Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 13/72/01. The contractual start date was in January 2014. The draft report began editorial review in August 2014 and was accepted for publication in May 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Wade et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Aetiology and prevention of deep-vein thrombosis
Venous thrombosis is a condition in which a blood clot forms in a vein, resulting in blockage of the affected vein. It most commonly occurs in the deep veins of the lower limbs, and this is known as deep-vein thrombosis (DVT). DVT can be asymptomatic (detected by screening) or symptomatic, usually presenting as leg pain and/or swelling as a result of occlusion of the vein. If the blood clot breaks off and travels through the venous system, an embolism is created; if the clot lodges in the lung, a pulmonary embolism (PE) arises. DVT and PE are collectively known as venous thromboembolism (VTE).
Deep-vein thrombosis can occur in hospitalised patients owing to changes in the blood vessel wall, changes in blood flow and changes in the properties of the blood, caused by factors such as immobilisation, decreased fluid intake and excessive body fluid loss. In addition, trauma and surgery can also cause activation of the coagulation system, leading to a higher risk of DVT. 1 It has been estimated that between 45% and 51% of patients undergoing orthopaedic surgery develop DVT if they are not provided with adequate thromboprophylaxis, as shown in Table 1. 2 However, these estimates are from out-dated studies in which patients were not receiving DVT prophylaxis. Estimates of baseline risk of DVT for patients on pharmacological prophylaxis have been presented below (see Chapter 4), along with the methods used to derive these more up-to-date, clinically relevant estimates.
| Specialty | DVT (%) (weighted mean) |
|---|---|
| General surgery | 25 |
| Orthopaedic surgery | 45–51 |
| Urology | 9–32 |
| Gynaecological surgery | 14–22 |
| Neurosurgery (including stroke) | 22–56 |
| Multiple trauma | 50 |
| General medicine | 17 |
Data from a UK prospective cohort study (Million Women Study3) showed that women undergoing an inpatient surgical procedure were 70 times more likely than those who had not undergone surgery to be admitted with VTE in the 6 weeks post surgery, while those undergoing a day-case procedure were 10 times more likely to be admitted. 3 Risks remained increased 7–12 weeks post surgery, and the pattern of risk was similar for PE and DVT. Risk varied considerably by surgery type. It is estimated that up to 25,000 people in England may die each year from potentially preventable VTE developed while in hospital. 2
Surgical patients and patients with trauma are at an increased risk of VTE if they meet one of the following criteria:4
-
surgical procedure with a total anaesthetic and surgical time of more than 90 minutes, or 60 minutes if the surgery involves the pelvis or lower limb
-
acute surgical admission with inflammatory or intra-abdominal condition
-
expected significant reduction in mobility
-
one or more of the following risk factors:
-
active cancer or cancer treatment
-
aged over 60 years
-
critical care admission
-
dehydration
-
known thrombophilias
-
obesity
-
personal or first-degree family history of VTE
-
use of oestrogen-containing oral contraceptives or hormone replacement therapy
-
varicose veins with phlebitis
-
one or more significant medical comorbidities (e.g. heart disease; metabolic, endocrine or respiratory pathologies; acute infectious diseases; inflammatory conditions).
-
In recent years, there have been changes in the factors that impact on the risk of postsurgery DVT. Surgical practice has changed so that the duration of general anaesthetic is shorter, or surgery is performed under local anaesthetic. The duration of a patient’s stay in hospital is much shorter, with many procedures now performed as day cases. Patients are mobilised more quickly, and patients discharged home are supported by community-based physiotherapists. In addition, new oral anticoagulants (NOACs) [e.g. dabigatran (Pradaxa®, Boehringer Ingelheim), rivaroxaban (Xarelto®, Bayer Healthcare), apixaban (Eliquis®, Bristol-Myers Squibb and Pfizer)] can be used for longer periods, offering extended protection to patients. 4 In March 2010, the Department of Health produced a Risk Assessment for Venous Thromboembolism tool for use in hospitalised patients. 5 It is also a National Institute for Health and Care Excellence (NICE) quality standard that all patients on admission to hospital receive an assessment of individual risk of VTE and bleeding using clinical risk assessment criteria described in the national tool. 6
Despite these efforts to prevent postsurgery DVT, other factors, such as the increasing numbers of older patients undergoing surgery and the increasing proportion of obese and morbidly obese patients, adds upwards pressure on the population risk of postsurgery DVT.
Consequences of deep-vein thrombosis
Deep-vein thrombosis on its own does not frequently result in death, but left untreated it can result in PE. 7 The number of hospitalised patients dying each year from PE following DVT in the UK has been estimated to be 25,000. 4 PE is the immediate cause of death in 10% of all patients who die in hospital. 8 Those who do survive DVT or PE are at increased risk of recurrence, particularly within the first 2 years. 9
Untreated patients may also be at risk of post-thrombotic syndrome (PTS) which can occur immediately or within 10–20 years of the initial episode. 4 Signs and symptoms of PTS include pain, swelling, oedema and ulcers. 10 These conditions can also have a significant impact on an individual’s quality of life. 9
Other long-term complications of VTE include pulmonary hypertension (PHT), abnormally elevated blood pressure within the pulmonary artery and stroke. 4 These long-term consequences have implications on extended prophylaxis and the costs arising from treatment, which will be discussed further below (see Chapter 4).
Thromboprophylaxis
There is evidence that routine prophylaxis reduces morbidity, mortality and health-service costs in hospitalised patients at risk of DVT and VTE. 11 Prophylaxis can be pharmacological [fondaparinux sodium, low-molecular-weight heparin (LMWH) or unfractionated heparin] and/or mechanical. Mechanical methods of prophylaxis include graduated compression stockings (GCSs), intermittent pneumatic compression devices (IPCDs) and pneumatic foot pumps (FPs). GCSs have been shown to reduce the incidence of postoperative DVT in surgical patients to approximately 11%, whereas low-dose heparin (LDH) administered via subcutaneous injection reduces the rate of DVT to around 9%; used together, the rate of DVT is reduced further. 12
Graduated compression stockings/antiembolism stockings
There are two different types of compression hosiery: antiembolism stockings and GCSs. Both products offer graduated compression and the two terms are often used interchangeably, although antiembolism stockings are designed for the prevention of VTE in immobile patients, whereas GCSs are designed for the management and treatment of conditions such as venous leg ulcers and lymphoedema in the ambulant patient. For consistency with the Health Technology Assessment (HTA) scope, we will use the more commonly used term GCS.
Graduated compression stockings exert graded pressure at a decreasing gradient from the ankle to the thigh, which increases blood flow velocity and promotes venous return. In addition, preventing passive venous distension is thought to prevent subendothelial tears and the activation of clotting factors. 4
The Sigel profile, which equates to a graduated compression pressure profile of 18 mmHg at the ankle, 14 mmHg at the mid-calf, 8 mmHg at the knee (popliteal break), 10 mmHg at the lower thigh and 8 mmHg at the upper thigh was found to increase deep venous flow velocity by 75%. 13 The current British and European Standards for antiembolism stockings [BS7672 (1); ENV 12719 (70)] do not replicate the Sigel profile and the British Standard requires pressure to be measured at only three points rather than the five specified by Sigel. 4
Graduated compression stockings are available as knee-length or thigh-length stockings. Patients report that both knee-length and thigh-length stockings are difficult to use, but knee-length stockings wrinkle less than thigh-length, and fewer patients report discomfort when using them. 14 Patient adherence is reported to be higher with knee-length stockings, and thigh-length stockings are more likely to be worn incorrectly. 15,16 Incorrectly worn stockings can be unsafe: thigh-length stockings that are fitted incorrectly or roll down can create a tourniquet effect. In addition, for some patient subgroups, one length of stocking may be more appropriate than the other; for example, it is widely believed that knee-length stockings are more likely to induce wound complications in patients undergoing knee replacement surgery. There are also some patients for whom GCSs are contraindicated, such as those who have peripheral arterial disease.
Existing guidelines and systematic reviews
A rapid appraisal of the review and guideline literature was undertaken to inform the protocol and give an indication of the size of the literature. We searched key resources for published systematic reviews and guidelines on GCSs, including The Cochrane Library, PROSPERO, Clinical Trials.gov, National Guidelines Clearinghouse, National Institute for Health Research HTA website, Turning Research into Practice, Clinical Evidence, NHS Evidence, NICE website and the NICE Clinical Knowledge Summaries Database. The search identified the NICE and Scottish Intercollegiate Gudielines Network (SIGN) guidelines for the prevention of VTE,4,11 and two relevant Cochrane reviews,1,17 described below. Guidelines were also identified for several other countries, including the USA and Australia.
National Institute for Health and Care Excellence guidelines
In January 2010, NICE published Clinical Guideline (CG) 92 on reducing the risk of VTE (DVT and PE) in patients admitted to hospital (updating previous CG46). 4 The key recommendations relating to thromboprophylaxis in surgical patients are detailed below.
If using mechanical VTE prophylaxis, base the choice of mechanical VTE prophylaxis on individual patient factors including clinical condition, surgical procedure and patient preference. Choose any one of thigh- or knee-length GCSs, foot impulse devices or IPCDs (thigh or knee length).
Further recommendations are made, for example regarding correct sizing and fitting of stockings. The guideline states that patients should be encouraged to wear their stockings day and night until they no longer have significantly reduced mobility.
Pharmacological VTE prophylaxis is also recommended for surgical patients at a low risk of major bleeding, taking into account individual patient factors and according to clinical judgement. Pharmacological VTE prophylaxis should also be continued until the patient no longer has significantly reduced mobility (generally 5–7 days), although for patients with hip fracture or undergoing elective hip replacement surgery, pharmacological VTE prophylaxis should be continued for 28–35 days (according to the summary of product characteristics for the individual agent being used) and, for patients undergoing knee replacement surgery, pharmacological prophylaxis should be continued for 10–14 days.
The NICE guideline states that the length of stockings is a controversial issue and there is no clear randomised evidence that one length of stocking is more effective than another. Clinical judgement, patient preference, concordance and surgical site are all important issues when deciding on stocking length.
Contraindications to GCS use are suspected or proven peripheral arterial disease; peripheral arterial bypass grafting; peripheral neuropathy or other causes of sensory impairment; any local conditions in which stockings may cause damage, such as gangrene or dermatitis; known allergy to material of manufacture; cardiac failure; severe leg oedema or pulmonary oedema from congestive heart failure; unusual leg size or shape; or major limb deformity preventing correct fit.
In February 2012, NICE published an evidence update to CG92. 18 New evidence was found (a Cochrane review by Sachdeva et al. 17) that supported the use of GCSs in surgical patients with or without other methods of thromboprophylaxis, which is in line with current recommendations in CG92. The evidence update stated that the review was not able to answer the question of the efficacy of thigh-length versus knee-length GCSs.
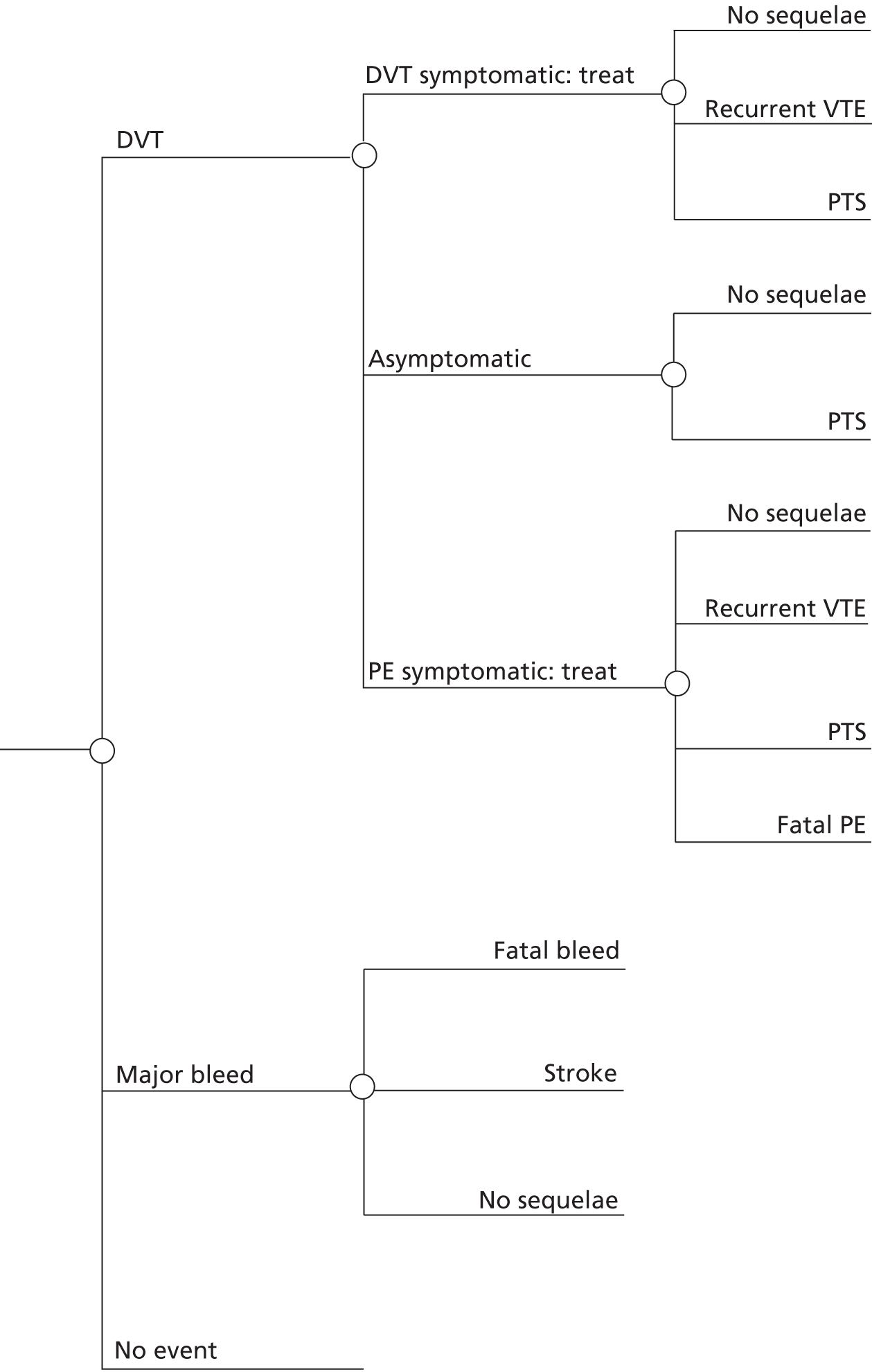
A decision-analytic model was also developed in CG92 to determine the most cost-effective thromboprophylaxis strategy for different hospital population subgroups [hip fracture surgery, total hip replacement (THR), total knee replacement (TKR), general surgery (GS) and general medical admissions]. VTEs and major bleeding events were modelled for the acute period [determined by the randomised controlled trial (RCT) follow-up, typically only 10–14 days) but quality-adjusted life-years (QALYs) and health-service costs arising from these events were modelled over the patient’s lifetime, including treatment of PTS and PHT. Results differed across the different population subgroups, although GCSs either alone or combined with pharmacological prophylaxis was consistently found to be the most clinically effective and cost-effective approach for the prevention of VTE. The different results were largely driven by population differences in terms of the baseline risks of major bleeding and PE. The cost of GCSs was assumed to be £6.36 per pair (2009 prices) but the length was not specified. In addition, no attempt was made to formally model the relative cost-effectiveness of different GCSs lengths.
Scottish Intercollegiate Guidelines Network guidelines
The SIGN published guideline 122 on the prevention and management of VTE in December 2010 (updating previous guidelines 62 and 36). 11 The key recommendations relating to thromboprophylaxis in surgical patients are detailed below.
Patients undergoing abdominal surgery who are at risk as a result of the procedure or personal risk factors should receive thromboprophylaxis with mechanical methods unless contraindicated and either subcutaneous LMWH, unfractionated heparin or fondaparinux.
Patients undergoing THR or TKR surgery should receive pharmacological prophylaxis (with LMWH, fondaparinux, rivaroxaban or dabigatran) combined with mechanical prophylaxis unless contraindicated. Extended prophylaxis should be given.
The SIGN guideline states that studies comparing above-knee with below-knee stockings have been too small to determine whether or not they are equally effective, although a meta-analysis suggested no major difference in efficacy in surgical patients. 19 The guideline recommends that above-knee or below-knee GCSs may be used for prophylaxis of DVT in surgical patients, provided that there are no contraindications and that attention is paid to correct fitting and application. Contraindications are massive leg oedema; pulmonary oedema (e.g. heart failure); severe peripheral arterial disease; severe peripheral neuropathy; major leg deformity; and dermatitis.
Cochrane review: knee-length versus thigh-length graduated compression stockings
A Cochrane review undertaken by Sajid et al. 1 included three small RCTs12,20,21 that compared the effectiveness of thigh-length versus knee-length GCSs in hospitalised postoperative surgical patients. There was no statistically significant difference in clinical effectiveness between the two stocking lengths in terms of reducing the incidence of DVT; however, there was significant heterogeneity among the trials and considerable methodological limitations. The authors concluded that there was insufficient high-quality evidence to determine whether or not thigh-length or knee-length stockings differ in their effectiveness in terms of reducing the incidence of DVT in hospitalised patients. They recommended that a large multicentre RCT be conducted to address this issue.
Cochrane review: elastic compression stockings for prevention of deep-vein thrombosis
A Cochrane review undertaken by Sachdeva et al. 17 included 18 RCTs that compared the effectiveness of GCSs, with or without another method of DVT prophylaxis, versus no stockings in hospitalised patients. Eight RCTs compared GCSs alone with no stockings; the incidence of DVT was statistically significantly lower in the stocking group than in the no stockings group. 22–29 Ten RCTs compared GCSs plus another prophylactic method versus the prophylactic method alone; the incidence of DVT was statistically significantly lower in the stocking plus other prophylactic method group than in the other prophylactic alone group. 30–39 The authors concluded that GCSs are effective at diminishing the risk of DVT in hospitalised patients. However, where stated, all of the included RCTs used thigh-length stockings. The authors of this review also recommended a RCT comparing thigh-length with knee-length GCSs.
The two previous Cochrane reviews did not answer our specific research question. The review by Sajid et al. 1 included only three RCTs and did not seek indirect evidence. The review by Sachdeva et al. 17 did not restrict the inclusion criteria to surgical patients or compare the clinical effectiveness of thigh- versus knee-length stockings; the length of stocking used in some of the included studies was unclear.
Research aims and objectives
The aim of the research was to establish the expected value of undertaking additional research comparing the relative effectiveness of thigh-length versus knee-length GCSs, in addition to standard pharmacological prevention, for prevention of DVT in surgical patients. There were two key objectives:
-
to undertake an evidence synthesis by systematic review to estimate clinical effectiveness and inform key clinical parameters for a decision model
-
to develop a decision model to estimate cost-effectiveness and to undertake a value of information (VOI) analysis.
Chapter 2 Methods of clinical evidence reviews
Four key clinical areas were assessed to inform the decision model:
-
the relative effectiveness of thigh-length versus knee-length stockings for prevention of DVT in surgical patients
-
baseline risk of DVT
-
the clinical consequences of DVT
-
patient adherence.
A systematic approach to identifying the evidence was undertaken to inform these parameters. In the first instance, for each question, existing systematic reviews and CGs were sought. Where the existing systematic reviews and CGs were considered out of date or not sufficiently directly relevant, the primary literature was then systematically reviewed. Further details of each of the reviews are outlined below.
The systematic reviews were conducted and reported following the general principles recommended in the Centre for Reviews and Dissemination (CRD)’s guidance for undertaking reviews in health care,40 and the reporting guidance of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement. 41 The research protocol was registered on the international prospective register of systematic reviews (PROSPERO registration number: CRD42014007202).
Clinical advice was provided by an advisory group, which included a vascular surgeon, an orthopaedic surgeon, and an anticoagulant and thrombosis consultant nurse. A patient representative also provided information on her experiences of using GCSs after two different types of surgery. We hoped to collaborate with a local cardiology rehabilitation clinic (York Hospital), so that attending postsurgery patients could provide us with their comments on our interpretation of the evidence and the first phase of the economic modelling and could discuss the gaps in the evidence and the proposed research from a patient’s perspective. Unfortunately, it was not possible to develop this collaboration.
Effectiveness of thigh-length versus knee-length stockings
A systematic review was undertaken to evaluate the relative effectiveness of thigh-length versus knee-length GCSs, in addition to standard pharmacological prevention, for surgical patients at risk of DVT. Owing to the anticipated paucity of research evidence directly comparing thigh-length stockings with knee-length stockings, data were also sought comparing thigh-length stockings with a control treatment and knee-length stockings with a control treatment, in addition to studies directly comparing the two types of stockings.
Search strategy
A systematic search of the relevant guideline and systematic review databases was undertaken between 31 July 2013 and 14 August 2013, and records were inserted into an EndNote® version 7.2 (Thomson Reuters, CA, USA) library. The following databases were searched: Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects (DARE), NHS Economic Evaluations Database (NHS EED), Cochrane Methods Register, PROSPERO, HTA Database, National Guidelines Clearinghouse, Turning Research Into Practice (TRIP), Clinical Evidence, NHS Evidence and NICE Clinical Knowledge Summaries. During protocol development, scoping searches identified two up-to-date relevant reviews; a Cochrane review of knee-length versus thigh-length GCSs for prevention of DVT in postoperative surgical patients1 and a Cochrane review of GCSs for prevention of DVT. 17 These reviews searched the Cochrane Central Register of Controlled Trials (CENTRAL) and the Cochrane Peripheral Vascular Diseases Group Specialised Register, which is constructed from weekly electronic searches of MEDLINE, EMBASE, Cumulative Index to Nursing and Allied Health (CINAHL), The Allied and Complementary Medicine Database (AMED) and through hand searching relevant journals. The included and excluded studies lists of these two reviews, and other relevant reviews identified by searching the guideline and systematic review databases, were added to the EndNote library for screening.
In order to bring the searches undertaken in these two Cochrane reviews up to date, systematic searches of electronic sources for RCTs published since January 2010 (the date of the search in the earlier Cochrane review17) were undertaken on 19 February 2014 and added to the EndNote library. The following databases were searched: MEDLINE, MEDLINE In-Process & Other Non-Indexed Citations, EMBASE, CINAHL, AMED and CENTRAL. In addition, information on studies in progress, unpublished research or research reported in the grey literature was sought by searching relevant databases including ClinicalTrials.gov and Current Controlled Trials.
The search strategy used for trials of effectiveness developed for Ovid MEDLINE can be found in Appendix 1. This strategy was modified to run appropriately on the other databases searched. The strategy combines terms for GCS, terms for thrombosis and terms for RCTs. No language restrictions were applied to the search strategies.
In addition, clinical advisors were consulted for additional potentially relevant studies, and reference lists of all included studies and relevant reviews and guidelines were also manually searched.
Titles and abstracts of studies identified by the searches were independently assessed for inclusion by two reviewers using the criteria outlined below. Disagreements were resolved through discussion and, where necessary, by consultation with a third reviewer. For studies of potential relevance, full papers were assessed independently by two reviewers, with disagreements resolved by the same procedure.
Inclusion criteria
Participants
Studies of surgical patients at risk of DVT were included; day surgery patients were included as well as inpatients. Studies were included regardless of the participants’ level of risk for DVT, and the issue of level of risk was planned to be addressed in the analysis, if sufficient data were available.
Interventions
Studies assessing thigh-length GCSs (with or without standard pharmacological prevention) or knee-length GCSs (with or without standard pharmacological prevention) were included. The length of stocking used had to be clearly stated.
Comparators
Studies comparing thigh-length with knee-length GCSs were included. In addition, studies comparing thigh-length or knee-length GCSs (with or without standard pharmacological prevention) with no GCSs (with the same standard pharmacological prevention as in the GCSs group) were also included, as long as the length of stocking used was clear, and if different lengths were used, they were analysed separately.
Setting
Hospital and community.
Outcomes
The primary outcome was incidence and type of DVT (i.e. symptomatic or asymptomatic). DVT data were included only if diagnosed using radioiodine (125I) fibrinogen uptake, venography, Doppler ultrasound or magnetic resonance imaging (MRI) (as used in the review for NICE guideline 9218). Complications and consequences associated with DVT, such as the incidence of PE, incidence of PTS (and its associated complications) and mortality, and adverse effects related to the use of GCSs were assessed. Patient adherence, preference and cost implications were also assessed.
Study design
Randomised controlled trials only were included to address this review question.
Data extraction
Data extraction was conducted by one reviewer using a piloted and standardised data extraction form in EPPI-Reviewer 4.0 (Evidence for Policy and Practice Information and Co-ordinating Centre, London, UK) and independently checked by a second reviewer. Discrepancies were resolved by discussion, with involvement of a third reviewer when necessary. In cases where the same study was reported in multiple publications, the most up-to-date or comprehensive publication was used for data extraction. Data were extracted on study details (e.g. author, year, location of study), patient characteristics (e.g. age, sex, type of surgery, baseline risk factors for VTE), details of intervention (e.g. type of stocking, duration of use, co-interventions, including pharmacological thromboprophylaxis) and reported outcomes (e.g. method of assessment and results).
Quality assessment
The quality of the individual trials was assessed by one reviewer and independently checked by a second reviewer. No primary study was excluded based on the result of the quality assessment; disagreements were resolved by consensus and, if necessary, a third reviewer was consulted. The quality of included trials was assessed using the Cochrane risk of bias tool. 42
Data analysis
Data on the incidence of DVT or VTE in the treatment and comparison groups were extracted into 2 × 2 tables in Microsoft Excel® 2010 (Microsoft Corporation, Redmond, WA, USA) by one reviewer. Data were checked for accuracy by a second reviewer. An analysis of the data was performed using odds ratios (ORs) along with 95% confidence intervals (CIs). A random-effects model was used owing to the clinical and methodological variation between trials. The statistical package used for analysis was RevMan 5.2 (The Cochrane Collaboration, The Nordic Cochrane Centre, Copenhagen, Denmark). Comparisons of results are presented in forest plots by type of comparison and separately by unit of analysis (patient or leg). Subtotals for comparisons and an overall effect estimate are presented for display purposes only. These results should be interpreted with caution because of methodological differences between the included trials, such as the use of the opposite limb as the control and the range of publication dates of the trials. The I2-statistic was used to quantify statistical heterogeneity.
Data were insufficient to assess the effect of duration of stocking use and baseline risk of DVT on the outcome.
Where meta-analysis of the data was considered inappropriate, data were tabulated. Data on the incidence of PE, mortality and adverse events related to the use of GCSs were tabulated and synthesised narratively.
Network meta-analysis
A network meta-analysis (NMA) was planned, first, to produce consistent effect estimates across different comparisons for the cost-effectiveness and VOI analyses (see Chapter 5, Interventions) and, second, to investigate if the utilisation of indirect evidence may increase the precision of the relative effect estimate for knee-length GCSs versus thigh-length GCSs. As stated previously (see Inclusion criteria), trials were included whether patients were day-case patients or inpatients and regardless of the participants’ level of risk of DVT. If either of these factors was an effect-modifier, then effect estimates from a NMA could potentially be biased if these factors are not controlled for. If there is sufficient evidence, then these will be controlled for in the analysis. If there is insufficient evidence to do so then a NMA consisting of loops may still be of value to a cost-effectiveness or VOI analysis. A high level of inconsistency between direct and indirect evidence, which suggests clinical or methodological heterogeneity, will increase the uncertainty in the effect estimates, which will better inform the decision uncertainty where there are multiple treatments.
In addition, the DVT risk in the trials may not reflect the DVT risk in the decision population in the cost-effectiveness analysis and VOI analysis, and including all the studies maximises the use of available evidence. Where the distribution of study characteristics does not represent the setting of the cost-effectiveness analysis then predictive distributions can be used to represent the uncertainty in the generalisability of the effect estimates to the cost-effectiveness analysis setting.
A NMA is an extension of meta-analysis, but where a meta-analysis includes only direct evidence, a NMA can draw on both direct and indirect evidence. The results from studies that compare interventions A and C are considered to be direct evidence for the treatment effect dAC. If a study X compares treatments A and B, and a study Y compares treatments B and C, and a treatment effect dAC is calculated from these two studies, then this result is referred to as indirect evidence.
A standard meta-analysis combines the results from two or more studies that have comparable populations, interventions, comparators and outcomes. Study quality and other study characteristics are also assumed to be similar. Similarly, to make indirect comparisons, it is assumed that the study characteristics are comparable. This is known as exchangeability, which can be investigated through the consistency of the direct and indirect evidence. 43–45 It assumes that, had treatment C been included in the study comparing A and B, then the treatment effect dAC would be the same as that found from the study of A and C. 46 Assuming consistency, the treatment effect dAC is the sum of the treatment effects dAB and dBC:
A NMA can combine both the direct evidence and the indirect evidence for dAC. 46 As in a meta-analysis, it is the summary treatment effect from each study that is utilised in the NMA; hence the benefit of randomisation in each study is retained.
Although several outcomes were investigated in this review, there was sufficient evidence to perform a NMA only for the outcome DVT. The systematic review of effectiveness included all trials that evaluated the effectiveness of a stocking treatment. The included trials evaluated the effectiveness of many interventions that did not include a stocking treatment when compared with a stocking treatment. The criterion for developing the networks for the NMAs was that interventions were included in the network only if the effectiveness evaluated in the corresponding study informed directly or indirectly the relative effectiveness of thigh-length versus knee-length stockings.
Full details of the trials included in the network are reported in Chapter 3, Network meta-analysis results. To create the network, interventions that were considered sufficiently similar relative to the interventions of interest were lumped together. The effectiveness of different drugs, LMWH, LDH and fondaparinux were assumed to be the same, and these were therefore lumped together in the network and will be referred to collectively as ‘heparin’. The interventions that formed part of comparisons that informed the effect estimates of interest are shown in Figure 1.
FIGURE 1.
The network of treatments included in the NMA. In the base case, every relative effect measure can be described in terms of the additive effects of thigh-length stockings (T), knee-length stockings (K) and heparin (H).
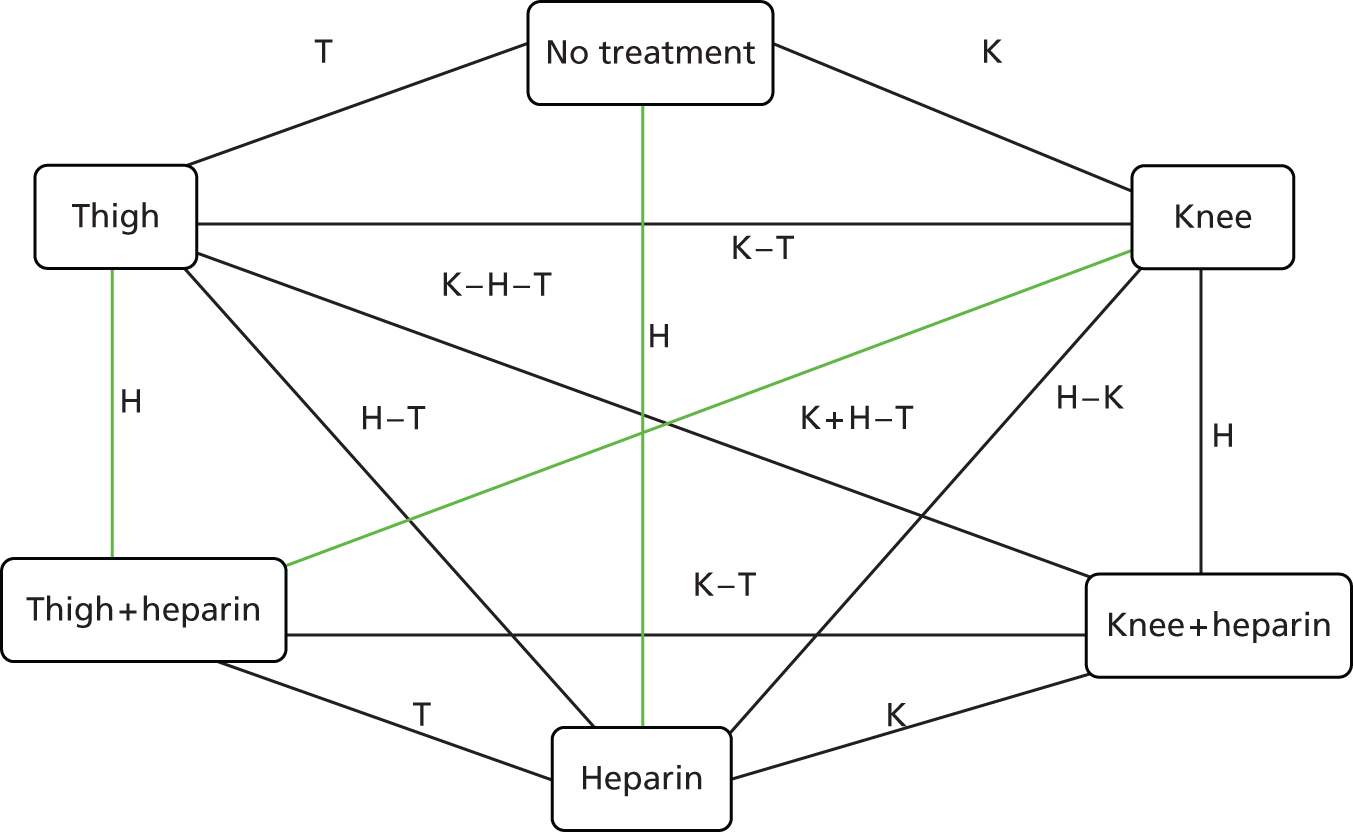
Based on the advice of the clinical advisors, it was assumed that there was no stocking–heparin interaction in the base case. This implies that the effect of thigh-length compared with knee-length stockings is the same as thigh-length stockings plus concomitant heparin compared with knee-length stockings plus concomitant heparin. The simplest way to model this is to lump thigh-length stockings and thigh-length stockings plus heparin together, knee-length stockings and knee-length stockings plus heparin together, and no treatment and heparin together. This approach potentially loses indirect evidence for thigh-length stockings compared with knee-length stockings from trials that compare thigh-length stockings with heparin and knee-length stockings plus heparin compared with knee-length stockings alone. Instead of lumping those interventions, another approach, which also assumes no interaction and is therefore almost an identical approach, is to assume that the effectiveness of each of the six interventions compared with each other can be described in terms of the additive treatment effects of thigh-length stockings, knee-length stockings and heparin. This follows the NMA methods for a no interaction assumption taken in Wolf et al. 47 In a sensitivity analysis, this assumption was relaxed and the relative effectiveness of each treatment compared with every other treatment was estimated.
The model, written in WinBUGS (MRC Biostatistics Unit, Cambridge, UK), was based on code presented in the NICE Technical Support Document 2. 48 The full code can be found in Appendix 5. DVT was a binary outcome and, therefore, a model with a binomial likelihood was adopted.
Assuming that there may be an interaction between stocking treatment and heparin, the model of the probability of a DVT pik for trial i and trial arm k on the log scale uses a log-link function.
where I is the baseline risk, dt is the effect of the treatment compared with the baseline treatment (no treatment), dc is the effect of the comparator compared with the baseline treatment and I{k ≠ 1} ensures that the treatment effect does not apply to the baseline trial arm.
Assuming that there is no interaction between stocking and heparin treatment, each treatment is coded as no treatment, thigh-length stocking or knee-length stocking with or without an additive heparin effect. So, for a trial comparing thigh-length stocking with heparin to knee-length stocking alone, the model of the probability of a DVT pik on the log-odds scale is:
The model produced ORs for every pairwise comparison between the interventions in the network. Given that the objective of this project was to evaluate the expected VOI of doing further research, the probability that each treatment would be the most effective given the results of a new trial is calculated, using the predictive distributions for each treatment effect. Predictive distributions are used because of the unexplained heterogeneity and the true treatment effect from a new trial may arise from anywhere in the random-effects distribution. This predictive distribution is broader than the posterior distribution of the average treatment effect estimate because of the trial heterogeneity. The probability of error in identifying the most effective treatment can be derived from these probabilities.
Finally, for different risks of DVT for patients on heparin the risk of DVT was calculated for patients on each treatment, and the number of patients needed to treat (NNT) with a selection of treatments to avoid an extra case of DVT beyond that achieved by the selected comparator was calculated. The selection of comparisons and baseline risks for DVT for patients on heparin for the NNT calculations was designed to illustrate the incremental benefits of the heparin combination treatments, which are evaluated in the cost-effectiveness analyses below (see Chapters 4–6).
The duration of stocking use and baseline DVT risk were both considered potential effect modifiers for the analysis, but the effect of these on the results was not investigated as there were insufficient data across the trials. The only potential effect modifiers for which there was evidence across the trials were publication in year 2003 or later, and whether or not patients had undergone orthopaedic surgery. Publication in or after 2003 was considered important owing to changes in clinical practice over the past decade, such as less invasive surgery and shorter recovery times, meaning that older trials may not be applicable to current NHS practice. This was on the advice of our clinical advisors. Orthopaedic surgery was considered because orthopaedic surgery carries a high risk of DVT and there were sufficient data available from the trials to compare orthopaedic with non-orthopaedic surgeries. Subgroup analyses were conducted for trials published before and after 2003, and for orthopaedic and non-orthopaedic surgery patients where a connected network existed that informed the relative effectiveness of thigh-length stockings versus knee-length stockings.
Random- and fixed-effects models were both considered. The random-effects analysis was chosen if there were adequate data to estimate the between-study variance and the model was a better fit according to the residual deviance statistic. For the random-effects model, the between-study variance was assumed to be common across all of the comparisons in the analysis. A uniform distribution was the primary choice for the prior distribution of the between-study standard deviation (SD) in the random-effects model. This had the range 0–10. An inverse gamma distribution was also tested for the prior distribution for the between-study variance as an alternative to the uniform distribution. The choice of prior distribution was based on model fit and sensitivity to the variance of the prior distribution. The results were not sensitive to different uniform prior distributions with upper limits 3–10, and the uniform distribution produced a better-fitting model, so the uniform prior distribution of 0–10 was used. The between-study variance was also compared with the between-study variance estimated for the nine trials that provided estimates for the effectiveness of thigh-length stockings versus no stockings using the Mantel–Haenszel method. 22,24,25,30,33,35–37,49
Model convergence was evaluated by reviewing the posterior densities of the model parameters and the Ruben–Gelman statistic. 50 In total, 20,000 iterations were discarded and the results were based on a further 50,000 iterations.
Inconsistency in the evidence was explored using the node-split method on appropriate edges of loops in the network. 43 The between-study SD for the network was compared with the between-study SD of the comparison of thigh-length stockings versus no stockings using a Bayesian analysis to see if any inconsistency increased its estimate. When assessing consistency for the base-case analysis where no stocking–heparin interaction was assumed, edges in the network with the same treatment effect were considered the same edge, for example, thigh-length stockings versus no stockings and thigh-length stockings plus heparin versus heparin.
Baseline risk of deep-vein thrombosis
It was anticipated that the review of clinical effectiveness of thigh-length and knee-length GCSs would provide limited data on baseline risk of DVT (both patient specific and procedure specific) from the no prophylaxis arms of the trials. Therefore, to supplement these data and ensure that the best available data were used for the economic model, existing guidelines on the risk of DVT in surgical populations were identified by searching national and international guidelines.
The searches aimed to identify the most appropriate source of evidence, which included evidence from large population-based studies that estimated the expected baseline risk of DVT in different patient population groups (e.g. different age groups) in the absence of prophylaxis. The source of synthesised evidence considered most appropriate was based on the scope and quality of the evidence, and was used to inform the economic model.
The clinical consequences of deep-vein thrombosis (mortality and morbidity)
To identify the evidence regarding the short-term and longer-term clinical consequences of DVT the EndNote version 7.2 library of records identified for the review of RCTs of effectiveness was screened, and clinical advisors were contacted. An additional specific search of the literature to identify the best available evidence to quantify the consequences of DVT was not undertaken because the records already included in the library contained relevant up-to-date systematic reviews and CGs, providing sufficient detail to inform the clinical aspects of the review. It is acknowledged that potentially relevant studies may have been missed. The source of synthesised evidence on the clinical consequences of DVT considered most appropriate to inform the economic model was identified based on the scope and quality of the review/guidelines.
Patient adherence and preference
Search strategy
The RCTs that met the criteria for inclusion in the review of effectiveness of thigh-length and knee-length GCSs were screened independently by two reviewers to identify those that also provided data on patient adherence and/or preference. The Endnote library of records identified for the review of effectiveness was checked for additional relevant studies (not limited to RCTs) on patient adherence and preference. An additional search of the literature for studies on patient adherence and preference was not undertaken. The findings from studies already identified from the Endnote library of records were consistent in terms of patient experiences with wearing different lengths of GCSs. It was therefore concluded that further searches would not have substantially added to the evidence base.
Data extraction
Data on patient adherence and preference were extracted from the RCTs into Eppi-Reviewer 4.0 by one reviewer. Data from the observational studies were extracted into a Microsoft Word 2010 (Microsoft Corporation, Redmond, WA, USA) document by one reviewer. A second reviewer checked all data for accuracy.
Quality assessment
The quality of the RCTs was assessed using the Cochrane risk of bias tool, as described above (see Quality assessment). 42 The quality of the observational studies was not formally assessed. The observational studies were generally small, provided limited data and the methods used to conduct the studies were not rigorous. These studies were therefore considered to be at high risk of bias and formal quality assessment was not deemed necessary.
Data analysis
Given the heterogeneity between the studies and the limited outcome data reported, the data are presented in tables and as a narrative synthesis.
Chapter 3 Results of clinical evidence reviews
Effectiveness of thigh-length versus knee-length stockings
Flow of studies through the review of effectiveness
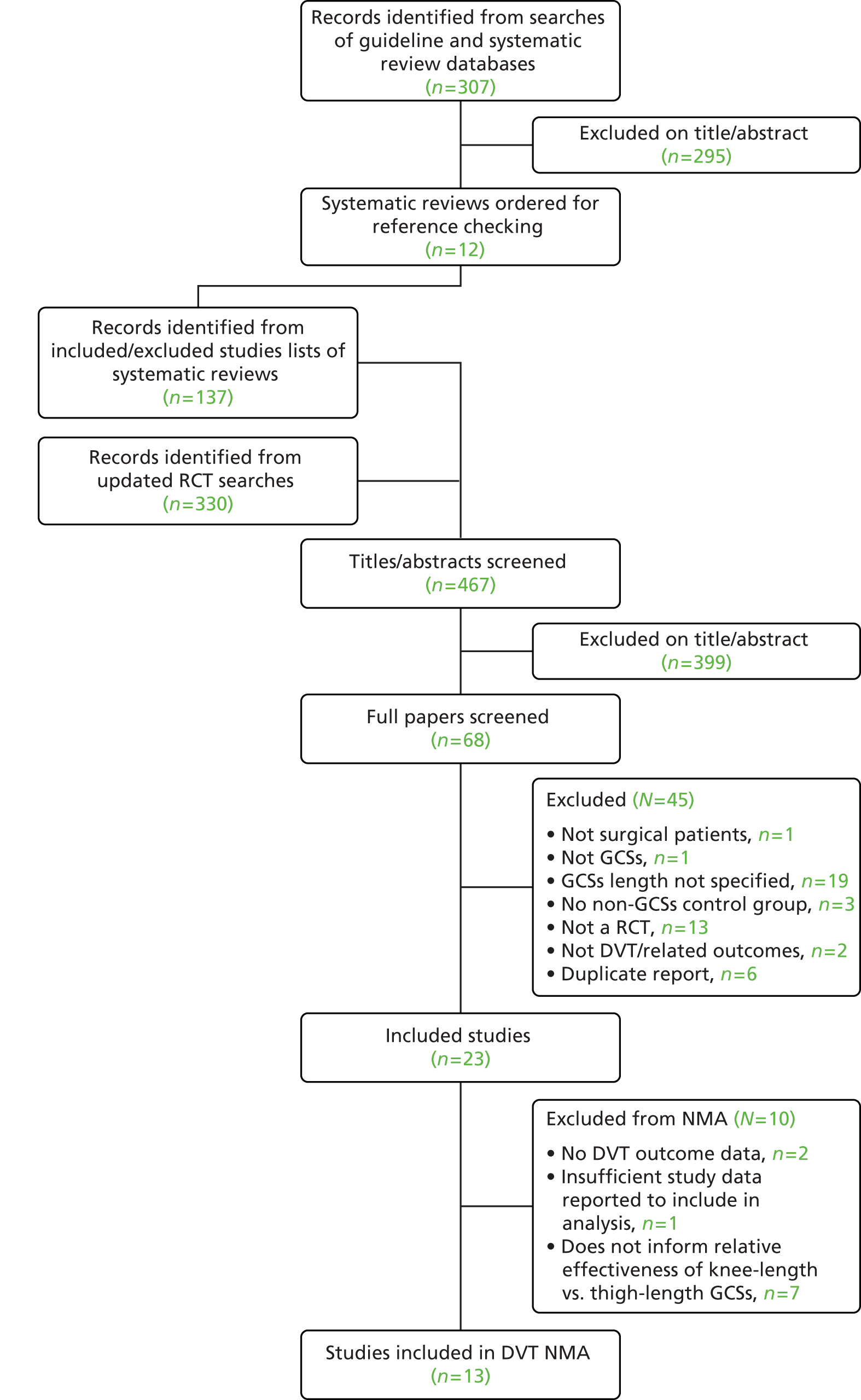
The electronic search of the review and guideline literature, undertaken to inform the protocol, identified the NICE guidelines for the prevention of VTE,4,18 and two particularly relevant Cochrane reviews. 1,17 Therefore, because of the existence of these systematic reviews (among others), many relevant trials were identified from their included and excluded studies lists, prior to running the update searches for primary studies.
The electronic search of the relevant systematic review and guideline databases identified 307 records, which were inserted into an EndNote library. From this EndNote library, 12 potentially relevant systematic reviews that appeared to assess GCSs in postoperative surgical patients (including the two reviews identified during the protocol development stage1,17) were obtained so that their lists of included and excluded studies could be systematically searched for potentially relevant primary studies. 1,17,19,51–59 A total of 137 records were added to the EndNote library from the included and excluded studies lists of the 12 relevant systematic reviews (after removal of duplicates).
Once the searches of existing systematic reviews and guidelines were completed, more recent primary studies were searched for. These update searches of electronic databases (from 2010 to 19 February 2014) identified an additional 330 records, which were also added to the EndNote library.
The full papers of 68 potentially eligible primary studies were screened for inclusion in the review. A total of 23 RCTs were included in the review of effectiveness of thigh-length versus knee-length stockings. 12,20–25,30–37,49,60–66
Of these 23 RCTs, 21 reported data for the outcome DVT. 12,20–25,30–37,49,60,61,63,65,66 However, one trial did not report sufficient data to be included in the meta-analysis or NMA, as total numbers of patients in treatment groups were not reported. 65 An additional seven trials did not add to the network of evidence comparing thigh-length with knee-length GCSs. 23,31,32,34,61,63,66 Therefore, 13 RCTs contained data that directly or indirectly informed the relative effectiveness of thigh-length versus knee-length stockings and were included in the NMA. 12,20–22,24,25,30,33,35–37,49,60
Figure 2 presents the flow of studies through the study selection process. Details of studies excluded at the full publication stage, with the reason for their exclusion, are provided in Appendix 2.
FIGURE 2.
Flow diagram of the study selection process.
Characteristics of studies included in the review of effectiveness
Detailed study characteristics for the 23 included trials are presented in Appendix 3.
There was substantial variation among the 23 included RCTs in terms of the patient characteristics, suggesting that the participants had a different baseline risk for DVT. Some trials included only patients with at least one VTE risk factor (usually age over 40 years),20,21,31,33,36,37,61–65 whereas others excluded patients with certain risk factors (usually history of prior VTE). 21,22,25,33,60 The majority of trials did not report the proportion of patients with known VTE risk factors, such as history of prior VTE, malignancy and obesity. The type of surgery and anaesthesia also varied between trials, which also alters the baseline risk for DVT, with orthopaedic surgery being associated with the highest risk.
There was also variation in the interventions used in the RCTs; in some trials, a GCS was worn on only one leg rather than on both legs,22,31,34,35,60,63 and the duration of use varied between trials. For most trials, GCSs were worn until full mobilisation or discharge from hospital, where reported. Patients received different brands of thigh-length or knee-length GCS, including Thrombex (medi GmbH & Co. KG, Bayreuth, Germany), Brevet TX (Mölnlycke Health Care Ltd, Dunstable, UK), Kendall TED [Kendall Company (UK) Ltd, Basingstoke, UK] and SaphenaMedical (Griffiths and Nielsen Ltd, Horsham, UK) antiDVT GCSs. Only four RCTs reported the pressure index of the stockings,21,22,31,60 which varied from 11.3 mmHg at the ankle,21 which is outside the British Standard range, to between 30 mmHg and 40 mmHg at the ankle. 60 Concomitant pharmacological prophylaxis also varied between trials; some trials used dextran, which is no longer used in NHS practice, and, therefore, the DVT results for these trials have been reported separately from those using LMWH, LDH or fondaparinux. 31,32,66 None of the included trials used the NOACs (dabigatran, rivaroxaban or apixaban).
The methods of assessing outcomes also varied between trials, with some trials assessing certain outcomes, such as PE, only if signs or symptoms were present. 30,36,37,60,66 The timing of outcome assessments was generally short, where reported; DVT was assessed up to the seventh postoperative day in nine RCTs,12,23,25,31,34–37,65 one RCT assessed DVT up to the ninth postoperative day,63 one RCT assessed DVT for 10 days,32 one assessed DVT up to the 12th postoperative day33 and two assessed DVT up to the 14th postoperative day. 24,66 The included trials assessed all DVTs, not just symptomatic DVTs. Where reported, the majority of DVTs were asymptomatic, the clinical consequences of which are unknown. Two RCTs that were included in the review for the outcomes PE and mortality also assessed DVT using the 99mTc-labelled plasmin test. However, owing to the unreliability of this test, our inclusion criteria stated that DVT data were included only if diagnosed using radioiodine (125I) fibrinogen uptake, venography, Doppler ultrasound or MRI. Therefore, the DVT results for these two RCTs are not reported. 62,64 Some trials also reported results relating to adverse events, quality of life and patient preference and adherence.
Summary study details are presented in Tables 2–6, categorised by the intervention and comparator assessed, with the most informative to the review question and most clinically relevant interventions presented first (corresponding to the groupings for meta-analysis presented in Results of studies included in the review). The tables demonstrate the clinical heterogeneity between the included trials for each of the meta-analyses.
| Study details | Location and number randomised/analysed | Patient characteristics | Type of surgery | Intervention | Control | Outcomes assessed | Risk of biasa |
|---|---|---|---|---|---|---|---|
| Thigh-length GCSs + LMWH vs. knee-length GCSs + LMWH | |||||||
| Howard et al. (2004)12 | UK 376/294 |
VTE risk factors: 77% high risk, 16% moderate risk, 7% low risk Average age: 58 years (range 16–88 years) Male: 42% |
GS | (1) Kendall TED thigh-length GCSs + enoxaparin LMWH (n = 127) (2) Medi thrombexin® climax thigh-length GCSs + enoxaparin LMWH (n = 121) |
Medi thrombexin® climax knee-length GCSs + enoxaparin (LMWH) (n = 128) | DVT (assessed by duplex ultrasound) PE Adverse events |
Unclear |
| Thigh-length GCSs + fondaparinux vs. knee-length GCSs + fondaparinux | |||||||
| Cohen et al. (2007)49 | Brazil, UK, Hong Kong and Spain 874/795 |
VTE risk factors: 20% obese, 3% had a history of VTE, 8% had varicose veins and/or chronic venous insufficiency, 3.5% had a family history of VTE Average age: 65 years (range 18–99 years) Male: 43% |
Orthopaedic surgery | (1) Thigh-length GCSs + fondaparinux (n = 266) | (1) Knee-length GCSs + fondaparinux (n = 123) (2) Fondaparinux alone (n = 400) |
VTE (demonstrated by bilateral proximal ultrasound or venography) Fatal PE Adverse events Quality of life |
Low |
| Thigh-length GCSs vs. knee-length GCS | |||||||
| Porteous et al. (1989)21 | UK 124/114 |
VTE risk factors: 40% had malignancy, 32% were smokers. Patients with a history of DVT were excluded from the trial Average age: 65 years Male: 43% |
Abdominal surgery | Thigh-length GCSs (pressure at the ankle: 11.3 mmHg) (n = 56) | Knee-length GCSs (n = 58) | DVT (assessed by radioiodine fibrinogen uptake test. Phlebography was performed if DVT was suspected) Adverse events Patient preference |
Unclear |
| Hui et al. (1996)25 | UK 177/138 |
VTE risk factors: 14% were smokers, average BMI was nearly 28 kg/m2 for patients undergoing TKR Average age: 69 years (range 49–88 years) Male: NR |
Orthopaedic surgery | Thigh-length GCSs (n = 44) | (1) Knee-length GCSs (n = 40) (2) No stocking (n = 54) |
DVT (assessed by bilateral ascending venography) Fatal PE (control group only) Patient adherence and preference |
High |
| Williams and Palfrey (1988)20 | UK NR/128 |
VTE risk factors: NR Average age: NR Male: NR |
Abdominal surgery | TED thigh-length GCSs (n = 44) | (1) Brevet TX knee-length GCSs (n = 44) (2) Brevet TX knee-length GCSs + LDH in high-risk patients (high risk not defined) (n = 40) |
DVT (assessed by radioiodine fibrinogen uptake test) | High |
| Ayhan et al. (2013)65 | Turkey 219/NR |
VTE risk factors: extremely high risk for postoperative DVT (not defined) Average age: NR Male: NR |
NR | Low-pressure thigh-length GCSs (n = not stated) | (1) Low-pressure knee-length GCSs (n = not stated) (2) Moderate-pressure knee-length GCSs (n = not stated) |
DVT (assessed by duplex ultrasound) Patient preference |
Unclear |
| Study details | Location and number randomised/analysed | Patient characteristics | Type of surgery | Intervention | Control | Outcomes assessed | Risk of biasa |
|---|---|---|---|---|---|---|---|
| Thigh-length GCSs + LMWH vs. LMWH | |||||||
| Kalodiki et al. (1996)33 | UK 93/78 |
VTE risk factors: 32% were obese, 45% had varicose veins, 5% had postphlebitic syndrome, 3% had history of previous DVT, 12% had leg oedema and 18% had chronic bronchitis. Patients with a history of recent DVT or active malignancy were excluded from the trial Average age: 69 years (range 53–85 years) Male: 49% |
Orthopaedic surgery | Kendall TED thigh-length GCSs + enoxaparin LMWH (n = 32) | Enoxaparin LMWH alone (n = 32) Placebo (n = 14) |
DVT (assessed by ascending venography) PE (assessed by perfusion lung scans) Adverse events |
Unclear |
| Thigh-length GCSs + LDH vs. LDH | |||||||
| Wille-Jørgensen et al. (1985)37 | Denmark 196/176 |
VTE risk factors: all patients had at least one thromboembolic risk factor Average age: 60 years (range 36–90 years) Male: 60% |
Abdominal surgery | TED thigh-length GCSs plus LDH (n = 86) | LDH (n = 90) | DVT (assessed by radioiodine fibrinogen uptake test, ascending phlebography was performed if DVT was suspected) PE (verified by pulmonary scintigraphy or autopsy) Mortality Patient adherence |
High |
| Wille-Jørgensen et al. (1991)36 | Denmark 276/245 |
VTE risk factors: all patients had at least one thromboembolic risk factor Average age: 72 years (range 37–95 years) Male: 36% |
Abdominal surgery | (1) Kendall TED thigh-length GCSs + LDH (n = 79) (2) Kendall TED thigh-length GCSs + dextran (n = 85) |
LDH (n = 81) | DVT (assessed by radioiodine fibrinogen uptake test, ascending phlebography was performed if DVT was suspected) PE (verified by pulmonary scintigraphy and roentgenograms, if patients had signs or symptoms of PE) Mortality Adverse events |
Unclear |
| Torngren (1980)35 | Sweden 110/98 |
VTE risk factors: 56% had malignancy Average age: 66 years (range 42–86 years) Male: 57% |
Abdominal surgery | Kendall thigh-length GCSs randomly allocated to right or left leg + LDH (n = 45 right leg, n = 53 left leg) | Unstockinged leg (patients were their own controls) | DVT (assessed by radioiodine fibrinogen uptake test) Fatal PE Adverse events |
High |
| Thigh-length GCSs + dextran vs. dextran | |||||||
| Fredin et al. (1989)32 | Sweden 150/144 |
VTE risk factors: NR Average age: 67 years Male: 40% |
Orthopaedic surgery | Comprinet thigh-length GCSs + dextran (n = 49) | (1) Dextran (n = 48) (2) Dextran + additional preoperative dextran (n = 47) |
DVT (assessed by radioiodine fibrinogen uptake test and ascending phlebography) PE (assessed by perfusion-ventilation scintigraphy) Mortality Adverse events Patient adherence |
Unclear |
| Ishak and Morley (1981)66 | UK 76/74 |
VTE risk factors: 26% had previous hip surgery or DVT, 67% had varicose veins and 28% were smokers Average age: 67 years Male: 54% |
Orthopaedic surgery | Kendall TED thigh-length GCSs (n = 35) Dextran was given to 26 patients |
No stocking (n = 41) Dextran was given to 33 patients |
DVT (assessed by venography) PE (assessed by chest radiograph followed by ventilation and perfusion lung scanning in symptomatic patients) Mortality |
High |
| Bergqvist and Lindblad (1984)31 | Sweden 88/80 |
VTE risk factors: 7.5% had history of VTE, 55% had malignant disease, 29% had varicose veins, 16% patients had major cardiopulmonary disease Average age: 68 years (range 52–85 years) Male: 53% |
GS | Thigh-length GCSs (16 mmHg at the ankle) randomly allocated to right or left leg + dextran (n = 41, right leg; n = 39, left leg) | Unstockinged leg (patients were their own controls) | DVT (assessed by radioiodine fibrinogen uptake test) PE (assessed by perfusion-ventilation scintigraphy) Mortality Adverse events |
Low |
| Study details | Location and number randomised/analysed | Patient characteristics | Type of surgery | Intervention | Control | Outcomes assessed | Risk of biasa |
|---|---|---|---|---|---|---|---|
| Thigh-length GCSs vs. no treatment | |||||||
| Barnes et al. (1978)30 | USA NR/18 |
VTE risk factors: 11% had a previous thrombophlebitis, 22% had a family predisposition, 22% had stasis changes, 33% had varicose veins and 67% patients were obese Average age: 66 years Male: 39% |
Orthopaedic surgery | Kendall TED thigh-length GCSs (n = 8) | No stocking (n = 10) | DVT (assessed by Doppler ultrasound, verified by contrast phlebography when DVT suspected) PE (assessed by chest roentgenograms, arterial blood gases and perfusion lung scanning in symptomatic patients) Adverse events |
Unclear |
| Turpie et al. (1989)24 | Canada 239/239 |
VTE risk factors: 3% had a history of DVT, 49% had a brain or spinal cord tumour and 23% had subarachnoid haemorrhage Average age: 50 years (range 16–90 years) Male: 60% |
Neurosurgery | (1) Kendall TED thigh-length GCSs (n = 80) (2) Kendall TED thigh-length GCSs + intermittent pneumatic compression (n = 78) |
No treatment (n = 81) | DVT (assessed by radioiodine fibrinogen uptake test and impedance plethysmography, confirmed using bilateral ascending venography) Mortality Patient adherence |
Unclear |
| Hui et al. (1996)25 | UK 177/138 |
VTE risk factors: 14% were smokers, average BMI was nearly 28 kg/m2 for patients undergoing TKR Average age: 69 years (range 49–88 years) Male: NR |
Orthopaedic surgery | Thigh-length GCSs (n = 44) | (1) Knee-length GCSs (n = 40) (2) No stocking (n = 54) |
DVT (assessed by bilateral ascending venography) Fatal PE (control group only) Patient adherence and preference |
High |
| Shirai (1985)22 | Japan 126/126 |
VTE risk factors: NR. Patients with a history of VTE were excluded from the trial Average age: 55 years (range 18–81 years) Male: 51% |
GS | Kendall TED thigh-length GCSs (pressure at the ankle: 18 mmHg) randomly allocated to right or left leg (n = 126 legs) | Unstockinged leg (patients were their own controls) | DVT (assessed by radioiodine fibrinogen uptake test) | Unclear |
| Knee-length GCSs vs. no treatment | |||||||
| Hui et al. (1996)25 Recruited: 177 patients Analysed: 138 patients |
UK 177/138 |
VTE risk factors: 14% were smokers, average BMI was nearly 28 kg/m2 for patients undergoing TKR Average age: 69 years (range 49–88 years) Male: NR |
Orthopaedic surgery | Thigh-length GCSs (n = 44) | (1) Knee-length GCSs (n = 40) (2) No stocking (n = 54) |
DVT (assessed by bilateral ascending venography) Fatal PE (control group only) Patient adherence and preference |
High |
| Tsapogas et al. (1971)23 | USA 95/95 |
VTE risk factors: average age: 56 years (range 40–83 years) Male: 98% |
Abdominal surgery | Knee-length GCSs (n = 51) In addition, the foot of the patient’s bed was elevated, early ambulation was encouraged and dorsi- and plantarflexion of the feet was instigated |
No treatment (n = 44) | DVT (assessed by radioiodine fibrinogen uptake test and phlebography) | Unclear |
| Thigh-length GCSs + LMWH vs. no treatment | |||||||
| Kalodiki et al. (1996)33 | UK 93/78 |
VTE risk factors: 32% were obese, 45% had varicose veins, 5% had postphlebitic syndrome, 3% had history of previous DVT, 12% had leg oedema and 18% had chronic bronchitis. Patients with a history of recent DVT or active malignancy were excluded from the trial Average age: 69 years (range 53–85 years) Male: 49% |
Orthopaedic surgery | Kendall TED thigh-length GCSs + enoxaparin LMWH (n = 32) | Enoxaparin LMWH alone (n = 32) Placebo (n = 14) |
DVT (assessed by ascending venography) PE (assessed by perfusion lung scans) Adverse events |
Unclear |
| Study details | Location and number randomised/analysed | Patient characteristics | Type of surgery | Intervention | Control | Outcomes assessed | Risk of biasa |
|---|---|---|---|---|---|---|---|
| Thigh-length GCSs vs. LMWH (different durations) | |||||||
| Camporese et al. (2008)60 | Italy 1761/1602 |
VTE risk factors: 26% were smokers, 1% had family history of VTE, 9% were using hormonal compounds and the average BMI was around 25.5 kg/m2. Patients with previous VTE or active malignancy were excluded from the trial Average age: 42 years Male: ratio around 1.6 : 1 |
Orthopaedic day surgery | Thigh-length GCSs (pressure at the ankle 30–40 mmHg) worn on the operated on leg (n = 597) | Nadroparin LMWH for 7 days (n = 603) Nadroparin LMWH for 14 days (n = 402). This arm was stopped early for safety reasons |
DVT (assessed by Doppler ultrasound) PE (assessed by ventilation perfusion lung scan when PE was suspected) Mortality Adverse events Patient adherence |
Low |
| Thigh-length GCSs vs. pneumatic compression device | |||||||
| Caprini et al. (1983)61 | USA 102/77 |
VTE risk factors: 22% had history of thromboembolism, 26% were obese, 18% had varicose veins, 17% had malignancy, 13% had oedema, 9% had history of cerebral vascular accident or myocardial infarction, 8% had major infection, 8% were taking hormones, 5% had leg ulcers and one patient was at a high risk of bleeding Average age: most > 60 years Male: 40% |
High-risk GS | TED thigh-length GCSs (n = 39) | Intermittent sequential compression device for 72 hours or until ambulation, then thigh-length GCSs (n = 38) | DVT (assessed by radioiodine fibrinogen uptake test; venography or angiography, or both, were completed when dictated by clinical signs and symptoms) PE Mortality |
Unclear |
| Mellbring and Palmer (1986)63 | Sweden 114/108 |
VTE risk factors: 36% had malignant disease and the average BMI was 25.3 kg/m2 Average age: 66 years (range 50–85 years) Male: 47% |
Abdominal surgery | LDH + dihydroergotamine (n = 54) Each patient wore a thigh-length GCSs randomly allocated to the right or left leg The comparison of interest to this review is the stockinged versus unstockinged leg of the 54 patients allocated to LDH + dihydroergotamine |
IPCC (n = 54) Each patient wore a thigh-length GCSs randomly allocated to the right or left leg |
DVT (assessed by radioiodine fibrinogen uptake test) Mortality Adverse events Patient adherence |
Unclear |
| Scurr et al. (1987)34 | UK 78/78 |
VTE risk factors: 31% had malignancy Average age: 61 years Male: 55% |
GS | Kendall TED thigh-length GCSs randomly allocated to right or left leg (51% right leg, 49% left leg) Once patients were fully ambulatory, GCSs were applied to both legs Patients also received intermittent pneumatic sequential compression |
Unstockinged leg (patients were their own controls) | DVT (assessed by radioiodine fibrinogen uptake test, Doppler ultrasound and strain-gauge plethysmography, with positive findings confirmed by contrast venography) PE |
Unclear |
| Study details | Location and number randomised/analysed | Patient characteristics | Type of surgery | Intervention | Control | Outcomes assessed | Risk of biasa |
|---|---|---|---|---|---|---|---|
| Rasmussen et al. (1988)64 | Denmark 249/248 |
VTE risk factors: around 58% of patients were obese, around 8.5% had a history of thrombosis, around 20% had varicose veins and around 43% were smokers Average age: 62 years (range 40–90 years) Male: 44% |
Abdominal surgery | (1) Kendall TED knee-length stockings (n = 74) (2) Kendall TED knee-length stockings + LDH (n = 89) |
LDH (n = 85) | PE assessed by clinical signs Mortality Note: this study also assessed DVT using 99mTc-labelled plasmin test. Owing to the unreliability of this test, DVT results are not reported for this study |
Unclear |
| Fasting et al. (1985)62 | Denmark 112/97 |
VTE risk factors: 16% had a previous DVT or varicose veins, 32% had malignancy, 14% had cardiopulmonary disorders, 4% were taking oestrogen and 21% were obese Average age: 60 years (range 39–87 years) Male: 51% |
GS | Kendall TED thigh-length GCSs (n = 52) | LDH (n = 45) | Fatal PE (assessed by autopsy) Mortality Adverse events Note: this study also assessed DVT using 99mTc-labelled plasmin test. Owing to the unreliability of this test, DVT results are not reported for this study |
Unclear |
Quality of studies included in the review
All of the included studies were RCTs. Results of the quality assessment, using the Cochrane risk of bias tool, are presented in Table 7. Each trial has been given an overall risk of bias judgement; trials that have a low risk of bias for all key domains (i.e. have a ‘yes’ response for each key domain) are judged to have a low overall risk of bias, trials that have a high risk of bias for one or more key domains (i.e. have a ‘no’ response) are judged to have a high overall risk of bias, and trials that have an unclear risk of bias for one or more key domains are judged to have an unclear overall risk of bias. The domains relating to allocation concealment and ‘other sources of bias’ were not judged to be ‘key domains’.
