Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 11/70/01. The contractual start date was in December 2012. The draft report began editorial review in August 2014 and was accepted for publication in July 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Joanne Lord is a member of the Health Technology Assessment Commissioning Board.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Nyssen et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
Therapeutic writing
Writing as a form of therapy to improve physical or mental health has a long history1 and is widely reported in psychology textbooks as being of therapeutic value. 2–5 It can take many formats including those from a psychotherapeutic background, such as therapeutic letter writing,6 specific controlled interventions, such as emotional disclosure/expressive writing,7 to more recent approaches, such as developmental creative writing8 and other epistolary approaches, such as blogging. 8 With the development of UK organisations such as Lapidus (Association for Literary Arts in Personal Development), dedicated to the promotion of therapeutic writing (TW) based on the premise that it has health benefits, and an increased interest in the potential of non-pharmacological adjunctive therapies, it is important to evaluate the effectiveness of a variety of different approaches within this field. These include two main categories: written emotional disclosure [or emotional writing (EW)]9 and creative writing, such as poetry. 7 Other forms of creative writing include alpha writes/poems (a poetic device in which each successive line of the poem starts with the next letter of the alphabet, or a predetermined word or phrase written vertically down the page);10 writing from published poems/narratives; acrostics; and haiku poems (traditionally a haiku contains three lines of five, seven and then five syllables, making a total of 17 syllables; the tradition is modified so that no more than 17 syllables are arranged in no more than three lines, but the shorter the better);11 autobiographical writing (such as reflective diaries, journaling); descriptive writing; genre writing (e.g. fairy tales); free writing; short stories; drama or fictional narratives; unsent letters; diary/journaling; collaborative writing (workshops); writing accompanying other art forms; life writing or memoirs (such as reminiscence, life review); list writing; redrafting or sentence stems writing; scribing for others; writing from visual/sound stimuli (e.g. writing from mindfulness); writing from the senses; and writing in form and writing from music (as part of a music therapy). 10,12 Newer forms of writing include blogging or participating in web-based forums. 13,14
Dimensions of therapeutic writing
Within each type of TW there may be significant process variability, for example in the flexibility and number of topics; the dose (frequency and duration); group or individual delivery; computerised compared with handwritten exercises; participant recruitment; and financial compensation. However, a major distinction lies in whether the writing is facilitated or unfacilitated.
Facilitated therapeutic writing
Facilitated TW interventions, when a facilitator is present at some stage before or during the writing, might be delivered in many different ways and contexts: in a health-care centre, as part of a programme in a rehabilitation clinic or within a group of people with common or different chronic conditions, face to face or via the internet. People using these therapeutic tools may receive feedback from someone else, a health-care professional, a group of persons or not receive feedback at all. 10
Furthermore, the topic of the writing can be varied, from positive to negative expression of emotions through neutral topics (e.g. childhood/birth, life aims and goals, places, relationships). 10 TW can also be used in children, adolescents or adults and among different clients, such as the chronically ill (e.g. cancer, mental health problems, chronic infections) or healthy individuals, and assessed from different angles such as community carers, doctors and nurses, peer training, patient’s family and/or friends or the participant him/herself – the most usual perspective. 10
The writing event should not be considered as solely an isolated exercise but as a sequence of exercises, not necessarily all of which encompass a written component. As such, a common practice is that writing starts with (visual) stimuli12 or with mindfulness meditation in order to inspire people and to act as a form of distraction from reality. 15 The following examples of the work of facilitated writing practitioners in the UK exemplify the variety of this type of TW (Box 1).
Writing practitioner Carol Ross (CR) facilitates weekly TW groups for inpatients in mental health units in a UK NHS Foundation Trust. CR has developed her own practice, influenced by a number of published research studies, e.g. on positive writing; and by established therapies such as mindfulness-based cognitive therapy and narrative therapy.
A typical session lasts 60 minutes, attended by one to seven self-referred inpatients, and comprising 25 minutes of writing interventions (duration 5–15 minutes each) and 25 minutes of reading aloud and group discussion, with the remaining time being taken up with introductions, explanations and evaluation forms. Flexible writing interventions are used to allow tailoring of interventions for individuals and give patients some freedom to choose what they write. The writing practitioner writes and reads aloud what they have written with the group.
Many of the writing interventions CR uses in acute mental health settings, e.g. mindful writing, are aimed at calming the individual, decreasing anxiety, increasing mental focus and lifting mood. With some writing interventions, another effect is intended, e.g. broadening of cognitive focus, reframing, insight, improved self-expression.
CR’s TW toolbox includes mindful writing with either an external or internal focus; positive writing about the past, present and future; perspective shift writing, including unsent letters; and responding to published poems. The broadest range of TW is used in the general adult ward. In the older people’s assessment unit, some interventions are designed to trigger positive/neutral memories in a low pressure way (see Appendix 1, Table 75, illustrating the types of TW interventions used by CR).
In the PICU, the sessions are typically one to one or one to two, with individuals experiencing acute symptoms, e.g. of psychosis or mania. The PICU writing group is held in an open area so that patients who decline to do any writing, or even sit at the table, still sometimes take part in a brief conversation with the practitioner or other patients, and look at whatever prompt materials are on display, e.g. photographs or objects. Data from an internal audit suggest that the writing group contributes to a reduction in violent incidents in the PICU.
It will be seen that the practice described differs markedly from the unfacilitated EW method described by Pennebaker and Beall1 (see section below on EW), e.g. writing interventions are facilitated and take place in a group. Patients are also never directed to write about trauma.
Poetry therapy for people with mild mental health problems: Victoria FieldPoetry therapy practitioner Victoria Field (VF) facilitates a weekly Words for Wellbeing group in the Beaney House of Art and Knowledge in Canterbury (part of Kent Library Service), aimed at people with mild mental health problems, often as a result of LTCs. She ran a similar group for some years at Falmouth Health Centre, with referrals from GPs. VF qualified in 2005 as a Certified Poetry Therapist, with the NFBPT, which works with the therapeutic potential of both the receptive (reading and listening) and expressive (writing and sharing) aspects of writing. The practice can be adapted for individuals and non-writers but is always interactive for reasons outlined. 16 She is now approved as a Provisional Mentor–Supervisor for the NFBPT, training others in these techniques. The aims of the group are closely aligned with the NHS Wellbeing agenda. 17 A typical session lasts 2 hours, including a break, attended by anything from 2 to 18 people. An ideal group size is around 10, fewer when participants are more unwell or distressed. The group follows a set format, and this predictability is valued by attendees:
-
Reflective writing This is the activity closest to a written emotional disclosure type of intervention as described by Pennebaker and Beall. 1 However, it is firmly contained. Participants are invited to write for 6 minutes or so from a given prompt. This might be as simple as ‘I can see’ or ‘Here now’, or more elaborated, such as a list of statements, ‘Then I was, now I am’ or working with a metaphor, e.g. a colour or weather ‘Today I am’ or ‘Red is . . .’ This initial writing is intended to be private, although participants are invited to talk about what might have come up, and sometimes some wish to read.
-
The reading aloud of a poem Not necessarily literary, which VF has chosen for that week, followed by discussion of what it suggests.
-
Writing in response to the poem Again for a short period of 6/7 minutes, typically from a choice of prompts. The writing that emerges is often fully formed, powerful, satisfying to the writer and helpful for the listeners.
Writing and reading in this way offers a container for complex emotions, catharsis, pleasure, connection, validation, self-expression and mastery that may improve mood, decrease anxiety, allow reframing, insight and encourage a more nuanced approach to life. The group dynamic is also a powerful therapeutic tool (see Appendix 1, outlining VF’s professional perspective).
Write to life at Freedom from Torture: Sheila HaymanSheila Hayman is a member of Lapidus, and has run creative and therapeutic workshops for elderly day-care patients, detention centre visitors, children and the general public. However, her main work for the past 11 years has been with Write to Life, a unique therapeutic creative writing programme based at, and funded by, Freedom from Torture, the UK’s only national charity dedicated to the support and rehabilitation of torture survivors from around the world.
In 12 years, the group has grown to about 20 members, of whom a dozen regularly attend bi-weekly group workshops and individual one-to-one sessions. Members are referred, while still in clinical treatment, by the clinical key worker, and while they remain in treatment the group works closely with the clinician. However, as the group is open-ended, clients can stay as long as they like, and there are members who have been with the group for 6 years or more. This enables them to make huge strides in what they can achieve.
When they arrive, many are still very traumatised, unable to trust others or communicate freely, unable to talk about their past or present experiences or make friends. Over time, they make friends inside and outside the group, begin to enjoy not just writing but performing their work, and are enabled to address large gatherings of all sorts about the effects of torture, asylum and other aspects of their situation, as well as perform in public in plays and other events. They report improved sleep, reduced headaches and other sorts of pain, and most of all the reduction or even elimination of the flashbacks, nightmares and other symptoms of their post-traumatic condition.
The writing falls into two parts: the first is the public setting of the group, which is run by a group of volunteers who are professional writers rather than clinicians. This group writing sometimes focuses on matters of interest to the client base, such as journeys, poverty, or trust, but equally could be an exercise in literary criticism, or an invitation to reflect on living in London. It usually takes the form of a short exercise and discussion, followed by a longer piece of writing which members are invited to read out. Everybody has to write, but not everybody has to read out, as sometimes they find that the subject has unearthed things they prefer to keep private.
It is noticeable that the framework, often quite unguided as to the form of writing, enables group members to dig as deeply into their feelings, including bad ones, as they wish. Some people will always find a way of writing about the source of their pain, no matter how the exercise is framed. And that is how it should be. Others may want to be more structured, or literary, or metaphorical.
The strong feelings, and the personal exploration and laying of ghosts, are dealt with in the one-to-one element of the work. Usually, on the same day as the workshop, and purely for practicality, each group member is offered one-to-one sessions with one of the six writer/mentors. This is an opportunity to write about whatever they choose, and to dig as deeply as they wish into their past or present trauma. This writing may remain private, or be published, as they choose. Leaving the level of introspection up to them gives much more sense of control and safety, as reported by more than one group member, compared with their clinical therapy sessions, which may leave them distressed when they need to be okay for a meeting, or may make them jump with unexpected reactions.
Sometimes the writing seems to gloss over, or miss out, a crucial painful moment or event, and on these occasions the mentor, in consultation with the writer, may guide them to look again at that portion of the writing and fill in the missing emotion. This is why it’s important to collaborate with a clinician, at least in the early stages when clients are still raw and vulnerable. But in practice, our work, and, by their own account, that of our clinical colleagues, is often guided as much by instinct, common sense and experience, as any theory or training.
Perhaps the last thing to add is that clinicians at Freedom from Torture continue to send more clients than can be coped with, which is some vindication of the practice. As a bridge between intense therapy and the outside world, giving clients a skill they can take with them and a means of self-discovery, self-healing and personal growth, it seems, as the Hippocratic Oath puts it, to do no harm, and a great deal of good.
Unfacilitated emotional writing
Unfacilitated EW means writing, completed without any assistance, feedback, comment or any other form of support. Therefore, in the current review, an unfacilitated writing intervention has been defined as when a facilitator was simply not present in person during the writing exercise, as opposed to facilitated writing (described above). Typically, in unfacilitated writing interventions, participants are instructed to write for 15–30 minutes on 3 to 4 consecutive days (or at weekly intervals). Instructions on these unfacilitated writing assignments can be delivered in writing via leaflets, verbally over the telephone or even via video or the internet. Participants are asked to do their writing unassisted and alone at home or on their own in a given clinic or laboratory setting. In the most commonly evaluated form of unfacilitated EW, there is a single writing topic that can be chosen (usually disease or treatment focused), for which participants are directed to write emotionally and disclose about their deepest thoughts and feelings or about a self-selected trauma. Thereafter, either the writings may be collected by the practitioner without any feedback or the participant can simply decide what to do with the writing. Sometimes, practitioners provide participants the option to make telephone calls during the writing exercise should any concerns emerge; however, this action has not been considered as facilitation in this review.
The Pennebaker writing paradigm: expressive writing or written emotional disclosure
This is the most common form of unfacilitated EW. It is a technique whereby people are encouraged to write (or talk into a tape recorder) in private about a traumatic, stressful or upsetting event, usually from their recent or distant past. They write for 15–30 minutes typically for 3 or 4 days within a relatively short period of time, such as on consecutive days or within 2 weeks. The format has been relatively consistent since the earliest randomised controlled trials (RCTs),1,18 but more recent studies have varied the duration, number of sessions and topic of writing, including positive events and thoughts and feelings about illnesses. 19 RCTs of expressive/emotional writing have been conducted in a wide variety of participants, including healthy students, people undergoing psychological stressors, such as bereavement or being in a caregiving role, or in people with long-term physical conditions, such as rheumatoid arthritis (RA) and asthma. Variants of the technique include disclosure in front of a listener, who can be a confederate, a researcher or a doctor. For the purposes of this project, these activities are not considered to be EW and lie outside the scope of this review. The presence of a listener is likely to affect outcomes, as it potentially adds a counselling dimension.
Positive writing
Positive writing can be delivered either as part of a facilitated TW or unfacilitated EW intervention. The exercise involves writing about positive topics only, including positive emotions, typically for 20–30 minutes, three or four times per week if delivered as an unfacilitated EW intervention. Otherwise, the duration and length of the positive writing can be very varied when facilitated (see Appendix 1). Pennebaker et al. 19 found in a review published in 1997 that the description of positive emotions could predict improvements in health outcomes. Since then, researchers have studied the positive effects of the positive emotional disclosure, advocating that participants writing about the positive aspects of past traumas (benefit finding by describing any positive outcomes of the disease experience or treatment in detail) or simply about positive life events, could achieve comparable health improvements as those writing about past traumas. 20
Bibliotherapy
Although the above require the individual to write as part of therapy, other forms of therapy use existing texts. The most commonly encountered type of bibliotherapy, Reading Bibliotherapy, involves reading material specifically selected for its therapeutic potential for that person. 21 In the UK, Books on Prescription Schemes have been running in primary care for several years, and in 2013 a national scheme was launched in England by the Society of Chief Librarians and the Reading Agency. 22 Such reading bibliotherapy is not covered by this review.
In contrast, interactive bibliotherapy has been defined as the use of literature to bring about a therapeutic interaction between participant and facilitator. 21 The triad of participant, literature and therapist is viewed as critical. In fact, interactive bibliotherapy does not restrict itself to the written word: it can include the spoken word, for example in film or theatre but it must involve the coherent use of language. When interactive bibliotherapy uses poetry, it is synonymous with poetry therapy and they are both encompassed by the term biblio/poetry therapy. 21 Sometimes the literature involved in biblio/poetry therapy is new writing generated by the participants themselves. This type of creative writing biblio/poetry therapy is the principal form of facilitated TW included in this review and it is the form of TW used by the practitioner experts collaborating in the current systematic reviews (see Box 1, in which the TW expert practitioners describe their different facilitated biblio/poetry therapy practices).
Nonetheless, little has been published around all the different types of facilitated TW, and literature shows that the most evaluated form of TW is the EW intervention, described by Pennebaker and Beall1 Comprehensive research around the writing paradigm18,23–27 and narrative analysis within the health-care setting28–31 has been performed through the last decades.
Long-term conditions
The prevalence of long-term conditions (LTCs) increases with ageing populations. In 2002, the leading chronic diseases [cardiovascular disease (CVD), cancer, chronic respiratory disease and diabetes] were responsible for 29 million deaths worldwide. 32 According to the UK Department of Health (DH),33 more than 15 million people in England (including half of all those aged > 60 years) are living with at least one LTC, and the risk of death is particularly high in those with three or more conditions occurring concurrently. 34 LTCs also result in a huge burden on UK NHS resources. Although some are preventable, for most LTCs the only realistic management strategy is continuing care, as biological and psychosocial mechanisms regulating disease progression are not yet fully understood. As LTCs are difficult to improve, especially for elderly populations, health-care programmes, such as self-management support and patient education, often combined with structured clinical follow-up, have been suggested as a way to improve the quality of life (QoL) of such patients. 35 New therapeutic approaches, such as TW, have the potential to improve the QoL in people with LTCs.
Possible pathways linking memory, emotions and physical health
There are several potential ways that writing might impact on physical health. For example, cognitive restructuring or behavioural mechanisms (e.g. reflection on health behaviours) may lead to improvement in outcomes. However, many of the types of TW described above engage emotions and memories (both positive or negative) and there are physiological pathways linking memory, emotions, chronic stress and physical health.
Two interdependent memory systems are thought to be associated with remembering events in humans. 36 Episodic memory is linked to the hippocampus and this structure is vital for processing events that eventually become long-term memories. 37 Emotional memory is linked to the amygdala, part of the limbic system involved with emotions, in particular fear-related responses and general pleasant and unpleasant emotional processing. 38 Although the episodic and emotional memory systems are independent, they affect each other in a variety of ways. 36 Emotion enhances perception of, and attention to, the memory-provoking stimulus, as well as the long-term storage of the memory. 36 Episodic memory also influences emotional memory by, for example, causing the autonomic effects of emotional arousal (e.g. the sweaty palms and dry mouth) when remembering a past situation. 36
The limbic system has links with the cerebral cortex, the brainstem and the pituitary gland (part of the hypothalamic–pituitary–adrenal axis). Parts of the cerebral cortex have a role in cognitive appraisal and the conscious awareness of emotional states, and can regulate amygdalar activity. 38 Through the brainstem, areas in the limbic system can control many internal conditions of the body, for example cardiovascular regulation. The hypothalamic–pituitary–adrenal axis is both responsive to psychological inputs and has significant influences on the immune system, which, in turn, influences physical health. 39 This pathway may be one of the ways chronic stress is linked to poor health. 39–42 It is therefore possible that a psychological intervention might improve aspects of physical health, and if modification of such pathways had even a small effect then this could have profound public health significance.
Realist synthesis
In this review, a conventional systematic review of the effectiveness of unfacilitated EW and facilitated TW was conducted, but, in addition, the findings of a realist synthesis are reported. Realist synthesis is a theory-driven interpretive approach to evidence synthesis. Rather than producing a judgement on whether (or not) an intervention works, realist syntheses attempt to explain outcome patterns in data using theory (or theories). It is particularly useful when interventions are complex and evidence is mixed or conflicting and provides little or no clues as to why the intervention worked or did not work when used in different contexts, by different stakeholders or when used for different purposes. 43
In brief, realist syntheses ask what works for whom in what circumstances, how and why? To do so, realist syntheses use a particular logic of analysis that deliberately breaks down how an outcome has arisen. An outcome is considered to have occurred because it is caused to do so by a causal process known as a mechanism. In addition, the contexts in which an outcome has occurred are also considered to be important as they cause mechanisms to be activated. This logic of analysis thus provides an approach for understanding how and why it is that context can influence outcomes. In summary, the realist logic of analysis used in a realist synthesis considers the interaction between context, mechanism and outcome (sometimes abbreviated as CMO). That is how particular contexts have triggered (or, conversely, interfered with) mechanisms to generate the observed outcomes. 43
To elaborate further, in order to understand how outcomes are generated, the roles of both external reality and human understanding and response need to be incorporated. Realism does this through the concept of mechanisms, whose precise definition is contested but for which a working definition is ‘. . . underlying entities, processes, or structures which operate in particular contexts to generate outcomes of interest.’44 Different contexts interact with different mechanisms to make particular outcomes more or less likely – hence, in general, a realist synthesis produces recommendations of the general format ‘In situations [X], complex intervention [Y], modified in this way and taking account of these contingencies, may be appropriate’. This approach, when done well, is widely recognised as a robust set of methods, which is particularly appropriate when seeking to explore the interaction between CMO in a complex intervention [e.g. see Berwick’s editorial explaining why experimental (RCT/meta-analysis) designs may need to be supplemented (or perhaps in some circumstances replaced) by realist studies aimed at elucidating CMOs]. 45
The philosophical basis underpinning a realist synthesis is realism. Realism assumes the existence of an external reality (a real world) but one that is filtered (i.e. perceived, interpreted and responded to) through human senses, volitions, language and culture. Such human processing initiates a constant process of self-generated change in all social institutions, a vital process that has to be accommodated in evaluating social programmes. In other words, the way individuals interpret and respond (or not) to the world around them has the potential to cause changes to this world around them. Such changes may then cause additional responses from individuals, potentially leading to a series of feedback loops. Within a realist synthesis, where possible, attempts are made to understand these feedback loops.
A realist approach is particularly useful for this project because TW is a complex intervention that could be useful in a variety of patient groups, and currently it is unclear whether it is effective for all or some, and how and why it might be effective.
Realist syntheses often use input from content experts to help develop the programme theories needed to explain how complex interventions work. In this project, input from practitioner experts was deliberately sought. During the second programme theory-building meeting with practitioner experts, they were asked for their feedback on what their views were on how TW was meant to work, for whom and why (see Chapter 5, Methods, for more details). Two practitioner experts [Carole Ross (CR) and Victoria Field (VF)] provided written responses (see Appendix 1, Tables 76 and 77, respectively) and have been included in this report as they provide an insight into how facilitated TW is used in the NHS and voluntary sector.
Previous systematic reviews on therapeutic writing in long-term conditions
There have been a number of systematic reviews on expressive writing,18,23,46,47 published in psychology journals, that have conducted meta-analyses according to normal practice in psychology, combining different types of participants and outcomes across different conditions, and using Cohen’s d or Hedges’ g statistics. Their results are difficult to interpret because effect sizes for specific populations and interventions are unclear. There have been three recent systematic reviews on TW in LTCs. One concerned post-traumatic stress disorder (PTSD) only and included five studies. 27 One of the included studies is on cognitive–behavioural therapy (CBT) rather than TW,48 and another49 is a very small, non-randomised study with students. A second, unpublished systematic review was accessed via the internet. 26 This assessed TW for psychological morbidity in people with long-term physical conditions. The review included 14 RCTs and searches were conducted up to May 2011. It is unclear why this review did not include a number of potentially includable studies including Abel et al. 50 [human immunodeficiency virus (HIV)], Graham et al. 51 (chronic pain), Halpert et al. 52 [inflammatory bowel syndrome (irritable bowel syndrome, IBS)], Henry et al. 53 (breast cancer), Hughes54 (breast cancer), Kraaij et al. 55 (HIV), Petrie et al. 56 (HIV), Stark57 [fibromyalgia (FM)] and Theadom et al. 58 (asthma), as all of these studies measure psychological morbidity and were published before the search end date. It may be that they did not include some of these because of their definition of long-term physical conditions, as there is no uniform definition as yet. It is unclear how the results might have differed if some of these studies had been included. The third systematic review evaluated the impact of support on the effectiveness of written cognitive–behavioural self-help59 and thus was not really focused on TW per se. It included 38 studies, none of which are included in this project.
Hypotheses tested in the review (research questions)
Overall aims and objectives of this review
-
What are the different types of TW that have been evaluated in comparative studies? What are their defining characteristics? How are they delivered? What underlying theories have been proposed for their effect(s)?
-
What is the clinical effectiveness of the different types of TW for LTCs compared with no writing or other suitable comparators?
-
How is heterogeneity in results of empirical studies accounted for in terms of patient and/or contextual factors, and what are the potential mechanisms responsible for the success, failure or partial success of interventions (i.e. what works for whom in what circumstances and why)?
-
What is the cost-effectiveness or cost–consequences of one or more types of TW, in one or more representative LTCs, when there is sufficient information on the intervention, comparator and outcomes to conduct an economic evaluation?
Chapter 2 Systematic effectiveness review methods
Expert advisory group
We invited practitioner experts in the area of the TW who approached us following our contact with Lapidus and/or publicity following the awarding of the grant to contribute to the project. On invitation to join the project we were unaware of the techniques of TW that they were employing. Although they were all working in different fields, and with slightly different techniques and approaches, they were all practitioners of facilitated TW. Indeed, we were unable to identify any UK-based practitioners of clinically-based unfacilitated TW to invite to join us as advisors. However, one of our authors, CM, had previously conducted a trial of unfacilitated TW. 60 The practitioner experts were invited to collaborate during all phases of this project in the role of advisors, in order to inform our understanding of the range of TW interventions and to help reach consensus within the Steering Group Committee (SGC).
Search strategy
All electronic and hand-searches were conducted up to March 2013 by the lead researcher (OPN) in collaboration with a librarian (JB). A mapping search was performed in order to determine the extent of relevant literature (looking for both qualitative and quantitative studies). From the list of studies, appropriately includable studies for the systematic review were selected according to the selection criteria. A single electronic search was performed for both the mapping search and the systematic reviews of effectiveness and economic studies. A further search was conducted by CM in January 2015 to cover the 2 years since the previous search.
Search engines
Studies were systematically identified by searching a total of 22 electronic medical and psychological electronic databases: MEDLINE, EMBASE, PsycINFO, CAB Abstracts, Physiotherapy Evidence Database (PEDro), Published International Literature on Traumatic Stress (PILOTS), The British Library’s Electronic Table of Contents (Zetoc), Science Citation Index (SCI), Social Sciences Citation Index (SSCI), Linguistics and Language Behaviour Abstracts, Periodicals Index Online, Applied Social Sciences Index and Abstracts (ASSIA), Education Resources Information Center (ERIC), Allied and Complementary Medicine Database (AMED), Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Central Register of Controlled Trials (CENTRAL) and Database of Abstracts of Reviews of Effects (DARE) for primary studies, and NHS Economic Evaluation Database (NHS EED) for economic studies. Grey literature was searched because of the possibility that effect size estimates might have been overestimated owing to selective reporting bias and unpublished studies are known to be less likely to have statistically significant results compared with published studies. 61 Information on studies in progress and unpublished research or research reported in the grey literature was also sought by searching relevant databases including the Inside Conferences, Open System for Information on Grey Literature in Europe, Dissertation Abstracts, Current Controlled Trials database and ClinicalTrials.gov, Cochrane Database of Systematic Reviews (CDSR), Health Technology Assessment (HTA) Database, and The Campbell Library was searched for systematic reviews and economic evaluations. In addition, internet searches were also carried out using a specialist search gateway (OMNI), general search engine (Google) and a meta-search engine (ReadCube).The search was first conducted in Ovid for MEDLINE and MEDLINE In-Process & Other Non-Indexed Citations and then translated into the other databases. Similarly, the search in The Cochrane Library retrieved papers from the CDSR, Cochrane DARE and NHS EED.
The update searches (January 2015) included only the databases that had found all of the relevant citations in the previous search (i.e. MEDLINE, EMBASE, PsycINFO, Web of Science and Social SSCI, CINAHL and The Cochrane Library databases).
Additional searches and cross-referencing
Reference lists of included studies and previous reviews of emotional disclosure were screened. Experts in the area were contacted to identify additional unpublished literature. All studies previously included in former systematic reviews were searched for, screened against the inclusion criteria and considered for inclusion in current systematic review.
Search terms
Medical subject headings together with key words and controlled vocabulary were combined to capture two components of the review question: the populations and the interventions of interest. The search was limited to humans and there were no restrictions regarding the study design. The search terms used for each of the databases are listed in Appendix 3. In the update searches (January 2015) sensitive searches using very wide search terms (writing, writ*, etc.) were used in order to find all relevant studies that had been recently published.
The population of interest: long-term conditions
No definite list of LTCs was pre-established, as the potential range of diseases of interest was both extensive and diverse and made it difficult to create an exhaustive list. For the purposes of the search strategy and subsequent steps of the review, the UK DH definition of a LTC was adopted. 33 The definition states: ‘Long term conditions are those conditions that cannot, at present, be cured, but can be controlled by medication and other therapies. They include diabetes, asthma, and chronic obstructive pulmonary disease’. Where it was unclear whether or not a condition met criteria discussion was held with the SGC and consensus reached (Table 1, column 1).
| Included LTCs after executive decision | Excluded LTCs after executive decision | Included LTCs but analysed in separate groupa |
|---|---|---|
| Acquired brain injury | Acute stress | Addictive conditions (such as drug, alcohol dependence) |
| Anorexia | Alexythimia | Aphasia/agraphia |
| Body dysmorphia | Benign prostate enlargement/hypertrophy | Asperger’s syndrome |
| Bulimia | Bereavement | Bladder papilloma resection (low-grade non-invasive cancer) |
| Chronic pain (at least 3 months) | Body dissatisfaction | Cancers including those newly diagnosed |
| Cystic fibrosis | Child sex abuse | Learning disabilities |
| Deafness/blindness | Chronic dieters | |
| Eating disorders | Domestic violence | |
| High BP | EBV | |
| HIV | Lesbian/gay-related stress | |
| IBS | Mild traumatic brain injury | |
| Infertility | Obesity | |
| MI | Overweight | |
| Serious traumatic brain injury | People found to be at increased risk of developing a LTC | |
| Personality traits | ||
| Smoking | ||
| Unresolved grief |
For inclusion, populations had to have received a clinical diagnosis of the condition. In some studies participants had symptoms of LTCs (e.g. student populations) but no formal evidence of a clinical diagnosis and study participants did not report having been diagnosed with these conditions. For such studies the full text was scrutinised before making a decision regarding inclusion. The chronic conditions in these studies included anxiety, chronic stress, closed head injury, depression (usually stated as symptoms of depression), insomnia or poor sleep, migraine or tension headache, and suicidality.
The authors also discussed whether to consider some diagnosed conditions as LTCs, for example newly diagnosed cancer, or whether congenital conditions might be seen by some to reflect a continuum of normality (e.g. congenital deafness). It was decided to include these conditions but to analyse them separately. These are listed below (see Table 1, column 3).
It was decided to include all other cancer studies because patients may receive palliative care for prolonged periods, and terminally ill patients in hospices may still be receiving active treatment. Thus the distinction between active treatment and palliation might be difficult to distinguish and, furthermore, disease trajectories are not always predictable. There is a debate around whether or not obesity in the absence of any comorbidity is a disease;62 therefore, studies in people with uncomplicated overweight and obesity were excluded. Studies of addictive conditions (alcohol, smoking, illegal drugs, legal drugs) and learning disability were also included because the results could be useful to the NHS, although these might not meet the current definition of LTC. The following conditions were excluded:
-
personality traits, such as alexithymia, body dissatisfaction
-
people who had undergone stressful life events, such as bereavement, domestic violence, child sex abuse (unless PTSD diagnosed)
-
people found to be at increased risk of developing a LTC.
The intervention of interest: therapeutic writing
Prior to the drafting of the definitive list of search terms used to develop the search strategy, consensus within the SGC was reached on the relevant and appropriate terms related to TW interventions. The terms under debate had been identified as part of the mapping search. The aim was to capture the published literature related to the different types of TW interventions; therefore the main key terms referring to TW were defined, discussed, agreed and validated with the expert advice (Table 2, column 1).
| Terms considered | Terms not considered |
|---|---|
| Blogging | Bibliotherapy |
| Catharsis | Emotional announcement |
| Creative writing | Emotional perspective |
| Descriptive writing | Emotional revelation, revealment |
| Diary | e-therapy |
| EW | Internet writing |
| Epistolary writing | Moral disclosure |
| Experimental disclosure | Patient-reported outcomes writing |
| Expressive writing | Therapeutic (or therapy) disclosure |
| Forum | Truth disclosure |
| Handwriting | Wellness writing |
| Health status writing | Writing (or written) exercise |
| Journal, journaling | Written confession |
| Letter writing | Written divulgation |
| Life reminiscence | Written exposé |
| Life review | Written information |
| Life writing | Written material |
| Memoirs | Written/emotional betrayal |
| Narratives | Written/emotional declaration |
| Poetry, poem, poetic | |
| Reactive writing | |
| Reflective writing | |
| Sensitive writing | |
| Story writing | |
| Typing, keying | |
| Writing (as such) | |
| Writing as self-concealment | |
| Writing as self-disclosure | |
| Writing as self-help or self-management | |
| Writing for healing | |
| Writing therapy | |
| Writing to cure | |
| Writing workshop | |
| Written (Pennebaker) paradigm | |
| Written emotion | |
| written emotional disclosure | |
| written expression |
Some terms were not considered because:
-
they had been already identified with a more common synonym thought to be equivalent (e.g. writing for healing/writing to cure vs. wellness writing)
-
the focus of the writing was thought not to be therapeutic (e.g. written divulgation, written exposé or written material/information).
Selection of papers
Results from the electronic searches (titles and abstracts where available) were transferred into a spreadsheet using Microsoft Excel® 2010 (Microsoft Corporation, Redmond, WA, USA) following automatic de-duplication within the citation manager EndNote X 4.02 (Thomson Reuters, CA, USA) and the manual removal of other duplicates.
Peer-reviewed articles and non-peer-reviewed papers (e.g. conference abstracts and dissertations) were then selected for potential inclusion in a two-stage process by one reviewer (OPN), with a random 10% selection of citations independently checked by a second reviewer (LB and CM). The two reviewers independently selected studies that met the predefined inclusion criteria. Disagreements were resolved by discussion and/or arbitration involving a third reviewer or by the full team, depending on the complexity of the issues. When it was not possible to determine the study eligibility by title and abstract alone the full text was retrieved for assessment. Authors of conference abstracts were contacted for full articles.
During the selection of studies, the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) approach was used. 63 A diagram was developed to show the numbers of studies in the different categories and the reasons for exclusion of full-text studies. Additionally, an expert in the field of TW was shown the list of included studies to check whether or not they believed that all relevant papers had been identified.
Inclusion criteria
Studies meeting the following inclusion criteria were included in the systematic review:
-
Studies assessing participants with at least one LTC as per DH definition. 33
-
Studies assessing any form of TW including emotional disclosure/expressive writing, poetry, diaries, etc., with inactive comparators or comparison groups thought to be inactive:
-
For example, if participants in the control arm were directed to write in a non-emotional way by using, for instance, neutral topics or by describing facts or how they managed their time. When the control group wrote about topics related to their illness or treatment, or when arousal of emotions might occur, these were not considered to be inactive controls and these studies were excluded. However, if descriptions of the comparators used were not provided, the paper was not be excluded on this basis alone.
-
-
Studies reporting any relevant clinical outcomes including both disease-specific outcomes and generic outcomes.
-
Outcomes related to physical (including physiological, haematological/immunological outcomes, pain, or disability), psychological, social and behavioural health. Performance, health-related quality of life (HRQoL), as well as participant mental status, satisfaction and both intervention safety and compliance to treatment for the LTC, were of interest. Resource-use or cost data were also collected for economic consideration. Outcomes could be self-reported or evaluated by a clinician or a carer.
-
If the study could report relevant outcomes without reporting any usable numerical data. In this particular case, the authors were contacted for unpublished data.
-
-
Full versions of prospective randomised or non-randomised trials or observational studies having any form of comparison group including, for instance, RCTs/non-RCTs, cohort, case–control studies and economic evaluations.
Exclusion criteria
The following were excluded:
-
Studies including participants with acute conditions, stress, bereavement or any acute event.
-
Studies assessing any form of psychotherapy, counselling, talking to a listener, talking into a tape recorder, mobile phone or similar, where this was the primary mode of delivering the intervention, expressive drama, dance or film-making.
-
Any study that evaluated other people’s writing.
-
Any study that evaluated any type of writing as a diagnostic tool instead of as a therapeutic tool in the course of a disease treatment (e.g. patients with agraphia).
-
-
A comparative study with any active or probably active control including any form of TW or talking into a tape recorder or mobile telephone.
-
Studies assessing only intermediate physiological outcomes such as salivary cortisol, immune parameters not routinely measured in the management of LTCs or studies not reporting relevant numerical and usable data and/or where unpublished data could not be obtained.
-
Inappropriate study design for this review: single case reports, case series (as both have no comparator arm) and studies where results for intervention and control groups were not presented separately. Studies only available in brief abstract form.
Data collection
The forms used for the data extraction are shown in Appendix 4.
Data extraction methods
Study findings were extracted and entered into a spreadsheet by one reviewer (OPN) and checked by a second reviewer (CM, ST, AH, LS and LB) working independently. A purpose-built data extraction form (Excel) was developed and piloted prior to data collection. Any disagreements were resolved by consensus and/or arbitration involving a third reviewer. Missing information was obtained from investigators if it was crucial to subsequent analysis (this was not possible for the five studies identified in the updated search to January 2015). The software GetData Graph Digitizer version 2.26.0.20 (GETDATA Graph Digitizer, Moscow, Russia) was used when numerical data had to be derived from graphs. To avoid introducing bias, unpublished information was coded in the same fashion as published information.
Quality assessment methods
Quality of studies was assessed based on accepted contemporary standards including the Newcastle–Ottawa Scale for case–control studies. 64 The Cochrane risk-of-bias tool65 was used for RCTs and quasi-randomised trials. Risk of bias was qualified as high, low or unclear. The first assessment was performed by one reviewer (OPN) on all studies, with a second reviewer (CM, LB, LS, SJCT) independently checking each study.
Data analysis
Synthesis of data
In order to collate, combine and summarise the information from the included studies, narrative and quantitative (meta-analysis) approaches were undertaken. After all included studies were identified, the SGC discussed organisation of the data for analysis. It became clear that the studies fell into two distinct categories: those that were facilitated (such as interactive biblio/poetry therapy) and those that were not (such as unfacilitated TW models and its various elaborations). Discussion with our expert practitioners and consideration of the literature revealed that facilitated and unfacilitated writing interventions are fundamentally different. As explained by the practitioner experts, facilitated TW interventions consist of one or more interactive activities (including TW) between the group facilitator and participant, which allows a live, in-person communication and an element of quality control and tailoring. Usually, the facilitator is in the same room as the participant, and may help with any unexpected concern and/or guide the participant in the usual process of the intervention. For unfacilitated writing, studies were categorised by ICD-10 (International Classification of Diseases, Tenth Edition) code according to the LTC assessed (see Chapter 3).
Analysis of studies
The numerical results from each of the included studies were checked to identify possible data entry problems. For each study, for continuous measures, either the mean and standard deviation (SD) at the various follow-ups, or any other statistic that could be used to calculate SD, such as the standard error (SE), were extracted for further analysis. For categorical measures, dichotomous or binary data, or counts and rates calculated from the number of events that each individual experienced, were collected.
Meta-analyses
Pooled-effect estimations were conducted using the standard software package Review Manager 5.2.6 (RevMan 2012, The Cochrane Collaboration, The Nordic Cochrane Centre, Copenhagen, Denmark). Analyses were stratified according to the type of outcome measured. A comparison was performed when at least three studies used the same (or a similar) instrument to assess the same (or similar) aspects of a given outcome and when sufficient numerical data were reported. In the case of different follow-up periods, results were combined using threshold intervals of ‘immediate’, ‘short term’, ‘medium term’ and ‘long term’, as shown in Table 3.
| Follow-up thresholdsa for meta-analysis, months | Equivalence, weeks | |
|---|---|---|
| Immediate | < 1 | < 4 |
| Short term | ≥ 1 and < 4 | ≥ 4 and < 17 |
| Medium term | ≥ 4 and < 8 | ≥ 17 and < 34 |
| Long term | ≥ 8 | ≥ 34 |
In cases where two studies reported short-term follow-up, and one study reported an immediate follow-up assessment, the studies were meta-analysed and combined into a short-term follow-up comparison. For continuous outcomes, standardised mean differences (SMDs) were used when outcomes were measured with different instruments. Random-effects models were used because of clinical heterogeneity. Statistical heterogeneity of results between studies was assessed using the I2-value. Conclusions regarding the estimates of effect sizes were interpreted cautiously if there was significant heterogeneity.
Unit of analysis issues
Only comparative studies were included. Participants were usually randomised to one group of two groups; however, some studies could compare one experimental TW intervention group against both a standard intervention (such as standard care) and one with placebo writing. Alternatively, two or more experimental interventions could be tested against a standard intervention (or with both a standard intervention and with placebo writing), giving a four-arm trial. There could be also trials with the same outcome assessed at different time points or just measured after the writing session or at the end of the treatment period.
For the systematic review, the interest lay only in the direct comparison between a TW intervention arm and an inactive comparator. If a trial had two intervention groups and two control groups, for meta-analysis the trial was treated as two separate trials one comparing, for instance, a more brief TW intervention against inactive comparator and one comparing a longer TW intervention against inactive comparator. Where there were two intervention groups and one control group, the TW intervention most widely used (i.e. the unfacilitated EW with the standard instructions was the one included in the meta-analysis).
Results across LTCs
Four analyses were performed:
-
physiological, disease-related and biomarker outcomes (results tabulated)
-
positive writing across LTCs (results tabulated)
-
depression (results tabulated and meta-analysed where possible)
-
anxiety (results tabulated and meta-analysed where possible).
Chapter 3 Systematic review results
Study selection
A total of 18,235 citations were initially retrieved from the searches in the different electronic databases. After removal of duplicates, 14,658 citations were initially screened. Based on the review of their corresponding titles and abstracts 14,374 records were excluded, while 284 full papers were marked for retrieval, either because they were potentially relevant or because insufficient information was reported in the title and abstract to make a final decision regarding inclusion in the systematic review. After screening the full papers, 64 publications relating to 64 unique studies were finally included in the systematic review: 58 from database searches and six from hand-searches. The duplicate checking of 10% of the titles and abstracts revealed no studies missed and excellent agreement on excluded studies. Therefore, no further checking was indicated.
All included studies were comparative studies evaluating a TW intervention in patients with different LTCs. A description of the process followed for the identification and selection of studies, and the number of studies identified through each step, is presented in the PRISMA diagram (Figure 1).
FIGURE 1.
Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) diagram. a, Final number of studies with no numerical results (after correspondence with authors); b, authors of the abstracts and ongoing studies were contacted to obtain a full-text version if available.

Included studies
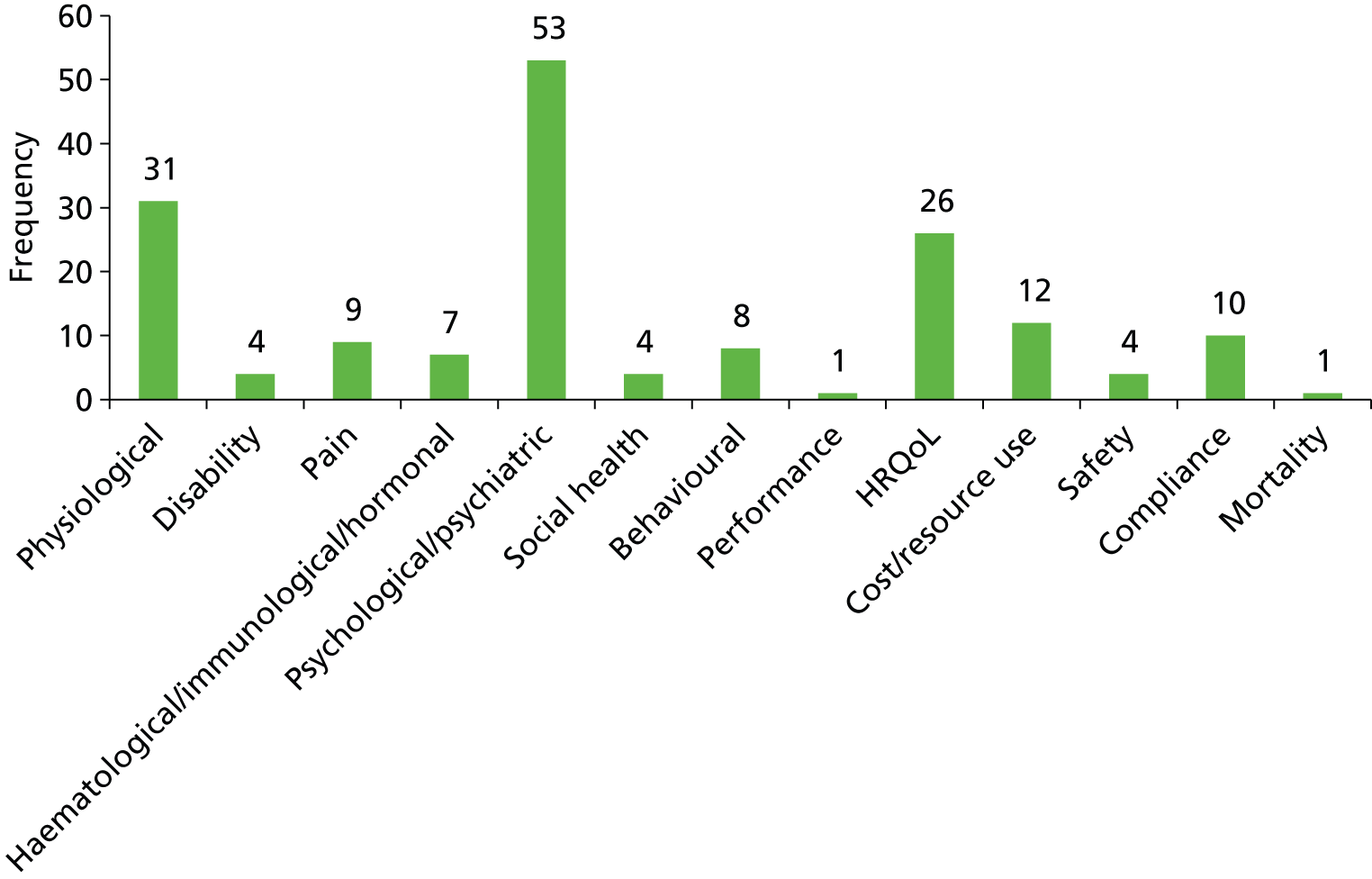
Details on the study design, participants’ chronic conditions, intervention types and processes, outcome measures, as well as the quality assessment of the included studies, are reported in Appendix 5. The number of studies categorised by ICD-10 code according to the LTC evaluated, together with the names of the studies in each category, are shown in Table 4. The number of studies published by year is shown in Figure 2, and the frequency of outcomes evaluated across the included studies is shown in Figure 3.
FIGURE 2.
Included studies by year of publication.

FIGURE 3.
Frequency of outcomes evaluated across the included studies.
| Condition | ICD-10 code | Number of unfacilitated EW studies (facilitated TW) | Authors |
|---|---|---|---|
| HIV | B24 | 6 | Abel 2004,50 Ironson 2013,71 Kraaij 2010,55 Mann 2001,72 Petrie 2004,56 Wagner 201073 |
| Breast cancer | C50 | 8 | Craft 2013,74 Gellaitry 2010,75 Henry 2010,53 Hughes 2007,54 Jensen-Johansen 2013,76 Mosher 2012,77 Park 2012,78 Walker 199979 |
| Gynaecological and genitourinary cancers | C57, C61, C62, C64 | 5 (1) | Arden-Close 2013,80 Milbury 2014,81 Pauley 2011,82 (Rickett 201166), Rosenberg 2002,83 Zakowski 200484 |
| Other cancers | C80 | 2 | Cepeda 2008,85 Rini 201486 |
| Sickle cell disease | D57 | 1 | McElligott 200687 |
| Type 2 diabetes mellitus | E11 | 1 | Dennick 201488 |
| Cystic fibrosis | E84 | 1 | Taylor 200389 |
| Dementia | F03 | (1) | (Hong 201167) |
| SUD | F14/F19 | 3 | Grasing 2010,90 Meshberg-Cohen 2010,91 Van Dam 201392 |
| Psychiatric disorders | F41–60 | 5 (1) | Bernard 2006,93 Canna 2006,94 (Golkaramnay 200768), Graf 2008,95 Krpan 2013,96 Richards 200097 |
| PTSD | F43 | 2 (2) | Gidron 1996,98 (Lange 200369), (Sloan 201270), Smyth 20089 |
| BN | F50 | 1 | Robinson 200899 |
| Amyotrophic lateral sclerosis | G12 | 1 | Averill 2013100 |
| Migraines and tension headaches | G43/G44 | 1 | D’Souza 2008101 |
| CVD | I51 | 3 | Bartasiuniene 2011,102 Hevey 2012,103 Willmott 2011104 |
| COPD and IPF | J44, J84 | 1 | Sharifabad 2010105 |
| Asthmaa | J45 | 4 | Harris 2005,106 aSmyth 1999,107 Theadom 2010,58 Warner 2006108 |
| IBS | K58 | 2 | Halpert 2010,52 Wallander 2011109 |
| Psoriasis | L40 | 3 | Paradisi 2010,110 Tabolli 2012,111 Vedhara 2007112 |
| Inflammatory arthropathiesa | M06/M45 | 6 | Broderick 2004,113 Hamilton-West 2007,114 Lumley 2011,115 Lumley 2014,116 aSmyth 1999,107 Wetherell 2005117 |
| FM and chronic pain | M79 | 4 | Broderick 2005,118 Gillis 2006,119 Graham 2008,51 Stark 201057 |
Regarding interventions, five used a facilitated type of TW66–70 and 59 studies71–119 used an unfacilitated type of EW therapy. Participants in the control groups were usually instructed to neutral writing; time-management writing; factual writing; non-writing; or waiting list. Most of the studies were published in the USA and, since 2008, the year with most studies published (n = 11) was 2010. Breast cancer and HIV were the most frequently evaluated conditions, followed by PTSD and rheumatoid arthritis (RA). The outcomes most frequently evaluated were, in descending order, psychological, physiological and HRQoL.
Of the 64 included studies,9,51–58,66–119 599,51,54–58,66–68,71–77,79–86,88,89,91,93–119 were RCTs, and four52,78,87,92 were non-randomised studies. The remaining study53 was a matched case–control study. Among the 64 studies,9,51–58,66–119 one was written not in the English language but in Korean. 78 Smyth et al. 107 and D’Souza120 evaluated the effect of TW in two groups of patients with different conditions and reported relevant outcomes independently. Data were extracted on the most recent paper, or the most complete piece of information in the case of duplicates of an abstract and when the corresponding published article of a PhD thesis was retrieved. Fifty papers required correspondence with authors in order to get relevant unpublished information (or adequate data for meta-analysis purposes): 32 authors could be contacted and 14 provided the sought information. All 64 studies9,51–58,66–119 provided information (numerical data) relating to the efficacy and/or effectiveness of TW. Among those, numerical results were derived from graphs in nine studies. 51,53,56,70,85,103,110,114,121 Several studies under-reported the numerical data (e.g. reporting the mean with no measure of variability, such as the SD) or used different statistics [such as the median, together with confidence intervals (CIs) and/or ranges or the mean together with the SE] to report the results. All 64 studies9,51–58,66–119 were considered for the quantitative analysis and 35 were finally included in the meta-analyses.
Excluded studies
Abstracts and ongoing studies were excluded from the systematic review and have been listed separately with details of all excluded papers, with their reasons for exclusion (see Appendix 6, List of excluded studies with reasons for exclusion).
Nine studies evaluated TW but reported no numerical results for any of the outcomes measured and were therefore excluded from the systematic review, as they could not contribute to estimation of efficacy or effectiveness (see Appendix 6, List of excluded studies with reasons for exclusion).
Results of the different therapeutic writing interventions
This section is organised as follows:
-
facilitated writing (in one or more arms of the study)
-
unfacilitated writing (standard type) categorisated by ICD-10 code122
-
positive unfacilitated writing
-
summaries across different LTCs for:
-
physiological, disease-related and biomarker outcomes
-
depression
-
anxiety.
-
Most of the current published research focuses usually on unfacilitated EW for disease intervention types encompassing many variants. When a study had two groups of patients with different conditions, for example asthma and RA, results for each condition were reported under the separate ICD-10 codes where possible.
Facilitated therapeutic writing
Overview
There were five studies66–70 evaluating facilitated TW. A summary of their main characteristics is presented in Table 5.
| First author, year | Country | Study design | LTC | Intervention group | Control group |
|---|---|---|---|---|---|
| Golkaramnay 200768 | Germany | Matched case–control study | Mental health disorders | Group therapy through internet chat | No interventiona |
| Hong 201167 | Korea | RCT | Dementia (Alzheimer’s disease/vascular dementia/Parkinson’s disease) | Songwriting | Waiting list |
| Lange 200369 | The Netherlands | Non-randomised trial | PTSD | Interapy | Waiting list |
| Rickett 201166 | Australia | Non-randomised trial | Primarily cancer | Poetry writing programme/workshop | Waiting list |
| Sloan 201270 | USA | RCT | PTSD | Written exposure therapy | Waiting list |
All studies66–70 evaluated one facilitated intervention group against one control group. All studies66–70 were conducted in a different country. Two studies69,70 concerned PTSD and involved writing on trauma-related topics, but the remaining studies examined different conditions [dementia,67 mental health problems68 and serious physical illness66 (primarily cancer)]. Although grouped together here as facilitated TW, the interventions studied were all very different and the type and amount of level of facilitation (and indeed actual writing) varied greatly.
The studies conducted by Golkaramnay et al. 68 and Lange et al. 69 were internet based. Golkaramnay et al. 68 studied a chat room through which groups of participants recently discharged from psychiatric hospital communicated with each other in writing during weekly 90-minute sessions, guided by experienced group therapists who knew all of the participants beforehand. The intervention in Lange et al. 69 (Interapy) involved psychoeducation and 10 structured writing assignments over 5 weeks, delivered one to one via a website, with seven lots of feedback on the writing assignments from a therapist. Hong and Choi67 studied weekly group songwriting sessions in care home residents with dementia, but it is not clear how much actual writing was involved. Rickett et al. 66 examined the impact of eight weekly 2-hour facilitated poetry-writing workshops. The intervention in Sloan et al. 70 involved five 30-minute writing exercises with the first session preceded by some scripted psychoeducation delivered over 1 hour. The facilitation was limited to reading verbatim writing instructions at the start of the session and answering questions at the end.
The duration of the therapy sessions ranged from 45 minutes in Lange et al. 69 to 210 minutes in Sloan et al. 70 The duration of the intervention varied from five sessions in Sloan et al. 70 up to 16 weeks in Hong and Choi. 67
The outcomes evaluated in the studies with a facilitated intervention are reported in Table 6.
| First author, year | Emotional distress | Physical well-being | Life satisfaction | Cognitive functioning | Intrusions and avoidance | Symptomatic distress/physical symptoms | PTSD symptom severity | Health-care utilisation | Prior trauma exposure |
|---|---|---|---|---|---|---|---|---|---|
| Golkaramnay 200768 | OQ-45.2 | GBB | FLZ | – | – | SCL-90-R (GSI) | – | LIFE | – |
| Hong 201167 | – | – | – | MMSE-K | – | – | – | – | – |
| Lange 200369 | – | – | – | – | IES | SCL-90 | – | – | – |
| Rickett 201166 | K-10 | – | – | – | – | – | – | – | – |
| Sloan 201270 | SAM | – | – | – | – | – | CAPS | – | TLEQa |
Physical symptoms were evaluated in two studies67,68 using the SCL-90-R (Symptom Checklist-90-Revised) although different subscales. The remaining studies66,69,70 evaluated different outcomes, although three studies assessed aspects of the participant’s emotional distress using different instruments [Kessler Psychological Distress Scale (K-10), Self-Assessment Manikin (SAM) and Outcome Questionnaire (OQ-45.2)] with different scales and scoring systems.
Quality of the included studies
A summary of the quality of the studies of facilitated TW is shown in Figures 4 and 5.
FIGURE 4.
Risk-of-bias summary in the studies of facilitated TW.

FIGURE 5.
Risk-of-bias graph in the studies of facilitated TW.
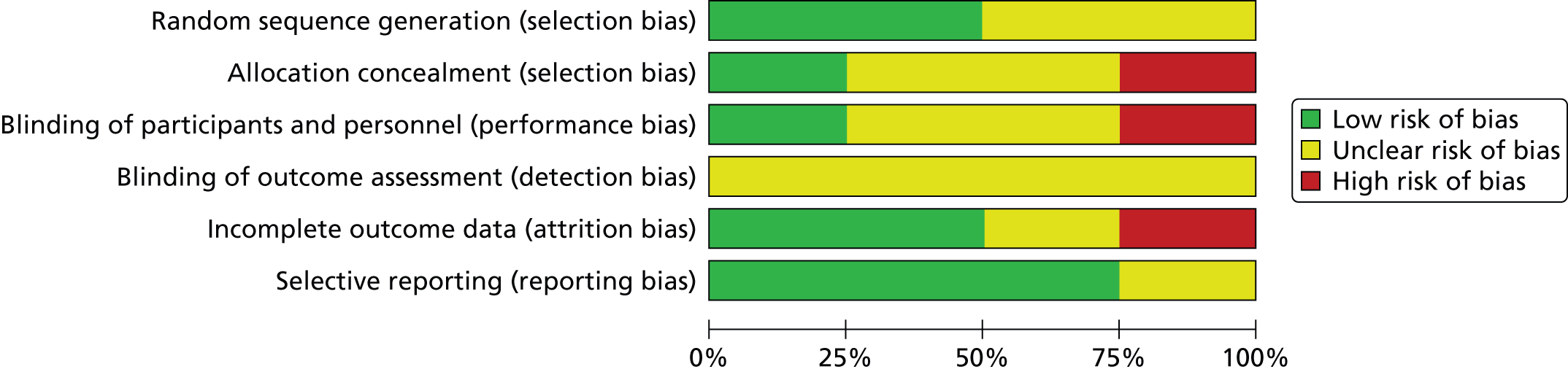
Golkaramnay et al. 68 was a matched case–control study; therefore, without allocation concealment (as it was not an RCT, it is not included in the risk-of-bias table). Participants and personnel were not blinded to the intervention performance. Blinding of the outcome assessment was unclear. The information related to the participation rates was unclear, thus the study was likely to introduce attrition bias. Similarity of groups at baseline was unclear. Selection was adequate, as the case definition and comparators were representative and comparable controls were selected from hospital records.
Two studies had allocation concealment. Hong and Choi67 may have introduced selection bias given the sequence generation was not concealed, whereas in Sloan et al. 70 randomisation was computerised and with allocation concealment. Selection bias was unclear in the remaining two studies. Participants and/or personnel masking was not performed in Hong and Choi,67 as opposed to Lange et al. ,69 in which masking was maintained at the intervention performance level. In the remaining studies, the information related to blinding was unclear. Rickett et al. 66 was the only study with a high risk of attrition bias. However, reporting bias was absent in all studies66,68–70 but Hong and Choi,67 in which it was assessed as unclear.
Numerical results
The numerical results reported in each of the five studies66–70 are summarised in Table 7.
| First author, year | Outcome measures | Follow-upa (weeks) | Facilitated intervention group | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||
|---|---|---|---|---|---|---|---|---|---|
| n totalb | Final mean scorea | SDa | n totalb | Final mean scorea | SDa | ||||
| Golkaramnay 200768 | SCL-90-R | 52 | 97 | 0.68 | 0.51 | 104 | 0.86 | 0.68 | SS |
| OQ-45.2 | 52 | 97 | 56.12 | 23.35 | 104 | 65.83 | 27.96 | SS | |
| GBB | 52 | 97 | 19.60 | 13.90 | 97 | 24.68 | 14.82 | SS | |
| n of patients accessing psychotherapeutic care | 52 | 97 | 53.60% | NA | 94 | 62.80% | NA | NS | |
| n of patients who received medication | 52 | 97 | 55.90% | NA | 94 | 60.40% | NA | NS | |
| Hong 201167 | MMSE-K | Just after writing | 15 | 18.40 | 3.00 | 15 | 14.13 | 2.95 | SS |
| Lange 200369 | IES-I | Just after writing | 69 | 11.12 | 9.27 | 32 | 21.97 | 8.60 | SS |
| IES-I | 6 | 57 | 10.46 | 9.42 | 32 | NRc | NRc | NA | |
| IES-Av | Just after writing | 69 | 6.17 | 7.14 | 32 | 17.28 | 8.29 | NS | |
| IES-Av | 6 | 57 | 5.70 | 7.51 | 32 | NRc | NRc | NA | |
| SCL-90-D | Just after writing | 69 | 26.42 | 10.33 | 32 | 37.25 | 9.67 | SS | |
| SCL-90-D | 6 | 57 | 25.70 | 12.28 | 32 | NRc | NRc | NA | |
| SCL-90-A | Just after writing | 69 | 15.32 | 5.65 | 32 | 20.41 | 7.38 | SS | |
| SCL-90-A | 6 | 57 | 14.84 | 7.33 | 32 | NRc | NRc | NA | |
| SCL-90-S | Just after writing | 69 | 17.52 | 6.34 | 32 | 22.88 | 7.74 | SS | |
| SCL-90-S | 6 | 57 | 16.34 | 7.02 | 32 | NRc | NRc | NA | |
| SCL-90-Sl pb | Just after writing | 69 | 5.80 | 2.96 | 32 | 5.50 | 2.40 | SS | |
| SCL-90-Sl pb | 6 | 57 | 5.18 | 2.79 | 32 | NRc | NRc | NA | |
| Rickett 201166 | K-10 | Just after writing | 14 | 4.30 | 0.62 | 14 | 3.90 | 0.77 | SS |
| Sloan 201270 | SAM | 6 | 22 | NRd | NRd | 24 | NRd | NRd | NA |
| SAM | 18 | 22 | NRd | NRd | 24 | NRd | NRd | NA | |
| SAM | 30 | 22 | NRd | NRd | 24 | NRd | NRd | NA | |
| CAPS | 6 | 22 | 19.30 | 22.23 | 24 | 73.68 | 35.43 | SS | |
| CAPS | 18 | 22 | 10.29 | 17.54 | 24 | 57.41 | 57.43 | SS | |
| CAPS | 30 | 22 | 10.46 | 17.54 | 24 | No follow-up at week 30 in control group | NA | ||
The follow-up assessment ranged from 5 weeks in Lange et al. 69 to 52 weeks in Golkaramnay et al. 92 In Sloan et al. ,70 data are available to only 18 weeks. Total sample sizes varied on each of the outcomes measured in Golkaramnay et al. ,68 in which initial total sample sizes were of 228 participants with a dropout rate of 10–15%. The remaining trials used intention-to-treat (ITT) analyses. All of the studies66–69 reported final mean scores together with corresponding SDs, except Sloan et al. ,70 in which SEs were reported in a graph. All studies66–70 reported improvement in favour of the intervention group across all outcomes and follow-ups (except on health-care use outcomes in Golkaramnay et al. 68). It must be noted that three of the studies66,67,70 were very small. None of the studies evaluating facilitated TW interventions could be meta-analysed owing to lack of consistency in measurement and heterogeneity in interventions and participants.
Unfacilitated emotional writing by International Classification of Diseases, Tenth Edition code
B24: human immunodeficiency virus
Overview
There were six studies50,55,56,71–73 evaluating unfacilitated EW in patients with HIV. A summary of main characteristics is presented in Table 8. All participants were diagnosed with HIV and were receiving active treatment at the time of the study. Some participants in Ironson et al. 71 also had PTSD (n = 85 men, n = 47 women).
| First author, year | Study design | Intervention group | Control group |
|---|---|---|---|
| Abel 200450 | RCT | Unfacilitated EW | Factual writing |
| Ironson 201371 | RCT | Unfacilitated EW | Factual writing |
| Kraaij 201055 | RCT | Computerised, structured, unfacilitated EW | Waiting list |
| Mann 200172 | RCT | Unfacilitated EW (positive writing) | Non-writing |
| Petrie 200456 | RCT | Unfacilitated EW | Time-management writing |
| Wagner 201073 | RCT | Unfacilitated EW | Factual and time-management writing |
Four studies were conducted in the USA,50,71–73 with Kraaij et al. 55 and Petrie et al. 56 conducted in the Netherlands and New Zealand, respectively. All studies50,56,71–73 except Kraaij et al. 55 had two groups and evaluated one EW intervention compared with one control. Kraaij et al. 55 also compared EW with a cognitive–behavioural self-help programme but this is not considered further here. Mann72 asked participants to write about a positive future with their HIV, in which they had to take only one tablet per day, and the remaining studies all explicitly involved standard EW writing. The studies by Abel et al. 50 and Kraaij et al. 55 used a disease-focus topic in the intervention arm, and the latter study was web based. The remaining studies56,71–73 used self-selected worst trauma for participants to write about. The length of the interventions varied across studies. In the studies by Abel et al. ,50 Petrie et al. 56 and Ironson et al. ,71 EW was conducted over 3 or 4 consecutive days, whereas in the remaining studies55,72,73 the writing exercises were distributed over 4 weeks (once or twice a week). Participants in the studies by Kraaij et al. ,55 Petrie et al. 56 and Wagner et al. 73 used computers or tablets to write, as opposed to the other studies in which EW was handwritten. Participants in the studies by Abel et al. ,50 Mann72 and Wagner et al. 73 were financially compensated for participation in the study.
The outcomes evaluated across the HIV studies of unfacilitated EW are reported in Table 9.
| First author, year | HIV-related physical symptoms | CD4+ count | VL | Psychosocial distress/perceived stress | Depression | Affects (mood states) | Optimism | Coherence | Stigma | QoL | Adherence and side effects | Resource use |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Abel 200450 | – | – | – | – | CES-D | – | – | – | Stigma Scale and Disclosure Scale | SF-36 | – | – |
| Ironson 201371 | Symptom checklist | Flow cytometry | Quantitative reverse-transcriptase PCR | PTSDTOTa | HAM-D | – | – | – | – | – | – | – |
| Kraaij 201055 | – | – | – | – | HADS-D | – | – | – | – | – | – | – |
| Mann 200172 | – | – | – | – | – | – | LOT | – | – | – | Adherence and side effects due to HIV medicationb | – |
| Petrie 200456 | Self-rated health status | Flow cytometry | Quantitative reverse-transcriptase PCR | PSSa | – | – | – | – | – | – | – | – |
| Wagner 201073 | – | – | – | PSSa | – | PANAS-X(a) | HIV-OS | SOC | – | MOS-HIV | – | – |
Psychological outcomes (e.g. depression or mood) were the most commonly evaluated outcomes, together with physiological (e.g. HIV symptoms) and biological outcomes [e.g. viral load (VL) and cluster of differentiation antigen 4-positive lymphocyte cell count (CD4+ count)].
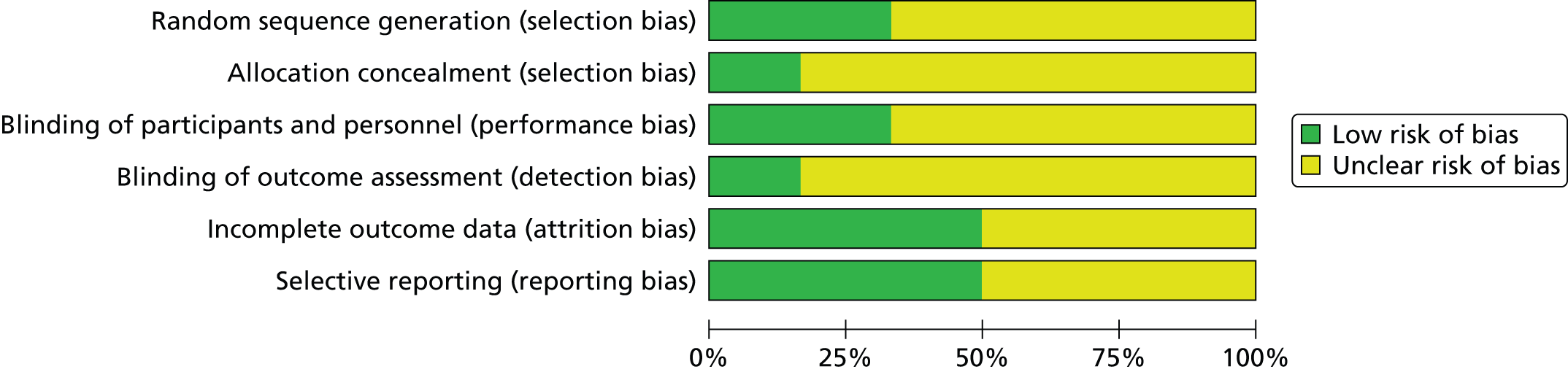
Quality assessment
A summary of the quality of the studies in HIV is shown in Figures 6 and 7. Two studies56,73 reported methods of randomisation. Allocation concealment was reported in only one study,56 and blinding was preserved in one other study. 50 The methods used were scarcely reported in almost all of the studies.
FIGURE 6.
Risk-of-bias summary in the HIV studies.

FIGURE 7.
Risk-of-bias graph in the HIV studies.
Numerical results
The numerical results reported in the HIV studies are summarised in Table 10. Follow-up assessments ranged from 2 weeks in Petrie et al. 56 to 52 weeks in Ironson et al. 71 Total sample sizes ranged from 11 participants in Abel et al. 50 to 212 participants in Ironson et al. 71 Petrie et al. 56 reported medians and SEs rather than means and SDs as in the other studies. Statistical significance of the follow-up results differences were not reported in the studies by Abel et al. ,50 Ironson et al. ,71 Mann,72 Petrie et al. 56 or Wagner et al. 73 The group-by-time interaction analysis in the Ironson et al. 71 and Kraaij et al. 55 studies was non-significant for the following outcomes: biomarkers, such as VL at long term only and CD4+ count at short, medium and long term, as well as depression [Hamilton Depression Scale (HAM-D)] or social distress [The Davidson PTSD scale (PTSDTOT)]. However, in the Petrie et al. 56 study, the CD4+ count increased significantly in the EW group compared with control subjects when assessed at 26 weeks only.
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||
|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean scoreb | SDb | n totala | Final mean scoreb | SDb | ||||
| Abel 200450 | Stigma Scale | 4.5 | 5 | 22.70 | 5.90 | 6 | 23.80 | 7.90 | NR |
| CES-D | 4.5 | 5 | 22.00 | 6.10 | 6 | 20.20 | 9.70 | NR | |
| SF-36 PCS | 4.5 | 5 | 525.00 | 141.10 | 6 | 610.00 | 277.00 | NR | |
| SF-36 MCS | 4.5 | 5 | 343.00 | 50.00 | 6 | 356.00 | 128.40 | NR | |
| Ironson 201371 | CD4+ count | 4 | 101 | 421.00 | 269.00 | 107 | 466.00 | 249.00 | NS |
| CD4+ count | 26 | 95 | 419.00 | 254.00 | 92 | 464.00 | 223.00 | NS | |
| CD4+ count | 52 | 78 | 429.00 | 251.00 | 87 | 491.00 | 302.00 | NS | |
| VL | 4 | 102 | 38,100.00 | 100.17 | 105 | 24,166.00 | 79,005.00 | NS | |
| VL | 26 | 96 | 47,406.00 | 114,877.00 | 89 | 28,743.00 | 94,105.00 | NS | |
| VL | 52 | 81 | 56,577.00 | 142,846.00 | 87 | 24,056.00 | 68,682.00 | NS | |
| HIV S-CL | 4 | 106 | 0.24 | 0.43 | 104 | 0.25 | 0.44 | NS | |
| HIV S-CL | 26 | > 93 | 0.19 | 0.40 | 94 | 0.27 | 0.45 | NS | |
| HIV S-CL | 52 | 81 | 0.22 | 0.42 | 88 | 0.26 | 0.44 | NS | |
| PTSDTOT | 4 | 104 | 20.63 | 23.72 | 108 | 23.84 | 21.93 | NS | |
| PTSDTOT | 26 | 94 | 17.66 | 20.13 | 96 | 19.83 | 21.73 | NS | |
| PTSDTOT | 52 | 82 | 18.08 | 20.41 | 91 | 17.89 | 22.42 | NS | |
| HAM-D | 4 | 103 | 8.41 | 6.26 | 104 | 8.99 | 7.27 | NS | |
| HAM-D | 26 | 95 | 8.13 | 6.46 | 94 | 8.30 | 6.60 | NS | |
| HAM-D | 52 | 82 | 7.54 | 6.24 | 89 | 7.09 | 5.56 | NS | |
| Kraaij 201055 | HADS-D | 4 | 16 | 7.06 | 4.81 | 15 | 7.73 | 3.88 | NS |
| Mann 200172 | LOT | 4 | 20 | 28.13 | 0.90 | 20 | 27.23 | 1.10 | NR |
| Adherence | 4 | 20 | 4.12 | 0.31 | 20 | 4.82 | 0.16 | NR | |
| Side effects | 4 | 20 | 37.7 | 5.71 | 20 | 35.85 | 4.76 | NR | |
| Petrie 200456 | VL | 2 | 20 | Median: 3.1 | 0.67 | 17 | Median: 3.36 | 0.66 | NR |
| VL | 13 | 20 | Median: 3.01 | 0.63 | 17 | Median: 3.08 | 1.40 | NR | |
| VL | 26 | 20 | Median: 3.03 | 0.63 | 17 | Median: 3.26 | 0.66 | NS | |
| CD4+ count | 2 | 20 | Median: 495.69 | 158.0 | 17 | Median: 513.79 | 74.57 | NR | |
| CD4+ count | 13 | 20 | Median: 509.48 | 161.85 | 17 | Median: 529.31 | 170.49 | NR | |
| CD4+ count | 26 | 20 | Median: 571.55 | 154.14 | 17 | Median: 533.62 | 301.79 | SS | |
| Wagner 201073 | PANAS-NA | 4 | 19 | 2.81 | 0.91 | 18 | 2.62 | 0.95 | NR |
| PANAS-PA | 4 | 19 | 2.92 | 1.05 | 18 | 3.36 | 0.60 | NR | |
| PSS | 4 | 19 | 3.10 | 0.60 | 18 | 2.90 | 0.60 | NR | |
| HIV-OS | 4 | 19 | 4.20 | 1.05 | 18 | 3.80 | 1.16 | NR | |
| SOC | 4 | 19 | 3.80 | 1.16 | 18 | 4.30 | 1.08 | NR | |
| MOS-HIV | 4 | 19 | 32.60 | 9.20 | 18 | 35.50 | 6.50 | NR | |
In the Mann study,72 the writing intervention was stated as a promising technique to increase medication adherence and decrease symptoms of distress in pessimistic individuals. However, these differences between the two groups at follow-up were not further reported. The studies by Petrie et al. 56 and Wagner et al. 73 did not report any association or interaction between groups in the outcomes evaluated [i.e. VL in Petrie et al. ;56 Positive and Negative Affect Schedule, positive subscale (PANAS-PA), Positive and Negative Affect Schedule, negative subscale (PANAS-NA), Perceived Stress Scale (PSS), HIV-Specific Optimism Scale (HIV-OS), Sense of Coherence Scale (SOC) and Short Form questionnaire-36 items (SF-36) in Wagner et al. 73]. In the Ironson et al. study,71 among the women, only the EW was associated with a significant reduction in PTSD symptoms, depression and physical symptoms, and this finding was more pronounced in the group with elevated PTSD symptom scores at baseline. Men, however, reported greater decrease in depression among control subjects than in the EW group.
Meta-analysis
The outcome depression was meta-analysed (Figure 8).
FIGURE 8.
Forest plot of depression at short-term follow-up in HIV. df, degrees of freedom; IV, inverse variance.

Three studies50,55,71 used different instruments each [Centre for Epidemiological Studies Depression Scale (CES-D), HAM-D and Hospital Anxiety and Depression Scale, depression subscale (HADS-D)] to measure similar aspects of depression.
-
Clinical differences between studies In Ironson et al. ,71 participants were diagnosed with both HIV falling into a CD4 range of 100–600. Additionally, some were also diagnosed with PTSD. In Abel et al. ,50 participants were taking antiretroviral therapy (ART) and reported their last VL < 80,000–100,000 copies/ml. All participants in all three studies were self-reportedly free of major psychiatric problems. There were no substantial clinical differences between the three studies50,51,55 regarding HIV diagnosis.
-
Follow-up length All three studies50,55,71 assessed depression at a short term, that is, at 4 weeks or at 4.5 weeks.
-
Forest plot A total of 249 participants were meta-analysed (124 in the EW group and 125 in the control group). The SMD was –0.08 [95% confidence interval (CI) –0.33 to 0.17] with a random-effects model and with no significant heterogeneity (I2 = 0%). The overall analysis suggests that there is no significant difference in depression for the EW group compared with the control group.
C50: breast cancer
Overview
There were eight studies53,54,74–79 evaluating unfacilitated EW in patients with breast cancer, including one very large study (507 participants) by Jensen-Johansen et al. 76 A summary of main characteristics is presented in Table 11.
| First author, year | Study design | Intervention group 1 | Intervention group 2 | Control group 1 | Control group 2 |
|---|---|---|---|---|---|
| Craft 201374 | RCT | Unfacilitated EWa | Unfacilitated EWb | Factual writing | Non-writing |
| Gellaitry 201075 | RCT | Unfacilitated EW plus positive writing | – | SMC | – |
| Henry 201053 | Case–control | Unfacilitated EW | – | SMC | – |
| Hughes 200754 | RCT | Unfacilitated EW | – | SMC | – |
| Jensen-Johansen 201376 | RCT | Unfacilitated EW | – | Time-management writing | – |
| Mosher 201277 | RCT | Unfacilitated EW | – | Factual writing | – |
| Park 201278 | Controlled cohort | Unfacilitated EW | – | No intervention | – |
| Walker 199979 | RCT | Unfacilitated EW | Unfacilitated EW | – | SMCc |
Most of the participants were women with breast cancer at stage 0–III, who were mainly receiving curative radiation therapy, but the patients in Mosher et al. 77 had stage IV breast cancer and presented with significant distress. The patients in Jensen-Johansen et al. 76 had recently completed treatment with surgery, radiotherapy or chemotherapy. Participants in Craft et al. ,74 Gellaitry et al. ,75 Hughes54 and Walker et al. 79 included patients with stage I–III breast cancer. Participants were reported to have completed definitive treatment,74 were receiving the last radiotherapy appointment75 or were still receiving curative radiotherapy. 54,59 In the remaining studies, participants in Henry et al. 53 had stage 0–III breast cancer and had completed radiation, and in Park and Yi78 they had stage II and III breast cancer and had undergone surgery, radiotherapy and hormone therapy. Participants in Henry53 were urban and rural women with breast cancer who were still attending radiation oncology clinics, whereas patients in Park and Yi,78 had been recruited from self-help groups.
Almost all studies were conducted in the USA except for Park and Yi,78 which was conducted in Korea and published in the Korean language (which was translated into English), and Jensen-Johansen et al. ,76 which was conducted in Denmark and published in English.
One study had four groups (two experimental and two control groups) and one other study evaluated three groups (two experimental and one control). The remaining studies evaluated one intervention group each against one control (see Table 11).
In six of the breast cancer studies, only unfacilitated EW was evaluated. Topics across all studies included disease-focused writing exercises. Participants were asked to write about their deepest thoughts and feelings about their cancer and treatment–related emotions during 20–30 minutes over 3/4 days at different intervals. Craft et al. 74 assessed two additional types of unfacilitated EW interventions in which topics changed: participants had to write about a self-selected trauma in one group and about facts of treatment and daily events related to breast cancer in the other group. One other study79 evaluated a modified version of the unfacilitated EW intervention using the same topic but feelings and emotions had to be expressed in a positive way. On the other hand, Gellaitry et al. 75 used a different form of EW, combining in 4 days the standard unfacilitated EW (first 2 days) and a positive writing type of EW (the remaining 2 days). Patients were instructed to change the topic throughout the writing sessions starting with an emotional disclosure exercise and cognitive appraisal related to their condition and moving to the benefit finding of it, looking into the future where they wrote about their experience being shared with others. Four studies delivered the intervention on 1,53 354,79 or 474,75 consecutive days. Three other studies delivered three or four sessions at weekly intervals. 76–78 Henry et al. 53 used one single session. Four studies53,54,70,74 used SMC as the control arm, two studies used a non-emotional factual writing,69,72 one study71 used a time-management writing as control, and in the remaining two studies the control group either did not write69 or did not receive an intervention73 at all. Patients were financially compensated in Mosher et al. 77 and Henry et al. 53
The outcomes evaluated in the breast cancer studies are reported in Table 12. QoL was assessed in four studies;54,74,75,77 two studies74,75 used the same instrument [Functional Assessment of Cancer Therapy, Breast Cancer Version (FACT-B)], which contains 10 specific breast cancer items (in addition to the 27 general items) addressing physical and psychological concerns related to breast cancer. The study by Mosher et al. 77 used the meaning/peace subscale of FACIT [Functional Assessment of Chronic Illness Therapy meaning/peace subscale (FACI-Sp)], an instrument tailored to measure the spiritual well-being of patients. Six studies53,54,75–77,79 evaluated affect (mood states). Two studies77,78 assessed anxiety with the same instrument (HADS). Depression was evaluated in four studies53,76–78 using three different instruments each [CES-D, Beck Depression Inventory-Short Form (BDI-SF) and HADS-D].
| First author, year | Physical health/symptoms | Perception of disclosure | General affect (mood states) | Positive mood | Negative mood | Social support | Intrusions/avoidance | Depression | Anxiety | Sleep disturbance/fatigue | QoL | Adverse events | Resource use |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Craft 201374 | – | – | – | – | – | – | – | – | – | – | FACT-B | – | – |
| Gellaitry 201075 | – | – | POMS | – | – | SOS | – | – | – | – | FACT-B | ✓ | – |
| Henry 201053 | Survey – 18 physical symptoms items | – | POMS | – | – | – | – | CES-D | – | – | – | – | – |
| Hughes 200754 | – | DIS | – | PANAS-PA | PANAS-NA | – | IES | – | – | – | SIP | – | – |
| Jensen-Johansen 201376 | IES | – | – | PPMS | POMS-NAa | – | – | BDI-SF | – | – | – | – | – |
| Mosher 201277 | – | – | DT | – | – | – | – | CES-D | HADS-A | PSQI, FACIT-F | FACIT-Sp (and demoralisation) | – | – |
| Park 201278 | PILL, MDASI | – | – | – | – | – | – | HADS-D | HADS-A | – | – | – | – |
| Walker 199979 | – | – | – | PANAS-PA | PANAS-n | – | IES | – | – | – | – | Side effect severity checklista | – |
Quality assessment
A summary of the quality of the studies in breast cancer is shown in Figures 9 and 10.
FIGURE 9.
Risk-of-bias summary in the breast cancer studies.
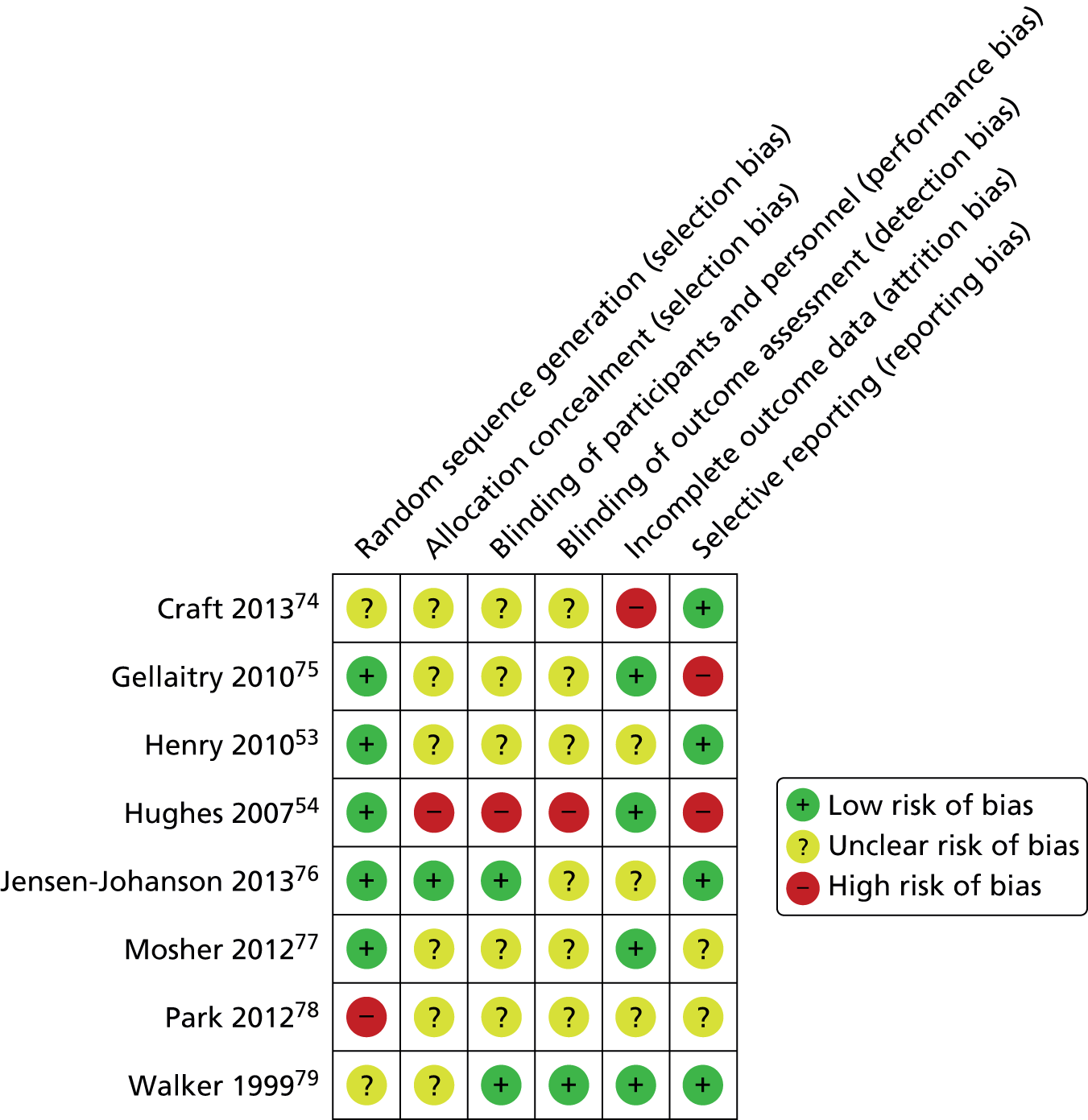
FIGURE 10.
Risk-of-bias graph in the breast cancer studies.

Almost all studies, except that of Park and Yi,78 were reported as RCTs. However, in the Walker et al. study,79 the method of randomisation was not provided. In the Craft et al. study,74 authors reported that randomisation was performed using sequential numbering, which remained unclear as a method of randomisation. The Hughes study54 was truly randomised, but allocation of the sequence generation was not concealed and there was no blinding. Among the remaining studies, almost all did not report on the allocation and blinding methods, except Jensen-Johansen et al. ,76 in which allocation was concealed, and blinding was conducted at both the performance and outcome assessment stages.
One study74 was more likely to have introduced attrition bias. Two other studies54,75 reported selectively on specific outcomes and the Henry et al. study53 reported outcomes but with insufficient detail for the data to be included in the meta-analysis. No measure of variability could be derived from the graphs.
Numerical results
The numerical results reported in the breast cancer studies are summarised in Table 13.
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group 1 | Intervention group 2 | Control group 1 | Control group 2 | Author’s reported statistical significance (group-by-time interaction) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean score | SDb | n totala | Final mean score | SDb | n totala | Final mean score | SDb | n totala | Final mean score | SDb | ||||
| Craft 201374 | FACT-B | 4 | 26 | 114.83 | 10.48 | 19 | 110.75 | 15.17 | 22 | 119.62 | 13.52 | 30 | 104.38 | 21.31 | SS |
| 26 | 26 | 112.60 | 9.12 | 19 | 106.63 | 12.08 | 22 | 112.04 | 10.31 | 30 | 101.69 | 24.70 | NS | ||
| Gellaitry 201075 | POMS | 4 | 38 | 26.54 | 32.99 | – | – | – | – | – | – | 42 | 32.36 | 43.06 | NR |
| 13 | 38 | 25.58 | 30.42 | – | – | – | – | – | – | 42 | 28.17 | 42.50 | NR | ||
| 26 | 38 | 20.63 | 32.28 | – | – | – | – | – | – | 42 | 24.21 | 36.97 | NS | ||
| SOSc | 4 | 38 | 11.40 | 1.56 | – | – | – | – | – | – | 42 | 11.34 | 1.78 | NR | |
| 13 | 38 | 11.28 | 1.55 | – | – | – | – | – | – | 42 | 11.07 | 2.24 | NR | ||
| 26 | 38 | 11.36 | 1.49 | – | – | – | – | – | – | 42 | 11.01 | 2.45 | SSd | ||
| FACT-B | 4 | 38 | 109.20 | 17.51 | – | – | – | – | – | – | 42 | 105.70 | 24.37 | NR | |
| 13 | 38 | 106.94 | 19.31 | – | – | – | – | – | – | 42 | 107.00 | 23.82 | NR | ||
| 26 | 38 | 109.56 | 19.81 | – | – | – | – | – | – | 42 | 108.03 | 21.36 | NS | ||
| Adverse events | Just after writing | 38 | NR | NR | – | – | – | – | – | – | 42 | NR | NR | NR | |
| Henry 201053 | Survey – 18 physical symptoms items | 13 | 40 | 1.85 | NR | – | – | – | – | – | – | 40 | 2.15 | NR | NS |
| 39 | 40 | 2.05 | NR | – | – | – | – | – | – | 40 | 2.09 | NR | NS | ||
| CES-D | 13 | 40 | 1.31 | NR | – | – | – | – | – | – | 40 | 1.55 | NR | NS | |
| 39 | 40 | 1.40 | NR | – | – | – | – | – | – | 40 | 1.47 | NR | NS | ||
| POMS | 13 | 40 | NR | NR | – | – | – | – | – | – | 40 | NR | NR | SS | |
| 39 | 40 | NR | NR | – | – | – | – | – | – | 40 | NR | NR | NS | ||
| Hughes 200754 | IES-I | 1 | 89 | 10.57 | 8.36 | – | – | – | – | – | – | 91 | 9.69 | 8.71 | NA |
| 17 | 89 | 9.71 | 8.54 | – | – | – | – | – | – | 91 | 9.26 | 9.14 | NA | ||
| 26 | 89 | 10.52 | 9.15 | – | – | – | – | – | – | 91 | 9.07 | 8.67 | NA | ||
| 52 | 89 | 7.53 | 7.24 | – | – | – | – | – | – | 91 | 7.39 | 6.88 | NA | ||
| IES-Av | 1 | 89 | 10.77 | 9.64 | – | – | – | – | – | – | 91 | 11.01 | 10.92 | NA | |
| 17 | 89 | 11.45 | 9.60 | – | – | – | – | – | – | 91 | 10.62 | 10.35 | NA | ||
| 26 | 89 | 10.37 | 10.06 | – | – | – | – | – | – | 91 | 10.84 | 10.29 | NA | ||
| 52 | 89 | 7.94 | 8.61 | – | – | – | – | – | – | 91 | 7.75 | 9.29 | NA | ||
| IES-home management | 1 | 89 | 46.96 | 36.58 | – | – | – | – | – | – | 91 | 48.33 | 36.28 | NA | |
| 17 | 89 | 40.01 | 37.79 | – | – | – | – | – | – | 91 | 41.25 | 34.84 | NA | ||
| 26 | 89 | 34.74 | 37.87 | – | – | – | – | – | – | 91 | 33.95 | 36.79 | NA | ||
| 52 | 89 | 22.62 | 33.75 | – | – | – | – | – | – | 91 | 24.89 | 34.20 | NA | ||
| SIP-m | 1 | 89 | 23.27 | 32.94 | – | – | – | – | – | – | 91 | 30.92 | 35.39 | NA | |
| 17 | 89 | 21.28 | 33.36 | – | – | – | – | – | – | 91 | 18.87 | 29.67 | NA | ||
| 26 | 89 | 12.71 | 27.33 | – | – | – | – | – | – | 91 | 13.29 | 28.73 | NA | ||
| 52 | 89 | 10.21 | 23.11 | – | – | – | – | – | – | 91 | 9.75 | 25.31 | NA | ||
| SIP-r&p-t | 1 | 89 | 41.02 | 32.18 | – | – | – | – | – | – | 91 | 42.50 | 33.51 | NA | |
| 17 | 89 | 36.64 | 33.19 | – | – | – | – | – | – | 91 | 35.90 | 34.29 | NA | ||
| 26 | 89 | 31.89 | 32.22 | – | – | – | – | – | – | 91 | 28.32 | 32.53 | NA | ||
| 52 | 89 | 20.99 | 29.56 | – | – | – | – | – | – | 91 | 19.86 | 29.33 | NA | ||
| PANAS-PA | 1 | 89 | 34.92 | 7.62 | – | – | – | – | – | – | 91 | 31.30 | 8.65 | NA | |
| 17 | 89 | 34.23 | 8.04 | – | – | – | – | – | – | 91 | 32.23 | 8.43 | NA | ||
| 26 | 89 | 36.26 | 7.61 | – | – | – | – | – | – | 91 | 32.85 | 8.75 | NA | ||
| 52 | 89 | 38.09 | 8.84 | – | – | – | – | – | – | 91 | 34.75 | 9.43 | NA | ||
| PANAS-NA | 1 | 89 | 16.41 | 6.84 | – | – | – | – | – | – | 91 | 17.67 | 7.48 | NA | |
| PANAS-NA | 17 | 89 | 16.48 | 6.75 | – | – | – | – | – | – | 91 | 17.11 | 7.50 | NA | |
| 26 | 89 | 16.77 | 7.54 | – | – | – | – | – | – | 91 | 16.72 | 6.82 | NA | ||
| 52 | 89 | 14.31 | 5.36 | – | – | – | – | – | – | 91 | 16.01 | 5.93 | NA | ||
| DIS | NR | NR | NR | NR | – | – | – | – | – | – | NR | NR | NR | NR | |
| Jensen-Johansen 201376 | IES-I | 13 | 199 | 7.50 | 7.40 | – | – | – | – | – | – | 222 | 8.00 | 7.60 | NS |
| IES-I | 39 | 207 | 7.50 | 7.40 | – | – | – | – | – | – | 223 | 7.30 | 7.70 | NS | |
| IES-Av | 13 | 199 | 8.20 | 7.90 | – | – | – | – | – | – | 222 | 9.70 | 8.80 | NS | |
| IES-Av | 39 | 207 | 8.10 | 8.00 | – | – | – | – | – | – | 223 | 8.80 | 8.70 | NS | |
| IES-T | 13 | 199 | 15.60 | 13.60 | – | – | – | – | – | – | 222 | 17.70 | 14.80 | NS | |
| 39 | 207 | 15.60 | 13.70 | – | – | – | – | – | – | 223 | 16.10 | 14.50 | NS | ||
| BDI-SF | 13 | 197 | 4.00 | 4.10 | – | – | – | – | – | – | 221 | 4.50 | 4.40 | NS | |
| 39 | 209 | 4.20 | 4.30 | – | – | – | – | – | – | 226 | 4.50 | 4.60 | NS | ||
| POMS-n | 13 | 198 | 4.50 | 18.50 | – | – | – | – | – | – | 215 | 5.30 | 20.80 | NS | |
| 39 | 206 | 4.60 | 18.80 | – | – | – | – | – | – | 225 | 6.70 | 22.10 | NS | ||
| PPMS | 13 | 198 | 19.40 | 7.00 | – | – | – | – | – | – | 215 | 19.80 | 7.00 | NS | |
| 39 | 206 | 19.60 | 6.80 | – | – | – | – | – | – | 225 | 19.50 | 6.90 | NS | ||
| Mosher 201277 | PSQI | 8 | 44 | 8.42 | 2.59 | – | – | – | – | – | – | 42 | 7.83 | 2.53 | NS |
| FACIT-F | 8 | 44 | 30.38 | 7.76 | – | – | – | – | – | – | 42 | 32.58 | 7.78 | NS | |
| HADS-A | 8 | 44 | 7.15 | 3.18 | – | – | – | – | – | – | 42 | 7.87 | 3.18 | NS | |
| CES-D | 8 | 44 | 17.99 | 8.95 | – | – | – | – | – | – | 42 | 17.87 | 8.94 | NS | |
| DT | 8 | 44 | 4.53 | 2.39 | – | – | – | – | – | – | 42 | 4.37 | 2.4 | NS | |
| FACIT-Sp | 8 | 44 | 21.60 | 3.91 | – | – | – | – | – | – | 42 | 22.58 | 3.89 | NS | |
| FACIT-d | 8 | 44 | 21.07 | 10.94 | – | – | – | – | – | – | 42 | 19.50 | 10.89 | NS | |
| Park 201278 | PILL | Post-test | 29 | 50.62 | 34.29 | – | – | – | – | – | – | 29 | 48.17 | 25.74 | NR |
| 4 | 29 | 45.41 | 28.18 | – | – | – | – | – | – | 29 | 52.17 | 28.51 | SS | ||
| MDASI | Post-test | 29 | 47.72 | 35.56 | – | – | – | – | – | – | 29 | 51.69 | 36.57 | NR | |
| 4 | 29 | 41.86 | 34.65 | – | – | – | – | – | – | 29 | 53.03 | 35.78 | NS | ||
| HADS-A | Post-test | 29 | 6.17 | 4.21 | – | – | – | – | – | – | 29 | 5.79 | 3.63 | NR | |
| 4 | 29 | 5.62 | 4.37 | – | – | – | – | – | – | 29 | 5.90 | 3.80 | NS | ||
| HADS-D | Post-test | 29 | 4.93 | 3.40 | – | – | – | – | – | – | 29 | 4.48 | 3.33 | NR | |
| 4 | 29 | 4.52 | 3.45 | – | – | – | – | – | – | 29 | 4.48 | 3.70 | NS | ||
| C-QoL | Post-test | 29 | 54.21 | 8.72 | – | – | – | – | – | – | 29 | 55.48 | 12.41 | NR | |
| 4 | 29 | 57.07 | 10.31 | – | – | – | – | – | – | 29 | 55.76 | 12.94 | SS | ||
| Walker 199979 | PANAS-NA | 4–6 | 11 | 16.70 | 5.31 | 14 | 15.50 | 4.86 | – | – | – | 14 | 13.90 | 5.24 | NS |
| 16 | 11 | 17.90 | 5.98 | 14 | 16.90 | 5.61 | – | – | – | 14 | 14.10 | 5.98 | NS | ||
| 28 | 11 | 17.10 | 5.98 | 14 | 17.10 | 5.98 | – | – | – | 14 | 14.10 | 6.36 | NS | ||
| PANAS-PA | 4–6 | 11 | 38.70 | 6.65 | 14 | 39.40 | 6.36 | – | – | – | 14 | 36.60 | 6.73 | NS | |
| 16 | 11 | 39.40 | 5.98 | 14 | 36.10 | 5.61 | – | – | – | 14 | 36.40 | 6.36 | NS | ||
| 28 | 11 | 39.10 | 6.31 | 14 | 36.40 | 5.98 | – | – | – | 14 | 34.80 | 6.73 | NS | ||
| IES-Av | 4–6 | 11 | 10.90 | 7.97 | 14 | 8.60 | 7.85 | – | – | – | 14 | 7.70 | 8.23 | NS | |
| 16 | 11 | 11.90 | 8.63 | 14 | 8.70 | 8.60 | – | – | – | 14 | 8.80 | 8.98 | NS | ||
| 28 | 11 | 10.70 | 9.30 | 14 | 9.50 | 8.98 | – | – | – | 14 | 9.30 | 9.35 | NS | ||
| IES-I | 4–6 | 11 | 8.10 | 6.31 | 14 | 8.40 | 5.98 | – | – | – | 14 | 7.30 | 6.36 | NS | |
| 16 | 11 | 10.30 | 6.64 | 14 | 7.30 | 6.36 | – | – | – | 14 | 7.60 | 7.11 | NS | ||
| 28 | 11 | 10.50 | 7.64 | 14 | 8.50 | 7.11 | – | – | – | 14 | 6.00 | 7.48 | NS | ||
The broadest range of outcomes measures were collected in Hughes54 on several occasions between 1 and 52 weeks’ follow-up. Almost all studies followed the patients for between 6 and 12 months, except those of Park and Yi78 and Mosher et al. ,77 for which follow-up after the writing intervention was performed at 1 and 2 months, respectively. The total sample sizes ranged from 56 in Craft et al. 74 to 435 participants in Jensen-Johansen et al. 76
Overall, there were significant improvements at short-term follow-up mainly (from 4 to 13 weeks) in favour of the EW groups compared with control subjects regarding QoL [Functional Assessment of Cancer Therapy, Breast Cancer Version (FACT-B) at 4 weeks only, Cancer Quality of Life (C-QoL)], physical symptoms [Pennebaker Inventory of Limbic Languidness (PILL)] particularly regarding nervousness, distress, and unhappiness and mood [Profile of Mood States (POMS) at 13 weeks]. No significant group-by-time interaction differences were reported in the following outcomes when evaluated at both shorter and longer follow-ups (up to 39 weeks): QoL, as measured by FACIT-sp at 8 weeks, FACT-B at 26 weeks in both Craft et al. 74 and Gellaitry et al. 75, mood (POMS at 13 and 39 weeks), immediate mood [PANAS-PA, PANAS-NA and Passive Positive Mood Scale (PPMS) at 11 and 39 weeks, respectively], depression (HADS-D, CES-D, BDI-SF at 4, 8, 13 and 39 weeks), sleep quality [Pittsburgh Sleep Quality Index (PSQI) at 8 weeks], fatigue [Functional Assessment of Chronic Illness Therapy, fatigue subscale (FACIT-F) at 8 weeks], anxiety [Hospital Anxiety and Depression Scale, anxiety subscale (HADS-A) at 4 and 8 weeks], physical symptoms including distress [Distress Thermometer (DT)] or measures of intrusions and avoidance [intrusion subscale of the Impact of Event Scale (IES; IES-I), avoidance subscale of the IES (IES-Av)]. The studies by Park and Yi78 and Mosher et al. 77 evaluated outcomes at shorter follow-ups (4 and 8 weeks, respectively) than in the remaining studies. For instance, Mosher et al. 77 evaluated the impact of the EW intervention on QoL, depression and general well-being at 8 weeks only.
In Mosher et al. ,77 participants in the intervention group reported greater use of mental health services during the study period than did those in the control group (24/44 vs. 11/42, respectively), and differences between groups were statistically significant [odds ratio (OR) = 3.40, 95% CI 1.05 to 11.08]. In the largest study, by Jensen-Johansen et al. ,76 no significant differences were found in the group-by-time interaction analysis on any of the outcomes evaluated (depression, mood, and symptoms such as intrusions or avoidance).
In Gellaitry et al. ,75 adverse events were assessed but not reported by group; however, four women of the total sample indicated that writing was difficult, not helpful and of no benefit to them personally. They also reported feeling negatively on completion of writing, but these negative feelings were not prolonged. In addition, separate studies reported significant differences [statistically significant (SS)] for the following outcomes: FACT-B at 4 weeks, Significant Others Scale (SOS) at 26 weeks, and PILL and QoL at 4 weeks, as shown in Table 13.
Meta-analysis
The outcomes positive and negative mood (Figures 11 and 12) and depression (Figure 13) were meta-analysed. In addition, three studies76–78 assessed general mood but the Henry et al. study53 did not report any numerical data on the POMS outcome, so meta-analysis was not performed for this outcome.
FIGURE 11.
Forest plot of positive mood at short-term follow-up in patients with breast cancer. df, degrees of freedom; IV, inverse variance.
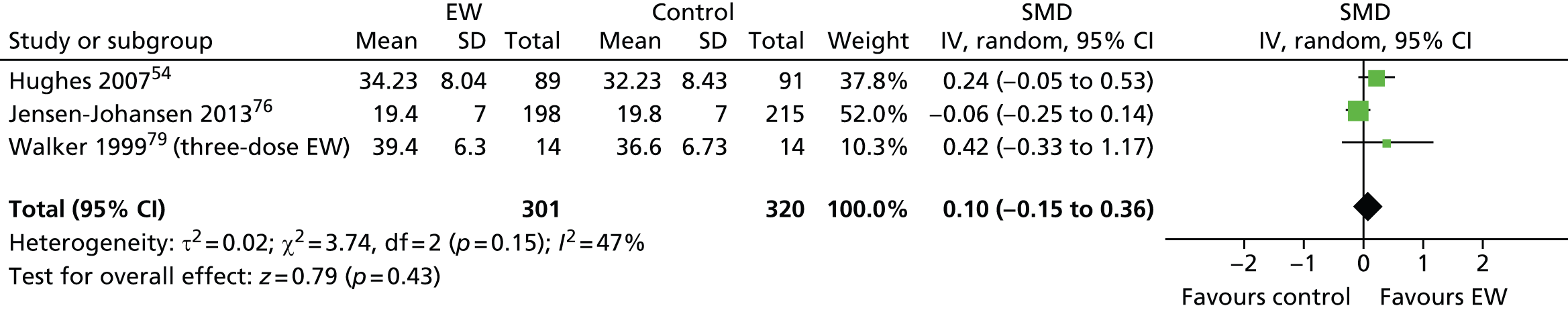
FIGURE 12.
Forest plot of negative mood at short-term follow-up in patients with breast cancer. df, degrees of freedom; IV, inverse variance.
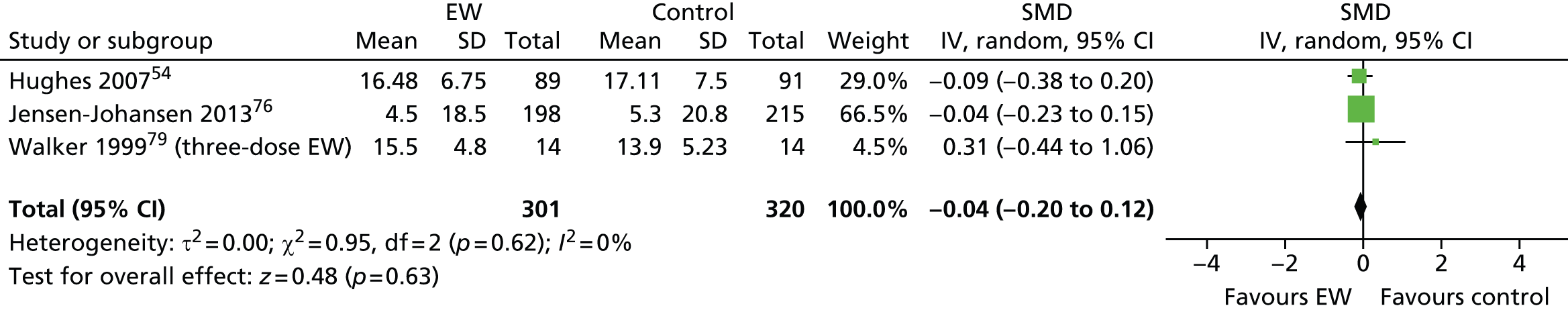
FIGURE 13.
Forest plot of depression at short-term follow-up in patients with breast cancer. df, degrees of freedom; IV, inverse variance.

