6 | 229 | 24.0 | 109 | 22.8 |
| 55–64 | 9933 | 15 | 456 | 14.9 | 210 | 22.0 | 140 | 29.2 |
| 65–85 | 6469 | 10 | 214 | 7.0 | 108 | 11.3 | 58 | 12.1 |
| Total | 65,937 | 100.0 | 3057 | 100.0 | 953 | 100.0 | 479 | 100.0 |
| Gender | ||||||||
| Female | 34,955 | 53 | 1710 | 55.9 | 531 | 55.7 | 267 | 55.7 |
| Male | 30,982 | 47 | 1347 | 44.1 | 422 | 44.3 | 212 | 44.3 |
| Total | 65,937 | 100.0 | 3057 | 100.0 | 953 | 100.0 | 479 | 100.0 |
| NSSEC | ||||||||
| Routine and manual occupations | 18,201 | 28 | 939 | 30.7 | 251 | 26.3 | 112 | 23.4 |
| Managerial/professional and intermediate occupations | 14,098 | 21 | 716 | 23.4 | 239 | 25.1 | 133 | 27.8 |
| Sick/disabled and unemployed | 14,932 | 23 | 660 | 21.6 | 188 | 19.7 | 86 | 18.0 |
| Other/unknown | 18,706 | 28 | 742 | 24.3 | 275 | 28.9 | 148 | 30.9 |
| Total | 65,937 | 100.0 | 3057 | 100.0 | 953 | 100.0 | 479 | 100.0 |
| Behavioural support | ||||||||
| Closed group | 541 | 1 | 102 | 3.3 | 30 | 3.1 | 18 | 3.8 |
| Open group | 2159 | 3 | 550 | 18.0 | 202 | 21.2 | 84 | 17.5 |
| Drop-in | 11,308 | 17 | 887 | 29.0 | 247 | 25.9 | 130 | 27.1 |
| One-to-one specialist | 21,796 | 33 | 1131 | 37.0 | 374 | 39.2 | 188 | 39.2 |
| GP practice | 16,412 | 25 | 269 | 8.8 | 75 | 7.9 | 45 | 9.4 |
| Pharmacy | 9821 | 15 | 97 | 3.2 | 23 | 2.4 | 9 | 1.9 |
| Other or unclear | 3900 | 6 | 21 | 0.7 | 2 | 0.2 | 5 | 1.0 |
| Total | 65,937 | 100.0 | 3057 | 100.0 | 953 | 100.0 | 479 | 100.0 |
| CO-validated quit at 52 weeks | ||||||||
| Not quit | – | – | 2772 | 90.7 | 775 | 81.3 | 351 | 73.3 |
| Quit | – | – | 285 | 9.3 | 178 | 18.7 | 128 | 26.7 |
| Total | – | – | 3057 | 100.0 | 953 | 100.0 | 479 | 100.0 |
Tables 46 and 47 present multivariable linear regression results, presenting client and service characteristics that were associated with well-being at baseline, 4 weeks and 12 months. Table 46 presents results of analyses of associates including the previous dependent variables and additionally ‘ontological security’. Ontological security was operationalised as 10 items intended to measure feelings of being protected, in control, prestige and response to change. The analysis with well-being at 4 weeks as the outcome includes ontological security collected in the 4-week postal survey and the analysis with well-being at 12 months as the outcome includes ontological security collected in the 12-month postal survey.