| Study | Sequence generation adequate | Allocation concealment adequate | Groups similar at baseline | Blinding of outcome assessors | Incomplete outcome data adequately addressed | Free of suggestion of selective outcome reporting | Apparently free from other sources of bias | Overall risk of bias |
|---|---|---|---|---|---|---|---|---|
| Howard et al. (2004)12 | Unclear | Unclear | Yes | Unclear | Yes | Yes | Unclear | Unclear |
| Cohen et al. (2007)49 | Yes | Unclear | Yes | Yes | Yes | Yes | Unclear | Low risk of bias |
| Porteous et al. (1989)21 | Yes | Unclear | Yes | Unclear | Yes | Yes | Yes | Unclear |
| Hui et al. (1996)25 | Unclear | Unclear | No | Unclear | No | Yes | Unclear | High risk of bias |
| Williams and Palfrey (1988)20 | Yes | Unclear | No | Unclear | Unclear | Unclear | Unclear | High risk of bias |
| Ayhan et al. (2013)65 | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear | Unclear |
| Kalodiki et al. (1996)33 | Unclear | Yes | Yes | Yes | Yes | Yes | Unclear | Unclear |
| Wille-Jørgensen et al. (1985)37 | Yes | Unclear | No | Yes | Yes | Yes | Unclear | High risk of bias |
| Wille-Jørgensen et al. (1991)36 | Yes | Unclear | Yes | Unclear | Yes | Noa | Unclear | Unclear |
| Torngren (1980)35 | No | No | Yes | Unclear | Yes | Yes | Unclear | High risk of bias |
| Fredin et al. (1989)32 | Unclear | Unclear | Yes | Yes | Yes | Yes | Unclear | Unclear |
| Ishak and Morley (1981)66 | No | No | Yes | Unclear | Unclear | Yes | Unclear | High risk of bias |
| Bergqvist and Lindblad (1984)31 | Yes | Unclear | Yes | Yes | Yes | Yes | Unclear | Low risk of bias |
| Barnes et al. (1978)30 | Unclear | Unclear | Yes | Unclear | Yes | Yes | Unclear | Unclear |
| Turpie et al. (1989)24 | Unclear | Unclear | Yes | Yes | Yes | Yes | Unclear | Unclear |
| Shirai (1985)22 | Unclear | Unclear | Yes | Unclear | Unclear | Yes | Unclear | Unclear |
| Tsapogas et al. (1971)23 | Yes | No | Unclear | Unclear | Yes | Yes | Unclear | Unclear |
| Camporese et al. (2008)60 | Yes | Yes | Yes | Yes | Yes | Yes | Unclear | Low risk of bias |
| Caprini et al. (1983)61 | Unclear | Unclear | Yes | Unclear | Yes | Unclear | Unclear | Unclear |
| Mellbring and Palmer (1986)63 | Unclear | Unclear | Yes | Unclear | Yes | Yes | Unclear | Unclear |
| Scurr et al. (1987)34 | Unclear | Unclear | Yes | Unclear | Yes | Yes | Yes | Unclear |
| Rasmussen et al. (1988)64 | Unclear | Unclear | Yes | Unclear | Yes | Yes | Unclear | Unclear |
| Fasting et al. (1985)62 | Unclear | Unclear | Yes | Unclear | Yes | Yes | Unclear | Unclear |
| Total | Yes = 8 No = 2 Unclear = 13 |
Yes = 2 No = 3 Unclear = 18 |
Yes = 18 No = 3 Unclear = 2 |
Yes = 7 No = 0 Unclear = 16 |
Yes = 18 No = 1 Unclear = 4 |
Yes = 19 No = 1 Unclear = 3 |
Yes = 2 No = 0 Unclear = 21 |
Generally, methods were poorly reported, with a high proportion of assessments for each domain having to be recorded as unclear (see Table 7). It was clear that the allocation sequence was adequately generated in eight RCTs; methods of sequence generation were inadequate in two RCTs and methods were unclear in 13 RCTs. Concealment of allocation was poorly reported; only two RCTs reported adequate methods, three RCTs reported inadequate methods and methods of concealment of allocation were unclear in 18 RCTs. Study groups were similar at baseline in 18 RCTs, there were differences between groups in important prognostic characteristics in three RCTs and insufficient data were available to assess similarity of baseline characteristics in two RCTs. Seven RCTs reported blinding of outcome assessors; the remainder of RCTs did not report whether or not outcome assessors were blinded to treatment group. Outcome data were either complete, or incomplete outcome data were adequately addressed, in 18 RCTs; only one RCT did not adequately address missing outcome data, and in four RCTs it was unclear whether or not missing outcome data were adequately addressed. Nineteen RCTs appeared to be free of the suggestion of selective outcome reporting and it was unclear whether or not three RCTs were free of the suggestion of selective outcome reporting. One RCT did not report results for one outcome; there were a large number of false-positive fibrinogen uptake test results in patients with stockings; therefore, the paper did not report results of fibrinogen uptake tests for any of the patients. None of the RCTs clearly contained other sources of bias.
Overall, three RCTs can be considered to have a low risk of bias,31,49,60 five have a high risk of bias20,25,35,37,66 and for 15 RCTs the reporting was inadequate to judge the risk of bias. 12,21–24,30,32–34,36,61–65
Eighteen of the RCTs randomised by patient. 12,20,21,23–25,30,32,33,36,37,49,60–62,64–66 Five RCTs randomised by leg;22,31,34,35,63 GCSs were worn on only one leg, rather than both legs in these trials. In addition to the RCTs that randomised by leg, one of the RCTs that randomised by patient applied GCSs to the operated leg only rather than to both legs. 60 In current practice, patients are advised to wear GCSs on both legs; therefore, these trials are not representative of clinical practice. In addition, outcomes such as PE cannot be adequately assessed in trials in which patients wore stockings only on one leg, with the other leg serving as the control, as it may not be clear whether the embolism arose from the stockinged leg or the unstockinged leg.
Many of the included RCTs date back to the 1970s23,30 and 1980s and20–22,24,31,32,34,35,37,61–64,66 therefore, their results may not be generalisable to current practice; surgical practice has changed over time with surgical procedures that are less invasive, shorter duration of hospitalisation and earlier mobilisation after surgery.
In addition, some trials excluded high-risk patients (usually patients with a history of prior VTE);21,22,25,33,60 therefore, the patients in the included trials may not be representative of patients likely to be seen in practice.
Results of studies included in the review
Deep-vein thrombosis
A total of 21 of the included trials reported rates of DVT, and a total of 20 trials provided sufficient data to be included in meta-analyses. The analyses and results of the included trials are reported below by specific treatment comparison.
Thigh-length graduated compression stockings (with or without pharmacological prophylaxis) versus knee-length graduated compression stockings (with or without pharmacological prophylaxis)
The trials by Cohen et al. 49 and Howard et al. 12 were the two most informative trials to answer the review question. Both trials used a combination of GCSs plus pharmacological prophylaxis, reflecting current practice for the treatment of patients at high risk of DVT but who are not at high risk of bleeding. The primary outcome of interest in both trials was VTE. However, all patients experienced DVTs and no PE events occurred. To avoid confusion, we have therefore reported outcomes as DVT events.
Cohen et al. 49 and Howard et al. 12 present inconsistent findings in terms of direction of effect (Figure 3), the first trial favouring knee-length GCSs for the prevention of DVT (OR 0.75, 95% CI 0.26 to 2.13) and the second favouring thigh-length GCSs (OR 2.92, 95% CI 1.14 to 7.52). Reasons for the inconsistent findings between the two trials were unclear and may be attributable to chance. The relatively small number of DVT events and variances in surgical procedure, type of pharmacological prophylaxis, patient risk factors and quality of the trials may have contributed to the inconsistent findings (see Table 2). Patients in the Howard et al. trial12 were slightly younger than patients in the Cohen et al. trial49 (mean age 58 years and 65 years, respectively). Patients in the Cohen et al. trial49 were undergoing THR or standard fracture surgery, whereas patients in the Howard et al. trial12 were recruited from general wards and were, therefore, undergoing various different types of surgery, including orthopaedic and abdominal surgery. Overall, the impact of the clinical heterogeneity is unclear and differences between the trials do not readily predict different treatment effects. Therefore, despite the substantial statistical heterogeneity, the pooled estimate of effect is presented here (see Figure 3).
FIGURE 3.
Rates of DVT comparing thigh-length GCSs (with pharmacological prophylaxis) vs. knee-length GCSs (with pharmacological prophylaxis). M–H, Mantel–Haenszel.
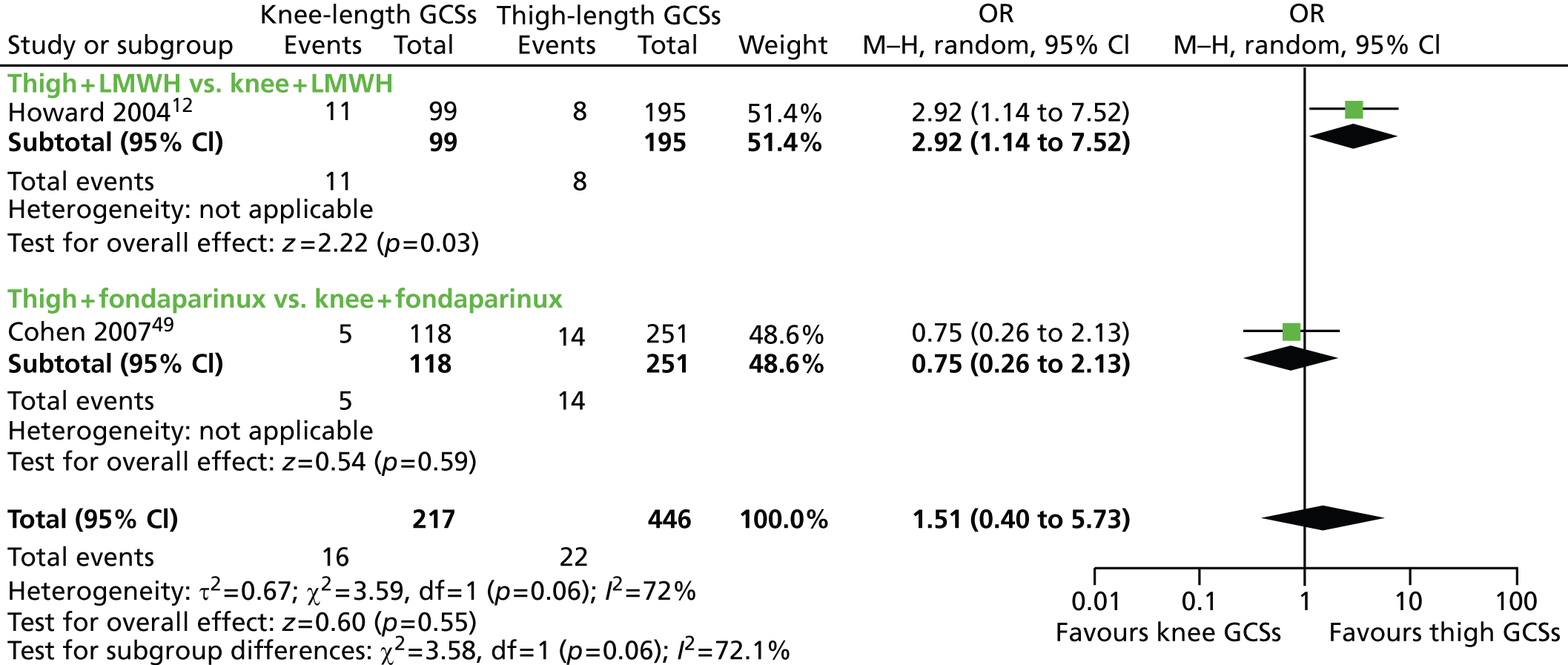
The summary estimate of effect indicated fewer DVT events in patients receiving thigh-length GCSs plus pharmacological prophylaxis than in patients receiving knee-length GCSs plus pharmacological prophylaxis (OR 1.51, 95% CI 0.40 to 5.73), but the result was not statistically significantly. As discussed above, there was substantial statistical heterogeneity (I2 = 72%).
Four additional RCTs that compared thigh-length with knee-length GCSs were identified, but these trials did not include additional pharmacological prophylaxis. 20,21,25,65 Unfortunately, the trial by Ayhan et al. 65 was reported only as an abstract and did not provide details on the number of patients in each treatment group; the abstract reported only that no DVTs occurred in either treatment arm. This trial was therefore excluded from meta-analyses. Few events occurred in the Porteous et al. 21 trial. Slightly more DVTs were observed in the Williams and Palfrey trial20 In contrast, Hui et al. 25 reported high DVT event rates in all three treatment arms.
Based on clinical advice, it was considered that the addition of pharmacological prophylaxis to GCSs was unlikely to affect the relative effectiveness of knee-length or thigh-length GCS. The five available RCTs12,20,21,25,49 comparing thigh-length with knee-length GCSs with or without additional pharmacological prophylaxis were therefore combined using meta-analysis (see Figure 4). The potential for a stocking drug interaction will be explored in the NMA, discussed below (see Network meta-analysis results).
FIGURE 4.
Rates of DVT (or VTE) comparing thigh-length GCSs (with or without pharmacological prophylaxis) with knee-length GCSs (with or without pharmacological prophylaxis). a, Number of events calculated from % of DVTs reported and it is unclear if any were bilateral and therefore whether or not double counting of patients has occurred. M–H, Mantel–Haenszel.
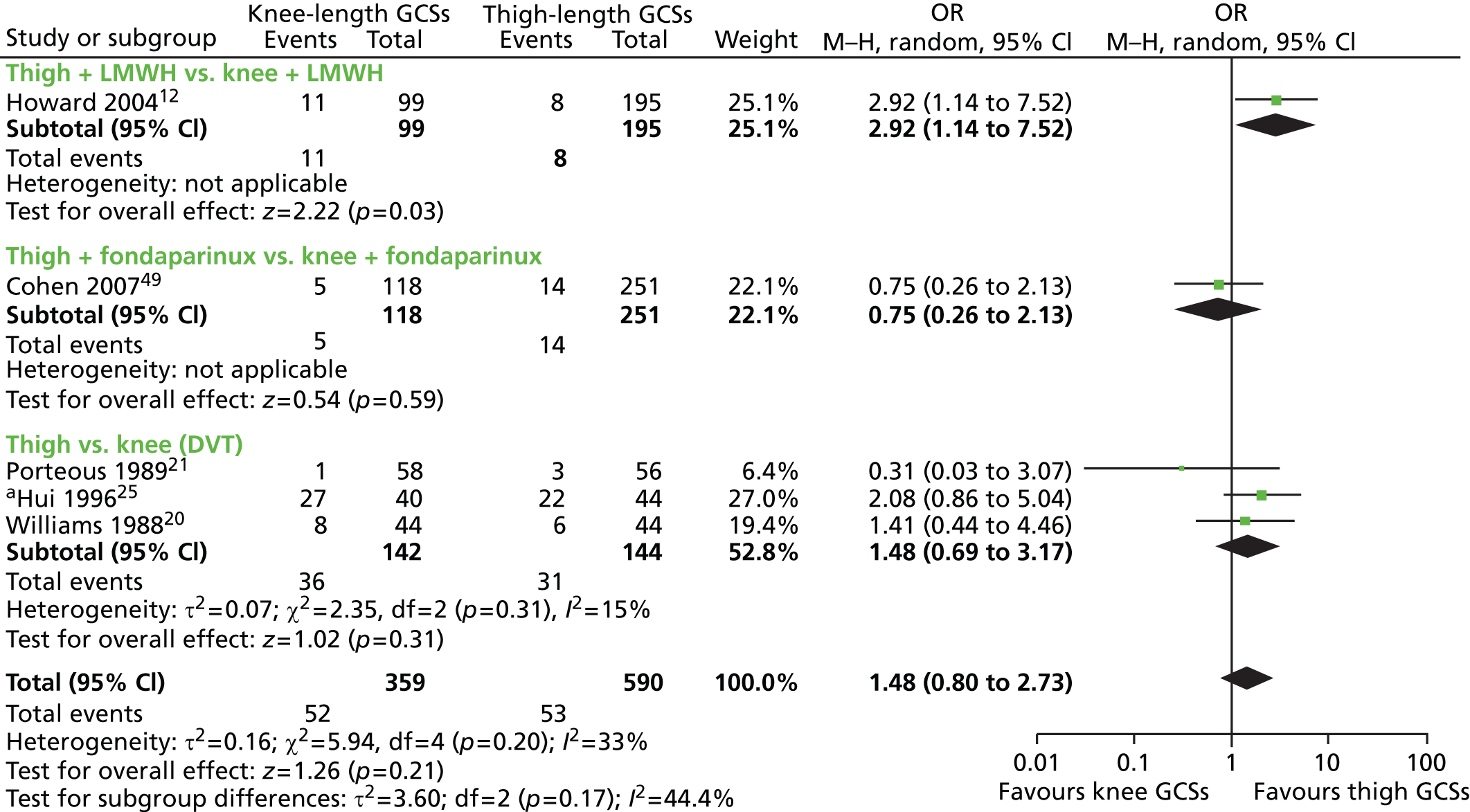
The summary estimate of effect for all five trials indicated a trend favouring thigh-length GCS, but, again, the findings were not statistically significant (OR 1.48, 95% CI 0.80 to 2.73) and some trials lacked precision (Figure 4). There was some evidence of statistical heterogeneity for the summary estimate of effect (I2 = 33%), which was greater when testing for differences between the trial groupings presented (I2 = 44.4%). There was some inconsistency in the direction of effect for trials assessing patients in similar surgical groups. The Cohen et al. 49 and Hui et al. 25 trial were in orthopaedic patients, and the Porteous et al. 21 and Williams and Palfrey20 trials were in patients undergoing abdominal surgery. The reasons for the inconsistency were unclear and may be attributable to chance.
Thigh-length or knee-length graduated compression stockings plus pharmacological prophylaxis versus pharmacological prophylaxis alone
Seven RCTs, comprising 928 surgical patients, compared thigh-length GCSs plus pharmacological prophylaxis with pharmacological prophylaxis alone and reported rates of DVT. 31–33,35–37,66 For study characteristics, see Characteristics of studies included in the review of effectiveness. No trials comparing knee-length GCSs plus pharmacological prophylaxis with pharmacological prophylaxis alone met criteria for inclusion in the review.
Dextran is no longer used in clinical practice; therefore, the three trials administering dextran (Bergqvist and Lindblad,31 Fredin et al. 32 and Ishak and Morley66) are presented for completeness only (see Figure 6) and are considered separately from more recent publications assessing pharmacological prophylaxis currently in use. These comparisons are also omitted from the NMA.
The summary estimate of effect indicated statistically significantly fewer DVT events in patients receiving thigh-length GCSs plus pharmacological prophylaxis than in those receiving pharmacological prophylaxis alone (OR 0.31, 95% CI 0.16 to 0.61), as shown in Figure 5. All trials were consistent for direction of effect. The test suggested no statistical heterogeneity (I2 = 0%) but some evidence for subgroup differences (I2 = 21.6%).
FIGURE 5.
Rates of DVT comparing thigh-length GCSs plus currently used pharmacological prophylaxis with pharmacological prophylaxis alone. M–H, Mantel–Haenszel.
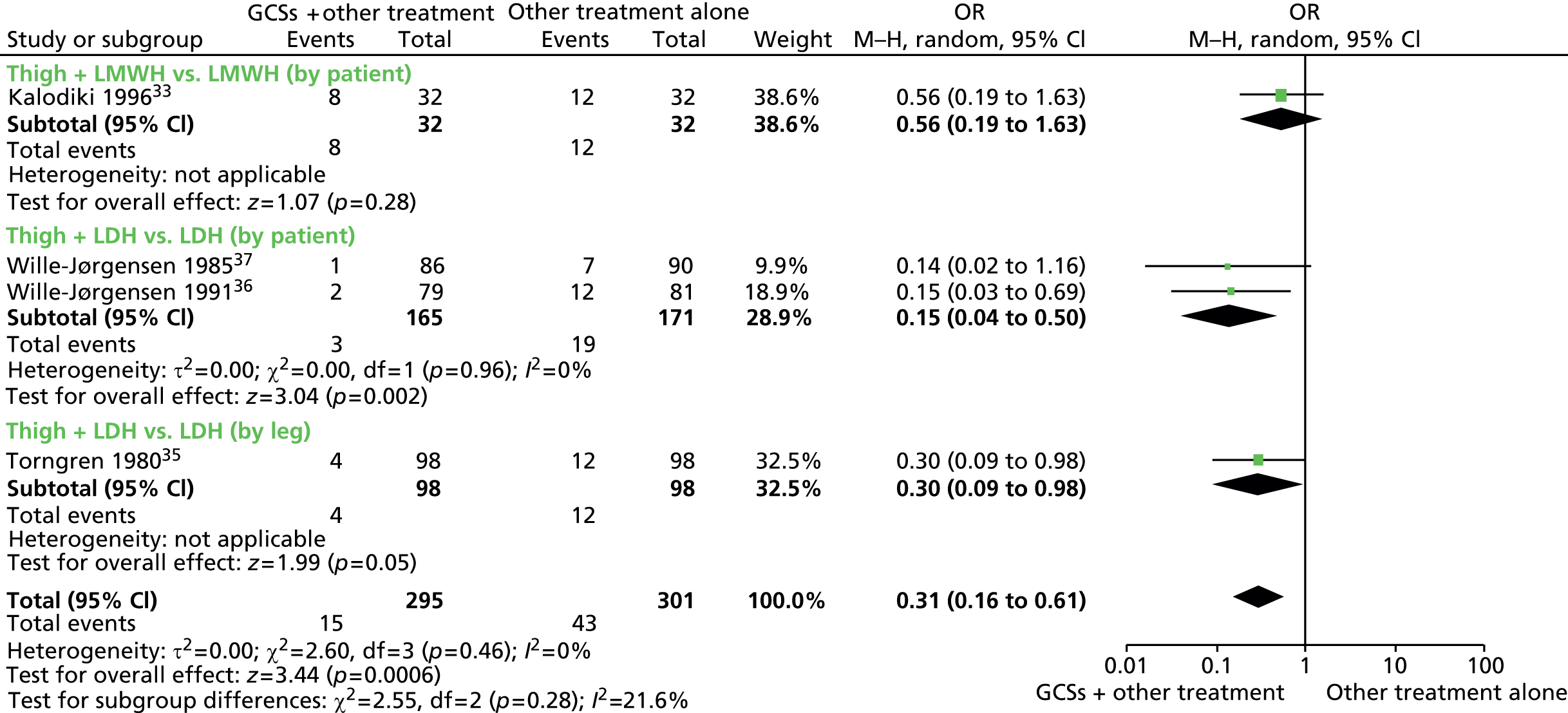
The summary estimate of effect indicated statistically significantly fewer DVT events in patients receiving thigh-length GCSs plus dextran than in those receiving dextran alone (OR 0.27, 95% CI 0.11 to 0.65), as shown in Figure 6. All trials were consistent for direction of effect. The test suggested some statistical heterogeneity (I2 = 33%), which was greater when testing for differences between the trial groupings presented (I2 = 40.7%).
FIGURE 6.
Rates of DVT comparing thigh-length GCSs plus dextran pharmacological prophylaxis with pharmacological prophylaxis alone. a, 26 patients (74%) in the stocking group and 33 (80%) in the control group received dextran 70. M–H, Mantel–Haenszel.
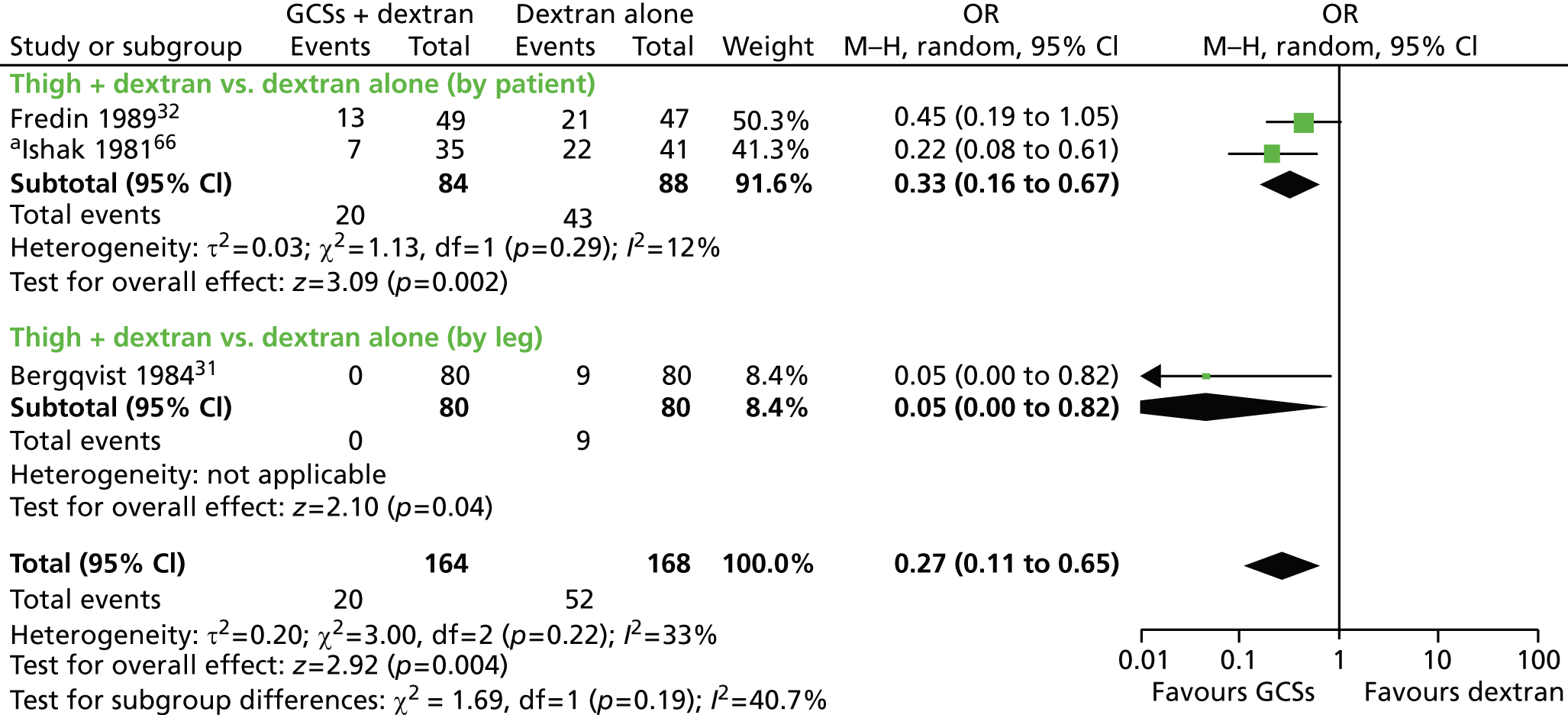
Thigh-length or knee-length graduated compression stocking versus no active treatment control
Six RCTs, comprising 710 surgical patients, compared thigh-length or knee-length GCSs with no stockings or a drug placebo (i.e. no active treatment control)22–25,30,33 for study characteristics.
Five trials compared thigh-length GCSs with no active treatment control22,24,25,30,33 (see Characteristics of studies included in the review of effectiveness for details). There are clinical and methodological differences between trials, including that trials were conducted in different surgical specialities and cover a wide range of publication dates (1978–96). Interpretation of the findings should, therefore, take into consideration the changes that have taken place in clinical practice in the intervening years, for example, the use of surgical procedures that are less invasive and reduction in length of patient hospitalisation.
As it is unclear how this clinical heterogeneity might impact on the treatment effect, the summary treatment effect for trials comparing thigh- or knee-length GCSs with no active treatment are presented separately. Comparisons between thigh-length GCSs and no active treatment (Figure 7) show statistically significantly fewer DVT events in patients wearing thigh-length stockings (OR 0.25, 95% CI 0.12 to 0.52). There was, however, some evidence of statistical heterogeneity (I2 = 41%) and it was higher when testing for differences between the trial groupings presented (I2 = 61.7%).
FIGURE 7.
Rates of DVT comparing thigh-length GCSs vs. no treatment control. a, Number of events calculated from% of DVTs reported and it is unclear if any were bilateral and therefore whether or not double counting of patients has occurred. M–H, Mantel–Haenszel.
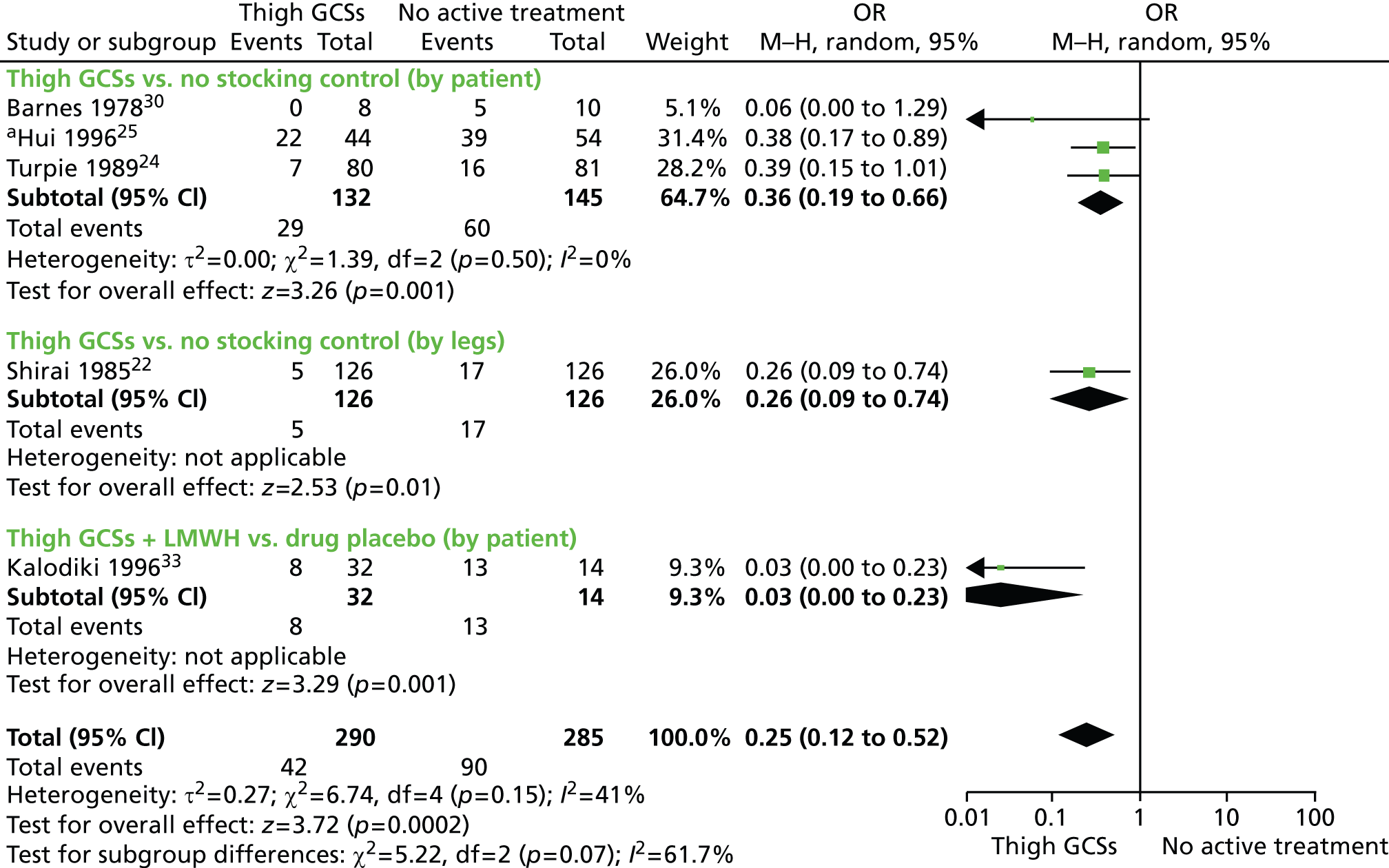
Two trials compared knee-length GCSs with no active treatment control. 23,25 As for the thigh-length trials versus no active treatment, there are clinical and methodological differences between trials, and both trials are old (1971 and 1996). Pooling the results of these two trials generated a non-significant result for patients wearing knee-length GCSs compared with no active treatment (by patient) (OR 0.57, 95% CI 0.21 to 1.57). There was some evidence of statistical heterogeneity (I2 = 28%) (Figure 8). This non-significant effect for knee-length GCSs versus no active treatment control is much smaller than the statistically significant effect reported for thigh-length GCSs versus no active treatment.
FIGURE 8.
Rates of DVT comparing knee-length GCSs with no treatment control. a, number of events calculated from percentage of DVTs reported and it is unclear if any were bilateral and therefore whether or not double counting of patients has occurred. M–H, Mantel–Haenszel.
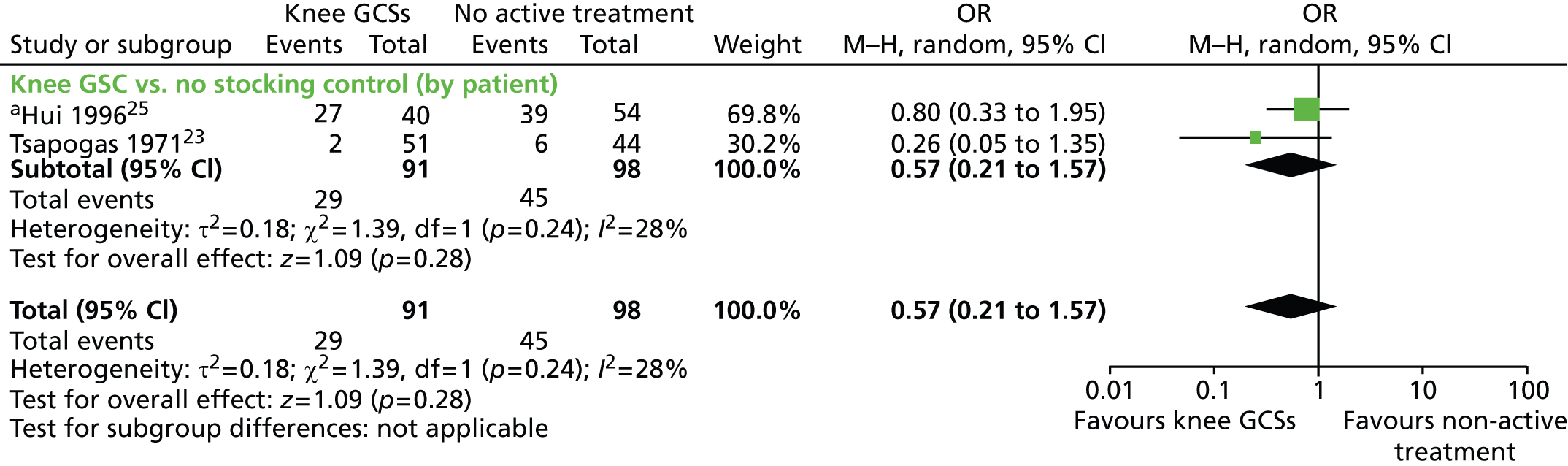
Graduated compression stockings alone versus pharmacological therapy alone
One RCT of patients undergoing orthopaedic day surgery compared GCSs alone with pharmacological therapy alone, specifically thigh-length GCSs worn on the operated-on leg only to LMWH administered for 7 days or 14 days. 60 This trial found that the rates of DVT were statistically significantly higher with thigh-length GCSs alone than with LMWH alone (OR 2.62, 95% CI 1.46 to 4.71), ignoring the differences in treatment duration for LMWH.
Other comparisons
Three RCTs compared thigh-length GCSs with an alternative mechanical prophylaxis [i.e. pneumatic compression device (Caprini et al. ,61 Mellbring and Palmer,63 Scurr et al. 34)]. Two RCTs randomised patients by leg, with the other leg serving as the control;34,63 the remaining RCT randomised by patient. 61 These comparisons are not included in the NMA as they do not inform the thigh-length versus knee-length GCSs question.
These three RCTs showed no statistically significant difference in DVT event rates between treatment groups. However, the direction of effect differed between trials; Mellbring and Palmer63 and Caprini et al. 61 had fewer DVT events in the pneumatic compression group, whereas Scurr et al. 34 reported fewer DVT events in the GCSs group (Figure 9).
FIGURE 9.
Rates of DVT comparing thigh-length GCSs with pneumatic compression device. M–H, Mantel–Haenszel.

Pulmonary embolism
Fifteen RCTs assessed PE or fatal PE; 12 assessed PE12,30–34,36,37,60,61,64,66 (four of which assessed PE only if patients were symptomatic)30,36,60,66 and three assessed fatal PE. 35,49,62 Three of the 12 RCTs that assessed PE reported that there were no cases of PE;12,34,64 two of the three RCTs that assessed fatal PE reported that there were no fatal PE events. 35,49
In the nine RCTs in which there were cases of PE, the number of patients with PE in thigh-length stocking groups, with or without additional pharmacological prophylaxis, ranged from 0 to two patients (0–6.5%). 30–33,36,37,60,61,66 The number of patients with PE in active control groups (LMWH, LDH, dextran or sequential compression device) ranged from 0 to six patients (0–10.3%) (seven RCTs32,33,36,37,60–62). The number of patients with PE in placebo or no treatment control groups ranged from three to five patients (30–41.7%) (two RCTs30,33).
In the trial that assessed and reported fatal PE events, there were no events in the thigh-length GCSs group and one event among the 45 patients in the LDH group. 62 In addition, two RCTs that assessed mortality reported fatal PE cases (see Mortality below). 37,61
Additional study details and results for trials assessing PE are presented in Table 8.
| Study details | Type of surgery | Intervention/control | Results | OR (95% CI) |
|---|---|---|---|---|
| Howard et al. (2004)12 | GS | Thigh-length GCSs plus LMWH (n = 248) | 0/248 | Not estimable |
| Knee-length GCSs plus LMWH (n = 128) | 0/128 | |||
| Cohen et al. (2007)49 | Orthopaedic surgery | Thigh-length GCSs plus fondaparinux (n = 266) | 0/266 (fatal PE) | Not estimable |
| Knee-length GCSs plus fondaparinux (n = 123) | 0/123 (fatal PE) | |||
| Fondaparinux alone (n = 400) | 0/400 (fatal PE) | |||
| Kalodiki et al. (1996)33 | Orthopaedic surgery | Thigh-length GCSs plus LMWH (n = 32) | 2/31 (6.5%) | 0.60 (0.09 to 3.86) |
| LMWH (n = 32) | 3/29 (10.3%) | |||
| Placebo (n = 14) | 5/12 (41.7%) | Thigh vs. placebo OR 0.10 (0.02 to 0.61) | ||
| Wille-Jørgensen et al. (1985)37 | Abdominal surgery | Thigh-length GCSs plus LDH (n = 86) | 2/86 (2.3%) (non-fatal PE) | 0.33 (0.07 to 1.70) |
| LDH (n = 90) | 6/90 (6.7%) (one case was fatal) | |||
| Wille-Jørgensen et al. (1991)36 | Abdominal surgery | Thigh-length GCSs plus LDH (n = 79) | 0/79 | Not estimable |
| Thigh-length GCSs plus dextran (n = 85) | 1/85 (1.2%) | |||
| LDH (n = 81) | 0/81 | |||
| Torngren (1980)35 | Abdominal surgery | Thigh-length GCSs randomly allocated to right or left leg plus LDH (n = 45, right leg; n = 53, left leg) | 0/98 (fatal PE) | Not applicable (patients were their own control) |
| Unstockinged leg | ||||
| Fredin et al. (1989)32 | Orthopaedic surgery | Thigh-length GCSs plus dextran (n = 49) | 0/49 | 0.19 (0.01 to 4.02) |
| Dextran (n = 48) | 2/48 (4.2%) | |||
| Dextran plus additional preoperative dextran (n = 47) | 0/47 | |||
| Ishak and Morley (1981)66 | Orthopaedic surgery | Thigh-length GCSs (n = 35). Dextran was given to 26 patients | 2/35 (5.7%) | 1.18 (0.16 to 8.86) |
| No stocking (n = 41). Dextran was given to 33 patients | 2/41 (4.9%) | |||
| Bergqvist and Lindblad (1984)31 | GS | Thigh-length GCSs randomly allocated to right or left leg plus dextran (n = 41, right leg; n = 39, left leg) | 1/80 | Not applicable (patients were their own control) |
| Unstockinged leg | ||||
| Barnes et al. (1978)30 | Orthopaedic surgery | Thigh-length GCSs (n = 8) | 0/8 | 0.13 (0.01 to 2.86) |
| No stocking (n = 10) | 3/10 (30%) | |||
| Camporese et al. (2008)60 | Orthopaedic day surgery | Thigh-length GCSs (n = 597) | 2/597 (0.3%) | 0.84 (0.15 to 4.60) |
| LMWH for 7 days (n = 603) LMWH for 14 days (n = 402) |
2/603 (0.3%) 2/402 (0.5%) |
|||
| Caprini et al. (1983)61 | High-risk GS | Thigh-length GCSs (n = 39) | 1/39 (2.6%) (non-fatal PE) | 0.97 (0.06 to 16.15) |
| Intermittent sequential compression device then thigh-length GCSs (n = 38) | 1/38 (2.6%) (fatal PE) | |||
| Scurr et al. (1987)34 | GS | Thigh-length GCSs randomly allocated to right or left leg (n = 78; 51% right leg, 49% left leg) | 0/78 | Not applicable (patients were their own control) |
| Unstockinged leg | ||||
| Rasmussen et al. (1988)64 | Abdominal surgery | Knee-length stockings (n = 74) | 0/74 | Not estimable |
| Knee-length stockings plus LDH (n = 89) | 0/89 | |||
| LDH (n = 89) | 0/89 | |||
| Fasting et al. (1985)62 | GS | Thigh-length GCSs (n = 52) | 0/52 | 0.28 (0.01 to 7.11) |
| LDH (n = 45) | 1/45 (2.2%) |
Mortality
Eleven RCTs assessed mortality;24,31,32,36,37,60–64,66 three reported that there were no deaths. 60,63,64 Of the eight RCTs in which there were deaths, five reported that thromboembolism was not suspected to be the cause of death,24,31,32,36,66 whereas three RCTs each reported one case of fatal PE37,61,62 (one of which is reported above; see Pulmonary embolism62); each fatal PE event occurred in the active control group (non-GCS).
Additional study details and results for trials assessing mortality are presented in Table 9.
| Study details | Type of surgery | Intervention/control | Results | OR (95% CI) | Comments |
|---|---|---|---|---|---|
| Wille-Jørgensen et al. (1985)37 | Abdominal surgery | Thigh-length GCSs + low dose heparin (n = 86) | 0/86 | 0.34 (0.01 to 8.58) | An additional two patients died within 30 days of surgery, without suspicion of thrombi-embolism. It was not stated which group they were in |
| LDH (n = 90) | 1/90 (1.1%) (fatal PE) | ||||
| Wille-Jørgensen et al. (1991)36 | Abdominal surgery | Thigh-length GCSs + LDH (n = 79) | 16/79 (20.3%) | GCSs + heparin vs. heparin 1.62 (0.70 to 3.74) | None of the patients who died was suspected of suffering from thromboembolism |
| Thigh-length GCSs + dextran (n = 85) | 17/85 (20%) | ||||
| LDH (n = 81) | 11/81 (13.6%) | ||||
| Fredin et al. (1989)32 | Orthopaedic surgery | Thigh-length GCSs + dextran (n = 49) | Not estimable | Two patients died within 30 days, both of myocardial infarction. The autopsies did not reveal any thromboembolic complications. It was not stated which group they were in | |
| Dextran (n = 48) | |||||
| Dextran plus additional preoperative dextran (n = 47) | |||||
| Ishak and Morley (1981)66 | Orthopaedic surgery | Thigh-length GCSs (n = 35) Dextran was given to 26 patients |
1/35 (2.9%) (unknown cause) | 3.61 (0.14 to 91.44) | |
| No stocking (n = 41) Dextran was given to 33 patients |
0/41 | ||||
| Bergqvist and Lindblad (1984)31 | GS | Thigh-length GCSs randomly allocated to right or left leg plus dextran (n = 41 right leg, n = 39 left leg) | Not estimable | Two patients died postoperatively. The autopsies did not reveal any thromboembolic complications. It was not stated which group they were in | |
| Unstockinged leg | |||||
| Turpie et al. (1989)24 | Neuron surgery | Thigh-length GCSs (n = 80) | 10/80 (12.5%); one of whom autopsy showed had PE but cause of death was reported to be massive cerebral oedema | GCSs vs. no treatment 2.75 (0.83 to 9.17) | |
| Thigh-length GCSs plus intermittent pneumatic compression (n = 78) | 4/78 (5.1%); none of whom died of PE | ||||
| No treatment (n = 81) | 4/81 (4.9%); none of whom died of PE | ||||
| Camporese et al. (2008)60 | Orthopaedic day surgery | Thigh-length GCSs (n = 597) | 0/597 | Not estimable | |
| LMWH for 7 days (n = 603) | 0/603 | ||||
| LMWH for 14 days (n = 402) | 0/402 | ||||
| Caprini et al. (1983)61 | High-risk GS | Thigh-length GCSs (n = 39) | 0/39 | 0.32 (0.01 to 8.01) | |
| Intermittent sequential compression device then thigh-length GCSs (n = 38) | 1/38 (2.6%) (fatal PE) | ||||
| Mellbring and Palmer (1986)63 | Abdominal surgery | LDH plus dihydroergotamine (n = 54) Each patient wore a thigh-length GCSs randomly allocated to the right or left leg |
0/54 | Not applicable (patients were their own control) | |
| IPCC (n = 54) Each patient wore a thigh-length GCSs randomly allocated to the right or left leg |
|||||
| Rasmussen et al. (1988)64 | Abdominal surgery | Knee-length stockings (n = 74) | 0/74 | Not estimable | |
| Knee-length stockings plus LDH (n = 89) | 0/89 | ||||
| LDH (n = 89) | 0/89 | ||||
| Fasting et al. (1985)62 | GS | Thigh-length GCSs (n = 52) | NR | Not estimable | |
| LDH (n = 45) | 1/45 (2.2%) (fatal PE) |
Adverse events
Twelve trials reported results relating to adverse events. 12,21,30–33,35,49,60,62,63 The majority of complications reported were minor bleeding complications associated with pharmacoprophylaxis and not with the GCSs, which are of interest here, although the proportion of patients reporting such events was low; between 1%12 and 4%. 35,60 Some trials merely reported that there were no significant differences between treatment groups in terms of blood loss, haemoglobin levels, wound haematomata or number of perioperative transfusions,33,36,62,63 although one trial reported that perioperative blood loss was, on average, 350 ml lower in the stockinged group than the dextran group (p < 0.01). 32
The proportion of patients experiencing GCS-related complications was also low, between 0%31,63 and 2%,21,49 in the six trials in which it was reported. 12,21,30,31,49,63 This does not include the Barnes et al. 30 trial, in which one patient developed an episode of syncope on the 14th postoperative day. Owing to the very small number of patients in the GCSs group in this trial (eight patients), this equates to 12.5%. 30 Where specified, complications were minor foot abrasions, superficial thrombophlebitis, the stocking slipping down or feeling hot.
Additional study details and results for trials assessing GCS-related adverse events are presented in Table 10.
| Study details | Type of surgery | Intervention | Control | Results |
|---|---|---|---|---|
| Howard et al. (2004)12 | GS | Thigh-length GCSs + LMWH (n = 248) | Knee-length GCSs + LMWH (n = 128) | Three patients reported minor foot abrasions from stockings |
| Cohen et al. (2007)49 | Orthopaedic surgery | Thigh-length GCSs + fondaparinux (n = 266) | (1) Knee-length GCSs + fondaparinux (n = 123) (2) Fondaparinux alone (n = 400) |
2% of patients reported complications with GCSs |
| Porteous et al. (1989)21 | Abdominal surgery | Thigh-length GCSs (n = 56) | Knee-length GCSs (n = 58) | One patient in the thigh-length GCSs group had a superficial thrombophlebitis with no evidence of DVT on phlebography |
| Torngren (1980)35 | Abdominal surgery | Thigh-length GCSs randomly allocated to right or left leg + LDH (n = 45, right leg; n = 53, left leg) | Unstockinged leg | The stockings resulted in no complications and did not cause complaints from the surgeons or nursing staff. Only a few complaints from the patients were noted, mostly because the stockings fell down easily, causing some disturbance to the ambulant patients |
| Bergqvist and Lindblad (1984)31 | GS | Thigh-length GCSs randomly allocated to right or left leg + dextran (n = 41, right leg; n = 39, left leg) | Unstockinged leg | No complications directly related to prophylaxis |
| Barnes et al. (1978)30 | Orthopaedic surgery | Thigh-length GCSs (n = 8) | No stocking (n = 10) | One patient in the thigh-length GCSs group developed an episode of syncope on the 14th postoperative day |
| Mellbring and Palmer (1986)63 | Abdominal surgery | LDH plus dihydroergotamine (n = 54) Each patient wore a thigh-length GCSs randomly allocated to the right or left leg |
IPCC (n = 54) Each patient wore a thigh-length GCSs randomly allocated to the right or left leg |
No leg complication arose that could be attributed to IPCC or wearing of GCSs |
| Fasting et al. (1985)62 | GS | Thigh-length GCSs (n = 52) | LDH (n = 45) | A few patients complained about stockings, which slipped down or felt hot |
Network meta-analysis results
Inclusion of trials in the network meta-analysis
Figure 10 presents the network of 20 trials that reported data for the outcome DVT and provided sufficient data to be included in the direct meta-analyses. The two trials that did not report DVT outcome data are not included in this figure or in the NMA. 62,64 In addition, the trial by Ayhan et al. ,65 which was only reported as an abstract, did not report sufficient data to be included in the direct meta-analyses or NMA, as total numbers of patients in treatment groups were not reported; therefore, this trial is also excluded from Figure 10.
FIGURE 10.
Network of trials presenting data on DVT. a, not current NHS practice. Shaded boxes represent interventions not included in the NMA as they do not add to the network of evidence comparing thigh-length with knee-length GCSs.

The shaded boxes in Figure 10 represent interventions that are not included in the NMA, as they do not add to the network of evidence comparing thigh-length with knee-length GCSs. After removing these seven trials that did not add to the network of evidence,23,31,32,34,61,63,66 13 RCTs were included in the NMA. 12,20–22,24,25,30,33,35–37,49,60 There is significant clinical heterogeneity across these trials in terms of the risk of DVT and whether patients are day-case patients or inpatients. The degree to which these factors are effect-modifiers is unclear and there are insufficient data to control for them in the analysis. The results of a NMA including these trials may still be of value to cost-effectiveness and VOI analyses because the network consists of loops and statistical heterogeneity and inconsistency will increase the uncertainty around the effect estimates. It will also allow for consistent estimates across multiple comparisons and the maximum use of available evidence. Furthermore, where the distribution of study characteristics does not represent the setting of the cost-effectiveness analysis, then predictive distributions can be used to represent the uncertainty in the generalisability of the effect estimates to the cost-effectiveness analysis setting.
Base-case analysis: assumption of no stocking–heparin treatment interaction
In Figure 10, the unshaded boxes represent the interventions included in the NMA. However, the effectiveness of different drugs (LMWH, LDH and fondaparinux) are assumed to be the same, and these were therefore lumped together in the network and are collectively referred to as ‘heparin’. The final network for the base-case analysis is presented in Figure 11. A total of 13 trials were included in the NMA, three of which were three-armed trials. The number of trials informing each comparison, including each possible comparison in a three-armed trial, is presented in Figure 11.
FIGURE 11.
The network of all studies comparing the treatments shown with the number of trials informing each comparison shown.
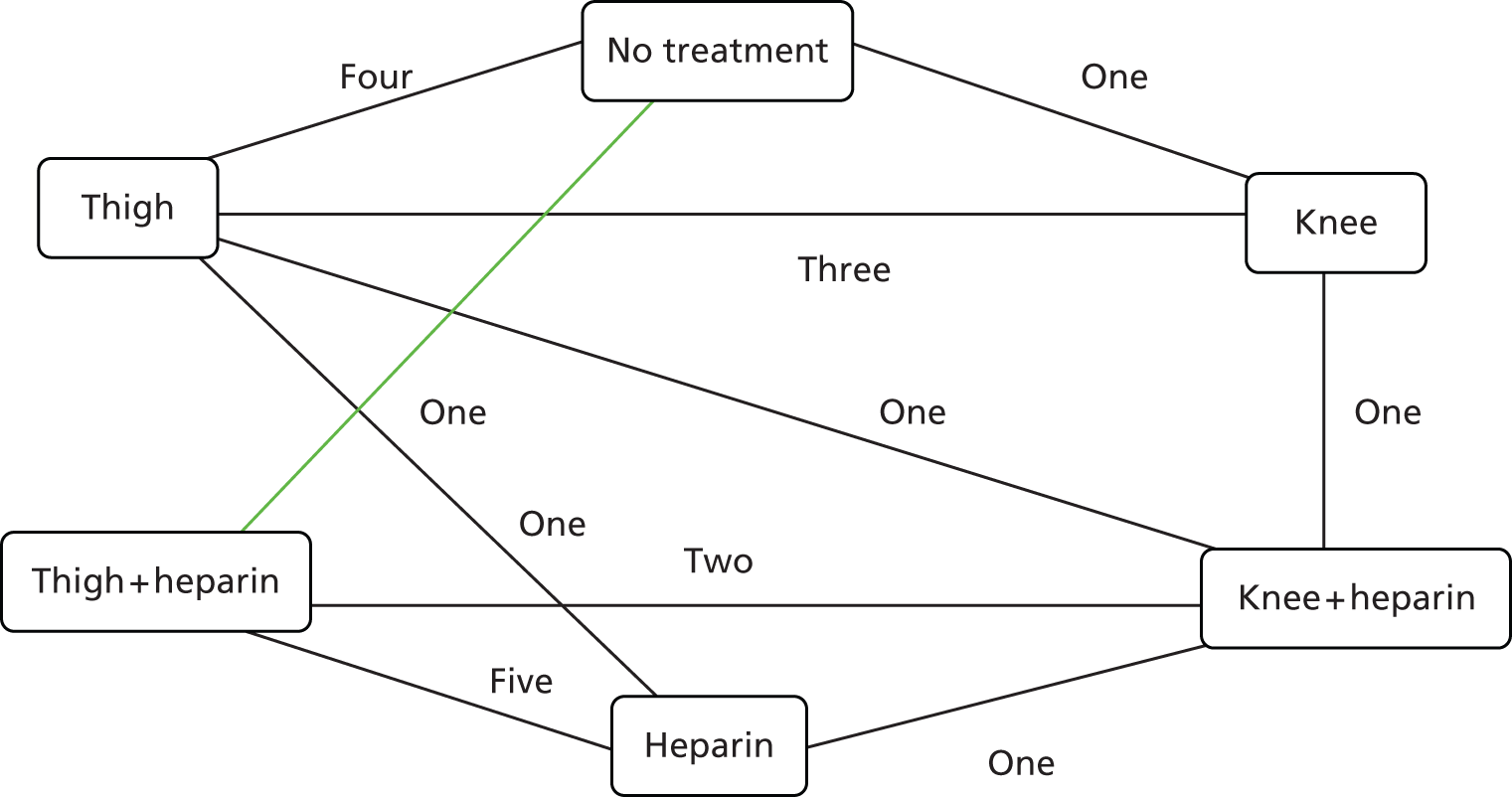
In the base-case analysis, it is assumed that there is no interaction between the effects of stocking and heparin. The result is that each possible pair-wise comparison between the six treatments in Figure 11 can be expressed in terms of three basic parameters as illustrated in Figure 1: thigh-length stockings versus no treatment, knee-length stockings versus no treatment and heparin versus no treatment.
