Notes
Article history
This issue of the Health Technology Assessment journal series contains a project commissioned/managed by the Methodology research programme (MRP). The Medical Research Council (MRC) is working with NIHR to deliver the single joint health strategy and the MRP was launched in 2008 as part of the delivery model. MRC is lead funding partner for MRP and part of this programme is the joint MRC–NIHR funding panel ‘The Methodology Research Programme Panel’.
To strengthen the evidence base for health research, the MRP oversees and implements the evolving strategy for high-quality methodological research. In addition to the MRC and NIHR funding partners, the MRP takes into account the needs of other stakeholders including the devolved administrations, industry R&D, and regulatory/advisory agencies and other public bodies. The MRP funds investigator-led and needs-led research proposals from across the UK. In addition to the standard MRC and RCUK terms and conditions, projects commissioned/managed by the MRP are expected to provide a detailed report on the research findings and may publish the findings in the HTA journal, if supported by NIHR funds.
The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Charles Abraham acknowledges funding from the UK National Institute for Health Research and the Peninsula Collaboration for Leadership in Applied Health Research and Care.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2015. This work was produced by Michie et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 General introduction
Behaviour change interventions: purpose and reporting
Preventable behaviours, such as smoking, physical inactivity, eating unhealthy diets and excessive alcohol consumption, have been identified as leading causes of morbidity and mortality. 1–4 Behaviour change interventions (BCIs) are typically complex, involving many interacting components. 5 This can make them challenging to replicate in research, to implement in practical settings and to synthesise in systematic literature reviews.
Behaviour change interventions are ‘Coordinated sets of activities designed to change specified behaviour patterns’. 6 The development, implementation and evaluation of effective BCIs are fundamental for advancing behavioural science and its application. 7,8 However, both science and practice depend on having a good understanding of the nature and content of interventions. This includes knowing what was delivered in the intervention [i.e. the ‘active ingredients’ or behaviour change techniques (BCTs)] and how it was delivered (i.e. who delivered, to whom, how often, for how long, in what format, and in what context). 9–11 Poorly described interventions in research protocols and published reports mean that the precise content of interventions is difficult to establish, with the possibility of the same labels (e.g. behavioural counselling) meaning different things to different researchers/implementers and different labels being used to describe the same BCTs. As a result, the content delivered in practice often deviates from that specified in the intervention protocol12 presenting a barrier to scientific progress and effective translation.
Guidance documents have been published aimed at improving methods of specifying and reporting interventions. For example, Consolidated Standards of Reporting Trials guidelines for reporting randomised controlled trials (RCTs)13 advise researchers to report the ‘precise details’ of the intervention as ‘actually administered’, and the Transparent Reporting of Evaluations with Nonrandomized Designs statement for reporting non-randomised trials14 emphasises the reporting of content and context and full description of comparison and intervention conditions. The UK Medical Research Council (MRC) guidance for developing and evaluating complex interventions calls for the specification of the active ingredients as a necessary step for investigating how interventions exert their effect and, therefore, for designing more effective interventions and applying them appropriately across target population group and setting. 5 The Workgroup for Intervention Development and Evaluation Research group has had some success in encouraging journal editors to ensure that transparent and accessible intervention descriptions are available before publication of intervention outcomes. 15 The Template for Intervention Description and Replication (TIDieR)16 provides a checklist of the minimum data required to report interventions, including surgical, pharmacological, psychotherapeutic as well as behavioural interventions. Although progress has been made in improving how intervention content is reported, if descriptions of BCIs are to be communicated effectively and successfully replicated, a shared and standardised method of classifying intervention content is needed. 17
Behaviour change techniques
A BCT is defined as an observable and replicable component designed to change behaviour. It is the smallest component compatible with retaining the postulated active ingredients and can be used alone or in combination with other BCTs. To enable interventions to be evaluated and effective interventions (i.e. those which bring about the desired change in the target behaviour or behaviours) to be implemented, a BCT should be well specified. BCTs are descriptors and vary in the extent to which they have been empirically investigated and the extent to which they bring about the desired change to behaviour(s) in different situations. BCT definitions used for coding have to be practical, non-overlapping and useful in the reliable reporting of interventions.
Specification of interventions according to component BCTs is beneficial for conducting primary research, implementing effective interventions and for conducting evidence syntheses. A comprehensive list of BCTs facilitates primary research, as intervention developers can draw on a wider range of BCTs than is likely to be considered without such a list. Specification of intervention and control conditions using BCTs can increase accurate replication of interventions found to be efficacious in RCTs. BCT methodology is also useful in assessing the fidelity of implementation of interventions. For systematic reviewers, BCTs provide a reliable method for extracting and coding information about intervention content. Reviewers can identify and synthesise discrete, replicable, potentially active ingredients associated with efficacy and multivariate statistical analysis can then be used to identify BCTs and BCT combinations associated with efficacy. By linking BCTs with theories of behaviour change, researchers and reviewers can investigate possible effect modifiers and/or mechanisms of action. There are some intervention components that can be thought of as ‘modifier BCTs’ in that they add value to BCTs but do not in themselves change behaviour, for example, tailoring, giving choice and homework tasks. Specifying intervention content with this degree of precision helps to maximise scientific as well as practical benefits of research investment into the development and evaluation of complex interventions.
Behaviour change technique taxonomies
To provide a more rigorous methodology for characterising intervention content, methods have been developed for specifying the potentially active ingredients in terms of BCTs. 18–20 Abraham and Michie’s20 taxonomy of 22 BCTs and four BCT packages observed in BCIs was demonstrated to have good intercoder reliability (i.e. the extent to which coders agreed on the presence/absence of BCTs) among the taxonomy developers and trained coders across 221 intervention descriptions in papers and manuals. This, and subsequent taxonomies developed for specific behavioural domains, have been widely used internationally to report interventions, synthesise evidence21–24 and design interventions. 25,26 BCT taxonomies have been developed in relation to smoking,27 physical activity and healthy eating,28 excessive alcohol use29 and condom use. 30 Taxonomies of BCTs have also been used to assess the extent to which published reports reflect intervention protocols12 and to assess fidelity of delivery. 31 They have enabled the specification of professional competences for delivering BCTs32,33 and as a basis for a national training programme. 34,35 Guidance has also been developed for incorporating BCTs in text-based interventions. 36
Previous classification systems have either been in the form of an unstructured list or have been linked to, or structured, according to theories and/or theoretical mechanisms19,20,32,33 judged to be the most appropriate by the authors.
A hierarchically structured list provides the advantage of making it more coherent to, and useable by, those applying it. 37 There are at least five potential benefits of developing a cross-domain, hierarchically structured and internationally supported taxonomy for specifying intervention content:
-
To promote the accurate replication of interventions and control conditions in comparative efficacy research, a key activity in accumulating scientific knowledge and investigating generalisability across behaviours, populations and settings.
-
To specify intervention content to facilitate faithful implementation of intervention protocols in research and, in practice, of interventions found to be effective.
-
To extract and synthesise information about intervention content in systematic reviews. BCT taxonomies, combined with the statistical technique of meta-regression or classification and regression tree (CART), have allowed reviewers to synthesise evidence from complex, heterogeneous interventions to identify effective component BCTs and BCT combinations. 21,23,24,38,39
-
To draw on a comprehensive list of BCTs in developing interventions (rather than relying on the limited set that can be brought to mind).
-
To investigate possible mechanisms of action by linking BCTs with theories of behaviour change and component theoretical constructs. 8,19,21,23
In this monograph, we present the development and evaluation of Behaviour Change Technique Taxonomy version 1 (BCTTv1): a cross-domain, hierarchically structured taxonomy based on interdisciplinary consensus as a method for the accurate and reliable reporting of interventions to change behaviour. 40
Phase 1: development
Chapter 2 Developing a comprehensive list of behaviour change techniques (study 1)
Abstract
Objectives: To develop an extensive, consensually agreed taxonomy of BCTs used in BCIs.
Methods: In a Delphi-type exercise, 14 experts rated labels and definitions of 124 BCTs from six published classification systems. 20,23,27,29,33,36 The resulting list was refined based on the feedback from group discussions of 16 members of the International Advisory Board (IAB).
Results: This resulting BCTTv1 comprised 93 distinct, non-redundant and non-overlapping BCTs.
Conclusions: BCTTv1 offers a step change in methods for specifying interventions using shared concepts and language. When sufficient data have been collected about its implementation and an international, interdisciplinary consortium established, v1 will be reviewed and v2 released as and when the need is judged by consensus.
Introduction
Literature reviews find that even essential elements of interventions are frequently omitted from intervention descriptions; an analysis of trials and reviews found that 67% of pharmacological intervention descriptions were adequate, compared with only 29% of non-pharmacological intervention descriptions. 41 While this occurs in descriptions of all types of intervention, it is an even more common problem in BCIs. Titles and abstracts of published interventions (i.e. the materials screened for inclusion in systematic reviews) have been found to mention the active components of the intervention in only 56% of published descriptions compared with over 90% in pharmacological interventions. 42 The TIDieR checklist and guide for reporting all types of interventions was developed using consensus methods with international participants from several disciplines and proposes a minimum set of information: brief name, why (rationale), what materials, what procedure, who provided, how, where, when and how much, tailoring, changes, how well monitored and how well delivered. 16 However, for BCIs, further information is required to specify the active ingredients, that is ‘components within an intervention that can be specifically linked to its effect on outcomes such that, if they were omitted, the intervention would be ineffective’. 42
The content, or active components, of BCIs are often described in intervention protocols and published reports with different labels (e.g. ‘self-monitoring’ may be labelled ‘daily diaries’) and the same labels may be applied to different techniques (e.g. ‘behavioural counselling’ may involve ‘educating patients’ or ‘feedback, self-monitoring, and reinforcement’). 43 This may lead to uncertainty, confusion and difficulties in determining the efficacy of specific change approaches; for example, Morton et al. 44 had considerable difficulty in identifying the necessary components of motivational interviewing and as a result found it difficult to synthesise evidence of efficacy. Further, behavioural medicine researchers and practitioners have reported low confidence in their ability to replicate highly effective behavioural interventions for type 2 diabetes mellitus prevention. 45 The absence of standardised definitions and labels for intervention components means that systematic reviewers develop their own systems for classifying behavioural interventions and synthesising study findings [e.g. Hardeman et al. ,18 Albarracín et al. ,19 Mischel (Presidential address given at the Association for Psychological Science Annual Convention, Washington, DC; 2012) and West et al. 46]. This proliferation of systems leads to duplication of effort and undermines the potential to accumulate evidence across reviews. It also points to the urgent need for consensus. Consequently, the UK MRC guidance5 for developing and evaluating complex interventions called for improved methods of specifying and reporting intervention content in order to address the problems of lack of consistency and consensus.
A method developed for this purpose is the reliable specification of interventions in terms of BCTs. 20 Previous classification systems have mainly been developed for particular behavioural domains (e.g. physical activity, smoking, alcohol consumption or safer sex). Abraham and Michie20 developed the first cross-behaviour BCT taxonomy, building on previous intervention content analyses. 18,19 The taxonomy demonstrated reliability in identifying 22 BCTs (e.g. ‘self-monitoring’) and four BCT packages (e.g. ‘relapse prevention’). Identifying the presence of BCTs in intervention descriptions included in systematic reviews and national datasets of outcomes has allowed the identification of BCTs associated with effective interventions. 46,47 Effective BCTs have been identified for interventions to increase physical activity and healthy eating,23,48 and to support smoking cessation,27,46 reduce excessive alcohol consumption,29 prevent sexually transmitted infections19,30 and change professional behaviour. 49
Although the subsequent development of classification systems of defined and reliably identifiable BCTs has been accompanied by a progressive increase in their comprehensiveness and clarity, this work has been conducted by only a few research groups, but with each developing their own methodology. For this method to maximise scientific advance, collaborative work was needed to develop agreed labels and definitions and reliable procedures for their identification and application across behaviours, disciplines and countries. Therefore, the aim of study 1 was to develop a taxonomy that comprises an extensive list of clearly labelled, well defined BCTs that (1) are proposed as the active components of BCIs, (2) are distinct (non-overlapping, non-redundant) and precise, (3) can be used with confidence to describe interventions, and (4) have a breadth of international and disciplinary agreement.
Method
This study is also published as Michie et al. 40
Participants
Participants were international behaviour change experts (i.e. active in their field and engaged in investigating, designing and/or delivering BCIs) who had agreed to take part in one or more of the project phases or were members of the IAB50 or of the study team (which included a ‘lay’ person). All board members, as leaders in their field, were eligible to take part as a behaviour change expert. However, in light of their advisory role commitments, members were not routinely approached for further participation except to help widen participation in terms of country, discipline and behavioural expertise.
For the Delphi exercise, 19 international behaviour change experts were invited to take part. Experts were identified from a range of scientific networks on the basis of breadth of knowledge of BCTs, experience of designing and/or delivering BCIs, and of being able to complete the study task in the allotted time. Recruitment was by e-mail, with an offer of an honorarium of £140 (approximately US$230; conversion as of March 2014) on completing the task. Of the 19 originally approached, 14 agreed to take part (response rate of 74%). Ten participants were female, with an age range of 37–62 years [mean = 50.57 years; standard deviation (SD) = 7.74 years]. Expert participants were from the UK (8), Australia (2), the Netherlands (2), Canada (1) and New Zealand (1). Eleven were psychologists (six health psychologists, one clinical psychologist, three clinical and health psychologists and one educational psychologist); one was a cognitive–behaviour therapist and two had backgrounds in health sciences or community health. Eleven were active practitioners in their discipline. Eleven had research or professional doctorates and two had registered psychologist status. There was a wide range of experience of using BCTs, with all having used at least six BCTs, more than half having used more than 30 BCTs and four having used more than 50 BCTs for intervention design, delivery and training.
For the international feedback phase, 16 out of the 30 IAB members took part in discussions to comment on a prototype BCT classification system. IAB members were identified by the study team as being leaders in their field within the key domains of interest (e.g. types of health-related behaviours, major disease types, disciplines such as behavioural medicine) following consultation of websites, journals, and scientific and professional organisations. IAB members were from the USA, Canada, Australia, UK, the Netherlands, Finland and Germany (see Appendix 2). Feedback was also provided by members of the study team, who had backgrounds in psychology and/or implementation science and a ‘lay’ person with a Bachelor of Arts with Honours [BA (Hons)] in English but no background in psychology or behaviour change.
Procedure
Participants provided written consent and were assured that their responses would remain confidential. All participants were asked to provide demographic information (i.e. age, sex and nationality). Delphi participants were also asked to provide their professional background (i.e. qualifications, registrations, job title and area of work) and how many BCTs they had used professionally in intervention design, face-to-face delivery and training (reported in increments of 5 up to 50 +).
A prototype classification system was developed by the study team based on all known published classifications of BCTs following a literature review37 (step 1). An online Delphi-type exercise51 with two ‘rounds’ was used for initial evaluation and development of the classification system. Participants worked independently and rated the prototype BCT labels and definitions on a series of questions designed to assess omission, overlap and redundancy (step 2). The results of step 2 subsequently informed the development of an improved BCT list. The BCTs identified as requiring further clarification were sent to the Delphi participants for the second round. They were asked to rate BCTs for clarity, precision, distinctiveness and confidence of use (step 3). The resulting list of BCTs was then scrutinised by the IAB, who submitted verbal and written feedback (step 4), and was assessed by the lay and expert members of the study team (step 5). Following each of steps 2–4, the results were synthesised by SM and MJ in preparation for the next step.
Step 1: developing the prototype classification system
The labels and definitions of distinct BCTs were extracted from six BCT classification systems identified by a literature search (the relevant papers are marked with an asterisk in the reference section). For BCTs with two or more labels (n = 24) and/or definitions (n = 37), five study team members rated their preferred labels and definitions. Where there was complete or majority agreement, the preferred label and/or definition was retained. Where there was some, little or no agreement, new labels and definitions were developed by synthesising the existing labels and definitions across classification systems. Definition wording was modified to include active verbs and to be non-directional (i.e. applicable to both the adoption of a new wanted behaviour and the removal of an unwanted behaviour).
Step 2: Delphi exercise first round
Participants were provided with the study definition of a BCT,8 that is having the following characteristics: (1) aim to change behaviour, (2) are proposed ‘active ingredients’ of interventions, (3) are the smallest components compatible with retaining the proposed active ingredients, (4) can be used alone or in combination with other BCTs, (5) are observable and replicable, (6) can have a measurable effect on a specified behaviour(s), and (7) may or may not have an established empirical evidence base. It was explained that BCTs could be delivered by someone else or self-delivered.
The BCTs (labels and definitions) from step 1 were presented in a random order and participants were asked five questions about each of them:
-
Does the definition contain what you would consider to be potentially active ingredients that could be tested empirically? Participants were asked to respond to this question using a 5-point scale (‘definitely no’, ‘probably no’, ‘not sure’, ‘probably yes’ and ‘definitely yes’).
-
Please indicate whether you are satisfied that the BCT is conceptually unique or whether you consider that it is redundant or overlapping with other BCTs. (With forced choice as to ‘whether it was conceptually unique, redundant, or overlapping’.)
-
If participants indicated that the BCT was ‘redundant’, they were asked to state why they had come to this conclusion.
-
If they indicated that the BCT was ‘overlapping’, they were asked to state: (1) with which BCT(s) and (2) whether or not they can be separated (‘yes’ or ‘no’)’.
-
If the BCTs were considered to be separate, participants were asked how the label or definition could be rephrased to reduce the amount of overlap or, if not separate, which label and which definition was better.
Participants were given an opportunity to make comments on the exercise and to detail any BCTs not included on the list. They were asked, ‘does the definition and/or label contain unnecessary characteristics and/or omitted characteristics?’ with an open-ended response format. The exercise was designed to take 2 hours, follow-up reminders were sent to participants after 2 weeks and all responses were submitted within 1 month of the initial request.
Frequencies, means and/or modes of responses to questions (1) and (2) were considered for each BCT. Based on the distribution of responses, BCTs for which (a) more than one-quarter of participants doubted that they contained active ingredients and/or (b) more than one-third considered them to be overlapping or redundant were flagged as ‘requiring further consideration’. These data, along with the responses to questions (3) to (4), guided the rewording of BCT labels and definitions, and the identification of omitted BCTs. The BCTs for reconsideration and the newly identified BCTs were presented in the second Delphi exercise round.
Step 3: Delphi exercise second round
The BCTs identified as requiring further consideration were presented. The rest of the BCTs were included for reference only, to assist judgement about distinctiveness. For each BCT, participants were asked three questions and asked to respond using a 5-point scale (‘definitely no’, ‘probably no’, ‘not sure’, ‘probably yes’ and ‘definitely yes’).
-
If you were asked to describe a BCI in terms of its component BCTs, would you think the following BCT was (a) clear, (b) precise, (c) distinct?
-
Would you feel confident in using this BCT to describe the intervention?
-
Would you feel confident that two behaviour change researchers or practitioners would agree in identifying this BCT?
If participants responded ‘probably no’, ‘definitely no’, or ‘not sure’, to any question, they were asked to state their suggestions for improvement.
Frequencies, means and/or modes were calculated for all questions for each BCT. BCTs for which more than one-quarter of participants responded ‘probably no’, ‘definitely no’ or ‘not sure’ to any question were flagged as needing to be given special attention. Using information on the distribution of ratings, the modal scores and suggestions for improvement, SM and MJ amended the wording of definitions and labels. This included changes to make BCTs more distinct from each other when this had been identified as a problem and to standardise wording across BCTs. When it was not obvious how to amend the BCT from the second round responses, other sources (e.g. Vandenbos52) were consulted for definitions of particular words or descriptions of BCTs.
Step 4: feedback from the International Advisory Board
Sixteen out of the 30 members of the IAB took part in one of three, 2-hour long teleconferences to give advice to the study team, and the BCT list was refined based on their feedback.
Step 5: feedback from study team members
The BCT definitions were checked to ensure that they contained an active verb specifying the action required to deliver the intervention. 53 The ‘lay’ member of the study team (FR, see Acknowledgments) read through the list to ensure syntactic consistency and general comprehensibility to those outside the field of behavioural science. Subsequently, the study team members made a final check of the resulting BCT labels and definitions.
Results
All data tables for this chapter are reported elsewhere, please refer to Michie et al. 40 The evolution of the taxonomy at the different steps of the procedure is summarised in Michie et al. 40
Step 1: developing the prototype classification system
Demographic information about the experts involved is summarised in Michie et al. 40 Of the 124 BCTs in the prototype classification system, 31 were removed: five composite BCTs and 26 BCTs overlapping with others, which were rated to have better definitions. One additional BCT was identified by the study team, given a label and definition and added to the system. This produced a list of 94 BCTs.
Step 2: Delphi exercise first round
The means, modes and frequencies of responses to the Delphi exercise first-round questions are shown in Michie et al. 40 On the basis of these scores, 21 BCTs were judged to be ‘satisfactory’ and 73 ‘requiring further consideration’. Of the 73 reconsidered BCTs, four were removed, four were divided and one BCT was added, giving 74 BCTs. During this process, one reason for overlap became evident: there was a hierarchical structure meaning that deleting overlapping BCTs would end up with only the superordinate BCT and a loss of specific variation (e.g. adopting the higher order BCT ‘consequences’ would have deleted ‘reward’).
Step 3: Delphi exercise second round
The means, modes and frequencies of responses to the five Delphi exercise second round questions are shown in Michie et al. 40 On the basis of these scores, 38 BCTs were judged to be ‘satisfactory’ and 32 ‘requiring further consideration’. Of the 70 BCTs reconsidered, seven labels were amended, 35 definitions were rephrased and seven BCTs were removed, giving 63 BCTs. Together with the 21 BCTs judged to be ‘satisfactory’ in the first round, there were 84 BCTs at the end of the Delphi exercise. Some further standardisation of wording across all BCTs was made by study team members (e.g. specifying ‘unwanted’ or ‘wanted’ behaviours rather than the more generic ‘target’ behaviours and ensuring that all definitions included active verbs).
Step 4: feedback from the International Advisory Board
The IAB members made two general recommendations: first, to make the taxonomy more usable by empirically grouping the BCTs and second, to consider publishing a sequence of versions of the taxonomy (with each version clearly labelled) that would achieve a balance between stability/usability and change/evolution. Feedback from members led to the addition of two and the removal of four BCTs.
Step 5: feedback from study team members
Further refinement of labels and definitions by study team members resulted in a list of 93 clearly defined, non-redundant BCTs (see Appendix 2, Table 19). The full evolution of the taxonomy across the five steps is shown in Figure 1.
FIGURE 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram to show evolution of the taxonomy: labels and definitions of BCTs modified.

Discussion
An extensive list of 93 distinct, non-redundant BCTs was developed with labels and definitions refined to capture the smallest components compatible with retaining the proposed active ingredients with the minimum of overlap: BCTTv1 (see Appendix 2, Table 19). Development comprised a series of consensus exercises involving 35 experts in delivering and/or designing BCIs. These experts were drawn from a variety of disciplines including psychology, behavioural medicine and health promotion, and from seven countries (the USA, Canada, Australia, UK, the Netherlands, Finland and Germany). Therefore, the resulting BCTs have relevance among experts from varied behavioural domains, disciplines and countries, and potential relevance to the populations from which they were drawn. Evidence is already emerging to suggest that some BCTs from BCTTv1 occur more frequently than others in descriptions of BCIs. 40 These BCTs are marked with an asterisk in Table 19 (see Appendix 2).
The extent to which BCTTv1 is applicable without adaptation across behaviours, disciplines and countries is an important question for future monitoring and research. The process of building a shareable consensus language and methodology is necessarily collaborative and will be an ongoing cumulative and iterative process, involving an international network of advisors and collaborators. 50 The balance of stability to allow accumulation of knowledge and development to incorporate significant bodies of new knowledge and experience means that classificatory systems are updated at strategic intervals. 37 Examples where this has happened are Linnaeus’s classification of plants and systems based on consensus such as the Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition54 or the International Classification of Diseases and Related Health Problems, Tenth Edition. 55
There was no prior agreed methodology for this work and there are limitations to the methods we have used. The purpose of the Delphi exercise was to develop a prototype taxonomy on which to build. It was the first in a series of exercises adapted to develop the taxonomy. Our Delphi-type methods involved 14 individuals, an appropriate number for these methods,51 but a number that makes the choice of participants important. We attempted to ensure adequate coverage of behaviour change experts. Although we had some diversity of expertise, we acknowledge the predominance of European experts from a psychological background within our sample. At various stages we made arbitrary decisions such as the cut-offs for amending BCT labels and descriptions. In the absence of agreed standards for such decisions, we were guided by the urgent need to develop an initial taxonomy that was fit for purpose and would therefore form a basis for future development. Our amendments of the BCT labels and definitions also depend on the expertise available and, therefore, we based our amendments on a wide range of inputs – the data we collected from Delphi participants and coders, expert modification, international advice and lay user improvements.
The BCTTv1 encompasses a greater number of BCTs than previous taxonomies. Therefore, it requires structure to facilitate recall and access to the BCTs, and thus increase speed and accuracy of use. A true, that is hierarchically structured, taxonomy provides the advantage of making it more coherent to, and useable by, those applying it. 37 As the number of identified BCTs has increased, so also has the need for such a structure, to improve the usability of the taxonomy.
Simple, reliable grouping structures have previously been used by three groups of authors. Dixon and Johnston33 grouped BCTs according to ‘routes to behaviour change’, ‘motivation’, ‘action’ and ‘prompts/cues’; Michie et al. 27 grouped according to ‘function’ in changing behaviour, ‘motivation’, ‘self-regulation capacity/skills’, ‘adjuvant’ and ‘interaction’; and Abraham et al. 30 grouped according to ‘change target’, that is ‘knowledge’, ‘awareness of own behaviour’, ‘attitudes’, ‘social norms’, ‘self-efficacy’, ‘intention formation’, ‘action control’, ‘behavioural maintenance’ and ‘change facilitators’. In order to achieve our aim of a structured taxonomy that is acceptable and useable over diverse disciplines and theoretical orientations, we used a basic method of grouping that does not depend on a theoretical structure. In the next study, we therefore adopted an empirical, ‘bottom-up’ method to developing a consensus of BCT groupings.
Chapter 3 Behaviour Change Technique Taxonomy version 1 with hierarchical structure (study 2)
Abstract
Objectives: To enhance understanding and use of BCTs by investigating the hierarchical structure of BCTTv1.
Methods: Participants grouped BCTs according to similarity of active ingredients in an open-sort task. This structure was examined for higher-order groupings using a dendrogram derived from hierarchical cluster analysis. This ‘bottom-up’ sort method was compared with a theory-based ‘top-down’ method in which 18 experts sorted BCTs into 14 theoretical domains in a closed-sort task. Discriminant content validity (DCV) was used to identify groupings and chi-squared tests, and Pearson’s residual values were used to examine the overlap between groupings.
Results: Participants created an average of 15.11 groupings (SD = 6.11 groupings, range 5–24 groupings). BCTs relating to ‘Reward and Punishment’ and ‘Cues and Cue Responses’ were perceived as markedly different from other BCTs. Fifty nine of the BCTs were reliably allocated to 12 of the 14 theoretical domains; 47 were significant and 12 were of borderline significance. Two domains had no BCTs significantly assigned to them. An additional grouping of ‘No Domain’ was included to represent these cases. There was a significant association between the 16 ‘bottom-up’ groupings and the 13 ‘top-down’ groupings (χ2 = 437.80; p < 0.001). Thirty-six of the 208 ‘bottom-up’ × ‘top–down’ pairings (i.e. 16 × 13) showed greater overlap than expected by chance. However, only six combinations achieved satisfactory evidence of similarity.
Conclusions: The moderate overlap between the groupings indicates some tendency to implicitly conceptualise BCTs in terms of the same theoretical domains. Understanding the nature of the overlap will aid the conceptualisation of BCTs in terms of theory and application. Further research into different methods of developing a hierarchical taxonomic structure of BCTs for international, interdisciplinary work is now required.
Introduction
Study 1 presented the synthesis of existing BCT taxonomies into a single comprehensive, cross-context, overarching BCT taxonomy: BCTTv1. 8,17,40 Previous BCTs groupings have been based on judgements made by the study author. 20,27,32,33 Given the 93 items of BCTTv1, it is necessary to group the BCTs to make the taxonomy more memorable and useable. To achieve this, we need an agreed method for identifying links between particular BCTs and theoretical constructs.
Two methods were investigated: (1) a ‘bottom-up’ linkage and (2) a ‘top-down’, theoretically guided linkage. The ‘bottom-up’ approach allows each respondent to propose linkages inductively and then identifies which linkages are common across respondents. It makes no assumptions about underlying theory and, therefore, the results should be accessible to users from diverse theoretical and disciplinary backgrounds. Nevertheless, it may reflect commonalities in theoretical approaches. The ‘top-down’ approach prompts each respondent to deduce theoretical linkages based on underlying theory. Common linkages across respondents are then identified.
Theories of behaviour change summarise what is known about the mechanisms of behaviour change and the conditions in which behaviour change is most likely to occur. 8 The importance of understanding the theoretical underpinnings of BCTs has been highlighted in previous research. 10,21,56,57 However, a recent meta-analysis found that BCIs are often not designed on a clear theoretical foundation; for example, only 22.5% of 235 implementation studies explicitly used theories of behaviour change58,59 and the majority of those doing so gave no clear explanation for why the selected theories had been used. Therefore, there is a clear need for improving methods for applying theory to intervention design to increase our understanding of how BCTs exert their influences. Grouping BCTs by theory would help guide understanding of the functional relationships between BCTs, the underlying mechanisms through which they exert their effects and the most effective ways in which BCTs can be applied.
In light of the 93 BCTs of BCTTv1 and the large number of behaviour change theories and component constructs,60 grouping by individual theoretical constructs is impractical. An alternative is to group by broader domains of theoretical constructs (e.g. knowledge, skills, etc.) as has been done in the theoretical domains framework (TDF). 45,61 The TDF is an integrative framework of theoretical constructs of behaviour change that was originally developed by 18 psychological theorists in collaboration with 16 health service researchers and 30 health psychologists. 45 It was developed to make theory more accessible to, and usable by, a range of disciplines and theoretical orientations. The first version of the TDF contains 12 theoretical domains synthesised from 128 theoretical constructs related to behaviour change; the validated version61 suggested minor modifications, with 14 domains.
The TDF has been used by research teams across many countries and health-care systems to investigate implementation problems and inform interventions to change professional practice. 62–72 The TDF was validated using two sort tasks,61 producing a refined TDF containing 87 theoretical constructs relevant to behaviour change categorised across 14 domains: knowledge, skills, social/professional role and identity, beliefs about capabilities, optimism, beliefs about consequences, reinforcement, intentions, goals, memory, attention and decision processes, environmental context and resources, social influences, and emotion and behavioural regulation. A previous study linking 35 BCTs to 11 theoretical domains from the original TDF showed good reliability across four researchers, with 71% agreement over the 385 possible links. 43 Building on this work, we aim to link BCTs from the more comprehensive BCTTv1 to the refined TDF, using a larger number of experts in behaviour change.
Study 2 aimed to:
-
investigate the hierarchical structure of the groupings of the taxonomy, which were obtained from an inductive ‘bottom-up’ method, using quantitative clustering methods
-
identify to what extent the taxonomy can be reliably grouped using a deductive, ‘top-down’ theory-based method into the 14 theory-based domains of the revised TDF
-
examine similarities and differences in the groupings that emerged using these two methods of developing a hierarchical structure.
Method
This study is also published as Cane et al. 73 Some text has been reproduced from Cane et al. 73 © 2014 The Authors. British Journal of Health Psychology published by John Wiley & Sons Ltd on behalf of the British Psychological Society. This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited.
Participants
For the ‘bottom-up’ method, participants were recruited from the pool of behaviour change experts used in study 1 (see Chapter 2) to take part in an online, open-sort grouping task. Eighteen of 19 participants approached from the pool of experts completed the task. Eight were women and 10 men, with an age range of 27–67 years (mean = 43.94 years); 16 were from the UK and two were from Australia.
For the ‘top-down’ method, 25 individuals were invited to take part in the closed-sort task. Participants were eligible to take part if they had (1) experience in designing interventions that specifically used BCTs, (2) experience in writing manuals or protocols of BCIs or (3) undertaken a narrative or systematic review of behaviour change literature. Participants were recruited via announcements through university networks and scientific societies’ mailing lists – the Society of Behavioural Medicine, the American Psychological Association Health Division and the Society for Academic Primary Care. Eighteen people (72%) met the eligibility criteria and all who were eligible consented to complete the task (Table 1 shows demographic information). There was no overlap in participants between the ‘bottom-up’ and ‘top-down’ sort tasks. The sample size for the closed-sort task was based on estimates given for content-validation exercises, with 2–24 participants being shown to be sufficient74–77 and more than five participants reducing the influence of rater outliers. 78
| Sort task | Open ‘bottom-up’ | Closed ‘top-down’ |
|---|---|---|
| Age (years) | ||
| Mean | 43.94 | 40.83 |
| SD | 13.58 | 10.47 |
| Range | 27–67 | 24–63 |
| Gender – number of participants | ||
| Women | 8 | 15 |
| Men | 10 | 3 |
| Country – number of participants | ||
| Australia | 2 | |
| Italy | 1 | |
| The Netherlands | 1 | |
| New Zealand | 1 | |
| UK | 16 | 5 |
| USA | 10 |
Procedure
Invitations included a brief overview of the study and participation consent form. Consenting participants were given detailed instructions on how to complete the task and were asked to provide demographic information (including age, sex and nationality) and to rate their expertise in behaviour change theory and in delivering BCIs on a 5-point scale (1 – ‘A great deal’, 2 – ‘quite a bit’, 3 – ‘some’, 4 – ‘a little’, 5 – ‘none’).
Open-sort task: the open-sort grouping task was delivered via an online computer program. Participants were asked to sort the list of BCTs into groupings (up to a maximum of 24) of their choice and label the groupings. Instructions guided the experts to ‘group together BCTs which have similar active ingredients i.e. by the mechanism of change, NOT the mode of delivery’. 73
Closed-sort task: participants sorted BCTs into the 14 domains specified in the revised version of the TDF:61 knowledge, skills, social/professional role and identity, beliefs about capabilities, optimism, beliefs about consequences, reinforcement, intentions, goals, memory, attention and decision processes, environmental context and resources, social influences, and emotion and behavioural regulation. The closed-sort task was delivered via a Microsoft Word document 1997–2003 (Microsoft Corporation, Redmond, WA, USA), comprising labels and definitions of the 14 theoretical domains and of the 87 BCTs from BCTTv1, which were randomly ordered. 40 The closed-sort task was conducted on an earlier version of the taxonomy containing 87 BCTs and the open-sort task an even earlier version containing 85 BCTs. Both were conducted while BCTTv1 was in development. Participants were required to indicate which domain was most relevant for each BCT and give a confidence rating for their allocation. Participants were asked to allocate each of the 87 BCTs to one or more of the 14 theoretical domain(s), giving a confidence rating for each allocation (from 1 – ‘not at all confident’ to 10 – ‘extremely confident’). After assigning all BCTs, participants were asked to review their BCT allocations and to revise any allocations if they wanted to. There was no time limit for the tasks and participants were debriefed about the study on completion.
Analysis
To analyse open-sort data, a binary dissimilarity matrix containing all possible BCT × BCT combinations was produced for each participant, for whom a score of one indicated BCTs that were not sorted into the same grouping, and a score of 0 indicated items that were sorted into the same grouping. Individual matrices were aggregated to produce a single dissimilarity matrix, which could be used to identify the optimal grouping of BCTs using cluster analysis. Using hierarchical cluster analysis, the optimal number of groupings (2–20) were examined for suitability using measures of internal validity (Dunn’s Index) and stability (figure of merit). 79 Bootstrap methods were used in conjunction with the hierarchical cluster analysis, whereby data were resampled 10,000 times, to identify which groupings were strongly supported by the data. The approximately unbiased p-values yielded by this method indicated the extent to which groupings were strongly supported by the data with higher approximately unbiased values (e.g. 95%) indicating stronger support for the grouping. 80 The words and phrases used in the labels given by participants were analysed to identify any common themes and to help identify appropriate labels for the groupings. For each grouping, labels were created based on their content and, when applicable, based on the frequency of word labels given by participants. After the labels were assigned to relevant groupings, the fully labelled groupings with the word frequency analysis were sent out to a subset of five of the original participants for refinement.
To analyse closed-sort data, mean confidence ratings for each BCT × domain pairing were calculated and analysed using DCV methods. 74,77 BCT × domain pairings that had no confidence rating from individual participants (i.e. BCT was not allocated to that domain by that participant) were scored zero and entered into the mean score for that pairing. A series of one-sample t-tests compared the mean confidence ratings for the assignment of BCTs to a value of zero. This established the extent to which BCTs were related to each domain. In cases for which no experts allocated a BCT to a specific domain (i.e. all scores for a BCT × domain pairing were zero) the BCT × domain pairings was excluded from t-test analyses.
The BCTs were considered to be reliably allocated to a domain if their mean confidence ratings were significantly greater than zero (p < 0.05) after Hochberg’s correction81 [applied using the p.adjust function in R version 3.0.1 (The R Foundation for Statistical Computing, Vienna, Austria)]. This was used to control for the family-wise error rate, given the large number of tests used, and provided a suitable criterion for inclusion and exclusion of BCTs to a particular domain, over and above the use of a subjective cut-off value. Hochberg’s correction also provides a conservative p-value that makes it less likely that a BCT × domain pairing achieving low confidence ratings across the majority of participants will achieve significance. The agreement of BCT allocation across participants was analysed using a two-way intraclass correlation coefficient (ICC) within each domain.
To identify any overlap between groupings, two types of comparisons were made between the ‘bottom-up’ groupings and the ‘top-down’ TDF derived groupings – comparison between the theoretically derived ‘top-down’ groupings and, (1) the higher order strategy groupings found in the ‘bottom-up’ sort task, and (2) the final groupings of the ‘bottom-up’ sort task. To test the possibility of overlap between groupings derived from using ‘bottom-up’ and ‘top-down’ methods, Pearson’s chi-squared test was adopted. To adjust for potential inaccuracy of the p-value estimation (resulting from the number of cells that had expected frequencies < 1), Monte Carlo simulation (using 2000 replications) was used. Pearson’s residual values [(observed – expected)/sqrt (expected)] were used to quantify the extent of overlap between individual BCTTv1 grouping × TDF domain pairings resulting from the ‘bottom-up’ and ‘top-down’ methods. Positive values indicate that the observed overlap in BCT assignment between the BCT taxonomy and TDF domain pairings is greater than expected by chance whereas negative values indicate that it is less than expected.
Results
Participants for the closed-sort task reported moderately high levels of expertise in behaviour change theory (mean = 3.17, SD = 0.71) and in delivering BCIs (mean = 2.17, SD = 1.38) as measured on 5-point scales (scores are reversed so a higher score indicates more experience). This was not significantly different from the level of expertise reported by participants in the open-sort task: behaviour change theory, mean = 3.00, SD = 0.88, t(34) = 0.64; p > 0.10; BCIs, mean = 2.42, SD = 0.96, t(34) = 0.63; p > 0.10. Although the age of participants did not differ significantly between the two sort tasks [t(34) = 0.77; p > 0.10] the number of female and male participants did [χ2(1) = 4.33; p < 0.05] as did the country of residence (χ2 = 20.76; p < 0.001) (Monte-Carlo simulation using 2000 replicates was used to compute the p-value given that a number of the expected cell values were < 1). This was an artefact of the selection process as there was no duplication of participants across the two sort tasks.
Developing a basic hierarchical structure within Behaviour Change Technique Taxonomy version 1 using an open-sort task (‘bottom-up’ method)
The BCTs were grouped using an inductive ‘bottom-up’ method based on the similarity of their active ingredients. This process yielded 16 distinct sets of BCTs, as follows (with number of BCTs in parentheses): scheduled consequences (10), reward/threat (7), repetition/replacement (7), antecedents (4), associations (8), covert learning (3), natural consequences (6), feedback and monitoring (5), goals and planning (9), social support (3), comparison of behaviour (3), self-belief (4), comparison of outcomes (3), identity (5), shaping knowledge (4) and adjunctive (4). The hierarchical structure is illustrated using a dendrogram (see Michie et al. 40). The distance between the groupings at each split is indicated by the ‘height’ on the y-axis of the dendrogram, with greater height values indicating greater distance and less similarity between the groupings, and lower height values indicating less distance and greater similarity between the groupings.
Within the reported 16-grouping open-sort solution of the taxonomy, there are six points at which groupings of BCTs split into groupings containing similar BCTs (creating seven split groupings, i.e. higher order strategy groupings). These groupings themselves contain more subtle distinct groupings as detailed in BCTTv1. The first split is at ‘split 1′ (height = 31.78), for which the body of BCTs split into two groupings, the grouping to the left containing the groupings of ‘scheduled consequences’ and ‘reward and threat’ that involve BCTs relating to the anticipation of a direct reward or punishment (e.g. social reward, negative reinforcement, extinction). The next split, ‘split 2’ (height = 14.16) reveals three groupings to the left of the remaining BCTs: ‘repetition and substitution’, ‘antecedents’ and ‘associations’ comprising BCTs relating to cues and cue responses. From split 3 onwards, the distance between the groupings is markedly smaller (height < 10), indicating that the groupings formed are less distinct from each other. At split 3 (height = 9.56) BCTs from the groupings ‘covert learning’ and ‘natural consequences’ are separated off from the remaining groupings. At split 4 (height = 7.69), the split includes the groupings ‘feedback and monitoring’, and ‘goals and planning’ and BCTs relating to goals, planning and feedback. At split 5 (height = 5.55), the split includes the groupings ‘social support’ and ‘comparison of behaviour’ and BCTs related to social factors. The final split occurs at split 6 (height = 4.18), where the groupings ‘self-belief’, ‘comparison of outcome’ and ‘identity’ (BCTs relating to the self and identity) are separated from the groupings of ‘shaping knowledge’ and ‘regulation’ (BCTs relating to knowledge and regulation).
Identifying whether or not behaviour change techniques can reliably be linked to theoretical domains using a closed-sort task (‘top-down’, theoretically driven method)
All TDF domains had BCTs allocated to them in the closed-sort task, with the number of BCTs allocated ranging from 15 for social/professional role and identity to 68 for behavioural regulation (Table 2). This allocation was reliable for 12 of the 14 domains, that is BCTs were allocated consistently with high confidence across experts, leading to p < 0.05 (see Table 2 for frequencies and see Table 4 for confidence ratings, ICC values and related p-values).
| Domain | Number of BCTs allocated | Number of BCTs allocated where p < 0.10 |
|---|---|---|
| Knowledge | 40 | 4 |
| Skills | 44 | 5 |
| Social/professional role and identity | 15 | 0 |
| Beliefs about capabilities | 46 | 2 |
| Optimism | 24 | 1 |
| Beliefs about consequences | 46 | 10 |
| Reinforcement | 45 | 17 |
| Intentions | 27 | 2 |
| Goals | 29 | 5 |
| Memory, attention and decision processes | 49 | 0 |
| Environmental context and resources | 42 | 5 |
| Social influences | 42 | 10 |
| Emotion | 44 | 4 |
| Behavioural regulation | 68 | 1 |
Within these domains, 59 (68%) of the BCTs were considered to be reliably allocated, with a further 12 (14%) BCTs having borderline statistical significance (p > 0.05 but p < 0.1) and six being allocated to multiple domains (Table 3). The domains, in order of number of BCT allocations obtaining statistical or marginal statistical significance, were (numbers of BCTs in brackets): reinforcement (17), beliefs about consequences (10), social influences (10), goals (6), environmental context and resources (6), skills (5), emotion (5), knowledge (4), beliefs about capabilities (2), intentions (2), optimism (1) and behavioural regulation (1). Two domains, ‘social/professional role and identity’ and ‘memory, attention and decision processes’ had no BCTs significantly assigned to them. This indicates that, although both of these domains had BCTs allocated to them during the sort process (15 and 49, respectively), experts did not consistently allocate or rate highly any of the BCTs to these two domains.
| Domain label and associated BCTs | Mean confidence rating | Associated probability | 95% confidence intervals | ICC (p < 0.005) | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Knowledge | |||||
| Health consequences | 6.06 | 0.001 | 3.80 | 8.32 | |
| Biofeedback | 3.78a | 0.066 | 1.66 | 5.90 | 0.15 |
| Antecedents | 3.72a | 0.051 | 1.71 | 5.74 | |
| Feedback on behaviour | 3.67a | 0.057 | 1.65 | 5.68 | |
| Skills | |||||
| Graded tasks | 4.89 | 0.014 | 2.62 | 7.16 | |
| Behavioural rehearsal/practice | 4.78 | 0.016 | 2.53 | 7.02 | 0.16 |
| Habit reversal | 4.33 | 0.018 | 2.27 | 6.40 | |
| Body changes | 4.06 | 0.020 | 2.08 | 6.03 | |
| Habit formation | 4.33a | 0.091 | 1.57 | 5.88 | |
| Social/professional role and identity | N/A | N/A | N/A | N/A | 0.07 |
| Beliefs about capabilities | |||||
| Verbal persuasion to boost self-efficacyb | 5.11 | 0.015 | 2.72 | 7.50 | 0.11 |
| Focus on past success | 4.33 | 0.040 | 2.07 | 6.60 | |
| Optimism | |||||
| Verbal persuasion to boost self-efficacyb | 3.83 | 0.049 | 1.62 | 6.05 | 0.09 |
| Beliefs about consequences | |||||
| Emotional consequencesb | 6.39 | 0.0001 | 4.48 | 8.30 | |
| Salience of consequences | 5.67 | 0.005 | 3.33 | 8.01 | |
| Covert sensitisation | 4.56 | 0.016 | 2.43 | 6.68 | |
| Anticipated regret | 4.44 | 0.018 | 2.34 | 6.55 | |
| Social and environmental consequences | 4.28 | 0.041 | 2.05 | 6.51 | 0.22 |
| Comparative imagining of future outcomes | 4.17 | 0.041 | 1.99 | 6.34 | |
| Vicarious reinforcement | 4.00a | 0.092 | 1.69 | 6.31 | |
| Threatb | 4.06 | 0.023 | 2.08 | 6.03 | |
| Pros and cons | 3.67a | 0.078 | 1.60 | 5.73 | |
| Covert conditioning | 3.50 | 0.041 | 1.68 | 5.32 | |
| Reinforcement | |||||
| Threatb | 6.78 | 0.00006 | 4.86 | 8.70 | |
| Self – reward | 5.50 | 0.006 | 3.20 | 7.80 | |
| Differential reinforcement | 5.33 | 0.014 | 2.88 | 7.79 | |
| Incentive | 5.39 | 0.008 | 3.06 | 7.72 | |
| Thinning | 5.28 | 0.008 | 2.99 | 7.56 | |
| Negative reinforcement | 5.28 | 0.008 | 3.00 | 7.56 | |
| Shaping | 5.06 | 0.017 | 2.67 | 7.44 | |
| Counter conditioning | 5.17 | 0.010 | 2.89 | 7.44 | 0.28 |
| Discrimination training | 5.06 | 0.012 | 2.77 | 7.34 | |
| Material reward | 4.89 | 0.024 | 2.48 | 7.30 | |
| Social rewardb | 4.94 | 0.015 | 2.65 | 7.24 | |
| Non-specific reward | 4.89 | 0.019 | 2.55 | 7.23 | |
| Response cost | 4.94 | 0.011 | 2.74 | 7.15 | |
| Anticipation of future rewards or removal of punishment | 4.67 | 0.022 | 2.40 | 6.94 | |
| Punishment | 4.56 | 0.025 | 2.30 | 6.81 | |
| Extinction | 4.33 | 0.018 | 2.28 | 6.39 | |
| Classical conditioning | 3.89a | 0.078 | 1.69 | 6.09 | |
| Intentions | |||||
| Commitment | 4.44 | 0.022 | 2.14 | 6.75 | 0.13 |
| Behavioural contract | 3.56a | 0.064 | 1.45 | 5.66 | |
| Goals | |||||
| Goal-setting (outcome) | 6.50 | 0.0007 | 4.13 | 8.87 | |
| Goal-setting (behaviour) | 5.50 | 0.008 | 2.98 | 8.02 | |
| Review of outcome goal(s) | 5.06 | 0.011 | 2.67 | 7.44 | 0.23 |
| Review behaviour goals | 4.28a | 0.057 | 1.82 | 6.74 | |
| Action planning (including implementation intentions) | 4.39 | 0.026 | 2.10 | 6.68 | |
| Memory, attention and decision processes | N/A | N/A | N/A | N/A | 0.22 |
| Environmental context and resources | |||||
| Restructuring the physical environment | 6.33 | 0.001 | 4.03 | 8.64 | |
| Discriminative (learned) cue | 5.33 | 0.006 | 3.06 | 7.61 | |
| Prompts/cues | 5.17 | 0.005 | 2.97 | 7.36 | 0.04 |
| Restructuring the social environmentb | 4.33 | 0.037 | 2.08 | 6.59 | |
| Avoidance/changing exposure to cues for the behaviour | 3.67a | 0.076 | 1.58 | 5.75 | |
| Social influences | |||||
| Social comparison | 6.11 | 0.001 | 3.86 | 8.36 | |
| Social support or encouragement (general) | 6.11 | 0.001 | 3.88 | 8.34 | |
| Information about others’ approval | 5.72 | 0.005 | 3.35 | 8.097 | |
| Social support (emotional)b | 5.50 | 0.004 | 3.23 | 7.77 | |
| Social support (practical) | 5.00 | 0.013 | 2.68 | 7.32 | |
| Vicarious reinforcement | 4.89 | 0.013 | 2.63 | 7.15 | |
| Restructuring the social environmentb | 4.67 | 0.013 | 2.50 | 6.84 | 0.19 |
| Modelling or demonstrating the behaviour | 4.44 | 0.014 | 2.37 | 6.52 | |
| Identification of self as role model | 4.22 | 0.040 | 2.00 | 6.44 | |
| Social rewardb | 3.89a | 0.088 | 1.63 | 6.14 | |
| Emotion | |||||
| Reduce negative emotions | 5.06 | 0.014 | 2.71 | 7.40 | |
| Emotional consequencesb | 5.11 | 0.007 | 2.90 | 7.32 | |
| Self-assessment of affective consequences | 4.78 | 0.016 | 2.52 | 7.04 | 0.03 |
| Social support (emotional)b | 3.94a | 0.061 | 1.77 | 6.12 | |
| Behavioural regulation | |||||
| Self-monitoring of behaviour | 4.50 | 0.022 | 2.39 | 6.61 | 0.32 |
Of the 24 most commonly occurring BCTs (see Michie et al. 40), 18 (75%) were reliably linked to seven of the theory domains, with a further two (8%) obtaining borderline statistical significance. These domains were (with number of BCTs in brackets): goals (5), social influences (4), environmental context and resources (3), knowledge (2), reinforcement (2), skills (1), and behavioural regulation (1). The following commonly identified BCTs were not linked to any of the theoretical domains: problem-solving, credible source, discrepancy between current behaviour, self-monitoring of outcome of behaviour, monitoring of outcome behaviour by others without feedback and pharmacological support.
Identifying overlap between the ‘bottom-up’ and ‘top-down’ groupings
The chi-squared analyses used for the grouping comparisons did not allow us to include domains in which no BCTs were assigned (i.e. not linked to domains through the DCV process); therefore, the domains of memory, attention and decision processes, and social/professional identity were excluded from these analyses. An additional grouping of ‘No domain’ was included in the ‘top-down’ groupings and represented cases for which BCTs included in BCTTv1 were not assigned to any TDF domain. Therefore, the chi-squared analysis was conducted first on 91 (7 × 13) possible pairings for the seven higher-order ‘bottom-up’ sorting strategy groupings and the 13 ‘top-down’ groupings, and second on 208 (16 × 13) possible pairings derived from the original 16 BCTTv1 ‘bottom-up’ groupings and the 13 ‘top-down’ groupings.