| Variables | Well-being at baseline | Well-being at 4 weeks | Well-being at 52 weeks | |||
|---|---|---|---|---|---|---|
| n | Beta (95% CI) | n | Beta (95% CI) | n | Beta (95% CI) | |
| Smoking cessation behavioural support | ||||||
| Specialist group | 634 | 2.31 (–0.81 to 5.43) | 232 | –0.68 (–6.19 to 4.82) | 102 | –5.07 (–13.24 to 3.11) |
| Specialist drop-in | 856 | –0.80 (–3.02 to 1.42) | 247 | –0.52 (–4.11 to 3.07) | 130 | 3.28 (–1.95 to 8.52) |
| Specialist one to one | 1090 | 0 | 374 | 0 | 188 | 0 |
| Provided by GP practice or pharmacy | 358 | 0.46 (–3.29 to 4.21) | 98 | 0.10 (–5.98 to 6.18) | 54 | –6.43 (–15.59 to 2.73) |
| Other or unclear | 21 | 9.60 (0.38 to 18.81) | 2 | 5.11 (–24.12 to 34.33) | 5 | –0.34 (–20.17 to 19.50) |
| Time of year | ||||||
| Other months | 736 | 1.11 (–2.38 to 4.61) | 227 | –0.37 (–6.15 to 5.40) | 135 | –6.42 (–15.71 to 2.88) |
| Summer – July and August | 933 | 1.75 (–1.70 to 5.21) | 300 | 0.29 (–5.22 to 5.80) | 168 | –5.58 (–14.82 to 3.66) |
| Back to school – September and October | 1100 | 2.24 (–1.12 to 5.60) | 354 | 2.56 (–2.87 to 7.98) | 149 | –3.77 (–12.95 to 5.42) |
| New Year – January and February | 190 | 0 | 72 | 0 | 27 | 0 |
| Age group (years) | ||||||
| 16–24 | 314 | 5.61 (2.66 to 8.57) | 65 | 9.05 (3.28 to 14.82) | 28 | 13.80 (4.72 to 22.88) |
| 25–34 | 651 | 3.46 (1.09 to 5.83) | 147 | 6.66 (2.34 to 10.97) | 47 | 3.77 (–3.67 to 11.21) |
| 35–44 | 734 | 2.33 (0.06 to 4.60) | 194 | 3.48 (–0.50 to 7.46) | 97 | 6.32 (0.33 to 12.31) |
| 45–54 | 608 | 0 | 229 | 0 | 109 | 0 |
| 55–64 | 442 | 1.60 (–1.00 to 4.19) | 210 | 2.27 (–1.61 to 6.15) | 140 | 3.96 (–1.53 to 9.44) |
| 65–85 | 210 | 5.62 (2.23 to 9.00) | 108 | 5.44 (0.66 to 10.23) | 58 | 7.71 (0.71 to 14.71) |
| Gender | ||||||
| Male | 1302 | 1.18 (–0.37 to 2.73) | 422 | 0.58 (–2.16 to 3.32) | 267 | 0.34 (–3.64 to 4.33) |
| Female | 1657 | 0 | 531 | 0 | 212 | 0 |
| SES | ||||||
| Low SES (unemployed/basic education/social rent) | 1179 | 0 | 333 | 0 | 134 | 0 |
| Mid SES | 1480 | 3.14 (1.48 to 4.79) | 503 | 1.39 (–1.63 to 4.41) | 276 | 4.10 (–0.51 to 8.72) |
| High SES (owns home and professional manager/tertiary education) | 300 | 3.92 (1.17 to 6.66) | 117 | 4.04 (–0.50 to 8.58) | 69 | 4.70 (–1.80 to 11.21) |
| Ethnicity | ||||||
| White British | 2776 | 3.49 (–1.63 to 8.61) | 895 | 3.10 (–5.93 to 12.14) | 454 | – |
| Other white | 66 | 0 | 21 | 0 | 8 | – |
| Asian (including mixed Asian and white) | 62 | 7.50 (0.04 to 14.96) | 9 | 21.83 (5.60 to 38.06) | 2 | – |
| Ethnicity other or unknown | 55 | 2.71 (–4.79 to 10.22) | 28 | 2.79 (–8.93 to 14.51) | 15 | – |
| Smoking dependence | ||||||
| Not recorded as dependent | 1634 | 3.19 (1.62 to 4.75) | 562 | 3.31 (0.55 to 6.07) | 276 | 5.31 (1.19 to 9.43) |
| Dependent | 1325 | 0 | 391 | 0 | 203 | 0 |
| Determination to quit | ||||||
| Determined | 2688 | 3.43 (0.77 to 6.10) | 873 | – | 425 | – |
| Not recorded as determined | 271 | 0 | 80 | – | 54 | – |
| Quit attempt supported by spouse/partner | ||||||
| Supported | 1530 | 2.50 (0.96 to 4.04) | 511 | 4.83 (2.14 to 7.53) | 235 | – |
| Other | 1429 | 0 | 442 | 0 | 244 | – |
| Proportion of friends and family who smoke | ||||||
| Half or more do not smoke | 2249 | 1.80 (–0.04 to 3.63) | 165 | – | 83 | – |
| Other | 710 | 0 | 788 | – | 396 | – |
| Took varenicline in first week | ||||||
| Took varenicline | 1356 | 2.48 (0.88 to 4.08) | 476 | – | 224 | – |
| Varenicline not recorded | 1603 | 0 | 477 | – | 255 | – |
| Mental health condition | ||||||
| Yes | 471 | 0 | 146 | 0 | 69 | – |
| Not recorded | 2488 | 9.95 (7.81 to 12.10) | 807 | 10.77 (7.05 to 14.49) | 410 | 9.94 (4.24 to 15.65) |
| Heart, blood or circulatory conditions | ||||||
| Yes | 512 | – | 196 | – | 101 | – |