The relative effects for no treatment, thigh-length stockings, knee-length stockings and heparin are presented in Table 11. Results are presented for all comparisons possible given the network. Note that the no interaction model assumes that thigh-length stockings versus no treatment is the same as thigh-length stockings plus heparin versus heparin, etc., and this is shown in the results. Where there was sufficient evidence to estimate the between-study variance, the random-effects models were a better fit than the fixed-effect models. As such, the credible intervals (CrIs) represent the uncertainty around the average treatment effect across trials conducted with unknown clinical and methodological heterogeneity. Given that there is statistical heterogeneity, the predictive distribution for the results from a new trial would be more widely dispersed than the posterior distribution for the random-effects estimates.
| Intervention | Comparator | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No treatment | Thigh | Knee | Heparin | Thigh + heparin | Knee + heparin | |||||||
| Med | CrI | Med | CrI | Med | CrI | Med | CrI | Med | CrI | Med | CrI | |
| No treatment | – | – | 2.60 | 1.58 to 4.87 | 1.48 | 0.72 to 3.69 | 3.81 | 1.15 to 10.55 | 9.88 | 2.47 to 38.04 | 5.62 | 1.44 to 22.75 |
| Thigha | 0.38 | 0.21 to 0.63 | – | – | 0.57 | 0.28 to 1.21 | 1.47 | 0.41 to 3.75 | 3.81 | 1.15 to 10.55 | 2.16 | 0.62 to 6.77 |
| Knee | 0.68 | 0.27 to 1.38 | 1.76 | 0.82 to 3.53 | – | – | 2.58 | 0.53 to 8.40 | 6.70 | 1.40 to 25.14 | 3.81 | 1.15 to 10.55 |
| Heparin | 0.26 | 0.09 to 0.87 | 0.68 | 0.27 to 2.42 | 0.39 | 0.12 to 1.89 | – | – | 2.60 | 1.58 to 4.87 | 1.48 | 0.72 to 3.69 |
| Thigh + heparina | 0.10 | 0.03 to 0.41 | 0.26 | 0.09 to 0.87 | 0.15 | 0.04 to 0.72 | 0.38 | 0.21 to 0.63 | – | – | 0.57 | 0.28 to 1.21 |
| Knee + heparin | 0.18 | 0.04 to 0.70 | 0.46 | 0.15 to 1.62 | 0.26 | 0.09 to 0.87 | 0.68 | 0.27 to 1.38 | 1.76 | 0.82 to 3.53 | – | – |
The median OR of heparin compared with no treatment was 0.26 (95% CrI 0.09 to 0.87). The median OR of thigh-length stockings with heparin compared with heparin alone was 0.38 (95% CrI 0.21 to 0.63). The median OR of knee-length stockings with heparin compared with heparin alone was 0.68 (95% CrI 0.27 to 1.38). The median OR of knee-length stockings with heparin compared with thigh-length stockings with heparin is 1.76 (95% CrI 0.82 to 3.53). This estimate favours thigh-length stockings slightly more than the direct estimate of 1.48 (95% CI 0.80 to 2.73) from the direct meta-analysis in Figure 4. These estimates are quite similar, but there appears to be greater heterogeneity across studies in the network than across the studies in the direct meta-analysis.
Given that the objective of this project is to evaluate the expected VOI of doing further research, Table 12 presents the probability that each treatment would be the most effective given the results of a new trial, using the predictive distributions for each treatment effect. Predictive distributions are used because of the unexplained heterogeneity and the true treatment effect from a new trial may arise from anywhere in the random-effects distribution. M1 represents the base case, no interaction model. Taking into account all the interventions simultaneously, there is a 0.73 probability that thigh-length stockings plus heparin is the most effective treatment combination within the population of the included trials.
| Intervention | P(Best) | ||
|---|---|---|---|
| M1a | M2b | M3c | |
| No treatment | 0.00 | – | 0.00 |
| Thigh | 0.04 | – | 0.00 |
| Knee | 0.02 | – | 0.02 |
| Heparin | 0.02 | 0.03 | 0.10 |
| Thigh + heparin | 0.73 | 0.82 | 0.75 |
| Knee + heparin | 0.20 | 0.16 | 0.12 |
Although there is little uncertainty that it is the most effective treatment, the marginal benefit of thigh-length stockings plus heparin over heparin alone is less than the marginal benefit of heparin over no treatment, as heparin has already reduced the risk of DVT substantially. Tables 13 and 14 present the estimated median risks of symptomatic DVT and of DVT given different treatments assuming different risk of symptomatic DVT and of DVT while on heparin. The tables also present the NNT to avoid an extra case of DVT beyond that achieved by the comparator for different comparisons. For example, if the risk of DVT while on heparin was 4.94%, implying a risk of 16.4% with no treatment, then nine people would need to be treated with heparin to avoid one case of DVT. Adding thigh-length stockings to heparin would require treating a further 34 patients to avoid one case of DVT over and above the cases of DVT avoided using heparin alone. The NNT with thigh-length stockings in addition to heparin to avoid an extra case of DVT is reasonably low, ranging from 9 to 34, depending on the level of risk for GS patients. The NNT with thigh-length stockings in addition to heparin to avoid an extra case of symptomatic DVT is extremely high, ranging from 133 to 524, depending on the level of risk for GS patients.
| 0.31% risk of DVT taking drugs | 0.61% risk of DVT taking drugs | 1.23% risk of DVT taking drugs | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Risk of DVT, % | Comparison | NNT | Intervention | Risk of DVT, % | Comparison | NNT | Intervention | Risk of DVT, % | Comparison | NNT |
| No treatment | 1.16 | H vs. NT | 114 | NT | 2.27 | H vs. NT | 59 | NT | 4.49 | H vs. NT | 30 |
| Knee | 0.79 | K + H vs. H | 785 | K | 1.56 | K + H vs. H | 399 | K | 3.11 | K + H vs. H | 199 |
| Thigh | 0.45 | T + H vs. K + H | 988 | T | 0.89 | T + H vs. K + H | 502 | T | 1.78 | T + H vs. K + H | 249 |
| Heparin | 0.31 | T + H vs. H | 524 | H | 0.61 | T + H vs. H | 267 | H | 1.23 | T + H vs. H | 133 |
| Knee + heparin (K + H) | 0.21 | K + H | 0.42 | K + H | 0.84 | ||||||
| Thigh + heparin (T + H) | 0.12 | T + H | 0.24 | T + H | 0.48 | ||||||
| 4.94% risk of DVT taking drugs | 9.88% risk of DVT taking drugs | 19.76% risk of DVT taking drugs | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Risk of DVT, % | Comparison | NNT | Intervention | Risk of DVT, % | Comparison | NNT | Intervention | Risk of DVT, % | Comparison | NNT |
| No treatment | 16.40 | H vs. NT | 9 | NT | 29.28 | H vs. NT | 5 | NT | 48.18 | H vs. NT | 3 |
| Knee | 11.80 | K + H vs. H | 51 | K | 22.01 | K + H vs. H | 26 | K | 38.79 | K + H vs. H | 14 |
| Thigh | 7.03 | T + H vs. K + H | 62 | T | 13.76 | T + H vs. K+H | 31 | T | 26.38 | T + H vs. K + H | 16 |
| Heparin | 4.94 | T + H vs. H | 34 | H | 9.88 | T + H vs. H | 17 | H | 19.76 | T + H vs. H | 9 |
| Knee + heparin (K + H) | 3.41 | K + H | 6.94 | K + H | 14.35 | ||||||
| Thigh + heparin (T + H) | 1.96 | T + H | 4.04 | T+ H | 8.64 | ||||||
Inconsistency
An inconsistency analysis was conducted and the results are presented in Figure 12. The inconsistency was considerable. The direct and indirect evidence for the thigh-length stocking compared with heparin comparison was almost completely inconsistent (0.003). Inconsistency would increase the between-study variance estimate if the variation in effect estimates increases as a result. The inconsistency adds to the suggestion of unknown clinical and methodological heterogeneity. The effect of excluding each trial on the consistency of the direct and indirect evidence for the thigh-length stockings compared with heparin effect was evaluated, which showed the highest inconsistency across the network. The trial that has the greatest effect on the inconsistency is Williams and Palfrey,20 a trial that provides direct evidence for the treatment effect of heparin, despite being a small trial. Eliminating the Williams and Palfrey20 trial increases consistency between the direct and indirect evidence for the thigh-length stockings compared with heparin effect from 0.003 to 0.39. There is clearly inconsistency between the heparin effect estimates. Another trial that provides evidence for the heparin effect is Kalodiki et al. 33 Excluding the Kalodiki et al. 33 trial increases consistency to 0.09. The Cohen et al. 49 trial informs the effect of thigh-length stockings with heparin versus knee-length stockings with heparin. Excluding the Cohen et al. 49 trial increases consistency to 0.22.
FIGURE 12.
No interaction NMA network. The direct effects on the log-scale, and direct and indirect effect consistency values in brackets. Key: the solid black lines represent comparisons included in the data set. The arrows indicate which treatment is most effective in the comparison for the direct estimate for that comparison. ‘Thigh → no treatment’ indicates that thigh is more effective than no treatment. The negative numbers are the effect estimates on the log-scale; negative represents more effective. Because of the no interaction assumption, the dashed lines show the implied direct estimate treatment effects. The numbers in brackets represent consistency level between direct and indirect evidence. 0 represents complete inconsistency and 1 represents complete consistency.

To explore inconsistency further, for the no interaction model, the six-node network was collapsed into a three-node network as shown in Figure 13; this represents the ‘No interaction, lumped model’. In this network, because the nodes have been lumped, no heparin effect estimates have been estimated.
FIGURE 13.
No interaction, lumped NMA network. The direct effects on the log-scale, and direct and indirect effect consistency values in brackets.

The ORs for each comparison in the network are presented in Table 15. The results are similar to the no interaction model in which the nodes are not lumped, with a little more precision in the estimates, possibly because of less inconsistency. The probability that thigh-length stockings with heparin would be the most effective treatment were a new trial to be conducted is presented in Table 12 in the M2 column. The probability that thigh-length stockings with heparin is the most effective treatment was slightly higher at 0.82. There is still a high level of inconsistency in this network, that is, approximately 0.11 for this loop. Although different trials have different influences on the inconsistency, there are no outlying trials that can be singled out as likely to be outliers and that would individually explain the inconsistency. For each edge of the network in Figure 13, the trials are fairly consistent. For the thigh-length stocking with heparin versus knee-length stocking with heparin comparison, the estimates of Cohen et al. 49 and Porteous et al. 21 favour knee-length stockings over of thigh-length stockings, whereas the other trials favour thigh-length stockings. However, the CIs overlap the other mean estimates (see Figure 4).
| Intervention | Comparator | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No treatment | Thigh | Knee | Heparin | Thigh + heparin | Knee + heparin | |||||||
| Med | CrI | Med | CrI | Med | CrI | Med | CrI | Med | CrI | Med | CrI | |
| No treatment | – | – | 2.79 | 1.77 to 5.18 | 1.66 | 0.84 to 4.09 | – | – | – | – | – | – |
| Thigha | 0.36 | 0.19 to 0.57 | – | – | 0.59 | 0.31 to 1.21 | – | – | – | – | – | – |
| Knee | 0.60 | 0.24 to 1.19 | 1.69 | 0.82 to 3.21 | – | – | – | – | – | – | – | – |
| Heparin | – | – | – | – | – | – | – | – | 2.79 | 1.77 to 5.18 | 1.66 | 0.84 to 4.09 |
| Thigh + heparina | – | – | – | – | – | – | 0.36 | 0.19 to 0.57 | – | – | 0.59 | 0.31 to 1.21 |
| Knee + heparin | – | – | – | – | – | – | 0.60 | 0.24 to 1.19 | 1.69 | 0.82 to 3.21 | – | – |
Sensitivity analysis: no assumption on stocking–heparin treatment interaction
A sensitivity analysis was conducted where a stocking–heparin treatment interaction was considered to be plausible. The network is shown in Figure 14 and each treatment effect is considered to be potentially different and the results are presented in Table 16.
FIGURE 14.
Interaction NMA network. The direct effects on the log-scale, and direct and indirect effect consistency values in brackets. The solid black lines represent comparisons included in the dataset. The arrows indicate which treatment is most effective in the comparison for the direct estimate for that comparison. ‘Thigh → no treatment’ indicates that thigh is more effective than no treatment. The negative numbers are the effect estimates on the log scale; negative represents more effective. Because of the no interaction assumption, the dashed lines show the implied direct estimate treatment effects. The numbers in brackets represent consistency level between direct and indirect evidence. 0 represents complete inconsistency and 1 represents complete consistency.
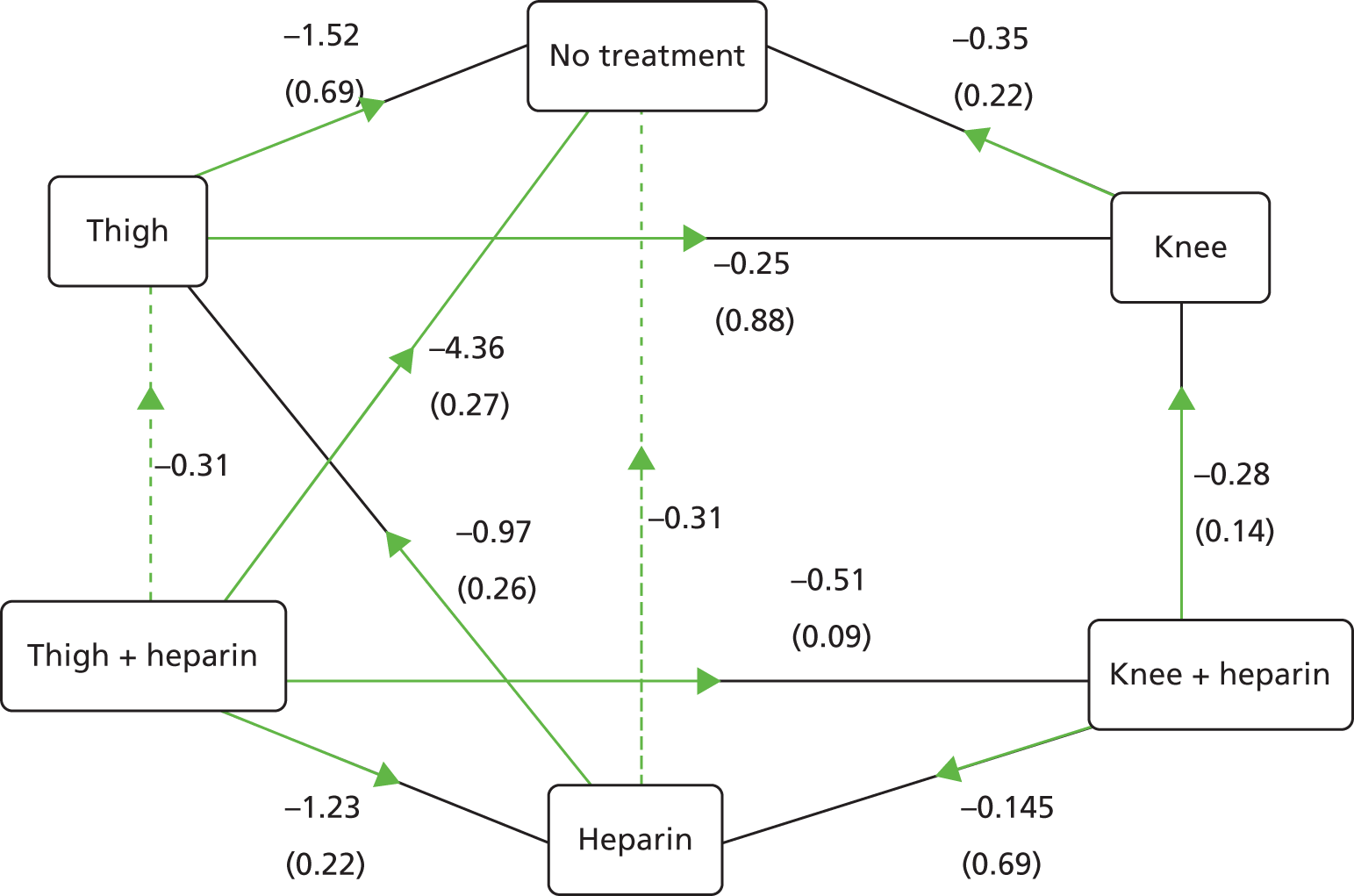
| Intervention | Comparator | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No treatment | Thigh | Knee | Heparin | Thigh + heparin | Knee + heparin | |||||||
| Med | CrI | Med | CrI | Med | CrI | Med | CrI | Med | CrI | Med | CrI | |
| No treatment | – | – | 3.64 | 1.69 to 9.99 | 2.78 | 0.96 to 11.37 | 7.91 | 2.45 to 31.50 | 19.60 | 5.96 to 95.05 | 7.61 | 2.14 to 36.61 |
| Thigh | 0.27 | 0.10 to 0.59 | – | – | 0.76 | 0.29 to 2.29 | 2.18 | 0.69 to 6.63 | 5.40 | 1.67 to 20.16 | 2.09 | 0.62 to 7.62 |
| Knee | 0.36 | 0.09 to 1.04 | 1.31 | 0.44 to 3.50 | – | – | 2.86 | 0.63 to 10.75 | 7.10 | 1.65 to 30.45 | 2.73 | 0.66 to 11.03 |
| Heparin | 0.13 | 0.03 to 0.41 | 0.46 | 0.15 to 1.46 | 0.35 | 0.09 to 1.59 | – | – | 2.48 | 1.21 to 6.13 | 0.96 | 0.33 to 3.15 |
| Thigh + heparin | 0.05 | 0.01 to 0.17 | 0.19 | 0.05 to 0.60 | 0.14 | 0.03 to 0.61 | 0.40 | 0.16 to 0.83 | – | – | 0.39 | 0.13 to 1.09 |
| Knee + heparin | 0.13 | 0.03 to 0.47 | 0.48 | 0.13 to 1.62 | 0.37 | 0.09 to 1.51 | 1.05 | 0.32 to 3.03 | 2.59 | 0.92 to 7.84 | – | – |
There is considerable uncertainty in many of the estimates in Table 16. There is greater uncertainty in the between-study SD estimate, which also has a higher median estimate than in the base case. The results of the inconsistency analysis are presented in Figure 14. There is less inconsistency evident in this analysis than the no interaction analyses, but this may be attributable to the same amount of evidence informing more parameters, and the lack of evidence of inconsistency does not prove there is not significant between-comparison heterogeneity. There is still significant inconsistency for two or three comparisons in the network. The median ORs of heparin compared with no treatment was 0.13 (95% CrI 0.03 to 0.41). The median OR of thigh-length stockings with heparin compared with heparin alone was 0.40 (95% CrI 0.16 to 0.83). The median OR of knee-length stockings with heparin compared with heparin alone was 1.05 (95% CrI 0.32 to 3.03). This result indicates there was very little evidence informing this estimate. The median OR of knee-length stockings with heparin compared with thigh-length stockings with heparin is 2.59 (95% CrI 0.92 to 7.84). This effect is significantly larger than that for knee-length stockings compared with thigh-length stockings, which was 1.31 (95% CI 0.44 to 3.50).
Table 12 presents the probability that each treatment would be the most effective given the results of a new trial. M3 represents the interaction model. Taking into account all the interventions simultaneously, there is a 0.75 probability that thigh-length stockings plus heparin is the most effective treatment combination within the population of the included trials.
Although there is little uncertainty that it is the most effective treatment, the incremental benefit of thigh-length stockings plus heparin over heparin alone is less than the incremental benefit of heparin over no treatment, as heparin has already reduced the risk of DVT substantially. Tables 17 and 18 present the estimated median risks of symptomatic DVT and of DVT given different treatments assuming different risk of symptomatic DVT and of DVT while on heparin. Tables 17 and 18 also present the NNT to avoid an extra case of DVT beyond that achieved by the comparator for different comparisons. For example, if the risk of DVT while on heparin was 4.94%, implying a risk of 29.24% with no treatment, then four people would need to be treated with heparin to avoid one case of DVT. Adding thigh-length stockings to heparin would require treating a further 35 patients to avoid one case of DVT over and above the cases of DVT avoided using heparin alone. The NNT with thigh-length stockings in addition to heparin to avoid an extra case of DVT is reasonably low, ranging from 9 to 35, depending on the level of risk for GS patients. The NNT with thigh-length stockings in addition to heparin to avoid an extra case of symptomatic DVT is extremely high, ranging from 137 to 541, depending on the level of risk for GS patients.
| 0.31% risk of DVT taking drugs | 0.61% risk of DVT taking drugs | 1.23% risk of DVT taking drugs | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Risk of DVT, % | Comparison | NNT | Intervention | Risk of DVT, % | Comparison | NNT | Intervention | Risk of DVT, % | Comparison | NNT |
| No treatment | 2.41 | H vs. NT | 47 | No treat | 4.65 | H vs. NT | 25 | No treat | 9.01 | H vs. NT | 13 |
| Knee | 0.88 | T + H vs. H | 541 | Knee | 1.73 | T + H vs. H | 275 | Knee | 3.45 | T + H vs. H | 137 |
| Thigh | 0.68 | T + H vs. K + H | 491 | Thigh | 1.33 | T + H vs. K + H | 250 | Thigh | 2.66 | T + H vs. K + H | 124 |
| Knee + heparin | 0.32 | Knee + heparin | 0.63 | Knee + heparin | 1.28 | ||||||
| Heparin | 0.31 | Heparin | 0.61 | Heparin | 1.23 | ||||||
| Thigh + heparin | 0.13 | Thigh + heparin | 0.25 | Thigh + heparin | 0.50 | ||||||
| 4.94% risk of DVT taking drugs | 9.88% risk of DVT taking drugs | 19.76% risk of DVT taking drugs | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Risk of DVT, % | Comparison | NNT | Intervention | Risk of DVT, % | Comparison | NNT | Intervention | Risk of DVT, % | Comparison | NNT |
| No treatment | 29.24 | H vs. NT | 4 | No treat | 46.58 | H vs. NT | 3 | No treat | 66.20 | H vs. NT | 2 |
| Knee | 12.97 | T + H vs. H | 35 | Knee | 23.92 | T + H vs. H | 18 | Knee | 41.40 | T + H vs. H | 9 |
| Thigh | 10.22 | T + H vs. K + H | 32 | Thigh | 19.37 | T + H vs. K + H | 16 | Thigh | 35.04 | T + H vs. K + H | 9 |
| Knee + heparin | 5.13 | Knee + heparin | 10.23 | Knee + heparin | 20.39 | ||||||
| Heparin | 4.94 | Heparin | 9.88 | Heparin | 19.76 | ||||||
| Thigh + heparin | 2.07 | Thigh + heparin | 4.26 | Thigh + heparin | 9.09 | ||||||
Orthopaedic surgery patients
Whether or not the trial population had undergone orthopaedic surgery was considered a potential effect modifier. A subgroup analysis was undertaken on the orthopaedic and non-orthopaedic groups, assuming both no stocking–heparin interaction and allowing for the interaction.
The network for the orthopaedic subgroup is shown in Figure 15 and included five trials. 25,30,33,49,60 The network for the non-orthopaedic subgroup is shown in Figure 16 and included eight trials. 12,20–22,24,35–37 Fixed-effect analyses were conducted for all of the subgroup analyses owing to a lack of trials with which to estimate the between-study variance. The uncertainty in the effectiveness estimates is likely to be underestimated, as between-study variance and inconsistency has been shown to be significant in this set of trials in the network.
FIGURE 15.
The network for the orthopaedic subgroup with the number of trials informing each comparison shown.
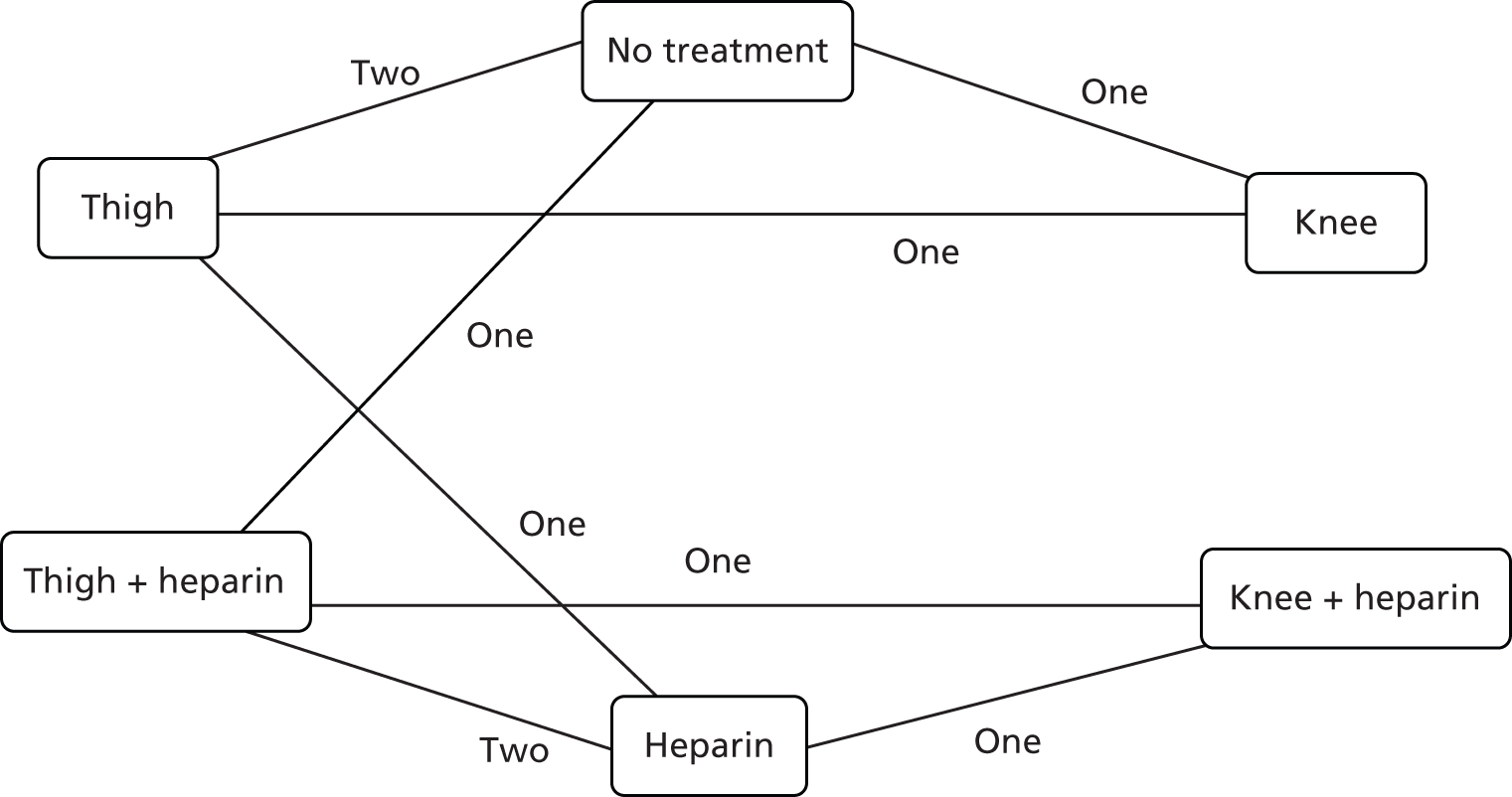
FIGURE 16.
The network for the non-orthopaedic subgroup with the number of trials informing each comparison shown.
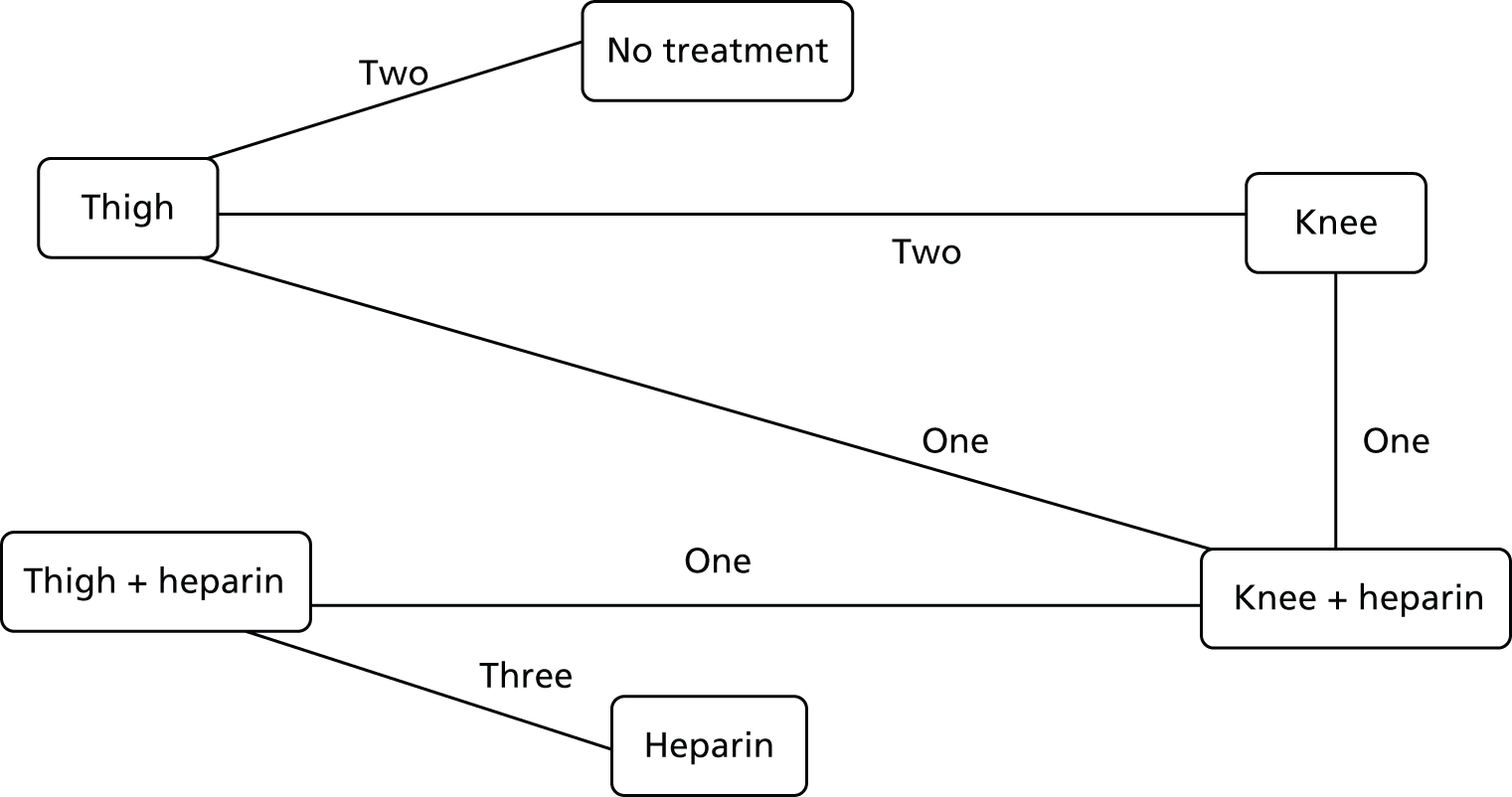
No stocking–heparin interaction
The results for the analysis assuming no stocking–heparin interaction for the orthopaedic subgroup of trials are presented in Table 19. The results for the non-orthopaedic group are presented in Table 20. The median ORs are slightly more in favour of both thigh- and knee-length stockings with heparin compared with heparin alone for the non-orthopaedic group compared with the orthopaedic group. The effectiveness of thigh-length stockings compared with knee-length stockings is slightly less in the orthopaedic group than the non-orthopaedic group. The median OR of knee-length stockings compared with thigh-length stockings is 1.55 (95% CrI 0.81 to 2.95) in the orthopaedic group and 1.78 (95% CrI 0.89 to 3.57) in the non-orthopaedic group. This compares with 1.76 (95% CrI 0.82 to 3.53) in the base case.
| Intervention | Comparator | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No treatment | Thigh | Knee | Heparin | Thigh + heparin | Knee + heparin | |||||||
| Med | CrI | Med | CrI | Med | CrI | Med | CrI | Med | CrI | Med | CrI | |
| No treatment | – | – | 2.05 | 1.32 to 3.23 | 1.32 | 0.72 to 2.46 | 6.30 | 3.32 to 12.42 | 12.92 | 5.03 to 35.16 | 8.34 | 3.24 to 22.20 |
| Thigha | 0.49 | 0.31 to 0.76 | – | – | 0.64 | 0.34 to 1.24 | 3.08 | 1.77 to 5.49 | 6.30 | 3.32 to 12.42 | 4.07 | 1.83 to 9.29 |
| Knee | 0.76 | 0.41 to 1.38 | 1.55 | 0.81 to 2.95 | – | – | 4.78 | 2.10 to 10.90 | 9.77 | 3.57 to 27.36 | 6.30 | 3.32 to 12.42 |
| Heparin | 0.16 | 0.08 to 0.30 | 0.33 | 0.18 to 0.57 | 0.21 | 0.09 to 0.48 | – | – | 2.05 | 1.32 to 3.23 | 1.32 | 0.72 to 2.46 |
| Thigh + heparina | 0.08 | 0.03 to 0.20 | 0.16 | 0.08 to 0.30 | 0.10 | 0.04 to 0.28 | 0.49 | 0.31 to 0.76 | – | – | 0.64 | 0.34 to 1.24 |
| Knee + heparin | 0.12 | 0.05 to 0.31 | 0.25 | 0.11 to 0.55 | 0.16 | 0.08 to 0.30 | 0.76 | 0.41 to 1.38 | 1.55 | 0.81 to 2.95 | – | – |
| Intervention | Comparator | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No treatment | Thigh | Knee | Heparin | Thigh + heparin | Knee + heparin | |||||||
| Med | CrI | Med | CrI | Med | CrI | Med | CrI | Med | CrI | Med | CrI | |
| No treatment | – | – | 3.83 | 2.29 to 6.66 | 2.16 | 0.90 to 5.21 | 1.41 | 0.49 to 4.53 | 5.41 | 1.65 to 19.52 | 3.04 | 0.89 to 11.39 |
| Thigha | 0.26 | 0.15 to 0.44 | – | – | 0.56 | 0.28 to 1.13 | 0.37 | 0.11 to 1.31 | 1.41 | 0.49 to 4.53 | 0.80 | 0.26 to 2.64 |
| Knee | 0.46 | 0.19 to 1.11 | 1.78 | 0.89 to 3.57 | – | – | 0.66 | 0.14 to 3.11 | 2.53 | 0.60 to 10.94 | 1.41 | 0.49 to 4.53 |
| Heparin | 0.71 | 0.22 to 2.05 | 2.72 | 0.76 to 8.99 | 1.52 | 0.32 to 6.99 | – | – | 3.83 | 2.29 to 6.66 | 2.16 | 0.90 to 5.21 |
| Thigh + heparina | 0.18 | 0.05 to 0.61 | 0.71 | 0.22 to 2.05 | 0.40 | 0.09 to 1.67 | 0.26 | 0.15 to 0.44 | – | – | 0.56 | 0.28 to 1.13 |
| Knee + heparin | 0.33 | 0.09 to 1.12 | 1.26 | 0.38 to 3.83 | 0.71 | 0.22 to 2.05 | 0.46 | 0.19 to 1.11 | 1.78 | 0.89 to 3.57 | – | – |
Allowing a stocking–heparin interaction
The results for the analysis assuming no stocking–heparin interaction for the orthopaedic subgroup of trials are presented in Table 21. The results for the non-orthopaedic group are presented in Table 22. Thigh-length stockings plus heparin appears to be significantly more effective in the non-orthopaedic group than in the orthopaedic group. The median ORs are slightly more in favour of both thigh- and knee-length stockings with heparin compared with heparin alone for the non-orthopaedic group compared with the orthopaedic group. The effectiveness of thigh-length stockings plus heparin is significantly higher relative to knee-length stockings plus heparin in the non-orthopaedic group compared with the orthopaedic group. The median OR of knee-length stockings compared with thigh-length stockings is 2.60 (95% CrI 1.11 to 6.34) in the orthopaedic group and 0.99 (95% CrI 0.36 to 2.75) in the non-orthopaedic group. This compares with 1.31 (95% CrI 0.44 to 3.50) when these groups are not distinguished.
| Intervention | Comparator | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No treatment | Thigh | Knee | Heparin | Thigh + heparin | Knee + heparin | |||||||
| Med | CrI | Med | CrI | Med | CrI | Med | CrI | Med | CrI | Med | CrI | |
| No treatment | – | – | 4.02 | 1.96 to 8.60 | 1.55 | 0.63 to 3.77 | 11.67 | 5.07 to 28.47 | 14.58 | 5.53 to 40.72 | 17.80 | 5.15 to 73.66 |
| Thigh | 0.25 | 0.12 to 0.51 | – | – | 0.39 | 0.16 to 0.90 | 2.90 | 1.66 to 5.19 | 3.63 | 1.66 to 8.14 | 4.38 | 1.52 to 15.75 |
| Knee | 0.65 | 0.27 to 1.60 | 2.60 | 1.11 to 6.34 | – | – | 7.57 | 2.80 to 21.14 | 9.45 | 3.08 to 30.06 | 11.58 | 2.96 to 53.16 |
| Heparin | 0.09 | 0.04 to 0.20 | 0.34 | 0.19 to 0.60 | 0.13 | 0.05 to 0.36 | – | – | 1.24 | 0.70 to 2.26 | 1.50 | 0.61 to 4.75 |
| Thigh + heparin | 0.07 | 0.02 to 0.18 | 0.28 | 0.12 to 0.60 | 0.11 | 0.03 to 0.32 | 0.80 | 0.44 to 1.42 | – | – | 1.21 | 0.46 to 3.98 |
| Knee + heparin | 0.06 | 0.01 to 0.19 | 0.23 | 0.06 to 0.66 | 0.09 | 0.02 to 0.34 | 0.67 | 0.21 to 1.65 | 0.83 | 0.25 to 2.19 | – | – |
| Intervention | Comparator | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No treatment | Thigh | Knee | Heparin | Thigh + heparin | Knee + heparin | |||||||
| Med | CrI | Med | CrI | Med | CrI | Med | CrI | Med | CrI | Med | CrI | |
| No treatment | – | – | 3.16 | 1.60 to 6.62 | 3.21 | 0.94 to 11.22 | 2.02 | 0.28 to 13.62 | 10.31 | 1.85 to 57.64 | 3.45 | 0.87 to 14.26 |
| Thigh | 0.32 | 0.15 to 0.62 | – | – | 1.01 | 0.36 to 2.81 | 0.63 | 0.10 to 3.72 | 3.23 | 0.68 to 15.59 | 1.08 | 0.33 to 3.76 |
| Knee | 0.31 | 0.09 to 1.06 | 0.99 | 0.36 to 2.75 | – | – | 0.63 | 0.10 to 3.68 | 3.22 | 0.69 to 15.33 | 1.07 | 0.33 to 3.65 |
| Heparin | 0.49 | 0.07 to 3.55 | 1.58 | 0.27 to 9.66 | 1.59 | 0.27 to 9.73 | – | – | 5.05 | 2.28 to 13.13 | 1.72 | 0.48 to 6.62 |
| Thigh + heparin | 0.10 | 0.02 to 0.54 | 0.31 | 0.06 to 1.47 | 0.31 | 0.07 to 1.45 | 0.20 | 0.08 to 0.44 | – | – | 0.34 | 0.12 to 0.88 |
| Knee + heparin | 0.29 | 0.07 to 1.15 | 0.92 | 0.27 to 3.00 | 0.93 | 0.27 to 3.03 | 0.58 | 0.15 to 2.09 | 2.97 | 1.13 to 8.06 | – | – |
Year of publication
Whether or not the trial was published prior to 2003 or from 2003 onwards was considered a potential effect modifier. Subgroup analysis was planned on the year 2003 and onwards and pre-2003 subgroups, assuming no stocking–heparin interaction and allowing for the interaction. However, the network for the year 2003 and onwards subgroup comprised only three trials,12,49,60 such that the network was very small and there was no indirect evidence to support direct evidence for any comparison. The analysis for the year 2003 and onwards subgroup was, therefore, not conducted. Consequently, the pre-2003 year subgroup analysis was rendered redundant and was not conducted either.
Summary of the network meta-analysis results
Thirteen trials were included in the base-case network. 12,20–22,24,25,30,33,35–37,49,60 Several comparisons in the network had direct evidence informed by one or two trials. Many of the trials in the network were quite small. The evidence informing the network was sparse. There was significant statistical heterogeneity in the models and inconsistency reflecting known clinical heterogeneity, as well as indicating that there may be further underlying unknown clinical and methodological heterogeneity across the trials. As such, it should be noted that the model estimates represent the average estimate across a distribution of trial estimates that may vary according to underlying differences between the trials. The CrIs represent the uncertainty in the average trial estimate.
There was little statistical uncertainty that heparin alone was more effective than no treatment. Whether or not a stocking–heparin interaction was assumed, thigh-length stockings with heparin was statistically significantly more effective than heparin alone in the whole population, and in the orthopaedic and non-orthopaedic populations. When no stocking–heparin interaction was assumed, knee-length stockings plus heparin was more effective than heparin alone but was not statistically significant at a 95% level of confidence. When a stocking–heparin interaction was assumed, there was little information to determine this effect estimate. Thigh-length stockings plus heparin was more effective for the average trial compared with knee-length stockings plus heparin, but this was not statistically significant at a 95% level of confidence.
The results of the different analyses for knee-length stockings with heparin compared with thigh-length stockings with heparin are presented in Table 23. The results are similar across the no stocking–heparin interaction models. The median ORs differ for the model allowing for a stocking–heparin interaction because of the heterogeneity across the trials and the fact that thigh-length stockings versus knee-length stockings are no longer directly informing this comparison of thigh- and knee- length stockings plus heparin. However, there is more uncertainty around the result, and so the interaction model is not inconsistent with the no interaction model. There is not sufficient information to test whether or not the interaction assumption makes a difference.
| Analysis | Median OR (CrI) of knee + heparin vs. thigh + heparin | |||||
|---|---|---|---|---|---|---|
| Whole NMA population | Orthopaedic population | Non-orthopaedic population | ||||
| No interaction meta-analysisa | 1.48 | (0.80 to 2.73) | – | – | – | – |
| No interaction NMA | 1.76 | (0.82 to 3.53) | 1.55 | (0.81 to 2.95) | 1.78 | (0.89 to 3.57) |
| No interaction NMA, lumped | 1.69 | (0.82 to 3.21) | – | – | – | – |
| Interaction NMA | 2.59 | (0.92 to 7.84) | 0.83 | (0.25 to 2.19) | 2.97 | (1.13 to 8.06) |
The results of the NMA are the average estimates across a heterogeneous set of trials. The trials may vary by population subgroup, protocol or what treatment outcomes are measured. The CrIs presented represent the uncertainty around that average. If a new trial were conducted the true value of that trial may come from anywhere in the random-effects distribution of the trials. It is possible to create a predictive distribution over the range of outcomes that may occur in a new trial. This predictive distribution is broader than the posterior distribution of the average treatment effect estimate because of the trial heterogeneity. It is a new trial that is of interest in this project and the reason for the VOI analysis in Chapter 7. Therefore, the probability that each treatment would be the most effective in a new trial was calculated. Overall, there was a probability of 0.73–0.82 that thigh-length stockings with heparin would be the most effective treatment in a new trial. The error probability of 0.18–0.27 is owing to the unexplained heterogeneity across the trials in the network.
Although thigh-length stockings with heparin is the most effective treatment, the incremental benefit of reducing the risk of DVT of adding thigh-length stockings to heparin is less than adding heparin to no treatment as heparin already reduces the risk of DVT significantly. For example, using the results of the base-case NMA, at a risk of DVT of 4.49% while on no treatment, you need to treat 30 patients with heparin to avoid a case of DVT. Adding thigh-length stockings to heparin, you need to treat a further 133 patients to avoid an extra case of DVT above that already achieved through heparin alone. The NNT with thigh-length stockings in addition to heparin to avoid an extra case of DVT is reasonably low ranging from 9 to 34, depending on the level of risk for GS patients. The NNT with thigh-length stockings in addition to heparin to avoid an extra case of symptomatic DVT is extremely high ranging from 133 to 524, depending on the level of risk for GS patients. The incremental cost-effectiveness of thigh-length stockings and heparin combined is evaluated in Chapters 4–6.
Baseline risk of deep-vein thrombosis
The searches identified a total of 13 potentially relevant guidelines. 4,8,11,18,67–77 These are summarised in Appendix 4. The synthesised evidence identified was considered current and relevant and further searches of the primary literature were not deemed necessary.
Two reviewers independently screened the full guidelines. The guidelines were assessed on whether or not a systematic literature review had been performed to inform the evidence base and the rigor of the review methods used. The guidelines were also checked for reporting of procedure- and/or patient-specific risks for DVT, baseline risk estimates in the absence of prophylaxis, or whether they did not list risk factors for DVT or baseline risk estimates. The results of this assessment are presented in Table 24.
| Author | Evidence based on systematic literature review? | Rigorous methods used | Procedure-specific risks for VTE | Patient-specific risks for VTE (e.g. age, obesity, anaesthetic duration and malignancy) | Provided estimates for baseline risk of VTE in the absence of prophylaxis | Reported methods to calculate baseline risks | Up-to-date evidence base for baseline risk estimates (2003 onwards) |
|---|---|---|---|---|---|---|---|
| American College of Chest Physicians Guidelines (2012)67 Non-orthopaedic patients | ✓ | ✓ | ✓ | ✓ | ✓ | Partly | ✓ |
| American College of Chest Physicians Guidelines (2012)68 Orthopaedic patients | ✓ | UC | ✓ | ✓ | ✓ | Partly | ✓ |
| Brazilian Society of Cardiology (2011)69 (AHRQ) | ✓ | UC | ✓ | ✗ | ✓ | ✗ | UC |
| Finnish Medical Society Duodecim (2010; 2011)70,71 | ✓ | UC | ✓ | ✓ | ✓ | ✗ | ✓ |
| International Consensus Statement, fifth revision (2013)72 | ✓ | UC | ✗ | ✓ | ✓ | ✓ | Partly |
| NICE guideline 92 (2010; 2012)4,18 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Partly |
| Royal College of Surgeons guideline (2007)73 | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | Partly |
| Agency for Information, Evaluation, and Quality in Health of Catalonia 201074 | ✓ | UC | ✗ | ✓ | ✗ | N/A | N/A |
| ENT UK (2010)75 | ✗ | ✗ | ✗ | ✓ | ✗ | N/A | N/A |
| Australian Government Clinical Practice Guideline (2009)76 | ✓ | ✓ | ✓ | ✓ | ✗ | N/A | N/A |
| SIGN (2010)11 | ✓ | ✗ | ✗ | ✓ | ✗ | N/A | N/A |
| Thromboembolic Risk Factors Consensus Group Lowe (1992)8 | ✗ | ✗ | ✓ | ✓ | ✗ | N/A | N/A |
| British Committee for Standards in Haematology Journal (2010)77 | ✗ | ✗ | ✗ | ✗ | ✗ | N/A | N/A |
The methodological limitations of the guidelines and the evidence on which they are based should be borne in mind, and these are briefly outlined in Appendix 4. Seven guidelines4,18,67–77 reported the procedure-specific risks for DVT, patient-specific risks for DVT (e.g. age, obesity, anaesthetic duration and malignancy) and also provided estimates for baseline risk of DVT in the absence of prophylaxis. The various guidelines calculated baseline risk estimates using different sources, including RCTs and non-RCTs; most were based on a systematic review (see Table 24). Six guidelines,8,11,74–77 including one set of guidelines relating to the prevention of DVT in children,77 listed only patient and/or surgical risk factors for DVT or risks for bleeding and did not provide data on baseline risks (see Table 24). These guidelines were therefore not useful to inform the economic model.
Of the 13 guidelines, the most comprehensive and rigorous guidelines were published by NICE4,18 and the American College of Chest Physicians (ACCP) for orthopaedic68 and non-orthopaedic patients. 67
The NICE guidelines4,18 used evidence from various sources (including RCTs), and indicated that major orthopaedic surgery carries a greater risk for DVT than cardiac, thoracic, vascular, gynaecological, neurological and GS. The ACCP guidelines for orthopaedic68 and non-orthopaedic patients67 recommend different types of prophylaxis based on levels of risk. It should be noted that the figures presented in Appendix 4 are sometimes calculated from outdated studies (pre-2003), and reflect baseline risk estimates in the absence of prophylaxis. Clinical practice has changed over time and current practice is to administer drug treatment to patients not at high risk of bleeding. The baseline risk estimates presented in Appendix 4 will therefore be high compared with more recent calculations and compared with baseline risk estimates in the presence of drug therapy.
For the economic model and VOI analysis, the ACCP guideline was chosen as a basis for the analysis of baseline risk because (1) it used more current studies to estimate baseline risk than NICE CG92; (2) it used heparin prophylaxis as the baseline; (3) it separated baseline risk into risk by surgery type, orthopaedic and non-orthopaedic; and (4) for the orthopaedic surgeries, VTEs were separated into PEs and DVTs.
The ACCP guidelines reported findings for orthopaedic and non-orthopaedic patients separately. Each guideline was further broken down into subgroups. The orthopaedic subgroups were THR surgery patients, TKR surgery patients and hip fracture patients. The non-orthopaedic subgroups were low-, moderate- and high-risk patients.
To estimate the baseline risk of VTE in orthopaedic patients the ACCP authors analysed all controlled trials since 1959 that had a placebo or no treatment group. However, it is expected that baseline risks post surgery will have changed because of changes in surgical care. RCT data showed a symptomatic VTE event rate of 15–30% without prophylaxis prior to 1980 and observational data showed a decrease in the event rate of 1–5% from 1989 to 2001. The authors reported that no large placebo-controlled trials or well-designed cohort studies that provided a baseline risk relevant to current practice had been undertaken in recent years. However, there are several large RCTs that have used LMWH. The authors estimated the baseline risk on LMWH of symptomatic DVT to be 0.8% and for PE to be 0.35% (1.15% VTE) by averaging the LMWH event rates from trials since 2003 with a total number of patients > 16,000. The year 2003 was selected because of a shift in surgical technique since that time to be less invasive and possibly less thrombogenic. The authors were concerned that these rates may be too low given the selective nature of clinical trials, so they compared this with data from a large observational study which found 133 of 19,586 (0.7%) VTE events during the initial hospitalisation for patients receiving prophylaxis, suggesting to the ACCP authors that the VTE rate of 1.15% is not too low.
For the orthopaedic surgery types, data were extracted from the original clinical trials reported in the ACCP guideline; some studies reported PE and VTE and some did not separate symptomatic and asymptomatic DVT. We contacted the ACCP authors for clarification and the lead author generously provided the data and suggestions for improving the baseline risk calculation. In re-estimating the baseline risks we have used the data provided and made some slight changes. First, we calculated the number of DVT events from trials that reported VTE by subtracting the number of PE events reported instead of just using VTE in the place of DVT. This resulted in fewer events being used in the DVT calculation and a lower estimate of the baseline risk. Second, we estimated fixed- and random-effects models weighting by the inverse of study variance, rather than calculating the average. Finally, we calculated separate estimates for THR and TKR; no trials were available for the hip fracture population (Table 25).
| Analysis | All orthopaedic (n = 16,031) | THR (n = 8414) | TKR (n = 7617) |
|---|---|---|---|
| DVT | |||
| ACCP average | 0.8 (NR) | NR | NR |
| Fixed effect | 0.70 (0.110) | 0.46 (0.180) | 0.89 (0.139) |
| Random effects | 0.55 (0.225) | 0.38 (0.351) | 0.72 (0.293) |
| PE | |||
| ACCP average | 0.35 (NR) | NR | NR |
| Fixed effect | 0.40 (0.153) | 0.26 (0.243) | 0.52 (0.197) |
| Random effects | 0.39 (0.178) | 0.25 (0.276) | 0.53 (0.233) |
For GS patients, the baseline risk estimates in the ACCP prevention of VTE in non-orthopaedic surgical patients guideline were based on a large retrospective study by Bahl et al. ,78 which aimed to validate the Caprini score (a model to estimate VTE risk) in a sample of general, vascular and urological surgery patients. These baseline risks were adjusted for LMWH within the non-orthopaedic ACCP guideline and were reported for low-, moderate- and high-risk GS patients (Table 26).
| Event | Low risk, % (95% CI) | Moderate risk, % (95% CI) | High risk, % (95% CI) |
|---|---|---|---|
| Non-fatal symptomatic VTE incidence | 0.47 (0.2 to 1.2) | 0.93 (0.4 to 2.4) | 1.86 (0.7 to 4.9) |
An issue with the non-orthopaedic baseline risk estimates from ACCP is that they are provided for overall VTE but are not reported separately by the type of event (i.e. baseline risk of symptomatic DVT or PE). To estimate the risk of symptomatic DVT and PE from the ACCP estimate of VTE, we used the proportions of DVT to PE that were reported in the overall orthopaedic population, 83 of 126. The baseline risks for GS are summarised in Table 27.
| Event | Low risk (%) | Moderate risk (%) | High risk (%) |
|---|---|---|---|
| Non-fatal symptomatic DVT | 0.31 | 0.61 | 1.23 |
| Non-fatal symptomatic PE | 0.16 | 0.32 | 0.63 |
From the ACCP guideline it was possible to estimate the risks of symptomatic DVT and PE, but asymptomatic DVTs were not reported. To estimate the total number of asymptomatic DVTs, we used the percentage of symptomatic DVTs from all DVTs reported in the NICE guidelines (Table 28).
| Event | THR (%) | TKR (%) | GS (%) |
|---|---|---|---|
| Symptomatic DVT | 21.0 | 5.0 | 6.2 |
The probabilities of symptomatic and asymptomatic DVT and PE are reported in Table 29. These probabilities are used in the sample size calculation and in the economic analysis.
| Risk | Orthopaedic surgery (%) | GS (%) | |||
|---|---|---|---|---|---|
| THR | TKR | Low risk | Moderate risk | High risk | |
| All DVT | 1.81 | 14.40 | 4.94 | 9.88 | 19.76 |
| Symptomatic | 0.38 | 0.72 | 0.31 | 0.61 | 1.23 |
| Asymptomatic | 1.43 | 13.70 | 4.63 | 9.27 | 18.54 |
| PE | 0.25 | 0.53 | 0.16 | 0.32 | 0.63 |
The clinical consequences of deep-vein thrombosis (mortality and morbidity)
The NICE guidelines were considered the most directly relevant sources of synthesised evidence for the economic model; the estimates of the consequences of DVT were based on a search for good-quality systematic reviews and economic evaluations into baseline risks for PTS, PHT and stroke. 4,9 The NICE guidelines did not provide estimates for recurrence of VTE. The trial by Baglin et al. 79 was identified as a source for recurrent VTE event rates and this, along with the NICE guideline estimates, were therefore used to inform the economic model described in Chapter 4.
Patient adherence and preference
Flow of studies through the review of patient adherence and preference
The review of RCTs on the clinical effectiveness of thigh-length and knee-length GCSs identified eight RCTs that also provided some data on patient adherence and/or preference. 21,24,25,32,37,60,63,65 One additional RCT14 and seven observational studies (eight articles) were identified. 15,16,80–85 These additional studies did not meet criteria for inclusion in the review of RCTs of clinical effectiveness, but did provide some data on patient adherence and/or preference.
Another trial included in the review of clinical effectiveness of thigh-length and knee-length GCSs (Cohen et al. 49) that compared knee-length GCSs plus fondaparinux versus thigh-length GCSs plus fondaparinux reported that the level of adherence for the continuous use of GCSs was 85% while patients were hospitalised, but this dropped to 76% once patients were discharged. The authors did not state levels of adherence by stocking length and, therefore, these results will not be discussed further here.
Characteristics of studies included in the review of patient adherence and preference
Detailed characteristics of the RCTs identified by the review of clinical effectiveness of thigh-length and knee-length GCSs have been previously described (see Characteristics of studies included in the review of effectiveness). Brief study characteristics for the observational studies are presented in Table 30.
| Author | Study design | Patient number/analysed | Type of surgery | Age (years) | % male | BMI | Intervention |
|---|---|---|---|---|---|---|---|
| Thigh-length GCSs vs. knee-length GCSs | |||||||
| Brady et al. (2007)15 | Single-centre survey | n = 137 | Mixed | Range 18–92 | 47 | NR | Thigh-length or knee-length TEDs and/or SCD |
| Hameed et al. (2002)16 | Single-centre prospective observational study | n = 72 | Mixed | Mean 51 (range 13–84) | 54 | NR | Kendall thigh-length or knee-length TED stockings |
| Parnaby (2004)80 | Single-centre survey and two trials | n = 218 (survey); n = 70 (trial 1); n = 20 (trial 2) | Mixed | NR | NR | NR | Knee-length or thigh-length SaphenaMedical antiDVT GCSs |
| Williams et al. (1994)81 and (1996)82 | Multicentre observational | n = 324 [131 (40%) wore stockings] | Orthopaedic | Median 67 | 40 | NR | Thigh-length TED (brand unknown) or Brevet GCSs, or knee-length Brevet GCSs |
| Williams and Owen (2006)83 | Single-centre prospective comparison | n = 50/n = 47 | Orthopaedic | Mean 71 | 53 | NR | Knee-length or thigh-length GCSs |
| Winslow and Brosz (2008)84 | Single-centre comparative descriptive design | n = 145/n = 142 | Mixed | Mean 57 (range 18–97) | 16 | 74% of patients overweight (BMI ≥ 25 kg/m2) | Knee-length or thigh-length TED GCSs |
| Knee-length GCSs | |||||||
| Thompson et al. (2011)85 | Audit and trial | n = 56/n = 56 (audit); n = 62 (trial)/n = 57 (trial) | Orthopaedic | NR | 44 | NR | Knee-length Preventex AES |
The objectives of the seven observational studies were specifically to assess the correct use of knee-length and thigh-length GCSs and to elicit patient perspectives about their use. 15,16,80–85 The observational studies reflect adherence only in a hospital setting in which patients are observed by health-care professionals.
Methods for measuring adherence, and definitions for this outcome, were inconsistent across RCTs and observational studies.
Quality of studies included in the review of patient adherence and preference
Detailed quality assessment results for the RCTs identified by the review of clinical effectiveness of thigh-length and knee-length GCSs have been previously described (see Characteristics of studies included in the review of effectiveness). The additional RCT by Benko et al. 14 was assessed for quality and was considered to have an unclear risk of bias. The quality of the observational studies was not formally assessed. The inherent problems associated with observational studies, and the poor reporting in the included observational studies, suggest that they should be considered low quality.