Three studies54,76,79 assessed positive mood using different instruments (PANAS-PA and PPMS).
-
Clinical differences between studies Jensen-Johansen et al. 76 included newly diagnosed patients with stage I or stage II breast cancer, who had been treated surgically within 3 weeks of their diagnosis (mastectomy or lumpectomy) and/or recently completed radiotherapy or chemotherapy. The patients in the other two studies were attending or completing radiation therapy.
-
Intervention differences Walker et al. 79 had two intervention groups. In one arm unfacilitated EW1 was administered as a single episode whereas in the other unfacilitated EW2 was administered in three episodes. Unfacilitated EW2 (three episodes) was selected as the closest intervention to the standard type of EW intervention and was therefore included in the meta-analysis. This also applies to the meta-analysis of the negative mood outcome comparison.
-
Duration of follow-up length All studies reported short-term outcome measures at 13, 17 and 16 weeks.
-
Forest plot A total of 621 participants were meta-analysed (301 in the EW group and 320 in the control group). The SMD was 0.10 (95% CI –0.15 to 0.36) with a random-effects model and with non-significant but substantial heterogeneity (I2 = 47%). It suggests that there is no statistically significant difference in positive mood at short term for the EW group compared with the control group.
The same three studies54,76,79 assessed negative mood using different instruments (PANAS-NA and Profile of Mood States – negative affect).
-
Forest plot A total of 621 participants were meta-analysed (301 in the EW group and 320 in the control group). The SMD was –0.04 (95% CI –0.20 to 0.12) with a random-effects model and with non-significant heterogeneity (I2 = 0%). This result suggests that there is no significant difference in negative mood at short term for the TW group compared with the control group.
Four studies53,76–78 assessed depression using different instruments (CES-D, BDI-SF and HADS-D).
-
Clinical and intervention group differences described above apply also in this section.
-
Follow-up All studies reported short-term outcome measures at 4, 8 and 13 weeks.
-
Study by Henry et al. 53 The mean value for depression was derived from a graph but data regarding variability could not be collected. Therefore, the individual effect size for this study could not be estimated.
-
Forest plot A total of 562 participants were meta-analysed (270 in the EW group and 292 in the control group). The SMD was –0.08 (95% CI –0.25 to 0.08) with a random-effects model and with non-significant, unimportant heterogeneity (I2 = 0%). This result suggests that there is no significant difference in depression at short term for the TW group compared with the control group.
C57, C61 and C62: gynaecological and genitourinary cancers
There were five studies80–84 included in this section with different ICD-10 codes; however, all were of gynaecological or genitourinary cancers:
Overview
All five studies80–84 evaluated unfacilitated EW. A summary of their main characteristics is presented in Table 14. In all except one of the studies, participants had undergone between 4 and 5 years of treatment. In the Rosenberg et al. 83 study, patients all had adenocarcinoma of the prostate (staging not given) and were being followed up after definitive local treatment (prostatectomy or radiotherapy) within the last 4 years. In Zakowski et al. 84 all patients were diagnosed with prostate or gynaecological cancer (no further details supplied) and had completed treatment within the last 5 years. No further details were available for Arden-Close et al. 80 and Pauley et al. 82 In Milbury et al. 81 participants were patients with newly diagnosed renal cell carcinoma (RCC), with stage I–IV disease and with a Zubrod performance status of < 2 points (i.e. either fully active and unrestricted by their disease, or only restricted in performing physically strenuous activities).
| First author, year | Study design | Intervention group 1 | Intervention group 2 | Control group 1 |
|---|---|---|---|---|
| Arden-Close 201380 | RCT | Unfacilitated EW | – | Time-management writinga |
| Milbury 201481 | RCT | Unfacilitated EW | – | Neutral topics |
| Pauley 201182 | RCT | Unfacilitated EW | Positive writing | Factual writing |
| Rosenberg 200283 | RCT | Unfacilitated EW | – | Non-writing |
| Zakowski 200484 | RCT | Unfacilitated EW | – | Factual writing |
Arden-Close et al. 80 was conducted in the UK, and the remaining studies were in the USA.
Four studies80,81,83,84 assessed one intervention group against one control but Pauley et al. 82 had two different intervention groups. All studies80–84 assessed the impact of the standard expressive writing intervention whereby participants were instructed to write about their experience with cancer and its treatment compared with a time-management or factual writing control group.
Additionally, Pauley et al. 82 also assessed the effect of a positive EW intervention, whereby participants were asked to write about any aspect of their cancer characterised as positive. In Rosenberg et al. 83 and Zakowski et al. ,84 all participants wrote for 20–30 minutes for 3 or 4 consecutive days. In Arden-Close et al. 80 and Pauley et al.,82 participants had to write at 1-week intervals over a 3-week period, and in Milbury et al. 81 participants had to complete the four writing assignments within 10 days. Participants in Pauley et al. 82 were recruited online, received EW instructions and submitted their writing via the internet. In the studies by Pauley et al. 82 and Milbury et al. ,81 participants were financially compensated for their participation in the study. Participants in the other studies82–84 did not receive financial compensation.
The outcomes evaluated in each of the studies on gynaecological/urinary cancer patients are reported in Table 15. Psychological symptoms, coping with cancer and QoL were the most frequently assessed outcomes. In the Milbury et al. study,81 intrusions and avoidance, as well as specific cancer physical symptoms, were evaluated using two different instruments. Sleep disturbance was also evaluated in addition to general HRQoL.
| First author, year | Immune function/disease markers | Pain | Sexual health/performance | Distress | Psychological symptoms | Social constraints | Coping | Mental health | QoL | Resource use |
|---|---|---|---|---|---|---|---|---|---|---|
| Arden-Close 201380 | – | – | – | PSS | IES | – | – | – | FACT-General | – |
| Milbury 201481 | – | – | – | – | IES, PSQI, BFI | – | – | CES-D | MOS-SF-36, MDASI | – |
| Pauley 201182 | – | – | 6-item measure | – | – | – | ARS-20 | GHQ-12 | QLQ-30 | – |
| Rosenberg 200283 | PSA levels, peripheral blood T-cell proliferation, Serum cytokine levels of TNF-α, IL-4 and IL-10 | BPI | – | – | SCL-90-R; Brief POMS, Rumination scale | – | Ways of Coping-Cancer Version | – | MOS-SF-36, FACT-P | NMCUES |
| Zakowski 200484 | – | – | – | BSI, GSI | IES | SCS | – | – | – | – |
Quality assessment
A summary of the quality of the studies in gynaecological and genitourinary cancers is shown in Figures 14 and 15.
FIGURE 14.
Risk-of-bias summary in the gynaecological and genitourinary cancers studies.
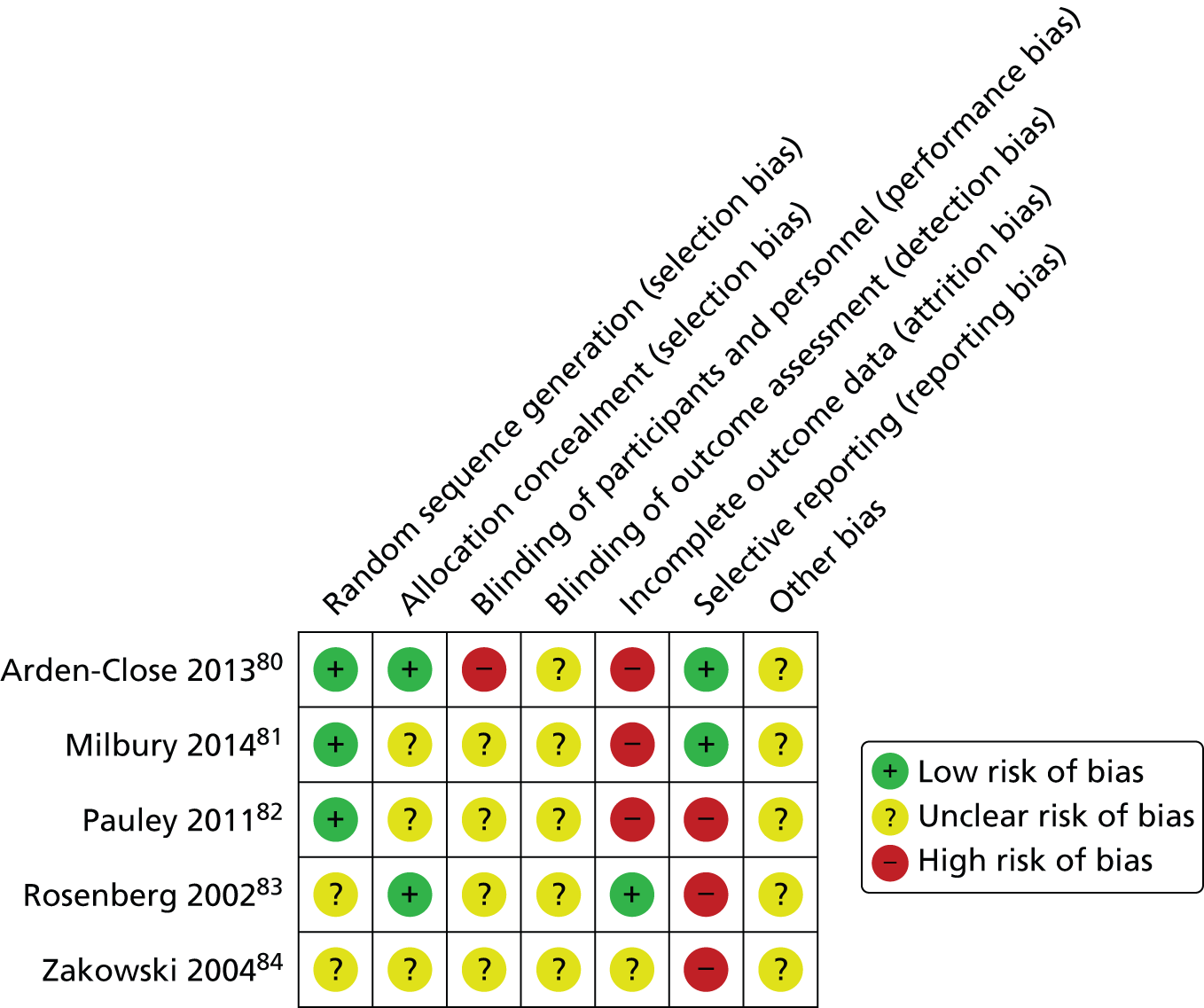
FIGURE 15.
Risk-of-bias graph in the gynaecological and genitourinary cancers studies.

In Arden-Close et al. ,80 Milbury et al. 81 and Pauley et al. ,82 the method of randomisation was adequately reported (Milbury et al. 81 used minimisation). Allocation concealment was not specified in Pauley et al. ,82 Milbury et al. 81 or Zakowski et al. ,84 as opposed to Arden-Close et al. 80 and Rosenberg et al. ,83 for which concealment of sequence generation was adequate. Blinding was not preserved at the performance level in Arden-Close et al. ,80 and was unclear in the rest of the studies. ITT analysis was performed in Arden-Close et al. ,80 Milbury et al. 81 and Zakowski et al. ,84 but not in the remaining studies. Almost all studies,81–84 except that of Arden-Close et al. ,80 were likely to introduce selective reporting as data for the outcomes assessed were under-reported or the information was unclear. In Milbury et al. ,81 there was substantial attrition and non-compliance in both arms at 10-month follow-up (approximately 50% of baseline cohort).
Numerical results
The numerical results reported in the gynaecological and genitourinary cancers studies are summarised in Table 16.
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group 1 | Intervention group 2 | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean scoreb | SD | Change score | SD | n totala | Final mean scoreb | SD | Change score | SD | n totala | Final mean scoreb | SD | Change score | SD | ||||
| Arden-Close 201380 | FACT-General | 13 | 53 | 56.00 | 15.30 | – | – | – | – | – | – | – | 49 | 60.26 | 11.77 | – | – | NS |
| 26 | 53 | 56.30 | 14.96 | – | – | – | – | – | – | – | 49 | 60.26 | 12.58 | – | – | NS | ||
| PSS | 13 | 53 | 18.95 | 7.68 | – | – | – | – | – | – | – | 49 | 15.09 | 6.92 | – | – | NS | |
| 26 | 53 | 18.85 | 7.74 | – | – | – | – | – | – | – | 49 | 16.23 | 7.82 | – | – | NS | ||
| IES-R | 13 | 53 | 10.68 | 8.00 | – | – | – | – | – | – | – | 49 | 9.06 | 6.55 | – | – | NS | |
| 26 | 53 | 11.40 | 7.59 | – | – | – | – | – | – | – | 49 | 9.36 | 6.90 | – | – | NS | ||
| Milbury 201481 | MDASI | 4 | 87 | 1.22 | 1.51 | NR | NR | – | – | – | – | – | 86 | 1.62 | 1.52 | NR | NR | NR |
| 17 | 84 | 1.31 | 1.48 | NR | NR | – | – | – | – | – | 84 | 1.4 | 1.44 | NR | NR | NR | ||
| 43 | 72 | 1.09 | 1.42 | NR | NR | – | – | – | – | – | 76 | 1.64 | 1.64 | NR | NR | SS | ||
| BFI | 4 | 87 | 2.6 | 2.3 | NR | NR | – | – | – | – | – | 86 | 3 | 2.3 | NR | NR | NR | |
| 17 | 84 | 2.7 | 2.2 | NR | NR | – | – | – | – | – | 84 | 2.9 | 2.2 | NR | NR | NR | ||
| 43 | 72 | 2.5 | 2.2 | NR | NR | – | – | – | – | – | 76 | 3.2 | 2.3 | NR | NR | SS | ||
| CES-D | 4 | 87 | 8.8 | 8.6 | NR | NR | – | – | – | – | – | 86 | 10.2 | 6.7 | NR | NR | NR | |
| 17 | 84 | 9.9 | 10.1 | NR | NR | – | – | – | – | – | 84 | 9.5 | 7.1 | NR | NR | NR | ||
| 43 | 72 | 9.5 | 9.6 | NR | NR | – | – | – | – | – | 76 | 10.5 | 7.4 | NR | NR | NS | ||
| PSQI | 4 | 87 | 6.4 | 3.9 | NR | NR | – | – | – | – | – | 86 | 6 | 3.3 | NR | NR | NR | |
| 17 | 84 | 6.4 | 4 | NR | NR | – | – | – | – | – | 84 | 6.4 | 3.6 | NR | NR | NR | ||
| 43 | 72 | 6.3 | 4.4 | NR | NR | – | – | – | – | – | 76 | 6.4 | 3.5 | NR | NR | NS | ||
| SF-36 MCS | 4 | 87 | 44.8 | 47.7 | NR | NR | – | – | – | – | – | 86 | 48.7 | 8.2 | NR | NR | NR | |
| SF-36 MCS | 17 | 84 | 48.9 | 9.3 | NR | NR | – | – | – | – | – | 84 | 48.4 | 7.3 | NR | NR | NR | |
| SF-36 MCS | 43 | 72 | 48.2 | 8.7 | NR | NR | – | – | – | – | – | 76 | 48.8 | 7 | NR | NR | NS | |
| SF-36 PCS | 4 | 87 | 43.2 | 12.04 | NR | NR | – | – | – | – | – | 86 | 42.2 | 11.4 | NR | NR | NR | |
| SF-36 PCS | 17 | 84 | 46.3 | 11.1 | NR | NR | – | – | – | – | – | 84 | 42.8 | 11.8 | NR | NR | NR | |
| SF-36 PCS | 43 | 72 | 46.2 | 11.1 | NR | NR | – | – | – | – | – | 76 | 42.3 | 12.6 | NR | NR | SS | |
| IES | 4 | 87 | 11.3 | 13.7 | NR | NR | – | – | – | – | – | 86 | 15.9 | 14 | NR | NR | NR | |
| IES | 17 | 84 | 12 | 12.9 | NR | NR | – | – | – | – | – | 84 | 13.4 | 14.4 | NR | NR | NR | |
| IES | 43 | 72 | 12.7 | 14.7 | NR | NR | – | – | – | – | – | 76 | 13.8 | 14.3 | NR | NR | NS | |
| Pauley 201182 | Sexual performance | 5 | 28 | NR | NR | NR | NR | 28 | NR | NR | NR | NR | 28 | NR | NR | NR | NR | NR |
| Sexual health | 5 | 28 | 5.68 | 1.48 | NR | NR | 28 | 6.05 | 1.48 | NR | NR | 28 | 5.66 | 1.69 | NR | NR | NSc | |
| GHQ-12 | 5 | 28 | 5.04 | 0.90 | 0 | 2.43 | 28 | 5.40 | 0.79 | 0.34 | 0.47 | 28 | 4.70 | 0.85 | 0.29 | 2.06 | SSc | |
| ARS-20 | 5 | 28 | NR | NR | NR | NR | 28 | NR | NR | NR | NR | 28 | NR | NR | NR | NR | NR | |
| QLQ-30 | 5 | 28 | 2.86 | 1.11 | NR | NR | 28 | 2.38 | 1.01 | NR | NR | 28 | 2.52 | 1.11 | NR | NR | NSc | |
| Rosenberg 200283 | BPI | 13 | 16 | 2.13 | 3.2 | – | – | – | – | – | – | – | 14 | 5.50 | 7.75 | – | – | SS |
| 26 | 16 | 3.19 | 3.95 | – | – | – | – | – | – | – | 14 | 9.43 | 8.08 | – | – | SS | ||
| PSA spec – CD4+ | 13 | 16 | 1.60 | 0.89 | – | – | – | – | – | – | – | 14 | 2.90 | 3.80 | – | – | NS | |
| 26 | 16 | 1.80 | 1.50 | – | – | – | – | – | – | – | 14 | 1.80 | 1.00 | – | – | NS | ||
| PSA spec – CD8+ | 13 | 16 | 0.50 | 0.20 | – | – | – | – | – | – | – | 14 | 1.10 | 1.40 | – | – | NS | |
| 26 | 16 | 0.40 | 0.50 | – | – | – | – | – | – | – | 14 | 0.60 | 0.60 | – | – | NS | ||
| n of pain medication/month | 13 | 16 | 9.44 | 3.82 | – | – | – | – | – | – | – | 14 | 13.64 | 8.84 | – | – | NS | |
| 26 | 16 | 4.94 | 2.66 | – | – | – | – | – | – | – | 14 | 6.05 | 4.70 | – | – | NS | ||
| n of visits clinician | 13 | 16 | 6.70 | 6.00 | – | – | – | – | – | – | – | 14 | 7.60 | 7.46 | – | – | NS | |
| 26 | 16 | 4.40 | 3.12 | – | – | – | – | – | – | – | 14 | 7.60 | 8.33 | – | – | NS | ||
| Zakowski 200484 | BSI/GSI | 26 | 62 | 0.35 | 0.40 | – | – | – | – | – | – | – | 42 | 0.34 | 0.40 | – | – | NS |
| IES-Av | 26 | 62 | 7.23 | 8.27 | – | – | – | – | – | – | – | 42 | 6.55 | 8.57 | – | – | NS | |
| IES-I | 26 | 62 | 6.53 | 7.30 | – | – | – | – | – | – | – | 42 | 4.98 | 6.33 | – | – | NS | |
| SCS | 34 | 62 | 20.51 | 4.66 | – | – | – | – | – | – | – | 42 | 19.71 | 6.41 | – | – | NS | |
Follow-up assessments ranged from 5 weeks in Pauley et al. ,82 to 34 weeks in Zakowski et al. 84 Total sample sizes ranged from 30 participants in Rosenberg et al. 83 up to 277 participants in Milbury et al. 81 In Milbury et al. 81 the total sample size varied throughout the study. There were 173 participants evaluated at 4 weeks, 168 participants evaluated at 17 weeks and 148 participants evaluated at 43 weeks.
Pauley et al. 82 and Rosenberg et al. 83 did show statistically significant differences between the two groups for the General Health Questionnaire (GHQ-12) and Brief Pain Inventory (BPI) outcomes, respectively. In Pauley et al. ,82 participants in the positive expression writing group scored higher in mental health than participants in the negative expression writing group or than those in the control group. However, no significant effects were reported regarding the QoL and sexual performance outcomes. In Milbury et al. ,81 there were significant group differences for the expressive writing group compared with the neutral writing group at the 10 months’ follow-up assessment for the following outcomes measures: the MD Anderson Symptom Inventory (MDASI), the Brief Fatigue Inventory (BFI) and the Short Form questionnaire-36 items physical composite score (SF-36 PCS).
Regarding the other outcomes assessed across the remaining studies, either no significant group-by-time interaction was reported or differences between groups were not addressed as in Pauley et al. 82 or Rosenberg et al. 83
Quality of life was assessed in four studies,80–82,84 in which instruments were sufficiently similar to pool in a meta-analysis. However, in Rosenberg et al. ,83 numerical data regarding the Functional Assessment of Cancer Therapy (FACT) or the Medical Outcomes Short-Form Health Survey (MOS-SF-36) were not reported, and the results for the other studies80–82,84 were at two different follow-up time periods and so no meta-analysis was performed for this outcome.
C80 and C96: other non-specified cancers
Overview
Three studies66,85,86 evaluated EW in participants with various types of cancer. The study by Rickett et al. 66 is reported in the Facilitated TW section. Here, the studies by Cepeda et al. 85 and Rini et al. 86 are described. A summary of main characteristics is presented in Table 17.
| First author, year | Study design | Intervention group | Control group |
|---|---|---|---|
| Cepeda 200885 | RCT | Unfacilitated EW | SMC |
| Rini 201486 | RCT | Unfacilitated EW | Non-EW |
Cepeda et al. 85 included participants with any type of cancer reporting average pain intensity levels of at least 5 on a 0–10 scale. Participants scored > 50% in the Karnofsky performance scale (ranging from having no evidence of their disease to requiring occasional assistance but able to care for most of their personal needs). The study was conducted in Colombia and published in English. The authors evaluated one intervention group against two control groups. However, only the group receiving standard medical care (SMC) was considered in the analysis, as the other group was an active control involving an educational intervention. The unfacilitated EW group (narrative group) had to write about a disease-focused topic during 20 minutes over 3 non-consecutive days (at 1-week intervals). Participants were not financially compensated.
Rini et al. 86 included participants who had had a stem cell transplant for any form of haematological cancer within the previous 9 months to 3 years and not in current relapse. The study was conducted in the USA. Participants were randomised to three intervention groups or one neutral writing control (factual writing about their experience). The three intervention groups were standard unfacilitated EW, peer helping and unfacilitated EW with peer helping. As the peer-helping component is not part of this systematic review, it is not discussed further. The unfacilitated EW group had to write about their deepest emotions and thoughts about the time before, during and after the transplant. Writing took place at the participants’ homes: one 20-minute episode of writing per week for 4 weeks. A researcher telephoned the participant before and after each writing episode. Participants were financially compensated.
The outcomes evaluated in the studies are reported in Table 18. For almost all of the outcomes in the Rini et al. study,86 the results were split into subgroups of high and low survivorship problems rather than whole scores for the groups.
| First author, year | Pain intensity | Well-being/QoL | Physical symptoms | Resource use |
|---|---|---|---|---|
| Cepeda 200885 | Verbal numerical rating scale | 7-point Likert scale | – | – |
| Rini 201486 | – | FACT, BSI/GSI | Deaths, Inventory of physical symptoms | – |
Quality assessment
A summary of the study quality is shown in Figure 16.
FIGURE 16.
Risk-of-bias summary in the cancer studies.
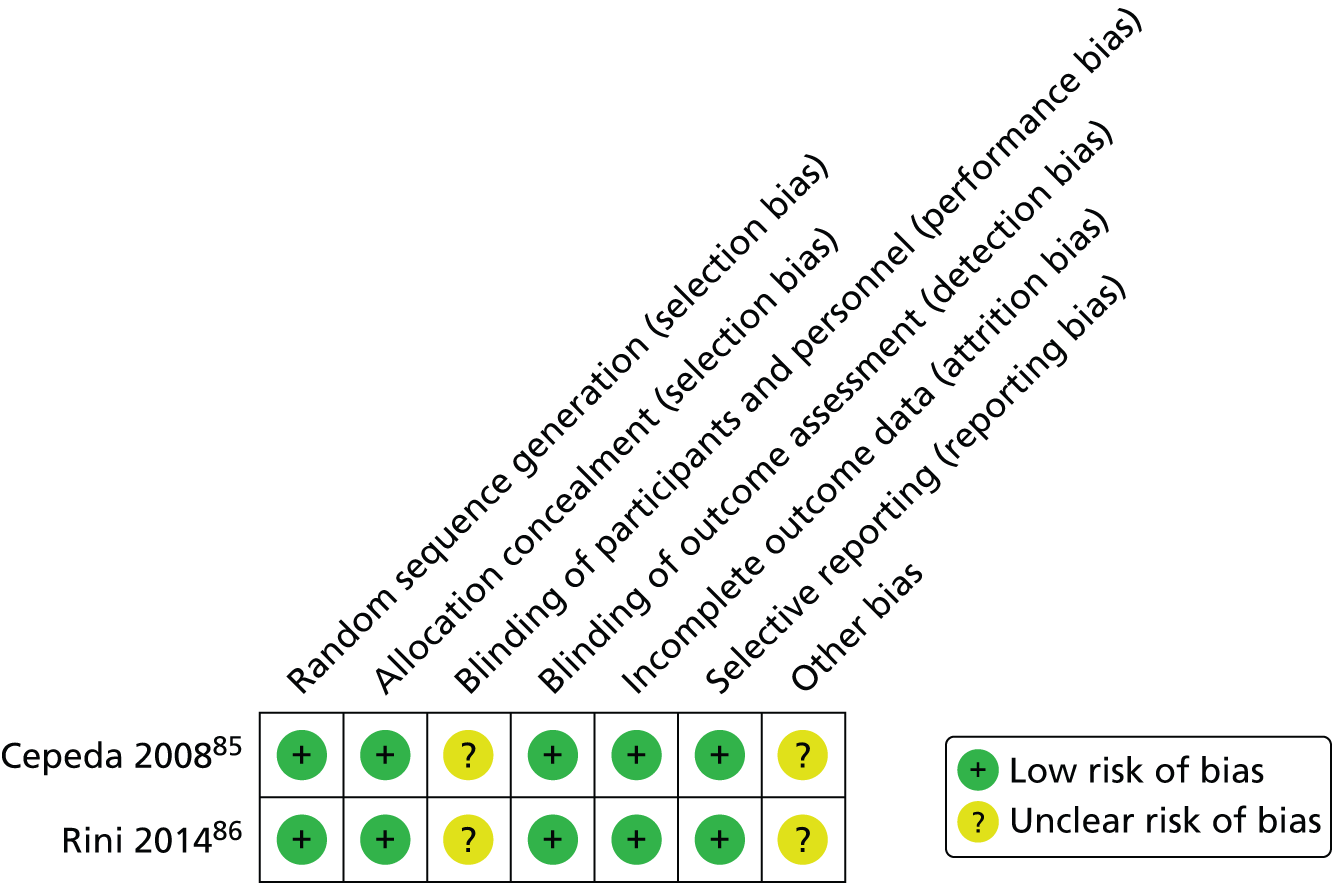
Both studies85,86 had the method of randomisation described. In Cepeda et al. ,85 allocation concealment was performed using opaque envelopes, and in Rini et al. 86 it was by sequentially numbered computer files. The personnel (evaluators) were blinded in both studies though participants were not. However, it was likely that selective reporting was introduced for the QoL outcome in Cepeda et al. 85 Therefore, the quality item referring to selection bias was rated as low risk in this study. ITT analysis was used in both studies. 85,86
Numerical results
The numerical results are reported in Table 19.
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean score | SD | Change score | SD | n totala | Final mean score | SD | Change score | SD | ||||
| Cepeda 200885 | Pain meter | 2 | 79 | 5.40 | NR | NR | NR | 78 | 5.50 | NR | NR | NR | NS |
| 4 | 79 | 5.00 | NR | NR | NR | 78 | 5.00 | NR | NR | NR | NS | ||
| 6 | 79 | 4.50 | NR | NR | NR | 78 | 4.50 | NR | NR | NR | NS | ||
| 8 | 79 | 4.60 | NR | NR | NR | 78 | 4.20 | NR | NR | NR | NS | ||
| Well-being | 4 | 79 | NR | NR | NR | NR | 78 | NR | NR | NR | NR | NR | |
| 8 | 79 | NR | NR | NR | NR | 78 | NR | NR | NR | NR | NR | ||
| Rini 201486 | Relapse | 13 | 75 | n = 1 | – | – | – | 76 | n = 2 | – | – | – | NR |
| Deaths | 13 | 75 | n = 1 | – | – | – | 76 | n = 2 | – | – | – | NR | |
In Cepeda et al. ,85 follow-up assessments were performed at 2, 4, 6 and 8 weeks post writing, whereas in Rini et al. 86 they were at carried out at 13 weeks only. The total sample size in Cepeda et al. 85 was 157 participants, and in Rini et al. 86 it was 151 participants in the unfacilitated EW and control groups.
In Cepeda et al. ,85 no significant differences in pain intensity or QoL were reported between the groups throughout the study. The authors used a single question with a Likert scale to measure HRQoL, as they reported it was minimally burdensome, but no numerical data were reported for this outcome. However, authors reported that those disclosing a high degree of emotion had better well-being and pain intensity level outcomes.
In Rini et al. ,86 there was one relapse and one death in the unfacilitated EW group, and two relapses and two deaths in the control group.
D57: sickle cell disease
Overview
There was one non-randomised study evaluating unfacilitated EW in participants with sickle cell disease. The participants in McElligott87 were adolescents, with an average age of 14.9 years (SD 2.3 years). The study87 was conducted in the USA. The authors evaluated an EW intervention for which participants had to write about their deepest thoughts and feelings related to their illness. The control group had to write about details of the previous day (factual writing). The written exercise ran over 3 weeks, with one session per week. Participants were financially compensated. The outcomes evaluated in McElligott87 are reported in Table 20.
| First author, year | Physical symptoms | Self-esteem | Depression | Behavioural problems | Anxiety | QoL | Resource use |
|---|---|---|---|---|---|---|---|
| McElligott 200687 | PSC, PSC-Y | ADSEI | CDI | ADSEI | RCMAS | Well-being | Number of patients hospitalised, number of visits to clinician |
Quality assessment
A summary of the quality of the study by McElligott87 is shown in Figure 17. The study87 was very likely to introduce various biases. All risk-of-bias items were unclear except for lack of blinding among outcome assessors and no evidence of selective reporting.
FIGURE 17.
Risk-of-bias summary in the sickle cell disease study.

Numerical results
The numerical results are reported in Table 21. The follow-up assessment in McElligott87 was performed at 2 weeks post writing. The total sample size was 36 participants.
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||
|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean score | SD | n totala | Final mean score | SD | ||||
| McElligott 200687 | ADSEI | 2 | 19 | 74 | 36.8 | 17 | 100 | 0 | NS |
| SEI | 2 | 19 | 84.6 | 9.4 | 17 | 64.4 | 19.8 | NS | |
| RCMAS | 2 | 19 | 8 | 5.9 | 17 | 9.5 | 5.7 | NS | |
| CDI | 2 | 19 | 5.9 | 5.6 | 17 | 7.2 | 6.1 | NS | |
| PSC-Y | 2 | 19 | 14.5 | 9.1 | 17 | 20 | 9.7 | NS | |
| PSC | 2 | 19 | 12.8 | 12.6 | 17 | 16.8 | 6.8 | NS | |
| Well-being | 2 | 19 | NR | NR | 17 | NR | NR | NS | |
| Number of visits to clinician | 2 | 19 | 0 | 0 | 17 | 0.38 | 0.65 | NS | |
| Number of days hospitalised | 2 | 19 | 0.17 | 0.71 | 17 | 0.12 | 1.1 | NS | |
Authors reported there were no significant differences between groups for any of the outcomes evaluated.
E11: diabetes mellitus
Overview
There was one RCT88 evaluating unfacilitated EW in participants who had been diagnosed with type 2 diabetes mellitus. The main characteristics are summarised in Table 22. Participants were adults attending a general practitioner (GP) practice in the UK. Unfacilitated EW for 20 minutes on 3 days was compared with the same amount of writing about the previous day’s activities (factual writing). Both groups wrote at home in private and then returned their writing to the researcher. They were not financially compensated.
| First author, year | Physical symptoms | Depression | Behavioural problems | QoL | Resource use |
|---|---|---|---|---|---|
| Dennick 201488 | PAID | CES-D | SDSCA | EQ-5D | – |
The outcomes evaluated in Dennick et al. 88 are reported in Table 22.
Quality assessment
A summary of the study88 quality is shown in Figure 18. Randomisation was using random numbers in sealed envelopes, stratified by recruitment approach and with random block sizes of four, six and eight per block. GPs were blinded to the group allocation. ITT was used. It was noticeable that of 1715 individuals who were given information about the study, only 41 consented to join the study88 and 32 completed the follow-up.
FIGURE 18.
Risk-of-bias summary for the diabetes mellitus study.

Numerical results
The numerical results are reported in Table 23. Follow-up assessment was performed at 3 months. The total sample size where all completed all writing and the follow-up was 27 participants. The study found that EW resulted in worse depression at follow-up for the intervention group. There were no significant differences in the other outcomes measured.
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||
|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean score | SD | n totala | Final mean score | SD | ||||
| Dennick 201488 | CES-D | 13 | 23 | 9.9 | 5.3 | 18 | 5.1 | 5.1 | 0.006 |
| EQ-5D utility | 13 | 23 | 0.92 | 0.1 | 18 | 0.87 | 0.1 | 0.907 | |
| EQ-5D VAS | 13 | 23 | 77.4 | 13.4 | 18 | 82.1 | 12.7 | 0.268 | |
| PAID | 13 | 23 | 35.3 | 6.7 | 18 | 34.4 | 6.8 | 0.658 | |
| SDSCA (general diet) | 13 | 23 | 5.8 | 1.2 | 18 | 5.8 | 1.1 | 0.826 | |
| SDSCA (specific diet) | 13 | 23 | 4.5 | 0.9 | 18 | 5.1 | 0.9 | 0.057 | |
| SDSCA (exercise) | 13 | 23 | 3.5 | 1.3 | 18 | 4.0 | 1.3 | 0.245 | |
| SDSCA blood glucose testing) | 13 | 23 | 2.5 | 1.9 | 18 | 2.5 | 2.0 | 0.922 | |
| SDSCA (foot care) | 13 | 23 | 3.2 | 1.2 | 18 | 3.0 | 1.1 | 0.755 | |
E84: cystic fibrosis
Overview
There was one RCT89 evaluating unfacilitated EW in participants that had been medically diagnosed with cystic fibrosis. Participants in Taylor et al. 89 were adolescents of at least 15 years of age. The study89 was conducted in the USA. A written self-disclosure intervention compared with usual care was assessed. Participants had to write about their deepest thoughts and feelings about the most distressing experience of their entire life and were encouraged to connect the topic to their relationships with others. They had to write for 20 minutes, three times over a 5-day period. The control was SMC. Participants were not financially compensated. The outcomes evaluated in Taylor et al. 89 are reported in Table 24.
| First author, year | Physical health status | Psychological health status | Patient’s satisfaction | QoL | Resource use |
|---|---|---|---|---|---|
| Taylor 200389 | FEV1, BMI | PHQ, Somatization Scale, SLESQ | VSQa | SF-12 | Outpatient use, inpatient use |
Quality assessment
A summary of the study quality is shown in Figure 19.
FIGURE 19.
Risk-of-bias summary in the cystic fibrosis study.
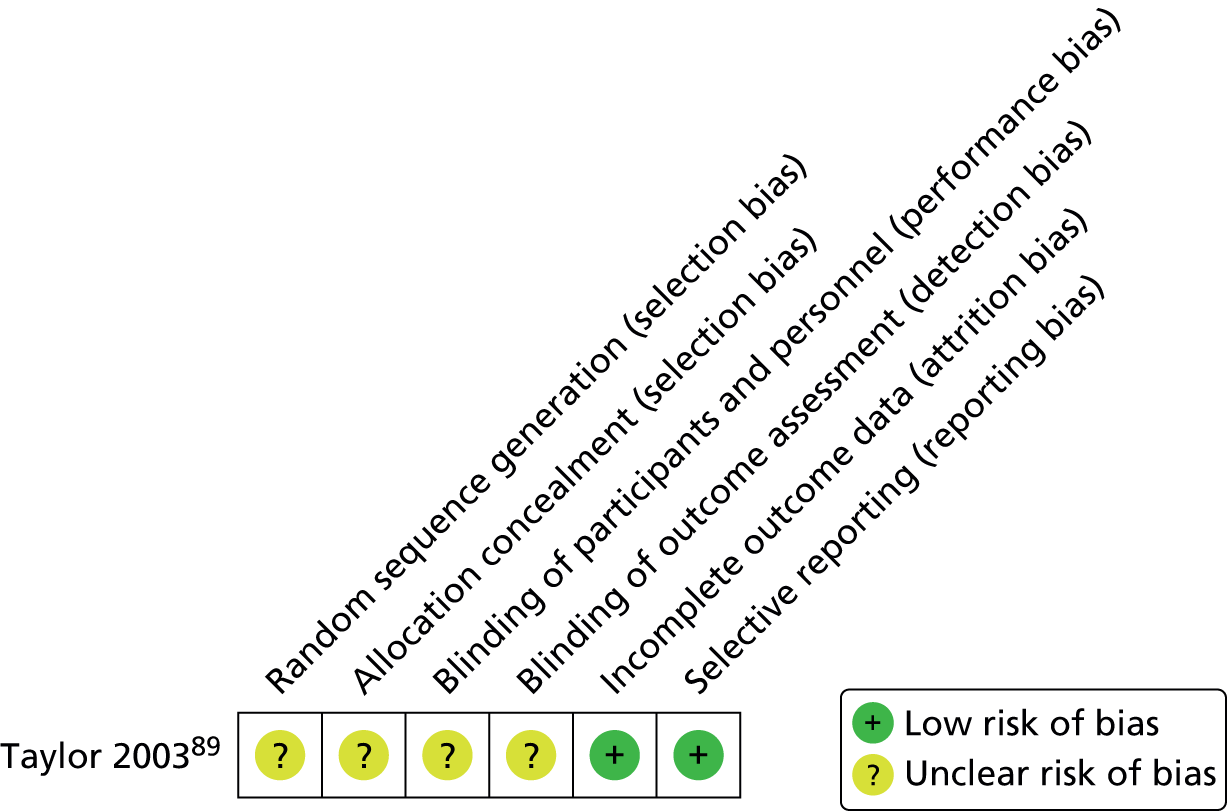
Taylor et al. 89 was reported as randomised. However, selection, performance and detection biases were possible as the information related to the method of randomisation, allocation concealment of the sequence generation or any statement regarding masking were unclear. The quality item selective reporting was rated as low risk [although data for the Visit Specific Satisfaction Questionnaire (VSQ) were not reported this was intended as a measure of the acceptability of the intervention]. ITT analysis was used.
Numerical results
The numerical results are reported in Table 25. Follow-up assessment was performed at 13 weeks post writing. The total sample size was 39 participants. The authors reported that participants in the written self-disclosure group had a significantly reduced number of inpatient days over a 3-month period after the intervention compared with before the intervention, which was not the case in the control group. However, the overall number of participants was small and the intervention group had a higher mean number of inpatient days than the control group at baseline. The physical or psychological health status remained unchanged over the study period and no changes were reported regarding QoL.
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||
|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean scoreb | SD | n totala | Final mean score | SD | ||||
| Taylor 200389 | FEV1 | 13 | 18 | 48.50 | 21.2 | 21 | 50.40 | 20.1 | NS |
| BMI | 13 | 18 | 19.30 | 3 | 21 | 19.00 | 2.1 | NS | |
| Somatisation scale | 13 | 18 | 3.90 | 3.4 | 21 | 7.00 | 3.8 | NS | |
| SLESQ | 13 | 18 | 14.80 | 6.9 | 21 | 14.30 | 3.1 | NS | |
| SF-12 MCS | 13 | 18 | 53.70 | 7.5 | 21 | 49.50 | 9.1 | NS | |
| SF-12 PCS | 13 | 18 | 43.80 | 10.3 | 21 | 43.30 | 10 | NS | |
| VSQ-modified | 13 | 18 | All good to very good, but one fair | NR | 21 | NR | NR | NR | |
| PHQ – depression | 13 | 18 | 12.40 | 4.1 | 21 | 13.90 | 4.2 | NS | |
| PHQ – anxiety | 13 | 18 | 15.30 | 1.4 | 21 | 16.10 | 3.1 | NS | |
| Outpatients use | 13 | 18 | 1.20 | 1 | 21 | 2.00 | 2.4 | NS | |
| Inpatients use | 13 | 18 | 5.60 | 7 | 21 | 8.40 | 9.6 | SS | |
F03: dementia
In the systematic review, one study67 evaluated participants diagnosed with dementia. However, it assessed a facilitated type of TW intervention and the study67 has been summarised in the facilitated TW section.
F14 and F19: substance use disorder
Overview
There were three studies90–92 (Meshberg-Cohen91 was a doctoral thesis) evaluating unfacilitated EW on patients with drug dependence (cocaine dependence, ICD-10 code – F14) or substance use disorder (SUD). A summary of their main characteristics is presented in Table 26.
| First author, year | Study design | Intervention group | Control group |
|---|---|---|---|
| Grasing 201090 | RCT | Unfacilitated EW | Time-management writing |
| Meshberg-Cohen 201091 | RCT | Unfacilitated EW | Factual writing |
| Van Dam 201392 | RCT | Unfacilitated EW | Treatment as usual |
Two studies90,91 were conducted in the USA and one study92 in the Netherlands. All three studies90–92 recruited individuals from residential drug treatment programmes. In a small, non-randomised, feasibility study by Grasing et al. ,90 participants (all military veterans and only one female) met DSM-IV (Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition) criteria for cocaine dependence at the time of admission or fulfilled criteria for a SUD following the structured clinical interview for DSM-IV-TR (Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition, Text Revision): Alcohol and Substance Use Disorders Module [Structured Clinical Interview for DSM Disorders (SCID)]. Meshberg-Cohen91 recruited women who fulfilled the DSM-IV criteria for a SUD with the SCID; 80% had cocaine as their primary drug of dependence and 57% were dependent on more than one drug. Van Dam et al. 92 recruited men and women who were addicted to a variety of substances including alcohol, cocaine and cannabis.
All three studies90–92 assessed an EW intervention for which participants had to write about a self-selected trauma. In Grasing et al. ,90 participants had to complete the exercise on 17 non-consecutive days, a longer period than in Meshberg-Cohen,91 when participants completed the task in 4 consecutive days. In Van Dam et al. 92 they wrote for 10 sessions, for unspecified amount of time that was < 45 minutes. The control group tasks emphasised objective, neutral and factual topics with no emotional component in Grasing et al. 90 and Meshberg-Cohen. 91 For Van Dam et al. ,92 the control was treatment as usual. Participants were financially compensated in Grasing90 and Meshberg-Cohen,92 but not in Van Dam et al. 93
The outcomes assessed in the studies on SUD are reported in Table 27. Drug craving, distress and general mood were the outcomes most frequently assessed in the studies. 90–92
| First author, year | Objective markers | Drug craving | Symptom severity | Distress | Mood | Depression | Resource use |
|---|---|---|---|---|---|---|---|
| Grasing 201090 | BP, heart rate | BSCS | – | PSS, BSI | POMS | – | Self-report use of cocaine |
| Meshberg-Cohen 201091 | – | BSCS | PDS, PILL | BSI/GSI | PANAS-X | CES-D | – |
| Van Dam 201392 | – | TLFB abstinence | PDS | – | – | – | – |
Quality assessment
A summary of the quality of the studies on SUD is shown in Figures 20 and 21. The study by Meshberg-Cohen91 was truly randomised; however, there was no information related to the concealment of the sequence generation or the masking. Therefore, this study91 was likely to introduce selection and performance biases. In addition, data were not reported or were under-reported, introducing high risk of reporting bias. The study by Grasing et al. 90 was evaluated in the same way for all of the quality items, except that the method of randomisation was not provided. In the Van Dam et al. study,92 the method of randomisation was by assignments in closed envelopes. These were opened at the start so that there was no allocation concealment. Blinding was not mentioned. The studies by Meshberg-Cohen91 and Van Dam et al. 92 used an ITT analysis, whereas in the Grasing et al. study90 this information was unclear.
FIGURE 20.
Risk-of-bias summary in the SUD studies.
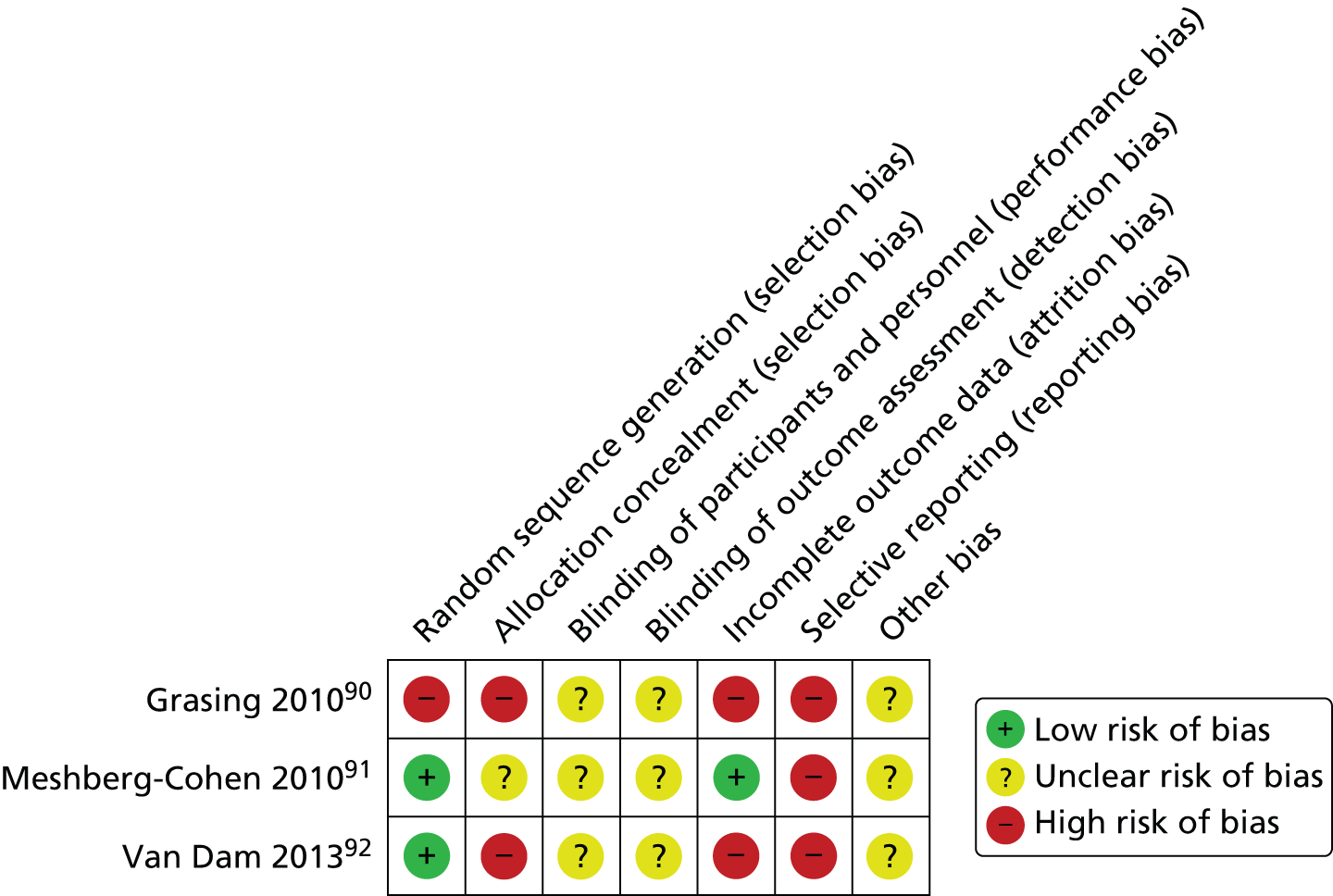
FIGURE 21.
Risk-of-bias graph in the SUD studies.

Numerical results
The numerical results reported in the studies on SUD are shown in Table 28. The follow-up assessment ranged from 4 weeks in Meshberg-Cohen91 to 13 weeks in Grasing et al. 90 The total sample size was 42 participants in Grasing et al. 90 and 141 participants in Meshberg-Cohen. 91 In Grasing et al. ,90 expressive writing participants reported a higher final average number of visits to the clinician than in the control group; however, it was not reported whether or not this difference was significant. Authors mentioned cocaine use differences based on self-reports but there were a very small number of participants assessed and a considerable attrition. There were no usable data reported for the remaining outcomes assessed in this study (results are shown in graphs only and the numbers of participants providing results are unclear).
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||
|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean scoreb | SD | n totala | Final mean scoreb | SD | ||||
| Grasing 201090 | Numebr of visits, clinician | 12 | 23 | 10.27 | 5.49 | 19 | 9.68 | 2.55 | NR |
| BP | 2, 4, 8 and 12 | NR | NR | NR | NR | NR | NR | NR | |
| Heart rate | 2, 4, 8 and 12 | NR | NR | NR | NR | NR | NR | NR | |
| BSI-18 | 2, 4, 8 and 12 | NR | NR | NR | NR | NR | NR | NR | |
| POMS | 2, 4, 8 and 12 | NR | NR | NR | NR | NR | NR | NR | |
| Craving – frequency | 2, 4, 8 and 12 | NR | NR | NR | NR | NR | NR | NR | |
| Craving – intensity | 2, 4, 8 and 12 | NR | NR | NR | NR | NR | NR | NR | |
| Self-report use of cocaine | 2 | 10 | Number of patients: 0 | – | 12 | Number of patients: 3 | – | SS | |
| 4 | 9 | Number of patients: 0 | – | 10 | Number of patients: 1 | – | NS | ||
| 8 | 9 | Number of patients: 0 | – | 9 | Number of patients: 1 | – | NS | ||
| 12 | 9 | Number of patients: 0 | – | 7 | Number of patients: 1 | – | NS | ||
| Meshberg-Cohen 201091 | PILL | 2 | 77 | 110.90 | 35.70 | 64 | 109.70 | 27.20 | NS |
| 4 | 77 | 103.70 | 39.10 | 64 | 108.20 | 35.70 | NS | ||
| PDS | 2 | 77 | 17.50 | 12.40 | 64 | 18.90 | 11.80 | SS | |
| 4 | 77 | 16.50 | 12.90 | 64 | 13.90 | 12.00 | NS | ||
| CES-D | 2 | 77 | 21.20 | 10.10 | 64 | 20.30 | 12.10 | NS | |
| 4 | 77 | 18.30 | 11.60 | 64 | 15.40 | 10.20 | NS | ||
| BSI/GSI | 2 | 77 | 1.00 | 0.70 | 64 | 1.00 | 0.80 | NR | |
| 4 | 77 | 0.90 | 0.60 | 64 | 0.70 | 0.80 | NR | ||
| BSI – anxiety | 2 | 77 | 0.90 | 0.90 | 64 | 0.90 | 0.80 | SS | |
| 4 | 77 | 0.90 | 1.00 | 64 | 0.60 | 0.60 | NS | ||
| PANAS-X | 2 | 74 | 15.20 | 5.10 | 58 | 13.80 | 4.80 | NR | |
| 4 | 70 | 15.30 | 7.00 | 58 | 13.10 | 4.60 | NR | ||
| Van Dam 201392 | PDS | 13 | 19 | 23.5 | 14.8 | 15 | 21.7 | 9.4 | NR |
| TLFB | 13 | 19 | 61.0 | 30.8 | 15 | 58.6 | 38.4 | NR | |
In Meshberg-Cohen,91 the EW group showed significantly greater reductions than control subjects only in post-traumatic symptom severity and anxiety scores at 2 weeks’ follow-up, but not at 1 month, when there was no difference in any measure between the two groups. No adjustments for multiple testing were made. At 1 month, there were significant improvements for both groups over the course of residential treatment, suggesting that there was little scope to detect any additional benefit from the intervention. In addition, the EW participants showed increased negative affect immediately after each writing session, but there were no differences in pre-writing negative affect scores between groups the following day.
Van Dam et al. 92 was a very small study, with a large number of rather unclear and complicated statistical tests reported. It is likely that no significant differences were seen at follow-up for the two outcome measures.
F40, F59 and F99: psychiatric disorders
Overview
There were five studies93–97 evaluating unfacilitated EW with patients with mental and/or psychiatric disorders. A summary of main characteristics is presented in Table 29. (Golkaramnay et al. 68 also assessed TW in patients with mental disorders but used facilitated EW so is reported in the Facilitated TW section.)
| First author, year | Study design | Intervention group 1 | Intervention group 2 | Control group 1 | Control group 2 |
|---|---|---|---|---|---|
| Bernard 200693 | RCT | Unfacilitated EW | – | Factual and time-management writing | – |
| Canna 200694 | RCT | Unfacilitated EW | – | Time-management writing | – |
| Graf 200895 | RCT | Unfacilitated EW | – | Time-management writing | SMC |
| Krpan 201396 | RCT | Unfacilitated EW | – | Time-management writing | – |
| Richards 200097 | RCT | Unfacilitated EW plus CBTa | CBTb | Factual writing plus CBTc | Waiting list |
All studies93–97 were described as RCTs. Study participants were very heterogeneous. The patients in Bernard et al. 93 had a first episode of psychosis conforming to broad ICD-10 categories (F20, F22, F23, F25) but, for ethical reasons, patients were not suicidal or acutely psychotic; rather they were in the recovery phase of their illness. The participants in Graf et al. 95 were recruited from a university-based outpatient psychiatric clinic and student counselling centre, and all participants were also undergoing psychotherapy. In Richards et al. 97 and Canna94 (a doctoral thesis), participants had an axis I anxiety or mood disorder primary diagnosis or were diagnosed with at least one mental disorder as classified by the [Diagnostic and Statistical Manual of Mental Disorders-Third Edition, Revised (DSM-III-R)]. In Krpan et al. ,96 all participants had major depressive disorder. In Richards et al. ,97 all participants were male psychiatric maximum security prison inmates (47% sex offenders).
Bernard et al. 93 had two groups: one standard EW intervention and one non-EW control in which participants had to write about facts of the day, describe the room they were in and their plans for the next week. Canna94 examined four groups: CBT with TW, CBT alone, CBT with inexpressive writing (activities of the day) and a waiting list control group. The CBT with TW compared with CBT with inexpressive writing was used in this systematic review, as both arms had CBT: its effect in each would be cancelled out when the two groups were compared. In Richards et al. ,97 one intervention group and two control groups were evaluated: trivial writing and no writing. For the systematic review, EW was compared with trivial writing. The remaining study95 assessed one intervention group compared with one control group. Intervention topics were disease-focused EW or participants were asked to write about their worst trauma. Participants in Krpan et al. 96 and Richards et al. 97 were financially compensated, whereas participants in the remaining studies were not. In Graf et al. ,95 the EW intervention lasted 14 non-consecutive days, whereas in the other four studies93,94,96,97 the intervention was delivered on 3 consecutive days. Follow-up assessments ranged from just after the writing exercise in Graf et al. ,95 up to 24 weeks after in Canna. 94
The results of the outcomes evaluated across the studies are given in Table 30.
| First author, year | Physical symptoms | PTSD symptoms | Positive affect | Negative affect | Depression | Anxiety | Distress | Panic | QoL | Social support | Recovery | Resource use |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bernard 200693 | – | IES | PANAS-PA | PANAS-NA | HADS-D | HADS-A | – | – | – | – | RSQ | – |
| Canna 200694 | PILL | – | PANAS-PA | PANAS-NA | BDI-II | BAI, STAI | BSI, GSI | PSWQ | QoL, life satisfaction | MSPSS | – | Number of treatment sessions |
| Graf 200895 | OQ-45.2 | – | – | – | DASS-D | DASS-A | DASS-S | – | – | – | – | – |
| Krpan 201396 | – | – | – | – | BDI, PHQ-9 | – | – | – | – | – | – | – |
| Richards 200097 | PILL | – | Self-report Q Sympt-p | – | – | CSAQ | – | – | – | – | – | – |
Quality assessment
A summary of the quality of the psychiatric disorders studies93–97 is shown in Figures 22 and 23. All studies93–97 were reported as randomised but Canna,94 Krpan et al. 96 and Richards et al. 97 did not provide information regarding the method of randomisation used. All studies93–97 were very likely to introduce performance and detection biases. All studies except Graf et al. 95 adequately addressed items related to the selection of participants. Krpan et al. 96 and Richards et al. 97 were the most likely to introduce biases that could affect outcomes, as randomisation and information related to masking, as well as assessment of outcomes, was under-reported. Participation rates were reported in Bernard et al. 93 and Graf et al. 95 but unclear information regarding withdrawals was provided in the other three studies. 94,96,97 Only Graf et al. 95 clearly used an ITT analysis.
FIGURE 22.
Risk-of-bias summary in the mental and psychiatric disorders studies.

FIGURE 23.
Risk-of-bias graph in the mental and psychiatric disorders studies.
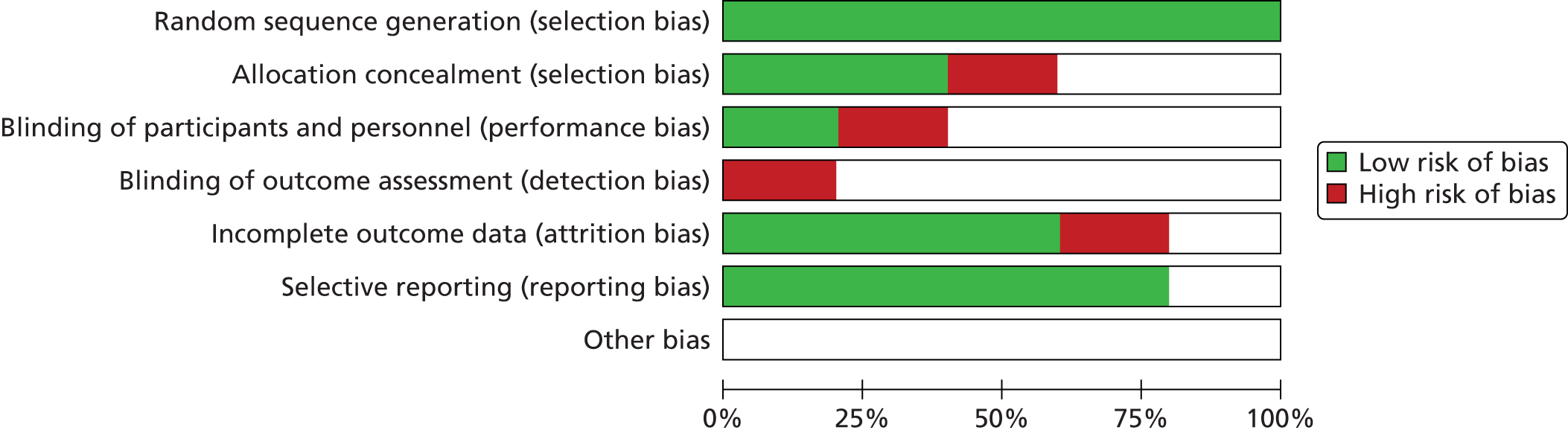
Numerical results
The numerical results reported in the studies evaluating mental disorders are summarised in Table 31. Total sample sizes ranged from 22 participants in Bernard et al. 93 to 65 participants in Richards et al. 97 Bernard et al. 93 reported significant differences between group-by-time interaction in the total IES score in favour of the intervention group (a reduction in PTSD – symptoms associated with the diagnosis of psychosis); no other differences between groups were seen. Canna94 and Graf et al. 95 reported significant improvements post treatment in a variety of measures of psychological distress in favour of the experimental condition. In the Canna study94 (a doctoral thesis), improvement was reported in a variety of measured of psychological distress, such as the Beck Anxiety Inventory (BAI); the revised Beck Depression Inventory (BDI-II), Brief Symptom Inventory (BSI)/Global Severity Index (GSI) and the Penn State Worry Questionnaire (PSWQ) at the final follow-up assessment (24 weeks), but the author stated that these improvements could not be attributed specifically to the writing intervention. Graf et al. 95 reported significant reductions in anxiety, depression and stress symptoms, as well as greater overall progress in psychotherapy, in the experimental group compared with the writing control group immediately after the third writing session (longer follow-up was not reported). However, in Richards et al. ,97 the written emotional disclosure participants reported significantly more physical symptoms and less anxiety at 6 weeks after the intervention than those in the control arm, with no other differences between groups.
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean score | SD | Change score | SD | n totala | Final mean score | SD | Change score | SD | ||||
| Bernard 200693 | PANAS-PA | Day 3 | 12 | – | – | –0.6 | 3.81 | 10 | – | – | –20.022 | 3.31 | NS |
| PANAS-NA | Day 3 | 12 | – | – | 0.8 | 1.69 | 10 | – | – | –0.56 | 1.81 | NS | |
| IES-T | 5 | 12 | 32.17 | 21.80 | – | – | 10 | 39.10 | 25.23 | – | – | SS | |
| IES-Av | 5 | 12 | 10.67 | 7.25 | – | – | 10 | 14.60 | 8.89 | – | – | NS | |
| IES-I | 5 | 12 | 12.83 | 9.41 | – | – | 10 | 14.10 | 11.40 | – | – | NS | |
| IES-Ar | 5 | 12 | 8.67 | 6.69 | – | – | 10 | 10.40 | 7.92 | – | – | NS | |
| RSQ | 5 | 12 | 1.92 | 1.16 | – | – | 10 | 2.20 | 1.23 | – | – | NS | |
| HADS-A | 5 | 12 | 8.75 | 5.83 | – | – | 10 | 8.11 | 5.44 | – | – | NS | |
| HADS-D | 5 | 12 | 5.92 | 4.54 | – | – | 10 | 7.11 | 4.65 | – | – | NS | |
| IS-8 | 5 | 12 | 14.23 | 20.60 | – | – | 10 | 12.08 | 2.93 | – | – | NS | |
| Canna 200694 | BAI | 8 | 22 | 17.6 | 9.88 | – | – | 18 | 23.2 | 14.59 | – | – | NR |
| – | 16 | 18 | 10.2 | 6.62 | – | – | 13 | 17.9 | 15.36 | – | – | NR | |
| – | 24 | 12 | 8.6 | 6.83 | – | – | 12 | 13.3 | 10.93 | – | – | SS | |
| BDI-II | 8 | 22 | 16.8 | 8.28 | – | – | 13 | 17.8 | 9.65 | – | – | NR | |
| – | 16 | 18 | 9.9 | 7.85 | – | – | 18 | 15.1 | 9.78 | – | – | NR | |
| – | 24 | 12 | 12.4 | 10.54 | – | – | 12 | 10.4 | 6.90 | – | – | SS | |
| BSI/GSI | 16 | 18 | 40.9 | 9.95 | – | – | 13 | 47.9 | 12.55 | – | – | NR | |
| – | 24 | 12 | 39.8 | 15.12 | – | – | 12 | 40.8 | 10.48 | – | – | SS | |
| STAI-S | 8 | 22 | 49.7 | 12.70 | – | – | 18 | 50.6 | 14.52 | – | – | NR | |
| – | 16 | 18 | 42.4 | 11.40 | – | – | 13 | 46.9 | 12.20 | – | – | NR | |
| – | 24 | 12 | 43.8 | 19.33 | – | – | 12 | 39.6 | 12.36 | – | – | NR | |
| STAI-T | 16 | 18 | 49.3 | 9.49 | – | – | 13 | 51.3 | 13.38 | – | – | NR | |
| – | 24 | 12 | 46.3 | 12.94 | – | – | 12 | 46.1 | 10.77 | – | – | NR | |
| BSI | 16 | 18 | 40.9 | 9.95 | – | – | 13 | 47.9 | 12.55 | – | – | NR | |
| – | 24 | 12 | 39.8 | 15.12 | – | – | 12 | 40.8 | 10.48 | – | – | NR | |
| PSWQ | 16 | 18 | 54.6 | 15.15 | – | – | 13 | 59.5 | 14.50 | – | – | NR | |
| – | 24 | 12 | 56.7 | 13.25 | – | – | 12 | 55.7 | 14.41 | – | – | SS | |
| PILL | 16 | 18 | 18.8 | 9.97 | – | – | 13 | 22.4 | 11.01 | – | – | NR | |
| – | 24 | 12 | 15.8 | 11.74 | – | – | 12 | 18.3 | 11.79 | – | – | NR | |
| QoLI | 16 | 18 | 42.3 | 8.99 | – | – | 13 | 36.9 | 14.00 | – | – | NR | |
| – | 24 | 12 | 43.7 | 16.73 | – | – | 12 | 40.6 | 9.31 | – | – | NR | |
| MSPSS | 16 | 18 | 65.1 | 10.28 | – | – | 13 | 53.9 | 14.83 | – | – | NR | |
| – | 24 | 12 | 65.5 | 14.07 | – | – | 12 | 55.8 | 13.07 | – | – | NR | |
| PANAS-PA | Day 3 | 22 | 21.4 | 6.87 | – | – | 18 | 15.9 | 5.21 | – | – | NR | |
| – | Day 4 | 22 | 21 | 6.55 | – | – | 18 | 17.7 | 5.64 | – | – | NR | |
| PANAS-NA | Day 3 | 22 | 20.7 | 6.94 | – | – | 18 | 17.9 | 9.70 | – | – | NR | |
| – | Day 4 | 22 | 20.2 | 8.35 | – | – | 18 | 16.6 | 8.82 | – | – | NR | |
| n of treatment sessions | 12 | 6.25 | 1.14 | – | – | 12 | 7.17 | 1.34 | – | – | NR | ||
| Graf 200895 | DASS-D | Just after final writing | 22 | 11.32 | 10.25 | – | – | 22 | 17.45 | 12.18 | – | – | SS |
| DASS-A | Just after final writing | 22 | 8.23 | 8.62 | – | – | 22 | 10.91 | 9.66 | – | – | NS | |
| DASS-S | Just after final writing | 22 | 12.32 | 8.45 | – | – | 22 | 18.64 | 10.74 | – | – | SS | |
| OQ-45.2 | Just after final writing | 22 | 52.91 | 20.45 | – | – | 22 | 78.09 | 24.55 | – | – | SS | |
| Krpan 201396 | BDI | 4 | 20 | 20.0 | 10.5 | – | – | 20 | 26.0 | 8.5 | – | – | 0.36 |
| PHQ-9 | 4 | 20 | 9.0 | 6.5 | – | – | 20 | 14.0 | 6.5 | – | – | 0.31 | |
| Richards 200097 | PILL | 6 | 36 | 17.29 | 7.85 | – | – | 29 | 11.92 | 7.96 | – | – | SS |
| CSAQ-t | 6 | 36 | 22.62 | 11.35 | – | – | 29 | 21.45 | 11.51 | – | – | NS | |
| CSAQ-cog | 6 | 36 | 11.93 | 6.94 | – | – | 29 | 10.98 | 7.04 | – | – | NS | |
| CSAQ-som | 6 | 36 | 9.99 | 5.38 | – | – | 29 | 8.84 | 5.46 | – | – | NS | |
| Self-report Q Sympt-p | Just after writing | 26 | 1.76 | 0.89 | – | – | 23 | 2.36 | 1.07 | – | – | NS | |
| Self-report Q Sympt-n | Just after writing | 26 | 2.73 | 0.65 | – | – | 23 | 1.93 | 0.75 | – | – | NS | |
Three studies93,94,97 evaluated positive affect and four studies93–96 assessed depression and three could be meta-analysed. With respect to the positive affect outcomes, Canna94 and Richards et al. 97 reported absolute scores but Bernard et al. 93 used change scores, and different instruments were used, so the meta-analysis could not be performed. Four studies93–95,97 reported information on physical symptoms and anxiety. The PILL and IES were not meta-analysed because the SGC considered that they were measuring different things. In total, three93,94,97 of the five studies93–97 assessed anxiety at short term and this outcome was meta-analysed.
Meta-analysis
The outcomes of anxiety and depression were meta-analysed separately (Figures 24 and 25).
FIGURE 24.
Forest plot of anxiety at short-term follow-up in the psychiatric/mental disorders studies. df, degrees of freedom; IV, inverse variance.

FIGURE 25.
Forest plot of depression at short-term follow-up in the psychiatric/mental disorder studies. df, degrees of freedom; IV, inverse variance.
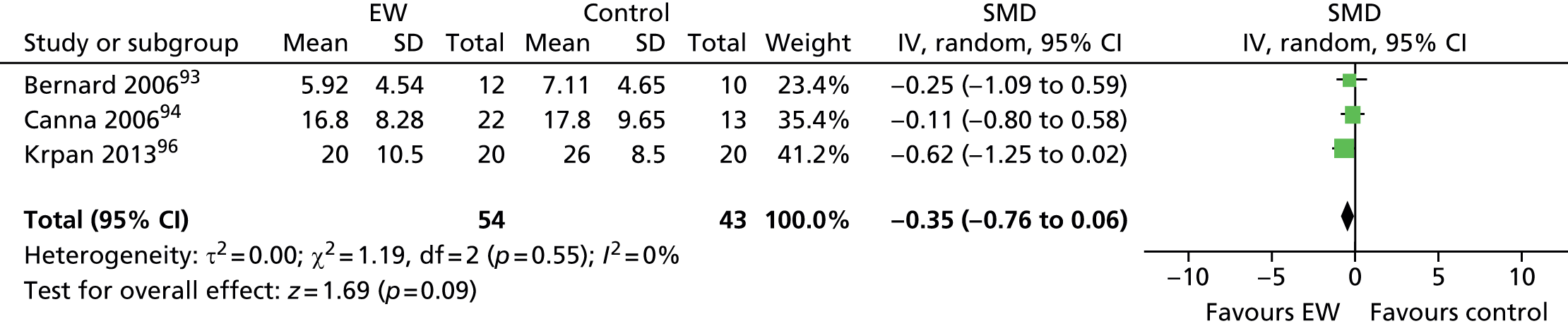
Four studies93–95,97 assessed anxiety: three of them at short term93,94,97 and the remaining one95 at immediate term. Canna94 also assessed anxiety at a medium term (16 weeks), but the 8-week assessment was chosen for consistency and proximity with the other two study follow-up times (5 and 6 weeks in the studies by Bernard et al. 93 and Richards et al. ,97 respectively). Bernard et al. 93 used the anxiety subscale of the Hospital Anxiety and Depression Scale (HADS-A) and Richards et al. 97 used the total score of the Cognitive–Somatic Anxiety Questionnaire (CSAQ). Canna94 used two instruments to assess anxiety: the BAI and the STAI – both are self-reported questionnaires. The BAI measures the severity of anxiety and provides a total score and the STAI, which has two subscales, measures state and trait anxiety. Thus, the BAI was chosen for inclusion in the meta-analysis.
-
Forest plot A total of 127 participants were meta-analysed (70 in the EW group and 57 in the control group) (see Figure 24). The SMD was –0.07 (95% CI –0.42 to 0.29) with a random-effects model, and with unimportant, non-significant heterogeneity, I2 = 2%. This result suggests that there is no significant difference in anxiety at short term for the EW group compared with the control group.
There was considerable clinical heterogeneity as follows:
-
Clinical differences between studies Participants in Bernard et al. 93 were first episode psychosis patients, those in Canna94 were diagnosed with Axis I anxiety or mood disorder, and those in Richards et al. 97 had at least one diagnosis of mental disorder and were different from the other study participants as they were psychiatric maximum-security prison inmates. They were reported to have had a higher use of health-care services than non-incarcerated men.
-
Intervention differences Bernard et al. 93 and Canna94 instructed their participants to write about a disease- and treatment-related topic, whereas the prison inmates in Richards et al. 97 had to write about their deepest thoughts and feelings, regarding an experience that had not been previously shared with others at all, or in very little detail. In addition, Richards et al. 97 evaluated two control groups, whereas one control group was evaluated in the other two studies. 93,94 The prison inmates were financially compensated, whereas participants in the other two studies were not.
Four studies measured depression:93,94,96,97 one study97 immediately after writing and three studies93,94,96 at short-term follow-up, which could be meta-analysed. Bernard et al. 93 measured the HADS-D at 5 weeks, and Canna94 measured the BDI-II at 8, 16 and 24 weeks so the 8-week value was used, and Krpan et al. 96 measured the Beck Depression Inventory (BDI) at 4 weeks. Krpan et al. 96 also measured depression with the Patient Health Questionnaire 9-item subscale (PHQ-9) but the BDI was used for the meta-analysis because it was similar to the BDI used by Canna. 94
-
Forest plot In the meta-analysis a total of 97 participants were included (54 in the EW groups and 43 in the control groups). The SMD was –0.35 (95% CI –0.76 to 0.06), suggesting that there is no significant difference in depression at short term for the EW group compared with the control group.
F43: post-traumatic stress disorder
Overview
There were two small studies evaluating unfacilitated EW on PTSD. 98,121 A summary of their main characteristics is presented in Table 32. Two other studies97,98 also evaluated patients with PTSD; however, they used facilitated TW and are reported in the facilitated TW section.
| First author, year | Study design | Intervention group | Control group |
|---|---|---|---|
| Gidron 199698 | RCT | Unfacilitated EW | Factual writing |
| Smyth 2008121 | RCT | Unfacilitated EW | Time-management writing |
One study121 was conducted in the USA and the other one98 in Israel. In Gidron et al. ,98 10 out of the 14 participants had PTSD following a motor vehicle accident (MVA), and the 25 participants in Smyth and Arigo121 were recruited from a veterans hospital and a community rape and trauma centre. In both studies,98,121 patients had been diagnosed with PTSD as defined by the DSM-IV.
The outcomes evaluated in each of the studies on PTSD patients are reported in Table 33.
| First author, year | Physical health/symptoms | PTSD symptoms | Positive mood | Negative mood | Depression | Biomarker of clinical course of disease | Various other | Adherence | Resource use |
|---|---|---|---|---|---|---|---|---|---|
| Gidron 199698 | PILL | IES | PANAS-PA | PANAS-NA | BDI-II | – | – | – | Number of visits to clinician |
| Smyth 2008121 | – | PSS-I (PTSD symptoms) | POMS-v | – | POMS-d | Cortisol reactivity | PTGI (positive changes) | ✓ | – |
The main outcomes assessed were related to the physical symptoms and to psychological factors, mostly depression.
Quality assessment
A summary of the quality of the studies on PTSD is shown in Figure 26. Both studies were randomised but the method of randomisation was not indicated in either study.
FIGURE 26.
Risk-of-bias summary in the PTSD studies.
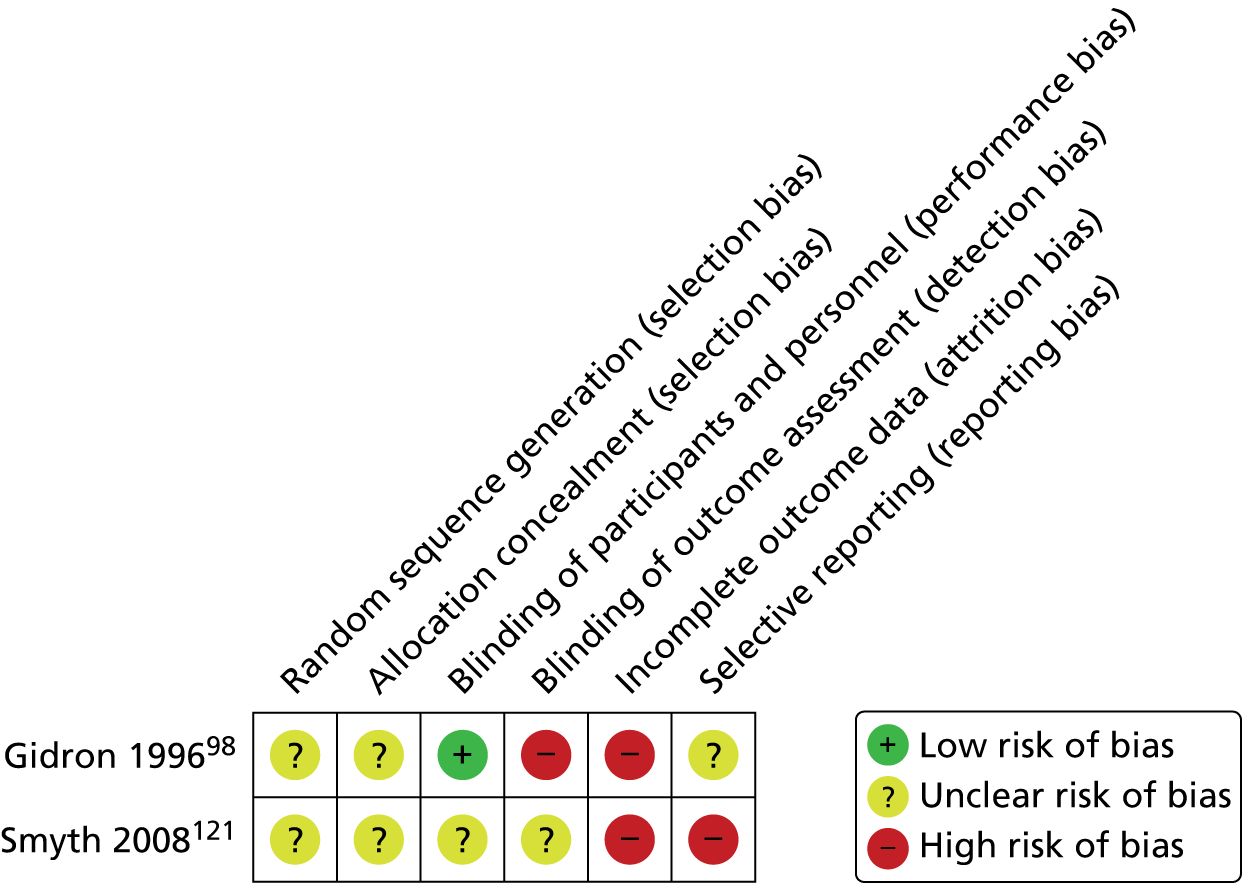
Gidron et al. 98 was likely to introduce both detection and attrition biases. The study by Smyth and Arigo121 was more likely to introduce attrition and selection biases. The remaining items in these two studies98,121 were unclear or not reported. Overall, the quality of the methods used in each of the studies was under-reported. Only participants in Gidron et al. 98 were analysed by ITT analysis.
Numerical results
The numerical results reported in the PTSD studies are summarised in Table 34. The follow-up periods were 5 weeks in Gidron et al. 98 and 13 weeks in Smyth and Arigo. 121 The final sample size was 14 participants in Gidron et al. 96 and 21 participants in Smyth and Arigo. 121
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean scoreb | SD | Change score | SD | n totala | Final mean scoreb | SD | Change score | SD | ||||
| Gidron 199698 | PILL | 5 | 8 | 138.50 | 34.70 | – | – | 6 | 116.00 | 28.90 | – | – | SS |
| IES-T | 5 | 8 | 40.90 | 16.10 | – | – | 6 | 27.30 | 21.60 | – | – | SS | |
| IES-I | 5 | 8 | 23.20 | 9.20 | – | – | 6 | 13.20 | 10.80 | – | – | NR | |
| IES-Av | 5 | 8 | 17.60 | 10.10 | – | – | 6 | 14.20 | 12.50 | – | – | SS | |
| PANAS-PA | 5 | 8 | 31.40 | 8.60 | – | – | 6 | 24.70 | 8.80 | – | – | NR | |
| PANAS-NA | 5 | 8 | 32.70 | 8.40 | – | – | 6 | 32.00 | 9.40 | – | – | SS | |
| BDI-II | 5 | 8 | 39.10 | 9.10 | – | – | 6 | 45.20 | 13.00 | – | – | NR | |
| Number of visits, clinician | 5 | 8 | 3.10 | 2.00 | – | – | 6 | 0.70 | 1.60 | – | – | SS | |
| Smyth 2008121 | Cortisol | 13 | 13 | 12.7 | NR | NR | NR | 8 | 16.3 | NR | NR | NR | SS |
| POMS-t | 13 | 13 | NR | NR | Mean change: –4.87 | NR | 8 | NR | NR | Mean change: NR | NR | SS | |
| POMS-d | 13 | 13 | NR | NR | Mean change: –3.3 | NR | 8 | NR | NR | Mean change: –0.5 | NR | NS | |
| POMS-a | 13 | 13 | NR | NR | Mean change: –5.51 | NR | 8 | NR | NR | Mean change: 0.5 | NR | SS | |
| POMS-v | 13 | 13 | NR | NR | Mean change: –0.5 | NR | 8 | NR | NR | Mean change: 3.6 | NR | NS | |
| POMS-f | 13 | 13 | NR | NR | Mean change: –1.7 | NR | 8 | NR | NR | Mean change: 1.3 | NR | NS | |
| POMS-c | 13 | 13 | NR | NR | Mean change: –2.1 | NR | 8 | NR | NR | Mean change: –3 | NR | NS | |
| PTGI | 13 | 13 | NR | NR | NR | NR | 8 | NR | NR | SS | |||
| PSS-I-v | 13 | 13 | NR | NR | 1.13 | NR | 8 | NR | NR | –0.8 | NR | SS | |
| PSS-I-a | 13 | 13 | NR | NR | 0.36 | NR | 8 | NR | NR | 0.2 | NR | SS | |
| Adherence (rate) | 13 | 15 | Number of patients: 14 | – | – | – | 10 | Number of patients: 10 | – | – | – | NR | |
Overall, a significant effect of group-by-time interaction in mood outcomes was reported in both studies. 98,121 In Smyth and Arigo,121 there was a significant improvement in mood in the TW group compared with control subjects, as opposed to Gidron et al. ,98 in which participants in the experimental group increased significantly the negative affect compared with control subjects.
F50: bulimia nervosa
Overview
There was one RCT99 on bulimia nervosa (BN), binge-eating disorder (BED) and other eating disorders evaluating unfacilitated EW. Participants in Robinson and Serfaly99 were UK university students and staff, recruited via e-mail, and diagnosed with the Questionnaire for Eating Disorders Diagnosis (QEDD) using DSM-IV. 123 Two interventions were assessed. One intervention was e-mail bulimia therapy (eBT), which did not involve TW, and is not considered further here. In the other active intervention, unsupported self-directed writing (SDW) participants were sent an e-mail and were asked to write about their self-selected difficulties at least twice a week and send it back to the authors. The duration of the intervention was not specified. Participants in the control group were placed in a waiting list for 3 months, after which they were offered eBT or SDW by random allocation. The outcomes evaluated in the studies on BN are reported in Table 35.
| First author, year | Diagnosis of eating disorder | Desired weight | Bulimia test | Depression | Resource use |
|---|---|---|---|---|---|
| Robinson 200899 | QEDD | BMIa | BITE | BDI | – |
Quality assessment
A summary of the study quality is shown in Figure 27. Robinson et al. 99 was truly randomised; however, the sequence generation was not concealed. Masking of participants was performed but information related to masking of outcome assessment was unclear. The study99 was likely to introduce high risk of selection bias and unclear risk of detection bias and high risk of attrition bias. Authors reported that they used an ITT analysis.
FIGURE 27.
Risk-of-bias summary in the BN study.
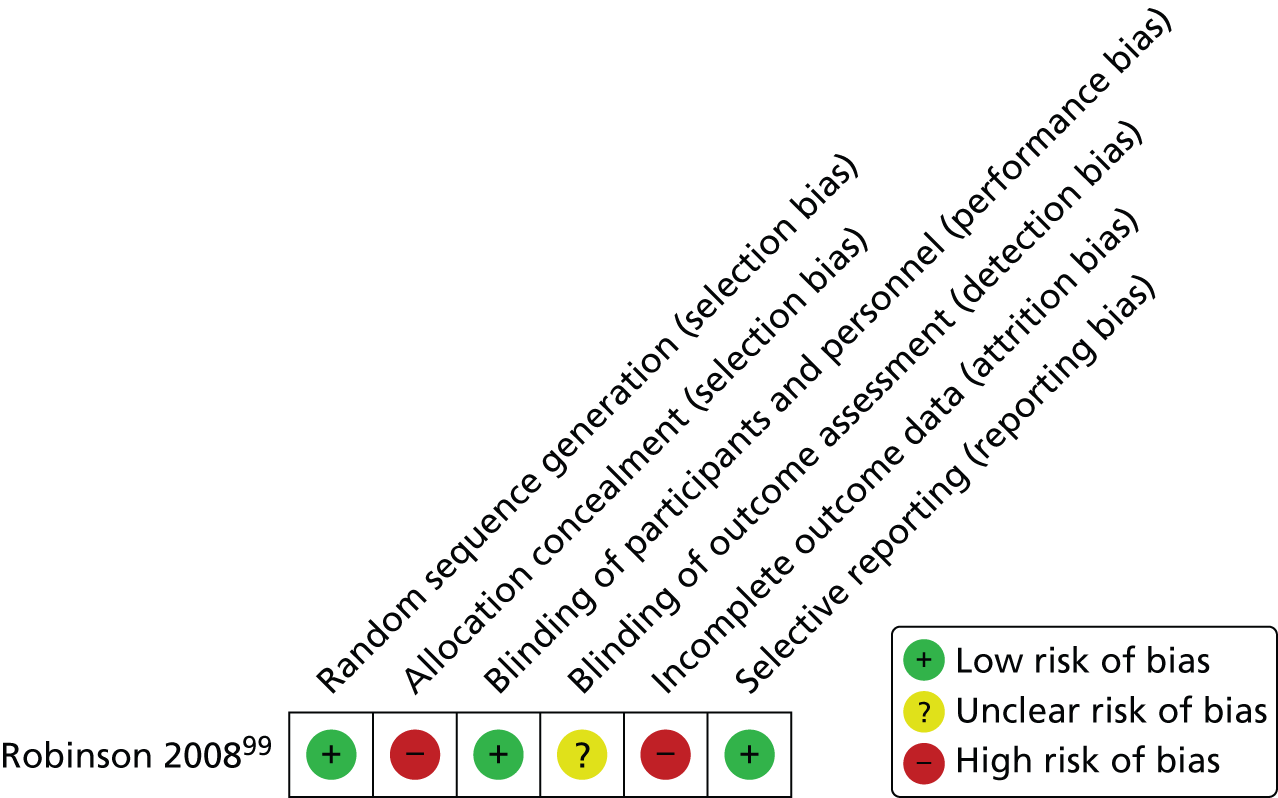
Numerical results
The numerical results reported in Robinson et al. 99 are summarised in Table 36. The follow-up assessments were performed at 13 weeks post writing. The total sample size in the study arms relevant to this review was 51 participants.
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||
|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean scoreb | 95% CIb | n totala | Final mean scoreb | 95% CIb | ||||
| Robinson 200899 | QEDD | 13 | 34 | Number of participants without EDD = 5; number of participants with EDD = 29 | – | 27 | Number of participants without EDD = 0; number of participants with EDD = 27 | – | SS |
| BDI-II | 13 | 34 | 18.30 | 14.1 to 22.6 | 27 | 23.3 | 19.8 to 28.6 | NS | |
| BITE-sev | 13 | 34 | 6.91 | 5.33 to 8.5 | 27 | 9.37 | 8.0 to 10.74 | NS | |
| BITE-symp | 13 | 34 | 21.70 | 19.3 to 24.1 | 27 | 24.19 | 22.9 to 25.5 | NS | |
| BMI | 13 | 34 | NR | NR | 27 | NR | NR | NR | |
Authors reported that overall severity scores were reduced within the intervention group but differences were not significant. However, the number of participants fulfilling DSM-IV eating disorder criteria tended to be lower (but was not significantly different) in the EW group than in the control group.
G12: amyotrophic lateral sclerosis/motor neurone disease
Overview
There was one RCT100 evaluating unfacilitated EW on patients who had been diagnosed with amyotrophic lateral sclerosis (ALS) (also known as motor neurone disease). Participants in the Averill et al. study100 were diagnosed with definite or probable ALS using El Escorial World Federation of Neurology criteria at least 6 months prior to study entry124 (World Federation of Neurology Research Group on Neuromuscular Diseases, 1994). The study100 was conducted in the USA. One intervention group was compared with one control group. Intervention group participants had to disclose, by handwriting (or orally), about a disease-focused topic during 20 minutes over 3 non-consecutive days. The control group did no writing and had to complete study outcome measures only. Participants were not financially compensated. The outcomes evaluated in Averill et al. 100 are reported in Table 37. Psychological outcomes were the most extensively assessed, together with QoL.
| First author, year | Affect | Coping | Depression | Various others | QoL | Resource use |
|---|---|---|---|---|---|---|
| Averill 2013100 | ABS | Likert scale | GDS | AEE, SCS | McGill QOL | – |
Quality assessment
A summary of the quality of the study in ALS is shown in Figure 28.
FIGURE 28.
Risk-of-bias summary in the ALS study.
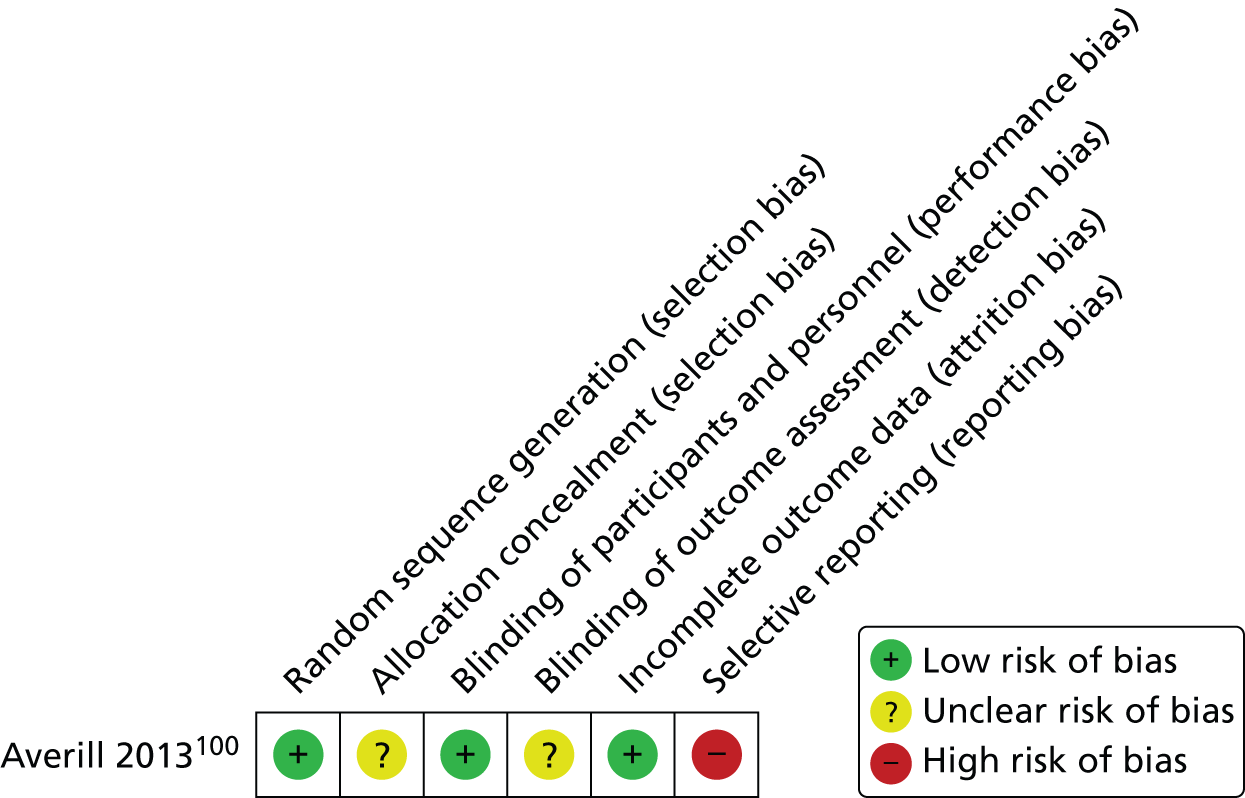
Averill et al. 100 was truly randomised but information relating to the allocation concealment of the sequence generation was unclear. There was no information reported regarding the masking of participants and/or personnel. Therefore, there was a possibility of selection and performance biases. Numerical outcome data were supplied for only the QoL measure; none of the remaining outcomes was reported. The authors did not perform ITT analysis.
Numerical results
The numerical results reported in Averill et al. 100 are summarised in Table 38.
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||
|---|---|---|---|---|---|---|---|---|---|
| n totala | Mean of standardised scores | SD unit | n totala | Mean of standardised scores | SD unit | ||||
| Averill 2013100 | QoL | 13 | 24 | 0.066 | NR | 24 | –0.164 | NR | NR |
| 26 | 24 | –0.031 | NR | 24 | 0.009 | NR | NS | ||
Follow-up assessments were performed at 13 and 26 weeks. The total sample size was 48 participants at both time points. At 13 weeks, there was a small but significant improvement in well-being measures in the intervention group compared with baseline, and a significant reduction in well-being (QoL) in the control group; both these differences had disappeared at 26 weeks. The authors pointed out that ALS is a progressive condition and it may be that the physical and emotional challenges faced by those with the condition at 6 months might be very different from those faced by them at baseline and it could be that booster sessions of EW are required in conditions such as this. Ambivalence Emotional Expression (or Ambivalence over Emotional Expression; AEE) appeared to moderate psychological well-being. Authors reported that those participants who were more ambivalent about expressing emotion appeared to benefit particularly from emotional disclosure at 13 weeks.
G43 and G44: migraine and tension headache
Overview
There was one RCT101 evaluating unfacilitated EW on patients diagnosed with migraine or tension headache, using the International Headache Society criteria. D’Souza et al. 101 was conducted in the USA on psychology students, who reported either tension or migraine headaches on screening. The majority (86.5%) of participants were female. Unfacilitated EW was compared with time-management writing; intervention participants were asked to write about their most significant trauma, upheaval or stressful experience for 20 minutes on four occasions over 2 weeks. A third arm (not reported further here) examined the effect of relaxation training. Control subjects had a time-management writing task. Participants received financial compensation for participating in the study. The outcomes evaluated in D’Souza et al. 101 are reported in Table 39. Physical symptoms were the main outcomes assessed.
| First author, year | Physical symptoms | Positive mood | Negative mood | Behavioural disability from headache | Resource use |
|---|---|---|---|---|---|
| D’Souza 2008101 | Headache frequency, disability and severity, SCL-90-R | PANAS-PA | PANAS-NA | MIDAS | – |
Quality assessment
A summary of the study quality is shown in Figure 29. D’Souza et al. 101 was truly randomised. Allocation concealment was performed, and blinding was preserved at the performance level. Withdrawals were adequately reported and outcomes were fully reported. This study101 was not likely to introduce any bias other than detection bias. ITT analyses were performed. However, numbers involved in the study101 were very small and no sample size calculation was reported.
FIGURE 29.
Risk-of-bias summary in the migraine and tension headache study.

