Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 10/69/05. The contractual start date was in June 2012. The draft report began editorial review in June 2014 and was accepted for publication in November 2014. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
Dr Panos Barlas received funding from training health professionals in acupuncture.
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Foster et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Introduction
Pregnancy-related low back pain (with and without pelvic girdle pain)
Low back pain in pregnancy is defined as pain in the lower back, located above the lumbosacral junction, with or without radiation in the legs,1 although this is a narrower definition than that used in the general population,2 in which low back pain is usually defined as pain and discomfort localised below the costal margin and above the inferior gluteal folds, with or without leg pain. Pelvic girdle pain (PGP) is musculoskeletal pain located within the pelvic area between the posterior iliac crest and the gluteal folds, particularly in the vicinity of the sacroiliac joints, that develops in relation to pregnancy. 3,4 The pain may radiate in the posterior thigh and can also occur in conjunction with or separately from pain in the pubic symphysis.
Low back pain and PGP during pregnancy are common and, although they can occur separately, many women experience both. Although prevalence estimates vary between studies owing to different definitions and diagnostic criteria, low back pain is reported to affect between 45% and 75% of women at some stage during their pregnancy,5,6 with a point prevalence of approximately 34%. 6 Prevalence estimates for PGP range widely and include 20% overall,3 35% to 50% in early pregnancy and 60% to 70% in late pregnancy. 3,7,8 The pain increases with advancing pregnancy, is usually worse at night and interferes with sleep, daily activities and work. 7 It is a common reason for sick leave, with reports suggesting that 20–23% of women take sick leave because of their pain. 6,9 Studies have shown that pregnant women with back pain have lower quality of life than pregnant women without back pain. 10 Hence, low back pain and PGP in pregnancy negatively affect activities of daily life and quality of life during pregnancy and are an important health problem. Some have reported an increasing number of affected women requesting induction of labour or elective caesarean section before the recommended 39th week of gestation in order to achieve symptomatic relief. 11 Although longitudinal data are limited, it has been estimated that in 1 in 10 women the pain becomes long-lasting and disability persists after childbirth. 12,13 Pregnancy-related low back pain has been found to reduce soon after delivery but it improves in few women later than 6 months post partum. 14 By 2 years after giving birth, the prevalence of back pain has been reported to fall to the same level found pre pregnancy (18%).
A range of biomedical, psychological and social factors may be important predictors of non-recovery from low back pain in pregnancy, but in general these have not been well studied. Cohort studies15,16 suggest that predictors of poor recovery from symptoms post partum include older age, work dissatisfaction and the presence of combined low back pain and PGP in comparison with pain in either location alone. There is some evidence that women with combined pubic symphysis pain and bilateral posterior PGP in pregnancy have a slower recovery than those women with fewer pain locations12,16 and that women with a high number of other bodily pain sites are more likely to have high pain intensity scores and postpartum non-recovery. 17 Guidelines3 suggest risk factors for PGP include a previous history of low back pain and previous trauma to the pelvis. Studies of low back pain in general have shown the important role of psychosocial obstacles to recovery18,19 and there is some evidence that psychological factors such as a lack of belief in improvement,20 exaggerated negative thoughts or catastrophising about the pain, fear avoidance beliefs21 and distress (anxiety and depression) are also important predictors of poor outcome in women with pregnancy-related back pain. 8
Current clinical management
Women experiencing these problems most often report them to their midwives; for example, in an Australian study 71% reported their pain to their maternity carer,6 but it appears that few receive much in the way of treatment. Pierce et al. 6 found that only 25% of women received any treatment. There are no high-quality UK data that describe current treatment for pregnancy-related low back pain or PGP. It is most often accepted as a ‘normal’ discomfort of pregnancy6,11 with some suggesting this may be related to health professionals’ lack of knowledge about available treatments and fear of possible harmful effects of treatment on the developing fetus. 11 Women are encouraged to believe that their pain is temporary and self-limiting (which may not always be the case), a part of the normal aches and pains of pregnancy,11 and those involved in their care tend to give women information on how to self-manage7 through postural changes, adaptations in lifting techniques, simple exercises to try at home, rest, heat and cold therapy, supportive belts and pillows, massage and relaxation. Some women, however, do proceed to use a range of treatments, such as physiotherapy-led exercise, manual therapy, acupuncture, massage, transcutaneous electrical nerve stimulation (TENS) and mobility aids as well as safe pharmacological options (mostly paracetamol) and, much less commonly, epidural injections. 6,7,11 None of these treatment options has been well researched in women with pregnancy-related back pain.
Current NHS practice varies across services and geographical regions. Most women are not referred from their midwives or general practitioners (GPs) to other health professionals for treatment, but are advised to self-manage. The self-management advice tends to follow the guidance from national associations such as the National Childbirth Trust (www.nct.org.uk) or the Association of Chartered Physiotherapists in Women’s Health (ACPWH; http://pogp.csp.org.uk/) and only the most severely affected women are referred to physiotherapists and receive individual assessment, advice or treatment. We estimate that approximately 10–20% of women are likely to be referred to see a NHS physiotherapist for help with severe back pain and/or PGP. In North Staffordshire, for example, 10% of women with back pain in pregnancy are referred by their midwife (and some cases by their GP), to women’s health physiotherapists, who invite them to a group advice and education session, and are offered individual care following the group session only if needed. The referral is left open for the duration of the pregnancy so that the woman can access further physiotherapy support if needed. In other services, physiotherapists offer individual assessment and individualised advice and treatment.