Results of studies included in the review of patient adherence and preference
Patient adherence
Patient adherence results are presented in Table 31.
| Author | Patient characteristics | Number of patients complying |
|---|---|---|
| RCTs | ||
| Benko et al. (2001)14 | Orthopaedic surgery (n = 200) | No difference between knee- and thigh-length stockings for independent management Thigh-length stockings wrinkled significantly more (p < 0.05) |
| Camporese et al. (2008)60 | Orthopaedic day surgery (n = 1761) | Sixty-three (9.6%) patients in the GCSs group, 54 (8.3%) patients in the 7-day LMWH group and 47 (10.6%) patients in the 14-day LMWH group declined to complete the prophylactic regimen |
| Fredin et al. (1989)32 | Orthopaedic surgery (n = 150) | Two (4%) patients in the thigh-length GCSs + dextran group discontinued wearing stockings because of discomfort. Control groups received dextran only |
| Hui et al. (1996)25 | Orthopaedic surgery (n = 177) | Twenty-three per cent of patients in the thigh-length stocking group and 16% in the knee-length stocking group found the stockings too uncomfortable and requested their removal |
| Mellbring and Palmer (1986)63 | Abdominal surgery (n = 114) | All patients tolerated wearing thigh-length GCSs |
| Turpie et al. (1989)24 | Neurosurgery (173 patients had neurosurgery; 66 patients did not have surgery) | Two (2.5%) patients did not wear thigh-length stockings correctly. Ten patients in the GCSs + IPC group did not tolerate treatment, although eight of these patients wore the GCSs as required |
| Wille-Jørgensen et al. (1985)37 | Major abdominal surgery (n = 196) | Two (2.3%) patients removed their thigh-length stockings after 5 days; otherwise they were well tolerated |
| Observational studies | ||
| Brady et al. (2007)15 | Mixed surgery (n = 137) | Fifty-one (37%) patients were not wearing stockings (most thigh length). There were 34 problems with fit among patients wearing thigh-length stockings, compared with 18 problems with knee-length stockings |
| Hameed et al. (2002)16 | Mixed surgery (n = 72) | A higher proportion of patients with thigh-length stockings than with knee-length stockings were wearing them incorrectly or rolled down (64.3% vs. 30%) |
| Parnaby (2004)80 | Mixed surgery: 218 (survey); 70 (trial 1); 20 (trial 2) | Of 218 patients, 119 (54%) were not wearing GCSs One-third of patients wearing above-knee stockings compared with 9% of patients wearing below-knee stockings wore the stockings incorrectly |
| Thompson et al. (2011)85 | Orthopaedic surgery: n = 56 (audit); n = 62 (trial) | Knee-length stockings were incorrectly sized in 28/38 (74%) patients. Twelve of 18 patients (67%) removed knee-length stockings as they were uncomfortable or too tight. Implementation of a standardised protocol reduced these problems |
| Williams et al. (1994,81 199682) | Orthopaedic surgery (n = 324) | Greater proportion of patients wearing thigh-length stockings too low or with wrinkles/bands. Satisfaction was greater in patients wearing knee-length GCSs |
| Winslow and Brosz (2008)84 | Mixed surgery (n = 145) | A greater proportion of patients in the thigh-length GCSs groups (particularly overweight patients) than in the knee-length GCSs groups were wearing GCSs incorrectly or wearing stockings of the incorrect size or reported skin problems |
Two RCTs comparing thigh-length versus knee-length stockings reported data on patient adherence. Hui et al. 25 reported that a higher proportion of patients wearing thigh-length GCSs than wearing knee-length GCSs removed stockings owing to discomfort. Benko et al. 14 reported that 50% of patients were unable to fit the stockings independently, with similar numbers of patients distributed between thigh-length and knee-length groups.
Three RCTs32,37,63 comparing thigh-length GCSs plus other treatment versus other treatment alone provided limited details on patient adherence. 32,63
The majority of patients in most of the observational studies were assigned to wear thigh-length stockings. Across the five studies that reported on adherence, this was relatively poor but varied. 15,16,80,81,84 The proportion of patients not wearing stockings or wearing stockings incorrectly appeared to be generally higher in patients receiving thigh-length GCSs (see Table 31).
Across the studies, reasons for not wearing stockings related to discomfort, stocking provision, removing stockings for bathing or no longer requiring them owing to ambulation. Incorrect use related to wearing incorrectly sized stockings or to the stocking rolling down, binding or wrinkling. In a study involving an audit and a trial of knee-length GCSs,85 74% of patients were wearing stockings that were incorrectly sized. Implementation of a standardised protocol within the study setting resulted in statistically significant reduction in this proportion to 34%.
Brady et al. 15 reported a strong correlation between age and adherence, indicating that older patients wore stockings more consistently than younger patients. None of the other studies assessed this association and the evidence is therefore insufficient to draw any conclusions.
From the two studies that compared thigh-length or knee-length stockings, non-adherence or incorrect use was worse with thigh-length stockings (16.7% vs. 3% and 54% vs. 20%). 16,84
Patient preference
Three RCTs14,21,65 and five observational studies15,16,80,83,84 presented findings on patient preference (Table 32). One RCT (Ayhan et al. 65) reported that patients found the low-pressure knee-length GCSs ‘very comfortable’ and the thigh-length GCSs ‘comfortable’, but patients reported that moderate-pressure knee-length GCSs were ‘uncomfortable’ (p < 0.001). 65 The remaining two RCTs14,21 reported that knee-length stockings were more acceptable and more comfortable than thigh-length stockings.
| Author | Patient characteristics | Patient preference |
|---|---|---|
| RCTs | ||
| Ayhan et al. (2013)65 | Patients at extremely high risk for postoperative DVT (n = 219) | Low-pressure knee- and thigh-length stockings reported to be very comfortable/comfortable. Moderate-pressure knee-length GCSs were reported to be uncomfortable (p < 0.001) |
| Benko et al. (2001)14 | Orthopaedic surgery (n = 200) | Significantly more patients reported discomfort with thigh-length Thrombex GCSs than knee-length Thrombex or Brevet TX GCSs (p < 0.05) |
| Porteous et al. (1989)21 | Major abdominal surgery (n = 124) | Brevet knee-length stockings were more acceptable and comfortable than thigh-length stockings |
| Observational studies | ||
| Brady et al. (2007)15 | Mixed surgery (n = 137) | Complaints of discomfort were highest among patients wearing thigh-length TED stockings compared with knee-length TED stockings and/or SCD |
| Hameed et al. (2002)16 | Mixed surgery (n = 72) | Patients were generally more satisfied with knee-length GCSs than with Kendall thigh-length GCSs |
| Parnaby (2004)80 | Mixed surgery: n = 218 (survey); n = 70 (trial 1); n = 20 (trial 2) | 95% patients would wear the modified thigh- or knee-length SaphenaMedical GCSs again. None of the patients wearing the modified heel design complained of heel friction |
| Williams and Owen (2006)83 | Orthopaedic surgery (n = 50) | All female patients would have preferred to wear below-knee-length than thigh-length GCSs |
| Winslow and Brosz (2008)84 | Mixed surgery (n = 145) | Higher proportion of patients (including overweight patients) rated thigh-length GCSs as uncomfortable or very uncomfortable compared with knee-length GCSs; p < 0.001 |
Parnaby80 undertook an initial survey and two subsequent trials of patients wearing a particular brand of knee- or thigh-length stocking. The second trial administered a modified stocking to incorporate changes to overcome problems identified by patients in the first trial, including a change in the heel design to prevent excess friction and the availability of an open toe version. Patients preferred the modified stockings and 95% stated that they would wear the stockings again (see Table 32).
Four observational studies reported patient preference in terms of comfort, ease of application and general satisfaction. A greater proportion of patients in the observational studies preferred knee-length GCSs, finding them more comfortable (see Table 32). 15,16,83,84
Of the eight studies, six reported on patients’ preference for length of stocking and all favoured knee-length stockings. 14,16,21,80,83,84
Adherence of doctors prescribing
A hospital audit showed that heparin was omitted in 43% of 106 patients; stockings were prescribed to 46.2% patients; and combined use was prescribed in 24.3% of patients. Stockings were used with inadequate fitting. After a protocol had been introduced, optimal prophylaxis was given to 88.1% of patients (p = 0.003). 12
Sample size of a new study
The NMA result for thigh-length stockings plus heparin compared with knee-length stockings plus heparin showed that, although the effect estimate favoured thigh-length stockings plus heparin, the result was not statistically significant. Furthermore, because the NMA results were no more precise than direct meta-analysis results, this emphasises the heterogeneity across the included trials. We have, therefore, estimated the sample size of a definitive trial using the treatment effect estimate from the base-case NMA analysis in Network meta-analysis results and the baseline risks of DVT and symptomatic DVT calculated in Baseline risk of deep-vein thrombosis (see Table 29).
In Baseline risk of deep-vein thrombosis, baseline risks of DVT were estimated for patients on heparin for low-, moderate- and high-risk GS patients. For this analysis, the risk of DVT (symptomatic and asymptomatic) and risk of symptomatic DVT are used. Symptomatic DVT is selected instead of asymptomatic DVT because it has more significant health implications for patients. The risks of DVT and symptomatic DVT for thigh-length stockings plus heparin and for knee-length stockings plus heparin were derived from the risks for patients on heparin and the median ORs for thigh- and knee-length stockings plus heparin versus heparin from the NMA base-case analysis. The risks for DVT and symptomatic DVT for the different treatments are presented in Table 33.
| Risk | Symptomatic DVT (%) | Patients/arm | Total DVT (%) | Patients/arm | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Heparin | Knee + heparin | Thigh + heparin | 80% power | 90% power | Heparin | Knee + heparin | Thigh + heparin | 80% power | 90% power | |
| Low | 0.31 | 0.22 | 0.12 | 26,428 | 35,261 | 4.94 | 3.58 | 1.99 | 1692 | 2258 |
| Moderate | 0.61 | 0.44 | 0.24 | 13,456 | 17,954 | 9.88 | 7.22 | 4.11 | 866 | 1156 |
| High | 1.23 | 0.89 | 0.49 | 6691 | 8927 | 19.76 | 14.73 | 8.75 | 456 | 608 |
A null hypothesis of no difference in treatment effect was used. Assuming that there is an equal number of patients in each trial arm and an OR of 0.57 (see Table 11) for thigh-length stockings plus heparin compared with knee-length stockings plus heparin, the sample size per arm for a trial comparing thigh-length stockings plus heparin with knee-length stockings plus heparin was calculated for a type I error of 0.05 and for two power values (0.8 and 0.9). The sample size estimates for both the risk of symptomatic DVT and DVT are reported in Table 33.
These estimates indicate that for symptomatic DVT, a definitive trial would require a minimum of 13,000 patients because of the very low risk of symptomatic DVT. For DVT (symptomatic and asymptomatic) the risk is much higher, and for high-risk patients a trial would need a minimum of 900 patients. The sample size numbers are much greater for moderate- and low-risk patients.
Summary of findings of the clinical evidence review
Four key clinical areas were assessed to inform the decision model:
-
the relative effectiveness of thigh-length versus knee-length stockings for prevention of DVT in surgical patients
-
baseline risk of DVT
-
the clinical consequences of DVT
-
patient adherence.
Twenty-three RCTs were included in the systematic review of thigh-length versus knee-length stockings,12,20–25,30–37,49,60–66 of which 20 provided sufficient data to be included in meta-analyses. 12,20–25,30–37,49,60,61,63,66 There was substantial variation between the included trials in terms of the patient characteristics, interventions and methods of outcome assessment.
Two trials directly compared knee-length versus thigh-length stockings plus pharmacological prophylaxis; their results were inconsistent in terms of the direction of effect and the pooled result was not statistically significant. 12,49 Reasons for the inconsistent findings between the two trials were unclear and may be due to chance.
To add strength to the comparison of thigh-length and knee-length stockings, additional comparisons of these stockings were reviewed. A total of five trials comparing thigh-length versus knee-length stockings with or without pharmacological prophylaxis were pooled;12,20,21,25,49 the summary estimate of effect for all five trials indicated a trend favouring thigh-length stockings, but the findings were not statistically significant. A pooled analysis of four trials found statistically significantly fewer DVT events in patients receiving thigh-length stockings plus heparin versus heparin alone. 33,35–37 Compared with no active treatment, both thigh-length (five trials24,25,30,33,53) and knee-length (two trials23,25) stockings reduced DVT events, but only with thigh-length stockings was the effect statistically significant.
All the relevant comparisons were combined in a NMA. Thirteen trials contained data that directly or indirectly informed the relative effectiveness of thigh-length versus knee-length stockings for the prevention of DVT and were included in the NMA, and the effect of removing the assumption of no interaction between GCSs and baseline heparin was explored in sensitivity analysis. 12,20–22,24,25,30,33,35–37,49,60 There was significant statistical heterogeneity in the models as well as inconsistency indicating that there may be underlying unknown clinical and methodological heterogeneity across the trials. Thigh-length stockings plus heparin were more effective than knee-length stockings plus heparin, but this result was not statistically significant. Thigh-length stockings plus heparin were statistically significantly more effective than heparin alone. Knee-length stockings plus heparin were more effective than heparin alone in the no stocking–heparin interaction model, which was not statistically significant, and there was little evidence for the effect estimate in the stocking–heparin interaction model.
The results of the NMA are the average estimates across a heterogeneous set of trials. The trials may vary by population subgroup, protocol or what treatment outcomes are measured. The CrIs represent the uncertainty around that average. Predictive distributions describe the probability that a range of outcomes may occur in a new trial. This predictive distribution is broader than the posterior distribution of the average treatment effect estimate because of the trial heterogeneity. Overall, there was a probability of 0.73–0.82 that thigh-length stockings with heparin would be the most effective treatment in a new trial. The error probability of 0.18–0.27 is because of the unexplained heterogeneity across the trials in the network.
Although thigh-length stockings plus heparin is the most effective treatment, the incremental benefit of reducing the risk of DVT of adding thigh-length stockings to heparin is less than adding heparin to no treatment, as heparin already reduces the risk of DVT significantly. For example, using the results of the base-case NMA, at a risk of DVT of 4.49% while on no treatment, 30 patients need to be treated with heparin to avoid a case of DVT. Adding thigh-length stockings to heparin, you need to treat a further 133 patients to avoid an extra case of DVT above that already achieved through heparin alone. The NNT with thigh-length stockings in addition to heparin to avoid an extra case of DVT is reasonably low, ranging from 9 to 34, depending on the level of risk for GS patients. The NNT with thigh-length stockings in addition to heparin to avoid an extra case of symptomatic DVT is extremely high, ranging from 133 to 524, depending on the level of risk for GS patients.
The results of the different analyses for the comparison of thigh- and knee-length stockings plus heparin are similar across the no stocking–heparin interaction models and the standard meta-analysis. The results also show that the precision of the estimate of effect is not improved by the NMA and, therefore, the analyses confirm that further research is needed to confirm precisely the difference in treatment effect of high- and knee-length stockings when used in combination with heparin. Given the uncertainty in the NMA, it is unlikely that an additional underpowered trial would be sufficient: only a new definitive trial would be worthwhile. The definitive trial would replace the existing heterogeneous evidence, as the results would be directly applicable to the decision question.
We estimated the sample size of any such definitive trial. The estimates indicate that for symptomatic DVT for the high-risk patients, a definitive trial would require a minimum of 13,000 patients because of the very low risk of symptomatic DVT. For DVT (symptomatic and asymptomatic) the risk is much higher, and for high-risk patients a trial would need a minimum of 900 patients. For patients at moderate or low risk of DVT, the sample sizes are much higher for both DVT and symptomatic DVT.
The review found that evidence relating to other clinical outcomes was sparse: PE events and VTE-related mortality events were generally rare in the included trials. Adverse events were also rarely reported and those related to GCSs were minor events, including minor foot abrasions, superficial thrombophlebitis, the stocking slipping down or feeling hot.
Nine RCTs14,21,24,25,32,37,60,63,65 and seven observational studies15,16,80–85 were identified that reported data on patient adherence and/or preference. Patient adherence was higher in the RCTs than the observational studies but across all studies the proportion of patients not wearing stockings or wearing stockings incorrectly appeared to be generally higher in patients receiving thigh-length stockings than in those receiving knee-length stockings. All of these studies reflect patient adherence in a hospital setting; it is likely that adherence is lower after patients have been discharged from hospital. In all six studies that reported on patients’ preference for length of stocking, patients preferred knee-length stockings over thigh-length stockings. Any new trial comparing thigh- and knee-length stockings when used in combination with heparin must take patient adherence into account in order to accurately reflect real-life practice.
Information on baseline risks of DVT was identified through searches of the guideline and systematic review literature. Of the 13 potentially relevant guidelines,4,8,11,18,67–77, the most comprehensive and rigorous were published by NICE4,18 and the ACCP67,68 for orthopaedic and non-orthopaedic patients. However, the studies used to calculate baseline risks in the NICE guidelines were considered to be out of date and not appropriate to inform the economic model, and the methods used to calculate baseline risks were not fully reported and the variance in results was not reported in the ACCP guidelines. Therefore, to inform the current modelling, the authors of the ACCP guidelines were contacted for further information and a meta-analysis undertaken of the studies included in the ACCP guidelines.
With regards to the clinical consequences of DVT (mortality and morbidity), the NICE guidelines were considered the most directly relevant sources of synthesised evidence for the economic model; the estimates of the consequences of DVT were based on a search for good-quality systematic reviews and economic evaluations into baseline risks for PTS, PHT and stroke. However, the NICE guidelines did not provide estimates for recurrence of VTE and a study by Baglin et al. 79 was used as the source for recurrent VTE event rates.
Chapter 4 Assessment of existing cost-effectiveness evidence
Systematic review of existing cost-effectiveness evidence
This chapter provides an overview of the evidence reporting the cost-effectiveness of GCSs for the prevention of DVT in postoperative surgical patients, and an assessment of the quality and relevance of the data from the perspective of the UK NHS and Personal Social Services (PSS). Summary data extraction tables were applied to the studies that met the inclusion criteria. The differences in the approaches and assumptions used across the studies were examined in order to explain any discrepancies in the findings and to identify key areas of remaining uncertainty. The findings from the review of the existing cost-effectiveness evidence provide the basis for the development of a new decision analytic model reported in Chapter 5. A discussion on the cost-effectiveness evidence and the key issues is provided at the end of the chapter.
Methods
Systematic searches of the literature were conducted to identify potentially relevant studies for inclusion in the assessment of the cost-effectiveness of GCSs for the prevention of DVT in postoperative surgical patients.
National Institute for Health and Care Excellence CG924 was published in 2010 and included a review of published cost-effectiveness studies using a comprehensive search strategy designed to find any applied study estimating the cost or cost-effectiveness of any VTE prophylaxis intervention. The searches for this guideline were undertaken up to December 2008; the search identified five non-UK studies, none of which included GCSs as a comparator. The search strategies used in the economics section of the NICE CG924 were rerun with minor amendments in order to update results. The following databases were searched: MEDLINE, EMBASE, Health Economics Evaluations Database and HTA. NICE CG924 searches were originally run in December 2008, so the updated search was limited to 2008–14. Additional searches were run in NHS EED, CENTRAL, EconLit, IDEAS and the NICE website. Results from these were also limited to 2008–14. Following the initial searches as per protocol, the results set was narrowed by conducting more focused searches with a cost-effectiveness study filter, to identify cost-effectiveness-related records within the results set.
Table 34 lists the inclusion criteria for the review of cost-effectiveness. Only full economic evaluations that considered both costs and consequences (including cost-effectiveness, cost–utility and cost–benefit analyses) were included. Full details of the search strategies are reported in Appendix 1. Identified studies were assessed in a stepwise manner; three types of studies in postoperative surgical patients were considered to meet the inclusion criteria for this review: (1) studies with a focus on the cost-effectiveness of different types (lengths) of GCSs, either with or without a background of pharmacological prophylaxis; (2) cost-effectiveness studies that have compared alternative DVT prophylaxis strategies and include either type of compression stockings as a comparator; (3) cost-effectiveness studies comparing alternative DVT prophylaxis strategies but which have not included either type of compression stockings. A UK filter was applied for type (2) and type (3) studies, whereas all studies were considered for type (1) studies. Although study types (2) and (3) do not directly inform questions relating to the cost-effectiveness of the different types of compression stockings, we considered that they may provide useful information in relation to the choice of model structure, key assumptions and source of inputs. Hence, a more focused review of these study types was planned with the intention to report on aspects of these studies which would assist in the conceptualisation and development of a new decision-analytic model.
| Category | Inclusion criteria |
|---|---|
| Study type | Only full economic evaluations (including cost-effectiveness, cost–utility and cost–benefit evaluations) were included |
| Population | Studies of postsurgical patients at risk of DVT were included |
| Interventions | The intervention of interest was thigh-length and knee-length GCSs |
| Comparators | Other DVT prophylaxis strategies |
| Study inclusion hierarchy |
|
| Outcomes | Incremental costs and consequences separately reported |
| Other | Only studies in the UK setting were included for study types (2) and (3). Study type (1) considered all identified studies. Abstracts, posters, editorials and reviews of economic evaluations were excluded |
Titles and abstracts were assessed independently by two reviewers for inclusion and any discrepancies were resolved by consensus. After a detailed review of titles and abstracts, the papers that appeared to meet the inclusion criteria were obtained for a secondary review; this involved the full article being assessed according to the inclusion criteria. Methods and inputs of the included studies were extracted by one reviewer using a standardised data extraction form and checked for accuracy by a second reviewer. This information is summarised within the text of the report, alongside a detailed critique of the main studies and their relevance to the UK NHS. The findings from the review provide the basis for the development of a new model reported in Chapter 5.
Results
A total of 687 records were identified from the systematic literature search of existing cost-effectiveness evidence. In addition, eight previous NICE technology appraisals were identified from a focused search in the NICE website. Figure 17 presents a flow diagram summarising the identification and selection of studies. A total of 659 records were excluded based on the review of titles and abstracts. After reviewing the full papers for the remaining 36 records, only three studies subsequently met the inclusion criteria and were included in the review. 4,73,86 A summary of the included studies is reported in Table 35.
FIGURE 17.
Flow diagram of the cost-effectiveness studies selection process.
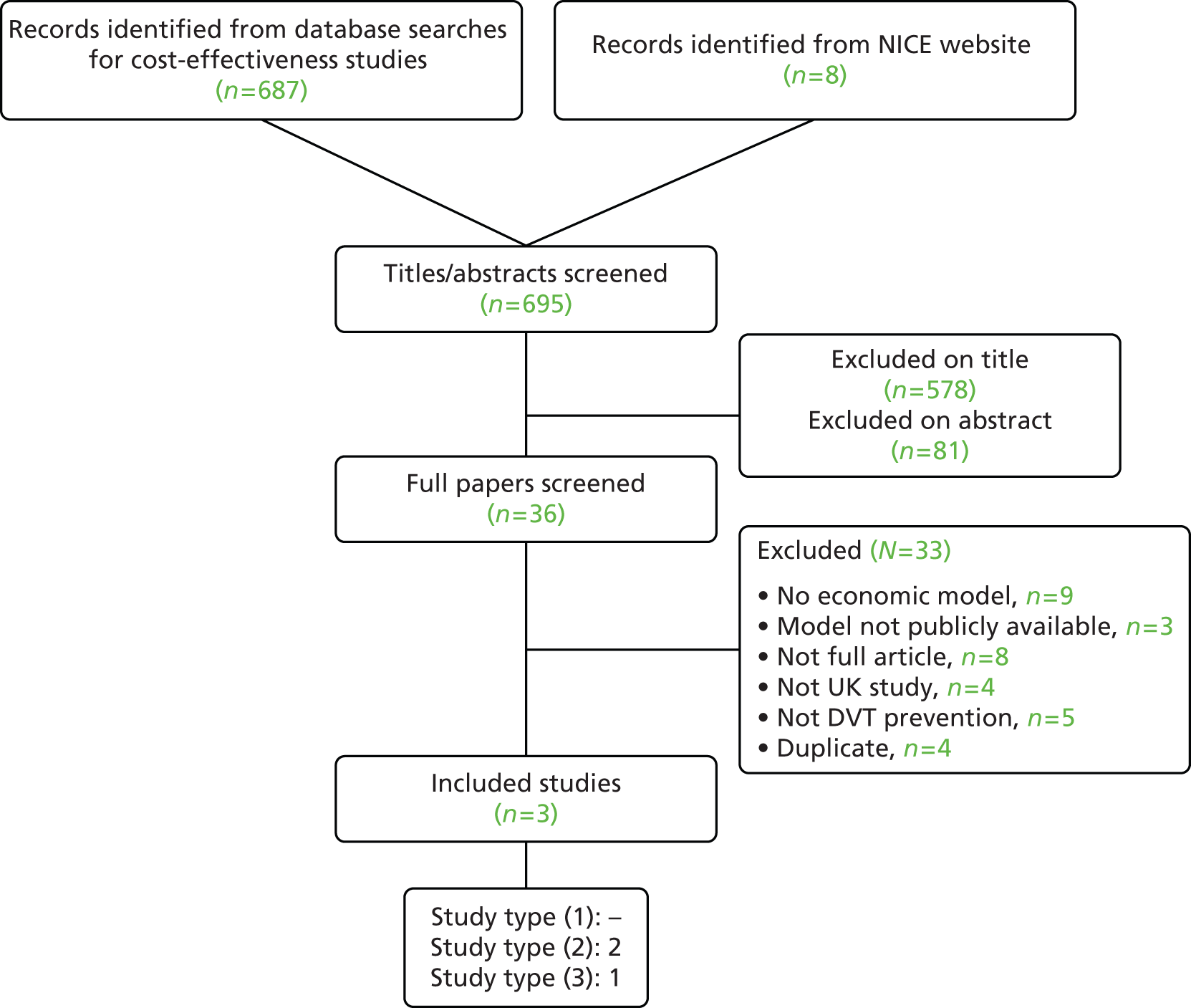
| Study details | NICE CG92 (2010)4 | Royal College of Surgeons CG (2007)73 | NICE TA245 apixaban for the prevention of VTE in adults who have undergone elective hip or knee replacement surgery (2011)86 |
|---|---|---|---|
| Economic evaluation type | Cost-effectiveness analysis | Cost-effectiveness analysis | Cost-effectiveness analysis |
| Currency, £ (year) | 2010 | 2007 | 2011 |
| Study design | Decision tree | Decision tree/Markov model for VTE recurrence in sensitivity analysis | Two-stage modelling approach: decision tree to model treatment in the acute phase (surgery to 90 days post surgery) and a Markov model for long-term events (90 days post surgery and beyond) |
| Perspective | NHS/PSS | NHS/PSS | NHS/PSS |
| Setting | UK | UK | UK |
| Patient population | Five population subgroups: (1) hip fracture surgery, (2) THR, (3) TKR, (4) GS (including other internal surgery), (5) general medical admissions | Four population subgroups: (1) hip fracture surgery, (2) elective hip, (3) gynaecological surgery (hysterectomy), (4) GS | Adults undergoing elective knee or hip replacement surgery |
| Time horizon |
|
|
90 days for acute phase and 35 years for long-term events |
| Comparators |
|
|
|
| Modelled events |
|
|
|
| Risk |
|
|
|
| Resources used and costs | Pharmacological prophylaxis costs, mechanical prophylaxis costs, prophylaxis testing and nurse time, VTE diagnosis and treatment costs, other events treatment costs (i.e. stroke, PTS, chronic thromboembolic PHT, major bleeding, reoperation) | Pharmacological prophylaxis costs, mechanical prophylaxis costs, prophylaxis testing and nurse time, VTE diagnosis and treatment costs, other treatment costs (i.e. stroke, PTS, recurrent VTE, major bleeding with reoperation, major bleeding without reoperation) | Intervention and comparator costs, testing costs, inpatient stay, postdischarge drug administration costs, VTE diagnosis and treatment costs, long-term costs in the long-term Markov model for PE, DVT, mild to moderate PTS and severe PTS |
| Source of resources used |
|
|
|
| Source of costs | Unit costs were taken from standard NHS sources: NHS reference costs,103 British National Formulary,104 NHS Electronic Drug Tariff,105 NHS Purchasing and Supplies Agency,106 Unit Costs of Health and Social Care 2007107 | Unit costs were taken from standard NHS sources: NHS reference costs,108 British National Formulary,104 NHS Electronic Drug Tariff,105 NHS Purchasing and Supplies Agency,106 Unit Costs of Health and Social Care 2005109 | |
| Clinical outcomes | The main outcomes considered were VTE events (asymptomatic and symptomatic DVT, symptomatic PE and fatal PE), bleeding events (major bleeding, fatal bleeding and stroke) and other long-term events occurring as a result of VTE (PHT and PTS) | Asymptomatic and symptomatic DVT, symptomatic PE and fatal PE, major bleeding, stroke, VTE recurrence, reoperation, all-cause mortality | Asymptomatic and symptomatic DVT (distal and proximal), PE, intracranial haemorrhage, bleeding events, PTS (moderate or severe), VTE recurrence, all-cause mortality |
| Source of clinical outcomes | Meta-analysis of RCTs included in the clinical review of the guideline. Published studies were referenced for symptomatic event rates irrespective of population subgroup | Meta-analysis of RCTs included in the clinical review of the guideline. Published studies were referenced for long-term events and symptomatic event rates irrespective of population subgroup | Baseline risk and apixaban risk from ADVANCE-2 and -387,88 trials; comparators clinical efficacy from RECORD,89–92 RE-MODEL,93 RE-NOVATE94,95 trials and ADVANCE87,88 trials |
| HRQoL | QALY | QALY | QALY |
| Source of HRQoL | Health-state utilities sourced from published studies and published NICE guidelines | Health-state utilities were taken from published studies and published NICE guidelines | Health-state utilities were taken from published studies and previous NICE TAs |
| Adverse events | The only complications of VTE prophylaxis included are major bleeding and HIT (only in sensitivity analysis), both of which are complications of pharmacological prophylaxis | The only adverse event explicitly modelled is major bleeding | Bleeding events are explicitly modelled: intracranial bleeds, major, non-major clinically relevant and minor bleeds |
| Subgroup analysis | Five population subgroups included: (1) hip fracture surgery, (2) THR, (3) TKR, (4) GS, (5) general medical admissions | Four population subgroups included (1) hip fracture surgery, (2) elective hip, (3) gynaecological surgery (hysterectomy), (4) GS | The analysis was segregated into knee replacement and hip replacement patients |
| Discounting | 3.5% (for both costs and QALYs) | 3.5% (for both costs and QALYs) | 3.5% (for both utilities and costs) |
| Approaches to quantifying decision uncertainty | Deterministic and probabilistic sensitivity analyses were performed | Deterministic and probabilistic sensitivity analyses were performed | Deterministic and probabilistic sensitivity analyses were performed |
No existing economic evaluations were found comparing the different types of GCSs, either with or without a background of pharmacological prophylaxis. The prevention of DVT in postoperative surgical patients, however, has been the subject of a full economic evaluation in two previous NICE CGs, comparing a range of thromboprophylaxis strategies which include compression stockings: NICE CG92, issued in 2010,4 and a 2007 CG produced by the National Collaborating Centre for Acute Care at the Royal College of Surgeons of England. 73
The prevention of DVT has also been the subject of three previous NICE single technology appraisals (STAs): TA157111 (Dabigatran etexilate for the prevention of venous thromboembolism after hip or knee replacement surgery in adults), TA170100 (Rivaroxaban for the prevention of venous thromboembolism after THR or TKR in adults) and TA24586 (Apixaban for the prevention of venous thromboembolism after total hip or knee replacement in adults). All three technology appraisals compared different pharmacological prophylaxis interventions for the prevention of DVT but did not explicitly include either type of GCSs as a comparator. The economic models were not publicly available [either in the manufacturer submission or in the Evidence Review Group (ERG) report] for TA157111 and TA170. 100 Thus, only the manufacturer submission and the ERG critique for TA24586 are reviewed and summarised here.
All included studies evaluated the cost-effectiveness of different thromboprophylaxis strategies from an NHS/PSS perspective. The patient population subgroups differed across studies: the NICE CG924 focused on four surgical patient groups and general medical admission patients; the Royal College of Surgeons guideline73 evaluated four surgical patient groups and the NICE TA24586 focused on adult total hip or knee replacement patients, reflecting the scope for the appraisal (see Table 35). In terms of comparators, the CGs from NICE4 and the Royal College of Surgeons73 included mechanical treatments (i.e. IPCDs, FPs and GCSs) in the comparators list, whereas in NICE TA24586 mechanical prophylaxis (e.g. GCSs) was assumed as background therapy for the anticoagulant treatments and thus not explicitly modelled.
The decision-analytic modelling approach used to estimate the cost-effectiveness of different thromboprophylaxis strategies differed between the three included studies. The CGs from NICE4 and the Royal College of Surgeons73 used a decision-tree structure for the cost-effectiveness analysis. Longer-term costs and consequences of these events captured within the decision tree were subsequently modelled within NICE CG92 by applying different ‘payoffs’ (i.e. longer-terms costs and outcomes) depending on particular pathways and events (see Table 35). However, these longer-term payoffs do not appear to have been modelled using a formal structure and instead simple adjustments appear to have been applied to estimate patients’ remaining life-expectancy and costs conditional on events occurring within the decision-tree structure. The model informing Royal College of Surgeons CG73 included longer-term costs and consequences only as part of a sensitivity analysis, where a separate formal Markov process was used to capture the long-term risk of recurrent VTE and PTS. Within NICE TA245,86 the manufacturer employed a two-stage modelling approach: a decision tree to model treatment in the acute phase (up to 90 days post surgery) and a Markov model for long-term events (90 days post surgery and beyond).
Table 35 provides a structured overview of the three included cost-effectiveness models. The three included studies are discussed in more detail below, focusing on key aspects of the economic modelling approach and the sources for key inputs.
Identified cost-effectiveness studies
Population
Although there were differences in the patient populations evaluated across the studies, there was also significant overlap in relation to specific patient subgroups. The 2007 Royal College of Surgeons guideline73 included four surgical population subgroups: (1) hip fracture surgery; (2) THR; (3) gynaecological surgery (hysterectomy); and (4) GS. The 2010 NICE CG924 modelled five population subgroups, four of which were surgical: (1) hip fracture surgery; (2) THR; (3) TKR; (4) GS; and (5) general medical patients. The patient population in NICE TA24586 reflected the marketing authorisation for the technology and consisted of adult patients undergoing THR or TKR surgery.
Comparators
The CGs from NICE4 and the Royal College of Surgeons73 included mechanical treatments (IPCDs, FPs and GCSs) in their list of comparators. Compression stockings in the two NICE guidelines were evaluated as a thromboprophylaxis strategy either independently or in combination with a drug intervention (e.g. heparin or warfarin). In the NICE TA245 for apixaban86 mechanical prophylaxis (defined within the manufacturer submission as graduated elasticated compression stockings, intermittent pneumatic foot compression or foot impulse devices) was considered as background therapy and assumed to be used equally in all patients regardless of pharmacological intervention; therefore, GCSs were not explicitly modelled as a comparator in their economic evaluation.
Model structure
The CGs from NICE4 and the Royal College of Surgeons73 employed similar decision-tree model structures. Figures 18 and 19 provide a schematic of each of the two economic models.
FIGURE 19.
National Institute for Health and Care Excellence CG92 model structure (adapted from CG). 4

The events modelled in the NICE CG924 economic model are: DVT, symptomatic DVT, asymptomatic DVT, PE, PTS, fatal PE, PHT, major bleed, fatal bleed and stroke. The Royal College of Surgeons73 economic model includes DVT, symptomatic DVT, asymptomatic DVT, PE, fatal PE, major bleed, fatal bleed and stroke. Recurrent VTE and PTS were modelled only as part of their sensitivity analysis. Therefore, the structural differences between the two economic models are that (1) DVT and PE have been modelled as different events in NICE CG92, whereas in the Royal College of Surgeons73 economic analysis, a combined event is first modelled and then split into symptomatic DVT, asymptomatic DVT and PE; (2) PHT is modelled as a PE consequence in the NICE CG92 economic model only; and (3) VTE recurrence is explicitly modelled only in the Royal College of Surgeons73 economic analysis and only in a sensitivity analysis scenario.
The apixaban appraisal (NICE TA24586) followed a two-stage modelling approach: a decision-tree structure was used to model treatment in the acute phase (up to 90 days post surgery) and a Markov model was developed for long-term events (90 days post surgery and beyond). The rationale was that postsurgery VTE and bleeding would be captured in the decision tree and future events would be modelled over the patients’ lifetime in the Markov model. The model schematic is provided in Figures 20 and 21. The modelled events in the decision tree (acute phase) included PE, proximal symptomatic DVT, distal symptomatic DVT, proximal asymptomatic DVT, distal asymptomatic DVT, intracranial haemorrhage (stroke), other major bleed, non-major clinically relevant bleed, minor bleed and death. The long-term phase (Markov model) included the following states: well, dead, disabled (having experienced intracranial haemorrhage), untreated VTE (after proximal or distal asymptomatic DVT), treated VTE (after PE, proximal or distal symptomatic DVT), mild to moderate PTS and severe PTS.
FIGURE 20.
National Institute for Health and Care Excellence TA24586 decision-tree structure (replicated from manufacturer submission).

FIGURE 21.
National Institute for Health and Care Excellence TA24586 long-term Markov model structure (replicated from manufacturer submission).
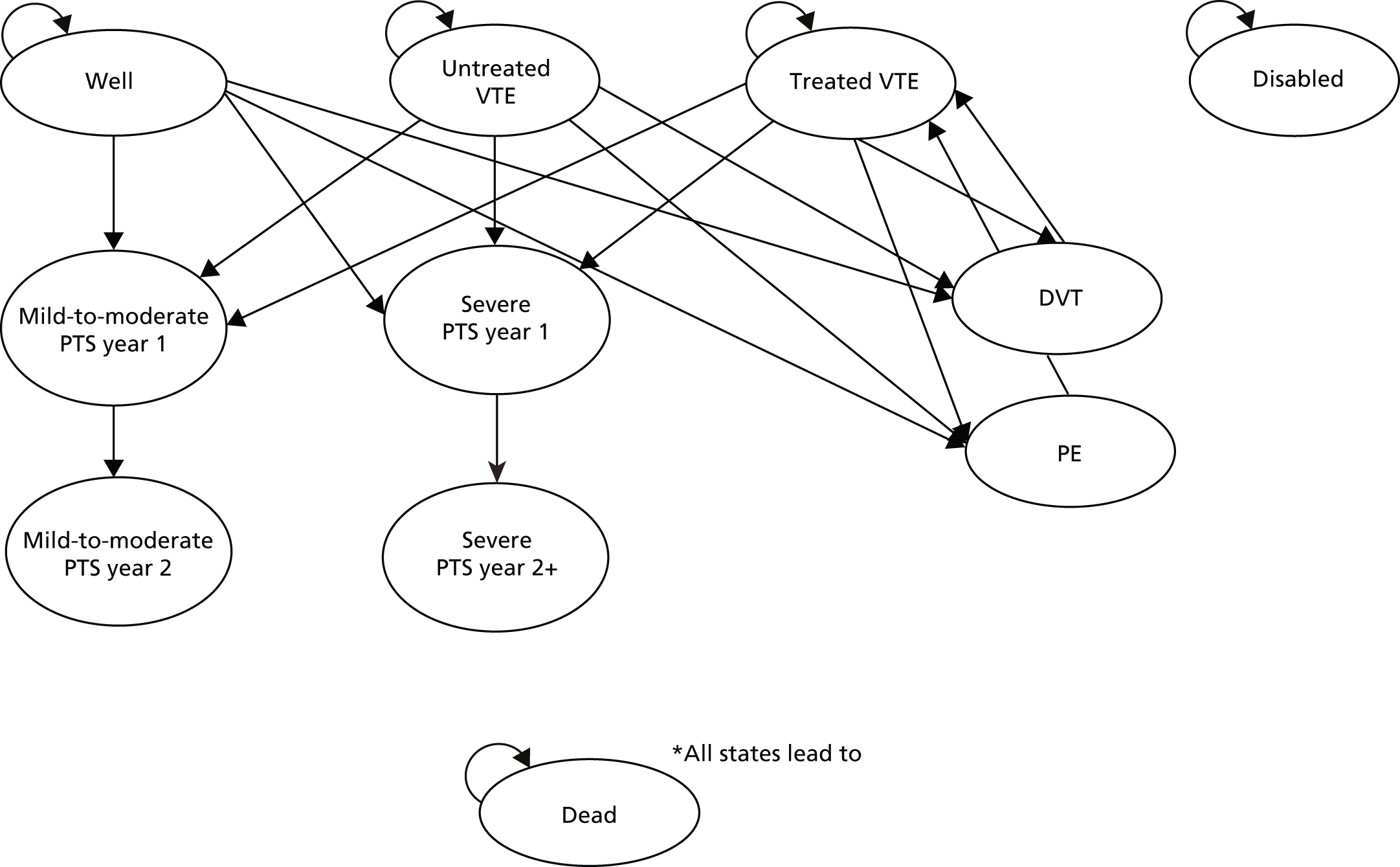
Long-term consequences
The three economic models varied in their approach for the inclusion of VTE long-term consequences. The CG from NICE4 modelled the long-term events of PTS and PHT in their base-case analysis but did not address VTE recurrence. The rates for PTS and PHT were sourced from a published meta-analysis of cohort studies (Wille-Jørgensen et al. 112) and a 2006 cohort study, respectively (Miniati et al. 113).
The base-case analysis of the Royal College of Surgeons economic model73 considered only the cost and health effects of events taking place during the observation period of the trials included in their clinical review, and hence did not address longer-term VTE consequences. As a sensitivity analysis, the model estimated events taking place over 5 years (recurrent VTE and PTS) under the hypothesis that strategies that reduce DVT would lead to a similar reduction in the incidence of recurrence and PTS. Symptomatic VTE recurrence rate and PTS rate after symptomatic VTE were derived from a published cohort study by Prandoni et al. 114 and the PTS rate after asymptomatic VTE from a meta-analysis of cohort studies (Wille-Jørgensen et al. 112). A Markov model was used in the sensitivity analysis to estimate long-term costs and effects; its structure is depicted in Figure 22.
FIGURE 22.
Royal College of Surgeons; Markov model structure for long-term events (adapted from CG). 73
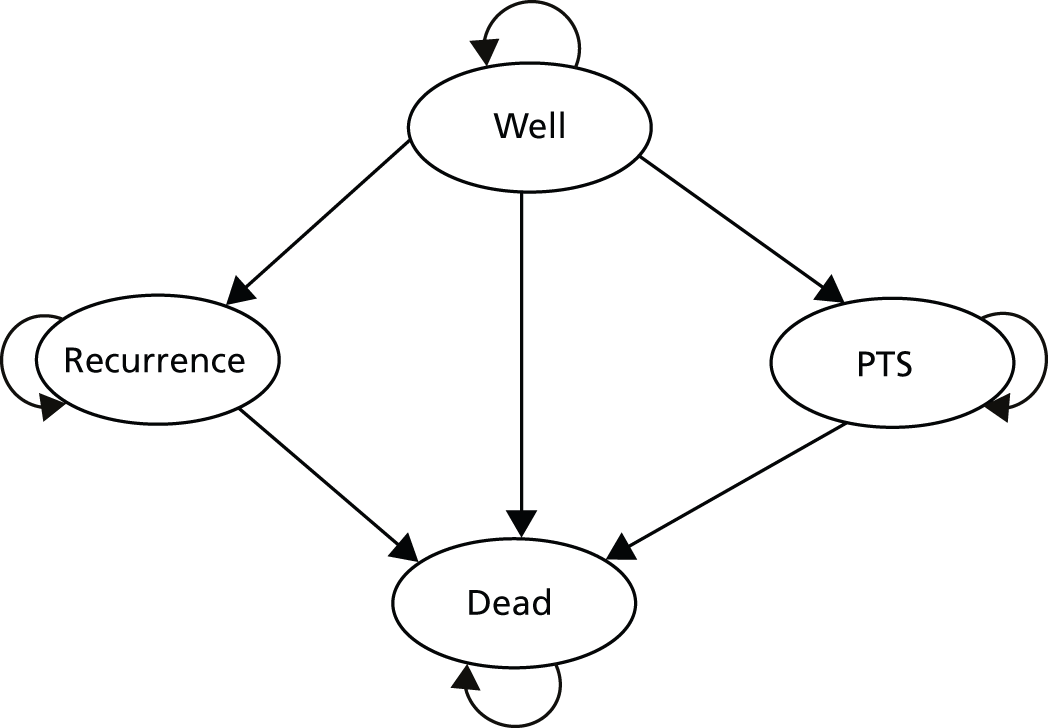
In the apixaban appraisal (NICE TA24586), long-term events were part of the two-stage modelling approach that was employed. The long-term Markov model structure has been presented in Figure 21. At 90 days post surgery, patients were assumed to leave the decision-tree model and enter the long-term Markov model. The event or events that patients experienced in the decision tree would define the state in which those patients would enter the Markov model [i.e. well, dead, disabled (after intracranial haemorrhage), untreated VTE (after asymptomatic DVT), treated VTE (after PE or symptomatic DVT)]. The events/consequences included in the long-term Markov model were: DVT (recurrent), PE (recurrent), mild to moderate PTS and severe PTS. Literature reviews were conducted to identify parameter estimates for the long-term risk of recurrent VTE and/or the development of PTS in patients who suffered an initial VTE event. For DVT recurrence rates, the source was Prandoni et al. ;96 for PE recurrence rate a published meta-analysis by Imperiale and Speroff97 was used; and for mild to moderate and severe PTS, Prandoni et al. 96 was referenced.
Risk of venous thromboembolism
The sections below discuss the approach and source of inputs for baseline risk and relative risk (RR) included in the cost-effectiveness analyses of the three identified studies.
Baseline risk
In the NICE CG924 analysis, data were extracted from three sources to assess the baseline risk of VTE during a surgical admission or soon after: (1) the RCTs identified in their clinical review (specifically from the no prophylaxis arm of the included RCTs), (2) registries of routinely collected clinical data (NHS Hospital Episode Statistics and US clinical registry data) and (3) prospective cohort studies (as identified in the previous NICE surgical guideline115). According to the CG development group, the incidence figures for VTE estimated using registry data were much lower than other estimates, implying under-reporting and/or undertreatment in the community. It was thus decided that the no prophylaxis arms of the RCTs were the best source for the baseline risk of DVT, symptomatic PE and major bleeding in the absence of any prophylaxis and these data were used to inform their cost-effectiveness analysis. For deriving baseline risks, RCTs were grouped according to type of surgery by the guideline development group and separate meta-analyses were performed for each of the five population subgroups.
A similar approach was followed in the Royal College of Surgeons CG,73 where the baseline risks of DVT, symptomatic PE and major bleeding in the absence of prophylaxis were also derived from the no prophylaxis arms of the RCTs included in their clinical review.
In the apixaban NICE technology appraisal (NICE TA24586), enoxaparin, the most widely studied and used LMWH in the UK,86 was used as the reference treatment for calculating baseline risk. Hence, baseline risk in NICE TA245 is not in the absence of prophylaxis, but considers patients on treatment with LMWH. The baseline risk in NICE TA24586 was sourced from the Apixaban Dose orally Vs. ANtiCoagulation with Enoxaparin (ADVANCE)-287 head-to-head trial for knee replacement patients, and from the ADVANCE-388 head-to-head trial for hip replacement surgery patients.
Relative risk
Deep-vein thrombosis RRs in the NICE CG924 analysis were estimated from the RCTs included in their clinical review, with separate NMAs performed for each of the five population subgroups. The estimated RR reductions were then applied within the model to symptomatic DVT, asymptomatic DVT, non-fatal PE, fatal PE, PTS and PHT. For estimating bleeding events RRs, studies were pooled across all population subgroups because data were sparse and a NMA of major bleeding risk was conducted. The estimated bleeding RR increases were applied to fatal bleeds and strokes as well as to non-fatal major bleeding events in the economic model.
The Royal College of Surgeons CG73 followed a different approach: an assumption was made that that the RR change of each prophylaxis strategy is constant regardless of type of surgery and, therefore, the CG development group pooled together the results of RCTs from all surgical categories. The RR reduction in symptomatic PE (fatal and other symptomatic) was assumed to be exactly the same as for DVT, owing to the rarity of the event and the fact that not every study collected PE data. Similarly, an assumption was made in the Royal College of Surgeons73 economic model that the RR increase in major bleeding overall would also be applied to fatal bleeds and strokes.
In the NICE TA24586 economic model, in the absence of head-to-head RCT evidence for apixaban versus rivaroxaban, dabigatran and fondaparinux, an adjusted indirect comparison approach using the Bucher method116 was performed to derive efficacy and safety RRs and inform the economic model. The RR rates were therefore obtained from a synthesis of the published and available data for rivaroxaban (RECORD trials89–92) dabigatran (RE-MODEL,93 RE-NOVATE94,95 trials) and apixaban (ADVANCE-287 and -3 trials88). A mixed-treatment comparison of the relevant trial data was also undertaken and the results were assessed in a sensitivity analysis in the economic model. The post-initial VTE event treatment-independent probabilities were also obtained, where possible, from a synthesis of the published and available data for rivaroxaban (RECORD89–92) dabigatran (RE-MODEL,93 RE-NOVATE,94,95) and apixaban (ADVANCE-287 and -388) trials. For end points that were not reported in the RECORD,89–92 RE-MODEL93 and RE-NOVATE94,95 trials, data were extracted from both arms of the apixaban trials (ADVANCE-287 and -388).
Resource use and costs associated with venous thromboembolism
The NICE CG924 cost-effectiveness analysis considered the following categories of cost and resource use: pharmacological prophylaxis costs; mechanical prophylaxis costs; prophylaxis testing and nurse time; VTE diagnosis and treatment costs; and treatment costs for other events (i.e. stroke, PTS, PHT, major bleeding, reoperation). The duration of prophylaxis included in the economic analysis reflected the average duration of prophylaxis in the RCTs. Unit costs were taken from standard NHS sources: NHS reference costs,103 British National Formulary,104 NHS Electronic Drug Tariff,105 NHS Purchasing and Supplies Agency106 and Unit Costs of Health and Social Care 2007. 107 The costs and resources used for diagnosing and treating VTEs were sourced from published guidelines: British Thoracic Society guidelines on the management of PE98 and British Committee for Standards in Haematology guidance on the prophylaxis and treatment of DVT. 99 For patients with stroke, the NICE acute stroke guideline117 was referenced. PTS and PHT were costed using relevant cohort studies and published HTAs and NICE technology appraisals.
The Royal College of Surgeons economic model73 included intervention costs (pharmacological and mechanical prophylaxis), prophylaxis testing and nurse time, VTE diagnosis and treatment costs and other treatment costs (i.e. stroke, PTS, recurrent VTE, major bleeding with or without reoperation). Unit costs were taken from standard NHS sources: NHS reference costs,103 British National Formulary,104 NHS Electronic Drug Tariff,105 NHS Purchasing and Supplies Agency106 and Unit Costs of Health and Social Care 2005. 109 The duration of prophylaxis modelled also reflected the average duration of prophylaxis in the RCTs included in the guideline’s clinical review. For costing VTE diagnosis and treatment, the same published guidelines as in NICE CG924 were considered. PTS, recurrence and stroke were costed using relevant patient cohort studies from the literature.
The economic model in NICE TA24586 for apixaban considered intervention and comparator costs, testing costs, inpatient stay, VTE diagnosis and treatment costs, postdischarge drug administration costs and costs associated with the long-term Markov model states for PE, DVT, mild to moderate and severe PTS. Drug acquisition costs were sourced from Monthly Index of Medical Specialties110 for comparator treatments and from the manufacturer (Bristol-Myers Squibb/Pfizer) for apixaban. Testing unit costs were taken from the rivaroxaban STA submission to NICE (TA170100). Treatment duration in the economic model was derived from the treatment duration in the relevant clinical trials (i.e. ADVANCE-287 and ADVANCE-388 for apixaban, RECORD89–92 and RE-MODEL93 for rivaroxaban and RE-NOVATE94,95 for dabigatran). NHS reference costs (2008/9)103 were used in the analysis for resource use estimation. The Healthcare Resource Group codes were selected based on those used in the NICE guideline (NICE CG924).
Health-related quality of life
In the NICE CG92,4 a literature search was performed for quality-of-life weightings to inform the economic model. For patients with no event, the population average quality of life for England and Wales measured using the European Quality of Life-5 Dimensions (EQ-5D) instrument was used. 118 For other health states, utility value scores from the published literature were used. A very similar approach was followed in the Royal College of Surgeons guideline. 73
In the apixaban NICE technology appraisal (NICE TA24586) utility decrements were used to model utility losses after patients experienced several events within the economic model. A systematic review was conducted to identify quality-of-life values and decrements for VTE-related events and health states. Utility values were identified for the health states of symptomatic distal DVT, symptomatic proximal DVT, PE, major bleed, well/treated VTE, mild to moderate and severe PTS, and intracranial haemorrhage/disability following intracranial haemorrhage. For fully recovered patients following surgery, the value for the health state of ‘well’ derived from EQ-5D UK population norms (Kind et al. 118) was assumed.
Life expectancy
The NICE CG924 and Royal College of Surgeons73 economic models estimated life expectancy using a combination of general population data and subgroup-specific estimates. For the initial postsurgical period, standardised mortality ratios were applied to the relevant age- and sex-specific England and Wales mortality rate. From that period onwards, the relevant age- and sex-specific life expectancy for England and Wales was assumed. In the NICE CG92,4 patients with PHT were assumed to have a life expectancy of 5 years based on evidence from the literature. 119,120 In the case of patients with stroke, a life expectancy of 4.5 years was assumed, based on the NICE acute stroke guideline. 117 In the case of patients dying during the initial hospitalisation, as a result of a fatal PE or fatal bleeding event, the number of expected life-years in the models was zero.
The economic model in NICE TA24586 for apixaban estimated all-cause mortality based on the relevant age- and sex-specific England and Wales mortality rates. 121 For patients dying during the acute period as a result of a fatal PE or fatal bleeding event, the life expectancy was zero. Minor or non-major clinically relevant bleeding events were not associated with higher mortality. Patients with mild/moderate or severe PTS in the long-term model were allowed to transition to the death state only.
Discussion of the existing cost-effectiveness evidence
Following the assessment of the existing evidence base for the cost-effectiveness of GCSs for the prevention of DVT in postoperative surgical patients, no existing studies were identified comparing different types (lengths) of GCSs; thus, no conclusions can be drawn on the cost-effectiveness of knee-length versus thigh-length GCSs as a thromboprophylaxis strategy in postoperative surgical patients.
The review of the three studies that met the review inclusion criteria, two of which included GCSs regardless of type as a comparator, identified a number of issues and limitations in terms of the structural and other assumptions of the economic modelling approach and the sources used to inform key inputs. These include:
-
Variability in the patient population subgroups considered across the studies. Common surgical patient groups were considered in the two CGs (NICE CG92, Royal College of Surgeons CG);4,73 the patient population in NICE TA24586 considered adult patients undergoing elective knee or hip replacement surgery and reflected the marketing authorisation for the technology.
-
A lack of consensus on the time horizon and the events included in the economic models. Although there is some degree of consensus in how the studies modelled the acute period, there is a differential approach in the inclusion of long-term consequences within the economic models. NICE CG924 models the long-term events of PTS and PHT but does not address VTE recurrence. The Royal College of Surgeons73 base-case analysis considered only events taking place during the observation period of the trials in their clinical review; they estimated only longer-term consequences (recurrent VTE and PTS) in a sensitivity analysis. In the apixaban appraisal (NICE TA24586), long-term events were an integral part of the two-stage modelling approach employed and a Markov model was developed to consider events taking place after the acute phase.
-
A differential approach in deriving baseline risk. The two CGs (NICE CG92,4 Royal College of Surgeons CG73)4,73 have considered patients in the absence of any prophylaxis as the source for estimating baseline risk, whereas the NICE TA14586 has estimated the baseline risk for patients being on-treatment with enoxaparin (LMWH). In addition, the studies that were used to inform baseline risk estimation in the NICE CGs have been critiqued as not being contemporary and not necessarily reflecting current clinical practice.
-
The only complications of thromboprophylaxis included in the economic models were bleeding events, which are associated with pharmacological prophylaxis, and their consequences. There is a lack of compression stockings evidence in the cost-effectiveness studies that could inform an economic model comparing different types of GCSs, such as patient adherence and compliance to GCSs or complications and adverse events related to the use of GCSs.
Chapter 5 Cost-effectiveness and value of information: development of the decision-analytic model
General approach
A decision-analytic model was developed to formally assess the cost-effectiveness of knee-length versus thigh-length GCSs for the prevention of DVT in postoperative surgical patients from the perspective of the UK NHS and PSS. Outcomes are expressed in terms of QALYs and costs are expressed in GBP. Both costs and QALYs are evaluated over a lifetime horizon and discounted using a 3.5% annual discount rate.
The expected cost and QALYs for each of the strategies were estimated and compared using incremental cost-effectiveness ratios (ICERs) where appropriate. The ICER represents the incremental cost per additional QALY associated with a more costly and effective strategy. The ICER can be compared with thresholds used by NICE to establish value for money in the NHS (currently in the region of £20,000–30,000 per additional QALY). These thresholds can be used to identify the optimal strategy in terms of cost-effectiveness considerations based on existing evidence.
The model is probabilistic in that input parameters are entered into the model as probability distributions to reflect parameter uncertainty (i.e. uncertainty in the mean estimates). Monte Carlo simulation is used to propagate uncertainty in input parameters through the model in such a way that the results of the analysis can also be presented with their associated uncertainty. The probabilistic analysis (PSA) also provides a formal approach to quantifying the consequences associated with the uncertainty surrounding the model results and can be used to identify priorities for future research.
A range of scenarios were undertaken to assess the impact of key uncertainties related to input parameters and assumptions. Consistent with available evidence, the model also assessed the variability in the cost-effectiveness of alternative strategies for specific subgroups of patients.
We used formal methods based on VOI approaches to identify potential research priorities and to establish whether or not investment in a large-scale RCT is likely to be cost-effective. These approaches can be used to inform the need for major investment in future research and also prioritise specific research questions. The methods and results of the VOI analyses are reported in Chapter 7.
Decision problem
This assessment aims to establish the expected value of undertaking additional research comparing the relative effectiveness of thigh-length GCSs with knee-length GCSs, in addition to standard pharmacological thromboprophylaxis, for the prevention of DVT in postsurgical patients. An evidence synthesis was undertaken to estimate clinical effectiveness and inform key clinical parameters for the decision model (see Chapter 2, Network meta-analysis). Here, we discuss the development of a decision-analytic model to formally assess the cost-effectiveness of knee-length versus thigh-length GCSs in addition to standard pharmacological prophylaxis for the prevention of DVT in surgical patients.
Interventions
The thromboprophylaxis strategies being compared in the economic model are:
-
LMWH, which is assumed to be the background pharmacological prophylaxis therapy, administered to all patients in the economic model
-
thigh-length GCSs in addition to standard pharmacological prophylaxis (i.e. LMWH)
-
knee-length GCSs in addition to standard pharmacological prophylaxis (i.e. LMWH).
Although the focus of the assessment was on the relative cost-effectiveness of the different lengths of GCSs as adjunctive treatments to standard pharmacological prophylaxis, owing to the requirements of the model it was necessary to include standard pharmacological prophylaxis alone as an additional comparator. This is because the model requires one of the strategies to function as a source of natural history (or baseline) data to which the relative treatment effects of the comparator strategy or strategies are then applied in order to estimate their predicted event rates. It would have been possible to use either thigh- or knee-length GCSs (in addition to standard pharmacological prophylaxis) as a source of baseline data and then to apply the relative treatment effect of the alternative length GCSs to estimate absolute event rates for both types of stockings. However, we considered that this would introduce additional uncertainty into the analysis, which was not warranted based on the best available evidence and the additional reviews undertaken. Given the relatively small number of trials for GCSs, using these studies to estimate both the baseline event rates and the relative effectiveness of the main strategies would inevitably have resulted in significant uncertainty surrounding both these elements. However, the clinical effectiveness review also identified other external sources of natural history data in relation to the VTE rate itself, which were derived from significantly larger studies and hence provided more precise estimates of the underlying rate of VTE. The external data also allowed variation in the rate of VTE to be explored in relation to specific subgroups. Therefore, it was decided that using external sources of data to provide a baseline in the model was more appropriate than using the RCTs of GCSs identified in our review.
The external sources, however, typically reported estimates for either a no treatment strategy or pharmacological therapy (e.g. LMWH). Consequently, it was necessary to incorporate an additional strategy within the economic model to populate the baseline event rate and then link to the different types of GCSs via the relative effect estimates derived from the synthesis reported above. The justification for including LMWH to function as a baseline in the model is discussed further below (see Baseline risks: acute phase model).
Population
The decision model evaluates the cost-effectiveness of knee-length versus thigh-length GCSs for five surgical population subgroups:
-
THR
-
TKR
-
GS: low-risk patients
-
GS: moderate-risk patients
-
GS: high-risk patients.