Numerical results
The numerical results are summarised in Table 40. Follow-up assessment was performed at 12 weeks post writing for all outcomes but for the Positive and Negative Affect Schedule (PANAS), which was evaluated just after writing as a manipulation check to verify that the conditions operated as expected. The total sample size was 62 participants. The results were reported separately for the two types of headache. If 12-week outcome data were missing then 4-week data were used. The intervention group had increased negative mood immediately after administration compared with control subjects but whether or not differences between groups were statistically significant was not reported.
| First author, year | LTC | Outcome measures | Follow-up (weeks) | Intervention group | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean score | SD | Change score | SD | n totala | Final mean score | SD | Change score | SD | |||||
| D’Souza 2008101 | Migraine headache | PANAS-PA | Just after writing | 29 | 24.72 | 9.07 | –1.35 | 8.12 | 27 | 26.15 | 7.39 | –1.65 | 5.54 | NR |
| PANAS-NA | Just after writing (SS) | 29 | 17.23 | 6.06 | –3.7 | 3.86 | 27 | 17.46 | 4.48 | –3.58 | 5.41 | NR | ||
| Headache frequency: n of days | 12 | 31 | 9.00 | 5.81 | – | – | 31 | 8.97 | 6.14 | – | – | NS | ||
| Headache severity: pain | 12 | 31 | 5.23 | 2.28 | – | – | 31 | 5.55 | 1.69 | – | – | NS | ||
| MIDAS | 12 | 31 | 9.87 | 8.79 | – | – | 31 | 10.13 | 11.49 | – | – | NS | ||
| SCL-90-R | 12 | 31 | 11.26 | 7.61 | – | – | 31 | 10.61 | 5.37 | – | – | NS | ||
| Tension headache | Headache frequency: n of days | 12 | 17 | 12.24 | 7.90 | – | – | 17 | 11.24 | 9.01 | – | – | NS | |
| Headache severity: Pain | 12 | 17 | 5.00 | 1.62 | – | – | 17 | 4.71 | 1.80 | – | – | NS | ||
| MIDAS | 12 | 17 | 8.35 | 8.89 | – | – | 17 | 7.29 | 7.82 | – | – | NS | ||
| SCL-90-R | 12 | 17 | 8.71 | 5.03 | – | – | 17 | 11.06 | 4.76 | – | – | NS | ||
No difference in any outcome was seen between intervention and control subjects for either type of headache at 4 or 12 weeks (only 12-week data were provided in full).
I51: cardiovascular disease
Overview
There were three studies102–104 evaluating unfacilitated EW on patients with CVD. A summary of their main characteristics is presented in Table 41. Participants in Willmott et al. 104 were patients with a first myocardial infarction (MI) receiving treatment at one of two acute hospital clinics. Participants in Hevey et al. 103 were patients with a confirmed MI, who had received treatment at a large teaching hospital. Bartasiuniene et al. 102 included rehabilitation hospital patients with CVD. Bartasiuniene et al. 102 was conducted in Lithuania, Hevey et al. 103 was conducted in Ireland and Willmott et al. 104 was conducted in the UK.
| First author, year | Study design | Intervention group | Control group |
|---|---|---|---|
| Bartasiuniene 2011102 | RCT | Unfacilitated EW | Factual writing |
| Hevey 2012103 | RCT | Unfacilitated EW | Factual writing |
| Willmott 2011104 | RCT | Unfacilitated EW | Factual writing |
All studies102–104 assessed an expressive writing intervention in which the topic was disease focused. Additionally, participants in Willmott et al. 104 had to express both positive and negative disease-related feelings, whereas in the remaining studies only negative thoughts were to be expressed. Factual writing was the control intervention in all three studies. Bartasiuniene et al. 102 also included a second, non-writing control group, in which participants received what the authors described as usual care. However, this latter control group was not included in current analyses, as the usual care consisted of aromatherapy and other activities that were considered active, in that participants would have been getting more attention than those receiving only usual care. Hevey et al. 103 and Willmott et al. 104 both implemented writing for 20 minutes over 3 consecutive days, whereas intervention group participants in Bartasiuniene et al. 102 wrote for 30 minutes on 4 consecutive days.
The outcomes evaluated in the studies102–104 are reported in Table 42. Negative affect and QoL were the most frequent outcomes measured.
| First author, year | Physical symptoms | Positive mood | Negative mood | Anxiety | Depression | Coping | QoL | Resource use |
|---|---|---|---|---|---|---|---|---|
| Bartasiuniene 2011102 | – | PANAS-X(b)–PA | PANAS-X(b)–NA | – | – | – | – | – |
| Hevey 2012103 | – | – | Type D negative affectivity | HADS–A | HADS–A | Brief COPE | Mac New HRQOL | – |
| Willmott 2011104 | SBP, DBP, cardiac symptoms | – | – | – | – | – | SF-36 | Number of visits to clinician, number of prescribed pain medications per month |
Quality assessment
A summary of the quality of the CVD studies102–104 is shown in Figures 30 and 31.
FIGURE 30.
Risk-of-bias summary in the CVD studies.
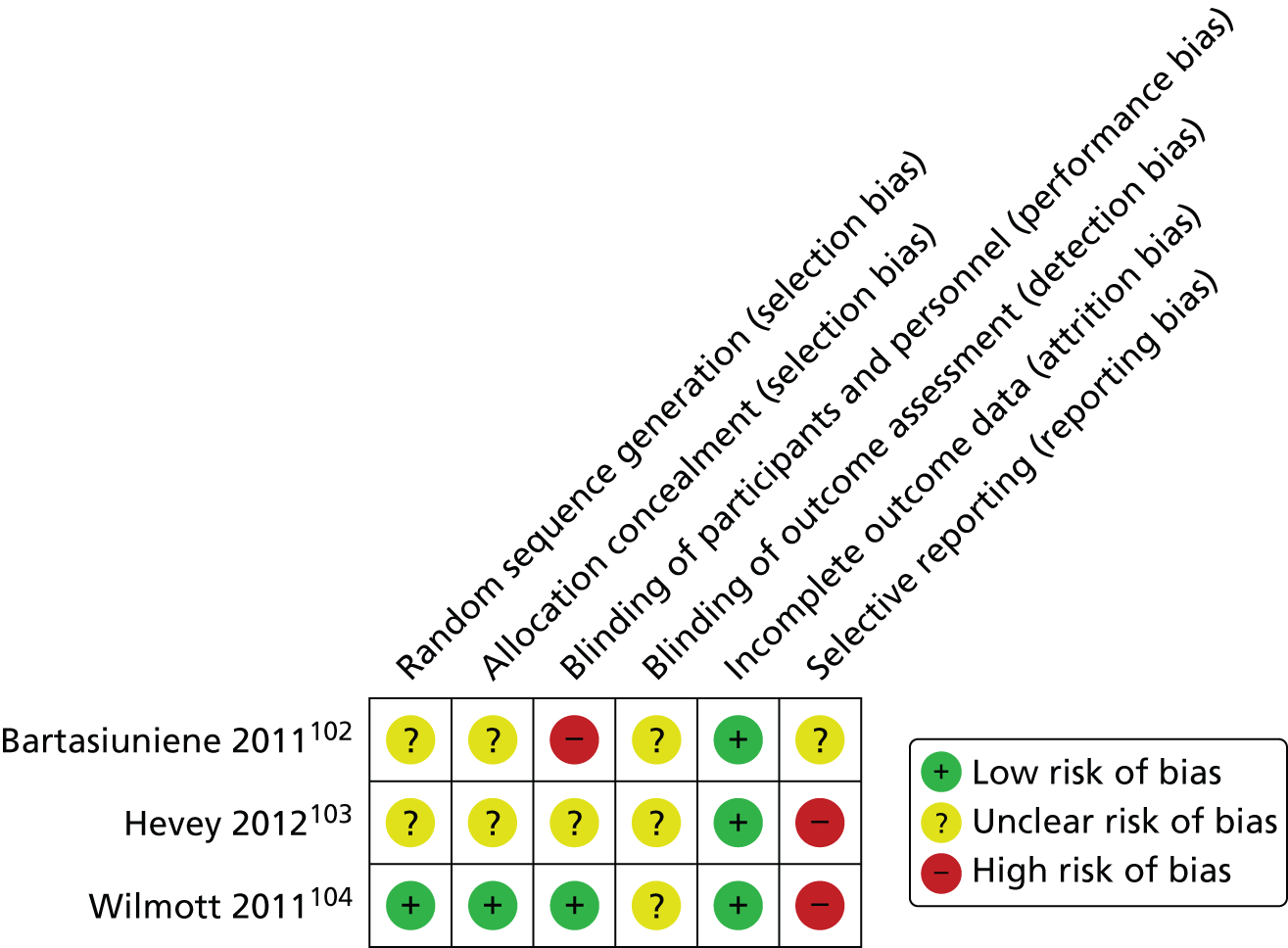
FIGURE 31.
Risk-of-bias graph in the CVD studies.

All three studies102–104 were randomised. However, Bartasiuniene et al. 102 and Hevey et al. 103 did not report the method of randomisation used or whether or not the sequence of the random generation was concealed. Willmott et al. ,104 however, reported adequately on all quality items except for the outcome assessment, which was unclear. In the remaining studies,102,103 selection, performance and detection biases were possible. Additionally, in Hevey et al. ,103 numerical data were reported for only QoL, and these data were derived from graphs so no measure of variability could be computed. Similarly, Bartasiuniene et al. 102 under-reported outcomes; it was also unclear whether or not the authors performed an ITT analysis, as they reported that only 48 out of 60 participants completed the study, and they did not report further on the 12 dropouts. The remaining studies103,104 reported on only those who continued to participate in the study.
Numerical results
The numerical results of the CVD studies are reported in Table 43. Follow-up assessments were performed from just after writing up to 21 weeks later. Total study sizes ranged from 30 participants in the Bartasiuniene et al. study102 to 128 participants in the Willmot et al. study. 104
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||
|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean score | SD | n totala | Final mean score | SD | ||||
| Bartasiuniene 2011102 | PANAS-PA | Day 4 | 15 | 28.53 | NR | 15 | 28.06 | NR | SSb |
| PANAS-NA | Day 4 | 15 | 15.93 | NR | 15 | 18.73 | NR | SSb | |
| Hevey 2012103 | QoL | Just after writing | 43 | 4.97 | NR | 46 | 4.84 | NR | NR |
| 13 | 43 | 5.65 | NR | 46 | 5.08 | NR | SS | ||
| HADS-D | Just after writing | 43 | NR | NR | 46 | NR | NR | NS | |
| 13 | 43 | NR | NR | 46 | NR | NR | NS | ||
| HADS-A | Just after writing | 43 | NR | NR | 46 | NR | NR | NS | |
| 13 | 43 | NR | NR | 46 | NR | NR | NS | ||
| Type D negative affectivity | Just after writing | 43 | NR | NR | 46 | NR | NR | NS | |
| 13 | 43 | NR | NR | 46 | NR | NR | NS | ||
| Type D social inhibition | Just after writing | 43 | NR | NR | 46 | NR | NR | NS | |
| 13 | 43 | NR | NR | 46 | NR | NR | NS | ||
| Brief COPE-ad | Just after writing | 43 | NR | NR | 46 | NR | NR | NS | |
| 13 | 43 | NR | NR | 46 | NR | NR | NS | ||
| Brief COPE-m | Just after writing | 43 | NR | NR | 46 | NR | NR | NS | |
| 13 | 43 | NR | NR | 46 | NR | NR | NS | ||
| Willmott 2011104 | n of visits clinician | 21 | 68 | 8.60 | 3.70 | 60 | 10.30 | 5.00 | NS |
| n of prescribed pain medication/month | 4 | 68 | 5.00 | 1.60 | 60 | 5.00 | 1.60 | NR | |
| 8 | 68 | 4.90 | 1.70 | 60 | 5.20 | 1.70 | NR | ||
| 21 | 68 | 4.80 | 1.70 | 60 | 5.30 | 1.70 | SS | ||
| n of cardiac symptoms | 4 | 68 | 0.62 | 0.70 | 60 | 0.96 | 0.90 | NR | |
| 8 | 68 | 0.73 | 1.00 | 60 | 1.10 | 0.90 | NR | ||
| 21 | 68 | 0.63 | 0.80 | 60 | 1.10 | 0.90 | NS | ||
| DBP | 4 | 68 | 73.70 | 9.00 | 60 | 73.10 | 8.80 | NR | |
| 8 | 68 | 71.80 | 8.40 | 60 | 74.20 | 8.80 | NR | ||
| 21 | 68 | 71.00 | 9.00 | 60 | 75.00 | 9.80 | SS | ||
| SBP | 4 | 68 | 126.50 | 16.20 | 60 | 126.50 | 17.00 | NR | |
| 8 | 68 | 125.20 | 17.30 | 60 | 129.90 | 16.40 | NR | ||
| 21 | 68 | 127.60 | 17.00 | 60 | 133.90 | 18.30 | NS | ||
| SF-36 PCS | 4 | 68 | 44.00 | 14.80 | 60 | 40.50 | 15.80 | NR | |
| 8 | 68 | 65.50 | 21.60 | 60 | 60.30 | 22.00 | NR | ||
| 21 | 68 | 68.10 | 22.50 | 60 | 63.60 | 16.30 | NS | ||
| SF-36 MCS | 4 | 68 | 48.30 | 16.20 | 60 | 47.80 | 16.00 | NR | |
| 8 | 68 | 66.80 | 21.60 | 60 | 64.80 | 21.60 | NR | ||
| 21 | 68 | 71.40 | 20.20 | 60 | 62.90 | 22.40 | SSb | ||
Differences between groups by time interaction were reported as statistically significant for the following outcomes measures: PANAS-PA/PANAS-NA; QoL; number of prescribed medication/month; diastolic blood pressure (DBP) and Short Form questionnaire-36 items mental composite score (SF-36 MCS). No other significant effect of group-by-time interaction was reported across the studies in CVD. Additionally, Willmott et al. 104 stated that the intervention group had significantly fewer symptoms than those in the control group (p < 0.001). Likewise, DBP in the control group was reported as significantly higher than in the experimental group at the 5-month follow-up (p < 0.008).
J44 and J84: chronic obstructive pulmonary disease and idiopathic pulmonary fibrosis
Overview
There was one RCT105 evaluating unfacilitated EW on patients medically diagnosed with chronic obstructive pulmonary disease (COPD) or idiopathic pulmonary fibrosis (IPF), who were recruited while participating in an 8-week pulmonary rehabilitation programme. Sharifabad et al. 105 was conducted in the USA. A written emotional disclosure intervention was evaluated, for which participants had to write about their most traumatic or upsetting life experiences for 20 minutes once a week for 3 consecutive weeks, whereas control participants had to write in detail about an assigned neutral topic (a specific event or an object) without referring to their emotions. The outcomes evaluated by Sharifabad et al. 105 are reported in Table 44. They include physical function, symptom and QoL.
| First author, year | Physical function | Physical symptoms | QoL | Resource use |
|---|---|---|---|---|
| Sharifabad 2010105 | 6MWD, FEV1, FVC | MMRC dyspnoea scale | CRQ, SGRQ | – |
Quality assessment
A summary of the quality of the COPD/ IPF studies is shown in Figure 32. Sharifabad et al. 105 was described as randomised but authors did not report the method of randomisation. They stated, ‘The pulmonary rehabilitation program had two morning sessions and one evening session. For one cycle of patients, those in the morning sessions were enrolled in the WDT group [i.e. intervention] and patients in the evening group were enrolled in the control group. Then, for the following cycle of patients the enrolment switched . . .’ Thus, it is not clear whether or not this study105 was truly randomised. The quality items assessed showed that this study105 was likely to introduce selection, performance, detection and attrition biases.
FIGURE 32.
Risk-of-bias summary in the COPD/IPF study.

Numerical results
The numerical results of this study are reported in Table 45. Follow-up assessments were performed at 8 and 26 weeks. The total sample size was 66 participants (no power calculation was provided). At 6 months, and adjusting for baseline differences, authors reported significant improvement between groups favouring the control group in the emotion domain of the Chronic Respiratory Disease Questionnaire, emotion subscale (CRQ-e). The remaining outcomes had non-significant differences in scores between groups.
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||
|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean score | SD | n totala | Final mean score | SD | ||||
| Sharifabad 2010105 | Modified MRC dyspnoea | 8 | 29 | 1.61 | 1.14 | 37 | 1.79 | 1.00 | NS |
| Modified MRC dyspnoea | 26 | 29 | 1.94 | 0.98 | 37 | 1.83 | 0.95 | NS | |
| SGRQ | 8 | 29 | 39.46 | 16.80 | 37 | 42.21 | 14.76 | NS | |
| SGRQ | 26 | 29 | 40.06 | 17.06 | 37 | 42.78 | 16.15 | NS | |
| CRQ-d | 8 | 29 | 4.39 | 1.37 | 37 | 4.17 | 1.45 | NS | |
| CRQ-d | 26 | 29 | 3.98 | 1.86 | 37 | 4.22 | 1.60 | NS | |
| CRQ-m | 8 | 29 | 5.42 | 1.03 | 37 | 5.39 | 1.18 | NS | |
| CRQ-m | 26 | 29 | 5.46 | 1.21 | 37 | 5.44 | 1.33 | NS | |
| CRQ-f | 8 | 29 | 4.67 | 1.16 | 37 | 4.54 | 1.03 | NS | |
| CRQ-f | 26 | 29 | 4.78 | 1.20 | 37 | 4.50 | 1.06 | NS | |
| CRQ-e | 8 | 29 | 5.20 | 1.06 | 37 | 5.26 | 0.99 | SS | |
| CRQ-e | 26 | 29 | 5.00 | 1.17 | 37 | 5.11 | 1.22 | SS | |
| 6MWD | 8 | 29 | 314.60 | 99.70 | 37 | 314.20 | 122.50 | NS | |
| 6MWD | 26 | 29 | 263.70 | 110.40 | 37 | 278.40 | 118.90 | NS | |
| FEV1 | 8 | 29 | 0.97 | 0.48 | 37 | 1.09 | 0.65 | NS | |
| FEV1 | 26 | 29 | 1.00 | 0.51 | 37 | 1.10 | 0.61 | NS | |
| FVC | 8 | 29 | 1.72 | 0.68 | 37 | 1.93 | 0.80 | NS | |
| FVC | 26 | 29 | 1.70 | 0.72 | 37 | 2.01 | 0.69 | NS | |
J45: asthma
Overview
There were four studies58,106–108 evaluating unfacilitated EW on patients with asthma (Table 46). A summary of main characteristics is presented in Table 46. Participants were diagnosed through a clinical history of asthma and confirmed by a physician. In all studies,58,106–108 patients were reported to be on regular inhaled medication to treat persistent symptoms. Three studies106–108 were conducted in the USA and Theadom et al. 58 was conducted in the UK.
| First author, year | Study design | Intervention group 1 | Intervention group 2 | Control group 1 |
|---|---|---|---|---|
| Harris 2005106 | RCT | Unfacilitated EW | Positive writing | Factual writing |
| Smyth 1999107 | RCT | Unfacilitated EW | – | Time-management writing |
| Theadom 201058 | RCT | Unfacilitated EW | – | Factual writing |
| Warner 2006108 | RCT | Unfacilitated EW | – | Time-management writing |
Three studies58,107,108 evaluated one intervention group compared with one control group but Harris et al. 106 assessed two intervention arms: in one group, participants had to write about stressful traumatic experiences, whereas in the other active group participants had to write about positive experiences such as events that stimulated feelings of happiness or joy. In the remaining studies58,107,108 the topic of the intervention arm was focused on a self-selected trauma/emotional issue or worst experience. Therefore, because of similarity to the other active interventions, only the intervention group which wrote about negative experiences in Harris et al. ,106 was used for meta-analysis. All control groups were focused on descriptions of neutral topics/events of previous day or on the management of time. Three studies58,107,108 delivered the intervention over 3 consecutive days except for Harris et al. ,106 which delivered the intervention once per week for 3 weeks. Patients in Smyth et al. ,107 Warner et al. 108 and Harris et al. 106 were financially compensated.
The outcomes assessed within the studies58,106–108 on asthma are reported in Table 47. Lung function was evaluated through spirometry in three studies. 106–108 The remaining outcomes were mostly evaluated once across studies.
| First author, year | Asthma symptoms | Lung function | General mood | Positive mood | Negative mood | Behaviour | Adherence | Resource use |
|---|---|---|---|---|---|---|---|---|
| Harris 2005106 | – | FEV1% pred, FVC | – | – | – | – | ✓ | – |
| Smyth 1999107 | – | FEV1% pred | – | – | – | – | – | – |
| Theadom 201058 | Asthma symptoms | – | – | – | – | – | – | – |
| Warner 2006108 | ASS | FEV1% pred | Five moods a | PANAS-PAb | PANAS-NAb | FDI, CBCL | ✓ | – |
Quality assessment
A summary of the quality of the studies in asthma is shown in Figures 33 and 34. All studies58,106–108 were randomised; however, in Theadom et al. 58 the method of randomisation was not reported. Two studies106,107 reported having protected the allocation sequence before and until assignment. The other two studies58,108 were unclear on this item. Additionally, information related to masking was not reported in any of the studies or the information given was scarce, making more likely to introduce certain risk of bias and to affect outcomes. Warner et al. 108 was contacted in order to get numerical data related to the outcome collected ‘five moods’, which were not reported in the published article. The information was supplied, and therefore the selective reporting item was rated as low risk of bias. All studies performed ITT analysis, but Harris et al. 106 did not reflect this clearly.
FIGURE 33.
Risk-of-bias summary in the asthma studies.

FIGURE 34.
Risk-of-bias graph in the asthma studies.
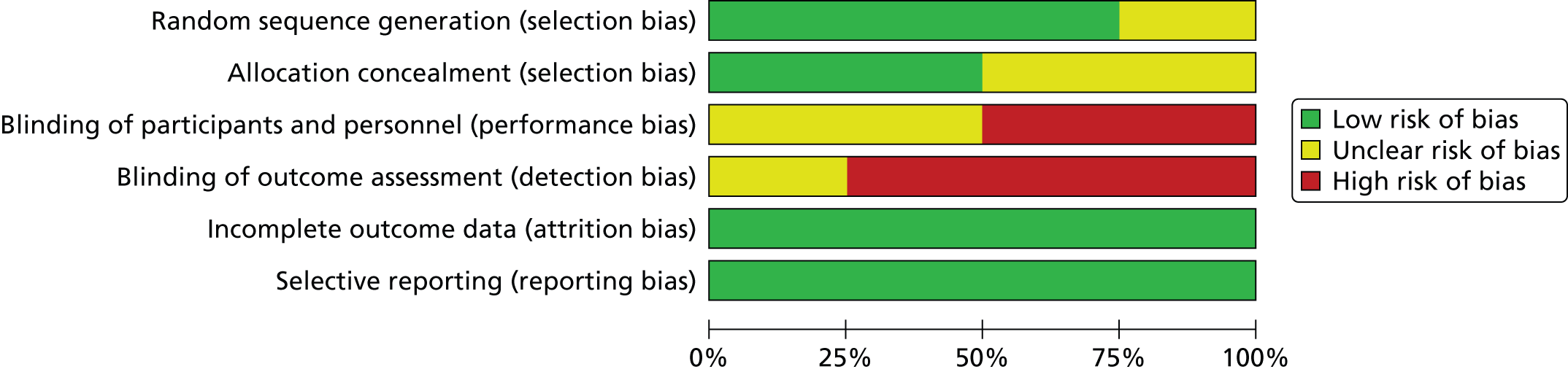
Numerical results
The numerical results reported in the asthma studies58,106–108 are summarised in Table 48. Follow-up assessments ranged from 2 weeks in Smyth et al. 107 to 28 weeks in Warner et al. 108 Total sample sizes ranged from 77 patients in Harris et al. 106 to 28 patients in Theadom et al. 58 The most frequent outcome evaluated was lung function through spirometry. The follow-up assessments for forced expiratory volume in 1 second (FEV1)/forced vital capacity (FCV) were performed immediately after the writing and at short term. Warner et al. 108 reported a statistically significant group-by-time interaction between the two groups for the positive affect subscale of the Positive and Negative Affect Schedule for Children (PANAS-PA) and on the Child Behavior Checklist (CBCL), in favour of the EW group. However, no differences between groups were found for lung function, the negative affect subscale of the Positive and Negative Affect Schedule for Children (PANAS-NA) or mood changes. In Warner et al. ,108 participants rated their mood and physical symptoms immediately before and after each day’s writing and change scores (after writing – before writing) were computed for all ratings, but were not reported. There were significant group main effects for two variables: the disclosure group participants rated themselves as significantly less calm and angrier after writing than did control group participants. A marginal group effect was also found for the physical symptom ratings, with the disclosure group reporting slightly higher levels of physical symptoms after writing compared with control subjects, who reported a slight decrease in physical symptoms following the writing. Finally, there was one significant early effect. Participants in both groups reported a greater increase in sadness after writing on the third day relative to the first and second days.
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group 1 | Intervention group 2 | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean scoreb | SDb | Change score | SDb | n totala | Final mean scoreb | SDb | Change score | SDb | n totala | Final mean scoreb | SDb | Change score | SDb | ||||
| Harris 2005106 | FEV1% pred | 8 | 41 | 76.2 | 18.9 | 4.2 | 8.2 | 37 | 75.5 | 17.2 | 1.3 | 7.3 | 36 | 77.1 | 17.1 | 3 | 4.4 | NSc |
| FVC | 8 | 41 | 80.2 | 20 | 3.1 | 10.1 | 37 | 79.2 | 14.5 | 3.6 | 9.0 | 36 | 78.5 | 15 | 2.4 | 4.6 | NSc | |
| Adherence | 8 | NR | NR | NR | – | – | – | – | – | – | – | NR | NR | NR | – | – | NS | |
| Smyth 1999107 | FEV1% pred | 2 | 39 | 74.1 | 3.3 | – | – | – | – | – | – | – | 19 | 58.8 | 3.9 | – | – | NS |
| FEV1% pred | 8 | 39 | 74.7 | 3.4 | – | – | – | – | – | – | – | 19 | 65.8 | 3.2 | – | – | NS | |
| FEV1% pred | 16 | 39 | 76.3 | 3.2 | – | – | – | – | – | – | – | 19 | 65.3 | 3.2 | – | – | NS | |
| Theadom 201058 | Asthma symptoms | 1 | 13 | NR | NR | – | – | – | – | – | – | – | 15 | NR | NR | – | – | NS |
| Warner 2006108 | ASS | 8 | 28 | 10.25 | 4.77 | – | – | – | – | – | – | – | 22 | 11.05 | 6.66 | – | – | NR |
| FEV1% pred | 8 | 15 | 95.67 | 13.73 | – | – | – | – | – | – | – | 17 | 94.76 | 10.56 | – | – | NS | |
| FDI | 8 | 28 | 5.36 | 6.09 | – | – | – | – | – | – | – | 22 | 7.27 | 5.71 | – | – | NS | |
| PANAS-NA | 8 | 28 | 1.59 | 0.44 | – | – | – | – | – | – | – | 22 | 1.66 | 0.62 | – | – | NS | |
| PANAS-PA | 8 | 28 | 3.35 | 0.75 | – | – | – | – | – | – | – | 22 | 3 | 0.57 | – | – | SS | |
| CBCL-youth | 8 | 28 | 49.07 | 10.17 | – | – | – | – | – | – | – | 22 | 50.86 | 11.4 | – | – | SS | |
| Adherenced (rate) | 8 | 28 | Number of patients: 27 | – | – | – | – | – | – | – | – | 22 | Number of patients: 22 | – | – | – | NR | |
| Mood – calm | Day 1 | 28 | – | – | –1 | 2.22 | – | – | – | – | – | 22 | – | – | – | – | NS | |
| Day 2 | 28 | – | – | –0.52 | 1.81 | – | – | – | – | – | 22 | – | – | 0 | 1.7 | NS | ||
| Day 3 | 28 | – | – | –0.44 | 1.83 | – | – | – | – | – | 22 | – | – | –0.19 | 1.81 | NS | ||
| Mood – enthusiastic | Day 1 | 28 | – | – | –0.7 | 1.32 | – | – | – | – | – | 22 | – | – | –0.43 | 2.04 | NS | |
| Day 2 | 28 | – | – | –0.2 | 1.8 | – | – | – | – | – | 22 | – | – | –0.48 | 1.83 | NS | ||
| Day 3 | 28 | – | – | –0.36 | 1.38 | – | – | – | – | – | 22 | – | – | –0.29 | 1.45 | NS | ||
| Mood – sad | Day 1 | 28 | – | – | 0.08 | 1.56 | – | – | – | – | – | 22 | – | – | –0.57 | 1.33 | NS | |
| Day 2 | 28 | – | – | –0.08 | 0.97 | – | – | – | – | – | 22 | – | – | –0.43 | 1.12 | NS | ||
| Day 3 | 28 | – | – | 0.29 | 1.04 | – | – | – | – | – | 22 | – | – | –0.48 | 1.78 | NS | ||
| Mood – afraid | Day 1 | 28 | – | – | –0.08 | 1.26 | – | – | – | – | – | 22 | – | – | –0.29 | 1.42 | NS | |
| Day 2 | 28 | – | – | –0.24 | 1.09 | – | – | – | – | – | 22 | – | – | –0.38 | 1.28 | NS | ||
| Day 3 | 28 | – | – | 0.16 | 1.11 | – | – | – | – | – | 22 | – | – | –0.05 | 1.2 | NS | ||
| Mood – angry | Day 1 | 28 | – | – | –0.16 | 1.84 | – | – | – | – | – | 22 | – | – | –0.81 | 1.66 | NS | |
| Day 2 | 28 | – | – | 0.4 | 1 | – | – | – | – | – | 22 | – | – | –0.38 | 0.67 | NS | ||
| Day 3 | 28 | – | – | 0.16 | 1.37 | – | – | – | – | – | 22 | – | – | –0.67 | 1.28 | NS | ||
| ASS | Day 1 | 28 | – | – | 0.1 | 0.44 | – | – | – | – | – | 22 | – | – | –0.18 | 0.4 | NS | |
| Day 2 | 28 | – | – | 0.04 | 0.39 | – | – | – | – | – | 22 | – | – | –0.06 | 0.36 | NS | ||
| Day 3 | 28 | – | – | –0.02 | 0.39 | – | – | – | – | – | 22 | – | – | –0.1 | 0.37 | NS | ||
The remaining studies did not report on any association between the groups across time for the outcomes assessed.
Meta-analysis
The percentage of predicted forced expiratory volume in 1 second (FEV1% pred) was the outcome meta-analysed (Figure 35). Three studies106–108 assessed lung function by means of spirometry.
FIGURE 35.
Forest plot of FEV1% at short term in asthma patients. df, degrees of freedom; IV, inverse variance.

-
Clinical differences between studies Participants in Warner et al. 108 were adolescents aged 12–17 years, whereas the other two studies106,107 included adults. In addition, all participants in Warner et al. 108 reported never having smoked, as opposed to the participants in the other studies,106,107 which had a proportion of non-smokers, ex-smokers and current smokers.
-
Follow-up length All studies included in the meta-analysis evaluated the impact of TW at 8 and 13 weeks (short-term follow-up). In addition, Smyth et al. 107 assessed FEV1% pred at 2 weeks (immediate follow-up).
-
Forest plot A total of 167 participants were meta-analysed (95 in the EW group and 72 in the control group). The SMD was 0.24 (95% CI –0.07 to 0.56) with a random-effects model and with no heterogeneity (I2 = 0%). This result suggests that there is no statistically significant difference in mean percentage of FEV1 at short term for the TW groups compared with the control groups.
K58: irritable bowel syndrome
Overview
There were two studies evaluating unfacilitated EW. A summary of main characteristics is presented in Table 49. Halpert et al. 52 evaluated young participants who were diagnosed with IBS using the Rome III Criteria for IBS. This study52 was conducted entirely online with participants recruited via adverts at IBS-related websites and the intervention writing submitted online. Wallander et al. 109 evaluated young participants who were diagnosed with gastrointestinal (GI) recurrent abdominal pain (RAP) meeting the Apley’s criteria for functional RAP. Both studies52,109 were conducted in the USA.
| First author, year | Study design | Intervention group | Control group |
|---|---|---|---|
| Halpert 201052 | Non-RCT | Unfacilitated EW (via internet) | Non-writing |
| Wallander 2011109 | RCT | Unfacilitated EW | SMC |
Halpert et al. 52 was conducted entirely online and only young participants were recruited. The separation of writing group compared with non-writing group was formed post hoc after completing the four writing exercises. Thus, participants completing all four writing assignments became the writing group (intervention group) and those who initially intended to write but did not write became the non-writing group (control group). For the purposes of the systematic review, this comparator group was considered as a suitable comparator, even though it seems that the researchers were not planning to have a comparator group and assumed that some participants did not write happened at random. The Wallander et al. study109 used a written standard disclosure intervention, whereby each young participant was taken to a private room in the clinic to perform the first session and then was sent home to complete the remaining two assignments. The control group received usual care.
The outcomes evaluated in the studies52,109 on IBS/GI RAP are reported in Table 50. QoL was evaluated in both studies. 52,109 The remaining outcomes were assessed once in each study.
| First author, year | Pain frequency | Pain severity | Somatisation severity | Cognition concerning their IBS | Catastrophising/coping | QoL | Resource use |
|---|---|---|---|---|---|---|---|
| Halpert 201052 | – | IBSSS | – | CG-FBD | CT3 | IBS-QoL | – |
| Wallander 2011109 | The abdominal pain frequency rating | – | CSI | – | – | PedsQL | Number of visits to clinician |
Quality assessment
A summary of the quality of the studies in IBS/GI RAP is shown in Figure 36. Halpert et al. 52 was described as an exploratory study, and was not randomised. It is likely to be at very high risk of selection bias because the intervention group included only those who completed the entire 4-day writing exercise (and those who did not were excluded as dropouts). On the other hand, the comparison group comprised participants recruited to the intervention but who did not even start it (the non-writers group). Wallander et al. ,109 which was a randomised trial, was at high risk of bias across some domains such as selection, detection and attrition biases. Neither study involved ITT analysis.
FIGURE 36.
Risk-of-bias summary in the IBS/GI RAP studies.

Numerical results
The numerical results reported in the IBS/GI RAP studies52,109 are summarised in Table 51. Follow-up assessments were 4 weeks in Halpert et al. 52 and 26 weeks in Wallander et al. 109 Total sample sizes were 103 and 56 participants in Halpert et al. 52 and Wallander et al. ,109 respectively.
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean score | SD | Change score | SD | n totala | Final mean score | SD | Change score | SD | ||||
| Halpert 201052 | CT3 | 4 | 82 | – | – | –2.15 | 0.62 | 21 | – | – | 0.28 | 1.23 | NS |
| 13 | 82 | – | – | –3.68 | 0.86 | 21 | – | – | –2.38 | 1.4 | NS | ||
| IBS-QoL | 4 | 82 | – | – | 1.85 | 1.68 | 21 | – | – | –0.83 | 3.41 | NS | |
| 13 | 82 | – | – | 5.69 | 2.38 | 21 | – | – | –0.27 | 3.94 | NS | ||
| CG-FBD | 4 | 82 | – | – | –0.19 | 0.08 | 21 | – | – | 0.13 | 0.15 | NS | |
| 13 | 82 | – | – | –0.43 | 0.11 | 21 | – | – | 0.15 | 0.17 | SS | ||
| CG-FBD Q16 | 4 | 82 | – | – | –0.23 | 0.12 | 21 | – | – | 0.52 | 0.25 | SS | |
| 13 | 82 | – | – | –0.27 | 0.17 | 21 | – | – | 0.35 | 0.27 | NS | ||
| CG-FBD Q31 | 4 | 82 | – | – | –0.11 | 0.15 | 21 | – | – | 0.16 | 0.59 | NS | |
| 13 | 82 | – | – | –0.46 | 0.2 | 21 | – | – | 0.46 | 0.33 | SS | ||
| IBSSS | 4 | 82 | – | – | –13.4 | 4.88 | 21 | – | – | 24.03 | 9.63 | SS | |
| 13 | 82 | – | – | –28.02 | 7.1 | 21 | – | – | 25.74 | 10.91 | SS | ||
| Wallander 2011109 | Abdominal Pain Frequency Rating | 13 | 32 | 1.54 | 1.40 | – | – | 24 | 1.96 | 1.51 | – | – | NS |
| 26 | 32 | 1.35 | 1.39 | – | – | 24 | 2.32 | 1.72 | – | – | SS | ||
| CSI | 13 | 32 | 16.85 | 10.83 | – | – | 24 | 17.64 | 10.07 | – | – | NS | |
| 26 | 32 | 14.14 | 9.06 | – | – | 24 | 15.42 | 8.59 | – | – | NS | ||
| Physical QoL | 13 | 32 | 23.96 | 4.38 | – | – | 24 | 23.75 | 5.83 | – | – | NS | |
| 26 | 32 | 26.32 | 4.69 | – | – | 24 | 23.81 | 6.11 | – | – | NS | ||
| Psychosocial QoL | 13 | 32 | 36.12 | 10.69 | – | – | 24 | 40.39 | 8.59 | – | – | SS | |
| 26 | 32 | 43.29 | 9.20 | – | – | 24 | 41.38 | 8.87 | – | – | NS | ||
| n of visits clinician | 26 | 32 | 1.00 | 2.36 | – | – | 24 | 2.36 | 2.21 | – | – | SS | |
In Halpert et al. ,52 there were statistically significant differences at 4 weeks for the following outcomes: the functional bowel disease-related cognition [Functional Bowel Disease-related Cognition questionnaire 31 (CG-FBD Q31)] and IBS severity [Irritable Bowel Syndrome Severity Scale (IBSSS)], where improvements were made in favour of the writing. Likewise, at 13 weeks differences between groups were significant for the following outcomes: the functional bowel disease-related cognition [Functional Bowel Disease-related Cognition (CG-FBD) and CG-FBD Q31]; IBS severity (IBSSS); and psychosocial QoL, where improvements were made in favour of the writing group. In addition, between-group differences were reported at 26 weeks as well for the abdominal pain frequency rating and number of visits to the clinician in favour of the writing group.
Physical symptoms and resource use were reported to be significantly reduced at short time points assessments in both studies. Wallander et al. 109 reported a significant reduction in pain and frequency of clinician visits in the intervention group at 26 weeks also, but no improvement in QoL at this time point. However, QoL was reported as not showing any between group difference when measured at 4 and 13 weeks in Halpert et al. 52 and at 26 weeks in Wallander et al. 109
L40: psoriasis
Overview
There were three studies110–112 evaluating unfacilitated EW in patients with psoriasis. A summary of their main characteristics is presented in Table 52. Paradisi et al. 110 and Tabolli et al. 111 were conducted in Italy, and Vedhara et al. 112 was conducted in New Zealand. In Vedhara et al. 112 and Tabolli et al. 111 a minority of patients were diagnosed with psoriatic arthritis (22% and 19%, respectively). In the latter study,111 psoriatic arthritis was significantly more prevalent in the control group than in the EW group. In Vedhara et al. ,112 patients had plaque-type psoriasis involving > 10% of the body area. In Paradisi et al. ,110 all participants were undergoing phototherapy for their psoriasis.
| First author, year | Study design | Intervention group 1 | Intervention group 2 | Control group 1 |
|---|---|---|---|---|
| Paradisi 2010110 | RCT | Unfacilitated EW | Positive writing | Non-EW |
| Tabolli 2012111 | RCT | Unfacilitated EW | – | Non-writing |
| Vedhara 2007112 | RCT | Unfacilitated EW | – | Factual writing |
The main intervention assessed across studies110–112 was disease-focused writing, including worst experience/trauma/stressful life events. All interventions were delivered on 3–4 consecutive days for 20 minutes each day and by handwriting. Patients were not financially compensated over the study period. One study110 also assessed one other active intervention based on an emotional positive writing technique focused on the best possible future self and achieving life-goals: ‘Think about your life in the future. Imagine that every-thing has gone as well as it possibly could, and the desires related to the psoriasis have been realised’.
The outcomes assessed within the studies110–112 on psoriasis are reported in Table 53. The most frequent outcome evaluated was disease severity from both the clinicians’ [Psoriasis Area and Severity Index (PASI)] and patients’ [Self-Administered Psoriasis Area and Severity Index (SAPASI)] perspectives. QoL was also measured in all three studies110–112 by either general or disease-specific instruments [SF-36, Dermatology Life Quality Index (DLQI) and Skindex-29].
| First author, year | Psoriasis severity | Physical global health | Mood | Psychological distress | Depression and anxiety | QoL | Resource use |
|---|---|---|---|---|---|---|---|
| Paradisi 2010110 | PASI, SAPASI | – | – | GHQ-12 | – | Skindex-29 Symptoms, Emotions and Functioning subscales | – |
| Tabolli 2012111 | PASI, SAPASI | PGA, PtGA, BMI | – | GHQ-12 | – | SF-36, Skindex-29 Symptoms, Emotions and Functioning subscales | – |
| Vedhara 2007112 | PASI | – | POMS | – | HADS-A, HADS-D | DLQI | – |
Quality assessment
All three studies110–112 were randomised, but allocation concealment was unclear in Vedhara et al. 112 Paradisi et al. 110 did not blind study personnel; the remaining studies111,112 were unclear about masking. All three studies110–112 were likely to introduce both performance and detection bias mainly (Figures 37 and 38). Paradisi et al. 110 under-reported data for PASI and data regarding SAPASI had to be derived from a graph, with no measure of variability reported. Vedhara et al. 112 performed ITT analysis, whereas per-protocol analyses were used in the other two studies. 110,111
FIGURE 37.
Risk-of-bias summary in the psoriasis studies.
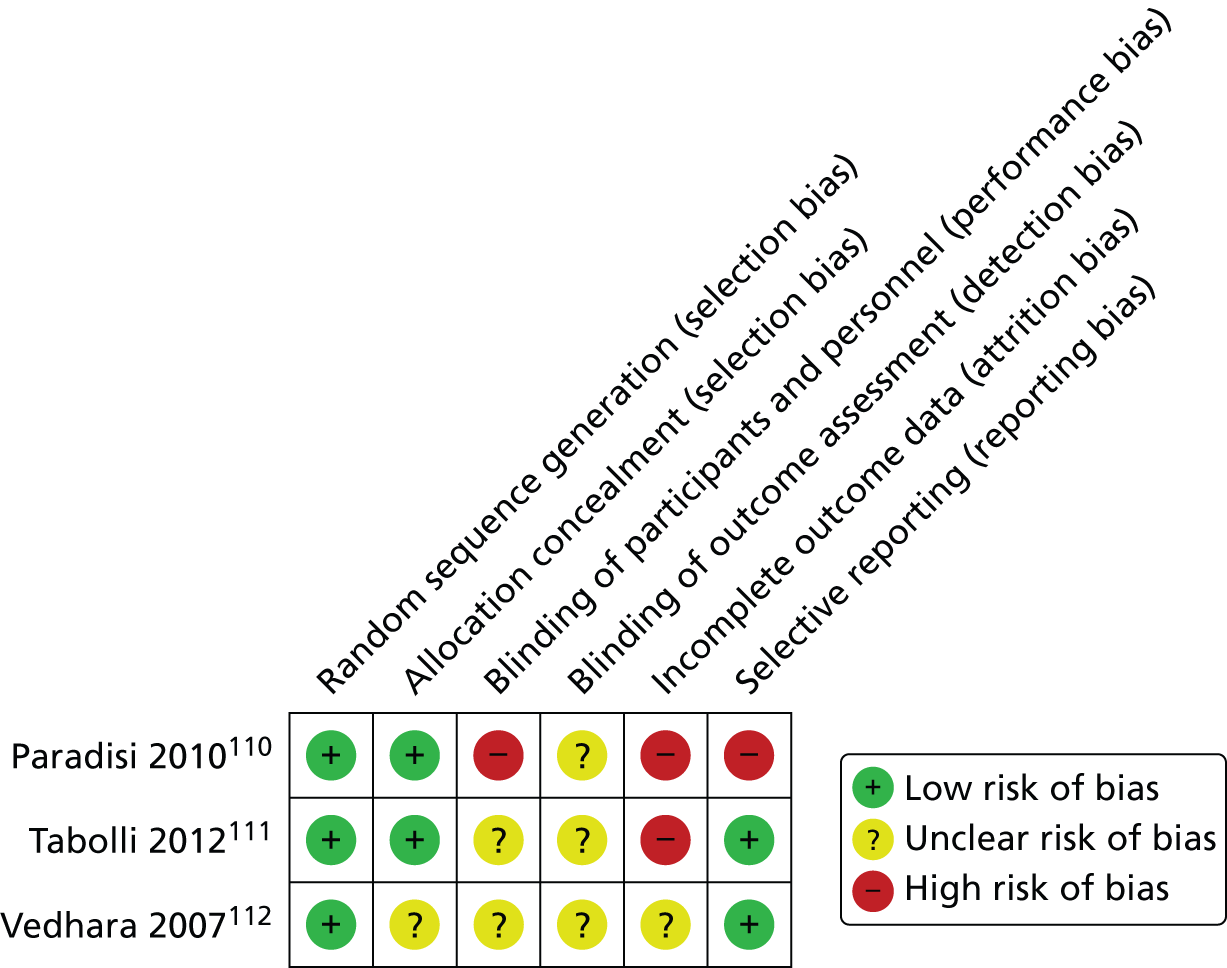
FIGURE 38.
Risk-of-bias graph in the psoriasis studies.

Numerical results
The numerical results reported in the studies on psoriasis are summarised in Table 54. Follow-up assessments were performed from 2 weeks in Vedhara et al. 112 up to 52 weeks in Tabolli et al. 111 Total samples were 78 participants randomised in Paradisi et al. 110 (taking into account both intervention groups), 67 participants in Tabolli et al. 111 and 59 participants in Vedhara et al. 112
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group 1 | Intervention group 2 | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean scoreb | SDb | Change score | SDb | n totala | Final mean scoreb | SDb | Change score | SD | n totala | Final mean scoreb | SDb | Change score | SD | ||||
| Paradisi 2010110 | PASI | 8 | 24 | NR | NR | – | – | 22 | NR | NR | – | – | 26 | NR | NR | – | – | SSc |
| 17 | 15 | NR | NR | – | – | 12 | NR | NR | – | – | 13 | NR | NR | – | – | NR | ||
| SAPASI | 8 | 24 | Median: 4 | NR | – | – | 22 | Median: 2 | NR | – | – | 26 | Median: 2 | NR | – | – | NSc | |
| 17 | 15 | Median: 4.8 | NR | – | – | 12 | Median: 5.8 | NR | – | – | 13 | Median: 6 | NR | – | – | SSc | ||
| GHQ-12 | 8 | 24 | Median: 8 | Range 5–16 | – | – | 22 | Median: 8 | Range: 2–19 | – | – | 26 | Median: 11 | Range 3–24 | – | – | NR | |
| 17 | 15 | Median: 9 | Range 0–17 | – | – | 12 | Median: 8 | Range: 4–28 | – | – | 13 | Median: 12 | Range: 3–27 | – | – | NR | ||
| Skindex-29 Symptoms | 8 | 24 | Median: 14 | Range 0–50 | – | – | 22 | Median: 21 | Range 0–46 | – | – | 26 | Median: 21 | Range: 0–60 | – | – | NR | |
| 17 | 15 | Median: 25 | Range 0–46 | – | – | 12 | Median: 20 | Range 0–64 | – | – | 13 | Median: 25 | Range 4–68 | – | – | NR | ||
| Skindex-29 Functioning | 8 | 24 | Median: 12 | Range 0–44 | – | – | 22 | Median: 3 | Range 0–71 | – | – | 26 | Median: 19 | Range 2–42 | – | – | NR | |
| 17 | 15 | Median: 23 | Range 0–58 | – | – | 22 | Median: 6 | Range 0–75 | – | – | 26 | Median: 19 | Range 2–67 | – | – | NR | ||
| Skindex-29 Emotions | 8 | 24 | Median: 25 | Range 0–42 | – | – | 22 | Median: 16 | Range 0–80 | – | – | 26 | Median: 30 | Range 5–80 | – | – | NR | |
| 17 | 15 | Median: 35 | Range 0–57 | – | – | 22 | Median: 21 | Range 0–82 | – | – | 26 | Median: 30 | Range 7–67 | – | – | NR | ||
| Tabolli 2012111 | PASI | 4 | 32 | 9.50 | 6.40 | – | – | – | – | – | – | – | 35 | 11 | 8.7 | – | – | NS |
| 26 | 32 | 5.80 | 7.90 | – | – | – | – | – | – | – | 35 | 8.6 | 9.5 | – | – | NS | ||
| 52 | 32 | 5.70 | 7.90 | – | – | – | – | – | – | – | 35 | 4.3 | 4.5 | – | – | NS | ||
| SAPASI | 4 | 32 | 10.30 | 7.50 | – | – | – | – | – | – | – | 35 | 12.3 | 9.5 | – | – | NS | |
| 26 | 32 | 5.40 | 9.10 | – | – | – | – | – | – | – | 35 | 10.1 | 11.7 | – | – | NS | ||
| 52 | 32 | 7.30 | 9.00 | – | – | – | – | – | – | – | 35 | 6 | 7.5 | – | – | NS | ||
| Skindex-29 Symptoms | 4 | 32 | 37.80 | 20.50 | – | – | – | – | – | – | – | 35 | 38.2 | 19.7 | – | – | NS | |
| 26 | 32 | 24.40 | 22.30 | – | – | – | – | – | – | – | 35 | 32.7 | 23.9 | – | – | NS | ||
| 52 | 32 | 26.90 | 22.50 | – | – | – | – | – | – | – | 35 | 24.3 | 21.1 | – | – | NS | ||
| Skindex-29 Emotions | 4 | 32 | 34.80 | 22.70 | – | – | – | – | – | – | – | 35 | 37.2 | 19.5 | – | – | NS | |
| 26 | 32 | 27.70 | 21.10 | – | – | – | – | – | – | – | 35 | 33.6 | 22.4 | – | – | NS | ||
| 52 | 32 | 27.70 | 19.90 | – | – | – | – | – | – | – | 35 | 28.5 | 21.9 | – | – | NS | ||
| Skindex-29 Functioning | 4 | 32 | 28.80 | 23.10 | – | – | – | – | – | – | – | 35 | 27.7 | 21.3 | – | – | NS | |
| 26 | 32 | 22.50 | 20.50 | – | – | – | – | – | – | – | 35 | 23.7 | 23.1 | – | – | NS | ||
| 52 | 32 | 21.40 | 20.80 | – | – | – | – | – | – | – | 35 | 21.3 | 22 | – | – | NS | ||
| GHQ-12 | 4 | 32 | 11.30 | 5.60 | – | – | – | – | – | – | – | 35 | 12.4 | 6.6 | – | – | NS | |
| 26 | 32 | 9.80 | 5.00 | – | – | – | – | – | – | – | 35 | 10.6 | 5.8 | – | – | NS | ||
| 52 | 32 | 10.60 | 4.50 | – | – | – | – | – | – | – | 35 | 10.7 | 5.6 | – | – | NS | ||
| SF-36 PCS | 4 | 32 | 50.00 | 6.30 | – | – | – | – | – | – | – | 35 | 48 | 11.4 | – | – | NS | |
| 26 | 32 | 52.40 | 5.60 | – | – | – | – | – | – | – | 35 | 49.4 | 7.8 | – | – | NS | ||
| 52 | 32 | 52.20 | 6.90 | – | – | – | – | – | – | – | 35 | 47.5. | 6.1 | – | – | SS | ||
| SF-36 MCS | 4 | 32 | 39.60 | 12.10 | – | – | – | – | – | – | – | 35 | 42.1 | 7.7 | – | – | NS | |
| 26 | 32 | 42.50 | 10.40 | – | – | – | – | – | – | – | 35 | 41.5 | 8.8 | – | – | NS | ||
| 52 | 32 | 42.70 | 9.10 | – | – | – | – | – | – | – | 35 | 42.5 | 7.3 | – | – | NS | ||
| BMI | 4 | 32 | 26.60 | 5.90 | – | – | – | – | – | – | – | 35 | 26.5 | 6.3 | – | – | NS | |
| 26 | 32 | 27.50 | 7.80 | – | – | – | – | – | – | – | 35 | 26.6 | 6.3 | – | – | NS | ||
| 52 | 32 | 27.00 | 5.70 | – | – | – | – | – | – | – | 35 | 26.8 | 6.5 | – | – | NS | ||
| PGA | 4 | 32 | 1.84 | 0.90 | – | – | – | – | – | – | – | 35 | 1.8 | 0.9 | – | – | NS | |
| 26 | 32 | 0.84 | 1.10 | – | – | – | – | – | – | – | 35 | 1.3 | 1.1 | – | – | NS | ||
| 52 | 32 | 1.03 | 1.40 | – | – | – | – | – | – | – | 35 | 0.8 | 1 | – | – | NS | ||
| PtGA | 4 | 32 | 1.65 | 0.90 | – | – | – | – | – | – | – | 35 | 1.9 | 0.8 | – | – | NS | |
| 26 | 32 | 0.94 | 1.20 | – | – | – | – | – | – | – | 35 | 1.4 | 1.2 | – | – | NS | ||
| 52 | 32 | 1.03 | 1.10 | – | – | – | – | – | – | – | 35 | 1 | 1 | – | – | NS | ||
| Vedhara 2007112 | PASI | 2 | 31 | 6.74 | 4.47 | – | – | – | – | – | – | – | 28 | 6.47 | 4.74 | – | – | NS |
| 8 | 31 | 6.09 | 3.40 | – | – | – | – | – | – | – | 28 | 5.69 | 2.77 | – | – | NS | ||
| 12 | 31 | 5.57 | 2.99 | – | – | – | – | – | – | – | 28 | 5.61 | 3.54 | – | – | NS | ||
| DLQI | 2 | 31 | 6.53 | 6.08 | – | – | – | – | – | – | – | 28 | 6.31 | 4.99 | – | – | NS | |
| 8 | 31 | 5.18 | 5.26 | – | – | – | – | – | – | – | 28 | 4.36 | 3.4 | – | – | NS | ||
| 12 | 31 | 5.39 | 4.59 | – | – | – | – | – | – | – | 28 | 4.82 | 3.82 | – | – | NS | ||
| POMS | 2 | 31 | 47.49 | 31.07 | – | – | – | – | – | – | – | 28 | 51.88 | 34.4 | – | – | NS | |
| 8 | 31 | 39.69 | 29.44 | – | – | – | – | – | – | – | 28 | 37.91 | 18.3 | – | – | NS | ||
| 12 | 31 | 38.20 | 26.83 | – | – | – | – | – | – | – | 28 | 40.27 | 21.05 | – | – | NS | ||
| HADS-A | 2 | 31 | 6.51 | 3.93 | – | – | – | – | – | – | – | 28 | 7.52 | 3.87 | – | – | NS | |
| 8 | 31 | 5.83 | 3.06 | – | – | – | – | – | – | – | 28 | 6.36 | 3.34 | – | – | NS | ||
| 12 | 31 | 5.81 | 3.14 | – | – | – | – | – | – | – | 28 | 6.54 | 3.66 | – | – | NS | ||
| HADS-D | 2 | 31 | 6.43 | 8.62 | – | – | – | – | – | – | – | 28 | 5.93 | 9.5 | – | – | NS | |
| 8 | 31 | 4.01 | 4.11 | – | – | – | – | – | – | – | 28 | 4.01 | 3.21 | – | – | NS | ||
| 12 | 31 | 4.38 | 4.44 | – | – | – | – | – | – | – | 28 | 3.68 | 3.36 | – | – | NS | ||
Few statistical differences between groups were reported in the three studies,110–112 although typically both control and intervention groups improved over time. Significant effects in favour of the written emotional disclosure groups compared with control subjects were reported on the following outcomes: PASI scores at 8 weeks, SAPASI scores at 17 weeks and SF-36 PCS. No effect between groups by time interaction was reported for the remaining outcome measures.
All three studies110–112 assessed psoriasis severity at short term (at 4 and 8 weeks) using PASI and SAPASI questionnaires. However, in Paradisi et al. ,110 data on the PASI (the clinician-rated version as opposite to the SAPASI, the participant self-rated index) were not reported and therefore a meta-analysis could not be performed.
M06 and M45: inflammatory arthropathies
Overview
There were six studies107,113–117 evaluating unfacilitated EW in inflammatory arthropathy patients. A summary of main characteristics is presented in Table 55. Hamilton-West and Quine114 assessed patients with ankylosing spondylitis (AS). The remaining studies involved patients diagnosed with RA. Four studies107,113,115,116 were conducted in the USA but Wetherell et al. 117 and Hamilton-West and Quine114 were conducted in the UK. All of the included studies107,113–117 examined the effect of unfacilitated EW about a stressful or traumatic event/s in an emotional way for 20 minutes on 3 or 4 consecutive days. Broderick et al. 113 included a second intervention group to assess the impact of EW about the meaning of the trauma. Lumley et al. 116 had four groups: two coping skills training (one EW intervention and one control) and two with arthritis education (one EW intervention and one control). These were combined in the publication to provide scores for the unfacilitated EW and control groups.
| First author, year | Study design | Intervention group 1 | Intervention group 2 | Control groups |
|---|---|---|---|---|
| Broderick 2004113 | RCT | Unfacilitated EW | EW with meaning writing | Time-management writing |
| Hamilton-West 2007114 | RCT | Unfacilitated EW | – | Time-management writing |
| Lumley 2011115 | RCT | Unfacilitated EW | Positive writing | Time-management writing |
| Lumley 2014116 | RCT | Unfacilitated EW with coping skills training | Unfacilitated EW with arthritis education | 1. Time-management writing with coping skills training 2. Time-management writing with arthritis education |
| Smyth 1999107 | RCT | Unfacilitated EW | – | Time-management writing |
| Wetherell 2005117 | RCT | Unfacilitated EW | – | Time-management writing |
In all studies except Lumley et al. ,116 the control group carried out time-management writing, writing in an unemotional way about their plans or activities on specific days (e.g. the next day, next week). Lumley et al. 115 used a second control arm, in which participants were asked to write about positive emotional events in their lives in an emotional way. Results for these two control groups were combined together in the paper but are presented separately here. This positive writing intervention is analysed separately in a later section of this systematic review. The effect of having an active intervention as a control is likely to have reduced the ability of this study to demonstrate an effect of EW, so we have presented results for the two different control interventions separately and have omitted the results for the combined control. It should be noted that Lumley et al. 115 was powered to compare the intervention against the two control interventions combined. (Neither Brodericks et al. ’s113 nor Lumleys et al. ’s115 alternative writing interventions are included in meta-analyses here.) Lumley et al. 115 also examined a spoken emotional disclosure intervention, which was compared with spoken control groups; however, these results are not discussed further here, as it appeared that the speaking intervention was not specifically designed for those who were unable write.
In Wetherell et al. ,117 participants were contacted at home by telephone at a prearranged time and told of the topic on which they would be writing on for the next 20 minutes. However, it is important to note that the facilitator (the term used in the paper to define the researcher delivering the intervention) was available only by telephone should the need arise.
The outcomes assessed within the studies on inflammatory arthropathies are reported in Table 56.
| First author, year | Disease activity/severity | Biomarker of inflammation | Affective/sensory pain | Pain behaviour | Physical symptoms | Mood or affect | Depression | QoL/well-being | Resource use |
|---|---|---|---|---|---|---|---|---|---|
| Broderick 2004113 | DAS | – | – | – | – | – | – | SF-36v2 Health Survey | – |
| Hamilton-West 2007114 | BASDAI | – | – | – | BASFI | – | HADS-D | BAS-G | – |
| Lumley 2011115 | Swollen joint count, walking speed, grip strength, physician’s global rating of disease activity (100-mm VAS) | ESR | McGill Pain Q-SF | OPB | AIMS2: physical dysfunction subscale | PANAS-X AIMS2: affective disturbance subscales |
– – |
– – |
– – |
| Lumley 2014116 | Walking speed, physician’s global rating of disease activity (100-mm VAS) | CRP | McGill Pain Q | – | AIMS2 | – | – | – | – |
| Smyth 1999107 | DAS | – | – | – | – | – | – | – | – |
| Wetherell 2005117 | Swollen and tender joint count, patients rating of disease activity (100-mm VAS), DAS | ESR, CRP | – | – | – | POMS-SF | – | – | – |
Quality assessment
A summary of the quality of the studies in inflammatory arthropathy is shown in Figures 39 and 40. All studies were described as randomised but Broderick et al. 113 did not provide the method of randomisation. Blinding of participants and personnel was performed only in Broderick et al. 113 and Smyth et al. 107 Almost all studies (except Lumley et al. 115) introduced reporting bias in several ways: either by omission of the outcomes, by providing subscales of a full measurement scale without providing the total score, or by under-reporting the data, that is not giving enough detail for the data to be included in the meta-analysis. For instance, in Hamilton-West and Quine,114 results regarding disease activity [Bath Ankylosing Spondylitis Disease Functional Index (BASFI)] were not adequately reported. Mean values were derived from a graph without no information regarding variability and no other data were provided among the outcomes a priori evaluated.
FIGURE 39.
Risk-of-bias summary in the inflammatory arthropathy studies.
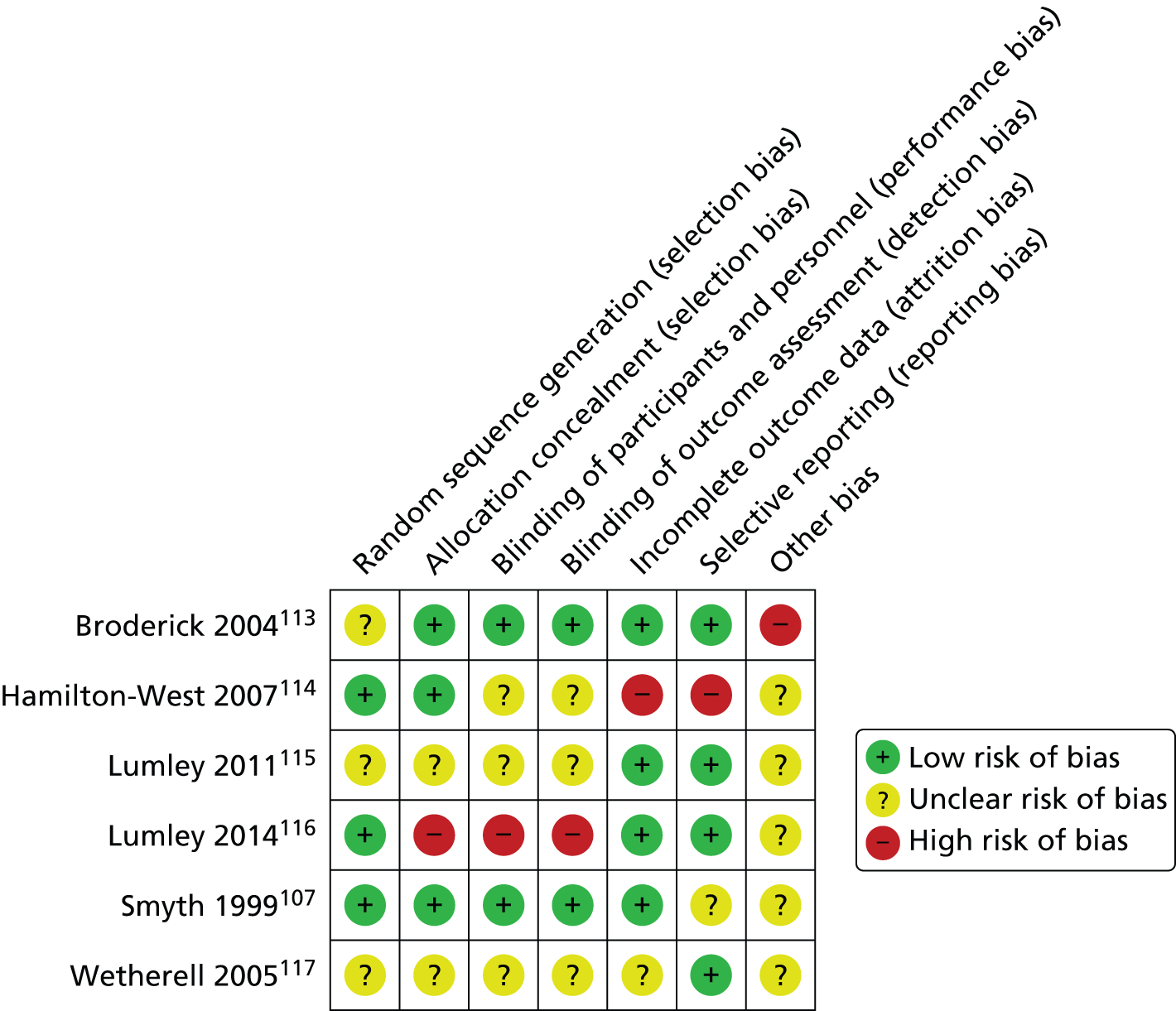
FIGURE 40.
Risk-of-bias graph in the inflammatory arthropathy studies.
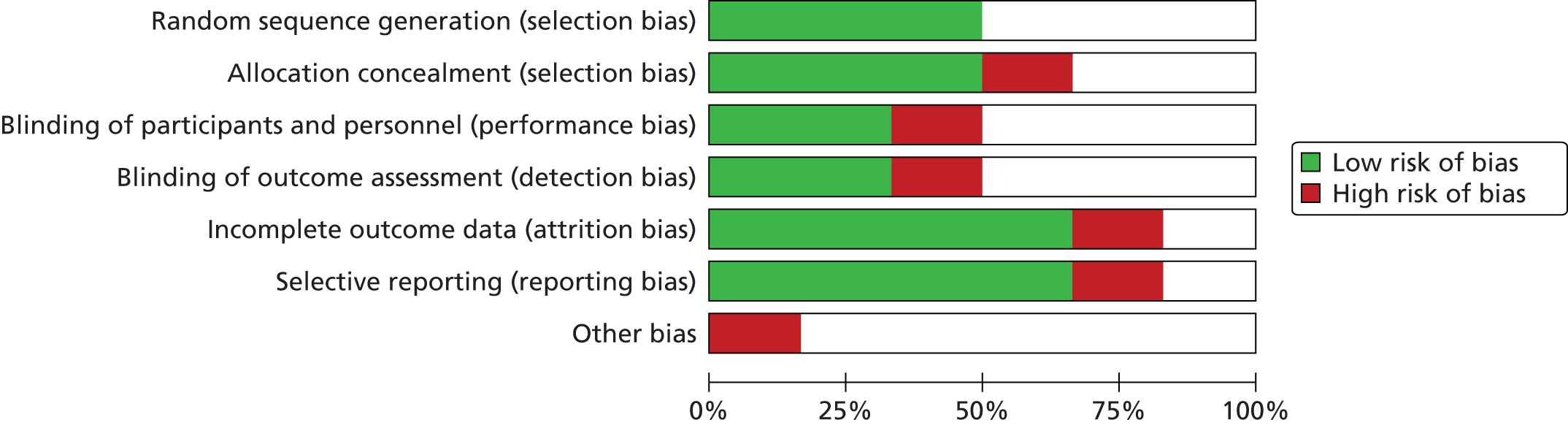
Numerical results
The numerical results reported in the studies on inflammatory arthropathies are summarised in Table 57. The shorter follow-up assessments was performed just after writing in Lumley et al. 115 when assessing immediate mood. Otherwise, the follow-up length varied from 1 week in Wetherell et al. 117 to 26 weeks in Broderick et al. 113 and Lumley et al. 115 The total sample sizes ranged from 34 participants in Wetherell et al. 117 to 218 participants in Broderick et al. 113
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group 1 | Intervention group 2 | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean score | SD | Change score | SD | n totala | Final mean score | SD | Change score | SD | n totala | Final mean score | SD | Change score | SD | ||||
| Broderick 2004113 | DASb | 26 | 78 | – | – | –0.31 | NR | 80 | – | – | –0.55 | 60 | – | – | –0.49 | NSc | ||
| SF-36 vs. SF-36 PCS | 26 | 76 | – | – | 0.27 | NR | 76 | – | – | –0.51 | NR | 58 | – | – | 0.14 | NSc | ||
| Hamilton-West 2007114 | BASDAI | 4 | 39 | NR | NR | – | – | – | – | – | – | – | 19 | NR | NR | – | – | NS |
| 13 | 30 | NR | NR | – | – | – | – | – | – | – | 15 | NR | NR | – | – | NS | ||
| HADS | 4 | 39 | NR | NR | – | – | – | – | – | – | – | 19 | NR | NR | – | – | NS | |
| 13 | 30 | NR | NR | – | – | – | – | – | – | – | 15 | NR | NR | – | – | NS | ||
| BASFI | 4 | 39 | 4.76 | NR | – | – | – | – | – | – | – | 19 | 5.33 | NR | – | – | NR | |
| 13 | 30 | 4.78 | NR | – | – | – | – | – | – | – | 15 | 5.62 | NR | – | – | SS | ||
| BAS-G | 4 | 39 | NR | NR | – | – | – | – | – | – | – | 19 | NR | NR | – | – | NS | |
| 13 | 30 | NR | NR | – | – | – | – | – | – | – | 15 | NR | NR | – | – | NS | ||
| Lumley 2011115 | PANAS-a | Just after writing | 43 | – | – | 0.4 | 0.99 | 24 | – | – | –0.36 | 1 | 21 | – | – | –0.02 | 0.84 | SSc |
| PANAS-f | Just after writing | 43 | – | – | 0.08 | 1.05 | 24 | – | – | –0.18 | 0.53 | 21 | – | – | 0.06 | 0.38 | NSc | |
| PANAS-s | Just after writing | 43 | – | – | 0.47 | 1.12 | 24 | – | – | –0.14 | 0.6 | 21 | – | – | 0 | 0.61 | SSc | |
| PANAS-g | Just after writing | 43 | – | – | 0.14 | 1 | 24 | – | – | –0.45 | 0.76 | 21 | – | – | –0.11 | 0.69 | SSc | |
| PANAS-pn | Just after writing | 43 | – | – | 5.08 | 0.9 | 24 | – | – | 4.94 | 1.3 | 21 | – | – | 3.4 | 2.14 | SSc | |
| PANAS-r | Just after writing | 43 | – | – | 4.88 | 0.88 | 24 | – | – | 4.7 | 1.25 | 21 | – | – | 3 | 2 | SSc | |
| PANAS-m | Just after writing | 43 | – | – | 4.79 | 1.05 | 24 | – | – | 4.98 | 0.94 | 21 | – | – | 2.75 | 1.9 | SSc | |
| PANAS-i | Just after writing | 43 | – | – | 3.02 | 1.57 | 24 | – | – | 1.91 | 1.68 | 21 | – | – | 1.93 | 1.61 | NR | |
| MPQ-s | 4 | 43 | 0.56 | 0.57 | – | – | 24 | 0.9 | 0.85 | – | – | 21 | 0.88 | 0.61 | – | – | NSc | |
| 13 | 43 | 0.71 | 0.59 | – | – | 24 | 0.8 | 0.74 | – | – | 21 | 0.56 | 0.5 | – | – | NSc | ||
| 26 | 43 | 0.59 | 0.52 | – | – | 24 | 0.99 | 0.84 | – | – | 21 | 0.68 | 0.65 | – | – | NSc | ||
| MPQ-a | 4 | 43 | 0.40 | 0.59 | – | – | 24 | 0.53 | 0.68 | – | – | 21 | 0.57 | 0.58 | – | – | NSc | |
| 13 | 43 | 0.31 | 0.43 | – | – | 24 | 0.52 | 0.76 | – | – | 21 | 0.3 | 0.28 | – | – | NSc | ||
| 26 | 43 | 0.24 | 0.35 | – | – | 24 | 0.6 | 0.75 | – | – | 21 | 0.43 | 0.56 | – | – | SSc | ||
| AIMS-ps | 4 | 43 | 2.12 | 0.65 | – | – | 24 | 2.05 | 0.69 | – | – | 21 | 2.07 | 0.85 | – | – | NSc | |
| 13 | 43 | 2.03 | 0.65 | – | – | 24 | 2.2 | 0.89 | – | – | 21 | 2.07 | 0.65 | – | – | NSc | ||
| 26 | 43 | 1.94 | 0.61 | – | – | 24 | 2.25 | 0.77 | – | – | 21 | 2.19 | 0.87 | – | – | NSc | ||
| AIMS-as | 4 | 43 | 2.36 | 0.81 | – | – | 24 | 2.27 | 0.7 | – | – | 21 | 2.12 | 0.65 | – | – | NSc | |
| 13 | 43 | 2.43 | 0.88 | – | – | 24 | 2.44 | 0.72 | – | – | 21 | 2.13 | 0.65 | – | – | NSc | ||
| 26 | 43 | 2.39 | 0.86 | – | – | 24 | 2.44 | 0.73 | – | – | 21 | 2.26 | 0.59 | – | – | NSc | ||
| OPB | 4 | 43 | 13.17 | 8.86 | – | – | 24 | 11.52 | 8.12 | – | – | 21 | 12.43 | 8.62 | – | – | NSc | |
| 13 | 43 | 10.55 | 7.28 | – | – | 24 | 10.6 | 7.28 | – | – | 21 | 13.21 | 6.03 | – | – | NSc | ||
| 26 | 43 | 14.83 | 10.11 | – | – | 24 | 15.5 | 8.09 | – | – | 21 | 13.61 | 6.95 | – | – | NS | ||
| Grip strength | 4 | 43 | 226.93 | 120.78 | – | – | 24 | 243.06 | 111.8 | – | – | 21 | 223.13 | 134.5 | – | – | NS | |
| 13 | 43 | 245.56 | 117.66 | – | – | 24 | 223.68 | 123.8 | – | – | 21 | 226.45 | 138.7 | – | – | NS | ||
| 26 | 43 | 232.04 | 117.54 | – | – | 24 | 235.83 | 109.6 | – | – | 21 | 211.05 | 118.1 | – | – | NS | ||
| Walking speed | 4 | 43 | 15.24 | 6.78 | – | – | 24 | 15.1 | 6.46 | – | – | 21 | 15.23 | 4.08 | – | – | NS | |
| 13 | 43 | 14.98 | 6.08 | – | – | 24 | 16.27 | 8.77 | – | – | 21 | 15.56 | 4.13 | – | – | NS | ||
| 26 | 43 | 13.70 | 3.44 | – | – | 24 | 15.26 | 3.6 | – | – | 21 | 17.43 | 5.89 | – | – | SS | ||
| Swollen joint count | 4 | 43 | 3.00 | 4.08 | – | – | 24 | 2.47 | 2.95 | – | – | 21 | 5.58 | 5.98 | – | – | NS | |
| 13 | 43 | 2.89 | 3.95 | – | – | 24 | 2.28 | 3.97 | – | – | 21 | 5 | 5.22 | – | – | NS | ||
| 26 | 43 | 3.61 | 4.22 | – | – | 24 | 4.39 | 3.97 | – | – | 21 | 3.47 | 3.81 | – | – | NS | ||
| Physician VAS | 4 | 43 | 24.60 | 21.60 | – | – | 24 | 18.67 | 15.02 | – | – | 21 | 29.39 | 23.86 | – | – | NS | |
| 13 | 43 | 19.44 | 14.91 | – | – | 24 | 19.56 | 18.92 | – | – | 21 | 24.76 | 18.25 | – | – | NS | ||
| 26 | 43 | 23.69 | 21.58 | – | – | 24 | 30.65 | 18.21 | – | – | 21 | 20.56 | 16.25 | – | – | NS | ||
| ESR | 4 | 43 | 49.03 | 22.79 | – | – | 24 | 41.23 | 31.26 | – | – | 21 | 34.44 | 28.46 | – | – | NS | |
| 13 | 43 | 40.00 | 21.72 | – | – | 24 | 38.14 | 30.61 | – | – | 21 | 26.29 | 24.03 | – | – | NS | ||
| 26 | 43 | 46.37 | 18.19 | – | – | 24 | 40.09 | 29.73 | – | – | 21 | 23.47 | 15.33 | – | – | NS | ||
| Lumley 2014116 | Disease activity | 4 | 136 | –0.06 | 0.77 | – | – | – | – | – | – | – | 128 | 0.06 | 1.00 | – | – | SS |
| 16 | 136 | 0.02 | 0.85 | – | – | – | – | – | – | – | 128 | –0.03 | 0.95 | – | – | NS | ||
| 52 | 136 | 0.00 | 0.82 | – | – | – | – | – | – | – | 128 | –0.00 | 0.92 | – | – | NS | ||
| AIMS2 pain subscale | 4 | 136 | 2.83 | 1.04 | – | – | – | – | – | – | – | 128 | 2.64 | 0.99 | – | – | NS | |
| 16 | 136 | 2.84 | 0.97 | – | – | – | – | – | – | – | 128 | 2.58 | 0.92 | – | – | SS | ||
| 52 | 136 | 2.93 | 1.04 | – | – | – | – | – | – | – | 128 | 2.66 | 0.99 | – | – | SS | ||
| MPQ-a | 4 | 136 | 0.39 | 0.46 | – | – | – | – | – | – | – | 128 | 0.41 | 0.48 | – | – | NS | |
| 16 | 136 | 0.37 | 0.47 | – | – | – | – | – | – | – | 128 | 0.40 | 0.47 | – | – | NS | ||
| 52 | 136 | 0.44 | 0.53 | – | – | – | – | – | – | – | 128 | 0.40 | 0.46 | – | – | NS | ||
| MPQ-s | 4 | 136 | 1.29 | 0.82 | – | – | – | – | – | – | – | 128 | 1.28 | 0.81 | – | – | NS | |
| 16 | 136 | 1.30 | 0.86 | – | – | – | – | – | – | – | 128 | 1.29 | 0.75 | – | – | NS | ||
| 52 | 136 | 1.34 | 0.83 | – | – | – | – | – | – | – | 128 | 1.28 | 0.77 | – | – | NS | ||
| AIMS physical disability | 4 | 136 | 1.75 | 0.56 | – | – | – | – | – | – | – | 128 | 1.86 | 0.69 | – | – | SS | |
| 16 | 136 | 1.79 | 0.57 | – | – | – | – | – | – | – | 128 | 1.82 | 0.71 | – | – | NS | ||
| 52 | 136 | 1.79 | 0.57 | – | – | – | – | – | – | – | 128 | 1.81 | 0.68 | – | – | NS | ||
| AIMS psychological symptoms | 4 | 136 | 2.05 | 0.64 | – | – | – | – | – | – | – | 128 | 2.14 | 0.75 | – | – | NS | |
| 16 | 136 | 2.07 | 0.69 | – | – | – | – | – | – | – | 128 | 2.07 | 0.70 | – | – | NS | ||
| 52 | 136 | 2.03 | 0.66 | – | – | – | – | – | – | – | 128 | 2.10 | 0.70 | – | – | NS | ||
| Walking speed | 4 | 136 | 11.91 | 3.63 | – | – | – | – | – | – | – | 128 | 12.44 | 4.43 | – | – | NS | |
| 16 | 136 | 11.87 | 3.24 | – | – | – | – | – | – | – | 128 | 12.31 | 4.00 | – | – | NS | ||
| 52 | 136 | 12.03 | 3.37 | – | – | – | – | – | – | – | 128 | 12.43 | 4.16 | – | – | NS | ||
| CRP | 4 | 136 | 5.14 | 9.91 | – | – | – | – | – | – | – | 128 | 5.93 | 12.8 | – | – | NS | |
| 16 | 136 | 5.17 | 11.1 | – | – | – | – | – | – | – | 128 | 6.21 | 14.1 | – | – | NS | ||
| 52 | 136 | 5.90 | 12.3 | – | – | – | – | – | – | – | 128 | 5.58 | 10.9 | – | – | NS | ||
| Smyth 1999107 | DAS | 2 | 30 | 1.90 | SE = 0.16 | – | – | – | – | – | – | – | 16 | 1.76 | SE = 0.23 | – | – | NS |
| 8 | 31 | 1.81 | SE = 0.09 | – | – | – | – | – | – | – | 17 | 1.65 | SE = 0.2 | – | – | NS | ||
| 16 | 31 | 1.19 | SE = 0.09 | – | – | – | – | – | – | – | 17 | 1.71 | SE = 0.17 | – | – | SS | ||
| Wetherell 2005117 | DAS | 1 | 19 | 3.90 | 1.60 | – | – | – | – | – | – | – | 15 | 3.8 | 1.3 | – | – | NS |
| 6 | 19 | 3.80 | 1.20 | – | – | – | – | – | – | – | 15 | 4.2 | 1.4 | – | – | NS | ||
| 10 | 19 | 4.00 | 1.30 | – | – | – | – | – | – | – | 15 | 4.9 | 1 | – | – | SS | ||
| Tender joints | 1 | 19 | 4.90 | 4.00 | – | – | – | – | – | – | – | 15 | 7 | 5.5 | – | – | NS | |
| 6 | 19 | 4.40 | 3.50 | – | – | – | – | – | – | – | 15 | 6.4 | 4.1 | – | – | NS | ||
| 10 | 19 | 4.60 | 4.40 | – | – | – | – | – | – | – | 15 | 7.4 | 3.8 | – | – | NS | ||
| Swollen joint count | 1 | 19 | 4.80 | 4.60 | – | – | – | – | – | – | – | 15 | 3.9 | 3 | – | – | NS | |
| 6 | 19 | 3.70 | 2.90 | – | – | – | – | – | – | – | 15 | 3.2 | 2.3 | – | – | NS | ||
| 10 | 19 | 3.70 | 3.50 | – | – | – | – | – | – | – | 15 | 4.7 | 4.6 | – | – | NS | ||
| Patient VAS | 1 | 19 | 30.00 | 22.30 | – | – | – | – | – | – | – | 15 | 28.8 | 23.9 | – | – | NS | |
| 6 | 19 | 31.20 | 25.20 | – | – | – | – | – | – | – | 15 | 35.5 | 20.3 | – | – | NS | ||
| 10 | 19 | 25.00 | 23.50 | – | – | – | – | – | – | – | 15 | 45 | 24.1 | – | – | NS | ||
| CRP | 1 | 19 | 25.60 | 16.20 | – | – | – | – | – | – | – | 15 | 14.8 | 8.1 | – | – | NS | |
| 6 | 19 | 20.30 | 13.70 | – | – | – | – | – | – | – | 15 | 25.8 | 30.8 | – | – | NS | ||
| 10 | 19 | 21.90 | 16.30 | – | – | – | – | – | – | – | 15 | 20.8 | 15.3 | – | – | NS | ||
| ESR | 1 | 19 | 29.40 | 23.30 | – | – | – | – | – | – | – | 15 | 19.5 | 15.4 | – | – | NS | |
| 6 | 19 | 21.20 | 16.30 | – | – | – | – | – | – | – | 15 | 25.6 | 27.6 | – | – | NS | ||
| 10 | 19 | 28.90 | 19.20 | – | – | – | – | – | – | – | 15 | 32.6 | 20.6 | – | – | NS | ||
| POMS-SF | 1 | 19 | 42.40 | 28.00 | – | – | – | – | – | – | – | 15 | 38.6 | 14.3 | – | – | NS | |
| 6 | 19 | 41.60 | 21.30 | – | – | – | – | – | – | – | 15 | 38.2 | 17.7 | – | – | NS | ||
| 10 | 19 | 33.90 | 26.10 | – | – | – | – | – | – | – | 15 | 43.5 | 19.9 | – | – | SS | ||
Differences between groups by time interaction were reported for the following outcomes – BASFI, PANAS, Disease Activity Score (DAS) and the Profile of Mood States Short Form (POMS-SF) – in Hamilton-West and Quine, 114 Lumley et al. ,115 Smyth et al. 107 and Wetherell et al. ,117 respectively (see Table 57). In Hamilton-West and Quine 114 the functional status (measured using BASFI) was reported as statistically greater at 3-month follow-up in the EW group than with the control subjects. However, the clinical improvement was not apparent in the previous measurement at 4 weeks. On the other hand, Lumley et al. 115 assessed also the functional status [measured using the Arthritis Impact Measurement Scale-2 (AIMS2) pain subscale (AIMS2-ps)] at the same time points as Hamilton-West and Quine. 114 No significant differences were reported between intervention and any control group (positive writing, time-management writing or combined – results not shown in this review) within this study at any of the time points.
Regarding mood outcomes in Lumley et al. ,115 in the writing sample, compared with combined control subjects, disclosure led to significantly larger increases in the anger, sadness and guilt subscales of PANAS, but not fear, during the sessions. The authors stated that these differences were probably due to differences between the disclosure and positive control groups, but not the neutral control group. However, Wetherell et al. 117 reported that measures of total mood disturbance (POMS-SF) did increase in the disclosure group at 1 month compared with control subjects.
Disease activity measures were reported in all studies. This outcome is meta-analysed in the corresponding heading.
Meta-analysis
Outcomes related to the disease activity and inflammation were meta-analysed (Figures 41–43).
FIGURE 41.
Forest plot of disease activity/severity at immediate follow-up in patients with inflammatory arthropathy. df, degrees of freedom; IV, inverse variance.
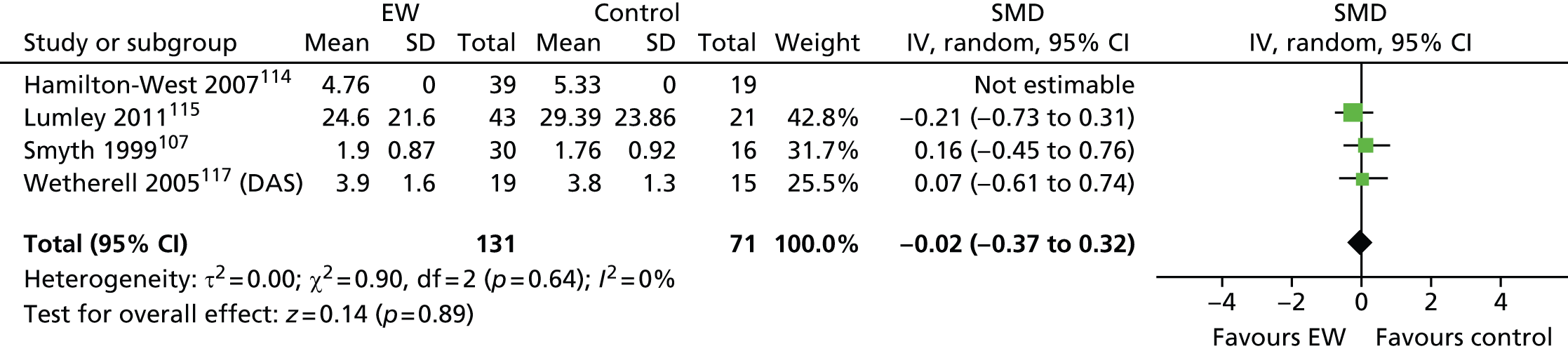
FIGURE 42.
Forest plot of disease activity/severity at short-term follow-up in patients with inflammatory arthropathy. df, degrees of freedom; IV, inverse variance.
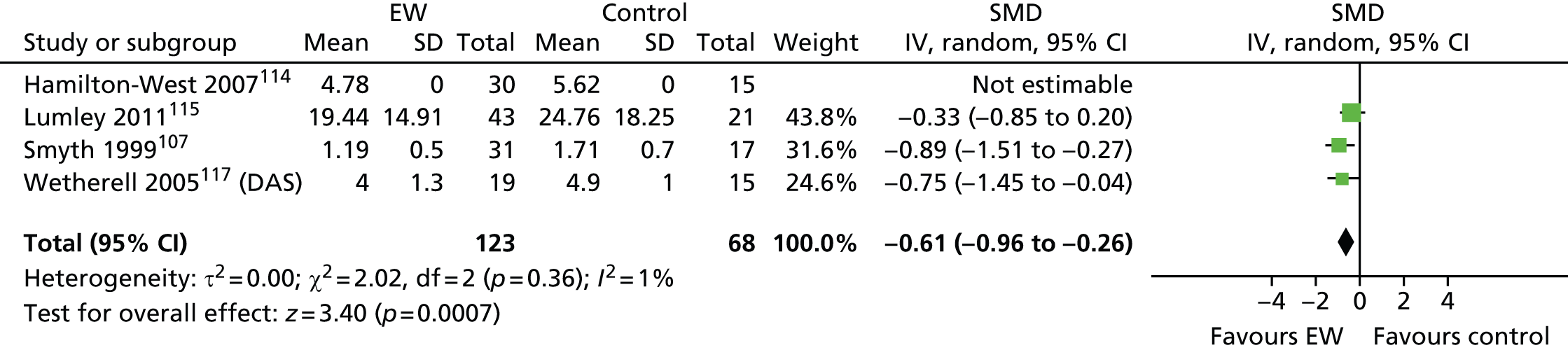
FIGURE 43.
Forest plot of inflammation at immediate follow-up in patients with inflammatory arthropathy. df, degrees of freedom; \IV, inverse variance.
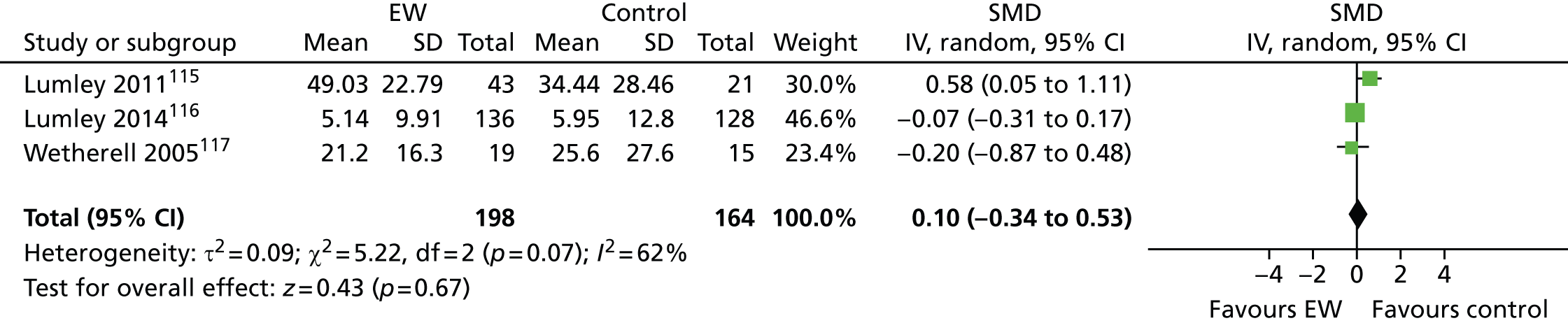
Six studies107,113–117 used different scales to measure similar aspects of the disease activity and severity. All of the studies, except Hamilton-West and Quine,114 reported complete numerical data regarding disease activity, but in Lumley et al. 116 some of the scores are minus numbers, which means they cannot be meta-analysed, as they may be change scores.
-
Clinical differences between studies All of the patients included in these studies had been diagnosed with RA and were free of other major illnesses. In Smyth et al. ,107 the sample consisted of volunteers recruited from local communities, whereas in the remaining studies113–117 patients were recruited from rheumatological clinics.
-
Follow-up length Disease activity was measured immediately after the writing and at short term.
The effect of the TW intervention on disease activity/severity was evaluated in Smyth et al. ,107 Hamilton-West and Quine,114 Wetherell et al. 117 and Lumley et al. 115 almost immediately after the writing exercise at 1, 2, 4 and 4 weeks.
-
Forest plot A total of 202 participants were meta-analysed (131 in the EW group and 71 in the control group). The SMD was –0.02 (95% CI –0.37 to 0.32) with a random-effects model and with non-significant heterogeneity (I2 = 0%). This result suggests that there is no statistically significant difference in disease activity when measured immediately after the writing exercise for the TW group compared with the control group (Figure 43).
The same studies evaluated the short-term effect of the TW intervention at 8, 10 and 13 weeks.
-
Forest plot A total of 191 participants were meta-analysed (123 in the EW group and 68 in the control group). The SMD was –0.61 (95% CI –0.96 to –0.26) with a random-effects model and with non-significant heterogeneity, (I2 = 1%). The result suggests that there are significant differences in disease activity in favour of the TW group at short-term follow-up (Figure 44).
The effect of inflammation [erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP)] was evaluated in Lumley et al. 115,116 and Wetherell et al. 117 at short-term follow-up (4, 4 and 6 weeks, respectively).
-
Clinical differences between studies All patients included in these studies had been diagnosed with RA and were free of other major illnesses. In Lumley et al. 116 the sample consisted of volunteers recruited from local communities as well as from a rheumatology clinic, whereas in the remaining studies patients were recruited only from rheumatological clinics.
-
Forest plot A total of 362 participants were meta-analysed (198 intervention, 164 control). The SMD was –0.10 (95% CI –0.34 to 0.53) with a random-effects model and with significant heterogeneity, (I2 = 62%). The result suggests that there are no significant differences in disease activity in favour of the TW group at short-term follow-up. Wetherell et al. 117 measured ESR and CRP and both made no significant difference to the meta-analysis result (Figure 45).
M79 and RSI: fibromyalgia and chronic pain and facial pain
Overview
There were two studies evaluating unfacilitated EW in fibromyalgia (FM)118,119 and two studies in chronic pain. 51,57 A summary of the main characteristics is presented in Table 58. All studies51,57,118,119 were conducted in the USA. Stark57 included facial pain patients (ICD-10 code: R51). Broderick et al. 118 and Gillis et al. 119 used a standard written emotional expression intervention. Stark57 combined a trauma writing exercise with a Change Theory-based positive writing technique. Graham et al. 51 was unique in the current systematic review in using a written anger expression exercise through a letter-writing format. This technique was based on Rusting and Nolen-Hoeksema’s type of EW125 and consisted of completing a pre-writing short exercise, where intervention group patients had to focus their attention on existing anger related to their pain experience. In this brief questionnaire, participants were asked to consider if they currently or recently felt anger towards a health-care provider, themselves, or someone or something else and, if so, to remember and/or focus on it. Participants were given a writing tablet and instructions to write a letter to the person at whom, or thing at which, they were most angry. They were instructed to focus on their anger rather than other emotions. Gillis et al. 119 and Stark57 delivered the intervention in three and four 20-minute consecutive sessions, respectively, whereas in Broderick et al. 118 and Graham et al. 51 the interventions were delivered at 1-week (three sessions) and 2.5-week (two sessions) intervals. All patients were financially compensated except for those in Gillis et al. 119
| First author, year | Study design | Intervention group | Control group 1 | Control group 2 |
|---|---|---|---|---|
| Broderick 2005118 | RCT | Unfacilitated EW | Time-management writing | SMCa |
| Gillis 2006119 | RCT | Unfacilitated EW | Time-management writing | – |
| Graham 200851 | RCT | Questionnaire plus unfacilitated EW | Factual goal writing | – |
| Stark 201057 | RCT | Unfacilitated EW (mixed writing) | Non-writing | – |
The outcomes assessed within the different studies are reported in Table 59. Pain severity, depression and resource use were the outcomes that were most frequently evaluated.
| First author, year | Physical global health | Pain severity/intensity | Anxiety | Depression | Affect | Social support | QoL | Various, other | Resource use |
|---|---|---|---|---|---|---|---|---|---|
| Broderick 2005118 | FIQ, CLINHAQ | McGill Pain Q-SF (MPQ-i) | STAI-S | BDI-II | – | – | MOS SF-36, QOL | – | – |
| Gillis 2006119 | FIQ, AIMS2 (dysfunction) | AIMS2-ps | – | – | PANAS-NA | AIMS2 | Sleep quality (4-item questionnaire) | FSS (fatigue) | Number of visits to clinician |
| Graham 200851 | – | MPI | – | CES-D | – | – | – | Expressed anger, SOPA | Number of years attending clinic |
| Stark 201057 | – | DDS, MPI | – | BDI-SF | POMS | – | – | SLESQ (distress), Pain Catastrophising Scale | Number of pain medications per month, number of psychotropic medications per month |
Quality assessment
A summary of the quality of the studies is shown in Figures 44 and 45. All studies51,57,118,119 were truly randomised and three studies51,118,119 out of four reported concealment of the allocation of the sequence generation. In one study,51 the outcome assessment was masked. In one other study,119 the blinding was preserved at the performance level. The remaining studies51,57,118 were likely to introduce both performance and detection bias, and one study51 was unclear regarding the reporting of pain severity, with data derived from a graph.
FIGURE 44.
Risk-of-bias summary in the FM/chronic pain studies.
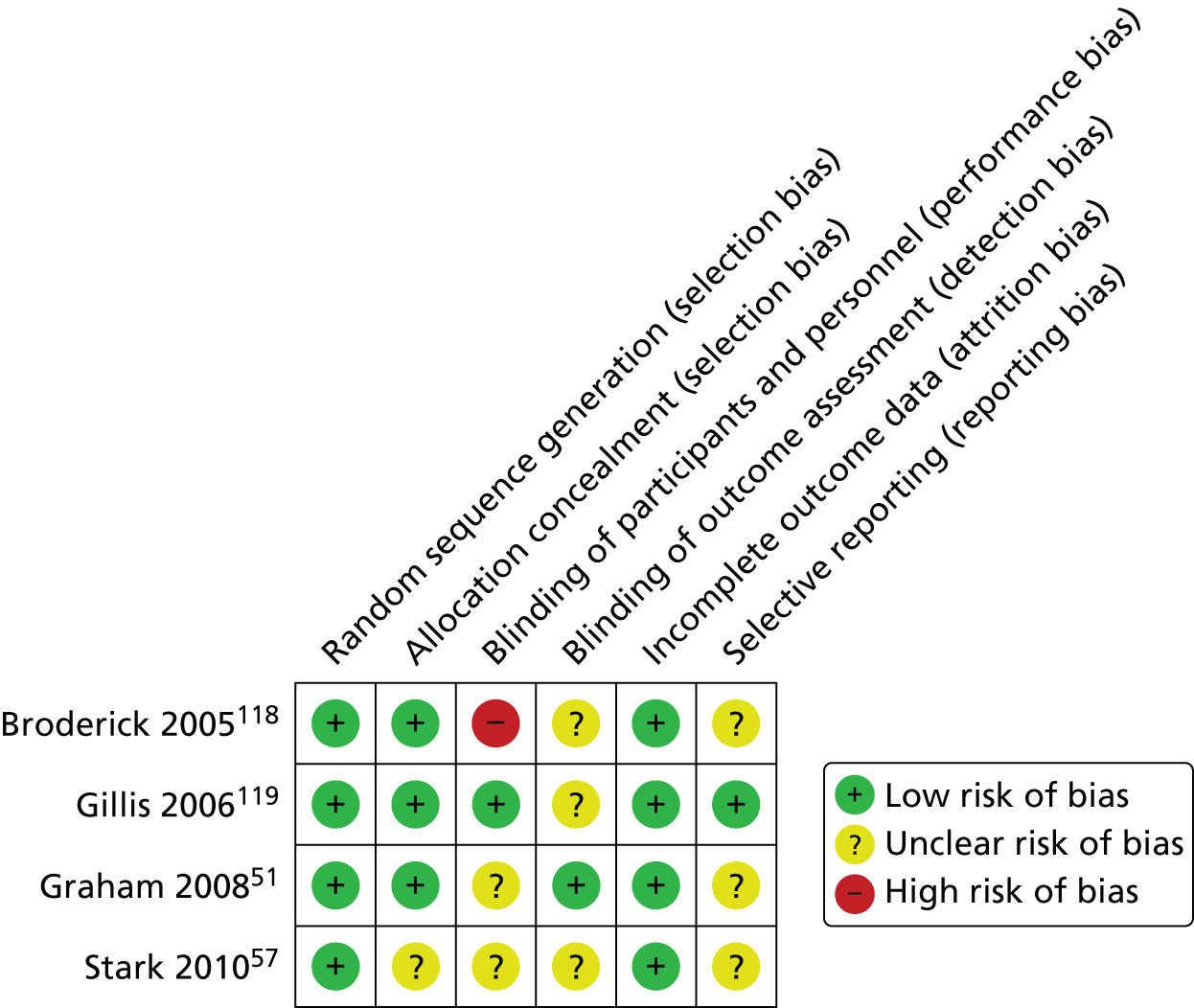
FIGURE 45.
Risk-of-bias graph in the FM/chronic pain studies.
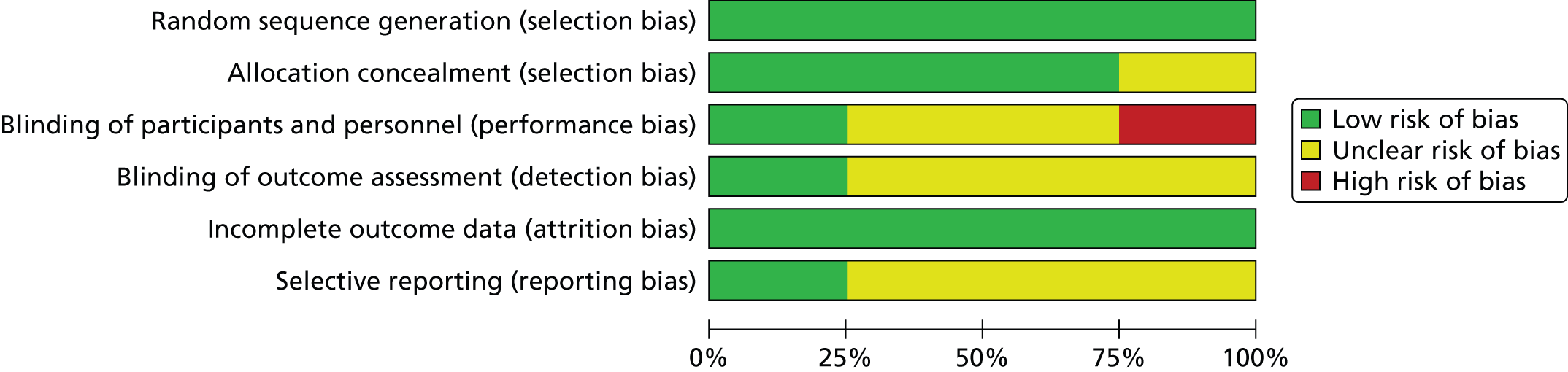
Numerical results
The numerical results reported in the FM/chronic pain studies are summarised in Table 60. Follow-up assessments ranged between 4 weeks in Gillis et al. 119 and Graham et al. 51 up to 17 weeks in Broderick et al. 118 Total sample sizes ranged from 42 patients in Stark57 to 102 patients in Graham et al. 51 Studies reported a statistical significant association of group-by-time interaction for the following outcomes: depression, control over pain in Graham et al. ,51 global impact, physical disability, poor sleep, health-care use in Gillis et al. ,119 and pain severity, fatigue and well-being in Broderick et al. 118
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group 1 | Control group 1 | Author’s reported statistical significance (group-by-time interaction) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean scoreb | SDb | Change score | SDb | n totala | Final mean scoreb | SDb | Change score | SDb | ||||
| Broderick 2005118 | FIQ-physical function | 17 | 28 | – | – | –0.7 | 0.3 | 55 | – | – | –0.3 | 0.2 | NS |
| CLINHAQ f-VAS | 17 | 28 | – | – | –1.2 | 0.4 | 55 | – | – | –0.7 | 0.3 | NS | |
| MOS-SF-36 | 17 | 28 | – | – | 1.4 | 3.6 | 55 | – | – | –2.1 | 2.6 | NS | |
| MPQ-s | 17 | 28 | – | – | –3.4 | 1 | 55 | – | – | –0.4 | 0.7 | SS | |
| MPQ-a | 17 | 28 | – | – | –0.6 | 0.5 | 55 | – | – | –0.2 | 0.4 | NS | |
| MPQ-VAS | 17 | 28 | – | – | –1 | 0.4 | 55 | – | – | 0.1 | 0.3 | SS | |
| MPQ-i | 17 | 28 | – | – | –0.6 | 0.2 | 55 | – | – | 0.1 | 0.2 | SS | |
| BDI-II | 17 | 28 | – | – | –5.8 | 1.7 | 55 | – | – | –1.1 | 1.2 | SS | |
| STAI-S | 17 | 28 | – | – | 3.7 | 2.4 | 55 | – | – | 7 | 1.7 | NS | |
| QoL | 17 | 28 | – | – | 0.6 | 2.1 | 55 | – | – | 7 | 1.5 | SS | |
| Gillis 2006119 | AIMS2 | 4 | 38 | 2.04 | 0.70 | – | – | 34 | 1.91 | 0.57 | – | – | NS |
| 13 | 38 | 20.30 | 0.72 | – | – | 34 | 1.90 | 0.59 | – | – | NS | ||
| AIMS2-ps | 4 | 38 | 3.32 | 0.98 | – | – | 34 | 3.20 | 0.88 | – | – | NS | |
| 13 | 38 | 3.51 | 0.91 | – | – | 34 | 3.34 | 0.87 | – | – | NS | ||
| FSS | 4 | 38 | 5.49 | 1.33 | – | – | 34 | 5.70 | 1.09 | – | – | NS | |
| 13 | 38 | 5.66 | 1.24 | – | – | 34 | 5.84 | 1.11 | – | – | NS | ||
| PANAS-NA | On day 3 | 38 | – | – | 0.74 | 1.51 | 34 | – | – | –0.16 | 0.59 | NS | |
| On day 4 | 38 | – | – | 0.43 | 1.14 | 34 | – | – | –0.17 | 0.75 | NS | ||
| PANAS-NA | 4 | 38 | 2.12 | 0.78 | – | – | 34 | 1.94 | 0.70 | – | – | NS | |
| 13 | 38 | 1.91 | 0.71 | – | – | 34 | 2.14 | 0.78 | – | – | NS | ||
| AIMS-social support | 4 | 37 | 2.84 | 1.16 | – | – | 32 | 2.72 | 1.14 | – | – | NR | |
| 13 | 36 | 2.52 | 1.05 | – | – | 32 | 2.84 | 1.24 | – | – | NR | ||
| Sleep quality scale-4 | 4 | 38 | 4.28 | 1.05 | – | – | 34 | 4.19 | 0.83 | – | – | SS | |
| 13 | 38 | 4.23 | 1.06 | – | – | 34 | 4.22 | 0.90 | – | – | SS | ||
| FIQ | 4 | 38 | 56.60 | 20.42 | – | – | 34 | 53.31 | 17.79 | – | – | NS | |
| 13 | 38 | 52.70 | 20.35 | – | – | 34 | 53.79 | 18.13 | – | – | SS | ||
| n of visits clinician | 4 | 38 | 1.66 | 1.51 | – | – | 34 | 2.16 | 2.23 | – | – | NS | |
| 13 | 38 | 1.13 | 1.07 | – | – | 34 | 1.80 | 2.21 | – | – | SS | ||
| Graham 200851 | CES-D | 4 | 51 | 25 | SE = 1.84 | – | – | 51 | 25.31 | SE = 1.08 | – | – | – |
| 9 | 51 | 20.44 | SE = 1.34 | – | – | 51 | 24.12 | SE = 2.05 | – | – | SS | ||
| Expressed anger | 4 | 51 | 21.33 | 9.37 | – | – | 51 | 19.02 | 7.42 | – | – | – | |
| 9 | 51 | 20.00 | 6.89 | – | – | 51 | 19.70 | 7.03 | – | – | NS | ||
| MPI | 4 | 51 | 4.67 | SE = 0.24 | – | – | 51 | 4.58 | SE = 0.27 | – | – | – | |
| 9 | 51 | 4.03 | SE = 0.21 | – | – | 51 | 4.49 | SE = 0.28 | – | – | NR | ||
| SOPA | 4 | 51 | 25.8 | SE = 1.61 | – | – | 51 | 25.28 | SE = 1.05 | – | – | – | |
| 9 | 51 | 26.89 | SE = 1.37 | – | – | 51 | 23.9 | SE = 1.17 | – | – | SS | ||
| n of years attending clinic | NR | NR | 2.90 | 2.40 | – | – | NR | 3.70 | 3.10 | – | – | NR | |
| Stark 201057 | MPI | 5 | 21 | 38.33 | 15.39 | – | – | 21 | 40.76 | 15.93 | – | – | NR |
| 10 | 21 | 41.52 | 15.26 | – | – | 21 | 40.76 | 13.87 | – | – | NR | ||
| DDS | 5 | 21 | 14.13 | NR | 1.58 | NR | 21 | 13.56 | NR | 0.19 | NR | NR | |
| 10 | 21 | 12.55 | NR | 2.66 | NR | 21 | 13.75 | NR | 1.34 | NR | NR | ||
| Pain Catastrophising Scale | 5 | 21 | 20.38 | 10.75 | 2.33 | NR | 21 | 24.48 | 13.20 | 4.095 | NR | NR | |
| 10 | 21 | 17.10 | 10.56 | 5.56 | NR | 21 | 20.38 | 12.40 | 4.46 | NR | NR | ||
| BDI-SF | 5 | 21 | 5.10 | 2.72 | – | – | 21 | 4.67 | 4.07 | – | – | NR | |
| 10 | 21 | 4.00 | 3.08 | – | – | 21 | 5.19 | 4.25 | – | – | NR | ||
| POMS | 5 | 21 | 11.29 | 3.68 | –1.48 | NR | 21 | 12.00 | 4.09 | –0.9 | NR | NR | |
| 10 | 21 | 12.67 | 3.18 | –1.38 | NR | 21 | 12.48 | 3.84 | –0.48 | NR | NR | ||
| n of pain medication/month | 5 | 21 | 148.50 | 114.27 | – | – | 21 | 188.30 | 123.52 | – | – | NR | |
| 10 | 21 | 144.50 | 110.44 | – | – | 21 | 169.90 | 128.99 | – | – | NR | ||
| n of psychotropic medication/month | 5 | 21 | 56.70 | 62.97 | – | – | 21 | 61.10 | 65.46 | – | – | NR | |
| 10 | 21 | 44.90 | 47.48 | – | – | 21 | 60.20 | 60.36 | – | – | NR | ||
Meta-analysis
It was decided not to combine data related to depression, as numerical outcomes could not be pooled together: studies were reporting change scores, median and SE and means and SD using different instruments each and at different follow-up times. The outcomes related to pain severity were meta-analysed (Figures 46 and 47).
FIGURE 46.
Forest plot of pain severity at 4/5 weeks’ follow-up in FM/chronic pain studies. df, degrees of freedom; IV, inverse variance.

