Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 11/35/06. The contractual start date was in May 2013. The draft report began editorial review in June 2015 and was accepted for publication in October 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interest of authors
Phillip J Cowen has, in the last 3 years, been a paid member of an advisory board of Lundbeck. Nick Freemantle has received funding for research and consultancy from a variety of governmental, industrial, and charitable sources. Cormac J Sammon has received funding for research from Novartis Vaccines and Diagnostics. Irene Petersen supervises a PhD student who is sponsored by Novo Nordisk. Irwin Nazareth is currently a member of the National Institute for Health Research Health Technology Assessment commissioning board.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Petersen et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background, aims and objectives
Background
Onset of psychoses and psychotropic treatment
The onset of psychoses (schizophrenia and bipolar disorder) in women usually occurs within childbearing age and long-term treatment is often required, including a mixture of psychotropic medication such as antipsychotics, lithium and anticonvulsant mood stabilisers, for example valproate, lamotrigine and carbamazepine (see Table 1 for trade names and manufacturers). 1–6 In 2007 in the UK, women with a diagnosis of schizophrenia aged between 18 and 44 years received antipsychotic treatment for more than 50% of the time they were registered with a general practice. However, antipsychotics are being increasingly prescribed not just for schizophrenia, but also for bipolar disorder and severe depression. 2,7,8 A second UK study revealed that in 2009, 233 out of 682 (34%) women of childbearing age who had bipolar disorder received two or more prescriptions of valproate. 2 Atypical antipsychotics in combination with lithium are also often prescribed to women of this age group. 2,4
Pregnancy and psychotropic treatment dilemma
Although many women treated with psychotropic medication become pregnant or plan pregnancy,9–11 no psychotropic medication has been licenced for use in pregnancy. 12,13 This leaves women and their health-care professionals in a treatment dilemma as they need to balance the health of the women with that of the unborn child. 1,14–16 Advice on treatment varies across countries and in some instances standard psychiatric advice is that women should maintain pharmacological treatment across the perinatal period,17 however, some psychotropic medications are known to have teratogenic and adverse neurodevelopmental effects. 4,12,18 Thus, the 2014 National Institute for Health and Care Excellence (NICE) guidelines12 for antenatal and postnatal mental health clearly state that valproate should not be offered for acute or long-term treatment of a mental health problem in women of childbearing potential. Likewise, the guidelines suggest that lithium should not be prescribed to women who are planning a pregnancy or who are pregnant, unless there has been a poor response to antipsychotic medication. 12 The evidence base for adverse effects of other psychotropic medications is sparse. Although antipsychotic drugs are often used in the treatment of both schizophrenia and bipolar disorder in pregnancy, several reviews conclude that there is a paucity of information on the risks and benefits of pharmacological treatment of psychoses in pregnancy in the absence of large and well-designed prospective studies. 1,14,17,19,20 This is further supported by a Cochrane review from 2004,21 updated in 2009,22 which concluded that no randomised controlled trials (RCTs) have been conducted to establish whether the benefits of taking antipsychotic drugs outweigh the risks for pregnant or postpartum women. Similarly, limited information is available for anticonvulsant mood stabilisers other than valproate,18 even though the prescribing of drugs such as lamotrigine has been on the rise for more than a decade.
In recognition of the lack of evidence on the risks and benefits of psychotropic medication in pregnancy and the difficulties encountered in evaluating this issue using a traditional RCT design, in 2001, the National Institute for Health Research Health Technology Assessment (HTA) programme commissioned research utilising information derived from established databases. The commissioned call was titled ‘What are the risks and benefits of psychotropic drugs in women treated for psychosis who become pregnant?’ (HTA reference number 11/35/06). The ‘health technology’ to be evaluated in this call was psychotropic medications that included antipsychotics, lithium and anticonvulsant mood stabilisers prescribed to women with psychosis (bipolar disorder or schizophrenia or overlap syndromes) and whose symptoms are controlled on treatment and who become pregnant. The focus of the investigation was to compare the relative benefits and harms of these different drugs on the mother and the child, when prescribed both during pregnancy and when discontinued.
This project was hence designed in response to this commissioned call. We used data from two large UK clinical databases – The Health Improvement Network (THIN) and the Clinical Practice Research Datalink (CPRD) – to study ‘real-life’ prescribing of psychotropic medication just before, during and after pregnancy and to examine the absolute and relative risks of adverse maternal and child outcomes in women who use psychotropic medication in pregnancy.
Structure of the report
In this chapter of the report we include a description of the overall aim and the specific objectives. Chapter 2 then presents the overall methodology: the data sources, the development of the pregnancy cohorts and the linked mother–child cohorts, the study sample and target populations, and the ‘health technology’ (i.e. the psychotropic medications). This will be followed by the results of five descriptive studies in Chapter 3 with a focus on psychotropic drug utilisation, discontinuation and restarting of treatment. In Chapter 4 we report the results of a series of cohort studies that examine the absolute and relative risks of adverse maternal and child outcomes associated with psychotropic medication that emerged from the analyses of the data, followed by a synthesis and discussion of strength and limitations (see Chapter 5), conclusions and recommendations for future research (see Chapter 6) and a descriptive account of our work with patients and the public (see Chapter 7).
Aim and objectives
The overall aim of the project was to ascertain the risks and benefits of psychotropic medication in women treated for psychosis who become pregnant.
The specific objectives were to:
-
provide a descriptive account of psychotropic medication prescribed before pregnancy, during pregnancy and up to 15 months after delivery in UK primary care from 1995 to 2012
-
identify risk factors predictive of discontinuation and restarting of lithium, anticonvulsant mood stabilisers and antipsychotic medication
-
examine the extent to which pregnancy is a determinant for discontinuation of psychotropic medication
-
examine prevalence of records suggestive of adverse mental health, deterioration or relapse 18 months before and during the course of pregnancy and up to 15 months after delivery
-
estimate absolute and relative risks of adverse maternal and child outcomes of psychotropic treatment in pregnancy.
Chapter 2 Methods
In this chapter we describe the data sources for the project (THIN and the CPRD) and how the pregnancy cohorts and mother–child cohorts were developed. We also describe our study samples and the ‘health technology’ under evaluation, that is, the psychotropic medication.
UK electronic primary care health records
We used data from two electronic health records data sources, THIN and the CPRD (formerly known as the General Practice Research Database). The Department of Primary Care and Population Health at University College London has a licence for full access to all of the THIN data. Hence, we used data from THIN to address four of our five objectives, but for our final objective (i.e. to calculate absolute and relative risks of adverse effects of discontinuation compared with continuation of psychotropic medication in pregnancy on maternal and child outcomes) we supplemented our sample of pregnant women and their children in THIN with a sample of pregnant women who have been prescribed psychotropic medication either before and/or during pregnancy and their linked children from the CPRD in order to obtain a larger study sample. Below, we provide a description of the two data sources and information about how the cohorts of pregnant women and the linked mother–child cohort were derived.
The Health Improvement Network primary care database and the Clinical Practice Research Datalink
The Health Improvement Network and the CPRD are two large primary care databases that provide continuous anonymised longitudinal general practice data on patients’ clinical and prescribing records and include data from > 10% of the UK population, (www.csdmruk.imshealth.com/; www.cprd.com/intro.asp). Both databases collect data from general practices that use Vision computer software (In Practice Systems, London) (www.inps4.co.uk/vision) to manage patient consultations and health records. Diagnoses and symptoms are recorded by practice staff using Read codes, which is a hierarchical coding system including more than 100,000 codes. 23,24 Although the Read code system can be mapped to the International Classification of Diseases, Tenth Edition (ICD-10), the Read codes also include a number of symptoms and administrative codes. 24 Information on weight, height, smoking habits, alcohol intake and illicit drug problems is also recorded as well as information on antenatal care and birth details, pregnancy outcomes and postnatal care. Prescriptions are issued electronically and directly recorded on the general practice computer systems and thus captured in specific therapy records that hold information on dates of prescription and generic names. Some information is also available on quantity and dosage, although this information is not always complete. In addition, the databases hold individual patient-level information about year of birth (month of birth for individuals < 15 years of age), date of registration, date of death and date of transfer out of the practice. There is also a household identifier, which is the same for individuals who are registered with the same practice and live in the same household. However, some household identifiers include more than one household. This may, for example, be the case where several people live in a block of flats (e.g. flat 2A, flat 2B). In THIN, social deprivation is recorded for each individual by quintiles of Townsend scores, based on information from the 2001 census25 In the CPRD, social deprivation information is available for practices that have signed up to their linkage scheme (www.cprd.com/recordLinkage/), but we did not have access to Townsend scores for this project from the CPRD.
Over 98% of the UK population are registered with a general practitioner (GP) (family doctor)26 and the databases are broadly representative of the UK population. 27,28 However, Blak et al. 27 demonstrated that THIN contains slightly more patients who lived in the most affluent areas (23.5% in THIN vs. 20% nationally). Although antenatal care is often shared between general practice staff and midwives, the GP remains responsible for women’s general medical care during pregnancy, including prescribing of medicines. Some women with psychosis also receive care from local NHS mental health trusts, but most mental health trusts have limited prescribing budgets; therefore, for most women, prescribing of psychotropic medication remains with GPs during pregnancy and hence this information is available in THIN and the CPRD.
Although computerisation of general practices started as early as the late 1980s, few practices used computers initially. It was, however, in the mid-1990s that an increasing number of general practices became fully computerised29 and in this study we utilised data from 1 January 1995, or when general practices met data quality standards. 28–30
Pregnancy cohort and mother–child cohorts
We created a cohort of pregnant women using data from THIN for the period 1 January 1995–31 December 2012. We subsequently linked the pregnant women’s clinical records to those of their children if they were registered with the same general practice. Details on how the cohort was created and the decisions that were made to identify a suitable cohort for further analysis are described below. We also describe how we linked mothers and children, and finally how we identified women receiving psychotropic treatments within these cohorts.
Pregnancy cohort
Our pregnancy cohort was based on the recorded date of delivery of the women, the postnatal care record, the first day of last menstrual periods (LMPs) and the estimated delivery dates (EDDs).
The Health Improvement Network includes records that are made as a part of clinical management in primary care; therefore, some pregnancy and antenatal records may not represent actual pregnancies, but they represent historical information. Furthermore, some pregnancies may result in early terminations (either selective or spontaneous abortions/miscarriages) and in these instances little information is recorded in the electronic health records, making it impossible to determine the start and duration of the pregnancy. We therefore derived a set of rules for the inclusion of pregnancies in our cohort. Every pregnancy was ascertained using two different types of information as follows:
-
LMP date
-
antenatal record
-
delivery record
-
postnatal care record
-
child whose GP record could be matched to the current pregnancy.
Further, we ensured that if we had information only on LMP and antenatal records, the latest antenatal record should be at least 105 days after the first date of the LMP (i.e. equivalent to 15 weeks’ gestation). Only a very small proportion (1%) of the pregnancy cohort was identified from LMP and antenatal records alone.
In total, we identified 495,953 pregnancies in 365,138 women who were permanently registered with one of the general practices that contributed data to THIN in the period between 1 January 1995 and 31 December 2012. This cohort was used as the basis for selecting the target population for our examination of psychotropic medication prescribed before pregnancy, during pregnancy and up to 15 months after delivery; changes in severity of illness during the course of pregnancy and in the period after delivery; and for assessing the absolute and relative risks of adverse maternal pregnancy outcomes.
Duration of pregnancy
In accordance with clinical practice in the UK, the first day of the LMP was considered as the start of pregnancy. As the clinical records do not always hold direct information about the pregnancy length, we estimated the duration of the pregnancy based on information on gestation and maturity of the fetus and/or baby as entered on the electronic record. For women where there was no information available on length of pregnancy or no indications that suggested a child was born pre or post term, we made the assumption that the pregnancy lasted the normal course of 280 days (40 weeks).
Linked mother–child cohorts
Pregnant women and their potential children were linked if they were both registered with the same general practice and shared the same family/household identifier. Furthermore, the date of delivery and the child’s month of birth were required to be near to each other (within 6 months) and the child should have been registered with the general practice within 6 months of birth.
We excluded mother–child pairs when several possible mothers could be linked to a child (< 0.2%). This could have occurred if two women from a block of flats (who would have shared the same household/family identifier) were pregnant at the same time. In cases where the child was registered with another general practice, linkage with the mother was not possible. This was also not done in instances where the mother and child moved to a different practice shortly after the birth of the child. We also excluded pregnancies from the mother–child cohort where there were two or more children associated with the same delivery.
We first identified mother–child pairs in THIN. They were combined with records from the CPRD and together used as the target populations to examine the absolute and relative risks of adverse effects of discontinuation compared with continuation of psychotropic medication on child outcomes.
Combining records from The Health Improvement Network and the Clinical Practice Research Datalink
Inspired by previous research that utilised data from both THIN and the CPRD and demonstrated that combining clinical records from these two databases is feasible,31 we combined our cohorts derived from THIN with data from the CPRD, including pregnant women who have been prescribed psychotropic medication before and/or during pregnancy as well as a cohort of linked mother–child pairs.
We provide a brief description on how we combined the data from THIN and the CPRD, and the process used to remove records that were duplicated from those practices that contributed to both databases.
Although THIN and the CPRD receive raw data from general practices that use the Vision clinical software system, the two databases are structured in slightly different ways. The CPRD data were first reformatted such that the data structure was similar to that of THIN. We then derived a matching algorithm between the two databases based on patient registration data, medical records and patient demographics. As the two databases overlap at practice level, practices deemed to have a sufficient number of matching individuals were taken to be the same practice. THIN records for such practices were excluded and the CPRD records maintained for further analysis. Further details are provided in Appendix 1.
Study sample and target population
The target population for this project was women with psychosis (bipolar disorder, schizophrenia or overlap syndromes) who are in receipt of antipsychotics, lithium and anticonvulsant mood stabilisers, and who became pregnant. Some women receive psychotropic medication prior to formal diagnoses and others may never have a diagnosis of psychosis recorded in their electronic primary care health records. For antipsychotics and lithium, we therefore opted for the most sensitive approach and included all women who were treated with these medications prior to pregnancy in our studies, irrespective of whether or not they had a record of psychosis in their electronic health records. On the other hand, anticonvulsant mood stabilisers are prescribed for various indications. We therefore identified all women prescribed an anticonvulsant mood stabiliser, but for some analyses then limited our analyses to those with a history of psychosis (including bipolar disorder) or a recent record of depression (in the 3 years prior to the start of pregnancy).
Psychotropic medication
The ‘health technology’ under investigation in this project was (1) antipsychotics (atypical and typical); (2) lithium; or (3) anticonvulsant mood stabilisers. Table 1 provides a list of the generic names of each of the treatments.
| Antipsychotics | |||
|---|---|---|---|
| Typical | Atypical | Lithium | Anticonvulsant mood stabilisers |
| Asenapine (Sycrest®, Lundbeck) | Amisulpride (Solian®, Sanofi Synthelabo) | Lithium Camcolit®, Norgine; Li-Liquid®, Rosemont; Liskonum®, GSK; Litarex®, Dumex; Lithonate®, Approve Prescription Services; Phasal®, Lagap; Priadel®, Sanofi) | Carbamazepine (Arbil®, Ranbaxy; Carbagen®, Generics; Epimaz®, Ivax; Tegretol®, Novartis; Teril®; Timonil®, CP Pharmaceuticals) |
| Benperidol (Anquil®, Archimedes; Benquil®, Concord) | Aripiprazole (Abilify®, Otsuka) | Lamotrigine (Lamictal®, GSK) | |
| Chlorpromazine (Chloractil®, DDSA Pharmaceuticals; Largactil®, Sanofi-Aventis) | Clozapine (Clozaril®, Novartis; Denzapine®, Merz; Zaponex®, Ivax) | Sodium valproate (Epilim®, Sanofi-Aventis; Epilim Chrono®, Sanofi-Aventis; Episenta®, Desitin; Orlept®, Wockhardt) | |
| Chlorprothixene | Olanzapine (Zypadhera®, Lilly; Zyprexa®, Lilly) | Valproic acid (Convulex®, Pharmacia; Depakote®, Sanofi Synthelabo) | |
| Droperidol (Thalamonal®, Janssen; Droleptan®, Janssen-Cilag; Xomolix®, ProStrakan) | Paliperidone (Invega®, Janssen-Cilag; Xeplion®, Janssen) | Valproate semisodium (Convulex®, Pharmacia; Depakote®, Sanofi Synthelabo) | |
| Flupentixol (Depixol®, Lundbeck; Fluanxol®, Lundbeck) | Quetiapine (Atrolak®, Accord; Biquelle®, Aspire; Ebesque®, Ashbourne; Mintreleq®, CEB Pharma Ltd; Seotiapim®, Sandoz; Seroqul®, AstraZeneca; Sondate®, Teva; Zaluron®, Fontus) | ||
| Fluphenazine (Decazate®, Berk; Modecate®, Sanofi Synthelabo; Moditen®, Sanofi-Aventis; Motipress®, Sanofi Synthelabo; Motival®, Sanofi-Aventis) | Risperidone (Risperdal®, Janssen-Cilag) | ||
| Fluspirilene (Redeptin®, Fluspirilene) | |||
| Haloperidol (Dozic®, Rosemont; Fortunan®, Steinhard; Haldol®, Janssen-Cilag; Serenace®, Ivax) | |||
| Levomepromazine (Levinan®, Link; Nozinan®, Sanofi-Aventis) | |||
| Loxapine (Loxapac®, Wyeth) | |||
| Oxypertine (Integrin®, Sterling Winthrop) | |||
| Pericyazine (Neulactil®, JHC Healthcare) | |||
| Perphenazine (Fentazin®, Goldshield; Triptafen®, AMCo) | |||
| Pimozide (Orap®, Eumedica) | |||
| Pipotiazine (Piportil®, JHC Healthcare) | |||
| Promazine (Sparine®, Genus) | |||
| Remoxipride (Roxima®, AstraZeneca) | |||
| Sertindole (Serdolect®, Lundbeck) | |||
| Sulpiride (Dolmatil®, Sanofi-Aventis; Sulparex®, BMS; Sulpitil®, Pfizer; Sulpor®, Rosemont) | |||
| Thiopropazate | |||
| Thioproperazine | |||
| Thioridazine (Melleril®, Novartis; Rideril®, DDSA Pharmaceuticals) | |||
| Trifluoperazine (Stelazine®, Goldshield) | |||
| Trifluperidol (Triperidol®, Lagap) | |||
| Zotepine (Zolpetil®, Movianto) | |||
| Zuclopenthixol (Clopixol®, Lundbeck) | |||
We used all antipsychotics listed in the British National Formulary (BNF)32 chapter 4.2.1, except prochlorperazine, which is primarily prescribed for morning sickness in pregnancy (nausea gravidarum, emesis gravidarum). For anticonvulsant mood stabilisers, we focused on the three most commonly prescribed anticonvulsant mood stabilisers;33 lamotrigine, carbamazepine and valproate (sodium valproate, valproic acid and valproate semisodium) listed in the BNF chapter 4.8. For lithium, we included lithium carbonate and lithium citrate listed in the BNF chapter 4.2.3.
Data analysis and statistical software
Data analysis conducted for each study is described in further detail in Chapters 3 and 4. Stata (version 13.1) (StataCorp LP, College Station, TX, USA) was used for all data management and analysis.
Ethics and scientific approvals
The scheme for THIN to obtain and provide anonymous patient data to researchers was approved by the NHS South-East Multicenter Research Ethics Committee in 2002. The CPRD has been granted Multiple Research Ethics Committee approval (05/MRE04/87) to undertake purely observational studies, with external data linkages, including Hospital Episode Statistics and Office for National Statistics (ONS) mortality data. The work of the CPRD is also covered by the National Information Governance Board for Health and Social Care – Ethics and Confidentiality Committee approval Ethics and Confidentiality Committee (a) 2012. Scientific approval for use of THIN data for this study was obtained from Cegedim Strategic Data Medical Research’s Scientific Review Committee (protocol number 13–059) and scientific approval for use of CPRD data was obtained from Independent Scientific Advisory Committee (protocol number 14_087R).
Chapter 3 Psychotropic medication prescribed before pregnancy, during pregnancy and up to 15 months after delivery
Introduction
In order to understand the risks and benefits of psychotropic medication in pregnancy, it is important to also have an overview of the utilisation of these medications before and during pregnancy. This has been the subject of a number of recent studies conducted in Europe and North America. 34–41 Epstein et al. 39 examined use of psychotropic medication using data from Tennessee Medicaid to conduct a retrospective cohort study of nearly 300,000 women enrolled in the database throughout pregnancy from 1985 to 2005. This study reported significant increases in the use of anticonvulsants among mothers with pain and other psychiatric disorders, but a decrease in the use of lithium and typical antipsychotics. 39 Two studies37,40 based on pharmacy dispensing data from the USA estimated the prevalence of anticonvulsant mood stabilisers and antipsychotics dispensed during pregnancy over the period 2001–7 from 11 US health plans participating in the Medication Exposure in Pregnancy Risk Evaluation Program involving 585,615 deliveries. One study37 reported a sharp increase in the use of atypical antipsychotics from 0.33% [95% confidence interval (CI) 0.29% to 0.37%)] in 2001 to 0.82% (95% CI 0.76% to 0.88%) in 2007, while the use of typical antipsychotics remained stable. The other study40 estimated that in 2001 there were 15.7 women receiving anticonvulsant mood stabilisers per 1000 deliveries in the USA, increasing to 21.9 per 1000 deliveries in 2007. A more recent study34 based on data from THIN demonstrated that for anticonvulsant mood stabilisers the overall prevalence of prescribing in pregnancy has remained at the same level, between 0.4% and 0.6% between 1994 and 2009; however, the prevalence of prescribing of individual types of anticonvulsants has changed over time with lamotrigine becoming increasingly common. 34
A study based on one of the UK primary care databases, the CPRD, including records from 1989 to 2010, found that among 420,000 pregnancies, treatment with antipsychotics (excluding prochlorperazine) followed a u-shaped pattern, with 0.15% of all women having a prescription in the 3 months before pregnancy, a decline during pregnancy (0.07–0.08% in the second and the third trimester) and an increase in the first 3 months after delivery, to 0.15%. 36 A dramatic decline in the dispensing of antipsychotics in the second and third trimester was also observed in the American dispensing data. 37 UK data suggest that the rate of discontinuation of anticonvulsant mood stabilisers depends on whether or not the woman has a record of epilepsy or bipolar disorder. 34 Thus, women with bipolar disorder were much more likely to discontinue treatment than women with epilepsy, although the medications were the same. 34 Petersen et al. 35 studied discontinuation of antidepressants in pregnancy and found that only 1060 (20%) out of 5229 women who were on antidepressant treatment 3 months before they became pregnant received further treatment after the first 6 weeks of their pregnancy (when the woman is likely to become aware of her pregnancy).
Limited information is available on the proportion of women who discontinued psychotropic medication just before or during pregnancy and who then restarted medication in either the course of being pregnant or in the post-partum period. However, studies on antidepressants indicate that reintroduction of antidepressant treatment in pregnancy is common. Cohen et al. 42 followed 54 non-depressed pregnant women who had discontinued antidepressant treatment around the time of conception. Of these women, 23 (42%) restarted antidepressant therapy during pregnancy, with nearly half of them (n = 11) doing so in the first trimester. Another study followed 70 women who discontinued antidepressants, and of these, 40 (57%) restarted treatment, almost half in the first trimester of pregnancy. 43 The major determinant of treatment reintroduction was relapse of the disorder, as noted from women who scored higher on depression and anxiety measures in cases where treatment was reintroduced. 39 Lithium and other mood stabilisers may on the other hand be introduced for preventative measures rather than to treat relapse. In fact, NICE guidance12 recommends that lithium may be stopped in early pregnancy, but reintroduced in the third trimester in the case of women at high risks of relapse.
Methods
Studies
We conducted five studies to evaluate utilisation and recording of mental health in primary care; these were (1) the prevalence, initiation and termination of prescribing of psychotropic medication at 6 months before pregnancy, during pregnancy and up to 15 months after delivery; (2) the patterns of recording that indicate worsening of mental health at 18 months before pregnancy, during the course of pregnancy and up to 15 months after delivery; (3) the time trends in prescribing of psychotropic medication around and during pregnancy over the calendar period 1995–2012; (4) the extent of discontinuation and factors associated with discontinuation of psychotropic medication in pregnancy; and (5) the extent of restarting and factors associated with restarting psychotropic medication in pregnancy. Below we provide further details on each study in turn.
Study participants
We used data from women in the pregnancy cohort derived from THIN. As a minimum inclusion criterion, we required that women were registered with the practice throughout their pregnancy. For each of the individual studies, we introduced further inclusion criteria, detailed in the analysis section.
For the studies on discontinuation and restarting psychotropic medication, we randomly selected one pregnancy from the women who had records of more than one eligible pregnancy (antipsychotics, n = 19; lithium, n = 1; and anticonvulsant mood stabilisers, n = 2). Pregnancies that ended in miscarriage or termination were excluded from all four studies as it was impossible to determine the start and end dates of these pregnancies.
Psychotropic medication, prescription intervals and dose
Most psychotropic prescribing occurred over monthly intervals. For > 98% of women prescribed antipsychotics in the year prior to pregnancy, the median gap between prescriptions was < 3 months (91 days) and similar patterns were observed for other psychotropic medication. We considered a new episode of treatment if a woman had not received psychotropic medication prescriptions in the past 3 months (91 days). Likewise, if a woman received no further prescriptions after 3 months, she was deemed to have discontinued an episode of treatment. The date of initiation was considered as the date the first prescription was issued for that episode. The date of termination was considered as the date of the last prescription issued in the episode.
For antipsychotics we also calculated the average daily dose during the period from 4–6 months before the start of pregnancy by dividing the total amount of drugs prescribed over the period by the expected total duration of the relevant prescriptions. Durations were estimated with the help of the enhanced dosage determination method developed by the University of Nottingham Division of Epidemiology and Public Health (further details can be obtained from the data providers of THIN, IMS Health). The mass of each antipsychotic drug was standardised into units of the defined daily dose (DDD) for maintenance treatment of psychosis. 44
Prevalence, initiation and termination of psychotropic treatment: study participants, outcomes and data analysis
Study participants
We included women from the pregnancy cohort who registered with their general practice in the relevant time periods.
Outcomes
Our outcomes were (1) prevalence of prescribing before pregnancy (6 months before), during pregnancy and after delivery [up to 15 months after delivery (approximately 24 months after conception)]; and (2) proportions of individuals who initiated, terminated or received isolated psychotropic prescriptions before and during pregnancy, and after delivery.
Data analysis
Prevalence
We provided estimates of the prevalence for each 3-month period (trimester in pregnancy) from 6 months prior to pregnancy to 15 months after delivery. Prevalence was estimated for each class of psychotropic medication as the number of women who received a prescription in the relevant time period (numerator), divided by the number of women in the cohort in the relevant time period (denominator). Women were included in the denominator for the prevalence estimates if they were registered with a practice for at least 1 day during the relevant period.
For antipsychotics and anticonvulsant mood stabilisers we further stratified the analyses according to treatment prescribed. For antipsychotics we stratified by typical and atypical antipsychotics, and for anticonvulsant mood stabilisers we stratified the analysis by lamotrigine, valproates and carbamazepine. We estimated prevalence ratios (PRs) for each 3-month period using the period from 1 to 3 months before pregnancy as a reference.
Multiple psychotropic medications
In order to gain a better understanding of drugs prescribed from the BNF chapter on the central nervous system, we explored prescription of multiple classes of drugs from antipsychotics (BNF chapter 4.2.1 and 4.2.2), lithium and anticonvulsants (BNF chapter 4.8.1), as well as antidepressants (BNF chapter 4.3), anxiolytics (BNF chapter 4.1.2) and hypnotics (BNF chapter 4.1.1). We estimated the number of women who were in receipt of more than one psychotropic medication in the 4–6 months before pregnancy.
Start and end of prescribing episodes and isolated prescriptions
For each 3-month period (trimester in pregnancy) we also estimated the number of individuals who started or ended a prescribing episode and the number of individuals who received an isolated prescription (no preceding or subsequent prescriptions within 91 days).
Patterns of recording that indicate worsening of mental health: 18 months before pregnancy, during the course of pregnancy and up to 15 months after delivery
Study participants
We included women from the pregnancy cohort who registered with their general practice in the relevant time periods.
Outcomes
Our outcomes were records of suicide attempts, overdose and deliberate self-harm, hospital admissions, invoking under the Mental Health Act45 and entries of Read codes for psychosis, mania and hypomania. We combined the codes into three sets of outcomes: (1) suicide attempts, overdose or deliberate self-harm; (2) hospital admissions or examination under section under Mental Health Act; and (3) entries of psychosis, mania or hypomania.
Further details regarding the definition of outcomes and Read codes are provided in Appendix 1.
Data analysis
We provided estimates of the prevalence for each outcome group for each 3-month period (trimester in pregnancy) from 18 months prior to pregnancy to 15 months after delivery. Prevalence estimates were made for each of the three sets of outcomes by dividing the number of women who had a relevant record(s) (numerator) by the number of women who were registered with their general practice and thus in the cohort in the relevant time period (denominator). Women were included in the denominator for the prevalence estimates if they were registered with a practice for at least 1 day during the relevant period. They were included in the numerator if they had a least one Read code within the relevant record group. Some women may have contributed to several record groups.
The prevalence for each record group was plotted against time in relation to the pregnancy. We estimated PRs for each 3-month period using the period 1–3 months before pregnancy as a reference.
Time trends in prevalence of psychotropic medication treatment around and during pregnancy
Study participants
We included women from the pregnancy cohort who were registered with their general practice in the relevant time periods.
Outcomes
Our outcomes were annual prevalence of psychotropic treatment in (1) the 6 months before pregnancy; (2) pregnancy after the first 6 weeks of gestation (when the pregnancy is likely to be known); and (3) the first 6 months after delivery. Separate estimates were made for antipsychotics, anticonvulsant mood stabilisers and lithium. We provided the estimates by year of delivery for every 2-year period.
Data analysis
Prevalence was estimated as described in the previous section (see Patterns of recording that indicate worsening of mental health: 18 months before pregnancy, during the course of pregnancy and up to 15 months after delivery). Estimates were made separately for the 6 months before pregnancy, during pregnancy (after the first 6 weeks of gestation) and in the first 6 months after delivery.
We accounted for variation in the denominator before and after pregnancy. Hence, for women to be included in the estimates for before pregnancy they had to be registered with their general practice for the 6 months before pregnancy. Likewise, women had to be registered for at least 6 months after pregnancy to be included in the estimates for after delivery.
Discontinuation and factors associated with discontinuation of psychotropic medication in pregnancy
Study participants
This study included both a cohort of pregnant women and a comparison cohort of women who were not pregnant but who were prescribed psychotropic drugs, in order to examine the impact of pregnancy on discontinuation of these medications.
We included women from the pregnancy cohort and selected women who:
-
contributed data for at least 6 months before the pregnancy and throughout their pregnancy
-
received continuous psychotropic medication before they became pregnant, that is, women were selected if they received prescriptions between 4 and 6 months (inclusive) before they became pregnant
-
received at least one further prescription in the 3 months before the start of pregnancy.
Thus, we focused on women who received two or more prescriptions of psychotropic medication in the 6 months leading up to pregnancy.
We excluded women with a miscarriage, abortion or delivery in the 6 months prior to the start of their pregnancy since these women’s decisions about whether or not to discontinue medication might have been influenced by their previous pregnancy.
For the comparison cohort, we identified a cohort of twice as many women also in receipt of the relevant psychotropic prescriptions, but who were not pregnant for at least 12 months before and 24 months after a randomly selected index date. We stratified these groups such that the age distribution was similar in the pregnant and non-pregnant samples.
Outcomes
Our outcomes were (1) the time to last consecutive prescription of psychotropic medication in pregnancy; and (2) the factors associated with continuation of prescribed psychotropic medication in pregnant women. These included age, the average daily dosage (for antipsychotics), the length of time that the medication had been prescribed prior to pregnancy, prescription of other psychotropic medication (antidepressants, mood stabilisers or antipsychotics), records of illicit drug or alcohol problems, obesity, parity, social deprivation and ethnicity). While there is no direct measurement of severity of illness, the average daily dosage of antipsychotics and length of time the treatment had been prescribed prior to pregnancy may be indicative of the severity of illness.
Many other factors may impact on the decision to continue or discontinue psychotropic medication in pregnancy. We chose, however, to examine the variables described above, as they were available from primary care electronic health records.
Data analysis
We used Kaplan–Meier plots to examine time to last psychotropic prescription, and performed separate analyses for each class of psychotropic medication (antipsychotics, lithium and anticonvulsant mood stabilisers). We followed pregnant and non-pregnant women who were prescribed any of the three classes of psychotropic medication from 3 months before the pregnancy (or the index date for the non-pregnant women) and identified when they had their last consecutive prescription (identified as < 91 days after the previous prescription). We ended follow-up after 220 days (2 months before delivery). In the case of a premature delivery this was sooner than 220 days with follow-up ending at the time of delivery. Although we defined stopping psychotropic medication as the date of issue of the last prescription, we are aware that some women would have continued taking the drug beyond this point. The data were further stratified for atypical and typical antipsychotics and for different dosages of antipsychotics. In the case of anticonvulsant mood stabilisers the data were stratified by lamotrigine, carbamazepine and valproate and also by indication for prescription (i.e. distinctions were made between those who had an electronic health record of epilepsy, psychosis/depression or none of these).
In the pregnant cohort we examined whether or not continuation of antipsychotic and anticonvulsant mood stabiliser prescribing beyond 6 weeks of pregnancy was associated with the factors listed above using a Poisson regression model. We estimated the univariate relative risk ratios (RRRs) for each of the variables as well as the RRR adjusted for age and average daily dose. For antipsychotics we also examined if women switched between typical and atypical treatments.
For lithium we provided percentages and their CIs, but did not embark on further statistical analyses, as so few women received lithium prescriptions beyond 6 weeks of pregnancy.
Restarting and factors associated with restarting psychotropic medication in pregnancy
Study participants
In this study we began by using the same cohorts of women as used in the studies on discontinuation (see Chapter 3, Discontinuation and factors associated with discontinuation of psychotropic medication in pregnancy), that is, women who were treated with psychotropic medication in the 6 months before they became pregnant. We then selected subsets of women who discontinued psychotropic treatments just before they reached 6 weeks of pregnancy.
Outcomes
Our outcomes were (1) time to first new psychotropic prescription; (2) the proportion of women who restarted psychotropic medication by 6 months after delivery; and (3) the factors/characteristics of the women associated with restarting of prescribed psychotropic medication. We included the following factors/characteristics: age, the average daily dosage (for antipsychotics), length of time the psychotropic medication had been prescribed prior to pregnancy and prescription of other psychotropic medication (antidepressants, mood stabilisers or antipsychotics).
Data analysis
We used Kaplan–Meier plots to examine time to renewal of prescribing the psychotropic prescriptions after the start of the pregnancy. Follow-up was censored at the earliest of the following: 15 months after delivery, 31 December 2012 or when the woman left the general practice. We conducted separate analyses for each class of psychotropic medication (antipsychotics, lithium and anticonvulsant mood stabilisers) and with antipsychotics we stratified our analyses for atypical and typical antipsychotics. For anticonvulsant mood stabilisers we performed the analysis for women who had a record of psychoses or depression.
We estimated the proportion with 95% CIs of women who had discontinued medication before 6 weeks of pregnancy and restarted treatment by 6 months after delivery. The characteristics of these women were tabulated and contrasted to women who had not restarted psychotropic medication by 6 months after delivery. For antipsychotics, we estimated the univariate RRRs for each of the variables as well as RRRs adjusted for age and average daily dose. For lithium and anticonvulsant mood stabilisers we did not attempt further analysis, as the numbers were too small to produce meaningful results.
Changes to the protocol
We originally planned to undertake an evaluation of changes in severity of mental illness from the period commencing 18 months before the start of pregnancy up to 15 months after the delivery of the baby. This analysis was deemed infeasible, as it was not possible to ‘grade’ the severity of mental illness in an individual merely from their Read code entries. Instead we decided to explore how the entries varied more generally over this time period by choosing a number of outcomes suggestive of adverse mental health, deterioration or relapse and we then estimated 3-month (trimester in pregnancy) prevalence.
Results
Below we report the results on:
-
prevalence, initiation and termination of psychotropic treatment
-
patterns of recording that indicate worsening of mental health
-
time trends in prevalence of psychotropic treatment around and during pregnancy over the calendar period 1995–2012
-
discontinuation and factors associated with continuation of psychotropic medication in pregnancy
-
restarting and factors associated with restarting psychotropic medication in pregnancy.
Prevalence, initiation and terminations of psychotropic treatment: 6 months before pregnancy, during pregnancy and up to 15 months after delivery
Overall, 495,953 pregnancies were included in the study from 1 January 1995 to 31 December 2012. Below we describe the results of our studies on the prevalence, initiation and termination of psychotropic treatment. Parts of this work have been published elsewhere. 46,47
Prevalence of psychotropic treatment before, during and after delivery
In the 1–3 months before the start of pregnancy 1051 out of 495,624 (0.21%) women were prescribed antipsychotics (Table 2), 78 out of 495,624 (0.015%) were prescribed lithium and 2046 out of 495,624 (0.41%) were prescribed anticonvulsant mood stabilisers (Table 3). Only 165 out of 52,998 (0.31%) of the women prescribed an anticonvulsant drug had a record of psychosis or depression (see Table 3).
| Prescribed antipsychotic | 4–6 months before pregnancy | 1–3 months before pregnancy | First trimester | Second trimester | Third trimester | 1–3 months after delivery | 4–6 months after delivery | 7–9 months after delivery | 10–12 months after delivery | 13–15 months after delivery |
|---|---|---|---|---|---|---|---|---|---|---|
| Any antipsychotic | 999 | 1051 | 992 | 554 | 509 | 987 | 1157 | 1127 | 1092 | 1065 |
| Any typical | 550 | 594 | 596 | 301 | 258 | 533 | 582 | 558 | 536 | 519 |
| Chlorpromazine | 120 | 134 | 185 | 110 | 81 | 114 | 117 | 109 | 98 | 101 |
| Trifluoperazine | 118 | 111 | 110 | 61 | 50 | 103 | 98 | 100 | 100 | 94 |
| Flupentixol | 112 | 125 | 86 | 28 | 15 | 108 | 123 | 123 | 115 | 130 |
| Promazine | 24 | 26 | 88 | 30 | 41 | 17 | 18 | 16 | 36 | 36 |
| Thioridazine | 96 | 97 | 52 | 20 | 17 | 83 | 114 | 97 | 89 | 77 |
| Haloperidol | 36 | 37 | 36 | 30 | 36 | 59 | 42 | 47 | 39 | 32 |
| Sulpiride | 15 | 11 | 9 | 10 | 10 | 30 | 33 | 24 | 23 | 17 |
| Pericyazine | 6 | 20 | 11 | 4 | 3 | 10 | 15 | 14 | 15 | 11 |
| Zuclopenthixol | 6 | 8 | 3 | 5 | 5 | 7 | 5 | 4 | 7 | 6 |
| Fluphenazine | 15 | 20 | 7 | 1 | 0 | 11 | 11 | 17 | 13 | 14 |
| Perphenazine | 11 | 10 | 5 | 2 | 2 | 6 | 10 | 14 | 9 | 8 |
| Levomepromazine | 2 | 2 | 6 | 2 | 0 | 2 | 3 | 5 | 5 | 4 |
| Droperidol | 1 | 4 | 2 | 0 | 0 | 1 | 3 | 3 | 3 | 2 |
| Loxapine | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Trifluperidol | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Pimozide | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 |
| Pipotiazine | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| Paliperidone | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 |
| Any atypical | 473 | 485 | 427 | 265 | 263 | 485 | 604 | 597 | 579 | 573 |
| Quetiapine | 173 | 200 | 171 | 113 | 112 | 177 | 209 | 211 | 209 | 214 |
| Olanzapine | 154 | 157 | 149 | 101 | 108 | 199 | 243 | 229 | 219 | 207 |
| Risperidone | 90 | 85 | 70 | 30 | 25 | 76 | 107 | 125 | 118 | 111 |
| Aripiprazole | 40 | 45 | 37 | 20 | 18 | 37 | 42 | 35 | 41 | 40 |
| Amisulpride | 21 | 17 | 9 | 4 | 3 | 13 | 28 | 19 | 17 | 19 |
| Clozapine | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| Total pregnancies | 476,270 | 495,624 | 495,953 | 495,953 | 493,672 | 495,894 | 473,358 | 456,040 | 439,313 | 423,192 |
| Prescribed drug | 4–6 months before pregnancy | 1–3 months before pregnancy | First trimester | Second trimester | Third trimester | 1–3 months after delivery | 4–6 months after delivery | 7–9 months after delivery | 10–12 months after delivery | 13–15 months after delivery |
|---|---|---|---|---|---|---|---|---|---|---|
| Lithium | 84 | 78 | 58 | 33 | 37 | 69 | 98 | 110 | 104 | 105 |
| Any of the three ACMS | 1991 | 2046 | 1991 | 1782 | 1741 | 1965 | 1957 | 1922 | 1862 | 1819 |
| Carbamazepine | 830 | 859 | 822 | 706 | 706 | 799 | 780 | 795 | 776 | 749 |
| Lamotrigine | 687 | 727 | 748 | 707 | 696 | 718 | 722 | 687 | 666 | 639 |
| Valproate | 629 | 607 | 556 | 472 | 436 | 562 | 577 | 555 | 545 | 556 |
| Total pregnancies | 476,270 | 495,624 | 495,953 | 495,953 | 493,672 | 495,894 | 473,358 | 456,040 | 439,313 | 423,192 |
| Women with a record of psychosis or depression | ||||||||||
| Any of the three ACMS | 160 | 165 | 135 | 57 | 55 | 121 | 151 | 159 | 149 | 152 |
| Carbamazepine | 77 | 82 | 65 | 23 | 26 | 59 | 61 | 68 | 61 | 53 |
| Valproate | 68 | 66 | 47 | 19 | 17 | 50 | 68 | 66 | 66 | 77 |
| Lamotrigine | 19 | 21 | 24 | 16 | 15 | 16 | 26 | 28 | 26 | 26 |
| Total pregnancies | 51,718 | 52,998 | 53,012 | 53,012 | 52,736 | 53,006 | 50,487 | 48,489 | 46,546 | 44,711 |
During pregnancy the prevalence of antipsychotics and lithium prescribing fell dramatically. Hence, 554 out of 495,953 (0.11%) were prescribed antipsychotics and 33 out of 495,953 (0.006%) lithium in the second trimester. The corresponding PRs of antipsychotics and lithium prescribing relative to the period from 1–3 months before pregnancy were 0.53 (95% CI 0.47 to 0.58) and 0.42 (95% CI 0.27 to 0.64), respectively (Table 4 and Figure 1). In the case of anticonvulsant mood stabilisers there was only a small decline in the prevalence of prescribing in pregnancy, 1782 out of 495,953 (0.36%) were prescribed in the second trimester and the PR was 0.87 (95% CI 0.82 to 0.93) (see Table 4 and Figure 1). In the case of those prescribed anticonvulsant mood stabilisers who had a record of psychosis or depression the level of prescribing in the second trimester fell dramatically, with 57 out of 53,012 (0.11%) being prescribed an anticonvulsant mood stabiliser in the second trimester. The PR in the second trimester was 0.35 (95% CI 0.25 to 0.47) (see Table 4 and Figure 1).
| Prescribed antipsychotic | 4–6 months before pregnancy | 1–3 months before pregnancy | First trimester | Second trimester | Third trimester | 1–3 months after delivery | 4–6 months after delivery | 7–9 months after delivery | 10–12 months after delivery | 13–15 months after delivery |
|---|---|---|---|---|---|---|---|---|---|---|
| Any antipsychotic | 0.99 (0.91 to 1.08) | 1 | 0.94 (0.86 to 1.03) | 0.53 (0.47 to 0.58) | 0.49 (0.44 to 0.54) | 0.94 (0.86 to 1.02) | 1.15 (1.06 to 1.25) | 1.17 (1.07 to 1.27) | 1.17 (1.08 to 1.28) | 1.19 (1.09 to 1.29) |
| Any typical | 0.96 (0.86 to 1.08) | 1 | 1.00 (0.89 to 1.13) | 0.51 (0.44 to 0.58) | 0.44 (0.38 to 0.51) | 0.90 (0.80 to 1.01) | 1.03 (0.91 to 1.15) | 1.02 (0.91 to 1.15) | 1.02 (0.90 to 1.15) | 1.02 (0.91 to 1.15) |
| Any atypical | 1.01 (0.89 to 1.15) | 1 | 0.88 (0.77 to 1.00) | 0.55 (0.47 to 0.64) | 0.54 (0.47 to 0.63) | 1.00 (0.88 to 1.14) | 1.30 (1.16 to 1.47) | 1.34 (1.18 to 1.51) | 1.35 (1.19 to 1.52) | 1.38 (1.22 to 1.56) |
| Lithium | 1.12 (0.81 to 1.55) | 1 | 0.74 (0.52 to 1.06) | 0.42 (0.27 to 0.64) | 0.48 (0.31 to 0.71) | 0.88 (0.63 to 1.24) | 1.32 (0.97 to 1.79) | 1.53 (1.14 to 2.08) | 1.50 (1.11 to 2.04) | 1.58 (1.17 to 2.14) |
| Any of the three ACMS | 1.01 (0.95 to 1.08) | 1 | 0.97 (0.91 to 1.03) | 0.87 (0.82 to 0.93) | 0.85 (0.80 to 0.91) | 0.96 (0.90 to 1.02) | 1.00 (0.94 to 1.07) | 1.02 (0.96 to 1.09) | 1.03 (0.96 to 1.09) | 1.04 (0.98 to 1.11) |
| Any of the three ACMS limited to women with SMI or recent depression | 0.99 (0.79 to 1.24) | 1 | 0.82 (0.65 to 1.03) | 0.35 (0.25 to 0.47) | 0.33 (0.24 to 0.46) | 0.73 (0.58 to 0.93) | 0.96 (0.77 to 1.21) | 1.05 (0.84 to 1.32) | 1.03 (0.82 to 1.29) | 1.09 (0.87 to 1.37) |
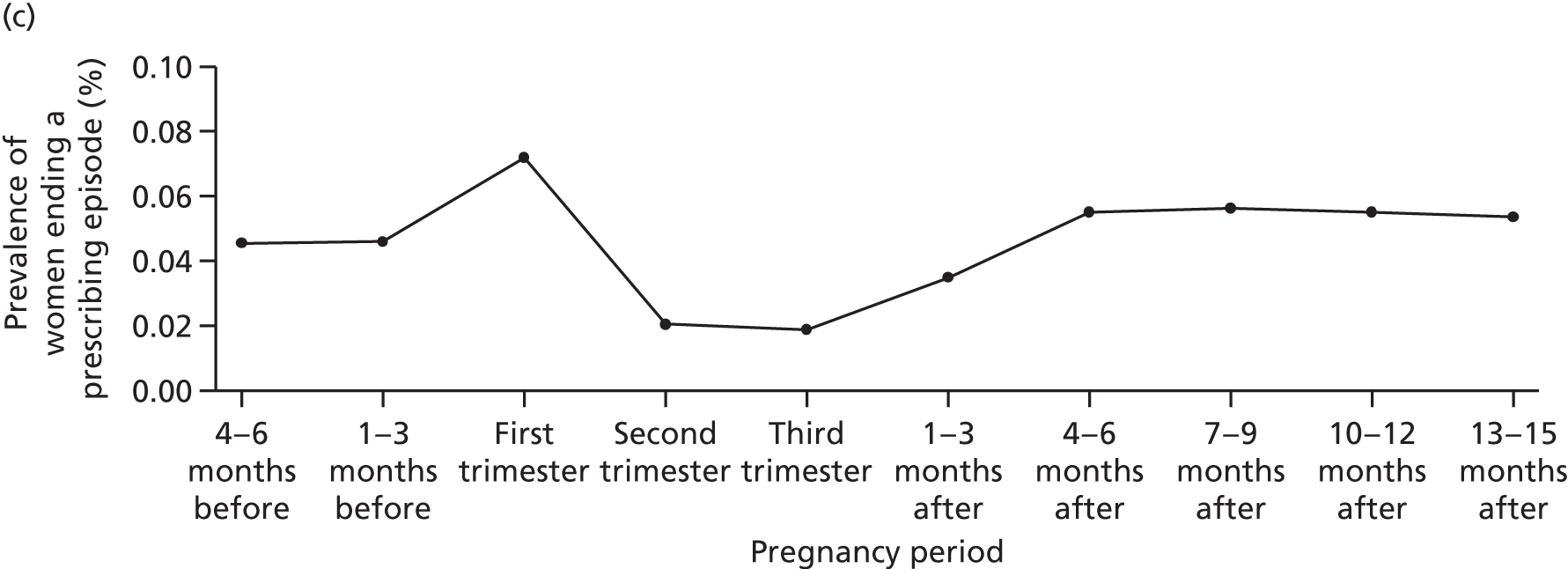
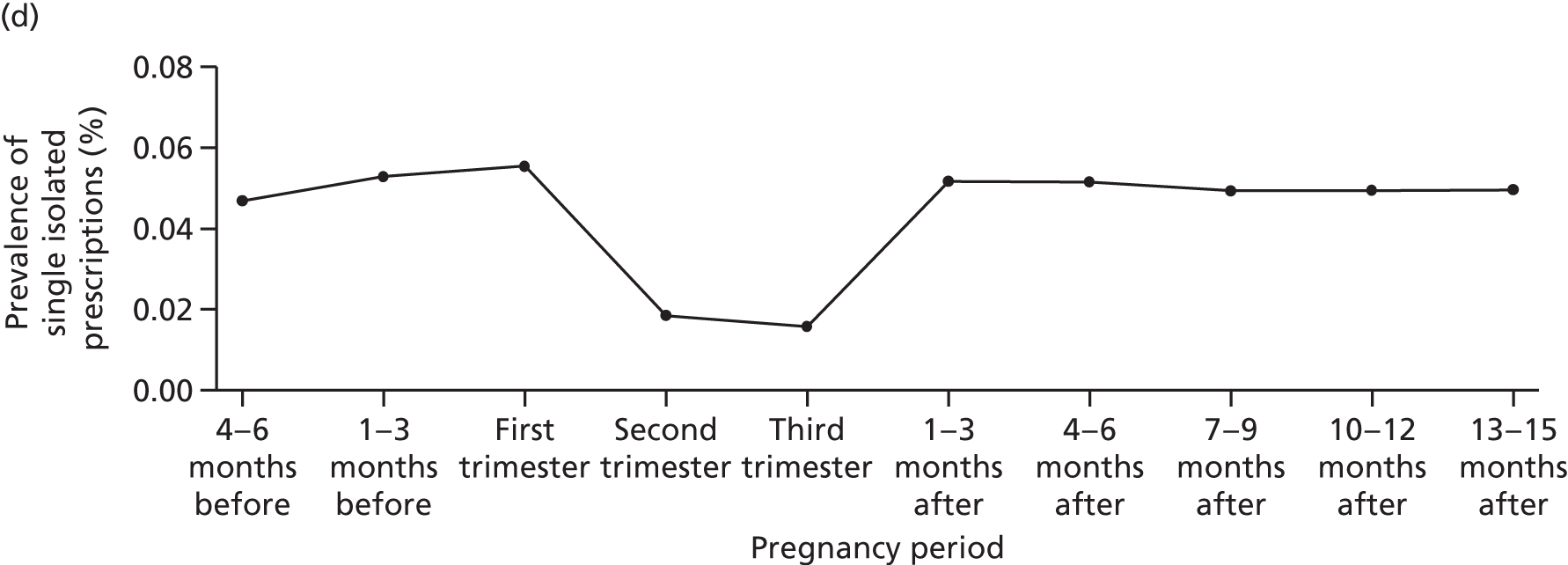
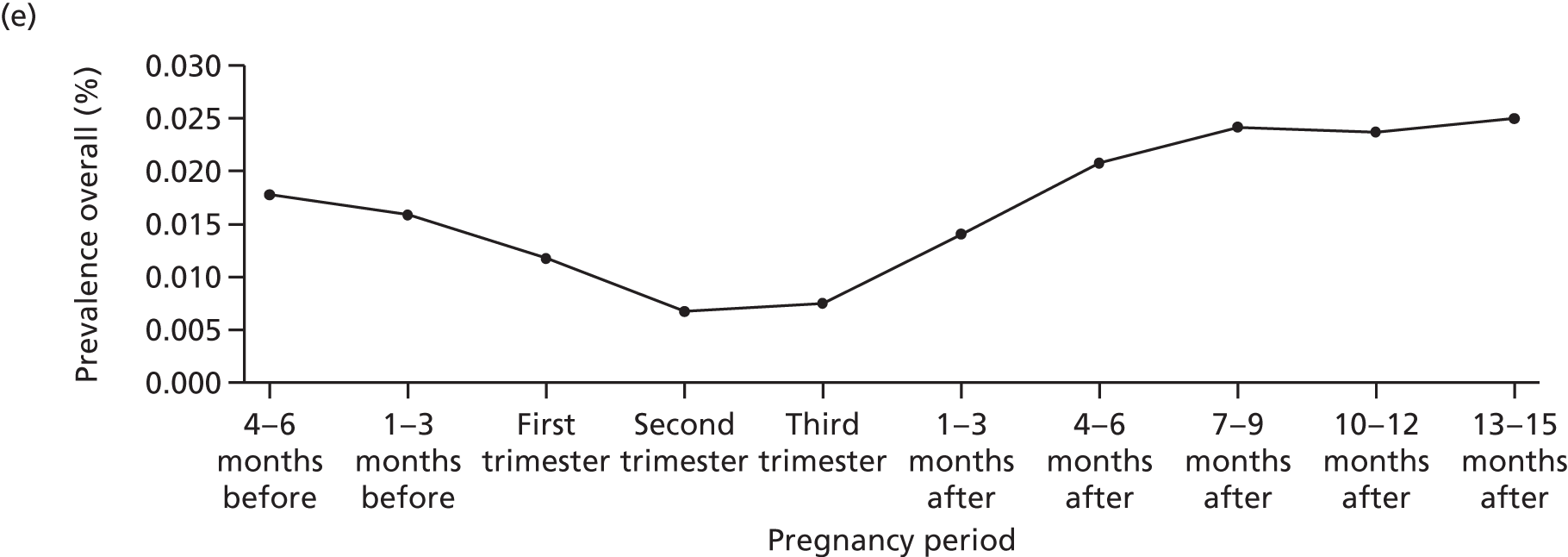
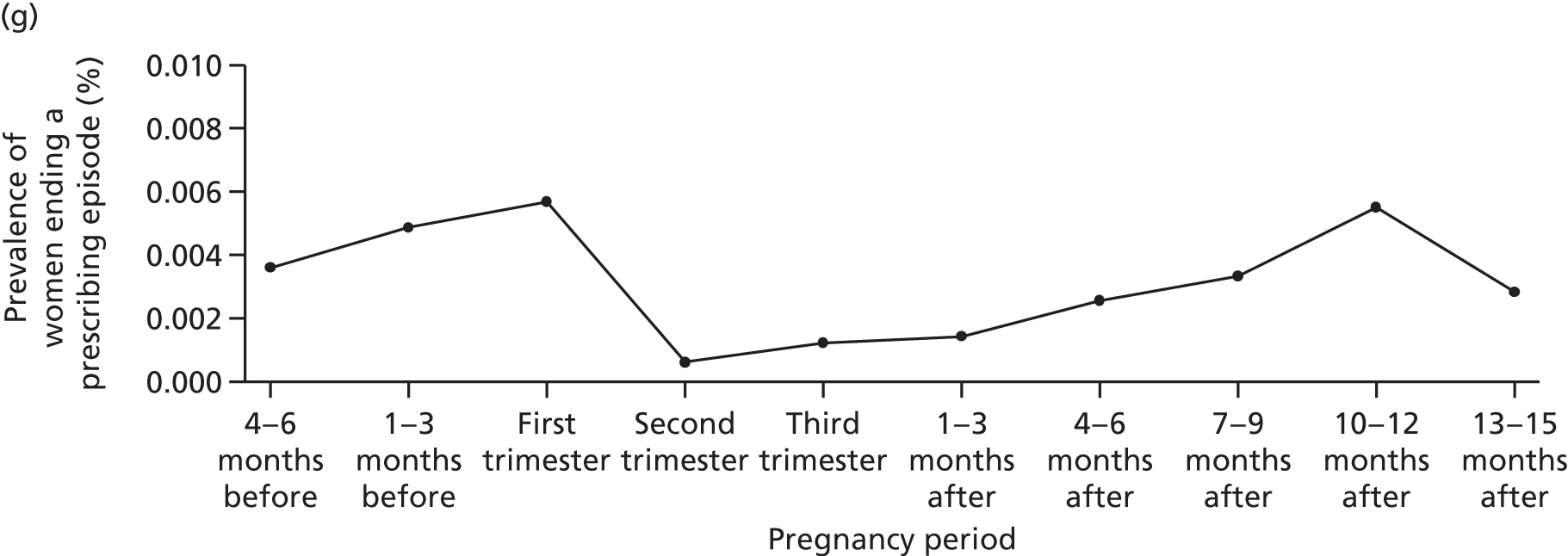
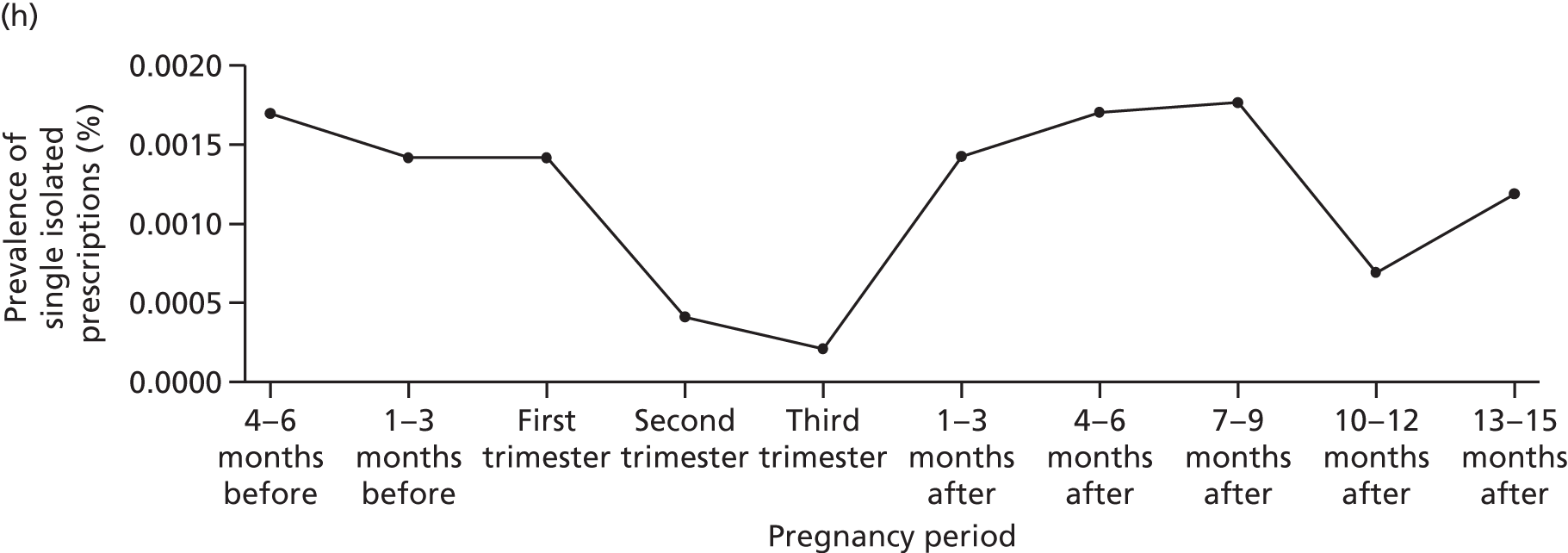
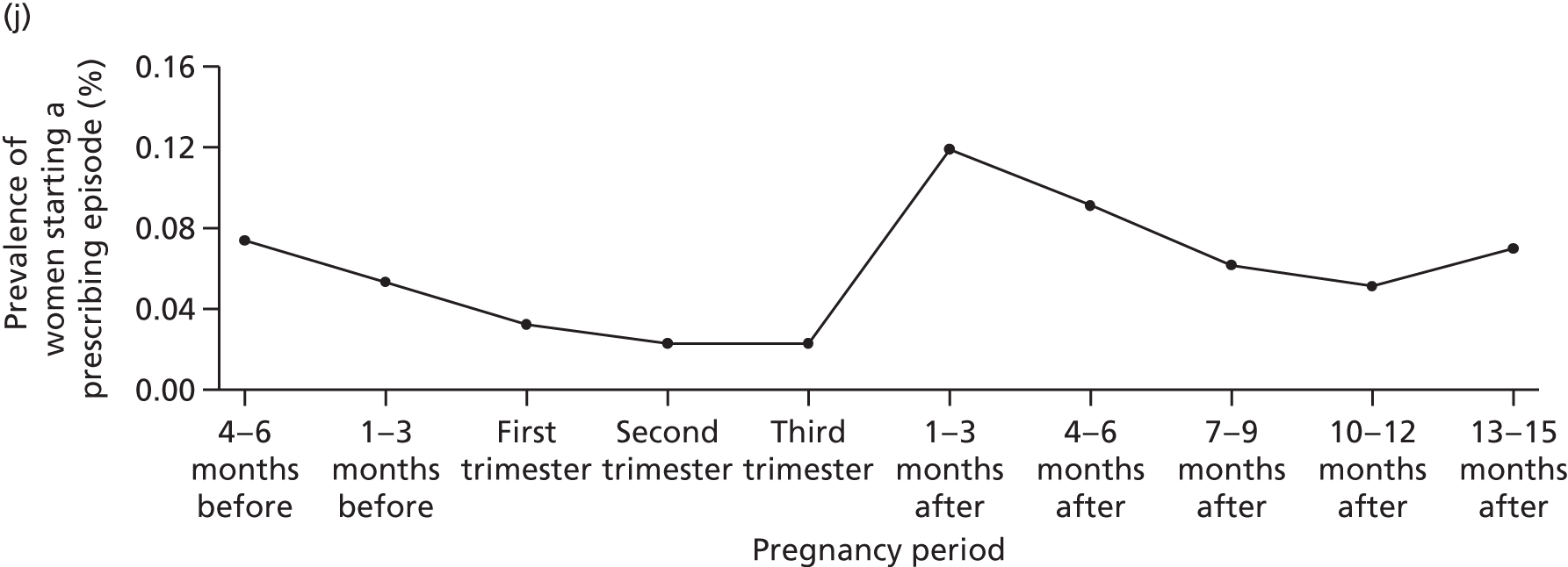
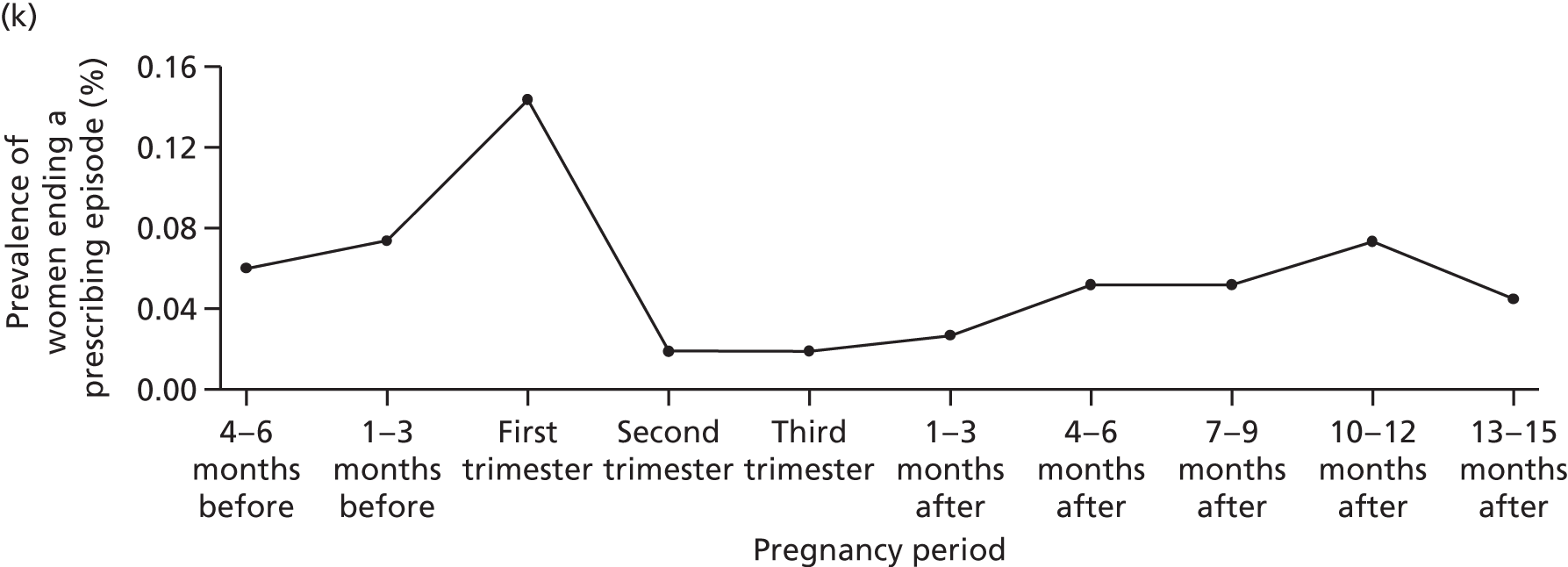
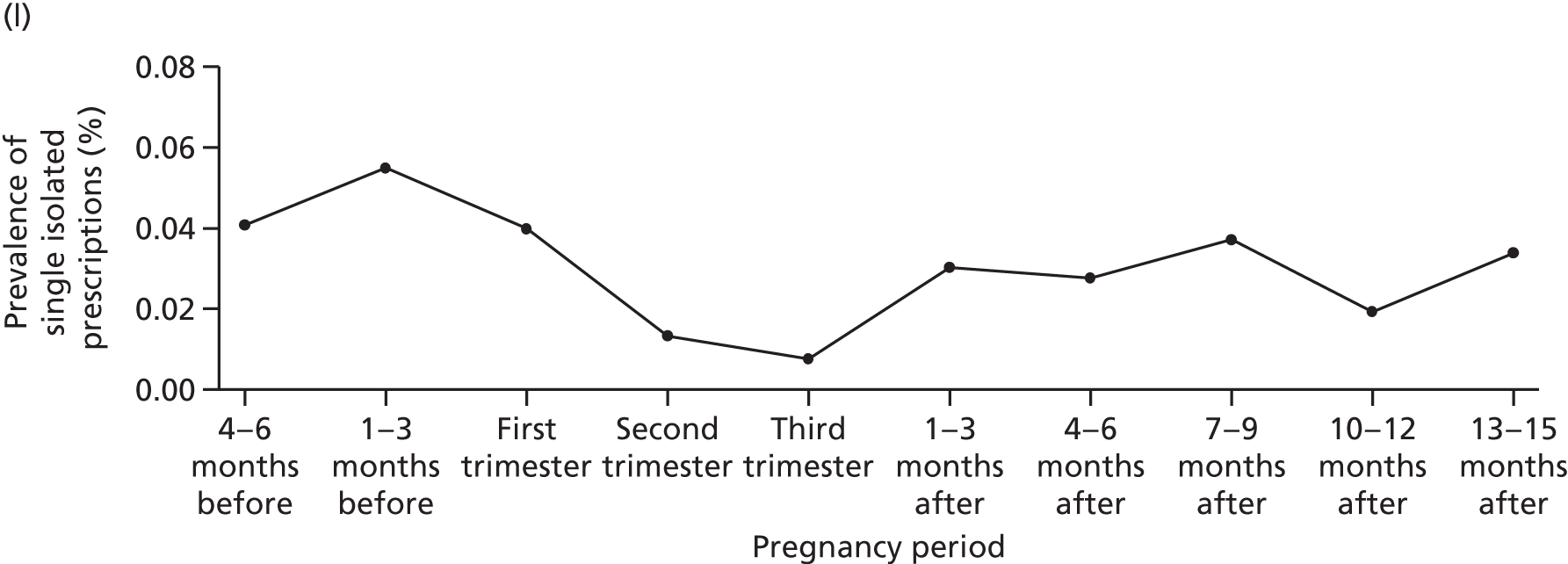
FIGURE 1.