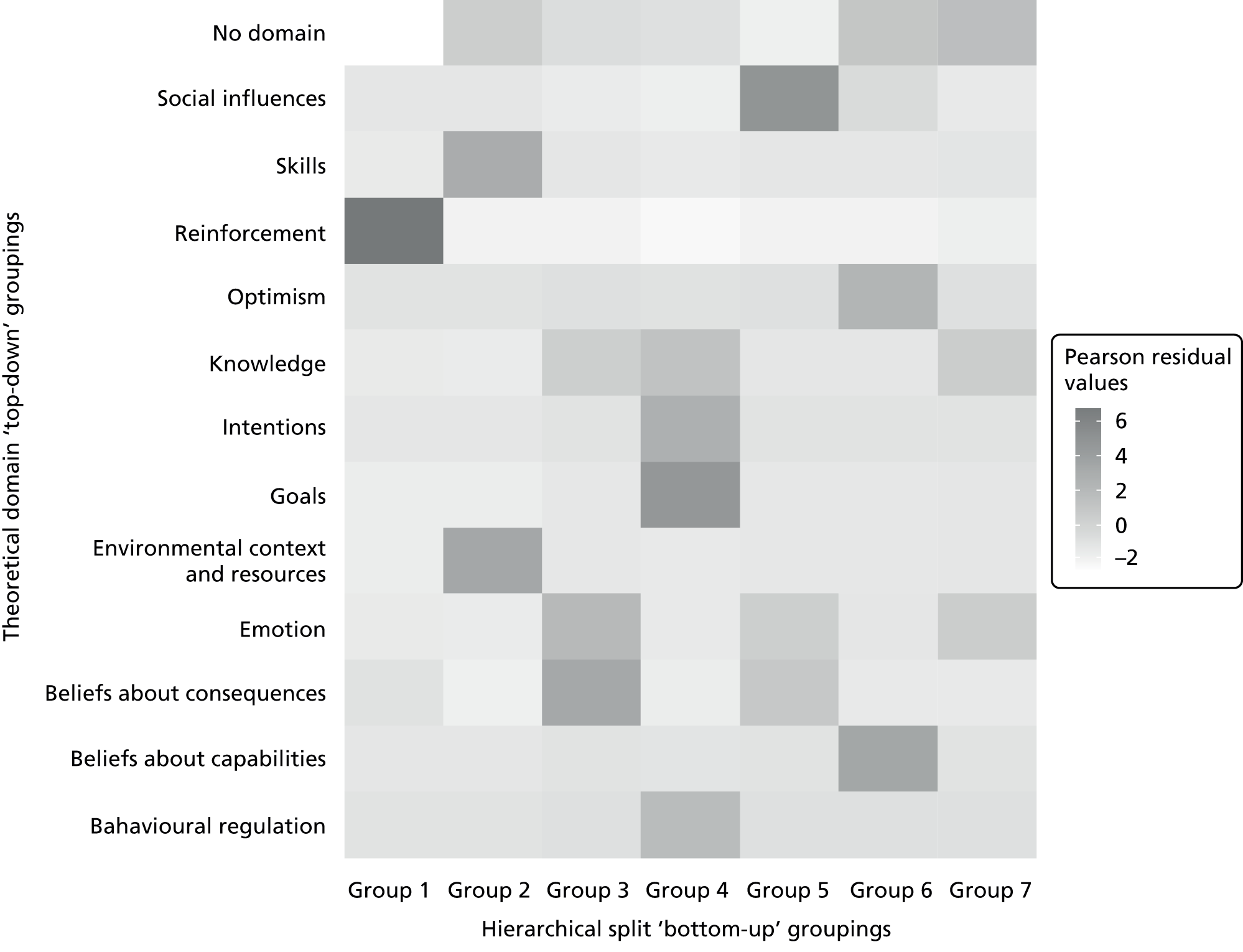
Comparison of the BCT groupings derived from the higher-order ‘bottom-up’ sorting strategies, shown in the dendrogram and the ‘top-down’ TDF derived groupings (see Table 3) revealed a significant association (χ2 = 236.13; p < 0.001). Figure 2 shows the level of overlap between each of the grouping × TDF pairings within each cell (Pearson’s residual value range –2.10 to 6.61).
FIGURE 2.
Pearson’s residual values for the association between BCT allocation to ‘top-down’ theoretical domain groupings and the ‘bottom-up’ higher-order hierarchical split groupings. Note: ‘No domain’ indicates BCTs contained within a ‘bottom-up’ higher-order grouping not assigned to any TDF domain. Reproduced from Cane et al. 73 © 2014 The Authors. British Journal of Health Psychology published by John Wiley & Sons Ltd on behalf of the British Psychological Society. This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited.

Twenty one of the 91 ‘bottom-up’ and ‘top-down’ TDF domain combinations showed a greater than expected overlap with positive Pearson’s residual values (Table 4). Only two combinations achieved Pearson’s residual values > 5, which were: ‘grouping 1′ with ‘reinforcement’ (Pearson’s residual value = 6.61) and ‘grouping 5′ with ‘social influences’ (Pearson’s residual value = 5.04).
| Taxonomy grouping | TDF domain | Pearson’s residual value |
|---|---|---|
| Repetition and substitution | Skills | 6.66 |
| Goals and planning | Goals | 6.41 |
| Covert learning | Beliefs about consequences | 5.76 |
| Self-belief | Beliefs about capabilities | 5.70 |
| Scheduled consequences | Reinforcement | 5.22 |
| Antecedents | Environmental context and resources | 5.20 |
| Comparison of behaviour | Social influences | 4.96 |
| Social support | Social influences | 4.14 |
| Reward and threat | Reinforcement | 4.10 |
| Goals and planning | Intentions | 4.05 |
| Feedback and monitoring | Behavioural regulation | 4.03 |
| Self-belief | Optimism | 4.03 |
| Feedback and monitoring | Knowledge | 3.80 |
| Comparison of outcomes | Beliefs about consequences | 3.68 |
| Natural consequences | Emotion | 3.05 |
| Associations | Environmental context and resources | 2.35 |
| Regulation | Emotion | 1.97 |
| Shaping knowledge | Knowledge | 1.97 |
| Social support | Emotion | 1.97 |
| Identity | No domain | 1.83 |
| Regulation | No domain | 1.46 |
| Shaping knowledge | No domain | 1.46 |
| Associations | No domain | 1.45 |
| Natural consequences | Knowledge | 1.25 |
| Antecedents | Social influences | 0.72 |
| Identity | Social influences | 0.72 |
| Natural consequences | Beliefs about consequences | 0.63 |
| Natural consequences | No domain | 0.46 |
| Repetition and substitution | No domain | 0.46 |
| Reward and threat | Beliefs about consequences | 0.37 |
| Feedback and monitoring | No domain | 0.27 |
| Self-belief | No domain | 0.27 |
| Reward and threat | Social influences | 0.12 |
| Comparison of outcomes | No domain | 0.01 |
There was also an association between the 16 ‘bottom-up’ groupings and the 13 ‘top-down’ groupings (χ2 = 437.80; p < 0.001). Figure 3 shows the level of overlap between structures; Pearson’s residual values range from –1.72 to 6.66. Thirty six of the 208 combinations showed greater than expected overlap, achieving positive Pearson’s residual values (see Table 4). Six combinations achieved Pearson’s residual values > 5 indicating a comparatively high level of overlap and these combinations were ‘repetition and substitution’ and ‘skills’ (Pearson’s residual value = 6.66), ‘goals and planning’ and ‘goals’ (Pearson’s residual value = 6.41), ‘covert learning’ and ‘beliefs about consequences’ (Pearson’s residual value = 5.76), ‘self-belief’ and ‘beliefs about capabilities’ (Pearson’s residual value = 5.70), ‘scheduled consequences’ and ‘reinforcement’ (Pearson’s residual value = 5.22), and ‘antecedents’ and ‘environmental context and resources’ (Pearson’s residual value = 5.20).
FIGURE 3.
Pearson’s residual values for the association between BCT allocation in ‘top-down’ theoretical domain groupings and ‘bottom-up’ groupings. Note: ‘No domain’ indicates BCTs within a ‘bottom-up’ BCTTv1 grouping not assigned to any domain. Reproduced from Cane et al. 73 © 2014 The Authors. British Journal of Health Psychology published by John Wiley & Sons Ltd on behalf of the British Psychological Society. This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited.
Discussion
Examination of the hierarchical structure of BCTTv1 uncovered a ‘higher-order’ grouping strategy taken by the behaviour change experts in the ‘bottom-up’ task and the dendrogram indicates that some groupings of BCTs within the 16-grouping solution can be considered as more clearly distinct from others. The grouping of BCTs in the ‘top-down’ sort task has helped illuminate relationships between particular BCTs and theoretical domains and could aid the selection of BCTs in the construction of theory-based interventions. There was a moderate overlap between the 16 BCT groupings derived from the ‘bottom-up’ inductive approach and the 12 groupings from the ‘top-down’ theoretically driven approach, indicating some common conceptualisation of BCTs across these two approaches. These findings may help to further our understanding of the relationships between BCTs and enable researchers to use common BCT grouping labels to discuss individual, or groupings of, BCTs in behaviour change research.
The grouping methods employed in the ‘bottom-up’ and ‘top-down’ sort tasks improve on previous attempts to group BCTs using consensus approaches. First, use of an open-sort grouping task allowed for the individual groupings of BCTs defined by participants to hold equal weight within the final solution and be aggregated using empirical techniques (hierarchical cluster analysis in the ‘bottom-up’ sort task and DCV methods in the ‘top-down’ sort task). As a result, the groupings reported here are potentially more robust than those derived using consensus methods among a few people. 43
A second advance was that a comprehensive, cross-behavioural domain taxonomy of BCTs was used rather than BCTs relevant for a single behavioural domain (e.g. road safety,82 smoking cessation,32 weight management83). Third, the BCTs were grouped according to the perceived active ingredients underlying BCTs, rather than by categorisations that may not have reflected how people think about BCTs.
In addition to providing 16 groupings, the ‘bottom-up’ open-sort task yielded systematic empirical estimates of how distinct the groupings are. Examination of this hierarchical structure revealed that BCTs related to reward and threat, and those related to cues and cue responses, were conceptualised quite distinctly from the other BCTs. The least distinct groupings (i.e. ‘social support’, ‘comparison of behaviour’, ‘self-belief’, ‘comparison of outcome’ and ‘identity’) comprised BCTs relating to social support, social comparisons, and self and identity, suggesting that there is less clarity about the BCTs within these theoretical domains. Four further groupings of BCTs (‘covert learning’ and ‘natural consequences’, and ‘feedback and monitoring’ and ‘goals and planning’) lay between these most distinct and least distinct groupings. BCTs in distinct groupings are clearly perceived to share a common mode of action in changing behaviour whereas BCTs in less distinct groupings may be viewed as having less distinct or more than one mode of action.
This difference in distinctiveness not only has implications for understanding how BCTs are conceptualised by behaviour change experts but also has implications for the practical use of BCTTv1 in behaviour change research. For example, the groupings increase the practical use of BCTs by aiding recall. Distinct sets of individual items with semantic similarity can be more easily recalled than a single list of individual items both in the short term and long term, particularly when the semantic category is cued. 84–86 This is especially useful when quick reference to BCTs is necessary, for instance when coding descriptions of interventions or in choosing BCTs to develop or report a BCI. Therefore, in those cases where the groupings are less distinct, adopting additional strategies to aid recall the groupings may be of particular advantage.
The ‘top-down’ mapping of BCTs to theoretical domains advances the limited consensus methods used by Michie et al. 43 by using an improved BCT taxonomy, an empirically validated TDF and a larger number of respondents. In this ‘top-down’ task, 59 out of 87 BCTs were reliably allocated to one or more of the TDF domains with a further 12 BCTs having borderline statistical significance. Thirty-seven BCTs were allocated to three domains that also had high confidence ratings and ICCs: ‘beliefs about consequences’, ‘reinforcement’ and ‘social influences’. This suggests that these are the theoretical domains for which there is the greatest number of agreed methods for bringing about change. Other domains also showed high agreement but had fewer associated BCTs – ‘behavioural regulation’ had only one assigned BCT but achieved good agreement, while ‘goals’ had five BCTs assigned with good agreement. In designing interventions, it may be more important to have a few agreed BCTs than to have a large choice of BCTs available to target change in a given theoretical determinant of behaviour. Further evidence is required to ensure that these ‘agreed’ BCTs do in fact achieve behaviour change by changing the proposed theoretical domain. For the two theoretical domains for which no BCTs were reliably assigned, there would appear to be no shared, or recognised, way of changing them.
Most of the commonly used BCTs were associated with a theoretical domain. Of the 24 most frequently identified BCTs in Michie et al. ,40 18 were clearly grouped into one of the 14 domains and the remaining seven BCTs were not reliably allocated to any domain even though they could be identified reliably in the intervention descriptions. This finding suggests that these BCTs may have evolved from several different behavioural domains, theoretical approaches or disciplines and, therefore, may be less associated with a particular theoretical domain.
Comparison of open and closed-sort tasks
Six of the open-sort tasks groupings, ‘repetition and substitution, ‘goals and planning’, ‘covert learning’, ‘self-belief’, ‘scheduled consequences’ and ‘antecedents’, showed a high level of overlap with the BCTs assigned to the equivalent TDF domains, suggesting that experts may have sorted BCTs by theoretical constructs or domains (implicitly or explicitly) across both tasks. This is supported by the fact that both groups of experts reported high levels of expertise in relation to behaviour change theory. For the higher-order groupings created by the top-down task, there were only two similarly strong overlaps with the BCTs allocated to the equivalent TDF domains indicating that the relationship between higher-order sorting strategies and theoretically derived groupings is not strong. It would appear that the lower-level groupings are more in line with the TDF domains than the empirically higher-order groupings, suggesting that the higher-level grouping shared by respondents does not align as well with the theoretical domains. It may be that the higher-order groupings of BCTs depended on considerations other than theory, for example target populations or behaviours.
The next step for this line of research is to evaluate the extent to which these groupings facilitate the usability of the taxonomy, and to do this for larger sample sizes and a greater disciplinary and geographical spread. It may be that different groupings may be useful for different tasks (e.g. identifying BCTs in reports of interventions vs. designing interventions) and/or be beneficial to different users in different contexts. It may be that for those applying BCTs to designing or specifying interventions without reference to theory, the open-sort groupings may be of more benefit as all of the BCTs were grouped. On the other hand, the closed-sort grouping of BCTs is likely to be more useful for those who are seeking a theoretical base for coding and designing interventions. Further work will be necessary to investigate the replicability and utility of these groupings, as well as their theoretical basis. As more evidence is gained from the application of BCTTv1, it may be that the BCT groupings will be modified to incorporate links between BCTs that are commonly used together in research practice and/or to reflect the ‘common mechanisms of action.’
The hierarchical structure and grouping of BCTs within the taxonomy has practical use in that it is predicted to increase the speed by which BCTs can be recalled by users. It also has theoretical interest in that links between BCTs and theory can be used to inform the design and evaluation of BCIs. Although BCTTv1 represents an advance in methods for specifying BCIs, reliable and valid application of BCTTv1 will require skills and, therefore, training. To investigate how best to train the skills of using BCTTv1, two programmes of user training were developed (face-to-face workshops and distance group tutorials). The next study reports the development and evaluation of these training programmes.
Phase 2: evaluation
Chapter 4 Training to code intervention descriptions using Behaviour Change Technique Taxonomy version 1 (study 3)
Abstract
Objectives: To evaluate two programmes of user training in improving reliable, valid and confident application of BCTTv1 to code BCTs in descriptions of BCIs.
Methods: 161 trainees (109 in face-to-face workshops and 52 in distance group tutorials) were trained to code frequently occurring BCTs. Training was evaluated by comparing three measures before and after training: (1) intercoder agreement, (2) trainee agreement with expert consensus and (3) confidence ratings. Coding was assessed for 12 BCTs in workshops and for 17 BCTs in tutorials. Trainees also completed a course evaluation.
Results: Workshop and tutorial training improved trainee agreement with expert consensus [workshops: mean prevalence- and bias-adjusted kappa (PABAK) before training = 0.39, after training = 0.50; tutorials: mean PABAK score = 0.57, after training = 0.72; both p < 0.05] but not intercoder agreement (p = 0.08 and p = 0.57, respectively) and increased confidence ratings for BCTs assessed in workshops (mean number of assessed BCTs, identified with high confidence before training = 8.38, after training = 9.56; p < 0.001). Training was evaluated positively by trainees; all components of both types of training were highly rated in terms of usefulness.
Conclusions: Both methods of training improved trainee agreement with expert consensus and confidence for BCTs assessed, but neither method improved intercoder agreement. This varied according to BCT.
Introduction
In order to enhance understanding and use of BCTs in BCIs, we have improved the quality of their labels and definitions, and developed a hierarchical structure of BCTTv1. 73 However, it is not only the content and form of the taxonomy that drives reliable and valid application of BCT labels/definitions but also the extent to which the user has been trained to use the taxonomy. Identifying (coding) BCTs involves a deductive process of categorising qualitative information (e.g. descriptions of interventions) using an established coding framework and instructions. The process of coding BCTs is a highly skilled task requiring familiarity with the BCT labels and definitions and one which requires coders to make a series of complex interpretative judgements. 87,88 Achievement of good intercoder reliability (i.e. the extent to which coders agree on the presence/absence of BCTs identified in intervention descriptions using the taxonomy as a coding framework) is therefore not only a function of the clarity of the taxonomy and its coding guidelines, but also of the competence of its coders.
Intercoder reliability has been demonstrated in using BCT taxonomies among coders with varying amounts of training and experience. 20,23,28–30,48 Training in taxonomies, when reported, has generally involved manual-based coding instructions, prompting of practice and one-to-one feedback from those familiar with using the taxonomy. Delivery and intensity of training has varied, with some coders receiving one-to-one feedback from experienced BCT coders whereas others have trained themselves using coding manuals. Systematic documentation of the training process and evaluation, involving the comparison of coding competence to apply BCT taxonomies with reliability and validity before and after training, will establish whether or not training can enhance coding competence.
One of the goals of training in the use of the taxonomy is to teach coders to recognise BCTs as defined by the taxonomy rather than relying on their own subjective judgements that are triggered by the BCT label. 89,90 Another goal of training is to enhance the ‘validity’ of coder judgements, that is the extent to which coders agree with expert BCT coders as to the presence or absence of BCTs. Expert coding, assessed here as a consensus between expert coders, is the nearest we have to an objective standard of ‘validity’. An effective training programme is therefore one that not only enhances intercoder agreement between trainees but also enhances agreement with expert consensus about BCTs identified.
The research literature suggests that collaborative or co-operative training strategies (i.e. working together in small groups towards a common goal) and active learning techniques such as discussion are more effective than traditional, lecture-style training for acquiring new knowledge, building skills and increasing motivation to continue to improve skills. 91 An effective training programme is built on four basic principles: (1) setting training goals involving provision of information or concepts to be learned, (2) demonstration of knowledge and skills to be learned, (3) practice or rehearsal of skills learned and (4) provision of feedback to trainees during and after practice. 92,93 Skills are more likely to be retained and improve future practice if trainees feel challenged, receive positive feedback and find the learning process interesting and enjoyable. 93,94 This evidence and these principles clearly reflect the relevance and use of BCTs such as feedback on behaviour, goal-setting, social support and behavioural practice/rehearsal directed at changing skilled behaviours. Coder training incorporating these principles and BCTs has previously been evaluated in applying the taxonomy to specify BCT content in written intervention descriptions of behavioural support in smoking cessation, and training in this context was a 3-hour workshop delivered to a mixture of research psychologists and non-psychologist practitioners. 95 This study found that training improved trainees’ coding competence (i.e. their agreement with expert consensus about which BCTs are present).
Developing user training for applying Behaviour Change Technique Taxonomy version 1
The increasing use of the BCT approach, in particular for specifying interventions in evidence synthesis, has prompted high demand for training in the reliable and valid application of BCTTv1. In response to this, training programmes have been developed building on previous BCT coder training conducted by the study team and integrating the principles drawn from the literature. 92–95 These training programmes are evaluated in this chapter. They were designed to train coders to identify the most frequently occurring BCTs from BCTTv1, that is those that were found to occur most frequently in intervention descriptions. The decision was made to train coders in the most frequently occurring BCTs as training in 93 BCTs was not feasible within the proposed training intensity and duration, and because frequently occurring BCTs would be more accessible to trainees as well as more useful for them to learn. Two methods of training were developed: workshops, which involved face-to-face group training for 1 day, and distance tutorials, which were usually delivered by telephone to groups of two to four people in four, 1-hour sessions held over 1–2 months. The latter allowed training of coders across the world. Two substudies evaluated these training programmes and addressed the following research questions (RQs):
Does face-to-face training (1-day workshops) and distance training (group tutorials) improve the specification of BCIs by BCT as assessed by increased:
-
Intercoder agreement about BCTs identified?
-
Agreement with BCTs identified by expert consensus?
-
Confidence ratings for BCTs identified as present?
-
Do trainees evaluate BCTTv1 training as a useful experience?
-
What proportion of trainees reach an acceptable standard of competence following training?
One-day workshops
Method
This study is also published as Wood et al. 96 Some of the text in this section is reproduced from Wood et al. 96 © The Author(s) 2014. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Design
Coding competence was assessed before and after each workshop by assessment tasks and evaluation of usefulness was assessed at the end of the training in a confidential questionnaire. To overcome potential practice effects, the assessments were administered in a counterbalanced design, so that a random 50% of trainees completed assessment task A at the beginning and B at the end, and the other half completed B followed by A.
Participants
Workshops were offered to those interested in investigating, reviewing, designing or delivering behavioural interventions, and no previous knowledge or experience was required. They were advertised via scientific and professional organisations and the BCT Taxonomy Project website. 97 Coders who had been involved in the development of BCTTv1 or in the sort tasks to determine hierarchical structure were not eligible for this training. Five workshops were conducted with groups of between 9 and 29 trainees (n = 109). A total of 64.9% were from the UK, 21.6% from other European countries, 7.2% from the USA, 4.5% from Asia, 0.9% from Australia and 0.9% from South Africa. A total of 35% of trainees had obtained a research or clinical doctorate and 11% identified themselves as active practitioners in their field. Trainees ranged in age from 21 years to 59 years (mean = 32.31 years, SD = 9.27 years) and 95% of trainees were female (Table 5).
| Workshops n = 109 | Tutorials n = 52 | ||
|---|---|---|---|
| Age, years [mean (SD)] | 32.31 (9.27) | 37.04 (7.82) | |
| Gender | Female | 103 | 35 |
| Male | 6 | 17 | |
| Professiona | Practitioner | 12 | 7 |
| Student | 57 | 3 | |
| Academic | 40 | 40 | |
| Highest qualification | BA/BSc | 23 | – |
| MA/MSc | 46 | 10 | |
| PhD | 35 | 33 | |
| Clinical | 4 | 9 | |
| Nationality | UK | 72 | 38 |
| European (non-UK) | 22 | 8 | |
| America | 8 | 4 | |
| Asia | 5 | – | |
| Australia | 1 | 1 | |
| South Africa | 1 | – | |
| Previous experience of taxonomy use, n (%) | Coding | 26 (24) | 28 (54) |
| Describing BCIs | 35 (32) | 36 (69) | |
| Expertise associated with BCIs [mean (SD)]b | Designing | 2.38 (1.10) | 3.60 (1.00) |
| Delivering | 2.46 (1.22) | 3.19 (1.04) | |
| Reporting | 2.45 (1.16) | 3.51 (0.87) | |
| Reviewing | 2.46 (1.13) | 3.45 (1.08) | |
| Using behaviour change theories | 3.30 (0.90) | 3.70 (0.77) |
Materials
Coding manuals of previous taxonomies20,95 were used to inform the development of the workshop training programme. Training involved trainees watching three short Microsoft PowerPoint® 1997–2003 (Microsoft Corporation, Redmond, WA, USA) presentations and participating in a series of interactive coding tasks as a group, individually and in pairs. Workshop tasks were delivered according to a number of different formats, for example via a ‘ready, steady, point!’ task in which trainees were shown a short excerpt on the presentation screen and, when prompted, were asked to point to the left if BCT X was present, to the right if BCT Y was present, or to the ceiling if they were unsure (Table 6). Content was structured around a series of learning objectives (e.g. ‘to learn the need for precise labels and definitions’ and ‘to learn appropriate levels of inference and discrimination’). The training was designed using BCTs associated with key learning principles and with changing skilled behaviour (e.g. graded tasks, behavioural practice/rehearsal, instruction on how to perform the behaviour, feedback on behaviour; for a full list of BCTs used, see Table 6).
| Content | Brief description | Learning objectives | BCTs used | |
|---|---|---|---|---|
| Presentation | Background to BCTs | Outlines the goals for the day, defines and conceptualises the term ‘BCT’ and communicates need for agreed standard list of BCTs in behavioural medicine |
|
|
| Assessment | Using the taxonomy | Trainees work individually to identify presence/absence of 12 BCTs in an intervention description |
|
|
| Task | Ready, Steady, Point! | Trainees shown a short excerpt on screen and, when prompted, asked to point left BCT1, right for BCT2 or to the ceiling if unsure |
|
|
| Morning break | ||||
| Presentation | Identifying behaviours and BCTs | Defines behaviour and the distinction between behaviour and behaviour outcome |
|
|
| Task | Identifying behaviours and BCTs | Trainees work in pairs to highlight exact words showing behaviour and BCT in two short excerpts |
|
|
| Task | Identifying BCTs in reports | BCTs 7–12 cards are placed around the room. Trainees shown five excerpts taken from real interventions; for reports one and two, trainees asked when prompted, to point at the correct BCT card. For reports three to five, trainees asked to identify presence of BCTs 7–12 |
|
|
| Task | Providing examples of BCTs | Trainees work in groups of four to generate their own examples of BCTs 7–12 and then feed back to the rest of the group |
|
|
| Lunch break | ||||
| Task | Role play | Expert tutors act out two role plays with six of BCTs 13–24 in each. Trainees asked to identify presence of BCTs |
|
|
| Task | Coding published descriptions | Trainees work in pairs to identify presence of BCTs 1–24 in two longer excerpts |
|
|
| Afternoon break | ||||
| Presentation | Moving from a list to a taxonomy | Introduces the idea of a hierarchical structure and outlines how it was developed |
|
|
| Assessment | Using the taxonomy | Trainees work individually to identify presence/absence of 12 BCTs in an intervention description |
|
|
Trainees were taught 24 of the frequently identified BCTs from BCTTv1. Furthermore, the early part of the workshop focused on simple coding tasks working up to more difficult tasks in an attempt to approach ‘errorless learning’ as this has been shown to be effective in learning new terms. 98 Each workshop was delivered by two experienced BCT coders (BCTTv1 project team members).
Measures
Prior experience
Trainees were asked if they had previously (1) designed or reported BCIs that specifically identified BCTs, (2) been involved in writing manuals or protocols of interventions, and (3) undertaken a narrative or systematic review of behaviour change literature. They also rated their expertise (i.e. knowledge, skills and familiarity) in the areas of designing, writing, reporting and systematic reviewing of BCIs using response options from 1 (‘no experience’) to 5 (‘a great deal of experience’).
Evaluating training effectiveness in increasing coding competence: coding competence for 12 frequently occurring BCTs (see Table 8) was assessed before and after training. Trainees were asked to identify the presence/absence of BCTs in descriptions of two BCIs that targeted physical activity and safe needle cleaning behaviour, respectively. They were asked to rate how confident they were that the BCT was present using +/++; whereby ‘+’ represented ‘BCT present in all probability but evidence not clear’ and ‘++’, ‘BCT present beyond all reasonable doubt; clear evidence available’. The descriptions were written (by CA and MR; see Acknowledgements) to exemplify particular BCTs, to highlight the learning principles and to ensure inclusion of the frequent BCTs targeted for training.
To assess trainees’ agreement with expert consensus, six experienced BCTTv1 coders who had been involved in developing BCTTv1 (study team members: MJ, SM, JF, WH, CA, MR), working in pairs, independently coded the descriptions using BCTTv1. Expert consensus was developed by discussion of any discrepancies within each of the pairs. If a resolution was not obvious, SM and the study researcher (MR) reviewed the remaining discrepancies and proposed a coding. The list of BCT codes resulting from this process was circulated to the whole study team who agreed the final codes. We used this consensus about the presence of BCTs in the descriptions as a criterion against which trained coder codings were judged and validity was assessed. The coders reached consensus about the presence of 12 BCTs in the descriptions: self-monitoring of behaviour, feedback on behaviour, behavioural practice/rehearsal, non-specific reward, goal-setting (outcome), material reward (behaviour), credible source, problem-solving, demonstration of the behaviour, information about health consequences, goal-setting (behaviour) and social support (unspecified).
Training effectiveness was evaluated by changes in intercoder agreement, in trainee agreement with expert consensus, in the proportion of high (i.e. ++) confidence ratings for the 12 BCTs assessed and in the proportion of trainees reaches an acceptable standard of competence. Effectiveness was assessed for 12 frequently observed BCTs. This task was considered an appropriate ‘challenge’ for trainees and one that was in line with the length and intensity of training undertaken. Agreement was assessed using PABAK99 (see Analysis). An acceptable standard of competence was defined in terms of trainee agreement with expert consensus (see Analysis for rationale).
Evaluating trainee experience of training: trainees rated the usefulness of each of the presentations, individual and group tasks in helping them to build skill and knowledge, using response options from 1, ‘not useful’ to 5 ‘useful’. All trainees were also asked to respond to four open-ended questions: (1) what part(s) of the training did you find the most useful?; (2) what part(s) or aspect(s) of the training, if any, did you find least useful?; (3) would you like future training? If so, do you have a specific proposal?; and (4) please provide any other feedback about using BCT taxonomies.
Procedure
Prior to attending the workshop, all trainees were sent two articles as preparatory reading. 17,100 At the start of the workshop, they were asked to complete a questionnaire with demographic information (age, sex, nationality, professional background and highest qualification). All trainees completed an assessment of their coding competence before and after training. They also completed a training evaluation questionnaire. They received a BCTTv1 training certificate at the end of the workshop and individual feedback on their coding competence via e-mail.
Distance group tutorials
Method
Design
Training was conducted over four, 1-hour sessions. Training was held over an average period of 6 weeks with a minimum of 1 week between sessions. Each group was led by an experienced BCT tutor and for 9 of the 10 groups took place via teleconference call. The 10 tutors included members of the BCTTv1 study team who had been involved in development of BCTTv1 (SM, MJ, JF, WH and MR) and five experts in behaviour change recruited via the BCTTv1 Project website. 97 The five experts had all been involved on at least one occasion as part of their own research and practice, in designing and reporting BCIs specifically identifying BCTs, in writing manuals or protocols of interventions, or had undertaken narrative or systematic reviews of published behaviour change studies. Trainees’ coding competence was assessed before and after training by assessment tasks and evaluation of usefulness was assessed after training in a confidential questionnaire.
Participants
Tutorial training was advertised as for workshops. BCTTv1 study team members were also asked to identify potential trainees from their own teams and networks. Those interested in taking part were asked to complete a self-evaluation form. Trainees (n = 52) were invited to join if they indicated that they had some previous experience in investigating, designing and/or delivering BCIs and were available over the training period. Those who had been involved in study 1 and/or 2 were not eligible for this training. Trainees were contacted via e-mail and offered an honorarium of £560 on completion of a coding task for research purposes (see Chapter 5) (estimated to take 2 days) following the group tutorial training programme. A total of 71% were from the UK, 15% from other European countries, 8% from the USA and 6% from Australia. A total of 81% had obtained a research or clinical doctorate and 13% identified themselves as active practitioners in their field. Trainees ranged in age from 24 years to 60 years (mean = 37.04 years, SD = 7.82 years) and 67% of the sample were female (see Table 5).
Previous experience: 24% (n = 26) of trainees had previously used a BCT taxonomy to code BCIs and 32% (n = 35) to describe BCIs. Trainees reported a low-to-moderate level of expertise associated with BCIs (mean = 2.62, SD = 0.86), with significant variation between workshops.
Materials
Training was structured around the same learning objectives as workshops (Table 7) with the manual adapted for the format and covering a more extensive range of 44 BCTs from BCTTv1. Training was piloted in a face-to-face format with one group of trainees and these data were included in the analyses as few changes were made. All other tutorial groups were conducted via teleconference call.
| Tutorial session | Learning principle | Learning objectives |
|---|---|---|
| 1 | Only code BCTs that are directly applied to the target behaviour(s) and population(s) |
|
| 2 | Do not infer the presence of a BCT. The description must correspond to the definition of the BCT given in the taxonomy. If you are unsure, DO NOT code the BCT as present |
|
| 3 | Take care distinguishing between BCTs that only differ in terms of their behaviour change type (i.e. behaviour vs. outcome) |
|
| 4 | Code technical terms and packages of BCTs that map onto BCTs in the taxonomy |
|
Tutorials were held over an average period of 6 weeks with a minimum of 1 week between each session. Each tutorial group had four trainees who were paired into two sets of ‘buddies’. The purpose of the buddy system was to provide trainees with both practical and emotional social support throughout the training and to foster independent problem-solving. Before each tutorial session, trainees independently completed and submitted a preparatory coding task (comprising one, two or three short exercises) before discussing it with their ‘buddy’. Each pair was asked to discuss their homework in advance, identifying key issues to discuss at the tutorial session in their ‘learning log’ to maximise the usefulness of the session and increase time for discussion and reflection. Discrepancies in coding between the trainees and BCTs agreed on as present by expert consensus were identified by the expert tutor and discussed during the session.
Measures
Evaluating training effectiveness in increasing competence: trainees were asked to identify the presence or absence of BCTs in intervention descriptions before and after training. Two descriptions were used (one for the before-training assessment and one for the after-training assessment), with the target behaviour for both descriptions being increasing physical activity. As for the workshops, descriptions were written by CA and MR to exemplify specific BCTs to highlight the learning principles and to ensure inclusion of the frequent BCTs targeted in training. Expert consensus was reached about the presence of 17 BCTs in each of the two descriptions (see Table 9): feedback on behaviour, credible source, information about health consequences, information about social and environmental consequences, social support (unspecified), monitoring of outcome(s) of behaviour without feedback, non-specific reward, demonstration of the behaviour, adding objects to the environment, goal-setting (behaviour), problem-solving, self-monitoring of outcome of the behaviour, goal-setting (outcome), behavioural practice/rehearsal, self-monitoring of behaviour, instruction on how to perform the behaviour and material reward (behaviour).
Trainees were provided with a training taxonomy (a shortened version of BCTTv1 comprising 44 BCTs) and coded the presence/absence of BCTs in the descriptions, rating their confidence in each BCT identification using the same +/++ ratings as for workshops.
Training effectiveness was evaluated by changes in intercoder agreement, in agreement with expert consensus and in the proportion of high (i.e. ++) confidence ratings for the 17 BCTs assessed. As additional evaluators, tutorial trainees completed measures of perceived confidence and reported intentions to use a taxonomy to code reports and describe BCIs, using response options ranging from 1 (‘strongly disagree’) to 5 (‘strongly agree’), before and after training. An acceptable standard of competence was defined in terms of trainee agreement with expert consensus (see Analysis).
Evaluating trainee experience of training: using the same response options as for 1-day workshops, trainees rated perceived usefulness of the reading materials provided prior to the first tutorial session, the materials provided for sessions 1 to 4, the content and the structure of the sessions and the preparatory coding tasks completed prior to each session, the buddy system and the learning log. They completed the same open-ended evaluation items as for workshops.
Procedure
Prior to their first tutorial session, trainees were sent the same preparatory reading and completed the same measures as for workshops. Tutorial trainees were also asked to read a short, introductory PowerPoint presentation on the advantages and challenges associated with the use of the BCT approach in specifying the content of BCIs. All trainees completed the coding competence assessment (see Measures) before training. After the final session, trainees completed the after-training coding competence assessment and a training evaluation questionnaire. Trainees received individual feedback on coding competence, generic feedback on the common coding discrepancies encountered within their coding groups across the four sessions and a BCTTv1 training certificate via e-mail.
Analysis
For both workshops and tutorials, the following analyses were conducted.
Intercoder agreement about BCTs identified was assessed by using the PABAK; see Byrt et al. 99 PABAK was used rather than Cohen’s kappa statistic101 or percentage agreement because it adjusts for (1) coders sharing bias in the use of categories and (2) high prevalence of negative agreement (i.e. when both coders agree the BCT is absent). Trainees were randomly allocated into coding pairs across tutorial groups using a random number generator. When both trainees identified the BCT as present or absent, agreement was recorded and when one trainee identified the BCT but the other did not identify the BCT, disagreement was recorded. The PABAK score was calculated for each trainee pairing and means reported across pairs and for each of the BCTs assessed.
Trainee agreement with expert consensus was assessed by calculating the number of BCTs identified by each trainee that were also identified by expert consensus and by using PABAK. Each trainee was paired with the expert consensus. The number of agreements and disagreements between trainees and expert consensus were recorded and were used to calculate the PABAK score. Means were reported across trainee–expert consensus pairings and for each of the BCTs assessed. When a trainee identified the BCT identified as present by expert consensus, agreement was recorded and when the trainee did not identify the BCT, or identified a BCT not included in the consensus, disagreement was recorded.
Confidence for BCTs identified was assessed by calculating the frequency and percentage of high confidence ratings (i.e. ‘++’: BCT present beyond all reasonable doubt and clear evidence available) for BCTs identified as present. High confidence ratings were included in the analysis so that we could easily distinguish BCTs identified with certainty.
Change following training: paired sample t-tests were used to assess change in (1) agreement between trainees about BCTs identified (intercoder PABAK), calculated across trainee pairings and across BCTs; (2) the number of BCTs identified by trainees also agreed on as present by expert consensus; (3) trainee agreement with expert consensus (trainee consensus PABAK) across trainee consensus pairings (i.e. each trainee paired with the expert consensus) and across the BCTs assessed; (4) high confidence ratings (i.e. ‘++’) for BCTs identified as present; (5) perceived confidence; and (6) reported intention to use BCT taxonomies in the future.
Previous experience: frequencies and percentages were calculated to describe the number and proportion of trainees with previous experience of BCT taxonomy use. Means and SDs were calculated to describe trainees’ expertise associated with BCIs (separate means were calculated for each of designing, delivering, reporting, reviewing experience and for use of behaviour change theories; an overall mean was calculated across these categories).
Evaluation of training: trainee ratings of the content of the training and ratings of the materials used were summarised using means and SDs. A content analysis of the written feedback was conducted to identify training components that participants reported to work well or not well. Given the novelty of this type and format of coder training, we decided that content analysis provided an appropriate first step for investigating patterns within coders’ initial feedback. CW conducted the first round of analysis, allocating coder feedback into categories based on similarity of content. KS (see Acknowledgments) then checked allocation of coder feedback to content categories. Any discrepancies were resolved through discussion between the two researchers.
Proportion of trainees reaching an acceptable standard of competence following training: an acceptable standard of competence was defined in terms of trainee agreement with expert consensus. Landis and Koch102 suggested that kappa values of 0.60–0.79 indicate ‘substantial’ reliability and those > 0.80 are ‘outstanding’. Thus, we used this as a guide and considered trainees achieving a PABAK score of at least 0.60 to have reached an acceptable standard of competence. To assess change in competence from before to after training, a one-way analysis of variance (ANOVA) was carried out. To evaluate the two training methods in increasing competence, a 2 (before vs. after training) × 2 (workshop vs. distance tutorial) ANOVA was carried out.
Results
Evaluating effect of training in increasing trainee competence
One-day workshops (Tables 5 and 8)
| BCT number and label (BCTs ordered according to mean PABAK intercoder agreement between trainees, after training) | Before training | After training | ||||||
|---|---|---|---|---|---|---|---|---|
| n trainees identifying BCT (max. = 109) | Mean PABAK agreement between trainees | Mean PABAK trainee agreement with expert consensus | % trainee identifications with high confidence ratings (i.e. ++) | n trainees identifying BCT (max. = 109) | Mean PABAK agreement between trainees | Mean PABAK trainee agreement with expert consensus | % trainee identifications with high confidence ratings (i.e. ++) | |
| 2.3. Self-monitoring of behaviour | 49 | 0.49 | –0.10 | 22 | 101 | 0.96 | 0.85 | 88 |
| 2.2. Feedback on behaviour | 56 | 0.49 | 0.03 | 57 | 93 | 0.93 | 0.71 | 92 |
| 8.1. Behavioural practice/rehearsal | 81 | 0.42 | 0.49 | 80 | 98 | 0.70 | 0.80 | 90 |
| 10.3. Non-specific reward | 74 | 0.48 | 0.36 | 86 | 75 | 0.56 | 0.38 | 88 |
| 1.3. Goal-setting (outcome) | 60 | 0.64 | 0.22 | 89 | 84 | 0.56 | 0.54 | 87 |
| 10.2. Material reward (behaviour) | 104 | 0.56 | 0.91 | 85 | 105 | 0.48 | 0.93 | 88 |
| 9.1. Credible source | 68 | 0.20 | 0.25 | 57 | 75 | 0.44 | 0.38 | 87 |
| 1.2. Problem-solving | 82 | 0.45 | 0.50 | 89 | 71 | 0.33 | 0.30 | 89 |
| 6.1. Demonstration of the behaviour | 76 | 0.27 | 0.39 | 89 | 100 | 0.30 | 0.83 | 93 |
| 5.1. Information about health consequences | 86 | 0.67 | 0.58 | 91 | 77 | 0.19 | 0.41 | 87 |
| 1.1. Goal-setting (behaviour) | 86 | 0.93 | 0.58 | 89 | 62 | 0.19 | 0.14 | 78 |
| 3.1. Social support (unspecified) | 89 | 0.78 | 0.63 | 86 | 47 | –0.11 | –0.13 | 94 |
Intercoder agreement between trainees: there was a trend for intercoder agreement to increase across trainees, t(54) = 1.77; p = 0.08 (before training: mean PABAK = 0.39, SD = 0.34); after training: mean PABAK = 0.50, SD = 0.26). Intercoder agreement increased for 6 out of the 12 BCTs assessed: self-monitoring of behaviour, feedback on behaviour, behavioural practice/rehearsal, non-specific reward, credible source and demonstration of the behaviour (average increase in PABAK for these six BCTs = 0.26, SD = 0.18; range = 0.03–0.47). However, change across the 12 BCTs was non-significant, t(11) = 0.90; p = 0.39. The BCT ‘material reward’ achieved good reliability before training and this was also achieved after training.
Agreement with expert consensus: overall, trainee agreement with expert consensus increased, t(108) = 3.26; p < 0.0001 (before training: mean PABAK = 0.39, SD = 0.29; after training: mean PABAK = 0.50, SD = 0.28). Across the BCTs assessed, agreement with expert consensus increased for 8 out of the 12 BCTs: self-monitoring of behaviour, feedback on behaviour, behavioural practice/rehearsal, non-specific reward, goal-setting (outcome), material reward (behaviour), credible source and demonstration of the behaviour (average increase in PABAK for these eight BCTs = 0.36, SD = 0.33; range = 0.02–0.95). However, change across the 12 BCTs was non-significant, t(11) = 0.56; p = 0.59.
Confidence for BCTs identified: the number of high confidence ratings (i.e. ‘++’) that trainees assigned increased, t(108) = 4.89; p < 0.001 (before training: mean number of BCTs = 8.38, SD = 1.91; after training: mean number of BCTs = 9.56, SD = 1.93). Across BCTs assessed, the number of high confidence ratings also increased, t(11) = 2.89; p < 0.05. The number of high confidence ratings increased for 6 out of the 12 BCTs: self-monitoring of behaviour, feedback on behaviour, behavioural practice/rehearsal, material reward, credible source and demonstration of the behaviour. Before training, one of the BCTs, ‘information about health consequences’ was rated with high confidence by over 90% of trainees. After training, four of the BCTs – ‘demonstration of the behaviour’, ‘material reward (behaviour)’, ‘behavioural practice/rehearsal’ and ‘self-monitoring of behaviour’ – were rated with high confidence by 90% or more of trainees.
Distance group tutorials (Tables 5 and 9)
| BCT number and label (ordered according to mean PABAK intercoder agreement between trainees, post-training) | Before training | After training | ||||||
|---|---|---|---|---|---|---|---|---|
| n trainees identifying BCT (max. = 52) | Mean PABAK intercoder agreement between trainees | Mean PABAK trainee agreement with expert consensus | % trainee identifications with high confidence ratings (i.e. ++) | n trainees identifying BCT (max. = 52) | Mean PABAK intercoder agreement between trainees | Mean PABAK trainee agreement with expert consensus | % trainee identifications with high confidence ratings (i.e. ++) | |
| 10.2. Material reward (behaviour) | 47 | 0.62 | 0.81 | 85 | 49 | 0.77 | 0.88 | 82 |
| 4.1. Instruction on how to perform behaviour | 19 | 0.00 | –0.27 | 63 | 44 | 0.69 | 0.69 | 82 |
| 2.3. Self-monitoring of behaviour | 47 | 0.62 | 0.81 | 91 | 48 | 0.69 | 0.85 | 92 |
| 8.1. Behavioural practice/rehearsal | 16 | 0.08 | –0.38 | 63 | 47 | 0.62 | 0.81 | 66 |
| 2.4. Self-monitoring of outcome(s) of the behaviour | 45 | 0.46 | 0.73 | 86 | 45 | 0.46 | 0.73 | 91 |
| 1.3. Goal-setting (outcome) | 42 | 0.38 | 0.62 | 88 | 45 | 0.46 | 0.73 | 91 |
| 1.2. Problem-solving | 49 | 0.77 | 0.88 | 78 | 42 | 0.38 | 0.62 | 71 |
| 1.1. Goal-setting (behaviour) | 49 | 0.77 | 0.88 | 76 | 40 | 0.38 | 0.54 | 78 |
| 12.5. Adding objects to the environment | 6 | 0.54 | –0.77 | 33 | 36 | 0.38 | 0.38 | 72 |
| 6.1. Demonstration of the behaviour | 27 | –0.31 | 0.04 | 78 | 40 | 0.38 | 0.54 | 83 |
| 10.3. Non-specific reward | 11 | 0.46 | –0.58 | 27 | 10 | 0.38 | –0.62 | 50 |
| 2.5. Monitoring of outcome(s) of behaviour without feedback | 37 | 0.31 | 0.42 | 51 | 41 | 0.31 | 0.58 | 71 |
| 3.1. Social support (unspecified) | 10 | 0.54 | –0.62 | 50 | 43 | 0.31 | 0.65 | 72 |
| 5.3. Information about social and environmental consequences | 4 | 0.85 | –0.85 | 25 | 30 | 0.23 | 0.15 | 60 |
| 5.1. Information about health consequences | 50 | 0.85 | 0.92 | 84 | 41 | 0.15 | 0.58 | 83 |
| 9.1. Credible source | 28 | –0.38 | 0.08 | 43 | 39 | 0.15 | 0.50 | 90 |
| 2.2. Feedback on behaviour | 27 | –0.31 | 0.04 | 74 | 19 | 0.00 | –0.27 | 58 |
Previous experience: 54% (n = 28) of trainees had previously used a BCT taxonomy to code BCIs and 69% (n = 36) to describe BCIs. The majority of tutorial trainees had a moderate level of expertise in BCIs (mean = 3.50, SD = 0.71).
Intercoder agreement between trainees: intercoder agreement across trainees did not change, t(25) =0 .57; p = 0.57. Across the BCTs assessed, intercoder agreement increased for 8 out of the 17 BCTs: feedback on behaviour, credible source, demonstration of the behaviour, goal-setting (outcome), behavioural practice/rehearsal, self-monitoring of behaviour, instruction on how to perform behaviour and material reward (behaviour) (average increase in PABAK for these eight BCTs = 0.38, SD = 0.26; range = 0.08–0.69). However, change across the 17 BCTs was non-significant, t(16) = 0.28; p = 0.78. As for workshops, the BCT ‘material reward’ achieved good reliability before training and this was also achieved after training. Two further BCTs – ‘self-monitoring of behaviour’ and ‘self-monitoring of outcome(s) of behaviour’ – achieved good reliability before and after training.
Agreement with expert consensus: trainee agreement with expert consensus increased, t(51) = 6.60; p < 0.001 (before training: mean PABAK = 0.57, SD = 0.11; after training: mean PABAK = 0.72, SD = 0.14). Across the BCTs assessed, trainee agreement with expert consensus also increased, t(16) = 2.35; p < 0.05. Agreement with expert consensus increased for 11 of the 17 BCTs: credible source, information about social and environmental consequences, social support (unspecified), monitoring of outcome(s) of behaviour without feedback, demonstration of the behaviour, adding objects to the environment, goal-setting (outcome), behavioural practice/rehearsal, self-monitoring of behaviour, instruction on how to perform the behaviour and material reward (behaviour) (average increase in PABAK for these 11 BCTs = 0.62, SD = 0.50; range = 0.04–1.27).
Confidence for BCTs identified: the number of high confidence ratings (i.e. ‘++’) that trainees assigned did not change, t(51) = –0.57; p = 0.57. Across the 17 BCTs assessed, the number of high confidence ratings increased, t(16) = –3.40; p < 0.001. Ratings increased for 13 out of the 17 BCTs: credible source, information about social and environmental consequences, social support (unspecified), monitoring of outcome(s) of behaviour without feedback, non-specific reward, demonstration of the behaviour, adding objects to the environment, goal-setting (behaviour), self-monitoring of outcome(s) of the behaviour, goal-setting (outcome), behavioural practice/rehearsal, self-monitoring of behaviour and instruction on how to perform the behaviour. Before training, one of the BCTs – ‘self-monitoring of behaviour’ – was rated with high confidence by over 90% of trainees. After training, four BCTs were rated with high confidence by over 90% of trainees: self-monitoring of outcome(s) of behaviour, self-monitoring of behaviour, goal-setting (outcome) and credible source.
There was an increase in self-reported confidence in using the taxonomy from before training: mean = 3.42, SD = 1.00 to after training: mean = 4.08, SD = 0.56, t(51) = –5.27; p < 0.001. Reported intention to use BCT taxonomies in the future remained high from before training: mean = 4.23, SD = 0.74 to after training: mean = 4.16, SD = 1.02; t(51) = 0.44; p = 0.66.
Proportion of trainees reaching acceptable standard of competence
Before training, 22% of workshop trainees and 35% of tutorial trainees achieved a PABAK score (in terms of agreement with expert consensus) of ≥ 0.60 (workshops: mean PABAK = 0.39, SD = 0.29; tutorials: mean PABAK = 0.57, SD = 0.11). After training, the proportion of trainees reaching this threshold increased across both methods: 46% of workshop trainees and 78% of tutorial trainees achieved a PABAK score of ≥ 0.60 therefore meeting the acceptable standard of competence (workshops: mean PABAK = 0.50, SD = 0.28; tutorials: mean PABAK = 0.72, SD = 0.14). Change from before to after training competence was significant for workshops, F(1,216) = 9.66; p < 0.05, and for tutorials, F(1,102) = 38.38; p < 0.001. Training methods were equally effective at increasing competence, F(1,318) = 0.35; p = 0.55.
Evaluating coder experience
Training was evaluated positively by trainees with all components receiving high ratings (on the scale of 1–5) in terms of usefulness (workshops: mean = 4.62, SD = 0.68; range = 3–5; tutorials: mean = 4.30, SD = 0.67; range 4–5). Trainees rated activities that used the taxonomy to code short excerpts and longer descriptions from published reports as being useful opportunities to apply their newly learned skills. In particular, trainees valued the combination of ‘working through practical examples’ alongside the ‘opportunity to clarify and discuss’ any coding they found unclear. A few trainees commented on the ‘Ready, steady, point!’ exercises as being a useful method to increase their ability to identify BCTs at speed.
Tutorial trainees reported that the combination of practical tasks and the opportunity for structured discussion during the tutorial sessions was particularly useful. Many of the trainees commented that the tutorials provided a useful opportunity to learn ‘the consensus answers and the rationale behind coding’ for specific BCTs and then ‘discuss any reasons for discrepancies with other members of the group’. The majority commented that having access to a wide range and number of excerpts taken from published reports provided a useful opportunity to practice applying the taxonomy. Although the majority agreed that the ‘Learning Log’ and ‘Buddy system’ components were both useful in principle, feedback suggested that trainees generally wanted more guidance on how to use them. Trainees commented that they occasionally found them difficult to put into practice owing to time constraints. This was particularly an issue for trainees from different time zones.
Discussion
Training in using BCTTv1 in the form of 1-day workshops or group tutorials held over 6 weeks increased average trainee agreement with expert consensus and doubled the proportion achieving the competence threshold to 46% and 78% respectively. Training also increased workshop trainees’ confidence in identifying BCTs assessed in descriptions of BCIs, but did not improve intercoder agreement for either method. The opportunity to apply new knowledge and skills in a number of coding tasks followed by group discussion was evaluated as being a useful approach by trainees.
The difference between training methods in the proportion of those achieving an acceptable standard of coding competence may be partly due to differences in the percentage showing competence before training. Workshops required less commitment and may have attracted participants with less involvement and less competence in BCT coding. The fact that tutorial training allows consolidation of learning and practice between sessions may account for the higher proportion of competent coders following training. This is the model that has been taken forward in developing an e-learning programme of training (see Chapter 7 and BCTTv1. Online Training103).
We identified BCTs for which training was effective, that is when agreement and intercoder agreement were poor before training but good after training; for example, behavioural practice/rehearsal. There was only one frequently used BCT that achieved good reliability without training for workshops and tutorials: material reward (behaviour). Two other BCTs achieved good reliability without training for tutorial trainees: self-monitoring of behaviour and self-monitoring of outcome(s) of behaviour. Overall, training achieved good validity and reliability for between one-quarter and one-third of the BCTs.
Some BCTs consistently achieved poor reliability before and/or after training, for example goal-setting (outcome), social support (unspecified), and information about social and environmental consequences. These BCTs may require further definition and/or refinement of labels and examples for trained coders to be able to identify them with high reliability and validity. For example, drawing on feedback from trainees, refinements could include further clarification of the distinction between BCTs with similar labels that also appear in the same taxonomy grouping [e.g. social support (unspecified) and social support (practical)] or addition of more examples to help coders distinguish between different ‘types’ of BCTs [i.e. ‘behaviour’ vs. ‘outcome’ BCTs such as goal-setting (behaviour) and goal-setting (outcome)]. It is therefore likely that the number of BCTs that can be effectively trained will increase as BCTTv1 develops.
Training increased confidence in identifying BCTs assessed for both training methods and significantly so among workshop trainees. Tutorial trainees also reported increased overall confidence in using the taxonomy. This may be due to the learning environment provided by tutorials which includes a support network built over the period of multiple and regular sessions, and more time for reflection and practice between sessions. In the current study, we did not compare differences in the efficacy of training across the tutorial groups. While guided by a training manual, it is feasible that the engagement style and delivery of support, guidance and feedback differed across expert tutors despite having a similar level of experience to one another. Confidence in applying BCTTv1 requires learning the complexities and challenges of applying it, which may decrease or increase confidence in the short term. Therefore, future research should examine how this changes with training, further experience and across different modes of training delivery.
Although a direct comparison of the two BCTTv1 training methods was not the focus of study 3, some reflections are possible about the comparative merits, acceptability and feasibility of each approach. Workshops may be considered the more cost-effective and time-effective option given that a relatively large group of coders can be trained over the course of a day. They may also be more accessible to participants who simply wish to learn about the approach but with less commitment to becoming expert BCT coders.
Compared with workshop trainees, tutorial trainees started with a greater level of experience and expertise in using BCT taxonomies. It may be that training involves a process of trainees changing their existing interpretations of a BCT as understood from their discipline’s perspective. Greater pre-existing experience may have meant that ‘unlearning’ needed to take place before competence could be reached. This could help to explain why some BCTs achieved poor reliability and validity before and/or after training. Small group tutorial training delivered over a longer period of time provides a learning environment which includes a support network built over the period of multiple and regular sessions and more time for reflection and practice between sessions. Having access to an interactive training resource that provides continued support and feedback beyond that of time spent with the tutorial group would provide the additional space and time that this level of learning requires. Such a resource has been developed and is described in more detail in Chapter 7.