Acupuncture
Acupuncture is based on needle stimulation of points on the surface of the body (acupuncture points) and originates from traditional Chinese medicine (TCM). It encompasses a variety of different procedures and techniques but most often is based on penetrating the skin at anatomical points on the body with thin, solid, metallic needles that are manipulated manually or by electrical stimulation. Since its introduction to the West several hundred years ago, many different styles of acupuncture have developed, including Japanese meridian therapy, French energetic acupuncture, Korean constitutional acupuncture and Lemington five-element acupuncture. 22 Although similar to traditional acupuncture, these various styles have their own distinct characteristics. In the past several decades, new forms and styles of acupuncture have evolved, including ear (auricular), hand, foot and scalp acupuncture. As a result of advances in the understanding of the neurophysiology of pain and acupuncture, the boundary between acupuncture and conventional medicine is changing. For example, a simplified and more empirical Western approach to acupuncture of local dry needling at the site of pain or at points in the vicinity of pain, called trigger points, is popular among conventional health professionals (medical doctors and physiotherapists). Modern acupuncturists typically use a combination of both TCM meridian acupuncture points and non-meridial (or extrameridial) points. Once appropriate points are selected, the therapist inserts a needle into each point by gently tapping it into place and rotating it until the patient experiences a needle sensation or de-qi, usually described as a tingling, numbness or dull ache sensation. A typical session with acupuncture includes treatment with a varying number of needles (1–30) inserted and kept in place for 20–30 minutes, during which period the therapist may stimulate the needles by rotating or tapping them. Some therapists may also use electrical stimulation (in which an electrical stimulator is connected to the acupuncture needles), injection acupuncture (herbal extracts are injected into acupuncture points), heat lamps or moxibustion. Although the neurophysiological mechanisms of acupuncture are well established in research for experimental pain, the exact mechanisms underlying the action of acupuncture in clinical practice are still unclear. 23 In terms of Western scientific principles, it is uncertain how acupuncture may help musculoskeletal pain such as back pain in pregnancy. Current theories suggest that acupuncture may produce its effects through the nervous system by stimulating the production of biochemicals such as endorphins and other neurotransmitters that influence pain sensation; that acupuncture works through the gate control theory of pain, in which the sensory input is inhibited in the central nervous system by another type of input (the needle); or that the presence of a foreign substance (the needle) within the tissue of the body stimulates vascular and immunomodulatory factors such as mediators of inflammation. 22
The use of acupuncture for musculoskeletal problems appears to be increasing and acupuncture has been recommended within recent UK national guidelines for the management of persistent non-specific low back pain. 24 One of the few randomised trials conducted within the UK25 concluded that there was weak evidence of an effect of a short course of acupuncture on persistent non-specific low back pain (rather than back pain in pregnancy) at 12 months, but that at 24 months there was stronger evidence of a small benefit compared with usual GP care. The health economic analysis conducted alongside that trial26 concluded that acupuncture confers a modest health benefit for minor extra cost to the NHS. The most recent Cochrane Review of acupuncture for low back pain27 included 35 trials, but only three of these were of acute low back pain. Overall, no firm conclusions could be drawn but there was some evidence of short-term pain relief and functional improvement from acupuncture compared with no treatment or sham treatment. There was also some evidence that acupuncture, added to other conventional therapies, relieves pain and improves function better than conventional therapies alone.
A small number of trials have evaluated acupuncture for low back pain and PGP during pregnancy. 28–33 To date, two rigorously conducted systematic reviews have been published. 7,34 The first of these was a Cochrane Review of eight studies (1305 participants) testing the effects of adding various pregnancy-specific exercises, physiotherapy, acupuncture and pillows to standard pre-natal care. 7 That review found positive results for the additional benefit of strengthening exercises, pelvic tilt exercises and exercise in water for women with low back pain. Both acupuncture and stabilising exercises relieved PGP more than usual pre-natal care, and acupuncture provided more relief from evening pain than exercise. One study found that acupuncture was more effective than physiotherapy for pain reduction,28 although it was unclear if this was a result of the type of treatment delivery (acupuncture was individually delivered while the physiotherapy was delivered in groups). A further study showed that 60% of those who received acupuncture reported less intense pain, compared with 14% who had standard pre-natal care. 31 The second systematic review34 focused on randomised trials of needle acupuncture for back pain and PGP in pregnancy and included only three trials (448 women), all from Sweden. 28,31,32 The conclusions were similar to the Cochrane Review by Pennick and Young. 7 Overall, there was limited, though promising, evidence for the effectiveness of acupuncture. Both systematic reviews highlighted the need for further high-quality trials given the weaknesses in the available evidence. Most previous trials have a moderate to high risk of bias, with unclear randomisation and allocation concealment and lack of full intention-to-treat analyses, and only one trial reported work outcomes, despite these clearly being an important outcome for both pregnant women and society more generally. The one trial with low risk of bias32 focused on Swedish women with PGP at 12–31 weeks’ gestation, and randomised them to standard treatment (information, advice about activities, a pelvic belt and a home exercise programme), standard treatment plus acupuncture (twice per week over 6 weeks using 10 local acupuncture points and seven extrasegmental points with the needles manipulated to evoke a de-qi sensation and left in situ for 30 minutes and stimulated every 10 minutes) or standard treatment plus stabilising exercise (individual stabilising exercises modified for pregnancy for a total of 6 hours over 6 weeks). Since the publication of the two systematic reviews in 2008, a small number of further studies were published. One small pilot study35 found auricular acupuncture to be more effective than either sham acupuncture or a waiting list control. Another further high-quality trial by Elden et al. 33 from Sweden compared standard treatment plus acupuncture with standard treatment plus sham (non-penetrating) acupuncture for women with PGP. In that trial, 12 acupuncture treatments were provided over 8 weeks and results showed no differences between groups on pain or sick leave, questioning the importance of needle penetration in the reported beneficial effects of acupuncture. The existing research clearly highlights the need for a high-quality randomised trial in the UK NHS setting, testing the clinical effectiveness and cost-effectiveness of the addition of acupuncture to standard care (SC) for pregnant women with low back pain (with or without PGP). It also highlights the importance of including a sham or non-penetrating acupuncture intervention.
Key methodological issues for the EASE Back study
Given the known limitations of previous trials of acupuncture, we followed published recommendations about methods and reporting trials of acupuncture,36 non-pharmacological interventions37 and sham interventions in trials of physical medicine and rehabilitation23 for our pilot trial. This was informed by the results of our pre-pilot work in phase 1 of the Evaluating Acupuncture and Standard carE for pregnant women with Back pain (EASE Back; a national survey and interviews) study and includes the rationale for acupuncture type, the details of the needling, the intervention protocol, other components of the treatment, practitioner background and experience, full details of the treatments, similar protocols for the true and sham acupuncture treatments and data on participants’ treatment preferences and expectations before they are randomised. There are several key methodological issues relevant to conducting trials of acupuncture (and, more broadly, non-pharmacological interventions for pain); these include sham treatment considerations, issues of blinding, safety, protocolising or standardising what is usually a highly individualised acupuncture treatment for the purposes of a trial and choosing the most appropriate package of SC for comparison. Each of these is discussed along with the implications for the EASE Back study.
Sham acupuncture
A key discussion in the existing research on acupuncture focuses on the challenge of adequate sham or placebo acupuncture treatments. 23 In fact, some believe that it is virtually impossible to construct a completely inert placebo that sufficiently mimics the insertion and manipulation of acupuncture needles; hence we use the term ‘sham’. The use of sham intervention helps to ensure participant blinding and reduces the risk of potential bias that can interfere with the observed outcomes. 23 We believe that any future large trial should include a treatment group that receives sham acupuncture to enable us to better understand the possible basis of acupuncture effects. Previous trials have used different methods of sham and there is little agreement on the best sham, given that some methods appear to induce physiological effects (e.g. inserting needles at non-acupuncture points or superficial needling at acupuncture points). 23 A perfect sham for acupuncture would induce the needle or de-qi sensation,23 but it is increasingly clear that inducing this needling sensation regardless of the stimulation point is associated with the physiological effects of acupuncture. A recent review38 concluded that the effect of acupuncture seems to be unrelated to the type of sham acupuncture used as control and that non-penetrating acupuncture shams are thought to be least likely to have physiological effects. We believe that using non-penetrating needles on a small number of the same acupuncture points that would be used for true acupuncture alongside the inclusion of acupuncture-naive participants are the best solutions to this challenge. Similar approaches have been used successfully in previous trials of acupuncture for musculoskeletal problems39 and pregnant women with PGP. 33 Thus, we included three treatment arms in the pilot EASE Back trial: SC, SC plus true acupuncture and SC plus sham acupuncture using non-penetrating needles. The use of sham in trials of acupuncture remains a matter of debate, and some may consider it an ethical dilemma. However, by ensuring that all our pilot trial participants received a package of SC, and that the acupuncture treatment (either true or non-penetrating) was in addition to this SC, we are confident that all participants received appropriate treatment for their pain.