Overall prevalence of antipsychotics (a–d), lithium (e–h) and anticonvulsant mood stabilisers (i–l) (women with a record of psychosis or depression) prescribing in the total pregnancy cohort along with levels of starting and ending a prescribing episode and single prescriptions.



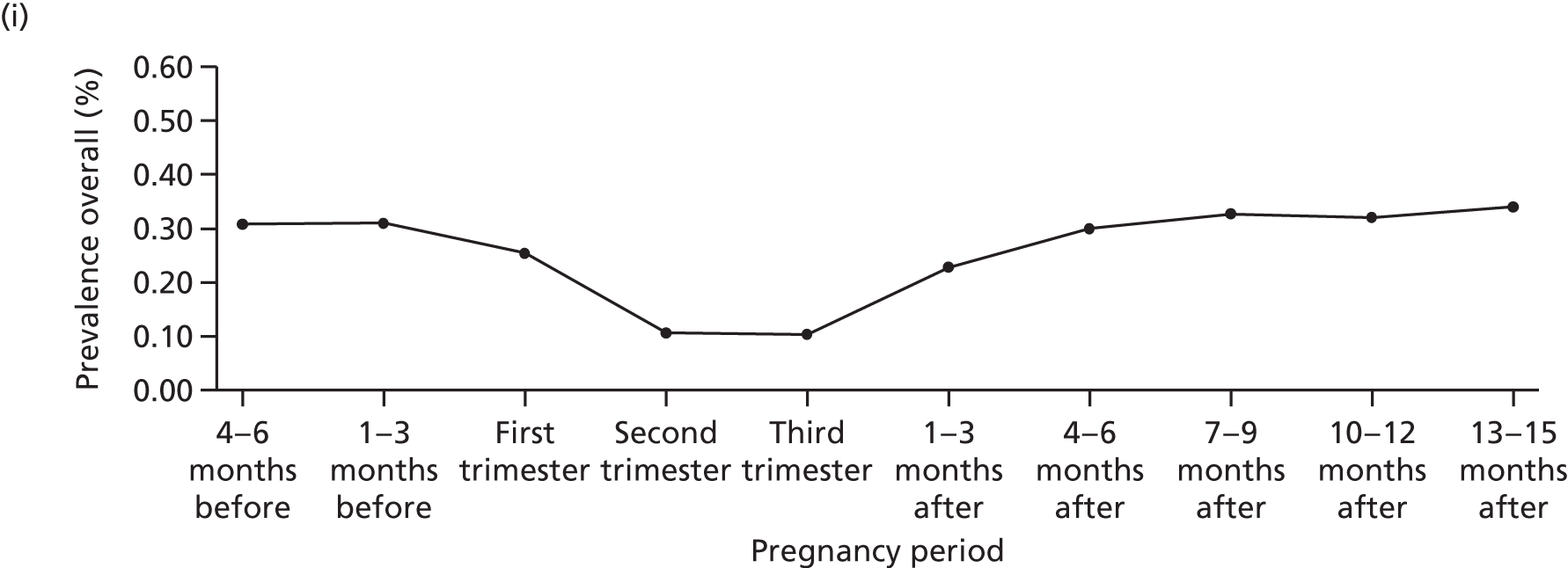
For the period after delivery the prevalence of both antipsychotic and lithium treatment were higher in the period between 4 months and 15 months after delivery than before pregnancy. In the case of anticonvulsant mood stabilisers the prevalence after pregnancy remained similar to that before pregnancy irrespective of whether or not the sample was limited to women with psychoses or depression (see Table 4 and Figure 1). The three most commonly prescribed typical antipsychotics in pregnancy were chlorpromazine, trifluoperazine and flupentixol and for atypical antipsychotics, it was quetiapine, olanzapine, and risperidone (see Table 2). For anticonvulsant mood stabilisers, carbamazepine was primarily prescribed in pregnancy followed by lamotrigine and valproate (see Table 3), but this has changed over time, see Time trends in prevalence of psychotropic medication treatment around and during pregnancy over the calendar period 1995–2012.
Multiple psychotropic medications
Considering the six relevant classes of drugs [antipsychotics (BNF chapters 4.2.1 and 4.2.2); lithium and anticonvulsants (BNF chapter 4.8.1); antidepressants (BNF chapter 4.3); anxiolytics (BNF chapter 4.1.2) and hypnotics (BNF chapter 4.1.1)], in about 6% (28,305/495,953) of all pregnancies, the women received one class of psychotropic medication in the 4–6 months before they became pregnant, whereas < 1% received prescriptions from two to five classes (Table 5). The most typical combinations were antidepressants and hypnotics [1256 (0.25%)] and antidepressants and anxiolytics [906 (0.18%)]. Antipsychotics and antidepressants were prescribed in combination to 387 individuals, equivalent to 0.08% of the full pregnancy cohort, but to 38% (387/999) of the women prescribed antipsychotics 4–6 months before pregnancy. Anticonvulsant and antidepressants were prescribed to 317 (0.06%) of the full pregnancy cohort (Table 6), but to 16% (317/1991) of those who received anticonvulsant mood stabilisers 4–6 months before pregnancy.
| Number of drug categories | Frequency | Per centa |
|---|---|---|
| 0 | 463,950 | 93.55 |
| 1 | 28,305 | 5.71 |
| 2 | 3156 | 0.64 |
| 3 | 456 | 0.09 |
| 4 | 73 | 0.01 |
| 5 | 13 | < 0.01 |
| Combination | Frequency | Per centa |
|---|---|---|
| Antidepressant and hypnotic | 1256 | 0.25 |
| Antidepressant and anxiolytic | 906 | 0.18 |
| Antipsychotic and antidepressant | 387 | 0.08 |
| Anticonvulsant and antidepressant | 317 | 0.06 |
| Antidepressant, anxiolytic and hypnotic | 187 | 0.04 |
| Anxiolytic and hypnotic | 122 | 0.02 |
| Antipsychotic, antidepressant and hypnotic | 80 | 0.02 |
| Antipsychotic, antidepressant and anxiolytic | 53 | 0.01 |
| Anticonvulsant and anxiolytic | 40 | 0.01 |
| Anticonvulsant, antidepressant and anxiolytic | 40 | 0.01 |
| Antipsychotic, antidepressant, anxiolytic and hypnotic | 35 | 0.01 |
| Antipsychotic, anticonvulsant and antidepressant | 34 | 0.01 |
Initiation of psychotropic treatment, termination of psychotropic treatment and isolated psychotropic prescriptions
Although very few women were prescribed a new episode of antipsychotics, lithium or anticonvulsant mood stabilisers immediately before and during pregnancy (see Figure 1), there was a sharp rise in the proportion of women initiating new episodes in the first 6 months after delivery (see Figure 1). In contrast, a large number of women terminated treatments before and during pregnancy. Thus, the highest proportion of women terminating treatments were found in the 1–3 months before pregnancy and during the first pregnancy trimester (see Figure 1).
In general there were few women who received a single isolated prescription of psychotropic medication and there were even fewer women who received such during the second and third pregnancy trimester (see Figure 1).
Patterns of recording that indicate worsening of mental health: 18 months before pregnancy, during the course of pregnancy and up to 15 months after delivery
Overall, 495,953 pregnancies were included in the study from 1 January 1995 to 31 December 2012.
Below, we describe the annual prevalence of each of the three sets of outcomes: (1) suicide attempts, overdose or deliberate self-harm; (2) mental health hospital admission or examination in relation to the Mental Health Act;45 and (3) psychosis, mania or hypomania before, during and after delivery over the calendar period 1995–2012.
In general, relatively few women had any entries in their records that suggested deterioration or change of severity of mental illnesses in the period before and during pregnancy as well as after delivery (see Figure 2). The recording of suicide attempts, overdose or deliberate self-harm was relatively constant in the 18 months prior to pregnancy (Figure 2 and Table 7). During pregnancy the prevalence declined and relative to the period of 1–3 months before pregnancy the PR was 0.11 (95% CI 0.08 to 0.14) in the third trimester. It rose after pregnancy, but was still only half of what it was prior to pregnancy (see Table 7). The entries made of mental health hospital admissions or invoking of the Mental Health Act45 more than tripled just after delivery in comparison to the period of 1–3 months before pregnancy (PR 3.16, 95% CI 1.86 to 5.60) (see Table 7). Records of psychosis, mania or hypomania followed similar patterns with a doubling just after delivery in comparison to the 1–3 months before pregnancy (PR 2.02, 95% CI 1.53 to 2.69) (see Table 7).
FIGURE 2.
Prevalence recording of (a) suicide attempts, overdose or self-harm; (b) mental health hospital admission; and (c) psychosis, mania or hypomania, from 18 months before the start of pregnancy up to 15 months after delivery.



| Prescribed antipsychotic | 4–6 months before pregnancy | 1–3 months before pregnancy | First trimester | Second trimester | Third trimester | 1–3 months after delivery | 4–6 months after delivery | 7–9 months after delivery | 10–12 months after delivery | 13–15 months after delivery |
|---|---|---|---|---|---|---|---|---|---|---|
| Suicide attempt, overdose or deliberate self-harm | 1.03 (0.92 to 1.15) | 1 | 0.50 (0.44 to 0.57) | 0.19 (0.15 to 0.23) | 0.11 (0.08 to 0.14) | 0.31 (0.26 to 0.36) | 0.43 (0.37 to 0.50) | 0.48 (0.42 to 0.55) | 0.50 (0.43 to 0.57) | 0.55 (0.48 to 0.63) |
| Hospital admissions or MHA examination | 1.53 (0.83 to 2.91) | 1 | 1.26 (0.66 to 2.44) | 0.79 (0.37 to 1.64) | 0.58 (0.25 to 1.28) | 3.16 (1.86 to 5.60) | 1.98 (1.11 to 3.66) | 1.26 (0.65 to 2.46) | 1.60 (0.86 to 3.05) | 1.79 (0.97 to 3.37) |
| Psychosis, mania or hypomania | 1.05 (0.76 to 1.46) | 1 | 0.86 (0.61 to 1.21) | 0.54 (0.36 to 0.79) | 0.53 (0.35 to 0.78) | 2.02 (1.53 to 2.69) | 1.38 (1.02 to 1.88) | 1.24 (0.90 to 1.70) | 1.13 (0.81 to 1.56) | 0.74 (0.50 to 1.07) |
Time trends in prevalence of psychotropic medication treatment around and during pregnancy over the calendar period 1995–2012
Overall, 495,953 pregnancies were included in the study from 1 January 1995 to 31 December 2012. Below we describe annual prevalence for each of the three classes of psychotropic medication (antipsychotics, lithium and anticonvulsant mood stabilisers) before, during and after delivery over the calendar period 1995–2012. The work on antipsychotics and lithium has been published in part elsewhere. 46,47
Overall, annual prescribing in the 6 months before pregnancy and during pregnancy of both antipsychotics and anticonvulsant mood stabilisers was relatively stable from 1995 to 2006, but increased from around 2007 (Figure 3). By 2011/12, just under 0.4% were prescribed antipsychotics in the 6 months before pregnancy and just under 0.3% received antipsychotic treatment in pregnancy by 2011/12, suggesting a more than 50% increase since 1995/6. For anticonvulsant mood stabilisers the prevalence figures for women with a record of psychoses or depression for 2011/12 were 0.6% before pregnancy, 0.26% during pregnancy and 0.36% after delivery. Hence the treatment prevalence has almost doubled since 1995/6 (see Figure 3).
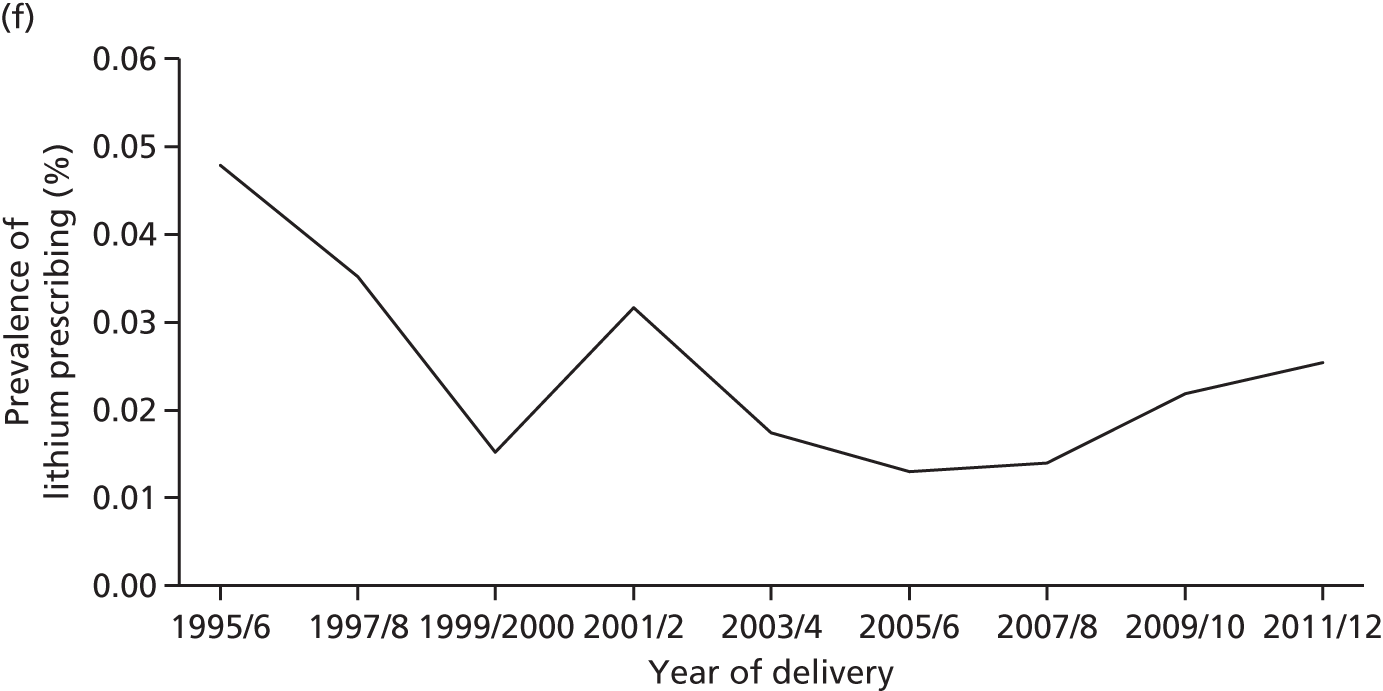
FIGURE 3.
Prevalence of prescribing over calendar period 1995–2012. Prescribing of antipsychotics (a) in the 6 months before pregnancy; (b) during pregnancy; (c) 6 months after delivery; lithium (d) in the 6 months before pregnancy; (e) during pregnancy; (f) 6 months after delivery; anticonvulsant mood stabilisers (g) in the 6 months before pregnancy; (h) during pregnancy; and (i) 6 months after delivery.
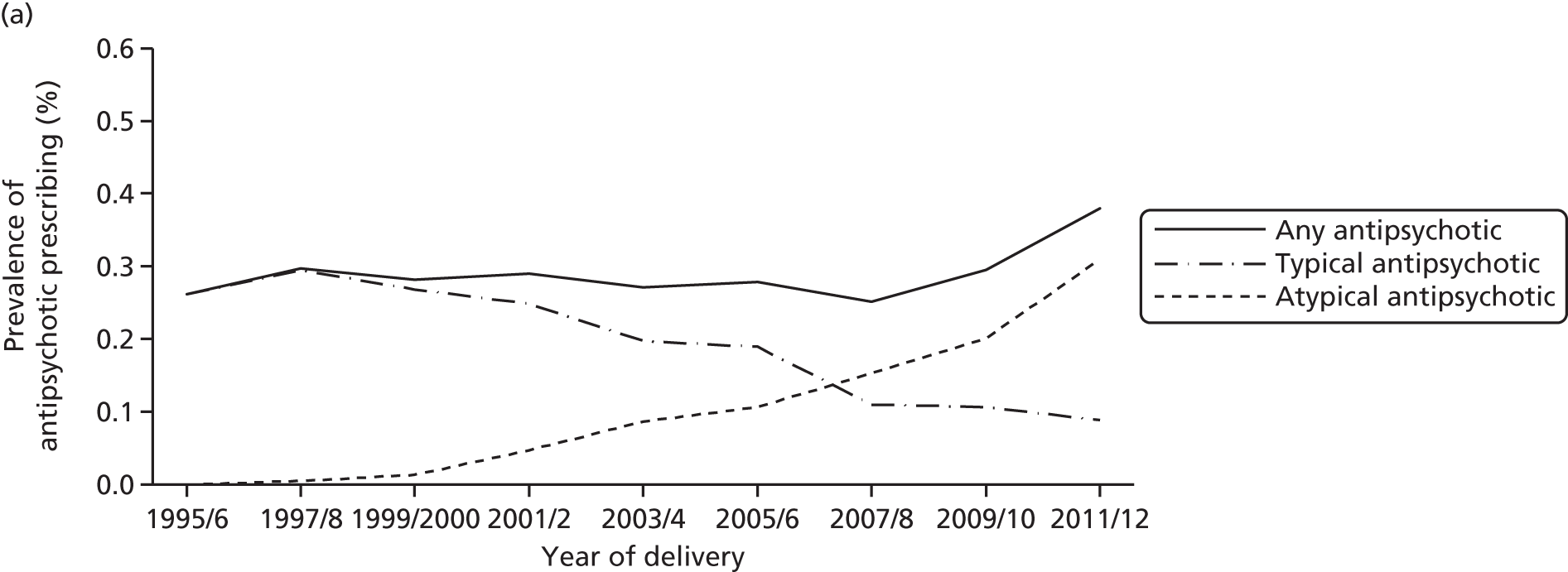




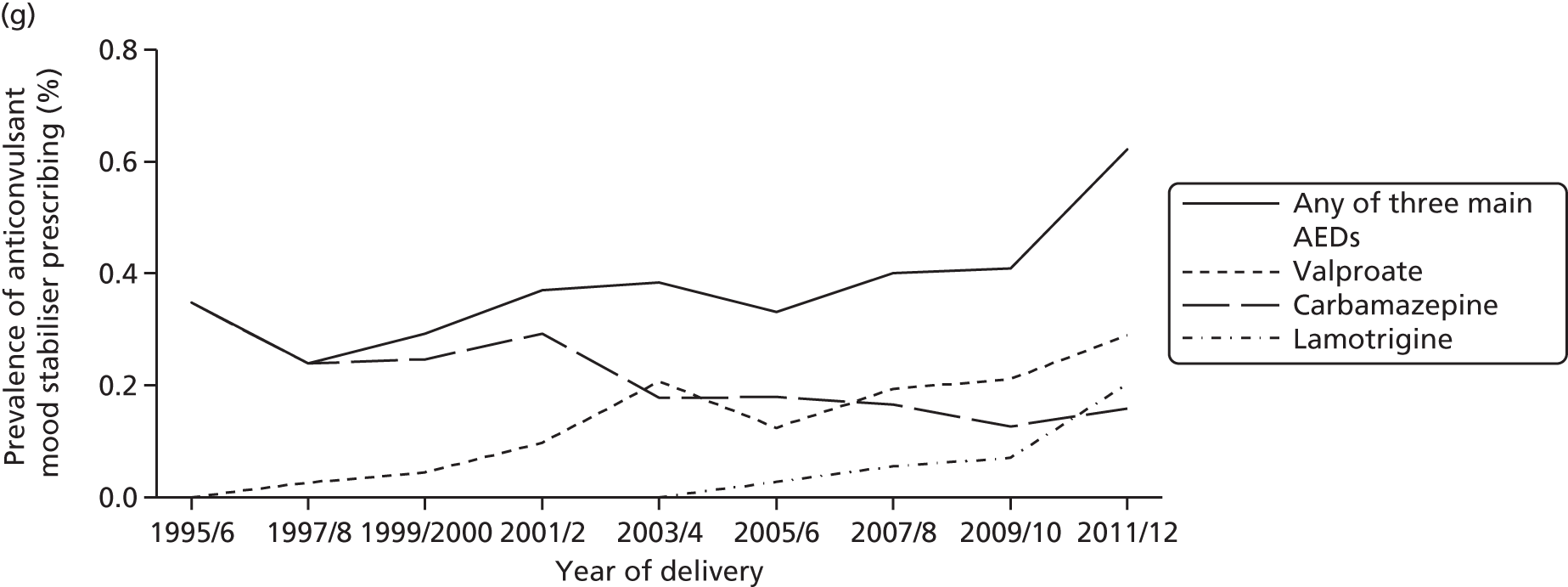

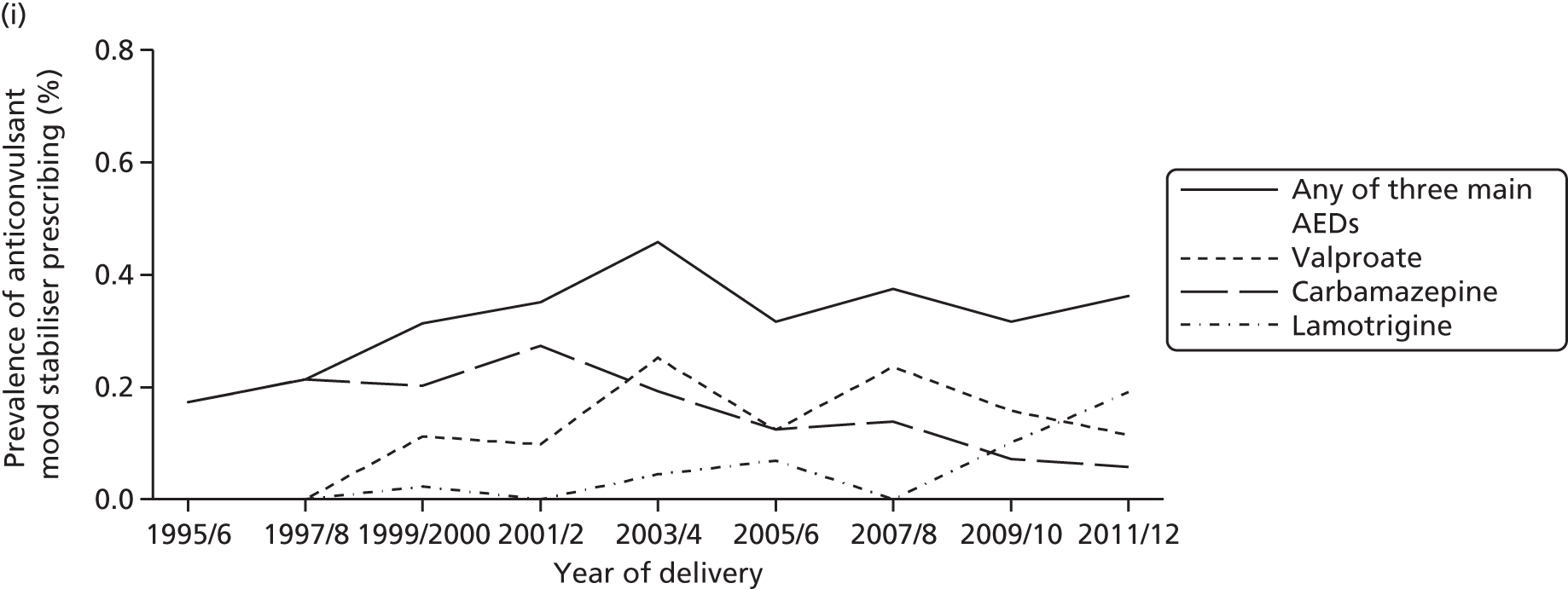
Prescribing of typical antipsychotics has been declining since 1997/8, whereas prescribing of atypical antipsychotics has been increasing. Thus, atypical antipsychotics were more commonly prescribed before pregnancy, during pregnancy and after delivery after 2007/8 (see Figure 3). For anticonvulsant mood stabilisers, prescribing of carbamazepine has declined, whereas both valproate and lamotrigine have gradually increased before pregnancy (see Figure 3). By 2011/12, carbamazepine was superseded by lamotrigine before, during and after pregnancy and valproate was the most commonly prescribed anticonvulsant mood stabiliser before pregnancy (see Figure 3).
Lithium was rarely prescribed; before pregnancy the annual prevalence of lithium prescribing ranged between 0.01% and 0.03%, and during pregnancy between 0.003% and 0.018%. The annual prevalence in the 6 months after delivery declined from 0.048% in 1995/6 to 0.015 in 1999/2000 (see Figure 3).
Discontinuation and factors associated with continuation of psychotropic medication in pregnancy
We identified 207 women receiving typical antipsychotics, 279 receiving atypical antipsychotics, 52 receiving lithium and 93 with a record of psychoses or depression receiving anticonvulsant mood stabilisers in the 4–6 months before the start of their pregnancy.
Although many women discontinued psychotropic medication either before or early in pregnancy the proportion varied between psychotropic treatments. Women prescribed atypical antipsychotics were least likely to discontinue treatment in pregnancy and 150 out of 279 (54%) received further prescriptions after 6 weeks of pregnancy (when the woman is likely to become aware of the pregnancy). In contrast, only 73 out of 207 (35%) women received further prescriptions of typical antipsychotics, 17 out of 52 (33%) lithium and 34 out of 93 (37%) anticonvulsant mood stabilisers after 6 weeks of pregnancy. By the start of the third trimester the figures were 107 out of 279 (38%) for atypical antipsychotics, 39 out of 207 (19%) for typical antipsychotics, 14 out of 52 (27%) for lithium and 13 out of 93 (14%) for anticonvulsant mood stabilisers.
We report below, additional results from studies on discontinuation of psychotropic medication in pregnancy and factors associated with continuation for each of the classes of psychotropic medication (antipsychotics, lithium and anticonvulsant mood stabilisers) Parts of this work have been published elsewhere. 46,47
Discontinuation of antipsychotics
Pregnant and non-pregnant women prescribed atypical antipsychotics discontinued at similar rates up to the start of pregnancy (or index date) (Figure 4). However, pregnant women were more likely to discontinue atypical antipsychotics than non-pregnant women (see Figure 4b).
FIGURE 4.
Discontinuation of antipsychotic drugs in pregnant and non-pregnant women by (a) typical; and (b) atypical antipsychotics.

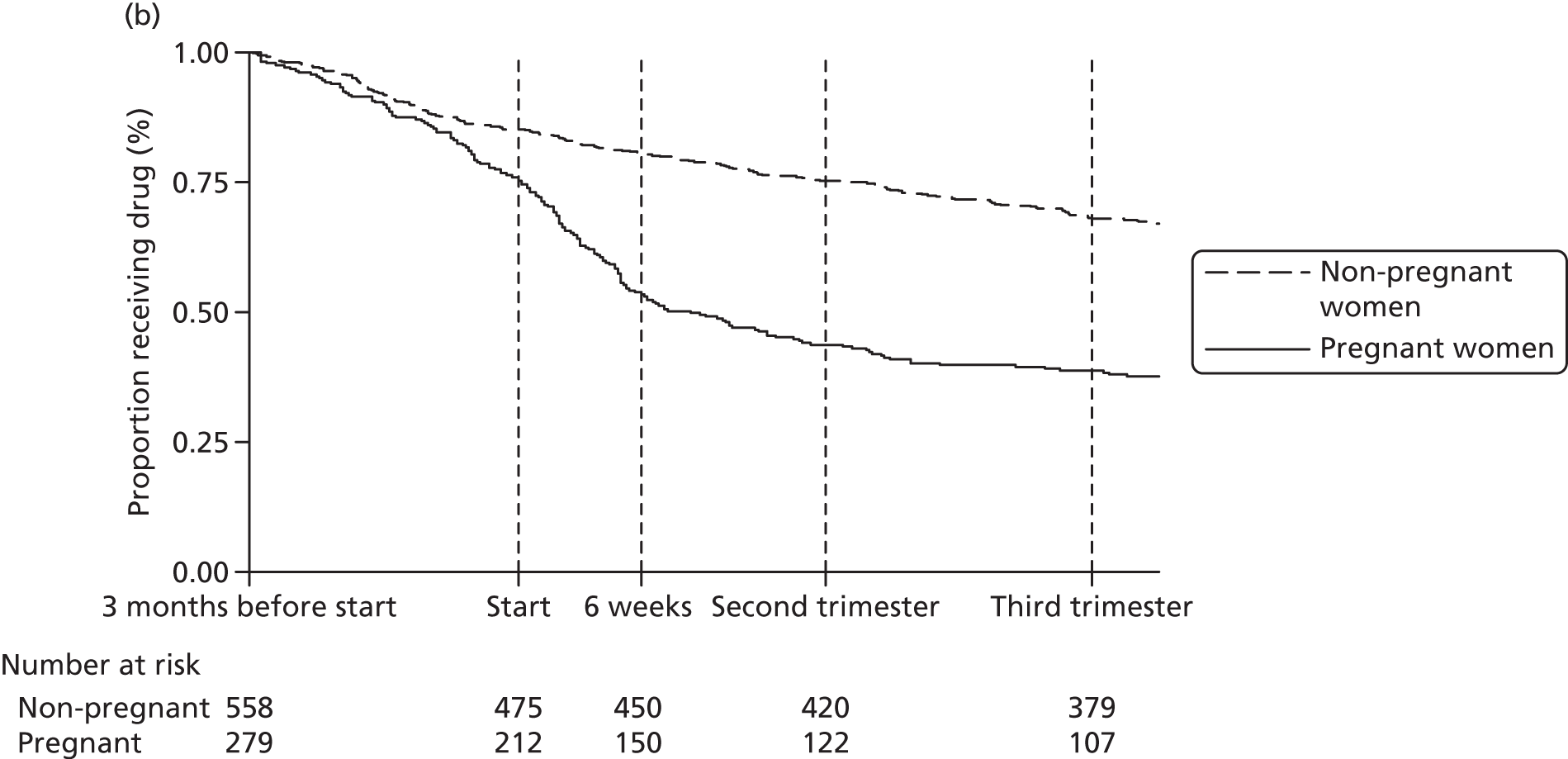
For women on typical antipsychotics there was a substantial difference in the rates of discontinuation between pregnant and non-pregnant women even before the pregnancy (see Figure 4a) and the gap became wider in early pregnancy (see Figure 4a). The comparisons with non-pregnant women, however, suggest that awareness of the pregnancy may not be the only reason for stopping antipsychotics. About 75% of non-pregnant women continued both typical and atypical antipsychotics throughout the follow-up period (see Figure 4).
The rates of discontinuation differed by dose and type of antipsychotics (Figure 5). Among women receiving prescriptions of less than one-quarter of the DDD of typical antipsychotics, only 29 out of 118 (25%) continued prescriptions after 6 weeks. For women on atypical antipsychotics the figure was 24 out of 52 (46%) after 6 weeks (see Figure 5).
FIGURE 5.
Discontinuation of antipsychotic drugs in pregnant women, by dose, in women who were prescribed (a) typical; and (b) atypical antipsychotics.
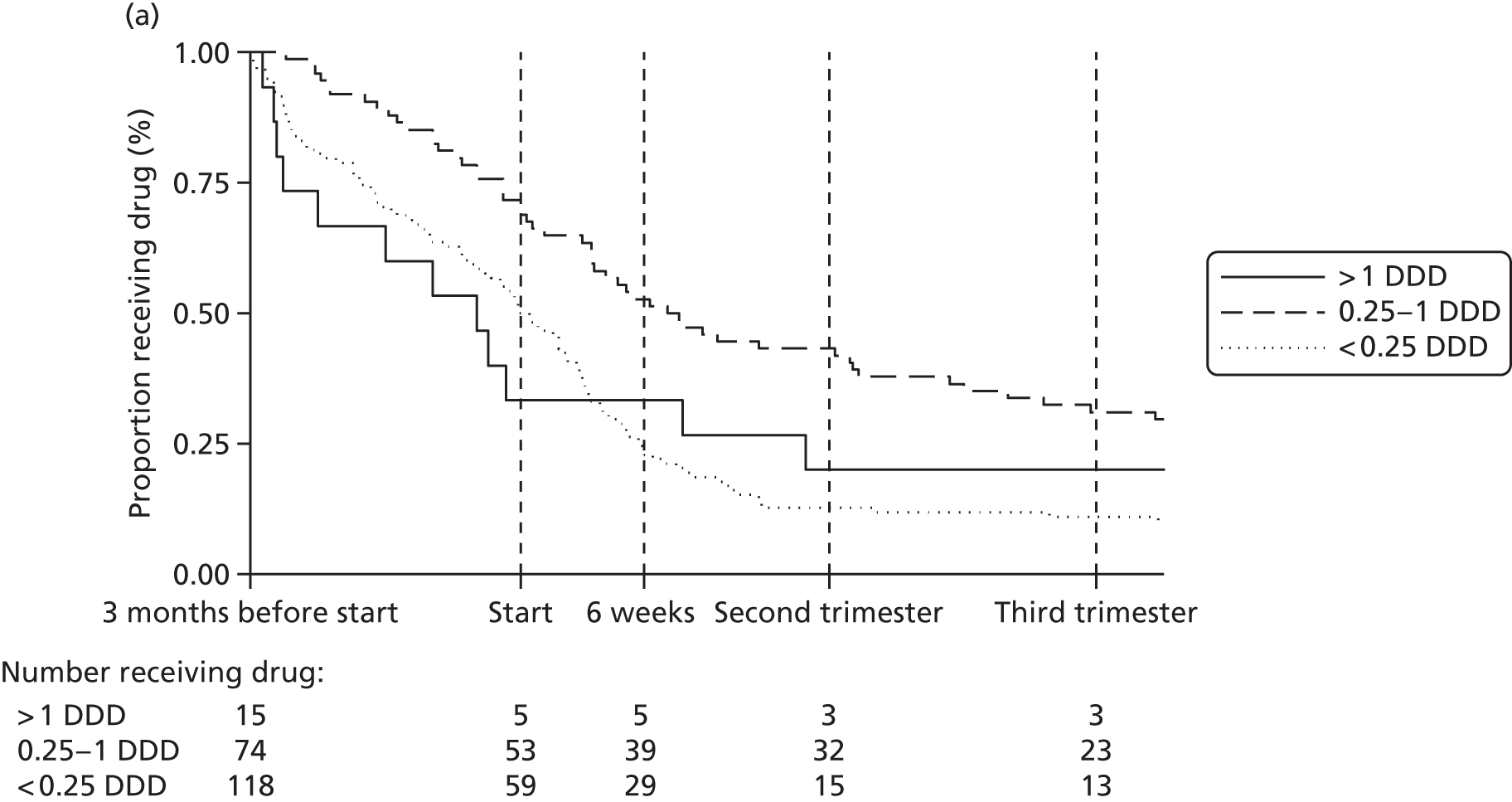
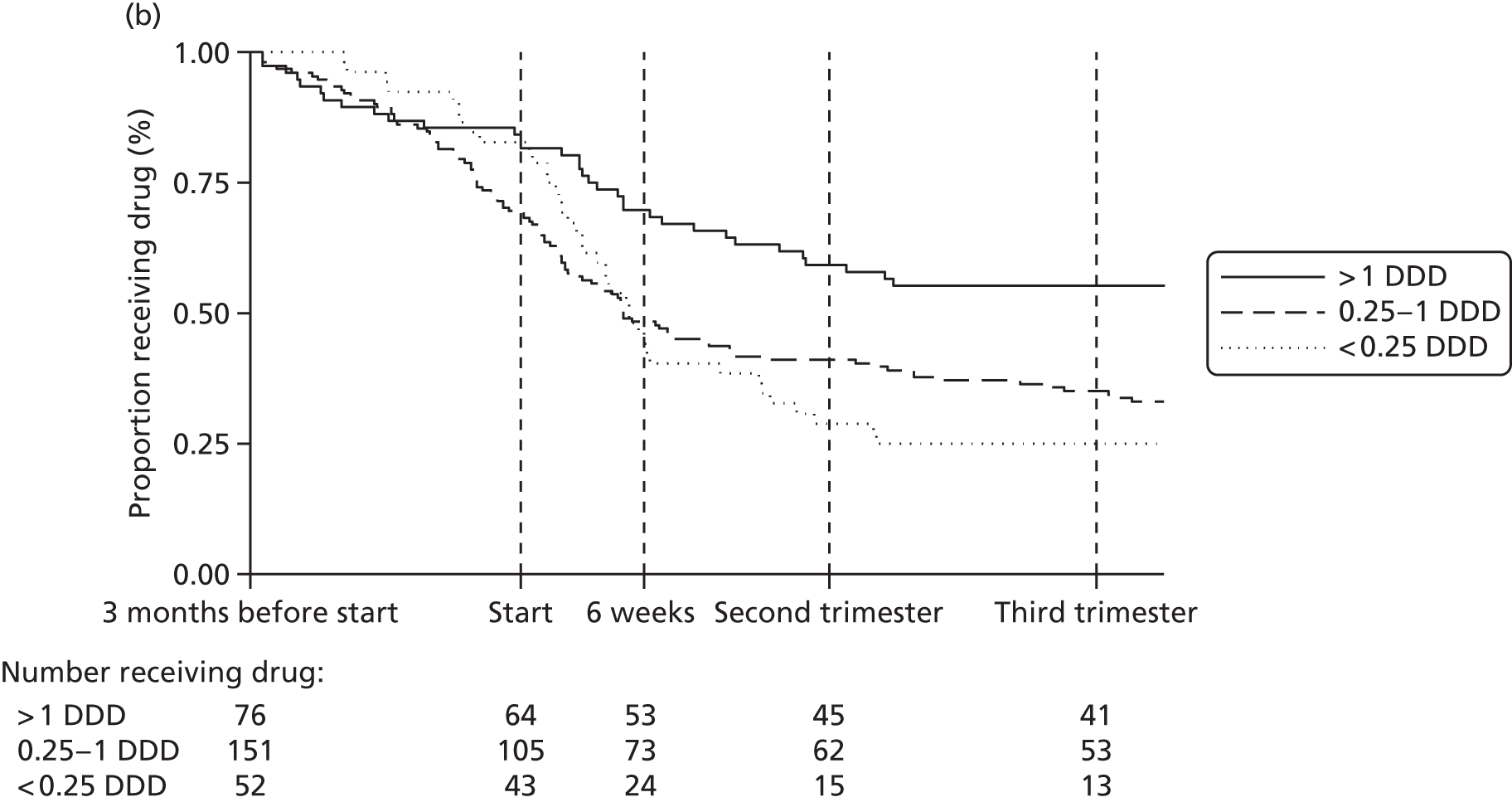
Women on a high dose (DDD > 1) of typical antipsychotics were highly likely to discontinue prescriptions prior to pregnancy in contrast to women on a high dose (DDD > 1) of atypical antipsychotics (see Figure 5). Three out of 15 women on high dose typical antipsychotics were on depots prior to the start of pregnancy.
Factors associated with continuation of antipsychotics
Factors associated with continuation of receiving antipsychotic prescriptions beyond 6 weeks of pregnancy for typical antipsychotics included age and durations of treatment prior to pregnancy (Table 8). Those aged ≥ 35 years were more than three times as likely to continue treatment compared with those < 25 years [risk ratio (RR) 3.09, 95% CI 1.76 to 5.44]. The effect of age attenuated slightly after adjustment for dose. Likewise, those who had received continuous treatment for > 12 months prior to pregnancy were also more likely to continue treatment in pregnancy compared with those who had received < 6 months of continuous treatment prior to pregnancy (RR 3.12, 95% CI 1.97 to 4.95). This was still the case after adjustment for age and dose (RR 2.48, 95% CI 1.54 to 3.99). For atypical antipsychotics, length and dose of prior prescribing were also associated with continuation in pregnancy (Table 9). However, those aged 30–34 years were the most likely to continue prescriptions in pregnancy (see Table 9). For other factors examined (diagnosis of severe mental illnesses, also taking antidepressants and mood stabilisers, social deprivation, estimated parity, obesity, smoking, records of alcohol problems, illicit drug use and ethnicity) none of the adjusted effect sizes was larger than 1.67 or lower than 0.64 (see Tables 8 and 9).
| Factors | Typical antipsychotics (N = 207) | ||||||
|---|---|---|---|---|---|---|---|
| n | Unadjusted | Adjusted | |||||
| RR | 95% CI | p-value | RR | 95% CI | p-value | ||
| Average daily dose (in units of DDD) | < 0.001 | 0.011 | |||||
| < 0.25 DDD | 118 | 1 | 1 | ||||
| 0.25–1 DDD | 74 | 2.14 | 1.46 to 3.15 | 1.78 | 1.22 to 2.60 | ||
| > 1 DDD | 15 | 1.36 | 0.62 to 2.97 | 1.25 | 0.58 to 2.68 | ||
| Age band | < 0.001 | < 0.001 | |||||
| < 25 years | 53 | 1 | 1 | ||||
| 25–29 years | 42 | 1.49 | 0.74 to 2.99 | 1.34 | 0.68 to 2.62 | ||
| 30–34 years | 59 | 1.22 | 0.62 to 2.43 | 1.15 | 0.58 to 2.29 | ||
| ≥ 35 years | 53 | 3.09 | 1.76 to 5.44 | 2.60 | 1.47 to 4.59 | ||
| Continuous prior time on antipsychotics | < 0.001 | 0.001 | |||||
| < 6 months | 98 | 1 | 1 | ||||
| 6–12 months | 34 | 1.92 | 1.03 to 3.57 | 1.78 | 0.97 to 3.26 | ||
| > 12 months | 75 | 3.12 | 1.97 to 4.95 | 2.48 | 1.54 to 3.99 | ||
| SMI diagnosis code | 0.018 | 0.404 | |||||
| No | 160 | 1 | 1 | ||||
| SMI diagnosis code | 47 | 1.57 | 1.08 to 2.27 | 1.17 | 0.81 to 1.71 | ||
| Also taking an antidepressant | 0.238 | 0.566 | |||||
| No | 66 | 1 | 1 | ||||
| Taking an antidepressant | 141 | 0.80 | 0.55 to 1.16 | 0.90 | 0.64 to 1.28 | ||
| Also taking a mood stabiliser | 0.033 | 0.281 | |||||
| No | 191 | 1 | 1 | ||||
| Taking a mood stabiliser | 16 | 1.68 | 1.04 to 2.71 | 1.31 | 0.80 to 2.12 | ||
| Townsend quintile | 0.562 | 0.440 | |||||
| 1 | 16 | 1 | 1 | ||||
| 2 | 22 | 0.85 | 0.35 to 2.05 | 0.72 | 0.32 to 1.61 | ||
| 3 | 36 | 0.67 | 0.28 to 1.56 | 0.64 | 0.29 to 1.43 | ||
| 4 | 61 | 1.14 | 0.57 to 2.28 | 1.07 | 0.57 to 1.99 | ||
| 5 | 68 | 0.98 | 0.48 to 1.99 | 0.89 | 0.47 to 1.68 | ||
| Unrecorded | 4 | ||||||
| Estimated parity | 0.103 | 0.159 | |||||
| 0 | 84 | 1 | 1 | ||||
| 1 | 57 | 1.47 | 0.91 to 2.40 | 1.34 | 0.87 to 2.08 | ||
| 2 | 44 | 1.82 | 1.13 to 2.93 | 1.65 | 1.06 to 2.57 | ||
| 3 or more | 22 | 1.39 | 0.72 to 2.69 | 1.52 | 0.80 to 2.90 | ||
| Obesity status | 0.771 | 0.759 | |||||
| Not obese | 186 | 1 | 1 | ||||
| Obese | 21 | 1.09 | 0.61 to 1.95 | 1.09 | 0.63 to 1.90 | ||
| Smoking status | 0.912 | 0.602 | |||||
| Non-smoker | 106 | 1 | 1 | ||||
| Smoker | 101 | 1.02 | 0.71 to 1.48 | 1.09 | 0.78 to 1.53 | ||
| Alcohol problems | 0.154 | 0.094 | |||||
| No | 191 | 1 | 1 | ||||
| Yes | 16 | 1.47 | 0.87 to 2.50 | 1.59 | 0.92 to 2.75 | ||
| Illicit drug use | 0.941 | 0.866 | |||||
| No | 181 | 1 | 1 | ||||
| Yes | 26 | 0.98 | 0.56 to 1.72 | 1.05 | 0.60 to 1.84 | ||
| Ethnicity | |||||||
| Other | 204 | 1 | 1 | ||||
| Black or minority ethnic | 3 | Could not be estimated – all three continue receiving prescriptions | |||||
| Factors | Atypical antipsychotics (N = 279) | ||||||
|---|---|---|---|---|---|---|---|
| n | Unadjusted | Adjusted | |||||
| RR | 95% CI | p-value | RR | 95% CI | p-value | ||
| Average daily dose (in units of DDD) | 0.002 | 0.003 | |||||
| < 0.25 DDD | 52 | 1 | 1 | ||||
| 0.25–1 DDD | 151 | 1.05 | 0.75 to 1.47 | 1.04 | 0.74 to 1.47 | ||
| > 1 DDD | 76 | 1.51 | 1.09 to 2.10 | 1.48 | 1.06 to 2.07 | ||
| Age band | 0.147 | 0.201 | |||||
| < 25 years | 53 | 1 | 1 | ||||
| 25–29 years | 74 | 1.24 | 0.84 to 1.83 | 1.23 | 0.84 to 1.80 | ||
| 30–34 years | 82 | 1.50 | 1.04 to 2.15 | 1.45 | 1.02 to 2.08 | ||
| ≥ 35 years | 70 | 1.34 | 0.92 to 1.97 | 1.31 | 0.90 to 1.92 | ||
| Continuous prior time on antipsychotics | < 0.001 | 0.001 | |||||
| < 6 months | 100 | 1 | 1 | ||||
| 6–12 months | 53 | 1.34 | 0.93 to 1.93 | 1.34 | 0.93 to 1.94 | ||
| > 12 months | 126 | 1.78 | 1.34 to 2.35 | 1.67 | 1.27 to 2.21 | ||
| SMI diagnosis code | 0.005 | 0.073 | |||||
| No | 136 | 1 | 1 | ||||
| SMI diagnosis code | 143 | 1.39 | 1.11 to 1.74 | 1.25 | 0.98 to 1.59 | ||
| Also taking an antidepressant | 0.097 | 0.402 | |||||
| No | 96 | 1 | 1 | ||||
| Taking an antidepressant | 183 | 0.83 | 0.67 to 1.03 | 0.91 | 0.73 to 1.13 | ||
| Also taking a mood stabiliser | 0.098 | 0.574 | |||||
| No | 232 | 1 | 1 | ||||
| Taking a mood stabiliser | 47 | 1.23 | 0.96 to 1.58 | 1.08 | 0.83 to 1.40 | ||
| Townsend quintile | 0.880 | 0.805 | |||||
| 1 | 26 | 1 | 1 | ||||
| 2 | 32 | 1.10 | 0.70 to 1.74 | 1.07 | 0.68 to 1.67 | ||
| 3 | 52 | 0.93 | 0.59 to 1.45 | 0.87 | 0.56 to 1.35 | ||
| 4 | 72 | 0.93 | 0.61 to 1.42 | 0.87 | 0.57 to 1.33 | ||
| 5 | 85 | 1.03 | 0.69 to 1.54 | 0.94 | 0.63 to 1.41 | ||
| Unrecorded | 12 | ||||||
| Estimated parity | 0.474 | 0.511 | |||||
| 0 | 110 | 1 | 1 | ||||
| 1 | 89 | 0.89 | 0.70 to 1.15 | 0.92 | 0.72 to 1.18 | ||
| 2 | 49 | 0.79 | 0.57 to 1.11 | 0.82 | 0.58 to 1.14 | ||
| 3 or more | 31 | 0.82 | 0.55 to 1.22 | 0.80 | 0.54 to 1.18 | ||
| Obesity status | 0.055 | 0.119 | |||||
| Not obese | 223 | 1 | 1 | ||||
| Obese | 56 | 1.26 | 1.00 to 1.59 | 1.21 | 0.95 to 1.53 | ||
| Smoking status | 0.875 | 0.935 | |||||
| Non-smoker | 142 | 1 | 1 | ||||
| Smoker | 137 | 0.98 | 0.79 to 1.22 | 0.99 | 0.80 to 1.23 | ||
| Alcohol problems | 0.595 | 0.385 | |||||
| No | 264 | 1 | 1 | ||||
| Yes | 15 | 1.12 | 0.73 to 1.73 | 1.22 | 0.78 to 1.90 | ||
| Illicit drug use | 0.370 | 0.340 | |||||
| No | 246 | 1 | 1 | ||||
| Yes | 33 | 1.15 | 0.85 to 1.55 | 1.16 | 0.85 to 1.58 | ||
| Ethnicity | 0.087 | 0.214 | |||||
| Other | 249 | 1 | 1 | ||||
| Black or minority ethnic | 30 | 1.28 | 0.97 to 1.69 | 1.20 | 0.90 to 1.59 | ||
Switch between typical and atypical antipsychotic treatment
In general, few women switched between typical and atypical antipsychotic treatment just before or in pregnancy. Only 5 out of 207 (2.4%) women switched from typical to atypical antipsychotics and 9 out of 279 (3.2%) switched from atypical to typical antipsychotics. However, among the more frequently used antipsychotics, switching levels were high for two drugs: 12 out of 50 women (24.0%) switched from risperidone to another antipsychotic, while 9 out of 48 (18.8%) switched from trifluoperazine to another antipsychotic.