It is important to remember that effect of training was evaluated on trainee coding of just one intervention description before and after training for each of the methods. The training materials used in 1-day workshops and tutorials were written to exemplify particular BCTs, to highlight the learning principles and to ensure inclusion of the frequent BCTs targeted for training. However, the quality of published intervention descriptions is generally poor,95 with techniques described using different terminology and referred to using different labelling. 104,105 As the use of BCT methodology increases, BCT content as reported in intervention descriptions is likely to become much clearer, leading to increased ease of identifying BCTs. 95 It is also important to acknowledge that, despite attempts to ensure diversity of trainees, our sample were predominantly female and from the UK. As the use of BCT methodology becomes more widely used, it will be possible to recruit a broader range of trainees for training evaluation.
For users to maintain good levels of accuracy and reliability after training, efforts should be made to maintain knowledge and skills over time. 106 Therefore, we recommend that coders already trained in use of BCTTv1 regularly review training materials and check their reliability and accuracy.
Chapter 5 Reliability of identification of behaviour change techniques in interventions using Behaviour Change Technique Taxonomy version 1 (study 4)
Abstract
Objectives: To assess frequency and reliability (intercoder and test–retest) of identifying BCTs in written intervention descriptions.
Methods: 40 coders were trained to identify BCTs defined in BCTTv1. Coders identified BCTs in 40 intervention descriptions published in protocols and repeated this task 1 month later. A consensus of judgements reached by coders who were experienced in coding BCTs (and also developed BCTTv1) were compared with those of trained coders and used as the index of current validity.
Results: 80 out of 93 (86%) defined BCTs were identified by at least one trained coder and 22 (28%) of these were identified in 16 or more of 40 descriptions. Good intercoder reliability was observed across 80 BCTs identified in the protocols; 64 (80%) achieved mean PABAK scores of ≥ 0.70 and 59 (74%) achieved mean scores of ≥ 0.80. There was good test–retest reliability; good within-coder agreement was observed between baseline and 1 month. For the 32 coders providing data at both time points, mean PABAK scores for the two occasions ranged from 0.84 to 0.99. Good concurrent validity for 15 BCTs was agreed to be present by the experienced coders and mean PABAK score of ≥ 0.70 was achieved for 14 out of the 15 BCTs.
Conclusions: BCTTv1 can be used by trained coders to identify BCTs in intervention descriptions reliably (both in terms of agreement with each other and over time) and validly (assessed by agreement with experienced coder consensus). Some BCT definitions require further clarification.
Introduction
Results from two initial phases of reliability testing indicated BCTTv1 to be reliable in specifying 26 frequently occurring BCTs when used by the taxonomy developers. 40 These findings helped to identify BCT labels and definitions requiring refinement. It also suggested that user training may be required as high reliability is not only dependent on the content of the taxonomy but also on the extent that the user is skilled in using it. Since this initial assessment of reliability, the taxonomy has been developed further and we have developed a user-training programme for BCTTv1 delivered through face-to-face workshops, distance group tutorials and more recently via an online training programme (see Chapter 4). Study 4 reports a detailed assessment of reliability of use of the taxonomy also reported in Abraham et al. 107 It investigates concurrent validity of BCTTv1 and evaluates the use of BCTTv1 by newly trained users (primary researchers, systematic reviewers and practitioners) in specifying BCTs across a wide range of complex BCIs.
Since Abraham and Michie’s20 initial paper, intercoder reliability has been demonstrated for various subsequent BCT taxonomies. 20,23,27,28,30,48 One indication of intercoder reliability is the percentage of BCTs for which there is agreement between coders that a BCT is present or absent. Abraham and Michie20 reported > 93% agreement between three pairs of coders (including the authors). As agreement scores tend to be inflated by the number of occasions on which neither coder reports the BCT to be present, Cohen’s kappa scores were calculated excluding BCTs agreed to be absent. Across 78 reliability tests (of identification of 26 defined BCTs and BCT clusters across 195 published intervention descriptions) the average kappa per technique was 0.79 with only three BCTs yielding kappa scores of < 0.70. Landis and Koch102 have suggested that kappa scores of 0.60–0.79 can be described as ‘substantial’ and that scores of ≥ 0.80 can be described as ‘outstanding’ but, conventionally, 0.70 is taken to indicative of acceptable intercoder reliability. Thus, these findings demonstrated that BCTs can be reliably identified in published descriptions. Similar methods were applied to BCTTv1.
Initial assessment of BCTTv1 used six experienced coders on the BCTTv1 study team and calculated kappa (PABAK, for full description see Analysis) when there were at least five identifications of a BCT in the 65 coded intervention descriptions. 40 We set the criteria of ‘at least five identifications’ because the more frequent the BCTs, the greater the confidence that PABAK is a useful indicator of reliability of judging the BCT to be present. Of the 26 BCTTv1 BCTs meeting this criterion, nine were found to have ‘outstanding’ and 14 ‘substantial’ reliabilities. Although these are good kappa results, they raise several questions. First, would equally good reliability be obtained by newly trained coders who have not been involved in the development of the taxonomy? The extensive discussions involved in taxonomy development described by Michie et al. 40 might result in enhanced agreement owing to tacit knowledge beyond the explicit BCT labels and definitions. therefore, it is important to examine the extent to which the BCT taxonomy enables newly trained coders (i.e. coders who have not been involved in the development of BCTTv1) to reach agreement about the content of interventions.
Second, are these levels of agreement good enough to enable replicable implementation of intervention content? Most researchers would probably accept that BCTs definitions generating kappa scores of 0.70 can be reliably identified but may have reservations about those with lower scores. 108 Although these reliability statistics indicate levels of agreement, they do not quantify the degree of error that might be incurred when scientists try to replicate interventions from their descriptions. When two practitioners read a report of an effective intervention with kappa agreement of 0.80, which is ‘outstanding’, how different might their implementation of the intervention be? For example, in coding 40 BCTs, it would be possible for each of two coders to identify two BCTs but for each to have identified different BCTs, or for one coder to identify and implement five BCTs while the other identified and implemented nine (i.e. a further four BCTs), would result in quite different interventions.
Third, it is possible to assess reliability of coding of specific BCTs, or of an intervention description as a whole. So, for example, if an intervention contained some BCTs that were reliably coded and some that were not, replication of the intervention might fail owing to the omission of poorly recognised BCTs. There might also be failure to replicate if the intervention description was badly written, either by omitting aspects of the intervention or by lack of clarity in the description. Improved coding systems cannot facilitate detection of a BCT if the description omits to mention that it was included in the intervention; Lorencatto et al. 12 found that published descriptions reported, on average, less than half the BCTs that were included in the longer protocol descriptions. BCTTv1 might enable authors to report fuller, clearer descriptions of their evaluated interventions. 17 On the other hand, when the description is simply unclear, BCTTv1 should enable agreement between coders as it clearly specifies that coders should not infer the presence of a BCT from vague descriptions. It is therefore important to assess not only the reliability of coding of each BCT, but also to investigate whether or not intervention descriptions are satisfactorily coded.
Fourth, it is quite possible for two coders to reach good agreement but be wrong, that is it is reliable but not valid. While reliability of use of BCT taxonomies has typically been evaluated, it is also important to assess the ‘validity’ of these judgements. Poor reliability or a good level of reliability between newly trained coders but without agreement with expert consensus would both be unsatisfactory outcomes. High reliability with poor validity might occur for a variety of reasons such as misleading pre-coding discussion or a misleading cue in the intervention description. Estimates of validity require a criterion against which the codes are judged, but in the case of intervention descriptions such a criterion does not exist.
Abraham and Michie20 assessed reliability between the two coders who developed the 26 BCT definitions (the authors) and also between the first author and two other coders trained to use the taxonomy. Findings showed no significant difference between reliability scores indicating that trained coders could identify BCTs as reliably as coders involved in defining BCTs. In order to assess concurrent validity of BCTTv1, we compared trained coders’ identification of BCTs with BCTs judged to be present in descriptions by a consensus of experienced coders. This consensus took as its starting point the independent coding by pairs from a pool of six taxonomy developers who were experienced in identifying BCTs in intervention descriptions. This resulted in the reliability data for 15 BCT definitions reported in both Michie et al. 40 (see Table 3) and Abraham et al. 107 It was then further developed by discussion of any discrepancies by each of the pairs. Further discrepancies were identified during BCT training of new coders. If a resolution was not obvious, SM and the study researcher (CW) reviewed the remaining discrepancies and proposed a coding. The list of BCT codes resulting from this process was circulated to the group of six researchers and each agreed the final codes. In the absence of any better criterion for valid codes, consensus regarding the presence for these 15 BCTs was used as a criterion by which to judge the validity of trained coders’ judgements across the same 40 intervention descriptions.
Fifth, BCT identifications rated with low confidence by coders could indicate problems with specific BCTs or ambiguity of specific intervention descriptions, which might prevent achievement of good intercoder reliability and accurate replication. However, our analyses have shown that reliability of BCT identification was not positively correlated with coder confidence and indeed tended to be negatively correlated. 109 Therefore, it is important to ascertain, if possible, whether or not codes made with high confidence are also reliable and valid ratings.
Finally, various authors have proposed different methods of assessing kappa that adjust for its limitations. Byrt et al. 99 proposed the ‘PABAK’, which results in considerably more meaningful indices for data such as BCT coding when the prevalence of each BCT is low and bias may occur; therefore, it was the statistic chosen by Michie et al. 40 as the most appropriate to measure intercoder reliability in applying BCTTv1. Gwet et al. 110 suggest that further adjustment should be made for chance agreement that might occur when two coders make random ratings and make allowance for this in the alternative chance – corrected statistic to kappa (AC1) statistic110 (see equations 7 and 8 in Gwet et al. 110 and equation 4.1 in Gwet et al. 111). We compare reliability results generated by applying the PABAK and AC1 formulae.
The aims of study 4 were:
-
To assess the reliability (intercoder and test–retest) and validity of labels and definitions in BCTTv1 when used by newly trained coders to specify BCTs across a range of intervention descriptions.
-
To assess whether or not confidence in codes relates to validity of codes.
-
To identify labels and definitions in BCTTv1 requiring further refinement.
First, we investigated how many of the 93 BCTs were used by participants to describe the interventions coded in order to ascertain whether or not BCTTv1 contained too many BCTs.
-
How often are particular behaviour change techniques identified in intervention descriptions?
We then addressed the following RQs.
Replicability of coding
-
To what extent do trained coders agree on BCTs indentified in intervention description; how good is intercoder reliability? And does their change over a 1-month period?
-
Does intercoder reliability vary across different intervention descriptions?
-
How good is test–retest reliability? Do coders identify the same BCTs at baseline as they do 1 month later?
-
Are meaningfully different patterns of reliability data generated by different indices of intercoder reliability?
Concurrent validity of coding
-
What is the extent of agreement between trained coders and a consensus reached by experienced coders about whether or not BCTs are present? Is this stable over a 1-month period?
Confidence of coding
-
How confident are trained coders in identifying BCTs from intervention descriptions and is this stable over a 1-month period?
-
How does confidence in identification relate to observed intercoder reliability?
-
How does trained coders’ confidence of BCT identification relate to trained coders’ agreement with experienced coders’ consensus about which BCTs are present?
Feedback on using Behaviour Change Technique Taxonomy version 1
-
Are there any BCT labels and definitions that trained coders judge to be in need of refinement and/or clarification? How do such judgements relate to observed intercoder reliability?
Method
This study is also published as Abraham et al. 107
Materials
Forty descriptions of BCIs were used to test reliability of identification of BCT labels and definitions. Protocols selected were from those published in three interdisciplinary journals that publish BCI protocols related to health improvement between 2009 and 2010 namely, BioMed Central (BMC) Public Health (n = 24), Implementation Science (n = 11) and BMC Health Services Research (n = 5). The 40 descriptions included interventions designed to promote or change behaviours to prevent illness (n = 13), behaviours to improve illness management (n = 13) and behaviours of health-care professionals (n = 14). Quota sampling ensured that protocols were selected from each of these three broad categories.
A coding task booklet (consisting of the 40 intervention descriptions and task instructions) was developed and sent to each coder. Coders used BCTTv140 to identify the absence/presence of BCTs in the intervention descriptions. For a list of the 40 protocols from which intervention descriptions were extracted, Table 10; for the coding booklet, see Appendix 2, Table 20.
| Year of publication | Authors and title | Journal |
|---|---|---|
| 2010 | Murphy S, Raisanen L, Moore G, Edwards RT, Linck P, Williams N, et al. A pragmatic randomised controlled trial of the Welsh National Exercise Referral Scheme: protocol for trial and integrated economic and process evaluation | BMC Public Health 112 |
| 2010 | Ahmad A, Hugtenburg J, Welschen LM, Dekker JM, Nijpels G. Effect of medication review and cognitive behaviour treatment by community pharmacists of patients discharged from the hospital on drug related problems and compliance: design of a randomized controlled trial | BMC Public Health 113 |
| 2010 | Ivers NM, Tu K, Francis J, Barnsley J, Shah B, Upshur R, et al. Feedback GAP: study protocol for a cluster-randomized trial of goal setting and action plans to increase the effectiveness of audit and feedback interventions in primary care | Implementation Science 114 |
| 2010a | Skouteris H, McCabe M, Swinburn B, Hill B. Healthy eating and obesity prevention for preschoolers: a randomised controlled trial | BMC Public Health 115 |
| 2010 | Castelnuovo G, Manzoni GM, Cuzziol P, Cesa GL, Tuzzi C, Villa V, et al. TECNOB: study design of a randomized controlled trial of a multidisciplinary telecare intervention for obese patients with type-2 diabetes | BMC Public Health 116 |
| 2010 | Wyers CE, Breedveld-Peters JJ, Reijven PL, van Helden S, Guldemond NA, Severens JL, et al. Efficacy and cost-effectiveness of nutritional intervention in elderly after hip fracture: design of a randomized controlled trial | BMC Public Health 117 |
| 2010 | Mckenzie JE, O’Connor DA, Page MJ, Mortimer DJ, French SD, Walker BE, et al. Improving the care for older people with acute low-back pain by allied health professionals (the ALIGN trial). a cluster randomised trial protocol | Implementation Science 71 |
| 2010 | Wyse RJ, Wolfenden L, Campbell E, Brennan L, Campbell KJ, Fletcher A, et al. A cluster randomised trial of a telephone-based intervention for parents to increase fruit and vegetable consumption in their 3- to 5-year-old children: study protocol | BMC Public Health 118 |
| 2010 | Sanfelix-Genoves J, Peiro S, Sanfelix-Gimeno G, Hurtado I, Pascual de la Torre M, Trillo-Mata JL, et al. Impact of a multifaceted intervention to improve the clinical management of osteoporosis. The ESOSVAL-F study | BMC Health Services Research 119 |
| 2010 | Siddiqi K, Khan A, Ahmad M, Shafiq-ur R. An intervention to stop smoking among patients suspected of TB--evaluation of an integrated approach | BMC Health 120 |
| 2010 | Mc Namara KP, George J, O’Reilly SL, Jackson SL, Peterson GM, Howarth H, et al. Engaging community pharmacists in the primary prevention of cardiovascular disease: protocol for the Pharmacist Assessment of Adherence, Risk and Treatment in Cardiovascular Disease (PAART CVD) pilot study | BMC Health Services Research 121 |
| 2010 | Spijkers W, Jansen DE, de Meer G, Reijneveld SA. Effectiveness of a parenting programme in a public health setting: a randomised controlled trial of the positive parenting programme (Triple P) level 3 versus care as usual provided by the preventive child healthcare (PCH) | BMC Public Health 122 |
| 2010 | McNamara R, Robling M, Hood K, Bennert K, Channon S, Cohen D, et al. Development and Evaluation of a Psychosocial Intervention for Children and Teenagers Experiencing Diabetes (DEPICTED): a protocol for a cluster randomised controlled trial of the effectiveness of a communication skills training programme for healthcare professionals working with young people with type 1 diabetes | BMC Health Services Research 123 |
| 2010 | Colagiuri S, Vita P, Cardona-Morrell M, Singh MF, Farrell L, Milat A, et al. The Sydney Diabetes Prevention Program: a community-based translational study | BMC Public Health 124 |
| 2010 | McAlister FA, Majumdar SR, Padwal RS, Fradette M, Thompson A, Tsuyuki R, et al. The preventing recurrent vascular events and neurological worsening through intensive organized case-management (PREVENTION) trial protocol [clinicaltrials.gov identifier: NCT00931788] | Implementation Science 125 |
| 2010 | Lau R, Stewart K, McNamara KP, Jackson SL, Hughes JD, Peterson GM, et al. Evaluation of a community pharmacy-based intervention for improving patient adherence to antihypertensives: a randomised controlled trial | BMC Health Services Research 126 |
| 2010 | Rost KM, Marshall D. Marketing depression care management to employers: design of a randomized controlled trial | Implementation Science 127 |
| 2010 | Garner BR, Godley SH, Dennis ML, Godley MD, Shepard DS. The Reinforcing Therapist Performance (RTP) experiment: study protocol for a cluster randomized trial | Implementation Science 128 |
| 2010 | Johnston V, Walker N, Thomas DP, Glover M, Chang AB, Bullen C, et al. The study protocol for a randomized controlled trial of a family-centred tobacco control program about environmental tobacco smoke (ETS) to reduce respiratory illness in Indigenous infants | BMC Public Health 129 |
| 2010 | Taylor RW, Brown D, Dawson AM, Haszard J, Cox A, Rose EA, et al. Motivational interviewing for screening and feedback and encouraging lifestyle changes to reduce relative weight in 4–8 year old children: design of the MInT study. Geimer N, Olson CE, Baumgarten D, Kepner JL, Mahoney MC. Use of a liquid nicotine delivery product to promote smoking cessation | BMC Public Health 130 |
| 2010 | Gonseth S, Abarca M, Madrid C, Cornuz J. A pilot study combining individual-based smoking cessation counseling, pharmacotherapy, and dental hygiene intervention | BMC Public Health 132 |
| 2010 | Geimer N, Olson CE, Baugarten D, Kepner JL, Mahoney MC. Use of a liquid delivery product to promote smoking cessation | BMC Public Health 131 |
| 2010 | Mann E, Kellar I, Sutton S, Kinmonth AL, Hankins M, Griffin S, et al. Impact of informed-choice invitations on diabetes screening knowledge, attitude and intentions: an analogue study | BMC Public Health 133 |
| 2010a | Menza TW, Jameson DR, Hughes JP, Colfax GN, Shoptaw S, Golden MR. Contingency management to reduce methamphetamine use and sexual risk among men who have sex with men: a randomized controlled trial | BMC Public Health 134 |
| 2010a | Rosenkranz RR, Behrens TK, Dzewaltowski DA. A group-randomized controlled trial for health promotion in Girl Scouts: healthier troops in a SNAP (Scouting Nutrition & Activity Program) | BMC Public Health 135 |
| 2010a | Werkman A, Hulshof PJ, Stafleu A, Kremers SP, Kok FJ, Schouten EG, et al. Effect of an individually tailored one-year energy balance programme on body weight, body composition and lifestyle in recent retirees: a cluster randomised controlled trial | BMC Public Health 136 |
| 2009 | Buis LR, Poulton TA, Holleman RG, Sen A, Resnick PJ, Goodrich DE, et al. Evaluating Active U: an internet-mediated physical activity program | BMC Public Health 137 |
| 2010 | Bull FC, Milton KE. A process evaluation of a ‘physical activity pathway’ in the primary care setting | BMC Public Health 138 |
| 2010 | Claesson IM, Josefsson A, Sydsjo G. Prevalence of anxiety and depressive symptoms among obese pregnant and postpartum women: an intervention study | BMC Public Health 139 |
| 2010 | Storrø O, Oien T, Dotterud CK, Jenssen JA, Johnsen R. A primary health-care intervention on pre- and postnatal risk factor behavior to prevent childhood allergy. The Prevention of Allergy among Children in Trondheim (PACT) study | BMC Public Health 140 |
| 2010 | Ramos M, Ripoll J, Estrades T, Socias I, Fe A, Duro R, et al. Effectiveness of intensive group and individual interventions for smoking cessation in primary health care settings: a randomized trial | BMC Public Health 141 |
| 2010 | Leon N, Naidoo P, Mathews C, Lewin S, Lombard C. The impact of provider-initiated (opt-out) HIV testing and counseling of patients with sexually transmitted infection in Cape Town, South Africa: a controlled trial | Implementation Science 142 |
| 2010 | Pilling SA, Williams MB, Brackett RH, Gourley R, Weg MW, Christensen AJ, et al. Part I, patient perspective: activating patients to engage their providers in the use of evidence-based medicine: a qualitative evaluation of the VA Project to Implement Diuretics (VAPID) | Implementation Science 143 |
| 2010 | Bilardi JE, Fairley CK, Temple-Smith MJ, Pirotta MV, McNamee KM, Bourke S, et al. Incentive payments to general practitioners aimed at increasing opportunistic testing of young women for chlamydia: a pilot cluster randomised controlled trial | BMC Public Health 144 |
| 2010 | Brousseau N, Sauvageau C, Ouakki M, Audet D, Kiely M, Couture C, et al. Feasibility and impact of providing feedback to vaccinating medical clinics: evaluating a public health intervention | BMC Public Health 145 |
| 2010 | Kauth MR, Sullivan G, Blevins D, Cully JA, Landes RD, Said Q, et al. Employing external facilitation to implement cognitive behavioral therapy in VA clinics: a pilot study | Implementation Science 146 |
| 2010 | Kennedy A, Rogers A, Chew-Graham C, Blakeman T, Bowen R, Gardner C, et al. Implementation of a self-management support approach (WISE) across a health system: a process evaluation explaining what did and did not work for organisations, clinicians and patients | Implementation Science 147 |
| 2010 | McCluskey A, Middleton S. Delivering an evidence-based outdoor journey intervention to people with stroke: barriers and enablers experienced by community rehabilitation teams | BMC Health Services Research 148 |
| 2010 | Ramsay CR, Thomas RE, Croal BL, Grimshaw JM, Eccles MP. Using the theory of planned behaviour as a process evaluation tool in randomised trials of knowledge translation strategies: a case study from UK primary care | Implementation Science 149 |
| 2010 | Shelley D, Cantrell J. The effect of linking community health centers to a state-level smoker’s quitline on rates of cessation assistance | BMC Health Services Research 150 |
Participants
For participant demographic data (Table 11). Forty-eight coders who had not been involved in the development of BCTTv1 were trained to use the taxonomy96 (for more details of recruitment and training, see Chapter 4, Materials). Of these, 72.5% were from the UK, 17.5% from other European countries, 5% from the USA and 5% from Australia. They ranged in age from 24 to 60 years (mean = 37.13 years, SD = 7.45 years) and 70% were women. Eighty per cent had obtained a research or clinical doctorate and 13% identified themselves as active practitioners in their field. Eight-eight per cent rated themselves as being highly confident in using the taxonomy to specify intervention content after training.
| Descriptor | Category | Value |
|---|---|---|
| Age, years [mean (SD)] | 36.32 (6.68) | |
| Gender | Female | 30 |
| Male | 10 | |
| Profession | Practitioner | 5 |
| Student | 2 | |
| Academic | 30 | |
| Other | 3 | |
| Highest qualification | MA/MSc | 7 |
| PhD | 25 | |
| Clinical | 7 | |
| Medical qualification | 1 | |
| Previous experience of taxonomy use n (%) | Coding | 26 (24) |
| Describing BCIs | 35 (32) | |
| Expertise associated with BCIs [mean (SD)]a | Designing | 3.47 (0.96) |
| Delivering | 3.32 (0.97) | |
| Reporting | 3.43 (0.78) | |
| Reviewing | 3.43 (0.90) | |
| Using behaviour change theories | 3.65 (0.70) |
Procedure
Development of expert consensus for behaviour change technique identification
During the development of BCTTv1, six experienced BCT coders (study team members: CA, SM, MJ, JF, WH and MR), working in pairs, independently identified BCTs in the intervention descriptions using BCTTv1. They used the same coding method as described above for trained coders. The agreement within pairs produced reliability data for the 86 BCTs available at that time, as reported in Michie et al. 40 The expert consensus for the current study took this as its starting point. Expert consensus was developed by discussion of any discrepancies within each of the pairs and was also informed by feedback from trained coders. If a resolution was not obvious, SM and the study researcher (CW) reviewed the remaining discrepancies and proposed a coding. The list of BCT codes resulting from this process was circulated to the whole study team who agreed the final codes. We used this consensus about the presence of BCTs in the descriptions as a criterion against which trained coder codings were judged and concurrent validity was assessed. 107
Behaviour change technique identification by trained coders
The trained coders (n = 48) were randomised into 24 pairs using a random number generator. Both members of the coding pair received the same set of 20 (out of the 40) intervention descriptions to code. A random number generator was also used to allocate descriptions to coder pairings. The trained coders completed the coding task at two time points, 1 month apart.
At time 1, 40 coders (20 coding pairs) of the 48 coders completed the exercise generating 8–12 (as opposed to the planned 12) sets of reliability data for each of the 40 intervention descriptions. Coders used BCTTv1 to identify BCTs in each intervention description. They indicated which BCT was identified, where in the description it was identified, and also rated their confidence in their identification, using ‘+’ to mean ‘present in all probability but evidence not clear’ and ‘++’ to mean ‘present beyond all reasonable doubt and clear evidence’. After completing the task for the first time (‘time 1’), coders returned all materials and were asked to delete any copies they had made.
One month later (‘time 2’), coders were resent coding materials (including the same 20 descriptions but in a different order) and completed the coding exercise again. Thirty-two coders completed the exercise at time 2 (16 coding pairs, comprising the same trained coders as time 1). Coding took approximately 1 day of work for each coder on each occasion. Coders were paid an honorarium for their time.
Feedback on behaviour change technique definitions and labels
After completing the coding exercise, coders were asked to provide free response written feedback about using BCTTv1. They were invited to identify BCT definitions and labels that they believed remained unclear.
Analysis
The extent to which coders agreed on the absence/presence of BCTs in the descriptions (‘intercoder reliability’) was assessed using PABAK. 99 Coders at time 1 were randomly allocated to pairs working on the same set of intervention descriptions. Mean PABAK scores for each trained coder pairing, for each BCT and for each intervention description were calculated using the number of agreements and disagreements between each coding pair. Trained coder agreement with expert consensus was calculated by pairing each individual trained coder with the expert consensus BCT identifications (as described above). Trained coder agreement with expert consensus was represented by mean PABAK scores for each trained coder–consensus pairing and for each BCT.
Test–retest reliability of trained coder judgements was also assessed using PABAK. Coders at time 1 were paired with themselves at time 2. Mean PABAK scores for each intervention description were calculated using the number of agreements and disagreements. A PABAK score for each coder was then calculated using the mean of these scores.
Prevalence- and bias-adjusted kappa was used rather than Cohen’s kappa statistic. 101 Many authors have discussed inter-rater agreement measures. 111 Kappa tends to underestimate identification reliability when the number of instances is small or has asymmetric distribution between agreements and disagreements, thus PABAK overcomes these problems. Guidance on interpretation of Cohen’s kappa and other reliability statistics has been published and, conventionally, 0.70 is regarded as indicative of acceptable of good inter-rater reliability as indicated by Cohen’s kappa. In the absence of evidence-based guidance on interpretation of PABAK scores, we report means above and below 0.70 and 0.80.
Test–retest of intercoder reliability between time 1 and time 2 and of trained coder agreement with experienced coder consensus was assessed by bivariate correlations, and stability of reliability was assessed by paired t-tests. For each of the BCTs identified, the number of high confidence ratings by each trained coder at time 1 and at time 2 was calculated. The percentage of high confidence ratings was then calculated for each BCT taking into account the frequency of BCT identification across the 40 intervention descriptions. Paired t-tests (i.e. by pairing percentage of high confidence ratings made at time 1 with percentage of high confidence ratings made at time 2) were used to assess stability of high confidence ratings. A multivariate ANOVA was carried out to assess whether or not percentage of high confidence ratings at time 1 and at time 2 differed according to frequency of BCT identification (i.e. between categories of frequently, occasionally and rarely).
A number of alternatives to Cohen’s kappa have been developed. Gwet110 tested a number of such reliability indices and concluded that the AC1 statistic (see equations 7 and 8 in Gwet110) had optimal output characteristics. This is particularly true when the frequencies of occurrence are small. In the present study, a two-tailed chi-squared test applying the Yates’ correction for continuity was used to explore which statistic, PABAK or AC1, gave the higher number of BCTs achieving good reliability (i.e. ≥ 0.70).
The free response feedback provided by coders was subjected to analyses. The lead researcher on these analyses (CW) read coders’ feedback and sorted responses into themes. Themes were developed during inspection of the data. Additional themes were added if data did not fit the existing themes. An independent coder (KS) then checked allocation of feedback to themes. Any discrepancies were resolved through discussion between the two researchers.
Results
Reliability of behaviour change technique identification by trained coders
Agreement rates were similar across the 20 trained coder pairs at time 1. All coding pair means fell within one SD of the overall PABAK mean scores (mean = 0.86, SD = 0.02) indicating that there were no outlying pairs. Consequently, all pairs were included in subsequent analyses.
Table 12 lists the 93 BCT labels from BCTTv1, ordered by the frequency of identification by trained coders at time 1. The columns in the table also show (i) the mean PABAK scores between trained coder pairs; (ii) the range of mean PABAK scores between trained coder pairs; (iii) the percentage of identifications made with high confidence ratings; (iv) the mean AC1 score between trained coder pairs; and (v) the number of intervention descriptions (out of 40) in which each BCT was identified. Time 2 data for (i) and (iii) are given in parentheses in the respective columns.
| BCT label | Mean PABAK (between trained coder pairs)a | Range of PABAK (between trained coder pairs) | % BCT identifications with high confidence ratings (i.e. ++)a | Mean AC1 (between trained coder pairs) | N descriptions where BCT identified by trained coders (max 40) | |
|---|---|---|---|---|---|---|
| Frequently identified by trained coder pairs (16+ descriptions) | 3.1. Social support (unspecified) | 0.30 (0.38) | –0.10 to 0.50 | 66 (70) | 0.69 | 36 |
| 4.1. Instruction on how to perform behaviour | 0.31 (0.36) | –0.20 to 0.60 | 68 (79) | 0.68 | 35 | |
| 3.2. Social support (practical) | 0.51 (0.53) | 0.10 to 0.90 | 57 (74) | 0.76 | 34 | |
| 9.1. Credible source | 0.40 (0.43) | –0.10 to 0.90 | 69 (68) | 0.71 | 32 | |
| 5.3. Information about social and environmental consequences | 0.50 (0.57) | –0.10 to 0.90 | 68 (76) | 0.78 | 31 | |
| 1.1. Goal-setting (behaviour) | 0.48 (0.58) | 0.10 to 0.90 | 68 (76) | 0.79 | 30 | |
| 5.1. Information about health consequences | 0.50 (0.40) | 0.10 to 0.80 | 71 (80) | 0.70 | 28 | |
| 12.5. Adding objects to the environment | 0.57 (0.49) | 0.00 to 1.00 | 69 (69) | 0.75 | 28 | |
| 2.2. Feedback on behaviour | 0.57 (0.58) | 0.00 to 0.80 | 73 (76) | 0.79 | 26 | |
| 1.2. Problem-solving | 0.68 (0.69) | 0.30 to 0.90 | 74 (76) | 0.85 | 26 | |
| 2.7. Feedback on outcome(s) of behaviour | 0.62 (0.65) | 0.00 to 0.90 | 62 (77) | 0.82 | 26 | |
| 1.4. Action planning | 0.68 (0.69) | 0.10 to 1.00 | 60 (60) | 0.84 | 25 | |
| 7.1. Prompts/cues | 0.66 (0.66) | 0.30 to 1.00 | 54 (65) | 0.83 | 24 | |
| 2.1. Monitoring of behaviour by others without feedback | 0.69 (0.67) | 0.40 to 1.00 | 40 (49) | 0.83 | 23 | |
| 1.3. Goal-setting (outcome) | 0.61 (0.61) | 0.30 to .90 | 65 (76) | 0.81 | 21 | |
| 2.3. Self-monitoring of behaviour | 0.72 (0.69) | 0.30 to 0.90 | 64 (68) | 0.84 | 21 | |
| 6.1. Demonstration of the behaviour | 0.70 (0.69) | 0.30 to 1.00 | 78 (80) | 0.85 | 20 | |
| 8.1. Behavioural practice/rehearsal | 0.68 (0.66) | 0.50 to 0.90 | 71 (89) | 0.83 | 19 | |
| 12.1. Restructuring the physical environment | 0.77 (0.79) | 0.50 to 1.00 | 65 (65) | 0.89 | 17 | |
| 2.5. Monitoring of outcome(s) of behaviour without feedback | 0.77 (0.68) | 0.70 to 0.90 | 56 (54) | 0.84 | 16 | |
| 1.5. Review behaviour goal(s) | 0.750 (0.74) | 0.50 to 1.00 | 53 (55) | 0.87 | 16 | |
| 1.7. Review outcome goal(s) | 0.80 (0.76) | 0.50 to 1.00 | 48 (68) | 0.88 | 16 | |
| Occasionally identified by trained coder pairs (6–15 descriptions) | 2.4. Self-monitoring of outcome(s) of the behaviour | 0.79 (0.76) | 0.50 to 0.90 | 61 (65) | 0.88 | 15 |
| 3.3. Social support (emotional) | 0.85 (0.85) | 0.40 to 1.00 | 62 (73) | 0.92 | 15 | |
| 4.2. Information about antecedents | 0.87 (0.93) | 0.70 to 1.00 | 43 (50) | 0.96 | 15 | |
| 8.3. Habit formation | 0.91 (0.94) | 0.70 to 1.00 | 52 (46) | 0.97 | 14 | |
| 11.1. Pharmacological support | 0.82 (0.87) | 0.40 to 1.00 | 82 (90) | 0.93 | 13 | |
| 6.2. Social comparison | 0.76 (0.83) | 0.50 to 1.00 | 75 (74) | 0.91 | 13 | |
| 2.6. Biofeedback | 0.83 (0.83) | 0.50 to 1.00 | 61 (72) | 0.92 | 13 | |
| 1.6. Discrepancy between current behaviour and goal | 0.87 (0.88) | 0.50 to 1.00 | 41 (64) | 0.94 | 11 | |
| 5.2. Salience of consequences | 0.87 (0.94) | 0.60 to 1.00 | 59 (64) | 0.95 | 11 | |
| 10.2. Material reward (behaviour) | 0.85 (0.85) | 0.70 to 1.00 | 80 (78) | 0.92 | 10 | |
| 13.2. Framing/reframing | 0.92 (0.89) | 0.70 to 1.00 | 61 (80) | 0.95 | 9 | |
| 10.1. Material incentive (behaviour) | 0.80 (0.89) | 0.40 to 1.00 | 66 (64) | 0.94 | 9 | |
| 15.1. Verbal persuasion about capability | 0.91 (0.91) | 0.70 to 1.00 | 38 (64) | 0.96 | 9 | |
| 12.2. Restructuring the social environment | 0.90 (0.92) | 0.60 to 1.00 | 64 (64) | 0.96 | 8 | |
| 10.3. Non-specific reward | 0.95 (0.91) | 0.70 to 1.00 | 55 (67) | 0.95 | 8 | |
| 11.2. Reduce negative emotions | 0.90 (0.90) | 0.60 to 1.00 | 71 (80) | 0.95 | 8 | |
| 1.9. Commitment | 0.95 (0.94) | 0.50 to 1.00 | 70 (71) | 0.97 | 7 | |
| 10.4. Social reward | 0.90 (0.91) | 0.70 to 1.00 | 60 (59) | 0.95 | 7 | |
| 1.8. Behavioural contract | 0.92 (0.94) | 0.80 to 1.00 | 44 (65) | 0.97 | 7 | |
| 10.6. Non-specific incentive | 0.94 (0.96) | 0.70 to 1.00 | 33 (50) | 0.98 | 7 | |
| 9.2. Pros and cons | 0.94 (0.94) | 0.70 to 1.00 | 84 (74) | 0.97 | 6 | |
| 6.3. Information about other's approval | 0.94 (0.93) | 0.50 to 1.00 | 31 (54) | 0.97 | 6 | |
| 11.3. Conserving mental resources | 0.96 (0.97) | 0.70 to 1.00 | 25 (76) | 0.98 | 6 | |
| 5.6. Information about emotional consequences | 0.99 (0.95) | 0.60 to 1.00 | 75 (50) | 0.97 | 6 | |
| 8.2. Behaviour substitution | 0.92 (0.90) | 0.70 to 1.00 | 87 (73) | 0.95 | 6 | |
| Rarely identified by trained coder pairs (5 descriptions or less) | 7.5. Remove aversive stimulus | 0.97 (0.98) | 0.80 to 1.00 | 29 (25) | 0.99 | 5 |
| 8.6. Generalization of target behaviour | 0.97 (0.95) | 0.70 to 1.00 | 33 (42) | 0.97 | 5 | |
| 10.8. Incentive (outcome) | 0.93 (0.96) | 0.80 to 1.00 | 63 (78) | 0.98 | 4 | |
| 5.4. Monitoring of emotional consequences | 0.98 (0.94) | 0.90 to 1.00 | 29 (47) | 0.97 | 4 | |
| 15.4. Self-talk | 0.98 (0.99) | 0.80 to 1.00 | 25 (0) | 1.00 | 4 | |
| 8.7. Graded tasks | 0.98 (0.98) | 0.80 to 1.00 | 0 (25) | 0.99 | 4 | |
| 8.4. Habit reversal | 0.96 (0.97) | 0.80 to 1.00 | 50 (60) | 0.98 | 4 | |
| 10.10. Reward (outcome) | 0.96 (0.91) | 0.80 to 1.00 | 62 (81) | 0.96 | 4 | |
| 13.1. Identification of self as role model | 0.98 (0.97) | 0.80 to 1.00 | 85 (94) | 0.98 | 3 | |
| 12.3. Avoidance/reducing exposure to cues for the behaviour | 0.98 (0.94) | 0.90 to 1.00 | 75 (57) | 0.97 | 3 | |
| 12.6. Body changes | 0.97 (0.97) | 0.80 to 1.00 | 38 (80) | 0.98 | 3 | |
| 14.10. Remove punishment | 0.99 (0.98) | 0.80 to 1.00 | 33 (25) | 0.99 | 3 | |
| 9.3. Comparative imagining of future outcomes | 0.97 (0.96) | 0.80 to 1.00 | 40 (90) | 0.98 | 3 | |
| 16.3. Vicarious consequences | 0.98 (0.99) | 0.50 to 1.00 | 50 (100) | 0.99 | 3 | |
| 7.2. Cue signaling reward | 1.00 (0.98) | 0.80 to 1.00 | 0 (75) | 0.99 | 2 | |
| 14.5. Rewarding completion | 0.96 (0.95) | 0.80 to 1.00 | 50 (50) | 0.97 | 2 | |
| 4.3. Re-attribution | 1.00 (0.94) | 0.90 to 1.00 | 50 (78) | 0.97 | 2 | |
| 13.4. Valued self-identity | 0.98 (0.95) | 0.90 to 1.00 | 14 (63) | 0.97 | 2 | |
| 7.3. Reduce prompts/cues | 0.98 (0.96) | 0.90 to 1.00 | 75 (71) | 0.98 | 2 | |
| 14.4. Reward approximation | 0.97 (0.98) | 0.80 to 1.00 | 67 (60) | 0.98 | 2 | |
| 16.6. Situation-specific reward | 1.00 (0.98) | 0.90 to 1.00 | 100 (67) | 0.99 | 2 | |
| 14.2. Punishment | 0.99 (0.99) | 0.90 to 1.00 | 67 (100) | 0.99 | 2 | |
| 15.3. Focus on past-success | 1.00 (0.99) | 0.90 to 1.00 | 0 (0) | 0.99 | 2 | |
| 7.4. Remove access to the reward | 0.98 (0.99) | 0.80 to 1.00 | 100 (100) | 0.99 | 2 | |
| 13.5. Identity associated with changed behaviour | 0.99 (0.97) | 0.90 to 1.00 | 33 (40) | 0.98 | 1 | |
| 10.5. Social incentive | 1.00 (0.98) | 0.90 to 1.00 | 8 (100) | 0.99 | 1 | |
| 14.3. Remove reward | 0.97 (0.98) | 0.90 to 1.00 | 79 (85) | 0.99 | 1 | |
| 10.11 Future punishment | 1.00 (0.99) | 0.90 to 1.00 | 50 (33) | 1.00 | 1 | |
| 4.4. Behavioural experiments | 1.00 (0.99) | 0.90 to 1.00 | 0 (50) | 0.99 | 1 | |
| 14.1. Behaviour cost | 0.98 (0.99) | 0.90 to 1.00 | 100 (50) | 0.99 | 1 | |
| 7.7. Exposure | 0.98 (0.98) | 0.90 to 1.00 | 40 (0) | 0.99 | 1 | |
| 14.9. Reduce reward frequency | 1.00 (0.99) | 0.90 to 1.00 | 100 (0) | 1.00 | 1 | |
| 12.4. Distraction | 1.00 (0.99) | 0.90 to 1.00 | 100 (0) | 1.00 | 1 | |
| 8.5. Overcorrection | – (0.98) | – | – (100) | – | – | |
| 13.3. Incompatible beliefs | – (0.99) | – | – (50) | – | – | |
| Not identified by coder pairs | 7.8. Associative learning | – | – | – | – | – |
| 14.8. Reward alternative behaviour | – | – | – | – | – | |
| 16.1. Imaginary punishment | – | – | – | – | – | |
| 11.4. Paradoxical instructions | – | – | – | – | – | |
| 7.6. Satiation | – | – | – | – | – | |
| 15.2. Mental rehearsal of successful performance | – | – | – | – | – | |
| 14.7. Reward incompatible behaviour | – | – | – | – | – | |
| 10.7. Self-incentive | – | – | – | – | – | |
| 10.9. Self-reward | – | – | – | – | – | |
| 5.5. Anticipated regret | – | – | – | – | – | |
| 16.2. Imaginary reward | – | – | – | – | – |
Number of behaviour change techniques identified
How often were specific behaviour change techniques identified?
Of the 93 BCTs in BCTTv1, 80 (86%) were identified by at least one trained coder, at time 1. Twenty-two BCTs were identified in 16 or more intervention descriptions (i.e. in at least 40% of the 40 descriptions; referred to as ‘frequently identified’). Twenty-five BCTs were identified in between 6 and 15 intervention descriptions (‘occasionally’ identified) and 33 BCTs were identified in 1–5 descriptions (‘rarely’ identified). Thirteen BCTs were not identified in any description at time 1, but two of these were identified at time 2.
Replicability of coding
To what extent do trained coders agree on BCTs identified in intervention descriptions; how good is intercoder reliability? And does this change over a 1-month period?
Mean PABAK scores ranged from 0.30 to 1.00 over the 80 BCTs identified, and 64 out of the 80 observed BCTs (80%) achieved mean PABAK scores of ≥ 0.70 and 59 (74%) achieved mean PABAK scores of ≥ 0.80 indicating that good intercoder reliability was observed across BCTs by trained coders. All of the BCTs under ‘occasionally’ and ‘rarely’ identified categories achieved mean PABAK scores of ≥ 0.70 but only 6 out of the 22 (27%) of the BCTs in the ‘frequently’ identified category reached the 0.70 threshold.
Sixteen BCTs failed to reach the 0.70 PABAK threshold with nine falling below 0.60. All were frequently identified. Four of these were very close to the threshold, scoring 0.68 or 0.69: problem-solving (0.68), action planning (0.68), behavioural practice/rehearsal (0.68) and monitoring of behaviour by others without feedback (0.69). The remaining 12 were goal-setting (outcome) (0.61), prompts/cues (0.66), feedback on outcome(s) of behaviour (0.62), adding objects to the environment (0.57), information about health consequences (0.50), feedback on behaviour (0.57), social support (practical) (0.51), goal-setting (behaviour) (0.48), information about social and environmental consequences (0.50), instruction on how to perform behaviour (0.31), credible source (0.40) and social support (unspecified) (0.30).
Intercoder reliability at time 1 and at time 2 was strongly correlated, r(14) = 0.97; p < 0.001. The pattern of mean PABAK scores at time 1 and time 2 did not significantly change, t(15) = −0.05; p = 0.97. The pattern of mean PABAK scores across the BCTs identified also did not significantly change, [t(79) = 0.56; p = 0.58, time 1 PABAK mean = 0.88, SD = 0.17; time 2 PABAK: mean = 0.87, SD = 0.17]. Twelve out of the 22 frequently observed BCTs at time 2 had mean PABAK scores < 0.70, and 10 out of these also fell below this threshold at time 1. This suggests that intercoder reliability remained stable over time.
Does intercoder reliability vary across different intervention descriptions?
We considered whether or not mean PABAK scores differed across descriptions (as opposed to BCTs). Across the 40 intervention descriptions, mean PABAK scores ranged between 0.73 and 0.96 (mean = 0.87, SD = 0.05). Four of the 40 descriptions had mean PABAK scores of < 0.80 (mean PABAK for the four descriptions = 0.76, SD = 0.04). All of the four descriptions were taken from protocols published in 2010 by BMC Public Health. Two described interventions targeting behaviours to prevent illness (physical activity: mean PABAK = 0.73, and healthy eating: mean PABAK = 0.77), one described an intervention targeting behaviours to improve illness management (reduction in the use of methamphetamine: mean PABAK = 0.79) and one described an intervention targeting the behaviour of health-care professionals (health promotion and obesity prevention: mean PABAK = 0.78). There was no indication therefore, that any particular description or subset of the descriptions influenced intercoder reliability.
How good is test-retest reliability? Do coders identify the same BCTs at baseline as they do 1 month later?
Over the 32 coders providing data at both time points, mean PABAK scores for the two occasions ranged from 0.84 to 0.99, and 14 out of the 32 coders (44%) achieved mean PABAK scores of ≥ 0.80 and 18 (56%) achieved mean PABAK scores of ≥ 0.90. Good test–retest reliability was observed across all coders, indicating that those coders who performed well at time 1 were also those who performed well at time 2.
Are meaningfully different patterns of reliability data generated by different indices of intercoder reliability?
Correlational analyses showed that the relationship between mean PABAK scores and mean AC1 scores across BCTs at time 1 was near perfect (r = 0.96; p < 0.001, two-tailed). This reflects the mathematical similarity of the two formulae. For all occasionally and rarely identified BCTs, both PABAK and AC1 statistics show reliable identification of BCTs (i.e. > 0.70). Twenty of the 22 of the BCTs from the ‘frequently’ identified category meet the threshold of 0.70 when reliability is represented by AC1 but only six meet this threshold when represented by PABAK [χ2 (degrees of freedom = 1, n = 44) = 15.89; p < 0.001]. For 59 of the BCTs, the AC1 statistic generated higher reliability scores but lower scores for 10 of the BCTs. AC1 was significantly more likely than PABAK to generate reliability scores that exceeded the 0.70 threshold [χ2 (degrees of freedom = 1, n = 160) = 10.58; p < 0.001].
Validity of coding
What is the agreement between trained coders and developer consensus about which behaviour change techniques are present? Is this stable over a 1-month period?
Table 13 shows data for 15 BCTs out of 86. These BCTs were identified at least five times across the 40 intervention descriptions by the experienced coders and appear in Table 13 ordered by frequency of identification. 40 Subsequent columns show (i) the mean PABAK scores for trained coder agreement with the experienced coders, (ii) the mean PABAK scores for experienced coders, (iii) the mean PABAK scores for the 15 BCTs, between trained coder pairs at time 1, (iv) the percentage of trained coder identifications for the 15 BCTs, made with high confidence ratings and, (v) the number of descriptions in which the BCT was identified (out of 40) by at least one of the experienced coders. For reference, time 2 data is provided in parentheses for each of (iii) and (iv).
| BCT label | Mean PABAK (trained coder agreement with experienced coder consensus) | Mean PABAK (between experienced coder pairs) | Mean PABAK (between trained coder pairs)a | % BCT identifications with high confidence ratings by trained coders (i.e. ++)a | N descriptions where BCT identified by expert consensus (max 40) |
|---|---|---|---|---|---|
| 1.2. Problem-solving | 0.74 | 0.75 | 0.68 (0.69) | 74 (76) | 12 |
| 9.1. Credible source | 0.49 | 0.60 | 0.40 (0.43) | 69 (68) | 11 |
| 2.3. Self-monitoring of behaviour | 0.71 | 0.75 | 0.72 (0.69) | 64 (68) | 10 |
| 8.1. Behavioural practice/rehearsal | 0.73 | 0.70 | 0.68 (0.66) | 71 (89) | 9 |
| 1.3. Goal-setting (outcome) | 0.64 | 0.85 | 0.61 (0.61) | 65 (76) | 7 |
| 11.1. Pharmacological support | 0.83 | 0.85 | 0.82 (0.87) | 82 (90) | 7 |
| 6.1. Demonstration of the behaviour | 0.70 | 0.75 | 0.70 (0.69) | 78 (80) | 7 |
| 6.2. Social comparison | 0.80 | 0.90 | 0.76 (0.83) | 75 (74) | 6 |
| 3.2. Social support (practical) | 0.62 | 0.70 | 0.57 (0.53) | 57 (74) | 5 |
| 1.5. Review behaviour goal(s) | 0.68 | 0.75 | 0.75 (0.74) | 53 (55) | 5 |
| 12.1. Restructuring the physical environment | 0.79 | 0.85 | 0.77 (0.79) | 69 (65) | 4 |
| 10.2. Material reward (behaviour) | 0.83 | 0.85 | 0.85 (0.85) | 80 (78) | 4 |
| 10.1. Material incentive (behaviour) | 0.82 | 0.80 | 0.80 (0.89) | 66 (64) | 4 |
| 2.5. Monitoring of outcome(s) of behaviour without feedback | 0.77 | 0.70 | 0.77 (0.68) | 40 (54) | 4 |
| 7.1. Prompts/cues | 0.70 | 0.70 | 0.66 (0.66) | 54 (65) | 3 |
Mean PABAK scores for experienced coders for the 15 BCTs (see Table 13) ranged from 0.60 to 0.90 (overall mean = 0.77); all but one BCT achieved a mean PABAK score of ≥ 0.70. Mean trained coders’ PABAK scores ranged from 0.40 to 0.85 (overall mean = 0.70). Six BCTs achieved mean PABAK scores < 0.70. The mean reliability scores for experienced coders and trained coders were correlated with a large effect size [r(13) = 0.69; p < 0.01, two tailed] but were significantly different [t(14) = 3.01; p < 0.01] with experienced coders achieving higher PABAK scores for 13 out of the 15 BCTs. The BCT ‘credible source’, reduced the overall intercoder reliability for both the experienced coders and the trained coders (PABAK score = 0.60 and 0.40 for experienced coders and trained coders, respectively). Discounting this particular BCT, the overall mean PABAK scores for the 15 BCTs would increase to 0.78 and 0.72 for experienced coders and trained coders, respectively.
Concurrent validity scores for the 15 BCTs at time 1 ranged from 0.49 to 0.83, with four BCTs having scores < 0.70. Three of these four were associated with BCTs having low reliabilities and the fourth, ‘review behaviour goal(s)’ had a validity score of 0.68. The poorest validity was for ‘credible source’, with ‘social support (practical)’ and ‘goals-setting (outcome)’ also being low and all three of these had also shown low intercoder reliability. The mean PABAK validity scores across trained coder consensus pairs did not significantly change with time [t(31) = 0.84; p = 0.41] and scores on the two occasions were correlated [r(30) = 0.67; p < 0.001]. Validity was reasonably high and remained stable over a 1-month period.
Confidence of coding
How confident are trained coders in identifying behaviour change techniques from intervention descriptions and is this stable over a one-month period?
The percentage of identifications judged by coders to have been made with high confidence (‘++’) across the 80 BCTs identified, ranged from 0% to 100% with an average percentage of 57%. The trained coders appeared to be more confident about identifying BCTs at time 2 than the same BCTs at time 1: t(79) = –2.08; p < 0.05 (mean percentage of judgements made with high confidence at time 1 mean = 57, SD = 23.65; time 2 mean = 63.04, SD = 23.11). The percentage of trained coders high confidence ratings also increased for the 15 BCTs agreed as present by the experienced coders. t(14) = –2.78; p < 0.05 (mean percentage of judgements made with confidence ‘++’: time 1 66.47, SD = 11.51; time 2 71.73, SD = 10.55).
The percentage of high confidence ratings did not differ according to frequency of BCT identification at time 1 [F(2,77) = 2.55; p = 0.08]; however, they significantly differed at time 2 [F(2,77) = 3.48; p < 0.05]. Frequently identified BCTs were rated with more confidence (mean percentage = 70.45, SD = 9.68) than those BCTs that were rarely identified BCTs [p < 0.05 (mean percentage = 55.33, SD = 32.53)] and there were no significant differences between categories of rarely and occasionally (p = 0.18), or between categories of occasionally and frequently (p = 1.00) identified BCTs.
How does confidence relate to intercoder reliability?
For the 80 BCTs identified by trained coders, confidence was not correlated with greater reliability. Perhaps surprisingly, mean PABAK scores were not positively correlated with confidence, but rather tended to be negatively correlated, r(78) = –0.37; p = 0.07 (two tailed).
How does trained coders’ confidence of behaviour change technique identification relate to trained coders’ agreement with experienced, coder consensus about which behaviour change techniques are present?
Confidence ratings were not associated with validity; trained coders’ confidence in their identification of the 15 BCTs agreed by experienced consensus was not associated with mean PABAK scores [r(13) = 0.27; p > 0.10].
Feedback on use of Behaviour Change Technique Taxonomy version 1
Are there any BCT labels and definitions that trained coders’ judge to be in need of refinement and/or clarification? How do such judgements relate to observed intercoder reliability?