The impact of patient heterogeneity (e.g. as a result of different clinical characteristics) is thus explored in separate analyses. This approach ensures that uncertainty in the decision owing to the imprecision in parameter inputs can be separated from uncertainty over whether or not an intervention is cost-effective for particular subgroups of the population.
Although the population subgroup of hip fracture surgery patients was evaluated in previous NICE guidelines (NICE CG924), we did not identify appropriate evidence to inform key parameter inputs for the current economic analysis (i.e. baseline risk for hip fracture surgery patients on LMWH, patient population numbers for hip fracture surgery). Therefore, the hip fracture surgery subgroup has not been evaluated as part of the current analysis.
Outcomes
The model was developed in accordance with the NICE reference case. 122 The primary outcomes of the analysis are QALYs gained and incremental cost. Costs were estimated from an NHS and PSS perspective. Both costs and QALYs are evaluated over a lifetime horizon and discounted using a 3.5% annual discount rate.
The model
A two-stage modelling approach was adopted to model the VTE pathway, informed by the findings of the cost-effectiveness review. In common with many of the existing model structures, we considered two related elements, reflecting an acute phase post surgery and longer-term consequences. Initial VTE episodes are modelled for the acute period (typically up to 14 days post surgery), but QALYs and health service costs associated with the long-term consequences following an initial VTE episode (i.e. PTS and PHT), as well as consequences of any recurrent VTE event, are modelled in the long-term Markov models, with a lifetime time horizon. Similarly, major bleeding events are modelled for the acute period, but costs and health benefits arising from these events are modelled over the patient’s lifetime.
-
Acute phase: a decision-tree structure has been used to model events taking place in the acute phase (up to 14 days post surgery) and a separate series of Markov models have been designed to model the long-term consequences and the recurrent events that patients can experience after having an initial VTE event. The decision-tree structure is depicted in Figure 23. Depending on the initial VTE event (i.e. symptomatic DVT, asymptomatic DVT, symptomatic PE), patients can experience different long-term consequences and different rates of recurrent VTE events; they are therefore assumed to enter separate Markov models.
-
Long term: conditional on the pathway during the acute phase, a Markov structure is subsequently used to characterise the long-term prognosis over the remainder of a patient’s lifetime. Annual cycles are employed to reflect the annual probability of further VTE events (and associated consequences) and death for each year after the acute period. Therefore, the extent to which the different thromboprophylaxis strategies reduce the risk of VTE events during the acute period will be translated into differences in long-term costs and QALYs on the basis of the long-term model.
FIGURE 23.
Decision-tree model structure.
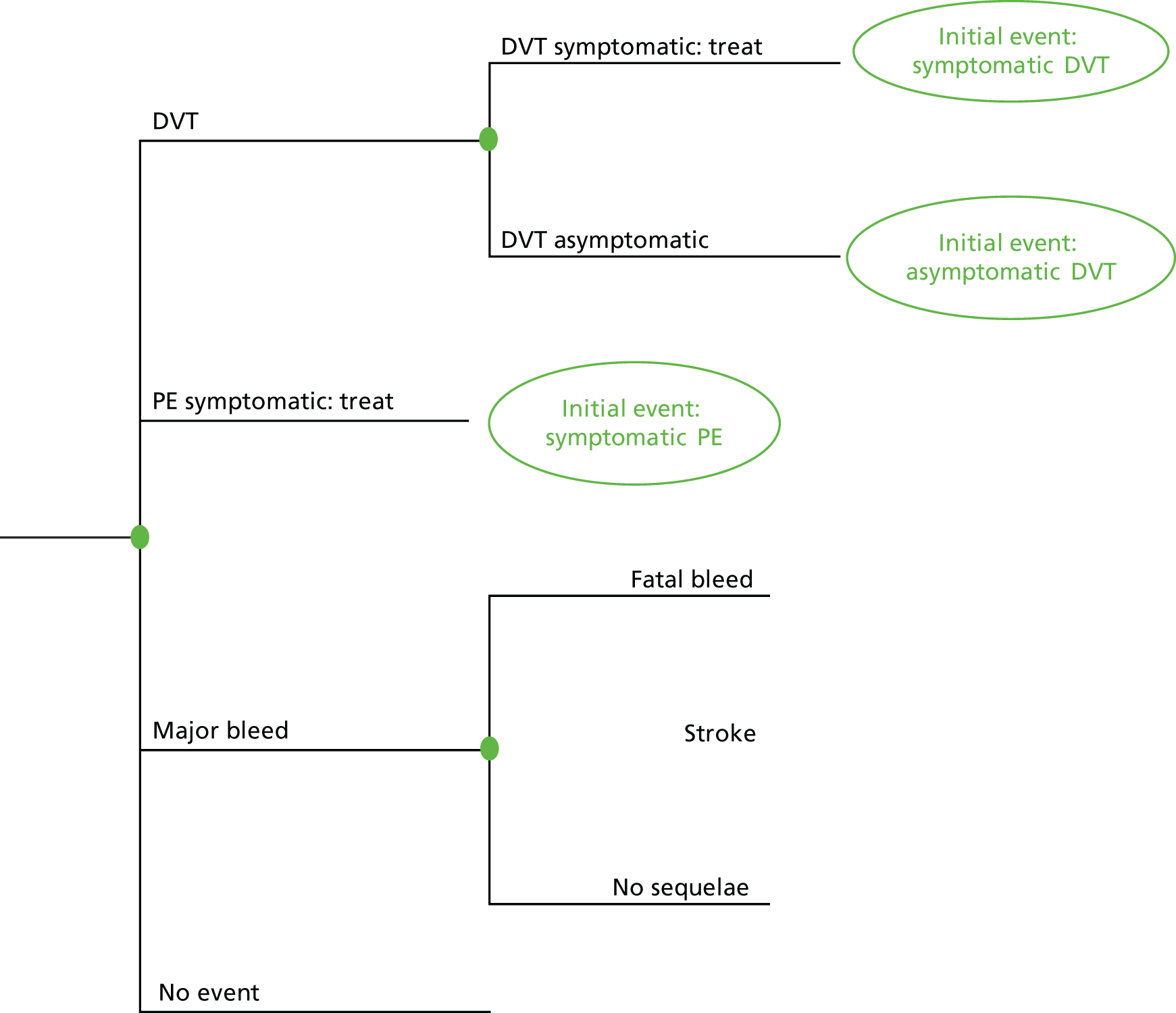
The Markov model schematics after an initial symptomatic PE, symptomatic DVT and asymptomatic DVT are presented in Figures 24–26. The various health states are represented using circles, and possible transitions between the health states are represented with arrows. Transition to the death state is possible from each of the separate health states and potentially differs depending on the particular state in which a patient resides during each cycle. For the purposes of simplifying the figures, the death state is represented separately for two of these. However, within these particular figures separate transitions are still applied.
FIGURE 24.
Long-term Markov model structure after an initial symptomatic PE event.

FIGURE 25.
Long-term Markov model structure after an initial symptomatic DVT event.

FIGURE 26.
Long-term Markov model structure after an initial asymptomatic DVT event.
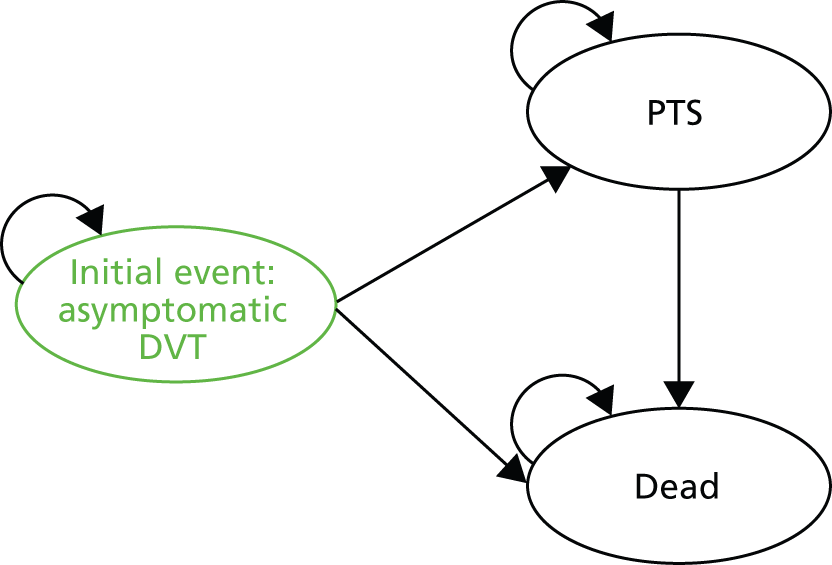
The economic model (decision tree and Markov) is populated with different parameter inputs for each prophylaxis strategy (i.e. LMWH prophylaxis alone, thigh-length GCSs plus LMWH prophylaxis, knee-length GCSs plus LMWH prophylaxis). As previously stated, LMWH is incorporated to provide a baseline source of data for the VTE event rates, and the results of the evidence syntheses reported above are used to estimate the equivalent event rates for the two GCSs strategies. Similarly, although the same structure is applied to each of the population subgroups, different parameter inputs are estimated for each of the population subgroups listed in Chapter 5, Population.
The key features of the economic evaluation are presented in Table 36.
| Factor | Approach employed |
|---|---|
| Time horizon | Decision tree: up to 14 days Markov models: lifetime |
| Cycle length (Markov) | 1 year |
| Half-cycle correction (Markov) | Yes |
| Were health effects measured in QALYs; if not, what was used? | Health effects were measured in QALYs and life-years |
| Discount of 3.5% for utilities and costs | Utilities and costs were discounted at 3.5% |
| Perspective | NHS and PSS |
Baseline risks: acute phase model
Venous thromboembolism events
The clinical effectiveness and cost-effectiveness of the different VTE prophylaxis strategies in the economic model depends not only on the differences between their relative effectiveness, but also on the change in terms of absolute risk for each strategy. Consequently, the baseline risk of VTE is an important determinant of the absolute risk and, hence, cost-effectiveness.
As discussed in Chapter 2, the review of RCTs of effectiveness of thigh-length and knee-length GCSs has provided some data on baseline risk of DVT from the no prophylaxis arms of the trials. To ensure that the best available data are used in the model, searches for existing systematic reviews of risk of DVT in surgical populations were also undertaken, as well as searches for national and international guidelines, for example the guidelines of the ACCP on the prevention of VTE. 123,124 In addition, the approaches used to estimate baseline risk in previous published cost-effectiveness studies were considered.
In terms of the previous cost-effectiveness studies, the NICE CG924 economic model derived estimates of the baseline risk of VTE from the no prophylaxis arms of the studies included in their clinical review. The Royal College of Surgeons CG73 followed a similar approach; the baseline risks of DVT, symptomatic PE and major bleeding in the absence of prophylaxis were also derived from the no prophylaxis arms of the RCTs included in their clinical review.
Although it would have been feasible to use a similar approach within this assessment, the use of ‘no prophylaxis’ as the source of baseline data was rejected on the following grounds:
-
Many of the RCTs that were used to inform the baseline risk estimates within the NICE CG924 date back to the 1970s and 1980s and, therefore, may not appropriately reflect current clinical practice and current surgery techniques. Consequently, there is a significant risk of bias if advances in clinical practice (independent from changes in prophylaxis management) have resulted in lower VTE rates.
-
Estimates linking both types of GCSs (in addition to conventional pharmacological management) are sparse and therefore highly uncertain. Results from the no interaction, random-effects NMA conducted and discussed in Chapter 3 reveal wide CrIs around the comparisons with no treatment. In addition, it would not be possible to link either type of GCSs to no treatment using the no interaction, lumped random-effect NMA.
The searches for systematic reviews of risk of DVT, and the searches for national and international guidelines addressing the risk of DVT identified several potentially relevant guidelines, risk models and risk algorithms; these have been presented in Chapter 3, Baseline risk of deep-vein thrombosis, and summarised in Appendix 4. Most of these approaches for calculating baseline risk of DVT, however, could not easily be applied within an economic model owing to their rather qualitative and descriptive nature.
The two guidelines from the ACCP for the prevention of VTE in orthopaedic surgery patients123 and the prevention of VTE in non-orthopaedic surgery patients124 were identified as the most comprehensive and rigorous guidelines and were considered to be the best source of VTE baseline risk estimates. The ACCP guidelines provide contemporary estimates for baseline risk of VTE events for patients on LMWH prophylaxis that can directly inform the economic model. These estimates were derived from large-scale RCTs that were considered to provide more precision and less bias than other alternatives considered. Table 25 summarises the baseline risk estimates from the ACCP guidelines for the orthopaedic123 and non-orthopaedic patients. 124
Relative effectiveness
The differences between prophylaxis strategies in terms of costs and health outcomes are driven by the relative effectiveness of each strategy in the reduction of VTE events. For example, the number of symptomatic DVT events occurring under the thigh-length GCSs plus LMWH strategy is the baseline risk of symptomatic DVT (i.e. the risk for patients being on LMWH prophylaxis only) adjusted for the relative effectiveness for thigh-length GCSs plus LMWH compared with LMWH alone.
Venous thromboembolism
The results of the clinical effectiveness review, discussed in Chapter 3, were used to estimate the relative effectiveness of thigh-length versus knee-length GCSs, in addition to standard pharmacological prophylaxis, for postsurgical patients at risk of DVT. Results from all analyses have been reported in Chapter 3, Network meta-analysis results.
The relative effectiveness inputs that were subsequently used within the economic model are sourced from:
-
The base-case NMA based on the no interaction, random-effect analysis, using the predictive distribution output. The impact of this type of analysis on the uncertainty around the results is further discussed in Chapter 7.
-
The direct meta-analysis comparing thigh-length GCSs (with pharmacological prophylaxis) with knee-length GCSs (with pharmacological prophylaxis).
The justification for using the predictive distribution and its impact are discussed in Chapter 7, Expected value of perfect information results.
In the absence of differential estimates for each type of VTE event, the relative effectiveness estimates were applied to all VTE events included in the model (i.e. symptomatic DVT, asymptomatic DVT and symptomatic PE). The relative effectiveness inputs used in the economic model are summarised in Tables 37 and 38. These relative effectiveness rates were assumed to be common for all population subgroups evaluated.
| Intervention | Thigh + drug, median (CrI) |
|---|---|
| Drug | 2.60 (1.58 to 4.87) |
| Knee-length GCSs + drug | 1.76 (0.82 to 3.53) |
| Intervention | Thigh-length GCSs + drug, median (CrI) |
|---|---|
| Knee-length GCSs + drug | 1.51 (0.40 to 5.73) |
It should be noted that, although the NMAs in Chapter 3, Network meta-analysis results, grouped LMWH, LDH and fondaparinux under the term ‘heparin’ as a comparator, the relative effectiveness results were subsequently applied to LMWH in the economic model. This is because of the strategies that are being compared in the analysis and the type of evidence that was used to inform the baseline risks (i.e. for patients on treatment with LMWH).
Bleeding
Bleeding events are a complication associated with pharmacological prophylaxis. Hence, we assumed that GCSs prophylaxis (thigh-length or knee-length stockings) in addition to standard LMWH prophylaxis is not expected to alter the incidence of bleeding events compared with LMWH prophylaxis alone. In the economic model, the bleeding event rates and their associated consequences are assumed to be the same across all three prophylaxis strategies (LMWH alone, LMWH plus thigh-length GCSs, LMWH plus knee-length GCSs).
Similarly to the baseline risks for VTE events, the baseline risks for bleeding events in the economic model have been sourced from the two guidelines from the ACCP for the prevention of VTE in orthopaedic surgery patients123 and the prevention of VTE in non-orthopaedic surgical patients. 124 These baseline risk rates for bleeding events refer to patients on treatment with LMWH and can be directly used in the economic model. Table 39 reports the baseline risk estimates for bleeding events used in the economic analysis.
| Population | Major bleeding risk: on LMWH (%) |
|---|---|
| Orthopaedic surgery patients | 1.50 |
| GS patients | 2.44 |
Other complications
The only complication of prophylaxis included in the economic model is major bleeding events, a complication of pharmacological prophylaxis. There may be other important complications associated with VTE prophylaxis but they are more difficult to quantify. Mechanical prophylaxis is not without potential complications. Chapter 3, Results of studies included in the review of patient adherence and preference, presented evidence of patients not adhering to compression stockings usage, with the main reasons being related to discomfort, provision of stockings, removing stockings for bathing or no longer requiring them owing to ambulation. Incorrect GCSs use is also an issue and is related to wearing incorrectly sized stockings, or to the rolling down, binding or wrinkling of the stocking.
Incorrect GCSs use suggests that some disutility (i.e. reduced quality of life) is associated with stockings, but this disutility is difficult to quantify and might be negligible compared with the patient’s underlying condition. Perhaps of more concern is that the discomfort might cause patients not to adhere to GCS use or to wear the stockings incorrectly (especially thigh-length stockings); this might mean that the effectiveness estimated in trial conditions might not be replicated in practice.
To account, to some extent, for those concerns, the cost of nurse time for checking that stockings are fitted correctly has been included in the economic model (see Prophylaxis costs). In addition, the potential impact of differential levels of adherence for thigh-length and knee-length stockings that may arise in a real-world setting has been explored in scenario analyses.
To explore the effect of differential adherence to thigh-length versus knee-length stockings that may occur in clinical practice settings rather than controlled trial settings, scenarios were run in which the adherence of patients to thigh-length stockings was varied. The levels of adherence in these scenarios were informed by the studies reporting comparative adherence rates of thigh-length versus knee-length stockings in Chapter 3, Results of studies included in the review of patient adherence and preference.
Post-thrombotic syndrome, pulmonary hypertension and stroke
The risk of longer-term events was estimated to be conditional on the initial acute risk of VTE (and the type of VTE). In the absence of evidence, the risk of longer-term events was assumed to be the same for each of the population subgroups evaluated. To estimate these probabilities in the current model, we employed a similar approach and data sources to previously published cost-effectiveness studies.
In particular, the NICE CG924 estimates for PTS after an initial VTE event, PHT after a symptomatic PE event and the proportion of major bleeding episodes that lead to stroke were used as inputs in the economic analysis for this assessment. These inputs are summarised in Table 40. It should be noted that the 5-year PTS rates and 2-year PHT rates were annualised and converted to probabilities prior to being used as inputs within the economic model.
| Event | Probability (%) | Source | Method |
|---|---|---|---|
| 5-year PTS rate after symptomatic DVT | 25.0 | Prandoni et al. (1997)114 | 528 consecutive patients with venographically confirmed symptomatic DVT followed for 8 years |
| 5-year PTS rate after symptomatic VTE | 25.0 | The incidence of PTS after symptomatic PE was assumed to be the same as after a symptomatic DVT | |
| 5-year PTS rate after asymptomatic VTE | 15.0 | Expert opinion: derived from Wille-Jørgensen et al. (2005)112 | Meta-analysis of cohort studies (n = 364). Follow-up was 2–10 years |
| 2-year chronic thromboembolic PHT rate after symptomatic PE | 0.75 | Expert opinion: derived from Miniati et al. (2006)113 | Cohort study of patients with proven PE (n = 320) compared with those without (n = 514) |
| Proportion of major bleeds that lead to chronic morbidity (i.e. non-fatal strokes) | 3.0 | Muntz et al. (2004)125 | Systematic review of thromboprophylaxis RCTs |
Venous thromboembolism recurrence
Patients who have had an initial symptomatic VTE event within the economic model (i.e. a symptomatic DVT or a symptomatic PE event) were assumed to be at risk of experiencing a recurrent VTE event. NICE CG924 did not address VTE recurrence within the economic model, and the RCTs included in their clinical review would be unsuitable to determine the baseline risk of VTE recurrence, because of their short follow-up time. Another source for VTE recurrence rates had, therefore, to be identified to inform the economic model.
The NICE CG1449 assessed the benefit of different durations of treatment for individuals with a first VTE episode. VTE recurrence was thus an integral part of their analysis. Recurrence rates in NICE CG1449 were sourced from a published study by Baglin et al. 79 These VTE recurrence rates were used to inform the current economic model and are listed in Table 41. The 5-year rates of recurrent VTE events were annualised and converted to probabilities prior to being included in the economic model.
| Recurrence rate (%) | Initial event: symptomatic PE | Initial event: symptomatic DVT | Source |
|---|---|---|---|
| VTE recurrence rate per year (years 1–5) | 5.1 | 6.0 | Baglin et al.;79 annual rate for years 1–5 (converted to probability) |
| PE recurrence rate per year (years 1–5) | 2.6 | 0.9 | |
| DVT recurrence rate per year (years 1–5) | 2.6 | 5.1 |
No evidence was identified to inform recurrence rates for VTE events after an initial asymptomatic DVT event. Patients experiencing an initial asymptomatic DVT event were therefore not assumed to be at risk of recurrence in the economic model.
Other parameters that vary by population subgroup
Table 42 summarises other inputs in the economic analysis that are assumed to vary by population subgroup.
| Parameters | THR | TKR | GS |
|---|---|---|---|
| Mean age (years) | 69a | 69a | 60b |
| Male (%) | 39a | 43a | 50b |
| Standardised mortality ratio (%) | Men: 85;c women: 98c (10 years) | 52d (1 year) | 100e (1 year) |
| Proportion of DVTs that are symptomatic (ratio of symptomatic DVTs to all DVTs) (%) | 21.0f | 5.0f | 6.2b |
| Major bleeding fatality rate (%) | 0.8g | 0.8g | 0.8b |
| PE fatality rate (%) | 6.00b | 6.00b | 6.00b |
| Reoperation rate after major bleed (%) | 13b | 13b | 21g |
Resource use and cost
Prophylaxis costs
The unit costs of LMWH and GCSs, and the respective sources of this information are provided in Table 43. LMWH prices were taken from the British National Formulary130 for the recommended dose and GCSs published prices were sourced from the NHS Electronic Drug Tariff. 131
| Item | Price | Source |
|---|---|---|
| LMWH (GS) | £2.72 per day | British National Formulary, June 2014130 |
| LMWH (orthopaedic surgery) | £3.14 per day | British National Formulary, June 2014130 |
| GCSs (thigh-length, 25–35 mmHg at ankle) | £14.28 per pair | NHS Electronic Drug Tariff, June 2014131 |
| GCSs (knee-length, 25–35 mmHg at ankle) | £12.28 per pair | NHS Electronic Drug Tariff, June 2014131 |
| GCS: thigh-length | £6.36 per pair | Clinical advisors/expert opinion |
| GCS: knee-length | £4.31 per pair | Clinical advisors/expert opinion |
With respect to the cost of GCSs, however, differences were identified between the published prices (sourced from the NHS Electronic Drug Tariff131) and the estimates of the actual prices paid, as obtained from our clinical advisors for this assessment. Those different price levels for GCSs are reported in Table 43 and their impact on the cost-effectiveness results is explored in scenario analyses in Chapter 6.
The duration of prophylaxis in the NICE CG924 economic model reflected the average duration of prophylaxis in the RCTs in their clinical review and was assumed to be subgroup specific. The same duration of prophylaxis was considered in the current economic analysis and ranged between 7 and 10 days (Table 44).
| Subgroup | Duration of prophylaxis in the economic model (days) |
|---|---|
| THR | 10 |
| TKR | 10 |
| GS | 7 |
To derive the total prophylaxis cost per strategy, the costs of nurse time and monitoring tests per strategy were added. These are reported in Table 45. For nursing time, the NICE CG924 assumed 5–10 minutes of nursing time per day for mechanical prophylaxis strategies (i.e. IPCDs, FPs and GCSs). In the current economic analysis, the lower end of this range was assumed (i.e. 5 minutes per day) owing to the fact that GCSs were assumed to be less complicated to fit and monitor than the other types of mechanical prophylaxis.
| Prophylaxis method | Tests required | Nurse time | Source |
|---|---|---|---|
| LMWH | Full blood count (at baseline, then every 2–4 days) | 2–3 minutes per injection | NICE CG924 |
| GCS | – | 5 minutes per day | NICE CG924 |
Table 46 summarises the total cost for each thromboprophylaxis strategy included in the economic model.
| Costs | THR | TKR | GS |
|---|---|---|---|
| Total prophylaxis cost: LMWH | 64.5 | 64.5 | 42.8 |
| Total prophylaxis cost: LMWH + thigh-length GCS | 148.1 | 148.1 | 109.9 |
| Total prophylaxis cost: LMWH + knee-length GCS | 144.1 | 144.1 | 105.9 |
Venous thromboembolism treatment costs
To estimate the resource use and costs for diagnosing and treating symptomatic VTE episodes, we applied NHS reference costs for the treatment of symptomatic DVT and symptomatic PE events (Table 47). 132
| Event | Cost (£) | Source |
|---|---|---|
| Symptomatic DVT | 974 | NHS reference costs 2012–13132 DVT HRGs (QZ20A–QZ20E): weighted average of costs for non-elective inpatient treatment of DVT; long and short stay |
| PE | 1481 | NHS reference costs 2012–13132 PE HRGs (DZ09D–DZ09H): weighted average of costs for non-elective inpatient treatment of PE; long and short stay |
In clinical practice, there would be no treatment cost associated with asymptomatic DVT. This has been a standard assumption in previous VTE prophylaxis models and was also assumed in the current analysis.
In the absence of more detailed information in the published literature, it is also assumed that the cost of treating a VTE episode does not vary by population subgroup (i.e. THR, TKR, GS).
Long-term costs
For PTS, PHT and stroke, the treatment pathways are varied and complex, and previous cost-effectiveness studies have used costs estimates from relevant cohort studies of patients from the literature. The NICE CG924 economic model identified these sources primarily through systematic reviews and rapid searches of the HEED and PubMed databases. No updated studies were identified to inform the current economic model; therefore, the NICE CG924 resource-use sources were updated and used to estimate the cost of long-term consequences of VTE and bleeding events (Table 48). All cost estimates have been inflated to 2012/13 prices, using the Hospital and Community Health Services Pay and Prices Index. 132
| Event | Cost £ (2012–13 values) | Source | Method |
|---|---|---|---|
| PTS | 762 (per year) | Average of: Bergqvist et al. (1997)133 Goodacre et al. (2006)134 (HTA report) |
Retrospective cohort study of 250 Swedish patients followed for 15 years after first symptomatic DVT Protocol derived for the NHS HTA cost-effectiveness analysis |
| PHT | 1422 (per month) | NICE technology appraisal on pulmonary arterial hypertension (adults)135 | |
| Major bleeding without reoperation | 1428 (per episode) | National Schedule of Reference Costs 2012–13132 | Mean cost of HRG codes for gastrointestinal bleed, without interventions (FZ38M, FZ38N, FZ38P) |
| Reoperation (GS) | 2719 (per episode) | National Schedule of Reference Costs 2012–13132 | Mean cost of HRG codes for gastrointestinal bleed, with single intervention (elective and non-elective) |
| Reoperation (orthopaedic surgery) | 3085 (per episode) | National Schedule of Reference Costs 2012–13132 | Average of HRG codes for minor hip procedures for non-trauma (HB15D, HB15E, HB16B, HB16C) |
| Stroke (first year) | 9793 (per year) | Grieve et al. (2000)136 | 328 NHS patients followed prospectively for 12 months after stroke |
| Stroke (subsequent years) | 5628 (per year) | NICE stroke guideline, 2008117 | Assuming that 38% dependent stroke and 62% independent stroke |
Bleeding events and stroke costs
The cost of treating major bleeding is assumed to vary primarily according to whether or not there is a decision to reoperate. Rates of reoperation after a bleeding episode differ per patient subgroup within the economic model and were sourced from the NICE CG924 economic model (see Table 48).
For patients with stroke, the NICE acute stroke guideline117 was used to inform the cost and resource use associated with stroke during the first year and for subsequent years (see Table 48).
Life expectancy
Fatal events
Naturally for patients dying during the initial hospitalisation, their expected life-years in the model is zero. This refers to patients who experience (1) a fatal PE or (2) a fatal bleeding event.
Patients without long-term consequences
For patients surviving surgery, life expectancy has been estimated using a combination of general population data and subgroup-specific estimates.
-
For TKR and GS patients, for the first 12 months standardised mortality ratios were applied to the relevant age- and sex-specific England and Wales mortality rate, so that for the first year after surgery disease-specific mortality was used. For these patients, from 12 months onwards, age- and sex-specific life expectancy for England and Wales was assumed using 2009–11 interim life tables for England and Wales137).
-
For THR patients, the standardised mortality ratio was applied for 10 years.
Patients surviving with long-term consequences
In the absence of specific evidence, it was assumed that the life expectancy of patients with PTS would be the same as for other patients in their population subgroup who did not experience PTS.
For patients with PHT, a life expectancy of 5 years was assumed based on evidence from the literature, as used in the NICE CG92 economic model. 119,120
For patients with stroke, a life expectancy of 4.5 years was assumed, based on the NICE acute stroke guideline. 117
Patients with recurrent venous thromboembolism events
Recurrent VTE events (i.e. recurrent symptomatic DVT and recurrent symptomatic PE) were assumed not to have an impact on the life expectancy of patients within the economic model, apart from the proportion of patients for whom a recurrent symptomatic PE event would be fatal.
Quality-of-life weightings
For patients with no event, the population average quality of life from EQ-5D UK population norms (Kind et al. 118) was assumed. For other health states, utility value scores from the published literature were used. This is a very similar approach to the NICE CG92 economic model. 4
The utility weights and utility values used in the economic model are summarised in Table 49.
| Health state | Utility | Source | Duration of health state after initial event |
|---|---|---|---|
| No event (general population average) | 0.82 | Kind et al. (1998)118 | Lifetime |
| Asymptomatic DVT/asymptomatic PE | 0.82 | Assumed no disutility | Lifetime |
| Warfarin treatment after a symptomatic VTE event | 0.82 × 0.99 = 0.81 | Gage et al. (1996)138 Time trade-off, 70 patients with atrial fibrillation |
3 months distal DVTa 6 months proximal DVTa 6 months PE (then return to usual quality of life) |
| Symptomatic PE | 0.82 × 0.94 = 0.771 | Goodacre et al. (2006)134 | 1 month, then treatment with warfarin |
| Recurrent PE | 0.82 – 0.06 = 0.760 | Goodacre et al. (2006)134 based on expert opinion on PE | 1 month (then return to usual quality of life) |
| Recurrent DVT | 0.820 | Assumed no disutility | Lifetime |
| PTS | 0.82 × 0.982 = 0.805 | O’Meara et al. (1994)139 | Lifetime |
| PE (symptomatic) | 0.82 × 0.94 = 0.771 | Goodacre et al. (2006)134 | 1 month then treatment with warfarin |
| PHT | 0.765 | NICE guideline on pulmonary arterial hypertension135 | Life expectancy: 5 years |
| Major bleeding | 0.50 | Sarasin et al. (2000)140 (based on expert opinion) | 1 month then return to usual quality of life |
| Stroke | 0.52 | The FOOD Trial Collaboration, (Lancet 2005 EQ-5D, 3086 stroke patients in a RCT141) | Life expectancy: 4.25 years |
| Fatal bleeding | N/A | ||
| Fatal PE | N/A |
Analytic methods
The model was developed in Microsoft Excel. The model was run several times to explore alternative scenarios. Owing to the model complexity and the number of scenario analyses, the Monte Carlo simulation was run for 1000 iterations across all scenarios. However, 10,000 iterations were run for the base-case scenario for each population subgroup to validate the consistency of the results. The main scenarios shown as represent the uncertainty surrounding the most appropriate assumptions and statistical model from the clinical effectiveness review.
-
the base-case NMA based on the no interaction, random-effects analysis, using the predictive distribution output
-
the direct meta-analysis comparing thigh-length GCSs (plus pharmacological prophylaxis) with knee-length GCSs (plus pharmacological prophylaxis).
Given the difference between the published list prices for GCSs and the actual price paid reported by our clinical advisors, cost-effectiveness and VOI results for these different scenarios were reported separately for the two cost estimates. Different scenarios also explore the impact of different levels of patient adherence for thigh-length stockings on the cost-effectiveness and VOI results.
The estimates of relative effectiveness (ORs) in the deterministic analysis were taken from the NMA; this method is simulation based and, therefore, the output gives not just a point estimate for each OR but also an entire distribution of 50,000 OR estimates. In each of the simulations in the PSA, values were sampled from the 50,000 estimates of OR from the NMA. For each simulation, values were selected from the same NMA iteration for the different strategies (e.g. LMWH vs. thigh-length GCSs plus LMWH; LMWH vs. knee-length GCSs plus LMWH) to preserve the covariance between the different relative effectiveness estimates.
For other model parameters, a distribution had to be defined. The distributions were chosen to reflect the nature of the data. All probabilistic variables in the model and their distribution parameters are detailed in Appendix 6. For logical consistency and simplicity, the following variables were left deterministic (i.e. were not varied in the PSA): age, proportion of male patients, standardised mortality ratio, drug and GCSs prices (the GCSs prices were subject to a deterministic sensitivity analysis), other cost estimates, the discount rates and cost-effectiveness threshold.
Model validation
The structure and assumptions of the model follow, to a large extent, those employed in previous published CGs and published peer-reviewed cost-effectiveness studies. The model was developed in Microsoft Excel by one analyst and independently checked by another. As part of an overall quality-assurance process, the internal validity of the model was assessed by extensively exploring the logical consistency of the model results. In addition, several parameter inputs used in the NICE CG924 economic model were applied in the current model to provide a measure of validation against previously published results.
Chapter 6 Cost-effectiveness analysis results
The results of the cost-effectiveness model are presented in two ways. First, mean lifetime costs and QALYs of the alternative strategies are presented and their cost-effectiveness compared, estimating ICERs as appropriate, using standard decision rules. 142 The ICER examines the additional costs that one strategy incurs over another and compares this with the additional benefits. When more than two strategies are being compared, the ICERs are calculated using the following process:
-
The strategies are ranked in terms of mean cost (from the least expensive to the most costly).
-
If a strategy is more expensive and less effective than the previous strategy, then this strategy is said to be dominated and is excluded from the calculation of the ICERs.
-
The ICERs are calculated for each successive alternative, from the least expensive to the most costly. If the ICER for a given strategy is higher than that of the next more effective strategy, then this strategy is ruled out on the basis of extended dominance.
-
Finally, the ICERs are recalculated excluding any strategies that are ruled out using the notions of dominance and extended dominance.
Second, to present the uncertainty in the cost-effectiveness of the alternative strategies, the probability that each strategy is the most cost-effective, when all strategies are compared simultaneously, are reported at cost-effectiveness thresholds of £20,000 and £30,000 per additional QALY. These thresholds represent the range that is conventionally applied to new technologies in determining whether or not they represent value for money in the NHS.
The cost-effectiveness results are presented separately for each of the five main populations previously outlined: (1) THR; (2) TKR; (3) GS: low risk; (4) GS: moderate risk; and (5) GS: high risk. Separate results are also presented for a base-case analysis and for a series of additional scenarios. Table 50 summarises the alternative scenarios considered. For each element, the position in the base-case analysis is outlined, alongside the alternative assumptions applied.
| Scenario | Element | Base-case assumption | Scenario assumption |
|---|---|---|---|
| 1 | Treatment effectiveness | Base-case NMA results | Relative effect estimate for thigh GCSs + LMWH vs. knee GCSs + LMWH from head-to-head studies only |
| 2 | Acquisition cost of stockings | National published prices | Local prices |
| 3a | Adherence | ITT results from trials | Adjusted ITT results (effect estimates for thigh GCSs assumed to be 90% of ITT estimates) |
| 3b | Adherence | ITT results from trials | Adjusted ITT results (effect estimates for thigh GCSs assumed to be 75% of ITT estimates) |
Base-case results
Table 51 reports the results for the base-case analysis. In three of the populations considered (TKR, GS: moderate risk and GS: high risk), thigh-length GCSs plus LMWH dominated the other strategies (i.e. lower mean costs and higher QALYs than knee-length GCSs plus LMWH and LMWH alone). In these three populations, the probability that thigh-length GCSs plus LMWH was the most cost-effective strategy ranged between 0.78 and 0.79 across the thresholds considered (i.e. an error probability of 0.21–0.22).
| Treatment | Total costs (£) | Total QALYs | Incremental costs (£) | Incremental QALYs | ICER (£) | Probability cost-effective £20,000 | Probability cost-effective £30,000 |
|---|---|---|---|---|---|---|---|
| THR | |||||||
| LMWH | 131 | 10.01024 | – | – | – | 0.61 | 0.35 |
| LMWH + thigh | 175 | 10.01168 | 44 | 0.00144 | 30,366 | 0.30 | 0.52 |
| LMWH + knee | 188 | 10.01050 | 13 | –0.00118 | Dominated | 0.09 | 0.14 |
| TKR | |||||||
| LMWH + thigh | 260 | 9.91228 | – | – | – | 0.78 | 0.78 |
| LMWH | 309 | 9.90757 | 48 | –0.00471 | Dominated | 0.05 | 0.04 |
| LMWH + knee | 346 | 9.90859 | 85 | –0.00369 | Dominated | 0.18 | 0.18 |
| GS: low risk | |||||||
| LMWH | 177 | 12.76887 | – | – | – | 0.09 | 0.07 |
| LMWH + thigh | 182 | 12.77087 | 5 | 0.00200 | 2632 | 0.74 | 0.75 |
| LMWH + knee | 217 | 12.76931 | 35 | –0.00156 | Dominated | 0.18 | 0.18 |
| GS: moderate risk | |||||||
| LMWH + thigh | 230 | 12.76890 | – | – | – | 0.78 | 0.78 |
| LMWH | 276 | 12.76486 | 46 | –0.00403 | Dominated | 0.05 | 0.04 |
| LMWH + knee | 306 | 12.76567 | 76 | –0.00322 | Dominated | 0.18 | 0.18 |
| GS: high risk | |||||||
| LMWH + thigh | 345 | 12.76439 | – | – | – | 0.78 | 0.79 |
| LMWH | 521 | 12.75535 | 176 | –0.00904 | Dominated | 0.04 | 0.04 |
| LMWH + knee | 522 | 12.75751 | 177 | –0.00688 | Dominated | 0.18 | 0.18 |
In two of the populations (THR and GS: low risk), thigh-length GCSs plus LMWH also dominated knee-length GCSs plus LMWH. However, thigh-length GCSs plus LMWH did not dominate LMWH alone. In both of these populations, LMWH alone was less effective than thigh-length GCSs plus LMWH but also less costly. Hence, the additional costs and additional effects of thigh-length GCSs plus LMWH were compared with LMWH alone. In the low-risk GS population, this ICER was £2632 per additional QALY, well within a cost-effectiveness threshold range of £20,000–£30,000. However, the ICER in the THR population was £30,366 and hence marginally exceeds the threshold range. Therefore, if the threshold range were to be strictly applied, LMWH alone would be the most cost-effective strategy in this population. The probability that thigh-length GCSs plus LMWH was the most cost-effective strategy in the low-risk GCSs population ranged between 0.74 and 0.75 (i.e. error probability of 0.25–0.26), consistent with the uncertainty estimates reported in the three populations in which thigh-length GCSs plus LMWH was the dominant strategy. However, there was considerably more decision uncertainty surrounding the probability that thigh-length GCSs plus LMWH was the most cost-effective strategy in the THR population, varying between 0.30 and 0.52 (error probability 0.48–0.70) across the lower and upper bounds of the cost-effectiveness threshold.
Given that the same relative effectiveness estimates were applied to each of the subpopulations based on the base-case NMA analysis, the differences between the cost-effectiveness results reported across the different subgroups are attributable to the different baseline VTE risks applied (i.e. risk of asymptomatic DVT, and symptomatic DVT and PE). That is, the cost-effectiveness results are driven by differences in the absolute risks of the separate VTE risks modelled for each of these strategies and these absolute risks are a function of different baseline risks and a common RR estimate. Hence, in populations with higher baseline VTE risks, thigh-length GCSs plus LMWH dominates the other strategies. However, in populations with lower baseline VTE risks, the additional acquisition and monitoring costs of using thigh stockings are not completely offset by cost savings attributable to a reduction in the subsequent VTE event risk.
It is important to appreciate that the relationship between cost-effectiveness and event risk is not solely driven by the risks of symptomatic DVT and PE but also the risk of asymptomatic DVT. Although the model does not assume that asymptomatic DVTs would be identified and treated in routine clinical practice, a proportion of these are assumed to lead subsequently to PTS and this would impact on longer-term cost and effect estimates. Indeed, the baseline risks of symptomatic DVT (0.31%) and PE (0.16%) assigned to the LMWH alone strategy were lower in the GS low-risk population than the equivalent estimates in the THR population (0.38% and 0.25%, respectively). However, the cost-effectiveness of thigh-length GCSs plus LMWH was more favourable in the GS low-risk population owing to the higher risk of asymptomatic DVTs (4.63% vs. 1.43%).
Finally, although thigh-length GCSs plus LMWH appeared to be the most cost-effective strategy in four of the five populations (and was only marginally over the threshold in THR), the differences between the strategies in terms of mean costs and QALYs were minimal, and there are issues regarding the clinical and/or economic significance of these differences. The mean cost differences between all three strategies ranged from £5 to £177, whereas the mean incremental QALY differences ranged between 0.001 and 0.009 QALYs. Given these small QALY differences, expressing these in terms of differences in days of perfect health (rather than years) may aid interpretation. The minimum and maximum differences between all three strategies represent differences of between 0.37 and 3.32 days of perfect health over a patient’s remaining lifetime, across all the separate populations.
In an additional analysis of the base-case models, results were generated for each subgroup using 10,000 simulations. Results for these analyses are reported in Appendix 7. Minor variations were found in the results compared with those from 1000 simulations; however, it was not expected that the differences would materially affect the general nature of the recommendations and further analyses were undertaken using 1000 simulations.
Scenario results
Scenario 1
In the base-case cost-effectiveness analysis, the estimates of relative effectiveness of thigh-length and knee-length GCSs as adjunctive treatments to LMWH, relative to LMWH alone, were obtained from the base-case NMA reported in Chapter 3 (random effect, no interaction). Chapter 3 concluded that the results of the NMA and the standard meta-analysis were similar regarding the relative effectiveness of thigh- versus knee-length GCSs and that the precision of the estimate of effect was not increased by the NMA. To ensure that this interpretation also applied to the cost-effectiveness results, a separate scenario was explored, which replaced the relative effectiveness estimate for thigh-length GCSs plus LMWH versus knee-length GCSs plus LMWH derived from the NMA, with the estimate derived from the standard meta-analysis.
Table 52 reports the probabilistic cost-effectiveness results for scenario 1. The results and interpretation of this scenario were consistent with those of the base-case and the interpretation of the clinical effectiveness results reported in Chapter 3.
| Treatment | Total costs (£) | Total QALYs | Incremental costs (£) | Incremental QALYs | ICER (£) | Probability cost-effective £20,000 | Probability cost-effective £30,000 |
|---|---|---|---|---|---|---|---|
| THR | |||||||
| LMWH | 131 | 10.01020 | – | – | – | 0.60 | 0.36 |
| LMWH + thigh | 175 | 10.01163 | 44 | 0.00143 | 30,683 | 0.24 | 0.42 |
| LMWH + knee | 186 | 10.01055 | 11 | –0.00108 | Dominated | 0.17 | 0.22 |
| TKR | |||||||
| LMWH + thigh | 257 | 9.91240 | – | – | – | 0.68 | 0.69 |
| LMWH | 305 | 9.90771 | 48 | –0.00468 | Dominated | 0.08 | 0.07 |
| LMWH + knee | 334 | 9.90909 | 77 | –0.00331 | Dominated | 0.24 | 0.24 |
| GS: low risk | |||||||
| LMWH | 178 | 12.76883 | – | – | – | 0.12 | 0.11 |
| LMWH + thigh | 182 | 12.77081 | 5 | 0.00198 | 2341 | 0.62 | 0.64 |
| LMWH + knee | 213 | 12.76940 | 31 | –0.00141 | Dominated | 0.26 | 0.25 |
| GS: moderate risk | |||||||
| LMWH + thigh | 229 | 12.76908 | – | – | – | 0.67 | 0.69 |
| LMWH | 276 | 12.76502 | 47 | –0.00406 | Dominated | 0.08 | 0.07 |
| LMWH + knee | 294 | 12.76634 | 66 | –0.00274 | Dominated | 0.24 | 0.24 |
| GS: high risk | |||||||
| LMWH + thigh | 345 | 12.76439 | – | – | – | 0.78 | 0.79 |
| LMWH | 521 | 12.75535 | 176 | –0.00904 | Dominated | 0.04 | 0.04 |
| LMWH + knee | 522 | 12.75751 | 177 | –0.00688 | Dominated | 0.18 | 0.18 |
Scenario 2
The national published prices of thigh- and knee-length GCSs were applied in the base-case. However, owing to local purchasing agreements, the national published prices may not appropriately reflect those actually being paid in practice. Hence, we undertook a separate scenario analysis which used local prices reported by our clinical advisors. Importantly, although the price of both stocking types in absolute terms was markedly lower in this scenario, the difference in price between the types of stockings (approximately £2) was exactly the same based on national and local prices. Therefore, it was not envisaged that this scenario would significantly alter the relative cost-effectiveness of thigh-length versus knee-length GCSs compared with the base case, but that the cost-effectiveness of both types of stockings compared with LMWH alone might be impacted. Hence, decision uncertainty surrounding all three strategies could also be significantly affected.
Table 53 presents the probabilistic results for scenario 2. In common with the base-case results, across all five of the populations, thigh-length GCSs plus LMWH appeared to dominate knee-length GCSs plus LMWH. However, in contrast to scenario 1, thigh-length GCSs plus LMWH either dominated or appeared cost-effective (i.e. ICER less than lower bound of the threshold) compared with LMWH alone in all five populations. Hence, applying lower stocking prices that may be more reflective of local prices improves the cost-effectiveness of both types of stockings compared with drug therapy alone (i.e. because the difference in acquisition costs between GCSs and drug-alone strategies reduces). Although there were two populations in the base-case for which thigh-length GCSs plus LMWH did not dominate LMWH alone (THR and low-risk GS), in this scenario thigh-length GCSs plus LMWH now also appeared to be the dominant strategy for the low-risk GS population. Although the lower VTE risks in the THR population meant that thigh-length GCSs plus LMWH did not dominate LMWH alone, the ICER was now more favourable and below conventional cost-effectiveness thresholds (£18,900 per QALY vs. £30,366 in the base case). Importantly, there was less decision uncertainty over whether or not thigh-length GCSs plus LMWH is the most cost-effective strategy compared with the base-case analysis. The error probability across the different populations ranged from between 0.21 and 0.47, compared with a range of between 0.21 and 0.70 in the base case.
| Treatment | Total costs (£) | Total QALYs | Incremental costs (£) | Incremental QALYs | ICER (£) | Probability cost-effective £20,000 | Probability cost-effective £30,000 |
|---|---|---|---|---|---|---|---|
| THR | |||||||
| LMWH | 131 | 10.01024 | – | – | – | 0.32 | 0.18 |
| LMWH + thigh | 159 | 10.01171 | 28 | 0.00147 | 18,900 | 0.53 | 0.66 |
| LMWH + knee | 172 | 10.01052 | 13 | –0.00119 | Dominated | 0.15 | 0.17 |
| TKR | |||||||
| LMWH + thigh | 242 | 9.91253 | – | – | – | 0.78 | 0.79 |
| LMWH | 304 | 9.90782 | 63 | –0.00471 | Dominated | 0.04 | 0.04 |
| LMWH + knee | 326 | 9.90884 | 85 | –0.00370 | Dominated | 0.18 | 0.18 |
| GS low risk | |||||||
| LMWH + thigh | 166 | 12.77080 | – | – | – | 0.76 | 0.77 |
| LMWH | 177 | 12.76882 | 11 | –0.00198 | Dominated | 0.05 | 0.05 |
| LMWH + knee | 201 | 12.76923 | 35 | –0.00158 | Dominated | 0.19 | 0.19 |
| GS moderate risk | |||||||
| LMWH + thigh | 212 | 12.76893 | – | – | – | 0.78 | 0.78 |
| LMWH | 274 | 12.76484 | 62 | –0.00409 | Dominated | 0.04 | 0.04 |
| LMWH + knee | 287 | 12.76565 | 75 | –0.00327 | Dominated | 0.18 | 0.18 |
| GS high risk | |||||||
| LMWH + thigh | 324 | 12.76458 | – | – | – | 0.79 | 0.79 |
| LMWH + knee | 493 | 12.75751 | 170 | –0.00708 | Dominated | 0.18 | 0.18 |
| LMWH | 507 | 12.75569 | 183 | –0.00890 | Dominated | 0.04 | 0.03 |
Scenario 3
The review of patient adherence studies reported in Chapter 3, Patient adherence and preference, reported that the proportion of patients not wearing stockings or wearing stockings incorrectly appeared to be higher in patients receiving thigh-length GCSs than in those receiving knee-length GCSs. In addition, patient adherence was reported to be higher in the RCTs than the observational studies. Given that the base-case analysis is based on the intention-to-treat results reported in the trials, it is assumed that differences in adherence between the types of stocking are at least partially captured in the model. However, because the model is based on the intention-to-treat results from RCTs, the analysis may not capture differences in adherence that might happen in routine clinical practice outside a trial environment. Consequently, a separate scenario was undertaken to explore the robustness of the cost-effectiveness results to alternative assumptions regarding patient adherence. This scenario explored the impact of differences between the types of stocking (i.e. assuming that adherence to thigh-length GCSs might be lower in clinical practice compared with a trial setting but that adherence to knee-length GCSs would be unaffected). A separate adjustment was thus employed to the relative effectiveness applied to thigh-length GCSs by reducing this relative to LMWH alone by 10% and 25% (i.e. equivalent to assuming an adherence rate for thigh GCSs of between 75% and 90% of that reported in the trials; see Chapter 3, Patient adherence and preference).
The adjustment applied to the relative effectiveness estimates of thigh-length GCSs (10–25%) is based on differences in adherence between the stocking types based on the range of quantitative estimates reported in Chapter 3. Although this scenario provides a useful exploratory analysis of the robustness of the results to higher differences in adherence between the stocking types that may occur in clinical practice settings rather than controlled trial settings, this analysis should be considered as exploratory in nature. It is important to recognise that the results from this analysis are potentially conservative towards thigh-length GCSs compared with knee-length GCSs. First, the evidence on the effectiveness of GCSs and the focus of the model relates to the use of GCSs during the acute postsurgical period (i.e. between 10 and 14 days), rather than the long-term use of GCSs in the postacute period. Consequently, because a significant proportion of this time may be spent in a hospital setting, differences in adherence may be less evident than over a longer time period when a patient has subsequently been discharged. Second, it is difficult to ascertain the potential impact on VTE risks of any reported differences in adherence. The assumption made in this scenario is akin to assuming that those patients who would not be adherent to thigh-length GCSs (but, importantly, would have been compliant with knee stockings) receive no additional clinical benefit compared with drug therapy alone. However, this may be a conservative assumption, because an incorrectly fitted stocking and/or failure to wear the stocking for the recommended duration may result not in a complete loss of benefit but rather some reduction in magnitude of the expected benefit.
Tables 54 and 55 report the results assuming 90% adherence and 75% adherence, respectively, for thigh-length GCSs. In three of the populations considered (TKR, moderate-risk GS and high-risk GS), the ICER results were consistent with the base-case analysis; thigh-length GCSs plus LMWH still dominated the other strategies. However, decision uncertainty was higher in these scenarios, with error probabilities across the thresholds and scenarios of between 0.25 and 0.35, compared with 0.21–0.22 in the base case. Therefore, although assuming a lower adherence rate for thigh-length GCSs did not alter the cost-effectiveness conclusions based on the mean ICER, the uncertainty that thigh-length GCSs plus LMWH was the optimal strategy did increase.
| Treatment | Total costs (£) | Total QALYs | Incremental costs (£) | Incremental QALYs | ICER (£) | Probability cost-effective £20,000 | Probability cost-effective £30,000 |
|---|---|---|---|---|---|---|---|
| THR | |||||||
| LMWH | 131 | 10.01023 | – | – | – | 0.64 | 0.39 |
| LMWH + thigh | 176 | 10.01156 | 45 | 0.00132 | 34,297 | 0.25 | 0.44 |
| LMWH + knee | 188 | 10.01057 | 11 | –0.00099 | Dominated | 0.11 | 0.17 |
| TKR | |||||||
| LMWH + thigh | 270 | 9.91193 | – | – | – | 0.73 | 0.74 |
| LMWH | 307 | 9.90766 | 37 | –0.00426 | Dominated | 0.07 | 0.05 |
| LMWH + knee | 342 | 9.90872 | 72 | –0.00321 | Dominated | 0.21 | 0.21 |
| GS: low risk | |||||||
| LMWH | 176 | 12.76885 | – | – | – | 0.11 | 0.08 |
| LMWH + thigh | 186 | 12.77065 | 10 | 0.00180 | 5774 | 0.68 | 0.70 |
| LMWH + knee | 216 | 12.76923 | 30 | –0.00141 | Dominated | 0.21 | 0.21 |
| GS: moderate risk | |||||||
| LMWH + thigh | 237 | 12.76856 | – | – | – | 0.73 | 0.74 |
| LMWH | 273 | 12.76497 | 36 | –0.00359 | Dominated | 0.06 | 0.05 |
| LMWH + knee | 301 | 12.76584 | 64 | –0.00272 | Dominated | 0.22 | 0.22 |
| GS: high risk | |||||||
| LMWH + thigh | 368 | 12.76337 | – | – | – | 0.75 | 0.75 |
| LMWH | 503 | 12.75571 | 135 | –0.00767 | Dominated | 0.04 | 0.04 |
| LMWH + knee | 505 | 12.75771 | 138 | –0.00567 | Dominated | 0.21 | 0.21 |
| Treatment | Total costs (£) | Total QALYs | Incremental costs (£) | Incremental QALYs | ICER (£) | Probability cost-effective £20,000 | Probability cost-effective £30,000 |
|---|---|---|---|---|---|---|---|
| THR | |||||||
| LMWH | 132 | 10.01020 | – | – | – | 0.72 | 0.53 |
| LMWH + thigh | 182 | 10.01124 | 51 | 0.00104 | 48,781 | 0.17 | 0.30 |
| LMWH + knee | 189 | 10.01051 | 6 | –0.00073 | Dominated | 0.12 | 0.17 |
| TKR | |||||||
| LMWH + thigh | 294 | 9.91111 | – | – | – | 0.65 | 0.66 |
| LMWH | 306 | 9.90777 | 12 | –0.00334 | Dominated | 0.08 | 0.08 |
| LMWH + knee | 343 | 9.90882 | 49 | –0.00228 | Dominated | 0.27 | 0.27 |
| GS: low risk | |||||||
| LMWH | 177 | 12.76879 | – | – | – | 0.15 | 0.11 |
| LMWH + thigh | 196 | 12.77022 | 20 | 0.00143 | 13,807 | 0.59 | 0.63 |
| LMWH + knee | 216 | 12.76920 | 20 | –0.00101 | Dominated | 0.25 | 0.27 |
| GS: moderate risk | |||||||
| LMWH + thigh | 256 | 12.76783 | – | – | – | 0.65 | 0.65 |
| LMWH | 271 | 12.76507 | 15 | –0.00275 | Dominated | 0.08 | 0.08 |
| LMWH + knee | 301 | 12.76588 | 44 | –0.00195 | Dominated | 0.27 | 0.27 |
| GS: high risk | |||||||
| LMWH + thigh | 368 | 12.76322 | – | – | – | 0.74 | 0.75 |
| LMWH | 515 | 12.75511 | 147 | –0.00812 | Dominated | 0.04 | 0.04 |
| LMWH + knee | 523 | 12.75681 | 155 | –0.00641 | Dominated | 0.21 | 0.21 |
In the GS low-risk population, thigh-length GCSs plus LMWH continued to dominate knee-length GCSs plus LMWH but remained more costly and more effective than LMWH alone. However, because the magnitude of the difference in QALYs decreased with lower adherence rates, the ICER estimates of thigh-length GCSs plus LMWH versus LMWH alone increased compared with the base-case analysis (£5774–13,807 across the two scenarios vs. £2632 in the base case). However, even assuming 75% adherence, these ICER estimates were still under the lower bound of the threshold (£20,000), indicating that thigh-length GCSs plus LMWH appeared cost-effective even when assuming lower adherence rates.
In the THR population, thigh-length GCSs plus LMWH continues to dominate knee-length GCSs plus LMWH, assuming either a 75% or 90% adherence rate. The ICER of interest from the fully incremental analysis was still estimated between thigh-length GCSs plus LMWH versus LWMH alone. Although in the base-case analysis this ICER was only marginally higher than the upper bound of the cost-effectiveness threshold, the ICER estimates in the scenarios increased to £34,297 per QALY (90% adherence) and £48,781 per QALY (75% adherence), such that there was significantly more decision uncertainty over whether or not thigh-length GCSs plus LMWH was the most cost-effective strategy.
Summary of findings of the cost-effectiveness analyses
Compared with LWMH alone, our findings suggest that the adjunctive use of compression stockings appears to represent good value for money to the NHS across the different populations considered. However, in the population with the lowest risk of DVT (THR), the cost-effectiveness of adding compression stockings to LMWH appeared more finely balanced. However, even within this population it seems likely that the use of compression stockings would be cost-effective, assuming that the local prices taken into account in the scenario analyses are more representative of prices actually paid in the NHS compared with the national published prices and that adherence in the real world would not be significantly different from that observed in existing RCT populations.
These general findings are consistent with the findings from the previous NICE CG,4 which reported favourable cost-effectiveness estimates for GCSs combined with pharmacological prophylaxis. However, in contrast to the previous NICE guideline, our analysis was also able to explore differences in cost-effectiveness between the different types of stockings. Importantly, our results consistently found that the use of thigh-length GCSs plus LMWH appeared to dominate knee-length GCSs plus LMWH. That is, although the use of thigh-length GCSs is associated with higher acquisition costs compared with knee-length GCSs, the differences in acquisition costs appear to be more than offset by cost savings that could be achieved by the expected reduction in the risk of DVT. These findings appeared robust to alternative assumptions relating to the acquisition costs and adherence.
Although the comparisons of mean cost and QALYs consistently indicated that thigh-length GCSs plus LMWH was the most cost-effective strategy, there remains significant uncertainty surrounding any decision to routinely recommend the use of thigh-length GCSs plus LMWH compared with knee-length GCSs plus LMWH and LMWH alone. Indeed, the error probability that thigh-length GCSs plus LMWH is the most cost-effective strategy varied between 0.21 and 0.70 in the base-case analysis. The scenarios explored indicated that this uncertainty would be lower if the local prices of GCSs reported by our clinical advisors are more representative of prices being paid nationally compared with the nationally reported published prices, but could also be higher if adherence to GCSs (and particularly thigh-length stockings) is lower in routine clinical practice compared with their use in a more controlled trial environment.
Another important finding from the cost-effectiveness analysis relates to the magnitude of differences in expected lifetime costs and QALYs between the alternative strategies. That is, although the expected estimates consistently found thigh-length GCSs plus LMWH to be the most cost-effective strategy, the differences in the expected cost and QALY estimates were small, and the clinical and economic significance of these needs to be considered. In the base case, the maximum differences reported (i.e. between the least effective and most effective strategy) in QALYs, across all the separate populations, was equivalent to a difference of between 0.37 and 3.32 days of perfect health over a patient’s remaining lifetime. Given that LMWH alone was consistently found to be the least effective strategy, the differences between the different types of stockings would be even lower than this range.
Hence, although the model results demonstrate that the use of thigh-length GCSs as an adjunctive treatment to pharmacological prophylaxis appears to be more cost-effective than the adjunctive use of knee-length GCSs and pharmacological prophylaxis alone, the importance of these findings in terms of informing clinical practice and relevant policies needs to also take into account both the high levels of decision uncertainty that currently exists and the clinical and economic significance of the differences in costs and QALYs.
The next chapter reports the methods and results of the VOI analyses that have also been conducted. A formal analytic framework is used to assess both the level of decision uncertainty, and the scale and magnitude of the consequences. It also provides an explicit basis to further inform clinical and policy decision-making.
Chapter 7 Value of information analysis results
Methods
Treatment choices have to be made in the face of uncertainty about clinical effectiveness, safety and economic implications. 143 There is always a chance that the wrong decision has been made with subsequent opportunity loss. 143,144 Policy-makers assessing interventions are keen to understand the level of decision uncertainty, and this can be quantified directly from the PSA results. 145 The level of decision uncertainty can be derived from the probability that a strategy is cost-effective based on conventional cost-effectiveness threshold estimates (£20,000–£30,000 per QALY). However, assessing the level of decision uncertainty is necessary, but not sufficient, in subsequently determining the significance of this uncertainty in terms of informing appropriate policy responses. An assessment of the significance of uncertainty also requires the consequences associated with the level of uncertainty to be established (i.e. in terms of the costs or equivalent health forgone if an incorrect decision is made) and the scale and magnitude of these consequences need to be reflected in the entire patient population who stand to be affected by a particular decision.