Discontinuation of lithium
For lithium, there was a substantial difference in the rates of discontinuation between pregnant and non-pregnant women (Figure 6). Only 14 out of 52 (27%) continued lithium treatment after the start of the third trimester. Of the non-pregnant women, 80 out of 104 (77%) continued lithium treatment beyond this period (see Figure 6).
FIGURE 6.
Discontinuation of lithium in pregnant and non-pregnant women.
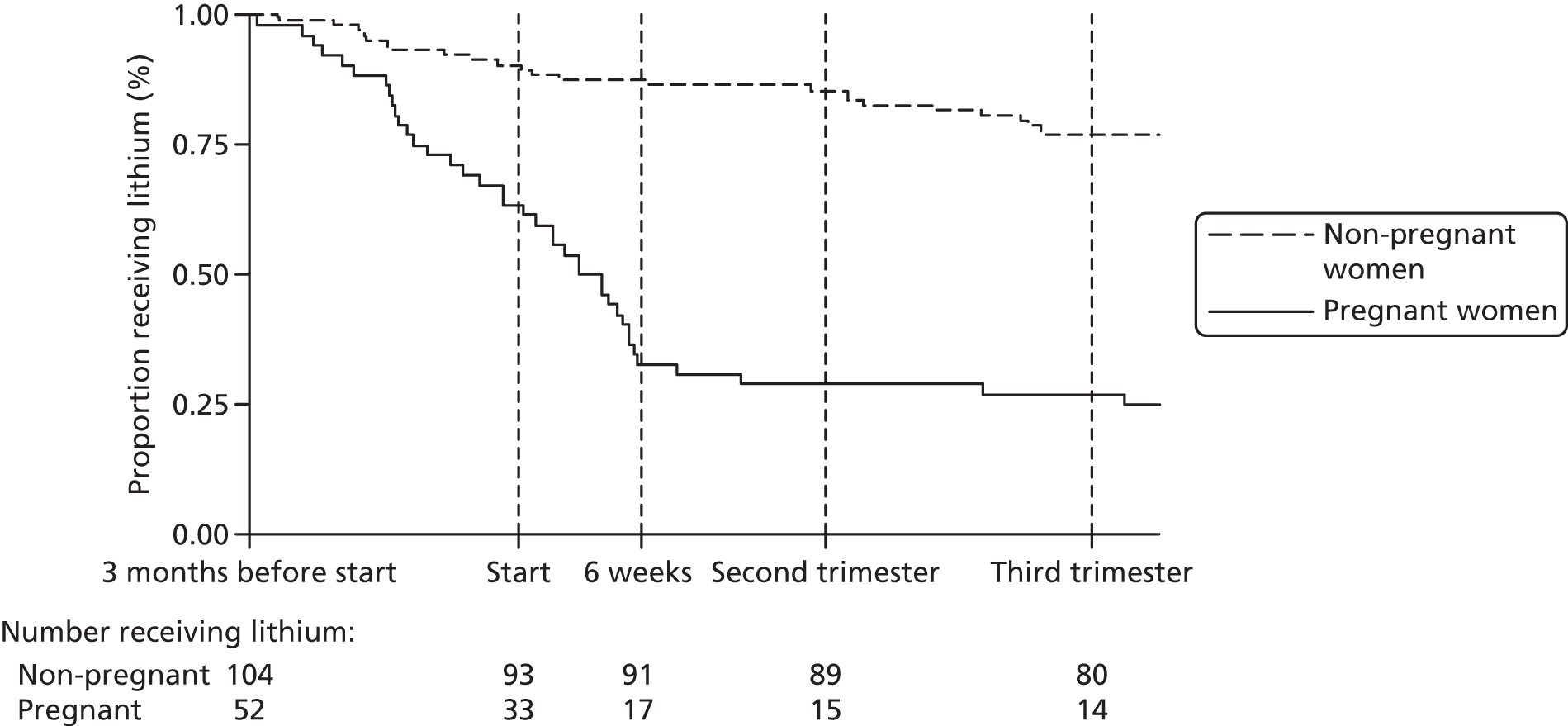
Factors associated with continuation of lithium
A greater proportion of those who continued lithium in pregnancy had been prescribed an antidepressant (47%) or antipsychotic (53%) in addition to lithium during the 4–6 months before pregnancy (compared with 34% prescribed antidepressants or antipsychotics in those who stopped). In addition, a greater proportion of those who continued lithium were having their first child (59% vs. 40%) or had been receiving continuous lithium prescriptions for < 6 months (47% vs. 31%). However, the small numbers of women involved mean that the CIs for these percentages are wide and generally overlap (Table 10).
| Factors | Stopped before 6 weeks (N = 35) | Continued beyond 6 weeks (N = 17) | ||||
|---|---|---|---|---|---|---|
| n | % | 95% CI | n | % | 95% CI | |
| Age band | ||||||
| < 25 years | 5 | 14.3 | 5.9 to 30.8 | 0 | 0.0 | – |
| 25–29 years | 8 | 22.9 | 11.5 to 40.2 | 4 | 23.5 | 8.6 to 50.1 |
| 30–34 years | 10 | 28.6 | 15.7 to 46.2 | 7 | 41.2 | 20.2 to 66.0 |
| ≥ 35 years | 12 | 34.3 | 20.2 to 51.9 | 6 | 35.3 | 16.0 to 60.9 |
| Prior continuous time on lithium | ||||||
| < 6 months | 11 | 31.4 | 17.9 to 49.0 | 8 | 47.1 | 24.5 to 70.8 |
| 6–12 months | 6 | 17.1 | 7.7 to 34.0 | 2 | 11.8 | 2.7 to 38.8 |
| > 12 months | 18 | 51.4 | 34.7 to 67.8 | 7 | 41.2 | 20.2 to 66.0 |
| Estimated parity | ||||||
| 0 | 14 | 40.0 | 24.8 to 57.4 | 10 | 58.8 | 34.0 to 79.8 |
| 1 | 13 | 37.1 | 22.5 to 54.6 | 4 | 23.5 | 8.6 to 50.1 |
| 2 | 6 | 17.1 | 7.7 to 34.0 | 3 | 17.6 | 5.4 to 44.4 |
| 3 or more | 2 | 5.7 | 1.4 to 21.1 | 0 | 0.0 | – |
| Also taking an antidepressant | 12 | 34.3 | 20.2 to 51.9 | 8 | 47.1 | 24.5 to 70.8 |
| Also taking an antipsychotic | 12 | 34.3 | 20.2 to 51.9 | 9 | 52.9 | 29.2 to 75.5 |
| Also taking an anticonvulsant | 6 | 17.1 | 7.7 to 34.0 | 3 | 17.6 | 5.4 to 44.4 |
Switch from lithium to antipsychotic treatment
Of the 39 women who discontinued lithium before the end of follow-up at 220 days, six received at least two prescriptions for an antipsychotic in the 91 days after lithium discontinuation. However, five of these were already receiving an antipsychotic prior to lithium discontinuation, so only one could be classed as having ‘switched’ treatment. We cannot exclude the possibility that some of the other five may have started a new antipsychotic while gradually tapering off lithium.
Discontinuation of anticonvulsant mood stabilisers
We identified 1175 women receiving anticonvulsant mood stabilisers in the period of 4–6 months before the start of their pregnancy. Of these, 1007 had a record of epilepsy, 62 had a record of psychosis, 31 had a record of depression and 75 did not have a record of any of these indications. Among the 93 women with a record of psychosis or depression, there was a substantial difference in the rates of discontinuation between pregnant and non-pregnant women (Figure 7). This was the case even before the pregnancy started (see Figure 7). As for antipsychotics and lithium, the comparisons with non-pregnant women suggest that awareness of the pregnancy may not be the only reason for stopping treatment, as about 70% of non-pregnant women continued anticonvulsant mood stabilisers throughout the follow-up period (see Figure 7).
FIGURE 7.
Discontinuation of anticonvulsant mood stabilisers in pregnant and non-pregnant women with a record of psychosis or depression.

Although the numbers were small, there appeared to be no substantial difference in the rate of discontinuation between women who were prescribed lamotrigine, carbamazepine or valproates (Figure 8).
FIGURE 8.
Discontinuation of anticonvulsant mood stabilisers in pregnant women with a record of psychosis or depression, by drug.

Discontinuation of anticonvulsant mood stabilisers in women with a record of epilepsy compared with women with other or unknown indications
There was a sharp contrast in rates of discontinuation between women with a record of epilepsy who were prescribed anticonvulsant mood stabilisers and women who had a record of psychosis or depression or unknown indications (Figure 9). Hence, among women who had a record of epilepsy 795 out of 1007 (79%) continued to be prescribed anticonvulsant mood stabilisers beyond 6 weeks of pregnancy (see Figure 9) compared with 34 out of 93 (37%) for women with records of psychoses or depression (see Figure 9).
FIGURE 9.
Discontinuation of anticonvulsant mood stabilisers in pregnant women with a record of epilepsy, psychosis, depression or unknown indications. SMI, severe mental illness.

Factors associated with continuation of anticonvulsant mood stabilisers
Factors associated with continuation of receiving anticonvulsant mood stabiliser prescriptions beyond 6 weeks of pregnancy for women with a record of psychoses or depression included duration of treatment prior to pregnancy, lithium treatment and obesity, although after adjustment for age the association with lithium was no longer statistically significant (Table 11). Those who had received continuous treatment for > 12 months prior to pregnancy were more likely to continue treatment in pregnancy compared with those who had received < 6 months of continuous treatment prior to pregnancy (RR 2.56, 95% CI 1.27 to 5.15) (see Table 11). This was still the case after adjustment for age (RR 2.47, 95% CI 1.23 to 4.95) (see Table 11). For other factors examined (age, diagnosis of severe mental illnesses, also taking antidepressants and antipsychotics, social deprivation, estimated parity, smoking, records of alcohol problems, illicit drug use and ethnicity) none of the adjusted effect sizes was statistically significant although the CIs were relatively wide for some estimates (see Table 11).
| Factors | n | Unadjusted | Adjusted | ||||
|---|---|---|---|---|---|---|---|
| RR | 95% CI | p-value | RR | 95% CI | p-value | ||
| Age band | 0.394 | ||||||
| < 25 years | 9 | 1 | |||||
| 25–29 years | 22 | 0.72 | 0.27 to 1.87 | ||||
| 30–34 years | 35 | 0.64 | 0.26 to 1.59 | ||||
| > 35 years | 27 | 1.08 | 0.47 to 2.49 | ||||
| Continuous prior time on ACMS | 0.026 | 0.020 | |||||
| < 6 months | 41 | 1 | 1 | ||||
| 6–12 months | 12 | 2.56 | 1.10 to 5.97 | 2.77 | 1.27 to 6.02 | ||
| > 12 months | 40 | 2.56 | 1.27 to 5.15 | 2.47 | 1.23 to 4.95 | ||
| SMI diagnosis code | 0.308 | 0.433 | |||||
| No | 31 | 1 | 1 | ||||
| SMI diagnosis code | 62 | 1.39 | 0.74 to 2.61 | 1.29 | 0.68 to 2.45 | ||
| Also taking an antidepressant | 0.699 | 0.733 | |||||
| No | 38 | 1 | 1 | ||||
| Taking an antidepressant | 55 | 1.12 | 0.64 to 1.95 | 1.10 | 0.63 to 1.91 | ||
| Also taking an antipsychotic | 0.152 | 0.247 | |||||
| No | 58 | 1 | 1 | ||||
| Taking an antipsychotic | 35 | 1.47 | 0.87 to 2.50 | 1.37 | 0.80 to 2.34 | ||
| Also taking lithium | 0.043 | 0.056 | |||||
| No | 87 | 1 | 1 | ||||
| Taking lithium | 6 | 1.93 | 1.02 to 3.66 | 2.21 | 0.98 to 4.97 | ||
| Townsend quintile | 0.933 | 0.886 | |||||
| 1 | 16 | 1 | 1 | ||||
| 2 | 11 | 1.16 | 0.40 to 3.40 | 0.96 | 0.32 to 2.90 | ||
| 3 | 15 | 0.85 | 0.28 to 2.61 | 0.71 | 0.24 to 2.15 | ||
| 4 | 30 | 1.17 | 0.49 to 2.80 | 1.09 | 0.46 to 2.58 | ||
| 5 | 17 | 1.32 | 0.52 to 3.33 | 1.18 | 0.48 to 2.90 | ||
| Unrecorded | 4 | ||||||
| Estimated parity | 0.383 | 0.425 | |||||
| 0 | 43 | 1 | 1 | ||||
| 1 | 29 | 0.86 | 0.48 to 1.53 | 0.85 | 0.47 to 1.53 | ||
| 2 | 12 | 0.38 | 0.10 to 1.41 | 0.37 | 0.10 to 1.34 | ||
| 3 or more | 9 | 0.50 | 0.14 to 1.80 | 0.56 | 0.15 to 2.08 | ||
| Obesity status | 0.020 | 0.010 | |||||
| Not obese | 80 | 1 | 1 | ||||
| Obese | 13 | 1.89 | 1.11 to 3.24 | 2.11 | 1.20 to 3.73 | ||
| Smoking status | 0.174 | 0.137 | |||||
| Non-smoker | 56 | 1 | 1 | ||||
| Smoker | 37 | 1.45 | 0.85 to 2.47 | 1.50 | 0.88 to 2.56 | ||
| Alcohol problems | 0.867 | 0.893 | |||||
| No | 88 | 1 | 1 | ||||
| Yes | 5 | 1.10 | 0.36 to 3.35 | 1.07 | 0.42 to 2.71 | ||
| Illicit drug use | 0.122 | 0.114 | |||||
| No | 80 | 1 | 1 | ||||
| Yes | 13 | 1.60 | 0.88 to 2.89 | 1.56 | 0.90 to 2.69 | ||
| Ethnicity | 0.376 | 0.454 | |||||
| Other | 87 | 1 | 1 | ||||
| Black or minority ethnic | 6 | 0.44 | 0.07 to 2.71 | 0.49 | 0.08 to 3.14 | ||
Restarting and factors associated with restarting psychotropic medication in pregnancy
We identified 134 women who discontinued typical antipsychotics and 129 women who discontinued atypical antipsychotics before 6 weeks of pregnancy. The figures were 35 for lithium and 59 for anticonvulsant mood stabilisers prescribed to women with a record of psychosis or depression. The proportion of women who restarted treatment (i.e. received additional prescriptions after > 91 days of a gap) varied between psychotropic treatments. At 15 months after delivery, the proportion of restarting treatment was highest for lithium (0.76) and lowest for typical antipsychotics (0.40). We report below additional results from studies on restarting of psychotropic medication in pregnancy and factors associated with restarting for each of the classes of psychotropic medication (antipsychotics, lithium and anticonvulsant mood stabilisers).
Restarting of antipsychotics
Of the 134 women who discontinued typical antipsychotics, the proportion of women who had restarted at the EDD, 6 months and 15 months after delivery was 0.17, 0.33 and 0.40, respectively (Figure 10). Of the 129 women who discontinued atypical antipsychotics, the proportion of women who had restarted treatment at the EDD was 0.23. The proportion of women who had restarted at 6 and 15 months after delivery was 0.44 and 0.52, respectively (see Figure 10).
FIGURE 10.
Proportions of women restarting antipsychotics among those who discontinued by 6 weeks of pregnancy (Kaplan–Meier failure functions). (a) Typical antipsychotics and (b) atypical antipsychotics.

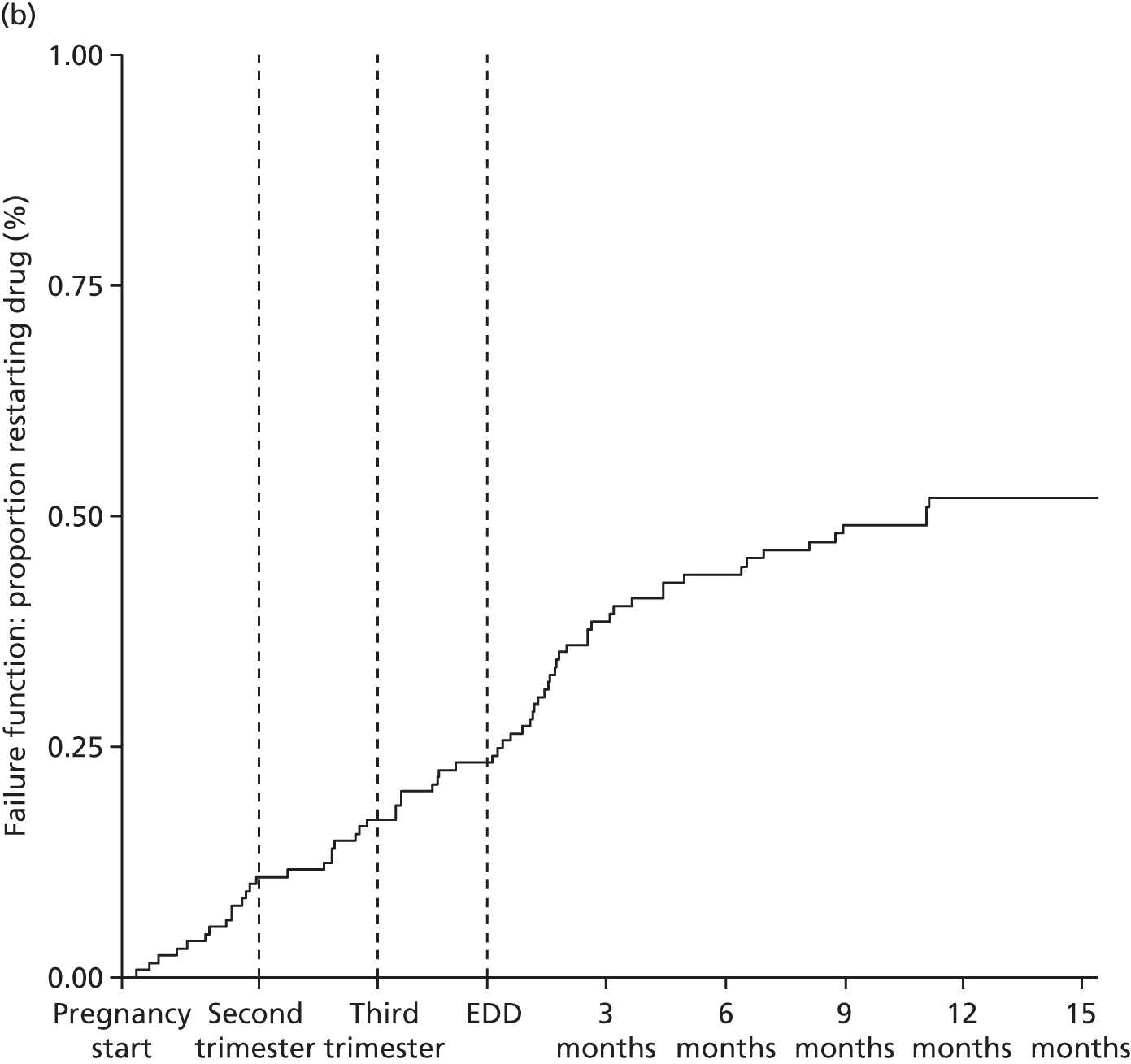
Factors associated with restarting treatment of antipsychotics
There were 44 individuals who had restarted typical antipsychotics and 55 who had restarted atypical antipsychotics by 6 months after delivery. The factors associated with restarting antipsychotic treatment for typical antipsychotics was the average daily dose prescribed and whether or not the women had been prescribed an anticonvulsant mood stabiliser before they became pregnant. Thus, women receiving the DDD or higher were nearly three times as likely to restart treatment by 6 months after delivery compared with women receiving less than one-quarter of the DDD level before and after pregnancy for typical antipsychotics (RR 2.88, 95% CI 1.75 to 4.74) (see Table 12). Women who were also receiving mood stabilisers (anticonvulsants or lithium) were twice as likely to restart typical antipsychotic treatment by 6 months after delivery (RR 2.09, 95% CI 1.21 to 3.59) (Table 12). There were no associations with age, prior duration of treatment or antidepressant treatment prior to pregnancy.
| Factors | Typical antipsychotics (N = 134, n = 44 restarted) | ||||||
|---|---|---|---|---|---|---|---|
| n | Unadjusted | Adjusted | |||||
| RR | 95% CI | p-value | RR | 95% CI | p-value | ||
| Age band | 0.494 | 0.536 | |||||
| < 25 years | 42 | 1 | 1 | ||||
| 25–29 years | 29 | 1.45 | 0.69 to 3.04 | 1.43 | 0.70 to 2.91 | ||
| 30–34 years | 44 | 1.53 | 0.78 to 2.98 | 1.49 | 0.79 to 2.80 | ||
| > 35 years | 19 | 1.77 | 0.83 to 3.77 | 1.65 | 0.79 to 3.46 | ||
| Average daily dose (in units of DDD) | < 0.001 | < 0.001 | |||||
| < 0.25 DDD | 89 | 1 | 1 | ||||
| 0.25–1 DDD | 35 | 1.27 | 0.72 to 2.26 | 1.20 | 0.67 to 2.15 | ||
| > 1 DDD | 10 | 2.97 | 1.87 to 4.71 | 2.88 | 1.75 to 4.74 | ||
| Continuous prior time on antipsychotics | 0.066 | 0.153 | |||||
| < 6 months | 80 | 1 | 1 | ||||
| 6–12 months | 22 | 1.82 | 1.00 to 3.30 | 1.72 | 0.92 to 3.21 | ||
| > 12 months | 32 | 1.75 | 1.01 to 3.03 | 1.55 | 0.89 to 2.68 | ||
| Also taking an antidepressant | 0.367 | 0.834 | |||||
| No | 39 | 1 | 1 | ||||
| Taking an antidepressant | 95 | 0.79 | 0.48 to 1.31 | 0.95 | 0.57 to 1.57 | ||
| Also taking a mood stabiliser | 0.002 | 0.008 | |||||
| No | 127 | 1 | 1 | ||||
| Taking a mood stabiliser | 7 | 2.33 | 1.36 to 3.99 | 2.09 | 1.21 to 3.59 | ||
For atypical antipsychotics there were no significant associations between any of the factors measured at 6 months prior to pregnancy (age, dose, prior duration of treatment, antidepressant treatment or mood stabilisers) and restarting treatment by 6 months after delivery (Table 13).
| Factors | Atypical antipsychotics (N = 129, n = 55 restarted) | ||||||
|---|---|---|---|---|---|---|---|
| n | Unadjusted | Adjusted | |||||
| RR | 95% CI | p-value | RR | 95% CI | p-value | ||
| Age band | 0.425 | 0.487 | |||||
| < 25 years | 31 | 1 | 1 | ||||
| 25–29 years | 36 | 0.86 | 0.45 to 1.64 | 0.91 | 0.48 to 1.73 | ||
| 30–34 years | 31 | 1.25 | 0.70 to 2.22 | 1.27 | 0.71 to 2.27 | ||
| ≥ 35 | 31 | 1.33 | 0.76 to 2.34 | 1.34 | 0.77 to 2.35 | ||
| Average daily dose (in units of DDD) | 0.364 | 0.454 | |||||
| < 0.25 DDD | 28 | 1 | 1 | ||||
| 0.25–1 DDD | 78 | 1.36 | 0.75 to 2.46 | 1.35 | 0.75 to 2.43 | ||
| > 1 DDD | 23 | 1.62 | 0.83 to 3.17 | 1.53 | 0.79 to 2.99 | ||
| Continuous prior time on antipsychotics | 0.836 | 0.840 | |||||
| < 6 months | 62 | 1 | 1 | ||||
| 6–12 months | 26 | 0.85 | 0.49 to 1.49 | 0.86 | 0.47 to 1.57 | ||
| > 12 months | 41 | 0.92 | 0.58 to 1.45 | 0.90 | 0.57 to 1.41 | ||
| Also taking an antidepressant | 0.646 | 0.353 | |||||
| No | 38 | 1 | 1 | ||||
| Taking an antidepressant | 91 | 1.11 | 0.70 to 1.76 | 1.25 | 0.78 to 1.98 | ||
| Also taking a mood stabiliser | 0.322 | 0.516 | |||||
| No | 112 | 1 | 1 | ||||
| Taking a mood stabiliser | 17 | 1.29 | 0.78 to 2.13 | 1.20 | 0.70 to 2.06 | ||
Restarting of lithium
Of the 35 women who discontinued lithium, the proportion of women who restarted treatment by the EDD was 0.26. The proportion of women who had restarted at 6 and 15 months after delivery was 0.64 and 0.76, respectively (Figure 11).
FIGURE 11.
Proportions of women restarting lithium among those who discontinued by 6 weeks of pregnancy (Kaplan–Meier failure functions).

Factors associated with restarting treatment of lithium
There were 22 women who had restarted lithium by 6 months after delivery. Tabulation of factors potentially associated with restarting of lithium treatment (age, prior duration of treatment, antidepressant treatment or antipsychotic treatment) by 6 weeks after delivery suggests some variation between women who restarted and those who did not (Table 14). However, the overall numbers were small and CIs were wide.
| Factors | Restarted before 6 months (N = 22) | Did not restart (N = 13) | ||||
|---|---|---|---|---|---|---|
| n | % | 95% CI | n | % | 95% CI | |
| Age band | ||||||
| < 25 years | 3 | 13.6 | 4.2 to 36.5 | 2 | 15.4 | 3.5 to 48.0 |
| 25–29 years | 5 | 22.7 | 9.3 to 45.9 | 3 | 23.1 | 6.9 to 54.7 |
| 30–34 years | 9 | 40.9 | 21.9 to 63.0 | 1 | 7.7 | 0.9 to 43.0 |
| ≥ 35 years | 5 | 22.7 | 9.3 to 45.9 | 7 | 53.8 | 26.5 to 79.1 |
| Continuous prior time on lithium | ||||||
| < 6 months | 8 | 36.4 | 18.5 to 59.0 | 3 | 23.1 | 6.9 to 54.7 |
| 6–12 months | 5 | 22.7 | 9.3 to 45.9 | 1 | 7.7 | 0.9 to 43.0 |
| > 12 months | 9 | 40.9 | 21.9 to 63.0 | 9 | 69.2 | 38.7 to 88.9 |
| Also taking an antidepressant | 6 | 27.3 | 12.2 to 50.4 | 6 | 46.2 | 20.9 to 73.5 |
| Also taking an anticonvulsant | 4 | 18.2 | 6.6 to 41.2 | 2 | 15.4 | 3.5 to 48.0 |
| Also taking an antipsychotic | 8 | 36.4 | 18.5 to 59.0 | 4 | 30.8 | 11.1 to 61.3 |
Restarting of anticonvulsant mood stabilisers
Of the 59 women with a record of psychosis or depression who discontinued anticonvulsant mood stabilisers the proportion of women who restarted treatment at the EDD was 0.29. The proportion of women who had restarted at 6 and 15 months after delivery was 0.58 and 0.64, respectively (Figure 12).
FIGURE 12.
Proportions of women restarting anticonvulsant mood stabilisers among those who discontinued by 6 weeks of pregnancy (Kaplan–Meier failure functions).

Factors associated with restarting treatment of anticonvulsant mood stabilisers
There were 34 women who had restarted anticonvulsant mood stabilisers by 6 months after delivery. Tabulation of factors potentially associated with restarting of treatment with anticonvulsant mood stabilisers (age, prior duration of treatment, antidepressant treatment or antipsychotic treatment) by 6 weeks after delivery suggest some differences between women who restarted and those who did not (Table 15). However, the overall numbers were small and CIs were wide.
| Factors | Restarted before 6 months (N = 34) | Did not restart (N = 25) | ||||
|---|---|---|---|---|---|---|
| n | % | 95% CI | n | % | 95% CI | |
| Age band | ||||||
| < 25 years | 4 | 11.8 | 4.3 to 28.2 | 1 | 4.0 | 0.5 to 25.1 |
| 25–29 years | 8 | 23.5 | 11.9 to 41.2 | 7 | 28.0 | 13.5 to 49.1 |
| 30–34 years | 13 | 38.2 | 23.2 to 55.9 | 12 | 48.0 | 28.9 to 67.7 |
| ≥ 35 years | 9 | 26.5 | 14.0 to 44.2 | 5 | 20.0 | 8.3 to 41.0 |
| Continuous prior time on anticonvulsants | ||||||
| < 6 months | 17 | 50.0 | 33.2 to 66.8 | 16 | 64.0 | 43.1 to 80.6 |
| 6–12 months | 4 | 11.8 | 4.3 to 28.2 | 2 | 8.0 | 1.9 to 28.2 |
| > 12 months | 13 | 38.2 | 23.2 to 55.9 | 7 | 28.0 | 13.5 to 49.1 |
| Also taking an antidepressant | 18 | 52.9 | 35.9 to 69.3 | 16 | 64.0 | 43.1 to 80.6 |
| Also taking lithium | 0 | 0 | – | 2 | 8.0 | 1.9 to 28.2 |
| Also taking an antipsychotic | 12 | 35.3 | 20.8 to 53.1 | 7 | 28.0 | 13.5 to 49.1 |
Discussion
In the previous section we reported the results of the five (drug utilisation) studies. Below we discuss the findings from each of these studies in turn.
Prevalence, initiation and termination of psychotropic treatment around and during pregnancy
Overall, the patterns of psychotropic medication prescribing before and during pregnancy and after delivery were remarkably similar, although the absolute prevalence estimates varied between classes of medication. Following a broad ‘u shape’ the prevalence was relatively constant before pregnancy, decreased sharply in early pregnancy and increased after delivery to the level of before or even higher. Hence, 0.11% were prescribed antipsychotics, 0.006% lithium and 0.11% were prescribed anticonvulsant mood stabilisers in the second trimester. The prevalence was higher after delivery for atypical antipsychotics and lithium, but remained at the same level before and after pregnancy for typical antipsychotics and anticonvulsant mood stabilisers.
Chlorpromazine, trifluoperazine and flupentixol were the three most commonly prescribed typical antipsychotics in pregnancy and quetiapine, olanzapine, and risperidone were the most commonly prescribed atypical antipsychotics.
We observed a peak in the starting of new prescribing episodes just after delivery for all three classes of psychotropic medication and likewise a peak in termination of prescribing episodes during the first trimester. Single isolated prescriptions were at the lowest during the second and third trimester and that was true of all three classes of psychotropic medications.
A US study based on pharmacy dispensing data from nearly 600,000 deliveries demonstrated a sharp increase in the use of atypical antipsychotics in pregnant women between 2001 and 2007, but estimated that atypical antipsychotics were, on average, dispensed to 26.7 out of 10,000 pregnancies in the second trimester, whereas typical antipsychotics were dispensed to 4.8 out of 10,000 pregnancies in the second trimester. 37 Our estimates are much lower, but in line with another study,36 also based on UK primary care data. This study, which covered the period from 1989 to 2010, found that 0.08% were prescribed antipsychotics in the second trimester. A Swedish study identified 570 women who reported use of antipsychotics out of 958,729 pregnancies (equivalent to 0.06%) from the Swedish birth registry between July 1995 and the end of 2005. 48 Maternal drug use in early pregnancy was recorded from interviews performed by the midwife at the first antenatal care visit, usually before the end of the first trimester. It is likely, however, that this study may have underestimated the prevalence of antipsychotic use in pregnant women in the Swedish population. 49 Another study also using Swedish registry data, but from 2005 to 2009 estimated atypical antipsychotic use during pregnancy to be approximately 0.1%. 50
We found that quetiapine, olanzapine and risperidone were the three most commonly prescribed atypical antipsychotics both before and after pregnancy. This mirrors the patterns of atypical antipsychotics dispensed in the USA37 and the general prescribing pattern of antipsychotics in the UK. 7
The utilisation of anticonvulsant mood stabilisers was examined in another US study also based on pharmacy dispensing data from nearly 600,000 pregnancies. 40 This study included benzodiazepines as one of the ‘older’ anticonvulsant mood stabilisers and the prevalence estimates were primarily driven by the dispensing of these drugs. They found that 0.9% received benzodiazepines at any time in pregnancy while 0.2% received valproic acid derivatives. 40 Of those who were dispensed an old anticonvulsant mood stabiliser 4024 out of 9001 (45%) had an indication of psychiatric disorder, while 2115 out of 3515 (60%) of those dispensed new anticonvulsant mood stabilisers had an indication of psychiatric disorder. Only between 21% and 25% had an indication of epilepsy. 40 A study by Kulaga et al. 41 identified 349 epileptic pregnant women within the Quebec Pregnancy Registry and divided these into three groups based on maternal use of anticonvulsant mood stabilisers during pregnancy. Like our study, Kulaga et al. 41 also found that the frequency of exposure to anticonvulsant mood stabilisers declined substantially during pregnancy, and in the second trimester was estimated to be 0.22% (95% CI 0.19 to 0.26%). 41 Most women were dispensed anticonvulsant mood stabilisers as monotherapy (79.6%) during pregnancy and the three most prevalent anticonvulsants were carbamazepine (29.9%), valproate (19.7%) and phenytoin (11.5%). 41
To our knowledge there are no recent estimates of lithium usage or prescribing in pregnancy. However, the study by Reis and Källén48 identified 79 lithium users among 958,729 pregnancies (< 0.01%) from the Swedish birth registry between July 1995 and the end of 2005. Another study on adverse birth outcome following lithium exposure in pregnancy identified 83 lithium-exposed pregnancies among women who contacted the Israeli Teratology Information Service between 1999 and 2010. 51 Both studies support our findings that lithium is still used by pregnant women, but rarely.
Patterns of recording that indicate worsening of mental health; 18 months before pregnancy, during the course of pregnancy and up to 15 months after delivery
In this exploratory study we observed that recording of suicide attempts, overdose or deliberate self-harm was relatively constant in the 18 months before pregnancy, but declined during pregnancy. Recording of psychosis, mania and hypomania was also slightly lower in the second and third trimester. However, entries increased substantially in the immediate period after delivery, while hospital admissions and the Mental Health Act45 examinations tripled compared with before pregnancy. Recording of psychosis, mania and hypomania followed similar patterns with a doubling just after delivery.
Comparing the results of this study with the prevalence of psychotropic medications around pregnancy there appears to be a strong correlation in terms of the timing of psychosis, mania and hypomania and the start of new prescribing episodes just after delivery (see Figure 1). In contrast, the low level of entries for suicide attempts, overdose or deliberate self-harm during pregnancy may suggest that there were fewer such events. However, it is also possible that some women were less likely to reveal these events to their GP during pregnancy, in particular if they were not in receipt of psychotropic medication.
Time trends in prevalence of psychotropic medication treatment around and during pregnancy
The overall annual prevalence of prescribing in the 6 months before and during pregnancy of both antipsychotics and anticonvulsant mood stabilisers was relatively stable from 1995 to 2006, but increased from around 2007. The total prevalence of antipsychotic treatment has increased by > 50% before and during pregnancy since 1995/6 and the prevalence of anticonvulsant mood stabilisers prescribing in women with a record of psychosis or depression has almost doubled since 1995/6. There has been a shift from typical to atypical antipsychotics in the study period. Likewise, for the anticonvulsant mood stabilisers, carbamazepine has recently been superseded by valproate and lamotrigine. Lithium was rarely prescribed and prescribing fluctuated over time with annual prescribing after delivery almost halved between 1995/6 and 2011/12. We observed a sharp increase in the prevalence of atypical antipsychotic prescribing in pregnancy although this only really ‘kicked off’ after 2007/8. However, the prescribing of atypical antipsychotics after delivery superseded typical antipsychotics by 2005/6.
Our study findings are consistent with an increase in atypical antipsychotics usage in the general population8 and an expansion of indications for usage including bipolar disorder and treatment-resistant depression. 2,52 However, there seems to be an even faster growth in dispensing of antipsychotics to pregnant women in the USA, which has increased 2.5-fold between 2001 and 2007. 37
As mentioned in Prevalence, initiation and termination of psychotropic treatment around and during pregnancy, there seem to be no recent estimates of lithium usage or prescribing in pregnancy. However, a UK study also based on primary care data suggests that lithium continues to be prescribed to women of childbearing age with bipolar disorder2 and that women were prescribed the drug for 30% of the time they were registered with the general practice, which remained constant between 1996 and 2009. 2
Pharmacy dispensing of anticonvulsant mood stabilisers before and during pregnancy in the USA increased by approximately 40% between 2001 and 2007, with 15.7 women receiving anticonvulsant mood stabilisers per 1000 pregnancies in 2001 and 21.9 per 1000 pregnancies in 2007. 40 As mentioned earlier these estimates include benzodiazepines, which account for a large proportion of the ‘older’ anticonvulsant mood stabilisers. However, it appears that our overall prevalence estimates for prescribing of anticonvulsant mood stabilisers are roughly the same for women prescribed anticonvulsant mood stabilisers with a record of psychosis or depression.
For some time there has been concern about potential teratogenic and neurodevelopmental effects of valproate. 15,53–58 We were therefore surprised to observe that valproate appears to be the most commonly prescribed mood stabilising anticonvulsant in the 4–6 months before pregnancy in women with a record of psychosis or depression in 2011/12. The NICE guidelines for antenatal and postnatal mental health and for management of bipolar disorders both issued in 201412,59 state clearly that valproate should not be prescribed to girls and women of childbearing potential. An American study based on Florida Medicaid beneficiaries suggested that use of valproate in pregnancy has declined for women with epilepsy over the period 1999 –2009, but not for other indications60 and a Danish registry study suggested that dispensing of lamotrigine has been sharply rising during pregnancy in the period 1996–2006 (the time period of the study). 61 Future investigations should monitor the impact of these guidelines on prescribing.
Discontinuation and factors associated with discontinuation of psychotropic medication in pregnancy
The overall patterns of discontinuation of psychotropic medication around pregnancy were remarkably similar. Thus, many women were not prescribed further psychotropic medication after 6 weeks of pregnancy, suggesting that pregnancy is a major determinant for stopping psychotropic prescribing. By the time the prescription would be due for renewal many women would have been aware of their pregnancy and have decided to stop the medication. Women prescribed lithium were most likely to discontinue treatment with only 17 out of 52 (33%) receiving further prescriptions after 6 weeks of gestation. For the other psychotropic medications the figures were 73 out of 207 (35%) for typical antipsychotics, 34 out of 93 (37%) for anticonvulsant mood stabilisers (in women with a record of psychosis or depression) and 150 out of 279 (54%) for atypical antipsychotics. By the start of third trimester the figures were 13 out of 93 (14%) for anticonvulsant mood stabilisers, 39 out of 207 (19%) for typical antipsychotics, 14 out of 52 (27%) for lithium and 107 out of 279 (38%) for atypical antipsychotics. However, women prescribed anticonvulsant mood stabilisers with an indication of epilepsy were far more likely to continue treatment in pregnancy than women with any other indications. Hence, of women with a record of epilepsy, 795 out of 1007 (79%) continued to be prescribed anticonvulsant mood stabilisers beyond 6 weeks of pregnancy.
Those most likely to continue antipsychotic treatment were those who had received continuous treatment for > 12 months prior to pregnancy. Other determinants for continuation of antipsychotic prescribing in pregnancy included women’s age and being on higher pre-pregnancy treatment doses. It appears that a greater proportion of those who continued lithium in pregnancy had also been prescribed antidepressants before they became pregnant, were pregnant with their first child and received lithium for < 6 months before pregnancy. However, the numbers were small and CIs were overlapping. Factors associated with continuation of anticonvulsant mood stabilisers in women with a record of psychosis or depression included duration of previous treatment and obesity.
Previous studies on utilisation of psychotropic medication in pregnancy suggest that many women discontinue treatment either just before or in early pregnancy. 36,37,39,40,49 As we describe in a Chapter 2, there was a peak in the termination of prescribing episodes for all three classes of psychotropic medications in the first pregnancy trimester.
The pregnant woman’s mental health team/consultant as well as the GP may play a pivotal role in advising an individual woman on continuation of psychotropic medication in pregnancy. This would be in keeping with the recommendations made by national formularies and the NICE guidelines. 12,32,59 As outlined earlier in this document, there are a few very specific recommendations in terms of prescribing of psychotropic medication to pregnant women, but most are non-specific. In many situations this leaves both health-care professionals and the women with a very difficult and complex decision. They will have to weigh up risks to the mother and child of continuation versus discontinuation of medication in each individual case.
The greatest risk of discontinuation of psychotropic medication is the possibility of relapse of mental illness in pregnancy and postpartum. An observational study of mood disorders in 2252 pregnancies and postpartum periods demonstrated that women with bipolar disorders were at particularly high risk of developing major depression in the postpartum period (prevalence: 19% and 29% in women with bipolar I disorder and bipolar II disorder, respectively). 62 Likewise, it has been shown that women with a history of psychotic disorder are at higher risk of postpartum psychiatric illness, in particular non-psychotic anxiety and depressive disorders. 63 The severity of these illnesses is highlighted by case reports of suicide among these women. 16 Aside from the direct effects of discontinuation of psychotropic medication on the mother, the indirect impact on the fetus and child of severe depression and puerperal psychosis also needs to be taken into consideration. Women may have different reasons to discontinue psychotropic medication in pregnancy; some may discontinue because they fear the medication will harm the unborn child and deem that uncertainty of risk to be higher than the potential risk of relapse. Thus, an international survey of nearly 10,000 women reveals a substantial disparity between women’s perceived risks and the actual risks of prescribed medication in pregnancy. 64 In this survey women rated the risks of antidepressants on par with smoking and alcohol and almost as dangerous as thalidomide. 64 Indeed only about 20% of around 5000 women who were prescribed antidepressants before pregnancy continued to receive treatment after 6 weeks of gestation. 35 However, some women may discontinue psychotropic medication in this period because they no longer need it. We also observed that a number of women on high-dose typical antipsychotics ceased receiving prescriptions before they became pregnant. This may be a part of pregnancy planning, but could also be explained by the fact that typical antipsychotics are known to reduce fertility by inducing hyperprolactinaemia. Finally, the comparison of discontinuation between non-pregnant and pregnant women revealed that pregnancy is not the only reason for women to discontinue psychotropic medication. Other factors, such as experience of adverse effects and stigmatisation associated with psychotropic medication may influence continuous prescribing in pregnant as well as non-pregnant women.
As previously demonstrated by Man et al. ,34 using a similar approach to this study, the rate of discontinuation of anticonvulsant mood stabilisers in pregnancy is associated with the indications for treatment. Thus, women with a record of epilepsy were much more likely to continue anticonvulsant mood stabilisers in pregnancy compared with women with a record of psychosis or depression. There may be several reasons why we see these differences such as alternative treatment options and advice from specialists. However, a detailed investigation of this was outside the remit of this project.
Restarting and factors associated with restarting of psychotropic medication in pregnancy
Of the women who discontinued psychotropic medication either before or in early pregnancy those who were prescribed lithium were most likely to restart treatment. Thus, within 15 months of delivery three-quarters of the women who had discontinued were again receiving lithium treatment. For anticonvulsant mood stabilisers the proportion of women who had restarted within 15 months after delivery was 0.64. On the other hand approximately half of the women prescribed atypical antipsychotics had restarted by 15 months after delivery and a slightly smaller proportion of women prescribed typical antipsychotics had restarted. Overall, there were no clear predictors of restarting of treatment within 6 months of delivery, although for typical antipsychotics women who received an average daily dose greater than the DDD before pregnancy were about three times as likely to restart treatment as women receiving an average daily dose less than one-quarter of the DDD.
With these data we were unable to determine whether women restarted medication in response to relapse of their mental illness or whether treatments were given to prevent major psychoses or other relapses in the postnatal period, but it is likely that it is a mixture of the two. As discussed in Discontinuation and factors associated with discontinuation of psychotropic medication in pregnancy previous research has demonstrated that both women with a psychotic disorder and women with mood disorders are at a particularly high risk of developing major depression and affective psychosis in the postpartum period. 62,63 Some observational studies have sought to compare the risks of relapse of mental illnesses during and after pregnancy in relation to psychotropic treatment. 65–68 Newport et al. 65 observed 16 women who stopped lamotrigine treatment for bipolar disorder in pregnancy. All 16 women experienced a new illness episode during the course of the pregnancy in contrast to 3 out of 10 women who continued treatment. 65 In another study66 more than half (52%) of 42 women who discontinued treatment with lithium in pregnancy experienced a recurrence of bipolar disorder in pregnancy compared with 21% in the year before treatment was discontinued. Viguera et al. 66 observed 89 pregnant women with bipolar disorder (euthymic at conception) treated with one or more mood stabilisers. Of these women, 62 discontinued treatment and 86% experienced at least one recurrence in pregnancy. In contrast only 37% of the 27 women who maintained treatment experienced recurrences in pregnancy66 and similar findings were reported by Cohen et al. 42 for antidepressants. The relationship between drug treatment and mental illness is intrinsically difficult to disentangle as the women who continue psychotropic medication during pregnancy may be more likely to be those who are at the highest risk of relapse; this may result in spurious findings suggesting that psychotropic medication may increase risks of adverse mental outcomes or suggest no difference as in the study by Yonkers et al. 68 on antidepressant prescribing in pregnancy.
It is likely that some women titrate their medication (for example take one tablet instead of two tablets) and hence ‘stretch’ a prescription for much longer during pregnancy. In such cases what may have appeared as a restart of treatment (prescription after more than 91 days gap), was actually a delay in picking up a subsequent prescription because of this prescription ‘stretching’ behaviour.
Chapter 4 Absolute and relative risks of adverse effects of psychotropic medication in pregnancy on maternal and child outcomes
Introduction
In the 1960s the large number of children born with severe birth defects as a result of women’s exposure to thalidomide during pregnancy brought focus on the adverse effects of medicines used in pregnancy. 69 Fifty years later, we still know little about the potential adverse effects of exposure to many medicines in pregnancy. For some time there has been concerns over whether or not certain psychotropic medications increase the risks of major congenital malformations. 15,48,53,54 Likewise, there has been some debate since the 1970s whether or not some anticonvulsant mood stabilisers may adversely impact on child development and increase the risk of behavioural disorders. 18 This leaves many pregnant women with serious psychiatric illnesses and also leaves them (and their health-care professionals) in a dilemma, as they have to consider their own health as well as that of their future child, and many women are conflicted in managing the two. The important question for many women who need treatment during pregnancy is whether some treatments are safer than others and although data from electronic health records do not indicate the reasons for discontinuation of psychotropic medication in pregnancy, it is likely, as discussed in Chapter 3, that the lack of evidence surrounding the safety of medication in pregnancy may have an impact on the decisions made.
In this chapter, we report the results of a number of studies in which we further examined the potential adverse effects of psychotropic medication prescribed in pregnancy on maternal and child outcome. These effects can broadly be divided into three categories: congenital malformations, adverse developmental and adverse perinatal outcomes. The adverse perinatal outcomes category can be further divided between adverse maternal and child outcomes.
We examined a range of maternal and child outcomes, which have previously been identified in the literature. 14,15,19,48,53–55,70,71 These included maternal outcomes such as pre-eclampsia, gestational diabetes, caesarean section, and perinatal death; child outcomes such as major congenital malformations and adverse birth outcomes such as low Apgar scores, preterm birth, low birthweight, tremor, agitation, any breathing problems; and problems with the infants’ muscle tone, which we divide into ‘poor birth outcomes’ and ‘transient poor birth outcomes’. We also conducted exploratory analyses to evaluate potential associations between psychotropic medication treatment in pregnancy and developmental and behavioural outcomes.
Most prior research on psychotropic medication in pregnancy has used ‘healthy women’, that is, women not prescribed psychotropic medication as their comparison group. 23,38,48 However, these women may differ in terms of individual characteristics and health and lifestyle factors which can confound the associations between psychotropic drug treatment and the pregnancy and birth outcomes. To overcome some of these issues we compared women treated with psychotropic medication in pregnancy with those with records of psychotropic treatment before they became pregnant, but not in pregnancy, as well as with women who had no records of psychotropic treatment up to 24 months before and during pregnancy.
Methods
Studies
For each class of psychotropic drugs (i.e. antipsychotics, lithium and anticonvulsant mood stabilisers) we performed two studies; one of which was based on the pregnancy cohorts to examine maternal outcomes, and another of which was based on the linked mother–child cohort to examine child outcomes.
Participants
Pregnancy cohorts
We included women from the pregnancy cohort who were registered with the general practice for at least 6 months before and throughout their pregnancy. Where a woman had two or more eligible pregnancies, we randomly selected one pregnancy for the analyses.
Mother–child cohorts
We included mothers and children in the mother–child cohort if the mothers were registered with the general practice for at least 6 months before the start of their pregnancy, throughout their pregnancy and had a singleton birth. We excluded mother–child pairs when the child had Down syndrome. If a woman had two or more eligible pregnancies, we randomly selected one for the analyses.
Psychotropic medication exposures
For each class of psychotropic medication (i.e. antipsychotics, lithium and anticonvulsant mood stabilisers) we created four cohorts based on medication prescribed. Figure 13 provides a graphical representation of how the exposure cohorts were constructed.
FIGURE 13.
Schematic describing the derivation of the four exposure cohorts in the pregnancy and mother-child linked cohorts. Rx, prescription.

Cohort A contained women with records of psychotropic treatment between 4 and 24 months before the start of pregnancy and no evidence of prescriptions issued after 4 weeks prior to pregnancy start.
Cohort B1 contained women with records of psychotropic treatments between 4 and 24 months before the start of pregnancy and with evidence of prescriptions issued between 31 and 105 days (inclusive) after the start of pregnancy (which is the critical period for many major congenital malformations).
Cohort B2 contained women with records of psychotropic treatment between 4 and 24 months prior to the start of pregnancy and records of psychotropic treatment within 92 days prior to the delivery date. Thus, cohort B1 and cohort B2 are not mutually exclusive.
Cohort C contained women with no records of psychotropic treatment from 24 months before the start of pregnancy through to the delivery date. Start of pregnancy was defined as the first day of LMP or 280 days before delivery if no indication suggested a different duration of pregnancy.
These cohorts were based on prescribing of the psychotropic medication, irrespective of the underlying indication for prescribing.
For the study of anticonvulsant mood stabilisers we defined an additional two sets of subcohorts: (1) cohorts limited to women with a record of psychosis or depression and no records of epilepsy and (2) a cohort of women prescribed valproate in the beginning of pregnancy. For the latter cohort we made comparisons against other anticonvulsant mood stabilisers (lamotrigine and carbamazepine) within cohort B1 as well as against cohort A and C. The reason to select more than one comparison cohort was to investigate the potential issues of confounding. Thus, we anticipated that women who had discontinued treatment (cohort A) just before pregnancy would be more similar both in terms of their measured, but also their unmeasured, characteristics to women who continued treatment in pregnancy (cohort B1 and B2) than women in cohort C.
Characteristics of the women and information on prescribed medication
We extracted information from the women’s electronic primary care health records in order to include the following information in the analyses: age at delivery, social deprivation (Townsend scores), calendar year of delivery, body mass index (BMI), illicit drug use, alcohol problem, smoking status, ethnicity, pre-existing medical conditions (depression, epilepsy, psychosis, hypertension, diabetes), prescriptions from medication listed in the BNF chapter 4, including antidepressants, anxiolytics, hypnotics, anticonvulsant mood stabilisers, antipsychotics and lithium.
Details on how the characteristics and information on prescribed medications were defined and relevant Read codes and drug codes are provided in Appendix 1.
Outcomes
We separated the outcomes into maternal and child outcomes. Below we describe these in further detail.
Maternal outcomes
Our outcomes were pre-eclampsia, gestational hypertension, gestational diabetes, perinatal death and caesarean section. These are all outcomes that have previously been examined in association with exposure to psychotropic medication in pregnancy. 19,48
Further details on how each of these outcomes were defined and relevant Read codes are provided in Appendix 1.
Child outcomes
First we considered major congenital malformations. Further, we considered the following outcomes: prematurity, low Apgar score (< 7), low birthweight, small for gestation age (SGA), tremor, agitation, any breathing problems and problems with the infants’ muscle tone. We combined prematurity, low Apgar score, low birthweight and SGA into one composite outcome, which we refer to as poor birth outcomes, and tremor, agitation, breathing and muscle tone problems into a second composite outcome, which we refer to as transient poor birth outcomes. This was done for several reasons. First, from a mother’s (and health professionals) perspective these outcomes are all signs of poor pregnancy outcomes and as they are all equally relevant, there is no obvious choice of one over the other as a primary outcome. Further, the clinical decision to stop psychotropic medication in pregnancy is often based on a general uncertainty about adverse effects rather than the risks of specific adverse outcomes. 72 Second, the use of composite outcomes reduces the number of statistical tests and improves the statistical power of the study, albeit with the potential disadvantage that results relate to a cluster of outcomes that make up the composite outcome, and cannot be extrapolated to the individual components. 73
Finally, we included an outcome, which we refer to as neurodevelopmental and behavioural outcomes. This outcome includes a broad range of Read codes describing developmental delay as well as behavioural problems recorded within the first 5 years of life.
Further details on how each of these outcomes were defined and relevant Read codes are provided in Appendix 1.
Data analysis
For each class of psychotropic medications, characteristics of the women and the maternal and child outcomes were tabulated for cohort A, B1 and C. For continuous variables, the means and standard deviations (SDs) were estimated and for categorical variables, the numbers of individuals in each category and percentage were estimated. As there was an overlap between the individuals in cohort B1 and B2, and as cohort B2 was only used for a few specific sets of analyses the characteristics of these cohorts are described in Appendix 1.
For each outcome we first estimated and tabulated the number and percentage of events as well as risk difference with 95% CIs where there were more than five events. We then estimated RRRs using Poisson regression. Comparisons were made between cohort B1 (women who had continued psychotropic medication in the first part of pregnancy) and cohort A (women who had discontinued treatment before pregnancy) using the latter as a reference category. Likewise, comparisons were made between cohort B1 (women who had continued psychotropic medication in the first part of pregnancy) and cohort C (women who had not been treated with psychotropic medication) using cohort C as a reference category.
For transient poor birth outcomes (tremor, agitation, breathing and muscle tone problems) the comparisons were made between cohort B2 (women who had received psychotropic medication in the later part of pregnancy) and cohort A, as well as between cohort B2 and cohort C. Specifically for anticonvulsant mood stabilisers we compared outcomes between women in cohort B1 who were prescribed valproate against women in cohort A and C as well as women in cohort B1 who were prescribed other anticonvulsant mood stabilisers.
Poisson regression models were developed, thus providing RRRs with 95% CIs. For all analyses we adopted the following sequence of analysis: model (a): examining crude associations, that is, with no adjustment; model (b): examining associations with adjustment for maternal age; model (c): examining associations with adjustment for ‘health and lifestyle’ factors, that is, adjustment for smoking, obesity, records of alcohol and illicit drug problems; model (d): examining associations with adjustment for concomitant prescriptions issued in the same time window as for cohort B1. For example, for the analyses on antipsychotics we accounted for prescription of antidepressants and anticonvulsant mood stabilisers; and model (e): examining associations with adjustment for all covariates. The results of model (a) and model (e) were tabulated. Further, we tabulated the associations between the health, lifestyle factors, concomitant medication and the outcomes from model (e). These are reported in Appendix 1.