FIGURE 47.
Forest plot of pain severity at short-term (9–13 weeks) follow-up in FM/chronic pain studies. df, degrees of freedom; IV, inverse variance.

Four studies51,57,118,119 used different scales [McGill Pain Questionnaire, impact (MPQ-i), AIMS2-ps and Multidimensional Pain Inventory (MPI)] to measure pain intensity. All of the studies except Broderick et al. 118 (reporting change scores only)51,57,119 reported data that could be pooled.
-
Clinical differences between studies In Gillis et al. ,119 patients had been diagnosed with FM for a mean of 5.9 years (range 1–20 years) before entering the study. In the other two studies, patients were diagnosed with chronic pain. For instance, in Graham et al. ,51 patients had chronic pain from diverse sources such as arthritis (22.4%), injury (57.2%), complex regional pain syndrome (9.7%), and other (27.5%), such as myofascial pain, pancreatitis and migraine; locations included back (65.5%), shoulder/arms (41.8%), neck (14.5), hips/pelvis (11.5%), hands/feet (12.7%), head (9.2%) and all over (6.9%). In Stark,57 patient’s condition was mainly related to muscle pain.
-
Follow-up length All three studies51,57,119 assessed pain intensity at short term, that is between 4 and 5 weeks up to 13 weeks. Although these measurements were in the same short-term follow-up category defined in Table 2, it was decided that two meta-analyses should be performed, one for outcomes at 4 or 5 weeks and one for outcomes between 9 and 13 weeks.
Short term, at 4/5 weeks:
-
Forest plot A total of 216 participants were meta-analysed (110 in the EW group and 106 in the control group). The SMD was –0.04 (95% CI –0.23 to 0.30) with a random-effects model and with no significant heterogeneity (I2 = 0%). This result suggests that there is no statistically significant difference in pain severity when measured at 4/5 weeks after the writing exercise for the TW group compared with the control group (Figure 48).
Short term, at 9, 10 and 13 weeks:
-
Forest plot A total of 216 participants were meta-analysed (110 in the EW group and 106 in the control group). The SMD was 0.18 (95% CI –0.09 to 0.44) with a random-effects model and with no significant heterogeneity (I2 = 0%). This result suggests that there is no statistically significant difference in pain severity when measured at 9/10 weeks to 13 weeks after the writing exercise for the EW group compared with the control group (Figure 49).
Positive therapeutic writing
Overview
Previously, Chapter 3 summarised the effect of the standard forms of unfacilitated EW and used those in meta-analyses where possible. In addition to these forms of writing, which were usually disease/treatment, or trauma-focused, seven of the included studies53,57,72,82,106,110,115 used a form of positive writing.
As mentioned in Chapter 1, positive writing is a form of expressive/emotional writing and is a more usual form of writing used among facilitated types of TW, although it can be used as part of an unfacilitated EW as evaluated here.
These seven studies53,57,72,82,106,110,115 have been already described in corresponding ICD-10 sections; however, Table 61 outlines the interventions evaluated. Four82,106,110,115 of the seven studies used positive writing as a second intervention group in addition to the unfacilitated EW. Two studies53,72 used positive writing only and the doctoral thesis by Stark57 used a combined form of expressive writing mixing both a form of emotional disclosure and positive writing. In this study, participants in the positive writing group had to write about a self-selected worst experience from a positive perspective. This intervention is unusual and was compared against a non-writing control group.
| First author, year | LTC | Intervention group 1 | Intervention group 2 | Control group |
|---|---|---|---|---|
| Harris 2005106 | Asthma | Unfacilitated EW | Positive writing | Factual writing |
| Henry 201053 | Breast cancer | Positive writing | – | Usual care |
| Lumley 2011115 | RA | Unfacilitated EW | Positive writing | Time-management writing |
| Pauley 201182 | Testicular cancer | Unfacilitated EW | Positive writing | Factual writing |
| Paradisi 2010110 | Psoriasis | Unfacilitated EW | Positive writing | Non-EW |
| Mann 200172 | HIV | Positive writing | – | Non-writing |
| Stark 201057 | FM and facial pain | Unfacilitated EW (mixed writing including positive writing) | – | Non-writing |
As shown in Table 62, the outcomes evaluated in all seven studies were very varied, although two studies110,117 evaluated mental health using the GHQ-12 and were among patients with psoriasis110 and testicular cancer. 77 In the remaining studies, three studies53,57,115 evaluated affect and mood states; two studies82,110 assessed QoL; two studies110,115 assessed disease severity; and three studies53,106,115 evaluated biomarkers.
| First author, year | Physiological/biomarkers outcomes | Disease severity | Pain severity | Sexual health | Coping | Depression | Affect | Mental health | Various others | QoL | Adherence and side effects | Resource use |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Harris 2005106 | FEV1% pred, FVC | – | – | – | – | – | – | – | – | – | ✓ | – |
| Henry 201053 | Survey–18 physical symptoms | – | – | – | – | CES-D | POMS | – | – | – | – | – |
| Lumley 2011115 | ESR | Swollen joint count, walking speed, grip strength, physicians global rating of disease activity (100-mm VAS) | – | – | – | – | PANAS-X AIMS2: affective disturbance subscales | – | AIMS2: physical dysfunction subscale, McGill Pain Q-SF | – | – | – |
| Mann 200172 | – | – | – | – | – | – | – | – | LOT (optimism) | – | Adherence and side effects due to HIV-medication | – |
| Pauley 201182 | – | – | – | 6-item measure | ARS-20 | – | – | GHQ-12 | – | QLQ-30 | – | – |
| Paradisi 2010110 | – | PASI, SAPASI | – | – | – | – | – | GHQ-12 | – | Skindex-29 Symptoms, Emotions and Functioning subscales | – | – |
| Stark 201057 | – | – | DDS, MPI | – | – | BDI-SF | POMS | – | – | SLESQ (distress), Pain Catastrophising Scale | – | Number of pain medications per month, number of psychotropic medications per month |
Numerical results
The numerical results on positive writing and controls are reported in Table 63. All studies on positive writing were of small sample sizes, with follow-ups conducted up to 26 weeks. All studies evaluated different LTC populations.
| First author, year | Outcome measures | Follow-up (weeks) | Intervention group | Control group | Author’s reported statistical significance (group-by-time interaction) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n totala | Final mean scoreb | SDb | Change score | SDb | n totala | Final mean scoreb | SDb | Change score | SDb | ||||
| Harris 2005106 | FEV1% pred | 8 | 37 | 75.5 | 17.2 | 1.3 | 7.3 | 36 | 77.1 | 17.1 | 3 | 4.4 | NS |
| FVC | 8 | 37 | 79.2 | 14.5 | 3.6 | 9.0 | 36 | 78.5 | 15 | 2.4 | 4.6 | NS | |
| Adherencec | NR | NR | NR | – | – | – | – | – | – | – | NR | ||
| Henry 201053 | Survey–18 physical symptoms items | 13 | 40 | 1.85 | NR | – | – | 40 | 2.15 | NR | – | – | NS |
| Survey–18 physical symptoms items | 39 | 40 | 2.05 | NR | – | – | 40 | 2.09 | NR | – | – | NS | |
| CES-D | 13 | 40 | 1.31 | NR | – | – | 40 | 1.55 | NR | – | – | NS | |
| CES-D | 39 | 40 | 1.40 | NR | – | – | 40 | 1.47 | NR | – | – | NS | |
| POMS | 13 | 40 | NR | NR | – | – | 40 | NR | NR | – | – | SS | |
| POMS | 39 | 40 | NR | NR | – | – | 40 | NR | NR | – | – | NS | |
| Lumley 2011115 | PANAS-a | Just after writing | 24 | – | – | –0.36 | 1 | 21 | – | – | –0.02 | 0.84 | NR |
| PANAS-f | Just after writing | 24 | – | – | –0.18 | 0.53 | 21 | – | – | 0.06 | 0.38 | NR | |
| PANAS-s | Just after writing | 24 | – | – | –0.14 | 0.6 | 21 | – | – | 0 | 0.61 | NR | |
| PANAS-g | Just after writing | 24 | – | – | –0.45 | 0.76 | 21 | – | – | –0.11 | 0.69 | NR | |
| PANAS-pn | Just after writing | 24 | – | – | 4.94 | 1.3 | 21 | – | – | 3.4 | 2.14 | NR | |
| PANAS-r | Just after writing | 24 | – | – | 4.7 | 1.25 | 21 | – | – | 3 | 2 | NR | |
| PANAS-m | Just after writing | 24 | – | – | 4.98 | 0.94 | 21 | – | – | 2.75 | 1.9 | NR | |
| PANAS-i | Just after writing | 24 | – | – | 1.91 | 1.68 | 21 | – | – | 1.93 | 1.61 | NR | |
| MPQ-s | 4 | 24 | 0.9 | 0.85 | – | – | 21 | 0.88 | 0.61 | – | – | NR | |
| 13 | 24 | 0.8 | 0.74 | – | – | 21 | 0.56 | 0.5 | – | – | NR | ||
| 26 | 24 | 0.99 | 0.84 | – | – | 21 | 0.68 | 0.65 | – | – | NR | ||
| MPQ-a | 4 | 24 | 0.53 | 0.68 | – | – | 21 | 0.57 | 0.58 | – | – | NR | |
| 13 | 24 | 0.52 | 0.76 | – | – | 21 | 0.3 | 0.28 | – | – | NR | ||
| 26 | 24 | 0.6 | 0.75 | – | – | 21 | 0.43 | 0.56 | – | – | NR | ||
| AIMS-ps | 4 | 24 | 2.05 | 0.69 | – | – | 21 | 2.07 | 0.85 | – | – | NR | |
| 13 | 24 | 2.2 | 0.89 | – | – | 21 | 2.07 | 0.65 | – | – | NR | ||
| 26 | 24 | 2.25 | 0.77 | – | – | 21 | 2.19 | 0.87 | – | – | NR | ||
| AIMS-as | 4 | 24 | 2.27 | 0.7 | – | – | 21 | 2.12 | 0.65 | – | – | NR | |
| 13 | 24 | 2.44 | 0.72 | – | – | 21 | 2.13 | 0.65 | – | – | NR | ||
| 26 | 24 | 2.44 | 0.73 | – | – | 21 | 2.26 | 0.59 | – | – | NR | ||
| OPB | 4 | 24 | 11.52 | 8.12 | – | – | 21 | 12.43 | 8.62 | – | – | NR | |
| 13 | 24 | 10.6 | 7.28 | – | – | 21 | 13.21 | 6.03 | – | – | NR | ||
| 26 | 24 | 15.5 | 8.09 | – | – | 21 | 13.61 | 6.95 | – | – | NR | ||
| Grip strength | 4 | 24 | 243.06 | 111.8 | – | – | 21 | 223.13 | 134.5 | – | – | NR | |
| 13 | 24 | 223.68 | 123.8 | – | – | 21 | 226.45 | 138.7 | – | – | NR | ||
| 26 | 24 | 235.83 | 109.6 | – | – | 21 | 211.05 | 118.1 | – | – | NR | ||
| Walking speed | 4 | 24 | 15.1 | 6.46 | – | – | 21 | 15.23 | 4.08 | – | – | NR | |
| 13 | 24 | 16.27 | 8.77 | – | – | 21 | 15.56 | 4.13 | – | – | NR | ||
| 26 | 24 | 15.26 | 3.6 | – | – | 21 | 17.43 | 5.89 | – | – | NR | ||
| Swollen joint count | 4 | 24 | 2.47 | 2.95 | – | – | 21 | 5.58 | 5.98 | – | – | NR | |
| 13 | 24 | 2.28 | 3.97 | – | – | 21 | 5 | 5.22 | – | – | NR | ||
| 26 | 24 | 4.39 | 3.97 | – | – | 21 | 3.47 | 3.81 | – | – | NR | ||
| Physician VAS | 4 | 24 | 18.67 | 15.02 | – | – | 21 | 29.39 | 23.86 | – | – | NR | |
| 13 | 24 | 19.56 | 18.92 | – | – | 21 | 24.76 | 18.25 | – | – | NR | ||
| 26 | 24 | 30.65 | 18.21 | – | – | 21 | 20.56 | 16.25 | – | – | NR | ||
| ESR | 4 | 24 | 41.23 | 31.26 | – | – | 21 | 34.44 | 28.46 | – | – | NR | |
| 13 | 24 | 38.14 | 30.61 | – | – | 21 | 26.29 | 24.03 | – | – | NR | ||
| 26 | 24 | 40.09 | 29.73 | – | – | 21 | 23.47 | 15.33 | – | – | NR | ||
| Mann 200172 | LOT | 4 | 20 | 28.13 | 0.9 | – | – | 20 | 27.23 | 1.1 | NR | – | NR |
| Adherence (mean) | 4 | 20 | 4.12 | 0.31 | – | – | 20 | 4.82 | 0.16 | NR | – | NR | |
| Side effects | 4 | 20 | 37.7 | 5.71 | – | – | 20 | 35.85 | 4.76 | NR | – | NR | |
| Pauley 201182 | Sexual performance | 5 | 28 | NR | NR | NR | NR | 28 | NR | NR | NR | NR | NR |
| Sexual health | 5 | 28 | 6.05 | 0.28 | NR | NR | 28 | 5.66 | 0.32 | NR | NR | NS | |
| GHQ-12 | 5 | 28 | 5.4 | 0.15 | 0.34 | 0.47 | 28 | 4.7 | 0.16 | 0.29 | 0.39 | SS | |
| ARS-20 | 5 | 28 | NR | NR | NR | NR | 28 | NR | NR | NR | NR | NR | |
| QLQ-30 | 5 | 28 | 2.38 | 0.19 | NR | NR | 28 | 2.52 | 0.21 | NR | NR | NS | |
| Paradisi 2010110 | PASI | 8 | 22 | NR | NR | – | – | 26 | NR | NR | – | – | SS |
| 17 | 12 | NR | NR | – | – | 13 | NR | NR | – | – | NR | ||
| SAPASI | 8 | 22 | Median: 2 | NR | – | – | 26 | Median: 2 | NR | – | – | NS | |
| 17 | 12 | Median: 5.8 | NR | – | – | 13 | Median: 6 | NR | – | – | SS | ||
| GHQ-12 | 8 | 22 | Median: 8 | Range: 2–19 | – | – | 26 | Median: 11 | Range 3–24 | – | – | NR | |
| 17 | 12 | Median: 8 | Range: 4–28 | – | – | 13 | Median: 12 | Range: 3–27 | – | – | NR | ||
| Skindex-29 Symptoms | 8 | 22 | Median: 21 | Range 0–46 | – | – | 26 | Median: 21 | Range: 0–60 | – | – | NR | |
| 17 | 12 | Median: 20 | Range 0–64 | – | – | 13 | Median: 25 | Range 4–68 | – | – | SS | ||
| Skindex-29 Functioning | 8 | 22 | Median: 3 | Range 0–71 | – | – | 26 | Median: 19 | Range 2–42 | – | – | NR | |
| 17 | 22 | Median: 6 | Range 0–75 | – | – | 26 | Median: 19 | Range 2–67 | – | – | NR | ||
| Skindex-29 Emotions | 8 | 22 | Median: 16 | Range 0–80 | – | – | 26 | Median: 30 | Range 5–80 | – | – | NR | |
| 17 | 22 | Median: 21 | Range 0–82 | – | – | 26 | Median: 30 | Range 7–67 | – | – | NR | ||
| Stark 201057 | MPI | 5 | 21 | 38.33 | 15.39 | – | – | 21 | 40.76 | 15.93 | – | – | NA |
| 10 | 21 | 41.52 | 15.26 | – | – | 21 | 40.76 | 13.87 | – | – | NA | ||
| DDS | 5 | 21 | 14.13 | NR | 1.58 | NR | 21 | 13.56 | NR | 0.19 | NR | NA | |
| 10 | 21 | 12.55 | NR | 2.66 | NR | 21 | 13.75 | NR | 1.34 | NR | NA | ||
| Pain Catastrophising Scale | 5 | 21 | 20.38 | 10.75 | 2.33 | NR | 21 | 24.48 | 13.2 | 4.095 | NR | NA | |
| 10 | 21 | 17.1 | 10.56 | 5.56 | NR | 21 | 20.38 | 12.4 | 4.46 | NR | NA | ||
| BDI-SF | 5 | 21 | 5.1 | 2.72 | – | – | 21 | 4.67 | 4.07 | – | – | NA | |
| 10 | 21 | 4 | 3.08 | – | – | 21 | 5.19 | 4.25 | – | – | NA | ||
| POMS | 5 | 21 | 11.29 | 3.68 | –1.48 | NR | 21 | 12 | 4.09 | –0.9 | NR | NA | |
| 10 | 21 | 12.67 | 3.18 | –1.38 | NR | 21 | 12.48 | 3.84 | –0.48 | NR | NA | ||
| n of pain medication/month | 5 | 21 | 148.5 | 114.27 | – | – | 21 | 188.3 | 123.52 | – | – | NA | |
| 10 | 21 | 144.5 | 110.44 | – | – | 21 | 169.9 | 128.99 | – | – | NA | ||
| n of psychotropic medication/month | 5 | 21 | 56.7 | 62.97 | – | – | 21 | 61.1 | 65.46 | – | – | NA | |
| 10 | 21 | 44.9 | 47.48 | – | – | 21 | 60.2 | 60.36 | – | – | NA | ||
Harris et al. 106 did not show significant differences between positive writing and control groups on lung function (similar results to the EW group compared with control subjects).
In Henry et al. ,53 there was a significant improvement in POMS scores for the writing group compared with the matched control subjects at 13 weeks but not at 39 weeks. No other outcomes measured showed significant differences.
In Pauley et al. ,82 as in the EW group, significant differences were found in mental health in favour of the positive writing group compared with control subjects.
In Paradisi et al. ,110 intragroup analyses show increases in SAPASI scores between the end of intervention and the final assessment in the positive writing group and control subjects, whereas no differences were found in the EW group participants. In addition, significant differences in Skindex-29 values between positive writing and the control group were reported (similarly to the EW group compared with control subjects) at final follow-up. Participants allocated to the EW group had a longer period of remission after phototherapy; this was not seen in the positive writing group participants.
Mann72 measured optimism and pessimism but differences between groups in the time-by-group interaction analysis were not reported.
Given the heterogeneity in conditions, outcomes measured and results, no meta-analysis could be performed for this subgroup of participants for whom positive writing was evaluated.
Outcomes measured across long-term conditions
As described in previous chapters, authors of included studies have used a wide range of instruments and outcome measures to illustrate how TW interventions may have affected the different LTCs assessed. The purpose of this section is to describe whether among the included studies with any LTC, TW improved people’s depression, anxiety and disease-based outcomes (Table 64).
| Disease area (total number of studies) | Number of studies reporting physiological and biomarker outcomes (listed) | Total number of patients (maximum number) | Whether EW showed statistically significant improvement, no difference or worsening | Comments |
|---|---|---|---|---|
| HIV (6) | 3a (VL, CD4+ count) | Abel50 (208) | Abel50 – NS | |
| Ironson71 (207) | Ironson71 – NS | |||
| Petrie56 (37) | Petrie56 – NS at 2 and 13 weeks, improvement at 26 weeks | |||
| Breast cancer (8) | 0 | NA | NA | |
| Gynaecological and genitourinary cancers (6) | 1 (PSA levels, peripheral blood T-cell proliferation, serum cytokine levels of TNF-α, IL-4 and IL-10) | Rosenberg83 (30) | Rosenberg83 – NS | |
| Cancer from various sources (2) | 0 | NA | NA | |
| Sickle cell disease (1) | 0 | NA | NA | |
| Type 2 diabetes mellitus (1) | 0 | NA | NA | |
| Cystic fibrosis (1) | 1 (FEV1, BMI) | Taylor89 (34) | Taylor89 – NS | |
| Dementia (1) | 0 | NA | NA | |
| SUD (2) | 1 (BP, heart rate) | Grasing90 (42) | Grasing90 – NS | |
| Psychiatric disorders (6) | 0 | NA | NA | |
| PTSD (4) | 0 | NA | NA | |
| BN (1) | 1 (BMI) | Robinson99 (61) | Robinson99 – NR | BMI was used as baseline moderator |
| ALS (1) | 0 | NA | NA | |
| Migraine and tension headache (1) | 1 (headache frequency and headache severity) | D’Souza120 – migraine headache sample (62) | D’Souza120 – migraine headache – NS | |
| D’Souza120 – tension headache sample (34) | D’Souza120 – tension headache – NS | |||
| CVD (3) | 1 (BP, cardiac symptoms) | Willmott104 (128) | Willmott104 – cardiac symptoms – NS | |
| Willmott104 – DBP – SS | ||||
| Willmott104 – SBP – NS | ||||
| COPD (1) | 1 (6MWD, FEV1, FVC) | Sharifabad105 (66) | Sharifabad105 – 6MWD – NR | |
| Sharifabad105 – FEV1 – NS | ||||
| Sharifabad105 – FVC – NS | ||||
| Asthma (4) | 4 (FEV1% predicted, FVC) | Harris106 (77)b | Harris106 – NS | |
| Smyth107 (58) | Smyth107 – NS | |||
| Theadom58 (114) | Theadom58 – NR | |||
| Warner108 (32) | Warner108 – NS | |||
| IBS (2) | 0 | NA | NA | |
| Psoriasis (3) | 3 (psoriasis severity) | Paradisi110 (50) | Paradisi110 – SS/NR | Paradisi100 – SS first follow-up only |
| Tabolii111 (67) | Tabolli111 – NS | |||
| Vedhara112 (59) | Vedhara112 – NS | |||
| Rheumatoid arthropathies (6) | 4 (swollen joint count, walking speed, grip strength, ESR) | Lumley115 (64)a | Lumley115 – NS | |
| Lumley116 (264) | Lumley116 – NS | |||
| Smyth107 (49) | Smyth107 – NS | |||
| Wetherell117 (34) | Wetherell117 – NS | |||
| FM and chronic pain (4) | 4 (chronic pain) | Broderick118 (83) | Broderick118 – NS/SS | Broderick118 – SS for some subsets of questionnaire only |
| Gillis119 (72) | Gillis119 – NS | |||
| Graham51 (102) | Graham51 – NR | |||
| Stark57 (42) | Stark57 – NR |
Therapeutic writing effect on disease-based outcomes
From all of the included studies on LTCs, only 25 measured disease-specific outcomes (see Table 64). Of these – the TW intervention – only two had a significant effect on outcomes: the DBP of patients following first MI in Willmott et al. 104 and PASI in Paradisi et al. 110 The effects were in favour of participants receiving unfacilitated EW compared with control subjects. None of the other outcomes showed statistical differences between groups, apart from when subsets of questionnaire measures were reported separately, such as in Broderick et al. 118
Therapeutic writing effect on depression
Overview of studies
Overall, 26 studies50,51,53,55–57,76–78,81,87–96,99,100,103,106,107,112,114,115,118 out of 64 included studies9,51–58,66–119 evaluated depression. These 26 studies evaluated participants with different chronic conditions: three studies50,55,56 evaluated HIV patients; four studies53,76–78 evaluated patients with breast cancer; one study81 evaluated renal cell carcinoma patients; one study87 evaluated sickle cell disease; one study88 evaluated type 2 diabetes mellitus; one study92 evaluated patients with SUD; three studies94–96 evaluated patients with psychiatric disorders; three studies93,98,107 evaluated PTSD patients; one study99 evaluated BN; one study100 evaluated amyotrophic lateral sclerosis; one study103 in patients with a first myocardial arrest; one study112 evaluated patients with psoriasis; two studies114,115 evaluated patients with inflammatory arthropathy; and three other studies51,57,118 evaluated patients with FM and chronic pain. Fourteen different conditions were included in the overall analysis of depression. Almost all of the studies evaluated an EW intervention whereby instructions to write about the most upsetting event related to their life or disease were given. But, in one study,57 participants were instructed to change the topic throughout the writing intervention to write in the same emotional way about the positive life/disease-related events. Instruments used varied across studies and included following: HAM-D, CES-D, HADS-D, BDI (including both the revised and short form versions), CDI, Depression Anxiety Stress Scales, depression subscale (DASS-D), POMS-d and Geriatric Depression Scale (GDS).
Numerical results
The numerical results reported in the included studies evaluating depression are summarised in Table 65.
| LTC | First author, year | Immediately after writing | Depression short term | Depression medium term | Depression long term | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TW | Control | TW | Control | TW | Control | TW | Control | ||||||||||||||||||
| n | Mean | SD | n | Mean | SD | n | Mean | SDa | n | Mean | SDa | n | Mean | SD | n | Mean | SD | n | Mean | SD | n | Mean | SD | ||
| HIV | Ironson 201371 | – | – | – | – | – | – | 103 | 8.41 | 6.26 | 104 | 8.99 | 7.27 | 95 | 8.13 | 6.46 | 94 | 8.3 | 6.6 | 82 | 7.54 | 6.24 | 89 | 7.09 | 5.56 |
| Kraiij 201055 | – | – | – | – | – | – | 16 | 7.06 | 4.81 | 15 | 7.73 | 3.88 | – | – | – | – | – | – | – | – | – | – | – | – | |
| Abel 200450 | – | – | – | – | – | – | 5 | 22 | 6.1 | 6 | 20.2 | 9.7 | – | – | – | – | – | – | – | – | – | – | – | – | |
| Breast cancer | Henry 201053 | – | – | – | – | – | – | 40 | 1.31 | NR | 40 | 1.55 | NR | – | – | – | – | – | – | 40 | 1.4 | NR | 40 | 1.47 | NR |
| Jensen-Johansen 201376 | – | – | – | – | – | – | 197 | 4 | 4.1 | 221 | 4.5 | 4.4 | – | – | – | – | – | – | 209 | 4.2 | 4.3 | 226 | 4.5 | 4.6 | |
| Mosher 201277 | – | – | – | – | – | – | 44 | 17.9 | 8.9 | 42 | 17.87 | 8.9 | – | – | – | – | – | – | – | – | – | – | – | – | |
| Park 201278 | 29 | 4.93 | 3.4 | 29 | 4.48 | 3.33 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | |
| RCC | Milbury 201481 | – | – | – | – | – | – | 87 | 8.8 | 8.6 | 86 | 10.2 | 6.7 | 84 | 9.9 | 10.1 | 84 | 9.5 | 7.1 | 72 | 9.5 | 9.6 | 76 | 10.5 | 7.4 |
| Sickle cell disease | McElligott 200687 | 19 | 5.9 | 5.6 | 17 | 7.2 | 6.1 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Diabetes mellitus | Dennick 201488 | – | – | – | – | – | – | 23 | 9.9 | 5.3 | 18 | 5.1 | 5.1 | – | – | – | – | – | – | – | – | – | – | – | – |
| SUD | Meshberg-Cohen 201091 | 77 | 21.2 | 10.1 | 64 | 20.3 | 12.1 | 77 | 18.3 | 11.6 | 64 | 15.4 | 10.2 | – | – | – | – | – | – | – | – | – | – | – | – |
| Psychiatric disorders | Canna 200694 | – | – | – | – | – | – | 22 | 16.8 | 8.28 | 13 | 17.8 | 9.65 | 18 | 9.9 | 7.85 | 18 | 15.1 | 9.78 | 12 | 12.4 | 10.54 | 12 | 10.4 | 6.9 |
| Graf 200895 | 22 | 11.32 | 10.25 | 22 | 17.45 | 12.18 | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | |
| Krpan 201396 | – | – | – | – | – | – | 20 | 20.0 | 10.5 | 20 | 26.0 | 8.5 | – | – | – | – | – | – | – | – | – | – | – | – | |
| PTSD | Bernard 200693 | – | – | – | – | – | – | 12 | 5.92 | 4.54 | 10 | 7.11 | 4.65 | – | – | – | – | – | – | – | – | – | – | – | – |
| Gidron 199698 | – | – | – | – | – | – | 8 | 39.1 | 9.1 | 6 | 45.2 | 13 | – | – | – | – | – | – | – | – | – | – | – | – | |
| Smyth 2008121 | – | – | – | – | – | – | POMS mean change reported only | – | – | – | – | – | – | – | – | – | – | – | – | ||||||
| BN | Robinson 200899 | – | – | – | – | – | – | 34 | 18.3 | 95% CI 14.1 to 22.6 | 27 | 9.37 | 95% CI 8.0 to 10.74 | – | – | – | – | – | – | – | – | – | – | – | – |
| ALS | Averill 2013100 | – | – | – | – | – | – | Numerical data not reported | – | – | – | – | – | – | – | – | – | – | – | – | |||||
| MI | Hevey 2012103 | Numerical data not reported | Numerical data not reported | – | – | – | – | – | – | – | – | – | – | – | – | ||||||||||
| Psoriasis | Vedhara 2007112 | 31 | 6.43 | 8.62 | 28 | 5.93 | 9.5 | 31 | 4.38 | 4.44 | 28 | 3.68 | 3.36 | – | – | – | – | – | – | – | – | – | – | – | – |
| Inflammatory arthritis | Hamilton-West 2007114 | – | – | – | – | – | – | Numerical data not reported | – | – | – | – | – | – | – | – | – | – | – | – | |||||
| FM | Broderick 2005118 | – | – | – | – | – | – | BDI-II mean change reported only | – | – | – | – | – | – | – | – | – | – | – | – | |||||
| bGraham 200851 | 51 | 25 | (24.23 to 26.07) | 51 | 25.31 | (24.45 to 25.53) | 51 | 20.44 | (19.68 to 21.20) | 51 | 24.12 | (23.04 to 25.09) | – | – | – | – | – | – | – | – | – | – | – | – | |
| Stark 201057 | – | – | – | – | – | – | 21 | 4 | 3.08 | 21 | 5.19 | 4.25 | – | – | – | – | – | – | – | – | – | – | – | – | |
Meta-analysis
Depression was assessed at immediate-, short-, medium- and long-term follow-up across studies (Figures 48–51).
FIGURE 48.
Forest plot of depression at immediate follow-up across included studies. df, degrees of freedom; IV, inverse variance.

FIGURE 49.
Forest plot of pain severity at short-term follow-up across included studies. df, degrees of freedom; IV, inverse variance.
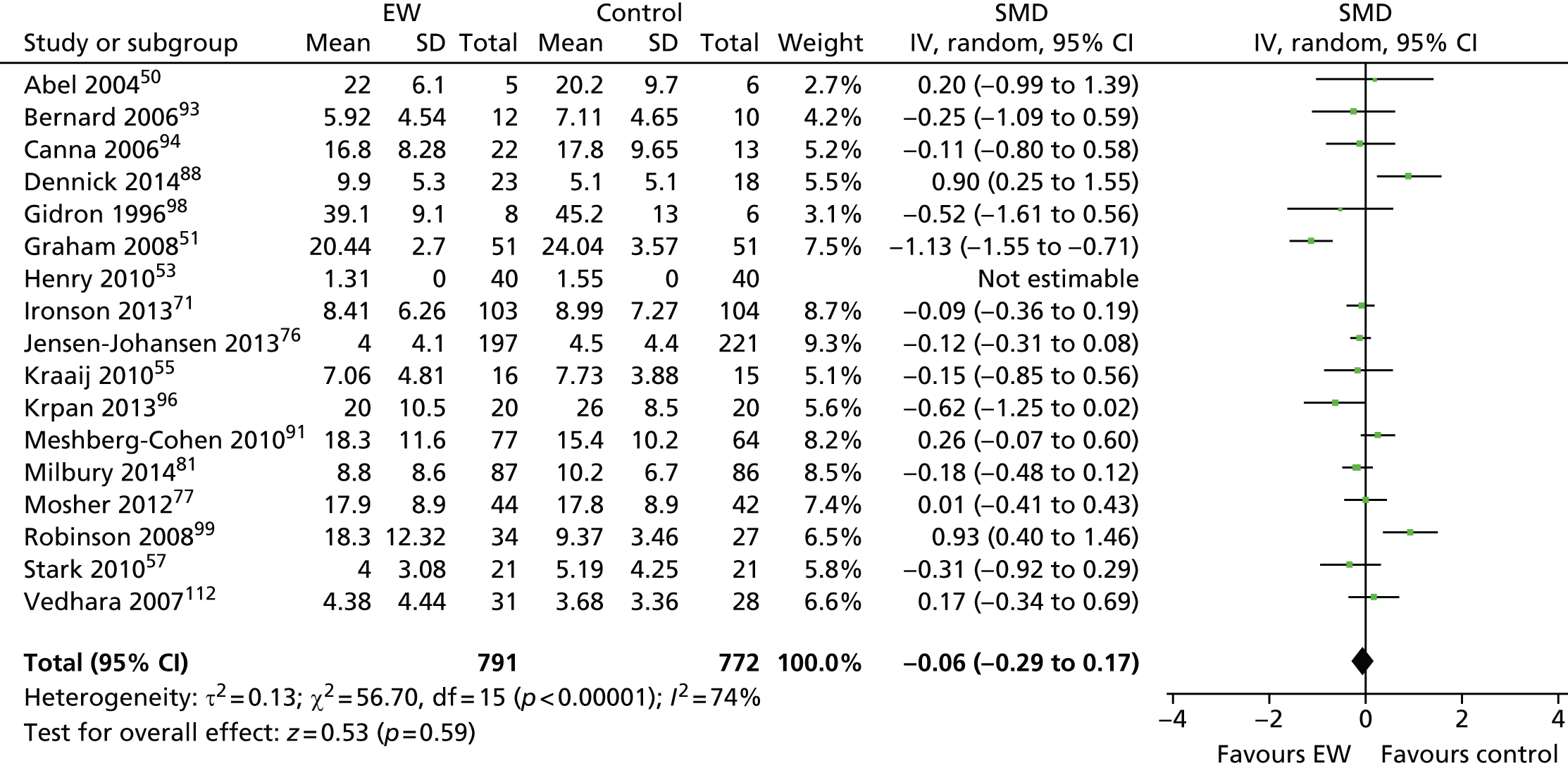
FIGURE 50.
Forest plot of depression at medium-term follow-up across included studies. df, degrees of freedom; IV, inverse variance.
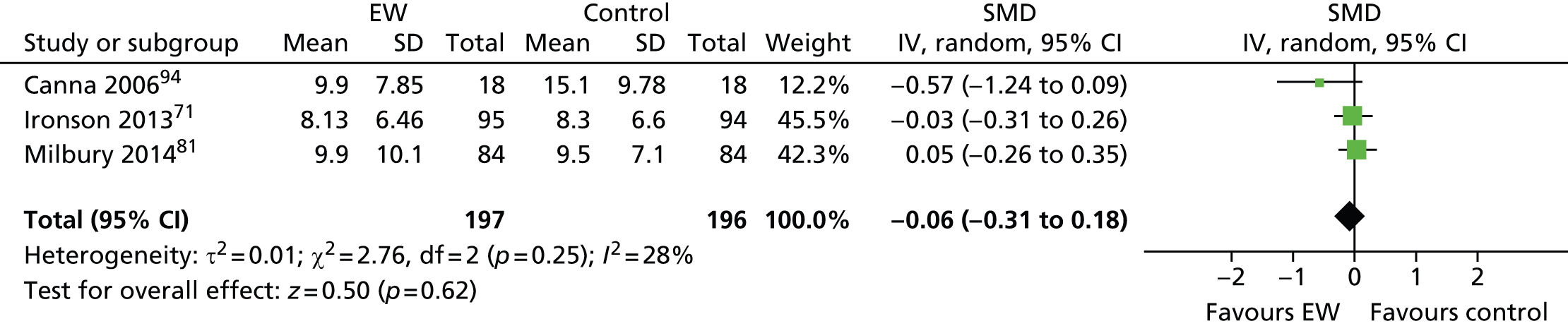
FIGURE 51.
Forest plot of depression at long-term follow-up across included studies. df, degrees of freedom; IV, inverse variance.
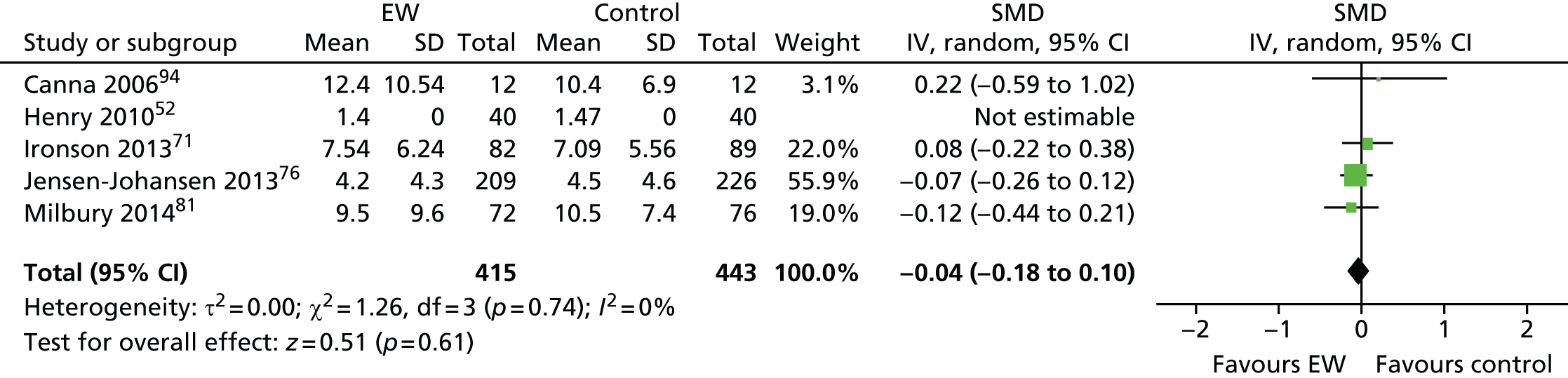
-
Immediate follow-up A total of 440 participants were meta-analysed (229 in the EW group and 211 in the control group). The SMD was –0.01 (95% CI –0.20 to 0.18) with no significant heterogeneity (I2 = 0%). This result suggests that there is no statistically significant difference in depressive symptoms up to 4 weeks after writing exercise in the TW group compared with the control group.
-
Short-term follow-up A total of 1563 participants were meta-analysed (791 in the EW group and 772 in the control group). The SMD was –0.06 (95% CI –0.29 to 0.17) with substantial, significant heterogeneity (I2 = 74%). This result suggests that there is no statistically significant difference in depressive symptoms between 4 and 17 weeks after the writing exercise in the TW group compared with the control group.
-
Medium-term follow-up A total of 393 participants were meta-analysed (197 in the EW group and 196 in the control group). The SMD was –0.06 (95% CI –0.31 to 0.18) with a significant heterogeneity (I2 = 28%). This result suggests that there is no statistically significant difference in depressive symptoms between 17 and 34 weeks after the writing exercise in the TW group compared with the control group.
-
Long-term follow-up A total of 778 participants were meta-analysed (375 in the EW group and 403 in the control group). The SMD was –0.04 (95% CI –0.18 to 0.10) with no significant heterogeneity (I2 = 0%). This result suggests that there is no statistically significant difference in depressive symptoms 34 weeks after the writing exercise in the TW group compared with the control group.
The overall analysis of the effect of TW on depression showed no significant differences between the TW group and the control subjects at any of the time points.
Therapeutic writing effect on anxiety
Overview of studies
Overall, 977,78,87,93–95,97,112,118 studies out of 59 evaluated anxiety across the included LTCs. These 9 studies evaluated participants with different chronic conditions: two studies77,78 evaluated patients with breast cancer; one study87 evaluated patients diagnosed with sickle cell disease; four93–95,97 evaluated participants with mental and psychiatric disorders; one study112 evaluated patients with psoriasis; and the remaining study118 assessed patients with fibromyalgia. Five different conditions were accounted in the overall analysis of anxiety. All studies evaluated an unfacilitated EW intervention. In one study,97 participants were instructed to write about the deepest thoughts and feelings, regarding an experience that had not been previously shared with others at all or in very little detail. Instruments used varied across studies and included the following: HADS-A, Revised Children’s Manifest Anxiety Scale (RCMAS), BAI, Depression Anxiety Stress Scales, anxiety subscale (DASS-A) and CSAQ.
Numerical results
The numerical results reported in the included studies evaluating anxiety are summarised in Table 66.
| LTC | First author, year | Immediately after writing | Short term | Medium term | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TW | Control | TW | Control | TW | Control | ||||||||||||||
| n | Mean | SD | n | Mean | SD | n | Mean | SDa | n | Mean | SDa | n | Mean | SD | n | Mean | SD | ||
| Breast cancer | Mosher 201277 | – | – | – | – | – | – | 44 | 7.15 | SE = 0.48 | 42 | 7.87 | SE = 0.49 | – | – | – | – | – | – |
| Park 201278 | 29 | 6.17 | 4.21 | 29 | 5.79 | 3.63 | 29 | 5.62 | 4.37 | 29 | 5.9 | 3.8 | – | – | – | – | – | – | |
| Sickle cell disease | McElligott 200687 | 19 | 8 | 5.9 | 17 | 9.5 | 5.7 | – | – | – | – | – | – | – | – | – | – | – | – |
| Mental and psychiatric disorders | Bernard 200693 | – | – | – | – | – | – | 12 | 8.75 | 5.83 | 10 | 8.11 | 5.44 | – | – | – | – | – | – |
| bCanna 200694 | – | – | – | – | – | – | 22 | 17.6 | 9.88 | 18 | 23.2 | 4.59 | 12 | 8.6 | 6.83 | 12 | 13.3 | 10.93 | |
| cCanna 200694 | – | – | – | – | – | – | 18 | 10.2 | 6.62 | 13 | 17.9 | 15.36 | – | – | – | – | – | – | |
| Graf 200895 | 22 | 8.23 | 8.62 | 22 | 10.91 | 9.66 | – | – | – | – | – | – | – | – | – | – | – | – | |
| Richards 200097 | – | – | – | – | – | – | 36 | 22.62 | 11.35 | 29 | 21.45 | 11.51 | – | – | – | – | – | – | |
| Psoriasis | dVedhara 2007112 | 31 | 6.51 | 3.93 | 28 | 7.52 | 3.87 | 31 | 5.83 | 3.06 | 28 | 6.36 | 3.34 | – | – | – | – | – | – |
| eVedhara 2007112 | – | – | – | – | – | – | 31 | 5.81 | 3.14 | 28 | 6.54 | 3.66 | – | – | – | – | – | – | |
| FM | Broderick 2005118 | – | – | – | – | – | – | 28 | Change score: 3.7 | 2.4 | 55 | Change score: 7 | 1.7 | – | – | – | – | – | – |
Meta-analysis
Anxiety was assessed with different instruments at immediate, short and medium term only (Figures 52 and 53). Only one study94 assessed anxiety in the medium term, so no meta-analysis was required.
FIGURE 52.
Forest plot of anxiety at immediate follow-up across included studies. df, degrees of freedom; IV, inverse variance.