Blinding
A further methodological challenge is the need to ensure adequate blinding: ideally, patients, therapists, outcome assessors and data analysts should be adequately blinded. In a trial of SC and acupuncture, clearly, the therapist cannot be blinded to treatment, but it is possible to blind acupuncture-naive patients to the type of acupuncture (true or non-penetrating), as well as those involved in collecting data and data analysis. Successful blinding has been achieved in a previous trial of acupuncture within the NHS39 and we incorporated this level of blinding into the EASE Back pilot trial. In particular, by gaining ethics approval to explain to potential participants that they would all receive SC and some would receive one of two forms of acupuncture, we were able to ensure that all participants expected to receive good treatment, thus maximising expectation and treatment credibility effects. We included measures of treatment preference and expectation in our pilot trial data set and captured information on treatment credibility at follow-up.
Safety/risks of acupuncture
Despite promising evidence for the effectiveness of acupuncture for relief of back pain and PGP in pregnant women, some clinicians express concerns about safety. One concern is that acupuncture might induce pre-term labour, but available data show this not to be the case. The normal risk of pre-term labour (before 37 weeks’ gestation) is 7–10%. In one of the Swedish trials, Elden et al. 40 assessed the adverse effects of acupuncture on the pregnancy, mother, delivery and fetus/neonate. Acupuncture that may be considered strong was used and treatment was started in the second trimester of pregnancy. Adverse effects were recorded during treatment and throughout the pregnancy. The results showed that there were no serious adverse events (SAEs) after any of the treatments, in either babies or mothers. Minor adverse events were common in the acupuncture group, but women rated acupuncture favourably despite this. Therefore, acupuncture administered with a stimulation that may be considered strong led to minor adverse complaints from the mothers and had no observable severe adverse influences on the pregnancy, mother, delivery or fetus/neonate. In addition, acupuncture in early pregnancy (for nausea and vomiting) has been shown to be safe, with no adverse effects on perinatal outcome, congenital abnormalities, pregnancy complications and other infant outcomes. 41 In the wider literature, most side effects associated with acupuncture are minor and transient, such as dizziness/light-headedness and slight bleeding after the needles are removed. 42 Although there have been reports of fatal events following acupuncture (14 cases in a review of literature over the last 50 years),43 these appear to have been related to cases of clear malpractice and negligence (e.g. as described by Halvorsen et al. 44). In the UK, acupuncture training for health professionals, including physiotherapists, is set at a high level, and in trained hands acupuncture is a safe intervention. In our pilot trial in phase 2 of the EASE Back study, the participant information leaflet and consent procedures made the known risks clear and explained the frequency of these risks where these data were available while reassuring pregnant women that even strong acupuncture stimulation has been shown to have no adverse effects on the pregnancy, mother, delivery or developing baby. In addition, the trial design ensured that all women received SC and that acupuncture was in addition to this SC. Therefore, we did not withhold SC from any woman in the EASE Back trial.
Standardising acupuncture treatment for a randomised controlled trial
Since the location and manipulation of the needles in acupuncture are thought to be important in achieving successful outcomes, the therapist usually individualises the treatment for each patient in clinical practice. For the purposes of a trial, however, some degree of standardisation is needed in order to be able to describe the treatment that participants were expected to receive (the intervention protocol) and then to be able to judge whether or not patients received the treatment as expected (protocol adherence). Previous trials of acupuncture have been criticised for lack of clarity about the acupuncture intervention provided as well as for being overly prescriptive with the selection of acupuncture points and needle manipulation to the point that those using acupuncture in clinical practice do not feel that the acupuncture provided in the trial reflects their practice. We believe the best solution to this challenge, for the purposes of a randomised controlled trial (RCT), is to agree a semiflexible acupuncture protocol, in which therapists assess the individual patient’s pain type and location, they palpate for tender points and then they select points from a large number of points that have been agreed to be suitable for inclusion in the protocol (including acupuncture and tender points). This approach has been used successfully in previous trials33,39 ensuring that the acupuncture treatment is individualised, reflecting clinical practice, and that it can be amended over a course of treatment sessions but can also be clearly described in publications.
Copy of the Health Technology Assessment commissioning brief (Health Technology Assessment number 10/69/05)
Question: what is the clinical effectiveness and cost-effectiveness of acupuncture in pregnant women with back pain, in comparison to SC?
Technology: a 6-week acupuncture package, as may plausibly be delivered in the NHS.
Patient group: pregnant women with back pain (including women attending antenatal clinics and outpatients clinics because of back pain).
Control or comparator treatment: sham acupuncture.
Design: a feasibility study to assess the acceptability and design of a trial in the NHS. Methods are likely to include a survey of current practice and qualitative work with clinicians, patients and commissioners. Researchers should identify an appropriate acupuncture intervention and control. They should explore the merits of a sham acupuncture arm.
Important outcomes of main study: pain.
Other outcomes: adverse events, consumption of analgesics, obstetric outcomes, absence from work, functional status, health-related quality of life and cost-effectiveness.
Outcome of the feasibility study: outline plan for a randomised controlled study with evidence supporting its design and delivery.
Minimum duration of follow-up of main study: 6 months after delivery.
Appropriate standard care comparison
The choice of the comparison treatment in acupuncture trials is critically important. Previous trials that compare acupuncture with waiting list controls, ongoing stable medication or minimal care packages tend to show that acupuncture is superior, whereas those that compare acupuncture with more intensive or active interventions have tended to conclude that there are no differences between acupuncture and comparisons. 39 We wanted to include a SC comparison that accurately reflected what currently happens in the UK for pregnant women with low back pain. Thus, we followed the recommendations of Ee et al. 34 that some form of consensus about treatments for these women is essential to inform clinical trials. Although usual care differs in different services and geographical regions, our interview and survey results from the phase 1 pre-pilot work in the EASE Back study provide the most useful information on which to base a trial protocol for SC. These data ensured that the pilot trial protocol for SC reflected current care in the UK and thus is a fair comparison in the trial.