Free response feedback was categorised into three themes: (1) BCT definitions and labels that remain unclear/require refinement, (2) improving reliable and valid application and (3) methods to improve the usability of BCTTv1.
Behaviour change technique definitions and labels that remain unclear/require refinement
Of the 93 BCTs in BCTTv1, trained coders highlighted 12 as being unclear or requiring further refinement. Nine of these (75%) BCTs were among the 12 BCTs achieving mean PABAK reliability scores of < 0.70 (listed above). Three of these were among the 15 BCTs identified by the experienced coders achieving mean PABAK validity scores of < 0.70. This suggests that there was considerable correspondence between coders' individual judgements of BCT definition clarity, BCT intercoder reliability and validity.
Fifty per cent of the BCT definitions judged by trained coders as being in need of further clarification belonged to the same BCT grouping in BCTTv1, therefore, referring to the same underlying mechanism of change. For example, coders noted that if distinctions between the three social support BCTs were clearer (i.e. Social support – unspecified, Social support – practical and Social support – emotional), users would find it easier to decide when unspecified forms of support could more accurately be specified as practical:
Make the definitions of ‘social support unspecified’ clearer and in tune with the definition of Social support (practical)
Participant 7
Would be useful to have ‘social support’ better defined
Participant 11
. . . still finding the social support BCTs vague – e.g. aside from the definition of ‘social support’, what defines ‘practical’ in practical social support?
Participant 4
Similar refinement was recommended for the three information provision BCT variants (i.e. Information about health consequences, Information about emotional consequences and Information about social and environmental consequences):
Some BCTs, e.g. social support (unspecified) or information about social and environmental consequences are too vague and used for too many techniques.
Participant 18
Improving reliable and valid application
Four BCTs achieved intercoder reliability mean PABAK scores of 0.68 and 0.69, at time 1. These were: problem-solving (0.69), demonstration of the behaviour (0.69), self-monitoring of behaviour (0.69) and monitoring of outcome(s) of behaviour without feedback (0.68). We considered these as being close enough to the 0.70 threshold to be counted as reliably identified. Three additional BCT definitions were identified by trained coders as being in need of clarification and/or refinement. These were: demonstration of the behaviour, action planning and restructuring the physical environment. Coders tended to find several ‘pairs’ of BCTs difficult to distinguish: instruction on how to perform the behaviour versus demonstration of the behaviour; goal-setting (behaviour) versus goal-setting (outcome); goal-setting (behaviour) versus action planning and restructuring the physical environment versus adding objects to the environment. To further facilitate reliable and valid specification of these BCTs, guidance was requested on when to code one rather than both of these BCT pairs:
Why is this (excerpt) not coded as ‘instruction on how to perform the behaviour’? (This is a wider question about how demonstration differs from instruction.) Does demonstration encompass instruction?
Participant 9
Two BCTs should not be inferred as always co-occurring. It is possible to have a demonstration of a behaviour without practice and vice versa. So the definitions of these two BCTs should be revised.
Participant 23
The BCT ‘credible source’, created considerable difficulty as indicated by low reliability and validity for coders, but also low reliability for the experienced coders. Coders noted that identification required inferences regarding intervention recipients’ evaluation of the credibility of those delivering interventions and that this could sometimes be unclear. They suggested that intercoder reliability could be improved if additional guidance documents were made available:
What determines/constitutes ‘credibility’ of a source? Is a parent providing information to a child a ‘credible source’? Also, is telling someone to do a behaviour a case of ‘presenting information . . . in favour of or against the behaviour’?
Participant 33
Methods to improve the usability of Behaviour Change Technique Taxonomy version 1
Coders’ suggestions for improving usability focused on improving the speed at which specific BCTs could be located in the taxonomy. Frequent suggestions included having a hyperlinked index page at the beginning of version 1 to minimise the need to manually search through BCTs:
Would be useful to have a first page list of all codes and where to find them and any linked codes as this was difficult to scroll back and forth finding the codes on each page during doing.
Participant 14
. . . presentation of the taxonomy – a front page with all BCT labels numbered and with page of definition to enable access
Participant 2
Discussion
Eighty of the 93 BCTs defined in BCTTv1 were identified in 40 intervention descriptions by at least one trained coder, 22 BCTs were identified in at least 16 descriptions and 47 BCTs were identified in at least six of 40 descriptions. Thus, coders made extensive use of BCTTv1, justifying the large number of BCTs included. Clearly specification of BCIs requires at least this range of BCTs to describe the active content.
Good intercoder reliability was observed across the 80 identified BCTs, with 80% achieving mean PABAK scores of at least 0.70 and 74% with scores of ≥ 0.80. Poorer reliabilities were more common for frequently occurring BCTs; just 12 of the 22 (55%) achieved mean PABAK scores of ≥ 0.68 and six (27%) achieved ≥ 0.70.
Intercoder reliability was equally good across intervention descriptions and remained similar across two tests separated by 1 month, indicating temporal stability. There was also good trained coder agreement with developer consensus about the 15 BCTs agreed on as present, thus indicating concurrent validity.
Trained coders’ confidence in their BCT identifications increased from time 1 to time 2, and varied across BCTs. There tended to be a negative correlation between trained coders’ confidence of BCT identification and intercoder agreement. Coders’ confidence in identifying BCTs was not related to either intercoder agreement or to agreement with experienced coders. This suggests that perceived confidence does not appear to be a useful indicator of accuracy of identification of BCTs in intervention descriptions. Reliability was consistently higher when represented by the AC1 statistic than the PABAK statistic.
The BCTTv1 taxonomy of BCT labels and definitions is an important development of previous work and provides the most comprehensive listing of BCTs to date. Of the 22 BCTs observed in 16 or more of 40 intervention descriptions, 18 (82%) were also identified in the Abraham and Michie20 BCT taxonomy, confirming the frequent occurrence of these 18 BCTs. However, while Abraham and Michie defined only 22 BCTs and four packages of BCTs, BCTTv1 defines 93 separate BCTs, 80 of which were identified by coders in 40 published intervention descriptions. The data reported here provide good overall intercoder and test–retest reliability for 80 of those definitions among trained coders. Furthermore, the data suggest that newly trained coders can code accurately as defined by agreement with experienced coder consensus. Given the expertise derived from the experience of developing BCT definitions and the previous experience of the developers in identifying BCTs in intervention descriptions, correspondence between trained coder judgements and experienced developers’ judgements was regarded as a measure of the validity of the trained coders’ judgements. Thus, validity of BCTTv1 is demonstrated among new users and does not depend on additional discussion and cues that may have influenced the experienced coders. Therefore, the BCTTv1 taxonomy can be used successfully, with appropriate training, by a wide range of users to identify a wide range of BCTs included in intervention descriptions.
Beyond testing the reliable and valid use of current BCT labels and definitions, a primary purpose of this research was to identify definitions that might be applied more reliably with further clarification or guidance. Sixteen frequently identified BCTs achieved PABAK scores of < 0.70 with nine of these falling below 0.60. These included four pairs of BCTs defining variants of the same underlying change mechanism, namely (1) Information about (a) health consequences and (b) social and environmental consequences; (2) goal-setting in relation to (a) outcomes and (b) behaviours; (3) feedback on (a) behaviour and (b) outcome(s) of behaviour; and (4) social support both (a) practical and (b) unspecified.
It may be appropriate to remain somewhat circumspect about trained coders’ feedback on clarity of BCT definitions as confidence in BCT identification was not related to observed intercoder reliability (and indeed tended to be negatively correlated) or to trained coder agreement with experienced coder consensus. Nonetheless, coders provided clear feedback suggesting that further distinction between such BCTs groupings was needed.
Intercoder reliability was poor for ‘instruction on how to perform behaviour’ and individual coder feedback suggested confusion with ‘demonstration of the behaviour’. This was one of four pairs of BCTs (including two goal-setting definitions) with which coders reported difficulty. Both prompts/cues and adding objects to the environment also fell below the 0.70 threshold. Further testing of the definitions of these BCTs is therefore warranted.
Trained coders commented on the definition of credible source. This BCT showed poor intercoder reliability among coders and poor validity. It was also the lowest intercoder reliability score among experienced BCT coders. This is clearly a BCT that requires further clarification and specification but should be retained because of its relevance to behaviour change. The importance of message–source credibility has been recognised for over half a century151 and coding for source characteristics in intervention descriptions has been shown to predict intervention effectiveness in meta-analytic studies. Perceived professional competence of intervention facilitators has also been found to predict effectiveness of human immunodeficiency virus-preventative interventions. 152 Similarities between intervention facilitators and recipients (e.g. age, ethnicity and behaviour risk group membership) explained differential effectiveness of interventions. This highlights that coding intervention descriptions for message source or facilitator characteristics is important. Plus it may be important to distinguish between perceived professional competence of those delivering the interventions and their ‘credibility’, which could also be based on common group membership. Finally, it may be important to distinguish between characteristics of those delivering interventions and the content of what they deliver. Certainly, further work on the label and/or definition of this BCT is needed.
The coders trained for this study seem typical of those likely to want to use BCT labels and definitions to identify intervention components associated with greater intervention effectiveness, for example when conducting meta-analyses. 20,23,48,56 Although we used data from 40 trained coders, we recommend that future studies continue to use at least two coders to check (and report) intercoder reliability.
We found that reliability was high and similar over the 40 intervention protocols coded. However, as reported above, we used a sample of descriptions included in well-cited journals that publish BCI protocols related to health improvement and this reliability might not be maintained in intervention descriptions of poorer quality.
We compared intercoder reliability assessments generated by the PABAK and AC1 statistics. Reassuringly, our findings indicate that these indices generate very similar patterns of intercoder scores across identified BCTs. We found, however, that for the most frequently indentified BCTs, the two indices differ significantly in their representation of reliability with PABAK generating lower reliability scores than AC1. These frequently identified BCTs were less reliably identified than other BCTs. Thus, our findings suggest that, at least in some contexts, the two statistics may not be directly interchangeable when data similar to the current data are investigated. Guessing may be more likely for frequently occurring BCTs than for rare BCTs meaning that random effects, such as those that AC1 controls for, could emerge. AC1 may therefore be a more appropriate index. It may also be helpful to interpret these statistics alongside other results (e.g. frequency of item observations). The consistently higher AC1 scores suggest that our data may have been influenced by random judgement effects that are controlled in AC1 but not PABAK, with resulting lower scores in PABAK. Nevertheless, even PABAK takes account of the high prevalence of negative codes and of the extent to which coders use similar marginal totals and, therefore, is more appropriate for this type of data than a simple kappa. The use of more than one statistic to assess agreement is a relatively new approach and the consistent difference between the scores indicates that the AC1 takes account of more sources of error in these data and, therefore, is more appropriate for establishing the level of agreement in BCT coding. The high correlation between the measures indicates that the pattern of relative agreement across BCTs is adequately represented by either score, although the PABAK may result in fewer frequently observed BCTs achieving reliability above thresholds such as 0.70, as used here.
Comparison of the pattern of results for frequent and rare BCTs suggests that PABAK is as good as AC1 for the rare but not for the frequent BCTs, while the poor reliabilities (using PABAK) were more common for frequently occurring BCTs. As was suggested by our comparison of confidence ratings across BCT categories, guessing may be more likely for common than for rare BCTs. This would result in occurrence of the random effects that AC1 controls and confirms the need to use AC1 rather than PABAK in studies assessing reliability. Further developments of reliability indices111 controlling for additional sources of error and more recently proposed indices may give an even better indication of the true reliability of coding.
In conclusion, our results show that BCTTv1 can be used by trained coders to reliably identify BCTs included in intervention descriptions. Feedback from our coders highlights several BCT definitions that require further classification and refinement before they can be identified reliably. BCTTv1 provides a uniquely comprehensive list of BCTs. The taxonomy can be used both by developers and implementers of BCIs and by those wishing to identify effective BCTs within complex interventions (e.g. systematic reviews).
Chapter 6 Reporting observed interventions using Behaviour Change Technique Taxonomy version 1: clarity and distinctiveness of intervention descriptions (studies 5a, 5b and 5c)
Abstract
Objectives: To assess whether or not use of BCTTv1 improves the reporting of observed BCIs.
Methods: 166 participants (‘writers’) watched videos of BCIs and wrote descriptions of the active content delivered. Three different study designs were used so we could assess effects of BCTTv1 provision, with and without training. The first two studies were RCTs: study 5a examined provision of BCTTv1 without training and study 5b examined the effects of training plus provision of BCTTv1 compared with a control group receiving neither the taxonomy nor training. Study 5c used a within-person design to assess change in the quality of descriptions before and after training. Writers provided with BCTTv1 for the task evaluated usability and acceptability of using BCTTv1 to write descriptions. Twelve ‘raters’ (untrained in BCTTv1) assessed description quality in terms of clarity and replicability, and 12 ‘coders’ (trained in BCTTv1) coded the descriptions for BCTs.
Results: Providing BCTTv1 did not improve the reliability or validity of the descriptions written by untrained writers (for all measures p > 0.05; study 5a) and resulted in poorer quality of descriptions (all p < 0.05). Compared with untrained writers, those who were trained and using BCTTv1 wrote descriptions that had no greater quality or validity but which resulted in more reliable BCT identification (all p < 0.05) (study 5b). Following training, writers’ descriptions did not increase in reliability or validity but were rated to be of higher quality (all p < 0.05 except replicability of mode of delivery) than those written before training (study 5c). Writers thought that using BCTTv1 to write intervention descriptions was a difficult task but considered it ‘useful’, ‘good’ and ‘desirable’, and that their descriptions would be clear and replicable if the taxonomy were to be used (all means above mid-point of the scale).
Conclusions: We did not find a clear benefit of using the BCTTv1 to report observed interventions. This may be owing to task demands, the nature of the task evaluated, omission of other intervention components in descriptions, lack of time and experience, or an insufficient training package. Further work is needed to evaluate its usefulness in this area.
Introduction
There is a lack of guidance about how to report intervention descriptions in terms of both the proposed active content (BCTs) and supportive content necessary to engage the participant. 32
It is important to examine whether or not the use of BCTTv1 can improve the reporting of intervention descriptions. Improved reporting of intervention content means specifying the content of all the BCTs delivered in the intervention in a manner that makes them recognisable and replicable. 153,154 We investigated whether or not using BCTTv1 improved communication of the content of observed interventions. We used observed interventions with the aim of providing all the information about the intervention without writing it down and thus providing the words to be used. However, this is a rather artificial scenario as usually interventions are developed in an iterative process of reading and discussion.
This chapter reports three substudies that investigated whether or not BCTTv1 improves the reporting of descriptions of observed BCIs. We focused on whether or not provision of BCTTv1 alone and/or BCTTv1 plus training has an impact on the quality of reporting and recognition of BCTs in written intervention descriptions. The writers of intervention descriptions (‘writers’) reflected a range of potential users of BCTTv1: primary researchers, systematic reviewers, funders, policy-makers and practitioners, and both trained and untrained users of the BCTTv1. Participants watched videos of BCIs as delivered in practice and were asked to write descriptions and rate the usefulness and acceptability of BCTTv1 for this purpose. We assessed intervention descriptions generated by the writers in multiple ways. We assessed their clarity and replicability using independent raters who were not familiar with the BCTTv1 (‘raters’) as they reflect the typical reader of intervention descriptions. Separately, trained coders (‘coders’) were asked to identify BCTs and we assessed how well their coding corresponded with the agreement reached by experienced coders from the BCTTv1 project team (‘expert consensus’). We used trained coders as we showed that training in BCTTv1 improves the identification of BCTs96 (see Chapter 4, Methods).
A series of three substudies addressed the following RQs:
-
Does provision of BCTTv1 or training in its use improve:
-
the quality (i.e. clarity and replicability) of intervention descriptions?
-
recognition of BCTs described in intervention descriptions (in terms of intercoder agreement)?
-
agreement with expert consensus about BCTs described?
-
-
Do users find BCTTv1 a useful and acceptable tool for reporting intervention descriptions?
Method
Design
Three studies were conducted to evaluate the effects of BCTTv1 on the reporting of BCI descriptions. Study 5a examined the effects of providing BCTTv1, without training, in a RCT. The experimental group was provided with BCTTv1 but no training while the control group wrote BCI descriptions with neither BCTTv1, nor training. Study 5b also used a RCT design and examined the effects of training plus provision of BCTTv1 compared with a control group who received neither BCTTv1 nor training. Study 5c used a within-person design to assess change in the quality of BCI descriptions before training, without provision of BCTTv1 and quality of descriptions after training, with provision of BCTTv1. In each study, writers watched a video of an intervention and wrote a short description of the active content being delivered. To counteract potential practice and ordering effects, we used two videos with the same target behaviour (smoking cessation) and these were administered in a counterbalanced design. For each study, the quality of the descriptions was assessed in terms of (1) clarity and distinctiveness, (2) reliability of BCT identification and (3) validity of BCT identification assessed against expert consensus.
Participants
There were three types of participant: writers, untrained raters and trained coders. As they were different for the three studies, participant details are given separately for each study (Table 14).
-
Writers were 166 health-care professionals and trainees with an interest in investigating, reviewing and designing or delivering BCIs but with little or no previous knowledge of using BCTTv1. All writers had signed up to complete a BCTTv1 training workshop and participated when they attended the workshop. Six workshops were delivered by two or three members of the BCTTv1 project team. They were held at Newcastle University (n = 26), the University of Oxford (n = 16), Queens University in Belfast (n = 45), the University of Aberdeen (n = 24), University College London (n = 15) and the University of Manchester (n = 16). Workshops were advertised via scientific and professional organisations, and via the BCTTv1 project website. 97
-
Untrained raters were 12 practitioners unfamiliar with BCTTv1. Because they were rating descriptions of smoking cessation interventions, they were recruited from the National Centre for Smoking Cessation and Training (NCSCT) database,35 an online training resource for smoking cessation advisors to support delivery of smoking cessation interventions. To help ensure unfamiliarity with BCTTv1, only practitioners who had registered but who had not yet started their training with the NCSCT were invited to take part.
-
Trained coders were 12 behaviour change researchers and practitioners, previously trained to code BCIs using BCTTv1 via distance group tutorial training. 96,107 Coders had all demonstrated competence in using BCTTv1 to reliably and validly specify the content of BCIs, that is they achieved criteria of satisfactory performance on coding intervention descriptions following training, in a formal assessment of coding competence. 107
| Study (location of workshops) | Participants | Total number | Condition | Age (years) | % UK | % doctorate | % practitioner | % use of BCT taxonomy | Expertise in BCIs, mean (SD) measured using a response scale | |
|---|---|---|---|---|---|---|---|---|---|---|
| Code | Describe | |||||||||
| 5a (Manchester and Belfast) | Writers | 42 | No tax | 37.37 | 83 | 61 | 18 | 4 | 7 | 2.52 (0.86) |
| Tax | 39.53 | 84 | 32 | 28 | 1 | 5 | 2.36 (1.15) | |||
| Raters | 4 | 30.50 | 100 | 0 | 100 | 0 | 0 | 2.00 (1.47) | ||
| Coders | 4 | 32.25 | 50 | 75 | 25 | 75 | 75 | 3.50 (0.37) | ||
| 5b (Aberdeen, Oxford and Belfast) | Writers | 85 | Untrained + no tax | 38.00 | 79 | 16 | 32 | 3 | 2 | 2.44 (0.66) |
| Trained + tax | 42.55 | 100 | 35 | 40 | 1 | 3 | 2.22 (0.99) | |||
| Raters | 4 | 32.50 | 100 | 0 | 100 | 0 | 0 | 2.00 (1.22) | ||
| Coders | 4 | 31.75 | 100 | 100 | 25 | 100 | 100 | 3.44 (0.59) | ||
| 5c (London and Newcastle) | Writers | 39 | Untrained + no tax | 36.43 | 73 | 43 | 16 | 14 | 14 | 2.11 (0.83) |
| Trained + tax | 29.33 | 67 | 17 | 17 | 16 | 7 | 2.00 (0.56) | |||
| Raters | 4 | 31.50 | 100 | 0 | 100 | 0 | 0 | 2.26 (0.82) | ||
| Coders | 4 | 44.25 | 75 | 100 | 50 | 100 | 100 | 3.50 (0.88) | ||
Materials
Videos: two videos were used, both addressing the same behaviour (smoking cessation) and including a range of frequently observed and clearly delivered BCTs. Both were approximately 9 minutes in duration and showed a smoking cessation practitioner delivering a smoking cessation intervention to a client. To overcome potential confounding effects of possible differences in task difficulty between videos, two videos were used and were shown in a counterbalanced design.
Consensus on BCTs delivered: to establish consensus about the presence of BCTs in the videos, four BCT coders who had been involved in developing BCTTv1 (MJ, JF, SM and WH) independently coded both videos using BCTTv1. Each video was coded by two coders and discrepancies were discussed within each of the pairs. If a resolution was not obvious, SM and the study researcher (CW) reviewed the remaining discrepancies and proposed a coding. Codings were then circulated and all coders agreed the final codings. This process established expert consensus about the presence/absence of 21 BCTs in video 1 and 15 BCTs in video 2.
BCTTv1: dependent on workshop design, some of the writers were provided with a copy of BCTTv1 for the writing task (see Appendix 2, Table 19).
Procedure
Workshops: at the beginning of the workshop, writers completed a questionnaire with demographic information (i.e. age, sex, nationality, professional background and highest qualification) and completed measures of previous BCTs/BCT taxonomy experience and expertise (see Measures).
Randomisation for RCTs (studies 5a and 5b): at the start of the workshop, writers were randomised into two groups to complete the writing task by selecting a letter (either A or B) from a bag containing equal numbers of A and B and a total equal to the number of workshop attendees.
Writing task: writers watched a video of a smoking cessation intervention being delivered (see Materials). While watching the video, writers were instructed to write notes about the ‘active components’ (i.e. content delivered that was likely to change behaviour). The video was only shown once. Following the video, they were then given 15 minutes to write a description in such a way that (1) the active components being delivered in the intervention could be understood and (2) the intervention could be replicated by someone else. Dependent on study design, some writers were provided with a copy of BCTTv1 for the task while others were not. These writers were given an additional 5 minutes at the start of the task to familiarise themselves with the taxonomy (i.e. briefly read labels, definitions and examples).
Ratings of written descriptions: raters were sent materials via e-mail and could complete and submit their ratings remotely. They provided demographic information (i.e. age, sex, nationality, professional background and highest qualification) and completed measures of previous BCT and/or BCT taxonomy experience and expertise (see Measures). They were randomly allocated a set of the descriptions written by the ‘writers’ (the number of descriptions in the set differed according to study). Allocation was stratified so that sets comprised an approximately equal number of descriptions that had been written by writers watching video 1 or video 2. For study 5a, they received equal numbers of descriptions written with or without BCTTv1 and for studies 5b and 5c, sets also contained the same number of descriptions written by untrained and trained writers. Raters were instructed to read each description carefully before rating it according to (1) ease of understanding and (2) adequacy of information required to undertake a replication (see Measures).
Behaviour change technique coding of written descriptions (coders): using the same randomisation methods as described for raters, coders were randomly allocated to a set of descriptions. They were sent materials and a copy of BCTTv1 via e-mail and could complete and submit remotely. Coders identified the presence or absence of BCTs using BCTTv1 (see Measures). The coding was estimated to take up to 1 day. Invitations were sent with an offer of an honorarium of £280 on completion of the coding.
Training
The workshop training programme and materials were based on 1-day workshops as reported in study 396 (see Chapter 4). The structure of the workshops was similar, with writers watching three short PowerPoint presentations and participating in a series of interactive coding tasks as a group, individually and in pairs. Workshop tasks were adapted slightly from those reported in study 3 to include 30 minutes of training in using BCTTv1 to write intervention descriptions (Table 15). Some of the content was modified so that learning objectives could be more directly addressed (e.g. for the objective ‘teach how to identify reliably in real and increasingly complex interventions’, writers identified BCTs delivered in short videos rather than written excerpts taken from intervention descriptions).
| Content | Brief description | Learning objectives | BCTs used | |
|---|---|---|---|---|
| Registration | Welcome and introductions. Writers complete a registration form | |||
| Writing task (all writers in study 5a; group A in study 5b and study 5c) | Using the taxonomy | Writers watch a clip of an intervention delivered by a practitioner to a client and make notes about the active content delivered. The clip is shown only once. They are given 15 minutes to write a clear and replicable description of the intervention as delivered | To generate descriptions written by untrained writers without and with BCTTv1 | Instruction on how to perform the behaviour |
| Behavioural practice/rehearsal | ||||
| Presentation | Background to BCTs | Outlines the goals for the day, defines and conceptualises the term ‘BCT’ and communicates need for agreed standard list of BCTs in behavioural medicine | To understand aims, objectives and learning outcomes | Credible source |
| To learn need for precise labels and definitions | Social reward | |||
| Pros and cons | ||||
| Comparative imagining of future outcomes | ||||
| Task | Ready, Steady, Point! | Writers shown a short excerpt of intervention descriptions on screen and, when prompted, asked to point left if they identify BCT 1, right for BCT 2 or to the ceiling if unsure | To learn BCTs 1–2 labels and definitions | Social comparison |
| To learn appropriate levels of inference and discrimination | Salience of consequences | |||
| Graded task | ||||
| Behaviour practice/rehearsal | ||||
| Feedback on behaviour | ||||
| Morning break | Writers to read through BCTs 1–12 | Writers to read through labels and definitions of BCTs 1–12 | ||
| Presentation | Identifying behaviours and BCTs | Defines behaviour and the distinction between behaviour and behavioural outcome | To learn what a behaviour is and the difference between a behaviour and a behaviour outcome | Behaviour practice/rehearsal |
| Task | Providing examples of BCTs | Writers work in groups of four to generate their own examples of BCTs 1–12 and then feed back to the rest of the group | To learn BCTs through detailed consideration of examples | Feedback on behaviour |
| Generalisation of target behaviour | ||||
| Social comparison | ||||
| Feedback on behaviour | ||||
| Social reward | ||||
| Task | Identifying BCTs in interventions as delivered in practice | Writers work individually to identify BCTs in two short videos showing an intervention delivered by a practitioner to a client | To consolidate previous learning of BCTs 1–12 | |
| To learn how to reliably identify BCTs as delivered in practice | ||||
| Task | Applying the BCT approach | Writers split into small groups to discuss use of the BCT approach as applied to their own work | To understand how the BCT approach can be applied to own research | |
| Lunch break | ||||
| Task | Feedback on discussion | Writers feedback on their group discussions held before the lunch break | To learn how other researchers/practitioners are using the BCT approach in their own work | Graded tasks |
| Task | Identifying BCTs in interventions as delivered in practice | Writers work in pairs to identify presence of BCTs 1–24 in two longer videos | To discuss questions arising | Feedback on behaviour |
| To consolidate previous learning of BCTs 1–24 | Demonstration of the behaviour | |||
| To consolidate previous learning of identifying BCTs and making inferential judgements in interventions as delivered in practice | Social reward | |||
| Feedback on outcome | ||||
| Task | Writing descriptions | Writers rewatch short video 1 and describe the BCT ‘problem-solving’ as delivered in practice, in their own words. They then refine their description using the definition from the taxonomy. Writers discuss their approach to this task in pairs and then feed back to the rest of the group | To learn how to describe BCTs as delivered in practice using definitions from the taxonomy | Problem-solving |
| Presentation | Moving from a list to a taxonomy | Introduces the idea of a hierarchical structure and outlines how it was developed | To become familiar with hierarchical structure of the taxonomy and the 24 BCTs within their clusters | Problem-solving |
| Afternoon break | ||||
| Writing task | Using the taxonomy | Writers watch a clip of an intervention delivered by a practitioner to a client and make notes about the active content delivered. The clip is only shown once. They are given 15 minutes to write a clear and replicable description of the intervention as delivered | To generate descriptions written by trained writers with BCTTv1 | Instruction on how to perform the behaviour |
| Behavioural practice/rehearsal | ||||
| Question and answer session and close | Learning outcomes are summarised. Writers complete an evaluation questionnaire | |||
Measures
The following measures were completed by writers/raters/coders (as indicated).
Previous experience and BCT taxonomy expertise (writers, raters and coders): previous experience of (1) designing or reporting BCIs that specifically identified BCTs, (2) writing manuals or protocols of interventions and (3) undertaking a narrative or systematic review of behaviour change literature. Expertise (i.e. knowledge, skills and familiarity) in the areas of designing, writing, reporting and systematic reviewing of BCIs was assessed for (1) designing or reporting BCIs that specifically identified BCTs, (2) involvement in writing manuals or protocols of interventions and (3) undertaking a narrative or systematic review of behaviour change literature. All used response options from 1 (‘no experience’) to 5 (‘a great deal of experience’).
Quality of intervention descriptions (raters): to assess clarity, raters rated the following statements ‘I can clearly visualise how the intervention was delivered (i.e. the mode of delivery)’ and ‘I can clearly visualise what was delivered in the intervention (i.e. the active ingredients)’. To assess replicability they rated: ‘Someone would be able to replicate how the intervention was delivered (i.e. the mode of delivery)’ and ‘Someone would be able to replicate what was delivered in the intervention (i.e. the active ingredients)’. Response options for both were a scale from –3 (strongly disagree) to + 3 (strongly agree). As each description was rated by two raters, scores for each of the items were added and divided by two to give a mean score. The items were entered as separate variables into the analyses.
Identification of BCTs described (coders): coders used BCTTv1 to identify the absence/presence of BCTs in each of the written descriptions.
Usefulness and acceptability of using BCTTv1 for writing intervention descriptions (writers): writers rated whether or not the time allocated for the writing task was sufficient from 1 ‘strongly disagree’ to 7 ‘strongly agree’. They also rated the difficulty of the writing task from 1 ‘very easy’ to 7 ‘very difficult’. Writers who had been provided with BCTTv1 for the writing task were presented with the statement: ‘Using BCTTv1 to describe the content of BCIs is . . .’ and responded by rating on 7-point bipolar adjective scales (i.e. pairs of opposites): difficult–easy, useful–worthless, good–bad and undesirable–desirable. Scores were averaged to give an overall evaluation scoring (mean = 5.42, SD = 0.82; range = 3.50–7.00). Finally, they rated ‘If I use BCTTv1 to describe the content of behaviour change intervention . . . ‘, ‘ . . . my description will be clear’ and ’. . . someone will be able to replicate the intervention after reading my description’ from 1 ‘strongly disagree’ to 7 ‘strongly agree’. Mean scores were calculated for each of the items.
Study 5a: randomised controlled trial evaluating the effect of provision of Behaviour Change Technique Taxonomy version 1 on the writing of descriptions
Analysis
Quality of written intervention descriptions (RQ 1a) was assessed by calculating the mean scores for (1) ease of understanding (i.e. clarity of active ingredients and of mode of delivery) and (2) adequacy of information required to undertake a replication (i.e. replicability of active ingredients and of mode of delivery). mean scores were entered as dependent variables in a 2 (video 1 vs. video 2) × 2 (no taxonomy vs. taxonomy) ANOVA.
Identification of BCTs in descriptions (RQ 1b) was assessed by calculating intercoder reliability between the pairs of coders using PABAK. 99 When both coders identified a BCT as present or absent, agreement was recorded and when one coder identified the BCT but the other did not identify the BCT, disagreement was recorded. The number of agreements and disagreements between each pair of coders was recorded and used to calculate PABAK for each description. Calculated PABAK was entered as a dependent variable in a 2 (video 1 vs. video 2) × 2 (no taxonomy vs. taxonomy) ANOVA.
Agreement with expert consensus (RQ 1c) was assessed using PABAK by pairing each coder with the expert consensus coding (see Materials). The number of agreements and disagreements between coders and expert consensus was recorded and used to calculate PABAK for each description. Calculated PABAK was entered as a dependent variable into a 2 (video 1 vs. video 2) × 2 (no taxonomy vs. taxonomy) ANOVA.
Usability and acceptability (RQ 3) was assessed by calculating mean scores to describe writers’ evaluations of (1) sufficiency of time allocated for the task and (2) difficulty of the task. The bipolar adjectives were recoded so that a high score represented a positive evaluation and mean scores were calculated for each of these items. mean scores were calculated to describe writers’ responses to the two statements: ‘if I use BCTTv1 to describe the content of behaviour change interventions, I think: (i) my description will be clear and, (ii) someone will be able to replicate the intervention after reading my description’.
Results
A total of 42 written intervention descriptions were assessed: 18 written by untrained writers using BCTTv1 and 24 written by untrained writers not using BCTTv1. Means and SDs for all dependent variables are summarised in Table 16.
| Study 5a, n = 42 | Study 5b, n = 85 | Study 5c, n = 39 | ||||||
|---|---|---|---|---|---|---|---|---|
| Effect of provision of BCTTv1 (RCT) | Effect of training and provision of BCTTv1 (RCT) | Effect of training and provision of BCTTv1 (within participants) | ||||||
| RQ number | Video number | Condition: untrained + no taxonomy | Condition: untrained + taxonomy | Condition: untrained + no taxonomy | Condition: trained + taxonomy | Untrained + no taxonomy | Trained + taxonomy | |
| 1a | Clarity of active ingredients | 1 and 2 | 0.83 (1.44) | 1.47 (1.18) | 1.76 (0.62) | 0.88 (1.07) | –0.13 (1.20) | 0.64 (1.48) |
| 1 | 1.75 (0.60) | 0.94 (1.40) | 1.71 (0.82) | 0.55 (1.19) | 0.26 (1.09) | 0.83 (1.52) | ||
| 2 | 0.38 (1.53) | 1.90 (0.81) | 1.45 (0.64) | 0.51 (1.23) | –0.53 (1.21) | 0.45 (1.44) | ||
| Clarity of mode of delivery | 1 and 2 | 1.02 (1.37) | 1.53 (1.16) | 1.14 (1.14) | 0.14 (1.09) | –0.17 (1.19) | 0.59 (1.61) | |
| 1 | 1.94 (0.62) | 0.94 (1.18) | 1.00 (1.03) | 0.00 (1.26) | 0.29 (1.14) | 0.68 (1.73) | ||
| 2 | 0.56 (1.42) | 2.00 (0.94) | 0.70 (1.64) | –0.42 (1.05) | –0.63 (1.04) | 0.50 (1.53) | ||
| Replicability of active ingredients | 1 and 2 | 0.69 (1.56) | 1.39 (1.30) | 1.64 (0.76) | 1.02 (0.86) | –0.18 (1.22) | 0.40 (1.50) | |
| 1 | 1.56 (0.42) | 0.87 (1.41) | 1.53 (0.92) | 1.05 (1.09) | 0.16 (1.07) | 0.38 (1.39) | ||
| 2 | 0.25 (1.74) | 1.80 (1.11) | 1.55 (0.69) | 0.81 (0.81) | –0.53 (1.29) | 0.43 (1.63) | ||
| Replicability of mode of delivery | 1 and 2 | 0.69 (1.56) | 1.42 (1.10) | 1.31 (0.88) | 0.47 (1.04) | –0.25 (1.17) | 0.45 (1.47) | |
| 1 | 1.50 (0.71) | 1.00 (1.10) | 1.18 (0.92) | 0.43 (1.20) | 0.11 (1.14) | 0.45 (1.41) | ||
| 2 | 0.28 (1.72) | 1.75 (1.03) | 1.05 (0.93) | 0.28 (1.01) | –0.61 (1.11) | 0.45 (1.56) | ||
| 1b | Reliability of BCT identification (PABAK between trained coders) | 1 and 2 | 0.86 (0.05) | 0.88 (0.05) | 0.84 (0.07) | 0.87 (0.06) | 0.85 (0.06) | 0.86 (0.06) |
| 1 | 0.87 (0.06) | 0.88 (0.06) | 0.84 (0.05) | 0.85 (0.04) | 0.86 (0.06) | 0.85 (0.06) | ||
| 2 | 0.86 (0.05) | 0.88 (0.05) | 0.84 (0.05) | 0.83 (0.09) | 0.85 (0.06) | 0.85 (0.06) | ||
| 1c | Validity of BCT identification (PABAK between trained coders and experienced BCT coders) | 1 and 2 | 0.69 (0.05) | 0.69 (0.06) | 0.67 (0.05) | 0.70 (0.05) | 0.67 (0.06) | 0.66 (0.06) |
| 1 | 0.65 (0.03) | 0.65 (0.07) | 0.66 (0.04) | 0.69 (0.05) | 0.63 (0.04) | 0.61 (0.04) | ||
| 2 | 0.72 (0.04) | 0.70 (0.05) | 0.66 (0.04) | 0.72 (0.05) | 0.72 (0.03) | 0.71 (0.04) | ||
| 2a | Sufficiency of time allocated for task | – | 5.43 (1.74) | 5.56 (1.32) | 6.06 (1.43) | 4.90 (1.41) | 5.36 (1.46) | 4.20 (1.90) |
| Difficulty of writing task | – | 4.71 (0.73) | 4.88 (1.03) | 4.72 (1.27) | 4.30 (1.22) | 5.00 (1.03) | 4.80 (0.68) | |
| Paired adjectives | ||||||||
| Difficult vs. easy | – | 4.25 (0.89) | 3.56 (1.32) | 4.40 (0.89) | 3.75 (1.25) | 3.86 (1.41) | 3.38 (1.31) | |
| Worthless vs. useful | – | 6.50 (0.53) | 6.25 (0.93) | 6.00 (1.00) | 4.70 (2.08) | 6.43 (0.65) | 6.00 (1.43) | |
| Bad vs. good | – | 6.75 (0.46) | 6.25 (0.86) | 6.00 (0.82) | 4.60 (1.98) | 6.29 (0.61) | 6.41 (1.04) | |
| Undesirable vs. desirable | – | 6.50 (0.76) | 5.31 (2.00) | 6.40 (0.89) | 5.85 (1.04) | 5.86 (1.29) | 6.38 (0.71) | |
| Description will be clear | – | 5.70 (1.49) | 5.20 (1.57) | 5.67 (0.52) | 5.68 (1.00) | 6.21 (0.80) | 5.54 (1.35) | |
| Description will be replicable | – | 5.70 (1.83) | 5.07 (1.49) | 5.50 (1.05) | 5.37 (1.26) | 6.07 (0.92) | 5.49 (1.30) | |
Quality of written intervention descriptions (RQ 1a): description quality in terms of clarity of active ingredients [F(1,38) = 0.82; p = 0.37], clarity of mode of delivery [F(1,38) = 0.35; p = 0.56], replicability of active ingredients [F(1,38) = 0.96; p = 0.33] and replicability of mode of delivery [F(1,38) = 1.31; p = 0.26], did not differ significantly for descriptions written by writers using BCTTv1 and for descriptions written by writers not using BCTTv1. There were no interaction effects between being trained and the video described for any of the dependent variables.
Identification of BCTs in descriptions (RQ 1b): agreement between trained coders about the presence/absence of BCTs did not differ significantly for descriptions written by writers using BCTTv1 and for descriptions written by writers not using BCTTv1, F(1,38) = 0.01; p = 0.93. There were no interaction effects between being trained and video F(1,38) = 0.07; p = 0.79.
Agreement with expert consensus (RQ 1c): trained coder agreement with expert consensus was not significantly different for descriptions written by writers using and not using BCTTv1, F(1,38) = 0.25; p = 0.62. There were no significant interaction effects between being trained and video, F(1,38) = 0.70; p = 0.41.
Usability and acceptability (RQ 2): means for sufficiency of time allocated were around the mid-point of the scale both for writers provided with BCTTv1 and for those who were not. Means for perceived difficulty of the writing task were also around the mid-point for both groups of writers. Writers thought that using BCTTv1 to write intervention descriptions was a ‘useful’, ‘good’ and ‘desirable’ concept and that their descriptions would be clear and replicable if the taxonomy were to be used (all means above mid-point of the scale). However, the data for the ‘easy–difficult’ paired adjective item suggest that both groups considered using BCTTv1 as being a difficult task as means were above the mid-point of the scale.
Study 5b: randomised controlled trial evaluating the effect training in, and provision of, Behaviour Change Technique Taxonomy version 1 on the writing of descriptions
Analysis
Analyses were conducted as for study 5a.
Results
A total of 85 written intervention descriptions were assessed; 29 written by untrained writers not using BCTTv1 and 56 written by trained writers using BCTTv1. Means and SDs for all dependent variables are summarised in Table 16.
Quality of written intervention descriptions (RQ 1a): quality, in terms of clarity of active ingredients, clarity of mode of delivery, replicability of active ingredients and replicability of mode of delivery, was judged to be greater for descriptions written by untrained writers not using BCTTv1: clarity of active ingredients [F(1,81) = 16.09; p < 0.001], clarity of mode of delivery [F(1,81) = 14.08; p < 0.001], replicability of active ingredients [F(1,81) = 8.05; p < 0.01], and replicability of mode of delivery [F(1,81) = 9.62; p < 0.005]. There were no interaction effects between being trained and video described for any of the dependent variables.
Identification of BCTs in descriptions (RQ 1b): agreement between trained coders about the absence/presence of BCTs was greater for descriptions written by trained writers using BCTTv1: F(1,81) = 5.02; p < 0.05 (trained: mean = 0.87, SD = 0.06; untrained: mean = 0.84, SD = 0.07). A marginally significant interaction effect was found, suggesting that agreement was greater for descriptions written by trained writers using BCTTv1 about video 2, F(1,81) = 3.59; p = 0.06.
Agreement with expert consensus (RQ 1c): trained coder agreement with expert consensus did not differ significantly for descriptions written by untrained writers not using BCTTv1 and for descriptions written by trained writers using BCTTv1, F(1,81) = 2.84; p = 0.10. There was no significant interaction effects between being trained and video described, F(1,81) = 3.24; p = 0.08.
Usability and acceptability (RQ 2): means for sufficiency of time allocated were above the mid-point of the scale both for writers provided with BCTTv1 and for those who were not. Means for perceived difficulty of the writing task were also above the mid-point for both groups of writers. Writers thought that using BCTTv1 to write intervention descriptions was a ‘useful’, ‘good’ and ‘desirable’ concept and that their descriptions would be clear and replicable if the taxonomy were to be used (all means above mid-point of the scale). However, the data for the ‘easy–difficult’ paired adjective item suggest that both groups considered using BCTTv1 as being a difficult task as means were above the mid-point of the scale.
Study 5c: within-person study of the effect of training in, and provision of, Behaviour Change Technique Taxonomy version 1 on the writing of descriptions
Analysis
The analyses were as for study 5a but using repeated measures ANOVA.
Results
A total of 78 written intervention descriptions were assessed; 39 written before training and 39 written by the same writers following training and using BCTTv1. Means and SDs for all dependent variables are summarised in Table 16.
Quality of written intervention descriptions (RQ 1a): quality, in terms of clarity of active ingredients, clarity of mode of delivery and replicability of mode of delivery was judged to be greater for descriptions written after training using BCTTv1: clarity of active ingredients [F(1,74) = 6.51; p < 0.05], clarity of mode of delivery [F(1,74) = 5.71; p < 0.05], and replicability of mode of delivery [F(1,74) = 5.46; p < 0.05]. For replicability of active ingredients, this was non-significant F(1,74) = 3.57; p = 0.06. There were no interaction effects between being trained and video described for any of the dependent variables.
Identification of BCTs in descriptions (RQ 1b): agreement between coders about the absence/presence of BCTs did not differ significantly for descriptions written before training and after training using BCTTv1, F(1,74) = 0.46; p = 0.50. There were no interaction effects between being trained and video described.
Agreement with expert consensus (RQ 1c): coder agreement with expert consensus was not significantly different for descriptions written before training and after training using BCTTv1, F(1,74) = 1.20; p = 0.28. There were no interaction effects between being trained and video described.
Usability and acceptability (RQ 2): means for sufficiency of time allocated were above the mid-point of the scale both before and after training. Means for perceived difficulty of the writing task were also above the mid-point on both occasions. Writers thought that using BCTTv1 to write intervention descriptions was a ‘useful’, ‘good’ and ‘desirable’ concept and that their descriptions would be clear and replicable if the taxonomy were to be used (all means above mid-point of the scale). However, the data for the ‘easy–difficult’ paired adjective item suggest that on both occasions they considered using BCTTv1 a difficult task as means were above the mid-point of the scale.
A summary of the results from across studies 5a, 5b and 5c is provided in Table 17.
| Measure | Study 5a (RCT of providing taxonomy), n = 42 | Study 5b (RCT of training and taxonomy), n = 85 | Study 5c (within-person study of training and taxonomy, n = 39 | ||
|---|---|---|---|---|---|
| Quality | Clarity of understanding | Active content | n.s. | U > T | T > U |
| Mode of delivery | n.s. | U > T | T > U | ||
| Replicability | Active content | n.s. | U > T | T > U | |
| Mode of delivery | n.s. | U > T | n.s. | ||
| BCT identification | Reliability | n.s. | T > U | n.s. | |
| Validity | n.s. | n.s. | n.s. | ||
| Usability and acceptability | Time | n.s. | n.s. | n.s. | |
| Difficulty | n.s. | n.s. | n.s. | ||
Discussion
In Study 5a, 5b and 5c we investigated the effect of the provision of BCTTv1 alone and training plus BCTTv1, using both randomised and within-participant designs. The results do not show clear benefit of providing BCTTv1 for reporting observed interventions. This is not simply due to lack of power as even Study 5a which had the largest number of writers did not show the benefit of training except for reliability of BCT identification. As Tables 16 and 17 show, the descriptions produced in the trained and/or BCTTv1 condition were only found to perform better than those of the control condition for the reliability of identification of BCTs (study 5b) and for the rated clarity and replicability of the descriptions (study 5c). Even so, the latter results report only a small effect, one that might not be meaningful in practice and could simply be due to practice effects as the trained writing followed the untrained writing. Furthermore, there might have been more room for some writers to improve their writing ability from baseline ability to after training. Baseline scores in study 5c, for example, were much lower than for the comparable group in study 5b.
In contrast, there was evidence of poorer performance among those who had been trained and had access to BCTTv1 than those who received no training and BCTTv1. Untrained writers produced descriptions that were rated to be of higher quality (clarity and replicability) than untrained writers in study 5b, in which participants were randomised and no practice effects were possible. These results were somewhat unexpected and difficult to explain. Although they appear to have made descriptions easier to recognise in one study, they appear to have done the opposite in another. Given the difficulty and uncertainty as to how best to report interventions, one would have expected that a structured and detailed method would have led to consistently improved report writing. There are a number of possible explanations for the results of study 5b:
-
Trained writers completed the task at the end of a workshop and may have been more tired than untrained writers. If so, then one might expect their descriptions to be shorter and less detailed. However, this result was not found in study 5a, in which both groups completed the writing task before the workshop.
-
Alternatively, trained writers may have written longer or more complex descriptions that made it more difficult for coders to identify the distinguishing elements.
-
Trained coders may have concentrated on reporting BCTs and omitted other descriptive elements such as detail about the delivery procedures, which might be more recognisable.
-
The time constraint may have seemed more restrictive for the trained than the untrained writers with the result that their descriptions were less clear. The demands of the task may have seemed especially high to trained writers, expected to implement new knowledge and skill from their training to use the taxonomy with 93 BCTs in addition to reporting the content of a 9-minute video, which was shown only once.
-
Immediately following training, writers may be unable to clearly report all of their ideas about the intervention and may need more time or experience with BCTTv1 to write good descriptions.
-
The training in reporting intervention descriptions using the BCTTv1 may have been insufficient in terms of time and content. Most of the training focused on identifying BCTs from written descriptions and videos; however, only 30 minutes was devoted to how to write sentences about active ingredients using the BCTTv1 with a single task, and no emphasis was placed on the importance of writing down other intervention components, e.g. delivery procedures, alongside the active ingredients.
These explanations can be tested by examining whether or not controlling for the following variables alters the findings: the number of words (explanations 1 and 2), the intelligibility of the text (explanation 2), the number of BCTs identified (explanation 3) and ratings of time pressure and difficulty (explanation 4). Testing explanation 5 would require a longitudinal study and testing explanation 6 would require the development and evaluation of an optimised training package for using the BCTTv1 to report intervention content. These will be investigated in future research.
There were limitations in the design, the measures and the writing task. In terms of design, these studies confounded training condition with time of day, which was inevitable given the resources of the study. This might have been improved by asking participants to write the descriptions at a later date at the same time of day, although this introduces the possibility of further confounders such as additional reading by either group.
In terms of measures, we were seeking quality measures that reflected the likelihood that readers of the descriptions would be able to envisage the intervention in such a way that they felt confident about being able to replicate it. Although there are guidelines which aid the assessment of whether or not intervention components are reported, the standardised measures for assessing the quality of reporting of active ingredients and mode of delivery in intervention descriptions is still developing. 155 Hence, we developed measures of clarity and replicability specifically for studies 5a, 5b and 5c and ensured that active content was rated separately from mode of delivery of the intervention. However, further work needs to be done to establish their psychometric properties. While the use of indices of reliability of BCT identification is an accepted method, assessing validity of BCT identification is less well established. We used consensus following independent judgements by experienced, ‘expert’, coders as our best approximation to a criterion of validity against which judgements could be evaluated.
In terms of the writing task, this was an unusual task and was outside the normal activities involved in intervention development and reporting. The normal practice would not be to describe an intervention after observing it on a video, it would be to describe it after reading and discussion, without a strict time pressure. The task was constrained by the time available within the workshop format and it was also difficult to decide on the appropriate time allowed for completing the task. Nevertheless, participants did not express dissatisfaction with this task in their feedback. However, in retrospect, a better test of BCTTv1 for this purpose would be to investigate whether use of BCTTv1 enhances existing intervention descriptions rather than using it to create descriptions simply from observation. For example, authors of published intervention protocols might be invited to rewrite the intervention description using BCTTv1 and research participants asked to choose the ‘better’ description from each pair of old and new descriptions.
The finding of unexpected negative effects of training is consistent with some of the counterintuitive findings reported in the psychology literature. For example, there is evidence of a paradoxical effect of incentives on skilled performance, described as a ‘choking effect’. 156 Participants under high mental load and in a stressful situation displayed greater levels of physiological stress reaction when asked to relax than participants who were not asked to relax. 157 Furthermore, therapists who participated in a training programme showed unexpected deterioration in skills after training. 158 The authors proposed that this was evidence of a ‘post-training phase in which [participants’] performance actually declined in certain ways as they struggled to naturally integrate new techniques into their existing styles and approaches’. 158 It is possible that the participants in our study similarly responded to the intervention writing task in ways that parallel a choking effect or the post-training effect described in these examples. Hence, it may be that measurable benefits of training occur after a period of integration and practice. Further follow-up research could explore this possibility.
In conclusion, we did not find a clear benefit of providing BCTTv1 for reporting observed interventions. This may be owing to task demands, the nature of the task evaluated, omission of other intervention components, lack of time and experience, or an insufficient training package. Further work is needed to improve its utility in this area. This includes further examination of the data to identify potential reasons for the unexpected findings, testing the utility of BCTTv1 in enhancing existing intervention descriptions, and potential improvements of the training package, such as more detailed guidance for how to use BCTTv1 to report the active content of interventions alongside mode of delivery and a wider range of interactive tasks to train users in reporting good quality descriptions. Further work is also needed to train users in how to use BCTTv1 to report descriptions of newly developed interventions.
Phase 3: supporting use of the taxonomy
Chapter 7 Facilitating application and usability of the Behaviour Change Technique Taxonomy version 1
The developed taxonomy (BCTTv1) lays the foundation for the reliable and systematic specification of BCTs in interventions. It is anticipated that further refinement and development of BCTTv1 will occur as a result of its use and feedback from trainees, researchers, systematic reviewers and practitioners. This chapter outlines the systems that have been put in place to support continued development of the taxonomy and provide ongoing training and support for its users.
Disseminating Behaviour Change Technique Taxonomy version 1 development and project progress
A static website was developed during the BCTTv1 project to serve as an informative repository for taxonomy users: www.ucl.ac.uk/health-psychology/bcttaxonomy. 97 Google (Google Inc., Mountain View, CA, USA) analytic statistics from 2010 to 2013: 820 page views, 173 visits, 127 unique visits. Supplementary to regular newsletters sent to contacts via e-mail, the website provided users with updates on project progress, featured related publications, useful links and advertised forthcoming training opportunities.
Project progress was widely disseminated at national and international conferences. The ‘Theories and Techniques of Behaviour Change’ special interest group was established in 2012 at the Society for Behavioral Medicine annual conference to provide a platform for developers and users to discuss application, usability and future development of BCTTv1. A similar group was formed at the European Health Psychology Conference in 2013. Individual studies from the BCTTv1 project have been published as peer-reviewed journal articles (see Publications). 40,73,96,107
Providing training in use of Behaviour Change Technique Taxonomy version 1
Studies 3 and 4 showed that BCTTv1 offers a generally reliable method for specifying the active ingredients of BCIs when used by trained coders. We recommend that coders already trained in the use of BCTTv1 regularly review training materials and check their own reliability. In order to give coders further practice and experience in applying relevant learning principles to coding BCTs, and in order to train new coders using BCTTv1, we have developed an interactive online training portal: www.bct-taxonomy.com. 103 It is based on the tutorial training model. This includes practice coding tasks with associated feedback, the possibility of structured discussion guided by an expert tutor and access to a social support network to foster continued learning. It trains coders on a greater number of frequently used BCTs than those taught and evaluated in the current study.
Demand for face-to-face training remains high. Since completion of the project, the team have facilitated a further 100 workshops, training approximately 3000 researchers, practitioners and policy-makers.
Increasing accessibility and usability of Behaviour Change Technique Taxonomy version 1
To further increase usability of the taxonomy, a digital version of BCTTv1 as a smartphone and tablet application has been developed. The application is available for download on all mobile platforms (see www.ucl.ac.uk/health-psychology/bcttaxonomy97 for more information). Since launching in early 2014, the app has received 500 downloads via the Google Play™ store and Apple AppSM store (Apple Inc., Cupertino, CA, USA).