FIGURE 53.
Forest plot of anxiety at short-term follow-up across included studies. df, degrees of freedom; IV, inverse variance.
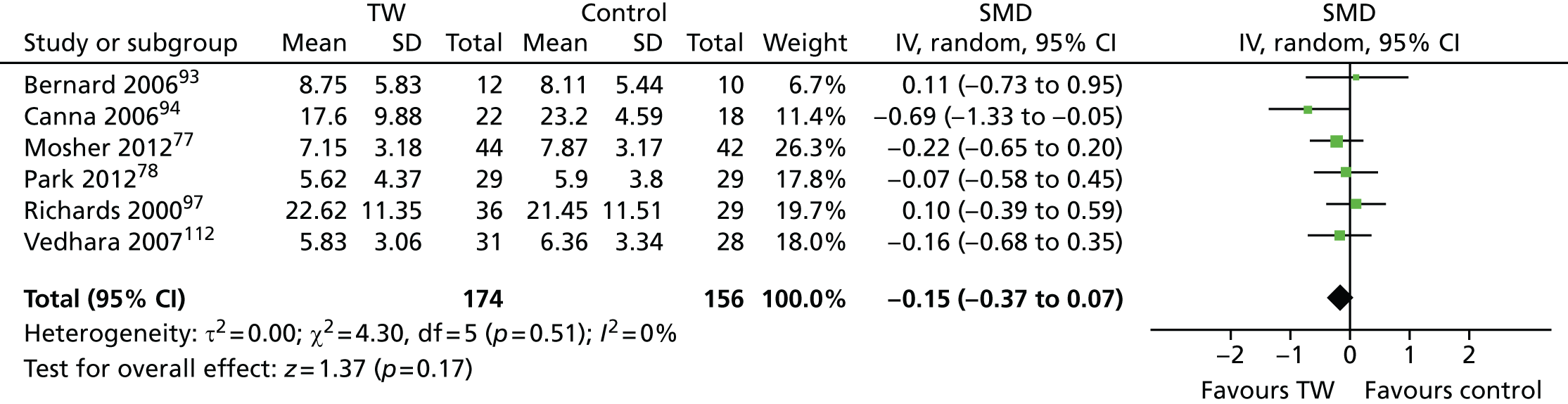
-
Immediate follow-up Four studies78,87,95,112 assessed anxiety at immediate follow-up, just after the writing exercise.
-
A total of 197 participants were meta-analysed (101 in the EW group and 96 in the control group). The SMD was –0.16 (95% CI –0.44 to 0.12) and with no significant heterogeneity, I2 = 0%. This result suggests that there is no statistically significant difference in anxiety at immediate follow-up in the EW group compared with the control group.
-
-
Short-term follow-up Six studies77,78,93,94,97,112 assessed anxiety at short-term follow-up. Broderick et al. ,113 however, was not included in the meta-analysis, as only change scores were reported. Canna94 reported anxiety at 8 and 16 weeks. Likewise, Vedhara et al. 112 reported anxiety at 8 and 12 weeks. For consistency among the studies included in the meta-analysis, the 8-week assessments were chosen.
-
A total of 330 participants were meta-analysed (174 in the EW group and 156 in the control group). The SMD was –0.15 (95% CI –0.37 to 0.07) with no significant heterogeneity (I2 = 0%). This result suggests that there is no statistically significant difference in anxiety at short-term follow-up for the EW group compared with the control group.
-
Chapter 4 Economic considerations
Introduction
In a health-care system such as the NHS it is important to consider not just the benefits and potential harms of interventions for the recipients, but also the impact that interventions may have on the use of limited health-care resources. In the previous chapter the available evidence on the effects of TW on health outcomes for people with a variety of LTCs is summarised. Here the evidence on the economic impacts of TW in these populations from a NHS perspective is reviewed. NHS provision of TW interventions would incur direct costs; the cost for staff training and time to deliver the intervention, or of payments to external experts; administrative costs; and costs for the use of a room and, possibly, some materials. There may also be some indirect costs or savings for the NHS if TW encouraged patients to increase or decrease their use of other health services. For example, patients might feel better able to manage their condition and consult their GP or hospital specialist less often or, conversely, TW might lead patients to recognise a need to make more use of available health services. The net effect on NHS expenditure might therefore be positive or negative.
In addition to financial costs and savings, a full economic evaluation would account for the intrinsic value of any impacts on patients’ health and well-being. For example, health gains or losses attributable to the intervention could be quantified in terms of quality-adjusted life-years (QALYs), where one QALY is defined as 1 year lived in perfect health for one person. The cost-effectiveness of the intervention could then be summarised as the additional cost per QALY gained, in relation to some appropriate comparator. For such a calculation, the magnitude and persistence of any effects of TW on HRQoL would need to be estimated. This calculation of QALYs from the studies in this review is problematic because although some of the studies reviewed in the preceding chapter reported on general HRQoL (23 out of 64 studies), only one study88 used a measure suitable for QALY estimation, such as the EQ-5D, and none used the Short Form questionnaire-6 Dimensions (SF-6D).
From the early stages of the project, the need for flexibility in the approach to the consideration of the economic evidence was apparent. Given the limitations of the evidence base, it was concluded that it was not possible to directly estimate QALY impacts of TW across the range of populations with LTCs. Consideration was given to the possibility of using a decision-analytic model to estimate the effects of the intervention on intermediate indicators of disease progression, and then to link to the effects of disease progression on health-care costs and outcomes. However, the lack of convincing or consistent evidence of such effects led us to conclude that such modelling exercises would not be appropriate or feasible. Instead, a more pragmatic approach was taken, making the most of the evidence available.
The economics section is in three parts:
-
a systematic review of TW studies reporting on economic outcomes (resource use, costs and/or cost-effectiveness)
-
an estimation of the cost of providing a range of TW interventions in a NHS context
-
case studies presenting balance sheets of available economic and clinical evidence for three conditions: PTSD, RA and breast cancer.
Systematic review of therapeutic writing studies with resource-use outcomes
Methods
A review across LTCs of the available literature on comparative studies of TW for patients with LTCs reporting economic outcomes was conducted. This resource-use systematic review was nested within the overall systematic review described in the previous chapter and the realist synthesis presented in the following chapter. The full search strategy is given in Appendix 3.
The inclusion criteria used for the economic systematic review are shown in Table 67.
| Inclusion criteria | Details |
|---|---|
| Patients | Any patients with at least one LTC |
| Intervention | Any form of TW |
| Comparator | Any inactive comparator |
| Outcomes | Resource use, costs or cost-effectiveness |
| Study design | Any fully published comparative study (PhD dissertations were not used) |
Titles and abstracts were checked by two reviewers to find relevant studies, data extraction was undertaken by one reviewer and checked by a second. If there were disagreements, a third senior systematic reviewer or health economist was consulted to make a decision. All of the studies in the economic review were also included in the effectiveness review, and critically appraised as part of that review (see Appendices 4 and 5). Quality assessment using a critical appraisal checklist for economic evaluations was planned if any economic evaluations were identified.
Where three or more studies presented outcomes in the same category (e.g. health centre visits, medications used), meta-analysis was conducted using the same methods as for the effectiveness systematic review.
Results of economic review (resource use)
No full economic evaluations (cost-effectiveness, cost–benefit or cost–utility studies) were identified. One study89 estimated that the cost of a writing intervention was US$130 per patient, based on a psychologist’s fee and some administration time. This study89 found a reduction in inpatient use for the EW intervention compared with SMC and estimated that this represented a cost saving of US$25,878 per patient per year. Another study113 estimated that the cost of delivering videotaped instructions for an EW intervention was approximately US$5 per patient. The basis for this estimate was unclear but it seems to be reasonable.
Twelve studies57,68,75,77,83,89,90,97,98,104,109,119 that reported on some element of health-care resource use were identified. One study reported on the cost of the TW intervention89 and none on monetary estimates of costs or savings relating to differences in health-care use between the study groups. Consequently, no additional economic quality assessment was conducted.
Study details
Details of the studies57,68,75,77,83,89,90,97,98,104,109,119 are outlined in Table 68. The publication dates ranged from 1996 to 2012: six studies57,75,77,90,104,109 were published after 2009. The majority of the studies57,77,83,89,90,97,109,119 were from the USA. Two studies75,104 were conducted in the UK. All patients were recruited via flyers distributed at disease-specific clinics or approached by health-care professionals during their treatment cycle. The disease areas varied, but can be broadly grouped into three categories: cancer (n = 3),75,77,83 chronic pain or FM (n = 3),57,109,119 or PTSD, mental health disorders or drug dependency (n = 4). 68,90,97,98 The remaining studies related to MI104 and cystic fibrosis. 89 One study68 was a case–control study and tested a facilitated form of TW – an internet discussion. The other studies57,75,77,83,89,90,97,98,104,109,119 were RCTs and tested unfacilitated EW. 1 The control interventions varied: seven studies68,75,83,89,97,98,109 included a normal care or non-writing control arm. Six studies57,77,89,90,104,119 used a non-emotional form of writing.
| First author, year | Country | Patient LTC | n total | Intervention | Comparator | Resource-use outcomes |
|---|---|---|---|---|---|---|
| Gellaitry 201075 | UK | Breast cancer | 80 | Unfacilitated EW | Normal care | Use of health-care facilities (6 months following completion of treatment) |
| Gidron 199698 | Israel | PTSD | 14 | Unfacilitated EW | Normal care | Number of health-care visits at 5 weeks |
| Gillis 2006119 | USA | FM | 155 | Unfacilitated EW | Time-management writing | Number of visits to health-care specialist at 1 and 3 months |
| Golkaramnay 200768 | Germany | Mental disorders | 228 | Internet chat (facilitated) | Normal care | Proportion accessing psychotherapeutic care during 12-month follow-up |
| Proportion receiving medication | ||||||
| Grasing 201090 | USA | Drug dependency | 42 | Unfacilitated EW | Time-management writing | Outpatient follow-up visits 12 weeks after discharge |
| Mosher 201277 | USA | Breast cancer | 87 | Unfacilitated EW | Factual writing | Proportion using mental health services at 8 weeks’ follow-up |
| Richards 200097 | USA | Mental disorders | 98 | Unfacilitated EW | Trivial writing Normal care |
Infirmary visits at 6 weeks |
| Rosenberg 200283 | USA | Prostate cancer | 30 | Unfacilitated EW | Non-writing | Number of health-care contacts at 3 months |
| Medication use | ||||||
| Stark 201057 | USA | FM | 43 | Unfacilitated EW | Time-management writing | Medication use at 5 and 10 weeks |
| Taylor 200389 | USA | Cystic fibrosis | 39 | Unfacilitated EW | Normal care | Number of days in hospital |
| Outpatient clinic visits over 3 months’ follow-up | ||||||
| Wallander 2011109 | USA | RAP | 63 | Unfacilitated EW | Normal care | Number of health-care contacts during 6 months’ follow-up |
| Willmott 2011104 | UK | MI | 156 | Unfacilitated EW | Inexpressive writing | GP and hospital visits during 5 months’ follow-up |
| Medication use | ||||||
| Attendance at cardiac rehabilitation sessions | ||||||
| Return to work |
Numerical results of resource-use studies
Numerical results are shown in Table 69. The quality and detail of studies reporting on health-care resource use varied widely across studies. The types of use recorded were broadly similar: almost all reported on contacts with health-care services, consultations with clinicians or inpatient stays (n = 11). Four papers57,68,83,104 also reported on use of medication. Willmott et al. 104 also reported the number of weeks’ absence from work as an outcome, which is an important indicator for the personal and broader economic impact of an intervention.
| First author, year | Resource use reported | Intervention: mean (SD) or percentages | Control: mean (SD) or percentages | Comments |
|---|---|---|---|---|
| Gellaitry 201075 | Number of medical visits in the 6 months following baseline | NR | NR | Authors report a significant time effect, i.e. health-care use decreasing in the 6 months following completion of treatment [F(3,213) = 5.43; p < 0.01]. Authors report no difference between groups in terms of resource usage. No numerical data are provided |
| Gidron 199698 | Number of health-care visits | 3.1 (2) (n = 8) | 0.7 (1.6) (n = 6) | Authors report a significant increase in health-care visits among patients in the intervention group (from 1.6 to 3.1) compared with a significant decrease among patients in the control group (from 1.3 to 0.7) |
| Gillis 2006119 | Number of health-care visits in the 3 months after baseline | 1.13 (1.07) (n = 38) | 1.80 (2.21) (n = 34) | Authors report a significant decrease in health service use for the intervention group at 3 months (p = 0.05) but not at 1 month (p = 0.16) |
| Golkaramnay 200768 | Proportion accessing psychotherapeutic care | 53.6% (52/97) | 62.8% (59/94) | Original sample was 114 in each group. NS |
| Proportion receiving medication | 55.9% (57/97) | 60.4% (57/94) | NS | |
| Grasing 201090 | Number of outpatient mental health clinic visits | 7 (15.3) (n = 23) | 2.36 (2.8) (n = 19) | Although resource use was higher among patients in the intervention group in all three categories, none of these differences were statistically significant. SEs were given in paper, converted here to SDs |
| Number of clinical support visits | 9.68 (12.2) | 10.27 (23.9) | ||
| Number of study follow-up visits | 2.05 (1.9) | 1.57 (1.7) | ||
| Mosher 201277 | Proportion of patients accessing mental health services | NR | NR | Intervention and control group numbers given combined only – 27/86 |
| Richards 200097 | Infirmary visits | NR | NR | Mean (SD) infirmary visit results given split by sex offender status only. No complete group results available |
| Rosenberg 200283 | Number of health-care contacts 6 months after baseline | 4.4 (3.12) (n = 16) | 7.6 (8.33) (n = 14) | Authors report a trend towards lower health-care utilisation and reduced use of medications based on these findings; however, the paper does not report on statistical significance |
| Number of medicines being used 6 months after baseline | 4.94 (2.66) | 6.05 (4.7) | ||
| Stark 201057 | Number of pain medications taken per month | 144.5 (110.44) (n = 21) | 169.9 (128.99) (n = 21) | |
| Number of psychotropic medications taken per month | 44.9 (47.48) | 60.20 (60.36) | ||
| Taylor 201389 | Number of days in hospital | 5.6 (NR) (n = 18) | 8.4 (NR) (n = 21) | Significant group-by-time interaction for inpatient hospital days; no significant interaction found for outpatient clinic visits |
| Wallander 2011109 | Number of health-care contacts | 1.0 (2.36) (n = 32) | 2.36 (2.21) (n = 24) | Authors report that 43% of intervention group had no contact with clinical services compared with 11% of the control group |
| Willmott 2011104 | Number of GP and hospital visits | 8.6 (3.7) (n = 79) | 10.3 (5.0) (n = 77) | Patients in the intervention group reported to make significantly fewer visits to GPs or hospital clinics than those in the control group. Although the number of prescribed medicines was lower in the intervention group, the difference was not significant; however, authors identified a significant interaction between group and time, suggesting that the number of medications decreased over time for the intervention group and increased over time for the control group. For the other two outcomes reported, the control group was associated with lower levels of resource usage. It was not reported if the difference in the number of attendances at cardiac rehabilitation sessions was significant. The difference in the number of weeks’ absence from work was not significant |
| Median number of GP and hospital visits in the 5 months following completion of treatment (range) | 8 (2–22) | 10 (3–25) | ||
| Mean number of prescribed medications 5 months following completion of treatment (SD) | 4.8 (1.7) | 5.3 (1.7) | ||
| Mean number of cardiac rehabilitation sessions attended (SD); p = 0.01 | 7.99 (5.26) | 5.68 (5.85) | ||
| Mean number of weeks absent from work (SD) | 12.2 (7.4) | 10.3 (6.9) |
Contact with health-care services
Of the 11 studies57,68,75,77,83,89,90,98,104,109,119 reporting on some form of contact with health-care professionals in a health-care setting, seven studies83,89,90,98,104,109,119 provided means and/or SDs that could be combined in a forest plot (Figure 54). Golkaramnay et al. 68 and Mosher et al. 77 reported proportions of patients accessing services. The meta-analysis results showed no significant differences (SMD –0.19, 95% CI –0.57 to 0.18). Willmott et al. 104 reported on two outcomes relating to health-care contact: median number of GP and hospital visits, which was higher in the control arm, and the mean number of cardiac rehabilitation sessions attended, which was higher in the intervention group. Overall, the results suggest that TW has little impact on health centre visits.
FIGURE 54.
Forest plot of health-care resource use. df, degrees of freedom; IV, inverse variance.
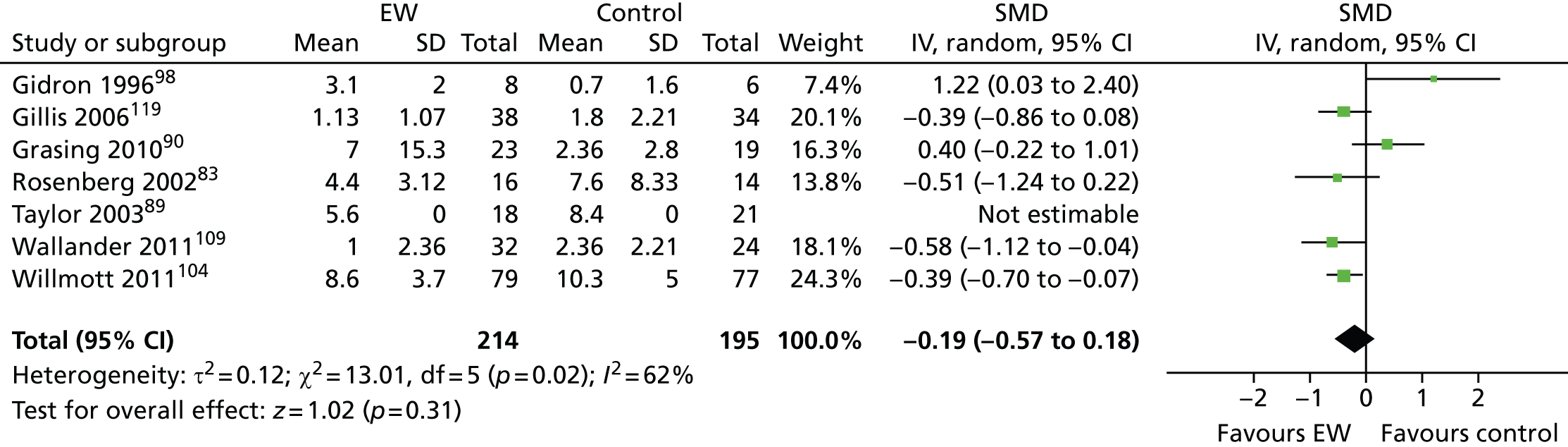
Use of medication
Three studies57,83,104 reported means and SDs for the impact of TW on use of medication, and Golkaramnay et al. 68 reported the proportion of participants receiving medication. Stark57 reported on the number of units of pain and psychotropic medication per patient per month, finding lower levels of use in the intervention group 10 weeks after baseline. Willmott et al. 104 and Rosenberg et al. 83 took a different approach, looking at the number of medications participants report using at similar time spans post baseline (5 and 6 months, respectively). In both cases, participants in the intervention group were identified as using fewer medications, although in Willmott et al. 104 this difference was not significant, and Rosenberg et al. 83 did not report on significance. Willmott et al. 104 also noted a potential time effect – medication use decreased in the intervention group but increased in the control group. The meta-analysis results (Figure 55) suggested that fewer medications were taken after TW (SMD –0.28, 95% CI –0.54 to –0.02).
FIGURE 55.
Forest plot of medication use. df, degrees of freedom; IV, inverse variance.
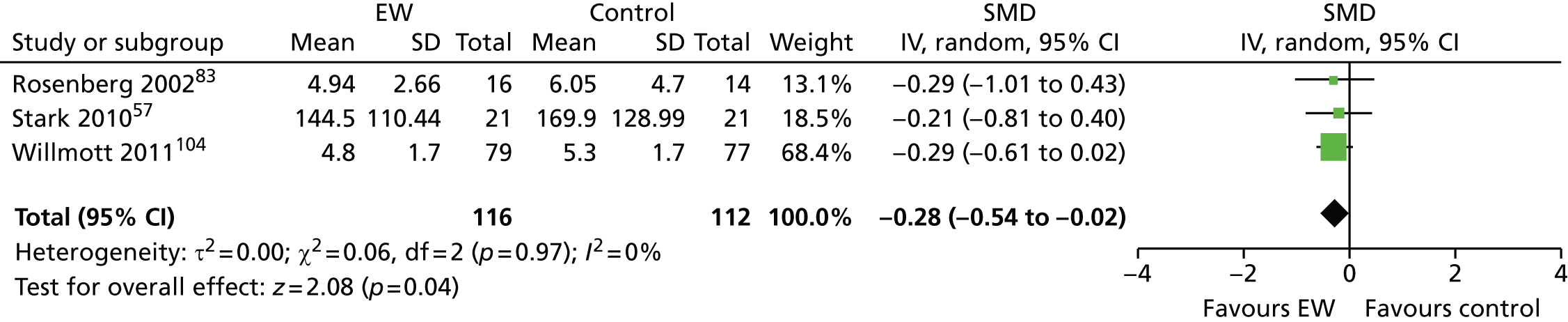
Many of the costs associated with the use of medication are indirect, and not examined in these studies, for example consultations with prescribers, and treatment for side effects. Although these add to the uncertainty around impact of decreased medication use, it also raises the possibility that there are potentially unacknowledged benefits associated with TW, which have not been explicitly accounted for here.
As with health-care contacts, this evidence base is not strong enough to draw conclusions about the likely impact of TW interventions on patient use of medication.
Costs of therapeutic writing interventions
None of the identified studies presented estimates of the cost of TW or EW in the UK. Therefore, estimates for a range of interventions in a NHS context were made, after discussion with practitioner experts.
The primary driver of costs is likely to be the staff costs associated with employing (or contracting) TW practitioners. TW practitioners come from a wide range of professional backgrounds, and many are self-employed, rather than NHS employees. However, for illustrative purposes, the costs for NHS occupational therapists published by the Personal Social Services Research Unit (PSSRU)126 were adapted (Table 70).
| Cost item (£) | Salary gradea | |||
|---|---|---|---|---|
| 5 | 6 | 7 | 8a | |
| Salary | 23,441 | 30,712 | 38,146 | 45,593 |
| On-costs | 5483 | 7184 | 8923 | 10,664 |
| Qualifications | 5531 | 5531 | 5531 | 5531 |
| Overheads: staff | 5585 | 7318 | 9089 | 10,863 |
| Overheads: non-staff | 12,139 | 15,905 | 19,755 | 23,611 |
| Overheads: capitalb | 4776 | 4776 | 4776 | 4776 |
| Total cost | 56,956 | 71,425 | 86,219 | 101,039 |
| Cost per hourc | 36 | 45 | 54 | 63 |
Costs were estimated for NHS staff at Agenda for Change pay bands 5, 6, 7 and 8a to reflect a range of levels of qualifications and experience. The estimated total cost per hour ranged from £36 to £63 (at 2012–13 prices). For comparison, the PSSRU report126 estimated a cost of £36 per hour for a hospital-based occupational therapist; £48 per hour for a counsellor in primary care; and £59 for a clinical psychologist.
All of the above costs were inclusive of staff training, as well as salary on-costs (employer’s national insurance plus 14% of salary for employer’s contribution to superannuation); management and administration overheads, and capital overheads (annuitised over 60 years at a discount rate of 3.5%). The capital cost included an allocation for patient care and non-patient care facilities within a NHS hospital, and can therefore be assumed to include the cost of a room for delivery of the individual or group TW sessions. There may be some other costs for materials, such as printed instructions, videos, pens and paper, but these are difficult to estimate.
The time required for a TW practitioner to prepare for a session was not quantified. The PSSRU report126 estimated the percentage of working time spent on face-to-face client contact: 77% for primary care counsellors and 45% for clinical psychologists (no estimates were available for occupational therapists). This implies that, for every hour of client contact, approximately 15–30 minutes will be spent on other activities. For cost estimates, it was assumed that it takes 10 minutes for a TW practitioner to prepare for a session with clients; this is not assumed to vary according to the length of the session or the number of participants in the session.
The majority of studies included in the systematic review used self-administered unfacilitated form of writing. This typically involves a brief initial consultation with the patient, either in person or over the telephone. Following this initial discussion, the patient is left to continue with the intervention on their own, writing unsupervised, often in their own home, for the prescribed time and on the prescribed topic. There is minimal subsequent interaction with practitioners – in some cases, the TW is not returned to, or read by, practitioners. Although this set of methods is used in the majority of studies – possibly due to its relative ease of implementation – this form of writing is not representative of current clinical practice in the UK. Practitioner experts advised that facilitated writing is much more common in a NHS setting: writing sessions run by trained experts. These sessions may be individual or group, and patients may attend multiple sessions.
The estimated costs for a range of TW interventions, with varying group sizes, numbers of sessions and contact times per session, are outlined in Table 71.
| Type of TW | Number of sessions | Preparation time per session (minutes) | Contact time per session (minutes) | Mean cost per participant (£), by grade of practitionera | |||
|---|---|---|---|---|---|---|---|
| 5 | 6 | 7 | 8a | ||||
| £36 | £45 | £54 | £63 | ||||
| Unfacilitated | 1 | 10 | 10 | 12 | 15 | 18 | 21 |
| 1 | 10 | 30 | 24 | 30 | 36 | 42 | |
| Facilitated: eight patients per session | 4 | 10 | 45 | 17 | 21 | 25 | 29 |
| 4 | 10 | 60 | 21 | 26 | 32 | 37 | |
| 4 | 10 | 120 | 39 | 49 | 59 | 68 | |
| 10 | 10 | 45 | 41 | 52 | 62 | 72 | |
| 10 | 10 | 60 | 53 | 66 | 79 | 92 | |
| 10 | 10 | 120 | 98 | 122 | 146 | 171 | |
| 16 | 10 | 45 | 66 | 83 | 99 | 116 | |
| 16 | 10 | 60 | 84 | 105 | 126 | 147 | |
| 16 | 10 | 120 | 156 | 195 | 234 | 273 | |
| Facilitated: four patients per session | 4 | 10 | 45 | 33 | 41 | 50 | 58 |
| 4 | 10 | 60 | 42 | 53 | 63 | 74 | |
| 4 | 10 | 120 | 78 | 98 | 117 | 137 | |
| 10 | 10 | 45 | 83 | 103 | 124 | 144 | |
| 10 | 10 | 60 | 105 | 131 | 158 | 184 | |
| 10 | 10 | 120 | 195 | 244 | 293 | 341 | |
| 16 | 10 | 45 | 132 | 165 | 198 | 231 | |
| 16 | 10 | 60 | 168 | 210 | 252 | 294 | |
| 16 | 10 | 120 | 312 | 390 | 468 | 546 | |
| Facilitated: one to one | 4 | 10 | 45 | 132 | 165 | 198 | 231 |
| 4 | 10 | 60 | 168 | 210 | 252 | 294 | |
| 4 | 10 | 120 | 312 | 390 | 468 | 546 | |
| 10 | 10 | 45 | 330 | 413 | 495 | 578 | |
| 10 | 10 | 60 | 420 | 525 | 630 | 735 | |
| 10 | 10 | 120 | 780 | 975 | 1170 | 1365 | |
| 16 | 10 | 45 | 528 | 660 | 792 | 924 | |
| 16 | 10 | 60 | 672 | 840 | 1008 | 1176 | |
| 16 | 10 | 120 | 1248 | 1560 | 1872 | 2184 | |
The upper and lower limits of these ranges are based on interventions described in the included studies in Chapter 3. Session length for facilitated TW ranged from 45 minutes in Lange et al. 69 to 120 minutes in Rickett et al. 66 and Sloan et al. 70 The length of the intervention varied from four sessions in Sloan et al. 70 to 16 sessions in Hong and Choi. 67 The number of participants in the interventions ranged from two to eight, based on advice from a TW practitioner that sessions range from one to seven participants, with four being the optimal number. It was assumed that the introductory session for unfacilitated writing would last for 10–30 minutes. Even the more resource-intensive, facilitated versions of TW seem to be low cost in relation to other health-care interventions. However, the range of estimated costs is wide: from £17 to about £2200 per patient. The estimated cost per patient for unfacilitated EW here is less than the US$130 estimated in Taylor et al. 89 In that study89 the cost was largely based on the psychologist’s fee of US$130 per hour, which is more than the £59 per hour for a UK clinical psychologist quoted above.
Without adequate evidence on the effects of TW on patients’ health and well-being, or its effect on other health-care expenditure, it is difficult to draw conclusions about whether or not TW is a cost-effective use of NHS resources.
Exploratory cost–consequence analyses
Methods
Studies included in the effectiveness review spanned a wide range of disease areas and populations, making it difficult to identify where TW may have value. Three disease areas were examined in more detail, bringing together effectiveness evidence alongside estimates of economic impacts (cost–consequence analyses). The areas chosen for further analysis were PTSD, inflammatory arthritis and breast cancer. These topics were chosen by the SGC before the results of the meta-analyses were known, with the aim of reflecting a range of different conditions for which TW has been used. There was also a pragmatic element to this choice – these topics contained a greater number of studies, including some of the higher-quality ones. It was felt that they were likely to provide a stronger evidence base than some other areas. It is important to note that these case studies are unlikely to be representative of the whole evidence base for TW.
For each case study, a summary of effectiveness evidence was prepared, and presented alongside estimates of costs and use of health-care resources. Where possible, costs were estimated using information about the intensity of practitioner input in the related clinical studies.
Case study 1: post-traumatic stress disorder
In total, four studies69,70,98,121 reported on the use of TW in the treatment of people with PTSD. Gidron et al. 98 and Smyth and Arigo121 tested unfacilitated TW to treat PTSD. Details of these studies are presented in Chapter 3 (pp. 78–83). Lange et al. 69 and Sloan et al. 70 evaluated a facilitated TW intervention in a PTSD population (see Chapter 3, F43: post-traumatic stress disorder).
Summary of study design and quality
Two studies69,70 evaluated individual forms of facilitated TW compared with waiting list controls (see Table 5). Both recruited from the community: Lange et al. 69 recruited online and screened for post-traumatic stress and grief; those in the Sloan et al. 70 study were recruited through local advertisement and had a primary diagnosis of PTSD related to a MVA. Study quality was mixed (see Figure 4). The Lange et al. study69 was at risk of bias because of non-reporting of randomisation, concealment of allocation or blinding of outcome assessment. Sloan et al. 70 was a randomised trial, but did not report on blinding of participants or outcome collection.
The unfacilitated studies compared EW with factual or time-management writing as control in patients with diagnosed PTSD (see Table 32). Smyth and Arigo121 was conducted in the USA, and Gidron et al. 98 in Israel. Both studies had methodological and reporting flaws that left them susceptible to bias (see Figure 26).
Estimated costs of intervention
The two studies69,70 of facilitated writing gave quite detailed information about the treatment protocol and therapist input, which was used for costing. Lange et al. 70 evaluated a 5-week internet programme (Interapy), consisting of 10 45-minute writing sessions. Feedback on submitted writing was sent to each patient by a therapist on seven occasions. The feedback consisted of about 450 words. The time taken by the therapists to prepare this feedback was not reported but is unlikely to have been much less than 1 hour. The mean basic salary for qualified clinical psychologists is £46,280, similar to Agenda for Change band 8a. 126 However, the therapists employed in this study were graduate and postgraduate students in clinical psychology (mean age 29 years), not yet fully qualified, but who had attended advanced courses in behavioural cognitive psychotherapy and received special training in using writing assignments in PTSD. For costing purposes we assumed a band 6 salary (£30,712), or £45 per hour including indirect costs and overheads (see Table 70). The estimated cost per participant is therefore in the region of £315 (7 × £45).
Sloan et al. 70 evaluated a written exposure therapy (WET) intervention consisting of five weekly sessions (one lasting 60 minutes and four lasting 40 minutes). Participants had individual contact with a clinician for approximately 25 minutes during the first session, and for 10 minutes in each of the remaining sessions. In addition, it was assumed that therapists would need some time to prepare for sessions: 10 minutes for the first session and 5 minutes for each remaining sessions. Total therapist time per participant is therefore approximately 95 minutes. Therapists were clinicians with masters or doctoral level qualifications and prior experience of treating PTSD with exposure-based therapies. Therefore, it was assumed that a band 8a salary, with a mean cost per hour of £63, was reasonable. The estimated cost participant is in the region of £100 (95/60 × £63).
It is more difficult to estimate the cost of the unfacilitated writing interventions. Participants were asked to write on three or four occasions, for 15–30 minutes per session. However, after an initial briefing, patients wrote on their own, either at home or in a health-care environment. Neither study of unfacilitated TW in PTSD reported who instructed participants on the writing tasks, or how long this took. A cost of between £12 and £42 for unfacilitated writing interventions was assumed (see Table 71).
Summary of costs and consequences
Table 72 presents an overall summary of evidence relating to the clinical effectiveness and cost of TW for people with PTSD. It can be seen that evidence for facilitated TW is sparse but promising: the included studies reported significant benefits for the intervention group compared with control, for a range of outcomes of importance to patients: PTSD symptoms, measures of emotion, anxiety, depression, sleep and somatisation. The estimated cost of delivering these interventions in a NHS context is relatively modest: in the region of £100–300. However, evidence about the impact of facilitated TW on patients’ overall QoL and well-being, and on their use of other health-care services is lacking.
| Cost/consequences | Facilitated EW | Unfacilitated EW | ||
|---|---|---|---|---|
| Lange 200369 | Sloan 201270 | Gidron 199698 | Smyth 2008107 | |
| Physical health | ||||
| Somatisation | ↑ SCL-90-S | ↓ PILL | ||
| Sleep/fatigue | ↑ SCL-90-Sl | ∼ POMS-f | ||
| Biomarkers | ↑ Cortisol | |||
| Psychological health | ||||
| PTSD symptoms | ↑ CAPS | |||
| Intrusion/avoidance | ? IES | ∼ IES | ∼ PSS-I | |
| Emotion | ? SAM | |||
| Positive mood | ? PANAS-p | ∼ POMS-v | ||
| Negative mood | ↓ PANAS-n | ↑ POMS-t, POMS-a | ||
| Anxiety | ↑ SCL-90-A | |||
| Depression | ↑ SCL-90-D | ? BDI | ∼ POMS-d | |
| QoL | ||||
| Well-being | ↑ PTGI | |||
| NHS resource use | ||||
| Cost of intervention (£) | 315 | 100 | 12–42 | 12–42 |
| Health-care use | ↑ Visits | |||
Evidence relating to unfacilitated forms of TW is sparse and inconsistent. Of the two included studies,98,107 one reported some positive effects on mood and a biomarker for stress (Smyth et al. 107). However, the other study98 reported negative effects on PTSD symptoms and somatisation and an increase in non-routine health visits.
Case study 2: inflammatory arthropathy
Six studies107,113–117 reported on the use of TW in the treatment of people with inflammatory arthropathy and five studies107,113–115,117 were used for this analysis (i.e. except Lumley et al. ’s116 which was found in the update searches). Details of the studies were presented Chapter 3.
Summary of study design and quality
All five studies107,113–115,117 evaluated an unfacilitated EW intervention compared with neutral writing (time-management control). In addition, Broderick et al. 113 included a second intervention group, who were asked to write about the meaning of the trauma, and Lumley et al. ’s115 included a second control group, who were asked to write about a positive emotional event. All studies recruited patients with diagnosed RA, except Hamilton-West and Quine114 which recruited participants with a diagnosis of AS. Follow-up ranged from 13 to 43 weeks, and outcomes included measures of disease activity, pain, function, mood depression and QoL. None of the studies reported on health-care use or costs. Wetherell et al. 117 and Hamilton-West and Quine114 were conducted in the UK, and the other four studies107,113,115,116 were conducted in the USA. The quality of the studies was mixed (see Figure 39). Three were classified as true RCTs,107,114,115 but all had design or reporting flaws that left them susceptible to bias.
Estimated costs of intervention
As in PTSD, it is difficult to assess the cost of the interventions because papers did not generally report on the grade or qualifications of the staff who gave patients instructions on the writing task, or specify how long this took. The location of the writing intervention varied: in Smyth et al. 107 participants wrote in a private room in a laboratory; Broderick et al. ,113 Wetherell et al. 117 and Lumley et al. 115 adapted the intervention for participants to write in their home; Hamilton-West and Quine114 did not report the location of the intervention.
Broderick et al. 113 produced a videotape to introduce the rationale for the writing task and to provide detailed instructions for patients. They noted that this method was chosen as there is evidence that patients respond well to video-based introductions, and because it was likely to be a cost-effective approach that could be reproduced across large numbers of patients with minimum input from professionals. However, Broderick et al. 113 noted that some physician time would still be required to introduce the idea of the intervention to participants, and to encourage them to participate. In addition, a cost would be incurred for each patient given a video: including the cost of materials and reproduction; and a proportion of the cost for the development and production of the video. The latter is very difficult to estimate, as it is unknown how many patients would use the video.
In Wetherell et al. 117 participants were contacted by telephone before and after each writing session. Assuming 10 minutes’ preparation, 10 minutes for the introductory conversation and 5 minutes per telephone call before and after each of four writing sessions, the total estimated practitioner time to deliver the intervention is approximately 60 minutes, incurring a cost in the region of £36–63 per patient, depending on the grade of the practitioner.
Summary of costs and consequences
Summary results for inflammatory arthropathy are presented in Table 73. In this case, the results look rather more promising for unfacilitated EW. The meta-analysis of measures of disease activity in the four RA studies107,114,115,117 found a significant benefit in the intervention group at short-term follow-up (8–10 weeks). Three of these studies114,115,117 also reported significant positive effects for some outcomes at some time points: measures of mood in Wetherell et al. 117 pain in Lumley et al. 115 and function in Hamilton-West and Quine. 114 However, no significant effects were found across a number of other outcomes – including QoL – and Lumley et al. 115 reported some negative effects on mood immediately after writing.
| Costs/consequences | First author, year | Meta-analysis SMD (95% CI) | ||||
|---|---|---|---|---|---|---|
| Smyth 1999107 | Broderick 2004113 | Wetherell 2005117 | Hamilton-West 2007114 | Lumley 2011115 | ||
| Physical health | ||||||
| Disease activity | ↑∼ DAS | ∼ DAS | ↑∼ DAS | ∼ BASDAI | ∼ VAS | –0.49 (–0.83 to –0.14) |
| Biomarkers | ∼ ESR, CRP | ∼ ESR | ||||
| Psychological health | ||||||
| Mood | ↑∼POMS-SF | ↓∼ PANAS-X | ||||
| Depression | ∼ HADS-D | ∼ AIMS-as | ||||
| Pain | ↑∼ MPQ | |||||
| Functioning | ↑ BASFI | ∼ AIMS | ||||
| QoL | ∼ SF-36 PCS | ∼ BAS-G | ||||
| NHS resource use | ||||||
| Cost of intervention (£) | 12–42 | Video | 36–63 | 12–42 | 12–42 | |
| Health-care use | Data absent | |||||
Case study 3: breast cancer
Eight studies53,54,74–79 reported on the use of unfacilitated EW in participants with breast cancer; see Chapter 3 for details.
Summary of study design and quality
The studies evaluated unfacilitated EW against a usual care comparator53,54,74,75,78 or against an un-EW control74,76,77,79 (note that Craft et al. 74 had two control groups). The participants were at various stages of disease and treatment: Jensen-Johansen et al. ,76 Gellaitry et al. 75 and Craft et al. 74 recruited women with early-stage breast cancer who had recently completed treatment; Mosher et al. 77 recruited women with metastatic breast cancer who were in significant distress. The studies were all conducted in the USA, with the exception of one Korean study78 and one Danish study. 76 There were three randomised studies,54,74,79 but all studies were subject to design or reporting bias (see Figure 9).
Estimated costs of intervention
Henry et al. 53 sent written instructions to participants by post, asking them to write for 20 minutes, on one occasion at home. The cost of this intervention would be minimal, say £5 for materials. Three studies74,75,79 reported a single face-to-face or telephone contact with participants, either before the first writing session74,79 or after the final session. 75 A cost of £12 for these three interventions74,75,79 was assumed. Two studies76,77 reported a rather more resource-intensive approach, with telephone calls to the participants before and after each writing session. Jensen-Johansen et al. 76 first contacted women participating in another study by mail. The intervention consisted of three 20-minute writing sessions at home over a 3-week period. Participants were telephoned by a research assistant, trained by a clinical psychologist, before and after each writing session. Assuming 10 minutes’ preparation, 10 minutes for the initial telephone call and 5 minutes for each subsequent call, the total contact time would be 45 minutes: costing £27 (at £36 per hour). Mosher et al. 77 included women with advanced disease and high levels of distress. Women were screened and recruited by telephone, and then sent written instructions, paper and envelopes to return their writing. The intervention consisted of four writing sessions over 4/7 weeks, each lasting from 20 to 40 minutes. The women were telephoned by a psychology research fellow before each writing session, after 20 minutes, and, sometimes, again after an additional 20 minutes. The contact time was therefore greater than in other unfacilitated writing interventions. Assuming that the initial telephone call lasted for 20 minutes, and that each subsequent call lasted for an average of 5–10 minutes, the total contact time would have been approximately 60–90 minutes. At £36 per hour, the total cost per patient would be around £36–100.
Summary of costs and consequences
Summary results for breast cancer are presented in Table 74. The evidence base for unfacilitated EW in breast cancer is rather larger than in the other case studies presented above, with eight comparative studies,53,54,74–79 but the results are not encouraging. Although some studies did report some significant effects, meta-analyses of measures of positive mood, negative mood and depression at short-term follow-up failed to find a significant treatment effect.
| Costs/consequences | First author, year | Meta-analysis SMD (95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Walker 199979 | Hughes 200754 | Gellaitry 201075 | Henry 201053 | Mosher 201277 | Park 201278 | Jensen-Johansen 201376 | Craft 201374 | ||
| Physical health | |||||||||
| Physical symptoms | ∼ 18 items | ↑∼ PILL, MDASI | |||||||
| Side effects | ∼ SEC | ||||||||
| Sleep/fatigue | ∼ PSQI | ||||||||
| ∼ FACIT-F | |||||||||
| Psychological health | |||||||||
| Intrusions/avoidance | ∼ IES | ? IES | ∼ IES | ||||||
| General mood | ∼ POMS | ↑∼ POMS | ∼ DT | ||||||
| Positive mood | ∼ PANAS-p | ∼ PANAS-p | ∼ PPMS | 0.34 (–0.16 to 0.84) | |||||
| Negative mood | ∼ PANAS-n | ∼ PANAS-n | ∼ POMS-n | 0.33 (–0.25 to 0.90) | |||||
| Depression | ∼ CES-D | ∼ CES-D | ∼ HADS-D | ∼ BDI-SF | –0.07 (–0.24 to 0.09) | ||||
| Anxiety | ∼ HADS-A | ∼ HADS-A | |||||||
| Social support | ↑ SOS | ||||||||
| QoL | ? SIP | ∼ FACT-B | ∼ FACIT-Sp | ↑ C-QoL | ↑∼ FACT-B | ||||
| NHS resource use | |||||||||
| Cost of intervention, (£) | 12 | ? | 12 | 5 | 36–100 | ? | 27 | 12 | |
| Health-care use | ∼ Health-care visits | ↑ Mental health services | |||||||
Chapter 5 Realist synthesis
Aims
The focus of the realist synthesis was to make sense of the outcomes observed in the studies included in the effectiveness review, in effect addressing the objective: How is heterogeneity in results of empirical studies accounted for in terms of patient and/or contextual factors, and what are the mechanisms and moderators responsible for the success, failure or partial success of interventions (i.e. what works for whom in what circumstances and why)?
Methods
The realist synthesis drew initially on the studies included in the original searches for the systematic review (i.e. searches ending March 2013), as its intended purpose was to try to explain the outcome patterns found within this review. The inclusion criteria for the realist synthesis were thus initially identical to that of the systematic review. Additional searching was planned if it was deemed necessary as the programme theory developed.
The central task of the realist synthesis was to develop and refine a realist programme theory of TW. In order to do this, a series of steps – needed to achieve the final desired outcome from a TW intervention in the form of a programme theory – was set out. For each step, a realist logic of analysis was applied, so as to explain how the (intermediate) outcome for each step was achieved in realist terms [i.e. what interaction between context and mechanism(s) led to that outcome]. The initial programme theory was iteratively developed and refined in two ways:
-
Consulting with our practitioner experts Two meetings were held, at which the project team met with external experts to discuss and develop the programme theory. In the first meeting – attended by members of the project team and all the practitioner experts – the discussion was open-ended and exploratory. The main goal of this meeting was to get an initial rough idea of what the various mechanisms might be. Practitioner experts were asked how they thought TW worked and why. This first meeting took place in March 2013 (month 3) of the 18-month project. Later on in the project (month 14), we held a second meeting with the practitioner experts. On this occasion, a series of questions was circulated prior to the meeting (see Appendix 2) to prime those attending on what the focus of the meeting would be. Those unable to attend the meeting were invited to submit written responses. During the latter meeting the comments provided by the experts were discussed and attempts were made to organise the comments into an initial programme theory. Both meetings were facilitated by GW, with GW and OPN taking contemporaneous notes. The contents of the notes were used as data for programme theory development. By analysing (see point 2 on p.118) and discussing the contents of these notes from the second meeting, we produced a draft programme theory. This was circulated to the practitioner experts and project team, and, from their feedback, it was revised (e.g. to include more details on the steps and mechanisms within specific TW methods). A further draft was circulated in a steering group meeting and, from feedback received, refinements made (e.g. the addition of potential harm as an intermediate outcome from TW). The draft programme theory was revised in response to all feedback received.
-
Interrogating the studies included in the effectiveness review A total of 59 studies were included in the systematic review (original searches). All of these studies were potentially eligible for the realist synthesis. Realist reviewers read all the papers included in the effectiveness review and data from the included studies were used if they were relevant to the realist analysis – that is, could inform some aspect of the programme theory (see Box 1). An assessment of rigour (how trustworthy were the data being used) was also made. 127 To illustrate how rigour was operationalised, if data had been generated using an instrument then the trustworthiness of the data was considered to be greater if the instrument had been previously tested, shown to be reliable and valid and had not been altered (or if alterations had been made subsequent testing had been undertaken).
Theorising is an interpretive process, requiring immersion in the data and abductive reasoning (considering what mechanisms might have been in play). The contents of all the included studies (except theses – as the decision was made not to obtain these in full-text for the systematic review) were read and re-read by GW, looking for data that informed the development and/or refinement of the programme theory. Relevant sections of texts relating to contexts, mechanisms and/or their relationships to outcomes were extracted into an Excel spreadsheet (see Appendix 4). The analytic and synthesis processes consisted of a series of questions that the reviewer asked of the contents of included documents. These questions were all asked sequentially of each section of text that was thought to be possibly relevant. Some section of text turned out not to be relevant after these questions were asked. The questions asked were as follows:
-
Relevance:
-
Are the contents of a section of text within an included document referring to data that might be relevant to programme theory development?
-
-
Interpretation of meaning:
-
If it is relevant, do the contents of a section of text provide data that may be interpreted as being context, mechanism or outcome?
-
-
Judgements about context, mechanism, outcome and configurations (CMOCs):
-
What is the CMOC (partial or complete) for the data?
-
Are these data to inform CMOCs contained within this document or other included documents?
-
If so, which other documents?
-
How does this CMOC relate to CMOCs than have already been developed?
-
-
Judgements about programme theory:
-
How does this (full or partial) CMOC relate to the programme theory?
-
Within this same document are there data that inform how the CMOC relates to the programme theory?
-
If not, are these data in other documents? Which ones?
-
In light of this CMOC, and any supporting data, does the programme theory need to be changed?
-
-
Rigour:
-
Are the data sufficiently trustworthy and rigorous to warrant making changes to the CMOC?
-
Are the data sufficiently trustworthy and rigorous to warrant making changes to the programme theory?
-
The process of configuring the data into a programme theory took place through the use of a Microsoft Word version 2010 (Microsoft Corporation, Redmund, WA, USA) document with text boxes and use of arrows. As analysis and synthesis progressed, text boxes were created that contained a context, mechanism or outcome. These were dragged around the Word document to construct (where possible) complete context, mechanism, outcome configurations. The locations and relationships between the text boxes were driven by the interpretations and judgements of the reviewer of the answers obtained to the questions listed above. Where necessary, some text boxes were removed and others added as driven by the data. The text boxes were also combined when it was judged to be indicated by the data. Lines with arrows were added to show the relationships between and within context, mechanism and outcome configurations.
As the programme theory was refined, included studies were re-read and rescrutinised to check if relevant data had been missed out that might inform the revised programme theory (Box 2). Where necessary (as directed by the programme theory), and within the resource constraints of the study, we reanalysed our initial searches looking for additional studies that might contain relevant data. Realist programme theory development and refinement occurred mainly between February and April 2014.
A suggestion was made during a steering group meeting that one of the possible outcomes for those participating in TW was harm (e.g. increase in negative emotions immediately following writing) and that this had been reported in the literature. This had not initially been included in the current version of the programme theory. The included studies were re-read with the specific goal of looking for examples of some form of harm (early or delayed). Six such examples were found. 69,70,73,74,119,121 Therefore, it was considered reasonable to refine the programme theory to include harm as a possible outcome.
Example 2During the second programme theory development meeting, the practitioner experts told that in their TW groups they put up very few barriers to attendance (i.e. participants could come and go as they pleased and did not necessarily have to undertake any TW). This context was not accounted for in the current version of the programme theory. As a response, an additional step to the programme theory was added, and sought data to support, refute or refine this change. Supporting data were found in only two documents,128,129 both of which were descriptions by practitioners of their experiences of running TW groups. The nature of these sources raised questions about the trustworthiness of these data and hence cast doubt on the change made. However, while on its own, the sources were of questionable trustworthiness, there was existing substantive theory that supported the rationale behind allowing potential participants to just attend a group. This was the concept of trialability from Diffusion of Innovations theory. 130 This theory suggested that when something is new and has not been used by a person before, the persons perceptions and feelings about it is influenced by being able to try and see it. Thus it was inferred that, for those unfamiliar with TW, its uptake might be influenced by individuals being allowed to try and see for themselves. The existence of substantive theory added coherence to the change we made. This change is only partially supported, however, by data from published documents and hence is less secure than other sections of the programme theory. It would benefit from refinement from additional data.
Results
Overview
The characteristics of the studies included in the effectiveness review and the document flow diagram have already been outlined (see Chapter 3 and Figure 1, respectively). Most used (some with minor modifications) the unfacilitated EW model. In this, there appeared to be a deliberate attempt to minimise the degree of support provided to participants. In other words, TW was something that participants were expected to undertake on their own with minimal input from anyone else. Five of the included studies used a different approach – facilitated TW.
The TW intervention that was used in all but the five facilitated writing studies differed significantly from the approach used by our practitioner expert. Within both the NHS and UK voluntary sector, when TW was being used, it was rarely, if ever, used as a stand-alone intervention (i.e. in the form of unfacilitated EW). Rather, different types of TW was used as one of the activities within a group setting, and facilitated by a practitioner with expertise in both TW and running groups. Such approaches were thus more akin to the activities and processes as described (e.g. in Rickett et al. 66) than the stand-alone, minimal-support approaches found with unfacilitated EW used in the majority of the studies included in the systematic review.
In subsequent analyses, two different programme theories were developed to reflect this: first, to explain how TW might work if introduced in a stand-alone context with minimal support (unfacilitated EW), and, second, what was almost certainly an elaboration of the first programme theory to explain how it might work when it was introduced with facilitation in a group setting (facilitated TW).
Discussions with the practitioner experts contributed to refinement of the programme theories. The initial meeting (held before a definitive list of studies to include in the systematic review was established) indicated that there was a great deal of uncertainty as to how TW was meant to work to achieved desired outcomes. By the second expert meeting, it had become clear that there was a difference between current NHS and UK voluntary sector use of TW. By this second meeting the studies that would be included in the systematic review had been arrived at and thus a body of literature to use for programme theory refinement was available.
Not all of the included studies were used in programme theory refinement. Six studies were PhD or MSc theses54,57,87,91,94,131 that did not appear to have led to publications in the peer-reviewed academic literature. One study was in Korean78 and a full translation was performed. Because the practitioner experts had highlighted the widespread use of facilitated TW, studies that had not met the inclusion criteria for the systematic review and thus had been excluded, were screened again (by GW and OPN) and 11 relevant documents that specifically explored facilitated TW were identified. 128,129,132–140 The reference lists within each included study was also searched to look for information on whether or not there were any additional studies (of any type) of the same intervention. One such study141 was retrieved.
What happens, how and why in unfacilitated emotional writing?
Analysis and interpretation of the data indicated that there are a number of processes that need to occur for TW to be effective, and that a TW intervention takes place within a wider context. In the following section, descriptions, explanations and evidence for the programme theory illustrated in Figure 56 are provided. The intermediate outcomes that may result from engaging in TW, as perceived by the participants, range from harm through to no benefit, and possible benefit to definite benefit, as illustrated, as intermediate outcomes 1–4, in Figure 56. The benefit perceived by a participant in a TW intervention can be broad, and, in particular, may go beyond the predefined outcomes that are measured in an included study. Furthermore, perceived benefits are sometimes delayed and appear to vary from person to person. It is of interest to note that none of the included studies had attempted to ask participants why the decided to take part in the study in the first place or what they hoped to gain from taking part. Supporting data below illustrate that (1) participants reported a range of different benefits from unfacilitated EW; (2) the benefits were not necessarily what the participants might have predicted they would have received; and (3) these benefits were not necessarily those measured in the studies by the researchers.
. . . this writing helped me get over, you know, my anger . . . 50
FIGURE 56.
Putative generic subprogramme theory for unfacilitated EW. Shading indicates mechanisms and dashed lines indicate where mechanisms have their influences.
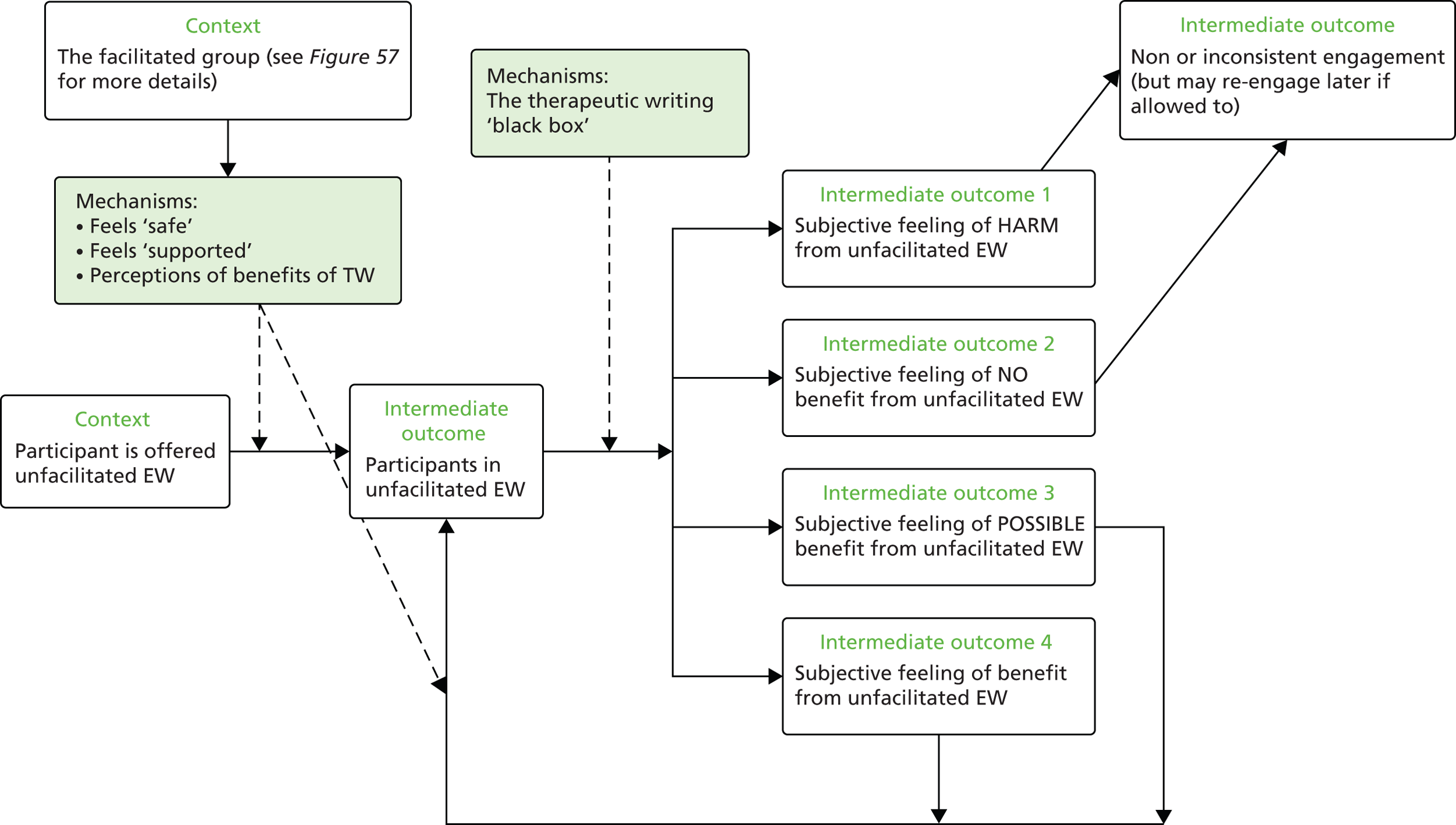
To questioning about whether or not the study was helpful, several responses included:
Yes, [it] has made me see how well I am doing; Yes, [it] reduced some stress; and Yes, I got to write about what I was feeling so I got it out and feel better afterwards not right after, but after. 142
Six months after the EW [Expressive Writing] intervention, we conducted interviews with 24 (57%) women about their experience of writing. Several women talked about the value of being able to express feelings that they had not acknowledged to themselves or to others; women also talked about the benefits of being able to process their experience of having breast cancer. Engaging in the EW process impacted on some women’s relationships in that the writing made them more aware of how much support they had had. We found that some women who had initially reported finding the writing difficult were able to reflect that there were benefits to writing which had not been immediately apparent. Several women expressed a sense of relief on the last day of writing indicating that something had been dealt with.
Copyright © 2009 John Wiley & Sons, Ltd. Reproduced with permission from Gellaitry G, Peters K, Bloomfield D, Horne R. Narrowing the gap: the effects of an expressive writing intervention on perceptions of actual and ideal emotional support in women who have completed treatment for early stage breast cancer. Psychooncology 2010;19:77–84. 75
Participants appreciated the opportunity to work together on something that they found challenging. They saw the poetry writing group as not simply a support mechanism, but a serious challenge to their intellects and creativity. 66
For the majority of the participants, disclosing their emotions resulted in perceived psychological benefits. Some participants recognised that writing was a therapeutic process that helped to reduce the burden of stressful events.
It was good for me to air these feelings, as they have been bottled up for a long time, I feel better now I have written about them [P17, Intervention]. Although I ended up with lots of what may have seemed negative stuff on the paper it has actually left me feeling quite strong, empowered, understanding, focused, lighter, however.
P15, Intervention. Copyright © 2009 John Wiley & Sons, Ltd. Reproduced with permission from Theadom A, Smith H, Horne R, Bowskill R, Apfelbacher CJ, Frew AJ. Participant experiences of a written emotional disclosure intervention in asthma. Stress Health 2010;26:45–50. 58
I found all the exercises to be very relaxing and helpful in clearing my mind of the day’s events.
P24, Control58
Difficult to say whether this [therapeutic writing] is helping my emotional or mental state – and what it is doing to my asthma – if anything.
P15, Intervention58
Some women reported that the writing provided them with a forum for expressing emotions they felt might be burdensome for family members or other confidants . . . Others indicated that writing helped them to identify priorities or focus concerns more specifically . . . Several women commented on the writing task itself, indicating that it was helpful or expressing surprised at the issues that came to mind as they wrote.
Reproduced with permission from Walker BL, Nail LM, Croyle RT. Does emotional expression make a difference in reactions to breast cancer? Oncol Nurs Forum 1999;26:1025–32. 79
Some studies revealed perceptions of harm (such as immediate negative feelings) or possible harm from TW. 69,70,73,74,119,121 Analysis indicates that when a person subjectively experienced harm or felt that they had not benefited from unfacilitated EW, they were likely to take no further part or engage inconsistently.
Contrary to the hypothesized outcome . . . the group who wrote about a self-selected trauma did not have a statistically significant benefit from the writing experience. This was true even though the majority of them did write about their breast cancer. This was also the group with the highest dropout rate. Having to make a choice about what to write about seemed to increase affective distress and alter the benefit that focusing on ones self might offer, even if choosing to write about the personal experience of breast cancer.
Copyright © 2012 Blackwell Publishing Ltd. Reproduced with permission from Craft MA, Davis GC, Paulson RM. Expressive writing in early breast cancer survivors. J Adv Nurs 2013;69:305–15. 74
. . . 13 persons (29.5%) dropped out because they experienced the writing about their stressful events to be too much of a burden. 69
One participant indicated that the reason she dropped out of WET [Written Exposure Therapy] (after 3 sessions) was because the treatment was making her think too much about her car accident, which she found unpleasant. The other participant reported that he dropped out of WET (after 2 sessions) because he was feeling better. 70
One experimental participant self-selected out of the study after the first writing session for iatrogenic reasons, indicating an unwillingness to continue writing due to distress. 121
When participants believed that they were gaining some benefit from using unfacilitated EW, they appeared to want to continue to engage with it. Within Figure 56, this has been illustrated by including a feedback loop to the intermediate outcome of participants in unfacilitated EW.
Some group 1 members had elected to keep on meeting regularly after their program had ended. 66
One participant started the course 2 years after being diagnosed with endometrial cancer:
One of the reasons I wanted to do this writing, I feel like I need to draw more strength from within . . . The oncologists are wonderful at what they do . . . it’s about killing the cancer cells and that’s really great, but there is also a place for having those other contacts for healing the illness.
Rickett C, Greive C, Gordon J. Something to hang my life on: the health benefits of writing poetry for people with serious illnesses. Australas Psychiatry vol. 19. pp. 265–8, Copyright © 2016 by The Royal Australian and New Zealand College of Psychiatrists. Reprinted by Permission of SAGE Publications, Ltd. 66
After the course, she said:
[It was] really enriching, because I’ve missed working and . . . it was really nice going to do something and exercising your brain . . . Poetry has given me an outlet to try to untangle some of the confusion within. 66
Finally, taking part in a writing intervention may have motivated some participants to start writing on their own. For example, one control participant said:
It kick-started me into entering some more things into my journal again, just got some feelings. But you didn’t really ask for thoughts and feelings in the writing exercises. But it had that side benefit but I didn’t write similar passages in my journal as I did for you. 143
Participants in both groups commented that they particularly appreciated having dedicated time to themselves. Completing the writing exercise necessitated them creating protected time and generated valuable time for reflection. It was a good time to reflect on how I feel about various issues [P25, Intervention]. Having 20 minutes a day to myself was quite a miracle and something I hope to continue in the future.
P20, Control. Copyright © 2009 John Wiley & Sons, Ltd. Reproduced with permission from Theadom A, Smith H, Horne R, Bowskill R, Apfelbacher CJ, Frew AJ. Participant experiences of a written emotional disclosure intervention in asthma. Stress Health 2010;26:45–50. 58
There appears to be an element here of emergence. The perception of benefit is an intermediate outcome from participating in unfacilitated EW, but appears to also act as a context to one of the mechanisms identified that appears to cause continuing use of unfacilitated EW.
In Figure 56, the inferred mechanisms are illustrated by shaded boxes. As alluded to above, and unsurprisingly, continuing use of unfacilitated EW occurs when participants perceive benefit from its use. Repeated beneficial experiences reinforce continuing use. However, perceiving benefit in TW is not the only mechanism that appears to be in operation. In order for participants to remain engaged, they also have to feel that it is safe to write and that they are supported. These mechanisms of feeling safe, supported and perceptions of benefits from TW seem to be important not only in encouraging participants to continue with TW, but also in starting to use it in the first place. Different contextual influences trigger the feeling safe and supported mechanisms and they are discussed in more detail in the next section (see What happens, how and why in facilitated therapeutic writing?).
From the analysis of included studies it is not immediately apparent what the mechanisms are within unfacilitated EW, as described by Pennebaker and Chung and in the various other models used in practice (e.g. mindfulness writing, positive writing, memory evoking, literary, reflective writing and perspective shifting writing). 10,144 In Figure 56, the TW has been termed as black box. Those studies that have used the approach to TW described by Pennebaker and Chung, or modifications of it, invariably cite one or more explanations proposed by Pennebaker and Chung145 for how TW was meant to work. The possible explanations for why expressive writing might work may be found in Box 3.
When people are encouraged to talk or write about a previously inhibited event, health improvements would be seen. Once people put their experience into words, they would no longer have the need to inhibit.
Emotions and emotional expressionThe emotional response from writing fosters important cognitive changes.
Habituation to emotional stimuliThe benefits of writing accrue because individuals habituate to the aversive emotions associated with the trauma that they are made to confront by writing.
Language and emotions: towards an A-to-D theory of emotional processingWhen an emotional event is represented in a language format, such as during expressive writing, verbal/conceptual processing becomes possible.
Use of emotion words in writingIndividuals who use very few emotional words or use a very high rate of them may be repressing their emotions of being unable to express their emotions, leading to being or remaining unwell.
Beyond emotions: the construction of a storyBeing able to structure emotions into a coherent story helps in the process of addressing the problem.
The components of a story: the analysis of cognitive wordsThe story created by the participant helps them to come to terms, explain and understand the behavioural and/or mental problem associated with their experiences.
Writing as a way to change perspectiveThe writing produced by a participant may help them stand back and look at the experience from a different perspective.
Expressive writing and social dynamicsAfter writing, participants continue to think about what they have written and this may lead to further changes, such as to their day-to-day behaviour.
The big picture: life course correctionThe change in perspective from writing may lead to participants re-examining how their life is progressing and how they may need to change.
Pennebaker and Chung145 state:
If you are expecting a clean and simple explanation for the effectiveness of writing, we have some very bad news: There is no single reason that explains it. Over the last two decades, a daunting number of explanations have been put forward and many have been found to be partially correct. Ultimately, there is no such thing as a single cause for a complex phenomenon. The reason is twofold. First, any causal explanation can be dissected at multiple levels of analysis ranging from social explanations to changes in neurotransmitter levels. Second, an event that takes weeks or even months to unfold will necessarily have multiple determinants that can inhibit or facilitate the process over time.
Oxford Handbook of Health Psychology edited by Howard S. Friedman (2011): Extract of 115 words (p. 426) from Chapter 18: ˝Expressive Writing: Connections to Physical and Mental Health˝ by James W. Pennebaker and Cindy K. Chung (pp. 417–437). Reproduced with permission. 145
The data reported within the included studies did not enable any coherent and plausible interpretations on what the possible mechanisms for unfacilitated EW approaches might be. Few of the included studies directly explored potential underlying mechanisms or provided data that would enable any inferences to be made. The challenge here is one of the absence of data in included studies.
In summary, it is reasonable to infer that the realist programme theory for unfacilitated EW is as follows. Participants are offered the option of undertaking unfacilitated EW. This forms the starting context. When offered this resource, participants make a choice about whether to participate. The reasoning in the participant in response to the resource offered is threefold: (1) an initial assessment as to whether or not the individual felt or thought there was any value in participating (i.e. will he/she gain any benefit); (2) was this a safe environment in which to write; and (3) was there any support on offer to them? These three responses form the most prominent mechanisms and their contextual triggers are discussed below. In unfacilitated EW, generally no attempts are made (by those offering this resource) to create a safe writing environment. Some studies did provide support should the participant require it (because they felt distressed) either face to face75 or by telephone. 113
Once a participant has decided to undertake unfacilitated EW, they are then in a position to experience for themselves its effects, which may range from harms to benefits. No benefit or perceptions of harm appeared to result in non-engagement or inconsistent engagement. When the individual perceives benefits, they seemed to engage in further TW. This perceived benefit seems to accumulate with repeated engagement and become a new contextual trigger for the mechanism related to perceptions of benefit.
What happens, how and why in facilitated therapeutic writing?
A consensus emerged from the programme theory planning meetings with practitioner experts. This was that within the NHS and voluntary sector writing groups, TW was routinely used in a group setting. The group formed part of the intervention in addition to the TW itself and this meant that the programme theory described above and in Figure 56 needed to be refined and elaborated on.
The practitioner experts contributed their insights into three areas that needed to be incorporated into the initial programme theory (as described above and illustrated in Figure 56). These were (1) the functions and purpose of the group; (2) the range of TW approaches used with participants; and (3) the range of outcomes that might be expected by participants. These are elaborated on below, and incorporated into a refined programme theory of facilitated TW (Figure 57). The information provided by the expert practitioners indicated that their groups had a range of similar characteristics. They were all voluntary, and, in addition, individuals were welcome to come and go and stay as long or as short a time as they pleased. Participation in TW was not always a compulsory condition for attending the group. There were rules for the group but they were designed to be as inclusive as possible, for example those that attended were expected not to disrupt the group. The groups existed in a context of tolerance. This meant that individuals were given permission to come and go as they please to the groups for the length of time that they chose, to as few or many group sessions, and to engage in TW or not.
The programme theory was refined to include steps that outline the processes involved with how and why individuals may wish to participate in facilitated TW group (left-hand side of Figure 57). In the section below, additional data from the 11 studies on facilitated TW128,129,132–140 found from additional purposive searching is provided to support the changes made to the programme theory. These supplement the data that were already presented to develop and refine the programme theory in Figure 56.
Individuals either would self-refer to TW groups or might be encouraged to do so by health-care professionals or another person. The mechanism that seemed to cause attendance and re-attendance might be termed trialability. This concept comes from work on the Diffusion of Innovations theory,130 and suggests that any new innovation may be more likely to be adopted when the user has opportunities to experiment with it. There are some data (from the studies included in the effectiveness review and from further searching for the realist synthesis) to indicate that, for many potential participants, TW in groups was not something in which they had engaged and participated in the past and so the opportunity to see what it was all about was important.
Our workshop became a space, a sandbox, in which they could come to play. 128
Patients who are generally withdrawn and reticent have found this [newsletter] a valuable means of communication and now are rarely short of ideas for articles. 135
Data from the practitioner experts indicated that attendance in TW groups in the real world was very fluid. Individuals would come and go to the groups, sometimes only to talk to other group members or to make use of other services being offered (e.g. the food provided). In some groups, individuals might be absent for some time, only to appear and attend more consistently later. Group attendance was thus a fluid affair, as indicated in Figure 57, and participation was driven more by the individuals own perceptions and feelings about what their needs were.
FIGURE 57.
Programme theory for facilitated TW. Light green shading indicates mechanisms and dashed lines indicate where mechanisms or contexts have their influences.
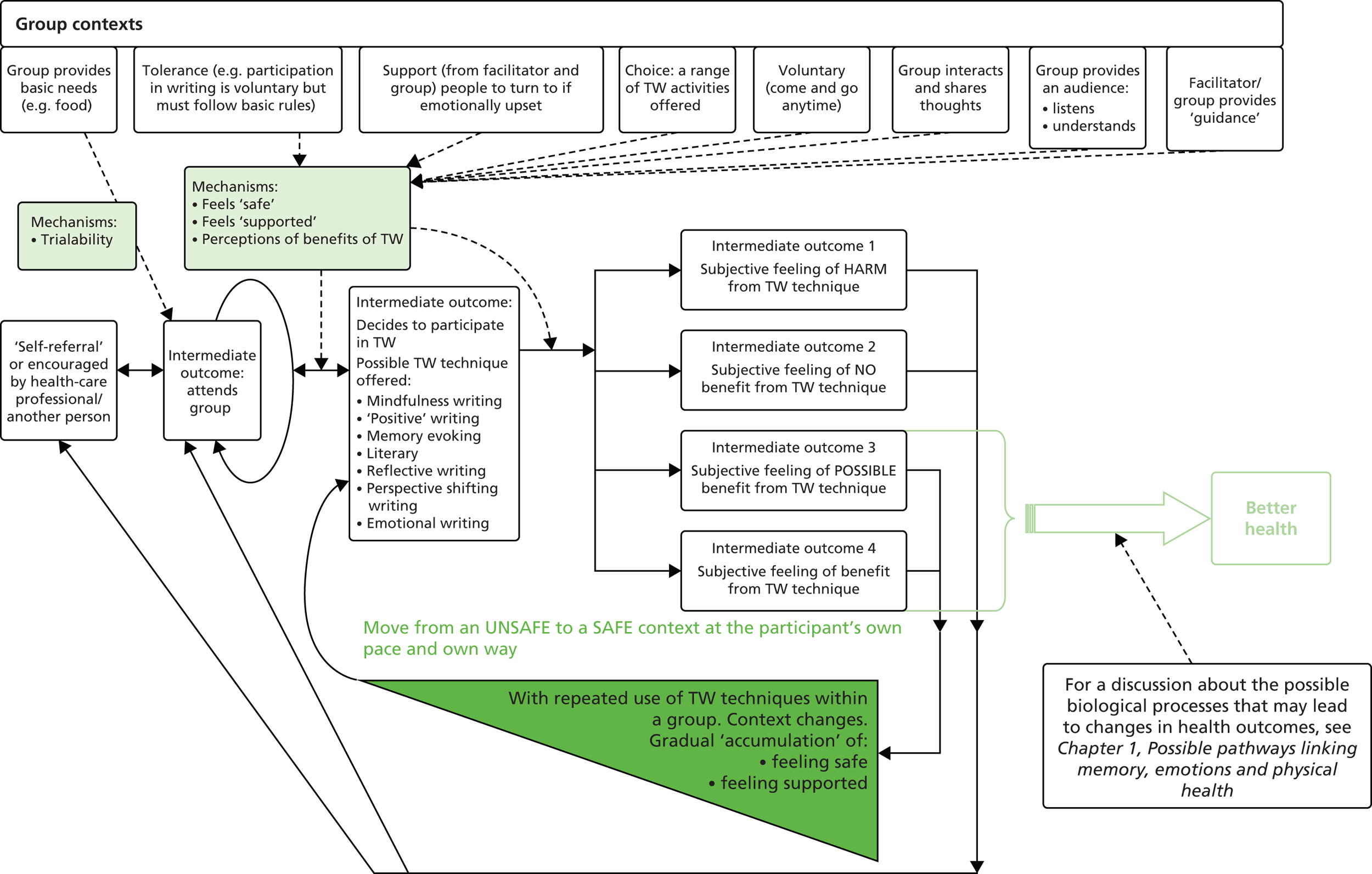
An important distinction has been made in the programme theory between group attendance and participation with TW. Those who attend may not necessarily undertake any TW. There appears to be complex interactions between contexts and mechanisms here when it comes to the intermediate outcome of whether or not an individual participates in a TW activity.
Group attendance enables an individual to make decisions about whether to participate in TW. In effect it exposes them to what TW is all about, and what benefits they might obtain from the TW activity itself and being an active participant in the a group.
Data from included studies indicate that the degree of tolerance of the group, the level of support on offer from the group, the range of therapeutic activities available, the voluntary nature of the group, interaction with the group, listening and understanding are all context influences that may trigger perceptions of benefits of TW.
The informal and relaxed atmosphere of the group encourages patients to read their work aloud and to welcome discussion, criticism and admiration. 135
Participants told us that they enjoyed the technical challenges of writing poetry and the opportunity to meet as a group to share their writing and get feedback. They were particularly proud to have the anthology of their own writing, interspersed with poems by recognized Australian poets, as a tangible outcome. 66
If I could think of any ideas of how the group can be improved, well, it’s to get more people. Like I know a lot of people are very shy or afraid of coming out and forcing themselves out there, thinking that they’re gonna be exposed, but it’s really an environmentally friendly place where we have the group. So it could be improved if more people would join and say how they really feel about living with HIV or AIDS [aquired immunodeficiency virus].
Reprinted from Arts Psychother, vol. 39, Fair CD, Connor L, Albright J, Wise E, Jones K. “I’m positive, I have something to say”: assessing the impact of a creative writing group for adolescents living with HIV. pp. 383–9. Copyright © 2012, with permission from Elsevier. 134
Perceiving that TW (or the group itself) may have benefits does not necessarily mean an individual will participate. Attendance at a group enables individuals to make subjective and/or objective judgements on some of the context influences mentioned above – degree of tolerance, support, nature and type of the interaction and so on. Another two mechanisms appear to be triggered if the context is right – individuals can not only perceive benefits from participating in TW, but will also feel that it is safe to do so and they will be supported. These mechanisms speak to the potential emotional costs of engaging in TW: embarrassment, ridicule, feeling exposure, upset, and so on.
Allowing persons to safely share their thoughts and feelings about themselves reassures them that it is okay to experience the feelings they have. 74
The paper became that space where the students could meet themselves and their concerns unimpeded by the predetermined expectations of others; the classroom became a safe place to read the stories that could not be heard elsewhere. 128
. . . many people were unable to write directly about significant, traumatic experiences without re-experiencing overwhelming emotions. One woman, an experienced licensed counsellor, wrote copious and beautiful poetry but became rigid and almost frantic when we worked with memoir. Interestingly, in her poetry, deep issues and memories would surface. She was able as well to write a fictional, third person story full of effective emotional content and events similar to her life. Yet to approach her past directly frightened her. There was clearly no safe place for her to go to in her own history.
Baker S. Tell it slant: history, memory, and imagination in the healing writing workshop. Traumatology vol. 15 pp. 15–23, 2009. Published by American Psychological Association and reprinted with permission. 128
. . . in reading this piece to a group who had been with her the better part of 6 months, she was able to reveal herself in a way that felt safe. 128
The interaction with a group of HIV-positive peers provided them with a safe place to talk openly about their experiences, which not only served to deepen their understanding of their illness, but also resulted in increased support. A 15-year old male explained that group members knew Everybody [in the group] was born with it [HIV], and we talked about how it was nobody’s fault.
Reprinted from Arts Psychother, vol. 39, Fair CD, Connor L, Albright J, Wise E, Jones K. “I’m positive, I have something to say”: assessing the impact of a creative writing group for adolescents living with HIV. pp. 383–9. Copyright © 2012, with permission from Elsevier. 134
An example of the safety of the group is seen in the following quotation from a group leader:
And so really the group became a way for them to help one another, and the older kids sort of took over in that regard, and kind of became peer counsellors in a way and were able to help them answer some responses to people . . . there was one girl, the oldest girl in the class, just felt like everyone should be out and open about it and perhaps that would release the stigma. So really a means for them to figure things out on their own and figure out how they wanted to represent themselves and HIV or if they wanted that to be a part of who they were.
Reprinted from Arts Psychother, vol. 39, Fair CD, Connor L, Albright J, Wise E, Jones K. “I’m positive, I have something to say”: assessing the impact of a creative writing group for adolescents living with HIV. pp. 383–9. Copyright © 2012, with permission from Elsevier. 134
Working in a group creates an inner/outer dynamic that can help people to make sense of illness. 66
Positive changes in the adolescent were attributed to the experience of meeting other young people living with HIV.
One mother stated participation in the group lets them know that there are other young people out there that are dealing with the same issues that they’re dealing with. Another mother agreed: more than anything else, being able to be around someone as themselves and see someone just like them and see that they’re doing things and going on with their lives and not having pity parties. I thought it was good.
Reprinted from Arts Psychother, vol. 39, Fair CD, Connor L, Albright J, Wise E, Jones K. “I’m positive, I have something to say”: assessing the impact of a creative writing group for adolescents living with HIV. pp. 383–9. Copyright © 2012, with permission from Elsevier. 134
Parents and guardians reported few concerns. Most had longstanding relationships with the social worker who first introduced the idea of a creative writing group; their trust in her contributed to their confidence that the group experience would be helpful.
One mother stated:
I knew she was in good hands it was going to be a good educational experience for her. I thought it was great. 134
In contrast, there are data to indicate that some potential participants in some context may find that the private nature of unfacilitated TW may be more suitable to their needs.
The structured, private nature of the intervention was particularly helpful to people who were unable to express emotion or who had ambivalent attitudes about expressing emotions to others. 100
As described above and illustrated in Figure 57, there are data to support the gradual accumulation of perceived and real benefits of TW, of being in a group, and feelings of safety and support. To reflect this reinforcing cycle – of engagement with TW, being in a group, accruing benefits, feeling safe and supported – the shaded triangle and text in Figure 57 have been used. Within a group with the relevant mix and balances of contexts, individuals move from an unsafe to a safe context at a pace that is under their control.
As previously mentioned, the practitioner experts pointed out that within the NHS and voluntary sector a broader range of TW techniques or activities were used (e.g. mindfulness writing, positive writing, memory evoking, literary, reflective writing and perspective shifting writing). The practitioner experts provided explanations on when these different techniques might be used and for what ends. An example of the information provided can be seen in Appendix 2.
There were no data within the included studies to inform the relevance and/or importance of these different TW techniques in the programme theory. Different TW techniques are used in the included studies, but the paucity of the reported data does not enable any firm conclusions to be made. This is one area of the programme theory that is thinnest and would benefit from the search for further relevant studies and documents.
Finally, the practitioner experts reported that the benefits an individual gains from engaging in TW can occur early and later as well as be broad and unpredictable. In the section above, data from the studies included in the systematic review, which support their observations, have already been presented. Below are data gleaned from studies on when TW was used in a group setting that provides further support.
My guiding principle is that the individuals healthy self will gravitate toward what it needs; that I as the practitioner cannot know whether this is ahead of time and that my job is to listen to the emerging self and allow it expression. 128
In summary, it is reasonable to infer that the realist programme theory when TW intervention is used as part of a group (facilitated TW) is as follows. Within the NHS and voluntary sector, TW is usually offered as an activity within a group context. Potential participants either self-refer or are encouraged to attend. These groups tend to operate in a context in which actual participation in TW is voluntary and non-participation is tolerated. Such a context enables potential participants to try out (the mechanism here being trialability) the group – seeing for themselves how it works and what goes on. A range of group-related contexts appear to be important in influencing potential participants to participate in a TW technique. With repeated attendance at the group, potential participants can subjectively and objectively assess the (contextual influences of) degree of tolerance, support and guidance (from others and the facilitator), the range of activities on offer, voluntariness, interactivity of the group, and so on. These appear to trigger the mechanisms of perceptions of benefits, safety and support. Potential participants feel that it is safe to take part in TW when they perceive that they are likely to receive support from the group if potentially troubling emotions are surfaced. If they perceive subjective benefits, continuing participation is more likely to occur.
Once a participant has decided to undertake TW, they are then in a position to experience for themselves its effects – from harms to benefits. No benefit or perceptions of harm will likely result in non-engagement or inconsistent engagement. When the individual perceives benefits, he/she is likely to engage in further TW. This perceived benefit seems to accumulate with repeated engagement and become a new contextual trigger for the mechanism related to perceptions of benefit. The range of benefits that a participant obtains from TW appears to be individually specific; they may be immediate or delayed to some degree and not necessarily predictable in advance or those that are measured by the researchers in the included studies.
Within the realist synthesis, we were unable to clarify further the mechanisms of how different TW techniques are meant to produce desired outcomes.
Chapter 6 Discussion
This is the first comprehensive systematic review of TW interventions for people with LTCs. There are many various forms of TW interventions that have been suggested as potential therapies for the treatment of mental and physical illnesses. However, in this systematic review, unfacilitated EW such as described in 1986 by Pennebaker and Beall1 was the most frequently used approach. As few as five studies66–70 reported a facilitated type of TW intervention. However, even these five studies are not that similar to the form of TW which has been described by TW practitioners as the most frequently used writing therapy in both NHS and voluntary sectors in the UK.
Statement of main findings
Systematic review
Five studies66–70 were identified which examined the effect of facilitated TW on four different disease areas (two studies in PTSD,69,70 and one each in dementia,67 psychiatric problems,68 and serious physical problems – primarily cancer66). The actual TW interventions studied were extremely varied, two being internet based. Three of the studies66,67,70 were very small, and across the studies quality was mostly unclear. The studies measured different outcomes but all reported positive outcomes in favour of the writing intervention, suggesting that facilitated TW may be beneficial but it requires much more evaluation, which should be conducted rigorously.
Unfacilitated EW was evaluated in 59 studies. 71–119 There was considerable heterogeneity in participants, interventions (context, content, delivery mode), comparators (factual writing, time management, non-writing, waiting list or SMC) and outcomes (type measured and length of follow-up). For measurement of outcomes, 172 instruments were used and more than 300 different measures were reported. All but four52,53,78,87 of the studies were RCTs. Methodological quality was frequently unclear, but most studies were likely to have introduced performance or detection biases that could have increased the likelihood of finding a positive result.
-
Of the six heterogeneous studies50,55,56,71–73 in patients with HIV, five were very small50,55,71–73 and all were of very unclear quality. Overall, there was no evidence of benefit in any of the outcomes examined (disease markers and psychological instruments), nor did a meta-analysis show any evidence of evidence of benefit on depressive symptoms.
-
Eight studies53,54,74–79 examined EW in patients with breast cancer: one was very large,76 and their quality ranged from unclear to poor (Hughes54). Most examined mood, depressive symptoms or QoL but there was no convincing evidence of benefit from EW across the studies or on meta-analysis of mood or depressive symptoms.
-
Five studies80–84 examined genitourinary and gynaecological cancers, and, again, quality ranged from unclear to poor. Across the wide variety of outcomes examined there was no consistent pattern of benefit from TW. Two other studies85,86 of unfacilitated EW in patients with various cancers also failed to identify any benefit from EW.
-
Three studies90–92 explored substance misuse: two were very small and study quality was unclear or poor; across a wide range of outcomes they found no evidence of benefit from EW.
-
Five small studies93–97 of variable quality examined EW in patients with various psychiatric conditions; there was little consistent evidence of benefit from TW across a variety of outcomes or on meta-analysis of the effect on anxiety or depression in the short term.
-
Two very small, low-/poor-quality studies9,98 looked at EW for PTSD; in the immediate or short term, both report inconsistent beneficial results on mood or PTSD symptoms with unfacilitated EW.
-
Three studies102–104 of variable quality found no consistent evidence of benefit in CVD.
-
Four studies58,106–108 (of mixed quality) investigated unfacilitated EW in patients with asthma but no evidence of benefit on a variety of outcomes was seen, and meta-analysis suggested that there was no benefit on short-term FEV1.
-
Two low-quality studies52,109 of IBS reported mostly positive results.
-
Three low-quality studies110–112 of psoriasis found little effect from the intervention.
-
For inflammatory arthropathies (six studies107,113–117) there was a reduction in disease severity (n = 191, SMD –0.61, 95% CI –0.96 to –0.26) in the short term on meta-analysis of four studies,107,114,115,117 with a random-effects model and with non-significant heterogeneity, I2 = 1%.
-
Four low-quality studies51,57,118,119 in FM and chronic pain showed mostly positive results.
-
Single studies looking at EW in sickle cell disease,87 diabetes mellitus,88 cystic fibrosis,89 BN,99 amyotrophic lateral sclerosis,100 migraine and tension headache,101 and chronic lung disease (COPD and IPF)105 were nearly all of low or unclear quality and found no evidence of benefit from EW.
-
The meta-analyses in the breast cancer studies53,54,74–79 showed no significant differences in depression (among 562 participants), positive and negative mood at short term (among 618 participants each) for the EW group compared with the control group. Likewise, the remaining meta-analyses on HIV (depression at short term in 249 participants); asthma (lung function at short term in 281 participants); mental and psychiatric disorders (anxiety at short term in 127 participants); inflammatory arthropathies (disease activity at both immediate and short term in 146 participants); and FM and chronic pain (pain severity at two different short term assessments in 216 participants) found no significant differences between EW groups and control subjects.
-
Twenty-four studies50,51,56–58,71,83,89,90,99,101,104–108,110–113,115–117,119 reported disease-based outcomes across different LTCs, and only two studies104,110 found a significant beneficial effect for EW: on DBP, but not SBP, in cardiovascular disease, and on the severity of psoriasis.
-
For anxiety and depression, across different LTCs, none of the meta-analyses showed significant effects.
Economic considerations
The review of economic evidence did not identify any true economic evaluations, quantifying both the monetary costs and health consequences of TW interventions. Only one of the studies89 included in the systematic review attempted to quantify the cost of delivering the TW intervention itself and made an estimate of cost savings. Some studies did report on the impact of TW on patients’ use of other health services: there was a significant reduction in reported use of medications with TW, but no significant effect on the use of other health services. Costs for delivering programmes of TW are likely to vary, depending principally on the amount of paid practitioner time per participant. The estimated direct cost to the NHS ranged from as little as £12 for unfacilitated interventions to > £2000 for a series of 16 one-to-one facilitated TW sessions. There is insufficient evidence to estimate how much, if any, of this cost would be offset by savings from reduced use of other NHS services. There is also insufficient evidence to estimate the overall cost-effectiveness of TW to the NHS. Cost–consequence analysis suggested that there might possibly be a favourable balance of participant benefits to NHS costs for selected interventions in selected LTC groups.
Realist synthesis
The realist synthesis was able to develop two programme theories that (to some extent) explained some of the findings within the studies included in the systematic review. Uncertainty continues to exist over why individuals with LTCs might wish to participate in TW (of any variety) and what, how, and in what way these individuals hope to gain from TW. For unfacilitated EW, there remains uncertainty as to how and why it generates any outcomes of interest, for whom, and in what circumstances. In facilitated TW the relative importance of the different processes within it (i.e. what processes need to be used – how and why – to generate desired outcomes) is unclear.
In unfacilitated EW, when participants were offered the option of undertaking EW, this formed the starting context. When offered this resource, participants made a choice about whether or not to participate. The participant reasoning in response to the resource offered might be threefold: (1) an initial assessment as to whether or not the individual felt or thought there was any value in participating (i.e. will he/she gain any benefit); (2) was this a safe environment in which to write; and (3) was there any support on offer to them? These three responses formed the most prominent mechanisms and their contextual triggers are discussed in more detail with reference to facilitated TW. Studies using unfacilitated EW generally did not attempt to create a safe writing environment or provide support. Once a participant had decided to undertake unfacilitated EW, they were then in a position to experience for themselves its effects – which may range from harms to benefits. No benefit or perceptions of harm appeared to result in non-engagement or inconsistent engagement. When the individual perceived benefits, he/she seemed to engage in further TW. This perceived benefit seemed to accumulate with repeated engagement and became a new contextual trigger for the mechanism related to perceptions of benefit. The range of benefits that a participant obtained from TW appeared to be individually specific; they may have been immediate or delayed to some degree, and not necessarily predictable in advance or those that were measured by the researchers in the included studies.
The programme theory for facilitated TW is an elaboration of that for unfacilitated EW. Within the NHS and voluntary sector, TW is usually offered as an activity within a group context. Potential participants either self-refer or are encouraged to attend. These groups tend to operate in a context in which actual participation in TW is voluntary and non-participation tolerated. Such contexts enables potential participants to try out (the mechanism here being trialability) the group – seeing for themselves how it works and what goes on. A range of group related contexts appear to be important in influencing potential participants to participate with a TW technique. With repeated attendance at the group, potential participants can subjectively and objectively assess the (contextual influences of) degree of tolerance, support and guidance (from others and the facilitator), the range of activities on offer, voluntariness, interactivity of the group, and so on. These appear to trigger the mechanisms of perceptions of benefits, safety and support. Potential participants feel safe to take part in TW, when they perceive that they are likely to receive support from the group if potentially troubling emotions arise. If they perceive subjective benefit, continuing participation is more likely to occur. The programme theory for facilitated TW and unfacilitated EW are the same once a participant has decided to undertake TW. Within the realist synthesis we were unable to clarify further the mechanisms of how different TW techniques are meant to produce desired outcomes.
Strengths
Systematic review
The systematic reviews and realist synthesis were supported during all phases by the expert advice of four TW professional practitioners. The systematic review has been undertaken following PRISMA criteria63 and was registered with PROSPERO at the start of the project. Comprehensive database searches were adopted, supplemented by checking citation lists, theses and grey literature and contacting experts in the field.
Selection criteria were developed to include only participants with documented diagnoses of LTCs and the list of LTCs considered was generous, with careful consideration of whether or not specific medical conditions could be considered long term (e.g. patients with bladder papilloma following resection). No restrictions were applied regarding the intervention (i.e. all types of therapies falling within the TW umbrella were considered). Included was any comparative study, not only RCTs, and careful consideration of appropriate comparators was given; where the control intervention appeared to have an inadvertent EW component, for example when patients with cancer were asked to write about the facts of their treatment, these studies were not included.
The assessment was not restricted to stated primary outcomes only. Independent double data extraction for all numerical data was used. The reporting of all results is very comprehensive and analyses were very thorough. Study authors (32 out of 64 included studies) were contacted for missing numerical data and 14 responded. In the report results were categorised by ICD-10 code as a systematic way of dealing with the very wide range of conditions in which TW had been investigated. Categorising by ICD-10 code is an unusual way to present systematic review results, and can be used sensibly only when an intervention can be applied to a wide range of conditions – in this case both psychiatric and physical conditions. Meta-analyses were conducted both within and across conditions to fully explore any potential effects of these interventions.
Economic considerations
The review of published economic evidence was nested within a thorough systematic review, following accepted methodological guidelines. An attempt was made to estimate the costs of TW from a NHS perspective, based on information about the range of interventions provided in the included studies and expert advice on how TW is used in practice. The cost–consequence summaries brought together best-available evidence of effects on outcomes of importance to patients with simple estimates of NHS costs for three illustrative case studies.
Realist synthesis
This realist synthesis has been undertaken following (where applicable) the RAMESES (Realist and Meta-review Evidence Synthesis: Evolving Standards) quality standards for realist syntheses. 146 Two programme theories have been developed. Document selection and appraisal applied the principles of relevance and rigour, and data extraction has focused on extracting data that are capable of supporting programme theory refinement. Where possible, a realist logic of analysis has been applied to the data and the synthesis has been reported following the RAMESES publication standards for realist syntheses. 146 Reporting for the realist synthesis has been distributed across different sections of this report as some of the processes used are similar to those of the systematic review. For example, the searching process of the systematic review was used as the starting point of the realist synthesis. This also meant that the document flow diagram is shared across both reviews. Additional searching (of a limited nature) was undertaken and this has not been shown in the main document flow diagram (see Figure 1). Based on the focus of the realist synthesis (to explain the outcome patterns found in the systematic review) no scoping of the literature was undertaken. No changes were made to the initially planned review process other than a much more limited additional searching due to time constraints. The RAMESES publication standards have been followed and an overview of compliance may be found in Appendix 7.
Weaknesses
Systematic review
We were not able to identify a UK-based therapeutic practitioner of unfacilitated EW as an expert advisor. We double checked only 10% of our retrieved titles and abstracts, so there is a risk that we missed relevant studies; however, our 10% checks did show excellent agreement between reviewers. We did not exclude studies in which the underlying condition was poorly described (e.g. patients with various cancers). The facilitated/unfacilitated TW split was a post hoc decision based on the background literature21 and discussion with the TW expert practitioners collaborating in the project. We tried to be consistent with our decisions around selection of interventions and comparators, particularly in the meta-analyses, but not all interventions and comparators were similar, introducing some heterogeneity. For example, when a study had two interventions – one with positive writing and one with standard unfacilitated EW – the latter group was selected. If a study had one intervention only, it would be included in the meta-analyses even if participants were asked to write about positive aspects of their experience, particularly on the last day of writing.
A disadvantage of using ICD-10 codes to categorise studies meant we had a large number of categories, often with relatively few studies in them, and this, in turn, constrained the sensitivity analyses that we could conduct within these categories.
Studies not reporting any numerical data (raw scores or proportions for any one of the outcomes) were excluded from the systematic review. Therefore, relevant studies might have been omitted. However, strenuous efforts were made to contact study authors regarding missing data. Authors were not contacted about study quality or when an explanation of a given instrument was not provided.
Many of the meta-analyses had high levels of statistical heterogeneity and should be interpreted with caution. Additionally, meta-analyses are on small numbers only. A post hoc decision was made to conduct overall meta-analyses across all LTCs for the outcomes of depression and anxiety. This decision was made before knowing the individual LTC meta-analyses results and was based on the large number of studies reporting these outcomes, and their clinical usefulness as an exploratory analysis.
Regarding the study designs, both RCTs and non-RCTs were included but no sensitivity analyses of randomisation compared with non-randomisation design were performed. This was because there were so few studies within each ICD-10 code that further subdivision was thought to be unhelpful. We also did not conduct any sensitivity analyses by study quality; we described study quality comprehensively but did not use it further in our analyses.
We made a pragmatic decision not to investigate subgroup analyses within the included studies because almost all appeared to be post hoc analyses, and the studies were not sufficiently powered for these analyses. Therefore, we did not look for moderators, which was in the aims and objectives in our original proposal. Regarding interventions, self-completion books were included as a TW intervention.
Economic considerations
The lack of evidence on cost and cost-effectiveness from published comparative studies was a major challenge. Most studies did not report impact on health-care resource use, only 12 out of 64 studies included such information. 57,68,75,77,83,89,90,97,98,104,109,119 In addition, the reporting standards for resource use in most papers were weak. It was also difficult to estimate the cost of the interventions in some studies, owing to a lack of detail on the level of practitioner input. The diversity of the studied populations, the inconsistent and sparse nature of the available effectiveness evidence, and, particularly, the lack of evidence on QoL outcomes, made de novo decision modelling an unrealistic prospect.
Realist synthesis
Although searches were exhaustive, selection criteria for the realist synthesis could have been identified earlier in order to conduct even more iterative searches. There was only one qualitative study147 identified as being useful for the realist synthesis process. Additional searching would have been desirable as it would have enabled more relevant data sources (especially those that contained potentially relevant existing substantive theories) to have been identified. However, because of time constraints, only one single round of additional searching specifically for the realist synthesis was undertaken. The absence of these additional searches is likely to have impacted on the degree of the explanatory powers of the realist synthesis. In addition, it was not possible to include the studies found in the updated search (to January 2015) in the realist synthesis.
The selection criteria for the realist review could have been more closely defined, or tailored earlier, in order to capture more relevant literature. Studies investigating healthy students and non-comparative studies were identified as a potentially useful tool for further programme theory development.
The development of the programme theory relied predominantly on the data contained within randomised, non-randomised and case–control study data. Previous review teams have identified that the data necessary for conducting a high-quality realist synthesis is often not found in RCTs. However, as the included studies consisted of a broader range of study types and much larger numbers of studies than that found in Dieleman et al. 148 and Kane et al. 149 it was anticipated during the project that sufficient data would be available. To supplement the data within the studies included in the effectiveness review, two additional searches were undertaken: one to look for studies on facilitated TW and the other for studies of any type that reported on one or more of the included studies. Despite these two additional searches, gaps in the data existed, which meant that it was not possible to fully elucidate and test a number of aspects of the programme theories, such as:
-
The mechanisms underlying the TW techniques encountered in this project. Additional searching for data from different disciplines (e.g. humanities) might have been more informative. In addition, there exists a large body of research on the use of unfacilitated EW in populations without LTCs and data from this body of work might have been valuable in mechanism identification and elucidation.
-
The role of the group in facilitated TW requires greater elucidation. The realist synthesis identified a number of contextual influences and mechanisms, but these are unlikely to be the only relevant ones. A large body of work exists on groups in general and on therapeutic groups specifically. Further searching in these areas would likely have provided further relevant data. The role and competencies of the group facilitator also needs further elucidation and additional searching for data on this topic area would have been helpful.
-
The value placed by participants in TW on the presence of an audience was noted in some of the data. This is another area with a large body of literature located within disciplines outside of health services research that is worthy of further attention.
This is the first realist synthesis that has sought to develop a realist programme theory that attempts to explain the outcome patterns for unfacilitated EW and facilitated TW when used for LTCs. In other words, it is the first attempt that tries to unpack the black box of TW when used in a population with LTCs. The programme theory provides potentially transferable knowledge about how these types of TW techniques might fare under different contexts. However, an important caveat on this programme theory is that it requires further development and refinement. This is because it includes only some of the relevant and important mechanisms and related contextual triggers. The paucity of relevant data in the studies used to develop and refine the programme theory has had an impact on both its detail and extent. In addition, the strength of the inferences made has been affected by the rigour of the included studies. Many of the outcomes reported within the included studies must be considered to be less trustworthy as a result of the conduct of the studies. For example, all reported findings of benefits, harms, correlations and/or associations were treated with caution when used in programme theory development. Findings that could reasonably be considered to be more trustworthy were those that had not been as a result of statistical manipulation and/or interpretation by the authors. Consideration was still given as to how such data were generated, for example the interview method for qualitative data. The result is that many of the inferences made in the development of the programme theory were often tentative. The implication is that further testing and refinement of the programme theory is needed, through future secondary or primary research.
This project faced two significant methodological challenges in trying to undertake both a systematic review and realist synthesis. The first related to the purpose of the realist synthesis and the other to human resources required. The purpose of the realist synthesis was to explain the outcome patterns reported in the studies included in the systematic review. Thus the realist synthesis was not able to proceed in earnest until it had been clearly decided what the final set of included studies were for the systematic review. This process for confirming the final set of included studies for the systematic review did not occur until month 11/12 of the project. This meant that the realist synthesis could only begin in the last third of the project. An additional related challenge that emerged from the focus of the realist synthesis was around the nature of the included studies. About midway through the project, the expert advisors had indicated that within the NHS and voluntary sector for LTCs, the main form of TW used was facilitated TW. Only when the final set of included studies for the systematic review had been finalised and were being analysed did it emerge that the vast majority of these related to the use of unfacilitated EW. This unexpected finding meant that additional unanticipated work was needed in the realist synthesis, as it had to develop one or more programme theories to make sense of both unfacilitated EW and facilitated TW.
In terms of human resource requirements, it must be kept in mind that both systematic reviews and realist syntheses are labour intensive. Within this project the majority of the researchers time was devoted to the systematic review. This meant that one of the two reviews had to be truncated – in this case the realist synthesis. Once the included studies had been identified, data extraction, analysis and synthesis took place in parallel for the systematic review and realist synthesis. As the project had only one full-time researcher (OPN) and almost all of her time was devoted to the systematic review, less human resources allocation, and time was available for the realist synthesis before the expected end date of the project. Within the 3-month time frame left to undertake the realist synthesis (especially in light of the additional work needed, as explained above), it was not possible to undertake the additional searches that would be needed to more fully develop the programme theories for unfacilitated EW and facilitated TW. These would have been especially important, as the studies included in the systematic review did not contain sufficient relevant data. There was simply not the spare human resources capacity or time to do so.
The challenges mentioned above provide important lessons to review teams and funders who wish to undertake both combined systematic reviews and realist syntheses.
-
Sequencing If the purpose for undertaking a realist synthesis is to explain the outcome patterns of studies included in a systematic review then additional time is likely to be needed to enable the rigorous execution of the realist synthesis component. Identifying the included studies takes time and the realist synthesis can pragmatically start only once it is clear what the included studies are. Its start is thus delayed and it is likely that an additional minimum of 9 months (ideally 12–18 months) is needed for a rigorous realist synthesis to take place. Review teams and funders need to expect that such combined reviews are going to take longer to complete.
-
Human resources Both systematic reviews and realist syntheses are labour intensive. Planning and budgeting needs to reflect the need for additional researcher(s) time when a project gets to the stage when data extraction, analysis and synthesis is taking place for both the systematic review and realist synthesis. Otherwise, one or the other of the reviews is likely to suffer. Ideally, two different individuals with sufficient funded time are needed with the necessary skill sets to undertake the systematic review and realist synthesis separately.
Uncertainties
Systematic review
Most interventions evaluated were unfacilitated EW and did not mirror those currently used by professional TW practitioners in clinical practice in the UK. The main uncertainty is the clinical effectiveness of TW as it is practised by therapeutic practitioners, including within the NHS. It must be noted that the facilitated TW interventions included in the systematic review do not mirror those used in current NHS practice. There is insufficient clinically relevant evidence on facilitated TW as practised within these studies to know whether or not it is beneficial. It is uncertain if unfacilitated EW might be harmful, particularly in psychotic patients, but there was little evidence of harm in the studies evaluated.
Economic considerations
The economic case for the NHS to fund TW interventions for people with LTCs remains unproven. Depending on the level of practitioner input, these interventions are likely to be relatively inexpensive, and there is some evidence suggestive of possible cost savings related to reduced use of other health care, although this evidence is sparse and inconsistent. The cost–consequence case studies also suggest that there may be positive impacts on measures of health and well-being for some types of TW in some patient groups but these are exploratory analyses. Until there is robust evidence of patient benefit, it is difficult to conclude that TW would be a cost-effective use of NHS money.
Realist synthesis
Unfacilitated TW appears to have some effect in that the people who took part did notice some changes to intermediate or more proximal outcomes. However, the outcome of interest was health functions of some form, but TW does not seem to have much of an effect on this final desired outcome.
Within another realist synthesis, one could try to work out what outcomes (final desired and/or intermediate/proximal) might be influenced by unfacilitated TW. This would be the programme theory development aspect of a realist synthesis of unfacilitated TW. In this project we could touch on this only because of insufficient relevant data. This further realist synthesis could try to build a more detailed realist programme theory [i.e. one that further explains what has caused each outcome (final/intermediate) and under what contexts], the causal force being the mechanism(s).
We did not look at unfacilitated EW on healthy students but these studies may or may not inform what outcomes (final/intermediate) might be possible with unfacilitated TW, under what contexts and what the mechanisms might be. So there may be contexts within which it is reasonable to extrapolate what can be learnt from the healthy students studies to those who are unhealthy – based on making (and if possible testing) the assumption that the same mechanism(s) might be in operation under these different contexts.