The maximum amount the NHS should be willing to invest to reduce uncertainty in the decision can be informed by the expected value of perfect information (EVPI). 143,145 The EVPI evaluates the expected cost of current uncertainty by accounting for both the probability that a decision based on existing evidence is wrong and for the magnitude of the consequences of making the wrong decision. The EVPI can then be used as a necessary requirement for determining the potential efficiency of further primary research. Applying this decision rule, additional research should be considered only if the EVPI exceeds the expected cost of the research. The EVPI can also be estimated for individual parameters (or groups of parameters) contained in the model, termed partial EVPI or expected value of partial perfect information (EVPPI). The EVPPI considers particular elements of the decision problem in order to direct and focus research towards the specific areas in which the elimination of uncertainty has the most value. This can be particularly relevant to the design of any future research. On the basis of EVPI and EVPPI calculations, the potential value of a future trial, or other research designs, can be evaluated.
As information can be of value to more than one individual, the EVPI can also be expressed for the total population who stand to benefit over the expected lifetime of the programme/technology. If the EVPI for the population of current and future patients exceeds the expected costs of additional research, then it is potentially cost-effective to conduct further research. Population EVPI is determined by applying the individual EVPI estimate to the number of people who would be affected by the information over the anticipated lifetime of the technology:
where I = incidence in period, t = period, T = total number of periods for which information from research would be useful and r = discount rate.
Population size estimates were calculated based on the number of procedures performed in the UK NHS for each of the population subgroups (i.e. THR, TKR, GS) according to the NHS Hospital Episode Statistics data 2012–13. 126 In order to derive the GS population, patients undergoing gastrointestinal, bariatric, gynaecological, laparoscopic, thoracic and urological surgery were considered, based on procedures included in NICE CG924 economic model. The total GS population was then stratified into low, moderate and high risk using the proportions of GS patients at different levels of DVT risk. 26 Further assumptions for the population level EVPI were that information would be valuable over a period of 10 years and that patient populations were discounted using the same discount rate as that used for costs and health benefits (i.e. 3.5% annually). Population EVPI estimates were calculated over a cost-effectiveness threshold range of £20,000–30,000 per QALY.
Expected value of perfect information results
Tables 56 and 57 provide a summary of the population EVPI estimates based on a cost-effectiveness threshold of £20,000 and £30,000 per QALY. These tables report the treatment strategy which appears most cost-effective based on expected (mean) estimates of costs and QALYs, the level of decision uncertainty (the error probability for this strategy) and the magnitude and scale of the consequences (i.e. the EVPI for an individual patient and total EVPI for the entire population over a 10-year period).
| Subgroup | Scenario | Population size (annual) | Optimal treatment (cost-effectiveness) | Error probability | Individual EVPI (£) | Total EVPI (£) |
|---|---|---|---|---|---|---|
| THR | Base case | 76,448 | LMWH | 0.39 | 7.22 | 4,748,998 |
| Base case, low prices | 76,448 | LMWH + thigh | 0.47 | 14.40 | 9,473,428 | |
| Base case, 75% adherence | 76,448 | LMWH | 0.28 | 5.23 | 3,440,162 | |
| TKR | Base case | 79,551 | LMWH + thigh | 0.22 | 41.20 | 28,213,062 |
| Base case, low prices | 79,551 | LMWH + thigh | 0.22 | 36.72 | 25,143,360 | |
| Base case, 75% adherence | 79,551 | LMWH + thigh | 0.35 | 68.17 | 46,682,189 | |
| GS: low risk | Base case | 42,208 | LMWH + thigh | 0.26 | 17.81 | 6,472,392 |
| Base case, low prices | 42,208 | LMWH + thigh | 0.24 | 16.94 | 6,154,213 | |
| Base case, 75% adherence | 42,208 | LMWH + thigh | 0.41 | 31.76 | 11,540,597 | |
| GS: moderate risk | Base case | 135,141 | LMWH + thigh | 0.22 | 34.73 | 40,396,307 |
| Base case, low prices | 135,141 | LMWH + thigh | 0.22 | 32.52 | 37,824,719 | |
| Base case, 75% adherence | 135,141 | LMWH + thigh | 0.35 | 57.27 | 66,614,738 | |
| GS: high risk | Base case | 192,900 | LMWH + thigh | 0.22 | 72.11 | 119,733,537 |
| Base case, low prices | 192,900 | LMWH + thigh | 0.21 | 68.97 | 114,518,588 | |
| Base case, 75% adherence | 192,900 | LMWH + thigh | 0.26 | 88.50 | 146,943,564 | |
| Subgroup | Scenario | Population size (annual) | Optimal treatment (cost-effectiveness) | Error probability | Individual EVPI (£) | Total EVPI (£) |
|---|---|---|---|---|---|---|
| THR | Base case | 76,448 | LMWH + thigh | 0.48 | 19.12 | 12,578,754 |
| Base case, low prices | 76,448 | LMWH + thigh | 0.35 | 14.90 | 9,802,690 | |
| Base case, 75% adherence | 76,448 | LMWH | 0.47 | 13.64 | 8,975,827 | |
| TKR | Base case | 79,551 | LMWH + thigh | 0.22 | 49.86 | 34,138,750 |
| Base case, low prices | 79,551 | LMWH + thigh | 0.22 | 44.16 | 30,238,722 | |
| Base case, 75% adherence | 79,551 | LMWH + thigh | 0.35 | 81.32 | 55,686,790 | |
| GS: low risk | Base case | 42,208 | LMWH + thigh | 0.25 | 20.57 | 7,471,697 |
| Base case, low prices | 42,208 | LMWH + thigh | 0.23 | 20.13 | 7,314,621 | |
| Base case, 75% adherence | 42,208 | LMWH + thigh | 0.38 | 36.99 | 13,437,606 | |
| GS: moderate risk | Base case | 135,141 | LMWH + thigh | 0.22 | 41.94 | 48,784,668 |
| Base case, low prices | 135,141 | LMWH + thigh | 0.22 | 39.20 | 45,604,829 | |
| Base case, 75% adherence | 135,141 | LMWH + thigh | 0.35 | 68.85 | £80,086,921 | |
| GS: high risk | Base case | 192,900 | LMWH + thigh | 0.21 | 87.86 | £145,890,839 |
| Base case, low prices | 192,900 | LMWH + thigh | 0.21 | 83.86 | £139,246,355 | |
| Base case, 75% adherence | 192,900 | LMWH + thigh | 0.25 | 107.83 | £179,041,840 | |
The results are based on treatment effectiveness estimates derived from the predictive distributions of the random-effect (no interaction) NMA model. The predictive distributions represent the effect size that would be estimated from a new trial in situations in which possible modifiers of relative effect (e.g. owing to population characteristics and study designs) are not known. Hence, rather than the effect estimate from an ‘average’ trial, which is obtained directly from the simulations in the NMA, the effect size estimates used in the model are derived from estimating the predictive distribution, which is more relevant when estimating the effect size in a new trial.
Expected value of perfect information estimates are reported based on the same assumptions employed in the base-case cost-effectiveness analysis. Separate EVPI estimates are also reported for key scenarios, reflecting the local prices of GCSs and assuming adherence to thigh-length stockings would be lower in routine clinical practice (75% adherence rate).
Given the relatively sparse network and the difficulties of attributing the existing between-study heterogeneity to specific effect modifiers relating to population or study design characteristics, a random-effects model was employed in the base-case approaches to both the NMA and the cost-effectiveness analysis. However, if the existing between-study heterogeneity is related to population and/or study design characteristics, then any new trial may not resolve uncertainty across the entire random-effect distribution. That is, a trial in a specific population (and designed in a specific way) may not ultimately reduce uncertainty in a broader context. Hence, applying the predictive distribution may overestimate the uncertainty that is likely to be addressed by a single study in a specific population. Tables 58 and 59 provide a summary of the same population EVPI estimates and scenarios based on the fixed-effects (no interaction) NMA results for the orthopaedic and non-orthopaedic populations. In contrast to the random-effects predictive distribution, this analysis assumes that the variation between studies is due entirely to study population characteristics (orthopaedic and non-orthopaedic populations).
| Subgroup | Scenario | Population size (annual) | Optimal treatment (cost-effectiveness) | Error probability | Individual EVPI (£) | Total EVPI (£) |
|---|---|---|---|---|---|---|
| THR | Orthopaedic NMA | 76,448 | LMWH | 0.17 | 2.09 | 1,378,405 |
| Orthopaedic NMA, low prices | 76,448 | LMWH | 0.45 | 6.61 | 4,350,705 | |
| Orthopaedic NMA, 75% adherence | 76,448 | LMWH | 0.08 | 1.02 | 672,179 | |
| TKR | Orthopaedic NMA | 79,551 | LMWH + thigh | 0.21 | 24.45 | 16,741,845 |
| Orthopaedic NMA, low prices | 79,551 | LMWH + thigh | 0.20 | 25.94 | 17,765,362 | |
| Orthopaedic NMA, 75% adherence | 79,551 | LMWH + thigh | 0.48 | 56.73 | 38,848,227 | |
| GS: low risk | Non-orthopaedic NMA | 42,208 | LMWH + thigh | 0.07 | 0.55 | 201,570 |
| Non-orthopaedic NMA, low prices | 42,208 | LMWH + thigh | 0.07 | 0.58 | 209,457 | |
| Non-orthopaedic NMA, 75% adherence | 42,208 | LMWH + thigh | 0.26 | 3.26 | 1,184,678 | |
| GS: moderate risk | Non-orthopaedic NMA | 135,141 | LMWH + thigh | 0.14 | 19.18 | 22,305,773 |
| Non-orthopaedic NMA, low prices | 135,141 | LMWH + thigh | 0.13 | 19.13 | 22,248,897 | |
| Non-orthopaedic NMA, 75% adherence | 135,141 | LMWH + thigh | 0.35 | 41.32 | 48,063,116 | |
| GS: high risk | Non-orthopaedic NMA | 192,900 | LMWH + thigh | 0.12 | 34.93 | 57,997,674 |
| Non-orthopaedic NMA, low prices | 192,900 | LMWH + thigh | 0.12 | 33.87 | 56,239,875 | |
| Non-orthopaedic NMA, 75% adherence | 192,900 | LMWH + thigh | 0.33 | 88.06 | 146,220,027 | |
| Subgroup | Scenario | Population size (annual) | Optimal treatment (cost-effectiveness) | Error probability | Individual EVPI (£) | Total EVPI (£) |
|---|---|---|---|---|---|---|
| THR | Orthopaedic NMA | 76,448 | LMWH | 0.44 | 8.04 | 5,289,716 |
| Orthopaedic NMA, low prices | 76,448 | LMWH + thigh | 0.37 | 4.73 | 3,110,282 | |
| Orthopaedic NMA, 75% adherence | 76,448 | LMWH | 0.22 | 3.91 | 2,575,798 | |
| TKR | Orthopaedic NMA | 79,551 | LMWH + thigh | 0.20 | 28.84 | 19,745,741 |
| Orthopaedic NMA, low prices | 79,551 | LMWH + thigh | 0.20 | 30.86 | 21,132,456 | |
| Orthopaedic NMA, 75% adherence | 79,551 | LMWH + thigh | 0.47 | 67.00 | 45,880,554 | |
| GS: low risk | Non-orthopaedic NMA | 42,208 | LMWH + thigh | 0.07 | 0.62 | 224,183 |
| Non-orthopaedic NMA, low prices | 42,208 | LMWH + thigh | 0.07 | 0.64 | 234,192 | |
| Non-orthopaedic NMA, 75% adherence | 42,208 | LMWH + thigh | 0.24 | 3.70 | 1,344,224 | |
| GS: moderate risk | Non-orthopaedic NMA | 135,141 | LMWH + thigh | 0.13 | 22.46 | 26,125,643 |
| Non-orthopaedic NMA, low prices | 135,141 | LMWH + thigh | 0.12 | 22.88 | 26,620,506 | |
| Non-orthopaedic NMA, 75% adherence | 135,141 | LMWH + thigh | 0.34 | 48.38 | 56,280,255 | |
| GS: high risk | Non-orthopaedic NMA | 192,900 | LMWH + thigh | 0.12 | 41.90 | 69,571,325 |
| Non-orthopaedic NMA, low prices | 192,900 | LMWH + thigh | 0.12 | 40.68 | 67,547,222 | |
| Non-orthopaedic NMA, 75% adherence | 192,900 | LMWH + thigh | 0.32 | 107.23 | 178,040,113 | |
Importantly, the results of the fixed-effect analysis should be seen as a form of sensitivity analysis. Given the sparse data that currently exist, it is not possible, a priori, to adequately identify key effect modifiers and, hence, it is possible that any new study may realise values across the entire predictive distribution. However, presenting the EVPI results based on both the random- and fixed-effects analyses represents a useful comparison by characterising the most optimistic (random effects) and pessimistic (fixed effect) assumptions regarding the uncertainty and associated value that could be resolved by a new trial.
The results demonstrate a considerable range in the population EVPI estimates, depending on the population and synthesis model applied to estimate the relative effectiveness of the different strategies. Based on the effectiveness estimates from the random effect, predictive distribution and applying a cost-effectiveness threshold of £20,000, total EVPI varies between approximately £3.4M and £146.9M across the separate populations (and between £7.3M and £179M at a threshold of £30,000). These results suggest that further primary research appears to be potentially worthwhile given the high cost of current decision uncertainty across all scenarios. The variation in the EVPI estimates across the populations is inextricably linked to the different baseline rates of VTE. That is, significantly higher EVPI estimates are reported in populations at higher baseline risk of VTE in the absence of mechanical prophylaxis. Hence, research potentially looks most worthwhile in the higher-risk populations considered (TKR, moderate- and high-risk GS).
As expected, the random-effects model results in higher EVPI estimates, given the additional between-study heterogeneity that is included. Based on the fixed-effect estimates (orthopaedic and non-orthopaedic results) and applying a cost-effectiveness threshold of £20,000, total EVPI varies between approximately £0.2M and £146.2M across the separate populations (and between £0.2M and £178M at a threshold of £30,000). Although research still appears most worthwhile in the higher-risk populations considered (TKR, moderate- and high-risk GS), the value of research in lower risk populations appears markedly lower and, hence, further research in these lower risk populations would appear unlikely to represent an efficient use of NHS resources.
The EVPI estimates reported in previous tables are based on decision uncertainty surrounding the decision problem involving all three strategies (thigh-length GCSs plus LMWH, knee-length GCSs plus LMWH and LMWH alone). The assumption underlying these analyses is that further research could address the uncertainties about the differential value of the different types of stockings as well as their value in relation to management with pharmacological prophylaxis alone. However, depending on the type of study and design that might be conducted in the future, not all of the causes and sources of uncertainty might be directly informed. For example, undertaking a head-to-head trial of thigh-length GCSs plus LMWH versus knee-length GCSs plus LMWH would inform uncertainties related to the differential value of the different stocking types but would not directly inform uncertainties related to their comparative value compared with pharmacological prophylaxis alone. Hence, the EVPI estimates reported in previous tables will overestimate the value of reducing uncertainties that could be addressed through research which is more focused on issues of comparative effectiveness and cost-effectiveness of the different types of stockings.
In order to more appropriately inform the value of further research that specifically focuses on the comparative value of the different types of stockings, EVPI estimates were re-estimated by restricting the relevant treatment strategies to a two-way comparison between thigh-length GCSs plus LMWH versus knee-length GCSs plus LMWH (i.e. cost-effectiveness estimates, error probabilities and consequences were re-estimated based on this two-way comparison). Tables 60 and 61 provide a summary of the population EVPI estimates based on a cost-effectiveness threshold of £20,000 and £30,000 per QALY and based on the random-effect, predictive distribution. Tables 62 and 63 report the equivalent results based on the fixed-effect analyses.
| Subgroup | Scenario | Population size (annual) | Optimal treatment (cost-effectiveness) | Error probability | Individual EVPI (£) | Total EVPI (£) |
|---|---|---|---|---|---|---|
| THR | Base case | 76,448 | LMWH + thigh | 0.22 | 8.30 | 5,461,287 |
| Base case, low prices | 76,448 | LMWH + thigh | 0.23 | 7.60 | 4,998,250 | |
| Base case, 75% adherence | 76,448 | LMWH + thigh | 0.32 | 14.73 | 9,691,393 | |
| TKR | Base case | 79,551 | LMWH + thigh | 0.19 | 32.43 | 22,207,882 |
| Base case, low prices | 79,551 | LMWH + thigh | 0.19 | 29.94 | 20,499,146 | |
| Base case, 75% adherence | 79,551 | LMWH + thigh | 0.30 | 54.40 | 37,247,969 | |
| GS: low risk | Base case | 42,208 | LMWH + thigh | 0.20 | 13.10 | 4,760,081 |
| Base case, low prices | 42,208 | LMWH + thigh | 0.21 | 13.28 | 4,825,603 | |
| Base case, 75% adherence | 42,208 | LMWH + thigh | 0.31 | 23.61 | 8,577,583 | |
| GS: moderate risk | Base case | 135,141 | LMWH + thigh | 0.19 | 27.88 | 32,432,928 |
| Base case, low prices | 135,141 | LMWH + thigh | 0.20 | 26.64 | 30,986,218 | |
| Base case, 75% adherence | 135,141 | LMWH + thigh | 0.30 | 45.59 | 53,027,997 | |
| GS: high risk | Base case | 192,900 | LMWH + thigh | 0.19 | 60.37 | 100,234,031 |
| Base case, low prices | 192,900 | LMWH + thigh | 0.19 | 58.40 | 96,969,427 | |
| Base case, 75% adherence | 192,900 | LMWH + thigh | 0.23 | 71.15 | 118,147,129 | |
| Subgroup | Scenario | Population size (annual) | Optimal treatment (cost-effectiveness) | Error probability | Individual EVPI (£) | Total EVPI (£) |
|---|---|---|---|---|---|---|
| THR | Base case | 76,448 | LMWH + thigh | 0.21 | 10.45 | 6,874,002 |
| Base case, low prices | 76,448 | LMWH + thigh | 0.22 | 9.46 | 6,223,853 | |
| Base case, 75% adherence | 76,448 | LMWH + thigh | 0.32 | 18.47 | 12,155,756 | |
| TKR | Base case | 79,551 | LMWH + thigh | 0.19 | 39.59 | 27,110,215 |
| Base case, low prices | 79,551 | LMWH + thigh | 0.19 | 36.38 | 24,909,531 | |
| Base case, 75% adherence | 79,551 | LMWH + thigh | 0.30 | 65.78 | 45,041,244 | |
| GS: low risk | Base case | 42,208 | LMWH + thigh | 0.20 | 15.73 | 5,715,851 |
| Base case, low prices | 42,208 | LMWH + thigh | 0.20 | 16.08 | 5,842,579 | |
| Base case, 75% adherence | 42,208 | LMWH + thigh | 0.31 | 28.52 | 10,360,049 | |
| GS: moderate risk | Base case | 135,141 | LMWH + thigh | 0.19 | 34.02 | 39,573,879 |
| Base case, low prices | 135,141 | LMWH + thigh | 0.19 | 32.34 | 37,617,324 | |
| Base case, 75% adherence | 135,141 | LMWH + thigh | 0.30 | 55.50 | 64,556,410 | |
| GS: high risk | Base case | 192,900 | LMWH + thigh | 0.19 | 73.79 | 122,514,249 |
| Base case, low prices | 192,900 | LMWH + thigh | 0.19 | 71.18 | 118,196,138 | |
| Base case, 75% adherence | 192,900 | LMWH + thigh | 0.22 | 87.18 | 144,760,513 | |
| Subgroup | Scenario | Population size (annual) | Optimal treatment (cost-effectiveness) | Error probability | Individual EVPI (£) | Total EVPI (£) |
|---|---|---|---|---|---|---|
| THR | Orthopaedic NMA | 76,448 | LMWH + thigh | 0.17 | 1.78 | 1,169,676 |
| Orthopaedic NMA, low prices | 76,448 | LMWH + thigh | 0.17 | 1.72 | 1,129,187 | |
| Orthopaedic NMA, 75% adherence | 76,448 | LMWH + thigh | 0.42 | 6.99 | 4,600,085 | |
| TKR | Orthopaedic NMA | 79,551 | LMWH + thigh | 0.13 | 4.39 | 3,003,311 |
| Orthopaedic NMA, low prices | 79,551 | LMWH + thigh | 0.13 | 4.62 | 3,161,608 | |
| Orthopaedic NMA, 75% adherence | 79,551 | LMWH + thigh | 0.37 | 20.22 | 13,847,143 | |
| GS: low risk | Non-orthopaedic NMA | 42,208 | LMWH + thigh | 0.07 | 0.55 | 200,986 |
| Non-orthopaedic NMA, low prices | 42,208 | LMWH + thigh | 0.07 | 0.58 | 209,457 | |
| Non-orthopaedic NMA, 75% adherence | 42,208 | LMWH + thigh | 0.25 | 3.20 | 1,161,782 | |
| GS: moderate risk | Non-orthopaedic NMA | 135,141 | LMWH + thigh | 0.06 | 1.06 | 1,230,292 |
| Non-orthopaedic NMA, low prices | 135,141 | LMWH + thigh | 0.06 | 1.21 | 1,405,075 | |
| Non-orthopaedic NMA, 75% adherence | 135,141 | LMWH + thigh | 0.22 | 7.73 | 8,997,013 | |
| GS: high risk | Non-orthopaedic NMA | 192,900 | LMWH + thigh | 0.05 | 2.24 | 3,716,565 |
| Non-orthopaedic NMA, low prices | 192,900 | LMWH + thigh | 0.05 | 2.34 | 3,879,973 | |
| Non-orthopaedic NMA, 75% adherence | 192,900 | LMWH + thigh | 0.21 | 15.14 | 25,130,884 | |
| Subgroup | Scenario | Population size (annual) | Optimal treatment (cost-effectiveness) | Error probability | Individual EVPI (£) | Total EVPI (£) |
|---|---|---|---|---|---|---|
| THR | Orthopaedic NMA | 76,448 | LMWH + thigh | 0.15 | 2.10 | 1,382,444 |
| Orthopaedic NMA, low prices | 76,448 | LMWH + thigh | 0.15 | 2.02 | 1,331,443 | |
| Orthopaedic NMA, 75% adherence | 76,448 | LMWH + thigh | 0.40 | 8.52 | 5,603,277 | |
| TKR | Orthopaedic NMA | 79,551 | LMWH + thigh | 0.13 | 5.23 | 3,584,204 |
| Orthopaedic NMA, low prices | 79,551 | LMWH + thigh | 0.13 | 5.55 | 3,803,184 | |
| Orthopaedic NMA, 75% adherence | 79,551 | LMWH + thigh | 0.37 | 24.49 | 16,769,620 | |
| GS low risk | Non-orthopaedic NMA | 42,208 | LMWH + thigh | 0.07 | 0.62 | 224,183 |
| Non-orthopaedic NMA, low prices | 42,208 | LMWH + thigh | 0.07 | 0.64 | 234,192 | |
| Non-orthopaedic NMA, 75% adherence | 42,208 | LMWH + thigh | 0.24 | 3.70 | 1,343,777 | |
| GS moderate risk | Non-orthopaedic NMA | 135,141 | LMWH + thigh | 0.05 | 1.25 | 1,454,251 |
| Non-orthopaedic NMA, low prices | 135,141 | LMWH + thigh | 0.05 | 1.44 | 1,671,041 | |
| Non-orthopaedic NMA, 75% adherence | 135,141 | LMWH + thigh | 0.22 | 9.20 | 10,700,716 | |
| GS high risk | Non-orthopaedic NMA | 192,900 | LMWH + thigh | 0.05 | 2.74 | 4,541,567 |
| Non-orthopaedic NMA, low prices | 192,900 | LMWH + thigh | 0.05 | 2.80 | 4,652,203 | |
| Non-orthopaedic NMA, 75% adherence | 192,900 | LMWH + thigh | 0.21 | 18.38 | 30,525,624 | |
Again, the results demonstrate a considerable range in the population EVPI estimates, depending on the population and synthesis model applied to estimate the relative effectiveness of the different strategies. In general, the value of reducing uncertainties related to a more restrictive decision problem was lower than those reported when uncertainties relating to all three strategies were considered. Based on the effectiveness estimates from the random-effect, predictive distribution and applying a cost-effectiveness threshold of £20,000, total EVPI varies between approximately £4.8M and £118.2M across the separate populations (and between £5.7M and £144.8M at a threshold of £30,000). Similar to previous results, research potentially looks most worthwhile in the higher-risk populations considered (TKR, moderate- and high-risk GS).
Expected value of partial perfect information results
Although estimates of the total EVPI provide a useful global estimate of the uncertainty surrounding the adoption decision, this estimate does not provide an indication of the area in which further research would be of most value. The value of reducing the uncertainty surrounding particular input parameters in the decision model can also be established by estimating partial EVPI. This type of analysis can be used to focus further research by identifying those inputs for which more precise estimates would be most valuable. The analysis of the VOI associated with each of the model inputs can be conducted in a very similar way to the EVPI for the decision as a whole in cases in which a linear relationship between the inputs and the expected costs and outcomes exists. However, where the relationship is non-linear, partial EVPI estimates require substantial additional computation. Owing to the complexity of the model presented here (and the number of separate populations considered), a linear relationship has been assumed for ease of exposition. Given that the results of the deterministic and probabilistic results were similar across populations, the assumption of linearity made here seems reasonable.
There are four groups of uncertain parameters considered in the partial EVPI analysis. These relate to:
-
baseline VTE risks during the acute period (up to 14 days) and longer-term risks (e.g. recurrent VTE events, PHT, PTS)
-
relative treatment effectiveness estimates (separated into the relative treatment effect between the types of stockings and between thigh-length GCSs plus LMWH vs. LMWH alone)
-
utilities
-
costs.
The groups of parameters also reflect potentially different research designs. For example, although a RCT would ideally be required to further inform the clinical effectiveness of GCSs, evidence on the other parameters could be generated using new cohort studies (e.g. to estimate the acute and longer-term VTE risks with pharmacological prophylaxis, quality of life and cost impact of VTE events).
Figures 27–31 report the EVPPI estimates for the groups of uncertain parameters for each of the clinical effectiveness models. These estimates are presented for the full decision problem relating to all three treatments (three-way comparison) and for a more restricted decision relating only to the different types of stockings (head-to-head comparison). The EVPPI associated with the relative treatment effect of the different types of stockings consistently emerges as having substantial influence on the overall decision uncertainty. However, in terms of the three-way comparison, the value of reducing uncertainty surrounding the relative effectiveness of the different types of stockings appears less valuable than evidence that would further inform their comparative value compared with pharmacological prophylaxis alone. Based on the findings from the two-way comparison, the value of resolving uncertainty surrounding the relative effectiveness of the different types of stockings appeared to be the only parameter that was associated with substantial value.
FIGURE 27.
Expected value of perfect parameter information: THR subgroup. RE, relative effect.

FIGURE 28.
Expected value of perfect parameter information: TKR subgroup. RE, relative effect.
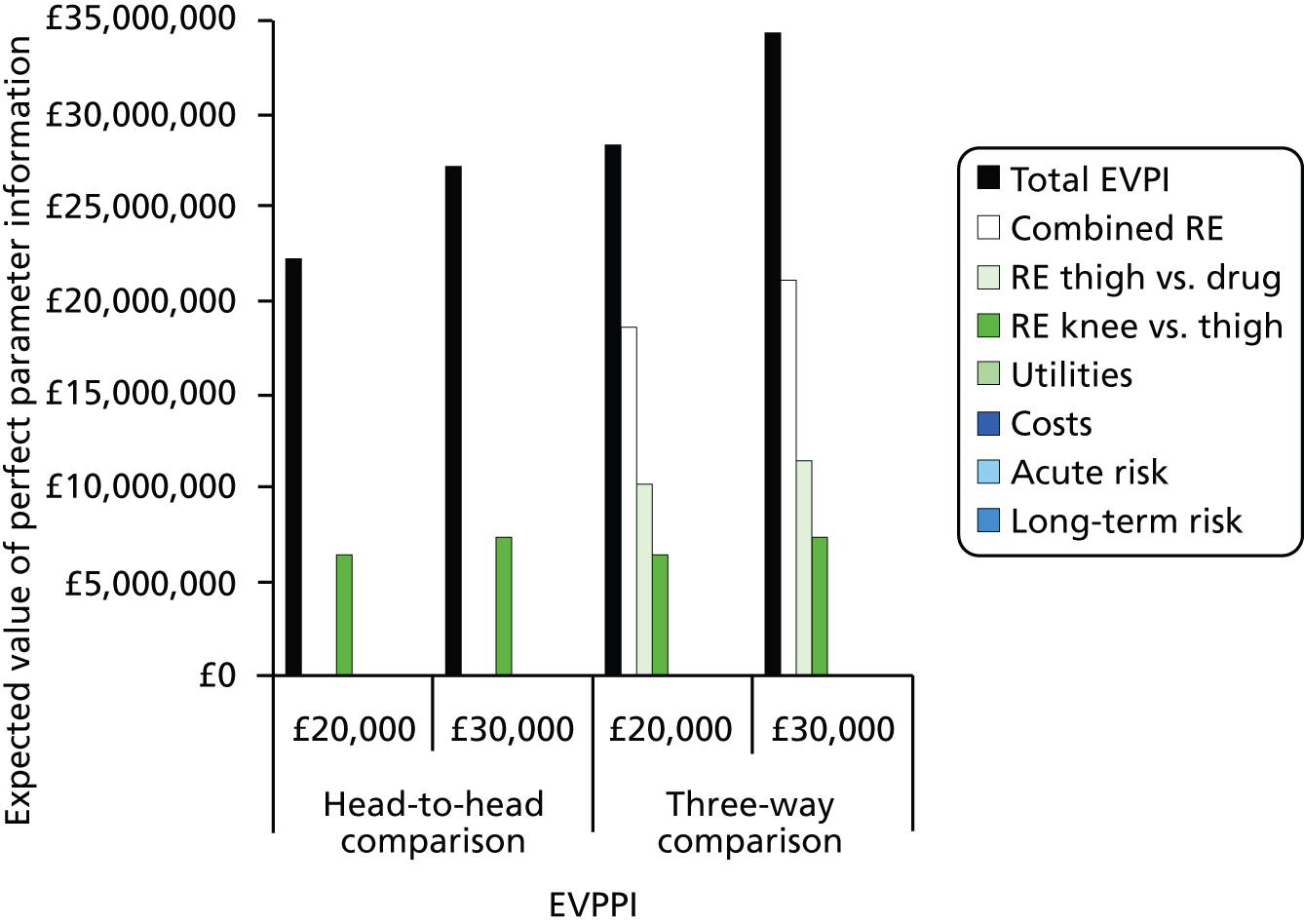
FIGURE 29.
Expected value of perfect parameter information: low-risk GS subgroup. RE, relative effect.

FIGURE 30.
Expected value of perfect parameter information: moderate-risk GS subgroup. RE, relative effect.

FIGURE 31.
Expected value of perfect parameter information: high-risk GS subgroup. RE, relative effect.

Figure 32 compares the EVPPI for relative effectiveness of thigh-length GCSs plus LMWH versus knee-length GCSs plus LMWH across the five populations based on the random-effect, predictive distributions (although not illustrated here, the fixed-effect estimates would be considerably lower than these). These estimates reflect the maximum value that could be resolved from a head-to-head trial that only informed uncertainty surrounding the relative effectiveness estimates. Similar to the findings from the total EVPI estimates, the maximum value varied across the populations, with higher values in populations with a higher baseline VTE. However, the range in values was considerably lower than the total EVPI estimates. Applying a cost-effectiveness threshold of £20,000, EVPPI for the relative effect parameter varies between approximately £2M and £32.9M across the separate populations (compared with total EVPI estimates that ranged between £3.4M and £146.9M). At a threshold of £30,000, EVPPI estimates varied between £3.37M and £39.42M (compared with total EVPI estimates of between £7.3M and £179M).
FIGURE 32.
Expected value of partial perfect information around the relative effectiveness of thigh-length vs. knee-length GCSs.

Hence, the value in resolving key uncertainties surrounding relative effectiveness of the different types of stockings is significantly lower than that indicated by the more global total EVPI estimate. However, there still exists significant potential value around relative effectiveness, particularly in the higher-risk populations (particularly high-risk GS). Hence, appropriate policy responses to these findings may be to target any future trial at a higher-risk population as opposed to recruiting lower-risk populations. Another alternative response might be to consider more efficient designs that might be less costly to undertake than a definitive trial appropriately powered on symptomatic end points. That is, it might be considered reasonable in this situation to power a future trial on total DVT events rather than symptomatic DVT events, requiring considerably smaller population sizes given the higher rate of asymptomatic events that would be expected, resulting in trial costs that might be considered more proportionate to the lower EVPPI estimates reported in the relative-effect parameters. The magnitude of the difference in trial sizes powered on symptomatic or total DVT events is discussed in more detail in Chapter 3, Sample size of a new study (see Table 33). Power calculations indicate that for symptomatic DVT for high-risk patients, a definitive trial would require a minimum of 13,000 patients because of the very low risk (1.23%) of symptomatic DVT. For total DVT (symptomatic and asymptomatic), the risk is much higher (19.76%), and for high-risk patients a trial would need a minimum of 900 patients. For both total DVT and symptomatic DVT, the sample size requirements are much greater for moderate- and low-risk patients.
However, powering the trial on asymptomatic DVT events will provide little information on symptomatic DVT events and is likely to resolve only the uncertainty around the asymptomatic DVT events. Given that the uncertainty and consequences differ between asymptomatic and symptomatic DVT, the specific value in reducing uncertainty surrounding asymptomatic DVTs can also be quantified. Figure 33 summarises the EVPPI estimates for relative effects that specifically relate to asymptomatic DVT events. As is evident, the value in resolving uncertainty surrounding the relative effectiveness of the different types of stocking relating to asymptomatic DVT events is markedly lower than the value of reducing uncertainty surrounding VTE events that include symptomatic events.
FIGURE 33.
Estimated value of partial perfect information around the relative effect of asymptomatic events for thigh-length vs. knee-length GCSs. RE, relative effect.

Summary of findings
Here, we have demonstrated the sensitivity of EVPI to different scenarios and across the five subgroups. Across all analyses, the EVPI remains highest in the high baseline risk subgroups (i.e. TKR and moderate- and high-risk GS). This indicates that further research is most valuable in populations at higher risk of VTE. The EVPPI undertaken supports this finding and suggests that further research may be worthwhile to resolve the uncertainty surrounding the relative treatment effect of the different types of stockings. However, this conclusion depends on the acquisition price of GCSs, the expected adherence with thigh-length GCSs and whether or not uncertainty can be resolved around possible effect modifiers.
Estimated value of perfect information and EVPPI do not take into account the specifics of trial design (e.g. the cost of the evidence collection or the amount of uncertainty that could be resolved given the sample size). Further methods such as expected value of sample information (EVSI), which estimates the expected value obtainable from collecting data on a sample of the population, might further inform the value of different trial types and sizes. However, the aim here was not to be prescriptive about trial design.
Chapter 8 Discussion
Summary of findings
The aim of the research was to establish the expected value of undertaking additional research comparing the relative effectiveness of thigh-length versus knee-length GCS, in addition to standard pharmacological prevention, for prevention of DVT in surgical patients. The two key objectives were to undertake an evidence synthesis by systematic review to estimate clinical effectiveness and inform key clinical parameters for a decision model and to develop a decision model to estimate cost-effectiveness and to undertake a VOI analysis.
Clinical effectiveness of thigh-length versus knee-length graduated compression stockings
Twenty-three RCTs were included in the systematic review of the clinical effectiveness of knee-length versus thigh-length GCSs.
Five RCTs that directly compared knee-length with thigh-length GCSs in surgical patients were pooled; the summary estimate of effect indicated a trend favouring thigh-length GCSs for the prevention of DVT, but the findings were not statistically significant. 12,20,21,25,49 There was substantial variation between the included trials in terms of patient characteristics (such as type of surgery) and interventions (such as concomitant pharmacoprophylaxis) and validity assessment suggested that most of the trials had an unclear or high risk of bias. This result is consistent with the Cochrane review1 comparing knee-length with thigh-length GCSs for the prevention of DVT in surgical patients, which included three of the five RCTs included here. 12,20,21
To add strength to the comparison of knee-length versus thigh-length stockings, additional analyses were undertaken. A pooled analysis of four RCTs found statistically significantly fewer DVT events in patients receiving thigh-length GCSs plus heparin versus heparin alone. 33,35–37 Compared with no active treatment, both thigh-length (five RCTs22,24,25,30,33) and knee-length (two RCTs23,25) GCSs reduced DVT events, but only with thigh-length stockings was the effect statistically significant. These results are consistent with the Cochrane review of GCSs for the prevention of DVT; although the Cochrane review did not separate trials of thigh-length stockings with trials of knee-length stockings; where reported, most of the included trials were of thigh-length stockings. 17
Thirteen trials contained data that directly or indirectly informed the relative effectiveness of knee-length versus thigh-length stockings for the prevention of DVT and were included in a NMA. 12,20–22,24,25,30,33,35–37,49,60 There was significant statistical heterogeneity in the models, as well as inconsistency reflecting clinical heterogeneity across the trials and indicating that there may be further underlying unknown clinical and methodological heterogeneity across the trials. Overall, thigh-length stockings plus heparin was the most effective treatment combination, but with a 0.2–0.27 probability that it would not be the most effective treatment in a new trial of all the treatments; this uncertainty is because of the unexplained heterogeneity across the trials in the network. Although thigh-length stockings plus heparin is the most effective treatment, the incremental benefit of reducing the risk of DVT of adding thigh-length stockings to heparin is less than adding heparin to no treatment, as heparin already reduces the risk of DVT significantly.
The results also show that the precision of the estimate of effect is not improved by the NMA, indicating clinical and methodological heterogeneity, and therefore the analyses confirm that further research is needed to confirm precisely the difference in treatment effect of thigh- and knee-length stockings when used in combination with heparin. Given the uncertainty in the NMA, it is unlikely that an additional underpowered trial would be sufficient: only a new definitive trial would be worthwhile. The definitive trial would replace the existing heterogeneous evidence, as the results would be directly applicable to the decision question.
Power calculations indicate that for symptomatic DVT for high-risk patients, a definitive trial would require a minimum of 13,000 patients because of the very low risk of symptomatic DVT. For DVT (symptomatic and asymptomatic), the risk is much higher, and for high-risk patients a trial would need a minimum of 900 patients. For both DVT and symptomatic DVT, the sample size requirements are much greater for moderate- and low-risk patients.
The review found that evidence relating to other outcomes was sparse: PE events and VTE-related mortality events were generally rare in the included trials. Adverse events were also rarely reported, and those related to GCSs were minor events, including minor foot abrasions, superficial thrombophlebitis, the stocking slipping down or feeling hot.
Nine RCTs14,21,24,25,32,37,60,63,65 and seven observational studies15,16,80–85 were identified that reported data on patient adherence and/or preference. Again, there was substantial variation between the included studies and most studies had an unclear or high risk of bias. Patient adherence (wearing stockings correctly) was generally higher in patients receiving knee-length stockings than patients receiving thigh-length stockings. Patients preferred knee-length stockings to thigh-length stockings.
Cost-effectiveness of thigh-length versus knee-length graduated compression stockings
Compared with LWMH alone, our findings suggested that the adjunctive use of compression stockings appeared to represent good value for money to the NHS across the different populations considered. However, in the population with the lowest risk of DVT (THR), the cost-effectiveness of adding compression stockings to LMWH alone appeared more finely balanced.
These general findings were consistent with the findings from the previous NICE CG, which reported favourable cost-effectiveness estimates for GCSs combined with pharmacological prophylaxis. However, in contrast to the previous NICE guideline,4 our analysis was also able to explore differences in cost-effectiveness between the different types of stockings. Importantly, our results consistently found that the use of thigh-length GCSs plus LMWH appeared to dominate knee-length GCSs plus LMWH. These findings appeared robust to alternative assumptions relating to the acquisition costs and adherence.
Although the comparisons of mean cost and QALYs consistently indicated that thigh-length GCSs plus LMWH was the most cost-effective strategy, there remains significant uncertainty surrounding any decision to routinely recommend the use of thigh-length GCSs plus LMWH compared with knee-length GCSs plus LMWH and LMWH alone. Indeed, the error probability that thigh-length stockings plus LMWH is the most cost-effective strategy varied between 0.48 and 0.70 in the base-case analysis. Another important finding from the cost-effectiveness analysis relates to the small differences in excepted lifetime costs and QALYs between the alternative strategies. In the base case, the maximum differences reported (i.e. between the least effective and most effective strategy) in QALYs, across all the separate populations, was equivalent to a difference of between 0.37 and 3.32 days of perfect health over a patient’s remaining lifetime.
Value of information analysis
The EVPI analysis was used to understand the uncertainty around the choice of treatment and the value of perfectly resolving that uncertainty. The values produced by EVPI are upper limits of the value of collecting further evidence, as research is unlikely to perfectly resolve the decision uncertainty. EVPI was estimated for different scenarios and across the five subgroups of interest. These analyses demonstrated that EVPI is sensitive to:
-
the subgroup
-
the price and adherence scenarios
-
the type of comparison (three way vs. head to head)
-
the type of NMA used to inform the relative effect (fixed-effect model versus the predictive distribution of a random-effects model)
-
the threshold (£20,000 vs. £30,000).
Across all analyses, the EVPI remained highest in the high baseline risk subgroups (i.e. TKR and moderate- and high-risk GS). This indicates that further research is potentially worthwhile in the higher-risk populations. EVPI also suggested that a three-way trial may be more valuable than a head-to-head trial and that a trial that could resolve uncertainty on possible treatment effect modifiers may be most valuable. This would require a trial powered to more formally address the presence and magnitude of possible effect modifiers (e.g. a trial stratified by different patient subgroups).
The acquisition price of GCSs also affected the EVPI estimates; however, the direction of its effect was not consistent. This is because when GCSs is estimated to be the most cost-effective option, lowering the acquisition price makes the decision more certain; however, if GCSs are not cost-effective, then lowering the price will make the decision more uncertain, as GCSs approach the cost-effectiveness threshold.
Although the scenarios around adherence have a substantial effect on decision uncertainty, how this should be interpreted to make decisions for further research raises a number of issues. First, it is not clear that it would be possible to detect differences in adherence given the control of a clinical trial; and second, the size of a trial needed to estimate the modifying effect of adherence on treatment may be unfeasible. In these cases, the value of resolving the uncertainty estimated in our adherence scenarios is unlikely.
Expected value of partial perfect analysis was used to better understand on which parameters to undertake further research. The EVPPI analysis presented considers four groups of uncertain parameters:
-
baseline VTE risks
-
relative treatment effect
-
utilities
-
costs.
The EVPPI associated with the relative treatment effect of the different types of stockings consistently emerged as having a substantial influence on the overall decision uncertainty. Similar to the EVPI findings, the maximum value varied across the populations, with higher value in populations with a higher baseline VTE risk. At a threshold of £30,000, the EVPPI for the relative effect parameter varied between approximately £3.37M and £39.42M. Further analysis demonstrated that the value of resolving the uncertainty surrounding the relative effectiveness of different stocking types on asymptomatic DVT is much lower than the value of reducing uncertainty surrounding total DVT.
Ongoing changes in pharmaceutical prophylaxis are important when determining the value of compression stocking use or the value of undertaking a trial comparing knee-length with thigh-length stockings. No studies were identified using compression stockings with NOACs and it is unclear to what extent improved surgical methods have been captured in the available studies, but clinical trials have demonstrated the improved efficacy of NOACs compared with LMWH. With an increased uptake in NOACs and improved surgical techniques, this may become the baseline on which future compression stockings are used. Given the increased efficacy of NOACs and improved surgical techniques, GSCs would be compared using a lower baseline risk of DVT. There was no evidence that different pharmaceutical prophylaxes changed the relative efficacy of the GCSs; however, the economic analysis consistently demonstrated that a lower baseline risk of DVT resulted in compression stockings having a higher ICER and lower VOI. This suggests that improved surgical techniques and NOAC use would result in GCSs being less likely to be cost-effective and lower value of resolving the uncertainty surrounding the relative effectiveness of different stocking types.
Strengths and limitations
Strengths
The systematic review of the clinical effectiveness of thigh-length versus knee-length GCSs used all available RCT evidence on thigh-length and knee-length stockings. Meta-analysis was used, when appropriate, as well as NMA to assess the relative effectiveness of thigh-length versus knee-length stockings for the prevention of DVT. The clinical effectiveness results were combined with the best available data on baseline risk, consequences of DVT, and patient adherence and preference study results, in order to model the cost-effectiveness of knee-length versus thigh-length stockings for the prevention of DVT.
Limitations
There was substantial variation across the RCTs assessing the clinical effectiveness of knee-length or thigh-length GCS, in terms of patient characteristics (suggesting that the participants had a different baseline risk for DVT) and interventions used (in terms of both stocking pressure and concomitant pharmacological prophylaxis). The timing of outcome assessments was generally short, where reported. The included trials assessed all DVTs, not just symptomatic DVTs. Where reported, the majority of DVTs were asymptomatic, the clinical consequences of which are unknown.
Generally the RCT methods were poorly reported, making risk-of-bias assessment difficult. Three RCTs were judged to have a low risk of bias,31,49,60 five to have a high risk of bias20,25,35,37,66 and for 15 RCTs the reporting was inadequate to judge the risk of bias. 12,21–24,30,32–34,36,61–65
There was some evidence of statistical heterogeneity for the summary estimate of effect for most of the meta-analyses undertaken.
Many of the included RCTs date back to the 1970s and 1980s and, therefore, they may not reflect current NHS practice. Surgical practice has changed over time, with surgical procedures that are less invasive shorter duration of hospitalisation with many procedures now performed as day cases and earlier mobilisation after surgery. Subgroup analysis was planned on the year 2003 and onwards and pre-2003 subgroups. However, the network for the year 2003 and onwards subgroup comprised only two trials. Therefore, the subgroup analysis was not conducted. In addition, none of the included trials used the NOACs (dabigatran, rivaroxaban or apixaban) and some trials excluded patients at high risk for DVT (e.g. patients with history of prior VTE). There are increasing numbers of older patients undergoing surgery, and an increasing proportion of obese and morbidly obese patients. Therefore, the results of the included studies may not be generalisable to patients seen in current NHS practice.
All of the studies assessing patient adherence reflect adherence in a hospital setting only, where patients are observed by health-care professionals; it is likely that adherence is lower after patients have been discharged from hospital. Therefore, the effectiveness estimated in trial conditions might not be replicated in practice.
Expected value of perfect information and EVPPI do not take into account the specifics of trial design, such as the cost of the evidence collection, or the amount of uncertainty that could be resolved given the sample size. Further methods such as EVSI, which estimates the expected value obtainable from collecting data on a sample of the population, might further inform the value of undertaking a specific trial.
Chapter 9 Conclusions
The evidence base for the relative treatment effect of knee-length versus thigh-length GCSs when used in combination with pharmacological prophylaxis (heparin) is weak and subject to considerable heterogeneity.
An analysis of all the available data using standard meta-analysis and NMA suggests that thigh-length stockings are more effective than knee-length stockings but that the benefit of GCSs over and above that achieved with heparin alone is small and may not be clinically significant. Furthermore, the results are subject to considerable uncertainty and the precision of the estimate of effect is not improved by the NMA. Further research could more precisely estimate the difference in treatment effect between knee-length and thigh-length stockings when used in combination with heparin, although the value and feasibility of a definitive trial is less clear. The sample size required for such a trial ranges from 900 to 13,000 patients.
Studies of patient adherence and preference found that the results favour knee-length stockings over thigh-length stockings.
The value of further research is most evident in the high-risk subgroups, and the effect of changes in patient characteristics and treatment patterns on DVT risk should be considered in any decision to undertake a trial. However, the efficiency of this research (i.e. whether or not this represents value for money) is dependent on several factors, the acquisition price of GCSs, the expected adherence to thigh-length GCSs and whether or not uncertainty can be resolved around possible effect modifiers as well as the feasibility and actual cost of undertaking the proposed research.
Implications for practice
Although the model results demonstrate that the use of thigh-length GCSs as an adjunctive treatment to pharmacological prophylaxis appears to be more cost-effective than the adjunctive use of knee-length GCSs and pharmacological prophylaxis alone, an assessment of the importance of these findings in terms of informing clinical practice and relevant policies needs also to take into account both the high levels of decision uncertainty that currently exists, and the clinical and economic significance of the differences in costs and QALYs.
Implications for research
The purpose of this analysis was not to be prescriptive about a potential trial design; however, methods such as EVSI might further inform the value of undertaking a specific trial. As discussed, the changes in clinical practice and the use of new drug technologies (i.e. NOACs) are likely to reduce the estimated value of further research on the use of knee-length versus thigh-length GCSs in combination with standard pharmacological prophylaxis, but a NMA of NOACs could be used in the model to better understand the VOI in this clinical environment.
Acknowledgements
We would like to thank members of our advisory group: Professor Gerard Stansby, Professor of Vascular Surgery at the Newcastle upon Tyne Hospitals NHS Foundation Trust; Mr Peter Millner, Consultant Orthopaedic and Spinal Surgeon at Leeds Teaching Hospitals NHS Trust; Ms Hayley Flavell, Anticoagulant and Thrombosis Consultant Nurse at the Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust; Mrs Camilla Smith, Sister at Leeds Teaching Hospitals NHS Trust; and Professor David Torgerson, Director of the York Trials Unit at the University of York. We would also like to thank Dr Yngve Falck-Ytter (Associate Professor, Case Western Reserve University, Cleveland, OH, USA) and the authors of the ACCP orthopaedic guidelines for providing baseline risk data. In addition, we would like to thank our patient representative, Mrs Kaye Norman, for advice.
Contributions of authors
Ros Wade wrote the protocol, performed study selection, data extraction, validity assessment and synthesis of the included studies and took responsibility for writing the report.
Eleftherios Sideris was the main economic analyst; he took the lead in the cost-effectiveness and VOI analyses, model programming and writing of the report.
Fiona Paton contributed to the protocol development, performed study selection, data extraction, validity assessment and synthesis of the included studies and contributed to the writing of the report.
Stephen Rice undertook the NMA and contributed to the writing of the report.
Stephen Palmer undertook an advisory role and provided input at all stages, and was involved in writing the protocol, developing the model and writing the report.
Dave Fox contributed to the protocol development, developed the search strategies, conducted a range of searches to locate studies and wrote the sections of the report relating to the searches.
Nerys Woolacott contributed to the protocol development, undertook an advisory role in the clinical reviews section and provided input to the project, provided comments on drafts of the report and took overall managerial responsibility for the project.
Eldon Spackman had overall responsibility for the cost-effectiveness and VOI analyses and contributed to the protocol development, economic data extraction, model programming and writing of the report.
Data sharing statement
Study characteristics and results of trials included in the systematic review of the effectiveness of thigh-length versus knee-length stockings are provided in Appendix 3. Details of guidelines reporting baseline risks are provided in Appendix 4. All data created during this research are available by request from the authors.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Sajid MS, Desai M, Morris RW, Hamilton G. Knee length versus thigh length graduated compression stockings for prevention of deep vein thrombosis in postoperative surgical patients. Cochrane Database Syst Rev 2012;5. http://dx.doi.org/10.1002/14651858.CD007162.pub2.
- The Prevention of Venous Thromboembolism in Hospitalised Patients: Second Report of Session 2004–05. London: The Stationery Office; 2005.
- Sweetland S, Green J, Liu B, de Gonzalez AB, Canonico M, Reeves G, et al. Duration and magnitude of the postoperative risk of venous thromboembolism in middle aged women: prospective cohort study. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b4583.
- NICE Clinical Guidance CG92: Venous Thromboembolism: Reducing the Risk: Reducing the Risk of Venous Thromboembolism (Deep Vein Thrombosis and Pulmonary Embolism) in Patients Admitted to Hospital. London: NICE; 2010.
- Risk Assessment for Venous Thromboembolism (VTE). London: DH; 2010.
- NICE Quality Standards: VTE and bleeding risk assessment. London: NICE; 2013.
- The Surgeon General’s Call to Action to Prevent Deep Vein Thrombosis and Pulmonary Embolism. Washington, DC: U.S. Department of Health and Human Services; 2008.
- Lowe GDO, Greer IA, Cooke TG, Dewar EP, Evans MJ, Forbes CD, et al. Regular review - risk of and prophylaxis for venous thromboembolism in hospital patients. BMJ 1992;305:567-74. http://dx.doi.org/10.1136/bmj.305.6853.567.
- NICE Clinical Guidance CG144: Venous Thromboembolic Diseases: the Management of Venous Thromboembolic Diseases and the Role of Thrombophilia Testing. London: NICE; 2012.
- Kanaan AO, Lepage JE, Djazayeri S, Donovan JL. Evaluating the role of compression stockings in preventing post thrombotic syndrome: a review of the literature. Thrombosis 2012. http://dx.doi.org/10.1155/2012/694851.
- SIGN Guideline 122: Prevention and Management of Venous Thromboembolism: A National Clinical Guideline. Edinburgh: SIGN; 2010.
- Howard A, Zaccagnini D, Ellis M, Williams A, Davies AH, Greenhalgh RM. Randomized clinical trial of low molecular weight heparin with thigh-length or knee-length antiembolism stockings for patients undergoing surgery. Br J Surg 2004;91:842-7. http://dx.doi.org/10.1002/bjs.4514.
- Sigel B, Edelstei Al, Felix WR, Memhardt CR. Compression of deep venous system of lower leg during inactive recumbency. Arch Surg 1973;106:38-43. http://dx.doi.org/10.1001/archsurg.1973.01350130040009.
- Benko T, Cooke EA, McNally MA, Mollan RAB. Graduated compression stockings – knee length or thigh length. Clin Orthop Relat Res 2001;383:197-203. http://dx.doi.org/10.1097/00003086-200102000-00022.
- Brady D, Raingruber B, Peterson J, Varnau W, Denman J, Resuello R, et al. The use of knee-length versus thigh-length compression stockings and sequential compression devices. Crit Care Nurs Q 2007;30:255-62. http://dx.doi.org/10.1097/01.CNQ.0000278926.67562.2f.
- Hameed MF, Browse DJ, Immelman EJ, Goldberg PA. Should knee-length replace thigh-length graduated compression stockings in the prevention of deep-vein thrombosis?. S Afr J Surg 2002;40:15-6.
- Sachdeva A, Dalton M, Amaragiri Sachiendra V, Lees T. Elastic compression stockings for prevention of deep vein thrombosis. Cochrane Database Syst Rev 2010;7. http://dx.doi.org/10.1002/14651858.cd001484.pub2.
- Venous Thromboembolism: Reducing the Risk. Evidence Update February 2012: A Summary of Selected New Evidence Relevant to NICE Clinical Guideline 92 ‘Reducing the Risk of Venous Thromboembolism (Deep Vein Thrombosis and Pulmonary Embolism) in Patients Admitted to Hospital’ (2010). London: NICE; 2012.
- Sajid MS, Tai NR, Goli G, Morris RW, Baker DM, Hamilton G. Knee versus thigh length graduated compression stockings for prevention of deep venous thrombosis: a systematic review. Eur J Vasc Endovasc Surg 2006;32:730-6. http://dx.doi.org/10.1016/j.ejvs.2006.06.021.
- Williams JT, Palfrey SM. Cost effectiveness and efficacy of below knee against above knee graduated compression stockings in the prevention of deep vein thrombosis. Phlebologie 1988;41:809-11.
- Porteous MJL, Nicholson EA, Morris LT, James R, Negus D. Thigh length versus knee length stockings in the prevention of deep-vein thrombosis. Br J Surg 1989;76:296-7. http://dx.doi.org/10.1002/bjs.1800760324.
- Shirai N. Study on prophylaxis of postoperative deep vein thrombosis. Acta Sch Med Univ Gifu 1985;33:1173-83.
- Tsapogas MJ, Goussous H, Peabody RA, Karmody AM, Eckert C. Postoperative venous thrombosis and effectiveness of prophylactic measures. Arch Surg 1971;103. http://dx.doi.org/10.1001/archsurg.1971.01350110059009.
- Turpie AGG, Hirsh J, Gent M, Julian D, Johnson J. Prevention of deep-vein thrombosis in potential neurosurgical patients – a randomized trial comparing graduated compression stockings alone or graduated compression stockings plus intermittent pneumatic compression with control. Arch Intern Med 1989;149:679-81. http://dx.doi.org/10.1001/archinte.1989.00390030131025.
- Hui ACW, Heras-Palou C, Dunn I, Triffitt PD, Crozier A, Imeson J, et al. Graded compression stockings for prevention of deep-vein thrombosis after hip and knee replacement. J Bone Joint Surg Br 1996;78B:550-4.
- Allan A, Williams JT, Bolton JP, Lequesne LP. The use of graduated compression stockings in the prevention of postoperative deep-vein thrombosis. Br J Surg 1983;70:172-4. http://dx.doi.org/10.1002/bjs.1800700311.
- Holford CP. Graded compression for preventing deep venous thrombosis. BMJ 1976;2:969-70. http://dx.doi.org/10.1136/bmj.2.6042.969.
- Scurr JH, Ibrahim SZ, Faber RG, Lequesne LP. Efficacy of graduated compression stockings in prevention of deep-vein thrombosis. Br J Surg 1977;64:371-3. http://dx.doi.org/10.1002/bjs.1800640521.
- Turner GM, Cole SE, Brooks JH. The efficacy of graduated compression stockings in the prevention of deep-vein thrombosis after major gynecological surgery. Br J Obstet Gynaecol 1984;91:588-91. http://dx.doi.org/10.1111/j.1471-0528.1984.tb04808.x.
- Barnes RW, Brand RA, Clarke W, Hartley N, Hoak JC. Efficacy of graded-compression anti-embolism stockings in patients undergoing total hip arthroplasty. Clin Orthop Relat Res 1978;132:61-7.
- Bergqvist D, Lindblad B. The thromboprophylactic effect of graded elastic compression stockings in combination with dextran 70. Arch Surg 1984;119:1329-31. http://dx.doi.org/10.1001/archsurg.1984.01390230095024.
- Fredin H, Bergqvist D, Cederholm C, Lindblad B, Nyman U. Thromboprophylaxis in hip-arthroplasty – dextran with graded compression or preoperative dextran compared in 150 patients. Acta Orthop Scand 1989;60:678-81. http://dx.doi.org/10.3109/17453678909149602.
- Kalodiki EP, Hoppensteadt DA, Nicolaides AN, Fareed J, Gill K, Regan F, et al. Deep venous thrombosis prophylaxis with low molecular weight heparin and elastic compression in patients having total hip replacement – a randomised controlled trial. Int Angiol 1996;15:162-8.
- Scurr JH, Coleridgesmith PD, Hasty JH. Regimen for improved effectiveness of intermittent pneumatic compression in deep venous thrombosis prophylaxis. Surgery 1987;102:816-20.
- Torngren S. Low-dose heparin and compression stockings in the prevention of postoperative deep venous thrombosis. Br J Surg 1980;67:482-4. http://dx.doi.org/10.1002/bjs.1800670710.
- Wille-Jørgensen P, Hauch O, Dimo B, Christensen SW, Jensen R, Hansen B. Prophylaxis of deep venous thrombosis after acute abdominal operation. Surg Gynecol Obstet 1991;172:44-8.
- Wille-Jørgensen P, Thorup J, Fischer A, Holstchristensen J, Flamsholt R. Heparin with and without graded compression stockings in the prevention of thromboembolic complications of major abdominal surgery: a randomized trial. Br J Surg 1985;72:579-81. http://dx.doi.org/10.1002/bjs.1800720726.
- Ohlund C, Fransson SG, Starck SA. Calf compression for prevention of thromboembolism following hip-surgery. Acta Orthop Scand 1983;54:896-9. http://dx.doi.org/10.3109/17453678308992929.
- Kierkegaard A, Norgren L. Graduated compression stockings in the prevention of deep vein thrombosis in patients with acute myocardial infarction. Eur Heart J 1993;14:1365-8. http://dx.doi.org/10.1093/eurheartj/14.10.1365.
- Systematic Reviews: CRD’s Guidance for Undertaking Reviews in Health Care. York: Centre for Reviews and Dissemination, University of York; 2009.
- Moher D, Liberati A, Tetzlaff J, Altman DG, Grp P. Preferred Reporting Items for Systematic Reviews and Meta-analyses: the PRISMA statement. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b2535.
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. Oxford: The Cochrane Collaboration; 2011.
- Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med 2010;29:932-44. http://dx.doi.org/10.1002/sim.3767.