Rationale for the EASE Back study
A high-quality randomised trial in the NHS is needed to test the clinical effectiveness and cost-effectiveness of adding acupuncture to SC for pregnant women with low back pain (with and without PGP). Before such a large trial can be conducted, however, a feasibility and pilot study was commissioned by the National Institute of Health Research (NIHR) Health Technology Assessment (HTA) programme to inform the design, recruitment, interventions and outcomes. A feasibility study is a research study carried out prior to a main study in order to answer the question ‘Can this study be done?’, and it is used to estimate important parameters needed to design the main study. 45 In the EASE Back study we wanted to find out whether or not pregnant women with low back pain would be willing to try acupuncture as a treatment and whether or not they had concerns about acupuncture or being involved in a trial. We also wanted to find out the likely proportions of eligible women from all of the pregnancies overseen by a large maternity centre and whether or not clinicians (community midwives and physiotherapists in particular) would be willing to recruit to, and treat, this patient population in a trial of acupuncture. We needed to test out all the processes of a future main trial and, therefore, the EASE Back study also involved a pilot RCT. A pilot study is a version of the main study run in miniature to test whether or not all the components of the main study can work together. 45 The EASE Back pilot RCT therefore tested the inclusion and exclusion criteria, the processes of identification of potentially eligible women, screening and recruitment, randomisation, training of participating research staff and physiotherapists, delivery of treatment, treatment fidelity and credibility of treatment. It allowed us to test whether or not pregnant women with back pain would be willing to be randomised, to test out the outcome measures that might be used in a future main trial, to explore the short-term effects of treatment on these outcomes, to determine short-term follow-up rate, to select a primary outcome measure for a future main trial and to estimate the sample size for a future main trial.
The EASE Back study was a mixed-methods feasibility and pilot study, designed in two phases over 24 months (June 2012 to May 2014), combining survey research (of current practice), qualitative research (focus groups and individual interviews) and a pilot randomised trial with pregnant women with back pain (with and without PGP) with short-term follow-up and audio-recordings of screening and consent meetings with a subsample of women. The results were shared at a dissemination event with stakeholders in May 2014 and consensus achieved about the feasibility and desirability of a main trial. Figure 1 provides a summary of the EASE Back study design.
FIGURE 1.
Summary of the EASE Back study design. AACP, Acupuncture Association of Chartered Physiotherapists; MIMDTP, McKenzie Institute of Mechanical Diagnosis and Therapy Practitioners; NP, non-penetrating.

Overall aim of the EASE Back study
The overall aim of the EASE Back study was to assess the feasibility of a future RCT to test the addition of acupuncture to SC in women with pregnancy-related low back pain.
Chapter 2 Phase 1 pre-pilot work
Objectives of phase 1 pre-pilot work
The specific objectives of phase 1 were to:
-
provide data on current UK SC and acupuncture treatment for low back pain in pregnant women
-
explore the views of pregnant women with back pain about the acceptability of the proposed interventions, the content and delivery of participant information, the outcomes most important to them and the most appropriate timing of outcome measurement
-
optimise trial information, recruitment and consent procedures by learning what works best from the perspectives of pregnant women with low back pain, midwives and physiotherapists
-
investigate the views of NHS health professionals regarding (1) the acceptability and feasibility of referring women with back pain in pregnancy to physiotherapists for acupuncture, (2) the proposed trial design and interventions and (3) ways in which to maximise recruitment and retention to a trial.
In order to address the above objectives, we used mixed research methods of a descriptive survey and qualitative interviews. Findings from the survey informed the semistructured interview schedule, and findings from both methods were integrated at the analysis stage to give additional validation. 46 The pre-pilot work in phase 1 was reviewed and approved by National Research Ethics Service Committee North West – Greater Manchester North (ref. 12/NW/0227).
National survey of chartered physiotherapists
Methods
Design and setting
This was a national cross-sectional survey of national samples of physiotherapists working in the UK from June to July 2012. Consent of respondents was assumed if they completed and returned the questionnaire; therefore, written consent was not sought from each participant.
Survey sample and mailing
The inclusion criteria were physiotherapists who:
-
were members of the Chartered Society of Physiotherapy
-
had experience of treating women with pregnancy-related low back pain.
We randomly sampled from three professional networks of the Chartered Society of Physiotherapy. Although the optimal approach to generate representative survey findings is to use a simple random sample, there is no comprehensive sampling frame for all UK-based physiotherapists available at the current time. The professional networks selected were those with interests relevant to low back pain, acupuncture and pregnancy/women’s health, with a total combined membership of around 7000 physiotherapists. This large sampling frame was required to access physiotherapists with a range of experience and clinical interests, to result in as generalisable a data set as possible about physiotherapy care for pregnancy-related back pain across the UK. The Chartered Society of Physiotherapy is the predominant professional trade union and educational body for physiotherapists in the UK and has 30 affiliated professional networks, usually with a specific clinical or occupational interest, which members have the option of joining. It was not possible to target only those physiotherapists working in the NHS. Random samples of members of the three professional networks (total n = 1093) were mailed by the administrators of each network and two reminder mailings were subsequently sent to non-responders. The professional networks were chosen to include physiotherapists with a special interest in (1) women’s health (ACPWH), (2) acupuncture (the Acupuncture Association of Chartered Physiotherapists) and (3) musculoskeletal pain conditions (McKenzie Institute of Mechanical Diagnosis and Therapy Practitioners). An initial filter question identified those respondents who had never treated a pregnant woman with low back pain in pregnancy, and only respondents with experience of treating this patient group were included in the analysis.
As the aim of this survey was primarily descriptive, a formal sample size calculation was not carried out. Previous surveys of physiotherapists in the UK indicated a likely response rate of 55–60%47–49 and so we expected approximately 600–650 overall responses from the mailing of 1093. This sample size is sufficient to estimate the proportions of the key survey variables within less than a 5% margin of error with 95% confidence.
Survey questionnaire
A previous national survey questionnaire of physiotherapy practice for non-specific low back pain (not related to pregnancy) was adapted for use in this study. 48 The questionnaire captured information about respondents’ demographics and clinical practice including years in practice, practice setting, postgraduate training in musculoskeletal pain, women’s health and acupuncture as well as experience of managing women with pregnancy-related back pain. The questionnaire investigated current clinical care using a patient vignette of a specific, typical case developed from a real patient example following recommendations from other studies50–52 and was pilot tested with 18 physiotherapists. The patient vignette is reproduced below, whereas the full questionnaire is provided in Appendix 1. Respondents were asked how they would manage this woman, including likely treatment approaches, advice offered and number of treatment sessions provided. Specific questions on their use of acupuncture were also included.
We additionally asked the physiotherapists whether or not they routinely used specific advice or self-management leaflets in the management of pregnancy-related low back pain and PGP and, if so, to enclose a copy of the leaflet in their response to the survey. This resulted in the research team receiving examples of 37 different advice and self-management leaflets currently used by physiotherapists. These were used to help develop the self-management booklet used in the pilot RCT in phase 2 of the EASE Back study (see The development of a standard care protocol).
A 34-year-old woman was referred from her GP with symptoms of intermittent sharp pain at her lower thoracic and lumbar regions and reports that the symptoms began a few weeks ago. She is 24 weeks pregnant with her first child. She is in good general health and of normal weight for her height and has never had back pain before.