We only report results from analyses where there were more than five events in each exposure group.
Changes to the project protocol
Although we have maintained the same cohorts as planned in our original proposal, A, B1 and B2 (originally called C), we decided to also include a cohort of women not treated with psychotropic medication (cohort C) in our comparisons. We then made the comparisons between B1 (and B2 for specific outcomes) and A as well as B1 and C. This allowed us to compare our results with other studies where similar comparisons were made. In general we did not conduct analyses on specific drugs as the sample sizes became small. However, we did perform specific analyses to examine child outcomes in women prescribed valproate in pregnancy (cohort B1) in contrast to other anticonvulsant mood stabilisers prescribed in pregnancy (cohort B1) as well as cohorts A and C.
We decided to use standard regression analyses methods rather than propensity score-matched methods in order to have direct estimates available for the covariates. In terms of the outcomes we still use composite outcomes, but have changed our groupings from the original proposal to form three groups of composite child outcomes: (1) poor birth outcome, (2) transient poor birth outcome and (3) neurodevelopmental and behavioural outcomes as described further in Chapter 4, Child outcomes. We were unable to identify child and maternal renal problems in a coherent way and decided to drop this as an outcome.
Results
In the case of antipsychotics there were 670 women who discontinued treatment before pregnancy (cohort A), 416 who received treatment in the beginning of pregnancy (cohort B1), 322 who received treatment towards the end of pregnancy (cohort B2) and 318,434 who did not receive antipsychotic treatment between 24 months before pregnancy and up to delivery (cohort C) (Table 16).
| Characteristics | Exposure cohort | ||
|---|---|---|---|
| A | B1 | C | |
| n (% or SD) | n (% or SD) | n (% or SD) | |
| Total | 670 (100) | 416 (100) | 318,434 (100) |
| Age (years) | |||
| Mean (SD) | 30 (5.9) | 32 (5.8) | 30 (5.9) |
| 12–19 | 21 (3.1) | 0 (0) | 14,004 (4.4) |
| 20–29 | 291 (43.4) | 136 (32.7) | 123,704 (38.8) |
| 30–39 | 326 (48.7) | 238 (57.2) | 165,353 (51.9) |
| 40–49 | 32 (4.8) | 42 (10.1) | 15,373 (4.8) |
| Year | |||
| 1995–9 | 42 (6.3) | 14 (3.4) | 46,548 (14.6) |
| 2000–4 | 184 (27.5) | 63 (15.1) | 80,542 (25.3) |
| 2005–9 | 232 (34.6) | 120 (28.8) | 99,765 (31.3) |
| 2010–12 | 212 (31.6) | 219 (52.6) | 91,579 (28.8) |
| Lifestyle variables | |||
| Smoker | 254 (37.9) | 195 (46.9) | 62,746 (19.7) |
| Illicit drug use | 56 (8.4) | 56 (13.5) | 2002 (0.6) |
| Alcohol problems | 37 (5.5) | 29 (7) | 1624 (0.5) |
| Obesity | 77 (11.5) | 72 (17.3) | 20,554(6.5) |
| BMI (kg/m2) | |||
| Mean (SD) | 27 (6.8) | 28 (6.5) | 26 (6.3) |
| Missing | 443 (66.1) | 241 (57.9) | 232,039 (72.9) |
| Townsend score | |||
| 1 | 24 (13.1) | 5 (5.7) | 71,024 (23.4) |
| 2 | 23 (12.6) | 13 (14.9) | 60,407 (19.9) |
| 3 | 37 (20.2) | 15 (17.2) | 64,868 (21.4) |
| 4 | 48 (26.2) | 29 (33.3) | 61,191 (20.2) |
| 5 | 51 (27.9) | 25 (28.7) | 45,942 (15.1) |
| Missing | 487 (72.7) | 329 (79.1) | 15,002 (4.7) |
| Ethnicity | |||
| White | 320 (47.8) | 212 (51) | 133,856 (42) |
| Mixed | 2 (0.3) | 0 (0) | 1786 (0.6) |
| Asian | 8 (1.2) | 12 (2.9) | 9937 (3.1) |
| Black | 7 (1) | 16 (3.8) | 4615 (1.4) |
| Other | 2 (0.3) | 3 (0.7) | 1803 (0.6) |
| Missing | 331 (49.4) | 173 (41.6) | 166,437 (52.3) |
| Use of psychiatric drugs during exposure period B1 | |||
| Anticonvulsant mood stabilisers | 15 (2.2) | 44 (10.6) | 1305 (0.4) |
| Lithium | 4 (0.6) | 13 (3.1) | 11 (0) |
| Antipsychotics | 0 (0) | 416 (100) | 0 (0) |
| Antidepressants | 150 (22.4) | 238 (57.2) | 5942 (1.9) |
| Anxiolytics | 33 (4.9) | 48 (11.5) | 805 (0.3) |
| Hypnotics | 32 (4.8) | 63 (15.1) | 598 (0.2) |
| Pre-existing medical conditions | |||
| Depression | 217 (32.4) | 105 (25.2) | 20,374 (6.4) |
| Epilepsy | 30 (4.5) | 31 (7.5) | 4846 (1.5) |
| SMI | 204 (30.4) | 250 (60.1) | 1480 (0.5) |
| Pre-existing hypertension | 66 (9.9) | 57 (13.7) | 26,232 (8.2) |
| Pre-existing diabetes | 9 (1.3) | 9 (2.2) | 2762 (0.9) |
For the studies on lithium there were 84 women in cohort A, 35 in cohort B1, 20 in cohort B2 and 320,853 in cohort C (Table 17).
| Characteristics | Exposure cohort | ||
|---|---|---|---|
| A | B1 | C | |
| n (% or SD) | n (% or SD) | n (% or SD) | |
| Total | 84 (100) | 35 (100) | 320,853 (100) |
| Age (years) | |||
| Mean (SD) | 33 (5.3) | 35 (5.4) | 30 (5.9) |
| 12–19 | 1 (1.2) | 0 (0) | 14,034 (4.4) |
| 20–29 | 22 (26.2) | 6 (17.1) | 124,982 (39) |
| 30–39 | 53 (63.1) | 21 (60) | 166,294 (51.8) |
| 40–49 | 8 (9.5) | 8 (22.9) | 15,543 (4.8) |
| Year | |||
| 1995–99 | 13 (15.5) | 3 (8.6) | 46,855 (14.6) |
| 2000–4 | 26 (31) | 8 (22.9) | 81,190 (25.3) |
| 2005–9 | 29 (34.5) | 11 (31.4) | 100,574 (31.3) |
| 2010–12 | 16 (19) | 13 (37.1) | 92,234 (28.7) |
| Lifestyle variables | |||
| Smoker | 24 (28.6) | 13 (37.1) | 63,778 (19.9) |
| Illicit drug use | 6 (7.1) | 1 (2.9) | 2167 (0.7) |
| Alcohol problems | 4 (4.8) | 3 (8.6) | 1718 (0.5) |
| Obesity | 9 (10.7) | 7 (20) | 20,870 (6.5) |
| BMI (kg/m2) | |||
| Mean (SD) | 27 (5.5) | 29 (4.5) | 26 (6.3) |
| Missing | 56 (66.7) | 22 (62.9) | 233,534 (72.8) |
| Townsend score | |||
| 1 | 3 (17.6) | 1 (16.7) | 71,307 (23.3) |
| 2 | 3 (17.6) | 0 (0) | 60,753 (19.9) |
| 3 | 4 (23.5) | 3 (50) | 65,291 (21.4) |
| 4 | 5 (29.4) | 1 (16.7) | 61,850 (20.2) |
| 5 | 2 (11.8) | 1 (16.7) | 46,548 (15.2) |
| Missing | 67 (79.8) | 29 (82.9) | 15,104 (4.7) |
| Ethnicity | |||
| White | 35 (41.7) | 19 (54.3) | 134,809 (42) |
| Mixed | 0 (0) | 0 (0) | 1788 (0.6) |
| Asian | 1 (1.2) | 1 (2.9) | 9978 (3.1) |
| Black | 1 (1.2) | 0 (0) | 4641 (1.4) |
| Other | 0 (0) | 0 (0) | 1822 (0.6) |
| Missing | 47 (56) | 15 (42.9) | 167,815 (52.3) |
| Use of psychiatric drugs during exposure period B1 | |||
| Anticonvulsant mood stabilisers | 7 (8.3) | 2 (5.7) | 1355 (0.4) |
| Lithium | 0 (0) | 35 (100) | 0 (0) |
| Antipsychotics | 17 (20.2) | 15 (42.9) | 457 (0.1) |
| Antidepressants | 24 (28.6) | 17 (48.6) | 6455 (2) |
| Anxiolytics | 4 (4.8) | 5 (14.3) | 907 (0.3) |
| Hypnotics | 5 (6) | 4 (11.4) | 690 (0.2) |
| Pre-existing medical conditions | |||
| Depression | 23 (27.4) | 9 (25.7) | 21,084 (6.6) |
| Epilepsy | 3 (3.6) | 3 (8.6) | 4925 (1.5) |
| SMI | 57 (67.9) | 31 (88.6) | 1945 (0.6) |
| Pre-existing hypertension | 8 (9.5) | 4 (11.4) | 26,362 (8.2) |
| Pre-existing diabetes | 3 (3.6) | 2 (5.7) | 2803 (0.9) |
For the studies of anticonvulsant mood stabilisers without restriction of the indication, there were 558 in cohort A, 1539 in cohort B1, 1375 in cohort B2 and 318,612 in cohort C (Table 18). For the study of valproate there were 558 women in cohort A, 398 women receiving valproate in pregnancy (cohort B1) and 1141 receiving other anticonvulsant mood stabilisers in pregnancy (Table 19). Finally, limited to women with a diagnosis of psychoses or depression there were 131 women in cohort A, 61 in cohort B1, 22 in cohort B2 and 318,612 in cohort C (Table 20).
| Characteristics | Exposure cohort | ||
|---|---|---|---|
| A | B1 | C | |
| n (% or SD) | n (% or SD) | n (% or SD) | |
| Total | 558 (100) | 1539 (100) | 318,612 (100) |
| Age (years) | |||
| Mean (SD) | 30 (5.8) | 30 (5.6) | 30 (5.9) |
| 12–19 | 24 (4.3) | 56 (3.6) | 14,008 (4.4) |
| 20–29 | 237 (42.5) | 645 (41.9) | 123,740 (38.8) |
| 30–39 | 276 (49.5) | 768 (49.9) | 165,396 (51.9) |
| 40–49 | 21 (3.8) | 70 (4.5) | 15,468 (4.9) |
| Year | |||
| 1995–9 | 41 (7.3) | 190 (12.3) | 46,638 (14.6) |
| 2000–4 | 114 (20.4) | 349 (22.7) | 80,466 (25.3) |
| 2005–9 | 218 (39.1) | 542 (35.2) | 100,009 (31.4) |
| 2010–12 | 185 (33.2) | 458 (29.8) | 91,499 (28.7) |
| Lifestyle variables | |||
| Smoker | 185 (33.2) | 378 (24.6) | 63,085 (19.8) |
| Illicit drug use | 17 (3) | 28 (1.8) | 2,110 (0.7) |
| Alcohol problems | 12 (2.2) | 22 (1.4) | 1653 (0.5) |
| Obesity | 47 (8.4) | 128 (8.3) | 18,018 (5.7) |
| BMI (kg/m2) | |||
| Mean (SD) | 27 (6.8) | 27 (6.3) | 26 (6.3) |
| Missing | 385 (69) | 1091 (70.9) | 234,733 (73.7) |
| Townsend score | |||
| 1 | 19 (18.8) | 44 (17.1) | 70,879 (23.3) |
| 2 | 19 (18.8) | 37 (14.4) | 60,417 (19.9) |
| 3 | 16 (15.8) | 53 (20.6) | 64,877 (21.4) |
| 4 | 23 (22.8) | 62 (24.1) | 61,357 (20.2) |
| 5 | 24 (23.8) | 61 (23.7) | 46,074 (15.2) |
| Missing | 457 (81.9) | 1282 (83.3) | 15,008 (4.7) |
| Ethnicity | |||
| White | 222 (39.8) | 604 (39.2) | 133,929 (42) |
| Mixed | 2 (0.4) | 13 (0.8) | 1772 (0.6) |
| Asian | 9 (1.6) | 25 (1.6) | 9943 (3.1) |
| Black | 51 (9.1) | 116 (7.5) | 4619 (1.4) |
| Other | 2 (0.4) | 13 (0.8) | 1827 (0.6) |
| Missing | 272 (48.7) | 768 (49.9) | 166,522 (52.3) |
| Use of psychiatric drugs during exposure period B1 | |||
| Anticonvulsant mood stabilisers | 42 (7.5) | 1539 (100) | 170 (0.1) |
| Lithium | 4 (0.7) | 2 (0.1) | 22 (0) |
| Antipsychotics | 26 (4.7) | 46 (3) | 423 (0.1) |
| Antidepressants | 68 (12.2) | 122 (7.9) | 6308 (2) |
| Anxiolytics | 12 (2.2) | 33 (2.1) | 859 (0.3) |
| Hypnotics | 19 (3.4) | 38 (2.5) | 670 (0.2) |
| Pre-existing medical conditions | |||
| Depression | 87 (15.6) | 138 (9) | 20,722 (6.5) |
| Epilepsy | 249 (44.6) | 1441 (93.6) | 3268 (1) |
| SMI | 97 (17.4) | 79 (5.1) | 1840 (0.6) |
| Pre-existing hypertension | 69 (12.4) | 155 (10.1) | 26,228 (8.2) |
| Pre-existing diabetes | 4 (0.7) | 24 (1.6) | 2767 (0.9) |
| Characteristics | Exposure cohort | |||
|---|---|---|---|---|
| A | Valproate | Other ACMS | C | |
| n (% or SD) | n (% or SD) | n (% or SD) | n (% or SD) | |
| Total | 558 (100) | 398 (100) | 1141 (100) | 318,612 (100) |
| Age (years) | ||||
| Mean (SD) | 30 (5.8) | 30 (5.7) | 30 (5.6) | 30 (5.9) |
| 12–19 | 24 (4.3) | 19 (4.8) | 37 (3.2) | 14,008 (4.4) |
| 20–29 | 237 (42.5) | 168 (42.2) | 477 (41.8) | 123,740 (38.8) |
| 30–39 | 276 (49.5) | 195 (49) | 573 (50.2) | 165,396 (51.9) |
| 40–49 | 21 (3.8) | 16 (4) | 54 (4.7) | 15,468 (4.9) |
| Year | ||||
| 1995–9 | 41 (7.3) | 78 (19.6) | 112 (9.8) | 46,638 (14.6) |
| 2000–4 | 114 (20.4) | 119 (29.9) | 230 (20.2) | 80,466 (25.3) |
| 2005–9 | 218 (39.1) | 123 (30.9) | 419 (36.7) | 100,009 (31.4) |
| 2010–12 | 185 (33.2) | 78 (19.6) | 380 (33.3) | 91,499 (28.7) |
| Lifestyle variables | ||||
| Obesity | 45 (8.1) | 32 (8) | 93 (8.2) | 17,058 (5.4) |
| Illicit drug use | 17 (3) | 13 (3.3) | 15 (1.3) | 2110 (0.7) |
| Alcohol problems | 12 (2.2) | 5 (1.3) | 17 (1.5) | 1653 (0.5) |
| Smoker | 185 (33.2) | 120 (30.2) | 258 (22.6) | 63,085 (19.8) |
| BMI (kg/m2) | ||||
| Mean (SD) | 27 (6.8) | 27 (6.7) | 27 (6.2) | 26 (6.3) |
| Missing | 385 (69) | 288 (72.4) | 803 (70.4) | 234,733 (73.7) |
| Townsend score | ||||
| 1 | 19 (18.8) | 6 (11.5) | 38 (18.5) | 70,879 (23.3) |
| 2 | 19 (18.8) | 4 (7.7) | 33 (16.1) | 60,417 (19.9) |
| 3 | 16 (15.8) | 4 (7.7) | 49 (23.9) | 64,877 (21.4) |
| 4 | 23 (22.8) | 19 (36.5) | 43 (21) | 61,357 (20.2) |
| 5 | 24 (23.8) | 19 (36.5) | 42 (20.5) | 46,074 (15.2) |
| Missing | 457 (81.9) | 346 (86.9) | 936 (82) | 15,008 (4.7) |
| Ethnicity | ||||
| White | 222 (39.8) | 131 (32.9) | 473 (41.5) | 133,929 (42) |
| Mixed | 2 (0.4) | 3 (0.8) | 10 (0.9) | 1772 (0.6) |
| Asian | 9 (1.6) | 9 (2.3) | 16 (1.4) | 9943 (3.1) |
| Black | 51 (9.1) | 21 (5.3) | 95 (8.3) | 4619 (1.4) |
| Other | 2 (0.4) | 3 (0.8) | 10 (0.9) | 1827 (0.6) |
| Missing | 272 (48.7) | 231 (58) | 537 (47.1) | 166,522 (52.3) |
| Use of psychiatric drugs during exposure period B1 | ||||
| Anticonvulsant mood stabilisers | 42 (7.5) | 398 (100) | 1141 (100) | 170 (0.1) |
| Lithium | 4 (0.7) | 0 (0) | 2 (0.2) | 22 (0) |
| Antipsychotics | 26 (4.7) | 13 (3.3) | 33 (2.9) | 423 (0.1) |
| Antidepressants | 68 (12.2) | 27 (6.8) | 95 (8.3) | 6308 (2) |
| Anxiolytics | 12 (2.2) | 10 (2.5) | 23 (2) | 859 (0.3) |
| Pre-existing medical conditions | ||||
| Hypnotics | 8 (1.4) | 8 (2) | 17 (1.5) | 693 (0.2) |
| Depression | 87 (15.6) | 38 (9.5) | 100 (8.8) | 20,722 (6.5) |
| Epilepsy | 249 (44.6) | 372 (93.5) | 1069 (93.7) | 3268 (1) |
| SMI | 97 (17.4) | 26 (6.5) | 53 (4.6) | 1840 (0.6) |
| Pre-existing hypertension | 69 (12.4) | 29 (7.3) | 126 (11) | 26,228 (8.2) |
| Pre-existing diabetes | 4 (0.7) | 5 (1.3) | 19 (1.7) | 2767 (0.9) |
| Characteristics | Exposure cohort | ||
|---|---|---|---|
| A | B1 | C | |
| n (% or SD) | n (% or SD) | n (% or SD) | |
| Total | 131 (100) | 61 (100) | 318,612 (100) |
| Age (years) | |||
| Mean (SD) | 32 (5.5) | 32 (5.4) | 30 (5.9) |
| 12–19 | 2 (1.5) | 1 (1.6) | 14,008 (4.4) |
| 20–29 | 43 (32.8) | 20 (32.8) | 123,740 (38.8) |
| 30–39 | 77 (58.8) | 36 (59) | 165,396 (51.9) |
| 40–49 | 9 (6.9) | 4 (6.6) | 15,468 (4.9) |
| Year | |||
| 1995–9 | 3 (2.3) | 3 (4.9) | 46,638 (14.6) |
| 2000–4 | 17 (13) | 10 (16.4) | 80,466 (25.3) |
| 2005–9 | 54 (41.2) | 24 (39.3) | 100,009 (31.4) |
| 2010–12 | 57 (43.5) | 24 (39.3) | 91,499 (28.7) |
| Lifestyle variables | |||
| Smoker | 49 (37.4) | 29 (47.5) | 63,085 (19.8) |
| Illicit drug use | 8 (6.1) | 4 (6.6) | 2110 (0.7) |
| Alcohol problems | 7 (5.3) | 5 (8.2) | 1653 (0.5) |
| Obesity | 14 (10.7) | 11 (18) | 18,018 (5.7) |
| BMI (kg/m2) | |||
| Mean (SD) | 27 (5.5) | 28 (7.9) | 26 (6.3) |
| Missing | 77 (58.8) | 38 (62.3) | 234,733 (73.7) |
| Townsend score | |||
| 1 | 5 (20) | 0 (0) | 70,879 (23.3) |
| 2 | 2 (8) | 4 (28.6) | 60,417 (19.9) |
| 3 | 5 (20) | 2 (14.3) | 64,877 (21.4) |
| 4 | 9 (36) | 5 (35.7) | 61,357 (20.2) |
| 5 | 4 (16) | 3 (21.4) | 46,074 (15.2) |
| Missing | 106 (80.9) | 47 (77) | 15,008 (4.7) |
| Ethnicity | |||
| White | 50 (38.2) | 21 (34.4) | 133,929 (42) |
| Mixed | 2 (1.5) | 1 (1.6) | 1772 (0.6) |
| Asian | 4 (3.1) | 2 (3.3) | 9943 (3.1) |
| Black | 14 (10.7) | 3 (4.9) | 4619 (1.4) |
| Other | 1 (0.8) | 0 (0) | 1827 (0.6) |
| Missing | 60 (45.8) | 34 (55.7) | 166,522 (52.3) |
| Use of psychiatric drugs during exposure period B1 | |||
| Anticonvulsant mood stabilisers | 0 (0) | 61 (100) | 170 (0.1) |
| Lithium | 4 (3.1) | 2 (3.3) | 22 (0) |
| Antipsychotics | 19 (14.5) | 29 (47.5) | 423 (0.1) |
| Antidepressants | 29 (22.1) | 33 (54.1) | 6308 (2) |
| Anxiolytics | 7 (5.3) | 5 (8.2) | 859 (0.3) |
| Hypnotics | 6 (4.6) | 8 (13.1) | 670 (0.2) |
| Pre-existing medical condition | |||
| Depression | 61 (46.6) | 20 (32.8) | 20,722 (6.5) |
| Epilepsy | 0 (0) | 0 (0) | 3268 (1) |
| SMI | 88 (67.2) | 57 (93.4) | 1840 (0.6) |
| Pre-existing hypertension | 16 (12.2) | 8 (13.1) | 26,228 (8.2) |
| Pre-existing diabetes | 2 (1.5) | 4 (6.6) | 2767 (0.9) |
Characteristics of the women in the pregnancy cohort
The characteristics of the women in cohort A, B1 and C are detailed in Tables 16–20. There was a substantial overlap between the women in cohort B1 and B2 (i.e. many of the women who received treatment in the beginning of pregnancy also received treatment towards the end). The details of the characteristics of women in cohort B2 can be found in Appendix 1.
Women who were prescribed antipsychotics, lithium or anticonvulsant mood stabilisers (with a record of psychosis or depression) in pregnancy were older {mean ages between 32 years (SD 5.6 years) and 35 years (SD 5.4 years) than women not prescribed psychotropic medication (cohort C) [mean age 30 years (SD 5.9 years)]}. Likewise, women who were prescribed antipsychotics and lithium in pregnancy were older than women who discontinued before pregnancy (cohort A). A large proportion of the women prescribed psychotropic medication in pregnancy were obese. For example, 72 out of 416 (17%) of the women who were prescribed antipsychotics were obese in contrast to 77 out of 670 (12%) in those who discontinued antipsychotics (cohort A) and 20,554 out of 318,434 (6.5%) in those not prescribed antipsychotics (cohort C) (see Table 16). Illicit drug use and alcohol problems were commonly recorded among women who continued psychotropic medication in pregnancy as well as those who discontinued. Hence, illicit drug use was recorded in 56 out of 416 (13.5%) of women who continued antipsychotics in pregnancy (see Table 16) and in 2–3% of women who continued anticonvulsant mood stabilisers and lithium. Less than 1% of the women not prescribed psychotropic medication had a record of illicit drug use or alcohol problems. More than 45% of women prescribed antipsychotics and anticonvulsant mood stabilisers in pregnancy (cohort B1) (with a record of psychosis or depression) were smokers. In women prescribed lithium in pregnancy (cohort B1) it was 37% and in the cohorts of women not prescribed psychotropic medication it was just under 20% (cohort C). Despite the fact that a large number of data on ethnicity was missing it appears that a relatively large proportion of women prescribed antipsychotics in pregnancy were black. Many women who continued antipsychotics, lithium or anticonvulsant mood stabilisers in pregnancy were also prescribed other medication listed in BNF chapter 4. For example, 238 out of 416 (57%) women who received antipsychotic treatment in pregnancy (cohort B1) also received antidepressant treatment in contrast to < 2% (5942/318,434) of the women in cohort C. Likewise, many received anticonvulsant mood stabilisers in the cohort of women receiving antipsychotics in pregnancy and vice versa.
Including all women, irrespective of indication, in anticonvulsant mood stabilisers cohorts slightly changed the characteristics of cohorts (see Table 18). In these cohorts the proportion of individuals with a record of obesity, alcohol problems and smoking was larger in those who discontinued treatment before pregnancy (cohort A) than in those who continued treatment (cohort B1).
Characteristics of the women in the mother–child cohorts
The mother–child cohorts were a subset of the pregnancy cohorts and included between 65% and 75% of the pregnancy cohorts. The characteristics of women in the mother–child cohorts varied slightly from the distribution in the pregnancy cohorts, but cohorts were overall similar for each class of psychotropic medication (Tables 21–25).
| Characteristics | Exposure cohort | ||
|---|---|---|---|
| A | B1 | C | |
| n (% or SD) | n (% or SD) | n (% or SD) | |
| Total | 492 (100) | 290 (100) | 210,966 (100) |
| Age (years) | |||
| Mean (SD) | 30 (5.7) | 32 (5.6) | 30 (5.9) |
| 12–19 | 12 (2.4) | 0 (0) | 8955 (4.2) |
| 20–29 | 222 (45.1) | 92 (31.7) | 80,491 (38.2) |
| 30–39 | 236 (48) | 166 (57.2) | 110,839 (52.5) |
| 40–49 | 22 (4.5) | 32 (11) | 10,681 (5.1) |
| Year | |||
| 1995–9 | 25 (5.1) | 9 (3.1) | 13,339 (6.3) |
| 2000–4 | 134 (27.2) | 40 (13.8) | 46,707 (22.1) |
| 2005–9 | 173 (35.2) | 82 (28.3) | 77,626 (36.8) |
| 2010–12 | 160 (32.5) | 159 (54.8) | 73,294 (34.7) |
| Lifestyle variables | |||
| Smoker | 183 (37.2) | 139 (47.9) | 42,502 (20.1) |
| Illicit drug use | 40 (8.1) | 37 (12.8) | 1354 (0.6) |
| Alcohol problems | 28 (5.7) | 23 (7.9) | 1124 (0.5) |
| Obesity | 62 (12.6) | 53 (18.3) | 15,363 (7.3) |
| BMI (kg/m2) | |||
| Mean (SD) | 27 (6.8) | 28 (6.7) | 26 (6.4) |
| Missing | 315 (64) | 164 (56.6) | 148,897 (70.6) |
| Townsend score | |||
| 1 | 16 (14.5) | 3 (5.9) | 47,381 (23.5) |
| 2 | 21 (19.1) | 10 (19.6) | 40,309 (20) |
| 3 | 19 (17.3) | 9 (17.6) | 43,152 (21.4) |
| 4 | 25 (22.7) | 11 (21.6) | 40,915 (20.3) |
| 5 | 29 (26.4) | 18 (35.3) | 30,120 (14.9) |
| Missing | 382 (77.6) | 239 (82.4) | 9089 (4.3) |
| Ethnicity | |||
| White | 256 (52) | 172 (59.3) | 104,928 (49.7) |
| Mixed | 2 (0.4) | 0 (0) | 1504 (0.7) |
| Asian | 7 (1.4) | 10 (3.4) | 7461 (3.5) |
| Black | 3 (0.6) | 11 (3.8) | 3446 (1.6) |
| Other | 2 (0.4) | 2 (0.7) | 1350 (0.6) |
| Missing | 222 (45.1) | 95 (32.8) | 92,277 (43.7) |
| Use of psychiatric drugs during exposure period B1 | |||
| Anticonvulsant mood stabilisers | 14 (2.8) | 27 (9.3) | 887 (0.4) |
| Lithium | 2 (0.4) | 11 (3.8) | 7 (0) |
| Antipsychotics | 0 (0) | 290 (100) | 0 (0) |
| Antidepressants | 124 (25.2) | 169 (58.3) | 4351 (2.1) |
| Anxiolytics | 24 (4.9) | 31 (10.7) | 523 (0.2) |
| Hypnotics | 28 (5.7) | 41 (14.1) | 423 (0.2) |
| Pre-existing medical conditions | |||
| Depression | 152 (30.9) | 79 (27.2) | 14,626 (6.9) |
| Epilepsy | 22 (4.5) | 17 (5.9) | 3254 (1.5) |
| SMI | 144 (29.3) | 180 (62.1) | 882 (0.4) |
| Pre-existing hypertension | 47 (9.6) | 42 (14.5) | 19,570 (9.3) |
| Pre-existing diabetes | 6 (1.2) | 7 (2.4) | 2005 (1) |
| Characteristics | Exposure cohort | ||
|---|---|---|---|
| A | B1 | C | |
| n (% or SD) | n (% or SD) | n (% or SD) | |
| Total | 57 (100) | 28 (100) | 212,531 (100) |
| Age (years) | |||
| Mean (SD) | 34 (5.1) | 36 (5.6) | 30 (5.9) |
| 12–19 | 0 (0) | 0 (0) | 8975 (4.2) |
| 20–29 | 14 (24.6) | 5 (17.9) | 81,287 (38.2) |
| 30–39 | 37 (64.9) | 15 (53.6) | 111,496 (52.5) |
| 40–49 | 6 (10.5) | 8 (28.6) | 10,773 (5.1) |
| Year | |||
| 1995–9 | 7 (12.3) | 1 (3.6) | 13,427 (6.3) |
| 2000–4 | 17 (29.8) | 6 (21.4) | 47,128 (22.2) |
| 2005–9 | 20 (35.1) | 11 (39.3) | 78,169 (36.8) |
| 2010–12 | 13 (22.8) | 10 (35.7) | 73,807 (34.7) |
| Lifestyle variables | |||
| Smoker | 15 (26.3) | 10 (35.7) | 43,146 (20.3) |
| Illicit drug use | 2 (3.5) | 1 (3.6) | 1453 (0.7) |
| Alcohol problems | 3 (5.3) | 3 (10.7) | 1188 (0.6) |
| Obesity | 8 (14) | 7 (25) | 15,619 (7.3) |
| BMI (kg/m2) | |||
| Mean, SD | 27 (6.1) | 30 (4.3) | 26 (6.4) |
| Missing | 36 (63.2) | 16 (57.1) | 149,792 (70.5) |
| Townsend score | |||
| 1 | 1 (8.3) | 0 (0) | 47,623 (23.4) |
| 2 | 3 (25) | 0 (0) | 40,530 (19.9) |
| 3 | 3 (25) | 3 (75) | 43,385 (21.3) |
| 4 | 3 (25) | 1 (25) | 41,380 (20.3) |
| 5 | 2 (16.7) | 0 (0) | 30,492 (15) |
| Missing | 45 (78.9) | 24 (85.7) | 9121 (4.3) |
| Ethnicity | |||
| White | 26 (45.6) | 17 (60.7) | 105,638 (49.7) |
| Mixed | 0 (0) | 0 (0) | 1505 (0.7) |
| Asian | 1 (1.8) | 1 (3.6) | 7476 (3.5) |
| Black | 1 (1.8) | 0 (0) | 3455 (1.6) |
| Other | 0 (0) | 0 (0) | 1360 (0.6) |
| Missing | 29 (50.9) | 10 (35.7) | 93,097 (43.8) |
| Use of psychiatric drugs during exposure period B1 | |||
| Anticonvulsant mood stabilisers | 4 (7) | 2 (7.1) | 916 (0.4) |
| Lithium | 0 (0) | 28 (100) | 0 (0) |
| Antipsychotics | 10 (17.5) | 14 (50) | 301 (0.1) |
| Antidepressants | 16 (28.1) | 17 (60.7) | 4694 (2.2) |
| Anxiolytics | 2 (3.5) | 4 (14.3) | 582 (0.3) |
| Hypnotics | 3 (5.3) | 4 (14.3) | 472 (0.2) |
| Pre-existing medical conditions | |||
| Depression | 17 (29.8) | 8 (28.6) | 15,100 (7.1) |
| Epilepsy | 2 (3.5) | 3 (10.7) | 3296 (1.6) |
| SMI | 40 (70.2) | 25 (89.3) | 1168 (0.5) |
| Pre-existing hypertension | 6 (10.5) | 4 (14.3) | 19,634 (9.2) |
| Pre-existing diabetes | 3 (5.3) | 2 (7.1) | 2022 (1) |
| Characteristics | Exposure cohort | ||
|---|---|---|---|
| A | B1 | C | |
| n (% or SD) | n (% or SD) | n (% or SD) | |
| Total | 429 (100) | 1108 (100) | 211,112 (100) |
| Age (years) | |||
| Mean (SD) | 30 (5.7) | 30 (5.5) | 30 (5.9) |
| 12–19 | 19 (4.4) | 41 (3.7) | 8951 (4.2) |
| 20–29 | 181 (42.2) | 454 (41) | 80,581 (38.2) |
| 30–39 | 217 (50.6) | 567 (51.2) | 110,873 (52.5) |
| 40–49 | 12 (2.8) | 46 (4.2) | 10,707 (5.1) |
| Year | |||
| 1995–9 | 24 (5.6) | 116 (10.5) | 13,389 (6.3) |
| 2000–4 | 83 (19.3) | 237 (21.4) | 46,601 (22.1) |
| 2005–9 | 168 (39.2) | 398 (35.9) | 77,886 (36.9) |
| 2010–12 | 154 (35.9) | 357 (32.2) | 73,236 (34.7) |
| Lifestyle variables | |||
| Smoker | 139 (32.4) | 264 (23.8) | 42,707 (20.2) |
| Illicit drug use | 10 (2.3) | 18 (1.6) | 1419 (0.7) |
| Alcohol problems | 9 (2.1) | 14 (1.3) | 1125 (0.5) |
| Obesity | 39 (9.1) | 104 (9.4) | 13,596 (6.4) |
| BMI (kg/m2) | |||
| Mean (SD) | 27 (6.7) | 27 (6.4) | 26 (6.4) |
| Missing | 296 (69) | 764 (69) | 150,820 (71.4) |
| Townsend score | |||
| 1 | 11 (16.7) | 22 (13.3) | 47,305 (23.4) |
| 2 | 16 (24.2) | 22 (13.3) | 40,308 (20) |
| 3 | 10 (15.2) | 35 (21.2) | 43,152 (21.4) |
| 4 | 17 (25.8) | 43 (26.1) | 41,067 (20.3) |
| 5 | 12 (18.2) | 43 (26.1) | 30,207 (15) |
| Missing | 363 (84.6) | 943 (85.1) | 9073 (4.3) |
| Ethnicity | |||
| White | 196 (45.7) | 471 (42.5) | 104,998 (49.7) |
| Mixed | 2 (0.5) | 13 (1.2) | 1489 (0.7) |
| Asian | 7 (1.6) | 18 (1.6) | 7468 (3.5) |
| Black | 36 (8.4) | 95 (8.6) | 3434 (1.6) |
| Other | 2 (0.5) | 7 (0.6) | 1375 (0.7) |
| Missing | 186 (43.4) | 504 (45.5) | 92,348 (43.7) |
| Use of psychiatric drugs during exposure period B1 | |||
| Anticonvulsant mood stabilisers | 31 (7.2) | 1108 (100) | 116 (0.1) |
| Lithium | 2 (0.5) | 2 (0.2) | 13 (0) |
| Antipsychotics | 22 (5.1) | 31 (2.8) | 268 (0.1) |
| Antidepressants | 49 (11.4) | 94 (8.5) | 4582 (2.2) |
| Anxiolytics | 9 (2.1) | 25 (2.3) | 551 (0.3) |
| Hypnotics | 13 (3) | 31 (2.8) | 454 (0.2) |
| Pre-existing medical conditions | |||
| Depression | 68 (15.9) | 104 (9.4) | 14,879 (7) |
| Epilepsy | 192 (44.8) | 1039 (93.8) | 2186 (1) |
| SMI | 78 (18.2) | 60 (5.4) | 1093 (0.5) |
| Pre-existing hypertension | 54 (12.6) | 120 (10.8) | 19,570 (9.3) |
| Pre-existing diabetes | 2 (0.5) | 19 (1.7) | 1998 (0.9) |
| Characteristics | Exposure cohort | |||
|---|---|---|---|---|
| A | Valproate | Other ACMS | C | |
| n (% or SD) | n (% or SD) | n (% or SD) | n (% or SD) | |
| Total | 429 (100) | 273 (100) | 835 (100) | 211,112 (100) |
| Age (years) | ||||
| Mean SD | 30 (5.7) | 30 (5.5) | 30 (5.6) | 30 (5.9) |
| 12–19 | 19 (4.4) | 13 (4.8) | 28 (3.4) | 8951 (4.2) |
| 20–29 | 181 (42.2) | 109 (39.9) | 345 (41.3) | 80,581 (38.2) |
| 30–39 | 217 (50.6) | 141 (51.6) | 426 (51) | 110,873 (52.5) |
| 40–49 | 12 (2.8) | 10 (3.7) | 36 (4.3) | 10,707 (5.1) |
| Year | ||||
| 1995–9 | 24 (5.6) | 50 (18.3) | 66 (7.9) | 13,389 (6.3) |
| 2000–4 | 83 (19.3) | 75 (27.5) | 162 (19.4) | 46,601 (22.1) |
| 2005–9 | 168 (39.2) | 86 (31.5) | 312 (37.4) | 77,886 (36.9) |
| 2010–12 | 154 (35.9) | 62 (22.7) | 295 (35.3) | 73,236 (34.7) |
| Lifestyle variables | ||||
| Obesity | 38 (8.9) | 26 (9.5) | 75 (9) | 12,831 (6.1) |
| Illicit drug use | 10 (2.3) | 7 (2.6) | 11 (1.3) | 1419 (0.7) |
| Alcohol problems | 9 (2.1) | 4 (1.5) | 10 (1.2) | 1125 (0.5) |
| Smoker | 139 (32.4) | 78 (28.6) | 186 (22.3) | 42,707 (20.2) |
| BMI (kg/m2) | ||||
| Mean, SD | 27 (6.7) | 27 (7.2) | 27 (6.2) | 26 (6.4) |
| Missing | 296 (69) | 193 (70.7) | 571 (68.4) | 150,820 (71.4) |
| Townsend score | ||||
| 1 | 11 (16.7) | 3 (9.7) | 19 (14.2) | 47,305 (23.4) |
| 2 | 16 (24.2) | 2 (6.5) | 20 (14.9) | 40,308 (20) |
| 3 | 10 (15.2) | 4 (12.9) | 31 (23.1) | 43,152 (21.4) |
| 4 | 17 (25.8) | 11 (35.5) | 32 (23.9) | 41,067 (20.3) |
| 5 | 12 (18.2) | 11 (35.5) | 32 (23.9) | 30,207 (15) |
| Missing | 363 (84.6) | 242 (88.6) | 701 (84) | 9,073 (4.3) |
| Ethnicity | ||||
| White | 196 (45.7) | 88 (32.2) | 383 (45.9) | 104,998 (49.7) |
| Mixed | 2 (0.5) | 3 (1.1) | 10 (1.2) | 1489 (0.7) |
| Asian | 7 (1.6) | 7 (2.6) | 11 (1.3) | 7468 (3.5) |
| Black | 36 (8.4) | 16 (5.9) | 79 (9.5) | 3434 (1.6) |
| Other | 2 (0.5) | 3 (1.1) | 4 (0.5) | 1375 (0.7) |
| Missing | 186 (43.4) | 156 (57.1) | 348 (41.7) | 92,348 (43.7) |
| Use of psychiatric drugs during exposure period B1 | ||||
| Anticonvulsant mood stabilisers | 31 (7.2) | 273 (100) | 835 (100) | 116 (0.1) |
| Lithium | 2 (0.5) | 0 (0) | 2 (0.2) | 13 (0) |
| Antipsychotics | 22 (5.1) | 8 (2.9) | 23 (2.8) | 268 (0.1) |
| Antidepressants | 49 (11.4) | 17 (6.2) | 77 (9.2) | 4582 (2.2) |
| Anxiolytics | 9 (2.1) | 6 (2.2) | 19 (2.3) | 551 (0.3) |
| Hypnotics | 5 (1.2) | 6 (2.2) | 14 (1.7) | 387 (0.2) |
| Pre-existing medical conditions | ||||
| Depression | 68 (15.9) | 28 (10.3) | 76 (9.1) | 14,879 (7) |
| Epilepsy | 192 (44.8) | 253 (92.7) | 786 (94.1) | 2186 (1) |
| SMI | 78 (18.2) | 19 (7) | 41 (4.9) | 1093 (0.5) |
| Pre-existing hypertension | 54 (12.6) | 21 (7.7) | 99 (11.9) | 19,570 (9.3) |
| Pre-existing diabetes | 2 (0.5) | 4 (1.5) | 15 (1.8) | 1998 (0.9) |
| Characteristics | Exposure cohort | ||
|---|---|---|---|
| A | B1 | C | |
| n (% or SD) | n (% or SD) | n (% or SD) | |
| Total | 103 (100) | 45 (100) | 211,112 (100) |
| Age (years) | |||
| Mean (SD) | 31 (5.3) | 31 (5.2) | 30 (5.9) |
| 12–19 | 2 (1.9) | 0 (0) | 8951 (4.2) |
| 20–29 | 35 (34) | 16 (35.6) | 80,581 (38.2) |
| 30–39 | 61 (59.2) | 27 (60) | 110,873 (52.5) |
| 40–49 | 5 (4.9) | 2 (4.4) | 10,707 (5.1) |
| Year | |||
| 1995–9 | 2 (1.9) | 1 (2.2) | 13,389 (6.3) |
| 2000–4 | 13 (12.6) | 8 (17.8) | 46,601 (22.1) |
| 2005–9 | 39 (37.9) | 16 (35.6) | 77,886 (36.9) |
| 2010–12 | 49 (47.6) | 20 (44.4) | 73,236 (34.7) |
| Lifestyle variables | |||
| Smoker | 39 (37.9) | 23 (51.1) | 42,707 (20.2) |
| Illicit drug use | 6 (5.8) | 3 (6.7) | 1419 (0.7) |
| Alcohol problems | 4 (3.9) | 4 (8.9) | 1125 (0.5) |
| Obesity | 12 (11.7) | 9 (20) | 13,596 (6.4) |
| BMI (kg/m2) | |||
| Mean (SD) | 28 (5.7) | 29 (8.1) | 26 (6.4) |
| Missing | 58 (56.3) | 26 (57.8) | 150,820 (71.4) |
| Townsend score | |||
| 1 | 5 (22.7) | 0 (0) | 47,305 (23.4) |
| 2 | 2 (9.1) | 4 (40) | 40,308 (20) |
| 3 | 4 (18.2) | 1 (10) | 43,152 (21.4) |
| 4 | 8 (36.4) | 3 (30) | 41,067 (20.3) |
| 5 | 3 (13.6) | 2 (20) | 30,207 (15) |
| Missing | 81 (78.6) | 35 (77.8) | 9073 (4.3) |
| Ethnicity | |||
| White | 48 (46.6) | 17 (37.8) | 104,998 (49.7) |
| Mixed | 2 (1.9) | 1 (2.2) | 1489 (0.7) |
| Asian | 3 (2.9) | 1 (2.2) | 7468 (3.5) |
| Black | 10 (9.7) | 3 (6.7) | 3434 (1.6) |
| Other | 1 (1) | 0 (0) | 1375 (0.7) |
| Missing | 39 (37.9) | 23 (51.1) | 92,348 (43.7) |
| Use of psychiatric drugs during exposure period B1 | |||
| Anticonvulsant mood stabilisers | 0 (0) | 45 (100) | 116 (0.1) |
| Lithium | 2 (1.9) | 2 (4.4) | 13 (0) |
| Antipsychotics | 16 (15.5) | 21 (46.7) | 268 (0.1) |
| Antidepressants | 22 (21.4) | 28 (62.2) | 4582 (2.2) |
| Anxiolytics | 6 (5.8) | 3 (6.7) | 551 (0.3) |
| Hypnotics | 5 (4.9) | 7 (15.6) | 454 (0.2) |
| Pre-existing medical conditions | |||
| Depression | 46 (44.7) | 17 (37.8) | 14,879 (7) |
| Epilepsy | 0 (0) | 0 (0) | 2186 (1) |
| SMI | 71 (68.9) | 42 (93.3) | 1093 (0.5) |
| Pre-existing hypertension | 12 (11.7) | 6 (13.3) | 19,570 (9.3) |
| Pre-existing diabetes | 1 (1) | 3 (6.7) | 1998 (0.9) |
Characteristics of children in the mother–child study cohorts
The characteristics of the children in the mother–child cohorts are detailed in Table 26. The median days of follow-up varied within and between drug exposures from 657 days [interquartile range (IQR) 286–1351 days] in children of women who were prescribed antipsychotics in pregnancy (cohort B1) to 1197 days (IQR 396–1671 days) in children of women who were prescribed lithium in pregnancy (cohort B1). The median follow-up for children of women not prescribed psychotropic medications (cohort C) was around 740 days depending on the comparison cohorts. The male-to-female ratio varied between cohorts. For example, more females (55%) than males (45%) were born to women who continued antipsychotic treatment in pregnancy (cohort B1) (see Table 26). Major congenital malformations were recorded relatively soon after birth and most records of neurodevelopmental/behavioural disorders were made around the age of 2–3 years (see Table 26).
| Characteristics | A | B1 | C |
|---|---|---|---|
| Antipsychotic cohorts | |||
| Total number of children, N (%) | 492 (100) | 290 (100) | 210,966 (100) |
| Sex, n (%) | |||
| Male | 253 (51.4) | 132 (45.5) | 107,979 (51.2) |
| Female | 239 (48.6) | 158 (54.5) | 102,987 (48.8) |
| Time to event (days), median (IQR) | |||
| Child follow-up | 834 (352.5–1758) | 657 (286–1351) | 738 (349–1416) |
| Major congenital malformation | 136 (33–1167) | 85 (21–110) | 50 (10–120) |
| NDBD | 1048 (710–1361) | 947 (778–1252) | 930 (619–1274) |
| Lithium cohorts | |||
| Total number of children, N (%) | 57 (100) | 28 (100) | 212,531 (100) |
| Sex, n (%) | |||
| Males | 24 (42.1) | 12 (42.9) | 108,797 (51.2) |
| Females | 33 (57.9) | 16 (57.1) | 103,734 (48.8) |
| Time to event (days), median (IQR) | |||
| Child follow-up | 879 (285–1595) | 1197 (396–1671) | 741 (350–1420) |
| Major congenital malformation | 242 (6–477) | 60 (22–97) | 50 (10–123) |
| NDBD | 1318 (805–1500) | 1252 (622–1642) | 937 (622–1280) |
| Limited anticonvulsant cohort | |||
| Total number of children, N (%) | 103 (100) | 45 (100) | 211,112 (100) |
| Sex, n (%) | |||
| Males | 49 (47.6) | 25 (55.6) | 108,015 (51.2) |
| Females | 54 (52.4) | 20 (44.4) | 103,097 (48.8) |
| Time to event (days), median (IQR) | |||
| Child follow-up | 667 (229–1265) | 957 (192.5–1692) | 738 (350–1420) |
| Major congenital malformation | 1047 (477–3961) | 22 (22–22) | 49 (10–120) |
| NDBD | 1360 (1051.5–1418) | 1087 (812–1361) | 934 (623–1270) |
| Anticonvulsant mood stabilisers cohort | |||
| Total number of children, N (%) | 429 (100) | 1108 (100) | 211,112 (100) |
| Sex, n (%) | |||
| Males | 207 (48.3) | 566 (51.1) | 108,015 (51.2) |
| Females | 222 (51.7) | 542 (48.9) | 103,097 (48.8) |
| Time to event (days), median (IQR) | |||
| Child follow-up | 740 (297–1465) | 924 (349–1741) | 738 (350–1420) |
| Major congenital malformation | 7 (1–477) | 65 (25–371) | 49 (10–120) |
| NDBD | 982 (666–1398) | 1042 (594–1370) | 934 (623–1270) |
Maternal outcomes
Antipsychotics
Absolute number of events, absolute risks (%) and risk differences with 95% CIs for the outcomes for each of the cohorts are listed in Table 27. The relative risk estimates with 95% CIs are listed in Table 28.
| Outcomes | Number of events and absolute risks (%) | Risk difference (95% CI) | |||
|---|---|---|---|---|---|
| A | B1 | C | B1 vs. A | B1 vs. C | |
| Maternal outcomes | |||||
| Pre-eclampsia | 28 (4.2) | 18 (4.3) | 9355 (2.9) | 0.1 (–2.3 to 2.6) | 1.4 (–0.6 to 3.3) |
| Gestational diabetes | 18 (2.7) | 11 (2.6) | 5227 (1.6) | 0 (–2 to 1.9) | 1 (–0.5 to 2.5) |
| Caesarean section | 145 (21.6) | 104 25) | 58,532 (18.4) | 3.4 (–1.8 to 8.6) | 6.6 (2.5 to 10.8) |
| Perinatal death | < 5 | < 5 | 931 (0.3) | – | – |
| Child outcomes | |||||
| MCM | 11 (2.2) | 10 (3.4) | 4162 (2) | 1.2 (–1.3 to 3.7) | 1.5 (–0.6 to 3.6) |
| PBO | 24 (4.9) | 31 (10.7) | 9244 (4.4) | 5.8 (1.8 to 9.8) | 6.3 (2.8 to 9.9) |
| Transient PBO | 20 (4.1) | 15 (5.2) | 4482 (2.1) | 1.1 (–2 to 4.2) | 3 (0.5 to 5.6) |
| NDBD | 50 (10.2) | 22 (7.6) | 10,107 (4.8) | –2.6 (–6.6 to 1.5) | 2.8 (–0.3 to 5.8) |
| Cohort comparisons | RRR (95% CI) | p-value | RRR (95% CI) | p-value |
|---|---|---|---|---|
| B vs. A | B vs. C | |||
| Pre-eclampsia | 1.03 (0.57 to 1.87) | 0.908 | 1.47 (0.92 to 2.33) | 0.100 |
| Pre-eclampsia (adjusted)a | 0.69 (0.37 to 1.29) | 0.248 | 1.24 (0.79 to 1.96) | 0.342 |
| Gestational diabetes | 0.98 (0.46 to 2.08) | 0.966 | 1.61 (0.89 to 2.91) | 0.114 |
| Gestational diabetes (adjusted)a | 0.43 (0.20 to 0.93) | 0.032 | 0.95 (0.53 to 1.69) | 0.867 |
| Caesarean section | 1.15 (0.89 to 1.48) | 0.261 | 1.36 (1.12 to 1.64) | 0.001 |
| Caesarean section (adjusted)a | 1.05 (0.82 to 1.34) | 0.671 | 1.09 (0.92 to 1.30) | 0.278 |
| Perinatal death | – | – | – | – |
| Perinatal death (adjusted)a | – | – | – | – |
Of the women who received antipsychotic treatment in pregnancy (cohort B1) 18 out of 416 (4.3%) developed pre-eclampsia/gestational hypertension and 11 out of 416 (2.6%) developed gestational diabetes. The proportions were similar for women who discontinued antipsychotics before pregnancy (cohort A) (see Table 27). After adjustment for concomitant medications, health and lifestyle characteristics, women who continued antipsychotic treatment in pregnancy were at lower risks of developing gestational diabetes than women who discontinued treatment [adjusted relative risk ratio (RRRadj) 0.43 (95% CI 0.20 to 0.93)] (see Table 28). Notably, obesity was strongly associated with gestational diabetes in this analysis [obesity RRRadj 5.49 (95% CI 2.67 to 11.2)]. Comparing women treated in pregnancy (cohort B1) to women not treated with antipsychotics (cohort C) there were small differences for pre-eclampsia/gestational hypertension and gestational diabetes in the treated group (cohort B1) (see Table 27). After adjustments for concomitant medications, health and lifestyle characteristics, the effects attenuated and the associations were not statistically significant [pre-eclampsia/gestational hypertension RRRadj 1.24 (95% CI 0.79 to 1.96) and gestational diabetes RRRadj 0.95 (95% CI 0.53 to 1.69)] (see Table 28). Notably there was an independent and strong association with obesity, antidepressant treatment and pre-eclampsia as well as gestational diabetes in the adjusted analyses (see Appendix 1).
Of the women who continued antipsychotics in pregnancy (cohort B1), 104 out of 416 (25%) had a caesarean section compared with 145 out of 670 (21.6%) of the women who discontinued treatment (cohort A), the figures for women not treated with antipsychotics were 58,532 out of 318,434 (18.4%) (see Table 27). After adjustments for concomitant prescriptions, health and lifestyle characteristics of the women, those who continued antipsychotic treatments in pregnancy were no longer at higher risk of having a caesarean section than women not treated [RRRadj 1.09 (95% CI 0.92 to 1.30)] or than women who discontinued treatment (cohort A) [RRRadj 1.05 (95% CI 0.82 to 1.34)] (see Table 28).
Of the women who continued antipsychotic treatment in pregnancy (cohort B1) and those who discontinued treatment before (cohort A) fewer than five women in each of the cohorts experienced a perinatal death and hence no further analyses were carried out.
Lithium
There were 8 out of 35 (23%) women who had a caesarean section among the women who continued lithium in pregnancy (cohort B1) in contrast to 11 out of 84 (13%) in those who discontinued treatment (cohort A) and 59,080 out of 320,853 (18%) among those not treated (cohort C). However, the RRRadj were not statistically significant [B1 vs. A: RRRadj 1.40 (95% CI 0.57 to 3.44)], [B1 vs. C: RRRadj 0.83 (95% CI 0.44 to 1.56)]. Of the cohort of women who received lithium in pregnancy (cohort B1) and the cohort of women who discontinued lithium treatment before pregnancy (cohort A) there were fewer than five individuals who experienced pre-eclampsia/gestational hypertension, gestational diabetes and perinatal death. Therefore, no further analyses were carried out for these outcomes.