The programme theory for unfacilitated EW and facilitated TW in LTCs highlights how complex these interventions are. It cannot and should not be assumed that they will work as expected when applied in differing contexts. The outcomes participants will get from TW are at present neither predictable nor necessarily achieved. In addition, these outcomes are rarely the ones hoped for by the researchers who have undertaken the primary studies included in the effectiveness reviews and realist synthesis. A number of contexts appear to influence whether or not individuals will choose to participate and continue with TW. In the real-world setting of clinical practice (such as in the NHS and voluntary sectors), due consideration needs to be given to ensuring that these contexts exist (or can be made to) if there is to be any hope that meaningful and continued participation in TW is to take place. Of note is that many of these contextual influences are beyond the TW technique itself and sit in the wider world that surrounds the individual and the TW technique. Despite the development of the programme theory, at present there is too much uncertainty surrounding too many aspects of it to enable a firm recommendation to be made about the benefits for the large-scale introduction of unfacilitated EW or facilitated TW into routine clinical practice.
Chapter 7 Conclusions
The systematic reviews and realist synthesis together with the economic considerations provided further and robust assessment of TW interventions across a broader range of chronic conditions than previously published research.
The clinical utility of TW interventions must be questioned, particularly the unfacilitated type of EW interventions frequently evaluated in different chronic conditions over almost two decades with no clear benefit on physiological, physical, psychological or QoL outcomes. In the UK, professional TW practitioners use other types of TW interventions, usually facilitated and with a variety of types of writing; however, such interventions have not yet been formally trialled. In addition, there is little information on any adverse effects of the evaluated TW and EW interventions, although increased negative mood immediately after the unfacilitated EW exercise was reported in nearly all of the included studies that looked at this, and may be worse among people with higher levels of baseline distress.
Further research
Realist synthesis
From the programme theory developed in the realist synthesis, it can be seen that further research might fruitfully be conducted in a number of areas. The primary research to date where TW (facilitated or not) is used to treat patients with LTCs appears to be highly under-theorised. Little is known about a number of aspects of these interventions. Although it is possible that a further dedicated realist synthesis might be able to make more sense of these intervention types, it is likely that greater mileage would be gained by first conducting additional primary research, particularly in patients with LTCs. This is especially the case if there is any intention to use unfacilitated EW for patients with LTCs. The existing studies demonstrate that greater attention is needed on theorising why it might be that such an intervention type would even work in the first place. In other words, in summary, better theorised TW interventions are first needed prior to undertaking any further realist synthesis. To provide guidance the following three questions are probably the most pressing areas to address with suitably designed primary research. This is because the answers to the following questions are most likely to provide data that are relevant for further programme theory refinement:
-
Why do people with LTCs want, or not want, to participate in TW (of any type or form)?
-
What do people with LTCs hope to get out of participating in TW (of any type or form)? How and why?
-
Which has a bigger influence on outcomes in facilitated TW, the group, the facilitator or the writing technique? How and why?
Unfacilitated emotional writing
-
There are large numbers of RCTs of unfacilitated TW in a variety of LTCs. The results suggest that there is no consistent and predictable benefit with this type of intervention. However, there may be some conditions where further robustly designed research with adequate sample sizes, comparing TW to usual care, might be useful, in particular, in people with substance misuse (because they may have experienced considerable trauma), and in PTSD (because there is weak evidence of possible benefit from the studies included in this review), or other areas in which people may have experienced traumatic events and have difficulty expressing themselves. If further research in unfacilitated writing is to be conducted, an explicit choice of patients and outcomes should be declared and CONSORT (Consolidated Standards of Reporting Trials) guidelines should be followed. 150 In view of the generally poor quality of the evidence to date, attention to statistical power and the maintenance of study quality are essential. Capturing any adverse events is important. Programme theory presented here might be a useful starting point to help researchers conceptualise unfacilitated EW. For example, if researchers are to investigate patients with COPD there needs to be a coherent and plausible reason as to why they think that FEV1 might be affected by TW. It would be very useful if standard outcomes for the different conditions were measured [COMET (Core Outcome Measures in Effectiveness Trials)]151 to facilitate comparison with other interventions and length of follow-up should be considered.
-
From the current research base, there are few data on patients understanding of, or expectations from, unfacilitated EW. Most of the trials appear to be explanatory and, in many cases, the researchers were at pains to withhold all information from participants about the possible nature of the intervention before they were randomised. If further research on unfacilitated EW in a health context is conducted, we recommend including qualitative studies to explore patients’ understanding of, and experience of undergoing, EW interventions.
Facilitated therapeutic writing
-
An audit of the types of TW currently being used in the NHS in both primary and secondary care would be very useful.
-
Further, robust research into the facilitated TW interventions that are used in clinical practice and the voluntary sector is recommended. Developmental work on the role of the facilitator, TW and group dynamics would be required. Some TW disciplines are very well developed but have not yet been formally evaluated in clinical settings. 16 Programme theory presented here might be a useful starting point to help researchers conceptualise facilitated TW. Development work and feasibility or pilot studies should probably be conducted prior to full evaluation. Cluster RCTs and studies of other appropriate designs could be conducted on these interventions, evaluating patients with chronic physical or mental ill health. The comparators could be standard practice without TW or other comparable therapeutic interventions, such as relaxation CDs or reading bibliotherapy. Outcomes would be the standard clinical outcomes for the patient’s medical condition, and patient satisfaction, HRQoL and costs. The sample sizes would need to be large enough to find a potentially modest effect.
Acknowledgements
Many thanks to the additional TW practitioner collaborating actively in this project, Dawn Coleman, for her professional and expert advice. Thanks also to Dr Jenny Basford (JB) for providing support with the electronic searches; Professor David Sheffield for checking the list of included studies against potential missing studies; content experts for providing technical support; and all study authors who responded to data requests.
Contributions of authors
Dr Olga P Nyssen Research Assistant, first reviewer, co-ordinated day-to-day running of the project, led on data extraction, conducted most of the statistical analyses, and wrote the first draft of the report.
Professor Stephanie JC Taylor Professor in Public Health and Primary Care, principal investigator, contributed to the design of the project, oversaw the project, conducted some data extraction and revised drafts of the report.
Dr Geoff Wong Clinical Senior Lecturer in Primary Health Care, led and conducted the realist synthesis, and revised drafts of the report.
Dr Elizabeth Steed Lecturer in Health Psychology, second reviewer, conducted some data extraction and revised drafts of the report.
Dr Liam Bourke Lecturer in Public Health Research, second reviewer, conducted some data extraction and revised drafts of the report.
Dr Joanne Lord Reader in Health Economics, led the health-economic considerations chapter and revised drafts of the report.
Ms Carol A Ross Expert Practitioner, advised on TW, contributed to the background chapter and revised drafts of the report.
Ms Sheila Hayman Expert Practitioner, advised on TW, contributed to the background chapter and revised drafts of the report.
Ms Victoria Field Expert Practitioner, advised on TW, contributed to the background chapter and revised drafts of the report.
Ms Ailish Higgins Research Fellow, wrote the first draft of the health-economic considerations chapter.
Professor Trisha Greenhalgh Professor of Primary Health Care, contributed to the design of the project, oversaw the realist synthesis, and commented on drafts of the report.
Dr Catherine Meads Reader in Health Technology Assessment, instigated the original proposal, contributed to the design of the project, oversaw some aspects of the project, conducted some data extraction and revised drafts of the report.
The final report and any errors remain the responsibility of Queen Mary University of London; Professor Stephanie JC Taylor, principal investigator of this 18-month research project, is guarantor.
Publications
Meads C. Does therapeutic writing help people with long term conditions? Systematics review, realist synthesis and economic modelling. Lapidus Journal 2013;7:6.
Meads C, Nyssen OP, Wong G, Steed L, Bourke L, Ross CA, et al. Protocol for an HTA report: Does therapeutic writing help people with long term conditions? Systematic review, realist synthesis and economic modelling. BMJ Open 2014;4:e004377.
Nyssen OP, Taylor S, Wong G, Steed L, Bourke L, Lord J, et al. Does therapeutic writing help people with long-term conditions? Systematic review, realist synthesis, and economic modelling. Cumbria Partnership Journal of Research Practice and Learning 2014;4:33–5.
Data sharing statement
No new data were generated from this project.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Pennebaker JW, Beall SK. Confronting a traumatic event: toward an understanding of inhibition and disease. J Abn Psycho 1986;95:274-81. http://dx.doi.org/10.1037/0021-843X.95.3.274.
- Kapstein A, Weinman J. Health Psychology. Oxford: Blackwell; 2008.
- Morrison VBP. An Introduction to Health Psychology. Harlow: Pearson; 2009.
- Ogden J. Health Psychology, a Textbook. Maidenhead: McGraw Hill; 2007.
- Abraham C, Conner M, Jones F, O’Connor D. Health Psychology: Topics in Applied Psychology. London: Hodder Education; 2008.
- Jolly M. What I never wanted to tell you: therapeutic letter writing in cultural context. J Med Humanit 2011;32:47-59. http://dx.doi.org/10.1007/s10912-010-9127-z.
- Nicholls S. Beyond expressive writing: evolving models of developmental creative writing. J Health Psychol 2009;14:171-80. http://dx.doi.org/10.1177/1359105308100201.
- Baker JR, Moore SM. Blogging as a social tool: a psychosocial examination of the effects of blogging. Cyberpsychol Behav 2008;11:747-9. http://dx.doi.org/10.1089/cpb.2008.0053.
- Smyth JM, Hockemeyer JR, Tulloch H. Expressive writing and post-traumatic stress disorder: effects on trauma symptoms, mood states, and cortisol reactivity. Br J Health Psychol 2008;13:85-93. http://dx.doi.org/10.1348/135910707X250866.
- Bolton G, Field V, Thompson K. Writing Works: A Resource Handbook for Therapeutic Workshops and Activities. London: Jessica Kingsley; 2006.
- Bolton G. The Therapeutic Potential of Creative Writing: Writing Myself. London: Jessica Kingsley; 1999.
- Bolton G, Field V, Thompson K. Writing Routes. A Resource Handbook of Therapeutic Writing. London: Jessica Kingsley; 2011.
- Pitts V. Illness and internet empowerment: writing and reading breast cancer in cyberspace. Health (London) 2004;8:33-59. http://dx.doi.org/10.1177/1363459304038794.
- Baker JR, Moore SM. Creation and validation of the personal blogging style scale. Cyberpsychol Behav Soc Netw 2011;14:379-85. http://dx.doi.org/10.1089/cyber.2010.0130.
- Silverton S. The Mindfulness Breakthrough: The Revolutionary Approach to Dealing with Stress, Anxiety and Depression. London: Watkins Publishing; 2012.
- Hynes AMC, Hynes-Berry M. Biblio-Poetry Therapy, The Interactive Process: A Handbook. St Cloud, MN: North Star Press; 1994.
- Anonymous . Five Steps to Mental Wellbeing 2014. www.nhs.uk/Conditions/stress-anxiety-depression/Pages/improve-mental-wellbeing.aspx#Evidence (accessed 23 June 2015).
- Frattaroli J. Experimental disclosure and its moderators: a meta-analysis. Psychol Bull 2006;132:823-65. http://dx.doi.org/10.1037/0033-2909.132.6.823.
- Pennebaker JW, Mayne TJ, Francis ME. Linguistic predictors of adaptive bereavement. J Pers Soc Psychol 1997;72:863-71. http://dx.doi.org/10.1037/0022-3514.72.4.863.
- King L, Miner KN. Writing about the perceived benefits of traumatic events: Implications for physical health. Pers Soc Psychol Bull 2000;26:220-30. http://dx.doi.org/10.1177/0146167200264008.
- McCarty Hynes A, Hynes-Berry M. Biblio/Poetry Therapy – The Interactive Process: A Handbook. St Cloud, MN: North Star Press; 2012.
- Anonymous . Reading Well 2014. http://readingagency.org.uk/adults/quick-guides/reading-well (accessed 23 June 2015).
- Frisina PG, Borod JC, Lepore SJ. A meta-analysis of the effects of written emotional disclosure on the health outcomes of clinical populations. J Nerv Ment Dis 2004;192:629-34. http://dx.doi.org/10.1097/01.nmd.0000138317.30764.63.
- Meads C, Nouwen A. Does emotional disclosure have any effects? A systematic review of the literature with meta-analyses. Int J Technol Assess Health Care 2005;21:153-64.
- Harris AHS. Does expressive writing reduce health care utilization? A meta-analysis of randomized trials. J Consult Clin Psychol 2006;74:243-52. http://dx.doi.org/10.1037/0022-006X.74.2.243.
- Bridle C, Dennick KJ, Sturt J. Written Emotional Disclosure for Psychological Morbidity Among People With Long-Term Physical Conditions: Systematic Review and Meta-Analysis of Randomised Controlled Trials 2011. www2.warwick.ac.uk/fac/med/staff/bridle/hta/bridle_wed_sept11.pdf (accessed 23 June 2015).
- Van Emmerik AAP, Reijntjes A, Kamphuis JH. Writing therapy for posttraumatic stress: a meta-analysis. Psychother Psychosom 2013;82:82-8. http://dx.doi.org/10.1159/000343131.
- Greenhalgh T, Hurwitz B. Narrative Based Medicine: Dialogue and Discourse in Clinical Practice. London: BMJ Books; 1998.
- Greenhalgh T. Writing as therapy. Effects on immune mediated illness need substantiation in independent studies. BMJ 1999;319:270-1. http://dx.doi.org/10.1136/bmj.319.7205.270.
- Greenhalgh T. What Seems to be the Trouble? Stories in Illness and Healthcare. Oxford: Radcliffe; 2006.
- Greenhalgh T, Collard A, Campbell-Richards D, Vijayaraghavan S, Malik F, Morris J, et al. Storylines of self-management: narratives of people with diabetes from a multiethnic inner city population. J Health Serv Res Policy 2011;16:37-43. http://dx.doi.org/10.1258/jhsrp.2010.009160.
- Yach D, Hawkes C, Gould CL, Hofman KJ. The global burden of chronic diseases: overcoming impediments to prevention and control. JAMA 2004;291:2616-22. http://dx.doi.org/10.1001/jama.291.21.2616.
- Anonymous . Ten Things You Need to Know about Long Term Conditions 2011. http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/Healthcare/Longtermconditions/DH_084294 (accessed 23 June 2015).
- Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012;380:37-43. http://dx.doi.org/10.1016/S0140-6736(12)60240-2.
- Ouwens M, Wollersheim H, Hermens R, Hulscher M, Grol R. Integrated care programmes for chronically ill patients: a review of systematic reviews. Int J Qual Health Care 2005;17:141-6. http://dx.doi.org/10.1093/intqhc/mzi016.
- Phelps EA. Human emotion and memory: interactions of the amygdala and hippocampal complex. Curr Opin Neurobiol 2004;14:198-202. http://dx.doi.org/10.1016/j.conb.2004.03.015.
- Bernstein DA, Clarke-Stewart A, Roy EJ, Wickens CD. Psychology. Boston, MA: Houghton Mifflin; 1997.
- Phan KL, Wager TD, Taylor SF, Liberzon I. Functional neuroimaging studies of human emotions. CNS Spectrum 2004;9:258-66.
- Evans P, Hucklebridge F, Clow A. Mind, Immunity and Health. The Science of Psychoneuroimmunology. London: Free Association Books; 2000.
- Jaremka LM, Lindgren ME, Kiecolt-Glaser JK. Synergistic relationships among stress, depression and troubled relationships: insights from psychoneuroimmunology. Depress Anxiety 2013;30:288-96. http://dx.doi.org/10.1002/da.22078.
- Mackner LM, Clough-Paabo E, Pajer K, Lourie A, Crandall WV. Psychoneuroimmunologic factors in inflammatory bowel disease. Inflamm Bowel Dis 2011;17:849-57. http://dx.doi.org/10.1002/ibd.21430.
- Broadbent E, Koschwanez HE. The psychology of wound healing. Curr Opin Psychiatry 2012;25:135-40. http://dx.doi.org/10.1097/YCO.0b013e32834e1424.
- Pawson R, Greenhalgh T, Harvey G, Walshe K. Realist review: a new method of systematic review designed for complex policy interventions. J Health Serv Res Pol 2005;10:21-34. http://dx.doi.org/10.1258/1355819054308530.
- Astbury B, Leeuw FL. Unpacking black boxes: mechanisms and theory building in evaluation. Am J Eval 2010;31:363-81. http://dx.doi.org/10.1177/1098214010371972.
- Berwick DM. The science of improvement. JAMA 2008;299:1182-4. http://dx.doi.org/10.1001/jama.299.10.1182.
- Frisina PG, Lepore SJ, Borod JC. Written emotional disclosure and clinical populations: confirming and updating our meta-analytic findings. J Nerv Mental Dis 2005;193:425-6. http://dx.doi.org/10.1097/01.nmd.0000165299.16000.0b.
- Smyth JM. Written emotional expression: effect sizes, outcome types, and moderating variables. J Consult Clin Psychol 1998;66:174-84. http://dx.doi.org/10.1037/0022-006X.66.1.174.
- Knaevelsrud C, Maercker A. Internet-based treatment for PTSD reduces distress and facilitates the development of a strong therapeutic alliance: a randomized controlled clinical trial. BMC Psychiatry 2007;7. http://dx.doi.org/10.1186/1471-244X-7-13.
- Lange A, Van de Ven JP, Schrieken B, Emmelkamp PMG. Interapy. Treatment of posttraumatic stress through the Internet: a controlled trial. J Behav Ther Exp Psychiatry 2001;32:73-90. http://dx.doi.org/10.1016/S0005-7916(01)00023-4.
- Abel E, Rew L, Gortner EM, Delville CL. Cognitive reorganization and stigmatization among persons with HIV. J Adv Nurs 2004;47:510-25. http://dx.doi.org/10.1111/j.1365-2648.2004.03134.x.
- Graham JE, Lobel M, Glass P, Lokshina I. Effects of written anger expression in chronic pain patients: making meaning from pain. J Behav Med 2008;31:201-12. http://dx.doi.org/10.1007/s10865-008-9149-4.
- Halpert A, Rybin D, Doros G. Expressive writing is a promising therapeutic modality for the management of IBS: a pilot study. Am J Gastroenterol 2010;105:2440-8. http://dx.doi.org/10.1038/ajg.2010.246.
- Henry EA, Schlegel RJ, Talley AE, Molix LA, Bettencourt BA. The feasibility and effectiveness of expressive writing for rural and urban breast cancer survivors. Oncol Nurs Forum 2010;37:749-57. http://dx.doi.org/10.1188/10.ONF.749-757.
- Hughes KN. Expressive writing and breast cancer: outcomes and linguistic analyses. Diss Abstr Int B 2007;68.
- Kraaij V, Emmerik A, Garnefski N, Shroevers MJ, Lo-Fo-Wong D, van Empelen P, et al. Effects of a cognitive behavioral self-help program and a computerized structured writing intervention on depressed mood for HIV-infected people: a pilot randomized controlled trial. Patient Educ Couns 2010;80:200-4. http://dx.doi.org/10.1016/j.pec.2009.08.014.
- Petrie KJ, Fontanilla I, Thomas MG, Booth RJ, Pennebaker JW. Effect of written emotional expression on immune function in patients with human immunodeficiency virus infection: a randomized trial. Psychosom Med 2004;66:272-5. http://dx.doi.org/10.1097/01.psy.0000116782.49850.d3.
- Stark HG. Expressive writing as an adjunct to multidisciplinary pain treatment in chronic pain patients. Diss Abstr Int B 2010;71.
- Theadom A, Smith H, Horne R, Bowskill R, Apfelbacher CJ, Frew AJ. Participant experiences of a written emotional disclosure intervention in asthma. Stress Health 2010;26:45-50. http://dx.doi.org/10.1002/smi.1255.
- Farrand P, Woodford J. Impact of support on the effectiveness of written cognitive behavioural self-help: a systematic review and meta-analysis of randomised controlled trials. Clin Psychol Rev 2013;33:182-95. http://dx.doi.org/10.1016/j.cpr.2012.11.001.
- Meads CA. Emotional Disclosure (Expressive Writing) and Health. Saarbrucken: VDM-Verlag; 2009.
- Egger M, Dickersin K, Davey-Smith G, Egger M, Dickersin K, Davey-Smith G. Systematic Reviews in Healthcare, Meta-analysis in Context. London: BMJ Books; 2001.
- Heshka S, Allison DB. Is obesity a disease?. Int J Obes Relat Metab Disord 2001;25:1401-4. http://dx.doi.org/10.1038/sj.ijo.0801790.
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006-12. http://dx.doi.org/10.1016/j.jclinepi.2009.06.005.
- Wells G, Brodsky L, O’Connell D, Robertson J, Peterson V, Welch V, et al. Evaluation of the Newcastle-Ottawa Scale (NOS): An Assessment Tool for Evaluating the Quality of Non-Randomized Studies n.d.
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 2011. www.cochrane-handbook.org (accessed 23 June 2015).
- Rickett C, Greive C, Gordon J. Something to hang my life on: the health benefits of writing poetry for people with serious illnesses. Australas Psychiatry 2011;19:265-8. http://dx.doi.org/10.3109/10398562.2011.562298.
- Hong I, Choi M. Songwriting oriented activities improve the cognitive functions of the aged with dementia. Art Psychother 2011;38:221-8. http://dx.doi.org/10.1016/j.aip.2011.07.002.
- Golkaramnay V, Bauer S, Haug S, Wolf M, Kordy H. The exploration of the effectiveness of group therapy through an internet chat as aftercare: a controlled naturalistic study. Psychother Psychosom 2007;76:219-25. http://dx.doi.org/10.1159/000101500.
- Lange A, Rietdijk D, Hudcovicova M, van de Ven JP, Schrieken B, Emmelkamp PM. Interapy: a controlled randomized trial of the standardized treatment of posttraumatic stress through the internet. J Consult Clin Psychol 2003;71:901-9. http://dx.doi.org/10.1037/0022-006X.71.5.901.
- Sloan DM, Marx BP, Bovin MJ, Feinstein BA, Gallagher MW. Written exposure as an intervention for PTSD: a randomized clinical trial with motor vehicle accident survivors. Behav Res Ther 2012;50:627-35. http://dx.doi.org/10.1016/j.brat.2012.07.001.
- Ironson G, O’Cleirigh C, Leserman J, Stuetzle R, Fordiani J, Fletcher M, et al. Gender-specific effects of an augmented written emotional disclosure intervention on posttraumatic, depressive, and HIV-disease-related outcomes: a randomized, controlled trial. J Consult Clin Psychol 2013;81:284-98. http://dx.doi.org/10.1037/a0030814.
- Mann T. Effects of future writing and optimism on health behaviors in HIV-infected women. Ann Behav Med 2001;23:26-33. http://dx.doi.org/10.1207/S15324796ABM2301_5.
- Wagner LJ, Hilker KA, Hepworth JT, Wallston KA. Cognitive adaptability as a moderator of expressive writing effects in an HIV sample. AIDS Behav 2010;14:410-20. http://dx.doi.org/10.1007/s10461-008-9427-8.
- Craft MA, Davis GC, Paulson RM. Expressive writing in early breast cancer survivors. J Adv Nurs 2013;69:305-15. http://dx.doi.org/10.1111/j.1365-2648.2012.06008.x.
- Gellaitry G, Peters K, Bloomfield D, Horne R. Narrowing the gap: the effects of an expressive writing intervention on perceptions of actual and ideal emotional support in women who have completed treatment for early stage breast cancer. Psychooncology 2010;19:77-84. http://dx.doi.org/10.1002/pon.1532.
- Jensen-Johansen MB, Christensen S, Valdimarsdottir H, Zakowski S, Jensen AB, Bovbjerg DH, et al. Effects of an expressive writing intervention on cancer-related distress in Danish breast cancer survivors: results from a nationwide randomized clinical trial. Psychooncology 2013;22:1492-500. http://dx.doi.org/10.1002/pon.3193.
- Mosher CE, DuHamel KN, Lam J, Dickler M, Li Y, Massie MJ, et al. Randomised trial of expressive writing for distressed metastatic breast cancer patients. Psychol Health 2012;27:88-100. http://dx.doi.org/10.1080/08870446.2010.551212.
- Park EY, Yi M. Development and effectiveness of expressive writing program for women with breast cancer in Korea. J Korean Acad Nurs 2012;42:269-79. http://dx.doi.org/10.4040/jkan.2012.42.2.269.
- Walker BL, Nail LM, Croyle RT. Does emotional expression make a difference in reactions to breast cancer?. Oncol Nurs Forum 1999;26:1025-32.
- Arden-Close E, Gidron Y, Bayne L, Moss-Morris R. Written emotional disclosure for women with ovarian cancer and their partners: randomised controlled trial. Psychooncology 2013;22:2262-9. http://dx.doi.org/10.1002/pon.3280.
- Milbury K, Spelman A, Wood C, Matin SF, Tannir N, Jonasch E, et al. Randomized controlled trial of expressive writing for patients with renal cell carcinoma. J Clin Oncol 2014;32:663-70. http://dx.doi.org/10.1200/JCO.2013.50.3532.
- Pauley PM, Morman MT, Floyd K. Expressive writing improves subjective health among testicular cancer survivors: a pilot study. Int J Mens Health 2011;10:199-21. http://dx.doi.org/10.3149/jmh.1003.199.
- Rosenberg HJ, Rosenberg SD, Ernstoff MS, Wolford GL, Amdur RJ, Elshamy MR, et al. Expressive disclosure and health outcomes in a prostate cancer population. Int J Psychiatry Med 2002;32:37-53. http://dx.doi.org/10.2190/AGPF-VB1G-U82E-AE8C.
- Zakowski SG, Ramati A, Morton C, Johnson P, Flanigan R. Written emotional disclosure buffers: the effects of social constraints on distress among cancer patients. Health Psychol 2004;23:555-63. http://dx.doi.org/10.1037/0278-6133.23.6.555.
- Cepeda MS, Chapman CR, Miranda N, Sanchez R, Rodriguez CH, Restrepo EA, et al. Emotional disclosure through patient narrative may improve pain and well-being: results of a randomized controlled trial in patients with cancer pain. J Pain Sympt Manage 2008;35:623-31. http://dx.doi.org/10.1016/j.jpainsymman.2007.08.011.
- Rini C, Austin J, Wu LM, Winkel G, Valdimarsdottir H, Stanton AL, et al. Harnessing benefits of helping others: a randomised controlled trial testing expressive helping to address survivorship problems after haemopoietic stem cell transplant. Health Psychol 2014;33:1541-51. http://dx.doi.org/10.1037/hea0000024.
- McElligott MD. Expressive writing as an intervention for adolescents with sickle cell disease. Diss Abstr Int B 2006;66.
- Dennick KJ, Bridle C, Sturt J. Written emotional disclosure for adults with type 2 diabetes: a primary care feasability study. Primary Health Care Res Dev 2014;6:1-9. http://dx.doi.org/10.1017/S1463423614000188.
- Taylor LA, Wallander JL, Anderson D, Beasley P, Brown RT. Improving health care utilization, improving chronic disease utilization, health status, and adjustment in adolescents and young adults with cystic fibrosis: a preliminary report. J Clin Psychol Med Settings 2003;10:9-16. http://dx.doi.org/10.1023/A:1022897512137.
- Grasing K, Mathur D, D’Souza C. Written emotional expression during recovery from cocaine dependence: group and individual differences in craving intensity. Subst Use Misuse 2010;45:1201-15. http://dx.doi.org/10.3109/10826080903474003.
- Meshberg-Cohen S. Expressive writing as a therapeutic process for drug dependent women. Diss Abstr Int B 2010;70. http://dx.doi.org/10.1080/08897077.2013.805181.
- Van Dam D, Ehring T, Vedel E, Emmelkamp P. Trauma-focused treatment for posttraumatic stress disorder combined with CBT for severe substance use disorder: a randomised controlled trial. BMC Psychiatry 2013;13. http://dx.doi.org/10.1186/1471-244X-13-172.
- Bernard M, Jackson C, Jones C. Written emotional disclosure following first-episode psychosis: effects on symptoms of post-traumatic stress disorder. Br J Clin Psychol 2006;45:403-15. http://dx.doi.org/10.1348/014466505X68933.
- Canna MA. Controlled evaluation of the effects of expressive writing on subsequent cognitive behavioral group treatment with an anxious/depressed sample. Diss Abstr In 2006;66.
- Graf MC, Gaudiano BA, Geller PA. Written emotional disclosure: a controlled study of the benefits of expressive writing homework in outpatient psychotherapy. Psychother Res 2008;18:389-99. http://dx.doi.org/10.1080/10503300701691664.
- Krpan KM, Kross E, Berman MG, Deldin PJ, Askren MK, Jonides J. An everyday activity as a treatment for depression: the benefits of expressive writing for people diagnosed with major depressive disorder. J Affect Disord 2013;15:1148-51. http://dx.doi.org/10.1016/j.jad.2013.05.065.
- Richards JM, Beal WE, Seagal JD, Pennebaker JW. Effects of disclosure of traumatic events on illness behavior among psychiatric prison inmates. J Abnorm Psychol 2000;109:156-60. http://dx.doi.org/10.1037/0021-843X.109.1.156.
- Gidron Y, Peri T, Connolly JF, Shalev AY. Written disclosure in posttraumatic stress disorder: is it beneficial for the patient?. J Nerv Ment Dis 1996;184:505-7. http://dx.doi.org/10.1097/00005053-199608000-00009.
- Robinson P, Serfaty M. Getting better byte by byte: a pilot randomised controlled trial of email therapy for bulimia nervosa and binge eating disorder. Eur Eat Disord Rev 2008;16:84-93. http://dx.doi.org/10.1002/erv.818.
- Averill AJ, Kasarskis EJ, Segerstrom SC. Expressive disclosure to improve well-being in patients with amyotrophic lateral sclerosis: a randomised, controlled trial. Psychol Health 2013;28:701-13. http://dx.doi.org/10.1080/08870446.2012.754891.
- D’Souza PJ, Lumley MA, Kraft CA, Dooley JA. Relaxation training and written emotional disclosure for tension or migraine headaches: a randomized, controlled trial. Ann Behav Med 2008;36:21-32. http://dx.doi.org/10.1007/s12160-008-9046-7.
- Bartasiuniene R, Sinkariova L, Petroliene R. Impact of expressive writing on emotional states of patients with cardiovascular disease. Rakstu Krajums Proc 2011.
- Hevey D, Wilczkiewicz E, Horgan JH. Type D moderates the effects of expressive writing on health-related quality of life (HRQOL) following myocardial infarction (MI). Irish J Psycho 2012;33:107-14. http://dx.doi.org/10.1080/03033910.2012.708901.
- Willmott L, Harris P, Gellaitry G, Cooper V, Horne R. The effects of expressive writing following first myocardial infarction: a randomized controlled trial. Health Psychol 2011;30:642-50. http://dx.doi.org/10.1037/a0023519.
- Sharifabad MA, Hurewitz A, Spiegler P, Bernstein M, Feuerman M, Smyth JM. Written disclosure therapy for patients with chronic lung disease undergoing pulmonary rehabilitation. J Cardiopulm Rehabil Prev 2010;30:340-5. http://dx.doi.org/10.1097/HCR.0b013e3181e174c4.
- Harris AH, Thoresen CE, Humphreys K, Faul J. Does writing affect asthma? A randomized trial. Psychosom Med 2005;67:130-6. http://dx.doi.org/10.1097/01.psy.0000146345.73510.d5.
- Smyth JM, Stone AA, Hurewitz A, Kaell A. Effects of writing about stressful experiences on symptom reduction in patients with asthma or rheumatoid arthritis: a randomized trial. JAMA 1999;281:1304-9. http://dx.doi.org/10.1001/jama.281.14.1304.
- Warner LJ, Lumley MA, Casey RJ, Pierantoni W, Salazar R, Zoratti EM, et al. Health effects of written emotional disclosure in adolescents with asthma: a randomized, controlled trial. J Pediatr Psychol 2006;31:557-68. http://dx.doi.org/10.1093/jpepsy/jsj048.
- Wallander JL, Madan-Swain A, Klapow J, Saeed S. A randomised controlled trial of written self-disclosure for functional recurrent abdominal pain in youth. Psychol Health 2011;26:433-47. http://dx.doi.org/10.1080/08870440903477212.
- Paradisi A, Abeni D, Finore E, Di Pietro C, Sampogna F, Mazzanti C, et al. Effect of written emotional disclosure interventions in persons with psoriasis undergoing narrow band ultraviolet B phototherapy. Eur J Dermatol 2010;20:599-605. http://dx.doi.org/10.1684/ejd.2010.1018.
- Tabolli S, Naldi L, Pagliarello C, Sampogna F, di Pietro C, Spagnoli A, et al. Evaluation of the impact of writing exercises interventions on quality of life in patients with psoriasis undergoing systemic treatments. Br J Dermatol 2012;167:1254-64. http://dx.doi.org/10.1111/j.1365-2133.2012.11147.x.
- Vedhara K, Morris RM, Booth R, Horgan M, Lawrence M, Birchall N. Changes in mood predict disease activity and quality of life in patients with psoriasis following emotional disclosure. J Psychosom Res 2007;62:611-19. http://dx.doi.org/10.1016/j.jpsychores.2006.12.017.
- Broderick JE, Stone AA, Smyth JM, Kaell AT. The feasibility and effectiveness of an expressive writing intervention for rheumatoid arthritis via home-based videotaped instructions. Ann Behav Med 2004;27:50-9. http://dx.doi.org/10.1207/s15324796abm2701_7.
- Hamilton-West KE, Quine L. Effects of written emotional disclosure on health outcomes in patients with ankylosing spondylitis. Psychol Health 2007;22:637-57. http://dx.doi.org/10.1080/14768320601020246.
- Lumley MA, Leisen JC, Partridge RT, Meyer TM, Radcliffe AM, Macklem DJ, et al. Does emotional disclosure about stress improve health in rheumatoid arthritis? Randomized, controlled trials of written and spoken disclosure. Pain 2011;152:866-77. http://dx.doi.org/10.1016/j.pain.2011.01.003.
- Lumley MA, Keefe FJ, Mosley-Williams A, Rice JR, McKee D, Waters SJ, et al. The effects of written emotional disclosure and coping skills training in rheumatoid arthritis: a randomised clinical trial. J Consult Clin Psychol 2014;82:644-58. http://dx.doi.org/10.1037/a0036958.
- Wetherell MA, Byrne-Davis L, Dieppe P, Donovan J, Brookes S, Byron M, et al. Effects of emotional disclosure on psychological and physiological outcomes in patients with rheumatoid arthritis: an exploratory home-based study. J Health Psychol 2005;10:277-85. http://dx.doi.org/10.1177/1359105305049778.
- Broderick JE, Junghaenel DU, Schwartz JE. Written emotional expression produces health benefits in fibromyalgia patients. Psychosom Med 2005;67:326-34. http://dx.doi.org/10.1097/01.psy.0000156933.04566.bd.
- Gillis ME, Lumley MA, Mosley-Williams A, Leisen JC, Roehrs T. The health effects of at-home written emotional disclosure in fibromyalgia: a randomized trial. Ann Behav Med 2006;32:135-46. http://dx.doi.org/10.1207/s15324796abm3202_11.
- D’Souza PJ. The effects of relaxation training and written emotional disclosure for people with migraine or tension headaches. Diss Abstr Int B 2003;63.
- Smyth JN, D. Arigo D, Nyklíček I, Vingerhoets AN, Denollet J. Emotion Regulation: Conceptual and Clinical Issues. Tilberg: Springer; 2008.
- International Classification of Diseases (ICD-10). Geneva: World Health Organization; 2014.
- Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: Arlington; 2004.
- Brooks B. El Escorial World Federation of Neurology criteria for the diagnosis of amyotrophic lateral sclerosis. Subcommittee on Motor Neuron Diseases/Amyotrophic Lateral Sclerosis of the World Federation of Neurology Research Group on Neuromuscular Diseases and the El Escorial ‘Clinical limits of amyotrophic lateral sclerosis’ workshop contributors. J Neurolog Sc 1994;124:96-107. http://dx.doi.org/10.1016/0022-510X(94)90191-0.
- Rusting CL, Nolen-Hoeksema S. Regulating responses to anger: effects of rumination and distraction on angry mood. J Pers Soc Psychol 1998;74:790-803. http://dx.doi.org/10.1037/0022-3514.74.3.790.
- Curtis L. Unit Costs of Health and Social Care 2013. Canterbury: PSSRU, University of Kent; 2013.
- Pawson R. Evidence-Based Policy: A Realist Perspective. London: Sage; 2006.
- Baker S. Tell it slant: history, memory, and imagination in the healing writing workshop. Traumatology 2009;15:15-23. http://dx.doi.org/10.1177/1534765609348912.
- Foster L. Writers’ workshops, the word processor and the psychiatric patient. Br J Occup Ther 1988;51:191-2. http://dx.doi.org/10.1177/030802268805100604.
- Rogers E. Diffusion of Innovations. New York, NY: Free Press; 2003.
- Macklem DJ. Exploration of emotion regulation styles as potential moderators of emotional disclosure in patients with rheumatoid arthritis: testing a model of emotional expression. Diss Abstr Int B 2008;68.
- Chidiac N. Writing of trauma or trauma of writing? (Two women, two stories, two ways of writing). Ann Med-Psychol 2008;166:308-14. http://dx.doi.org/10.1016/j.amp.2008.03.003.
- Cureton A, Schick E. Survivors writing together: a pilot study. Psychooncology 2009;18:S67-8.
- Fair CD, Connor L, Albright J, Wise E, Jones K. “I’m positive, I have something to say”: assessing the impact of a creative writing group for adolescents living with HIV. Arts Psychother 2012;39:383-9. http://dx.doi.org/10.1016/j.aip.2012.06.010.
- Mazza N. Poetry: a therapeutic tool in the early stages of alcoholism treatment. J Stud Alcohol 1979;40:123-8. http://dx.doi.org/10.15288/jsa.1979.40.123.
- Goldstein SL. A songwriting assessment for hopelessness in depressed adolescents: a review of the literature and a pilot study. Arts Psychother 1990;17:117-24. http://dx.doi.org/10.1016/0197-4556(90)90021-H.
- Jones JD. A comparison of songwriting and lyric analysis techniques to evoke emotional change in a single session with people who are chemically dependent. J Music Ther 2005;42:94-110. http://dx.doi.org/10.1093/jmt/42.2.94.
- Nortemann M, Friedrichs O, Wiethuchter B, Dietl T, Hohn D, Nortemann S. Therapeutic writing in the stationary psychiatric psychotherapeutic treatment. Nervenarz 2007;78.
- Smith C, Holcroft C, Rebeck S, Thompson N, Werkowitch M. Journal writing as a complementary therapy for reactive depression: a rehabilitation teaching program. Rehabil Nurs 2000;25:170-6. http://dx.doi.org/10.1002/j.2048-7940.2000.tb01901.x.
- Luber RFJ. Poetry therapy helps patients express feelings. Hosp Community Psychiatry 1973;24. http://dx.doi.org/10.1176/ps.24.6.387.
- Byrne-Davis LMT, Wetherell MA, Dieppe P, Weinmann J, Byron M, Donovan J, et al. Emotional disclosure in rheumatoid arthritis: participants’ views on mechanisms. Psychol Health 2006;21:667-82. http://dx.doi.org/10.1080/14768320500444315.
- Anderson SS. The effect of written emotional expression on depression following mild traumatic brain injury: a pilot study. Diss Abstr Int B 2009;69.
- Rivkin ID, Gustafson J, Weingarten I, Chin D. The effects of expressive writing on adjustment to HIV. AIDS Behav 2006;10:13-26. http://dx.doi.org/10.1007/s10461-005-9051-9.
- Bolton CE, Bevan-Smith EF, Blakey JD, Crowe P, Elkin SL, Garrod R, et al. British Thoracic Society guideline on pulmonary rehabilitation in adults. Thorax 2013;68:1-30. http://dx.doi.org/10.1136/thoraxjnl-2013-203809.
- Pennebaker JW, Chung CK, Friedman HS. Oxford Handbook of Health Psychology. New York, NY: Oxford University Press; 2011.
- Wong G, Greenhalgh T, Westhorp G, Buckingham J, Pawson R. RAMESES publication standards: realist syntheses. BMC Med 2013;11. http://dx.doi.org/10.1186/1741-7015-11-21.
- Furnes B, Dysvik E. Therapeutic writing and chronic pain: experiences of therapeutic writing in a cognitive behavioural programme for people with chronic pain. J Clin Nurs 2012;21:3372-81. http://dx.doi.org/10.1111/j.1365-2702.2012.04268.x.
- Dieleman M, Gerretsen B, van der Wilt GJ. Human resource management interventions to improve health workers’ performance in low and middle income countries: a realist review. Health Res Policy Syst 2009;7. http://dx.doi.org/10.1186/1478-4505-7-7.
- Kane SS, Gerretsen B, Scherpbier R, Dal Poz M, Dieleman M. A realist synthesis of randomised control trials involving use of community health workers for delivering child health interventions in low and middle income countries. BMC Health Serv Res 2010;10. http://dx.doi.org/10.1186/1472-6963-10-286.
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Int J Surg 2011;9:672-7. http://dx.doi.org/10.1016/j.ijsu.2011.09.004.
- Williamson P, Clarke M. The COMET (Core Outcome Measures in Effectiveness Trials) initiative: its role in improving Cochrane Reviews. Cochrane Database Syst Rev 2012;5. http://dx.doi.org/10.1002/14651858.ed000041.
- Burton CM, King LA. Effects of (very) brief writing on health: the two-minute miracle. Br J Health Psychol 2008;13:9-14. http://dx.doi.org/10.1348/135910707X250910.
- Burton CM, King LA. The health benefits of writing about positive experiences. J Res Pers 2004;38:150-63. http://dx.doi.org/10.1016/S0092-6566(03)00058-8.
- Burton CM, King LA. The health benefits of writing about positive experiences: the role of broadened cognition. Psychol Health 2009;24:867-79. http://dx.doi.org/10.1080/08870440801989946.
- Mackenzie CS, Wiprzycka UJ, Hasher L, Goldstein D. Seeing the glass half full: optimistic expressive writing improves mental health among chronically stressed caregivers. Br J Health Psychol 2008;13:73-6. http://dx.doi.org/10.1348/135910707X251153.
- McKay M, Wood JC, Brantley J. The Dialectical Behaviour Therapy Skills Workbook. Oakland, CA: New Harbinger Publications; 2007.
- Poon A, Danoff-Burg S. Mindfulness as a moderator in expressive writing. J Clin Psychol 2011;67:881-95. http://dx.doi.org/10.1002/jclp.20810.
- East P, Startup H, Roberts C, Schmidt U. Expressive writing and eating disorder features: a preliminary trial in a student sample of the impact of three writing tasks on eating disorder symptoms and associated cognitive, affective and interpersonal factors. Eur Eat Disord Rev 2010;18:180-96. http://dx.doi.org/10.1002/erv.978.
- King LA, Milner KN. Writing about the perceived benefits of traumatic events: implications for physical health. Pers Soc Psychol Bull 2000;26:220-30. http://dx.doi.org/10.1177/0146167200264008.
- Danoff-Burg S, Mosher CE. Predictors of tanning salon use: behavioral alternatives for enhancing appearance, relaxing and socializing. J Health Psychol 2006;11:511-18. http://dx.doi.org/10.1177/1359105306063325.
- Zakowski SG, Herzer M, Barrett SD, Milligan JG, Beckman N. Who benefits from emotional expression? An examination of personality differences among gynaecological cancer patients participating in a randomized controlled emotional disclosure intervention trial. Br J Psychol 2011;102:355-72. http://dx.doi.org/10.1348/000712610X524949.
- Hyland ME, Ley A, Fisher DW, Woodward V. Measurement of psychological distress in asthma and asthma management programmes. Br J Clin Psychol 1995;34:601-11. http://dx.doi.org/10.1111/j.2044-8260.1995.tb01494.x.
- Bradburn NM. The Structure of Psychological Well-being. Chicago, IL: Aldine; 1969.
- Ryden MB. An adult version of the Coopersmith Self-Esteem Inventory: test-retest reliability and social desirability. Psychological Reports 1978;43:1189-90. http://dx.doi.org/10.2466/pr0.1978.43.3f.1189.
- Coopersmith S. The Antecedents of Self-esteem. San Francisco, CA: W. H. Freeman and Company; 1967.
- King LA, Emmons RA. Conflict over emotional expression: psychological and physical correlates. J Pers Soc Psychol 1990;58:864-77. http://dx.doi.org/10.1037/0022-3514.58.5.864.
- Richmond VP, Mccroskey JC. Reliability and separation of factors on the assertiveness-responsiveness measure. Psychological Reports 1990;67:449-50. http://dx.doi.org/10.2466/PR0.67.6.449-450.
- Beck AT, Steer RA. Manual for the Beck Anxiety Inventory. San Antonio, TX: Psychological Corporation; 1990.
- Jones SD, Steiner A, Garrett SL, Calin A. The Bath Ankylosing Spondylitis Patient Global Score (BAS-G). Br J Rheumatol 1996;35:66-71. http://dx.doi.org/10.1093/rheumatology/35.1.66.
- Calin A, Garrett S, Whitelock H, Kennedy LG, O’Hea J, Mallorie P, et al. A new approach to defining functional ability in ankylosing spondylitis: the development of the Bath Ankylosing Spondylitis Functional Index. J Rheumatol 1994;21:2281-5.
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry 1961;4:561-71.
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York, NY: Guilford Press; 1979.
- Beck AT. The past and future of cognitive therapy. J Psychother Pract Res 1997;6:276-84.
- Furlanetto LM, Mendlowicz MV, Romildo Bueno J. The validity of the Beck Depression Inventory-Short Form as a screening and diagnostic instrument for moderate and severe depression in medical inpatients. J Affect Disord 2005;86:87-91. http://dx.doi.org/10.1016/j.jad.2004.12.011.
- Mendoza TR, Wang XS, Cleeland CS, Morrissey M, Johnson BA, Wendt JK, et al. The rapid assessment of fatigue severity in cancer patients: use of the Brief Fatigue Inventory. Cancer 1999;85:1186-96. http://dx.doi.org/10.1002/(SICI)1097-0142(19990301)85:5<1186::AID-CNCR24>3.0.CO;2-N.
- Henderson M, Freeman CP. A self-rating scale for bulimia. The ’BITE’. Br J Psychiatry 1987;150:18-24. http://dx.doi.org/10.1192/bjp.150.1.18.
- Carver CS. You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med 1997;4:92-100. http://dx.doi.org/10.1207/s15327558ijbm0401_6.
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med 1983;13:595-60. http://dx.doi.org/10.1017/S0033291700048017.
- Lee EH. Development and psychometric evaluation of a quality of life scale for Korean patients with cancer (C-QOL). Taehan Kanho Hakhoe Chi 2007;37:324-33.
- Weathers FW, Keane TM, Davidson JR. Clinician-administered PTSD scale: a review of the first ten years of research. Depress Anxiety 2001;13:132-56. http://dx.doi.org/10.1002/da.1029.
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991.
- Radloff LS. The CES-D Scale. A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement 1977;1:385-401. http://dx.doi.org/10.1177/014662167700100306.
- Geisser ME, Roth RS, Robinson ME. Assessing depression among persons with chronic pain using the Center for Epidemiological Studies-Depression Scale and the Beck Depression Inventory: a comparative analysis. Clin J Pain 1997;13:163-70. http://dx.doi.org/10.1097/00002508-199706000-00011.
- Wolfe F, Wolfe F, Pincus T, Dekker M. Rheumatoid Arthritis: Pathogenesis, Assessment, Outcome and Treatment. New York, NY: Marcel Dekker; 1994.
- Fries JF, Spitz P, Kraines RG, Holman HR. Measurement of patient outcome in arthritis. Arthritis Rheum 1980;23:137-45. http://dx.doi.org/10.1002/art.1780230202.
- Hawley DJ, Wolfe F. Depression is not more common in rheumatoid arthritis: a 10-year longitudinal study of 6,153 patients with rheumatic disease. J Rheumatol 1993;20:2025-31.
- DeVellis RF, DeVellis BM, Blanchard LW, Klotz ML, Luchok K, Voyce C. Development and validation of the Parent Health Locus of Control scales. Health Educ Q 1993;20:211-25. http://dx.doi.org/10.1177/109019819302000213.
- Burckhardt CS, Clark SR, Bennett RM. The fibromyalgia impact questionnaire: development and validation. J Rheumatol 1991;18:728-33.
- Kushner I. C-reactive protein in rheumatology. Arthritis Rheum 1991;34:1065-8. http://dx.doi.org/10.1002/art.1780340819.
- Schwartz GE, Davidson RJ, Goleman DJ. Patterning of cognitive and somatic processes in the self-regulation of anxiety: effects of meditation versus exercise. Psychosom Med 1978;40:321-8. http://dx.doi.org/10.1097/00006842-197806000-00004.
- Fuchs HA. The use of the disease activity score in the analysis of clinical trials in rheumatoid arthritis. J Rheumatol 1993;20:1863-6.
- Davidson JR, Book SW, Colket JT, Tupler LA, Roth S, David D, et al. Assessment of a new self-rating scale for post-traumatic stress disorder. Psychol Med 1997;27:153-60. http://dx.doi.org/10.1017/S0033291796004229.
- Zlotnick C, Davidson J, Shea MT, Pearlstein T. Validation of the Davidson Trauma Scale in a sample of survivors of childhood sexual abuse. J Nerv Ment Dis 1996;184:255-7. http://dx.doi.org/10.1097/00005053-199604000-00010.
- Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI) -- a simple practical measure for routine clinical use. Clin Exp Dermatol 1994;19:210-6. http://dx.doi.org/10.1111/j.1365-2230.1994.tb01167.x.
- Denollet J. DS14: standard assessment of negative affectivity, social inhibition, and Type D personality. Psychosom Med 2005;67:89-97. http://dx.doi.org/10.1097/01.psy.0000149256.81953.49.
- Denollet J, Schiffer AA, Spek V. A general propensity to psychological distress affects cardiovascular outcomes. Evidence from research on the Type D (Distressed) Personality Profile. Circ Cardiovasc Qual Outcomes 2010;3:546-57. http://dx.doi.org/10.1161/CIRCOUTCOMES.109.934406.
- Roth AJ, Kornblith AB, Batel-Copel L, Peabody E, Scher HI, Holland JC. Rapid screening for psychologic distress in men with prostate carcinoma: a pilot study. Cancer 1998;82:1904-8. http://dx.doi.org/10.1002/(SICI)1097-0142(19980515)82:10<1904::AID-CNCR13>3.0.CO;2-X.
- Stanton AL, Kirk SB, Cameron CL, Danoff-Burg S. Coping through emotional approach: scale construction and validation. J Pers Soc Psychol 2000;78:1150-69. http://dx.doi.org/10.1037/0022-3514.78.6.1150.
- Yellen SB, Cella DF, Webster K, Blendowski C, Kaplan E. Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. J Pain Symptom Manage 1997;13:63-74. http://dx.doi.org/10.1016/S0885-3924(96)00274-6.
- Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy--Spiritual Well-being Scale (FACIT-Sp). Ann Behav Med 2002;24:49-58. http://dx.doi.org/10.1207/S15324796ABM2401_06.
- Basen-Engquist K, Bodurka-Bevers D, Fitzgerald MA, Webster K, Cella D, Hu S, et al. Reliability and validity of the functional assessment of cancer therapy-ovarian. J Clin Oncol 2001;19:1809-17.
- Brady MJ, Cella DF, Mo F, Bonomi AE, Tulsky DS, Lloyd SR, et al. Reliability and validity of the Functional Assessment of Cancer Therapy-Breast quality-of-life instrument. J Clin Oncol 1997;15:974-86.
- Walker LS, Greene JW. The functional disability inventory: measuring a neglected dimension of child health status. J Pediatr Psychol 1991;16:39-58. http://dx.doi.org/10.1093/jpepsy/16.1.39.
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 1983;17:37-49. http://dx.doi.org/10.1016/0022-3956(82)90033-4.
- Goldberg DP, Gater R, Satorius N, Ustun TB, Piccinelli M, Gureje O, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 1997;27:191-7. http://dx.doi.org/10.1017/S0033291796004242.
- Goldberg DP, Oldhinkel T, Ormel J. Why GHQ threshold varies from one place to another. Psychol Med 1998;28:915-21. http://dx.doi.org/10.1017/S0033291798006874.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. http://dx.doi.org/10.1111/j.1600-0447.1983.tb09716.x.
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry 1960;23:56-62. http://dx.doi.org/10.1136/jnnp.23.1.56.
- Scheier MF, Carver CS. Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychol 1985;4:219-47. http://dx.doi.org/10.1037/0278-6133.4.3.219.
- Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther 1997;11:395-402. http://dx.doi.org/10.1046/j.1365-2036.1997.142318000.x.
- Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med 1979;41:209-18. http://dx.doi.org/10.1097/00006842-197905000-00004.
- Weiss DS, Marmar CR, Wilson JP, Keane TM. Assessing Psychological Trauma and PTSD. New York, NY: Guilford Press; 1997.
- Birchwood M, Smith J, Drury V, Healy J, Macmillan F, Slade M. A self-report Insight Scale for psychosis: reliability, validity and sensitivity to change. Acta Psychiatr Scand 1994;89:62-7. http://dx.doi.org/10.1111/j.1600-0447.1994.tb01487.x.
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, et al. The Longitudinal Interval Follow-up Evaluation. A comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry 1987;44:540-8. http://dx.doi.org/10.1001/archpsyc.1987.01800180050009.
- Valenti L, Lim L, Heller RF, Knapp J. An improved questionnaire for assessing quality of life after acute myocardial infarction. Qual Life Res 1996;5:151-61. http://dx.doi.org/10.1007/BF00435980.
- Dixon T, Lim LL, Oldridge NB. The MacNew heart disease health-related quality of life instrument: reference data for users. Qual Life Res 2002;11:173-83. http://dx.doi.org/10.1023/A:1015005109731.
- Marks GB, Dunn SM, Woolcock AJ. An evaluation of an asthma quality of life questionnaire as a measure of change in adults with asthma. J Clin Epidemiol 1993;46:1103-11. http://dx.doi.org/10.1016/0895-4356(93)90109-E.
- Juniper EF, Guyatt GH, Epstein RS, Ferrie PJ, Jaeschke R, Hiller TK. Evaluation of impairment of health related quality of life in asthma: development of a questionnaire for use in clinical trials. Thorax 1992;47:76-83. http://dx.doi.org/10.1136/thx.47.2.76.
- Melzack R. The short-form McGill Pain Questionnaire. Pain 1987;30:191-7. http://dx.doi.org/10.1016/0304-3959(87)91074-8.
- Cleeland CS, Mendoza TR, Wang XS, Chou C, Harle MT, Morrissey M, et al. Assessing symptom distress in cancer patients: the M.D. Anderson Symptom Inventory. Cancer 2000;89:1634-46. http://dx.doi.org/10.1002/1097-0142(20001001)89:7<1634::AID-CNCR29>3.0.CO;2-V.
- Yun YH, Mendoza TR, Kang IO, You CH, Roh JW, Lee CG, et al. Validation study of the Korean version of the M. D. Anderson Symptom Inventory. J Pain Symptom Manage 2006;31:345-52. http://dx.doi.org/10.1016/j.jpainsymman.2005.07.013.
- Wu AW, Revicki DA, Jacobson D, Malitz FE. Evidence for reliability, validity and usefulness of the Medical Outcomes Study HIV Health Survey (MOS-HIV). Qual Life Res 1997;6:481-93. http://dx.doi.org/10.1023/A:1018451930750.
- Kerns RD, Turk DC, Rudy TE. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI). Pain 1985;23:345-56. http://dx.doi.org/10.1016/0304-3959(85)90004-1.
- Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. J Personal Assess 1988;52:30-41. http://dx.doi.org/10.1207/s15327752jpa5201_2.
- National Medical Care Utilization and expenditure Survey. Washington, DC: National Center for Health Statistics; 1985.
- Lambert MJ, Burlingame GM, Umphress V, Hansen NB, Vermeersch DA, Clouse GC, et al. The reliability and validity of the Outcome Questionnaire. Clin Psychol Psychother 1996;3:249-58. http://dx.doi.org/10.1002/(SICI)1099-0879(199612)3:4<249::AID-CPP106>3.0.CO;2-S.
- Polonsky WH, Anderson BJ, Lohrer PA, Welch G, Jacobson AM, Aponte JE, et al. Assessment of diabetes-related distress. Diabetes Care 1995;18:754-60. http://dx.doi.org/10.2337/diacare.18.6.754.
- McDaniel LK, Anderson KO, Bradley LA, Young LD, Turner RA, Agudelo CA, et al. Development of an observation method for assessing overt pain behaviour in rheumatoid arthritis patients. Pain 1986;24:165-84.
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol 1988;54:1063-70. http://dx.doi.org/10.1037/0022-3514.54.6.1063.
- Watson D, Clark LA. PANAS-X: Manual for the Positive and Negative Affect Schedule-Expanded Form. n.d. http://ir.uiowa.edu/cgi/viewcontent.cgi?article=1011&context=psychology_pubs (accessed 15 March 2016).
- Laurent J, Catanzaro SJ, Joiner TE, Rudolph KD, Potter KI, Lambert S, et al. A measure of positive and negative affect for children: scale development and preliminary validation. Psychol Assess 1999;11:326-38. http://dx.doi.org/10.1037/1040-3590.11.3.326.
- Watson D, Clark LA. The PANAS-X: Manual for the positive and negative affect schedule-Expanded Form. Iowa City, IA: University of Iowa; 1994.
- Feldman SR, Fleischer AB, Reboussin DM, Rapp SR, Exum ML, Clark AR, et al. The self-administered psoriasis area and severity index is valid and reliable. J Invest Dermatol 1996;106:183-6. http://dx.doi.org/10.1111/1523-1747.ep12329912.
- Foa EB, Molnar C, Cashman L. Change in rape narratives during exposure therapy for posttraumatic stress disorder. J Trauma Stress 1995;8:675-90. http://dx.doi.org/10.1002/jts.2490080409.
- Spitzer RL, Williams JB, Kroenke K, Linzer M, deGruy FV, Hahn SR, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA 1994;272:1749-56. http://dx.doi.org/10.1001/jama.1994.03520220043029.
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 1999;282:1737-44. http://dx.doi.org/10.1001/jama.282.18.1737.
- McNair DM, Lorr M, Droppleman LF. Profile of Mood States (POMS) Manual. San Diego, CA: Education and Industrial Testing Service; 1971.
- Zevon MA, Auke T. The structure of mood change: An idiographic/nomothetic analysis. J Pers Soc Psychol 1982;43:111-22. http://dx.doi.org/10.1037/0022-3514.43.1.111.
- DiLorenzo TM, Williamson HA, Haber JD, Mitchell GE. Primary Care/Behavioral Health Integration Handbook. Tiburon, CA: CentraLink Publications; 1997.
- Shacham S. A shortened version of the Profile of Mood States. J Pers Assess 1983;47:305-6. http://dx.doi.org/10.1207/s15327752jpa4703_14.
- Little M, Murphy JM, Jellinek MS, Bishop SJ, Arnett HL. Screening 4- and 5-year-old children for psychosocial dysfunction: a preliminary study with the Pediatric Symptom Checklist. J Dev Behav Pediatr 1994;15:191-7. http://dx.doi.org/10.1097/00004703-199406000-00007.
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193-21. http://dx.doi.org/10.1016/0165-1781(89)90047-4.
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. J Traum Stress 1993;6:459-73. http://dx.doi.org/10.1002/jts.2490060405.
- Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: measuring the positive legacy of trauma. J Trauma Stress 1996;9:455-71. http://dx.doi.org/10.1002/jts.2490090305.
- Mintz LB, O’Halloran SM, Mulholland AM, Schneider PA. Questionnaire for Eating Disorder Diagnoses: Reliability and validity of operationalizing DSM-IV criteria into a self-report format. J Couns Psychol 1997;44:63-79. http://dx.doi.org/10.1037/0022-0167.44.1.63.
- Burckhardt CS, Woods SL, Schultz AA, Ziebarth DM. Quality of life of adults with chronic illness: A psychometric study. Res Nurs Health 1989;12:347-54. http://dx.doi.org/10.1002/nur.4770120604.
- Reynolds CR, Richmond BO. What I think and feel: a revised measure of children’s manifest anxiety. J Abnorm Child Psychol 1978;6:271-80. http://dx.doi.org/10.1007/BF00919131.
- Drayton M, Birchwood M, Trower P. Early attachment experience and recovery from psychosis. Br J Clin Psychol 1998;37:269-84. http://dx.doi.org/10.1111/j.2044-8260.1998.tb01385.x.
- McGlashan TH, Levy ST, Carpenter WT. Integration and sealing over. Clinically distinct recovery styles from schizophrenia. Arch Gen Psychiatry 1975;32:1269-72. http://dx.doi.org/10.1001/archpsyc.1975.01760280067006.
- McIntosh WD, Harlow TF, Martin LL. Linkers and nonlinkers: goal beliefs as a moderator of the effects of everyday hassles on rumination, depression, and physical complaints. J Appl Soc Psychol 1995;25:1231-44. http://dx.doi.org/10.1111/j.1559-1816.1995.tb02616.x.
- Bradley MM, Lang PJ. Measuring emotion: the Self-Assessment Manikin and the Semantic Differential. J Behav Ther Exp Psychiatry 1994;25:49-5. http://dx.doi.org/10.1016/0005-7916(94)90063-9.
- Sampogna F, Sera F, Mazzotti E, Pasquini P, Picardi A, Abeni D, et al. Performance of the self-administered psoriasis area and severity index in evaluating clinical and sociodemographic subgroups of patients with psoriasis. Arch Dermatol 2003;139:353-8. http://dx.doi.org/10.1001/archderm.139.3.353.
- Lepore SJ, Ituarte PHG. Optimism about cancer enhances mood by reducing negative social interactions. Cancer Research, Therapy and Control 1999;8:165-74.
- Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care 2000;23:943-50. http://dx.doi.org/10.2337/diacare.23.7.943.
- Ware JE, Snow KK, Kosinski M, Gandek B. SF-36® Health Survey: Manual and Interpretation Guide. Boston, MA: The Health Institute; 1993.
- Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care 1992;30:473-83. http://dx.doi.org/10.1097/00005650-199206000-00002.
- Ware JE. SF-36 health survey update. Spine 2000;25:3130-9. http://dx.doi.org/10.1097/00007632-200012150-00008.
- de Bruin AF, Buys M, de Witte LP, Diederiks JP. The sickness impact profile: SIP68, a short generic version. First evaluation of the reliability and reproducibility. J Clin Epidemiol 1994;47:863-71. http://dx.doi.org/10.1016/0895-4356(94)90189-9.
- Chren MM, Lasek RJ, Flocke SA, Zyzanski SJ. Improved discriminative and evaluative capability of a refined version of Skindex, a quality-of-life instrument for patients with skin diseases. Arch Dermatol 1997;133:1433-40. http://dx.doi.org/10.1001/archderm.1997.03890470111018.
- Abeni D, Picardi A, Pasquini P, Melchi CE, Chren MM, Evans GC, et al. Further evidence of the validity and reliability of the Skindex-29: an Italian study on 2242 dermatological outpatients. Dermatology 2002;204:43-9.
- Antonovsky A. The structure and properties of the sense of coherence scale. Soc Sci Med 1993;36:725-33. http://dx.doi.org/10.1016/0277-9536(93)90033-Z.
- Lepore SJ, Silver RC, Wortman CB, Wayment HA. Social constraints, intrusive thoughts, and depressive symptoms among bereaved mothers. J Pers Soc Psychol 1996;70:271-82. http://dx.doi.org/10.1037/0022-3514.70.2.271.
- Jensen MP, Karoly P, Huger R. The development and preliminary validation of an instrument to assess patients’ attitudes toward pain. J Psychosom Res 1987;31:393-400. http://dx.doi.org/10.1016/0022-3999(87)90060-2.
- DeGood DE, Tait RC, Turk DC, Melzack R. Handbook of Pain Assessment. New York, NY: Guilford Press; 2001.
- Andersen BL, Tewfik HH. Psychological reactions to radiation therapy: reconsideration of the adaptive aspects of anxiety. J Pers Soc Psychol 1985;48:1024-32. http://dx.doi.org/10.1037/0022-3514.48.4.1024.
- Ganz PA, Coscarelli A, Dimsdale JE, Baum A. Quality of Life in Behavioral Medicine Research. Hillsdale, NJ: Lawrence Erlbaum Associates; 1995.
- Whelan TJ, Mohide EA, Willan AR, Arnold A, Tew M, Sellick S, et al. The supportive care needs of newly diagnosed cancer patients attending a regional cancer center. Cancer 1997;80:1518-24. http://dx.doi.org/10.1002/(SICI)1097-0142(19971015)80:8<1518::AID-CNCR21>3.0.CO;2-7.
- Vinokur AD, van Ryn M. Social support and undermining in close relationships: their independent effects on the mental health of unemployed persons. J Pers Soc Psychol 1993;65:350-9. http://dx.doi.org/10.1037/0022-3514.65.2.350.
- Kubany ES, Haynes SN, Leisen MB, Owens JA, Kaplan AS, Watson SB, et al. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: the Traumatic Life Events Questionnaire. Psychol Assess 2000;12:210-24. http://dx.doi.org/10.1037/1040-3590.12.2.210.
- Wyatt GE, Chin D. HIV and ethnic minority women, families, and communities: an overview. Cult Divers Ethnic Minority Psychol 1999;53:179-82. http://dx.doi.org/10.1037/h0092586.
- Ware JE, Hays RD. Methods for measuring patient satisfaction with specific medical encounters. Med Care 1988;26:393-402. http://dx.doi.org/10.1097/00005650-198804000-00008.
- Kerns RD, Turk DC, Rudy TE. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI). Pain 1985;23:345-56. http://dx.doi.org/10.1016/0304-3959(85)90004-1.
Appendix 1 Therapeutic writing experts’ perspectives
Carol Ross’s perspective
| Symptoms/diagnosis/detail | Mindful writing | Free writing | Reflective writing | Writing inspired by metaphors/symbols | Journaling | Unsent letters | Positive memories | Traumatic memories | Fictional characters | Creative writing | Collaborative poems | Responding to published poetry | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Descriptive | Expressive | Celebrating positives | Expressive writing | |||||||||||
| Depression: mild/moderate | *** | *** | *** | *** | *** | *** | ||||||||
| Depression: severe | *** | *** | *** | *** | *** | |||||||||
| Entirely negative thinking | *** | *** | *** | *** | *** | |||||||||
| Anxiety/agitation | *** | *** | *** | *** | ||||||||||
| Heightened psychological arousal | *** | *** | *** | |||||||||||
| Difficulty with self expression | *** | *** | *** | *** | *** | *** | *** | |||||||
| Manic episode | *** | *** | *** | |||||||||||
| Psychotic episode | *** | *** | *** | |||||||||||
| Schizophrenia | *** | *** | *** | |||||||||||
| Obsessive compulsive disorder | *** | *** | *** | |||||||||||
| Personality disorder | *** | *** | *** | *** | *** | *** | *** | *** | ||||||
| Detox | *** | *** | *** | *** | *** | *** | *** | |||||||
| Grief | *** | *** | *** | *** | *** | |||||||||
Victoria Field’s perspective
A practitioner’s perspective: some snapshots
Types of writing
I concur with the list that Carol Ross provided – these are tried-and-tested writing suggestions that have therapeutic potential.
Rather than techniques being necessarily applicable to certain diagnoses, my own model is more to do with the level of wellness of the person or the group. The techniques are adapted according to the following continuums:
1. Containing factors
These keep the process safe and accessible.
-
Length of time For someone in distress, writing for a minute might be sufficient.
-
Length of writing Sometimes, for someone withdrawn, one word might be the starting point.
-
Amount of direction/structure Structured suggestions can help with inchoate material.
2. Complexity
Tolerance of complexity is a marker of mental health and I would use TW techniques that encourage nuanced responses with a more well population or with a group that has been meeting for a while. This determines the kinds of writing suggestions I make, such as:
-
metaphor – narrative
-
direct – elaborated
-
first-person – second-person – third-person writing
-
single perspective – multiple perspective.
3. Focus
-
Self – others – wider world These dimensions are all important to understanding experience – as a practitioner, I make judgements about when it is appropriate to encourage writing in a different direction.
-
Pain/distress – positive aspects of life – as above There is evidence that it is important to acknowledge a sense of victimhood before beginning to write a new story.
-
Past – present – future Again all are important but for example, the very elderly often appreciate writing that stays in the moment, especially nature writing.
Settings
My experience with TW includes the following health-care settings in which patients had LTCs, and we worked in groups unless otherwise stated:
-
stroke rehabilitation unit – some group work and one-to-one at the bedside
-
Arts for Older People – in care homes
-
Age Concern day centre
-
day treatment centre for people with severe and enduring mental illness
-
primary care – a health centre attached to a GP practice
-
one-to-one with a dementia patient in her home (referred by an occupational therapist) and, subsequently, on a psychogeriatric inpatient ward.
I have also worked in the following community settings in which participants have often had mental health issues, some severe and enduring, and other LTCs, but these were not the primary reason for attending. For example, the library promotional literature said service users welcome but people were not required to self-identify.
-
St Petroc’s Centre, offering services for street homeless people
-
open-access sessions in public libraries
-
Adult education Writing for Self-Discovery courses
-
Truro Cathedral (was writer-in-residence in 2006).
I also supervised a number of pilot projects in TW by other practitioners, which included the following client groups as part of an Arts Council England-funded Arts in Health project:
-
prisoners at risk of self-harm
-
children in hospital long term
-
long-term unemployed
-
patients at a GP surgery with mild depression
-
women at a clinic for pelvic pain.
The model for my intervention is a psychosocial rather than medical one. However, the outcomes can be measured in medical terms.
There follows a couple of examples that might exemplify some of approaches, justifications and outcomes:
-
On the stroke unit, I was part of a multi-art form team offering afternoon sessions for a year as a way of preventing boredom and depression, which, in turn, had an impact on motivation to get well, which, in turn, impacts on length of stay. Elevated mood was seen as a way of making it more likely patients would do the physiotherapy prescribed, for example.
The different art forms worked best with different patients but one characteristic of the writing was that it enabled catharsis and safe expression of emotions, such as despair and hopelessness, which were not permitted with medical staff or family: permission to be oneself is a characteristic of TW.
The average length of time on the unit was 96 days; to justify the intervention financially, this would need to reduce by 4.4 days per patient. The full report is available from: www.artsforhealthcornwall.org.uk/wp-content/uploads/2010/10/Arts-for-Stroke-Rehabilitation-Evaluation.pdf
-
On the Arts for Older People project in care homes (also an Arts for Health Cornwall and Isles of Scilly initiative), the improvements were mostly social and psychological – I feel all twinkly (care home resident) – but there are benefits from just moving residents into a group setting that indirectly led to more interaction and motivation to be more mobile, which, in turn, might help with constipation and the other common problems of being sedentary (summarised as poetry makes you poo).
The work can also change perceptions and lead to better care. One participant, relatively young, a retired headmaster, who had had a stroke and was severely depressed, was wheeled in to weekly care home sessions and never spoke nor made eye contact until the sixth session when he contributed one word and then smiled; subsequently, speech therapy was accessed and he made considerable progress.
Victoria Field, 9 May 2013
Appendix 2 Realist synthesis: expert practitioners’ feedback
| INTERVENTION PROCESS/ASPECTS OF THE INTERVENTION: What do you do and why? | RECRUITMENT/SUITABILITY: Who is it suitable for and why? | OUTCOMES IMPACT: What do you hope to achieve and why? |
|---|---|---|
| Note on duration of writing: In my sessions in MH units, the writing done in the exercises listed below lasts from 2-minute bursts to 15 minutes. Most often writing is 5–10 minutes in duration and 25–30 minutes in total for a 1-hour session (very brief writing is the subject of this research article: Burton and King152) | ||
| Writing about positive experiences, or positive aspects of situations Why: People with MH problems can become totally focused on their problems and lose interest in their normal life. I have been influenced by the research of Laura King and collaborators (e.g. Burton and King, 153,154 Mackenzie et al.155) |
Flexible enough to be used in PICU and adult and older people’s MH units. The technique is good for most MH problems, but I do not use, or else use with caution, when people are severely depressed because they can turn even positive writing around to be negative | Increased positivity and motivation Lifted mood Rediscovery of remembered interests and pleasures Focus on exceptions to their problem-saturated life Hope |
| Mindful writing about the world – notice something in the world and write to describe it in detail Why: Mindfulness is recognised to be useful in MH conditions and has been incorporated into therapies such as Dialectical Behaviour Therapy (McKay et al.,156 chapter 3) |
Very helpful in all of the MH units in which I work, and something I recommend as daily practice. I use an adapted form frequently in PICU – writing to describe large landscape photographs. Especially useful when someone is experiencing symptoms of mania, psychosis, anxiety, agitation, stress | Calming Increased mental focus Increased interest in the real world Grounding External perspective Respite/distraction |
| Mindful expressive writing – how I feel right now In a ward situation I would say scan body from toes to top of head writing about how each part of the body feel, and then move on to write about thoughts and feelings right now Why: Mindfulness is recognised to be useful in MH conditions and has been incorporated into therapies such as Dialectical Behaviour Therapy (McKay et al.,156 chapter 3). See also Poon and Danoff-Burg157 |
Not something I use in PICU or, so far, with older people but I do use it in the general adult MH unit with people who are well enough to manage to do it. When these individuals are sufficiently recovered, I recommend this, along with mindful writing about the world, as daily practice to people with MH issues. Many people who find meditation difficult are able to do mindful writing instead | Calming Shift of focus from past/present worries to the here and now Insight Clarification of thoughts and feelings With regular practice can look back at how things have changed |
| Creating a fictional character and writing about them. I start with a variety of prompts such as photographs of (unknown) people, pieces of fabric, a character questionnaire Why: To raise awareness of others’ lives and shift focus away from self. No reference – I developed this one based on my own observations of MH inpatients |
I find this useful in all of the MH units in which I work. Especially useful where someone is completely wrapped up in themselves and their own problems. I have found this useful in individuals with MH problems from severe depression to personality disorder to paranoid schizophrenia | Perspective shift away from self and own problems External focus Could help with emotional connections and relationships Respite/distraction |
| Neutral writing exercises that I expect will elicit memories in many individuals, e.g. older people writing about objects they would have used in the past Why: This is a low pressure way of eliciting memories – rather than show an object and asking people to write about a memory evoked by the object, I ask individuals to write about the object and what it makes them think of |
Suitable in all MH units as above but particularly helpful with older people and people with Alzheimer’s disease if they are able to do it | Stimulation of memory Enjoyment Comfort Social benefits – past experiences the individual remembers can then form topics of conversation with family/visitors/other patients and so help with emotional connections and relationships |
| Second- and third-person writing and unsent letters This type of writing is very varied, e.g. someone could write a letter from a future version of him/her, who is well, to a person who helped and inspired them in their recovery, or someone could write a third-person account of a conversation from the other person’s point of view Why: To change perspective in some way, e.g. externalising a problem. Example reference: East et al.158 |
Very useful in MH settings. I do not use often in PICU because the inpatients tend to be too unwell to do this sort of writing. I have found this type of writing helpful with people with different problems from personality disorder to bereavement. Some voice-hearing patients find it helpful to write letters to their voice, for example | Insight Externalisation of problem Closure Catharsis Acceptance Empathy Hope Perspective shift Could help with emotional connections and relationships |
| Visualisation writing, e.g. imagining oneself into a landscape or building or on a journey I prompt the writing with a photograph or a short piece of writing about their favourite way of travelling, or (occasionally) with a guided visualisation Why: Stimulating the imagination, a positive flight of fancy, a visit to a world outside the ward environment |
I often use variations on this idea with working age MH inpatients, and have had some success even with someone who was severely depressed | Stimulating interest in the world Motivation Respite/distraction |
| Writing in response to a fairly random prompt such as single words, symbols, shapes, colours Often the writing is freewriting (writing fast without stopping to think or correct anything) Why: Very flexible, minimal structure, freeing up the writing and allowing the individual to write whatever comes into their mind |
I use this in the adult MH unit mainly, but also with some patients in PICU. This type of writing, e.g. using symbols and metaphor, can be especially useful with people who have schizophrenia. However, I would not use where individuals are clearly manic, psychotic or voice hearing at the time of the session | It’s difficult to predict what the effects will be with this sort of exercise but it can bring out unexpected/subconscious thoughts and can spark an interest in doing more writing – which can be helpful Could help with freeing up mental blocks |
| Poetry therapy – writing in response to selected published poems Why: They can reflect common experiences, clear or metaphorical. Also thought provoking and stimulates group discussion |
Suitable for anyone in a MH unit who is capable of doing the exercise | Recognition that others have similar problems Stimulating interest in the world apart from self and problems Self-expression Insight Hope Positivity |
| Re-writing a memory – not to change or block it but to express the memory with a shift of perspective, e.g. re-writing a memory to show how the individuals strengths helped them get through it Why: To shift perspective about a traumatic or difficult memory so that it can become less dominant |
I believe this could be very useful in conditions such as PTSD and for survivors of abuse (as many MH patients are). This kind of idea, although not written, is at the heart of narrative therapy. I have suggested this kind of writing to one or two individuals as something they might try for themselves, but have not as yet used it in a group setting | Externalising and reducing the emphasis on problems Seeing the past from a more helpful perspective Seeing the future in a more hopeful light |
| Structured journal techniques, e.g. write one word every hour, for a whole day, which sums up how you feel right then, or write a daily journal containing only positives | Suitable for anyone, I would think, as long as the techniques are tailored for the individual. Unstructured journals can also be very helpful too – pouring out one’s thoughts and feelings to an impartial observer. I would worry about people, who are of completely negative thinking, writing an unstructured journal, however, because writing down negative thoughts repeatedly is likely to reinforce them | Depends on technique used: self-expression, positive thinking, motivation, insight, catharsis, clarification of thoughts and feelings, coming to terms with things |
| Creative writing in a group, e.g. collaborative poems, each writing the story depicted by a picture Why: To give participants a thought-provoking, surprising, enjoyable group experience |
This is a bit different. This kind of exercise works best with a group in which all participants are well enough, and thinking clearly enough, to manage it. Of all the exercises, this one is as much about group members sharing and relating to each other as about what is actually written in the exercise | Lifted mood Increased self-esteem and confidence Group bonding External focus Could help with emotional connections and relationships Respite/distraction |
| Benefit finding about an illness or problem, for example what are you able to do, or do more of, since having the illness that you couldn’t do previously Why: Change perception of illness to help with acceptance. Example references: King and Milner;159 Danoff-Burg and Mosher160 |
Not something I use with MH inpatients but I can see it could be helpful with some long-term physical conditions | Increased positivity and motivation Improved acceptance of illness Decreased focus on illness Insight |
| Head chatter – writing everything that comes into your head for a timed period, say 5 minutes Why: To clear the mind, for example before going to bed or before doing a writing session |
I believe this to be a good daily journal practice for many people, e.g. doing this late evening every day could help with sleep. However, I never use this in MH units because it is too unstructured, which means it is difficult for most inpatients to do and could well give opportunity for a voice or negative thoughts to dominate the writing | Clearing the mind of a confused jumble of thoughts Calming Increased mental focus Can bring out unexpected/subconscious thoughts and help with freeing up mental blocks |
| Expressive writing about illness/problem/trauma – write your deepest thoughts about . . . along the lines of Pennebaker and Beal1 Why: Expressing one’s deepest thoughts and feelings in writing can be easier than speaking them aloud |
Not something I use in inpatient MH units but I can see that it could be helpful, e.g. in long-term physical conditions and with undisclosed trauma. In inpatient MH units, I believe this kind of writing should be either at the individual’s instigation or that of his/her clinical psychologist/psychiatrist and under that clinician’s guidance. Some individuals write in this way during sessions or in between group sessions, but not at my direction. Some individuals ask me to pass this type of writing to their named nurse, or to shred it, which I do | Insight Catharsis Getting to the point of being able to talk to therapist Improved self-expression Clarification of thoughts and feelings Coming to terms with illness/problem Acceptance |
| RECRUITMENT/SUITABILITY: Who is it suitable for and why? | INTERVENTION PROCESS/ASPECTS OF THE INTERVENTION: What do you do and why? | OUTCOMES IMPACT: What do you hope to achieve and why? |
|---|---|---|
| General population with mild anxiety and/or depression: Can be due to ongoing mental health problems, life circumstances, such as bereavement, divorce, or caring responsibilities, or LTCs or adjustment to disability or just being at that difficult stage between birth and death | Reflective writing – a whole variety of writing prompts (including lists, free writing, acrostics, dialogues, mind maps, responding to images, music, environment, realia, fictionalising) – this writing may be kept private or shared
|
Connection with self and inner processes
|
Appendix 3 Original systematic review searches
| Database | Time span of the search (mapping search) | Provider (platform) |
|---|---|---|
| AMED | From 1985 to March 2013 | Ovid |
| ASSIA | 1987–week 12 2013 | ProQuest |
| CAB Abstracts | From 1973 to week 11 2013 | Ovid |
| The Campbell Collaboration Library of Systematic Reviews | From 2005 to Issue #4, Volume 9 2013 | The Campbell Library |
| CENTRAL | From 1992 to Issue 1 of 12, January 2013 | The Cochrane Library |
| CDSR | From 1992 to Issue 2 of 12, February 2013 | The Cochrane Library |
| CINAHL | 1981–week 12 March 2013 | EBSCOhost |
| DARE | From 1994 to Issue 1 of 4, January 2013 | The Cochrane Library |
| EMBASE | From 1974 to 11 March 2013 | Ovid |
| ERIC | 1966–18 March 2013 | ProQuest |
| HTA Database | Issue 1 of 4, January 2013 | The Cochrane Library |
| Linguistic and Language Behaviour Abstracts (LLBA) | 1973–18 March 2013 | ProQuest |
| MEDLINE | From 1946 to 11 March 2013 | Ovid |
| NHS EED | From 1995 to February 2013 | The Cochrane Library |
| PEDro | 1929–4 March 2013 | Centre for Evidence-Based Physiotherapy/University of Sydney |
| Periodicals Index Online (PIO) | 1665–95 | ProQuest |
| PILOTS | 1871–18 March 2013 | ProQuest |
| PsycINFO | From 1806 to March week 2 2013 | Ovid |
| SSCI | 1970–15 March 2013 | Web of Knowledge |
| SCI | 1970–15 March 2013 | Web of Knowledge |
| Zetoc | 1993–18 March 2013 | Mimas |
Search strategy
| # | Search term |
|---|---|
| 1 | chronic*.mp |
| 2 | ((persistent or (long* adj term) or ongoing or degenerative) adj3 (disease* or disab* or ill* or condition* or (health adj condition*) or (medical adj condition*) or impairment)).tw. |
| 3 | LONG TERM CARE/ |
| 4 | (long* adj term adj care).tw. |
| 5 | exp CARDIOVASCULAR DISEASE/ |
| 6 | ((heart adj disease*) or (heart adj failure) or (myocardial adj ischemia) or (angina adj pectoris) or (coronary adj disease*) or (coronary adj artery adj disease*) or (myocardial adj infarction) or hypertension or (high adj blood adj pressure)).tw. |
| 7 | exp LUNG DISEASES OBSTRUCTIVE/ |
| 8 | ((obstructive adj lung adj disease*) or (obstructive adj pulmonary adj disease*) or copd or asthma or bronchitis).tw. |
| 9 | exp EMPHYSEMA/ |
| 10 | exp PULMONARY EMPHYSEMA/ |
| 11 | emphysema.tw. |
| 12 | exp CEREBROVASCULAR DISORDERS/ |
| 13 | ((cerebrovascular adj disease*) or (cerebrovascular adj disorder*) or (brain adj ischemia) or (cerebral adj infarction) or (carotid adj artery adj disease*) or stroke or epilep*).tw. |
| 14 | exp NEURODEGENERATIVE DISEASES/ |
| 15 | (neurodegenerative or (Huntington* adj disease) or (Parkinson* adj disease) or (amyotrophic adj lateral adj sclerosis) or (motor adj neuron* adj disease)).tw. |
| 16 | exp MULTIPLE SCLEROSIS/ |
| 17 | (multiple adj sclerosis).tw. |
| 18 | exp INFLAMMATORY BOWEL DISEASES/ |
| 19 | IRRITABLE BOWEL SYNDROME/ |
| 20 | ((inflammatory adj bowel) or (irritable adj bowel)).tw. |
| 21 | Kidney disease/ |
| 22 | ((renal adj failure*) or (renal adj insufficienc*) or (kidney adj failure*) or (kidney adj insuffcienc*)).tw. |
| 23 | DIABETES MELLITUS/ |
| 24 | (diabetes or diabetic*).tw. |
| 25 | exp ARTHRITIS/ |
| 26 | exp RHEUMATIC DISEASE/ |
| 27 | (arthritis or osteoarthritis or rheumati* or fibromyalgia).tw. |
| 28 | exp low back pain/ |
| 29 | exp backache/ |
| 30 | NECK PAIN/ |
| 31 | ((back adj pain) or (neck adj pain)).tw. |
| 32 | exp OSTEOPOROSIS/ |
| 33 | osteoporosis.tw. |
| 34 | exp THYROID DISEASE/ |
| 35 | exp NEOPLASMS/ |
| 36 | (cancer* or oncolog* or neoplasm* or carcinom* or tumo?r* or malignan*).tw. |
| 37 | exp HIV INFECTIONS/ |
| 38 | ((hiv adj infect*) or (hiv adj disease*)).tw. |
| 39 | ENDOMETRIOSIS/ |
| 40 | endometriosis.tw. |
| 41 | exp MENTAL DISORDERS/ |
| 42 | DEPRESSION/ |
| 43 | ((mental* adj ill*) or (mental adj disorder*) or (mental adj disease*) or (mental adj distress*) or (mental adj disab*) or (mental adj problem*) or (mental adj health*) or (mental adj patient*) or (mental adj treatment) or (psychiatr* adj ill*) or (psychiatr* adj disorder*) or (psychiatr* adj disease*) or (psychiatr* adj distress*) or (psychiatr* adj disab*) or (psychiatr* adj problem*) or (psychiatr* adj health*) or (psychiatr* adj patient*) or (psychiatr* adj treatment) or (psychological* adj ill*) or (psychological*ADJ and disorder*) or (psychological* adj disease*) or (psychological* adj distress*) or (psychological* adj disab*) or (psychological* adj problem*) or (psychological* adj health*) or (psychological* adj patient*) or (psychological* adj treatment)).tw. |
| 44 | ((personality adj disorder*) or (mood adj disorder*) or (dysthymic adj disorder*) or (cognit* adj disorder*) or (anxiety adj disorder*) or (stress adj disorder*) or (eating adj disorder*) or (adjustment adj disorder*) or (reactive adj disorder*) or (somatoform adj disorder*) or (conversion adj disorder*) or (behavio* adj disorder*) or (percept* adj disorder*) or (psycho* adj disorder*) or (impulse adj control adj disorder*) or (development* adj disorder*)).tw. |
| 45 | (psychos#s or psychotic* or paranoi* or schizo* or neuros#s or neurotic* or delusion* or depression or depressive or bipolar or mania or manic or obsessi* or compulsi* or panic or phobic or phobia or anorexia or bulimia or neurastheni* or dissociative or affective or borderline or narcissis* or suicid* or (self adj injur*) or (self adj harm) or dementia or Alzheimer*).tw. |
| 46 | or/1-45 |
| 47 | ((writ* adj therap*) or (therapeutic* adj writ*) or (writ* adj cure*) or (writ* adj heal*) or (self adj management adj writ*) or (self adj help adj writ*) or (self adj conceal* adj writ*) or (self adj disclosure adj writ*) or (creative adj writ*) or (expressi* adj writ*) or (emoti* adj writ*) or (EMO adj writ*) or (sensitiv* adj writ*) or (sensor* adj writ*) or (reactive adj writ*) or (reflective adj writ*) or (descriptive adj writ*) or (biography* adj writ*) or (workshop adj writ*) or (epistolar* adj writ*) or (fiction* adj writ*) or (paradigm adj writ*) or (group adj writ*) or (letter* adj writ*) or (Pennebaker adj writ*) or (reminiscence adj review*) or (story adj writ*) or (stories adj writ*) or blog* or forum* or (memoir* adj writ*) or (journal* adj writ*) or (narrative* adj writ*) or (hand adj writ*) or (poe* adj writ*) or (health adj status adj writ*) or “program* writ*”).tw. |
| 48 | ((emoti* adj disclosure adj tip*) or (emoti* adj disclosure adj key*) or (emotional adj disclosure adj writ*) or (emotio* adj disclosure) or catharsis).tw. |
| 49 | ((express* or creativ* or emoti* or sensitiv* or reflect* or therap* or disclos* or conceal* or manag* or pennebaker or cathar* or “writing paradigm”) adj2 (writ* or “hand writ*” or blog or epistol* or letter* or story or stories or memoir* or narrat* or diary or diaries or poem or poet* or reminisc* or “life review” or “life writing” or journaling or “Journal Writing” or (“health status” adj2 writ*) or “program* writ*”)).tw. |
| 50 | 46 and 49 |
| 51 | 47 and 48 |
| 52 | Writing/ |
| 53 | 46 and 52 |
| 54 | 50 or 51 or 52 |
| # | Search term |
|---|---|
| 1 | chronic*.mp. |
| 2 | ((persistent or (long* adj term) or ongoing or degenerative) adj3 (disease* or disab* or ill* or condition* or (health adj condition*) or (medical adj condition*) or impairment)).tw. |
| 3 | LONG TERM CARE/ |
| 4 | (long* adj term adj care).tw. |
| 5 | exp CARDIOVASCULAR DISEASE/ |
| 6 | ((heart adj disease*) or (heart adj failure) or (myocardial adj ischemia) or (angina adj pectoris) or (coronary adj disease*) or (coronary adj artery adj disease*) or (myocardial adj infarction) or hypertension or (high adj blood adj pressure)).tw. |
| 7 | exp LUNG DISEASES OBSTRUCTIVE/ |
| 8 | ((obstructive adj lung adj disease*) or (obstructive adj pulmonary adj disease*) or copd or asthma or bronchitis).tw. |
| 9 | exp EMPHYSEMA/ |
| 10 | exp PULMONARY EMPHYSEMA/ |
| 11 | emphysema.tw. |
| 12 | exp CEREBROVASCULAR DISORDERS/ |
| 13 | ((cerebrovascular adj disease*) or (cerebrovascular adj disorder*) or (brain adj ischemia) or (cerebral adj infarction) or (carotid adj artery adj disease*) or stroke or epilep*).tw. |
| 14 | exp NEURODEGENERATIVE DISEASES/ |
| 15 | (neurodegenerative or (Huntington* adj disease) or (Parkinson* adj disease) or (amyotrophic adj lateral adj sclerosis) or (motor adj neuron* adj disease)).tw. |
| 16 | exp MULTIPLE SCLEROSIS/ |
| 17 | (multiple adj sclerosis).tw. |
| 18 | exp INFLAMMATORY BOWEL DISEASES/ |
| 19 | IRRITABLE BOWEL SYNDROME/ |
| 20 | ((inflammatory adj bowel) or (irritable adj bowel)).tw. |
| 21 | Kidney disease/ |
| 22 | ((renal adj failure*) or (renal adj insufficienc*) or (kidney adj failure*) or (kidney adj insuffcienc*)).tw. |
| 23 | DIABETES MELLITUS/ |
| 24 | (diabetes or diabetic*).tw. |
| 25 | exp ARTHRITIS/ |
| 26 | exp RHEUMATIC DISEASE/ |
| 27 | (arthritis or osteoarthritis or rheumati* or fibromyalgia).tw. |
| 28 | exp low back pain/ |
| 29 | exp backache/ |
| 30 | NECK PAIN/ |
| 31 | ((back adj pain) or (neck adj pain)).tw. |
| 32 | exp OSTEOPOROSIS/ |
| 33 | osteoporosis.tw. |
| 34 | exp THYROID DISEASE/ |
| 35 | exp NEOPLASMS/ |
| 36 | (cancer* or oncolog* or neoplasm* or carcinom* or tumo?r* or malignan*).tw. |
| 37 | exp HIV INFECTIONS/ |
| 38 | ((hiv adj infect*) or (hiv adj disease*)).tw. |
| 39 | ENDOMETRIOSIS/ |
| 40 | endometriosis.tw. |
| 41 | exp MENTAL DISORDERS/ |
| 42 | DEPRESSION/ |
| 43 | ((mental* adj ill*) or (mental adj disorder*) or (mental adj disease*) or (mental adj distress*) or (mental adj disab*) or (mental adj problem*) or (mental adj health*) or (mental adj patient*) or (mental adj treatment) or (psychiatr* adj ill*) or (psychiatr* adj disorder*) or (psychiatr* adj disease*) or (psychiatr* adj distress*) or (psychiatr* adj disab*) or (psychiatr* adj problem*) or (psychiatr* adj health*) or (psychiatr* adj patient*) or (psychiatr* adj treatment) or (psychological* adj ill*) or (psychological*ADJ and disorder*) or (psychological* adj disease*) or (psychological* adj distress*) or (psychological* adj disab*) or (psychological* adj problem*) or (psychological* adj health*) or (psychological* adj patient*) or (psychological* adj treatment)).tw. |
| 44 | ((personality adj disorder*) or (mood adj disorder*) or (dysthymic adj disorder*) or (cognit* adj disorder*) or (anxiety adj disorder*) or (stress adj disorder*) or (eating adj disorder*) or (adjustment adj disorder*) or (reactive adj disorder*) or (somatoform adj disorder*) or (conversion adj disorder*) or (behavio* adj disorder*) or (percept* adj disorder*) or (psycho* adj disorder*) or (impulse adj control adj disorder*) or (development* adj disorder*)).tw. |
| 45 | (psychos#s or psychotic* or paranoi* or schizo* or neuros#s or neurotic* or delusion* or depression or depressive or bipolar or mania or manic or obsessi* or compulsi* or panic or phobic or phobia or anorexia or bulimia or neurastheni* or dissociative or affective or borderline or narcissis* or suicid* or (self adj injur*) or (self adj harm) or dementia or Alzheimer*).tw. |
| 46 | or/1-45 |
| 47 | ((writ* adj therap*) or (therapeutic* adj writ*) or (writ* adj cure*) or (writ* adj heal*) or (self adj management adj writ*) or (self adj help adj writ*) or (self adj conceal* adj writ*) or (self adj disclosure adj writ*) or (creative adj writ*) or (expressi* adj writ*) or (emoti* adj writ*) or (EMO adj writ*) or (sensitiv* adj writ*) or (sensor* adj writ*) or (reactive adj writ*) or (reflective adj writ*) or (descriptive adj writ*) or (biography* adj writ*) or (workshop adj writ*) or (epistolar* adj writ*) or (fiction* adj writ*) or (paradigm adj writ*) or (group adj writ*) or (letter* adj writ*) or (Pennebaker adj writ*) or (reminiscence adj review*) or (story adj writ*) or (stories adj writ*) or blog* or forum* or (memoir* adj writ*) or (journal* adj writ*) or (narrative* adj writ*) or (hand adj writ*) or (poe* adj writ*) or (health adj status adj writ*) or “program* writ*”).tw. |
| 48 | ((emoti* adj disclosure adj tip*) or (emoti* adj disclosure adj key*) or (emotional adj disclosure adj writ*) or (emotio* adj disclosure) or catharsis).tw. |
| 49 | ((express* or creativ* or emoti* or sensitiv* or reflect* or therap* or disclos* or conceal* or manag* or pennebaker or cathar* or “writing paradigm”) adj2 (writ* or “hand writ*” or blog or epistol* or letter* or story or stories or memoir* or narrat* or diary or diaries or poem or poet* or reminisc* or “life review” or “life writing” or journaling or “Journal Writing” or (“health status” adj2 writ*) or “program* writ*”)).tw. |
| 50 | 46 and 49 |
| 51 | 47 and 48 |
| 52 | Writing/ |
| 53 | 46 and 52 |
| 53 | 50 or 51 or 53 |
| # | Search term |
|---|---|
| 1 | chronic* |
| 2 | ((persistent or “long* term” or ongoing or degenerative) near/2 (disease* or disab* or ill* or condition* or “health condition*” or “medical condition*” or impairment)) |
| 3 | MeSH descriptor: [Long-Term Care] explode all trees |
| 4 | long* term care |
| 5 | MeSH descriptor: [Cardiovascular Diseases] explode all trees |
| 6 | “heart disease*” or “heart failure” or “myocardial ischemia” or “angina pectoris” or “coronary disease*” or “coronary artery disease*” or “myocardial infarction*” or hypertension or “high blood pressure” |
| 7 | MeSH descriptor: [Lung Diseases, Obstructive] explode all trees |
| 8 | “obstructive lung disease*” or “obstructive pulmonary disease*” or copd or asthma or bronchitis |
| 9 | MeSH descriptor: [Emphysema] explode all trees |
| 10 | MeSH descriptor: [Pulmonary Emphysema] explode all trees |
| 11 | emphysema |
| 12 | MeSH descriptor: [Cerebrovascular Disorders] explode all trees |
| 13 | “cerebrovascular disease*” or “cerebrovascular disorder*” or “brain ischemia” or “cerebral infarction” or stroke or epilep* |
| 14 | MeSH descriptor: [Neurodegenerative Diseases] explode all trees |
| 15 | neurodegenerative or “Huntington* disease” or “Parkinson* disease” or “amyotrophic lateral sclerosis” or “motor neuron* disease” |
| 16 | MeSH descriptor: [Multiple Sclerosis] explode all trees |
| 17 | Multiple Sclerosis |
| 18 | MeSH descriptor: [Irritable Bowel Syndrome] explode all trees |
| 19 | MeSH descriptor: [Inflammatory Bowel Diseases] explode all trees |
| 20 | inflammatory bowel or “irritable bowel” |
| 21 | MeSH descriptor: [Kidney Diseases] explode all trees |
| 22 | MeSH descriptor: [Renal Insufficiency] explode all trees |
| 23 | “renal failure*” or “renal insufficienc*” or “kidney failure*” or “kidney insufficienc*” |
| 24 | MeSH descriptor: [Diabetes Mellitus] explode all trees |
| 25 | diabetes or diabetic* |
| 26 | MeSH descriptor: [Arthritis] explode all trees |
| 27 | MeSH descriptor: [Arthritis, Rheumatoid] explode all trees |
| 28 | arthritis or osteoarthritis or rheumati* or fibromyalgia |
| 29 | MeSH descriptor: [Back Pain] explode all trees |
| 30 | MeSH descriptor: [Neck Pain] explode all trees |
| 31 | “back pain” or “neck pain” |
| 32 | MeSH descriptor: [Osteoporosis] explode all trees |
| 33 | Osteoporosis |
| 34 | MeSH descriptor: [Thyroid Diseases] explode all trees |
| 35 | MeSH descriptor: [Neoplasms] explode all trees |
| 36 | cancer* or oncolog* or neoplasm* or carcinom* or tumo?r* or malignan* |
| 37 | MeSH descriptor: [HIV] explode all trees |
| 38 | “hiv infect*” or “hiv disease*” |
| 39 | MeSH descriptor: [Endometriosis] explode all trees |
| 40 | endometriosis |
| 41 | MeSH descriptor: [Mental Disorders] explode all trees |
| 42 | MeSH descriptor: [Depression] explode all trees |
| 43 | “mental* ill*” or “mental disorder*” or “mental disease*” or “mental distress*” or “mental disab*” or “mental problem*” or “mental health*” or “mental patient*” or “mental treatment” or “psych* ill*” or “psych* disorder*” or “psych* disease*” or “psych* distress*” or “psych* disab*” or “psych* problem*” or “psych* health*” or “psych* patient*” or “psych* treatment” |
| 44 | “personality disorder*” or “mood disorder*” or “dysthymic disorder*” or “cognit* disorder*” or “anxiety disorder*” or “stress disorder*” or “eating disorder*” or “Nustment disorder*” or “reactive disorder*” or “somatoform disorder*” or “conversion disorder*” or “behavio* disorder*” or “percept* disorder*” or “psycho* disorder*” or “impulse control disorder*” or “development* disorder*” |
| 45 | psychos?s or psychotic* or paranoi* or schizo* or neuros?s or neurotic* or delusion* or depression or depressive or bipolar or mania or manic or obsessi* or compulsi* or panic or phobic or phobia or anorexia or bulimia or neurastheni* or dissociative or affective or borderline or narcissis* or suicid* or “self injur*” or “self harm” or dementia or Alzheimer* |
| 46 | #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44 or #45 |
| 47 | ((express* or creativ* or emoti* or sensitiv* or reflect* or therap* or disclos* or conceal* or manag* or pennebaker or cathar* or “writing paradigm”) near/2 (writ* or “hand writ*” or blog or epistol* or letter* or story or stories or memoir* or narrat* or diary or diaries or poem or poet* or reminisc* or “life review” or “life writing” or journaling or “Journal Writing” or (“health status” adj2 writ*) or “program* writ*”)) |
| 48 | MeSH descriptor: [Writing] this term only |
| 49 | #47 or #48 |
| 50 | #46 and #49 |
| # | Search term |
|---|---|
| 1 | chronic*.mp. |
| 2 | ((persistent or (long* adj term) or ongoing or degenerative) adj3 (disease* or disab* or ill* or condition* or (health adj condition*) or (medical adj condition*) or impairment)).tw. |
| 3 | LONG TERM CARE/ |
| 4 | (long* adj term adj care).tw. |
| 5 | exp cardiovascular disorders/ |
| 6 | ((heart adj disease*) or (heart adj failure) or (myocardial adj ischemia) or (angina adj pectoris) or (coronary adj disease*) or (coronary adj artery adj disease*) or (myocardial adj infarction) or hypertension or (high adj blood adj pressure)).tw. |
| 7 | exp lung disorders/ |
| 8 | ((obstructive adj lung adj disease*) or (obstructive adj pulmonary adj disease*) or copd or asthma or bronchitis).tw. |
| 9 | exp EMPHYSEMA/ |
| 10 | exp PULMONARY EMPHYSEMA/ |
| 11 | emphysema.tw. |
| 12 | exp CEREBROVASCULAR DISORDERS/ |
| 13 | ((cerebrovascular adj disease*) or (cerebrovascular adj disorder*) or (brain adj ischemia) or (cerebral adj infarction) or (carotid adj artery adj disease*) or stroke or epilep*).tw. |
| 14 | exp NEURODEGENERATIVE DISEASES/ |
| 15 | (neurodegenerative or (Huntington* adj disease) or (Parkinson* adj disease) or (amyotrophic adj lateral adj sclerosis) or (motor adj neuron* adj disease)).tw. |
| 16 | exp MULTIPLE SCLEROSIS/ |
| 17 | (multiple adj sclerosis).tw. |
| 18 | exp colon disorders/ |
| 19 | IRRITABLE BOWEL SYNDROME/ |
| 20 | ((inflammatory adj bowel) or (irritable adj bowel)).tw. |
| 21 | Kidney disease/ |
| 22 | ((renal adj failure*) or (renal adj insufficienc*) or (kidney adj failure*) or (kidney adj insuffcienc*)).tw. |
| 23 | DIABETES MELLITUS/ |
| 24 | (diabetes or diabetic*).tw. |
| 25 | exp ARTHRITIS/ |
| 26 | exp rheumatoid arthritis/ |
| 27 | exp joint disorders/ |
| 28 | (arthritis or osteoarthritis or rheumati* or fibromyalgia).tw. |
| 29 | exp back pain/ |
| 30 | chronic pain/ |
| 31 | ((back adj pain) or (neck adj pain)).tw. |
| 32 | exp OSTEOPOROSIS/ |
| 33 | osteoporosis.tw. |
| 34 | exp thyroid disorders/ |
| 35 | exp NEOPLASMS/ |
| 36 | (cancer* or oncolog* or neoplasm* or carcinom* or tumo?r* or malignan*).tw. |
| 38 | ((hiv adj infect*) or (hiv adj disease*)).tw. |
| 39 | gynecological disorders/ |
| 40 | endometriosis.tw. |
| 41 | exp MENTAL DISORDERS/ |
| 42 | DEPRESSION/ |
| 43 | ((mental* adj ill*) or (mental adj disorder*) or (mental adj disease*) or (mental adj distress*) or (mental adj disab*) or (mental adj problem*) or (mental adj health*) or (mental adj patient*) or (mental adj treatment) or (psychiatr* adj ill*) or (psychiatr* adj disorder*) or (psychiatr* adj disease*) or (psychiatr* adj distress*) or (psychiatr* adj disab*) or (psychiatr* adj problem*) or (psychiatr* adj health*) or (psychiatr* adj patient*) or (psychiatr* adj treatment) or (psychological* adj ill*) or (psychological*ADJ and disorder*) or (psychological* adj disease*) or (psychological* adj distress*) or (psychological* adj disab*) or (psychological* adj problem*) or (psychological* adj health*) or (psychological* adj patient*) or (psychological* adj treatment)).tw. |
| 44 | ((personality adj disorder*) or (mood adj disorder*) or (dysthymic adj disorder*) or (cognit* adj disorder*) or (anxiety adj disorder*) or (stress adj disorder*) or (eating adj disorder*) or (adjustment adj disorder*) or (reactive adj disorder*) or (somatoform adj disorder*) or (conversion adj disorder*) or (behavio* adj disorder*) or (percept* adj disorder*) or (psycho* adj disorder*) or (impulse adj control adj disorder*) or (development* adj disorder*)).tw. |
| 45 | (psychos#s or psychotic* or paranoi* or schizo* or neuros#s or neurotic* or delusion* or depression or depressive or bipolar or mania or manic or obsessi* or compulsi* or panic or phobic or phobia or anorexia or bulimia or neurastheni* or dissociative or affective or borderline or narcissis* or suicid* or (self adj injur*) or (self adj harm) or dementia or Alzheimer*).tw. |
| 46 | or/1-45 |
| 47 | ((writ* adj therap*) or (therapeutic* adj writ*) or (writ* adj cure*) or (writ* adj heal*) or (self adj management adj writ*) or (self adj help adj writ*) or (self adj conceal* adj writ*) or (self adj disclosure adj writ*) or (creative adj writ*) or (expressi* adj writ*) or (emoti* adj writ*) or (EMO adj writ*) or (sensitiv* adj writ*) or (sensor* adj writ*) or (reactive adj writ*) or (reflective adj writ*) or (descriptive adj writ*) or (biography* adj writ*) or (workshop adj writ*) or (epistolar* adj writ*) or (fiction* adj writ*) or (paradigm adj writ*) or (group adj writ*) or (letter* adj writ*) or (Pennebaker adj writ*) or (reminiscence adj review*) or (story adj writ*) or (stories adj writ*) or blog* or forum* or (memoir* adj writ*) or (journal* adj writ*) or (narrative* adj writ*) or (hand adj writ*) or (poe* adj writ*) or (health adj status adj writ*) or “program* writ*”).tw. |
| 48 | ((emoti* adj disclosure adj tip*) or (emoti* adj disclosure adj key*) or (emotional adj disclosure adj writ*) or (emotio* adj disclosure) or catharsis).tw. |
| 49 | ((express* or creativ* or emoti* or sensitiv* or reflect* or therap* or disclos* or conceal* or manag* or pennebaker or cathar* or “writing paradigm”) adj2 (writ* or “hand writ*” or blog or epistol* or letter* or story or stories or memoir* or narrat* or diary or diaries or poem or poet* or reminisc* or “life review” or “life writing” or journaling or “Journal Writing” or (“health status” adj2 writ*) or “program* writ*”)).tw. |
| 50 | 46 AND 49 |
| 51 | 47 AND 48 |
| 52 | exp Creative Writing/ |
| 53 | exp Journal Writing/ |
| 54 | 46 and (52 OR 53) |
| 55 | 50 or 51 or 54 |
| # | Search term |
|---|---|
| 1 | chronic*.mp. |
| 2 | ((persistent or (long* adj term) or ongoing or degenerative) adj3 (disease* or disab* or ill* or condition* or (health adj condition*) or (medical adj condition*) or impairment)).tw. |
| 3 | LONG TERM CARE/ |
| 4 | (long* adj term adj care).tw. |
| 5 | exp CARDIOVASCULAR DISEASE/ |
| 6 | ((heart adj disease*) or (heart adj failure) or (myocardial adj ischemia) or (angina adj pectoris) or (coronary adj disease*) or (coronary adj artery adj disease*) or (myocardial adj infarction) or hypertension or (high adj blood adj pressure)).tw. |
| 7 | exp LUNG DISEASES OBSTRUCTIVE/ |
| 8 | ((obstructive adj lung adj disease*) or (obstructive adj pulmonary adj disease*) or copd or asthma or bronchitis).tw. |
| 9 | exp EMPHYSEMA/ |
| 10 | exp PULMONARY EMPHYSEMA/ |
| 11 | emphysema.tw. |
| 12 | exp CEREBROVASCULAR DISORDERS/ |
| 13 | ((cerebrovascular adj disease*) or (cerebrovascular adj disorder*) or (brain adj ischemia) or (cerebral adj infarction) or (carotid adj artery adj disease*) or stroke or epilep*).tw. |
| 14 | exp nervous system disease/ |
| 15 | (neurodegenerative or (Huntington* adj disease) or (Parkinson* adj disease) or (amyotrophic adj lateral adj sclerosis) or (motor adj neuron* adj disease)).tw. |
| 16 | exp MULTIPLE SCLEROSIS/ |
| 17 | (multiple adj sclerosis).tw. |
| 18 | exp INFLAMMATORY BOWEL DISEASE/ |
| 19 | IRRITABLE BOWEL SYNDROME/ |
| 20 | ((inflammatory adj bowel) or (irritable adj bowel)).tw. |
| 21 | Kidney disease/ |
| 22 | ((renal adj failure*) or (renal adj insufficienc*) or (kidney adj failure*) or (kidney adj insuffcienc*)).tw. |
| 23 | DIABETES MELLITUS/ |
| 24 | (diabetes or diabetic*).tw. |
| 25 | exp ARTHRITIS/ |
| 26 | exp RHEUMATIC DISEASE/ |
| 27 | (arthritis or osteoarthritis or rheumati* or fibromyalgia).tw. |
| 28 | exp low back pain/ |
| 29 | exp backache/ |
| 30 | NECK PAIN/ |
| 31 | ((back adj pain) or (neck adj pain)).tw. |
| 32 | exp OSTEOPOROSIS/ |
| 33 | osteoporosis.tw. |
| 34 | exp THYROID DISEASE/ |
| 35 | exp NEOPLASMS/ |
| 36 | (cancer* or oncolog* or neoplasm* or carcinom* or tumo?r* or malignan*).tw. |
| 37 | exp HIV INFECTIONS/ |
| 38 | ((hiv adj infect*) or (hiv adj disease*)).tw. |
| 39 | ENDOMETRIOSIS/ |
| 40 | endometriosis.tw. |
| 41 | exp MENTAL DISORDERS/ |
| 42 | DEPRESSION/ |
| 43 | ((mental* adj ill*) or (mental adj disorder*) or (mental adj disease*) or (mental adj distress*) or (mental adj disab*) or (mental adj problem*) or (mental adj health*) or (mental adj patient*) or (mental adj treatment) or (psychiatr* adj ill*) or (psychiatr* adj disorder*) or (psychiatr* adj disease*) or (psychiatr* adj distress*) or (psychiatr* adj disab*) or (psychiatr* adj problem*) or (psychiatr* adj health*) or (psychiatr* adj patient*) or (psychiatr* adj treatment) or (psychological* adj ill*) or (psychological*ADJ and disorder*) or (psychological* adj disease*) or (psychological* adj distress*) or (psychological* adj disab*) or (psychological* adj problem*) or (psychological* adj health*) or (psychological* adj patient*) or (psychological* adj treatment)).tw. |
| 44 | ((personality adj disorder*) or (mood adj disorder*) or (dysthymic adj disorder*) or (cognit* adj disorder*) or (anxiety adj disorder*) or (stress adj disorder*) or (eating adj disorder*) or (adjustment adj disorder*) or (reactive adj disorder*) or (somatoform adj disorder*) or (conversion adj disorder*) or (behavio* adj disorder*) or (percept* adj disorder*) or (psycho* adj disorder*) or (impulse adj control adj disorder*) or (development* adj disorder*)).tw. |
| 45 | (psychos#s or psychotic* or paranoi* or schizo* or neuros#s or neurotic* or delusion* or depression or depressive or bipolar or mania or manic or obsessi* or compulsi* or panic or phobic or phobia or anorexia or bulimia or neurastheni* or dissociative or affective or borderline or narcissis* or suicid* or (self adj injur*) or (self adj harm) or dementia or Alzheimer*).tw. |
| 46 | or/1-45 |
| 47 | ((writ* adj therap*) or (therapeutic* adj writ*) or (writ* adj cure*) or (writ* adj heal*) or (self adj management adj writ*) or (self adj help adj writ*) or (self adj conceal* adj writ*) or (self adj disclosure adj writ*) or (creative adj writ*) or (expressi* adj writ*) or (emoti* adj writ*) or (EMO adj writ*) or (sensitiv* adj writ*) or (sensor* adj writ*) or (reactive adj writ*) or (reflective adj writ*) or (descriptive adj writ*) or (biography* adj writ*) or (workshop adj writ*) or (epistolar* adj writ*) or (fiction* adj writ*) or (paradigm adj writ*) or (group adj writ*) or (letter* adj writ*) or (Pennebaker adj writ*) or (reminiscence adj review*) or (story adj writ*) or (stories adj writ*) or blog* or forum* or (memoir* adj writ*) or (journal* adj writ*) or (narrative* adj writ*) or (hand adj writ*) or (poe* adj writ*) or (health adj status adj writ*) or “program* writ*”).tw. |
| 48 | ((emoti* adj disclosure adj tip*) or (emoti* adj disclosure adj key*) or (emotional adj disclosure adj writ*) or (emotio* adj disclosure) or catharsis).tw. |
| 49 | ((express* or creativ* or emoti* or sensitiv* or reflect* or therap* or disclos* or conceal* or manag* or pennebaker or cathar* or “writing paradigm”) adj2 (writ* or “hand writ*” or blog or epistol* or letter* or story or stories or memoir* or narrat* or diary or diaries or poem or poet* or reminisc* or “life review” or “life writing” or journaling or “Journal Writing” or (“health status” adj2 writ*) or “program* writ*”)).tw. |
| 50 | 46 and 49 |
| 51 | 47 and 48 |
| 52 | Writing/ |
| 53 | 46 and 52 |
| 54 | 50 or 51 or 52 |
| # | Search term |
|---|---|
| 1 | ((chronic*) OR (persistent) OR (long* term) OR (ongoing) OR (degenerative)) |
| 2 | (catharsis AND (writ* OR typ* OR key*)) OR ((emoti* disclos* typ*) OR (emoti* disclos* key*) OR (emotion* disclos* writ*)) |
| 3 | ((writ* therap*) OR (therapeutic* writ*) OR (“writ* cure*”) OR (“writ* heal*”) OR (“self management writ*”) OR (“self help writ*”) OR (“self conceal* writ*”) OR (“self disclosure writ*”) OR (“creative writ*”) OR (“expressi* writ*”) OR (“emoti* writ*”) OR (“Emotion* writ*”) OR (“sensitiv* writ*”) OR (“sensor* writ*”) OR (“reactive writ*”) OR (“reflective writ*”) OR (“descriptive writ*”) OR (“biography* writ*”) OR (“workshop writ*”) OR (“epistolar* writ*”) OR (“fiction* writ*”) OR (“paradigm writ*”) OR (“group writ*”) OR (“letter* writ*”) OR (Pennebaker writ*) OR (“reminiscence review*”) OR (writ* reminisc*) (“story writ*”) OR (“writ* stories”) OR (blog*) OR (forum*) OR (memoir* writ*) OR (“journal* writ*”) OR (“narrative* writ*”) OR (“writ* narrative*”) OR (“hand writ*”) OR (poe* writ*) OR (“health status writ*”) OR (“program* writ*”) OR (writ* diar*)) |
| 4 | 1 and (2 or 3) |
| # | Search term |
|---|---|
| 1 | ((chronic*) OR (persistent) OR (long* term) OR (degenerative)) AND ((disease*) OR (disab*) OR (ill*) OR (condition*) OR (“health condition*”) OR (“medical condition*”) OR (impairment)) |
| 2 | (catharsis AND (writ* OR typ* OR key*)) OR ((emoti* disclos* typ*) OR (emoti* disclos* key*) OR (emotion* disclos* writ*)) |
| 3 | ((“writ* therap*”) OR (“therapeutic* writ*”) OR (“writ* cure*”) OR (“writ* heal*”) OR (“self management writ*”) OR (“self help writ*”) OR (“self conceal* writ*”) OR (“self disclosure writ*”) OR (“creative writ*”) OR (“expressi* writ*”) OR (“emoti* writ*”) OR (“Emotion* writ*”) OR (“sensitiv* writ*”) OR (“sensor* writ*”) OR (“reactive writ*”) OR (“reflective writ*”) OR (“descriptive writ*”) OR (“biography* writ*”) OR (“workshop writ*”) OR (“epistolar* writ*”) OR (“fiction* writ*”) OR (“paradigm writ*”) OR (“group writ*”) OR (“letter* writ*”) OR (Pennebaker writ*) OR (“reminiscence review*”) OR (writ* reminisc*) (“story writ*”) OR (“writ* stories”) OR (blog*) OR (forum*) OR (memoir* writ*) OR (“journal* writ*”) OR (“narrative* writ*”) OR (“writ* narrative*”) OR (“hand writ*”) OR (poe* writ*) OR (“health status writ*”) OR (“program* writ*”) OR (writ* diar*)) |
| 4 | 1 AND (2 OR 3) |
| # | Search term |
|---|---|
| 1 | ((chronic*) OR (persistent) OR (long* term) OR (degenerative)) AND ((disease*) OR (disab*) OR (ill*) OR (condition*) OR (“health condition*”) OR (“medical condition*”)) |
| 2 | (catharsis AND (writ* OR typ* OR key*)) OR ((emoti* disclos* typ*) OR (emoti* disclos* key*) OR (emotion* disclos* writ*)) |
| 3 | (“writ* therap*”) OR (“therapeutic* writ*”) OR (“writ* cure*”) OR (“writ* heal*”) OR (“self management writ*”) OR (“self help writ*”) OR (“self conceal* writ*”) OR (“self disclosure writ*”) OR (“creative writ*”) OR (“expressi* writ*”) OR (“emoti* writ*”) OR (“Emotion* writ*”) OR (“sensitiv* writ*”) OR (“sensor* writ*”) OR (“reactive writ*”) OR (“reflective writ*”) OR (“descriptive writ*”) OR (“biography* writ*”) OR (“workshop writ*”) OR (“epistolar* writ*”) OR (“fiction* writ*”) OR (“paradigm writ*”) OR (“group writ*”) OR (“letter* writ*”) OR (Pennebaker writ*) OR (“reminiscence review*”) OR (writ* reminisc*) (“story writ*”) OR (“writ* stories”) OR (blog*) OR (forum*) OR (memoir* writ*) OR (“journal* writ*”) OR (“narrative* writ*”) OR (“writ* narrative*”) OR (“hand writ*”) OR (poe* writ*) OR (“health status writ*”) OR (“program* writ*”) |
| 4 | 1 AND (2 OR 3) |
| # | Search term |
|---|---|
| 1 | therap* writ* |
| 2 | written emotional disclosure |
| 3 | expressive writing |
| 4 | pennebaker writing |
| 5 | writing emotion |
| 6 | 1 OR 2 OR 3 OR 4 OR 5 [NB: have to be collated separately, this function cannot be performed by Zetoc] |
| # | Search term |
|---|---|
| 1 | Therapeutic writing |
| 2 | Written emotional disclosure |
| 3 | Expressive writing |
| # | Search term |
|---|---|
| 1 | (writing or written or blog or story) and (disease or disorder) and (chronic or long-term) |
Appendix 4 Data extraction form and quality assessment methods used
Systematic review data extraction forms
Baseline data
| # (reference number in the citation manager) | ||
|---|---|---|
| Publication details | Author(s) | |
| Year | ||
| Title | ||
| Journal | ||
| Volume | ||
| Issue | ||
| Pages | ||
| Format of publication | ||
| Study overview | Study name | |
| Study objectives | ||
| Study overall conclusions | ||
| DID TW WORK? | ||
| Why does it work? Why not? Who do they think it works for? | ||
| Country/region of the study | ||
| Time span of the study | ||
| Number of sites | ||
| Funding | Description of funding (public/private, etc.) | |
| Funded? Yes/No | ||
| Study moderators and/or mediators | Moderator(s) effect? Including: effect moderators (patients’ characteristics) interacting with the intervention to change outcome – baseline variables that affect outcome but not interact with intervention | |
| Mediator(s) effect? Including: change-in-process factors impacting outcome with or without interaction with intervention | ||
| Study intervention: exposure and comparator | Intervention type(s) | |
| Definition | ||
| Site of the intervention(s) | ||
| Intervention(s) exposure episode and duration | ||
| Length of the intervention(s) | ||
| Comparator type | ||
| Comparator definition | ||
| Time of assessment | ||
| Concomitant therapies | ||
| Intervention fidelity | ||
| Intervention credibility or subjective essay evaluation or manipulation checks | ||
| Participant(s) type | Target population | LTC category |
| LTC type and diagnostic criteria | ||
| LTC category | ||
| ITT (and PP) sample size | ||
| ITT sample size by groups (treatment arms) | ||
| Participants selection criteria | Main inclusion criteria | |
| Main exclusion criteria | ||
| Participants baseline characteristics | Baseline characteristics | Age |
| Gender | ||
| Ethnicity | ||
| Disease status and severity | ||
| Comorbidities | ||
| Other characteristics | ||
| Study flow diagram | Study participation [based on Sohanpal et al., www.systematicreviewsjournal.com/content/1/1/66 (accessed June 2014)] | # participants ELIGIBLE to the study (and # of non-participants) |
| # participants RECRUITED (# of study participants willing to take part) | ||
| # study participants NON-ATTENDERS (recruited not willing to attend intervention) | ||
| # study ATTENDERS (attending at least one session of the intervention) | ||
| # study attenders DROPPING OUT (after one session or more) | ||
| # programme COMPLETERS (# participants completing all sessions of the intervention) | ||
| Study DROP-OUTs (# non-attenders or programme dropouts or programme completers that drop out also from the study) | ||
| Recruitment method(s) | ||