Informing future development of Behaviour Change Technique Taxonomy version 1
An interactive system is now being developed within the website to receive feedback from users which will inform development of BCTTv2. Discussions are under way to develop an international consortium to receive, synthesize and disseminate feedback from the use of BCTTv1 across populations, settings, behaviours and countries, and to develop a methodology for BCTTv2.
Chapter 8 General discussion and conclusions
We have outlined the need for a reliable method for specifying the content, or ‘active ingredients’, of BCIs, a difficult task given that they are complex and often involve several interacting techniques. However, such a method is necessary to enable more effective evaluations of intervention effectiveness, improved evidence synthesis and more accurate replication of intervention content in science and delivery.
When this project began, there was widespread and growing use of the taxonomy developed by Abraham and Michie20 and various research groups were developing their own taxonomies for application to different kinds of intervention. Therefore, it was important to co-ordinate this activity to ensure that a proliferation of taxonomies did not create the same ‘Tower of Babel’ as that produced by previous unco-ordinated methods of reporting. In order to achieve this, our starting point was all the published BCT taxonomies (e.g. smoking,27 physical activity and healthy eating,28 excessive alcohol use29 and condom use30), which we then developed into BCTTv1 using a systematic process and involving authors from each of these taxonomies. In order to ensure international input and to build international consensus for the work, a further early step was to invite world experts across a range of countries, disciplines and research areas to join an IAB. A wide range of experts from multiple disciplines and countries were involved throughout the project.
The major output of this work, BCTTv1, is a resource for intervention designers, researchers, practitioners, systematic reviewers and all those wishing to communicate effectively about the content of BCIs. This taxonomy was developed and evaluated in a series of stages involving 400 behaviour change experts. The stages consisted of:
-
initial prototype development
-
a two-round modified Delphi procedure
-
Feedback from the IAB
-
feedback from study team members
-
investigating hierarchical structure within the taxonomy using both an open-sort and a theory-driven methodology
-
developing and evaluating training in the use of BCTTv1 for coding intervention descriptions
-
testing the reliability and validity of using the taxonomy to specify intervention content
-
testing the utility of the taxonomy in reporting intervention descriptions.
This resulted in a hierarchical taxonomy of 93 distinctive, non-overlapping BCTs clustered into 16 groupings, each with a clear label, definition and examples. The value of this resource is demonstrated by the number of people wishing training in its use. To date, we have trained 350 people in eight full- and four half-day workshops and 75 people in group tutorials. Owing to increasing demand, we have launched a free, open-access online training resource and smart phone application to allow easy retrieval of BCTs (see www.ucl.ac.uk/health-psychology/bcttaxonomy/97).
The process of development was intensive, effortful and time-consuming, reflecting its complex nature and the need to achieve broad, international consensus. In effect we were producing a new dictionary and so had to reconcile nuances and ambiguities in the meanings of words to ensure that the BCT labels were understood by all users in the same way. The process involved much iteration through testing, refinement and consultation with 77 users and training 351 coders and writers in the taxonomy to identify BCTs in descriptions and report observed interventions. The amount of work involved should not be underestimated but it has produced BCTTv1, a comprehensive cross-behaviour and consensus-based BCT taxonomy representing significant progress towards a shared language for reliable and accurate description of intervention content.
The large number of distinct BCTs generated, combined with the detail needed to achieve precision in the definitions, raised the need for structure within the taxonomy. The reliability testing revealed that reliable use of BCTTv1 would be enhanced by training in addition to simply publishing BCTTv1 as a list of BCTs for people to use. The following sections discuss the work we did to develop the structure of the taxonomy and a comprehensive training programme, and assess its reliability, validity and usefulness for writing observed interventions.
Creating a structure for Behaviour Change Technique Taxonomy version 1
The recognised need by the BCCTv1 study team and the IAB to produce a structure for BCTTv1 to make it more usable and BCTs easier to find raised several issues. The first was whether to create a theory-driven, top-down structure or whether to create a more pragmatic, bottom-up structure that reflected a shared way of thinking about BCTs among users with different theoretical perspectives and/or disciplinary backgrounds. The general view of the IAB and the study team was that it would be more important to start by adopting a pragmatic, bottom-up structure as it would enable use of the structured taxonomy by users with very different backgrounds and would form a basis for consensus on its use and future development.
The second issue concerned the nature of the groupings produced. Despite not explicitly drawing on theory, the BCT groupings appeared to make theoretical sense. Therefore, we explored the relationship between the obtained structure and an alternative structure generated by people using a simple integrated classification of theoretical constructs. We found moderate overlap between the two structures, suggesting that apparently a theoretical use of BCTs may involve implicit theory.
To increase the applications and impact of BCTTv1, work has begun to establish linkage between BCTs and behaviour change theory in order to increase the BCTTv1’s usefulness for designing theory-based interventions,45 as well as understanding effective interventions in terms of theoretical mechanisms21,24,49,159 testing theory. A large number of theories have been used to explain behaviour change, with a recent review identifying 83. 160,161 Just as developing a consensus list of BCT labels and definitions required intensive work to develop a methodology, so developing a consensus about how BCTs link to theoretical mechanisms will require intensive work to develop a methodology. This work has begun, funded by the UK’s MRC. 138
Coding of behaviour change techniques as a trainable competence
Our experience has shown that a large number of users and potential users wish to undergo formal training in the use of BCTTv1. We showed that both workshop and distance group tutorial training formats increased validity of coding BCTs in intervention descriptions. Although there is room for improvement, we showed that training by either method increased the percentage of trainees achieving an acceptable standard of coding competence as indicated by agreement with expert consensus (75% for tutorials and 45% for workshops). In study 4 (see Chapter 5), a subgroup of trained coders then went on to successfully apply their knowledge and skills to a more extensive coding exercise, achieving good reliability at baseline and at 1 month later. The likely future identification of further BCTs in addition to the already extensive nature of BCTTv1 mean that maintaining reliability and accuracy in using the taxonomy becomes more challenging. Data from the training evaluation and trainee feedback have informed the development of an open-access, online assessment and training course based on our tutorial training model96 (see Chapter 4, Methods; see www.ucl.ac.uk/health-psychology/bcttaxonomy/97). As face-to-face training, delivered either in a 1-day workshop or distance group tutorial format, is labour intensive for the trainers, the study team has been unable to meet the demand from users wanting to be trained. The online training course will allow new users to develop BCT coding competence and will allow experienced users to upgrade their skills and assess their level and pattern of competence. This remains to be evaluated and we are not yet in a position to offer training or assessment of skills in using BCTTv1 to report intervention descriptions.
Reporting interventions
We expected that training in BCTTv1 would lead to better, that is clearer, more readily replicable and more recognisable intervention descriptions. This is not what we found. Our training was as likely to make the descriptions worse as it was to improve them, although it was limited to the context of reporting interventions for which the only source of information was watching a brief video. Therefore, although the findings of our studies did not support the added value of using BCTTv1 in reporting observed interventions, the nature of the task was rather artificial and so probably not a good test. Therefore, we can make no recommendations for using the BCTTv1 at this stage and further research to investigate this is urgently needed.
However, we continue to think that this is an important objective and, as indicated in Chapter 6, there are certain avenues that we would wish to explore to achieve a better understanding of the results we obtained. There are issues to do with the design, the assessment measures and the training package we used, but perhaps a key issue is the nature of the reporting task we used. While the task involved reporting an intervention, it is not a task that would normally be undertaken in either a practice or a research setting. We would not normally produce a description of an intervention after observing it, unless it is an existing intervention in clinical practice or policy settings and no manual or protocols are available. We would be much more likely to write an intervention description before its delivery (i.e. for inclusion in the study protocol) and once intervention delivery has been completed (i.e. when reporting for evaluation and publication). In retrospect, a better test of BCTTv1 for this purpose would be to investigate whether use of BCTTv1 enhances existing intervention descriptions rather than using it to create descriptions simply from observation, or whether it enhances intervention reporting after trainees have had the opportunity to integrate the taxonomy into their normal reporting style. For example, authors of published intervention protocols or existing manuals routinely used in clinical practice or policy settings might be invited to rewrite the intervention description using BCTTv1 and research participants asked to choose the ‘better’ description from each pair of old and new descriptions.
Strengths and limitations
The work conducted in this series of studies represents a step-change in the methodology for reporting the content of BCIs. However, it also has limitations in both the methods used and the product. Constraints in terms of both time and financial resources meant that recruitment was conducted via known networks and contacts, with the result that the 400 people involved in the work were predominantly from Europe and the USA, with only a sprinkling from countries beyond this. There was also an unevenness of disciplines involved in the work, the majority being psychologists. Whilst psychologists are likely to be familiar with behaviour change concepts and therefore likely to be relatively easy to train to use the taxonomy, its wide application will require usability across a range of backgrounds and expertise. We engaged one lay participant in the study to check comprehensibility of materials. Future work should extend this to a wider range of lay perspectives and to engagement with dissemination as well as development activities.
The aim of the work was to develop and evaluate the usefulness of the BCT approach to specifying interventions, that is demonstrate ‘proof of principle’ rather than to produce a finished product and training programme. In fact, when we designed the studies we had not envisaged developing a training programme; the need for this emerged as the size of the taxonomy emerged. Given resource constraints, we decided to train participants in 24 of the most common of the 93 BCTs, as this would be likely to be most useful and familiar to them and, therefore, likely to be learned most quickly. It may be that the less-familiar BCTs are more difficult to teach to the competence criteria and would need more intensive and longer training than was provided in this project.
The training was four distance group tutorials, which is substantially less than the training that the authors’ research groups used when applying precursor taxonomies. Although this is sufficient to train the principles underlying the use of the taxonomy and to get an acceptable degree of inter-rater reliability and agreement with expert judgements, our findings show that more training is required to become expert in using the method. To make the methodology as accessible as possible, we developed an e-learning programme based on our tutorial materials and methods. 103 However, we consider that this programme, and 1-day workshops, are good introductions but unlikely, on their own, to bring participants to the level of expertise required for research and implementation. Further, coding BCTs alongside another independent coder will allow discrepancies to be identified and accuracy to be improved.
More widespread use of BCTTv1 is likely to identify ambiguities or uncertainties about labels, definitions and examples, and ways in which they can be improved. Although we are gathering this information where we can via the online training and the study website, we recognise that we require an international consortium to systematically gather and review user feedback, draw in a wider group of users, and oversee the development and refinement of BCTTv2 in a few years. This will include a detailed and transparent log of all changes with their rationales. This approach will allow the international research community to move forward in a co-ordinated fashion, which will maximise communication between groups of users and the efficiency and effectiveness with which new evidence is generated.
As mentioned earlier, there were limitations in the methods used in study 5 that limit our confidence in the findings. We aimed to evaluate BCTTv1 for writing intervention descriptions and used a variety of study designs to do this, gathering data from training workshops. We decided to show participants the intervention in video form so that we did not cue them with the written word. However, taking in detailed information about an intervention by watching an intervention is not something participants were experienced in doing. Additionally, the time pressure of the workshops meant that the videos were very brief and there was not time to show them more than once (which many participants requested). In retrospect, this experimental paradigm was probably too artificial and implemented too hastily for it to have been a good basis for the evaluation. Intervention descriptions usually emerge from reading and discussions, and a better evaluation would be to investigate the impact on this process of using BCTTv1. Given the challenge of control conditions, it is likely that future studies will seek to involve large groups of naive participants, that is those who are new to designing BCIs (e.g. students). An alternative approach, as mentioned earlier, would be to investigate intervention description enhancement than intervention descriptions de novo.
Implications for using Behaviour Change Technique Taxonomy version 1 in evidence synthesis and primary studies
Although BCTTv1 provides a means of characterising intervention content to facilitate intervention implementation, delivery and evaluation, and it is also useful for synthesising evidence. It allows both intervention and control conditions to be coded in terms of BCTs which allows the identification of the BCTs that were used in the intervention over and above those used in the control or usual-care conditions. For example, de Bruin et al. 162 found that by coding control conditions, it was possible not only to explain differences in outcomes between conditions but it was also possible to explain variation in outcomes in control conditions. The key point here is that many active controls such as ‘usual care’ involve implementation of multiple BCTs, overlapping with those that constitute the intervention itself.
Behaviour change technique methodology is a starting point for investigating the effectiveness of single BCTs and the combinations of BCTs that typically characterise interventions in evidence synthesis. It is also a starting point for investigating how other factors, such as mode of delivery, intervention intensity, target behaviour, target population and context, may make BCTs more or less effective. 163–165 However, given the typically small number of studies that have used any particular BCT and potential influence of confounders, there are limits to this methodology. Meta-analyses lack power to test the effectiveness of most BCTs, as was evident in the National Institute for Health and Care Excellence (NICE) 2014 Behaviour Change guidance which used BCT methodology. 166 Therefore, it is important to be careful not to conclude that a BCT is ineffective when the conclusion should be that there is insufficient evidence to test for effectiveness. However, the importance of BCT methodology for advancing the field is reflected in the research recommendations within NICE’s Behaviour Change Guidance. 167 NICE recommend that research should seek to investigate which combinations of BCTs and which modes of delivery are effective and cost-effective in (1) changing behaviour and (2) in maintaining behaviour change. They recommend seeking to determine how effectiveness varies among people from different sociodemographic backgrounds, those with different skill sets, levels of motivation or with access to different information. Finally, research should include studies that build the evidence base on the effectiveness of each BCT, e.g. using experimental and meta-analytic work to clarify which BCTs work when and for whom.
Investigating behaviour change technique combinations in evidence synthesis and experimental studies
There are several examples of meta-analyses which have investigated both individual BCTs and combinations of BCTs that theory predicts would work synergistically together. 21,24,49,168,169 For example, in reviews of interventions to increase physical activity and healthy eating, Michie et al. 24 and Dombrowski et al. 21 investigated a combination of BCTs predicted by control theory170 and found similar results in two different populations. They found that interventions with the combination of self-monitoring, goal-setting and action planning were twice as effective as those that were not. A similar analytic approach was used to investigate audit and feedback interventions168 in a recent Cochrane review,49 finding that adding the BCTs of goal-setting and action planning to interventions increased the effect of feedback. The theoretically based combination of BCTs associated with provision of information, increasing motivation and enhancing behavioural skills171 has been found to reduce the frequency of sexual interactions that increase health risk. 169
An alternative method of combining BCTs is to use CARTs, referred to as Meta-CART,39 to analyse meta-analytic data. This has been used to identify groups of BCTs to predict intervention effects in a reanalysis of data from Michie et al. 23 Results showed that providing information about the links between behaviour and health was effective if combined with either setting goals or with providing information on the consequences of the behaviour and using follow-up prompts.
Very brief interventions offer a pragmatic context in which to test whether specific BCTs add to or dilute intervention effectiveness as they tend to include only a small number of BCTs. Such work is being conducted as part of a research programme into very brief interventions to promote physical activity in primary care. 172 A similar programme of research, supported by a meta-analysis,173 has identified BCTs in very brief advice interventions to promote smoking cessation. 174
With increasingly sophisticated designs, experimental methods can begin to unpack the ‘black box’ of complex interventions. For example, Collins et al. 175 have proposed an experimental paradigm, known as the MOST approach (the Multiphase Optimisation Strategy approach) that tests combinations of BCTs as a basis for optimising interventions. Using fractional factorial designs, they advocate selecting combinations of BCTs for testing based on both theory and accumulated evidence. These methods have the advantage that they not only provide evidence of effective combinations, but they also efficiently test theoretical propositions about the synergistic effects of constructs.
Behaviour change techniques and theory
Behaviour change techniques are technologies and in themselves are agnostic with regard to the role of theories. In most cases, there is no attempt to link specific BCTs to theoretical mechanisms. For example, a meta-analysis of 190 interventions to increase physical activity and healthy eating interventions found that 56% of studies claimed the interventions were based on a theory. 58 However, 90% of these did not report links between all of the BCTs and specific theoretical constructs. 58 When links are made, this is usually the result of the researchers’ judgement rather than being based on evidence, pilot work or a systematic methodology of establishing this. Establishing links between BCTs and theoretical constructs (their mechanisms of action) is a much needed step to advance the science of behaviour change. It is needed to translate theory into intervention design,43,45,161 to explain effective interventions in terms of their theoretical mechanisms,21,24,49,159 to aid practitioners and policy-makers in selecting effective BCTs to target specific behaviours, and to test theory. A large number of theories have been used to explain behaviour change, with a cross-disciplinary review identifying 83. 160,176 Just as developing a consensus list of BCT labels and definitions required intensive work to develop a methodology, so developing a consensus about how BCTs link to theoretical mechanisms will require intensive work to develop a methodology. Developing a consensus-based methodology to establish BCT theory links is the aim of a follow-up study to the current BCT study, funded by UK’s MRC (Michie S, Carey R, Johnston M, Rothman A, Kelly M, de Bruin M, et al. University College London, 2015, personal communication). This forms the basis of a larger programme of work, developing a Behaviour Change Ontology identifying the links between five levels of intervention characteristic: target behaviours, BCTs, theoretical mechanisms, modes of delivery and contexts. Given the enormity and complexity of the task, this requires collaboration between behavioural and computer scientists. By using computational machine learning methods of literature interrogation and data mining, it is possible to develop a virtual rapid learning environment to (1) optimise BCIs in the real world and (2) create an updatable open source intervention library for users to identify which combinations of intervention characteristics are most relevant to, and likely to be most effective for, their own behavioural targets and contexts.
Behaviour change techniques, replication and implementation
Given that published reports and existing manuals can effectively be coded into BCTs, there are likely to be benefits of using BCT methodology. These include intervention development, evidence synthesis, assessing and improving the replication of interventions within scientific investigation and the faithful delivery of interventions and treatments in practice. Behavioural interventions to increase fidelity of intervention delivery have the potential to bring about as great, or greater, health gains than medical advances on their own. 177 The importance of scientific journals ensuring that intervention content is well specified for replication and implementation has been recognised across the research community. 15 At least two journals have editorial policies stating that trials of interventions will only be published if the interventions are described in sufficient detail for replication and implementation, citing BCT methodology as an example. 10,178 Guidance by funding bodies would also support the adoption of BCT methodology for specifying and reporting BCIs.
There is ample evidence from reviews and primary studies that intervention protocols are often implemented with insufficient fidelity. 12,179–182 For example, in an intervention to increase physical activity among sedentary adults at risk of type 2 diabetes mellitus delivered by trained and quality-assured facilitators, 58% of BCTs specified in the intervention protocol were not faithfully delivered. 182 This was particularly the case for BCTs directed at maintenance of behaviour change. 183 Coding the delivery of BCTs using observations, audio or video recordings, of interventions allows researchers and practitioners to find out how many of the intervention’s proposed active ingredients are actually delivered. Such information can be used to improve the training of those who deliver interventions and their long-term implementation. It also aids the interpretation of trial results, e.g. the extent to which any lack of effects is due to the intervention itself or poor fidelity of delivery. BCTTv1 may also be used to inform the development of measures for assessing delivery of BCTs. 31
Behaviour change techniques and designing interventions
Having access to the 93 BCTs of BCTTv1 allows intervention designers to consider a large range of BCTs that might be effective and appropriate for their target behaviour and population. An example of a step-by-step guide for designing BCIs incorporating BCTs is The Behaviour Change Wheel: A Guide to Designing Interventions. 161 It links BCTs to intervention functions with the behaviour change wheel framework and to the 14 theoretical domains of the TDF. Intervention designers are encouraged to start their selection of BCTs by conducting a ‘behavioural diagnosis’ of the problem at hand. Because 93 BCTs are likely to be too many to easily work with, we recommend starting with a minimum set composed of the 22 frequently occurring BCTs and/or those shown to be effective in the specific area under investigation. These 22 found to frequently occur in 40 intervention descriptions include 18 of the 22 BCTs including in the Abraham and Michie taxonomy20 based on more than 200 intervention descriptions. Nevertheless, coders in study 4 used 80 BCTs to describe the 40 intervention descriptions and it may therefore be important to expand from the initial 22 BCTs to fully specify the intervention. Another issue is whether or not to use the earlier, shorter taxonomies that have been developed for specific behavioural domains,23,27,29,30 given that these BCTs will have high relevance and include the frequently occurring BCTs for that domain. This needs to be balanced with the potential problem that the scientific study of behaviours sometimes occurs in ‘silos’ so that one may miss potentially effective BCTs that are used in other behaviours. For example, ‘behavioural substitution’ was identified from a systematic review of brief alcohol interventions,29 but this effective BCT had not been identified in several reviews of physical activity, healthy eating and smoking cessation interventions, e.g. Carroll et al. 183 A second limitation of sticking with behaviour domain taxonomies is that it limits generalisation of all potential BCTs across behaviours and, therefore, the possibility of generating general models of behaviour change or investigating ways in which BCTs influence different behaviours. Finally, in contrast to earlier taxonomies, BCTTv1 was developed using robust methods and is based on expert consensus, and BCTs in earlier taxonomies (e.g. motivational interviewing) were removed from BCTTv1 as they did not meet the definition of a BCT.
Need for maintenance and updating
The overarching aim of developing BCTTv1 was to maximise the co-ordinated building of evidence and hence the rate at which we can develop more effective BCIs to improve health and well-being, and quality of health care. The aim is to achieve maximum consensus across disciplines, topic areas and countries in order to synthesise and share evidence more efficiently across them. BCTTv1 was termed v1 for a purpose. As BCTTv1 is applied to a wider range of populations, settings and behaviours, adaptations of language and possibly concepts will be needed and new BCTs will be identified. Wider application also involves delivering interventions at different ‘levels’ (e.g. individual, community, organisational, population), as illustrated in Table 18. As BCTTv1 is used to design and specify the content of interventions across wider ranges of delivery modes and contexts, it is likely that additional BCTs will be identified.
| BCT | Target behaviour | Mode of delivery |
|---|---|---|
| 5.1. Information about health consequences | Sedentary behaviours | Via GP/clinician |
| Posters: in health care or public settings | ||
| TV advertisements | ||
| Notices by stairs or elevators | ||
| 7.1. Prompts/cues | Smoking | Via GP/clinician |
| Posters | ||
| TV advertisements | ||
| Smoking ban | ||
| Sale of electronic cigarettes |
Therefore, we need an international consortium, appropriately resourced, to monitor and collate experiences, adaptations and findings so that BCTTv2 can be developed and released. The timing of this will depend on judgement: balancing the needs for stability and accumulation of evidence using a shared method with the weight of evidence of need for refinement and extension. Discussions are under way with international funding agencies to achieve this.
Final conclusion
The BCTTv1 is a technological advance that represents a step change in the translation of behavioural science into practice and in strengthening the science itself. Like all technologies, its usefulness will be determined by its application and dissemination by researchers, those designing and delivering interventions, funding agencies, journal editors and policy-makers.
Recommendations
The findings from this programme of research point to several recommendations for practice and future research. These are listed below in priority order, starting with the highest priority.
Recommendations for practice:
-
Characterising interventions – to facilitate accuracy, ease and speed of applying BCTTv1 to characterising intervention content, we recommend that users start their coding or other task (e.g. evidence synthesis, reporting interventions) with the list of the 22 most frequent BCTs (see Table 12). If behaviour-specific taxonomies are used, we suggest supplementing them with additional BCTs from BCTTv1.
-
Intervention design – we recommend considering the full range of BCTs in BCTTv1 in the design process, with selection of BCTs guided by theoretical and pragmatic criteria (see the behaviour change wheel guide161).
-
Evidence synthesis – BCTTv1 should be used to specify BCTs in both the active and the control arms of the evaluation trial. The effects of combinations of BCTs can be investigated, e.g. by theoretically informed metaregression and/or Meta-CART analyses.
-
Implementation – to assess and improve implementation (i.e. delivery that is faithful to the protocol), those reporting interventions should specify the content in terms of BCTs and assess delivery, using reliable methodology.
Recommendations for research:
-
Structure of BCTTv1 – a consensus concerning the linkages between BCTs and behaviour change theory is needed to increase BCTTv1’s usefulness for designing theory-based interventions, understanding interventions and testing theory. Work is already under way to address this need (Michie S, Carey R, Johnston M, Rothman A, Kelly M, de Bruin M, et al. University College London, 2015).
-
Reporting interventions – further research is needed to understand the potential usefulness of using BCTTv1 to report BCIs.
-
Understanding effects of BCTs – we recommend that systematic reviews with meta-analyses are developed for each BCT (for those which this has not already been done), starting with the most frequent BCTs.
-
User training – we recommend that further research is needed to evaluate user training, for all 93 BCTs in BCTTv1. This will help to increase understanding as to which BCTs require more/less training and will inform improvement of future training programmes.
-
BCTTv2 – precise documentation of the adaptations of BCTTv1 for specific settings, behaviours and populations is required to inform the development of BCTTv2.
Acknowledgements
This research was funded by the MRC via its Methodology Panel: ‘Strengthening evaluation and implementation by specifying components of behaviour change interventions’ Ref: G0901474/1. 17 We thank the 30 members of our IAB (see Appendix 2) who gave invaluable advice at strategic points during the project and the 36 experts from across the world who took part in the Delphi and coding exercises which provided the key data for developing BCTTv1. We are also grateful to Felicity Roberts (FR), Kate Sheals (KS), Linda Duffy and Elena Panagiotopoulou for their previous work on the project and help, especially with proofing early versions of the taxonomy and with coding; to Professor Tania Huedo-Medina, Department of Statistics, University of Connecticut, CT, USA, for sharing her AC1 calculator with us; and to Michelle Richardson (MR) for her previous work on the project. Finally, we thank Martin Eccles, a coapplicant on the proposal, for his invaluable contribution in developing the proposal and to the early stages of the research, before his retirement from his academic post.
Contributions of authors
Susan Michie (Professor of Health Psychology and principal investigator) and Marie Johnston (Professor of Health Psychology) led the development of the research proposal and protocol.
Susan Michie, Caroline E Wood and Marie Johnston wrote the first draft of this monograph.
Marie Johnston, Caroline E Wood and Charles Abraham conducted statistical analyses for studies 3, 4 and 5a, 5b, 5c.
Wendy Hardeman and Jill Francis contributed to the development of the study proposal, overseeing the studies and writing the final monograph.
All authors contributed to the development of the study proposal, overseeing of the studies and the writing of the final monograph.
Contribution of others
Statistical analyses for each of the studies were carried out as follows: study 1 by Michelle Richardson (Senior Research Fellow); study 2 by Ruhina Lahda (Research Assistant), James Cane (Lecturer; Senior Research Fellow) and Michelle Richardson; study 3 by Caroline Wood (Senior Research Associate); study 4 by Caroline Wood and Charles Abraham (Professor of Health Psychology); and studies 5a, 5b and 5c by Caroline Wood and Marie Johnston. Statistical guidance was provided by Beth Pollard (Statistical Expert).
Publications
Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behaviour change interventions. Ann Behav Med 2013;46:81–95.
Cane J, Richardson M, Johnston M, Lahda R, Michie S. From lists of behaviour change techniques (BCTs) to structured hierarchies: comparison of two methods of developing a hierarchy of BCTs. Br J Health Psychol 2015;20:130–50.
Wood CE, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. Applying the Behaviour Change Technique (BCT) Taxonomy v1: a study of user training. Transl Behav Med 2014;5:134–48.
Abraham C, Wood CE, Johnston M, Francis J, Hardeman W, Richardson M, et al. Reliability of identification of behavior change techniques in intervention descriptions. Ann Behav Med 2015 [published online ahead of print 20 August 2015].
Data sharing statement
All available data can be obtained from the corresponding author of this report.
Disclaimers
This report presents independent research funded under a MRC–NIHR partnership. The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, the MRC, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, the MRC, NETSCC, the HTA programme or the Department of Health.
References
- Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2095-128. http://dx.doi.org/10.1016/S0140-6736(12)61728-0.
- Murray C, Richards M, Newton J, Fenton K, Anderson H, Atkinson C, et al. UK health performance: findings of the Global Burden of Disease Study 2010. Lancet 2013;381:997-1020. http://dx.doi.org/10.1016/S0140-6736(13)60355-4.
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA 2004;291:1238-45. http://dx.doi.org/10.1001/jama.291.10.1238.
- Behaviour Change: The Principles for Effective Interventions (PH6). London: NICE; 2007.
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337.
- Michie S, van Stralen M, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6. http://dx.doi.org/10.1186/1748-5908-6-42.
- Rothman A. ‘Is there nothing more practical than a good theory?’: why innovations and advances in health behavior change will arise if interventions are used to test and refine theory. Int J Behav Nutr Phys Act 2004;1. http://dx.doi.org/10.1186/1479-5868-1-11.
- Michie S, Johnston M. Theories and techniques of behaviour change: developing a cumulative science of behaviour change. Health Psychol Rev 2012;6:1-6. http://dx.doi.org/10.1080/17437199.2012.654964.
- Davidson K, Goldstein M, Kaplan R, Kaufmann P, Knatterud G, Orleans C, et al. Evidence-based behavioral medicine: what is it and how do we achieve it?. Ann Behav Med 2003;26:161-71. http://dx.doi.org/10.1207/S15324796ABM2603_01.
- Michie S, Fixsen D, Grimshaw J, Eccles M. Specifying and reporting complex behaviour change interventions: the need for a scientific method. Implement Sci 2009;4. http://dx.doi.org/10.1186/1748-5908-4-40.
- Hoffmann T, English T, Glasziou P. Reporting of interventions in randomised trials: an audit of journal instructions to authors. Trials 2014;15. http://dx.doi.org/10.1186/1745-6215-15-20.
- Lorencatto F, West R, Christopherson C, Michie S. Assessing fidelity of delivery of smoking cessation behavioural support in practice. Implement Sci 2013;8. http://dx.doi.org/10.1186/1748-5908-8-40.
- Moher D, Schulz K, Altman D. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Clin Oral Investig 2003;7:2-7.
- Des Jarlais D, Lyles C, Crepaz N. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health 2004;94:361-6. http://dx.doi.org/10.2105/AJPH.94.3.361.
- Albrecht L, Archibald M, Arseneau D, Scott SD. Development of a checklist to assess the quality of reporting of knowledge translation interventions using the Workgroup for Intervention Development and Evaluation Research (WIDER) recommendations. Implement Sci 2013;8. http://dx.doi.org/10.1186/1748-5908-8-52.
- Hoffmann T, Glasziou P, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:1-13. http://dx.doi.org/10.1136/bmj.g1687.
- Michie S, Abraham C, Eccles MP, Francis JJ, Hardeman W, Johnston M. Strengthening evaluation and implementation by specifying components of behaviour change interventions: a study protocol. Implement Sci 2011;6. http://dx.doi.org/10.1186/1748-5908-6-10.
- Hardeman W, Griffin S, Johnston M, Kinmonth A, Wareham N. Interventions to prevent weight gain: a systematic review of psychological models and behaviour change methods. Int J Obes (Lond) 2000;24:131-43. http://dx.doi.org/10.1038/sj.ijo.0801100.
- Albarracín D, Gillette JC, Earl AN, Glasman LR, Durantini MR, Ho M-H. A test of major assumptions about behavior change: a comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychol Bull 2005;131:856-97. http://dx.doi.org/10.1037/0033-2909.131.6.856.
- Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol 2008;27:379-87. http://dx.doi.org/10.1037/0278-6133.27.3.379.
- Dombrowski SU, Sniehotta FF, Johnston M, Broom I, Kulkarni U, Brown J, et al. Optimizing acceptability and feasibility of an evidence-based behavioral intervention for obese adults with obesity-related co-morbidities or additional risk factors for co-morbidities: an open-pilot intervention study in secondary care. Patient Educ Couns 2012;87:108-19. http://dx.doi.org/10.1016/j.pec.2011.08.003.
- Quinn J, Johnston M, Johnston DW. Testing an integrated behavioural and biomedical model of disability in N-of-1 studies with chronic pain. Psychol Health 2013;28:1391-406. http://dx.doi.org/10.1080/08870446.2013.814773.
- Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol 2009;28:690-701. http://dx.doi.org/10.1037/a0016136.
- Michie S, Jochelson K, Markham W, Bridle C. Low-income groups and behaviour change interventions: a review of intervention content, effectiveness and theoretical frameworks. J Epidemiol Community Health 2009;63:610-22. http://dx.doi.org/10.1136/jech.2008.078725.
- Araujo-Soares V, McIntyre T, MacLennan G, Sniehotta FF. Development and exploratory cluster-randomised opportunistic trial of a theory-based intervention to enhance physical activity among adolescents. Psychol Health 2009;24:805-22. http://dx.doi.org/10.1080/08870440802040707.
- Cahill K, Moher M, Lancaster T. Workplace interventions for smoking cessation. Cochrane Database Syst Rev 2008;4. http://dx.doi.org/10.1002/14651858.cd003440.pub3.
- Michie S, Hyder N, Walia A, West R. Development of a taxonomy of behaviour change techniques used in individual behavioural support for smoking cessation. Addict Behav 2011;36:315-19. http://dx.doi.org/10.1016/j.addbeh.2010.11.016.
- Michie S, Ashford S, Sniehotta F, Dombrowski S, Bishop A, French D. A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health 2011;26:1479-98. http://dx.doi.org/10.1080/08870446.2010.540664.
- Michie S, Whittington C, Hamoudi S, Zarnani F, Tober G, West R. Identification of behaviour change techniques to reduce excessive alcohol consumption. Addiction 2012;107:1431-40. http://dx.doi.org/10.1111/j.1360-0443.2012.03845.x.
- Abraham C, Good A, Huedo-Medina T, Warren M, Johnson B. Reliability and utility of the SHARP taxonomy of behaviour change techniques. Psychol Health 2012;27:1-2.
- Lorencatto F, West R, Bruguera C, Michie S. A method for assessing fidelity of delivery of telephone behavioral support for smoking cessation. J Consult Clin Psychol 2014;82:482-91. http://dx.doi.org/10.1037/a0035149.
- Michie S, Churchill S, West R. Identifying evidence-based competencies required to deliver behavioural support for smoking cessation. Ann Behav Med 2011;41:59-70. http://dx.doi.org/10.1007/s12160-010-9235-z.
- Dixon D, Johnston M. Health Behavior Change Competency Framework: Competences to Deliver Interventions to Change Lifestyle Behaviors That Affect Health. Edinburgh: NHS Scotland; 2012.
- West R, Michie S. Carbon monoxide verified 4-week quit rates in the English Stop Smoking Services before versus after establishment of the National Centre for Smoking Cessation and Training. Smok Br 2013;1:1-5.
- NCSCT . National Centre for Smoking Cessation and Training n.d. www.ncsct.co.uk (accessed 6 July 2015).
- Abraham C, Abraham C, Kools M. Writing Health Communication: An Evidence-Based Guide. London: SAGE Publications Ltd.; 2012.
- Stavri Z, Michie S. Classification systems in behavioural science: current systems and lessons from the natural, medical and social sciences. Health Psychol Rev 2012;6:113-40. http://dx.doi.org/10.1080/17437199.2011.641101.
- de Bruin M, Viechtbauer W. The meaning of adherence when behavioral risk patterns vary: obscured use- and method-effectiveness in HIV-prevention trials. PLOS One 2012;7. http://dx.doi.org/10.1371/journal.pone.0044029.
- Dusseldorp E, van Genugten L, van Buuren S, Verheijden MW, van Empelen P. Combinations of techniques that effectively change health behavior: evidence from Meta-CART analysis. Health Psychol 2014;33:1530-40. http://dx.doi.org/10.1037/hea0000018.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95. http://dx.doi.org/10.1007/s12160-013-9486-6.
- Glasziou P, Meats E, Heneghan C, Shepperd S. What is missing from descriptions of treatment in trials and reviews?. BMJ 2008;336:1472-4. http://dx.doi.org/10.1136/bmj.39590.732037.47.
- McCleary N, Duncan EM, Stewart F, Francis JJ. Active ingredients are reported more often for pharmacologic than non-pharmacologic interventions: an illustrative review of reporting practices in titles and abstracts. Trials 2013;14. http://dx.doi.org/10.1186/1745-6215-14-146.
- Michie S, Johnston M, Francis J, Hardeman W, Eccles M. From theory to intervention: mapping theoretically derived behavioural determinants to behaviour change techniques. Appl Psychol 2008;57:660-80. http://dx.doi.org/10.1111/j.1464-0597.2008.00341.x.
- Morton K, Beauchamp M, Prothero A, Joyce L, Saunders L, Spencer-Bowdage S, et al. The effectiveness of motivational interviewing for health behaviour change in primary care settings: a systematic review [published online ahead of print 2014]. Health Psychol Rev 2015;9:205-23. http://dx.doi.org/10.1080/17437199.2014.882006.
- Michie S, Johnston M, Francis J, Hardeman W. Behaviour Change Interventions: Developing a Classification System 2005.
- West R, Walia A, Hyder N, Shahab L, Michie S. Behavior change techniques used by the English Stop Smoking Services and their associations with short-term quit outcomes. Nicotine Tob Res 2010;12:742-7. http://dx.doi.org/10.1093/ntr/ntq074.
- West R, Evans A, Michie S. Behavior change techniques used in group-based behavioral support by the English stop-smoking services and preliminary assessment of association with short-term quit outcomes. Nicotine Tob Res 2011;13:1316-20. http://dx.doi.org/10.1093/ntr/ntr120.
- Dombrowski SU, Sniehotta FF, Avenell A, Johnston M, MacLennan G, Araújo-Soares V. Identifying active ingredients in complex behavioural interventions for obese adults with obesity-related co-morbidities or additional risk factors for co-morbidities: a systematic review. Health Psychol Rev 2010;6:7-32. http://dx.doi.org/10.1080/17437199.2010.513298.
- Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev 2012;6. http://dx.doi.org/10.1002/14651858.cd000259.pub3.
- University College London . The Behaviour Change Technique Taxonomy Project. Collaborators n.d. www.ucl.ac.uk/health-psychology/bcttaxonomy/collaborators (accessed 6 July 2015).
- Pill J. The Delphi method: Substance, context, a critique and an annotated bibliography. Socio Econ Plan Sci 1971;5:57-71. http://dx.doi.org/10.1016/0038-0121(71)90041-3.
- Vandenbos G. APA Dictionary of Psychology. Washington, DC: American Psychological Association; 2006.
- Michie S, Johnston M. Changing clinical behaviour by making guidelines specific. BMJ 2004;328:343-5. http://dx.doi.org/10.1136/bmj.328.7435.343.
- Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychological Association; 2000.
- ICD-10 International Statistical Classification of Diseases and Related Health Problems. Geneva, Switzerland: World Health Organization; 1992.
- Taylor N, Conner M, Lawton R. The impact of theory on the effectiveness of worksite physical activity interventions: a meta-analysis and meta-regression. Health Psychol Rev 2012;6:33-7. http://dx.doi.org/10.1080/17437199.2010.533441.
- Webb T, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res 2010;12. http://dx.doi.org/10.2196/jmir.1376.
- Prestwich A, Sniehotta F, Whittington C, Dombrowski S, Rogers L, Michie S. Does theory influence the effectiveness of health behavior interventions? Meta-analysis. Health Psychol 2014;33:465-74. http://dx.doi.org/10.1037/a0032853.
- Davies P, Walker AE, Grimshaw JM. A systematic review of the use of theory in the design of guideline dissemination and implementation strategies and interpretation of the results of rigorous evaluations. Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-14.
- Hobbs L, Campbell R, Hildon Z, Michie S. Behaviour Change Theories Across Psychology, Sociology, Anthropology and Economics: A Systematic Review. Crete: Conference presentation given at 25th Annual Conference of the European Health Psychology Society; 2011.
- Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012;7. http://dx.doi.org/10.1186/1748-5908-7-37.
- Francis J, O’Connor D, Curran J. Theories of behaviour change synthesised into a set of theoretical groupings: introducing a thematic series on the theoretical domains framework. Implement Sci 2012;7. http://dx.doi.org/10.1186/1748-5908-7-35.
- Amemori M, Michie S, Korhonen T, Murtomaa H, Kinnunen TH. Assessing implementation difficulties in tobacco use prevention and cessation counselling among dental providers. Implement Sci 2011;6. http://dx.doi.org/10.1186/1748-5908-6-50.
- Beenstock J, Sniehotta FF, White M, Bell R, Milne EM, Araujo-Soares V. What helps and hinders midwives in engaging with pregnant women about stopping smoking? A cross-sectional survey of perceived implementation difficulties among midwives in the North East of England. Implement Sci 2012;7. http://dx.doi.org/10.1186/1748-5908-7-36.
- Bussieres AE, Patey AM, Francis JJ, Sales AE, Grimshaw JM, Brouwers M, et al. Identifying factors likely to influence compliance with diagnostic imaging guideline recommendations for spine disorders among chiropractors in North America: a focus group study using the Theoretical Domains Framework. Implement Sci 2012;7. http://dx.doi.org/10.1186/1748-5908-7-82.
- Dyson J, Lawton R, Jackson C, Cheater F. Does the use of a theoretical approach tell us more about hand hygiene behaviour? The barriers and levers to hand hygiene. J Infect Prev 2011;12:17-24. http://dx.doi.org/10.1177/1757177410384300.
- Francis J, Tinmouth A, Stanworth S, Grimshaw J, Johnston M, Hyde C, et al. Using theories of behaviour to understand transfusion prescribing in three clinical contexts in two countries: development work for an implementation trial. Implement Sci 2009;4. http://dx.doi.org/10.1186/1748-5908-4-70.
- French S, Green S, O’Connor D, McKenzie J, Francis J, Michie S, et al. Developing theory-informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implement Sci 2012;7. http://dx.doi.org/10.1186/1748-5908-7-38.
- Patey A, Islam R, Francis J, Bryson G, Grimshaw J. Anesthesiologists’ and surgeons’ perceptions about routine pre-operative testing in low-risk patients: application of the Theoretical Domains Framework (TDF) to identify factors that influence physicians’ decisions to order pre-operative tests. Implement Sci 2012;7. http://dx.doi.org/10.1186/1748-5908-7-52.
- McKenzie JE, French SD, O’Connor DA, Grimshaw JM, Mortimer D, Michie S, et al. IMPLEmenting a clinical practice guideline for acute low back pain evidence-based manageMENT in general practice (IMPLEMENT): cluster randomised controlled trial study protocol. Implement Sci 2008;3. http://dx.doi.org/10.1186/1748-5908-3-11.
- McKenzie JE, O’Connor DA, Page MJ, Mortimer DS, French SD, Walker BF, et al. Improving the care for people with acute low-back pain by allied health professionals (the ALIGN trial): a cluster randomised trial protocol. Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-86.
- Francis J, Stockton C, Eccles M, Johnston M, Cuthbertson B, Grimshaw J, et al. Evidence-based selection of theories for designing behaviour change interventions: using methods based on theoretical construct domains to understand clinicians’ blood transfusion behaviour. Br J Health Psychol 2009;14:625-46. http://dx.doi.org/10.1348/135910708X397025.
- Cane J, Richardson M, Johnston M, Lahda R, Michie S. From lists of behaviour change techniques (BCTs) to structured hierarchies: comparison of two methods of developing a hierarchy of BCTs. Br J Health Psychol 2015;20:130-50. http://dx.doi.org/10.1111/bjhp.12102.
- Johnston M, Dixon D, Hart J, Glidewell L, Schroder C, Pollard B. Discriminant content validity: a quantitative methodology for assessing content of theory-based measures, with illustrative applications. Health Psychol 2014;19:240-57. http://dx.doi.org/10.1111/bjhp.12095.
- Dixon D, Pollard B, Johnston M. What does the chronic pain grade questionnaire measure?. Pain 2007;130:249-53. http://dx.doi.org/10.1016/j.pain.2006.12.004.
- Waltz C, Strickland O, Lenz ER. Measurement in Nursing Research. Philadelphia, PA: F.A. Davis Company; 1991.
- Dixon D, Johnston M, McQueen M, Court-Brown C. The Disabilities of the Arm, Shoulder and Hand Questionnaire (DASH) can measure the impairment, activity limitations and participation restriction constructs from the International Classification of Functioning, Disability and Health (ICF). BMC Musculoskelet Disord 2008;9. http://dx.doi.org/10.1186/1471-2474-9-114.
- Carmines EG, Zeller RA. Reliability and Validity Assessment. Thousand Oaks, CA: Sage Publications; 1979.
- Brock G, Pihur V, Datta S, Datta S. clValid, an R package for cluster validation. J Stat Soft 2008;25:1-22. http://dx.doi.org/10.1002/bdra.20684.
- Suzuki R, Shimodaira H. Pvclust: an R package for assessing the uncertainty in hierarchical clustering. Bioinformatics 2006;22:1540-2. http://dx.doi.org/10.1093/bioinformatics/btl117.
- Hochberg Y. A sharper Bonferroni procedure for multiple tests of significance. Biometrika 1988;75:800-2. http://dx.doi.org/10.1093/biomet/75.4.800.
- Ludwig TD, Geller ES, Mawhinney TC. Intervening to Improve the Safety of Occupational Driving: A Behavior-Change Model and Review of Empirical Evidence. Stroud: Haworth Press; 2001.
- Hardeman W, Kinmonth AL, Michie S, Sutton S. Impact of a physical activity intervention program on cognitive predictors of behaviour among adults at risk of type 2 diabetes (ProActive randomised controlled trial). Int J Behav Nutr Phys Act 2009;6. http://dx.doi.org/10.1186/1479-5868-6-16.
- Baddeley A. The influence of acoustic and semantic similarity on long-term memory for word sequences. Q J Exp Psychol 1966;18:302-9. http://dx.doi.org/10.1080/14640746608400047.
- Polyn SM, Erlikhman G, Kahana MJ. Semantic cuing and the scale insensitivity of recency and contiguity. J Exp Psychol Learn Mem Cogn 2011;37:766-75. http://dx.doi.org/10.1037/a0022475.
- Tulving EP, Pearlstone Z. Availability versus accessibility of information in memory for words. J Verbal Learning Verbal Behav 1966;5:381-91. http://dx.doi.org/10.1016/S0022-5371(66)80048-8.
- Hak T, Bernts T. Coder training: theoretical training or practical socialization?. Qual Sociol 1996;19:235-57. http://dx.doi.org/10.1007/BF02393420.
- Bernard RM, Abrami PC, Lou Y, Borokhovski E, Wade A, Wozney L, et al. How does distance education compare with classroom instruction? A meta-analysis of the empirical literature. Rev Educ Res 2004;74:379-43. http://dx.doi.org/10.3102/00346543074003379.
- Potter WJ, Levine-Donnerstein D. Rethinking validity and reliability in content analysis. J Appl Commun Res 1999;27:258-84. http://dx.doi.org/10.1080/00909889909365539.
- Murphy E, Ciszewska-Carr J. Contrasting syntactic and semantic units in the analysis on online discussions. Australasian J Educ Tech 2005;21:546-66.
- Pollock PH, Hamann K, Wilson BM. Learning through discussions: comparing the benefits of small-group and large-class settings. J Polit Sci Educ 2011;7:48-64. http://dx.doi.org/10.1080/15512169.2011.539913.
- Salas E, Cannon-Bowers JA. The science of training: a decade of progress. Annu Rev Psychol 2001;52:471-99. http://dx.doi.org/10.1146/annurev.psych.52.1.471.
- Salas E, Kosarzycki MP, Burke CS, Fiore SM, Stone DL. Emerging themes in distance learning research and practice: some food for thought. Int J Manag Rev 2002;4:135-53. http://dx.doi.org/10.1111/1468-2370.00081.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84:191-215. http://dx.doi.org/10.1037/0033-295X.84.2.191.
- Lorencatto F, West R, Seymour N, Michie S. Developing a method for specifying the components of behavior change interventions in practice: the example of smoking cessation. J Consult Clin Psych 2013;81:528-44. http://dx.doi.org/10.1037/a0032106.
- Wood CE, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. Applying the Behaviour Change Technique (BCT) Taxonomy v1: a study of user training. Transl Behav Med 2014;5:134-48. http://dx.doi.org/10.1007/s13142-014-0290-z.
- University College London . The Behaviour Change Technique Taxonomy Project n.d. www.ucl.ac.uk/health-psychology/bcttaxonomy (accessed 6 July 2015).
- Warmington M, Hitch GJ. Enhancing the learning of new words using an errorless learning procedure: evidence from typical adults. Memory 2014;22:582-94. http://dx.doi.org/10.1080/09658211.2013.807841.
- Byrt T, Bishop J, Carlin JB. Bias, prevalence and kappa. J Clin Epidemiol 1993;46:423-9. http://dx.doi.org/10.1016/0895-4356(93)90018-V.
- Michie S, Johnston M, Gellman M, Turner RJ. Encyclopeadia of Behavioural Medicine. London: Springer; 2013.
- Cohen J. Weighted kappa: nominal scale agreement provision for scaled disagreement or partial credit. Psychol Bull 1968;70:213-20. http://dx.doi.org/10.1037/h0026256.
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-74. http://dx.doi.org/10.2307/2529310.
- British Websites . BCTTv1. Online Training n.d. www.bct-taxonomy.com (accessed 8 July 2015).
- Glasziou P, Chalmers I, Altman D, Bastian H, Boutron I, Brice A, et al. Taking healthcare interventions from trial to practice. BMJ 2010;341. http://dx.doi.org/10.1136/bmj.c3852.
- Hoffmann T, Erueti C, Glasziou P. Poor description of non-pharmacological interventions: analysis of consecutive sample of randomised trials. BMJ 2013;347. http://dx.doi.org/10.1136/bmj.f3755.
- Aguinis H, Kraiger K. Benefits of training and development for individuals and teams, organizations, and society. Annu Rev Psychol 2009;60:451-74. http://dx.doi.org/10.1146/annurev.psych.60.110707.163505.
- Abraham C, Wood CE, Johnston M, Francis J, Hardeman W, Richardson M, et al. Reliability of identification of behavior change techniques in intervention descriptions [published online ahead of print August 20 2015]. Ann Behav Med 2015. http://dx.doi.org/10.1007/s12160-015-9727-y.
- Johnston M, Michie S. Specifying the active content of behaviour change interventions: the Behaviour Change Technique Taxonomy v1 (BCTTv1). Revista De Psicología De La Salud (New Age) 2013;1:131-4. http://dx.doi.org/10.1007/s12160-013-9486-6.
- Wynne G, Marteau TM, Johnston M, Whiteley CA, Evans TR. Inability of trained nurses to perform basic life support. BMJ 1987;294:1198-9. http://dx.doi.org/10.1136/bmj.294.6581.1198.
- Gwet K. Inter-rater reliability: dependency on trait prevalence and marginal homogeneity. Statistical Methods for Inter-Rater Reliability Assessment Series 2002;2:1-9.
- Gwet KL. Handbook of Inter-Rater Reliability: The Definitive Guide to Measuring the Extent of Agreement Among Multiple Raters. Gaithersburg, MD: Advanced Analytics LLC; 2012.
- Murphy S, Raisanen L, Moore G, Edwards RT, Linck P, Williams N, et al. A pragmatic randomised controlled trial of the Welsh National Exercise Referral Scheme: protocol for trial and integrated economic and process evaluation. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-352.
- Ahmad A, Hugtenburg J, Welschen LM, Dekker JM, Nijpels G. Effect of medication review and cognitive behaviour treatment by community pharmacists of patients discharged from the hospital on drug related problems and compliance: design of a randomized controlled trial. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-133.
- Ivers NM, Tu K, Francis J, Barnsley J, Shah B, Upshur R, et al. Feedback GAP: study protocol for a cluster-randomized trial of goal setting and action plans to increase the effectiveness of audit and feedback interventions in primary care. Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-98.
- Skouteris H, McCabe M, Swinburn B, Hill B. Healthy eating and obesity prevention for preschoolers: a randomised controlled trial. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-220.
- Castelnuovo G, Manzoni GM, Cuzziol P, Cesa GL, Tuzzi C, Villa V, et al. TECNOB: study design of a randomized controlled trial of a multidisciplinary telecare intervention for obese patients with type-2 diabetes. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-204.
- Wyers CE, Breedveld-Peters JJ, Reijven PL, van Helden S, Guldemond NA, Severens JL, et al. Efficacy and cost-effectiveness of nutritional intervention in elderly after hip fracture: design of a randomized controlled trial. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-212.
- Wyse RJ, Wolfenden L, Campbell E, Brennan L, Campbell KJ, Fletcher A, et al. A cluster randomised trial of a telephone-based intervention for parents to increase fruit and vegetable consumption in their 3- to 5-year-old children: study protocol. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-216.
- Sanfélix-Genovés J, Peiro S, Sanfelix-Gimeno G, Hurtado I, Pascual de la Torre M, Trillo-Mata JL, et al. Impact of a multifaceted intervention to improve the clinical management of osteoporosis. The ESOSVAL-F study. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-292.
- Siddiqi K, Khan A, Ahmad M, Shafiq-ur R. An intervention to stop smoking among patients suspected of TB -- evaluation of an integrated approach. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-160.
- Mc Namara KP, George J, O’Reilly SL, Jackson SL, Peterson GM, Howarth H, et al. Engaging community pharmacists in the primary prevention of cardiovascular disease: protocol for the Pharmacist Assessment of Adherence, Risk and Treatment in Cardiovascular Disease (PAART CVD) pilot study. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-264.
- Spijkers W, Jansen DE, de Meer G, Reijneveld SA. Effectiveness of a parenting programme in a public health setting: a randomised controlled trial of the positive parenting programme (Triple P) level 3 versus care as usual provided by the preventive child healthcare (PCH). BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-131.
- McNamara R, Robling M, Hood K, Bennert K, Channon S, Cohen D, et al. Development and Evaluation of a Psychosocial Intervention for Children and Teenagers Experiencing Diabetes (DEPICTED): a protocol for a cluster randomised controlled trial of the effectiveness of a communication skills training programme for healthcare professionals working with young people with type 1 diabetes. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-36.
- Colagiuri S, Vita P, Cardona-Morrell M, Singh MF, Farrell L, Milat A, et al. The Sydney Diabetes Prevention Program: a community-based translational study. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-328.
- McAlister FA, Majumdar SR, Padwal RS, Fradette M, Thompson A, Tsuyuki R, et al. The preventing recurrent vascular events and neurological worsening through intensive organized case-management (PREVENTION) trial protocol [clinicaltrials.gov identifier: NCT00931788]. Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-27.