Her back pain presents as occasional sharp sensations at the lumbar/lower thoracic regions of her spine and seems to be unrelated to posture or activity. She also has some dull pain in the lower back region, which is more persistent but of lesser intensity than the sharp pain she occasionally experiences. Her symptoms are worse if she maintains a sitting posture for prolonged periods. She is reluctant to use any analgesic medication because of her pregnancy.
Upon examination there is no exacerbation with movement or any directional preference. She has normal range of movement and is moderately tender on the paraspinal muscles of her lower back. Straight-leg raise and slump tests are negative.
Statistical analysis
Analysis was primarily descriptive, using summary statistics to describe physiotherapists’ characteristics and provide data on current practice, including SC and their use of acupuncture. As treatment has been shown to differ across practice settings,53 treatment approaches used by respondents working in NHS and non-NHS settings were compared using Pearson’s chi-squared tests. This survey was not designed to test for differences between members of different professional networks. However, as the survey sample was not a simple random sample of physiotherapists in the UK, some exploratory comparisons between the professional networks were undertaken to explore any internetwork differences. All analyses were performed using Stata version 13 (StataCorp LP, College Station, TX, USA).
Results
Response rate and characteristics of responders
Responses were received from 629 (58%) of those mailed. Of these, 499 had treated at least one woman with pregnancy-related low back pain and were included in the analysis. The demographic and practice characteristics of the respondents are presented in Table 1. The respondents were very experienced (mean of 22 years in practice) and most were female. Respondents worked in a variety of settings: NHS only, non-NHS only or a combination of practice settings. Referrals of women with pregnancy-related back pain were received by respondents from a variety of other health-care practitioners and self-referral to physiotherapy by women themselves was also commonly reported. Approximately one-third of respondents reported seeing a pregnant woman with back pain at least once a month.
| Characteristic (denominator)a | n | % |
|---|---|---|
| Years of experience (456) | 21.5 (mean) | 10.4 (SD) |
| Female (499) | 459 | 92.0 |
| Work setting (498) | ||
| Exclusively NHS | 201 | 40.4 |
| Exclusively non-NHS | 159 | 31.9 |
| Combination of NHS and non-NHS | 138 | 27.7 |
| Frequency of treating pregnant women with back pain (499) | ||
| Infrequent – at most one in last 6 months | 173 | 34.7 |
| Somewhat frequent – between two and five in last 6 months | 148 | 29.7 |
| Frequent – at least one per month | 70 | 14.0 |
| Very frequent – at least one per week | 108 | 21.6 |
| Referral sourceb (499) | ||
| Referral from GP | 347 | 69.5 |
| Referral from midwife | 241 | 48.3 |
| Self-referral | 240 | 48.1 |
| Referral from a physiotherapy colleague | 147 | 29.5 |
| Referral from obstetrician | 137 | 27.5 |
| Other | 38 | 7.6 |
| Trainingb | ||
| Specific postgraduate training in low back pain in general (491) | 444 | 89.0 |
| Specific postgraduate training in acupuncture (497) | 370 | 74.5 |
| Specific postgraduate training in women’s health (492) | 327 | 65.5 |
| Specific postgraduate training in low back pain in pregnancy (496) | 264 | 52.9 |
| Use of acupuncture in management of musculoskeletal pain (496) | 338 | 68.2 |
Standard care management