| Not recorded | 2447 | 3.39 (1.19 to 5.59) | 757 | – | 378 | – |
| Respiratory or lung condition | ||||||
| Yes | 624 | – | 216 | – | 116 | – |
| Not recorded | 2335 | 6.30 (4.37 to 8.23) | 737 | – | 363 | 6.60 (1.84 to 11.36) |
| Has other condition not included above | ||||||
| Yes | 349 | – | 121 | – | 71 | – |
| No condition or has one of above conditions | 2610 | 2.79 (0.32 to 5.25) | 832 | – | 408 | – |
| CO-validated quit rate | ||||||
| Quit at 4 weeks | 1315 | N/A | 268 | 0 | 304 | N/A |
| Not quit at 4 weeks | 1644 | – | 685 | 6.11 (3.05 to 9.17) | 175 | – |
| CO-validated quit rate | ||||||
| Quit at 52 weeks | 282 | N/A | 178 | N/A | 351 | – |
| Not quit at 52 weeks | 2677 | – | 775 | – | 128 | 11.76 (7.23 to 16.29) |
| Practitioner variance | – | 11.4 (4.2) | – | 0.9 (4.4) | – | 10.2 (12.4) |
| Client-level unexplained variance (standard error) | – | 422.3 (11.2) | – | 415.6 (19.5) | – | 444.9 (30.6) |
| –2log likelihood | – | 26338.65 | – | 8453.027 | – | 4290.095 |
| Total (N) | 2959 | – | 953 | – | 479 | – |
| Variables | Well-being at 4 weeks | Well-being at 52 weeks | ||
|---|---|---|---|---|
| n | Beta (95% CI) | n | Beta (95% CI) | |
| Smoking cessation behavioural support | ||||
| Specialist group | 232 | 1.69 (–1.18 to 4.57) | 102 | –0.89 (–6.64 to 4.85) |
| Specialist drop-in | 247 | –0.50 (–5.34 to 4.33) | 130 | 2.81 (–0.87 to 6.49) |
| Specialist one to one | 374 | 0 | 188 | 0 |
| Provided by GP practice or pharmacy | 98 | 4.07 (–19.04 to 27.18) | 54 | –0.24 (–6.68 to 6.19) |
| Other or unclear | 2 | –0.67 (–5.97 to 4.63) | 5 | 8.42 (–5.33 to 22.17) |
| Time of year | ||||
| Other months | 227 | –1.55 (–6.12 to 3.02) | 135 | –2.89 (–9.32 to 3.55) |
| Summer – July and August | 300 | 0.16 (–4.21 to 4.53) | 168 | –1.65 (–8.04 to 4.75) |
| Back to school – September and October | 354 | 0.73 (–3.56 to 5.01) | 149 | –2.65 (–8.99 to 3.68) |
| New Year – January and February | 72 | 0 | 27 | 0 |
| Age group (years) | ||||
| 16–24 | 65 | 4.38 (–0.22 to 8.99) | 28 | 4.97 (–1.34 to 11.27) |
| 25–34 | 147 | 3.70 (0.25 to 7.15) | 47 | 1.52 (–3.62 to 6.66) |
| 35–44 | 194 | 1.96 (–1.20 to 5.13) | 97 | 1.76 (–2.45 to 5.96) |
| 45–54 | 229 | 0 | 109 | 0 |
| 55–64 | 210 | 1.17 (–1.92 to 4.26) | 140 | –0.22 (–4.06 to 3.62) |
| 65–85 | 108 | 3.43 (–0.41 to 7.28) | 58 | 1.79 (–3.10 to 6.69) |
| Gender | ||||
| Male | 422 | 0.32 (–1.83 to 2.47) | 267 | 1.05 (–1.75 to 3.84) |
| Female | 531 | 0 | 212 | 0 |
| SES | ||||
| Low SES (unemployed/basic education/social rent) | 333 | 0 | 134 | 0 |
| Mid SES | 503 | –2.26 (–4.64 to 0.12) | 276 | –2.09 (–5.32 to 1.15) |
| High SES (owns home and professional managerial/tertiary education) | 117 | –2.08 (–5.70 to 1.53) | 69 | –0.63 (–5.14 to 3.89) |
| Ethnicity | ||||
| White British | 895 | 3.68 (–3.50 to 10.87) | 454 | N/A |
| Other white | 21 | 0 | 8 | – |
| Asian (including mixed Asian and white) | 9 | 20.43 (7.50 to 33.36) | 2 | – |
| Ethnicity other or unknown | 28 | 3.04 (–6.23 to 12.32) | 15 | – |
| Smoking dependence | ||||
| Not recorded as dependent | 562 | – | 276 | – |
| Dependent | 391 | – | 203 | – |
| Determination to quit | ||||
| Determined | 873 | – | 425 | – |
| Not recorded as determined | 80 | – | 54 | – |
| Quit attempt supported by spouse/partner | ||||
| Supported | 511 | – | 235 | – |
| Other | 442 | – | 244 | – |
| Proportion of friends and family who smoke | ||||
| Half or more do not smoke | 165 | – | 83 | – |
| Other | 788 | – | 396 | – |
| Took varenicline in first week | ||||
| Took varenicline | 476 | – | 224 | – |
| Varenicline not recorded | 477 | – | 255 | – |
| Mental health condition | ||||
| Yes | 146 | – | 69 | – |
| Not recorded | 807 | – | 410 | – |
| Heart, blood or circulatory conditions | ||||