|---|---|---|
| Type(s) of outcome(s) reported (by responding Yes/No) | Outcomes assessed | |
| Physical health | Physiological | |
| Haematological/immunological/hormonal | ||
| Disability/handicap | ||
| Pain | ||
| Non-physical health | Psychological | |
| Social health | ||
| Mental status | ||
| Behavioural | ||
| Performance | ||
| HRQoL | ||
| Costs/resource use | ||
| Safety | ||
| Compliance | ||
| Other | ||
Results section
| Physiological outcomes | Description | Selected end point(s) |
| Definition(s) and type of outcome | ||
| Time of assessment(s) and overall outcome follow-up | ||
| Type of analysis | ||
| Results | Values | |
| Summary of the impact of intervention(s) on patient-reported outcomes | ||
| Haematological/immunological outcomes | Description | Selected end point(s) |
| Definition(s) | ||
| Time of assessment(s) and overall outcome follow-up | ||
| Type of analysis | ||
| Results | Values | |
| Summary of the impact of intervention(s) on patient-reported outcomes | ||
| Physical disability/handicap assessment | Description | Selected end point(s) |
| Definition(s) | ||
| Time of assessment(s) and overall outcome follow-up | ||
| Type of analysis | ||
| Results | Values | |
| Summary of the impact of the intervention | ||
| Pain measurement | Description | Selected end point(s) |
| Definition(s) | ||
| Time of assessment(s) and overall outcome follow-up | ||
| Type of analysis | ||
| Results | Values | |
| Summary of the impact of intervention(s) on patient-reported outcomes | ||
| Psychological assessment | Description | Selected end point(s) |
| Definition(s) | ||
| Time of assessment(s) and overall outcome follow-up | ||
| Type of analysis | ||
| Results | Values | |
| Summary of the impact of intervention(s) on patient-reported outcomes | ||
| Social health assessment | Description | Selected end point(s) |
| Definition(s) | ||
| Time of assessment(s) and overall outcome follow-up | ||
| Type of analysis | ||
| Results | Values | |
| Summary of the impact of intervention(s) on patient-reported outcomes | ||
| Mental status assessment | Description | Selected end point(s) |
| Definition(s) | ||
| Time of assessment(s) and overall outcome follow-up | ||
| Type of analysis | ||
| Results | Values | |
| Summary of the impact of intervention(s) on patient-reported outcomes | ||
| Behavioural assessment | Description | Selected end point(s) |
| Definition(s) | ||
| Time of assessment(s) and overall outcome follow-up | ||
| Type of analysis | ||
| Results | Values | |
| Summary of the impact of intervention(s) on patient-reported outcomes | ||
| Performance assessment | Description | Selected end point(s) |
| Definition(s) | ||
| Time of assessment(s) and overall outcome follow-up | ||
| Type of analysis | ||
| Results | Values | |
| Summary of the impact of intervention(s) on patient-reported outcomes | ||
| General health status and quality of life | Description | Instrument(s) type |
| Definition | ||
| Time of assessment(s) and overall outcome follow-up | ||
| Type of analysis | ||
| Results | Values | |
| Summary of the impact of intervention(s) on patient-reported outcomes | ||
| Assessment of adverse events due to intervention (and not related to concomitant therapy) | Description and identification of AEs | Selected end point(s) |
| Definition(s)/reported categories of AEs | ||
| Time of assessment(s) | ||
| Type of analysis | ||
| Results | ||
| Assessment of compliance (adherence) | Description | Selected end point(s) |
| Definition(s) | ||
| Time of assessment | ||
| Results | ||
| Costs and levels of resource use (related to specific intervention) | Resource use | Type |
| Analysis | ||
| Levels of resource used | ||
| Summary of the impact of intervention(s) on resource used | ||
| Perspective | ||
| Currency | Currency | |
| Price year | ||
| If inflated, inflator | ||
| Time period to which costs relate | ||
| Unit cost | ||
| Total costs | ||
| Specific findings helping programme theory | Theories or mechanisms postulated by study’s authors to explain the success of the intervention | |
| Process factors identified by study authors helping the successful theory | ||
| Theories or mechanisms postulated by study’s authors to explain the failure(s) of the intervention | ||
| Process factors identified by study authors helping the failure of the theory | ||
| How study contributes to realist review | ||
| Summary of the impact of intervention(s) on patient-reported outcomes | ||
| Additional comments to the study (does the study support previous research?) | ||
| Correspondence required with authors for missing data? | ||
| References not captured by the review (cross-referencing) | ||
| Notes | ||
Realist synthesis data extraction forms
| First author, date | Data to support programme theory included in the systematic review | Primary study author’s explanation for how TW works |
| Recruitment/suitability | Intervention process/aspects of the intervention | Outcomes impact |
|---|---|---|
| Who is it suitable for and why? | What do you do and why? | What do you hope to achieve and why? |
Quality assessment tools
Clinical trials: Cochrane Handbook for Systematic Reviews of Interventions
| Study design | Trial design | |
|---|---|---|
| Study quality checklist (based on the checklist in the Cochrane Handbook) | Randomisation | Sequence generation (selection bias) |
| Allocation concealment (selection bias) | ||
| Blinding | Outcome | |
| Performance | ||
| ITT analysis? (Yes/No) | ||
| Description of outcomes differences between groups (selective reporting) | ||
| Description of withdrawals (attrition bias) | ||
| Pre-specified criteria for eligibility of patients | ||
| Similarity of groups at baseline regarding prognostic factors | ||
| Statement supporting the quality of the methods used | ||
Observational studies: Newcastle–Ottawa checklist
| Study quality checklist | Case–control studies | Selection | Is the case definition adequate? |
| Representativeness of the cases | |||
| Selection of controls | |||
| Definition of controls | |||
| Comparability | Comparability of cases and controls on the basis of the design or analysis | ||
| Factor(s) | |||
| Exposure | Ascertainment of exposure | ||
| Same method of ascertainment for cases and controls | |||
| Non-response rate | |||
| Cohort (and cross-sectional) studies | Selection | Representativeness of the exposed cohort | |
| Selection of the non-exposed cohort | |||
| Ascertainment of exposure | |||
| Demonstration that outcome of interest was not present at start of study | |||
| Comparability | Comparability of exposed and unexposed (design or analysis) | ||
| Factor(s) | |||
| Outcome | Assessment of outcome | ||
| Was follow-up long enough for outcome to occur | |||
| Adequacy of follow-up |
Appendix 5 Characteristics of included studies
Study design
| First author, year | Country | Study design | n of intervention groups | n of control groups |
|---|---|---|---|---|
| Abel 200450 | USA | RCT | 1 | 1 |
| Arden-Close 201380 | UK | RCT | 1 | 1 |
| Averill 2013100 | USA | RCT | 1 | 1 |
| Bartasiuniene 2011102 | Lithuania | RCT | 1 | 2 |
| Bernard 200693 | UK | RCT | 1 | 1 |
| Broderick 2004113 | USA | RCT | 2 | 1 |
| Broderick 2005118 | USA | RCT | 1 | 1 |
| Canna 200694 | USA | RCT | 2 | 2 |
| Cepeda 200885 | Colombia | RCT | 1 | 2 |
| Craft 201374 | USA | RCT | 2 | 2 |
| Dennick 201488 | UK | RCT | 1 | 1 |
| D’Souza 2008101 | USA | RCT | 1 | 1 |
| Gellaitry 201075 | UK | RCT | 1 | 1 |
| Gidron 199698 | Israel | RCT | 1 | 1 |
| Gillis 2006119 | USA | RCT | 1 | 1 |
| Golkaramnay 200768 | Germany | Controlled cohort | 1 | 1 |
| Graf 200895 | USA | RCT | 1 | 1 |
| Graham 200851 | USA | RCT | 1 | 1 |
| Grasing 201090 | USA | RCT | 1 | 1 |
| Halpert 201052 | USA | Controlled cohort | 1 | 1 |
| Hamilton-West 2007114 | UK | RCT | 1 | 1 |
| Harris 2005106 | USA | RCT | 2 | 1 |
| Henry 201053 | USA | Case–control | 1 | 1 |
| Hevey 2012103 | Ireland | RCT | 1 | 1 |
| Hong 201167 | Korea | RCT | 1 | 1 |
| Hughes 200754 | USA | RCT | 1 | 1 |
| Ironson 201371 | USA | RCT | 1 | 1 |
| Jensen-Johansen 201376 | Denmark | RCT | 1 | 1 |
| Kraaij 201055 | Netherlands | RCT | 1 | 1 |
| Krpan 201396 | USA | RCT | 1 | 1 |
| Lange 200369 | Netherlands | RCT | 1 | 1 |
| Lumley 2011115 | USA | RCT | 2 | 1 |
| Lumley 2014116 | USA | RCT | 2 | 2 |
| Mann 200172 | USA | RCT | 1 | 1 |
| McElligott 200687 | USA | Non-RCT | 1 | 1 |
| Meshberg-Cohen 201091 | USA | RCT | 1 | 1 |
| Milbury 201481 | USA | RCT | 1 | 1 |
| Mosher 201277 | USA | RCT | 1 | 1 |
| Paradisi 2010110 | Italy | RCT | 2 | 1 |
| Park 201278 | Korea | Controlled cohort | 1 | 1 |
| Pauley 201182 | USA | RCT | 2 | 1 |
| Petrie 200456 | New Zealand | RCT | 1 | 1 |
| Richards 200097 | USA | RCT | 1 | 2 |
| Rickett 201166 | Australia | RCT | 1 | 1 |
| Rini 201486 | USA | RCT | 3 | 1 |
| Robinson 200899 | UK | RCT | 1 | 1 |
| Rosenberg 200283 | USA | RCT | 1 | 1 |
| Sharifabad 2010105 | USA | RCT | 1 | 1 |
| Sloan 201270 | USA | RCT | 1 | 1 |
| Smyth 1999107 | USA | RCT | 1 | 1 |
| Smyth 2008121 | USA | RCT | 1 | 1 |
| Stark 201057 | USA | RCT | 3 | 1 |
| Tabolli 2012111 | Italy | RCT | 1 | 1 |
| Taylor 200389 | USA | RCT | 1 | 1 |
| Theadom 201058 | UK | RCT | 1 | 1 |
| Van Dam 201392 | Netherlands | RCT | 1 | 1 |
| Vedhara 2007112 | New Zealand | RCT | 1 | 1 |
| Wagner 201073 | USA | RCT | 1 | 1 |
| Walker 199979 | USA | RCT | 2 | 1 |
| Wallander 2011109 | USA | RCT | 1 | 1 |
| Warner 2006108 | USA | RCT | 1 | 1 |
| Wetherell 2005117 | UK | RCT | 1 | 1 |
| Willmott 2011104 | UK | RCT | 1 | 1 |
| Zakowski 200484 | USA | RCT | 1 | 1 |
Participants’ conditions
| First author, year | LTC | ICD-10 code | LTC: inclusion criteria/diagnostic tool(s) |
|---|---|---|---|
| Abel 200450 | HIV | B24 | Taking ART for their diagnosis, able to report their last VL of < 80 000–100,000 copies/ml, free of major psychiatric problems (self-report) |
| Arden-Close 201380 | Ovarian cancer | C56 | Disease stage from I to IV, with CA125 level checked by oncologist and categorised above or below 35 U/ml for the prognosis of the cancer and within 5 years of treatment |
| Averill 2013100 | ALS | G12 | Definite or probable ALS using El Escorial criteria at least 6 months prior to study entry (World Federation of Neurology Research Group on Neuromuscular Diseases, 1994); FVC in the 50th percentile or higher |
| Bartasiuniene 2011102 | CVD | I51 | |
| Bernard 200693 | PTSD | F43 | First episode of psychosis conforming to broad ICD-10 criteria (F20, F22, F23, F25) |
| Broderick 2004113 | RA | M06 | Formal diagnosis of RA |
| Broderick 2005118 | FM | M79 | Formal diagnosis of FM by a physician |
| Canna 200694 | Axis I anxiety or mood disorder | F41 | Individuals with axis I anxiety or mood disorder primary diagnosis |
| Cepeda 200885 | Cancer | C80 | Any type of cancer and reporting average pain intensity levels of at least 5/10 on a 0–10 scale; scored > 50% in the Karnofsky scale |
| Craft 201374 | Breast cancer | C50 | Invasive or non-invasive early stage breast cancer, definitive treatment (surgery, chemotherapy and/or radiation therapy) completed, time from diagnosis < 2 years |
| Dennick 201488 | Type 2 diabetes mellitus | E11 | |
| D’Souza 2008101 | Tension/migraine headaches | G43/G44 | International Headache Society criteria for either tension or migraine headaches |
| Gellaitry 201075 | Breast cancer | C50 | Patients with early-stage breast cancer, attending the last radiotherapy appointment at the outpatient clinic and without a defined psychiatric disorder |
| Gidron 199698 | PTSD | F43 | PTSD assessed with the Mississippi Scale for PTSD |
| Gillis 2006119 | FM | M79 | Rehabilitation hospital patients with CVD |
| Golkaramnay 200768 | Mental disorders | F41–F60 | Inpatient from hospital with mental health conditions according to the ICD-10 criteria |
| Graf 200893 | Psychiatric disorder | F99 | Participants from an university-based outpatients’ psychiatric clinic and student counselling centre |
| Graham 200851 | Chronic pain | Unclassifiable | Patients had experience for at least 6 months and were recruited during routine visits to a university hospital-affiliated outpatient pain centre |
| Grasing 201090 | Cocaine dependence | F14 | Meeting DSM-IV criteria for cocaine dependence at the time of admission |
| Halpert 201052 | IBS | K58 | Fulfilled the Rome III Criteria for IBS |
| Hamilton-West 2007114 | AS | M45 | Inflammation of the joints in the pelvis; low back pain and stiffness for > 3 months, which improves with exercise but is not relieved by rest; limited movement of the lower back and restricted chest expansion |
| Harris 2005106 | Asthma | J45 | Asthma was confirmed by a history of asthma diagnosed by a physician and either evidence of reduced expiratory volume and reversibility obtained through medical records or evidence of reduced expiratory volume evaluated by study staff |
| Henry 201053 | Breast cancer | C50 | Female breast cancer survivors attending radiation oncology clinics |
| Hevey 2012103 | MI | I21 | Patients with confirmed MI, who received treatment at a large teaching hospital |
| Hong 201167 | Dementia (Alzheimer’s disease/vascular dementia/Parkinson’s disease) | F03 (F00/F01/F02) | Elderly people housed in a nursing home and already medically diagnosed with dementia, and scoring ≤ 19 on the MMSE-K |
| Hughes 200754 | Breast cancer | C50 | Stage I, II or III breast cancer women receiving curative radiation therapy for breast cancer |
| Ironson 201371 | HIV (plus PTSD) | B24 (plus F43) | HIV-positive, falling into a CD4 range of 100–600. Included were also those with one Category C symptom (AIDS defining) but without C symptoms 1 year prior to study entry. The stress of HIV was considered sufficient to enter the study and no other trauma was required |
| Jensen-Johansen 201376 | Breast cancer | C50 | Female Danish residents, able to read and write Danish, aged 18–70 years, and treated surgically within 3 weeks of their diagnosis (mastectomy or lumpectomy) for invasive breast cancer, stages I and II |
| Kraaij 201055 | HIV | B24 | HIV-diagnosed patients. No restricted criteria regarding the VL or the CD4+ count |
| Krpan 201396 | Depression | F41 | According to SCID |
| Lange 200369 | PTSD | F43 | Participants had to score below the cut-off scores of the Depression subscale of the SCL-90 in the Dutch norm, the SDQ-5, and the Dutch Screening Device for Psychotic Disorder of the Dutch norm group |
| Lumley 2011115 | RA | M06 | Patients with RA who met American College of Rheumatology criteria for non-juvenile RA. Patients had to report experience pain or disability due to their RA in the preceding week |
| Lumley 2014116 | RA | M06 | RA patients meeting American College of Rheumatology criteria for non-juvenile RA. Patients had to report experience pain or disability due to their RA in the preceding week |
| Mann 200172 | HIV | B24 | Women being treated for HIV or diagnosed with AIDS |
| McElligott 200687 | Sickle cell disease | D57 | Medically diagnosed with sickle cell disease |
| Meshberg-Cohen 201091 | SUD | F19 | The Structured Clinical Interview for DSM-IV-TR – Alcohol and Substance Use Disorders Module (SCID) was used as the diagnostic interview assessing SUD diagnosis, including alcohol and other drugs |
| Milbury 201481 | RCC | C64 | Newly diagnosed with stage I–IV RCC and with a Zubrod performance status of < 2 |
| Mosher 201277 | Breast cancer | C50 | Distressed women with stage IV breast cancer |
| Paradisi 2010110 | Psoriasis | L40 | Plaque-type psoriasis involving > 10% of body area |
| Park 201278 | Breast cancer | C50 | Stage II and III, breast cancer survivors, women. No restriction to staging, surgery or drugs intake |
| Pauley 201182 | Testicular cancer | C62 | Testicular cancer survivors, men. No restriction to staging, surgery or drugs intake |
| Petrie 200456 | HIV | B24 | Documented HIV infection and not had their classified oral drug regimen changed in the previous 12 months |
| Richards 200097 | Mental disorder | F41–F60 | Diagnosed with at least one mental disorder, as classified with the DSM-III-R |
| Rickett 201166 | Cancer | C80 | All diagnosed with cancer except for one participant with a history of severe CVD, and one with an autoimmune disorder |
| Rini 201486 | Following stem cell transplant | C80 | |
| Robinson 200899 | BN | F50 | Diagnosis was made using information from the QEDD using DSM-IV (American Psychiatric Association, 1994) for definitions of disorders. Included were those with a diagnosis of BN (purging or non-purging) |
| Rosenberg 200283 | Prostate cancer | C61 | Histological diagnosis of adenocarcinoma of the prostate being followed with serial PSAs. Previously local treatment (prostatectomy or radiation) within the last 4 years |
| Sharifabad 2010105 | COPD plus IPF | J44 plus J84 | Medically diagnosed with COPD or IPF |
| Sloan 201270 | PTSD | F43 | Participants met DSM-IV PTSD Criterion A for a traumatic stressor (American Psychiatric Association, 1994) |
| Smyth 1999107 | Asthma/RA | J45/M06 | RA diagnosis was confirmed by board-certified rheumatologists and all patients met American College of Rheumatology criteria Asthma was diagnosed by a history of asthma, confirmed by a physician; patients were also required to provide a documented reduction in expiratory function (either in physician records or when evaluated by study staff) |
| Smyth 2008121 | PTSD | F43 | Based on PTSD diagnosis verification defined by the DSM-IV |
| Stark 201057 | FM plus facial pain | M79 | Diagnosis made by the referring physician |
| Tabolli 2012111 | Psoriasis | L40 | Diagnosis by an experienced staff dermatologist, according to established internationally accepted criteria, with ≥ 10% of body surface affected |
| Taylor 200389 | Cystic fibrosis | E84 | Medically diagnosed with cystic fibrosis |
| Theadom 201058 | Asthma | J45 | Diagnosed with asthma and requiring regular inhaled medication (British Thoracic Society step 2 or higher; British Thoracic Society and Scottish Intercollegiate Guidelines Network, 2005) |
| Van Dam 201392 | SUD | F14 | Diagnosed with SUD |
| Vedhara 2007112 | Psoriasis | L40 | A clinically verified diagnosis of psoriasis for at least 6 months |
| Wagner 201073 | HIV | B24 | Diagnosed with HIV only |
| Walker 199979 | Breast cancer | C50 | Women completing radiation therapy for breast cancer stage I or II with a Karnofsky performance status of ≥ 70% |
| Wallander 2011109 | GI RAP | R10 | Patients with GI RAP, who met Apley’s (1975) criteria for functional RAP as determined by a paediatric GI specialist |
| Warner 2006108 | Asthma | J45 | Participants classified with mild, persistent asthma (i.e. asthma symptom activity at least 2 days per week and nocturnal symptoms at least twice monthly) |
| Wetherell 2005117 | RA | M06 | Diagnosed with RA |
| Willmott 2011104 | MI | I21 | Participants were the first patients with MI who were receiving treatment at two acute hospital clinics |
| Zakowski 200484 | Prostate plus gynaecological cancer | C61 (prostate) plus C55 (uterus), C56 (ovary), C53 (cervix) | Participants with a first-time diagnosis of prostate or gynaecological cancer within the last 5 years |
Included studies categorised by International Classification of Diseases, Tenth Edition code by the reviewers
| First author, year | LTC | ICD-10 code |
|---|---|---|
| Abel 200450 | HIV | B24 |
| Kraaij 201055 | HIV | B24 |
| Mann 200172 | HIV | B24 |
| Petrie 200456 | HIV | B24 |
| Wagner 201073 | HIV | B24 |
| Ironson 201371 | HIV (plus PTSD) | B24 |
| Craft 201374 | Breast cancer | C50 |
| Gellaitry 201075 | Breast cancer | C50 |
| Henry 201053 | Breast cancer | C50 |
| Hughes 200754 | Breast cancer | C50 |
| Jensen-Johansen 201376 | Breast cancer | C50 |
| Mosher 201277 | Breast cancer | C50 |
| Park 201278 | Breast cancer | C50 |
| Walker 199979 | Breast cancer | C50 |
| Arden-Close 201380 | Gynaecological and genitourinary cancer | C57 (ovarian) |
| Rosenberg 200283 | Gynaecological and genitourinary cancer | C61(prostate) |
| Zakowski 200484 | Gynaecological and genitourinary cancer | C61 (prostate) plus C55 (uterus), C56 (ovary), C53 (cervix) |
| Pauley 201182 | Gynaecological and genitourinary cancer | C62 (testicular) |
| Milbury 201481 | Gynaecological and genitourinary cancer | C64 |
| Cepeda 200885 | Cancer from various sources | C80 |
| Rickett 201166 | Cancer from various sources | C80 |
| Rini 201486 | Cancer from various sources | C80 |
| McElligott 200687 | Sickle cell disease | D57 |
| Taylor 200389 | Cystic fibrosis | E84 |
| Hong 201167 | Dementia (Alzheimer’s disease/vascular dementia/Parkinson’s disease) | F03 (F00/F01/F02) |
| Grasing 201090 | Cocaine dependence | F14 |
| Meshberg-Cohen 201091 | SUD | F19 |
| Van Dam 201392 | SUD | F19 |
| Bernard 200693 | First episode psychosis | F41–F60 |
| Canna 200694 | Mental disorder (Axis I anxiety or mood disorder) | F41–F60 |
| Golkaramnay 200768 | Mental disorder | F41–F60 |
| Richards 200097 | Mental disorder | F41–F60 |
| Graf 200895 | Mental disorder (psychiatric disorder) | F41–F60 (F99) |
| Krpan 201396 | Depression | F41 |
| Gidron 199698 | PTSD | F43 |
| Lange 200369 | PTSD | F43 |
| Sloan 201270 | PTSD | F43 |
| Smyth 2008121 | PTSD | F43 |
| Robinson 200899 | BN | F50 |
| Averill 2013100 | ALS | G12 |
| D’Souza 2008101 | Tension/migraine headaches | G43/G44 |
| Hevey 2012103 | MI | I21 |
| Willmott 2011104 | MI | I21 |
| Bartasiuniene 2011102 | CVD | I51 |
| Sharifabad 2010105 | COPD plus IPF | J44 plus J84 |
| Harris 2005106 | Asthma | J45 |
| Theadom 201058 | Asthma | J45 |
| Warner 2006108 | Asthma | J45 |
| aSmyth 1999107 | Asthma/RA | J45/M06 |
| Halpert 201052 | IBS | K58 |
| Wallander 2011109 | IBS (GI RAP) | K58 (R10) |
| Paradisi 2010110 | Psoriasis | L40 |
| Tabolli 2012111 | Psoriasis | L40 |
| Vedhara 2007112 | Psoriasis | L40 |
| Broderick 2004113 | RA | M06 |
| Lumley 2011115 | RA | M06 |
| Lumley 2014116 | RA | M06 |
| Wetherell 2005117 | RA | M06 |
| Hamilton-West 2007114 | AS | M45 |
| Broderick 2005118 | FM | M79 |
| Gillis 2006119 | FM | M79 |
| Stark 201057 | FM | M79 |
| Graham 200851 | Chronic pain | M79 |
Interventions assessed
Interventions assessed
| First author, year | Experimental condition | Control condition | ||
|---|---|---|---|---|
| Intervention group 1 | Intervention group 2 | Control group 1 | Control group 2 | |
| Abel 200450 | EW disclosure (unfacilitated type of TW) | Daily activities writing | ||
| Arden-Close 201380 | Written emotional disclosure (unfacilitated type of TW) | Details of previous day writing | ||
| Averill 2013100 | Written or oral expressive disclosure (unfacilitated type of TW) plus completion of study measures | Attentional control writing (completion of study measures) | ||
| Bartasiuniene 2011102 | Expressive writing (unfacilitated type of TW) | Daily events writing | Non-writing group (wrote nothing) | |
| Bernard 200693 | Written emotional disclosure (unfacilitated type of TW) | Non-EW (activities that day, the room they were in, and plans for the next week) | ||
| Broderick 2004113 | Standard expressive writing (unfacilitated type of TW) | Enhanced meaning writing | Day-to-day activities in relation to the time invested | Educational attention control group |
| Broderick 2005118 | Written emotional expression with cognitive reappraisal | Day-to-day activities in relation to the time invested | Non-writing (usual care) | |
| Canna 200694 | Expressive writing plus CBT | CBT | Inexpressive writing plus CBT | Waiting list |
| Cepeda 200885 | Narrative emotional disclosure | Questionnaire writing | Usual care | |
| Craft 201374 | Breast-cancer trauma writing (unfacilitated type of TW) | Self-selected trauma writing (unfacilitated type of TW) | Breast cancer factual writing (unfacilitated type of TW) | Non-writing |
| Dennick 201488 | Written emotional disclosure | Previous day’s activities | ||
| D’Souza 2008101 | Written emotional disclosure (unfacilitated type of TW) | Time-management control writing | ||
| Gellaitry 201075 | Expressive writing (unfacilitated type of TW) | Routine care | ||
| Gidron 199698 | Written disclosure (unfacilitated type of TW) plus oral disclosure of most severe event | Casual daily agenda writing plus oral disclosure of daily activity | ||
| Gillis 2006119 | Written emotional disclosure (unfacilitated type of TW) | Time-management writing | ||
| Golkaramnay 200768 | Group therapy through internet chat | No intervention | ||
| Graf 200895 | Written emotional disclosure (unfacilitated type of TW) | Plans for the rest of the day writing | ||
| Graham 200851 | Written anger expression through letter-writing format (Rusing and Nolen-Hoeksema type of TW) | Goals writing through letter-writing format | ||
| Grasing 201090 | Written emotional expression (Pennebaker type of TW) | Time-management writing | ||
| Halpert 201052 | Expressive writing (unfacilitated type of TW) | Non-writing | ||
| Hamilton-West 2007114 | EW exercise (unfacilitated type of TW not approved by ethics committee – adapted version used) | Time-management exercise | ||
| Harris 2005106 | Stressful experiences writing | Positive writing | Neutral topic writing | |
| Henry 201053 | Positive expressive writing (single episode unfacilitated type of TW) | Usual care | ||
| Hevey 2012103 | Expressive writing (single episode unfacilitated type of TW) | Daily activities writing in the year prior to heart attack | ||
| Hong 201167 | Songwriting | Waiting list | ||
| Hughes 200754 | Expressive writing | Usual care | ||
| Ironson 201371 | Augmented trauma writing (unfacilitated type of TW) plus processing probes | Daily event writing | ||
| Jensen-Johansen 201376 | Expressive writing (unfacilitated type of TW) | Daily activities writing | ||
| Kraaij 201055 | Structured writing intervention (through website) | Cognitive–behavioural self-help programme | Waiting list | |
| Krpan 201396 | Expressive writing (deepest thoughts and feelings) | How they organised their day | ||
| Lange 200369 | Interapy | Waiting list | ||
| Lumley 2011115 | Written or oral emotional disclosure | Positive writing (or talking) | Neutral topic writing (or talking) | |
| Lumley 2014116 | Expressive writing, coping skills training | Neutral writing, coping skills training | ||
| Mann 200172 | Positive future writing | Non-writing | ||
| McElligott 200687 | Expressive writing (unfacilitated type of TW) | Details of previous day writing | ||
| Meshberg-Cohen 201091 | Expressive writing (unfacilitated type of TW) | Neutral topic writing | ||
| Milbury 201481 | Expressive writing (unfacilitated type of TW) | Neutral topic writing | ||
| Mosher 201272 | Expressive writing | Neutral topic writing | ||
| Paradisi 2010110 | Written emotional disclosure (unfacilitated type of TW) | Positive future writing (unfacilitated type of positive TW) | Non-emotional disclosure | |
| Park 201278 | Expressive writing programme (unfacilitated type of TW) | No intervention | ||
| Pauley 201182 | Negative expressive writing (unfacilitated type of TW) | Positive expressive writing (unfacilitated type of TW) | Innocuous writing | |
| Petrie 200456 | Written emotional expression (unfacilitated type of TW) | Time-management writing | ||
| Richards 200097 | Trauma writing (unfacilitated type of TW) | Trivial writing | Usual routine | |
| Rickett 201166 | Poetry writing programme/workshop | Waiting list | ||
| Rini 201486 | Expressive writing | Peer helping, expressive helping | Neutral writing | |
| Robinson 200899 | eBT | Unsupported SDW (unfacilitated type of TW) | Waiting list | |
| Rosenberg 200283 | Expressive writing (unfacilitated type of TW) | Non-disclosure | ||
| Sharifabad 2010105 | Written emotional disclosure (unfacilitated type of TW) | Neutral topic writing | ||
| Sloan 201270 | WET | Waiting list | ||
| Smyth 1999107 | Disclosure exercise (unfacilitated type of TW) | Neutral topic writing | ||
| Smyth 2008121 | Expressive writing (unfacilitated type of TW) | Daily plans writing | ||
| Stark 201057 | Trauma writing (unfacilitated type of TW) plus Change Theory (King type of TW) | Time management (factual writing) | ||
| Tabolli 2012111 | Writing exercise (unfacilitated type of TW) | Non-writing | ||
| Taylor 200389 | Written self-disclosure intervention (unfacilitated type of TW) | SMC | ||
| Theadom 201058 | Written emotional disclosure (unfacilitated type of TW) | Details of previous day writing | ||
| Van Dam 201392 | Expressive writing (unfacilitated type of TW) | Treatment as usual | ||
| Vedhara 2007112 | Written emotional disclosure (unfacilitated type of TW) | Details of previous day writing | ||
| Wagner 201073 | Expressive writing (unfacilitated type of TW) | Trivial writing | ||
| Walker 199979 | Single-episode written emotional expression (unfacilitated type of TW) | Three-episode written emotional expression (unfacilitated type of TW) | Attentional control (standard care) | |
| Wallander 2011109 | WSD (unfacilitated type of TW) | SMC | ||
| Warner 2006108 | Written emotional disclosure (unfacilitated type of TW) | Time management | ||
| Wetherell 2005117 | Emotional disclosure (writing or talking) (unfacilitated type of TW) | Time-management writing | ||
| Willmott 2011104 | Written emotional expression – positive and negative (unfacilitated type of TW) | Details of previous day’s prior to heart attack | ||
| Zakowski 200484 | Written emotional disclosure (unfacilitated type of TW) | Details of daily activity writing | ||
Interventions definitions
| First author, year | Experimental condition | Control condition | |||
|---|---|---|---|---|---|
| Definition group 1 | Definition group 2 | Definition group 3 | Definition group 1 | Definition group 2 | |
| Abel 200450 | To write about innermost thoughts related to diagnosis of HIV and living with the disease | – | – | To write about their daily activities | Inexpressive writing |
| Arden-Close 201380 | To write about the patient’s diagnosis and treatment as follows: Day 1: describe the diagnosis and treatment chronologically and what led to what, without mentioning emotions Day 2: part 1, describe how you felt and what you thought at the time of the diagnosis. Part 2, what impact has your diagnosis and treatment had on your life, and has it caused you to change priorities? Day 3: how do you currently feel and think about the diagnosis and treatment? Are your current thoughts and feelings the same as at diagnosis? Would you be able to cope with similar situations better because you have experienced it? |
– | – | To write about what the patient did the previous day (time management) | – |
| Averill 2013100 | To write on traumatic and upsetting life experiences: Session 1: the most traumatic and upsetting experience of the patient’s life Session 2: continue writing about the topic described in session 1, or choose an alternate topic Session 3: continue writing about the topic described in session 1, or choose an alternate topic Session 4: as above, but a suggestion is made to relate experiences to subsequent life events Study measures were also completed |
– | – | To complete the study measures | – |
| Bartasiuniene 2011102 | Disease (self-focused): to write about their deepest thoughts and feelings related to their illness | – | – | To write about daily routine until illness | Participants in this group did not write anything but received usual care: received standard psychological care, pointed mostly for relaxation (e.g. aromatherapy, music therapy) |
| Bernard 200593 | To write about the most stressful and upsetting aspects of their illness and treatment (or whatever they had reported on the IES-R, e.g. psychosis, paranoia) using a protocol adapted from Pennebaker and Beall1 | – | – | To write about different non-emotional topics (activities that day, the room they were in and plans for next week) on each day in a factual manner | – |
| Broderick 2005118 | To write about any traumatic event, current or past, in their life | To write focusing more on the meaning of their past trauma | To write about day-to-day activities in relation to the time invested. Only facts should be written, excluding any emotions associated with them | Comprised viewing an educational videotape about RA [Education (ED)] | |
| Broderick 2005118 | The exercise was focused on factual retelling of an important current or past traumatic event, along with emotional expression and cognitive reappraisal. The writing should involve deep thoughts and feelings about the event | – | – | To write without concern about spelling or grammar about day-to-day activities in relation to the time invested Session 1 asked for a description of plans for the past week Session 2 focused on the previous 24 hours Session 3 focused on the upcoming week It was emphasised that only facts should be written, not any emotions associated with them |
– |
| Canna 200694 | To write about their deepest thoughts and feelings related to their illness | – | – | Participants in this group were assigned to a non-emotional task, for which they had to describe in detail what they had done since they wake up | – |
| Cepeda 200888 | To write, while at home, for at least 20 minutes, once a week, for 3 weeks, a story about how cancer affected their lives | – | – | As an attention control group, patients were asked to complete, while at home, the McGill Pain Q | Patients were asked simply to attend weekly medical follow-up visits (i.e. the same clinic schedule as the other two groups) to receive usual customary care |
| Craft 201374 | To write about the deepest thoughts and feelings about breast cancer | To write about the deepest thoughts and feelings about a self-selected worst trauma | – | To write about facts of treatment only: day 1, diet; day 2, exercise; day 3, sleep pattern; day 4, medications | Non-writing |
| Dennick 201484 | To write about their thoughts and feelings about any stressful experience over the last month or current concern (i.e. not specifically diabetes related) | Description of the previous day’s activities, without prompt to discuss thoughts or feelings | |||
| D’Souza 2008101 | To write about a trauma or upheaval or stressful experience that you may be experiencing right now, or that you experienced at some other time in your life, particularly the most stressful that you have experienced and is the most significant to you, and ideally one that you have not talked about in detail with others. Participants were encouraged to write about the facts as well as their deepest feelings, and to try to write about the same events for all 4 writing days | – | – | To write about their activities for the past week (session 1) and past 24 hours (session 2), and their planned activities for the next 24 hours (session 3) and next week (session 4) Instructions asked participants to write only about their actions, but to refrain from writing about their feelings or opinions |
– |
| Gellaitry 201075 | This intervention comprises several types of expressive writing performed in a 4-day treatment Day 1: emotional disclosure – exploring deepest thoughts and feelings about your experience of breast cancer Day 2: cognitive appraisal – making sense of your illness. What does having breast cancer mean to you? Day 3: benefit finding – perceived benefits of your experience; challenges you have overcome; changed outlook on life/priorities? Day 4: looking to the future – coping strategies; sharing experience with others |
– | – | – | – |
| Gidron 199698 | To write about their most traumatic experiences and then in a brief predetermined format to elaborate orally on the most severe event about which they wrote | – | – | To write about their casual daily agenda without affective content and then describe daily activity orally | – |
| Gillis 2006119 | Participants were asked to identify a stressful experience that continues to bother them, and they were given additional guidance on how to identify such an experience (e.g. it is difficult to think or talk about, makes them feel anxious or upset when encountering reminders of the experience or prompts intrusive thoughts). They were instructed to make the memories, images and emotions as vivid as possible, and to write both the facts and their deepest feelings about the experience. In addition, they were instructed to explore how the stressful experience has affected your FM or how you deal with having FM or you might want to explore how the experience has affected your relationships with others. Participants were encouraged to work on and resolve one stressful experience at a time, and this means that you might write about the same experience over several days or all 4 days. However, if they find that they had worked it out or feel better about one experience, they should go on and write about another stressful experience | – | – | To write about different time periods for each of the 4 writing days and to write about only their actual behaviours or planned actions rather than their feelings or opinions These four time periods were: Day 1: what they did with their time over the last week Day 2: what they did with their time over the last 24 hours DAY 3: what they plan to do with their time over the next 24 hours Day 4: what they plan to do with their time over the next week |
– |
| Golkaramnay 200768 | The group members met in virtual chat rooms through which they communicated through written messages. The text-based communication was synchronous and in real time | – | – | No intervention | – |
| Graf 200895 | To write about the most stressful and upsetting experiences of your entire life | – | – | To write about their plans for the rest of today for 20 minutes. You may or may not want to discuss your writing or the themes of your writing with your therapist. This is your choice. Your writing will be kept completely confidential. Do not worry about spelling, sentence structure, or grammar | – |
| Graham 200851 | Before writing each letter, intervention group participants completed a short exercise designed to focus their attention on existing anger related to their pain experience. In this brief questionnaire, participants were asked to consider if they currently or recently felt anger towards a health-care provider, themselves, or someone or something else and, if so, to remember and/or focus on it. Participants were given a writing tablet and instructions to write a letter to the person at whom or thing at which they were most angry. They were instructed to focus on their anger rather than other emotions | – | – | Participants in the control group did not complete the short anger-focusing exercise and were instructed to write a letter to a person of their choosing, describing their plans for the upcoming day. They were instructed to write about their goals in detail but without discussing any of their thoughts and feelings. Control group participants believed they were providing information about what they were able to do in a given day | – |
| Grasing 201090 | The writing task focused on traumatic and upsetting life experiences Session 1: the most traumatic and upsetting experience of the patient’s life Session 2: continue writing about the topic described in session 1, or choose an alternative topic Session 3: continue writing about the topic described in session 1, or choose an alternative topic Session 4: as above, but a suggestion is made to relate experiences to subsequent life events |
– | – | The time-management task emphasised objective, factual events. Time-management control group wrote about how time was spent during the previous day; current day (prior to the session); during the remainder of the current day (after the session); during the upcoming week | – |
| Halpert 201052 | To write about the thoughts and feelings about IBS. They had to really let go, and explore the very deep emotions and thoughts | – | – | Participants who intended to write but did not start writing were offered the option to remain in the study and complete the follow-up questionnaires without writing formed the non-writing group | – |
| Harris 2005106 | Trauma writing described as writing about stressful of traumatic experiences | To write about positive experiences such as events that stimulated feelings of happiness or joy | To write on neutral topics focused on the events of the previous day (control group) | – | |
| Hamilton-West 2007114 | To write about any stressful experiences encountered over the last month, or any worries or concerns that are currently troubling you These might be related to the AS or not |
– | – | To write in detail about the plans for the following day. Participants were permitted to write about one topic only, or move from one topic to another | – |
| Henry 201053 | To write about positive thoughts and feelings regarding their experience with breast cancer | – | – | Participants did not write, just received treatment as usual | – |
| Hevey 2012103 | They were asked to write about their thoughts and feelings in relation to having had a heart attack | – | – | To described daily activities in the year prior to their heart attack | – |
| Hong 201167 | Music therapy programme, using songwriting-related activities consisted of three stages: Stage 1: preparing songwriting for finding preferred songs Stage 2: doing songwriting Stage 3: reinforcing songwriting |
– | – | Free time was given to the participants allocated to the control group for the 16 weeks the intervention took place. Subjects just underwent the usual daily life at the nursing home | – |
| Hughes 200754 | To write about their very deepest thoughts and feelings about [their] cancer and cancer treatment | – | – | Participants were given general health information typically offered to patients by their health-care providers, and was considered a treatment as usual control | – |
| Ironson 201371 | To write about their worst trauma/current conflicts and then to write about what they did and future plans | – | – | To write about daily events | – |
| Jensen-Johansen 201376 | To write about a traumatic or distressing event and to explore their deepest feelings and emotions associated with this experience. They were free to write about their breast cancer as well as non-cancer experiences, and to switch topics during the intervention | – | – | To write as objectively and as detailed as possible in an emotionally neutral manner about their daily activities | – |
| Krpan 201396 | To write about their deepest thoughts and feelings about an extremely important emotional issue that had affected them and their life | – | – | How they organised their day | |
| Kraaij 201055 | To describe their deepest thoughts and feelings regarding their HIV-positive status or any other emotionally significant topic. Participants were instructed to pay special attention to issues that they had not previously disclosed to others. All writing assignments were completed through a website that was especially designed for the present study | The self-help programme consisted of a workbook, a work programme and a CD-ROM. In the first week, participants were asked to do mindfulness-based relaxation exercises, and to continue these exercises in the following 3 weeks. In the second and third week, participants learned to identify and change irrational cognitions and to practise counterconditioning. In the fourth week, they were guided to formulate a realistic, concrete goal and to improve their self-efficacy to reach this goal | Participants on the waiting list did not receive any intervention. They were offered the interventions after completion of the study | – | |
| Lange 200369 | To stimulate self-confrontation, participants had to write in the first person and in the present tense, describing in as much detail as possible the sensory perceptions that they experienced at the time of the traumatic event, including olfactory, visual and auditory sensations | – | – | For ethical reasons, the participants in the control condition were not kept waiting until the treatment group had completed the follow-up. They received treatment directly after the treatment group had terminated treatment | – |
| Lumley 2011115 | To write (or speak) in a journal about this stressful experience, incorporating both facts and deepest feelings | To write (or speak) about positive emotional events in their lives, including both facts and feelings, and to describe their memories as vividly as possible | – | To write (or speak) about their daily activities over four different time intervals: day 1, the previous week; day 2, the previous day; day 3, their plans for the next day; day 4, their plans for the next week Time-management type of control |
– |
| Lumley 2014116 | To identify a stressful or traumatic experience that continued to cause them stress and to write about their most vivid memories and innermost thoughts and feelings about that experience. Also about finding meaning from it and anything they had learned, and how they coped with it now | Coping skills training | How they spent and managed their time over the previous week, including eating, physical activity and sleep | Arthritis education | |
| Mann 200172 | To write about a somewhat positive future To write in journals nor were told to imagine an optimistic future in which they would only have to take one pill per day for HIV | – | – | Participants did not write nor were told to imagine an optimistic future in which they would only have to take one pill per day for HIV. However, efforts were made to equalise the amount of time that researchers spent with participants in the two conditions | – |
| McElligott 200687 | To write about their deepest thoughts and feelings related to their illness | – | – | To write about details of previous day | – |
| Meshberg-Cohen 201091 | To write about personal traumatic/stressful experiences | – | – | To write on neutral topics (e.g. what they ate on the previous day, what they did since waking up yesterday) | – |
| Milbury 201481 | To write about their deepest emotions and thoughts regarding their cancer experience with slightly different probes at each session (e.g. how the diagnosis and treatment interfere with their lives; treatment-related decision-making; and fears about the future) | – | – | To write about four neutral topics: dietary behaviours, physical activity and exercise behaviours, attitudes towards smoking and other substance use, and sleep habits | – |
| Mosher 201277 | Writing about their deepest thoughts and feelings regarding their cancer | – | – | To describe yesterday’s activities in a factual manner | – |
| Paradisi 2010110 | To describe the worst experience in their lives related to their disease. After each writing session patients were directed to phototherapy | To write about their best possible future self and life goals. After each writing session patients were directed to phototherapy | – | Non-emotional control group. No definition given | – |
| Park 201278 | Express with writing about cancer-related emotion in 20 minutes | – | No intervention | – | |
| Pauley 201182 | To write about any aspect of their cancer that they would characterise as positive | To indicate what was negative about their experience | – | To write about the events of the day, the layout of their homes, or the responsibilities at their current position | – |
| Petrie 200456 | To write about the most traumatic and emotional experiences of their lives, about deepest thoughts and feelings about an event that they had not previously discussed with others. They could write about HIV-related topics or any other issues of emotional importance to them | – | – | To write about how they used their time, but with slightly different orientations each day: what they had done in the previous 24 hours, and what their plans were for the next 24 hours, the next week, and the next 12 months. They were encouraged to write in a purely descriptive and objective way with minimum expression of emotions | – |
| Richards 200097 | To write about the deepest thoughts and feelings, regarding an experience that had not been previously shared with others at all or in very little detail | – | – | To write about an assigned topic usually on how they manage their time | Participants were asked to go about their daily routine |
| Rickett 201166 | Workshop series in two groups, split in first and second (control group) workshop times. Participants in group 1 undertook the first poetry writing programme, while the remaining participants in group 2 undertook the second During each meeting, participants read poetry selections, discussed aspects of poetry writing, wrote poems and read them aloud to the group |
– | – | The second group was wait-listed to enable comparison with the first group in the workshop | – |
| Rini 201486 | To explore their deepest emotions and emotions about the time before, during and after transplant and then any aspect of their transplant | Peer helping | Expressive helping | They wrote a factual account of their experience before, during and after their transplant | |
| Robinson 200899 | Participants were assigned an e-mail therapist. eBT was administered by a team of therapists of different backgrounds. The therapy included online supervision and feedback from the participants. All treatment included eliciting history; asking participants to keep a dietary and feelings diary; identifying and modifying negative automatic thoughts and other cognitive styles common in eating disorders; encouraging regular meals with adequate carbohydrate; examining relationships and aspects of the participants behaviour which might exacerbate the eating disorder; managing the ending | Participants were sent an e-mail and had to spend some time at least twice a week, writing about their difficulties and to send it to one of the authors | – | Participants were placed on a waiting list. After 3 months they were reassessed and offered either eBT or SDW by random allocation | – |
| Rosenberg 200283 | To write about their experience with cancer and its treatment. They were allowed to write about other experiences in their life | – | – | Any type of writing was performed | – |
| Sharifabad 2010105 | To write about their most traumatic or upsetting life experiences | – | – | To write about an assigned neutral topic, describing the specific event or object in detail without describing thoughts or feelings relating to the topic | – |
| Sloan 201270 | To write about the same MVA event during each writing session, about their deepest emotions and thoughts at the time of the MVA was emphasised, as well as the importance of providing detailed information about the MVA. During the second session, they had to add information about what they were thinking or feeling as the event was happening | – | – | Participants in the waiting list were encouraged to contact the project coordinator any time if they were having problems | – |
| Smyth 1999107 | To write about the most stressful experience that they had ever undergone | – | – | To describe their plans for the day (framed as a time-management exercise to reduce stress) | – |
| Smyth 2008121 | To write about their traumatic experience | – | – | To write about a neutral topic: time-management control writing related to their daily plans | – |
| Stark 201057 | To write about their most traumatic experience (based on Broderick et al.118). Concepts of the Change Theory were incorporated by asking also patients to write their experiences as a story with a clear beginning, middle and end, as well as incorporate their deepest thoughts and emotions regarding this event, to try to perceive themselves as survivors and attempts to find any positive results that may have occurred as a result of this traumatic experience | – | – | – | |
| Tabolli 2012111 | To write longhand, continuously, about the most stressful event in their life, about the experiences with psoriasis After the intervention, participants received information and educational material on the disease and its management |
– | – | Control patients received only an educational intervention: patients received information and educational materials | – |
| Taylor 200389 | To write about their deepest thoughts and feelings about the most distressing experience of their entire life for a period of 20 minutes Participants were encouraged to connect their topic to relationships with others (e.g. parents, caregivers, lovers, friends, relatives) and to their past, present, or future |
– | – | – | |
| Theadom 201058 | To write about your very deepest thoughts and feelings about an extremely important emotional issue that has affected you and your life | - | – | Day 1: to write about exactly what you did yesterday from the time you got up until the time you went to bed Day 2: to write about what they had eaten the day before Day 3: to write about the physical activity they had undertaken the previous day |
– |
| Van Dam 201392 | Ten individual sessions of writing: 1. In detail about the most traumatic event(s) they had experienced. The writing had to be in the first person and in the present tense, addressing sensory experiences, painful facts thoughts and emotions experienced during the trauma 2. To write a letter of advice to a friend or loved one, imagining that they had experienced the same event. Patients were asked to give advice on how to handle the thoughts and emotions 3. Write a similar letter to themselves 4. Writing a reflective letter about the trauma and its impact on their life, and their resolutions for dealing with the trauma in future |
Treatment as usual | |||
| Vedhara 2007112 | To write or talk about traumatic and stressful events | – | – | To provide a factual descriptive (i.e. non-emotional) account of their activities in a specified time period (e.g. yesterday) | - |
| Wagner 201073 | To write about some extremely upsetting or traumatic event that they had experienced in their life | – | – | To describe in detail, as objectively as possible (a) their plans for the remainder of the day; (b) the clothes they are wearing; (c) any particular object or event of their choosing; or (d) the contents of their closet | – |
| Walker 199979 | To write about the deepest thoughts and feelings about their cancer experience (during 1 day only) | To write about the deepest thoughts and feelings about their cancer experience (during 3 separate days) | – | The attentional control received usual care and on their final day of treatment the researcher met with them to chat about plans for trips or current events not related to cancer | – |
| Wallander 2011109 | WSD was administered in three 20-minute sessions: one in the clinic and two by telephone in the home (no additional information was reported) | – | – | Participants received SMC appropriate to their health status from a paediatric GI specialist. SMC for RAP generally consists of follow-up office visits and/or telephone consultations, education support, dietary instructions, as well as possible oral medication and supplements to increase dietary bulk, decreased acid or increase motility, as deemed medically appropriate by treating GI specialist | – |
| Warner 2006108 | To write about past negative events, about a trauma or problem that they may be experiencing at the moment of the intervention, or that they had experienced at some other time in their life | – | – | To write privately about how you manage their time, writing about a different topic every day | – |
| Wetherell 2005117 | To write about their deepest emotions and thoughts about the most upsetting experience in their life, to really let go explore their feelings and thoughts about it. If they were not able to write about it they were prompted to write about anything that had upset them significantly in the past (it had to be a new topic, never discussed) | – | – | To write or talk about one of three topics. To describe, in detail: (1) everything they had done during that day (2) were planning to do the following day or (3) during the forthcoming weekend Control patients were instructed that the description should be detailed and factual and to avoid emotion during their accounts |
– |
| Willmott 2011104 | To write about their thoughts and feelings in relation to having had a heart attack including any emotions (positive and negative) and thoughts about how they might cope Note that on day 3, additionally, they were encouraged to try to wrap things up by, for example, thinking about how the heart attack may affect their future and again the importance of exploring thoughts and feelings was emphasised |
– | – | To describe what they usually did on a Saturday, Sunday and Monday before they experienced a heart attack (each day forming the focus of one session’s writing) They were asked to describe their activities in detail and encouraged to be as objective as possible when doing so They were told that the important thing was not to get distracted by emotions but to focus on simple descriptions of what they did, such as where they went and the things they ate |
– |
| Zakowski 200484 | To write continuously for 20 minutes about their deepest thoughts and feelings regarding their cancer experience | – | – | To describe in detail their daily activities in a non-emotional manner in accord with previously published procedures | – |
Interventions as evaluated by the reviewers
| First author, year | Experimental condition | Control condition | |||
|---|---|---|---|---|---|
| Intervention group 1 | Intervention group 2 | Control group 1 | Control group 2 | Facilitated intervention? Yes/No | |
| Abel 200450 | Unfacilitated EW | Factual writing | No | ||
| Arden-Close 201380 | Unfacilitated EW | Time-management writing | No | ||
| Averill 2013100 | Unfacilitated EW | Non-writing | No | ||
| Bartasiuniene 2011102 | Unfacilitated EW | Factual writing | Non-writing | No | |
| Bernard 200693 | Unfacilitated EW | Factual and time-management writing | No | ||
| Broderick 2004113 | Unfacilitated EW | Unfacilitated EW | Time-management writing | Attention controla | No |
| Broderick 2005118 | Unfacilitated EW | Time-management writing | SMC | No | |
| Canna 200694 | Unfacilitated EW | Factual writing | ? | ||
| Cepeda 200885 | Unfacilitated EW | Attention controla | SMC | No | |
| Craft 201374 | Unfacilitated EW | Unfacilitated EW | Factual writing | Non-writing | No |
| Dennick 201488 | Unfacilitated EW | Factual writing | No | ||
| D’Souza 2008101 | Unfacilitated EW | Time-management writing | No | ||
| Gellaitry 201075 | Unfacilitated EW | SMC | No | ||
| Gidron 199698 | Unfacilitated EW | Factual writing | No | ||
| Gillis 2006119 | Unfacilitated EW | Time-management writing | No | ||
| Golkaramnay 200768 | Internet chat room | No intervention | Yes | ||
| Graf 200895 | Unfacilitated EW | Time-management writing | No | ||
| Graham 200851 | Questionnaire plus unfacilitated EW | Factual goal writing | No | ||
| Grasing 201090 | Unfacilitated EW | Time-management writing | No | ||
| Halpert 201052 | Unfacilitated EW | Non-writing | No | ||
| Hamilton-West 2007114 | Unfacilitated EW | Time-management writing | No | ||
| Harris 2005106 | Unfacilitated EW | Positive writing | Factual writing | No | |
| Henry 201053 | Positive writing | SMC | No | ||
| Hevey 2012103 | Unfacilitated EW | Factual writing | No | ||
| Hong 201167 | Songwriting | Waiting list | Yes | ||
| Hughes 200754 | Unfacilitated EW | SMC | No | ||
| Ironson 201371 | Unfacilitated EW | Factual writing | No | ||
| Jensen-Johansen 201376 | Unfacilitated EW | Time-management writing | No | ||
| Kraaij 201055 | Website structured writing | Waiting list | No | ||
| Krpan 201396 | Unfacilitated EW | Time management writing | No | ||
| Lange 200369 | Website Interapy | Waiting list | Yes | ||
| Lumley 2011115 | Unfacilitated EW | Positive writing | Time-management writing | No | |
| Lumley 2014116 | Unfacilitated EW | Time-management writing | No | ||
| Mann 200172 | Positive writing | Non-writing | No | ||
| McElligott 200687 | Unfacilitated EW | Factual writing | No | ||
| Meshberg-Cohen 201091 | Unfacilitated EW | Factual writing | No | ||
| Milbury 201481 | Unfacilitated EW | Factual writing | No | ||
| Mosher 201277 | Unfacilitated EW | Factual writing | No | ||
| Paradisi 2010110 | Unfacilitated EW | Positive writing | Non-EW | No | |
| Park 201278 | Unfacilitated EW | No intervention | No | ||
| Pauley 201182 | Unfacilitated EW | Positive writing | Factual writing | No | |
| Petrie 200456 | Unfacilitated EW | Time-management writing | No | ||
| Richards 200097 | Unfacilitated EW | Time-management writing | SMC | No | |
| Rickett 201166 | Poetry writing | Waiting list | Yes | ||
| Rini 201486 | Unfacilitated EW | Factual writing | No | ||
| Robinson 200899 | Unfacilitated EW | Waiting list | No | ||
| Rosenberg 200283 | Unfacilitated EW | Non-writing | No | ||
| Sharifabad 2010105 | Unfacilitated EW | Factual writing | No | ||
| Sloan 201270 | Written exposure therapy | Waiting list | Yes | ||
| Smyth 1999107 | Unfacilitated EW | Time-management writing | No | ||
| Smyth 2008121 | Unfacilitated EW | Time-management writing | No | ||
| Stark 201057 | Unfacilitated EW (mixed writing) | Non-writing | ? | ||
| Tabolli 2012111 | Unfacilitated EW | Non-writing | No | ||
| Taylor 200389 | Unfacilitated EW | SMC | No | ||
| Theadom 201058 | Unfacilitated EW | Factual writing | No | ||
| Van Dam 201392 | Unfacilitated EW | Treatment as usual | No | ||
| Vedhara 2007112 | Unfacilitated EW | Factual writing | No | ||
| Wagner 201073 | Unfacilitated EW | Factual and time-management writing | No | ||
| Walker 199979 | Unfacilitated EW | Positive writing | SMC | No | |
| Wallander 2011109 | Unfacilitated EW | SMC | No | ||
| Warner 2006108 | Unfacilitated EW | Time-management writing | No | ||
| Wetherell 2005117 | Unfacilitated EW | Time-management writing | No | ||
| Willmott 2011104 | Unfacilitated EW | Factual writing | No | ||
| Zakowski 200484 | Unfacilitated EW | Factual writing | No | ||
Additional information on the interventions assessed
| First author, year | Funding | Financial compensationa | Method of instruction | Topic of the intervention | Number of topics | Topic change allowed | Duration (minutes) | Length | In a group | Type of writing | Collection of writings | Carer feedback |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Abel 200450 | Yes | Yes | Verbally | Disease self-focused | 1 | No | 20 | Three consecutive | NR | Handwriting | NR | NR |
| Arden-Close 201380 | No | No | Telephone | Disease and treatment self-focused | 1 (with variations each day) | Yes | 20 | Three non-consecutive (over 3-week period) | No | Handwriting | Yes | NR |
| Averill 2013100 | Yes | No | Telephone | Disease self-focused | 1 | No | 20 | Three non-consecutive (over 1 week) | No | Handwriting | NR | No |
| Bartasiuniene 2011102 | No | No | In writing | Disease self-focused | 1 | NR | 30 | Four consecutive | No | Handwriting | NR | NR |
| Bernard 200693 | No | No | Telephone | Disease and treatment self-focused | 1 | No | 15 | Three non-consecutive (over 10 days) | No | Handwriting | No | Yes |
| Broderick 2004113 | Yes | No | Videotape | 1. Self-selected trauma 2. Enhanced meaning self-selected trauma |
2 | No | 20 | Three consecutive | No | Handwriting | No | No |
| Broderick 2005118 | Yes | Yes | Verbally | Self-selected trauma | 1 | No | 20 | Three non-consecutive (at 1-week intervals) | No | Handwriting | Yes | Yes |
| Canna 200694 | Yes | No | ||||||||||
| Cepeda 200885 | Yes | No | Verbally | Disease self-focused | 1 | No | 20 | Three non-consecutive (at 1-week intervals) | No | Handwriting | Yes | NR |
| Craft 201374 | No | No | In writing | 1. Disease self-focused 2. Self-selected worst trauma |
2 | No | 20 | Four consecutive | No | By hand or word processor | Yes | NR |
| Dennick 201488 | Part | No | In writing | Self-selected trauma | 1 | Yes | 20 | 3 days over 1 week | No | Handwriting | NR | Yes |
| D’Souza 2008101 | Yes | Yes | In writing | Self-selected trauma | 1 | No | 20 | Four non-consecutive (at 2-week intervals) | No | Handwriting | Yes | NR |
| Gellaitry 201075 | Yes | Disease self-focused | 2 | Yes | 20 | Four consecutive | No | Handwriting | Yes | Yes | ||
| Gidron 199698 | No | No | Verbally | Self-selected trauma | 1 | No | 20 | Three consecutive | No | Handwriting and oral | NR | NR |
| Gillis 2006119 | No | No | In writing | Self-selected social trauma disease self-focused | 3 | Yes | 15–20 | Four consecutive | No | Handwriting | Yes | NR |
| Golkaramnay 200768 | Yes | No | In writing | Here-and-now tasks | 1 | NR | 90 | Weekly for 12–15 weeks | Yes | Word processor | Yes | Yes |
| Graf 200895 | No | No | In writing | Self-selected worst trauma | 1 | No | 20 | Two sessions (2 weeks apart) | No | Handwriting | Yes | Yes |
| Graham 200851 | Yes | Yes | In writing | Self-selected anger | 1 | No | 20 | Two sessions (2.5 weeks apart) | No | Word processor | Yes | NR |
| Grasing 201090 | No | Yes | In writing | Self-selected trauma | 1 | Yes | 20 | Four sessions over 17 days | No | Handwriting | Yes | NR |
| Halpert 201052 | No | No | In writing | Disease self-focused | 1 | Yes | 30 | Four consecutive | No | Handwriting | NR | NR |
| Hamilton-West 2007114 | No | NR | In writing | Disease self-focused | 1 | Yes | 20 | Three consecutive | No | Handwriting | NR | NR |
| Harris 2005106 | Yes | Yes | 1. Self-selected trauma 2. Self-selected positive experience | 1 | No | 20 | Three non-consecutive (at 1-week intervals) | No | Handwriting | Yes | NR | |
| Henry 201053 | Yes | Yes | In writing | Disease, positive self-focused | 1 | No | 20 | One session | No | Handwriting | Yes | NR |
| Hevey 2012103 | No | NR | In writing | Disease self-focused | 1 | No | 20 | Three consecutive | No | Handwriting | Yes | NR |
| Hong 201167 | No | No | Verbally | Self-selected past experience or everyday live | > 1 | Yes | 60 | Sixteen sessions at weekly intervals | Yes | Handwriting | NR | |
| Hughes 200754 | No | No | In writing | Disease self-focused | 1 | NR | 30 | Three consecutive (over a five-time period) | Handwriting | NR | Yes | |
| Ironson 201371 | Yes | No | In writing | Self-selected worst trauma (or current conflicts) | 1 | Yes | 20 | Four consecutive | No | Handwriting | Yes | NR |
| Kraaij 201055 | No | No | NR | Disease self-focused | 1 | Yes | 30 | Four non-consecutive (at 1-week intervals) | No | Word processor | Yes | NR |
| Krpan 201396 | Yes | Yes | NR | Self-selected past trauma | 1 | NR | 20 | 3 consecutive days | NR | Handwriting | NR | NR |
| Jensen-Johansen 201371 | Yes | No | Telephone | Self-selected trauma | 1 | Yes | 20 | Three non-consecutive (over a 3-week period) | No | Handwriting | Yes | NR |
| Lange 200369 | Yes | No | In writing | Self-selected trauma: description of sensory perceptions including olfactory, visual and auditory sensations | 1 | NR | 45 | 10 non-consecutive (over 5 weeks at 2-week intervals) | No | Word processor | Yes | Yes |
| Lumley 2011115 | Yes | Yes | Verbally and in writing | 1. Self-selected stressful event 2. Self-selected positive event | 1 | No | 20 | Four consecutive | No | Handwriting | Yes | NR |
| Lumley 2014116 | Yes | Yes | Verbally and in writing | Self-selected trauma | 4 | No | 20 | Four within 1 week | No | Handwriting | Yes | NR |
| Mann 200172 | Yes | Yes | In writing | Self-selected positive future | 1 | NR | 10 | Four non-consecutive (twice a week) | NR | Handwriting | NR | NR |
| McElligott 200687 | No | Yes | Verbally and in writing | Disease self-focused | 1 | No | NR | Three (at 1-week intervals) | No | Handwriting | No | NR |
| Meshberg-Cohen 201091 | Yes | No | In writing | Self-selected trauma | 1 | NR | 20 | Four consecutive | No | Handwriting | Yes | NR |
| Milbury 201481 | Yes | Yes | In writing | Disease and treatment self-focused | 1 | NR | 20 | Four non-consecutive (over 10 days) | No | Handwriting | Yes | NR |
| Mosher 201277 | No | Yes | In writing | Disease (self-focused): deepest thoughts and feelings regarding their cancer | 1 | NR | 20 | Four non-consecutive (over 8 weeks) | No | Handwriting | Yes | Yes |
| Paradisi 2010110 | Yes | NR | In writing | 1. Disease self-focused worst experience 2. Best possible future self and life goals |
1 | No | 20 | 3 consecutive days | No | Handwriting | No | NR |
| Park 201278 | No | NR | In writing | Disease self-focused | 1 | NR | 20 | Four non-consecutive (at 1-week intervals) | Yes | Handwriting | NR | NR |
| Pauley 201182 | Yes | Yes | In writing | 1. Disease, positive self-focused 2. Disease, negative self-focused |
1 | NR | 20 | 3 days (at 1-week intervals) | No | Handwriting and word processor | Yes | NR |
| Petrie 200456 | Yes | NR | In writing | Self-selected worst trauma or self-focused disease | 1 | Yes | 30 | 4 consecutive days | No | Word processor | Yes | No |
| Richards 200097 | Yes | Yes | In writing | Disease self-focused | 1 | NR | 20 | 3 consecutive days | No | Handwriting | Yes | NR |
| Rickett 201166 | Yes | NR | In writing and verbally | Discussed aspects of poetry writing, wrote poems | 1 | NR | 120 | Weekly for 8 weeks | Yes | Handwriting | Yes | Yes |
| Rini 201486 | Yes | Yes | In writing | Disease and treatment focused | 4 | No | 20 | Weekly, over 4 weeks | No | handwriting | Yes | NR. |
| Robinson 200899 | No | No | In writing | Self-selected difficulties (not further specified) | 1 | NR | NR | Two sessions (over 1 week) | No | Handwriting | Yes | Yes |
| Rosenberg 200283 | Yes | No | In writing | Disease and treatment self-focused | 1 | Yes | 20–30 | 4 consecutive days | No | Handwriting | NR | NR |
| Sharifabad 2010105 | Yes | No | In writing and verbally | Self-selected worst experience | 1 | NR | 20 | Three sessions (at 1-week intervals) | Yes | Handwriting | NR | NR |
| Sloan 201270 | Yes | Yes | In writing and verbally | Disease self-focused | 2 | Yes | 120 | Four sessions | No | Handwriting | NR | Yes |
| Smyth 1999107 | Yes | Yes | In writing | Self-selected worst experience | 1 | NR | 20 | 3 consecutive days | No | Handwriting | Yes | No |
| Smyth 2008121 | No | Yes | In writing | Self-selected experience | 1 | NR | 20 | Three consecutive sessions (with 15-minute rest interval between each session) | No | Handwriting | NR | NR |
| Stark 201057 | No | Yes | In writing | Self-selected worst experience from a positive perspective | 1 | No | 20 | 3 consecutive days | No | Handwriting | NR | NR |
| Tabolli 2012111 | Yes | No | In writing | Disease self-focused | 1 | NR | 20 | 3 consecutive days | No | Handwriting | NR | Yes |
| Taylor 200389 | Yes | No | In writing | Self-selected worst experience | 1 | NR | 20 | 3 consecutive days | No | Handwriting | Yes | NR |
| Theadom 201058 | Yes | No | In writing | Self-selected emotional issue | 1 | No | 20 | 3 consecutive days | No | Handwriting | Yes | Yes |
| Van Dam 201392 | Yes | No | Verbally | Self-selected trauma | 4 | No | 45–60 | 10 sessions, 1 per week | No | Handwriting | Yes | Yes |
| Vedhara 2007112 | Yes | No | In writing | Self-selected traumatic and stressful events | 1 | Yes | 20 | 4 consecutive days | No | Handwriting | Yes | NR |
| Wagner 201073 | No | Yes | In writing | Self-selected trauma, past negative events, problem | 1 | Yes | 20 | Four non-consecutive (at 1-week intervals) | No | Word processor | Yes | NR |
| Walker 199979 | No | In writing | Disease self-focused | 1 | NR | 30 | 2–3 consecutive days | No | Handwriting | Yes | NR | |
| Wallander 2011109 | Yes | No | In writing and verbally | NR | NR | NR | 20 | Three sessions (in 6 days) | No | Handwriting | Yes | NR |
| Warner 2006108 | Yes | Yes | In writing | Self-selected trauma | > 1 | NR | 15–20 | 3 consecutive days | No | Handwriting | Yes | Yes |
| Wetherell 2005117 | Yes | No | Verbally | Self-selected most upsetting experience | 1 | NR | 20 (with so many breaks as wished) | 1 day | No | Handwriting or tape recording | Yes | Yes |
| Willmott 2011104 | Yes | No | In writing | Disease self-focused | 2 | NR | 10–20 (time spent writing in each session had to be recorded) | 3 consecutive days | No | Handwriting | Yes | NR |
| Zakowski 200484 | Yes | No | In writing and verbally | Disease self-focused | 1 | No | 20 | 3 consecutive days | No | Handwriting | Yes | NR |
Outcomes assessed
| First author, year | Physiological measures | Biomarkers measures of disease progression | Patient-reported outcome measures | Resource-use measures | Adherence | Comments |
|---|---|---|---|---|---|---|
| Abel 200450 | Cognitive reorganisation Social stigma (stigma scale) Depression (CES-D) QoL (SF-36) |
|||||
| Arden-Close 201380 | Perceived stress (PSS) Intrusive thoughts (IES) QoL (FACT-General) |
|||||
| Averill 2013100 | Affect (ABS) Emotional approach coping (specific scale) Depression (GDS) Ambivalence over emotional expression (AEE) Social support (Social Constraints scale) QoL (McGill QOL) |
|||||
| Bartasiuniene 2011102 | Emotional states [PANAS-X(b)] | |||||
| Bernard 200693 | Trauma of psychosis (IES-R) Recovery style (RSQ) Insight (IS) Anxiety – depression (HADS) Mood [PANAS- X(a)] |
|||||
| Broderick 2004118 | Disease activity (Disease Activity Rating scale) | QoL (SF-36v2 Health Survey) | ||||
| Broderick 2005118 | Anxiety and depression (STAI-S, BDI-II) Physical health (FIQ, CLINHAQ) QoL (MOS-SF-36, QOL) Pain (McGill Pain Q-SF, MPI) |
|||||
| Canna 200694 | Anxiety (BAI, STAI) Depression (BDI-II) Distress symptoms (BSI, GSI) Panic symptoms (PSWQ) Physical symptoms (PILL) Mood (PANAS) Life satisfaction (QoLI) Social support (MSPSS) |
Number of treatment sessions | ||||
| Cepeda 200885 | Average pain intensity, well-being | |||||
| Craft 201374 | QoL (FACT-B) | |||||
| Dennick 201488 | CES-D PAID EQ-5D VAS and utility SDSCA |
|||||
| D’Souza 2008101 | Headache frequency, disability and severity | Physical symptoms (SCL-90-R) Immediate mood [PANAS-X(d)] Behavioural disability from headache (MIDAS) |
||||
| Gellaitry 201075 | Social support (SOS) QoL (FACT-B) Mood (POMS) AEs |
Number of all medical visits (scheduled and unscheduled hospital appointments, GP appointments and visits to the nurse), regardless of whether they were cancer related or not | ||||
| Gidron 199698 | Physical symptoms (PILL, Mississippi scale for PTSD) Mood, depression, negative and positive affect [PANAS-X(a), IES, BDI-II] |
Health-care visits [mean (SD) number of health-care visits in the last month] | ||||
| Gillis 2006119 | Immediate negative mood (PANAS-X) Negative affect (NA subscale of PANAS-X) Pain (pain subscale of AIMS2) Fatigue (FSS) Social support (subscale of AIMS2) Global health status (FIQ) Physical dysfunction (AIMS2) Sleep quality (4-item scale) |
Total number of visits to specialist – related or not to FM – during the last month | ||||
| Golkaramnay 200768 | Patient distress (OQ-45.2) Symptomatic distress [SCL-90-R (GSI)] Subjective physical well-being (GBB) Life satisfaction (FLZ) |
|||||
| Graf 200895 | Mood (DASS) Functioning (OQ-45.2) |
|||||
| Graham 200851 | Anger expression and meaning making (expressed anger) Sadness/anxiety, depressed mood (CES-D) Pain severity (WHYMPI) Feelings of personal control over pain (SOPA) Resource use (number of years attending the centre) |
|||||
| Grasing 201090 | BP and heart rate (measured with patients in a sitting position) | Craving intensity (BSCS) Mood (POMS, BSI) Stress (PSS) |
Total number of contacts completed outpatient mental health clinic visits for treatment of substance abuse disorders | |||
| Halpert 201052 | Cognition (CG-FBD) Catastrophising/coping (CT3) IBS-specific QoL (IBS-QoL) IBS severity (IBSSS) |
|||||
| Hamilton-West 2007114 | Physical status – fatigue and pain mainly (BASDAI, BASFI, BAS-G) Depression (HADS) |
|||||
| Harris 2005106 | Lung function through spirometry (FEV1, FVC) | Adherence to probes | ||||
| Henry 201053 | Depressive symptomatology (CES-D) Mood states (POMS) Physical health (Survey – 18 physical symptoms items) |
|||||
| Hevey 2012103 | Anxiety and depression (HADS) Coping (Brief COPE) Negative affectivity (DS-14) QoL (Mac New HRQOL) |
|||||
| Hong 201167 | Cognitive functioning (MMSE-K) | |||||
| Hughes 200754 | Mood (PANAS) Sickness related dysfunction (SIP) Avoidant and intrusive thoughts (IES) Patient’s history of prior disclosure (DIS) |
|||||
| Ironson 201371 | CD4+ count (flow cytometry) and VL (quantitative reverse-transcriptase PCR) | HIV-related physical symptoms of HIV (checklist) Psychosocial distress (Davidson PTSD scale), depression (HAM-D) |
Yes | |||
| Jensen-Johansen 201376 | Distress (IES) Depression (BDI-SF) Negative mood (POMS) Vigour (POMS-v) Positive mood (PPMS) |
|||||
| Kraaij 201055 | Depressive symptoms (HADS) | |||||
| Krpan 201396 | – | – | PHQ BDI |
|||
| Lange 200369 | Intrusions and avoidance (IES) Physical symptoms (SCL-90-R) |
|||||
| Lumley 2011115 | RA severity (swollen joint count, walking speed and grip strength). Physician’s global rating of disease activity (100-mm VAS) | ESR | Self-reported physical and psychological functioning (AIMS2) Affective and sensory pain (McGill Pain Q-SF) Pain behaviour (structured observation system) Immediate mood (PANAS-X) |
|||
| Lumley 2014116 | RA severity (swollen joint count, walking speed and grip strength). Physician’s global rating of disease activity (100-mm VAS) | Inflammation (CRP) | Self-reported physical and psychological functioning (AIMS2) Affective and sensory pain (McGill Pain Q-SF) |
|||
| Mann 200172 | Optimism (LOT) | Yes | ||||
| McElligott 200687 | Self-esteem (ADSEI) Depression (CDI) Behavioural problems (ADSEI) Anxiety (RCMAS) Physical symptoms (PSC, PSC-Y) Physical well-being |
Number of visits to the clinic and number of days in hospital | ||||
| Meshberg-Cohen 201091 | Physical health problems (PILL) Distress (BSI, GSI) Depression (CES-D) Affect (PANAS-X) Drug craving (BSCS) PTSD severity (PDS) |
|||||
| Milbury 201481 | Fatigue (BFI) Intrusions and avoidance (IES) Psychological well-being (CES-D) Cancer-related symptoms (MDASI) Sleep disturbance (PSQI) QoL (SF-36) |
|||||
| Mosher 201277 | Existential well-being (FACIT-Sp) Psychological well-being (DT, HADS-A) Sleep disturbance and fatigue (PSQI, FACIT-F) |
The total Global Sleep Quality score was used in this study | ||||
| Paradisi 2010110 | Psoriasis severity (PASI) | QoL (Skindex-29, GHQ-12) Psoriasis severity (SAPASI) |
||||
| Park 201278 | Physical symptoms (PILL, MDASI) Anxiety/depression (HADS) |
|||||
| Pauley 201182 | Expressiveness (ARS-20) Mental health (GHQ-12) General QoL (QLQ-30) Sexual Health and performance (specific measure) |
|||||
| Petrie 200456 | HIV VL (quantitative reverse-transcriptase PCR); CD4+ count (flow cytometry) | Perceived stress (PSS) Self-rated health status |
||||
| Richards 200097 | Symptom and emotion self-report survey Somatic and cognitive anxiety (CSAQ) Frequency of physical symptoms (PILL) |
|||||
| Rickett 201166 | Non-specific emotional distress (K-10) | |||||
| Rini 201486 | Relapse Mortality |
|||||
| Robinson 200899 | Eating disorder diagnosis (QEDD) Desired weight (BMI) Bulimia test (BITE) |
Depression (BDI) | ||||
| Rosenberg 200283 | Immune function/disease markers (PSA levels, peripheral blood T-cell proliferation) Serum cytokine levels of TNF-α. IL-4 and IL-10 | Health-care utilisation (NMCUES) Pain (BPI) Health-related functioning and QoL (MOS-SF-36, FACT) Psychological symptoms (SCL-90-R; Brief POMS) Rumination (Rumination scale) Coping (The Ways of Coping-Cancer Version) |
||||
| Sharifabad 2010105 | Exercise capacity (6MWD), lung function through spirometry (FEV1, FVC) | QoL (CRQ) Impact on overall health, daily life and perceived well-being (SGRQ) Subjective feeling of shortness of breath (MMRC dyspnoea scale) |
||||
| Sloan 201270 | PTSD diagnostic status (CAPS) Self-reported emotion (SAM) Prior trauma exposure (TLEQ) |
|||||
| Smyth 1999107 | Lung function through spirometry (FEV1), disease severity (DAS) | |||||
| Smyth 2008121 | Cortisol (saliva sample) | Mood (POMS) Positive changes (PTGI) PTSD symptoms (PSS-I) |
||||
| Stark 201057 | Affect (POMS) Chronic pain experience (MPI) Pain distress (SLESQ) Pain Catastrophising Scale Pain intensity/severity (DDS) Depression (BDI-SF) Mood/affect (POMS) |
Number of health centre visits missed Quantity of pain medications taken per month Quantity of psychotropic medication taken per month |
||||
| Tabolli 2012111 | Psoriasis clinical severity (PASI) | Symptoms and emotions (Skindex-29 Symptoms and Emotions scales) General health (GHQ-12, SF-36) Psoriasis severity (SAPASI) |
||||
| Taylor 200389 | Health status (FEV1, BMI) | Perceived symptoms (PHQ) Physical complaints (SLESQ), physical, mental health and perceived health status (SF-12) Feasibility and acceptability of the intervention (VSQ) |
||||
| Theadom 201058 | Lung function through spirometry (FEV1, FVC) | Asthma-specific QoL instrument (Marks, SSQ Asthma, SSQ Awakenings) Asthma control (ACT) Asthma distress (ABP) Beta-agonist use Corticosteroids use |
Number of visits to the clinician (%) | |||
| Van Dam 201392 | PDS Number of abstinent days |
|||||
| Vedhara 2007112 | Psoriasis clinical severity (PASI) | Skin condition consequences in QoL (DLQI) Mood (POMS, HADS) |
||||
| Wagner 201073 | Affect [PANAS-X(a)] Stress (PSS) Optimism (HIV-OS) Coherence (SOC) HIV – QoL (MOS-HIV) |
|||||
| Walker 199979 | Affect [PANAS-X(a)] Intrusive thoughts and avoidance (IES) |
|||||
| Wallander 2011109 | GI pain frequency (the Abdominal Pain Frequency Rating) Somatisation severity (the Children’s Somatisation Inventory) QoL (PedsQL) |
GI clinic outpatient visit | ||||
| Warner 2006108 | Lung function through spirometry (FEV1) | Asthma symptoms (ASS) Affect [PANAS-X(c)] Behavioural disability (FDI) Internalising behaviour problems (CBCL) |
Adherence rate to the writing assignments | |||
| Wetherell 2005117 | RA severity (swollen and tender joint count), physician global rating of disease activity (100-mm VAS) Disease activity (DAS) |
ESR, CRP | Mood (POMS-SF) | |||
| Willmott 2011104 | Cardiac symptoms (SBP and DBP) | QoL (MOS-SF-36) | GP and attendance at cardiac rehabilitation sessions | Adherence to writing instructions | ||
| Zakowski 200484 | Personality factors (NEO-FFI) Distress symptoms (BSI, GSI) Intrusive thoughts and avoidance (IES) Positive and negative moods (POMS-SV) |
Outcomes measures definitions
| Acronym | Definitions given in the primary studies | Scale and scoring | Meaning |
|---|---|---|---|
| 6MWD | Changes in 6 Minutes’ Walk Distance (6MWD) over the study period | Values are given in metres | The longer the distance in the 6MWD, the higher the performance |
| ABP | The Asthma Bother Profile (ABP) is a 23-item self-administered questionnaire (Hyland et al.162) designed to measure level of distress caused by asthma. It covers two domains: distress and asthma management measured with a unidimensional scale | 6-point Likert scale with 0 (no) and 5 (yes); with use of 0–5 scale. All scores are added up with a maximum of 75 and minimum of 0 | Higher scores indicate higher distress caused by asthma |
| ABS | The Affects Balance Scale (ABS; Bradburn163) is a self-reported measure, which rates the degree to which participants experienced 20 positive and 20 negative emotions during the past week through two subscales: Positive Affect Scale (PAS) and Negative Affect Scale (NAS). It is a 10-item outcome measure: it contains five statements reflecting positive feelings and five statements reflecting negative feelings | An affect balance score is calculated based on the difference between the number of yes responses to positive-feeling questions minus the number of yes responses to negative-feeling questions | The greater the score difference, the higher the affect unbalance |
| Abdominal pain frequency | Stomach pain frequency was rated when it was sufficiently bad not to pursue with normal activity | From 0 to 5 With 0 (not at all), 1 (once), 2 (once a week), 3 (about two or three times a week), 4 (about every other day), 5 (every day) |
Higher scores indicate more frequency of abdominal pain |
| ACT | The Asthma Control Test (ACT), a five-question survey (with 4-week recall) on symptoms and daily functioning, which is self-administered by the patient to measure asthma control in individuals of ≥ 12 years. The survey measures the elements of asthma control as defined by the National Heart, Lung, and Blood Institute: frequency of shortness of breath and general asthma symptoms, use of rescue medications, the effect of asthma on daily functioning, and overall self-assessment of asthma control. ACT is clinically validated by specialist assessment and spirometry (www.thoracic.org/assemblies/srn/questionaires/act.php) | 5-point scale for symptoms and activities from 1 (all the time) to 5 (not at all); for asthma control rating from 1 (not controlled at all) to 5 (completely controlled). The scores range from 5 (poor control of asthma) to 25 (complete control of asthma) | Higher scores reflecting greater asthma control. An ACT score of > 19 indicates well-controlled asthma |
| Adherence | Self-reported adherence in the study by Mann72 was measured using the general measure of adherence from the RAND Medical Outcomes Study. It consists of five items | 6-point Likert scale ranging from 1 (none of the time) to 6 (all of the time) | NA |
| ADSEI | An adult version (Ryden164) of the Coopersmith Self-Esteem Inventory (SEI; Coopersmith165): test–retest reliability and social desirability The Coopersmith Self-Esteem Inventory (SEI): 58 short statements that are answered by checking the box like me or unlike me. These items consist of 50 self-esteem items and eight items that compose a lie scale, anxiety, depression, behavioural problems and physical well-being |
The test has a built-in lie scale that helps to determine if the participant is trying too hard to appear to have high self-esteem | The higher the number of like me, the greater the participant’s self-reports are markedly influenced by the social desirability factor |
| AEE | The Ambivalence Emotional Expression (AEE; King and Emmons166) Questionnaire is a 28-item questionnaire used to assess the extent to which participants feel uncomfortable or regret expressing their emotions (e.g. I’d like to talk about my problems with others but at times I just cannot, I feel guilty after I have expressed anger to someone) | The test predicts more benefit from disclosure | NA |
| AIMS2 | The Arthritis Impact Measurement Scale-2 (AIMS2) is a 28-item scale that surveys the effects of arthritis on multiple domains of functioning during the previous month. It uses six subscales: mobility level (e.g. you were in bed or chair for most of the day), walking and bending (e.g. you had trouble either bending, lifting, or stooping), hand and finger function, arm function, self-care tasks, and household tasks. In the study by Lumley et al.115 they analyse two scales: (1) physical dysfunction, which assesses dysfunction in mobility, walking/bending, hand and finger function, arm functioning, ability to perform household tasks, and self-care; and (2) affective disturbance, which assesses both anxious and depressive symptoms | 5-point scale with respect to the frequency (number of days in a week) that a particular behaviour or symptom was experienced from 1 (all days) to 5 (no days). Ratings are averaged | Higher scores indicate greater dysfunction |
| AIMS2: lack of social support subscale | The 4-item subscale from the AIMS2 assesses one’s perceptions that family and friends are available if needed, are sensitive to needs, interested in helping, and understand the effects of the FM. Items were rated regarding how frequently support is available | From 1 (all days) to 5 (no days) and averaged | Higher values indicate less social support |
| AIMS2: pain subscale | The 5-item pain subscale from the AIMS2, a widely-used instrument that measures health status in rheumatic diseases during the past month. Items were worded for FM rather than arthritis (e.g. you had severe pain from your FM) | 5-point scale from 1 (all days) to 5 (no days), reverse scored and averaged | Higher values indicate more pain |
| AIMS2 for physical dysfunction | The AIMS2 was used and assessed 28 items from six subscales: mobility level (you were in bed or chair for most of the day), walking and bending (you had trouble either bending, lifting, or stooping), hand and finger function, arm function, self-care tasks and household tasks | 5-point scale from 1 (all days) to 5 (no days) and scored | Higher scores indicate greater physical dysfunction |
| ARS-20 | The Assertiveness/Responsiveness scale (ARS-20; Richmond and McCroskey167) is a 20-item scale consisting of two subscales, one for each trait, with 10 items each | Both scales ask respondents to rate how much they identify with a list of representative behaviours. Behaviours for the Assertiveness scale include items like defend own beliefs and have strong personality, whereas items from the Responsiveness scale include items such as sympathetic and sensitive to the needs of others | Higher scores indicate greater levels |
| ASS | The Asthma Sum Scale (ASS) is a 9-item scale used to report both asthma and nasal or allergy symptoms during the past 2 weeks | 5-point scale from 0 (none) to 4 (severe) | Higher scores indicate greater symptoms |
| BA use | Beta-agonist use, measured as puffs per day | Numbers of puffs per day were summed up | Higher number of puffs indicated greater symptoms |
| BAI | The Beck Anxiety Inventory (BAI; Beck and Steer168) is a 21-item self-report measure that uses a 4-point Likert scale with ratings from not at all to severely to measure physical and cognitive symptoms of anxiety | Each BAI item is rated on a 4-point scale: 0 (not at all) to 3 (severely, I could barely stand it) | Higher total scores indicate more severe anxiety symptoms |
| BAS-G | The Bath Ankylosing Spondylitis Disease Global Score (BAS-G; Jones et al.169) requires patients to respond to two questions regarding the effect of their disease on their health: over the past week, and over the past 6 months. Responses to these scales are indicated by marking a line on a 100-mm VAS | Scale 0–10 VAS, best 10 Total score range from 0 to 10 |
Higher scores indicate greater effect of AS on the patient’s life |
| BASDAI | The Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) comprises six questions relating to individual domains of fatigue, spinal pain, joint pain and symptoms, together with perception of pain relating to bony areas of the body and to morning stiffness BASFI comprises 10 questions regarding function in AS and ability to meet the physical demands of everyday life. Responses to these scales are indicated by marking a line on a 100-mm VAS |
Scale 0–10 VAS, best 10 Total score ranges from 0 to 10 |
Higher scores indicate higher levels of disease activity |
| BASFI | The Bath Ankylosing Spondylitis Disease Functional Index (BASFI; Calin et al.170). Responses to these scales are indicated by marking a line on a 100-mm VAS | Scale 0–10 VAS, best 10 Total score range from 0 to 10 |
Higher scores indicate to greater limitation of function |
| BDI | The Beck Depression Inventory (BDI; Beck et al.171). The full BDI has 21 items, which stress cognitive symptoms of depression, each with four Guttman-type responses choices in the form of statements, ranked in order of severity. In some categories, two alternative statements are assigned the same score | Scale 0–3, reflecting severity Total scores range from 0 to 63 |
Higher total scores indicate more severe depressive symptoms |
| BDI-II | The revised Beck Depression Inventory (BDI-II; Beck et al.172) is a 21-item self-report measure incorporating cognitive, affective and somatic aspects of depressed mood. In this revised version, there is one alternative score for each level (so no statement is assigned the same weight) | Four alternatives for the 21 items ranging from 0 (low) to 3 (high). Total scores range from 0 to 63 | Higher total scores indicate more severe depressive symptoms |
| BDI-SF | The short 13-item version of Beck Depression Inventory (BDI-SF; Beck et al.173 and Furlanetto et al.174) measures depressive symptoms during the last 7 days | NA | Higher total scores indicate more severe depressive symptoms |
| BFI | The Brief Fatigue Inventory (BFI; Mendoza et al.175) is a 10-item questionnaire asking participants to rate the severity of their fatigue and the degree to which it interferes with their lives. BFI has been specifically developed for cancer patient populations | Response to the first question, ‘Are you usually tired?’ is either yes or no. The remaining nine items are measured on a 11-point Likert scale ranging from 0 (no fatigue) to 10 (worst that you can even imagine). Individual scores are added up in a total score | Higher scores indicate worse fatigue, and a score of > 3 indicates clinically significant fatigue |
| BITE | The Bulimia Investigatory Test Edinburgh (BITE; Henderson and Freeman176). This 33-item scale provides a rating of symptoms of BN and BED, and has a symptom and severity subscale. BITE was used to measure symptoms over the past month, as a response to treatment. The symptom scale comprised 27 items and the severity scale comprised three items |
|
|
| BMI | In the study by Taylor et al.,89 the body mass index (BMI) was recorded as kg body weight (kg)/height (m2) | NA | A reduction in the BMI indicated disease progression and/or exacerbation |
| BPI | The Brief Pain Inventory (BPI), short form, is a 11-item self-report rating scale using simple numeric rating scales to assess the severity of pain (four questions) and impact of pain (seven questions) | From 0 to 10 | Higher scores indicate greater pain |
| Brief COPE | The Brief COPE is a 28-item measure of 14 coping responses (Carver177). The responses can be categorised as adaptive coping (e.g. active coping, planning, use of emotional support) and maladaptive coping (e.g. denial, self-blame and behavioural disengagement) | 5-point Likert scale ranging from 1 (I haven’t been doing this at all) to 5 (I have been doing this a lot) Items are calculated into 14 separate indices |
Higher scores indicate greater active coping |
| Brief POMS | The Brief Profile of Mood States (Brief POMS) provides a summary measure of distress or mood. The original 65-item POMS has been widely used with cancer patients | 5-point Likert scale ranging from 0 (not at all); 1 (a little); 2 (moderately); 3 (quite a bit); 4 (extremely) | Higher scores indicate higher distress |
| BSCS | The Brief Substance Craving Scale (BSCS) is a 12-item self-report instrument assessing intensity, frequency and length of craving over a 24-hour period for substances of abuse. Each of the three items is related to the intensity, frequency and length of craving during the prior 24 hours. In Grasing et al.,90 the reductions in craving intensity were measured and those are calculated by subtracting baseline measures recorded during screening from results obtained at the initial outpatient visit | 5-point Likert scale ranging from 0 (not at all) to 4 (extremely). The total score ranges from 0 to 12 | Higher scores indicate higher craving |
| BSI | The Brief Symptom Inventory (BSI; Derogatis and Melisaratos178) is a 53-item scale, a shortened version of the SCL-90 (Symptom Checklist-90) that assesses nine symptoms of distress and provides three global distress indices. The BSI measures symptoms associated with distress on nine symptom dimensions (including somatisation, obsessive–compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation and psychoticism). Participants report the extent to which they experienced each of the symptoms in the past week including today. The scale also includes a global index of distress, the Global Severity Index (GSI) used in both studies by Zakowski et al. published in 200484 and 2011161 | Likert-type scale ranging from 0 (not at all) to 4 (extremely) | Higher scores indicate higher symptoms |
| C-QoL | Cancer Quality of Life (C-QoL; Lee179) is a cancer-specific type of QoL measurement tool developed in Korea to better reflect the cultural characteristics of the country. The C-QoL was used in Park and Yi78 and consists of 21 items with specific questions: physical conditions (n = 6), emotional states (n = 6), social role (n = 3), social status (n = 3) and coping ability (n = 4) | 5-point scale (0 = not at all, 1 = a little yes, 2 = moderate, 3 = quite a lot and 4 = very much so) Range from 0 to 84 |
Higher scores indicate greater QoL |
| CAPS | The Clinician-Administered PTSD Scale (CAPS; Weathers et al.180) used to assess PTSD symptom severity. CAPS rates the frequency and intensity of each symptom along 5-point ordinal scales, the impact of symptoms on the patient’s social and occupational functioning, the overall severity of the symptom complex, and the global validity of ratings obtained. There is a total score for the CAPS PTSD ratings (frequency and intensity). The CAPS yields both dichotomous (i.e. present or absent) and continuous (i.e. severity) scores for each symptom and for the disorder as a whole | 5-point scale ranging from 0 to 136 | Higher scores indicate greater severity of PTSD symptoms |
| CBCL | The Child Behavior Checklist (CBCL) and by youth on the Youth Self-Report of the CBCL (Achenbach181) consists of 113 questions used to detect emotional and behavioural problems in children and adolescents | 3-point Likert scale ranging from 0 (absent), 1 (occurs sometimes), 2 (occurs often) | Higher scores indicate more emotional and behavioural problems |
| CD4+ count | CD4+ lymphocyte count was determined by flow cytometry. A square root transformation was used on the CD4+ counts to give an approximately normal distribution. Data were analysed as a multivariate hierarchical model using the hierarchical linear modelling programme HLM 5.04. In Ironson et al.,71 flow cytometry was performed in one laboratory to enumerate CD3+/CD4+ lymphocytes with fluorochrome conjugated monoclonal antibodies in a four-colour system | Threshold used in the study was not reported but used as a predictor of disease progression | Higher count in CD4+ cells when associated with improved immune status and better health |
| CDI | The Children Depression Inventory (CDI) contains 27 items that represent a range of depressive symptoms including disturbed mood, hedonic capacity, vegetative functions, self-evaluation and interpersonal problems. The child is asked to choose the item that best describes him or her for the past 2 weeks. The five factors for the CDI are negative mood, interpersonal problems, ineffectiveness, anhedonia and negative self-esteem | Each item consists of three statements that are keyed 0, 1 or 2 | Higher scores indicating increased severity |
| CES-D | The Centre for Epidemiological Studies Depression Scale (CES-D; Radloff182) is a 20-item scale; participants rated the intensity and frequency of depressive symptoms they had experienced in the past week. The CES-D has been used to measure clinical and subclinical levels of depression in medical populations and effectively identifies depression among patients with chronic pain (Geisser et al.183). It includes four factors: dysphoria, positive affect, a somatic factor, and an interpersonal factor. In Henry et al.,53 four subscales were calculated from the CES-D: depressed mood (seven items, α = 0.83–0.92), (lack of) positive affect (four items, α = 0.71–0.9), somatisation or retarded activity (seven items, α = 0.5–0.9), and (lack of) interpersonal relations (two items) | 4-point Likert-type scale from 0 (rarely or none of the time) to 3 (most or all of the time) | Higher scores indicates the greatest frequency of depressed mood over the past week |
| CG-FBD | The functional bowel disease-related cognition consisted of CG-FBD Q16 My bowel symptoms make me feel out of control and CG-FBD Q31 Nothing seems to help my bowel symptoms | Scale 0–7, worse cognition 7 | Higher scores indicate worse adaptive cognition |
| CLINHAQ | Three items from the Clinical Health Assessment Questionnaire (CLINHAQ; Wolfe184) were used in Broderick et al.118 to assess GI, headache and fatigue symptoms. The CLINHAQ contains self-reports for the Health Assessment Questionnaire (HAQ; Fries185) disability index, Arthritis Impact Measurement Scale (AIMS) anxiety and depression index (Hawley and Wolfe186), VAS pain, VAS global severity, VAS GI symptoms, VAS sleep problems, VAS fatigue, satisfaction with health, and patient estimate of health status. In 1996, the helplessness subscale of the RAI was added to the CLINHAQ (deVellis et al.187). The variables contained in this questionnaire consider factors that are thought to be of major importance in FM (Burckhardt et al.188) | On a 100-point VAS | Higher scales indicate greater symptoms |
| Cortisol | Cortisol reactivity was assessed in Smyth et al.9 by asking participants to collect saliva by placing a sterile cotton wad in their mouth for a few minutes and then sealing the cotton in a salivette, a test tube-like container (Sartstedt, Rommelsdorf, Germany). Samples were kept frozen until shipped for assay at a clinical laboratory | Cortisol levels were assessed in response to imagery-based trauma re-exposure | Lower levels indicate greater health improvement |
| CRP | The C-reactive protein (CRP), which is another serum measure of inflammation, was measured in Wetherell et al.117 CRP is an acute phase protein, levels of which fluctuate over a shorter time period than ESR (Kushner189). CRP therefore provides an objective marker of disease activity in addition to the components of the DAS | CRP is a measure of inflammation and provide markers for clinical status in rheumatic disease. CRP is sensitive and is only raised during periods of acute inflammation | Higher CRP levels indicate greater transitory acute inflammation |
| CRQ | The Chronic Respiratory Disease Questionnaire (CRQ) is an interviewer-administered questionnaire measuring both physical and emotional aspects of chronic respiratory disease. It has 20 questions in four categories: dyspnoea, fatigue, emotional function and mastery | 7-point scale, with 7 indicating no health impairment. A change of 0.5 for each is considered the minimal clinically significant change | Higher scores indicate better HRQoL |
| CS use | Corticosteroid use, measured as puffs per day | CS use is an indicator of disease status | The higher the use of CS, the worst the disease course |
| CSAQ | The Cognitive-Somatic Anxiety Questionnaire (CSAQ; Schwartz190) a trait anxiety inventory, is a 14-item self-report inventory that is divided into two 7-item scales (cognitive and somatic) that appear to reflect cognitive or somatic anxiety. Participants are asked to rate the degree to which they are generally or typically experiencing symptoms of anxiety by circling a number from 1 through to 5 | 5-point Likert scale ranging from 1 (not at all) to 5 (very much so). The sums of the circled rating are separately computed for the cognitive and somatic items, and constituted the main dependent measures | Higher total scores indicate higher symptoms |
| CSI | The Children’s Somatisation Inventory (CSI) includes 36 symptoms from the criteria for Somatisation Disorder and the Somatisation factor of the Hopkins Symptom Checklist. Ratings are obtained on the severity with which the youth have experienced each symptom (e.g. headaches, pains in the heart, muscle aches) in the past 2 weeks | 5-point scale from 0 (not at all) to 4 (a whole lot). A total score was calculated in the standard fashion to measure severity of general somatisation symptoms | Higher scores indicate higher severity of symptoms |
| CT3 | Catastrophising (maladaptive coping) | Scale 0–36; worse catastrophising, 36 | Higher scores indicate worse catastrophising |
| DAS | The Disease Activity Score (DAS) involves measurement of four variables: counts of the number of swollen and tender joints (assessed by physical examination); a patient self-report measure (All things considered, how are you feeling?), measured using a 100-mm VAS; and a serum measure of inflammation, i.e. ESR. ESR is an indirect measure of acute phase reactions and provides a standardised and validated clinical index for assessing disease activity in RA (Fuchs191). A total score can be computed or individual components of the DAS can be used | The DAS ranges from 2 to 10 | Scores of < 2.6 indicate disease remission and scores of > 5.1 indicate high disease activity |
| DASS | The Depression Anxiety Stress Scales (DASS) is a 42-item self-report measure used to assess depression, anxiety and stress in clinical samples over the previous week | 4-point Likert scale from 0 (did not apply to me at all) to 3 (applied to me very much, or most of the time) | Higher scores indicate greater symptoms |
| Davidson PTSD scale | The Davidson PTSD scale (PTSDTOT; Davidson et al.,192 Zlotnick et al.193) is a 17-item, interview-administered measure based on the PTSD symptom clusters defined by DSM-IV. Respondents are asked to rate each of the 17 items referring to a particular traumatic event, or series of events, according to level of distress based on their ratings of symptoms that have occurred during the past week. Both frequency and severity are rated for each item. If the respondent has experienced multiple traumatic episodes, multiple copies of the scale may be administered | From 0 to 4 for both frequency and severity during the past week Items are summed for a total score, and subscales measure re-experiencing, avoidance and arousal |
Higher scores indicate greater symptoms |
| DBP | Diastolic blood pressure (DBP), measured in mmHg | BP is indicative of chronic complications post MI, such as cardiac arrhythmias and left ventricular failure | Higher DBP indicated greater post-MI complications |
| DIS | The Perception of Disclosure Scale (DIS) measures the perception of the extent to which participants had already expressed their deepest thoughts and feelings about their cancer experience through writing or discussion with others | Scale ranges from 0 (not all) to 10 (complete disclosure) | Higher scores indicate more complete disclosure |
| Disease Activity Rating Scale | The Disease Activity Rating Scale is a scale used by physicians to indicate the current status of the patient’s RA. Factors that physicians would take into account in making this rating include number of tender and swollen joints, and degree of inflammation and pain | 5-point rating scale ranging from 0 (asymptomatic) to 4 (very severe) A 1-point change is considered clinically significant |
Higher scores indicate greater disease activity |
| DLQI | The Dermatology Life Quality Index (DLQI; Finlay and Khan194) is used widely in patients with dermatological conditions, including psoriasis. It examines respondents views on the functional consequences of their skin condition on their lives in the previous week. It correlates well with clinical measures of disease severity and boasts of good reliability statistics. It measures how much the skin problem has affected your life. It is designed for young people aged > 16 years and for adults | 4-point Likert scale ranging from very much to not at all The scoring is:
|
The higher the score, the more QoL is impaired |
| DS-14 | The DS-14 is a 14-item measure of negative affectivity (seven items) and social inhibition (seven items) (Denollet195) The DS-14 has good psychometric properties and is widely used with cardiac populations (e.g. Denollet et al.196) |
5-point Likert scale from 0 to 4 | A score of ≥ 10 on both the negative affectivity and social inhibition scales indicates Type D personality |
| DT | The Distress Thermometer (DT; Roth et al.197) assessed general distress | 11-point Likert scale from 0 (no distress) to 10 (extreme distress) | Higher scores indicate greater distress |
| Emotional approach coping | In Averill et al.,100 the emotional approach coping (Stanton et al.198) was measured to assess emotional processing (four items: e.g. I take time to figure out what I am really feeling; α = 0.76) and emotional expression (four items; e.g. I feel free to express my emotions; α = 0.89). Because the two subscales were correlated only 0.61, they were used separately in analysis | 8-item scale | Lower emotional approach copying are related to lower psychological well-being |
| EQ-5D | QoL measured by utility and VAS. A measure of perceived health status | Utility: 0–1, where 0 is death and 1 is perfect perceived health VAS: 0–100, where 0 is death and 100 is perfect perceived health |
Higher scores indicate better health |
| ESR | The erythrocyte sedimentation rate (ESR) | ESR is an indicator of inflammation and disease activity | Values of > 20 mm/hour indicate elevated inflammation and disease activity |
| Expressed anger | In Graham et al.,51 the degree of express anger was uniquely accounted for intervention effects and meaning making mediated effects on depressed mood | From 0 (none) to 4 (very much) A code of 4 was given when the letter included an explicit statement indicating that the participant was, for instance, very angry or furious or if the participant had used many examples that sounded frustrating and/or used underlining, exclamation points, or other techniques for emphasis A code 0 was given when the participant neither identified at all with an anger-related emotion (including frustration) nor gave any examples that seemed frustrating |
Higher scores indicate higher expression of anger |
| FACIT-F | The Functional Assessment of Chronic Illness Therapy Fatigue subscale version 4 (FACIT-F; Yellen199) assessed fatigue during the past 7 days. It measures physical well-being, social/family well-being, emotional well-being, functional well-being and additional concerns | All items are measured on a 5-point Likert scale ranging from 0 (not at all) to 4 (very much) | Higher scores indicate greater fatigue |
| FACIT-Sp | The meaning/peace subscale of the Functional Assessment of Chronic Illness Therapy–Spiritual Well-Being scale (FACIT-Sp; Peterman et al.200) A 12-item self-report measure comprises two subscales: one measuring a sense of meaning and peace and the other assessing the role of faith in illness A total score for spiritual well-being is produced. In Mosher et al.,77 the FACIT-Sp is used to measure existential well-being by assessing participant’s degree of purpose in life and inner peace |
Scale ranging from 0 to 48 Two subscales:
|
Higher scores signifying greater spiritual well-being |
| FACT-General | The Functional Assessment of Cancer Therapy (FACT; Basen-Engquist et al.201) questionnaire is a 34-item general cancer QoL measure for evaluating patients receiving cancer treatment. It covers five general cancer-related domains (physical well-being, social family well-being, relationship with health-care provider, emotional well-being, and functional well-being) and one disease/site-specific domain | 5-point scale from 0 (not at all) to 4 (very much) | Higher scores indicate better QoL |
| FACT-B | The Functional Assessment of Cancer Therapy-Breast Cancer Version (FACT-B) is a 37-item self-report instrument, with known validity and reliability, containing 27 general items (from the FACT-General) plus 10 breast cancer-specific items (Brady et al.202) Subscales include physical well-being (seven items), social/family well-being (seven items), emotional well-being (six items) and functional well-being (seven items) The 10 additional items address physical and psychological concerns related to breast cancer Respondents are asked to rate how true each statement had been for them over the past 7 days |
5-point Likert-type scale from 0 (not at all) to 4 (very much). All 37 items can be combined for a total QoL score, and subscale scores may be computed as well | Higher scores indicate higher QoL |
| FDI | The Functional Disability Inventory (FDI; Walker and Greene203) is a 15-item assessing difficulty performing various routine behaviours during the last few weeks | Items range from 0 (no trouble) to 4 (impossible) and totalled | Higher scores indicate greater disability |
| FEV1 | The forced expiratory volume in 1 second (FEV1) | FEV1 is one of the primary indicators of health status and disease progression for cystic fibrosis or patients with asthma, for instance | A decrease in FEV1 indicates disease exacerbation and/or reduction of lung functioning |
| FIQ | The Fibromyalgia Impact Questionnaire (FIQ) evaluates the global health status using a 10-item survey assessing those components of health that are most affected by FM (physical functioning, work status, depression, anxiety, sleep, pain, stiffness, fatigue and well-being) during the prior week FIQ is an adaptation of the HAQ and the AIMS In Broderick et al.,118 items assessing physical functioning and stiffness were used |
Scores range from 0 to 100 | Higher scores indicate poorer health or functioning |
| FLZ | The Fragebogen zur Erfassung des Lebenszufriendenheit (FLZ) is a Life Satisfaction Scale used to measure life satisfaction The FLZ uses eight items assessing patient’s satisfaction with different areas of their life (e.g. social contacts, partnership, financial situation) |
7-point Likert scale from 1 (very satisfied) to 7 (very unsatisfied) The sum score indicates overall life satisfaction |
Higher scores indicate less life satisfaction |
| FSS | The 9-item Fatigue Severity Scale (FSS) assesses the frequency and severity of fatigues interference with physical functioning | Items were rated on a 1–7 scale and averaged | Higher scores indicate greater fatigue |
| FVC | The forced vital capacity (FVC) | FVC is one of the primary indicators of health status and disease progression for cystic fibrosis or patients with asthma, for instance | A decrease in FVC indicates disease exacerbation and/or reduction of lung functioning |
| GBB | The Giessener Beschwerdebogen (GBB) is a 24-item scale assessing various symptomatic complaints The sum score measures subjective physical well-being |
5-point Likert scale ranging from 0 (not applicable) to 4 (strongly) The total score ranges from 0 to 12 |
Higher scores indicate greater symptoms, decreased subjective physical health |
| GDS | The Geriatric Depression Scale (GDS; Yesavage et al.204) is a 30-item scale that is more appropriate for use with people with ALS than other depression instruments that include somatic symptoms regularly experienced in ALS |
|
Higher scores indicate higher symptoms of depression |
| GHQ-12 | The General Health Questionnaire (GHQ-12; Goldberg et al.205) was used as an indicator of overall mental health in hundreds of studies that assessed both clinical and non-clinical populations Items from the GHQ-12 included: Have you recently been able to concentrate on what you are doing? Have you been able to face up to your normal problems? Owing to the various thresholds of the GHQ-12, the mean GHQ score for a population of respondents was suggested as a rough indicator for the best cut-off point (Goldberg et al.206). Therefore, based on the mean GHQ score for this sample, the cut-off point is used to determine the respondent’s level of psychological well-being |
4-point Likert scale The scores are summed up by adding all the items on the scale ranging from 0 to 12 |
NA |
| GSI | The Global Severity Index (GSI) is a widely used index of stress and is highly correlated with the BSI subscales. Individuals report the extent to which they experienced each of the symptoms in the past week including today | 5-point Likert scale Ranges from 0 (not at all) to 4 (extremely) |
Higher scores indicate greater severity |
| HADS | The Hospital Anxiety and Depression Scale (HADS; Zigmond and Snaith207), which contains 14 items (seven anxiety items and seven depression items) This scale requires participants to indicate how they have been feeling during the past week. In Wallander et al.,109 participants with a HADS total score of 15 were classified as being clinically distressed |
4-point scale ranging from 0 (not at all) to 3 (most of the time) Total score ranges from 0 to 21 |
Higher scores indicate higher anxiety/depression |
| HADS-A | The anxiety subscale of the Hospital Anxiety and Depression Scale (HADS-A; Zigmond and Snaith207) | A score of 0–7 is considered to be normal Scores of ≥ 20 indicate moderate, severe or very severe anxiety |
Higher scores on each individual scale or the entire scale indicate greater anxiety or mood disorder |
| HADS-D | The depression subscale of the Hospital Anxiety and Depression Scale (HADS-A; Zigmond and Snaith207) | A score of 0–7 is considered to be normal Scores of ≥ 20 indicate moderate, severe or very severe depression |
Higher scores on each individual scale or the entire scale indicate greater depression or mood disorder |
| HAM–D | The Hamilton Depression Scale (HAM–D; Hamilton208) is a 17-item, interview-based measure, considered the gold standard for assessing severity of depression | A score of 0–7 is considered to be normal Scores of ≥ 20 indicate moderate, severe, or very severe depression |
Higher scores indicate more depression or mood disorder |
| Headache frequency | Number of days in the last month with a headache | NA | The higher the frequency the worst the health status |