Anticonvulsant mood stabilisers
Absolute numbers of events, absolute risks (%) and risk differences with 95% CIs for the outcomes for each of the cohorts are listed in Tables 29–31. The relative risk estimates with 95% CIs are listed in Tables 32–34.
| Outcome | Absolute risk (%) | Risk difference (95% CI) | |||
|---|---|---|---|---|---|
| A | B1 | C | B1 vs. A | B1 vs. C | |
| Maternal outcome | |||||
| Pre-eclampsia | 15 (2.7) | 57 (3.7) | 9381 (2.9) | 1 (–0.6 to 2.7) | 0.8 (–0.2 to 1.7) |
| Gestational diabetes | 6 (1.1) | 34 (2.2) | 5200 (1.6) | 1.1 (0 to 2.3) | 0.6 (–0.2 to 1.3) |
| Caesarean section | 111 (19.9) | 329 (21.4) | 58456 (18.3) | 1.5 (–2.4 to 5.4) | 3 (1.0 to 5.1) |
| Perinatal death | 4 (0.7) | 7 (0.5) | 947 (0.3) | –0.3 (–1 to 0.5) | 0.2 (–0.2 to 0.5) |
| Child outcomes | |||||
| MCM | 9 (2.1) | 45 (4.1) | 4119 (2.0) | 2 (0.2 to 3.7) | 2.1 (0.9 to 3.3) |
| PBO | 23 (5.4) | 69 (6.2) | 9186 (4.4) | 0.9 (–1.7 to 3.4) | 1.9 (0.5 to 3.3) |
| Transient PBO | 15 (3.5) | 44 (4.0) | 4543 (2.2) | 0.5 (–1.6 to 2.6) | 1.8 (0.7 to 3.0) |
| NDBD | 33 (7.7) | 96 (8.7) | 10217 (4.8) | 1 (–2.0 to 4.0) | 3.8 (2.2 to 5.5) |
| Outcome | Absolute risk (%) | Risk difference (95% CI) | |||||
|---|---|---|---|---|---|---|---|
| A | Valproate (B1) | Other ACMS (B1) | C | Valproate (B1) vs. Other ACMS (B1) | Valproate (B1) vs. A | Valproate (B1) vs. C | |
| Maternal outcomes | |||||||
| Pre-eclampsia | 15 (2.7) | 13 (3.3) | 44 (3.9) | 9381 (2.9) | –0.6 (–2.7 to 1.5) | 0.6 (–1.6 to 2.8) | 0.3 (–1.4 to 2.1) |
| Gestational diabetes | 6 (1.1) | 9 (2.3) | 25 (2.2) | 5200 (1.6) | 0.1 (–1.6 to 1.8) | 1.2 (–0.5 to 2.9) | 0.6 (–0.8 to 2.1) |
| Caesarean section | 111 (19.9) | 81 (20.4) | 248 (21.7) | 58,456 (18.3) | –1.4 (–6 to 3.2) | 0.5 (–4.7 to 5.6) | 2 (–2.0 to 6.0) |
| Perinatal death | 4 (0.7) | 3 (0.8) | 4 (0.4) | 947 (0.3) | 0.4 (–0.5 to 1.3) | 0 (–1.1 to 1.1) | 0.5 (–0.4 to 1.3) |
| Child outcomes | |||||||
| MCM | 9 (2.1) | 17 (6.2) | 28 (3.4) | 4119 (2) | 2.9 (–0.2 to 6) | 4.1 (1.0 to 7.3) | 4.3 (1.4 to 7.1) |
| PBO | 23 (5.4) | 15 (5.5) | 54 (6.5) | 9186 (4.4) | –1 (–4.1 to 2.2) | 0.1 (–3.3 to 3.6) | 1.1 (–1.6 to 3.8) |
| Transient PBO | 15 (3.5) | 16 (5.9) | 28 (3.4) | 4543 (2.2) | 2.5 (–0.5 to 5.5) | 2.4 (–0.9 to 5.6) | 3.7 (0.9 to 6.5) |
| NDBD | 33 (7.7) | 39 (14.3) | 57 (6.8) | 10,217 (4.8) | 7.5 (3.0 to 11.9) | 6.6 (1.7 to 11.5) | 9.4 (5.3 to 13.6) |
| Outcome | Absolute risk (%) | Risk difference (95% CI) | |||
|---|---|---|---|---|---|
| A | B1 | C | B1 vs. A | B1 vs. C | |
| Maternal outcomes | |||||
| Pre-eclampsia | 6 (4.6) | < 5 | 9381 (2.9) | ||
| Gestational diabetes | 2 (1.5) | < 5 | 5200 (1.6) | ||
| Caesarean section | 22 (16.8) | 13 (21.3) | 58,456 (18.3) | 4.5 (–7.6 to 16.6) | 3 (–7.3 to 13.2) |
| Perinatal death | < 5 | < 5 | 947 (0.3) | ||
| Child outcomes | |||||
| MCM | 3 (2.9) | < 5 | 4119 (2.0) | ||
| PBO | 5 (4.9) | 8 (17.8) | 9186 (4.4) | 12.9 (1.0 to 24.8) | 13.4 (2.3 to 24.6) |
| Transient PBO | 4 (3.9) | < 5 | 4543 (2.2) | ||
| NDBD | 4 (3.9) | < 5 | 10,217 (4.8) | ||
| Cohort comparisons | RRR (95% CI) | p-value | RRR (95% CI) | p-value |
|---|---|---|---|---|
| B vs. A | B vs. C | |||
| Pre-eclampsia | 1.37 (0.78 to 2.43) | 0.269 | 1.25 (0.96 to 1.63) | 0.084 |
| Pre-eclampsia (adjusted)a | 1.34 (0.76 to 2.36) | 0.299 | 1.22 (0.95 to 1.58) | 0.112 |
| Gestational diabetes | 2.05 (0.86 to 4.89) | 0.103 | 1.35 (0.96 to 1.89) | 0.078 |
| Gestational diabetes (adjusted)a | 2.17 (0.93 to 5.10) | 0.072 | 1.26 (0.90 to 1.76) | 0.165 |
| Caesarean section | 1.07 (0.86 to 1.33) | 0.511 | 1.16 (1.04 to 1.29) | 0.005 |
| Caesarean section (adjusted)a | 1.07 (0.88 to 1.30) | 0.450 | 1.14 (1.04 to 1.26) | 0.004 |
| Perinatal death | – | – | 1.53 (0.72 to 3.21) | 0.262 |
| Perinatal death (adjusted)a | – | – | 1.42 (0.67 to 2.99) | 0.356 |
| Cohort comparisons | Valproate (B1) vs. other ACMS (B1) | Valproate (B1) vs. A | Valproate (B1) vs. C | ||
|---|---|---|---|---|---|
| RRR (95% CI) | p-value | RRR (95% CI) | p-value | RRR (95% CI) | |
| Pre-eclampsia | 0.84 (0.45 to 1.57) | 0.598 | 1.21 (0.57 to 2.55) | 0.607 | 1.10 (0.64 to 1.91) |
| Pre-eclampsia (adjusted)a | 0.85 (0.46 to 1.56) | 0.600 | 1.30 (0.62 to 2.70) | 0.477 | 1.10 (0.64 to 1.87) |
| Gestational diabetes | 1.03 (0.48 to 2.21) | 0.935 | 2.10 (0.74 to 5.90) | 0.158 | 1.38 (0.72 to 2.66) |
| Gestational diabetes (adjusted)a | 1.17 (0.54 to 2.52) | 0.683 | 2.73 (0.98 to 7.63) | 0.054 | 1.34 (0.70 to 2.56) |
| Caesarean section | 0.93 (0.72 to 1.20) | 0.607 | 1.02 (0.76 to 1.36) | 0.875 | 1.10 (0.89 to 1.37) |
| Caesarean section (adjusted)a | 0.96 (0.77 to 1.20) | 0.770 | 1.03 (0.80 to 1.33) | 0.782 | 1.11 (0.91 to 1.34) |
| Perinatal death | – | – | – | – | 2.53 (0.81 to 7.87) |
| Perinatal death (adjusted)a | – | – | – | – | 2.30 (0.74 to 7.17) |
| Cohort comparisons | RRR (95% CI) | p-value | RRR (95% CI) | p-value |
|---|---|---|---|---|
| B vs. A | B vs. C | |||
| Pre-eclampsia | – | – | – | – |
| Pre-eclampsia (adjusted)a | – | – | – | – |
| Gestational diabetes | – | – | – | – |
| Gestational diabetes (adjusted)a | – | – | – | – |
| Caesarean section | 1.26 (0.63 to 2.51) | 0.495 | 1.16 (0.67 to 2.00) | 0.589 |
| Caesarean section (adjusted)a | 0.80 (0.44 to 1.45) | 0.464 | 0.92 (0.58 to 1.45) | 0.732 |
| Perinatal death | – | – | – | – |
| Perinatal death (adjusted)a | – | – | – | – |
Comparing women who continued anticonvulsant mood stabilisers in pregnancy, irrespective of whether or not they had a record of psychosis or depression (cohort B1) to women who were not prescribed anticonvulsant mood stabilisers (cohort C), there were small differences (< 1%) in the proportions of women experiencing pre-eclampsia/gestational hypertension, gestational diabetes and perinatal death (see Table 29). However, women who continued prescribing in pregnancy (cohort B) were more likely to have a caesarean section than women not treated (cohort C), but there were no statistically significant differences between women who discontinued and women who continued treatment after accounting for health and lifestyle factors (see Table 32). Likewise, when contrasting women prescribed valproate to other anticonvulsant mood stabilisers and when restricting the cohort to women with a record of psychosis or recent depression there were no significant associations with maternal outcomes (see Tables 30 and 31).
Child outcomes
Antipsychotics
Absolute number of events, absolute risks (%) and risk differences with 95% CIs for the outcomes for each of the cohorts are listed in Table 27. The relative risk estimates with 95% CIs are listed in Table 35.
| Cohort comparisons | RRR (95% CI) | p-value | RRR (95% CI) | p-value |
|---|---|---|---|---|
| B vs. A | B vs. C | |||
| MCM | 1.54 (0.65 to 3.63) | 0.321 | 1.74 (0.93 to 3.25) | 0.077 |
| MCM (adjusted)a | 1.79 (0.72 to 4.47) | 0.207 | 1.59 (0.84 to 3.00) | 0.148 |
| PBO | 2.19 (1.28 to 3.73) | 0.003 | 2.44 (1.71 to 3.47) | < 0.001 |
| PBO (adjusted)a | 1.83 (1.05 to 3.20) | 0.031 | 1.39 (0.98 to 1.97) | 0.061 |
| Transient PBOb | 1.37 (0.68 to 2.75) | 0.374 | 2.62 (1.52 to 4.52) | < 0.001 |
| Transient PBO (adjusted)a,b | 1.20 (0.57 to 2.53) | 0.625 | 1.59 (0.92 to 2.74) | 0.091 |
| NDBD | 0.74 (0.45 to 1.23) | 0.253 | 1.58 (1.04 to 2.40) | 0.031 |
| NDBD (adjusted)a | 0.83 (0.49 to 1.39) | 0.487 | 1.22 (0.80 to 1.84) | 0.344 |
Out of 290 women prescribed antipsychotics in pregnancy (cohort B1), 10 (3.4%) gave birth to a child with a major congenital malformation in comparison to 11 out of 492 (2.2%) in the cohort of women who discontinued treatment before pregnancy (cohort A), and 4162 out of 210,966 (2.0%) in the cohort of women not treated with antipsychotics (cohort C) (see Table 27). Thus, the risk differences and RRRs were non-significant both before and after adjustments for concomitant medications, health and lifestyle characteristics (see Tables 27 and 35).
The proportion of women that were prescribed antipsychotics in pregnancy (cohort B1) who gave birth to a child with poor birth outcomes was 31 out of 290 (10.7%), double the proportion [24/492 (4.9%)] in women who discontinued treatment (cohort A) and nearly triple the proportion [9244/210,966 (4.4%)] in women who were not treated with antipsychotics (see Table 35). After adjustment for concomitant medication and health and lifestyle factors the relative risks remained elevated in comparison with cohort A (RRRadj 1.83, 95% CI 1.05 to 3.20), but not in comparison with cohort C (RRRadj 1.39, 95% CI 0.98 to 1.97) (see Table 35). Notably, obesity, smoking, alcohol problems and illicit drug use, as well as concomitant medications, all remained independently associated with poor birth outcomes in the comparison between cohort B1 and cohort C (see Appendix 1).
The proportion of women who were prescribed antipsychotics in the later stages of pregnancy (cohort B2) who gave birth to a child with transient poor birth outcomes was 13 out of 233 (5.6%) compared with 20 out of 492 (4.1%) in women who discontinued treatment before pregnancy (cohort A) and 4482 out of 210,966 (2.1%) in women not treated with antipsychotics (cohort C). However, after adjustments, relative risk estimates were not statistically significant [cohort B2 vs. cohort A: RRRadj 1.20 (95% CI 0.57 to 2.53) and cohort B2 vs. cohort C: RRRadj 1.59 (95% CI 0.92 to 2.74)] (see Table 35). Age, obesity, smoking, illicit drug and concomitant medications, however, all remained independently associated with transient poor pregnancy outcomes in the comparison between cohort B1 and cohort C.
Finally, we observed a similar pattern for neurodevelopmental and behavioural disorders. Thus, in the unadjusted analysis the association was significant, but after adjustment the relative risk estimates attenuated and were no longer statistically significant (see Table 35).
Lithium
For all child outcomes there were fewer than five women prescribed lithium in pregnancy (cohort B1) who experienced the outcomes and therefore no further analyses were carried out.
Anticonvulsant mood stabilisers
Absolute number of events, absolute risk (%) and risk differences with 95% CIs for the outcomes for each of the cohorts are listed in Tables 29–31.
When including all women, irrespective of indication, 45 out of 1108 (4.1%) women prescribed anticonvulsant mood stabilisers in pregnancy (cohort B1) gave birth to a child with major congenital malformations (see Table 29). In contrast, 4119 out of 211,112 (2%) women not treated (cohort C) gave birth to a child with major congenital malformations. Thus, relative risks more than doubled when comparing cohort B1 and cohort C (RRRadj 2.05, 95% CI 1.53 to 2.74) (Table 36). There was no significant difference in the proportions with major congenital malformations between women who discontinued treatment before pregnancy (cohort A) and those who continued treatment in pregnancy (cohort B1) (see Tables 29 and 36).
| Cohort comparisons | RRR (95% CI) | p-value | RRR (95% CI) | p-value |
|---|---|---|---|---|
| B vs. A | B vs. C | |||
| MCM | 1.93 (0.94 to 3.96) | 0.070 | 2.08 (1.55 to 2.79) | < 0.001 |
| MCM (adjusted)a | 1.89 (0.93 to 3.85) | 0.077 | 2.05 (1.53 to 2.74) | < 0.001 |
| PBO | 1.16 (0.72 to 1.86) | 0.533 | 1.43 (1.12 to 1.81) | 0.003 |
| PBO (adjusted)a | 1.25 (0.78 to 2.01) | 0.340 | 1.33 (1.06 to 1.67) | 0.013 |
| Transient PBOb | 1.14 (0.63 to 2.07) | 0.654 | 1.86 (1.36 to 2.54) | < 0.001 |
| Transient PBO (adjusted)a,b | 1.41 (0.78 to 2.53) | 0.250 | 1.76 (1.30 to 2.38) | < 0.001 |
| NDBD | 1.12 (0.75 to 1.67) | 0.555 | 1.79 (1.46 to 2.18) | < 0.001 |
| NDBD (adjusted)a | 1.10 (0.75 to 1.61) | 0.604 | 1.73 (1.42 to 2.09) | < 0.001 |
When we compared women in cohort B1 who were prescribed valproate with women who were prescribed other anticonvulsant mood stabilisers (lamotrigine and carbamazepine) the relative risk of giving birth to a child with major congenital malformations nearly doubled (RRRadj 1.85, 95% CI 1.02 to 3.36) (Table 37). It was further elevated when comparing women prescribed valproate in pregnancy (B1) with women who discontinued treatment before pregnancy (cohort A) and more than a threefold increase was observed when comparing with women not prescribed anticonvulsant mood stabilisers (cohort C) [RRRadj 3.15 (95% CI 1.98 to 5.00)] (see Table 37).
| Cohort comparisons | RRR (95% CI) | p-value | RRR (95% CI) | p-value | RRR (95% CI) | p-value |
|---|---|---|---|---|---|---|
| Valproate (B1) vs. other ACMS (B1) | Valproate (B1) vs. A | Valproate (B1) vs. C | ||||
| MCM | 1.85 (1.01 to 3.39) | 0.044 | 2.96 (1.32 to 6.65) | 0.008 | 3.19 (1.98 to 5.13) | < 0.001 |
| MCM (adjusted)a | 1.85 (1.02 to 3.36) | 0.040 | 2.93 (1.36 to 6.34) | 0.006 | 3.15 (1.98 to 5.00) | < 0.001 |
| Poor birth outcome | 0.85 (0.47 to 1.50) | 0.576 | 1.02 (0.53 to 1.96) | 0.941 | 1.38 (0.72 to 2.66) | 0.328 |
| Poor birth outcome (adjusted)a | 0.82 (0.47 to 1.44) | 0.506 | 1.06 (0.55 to 2.04) | 0.841 | 1.34 (0.70 to 2.56) | 0.365 |
| Transient PBOb | 1.74 (0.94 to 3.23) | 0.074 | 1.67 (0.82 to 3.39) | 0.150 | 2.72 (1.66 to 4.44) | < 0.001 |
| Transient PBO (adjusted)a,b | 1.68 (0.96 to 2.93) | 0.067 | 1.75 (0.90 to 3.39) | 0.094 | 2.49 (1.55 to 4.00) | < 0.001 |
| NDBD | 2.09 (1.39 to 3.14) | < 0.001 | 1.85 (1.16 to 2.95) | 0.008 | 2.95 (2.15 to 4.04) | < 0.001 |
| NDBD (adjusted)a | 2.10 (1.43 to 3.08) | < 0.001 | 1.76 (1.14 to 2.72) | 0.010 | 2.83 (2.11 to 3.81) | < 0.001 |
Fewer than five women with a record of psychoses or depression and prescribed anticonvulsant mood stabilisers in pregnancy (cohort B1) gave birth to a child with major congenital malformations and therefore no further analyses were carried out.
The risks of giving birth to a child with poor birth outcomes were elevated for all women who were prescribed anticonvulsant mood stabilisers in pregnancy [69/1108 (6.2%)] compared with women who were not prescribed anticonvulsant mood stabilisers (cohort C) [9186/211,112 (4.4%)] (see Table 29). This remained significant after adjustments for health and lifestyle factors and concomitant medications for cohort B vs. C (RRRadj 1.33, 95% CI 1.06 to 1.67) (see Table 36). Notably, obesity, smoking and illicit drug use as well as concomitant medications were all independently associated with poor pregnancy outcomes in the comparison between cohort B1 and cohort C (see Appendix 1). There were no significant differences when the comparisons were made between cohort B and cohort A (see Tables 29 and 36). Very similar patterns were observed for transient poor birth outcomes and neurodevelopmental and behavioural disorders. Hence, of the women prescribed anticonvulsant mood stabilisers in pregnancy (cohort B1), 96 out of 1108 (9%) gave birth to a child who later had records of neurodevelopmental or behavioural disorders, in contrast to 10,217 out of 211,112 (4.8%) among women not prescribed anticonvulsant mood stabilisers (cohort C), resulting in RRRadj of 1.73 (95% CI 1.42 to 2.09) (see Table 36).
When comparing women in cohort B1, who were prescribed valproate, with women who were prescribed other anticonvulsant mood stabilisers (lamotrigine and carbamazepine), the relative risk of giving birth to a child who later had records of neurodevelopmental or behavioural disorders doubled RRRadj 2.10 (95% CI 1.43 to 3.08) (see Table 37). It was also elevated when comparing women prescribed valproate in pregnancy (cohort B1) with women who discontinued treatment before pregnancy (cohort A), but an almost threefold increase was observed when comparing with women not prescribed anticonvulsant mood stabilisers (cohort C) (RRRadj 2.83, 95% CI 2.11 to 3.81) (see Table 37).
The proportion of all women prescribed anticonvulsant mood stabilisers in the later stages of pregnancy (cohort B2) who gave birth to a child with transient poor birth outcomes was 44 out of 1108 (4.0%) compared with 4543 out of 211,112 (2.2%) in women not treated with anticonvulsant mood stabilisers (cohort C). After adjustments, the RRR estimate was 1.76 (95% CI 1.30 to 2.38). However, there were no significant differences between women prescribed anticonvulsant mood stabilisers in pregnancy (cohort B2) and women who discontinued treatment before pregnancy, although the relative risk estimates increased after adjustments (see Table 37).
The risks of giving birth to a child with poor birth outcomes were particularly high among women with a record of psychosis or depression who continued treatment in pregnancy (cohort B1) [8/45 (17.8%)]. This was in contrast to 5 out of 103 (4.9%) of the women who discontinued treatment in pregnancy (cohort A) and 9186 out of 211,112 (4.4%) of the women who were not prescribed anticonvulsant mood stabilisers (cohort C) resulting in a two- to threefold increase in relative risks [RRRadj cohort B1 vs. cohort A: 2.97 (95% CI 0.96 to 9.12) and cohort B1 vs. cohort C: 2.38 (95% CI 1.27 to 4.47) (Table 38).
| Cohort comparisons | RRR (95% CI) | p-value | RRR (95% CI) | p-value |
|---|---|---|---|---|
| B vs. A | B vs. C | |||
| MCM | – | – | – | – |
| MCM (adjusted)a | – | – | – | – |
| PBO | 3.66 (1.19 to 11.1) | 0.022 | 4.08 (2.04 to 8.17) | < 0.001 |
| PBO (adjusted)a | 2.97 (0.96 to 9.12) | 0.056 | 2.38 (1.27 to 4.47) | 0.006 |
| Transient PBOb | – | – | – | – |
| Transient PBO (adjusted)a,b | – | – | – | – |
| NDBD | – | – | – | – |
| NDBD (adjusted)a | – | – | – | – |
There were fewer than five children with a record of the remaining child outcomes among women who had a record of psychosis or depression and were prescribed anticonvulsant mood stabilisers in pregnancy and no further analyses were done.
Discussion
The characteristics of the women varied between as well as within different classes of psychotropic medication. Thus, women prescribed psychotropic medication in pregnancy (cohort B1) were in general older than women not prescribed psychotropic medication (cohort C) and a larger proportion were obese and were recorded as having illicit drug and/or alcohol problems. More than 45% of women prescribed antipsychotics and anticonvulsant mood stabilisers in pregnancy were smokers compared with 37% of women prescribed lithium and 20% in the cohort of women not prescribed psychotropic medication. Concomitant prescription of other psychotropic medications was common. For example, 57% of women who received antipsychotic treatment in pregnancy (cohort B1) also received antidepressant treatment.
Including all women, irrespectively of indication, in anticonvulsant mood stabilisers cohorts slightly changed the characteristics of cohorts. In these cohorts the proportions of individuals with a record of obesity, alcohol problems and smoking were larger in those who discontinued treatment before pregnancy (cohort A) compared with those who continued treatment (cohort B1).
Below we summarise the results of the analyses examining the associations with psychotropic drug treatment in pregnancy for each class of psychotropic medication.
Antipsychotics
Women prescribed antipsychotics in pregnancy (cohort B1) were at higher risks of delivering by caesarean section and giving birth to a child with poor birth outcomes, transient poor birth outcomes, and neurodevelopmental and behavioural disorders than women not prescribed antipsychotics (cohort C). After adjustment for health and lifestyle factors and concomitant medication prescribed, these effects were attenuated and none of the associations were statistically significant. For the remaining pregnancy and birth outcomes, including major congenital malformations, no differences were found between women prescribed antipsychotics in pregnancy and those who were not.
When comparing women who were prescribed antipsychotics in pregnancy (cohort B1) to those who discontinued treatment before pregnancy (cohort A), the former were at lower risk of developing gestational diabetes than women who discontinued treatment after adjustments were made for health, lifestyle factors and concomitant medication prescribed in pregnancy. For the child outcomes the only significant association was between treatment in pregnancy and poor birth outcomes; this association remained after adjustments for concomitant medication, health and lifestyle factors.
Lithium
In terms of caesarean sections, there was no difference between women who were prescribed lithium in pregnancy (cohort B1) and those that discontinued treatment (cohort A) or were not prescribed lithium (cohort C). The numbers prescribed lithium both before and during pregnancy, however, were too few for us to conduct further analyses as there were far too few events that were recorded for both maternal and child outcomes.
Anticonvulsant mood stabilisers
Women prescribed anticonvulsant mood stabilisers in pregnancy (cohort B1) were at a greater risk of having caesarean sections than women not prescribed the drug (cohort C). However, there were no significant differences between cohort B1 and cohort C for the remaining maternal outcomes or between women who continued treatment (cohort B) and those who discontinued treatment (cohort A). In terms of adverse child outcomes, women who continued anticonvulsant mood stabiliser treatment in pregnancy were at higher risks of all child outcomes than women not treated (cohort C) and this persisted after adjustments for health and lifestyle factors, and concomitant medication. There were no significant differences, however, in terms of the child outcomes when comparing women in cohort B with women who discontinued treatment before pregnancy (cohort A).
The comparison between women who were prescribed valproate in pregnancy and women who were prescribed other anticonvulsant mood stabilisers in pregnancy suggests an almost doubling in the risk of giving birth to a child with major congenital malformations in the group prescribed valproate as well as a doubling in the risk of giving birth to a child who later had records of neurodevelopmental or behavioural disorders. The RR was slightly lower when comparing women prescribed valproate in pregnancy (B1) with women who discontinued treatment before pregnancy (cohort A) and an almost threefold increase was observed when comparing with women not prescribed anticonvulsant mood stabilisers (cohort C).
On limiting our analyses for anticonvulsant mood stabilisers to women with a record of psychosis or depression we were unable to conduct most analyses owing to the small number of events. The risk of giving birth to a child with poor birth outcomes was two- to threefold higher in women who continued treatment in pregnancy both than in those who discontinued treatment (cohort A) and those not prescribed anticonvulsant mood stabilisers (cohort C).
Comparisons with existing literature
Antipsychotics
A review of the literature up to 2008 on the use and safety of individual antipsychotics prescribed in pregnancy found no definite associations between antipsychotic use during pregnancy and adverse perinatal or neurodevelopmental outcomes. 1 However, the review highlighted the occurrence of weight gain in women on second-generation antipsychotics; a risk factor for both hypertension and diabetes that exert their own risks on pregnancy outcomes. 74,75 We found that a much larger proportion of women who were prescribed antipsychotics in pregnancy were obese compared with women not prescribed antipsychotics or who discontinued treatment before pregnancy (17.3% in cohort B1 vs. 6.5% in cohort C and 11.5% in cohort A). Other research on antipsychotic treatment in pregnancy includes pharmacovigilance studies from drug companies’ safety databases76,77 as well as cohort studies based on various data sources. 38,50,78–85 A systematic review19 of many of these studies suggested that women requiring antipsychotic treatment during pregnancy have a higher risk of adverse birth outcomes. However, there was substantial heterogeneity between the studies and Coughlin et al. 19 emphasise that most studies had limited adjustment for potential confounding and therefore the observed associations may not be causal. A recent large Canadian study86 based on health administrative data sought to account for confounding factors and included 1021 women on antipsychotics matched to 1021 non-users on a range of parameters using propensity score matching. The study did not find significant differences in the rates of gestational diabetes, hypertensive disorders and venous thromboembolism, nor did they identify significant differences in child outcomes, such as preterm birth or birthweight, between the matched samples, although the absolute rates of these outcomes were high. 86
The results of our study are remarkably similar to another large study on antipsychotic treatment in pregnancy and adverse pregnancy and birth outcomes based on the Swedish birth register. 48 Reis and Källén48 identified 570 women, who when interviewed by midwives, indicated that they were prescribed antipsychotics in early pregnancy. While we cannot directly compare the characteristics of the women in the two studies, there was a large proportion of women on antipsychotics in pregnancy in the Swedish study who were smoking [219 out of 570 (38%)] and the use of other psychotropic medication was also common. They reported that 172 out of 570 (30%) used antidepressants, 79 out of 570 (14%) used lithium and 23 out of 570 (4%) used anticonvulsant mood stabilisers. In terms of maternal perinatal outcomes, the proportion of women with pre-eclampsia [27/570 (4.7%)], gestational diabetes [14/570 (2.5%)] and caesarean section [135/570 (23.7%)] among women prescribed antipsychotics in pregnancy were almost identical to our findings. 48 In terms of child outcomes, the Swedish study also observed elevated risks of low Apgar scores, low birthweight and preterm birth among women who used antipsychotics in pregnancy. The Swedish study reported an absolute risk of severe congenital malformations of 5.21% among women who continued antipsychotics in pregnancy, which was slightly higher than our estimates of major congenital malformations (3.4%). 48 Odds ratios estimating the risk in women who received antipsychotics in pregnancy relative to women not treated with antipsychotics were 1.78 (95% CI 1.04 to 3.01) for gestational diabetes, 1.43 (95% CI 1.17 to 1.74) for caesarean section and 1.52 (95% CI 1.05 to 2.19), relatively severe congenital malformations, mainly because of cardiovascular defects (atrium or ventricular septum defects). The study authors highlighted the non-specificity of the associations and suggested the excess risks may be because of confounding. When the comparison was made after exclusion of women exposed to concomitant anticonvulsant medication, the difference was no longer statistically significant. 48
Risks of extrapyramidal and withdrawal syndromes associated with third trimester exposure of first-generation antipsychotics have long been recognised87 and the US Food and Drug Administration and UK Medicines and Healthcare products Regulatory Agency updated their advice on the risks of extrapyramidal and withdrawal syndromes in 2011 for the entire class of antipsychotic drugs to inform health-care professionals. 88 Our estimates of transient poor pregnancy outcomes, however, were no longer significant after adjustment for concomitant medication, and health and lifestyle factors. Likewise, Vigod et al. 86 observed a sevenfold increased risk for neonatal adaptation syndrome, but this was reduced to a small non-significant relative risk in a matched cohort analysis, suggesting that the observed patterns may be attributed to confounding by concomitant medication use as well as alcohol and substance misuse. We, in keeping with others, found a high prevalence of smokers and individuals with illicit drug problems among women who were prescribed antipsychotics in pregnancy, which may have an inverse impact on pregnancy outcomes. 89
Little is known about adverse developmental effects of antipsychotic exposure in pregnancy. 90 After adjustments for concomitant medication, health and lifestyle factors we found that the association between antipsychotic prescribing in pregnancy and neurodevelopmental disorders attenuated and was not statistically significant.
Lithium
There is very limited information available on pregnancy outcomes in women exposed to lithium, with most evidence coming from case reports. 71 Initial research suggested a substantial increase in Ebstein’s anomaly, a rare cardiovascular anomaly, following lithium exposure in pregnancy. 91 However, these findings may be caused by bias in reporting, as four subsequent case–control studies of Ebstein’s anomalies did not identify any children born to women who took the drug during pregnancy. 92 One of the largest prospective studies on lithium in pregnancy (including 138 exposed women) did not find any difference in the rates of major congenital malformations among children born to women exposed (2.8%) compared with children exposed to treatment not considered to be teratogenic (2.4%). 93 The Swedish study discussed previously48 included 79 women using lithium in pregnancy and identified four children with congenital cardiac malformations equivalent to a prevalence rate of 5.1% (95% CI 1.4% to 12.5%). A recent study51 based on 183 women exposed to lithium during pregnancy who contacted the Israeli Teratology Information Service also suggests lithium treatment in pregnancy is associated with a higher rate of cardiovascular anomalies. We had only 28 mother–child pairs in our study in which the mother had been prescribed lithium in pregnancy and were therefore unable to conduct further analysis on congenital malformations.
Lithium exposure in pregnancy has been associated with high birthweight (large for gestation) even though these women were more likely to be smokers than those not exposed to the drug (32% vs. 16%). 93 However, this did not hold true in another comparative study of lithium-treated women with that of the general population and with another group of women with manic-depressive illness not treated with lithium. 94 A review of the records from the International Register of Lithium Babies published in 199394 suggested that more than one out of three of the children exposed to lithium experience preterm (< 37 weeks) births. Some case reports suggest that lithium toxicity can occur, which often presents as a ‘floppy infant syndrome’, characterised by lethargy, poor sucking, tachypnea, tachycardia and respiratory distress syndrome. 95
As for antipsychotics, limited information is available on potential physical and developmental anomalies in children whose mothers were exposed to lithium in pregnancy. 96 One study97 published in 1976 followed 60 children enrolled at the lithium registry at birth and up to 7 years old. This study compared physical and mental anomalies in these children with their 57 siblings not exposed to lithium during pregnancy, but did not find any differences.
Anticonvulsant mood stabilisers
For some time there has been concerns whether or not treatment with anticonvulsant mood stabilisers, in particular valproate, in pregnancy may increase the risks of major congenital malformations. 15,53–58 The NICE guidelines12,59 for both antenatal mental health care and bipolar disorder issued in 2014 recommend valproate not be prescribed to girls and women of childbearing potential. Limited research has been carried out specifically on women receiving anticonvulsant mood stabilisers for psychiatric illnesses, but a number of observational studies have examined the risks of congenital malformations in women with epilepsy treated with anticonvulsant mood stabilisers. In general, cardiovascular defects, in particular ventricular septal defects, are the most common congenital malformations for children born to both healthy women and women with epilepsy. 33,54,98,99 Neural tube defects, cleft palate and cleft lip, and hypospadias have also been associated with exposure to anticonvulsant mood stabilisers although they are rare events and the estimates vary considerably. 18,98
Our estimates of absolute risks and risk differences for major congenital malformations match closely with previous reports from UK epilepsy registries. 33 Thus, we identified 6.8% with major congenital malformations among children of women receiving prescriptions of valproate in pregnancy (cohort B1) and 3.1% among children of women who had discontinued anticonvulsant mood stabilisers before pregnancy (cohort A). Morrow et al. 33 reported a rate of 6.2% (95% CI 4.6% to 8.2%) for major congenital malformation in women exposed to valproate in pregnancy and 3.5% (95% CI 1.8% to 6.8%) in women with epilepsy who had not taken anticonvulsant mood stabilisers during pregnancy (n = 239). Like us, Morrow et al. 33 demonstrated that the risks of giving birth to a child with major congenital malformation more than doubled for women exposed to valproate versus carbamazepine. Similar findings have emerged from other registries and population-based samples and have been summarised in a review by Tomson and Battino. 18 One constraint of many registry studies is that they include limited information on general health and lifestyle factors that may confound the associations between drug exposure and congenital malformations. 18 Our comparative studies utilising different cohorts of women with different exposure status demonstrate that confounding may be an issue, as we observed much smaller effects estimates when we made comparisons between women prescribed different anticonvulsants than when we compared with women not prescribed anticonvulsant mood stabilisers. It has been suggested that the risks of major congenital malformations may increase with polytherapy involving valproate as well as with increasing dose. 33 However, we did not examine potential effects of dose or polytherapy.
There has been some debate since the 1970s whether or not exposure to anticonvulsant mood stabilisers during pregnancy can adversely affect neurodevelopment and increase the risk of behavioural disorders in children. Adverse neurodevelopmental outcomes in children which has been linked with anticonvulsant mood stabilisers range from global reduction in intelligence quotient (IQ) to specific developmental concerns such as autism, memory and attention. 15,61,100–105 A first Cochrane review,102 published in 2004, concluded that there was little evidence of differences between anticonvulsant mood stabilisers in terms of their effects on cognitive development in utero, but highlighted that there were few studies available on valproate. Subsequently, the Neurodevelopmental Effects of Antiepileptic Drugs study,103,104 examined cognitive outcomes at 3 and 6 years of age after in-utero exposure to valproate, carbamazepine, lamotrigine or phenytoin. Initial results of the interim analyses on 309 children controlling for maternal IQ and gestational age demonstrated that children exposed to valproate had an average IQ score substantially lower than children exposed to lamotrigine, phenytoin and carbamazepine. IQ scores did not differ significantly between the latter three anticonvulsant mood stabilisers. 104 Another Cochrane review,105 published in 2014, evaluated 22 prospective cohort studies and six registry-based studies. The review presented the results of a number of comparisons. The main conclusion was that there is a reduction in the IQ in children exposed to valproate in pregnancy compared with other anticonvulsant mood stabilisers. 105 In their summary of the literature, Tomson and Battino18 also reported poorer performance in children of mothers exposed to valproate in pregnancy, although the studies they reported on were heterogeneous in terms of age at assessment and methods.
Use of anticonvulsant mood stabilisers during pregnancy has also been associated with autism, child behavioural problems and socialising skills. 18,61,106 Thus, a Danish registry study61 identified 655,615 children born from 1996 through to 2006, of which 5437 were identified with autism spectrum disorder, including 2067 with childhood autism. Exposure to valproate was identified via linkage to their mothers’ records during pregnancy from the Danish Prescription Register, which holds information on all prescriptions filled since 1996. 61 The Danish study suggested a substantial increase in diagnoses of autism spectrum disorder (adjusted hazard ratios 2.9, 95% CI 1.7 to 4.9) as well as childhood autism (adjusted hazard ratios 5.2, 95% CI 2.7 to 10.0) in comparison with children of ‘healthy mothers’. 61 The association persisted when comparisons were made with women who discontinued treatment before pregnancy. However, the absolute rates of both autism spectrum disorder and childhood autism were doubled in children of mothers with epilepsy, but not treated with valproate, in comparison with the overall population rates. 61
In our study we used a broad measure for neurodevelopmental and behavioural disorders as we felt it unlikely that we would be able to capture very specific diagnoses/measurements of these disorders in primary care electronic health records. Nonetheless, our relative comparisons are similar to previous findings from the Danish registry study,61 suggesting a threefold increase in neurodevelopmental and behavioural disorders in children of women who were prescribed valproate in pregnancy (cohort B1) compared with women who were not (cohort C). As for our estimates of major congenital malformations, the risk estimates of neurodevelopmental and behavioural disorders attenuated when comparisons were made with children of women receiving other anticonvulsant mood stabilisers during pregnancy, suggesting that exposures to valproate cannot solely explain the elevated risks.
Finally, a number of prospective cohort studies have examined perinatal outcomes associated with exposure to anticonvulsant mood stabilisers in pregnancy. 15 The use of carbamazepine in pregnancy was significantly related to reduction in head circumference, lower birthweight and reduced length,107–109 and similarly the use of valproate was associated with neonatal hypoglycaemia and reduced birth dimensions. 110,111 A study based on Swedish Medical Birth registry data from 1995 to 2001 identified a higher proportion of caesarean section (odds ratio 1.64, 95% CI 1.43 to 1.88), pre-eclampsia (odds ratio 1.66, 95% CI 1.32 to 2.08) among women exposed to anticonvulsant mood stabilisers than among women not exposed. 71 Pilo et al. 71 demonstrated a higher rate of children born with respiratory distress (odds ratio 2.06, 95% CI 1.62 to 2.63). Another Swedish study112 also based on national health registries demonstrated that women with bipolar disorder treated with psychotropic medication (anticonvulsant mood stabilisers, lithium or antipsychotics) were more likely to experience caesarean section and preterm delivery.
Chapter 5 Synthesis
Summary of the findings
In this project our aim was to ascertain the risks and benefits of psychotropic medication in women treated for psychosis who become pregnant. The project was divided into two parts. First, we conducted five descriptive studies with a focus on psychotropic drug utilisation, discontinuation and restarting of treatment. This was followed by a series of cohort studies that examined the absolute and relative risks of adverse maternal and child outcomes associated with psychotropic medication. Our studies were based on data from UK primary care using two large databases: THIN and the CPRD. Below we summarise our main findings.
Prevalence, initiation and termination of psychotropic treatment
-
The overall patterns of prescribing of psychotropic medication around pregnancy were similar for the three classes of psychotropic medication, following a broad ‘u shape’. Thus, prescribing of psychotropic medication was relatively constant before pregnancy, decreased sharply in early pregnancy and then increased after delivery to equal or even surpass pre-pregnancy levels.
-
In the 1–3 months before the start of pregnancy, 0.21% of the women were prescribed antipsychotics, 0.015% were prescribed lithium and 0.41% were prescribed anticonvulsant mood stabilisers.
-
In the second trimester of pregnancy the figures for psychotropic prescribing were 0.11% for antipsychotics, 0.006% for lithium and 0.11% for anticonvulsant mood stabilisers.
-
Quetiapine, olanzapine, risperidone, chlorpromazine, trifluoperazine and flupentixol were the most commonly prescribed atypical and typical antipsychotics. Initially carbamazepine was the most commonly prescribed anticonvulsant mood stabiliser, but was replaced by lamotrigine and valproate.
Patterns of recording that indicate worsening of mental health
-
The recording of suicide attempts, overdose or deliberate self-harm was relatively constant in the 18 months prior to pregnancy, but declined during pregnancy. The recording rose after pregnancy, but only to half of what it was prior to pregnancy.
Entries made for mental health hospital admission or invoking of the Mental Health Act45 more than tripled just after delivery in comparison to the period just before pregnancy and recording of psychosis, mania and hypomania followed similar patterns with a doubling just after delivery.
Time trends in prevalence of psychotropic treatment around and during pregnancy over the calendar period 1995–2012
-
Overall, antipsychotic treatment has increased by > 50% before and during pregnancy from 1995/6 to 2011/12 with a shift from typical to atypical antipsychotics in the study period.
-
Anticonvulsant mood stabilisers prescribing to women with a record of psychosis or depression has almost doubled since 1997/8. Carbamazepine has recently been superseded by valproate and lamotrigine.
-
Lithium was rarely prescribed and prescribing fluctuated over time with annual prescribing after delivery almost halving between 1995/6 and 2011/12.
Discontinuation and factors associated with continuation of psychotropic medication in pregnancy
-
The overall patterns of discontinuation of psychotropic medication were remarkably similar between classes of psychotropic medication.
-
Both pregnant and non-pregnant women discontinue psychotropic medication, but women who become pregnant discontinue psychotropic medication at a much faster rate just before or in early pregnancy compared with non-pregnant women, suggesting that pregnancy is a strong determinant for discontinuation of psychotropic medication.
-
By the sixth week of pregnancy (when the women are likely to become aware of the pregnancy) only 54% received further atypical antipsychotic prescriptions, 37% anticonvulsant mood stabilisers, 35% typical antipsychotics and 33% lithium. By the start of the third trimester the figures were 38% for atypical antipsychotics, 27% for lithium, 19% for typical antipsychotics and 14% for anticonvulsant mood stabilisers.
-
Women with a record of epilepsy who were prescribed anticonvulsants were much more likely to continue medication in pregnancy than women with a record of psychosis, depression or other indications.
-
Factors associated with continuation of treatment in pregnancy included duration of prior treatment, dose, age and comedication.
-
In general, few women switched between typical and atypical antipsychotic treatment just before or in pregnancy. Likewise, few women switched from lithium to antipsychotics.
Restarting and factors associated with restarting psychotropic medication in pregnancy
-
Depending on the psychotropic drug prescribed, between 40% and 76% of women who discontinued psychotropic medication before or in early pregnancy had restarted treatment at 15 months after delivery.
-
Overall, there were no clear predictors of restarting of treatment within 6 months of delivery, except for typical antipsychotics in which women who were on a high dose before pregnancy were most likely to restart treatment.
Absolute and relative risks of adverse effects of psychotropic medication in pregnancy on maternal and child outcomes
Characteristics of women
-
Women prescribed psychotropic medication in pregnancy were in general older than women not prescribed psychotropic medication. A large proportion of the women prescribed psychotropic medication in pregnancy were obese and many had records of illicit drug use and alcohol problems.
-
More than 45% of women prescribed antipsychotics and anticonvulsant mood stabilisers in pregnancy were smokers compared with 37% of women prescribed lithium and 20% in the cohorts of women not prescribed psychotropic medication.
-
Concomitant prescriptions of other psychotropic medications were common. For example, 57% of women who received antipsychotic treatment in pregnancy also received antidepressant treatment.
Associations between prescribed psychotropic medication in pregnancy and adverse maternal and child outcomes
-
Women prescribed antipsychotic medication in pregnancy were not at higher risk of giving birth to a child with major congenital malformation than women not prescribed antipsychotics.
-
Women who were prescribed antipsychotics in pregnancy were at a higher risk of delivering by caesarean section and giving birth to a child with poor birth outcomes, transient poor birth outcomes, and neurodevelopmental and behavioural disorders than women not prescribed antipsychotics. However, these associations were confounded by health, lifestyle and concomitant medication and after adjustment the effects attenuated and none of the associations was statistically significant.
-
There was no significant difference in the risk of developing gestational diabetes between women who continued antipsychotics in pregnancy and those who discontinued. However, gestational diabetes appears to be strongly associated with obesity and after adjustment for health, lifestyle factors and concomitant medication, women who continued antipsychotics in pregnancy were at lower risk of developing gestational diabetes.
-
Few women were prescribed lithium before and during pregnancy and we were unable to conduct further analyses owing to the small number of events.
-
Women prescribed anticonvulsant mood stabilisers in pregnancy were at higher risk of giving birth by caesarean section than women not prescribed anticonvulsant mood stabilisers.
-
There were no significant differences for the remaining maternal outcomes or between women who continued treatment and those who discontinued treatment.
-
Women who continued anticonvulsant mood stabiliser treatment in pregnancy experienced higher risks of all child outcomes in comparison to women not treated, but no difference was observed when comparing with women who discontinued treatment before pregnancy.
-
Comparing women who were prescribed valproate in pregnancy with women who were prescribed other anticonvulsant mood stabilisers in pregnancy suggested a doubling in the risk of giving birth to a child with major congenital malformations or giving birth to a child who later had records of neurodevelopmental or behavioural disorders.
-
The risk of giving birth to a child with major congenital malformations and the risk of giving birth to a child who later had records of neurodevelopmental or behavioural disorders were increased threefold in comparison with women not prescribed anticonvulsant mood stabilisers.
-
By limiting the analyses to women with a record of psychosis or depression we were unable to conduct most analyses owing to the small number of events. However, the risk of giving birth to a child with poor birth outcomes was two- to threefold higher in women who continued treatment in pregnancy both in comparison with those who discontinued treatment and those not prescribed anticonvulsant mood stabilisers. The increased risk persisted after adjustment for health and lifestyle factors.
Risks and benefits of psychotropic medication in pregnancy
Many women treated with psychotropic medication face a dilemma on getting pregnant as they must decide whether or not to continue their medication in pregnancy. 12,18,20 In this project we demonstrated that the majority of these women discontinue psychotropic medication either before or in early pregnancy. 46,47 For each individual woman this is likely to result from an informal ‘risk–benefit’ evaluation, which may include a range of factors such as previous medical history, current state of illness, likelihood of relapse in pregnancy and postpartum, family circumstances, known teratogenic risks and fear of doing harm to the unborn child. 4,14,20 For some women the answer to this evaluation is ‘clear-cut’ with the benefits of continuing treatment in pregnancy noticeably outweighing the potential risks. 4,12,18,20 For example, this may be the case if they were to experience an acute psychiatric episode or have previously experienced postnatal psychosis. For other women potential teratogenic risks will clearly outweigh the potential benefits to the mother’s health of continued psychotropic treatment. One might expect such women to discontinue treatment at the beginning of pregnancy and then restart treatment when the perceived teratogenic risk is lower, such as after the first trimester, after delivery or after they finish breastfeeding. Yet, although our study on restarting of treatment suggested that a large proportion of the women restarted treatment, no clear patterns in the timing of restarting were observed. This suggests that for many women it may be far less straightforward to balance the risks and benefits of using psychotropic medication in pregnancy. The occurrence of an acute event/relapse of mental illness after discontinuation may further complicate decisions around restarting of psychotropic medication. However, our analyses shows that little of the information recorded in the women’s electronic health records prior to pregnancy were predictive of continuation as well as restarting of psychotropic medication.
We performed comprehensive studies on the risks associated with prescribing of psychotropic medication in pregnancy. The results of our cohort studies on antipsychotics and anticonvulsant mood stabilisers demonstrate on the one hand that women prescribed anticonvulsant mood stabilisers, in particular valproate, were at increased risk of giving birth to a child with major congenital malformation in comparison with women who were not prescribed these medications and women who discontinued treatment before pregnancy. Our analyses also suggest that children born to women prescribed anticonvulsant mood stabilisers, and again in particular valproate, were at elevated risk of giving birth to a child who later had records of neurodevelopmental or behavioural disorders. On the other hand, we observed no risk of major congenital malformations for women prescribed antipsychotics in pregnancy. This confirms previous research and recent guidelines. 12,18,19,56,58,59 There are, however, some studies that suggest associations between antipsychotic treatment in pregnancy and adverse maternal and child outcomes, but most previous research has not been able to account for potential confounding19 and our research reveals that these associations are likely to be confounded by the health, lifestyle characteristics and concomitant medication. In addition, it is important to recognise that although antipsychotics may not increase the risk of adverse maternal and child outcomes per se, many of the women prescribed antipsychotics in pregnancy may be more likely to experience some of the adverse outcomes because of other factors such as obesity, alcohol problems, smoking and illicit drug use.
In this project we have not been able to fully address the question about benefits of psychotropic medication in pregnancy. One obvious benefit of continuation of psychotropic medication in pregnancy would be prevention of relapse of mental illnesses in pregnancy and postpartum psychosis. However, electronic health records, such as THIN and the CPRD, are not well suited to address questions about the benefits of treatment with psychotropic medication in pregnancy for various reasons. First, the decision to prescribe psychotropic medication in pregnancy is likely to be driven by the prognosis of future illness (as well as the current status of the women’s mental health). This clinical judgement is not recorded well in electronic health records and, therefore, it is difficult, if not impossible, to identify comparison groups to evaluate effectiveness of psychotropic drugs in preventing relapse and/or postpartum psychosis using data that are based on clinical management. 113 Second, it may be challenging to clearly define what constitutes a relapse or deterioration of mental illnesses based on the records in primary care databases, as GPs may not enter this directly in the patient electronic records. Finally, as we highlight in Chapter 7, Lived experience advisory panel meetings, the evaluation of risks and benefits of psychotropic medication may reach much further for the individual woman and include a number of social aspects as well as medical conditions/outcomes. However, the social aspects are unlikely to be well defined/recorded in electronic health records.
Strengths and limitations
The overall strength of this project is that it relies on ‘real-life’ data on psychotropic medication prescribed to women of childbearing potential in UK primary care. To our knowledge it is the largest study to date and most comprehensive study of its kind. The study utilised the detailed prescribing information available in primary care databases to thoroughly investigate the prescribing of psychotropic medication in and around pregnancy. Below we outline some of the challenges and limitations specific to this project, including the identification of pregnancies, misclassification of exposures, outcomes and covariates, confounding and comparison cohorts, and statistical testing. Notably, most of these limitations are linked to the fact that primary care electronic health records are designed for clinical management rather than research, and therefore data on important factors are often incomplete.
Identification of pregnancies
The primary care databases used in this project are broadly representative of the UK population. 27,28 However, any subcohorts selected from within these databases may have been selective in terms of inclusion/exclusion of certain individuals. Although we made a great effort to ensure that our algorithm would have captured the vast majority of eligible pregnancies recorded in primary care electronic health records, we cannot exclude that a few women would have received parts of their antenatal and postnatal care in specialist and hospital settings. This may not be fully captured in their primary care records. Likewise, we were only able to capture mother–child dyads if the child was registered with the same general practice as the mother.
Many pregnancy studies using electronic healthcare records, including our study, exclude pregnancies ending in spontaneous or induced terminations as it is difficult to accurately identify the duration of many of these pregnancies. This can lead to selection bias whereby major congenital malformations that are more likely to result in terminations are not accounted for. 114 In short, a selection bias can arise if two conditions are met: (1) the proportion of, for example, major congenital malformations are different in those who terminated compared with those who did not terminate and (2) the proportion of those who terminated are different among exposed and unexposed. If just one of these conditions is met the effects will cancel out in relative estimates. There are some studies that suggest women on antipsychotic treatment are more likely to terminate pregnancies than women not treated with antipsychotics in different parts of the world. 77,115 However, our sensitivity analyses to evaluate the potential impact on excluding pregnancies that ended in terminations suggest that these were unlikely to have a major impact on our study findings (see Appendix 1).
Misclassification of exposure, outcome and covariates
As we utilised data recorded for the purpose of clinical management of patients, it is likely that some misclassification of exposure, outcome and covariate status may have occurred. In particular, there may be some discrepancies between prescribing data and actual drug consumption. Studies from different countries including the UK, the USA and the Netherlands have thus reported varying rates of prescription redemption. 116–120 We are aware that pregnancy may be a period during which women are particularly susceptible to non-adherence/non-compliance and if there is a genuine effect of a drug exposure this effect may be diluted by such exposure misclassification. In our studies women in cohort B would have received prescriptions of psychotropic medication both before and during the first trimester. This may increase the likelihood that the women were actually using the treatment. In terms of our outcomes we were unable to validate the prevalence of each outcome, but we noted that several of our prevalence estimates were close to previous published prevalence figures associated with specific drug exposures. 33,48 On the other hand, our prevalence rates for perinatal death were lower than figures from the ONS suggesting that not all events have been captured in primary care records.
For some of our covariates we observed a large proportion of missing data, for example, for ethnicity and deprivation scores (Townsend). We reported the level of missing data on each of these variables, but the high proportion of missing data limited the use of these variables in the further analysis. Therefore, we cannot exclude confounding by ethnicity and social deprivation.
Confounding and comparison cohorts
As mentioned previously (see Chapter 4, Psychotropic medication exposures), one way we sought to investigate the potential issues of confounding was by selecting multiple comparison groups (cohorts A and C) and, specifically for anticonvulsant mood stabilisers, by comparing the risks of adverse maternal and child outcomes between women prescribed valproate compared with other anticonvulsant mood stabilisers. For other classes of psychotropic medication we felt the sample sizes would have been too small for between-drug comparisons. As we noted previously (see Chapter 4, Characteristics of the women in the pregnancy cohort and Characteristics of the children in the mother–child study cohorts), the measured characteristics of women who continued treatment in pregnancy (cohort B1) and women who were not on treatment (cohort C) differed substantially. In general, the women in cohort A and B1 were more similar to each other than to women in cohort C; therefore, it seems likely that cohort A and B1 (B2) were closer to each other in terms of unmeasured characteristics and the resulting analysis less likely to be subject to confounding. Thus, in the analysis of valproate (see Table 37) we observed a twofold increase in major congenital malformations when comparing cohort B with cohort C. However, the effect attenuated when we compared cohort B with A and when we compared women prescribed valproate with other anticonvulsants. We are aware, however, that there is still likely to be some substantial differences between women who discontinue treatment before pregnancy and those who continue psychotropic medication in pregnancy, which will result in residual confounding.
Statistical testing and type 1 errors
Owing to the large number of statistical analyses included in this project we cannot exclude that some of the results might be statistically significant by chance (with an alpha level of 5% this may be the case for approximately 1 out of 20 tests). However, we have sought to minimise the number of tests by combining various child outcomes into poor birth outcomes, transient poor birth outcomes, and neurodevelopmental and behavioural outcomes. We discuss the limitations of this approach in Chapter 4, Child outcomes. In general we have sought to provide more emphasis on the actual estimates and their 95% CIs rather than p-values when we interpreted the results of the analyses.
Chapter 6 Conclusions and recommendations
Conclusions
The use of psychotropic drugs around pregnancy has increased with an increasing number of women using atypical antipsychotics, lamotrigine and, the potentially teratogenic drug, valproate. However, our findings indicate that many women discontinue treatment before or during early pregnancy and then restart again in late pregnancy or after delivery. Lithium continues to be prescribed around pregnancy but its use is decreasing.
Our results support previous findings of associations between valproate prescribed in pregnancy and major congenital malformations as well as neurodevelopmental or behavioural disorders. In contrast, our study offers no support for the discontinuation of antipsychotic medication in pregnancy in order to reduce the risk of gestational diabetes. The increased risk of adverse maternal and child outcomes in women who continue antipsychotic treatment in pregnancy may be associated with health and lifestyle factors (obesity, smoking, alcohol abuse and illicit drug use, and concomitant medication) rather than specific drug effects. It was not possible to investigate the risk associated with lithium use or anticonvulsant use specifically for psychoses owing to the small numbers of women in these groups.
Recommendations
Below we outline our recommendations for further research and implications of our research for clinical practice.
Valproate
Our findings suggest that women who are prescribed valproate in pregnancy are at an increased risk of giving birth to a child with major congenital malformations as well as neurodevelopmental and behavioural disorders. At the same time, we observed that valproate was still commonly prescribed both before and during pregnancy in women with a record of psychosis or recent depression. Therefore, we recommend further research is conducted to: (1) describe the utilisation of valproate in women of childbearing potential in terms of sociodemographics and underlying illnesses and (2) investigate how use of valproate can be curtailed in women of childbearing potential.
Benefits of continuing psychotropic medication
Further studies are needed to quantify the potential benefits of continuation of psychotropic treatment in pregnancy, but as we outlined in Chapter 5, Risks and benefits of psychotropic medication in pregnancy, it is difficult to address this in data collected for clinical management owing to confounding, that is, women who are at high risk of relapse and/or postpartum psychoses may be more likely to continue psychotropic medication in pregnancy. We recommend that a study be set up to evaluate the feasibility of a RCT to examine if the use of antipsychotics in pregnancy can reduce the risk of relapse and/or postpartum psychoses. Such a study should evaluate sample size for the RCT, whether or not it would be feasible to recruit women and potential barriers for recruitment. This should be done by interviewing health-care professionals (psychiatrists, GPs, obstetricians and midwives) as well as women prescribed psychotropic medication.
Associations between health and lifestyle factors, and adverse pregnancy outcomes
Our findings highlight that the characteristics of many women who continue psychotropic medication in pregnancy differed substantially from women who discontinued or were not prescribed psychotropic medication. Further research is needed to investigate the risks associated with alcohol abuse, illicit drug use and obesity in women with psychosis who then become pregnant.
Implication for clinical practice
The results of our research reinforce the guidance provided in the 2014 NICE guidelines. 12,59 Furthermore, our studies highlight the relationship between general health and lifestyle factors and the risks of adverse maternal and child outcomes in women who are prescribed psychotropic medication in pregnancy. Health-care providers should be alerted to the fact that many of the women prescribed psychotropic medication may be at a heightened risk of giving birth to a child with major congenital malformations caused by obesity, alcohol abuse, illicit drug use and concomitant use of anticonvulsants.
Chapter 7 Patient and public involvement
Introduction
Patient and public involvement (PPI) in research is a part of the National Institute for Health Research HTA programme and is actively supported by major UK funding bodies. The level and type of involvement and engagement varies between projects. It is now common to see service user representatives on research study steering groups and other approaches to PPI are increasingly being applied to UK-funded research. In this project we developed a plan for extensive engagement with service users through the charity Rethink Mental Illness. This involved recruiting a lived experience advisory panel (LEAP) of mental health service users to follow the study and examine its results in order to assist the research team with developing practical guidance and communication based on the findings. At the start of the project we initiated discussions with members of staff from Rethink Mental Illness to set up and develop the LEAP. However, in 2013, Rethink Mental Illness underwent a restructure and was no longer able to support these activities. Rather, they recommended that we continued our PPI with The McPin Foundation, which is a mental health research charity. In this chapter we report on the work with The McPin Foundation and the LEAP at key stages of the research.
Lived experience advisory panel
Recruitment of lived experience advisory panel
The LEAP was recruited by The McPin Foundation through open advert. We sought to work with women who would be able to draw on their own experiences. The following criteria were therefore developed:
-
women who currently or recently have been prescribed psychotropic medication (antipsychotics, lithium or anticonvulsant mood stabilisers)
-
women who have been pregnant or considered becoming pregnant
-
women who have experienced, or have a demonstrable interest in research.
The selection of the panel was carried out by staff at The McPin Foundation and in this process they carefully considered the experiences the women were able to share with the project team and how comfortable they felt using lived experience in a research study as advisors. It was also a requirement that they were willing to commit to the study for 12 months and be available to work flexibly, as meetings would happen in stages. The members of the LEAP were paid for their travel and their time participating in meetings.
Lived experience advisory panel meetings
An information meeting was held at The McPin Foundation in summer 2013 for four women who were interested in this study, and all women decided to join the LEAP. The women had a range of experiences relevant to the study. One member had experienced pregnancy and had children, whereas others had considered, or were considering, starting a family. The initial function of the LEAP was to provide advice and guidance on the risks and benefits of psychotropic medication use and pregnancy from the mental health service user’s perspective. The full advisory panel met face to face with members of the research team on four occasions – July 2013, August 2013, May 2014 and September 2014. Two members of the advisory panel also met with IP in May 2015 to discuss key findings from the project and one further meeting is planned to focus on dissemination of study findings.