- Lau R, Stewart K, McNamara KP, Jackson SL, Hughes JD, Peterson GM, et al. Evaluation of a community pharmacy-based intervention for improving patient adherence to antihypertensives: a randomised controlled trial. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-34.
- Rost KM, Marshall D. Marketing depression care management to employers: design of a randomized controlled trial. Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-22.
- Garner BR, Godley SH, Dennis ML, Godley MD, Shepard DS. The Reinforcing Therapist Performance (RTP) experiment: study protocol for a cluster randomized trial. Implement Sci 2010;5:1-12. http://dx.doi.org/10.1186/1748-5908-5-5.
- Johnston V, Walker N, Thomas DP, Glover M, Chang AB, Bullen C, et al. The study protocol for a randomized controlled trial of a family-centred tobacco control program about environmental tobacco smoke (ETS) to reduce respiratory illness in Indigenous infants. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-114.
- Taylor RW, Brown D, Dawson AM, Haszard J, Cox A, Rose EA, et al. Motivational interviewing for screening and feedback and encouraging lifestyle changes to reduce relative weight in 4–8 year old children: design of the MInT study. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-271.
- Geimer N, Olson CE, Baumgarten D, Kepner JL, Mahoney MC. Use of a liquid nicotine delivery product to promote smoking cessation. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-155.
- Gonseth S, Abarca M, Madrid C, Cornuz J. A pilot study combining individual-based smoking cessation counseling, pharmacotherapy, and dental hygiene intervention. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-348.
- Mann E, Kellar I, Sutton S, Kinmonth AL, Hankins M, Griffin S, et al. Impact of informed-choice invitations on diabetes screening knowledge, attitude and intentions: an analogue study. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-768.
- Menza TW, Jameson DR, Hughes JP, Colfax GN, Shoptaw S, Golden MR. Contingency management to reduce methamphetamine use and sexual risk among men who have sex with men: a randomized controlled trial. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-774.
- Rosenkranz RR, Behrens TK, Dzewaltowski DA. A group-randomized controlled trial for health promotion in Girl Scouts: healthier troops in a SNAP (Scouting Nutrition & Activity Program). BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-81.
- Werkman A, Hulshof PJ, Stafleu A, Kremers SP, Kok FJ, Schouten EG, et al. Effect of an individually tailored one-year energy balance programme on body weight, body composition and lifestyle in recent retirees: a cluster randomised controlled trial. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-110.
- Buis LR, Poulton TA, Holleman RG, Sen A, Resnick PJ, Goodrich DE, et al. Evaluating Active U: an internet-mediated physical activity program. BMC Public Health 2009;9. http://dx.doi.org/10.1186/1471-2458-9-331.
- Bull FC, Milton KE. A process evaluation of a ‘physical activity pathway’ in the primary care setting. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-463.
- Claesson IM, Josefsson A, Sydsjo G. Prevalence of anxiety and depressive symptoms among obese pregnant and postpartum women: an intervention study. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-766.
- Storrø O, Oien T, Dotterud CK, Jenssen JA, Johnsen R. A primary health-care intervention on pre- and postnatal risk factor behavior to prevent childhood allergy. The Prevention of Allergy among Children in Trondheim (PACT) study. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-443.
- Ramos M, Ripoll J, Estrades T, Socias I, Fe A, Duro R, et al. Effectiveness of intensive group and individual interventions for smoking cessation in primary health care settings: a randomized trial. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-89.
- Leon N, Naidoo P, Mathews C, Lewin S, Lombard C. The impact of provider-initiated (opt-out) HIV testing and counseling of patients with sexually transmitted infection in Cape Town, South Africa: a controlled trial. Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-8.
- Pilling SA, Williams MB, Brackett RH, Gourley R, Weg MW, Christensen AJ, et al. Part I, patient perspective: activating patients to engage their providers in the use of evidence-based medicine: a qualitative evaluation of the VA Project to Implement Diuretics (VAPID). Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-23.
- Bilardi JE, Fairley CK, Temple-Smith MJ, Pirotta MV, McNamee KM, Bourke S, et al. Incentive payments to general practitioners aimed at increasing opportunistic testing of young women for chlamydia: a pilot cluster randomised controlled trial. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-70.
- Brousseau N, Sauvageau C, Ouakki M, Audet D, Kiely M, Couture C, et al. Feasibility and impact of providing feedback to vaccinating medical clinics: evaluating a public health intervention. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-750.
- Kauth MR, Sullivan G, Blevins D, Cully JA, Landes RD, Said Q, et al. Employing external facilitation to implement cognitive behavioral therapy in VA clinics: a pilot study. Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-75.
- Kennedy A, Rogers A, Chew-Graham C, Blakeman T, Bowen R, Gardner C, et al. Implementation of a self-management support approach (WISE) across a health system: a process evaluation explaining what did and did not work for organisations, clinicians and patients. Implement Sci 2014;9. http://dx.doi.org/10.1186/s13012-014-0129-5.
- McCluskey A, Middleton S. Delivering an evidence-based outdoor journey intervention to people with stroke: barriers and enablers experienced by community rehabilitation teams. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-18.
- Ramsay CR, Thomas RE, Croal BL, Grimshaw JM, Eccles MP. Using the theory of planned behaviour as a process evaluation tool in randomised trials of knowledge translation strategies: a case study from UK primary care. Implement Sci 2010;5. http://dx.doi.org/10.1186/1748-5908-5-71.
- Shelley D, Cantrell J. The effect of linking community health centers to a state-level smoker’s quitline on rates of cessation assistance. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-25.
- Hovland CI, Janis IL, Kelley HH. Communication and Persuasion: Psychological Studies of Opinion Change. Santa Barbara, CA: Greenwood Press; 1953.
- Durantini MR, Albarracin D, Mitchell AL, Earl AN, Gillette JC. Conceptualizing the influence of social agents of behavior change: a meta-analysis of the effectiveness of HIV-prevention interventionists for different groups. Psychol Bull 2006;132:212-48. http://dx.doi.org/10.1037/0033-2909.132.2.212.
- Ley P, Broome AK. Health Psychology: Processes and Applications. London: Nelson Thornes Ltd; 1989.
- Schofield PB, Butow PN. Towards better communication in cancer care: a framework for developing evidence-based interventions. Patient Educ Couns 2004;55:32-9. http://dx.doi.org/10.1016/j.pec.2003.07.001.
- Chan A, Tetzlaff JM, Gotzsche PC, Altman DG, Mann, H, Berlin JA, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346. http://dx.doi.org/10.1136/bmj.e7586.
- Baumeister RF. Choking under pressure: self-consciousness and paradoxical effects of incentives on skillful performance. J Pers Soc Psychol 1984;46:610-20. http://dx.doi.org/10.1037/0022-3514.46.3.610.
- Wegner DM, Broome A, Blumberg SJ. Ironic effects of trying to relax under stress. Behav Res Ther 1997;35:11-2. http://dx.doi.org/10.1016/S0005-7967(96)00078-2.
- Henry WP, Schacht TE, Strupp HH, Butler SF, Binder JL. Effects of training in time-limited dynamic psychotherapy: mediators of therapists’ responses to training. J Consult Clin Psych 1993;61:441-7. http://dx.doi.org/10.1037/0022-006X.61.3.441.
- McEachan RRC, Conner M, Taylor NJ, Lawton RJ. Prospective prediction of health-related behaviours with the Theory of Planned Behaviour: a meta-analysis. Health Psychol Rev 2011;5:97-144. http://dx.doi.org/10.1080/17437199.2010.521684.
- Davis R, Campbell R, Hildon Z, Michie S. Theories of behaviour and behaviour change across disciplines: a systematic review. Health Psychol Rev 2014. http://dx.doi.org/10.1080/17437199.2014.941722.
- Michie S, Atkins L, West R. The Behaviour Change Wheel: A Guide to Designing Interventions. London: Silverback Publishing; 2014.
- de Bruin M, Viechtbauer W, Hospers HJ, Schaalma HP, Kok G. Standard care quality determines treatment outcomes in control groups of HAART-adherence intervention studies: implications for the interpretation and comparison of intervention effects. Health Psychol 2009;28:668-74. http://dx.doi.org/10.1037/a0015989.
- Peters G-JY, de Bruin M, Crutzen R. Everything should be as simple as possible, but no simpler: towards a protocol for accumulating evidence regarding the active content of health behaviour change interventions. Health Psychol Rev 2013;9:1-14. http://dx.doi.org/10.1080/17437199.2013.848409.
- Michie S, Johnson B, Johnston M. Advancing cumulative evidence on behaviour change techniques and interventions. Health Psychol Rev 2015;9:25-9. http://dx.doi.org/10.1080/17437199.2014.912538.
- Johnson BT, Mitchie S. Toward Healthy Theorizing about health behaviours in the maze of messy reality: a reaction to Peters, de Bruin, and Crutzen. Health Psychol Rev 2015;9:21-4. http://dx.doi.org/10.1080/17437199.2014.900722.
- Behaviour Change: The Principles for Effective Interventions (PH6). London: NICE; 2014.
- Behaviour Change: Individual Approaches (PH49). London: NICE; 2014.
- Gardner B, Whittington C, McAteer J, Eccles M, Michie S. Using theory to synthesise evidence from behaviour change interventions: the example of audit and feedback. Soc Sci Med 2010;70:1618-25. http://dx.doi.org/10.1016/j.socscimed.2010.01.039.
- Smoak ND, Scott-Sheldon LA, Johnson BT, Carey MP. Sexual risk reduction interventions do not inadvertently increase the overall frequency of sexual behavior: a meta-analysis of 174 studies with 116,735 participants. J Acquir Immune Defic Syndr 2006;41:374-84. http://dx.doi.org/10.1097/01.qai.0000185575.36591.fc.
- Carver CS, Scheier MF. Control theory: a useful conceptual framework for personality – social, clinical, and health psychology. Psychol Bull 1982;92:111-35. http://dx.doi.org/10.1037/0033-2909.92.1.111.
- Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull 1992;111. http://dx.doi.org/10.1037/0033-2909.111.3.455.
- Pears S, Morton K, Bijker M, Sutton S, Hardeman W. VBI Programme Team . Development and feasibility study of very brief interventions for physical activity in primary care. BMC Public Health 2015;15. http://dx.doi.org/10.1186/s12889-015-1703-8.
- Aveyard P, Begh R, Parsons A, West R. Brief opportunistic smoking cessation interventions: a systematic review and meta-analysis to compare advice to quit and offer of assistance. Addiction 2012;107:1066-73. http://dx.doi.org/10.1111/j.1360-0443.2011.03770.x.
- NCSCT . Very Brief Advice Training Module n.d. www.ncsct.co.uk/publication_very-brief-advice,php (accessed 13 July 2015).
- Collins L, Murphy S, Strecher V. The multiphase optimization strategy (MOST) and the sequential multiple assignment randomized trial (SMART): new methods for more potent eHealth interventions. Am J Prev Med 2007;32:S112-18. http://dx.doi.org/10.1016/j.amepre.2007.01.022.
- Michie S, Campbell R, Brown J, West R, Gainforth H. ABC of Behaviour Change Theories. Sutton: Silverback Publishing; 2014.
- Woolf SH, Johnson RE. The break-even point: when medical advances are less important than improving the fidelity with which they are delivered. Ann Fam Med 2005;3:545-52. http://dx.doi.org/10.1370/afm.406.
- West R. Providing full manuals and intervention descriptions: addiction policy. Addiction 2008;103. http://dx.doi.org/10.1111/j.1360-0443.2008.02341.x.
- Borrelli B. The assessment, monitoring, and enhancement of treatment fidelity in public health clinical trials. J Public Health Dent 2011;71:S52-63. http://dx.doi.org/10.1111/j.1752-7325.2011.00233.x.
- Dane AV, Schneider BH. Program integrity in primary and early secondary prevention: are implementation effects out of control?. Clin Psychol Rev 1998;18:23-45. http://dx.doi.org/10.1016/S0272-7358(97)00043-3.
- Dusenbury L, Brannigan R, Falco M, Hansen WB. A review of research on fidelity of implementation: implications for drug abuse prevention in school settings. Health Educ Res 2003;18:237-56. http://dx.doi.org/10.1093/her/18.2.237.
- Hardeman W, Michie S, Fanshawe T, Prevost T, McLoughlin K, Kinmonth A. Fidelity of delivery of a physical activity intervention: predictors and consequences. Psychol Health 2007;23:11-24. http://dx.doi.org/10.1080/08870440701615948.
- Carroll KM, Kadden RM, Donovan DM, Zweben A, Rounsaville BJ. Implementing treatment and protecting the validity of the independent variable in treatment matching studies. J Stud Alcohol Suppl 1994;12:149-55. http://dx.doi.org/10.15288/jsas.1994.s12.149.
Appendix 1 Changes to protocol
| Section of protocol | Details of changes made (e.g. addition, substitution, elaboration) | Rationale for change |
|---|---|---|
| Methods: phases 2a, 2b and 2c | In the protocol, we refer to phase 1 (1a and 1b), 2 (2a and 2b) and 3 as markers for phases of development, evaluation and prototyping the developed taxonomy (or ‘nomenclature’ as referred to in the protocol). In this report, we refer to the phases but omit the subphases (i.e. 1a, 1b, 2a and 2b), instead referring to study 1, study 2, study 3, etc. | To keep the structure of the report, simple and coherent |
| Methods: phase 2a – nomenclature training resource materials | Substitution: we proposed development of ‘training videos’ for use in phase 2c. Rather than developing videos, we were able to source existing videos | The existing videos contained an appropriate range of BCTs (from NCSCT www.ncsct.co.uk35) suitable for use in this phase |
| Methods: phase 3 – prototype nomenclature | Elaboration: we proposed production of a web-based user’s resource and user manual (to include the full, developed taxonomy, guidance on its use, and evidence of reliability, consensus and examples of each BCT from interventions). We developed this idea further and produced (1) a project website, (2) an online, interactive training resource for taxonomy users and (3) a smartphone application version of the full BCTTv1 | The rapid development of technology over the course of the project provided us the opportunity to produce interactive resources and engage with a much wider audience than originally proposed |
| Analyses: phase 2b – decoding/interpreting BCI protocols | Substitution: we proposed examining reliability ranges across type of coder as well as type of protocol. We focused on examining reliability across types of protocol | The unevenness in our sample of coders (as discussed in Chapter 8) prevented us from examining reliability across types of coder |
| Analyses: phase 2c – encoding/writing BCI protocols | Elaboration: we proposed that ‘raters’ would judge (1) ease of understanding, (2) adequacy of information required to undertake a replication and (3) ease of identification of discrete BCTs. In the report, we refer to two separate groups of participants completing this assessment: ‘raters’ and ‘coders’ | We considered that the most appropriate method of assessing (3) would be to ask participants to code intervention descriptions into component BCTs. Therefore, for clarity we refer to participants assessing (1) and (2) as ‘raters’ and those assessing (3) as ‘coders’ |
| Analyses: phase 2c – encoding/writing BCI protocols | Substitution: proposed using Q sort methods (a research method used to examine how people think about a specific topic) to identify whether or not availability of the taxonomy when reporting leads to better written intervention descriptions. In the report, we do not report use of these methods | Given the complex nature of the proposed analyses, we have decided to publish this study as a separate paper (Johnston M, Johnston DW, Wood CE, Hardeman W, Francis J, Michie S. University of Aberdeen, 2015) |
Appendix 2 International Advisory Board members
| Name | Institution |
|---|---|
| Professor Arja Aro | University of Southern Denmark, Odense, Denmark |
| Professor David Barlow | Boston University, Boston, MA, USA |
| Professor Christine Barrowclough | University of Manchester, Manchester, UK |
| Professor Ron Borland | University of Melbourne, Melbourne, VIC, Australia |
| Professor Belinda Borrelli | Brown University, Providence, RI, USA |
| Professor Linda Collins | Penn State University, State College, PA, USA |
| Professor Karina Davidson | Columbia University Medical Centre, New York, NY, USA |
| Professor Joost Dekker | VU University Medical Centre, Amsterdam, the Netherlands |
| Professor Hege Eriksen | University of Bergen, Bergen, Norway |
| Professor Jeffrey Fisher | University of Connecticut, Storrs, CT, USA |
| Professor Paul Glasziou | Bond University, Robina, QLD, Australia |
| Professor Gaston Godin | University of Laval, Québec, QC, Canada |
| Professor Jeremy Grimshaw | University of Ottawa, Ottawa, ON, Canada |
| Professor Nick Heather | Northumbria University, Northumbria, UK |
| Professor Blair Johnson | University of Connecticut, Storrs, CT, USA |
| Professor Robert Kaplan | UCLA School of Public Health, Los Angeles, CA, USA |
| Professor Francis Keefe | Duke University, Durham, NC, USA |
| Professor Gerjo Kok | Maastricht University, Maastricht, the Netherlands |
| Dr Helen Lindner | La Trobe University, Melbourne, VIC, Australia |
| Professor Steve Pilling | University College London, London, UK |
| Professor Miquel Porta | Municipal Institute of Medical Research, Barcelona, Spain |
| Professor Tony Roth | University College London, London, UK |
| Professor Rob Sanson-Fischer | The University of Newcastle, Callaghan, NSW, Australia |
| Professor Neil Schneiderman | University of Miami, Coral Gables, FL, USA |
| Professor Ralf Schwarzer | Free University of Berlin, Berlin, Germany |
| Professor Bonnie Spring | Northwestern University, Evanston, IL, USA |
| Professor Nick Tarrier | Institute of Psychiatry, King’s College London, London, UK |
| Professor Antti Uutela | National Institute for Health and Welfare, Helsinki, Finland |
| Professor Reinout Wiers | University of Amsterdam, Amsterdam, the Netherlands |
| Professor Redford Williams | Duke University, Durham, NC, USA |
The following two tables (Tables 19 and 20) present supplementary data relevant to the chapters in this report.
| Grouping and BCTs | Grouping and BCTs | Grouping and BCTs | |
|---|---|---|---|
| 1. Goals and planning | 6. Comparison of behaviour | 12. Antecedents | |
| 1.1 Goal-setting (behaviour) | 6.1. Demonstration of the behaviour | 12.1. Restructuring the physical environment | |
| 1.2. Problem-solving | 6.2. Social comparison | 12.2. Restructuring the social environment | |
| 1.3. Goal-setting (outcome) | 6.3. Information about others’ approval | 12.3. Avoidance/reducing exposure to cues for the behaviour | |
| 1.4. Action planning | 7. Associations | 12.4. Distraction | |
| 1.5. Review behaviour goal(s) | 7.1. Prompts/cues | 12.5. Adding objects to the environment | |
| 1.6. Discrepancy between current behaviour and goal | 7.2. Cue signalling reward | 12.6. Body changes | |
| 1.7. Review outcome goal(s) | 7.3. Reduce prompts/cues | 13. Identity | |
| 1.8. Behavioural contract | 7.4. Remove access to the reward | 13.1. Identification of self as role model | |
| 1.9. Commitment | 7.5. Remove aversive stimulus | 13.2. Framing/reframing | |
| 2. Feedback and monitoring | 7.6. Satiation | 13.3. Incompatible beliefs | |
| 2.1. Monitoring of behaviour by others without feedback | 7.7. Exposure | 13.4. Valued self-identify | |
| 2.2. Feedback on behaviour | 7.8. Associative learning | 13.5. Identity associated with changed behaviour | |
| 2.3. Self-monitoring of behaviour | 8. Repetition and substitution | 14. Scheduled consequences | |
| 2.4. Self-monitoring of outcome(s) of behaviour | 8.1. Behavioural practice/rehearsal | 14.1. Behaviour cost | |
| 2.5. Monitoring of outcome(s) of behaviour without feedback | 8.2. Behaviour substitution | 14.2. Punishment | |
| 2.6. Biofeedback | 8.3. Habit formation | 14.3. Remove reward | |
| 2.7. Feedback on outcome(s) of behaviour | 8.4. Habit reversal | 14.4. Reward approximation | |
| 3. Social support | 8.5. Overcorrection | 14.5. Rewarding completion | |
| 3.1. Social support (unspecified) | 8.6. Generalisation of target behaviour | 14.6. Situation-specific reward | |
| 3.2. Social support (practical) | 8.7. Graded tasks | 14.7. Reward incompatible behaviour | |
| 3.3. Social support (emotional) | 9. Comparison of outcomes | 14.8. Reward alternative behaviour | |
| 4. Shaping knowledge | 9.1. Credible source | 14.9. Reduce reward frequency | |
| 4.1. Instruction on how to perform the behaviour | 9.2. Pros and cons | 14.10. Remove punishment | |
| 4.2. Information about antecedents | 9.3. Comparative imagining of future outcomes | 15. Self-belief | |
| 4.3. Re-attribution | 10. Reward and threat | 15.1. Verbal persuasion about capability | |
| 4.4. Behavioural experiments | 10.1. Material incentive (behaviour) | 15.2. Mental rehearsal of successful performance | |
| 5. Natural consequences | 10.2. Material reward (behaviour) | 15.3. Focus on past success | |
| 5.1. Information about health consequences | 10.3. Non-specific reward | 15.4. Self-talk | |
| 5.2. Salience of consequences | 10.4. Social reward | 16. Covert learning | |
| 5.3. Information about social and environmental consequences | 10.5. Social incentive | 16.1. Imaginary punishment | |
| 5.4. Monitoring of emotional consequences | 10.6. Non-specific incentive | 16.2. Imaginary reward | |
| 5.5. Anticipated regret | 10.7. Self-incentive | 16.3. Vicarious consequences | |
| 5.6. Information about emotional consequences | 10.8. Incentive (outcome) | ||
| 10.9. Self-reward | |||
| 10.10. Reward (outcome) | |||
| 10.11. Future punishment | |||
| 11. Regulation | |||
| 11.1. Pharmacological support | |||
| 11.2. Reduce negative emotions | |||
| 11.3. Conserving mental resources | |||
| 11.4. Paradoxical instructions | |||
| Number | Label | Definition | Examples |
| 1. Goals and planning | |||
| 1.1 | Goal-setting (behaviour) | Set or agree on a goal defined in terms of the behaviour to be achieved Note: only code goal-setting if there is sufficient evidence that goal set as part of intervention; if goal unspecified or a behavioural outcome, code 1.3, goal-setting (outcome); if the goal defines a specific context, frequency, duration or intensity for the behaviour, also code 1.4, action planning |
Agree on a daily walking goal (e.g. 3 miles) with the person and reach agreement about the goal. Set the goal of eating five pieces of fruit per day as specified in public health guidelines |
| 1.2* | Problem-solving | Analyse, or prompt the person to analyse, factors influencing the behaviour and generate or select strategies that include overcoming barriers and/or increasing facilitators (includes ‘relapse prevention ’ and ‘coping planning’) Note: barrier identification without solutions is not sufficient. If the BCT does not include analysing the behavioural problem, consider 12.3, avoidance/changing exposure to cues for the behaviour; 12.1, restructuring the physical environment; 12.2, restructuring the social environment; or 11.2, reduce negative emotions |
Identify specific triggers (e.g. being in a pub, feeling anxious) that generate the urge/want/need to drink and develop strategies for avoiding environmental triggers or for managing negative emotions, such as anxiety, that motivate drinking. Prompt the patient to identify barriers preventing them from starting a new exercise regime, e.g. lack of motivation, and discuss ways in which they could help overcome them, e.g. going to the gym with a buddy |
| 1.3* | Goal-setting (outcome) | Set or agree on a goal defined in terms of a positive outcome of wanted behaviour Note: only code guidelines if set as a goal in an intervention context; if goal is a behaviour, code 1.1, goal-setting (behaviour); if goal unspecified code 1.3, goal-setting (outcome) |
Set a weight loss goal (e.g. 0.5 kg over 1 week) as an outcome of changed eating patterns |
| 1.4* | Action planning | Prompt detailed planning of performance of the behaviour (must include at least one of context, frequency, duration and intensity). Context may be environmental (physical or social) or internal (physical, emotional or cognitive includes ‘implementation intentions’) Note: evidence of action planning does not necessarily imply goal-setting, only code latter if sufficient evidence |
Encourage a plan to carry condoms when going out socially at weekends. Prompt planning the performance of a particular physical activity (e.g. running) at a particular time (e.g. before work) on certain days of the week |
| 1.5* | Review behaviour goal(s) | Review behaviour goal(s) jointly with the person and consider modifying goal(s) or behaviour change strategy in light of achievement. This may lead to resetting the same goal, a small change in that goal or setting a new goal instead of (or in addition to) the first, or no change Note: if goal specified in terms of behaviour, code 1.5, review behaviour goal(s), if goal unspecified, code 1.7, review outcome goal(s); if discrepancy created consider also 1.6, discrepancy between current behaviour and goal |
Examine how well a person’s performance corresponds to agreed goals, e.g. whether or not they consumed less than one unit of alcohol per day, and consider modifying future behavioural goals accordingly, e.g. by increasing or decreasing alcohol target or changing type of alcohol consumed |
| 1.6 | Discrepancy between current behaviour and goal | Draw attention to discrepancies between a person’s current behaviour (in terms of the form, frequency, duration or intensity of that behaviour) and the person’s previously set outcome goals, behavioural goals or action plans (goes beyond self-monitoring of behaviour) Note: if discomfort is created only code 13.3, incompatible beliefs and not 1.6, discrepancy between current behaviour and goal if goals are modified, also code 1.5, review behaviour goal(s) and/or 1.7, review outcome goal(s); if feedback is provided, also code 2.2, feedback on behaviour |
Point out that the recorded exercise fell short of the goal set |
| 1.7* | Review outcome goal(s) | Review outcome goal(s) jointly with the person and consider modifying goal(s) in light of achievement. This may lead to resetting the same goal, a small change in that goal or setting a new goal instead of, or in addition to the first Note: if goal specified in terms of behaviour, code 1.5, review behaviour goal(s), if goal unspecified, code 1.7, review outcome goal(s); if discrepancy created consider also 1.6, discrepancy between current behaviour and goal |
Examine how much weight has been lost and consider modifying outcome goal(s) accordingly, e.g. by increasing or decreasing subsequent weight loss targets |
| 1.8 | Behavioural contract | Create a written specification of the behaviour to be performed, agreed on by the person, and witnessed by another Note: also code 1.1, goal-setting (behaviour) |
Sign a contract with the person, e.g. specifying that they will not drink alcohol for 1 week |
| 1.9 | Commitment | Ask the person to affirm or reaffirm statements indicating commitment to change the behaviour Note: if defined in terms of the behaviour to be achieved also code 1.1, goal-setting (behaviour) |
Ask the person to use an ‘I will’ statement to affirm or reaffirm a strong commitment (i.e. using the words ‘strongly’, ‘committed’ or ‘high priority’) to start, continue or restart the attempt to take medication as prescribed |
| 2. Feedback and monitoring | |||
| 2.1 | Monitoring of behaviour by others without feedback | Observe or record behaviour with the person’s knowledge as part of a behaviour change strategy Note: if monitoring is part of a data collection procedure rather than a strategy aimed at changing behaviour, do not code; if feedback given, code only 2.2, feedback on behaviour, and not 2.1, monitoring of behaviour by others without feedback; if monitoring outcome(s) code 2.5, monitoring outcome(s) of behaviour by others without feedback; if self-monitoring behaviour, code 2.3, self-monitoring of behaviour |
Watch hand washing behaviours among health-care staff and make notes on context, frequency and technique used |
| 2.2* | Feedback on behaviour | Monitor and provide informative or evaluative feedback on performance of the behaviour (e.g. form, frequency, duration, intensity) Note: if biofeedback, code only 2.6, biofeedback and not 2.2, feedback on behaviour; if feedback is on outcome(s) of behaviour, code 2.7, feedback on outcome(s) of behaviour; if there is no clear evidence that feedback was given, code 2.1, monitoring of behaviour by others without feedback; if feedback on behaviour is evaluative e.g. praise, also code 10.4, social reward |
Inform the person of how many steps they walked each day (as recorded on a pedometer) or how many calories they ate each day (based on a food consumption questionnaire) |
| 2.3* | Self-monitoring of behaviour | Establish a method for the person to monitor and record their behaviour(s) as part of a behaviour change strategy Note: if monitoring is part of a data collection procedure rather than a strategy aimed at changing behaviour, do not code; if monitoring of outcome of behaviour, code 2.4, self-monitoring of outcome(s) of behaviour; if monitoring is by someone else (without feedback), code 2.1, monitoring of behaviour by others without feedback |
Ask the person to record daily, in a diary, whether or not they have brushed their teeth for at least two minutes before going to bed. Give patient a pedometer and a form for recording daily total number of steps |
| 2.4 | Self-monitoring of outcome(s) of behaviour | Establish a method for the person to monitor and record the outcome(s) of their behaviour as part of a behaviour change strategy Note: if monitoring is part of a data collection procedure rather than a strategy aimed at changing behaviour, do not code; if monitoring behaviour, code 2.3, self-monitoring of behaviour; if monitoring is by someone else (without feedback), code 2.5, monitoring outcome(s) of behaviour by others without feedback |
Ask the person to weigh themselves at the end of each day, over a 2 week period, and record their daily weight on a graph to increase exercise behaviours |
| 2.5* | Monitoring outcome(s) of behaviour by others without feedback | Observe or record outcomes of behaviour with the person’s knowledge as part of a behaviour change strategy Note: if monitoring is part of a data collection procedure rather than a strategy aimed at changing behaviour, do not code; if feedback given, code only 2.7, feedback on outcome(s) of behaviour; if monitoring behaviour code 2.1, monitoring of behaviour by others without feedback; if self-monitoring outcome(s), code 2.4, self-monitoring of outcome(s) of behaviour |
Record blood pressure, blood glucose, weight loss, or physical fitness |
| 2.6 | Biofeedback | Provide feedback about the body (e.g. physiological or biochemical state) using an external monitoring device as part of a behaviour change strategy Note: if biofeedback, code only 2.6, biofeedback and not 2.2, feedback on behaviour or 2.7, feedback on outcome(s) of behaviour |
Inform the person of their blood pressure reading to improve adoption of health behaviours |
| 2.7* | Feedback on outcome(s) of behaviour | Monitor and provide feedback on the outcome of performance of the behaviour Note: if biofeedback, code only 2.6, biofeedback and not 2.7, feedback on outcome(s) of behaviour; if feedback is on behaviour code 2.2, feedback on behaviour; if there is no clear evidence that feedback was given code 2.5, monitoring outcome(s) of behaviour by others without feedback; if feedback on behaviour is evaluative e.g. praise, also code 10.4, social reward |
Inform the person of how much weight they have lost following the implementation of a new exercise regime |
| 3. Social support | |||
| 3.1* | Social support (unspecified) | Advise on, arrange or provide social support (e.g. from friends, relatives, colleagues, ‘buddies’ or staff) or non-contingent praise or reward for performance of the behaviour. It includes encouragement and counselling, but only when it is directed at the behaviour Note: attending a group class and/or mention of ‘follow-up’ does not necessarily apply this BCT, support must be explicitly mentioned; if practical, code 3.2, social support (practical); if emotional, code 3.3, social support (emotional) (includes ‘motivational interviewing’ and ‘cognitive–behavioural therapy’) |
Advise the person to call a ‘buddy’ when they experience an urge to smoke. Arrange for a housemate to encourage continuation with the behaviour change programme. Give information about a self-help group that offers support for the behaviour |
| 3.2* | Social support (practical) | Advise on, arrange or provide practical help (e.g. from friends, relatives, colleagues, ‘buddies’ or staff) for performance of the behaviour Note: if emotional, code 3.3, social support (emotional); if general or unspecified, code 3.1, social support (unspecified). If only restructuring the physical environment or adding objects to the environment, code 12.1, restructuring the physical environment or 12.5, adding objects to the environment; attending a group or class and/or mention of ‘follow-up’ does not necessarily apply this BCT, support must be explicitly mentioned |
Ask the partner of the patient to put their tablet on the breakfast tray so that the patient remembers to take it |
| 3.3 | Social support (emotional) | Advise on, arrange or provide emotional social support (e.g. from friends, relatives, colleagues, ‘buddies’ or staff) for performance of the behaviour Note: if practical, code 3.2, social support (practical); if unspecified, code 3.1, social support (unspecified) |
Ask the patient to take a partner or friend with them to their colonoscopy appointment |
| 4. Shaping knowledge | |||
| 4.1* | Instruction on how to perform a behaviour | Advise or agree on how to perform the behaviour (includes ‘skills training’) Note: when the person attends classes such as exercise or cookery, code 4.1, instruction on how to perform the behaviour, 8.1, behavioural practice/rehearsal and 6.1, demonstration of the behaviour |
Advise the person how to put a condom on a model of a penis correctly |
| 4.2 | Information about antecedents | Provide information about antecedents (e.g. social and environmental situations and events, emotions, cognitions) that reliably predict performance of the behaviour | Advise to keep a record of snacking and of situations or events occurring prior to snacking |
| 4.3 | Re-attribution | Elicit perceived causes of behaviour and suggest alternative explanations (e.g. external or internal and stable or unstable) | If the person attributes their over-eating to the frequent presence of delicious food, suggest that the ‘real’ cause may be the person’s inattention to bodily signals of hunger and satiety |
| 4.4 | Behavioural experiments | Advise on how to identify and test hypotheses about the behaviour, its causes and consequences, by collecting and interpreting data | Ask a family physician to give evidence-based advice rather than prescribe antibiotics and to note whether the patients are grateful or annoyed |
| 5. Natural consequences | |||
| 5.1* | Information about health consequences | Provide information (e.g. written, verbal, visual) about health consequences of performing the behaviour Note: consequences can be for any target, not just the recipient(s) of the intervention; emphasising importance of consequences is not sufficient; if information about emotional consequences, code 5.6, information about emotional consequences; if about social, environmental or unspecified consequences code 5.3, information about social and environmental consequences |
Explain that not finishing a course of antibiotics can increase susceptibility to future infection. Present the likelihood of contracting a sexually transmitted infection following unprotected sexual behaviour |
| 5.2 | Salience of consequences | Use methods specifically designed to emphasise the consequences of performing the behaviour with the aim of making them more memorable (goes beyond informing about consequences) Note: if information about consequences, also code 5.1, information about health consequences, 5.6, information about emotional consequences or 5.3, information about social and environmental consequences |
Produce cigarette packets showing pictures of health consequences, e.g. diseased lungs, to highlight the dangers of continuing to smoke |
| 5.3* | Information about social and environmental consequences | Provide information (e.g. written, verbal, visual) about social and environmental consequences of performing the behaviour Note: consequences can be for any target, not just the recipient(s) of the intervention; if information about health or consequences, code 5.1, information about health consequences; if about emotional consequences, code 5.6, information about emotional consequences; if unspecified, code 5.3, information about social and environmental consequences |
Tell family physician about financial remuneration for conducting health screening. Inform a smoker that the majority of people disapprove of smoking in public places |
| 5.4 | Monitoring of emotional consequences | Prompt assessment of feelings after attempts at performing the behaviour | Agree that the person will record how they feel after taking their daily walk |
| 5.5 | Anticipated regret | Induce or raise awareness of expectations of future regret about performance of the unwanted behaviour Note: not including 5.6, information about emotional consequences; if suggests adoption of a perspective or new perspective in order to change cognitions also code 13.2, framing/reframing |
Ask the person to assess the degree of regret they will feel if they do not quit smoking |
| 5.6 | Information about emotional consequences | Provide information (e.g. written, verbal, visual) about emotional consequences of performing the behaviour Note: consequences can be related to emotional health disorders (e.g. depression, anxiety) and/or states of mind (e.g. low mood, stress); not including 5.5, anticipated regret; consequences can be for any target, not just the recipient(s) of the intervention; if information about health consequences code 5.1, information about health consequences; if about social, environmental or unspecified code 5.3, information about social and environmental consequences |
Explain that quitting smoking increases happiness and life satisfaction |
| 6. Comparison of behaviour | |||
| 6.1* | Demonstration of the behaviour | Provide an observable sample of the performance of the behaviour, directly in person or indirectly e.g. via film, pictures, for the person to aspire to or imitate (includes ‘modelling’) Note: if advised to practice, also code, 8.1, behavioural practice and rehearsal; if provided with instructions on how to perform, also code 4.1, instruction on how to perform the behaviour |
Demonstrate to nurses how to raise the issue of excessive drinking with patients via a role play exercise |
| 6.2 | Social comparison | Draw attention to others’ performance to allow comparison with the person’s own performance Note: being in a group setting does not necessarily mean that social comparison is actually taking place |
Show the doctor the proportion of patients who were prescribed antibiotics for a common cold by other doctors and compare with their own data |
| 6.3 | Information about others’ approval | Provide information about what other people think about the behaviour. The information clarifies whether others will like, approve or disapprove of what the person is doing or will do | Tell the staff at the hospital ward that staff at all other wards approve of washing their hands according to the guidelines |
| 7. Associations | |||
| 7.1* | Prompts/cues | Introduce or define environmental or social stimulus with the purpose of prompting or cueing the behaviour. The prompt or cue would normally occur at the time or place of performance Note: when a stimulus is linked to a specific action in an if–then plan including one or more of frequency, duration or intensity also code 1.4, action planning |
Put a sticker on the bathroom mirror to remind people to brush their teeth |
| 7.2 | Cue signalling reward | Identify an environmental stimulus that reliably predicts that reward will follow the behaviour (includes ‘discriminative cue’) | Advise that a fee will be paid to dentists for a particular dental treatment of 6–8 year old, but not older, children to encourage delivery of that treatment (the 6- to 8-year-old children are the environmental stimulus) |
| 7.3 | Reduce prompts/cues | Withdraw gradually prompts to perform the behaviour (includes ‘fading’) | Reduce gradually the number of reminders used to take medication |
| 7.4 | Remove access to the reward | Advise or arrange for the person to be separated from situations in which unwanted behaviour can be rewarded in order to reduce the behaviour (includes ‘time out’) | Arrange for cupboard containing high calorie snacks to be locked for a specified period to reduce the consumption of sugary foods in between meals |
| 7.5 | Remove aversive stimulus | Advise or arrange for the removal of an aversive stimulus to facilitate behaviour change (includes ‘escape learning’) | Arrange for a gym buddy to stop nagging the person to do more exercise in order to increase the desired exercise behaviour |
| 7.6 | Satiation | Advise or arrange repeated exposure to a stimulus that reduces or extinguishes a drive for the unwanted behaviour | Arrange for the person to eat large quantities of chocolate, in order to reduce the person’s appetite for sweet foods |
| 7.7 | Exposure | Provide systematic confrontation with a feared stimulus to reduce the response to a later encounter | Agree a schedule by which the person who is frightened of surgery will visit the hospital where they are scheduled to have surgery |
| 7.8 | Associative learning | Present a neutral stimulus jointly with a stimulus that already elicits the behaviour repeatedly until the neutral stimulus elicits that behaviour (includes ‘classical/Pavlovian conditioning’) Note: when a BCT involves reward or punishment, code one or more of: 10.2, material reward (behaviour); 10.3, non-specific reward; 10.4, social reward; 10.9, self-reward; 10.10, reward (outcome) |
Present repeatedly fatty foods with a disliked sauce to discourage the consumption of fatty foods |
| 8. Repetition and substitution | |||
| 8.1* | Behavioural practice/rehearsal | Prompt practice or rehearsal of the performance of the behaviour one or more times in a context or at a time when the performance may not be necessary, in order to increase habit and skill Note: if aiming to associate performance with the context, also code 8.3, habit formation |
Prompt asthma patients to practice measuring their peak flow in the nurse’s consulting room |
| 8.2 | Behaviour substitution | Prompt substitution of the unwanted behaviour with a wanted or neutral behaviour Note: if this occurs regularly, also code 8.4, habit reversal |
Suggest that the person goes for a walk rather than watches television |
| 8.3 | Habit formation | Prompt rehearsal and repetition of the behaviour in the same context repeatedly so that the context elicits the behaviour Note: also code 8.1, behavioural practice/rehearsal |
Prompt patients to take their statin tablet before brushing their teeth every evening |
| 8.4 | Habit reversal | Prompt rehearsal and repetition of an alternative behaviour to replace an unwanted habitual behaviour Note: also code 8.2, behaviour substitution |
Ask the person to walk up stairs at work where they previously always took the lift |
| 8.5 | Overcorrection | Ask to repeat the wanted behaviour in an exaggerated way following an unwanted behaviour | Ask to eat only fruit and vegetables the day after a poor diet |
| 8.6 | Generalisation of a target behaviour | Advise to perform the wanted behaviour, which is already performed in a particular situation, in another situation | Advise to repeat toning exercises learned in the gym when at home |
| 8.7 | Graded tasks | Set easy-to-perform tasks, making them increasingly difficult, but achievable, until behaviour is performed | Ask the person to walk for 100 yards a day for the first week, then half a mile a day after they have successfully achieved 100 yards, then two miles a day after they have successfully achieved one mile |
| 9. Comparison of outcomes | |||
| 9.1* | Credible source | Present verbal or visual communication from a credible source in favour of or against the behaviour Note: code this BCT if source generally agreed on as credible, e.g. health professionals, celebrities or words used to indicate expertise or leader in field and if the communication has the aim of persuading; if information about health consequences, also code 5.1, information about health consequences, if about emotional consequences, also code 5.6, information about emotional consequences; if about social, environmental or unspecified consequences also code 5.3, information about social and environmental consequences |
Present a speech given by a high status professional to emphasise the importance of not exposing patients to unnecessary radiation by ordering radiographs for back pain |
| 9.2 | Pros and cons | Advise the person to identify and compare reasons for wanting (pros) and not wanting to (cons) change the behaviour (includes ‘decisional balance’) Note: if providing information about health consequences, also code 5.1, information about health consequences; if providing information about emotional consequences, also code 5.6, information about emotional consequences; if providing information about social, environmental or unspecified consequences also code 5.3, information about social and environmental consequences |
Advise the person to list and compare the advantages and disadvantages of prescribing antibiotics for upper respiratory tract infections |
| 9.3 | Comparative imagining of future outcomes | Prompt or advise the imagining and comparing of future outcomes of changed vs. unchanged behaviour | Prompt the person to imagine and compare likely or possible outcomes following attending vs. not attending a screening appointment |
| 10. Reward and threat | |||
| 10.1 | Material incentive (behaviour) | Inform that money, vouchers or other valued objects will be delivered if and only if there has been effort and/or progress in performing the behaviour (includes ‘positive reinforcement’) Note: if incentive is social, code 10.5, social incentive if unspecified code 10.6, non-specific incentive, and not 10.1, material incentive (behaviour); if incentive is for outcome, code 10.8, incentive (outcome). If reward is delivered also code one of: 10.2, material reward (behaviour); 10.3, non-specific reward; 10.4, social reward, 10.9, self-reward; 10.10, reward (outcome) |
Inform that a financial payment will be made each month in pregnancy that the woman has not smoked |
| 10.2 | Material reward (behaviour) | Arrange for the delivery of money, vouchers or other valued objects if and only if there has been effort and/or progress in performing the behaviour (includes ‘positive reinforcement’) Note: if reward is social, code 10.4, social reward, if unspecified code 10.3, non-specific reward, and not 10.1, material reward (behaviour); if reward is for outcome, code 10.10, reward (outcome). If informed of reward in advance of rewarded behaviour, also code one of: 10.1, material incentive (behaviour); 10.5, social incentive; 10.6, non-specific incentive; 10.7, self-incentive; 10.8, incentive (outcome) |
Arrange for the person to receive money that would have been spent on cigarettes if and only if the smoker has not smoked for 1 month |
| 10.3 | Non-specific reward | Arrange delivery of a reward if and only if there has been effort and/or progress in performing the behaviour (includes ‘positive reinforcement’) Note: if reward is material, code 10.2, material reward (behaviour), if social, code 10.4, social reward, and not 10.3, non-specific reward; if reward is for outcome code 10.10, reward (outcome). If informed of reward in advance of rewarded behaviour, also code one of: 10.1, material incentive (behaviour); 10.5, social incentive; 10.6, non-specific incentive; 10.7, self-incentive; 10.8, incentive (outcome) |
Identify something (e.g. an activity such as a visit to the cinema) that the person values and arrange for this to be delivered if and only if they attend for health screening |
| 10.4 | Social reward | Arrange verbal or non-verbal reward if and only if there has been effort and/or progress in performing the behaviour (includes ‘positive reinforcement’) Note: if reward is material, code 10.2, material reward (behaviour), if unspecified code 10.3, non-specific reward, and not 10.4, social reward; if reward is for outcome code 10.10, reward (outcome). If informed of reward in advance of rewarded behaviour, also code one of: 10.1, material incentive (behaviour); 10.5, social incentive; 10.6, non-specific incentive; 10.7, self-incentive; 10.8, incentive (outcome) |
Congratulate the person for each day they eat a reduced fat diet |
| 10.5 | Social incentive | Inform that a verbal or non-verbal reward will be delivered if and only if there has been effort and/or progress in performing the behaviour (includes ‘positive reinforcement’) Note: if incentive is material, code 10.1, material incentive (behaviour), if unspecified code 10.6, non-specific incentive, and not 10.5, social incentive; if incentive is for outcome code 10.8, incentive (outcome). If reward is delivered also code one of: 10.2, material reward (behaviour); 10.3, non-specific reward; 10.4, social reward, 10.9, self-reward; 10.10, reward (outcome) |
Inform that they will be congratulated for each day they eat a reduced fat diet |
| 10.6 | Non-specific incentive | Inform that a reward will be delivered if and only if there has been effort and/or progress in performing the behaviour (includes ‘positive reinforcement’) Note: if incentive is material, code 10.1, material incentive (behaviour), if social, code 10.5, social incentive and not 10.6, non-specific incentive; if incentive is for outcome code 10.8, incentive (outcome). If reward is delivered also code one of: 10.2, material reward (behaviour); 10.3, non-specific reward; 10.4, social reward, 10.9, self-reward; 10.10, reward (outcome) |
Identify an activity that the person values and inform them that this will happen if and only if they attend for health screening |
| 10.7 | Self-incentive | Plan to reward self in future if and only if there has been effort and/or progress in performing the behaviour Note: if self-reward is material, also code 10.1, material incentive (behaviour), if social, also code 10.5, social incentive, if unspecified, also code 10.6, non-specific incentive; if incentive is for outcome code 10.8, incentive (outcome). If reward is delivered also code one of: 10.2, material reward (behaviour); 10.3, non-specific reward; 10.4, social reward, 10.9, self-reward; 10.10, reward (outcome) |
Encourage to provide self with material (e.g. new clothes) or other valued objects if and only if they have adhered to a healthy diet |
| 10.8 | Incentive (outcome) | Inform that a reward will be delivered if and only if there has been effort and/or progress in achieving the behavioural outcome (includes ‘positive reinforcement’) Note: this includes social, material, self- and non-specific incentives for outcome; if incentive is for the behaviour code 10.5, social incentive, 10.1, material incentive (behaviour), 10.6, non-specific incentive or 10.7, self-incentive and not 10.8, incentive (outcome). If reward is delivered also code one of: 10.2, material reward (behaviour); 10.3, non-specific reward; 10.4, social reward, 10.9, self-reward; 10.10, reward (outcome) |
Inform the person that they will receive money if and only if a certain amount of weight is lost |
| 10.9 | Self-reward | Prompt self-praise or self-reward if and only if there has been effort and/or progress in performing the behaviour Note: if self-reward is material, also code 10.2, material reward (behaviour), if social, also code 10.4, social reward, if unspecified, also code 10.3, non-specific reward; if reward is for outcome code 10.10, reward (outcome). If informed of reward in advance of rewarded behaviour, also code one of: 10.1, material incentive (behaviour); 10.5, social incentive; 10.6, non-specific incentive; 10.7, self-incentive; 10.8, incentive (outcome) |
Encourage to reward self with material (e.g. new clothes) or other valued objects if and only if they have adhered to a healthy diet |
| 10.10 | Reward (outcome) | Arrange for the delivery of a reward if and only if there has been effort and/or progress in achieving the behavioural outcome (includes ‘positive reinforcement’) Note: this includes social, material, self- and non-specific rewards for outcome; if reward is for the behaviour code 10.4, social reward, 10.2, material reward (behaviour), 10.3, non-specific reward or 10.9, self-reward and not 10.10, reward (outcome). If informed of reward in advance of rewarded behaviour, also code one of: 10.1, material incentive (behaviour); 10.5, social incentive; 10.6, non-specific incentive; 10.7, self-incentive; 10.8, incentive (outcome) |
Arrange for the person to receive money if and only if a certain amount of weight is lost |
| 10.11 | Future punishment | Inform that future punishment or removal of reward will be a consequence of performance of an unwanted behaviour (may include fear arousal) (includes ‘threat’) | Inform that continuing to consume 30 units of alcohol per day is likely to result in loss of employment if the person continues |
| 11. Regulation | |||
| 11.1 | Pharmacological support | Provide, or encourage the use of or adherence to, drugs to facilitate behaviour change Note: if pharmacological support to reduce negative emotions (i.e. anxiety) then also code 11.2, reduce negative emotions |
Suggest the patient asks the family physician for nicotine replacement therapy to facilitate smoking cessation |
| 11.2 | Reduce negative emotions a | Advise on ways of reducing negative emotions to facilitate performance of the behaviour (includes ‘stress management’) Note: if includes analysing the behavioural problem, also code 1.2, problem-solving |
Advise on the use of stress management skills, e.g. to reduce anxiety about joining Alcoholics Anonymous |
| 11.3 | Conserving mental resources | Advise on ways of minimising demands on mental resources to facilitate behaviour change | Advise to carry food calorie content information to reduce the burden on memory in making food choices |
| 11.4 | Paradoxical instructions | Advise to engage in some form of the unwanted behaviour with the aim of reducing motivation to engage in that behaviour | Advise a smoker to smoke twice as many cigarettes a day as they usually do tell the person to stay awake as long as possible in order to reduce insomnia |
| 12. Antecedents | |||
| 12.1* | Restructuring the physical environment | Change, or advise to change the physical environment in order to facilitate performance of the wanted behaviour or create barriers to the unwanted behaviour (other than prompts/cues, rewards and punishments) Note: this may also involve 12.3, avoidance/reducing exposure to cues for the behaviour; if restructuring of the social environment code 12.2, restructuring the social environment; if only adding objects to the environment, code 12.5, adding objects to the environment |
Advise to keep biscuits and snacks in a cupboard that is inconvenient to get to arrange to move vending machine out of the school |
| 12.2 | Restructuring the social environment | Change, or advise to change the social environment in order to facilitate performance of the wanted behaviour or create barriers to the unwanted behaviour (other than prompts/cues, rewards and punishments) Note: this may also involve 12.3, avoidance/reducing exposure to cues for the behaviour; if also restructuring of the physical environment also code 12.1, restructuring the physical environment |
Advise to minimise time spent with friends who drink heavily to reduce alcohol consumption |
| 12.3 | Avoidance/reducing exposure to cues for the behaviour | Advise on how to avoid exposure to specific social and contextual/physical cues for the behaviour, including changing daily or weekly routines Note: this may also involve 12.1, restructuring the physical environment and/or 12.2, restructuring the social environment; if the BCT includes analysing the behavioural problem, only code 1.2, problem-solving |
Suggest to a person who wants to quit smoking that their social life focus on activities other than pubs and bars which have been associated with smoking |
| 12.4 | Distraction | Advise or arrange to use an alternative focus for attention to avoid triggers for unwanted behaviour | Suggest to a person who is trying to avoid between-meal snacking to focus on a topic they enjoy (e.g. holiday plans) instead of focusing on food |
| 12.5* | Adding objects to the environment | Add objects to the environment in order to facilitate performance of the behaviour Note: provision of information (e.g. written, verbal, visual) in a booklet or leaflet is insufficient. If this is accompanied by social support, also code 3.2, social support (practical); if the environment is changed beyond the addition of objects, also code 12.1, restructuring the physical environment |
Provide free condoms to facilitate safe sex. Provide attractive toothbrush to improve tooth brushing technique |
| 12.6 | Body changes | Alter body structure, functioning or support directly to facilitate behaviour change | Prompt strength training, relaxation training or provide assistive aids (e.g. a hearing aid) |
| 13. Identity | |||
| 13.1 | Identification of self as role model | Inform that one’s own behaviour may be an example to others | Inform the person that if they eat healthily, that may be a good example for their children |
| 13.2 | Framing/reframing | Suggest the deliberate adoption of a perspective or new perspective on behaviour (e.g. its purpose) in order to change cognitions or emotions about performing the behaviour (includes ‘cognitive structuring’) Note: if information about consequences then code 5.1, information about health consequences, 5.6, information about emotional consequences or 5.3, information about social and environmental consequences instead of 13.2, framing/reframing |
Suggest that the person might think of the tasks as reducing sedentary behaviour (rather than increasing activity) |
| 13.3 | Incompatible beliefs | Draw attention to discrepancies between current or past behaviour and self-image, in order to create discomfort (includes ‘cognitive dissonance’) | Draw attention to a doctor’s liberal use of blood transfusion and their self-identification as a proponent of evidence-based medical practice |
| 13.4 | Valued self-identity | Advise the person to write or complete rating scales about a cherished value or personal strength as a means of affirming the person’s identity as part of a behaviour change strategy (includes ‘self-affirmation’) | Advise the person to write about their personal strengths before they receive a message advocating the behaviour change |
| 13.5 | Identity associated with changed behaviour | Advise the person to construct a new self-identity as someone who ‘used to engage with the unwanted behaviour’ | Ask the person to articulate their new identity as an ‘ex-smoker’ |
| 14. Scheduled consequences | |||
| 14.1 | Behaviour cost | Arrange for withdrawal of something valued if and only if an unwanted behaviour is performed (includes ‘response cost’) Note: if withdrawal of contingent reward code, 14.3, remove reward |
Subtract money from a prepaid refundable deposit when a cigarette is smoked |
| 14.2 | Punishment | Arrange for aversive consequence contingent on the performance of the unwanted behaviour | Arrange for the person to wear unattractive clothes following consumption of fatty foods |
| 14.3 | Remove reward | Arrange for discontinuation of contingent reward following performance of the unwanted behaviour (includes ‘extinction’) | Arrange for the other people in the household to ignore the person every time they eat chocolate (rather than attending to them by criticising or persuading) |
| 14.4 | Reward approximation | Arrange for reward following any approximation to the target behaviour, gradually rewarding only performance closer to the wanted behaviour (includes ‘shaping’) Note: also code one of 59–63 |
Arrange reward for any reduction in daily calories, gradually requiring the daily calorie count to become closer to the planned calorie intake |
| 14.5 | Rewarding completion | Build up behaviour by arranging reward following final component of the behaviour; gradually add the components of the behaviour that occur earlier in the behavioural sequence (includes ‘backward chaining’) Note: also code one of 10.2, material reward (behaviour); 10.3, non-specific reward; 10.4, social reward, 10.9, self-reward; 10.10, reward (outcome) |
Reward eating a supplied low calorie meal; then make reward contingent on cooking and eating the meal; then make reward contingent on purchasing, cooking and eating the meal |
| 14.6 | Situation-specific reward | Arrange for reward following the behaviour in one situation but not in another (includes ‘discrimination training’) Note: also code one of 10.2, material reward (behaviour); 10.3, non-specific reward; 10.4, social reward, 10.9, self-reward; 10.10, reward (outcome) |
Arrange reward for eating at mealtimes but not between meals |
| 14.7 | Reward incompatible behaviour | Arrange reward for responding in a manner that is incompatible with a previous response to that situation (includes ‘counter-conditioning’) Note: also code one of 10.2, material reward (behaviour); 10.3, non-specific reward; 10.4, social reward, 10.9, self-reward; 10.10, reward (outcome) |
Arrange reward for ordering a soft drink at the bar rather than an alcoholic beverage |
| 14.8 | Reward alternative behaviour | Arrange reward for performance of an alternative to the unwanted behaviour (includes ‘differential reinforcement’) Note: also code one of 10.2, material reward (behaviour); 10.3, non-specific reward; 10.4, social reward, 10.9, self-reward; 10.10, reward (outcome); consider also coding 1.2, problem-solving |
Reward for consumption of low fat foods but not consumption of high fat foods |
| 14.9 | Reduce reward frequency | Arrange for rewards to be made contingent on increasing duration or frequency of the behaviour (includes ‘thinning’) Note: also code one of 10.2, material reward (behaviour); 10.3, non-specific reward; 10.4, social reward, 10.9, self-reward; 10.10, reward (outcome) |
Arrange reward for each day without smoking, then each week, then each month, then every 2 months and so on |
| 14.10 | Remove punishment | Arrange for removal of an unpleasant consequence contingent on performance of the wanted behaviour (includes ‘negative reinforcement’) | Arrange for someone else to do housecleaning only if the person has adhered to the medication regimen for a week |
| 15. Self-belief | |||
| 15.1 | Verbal persuasion about capability | Tell the person that they can successfully perform the wanted behaviour, arguing against self-doubts and asserting that they can and will succeed | Tell the person that they can successfully increase their physical activity, despite their recent heart attack |
| 15.2 | Mental rehearsal of successful performance | Advise to practise imagining performing the behaviour successfully in relevant contexts | Advise to imagine eating and enjoying a salad in a work canteen |
| 15.3 | Focus on past success | Advise to think about or list previous successes in performing the behaviour (or parts of it) | Advise to describe or list the occasions on which the person had ordered a non-alcoholic drink in a bar |
| 15.4 | Self-talk | Prompt positive self-talk (aloud or silently) before and during the behaviour | Prompt the person to tell themselves that a walk will be energising |
| 16. Covert learning | |||
| 16.1 | Imaginary punishment | Advise to imagine performing the unwanted behaviour in a real-life situation followed by imagining an unpleasant consequence (includes ‘covert sensitisation’) | Advise to imagine overeating and then vomiting |
| 16.2 | Imaginary reward | Advise to imagine performing the wanted behaviour in a real-life situation followed by imagining a pleasant consequence (includes ‘covert conditioning’) | Advise the health professional to imagine giving dietary advice followed by the patient losing weight and no longer being diabetic |
| 16.3 | Vicarious consequences | Prompt observation of the consequences (including rewards and punishments) for others when they perform the behaviour Note: if observation of health consequences, also code 5.1, information about health consequences; if of emotional consequences, also code 5.6, information about emotional consequences, if of social, environmental or unspecified consequences, also code 5.3, information about social and environmental consequences |
Draw attention to the positive comments other staff get when they disinfect their hands regularly |

|
This booklet will also be included as a supplementary file in Abraham et al. 107
Target behaviour/s: physical activity.