- Cooper NJ, Sutton AJ, Morris D, Ades AE, Welton NJ. Addressing between-study heterogeneity and inconsistency in mixed treatment comparisons: Application to stroke prevention treatments in individuals with non-rheumatic atrial fibrillation. Stat Med 2009;28:1861-81. http://dx.doi.org/10.1002/sim.3594.
- Lu GB, Ades AE. Assessing evidence inconsistency in mixed treatment comparisons. J Am Stat Assoc 2006;101:447-59. http://dx.doi.org/10.1198/016214505000001302.
- Sutton A, Ades AE, Cooper N, Abrams K. Use of indirect and mixed treatment comparisons for technology assessment. Pharmacoeconomics 2008;26:753-67. http://dx.doi.org/10.2165/00019053-200826090-00006.
- Wolf J, Prüss-Ustün A, Cumming O, Bartram J, Bonjour S, Cairncross S, et al. Systematic review: assessing the impact of drinking water and sanitation on diarrhoeal disease in low- and middle-income settings: systematic review and meta-regression. Trop Med Int Health 2014;19:928-42. http://dx.doi.org/10.1111/tmi.12331.
- Dias S, Welton N, Sutton A, Ades AE. NICE DSU Technical Support Document 2: A Generalised Linear Modelling Framework for Pairwise and Network Meta-analysis of Randomised Controlled Trials. Sheffield: Decision Support Unit, ScHARR, University of Sheffield; 2011.
- Cohen AT, Skinner JA, Warwick D, Brenkel I. The use of graduated compression stockings in association with fondaparinux in surgery of the hip – a multicentre, multinational, randomised, open-label, parallel-group comparative study. J Bone Joint Surg Br 2007;89B:887-92. http://dx.doi.org/10.1302/0301-620X.89B7.18556.
- Brooks SP, Gelman A. General methods for monitoring convergence of iterative simulations. J Comp Graph Stat 1998;7:434-55.
- Ramos J, Perrotta C, Badariotti G, Berenstein G. Interventions for preventing venous thromboembolism in adults undergoing knee arthroscopy. Cochrane Database Syst Rev 2008;4. http://dx.doi.org/10.1002/14651858.cd005259.pub3.
- Wille-Jørgensen P, Rasmussen Morten S, Andersen Betina R, Borly L. Heparins and mechanical methods for thromboprophylaxis in colorectal surgery. Cochrane Database Syst Rev 2004;1. http://dx.doi.org/10.1002/14651858.cd001217.
- Byrne B. Deep vein thrombosis prophylaxis: the effectiveness and implications of using below-knee or thigh-length graduated compression stockings. Heart Lung 2001;30:277-84. http://dx.doi.org/10.1067/mhl.2001.116009.
- Elvaas IKO, Graff BA, Harboe I, Norderhaug IN. Graduated Compression Stockings for Prevention of Deep Vein Thrombosis. Hamar: The Norwegian Knowledge Centre for the Health Services; 2008.
- Scott A, Argaez C. Knee-high versus thigh-high compression devices: a review of the clinical and cost-effectiveness. Ottawa: Canadian Agency for Drugs and Technologies in Health; 2008.
- Agarwal R, Umscheid CA. Mechanical Prophylaxis for Venous Thromboembolism After Ambulatory Surgery. Philadelphia, PA: Center for Evidence-Based Practice; 2009.
- Amaragiri SV, Lees TA. Elastic compression stockings for prevention of deep vein thrombosis (Cochrane Review). J Am Coll Surg 2003;196.
- Loomba RS, Arora RR, Chandrasekar S, Shah PH. Thigh-length versus knee-length compression stockings for deep vein thrombosis prophylaxis in the inpatient setting. Blood Coagul Fibrinolysis 2012;23:168-71. http://dx.doi.org/10.1097/MBC.0b013e32834cb25b.
- Johnston R. The Effectiveness of Below Knee Thromboembolic Deterrent Garments Compared to Full Length Garments in Preventing Deep Vein Thrombosis. Clayton, VIC: Centre for Clinical Effectiveness; 2001.
- Camporese G, Bernardi E, Prandoni P, Noventa F, Verlato F, Simioni P, et al. Low-molecular-weight heparin versus compression stockings for thromboprophylaxis after knee arthroscopy: a randomized trial. Ann Int Med 2008;149:73-82. http://dx.doi.org/10.7326/0003-4819-149-2-200807150-00003.
- Caprini JA, Chucker JL, Zuckerman L, Vagher JP, Franck CA, Cullen JE. Thrombosis prophylaxis using external compression. Surg Gynecol Obstet 1983;156:599-604.
- Fasting H, Andersen K, Nielsen HK, Husted SE, Koopmann HD, Simonsen O, et al. Prevention of postoperative deep venous thrombosis – low-dose heparin versus graded pressure stockings. Acta Chir Scand 1985;151:245-8.
- Mellbring G, Palmer K. Prophylaxis of deep-vein thrombosis after major abdominal-surgery – comparison between dihydroergotamine-heparin and intermittent pneumatic calf compression and evaluation of added graduated static compression. Acta Chir Scand 1986;152:597-600.
- Rasmussen A, Hansen PT, Lindholt J, Poulsen TD, Toftdahl DB, Gram J, et al. Venous thrombosis after abdominal-surgery – a comparison between subcutaneous heparin and antithrombotic stockings, or both. J Med 1988;19:193-201.
- Ayhan H, Iyigun E, Ince S, Can MF, Hatipoglu S, Saglam M. Comparison of three different protocols in the prevention of postoperative deep vein thrombosis in patients at high-risk: randomized clinical study. Eur Surg Res 2013;50:64-5.
- Ishak MA, Morley KD. Deep venous thrombosis after total hip-arthroplasty: a prospective controlled-study to determine the prophylactic effect of graded pressure stockings. Br J Surg 1981;68:429-32. http://dx.doi.org/10.1002/bjs.1800680622.
- Kahn SR, Lim W, Dunn AS, Cushman M, Dentali F, Akl EA. Prevention of VTE in nonorthopedic surgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012;141:e195S-e226S.
- Bates SM, Greer IA, Middeldorp S, Veenstra DL, Prabulos A-M, Vandvik PO. VTE, thrombophilia, antithrombotic therapy, and pregnancy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012;141:e691S-e736S. http://dx.doi.org/10.1378/chest.11-2300.
- Brazilian Society of Cardiology . Steps to reduce surgical risk. In: II guidelines for perioperative evaluation. Arq Bras Cardiol 2011;96:S23-41.
- Prevention of venous thromboembolism. Helsinki: Wiley Interscience; 2010.
- Deep Vein Thrombosis. Helsinki: Wiley Interscience; 2011.
- Nicolaides AN, Fareed J, Kakkar AK, Breddin HK, Goldhaber SZ, Hull R, et al. Prevention and treatment of venous thromboembolism International Consensus Statement (Guidelines according to scientific evidence). Int Angiol 2013;32:111-14. http://dx.doi.org/10.1177/1076029612474840.
- Venous Thromboembolism. London: Royal College of Surgeons; 2007.
- Clinical Practice Guideline for the Patient Safety at Surgery Settings. Barcelona: Agency for Information, Evaluation, and Quality in Health of Catalonia; 2010.
- Venous thromboembolism (VTE) prophylaxis ENT Guideline. London: ENT UK; 2010.
- Clinical Practice Guideline for the Prevention of Venous Thromboembolism (Deep Vein Thrombosis and Pulmonary Embolism) in Patients Admitted to Australian Hospitals. Canberra: NHMRC; 2009.
- Chalmers EA, Ganesen VJ, Liesner R, Maroo S, Nokes TJC, Saunders D, et al. The Investigation, Management and Prevention of Venous Thrombosis in Children. London: British Committee for Standards in Haematology; 2010.
- Bahl V, Hu HM, Henke PK, Wakefield TW, Campbell DA, Caprini JA. A validation study of a retrospective venous thromboembolism risk scoring method. Ann Surg 2010;251:344-50. http://dx.doi.org/10.1097/SLA.0b013e3181b7fca6.
- Baglin T, Douketis J, Tosetto A, Marcucci M, Cushman M, Kyrle P, et al. Does the clinical presentation and extent of venous thrombosis predict likelihood and type of recurrence? A patient-level meta-analysis. J Thromb Haemost 2010;8:2436-42. http://dx.doi.org/10.1111/j.1538-7836.2010.04022.x.
- Parnaby C. A new anti-embolism stocking. Use of below-knee products and compliance. Br J Perioper Nurs 2004;14:302-4.
- Williams AM, Rhys-Davies P, Sweetham D. Graduated compression stockings in the prevention of deep vein thrombosis and the case for knee length versus thigh length stockings. J Bone Joint Surg Br 1994;76B.
- Williams AM, Davies PR, Sweetnam DIS, Harper G, Pusey R, Lightowler CDR. Knee-length versus thigh-length graduated compression stockings in the prevention of deep vein thrombosis. Br J Surg 1996;83. http://dx.doi.org/10.1002/bjs.1800831119.
- Williams LA, Owen TD. Above-knee versus below-knee stockings in total knee arthroplasty. Ann R Coll Surg Engl 2006;88:302-5. http://dx.doi.org/10.1308/003588406X98676.
- Winslow EH, Brosz DL. Graduated compression stockings in hospitalized postoperative patients: correctness of usage and size. Am J Nurs 2008;108:40-51. http://dx.doi.org/10.1097/01.NAJ.0000334973.82359.11.
- Thompson A, Walter S, Brunton LR, Pickering GT, Mehendale S, Smith AJ, et al. Anti-embolism stockings and proximal indentation. Br J Nurs 2011;20:1426-30. http://dx.doi.org/10.12968/bjon.2011.20.22.1426.
- NICE Technology Appraisal TA245: Apixaban (Eliquis®) for the Prevention of Venous Thromboembolic Events in Adult Patients Who Have Undergone Elective Hip or Knee Replacement Surgery: Submitted by Bristol-Myers Squibb Pharmaceuticals Ltd. and Pfizer Ltd. London: NICE; 2011.
- Lassen MR, Raskob GE, Gallus A, Pineo G, Chen D, Hornick P. Apixaban versus enoxaparin for thromboprophylaxis after knee replacement (ADVANCE-2): a randomised double-blind trial. Lancet 2010;375:807-15. http://dx.doi.org/10.1016/S0140-6736(09)62125-5.
- Lassen MR, Gallus A, Raskob GE, Pineo G, Chen D, Ramirez LM. Apixaban versus enoxaparin for thromboprophylaxis after hip replacement. N Engl J Med 2010;363:2487-98. http://dx.doi.org/10.1056/NEJMoa1006885.
- Eriksson BI, Borris LC, Friedman RJ, Haas S, Huisman MV, Kakkar AK, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after hip arthroplasty. N Engl J Med 2008;358:2765-75. http://dx.doi.org/10.1056/NEJMoa0800374.
- Lassen MR, Ageno W, Borris LC, Lieberman JR, Rosencher N, Bandel TJ, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty. N Engl J Med 2008;358:2776-86. http://dx.doi.org/10.1056/NEJMoa076016.
- Kakkar AK, Brenner B, Dahl OE, Eriksson BI, Mouret P, Muntz J, et al. Extended duration rivaroxaban versus short-term enoxaparin for the prevention of venous thromboembolism after total hip arthroplasty: a double-blind, randomised controlled trial. Lancet 2008;372:31-9. http://dx.doi.org/10.1016/S0140-6736(08)60880-6.
- Turpie AG, Lassen MR, Davidson BL, Bauer KA, Gent M, Kwong LM, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after total knee arthroplasty (RECORD4): a randomised trial. Lancet 2009;373:1673-80. http://dx.doi.org/10.1016/S0140-6736(09)60734-0.
- Eriksson BI, Dahl OE, Rosencher N, Kurth AA, Van Dijk N, Frostick SP, et al. Oral dabigatran etexilate vs. subcutaneous enoxaparin for the prevention of venous thromboembolism after total knee replacement: the RE-MODEL randomized trial. Thromb Haemost 2007;5:2178-85. http://dx.doi.org/10.1111/j.1538-7836.2007.02748.x.
- Eriksson BI, Dahl OE, Rosencher N, Kurth AA, van Dijk CN, Frostick SP, et al. Dabigatran etexilate versus enoxaparin for prevention of venous thromboembolism after total hip replacement: a randomised, double-blind, non-inferiority trial. Lancet 2007;370:949-56. http://dx.doi.org/10.1016/S0140-6736(07)61445-7.
- Eriksson BI, Dahl OE, Huo MH, Kurth AA, Hantel S, Hermansson K, et al. Oral dabigatran versus enoxaparin for thromboprophylaxis after primary total hip arthroplasty (RE-NOVATE II*). A randomised, double-blind, non-inferiority trial. Thromb Haemost 2011;105:721-9. http://dx.doi.org/10.1160/TH10-10-0679.
- Prandoni P, Lensing AWA, Cogo A, Cuppini S, Villalta S, Carta M, et al. The long-term clinical course of acute deep venous thrombosis. Ann Int Med 1996;125:1-7. http://dx.doi.org/10.7326/0003-4819-125-1-199607010-00001.
- Imperiale TF, Speroff T. A meta-analysis of methods to prevent venous thromboembolism following total hip-replacement. JAMA 1994;271:1780-5. http://dx.doi.org/10.1001/jama.1994.03510460072036.
- Campbell IA, Fennerty A, Miller AC. British Thoracic Society Standards of Care Committee . British Thoracic Society guidelines for the management of suspected acute pulmonary embolism. Thorax 2003;58:470-83. http://dx.doi.org/10.1136/thorax.58.6.470.
- Baglin TP, Brush J, Streiff M. British Commitee for Standards in Haematology . Guidelines on use of vena cava filters. Br J Haematol 2006;134:590-5. http://dx.doi.org/10.1111/j.1365-2141.2006.06226.x.
- NICE Technology Appraisal TA170: Rivaroxaban for the Prevention of Venous Thromboembolism After Total Hip or Total Knee Replacement in Adults. London: NICE; 2009.
- Cohen A, Botteman M, Nadipelli V, Stephens J, Ewing M, Collier P. Estimating the economic burden of pts and recurrent VTE following DVT in the UK n.d.
- Youman P, Wilson K, Harraf F, Kalra L. The economic burden of stroke in the United Kingdom. Pharmacoeconomics 2003;21:43-50. http://dx.doi.org/10.2165/00019053-200321001-00005.
- NHS Reference Costs 2007–2008. London: Department of Health; 2008.
- British National Formulary. London: BMJ Group and Pharmaceutical Press; 2008.
- NHS Electronic Drug Tariff 2008. London: NHS Prescription Services, Department of Health; 2008.
- NHS Purchasing and Supplies Agency (PASA) Catalogue. London: NHS Purchasing and Supplies Agency, Department of Health; 2007.
- Curtis L, Netten A. Unit Costs of Health and Social Care. Canterbury: PSSRU, University of Kent; 2007.
- NHS Reference Costs 2005–2006. London: Department of Health; 2006.
- Curtis L, Netten A. Unit Costs of Health and Social Care. Canterbury: PSSRU, University of Kent; 2005.
- MIMS online. Middlesex: Haymarket Medical Media; n.d.
- NICE Technology Appraisal TA157: Dabigatran Etexilate for the Prevention of Venous Thromboembolism After Hip or Knee Replacement Surgery in Adults. London: NICE; 2008.
- Wille-Jørgensen P, Jorgensen LN, Crawford M. Asymptomatic postoperative deep vein thrombosis and the development of postthrombotic syndrome – a systematic review and meta-analysis. Thromb Haemost 2005;93:236-41. http://dx.doi.org/10.1160/th04-09-0570.
- Miniati M, Monti S, Bottai M, Scoscia E, Bauleo C, Tonelli L, et al. Survival and restoration of pulmonary perfusion in a long-term follow-up of patients after acute pulmonary embolism. Medicine 2006;85:253-62. http://dx.doi.org/10.1097/01.md.0000236952.87590.c8.
- Prandoni P, Villalta S, Bagatella P, Rossi L, Marchiori A, Piccioli A, et al. The clinical course of deep-vein thrombosis. Prospective long-term follow-up of 528 symptomatic patients. Haematologica 1997;82:423-8.
- National Clinical Guideline: Venous Thromboembolism: Reducing the risk of venous thromboembolism (deep vein thrombosis and pulmonary embolism) in inpatients undergoing surgery. London: NCC AC at The Royal College of Surgeons of England; 2007.
- Bucher HC, Guyatt GH, Griffith LE, Walter SD. The results of direct and indirect treatment comparisons in meta-analysis of randomized controlled trials. J Clin Epidemiol 1997;50:683-91. http://dx.doi.org/10.1016/S0895-4356(97)00049-8.
- NICE Clinical Guidance CG68: Stroke: Diagnosis and Initial Management of Acute Stroke and Transient Ischaemic Attack (TIA). London: NICE; 2008.
- Kind P, Dolan P, Gudex C, Williams A. Variations in population health status: results from a United Kingdom national questionnaire survey. BMJ 1998;316:736-41. http://dx.doi.org/10.1136/bmj.316.7133.736.
- Bonderman D, Skoro-Sajer N, Jakowitsch J, Adlbrecht C, Dunkler D, Taghavi S, et al. Predictors of outcome in chronic thromboembolic pulmonary hypertension. Circulation 2007;115:2153-8. http://dx.doi.org/10.1161/CIRCULATIONAHA.106.661041.
- Condliffe R, Kiely DG, Gibbs JSR, Corris PA, Peacock AJ, Jenkins DP, et al. Prognostic and aetiological factors in chronic thromboembolic pulmonary hypertension. Eur Respir J 2009;33:332-7. http://dx.doi.org/10.1183/09031936.00092008.
- Interim Life Tables, England and Wales, 1980–82 to 2007–09. London: ONS; 2010.
- Guide to the Methods of Technology Appraisal 2013. London: NICE; 2013.
- Falck-Ytter Y, Francis CW, Johanson NA, Curley C, Dahl OE, Schulman S, et al. Prevention of VTE in orthopedic surgery patients antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012;141:E278S-E325S. http://dx.doi.org/10.1378/chest.11-2404.
- Gould MK, Garcia DA, Wren SM, Karanicolas PJ, Arcelus JI, Heit JA, et al. Prevention of VTE in nonorthopedic surgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2012;141:E227S-77S. http://dx.doi.org/10.1378/chest.11-2297.
- Muntz J, Scott DA, Lloyd A, Egger M. Major bleeding rates after prophylaxis against venous thromboembolism: systematic review, meta-analysis, and cost implications. Int J Technol Assess Health Care 2004;20:405-14. http://dx.doi.org/10.1017/S026646230400128X.
- Hospital Episode Statistics, Admitted patient care – England, 2012–13 [NS]. London: DH; 2013.
- Ramiah RD, Ashmore AM, Whitley E, Bannister GC. Ten-year life expectancy after primary total hip replacement. J Bone Joint Surg Br 2007;89B:1299-302. http://dx.doi.org/10.1302/0301-620X.89B10.18735.
- Nunley RM, Lachiewicz PF. Mortality after total hip and knee arthroplasty in a medium-volume university practice. J Arthroplasty 2003;18:278-85. http://dx.doi.org/10.1054/arth.2003.50095.
- Quinlan DJ, Eikelboom JW, Dahl OE, Eriksson BI, Sidhu PS, Hirsh J. Association between asymptomatic deep vein thrombosis detected by venography and symptomatic venous thromboembolism in patients undergoing elective hip or knee surgery. Thromb Haemost 2007;5:1438-43. http://dx.doi.org/10.1111/j.1538-7836.2007.02571.x.
- British National Formulary. London: BMJ Group and Pharmaceutical Press; 2014.
- NHS Electronic Drug Tariff 2014. London: NHS Prescription Services, DH; 2014.
- NHS Reference Costs 2012–2013. London: DH; 2013.
- Bergqvist D, Jendteg S, Johansen L, Persson U, Odegaard K. Cost of long-term complications of deep venous thrombosis of the lower extremities: an analysis of a defined patient population in Sweden. Ann Int Med 1997;126:454-7. http://dx.doi.org/10.7326/0003-4819-126-6-199703150-00006.
- Goodacre S, Sampson F, Stevenson M, Wailoo A, Sutton A, Thomas S, et al. Measurement of the clinical and cost-effectiveness of non-invasive diagnostic testing strategies for deep vein thrombosis. Health Technol Assess 2006;10. http://dx.doi.org/10.3310/hta10150.
- NICE Guidance in Development (Discontinued 2008): Pulmonary Arterial Hypertension (Adults) – Drugs. London: NICE; 2008.
- Grieve R, Porsdal V, Hutton J, Wolfe C. A comparison of the cost-effectiveness of stroke care provided in London and Copenhagen. Int J Technol Assess Health Care 2000;16:684-95. http://dx.doi.org/10.1017/S0266462300101242.
- Interim Life Tables, England and Wales, 2009–2011. London: ONS; 2011.
- Gage BF, Cardinalli AB, Owens DK. The effect of stroke and stroke prophylaxis with aspirin or warfarin on quality of life. Arch Intern Med 1996;156:1829-36. http://dx.doi.org/10.1001/archinte.1996.00440150083009.
- O’Meara JJ, McNutt RA, Evans AT, Moore SW, Downs SM. A decision-analysis of streptokinase plus heparin as compared with heparin alone for deep-vein thrombosis. N Engl J Med 1994;330:1864-9. http://dx.doi.org/10.1056/NEJM199406303302605.
- Sarasin FP, Gaspoz JM, Bounameaux H. Cost-effectiveness of new antiplatelet regimens used as secondary prevention of stroke or transient ischemic attack. Arch Intern Med 2000;160:2773-8. http://dx.doi.org/10.1001/archinte.160.18.2773.
- Dennis M, Lewis SC, Warlow C, Collaboration FT. Routine oral nutritional supplementation for stroke patients in hospital (FOOD): a multicentre randomised controlled trial. Lancet 2005;365:755-63. http://dx.doi.org/10.1016/S0140-6736(05)70998-3.
- Johannesson M, Weinstein MC. On the decision rules of cost-effectiveness analysis. J Health Econ 1993;12:459-67. http://dx.doi.org/10.1016/0167-6296(93)90005-Y.
- Claxton K. Exploring uncertainty in cost-effectiveness analysis. Pharmacoeconomics 2008;26:781-98. http://dx.doi.org/10.2165/00019053-200826090-00008.
- Hoomans T, Fenwick EA, Palmer S, Claxton K. Value of information and value of implementation: application of an analytic framework to inform resource allocation decisions in metastatic hormone-refractory prostate cancer. Value Health 2009;12:315-24. http://dx.doi.org/10.1111/j.1524-4733.2008.00431.x.
- Barton GR, Briggs AH, Fenwick EA. Optimal cost-effectiveness decisions: the role of the cost-effectiveness acceptability curve (CEAC), the cost-effectiveness acceptability frontier (CEAF), and the expected value of perfection information (EVPI). Value Health 2008;11:886-97. http://dx.doi.org/10.1111/j.1524-4733.2008.00358.x.
- Browse NL, Jackson BT, Mayo ME, Negus D. Value of mechanical methods of preventing postoperative calf vein-thrombosis. Br J Surg 1974;61:219-23. http://dx.doi.org/10.1002/bjs.1800610312.
- Brunkwall J, Bergqvist D, Takolander R. Deep-vein thrombosis after renal-transplantation is not reduced by graded compression stockings. Thromb Haemost 1991;65.
- Chandhoke PS, Gooding GAW, Narayan P. Prospective randomized trial of coumadin vs. sequential compression stockings as prophylaxis for postoperative deep venous thrombosis in major urological surgery. J Urol 1991;145.
- Douketis JD, Kearon C, Bates S, Duku EK, Ginsberg JS. Risk of fatal pulmonary embolism in patients with treated venous thromboembolism. JAMA 1998;279:458-62. http://dx.doi.org/10.1001/jama.279.6.458.
- Ellis H, Scurr JH. Prophylaxis of venous thrombosis. Phlebologie 1982;35:135-42.
- Flanc C, Kakkar VV, Clarke MB. Postoperative deep-vein thrombosis effect of intensive prophylaxis. Lancet 1969;1:477-8. http://dx.doi.org/10.1016/S0140-6736(69)91585-2.
- Hansberry KL, Thompson IM, Bauman J, Deppe S, Rodriguez FR. A prospective comparison of thromboembolic stockings, external sequential pneumatic compression stockings and heparin sodium dihydroergotamine mesylate for the prevention of thromboembolic complications in urological surgery. J Urol 1991;145:1205-8.
- Hou LL, Yao LW, Niu QM, Xu L, Yu QH, Sun WQ, et al. Preventive effect of electrical acupoint stimulation on lower-limb thrombosis: a prospective study of elderly patients after malignant gastrointestinal tumor surgery. Cancer Nurs 2013;36:139-44. http://dx.doi.org/10.1097/NCC.0b013e3182483415.
- Hui ACW, Gregg PJ, Triffitt PD, Armstrong L, Sinclair M, Mitchell V. Graded compression stockings in the prevention of deep-vein thrombosis. J Bone Joint Surg Br 1993;75B.
- Kahn SR, Morrison DR, Cohen JM, Emed J, Tagalakis V, Roussin A, et al. Interventions for implementation of thromboprophylaxis in hospitalized medical and surgical patients at risk for venous thromboembolism. Cochrane Database Syst Rev 2013;7. http://dx.doi.org/10.1002/14651858.cd008201.pub2.
- Kalodiki E, Gill K, Alkutoubi A, Birch B, Harris N, Hunt D. Low molecular weight heparin with or without graduated elastic compression in deep vein prophylaxis after elective hip replacement. Br J Surg 1992;79.
- Kalodiki E, Nicolaides A, Alkutoubi A, Birch B, Harris N, Hunt D, et al. Low-molecular-weight heparin (LMWH) and LMWH plus graduated elastic compression for deep venous thrombosis (DVT) prophylaxis in total hip-replacement. Thromb Haemost 1993;69.
- Kalodiki E, Nicolaides AN, Alkutoubi A, Birch R, Harris N, Hunt D, et al. LMWH and LMWH plus graduated elastic compression for DVT prophylaxis in total hip-replacement. Thromb Haemost 1993;69.
- Koopmann HD, Andersen K, Husted SE, Nielsen HK, Fasting H, Simonsen O, et al. Prevention of postoperative venous thrombosis. A comparison between low-dose heparin and graduated compression stockings. Ugeskr Laeger 1985;147:2296-8.
- Lewis CE, Antoine J, Mueller C, Talbot WA, Swaroop R, Edwards WS. Elastic compression in prevention of venous stasis – critical re-evaluation. Am J Surg 1976;132:739-43. http://dx.doi.org/10.1016/0002-9610(76)90447-5.
- Liavag I, Fotland K. [Prevention of postoperative thrombo-embolism by elastic compression bandage of the legs]. Tidsskrift Nor LAgeforen 1972;92:239-41.
- McNally MA, Cooke EA, O’Connel BM, Mollan RAB. Thigh versus knee length compression stockings in the prevention of venous stasis. J Bone Joint Surg Am 1995;77.
- Meneilly Z, McCutcheon K. Deep vein thrombosis and caesarean section. J Perioper Pract 2013;23:17-21.
- Moser G, Froidevaux A. Prophylaxis of post-operative deep venous thrombosis using small sub-cutaneous heparin doses, associated or not with compressive stockings: comparative study and results. Schweiz Rundsch Med Prax 1976;65:1015-20.
- Nelson LD, Montgomery SP, Dameron TB, Nelson RB. Deep vein thrombosis in lumbar spinal fusion: a prospective study of antiembolic and pneumatic compression stockings. J South Orthop Assoc 1996;5:181-4.
- Patel A, Couband D, Feron JM, Signoret F. Prevention of deep-vein thrombosis in surgery of the hip, using heparin and an anti-thrombosis stocking. Presse Med 1988;17:1201-3.
- Ryan MG, Westrich GH, Potter HG, Sharrock N, Maun LM, Macaulay W, et al. Effect of mechanical compression on the prevalence of proximal deep venous thrombosis as assessed by magnetic resonance venography. J Bone Joint Surg Am 2002;84A:1998-2004.
- San Norberto Garcia EM, Merino B, Taylor JH, Vizcaino I, Vaquero C. Low-molecular-weight heparin for prevention of venous thromboembolism after varicose vein surgery in moderate-risk patients: A randomized, controlled trial. Ann Vasc Surg 2013;27:940-6. http://dx.doi.org/10.1016/j.avsg.2013.03.006.
- Sharma U. Diving for PURLs: thigh-length stockings uncomfortable and show no patient-oriented benefit. Evid Based Pract 2011;14.
- Sharma M, Carpenter SL. Thromboprophylaxis in a pediatric hospital. Current Problems in Pediatric and Adolescent Health Care 2013;43:178-83. http://dx.doi.org/10.1016/j.cppeds.2013.05.006.
- Silbersack Y, Taute BM, Hein W, Podhaisky H. Prevention of deep-vein thrombosis after total hip and knee replacement – low-molecular-weight heparin in combination with intermittent pneumatic compression. J Bone Joint Surg Br 2004;86B:809-12. http://dx.doi.org/10.1302/0301-620X.86B6.13958.
- Sobieraj DM, Coleman CI, Tongbram V, Chen W, Colby J, Lee S, et al. Comparative effectiveness of combined pharmacologic and mechanical thromboprophylaxis versus either method alone in major orthopedic surgery: a systematic review and meta-analysis. Pharmacotherapy 2013;33:275-83. http://dx.doi.org/10.1002/phar.1206.
- Tasi SF, Lu PY, Chang CR. The effects of intermittent pneumatic compression system and elastic bandage compression of deep vein thrombosis prevention in urologic patient with lithotomy position. Int J Urol 2010;17:A360-A1.
- Turpie AG, Hirsh J, Gent M, Julian DH, Johnson JA. A randomized trial comparing graduated compression stockings alone or graduated compression stockings plus intermittent pneumatic compression with control in the prevention of deep-vein thrombosis in neurosurgical patients. Arteriosclerosis 1988;8.
- Wilkins RW, Mixter G, Stanton JR, Litter J. Elastic stockings in the prevention of pulmonary embolism - a preliminary report. N Engl J Med 1952;246:360-4. http://dx.doi.org/10.1056/NEJM195203062461002.
- Yokote R, Matsubara M, Hirasawa N, Hagio S, Ishii K, Takata C. Is routine chemical thromboprophylaxis after total hip replacement really necessary in a Japanese population?. J Bone Joint Surg Br 2011;93:251-6. http://dx.doi.org/10.1302/0301-620X.93B2.25795.
- Venous Thromboembolism – Reducing the Risk of Venous Thromboembolism (Deep Vein Thrombosis and Pulmonary Embolism) in Inpatients Undergoing Surgery. London: NICE; 2007.
- Salzman E, Hirsh J, Colman R, Hirsh J, Marder V, Salzman E. Hemostasis and Thrombosis: Basic Principles and Clinical Practice. New York, NY: Lippincott; 1982.
Appendix 1 Search strategies
Cochrane Library (Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects, Health Technology Assessment, Cochrane Methodology Register, NHS Economic Evaluation Database, Cochrane Central Register of Controlled Trials, CENTRAL)
http://onlinelibrary.wiley.com/cochranelibrary/search/advanced
Searched 7 August 2013 using strategy:
#1 (compression near/3 (stocking* or hose)):ti,ab,kw (Word variations have been searched) (428)
#2 MeSH descriptor: [Stockings, Compression] explode all trees (124)
#3 #1 or #2 (428)
PROSPERO
Searched 14 August 2013 using terms stocking, stockings, compression.
Centre for Reviews and Dissemination CMS2 system
Internal CRD DARE database production system searched for relevant rejected or provisional DARE records. Strategy:
-
Compression stock*
-
Compression hos*
-
MeSH Descriptor Stockings, Compression
-
MeSH DESCRIPTOR Intermittent Pneumatic Compression Devices
-
1 or 2 or 3 or 4
ClinicalTrials.gov
Searched online 7 August 2013 using term compression stocking*
National Guidelines Clearinghouse
Searched online 12 August 2013 using terms (compression stocking* and venous thrombo*)
National Insitute for Health Research Health Technology Assessment programme
Searched online 14 August 2013 using terms compression AND stocking
Turning Research into Practice
Searched online 14 August 2013 using terms: “compression stockings thrombosis”
NHS Evidence
Searched online 14 August 2013 using terms “compression stocking*” AND thromb*
MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations
Database: Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations and Ovid MEDLINE(R) <1946 to present>.
Searched via Ovid interface 19 February 2014.
Date limited to 2010 onwards.
Search strategy
-
exp “embolism and thrombosis”/ (172,610)
-
(thrombos$ or thrombus$ or thrombotic or thrombolic$ or thromboemboli$ or thromboprophyla$ or embol$).ti,ab. (232,741)
-
(DVT$ or PE or PTS).ti,ab. (34,899)
-
1 or 2 or 3 (317,779)
-
Stockings, Compression/ or Compression Bandages/ (1165)
-
(stocking$ or hose or hosiery or tights or sock$ or TEDS).ti,ab. (10,451)
-
(compression adj3 bandage$).ti,ab. (486)
-
5 or 6 or 7 (11,541)
-
4 and 8 (1418)
-
randomized controlled trial.pt. (362,662)
-
controlled clinical trial.pt. (87,530)
-
randomized.ab. (282,970)
-
placebo.ab. (149,727)
-
drug therapy.fs. (1,661,607)
-
randomly.ab. (205,717)
-
trial.ab. (291,784)
-
groups.ab. (1,315,795)
-
10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 (3,250,729)
-
9 and 18 (518)
-
limit 19 to yr=“2010 -Current” (141)
EMBASE
Database: EMBASE <1996 to 2014 Week 7>.
Searched via Ovid interface 19 February 2014.
Date limited to 2010 onwards.
Search strategy
-
exp thromboembolism/ (243,327)
-
(thrombos$ or thrombus$ or thrombotic or thrombolic$ or thromboemboli$ or thromboprophyla$ or embol$).ti,ab. (230,788)
-
(DVT$ or PE or PTS).ti,ab. (77,082)
-
1 or 2 or 3 (386,878)
-
compression stocking/ (571)
-
compression bandage/ (1103)
-
(stocking$ or hose or hosiery or tights or sock$ or TEDS).ti,ab. (9402)
-
(compression adj3 bandage$).ti,ab. (552)
-
5 or 6 or 7 or 8 (10,995)
-
(random$ or factorial$ or crossover$ or cross over$ or cross-over$ or placebo$ or (doubl$ adj blind) or (singl$ adj blind$) or assign$ or allocat$ or volunteer$).ti,ab,kw. (1,092,434)
-
crossover-procedure/ or double-blind procedure/ or randomized controlled trial/ or single-blind procedure/ (344,502)
-
10 or 11 (1,159,128)
-
4 and 9 and 12 (414)
-
limit 13 to (embase and yr=“2010 -Current”) (158)
Cumulative Index to Nursing and Allied Health Literature Plus
Database: CINAHL Plus.
Searched via EBSCOhost interface 19 February 2014.
Date limited to 2010 onwards.
Search strategy
S27 S6 AND S13 AND S25 Limiters - Published Date: 20100101-20140231 (82)
S26 S6 AND S13 AND S25 (256)
S25 S14 or S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 (872,307)
S24 TX allocat* random* (3800)
S23 (MH “Quantitative Studies”) (11,572)
S22 (MH “Placebos”) (8585)
S21 TX placebo* (30,948)
S20 TX random* allocat* (3800)
S19 (MH “Random Assignment”) (36,604)
S18 TX randomi* control* trial* (68,813)
S17 TX ( (singl* n1 blind*) or (singl* n1 mask*) ) or TX ( (doubl* n1 blind*) or (doubl* n1 mask*) ) or TX ( (tripl* n1 blind*) or (tripl* n1 mask*) ) or TX ( (trebl* n1 blind*) or (trebl* n1 mask*) ) (702,165)
S16 TX clinic* n1 trial* (160,753)
S15 PT Clinical trial (75,415)
S14 (MH “Clinical Trials+”) (171,168)
S13 S7 or S8 or S9 or S10 or S11 or S12 (3158)
S12 AB compression N3 bandage* (162)
S11 TI compression N3 bandage* (56)
S10 AB (stocking* or hose or hosiery or tights or sock* or TEDS) (1229)
S9 TI (stocking* or hose or hosiery or tights or sock* or TEDS) (945)
S8 (MH “Elastic Bandages”) (14)
S7 (MH “Compression Garments”) (1527)
S6 S1 or S2 or S3 or S4 or S5 (37,458)
S5 AB (DVT* or PE or PTS) (3032)
S4 TI (DVT* or PE or PTS) (1026)
S3 AB (thrombos* or thrombus* or thrombotic or thrombolic* or thromboemboli* or thromboprophyla* or embol*) (13,784)
S2 TI (thrombos* or thrombus* or thrombotic or thrombolic* or thromboemboli* or thromboprophyla* or embol*) (15,339)
S1 (MH “Embolism+”) OR (MH “Thromboembolism+”) OR (MH “Thrombosis+”) (25,199)
Cochrane Central Register of Controlled Trials
Searched online via http://onlinelibrary.wiley.com/cochranelibrary/search/advanced on 19 February 2014.
Limited to 2010 onwards.
Search strategy
#1 MeSH descriptor: [Embolism and Thrombosis] explode all trees
#2 (thrombos* or thrombus* or thrombotic or thrombolic* or thromboemboli* or thromboprophyla* or embol*):ti,ab
#3 (DVT* or PE or PTS):ti,ab
#4 #1 or #2 or #3
#5 MeSH descriptor: [Stockings, Compression] this term only
#6 MeSH descriptor: [Compression Bandages] this term only
#7 (stocking* or hose or hosiery or tights or sock* or TEDS):ti,ab
#8 (compression near/3 bandage*):ti,ab
#9 #5 or #6 or #7 or #8
#10 #4 and #9 from 2010 to 2014, in Trials
Allied and Complementary Medicine
Database: AMED <1985 to February 2014>.
Searched via Ovid interface 19 February 2014.
Date limited to 2010 onwards.
Search strategy
-
exp “embolism and thrombosis”/ (295)
-
(thrombos$ or thrombus$ or thrombotic or thrombolic$ or thromboemboli$ or thromboprophyla$ or embol$).ti,ab. (581)
-
(DVT$ or PE or PTS).ti,ab. (382)
-
1 or 2 or 3 (937)
-
(stocking$ or hose or hosiery or tights or sock$ or TEDS).ti,ab. (400)
-
(compression adj3 bandage$).ti,ab. (20)
-
5 or 6 (418)
-
(randomised controlled trial or randomized controlled trial).pt. (2920)
-
(clinical trial or clinical trial phase iii or clinical trialb or clinical trials or controlled clinical trial or controlled trial).pt. (1202)
-
(randomized or randomised).ab. (7694)
-
placebo.ab. (2128)
-
randomly.ab. (4451)
-
trial.ab. (6299)
-
groups.ab. (18,390)
-
8 or 9 or 10 or 11 or 12 or 13 or 14 (27,890)
-
4 and 7 and 15 (3)
-
(“2010” or “2011” or “2012” or “2013”).yr. (40,300)
-
16 and 17 (0)
Current Controlled Trials
Searched online at www.controlled-trials.com/.
Searched February 2014.
Search strategy
((thrombosis OR thrombus OR thrombotic OR thrombolic OR thromboembolism OR thromboembolisms OR thromboprophylaxis OR embolism OR embolisms OR DVT OR PTS) AND (stocking OR stockings OR hose OR hosiery OR tights OR sock OR socks OR TEDS))
43 results.
Economics searches
The Cochrane Library (includes NHS Economic Evaluations Database, Health Technology Assessment, Cochrane Central Register of Controlled Trials)
Searched online via http://onlinelibrary.wiley.com/cochranelibrary/search/advanced
Searched 4 February 2014.
Limited to 2008 onwards.
Search strategy
#1 MeSH descriptor: [Pulmonary Embolism] this term only (887)
#2 MeSH descriptor: [Venous Thrombosis] this term only (980)
#3 (((venous or vein) near (thrombosis or thrombus or thromboembolism)) or (dvt or vte) or ((pulmonary or lung) near (embolism or emboli))) (6672)
#4 #1 or #2 or #3 (6672)
#5 thromboprophyla*:ti,ab (518)
#6 (prophylaxis or prevention):ti,ab (42,766)
#7 pc.fs. (9)
#8 MeSH descriptor: [Anticoagulants] explode all trees (3703)
#9 MeSH descriptor: [Fibrinolytic Agents] explode all trees (1861)
#10 MeSH descriptor: [Platelet Aggregation Inhibitors] explode all trees (2957)
#11 MeSH descriptor: [Antithrombins] explode all trees (220)
#12 (anticoagula* or anti coagula* or antithromb* or anti thromb* or antiemboli* or anti emboli* or thrombin inhibit* or direct thrombin):ti,ab (6906)
#13 (Dabigatran or dabigatran etexilate or Rendix or lepirudin or refludan):ti,ab (191)
#14 MeSH descriptor: [Heparin] this term only (2935)
#15 MeSH descriptor: [Dalteparin] this term only (213)
#16 MeSH descriptor: [Enoxaparin] this term only (607)
#17 MeSH descriptor: [Nadroparin] this term only (95)
#18 MeSH descriptor: [Heparinoids] this term only (52)
#19 MeSH descriptor: [Heparinoids] this term only (52)
#20 MeSH descriptor: [Heparin, Low-Molecular-Weight] this term only (933)
#21 (Calciparine or Monoparin or Calcium Multiparin or Bemiparin or Zibor or Dalteparin or Fragmin or Enoxaparin or Clexane or Lovenox or Tinzaparin or Innohep or Antixarin or CY 222 or Embolex or monoembolex or Fragmin or Tinzaparin or Suleparoide or Ardeparin or Certoparin or Nadroparin or Parnaparin or Reviparin or Tedelparin):ti,ab (1794)
#22 MeSH descriptor: [Coumarins] this term only (137)
#23 MeSH descriptor: [Warfarin] this term only (1179)
#24 (fondaparinux or idraparinux or rivaroxaban or arixtra or xarelito or apixaban):ti,ab (488)
#25 (acenocoumarol or brodifacoum or bromadiolone or cloricromen or coumafos or coumadin or coumarin or coumatetralyl or coumetarol or dicoumarol or difenacoum or ethyl-biscoumacetate or flocoumafen or galbanic-acid or nicoumalone or phenindione or phenprocoumon or phepromaron or tioclomarol or sinthrone or warfarin):ti,ab (2086)
#26 (pentasaccharide or pentasaccharides):ti,ab (34)
#27 MeSH descriptor: [Aspirin] this term only (4439)
#28 (aspirin or acetylsalicylic acid or antiplatelet or anti platelet):ti,ab (8748)
#29 MeSH descriptor: [Bandages] this term only (1421)
#30 mechanical:ti,ab (7076)
#31 MeSH descriptor: [Intermittent Pneumatic Compression Devices] this term only (88)
#32 (stocking or stockings or hose or hosiery):ti,ab (716)
#33 (((calf or elastic or graded or limb or leg or pneumatic or plantar or foot) near compression) or (compression near device)):ti,ab (908)
#34 (((foot near pump) or foot) near pumps):ti,ab (45)
#35 flowtron:ti,ab (3)
#36 MeSH descriptor: [Motion Therapy, Continuous Passive] this term only (106)
#37 MeSH descriptor: [Early Ambulation] this term only (281)
#38 (mobilisation or mobilization or physiotherapy or ambulation or kinetic therapy or ((continuous or lateral) near rotation) or ((therapeutic or specialised or specialized) near bed) or air loss mattress or bedrest or bed rest or immobili* or leg exercises):ti,ab (9110)
#39 MeSH descriptor: [Hindlimb Suspension] this term only (3)
#40 ((foot or feet or limb or leg or legs) near (elevat* or raise* or suspend*)):ti,ab (280)
#41 MeSH descriptor: [Fluid Therapy] this term only (1170)
#42 MeSH descriptor: [Rehydration Solutions] this term only (255)
#43 (hydrat* or rehydrat*):ti,ab (2146)
#44 MeSH descriptor: [Anesthesia] this term only (1251)
#45 MeSH descriptor: [Anesthesia and Analgesia] this term only (1)
#46 MeSH descriptor: [Analgesia, Epidural] this term only (1752)
#47 MeSH descriptor: [Anesthesia, Conduction] this term only (364)
#48 (anaesthesia or anesthesia or anaesthetic* or anesthetic* or anaesthetise* or anesthetise* or analgesi* or spinal or epidural or extradural):ti,ab 50,557
#49 #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44 or #45 or #46 or #47 or #48 (124,759)
#50 #4 and #49 from 2008 to 2014 (1204)
Total 1204 results in Cochrane Library included 63 from NHSEED, 42 from HTA Database and 672 from CENTRAL.
Health Economic Evaluation Database
Searched online at http://heed.onlinelibrary.wiley.com/
Searched 12 April 2014.
Search strategy
Search All data: ‘venous thrombosis’ or ‘venous thrombus’ or ‘venous thromboembolism’ or ‘vein thrombosis’ or ‘vein thrombus’ or ‘vein thromboembolism’ or dvt or vte or ‘pulmonary embolism’ or ‘lung embolism’
AND Journal Date: 2008 or 2009 or 2010 or 2011 or 2012 or 2013 or 2014.
128 results.
MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations
Database: Ovid MEDLINE(R) In-Process & Other Non-Indexed Citations and Ovid MEDLINE(R) <1946 to Present>.
Searched via Ovid interface 4 February 2014.
Date limited to 2008 onwards.
Search strategy
-
Pulmonary Embolism/ or Venous Thrombosis/ (44,551)
-
(((venous or vein) adj (thrombosis or thrombus or thromboembolism)) or (dvt or vte) or ((pulmonary or lung) adj6 (embolism or emboli))).ti,ab. (60,606)
-
1 or 2 (77,187)
-
thromboprophyla$.ti,ab. (2792)
-
(prophylaxis or prevention).ti,ab. (399,800)
-
pc.fs. (990,842)
-
exp anticoagulants/ or exp fibrinolytic agents/ or exp platelet aggregation inhibitors/ (296314)
-
exp Antithrombins/ (13,005)
-
(anticoagula$ or anti coagula$ or antithromb$ or anti thromb$ or antiemboli$ or anti emboli$ or thrombin inhibit$ or direct thrombin).ti,ab. (84,858)
-
(Dabigatran or dabigatran etexilate or Rendix or lepirudin or refludan).ti,ab,kw. (1795)
-
heparin/ or heparin, low-molecular-weight/ or dalteparin/ or enoxaparin/ or nadroparin/ or heparinoids/ (55,615)
-
(Calciparine or Monoparin or Calcium Multiparin or Bemiparin or Zibor or Dalteparin or Fragmin or Enoxaparin or Clexane or Lovenox or Tinzaparin or Innohep or Antixarin or CY 222 or Embolex or monoembolex or Fragmin or Tinzaparin or Suleparoide or Ardeparin or Certoparin or Nadroparin or Parnaparin or Reviparin or Tedelparin).ti,ab,kw. (4434)
-
coumarins/ or warfarin/ (24,546)
-
(fondaparinux or idraparinux or rivaroxaban or arixtra or xarelito or apixaban).ti,ab,kw. (2275)
-
(acenocoumarol or brodifacoum or bromadiolone or cloricromen or coumafos or coumadin or coumarin or coumatetralyl or coumetarol or dicoumarol or difenacoum or ethyl-biscoumacetate or flocoumafen or galbanic-acid or nicoumalone or phenindione or phenprocoumon or phepromaron or tioclomarol or sinthrone or warfarin).ti,ab,kw. (24,246)
-
(pentasaccharide or pentasaccharides).ti,ab. (1869)
-
Aspirin/ (37,333)
-
(aspirin or acetylsalicylic acid or antiplatelet or anti platelet).ti,ab,kw. (54,825)
-
Bandages/ (13,384)
-
mechanical.ti,ab. (195,781)
-
Intermittent Pneumatic Compression Devices/ (388)
-
(stocking or stockings or hose or hosiery).ti,ab. (4036)
-
(((calf or elastic or graded or limb or leg or pneumatic or plantar or foot) adj compression) or (compression adj device)).ti,ab. (2089)
-
(((foot adj pump) or foot) adj pumps).ti,ab. (40)
-
flowtron.ti,ab. (15)
-
Motion Therapy, Continuous Passive/ (548)
-
Early Ambulation/ (1865)
-
(mobilisation or mobilization or physiotherapy or ambulation or kinetic therapy or ((continuous or lateral) adj rotation) or ((therapeutic or specialised or specialized) adj bed) or air loss mattress or bedrest or bed rest or immobili$ or leg exercises).ti,ab. (146,288)
-
Hindlimb Suspension/ (1447)
-
((foot or feet or limb or leg or legs) adj3 (elevat$ or raise$ or suspend$)).ti,ab. (1442)
-
Fluid Therapy/ (14,031)
-
Rehydration Solutions/ (1187)
-
(hydrat$ or rehydrat$).ti,ab. (46,475)
-
Anesthesia-and-Analgesia/ or Analgesia-Epidural/ or Anesthesia/ or exp Anesthesia-Conduction/ (100,187)
-
(anaesthesia or anesthesia or anaesthetic$ or anesthetic$ or anaesthetise$ or anesthetise$ or analgesi$ or spinal or epidural or extradural).ti,ab. (459,078)
-
4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 (2,302,491)
-
exp “Costs and Cost Analysis”/ (175,838)
-
Economics/ (26,421)
-
Economics, Nursing/ or Economics, Medical/ or Economics, Hospital/ or Economics, Pharmaceutical/ (24,426)
-
exp “Fees and Charges”/ (26,504)
-
exp Budgets/ (11,910)
-
budget$.ti,ab. (18,555)
-
cost$.ti. (78,950)
-
(cost$ adj2 (effective$ or utilit$ or benefit$ or minimi$)).ab. (82,337)
-
(economic$ or pharmacoeconomic$ or pharmaco-economic$).ti. (32,023)
-
(price$ or pricing$).ti,ab. (24,068)
-
(financial or finance or finances or financed).ti,ab. (53,074)
-
(fee or fees).ti,ab. (11,870)
-
(value adj2 (money or monetary)).ti,ab. (1285)
-
Value of Life/ (5357)
-
quality adjusted life.ti,ab. (5952)
-
(qaly$ or qald$ or qale$ or qtime$).ti,ab. (4942)
-
disability adjusted life.ti,ab. (1201)
-
daly$.ti,ab. (1186)
-
Health Status Indicators/ (19,375)
-
(sf36 or sf 36 or short form 36 or shortform 36 or sf thirtysix or sf thirty six or shortform thirtysix or shortform thirty six or short form thirtysix or short form thirty six).ti,ab. (15,414)
-
(sf6 or sf 6 or short form 6 or shortform 6 or sf six or sfsix or shortform six or short form six).ti,ab. (1337)
-
(sf12 or sf 12 or short form 12 or shortform 12 or sf twelve or sftwelve or shortform twelve or short form twelve).ti,ab. (2645)
-
(sf16 or sf 16 or short form 16 or shortform 16 or sf sixteen or sfsixteen or shortform sixteen or short form sixteen).ti,ab. (22)
-
(sf20 or sf 20 or short form 20 or shortform 20 or sf twenty or sftwenty or shortform twenty or short form twenty).ti,ab. (332)
-
(euroqol or euro qol or eq5d or eq 5d).ti,ab. (3811)
-
(hql or hqol or h qol or hrqol or hr qol).ti,ab. (7584)
-
(hye or hyes).ti,ab. (54)
-
(hui or hui1 or hui2 or hui3).ti,ab. (885)
-
utilit$.ti,ab. (114,870)
-
disutilit$.ti,ab. (207)
-
rosser.ti,ab. (71)
-
quality of wellbeing.ti,ab. (7)
-
qwb.ti,ab. (163)
-
willingness to pay.ti,ab. (2208)
-
standard gamble$.ti,ab. (650)
-
time trade off.ti,ab. (738)
-
time tradeoff.ti,ab. (202)
-
tto.ti,ab. (594)
-
exp models, economic/ (9706)
-
models, theoretical/ or models, organizational/ (115,389)
-
economic model$.ti,ab. (1698)
-
markov chains/ (9181)
-
markov$.ti,ab. (12,925)
-
Monte Carlo Method/ (18,992)
-
monte carlo.ti,ab. (28,034)
-
exp Decision Theory/ (9373)
-
(decision$ adj2 (tree$ or analy$ or model$)).ti,ab. (12,275)
-
or/37-83 (706,793)
-
3 and 36 and 84 (1547)
-
limit 85 to yr=“2008 -Current” (533)
533 results.
EMBASE
Database: EMBASE <1996 to 2014 week 5>.
Searched via Ovid interface 4 February 2014.
Date limited to 2008 onwards.
Search strategy
-
Thromboembolism/ or Vein Thrombosis/ (56,524)
-
(((venous or vein) adj (thrombosis or thrombus or thromboembolism)) or (dvt or vte) or ((pulmonary or lung) adj (embolism or emboli))).ti,ab. (63,565)
-
1 or 2 (102,138)
-
thromboprophyla$.ti,ab. (4176)
-
(prophylaxis or prevention).ti,ab. (394,468)
-
pc.fs. (738,578)
-
exp anticoagulant agent/ or exp fibrinolytic agent/ or exp antithrombocytic agent/ (377,108)
-
exp antithrombin/ (6031)
-
(anticoagula$ or anti coagula$ or antithromb$ or anti thromb$ or antiemboli$ or anti emboli$ or thrombin inhibit$ or direct thrombin).ti,ab. (84,632)
-
(Dabigatran or dabigatran etexilate or Rendix or lepirudin or refludan).ti,ab,kw. (3417)
-
heparin/ or heparin, low-molecular-weight/ or dalteparin/ or enoxaparin/ or nadroparin/ or heparinoid/ (92,225)
-
(Calciparine or Monoparin or Calcium Multiparin or Bemiparin or Zibor or Dalteparin or Fragmin or Enoxaparin or Clexane or Lovenox or Tinzaparin or Innohep or Antixarin or CY 222 or Embolex or monoembolex or Fragmin or Tinzaparin or Suleparoide or Ardeparin or Certoparin or Nadroparin or Parnaparin or Reviparin or Tedelparin).ti,ab,kw. (6708)
-
coumarin derivative/ or warfarin/ (57,173)
-
(fondaparinux or idraparinux or rivaroxaban or arixtra or xarelito or apixaban).ti,ab,kw. (4396)
-
(acenocoumarol or brodifacoum or bromadiolone or cloricromen or coumafos or coumadin or coumarin or coumatetralyl or coumetarol or dicoumarol or difenacoum or ethyl-biscoumacetate or flocoumafen or galbanic-acid or nicoumalone or phenindione or phenprocoumon or phepromaron or tioclomarol or sinthrone or warfarin).ti,ab,kw. (26,867)
-
(pentasaccharide or pentasaccharides).ti,ab. (1643)
-
acetylsalicylic acid/ (111,903)
-
(aspirin or acetylsalicylic acid or antiplatelet or anti platelet).ti,ab,kw. (57,199)
-
Bandage/ (5843)
-
mechanical.ti,ab. (181,837)
-
Intermittent Pneumatic Compression Device/ (646)
-
(stocking or stockings or hose or hosiery).ti,ab. (4295)
-
(((calf or elastic or graded or limb or leg or pneumatic or plantar or foot) adj compression) or (compression adj device)).ti,ab. (2052)
-
(((foot adj pump) or foot) adj pumps).ti,ab. (48)
-
flowtron.ti,ab. (16)
-
movement therapy/ (1320)
-
mobilization/ (15959)
-
(mobilisation or mobilization or physiotherapy or ambulation or kinetic therapy or ((continuous or lateral) adj rotation) or ((therapeutic or specialised or specialized) adj bed) or air loss mattress or bedrest or bed rest or immobili$ or leg exercises).ti,ab. (133,006)
-
mobilization/ (15,959)
-
((foot or feet or limb or leg or legs) adj3 (elevat$ or raise$ or suspend$)).ti,ab. (1358)
-
Fluid Therapy/ (11,885)
-
oral rehydration solution/ (1545)
-
(hydrat$ or rehydrat$).ti,ab. (38,745)
-
Anesthesia/ or exp Epidural-Anesthesia/ or exp Local-Anesthesia/ (73,543)
-
(anaesthesia or anesthesia or anaesthetic$ or anesthetic$ or anaesthetise$ or anesthetise$ or analgesi$ or spinal or epidural or extradural).ti,ab. (367,490)
-
or/4-35 (1,961,482)
-
exp economic aspect/ (810,345)
-
cost$.ti,ab. (370,638)
-
(price$ or pricing$).ti,ab. (24,922)
-
(fee or fees).ti,ab. (10,156)
-
(financial or finance or finances or financed).ti,ab. (56,498)
-
(value adj2 (money or monetary)).ti,ab. (1558)
-
resourc$ allocat$.ti,ab. (5021)
-
expenditure$.ti,ab. (35,118)
-
(fund or funds or funding or fundings or funded).ti,ab. (57,175)
-
(ration or rations or rationing or rationings or rationed).ti,ab. (6602)
-
(saving or savings).ti,ab. (43,859)
-
Quality of Life/ (230,283)
-
quality of life.ti,ab. (198,003)
-
life quality.ti,ab. (5846)
-
quality adjusted life.ti,ab. (8397)
-
(qaly$ or qald$ or qale$ or qtime$).ti,ab. (8298)
-
disability adjusted life.ti,ab. (1526)
-
daly$.ti,ab. (1570)
-
(sf36 or sf 36 or short form 36 or shortform 36 or sf thirtysix or sf thirty six or shortform thirtysix or shortform thirty six or short form thirtysix or short form thirty six).ti,ab. (22,554)
-
(sf6 or sf 6 or short form 6 or shortform 6 or sf six or sfsix or shortform six or short form six).ti,ab. (988)
-
(sf12 or sf 12 or short form 12 or shortform 12 or sf twelve or sftwelve or shortform twelve or short form twelve).ti,ab. (4037)
-
(sf16 or sf 16 or short form 16 or shortform 16 or sf sixteen or sfsixteen or shortform sixteen or short form sixteen).ti,ab. (23)
-
(sf20 or sf 20 or short form 20 or shortform 20 or sf twenty or sftwenty or shortform twenty or short form twenty).ti,ab. (256)
-
(euroqol or euro qol or eq5d or eq 5d).ti,ab. (6547)
-
(hql or hqol or h qol or hrqol or hr qol).ti,ab. (11,410)
-
(hye or hyes).ti,ab. (62)
-
health$ equivalent$ year$.ti,ab. (1)
-
(hui or hui1 or hui2 or hui3).ti,ab. (1141)
-
health utilit$.ti,ab. (1528)
-
disutilit$.ti,ab. (339)
-
rosser.ti,ab. (61)
-
(quality of wellbeing or quality of well being).ti,ab. (333)
-
qwb.ti,ab. (169)
-
willingness to pay.ti,ab. (3145)
-
standard gamble$.ti,ab. (738)
-
time trade off.ti,ab. (946)
-
time tradeoff.ti,ab. (212)
-
tto.ti,ab. (821)
-
factor analy$.ti,ab. (26,802)
-
preference based.ti,ab. (867)
-
(state adj2 valu$).ti,ab. (1491)
-
Life Expectancy/ (24,870)
-
life expectancy$.ti,ab. (20,405)
-
((duration or length or period of time or lasting or last or lasted) adj4 symptom$).ti,ab. (16,265)
-
exp model/ (1,414,953)
-
exp Mathematical Model/ (188,568)
-
markov$.ti,ab. (14747)
-
Monte Carlo Method/ (21,137)
-
monte carlo.ti,ab. (24,402)
-
exp Decision Theory/ (1132)
-
(decision$ adj2 (tree$ or analy$ or model$)).ti,ab. (14,235)
-
model$.ti,ab. (1,705,162)
-
or/37-88 (3,512,697)
-
3 and 36 and 89 (10641)
-
limit 90 to yr=“2008 -Current” (5933)
-
limit 91 to embase (5401)
5401 results.
EconLit
Database: EconLit <1886 to January 2014>.
Searched via Ovid interface 7 February 2014.
Date limited to 2008 onwards.