Initially, the members of the advisory panel were invited to comment on women’s discontinuation of psychotropic medication and the advisory panel were shown graphs from our work on discontinuation of psychotropic medication in pregnancy (see Chapter 3, Discontinuation and factors associated with continuation of psychotropic medication in pregnancy). The advisory panel then drew on their own experiences and reflected on factors that may influence discontinuation of psychotropic medication. A summary of the factors that the panel felt may be associated with the decision to continue or discontinue psychotropic medication is listed below:
-
Planned versus unplanned pregnancies.
-
Who is prescribing the psychotropic medicine, for example consultant or GP?
-
Where do women seek their advice?
-
Current dose of psychotropic medication.
-
Length of diagnosis history.
-
Relapse history (number of relapses).
-
Moving to other psychotropic medication as an option. Experience of this in the past.
-
Have they been offered alternative therapy if coming off medicine, for example cognitive–behavioural therapy?
-
Relationship status: partner/married/no stable relationship.
-
Culture, ethnicity factors linked to beliefs about medication.
-
Age.
-
Previous pregnancy history.
-
Previous miscarriages.
-
Number of different psychotropic medications, for example a woman might come off antipsychotics but stay on antidepressants.
-
Weight loss/gain/obesity (strategy for weight management).
-
History of postpartum psychosis.
-
Some women may restart medication in second or third trimester?
-
Are women who are told they cannot come off psychotropic medication more likely to terminate?
-
Social issues: friends, family and their opinion of whether or not you should continue your medication when you are pregnant.
-
Social class: stigma of mental health medication – the way women who take medication perceive themselves.
-
-
Past experiences of medication discontinuation.
We found this discussion very helpful and were able to incorporate some of these factors, where possible, in our further analysis and discussion (see Chapter 3, Discontinuation and factors associated with continuation of psychotropic medication and Chapter 3, Discussion).
We also sought the advisory panel’s opinion about adverse outcomes of pregnancy and how to classify these. During these discussions it became clear that the advisory panel felt that it was necessary to take a broader perspective on the mother’s general functioning, well-being and the wider family. Hence, it was not enough just to focus on adverse pregnancy outcomes such as birth defects. It was discussed whether or not it would be possible to ‘rank’ the adverse outcomes, but the LEAP did not feel that was neither possible nor appropriate. Some of the points raised in the discussion are listed below:
-
Obstetricians are likely to have a very different focus from the pregnant woman – likely to focus on health only
-
Women are more interested in social aspects, for example:
-
they want to be well functioning mothers
-
they want to meet other new mothers
-
they want to provide consistent care to their baby
-
they want to breastfeed.
-
-
Concern about the involvement of social services.
-
Fear of a major deterioration in the long term after pregnancy – this is not just a fear of relapse, but a fear that it might take longer to find stability after pregnancy than before.
-
Women want to enjoy pregnancy – they do not want to come off drugs that keep them happy.
-
Some mothers would not mind a disabled child – it would be loved just as much. Others would feel guilt for having taken drugs.
-
‘Whatever you do will be wrong.’
-
Quality of life is a key factor for women – what is the point of having a baby if you are too ill to enjoy it?
-
The quality of mental health input is important, just as much as what is provided.
-
The experience of a first pregnancy may affect the choice to have further children.
-
Some women may decide not to have children – there is no right decision to make.
-
Concern about having a premature baby.
-
Concern about bonding with the baby if the mother is poorly or in hospital.
-
Concern about not being able to breastfeed if on medication – the child will miss out on the benefits of breastfeeding.
-
Concern about the mother harming the baby when she is ill.
-
Concern about neglect of the child but also the mother neglecting herself.
-
Support for new mothers tails off over time, but the baby’s needs actually get more complex over time – language and social development.
-
The biggest fear is an incapacitating relapse – psychosis or depression. If you do not get the early bonding days you can never get them back.
-
Concern about social services taking the child away at birth.
-
Adverse outcomes for the child include:
-
permanent disability
-
lack of stability
-
losing mother to suicide
-
not having care needs met
-
being harmed by mother during a psychotic episode.
-
-
Fear about having a disabled child – if this happened, the mother would feel guilty that medication might have caused it, and this guilt might impair the mother’s relationship with the child. The mother may also feel anxiety that some disability might show up later – this anxiety might have a further impact on the relationship with the child.
-
Concern about passing on the mental illness to the child.
-
Concern about drug withdrawal for the child after birth.
-
This is a great big spider’s web – drugs are just one tiny part.
-
Does the baby get brothers and sisters? The woman must decide whether or not to have further children. Is a woman more likely to keep taking medication if she did this in a previous pregnancy?
-
The woman’s partner does not want to see her go through the struggle again – this may lead to a decision to have no further children.
-
A lot of the adverse outcomes are actually risk factors for future illness rather than actual negative outcomes themselves.
-
Pre-eclampsia can be managed.
Finally, we sought the opinion from the advisory panel on the interpretation of some of the key findings from the project and decisions around the cohort definitions. For example, we discussed reasons why some women may not have a record of psychosis despite being prescribed psychotropic medication and the panel provided a range of explanations. The panel felt it is likely that many GPs would not want to label women with a diagnosis early on and may decide to try antipsychotic treatment, for example to deal with the symptoms before making a more definite diagnosis. We also sought the panel’s opinion on the characteristics of cohorts of women who continued psychotropic medication in pregnancy (cohort B) in our studies of absolute and relative risks of psychotropic medication in pregnancy (see Chapter 4). The advisory panel highlighted that the findings from our study did match up with the ‘picture’ of mental health service users on antipsychotics in terms of health and lifestyle factors as well as concomitant medication. Again, the advisory panel emphasised that drug exposure in pregnancy should be considered in a much broader context and we discussed the potential of ‘self-medication’ with alcohol and the impact of illicit drug use/methadone on potential adverse pregnancy and birth outcomes. As one member of the advisory panel suggested ‘for some women the antipsychotics is the least of their problems’.
Inspired by this project and the preliminary findings, The McPin Foundation decided to work with the four members of the advisory panel on an independent study. In this study the women interviewed other women with severe mental illnesses, who had given birth in the previous 5 years, about their decision to continue or discontinue psychotropic medication in pregnancy. The women from the advisory panel developed a protocol and, following ethical approval, interviewed 12 women with support from The McPin Foundation and University College London staff during 2013 and 2014. Although these interviews were not a part of this project, the advisory panel drew on the experiences and insights that they gained from these interviews in our subsequent discussions about risks and benefits of psychotropic medication in pregnancy. For example, it came out of these interviews that many women find it very difficult to access information on risks and benefits of psychotropic medication in pregnancy. Many websites were based on US data and drug names and, therefore, proved difficult to apply into UK settings.
Lived experience advisory panel impact on project and vice versa
The discussions with the advisory panel have helped inform the interpretations and discussion sections of this report and published papers. 46,47 Our work with the advisory panel has, in particular, drawn our attention to the women’s dilemma in balancing their own health needs with that of the unborn child.
At the first advisory panel meeting, IP gave a presentation to introduce electronic health records research and the project on risks and benefits of psychotropic medication. Although some of the advisory panel members had previous experience of research methodology from Doctor of Philosophy and/or Master’s courses, electronic health records research and the challenges of working with clinical records were new to the majority of the panel members. We also hosted a specific session where RLM gave an introduction to statistical analysis to help advisory panel members understand the methodologies being applied in the project and for appraisal of scientific papers. One member of the advisory panel was fully versed with statistical procedures, but welcomed the opportunity to discuss these in further detail. Another member commented: ‘I found this a valuable development opportunity which helped me as a LEAP member feel more confident’.
The advisory panel members sometimes found it emotionally demanding, as talking about their personal experiences of managing severe mental illness, decisions around motherhood and medication use involved considerable challenges. This was something that the staff at The McPin Foundation was aware of and provided support for the individual women as necessary.
We plan to continue our work with the advisory panel to develop material for dissemination and will also seek feedback from the advisory panel on the contents of scientific papers arising from this project.
Strengths, limitations and recommendations for future public and patient engagement
We found the experience of working with the advisory panel valuable in many ways. In particular, we have benefited from listening to debates among the members of the advisory panel. We also found it helpful to be able to pose specific questions relating to use of psychotropic medication. It would have been difficult to have had the same level of discussions and insight from the service users had we just had a single individual attending steering group meetings.
A lived experienced advisory panel requires substantial resources and time from both organisers and participants. Over the course of the project we saw changes in the staff at The McPin Foundation who managed the advisory panel and there were periods where members of the advisory panel were less active because of relapse of illness or other demands on their time (work and/or studies). However, despite this, all women took an active part in the advisory panel over the course of the study.
Although the work of the advisory panel informed the development of the project and the discussion and synthesis of the study results, we did not expect direct involvement from the advisory panel in the research process or write up of the project. For future projects involving a LEAP the level of direct engagement in the research process may vary and we recommend that the role and activities of the advisory panel be clearly mapped out at the planning stage and evaluated over the course of the project.
Acknowledgements
Contributions of authors
Irene Petersen (Reader in Epidemiology and Statistics). IP was principal investigator on the project and managed the project on a day-to-day basis. She led the development of the original project protocol, developed data management and analysis plans for the individual studies in collaboration with RLM, CJS and IN. IP drafted the first version of the report with input from the remaining authors. She also led the write-up of the first paper arising from this project and was senior author on the second paper. 46,47 IP first developed the pregnancy and mother–child cohorts that were the basis for this project. She later worked with RLM and CS on further development of the cohorts and to identify and remove duplicates in THIN and the CPRD. IP worked with the LEAP together with RLM and FS.
Rachel L McCrea (Research Associate in Statistics). RLM developed the data management and analysis plans in collaboration with IP, CJS and IN. RLM conducted the data extraction and analysis on the studies described in Chapter 3 and contributed to the writing of this document. Furthermore, RLM led the write-up of the results from the study on Lithium prescribing during pregnancy for publication in PLOS ONE. 46 RLM participated in meetings with the LEAP and provided training for the panel on statistical analysis methodology.
Cormac J Sammon (Research Associate in Epidemiology and Statistics). CJS joined the team in September 2014 and conducted the data extraction and analysis on the studies described in Chapter 4 and contributed to the writing of this document. He combined the records from THIN and the CPRD, and removed the duplicates. He worked with IP, RLM and IN in developing data management and analysis plans for the individual studies.
David PJ Osborn (Professor of Psychiatry). DO was a coapplicant on the project and a member of the steering committee. He contributed to the discussion and interpretation of the study results from a clinical perspective.
Stephen J Evans (Professor of Statistics). SE was a coapplicant on the project and a member of the steering committee. He contributed to the development of the study design, discussion and interpretation of the study results from a pharmacoepidemiological perspective.
Phillip J Cowen (Professor of Psychiatry) PJC was a coapplicant on the project and a member of the steering committee. He contributed to the discussion and interpretation of the study results from a clinical perspective.
Nick Freemantle (Professor of Clinical Statistics). NF was a coapplicant on the project and a member of the steering committee. He helped in developing the study design and contributed to the discussion of the study results.
Irwin Nazareth (Professor of Primary Care). IN was a coapplicant on the project and a member of the steering committee and project management group. He contributed to the development of the cohort definitions, reviewed Read code lists and contributed to the development of the data management and analysis plans in collaboration with IP, CJS and RLM. He contributed to the discussion and interpretation of the study results from a clinical perspective.
Other contributions and publications
We thank Charlotte Walker, Ceri Dare, Ruth Lambley and Harminder Kaur for providing feedback and input to the project as a member of a LEAP. We would also like to thank Vanessa Pinfold, director of The McPin Foundation, Sarah Hamilton and other members of staff at The McPin Foundation for setting up and managing the LEAP. Finally, we would like to thank Fiona Stevenson (senior lecturer), University College London for supporting meetings with the LEAP.
Publications
The work from this project has so far resulted in two publications:
Petersen I, McCrea RL, Osborn DJP, Evans S, Pinfold V, Cowen PJ, et al. Discontinuation of antipsychotic medication in pregnancy: a cohort study. Schizophr Res 2014;59:218–25.
McCrea RL, Nazareth I, Evans SJW, Osborn DPJ, Pinfold V, Cowen PJ, et al. Lithium prescribing during pregnancy: a UK primary care database study. PLOS ONE 2015;10:e0121024.
Data sharing statement
Data for this study were obtained from THIN primary care database and the CPRD. A licence to the data can be obtained from Cegedim Strategic Data Medical research, for further details please see (www.csdmruk.imshealth.com) or CPRD www.cprd.com/intro.asp. Access to the data is subject to a licence fee.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Einarson A, Boskovic R. Use and safety of antipsychotic drugs during pregnancy. J Psychiatr Pract 2009;15:183-92. http://dx.doi.org/10.1097/01.pra.0000351878.45260.94.
- Hayes J, Prah P, Nazareth I, King M, Walters K, Petersen I, et al. Prescribing trends in bipolar disorder: cohort study in the United Kingdom THIN primary care database 1995–2009. PLOS ONE 2011;6. http://dx.doi.org/10.1371/journal.pone.0028725.
- Prah P, Petersen I, Nazareth I, Walters K, Osborn D. National changes in oral antipsychotic treatment for people with schizophrenia in primary care between 1998 and 2007 in the United Kingdom. Pharmacoepidemiol Drug Saf 2012;21:161-9. http://dx.doi.org/10.1002/pds.2213.
- Epstein RA, Moore KM, Bobo WV. Treatment of bipolar disorders during pregnancy: maternal and fetal safety and challenges. Drug Healthc Patient Saf 2015;7:7-29. http://dx.doi.org/10.2147/DHPS.S50556.
- Gitlin M, Frye MA. Maintenance therapies in bipolar disorders. Bipolar Disord 2012;14:51-65. http://dx.doi.org/10.1111/j.1399-5618.2012.00992.x.
- Yonkers KA, Wisner KL, Stowe Z, Leibenluft E, Cohen L, Miller L, et al. Management of bipolar disorder during pregnancy and the postpartum period. Am J Psychiatry 2004;161:608-20. http://dx.doi.org/10.1176/appi.ajp.161.4.608.
- Marston L, Nazareth I, Petersen I, Walters K, Osborn DPJ. Prescribing of antipsychotics in UK primary care: a cohort study. BMJ Open 2014;4. http://dx.doi.org/10.1136/bmjopen-2014-006135.
- Verdoux H, Tournier M, Bégaud B. Antipsychotic prescribing trends: a review of pharmaco-epidemiological studies. Acta Psychiatr Scand 2010;121:4-10. http://dx.doi.org/10.1111/j.1600-0447.2009.01425.x.
- Howard LM. Fertility and pregnancy in women with psychotic disorders. Eur J Obstet Gynecol Reprod Biol 2005;119:3-10. http://dx.doi.org/10.1016/j.ejogrb.2004.06.026.
- Howard LM, Kumar R, Thornicroft G. Psychosocial characteristics and needs of mothers with psychotic disorders. Br J Psychiatry 2001;178:427-32. http://dx.doi.org/10.1192/bjp.178.5.427.
- McGrath JJ, Hearle J, Jenner L, Plant K, Drummond A, Barkla JM. The fertility and fecundity of patients with psychoses. Acta Psychiatr Scand 1999;99:441-6. http://dx.doi.org/10.1111/j.1600-0447.1999.tb00990.x.
- Antenatal and Postnatal Mental Health: Clinical Management and Service Guidance. London: NICE; 2014.
- Altshuler LL, Cohen L, Szuba MP, Burt VK, Gitlin M, Mintz J. Pharmacologic management of psychiatric illness during pregnancy: dilemmas and guidelines. Am J Psychiatry 1996;153:592-606. http://dx.doi.org/10.1176/ajp.153.5.592.
- Gentile S. Antipsychotic therapy during early and late pregnancy. A systematic review. Schizophr Bull 2008;36:518-44. http://dx.doi.org/10.1093/schbul/sbn107.
- Galbally M, Roberts M, Buist A. Perinatal Psychotropic Review Group . Mood stabilizers in pregnancy: a systematic review. Aust N Z J Psychiatry 2010;44:967-77. http://dx.doi.org/10.3109/00048674.2010.506637.
- Jones I, Craddock N. Bipolar disorder and childbirth: the importance of recognising risk. Br J Psychiatry 2005;186:453-4. http://dx.doi.org/10.1192/bjp.186.6.453.
- Galbally M, Snellen M, Lewis AJ. A review of the use of psychotropic medication in pregnancy. Curr Opin Obstet Gynecol 2011;23:408-14. http://dx.doi.org/10.1097/GCO.0b013e32834b92f3.
- Tomson T, Battino D. Teratogenic effects of antiepileptic drugs. Lancet Neurol 2012;11:803-13. http://dx.doi.org/10.1016/S1474-4422(12)70103-5.
- Coughlin CG, Blackwell KA, Bartley C, Hay M, Yonkers KA, Bloch MH. Obstetric and neonatal outcomes after antipsychotic medication exposure in pregnancy. Obstet Gynecol 2015;125:1224-35. http://dx.doi.org/10.1097/AOG.0000000000000759.
- Jones I, Chandra PS, Dazzan P, Howard LM. Bipolar disorder, affective psychosis, and schizophrenia in pregnancy and the post-partum period. Lancet 2014;384:1789-99. http://dx.doi.org/10.1016/S0140-6736(14)61278-2.
- Webb RT, Howard L, Abel KM. Antipsychotic drugs for non-affective psychosis during pregnancy and postpartum. Cochrane Database Syst Rev 2004;2. http://dx.doi.org/10.1002/14651858.cd004411.pub2.
- Webb RT, Howard L, Abel KM. Antipsychotic drugs for non-affective psychosis during pregnancy and postpartum. Cochrane Database Syst Rev 2009;2.
- Chisholm J. The Read clinical classification. Br Med J 1990;300. http://dx.doi.org/10.1136/bmj.300.6732.1092.
- Davé S, Petersen I. Creating medical and drug code lists to identify cases in primary care databases. Pharmacoepidemiol Drug Saf 2009;18:704-7. http://dx.doi.org/10.1002/pds.1770.
- Office for National Statistics . Census 2001. www.ons.gov.uk/ons/guide-method/census/census-2001/index.html (accessed 1 February 2016).
- Lis Y, Mann RD. The VAMP research multi-purpose database in the UK. J Clin Epidemiol 1995;48:431-43. http://dx.doi.org/10.1016/0895-4356(94)00137-F.
- Blak BT, Thompson M, Dattani H, Bourke A. Generalisability of The Health Improvement Network (THIN) database: demographics, chronic disease prevalence and mortality rates. Inform Prim Care 2011;19:251-5. http://dx.doi.org/10.14236/jhi.v19i4.820.
- Williams T, van Staa T, Puri S, Eaton S. Recent advances in the utility and use of the General Practice Research Database as an example of a UK Primary Care Data resource. Ther Adv Drug Saf 2012;3:89-9. http://dx.doi.org/10.1177/2042098611435911.
- Horsfall L, Walters K, Petersen I. Identifying periods of acceptable computer usage in primary care research databases. Pharmacoepidemiol Drug Saf 2013;22:64-9. http://dx.doi.org/10.1002/pds.3368.
- Maguire A, Blak BT, Thompson M. The importance of defining periods of complete mortality reporting for research using automated data from primary care. Pharmacoepidemiol Drug Saf 2009;18:76-83. http://dx.doi.org/10.1002/pds.1688.
- Cai B, Xu W, Bortnichak E, Watson DJ. An algorithm to identify medical practices common to both the General Practice Research Database and The Health Improvement Network database. Pharmacoepidemiol Drug Saf 2012;21:770-4. http://dx.doi.org/10.1002/pds.3277.
- British National Formulary. London: BMJ Group and Pharmaceutical Press; n.d.
- Morrow J, Russell A, Guthrie E, Parsons L, Robertson I, Waddell R, et al. Malformation risks of antiepileptic drugs in pregnancy: a prospective study from the UK Epilepsy and Pregnancy Register. J Neurol Neurosurg Psychiatry 2006;77:193-8. http://dx.doi.org/10.1136/jnnp.2005.074203.
- Man S-L, Petersen I, Thompson M, Nazareth I. Antiepileptic drugs during pregnancy in primary care: a UK population based study. PLOS ONE 2012;7. http://dx.doi.org/10.1371/journal.pone.0052339.
- Petersen I, Gilbert RE, Evans SJW, Man S-L, Nazareth I. Pregnancy as a major determinant for discontinuation of antidepressants. J Clin Psychiatry 2011;72:979-85. http://dx.doi.org/10.4088/JCP.10m06090blu.
- Margulis AV, Kang EM, Hammad TA. Patterns of prescription of antidepressants and antipsychotics across and within pregnancies in a population-based UK cohort. Matern Child Health J 2014;18:1742-52. http://dx.doi.org/10.1007/s10995-013-1419-2.
- Toh S, Li Q, Cheetham TC, Cooper WO, Davis RL, Dublin S, et al. Prevalence and trends in the use of antipsychotic medications during pregnancy in the U.S., 2001–2007: a population-based study of 585,615 deliveries. Arch Womens Ment Health 2013;16:149-57. http://dx.doi.org/10.1007/s00737-013-0330-6.
- Kallen B, Borg N, Reis M. The use of central nervous system active drugs during pregnancy. Pharmaceuticals 2013;6:1221-86. http://dx.doi.org/10.3390/ph6101221.
- Epstein RA, Bobo WV, Shelton RC, Arbogast PG, Morrow JA, Wang W, et al. Increasing use of atypical antipsychotics and anticonvulsants during pregnancy. Pharmacoepidemiol Drug Saf 2013;22:794-801. http://dx.doi.org/10.1002/pds.3366.
- Bobo WV, Davis RL, Toh S, Li D-K, Andrade SE, Cheetham TC, et al. Trends in the use of antiepileptic drugs among pregnant women in the US, 2001–2007: a medication exposure in pregnancy risk evaluation program study. Paediatr Perinat Epidemiol 2012;26:578-88. http://dx.doi.org/10.1111/ppe.12004.
- Kulaga S, Sheehy O, Zargarzadeh AH, Moussally K, Bérard A. Antiepileptic drug use during pregnancy: perinatal outcomes. Seizure n.d.;20:667-72. http://dx.doi.org/10.1016/j.seizure.2011.06.012.
- Cohen LS, Altshuler LL, Stowe ZN, Faraone SV. Reintroduction of antidepressant therapy across pregnancy in women who previously discontinued treatment. A preliminary retrospective study. Psychother Psychosom 2004;73:255-8. http://dx.doi.org/10.1159/000077745.
- Roca A, Imaz ML, Torres A, Plaza A, Subirà S, Valdés M, et al. Unplanned pregnancy and discontinuation of SSRIs in pregnant women with previously treated affective disorder. J Affect Disord 2013;150:807-13. http://dx.doi.org/10.1016/j.jad.2013.02.040.
- WHO Collaborating Centre for Drug Statistics Methodology . WHOCC – ATC DDD Index 2013. www.whocc.no/atc_ddd_index/ (accessed 15 December 2015).
- Mental Health Act 1983. London: The Stationery Office; 1983.
- McCrea RL, Nazareth I, Evans SJW, Osborn DPJ, Pinfold V, Cowen PJ, et al. Lithium prescribing during pregnancy: a UK primary care database study. PLOS ONE 2015;10. http://dx.doi.org/10.1371/journal.pone.0121024.
- Petersen I, McCrea RL, Osborn DJP, Evans S, Pinfold V, Cowen PJ, et al. Discontinuation of antipsychotic medication in pregnancy: a cohort study. Schizophr Res n.d.;159:219-25. http://dx.doi.org/10.1016/j.schres.2014.07.034.
- Reis M, Källén B. Maternal use of antipsychotics in early pregnancy and delivery outcome. J Clin Psychopharmacol 2008;28:279-88. http://dx.doi.org/10.1097/JCP.0b013e318172b8d5.
- Stephansson O, Granath F, Svensson T, Haglund B, Ekbom A, Kieler H. Drug use during pregnancy in Sweden – assessed by the Prescribed Drug Register and the Medical Birth Register. Clin Epidemiol 2011;3:43-50. http://dx.doi.org/10.2147/CLEP.S16305.
- Boden R, Lundgren M, Brandt L, Reutfors J, Kieler H. Antipsychotics during pregnancy: relation to fetal and maternal metabolic effects. Arch Gen Psychiatry 2012;69:715-21. http://dx.doi.org/10.1001/archgenpsychiatry.2011.1870.
- Diav-Citrin O, Shechtman S, Tahover E, Finkel-Pekarsky V, Arnon J, Kennedy D, et al. Pregnancy outcome following in utero exposure to lithium: a prospective, comparative, observational study. Am J Psychiatry 2014;171:785-94. http://dx.doi.org/10.1176/appi.ajp.2014.12111402.
- Nelson JC, Papakostas GI. Atypical antipsychotic augmentation in major depressive disorder: a meta-analysis of placebo-controlled randomised trials. Am J Psychiatry 2009;166:980-91. http://dx.doi.org/10.1176/appi.ajp.2009.09030312.
- Walker S, Permezel M, Berkovic S. The management of epilepsy in pregnancy. BJOG Int J Obstet Gynaecol 2009;116:758-67. http://dx.doi.org/10.1111/j.1471-0528.2009.02141.x.
- Meador K, Reynolds MW, Crean S, Fahrbach K, Probst C. Pregnancy outcomes in women with epilepsy: a systematic review and meta-analysis of published pregnancy registries and cohorts. Epilepsy Res 2008;81:1-13. http://dx.doi.org/10.1016/j.eplepsyres.2008.04.022.
- Harden CL, Meador KJ, Pennell PB, Hauser WA, Gronseth GS, French JA, et al. Practice parameter update: management issues for women with epilepsy – focus on pregnancy (an evidence-based review): teratogenesis and perinatal outcomes report of the Quality Standards Subcommittee and Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and American Epilepsy Society. Neurology 2009;73:133-41. http://dx.doi.org/10.1212/WNL.0b013e3181a6b312.
- Hernández-Díaz S, Smith CR, Shen A, Mittendorf R, Hauser WA, Yerby M, et al. Comparative safety of antiepileptic drugs during pregnancy. Neurology 2012;78:1692-9. http://dx.doi.org/10.1212/WNL.0b013e3182574f39.
- Tomson T, Marson A, Boon P, Canevini MP, Covanis A, Gaily E, et al. Valproate in the treatment of epilepsy in girls and women of childbearing potential. Epilepsia 2015;56:1006-19. http://dx.doi.org/10.1111/epi.13021.
- Wide K, Winbladh B, Källén B. Major malformations in infants exposed to antiepileptic drugs in utero, with emphasis on carbamazepine and valproic acid: a nation-wide, population-based register study. Acta Paediatrica 2004;93:174-6. http://dx.doi.org/10.1111/j.1651-2227.2004.tb00701.x.
- National Institute for Health and Care Excellence . Bipolar Disorder: The Assessment and Management of Bipolar Disorder in Adults, Children and Young People in Primary and Secondary Care 2014. http://guidance.nice.org.uk/cg185 (accessed 1 February 2016).
- Wen X, Meador KJ, Hartzema A. Antiepileptic drug use by pregnant women enrolled in Florida Medicaid. Neurology 2015;84:944-50. http://dx.doi.org/10.1212/WNL.0000000000001304.
- Christensen J, Grønborg TK, Sørensen MJ, Schendel D, Parner ET, Pedersen LH, et al. Prenatal valproate exposure and risk of autism spectrum disorders and childhood autism. JAMA 2013;309:1696-703. http://dx.doi.org/10.1001/jama.2013.2270.
- Viguera AC, Tondo L, Koukopoulos AE, Reginaldi D, Lepri B, Baldessarini RJ. Episodes of mood disorders in 2,252 pregnancies and postpartum periods. Am J Psychiatry 2011;168:1179-85. http://dx.doi.org/10.1176/appi.ajp.2011.11010148.
- Howard LM, Goss C, Leese M, Appleby L, Thornicroft G. The psychosocial outcome of pregnancy in women with psychotic disorders. Schizophr Res 2004;71:49-60. http://dx.doi.org/10.1016/j.schres.2004.01.003.
- Petersen I, McCrea RL, Lupattelli A, Nordeng H. Women’s perception of risks of adverse fetal pregnancy outcomes: a large-scale multinational survey. BMJ Open 2015;5. http://dx.doi.org/10.1136/bmjopen-2014-007390.
- Newport DJ, Stowe ZN, Viguera AC, Calamaras MR, Juric S, Knight B, et al. Lamotrigine in bipolar disorder: efficacy during pregnancy. Bipolar Disord 2008;10:432-6. http://dx.doi.org/10.1111/j.1399-5618.2007.00565.x.
- Viguera MD, Whitfield SD, Baldessarini MD, Newport MD, Stowe MD, Reminick BA, et al. Risk of recurrence in women with bipolar disorder during pregnancy: prospective study of mood stabilizer discontinuation. Am J Psychiatry 2007;164:1817-24. http://dx.doi.org/10.1176/appi.ajp.2007.06101639.
- Viguera AC, Nonacs R, Cohen LS, Tondo L, Murray A, Baldessarini RJ. Risk of recurrence of bipolar disorder in pregnant and nonpregnant women after discontinuing lithium maintenance. Am J Psychiatry 2000;157:179-84. http://dx.doi.org/10.1176/appi.ajp.157.2.179.
- Yonkers KA, Gotman N, Smith MV, Forray A, Belanger K, Brunetto WL, et al. Does antidepressant use attenuate the risk of a major depressive episode in pregnancy?. Epidemiology 2011;22:848-54. http://dx.doi.org/10.1097/ede.0b013e3182306847.
- McBride W. Thalidomide and congenital abnormalities. Lancet 1961;2. http://dx.doi.org/10.1016/S0140-6736(61)90927-8.
- Meador KJ, Baker G, Cohen MJ, Gaily E, Westerveld M. Cognitive/behavioral teratogenetic effects of antiepileptic drugs. Epilepsy Behav 2007;11:292-30. http://dx.doi.org/10.1016/j.yebeh.2007.08.009.
- Pilo C, Wide K, Winbladh B. Pregnancy, delivery, and neonatal complications after treatment with antiepileptic drugs. Acta Obstet Gynecol Scand 2006;85:643-6. http://dx.doi.org/10.1080/00016340600604625.
- Nordeng H, Ystrøm E, Einarson A. Perception of risk regarding the use of medications and other exposures during pregnancy. Eur J Clin Pharmacol 2010;66:207-14. http://dx.doi.org/10.1007/s00228-009-0744-2.
- Freemantle N, Calvert M, Wood J, Eastaugh J, Griffin C. Composite outcomes in randomized trials: greater precision but with greater uncertainty?. JAMA 2003;289:2554-9. http://dx.doi.org/10.1001/jama.289.19.2554.
- Henderson DC. Weight gain with atypical antipsychotics: evidence and insights. J Clin Psychiatry 2007;68:18-26.
- Anderson JL, Waller DK, Canfield MA, Shaw GM, Watkins ML, Werler MM. Maternal obesity, gestational diabetes, and central nervous system birth defects. Epidemiology 2005;16:87-92. http://dx.doi.org/10.1097/01.ede.0000147122.97061.bb.
- Brunner E, Falk DM, Jones M, Dey DK, Shatapathy CC. Olanzapine in pregnancy and breastfeeding: a review of data from global safety surveillance. BMC Pharmacol Toxicol 2013;14. http://dx.doi.org/10.1186/2050-6511-14-38.
- Goldstein DJ, Corbin LA, Fung MC. Olanzapine-exposed pregnancies and lactation: early experience. J Clin Psychopharmacol 2000;20:399-403. http://dx.doi.org/10.1097/00004714-200008000-00002.
- Kulkarni J, Worsley R, Gilbert H, Gavrilidis E, Van Rheenen TE, Wang W, et al. A prospective cohort study of antipsychotic medications in pregnancy: the first 147 pregnancies and 100 one year old babies. PLOS ONE 2014;9. http://dx.doi.org/10.1371/journal.pone.0094788.
- Newham JJ, Thomas SH, MacRitchie K, McElhatton PR, McAllister-Williams RH. Birth weight of infants after maternal exposure to typical and atypical antipsychotics: prospective comparison study. Br J Psychiatry n.d.;192:333-7. http://dx.doi.org/10.1192/bjp.bp.107.041541.
- Lin HC, Chen IJ, Chen YH, Lee HC, Wu FJ. Maternal schizophrenia and pregnancy outcome: Does the use of antipsychotics make a difference?. Schizophr Res 2010;116:55-60. http://dx.doi.org/10.1016/j.schres.2009.10.011.
- Habermann F, Fritzsche J, Fuhlbruck F, Wacker E, Allignol A, Weber-Schoendorfer C, et al. Atypical antipsychotic drugs and pregnancy outcome: a prospective, cohort study. J Clin Psychopharmacol 2013;33:453-62. http://dx.doi.org/10.1097/JCP.0b013e318295fe12.
- Diav-Citrin O, Shechtman S, Ornoy S, Arnon J, Schaefer C, Garbis H, et al. Safety of haloperidol and penfluridol in pregnancy: a multicenter, prospective, controlled study. J Clin Psychiatry 2005;66:317-22. http://dx.doi.org/10.4088/JCP.v66n0307.
- McKenna K, Koren G, Tetelbaum M, Wilton L, Shakir S, Diav-Citrin O, et al. Pregnancy outcome of women using atypical antipsychotic drugs: a prospective comparative study. J Clin Psychiatry 2005;66:444-9. http://dx.doi.org/10.4088/JCP.v66n0406.
- Sadowski A, Todorow M, Yazdani Brojeni P, Koren G, Nulman I. Pregnancy outcomes following maternal exposure to second-generation antipsychotics given with other psychotropic drugs: a cohort study. BMJ Open 2013;3. http://dx.doi.org/10.1136/bmjopen-2013-003062.
- Munk EM, Norgaard B, Gislum M, Mortensen PB, Sorensen HT. Use of antipsychotic drugs during pregnancy and the risk of adverse birth outcomes: a population-based cohort study. Schizophr Bull 2005;31:233-.
- Vigod SN, Gomes T, Wilton AS, Taylor VH, Ray JG. Antipsychotic drug use in pregnancy: high dimensional, propensity matched, population based cohort study. BMJ 2015;350. http://dx.doi.org/10.1136/bmj.h2298.
- Falterman CG, Richardson CJ. Small left colon syndrome associated with maternal ingestion of psychotropic drugs. J Pediatr 1980;97:308-10. http://dx.doi.org/10.1016/S0022-3476(80)80504-X.
- Medicines and Healthcare products Regulatory Agency . Drug Safety Update: Antipsychotics: Risk of Extrapyramidal Effects or Withdrawal Symptoms in Newborns n.d. www.gov.uk/drug-safety-update/antipsychotics-risk-of-extrapyramidal-effects-or-withdrawal-symptoms-in-newborns#further-information (accessed 14 November 2015).
- Taylor CL, Stewart R, Ogden J, Broadbent M, Pasupathy D, Howard LM. The characteristics and health needs of pregnant women with schizophrenia compared with bipolar disorder and affective psychoses. BMC Psychiatry 2015;15. http://dx.doi.org/10.1186/s12888-015-0451-8.
- Coppola D, Russo LJ, Kwarta RF, Varughese R, Schmider J. Evaluating the postmarketing experience of risperidone use during pregnancy – pregnancy and neonatal outcomes. Drug Saf 2007;30:247-64. http://dx.doi.org/10.2165/00002018-200730030-00006.
- Weinstein MR, Goldfield M. Cardiovascular malformations with lithium use during pregnancy. Am J Psychiatry 1975;132:529-31. http://dx.doi.org/10.1176/ajp.132.5.529.
- Cohen LS, Friedman JM, Jefferson JW, Johnson EM, Weiner ML. A reevaluation of risk of in utero exposure to lithium. JAMA 1994;271:146-50. http://dx.doi.org/10.1001/jama.1994.03510260078033.
- Jacobson SJ, Jones KL, Johnson K, Ceolin L, Kaur P, Sahn D, et al. A prospective multicenter study of pregnancy outcome following lithium exposure during the first trimester of pregnancy. Reprod Toxicol 1993;7. http://dx.doi.org/10.1016/0890-6238(93)90263-7.
- Troyer WA, Pereira GR, Lannon RA, Belik J, Yoder MC. Association of maternal lithium exposure and premature delivery. J Perinatol Off J Calif Perinat Assoc 1993;13:123-7. http://dx.doi.org/10.1097/00006254-199311000-00003.
- Kozma C. Neonatal toxicity and transient neurodevelopmental deficits following prenatal exposure to lithium: another clinical report and a review of the literature. Am J Med Genet A 2005;132A:441-4. http://dx.doi.org/10.1002/ajmg.a.30501.
- van der Lugt NM, van de Maat JS, van Kamp IL, Knoppert-van der Klein EA, Hovens JGFM, Walther FJ. Fetal, neonatal and developmental outcomes of lithium-exposed pregnancies. Early Hum Dev 2012;88:375-8. http://dx.doi.org/10.1016/j.earlhumdev.2011.09.013.
- Schou M. What happened later to the lithium babies? A follow-up study of children born without malformations. Acta Psychiatr Scand 1976;54:193-7. http://dx.doi.org/10.1111/j.1600-0447.1976.tb00112.x.
- Dolk H, Jentink J, Loane M, Morris J, de Jong-van den Berg LTW. EUROCAT Antiepileptic Drug Working Group . Does lamotrigine use in pregnancy increase orofacial cleft risk relative to other malformations?. Neurology 2008;71:714-22. http://dx.doi.org/10.1212/01.wnl.0000316194.98475.d8.
- Tomson T, Xue H, Battino D. Major congenital malformations in children of women with epilepsy. Seizure 2015;28:46-50. http://dx.doi.org/10.1016/j.seizure.2015.02.019.
- Eriksson K, Viinikainen K, Mönkkönen A, Äikiä M, Nieminen P, Heinonen S, et al. Children exposed to valproate in utero – population based evaluation of risks and confounding factors for long-term neurocognitive development. Epilepsy Res 2005;65:189-200. http://dx.doi.org/10.1016/j.eplepsyres.2005.06.001.
- Bromley RL, Mawer G, Clayton-Smith J, Baker GA. Autism spectrum disorders following in utero exposure to antiepileptic drugs. Neurology 2008;71:1923-4. http://dx.doi.org/10.1212/01.wnl.0000339399.64213.1a.
- Adab N, Tudur SC, Vinten J, Williamson P, Winterbottom J. Common antiepileptic drugs in pregnancy in women with epilepsy. Cochrane Database Syst Rev 2004;3. http://dx.doi.org/10.1002/14651858.cd004848.
- Meador KJ, Baker GA, Browning N, Cohen MJ, Bromley RL, Clayton-Smith J, et al. Fetal antiepileptic drug exposure and cognitive outcomes at age 6 years (NEAD study): a prospective observational study. Lancet Neurol 2013;12:244-52. http://dx.doi.org/10.1016/S1474-4422(12)70323-X.
- Meador KJ, Baker GA, Browning N, Clayton-Smith J, Combs-Cantrell DT, Cohen M, et al. Cognitive function at 3 years of age after fetal exposure to antiepileptic drugs. N Engl J Med 2009;360:1597-605. http://dx.doi.org/10.1056/NEJMoa0803531.
- Bromley R, Weston J, Adab N, Greenhalgh J, Sanniti A, McKay AJ, et al. Treatment for epilepsy in pregnancy: neurodevelopmental outcomes in the child. Cochrane Database Syst Rev 2014;10. http://dx.doi.org/10.1002/14651858.cd010236.pub2.
- Vinten J, Bromley RL, Taylor J, Adab N, Kini U, Baker GA. The behavioral consequences of exposure to antiepileptic drugs in utero. Epilepsy Behav 2009;14:197-201. http://dx.doi.org/10.1016/j.yebeh.2008.10.011.
- Hiilesmaa VK, Teramo K, Granström M-L, Bardy AH. Fetal head growth retardation associated with maternal antiepileptic drugs. Lancet 1981;318:165-7. http://dx.doi.org/10.1016/S0140-6736(81)90354-8.
- Wide K, Winbladh B, Tomson T, Källén B. Body dimensions of infants exposed to antiepileptic drugs in utero: observations spanning 25 years. Epilepsia 2000;41:854-61. http://dx.doi.org/10.1111/j.1528-1157.2000.tb00253.x.
- Hvas CL, Henriksen TB, Østergaard JR, Dam M. Epilepsy and pregnancy: effect of antiepileptic drugs and lifestyle on birthweight. BJOG Int J Obstet Gynaecol 2000;107:896-902. http://dx.doi.org/10.1111/j.1471-0528.2000.tb11089.x.
- Ebbesen F, Joergensen A, Hoseth E, Kaad P, Moeller M, Holsteen V, et al. Neonatal hypoglycaemia and withdrawal symptoms after exposure in utero to valproate. Arch Dis Child Fetal Neonatal Ed 2000;83:F124-9. http://dx.doi.org/10.1136/fn.83.2.F124.
- Nau H, Rating D, Koch S, Häuser I, Helge H. Valproic acid and its metabolites: placental transfer, neonatal pharmacokinetics, transfer via mother’s milk and clinical status in neonates of epileptic mothers. J Pharmacol Exp Ther 1981;219:768-77.
- Boden R, Lundgren M, Brandt L, Reutfors J, Andersen M, Kieler H. Risks of adverse pregnancy and birth outcomes in women treated or not treated with mood stabilisers for bipolar disorder: population based cohort study. BMJ 2012;345. http://dx.doi.org/10.1136/bmj.e7085.
- Freemantle N, Marston L, Walters K, Wood J, Reynolds MR, Petersen I. Making inferences on treatment effects from real world data: propensity scores, confounding by indication, and other perils for the unwary in observational research. BMJ 2013;347. http://dx.doi.org/10.1136/bmj.f6409.
- Levy A, Matok I, Gorodischer R, Sherf M, Wiznitzer A, Uziel E, et al. Bias toward the null hypothesis in pregnancy drug studies that do not include data on medical terminations of pregnancy: the folic acid antagonists. J Clin Pharmacol 2012;52:78-83. http://dx.doi.org/10.1177/0091270010390806.
- Gissler M, Artama M, Ritvanen A, Wahlbeck K. Use of psychotropic drugs before pregnancy and the risk for induced abortion: population-based register-data from Finland 1996–2006. BMC Public Health 2010;10. http://dx.doi.org/10.1186/1471-2458-10-383.
- van Geffen EC, Gardarsdottir H, van Hulten R, van Dijk L, Egberts AC, Heerdink ER. Initiation of antidepressant therapy: do patients follow the GP’s prescription?. Br J Gen Pract 2009;59:81-7. http://dx.doi.org/10.3399/bjgp09X395067.
- Beardon PH, McGilchrist MM, McKendrick AD, McDevitt DG, MacDonald TM. Primary non-compliance with prescribed medication in primary care. BMJ 1993;307:846-8. http://dx.doi.org/10.1136/bmj.307.6908.846.
- Fischer MA, Stedman MR, Lii J, Vogeli C, Shrank WH, Brookhart MA, et al. Primary medication non-adherence: analysis of 195,930 electronic prescriptions. J Gen Intern Med 2010;25:284-90. http://dx.doi.org/10.1007/s11606-010-1253-9.
- Leclerc E, Mansur RB, Brietzke E. Determinants of adherence to treatment in bipolar disorder: a comprehensive review. J Affect Disord 2013;149:247-52. http://dx.doi.org/10.1016/j.jad.2013.01.036.
- Prescribing Compliance, A Review of the Proportion of Prescriptions Dispensed. Leeds: NHS Information Centre for Health and Social Care; 2011.
- Hernán MA, Hernández-Díaz S, Werler MM, Mitchell AA. Causal knowledge as a prerequisite for confounding evaluation: an application to birth defects epidemiology. Am J Epidemiol 2002;155:176-84. http://dx.doi.org/10.1093/aje/155.2.176.
- Johnson CY, Honein MA, Dana Flanders W, Howards PP, Oakley GP, Rasmussen SA. Pregnancy termination following prenatal diagnosis of anencephaly or spina bifida: a systematic review of the literature. Birth Defects Res A Clin Mol Teratol 2012;94:857-63. http://dx.doi.org/10.1002/bdra.23086.
- Department of Health . Abortion Statistics, England and Wales: 2013 2014. www.gov.uk/government/statistical-data-sets/abortion-statistics-england-and-wales-2013 (accessed 1 February 2016).
- Office for National Statistics . Birth Summary Tables, England and Wales, 2013 2014. www.ons.gov.uk/ons/publications/re-reference-tables.html?edition=tcm%3A77-317529 (accessed 1 February 2016).
- EUROCAT . Prevalence Tables n.d. www.eurocat-network.eu/accessprevalencedata/prevalencetables (accessed 1 February 2016).
Appendix 1 Additional information
Details of combining records from The Health Improvement Network and Clinical Practice Research Datalink
Transformation of Clinical Practice Research Datalink into The Health Improvement Network data format
Although THIN and the CPRD contain data from general practices using similar software for patient management (Vision), the providers of each database restructure their data somewhat differently before releasing it for research use. As a result, before deduplication and analysis could be carried out it was necessary to transform the CPRD and THIN data into a similar format. This was a time-consuming process that required a good knowledge of the structure of both databases (a fact that should be taken into account by any researchers intending to carry out an analysis on a combined CPRD–THIN dataset in the future). Notably, while a single Read code list can be used to identify clinical events in both databases, no common identifiers for therapy (drugs) records and additional health data (AHD) records are available. As a result, separate lists of drug and AHD codes were derived for each database using the same search criteria.
Removal of duplicate practices
The datasets from THIN and the CPRD used in this study contain neither a common patient identifier nor a practice identifier. As a result, straightforward matching of patients on a single variable could not be carried out and alternative means of deduplication had to be pursued. The overlap between the two databases occurs at a practice level, that is, entire practices contribute to either one or both datasets. Our approach was therefore to identify those practices contributing to both datasets and ensure patients from these practices were included only once in the analysis. We combined patient- and practice-level comparisons; making patient-to-patient comparisons of longitudinal clinical records and then assessing whether or not these comparisons indicated the population of patients in the two practices matched to a sufficient extent. First, we identified practices where there was an overlap between individuals based on a subset of 20 Read coded events and their dates per individual. After running this pre-screening step the longitudinal medical record of each of the women in THIN was compared with the longitudinal records of the women in the dataset from the CPRD where we had initially identified an overlap. However, we excluded Read codes from chapter 8 as these are administrative codes which are likely to be common across many patients. We noticed there were a few individuals who matched across two or more practices, but few individuals matched within these practices. After manual review of these records we were able to exclude unlikely matches resulting in the identification of 358 practices which were likely to provide data to both THIN and the CPRD, equivalent to 63% of the THIN practices and 54% of the CPRD practices. We excluded records from THIN where these were duplicated in the CPRD in our further analyses.