Target population/s: participants.
Excerpt from: Murphy et al. 112 © 2010 Murphy et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
NERS [National Exercise Referral Scheme] consists of a series of motivational interviewing (MI) consultations with an EP [exercise professionals] based in a community sports centre and access to a tailored, subsidised 16 week activity programme. To be eligible for NERS, participants must be sedentary (defined as not moderately active for 3 or more times per week or deconditioned through age or inactivity), and have at least one medical condition, covering CHD [coronary heart disease] risk factors, mental health, musculoskeletal, respiratory/pulmonary and neurological conditions. The primary aim of NERS is for participants to achieve 30 minutes of moderate physical activity on at least 5 days per week. Common features of the scheme are detailed below.
Delivery of the Welsh national exercise referral scheme:
16 week programme of exercise supervised by a qualified EP
-
Initial face to face consultation with EP on entry – lifestyle questionnaire, health check (resting heart rate, blood pressure, BMI [body mass index], and waist circumference), introduction to facilities, MI and goal setting
-
Access to one to one exercise instruction and/or group exercise classes
-
Discounted rate for exercise activities £1 per session.
-
Four week telephone consultation with EP – review of goals and MI [motivational interviewing]
-
Sixteen week face to face consultation with EP – review of goals, MI, health check, lifestyle questionnaire, service evaluation questionnaire and signposted to exit routes
-
Post 16 week activities
-
Range and cost of exit routes dependent on area
-
8 months contact by phone to check progress
-
12 months face to face review including Chester fitness step test.
Consultations occur at entry, 4 weeks (by phone) and 16 weeks. Following this, participants are contacted by telephone at 8 months to monitor progress and at 12 months they are invited to attend a review session. Routine programme monitoring systems are maintained by EPs and capture the dates of and records from initial, 4 and 16 week and 8 and 12 month consultations
Target behaviour/s: management of children’s healthy eating and physical activity (encompassing a range of behaviours).
Target population/s: parents.
Extract from: Skouteris et al. 115 © 2010 Skouteris et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
The MEND 2–4 program involves 10 weekly 90 minute workshops relating to general nutrition, and physical activity behaviours, that are typically held at community health and maternal and child health centres, where parents and their preschool-aged children attend together. Each program group will consist of 6–10 child-parent dyads and a MEND 2–4 trained program leader. Program leaders, who are trained extensively by MEND Australia prior to starting with a group, will be monitored and evaluated by MEND Australia staff to ensure their practice is in accordance with MEND 2–4 guidelines; parental feedback on program leaders will also be obtained. Each session involves 30 minutes of guided active play, where parents can learn how to play with their children; 15 minutes of healthy snack time based on an evidence-based exposure-based technique to promote acceptance and increased intake of fruit and vegetables and 45 minutes where the children participate in supervised crèche-style, creative play activities. Concurrently the parents attend an interactive education and skill development session, based on evidence-based group-based parent-training principles. Table A outlines the weekly education topics, and parents will receive handouts on these topics weekly. Pilot data reveals low attrition and that parents value the program and attend all 10 sessions. In the initial MEND 2–4 trials (UK) the participation rate was 87.6% which is high for developmental research.
| Week | Workshop title | Discussion topic(s) | Intervention content |
|---|---|---|---|
| 1 | Welcome & introduction | Meet the leader and pre-program measurements | Meet and welcome the families to their first MEND 2–4 physical activity and snack-time session; parents complete all pre-program forms and questionnaires and accurate child and parent anthropometric measurements (height and weight) taken |
| 2 | Introduction | Introductions and individual expectations | Discussion of individual expectations and introduction of MEND 2–4 program and practicalities; introduction of parents/carers to the behavioural model of parenting [customised as the 4Cs model (Causes, Consequences, Consistency and Copying) for the purposes of MEND 2–4] |
| 3 | Healthy eating for families | Healthy eating | Introduction to the five food groups, visual samples of excess sugar and fat found in foods. Discussion of appropriate treats and rewards and toddler intake of drinks |
| 4 | Be healthy, get active! | Non-TV activities for toddlers | Importance of limiting TV watching among toddlers; goal setting activity towards achievement of MEND 2–4 TV time guidelines (maximum of 1–2 hours of TV per day). Discussion of active play and activity ideas to replace time spent previously watching TV |
| 5 | What’s in your child’s food? | Reading food labels | Reading food labels; MEND 2–4 label reading guidelines and identification of MEND 2–4 friendly food |
| 6 | Food without fuss | Dealing with fussy eaters | Normalisation of fussy eating and common causes; importance of consistency around mealtimes and ideas for managing fussy eating behaviour. Strategies to reduce fear and unhelpful parenting behaviour around food at mealtimes |
| 7 | Portion sizes | Healthy eating and portion sizes | Introduction to the MEND 2–4 portion sizes with visual demonstration; demonstration of difference between toddler and adult portion sizes |
| 8 | Fun with food | Cooking together | Demonstration of ideas for making food preparation fun and including fruits and vegetables, how to actively involve children in preparation of snacks and parents/carers and child having fun with food together |
| 9 | Encouraging healthy habits | Rules, routines and tantrum management | Establishing health as a priority within the family life-cycle. Helpful strategies for dealing with behaviours that may be resistant to change. MEND 2–4 sleep guidelines for toddlers |
| 10 | Farewell and graduation | Evaluation and measurement | Collection of post-program measurements; MEND 2–4 certificates provided; information about follow-up activities or other local groups they may like to attend at the end of the MEND 2–4 Program |
Target behaviour/s: management of 3–5-year old children’s fruit and vegetable intake (encompassing a range of behaviours).
Target population/s: parents.
Extract from: Wyse et al. 118 © 2010 Wyse et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Intervention content
The telephone intervention script is designed to help parents modify their home food environments through addressing three key domains listed in Table B. The first column of the table lists each domain at the point at which it appears in the schedule of support calls, while the second column lists the specific topics that are used to explore each of the given domains. Each domain has been associated with increased fruit and vegetable consumption in children as described below.
| Key theme | Content | Behaviour change technique | Application of behaviour change technique |
|---|---|---|---|
| WEEK 1 Availability and Accessibility | Dietary recommendations and serving sizes | ||
| Children’s food diary | Prompt self-monitoring of behaviour | Parents are asked to monitor their children’s intake of fruit, and vegetables over 3 days | |
| Ways to provide fruit and vegetables throughout the day | |||
| Setting goals | Prompt specific goal-setting | Parents are encouraged to set a program goal | |
| WEEK 2 Availability and Accessibility, Supportive Family Eating Routines | Changing the family routine | Prompt intention formation | Parents decide which activities they will attempt in the coming week |
| Availability and accessibility of foods in the home | Provide general encouragement | Interviewers provide positive feedback about any helpful practices occurring in the home | |
| Mealtime practices | Teach to use prompts or cues | Parents learn the HELPS acronym, i.e. try to eat when Hungry, not attempting anything else at the same time (focus on Eating), at an appropriate Location to eat, from a Plate, and while Sitting | |
| Meal planning | |||
| Review of goals | Prompt review of behavioural goals | Parents review the goals they set during the previous calls and evaluate their progress | |
| WEEK 3 Parental role-modelling, Supportive Family Eating Routines | The Ps and Cs division of feeding responsibility | Teach to use prompts or cues | Parents learn the Ps and Cs: Parents are encouraged to Plan, Prepare and Provide. Children are encouraged to Choose (whether, what and how much to eat) |
| Mealtime strategies to encourage vegetable consumption | Prompt intention formation | Parents decide which activities they will attempt in the coming week | |
| Provide general encouragement | Interviewers provide positive feedback about any helpful practices occurring in the home | ||
| Role-modelling of fruit and vegetable consumption | Prompt identification as a role model | Parents are provided information About their importance in role-modelling fruit and vegetable consumption. Their consumption is compared with national nutrition recommendations. Tailored feedback is provided |
|
| WEEK 4 Availability and Accessibility Parental role-modelling, Supportive Family Eating Routines | Review of weeks 1–3 | Provide general encouragement | Interviewers provide positive feedback about any helpful practices occurring in the home |
| Planning for the future and dealing with difficult situations | Prompt barrier identification | Parents are encouraged to identify barriers that will prevent them implementing what they have learnt and to generate solutions | |
| Review of goals | Prompt review of behavioural goals | Parents review their program goal, evaluate their progress and identify how they can maintain the change |
Availability and accessibility of fruit and vegetables
The telephone intervention encourages parents to ensure that fruit and vegetables are available and accessible in the home and that they are prepared, presented or maintained in a ready-to-eat form that encourages their consumption. This could include offering cut-up pieces of fruit or vegetable at snack times, and ensuring fruit is visible by storing it in fruit bowls.
Supportive family eating routines
The intervention will seek to improve parent knowledge and facilitate the acquisition of skills to support parents to eat meals as a family without the television on, establish and enforce family rules about eating and develop boundaries regarding when and how food is offered to their children.
Parental role-modelling of fruit and vegetable consumption
Parents will be encouraged to increase the number of serves of fruit and vegetables that they consume in front of their children and to express supportive attitudes toward the consumption of fruit and vegetables to their children, for example, by making positive and encouraging comments.
Participants will also be asked to undertake homework activities to encourage them to apply, directly into their home environment, the strategies and information covered in the telephone calls. Incorporating homework assignments into health behaviour interventions has been found to increase the size of the intervention effect. Homework activities will be optional and tailored to the needs of the participant, based on recommended home food environment practices not currently undertaken by the participant.
Intervention resources
Based on evidence indicating telephone-based dietary interventions are more effective when used in conjunction with print and other resources, all intervention participants will be mailed resource kits following completion of the baseline survey. The kit comprises a participant workbook containing information and activities, a pad of meal planners, and a cookbook including recipes high in fruit and vegetables. The resources will be used to facilitate participant engagement in the telephone support calls and assist participants to complete intervention activities between telephone contacts.
Conceptual model
The telephone-based intervention accords with the model of family-based intervention proposed by Golan et al. (2001) in the treatment and prevention of childhood obesity. Their model, which draws upon socioecological theory, focuses on introducing new familial norms associated with healthy eating. This is achieved through making changes within the home food environment, providing positive parental role-modelling and increasing parenting- and nutrition-related knowledge and skills. Interventions based on such a model have been shown to be effective in bringing about environmental changes in participants’ homes to support healthy eating and in reducing poor eating habits of overweight and obese children of participants.
The intervention utilises a number of specific behaviour change techniques to initiate the change process as described in Table A. The third column lists the behaviour change techniques used and the fourth column links each technique to its application in the context of the topic listed in column 2. These behaviour change techniques include prompting intention formation, barrier identification, specific goal-setting and the reviewing of such goals, self-monitoring of behaviour and identification as a role-model, teaching to use prompts or cues, and providing general encouragement, as described in the taxonomy proposed by Abraham and Michie (2008).
Target behaviour/s: management of discrete child problem behaviours (specific behaviours unspecified).
Target population/s: parents.
Excerpt from: Spijkers et al. 122 © 2010 Spijkers et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Intervention
The intervention to be evaluated is Triple P level 3. Triple P is a multilevel system of family intervention which provides five levels of intervention of increasing strength. Triple P intervention at level 3 (Primary Care Triple P) is a brief, narrow-focus parent programme that is aimed at parents with specific concerns about their child’s behaviour or development. It combines advice, rehearsal and self-evaluation to teach parents to manage discrete child problem behaviour during four individual consultations of 20–30 minutes with the parents and their child (Table C).
| Session | Contents | Duration |
|---|---|---|
| 1. Assessment of the presenting problem | Intake interview | 15–30 minutes |
| Options for intervention | ||
| Keeping track of the children’s behaviour | ||
| 2. Developing a parenting plan | Feedback of assessment results | 15–30 minutes |
| Causes of child behaviour problems | ||
| Goals for change | ||
| Parenting plan (with active skills training) | ||
| 3. Review of implementation | Update on progress | 15–30 minutes |
| Refining parenting plan (with active skills training) | ||
| Identifying and overcoming obstacles | ||
| Other issues | ||
| 4. Follow-up | Update on progress | 15–30 minutes |
| Maintaining progress made | ||
| Other issues |
Target behaviour/s: health related behaviours including physical activity and dietary intake (encompassing a range of behaviours).
Target population/s: participants.
Extract from: Colagiuri et al. 124 © 2010 Colagiuri et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Intervention – Lifestyle Modification Program
The five aims of the lifestyle modifications are:
-
At least 30 min/day of moderate to vigorous intensity physical activity, including aerobic exercise 3 or more days/week plus strength training at least twice/week (210 min/week total structured exercise)
-
Reduction in the intake of energy from total fat to less than 30%
-
Reduction in the intake of energy from saturated fat to less than 10%
-
Fibre intake of at least 15 g/1000 kcal
-
Achievement of a 5% reduction in body weight at 12 months.
In addition to the 210 min/week structured exercise goal, participants are encouraged to increase incidental physical activity in ways which would enhance both cardiovascular and musculoskeletal fitness.
These five goals are entirely concordant with the Finnish DPS [Diabetes Prevention Service] which was one of the most successful diabetes prevention trials. The physical activity goal, which has been modified slightly from the Finnish DPS is based on a review of the physical activity prescriptions utilised in relation to outcomes achieved in all of the successful trials of diabetes prevention, considerations of cost and feasibility in this translational setting, as well as other literature regarding modality, volume, and intensity of exercise required to improve metabolic risk and body composition in similar cohorts. Both the Finnish DPS and the US DPP [Diabetes Prevention Programme] included resistance training (strength training) in their supervised exercise sessions and is explicitly specified within the physical activity goal of the SDPP [Sydney Diabetes Prevention Programme]. Resistance training is an anabolic form of exercise, differing substantially from aerobic exercise in its ability to induce muscle hypertrophy and associated metabolic and functional changes. It improves insulin sensitivity, glucose homeostasis, blood pressure, dyslipidaemia, markers of inflammation and catabolism, and visceral obesity, thus addressing the key metabolic abnormalities in adults at high risk of type 2 diabetes. Importantly, resistance training (but not aerobic exercise) attenuates or prevents the loss of lean tissue (muscle and bone) accompanying weight loss diets such as those prescribed in this study.
The behavioural components are based on stages of change and social cognitive theories. The intervention is delivered by dedicated program lifestyle officers from a variety of health backgrounds including dietetics, nursing, psychology and exercise physiology. The lifestyle officers undergo specific training in health coaching, group program delivery and standardized data collection used for evaluation. The health coaching approach incorporates principles from self-management, removing psychological blocks to change and confidence.
High risk individuals agreeing to participate in the lifestyle modification program complete an initial computer assisted telephone interview (CATI) survey. This survey includes socio-economic and demographic information, physical activity habits, quality of life and self-efficacy, as well as recent health service utilisation and current medication use. Participants are then scheduled to attend an individual consultation with a lifestyle officer. At this consultation, the lifestyle officers measure height, weight and waist circumference using calibrated stadiometers, scales and tape measures, following a standardized anthropometric protocol as specified by the International Society for the Advancement of Kinanthropometry (ISAK). The individual consultation includes a general discussion about diabetes risk and prevention, an overview of the program, and uses motivational interviewing techniques to assist participants to set goals and develop tools to self-monitor. Following this session, arrangements are made for participants to attend three two-hour group programs held over a six to eight week period. Lifestyle officers conduct these group sessions of approximately 10 people, which cover theoretical, behavioural and practical aspects of diet and physical activity. The overall program motto is: ‘Eat better and move more’. Those who are not able to or do not want to attend a group program are offered the option of three individual health coaching sessions by telephone, covering the same material. The intervention delivered to indigenous participants will be slightly modified to take account of cultural issues.
Follow up telephone calls are made by the lifestyle officers to each participant at 3, 6 and 9 months to enquire about progress, assist with behaviour change and offer participants additional support as required. In addition, participants are provided with details of local community-based lifestyle programs which have been evaluated by the research staff and found to be consistent with the goals of the SDPP. Participants have the option of enrolling in such programs as one way to assist in achieving the SDPP physical activity and dietary goals.
At 12 months the CATI survey is repeated and participants undergo an individual assessment with the lifestyle officer and their general practitioner.
Target behaviour/s: smoking cessation.
Target population/s: family members and caregivers.
Extract from: Johnston et al. 129 © 2010 Johnston et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Treatment group
The intervention program will (i) provide information and education about the health effects of ETS [environmental tobacco smoke] exposure and use behavioural ‘coaching’ techniques to help mothers/caregivers and family members implement strategies to reduce the infant’s ETS exposure, as well as (ii) identify the smokers among other household members and deliver culturally appropriate smoking cessation advice, counseling and treatment options as requested. An eight weeks supply of free nicotine replacement therapy (NRT) (patches or gum) will be available to participants and other household members for whom such drug therapy is indicated (i.e. they are motivated to quit, are nicotine dependent and have no contraindications to taking NRT). NRT will be provided by the IHW [indigenous health worker] with appropriate counseling and follow-up. Furthermore, for those that are interested a fax referral to Quitline will be offered, with proactive call back by Quitline.
The intervention program will be delivered during three face-to-face home visits (of approximately 45–60 minutes) conducted over the first three months of the infant’s life. Culturally appropriate resources (e.g. flip charts, ‘No Smoking’ stickers, posters, etc.) will be used to assist in both education and behavioural ‘coaching’. These resources will be obtained from relevant health groups in each country who hold a repository of such resources (e.g. QUIT Victoria, the Northern Territory Department of Health and Families, Auckland Regional Public Health Service). IHWs will deliver the program after appropriate training, and will complete standardized progress reports after each program session, which will be used at a weekly team meeting with the health workers and study personnel for discussion and ongoing training.
Target behaviour/s: health behaviours including dietary intake, physical activity/inactivity, and parenting behaviour to help reduce weight in 4–8 year old children (encompassing a range of behaviours).
Target population/s: family members.
Extract from: Taylor et al. 130 © 2010 Taylor et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Phase 2: Treatment
Tailored Package group – treatment phase
The Tailored package is modelled in part on our successful HEAT study and from the literature and is designed to be suitable for incorporation into primary care. Three main areas of interest will be assessed and targeted; dietary intake, physical activity/inactivity, and parenting/behaviour (Table D). In the Tailored Package condition, parents will attend one session with a multi-disciplinary team (consultant session) then all further contact will be with their MInT mentor.
| Diet | Behaviour management |
|---|---|
| Making water the main drink | Stress management for parents |
| Eating more fruit and vegetables | Using attention and effective commands |
| Changing fast food choices | Using ground rules and rewards |
| Healthy snacks | Discipline and consequences |
| Appropriate portion size | Developing action plans |
| Family meals | |
| Physical activity/inactivity | Other |
| Motivating kids to be active | Helping children sleep |
| Reducing screen time | |
| Increasing moderate/vigorous activity | |
| Increasing family activity |
Consultant session
Information obtained from the screening, follow-up and baseline assessments (family structure, economic situation, dietary intake, physical activity, child behaviour, motivation, parental weight, parenting) will be used by the clinical psychologist to develop a formulation that is specific for each family. This formulation will provide an explanation of factors that may have contributed to the development of the child’s weight, and may be maintaining the situation, as well as identifying strengths and resources in the family. The family will then meet with the ‘expert’ team, consisting of the clinical psychologist, a dietitian, an exercise specialist and the MInT mentor to discuss and modify the formulation as appropriate and to reflect on the implications of this for possible goals for change. The main objective of this session is to assist the family in developing an understanding of their current situation, and to collaboratively identify areas in which they may wish to make changes in. Once the goals have been identified, the session will focus on developing an individualized plan for each family consisting of strategies that they can use to achieve the goals they have identified.
Mentor sessions – timing
The MInT mentor will then become the main contact for each family. To aid in establishing new routines during the first phase of the treatment period (4 months) the mentor will contact the family each week, using an alternating but flexible schedule of in-person consultations and telephone calls. Frequency of contact will be gradually reduced over the subsequent 20 months of the intervention (fortnightly for months 5–8, monthly for months 9–12, and 3-monthly for months 13–24).
Mentor sessions – structure
During the sessions the mentor will assess progress with each goal since last contact, problem-solve with the family any difficulties arising, and negotiate goals for the next session. Each family will receive a different package of resources over time depending on identified need and there is some scope for resources to be tailored to individual families. Across the period of intervention the mentor may also (in consultation with the expert team) facilitate the introduction of new behavioural goals. The intervention will be conducted in the ‘spirit’ of MI, taking a client-centred collaborative approach, which has been identified as just as important as the specific techniques, by adhering to the four general principles of expressing empathy, supporting self-efficacy, rolling with resistance and developing discrepancy. MI will be used as required through the life of the intervention, in consultation with the supervisors, when motivation and/or engagement is waning, and when at the transition from one target behaviour to the next (where multiple goals have been identified).
Target behaviour/s: medication use/adherence.
Target population/s: patients.
Extract from: Ahmad et al. 113 © 2010 Ahmad et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Study procedures
Intervention group
Medication review
The medication of patients in the intervention group will be reviewed by the community pharmacist using the full record of prescription only drugs which were dispensed by the patients’ pharmacy and the patients medication evaluation profile. This profile shows when the patient has obtained his medication from the pharmacy. The GP [general practitioner] will be consulted by telephone for details about indications for drugs and results from laboratory tests. When prescribed by a medical specialist, details about the indication for the drug will be obtained from the specialist, who will be consulted by the community pharmacist. The National guidelines for treatment of diseases will be used by community pharmacists as a method for performing medication review.
The Pharmaceutical care network Europe DRP-score [drug-related problem score] form will be used to record drug problems. Each drug will be evaluated on adverse reactions, drug choice problems, dosing problems, drug use problems, drug-interactions or other problems. Causes for drug related problems will be assessed and interventions will be made. During the medication review the patient will be involved as a full partner. Any changes made will be communicated with the patient. This method for medication review will be pilot tested before use.
The occurrence of drug related problems will be discussed with the GP. The result may be an adaptation of the drug regimen. The medication review will take 10–30 minutes per patient and will depend on the complexity of the medication regimen and problems detected.
Cognitive behaviour treatment
Patients randomised to the intervention group will also receive cognitive behaviour treatment (CBT) at baseline and 1, 3, 6, 9 and 12 months by a pharmacy technician, with help of a structured interview protocol and with use of communication and motivational interviewing skills at home or in the pharmacy. The first session will be within one week of inclusion in order not to delay participant program admission. During these sessions the result of the medication review will be discussed with the patient. The patient will be informed about the effects, side effects and use of the drugs. Patients will be counselled according to the motivational interviewing principle to sustain or improve their drug adherence. The patients understanding of his or hers condition and its treatment are considered when appropriate. If possible, home supplies of drugs are checked and rationalised at each visit. All patients receive a written outline of their drug regimen. Cancelled and redundant drugs are taken in. During the session over the counter remedies will be included in the medication review. All sessions are done by pharmacist technicians with help of a structured protocol. The patient visit will take 30–60 minutes.
Target behaviour/s: healthy eating and physical activity for weight loss (encompassing a range of behaviours).
Target population/s: patients.
Extract from: Castelnuovo et al. 116 © 2010 Castelnuovo et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Intervention
The TECNOB clinical program has a total duration of 13 months and consists of two stepped down phases: inpatient (1 month) and out-patient (the following 12 months). During the in-patient phase, participants undergo an intensive four-week hospital-based and medically-managed program for weight reduction and rehabilitation. Along this period, participants live in a medical hospital-like environment located on a mountain highland and far away from towns and cities. Visits from parents are allowed only in the afternoon. All patients are placed on a hypocaloric nutritionally balanced diet tailored to the individual after consultation with a dietitian (energy intake around 80% of the basal energy expenditure estimated according to the Harris-Benedict equation and a macronutrient composition of about 16% proteins, 25% fat and 59% carbohydrates). Furthermore, they receive nutritional counseling provided by a dietitian, psychological counseling provided by a clinical psychologist and have physical activity training provided by a physiotherapist.
Nutritional rehabilitation program aims to improve and promote change in eating habits and consists of both individual sessions (dietary assessment, evaluation of nutrient intake and adequacy, nutritional status, anthropometric, eating patterns, history of overweight, readiness to adopt change) and group sessions (45 minutes each twice a week) including: information on obesity and related health risks, setting of realistic goals for weight loss, healthy eating in general, general nutrition and core food groups, weight management and behavior change strategies for preventing relapse).
Psychological counseling is provided once a week both individually and in group setting. Individual sessions, lasting 45 minutes each, are mainly based on the cognitive-behavioral approach described by Cooper and Fairburn (1990) and emphasize the techniques of self-monitoring, goal setting, time management, prompting and cueing, problem solving, cognitive restructuring, stress management and relapse prevention. Group sessions (‘closed’ groups of 5/6 persons), lasting 1 hour each, focus on issues such as motivation, assertiveness, self-esteem, self-efficacy and coping.
Physical activity takes place once a day except for weekend and consists of group programs (20 subjects) based on postural gymnastics, aerobic activity and walks in the open. Inpatients with specific orthopedic complications carry out individual activities planned by physiotherapists and articulated in programs of physical therapy, assisted passive and active mobilization and isokinetic exercise.
Low to moderate weight losses are expected at the end of the in-patient phase, but it is important to note that weight loss is not the primary goal of the in-patient program and each patient is made clear about this point at the very beginning of the treatment. Beyond the medical management of metabolic risk factors for health such as type 2 diabetes, developing a sense of autonomy and competence are the primary purposes of the in-hospital interventions. Patients are afforded the skills and tools for change and are supported in assigning positive values to healthy behaviours and also in aligning them with personal values and lifestyle patterns.
In the last week, just before discharge from hospital, participants are instructed for the out-patient phase of the program. They receive a multisensory armband (SenseWear® Pro2 Armband), an electronic tool that enables automated monitoring of total energy expenditure (calories burned), active energy expenditure, physical activity duration and levels (METs) and sleep/wake states duration. Patients are instructed to wear this device on the back of the upper arm and to record data for 36 hours every two weeks in a free-living context. The Armband holds up to 12 days of continuous data which the outpatients are instructed to download into their personal computer and to transmit online to a web-site specifically designed for data storing. Outpatients are also told that they can review their progress using the InnerView® Software which analyzes and organizes data into graphs and reports. Participants are then instructed to use the TECNOB platform, an interactive web-site developed by TELBIOS S.P.A. The TECNOB web-platform supports several functions and delivers many utilities, such as questionnaires, an animated food record diary, an agenda and a videoconference virtual room. In the ‘questionnaires’ section, patients fill in the Outcome Questionnaire and submit data concerning weight and glycated hemoglobin. In the ‘food record diary’ participants submit actual food intake day by day through the selection of food images from a comprehensive visual database provided by METEDA S.P.A. The same procedure is also possible through a software program called METADIETA (Meteda s.p.a.) previously installed on the outpatients’ mobile phones before discharge. Through the mobile phones outpatients maintain the contact with the dietitian who regularly sends them SMS containing syntax codes that METADIETA, the software previously installed into the outpatients’ mobile phones, uses in order to visually display the food choices (frequency and portions) outpatients have to adhere according to diet prescriptions. By this way, outpatients can keep a food record diary allowing comparisons between current eating and the recommended hypocaloric diet along the whole duration of the program. The ‘agenda’ allows the patients to remember the videoconference appointments with the clinicians and the days when to fill in the questionnaires. Moreover, the patients can use the ‘memo’ space to note down any important event occurred to him/her in the previous week/month. Indeed, some research indicates that changes in behaviour (eating and exercise) often follow discrete moments which have been variably described as life events, life crises, teachable moments or epiphanies. Life events can lead to weight loss but also to weight gain and qualitative research shows that it is not the event per se that results in behaviour change but the ways in which this event is appraised and interpreted by the individual. The clinical psychologist has thus the opportunity to discuss with the outpatients about the significant events reported in the ‘memo’ space during the videoconference sessions and cognitively reconstruct dysfunctional appraisals in functional ways. Finally, outpatients are instructed to use the videoconference tool. Thanks to this medium, they receive nutritional and cognitive-behavioural tele-counseling with the dietitian and the clinical psychologist who attended the patients inside the hospital. In particular, just after discharge, participants have 6 videoconference contacts with both clinicians along 3 months. From the 3rd to the 6th month sessions are scheduled every 30 days and then even more spaced up to an interval of 60 days. During tele-sessions, clinicians (psychologist and dietitian) test the outpatients’ progress, their mood, the maintenance of the ‘good alimentary and physical activity habits’, the loss/increase of weight and ask about critical moments, especially those ones reported on the ‘memo’ web-space. In particular, tele-sessions with the clinical psychologist aim to consolidate strategies and abilities acquired during the in-patient phase, to improve self-esteem and self-efficacy, to support motivation, to prevent relapse and to provide problem-solving and crisis counseling. On the other hand, dietitian assesses adherence and compliance to dietary therapy with a special focus on normal eating behaviour, sufficient fluid intake, hunger and fullness regulation, appropriate eating/etiquette (pace and timing of meals), slow rate of eating, and addresses critical points such as plateau in weight loss or lack of readiness to improve dietary habits.
In addition to videoconference, outpatients can further contact clinicians by e-mail. Indeed, each patient is given the possibility to join his clinician beyond the established videoconference contacts in case of urgency or emergency. According to the e-message’s content, clinicians choose the most appropriate format for delivering feedback among e-mail or telephone. In order to avoid excessive dependence and to contain costs, a maximum number of 1 non-scheduled contact per week is established a priori.
As described, in the outpatient phase of the TECNOB program great relevance is given to the clinicians–patient relationship as an important medium and vehicle of change. After discharge, out-patients begin to experience the autonomy and competence to change they develop during the in-patient phase and inevitably face resistances and barriers. Thanks to videoconferences, out-patients are supported by the clinicians who attended them during the in-hospital phase in exploring resistances and barriers they experience and in finding functional pathways to cope. Furthermore, out-patients are helped to experience mastery in terms of the health behaviour change that needs to be engaged.
Target behaviour/s: consumption of oral nutritional supplements and food intake.
Target population/s: patients.
Extract from: Wyers et al. 117 © 2010 Wyers et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Nutritional intervention
The nutritional intervention is a combination of dietetic counseling and oral nutritional supplements for three months. The intervention starts during hospital admission and continues after discharge during the stay at the rehabilitation clinic or at the patient’s home. During hospitalization, the study dietician visits the patient twice. At the first visit, two to five days after surgery and immediately after baseline measurements, the dietician interviews the patient regarding medical and social status, and pre-fracture mobility. The dietician also performs a 24-hour recall and takes a general dietary history of the patients’ diet before hospitalization. Next, the patient receives the nutritional supplement, a milk-based supplement providing 21 kJ (500 kcal) and 40 g of protein. The dietician advises the patient on the consumption of the supplement and arranges extra care or services to optimize the food intake if necessary. Before hospital discharge, the dietician visits the patient for the second time. During this visit, a 24-hour recall is performed and the consumption of the nutritional supplement is evaluated. Furthermore, arrangements are made to continue the dietetic advice and the consumption of the nutritional supplement at home or during the stay at the rehabilitation clinic. At home or during the stay in a rehabilitation clinic, the dietician visits the patient three times (one week, two weeks and six weeks after discharge) and makes five telephone calls with the patient (three, four, five, eight and ten weeks after discharge). During these visits, food intake and supplement use is assessed by a 24-hour dietary recall, and tailor-made dietetic advice is given to optimize the amount and composition of the diet. As soon as the patient meets nutritional requirements with a normal diet, the use of the nutritional supplement is stopped. Compliance with the nutritional supplement is evaluated by the 24-hour dietary recalls, patients’ registration of the consumption in a diary and by collecting the capsules of the cans of the nutritional supplement during the home visits.
Target behaviour/s: smoking cessation.
Target population/s: patients.
Extract from: Siddiqi et al. 120 © 2010 Siddiqi et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
The Intervention and its key components
FIVE STEPS TO QUIT – The Intervention Model: This is based on the evidence-based recommendations for treatment of tobacco addiction published by WHO in 2001. The same approach is being advocated by IUATLD, National US guidelines and NICE in the UK. This model relies on assessing personal motivation to quit tobacco use and uses it as the basis for assessing suitability for the different therapeutic options for tobacco dependence. Thus, the approach maximizes the efficient use of nicotine replacement therapy (NRT) and bupropion.
Key Components: We would like to develop components of the ‘Five Steps to Quit’ intervention model on the basis of the following principles:
-
Based on best available evidence and following an approach recommended by international agencies such as WHO and IUATLD.
-
Can be delivered in primary care setting by non-specialist health care staff (doctors or other non-medical personnel) integrated in their routine healthcare provision.
The intervention model consists of five key steps
-
Asking about the status of nicotine use;
-
Advising about the benefits of stopping nicotine use;
-
Assessing the motivation to stop its use;
-
Assisting in stop attempts through various therapeutic options; and
-
Arranging follow-up
Examples of the specific components for each step of the intervention are given in Appendix A; this is a general guide only and modifications will be made during the development of the intervention.
Delivery of the intervention
We propose to use a systematic, standardised approach to deliver ‘five steps to quit’ to make it effective and equitable. It is envisaged that the intervention will be primary delivered by the TB DOTS facilitator based in the diagnostic centre with the help and under the supervision of the primary care doctor (Table E). He will assess patients’ eligibility for the study and send them to the TB DOTS facilitator for further assessment. All eligible patients will be provided with verbal and written information about the study and invited to participate. Patients who agree to take part will be taken through different components of the ‘five steps to quit’ programme in two appointments. Patients in intervention arm 1 will also be offered therapeutic option (Bupropion) and such patients will be referred to the primary care doctor for assessing suitability and prescribing Bupropion.
| Trial arms | First contact | FU at week 1 | FU at week 5 | FU at week 8 | FU at week 25 |
|---|---|---|---|---|---|
| Intervention 1 (brief psychological intervention + therapeutics) | Assess eligibility at the laboratory | TB DOTS facilitator | TB DOTS facilitator | TB DOTS facilitator | TB DOTS facilitator |
| TB DOTS facilitator | Doctor | Doctor (if necessary) | |||
| Doctor | |||||
| Intervention 2 (brief psychological intervention only) | Recruitment at the laboratory | TB DOTS facilitator | TB DOTS facilitator | TB DOTS facilitator | |
| TB DOTS facilitator |
In the intervention arm 1, the primary care doctors, in addition to supervising TB DOTS facilitators, will be responsible for assessing and prescribing therapeutics (Bupropion) to patients who wish to quit and are being referred by the TB DOTS facilitators. All patients on treatment will have an additional follow up visit at week 8. In intervention arm 2, doctors will be only responsible for supervising TB DOTS facilitators. They will be provided with the appropriate training and relevant materials.
Apart from the relevant training and materials, health professionals will not be provided with any other incentive, financial or otherwise. However, treatments packs will be provided from the research budget. The research officer will also organise regular supervisory visits to oversee patient management and data collection procedures. Monthly cluster meetings of the health professionals involved will also be organised to discuss progress and potential problems.
Appendix A
| Steps of care | Objective | Key components | Components (examples) |
|---|---|---|---|
| 1. Ask | To assess current status of nicotine use and record | Use of simple questions to ask about the form, quantities and duration of nicotine use | Tobacco use questionnaire/register |
| 2. Advise | To provide evidence based advice to patients on the benefits of stopping nicotine use | Health professional explaining these benefits using patient education materials | A glossy desktop tool helping health professionals in explaining the benefits of quitting and an educational leaflets for patient to keep with professional’s signature once the advice has been given |
| 3. Assess | To assess the motivation to stop smoking (as well as dependence) | Health professional asking simple questions to assess patient’s desire to quit | A simple scoring card for health professionals to assess this motivation. Fagerström Test for Nicotine Dependence or Hooked on Nicotine Checklist can be adapted |
| 4. Assist | To offer a range of treatment options who wish to quit | Brief counseling, nicotine replacement therapy or bupropion | A desk-guide explaining different treatment options e.g. full seven week course of bupropion i.e. six tablet 150 mg for six days first and then 150 mg tablet twice a day for the next six weeks |
| 5. Arrange | To arrange a follow up to review smoking status and therapeutic options | Follow up visits arranged at regular intervals | For patients on TB treatment; during the treatment at week 1; during the treatment at week 5, on completion of the treatment at week 8; and after the treatment at week 25 |
Target behaviour/s: medication use/adherence to help prevent cardiovascular disease (CVD).
Target population/s: patients.
Extract from: Mc Namara et al. 121 © 2010 Mc Namara et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Intervention part two: community pharmacist facilitating patient change
Community pharmacists will be trained to deliver their interventions in accordance with the Health Action Process Approach (HAPA) to behaviour change over five counselling sessions conducted at monthly intervals. The emphasis in counselling progresses from change motivation initially (via improved self-efficacy, belief in the need for change and belief that change will generate positive outcomes), through to change maintenance and relapse prevention strategies. Written, achievable goals will be encouraged.
The first session with the patient will prioritise basic health education regarding individual CVD risk and the benefits of potential treatments. It also establishes acceptable goals for the treatment process through patient consultation, and how these might be achieved. Finally, the pharmacist will discuss with the patient any specific medication changes identified in the baseline report that are recommended to improve adherence to CVD guidelines. Community pharmacists will not be trained or asked to make interventions related specifically to diabetes or mental health issues, but will be alerted to any suboptimal assessment results in these areas and asked to discuss with the patient the potential need for GP input. Such issues will also be identified in the baseline assessment summary provided to the GP.
If a patient’s overall 5-year CVD risk score is 5% or less (considered very low risk) they will be advised to discuss with their pharmacist whether they are likely to benefit from continuing with the intervention. The decision to continue will be left to the pharmacist and the patient. Pharmacists will be expected to assess and document patient motivation to undertake various medication and lifestyle changes. Following discussion with each patient, the pharmacist will then forward the clinical summary to the patient’s GP with any additional comments considered relevant.
Subsequent sessions will involve: ensuring necessary changes to medicines have been made; monitoring of medicines adherence especially for new medicines; linking patients with local health and other services that provide relevant patient support; initiating lifestyle change and supporting maintenance and relapse prevention. Throughout these sessions, patient progress towards goals will be continually reassessed, as will be the goals themselves. GP input to patient treatment plans will also be invited.
Target behaviour/s: medication and lifestyle adherence.
Target population/s: patients.
Extract from: McAlister et al. 125 © 2010 McAlister et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Experimental arms
Intervention
Over and above usual care, our intervention will include intensive pharmacist case-management, consisting of monthly follow-up visits with the study pharmacist for six months that will be independent of any planned follow-up with the SPC [Stroke Prevention Clinic] or family physicians. At each visit, the study pharmacist will monitor the patient’s BP [blood pressure] and lipid levels and will initiate and/or titrate antihypertensive and/or hypo-lipidemic therapy as appropriate. The study pharmacist will follow treatment algorithms consistent with current Canadian national guidelines. The pharmacist will emphasize medication and lifestyle adherence with patients and their caregivers, using the cardiovascular risk profile as an educational aid as per prior studies by our group. The pharmacist will also send a fax to the primary care physician after each study visit outlining the status of that patient’s atherosclerosis risk factors and any therapy adjustments made at that visit.
Target behaviour/s: medication use/adherence.
Target population/s: patients.
Extract from: Lau et al. 126 © 2010 Lau et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Pharmacist Care Group (PCG)
The PCG participants receive a package of interventions from the pharmacist for enhancing their antihypertensive medication adherence, which includes:
-
A home BP monitor (Omron®T9IT) with the capacity to store and download BP readings to be used for discussion at three- and six-month follow-ups;
-
Training by the pharmacist on self-monitoring of BP;
-
Motivational interviewing and education by the pharmacist to help patients improve their medication adherence and achieve target BP;
-
Pharmacist-initiated home medicines review (HMR), dose administration aid (DAA) and/or patient medication profile (PMP), where necessary;
-
Medication use review (MUR) to identify and resolve possible medication-related hypertension (e.g. due to non-steroidal anti-inflammatory drugs, cold preparations, complementary medicines, etc.);
-
Referral to a GP when needed (e.g. very high blood pressure); and
-
Refill reminders (by either SMS, telephone or mail) from their pharmacist at a chosen number of days before their antihypertensive medication dispensing is due.
HMRs are designed to assist consumers living at home to maximise the benefits of their medication regimen and prevent medication related problems. The review involves the consumer’s general practitioner (GP) and preferred community pharmacy, and in some cases other relevant members of the healthcare team. The GP refers the consumer to the community pharmacy and an accredited pharmacist visits the consumer at home, reviews their medication regimen, and provides the GP with a report. The GP and consumer then agree on a medication management plan. A DAA is a device developed to assist patients in better managing their medicines by arranging their medicines into individual doses according to the prescribed dose schedule throughout the day. The aim of the DAA Program is to reduce medication-related hospitalisation and adverse events through improving medication management and adherence for people in the community. A PMP is a comprehensive written summary of all regular medicines taken by a patient that assists them in understanding and managing their medicines by informing them how, when and why to take their medicines. The aim of the PMP Program is to reduce the risk of medication-related adverse events by assisting people to understand and manage their medications, including prescription, over-the-counter and complementary medicines. A MUR usually takes place in the pharmacy and it involves the pharmacist checking the patient’s medication, making sure that the patient knows how and why they should be taking their medication, as well as identifying any problems. It provides the patient with an opportunity to ask questions and the pharmacist an opportunity to improve the patient’s medication understanding and adherence, as well as being able to highlight problems and provide appropriate solution.
Target behaviour/s: improvement of quality of care delivered to patients with diabetes and/or ischemic heart disease (encompassing a range of behaviours).
Target population/s: physicians.
Extract from: Ivers et al. 114 © 2010 Ivers et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Intervention
Participants in both arms of the trial will each receive an information package by courier every six months for two years with multiple components, including a one page cover letter, a one-page explanation of how the patient information was identified from EMRALD, a one-page handout reviewing generic clinical and quality improvement strategies for patients with diabetes and/or IHD [ischemic heart disease] (based in part on the chronic care model), and two separate feedback reports. The first report will describe the percentage of the participating physician’s patients with diabetes who are meeting evidence-based quality targets. The second will present similar information regarding their patients with IHD. The quality targets used were chosen to be consistent with those used by concurrent quality improvement interventions in Ontario (Quality Improvement and Innovation Partnership) and with current guidelines (see Outcomes section below). The reports will present information comparing the performance achieved by the participating physician to the average achieved by the top 10% of participants for any given measure. This type of comparator is similar to the achievable benchmark of care previously shown to improve the effectiveness of feedback reports. See Additional File 1 for prototype feedback reports.
Participants randomized to the enhanced feedback arm will receive exactly the same materials as the simple feedback arm, plus a one-page worksheet. This theory informed worksheet is designed to facilitate participants in setting specific but challenging goals and help participants develop action-plans through the creation of implementation intentions (see Additional File 2 for prototype of worksheet). An evaluation to assess the theoretical validity of the intervention will be reported separately.
Based on our review of the literature, the largest effects from goal setting and action planning seem to come from actually developing the plan (and linking it to a specific context to carry it out). For this reason, we chose not to provide participants with a list of possible actions. The participants, not the investigators, decide how to improve upon a care gap that they identify as important. Important mediators of the success of implementation intentions seem to be participant adherence to instructions to develop an appropriate plan, participant self-efficacy, and the inclusion of ‘coping plans’ to help participants plan ahead for situations that could interrupt goal-oriented behaviours. These factors will be addressed explicitly in this trial by: offering six ‘Main-Pro-C’ continuing medical education credits to encourage full completion of the worksheet and to permit monitoring of plans by the investigators; allowing participants to set their own goals for improvement; and requiring participants to develop a coping plan in the intervention worksheet. The format in this aspect of the worksheet is similar to previous studies, although to our knowledge the application of this type of intervention to family physicians is novel.
The worksheet in this intervention is similar in concept to commitment-to-change procedures that are increasingly used in the continuing medical education field, based on multiple theories related to adult learning. Rigorous evaluations of such procedures are few, but one study indicated that commitment-to-change can mediate the effect of an educational intervention for prescriptions. Although a signature has not been proven to increase the effectiveness of the commitment-to-change procedure, it is included in the worksheet because it offers an opportunity to explicitly use the word ‘commitment;’ this is thought to be a necessary feature for the procedure to successfully generate behaviour change (see Additional File 2 for prototype of worksheet). We tested the worksheet design and all other intervention materials with a group of non-participating family physicians and they found it easy to use. Specifically, they reported that they found the instructions clear and advised no changes to the design. To our knowledge, the application of this type of worksheet as a means of ‘enhancing’ the effectiveness of audit and feedback is novel.
PHYSICIAN ID#: Approximately 12% of your rostered adult patients have diabetes, and 30% of these patients also have ischemic heart disease
Overall in this study, 7% of rostered adult patients have diabetes, and 19% of these patients also have ischemic heart disease
Your diabetic patients are 68 years old on average and are 57% male. All diabetic patients in the study average 63 years and are 55% male
| Targets | Your Practice | Top 10% | |
|---|---|---|---|
| A1C ≤ 7.0% | 62% | 67% | ‘Top 10%’ = the score achieved by 10% of physicians with the best score for each target. (This data is based on your most recent EMR data upload, May, 2010) ACR = urinary albumin creatinine ratio (microalbumin) |
| A1C test in 6M | 81% | 91% | |
| BP < 130/80 | 48% | 72% | |
| BP test in 6M | 86% | 98% | |
| Rx ACE/ARB | 77% | 88% | |
| LDL ≤ 2.0 | 38% | 55% | |
| LDL test in 12M | 55% | 80% | |
| Rx Statin | 72% | 83% | |
| ACR test in 12M | 84% | 85% |
PHYSICIAN ID#: Approximately 9% of your rostered adult patients have ischemic heart disease, and 41% of these patients also have diabetes
Overall in this study, 5% of rostered adult patients have ischemic heart disease, and 28% of these patients also have diabetes
Your IHD patients are 71 years old on average and are 74% male. All IHD patients in the study average 70 years and are 65% male
| Targets | Your Practice | Top 10% | |
|---|---|---|---|
| Rx ASA | 33% | 69% | ‘Top 10%’ = the score achieved by 10% of physicians with the best score for each target. (This data is based on your most recent EMR data upload, May, 2010) |
| BP < 140/90 | 75% | 89% | |
| BP test in 6M | 83% | 95% | |
| Rx ACE/ARB | 72% | 85% | |
| Rx B-Blocker | 57% | 72% | |
| LDL ≤ 2.0 | 39% | 56% | |
| LDL test 12M | 58% | 91% | |
| Rx Statin | 77% | 89% |
Additional file: prototype of theory-informed worksheet for enhanced feedback group
1. Describe a goal that you will achieve within the next 6 months for your diabetic patients and for your IHD patients. Your goal must be challenging but achievable. Be very specific
[Phrase your goal as follows: ‘I will improve (choose one of the outcomes in the practice profile e.g.% at target BP)
to the goal of (state a target for your efforts e.g. by 20 percentage points)’]
For Diabetes, I will improve:
To the goal of:
For Ischemic heart disease (IHD), I will improve:
To the goal of:
2. Complete the following statements by describing a specific action you will take to help you achieve your goal
To identify on an ongoing basis the specific patients in my practice who are not meeting targets, I will:
If a patient with Diabetes and/or IHD comes to clinic (for any reason) and is not meeting targets, I will:
If I am too busy during an office visit to address all aspects of managing the patient’s diabetes and/or IHD, I will:
If I’m not making progress with respect to implementing my plan for achieving my goals, I will:
In signing below, I confirm my commitment to achieve this goal and my intention to carry out this action plan
___________________________
Signature
Target behaviour/s: diagnoses and management of lower back pain (encompassing a range of behaviours).
Target populations/s: practitioners (physiotherapists and chiropractors).
Extract from: McKenzie et al. 71 © 2010 McKenzie et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Intervention group
Both the findings of interviews and survey informed the design of the intervention, and will be published elsewhere.
The intervention consisted of: a full-day symposium-style event involving a combination of didactic lectures delivered by peer opinion leaders (identified in consultation with representatives from the physiotherapy and chiropractic associations), small group discussion led by trained clinical facilitators, and practical sessions; supporting written material; and a follow-up phone call. Separate symposia were held for physiotherapists and chiropractors. All practitioners in the intervention group, including those who were not able to attend the symposium, received a DVD including videos of the didactic sessions and printed resources about LBP [lower back pain] management. A clinical member of the project team attempted to follow-up all practitioners with a telephone call to discuss difficulties encountered in implementing behaviours and strategies to overcome these. More detail on the intervention, including the development process, will be reported in a separate publication. Symposia details are available in Additional File 1 – ‘ALIGN intervention content.’
Finally, while not formally a component of the intervention or control group, the practitioner data collection procedure involves completion of patient checklists about LBP management and may act as a prompt to change practitioner behaviour. The checklist includes a broad range of diagnostic procedures and interventions potentially used for patients with acute non-specific LBP, irrespective of supporting evidence.
Timing of recruitment, intervention delivery, and follow-up
The physiotherapist and chiropractic symposia took place on 20 and 27 February 2010, respectively. Practitioners in the intervention group were mailed a DVD of material from the symposium for their professional group on 29 March 2010. Practitioners in the intervention group received a follow-up phone call two to four weeks after either attending the symposium or being sent the DVD.
Patient participant recruitment will take place over a five-week period, beginning at least three months post-symposium delivery (31 May 2010). Each practice will recruit patients for a period of two weeks (a longer period was judged to place too great a burden on practitioners). Practices will be randomly allocated to recruit patients in either the first (31 May to 11 June 2010) or second (21 June to 2 July 2010) data collection period. Practitioners who are not able to collect data in either of these periods (e.g., on holiday), will be invited to select an alternative fortnight of data collection between July and September 2010.