Search strategy
-
(((venous or vein) adj (thrombosis or thrombus or thromboembolism)) or (dvt or vte) or ((pulmonary or lung) adj6 (embolism or emboli))).ti,ab. (21)
-
thromboprophyla$.ti,ab. (1)
-
(prophylaxis or prevention).ti,ab. (2311)
-
(anticoagula$ or anti coagula$ or antithromb$ or anti thromb$ or antiemboli$ or anti emboli$ or thrombin inhibit$ or direct thrombin).ti,ab. (8)
-
(Dabigatran or dabigatran etexilate or Rendix or lepirudin or refludan).ti,ab,kw. (0)
-
(Calciparine or Monoparin or Calcium Multiparin or Bemiparin or Zibor or Dalteparin or Fragmin or Enoxaparin or Clexane or Lovenox or Tinzaparin or Innohep or Antixarin or CY 222 or Embolex or monoembolex or Fragmin or Tinzaparin or Suleparoide or Ardeparin or Certoparin or Nadroparin or Parnaparin or Reviparin or Tedelparin).ti,ab,kw. (10)
-
(fondaparinux or idraparinux or rivaroxaban or arixtra or xarelito or apixaban).ti,ab,kw. (1)
-
(acenocoumarol or brodifacoum or bromadiolone or cloricromen or coumafos or coumadin or coumarin or coumatetralyl or coumetarol or dicoumarol or difenacoum or ethyl-biscoumacetate or flocoumafen or galbanic-acid or nicoumalone or phenindione or phenprocoumon or phepromaron or tioclomarol or sinthrone or warfarin).ti,ab,kw. (4)
-
(pentasaccharide or pentasaccharides).ti,ab. (0)
-
(aspirin or acetylsalicylic acid or antiplatelet or anti platelet).ti,ab,kw. (18)
-
mechanical.ti,ab. (686)
-
(stocking or stockings or hose or hosiery).ti,ab. (207)
-
(((calf or elastic or graded or limb or leg or pneumatic or plantar or foot) adj compression) or (compression adj device)).ti,ab. (0)
-
(((foot adj pump) or foot) adj pumps).ti,ab. (0)
-
flowtron.ti,ab. (0)
-
(mobilisation or mobilization or physiotherapy or ambulation or kinetic therapy or ((continuous or lateral) adj rotation) or ((therapeutic or specialised or specialized) adj bed) or air loss mattress or bedrest or bed rest or immobili$ or leg exercises).ti,ab. (1975)
-
((foot or feet or limb or leg or legs) adj3 (elevat$ or raise$ or suspend$)).ti,ab. (0)
-
(hydrat$ or rehydrat$).ti,ab. (28)
-
(anaesthesia or anesthesia or anaesthetic$ or anesthetic$ or anaesthetise$ or anesthetise$ or analgesi$ or spinal or epidural or extradural).ti,ab. (52)
-
or/2-19 (5267)
-
1 and 20 (10)
-
limit 21 to yr=“2008 -Current” (0)
No results.
IDEAS
Searched online at http://ideas.repec.org/
Searched 4 February 2014.
Search strategy
thrombosis thrombus thromboembolism dvt vte embolism
Match: Any
Search: Whole word
In: Whole record
Words forms: All
Use synonyms: No
Publication dates: from 2008 to no limit inclusive.
30 results.
Appendix 2 Studies excluded at full paper stage
| Study details (first author and year) | Reason for exclusion |
|---|---|
| Allan (1983)26 | GCSs length not specified |
| Benko (2001)14 | No DVT/related outcomes reported |
| Brady (2007)15 | Not a RCT |
| Browse (1974)146 | GCSs length not specified |
| Brunkwall (1991)147 | GCSs length not specified |
| Chandhoke (1991)148 | GCSs length not specified |
| Douketis (1998)149 | Not a RCT |
| Ellis (1982)150 | GCSs length not specified |
| Flanc (1969)151 | Not GCS |
| Hameed (2002)16 | Not a RCT |
| Hansberry (1991)152 | GCSs length not specified |
| Holford (1976)27 | GCSs length not specified |
| Hou (2013)153 | GCSs length not specified |
| Hui (1993)154 | GCSs length not specified |
| Kahn (2013)155 | Not a RCT |
| Kalodiki (1992)156 | Duplicate report |
| Kalodiki (1993)157 | Duplicate report |
| Kalodiki (1993)158 | Duplicate report |
| Koopmann (1985)159 | Duplicate report |
| Lewis (1976)160 | No DVT/related outcomes reported |
| Liavag (1972)161 | GCSs length not specified |
| McNally (1995)162 | Duplicate report |
| Meneilly (2013)163 | Not a RCT |
| Moser (1976)164 | GCSs length not specified |
| Nelson (1996)165 | No non-GCSs comparator group |
| Ohlund (1983)38 | GCSs length not specified |
| Parnaby (2004)80 | Not a RCT |
| Patel (1988)166 | GCSs length not specified |
| Ryan (2002)167 | GCSs length not specified |
| San Norberto Garcia (2013)168 | No non-GCSs comparator group |
| Scurr (1977)28 | GCSs length not specified |
| Sharma (2011)169 | Not surgical patients |
| Sharma (2013)170 | Not a RCT |
| Silbersack (2004)171 | GCSs length not specified |
| Sobieraj (2013)172 | Not a RCT |
| Tasi (2010)173 | GCSs length not specified |
| Thompson (2011)85 | Not a RCT |
| Turner (1984)29 | GCSs length not specified |
| Turpie (1988)174 | Duplicate report |
| Wilkins (1952)175 | GCSs length not specified |
| Williams (1994)81 | Not a RCT |
| Williams (1996)82 | Not a RCT |
| Williams (2006)83 | Not a RCT |
| Winslow (2008)84 | Not a RCT |
| Yokote (2011)176 | No non-GCSs comparator group |
Appendix 3 Effectiveness of thigh-length versus knee-length stockings: summary of study characteristics and results
| Study details (first author and year) | Patient characteristics | Knee-length GCSs | Thigh-length GCSs | Non-stocking control | Outcomes assessed | Results |
|---|---|---|---|---|---|---|
| Thigh-length GCSs + pharmacological prophylaxis vs. knee-length GCSs + pharmacological prophylaxis | ||||||
| Howard (2004)12 Location: UK |
Low-, moderate- and high-risk patients undergoing any surgery (n = 376 recruited; n = 294 analysed) | Medi thrombexin® climax knee-length GCSs plus single daily subcutaneous injection of 20 mg of enoxaparin sodium (LMWH) until discharge from hospital (n = 128) | (1) Kendall TED thigh-length GCSs plus single daily subcutaneous injection of 20 mg of enoxaparin sodium (LMWH) until discharge from hospital (n = 127) (2) Medi thrombexin® climax thigh-length GCSs plus single daily subcutaneous injection of 20 mg of enoxaparin sodium (LMWH) until discharge from hospital (n = 121) |
N/A | DVT assessed by duplex ultrasound on postoperative day 5 to 7 PE Adverse events |
DVT events: Kendall TED thigh-length GCSs: six patients developed DVT in the calf (five unilateral and one bilateral; all patients were in the high-risk group). No significant difference between this group and knee-length stocking group (OR 0.5, 95% CI 0.18 to 1.41; p = 0.19) Medi thrombexin® climax thigh-length GCSs: two patients developed DVT in the calf (both unilateral; both patients were in the high-risk group). Statistically significant improvement in preventing postoperative DVT versus knee-length stockings (OR 0.18, 95% CI 0.04 to 0.82; p = 0.026) Medi thrombexin® climax knee-length GCS: 11 patients developed DVT; 10 in the calf, 1 in the thigh (10 unilateral and 1 bilateral; all patients were in the high-risk group) No PE events Adverse events: One significant bleeding complication, two minor haematomas and minor foot abrasions from stockings in three patients |
| Cohen (2007)49 Location: Brazil, UK, Hong Kong and Spain |
Patients aged at least 18 years undergoing primary or revision THR or surgery for fracture of the proximal third of the femur were eligible for inclusion (n = 874 recruited; n = 795 analysed) | Knee-length GCSs (worn until the last follow-up visit; 35–49 days) plus fondaparinux (2.5 mg daily for between 5 and 9 days) (n = 123) | Thigh-length GCSs (worn until the last follow-up visit; 35–49 days) plus fondaparinux (2.5 mg daily for between 5 and 9 days) (n = 266) | Fondaparinux (2.5 mg daily for between 5 and 9 days) alone (n = 400) | VTE (objectively verified, symptomatic thromboembolism or asymptomatic proximal DVT demonstrated by bilateral proximal ultrasound or venography) Fatal PE Quality-of-life measures and adverse events were reported, but not separately for different GCSs lengths |
VTE events: Thigh-length GCSs: 14/251 (5.6%) Knee-length GCSs: 5/118 (4.2%) Fondaparinux: 22/400 (5.5%) No fatal PE events Adverse events: 2% of patients reported complications with GCSs |
| Thigh-length GCSs vs. knee-length GCSs | ||||||
| Porteous (1989)21 Location: UK |
Patients over 40 years of age undergoing major abdominal surgery (n = 124 recruited; n = 114 analysed) | Knee-length GCSs worn until discharge (n = 58) | Brevet thigh-length GCSs worn until discharge [pressure at the ankle: 11.3 mmHg (SD ± 2.8)] (n = 56) | N/A | DVT assessed by radioiodine fibrinogen uptake test. Phlebography was performed if DVT was suspected Adverse events Patient preference (results presented in Chapter 3) |
Calf thrombosis events: Thigh-length GCSs: 3/56 (5.4%); one was clinically overt Knee-length GCSs: 1/58 (1.7%), which was clinically overt Adverse events: 1/56 patient in the thigh-length GCSs group had a superficial thrombophlebitis with no evidence of DVT on phlebography |
| Hui (1996)25 Location: UK |
Patients undergoing primary THR or TKR (n = 177 recruited, n = 138 analysed) | Knee-length GCSs (n = 40) | Thigh-length GCSs (n = 44) | No treatment control (n = 54) | DVT assessed by bilateral ascending venography on fifth and seventh postoperative days Fatal PE reported for control group only Patient adherence and patient preference (results presented in Chapter 3) |
Rates of thrombosis (% of the number of legs with a successful venogram): Knee-length GCSs: THR patients – operated on leg: 50% Non-operated on leg: 7%. TKR patients – operated on leg: 68%; non-operated on leg: 10% Thigh-length GCSs: THR patients – operated on leg: 22%; non-operated on leg: 9%. TKR patients – operated on leg: 65%; non-operated on leg: 12% No treatment control: THR patients – operated on leg: 27%; non-operated on leg: 10%. TKR patients – operated on leg: 78%; non-operated on leg: 20% Fatal PE events: One event in no treatment control group (TKR patient) |
| Williams (1988)20 Location: UK |
Patients above the age of 40 years undergoing an abdominal operation (n = 128 analysed, number recruited not reported) | (1) Brevet TX knee-length GCSs (n = 44) (2) Brevet TX knee-length GCSs plus twice a day heparin (5000 U) in high-risk patients (high-risk patients not defined) (n = 40) |
TED thigh-length GCSs (n = 44) | N/A | DVT assessed by radioiodine fibrinogen uptake test Cost of stockings |
DVT events: Knee-length GCSs group: 8/44 patients (18.2%); 12/88 legs (13.6%), therefore four patients had bilateral DVT (9%) High-risk knee-length GCSs + heparin group: 6/40 patients (15%); 6/80 legs (7.5%), therefore no patients had bilateral DVT Thigh-length GCSs group: 6/44 patients (13.6%); 9/88 legs (10.2%), therefore three patients had bilateral DVT (7%). The difference between groups was not statistically significant Cost: The cost of the stockings was £5.44 per pair for TED thigh-length stockings and £2.75 per pair for Brevet TX below-knee stockings at the time of the trial |
| Ayhan (2013)65 Location: Turkey |
Patients at extremely high-risk for postoperative DVT (n = 219 recruited, number analysed not reported) | (1) Low pressure knee-length GCSs (n = not stated) (2) Moderate pressure knee-length GCSs (n = not stated) |
Low pressure thigh-length GCSs (n = not stated) | N/A | DVT assessed by duplex ultrasound within postoperative days 5–7 Patient preference (results presented in Chapter 3) |
No DVT events |
| Thigh-length GCSs + pharmacological prophylaxis vs. pharmacological prophylaxis alone | ||||||
| Kalodiki (1996)33 Location: UK |
Patients older than 40 years who were having unilateral THR for the first time or without cement under general anaesthetic (n = 93 recruited; n = 78 analysed) | N/A | Thigh-length GCSs (TEDR, Kendall) applied before operation on both legs and not taken off until the patient was discharged from hospital (days 8–12). All patients also received 40 mg of subcutaneous enoxaparin LMWH administered 12 hours before operation and once daily until discharge (n = 32) | (1) LMWH 40 mg of subcutaneous enoxaparin administered 12 hours before operation and once daily until discharge (n = 32) (2) Placebo normal saline injections (n = 14) |
DVT assessed by ascending venography up to the 12th postoperative day PE assessed by perfusion lung scans Adverse events |
DVT events: Thigh-length GCSs group: calf and proximal thrombi: 8/32 (25%); DVT proximal to the calf: 4/32 (13%) LMWH group (1): calf and proximal thrombi: 12/32 (38%); DVT proximal to the calf: 9/32 (28%) Placebo group (2): calf and proximal thrombi: 13/14 (93%); DVT proximal to the calf: 8/14 (57%) PE events: Thigh-length GCSs group: 2/31 (6%) LMWH group (1): 3/29 (10%) Placebo group (2): 5/12 (42%) Adverse events: There were no differences in the haemoglobin levels and wound haematomata in the three groups |
| Wille-Jørgensen (1985)37 Location: Denmark |
Patients scheduled for elective major abdominal surgery who fulfilled one of the following criteria: aged above 39 years, malignancy suspected, weight more than 19% above normal, varicose veins of the lower extremities, diabetes mellitus, hypertension, previous thromboembolism or cardiac failure (n = 196 recruited; n = 176 analysed; 64 patients were observed for fewer than 7 days) | N/A | Thigh-length GCSs (TED stockings) worn during the observation period (median 5 days, range 3–6 days) (n = 86) 5000 units of LDH (Noparin) administered twice daily subcutaneously, starting 1 hour preoperatively and continued for 7 days or until discharge |
All patients received LDH as per the thigh-length GCSs group (n = 90) Heparin was from the same batch in intervention and control groups |
DVT assessed by radioiodine fibrinogen uptake test up to seventh postoperative day. Whenever fibrinogen uptake test was abnormal, or when clinical signs were present, ascending phlebography and perfusion and ventilation scintigraphy of the lungs were performed Thromboembolism (defined as DVT, PE or both) PE verified by pulmonary scintigraphy or autopsy Mortality (assessed within first 30 days) Patient adherence (results presented in Chapter 3) |
DVT events: Thigh-length GCSs group: 5/86 patients (6%) had an abnormal fibrinogen uptake test. 1/86 patients (1%) had phlebographically verified DVT Heparin group: 12/90 patients (13%) had an abnormal fibrinogen uptake test (p = NS between groups). 7/90 patients (8%) had phlebographically verified DVT (difference between GCSs and heparin group p < 0.05) Thromboembolism events: Thigh-length GCSs group: 2/86 patients (2%) Heparin group: 11/90 patients (12%) (difference between GCSs and heparin group p < 0.05) PE events: Thigh-length GCSs group: 2/86 patients (2%) Heparin group: 6/90 patients (7%) (p = NS between groups) Mortality: No patients in GCSs group and one patient in heparin group had fatal PE |
| Wille-Jørgensen (1991)36 Location: Denmark |
Patients undergoing acute abdominal operations (lasting more than 1 hour) who fulfilled at least one of the following risk factors: over 39 years of age, malignant lesions suspected, varicose veins, cardiac disease or hypertension, diabetes mellitus, obesity or earlier thromboembolic episodes (n = 276 recruited; n = 245 analysed) | N/A | (1) Thigh-length TED stockings (Kendall) worn until full mobilisation (n = 79) In addition, patients received LDH (5000 units of Noparin) administered subcutaneously preoperatively and continued twice daily for 7 days or until the patient was fully mobile (2) Thigh-length TED stockings (Kendall) (n = 85) In addition patients received dextran (Macrodex 70) 500-ml infusion intraoperatively and repeated on the first and third postoperative days |
LDH, as per the thigh-length GCSs group (1) (n = 81) | DVT assessed by radioiodine fibrinogen uptake test up to seventh postoperative day. Whenever fibrinogen uptake test was abnormal, or when clinical signs were present, ascending phlebography was performed If patients had signs or symptoms of PE, perfusion pulmonary scintigrams combined with roentgenograms of the chest were performed Mortality Adverse events |
DVT events: Thigh-length GCSs and LDH group: 2/79 patients (3%) Thigh-length GCSs and dextran group: 12/85 patients (14%) LDH group: 12/81 patients (15%) PE events: Thigh-length GCSs and LDH group: 0/79 patients (0%) Thigh-length GCSs and dextran group: 1/85 patients (1%) LDH group: 0/81 patients (0%) The difference in incidence of thromboembolism (DVT or PE) between GCSs + LDH and GCSs + dextran groups was statistically significant (p = 0.002). The difference in incidence of thromboembolism between GCSs + LDH and LDH alone groups was statistically significant (p = 0.013) Mortality: 16 patients in the GCSs + LDH group, 17 patients in the GCSs + dextran group and 11 patients in the LDH group died within 30 days of surgery. None of the patients who died was suspected of suffering from thromboembolism Adverse events: more postoperative transfusions were given to patients in the GCSs + dextran group (n = 28) than the LDH group (n = 18) or GCSs + LDH group (n = 19), but the difference between groups was not statistically significant. One patient in the GCSs + dextran group had extensive postoperative bleeding, dextran was withdrawn but the patient had to be reoperated on. The reason for bleeding was considered surgical. Median perioperative blood loss and total number of perioperative transfusions were similar between groups |
| Torngren (1980)35 Location: Sweden |
Patients undergoing major abdominal surgery (n = 110 recruited; n = 98 analysed) | N/A | Thigh-length GCSs worn until the sixth postoperative day (n = 45 right leg, n = 53 left leg) All patients also received low dose of heparin 5000 IU/ml, 1 ml subcutaneously 2 hours before surgery and subsequently every 12th hour for 5–7 days postoperatively |
All patients received LDH as per the thigh-length GCSs group | DVT assessed by radioiodine fibrinogen uptake test up to seventh postoperative day Fatal PE Adverse events |
DVT events: Thigh-length GCSs group: unilateral DVT occurred in no stockinged legs No stocking control group: unilateral DVT occurred in eight unstockinged legs (difference in unilateral DVT between control and stockinged legs p < 0.004). Bilateral DVT occurred in four patients No fatal PE events Adverse events: the stockings resulted in no complications and did not cause complaints from the surgeons or nursing staff. Only a few complaints from the patients were noted, mostly because the stockings fell down easily causing some disturbance to the ambulant patients |
| Fredin (1989)32 Location: Sweden |
Total hip arthroplasty patients (n = 150 recruited; n = 144 analysed) | N/A | Bilateral graded compression stockings (Comprinet S Reg/BDF Hamburg-West Germany) worn for 14 days (n = 49) All patients had dextran 70 Macrodex (R) 6% in NaCl, 500 ml perioperatively and 500 ml during the first 12 hours postoperatively. Another unit of 500 ml was given on the first and third postoperative days. If perioperative blood loss exceeded 2 litres, another 500 ml was given on the second postoperative day |
(1) Dextran as per the thigh-length GCSs group (n = 48) (2) Dextran as per the thigh-length GCSs group, also additional preoperative dextran administered for 2–3 hours on the evening before the operation (n = 47) |
DVT assessed by radioiodine fibrinogen uptake test and ascending phlebography for 10 days PE assessed by perfusion-ventilation scintigraphy Mortality Adverse events Patient adherence (results presented in Chapter 3) |
DVT events: Thigh-length GCSs group: 13/49 patients; p < 0.05 compared with the non-stocking control groups Dextran group (1): 21/47 patients Additional dextran group (2): 24/46 patients PE events: Thigh-length GCSs group: 0 Dextran group (1): Two patients had clinical symptoms and scintigraphic signs of PE Additional dextran group (2): 0 Mortality: Two patients died within 30 days; neither had thromboembolic complications at autopsy Adverse events: perioperative blood loss on average 350 ml lower in stockinged group (p < 0.01) |
| Ishak (1981)66 Location: UK |
Patients undergoing total hip arthroplasty (n = 76 recruited; n = 74 analysed) | N/A | Kendall TED thigh-length GCSs worn until discharge from hospital (n = 35) Dextran 70 solution in normal saline was given to 26 patients. Patients began passive calf and thigh exercises immediately after recovery from anaesthesia. Traction was applied for 2 or 3 days in 10 patients and these patients started walking on the 14th day. The remaining patients began active mobilisation after 48 hours |
No stocking (n = 41) Dextran 70 solution in normal saline given to 33 patients. Patients began passive calf and thigh exercises immediately after recovery from anaesthesia. Traction was applied for 2 or 3 days in 10 patients and these patients started walking on the 14th day. The remaining patients began active mobilisation after 48 hours |
DVT assessed by venography between 10th and 14th postoperative day All patients thought to have sustained PE had chest radiography followed by ventilation and perfusion lung scans Mortality |
DVT events: Thigh-length GCSs group: 7/35 (20%) No stocking group: 22/41 (54%) Significant difference between GCSs vs. control; p < 0.01 PE events: Thigh-length GCSs group: 2/35 (both in the late mobilisation group) No stocking group: 2/41 (both in the late mobilisation group) Mortality: Thigh-length GCSs group: 1/35 (unknown cause 15 hours after operation) No stocking group: 0/41 |
| Bergqvist (1984)31 Location: Sweden |
Surgical patients over 50 years of age (n = 88 recruited; n = 80 analysed) | N/A | Thigh-length GCSs worn for 7 days (16 mmHg at the ankle and 7 mmHg at the groin) (n = 41 right leg, n = 39 left leg) All patients received dextran 70; 500 ml intraoperatively, 500 ml immediately postoperatively, 500 ml on the first and third postoperative days. Early mobilisation in accordance with ward routine |
All patients received dextran 70, as per the thigh-length GCSs group | DVT assessed by radioiodine fibrinogen uptake test for 7 days PE assessed by perfusion-ventilation scintigraphy Mortality Adverse events |
DVT events: Thigh-length GCSs group: 0 No stocking control group: 9; 8 of which were detected by fibrinogen uptake test (one in thigh, seven in calf). One additional patient had clinical signs of thrombosis on postoperative day 8, although previous fibrinogen 125I test had been negative; the thrombosis was verified by phlebography PE events: One patient in thigh-length GCSs group had symptoms suggesting PE on postoperative day 17; the fibrinogen uptake test had been negative. Perfusion-ventilation scintigraphy strengthened the suspicion of PE. The patient made an uneventful recovery after oral administration of anticoagulants Mortality: Two patients died postoperatively; neither had thromboembolic complications at autopsy Adverse events: no complications directly related to prophylaxis |
| Thigh- or knee-length GCSs vs. no treatment control | ||||||
| Barnes (1978)30 Location: USA |
Patients undergoing THR (n = 18 analysed, number recruited not reported) | N/A | Kendall TED thigh-length GCSs worn for the duration of hospitalisation (n = 8) | No treatment control (n = 10) | DVT assessed by Doppler ultrasound. Patients with symptoms or Doppler evidence of VTE underwent contrast phlebography Patients with clinical manifestations of PE were evaluated with chest roentgenograms, arterial blood gases and perfusion lung scanning Adverse events |
DVT events: Thigh-length GCSs group: 0/8 No stocking group: 5/10 (50.0%), four in the operated on leg, and two in the non-operated on leg (one patient had bilateral DVT); p = 0.029 PE events: Thigh-length GCSs group: 0/8 No stocking group: 3/10 (all with documented DVT) Adverse events: one patient in the stocking group developed an episode of syncope on the 14th postoperative day |
| Turpie (1989)24 Location: Canada |
Patients aged 16 years or over admitted to the Regional Neurosciences Centre with brain tumour, spinal cord tumour, head injury, spinal cord injury or subarachnoid haemorrhage (n = 239 recruited; n = 239 analysed) | N/A | (1) Kendall TED thigh-length GCSs worn for 14 days after surgery or until discharge, if earlier (n = 80) (2) Kendall TED thigh-length GCSs worn for 14 days after surgery or until discharge, if earlier (n = 78). Patients also received intermittent pneumatic compression using the TED sequential compression device (Kendall Company); compression was applied sequentially from the ankle to the thigh (further details reported) |
No treatment control (n = 81) | DVT assessed by radioiodine fibrinogen uptake test and impedance plethysmography to day 14 or discharge. If radioiodine fibrinogen uptake test or impedance plethysmography were abnormal, bilateral ascending venography was carried out Mortality Patient adherence (results presented in Chapter 3) |
DVT events: Thigh-length GCSs group: 7/80; one was proximal. Difference in DVT rate was statistically significant compared with control (p = 0.023) Thigh-length GCSs plus intermittent pneumatic compression: 7/78; one was proximal. Difference in DVT rate was statistically significant compared with control (p = 0.027) No stocking group: 16/81; two were proximal Mortality: Thigh-length GCSs group: 10/80; one of whom autopsy showed had PE but whose cause of death was reported to be massive cerebral oedema Thigh-length GCSs plus intermittent pneumatic compression: 4/78; none of whom died of PE No stocking group: 4/81; none of whom died of PE |
| Shirai (1985)22 Location: Japan |
Patients who were admitted to GS wards (n = 126 recruited; n = 126 analysed) | N/A | Kendall TED thigh-length GCSs worn until patient ambulation (ankle: 18 mmHg, sural region: 14 mm Hg, knee: 8 mmHg, lower thigh: 10 mmHg, middle thigh: 8 mmHg) (n = 126 legs) | No treatment control (n = 126 legs) | DVT assessed by radioiodine fibrinogen uptake test | DVT events: Thigh-length GCSs group: five legs (4.0%) No stocking group: 17 legs (13.5%) |
| Tsapogas (1971)23 Location: USA |
Postoperative patients. Most patients underwent major abdominal procedures such as colectomies, abdominoperineal resections and biliary tract operations (n = 95 recruited, n = 95 analysed) | Knee-length GCSs worn until discharge from hospital (n = 51) In addition, the foot of the patient’s bed was elevated 30°, early postoperative active ambulation was encouraged, passive and active dorsi- and plantarflexion of the feet was started in the recovery room and continued for 5 minutes at 2-hour intervals throughout the day |
N/A | No treatment control (n = 44) | DVT assessed by radioiodine fibrinogen uptake test up to seventh postoperative day Phlebography was also performed up to seventh postoperative day |
DVT events: Knee-length GCSs group: 2/51 patients (4%) developed DVT within 7 days of surgery. In addition, 2/51 patients developed superficial-vein thrombosis. Both patients developing DVT only had small thrombi, which were non-occlusive and had no clinical signs No prophylaxis group: 6/44 patients (14%) developed DVT within 7 days of surgery. In addition, 1/44 patients developed superficial vein thrombosis. Four of the six DVTs were occlusive and two developed clinical signs |
| Other comparisons | ||||||
| Camporese (2008)60 Location: Italy |
Patients undergoing diagnostic arthroscopy or arthroscopy-assisted knee surgery for partial meniscectomy, cartilage shaving, cruciate ligament reconstruction, synovial resection or combined surgical procedures (n = 1761 recruited; n = 1602 analysed) All patients were mobile and discharged home on the same day as the procedure |
N/A | Thigh-length GCSs (30–40 mmHg at the ankle) worn on the operated on leg for 7 days (n = 597) | (1) Nadroparin LMWH (3800 anti-Xa IU) for 7 days (n = 603) (2) Nadroparin LMWH (3800 anti-Xa IU) for 14 days NB: this trial arm was stopped during interim analysis by the Data and Safety Monitoring Board (n = 402) |
DVT assessed by Doppler ultrasound PE assessed by ventilation perfusion lung scan when PE was suspected Mortality Adverse events Patient adherence (results presented in Chapter 3) |
DVT events: Thigh-length GCSs group: 29 (4.4%) (all in the operated on leg) LMWH 7 days group: 10 (1.5%) (all in the operated on leg) LMWH 14 days group: 9 (2.0%) (all in the operated on leg) PE events: Thigh-length GCSs group: symptomatic PE (non-fatal): 2 (0.3%) LMWH 7 days group: symptomatic PE (non-fatal): 2 (0.3%) LMWH 14 days group: symptomatic PE (non-fatal): 2 (0.5%) No deaths Adverse events: major bleeding: GCS: 1 (0.2%); LMWH 7 days: 2 (0.3%); LMWH 14 days: 1 (0.2%). Clinically relevant bleeding event: GCS: 1 (0.2%); LMWH 7 days: 4 (0.6%); LMWH 14 days: 1 (0.2%). Minor bleeding event: GCS: 20 (3.0%); LMWH 7 days: 23 (3.5%); LMWH 14 days: 16 (3.6%) |
| Caprini (1983)61 Location: USA |
Patients undergoing elective surgical procedures, considered to be at high risk (n = 102 recruited, n = 77 analysed) | N/A | TED thigh-length GCSs worn throughout hospital stay (n = 39) | Patients wore thigh-length TED stockings preoperatively. Prior to onset of anaesthesia, stockings were removed, and an intermittent sequential compression device (35–55 mmHg) was applied and maintained for at least 72 hours postoperatively or until ambulation, when a TED stocking was reapplied until hospital discharge (n = 38) | DVT assessed by radioiodine fibrinogen uptake test Venography or angiography, or both, were completed when dictated by clinical signs and symptoms PE Mortality |
DVT events: Thigh-length GCSs group: 4/39 (10.2%) Sequential compression device group: 1/38 (2.6%) PE events: Thigh-length GCSs group: 1/39 (non-fatal PE) Sequential compression device group: 1/38 (fatal PE) Mortality: Thigh-length GCSs group: 0/39 Sequential compression device group: 1/38 (patient with fatal PE) |
| Mellbring (1986)63 Location: Sweden |
Patients older than 50 years undergoing operation for benign or malignant abdominal disease (n = 114 recruited; n = 108 analysed) | N/A | (1) Thigh-length GCSs worn until the patient was fully mobile. In addition, IPCC given during surgery, beginning immediately after induction of anaesthesia (n = 54 randomly allocated to right or left leg) (2) Thigh-length GCSs worn until the patient was fully mobile. In addition, DHE plus LDH (0.5 mg + 5000 IU) subcutaneously two hours before surgery and subsequently twice daily until the patient was fully mobilised (n = 54 randomly allocated to right or left leg) |
(1) IPCC, as per the thigh-length GCSs group (1) (n = 54) (2) DHE + LDH, as per the thigh-length GCSs group (2) (n = 54) |
DVT assessed by radioiodine fibrinogen uptake test to day 9 or last day of hospitalisation, whichever was earlier Mortality Adverse events Patient adherence (results presented in Chapter 3) |
DVT events: Thigh-length GCSs + IPCC group (1): 7/54 Thigh-length GCSs + DHE plus LDH group (2): 1/54 IPCC control group (1): 6/54 DHE plus LDH control group (2): 2/54 No deaths Adverse events: no major bleeding complication occurred and bleeding during surgery showed no significant intergroup difference. No leg complication arose that could be attributed to IPCC or wearing of GCSs |
| Scurr (1987)34 Location: UK |
Patients undergoing general surgical procedures (n = 78 recruited; n = 78 analysed) | N/A | Thigh-length TED stockings (Kendall) worn for the study period (51% right leg, 49% left leg) | At the time of surgery, the stocking was removed from one leg and intermittent pneumatic SCDs with full leg sleeves (Kendall) applied to both legs. SDC continued until patients fully ambulatory. When SCDs were discontinued, the previously removed stocking was reapplied and patients continued to wear on both legs for the remainder of the study period | DVT assessed by radioiodine fibrinogen uptake test, Doppler ultrasound and strain-gauge plethysmography up to the seventh postoperative day, with positive findings confirmed by contrast venography PE |
DVT events: Thigh-length GCSs group: unilateral: 0/78 (0%); bilateral: 1/78 Pneumatic compression device group: unilateral: 6/78 (7.7%); p = 0.0156; bilateral: 1/78 No PE events |
| RCTs not included in DVT results | ||||||
| Rasmussen (1988)64 Location: Denmark |
Patients aged over 40 years undergoing major abdominal surgery, with a duration of general anaesthesia of more than 1 hour (n = 249 recruited; n = 248 analysed) | (1) Bilateral TED (Kendall) stockings worn until complete mobilisation, or for not fewer than 5 days postoperatively (n = 74) (2) Bilateral TED (Kendall) stockings worn until complete mobilisation, or for not fewer than 5 days postoperatively plus sodium heparin 5000 IU administered subcutaneously every 12 hours until complete mobilisation, or for not less than 5 days postoperatively (n = 89) |
N/A | Sodium heparin 5000 IU administered subcutaneously every 12 hours until complete mobilisation, or for not fewer than 5 days postoperatively (n = 89) | DVT assessed by 99mTc-labelled plasmin test PE assessed by clinical signs Mortality |
DVT events: Knee-length GCSs group: 22/74 (29.7%) (95% CI 19.7% to 41.5%); none had clinical signs of DVT Knee-length GCSs plus heparin group: 23/89 (25.8%) (95% CI 17.1% to 36.2%); one patient had clinical signs of DVT Heparin alone group: 25/85 (29.4%) (95% CI 20.0% to 44.3%); none had clinical signs of DVT. There were no statistically significant differences between any of the three treatment groups in the incidence of DVT (p > 0.05) No PE events No deaths |
| Fasting (1985)62 Location: Denmark |
Patients aged above 40 years undergoing elective GS, involving general anaesthesia of more than 1 hour (n = 112 recruited; n = 97 analysed) | N/A | Kendall TED thigh-length GCSs worn for at least 5 days after surgery and only stopped when patients were mobile (n = 52) | Sodium heparin 5000 IU (subcutaneously) given every 12 hours for at least 5 days after surgery and stopped only when patients were mobile (n = 45) | VTE (DVT was assessed by 99mTc-labelled plasmin test) Fatal PE assessed by autopsy Mortality Adverse events |
VTE events: Thigh-length GCSs group: 3/52 patients (5.8%); all were detected by positive plasmin test Heparin group: 4/45 patients (8.9%); 3/4 were detected by positive plasmin test PE events: Thigh-length GCSs group: 0/52 Heparin group: 1/45 patients died on the second postoperative day from PE Mortality: one patient in the heparin group died from PE Adverse events: there was a slightly, but insignificantly, higher number of patients with perioperative bleeding and total number of blood transfusions in the heparin compared with the GCSs group. No patients experienced major postoperative haemorrhagic complications. A few patients in the heparin group complained of discomfort from the injections. A few patients complained about stockings, which slipped down or felt hot |
Appendix 4 Evidence on baseline risk from published guidelines
| Study details | Evidence methods | Evidence base | Limitations reported by authors | Risk factors/risk models used | Data on patient adherence/preference, or consequences of DVT |
|---|---|---|---|---|---|
| Guidelines reporting baseline risk factors for DVT/VTE and baseline risk estimates | |||||
| ACCP guidelines (2012)67 Non-orthopaedic patients |
Search: MEDLINE, Cochrane, DARE, reference lists (to 2010) Inclusion criteria: yes Quality: Cochrane, GRADE Synthesis: RRs Study details: yes Duplication: study selection Assesses cost-effectiveness |
Large, population-based, observational studies on baseline risks of VTE and bleeding Objectively measured patient outcomes over 1–3 months |
Studies estimating baseline risk: small samples, referral centre bias, retrospective, short time horizons, missing or incomplete data, heterogeneity | Procedure-specific risks for DVT: Low-risk procedures: laparoscopic cholecystectomy, appendectomy, transurethral prostatectomy, inguinal herniorrhaphy, mastectomy High-risk procedures: open abdominal and open-pelvic procedures Patient-specific risks for DVT: Age > 60 years Obesity Male sex (bariatric surgery) Obstructive sleep apnoea/obesity hyperventilation syndrome (bariatric surgery) Prior VTE Anaesthesia ≥ 2 hours Bed rest ≥ 4 days Male sex Longer length of hospital stay Higher Charlson comorbidity score Sepsis Pregnancy/postpartum Central venous access Malignancy Risk of bleeding Risk models: Rogers score (not externally validated) Caprini score (validated in general, vascular, urological, plastic and reconstructive surgery) Estimates for baseline risk of DVT in the absence of prophylaxis (general, abdominal-pelvic, bariatric, vascular, and plastic and reconstructive surgery) VTE risk category (in the absence of prophylaxis): low (1.5%); moderate (3.0%); high (6.0%) |
NR |
| ACCP guidelines (2012)68 Orthopaedic patients Recommend IPCD as mechanical prophylaxis rather than GCSs |
Search: MEDLINE, Cochrane, abstracts, conference proceedings, reference lists (to 2010) Inclusion criteria: yes Quality: levels of evidence Synthesis: RRs Study details: no Duplication: NR |
SRs, RCTs Evidence based on patients undergoing hip or knee replacement |
NR | Estimates for baseline risk of DVT in the absence of prophylaxis Days 0–14: symptomatic DVT risk (with LMWH) 0.80% for THA, TKA and hip fracture surgery Symptomatic PE risk (with LMWH) 0.35% for THA, TKA and hip fracture surgery Estimated combined 35-day untreated baseline risk for symptomatic VTE: 4.3% for THA, TKA, and hip fracture surgery Estimates for baseline risk for major bleeding events 1.5% |
Limited data on adherence and not on GCSs |
| Brazilian Society of Cardiology (2011)69 Agency for Healthcare Research and Quality |
Search: PubMed, Scielo, LILACS (to 2010) Inclusion criteria: limited Quality: levels of evidence Synthesis: levels of risk in the absence of prophylaxis Study details: no Duplication: NR |
RCTs, non-RCTs | NR | Estimates for baseline risk of DVT in the absence of prophylaxis Low risk: minor surgery in patients who can walk (approximate risk of DVT in the absence of thromboprophylaxis: < 10%)a Moderate risk: Most general, gynaecological and open urological surgeries (approximate risk of DVT in the absence of thromboprophylaxis: 10–40%)a High risk: Hip or knee arthroplasty, hip fracture surgery, major traumas, spinal cord injury (approximate risk of DVT in the absence of thromboprophylaxis: 40–80%)a |
NR |
| Finnish Medical Society Duodecim (2010; 2011)70,71 | Search: CDSR, Cochrane Library, hand searching Inclusion criteria: limited Quality: GRADE levels of evidence Synthesis: levels of recommendations Study details: NR Duplication: NR |
Cochrane Reviews | NR | Risk factors for DVT Previous VTE Dehydration Heart failure and inactivity Stroke, paralysis Malignancy Severe infections Severe pulmonary disease Inflammatory bowel and rheumatic diseases Nephrotic syndrome Immobility Hormonal contraception or replacement therapy Pregnancy Surgical procedures and tissue damage Spinal injury Polycythaemia vera, essential thrombocythaemia, paroxysmal nocturnal haemoglobinuria, myeloma Venous insufficiency Obesity Smoking Clozapine medication Central venous catheter Estimates for baseline risk of DVT in the absence of prophylaxis Low risk: [risk of VTE 2%–3(–10)%]: Minor surgery (< 30 minutes), no additional risk factors Non-major surgery, age < 40 years, no additional risk factors Moderate risk: (risk of VTE 10%–30%): Minor surgery, additional risk factors Non-major surgery, age 40–60 years, no additional risk factors Major surgery, age < 40 years, no additional risk factors High risk: (risk of VTE 50–80%): Major surgery, age > 40 years or a history of DVT or PE or cancer, cancer surgery; thrombophilia; knee or hip arthroplasty, hip fracture; major trauma, spinal injury; immobility |
NR |
| International Consensus Statement, fifth revision (2013)72 | Search: MEDLINE/PubMed, Cochrane Library (to August 2012) Inclusion criteria: limited Quality: levels of evidence Synthesis: RRs Study details: NR Duplication: levels of evidence |
SRs, RCTs, observational studies or results from registries DVT/fatal PE diagnosed using fibrinogen uptake test |
NR | Risk category: High: major GS, age > 60 years; major GS, age 40–60 years, cancer or history of DVT/PE, or other risk factors including thrombophilia Moderate: major GS, age 40–60 years without other risk factors; minor surgery, age > 60 years; minor surgery, age 40–60 years with history of DVT/PE or other risk factor Low: major GS, age < 40 years, no other risk factors; minor surgery, age 40–60 years, no other risk factors Estimates for baseline risk of DVT in the absence of prophylaxis – GS (frequency of outcome): High risk: 40–80% (calf vein thrombosis), 10–30% (proximal vein thrombosis), > 1% (fatal PE) Moderate risk: 10–40% (calf vein), 1–10% (proximal vein), 0.1–1% (fatal PE) Low risk: < 10% (calf vein), < 1% (proximal vein), < 0.1% (fatal PE)b |
NR |
| NICE guideline 92 (2010; 2012)4,18 Refers to antiembolism stockings only (prevention in immobile patients) rather than graduated compression stockings (in mobile patients) British and European standards do not replicate the Sigel profile |
Search: Five electronic databases, guidelines, experts (to June 2009). Restricted to English. Updated to 2012 Inclusion criteria: yes Includes questions to address risk factors for VTE associated with surgical procedure, medical conditions, and individual patient risk factors. Search for SRs in surgical and non-surgical populations, and other guidelines Quality: levels of evidence Synthesis: RRs, Bayesian NMA Study details: appendices A–D Duplication: no Literature review on health economics |
RCTs, observational studies, registries in surgical and medical patients Evidence from patients undergoing the following surgical procedures: hip replacement; knee replacement; hip fracture; other orthopaedic; cranial or spinal (neurological) DVT diagnosed using radioiodine fibrinogen uptake; venography; Doppler ultrasound; MRI GCSs vs. no prophylaxis (nine RCTs); GCSs vs. IPCD/FID (one RCT); GCSs vs. LMWH (one RCT); GCSs vs. UFH (three RCTs); GCSs vs. mechanical + pharmacological (17 RCTs) Identify evidence comparing thigh vs. knee-length GCSs (three RCTs) 2012 update: identifies meta-analysis and Cochrane reviews |
Populations may not be representative of surgical patients in general, incidence of VTE fallen, dated evidence, heterogeneity Limitations of patient view studies included lack of detail on questionnaire design and validity Adherence may have been better in RCTs |
Risk factors for DVT: Active cancer or cancer treatment > 60 years Critical care admission Dehydration Known thrombophilias Obesity (BMI of > 30 kg/m2) One or more significant medical comorbidities (e.g. metabolic syndrome) History of VTE Use of HRT Use of oestrogen-containing contraceptive therapy Varicose veins with phlebitis Pregnancy/postpartum Also reduced mobility, surgical procedure and duration of surgery Risk of bleeding and other increased risk factors AESs contraindicated in patients with peripheral arterial disease, arteriosclerosis, severe peripheral neuropathy, massive leg oedema or pulmonary oedema, oedema secondary to congestive cardiac failure, local skin/soft-tissue diseases, extreme deformity of the leg, gangrenous limb and Doppler pressure index of < 0.8, or cellulitis Estimates for baseline risk in the absence of prophylaxis: DVT Hip fracture (39.8%) THR: (45%) TKR (60%) GS (20.9%) Symptomatic PE Hip fracture (7.9%) THR: (3.4%) TKR (1%) GS (1.3%) Major bleed Hip fracture (3.2%) THR: (1.6%) TKR (1.9%) GS (1.4%) |
Patient views (effectiveness and acceptability) and preferences regarding all the interventions GCSs (one RCT, one survey, one interview); GCSs/IPCD (one observational study) Adherence GCSs (one observational) |
| Royal College of Surgeons Guideline (2007)73 Orthopaedic and non-orthopaedic patients (excluding day-case patients): part of NICE guidelines (2008) |
Search: four electronic databases (to August 2006), references, guidelines Inclusion criteria: yes Includes a question to address risk of surgical procedure and individual risk factors Quality: levels of evidence Synthesis: RRs, MTC Study details: appendices Duplication: study selection Cost-effectiveness review |
RCTs, registries, observational studies | Data may not be generalisable, small sample size, incidence of VTE fallen, dated evidence, heterogeneity | Patient risk factors:
DVT Cardiac: 14% (7–24%) General: 24% (23–26%) Gynaecology: 16% (13–19%) Neurological: 20% (17–24%) Orthopaedic (elective hip): 44% (42–47%) Orthopaedic (hip fracture): 37% (35–40%) Orthopaedic (elective knee): 27% (22–32%) Orthopaedic (mixed): 47% (39–55%) Urological: 10% (6–15%) Vascular: (no estimate) Mixed: 22% (19–24%) Not known: 36% (31–42%) Symptomatic PE Cardiac: (0) General: 1% (1–2%) Gynaecology: 1% (0–3%) Neurological: (0) Orthopaedic (elective hip): 3% (2–5%) Orthopaedic (hip fracture): 6% (4–7%) Orthopaedic (elective knee): (0) Orthopaedic (mixed): 19% (13–25%) Urological: 9% (3–19%) Vascular: (0) Mixed: 1% (1–2%) Not known: (0) |
Some evidence on patient adherence and patient views (1 RCT, 1 survey) |
| Guidelines only risk factors for DVT/VTE | |||||
| Agency for Information, Evaluation, and Quality in Health of Catalonia 201074 Agency for Healthcare Research and Quality |
Search: CDSR, CENTRAL, DARE, HTA, NHS EED, MEDLINE, EMBASE, 16 websites (to December 2008) Inclusion criteria: yes (excludes emergency surgical procedures) Quality: GRADE, strength of recommendation Synthesis: RRs Study details: no Duplication: NR |
RCTs, observational studies General recommendations reported (do not distinguish between knee and thigh-length stockings or surgical procedure) |
NR | GCSs should not be used in patients with peripheral arterial disease, atherosclerosis, serious peripheral neuropathy, massive oedema in the lower extremities, pulmonary oedema, oedema caused by congestive cardiac failure, local diseases affecting the skin or soft tissue, gangrenous extremities, Doppler pressure reading of < 0.8, and excessive cellulitis Estimates for baseline risk of DVT in the absence of prophylaxis NR |
NR |
| ENT UK (2010)75 | N/A | N/A | N/A | Risk factors for DVT: Significant reduction in mobility for ≥ 3 days Total anaesthetic + surgical time > 90 minutes Active cancer or treatment Age > 60 years Critical care admission Dehydration Thrombophilia Obesity Medical comorbidities Personal or family history of VTE Use of HRT Use of oestrogen containing contraceptive Varicose veins with phlebitis Risks for bleeding: Active bleeding Acquired bleeding disorders Use of anticoagulants known to increase risk of bleeding Lumbar puncture/epidural/spinal anaesthesia Acute stroke Thrombocytopenia Uncontrolled systolic hypertension Untreated inherited bleeding disorders Estimates for baseline risk of DVT in the absence of prophylaxis NR |
NR |
| National Health and Medical Research Council Australian Government Clinical Practice Guideline (2009)76 Do not distinguish between knee- and thigh-length stockings |
Search: International guideline databases (not specified) to January 2009, but based on NICE 2007 guideline searches177 Inclusion criteria: yes (PICOS) Quality: Cochrane risk of bias tool Synthesis: RRs by surgical procedure Study details: yes Duplication: inclusion criteria |
SRs of RCTs, RCTs in medical and surgical patients Diagnostic methods: compression ultrasonography, ascending venography Evidence based on THR (seven RCTs), knee arthroscopy (one RCT), GS (12 RCTs), urological surgery (one RCT), gynaecological (one RCT), abdominal surgery (four RCTs), neurosurgery (one RCT) No evidence on GCSs for hip fracture surgery, TKR, lower leg fractures, mixed orthopaedic surgery, cardiac/thoracic/vascular, trauma/spinal GCSs vs. no GCSs GCSs plus fondaparinux vs. fondaparinus only IPC vs. GCSs; GCSs vs. UFH |
Small sample sizes, age of evidence, different diagnosis methods and end points Evidence lacking on knowledge relating to the prevalence of known risk factors for VTE and magnitude of risk, evidence on the effectiveness of VTE prevention in specific situations |
Patient related risks for DVT: Age Pregnancy and puerperium Active or occult malignancy Previous VTE Varicose veins Marked obesity Prolonged severe immobility Use of oestrogen-containing hormone replacement therapy or oral contraceptives Thrombophilia Surgical procedure/injury: All surgical procedures, especially abdominal, pelvic, thoracic or orthopaedic procedures Type of surgery, anaesthesia, duration of immobility, and surgical complications Bleeding risk Estimates for baseline risk of DVT in the absence of prophylaxis NR |
NR |
| SIGN (2010)11 | Search: five electronic databases, guidelines (to 2009) Inclusion criteria: NR No specific search/inclusion criteria to identify risk assessment tools or risk factors Quality: NR Synthesis: unclear Study details: NR Duplication: study selection |
NR | Insufficient evidence to show whether interactions between risk factors are additive or greater. | Risk factors for DVT:
Algorithm for assessing the risk of venbous thromboemoblism: Grampian risk assessment tool (age; obesity; varicose veins; family history of VTE; thrombophilias; other thrombotic states; combined oral contraceptives, hormone replacement therapy and antioestrogens; pregnancy, puerperium; immobility; hospitalisation; anaesthesia; central venous catheters) Estimates for baseline risk of DVT in the absence of prophylaxis NR GS (frequency of outcome): High risk: 40–80% (calf vein thrombosis), 10–30% (proximal vein thrombosis), > 1% (fatal PE) Moderate risk: 10–40% (calf vein), 1–10% (proximal vein), 0.1–1% (fatal PE) Low risk: < 10% (calf vein), < 1% (proximal vein), < 0.1% (fatal PE)b |
NR |
| Thromboembolic Risk Factors (THRIFT) Consensus Group Lowe (1992)8 |
Search: NR Inclusion criteria: NR Quality: NR Synthesis: unclear Study details: NR Duplication: NR |
Controlled trials | NR | Patient risk factors for DVT:
NR |
NR |
| Guidelines not reporting risk factors for DVT/VTE or baseline risk estimates | |||||
| British Committee for Standards in Haematology Journal (2010)77 Investigation, management and prevention of VTE in children (usually older or larger children > 40 kg) Does not distinguish between knee- and thigh-length stockings |
Search: PubMed (1990–2010) Inclusion criteria: NR Quality: GRADE Synthesis: narrative Study details: NR Duplication: NR |
NR | NR | NR | NR |
Appendix 5 Network meta-analysis code
Model that allows for a stocking–heparin interaction
This model has a binomial likelihood, logit link, random-effects and multiarm trials. This is as stated in the NICE technical support document 2. 48
model{
for(i in 1:ns){
w[i,1]<-0
delta[i,1]<-0
mu[i]∼dnorm(0,0.0001)
for (k in 1:na[i]){
r[i,k]∼dbin(p[i,k],n[i,k])
logit(p[i,k])<-mu[i]+delta[i,k]
rhat[i,k]<-p[i,k]*n[i,k]
dev[i,k]<-2*(r[i,k]*(log(r[i,k])-log(rhat[i,k]))+
(n[i,k]-r[i,k])*(log(n[i,k]-r[i,k])-log(n[i,k]-rhat[i,k])))
}
resdev[i]<-sum(dev[i,1:na[i]])
for (k in 2:na[i]) {
delta[i,k]∼dnorm(md[i,k],taud[i,k])
md[i,k]<-d[t[i,k]]-d[t[i,1]]+sw[i,k]
taud[i,k]<-tau*2*(k-1)/k
w[i,k]<-(delta[i,k]-d[t[i,k]]+d[t[i,1]])
sw[i,k]<-sum(w[i,1:k-1])/(k-1)
}
}
Model that assumes no stocking–heparin interaction
Each treatment is assumed to be composed of two effects, e.g. thigh stocking + heparin. Thigh stocking is considered ‘thigh stocking + no treatment’, since, as no treatment is the reference treatment, it is defined as equal to 0.
model{
for(i in 1:ns){
w[i,1]<-0
delta[i,1]<-0
mu[i]∼dnorm(0,0.0001)
for (k in 1:na[i]){
r[i,k]∼dbin(p[i,k],n[i,k])
logit(p[i,k])<-mu[i]+delta[i,k]
rhat[i,k]<-p[i,k]*n[i,k]
dev[i,k]<-2*(r[i,k]*(log(r[i,k])-log(rhat[i,k]))+
(n[i,k]-r[i,k])*(log(n[i,k]-r[i,k])-log(n[i,k]-rhat[i,k])))
}
resdev[i]<-sum(dev[i,1:na[i]])
for (k in 2:na[i]) {
delta[i,k]∼dnorm(md[i,k],taud[i,k])
md[i,k]<-d[t1[i,k]]+d[t2[i,k]]-d[t1[i,1]]-d[t2[i,1]]+sw[i,k]
taud[i,k]<-tau*2*(k-1)/k
w[i,k]<-(delta[i,k]-d[t1[i,k]]-d[t2[i,k]]+d[t1[i,1]]+d[t2[i,1]])
sw[i,k]<-sum(w[i,1:k-1])/(k-1)
}
}
Appendix 6 Parameters and parameter distributions used in the probabilistic analysis
| Parameter description | Point estimate, % | Probability distribution | Distribution parameters |
|---|---|---|---|
| THR | |||
| Symptomatic DVT risk: on LMWH | 0.38 | Log-normal | SE = 0.351 |
| Symptomatic PE risk: on LMWH | 0.25 | Log-normal | SE = 0.276 |
| Proportion of DVTs that are symptomatic | 21.00 | Beta | α = 223, β = 840 |
| Major bleeding fatality rate | 0.80 | Beta | α = 5, β = 627 |
| PE fatality rate | 6.00 | Beta | α = 11, β = 173 |
| TKR | |||
| Symptomatic DVT risk: on LMWH | 0.72 | Log-normal | SE = 0.293 |
| Symptomatic PE risk: on LMWH | 0.53 | Log-normal | SE = 0.233 |
| Proportion of DVTs that are symptomatic | 5.00 | Beta | α = 17, β = 320 |
| Major bleeding fatality rate | 0.80 | Beta | α = 5, β = 627 |
| PE fatality rate | 6.00 | Beta | α = 11, β = 173 |
| GS: low risk | |||
| Symptomatic DVT risk: on LMWH | 0.31 | Log-normal | NR |
| Symptomatic PE risk: on LMWH | 0.16 | Log-normal | NR |
| Proportion of DVTs that are symptomatic | 6.20 | Beta | α = 40, β = 604 |
| Major bleeding fatality rate | 0.80 | Beta | α = 5, β = 627 |
| PE fatality rate | 6.00 | Beta | α = 11, β = 173 |
| GS: moderate risk | |||
| Symptomatic DVT risk: on LMWH | 0.61 | Log-normal | NR |
| Symptomatic PE risk: on LMWH | 0.32 | Log-normal | NR |
| Proportion of DVTs that are symptomatic | 6.20 | Beta | α = 40, β = 604 |
| Major bleeding fatality rate | 0.80 | Beta | α = 5, β = 627 |
| PE fatality rate | 6.00 | Beta | α = 11, β = 173 |
| GS: high risk | |||
| Symptomatic DVT risk: on LMWH | 1.23 | Log-normal | NR |
| Symptomatic PE risk: on LMWH | 0.63 | Log-normal | NR |
| Proportion of DVTs that are symptomatic | 6.20 | Beta | α = 40, β = 604 |
| Major bleeding fatality rate | 0.80 | Beta | α = 5, β = 627 |
| PE fatality rate | 6.00 | Beta | α = 11, β = 173 |
| Parameter description | Point estimate, % | Probability distribution | Distribution parameters |
|---|---|---|---|
| Relative effectiveness parameters | N/A | Output from WinBUGS simulation | |
| Duration of prophylaxis: orthopaedic | 10.0 | Log-normal | Log (mean) = 2.30, se = 0.13 |
| Duration of prophylaxis: GS | 7.0 | Log-normal | Log (mean) = 1.94, se = 0.13 |
| Re-operation (GS) | 21 | Beta | α = 25, β = 93 |
| Re-operation (orthopaedic surgery) | 13 | Beta | α = 32, β = 214 |
| PTS rate after symptomatic DVT (5 year) | 25 | Beta | α = 132, β = 396 |
| PTS rate after asymptomatic DVT (5 year) | 15 | Beta | α = 77, β = 436 |
| PHT rate after symptomatic PE (2 year) | 0.75 | Beta | α = 99, β = 13,133 |
| VTE recurrence after initial PE | 5.1 | Beta | α = 42.1, β = 783.3 |
| Probability that VTE recurrence is PE | 50.0 | Beta | α = 12.50, β = 12.51 |
| VTE recurrence after initial symptomatic DVT | 6.0 | Beta | α = 160.4, β = 2513.5 |
| Probability that VTE recurrence is PE | 15.5 | Beta | α = 12.69, β = 69.31 |
| Utility: DVT | 0.99 | Beta | α = 36.58, β = 0.48 |
| Utility: PE | 0.94 | Beta | α = 19.43, β = 1.24 |
| Utility: PTS | 0.98 | Beta | α = 232.65, β = 5.48 |
| Utility: PHT | 0.77 | Beta | α = 262.06, β = 80.50 |
| Utility: major bleeding | 0.50 | Beta | α = 49.5, β = 49.5 |
| Utility: stroke | 0.52 | Beta | α = 3.44, β = 3.17 |
| Disutility: recurrent PE | 0.06 | Beta | α = 93.94, β = 1471.73 |
Appendix 7 Base-case results: 10,000 simulations
| Treatment | Total | Incremental | ICER, £ | Probability cost-effective £20,000 | Probability cost-effective £30,000 | ||
|---|---|---|---|---|---|---|---|
| Costs, £ | QALYs | Costs, £ | QALYs | ||||
| THR | |||||||
| LMWH | 131 | 10.01023 | – | – | – | 0.59 | 0.35 |
| LMWH + thigh | 175 | 10.01164 | 44 | 0.00141 | 31,225 | 0.29 | 0.49 |
| LMWH + knee | 186 | 10.01063 | 11 | –0.00101 | Dominated | 0.12 | 0.17 |
| TKR | |||||||
| LMWH + thigh | 263 | 9.91221 | – | – | – | 0.74 | 0.75 |
| LMWH | 309 | 9.90763 | 45 | –0.00458 | Dominated | 0.04 | 0.04 |
| LMWH + knee | 338 | 9.90899 | 75 | –0.00322 | Dominated | 0.22 | 0.22 |
| GS: low risk | |||||||
| LMWH | 177 | 12.76884 | – | – | – | 0.08 | 0.06 |
| LMWH + thigh | 184 | 12.77076 | 7 | 0.00191 | 3461 | 0.70 | 0.72 |
| LMWH + knee | 213 | 12.76940 | 30 | –0.00136 | Dominated | 0.22 | 0.22 |
| GS: moderate risk | |||||||
| LMWH + thigh | 231 | 12.76881 | 0.74 | 0.74 | |||
| LMWH | 275 | 12.76488 | 43 | –0.00392 | Dominated | 0.04 | 0.03 |
| LMWH + knee | 297 | 12.76605 | 65 | –0.00276 | Dominated | 0.22 | 0.22 |
| GS: high risk | |||||||
| LMWH + thigh | 343 | 12.76432 | 0.75 | 0.75 | |||
| LMWH + knee | 498 | 12.75796 | 155 | –0.00636 | Dominated | 0.22 | 0.22 |
| LMWH | 504 | 12.75567 | 161 | –0.00865 | Dominated | 0.03 | 0.03 |
List of abbreviations
- ACCP
- American College of Chest Physicians
- ADVANCE
- Apixaban Dose orally Vs. ANtiCoagulation with Enoxuprin
- AMED
- Allied and Complementary Medicine Database
- CENTRAL
- Cochrane Central Register of Controlled Trials
- CG
- clinical guideline
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health
- CRD
- Centre for Reviews and Dissemination
- CrI
- credible interval
- DARE
- Database of Abstracts of Reviews of Effects
- DVT
- deep-vein thrombosis
- EQ-5D
- European Quality of Life-5 Dimensions
- ERG
- Evidence Review Group
- EVPI
- expected value of perfect information
- EVPPI
- expected value of partial perfect information
- EVSI
- expected value of sample information
- FP
- foot pump
- GCS
- graduated compression stocking
- GS
- general surgery
- HEED
- Health Economics Evaluations Database
- HRG
- Healthcare Resource Group
- HTA
- Health Technology Assessment
- ICER
- incremental cost-effectiveness ratio
- IPCD
- intermittent pneumatic compression device
- LDH
- low-dose heparin
- LMWH
- low-molecular-weight heparin
- MRI
- magnetic resonance imaging
- NHS EED
- NHS Economic Evaluations Database
- NICE
- National Institute for Health and Care Excellence
- NMA
- network meta-analysis
- NNT
- number of patients needed to treat
- NOAC
- new oral anticoagulant
- OR
- odds ratio
- PE
- pulmonary embolism
- PHT
- pulmonary hypertension
- PSA
- probabilistic analysis
- PSS
- Personal Social Services
- PTS
- post-thrombotic syndrome
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- RR
- relative risk
- SD
- standard deviation
- SIGN
- Scottish Intercollegiate Guidelines Network
- STA
- single technology appraisal
- THR
- total hip replacement
- TKR
- total knee replacement
- VOI
- value of information
- VTE
- venous thromboembolism