| Yes | 196 | 2.83 (0.10 to 5.56) | 101 | – |
| Not recorded | 757 | 0 | 378 | – |
| Respiratory or lung condition | ||||
| Yes | 216 | – | 116 | – |
| Not recorded | 737 | – | 363 | – |
| Has other condition not included above | ||||
| Yes | 121 | – | 71 | – |
| No condition or has one of above conditions | 832 | – | 408 | – |
| Ontological security | ||||
| I enjoy a challenge | – | 2.40 (0.88 to 3.93) | – | 2.21 (0.32 to 4.10) |
| I can deal with stress | – | 4.28 (3.01 to 5.56) | – | – |
| I’m frightened of change (reversed) | – | – | – | – |
| I can do what I want, when I want | – | – | – | 2.75 (1.27 to 4.23) |
| Most people would like a life like mine | – | 2.32 (0.98 to 3.66) | – | |
| I feel in control | – | 5.49 (3.86 to 7.13) | – | 6.78 (4.40 to 9.16) |
| I feel safe | – | – | – | 3.46 (1.34 to 5.57) |
| I worry about things going wrong (reversed) | – | – | – | 1.92 (0.56 to 3.29) |
| I feel I’m doing well in life | – | 6.02 (4.51 to 7.52) | – | 5.59 (3.43 to 7.75) |
| My life has a sense of routine | – | – | – | 2.16 (0.35 to 3.97) |
| CO-validated quit rate | ||||
| Quit at 4 weeks | 268 | 2.88 (0.45 to 5.31) | 304 | N/A |
| Not quit at 4 weeks | 685 | 0 | 175 | – |
| CO-validated quit rate | ||||
| Quit at 52 weeks | 178 | N/A | 351 | 5.24 (2.03 to 8.46) |
| Not quit at 52 weeks | 775 | – | 128 | 0 |
| Practitioner variance | – | 1.41 (3.0) | – | 8.7 (6.9) |
| Client-level unexplained variance (standard error) | – | 258.7 (12.2) | – | 209.5 (14.5) |
| –2log-likelihood | – | 8003.832 | – | 3936.1 |
| Total | 953 | – | 479 | – |
Glossary
- Adjusted odds ratio
- Odds ratio from a logistic regression model where other variables have been taken into account.
- Level 2 practitioner
- Practitioner who is employed by an organisation other than the Stop Smoking Service (usually a general practitioner practice or pharmacy), but is trained in assisting with quit attempts as one of a number of job roles (e.g. practice nurses, pharmacy assistants). They are sometimes called ‘community practitioners’ or ‘local enhanced service practitioners.’
- Service provider
- An organisation commissioned to provide smoking cessation interventions, specifically behavioural support and access to medication.
- Specialist practitioner
- Practitioner who is employed directly by the Stop Smoking Service management and assisting with quit attempts is the sole or main part of their role.
- Stop Smoking Services
- These are government-funded smoking cessation services. At the time of the data collection they were administered through the NHS but are now administered through local authorities.
List of abbreviations
- aOR
- adjusted odds ratio
- CI
- confidence interval
- CO
- carbon monoxide
- CSS
- client satisfaction survey
- DH
- Department of Health
- e-cigarette
- electronic cigarette
- ELONS
- Evaluating Long-term Outcomes of NHS Stop Smoking Services study
- FCTC
- Framework Convention on Tobacco Control
- GP
- general practitioner
- HTA
- Health Technology Assessment
- IGLS
- iterative generalised least squares
- IMD
- Index of Multiple Deprivation
- NCSCT
- National Centre for Smoking Cessation and Training
- NICE
- National Institute for Health and Care Excellence
- NIHR
- National Institute for Health Research
- NRT
- nicotine replacement therapy
- NSSEC
- National Statistics Socio-Economic Classification
- OR
- odds ratio
- PCRN
- Primary Care Research Network
- PCT
- primary care trust
- p.p.m.
- parts per million
- R&D
- research and development
- SES
- socioeconomic status
- SSS
- Stop Smoking Service
- TNS BMRB
- Taylor Nelson Sofres, British Market Research Bureau
- UKCTAS
- UK Centre for Tobacco and Alcohol Studies
- vif
- variance inflation factor
- WHO
- World Health Organization