Additional file 1
ALIGN CRT Intervention Content
The intervention for the ALIGN CRT consisted of a full-day weekend symposium-style event (with program and written material supporting presentations/content covered). The first half of the symposium focused on awareness rising and address the following theoretical domains: beliefs about professional role, social influences, beliefs about consequences and knowledge. The second half of symposium included more small group/interactive activity to address beliefs about capabilities and to allow for skill development regarding both target behaviours.
| Time | Content |
|---|---|
| 9:00am | Welcome and introductions (by study investigator) |
| 9:20am | Audience straw poll #1 (lead by study investigator) Using audience response system software, 10 questions measuring knowledge, attitudes, beliefs and intentions about acute low-back pain management were posed to the audience, who could respond anonymously using wireless keypads, and aggregated results of participants were presented in real time |
| 9:35am | Keynote speech by peer opinion leader Speech given by high status person recognised within the profession to discuss professional standards, state-of-the-art in diagnosis and/or communicating with patients with acute low-back pain, including use of latest research evidence and clinical practice guidelines |
| 10:20am | Video recording by peer opinion leader Pre-recorded video of well-respected clinician conveying confidence in diagnosis without plain X-ray, dispelling fears around missed pathology and/or litigation, and conveying importance of reassuring patients |
| 10:30am | Video recording by radiologist Pre-recorded video of radiologist outlining the amount of radiation delivered by plain X-ray and its poor utility in acute uncomplicated low-back pain |
| 10:35am | Video recording by consumer advocate Pre-recorded video or consumer advocate describing their expectation of a good health professional (those who are good listeners/ communicators, provide good explanations/reassurance, and provide evidence-informed best care) |
| 10:40am | Morning tea |
| 11:00am | Small group discussion Discussion between six participants lead by a clinician table facilitator, to discuss how the participants currently manage people with acute low-back pain, what participants think of the guideline and its recommendations, any scenarios participants find difficult managing patients in a manner consistent with the guideline (i.e., less plain X-rays, giving advice to stay active) difficult, and strategies to overcome these |
| 12:00pm | Skills demonstration (managing acute LBP patients without X-ray) Demonstration/modelling of skills needed to diagnose and manage patients without plain X-ray by an experienced clinician |
| 12:15pm | Skills demonstration (advising acute LBP patients to stay active) Demonstration/modelling of relevant skills in a successful communication encounter (giving advice to stay active) with patient (e.g. strategies on how to develop rapport, convey empathy, confidence, reassure patient, give message that patient will improve over time etc) by experienced clinician |
| 12:40pm | Lunch |
| 1:45pm | Small group practical: Simulated patients Rehearsal of diagnostic and communication skills on trained simulated patients (x4) in groups of six participants, led by a clinician table facilitator |
| 3:00pm | Afternoon Tea |
| 3:15pm | Reflection lead by peer opinion leader Brief summary/reflection of the key messages presented throughout the day, with opportunity for questions from the audience |
| 3:45pm | Audience straw poll #2 (lead by study investigator) Using audience response system software, 3 questions measuring beliefs about the extent to which participants believe their management of acute low-back pain patients will change were posed to the audience, who could respond anonymously using wireless keypads, and aggregated results of participants were presented in real time |
| 4:00pm | Summary and evaluation |
| 4:30pm | Close |
Two-four weeks following the symposium, participants received a follow-up telephone call by a clinician member of project team to enquire about any difficulties encountered in implementing behaviours (and strategies to overcome these) and to discuss how practice has changed (academic detailing style).
Target behaviour/s: clinicians management of osteoporosis (encompassing a range of behaviours).
Target populations/s: practitioners (physiotherapists and chiropractors).
Extract from: Sanfélix-Genovés et al. 119 © 2010 Sanfélix-Genovés et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Intervention
Given the characteristics of the ESOSVAL project linked to the Regional’s Plan of Osteoporosis, both the Intervention and the Control Group will receive some form of intervention aimed at improving care. The Control Group will benefit from the improvements introduced by the ESOSVAL project in the ABUCASIS Electronic Clinical Records system, since they affect all the system’s users, the doctors and nurses providing healthcare, including those in the Control Groups. These improvements consist in the incorporation of a new follow-up sheet for patients with osteoporosis or risk factors for osteoporosis, and a series of tables, scales and variables that can be monitored to improve the care and follow-up of these patients. The implementation of this change in the patients’ clinical records will be done through the usual training process used by the Valencia Healthcare Agency to introduce any change in recordkeeping (an informational session, and the option to have any individual questions answered).
The intervention group, and apart from the above mentioned changes to the recordkeeping system, receive a multifaceted intervention: 1) The participating clinicians took a four-hour classroom course in the last quarter of 2009, held in each Department; 2) Next, they participated in recruiting and following-up on patients for the ESOSVAL-R study. This requires the healthcare providers to include relevant information in the clinical records of 18 patients, and involves a hands-on practicum in obtaining information about osteoporosis and its incorporation into the clinical records; 3) participation in the study has been included as an ‘indicator’ towards gaining points in the Valencia Health Agency’s Management Contract, that will lead to economic incentives; 4) An on-line course on osteoporosis will be given during the first, third and fourth quarters of 2010. It is organized in modules prepared by recognized national experts; 5) During the first quarter of 2011, after all the participating healthcare providers have completed the on-line course, another classroom course will be given to reinforce training and to divulge the results collected so far during the intervention (Table G). The courses will be given to the doctors and nurses in the Region’s Healthcare Departments who volunteer for participation in the project and who work with the medical practices selected.
| Year | 2009 | 2010 | 2011 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Quarter | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | 1 | 2 |
| Design of the Training Plan | ► | ► | ►▐ | |||||||
| Design of the Research Project: ESOSVAL-F | ►▐ | |||||||||
| Presentation to Ethical Committee | ►▐ | |||||||||
| Changes to the electronic clinical history system to improve recordkeeping on osteoporosis | ► | ► | ►▐ | |||||||
| In-class training courses in the Healthcare Departments | ►▐ | ►▐ | ||||||||
| ‘On-line’ training | ► | ► | ►▐ | |||||||
| Statistical analysis | ► | ►▐ | ||||||||
| Issue of report on results | ►► | |||||||||
Target behaviour/s: communication strategies and skills for encouraging behaviour change among young people with diabetes including how to use a communication device (3 T: Time to Talk).
Target population/s: health care professionals.
Extract from: McNamara et al. 123 © 2010 McNamara et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Trial procedures
Intervention
Members of clinical teams allocated to the intervention arm will undergo a blended training programme comprising web-based material and face-to-face seminars (The Talking Diabetes Programme). The training course aims to prepare practitioners for constructive behaviour change conversations with patients and to provide practitioners with strategies and skills for encouraging behaviour change. The training emphasises the importance of shared agenda-setting, and drawing upon the Motivational Interviewing approach, emphasises the importance of a guiding style when consulting with patients about behaviour change. Practitioners work their way through a number of distinct programme parts with an approximate total duration of 1.5 hours (delivered via three main e-learning modules). In addition, more interactive web-based components of the course allow practitioners to record their thoughts and experiences as they proceed through the programme. Two face-to-face seminars (approximately 2 weeks apart) with combined clinical teams also form part of the training course. Time spent on off-line learning activities such as discussing the training content in pairs, is recorded online. Following the second face-to-face workshop, participants will be invited to submit reports of three consultations in which they use their newly acquired skills and feedback will be provided by pre-assigned trainers.
The training programme shows practitioners how to use a device (3 T: TimeToTalk) for promoting shared agenda-setting during clinical encounters with patients. This consists of a rigid folder and an inserted paper agenda pad of tear-off sheets which can be completed in advance by patients and carers to record topics of importance to be raised within consultations. Practitioners have the option to complete a pro-forma on which general topics discussed at clinic visits can be recorded and kept with patient notes, to facilitate clinical record keeping and communication between healthcare professionals. Copies of the paper agenda-setting pad (without folder) have been made available to each clinic to refill or replace folders as required and for patients not otherwise recruited to the study.
Target behaviour/s: management of depression in the workplace (encompassing a range of behaviours)
Target population/s: employers
Extract from: Rost and Marshal. 127 © 2010 Rost and Marshall; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Intervention
The intervention consists of a presentation and technical assistance delivered to employer representatives at local meetings sponsored by regional coalitions. Employers randomized to the VB [value-based] condition receive the Depression Management in the Workplace (DMW) presentation. All interested employer representatives are offered condition-specific technical assistance free of charge during the 24 months after the presentation.
Presentations
The DMW presentations present the content summarized in Table H utilizing high quality graphic material recently awarded The Communicators Award of Excellence in an international competition.
DMW presentation
The two-hour DMW presentation educates employer representatives about DMW Care and its evidence based impact on clinical and work outcomes. Employer representatives receive a company-specific return on investment (ROI) estimate associated with DMW Care. This estimate is generated by a calculator the research team developed in its earlier studies by translating scientifically derived estimates of DMW Care’s impact on absenteeism and productivity at work to a monetized savings in lost work days, varying pertinent employee, organizational, and vendor characteristics. During the presentation, employers are encouraged to explore purchasing a depression product for their company and to request free technical assistance to help them purchase a DMW Care quality product.
Technical assistance (TA)
TA is the provision of individualized consultation to enable employers to improve the depression care their employees receive. When an employer representative requests TA, the TA consultant schedules a two-hour phone call to conduct the initial consultation followed by a second call approximately one month later. In the VB condition, the TA assists employer representatives in building broad support within their organization for the purchase, in identifying DMW vendors, and in developing contracts for the program.
Research Design
| Sequence of Initial Activities | VB Presentation |
|---|---|
| Presentation | Prevalence in the workplace |
Depression burden to
|
|
| Problems treating depression in usual care | |
| DMW as an indicator of high quality care | |
| Clinical effectiveness of DMW Care Organizational effectiveness of DMW | |
| DMW Calculator | |
| Description of Technical Assistance | |
| Discussion | Open discussion of value of DMW Care |
Target behaviour/s: delivery of the target adolescent community reinforcement approach (A-CRA) (encompassing a range of behaviours).
Target population/s: therapists.
Extract from: Garner et al. 128 © 2010 Garner et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Study intervention
Implementation as usual (IAU)
Both groups receive the same training and technical assistance model they have been receiving since the inception of the Assertive Adolescent Family Treatment (AAFT) initiative. This state-of-the-art training and technical assistance model consists of a 3.5-day workshop training, bi-weekly telephone coaching calls with model experts, and on-going monitoring and feedback (both quantitative and qualitative) as part of a standardized certification process.
Pay-for-performance (P4P)
In addition to the above, the P4P group has the opportunity to earn monetary bonuses for two sets of measurable behaviours related to quality implementation of the model. These two behaviours are: delivering Target Adolescent Community Reinforcement Approach (A-CRA) and demonstrating Monthly A-CRA. Descriptions of the rationale and reinforcement schedules for these two targeted behaviours are described in the sections below; however, detailed descriptions of Target A-CRA and Monthly A-CRA competency are provided in the study measures section.
Rationale and reinforcement schedule for target A-CRA
Research has suggested that the degree of implementation can be as important as the efficacy of the EBT, with the biggest effects coming from well-implemented, highly efficacious interventions. Similarly, our prior research has shown that adolescents who received a threshold exposure of A-CRA were significantly more likely to be in recovery at follow-up. Increasing the number of adolescents who receive Target A-CRA would be expected to result in a higher likelihood that adolescents would have more positive treatment outcomes. Thus, one of the questions the study was designed to examine is the extent to which monetary bonuses could increase the probability that an adolescent receives Target A-CRA. As part of the RTP [Reinforcing Therapist Performance], study therapists in the P4P condition receive a $200 bonus for each adolescent who receives Target A-CRA within the first 14 weeks of AAFT and in no fewer than seven A-CRA sessions. In order to attribute improvements in adolescent outcomes to the incentives, only outcome data from adolescents admitted to the AAFT project after sites were randomly assigned to the study conditions will be used in Target A-CRA-related analyses.
Rationale and reinforcement schedule for monthly A-CRA competency
In addition to reinforcing exposure to a threshold number of procedures, we believed it was important to reinforce the quality of delivery (i.e., competence). Thus, P4P therapists also are provided the opportunity to earn a $50 bonus for each month that a randomly selected session recording has at least one core procedure rated at or above the minimum level of competence required for certification. Importantly, in order to ensure a representative sample of session recordings, only those therapists who submit at least 80% or more of treatment session recordings are eligible to have a session rated for competence. Because it would take approximately three months after randomization before P4P participants would be eligible to begin receiving their first bonus associated with delivery of Target A-CRA, reinforcing Monthly A-CRA competency is important as it can be reinforced sooner and more frequently.
Therapist implementation measures
The two implementation measures being reinforced as part of the study are Target A-CRA and Monthly ACRA Competency. Developed using existing AAFT data, Target A-CRA is a dichotomous (1 = yes, 0 = no) measure. It is defined as the delivery of 10 or more of the following 12 A-CRA procedures: functional analysis of substance using behaviour; functional analysis of pro-social behaviour; happiness scale; treatment plan/goals of counselling; communication skills; problem solving skills; adolescent–caregiver relationship skills; caregiver overview, rapport building, and motivation; homework reviewed; drink/drug refusal skills; relapse prevention; and increasing pro-social recreation during the first 14 weeks of an adolescent’s AAFT treatment experience (but in no fewer than seven sessions). See the A-CRA treatment manual for a description of these A-CRA procedures. 77 Additionally, because identifying, discussing, and reviewing the adolescent’s re-enforcers is considered a central mechanism of change within the A-CRA philosophy, as part of Target A-CRA, therapists also must, demonstrate one of these three components in at least 50% or more of the sessions conducted during this time period. Therapist-reported data on more than 450 adolescents uploaded to AAFT’s implementation tracking system (i.e., https://www.EBTx.org) indicated adolescents who received Target A-CRA had significantly (p < 0.05) greater reductions in days abstinent at both three- and six- month post-intake assessments. Importantly, although therapist reports are used to identify adolescents who appear to have received Target A-CRA, official achievement of Target A-CRA for the study requires independent verification (via listening to DSR) by a trained A-CRA rater. See Garner, Barnes, and Godley for complete details regarding the training process for A-CRA raters. Monthly A-CRA Competency is a dichotomous (1 = yes, 0 = no) measure and indicates whether or not a randomly selected session recording was rated at or above the minimum level of competence required for ACRA certification (i.e., rating of 3 or higher on all components of the procedure). As described in the A-CRA coding manual,79 each component of an attempted A-CRA procedure is rated using the following categories: 1 = poor, 2 = needs improvement, 3 = satisfactory, 4 = very good, and 5 = excellent. To ensure a representative sample of session recordings, only those therapist participants who submitted at least 80% or more of treatment sessions (minimum of five sessions per month) are eligible to have a session randomly selected and rated for competence. This requirement was implemented in order to reduce the risk of therapists trying to manipulate the criterion being reinforced by only uploading those sessions they expected would pass the competency rating.
Target behaviour/s: use of a liquid nicotine product to promote smoking cessation.
Target population/s: participants.
Extract from: Geimer et al. 131 © 2010 Geimer et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Intervention
Participants were provided with liquid nicotine cigarettes (e.g., Smoke-Break product) which are plastic tubes containing a 1.5 milligram (mg) dose of nicotine in a naturally flavoured, artificially sweetened gel. All components are FDA-approved for use in food and pharmaceutical products. Subjects were advised on use of Smoke-Break liquid cigarette tubes based on their daily nicotine intake estimated using the published nicotine content (in milligrams, mg) of their usual cigarette brand multiplied by the number of cigarettes smoked per day. This estimate of total daily nicotine intake was divided by 1.5 (the amount of nicotine (in mg) in each liquid cigarette tube to yield the total tubes of product to be used each day. Participants were advised not to exceed 4 tubes within a one hour period or 40 liquid cigarette tubes in a day. Subjects were provided a sufficient number of tubes to last 2 weeks. Participants returned at 2 week intervals for follow-up visits where vital signs, potential side effects, use of the liquid cigarette product and carbon monoxide levels were assessed; additional nicotine replacement product (a 2 week supply) was distributed at these visits for a total of 12 weeks of treatment. Subjects also rated the liquid cigarette product on taste and overall satisfaction, each based on a 10 point scale (1-worst, 10-best) at each follow-up visit.
Target behaviour/s: smoking cessation.
Target population/s: participants.
Extract from: Gonseth et al. 132 © 2010 Gonseth et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Smoking cessation intervention
All participants received an 8-week smoking cessation intervention including individual-based intervention combining replacement therapy and/or bupropion and 4 sessions of counseling. Counseling was based on national and international current guidelines, targeting increasing the motivation to quit smoking, the identification of barriers, and the prevention of relapse. A counseling session lasted thirty minutes in average. Participants received a combination of nicotine replacement therapy (transdermal patch 16-hour/day or 24-hour/day, 1-mg or 2-mg lozenge, 2-mg or 4-mg gum, 10-mg inhaler) and/or bupropion, according to the participant’s past experiences and preferences. Four visits (at week # 1, 2, 4, and 8) were scheduled and participants were asked to plan a quit date from the inclusion day until the 4th visit at week 8. They were considered as smokers if they failed to quit or if they relapsed to smoking afterwards. Participants lost during follow-up were called and received a letter explaining the scientific implications and the need for follow-up, and were invited to contact us.
Dentist’s Intervention
The dental intervention was provided by a dentist trained in periodontology (MA) and included two visits. At the first visit, the dentist performed an oro-dental exam to rule out oro-dental lesions, e.g. periodontitis, gingivitis, and other oral or dental lesions. At the end of this visit, the dentist orally explained the results of the oro-dental exam, i.e. detailed explanations of the lesion(s) related to smoking, and recommended treatment if necessary. He also provided standardized information about chronic effects of smoking on oral hygiene (e.g. bad breath, esthetic sequelae), chronic effects of smoking on oral health (e.g. increased risk of oral cancers or periodontitis), and a brief explanation about periodontitis (a chronic infection of periodontal tissues, beginning with gingivitis and gingival bleeding, that is often hidden by smoking). The dentist also provided oral and illustrated explanations of dental plaque and made a practical and individualized demonstration of oral hygiene techniques, e.g. correct teeth and tongue washing, correct dental floss/sticks use. The first visit lasted about one hour. At the second visit, one week later, the dentist performed a simple oral hygiene treatment – which was not a treatment of periodontitis – using the full mouth periodontal debridement technique with an ultrasound device (EMS®-Air Flow® S2). In terms of treatment and potential physical annoyances, results of full mouth disinfection and classic approach are similar for the patient. During this visit, a second verbal intervention reinforcing the importance and the correlation of potential periodontal and oral lesions and smoking was performed by the dentist.
Target behaviour/s: screening attendance for diabetes.
Target population/s: participants.
Extract from: Mann et al. 133 © 2010 Mann et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Intervention materials
Two invitations to attend for diabetes screening were developed for this study: a standard invitation (control group), and an invitation designed to facilitate informed choice (see additional files 1 and 2). Two versions of the informed choice invitation were developed. In the first, participants were asked to list ‘good things’ and ‘bad things’ about screening for diabetes. In the second, participants were asked to list ‘good feelings’ and ‘bad feelings’. There were no significant effects of this manipulation and the two groups were treated as a single group in the analysis reported here.
Standard invitation
The standard invitation, shown in additional file 1, was based upon invitations commonly used to invite people for diabetes and coronary heart disease screening. It presented a brief didactic argument, describing only benefits of attending for screening. It explained that the participant might have a higher chance of developing type 2 diabetes and that diabetes has serious long term consequences.
Informed choice invitation
The informed choice invitation, shown in additional file 2, contained the information described above, plus information which included the limited benefits and potential harms of attending for screening. The text of the invitation explained both absolute risks and relative risk using frequencies, e.g. ‘If 100 people had the test, about 63 would get this result’. Previous studies have shown that risk information is most readily understood using frequencies in this way. Participants were encouraged to make a choice that reflected their values by prompting them to evaluate the consequences and asking them to record their decision to attend or not.
Providing information about diabetes risk and consequences of screening
This section was developed from the UK General Medical Council (GMC) guidelines for providing sufficient information when gaining patient consent. These guidelines include purpose of screening, details of diagnosis and prognosis with and without treatment, probability of benefits and risks, and emphasis on patient choice. The invitation began with an emphasis on patient choice ‘Screening for diabetes. It’s your decision’, and a statement that the participant was being offered screening for type 2 diabetes because they might have a higher chance of developing the condition. An explanation of diabetes and the screening procedure followed, then an explanation of the expected results and what they mean for the patient. Finally, the benefits and harms of attending for screening were outlined, including likely prognosis of early treatment compared to standard treatment following clinical diagnosis and the potential for unnecessary worry following false positive results.
Encouraging participants to make a choice
At the end of the hypothetical invitation letter, participants were asked to consider the consequences of their attending diabetes screening and to indicate their decision as to whether to go for screening or not, or to think more about the decision.
The content and format of the informed choice invitation were refined through extensive piloting using ‘think aloud’ techniques. Both invitations were designed to be comprehensible to those with a reading age of 11 or above (Flesch Reading Ease score was 71.52 and 72.88 for the standard and the informed choice invitations, respectively). Rates of informed choice were significantly higher after reading the informed choice invitation compared to the standard invitation.
Target behaviour/s: reduction in the use of methamphetamine.
Target population/s: participants.
Extract from: Menza et al. 134 © 2010 Menza et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Study intervention and design
The study intervention was a 12-week contingency management (CM) program, adapted from previous studies, in which vouchers of escalating value were offered for consecutive urine samples that did not contain methamphetamine or crack or cocaine (herein referred to as cocaine) metabolites. Initially, the intervention consisted of thrice-weekly drop-in urine testing visits for a total of 36 visits. Vouchers started at $2.50 for the first stimulant-free sample and increased by $1.25 for every consecutive stimulant-free sample thereafter up to a maximum of $10.00. Participants submitting three stimulant-free urine samples in a row earned a $10.00 bonus. The maximum payout for this program was $453.75, similar to the payout in other programs. When participants submitted a stimulant-containing sample, or missed a visit, no vouchers were issued and the value of the voucher for the subsequent stimulant-free sample was reset to $2.50. If a participant submitted a week of stimulant-free samples after submitting a sample containing stimulant metabolites, he returned to the voucher value prior to the stimulant-containing sample (‘rapid reset’). Vouchers were redeemable immediately upon accrual for pre-paid gift cards and goods and services; we never offered cash. All CM participants signed a contract delineating the expectations of the CM program. Study personnel administering the CM intervention followed a simple, scripted protocol for the reporting of results of urine testing and administering vouchers. Such a protocol was used to avoid the provision of counseling around the results of the urine testing. The protocol, which required no formal training, was developed by one of us (SS) who has extensive expertise in delivering CM interventions.
All seven participants enrolled in the study while the above procedures were in place reported difficulty adhering to the intervention schedule, and only two attended ≥ 12 of their 36 visits. In response, in September 2007, we reduced the number of weekly urine testing visits to two (24 visits over the 12-week intervention) and increased the value of vouchers for the first stimulant-free urine sample to $7.50; other studies have employed a similar schedule. As before these vouchers increased by $1.25 for each consecutive stimulant-free sample to a maximum of $10.00. Additionally, we gave participants a $20.00 bonus for two consecutive stimulant-free samples. The maximum pay-out for this program was $476.25. We continued to withhold vouchers and reset voucher values to baseline for urines containing stimulants and for missed visits; however, to encourage participants to attend visits, we gave men submitting stimulant-positive samples a voucher worth $2.50.
Under the initial CM intervention schedule, drop-in urine-testing visits were available from 10:00 am to 6:00 pm on Tuesdays, Thursdays, and Saturdays; we offered extended hours for working participants. After the enrollment visit, we sent postcards or e-mails to all participants encouraging participation in the intervention. We reminded participants who did not attend urine-testing visits for the first week by phone or e-mail. We sent postcards, phoned, or e-mailed all CM participants again at the midpoint of the intervention period. Under the revised CM intervention schedule, drop-in urine testing visits were available from 10:00 am to 6:00 pm on Tuesdays and Saturdays with flexible hours for working participants. Postcard, phone, and e-mail reminder strategies remained the same.
We tested urine samples with the QuickScreen Pro Multi-Drug Screening Test (Phamatech, Inc., San Diego, CA), a point-of-care test used to qualitatively detect stimulant metabolites. For this assay, the estimated mean detection time in urine ranges from 43.6 to 66.9 hours for methamphetamine and is 88.4 hours for benzoylecgonine, a cocaine metabolite. We repeated 10% of all urine tests; none were discordant. Study staff monitored the collection of all urine samples and tested the samples immediately after their provision.
Participants randomized to both control and CM arms received a printed list of local counseling, treatment, and outreach services at baseline and at each study visit. Study staff offered all participants assistance accessing services. Control participants did not submit twice-weekly urine samples and did not receive vouchers during the first 12 weeks of the study.
Target behaviour/s: health promotion and obesity prevention including physical activity (PA)/inactivity and healthy eating (encompassing a range of behaviours).
Target population/s: junior girl scouts.
Extract from: Rosenkranz et al. 135 © 2010 Rosenkranz et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Description of Intervention
Our intervention was based on core components of Social Cognitive Theory, including: Role modelling by peers, troop leaders, and parents; skill building through active mastery experiences; enhancement of self-efficacy and proxy efficacy through role playing and active mastery experiences; and reinforcement of behaviour through verbal praise and merit badges. The intervention consisted of three main components: 1) An interactive educational curriculum delivered by troop leaders; 2) Troop meeting policies implemented by troop leaders; and 3) Badge assignments completed at home by Girl Scouts with parental assistance. The educational curriculum consisted of eight modules, delivered over the course of about four months. This intervention curriculum is an expanded version of our previously published work used in summer programs.
Each module consisted of a discussion of intervention target behaviours, worksheet for goal setting and self-monitoring, physically active recreation session (e.g., walking, dancing, yoga, and active games), FV (fruits and vegetables) snack recipe preparation, FM (family meals) role-playing, clean-up period, and description of the take-home assignment. The modules were designed to require 60–90 minutes to deliver, with flexibility allowed for specified program activities and module order. Troop leaders underwent two hours of training by the first author prior to intervention commencement. Regular and ongoing email and phone support took place throughout the intervention time period.
Target behaviours of the intervention included: 1) Frequent FM; 2) Parent-child shared PA (physical activity); 3) Elimination of TV during mealtime; 4) Drinking water instead of SSB (sugar-sweetened beverages) at mealtime; 5) Including FV in FM; 6) Practicing good manners during FM; 7) Helping parents prepare FM and cleaning up afterwards.
Troop meeting policies included: 1) Providing 15 minutes per meeting for physically active recreation; 2) Troop leaders participating in physically active recreation with girls; 3) Provision of a FV snack prepared by girls; 4) Troop leaders eating FV snack with girls; 5) Troop leaders verbally promoting PA, FV consumption in troop meetings and for home, and verbally promoting FM for home; and 6) Prohibition of SSB, candy, and TV watching during meetings.
Target behaviour/s: physical activity and dietary intake (encompassing a range of behaviours).
Target population/s: participants.
Extract from: Werkman et al. 136 © 2010 Werkman et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Intervention group
Five programme modules were provided to participants of the intervention group during the 1-year intervention period. Participants could freely choose to make use of the modules or not. Modules 1 and 2 aimed to increase awareness of the energy balance concept and module 3 aimed to improve dietary and/or physical activity behaviour. Module 1 (sent within two weeks after the baseline measurement) was provided as a toolbox and included an information leaflet and several energy balance tools, e.g. a pedometer and a waist tape. Module 2 (sent 3 months after baseline) was a CD-ROM providing individually computer-tailored feedback on BMI, its health consequences and energy balance behaviour. In module 3 participants could receive computer-tailored feedback regarding: physical activity, fibre consumption, portion sizes of energy dense foods and fat consumption. This module was sent 6 months after baseline. Participants without access to a computer (n = 22) were interviewed and received printed feedback by mail. Modules 4 and 5 were accessible via the study website which was available during the two-year study period. After login, participants could find more information about diet and physical activity behaviour, participate in a forum and use links to other websites (module 4). Module 5 was an interactive weight maintenance programme (Weight Co@ch) that provided a written tailored advice based on reported body weight, a food frequency questionnaire and a physical activity questionnaire. Finally, the intervention group received newsletters every 2–3 months that contained study information, information about diet and physical activity and encouragements to use the modules.
Overview of the one-year intervention programme. Note: + 2w = 2 weeks from baseline, + 3 of + 6 m = 3 or 6 months from baseline. No additional information related to diet, exercise or a healthy weight was provided between 12 m – 24 m follow-up period. Both intervention and control group received general newsletters (NL) to increase compliance at 24 m follow up.
Target behaviour/s: physical activity.
Target population/s: participants.
Extract from: Buis et al. 137 © 2009 Buis et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Active U Description
To promote physical activity, Active U utilizes an online, self-reported physical activity-tracking log combined with goal setting, team competition, and weekly motivational emailed newsletters that support continued physical activity. The physical activity log and goal setting components of this program facilitate self-monitoring and self-regulation and are the main theoretically based intervention components. Experts in health promotion wrote the newsletter content, which was not limited to a single theoretical framework.
To authenticate eligible University of Michigan faculty, staff, and graduate students, participants registered online for the Active U program by logging on with their university ID and password and filling out a questionnaire assessing baseline levels of physical activity and weight, as well as height, age, employment type, health status, and gender. During the enrolment process, participants had the opportunity to create a new team and to send out email invitations to others to join. Team competitions were introduced to the program to enhance social support and motivation. Those who did not want to start their own team could apply to join an existing team, which required the approval of the team captain. Teams tended to form around pre-existing affiliations such as departments, lab groups, or buildings. In some cases, department and school email lists were used to recruit team members, and it was not unusual for an individual to receive invitations from several different teams, but each participant was only allowed to join one team. Participants were able to track the collective goal attainment of each competitive team of five or more individuals. Competitive teams were ranked according to the average team percentage of goal met for each week. Each week, the teams with the highest percentage of team members meeting their goals were recognized, but no monetary incentives or prizes were given.
At the beginning of the program, participants were assigned an automated physical activity goal expressed as minutes per week of moderate- to vigorous-intensity physical activity. Individuals who self-reported less than 60 minutes of moderate to vigorous physical activity per week at baseline were assigned a physical activity goal of 60 minutes. Individuals who self-reported more than 60 minutes of moderate to vigorous physical activity per week at baseline were assigned a physical activity goal equal to their self-reported baseline amount. Participants had the option to decrease or increase their weekly goal whenever they wanted, as long as the goal was at least 60 minutes per week. During the Active U program, participants recorded each episode of physical activity into the activity log including the type of activity, as well as the minutes of activity. Participants selected activities from a dropdown list with 27 selections and included items such as running/jogging, aerobics, organized sports, cardio equipment, martial arts, dancing, or other moderate- or vigorous-intensity physical activity. Only bouts of activity that lasted for 10 minutes or longer, counted toward achieving weekly goals.
Finally, participants received a weekly email containing competitive team rankings, information about the health benefits of physical activity, tips about how to increase and maintain a physically active lifestyle, and a reminder to enter physical activity data.
Target behaviour/s: physical activity (encompassing a range of behaviours).
Target population/s: patients.
Extract from: Bull and Milton. 138 © 2010 Bull and Milton; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Patients who were not classified as ‘active’ were eligible to receive the brief intervention (BI), and this could be provided either as an extension to the screening (recruitment) consultation or booked as a separate appointment.
The purpose of the BI was for the practitioner to utilise adapted motivational interviewing methods to enhance patients’ willingness and confidence to change their physical activity behaviour. The BI involved discussing the importance and benefits of physical activity, goal setting and directing (or ‘signposting’) patients to local physical activity opportunities.
Practitioners used set criteria to assess the potential risk to each patient of taking part in physical activity based on their disease status. Protocols for patients identified as ‘high risk’ indicated supervised activity such as Exercise Referral schemes. ‘Medium’ and ‘low risk’ patients could be directed towards a variety of opportunities including structured (e.g., health walks, sports clubs, and local leisure facilities) and self-directed activities (e.g., pedometer loan schemes and ‘green exercise’). Although ‘high risk’ patients were restricted to clinically supervised activity, the underlying principle of the ‘signposting’ was that decisions were made in collaboration with the patient.
All patients were given a resource booklet containing information on the benefits of physical activity, details of local physical activity opportunities, and a local area map. The Let’s Get Moving protocols specified patient follow-up consultations at three and six months, however due to the timelines of the pilot study, practices were asked to undertake a three month follow-up only. The purpose of the follow-up consultation was to provide on-going support to facilitate sustained behaviour change.
Target behaviour/s: eating/food intake and physical activity to manage weight gain.
Target population/s: pregnant obese women.
Extract from: Claesson et al. 139 © 2010 Claesson et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Intervention
The obesity intervention program for pregnant women was based on extra visits to a specially trained midwife. The women in the intervention group made an average of 22 visits during their pregnancy. The motivational interview/talk followed guidelines set forth by Miller and Rollnick (2002); the goal of this interview was to motivate the obese pregnant woman to change their behaviour and to obtain information useful in meeting their needs. The weight gain goal for the study was less than 7 kg and this target was only discussed once during the intervention and that was at the first visit to the midwife. The midwife worked throughout the whole program with assessing the pregnant woman’s knowledge of obesity in general and as a risk factor for her pregnancy and delivery outcome as well as for the wellbeing of her child. If the woman lacked sufficient knowledge, she was offered information and given accurate facts. The woman was also informed about the potential consequences of different behaviours associated with eating and food intake; written information was supplied if needed.
All women were given the opportunity to attend an individual 30-min session every week. The session included weight control and counseling characterized by its collaborative structure i.e. counseling based on creating a partnership that honors the woman’s expertise and perspectives and enables the counselor to provide an atmosphere that is conducive rather than coercive to change. The woman’s own judgement of her motivation and the possibility of changing a behaviour, the advantages and disadvantages of changing a behaviour, the choice of strategies for adopting and maintaining a new behaviour were all topics of the sessions. All women who attended the program were also invited to an aqua aerobics class (once or twice a week), especially designed for obese women. The obese women in the control group attended the routine antenatal care program.
Target behaviour/s: reducing risk behaviours of developing allergies during pregnancy (encompassing a range of behaviours).
Target population/s: women and infants.
Extract from: Storrø et al. 140 © 2010 Storrø et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Interventional topics and strategies
All interventions were initiated at first scheduled consultation in pregnancy as soon as the informed consent form was signed. In Norway a daily supplement of cod-liver oil is very common and already recommended for children and adults alike. In the intervention program we aimed for a dietary intake of n3-PUFAs of at least two meals of oily fish a week and 5 ml cod-liver oil a day during pregnancy (5 ml cod liver oil = 1.2 g N-3 PUFA). Cod liver oil was to be introduced to the child from 4–6 weeks of age increasing to 5 ml/day, and oily fish at least twice a week from 6 months of age as dinner or sandwich spread. We did not intervene on intake of vegetables, breastfeeding, formula or other dietary factors. In the smoking cessation and SHS intervention the group adapted a clinic-based brief ‘5A’ office intervention based on the ‘A Clinical Practice Guideline for Treating Tobacco Use and Dependence’. The indoor dampness interventional strategy provided advice on how to detect and advice on how to reduce indoor dampness and its consequences. Simple advice regarding inspection of signs of dampness as damage due to moisture on walls and floors, mould and/or musty smell was given. Solutions such as simple ventilation by opening windows regularly and avoiding drying of clothes in living rooms were recommended.
Target behaviour/s: smoking cessation.
Target population/s: smokers.
Extract from: Ramos et al. 141 © 2010 Ramos et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Intervention
Three were conducted: intensive individual intervention (III), intensive group intervention (IGI) and minimal intervention (MI). In all three, pharmacological treatment with nicotine derivatives or bupropion was offered as an option at the physician’s discretion. Both the III and the IGI consisted of six visits during which the following were provided: counseling, psychological support and standard follow-up. Counseling and psychological support were based on motivational interview techniques that sought to: (a) reinforce in the smoker the motivation to quit smoking before D day (the day fixed for quitting by the smoker) and (b) prevent relapses after smoking cessation. Intensive interventions followed clinical guidelines developed in the Balearic Islands.
Target behaviour/s: HIV [human immunodeficiency virus] screening.
Target population/s: patients.
Extract from: Leon et al. 142 © 2010 Leon et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
The PITC intervention
This intervention is an adapted version of the ‘ACTS’ approach which includes four brief steps: assess, get consent, test, and provide supportive services. In this PITC intervention, the STI [sexually transmitted infection] nurse offered HIV testing as a standard part of STI care for all STI clients, and the client had to decline or ‘opt-out’ of this testing. According to policy in South Africa, written consent was required (although the WHO guidelines for PITC allow for only verbal consent). Abbreviated pre-test counseling consisted of informing patients that HIV is an STI and recommending that they test for HIV at this consultation. If they agreed, the nurse would do a brief test readiness assessment, obtain written informed consent, and perform the rapid test along with other routine blood tests such as those for syphilis.
Target behaviour/s: communication with medication provider (in order to change provider prescribing behaviour)
Target population/s: patients
Extract from: Pilling et al. 143 © 2010 Pilling et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
The parent study involved a randomized controlled trial of a patient activation intervention to encourage hypertensive patients to speak with their provider about obtaining a prescription for a thiazide diuretic, first-line therapy for hypertension. The objective of the parent study was to change provider prescribing behavior and increase implementation of clinical practice guidelines. Patients were randomized to a control arm or one of three intervention arms who received: (arm A) an individualized letter discussing their latest blood pressure, their 10-year cardiovascular risk score, and education about the value of thiazides; (arm B) the same individualized letter plus an offer of a $20 financial incentive if they talked with their provider about a thiazide prescription, and, if applicable, a copayment reimbursement for six months ($48) if prescribed a thiazide; and (arm C) the individualized letter, the financial incentive, plus a phone call from a health educator to answer questions about the intervention. Patients were asked to return a postcard (themselves or by giving it to their provider to complete) indicating whether they talked with their provider about their hypertension, whether they were prescribed a thiazide diuretic, and, if not, their understanding of their provider’s rationale for not initiating thiazide treatment.
Target behaviour/s: treatment of Chlamydia (encompassing a range of behaviours).
Target population/s: general practitioners (GPs).
Extract from: Bilardi et al. 144 © 2010 Bilardi et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Intervention and control
GPs in both the intervention and control groups were required to complete a pre-trial questionnaire, a clinical audit and an education session prior to the commencement of the trial. The self-completed pre-trial questionnaire collected information about GPs characteristics, knowledge, attitudes and practices regarding chlamydia testing and was conducted both pre and post-trial by all participating GPs. A clinical audit was undertaken at each practice to collect details about issues likely to have an impact on chlamydia testing in that clinic. Audit data were used to develop an ideal individualized chlamydia testing pathway for each clinic, which incorporated current best practice for testing in the primary care setting of annual chlamydia testing for sexually active women aged 16 to 24 years. GPs were advised to collect specimens for testing by first pass urine, self-collected vaginal swab or endocervical swab. Participating GPs were eligible to enrol in related chlamydia education activities accredited under the RACGP Quality Assurance and Continuing Professional Development Program (QA&CPD).
Following the audit, an education session was held at each practice to further inform GPs about chlamydia testing, management of test results and methods of introducing the subject of testing to patients. Practices were provided with waiting room chlamydia posters, pamphlets and chlamydia screening flow charts. A DVD recording of the education session was available for doctors unable to attend. At the request of GPs, tear off pads with brief information sheets for patients specifically about the reasons for testing and the simplicity of testing and treatment were produced and distributed to the practices.
Mid trial, GPs in the intervention group received a letter to remind them of the incentive offered for chlamydia testing. They were not provided with any information about the number of tests performed to date nor the amount of money they had accrued through testing. Payment was made to GPs at the end of the trial period. All practices received an honorarium amount of $AUD1000 in recognition of GPs time spent out of usual roles in participating in the trial.
Target behaviour/s: administration of vaccinations.
Target population/s: staff at medical clinics.
Extract from: Brousseau et al. 145 © 2010 Brousseau et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Intervention
In April and May 2008, a one-hour feedback session, led by a physician and a public health nurse, was carried out with the physicians, nurses and secretaries in each participating medical clinic. This feedback dealt with VD [vaccination delays] for infants at the clinic for the year 2007. Data on the proportion of doses administered without delay were presented for the first doses of three vaccines (DTaP-Polio-Hib, pneumococcal and meningococcal). Vaccination delays for each clinic were presented both in terms of the Quebec standard (one week) and the proposed Canadian standard (one month). Graphs showing the cumulative percentage of children vaccinated according to age were also presented for vaccines scheduled at 2 and 12 months, including measles, mumps and rubella vaccine (MMR). During preparation of the feedback, it became clear that certain clinics were not administering vaccines scheduled at one year during a single visit. Consequently, information on the importance of multiple injections was transmitted to these medical clinics.
Target behaviour/s: implementation of cognitive behavioural therapy (CBT).
Target population/s: therapists.
Extract from: Kauth et al. 146 © 2010 Kauth et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
The facilitation intervention
In addition to training, 12 therapists at 10 sites received facilitation. The facilitator met with them in person or by telephone or email before and during the workshop and at least monthly (twice the first month) after the workshop for six months. The facilitator (TAT) had an education and public health background (DrPH), but by design was not an expert in cognitive behavioural therapy (CBT) or a clinician. The facilitator was trained by the first author, who is an experienced facilitator in multi-site, complex behavioral adoption projects. Although the facilitator was located at one site where facilitation took place, the individual was not in mental health and functioned as an external facilitator for all facilitated sites.
The facilitator’s tasks and interventions varied by the phase of the project and by the needs of individual therapists (Table I). We viewed application of CBT training and development of skill competency as complex, developmental tasks that would require the facilitator to employ a range of enabling strategies varying with the therapist’s self-efficacy, skill competency, and situation. Prior to the workshop, the facilitator held two conference calls with the 12 therapists to introduce the concept of facilitation and begin to develop rapport. At the workshop, the facilitator met with the 12 therapists and addressed topics related to the facilitator’s role (e.g., will the facilitator evaluate my job performance?), benefits of facilitation, project expectations for therapists (e.g., attend facilitation calls, conduct CBT after the workshop), and anticipated barriers to conducting CBT and potential solutions. Initial post-workshop facilitation calls focused on setting individual goals for CBT implementation, attempting CBT quickly, and reinforcing all efforts to get started. The facilitator solicited barriers to getting started and helped to generate possible solutions. Later calls focused on maintaining motivation and overcoming barriers to achieving individual goals, such as challenges to providing weekly therapy sessions. In addition to scheduled calls, the facilitator received and responded to individual queries via email or telephone and sent email announcements and reminders to the group. The facilitator maintained a detailed time-log of all facilitation activities, including contacting the therapists and responding to queries.
| Interventions | Pre-workshop | Workshop | Post-workshop months: | |||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |||
| Develop rapport with therapists and answer questions | ✗ | ✗ | ✗ | |||||
| Provide education about facilitation and its benefits | ✗ | ✗ | ✗ | ✗ | ||||
| Identify goals for participating in this training | ✗ | ✗ | ✗ | ✗ | ||||
| Anticipate obstacles in meeting goals | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| Provide general encouragement and praise | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| Review goals and assess progress | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| Provide feedback on goal attainment | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ||
| Use email reminders of calls and study deadlines | ✗ | ✗ | ✗ | ✗ | ✗ | |||
| Provide opportunities for social comparison and support | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
| Employ motivational interviewing techniques to encourage rapid application of CBT | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | ✗ | |
Target behaviour/s: creating, finding, and implementing self-care support for people with long-term health conditions (encompassing a range of behaviours).
Target population/s: general practitioners, nurses, practice managers, clerical and reception staff.
Extract from: Kennedy et al. 147 © 2014 Kennedy et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Development of the WISE training package
The aims of the training are outlined in Table J.
Training session one
-
Introduction to WISE
-
Exercise one: ‘from reception to self-management’
-
Task one: Can we map out the process?
-
Task two: Where are the problems in the process?
-
-
Introduce self-management support options and tools
-
Demonstration DVD
-
Group one = GPs and nurses: Skills practice using difficult scenarios
-
Group two = receptionists, practice manager, IT [information technology] staff, and one clinician:
-
Begin to develop
-
List of local resources practice staff can access
-
Computer templates staff can access
-
-
Homework: Agree priorities for practice to work on. Audit patients to come up with some case studies for the role play sessions
Training session two
-
Feedback from session one – what has happened?
-
Group one
-
Skills practice using role play techniques to practice the consultation skills needed to provide motivation and support to patients to enable them to self-manage.
-
-
Group two
-
Reflect on the priorities the practice agreed to work on. Use problem-solving techniques
-
Problem solve on barriers to making support options for patients and/or use of PRISMS forms work in the practice
-
-
Summary
| Aim | Method | How |
|---|---|---|
| Understand the WISE approach and implications for practice | Presentation and discussion plus introduction of manual | Involving whole practice |
| Learn about people’s roles in the practice and their impact on the way patients with long-term conditions participate in health care | Interactive exercise using simplified process mapping | Small groups |
| For clinicians--learn: | ||
|
Interactive role play | Small groups |
|
Interactive role play | Small groups |
|
||
|
Brief presentation with discussion. DVD exemplar of use plus manual | Involving whole group |
|
Presentation with discussion. DVD exemplar of use plus manual | Involving whole group |
|
Presentation with discussion. DVD exemplar of use plus manual | Involving whole group |
|
Presentation with discussion. DVD exemplar of use plus manual | Involving whole group |
| As a practice--develop: | ||
|
Problem-solving techniques | Involving whole practice |
|
Problem-solving techniques | Involving whole practice |
|
Problem-solving techniques | Involving whole practice |
|
Ongoing activity and support | With WISE leads in the practice |
Target behaviour/s: delivery of the ‘Out-and-About Implementation Program’ including medical record audits followed by feedback, barrier identification, and education to target known local barriers (encompassing a range of behaviours).
Target population/s: rehabilitation therapists.
Extract from: McCluskey et al. 148 © 2010 McCluskey and Middleton; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited. The out-and-about implementation program Under Creative commons licence. (http://creativecommons.org/licenses/by/2).
The intervention provided to help rehabilitation therapists implement the outdoor journeys was named the ‘Out-and-About Implementation Program’. The program aimed to change practice and included three active components: medical record audits followed by feedback, barrier identification, and education to target known local barriers.
Medical record audits were conducted retrospectively by AM and two professionals from each team. We requested 100 consecutive records (20 records for each of the five teams) of people with stroke who had received therapy (for any reason) in the previous 12 months from a team occupational therapist, physiotherapist, or both. One exception was a new team that had been established six months earlier, and had only seen 10 people with stroke. In that case, we requested all of their records for people with stroke seen since service commencement. Multiple auditors were used to raise professionals’ awareness of their practice, and the practice of their team, by engaging them in audits. Each professional audited at least three medical records. Two medical files from the total sample were double coded by the first investigator to check for consistency. Differences were discussed and consensus reached when necessary. No formal study of rater agreement was conducted.
Audit criteria were rated using yes/no response options. Questions were asked about screening and assessments conducted, intervention provided, goals set and outcomes measured in relation to transport, outdoor mobility, and outings. Any occasions of service that focussed on improving outdoor journeys were counted. A written summary of each team’s performance was provided to teams within eight weeks by AM.
Feedback of results from the first audit was provided to each team about their compliance with key criteria, with comparison to the overall compliance by the five teams. Each team then set targets for the next 12 months (e.g., ‘50% of people with stroke will have written evidence that driving has been discussed’).
A second retrospective audit of medical records was conducted 12 months later using identical tools and processes to the first audit. Medical files were requested of 100 people with stroke treated after the half-day implementation training workshop (20 consecutive records for each of the five teams). Nine rehabilitation professionals audited the medical records in addition to AM.
Barrier identification was conducted concurrently with the audit process. To identify barriers, we used two methods that have been recommended for implementation research. First, we conducted in-depth interviews (described elsewhere) with allied health professionals from two teams, and then transcribed and analysed the content. Interviewees were asked to describe what they knew about the outdoor journey intervention, including the published evidence, and factors that might help or hinder their team from implementing the outdoor journey intervention. Prompt questions were used to enquire about skills and knowledge, staffing, resources, assessment procedures, screening and report-writing systems, and treatment routines. Findings were then used to inform the content of a workshop.
Education
A half-day workshop was run in August 2007. The workshop was led by AM. First, we presented a critical appraisal of the original randomised trial by Logan et al. (2006), and a description of the complex outdoor journey intervention. Therapists were alerted to the national clinical guideline recommendation about the intervention.
Second, baseline audit data were presented with the permission of the five teams. Based on the review by Grimshaw et al. (2006), consensus was reached at the workshop that a 10% improvement in the target practice behaviours would be the goal for teams following the implementation program (i.e., the pre-determined minimum clinically worthwhile difference).
Third, a written document was presented and discussed (‘Increasing outdoor journeys after stroke: Protocols for use by rehabilitation professionals’). Protocols were provided for upgrading walking, bus and train travel training, trialling motorised scooters, addressing return to driving, and providing written information about transport options. These protocols had been prepared by the AM with advice from local team members.
Fourth, two case studies were presented by occupational therapists who had delivered escorted journeys to people with stroke. Each case study included goals of the person with stroke, treatment progression, and safety tips. A videotaped interview was also presented showing a person with stroke who described the benefits of being assisted to get out of the house. Participants then practiced writing sample goals related to outdoor journeys and community participation.
Finally, potential barriers and enablers to delivering the outdoor journeys were identified, then discussed by workshop participants in pairs or teams. Examples and quotes were presented from the earlier in-depth interviews conducted with team members. Participants identified strengths, weaknesses, opportunities, and threats affecting their team’s ability to provide the evidence-based outdoor journey intervention. Solutions were proposed, discussed and documented by team leaders.
Target behaviour/s: test requesting behavior.
Target population/s: primary care doctors.
Extract from: Ramsay et al. 149 © 2010 Ramsay et al. ; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Methods
Description of the main trial interventions
Feedback consisted of a six-sided colour booklet (e.g., see Additional File 1) presenting graphs of practice level data for each of the nine targeted tests and for each laboratory discipline as a whole. Every graph showed rates of test requesting over the previous three years for the practice compared with the regional rates. The feedback was enhanced with brief educational messages that described specific clinical circumstances where it was inappropriate to request the test. These messages were included alongside the graphs for each of the targeted tests. The booklets were posted to each primary care doctor within each intervention group practice on four occasions (updated every three months from the start of the intervention period).
The brief educational messages were added as reminders to the test result reports sent to the requesting practice (e.g., see Additional File 2). The laboratory information system was programmed to recognise the relevant cues for each of the targeted tests and automatically add the brief educational reminder messages to the relevant printed and electronic test result reports. The messages were activated every time the cue occurred and were presented at the same time as the test result. The reminder messages were intended to influence future requests for the targeted tests.
Additional file 2: Example of the reminders intervention
Target behaviour/s: provision of smoking cessation assistance (encompassing a range of behaviours).
Target population/s: providers within ACRN Community Health Centers.
Extract from: Shelley and Cantrell. 150 © 2010 Shelley and Cantrell; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
Usual care
Prior to the study, as part of a quality improvement (QI) initiative to disseminate tobacco use treatment guidelines, all CHCs (Community Health Centers) within the ACRN (Ambulatory Care Research Network implemented an expanded vital sign chart stamp that prompted providers to ask patients about tobacco use, advise them to quit, assess readiness to quit and offer assistance (4As) (Additional file 1). The prompt to provide assistance was divided into two components on the chart stamp: prescription given and referral made. This approach was meant to simplify the documentation process and operationalize the 4th A, Assist, to make it clear that referral and prescription were the two primary options available to the provider and patient. After implementation of the new chart system, all providers attended a 60 minute physician led presentation on current evidence based practice guidelines for treating tobacco dependence and systems level changes to support identification and referral of smokers for cessation treatment. At the conclusion of this visit, each practice received a tool kit consisting of patient education materials and provider materials (e.g. pharmacotherapy guide) and wallet cards with the Quitline number.
Intervention
The intervention was comprised of four components: 1) usual care plus the fax referral system that linked smokers to the New York State Quitline for proactive tailored counseling, 2) a 30 minute training for physicians, nurses and medical assistants on how to use the Fax-to-Quit program, 3) two site visits from research staff that involved meeting with clinic staff to elicit any barriers to implementation, provide additional materials and offer further educational information as needed, and 4) provider feedback on their adherence to the 4As and use of the Fax-to-Quit program compared with other providers in their clinical site. Feedback data was embedded in two separate emails sent during the four month intervention period.
The New York State Quitline service includes proactive telephone calls with mailing of self-help material, free nicotine replacement therapy for those who qualify and referrals to local treatment programs. The Quitline faxes a report back to the provider describing the treatment plan. Providers are also notified if the patient cannot be reached. The Quitline makes up to five attempts to contact patients.
Additional file 1: Figure s1 – Expanded vital sign chart stamp
BP: __________ Weight: _______
Ht: _______ BMI:_____
Tobacco Use: Yes No Former
Advise to quit: Yes No
Ready to quit? Yes No
Rx given: Yes No
Referral made: Yes No
List of abbreviations
- AC1
- alternative chance – corrected statistic to kappa
- ANOVA
- analysis of variance
- BCI
- behaviour change intervention
- BCT
- behaviour change technique
- BCTTv1
- Behaviour Change Technique Taxonomy version 1
- BMC
- BioMed Central
- CART
- classification and regression tree
- DCV
- discriminant content validity
- IAB
- International Advisory Board
- ICC
- intraclass correlation coefficient
- MRC
- Medical Research Council
- NCSCT
- National Centre for Smoking Cessation and Training
- NICE
- National Institute for Health and Care Excellence
- PABAK
- prevalence- and bias-adjusted kappa
- RCT
- randomised controlled trial
- RQ
- research question
- SD
- standard deviation
- TDF
- theoretical domains framework
- TIDieR
- Template for Intervention Description and Replication