Standard care was explored by asking respondents to indicate the management options they would use for the typical patient described in the vignette. Most respondents (88%, n = 430) reported that they would be responsible for the care of such a patient, but 12% (n = 58) reported it was not their role and that this type of patient would be specifically referred to a women’s health specialist physiotherapist. A large majority of respondents (85%, n = 364) reported that they would manage this patient in one-to-one treatment sessions. The remainder reported that they would manage this patient as part of a group or class and that they would use one-to-one sessions for initial patient assessment only or only if required. This typical patient would be seen three or four times over a period of 3–6 weeks, although the episode would be left open for the duration of the pregnancy so that a woman could reconsult the physiotherapist if needed until after the birth of her baby. Table 2 summarises the episode of SC by physiotherapists.
| Characteristics of care (denominator)a | n | % |
|---|---|---|
| Number of times patient typically seen (425) | ||
| Once | 51 | 12 |
| Twice | 103 | 24.2 |
| Three or four times | 205 | 48.2 |
| Five or more times | 66 | 15.5 |
| Time period over which patient would typically be treated (415) | ||
| 1–2 weeks | 79 | 19 |
| 3–6 weeks | 221 | 53.3 |
| 7–10 weeks | 70 | 16.9 |
| > 10 weeks | 45 | 10.8 |
| Typical episode of care (428) | ||
| Finished after treatment, re-referral required for further treatment | 27 | 6.3 |
| Left open for duration of the pregnancy | 258 | 60.3 |
| Left open for a defined period after end of treatment | 66 | 15.4 |
| Other | 77 | 18.0 |
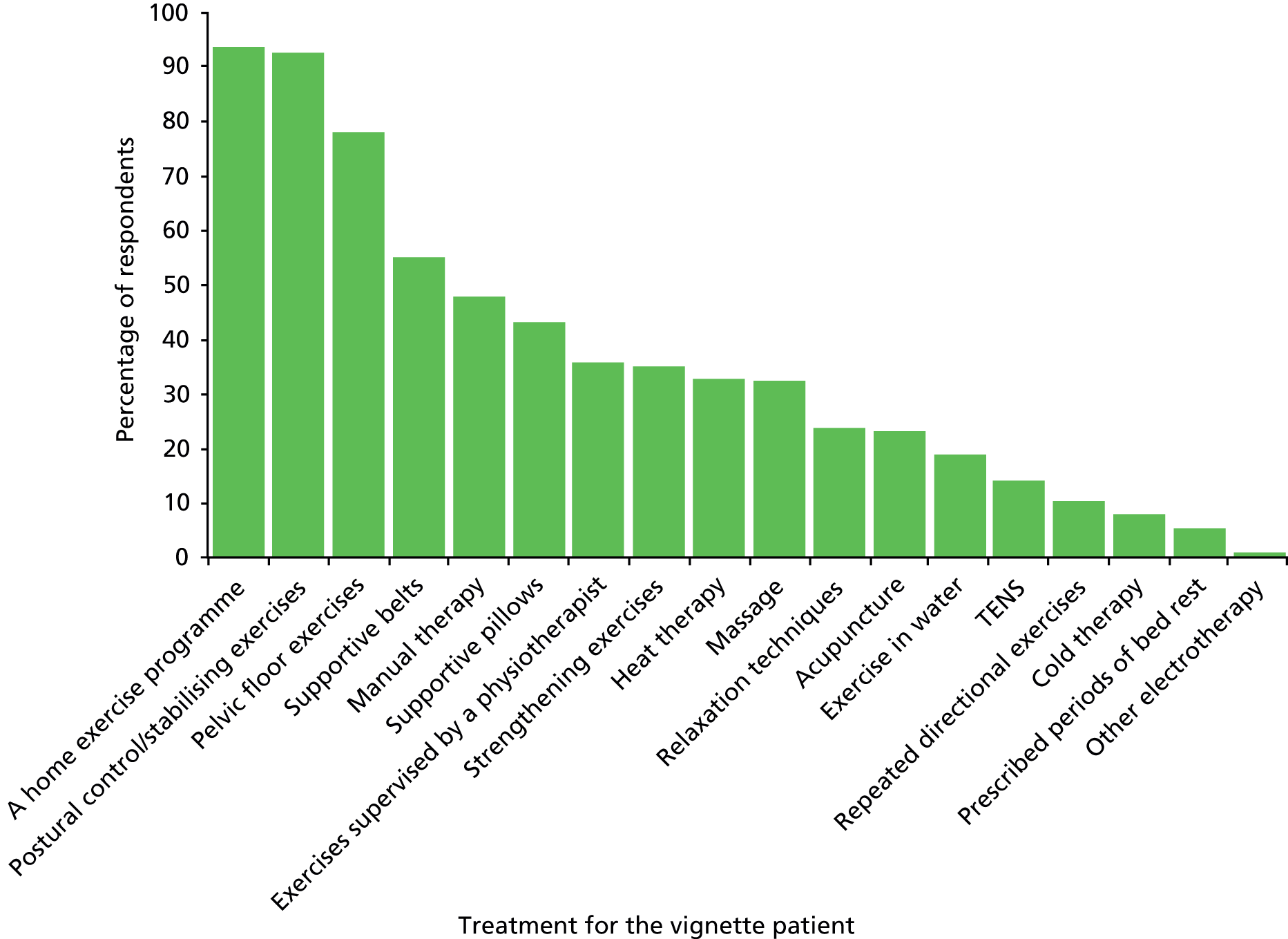
Many advice and treatment options were reported for the management of the typical patient described in the vignette, and combinations of advice and treatments were commonly reported. Advice on aspects of pregnancy, low back pain and activities of daily living was reported by the respondents and, although combinations of treatments were described in packages of care, most physiotherapists reported using exercise approaches to manage women with pregnancy-related low back pain (Figures 2 and 3).
FIGURE 2.
Survey findings: advice for the vignette patient.
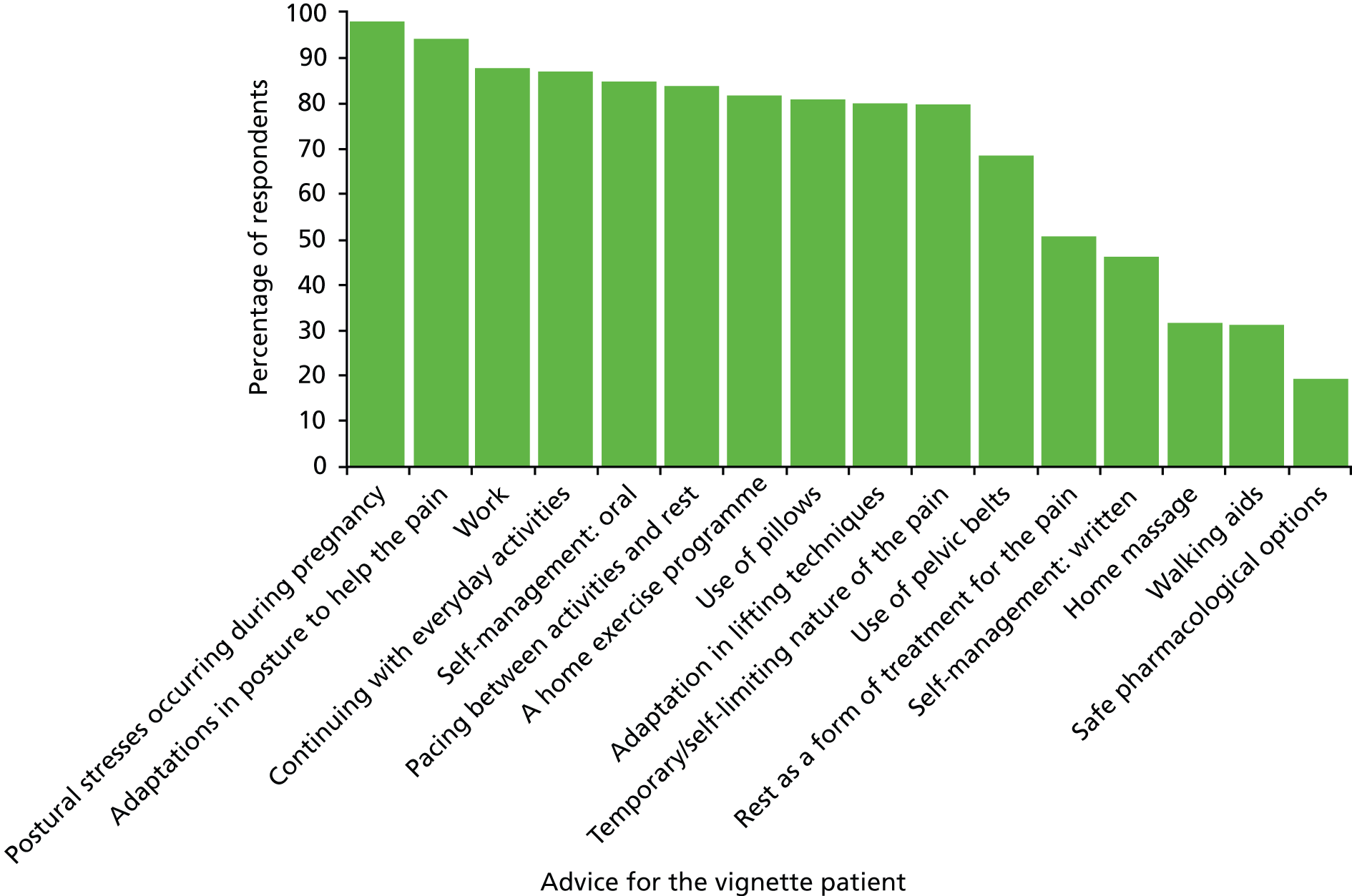
FIGURE 3.
Survey findings: treatment for the vignette patient.
Acupuncture management
Regarding use of acupuncture, of the 469 individuals who responded to this item, 68% (n = 338) reported that they used it in the management of patients with musculoskeletal conditions, including low back pain not related to pregnancy, whereas 37% (n = 126 of 337 responses to this question) reported that they used it to treat women with pregnancy-related low back pain. However, when asked about the treatment they would provide to the specific patient described in the vignette (430 responses), 24% (n = 101) reported that acupuncture would be part of their treatment. Respondents had a mean of 11 [standard deviation (SD) 6.2] years’ experience of using acupuncture in clinical practice. The majority of respondents (298 responses) used Western/medical acupuncture (71%, n = 212), 16% (n = 48) used TCM/traditional acupuncture and 11% (n = 32) used trigger point/myofascial acupuncture. Of 336 respondents completing details about acupuncture training, 37.5% had completed up to 80 hours of acupuncture training (the national minimum requirement for physiotherapists), 53% had completed more than 80 hours but less than 200 hours and 9.5% had completed a degree/diploma in acupuncture or equivalent.