Characteristics of women in exposure cohort B2
| Characteristics | Exposure cohort | ||
|---|---|---|---|
| A | B2 | C | |
| n (% or SD) | n (% or SD) | n (% or SD) | |
| Total | 670 (100) | 322 (100) | 318,434 (100) |
| Age (years) | |||
| Mean (SD) | 30 (5.9) | 33 (5.9) | 30 (5.9) |
| 12–19 | 21 (3.1) | 0 (0) | 14,004 (4.4) |
| 20–29 | 291 (43.4) | 107 (33.2) | 123,704 (38.8) |
| 30–39 | 326 (48.7) | 175 (54.3) | 165,353 (51.9) |
| 40–49 | 32 (4.8) | 40 (12.4) | 15,373 (4.8) |
| Year | |||
| 1995–9 | 42 (6.3) | 11 (3.4) | 46,548 (14.6) |
| 2000–4 | 184 (27.5) | 44 (13.7) | 80,542 (25.3) |
| 2005–9 | 232 (34.6) | 77 (23.9) | 99,765 (31.3) |
| 2010–12 | 212 (31.6) | 190 (59) | 91,579 (28.8) |
| Lifestyle variables | |||
| Obesity | 73 (10.9) | 56 (17.4) | 16,979 (5.3) |
| Illicit drug use | 56 (8.4) | 35 (10.9) | 2002 (0.6) |
| Alcohol problems | 37 (5.5) | 18 (5.6) | 1624 (0.5) |
| Smoker | 254 (37.9) | 152 (47.2) | 62,746 (19.7) |
| BMI (kg/m2) | |||
| Mean (SD) | 27 (6.8) | 29 (6.7) | 26 (6.3) |
| Underweight | 5 (0.7) | 4 (1.2) | 3632 (1.1) |
| Normal weight | 89 (13.3) | 40 (12.4) | 42,138 (13.2) |
| Overweight | 56 (8.4) | 39 (12.1) | 20,071 (6.3) |
| Obese | 77 (11.5) | 63 (19.6) | 20,554 (6.5) |
| Missing | 443 (66.1) | 176 (54.7) | 232,039 (72.9) |
| Townsend score | |||
| 1 | 24 (13.1) | 4 (6.7) | 71,024 (23.4) |
| 2 | 23 (12.6) | 10 (16.7) | 60,407 (19.9) |
| 3 | 37 (20.2) | 12 (20) | 64,868 (21.4) |
| 4 | 48 (26.2) | 14 (23.3) | 61,191 (20.2) |
| 5 | 51 (27.9) | 20 (33.3) | 45,942 (15.1) |
| Missing | 487 (72.7) | 262 (81.4) | 15,002 (4.7) |
| Ethnicity | |||
| White | 320 (47.8) | 176 (54.7) | 133,856 (42) |
| Mixed | 2 (0.3) | 1 (0.3) | 1786 (0.6) |
| Asian | 8 (1.2) | 9 (2.8) | 9937 (3.1) |
| Black | 7 (1) | 12 (3.7) | 4615 (1.4) |
| Other | 2 (0.3) | 2 (0.6) | 1803 (0.6) |
| Missing | 331 (49.4) | 122 (37.9) | 166,437 (52.3) |
| Use of psychiatric drugs during exposure period B2 | |||
| Hypnotics | 32 (4.8) | 42 (13) | 598 (0.2) |
| Anticonvulsant mood stabilisers | 11 (1.6) | 27 (8.4) | 1346 (0.4) |
| Lithium | 3 (0.4) | 8 (2.5) | 13 (0) |
| Antipsychotics | 0 (0) | 322 (100) | 0 (0) |
| Antidepressants | 145 (21.6) | 165 (51.2) | 4525 (1.4) |
| Anxiolytics | 22 (3.3) | 35 (10.9) | 612 (0.2) |
| Pre-existing medical conditions | |||
| Depression | 217 (32.4) | 69 (21.4) | 20,374 (6.4) |
| Epilepsy | 30 (4.5) | 27 (8.4) | 4846 (1.5) |
| SMI | 204 (30.4) | 220 (68.3) | 1480 (0.5) |
| Pre-existing hypertension | 66 (9.9) | 46 (14.3) | 26,232 (8.2) |
| Pre-existing diabetes | 9 (1.3) | 11 (3.4) | 2762 (0.9) |
| Characteristics | Exposure cohort | ||
|---|---|---|---|
| A | B2 | C | |
| n (% or SD) | n (% or SD) | n (% or SD) | |
| Total | 492 (100) | 233 (100) | 210,966 (100) |
| Age (years) | |||
| Mean (SD) | 30 (5.7) | 33 (5.9) | 30 (5.9) |
| 12–19 | 12 (2.4) | 0 (0) | 8955 (4.2) |
| 20–29 | 222 (45.1) | 77 (33) | 80,491 (38.2) |
| 30–39 | 236 (48) | 124 (53.2) | 110,839 (52.5) |
| 40–49 | 22 (4.5) | 32 (13.7) | 10,681 (5.1) |
| Year | |||
| 1995–9 | 25 (5.1) | 8 (3.4) | 13,339 (6.3) |
| 2000–4 | 134 (27.2) | 25 (10.7) | 46,707 (22.1) |
| 2005–9 | 173 (35.2) | 55 (23.6) | 77,626 (36.8) |
| 2010–12 | 160 (32.5) | 145 (62.2) | 73,294 (34.7) |
| Lifestyle variables | |||
| Obesity | 61 (12.4) | 42 (18) | 12,766 (6.1) |
| Illicit drug use | 40 (8.1) | 26 (11.2) | 1354 (0.6) |
| Alcohol problems | 28 (5.7) | 14 (6) | 1124 (0.5) |
| Smoker | 183 (37.2) | 115 (49.4) | 42,502 (20.1) |
| BMI (kg/m2) | |||
| Mean (SD) | 27 (6.8) | 29 (6.7) | 26 (6.4) |
| Underweight | 5 (1) | 3 (1.3) | 2494 (1.2) |
| Normal weight | 67 (13.6) | 27 (11.6) | 29,603 (14) |
| Overweight | 43 (8.7) | 29 (12.4) | 14,609 (6.9) |
| Obese | 62 (12.6) | 48 (20.6) | 15,363 (7.3) |
| Missing | 315 (64) | 126 (54.1) | 148,897 (70.6) |
| Townsend score | |||
| 1 | 16 (14.5) | 3 (7.5) | 47,381 (23.5) |
| 2 | 21 (19.1) | 8 (20) | 40,309 (20) |
| 3 | 19 (17.3) | 7 (17.5) | 43,152 (21.4) |
| 4 | 25 (22.7) | 8 (20) | 40,915 (20.3) |
| 5 | 29 (26.4) | 14 (35) | 30,120 (14.9) |
| Missing | 382 (77.6) | 193 (82.8) | 9089 (4.3) |
| Ethnicity | |||
| White | 256 (52) | 146 (62.7) | 104,928 (49.7) |
| Mixed | 2 (0.4) | 1 (0.4) | 1504 (0.7) |
| Asian | 7 (1.4) | 9 (3.9) | 7461 (3.5) |
| Black | 3 (0.6) | 9 (3.9) | 3446 (1.6) |
| Other | 2 (0.4) | 1 (0.4) | 1350 (0.6) |
| Missing | 222 (45.1) | 67 (28.8) | 92,277 (43.7) |
| Use of psychiatric drugs during exposure period B2 | |||
| Hypnotics | 28 (5.7) | 30 (12.9) | 423 (0.2) |
| Anticonvulsant mood stabilisers | 9 (1.8) | 18 (7.7) | 910 (0.4) |
| Lithium | 2 (0.4) | 7 (3) | 7 (0) |
| Antipsychotics | 0 (0) | 233 (100) | 0 (0) |
| Antidepressants | 115 (23.4) | 118 (50.6) | 3277 (1.6) |
| Anxiolytics | 17 (3.5) | 21 (9) | 373 (0.2) |
| Pre-existing medical conditions | |||
| Depression | 152 (30.9) | 54 (23.2) | 14,626 (6.9) |
| Epilepsy | 22 (4.5) | 15 (6.4) | 3254 (1.5) |
| SMI | 144 (29.3) | 158 (67.8) | 882 (0.4) |
| Pre-existing hypertension | 47 (9.6) | 37 (15.9) | 19,570 (9.3) |
| Pre-existing diabetes | 6 (1.2) | 8 (3.4) | 2005 (1) |
| Characteristics | Exposure cohort | ||
|---|---|---|---|
| A | B2 | C | |
| n (% or SD) | n (% or SD) | n (% or SD) | |
| Total | 57 (100) | 18 (100) | 212,531 (100) |
| Age (years) | |||
| Mean (SD) | 34 (5.1) | 35 (6.6) | 30 (5.9) |
| 12–19 | 0 (0) | 0 (0) | 8975 (4.2) |
| 20–29 | 14 (24.6) | 4 (22.2) | 81,287 (38.2) |
| 30–39 | 37 (64.9) | 10 (55.6) | 111,496 (52.5) |
| 40–49 | 6 (10.5) | 4 (22.2) | 10,773 (5.1) |
| Year | |||
| 1995–9 | 7 (12.3) | 2 (11.1) | 13,427 (6.3) |
| 2000–4 | 17 (29.8) | 4 (22.2) | 47,128 (22.2) |
| 2005–9 | 20 (35.1) | 5 (27.8) | 78,169 (36.8) |
| 2010–12 | 13 (22.8) | 7 (38.9) | 73,807 (34.7) |
| Lifestyle variables | |||
| Obesity | 8 (14) | 4 (22.2) | 12,982 (6.1) |
| Illicit drug use | 2 (3.5) | 0 (0) | 1453 (0.7) |
| Alcohol problems | 3 (5.3) | 2 (11.1) | 1188 (0.6) |
| Smoker | 15 (26.3) | 7 (38.9) | 43,146 (20.3) |
| BMI (kg/m2) | |||
| Mean (SD) | 27 (6.1) | 29 (4.5) | 26 (6.4) |
| Underweight | 0 (0) | 0 (0) | 2565 (1.2) |
| Normal weight | 8 (14) | 3 (16.7) | 29,842 (14) |
| Overweight | 5 (8.8) | 3 (16.7) | 14,713 (6.9) |
| Obese | 8 (14) | 4 (22.2) | 15,619 (7.3) |
| Missing | 36 (63.2) | 8 (44.4) | 149,792 (70.5) |
| Townsend score | |||
| 1 | 1 (8.3) | 0 (0) | 47,623 (23.4) |
| 2 | 3 (25) | 0 (0) | 40,530 (19.9) |
| 3 | 3 (25) | 3 (75) | 43,385 (21.3) |
| 4 | 3 (25) | 1 (25) | 41,380 (20.3) |
| 5 | 2 (16.7) | 0 (0) | 30,492 (15) |
| Missing | 45 (78.9) | 14 (77.8) | 9121 (4.3) |
| Ethnicity | |||
| White | 26 (45.6) | 13 (72.2) | 105,638 (49.7) |
| Mixed | 0 (0) | 0 (0) | 1505 (0.7) |
| Asian | 1 (1.8) | 1 (5.6) | 7476 (3.5) |
| Black | 1 (1.8) | 0 (0) | 3455 (1.6) |
| Other | 0 (0) | 0 (0) | 1360 (0.6) |
| Missing | 29 (50.9) | 4 (22.2) | 93,097 (43.8) |
| Use of psychiatric drugs during exposure period B2 | |||
| Hypnotics | 3 (5.3) | 2 (11.1) | 472 (0.2) |
| Anticonvulsant mood stabilisers | 3 (5.3) | 0 (0) | 932 (0.4) |
| Lithium | 0 (0) | 18 (100) | 0 (0) |
| Antipsychotics | 11 (19.3) | 8 (44.4) | 218 (0.1) |
| Antidepressants | 16 (28.1) | 9 (50) | 3574 (1.7) |
| Anxiolytics | 2 (3.5) | 3 (16.7) | 415 (0.2) |
| Pre-existing medical conditions | |||
| Depression | 17 (29.8) | 0 (0) | 15,100 (7.1) |
| Epilepsy | 2 (3.5) | 2 (11.1) | 3296 (1.6) |
| SMI | 40 (70.2) | 17 (94.4) | 1168 (0.5) |
| Pre-existing hypertension | 6 (10.5) | 2 (11.1) | 19,634 (9.2) |
| Pre-existing diabetes | 3 (5.3) | 2 (11.1) | 2022 (1) |
| Characteristics | Exposure cohort | ||
|---|---|---|---|
| A | B2 | C | |
| n (% or SD) | n (% or SD) | n (% or SD) | |
| Total | 84 (100) | 20 (100) | 320,853 (100) |
| Age (years) | |||
| Mean (SD) | 33 (5.3) | 35 (6.3) | 30 (5.9) |
| 12–19 | 1 (1.2) | 0 (0) | 14,034 (4.4) |
| 20–29 | 22 (26.2) | 4 (20) | 124,982 (39) |
| 30–39 | 53 (63.1) | 12 (60) | 166,294 (51.8) |
| 40–49 | 8 (9.5) | 4 (20) | 15,543 (4.8) |
| Year | |||
| 1995–9 | 13 (15.5) | 2 (10) | 46,855 (14.6) |
| 2000–4 | 26 (31) | 4 (20) | 81,190 (25.3) |
| 2005–9 | 29 (34.5) | 5 (25) | 100,574 (31.3) |
| 2010–12 | 16 (19) | 9 (45) | 92,234 (28.7) |
| Lifestyle variables | |||
| Obesity | 9 (10.7) | 4 (20) | 17,241 (5.4) |
| Illicit drug use | 6 (7.1) | 0 (0) | 2167 (0.7) |
| Alcohol problems | 4 (4.8) | 2 (10) | 1718 (0.5) |
| Smoker | 24 (28.6) | 7 (35) | 63,778 (19.9) |
| BMI (kg/m2) | |||
| Mean (SD) | 27 (5.5) | 28 (4.5) | 26 (6.3) |
| Underweight | 0 (0) | 0 (0) | 3741 (1.2) |
| Normal weight | 10 (11.9) | 4 (20) | 42,462 (13.2) |
| Overweight | 9 (10.7) | 3 (15) | 20,246 (6.3) |
| Obese | 9 (10.7) | 4 (20) | 20,870 (6.5) |
| Missing | 56 (66.7) | 9 (45) | 233,534 (72.8) |
| Townsend score | |||
| 1 | 3 (17.6) | 0 (0) | 71,307 (23.3) |
| 2 | 3 (17.6) | 0 (0) | 60,753 (19.9) |
| 3 | 4 (23.5) | 3 (60) | 65,291 (21.4) |
| 4 | 5 (29.4) | 1 (20) | 61,850 (20.2) |
| 5 | 2 (11.8) | 1 (20) | 46,548 (15.2) |
| Missing | 67 (79.8) | 15 (75) | 15,104 (4.7) |
| Ethnicity | |||
| White | 35 (41.7) | 15 (75) | 134,809 (42) |
| Mixed | 0 (0) | 0 (0) | 1788 (0.6) |
| Asian | 1 (1.2) | 1 (5) | 9978 (3.1) |
| Black | 1 (1.2) | 0 (0) | 4641 (1.4) |
| Other | 0 (0) | 0 (0) | 1822 (0.6) |
| Missing | 47 (56) | 4 (20) | 167,815 (52.3) |
| Use of psychiatric drugs during exposure period B2 | |||
| Hypnotics | 5 (6) | 2 (10) | 690 (0.2) |
| Anticonvulsant mood stabilisers | 5 (6) | 0 (0) | 1389 (0.4) |
| Lithium | 0 (0) | 20 (100) | 0 (0) |
| Antipsychotics | 15 (17.9) | 8 (40) | 336 (0.1) |
| Antidepressants | 25 (29.8) | 9 (45) | 4983 (1.6) |
| Anxiolytics | 3 (3.6) | 3 (15) | 683 (0.2) |
| Pre-existing medical conditions | |||
| Depression | 23 (27.4) | 0 (0) | 21,084 (6.6) |
| Epilepsy | 3 (3.6) | 2 (10) | 4925 (1.5) |
| SMI | 57 (67.9) | 19 (95) | 1945 (0.6) |
| Pre-existing hypertension | 8 (9.5) | 2 (10) | 26,362 (8.2) |
| Pre-existing diabetes | 3 (3.6) | 2 (10) | 2803 (0.9) |
| Characteristics | Exposure cohort | ||
|---|---|---|---|
| A | B2 | C | |
| n (% or SD) | n (% or SD) | n (% or SD) | |
| Total | 131 (100) | 22 (100) | 318,612 (100) |
| Age (years) | |||
| Mean (SD) | 32 (5.5) | 32 (4.9) | 30 (5.9) |
| 12–19 | 2 (1.5) | 0 (0) | 14,008 (4.4) |
| 20–29 | 43 (32.8) | 5 (22.7) | 123,740 (38.8) |
| 30–39 | 77 (58.8) | 17 (77.3) | 165,396 (51.9) |
| 40–49 | 9 (6.9) | 0 (0) | 15,468 (4.9) |
| Year | |||
| 1995–9 | 3 (2.3) | 1 (4.5) | 46,638 (14.6) |
| 2000–4 | 17 (13) | 4 (18.2) | 80,466 (25.3) |
| 2005–9 | 54 (41.2) | 10 (45.5) | 100,009 (31.4) |
| 2010–12 | 57 (43.5) | 7 (31.8) | 91,499 (28.7) |
| Lifestyle variables | |||
| Obesity | 14 (10.7) | 6 (27.3) | 17,058 (5.4) |
| Illicit drug use | 8 (6.1) | 1 (4.5) | 2110 (0.7) |
| Alcohol problems | 7 (5.3) | 1 (4.5) | 1653 (0.5) |
| Smoker | 49 (37.4) | 11 (50) | 63,085 (19.8) |
| BMI (kg/m2) | |||
| Mean (SD) | 27 (5.5) | 33 (4.1) | 26 (6.3) |
| Underweight | 2 (1.5) | 0 (0) | 3685 (1.2) |
| Normal weight | 18 (13.7) | 0 (0) | 42,093 (13.2) |
| Overweight | 20 (15.3) | 0 (0) | 20,083 (6.3) |
| Obese | 14 (10.7) | 6 (27.3) | 18,018 (5.7) |
| Missing | 77 (58.8) | 16 (72.7) | 234,733 (73.7) |
| Townsend score | |||
| 1 | 5 (20) | 0 (0) | 70,879 (23.3) |
| 2 | 2 (8) | 1 (20) | 60,417 (19.9) |
| 3 | 5 (20) | 2 (40) | 64,877 (21.4) |
| 4 | 9 (36) | 2 (40) | 61,357 (20.2) |
| 5 | 4 (16) | 0 (0) | 46,074 (15.2) |
| Missing | 106 (80.9) | 17 (77.3) | 15,008 (4.7) |
| Ethnicity | |||
| White | 50 (38.2) | 8 (36.4) | 133,929 (42) |
| Mixed | 2 (1.5) | 0 (0) | 1772 (0.6) |
| Asian | 4 (3.1) | 0 (0) | 9943 (3.1) |
| Black | 14 (10.7) | 1 (4.5) | 4619 (1.4) |
| Other | 1 (0.8) | 0 (0) | 1827 (0.6) |
| Missing | 60 (45.8) | 13 (59.1) | 166,522 (52.3) |
| Use of psychiatric drugs during exposure period B2 | |||
| Hypnotics | 6 (4.6) | 4 (18.2) | 670 (0.2) |
| Anticonvulsant mood stabilisers | 0 (0) | 22 (100) | 145 (0) |
| Lithium | 2 (1.5) | 0 (0) | 24 (0) |
| Antipsychotics | 29 (22.1) | 12 (54.5) | 301 (0.1) |
| Antidepressants | 36 (27.5) | 13 (59.1) | 4872 (1.5) |
| Anxiolytics | 4 (3.1) | 2 (9.1) | 645 (0.2) |
| Pre-existing medical conditions | |||
| Depression | 61 (46.6) | 5 (22.7) | 20,722 (6.5) |
| Epilepsy | 0 (0) | 0 (0) | 3268 (1) |
| SMI | 88 (67.2) | 20 (90.9) | 1840 (0.6) |
| Pre-existing hypertension | 16 (12.2) | 2 (9.1) | 26,228 (8.2) |
| Pre-existing diabetes | 2 (1.5) | 1 (4.5) | 2767 (0.9) |
| Characteristics | Exposure cohort | ||
|---|---|---|---|
| A | B2 | C | |
| n (% or SD) | n (% or SD) | n (% or SD) | |
| Total | 103 (100) | 16 (100) | 211,112 (100) |
| Age (years) | |||
| Mean (SD) | 31 (5.3) | 32 (4.9) | 30 (5.9) |
| 12–19 | 2 (1.9) | 0 (0) | 8951 (4.2) |
| 20–29 | 35 (34) | 4 (25) | 80,581 (38.2) |
| 30–39 | 61 (59.2) | 12 (75) | 110,873 (52.5) |
| 40–49 | 5 (4.9) | 0 (0) | 10,707 (5.1) |
| Year | |||
| 1995–9 | 2 (1.9) | 1 (6.3) | 13,389 (6.3) |
| 2000–4 | 13 (12.6) | 4 (25) | 46,601 (22.1) |
| 2005–9 | 39 (37.9) | 6 (37.5) | 77,886 (36.9) |
| 2010–12 | 49 (47.6) | 5 (31.3) | 73,236 (34.7) |
| Lifestyle variables | |||
| Obesity | 12 (11.7) | 5 (31.3) | 12,831 (6.1) |
| Illicit drug use | 6 (5.8) | 0 (0) | 1419 (0.7) |
| Alcohol problems | 4 (3.9) | 0 (0) | 1125 (0.5) |
| Smoker | 39 (37.9) | 8 (50) | 42,707 (20.2) |
| BMI (kg/m2) | |||
| Mean (SD) | 28 (5.7) | 33 (4.5) | 26 (6.4) |
| Underweight | 1 (1) | 0 (0) | 2522 (1.2) |
| Normal weight | 14 (13.6) | 0 (0) | 29,546 (14) |
| Overweight | 18 (17.5) | 0 (0) | 14,628 (6.9) |
| Obese | 12 (11.7) | 5 (31.3) | 13,596 (6.4) |
| Missing | 58 (56.3) | 11 (68.8) | 150,820 (71.4) |
| Townsend score | |||
| 1 | 5 (22.7) | 0 (0) | 47,305 (23.4) |
| 2 | 2 (9.1) | 1 (25) | 40,308 (20) |
| 3 | 4 (18.2) | 1 (25) | 43,152 (21.4) |
| 4 | 8 (36.4) | 2 (50) | 41,067 (20.3) |
| 5 | 3 (13.6) | 0 (0) | 30,207 (15) |
| Missing | 81 (78.6) | 12 (75) | 9073 (4.3) |
| Ethnicity | |||
| White | 48 (46.6) | 6 (37.5) | 104,998 (49.7) |
| Mixed | 2 (1.9) | 0 (0) | 1489 (0.7) |
| Asian | 3 (2.9) | 0 (0) | 7468 (3.5) |
| Black | 10 (9.7) | 1 (6.3) | 3434 (1.6) |
| Other | 1 (1) | 0 (0) | 1375 (0.7) |
| Missing | 39 (37.9) | 9 (56.3) | 92,348 (43.7) |
| Use of psychiatric drugs during exposure period B2 | |||
| Hypnotics | 5 (4.9) | 3 (18.8) | 454 (0.2) |
| Anticonvulsant mood stabilisers | 0 (0) | 16 (100) | 97 (0) |
| Lithium | 1 (1) | 0 (0) | 13 (0) |
| Antipsychotics | 21 (20.4) | 9 (56.3) | 197 (0.1) |
| Antidepressants | 27 (26.2) | 8 (50) | 3509 (1.7) |
| Anxiolytics | 3 (2.9) | 1 (6.3) | 393 (0.2) |
| Pre-existing medical conditions | |||
| Depression | 46 (44.7) | 5 (31.3) | 14,879 (7) |
| Epilepsy | 0 (0) | 0 (0) | 2186 (1) |
| SMI | 71 (68.9) | 14 (87.5) | 1093 (0.5) |
| Pre-existing hypertension | 12 (11.7) | 1 (6.3) | 19,570 (9.3) |
| Pre-existing diabetes | 1 (1) | 0 (0) | 1998 (0.9) |
| Characteristics | Exposure cohort | ||
|---|---|---|---|
| A | B2 | C | |
| n (% or SD) | n (% or SD) | n (% or SD) | |
| Total | 558 (100) | 1375 (100) | 318,612 (100) |
| Age (years) | |||
| Mean (SD) | 30 (5.8) | 30 (5.6) | 30 (5.9) |
| 12–19 | 24 (4.3) | 50 (3.6) | 14,008 (4.4) |
| 20–29 | 237 (42.5) | 563 (40.9) | 123,740 (38.8) |
| 30–39 | 276 (49.5) | 705 (51.3) | 165,396 (51.9) |
| 40–49 | 21 (3.8) | 57 (4.1) | 15,468 (4.9) |
| Year | |||
| 1995–9 | 41 (7.3) | 175 (12.7) | 46,638 (14.6) |
| 2000–4 | 114 (20.4) | 320 (23.3) | 80,466 (25.3) |
| 2005–9 | 218 (39.1) | 486 (35.3) | 100,009 (31.4) |
| 2010–12 | 185 (33.2) | 394 (28.7) | 91,499 (28.7) |
| Lifestyle variables | |||
| Obesity | 45 (8.1) | 110 (8) | 17,058 (5.4) |
| Illicit drug use | 17 (3) | 18 (1.3) | 2110 (0.7) |
| Alcohol problems | 12 (2.2) | 14 (1) | 1653 (0.5) |
| Smoker | 185 (33.2) | 315 (22.9) | 63,085 (19.8) |
| BMI (kg/m2) | |||
| Mean (SD) | 27 (6.8) | 27 (6.2) | 26 (6.3) |
| Underweight | 6 (1.1) | 12 (0.9) | 3685 (1.2) |
| Normal weight | 73 (13.1) | 158 (11.5) | 42,093 (13.2) |
| Overweight | 47 (8.4) | 117 (8.5) | 20,083 (6.3) |
| Obese | 47 (8.4) | 112 (8.1) | 18,018 (5.7) |
| Missing | 385 (69) | 976 (71) | 234,733 (73.7) |
| Townsend score | |||
| 1 | 19 (18.8) | 43 (19.2) | 70,879 (23.3) |
| 2 | 19 (18.8) | 32 (14.3) | 60,417 (19.9) |
| 3 | 16 (15.8) | 51 (22.8) | 64,877 (21.4) |
| 4 | 23 (22.8) | 50 (22.3) | 61,357 (20.2) |
| 5 | 24 (23.8) | 48 (21.4) | 46,074 (15.2) |
| Missing | 457 (81.9) | 1151 (83.7) | 15,008 (4.7) |
| Ethnicity | |||
| White | 222 (39.8) | 541 (39.3) | 133,929 (42) |
| Mixed | 2 (0.4) | 6 (0.4) | 1772 (0.6) |
| Asian | 9 (1.6) | 21 (1.5) | 9943 (3.1) |
| Black | 51 (9.1) | 114 (8.3) | 4619 (1.4) |
| Other | 2 (0.4) | 14 (1) | 1827 (0.6) |
| Missing | 272 (48.7) | 679 (49.4) | 166,522 (52.3) |
| Use of psychiatric drugs during exposure period B2 | |||
| Hypnotics | 19 (3.4) | 28 (2) | 670 (0.2) |
| Anticonvulsant mood stabilisers | 41 (7.3) | 1375 (100) | 145 (0) |
| Lithium | 3 (0.5) | 0 (0) | 24 (0) |
| Antipsychotics | 35 (6.3) | 22 (1.6) | 301 (0.1) |
| Antidepressants | 72 (12.9) | 68 (4.9) | 4872 (1.5) |
| Anxiolytics | 7 (1.3) | 23 (1.7) | 645 (0.2) |
| Pre-existing medical conditions | |||
| Depression | 87 (15.6) | 106 (7.7) | 20,722 (6.5) |
| Epilepsy | 249 (44.6) | 1326 (96.4) | 3268 (1) |
| SMI | 97 (17.4) | 38 (2.8) | 1840 (0.6) |
| Pre-existing hypertension | 69 (12.4) | 135 (9.8) | 26,228 (8.2) |
| Pre-existing diabetes | 4 (0.7) | 20 (1.5) | 2767 (0.9) |
| Characteristics | Exposure cohort | ||
|---|---|---|---|
| A | B2 | C | |
| n (% or SD) | n (% or SD) | n (% or SD) | |
| Total | 429 (100) | 999 (100) | 211,112 (100) |
| Age (years) | |||
| Mean (SD) | 30 (5.7) | 30 (5.5) | 30 (5.9) |
| 12–19 | 19 (4.4) | 37 (3.7) | 8951 (4.2) |
| 20–29 | 181 (42.2) | 394 (39.4) | 80,581 (38.2) |
| 30–39 | 217 (50.6) | 529 (53) | 110,873 (52.5) |
| 40–49 | 12 (2.8) | 39 (3.9) | 10,707 (5.1) |
| Year | |||
| 1995–9 | 24 (5.6) | 112 (11.2) | 13,389 (6.3) |
| 2000–4 | 83 (19.3) | 218 (21.8) | 46,601 (22.1) |
| 2005–9 | 168 (39.2) | 363 (36.3) | 77,886 (36.9) |
| 2010–12 | 154 (35.9) | 306 (30.6) | 73,236 (34.7) |
| Lifestyle variables | |||
| Obesity | 38 (8.9) | 88 (8.8) | 12,831 (6.1) |
| Illicit drug use | 10 (2.3) | 13 (1.3) | 1419 (0.7) |
| Alcohol problems | 9 (2.1) | 6 (0.6) | 1125 (0.5) |
| Smoker | 139 (32.4) | 224 (22.4) | 42,707 (20.2) |
| BMI (kg/m2) | |||
| Mean (SD) | 27 (6.7) | 27 (6.5) | 26 (6.4) |
| Underweight | 4 (0.9) | 11 (1.1) | 2522 (1.2) |
| Normal weight | 54 (12.6) | 120 (12) | 29,546 (14) |
| Overweight | 36 (8.4) | 85 (8.5) | 14,628 (6.9) |
| Obese | 39 (9.1) | 90 (9) | 13,596 (6.4) |
| Missing | 296 (69) | 693 (69.4) | 150,820 (71.4) |
| Townsend score | |||
| 1 | 11 (16.7) | 23 (15.2) | 47,305 (23.4) |
| 2 | 16 (24.2) | 20 (13.2) | 40,308 (20) |
| 3 | 10 (15.2) | 34 (22.5) | 43,152 (21.4) |
| 4 | 17 (25.8) | 38 (25.2) | 41,067 (20.3) |
| 5 | 12 (18.2) | 36 (23.8) | 30,207 (15) |
| Missing | 363 (84.6) | 848 (84.9) | 9073 (4.3) |
| Ethnicity | |||
| White | 196 (45.7) | 419 (41.9) | 104,998 (49.7) |
| Mixed | 2 (0.5) | 6 (0.6) | 1489 (0.7) |
| Asian | 7 (1.6) | 16 (1.6) | 7468 (3.5) |
| Black | 36 (8.4) | 94 (9.4) | 3434 (1.6) |
| Other | 2 (0.5) | 8 (0.8) | 1375 (0.7) |
| Missing | 186 (43.4) | 456 (45.6) | 92,348 (43.7) |
| Use of psychiatric drugs during exposure period B2 | |||
| Hypnotics | 13 (3) | 23 (2.3) | 454 (0.2) |
| Anticonvulsant mood stabilisers | 32 (7.5) | 999 (100) | 97 (0) |
| Lithium | 1 (0.2) | 0 (0) | 13 (0) |
| Antipsychotics | 27 (6.3) | 16 (1.6) | 197 (0.1) |
| Antidepressants | 51 (11.9) | 50 (5) | 3509 (1.7) |
| Anxiolytics | 4 (0.9) | 16 (1.6) | 393 (0.2) |
| Pre-existing medical conditions | |||
| Depression | 68 (15.9) | 78 (7.8) | 14,879 (7) |
| Epilepsy | 192 (44.8) | 964 (96.5) | 2186 (1) |
| SMI | 78 (18.2) | 28 (2.8) | 1093 (0.5) |
| Pre-existing hypertension | 54 (12.6) | 110 (11) | 19,570 (9.3) |
| Pre-existing diabetes | 2 (0.5) | 16 (1.6) | 1998 (0.9) |
Results on relative risks for health, lifestyle and concomitant medication in the fully adjusted models in Chapter 4, Results
| Maternal outcomes | Cohort B1 vs. cohort A | Cohort B1 vs. cohort C | ||
|---|---|---|---|---|
| RRadj | 95% CI | RRadj | 95% CI | |
| Gestational hypertension and/or pre-eclampsia | ||||
| Cohort comparison | 0.69 | 0.37 to 1.29 | 1.24 | 0.79 to 1.96 |
| Age (tertiles) | ||||
| 1 | 1 | 1 | ||
| 2 | 1.11 | 0.54 to 2.30 | 0.99 | 0.94 to 1.04 |
| 3 | 1.17 | 0.55 to 2.47 | 1.19 | 1.13 to 1.24 |
| Lifestyle variables | ||||
| Obesity | 2.37 | 1.27 to 4.41 | 1.92 | 1.80 to 2.06 |
| Alcohol problems | 1.27 | 0.43 to 3.74 | 0.77 | 0.56 to 1.07 |
| Smoker | 0.92 | 0.52 to 1.63 | 0.83 | 0.78 to 0.88 |
| Illicit drug use | 1.49 | 0.68 to 3.28 | 0.94 | 0.72 to 1.22 |
| Use of psychiatric drugs during exposure period B1 | ||||
| Antidepressant drugs | 2.26 | 1.19 to 4.29 | 1.20 | 1.05 to 1.37 |
| Antiepileptic drugs | 1.02 | 0.35 to 2.98 | 1.13 | 0.85 to 1.51 |
| Gestational diabetes | ||||
| Cohort comparison | 0.43 | 0.20 to 0.933 | 0.95 | 0.53 to 1.69 |
| Age (tertiles) | ||||
| 1 | 1 | 1 | ||
| 2 | 2.17 | 0.71 to 6.61 | 1.59 | 1.48 to 1.71 |
| 3 | 3.17 | 1.01 to 9.90 | 2.46 | 2.30 to 2.64 |
| Lifestyle variables | ||||
| Obesity | 5.49 | 2.67 to 11.2 | 3.32 | 3.08 to 3.57 |
| Alcohol problems | 0.50 | 0.07 to 3.56 | 0.92 | 0.61 to 1.37 |
| Smoker | 1.39 | 0.64 to 3.02 | 0.86 | 0.80, 0.93 |
| Illicit drug use | 1.21 | 0.87 to 1.67 | ||
| Use of psychiatric drugs during exposure period B1 | ||||
| Antidepressant drugs | 3.73 | 1.75 to 7.96 | 1.51 | 1.29 to 1.75 |
| Antiepileptic drugs | 1.54 | 0.53 to 4.45 | 0.96 | 0.65 to 1.42 |
| Caesarean section | ||||
| Cohort comparison | 1.05 | 0.82 to 1.34 | 1.09 | 0.92 to 1.30 |
| Age (tertiles) | ||||
| 1 | 1 | 1 | ||
| 2 | 1.23 | 0.89 to 1.68 | 1.32 | 1.29 to 1.34 |
| 3 | 1.79 | 1.34 to 2.40 | 1.67 | 1.64 to 1.70 |
| Lifestyle variables | ||||
| Obesity | 1.45 | 1.10 to 1.90 | 1.55 | 1.51 to 1.59 |
| Alcohol problems | 0.97 | 0.61 to 1.54 | 0.98 | 0.88 to 1.09 |
| Smoker | 0.99 | 0.78 to 1.25 | 0.98 | 0.96 to 1.00 |
| Illicit drug use | 1.21 | 0.85 to 1.72 | 0.98 | 0.89 to 1.08 |
| Use of psychiatric drugs during exposure period B1 | ||||
| Antidepressant drugs | 0.95 | 0.74 to 1.22 | 1.16 | 1.10 to 1.21 |
| Antiepileptic drugs | 1.02 | 0.64 to 1.62 | 1.17 | 1.06 to 1.29 |
| Perinatal death | ||||
| Cohort comparison | 0.94 | 0.22 to 3.88 | ||
| Age (tertiles) | ||||
| 1 | 1 | |||
| 2 | 0.93 | 0.79 to 1.09 | ||
| 3 | 1.26 | 1.08 to 1.46 | ||
| Lifestyle variables | ||||
| Obesity | 1.50 | 1.18 to 1.89 | ||
| Alcohol problems | 2.35 | 1.37 to 4.01 | ||
| Smoker | 1.49 | 1.28 to 1.73 | ||
| Illicit drug use | 1.07 | 0.54 to 2.10 | ||
| Use of psychiatric drugs during exposure period B1 | ||||
| Antidepressant drugs | 1.41 | 0.97 to 2.05 | ||
| Antiepileptic drugs | 1.39 | 0.61 to 3.13 | ||
| Child outcomes | Cohort B1 vs. cohort A | Cohort B1 vs. cohort C | ||
|---|---|---|---|---|
| RRadj | 95% CI | RRadj | 95% CI | |
| Major congenital malformations | ||||
| Cohort comparison | 1.79 | 0.72 to 4.47 | 1.59 | 0.84 to 3.00 |
| Age (tertiles) | ||||
| 1 | 1 | 1 | ||
| 2 | 1.33 | 0.42 to 4.16 | 0.92 | 0.86 to 1.00 |
| 3 | 1.28 | 0.41 to 3.96 | 1.01 | 0.94 to 1.09 |
| Lifestyle variables | ||||
| Obesity | 0.57 | 0.13 to 2.53 | 0.99 | 0.87 to 1.12 |
| Alcohol problems | 1.10 | 0.75 to 1.62 | ||
| Smoker | 0.14 | 0.03 to 0.623 | 1.03 | 0.95 to 1.11 |
| Illicit drug use | 1.03 | 0.72 to 1.48 | ||
| Use of psychiatric drugs during exposure period B1 | ||||
| Antidepressant drugs | 0.89 | 0.37 to 2.17 | 1.01 | 0.82 to 1.24 |
| Antiepileptic drugs | 1.68 | 1.18 to 2.40 | ||
| Poor birth outcomes | ||||
| Cohort comparison | 1.83 | 1.05 to 3.20 | 1.39 | 0.98 to 1.97 |
| Age (tertiles) | ||||
| 1 | 1 | 1 | ||
| 2 | 1.08 | 0.55 to 2.12 | 0.93 | 0.88 to 0.982 |
| 3 | 1.28 | 0.67 to 2.45 | 1.04 | 0.99 to 1.09 |
| Lifestyle variables | ||||
| Obesity | 0.80 | 0.38 to 1.65 | 1.11 | 1.03 to 1.20 |
| Alcohol problems | 0.34 | 0.08 to 1.35 | 1.31 | 1.07 to 1.61 |
| Smoker | 1.06 | 0.62 to 1.80 | 1.37 | 1.31 to 1.44 |
| Illicit drug use | 2.14 | 1.15 to 3.98 | 1.86 | 1.58 to 2.18 |
| Use of psychiatric drugs during exposure period B1 | ||||
| Antidepressant drugs | 1.38 | 0.79 to 2.41 | 1.54 | 1.39 to 1.72 |
| Antiepileptic drugs | 1.27 | 0.53 to 3.00 | 1.35 | 1.06 to 1.72 |
| Transient poor birth outcomes | ||||
| Cohort comparison | 1.20 | 0.57 to 2.53 | 1.59 | 0.92 to 2.74 |
| Age (tertiles) | ||||
| 1 | 1 | 1 | ||
| 2 | 1.66 | 0.73 to 3.75 | 0.85 | 0.79 to 0.913 |
| 3 | 1.06 | 0.42 to 2.62 | 0.92 | 0.85 to 0.987 |
| Lifestyle variables | ||||
| Obesity | 1.61 | 0.74 to 3.52 | 1.45 | 1.30 to 1.60 |
| Alcohol problems | 1.76 | 0.53 to 5.87 | 1.36 | 1.01 to 1.85 |
| Smoker | 1.48 | 0.74 to 2.96 | 1.26 | 1.17 to 1.35 |
| Illicit drug use | 0.77 | 0.25 to 2.39 | 1.78 | 1.39 to 2.28 |
| Use of psychiatric drugs during exposure period B1 | ||||
| Antidepressant drugs | 0.78 | 0.38 to 1.61 | 1.48 | 1.24 to 1.78 |
| Antiepileptic drugs | 3.62 | 1.29 to 10.1 | 1.70 | 1.23 to 2.34 |
| Neurodevelopmental/behavioural disorders | ||||
| Cohort comparison | 0.83 | 0.49 to 1.39 | 1.22 | 0.80 to 1.84 |
| Age (tertiles) | ||||
| 1 | 1 | 1 | ||
| 2 | 0.60 | 0.33 to 1.07 | 0.94 | 0.89 to 0.988 |
| 3 | 0.85 | 0.51 to 1.41 | 1.00 | 0.96 to 1.05 |
| Lifestyle variables | ||||
| Obesity | 0.93 | 0.48 to 1.81 | 1.15 | 1.07 to 1.24 |
| Alcohol problems | 1.69 | 0.84 to 3.40 | 1.14 | 0.90 to 1.43 |
| Smoker | 1.11 | 0.70 to 1.76 | 1.16 | 1.11 to 1.21 |
| Illicit drug use | 1.45 | 0.77 to 2.75 | 1.01 | 0.80 to 1.26 |
| Use of psychiatric drugs during exposure period B1 | ||||
| Antidepressant drugs | 0.65 | 0.37 to 1.11 | 1.26 | 1.12 to 1.42 |
| Antiepileptic drugs | 0.95 | 0.31 to 2.95 | 1.52 | 1.21 to 1.92 |
| Maternal outcomes | Cohort B1 vs. cohort A | Cohort B1 vs. cohort C | ||
|---|---|---|---|---|
| RRadj | 95% CI | RRadj | CI95 | |
| Gestational hypertension and/or pre-eclampsia | ||||
| Cohort comparison | 1.34 | 0.76 to 2.36 | 1.22 | 0.95 to 1.58 |
| Age (tertiles) | ||||
| 1 | 1 | 1 | 0 | |
| 2 | 0.93 | 0.53 to 1.63 | 0.97 | 0.92 to 1.02 |
| 3 | 1.23 | 0.69 to 2.20 | 1.17 | 1.11 to 1.22 |
| Lifestyle variables | ||||
| Obesity | 2.66 | 1.53 to 4.61 | 1.91 | 1.78 to 2.04 |
| Alcohol problems | 1.02 | 0.11 to 8.77 | 0.67 | 0.47 to 0.952 |
| Smoker | 0.61 | 0.33 to 1.13 | 0.81 | 0.77 to 0.865 |
| Illicit drug use | 1.52 | 0.38 to 6.10 | 1.04 | 0.81 to 1.34 |
| Use of psychiatric drugs during exposure period B1 | ||||
| Antidepressant drugs, lithium or antipsychotics | 1.14 | 0.59 to 2.20 | 1.21 | 1.07 to 1.38 |
| Gestational diabetes | ||||
| Cohort comparison | 2.17 | 0.93 to 5.10 | 1.26 | 0.90 to 1.76 |
| Age (tertiles) | ||||
| 1 | 1 | 1 | 0 | |
| 2 | 1.16 | 0.49 to 2.77 | 1.59 | 1.48 to 1.72 |
| 3 | 2.40 | 1.05 to 5.46 | 2.48 | 2.31 to 2.66 |
| Lifestyle variables | ||||
| Obesity | 2.05 | 0.95 to 4.41 | 3.26 | 3.03 to 3.51 |
| Alcohol problems | 0.86 | 0.57 to 1.30 | ||
| Smoker | 0.42 | 0.16 to 1.12 | 0.87 | 0.81 to 0.942 |
| Illicit drug use | 1.24 | 0.90 to 1.69 | ||
| Use of psychiatric drugs during exposure period B1 | ||||
| Antidepressant drugs, lithium or antipsychotics | 3.20 | 1.61 to 6.35 | 1.49 | 1.29 to 1.72 |
| Caesarean section | ||||
| Cohort comparison | 1.07 | 0.88 to 1.30 | 1.14 | 1.04 to 1.26 |
| Age (tertiles) | ||||
| 1 | 1 | 1 | 0 | |
| 2 | 1.27 | 1.02 to 1.59 | 1.32 | 1.29 to 1.34 |
| 3 | 1.86 | 1.50 to 2.32 | 1.67 | 1.64 to 1.70 |
| Lifestyle variables | ||||
| Obesity | 1.49 | 1.16 to 1.89 | 1.55 | 1.51 to 1.59 |
| Alcohol problems | 0.56 | 0.23 to 1.38 | 0.98 | 0.89 to 1.09 |
| Smoker | 0.89 | 0.73 to 1.09 | 0.98 | 0.96 to 0.998 |
| Illicit drug use | 1.02 | 0.54 to 1.92 | 1.02 | 0.93 to 1.12 |
| Use of psychiatric drugs during exposure period B1 | ||||
| Antidepressant drugs, lithium or antipsychotics | 1.16 | 0.91 to 1.49 | 1.18 | 1.13 to 1.23 |
| Perinatal death | ||||
| Cohort comparison | 1.42 | 0.67 to 2.99 | ||
| Age (tertiles) | ||||
| 1 | 1 | 0 | ||
| 2 | 0.95 | 0.81 to 1.11 | ||
| 3 | 1.28 | 1.10 to 1.49 | ||
| Lifestyle variables | ||||
| Obesity | 1.54 | 1.22 to 1.94 | ||
| Alcohol problems | 1.91 | 1.07 to 3.40 | ||
| Smoker | 1.45 | 1.25 to 1.68 | ||
| Illicit drug use | 1.31 | 0.71 to 2.39 | ||
| Use of psychiatric drugs during exposure period B1 | ||||
| Antidepressant drugs, lithium or antipsychotics | 1.41 | 0.98 to 2.02 | ||
| Child outcomes | Cohort B1 vs. cohort A | Cohort B1 vs. cohort C | ||
|---|---|---|---|---|
| RRadj | 95% CI | RRadj | 95% CI | |
| Major congenital malformations | ||||
| Cohort comparison | 1.89 | 0.93 to 3.85 | 2.05 | 1.53 to 2.74 |
| Age (tertiles) | ||||
| 1 | 1 | 1 | 0 | |
| 2 | 0.79 | 0.41 to 1.53 | 0.91 | 0.84 to 0.982 |
| 3 | 1.36 | 0.74 to 2.51 | 1.03 | 0.95 to 1.10 |
| Lifestyle variables | ||||
| Obesity | 0.39 | 0.09 to 1.63 | 1.06 | 0.93 to 1.19 |
| Alcohol problems | 1.18 | 0.81 to 1.70 | ||
| Smoker | 0.87 | 0.46 to 1.67 | 1.03 | 0.96 to 1.12 |
| Illicit drug use | 1.09 | 0.78 to 1.54 | ||
| Use of psychiatric drugs during exposure period B1 | ||||
| Antidepressant drugs, lithium or antipsychotics | 0.71 | 0.26 to 1.97 | 1.14 | 0.95 to 1.38 |
| Poor birth outcomes | ||||
| Cohort comparison | 1.25 | 0.78 to 2.01 | 1.33 | 1.06 to 1.67 |
| Age (tertiles) | ||||
| 1 | 1 | 1 | 0 | |
| 2 | 0.85 | 0.50 to 1.43 | 0.94 | 0.90,.994 |
| 3 | 1.72 | 1.07 to 2.76 | 1.04 | 0.99 to 1.10 |
| Lifestyle variables | ||||
| Obesity | 1.28 | 0.69 to 2.37 | 1.13 | 1.04 to 1.22 |
| Alcohol problems | 1.01 | 0.26 to 3.80 | 1.31 | 1.06 to 1.60 |
| Smoker | 1.85 | 1.20 to 2.85 | 1.37 | 1.30 to 1.43 |
| Illicit drug use | 1.63 | 0.62 to 4.26 | 1.89 | 1.61 to 2.21 |
| Use of psychiatric drugs during exposure period B1 | ||||
| Antidepressant drugs, lithium or antipsychotics | 1.28 | 0.76 to 2.15 | 1.54 | 1.39 to 1.70 |
| Transient poor birth outcomes | ||||
| Cohort comparison | 1.28 | 0.73 to 2.26 | 1.71 | 1.28 to 2.29 |
| Age (tertiles) | ||||
| 1 | 1 | 1 | 0 | |
| 2 | 0.55 | 0.28 to 1.07 | 0.87 | 0.81 to 0.934 |
| 3 | 1.25 | 0.70 to 2.20 | 0.90 | 0.84 to 0.972 |
| Lifestyle variables | ||||
| Obesity | 1.47 | 0.67 to 3.24 | 1.43 | 1.29 to 1.58 |
| Alcohol problems | 1.26 | 0.93 to 1.72 | ||
| Smoker | 2.71 | 1.61 to 4.53 | 1.24 | 1.16 to 1.33 |
| Illicit drug use | 1.81 | 0.59 to 5.54 | 1.85 | 1.46 to 2.34 |
| Use of psychiatric drugs during exposure period B1 | ||||
| Antidepressant drugs, lithium or antipsychotics | 1.52 | 0.79 to 2.93 | 1.48 | 1.27 to 1.72 |
| Neurodevelopmental/behavioural disorders | ||||
| Cohort comparison | 1.10 | 0.75 to 1.61 | 1.73 | 1.42 to 2.09 |
| Age (tertiles) | ||||
| 1 | 1 | 1 | 0 | |
| 2 | 1.07 | 0.72 to 1.59 | 0.94 | 0.89, 0.985 |
| 3 | 0.97 | 0.63 to 1.49 | 1.00 | 0.95 to 1.04 |
| Lifestyle variables | ||||
| Obesity | 0.96 | 0.53 to 1.74 | 1.14 | 1.06 to 1.23 |
| Alcohol problems | 1.21 | 0.33 to 4.46 | 1.15 | 0.91 to 1.44 |
| Smoker | 1.01 | 0.68 to 1.50 | 1.16 | 1.11 to 1.22 |
| Illicit drug use | 0.96 | 0.25 to 3.57 | 1.07 | 0.87 to 1.32 |
| Use of psychiatric drugs during exposure period B1 | ||||
| Antidepressant drugs, lithium or antipsychotics | 0.60 | 0.30 to 1.23 | 1.31 | 1.17 to 1.46 |
Sensitivity analysis exploring the potential impact of excluding non-live births
In an ideal study of adverse pregnancy outcomes we would identify all pregnancies from conception and follow these up to their various outcomes (termination, miscarriage, live birth, stillbirth). For pragmatic reasons this approach is rarely possible, with studies instead typically identifying pregnancies ending in live births and occasionally stillbirths, terminations and/or miscarriages. However, the exclusion of non-live births can potentially produce a selection bias. 121,122 Here we provide an example of how a selection bias might work for terminations of pregnancy in our study setting. Antenatal scanning now allows potential parents to identify whether or not a fetus has certain congenital malformations. This may lead to an increase in the termination of malformed pregnancies and hence a lower rate of malformations in pregnancies resulting in live birth. Figures supporting this theory are not directly available, however, based on extrapolations from Department of Health123 and ONS data124 for England and Wales, and the European surveillance of congenital abnormalities (EUROCAT),125 we estimate that in 2013 approximately 29% of terminated pregnancies were malformed whereas only 20% of live and stillbirths were malformed (Table 51).
| Estimates | Data source |
|---|---|
| 698,512 births in England and Wales in 2013 | ONS |
| 2% malformations (≈ 14,000) | EUROCAT |
| 168,000 terminations before gestational week 13 | DoH |
| 0.2% (389) of which are grounds Ea | DoH |
| Many may have terminated before malformation were observed. We therefore make the assumption that the true rate was the same as in general population ≈ 2% (≈ 3360) | |
| 15,716 terminations after gestational week 13 | DoH |
| 15% (2,343) of which are grounds Ea | DoH |
This discrepancy in malformation rates among terminations does not bias relative risk estimates by itself, as a selection bias will only arise if two conditions are met: (1) the proportion of, for example, major congenital malformations are different in those who terminated compared with those who did not terminate and (2) the proportion of those who terminated are different among exposed and unexposed. If just one of these conditions is met, the effects will cancel out in relative estimates.
By making assumptions such as those described in Table 51, we can model the impact of a potential selection bias and estimate the potential direction and magnitude.
Below we provide two examples of sensitivity analyses based on the results presented in Chapter 4, Child outcomes, comparing the risk of major congenital malformations in women who continued antipsychotics in pregnancy (cohort B1) to the risk in women who discontinued antipsychotics before pregnancy (cohort A) and women who were unexposed to antipsychotics both before and during pregnancy (cohort C).
Based on the information in Table 51 we make the assumption that the probability is 0.21 for a non-malformed, unexposed pregnancy to be terminated. We then vary the probability for a malformed unexposed pregnancy to be terminated between 0.20 and 0.50 as well as the difference in termination probabilities between exposed and unexposed. Figures 14 and 15 demonstrate that if there is no difference between termination probabilities between women who continue antipsychotics (cohort B) and women who discontinue antipsychotics (cohort A) or are not treated with antipsychotics (cohort C), the risk estimate will remain unaltered at 1.54 and 1.74, respectively. Likewise, convergence of the five lines in the figures illustrate that if the probability of a malformed and non-malformed pregnancy being aborted was the same (i.e. 0.20) then unbiased estimates are obtained regardless of the exclusion of non-live births. On the other hand, using the probability of 0.29 as a reference point, it is clear that even if the probability of termination in cohort B1 is 20% greater or smaller than in the other two cohorts, changes in the relative risk estimates are minimal. Using more extreme assumptions, as shown towards the right of these figures, may result in changes in relative risk estimates. However, these assumptions may not be plausible, for example a probability of 0.5 for termination of malformed pregnancies among unexposed and a 20% increase among exposed pregnancies.
FIGURE 14.
Sensitivity analysis assessing potential selection bias introduced by excluding terminations from the analyses comparing the risk of major congenital malformations in women continuing antipsychotic use in pregnancy (cohort B1) and women who discontinued antipsychotic use before pregnancy (cohort A). OR, odds ratio.
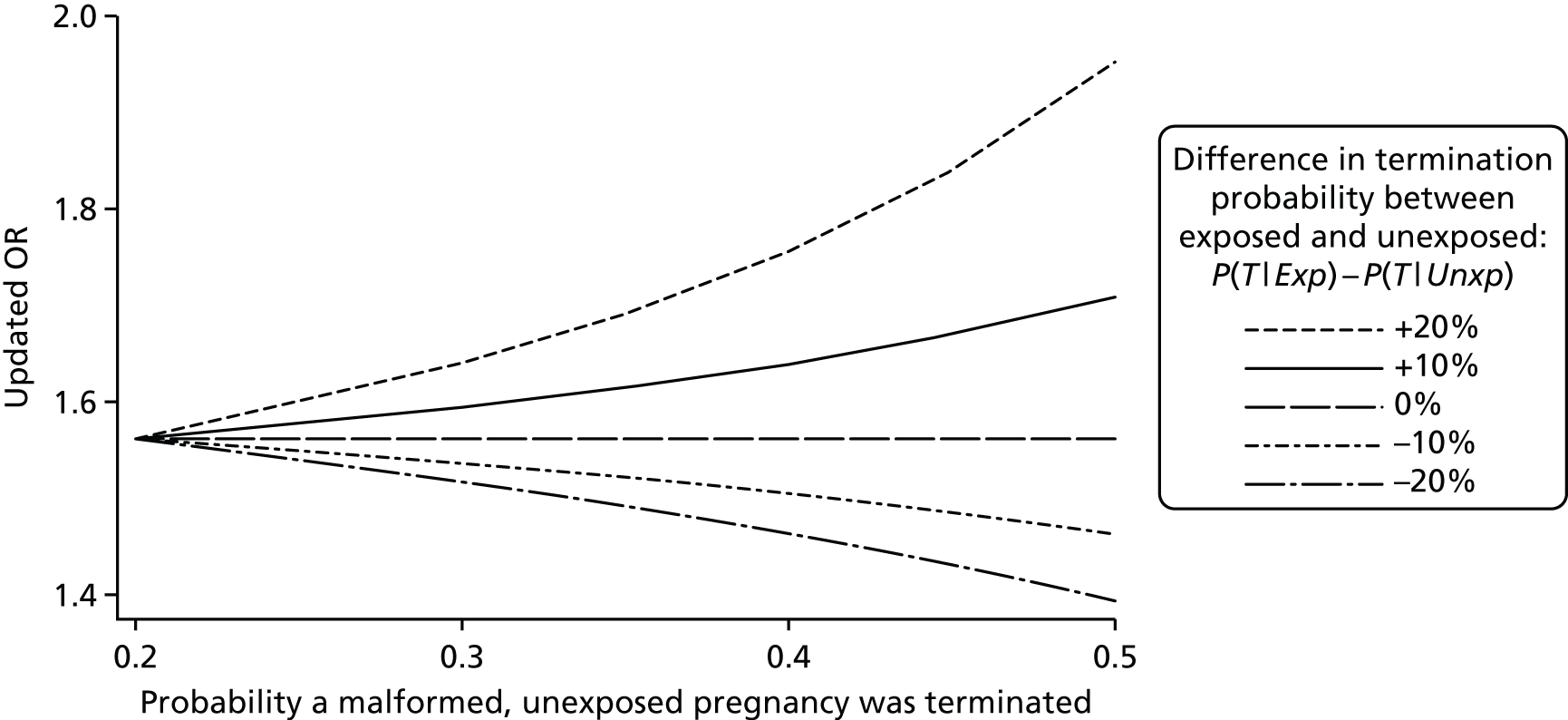
FIGURE 15.
Sensitivity analysis assessing potential selection bias introduced by excluding terminations from the analyses comparing the risk of major congenital malformations in women continuing antipsychotic use in pregnancy (cohort B1) and women who did not use antipsychotic before/during pregnancy (cohort C). OR, odds ratio.
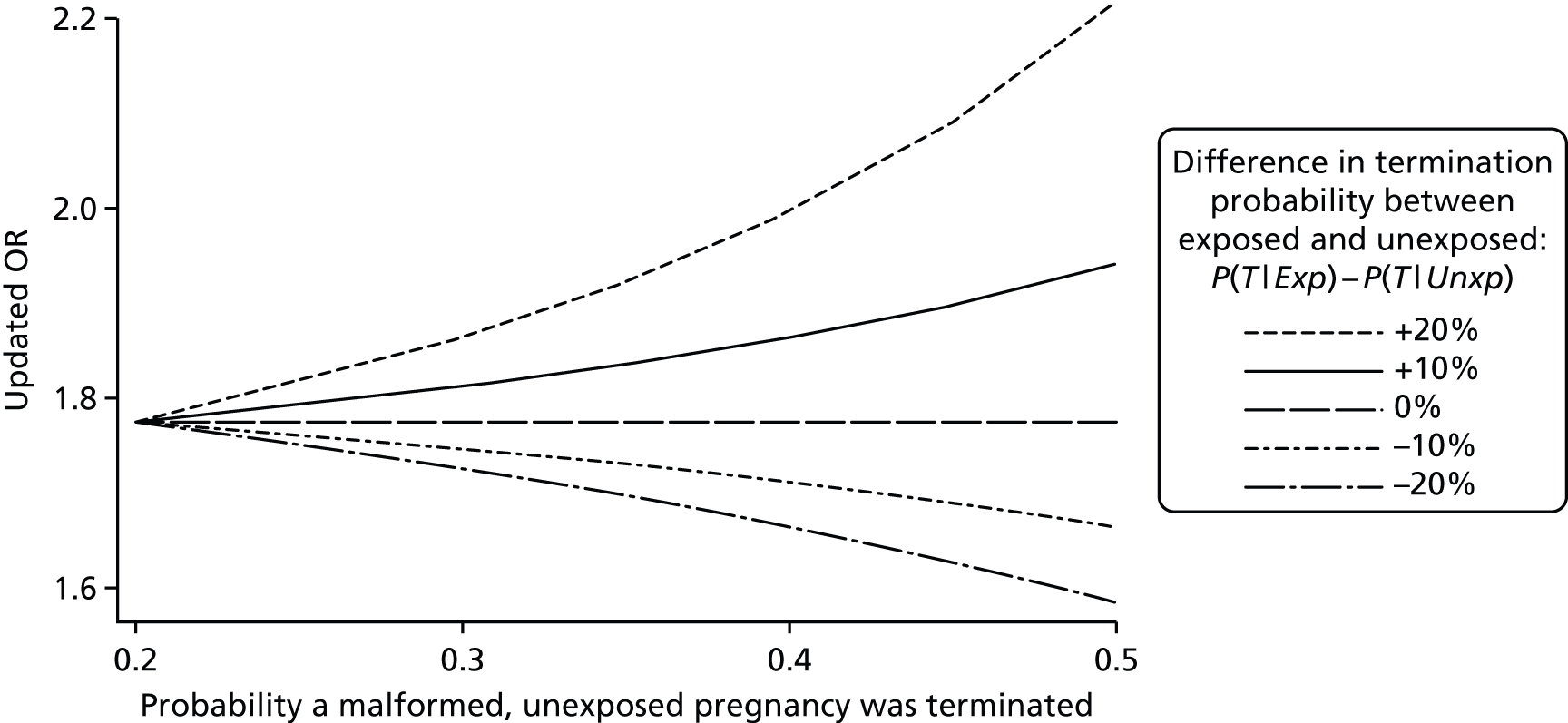
Variable definitions for Chapter 3
Below we provide information on how each of the outcomes were defined for the studies describing patterns of recording that indicate worsening of mental health; 18 months before, during the course of pregnancy and up to 15 months after delivery.
We examined the medical records in THIN for the presence of Read codes for symptoms or illness-related events within each 3-month period from 18 months before pregnancy to 15 months after delivery. We did not make any distinction between new codes and repeated codes. For each 3-month period we looked for the following categories of codes:
-
Attempted suicide, overdose or deliberate self-harm, including ‘events of undetermined intent’ (Table 52). For this outcome we also searched the medical records for any entries associated with the single word free-text comment ‘OVERDOSE’.
-
Psychiatric hospital admission or Mental Health Act examination (Table 53).
-
Psychosis, psychotic disorders and psychotic symptoms, including psychotic depression, mania and hypomania (Table 54).
| Read code | Description |
|---|---|
| SL. . .15 | Overdose of drug |
| TK05.00 | Suicide + selfinflicted poisoning by drug or medicine |
| U20..11 | [X]Deliberate drug overdose/other poisoning |
| TK. . .11 | Cause of overdose – deliberate |
| U2. . .00 | [X]Intentional self-harm |
| ZX1..13 | Deliberate self-harm |
| TK. . .15 | Attempted suicide |
| U20..00 | [X]Intentional self poisoning/exposure to noxious sub |
| U29..00 | [X]Intentional self harm by sharp object |
| U200.11 | [X]Overdose – paracetamol |
| ZX. . .00 | Self-harm |
| U2. . .11 | [X]Self inflicted injury |
| TK. . .00 | Suicide and selfinflicted injury |
| TK60100 | Self inflicted lacerations to wrist |
| SL. . .14 | Overdose of biological substance |
| TK. . .13 | Poisoning – self-inflicted |
| TK00.00 | Suicide + selfinflicted poisoning by analgesic/antipy |
| ZX14200 | Pulling out sutures |
| TK. . .12 | Injury – self-inflicted |
| U2E..00 | [X]Self mutilation |
| TKz..00 | Suicide and selfinflicted injury NOS |
| TN82.00 | Injury?accidental, by scald |
| TK. . .17 | Para-suicide |
| ZX13100 | Cutting own wrists |
| TN81.00 | Injury?accidental, by burns or fire |
| ZX13.00 | Cutting self |
| U2. . .15 | [X]Para-suicide |
| U200.00 | [X]Intent self poison/exposure to nonopioid analgesic |
| TK. . .14 | Suicide and self harm |
| TK0..00 | Suicide + selfinflicted poisoning by solid/liquid sub |
| U30..11 | [X]Deliberate drug poisoning |
| TK60111 | Slashed wrists self inflicted |
| TN61.00 | Injury?accidental, by stabbing instrument |
| TK6..00 | Suicide and selfinflicted injury by cutting and stabb |
| TK60.00 | Suicide and selfinflicted injury by cutting |
| U2. . .14 | [X]Attempted suicide |
| TK04.00 | Suicide + selfinflicted poisoning by other drugs/medi |
| U2. . .12 | [X]Injury – self-inflicted |
| U209.00 | [X]Intent self poison/exposure to alcohol |
| ZX1P.00 | Swallowing substances |
| 14K1.00 | Intentional overdose of prescription only medication |
| U200.13 | [X]Overdose – aspirin |
| ZX1..00 | Self-injurious behaviour |
| ZX11500 | Biting own tongue |
| TK03.00 | Suicide + selfinflicted poisoning tranquilliser/psych |
| U21..00 | [X]Intent self harm by hanging strangulation/suffoc |
| ZX1D.00 | Picking own skin |
| U208z00 | [X]Intent self poison oth/unsp drug/medic unspecif pl |
| ZX17100 | Banging own head against object |
| ZX1G.00 | Scratches self |
| Read code | Description |
|---|---|
| 13Hj.00 | Sub com trt ordr S17 A MHA 1983 |
| 69F..00 | Mental Health Act examination |
| 69F..11 | Section’ exam,Ment Health Act |
| 69F1.00 | Section’ exam – patient’s GP |
| 69F2.00 | Section’ exam-approved doctor |
| 69F3.00 | Section’ exam – social worker |
| 69FZ.00 | Mental Health Act exam NOS |
| 8H23.00 | Admit psychiatric emergency |
| 8H23000 | Emerg psychiatric admiss MHA |
| 8H2 T.00 | Emergency voluntary psychiatric admission Mental Heal |
| 8H38.00 | Non-urgent psychiatric admisn. |
| 8HM9.00 | Listed for Psychiatric admissn |
| 8Ha..00 | Voluntary admission |
| 8Hb..00 | Involuntary admission |
| 9H. . .11 | Patient ‘sectioned’ |
| 9H1..00 | Form 4-admit to hosp-assess |
| 9H11.00 | Form 4 completed |
| 9H12.00 | Form 4 passed to social worker |
| 9H1Z.00 | Form 4 NOS |
| 9H2..00 | Form 5/7-emerg admit-assess |
| 9H21.00 | Form 7-medical recommendation |
| 9H22.00 | Form 5-nearest relative recom |
| 9H23.00 | Form 7-fee to soc services |
| 9H2Z.00 | Form 5/7 – NOS |
| 9H4..00 | Section 2 form – compulsory admission for assessment |
| 9H41.00 | Form 2 completed |
| 9H42.00 | Form 2 passed to social worker |
| 9H43.00 | Form 2 passed to nearest relative |
| 9H4Z.00 | Form 2 NOS |
| 9H5..00 | Section 3 form – compulsory admission for treatment |
| 9H51.00 | Form 3 completed |
| 9H52.00 | Form 3 passed to social worker |
| 9H53.00 | Form 3 passed to nearest relative |
| 9H5Z.00 | Form 3 NOS |
| 9Ng5.00 | Aftercare under Section 117 MHA 1983 |
| 9Ng5.11 | Section 117 aftercare |
| Z171100 | Aftercare under Section 117 MHA 1983 |
| Z171111 | S117 MHA – Aftercare under Section 117 MHA 1983 |
| Z922.00 | Care planning under section 117 of Mental Health Act |
| Z922.11 | S117 MHA – Care plan s117 MHA |
| Read code | Description |
|---|---|
| 1B1E.00 | Hallucinations |
| Eu30000 | [X]Hypomania |
| E10..00 | Schizophrenic disorders |
| E13z.11 | Psychotic episode NOS |
| Eu2z.11 | [X]Psychosis NOS |
| R001000 | [D]Hallucinations, auditory |
| Eu22015 | [X]Paranoia |
| 1BH3.00 | Paranoid ideation |
| Eu25.00 | [X]Schizoaffective disorders |
| E13z.00 | Nonorganic psychosis NOS |
| E103.00 | Paranoid schizophrenia |
| E11..12 | Depressive psychoses |
| E12..00 | Paranoid states |
| Eu32300 | [X]Severe depressive episode with psychotic symptoms |
| Eu53111 | [X]Puerperal psychosis NOS |
| 1BH..00 | Delusions |
| Eu22011 | [X]Paranoid psychosis |
| Eu30.00 | [X]Manic episode |
| E10z.00 | Schizophrenia NOS |
| 1BY..00 | Elevated mood |
| E120.00 | Simple paranoid state |
| E130.11 | Psychotic reactive depression |
| E107.00 | Schizo-affective schizophrenia |
| R001.00 | [D]Hallucinations |
| R001400 | [D]Visual hallucinations |
| Eu23.00 | [X]Acute and transient psychotic disorders |
| E110100 | Single manic episode, mild |
| Eu30z11 | [X]Mania NOS |
| E12z.00 | Paranoid psychosis NOS |
| F481K00 | Visual hallucinations |
| Eu20.00 | [X]Schizophrenia |
| E1. . .00 | Non-organic psychoses |
| E110.11 | Hypomanic psychoses |
| Eu30100 | [X]Mania without psychotic symptoms |
| E116.00 | Mixed bipolar affective disorder |
| Eu31000 | [X]Bipolar affective disorder, current episode hypoma |
| 1S42.00 | Manic mood |
| E110000 | Single manic episode, unspecified |
| 1BH..11 | Delusion |
| Eu33311 | [X]Endogenous depression with psychotic symptoms |
| Eu30.11 | [X]Bipolar disorder, single manic episode |
| Eu22012 | [X]Paranoid state |
| E113400 | Recurrent major depressive episodes, severe, with psy |
| Eu30200 | [X]Mania with psychotic symptoms |
| Eu22000 | [X]Delusional disorder |
| E130.00 | Reactive depressive psychosis |
| R001z00 | [D]Hallucinations NOS |
| Eu33300 | [X]Recurrent depress disorder cur epi severe with psy |
| Eu20000 | [X]Paranoid schizophrenia |
| E100000 | Unspecified schizophrenia |
For each Read code list we provide a maximum of the 50 most frequently used codes.