| HIV symptom checklist | In Ironson et al.,71 experimenters assessed symptoms relevant to HIV (based on the Centre for Disease Control and Prevention criteria for Category B symptoms) by interview using a HIV symptom checklist Symptoms were assessed for the previous month at baseline and the 1-month visit, and for the previous 6 months, at the 6- and 12-month visits; thus, symptoms were assessed during the complete follow-up period |
Examples of symptoms are herpes zoster (shingles), oral thrush, cervical dysplasia, pelvic inflammatory disease, low platelet count (50,000), peripheral neuropathy, chronic unexplained fever and chronic unexplained diarrhoea | More symptoms indicate a worse health |
| HIV VL | HIV VL was determined using a quantitative reverse-transcriptase PCR assay (Amplicor HIV-1 Monitor, Roche Diagnostic Systems), which measures down to 400 copies of HIV RNA in plasma | Threshold not reported | A reduction in VL indicates better health |
| HIV-OS | The HIV-Specific Optimism Scale (HIV-OS) is a self-report measure of optimistic beliefs related to HIV issues Seven items were adapted from the LOT (Scheier and Carver209) specifically for Wagner et al.73 Sample HIV-OS items include ‘I am not counting on things going my way in the course of my HIV infection’ and ‘Although the future course of my HIV infection is uncertain, I expect the best’ |
6-point Likert scale ranging from strongly disagree to strongly agree | Higher scores indicate higher levels of optimism related to HIV issues |
| IBS-QoL | The Irritable Bowel Syndrome QoL | Scale 0–100, best = 100 | Higher scores indicate better QoL |
| IBSSS | The irritable bowel severity (IBS) scale/scoring system (IBSSS; Francis et al.210) is a 9-item survey designed to enable clinicians to record and monitor the severity of IBS Participants have to answer the questions based on how they feel currently (i.e. over the last 10 days or so) A total IBS severity score is given |
|
Higher scores indicate increase in IBS severity |
| IES | The Impact of Event Scale (IES; Horowitz et al.211) assesses frequency of intrusive thoughts and avoidance over the past week including today. Participants are asked to specifically refer to their cancer experience when answering the questions | Responses for each item are 0 (not at all); 1 (rarely); 3 (sometimes); 5 (often) Possible score ranges from 0 to 40 |
Higher scores indicate the greater extent to which participants have experienced each item, in the preceding 7 days |
| IES-R | The Impact of Event Scale-Revised (IES-R; Weiss and Marmar212), which contains 22 items that measure avoidance, intrusive re-experiences and arousal associated with a traumatic event | 5-point scale ranging from 0 (not at all) to 4 (extremely) | Higher scores indicate greater extent to which participants have experienced each item in the preceding 7 days in relation to their psychotic experiences and treatment |
| IS | The 8-item Insight Scale (IS; Birchwood et al.213), which measures three dimensions of insight: perceived need for treatment, awareness of illness and relabelling of symptoms as pathological | Response to each item reported as agree, disagree or unsure | NA |
| K-10 | The Kessler Psychological Distress Scale (K-10) detects non-specific emotional distress and has been used in a number of population health surveys in Australia. It contains 10 statements covering the preceding 4 weeks | 5-point Likert scale from 1 (none of the time) to 5 (all the time) Possible scores range from 10 (no distress) to 50 (maximal distress) |
Higher scores indicate higher distress |
| LIFE | The Longitudinal Interval Follow-Up Evaluation (LIFE; Keller et al.214) is a semistructured interview for assessing the longitudinal course of psychiatric disorders It consists of a semistructured interview, an Instruction booklet, a coding sheet, and a set of training materials. An interviewer uses the LIFE to collect detailed psychosocial, psychopathological, and treatment information for a 6-month follow-up interval The weekly psychopathology measures (psychiatric status ratings) are ordinal symptom-based scales with categories defined to match the levels of symptoms used in the Research Diagnostic Criteria The ratings provide a separate, concurrent record of the course of each disorder initially diagnosed in patients or developing during the follow-up Any DSM-III or Research Diagnostic Criteria disorder can be rated with the LIFE, and any length or number of follow-up intervals can be accommodated. The psychosocial and treatment information is recorded so that these data can be linked temporally to the psychiatric status ratings |
NA | NA |
| LIWC | The Linguistic Inquiry and Word Count (LIWC) is a text analysis software program designed by Pennebaker et al.19 LIWC calculates the degree to which people use different categories of words across a wide array of texts, including e-mails, speeches, poems, or transcribed daily speech. With a click of a button, you can determine the degree any text uses positive or negative emotions, self-references, causal words, and 70 other language dimensions (www.liwc.net/) |
NA | NA |
| LOT | The Life Orientation Test (LOT) assesses generalised positive outcome experiences measures optimism on eight items to indicate the extent to which they agree with each statement | 5-point Likert scales ranging from 1 (strongly agree) to 5 (strongly disagree) The items are summed to create a score ranging from 8 to 40 |
Higher numbers indicate more optimism |
| Mac New HRQOL | The Mac New Health Related Quality Of Life (Mac New HRQOL) scale is a 27-item measure of physical, emotional and social QoL (Valenti et al.215) In addition to separate physical, emotional and social QoL subscales, an overall index of QoL is provided. It has been extensively used in cardiac populations, and based on data from over 1000 cardiac patients |
7-point Likert scale. A change of 0.5 units reflects a minimal clinically important difference (Dixon et al.216) | Higher scores indicate better health |
| Marks | The Marks Asthma Quality of Life Questionnaire (Marks; Marks et al.217) is a self-administered questionnaire intended for use with adults Respondents are asked to describe how troubling particular items have been over the past 4 weeks. Covers both physical and emotional impact Should not be confused with the Asthma Quality of Life Questionnaire (AQLQ; Juniper et al.218) |
Scaling of items from 1 to 5 | NA |
| McGill Pain Q-SF | The McGill Pain Questionnaire-Short Form (McGill Pain Q-SF; Melzack219) assesses these two dimensions of pain, as currently experienced by the patient. It contains 11 items assessing several domains of pain experience: intensity, sensory and affective | Scale from 0 (none) to 3 (severe) scale Ratings were averaged |
Higher scores indicate greater severity |
| McGill QOL | In Averill et al.,100 psychological and existential QoL were measured with the McGill QOL questionnaire to assess the subjective QoL of patients with terminal illness. Psychological QoL reflects the extent to which patients have experienced symptoms of depression, anxiety, sadness and hopelessness. There were six measures of psychological well-being that were highly correlated with each other: positive affect, negative affect, depression, psychological QoL, existential QoL and spirituality Existential QoL reflects patients’ ratings of the worth and meaning of their life, their progress towards their goals, their control over their life and the value of each day |
11-point Likert scale ranging from 0 to 10 Scores are summed up into a total score |
Lower scores indicate better health |
| MDASI | The MD Anderson Symptom Inventory (MDASI; Cleeland et al.220) is used to assess multiple symptoms experienced by cancer patients and the interference with daily living caused by these symptoms. Participants rate the severity of 13 core symptoms (in the last 24 hours) common across all cancer diagnoses and treatments and the extent to which these symptoms interfere with daily activities In Park and Yi78 a Korean version (Yun et al.221) was adapted |
From 0 (symptom has not been present) to 10 (the symptom was as bad as you can imagine it could be) | Higher scores indicate greater severity and interference |
| MIDAS | The Migraine Disability Assessment Scale (MIDAS) is a 5-item inventory that assesses the number of days in the past month when the respondents functioning was reduced or impaired because of headaches (behavioural disability from headaches) including days of work (including housework), school or other activities missed, as well as the number of days for which productivity was reduced by half A total of five items are calculated and analysed |
The number of days is added up, totalling a final number of days from questions 1–5 MIDAS scores thresholds are as follows:
|
Higher scores indicate greater migraine disability |
| Mississippi Scale for PTSD | The Mississippi Scale for combat-related PTSD (Hebrew version) is a 35-item self-reported questionnaire describing participant’s feeling on each of the items Items 2, 6, 11, 17, 19, 22, 24, 27, 30 and 34 are scored in reverse order The cut-off score for PTSD is set at 107, a score that correctly classifies 90% of all subjects as PTSD or non-PTSD Means for the three validation groups are as follows: PTSD 130 (SD = 18); psychiatric 86 (SD = 26); well adjusted 76 (SD = 18) |
Each item receives a score of 1–5 Add all items to obtain the total score |
A total score of > 107 indicates a diagnosis of PTSD |
| MMSE-Korean | The Mini Mental State Examination (MMSE) is often taken to rate cognitive functioning difficulties in a relatively short time: in the present study, the Korean version of MMSE, named MMSE-K, was used in the included study by Hong and Choi67 The MMSE-K has 30 questions for rating and each question is counted as one point. The full score of MMSE-K is 30 points. It consists of seven subitems. The standard MMSE-K was slightly modified, combining time orientation and space orientation into orientation to which 10 points were allocated, and also unifying memory registration and memory recall to memory to which six points were allocated Diagnostic criteria of dementia in terms of the MMSE-K score are given as follows: a total score of > 23 points is classified as normal, 20–23 points as doubted as dementia and < 20 points as dementia |
The score of each item is allocated as follows: (1) 5 points for time orientation, (2) 5 points for space orientation, (3) 3 points for memory registration, (4) 3 points for memory recall, (5) 5 points for attention and calculation, (6) 7 points for language, and (7) 2 points for comprehension and judgement | A total score of < 20 indicates dementia |
| Modified MRC dyspnoea scale | The Modified Medical Research Council dyspnoea scale (MMRC) is an instrument to document subjective feeling of shortness of breath | From 0 (shortness of breath only with strenuous activity) to 4 (shortness of breath with minimal activity, even dressing or undressing) | Higher scores indicate higher subjective feeling of shortness of breath |
| MOS-HIV | The Medical Outcomes Study HIV Health Survey, a brief, multidimensional and comprehensive measure of HRQoL used extensively in HIV/AIDS research (MOS-HIV; Wu et al.222) It measured the physical functioning, pain, and mental health using three subscales:
|
|
|
| MPI | The Multidimensional Pain Inventory (MPI; Kerns223) is a 48-item self-reported questionnaire, divided in three sections In the first section, the participant responds about their pain, and how it affects their lives In the second section, the participant responds about how his/her spouse or significant others respond to them in that particular way when they are in pain In the third section, the participant responds to how often they do different daily tasks (such as washing dishes, going to the cinema, take a trip, or engage in sexual activities) Participants can also list any other pain-related problem |
Section 1: 7-point Likert scale ranging from 0 (not at all) to 6 (extremely) Section 2: range from never to often Section 3: range from never to often The scoring procedure produces a mean score for each scale |
Higher scores indicate greater pain |
| MSPSS | The Multidimensional Scale of Perceived Social Support (MSPSS; Zimet et al.224) is a 12-item self-report measure used to measure perceived social support | 7-point Likert scale from 1 (very strongly disagree) to 7 (very strongly agree) | Higher scores indicate higher perceived social support |
| NMCUES | The National Medical Care Utilisation Expenditure Survey (NMCUES; National Centre for Health Statistics225) It assesses multiple forms of health-care utilisation and behaviours over a period (3 months in Rosenberg et al.83) Questions addressed health-care utilisation patterns, current use of medicines and health-related behaviours (e.g. smoking, substance use) |
NA | NA |
| OQ-45.2 | The Outcome Questionnaire (OQ-45.2; Lambert et al.226) is a 45-item self-report measure intended for weekly assessment of client progress through the course of psychotherapy The OQ-45.2 produces a total score and three subscale scores (symptom distress, interpersonal relations and social role) |
The total score is calculated by summing the patient’s ratings across all 45 items (range 0–180) | Higher scores indicate greater clinical improvement |
| PAID | Problem Areas In Diabetes scale (PAID; Polonsky et al.227), otherwise not described | NA | NA |
| Pain behaviour | In both included studies by Lumley et al.115 and Macklem,131 a structured observation system228 which was designed for RA patients, assessed overt pain behaviour At each evaluation, patients were videotaped in the examination room for 10 minutes by a camera in the doorway while they engaged in four standardised manoeuvres (walking, sitting, standing and reclining), which were presented in a random order. The research assistant operated the camera and refrained from interacting with the patient other than to give directions for the next behaviour Raters were trained to code these videotapes by the developer of the system (Francis J Keefe) and achieved high inter-rater reliability during training. Next, these raters, blind to experimental condition, reviewed study videotapes for the presence of seven pain behaviours: guarding, bracing, grimacing, sighing, rigidity, passive rubbing and active rubbing The 10-minute tapes were divided into 20 30-second epochs; the presence or absence of each pain behaviour during each epoch was recorded, and a total score of all behaviours across all epochs was calculated |
NA | NA |
| Pain intensity | In the included study by Cepeda et al.,85 patients rated their average pain intensity using a verbal numerical rating scale In the included study by Macklem,131 pain intensity was measured using a 100-mm VAS |
Verbal numerical rating scale from 0 (no pain) to 10 (the worst pain imaginable) 100-mm VAS ranges from 0 (no pain) to 100 (pain as bad it can be) |
Higher scores indicate more pain intensity |
| PANAS-X(a) | The Positive and Negative Affect Schedule (PANAS; Watson et al.229) which contains 16 items (eight positive items and eight negative items) In Wagner et al.73 the same scale is reported as PANAS and defined as a 20-item scale with the same 5-point response options. Words that describe feelings and emotions, such as interested, distressed, and proud load on either the positive or negative affect factor (10 items each). In this study, participants were asked to rate their feelings during the past week, including today |
5-point scale ranging from 1 (very slightly or not at all) to 5 (extremely) | Higher scores indicate greater mood change |
| PANAS-X(b) | The Positive and Negative Affect Schedule–Expanded Form (PANAS-X, Watson and Clark230) was applied to assess emotional states of patients: 60-item scale, which was created to assess not only general dimensions of emotional experience, but specific emotional states too It included the original PANAS assessing short-term mood fluctuations, with consistent psychometric results in varying populations and over various time frames: this measure consists of two 10-item scales for positive and negative affect In addition to the two original higher order scales, the PANAS-X measures 11 specific affects: joviality, self-assurance, attentiveness, fear, sadness, guilt, hostility, shyness, fatigue, serenity, surprise |
5-point scale ranging from 1 (very slightly or not at all) to 5 (extremely) | Higher scores indicate greater mood change |
| PANAS-X(c) | The Positive and Negative Affect Schedule for Children [PANAS-X(c); Laurent et al.231] is a 30-item scale, through which items are rated for affect during the past few weeks and averaged separately for positive affect (PA) and negative affect (NA) measures | 6-point scale from 0 (very slightly or not at all) to 5 (extremely) | Higher scores indicate greater mood change |
| PANAS-X(d) | The Positive and Negative Affect Schedule–Abbreviated version of the expanded version [PANAS-X(d), Watson and Clark232] was used in the included study by D’Souza et al.101 The four negative moods were highly correlated (e.g. alpha for session 1 was 0.75 for tension and 0.73 for migraine samples), so the four ratings were averaged into one negative mood score and analysed it separately from calmness |
Items rated from 1 (not at all) to 7 (a great deal) for four negative moods (anger, guilt, sadness, fear) and for calmness | Higher scores indicate greater mood change |
| PANAS-X NA subscale | The 10-item negative affect subscale from the 60-item PANAS-X rated the frequency that they experienced each item during the prior 2 weeks | 5-point Likert scale ranging from 1 (not at all) to 5 (extremely) | Higher scores indicate greater mood change |
| PASI | The Psoriasis Area and Severity Index (PASI; Feldman et al.233) is an internationally accepted, clinician-rated, psoriasis-specific score, based on the body surface area involved and on semi-quantitative estimation of erythema, infiltration and scaling; it is by far the most common tool in clinical studies and in daily practice. The head, trunk, and upper and lower extremities are assessed | Scores range from 0 (no psoriasis) to 72 (extremely severe psoriasis) | Higher scores indicate greater psoriasis severity |
| PDS | The Posttraumatic Stress Diagnostic Scale (PDS; Foa et al.234), a 49-item self-reported measure, aids in PTSD diagnosis and symptom severity, with items that parallel DSM-IV criteria A diagnosis of PTSD is made only when DSM-IV criteria A–F are met The PDS includes a symptom severity score. Respondents rate 17 items representing the cardinal symptoms of PTSD experienced in the past 30 days. Finally, respondents rate the level of impairment caused by their symptoms across nine areas of life functioning |
4-point scale Scores range from 0 to 51, and this is obtained by adding up the individuals responses of selected items The cut-off points for symptom severity rating are:
|
Higher scores indicate higher PTSD symptoms |
| PedsQL | The Paediatric Quality of Life (PedsQL) is a 23-item well-validated scale with excellent internal consistency – how much of a problem various physical activities, feelings, social situations, and school activities have been in the past month QoL domains were restricted to (a) physical (eight items) and (b) psychosocial (15 items) |
5-point scale from 0 (never a problem) to 4 (almost always a problem) | Lower scores indicate better health |
| PSA spec – CD4+/8+ | Peripheral blood T-cell proliferation to specified antigens This technique was assessed by the cell census proliferation assay method. It involves the use of a fluorescent membrane dye that partitions between daughter cells at division, in conjunction with flow cytometry to measure the proliferation of cells With mathematical deconvolution of the fluorescence histograms, the precursor frequency of cells in the original population that responded to a specific stimulus can be derived By using a second tagged fluorescent antibody to stain for lymphocyte subsets, the proliferation of specific phenotypes (CD4+/CD8+) of responding cells can be examined |
NA | NA |
| PHQ | The Patient Health Questionnaire (PHQ; Spitzer et al.,235,236) is designed as a screening instrument for use with health-care seeking populations It provides information on perceived symptoms of (a) depression, (b) anxiety, (c) somatic complaints, and (d) psychological distress The two subscales that measure symptoms of depression (nine items) and anxiety (15 items) employ DSM-IV criteria to screen for the presence of these psychiatric illnesses |
For each item:
|
Depression severity:
|
| Physician’s global rating of disease activity | In Lumley et al.,115 the evaluating physician-rated patient’s overall disease activity with a 100-mm VAS In Macklem,131 scoring was done on a 5-point Likert scale |
From 0 to 100 VAS, with anchors of 0 (no activity) to 100 (most activity) Range from 0 (asymptomatic), 1 (mild), 2 (moderate), 3 (severe) to 4 (very severe) |
Higher scores indicate higher activity |
| PILL | The Pennebaker Inventory of Limbic Languidness (PILL), a self-report questionnaire that assess the frequency of each of the most 54 physical symptoms The PILL can be scored by summing up the total number of items on which individuals score C, D or E (every month or so or higher) With this strategy, the mean score is 17.9 (SD = 4.5) based on a sample of 939 college students. You can also simply sum up the 54 items resulting in a mean score of 112.7 (SD = 24.7) (http://homepage.psy.utexas.edu/HomePage/Faculty/Pennebaker/Questionnaires/PILL.pdf) |
From 0 to 216:
|
Higher scores indicate participants are more nervous, distressed and unhappy |
| POMS | The Profile of Mood States (POMS) (McNair et al.237) consists of 34 items aimed at assessing global negative and positive affect Participants indicate how often they experienced a particular feeling (e.g. liveliness, forgetfulness, unhappiness) since their cancer diagnosis or their last survey (for subsequent waves) In the included study by Henry et al.,53 mood disturbance was calculated by summing the negative affect subscales (e.g. anger, depression, tension, fatigue, confusion) and then subtracting the positive affect subscale score (e.g. vigour) In the included study by Smyth et al.,9 the POMS assessed current mood states using subscales for depression–dejection, tension–anxiety, fatigue–inertia, vigour–activity, anger–hostility and confusion–bewilderment |
Scale from 0 (not at all) to 4 (extremely often) | Higher scores indicate greater mood disturbance |
| POMS-n | The negative affect subscale of the Profile of Mood States (POMS; Zevon and Auke238) was measured in Jensen-Johansen et al.76 with a 37-item version validated for use with patients with breast cancer (Di Lorenzo and Williamson239) | Scale from 0 (not at all) to 4 (extremely often) | Higher scores indicate greater negative affect |
| POMS-SF | The Short Form of the Profile of Mood States (POMS-SF; Shacham240) is a 37-item questionnaire that comprises six subscales measuring transient states of six moods: tension–anxiety, depression–dejection, anger–hostility, vigour–activity, fatigue–inertia and confusion–bewilderment Total mood disturbance is assessed as the sum of the scores for these six moods |
5-point Likert scale, ranging from 0 (not at all) to 4 (extremely) | Higher scores representing greater mood disturbance, except for vigour/activity, where higher scores indicate lesser mood disturbance and the score of this subscale is subtracted from the sum of the rest to provide the total mood disturbance |
| Poor sleep quality | The poor sleep quality scale used a 4-item scale designed to evaluate the previous night’s sleep regarding sleep quality, degree to which sleep was restorative, waking daytime level of alertness, and ability to concentrate | 1–7 scale and averaged | Higher values indicate poorer sleep |
| Post mTBI Symptom Checklist | The Post Mild Traumatic Brain Injury (mTBI) Symptom Checklist comprised 30 items, describing symptoms that are commonly experienced in the following days or weeks after a mTBI The list comprises questions about physical changes, changes in thinking, changes in emotions or behaviours |
NA | The higher number of items ticked, the greater post-mTBI symptoms |
| PPMS | A Passive Positive Mood Scale (PPMS) was developed for the study by Jensen-Johansen et al.,76 using words reflecting non-active positive mood to supplement the active positive mood items of the POMS vigour subscale The PPMS consists of items reflecting passive positive mood in the past 7 days (positive/bright, balanced, glad, peaceful, relaxed, at ease, calm, contented) |
NA | Higher scores indicate better passive positive mood |
| PSC | The Paediatric Symptom Checklist (PSC) is a 35-item psychosocial screen designed to facilitate the recognition of cognitive, emotional and behavioural problems The PSC is the parent-completed version, as opposite to the Paediatric Symptom Checklist-Youth Report form (PSC-Y), which is the children-completed version (see p. 317) |
Items are rated as never, sometimes or often present and scored 0, 1 and 2, respectively The total score is calculated by adding together the score for each of the 35 items |
A positive score on the PSC indicates need of further evaluation by a qualified health or mental health professional Both false positive and false negative can occur and this should be interpreted by the appropriate professional |
| PSC-Y | The Paediatric Symptom Checklist-Youth Report form (PSC-Y; Little et al.241) contains 35 items to obtain a child’s report of their emotional and behavioural problems The items describe specific emotions and behaviours, and the respondent is asked to indicate how often the items apply to them by checking always, sometimes or never |
|
A positive score on the PSC-Y indicates need of further evaluation by a qualified health or mental health professional. Both false positive and false negative can occur and this should be interpreted by the appropriate professional |
| PSQI | The Pittsburgh Sleep Quality Index (PSQI; Buysse et al.242) evaluated habitual sleep disturbances over a 1-month period It differentiates poor from good sleep quality by measuring seven areas (components): subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medications, and daytime dysfunction over the last month |
Responses for each item are: 0 (very good); 1 (fairly good); 2 (fairly bad); 3 (very bad) The total score sums the seven item scores together |
A total score of ≥ 5 is indicative of poor sleep quality |
| PSS | The 14-item Perceived Stress Scale (PSS) measure was used to assess the degree to which participants found their daily lives over the period of the past 4 weeks to be unpredictable, uncontrollable and overloading The questionnaire is designed to quantify non-specific appraised stress over the previous month |
From 1 (never) to 5 (very often) | Higher scores indicate higher levels of appraised stress |
| PSS-I | The Post-Traumatic Stress Disorder Symptom Scale Interview (PSS-I; Foa et al.243) The PSS-I was used to generate three PTSD subscale scores for re-experiencing, avoidance, and arousal symptoms The PSS-I is a 17-item semistructured interview that assesses the presence and severity of DSM-IV PTSD symptoms related to a single identified traumatic event in individuals with a known trauma history. Each item is assessed with a brief, single question. There are no probes or follow-up questions. Interviewees are asked about symptoms they have experienced in the past 2 weeks |
For each item, the interviewer assigns a rating to reflect a combination of frequency and severity from 0 (not at all) to 3 (five or more times per week/very much) | Higher scores indicate greater symptoms |
| PTGI | The Post-Traumatic Growth Inventory (PTGI; Tedeschi and Calhoun244) measures the degree of positive changes reported after experiencing a traumatic event The PTGI measures growth in five domains: new possibilities, relating to others, appreciation of life, personal strength, and spiritual changes PTGI is a 21-item self-report inventory. In addition to an overall scale score, the PTGI comprises five factors:
|
6-point Likert type scale, ranging from 0 (I did not experience this change as a result of my crisis) to 5 (a very great degree as a result of my crisis) | Higher scores indicate greater positive changes |
| QEDD | The diagnosis of eating disorder on the Questionnaire for Eating Disorder Diagnosis (QEDD; Mintz et al.245) is a 50-item diagnostic instrument based on DSM-I criteria | NA | NA |
| QOL | The Quality of Life Scale (QOL; Burckhardt et al.246), used in Broderick et al.,118 is a 16-item instrument (rather than the 15-item one found in the Flanagan version) designed to measure QoL across a broad array of life domains in patients with chronic illness Independence, doing for yourself was added after a qualitative study indicated that the instrument had content validity in chronic illness groups but that it needed an item that reflected the importance to these people of remaining independent and able to care for themselves |
7-point Likert scale ranging from 1 (terrible) to 7 (delighted) The instrument is scored by summing the items to make a total score |
Higher scores indicate better QoL |
| RCMAS | The Revised Children’s Manifest Anxiety Scale (RCMAS; Reynolds and Richmond247) is subtitled What I Think and Feel, and contains 37 written statements describing feelings or behaviours that the individual is asked to respond to by circling yes or no This measure assesses the level and nature of children’s anxiety. The yes responses are counted to determine a total anxiety score. There a four subscales (for which scores can be calculated separately): physiological anxiety; worry/oversensitivity; social concerns/concentration; lie |
NA |
|
| RSQ | The Recovery Style Questionnaire (RSQ; Drayton et al.248) is a 39-item self-report measure with the categories developed by McGlashan et al.249 integration vs. sealing over styles of adaptation to psychotic illness The RSQ includes 13 aspects of recovery style, each of which is assessed by three items |
Using a formula (Drayton 1998), the scores on each of these aspects are combined into the six following classifications along one dimension:
|
Higher scores indicate greater recovery style |
| Rumination Scale | The Rumination Scale (McIntosh et al.,250) consists of a 10-item report that assesses people’s tendency to engage in ruminative thinking | NA | NA |
| SAM | The paper-and-pencil version of the Self-Assessment Manikin (SAM; Bradley and Lang251) obtains participant’s ratings of valence (pleasantness) and arousal in response to each session (self-reported emotion) | 9-point Likert-type scale:
|
Higher scores indicate greater pleasantness |
| SAPASI | The Self-Administered Psoriasis Area and Severity Index (SAPASI; Sampogna et al.252), a patient-rated, psoriasis-specific outcome measure, is a widely validated instrument that provides an objective measure of disease severity, and has been effectively used in previous studies Participants rate the colour, induration, and scaliness of an average psoriatic lesion using three modified VASs. As in the original PASI, the SAPASI weights the involvement of the head (H), upper extremities (U), trunk (T) and legs (L) as 10%, 20%, 30%, and 40% of the total body area, respectively |
SAPASI = (0,1 × AH) + (0,2 × AU) + (0,3 × AT) + (0,4 × AL) | Higher scores indicate greater severity |
| SCL-90-R | The Symptom Checklist-90-Revised (SCL-90-R) is a 90-item, self-report measure of current psychological symptomatology, including global psychological distress It is a multidimensional complaint list based on a self-assessment covering an important part of the compliant that can be seen in the psychiatric inpatient clinic |
5-point Likert scale ranging from 0 (not at all) to 4 (extremely) Items are summed for a total score |
Higher scores indicate greater distress and psychological symptoms |
| SCS | The Social Constraints Scale (SCS; Lepore and Ituarte253) is a 15-item scale assessing perceived inadequacy of social support resulting in reluctance among individuals to express thoughts and feelings about a specific stressor, in this case their cancer experience Example items include: How often did they avoid you? How often did they minimise your problems? How often did they tell you to try not to think about your cancer? and How often did they make you feel as though you had to keep feelings about your cancer to yourself, because they made him/her feel uncomfortable? In Zakowski et al.,84 two forms of the SCS were used: one asking about constraints from patient’s spouse or partner and one asking about constraints from people in their lives other than their spouse or partner (e.g. friends or family members) The mean of the two constraint scores in all analyses (among the 19 patients who had no current spouse or partner, the constraints from others score was used, in that we considered this score to be reflective of their average constraint level) were used in the aforementioned study |
Scores range from 15 (low constraints) to 60 (high constraints) | Higher scores indicate higher social constraints |
| SDSCA | Summary of Diabetes Self-Care Activities scale (revised) (SDSCA; Toobert et al.254) Splits into general diet, specific diet, exercise, blood glucose testing and foot care subscales |
NA | NA |
| Self-rated health status (a) | Compared with the person in excellent health, how would you rate your health at the present time? | 7-point scale from 1 (terrible) to 7 (excellent) | Higher scores indicate better health |
| Self-rated health status (b) | How you rate your health overall? | From 1 (very bad) to 5 (very good) | Higher scores indicate better health |
| Serum cytokine levels of TNF-α, IL-4 and IL-10 | Levels were determined using a high sensitivity ELISA sandwich essay In this method, the concentration of the selected cytokine in the serum is calculated from the linear portion of a standard curve of purified cytokine at known concentrations |
The detection limits of the assay were < 0.25 pg/ml | The detectable range for TNF-α was 0.5–32 pg/ml and for IL-10 0.8–50 pg/ml |
| Sexual health and performance | In the included study by Pauley et al.,82 sexual health and performance was assessed by a designed 6-item measure created by the authors The scale was intended to work as two separate subscales: one measuring performance and the other measuring sexual desire |
NA | Higher scores indicate greater levels |
| SF-12 | The Short Form questionnaire-12 items (SF-12; Ware et al.255) is a widely used, brief generic measure of self-reported health status derived from the larger SF-36 survey Self-ratings are made of severity and frequency of 12 physical and mental health problems, as well as of their impact on the patient’s overall perceived health status This modified version of the SF-36 has consistently been shown to have good reliability and validity |
It yields both physical health and mental health summary scores, which are reported as standard scores | Slower scores indicated positive psychological and physical health |
| SF-36 | The Medical Outcomes Short Form questionnaire-36 items (SF-36; Ware and Sherbourne256) is used to evaluate psychological (SF mental), physical health (SF physical) and general health The eight subscales include (a) limitations in physical activities because of health problems; (b) limitations in social activities because of physical or emotional problems; (c) limitations in usual role activities because of physical health problems; (d) bodily pain; (e) general mental health (psychological distress and well-being); (f) limitations in usual role activities because of emotional problems; (g) vitality (energy and fatigue); and (h) general health perceptions A physical health composite score embodies concepts (a), (c), (e) and (g) and a mental health composite score embodies concepts (b), (d), (e) and (f) This instrument has been also used a measure of HRQoL In the included study by Broderick et al.,118 four additional subscales from the MOS-SF-36 General Health Survey were selected: overall health, social functioning, health distress, and cognitive dysfunction. Three additional items assessing tiredness on awakening, tiredness during the day, and quality of sleep were rated over the past week on 4-point scales |
6-point Likert scale from 1 (excellent) to 5 (worst) | Lower scores indicated positive psychological and physical health |
| SF-36v2 Health Survey | The SF-36v2 Health Survey (Ware257) is a 36-item inventory that yields eight scale scores and two summary scores for physical and mental health The 1998 US norm-based scoring in version 2 allows for ready interpretation of scores relative to general population norms The eight scaled scores are the weighted sums of the questions in their section. Each scale is directly transformed into a 0–100 scale. The eight sections are vitality, physical functioning, bodily pain, general health perceptions, physical role functioning, emotional role functioning, social role functioning and mental health In the included study by Broderick et al.,118 the Pain Catastrophising Scale served as a primary outcome, because it measures the physical health status of the patient. The Mental Component Summary (MCS) was also examined to determine whether a psychological impact of the intervention was observed |
Total score in each component ranges from 0 to 100 | The higher the score the less disability |
| SGRQ | The St George’s Respiratory Questionnaire (SGRQ) is a disease-specific instrument designed to measure impact on overall health, daily life and perceived well-being, to be used in patients with fixed and reversible airway obstruction It has 76 questions in three sections: symptoms (frequency and severity), activity (activities that cause or are limited by breathlessness) and impacts (social functioning and psychological disturbances resulting from airways disease) |
Total score ranges from 0 to 100 | Higher scores indicate poor health |
| SIP | The Sickness Impact Profile (SIP; de Bruin et al.258) used in the included study by Hughes54 is 136 items The SIP contains three items: the physical functioning scale, mobility subscale (SIP-m), and the recreation and pastimes subscale (SIP-r&p-t) The SIP describes activities of daily living divided in 12 categories |
Numerical scale | Higher scores indicate greater dysfunction |
| Skindex-29 | The Skindex-29 (Chren et al.259) has been shown to be a valuable tool for measuring HRQoL (QoL) in dermatological patients, as reported in the included study by Paradisi et al.110 Its Italian version was developed following guidelines for the cross-cultural adaptation of HRQoL measures and validated in a previous survey260 |
VAS scale from 0 (no pain) to 10 (worst possible) | Higher scores indicate poorer QoL |
| SOC | The Sense of Coherence Scale (SOC) is a 13-item self-report instrument (Antonovsky261) based on the following underlying constructs: comprehensibility, manageability and meaningfulness The SOC items are scored along the 7-point scale |
7-point scale with two anchoring phrases: ‘until now life has had no clear goals or purpose at all’ and ‘until now life has had very clear goals and purpose’ | Higher scores indicate a strong sense of coherence |
| Social Constraints Scale | The Social Constraints Scale (Lepore et al.262) is a 15-item scale assessing perceived inadequacy of social support resulting in reluctance to express thoughts and feelings about a specific stressor, in this case, experience with amyotrophic lateral sclerosis (e.g. How often did they tell you not to think about amyotrophic lateral sclerosis?) All items referred to respondent’s experiences over the prior week |
5-point scale ranging from 1 (almost never) to 5 (almost always) | Higher scores indicate greater social constraint |
| Somatisation Scale | The Somatisation Scale (13 items) includes 13 common physical complaints (e.g. stomach pain, back pain, headaches), from which a severity score can be calculated | Range 0–4 | NR |
| SOPA | The control subscale of the Survey of Pain Attitudes (SOPA; Jensen et al.263) is a questionnaire to measure feelings of personal control over pain The SOPA is the most widely used measure of pain-related attitudes (De Good and Tait;264 Jensen et al.263) |
5-point scale from 0 (this is very untrue for me) to 4 (this is very true for me) After reversing responses on the four absence of control items, responses are summed to create a total score |
Higher scores indicate greater control over pain |
| SOS | The Significant Others Scale (SOS) measured how much practical and emotional support that individual provided responding to two questions for each item: Emotional support answered by:
|
From 1 (never) to 7 (always) scale | Higher scores indicate greater emotional support |
| SSQ Asthma | The Wasserfallen Symptom Score Questionnaire (SSQ): asthma subscale | NA | NA |
| SSQ Awakenings | The Wasserfallen Symptom Score Questionnaire (SSQ): awakenings subscale | NA | NA |
| STAI-S | The State/Trait Anxiety Scale (STAI-S) is a 20-item, self-report instrument that assesses the subjective feelings of apprehension, nervousness and anxiety at the moment | 4-point Likert scale ranging from not at all, somewhat, moderately so, to very much so | Higher scores indicate greater state anxiety |
| Stigma Scale | The Stigma Scale, designed for individuals diagnosed with HIV/AIDS, consisted of 13 items that evaluated fear, avoidance, and perceived negative responses related to HIV status | 1–4 ordinal scale reported as strongly, not at all, rarely, sometimes, often Total scores ranging from a low of 13 to a high of 52 |
Higher scores equating to greater stigma |
| Survey–18 physical symptoms items | The Survey–18 physical symptoms items includes items derived from other reports for their appropriateness for the sample in the included study by Henry et al.53 (Anderson and Tewfik;265 Ganz and Coscarelli;266 Whelan et al.267) Example symptoms included fatigue, nausea, appetite loss, breast pain, hair loss, weight gain, hot flashes, itchiness or discomfort of the skin, decreased arm mobility and swelling of the arm |
A 7-point scale was used, ranging from 1 (not at all) to 7 (severe) | Higher scores indicate greater physical symptoms |
| SUS | The Social Undermining Scale (SUS; Vinokur and van Ryn268) assesses the extent to which each of the four most important people in participant’s lives caused them distress by acting in an unpleasant or angry manner towards them, criticising them or making their life difficult | 5-point scale | |
| Swollen joint count | Joint swelling reflects local inflammation and limited motion in affected areas. The patient’s rheumatologist, blind to the patient’s experimental condition, evaluated 16 joints bilaterally (five interphalangeal and five metacarpal phalangeal joints in addition to shoulder, elbow, wrist, knee ankle and metatarsals, for a total of 32 joints) and the presence or absence of swelling was recorded for each joint | ||
| Symptom and Emotion Self-report Survey | Participants rated the degree to which they were currently experiencing physical symptoms and emotions. The symptom items were averaged to yield a symptom score, and emotion items were averaged to form positive and negative emotion scores | 5-point scale from 1 (not at all) to 5 (a great deal) and scored | |
| Symptom Checklist-90-Revised | Physical symptoms are reported on a 12-item somatisation subscale of the Symptom Checklist-90-Revised (SCL-90-R) In the included study by D’Souza et al.101 symptoms were rated regarding the past month, and ratings were totalled |
Rated from 0 (not at all) to 4 (extremely) | |
| SLESQ | The Stressful Life Events Screening Questionnaire (SLESQ) (10 items) includes 10 psychosocial complaints common among health-care seeking populations (e.g. difficulties with family support, problems with significant others, and financial concerns) | Range 1–4 | NR |
| The Ways of Coping-Cancer Version | The Ways of Coping-Cancer Version is a self-report checklist of coping responses to cancer-related stressors It assesses the frequency of problem-focused and emotion-focused coping efforts |
||
| TLEQ | The Trauma Life Experience Questionnaire (TLEQ; Kubany et al.269) is a 23-item self-report measure of 22 types of potentially traumatic events including natural disasters, exposure to warfare, robbery involving a weapon, physical abuse and being stalked TLEQ measures type and frequency of trauma event exposures, and responses to these exposures The TLEQ has strong psychometric properties (Kubany et al.269) and was completed at the baseline assessment Trauma exposure was scored only if the person indicated exposure to the traumatic event and a response to the event that was consistent with DSM-IV PTSD criterion A2 |
For each event, respondents are asked to provide the number of times it occurred, ranging from never to more than five times, and whether fear, helplessness or horror was present: yes/no | Higher scores indicate greater trauma |
| TLFB abstinence | Timeline Followback Method (TLFB) of assessing number of abstinent days | Larger number means longer abstinence | |
| UCLA-Charles | The UCLA-Charles R Drew University Women and Family Project (Wyatt and Chin270) was adapted to assess changes in meaning and perceived benefits Participants were asked how, if at all, being HIV positive changed the way they think about themselves, changed them as a person, changed the way they are with other people, and changed their priorities Different categories were developed, based on the literature and on an initial analysis of 14 patients |
Ten categories of positive changes, six categories of negative changes and three categories of mixed or neutral changes, as well as codes for uncategorised positive and negative changes The number of changes falling into the positive categories and negative categories was computed for each participant |
Higher scores indicate greater changes? |
| VSQ-9 | The Visit Specific Satisfaction Questionnaire (VSQ; Ware and Hays271), a self-report measure administered to participants and providers at the conclusion of the 3-month follow-up period | To score the VSQ-9, the responses from each individual should be transformed linearly to a 0–100 scale, with 100 corresponding to excellent and 0 corresponding to poor Responses to the nine VSQ items should then be averaged together to create a VSQ-9 score for each person |
Higher scores indicate greater satisfaction related to the visits |
| Walking speed and grip strength | In the included study by Lumley et al.,115 patients were instructed to walk as quickly as possible, but safely down a 50-foot corridor, and recorded the time to do so in seconds In addition, patient’s grip strength was assessed by having them squeeze, as firmly as possible, a sphygmomanometer bulb, and the pressure generated was recorded from two trials with each hand; all four values were averaged to a single score |
NA | Walking speed: higher values mean slower walking Grip strength: higher values indicate better functioning |
| Well-being | In the included study by Cepeda et al.85 each patient’s sense of general well-being was rated | 7-point Likert scale from awful to excellent | Higher scores indicate better well-being |
| WHYMPI –pain subscale | The Pain Severity subscale of the West Haven-Yale Multidimensional Pain Inventory (WHYMPI; Kerns et al.272) is a 61-item self-report inventory across three domains The WHYMPI is for use in chronic pain populations. It generates 13 empirically derived scale scores, including pain severity, perception of how pain interferes with daily life activities, appraisals of the support received from significant others, and perception of how significant others respond to their displays of pain |
From 0 to 6 | Higher scores indicate more extreme pain |
Quality assessment
| First author, year | Randomisation | Blinding | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sequence generation? (Selection bias) | Method description given? | Allocation concealment? (Selection bias) | Outcome | Performance | ITT analysis? | Selective reporting? (Description of outcomes differences between groups) | Attrition bias? (Description of withdrawals) | Pre-specified criteria for eligibility of patients? | Similarity of groups at baseline regarding prognostic factors? | |
| Abel 200450 | Y | N | U | U | U | Y | N | U | U | Y |
| Arden-Close 201380 | Y | Y | Y | U | N | Y | N | N | Y | N |
| Averill 2013100 | Y | Y | U | U | Y | N | Y | Y | Y | N |
| Bartasiuniene 2011102 | Y | N | U | U | N | Y | N | N | U | Y |
| Bernard 200693 | Y | Y | Y | U | U | N | N | N | Y | N |
| Broderick 2004113 | Y | N | Y | U | N | Y | Y | Y | Y | Y |
| Broderick 2005118 | Y | Y | Y | U | N | N | U | Y | Y | Y |
| Canna 200694 | Y | N | Y | N | Y | N | N | U | Y | Y |
| Cepeda 200885 | Y | N | Y | Y | U | Y | Y | Y | Y | Y |
| Craft 201374 | Y | Y | U | U | U | N | N | Y | Y | Y |
| Dennick 201488 | Y | Y | Y | Y | Y | Y | N | N | Y | Y |
| D’Souza 2008101 | Y | Y | Y | N | Y | Y | N | N | N | Y |
| Gellaitry 201075 | Y | Y | U | U | U | N | Y | N | Y | Y |
| Gidron 199698 | Y | N | U | N | Y | Y | U | Y | U | N |
| Gillis 2006119 | Y | Y | Y | U | Y | Y | Y | Y | Y | N |
| Golkaramnay 200768 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Graf 200895 | Y | Y | N | U | N | Y | N | N | Y | N |
| Graham 200851 | Y | Y | Y | Y | U | N | Y | Y | Y | Y |
| Grasing 201090 | N | N | N | U | U | U | Y | Y | Y | N |
| Halpert 201052 | N | Y | N | U | N | N | N | Y | Y | N |
| Hamilton-West 2007114 | Y | Y | Y | Y | N | Y | Y | Y | Y | U |
| Harris 2005106 | Y | Y | Y | N | N | N | N | Y | N | N |
| Henry 201053 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Hevey 2012103 | Y | N | U | U | U | N | Y | N | U | U |
| Hong 201167 | Y | Y | N | U | U | Y | U | U | Y | N |
| Hughes 200754 | Y | U | N | N | N | Y | N | Y | Y | Y |
| Ironson 201371 | Y | N | U | U | U | U | N | U | Y | N |
| Jensen-Johansen 201376 | Y | Y | Y | U | Y | N | N | U | ||
| Kraaij 201055 | Y | N | U | U | U | N | Y | Y | U | N |
| Krpan 201396 | Y | U | U | U | U | U | N | U | U | U |
| Lange 200369 | Y | N | U | U | Y | N | Y | Y | N | Y |
| Lumley 2011115 | Y | N | U | U | U | Y | Y | Y | N | Y |
| Lumley 2014116 | Y | N | N | U | U | Y | Y | Y | N | Y |
| Mann 200172 | Y | N | U | U | U | N | N | Y | N | N |
| McElligott 200687 | Y | U | N | N | U | Y | N | U | Y | Y |
| Meshberg-Cohen 201091 | Y | U | U | U | U | Y | Y | N | Y | Y |
| Milbury 201481 | Y | Y | U | U | U | N | N | Y | Y | Y |
| Mosher 201277 | Y | Y | U | U | U | Y | U | Y | Y | Y |
| Pauley 201182 | Y | Y | U | U | U | N | Y | N | Y | U |
| Paradisi 2010110 | Y | Y | U | U | N | N | Y | Y | Y | Y |
| Park 201278 | N | U | U | U | U | Y | U | U | Y | N |
| Petrie 200456 | Y | Y | Y | U | U | U | N | U | Y | Y |
| Richards 200097 | Y | N | U | U | U | N | U | Y | Y | Y |
| Rickett 201166 | Y | N | U | U | U | N | N | Y | N | U |
| Rini 201486 | Y | Y | Y | Y | Y | Y | U | U | Y | Y |
| Robinson 200899 | Y | Y | N | U | Y | Y | N | N | Y | N |
| Rosenberg 200283 | Y | N | Y | U | U | U | Y | U | Y | N |
| Sharifabad 2010105 | Y | N | U | U | U | Y | N | U | Y | N |
| Sloan 201270 | Y | Y | Y | U | U | U | N | Y | Y | Y |
| Smyth 1999107 | Y | Y | Y | N | U | N | N | Y | Y | Y |
| Smyth 2008121 | Y | N | U | U | U | U | Y | Y | N | U |
| Stark 201057 | Y | Y | U | U | U | N | U | Y | Y | Y |
| Tabolli 2012111 | Y | Y | Y | U | U | N | N | Y | Y | N |
| Taylor 200389 | Y | N | U | U | U | Y | N | N | N | N |
| Theadom 201058 | Y | N | U | U | U | N | N | Y | Y | |
| Van Dam 201392 | Y | Y | Y | U | U | N | N | U | U | Y |
| Vedhara 2007112 | Y | Y | U | U | U | Y | N | Y | N | Y |
| Wagner 201073 | Y | Y | U | Y | Y | N | Y | Y | Y | U |
| Walker 199979 | Y | N | U | Y | Y | N | N | Y | Y | N |
| Wallander 2011109 | Y | Y | N | N | U | N | N | Y | N | Y |
| Warner 2006108 | Y | Y | U | N | N | N | U | Y | Y | Y |
| Wetherell 2005117 | Y | N | U | Y | U | N | Y | Y | Y | Y |
| Willmott 2011104 | Y | Y | Y | U | Y | N | Y | N | Y | N |
| Zakowski 200484 | Y | N | U | U | U | Y | Y | U | N | Y |
| Number of studies | Quality assessment items |
|---|---|
| 53 | Studies were truly randomised (a valid method of randomisation was reported) |
| 24 | Studies were reported as randomised but the method of randomisation was not given |
| 18 | Studies were reported as having concealed the allocation of the sequence randomisation |
| 6 | Studies preserved blinding for outcome assessment |
| 11 | Studies preserved blinding during performance |
| 25 | Studies analysed the outcomes using the ITT approach |
| 44 | Studies reported outcomes differences between groups |
| 44 | Studies provided a description of withdrawals |
| 44 | Studies reported the prespecified criteria for eligibility of patients |
| 33 | Studies reported assessing similar groups at baseline |
Appendix 6 Excluded studies
List of excluded studies with reasons for exclusion
| Author(s) | Year | Title | Journal | Volume | Issue | Page(s) | Reason for exclusion |
|---|---|---|---|---|---|---|---|
| Anon | 1999 | Can writing about stressful experiences reduce symptoms of chronic disease? | Joint letter | 5 | 4 | 37–9 | Not the study type of interest |
| Abel E | 2007 | Women with HIV and stigma | Family and Community Health | 30 | Suppl. 1 | S104–14 | No numerical data reported |
| Adenauer H, Catani C, Gola H, Keil J, Ruf M, Schauer M, et al. | 2011 | Narrative exposure therapy for PTSD increases top-down processing of aversive stimuli – evidence from a randomized controlled treatment trial | BMC Neuroscience | 12 | 127 | 43–56 | Not TW |
| Adkins MH, Gavins MV | 2012 | Self-regulated strategy development and generalization instruction: effects on story writing and personal narratives among students with severe emotional and behavioral disorders | Exceptionality | 20 | 4 | 235–49 | Not the study type of interest |
| Adleman CS | 2006 | A write choice for stroke recovery | Beginnings (American Holistic Nurses Association) | 26 | 3 | 14–15 | Not the study type of interest |
| Adler JM, McAdams DP | 2007 | The narrative reconstruction of psychotherapy | Narrative Inquiry | 17 | 2 | 179–202 | Not a LTC |
| Allen NB, Bradley BS | 1993 | The place of emotion in stories told by children: an exploratory study | The Journal of Genetic Psychology: Research and Theory on Human Development | 154 | 3 | 397–406 | Not the comparator of interest |
| Almeida JP, Mendes R, Henriques M | 2009 | The impact of expressive writing on glycaemia control of diabetic adolescents | Psychology & Health | 24 | NA | 77–8 | Abstract |
| Andersson MA, Conley CS | 2013 | Optimizing the perceived benefits and health outcomes of writing about traumatic life events | Stress and Health: Journal of the International Society for the Investigation of Stress | 29 | 1 | 40–9 | Not a LTC |
| Anderson SS | 2009 | The effect of written emotional expression on depression following mild traumatic brain injury: a pilot study | Dissertation Abstracts International: Section B: The Sciences and Engineering | 69 | 9-B | 57–66 | No numerical data reported |
| Anonymous | 1999 | Writing for better health | Health News | 5 | 6 | 10 | Not available |
| Anschel DJ, Pike B, Dolce S, Schwartzman A | 2006 | Analysis of writing in an epilepsy center population: a prospective blinded study | Epilepsy and Behavior | 9 | 3 | 464–8 | Not the study type of interest |
| Austenfeld JL | 2007 | Effects of writing about emotions versus goals on hostility, depressive symptoms and physical health parameters: the moderating role of emotional approach coping | Dissertation Abstracts International: Section B: The Sciences and Engineering | 68 | 4-B | 2636 | Not a LTC |
| Bacigalupe G | 1996 | Writing in therapy: a participatory approach | Journal of Family Therapy | 18 | 4 | 361–73 | Not the study type of interest |
| Baikie KA, Geerligs L, Wilhelm K | 2012 | Expressive writing and positive writing for participants with mood disorders: an online randomized controlled trial | Journal of Affective Disorders | 136 | 3 | 310–19 | Duplicate |
| Baikie KA, Geerligs L, Wilhelm K | 2012 | Expressive writing and positive writing for participants with mood disorders: an online randomized controlled trial | Journal of Affective Disorders | 136 | 3 | 310–19 | Not a LTC |
| Baikie KA, Wilhelm K, Johnson B, Boskovic M, Wedgwood L, Finch A, et al. | 2006 | Expressive writing for high-risk drug dependent patients in a primary care clinic: a pilot study | Harm Reduction Journal | 3 | NA | 34 | Not the study type of interest |
| Baker S | 2009 | Tell it slant: history, memory, and imagination in the healing writing workshop | Traumatology | 15 | 4 | 15–23 | Not the study type of interest |
| Bartasiuniene R, Sinkariova L, Petroliene R | 2011(a) | The impact of expressive writing intervention on the changes of blood pressure of patients with cardiovascular disease | Psychology & Health | 26 | NA | 88 | Abstract |
| Bauer-Wu S, Norris R, Healey M, Powell M, Habin K, Partridge A, et al. | 2007 | An innovative expressive writing intervention for young breast cancer patients: feasibility, preference and psychological effects | Psycho-Oncology | 16 | 3 | S78–9 | Abstract |
| Baum ES, Rude SS | 2013 | Acceptance-enhanced expressive writing prevents symptoms in participants with low initial depression | Cognitive Therapy and Research | 37 | 1 | 35–42 | Not a LTC |
| Beckwith KM | 2003 | The effects of expressive writing on blood pressure, psychosocial adjustment, and heart rate variability in high normal to moderate high blood pressure | Dissertation Abstracts International: Section B: The Sciences and Engineering | 64 | 2-B | 995 | Not a LTC |
| Bedard-Gilligan MA, Blayney JA, Kaysen DL | 2011 | Feasibility of a trauma narrative writing exercise during treatment for alcohol dependence: pattern of alcohol cravings and emotions | Alcoholism: Clinical and Experimental Research | 35 | NA | 81A | Ongoing study |
| Behrns I, Ahlsen E, Wengelin A | 2010 | Aphasia and text writing | International Journal of Language & Communication Disorders | 45 | 2 | 230–43 | Not TW |
| Bennett PR, Elliott M | 2013 | God give me strength: exploring prayer as self-disclosure | Journal of Religious Health | 52 | – | 128–42 | Not LTC participants |
| Bhullar N, Schutte NS, Malouff JM | 2011 | Writing about satisfaction processes increases well-being | Individual Differences Research | 9 | 1 | 22–32 | Not a LTC |
| Bodor NZ | 2004 | The health effects of emotional disclosure for individuals with type 1 diabetes | Dissertation Abstracts International: Section B: The Sciences and Engineering | 64 | 10-B | 5207 | Not the comparator of interest |
| Bohlmeijer E, Valenkamp M, Westerhof G, Smit F, Cuijpers P | 2005 | Creative reminiscence as an early intervention for depression: results of a pilot project | Aging and Mental Health | 9 | 4 | 302–4 | Not the study type of interest |
| Boritz TZ, Angus L, Monette G, Hollis-Walker L, Warwar S | 2011 | Narrative and emotion integration in psychotherapy: investigating the relationship between autobiographical memory specificity and expressed emotional arousal in brief emotion-focused and client-centred treatments of depression | The Cochrane Library | 21 | 1 | 16–26 | Not TW |
| Bowers MJ, Buchanan MJ | 2007 | A group-based program of emotional recovery for younger women following myocardial infarction | Canadian Journal of Counselling | 41 | 2 | 77–90 | Not the study type of interest |
| Brandenstein JS, Cope E, Kerr AJ, Boynes AM, Popp CD, Knapp L | 2010 | Utilizing social media to reach young arthritis patients | Arthritis and Rheumatism | 62 | NA | 1345 | Not TW |
| Bray MA, Kehle TJ, Peck HL, Margiano SG, Dobson R, Peczynski K, et al. | 2005 | Written emotional expression as an intervention for asthma: a replication | Journal of Applied School Psychology | 22 | 1 | 141–65 | Not the study type of interest |
| Bray MA, Theodore LA, Patwa SS, Margiano SG, Alric JM, Peck HL | 2003 | Written emotional expression as an intervention for asthma | Psychology in the Schools | 40 | 2 | 193–207 | Not the study type of interest |
| Brinkman BS, Hateren KJ, Kleefstra N, Houweling ST, Groenier KH, Bilo HJ | 2014 | Effects of writing down the request for help: a randomised controlled trial | European Journal of General Practice | 20 | 3 | 214–18 | Not TW |
| Brown BT | 2008 | The content and structure of autobiographical memories in children with and without Asperger syndrome | Dissertation Abstracts International: Section B: The Sciences and Engineering | 68 | 12-B | 8427 | Not TW |
| Brown CA, Dick BD | 2010 | How do you write pain? A preliminary study of narrative therapy for people with chronic pain | Pain Research and Management Conference | 15 | 2 | NA | Not the study type of interest |
| Bruera E, Willey J, Cohen M, Palmer JL | 2008 | Expressive writing in patients receiving palliative care: a feasibility study | Journal of Palliative Medicine | 11 | 1 | 15–19 | Not the comparator of interest |
| Bugg A, Turpin G, Mason S, Scholes C | 2009 | A randomised controlled trial of the effectiveness of writing as a self-help intervention for traumatic injury patients at risk of developing post-traumatic stress disorder | Behaviour Research and Therapy | 47 | 1 | 6–12 | Not a LTC |
| Burger A, Stout R, Williams R, Lumley M | 2008 | The effect of internet-based guided written emotional disclosure on migraine headaches | Annals of Behavioral Medicine | 35 | NA | S29 | Abstract |
| Burger AJ | 2011 | Evaluating outcomes and response profiles of a psychological treatment for people with chronic pain | Dissertation Abstracts International: Section B: The Sciences and Engineering | 71 | 10-B | 6433 | Not the comparator of interest |
| Byrne-Davis LMT, Wetherell MA, Dieppe P, Weinman J, Byron M, Donovan J, et al. | 2006 | Emotional disclosure in rheumatoid arthritis: participants views on mechanisms | Psychology & Health | 21 | 5 | 667–82 | Not the study type of interest |
| Carmack CL, Basen-Engquist K, Yuan Y, Greisinger A, Rodriguez-Bigas M, Wolff RA, et al. | 2011 | Feasibility of an expressive-disclosure group intervention for post-treatment colorectal cancer patients: results of the Healthy Expressions study | The Cochrane Library | 117 | 21 | 4993–5002 | Not TW |
| Cash TV, Mickens MN, Lageman SK | 2013 | Expressive writing improves psychosocial functioning of patients with Parkinson’s disease and their caregivers | Journal of Parkinson’s Disease | 3 | – | 203 | Conference abstract |
| Cashin A, Browne G, Bradbury J, Mulder A | 2013 | The effectiveness of narrative therapy with young people with autism | Journal of Child & Adolescent Psychiatric Nursing | 26 | 1 | 32–41 | Not the study type of interest |
| Chan KM, Horneffer K | 2006 | Emotional expression and psychological symptoms: a comparison of writing and drawing | Arts in Psychotherapy | 33 | 1 | 26–36 | Not a LTC |
| Cheli S, Focardi F, Velicogna F, Fioretto L | 2011 | Narratives and interpreters in psycho-oncology: a pilot study | Psycho-Oncology | 20 | NA | 136 | Abstract |
| Chen TJ, Li HJ, Li J | 2012 | The effects of reminiscence therapy on depressive symptoms of Chinese elderly: study protocol of a randomized controlled trial | BMC Psychiatry | 12 | 189 | NA | Not TW |
| Chen YY, Contrada RJ | 2009 | Framing written emotional expression from a religious perspective: effects on depressive symptoms | International Journal of Psychiatry in Medicine | 39 | 4 | 427–38 | Not a LTC |
| Chidiac N | 2008 | Writing of trauma or trauma of writing? (two women, two stories, two ways of writing) | Annales Medico-Psychologiques | 166 | 4 | 308–14 | Not the study type of interest |
| Chippendale T | 2012(a) | The effects of life review writing on depressive symptoms: a randomized control trial | Journal of the American Geriatrics Society | 60 | NA | S81 | Not a LTC |
| Chippendale T | 2012 | The effects of life review through writing on depressive symptoms and life satisfaction in older adults | Dissertation Abstracts International: Section B: The Sciences and Engineering | 73 | 1-B | 237 | Duplicate |
| Clausen NS, Beeson PM | 2003 | Conversational use of writing in severe aphasia: a group treatment approach | Aphasiology | 17 | 6–7 | 625–44 | Not TW |
| Cohen L, Tannir N, Jonasch E, Pisters L, Matin S, Spelman A, et al. | 2012 | Short-and long-term effects of expressive writing in patients with renal cell carcinoma | BMC Complementary and Alternative Medicine | 12 | NA | NA | Duplicate |
| Combe D | 2005 | The use of patient diaries in an intensive care unit | Nursing in Critical Care | 10 | 1 | 31–4 | Not TW |
| Conrad R, Allam J, Geiser F, Haidl G, Karpawitz-Godt A, Ven H | 2012 | Expressive writing in male infertility – a randomized controlled study | Journal of Psychosomatic Research | 72 | 6 | 475 | Abstract |
| Cooper C, Stringer R | 2012 | An evaluation of an upper limb/handwriting group for people with Parkinson’s disease | Movement Disorders | 27 | NA | S300 | Not TW |
| Cornoldi C, Del Prete F, Gallani A, Sella F, Re AM | 2010 | Components affecting expressive writing in typical and disabled writers | Advances in Learning and Behavioral Disabilities: Literacy and Learning | 23 | NA | 269–86 | Not the study type of interest |
| Craft M | 2007 | Expressive writing in newly diagnosed breast cancer patients | Oncology Nursing Forum | 34 | 2 | 507 | Duplicate |
| Creswell JD, Lam S, Stanton AL, Taylor SE, Bower JE, Sherman DK | 2007 | Does self-affirmation, cognitive processing, or discovery of meaning explain cancer-related health benefits of expressive writing? | Personality and Social Psychology Bulletin | 33 | 2 | 238–50 | Not the study type of interest |
| Cunha C, Goncalves MM, Hill CE, Mendes I, Ribeiro AP, Sousa I, et al. | 2012 | Therapist interventions and client innovative moments in emotion-focused therapy for depression | Psychotherapy: Theory, Research, Practice, Training | 49 | 4 | 536–48 | Not the study type of interest |
| Cunningham LLC | 2000 | Emotional expressivity, cognitive processing, and psychological distress in women with breast cancer | Dissertation Abstracts International: Section B: The Sciences and Engineering | 60 | 11-B | 5767 | Not the comparator of interest |
| Cureton A, Schick E | 2009 | Survivors writing together: a pilot study | Psycho-Oncology | 18 | S1 | S67–8 | Not the study type of interest |
| Danoff-Burg S, Agee JD, Romanoff NR, Kremer JM, Strosberg JM | 2006 | Benefit finding and expressive writing in adults with lupus or rheumatoid arthritis | Psychology & Health | 21 | 5 | 651–65 | Not the comparator of interest |
| Davidson JU, Robison B | 2008 | Scrapbooking and journaling interventions for chronic illness: a triangulated investigation of approaches in the treatment of PTSD | The Kansas Nurse | 83 | 3 | 6–11 | Not the study type of interest |
| Davis MC | 1998 | Life review therapy as an intervention to manage depression and enhance life satisfaction in individuals with right hemisphere cerebral vascular accidents | Dissertation Abstracts International Section A: Humanities and Social Sciences | 58 | 7-A | 2545 | Not TW |
| Davis MS | 1979 | Poetry group therapy versus interpersonal group therapy: comparison of treatment effectiveness with depressed women | Dissertation Abstracts International | 39 | 11-B | 5543 | Not a LTC |
| De Moor C, Sterner J, Hall M, Warneke C, Gilani Z, Amato R, et al. | 2002 | A pilot study of the effects of expressive writing on psychological and behavioural adjustment in patients enrolled in a Phase II trial of vaccine therapy for metastatic renal cell carcinoma | Health Psychology | 21 | 6 | 615–19 | Not the comparator of interest |
| De Moor C, Warneke C, Sterner J, Gilani Z, Amato RJ, Cohen L | 2001 | An emotional expression writing program for cancer patients | Psychosomatic Medicine | 63 | 1 | 124–5 | Duplicate |
| De Moor JS, Moye L, Low MD, Rivera E, Singletary SE, Fouladi RT, et al. | 2008 | Expressive writing as a presurgical stress management intervention for breast cancer patients | Journal of the Society for Integrative Oncology | 6 | 2 | 5966 | Not the comparator of interest |
| De Roos C, Greenwald R, den Hollander-Gijsman M, Noorthoorn E, van Buuren S, de Jongh A | 2011 | A randomised comparison of cognitive behavioural therapy (CBT) and eye movement desensitisation and reprocessing (EMDR) in disaster-exposed children | European Journal of Psychotraumatology | 47 | 2 | 1–8 | No TW intervention |
| De Wit R, van Dam F, Zandbelt L, van Buuren A, van der Heijden K, Leenhouts G, et al. | 1997 | A pain education program for chronic cancer pain patients: follow-up results from a randomized controlled trial | Pain | 73 | 1 | 55–69 | Not TW |
| Deters PB, Range LM | 2003 | Does writing reduce posttraumatic stress disorder symptoms? | Violence and Victims | 18 | 5 | 569–80 | Not a LTC |
| D’Souza PJ | 2003 | The effects of relaxation training and written emotional disclosure for people with migraine or tension headaches | Dissertation Abstracts International: Section B: The Sciences and Engineering | 63 | 11-B | 5509 | Duplicate |
| Donovan HS, Ward SE, Serieka SM, Knapp JE, Sherwood PR, Bender CM, et al. | 2014 | Web-based symptom management for women with recurrent ovarian cancer: a pilot randomised controlled trial of the WRITE symptoms intervention | Journal of Pain and Symptoms Management | 47 | 2 | 35–42 | Not TW |
| East P, Startup H, Roberts C, Schmidt U | 2010 | Expressive writing and eating disorder features: a preliminary trial in a student sample of the impact of three writing tasks on eating disorder symptoms and associated cognitive, affective and interpersonal factors | The Cochrane Library | 18 | 3 | 180–96 | Not a LTC |
| Eid J, Johnsen BH, Saus ER | 2005 | Trauma narratives and emotional processing | Scandinavian Journal of Psychology | 46 | 6 | 503–10 | Not the study type of interest |
| Emmerik A, Kamphuis JH, Emmelkamp P | 2004 | CBT and structured writing therapy in preventing chronic PTSD (RCT) | 20th Annual Meeting, International Society for Traumatic Stress Studies, November 14–18, New Orleans, LA, 2004: War as a universal trauma: the International Society for Traumatic stress studies | NA | NA | NA | Not TW |
| Engel-Yeger B, Nagauker-Yanuv L, Rosenblum S | 2009 | Handwriting performance, self-reports, and perceived self-efficacy among children with dysgraphia | American Journal of Occupational Therapy | 63 | 2 | 182–92 | Not TW |
| Eonta A | 2014 | Heart rate variability as a moderator of trauma writing outcome | Dissertation | 75 | 5 B(E) | – | Not a LTC |
| Estilaee F, Sadeghi MM, Ghaffarinejad A | 2012 | The patient with schizophrenia writes blog; new way for thought pattern perception or the risk in figurative world? | European Psychiatry | 27 | NA | NA | Abstract |
| Fabricant LE, Abramowitz JS, Dehlin JP, Twohig MP | 2013 | A comparison of two brief interventions for obsessional thought: exposure and acceptance | Journal of Cognitive Psychotherapy | 27 | 3 | 195–209 | No inactive control |
| Fair CD, Connor L, Albright J, Wise E, Jones K | 2012 | I’m positive, I have something to say: assessing the impact of a creative writing group for adolescents living with HIV | Arts in Psychotherapy | 39 | 5 | 383–9 | Not the study type of interest |
| Fernandez I, Paez D | 2008 | The benefits of expressive writing after the Madrid terrorist attack: implications for emotional activation and positive affect | British Journal of Health Psychology | 13, Part 1 | NA | 31–4 | Not a LTC |
| Fernandez I, Paez D, Pennebaker J | 2004 | Expressive writing about the terrorist attacks of March-Eleven 2004 in Madrid: a longitudinal study | Ansiedad Y Estres | 10, no. 2 | NA | 233–45 | Not a LTC |
| Flood EM, Zazzali JL, Devlen J | 2013 | Demonstrating measurement equivalence of the electronic and paper formats of the urticaria patient daily diary in patients with chronic idiopathic urticaria | The Patient | 6 | – | 225–31 | No inactive control |
| Foster L | 1988 | Writers workshops, the word processor and the psychiatric patient | British Journal of Occupational Therapy | 51 | 6 | 191–2 | Not the study type of interest |
| Fraas M, Balz MA | 2008 | Expressive electronic journal writing: freedom of communication for survivors of acquired brain injury | Journal of Psycholinguistic Research | 37 | 2 | 115–24 | Not the study type of interest |
| Franz RA | NA | Processing traumatic events: a model of emotional processing and account complexification (dissertation) | NA | NA | NA | 156 | Not a LTC |
| Frayne A, Wade TD | 2006 | A comparison of written emotional expression and planning with respect to bulimic symptoms and associated psychopathology | The Cochrane Library | 14 | 5 | 329–40 | Not a LTC |
| Frederiksen Y, Zachariae R, Schmidt L, Ingerslev HJ | 2011 | Effects of expressive writing intervention on infertility-related symptoms in couples undergoing assisted reproductive technology treatment: a feasibility study | Human Reproduction | 26 | NA | i262 | Duplicate |
| Freyd JJ, Klest B, Allard CB | 2005 | Betrayal trauma: relationship to physical health, psychological distress, and a written disclosure intervention | Journal of Trauma & Dissociation | 6 | 3 | 83–104 | Not the comparator of interest |
| Furnes B, Dysvik E | 2012 | Therapeutic writing and chronic pain: experiences of therapeutic writing in a cognitive behavioural programme for people with chronic pain | Journal of Clinical Nursing | 21 | – | 3372–81 | No numerical results |
| Gabert-Quillen CA | 2012 | The efficacy of written emotional expression at reducing back and headache pain in college students | PhD thesis, Kent State University, USA | – | – | – | Not a formally diagnosed LTC |
| Gandhi N, Tosiello L | 1999 | Symptom reduction after writing about stressful experiences | JAMA | 282 | 19 | 1811; author reply 1811–12 | Not the study type of interest |
| Garcia-Palacios A, Herrero R, Belmonte MA, Castilla D, Guixeres J, Molinari G, et al. | 2013 | Ecologic momentary assessment for chronic pain in fibromyalgia using a smartphone: a randomised crossover study | European Journal of Pain | 18 | – | 862–72 | No inactive control |
| Giannotta F, Settanni M, Kliewer W, Ciairano S | 2009 | Results of an Italian school-based expressive writing intervention trial focused on peer problems | Journal of Adolescence | 32 | 6 | 1377–89 | Not a LTC |
| Gillis ME, Lumley MA, Koch H, Roehrs TA, Mosley-Williams AD, Leisen JC | 2002 | Written emotional disclosure in fibromyalgia: effects on sleep quality and fatigue | Sleep | 25 | NA | A384–5 | Duplicate |
| Gillis ME, Roehrs TA, Lumley MA | 2005 | Physiological reactivity of insomniacs participating in written emotional disclosure: salivary cortisol and respiration | Sleep | 28 | NA | A234 | Abstract |
| Gillis ME | 2002(a) | The effects of written emotional disclosure on adjustment in fibromyalgia syndrome | Dissertation Abstracts International: Section B: The Sciences and Engineering | 63 | 3-B | 1562 | Duplicate |
| Goldstein SL | 1990 | A songwriting assessment for hopelessness in depressed adolescents: a review of the literature and a pilot study | Arts in Psychotherapy | 17 | 2 | 117–24 | Not the study type of interest |
| Gortner E-M | 2006 | The mental and physical well-being of formerly depressed college students: a preventive intervention study | Dissertation Abstracts International: Section B: The Sciences and Engineering | 66 | 12-B | 6921 | Not a LTC |
| Graf MC | 2004 | Written emotional disclosure: what are the benefits of expressive writing in psychotherapy? | Dissertation Abstracts International: Section B: The Sciences and Engineering | 65 | 2-B | 1028 | Duplicate |
| Graham JE | 2004 | Effects of written constructive anger expression on health and coping in patients with chronic pain | Dissertation Abstracts International: Section B: The Sciences and Engineering | 64 | 9-B | 4601 | Duplicate |
| Greenhalgh T, Collard A, Campbell-Richards D, Vijayaraghavan S, Malik F, Morris J, et al. | 2011 | Storylines of self-management: narratives of people with diabetes from a multi-ethnic inner city population | Journal of Health Services Research and Policy | 16 | 1 | 37–43 | Not TW |
| Halpert A, Godena E | 2011 | Irritable bowel syndrome patients’ perspectives on their relationships with healthcare providers (HCP) | Gastroenterology | 1 | NA | S465–6 | Not TW |
| Halpert A, Rybin D | 2009 | Expressive writing is a promising therapeutic modality for irritable bowel syndrome (IBS) | Gastroenterology | 1 | NA | A118 | Duplicate |
| Harvey AG, Farrell C | 2003 | The efficacy of a Pennebaker-like writing intervention for poor sleepers | The Cochrane Library | 1 | 2 | 115–24 | Not a LTC |
| Heimes S | 2013 | Does expressive writing about best possible self have an influence on affect, coping, and self-efficacy? | Musik, Tanz und Kunsttherapie | 24 | 3 | 117–27 | Not a LTC |
| Hennighausen A, Schilling G | 2007 | Effect of a expressive writing (Pennebaker-Paradigm) for chronic backpain | Nervenarzt | 78 | Issue 2 supplement | 491 | Abstract |
| Herbst N, Voderholzer U, Theil N, Schaub R, Knaevelsrud C, Stracke S, et al. | 2014 | No talking, just writing. Efficacy of an internet-based cognitive behavioural therapy with exposure and response prevention in obsessive compulsive disorder | Psychotherapy and Psychosomatics | 83 | 165–75 | Not TW | |
| Hofmann AD, Lewis NR | 1981 | The needle of caring, the thread of love: creative writing on an adolescent medical ward | Adolescent Psychiatry | 9 | NA | 88–116 | Not the study type of interest |
| Horne R, Wilmott L, Harris P | 2003 | The positive effects of writing about the experience of a first myocardial infarction on clinical variables and healthcare utilisation: a randomised controlled trial with six-month follow-up | Fifth International Congress on coronary Artery Disease From Prevention to Intervention, Florence, Italy | NA | NA | NA | Abstract |
| Ironson G, O’Cleirigh C, Leserman J, Fordiani J, Balbin E, Schneiderman N, et al. | 2010 | Augmented trauma writing effects HIV symptoms and VL in women with PTSD and HIV | Brain, Behavior and Immunity | 24 | NA | S62 | Duplicate |
| Ironson G, O’Cleirigh C, Leserman J, Stuetzle R, Fordiani J, Fletcher M, et al. | 2012 | Gender-specific effects of an augmented written emotional disclosure intervention on posttraumatic, depressive, and hiv-disease-related outcomes: a randomized, controlled trial | Journal of Consulting and Clinical Psychology | NA | – | No pagination specified | Duplicate |
| Jelicic M, Frederix M, Merckelbach H | 2013 | Brief report: writing about chronic fatigue increases somatic complaints | Psihologijske teme | 22 | 3 | 405–12 | Not a LTC |
| Johansen MB, Zachariae R, Valdimarsdottir H, Bovbjerg D, Zkowski S | 2006 | Expressive writing and breast cancer: associations between cognitive and positive emotional words and changes in perceived social support | Psycho-Oncology | 15 | 2 | S278 | Abstract |
| Johnston O, Startup H, Lavender A, Godfrey E, Schmidt U | 2010 | Therapeutic writing as an intervention for symptoms of bulimia nervosa: effects and mechanism of change | The Cochrane Library | 43 | 5 | 405–19 | Not a LTC |
| Jones C, Smith H, Theadom A, Bowskill R, Hankins M, Horne R, et al. | 2010(a) | Are the benefits of written emotional disclosure sustained at 12-months? A randomised controlled trial | Allergy: European Journal of Allergy and Clinical Immunology | 65 | NA | 190 | Abstract |
| Jones C, Bäckman C, Capuzzo M, Egerod I, Flaatten H, Granja C, et al. | 2010 | Intensive care diaries reduce new onset post traumatic stress disorder following critical illness: a randomised, controlled trial | Critical Care | 14 | NA | Article R168 | Not TW |
| Jones JD | 2005 | A comparison of songwriting and lyric analysis techniques to evoke emotional change in a single session with people who are chemically dependent. [Erratum appears in J Music Ther 2005;42:320] | Journal of Music Therapy | 42 | 2 | 94–110 | Not the study type of interest |
| Joplin J | 2000 | The therapeutic benefits of expressive writing | Executive | 14, part 2 | NA | 124–5 | Not the study type of interest |
| Juknelyte A, Cerniauskaite R, Sinkariova L, Milinaviciene E, Bagdone I | 2014 | The changes in illness perception, negative emotions and arterial blood pressure applying the method of expressive writing in the patients of ischaemic heart disease | Annals of Physical and Rehabilitation Medicine | 57 | E298 | Conference abstract | |
| Junghaenel DU, Schwartz JE, Broderick JE | 2008 | Differential efficacy of written emotional disclosure for subgroups of fibromyalgia patients | British Journal of Health Psychology | 13 | Part 1 | 57–60 | No numerical data reported |
| Kallay E, Baban A | 2008 | Emotional benefits of expressive writing in a sample of Romanian female cancer patients | Cognitie Creier Comportament | 12, number 1 | NA | 115–30 | Not the study type of interest |
| Kallay E | 2011 | Benefits of expressive writing in a sample of Romanian female cancer patients | Psychology & Health | 26 | 2 | 37 | Ongoing study |
| Knowles RE, Tarrier N | 2009 | Evaluation of the effect of prospective patient diaries on emotional well-being in intensive care unit survivors: a randomized controlled trial | Critical Care Medicine | 37 | 1 | 184–91 | Not TW |
| Konig A, Eonta A, Dyal SR, Vrana SR | 2014 | Enhancing the benefits of written emotional disclosure through response training | Behavior Therapy | 45 | 3 | 344–57 | Not a LTC |
| Koopman C, Ismailji T, Holmes D, Classen CC, Palesh O, Wales T | 2005 | The effects of expressive writing on pain, depression and posttraumatic stress disorder symptoms in survivors of intimate partner violence | The Cochrane Library | 10 | 2 | 211–21 | Not a LTC |
| Kovac SH, Range LM | 2002 | Does writing about suicidal thoughts and feelings reduce them? | The Cochrane Library | 32 | 4 | 428–40 | Not a LTC |
| Kraft CA, Lumley MA, D’Souza PJ, Dooley JA | 2008 | Emotional approach coping and self-efficacy moderate the effects of written emotional disclosure and relaxation training for people with migraine headaches | British Journal of Health Psychology | 13 | 1 | 67–71 | No numerical data reported |
| Kristjansdottir OB, Fors EA, Eide E, Finset A, Stensrud TL, van Dulmen S, et al. | 2013 | A smartphone based intervention with diaries and therapist-feedback to reduce catastrophizing and increase functioning in women with chronic widespread pain: a randomised controlled trial | Journal of Medical Internet Research | 5 | 1 e5 | 1–22 | Not just writing in the intervention; no appropriate control |
| Kristjansdottir OB, Fors EA, Eide E, Finset A, Stensrud TL, van Dulmen S, et al. | 2013 | A smartphone based intervention with diaries and therapist-feedback to reduce catastrophizing and increase functioning in women with chronic widespread pain. Part 2: 11-month follow up results of a randomised controlled trial | Journal of Medical Internet Research | 15 | 3 e72 | 1–19 | Not just writing in the intervention; no appropriate control |
| Lammerts van Bueren N | 2007 | Writing assignments about stressful and/or traumatic events do not benefit patients with anxiety disorders (in Dutch) | Tijdschrift voor Psychiatrie | 49 | 2 | 75–84 | No numerical data reported |
| Lange A, Van de Ven JP, Schrieken B, Emmelkamp PMG | 2001 | Interapy. Treatment of posttraumatic stress through the Internet: a controlled trial | Journal of Behaviour Therapy and Experimental Psychiatry | 32 | 2 | 73–90 | Duplicate |
| Lange A, Schoutrop M, Schrieken B, Van de Ven J-P | 2002 | Interapy: a model for therapeutic writing through the Internet | NA | NA | NA | 215–38 | Not a LTC |
| Lorenz TA, Pulverman CS, Meston CM | 2013 | Sudden gains during patient-directed expressive writing treatment predicts depression reduction in women with history of childhood sexual abuse: results from a randomized clinical trial | Cognitive Therapy and Research | 37 | 4 | 690–6 | Not a LTC |
| Low CA, Stanton AL, Bower JE, Gyllenhammer L | 2010 | A randomized controlled trial of emotionally expressive writing for women with metastatic breast cancer | The Cochrane Library | 29 | 4 | 460–6 | Not the comparator of interest |
| Low CA, Stanton AL, Danoff-Burg S | 2006 | Expressive disclosure and benefit finding among breast cancer patients: mechanisms for positive health effects | The Cochrane Library | 25 | 2 | 181–9 | Not the comparator of interest |
| Lu QA, Stanton AL | 2010 | How benefits of expressive writing vary as a function of writing instructions, ethnicity and ambivalence over emotional expression | Psychology & Health | 25 | 6 | 669–84 | Not a LTC |
| Lu Q, Man J, Yeung N, You J, Young L, Loh A | 2012 | Sources of distress and culturally sensitive interventions to reduce distress among Chinese-speaking breast cancer survivors | Psycho-Oncology | 21 | NA | 36 | Duplicate |
| Luber RF Jr | 1973 | Poetry therapy helps patients express feelings | Hospital & Community Psychiatry | 24 | 6 | NA | Not the study type of interest |
| Lumley MA, Keefe FJ, Slatcher R, Mosley-Williams A, Rice J, Mayo A, et al. | 2011(a) | The raised trial: effects of coping skills training and written emotional disclosure on daily diary outcomes for patients with rheumatoid arthritis | Psychosomatic Medicine | 73 (3) | NA | A120 | Abstract |
| Lumley MA, Sklar ER, Carty JN | 2012 | Emotional disclosure interventions for chronic pain: from the laboratory to the clinic | Translational Behavioral Medicine | 2, number 1 | NA | 73–81 | Not the study type of interest |
| Macklem DJ | 2008 | Exploration of emotion regulation styles as potential moderators of emotional disclosure in patients with rheumatoid arthritis: testing a model of emotional expression | Dissertation Abstracts International: Section B: The Sciences and Engineering | 68 | 10-B | 6971 | No numerical data reported |
| MacRobert M | 2012 | Exploring an acting method to contain the potential madness of the creative writing process: mental health and writing with emotion | New Writing | 9, number 3 | NA | 349–60 | Not the study type of interest |
| Maestas KL | 2014 | The benefits of expressive writing on overgeneral memory and depressive symptoms | PhD dissertation | NA | NA | NA | Not a LTC |
| Manzoni GM, Castelnuovo G, Molinari E | 2011 | The WRITTEN-HEART study (expressive writing for heart healing): rationale and design of a randomized controlled clinical trial of expressive writing in coronary patients referred to residential cardiac rehabilitation | The Cochrane Library | 9 | NA | 51 | Ongoing study |
| Marston CB | 2003 | Written emotional expression, and its relation to psychological and physical health variables among people with HIV disease | Dissertation Abstracts International: Section B: The Sciences and Engineering | 64 | 2-B | 969 | Not the comparator of interest |
| Mastel-Smith BA, McFarlane J, Sierpina M, Malecha A, Haile B | 2007 | Improving depressive symptoms in community-dwelling older adults: a psychosocial intervention using life review and writing | The Cochrane Library | 33 | 5 | 13–19 | Not a LTC |
| Matthiesen S, Klonoff-Cohen H, Zachariae R, Jensen-Johansen MB, Nielsen BK, Frederiksen Y, et al. | 2012 | The effect of an expressive writing intervention (EWI) on stress in infertile couples undergoing assisted reproductive technology (ART) treatment: a randomized controlled pilot study | British Journal of Health Psychology | 17 | NA | 362–78 | Not a LTC |
| Maultsby MC Jr | 1971 | Written homework for the patient with an emotional crisis | American Family physician | 4 | 6 | 69–75 | Not the study type of interest |
| Mazza N | 1979 | Poetry: a therapeutic tool in the early stages of alcoholism treatment | Journal of Studies on Alcohol | 40 | 1 | 123–8 | Not the study type of interest |
| McGuire KMB, Greenberg MA, Gevirtz R | 2005 | Autonomic effects of expressive writing in individuals with elevated blood pressure | The Cochrane Library | 10 | 2 | 197–209 | Not a LTC |
| Melton BF, Bigham LE, Bland HW | 2013 | The feasibility of using video journaling to collect ecological momentary assessment data: application to health behaviour change interventions | Journal of Computing in Higher Education | 25 | – | 12–26 | No inactive control |
| Meston CM, Lorenz TA, Stevenson KR | 2013 | Effects of expressive writing on sexual dysfunction, depression and PTSD in women with a history of childhood sexual abuse: results from a randomised clinical trial | Journal of Sexual Medicine | 10 | – | 2177–89 | No inactive control |
| Mitchell SL | NA | The effects of journal-writing and story-listening on world assumptions, health, and religiousness following the terrorist attacks of 11 September 2001 (dissertation) | NA | NA | NA | 205 | Not a LTC |
| Mooney P, Espie CA, Broomfield NM | 2009 | An experimental assessment of a Pennebaker writing intervention in primary insomnia | Behavioral Sleep Medicine | 7 | 2 | 99–105 | Not the comparator of interest |
| Mosher CE, DuHamel K, Lam J, Massie MJ, Dickler M, Norton L | 2010 | Does expressive writing benefit distressed women with metastatic breast cancer? | Annals of Behavioral Medicine | 39 | NA | 80 | Duplicate |
| Mugerwa S, Holden JD | 2012 | Writing therapy: a new tool for general practice? | British Journal of General Practice | 62 | 605 | 661–3 | Not the study type of interest |
| Muller R, Gertz K, Molton I, Terrill A, Bombardier C, Ehde DM, et al. | 2014 | Pilot testing a positive psychology intervention in individuals with chronic disability-related pain | Archives of Physical Medicine and Rehabilitation | E9 | Conference abstract | ||
| Muresan A, Baban A, Dumitrascu D | 2012 | The effectiveness of an expressive writing intervention for irritable bowel syndrome in a Romanian sample | Psychology & Health | 27 | NA | 286 | Abstract |
| Nes AA, Eide H, Kristjansdottir OB, van Dulmen S | 2013 | Web-based, self-management enhancing interventions with e-diaries and personalised feedback for persons with chronic illness: a tale of three studies | Patient Education and Counselling | 93 | – | 451–8 | Not TW |
| Nitkin-Kaner Y | 2009 | Relationships between expressive writing about traumatic events and reduction in depressive symptomatology | Dissertation Abstracts International: Section B: The Sciences and Engineering | 69 | 7-B | 4436 | Not a LTC |
| Nitkin-Kaner Y, Cruess Dean G | 2008 | Using the expressive writing paradigm as a means to enhance perceived control in women with depression | NA | NA | NA | 11–37 | No outcome of interest |
| Norman SA, Lumley MA, Dooley JA, Diamond MP | 2004 | For whom does it work? Moderators of the effects of written emotional disclosure in a randomized trial among women with chronic pelvic pain | Psychosomatic Medicine | 66 | 2 | 174–83 | Not the comparator of interest |
| Norman S, Lumley M, Dooley J, Schram L, Diamond M | 2001 | Written emotional disclosure in women with chronic pelvic pain | Psychosomatic Medicine | 63 | 1 | 131 | Duplicate |
| Norman SA | 2001 | The effects of emotional disclosure in women with chronic pelvic pain | Dissertation Abstracts International: Section B: The Sciences and Engineering | 61 | 10-B | 131 | Duplicate |
| Nortemann M, Friedrichs O, Wiethuchter B, Dietl T, Hohn D, Nortemann S | 2007 | Therapeutic writing in the stationary psychiatric psychotherapeutic treatment | Nervenarzt | 78 | NA | 328 | Not the comparator of interest |
| O’Cleirigh C, Ironson G, Antoni M, Fletcher MA, McGuffey L, Balbin E, et al. | 2003 | Emotional expression and depth processing of trauma and their relation to long-term survival in patients with HIV/AIDS | Journal of Psychosomatic Research | 54 | 3 | 225–35 | Not the comparator of interest |
| O’Cleirigh C, Ironson G, Fletcher MA, Schneiderman N | 2008 | Written emotional disclosure and processing of trauma are associated with protected health status and immunity in people living with HIV/AIDS | British Journal of Health Psychology | 13 | 1 | 81–4 | Not the comparator of interest |
| O’Connor DB, Ashley L, Jones F, Ferguson E | 2014 | Maladaptive rumination moderates the effects of written emotional disclosure on ambulatory blood pressure levels in females | Health Psychology and Behavioural Medicine | 2 | 1 | 1067–77 | Not a LTC |
| Panagopoulou E, Montgomery A, Tarlatzis B | 2009 | Experimental emotional disclosure in women undergoing infertility treatment: are dropouts better off? | Social Science & Medicine | 69 | 5 | 678–81 | Not a LTC |
| Passalacqua S, Dolcetti FR, Pagliarello C, Di Pietro C, Tabolli S | 2011 | The illness experience in patients with psoriasis: suggestions for strategies to develop quality of care | British Journal of Dermatology | 165 | 6 | e35 | Abstract |
| Peterkin A, Esplen MJ, Hann J, Lawson A | 2013 | A pilot study of a narrative competence group to enhance coping and quality of life in patients with HIV | Arts & Health: an international journal for research, policy and practice | 5 | 1 | 5–18 | No comparator |
| Pitblado E, McConnachie F, Maxwell S | 2005 | What are the benefits of participating in creative writing workshops for people with epilepsy | Epilepsia | 46 | NA | 188 | Not TW |
| Possemato KA | 2008 | An internet-based expressive writing intervention for kidney transplant recipients | Dissertation Abstracts International: Section B: The Sciences and Engineering | 68 | 7-B | 4842 | Duplicate |
| Possemato K, Ouimette P, Geller PA | 2010 | Internet-based expressive writing for kidney transplant recipients: effects on posttraumatic stress and quality of life | Traumatology | 16 | 1 | 49–54 | Not the comparator of interest |
| Possis EA, Kemp JJ, Lickel JJ, Sy JT, Dixon LJ, Deacon BJ | 2013 | A comparison of cognitive and behavioural approaches for reducing cost bias in social anxiety | Journal of Cognitive Psychotherapy: an International Quarterly | 27 | 3 | 210–20 | Not TW intervention |
| Ressler PK, Bradshaw YS, Gualtieri L, Chui KK | 2012 | Communicating the experience of chronic pain and illness through blogging | Journal of Medical Internet Research | 14 | 5 | NA | Not the study type of interest |
| Rivkin ID, Gustafson J, Weingarten I, Chin D | 2006 | The effects of expressive writing on adjustment to HIV | AIDS and Behavior | 10 | 1 | 13–26 | No numerical data reported |
| Robinson P | 2001 | Using the internet as a vehicle for treatment of bulimia nervosa: a randomised control trial of cognitive behaviour therapy versus therapeutic writing | The Cochrane Library | NA | NA | NA | Not the study type of interest |
| Schmitter-Edgecombe M, Fahy JF, Whelan JP, Long CJ | 1995 | Memory remediation after severe closed head injury: notebook training versus supportive therapy | Journal of Consulting and Clinical Psychology | 63 | 3 | 484–9 | Not the comparator of interest |
| Schoutrop MJ, Lange A, Hanewald G, Davidovich U, Salomon H | 2002 | Structured writing and processing major stressful events: a controlled trial | Psychotherapy and Psychosomatics | 71 | 3 | 151–7 | Not a LTC |
| Segerstrom SC, Averill AJ, Kasarskis EJ | 2011 | Expressive writing and psychological well-being in amyotrophic lateral sclerosis (ALS) | Psychosomatic Medicine | 73 | 3 | A83 | Duplicate |
| Sehgal S, Casden D, Bardwell W, Hickman S | 2008 | The effects of expressive writing on physical and mental functioning in cancer patient survivors | Psycho-Oncology | 17 | 3 | S94 | Not the study type of interest |
| Seitz DC, Knaevelsrud C, Duran G, Waadt S, Loos S, Goldbeck L | 2014 | Efficacy of an internet-based cognitive–behavioural intervention for long-term survivors of paediatric cancer: a pilot study | Support Care cancer | 22 | – | 2075–83 | No control group |
| Serchia P | 2000 | The write stuff. APLAs Writers Workshop begins its second decade | Positive Living (Los Angeles, CA) | 9 | 9 | 16–19, 51–2 | Not available |
| Sloan DM, Epstein EM, Dobbs JM, Pontoski KE | 2006 | Written disclosure as an intervention for PTSD | Psychophysiology | 43 | NA | S93 | Duplicate |
| Sloan DM, Marx BP, Epstein EM | 2005 | Further examination of the exposure model underlying the efficacy of written emotional disclosure | Journal of Consulting and Clinical Psychology | 73 | 3 | 549–54 | Not a LTC |
| Sloan DM, Marx BP, Epstein EM, Lexington JM | 2007 | Does altering the writing instructions influence outcome associated with written disclosure? | The Cochrane Library | 38 | 2 | 155–68 | Not a LTC |
| Sloan DM, Marx BP, Greenberg EM | 2011 | A test of written emotional disclosure as an intervention for posttraumatic stress disorder | The Cochrane Library | 49 | 4 | 299–304 | Not a LTC |
| Smith CE, Holcroft C, Rebeck Sl, Thompson NC, Werkowitch M | 2000 | Journal writing as a complementary therapy for reactive depression: a rehabilitation teaching program | Rehabilitation Nursing | 25 | 5 | 170–6 | Not the study type of interest |
| Smith H | 2005 | Writing about emotional experience to reduce symptoms and improve lung function and quality of life in patients with asthma – pilot phase of a randomised controlled trial | The Cochrane Library | NA | NA | NA | Duplicate |
| Smith HE, Jones CJ, Theadom A, Horne R, Bowskill R, Hankins M, et al. | 2009 | Writing about emotional experiences reduces beta-agonist use in patients with asthma – 3-month follow up of a randomised controlled trial | Journal of Allergy and Clinical Immunology | 1 | NA | S80 | Abstract |
| Smyth JM | 1999 | Written emotional disclosure: effects on symptoms, mood, and disease status in patients with asthma or rheumatoid arthritis | Dissertation Abstracts International: Section B: The Sciences and Engineering | 59 | 8-B | 4543 | Duplicate |
| Solano L, Donati V, Pecci F, Persichetti S, Colaci A | 2003 | Postoperative course after papilloma resection: effects of written disclosure of the experience in subjects with different alexithymia levels | Psychosomatic Medicine | 65 | 3 | 477–84 | Not a LTC |
| Solano L, Pepe L, Donati V, Persichetti S, Laudani G, Colaci A | 2007 | Differential health effects of written processing of the experience of a surgical operation in high- and low-risk conditions | Journal of Clinical Psychology | 63 | 4 | 357–69 | Not a LTC |
| Spiegel D | 1999 | Healing words: emotional expression and disease outcome | JAMA | 281 | 14 | 1328–9 | Not the study type of interest |
| Stanton AL, Danoff-Burg S, Sworowski LA, Collins CA, Branstetter AD, Rodriguez-Hanley A, et al. | 2002 | Randomized, controlled trial of written emotional expression and benefit finding in breast cancer patients | Journal of Clinical Oncology | 20 | 20 | 4160–8 | Not the comparator of interest |
| Stice E, Burton E, Bearman SK, Rohde P | 2007 | Randomized trial of a brief depression prevention program: an elusive search for a psychosocial placebo control condition | The Cochrane Library | 45 | 5 | 863–76 | Not a LTC |
| Stone AA, Smyth JM, Kaell A, Hurewitz A | 2000 | Structured writing about stressful events: exploring potential psychological mediators of positive health effects | The Cochrane Library | 19 | 6 | 619–24 | Not TW |
| Tabolli S, Naldi L, Di Pietro C, Pagliarello C, Paradisi A, Sampogna F, et al. | 2011 | The impact of writing exercises on quality of life in patients with psoriasis undergoing systemic treatments | British Journal of Dermatology | 165 | 6 | e33–4 | Duplicate |
| Tamagawa R, Moss-Morris R, Martin A, Robinson E, Booth RJ | 2013 | Dispositional emotion coping styles and physiological responses to expressive writing | British Journal of Health Psychology | 18 | – | 574–92 | Not a LTC |
| Thompson T, Kreuter MW | 2014 | Using written narratives in public health practice: a creative writing perspective | Preventing Chronic Disease: Public Health Research, Practice, and Policy | 11 | – | 7–14 | Not a primary study |
| Torres GF, Otalvaro MI, Vargas JC, Castellanos Y, Garcia JX, Triana JD, et al. | 2012 | Devising and validating a headache diary in a series of patients with chronic daily headache from Colombia | NA | NA | NA | NA | Not TW |
| Toussaint L, Barry M, Bornfield L, Markman M | 2014 | Restore: the journey towards self forgiveness: a randomised trial in patient education on self-forgiveness in cancer patients and caregivers | Journal of Healthcare Chaplaincy | 20 | – | 54–74 | Not TW |
| Tsai Y-C, Chaung M-T | 2013 | Fostering revision of argumentative writing through structured peer-assessment | Perceptual and Motor Skills | 1 | – | 210–21 | Not a LTC |
| Ulbrect JS, Trief PM, Wallston KA, Heron KE, Smyth JA | 2014 | Short term effects of expressive writing as adjuvant treatment in T2DM on clinical status and patient wellbeing | ADA | 8 | – | A2 | Conference abstract |
| Van der Houwen K, Schut H, van den Bout J, Stroebe M, Stroebe W | 2010 | The efficacy of a brief internet-based self-help intervention for the bereaved | Behaviour Research & Therapy | 48 | 5 | 359–67 | Not a LTC |
| Van Middendorp H, Sorbi MJ, van Doornen LJP, Bijlsma JWJ, Geenen R | 2007 | Feasibility and induced cognitive-emotional change of an emotional disclosure intervention adapted for home application | Patient Education and Counseling | 66 | 2 | 177–87 | Not TW |
| Verrept H, Rogier C, Stuer H, Schillemans L | 1990 | Writing therapy for chronic disease patients (Dutch) | NA | NA | NA | NA | Not the study type of interest |
| Wagner LJ | 2004 | Moderating effects of cognitive adaptability on expressive writing outcomes among persons infected with human immunodeficiency virus | Dissertation Abstracts International: Section B: The Sciences and Engineering | 65 | 3-B | 1254 | Duplicate |
| Warner LJ | 2003 | Expressive writing and health in pediatric asthma (dissertation) | The Cochrane Library | NA | NA | 175 | Duplicate |
| Wilson BM, Proctor A | 2002 | Written discourse of adolescents with closed head injury | Brain Injury | 16 | 11 | 1011–24 | Not TW |
| Wilson BM, Smith R, Proctor A | 2001 | The validity of cognitive distance in oral and written discourse | Brain and Cognition | 46 | 1–2 | 304–7 | Not TW |
| You DS, Creech SK, Vichaya EG, Young EE, Smith JS, Meagher MW | 2014 | Effect of written emotional disclosure on secondary hyperalgesia in women with trauma history | Psychosomatic Medicine | 76 | 5 | 337–46 | Not a LTC |
| Young CM, Rodruigez LM, Neighbours C | 2013 | Expressive writing as a brief intervention for reducing drinking intentions | Addictive Behaviours | 38 | 12 | 25–32 | Not diagnosed LTC |
| Zakowski SG, Herzer M, Barrett SD, Milligan JG, Beckman N | 2011 | Who benefits from emotional expression? An examination of personality differences among gynaecological cancer patients participating in a randomized controlled emotional disclosure intervention trial | British Journal of Psychology | 102 | 3 | 355–72 | No numerical data reported |
| Zakowski SG, Morton C, Ramati A, Felch N | 2002 | Expressive writing moderates the effects of negative social interactions on distress in cancer patients | Psychosomatic Medicine | 64 | 1 | 102 | Duplicate |
| Ziviani J, Hayes A, Chant D | 1990 | Handwriting: a perceptual-motor disturbance in children with myelomeningocele | Occupational Therapy Journal of Research | 10 | 1 | 12–26 | Not TW |
Appendix 7 List of items required when reporting a realist synthesis (RAMESES checklist)
| Reporting item | Description of item | Reported on page(s) | |
|---|---|---|---|
| Title | |||
| 1 | In the title, identify the document as a realist synthesis or review | i | |
| Abstract | |||
| 2 | While acknowledging publication requirements and house style, abstracts should ideally contain brief details of: the study’s background, review question or objectives; search strategy; methods of selection, appraisal, analysis and synthesis of sources; main results; and implications for practice | vii and viii | |
| Introduction | |||
| 3 | Rationale for review | Explain why the review is needed and what it is likely to contribute to existing understanding of the topic area | 6 and 7 |
| 4 | Objectives and focus of review | State the objective(s) of the review and/or the review question(s). Define and provide a rationale for the focus of the review | 169–71 |
| Methods | |||
| 5 | Changes in the review process | Any changes made to the review process that was initially planned should be briefly described and justified | 169–71 |
| 6 | Rationale for using realist synthesis | Explain why realist synthesis was considered the most appropriate method to use | 169–71 |
| 7 | Scoping the literature | Describe and justify the initial process of exploratory scoping of the literature | Not undertaken |
| 8 | Searching processes | While considering specific requirements of the journal or other publication outlet, state and provide a rationale for how the iterative searching was done. Provide details on all of the sources accessed for information in the review. Where searching in electronic databases has taken place, the details should include, for example, name of database, search terms, dates of coverage and date last searched. If individuals familiar with the relevant literature and/or topic area were contacted, indicate how they were identified and selected | 169–71 |
| 9 | Selection and appraisal of documents | Explain how judgements were made about including and excluding data from documents, and justify these | 169–71 |
| 10 | Data extraction | Describe and explain which data or information were extracted from the included documents and justify this selection | 169–71 |
| 11 | Analysis and synthesis processes | Describe the analysis and synthesis processes in detail. This section should include information on the constructs analysed and describe the analytic process | 169–71 |
| Results | |||
| 12 | Document flow diagram | Provide details on the number of documents assessed for eligibility and included in the review, with reasons for exclusion at each stage, as well as an indication of their source of origin (e.g. from searching databases, reference lists and so on). You may consider using the example templates (which are likely to need modification to suit the data) that are provided | 172–82 |
| 13 | Document characteristics | Provide information on the characteristics of the documents included in the review | 172–82 |
| 14 | Main findings | Present the key findings with a specific focus on theory building and testing | 172–82 |
| Discussion | |||
| 15 | Summary of findings | Summarise the main findings, taking into account the reviews objective(s), research question(s), focus and intended audience(s) | 183–90 |
| 16 | Strengths, limitations and future research directions | Discuss both the strengths of the review and its limitations. These should include (but need not be restricted to) (a) consideration of all the steps in the review process and (b) comment on the overall strength of evidence supporting the explanatory insights which emerged The limitations identified may point to areas where further work is needed |
183–90 183–90 |
| 17 | Comparison with existing literature | Where applicable, compare and contrast the reviews findings with the existing literature (e.g. other reviews) on the same topic | 183–90 |
| 18 | Conclusion and recommendations | List the main implications of the findings and place these in the context of other relevant literature. If appropriate, offer recommendations for policy and practice | 183–90 |
| 19 | Funding | Provide details of funding source (if any) for the review, the role played by the funder (if any) and any conflicts of interests of the reviewers | xxxvii |
Appendix 8 Project details
Title
Does therapeutic writing help people with long-term conditions? Systematic review, realist synthesis and economic considerations
Funding body
NIHR HTA 11/70/01
Simon Bevan
Programme Manager
NETSCC, Health Technology Assessment
Alpha House
University of Southampton Science Park
Southampton
SO16 7NS
Project Steering Group Committee
The SGC was formed by the advisors (Carol Ross, Sheila Hayman, Victoria Field) and the Research Team (Olga Perez Nyssen, Stephanie Taylor, Geoff Wong, Elizabeth Steed, Liam Bourke, Joanne Lord, Ailish Higgins, Trisha Greenhalgh and Catherine Meads).
The SGC met every 4 weeks, starting February 2013 until the end of the project. Additionally, regular weekly catch-up meetings were undertaken between Stephanie Taylor and Olga Perez Nyssen.
Glossary
Technical terms, abbreviations and/or acronyms are used throughout this report with definitions provided. In some cases, usage may differ in the literature, but the term has a constant meaning throughout this review.
- Context
- In realist synthesis, context refers to the backdrop of programmes and research. As these conditions change over time, the context may reflect aspects of those changes while the programme is implemented. Context can be broadly understood as any condition that triggers and/or modifies the behaviour of a mechanism.
- Facilitated therapeutic writing
- Writing activities involving a facilitator, such as a trained writing practitioner or a psychologist. It may be a group activity or one to one, and can be delivered face to face or remotely, for example over the web.
- Mechanism
- In realist synthesis, mechanisms are underlying entities, processes or structures, which operate in particular contexts to generate outcomes of interest. Mechanisms (1) are usually hidden; (2) are sensitive to variations in context; and (3) generate outcomes.
- Positive writing
- Involves writing about positive experiences such as events that stimulated happiness or joy and it may be facilitated or unfacilitated.
- Programme theory
- In realist synthesis, the term programme theory refers to an abstracted description and/or diagram that lays out what a programme (or family of programmes or interventions) comprises and how it is expected to work.
- Unfacilitated emotional writing
- Also known as unfacilitated expressive writing or written emotional disclosure, a type of unfacilitated therapeutic writing, as described by Pennebaker and Beall (Pennebaker JW, Beall SK. Confronting a traumatic event: towards an understanding of inhibition and disease. J Abnorm Psychol 1986;95:274–81) or a variant thereof.The trauma–emotion subjects were asked to write about a personally upsetting experience and to describe the feelings they had about the experience. It was emphasized that they were to write only about their feelings, with no mention of what actually happened.
List of abbreviations
- AEE
- Ambivalence Emotional Expression (or Ambivalence over Emotional Expression)
- AIMS2
- Arthritis Impact Measurement Scale-2
- AIMS2-ps
- Arthritis Impact Measurement Scale-2, pain subscale
- ALS
- amyotrophic lateral sclerosis (in the UK referred to as ‘motor neurone disease’)
- AMED
- Allied and Complementary Medicine Database
- ART
- antiretroviral therapy
- AS
- ankylosing spondylitis
- ASSIA
- Applied Social Sciences Index and Abstracts
- BAI
- Beck Anxiety Inventory
- BASFI
- Bath Ankylosing Spondylitis Disease Functional Index
- BDI
- Beck Depression Inventory
- BDI-II
- revised Beck Depression Inventory
- BDI-SF
- Beck Depression Inventory-Short Form
- BED
- binge-eating disorder
- BFI
- Brief Fatigue Inventory
- BN
- bulimia nervosa
- BPI
- Brief Pain Inventory
- BSI
- Brief Symptom Inventory
- CBCL
- Child Behavior Checklist
- CBT
- cognitive–behavioural therapy
- CD4+
- cluster of differentiation antigen 4-positive
- CD4+ count
- CD4+ cell count
- CDI
- Children Depression Inventory
- CDSR
- Cochrane Database of Systematic Reviews
- CENTRAL
- Cochrane Central Register of Controlled Trials
- CES-D
- Centre for Epidemiological Studies Depression Scale
- CG-FBD
- Functional Bowel Disease-related Cognition
- CG-FBD Q31
- Functional Bowel Disease-related Cognition questionnaire 31
- CI
- confidence interval
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CMO
- context, mechanism and outcome
- CMOC
- context, mechanism, outcome andconfiguration
- COPD
- chronic obstructive pulmonary disease
- C-QoL
- Cancer Quality of Life
- CRP
- C-reactive protein
- CRQ-e
- Chronic Respiratory Disease Questionnaire, emotion subscale
- CSAQ
- Cognitive–Somatic Anxiety Questionnaire
- CVD
- cardiovascular disease
- DARE
- Database of Abstracts of Reviews of Effects
- DAS
- Disease Activity Score
- DASS-A
- Depression Anxiety Stress Scales, anxiety subscale
- DASS-D
- Depression Anxiety Stress Scales, depression subscale
- DBP
- diastolic blood pressure
- DH
- Department of Health
- DLQI
- Dermatology Life Quality Index
- DSM-III-R
- Diagnostic and Statistical Manual of Mental Disorders-Third Edition, Revised
- DSM-IV
- Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition
- DSM-IV-TR
- Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition, Text Revision
- DT
- Distress Thermometer
- eBT
- e-mail bulimia therapy
- EQ-5D
- European Quality of Life-5 Dimensions
- ERIC
- Education Resources Information Center
- ESR
- erythrocyte sedimentation rate
- EW
- emotional writing
- FACIT-F
- Functional Assessment of Chronic Illness Therapy, fatigue subscale
- FACT
- Functional Assessment of Cancer Therapy
- FACT-B
- Functional Assessment of Cancer Therapy, Breast Cancer Version
- FDI
- Functional Disability Inventory
- FEV1
- forced expiratory volume in 1 second
- FEV1% pred
- percentage of predicted forced expiratory volume in 1 second
- FM
- fibromyalgia
- FVC
- forced vital capacity
- GBB
- ‘Giessener Beschwerdebogen’ (Symptomatic Complaints)
- GDS
- Geriatric Depression Scale
- GHQ-12
- General Health Questionnaire
- GI
- gastrointestinal
- GI RAP
- gastrointestinal recurrent abdominal pain
- GP
- general practitioner
- GSI
- Global Severity Index
- HADS
- Hospital Anxiety and Depression Scale
- HADS-A
- Hospital Anxiety and Depression Scale, anxiety subscale
- HADS-D
- Hospital Anxiety and Depression Scale, depression subscale
- HAM-D
- Hamilton Depression Scale
- HIV
- human immunodeficiency virus
- HIV-OS
- HIV-Specific Optimism Scale
- HRQoL
- health-related quality of life
- HTA
- Health Technology Assessment
- IBS
- irritable bowel syndrome
- IBSSS
- Irritable Bowel Syndrome Severity Scale
- ICD-10
- International Classification of Diseases, Tenth Edition
- IES
- Impact of Event Scale
- IES-Av
- avoidance subscale of the IES
- IES-I
- intrusion subscale of the IES
- IL
- interleukin
- IPF
- idiopathic pulmonary fibrosis
- ITT
- intention to treat
- K-10
- Kessler Psychological Distress Scale
- LTC
- long-term condition
- MDASI
- MD Anderson Symptom Inventory
- MI
- myocardial infarction
- MOS-SF-36
- Medical Outcomes Short-Form Health Survey
- MPI
- Multidimensional Pain Inventory
- MPQ-i
- McGill Pain Questionnaire, impact
- MVA
- motor vehicle accident
- NHS EED
- Economic Evaluation Database
- OQ-45.2
- Outcome Questionnaire
- OR
- odds ratio
- PANAS
- Positive and Negative Affect Schedule
- PANAS-NA
- Positive and Negative Affect Schedule, negative subscale
- PANAS-PA
- Positive and Negative Affect Schedule, positive subscale
- PASI
- Psoriasis Area and Severity Index
- PEDro
- Physiotherapy Evidence Database
- PHQ-9
- Patient Health Questionnaire, 9-item subscale
- PILL
- Pennebaker Inventory of Limbic Languidness
- PILOTS
- Published International Literature On Traumatic Stress
- POMS
- Profile of Mood States
- POMS-d
- Profile of Mood States depression subscale
- POMS-SF
- Profile of Mood States Short Form
- PPMS
- Passive Positive Mood Scale
- PRISMA
- Preferred Reporting Items for Systematic reviews and Meta-Analyses
- PSQI
- Pittsburgh Sleep Quality Index
- PSS
- Perceived Stress Scale
- PSWQ
- Penn State Worry Questionnaire
- PTSD
- post-traumatic stress disorder
- PTSDTOT
- The Davidson PTSD scale
- QALY
- quality-adjusted life-year
- QEDD
- Questionnaire for Eating Disorders Diagnosis
- QoL
- quality of life
- RA
- rheumatoid arthritis
- RAMESES
- Realist and Meta-review Evidence Synthesis: Evolving Standards
- RAP
- recurrent abdominal pain
- RCC
- renal cell carcinoma
- RCMAS
- Revised Children’s Manifest Anxiety Scale
- RCT
- randomised controlled trial
- SAM
- Self-Assessment Manikin
- SAPASI
- Self-Administered Psoriasis Area and Severity Index
- SBP
- systolic blood pressure
- SCI
- Science Citation Index
- SCID
- Structured Clinical Interview for DSM Disorders
- SCL-90-R
- Symptom Checklist-90-Revised
- SD
- standard deviation
- SDW
- self-directed writing
- SE
- standard error
- SF-36
- Short Form questionnaire-36 items
- SF-36 MCS
- Short Form questionnaire-36 items mental composite score
- SF-36 PCS
- Short Form questionnaire-36 items physical composite score
- SF-6D
- Short Form questionnaire-6 Dimensions
- SGC
- Steering Group Committee
- SMC
- standard medical care
- SMD
- standardised mean difference
- SOC
- Sense of Coherence Scale
- SOS
- Significant Others Scale
- SS
- statistically significant
- SSCI
- Social Sciences Citation Index
- STAI
- State/Trait Anxiety Scale
- SUD
- substance use disorder
- TW
- therapeutic writing
- VL
- viral load
- VSQ
- Visit Specific Satisfaction Questionnaire
- WET
- written exposure therapy