If acupuncture was a treatment option selected by respondents for the vignette patient, further details about acupuncture management were requested in the questionnaire. The mean number of acupuncture points used in a treatment session was 7 (SD 2.6), with the needles being left in situ for a mean of 20 (SD 6.0) minutes, and 84% of respondents would elicit a de-qi needle sensation. The selection of acupuncture points varied considerably for the vignette patient, and the 10 most commonly reported local and distal acupuncture points are summarised in Table 3. Only two acupuncture points (BL25 and BL23) were reported by more than one-third of respondents. Of those using acupuncture in the treatment of pregnant women, 22 respondents (4%) reported they had observed some minor adverse effects during treatment. These included the patient feeling lightheaded/dizzy (n = 8) or fainting (n = 5), mild bruising at needle site (n = 3), worsening of symptoms (n = 3), vomiting (n = 2) and significant pain at a needle site (n = 1). One respondent reported that a patient she had treated with acupuncture miscarried the day after acupuncture treatment, but reported that the treatment was not thought to contribute to this.
| Acupuncture points | n | % |
|---|---|---|
| Local acupuncture points (n = 93) | ||
| BL25 | 33 | 35.5 |
| BL23 | 31 | 33.3 |
| GB30 | 24 | 25.8 |
| BL26 | 22 | 23.7 |
| BL24 | 18 | 19.4 |
| BL28 | 13 | 14.0 |
| BL27 | 12 | 12.9 |
| HJJ | 10 | 10.8 |
| BL54 | 7 | 7.5 |
| BL22 | 7 | 7.5 |
| Distal acupuncture points (n = 81) | ||
| GB34 | 25 | 30.9 |
| LI4 | 20 | 24.7 |
| BL60 | 16 | 19.8 |
| LR3 | 16 | 19.8 |
| BL62 | 14 | 17.3 |
| ST36 | 13 | 16.0 |
| BL40 | 11 | 13.6 |
| GB41 | 7 | 8.6 |
| BL57 | 6 | 7.4 |
| SI3 | 5 | 6.2 |
Differences between respondents working in different practice settings (exclusively NHS or exclusively non-NHS) were few. However, those working exclusively in the NHS were more likely than those in non-NHS settings to report that they saw the patient only once or twice (52% compared with 17%). Conversely, physiotherapists reporting the most patient treatment visits (more than five) were more likely to be working in non-NHS settings (24%, compared with 7% in exclusively NHS settings). In addition, physiotherapists working in non-NHS settings more commonly than those working exclusively in NHS settings reported using treatment approaches that were classified as ‘hands-on’. Overall, the proportion of respondents who would offer the patient any hands-on treatment approaches was significantly higher among those who worked exclusively in non-NHS settings than among those working exclusively in NHS settings (Table 4). For example, of the 33% (101 out of 304) of respondents who would offer massage, 71 (70%) worked exclusively in non-NHS settings, compared with 30 (30%) who worked exclusively in the NHS.
| Treatment offered (total responses, n = 304) | Overall, n (%) | NHS, n (%) | Non-NHS, n (%) | Significancea |
|---|---|---|---|---|
| Manual therapy | 134 (44.1) | 53 (32.9) | 81 (56.6) | p < 0.001 |
| Acupuncture | 69 (22.7) | 23 (14.3) | 46 (32.2) | p < 0.001 |
| Massage | 101 (33.2) | 30 (18.6) | 71 (49.7) | p < 0.001 |
Differences between professional networks
Exercise was the most common treatment reported by respondents from all three professional networks. Data about the typical episode of care (number of treatment sessions, length of sessions, length of episode of care) were also similar across all networks. The one area in which reported practice differed between professional networks was in the use of acupuncture for the typical patient described in the vignette, with respondents from the acupuncture professional network (the Acupuncture Association of Chartered Physiotherapists) being more likely to report using acupuncture (43.9%) than those from either a general musculoskeletal (the McKenzie Institute of Mechanical Diagnosis and Therapy Practitioners; 9.0%) or a women’s health professional network (ACPWH; 6.2%).
These survey findings, particularly those from NHS-based clinicians, were used to help develop the treatment content and intervention protocols for the pilot EASE Back trial in phase 2 of the EASE Back study (see The development of a standard care protocol).
Qualitative focus groups and individual interviews
Methods
The qualitative research was guided by our initial research objectives but retained the flexibility to explore previously unforeseen avenues of enquiry. 54,55 Methods consisted of focus groups or individual interviews (in person or by telephone) with pregnant women, midwives and physiotherapists. Given that both health-care professionals56 and women57 can be difficult to engage in research, the offer of choice over interview format was pragmatic rather than methodological and intended to meet the needs of participants in terms of convenience. All participants were given full information about the study ahead of deciding to participate, with the option of focus groups or individual face-to-face or telephone interviews. The health-care practitioners were invited to complete a brief questionnaire to describe their qualifications and experience (see Appendix 2). Semistructured interview guides were developed from the research objectives and from the findings of the national survey. They focused on exploring the acceptability of acupuncture, the sort of information that might be required to reach a decision around participation in a trial, the most important outcomes and the most appropriate timing of outcome measures for the pilot trial. In addition, participants were also invited to talk about the care and support they considered available for this population (see Appendix 3 for copies of the topic guides). All interviews were audio-recorded with consent and the focus groups were facilitated by two members of the research team. Data collection was concurrent with all three sets of participants and ceased when data saturation was reached.
Interviews with pregnant women
For pregnant women, the original intention had been to hold a series of focus groups, offering individual interviews if these were more convenient. In the planned recruitment period for phase 1 of the study (June to September 2012) it was estimated that there might be as many as 600 pregnant women with low back pain under the care of the participating maternity hospital who could be invited to participate; however, owing to poor response to the invitation to participate in the interviews, we extended the recruitment phase by a further 2 months to November 2012. A convenience sampling strategy58 was adopted and any pregnant woman with back pain could either self-refer or agree for the health-care practitioner caring for her to pass on her contact details to the research team. A flyer and poster were designed outlining the study and providing contact details of the research team. In total, 3000 flyers and 100 posters were distributed through a variety of means: general maternity information packs when the woman first booked in with her community midwife; local antenatal clinics; community midwives giving the flyers directly to pregnant women under their care; and the women’s health physiotherapy service back class for pregnant women at the local hospital. In addition, an invitation to participate was also posted on internet sites [Mumsnet (www.mumsnet.com) and the Pelvic Pain Support Network (www.pelvicpain.org.uk)]. Contact was also made with the National Childbirth Trust (www.nct.org.uk) and the Pelvic Partnership (www.pelvicpartnership.org.uk), but administrative difficulties on the part of these organisations meant it was not possible for them to collaborate with the research team within the time frame of phase 1.