Variable definitions for Chapter 4
Below we provide information on how each of the outcomes was defined for the studies in Chapter 4. For each Read code list we provide a maximum of 50 codes. These were the most frequent codes used.
Maternal outcomes
Pre-eclampsia and/or gestational hypertension
Read codes for eclampsia, pre-eclampsia or proteinuric hypertension of pregnancy (Table 55) recorded in the mother’s medical or AHD record between the 20th week of pregnancy and 3 months after delivery were identified as having pre-eclampsia.
| Read code | Description |
|---|---|
| L124600 | Pre-eclampsia, unspecified |
| L125.00 | Severe pre-eclampsia |
| L124.11 | Mild pre-eclampsia |
| L129.00 | Moderate pre-eclampsia |
| L124.12 | Toxaemia NOS |
| L126.00 | Eclampsia |
| L124.00 | Mild or unspecified pre-eclampsia |
| L124z00 | Mild or unspecified pre-eclampsia NOS |
| L12B.00 | Proteinuric hypertension of pregnancy |
| L124100 | Mild or unspecified pre-eclampsia – delivered |
| L124000 | Mild or unspecified pre-eclampsia unspecified |
| L126500 | Eclampsia in pregnancy |
| L126300 | Eclampsia – not delivered |
| L125100 | Severe pre-eclampsia – delivered |
| L125z00 | Severe pre-eclampsia NOS |
| L127100 | Pre-eclampsia or eclampsia with hypertension – delive |
| L124300 | Mild or unspecified pre-eclampsia – not delivered |
| L126600 | Eclampsia in labour |
| L127000 | Pre-eclampsia or eclampsia with hypertension unspecif |
| L126000 | Eclampsia unspecified |
| L126100 | Eclampsia – delivered |
| L125000 | Severe pre-eclampsia unspecified |
| L127.00 | Pre-eclampsia or eclampsia with pre-existing hyperten |
| L125300 | Severe pre-eclampsia – not delivered |
| L126400 | Eclampsia with postnatal complication |
| L126z00 | Eclampsia NOS |
| L125400 | Severe pre-eclampsia with postnatal complication |
Women with evidence of gestational hypertension were identified separately by searching for any of the following records between the 20th week of pregnancy and 3 months after delivery:
-
Read codes specific to hypertension in pregnancy (Table 56) both in the medical records and in the AHD records
-
Read codes for hypertension and hypertension monitoring that are not specific to pregnancy (Table 57), again both in the medical records and in the AHD records
-
two blood pressure measurements with systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg
-
any of the women identified as having gestational hypertension above were reclassified as having pre-existing hypertension if they had:
-
a diagnosis of hypertension or a code for hypertension monitoring prior to pregnancy
-
two blood pressure measurements with systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg prior to pregnancy
-
a prescription from the BNF chapter 2.5 in the 6 months prior to pregnancy.
-
| Read code | Description |
|---|---|
| L12..00 | Hypertension complicating pregnancy/childbirth/puerpe |
| L12z300 | Unspecified hypertension in preg/childb/puerp – not d |
| L123500 | Gestational hypertension |
| L123.00 | Transient hypertension of pregnancy |
| L120.00 | Benign essential hypertension in pregnancy/childbirth |
| L12z.00 | Unspecified hypertension in pregnancy/childbirth/puer |
| L120000 | Benign essential hypertension in preg/childb/puerp un |
| L12zz00 | Unspecified hypertension in preg/childb/puerp NOS |
| L123z00 | Transient hypertension of pregnancy NOS |
| L12z100 | Unspecified hypertension in preg/childb/puerp – deliv |
| L123100 | Transient hypertension of pregnancy – delivered |
| L120z00 | Benign essential hypertension in preg/childb/puerp NO |
| L12z000 | Unspecified hypertension in preg/childb/puerp unspeci |
| L123400 | Transient hypertension of pregnancy + postnatal compl |
| L120300 | Benign essential hypertension in preg/childb/puerp-no |
| L120400 | Benign essential hypertension in preg/childb/puerp +p |
| L121.00 | Renal hypertension in pregnancy/childbirth/puerperium |
| L123300 | Transient hypertension of pregnancy – not delivered |
| Read code | Description |
|---|---|
| 662P.00 | Hypertension monitoring |
| G20..00 | Essential hypertension |
| G2. . .00 | Hypertensive disease |
| G20..11 | High blood pressure |
| 9OI4.00 | Hypertens.monitor.1st letter |
| 9OIA.00 | Hypertension monitor.chck done |
| G20z.00 | Essential hypertension NOS |
| G20z.11 | Hypertension NOS |
| 662d.00 | Hypertension annual review |
| 9N1y200 | Seen in hypertension clinic |
| G2z..00 | Hypertensive disease NOS |
| 246M.00 | White coat hypertension |
| 9OI5.00 | Hypertens.monitor 2nd letter |
| 9OI..00 | Hypertension monitoring admin. |
| 662G.00 | Hypertensive treatm.changed |
| 9N4L.00 | DNA – Did not attend hypertension clinic |
| 9h32.00 | Excepted from hypertension qual indicators: Informed |
| 662O.00 | On treatment for hypertension |
| 662c.00 | Hypertension six month review |
| G24..00 | Secondary hypertension |
| 9OI6.00 | Hypertens.monitor 3rd letter |
| 9h31.00 | Excepted from hypertension qual indicators: Patient u |
| 6627 | Good hypertension control |
| G201.00 | Benign essential hypertension |
| 6146200 | Hypertension induced by oral contraceptive pill |
| 6628 | Poor hypertension control |
| G2. . .11 | BP – hypertensive disease |
| 8B26.00 | Antihypertensive therapy |
| 662H.00 | Hypertension treatm.stopped |
| 9OI1.00 | Attends hypertension monitor. |
| 8BL0.00 | Patient on maximal tolerated antihypertensive therapy |
| 662F.00 | Hypertension treatm. started |
| 9OI8.00 | Hypertens.monitor phone invite |
| G24z100 | Hypertension secondary to drug |
| G2y..00 | Other specified hypertensive disease |
| 8HT5.00 | Referral to hypertension clinic |
| G22z.00 | Hypertensive renal disease NOS |
| G22..00 | Hypertensive renal disease |
| G24zz00 | Secondary hypertension NOS |
| 662b.00 | Moderate hypertension control |
| G200.00 | Malignant essential hypertension |
| 9OIA.11 | Hypertension monitored |
| 9h3..00 | Exception reporting: hypertension quality indicators |
| L128200 | Pre-exist 2ndry hypertens comp preg childbth and puer |
| 9OI7.00 | Hypertens.monitor verbal inv. |
| TJC7.00 | Adverse reaction to other antihypertensives |
| G241z00 | Secondary benign hypertension NOS |
| Gyu2000 | [X]Other secondary hypertension |
| G202.00 | Systolic hypertension |
| G21z011 | Other codes |
Gestational diabetes
Women with gestational diabetes were identified as those with any of the following records:
-
Read codes for gestational diabetes or diabetes mellitus in pregnancy (Table 58), either in the medical records or in the AHD records between the 24th week of pregnancy and 3 months after delivery
-
Read code for diabetes or diabetes monitoring more generally (Table 59), either in the medical records or in the AHD records between the 24th week of pregnancy and 3 months after delivery
-
prescription for insulin from the BNF chapter 6.1.1 between the 24th week of pregnancy and delivery.
| Read code | Description |
|---|---|
| L180811 | Gestational diabetes mellitus |
| L180.00 | Diabetes mellitus during pregnancy/childbirth/puerper |
| L180800 | Diabetes mellitus arising in pregnancy |
| L180z00 | Diabetes mellitus in pregnancy/childbirth/puerperium |
| L180300 | Diabetes mellitus during pregnancy – baby not yet del |
| L180100 | Diabetes mellitus during pregnancy – baby delivered |
| Read code | Description |
|---|---|
| 9N1Q.00 | Seen in diabetic clinic |
| 9OL..00 | Diabetes monitoring admin. |
| 66 A..00 | Diabetic monitoring |
| C10..00 | Diabetes mellitus |
| 66AS.00 | Diabetic annual review |
| C10E.00 | Type 1 diabetes mellitus |
| 68A7.00 | Diabetic retinopathy screening |
| C109.12 | Type 2 diabetes mellitus |
| C108.00 | Insulin dependent diabetes mellitus |
| 66A2.00 | Follow-up diabetic assessment |
| 9OL4.00 | Diabetes monitoring 1st letter |
| 66A5.00 | Diabetic on insulin |
| 9NND.00 | Under care of diabetic foot screener |
| 66AQ.00 | Diabetes: shared care programme |
| 9OL5.00 | Diabetes monitoring 2nd letter |
| C101.00 | Diabetes mellitus with ketoacidosis |
| 66AJ.00 | Diabetic – poor control |
| 2G5E.00 | O/E – Right diabetic foot at low risk |
| F420.00 | Diabetic retinopathy |
| 2G5I.00 | O/E – Left diabetic foot at low risk |
| 9h42.00 | Excepted from diabetes quality indicators: Informed d |
| 8B3l.00 | Diabetes medication review |
| 9OL6.00 | Diabetes monitoring 3rd letter |
| 9OL1.00 | Attends diabetes monitoring |
| 9N2d.00 | Seen by diabetologist |
| 66AZ.00 | Diabetic monitoring NOS |
| 9h41.00 | Excepted from diabetes qual indicators: Patient unsui |
| 66AU.00 | Diabetes care by hospital only |
| 66Ac.00 | Diabetic peripheral neuropathy screening |
| 66AD.00 | Fundoscopy – diabetic check |
| 2BBJ.00 | O/E – no right diabetic retinopathy |
| 2BBK.00 | O/E – no left diabetic retinopathy |
| C109.00 | Non-insulin dependent diabetes mellitus |
| 66AP.00 | Diabetes: practice programme |
| 66AR.00 | Diabetes management plan given |
| 8H4F.00 | Referral to diabetologist |
| 13B1.00 | Diabetic diet |
| 1434.00 | H/O: diabetes mellitus |
| 9N4I.00 | DNA – Did not attend diabetic clinic |
| 8I3X.00 | Diabetic retinopathy screening refused |
| 2BBP.00 | O/E – right eye background diabetic retinopathy |
| 66A4.00 | Diabetic on oral treatment |
| C108.11 | IDDM-Insulin dependent diabetes mellitus |
| 2BBQ.00 | O/E – left eye background diabetic retinopathy |
| F420000 | Background diabetic retinopathy |
| 9N1v.00 | Seen in diabetic eye clinic |
| C10EM00 | Type 1 diabetes mellitus with ketoacidosis |
| 66AI.00 | Diabetic – good control |
| 66Aq.00 | Diabetic foot screen |
Any of the women identified as having gestational diabetes above were reclassified as having pre-existing diabetes if they had:
-
a Read code for diabetes or diabetes monitoring prior to pregnancy (but no codes specific to pregnancy), either in the medical records or in the AHD records
-
insulin prescriptions in the 6 months before pregnancy from the BNF chapter 6.1.1.
The Read codes that were used to identify pre-existing diabetes included diabetes monitoring and administration codes to be as sensitive as possible.
Caesarean section
Pregnancies ending in a caesarean section were identified in one of three ways:
-
by searching for relevant Read codes (Table 60) in the mother’s or child’s medical records between 4 weeks prior to the EDD and 6 months after the delivery date
-
by searching for relevant Read codes (see Table 60) in the mother’s or child’s AHD records between 4 weeks prior to the EDD and 6 months after the delivery date
-
by searching the mother’s or child’s AHD records for AHD codes for ‘CHS [Child Health Surveillence] – delivery details’ recorded between 4 weeks prior to the EDD and 6 months after the delivery date, and identifying whether or not the values recorded against the AHD code indicated the mode of delivery was caesarean.
| Read code | Description |
|---|---|
| 14Y0.00 | Born by caesarean section |
| 14Y2.00 | Born by elective caesarean section |
| 14Y6.00 | Born by emergency caesarean section |
| 7F12.00 | Elective caesarean delivery |
| 7F12000 | Elective upper uterine segment caesarean delivery |
| 7F12100 | Elective lower uterine segment caesarean delivery |
| 7F12111 | Elective lower uterine segment caesarean section (LSC |
| 7F12y00 | Other specified elective caesarean delivery |
| 7F12z00 | Elective caesarean delivery NOS |
| 7F13.00 | Other caesarean delivery |
| 7F13000 | Upper uterine segment caesarean delivery NEC |
| 7F13100 | Lower uterine segment caesarean delivery NEC |
| 7F13111 | Lower uterine segment caesarean section (LSCS) NEC |
| 7F13200 | Extraperitoneal caesarean section |
| 7F13300 | Emergency caesarean section |
| 7F13y00 | Other specified other caesarean delivery |
| 7F13z00 | Other caesarean delivery NOS |
| 7F1A000 | Caesarean hysterectomy |
| L213200 | Multiple delivery, all by caesarean section |
| L398.00 | Caesarean delivery |
| L398000 | Caesarean delivery unspecified |
| L398100 | Caesarean delivery – delivered |
| L398200 | Caesarean section – pregnancy at term |
| L398300 | Delivery by elective caesarean section |
| L398400 | Delivery by emergency caesarean section |
| L398500 | Delivery by caesarean hysterectomy |
| L398600 | Caesarean delivery following previous Caesarean deliv |
| L398z00 | Caesarean delivery NOS |
| L441.00 | Caesarean wound disruption |
| L441000 | Caesarean wound disruption unspecified |
| L441100 | Caesarean wound disruption – delivered with p/n compl |
| L441200 | Caesarean wound disruption with postnatal complicatio |
| L441z00 | Caesarean wound disruption NOS |
| Lyu5200 | [X]Other single delivery by caesarean section |
| Lyu6A00 | [X]Infection of caesarean section wound following del |
| Q021300 | Fetus/neonate affected by placental damage-caesarean |
| Q034.00 | Fetus or neonate affected by caesarean section |
| Z254500 | Delivered by caesarean section – pregnancy at term |
| Z254600 | Deliv caes following prev caes |
Perinatal death
Fetal losses and neonatal deaths were identified in one of three ways:
-
by searching for relevant Read codes (Table 61) in the mother’s medical records between 20 weeks’ gestation and 1 week after birth
-
by searching for relevant Read codes (see Table 61) in the mother’s AHD records between 20 weeks’ gestation and 1 week after birth
-
by searching the mother’s AHD records for AHD codes for ‘maternity outcome’ and ‘maternity infant details’ recorded between 20 weeks’ gestation and 1 week after birth, and identifying whether or not the values recorded against the AHD code indicated a stillbirth had occurred.
| Read code | Description |
|---|---|
| 633..12 | stillbirth [prevention record] |
| 6332.00 | single stillbirth |
| 6335.00 | twins – both still born |
| 6339.00 | triplets – 3 still born |
| L264.00 | intrauterine death |
| L264.11 | fetal death in utero |
| L264000 | intrauterine death unspecified |
| L264100 | intrauterine death – delivered |
| L264200 | intrauterine death with antenatal problem |
| L264z00 | intrauterine death nos |
| Q48D.00 | [x] stillbirth |
| Q48D000 | [x]fresh stillbirth |
| Q48D100 | [x]macerated stillbirth |
| Q48y600 | early neonatal death |
| Q48y700 | late neonatal death |
| Q4z..11 | infant death |
| Q4z..12 | neonatal death |
| Q4z..13 | newborn death |
| Q4z..14 | perinatal death |
| Q4z..15 | stillbirth nec |
| ZV27.12 | [v]stillbirth |
| ZV27100 | [v]single stillbirth |
| ZV27400 | [v]twins, both stillborn |
| ZV27700 | [v]other multiple birth, all stillborn |
| ZVu2C00 | [x]other multiple births, all stillborn |
| L39X.00 | obstetric death of unspecified cause |
| Lyu7500 | [x]obstetric death of unspecified cause |
| Q210.00 | fetal death due to prelabour anoxia |
| Q211.00 | fetal death due to labour anoxia |
For the pregnancies in THIN only, all free text recorded in pregnancy in either the medical or AHD records of the unlinked pregnancies was obtained and a string search used to identify any more perinatal deaths. No free text was available from the CPRD.
Child outcomes
Major congenital anomalies
Read codes starting with ‘P’ (indicating some form of congenital anomaly) recorded in our study population during the first year of a linked child’s life were identified. Read codes for malformations recorded in the mother’s notes at any time during pregnancy were also identified. These Read code lists were then compared with the EUROCAT guidelines and reviewed by a GP (IN) to identify whether the codes indicated a major or minor malformation occurred. Following this review a number of Read codes remained that were too vague to allow for a decision whether the malformation was major or minor. In the THIN cohort, the free-text record of children with these vague codes was obtained and reviewed, whereas in the CPRD cohort the Read coded medical record of children with these codes was reviewed without additional free-text information. Children in whom the free-text or coded record indicated that the malformation was major were included as a case; children in whom the record did not provide evidence the malformation was major were not included as a case. The list of Read codes used in the final extraction is provided in Table 62.
| Read code | Description |
|---|---|
| P54..00 | Ventricular septal defect |
| PC60.00 | Hypospadias |
| PA5..00 | Congenital hypertrophic pyloric stenosis |
| P550.00 | Atrial septal defect NOS |
| P90..00 | Cleft palate |
| PD23.11 | Congenital dilated renal pelvis |
| PE1..12 | Sternomastoid tumour |
| P71..00 | Coarctation of aorta |
| PD34.11 | Duplex kidneys |
| P52..00 | Tetralogy of Fallot |
| PF0..00 | Polydactyly – supernumerary digits |
| PG0y000 | Brachycephaly |
| P92..00 | Cleft palate with cleft lip |
| PD23.00 | Congenital hydronephrosis |
| P55..00 | Ostium secundum atrial septal defect |
| PG0z.11 | Dysmorphic features |
| PB26.00 | Imperforate anus |
| PF1..00 | Syndactyly – webbing of digits |
| PG71.00 | Gastroschisis |
| P6y2.00 | Pulmonary infundibular stenosis |
| PB30.00 | Hirschsprung’s disease |
| PC33.00 | Bicornuate uterus |
| PF13.11 | Webbed toes |
| P9. . .00 | Cleft palate and lip |
| PF01.00 | Accessory fingers |
| P21..00 | Microcephalus |
| P91..00 | Cleft lip (harelip) |
| PD11.00 | Polycystic kidney disease |
| P360.00 | Congenital ptosis |
| PG03.00 | Craniosynostosis |
| P1. . .00 | Spina bifida |
| PD02.00 | Congenital absence of kidney |
| PG0C.00 | Pierre – Robin syndrome |
| PD13.11 | Multicystic kidney |
| P6z..00 | Congenital heart anomaly NOS |
| PH3y200 | Epidermolysis bullosa |
| P51..00 | Transposition of great vessels |
| PKy9300 | Prader – Willi syndrome |
| P641.00 | Bicuspid aortic valve |
| P67..00 | Hypoplastic left heart syndrome |
| P602.00 | Congenital pulmonary stenosis |
| PK5..00 | Tuberous sclerosis |
| P31..00 | Microphthalmos |
| P63..00 | Congenital aortic valve stenosis |
| PH1..00 | Ichthyosis congenital |
| P344200 | Coloboma of iris |
| P3y0.00 | Ocular albinism |
| P80..00 | Choanal atresia |
| PA30.00 | Atresia of oesophagus |
| PC60312 | Hypospadias, glandular |
Preterm birth (< 37 weeks)
Preterm births were identified in one of the following ways:
-
by searching for relevant Read codes (Table 63) in the mother’s and child’s medical records between 4 weeks prior to delivery and 6 months after delivery
-
by searching for relevant Read codes (see Table 63) in the mother’s and child’s AHD records between 4 weeks prior to delivery and 6 months after delivery
-
by searching the mother’s and child’s AHD records for AHD codes for ‘CHS [Child Health Surveillence] – gestation’ and ‘Maternity outcome gestational age of baby’ recorded between 4 weeks prior to delivery and 6 months after delivery, and identifying whether or not the values recorded against the AHD code indicated the pregnancy ended prematurely
-
by using the LMP dates, or the dates on which antenatal and postnatal codes were recorded to estimate whether or not the delivery date occurred before 37 weeks’ gestation.
| Read code | Description |
|---|---|
| 635..13 | Premature baby |
| 6352.00 | Baby v. premature 32–36 weeks |
| 6353.00 | Baby extremely prem.28–32 week |
| 6356.00 | Baby premature 26–28 weeks |
| 6357.00 | Baby premature 24–26 weeks |
| 635B.00 | Baby premature 36 weeks |
| F422011 | Retinopathy of prematurity |
| L142.00 | Early onset of delivery |
| L142.11 | Premature delivery |
| L142000 | Early onset of delivery unspecified |
| L142100 | Early onset of delivery – delivered |
| L142z00 | Early onset of delivery NOS |
| L143.00 | Premature labour and delivery |
| L143100 | Premature labour with premature delivery |
| L143300 | Premature delivery without labour |
| Q11..00 | Short gestation and unspecified low birthweight probl |
| Q11..11 | Baby born premature |
| Q110.00 | Very premature – less than 1000 g or less than 28 week |
| Q110.11 | Immature baby |
| Q111.00 | Premature – weight 1000 g-2499 g or gestation of 28–37w |
| Q112.00 | Extreme immaturity |
| Q112.11 | Extreme prematurity – less than 28 weeks |
| Q116.00 | Premature infant 28–37 weeks |
| Q11z.00 | Born premature NOS |
| Q317100 | Prematurity with interstitial pulmonary fibrosis |
| Q432.00 | Preterm delivery associated jaundice |
| Q456.00 | Anaemia of prematurity |
| Qyu1100 | [X]Other preterm infants |
Low birthweight (< 2500 g)
Children born with a low birthweight were identified in one of the following ways:
-
by searching for relevant Read codes (Table 64) in the mother’s and child’s medical records between 4 weeks prior to delivery and 6 months after delivery
-
by searching for relevant Read codes (see Table 64) in the mother’s and child’s AHD records between 4 weeks prior to delivery and 6 months after delivery
-
by searching the mother’s and child’s AHD records for AHD codes for ‘Maternity infant details’ recorded between 4 weeks prior to delivery and 6 months after delivery, and identifying whether or not the values recorded against the AHD code indicated the child weighed < 2500 g.
| Read code | Description |
|---|---|
| 6361.00 | Baby BW = < 3% (under 2500 g) |
| 636 A.00 | Baby BW = below 751gm |
| 636B.00 | Baby BW = 751g-1kg |
| 636C.00 | Baby BW = 1.0–1.5kg |
| 636D.00 | Baby BW = 1.5–2.0kg |
| 636E.00 | Baby BW = 2.0 – 2.5kg |
| Q114.00 | Low birthweight |
| Q114000 | Birth weight 1000–2499 g |
| Q115.00 | Extremely low birth weight infant |
| Q115000 | Birth weight 999 g or less |
| Qyu1000 | [X]Other low birth weight |
Low weight for gestation/poor fetal growth
Children born small for their gestational age were identified in one of the following ways:
-
by searching for relevant Read codes (Table 65) in the mother’s and child’s medical record between 2 weeks prior to delivery and 8 weeks after delivery.
-
by searching for relevant Read codes (see Table 65) in the mother’s and child’s AHD record between 2 weeks prior to delivery and 8 weeks after delivery.
| Read code | Description |
|---|---|
| L265.00 | Small-for-dates fetus in pregnancy |
| L265000 | Small-for-dates unspecified |
| L265100 | Small-for-dates – delivered |
| L265200 | Small-for-dates with antenatal problem |
| L265300 | Maternal care for poor fetal growth |
| L265311 | Maternal care for intrauterine growth retardation |
| L265z00 | Small-for-dates NOS |
| L514.00 | Maternal care for poor fetal growth |
| Q10..00 | Slow fetal growth and fetal malnutrition |
| Q100.00 | Fetus small-for-dates, without mention of malnutritio |
| Q100.11 | Fetus small-for-dates (SFD), without mention of malnu |
| Q101.00 | Fetus small-for-dates with signs of malnutrition |
| Q101.11 | Fetus small-for-dates (SFD) with signs of malnutritio |
| Q10z.00 | Fetal growth retardation NOS |
| Q10z.11 | Intrauterine growth retardation |
| Q113.00 | Light for gestational age |
| Q13..00 | Light for gestational age |
Low Apgar scores (< 7) at 5 minutes
Children born with a low Apgar score were identified in one of the following ways:
-
by searching for relevant Read codes (Table 66) in the mother’s and child’s medical records between 4 weeks prior to delivery and 6 months after delivery.
-
by searching for relevant Read codes (see Table 66) in the mother’s and child’s AHD records between 4 weeks prior to delivery and 6 months after delivery.
-
by searching the mother’s and child’s AHD records for AHD codes for ‘CHS – APGAR Score At 5 Minutes’ and ‘Maternity infant details’ recorded between 4 weeks prior to delivery and 6 months after delivery, and identifying whether or not the values recorded against the AHD code indicated the Apgar score was ≥ 0 and ≤ 6.
| Read code | Description |
|---|---|
| 63A1.00 | Apgar at 5 minutes = 0 |
| 63A2.00 | Apgar at 5 minutes = 1 |
| 63A3.00 | Apgar at 5 minutes = 2 |
| 63A4.00 | Apgar at 5 minutes = 3 |
| 63A5.00 | Apgar at 5 minutes = 4 |
| 63A6.00 | Apgar at 5 minutes = 5 |
| 63A7.00 | Apgar at 5 minutes = 6 |
Extrapyramidal syndromes/signs/symptoms/effects or withdrawal symptoms in neonate to be included in ‘transient’ poor birth outcomes.
Preliminary investigations suggested it would not be possible to reliably identify cases of neonatal abstinence syndrome in primary care databases. Instead, an outcome of extrapyramidal-type symptoms was defined to include children with any record for a symptom related to the syndrome.
Operationally this outcome was defined as any child with a Read code for one of the following symptoms recorded in the medical or AHD records in the three months after birth:
-
abnormally increased or decreased muscle tone
-
agitation, restlessness and irritability
-
tremor/shaking and abnormal movements
-
difficulty breathing/respiratory distress – we will look at respiratory distress syndrome separately.
The full list of Read codes related to these symptoms is provided in Table 67.
| Read code | Description |
|---|---|
| Q30..00 | Respiratory distress syndrome |
| 1738.00 | Difficulty breathing |
| 1B15.11 | Irritable – symptom |
| 232C.00 | Noisy breathing |
| Q316.00 | Newborn transitory tachypnoea |
| R060600 | [D]Respiratory distress |
| R060400 | [D]Apnoea |
| Q31yz11 | Grunting baby |
| Q48B.00 | Jittery baby |
| 1739.00 | Shortness of breath |
| Q31y200 | Perinatal respiratory distress NOS |
| 2324.00 | O/E – respiratory distress |
| Q31y600 | Apnoea of newborn |
| R060300 | [D]Tachypnoea |
| Q31y611 | Neonatal apnoeic attack |
| R025.00 | [D]Cyanosis |
| 2326.00 | O/E – expiratory wheeze |
| R060800 | [D]Shortness of breath |
| Q31y111 | Cyanotic attacks of the newborn |
| F132300 | Myoclonic jerks |
| 225 A.00 | O/E – irritable |
| 1B22.12 | Shaking |
| Q31y000 | Perinatal apnoeic spells NOS |
| Q310.00 | Congenital pneumonia |
| 1B1O.00 | Restless |
| Q48y211 | Floppy infant |
| 173..13 | Shortness of breath symptom |
| N135.00 | Torticollis unspecified |
| F132.00 | Myoclonus |
| F13z500 | Benign neonatal sleep myoclonus |
| Q31y100 | Perinatal cyanotic attacks NOS |
| Q48y200 | Congenital hypotonia |
| R060900 | [D]Wheezing |
| R010.00 | [D]Abnormal involuntary movements |
| 16A3.11 | Torticollis – symptom |
| 1673.11 | Blue – symptom |
| PE1..00 | Congenital sternomastoid torticollis |
| F138200 | Spasmodic torticollis |
| 232F.00 | O/E – subcostal recession |
| 173..12 | Dyspnoea – symptom |
| Q3z..00 | Fetal or newborn respiratory problems NOS |
| 2276000.00 | Blue lips |
| 2276.00 | O/E – central cyanosis |
| R010300 | [D]Tremor NOS |
| 1B15.00 | Irritable |
| 1B22.11 | Tremor symptom |
| N23y400 | Spasm of muscle |
| R060z00 | [D]Respiratory abnormalities NOS |
| Q3. . .00 | Fetus and newborn respiratory conditions |
Neurodevelopmental and behavioural disorders
Children with neurodevelopmental and/or behavioural disorders were identified in one of three ways:
-
by searching for relevant Read codes (Table 68) in the child’s medical records up to 5 years after the delivery date
-
by searching for relevant Read codes (see Table 68) in the child’s AHD records up to 5 years after the delivery date
-
by searching the mother’s or child’s AHD records for AHD codes for ‘CHS – Gait’, ‘CHS – Language 3 Years’, ‘CHS – Speech & Language’, ‘CHS – Speech 3 Years’ or ‘CHS – Behaviour’ recorded up to 5 years after the delivery date, and identifying whether the values recorded against the AHD code indicate there a problem was identified.
| Read code | Description |
|---|---|
| 9N29.00 | Seen by speech therapist |
| R012.00 | [D]Gait abnormality |
| 1B9..00 | Speech problem |
| ZV40.11 | [V]Behavioural problems |
| ZS67300 | Speech delay |
| E2C..11 | Behaviour disorder |
| E2Cy000 | Breath holder |
| 1B1X.00 | Behavioural problem |
| E2F..00 | Specific delays in development |
| E2Fy.00 | Other development delays |
| ZD. . .00 | Speech and language therapy |
| R012z00 | [D]Gait abnormality NOS |
| 1469.00 | H/O: behaviour problem |
| E2C1200 | Tantrums |
| E140.12 | Autism |
| 64R3.11 | Child referral- speech therapy |
| Eu84011 | [X]Autistic disorder |
| 1B9..11 | Speech problem – symptom |
| 1P00.00 | Hyperactive behaviour |
| E2F5.11 | Global delay |
| 1B92.11 | Stammer – symptom |
| Eu95300 | [X]Involuntary excessive blinking |
| R034700 | [D]Gross motor development delay |
| ZS7B400 | Developmental language delay |
| 1B92.12 | Stutter – symptom |
| Eu85.00 | [X]Global developmental delay |
| 64R3.00 | Child: speech therapy |
| ZV57300 | [V]Speech therapy |
| E2F3.12 | Speech development disorder |
| ZS7B100 | Expressive language delay |
| ZL4C.00 | Under care of speech and language therapist |
| E2Fz.00 | Developmental disorder NOS |
| 918e.00 | On learning disability register |
| 13Z4E00 | Learning difficulties |
| 2B4 A.00 | O/E – speech delay |
| E2E..00 | Childhood hyperkinetic syndrome |
| Eu90011 | [X]Attention deficit hyperactivity disorder |
| E2F3.11 | Language development disorder |
| ZV40300 | [V]Other behavioural problems |
| 13ZA.00 | Language difficulty |
| Eu80.00 | [X]Specific developmental disorders of speech and lan |
| 13Z4C00 | Behavioural problems at school |
| E2F3.00 | Speech or language developmental disorder |
| E140.00 | Infantile autism |
| Eu81z11 | [X]Learning disability NOS |
| R034A00 | [D]Communication skills development delay |
| ZS. . .00 | Speech and language disorder |
| E2E0.00 | Child attention deficit disorder |
| ZT45.00 | Difficulty communicating |
Note that Read codes for neurodevelopmental and behavioural disorders were identified as those relating to conditions listed as neurodevelopmental or behavioural disorders in Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition.
Covariates
Down syndrome (for exclusion from cohort)
Children with Down syndrome or trisomy 21 were identified by searching for relevant Read codes (Table 69) anywhere in the child’s medical record. As this is a congenital condition, and was being used as an exclusion criterion, individuals with a code recorded against a missing date were considered to have the condition.
| Read code | Description |
|---|---|
| PJ0..00 | Down’s syndrome – trisomy 21 |
| PJ0..11 | Mongolism |
| PJ0..12 | Trisomy 21 |
| PJ00.00 | Trisomy 21, meiotic nondisjunction |
| PJ01.00 | Trisomy 21, mosaicism |
| PJ01.11 | Trisomy 21, mitotic nondisjunction |
| PJ02.00 | Trisomy 21, translocation |
| PJ02.11 | Partial trisomy 21 in Down’s syndrome |
| PJ0z.00 | Down’s syndrome NOS |
| PJ0z.11 | Trisomy 21 NOS |
Children whose mothers had codes recorded in their medical record during pregnancy were not considered to have Down syndrome or trisomy 21 as exploratory work revealed that some practices are using the Read codes for Down syndrome to record (negative) screening tests for Down syndrome.
Townsend score
Townsend scores and Townsend quintiles are provided by the THIN data provider for any consenting practice. These data were therefore directly extracted from the relevant table for each pregnancy. The CPRD also provides Townsend score data for consenting English practices. However, these data were not available at the time of analysis.
Pre-pregnancy body mass index
The pre-pregnancy BMI of women was identified in one of two ways:
-
By searching the mother’s AHD records for AHD codes for ‘Weight’ and identifying whether or not a valid BMI was recorded against it in the year prior to the estimated LMP.
-
By searching the mother’s AHD records for AHD codes for ‘Weight’ and identifying whether or not a weight in kilograms was recorded against it in the year prior to the estimated LMP. If a weight was recorded in the year prior to the estimated LMP, the mother’s records were searched for a height record. If height records were identified, the closest one to the estimated LMP was used to calculate the BMI.
As part of the data cleaning process BMI records ≥ 70 kg/m2, weight records > 180 kg or < 40 kg, and height records > 1.95 cm and < 1.4 cm were excluded.
Pre-pregnancy obesity
Women with pre-pregnancy obesity were identified in one of four ways:
-
By searching for relevant Read codes (Table 70) in the mother’s medical records up to 1 year before the estimated LMP.
-
By searching for relevant Read codes (see Table 70) in the mother’s AHD records up to 1 year before the estimated LMP.
-
By searching the mother’s AHD records for AHD codes for ‘Weight’ and identifying whether a BMI ≥ 30 kg/m2 was recorded against it in the year prior to the estimated LMP.
-
By searching the mother’s AHD record for AHD codes for ‘Weight’ and identifying whether or not a weight in kilograms was recorded against it in the year prior to the estimated LMP. If a weight was recorded in the year prior to the estimated LMP the mother’s record was searched for a height record. If height records were identified the closest one to the estimated LMP was used to calculate the BMI. If the BMI was ≥ 30 kg/m2 the woman was classified as obese.
| Read code | Description |
|---|---|
| 222 A.00 | O/E – obese |
| 22A5.11 | O/E – obese |
| 22K5.00 | Body mass index 30 + – obesity |
| 22K7.00 | Body mass index 40 + – severely obese |
| 66C..00 | Obesity monitoring |
| 66C1.00 | Initial obesity assessment |
| 66C2.00 | Follow-up obesity assessment |
| 66C4.00 | Has seen dietitian – obesity |
| 66C5.00 | Treatment of obesity changed |
| 66C6.00 | Treatment of obesity started |
| 66C7.00 | Treatment of obesity stopped |
| 66CE.00 | Reason for obesity therapy – occupational |
| 66CZ.00 | Obesity monitoring NOS |
| 9OK..00 | Obesity monitoring admin. |
| 9OK..11 | Obesity clinic administration |
| 9OK1.00 | Attends obesity monitoring |
| 9OK2.00 | Refuses obesity monitoring |
| 9OK3.00 | Obesity monitoring default |
| 9OK4.00 | Obesity monitoring 1st letter |
| 9OK5.00 | Obesity monitoring 2nd letter |
| 9OK6.00 | Obesity monitoring 3rd letter |
| 9OK7.00 | Obesity monitoring verbal inv. |
| 9OK8.00 | Obesity monitor phone invite |
| 9OK9.00 | Obesity monitoring deleted |
| 9OKA.00 | Obesity monitoring check done |
| 9OKZ.00 | Obesity monitoring admin.NOS |
| 9hN..00 | Exception reporting: obesity quality indicators |
| 9hN0.00 | Excepted from obesity quality indicators: patient uns |
| 9hN1.00 | Excepted from obesity quality indicators: informed di |
| C380.00 | Obesity |
| C380000 | Obesity due to excess calories |
| C380100 | Drug-induced obesity |
| C380200 | Extreme obesity with alveolar hypoventilation |
| C380300 | Morbid obesity |
| C380400 | Central obesity |
| C380500 | Generalised obesity |
| C380600 | Adult-onset obesity |
| C380700 | Lifelong obesity |
| C38y011 | Obesity hypoventilation syndrome |
| C38z000 | Simple obesity NOS |
| Cyu7000 | [X]Other obesity |
| ZC2CM00 | Dietary advice for obesity |
| ZV65319 | [V]Dietary counselling in obesity |
As part of the data cleaning process BMI records > 70 kg/m2, weight records > 180 kg or < 40 kg, and height records > 1.95 m and < 1.4 m were excluded.
Pre-pregnancy smoking status
Pre-pregnancy smoking status was identified by searching the mother’s AHD records for AHD codes for ‘Smoking’ in the 3 years prior to the estimated LMP.
Pre-pregnancy alcohol abuse
Women with pre-pregnancy alcohol abuse were identified in one of three ways:
-
by searching for relevant Read codes (Table 71) in the mother’s medical records up to 3 years before the estimated LMP
-
by searching for relevant Read codes (see Table 71) in the mother’s AHD records up to 3 years before the estimated LMP
-
by searching the mother’s AHD records for AHD codes for ‘Alcohol’ and identifying whether or not the value recorded against it was indicative of alcohol abuse.
| Read code | Description |
|---|---|
| 1365.00 | Heavy drinker – 7–9u/day |
| 1366.00 | Very heavy drinker – > 9u/day |
| 1369.00 | Suspect alcohol abuse – denied |
| 136P.00 | Heavy drinker |
| 136Q.00 | Very heavy drinker |
| 136S.00 | Hazardous alcohol use |
| 136 T.00 | Harmful alcohol use |
| 136 W.00 | Alcohol misuse |
| 136Y.00 | Drinks in morning to get rid of hangover |
| 13Y8.00 | Alcoholics anonymous |
| 66e..00 | Alcohol disorder monitoring |
| 7P22100 | Delivery of rehabilitation for alcohol addiction |
| 8BA8.00 | Alcohol detoxification |
| 8H7p.00 | Referral to community alcohol team |
| 8HHe.00 | Referral to community drug and alcohol team |
| 9NN2.00 | Under care of community alcohol team |
| 9k1..00 | Alcohol misuse – enhanced services administration |
| E01y000 | Alcohol withdrawal syndrome |
| E23..00 | Alcohol dependence syndrome |
| E23..11 | Alcoholism |
| E23..12 | Alcohol problem drinking |
| E230.00 | Acute alcoholic intoxication in alcoholism |
| E231.00 | Chronic alcoholism |
| E231000 | Unspecified chronic alcoholism |
| E231100 | Continuous chronic alcoholism |
| E231200 | Episodic chronic alcoholism |
| E231300 | Chronic alcoholism in remission |
| E231z00 | Chronic alcoholism NOS |
| E23z.00 | Alcohol dependence syndrome NOS |
| E250.00 | Nondependent alcohol abuse |
| E250.14 | Intoxication – alcohol |
| E250000 | Nondependent alcohol abuse, unspecified |
| E250200 | Nondependent alcohol abuse, episodic |
| Eu10011 | [X]Acute alcoholic drunkenness |
| Eu10211 | [X]Alcohol addiction |
| J153.00 | Alcoholic gastritis |
| R103.00 | [D]Alcohol blood level excessive |
Pre-pregnancy illicit drug use
Women with pre-pregnancy illicit drug use were identified in one of three ways:
-
by searching for relevant Read codes (Table 72) in the mother’s medical records up to 3 years before the estimated LMP
-
by searching for relevant Read codes (see Table 72) in the mother’s AHD records up to 3 years before the estimated LMP
-
by searching the mother’s prescription records for drugs used in the treatment of illicit drug use.
| Read code | Description |
|---|---|
| 8B23.00 | Drug addiction therapy |
| 46QB.00 | Urine methadone |
| 46QA.00 | Urine cocaine |
| E24..00 | Drug dependence |
| 46Q5.00 | Urine amphetamine |
| E24z.00 | Drug dependence NOS |
| 8B23.12 | FP10(MDA) issued |
| 8B23.11 | Drug addictn therap-methadone |
| E240.00 | Opioid type drug dependence |
| ZV6D700 | [V]Drug abuse counselling and surveillance |
| 46QH.00 | Urine cocaine metabolite screen |
| 46Qf.00 | Urine methadone metabolite level |
| 46Q5.11 | Amphetamine in urine |
| E240.11 | Heroin dependence |
| E24..11 | Drug addiction |
| 13c..00 | Drug user |
| E25z.00 | Misuse of drugs NOS |
| Eu11212 | [X]Heroin addiction |
| 1463.00 | H/O: drug dependency |
| E020.00 | Drug withdrawal syndrome |
| 8HHe.00 | Referral to community drug and alcohol team |
| 9NN1.00 | Under care of community drug team |
| 146F.00 | H/O: drug abuse |
| 8BA9.00 | Detoxification dependence drug |
| E240z00 | Opioid drug dependence NOS |
| 1J1..00 | Suspected drug abuse |
| 8H7x.00 | Referral to drug abuse counsellor |
| 9N0Z.00 | Seen in drug rehabilitation centre |
| E25..00 | Nondependent abuse of drugs |
| Eu11211 | [X]Drug addiction – opioids |
| 46Qr.00 | Urine buprenorphine level |
| E252.00 | Nondependent cannabis abuse |
| 44uK.00 | Plasma methadone level |
| E243.00 | Cannabis type drug dependence |
| ZV4K100 | [V]Drug use |
| 8B2P.00 | Drug addiction maintenance therapy – methadone |
| E240.12 | Methadone dependence |
| E244.00 | Amphetamine or other psychostimulant dependence |
| 13cM.00 | Substance misuse |
| E242.00 | Cocaine type drug dependence |
| Eu12211 | [X]Drug addiction – cannabis |
| 1T8..00 | H/O cannabis misuse |
| 9OhB.00 | Non-steroidal anti-inflammatory drug risk assessmnt completd |
| L183.00 | Drug dependence in pregnancy, childbirth and the puerperium |
| ZG23200 | Advice on drugs of addiction |
| Eu19211 | [X]Drug addiction NOS |
| 146E.00 | H/O: recreational drug use |
| ZV57B00 | [V]Drug rehabilitation |
Ethnicity
The ethnicity of a pregnancy was determined in one of two ways:
-
by searching for relevant Read codes (Table 73) in the mother’s or child’s medical records and using the one closest to the estimated LMP
-
by searching for relevant Read codes (see Table 73) in the mother’s or child’s medical records and using the one closest to the estimated LMP.
| Read code | Description |
|---|---|
| 9S10.00 | White British |
| 9i0..00 | British or mixed British – ethnic category 2001 census |
| 9S13.00 | White Scottish |
| 9S1..00 | White |
| 9i20.00 | English – ethnic category 2001 census |
| 9i2..00 | Other White background – ethnic category 2001 census |
| 9S12.00 | Other white ethnic group |
| 9i7..00 | Indian or British Indian – ethnic category 2001 census |
| 9i8..00 | Pakistani or British Pakistani – ethnic category 2001 census |
| 9S7..00 | Pakistani |
| 9S6..00 | Indian |
| 9iC..00 | African – ethnic category 2001 census |
| 9i9..00 | Bangladeshi or British Bangladeshi – ethn categ 2001 census |
| 9i24.00 | Northern Irish – ethnic category 2001 census |
| 9S3..00 | Black African |
| 9i2F.00 | Polish – ethnic category 2001 census |
| 9SJ..00 | Other ethnic group |
| 9i2R.00 | Oth White European/European unsp/Mixed European 2001 census |
| 9i1..00 | Irish – ethnic category 2001 census |
| 9i2 T.00 | Other White or White unspecified ethnic category 2001 census |
| 9i22.00 | Welsh – ethnic category 2001 census |
| 9SH..00 | Other Asian ethnic group |
| 9S8..00 | Bangladeshi |
| 9i21.00 | Scottish – ethnic category 2001 census |
| 9iA..00 | Other Asian background – ethnic category 2001 census |
| 134 N.00 | RACE: White |
| 9iB..00 | Caribbean – ethnic category 2001 census |
| 9S11.00 | White Irish |
| 9iAA.00 | Other Asian or Asian unspecified ethnic category 2001 census |
| 9i6..00 | Other Mixed background – ethnic category 2001 census |
| 9i3..00 | White and Black Caribbean – ethnic category 2001 census |
| 9iA8.00 | British Asian – ethnic category 2001 census |
| 9S2..00 | Black Caribbean |
| 9S14.00 | Other white British ethnic group |
| 9i2B.00 | Italian – ethnic category 2001 census |
| 9i4..00 | White and Black African – ethnic category 2001 census |
| 9iF..00 | Other – ethnic category 2001 census |
| 9i5..00 | White and Asian – ethnic category 2001 census |
| 9iD2.00 | Black British – ethnic category 2001 census |
| 9S9..00 | Chinese |
| 9iE..00 | Chinese – ethnic category 2001 census |
| 9SB2.00 | Other ethnic, Asian/White orig |
| 9iD0.00 | Somali – ethnic category 2001 census |
| 9iFK.00 | Any other group – ethnic category 2001 census |
| 9iF2.00 | Filipino – ethnic category 2001 census |
| 9iF7.00 | Muslim – ethnic category 2001 census |
| 9iD..00 | Other Black background – ethnic category 2001 census |
| 134B.00 | RACE: Caucasian |
| 9SAC.00 | Other European (NMO) |
Pregnancies were then classified into one of five ethnicity categories from the ONS based on the information in the Read code description.
Covariate drug use
Covariate drug use was identified within the same time periods as the exposure of interest, therefore, for comparisons involving the B1 exposure cohorts covariate use of anticonvulsant mood stabilisers, lithium, antipsychotics, antidepressants, hypnotics and anxiolytics was identified by searching for prescriptions for these drugs between 31 days (≈ 1 month) and 105 days (15 weeks) (inclusive) after pregnancy start. Likewise, for the B2 exposure cohorts, covariate drug use was identified by searching for women with prescriptions for these drugs within the 92 days prior to the delivery date.
Pre-existing hypertension
The definition of pre-existing hypertension is described under the outcome Pre-eclampsia and/or gestational hypertension.
Pre-existing diabetes
The definition of pre-existing hypertension is described under the outcome Gestational diabetes.
Recent depression
Women with a recent history of depression were identified by searching the mother’s medical records for relevant Read codes (Table 74) in the 3 years prior to the estimated LMP.
| Read code | Description |
|---|---|
| E2B..00 | depressive disorder nec |
| Eu32z11 | [x]depression nos |
| E200300 | anxiety with depression |
| E204.11 | postnatal depression |
| 1B17.00 | Depressed |
| 9H92.00 | depression interim review |
| 1465.00 | h/o: depression |
| 1BT..00 | depressed mood |
| Eu32.00 | [x]depressive episode |
| E204.00 | neurotic depression reactive type |
| 2257.00 | o/e – depressed |
| E113.11 | endogenous depression – recurrent |
| 8BK0.00 | depression management programme |
| E112.11 | agitated depression |
| Eu32z00 | [x]depressive episode, unspecified |
| Eu32100 | [x]moderate depressive episode |
| E112.13 | endogenous depression first episode |
| Eu32z14 | [x] reactive depression nos |
| E113700 | recurrent depression |
| E112.14 | endogenous depression |
| Eu33.00 | [x]recurrent depressive disorder |
| E2B1.00 | chronic depression |
| Eu41200 | [x]mixed anxiety and depressive disorder |
| 9H91.00 | depression medication review |
| E112.00 | single major depressive episode |
| Eu32000 | [x]mild depressive episode |
| 62T1.00 | puerperal depression |
| Eu32200 | [x]severe depressive episode without psychotic symptoms |
| E113.00 | recurrent major depressive episode |
| 9k4..00 | depression – enhanced services administration |
| Eu32z12 | [x]depressive disorder nos |
| 8CAa.00 | patient given advice about management of depression |
| 9Ov0.00 | depression monitoring first letter |
| 9Ov..00 | depression monitoring administration |
| 9hC0.00 | excepted from depression quality indicators: patient unsuita |
| Eu53011 | [x]postnatal depression nos |
| 9H90.00 | depression annual review |
| 9hC1.00 | excepted from depression quality indicators: informed dissen |
| 9HA0.00 | on depression register |
| E113200 | recurrent major depressive episodes, moderate |
| 9Ov1.00 | depression monitoring second letter |
| Eu32400 | [x]mild depression |
| Eu34114 | [x]persistant anxiety depression |
| Eu32.11 | [x]single episode of depressive reaction |
| E112200 | single major depressive episode, moderate |
| 9Ov2.00 | depression monitoring third letter |
| 9k40.00 | depression – enhanced service completed |
| Eu33.11 | [x]recurrent episodes of depressive reaction |
| Eu33100 | [x]recurrent depressive disorder, current episode moderate |
Severe mental illness
Women with a history of a severe mental illness were identified by searching the mother’s medical records for relevant Read codes (Table 75) recorded at any point before the estimated LMP.
| Read code | Description |
|---|---|
| Eu31.00 | [x]bipolar affective disorder |
| 9H8..00 | on severe mental illness register |
| E10..00 | schizophrenic disorders |
| 9H6..00 | on national service framework mental health |
| Eu2z.11 | [x]psychosis nos |
| Eu30000 | [x]hypomania |
| E13z.11 | psychotic episode nos |
| E11..11 | bipolar psychoses |
| Eu25.00 | [x]schizoaffective disorders |
| Eu22015 | [x]paranoia |
| E103.00 | paranoid schizophrenia |
| E13z.00 | nonorganic psychosis nos |
| Eu31.11 | [x]manic-depressive illness |
| E10z.00 | schizophrenia nos |
| Eu32300 | [x]severe depressive episode with psychotic symptoms |
| E117.00 | unspecified bipolar affective disorder |
| Eu22011 | [x]paranoid psychosis |
| E12..00 | paranoid states |
| 1464.00 | h/o: schizophrenia |
| E110100 | single manic episode, mild |
| E107.00 | schizo-affective schizophrenia |
| 146H.00 | h/o: psychosis |
| E11..12 | depressive psychoses |
| Eu30.00 | [x]manic episode |
| E11..00 | affective psychoses |
| E130.11 | psychotic reactive depression |
| E12z.00 | paranoid psychosis nos |
| Eu20.00 | [x]schizophrenia |
| Eu23.00 | [x]acute and transient psychotic disorders |
| Eu31700 | [x]bipolar affective disorder, currently in remission |
| E13..00 | other nonorganic psychoses |
| Eu30z11 | [x]mania nos |
| E110.11 | hypomanic psychoses |
| E120.00 | simple paranoid state |
| 146D.00 | h/o: manic depressive disorder |
| E116.00 | mixed bipolar affective disorder |
| Eu30100 | [x]mania without psychotic symptoms |
| Eu2..00 | [x]schizophrenia, schizotypal and delusional disorders |
| E110000 | single manic episode, unspecified |
| E115.11 | manic-depressive – now depressed |
| Eu33300 | [x]recurrent depress disorder cur epi severe with psyc symp |
| E114.11 | manic-depressive – now manic |
| Eu30.11 | [x]bipolar disorder, single manic episode |
| Eu32313 | [x]single episode of psychotic depression |
| E100000 | unspecified schizophrenia |
| E1. . .00 | non-organic psychoses |
| E100200 | chronic schizophrenic |
| Eu20000 | [x]paranoid schizophrenia |
| Eu31000 | [x]bipolar affective disorder, current episode hypomanic |
Epilepsy
Women with a history of epilepsy were identified by searching the mother’s medical records for relevant Read codes (Table 76) recorded at any point before the estimated LMP.
| Read code | Description |
|---|---|
| F25..00 | Epilepsy |
| 8BIF.00 | epilepsy medication review |
| 667F.00 | seizure free > 12 months |
| 6675.00 | fit frequency |
| 667..00 | epilepsy monitoring |
| 6676.00 | last fit |
| 6110.00 | contraceptive advice for patients with epilepsy |
| 67IJ000 | pre-conception advice for patients with epilepsy |
| 67AF.00 | pregnancy advice for patients with epilepsy |
| 9Of0.00 | epilepsy screen invite 1 |
| R003z11 | [d]seizure nos |
| 9Of1.00 | epilepsy screen invite 2 |
| 8IB4.00 | pregnancy advice for patients with epilepsy not indicated |
| 8IB3.00 | pre-conception advic fr patients with epilepsy not indicated |
| 9h62.00 | excepted from epilepsy quality indicators: informed dissent |
| 8IB2.00 | Contraceptive advice for patients with epilepsy not indicated |
| 667Q.00 | 1–12 seizures a year |
| 1473.00 | h/o: epilepsy |
| F25z.11 | Fit (in known epileptic) nos |
| 9N0r.00 | Seen in epilepsy clinic |
| F251600 | Grand mal seizure |
| F251000 | Grand mal (major) epilepsy |
| 9Of2.00 | Epilepsy screen invite 3 |
| 9h61.00 | Excepted from epilepsy quality indicators: patient unsuitabl |
| F254000 | Temporal lobe epilepsy |
| 667P.00 | No seizures on treatment |
| 6672.00 | Follow-up epilepsy assessment |
| F250000 | petit mal (minor) epilepsy |
| 667R.00 | Two to four seizures a month |
| 667C.00 | Epilepsy control good |
| 667S.00 | One to seven seizures a week |
| 282..13 | o/e – a seizure |
| 667Z.00 | Epilepsy monitoring nos |
| F25z.00 | Epilepsy nos |
| 9Of5.00 | Epilepsy monitoring call first letter |
| 2828.00 | Absence seizure |
| 8IAh.00 | Pre-conception advice for patients with epilepsy declined |
| 8IAg.00 | Contraceptive advice for patients with epilepsy declined |
| F254500 | Complex partial epileptic seizure |
| 8IAi.00 | Pregnancy advice for patients with epilepsy declined |
| 9Of..00 | Epilepsy screen administration |
| F251400 | Epileptic seizures – tonic |
| F250011 | Epileptic absences |
| 9Of6.00 | Epilepsy monitoring call second letter |
| 9N4 V.00 | DNA – did not attend epilepsy clinic |
| F251011 | Tonic–clonic epilepsy |
| 667 T.00 | Daily seizures |
| F255011 | Focal epilepsy |
| F251200 | Epileptic seizures – clonic |
List of abbreviations
- AHD
- additional health data
- BMI
- body mass index
- BNF
- British National Formulary
- CI
- confidence interval
- CPRD
- Clinical Practice Research Datalink
- DDD
- defined daily dose
- EDD
- estimated delivery date
- EUROCAT
- European surveillance of congenital abnormalities
- GP
- general practitioner
- HTA
- Health Technology Assessment
- ICD
- International Classification of Diseases
- IQ
- intelligence quotient
- IQR
- interquartile range
- LEAP
- lived experience advisory panel
- LMP
- last menstrual period
- NICE
- National Institute for Health and Care Excellence
- ONS
- Office for National Statistics
- PPI
- patient and public involvement
- RCT
- randomised controlled trial
- RR
- risk ratio
- RRR
- relative risk ratio
- RRRadj
- adjusted relative risk ratio
- SD
- standard deviation
- SGA
- small for gestational age
- THIN
- The Health Improvement Network