In total, 43 women gave consent to contact, which was attempted through telephone calls at differing times of the day, including in the evening, and a total of 18 women agreed to telephone interviews. On contact, if they were still willing to be interviewed, a convenient interview time was arranged. At that point, a letter confirming the interview arrangements, detailed information about the study and two copies of the consent form together with a stamped addressed envelope for the return of a signed copy of the consent form, were posted out. The information and consent form were discussed at the time of the interview and audio consent was also recorded then.
Interviews with midwives and physiotherapists
For the health professionals, a purposive sampling strategy was adopted to ensure a range of experience and perspectives. 59 Two teams of community midwives were approached, together with the group of research midwives working in the local maternity hospital who would be involved in recruiting women into the EASE Back pilot RCT. Physiotherapists from the local community musculoskeletal outpatient services and from the local hospital’s women’s health physiotherapy service were also invited to participate. In addition, a sample of those physiotherapists (n = 30) who consented to further contact on returned questionnaires from the national survey were also invited to take part. Owing to geographical spread and participant convenience, these individuals were also interviewed by telephone. The individual interviews took place after the focus groups with physiotherapists and, because of data saturation, were limited to three individuals. In total, 15 midwives and 21 physiotherapists took part, giving a total of 53 individuals interviewed in phase 1 (Table 5).
| Participants | Individual interviews (telephone) | Focus group interviews (face to face) |
|---|---|---|
| Pregnant women | 17 participants | 0 focus groups |
| Midwives | 0 participants | 3 focus groups (2 with community midwives, 1 with research midwives), 15 participants in total (2 were maternity assistants) |
| Physiotherapists | 3 participants | 3 focus groups (2 with community physiotherapists, 1 with women’s health physiotherapists), 18 participants in total (1 was a physiotherapy technician) |
Analysis
An exploratory thematic analysis was adopted, within a constructivist grounded theory framework. Emergent findings were checked out in subsequent interviews across all three groups of participants in an iterative cycle. 60,61 All interviews were digitally recorded, lasted between 20 and 60 minutes and were transcribed in full. To preserve participants’ anonymity, all were given unique identification numbers. To maximise the benefits of the interdisciplinary research team, the interview coders brought differing disciplinary perspectives to bear on the qualitative data (BB, social science; PB, acupuncture; and JW, physiotherapy). To ensure intercoder reliability, each independently coded a random selection of interviews as part of agreeing the initial coding frame, which was then applied across the whole data set, checking for consistencies and confounding cases and for further refinements of the coding frame. The findings were then compared with those from the national survey to identify areas of corroboration and contradiction.
Results
Engagement in the interviews
Despite the many flyers, posters and efforts on the part of clinical staff to discuss the study with potentially eligible women, and extending the recruitment period by 2 months, only 43 women agreed to contact by (or contacted) the research team. Of these, two self-referred, two were referred by physiotherapists, three were referred by obstetricians and 20 were referred to the research team by community midwives. The remaining 16 were identified through members of the research team attending the back education class within the women’s health physiotherapy service in the local hospital. We received no responses to the online invitations to participate that had been posted on Mumsnet or the Pelvic Pain Support Network. There were also challenges in making contact with the 43 women and in setting up focus groups. On average, it took five telephone calls spread over different times of day, including the evenings, to make initial contact. Two women declined to be interviewed during their first telephone contact (one no longer had low back pain and the husband of the other was ill) and 22 women were not contactable despite the five contact attempts. The difficulties in contacting these women were discussed at the focus groups with midwives and physiotherapists. They expressed little surprise, which they attributed to a patient population struggling to cope with everyday life and, moreover, discussions suggested that travelling to a focus group meeting would be an additional and unacceptable burden for pregnant women. The decision to offer individual telephone interviews instead of focus groups was made. Eighteen women agreed to interview, one was unavailable at the agreed time, and so a total of 17 women were interviewed over the 6-month period from June to November 2012, representing 39% of those who consented to further contact.
Characteristics of participants
Despite the initial difficulties in contacting women, the interview sample of 17 women was diverse and sufficient for data saturation. The average age was 26 years, with a range from 22 to 34 years; gestation ranged from 15 to 39 weeks, with a mean of 32 weeks; and for eight women it was their first pregnancy. In terms of ethnicity, eight described themselves as English, five were ‘other British’, three were ‘other white’ and one was ‘African’. All were either married or living with a partner and employment included health professional and clerical worker.
Analysis of the midwives’ profiles questionnaires indicated that the average length of practice was 18 years, with the majority (n = 9) qualified for over 12 years. The least experienced person had been qualified for 3 years, and there were also two maternity assistants included in the focus groups. None reported any specific postgraduate training around the area of back pain in pregnancy. Six midwives reported that they saw pregnant women with back pain either very frequently (at least one per week) or frequently (at least one per month). Just one midwife reported seeing such patients infrequently (at most one in the last 6 months).
As with the midwives, the physiotherapists were experienced practitioners. Their average length of practice was 12 years, nine had been qualified for 12 years or more (one for 36 years) and the least experienced person had been qualified for over 3 years. Fourteen individuals had a Bachelor of Science in Physiotherapy, of whom one also had a Master of Science in Musculoskeletal Healthcare, one a Master of Science in Acupuncture, one an Advanced Critical Care Practitioner (ACCP) foundation qualification in acupuncture and one Higher National Diploma in Sports Science. Another person had a Diploma in Physiotherapy, two individuals reported themselves simply as members of the Chartered Society of Physiotherapists (MCSP), and the final person was a physiotherapy technician with National Vocational Training Qualifications at Levels 1, 2 and 3. In terms of their contact with pregnant women, seven reported seeing such patients infrequently. All seven were community physiotherapists, and all apart from one reported that they had no specific postgraduate training in the topic of back pain in pregnancy. Unsurprisingly, the women’s health physiotherapists leading the hospital-based back class for pregnant women reported seeing such patients frequently. They identified that their education around treating pregnant women came from either in-house training or short (1-day) courses (the exact nature of these was not specified).
Key themes
We identified three main themes from the qualitative data in phase 1: the high burden of back pain in pregnancy and outcomes most important to women; the paucity of treatment options; and acupuncture as an acceptable intervention for women and midwives but generating concerns for many physiotherapists. Each of these main themes is presented briefly below with example quotations from the transcripts.
Theme 1: high burden of back pain in pregnancy and outcomes most important to women
During the interviews with these women a picture of the burden of low back pain in pregnancy and its often wide-ranging impact on daily life emerged strongly, corroborating the views of the midwives and physiotherapists, and highlighting the importance of flexibility in appointment times and treatment locations for the pilot RCT. The interview data highlighted the severely disabling effects of back pain during pregnancy, which can affect all aspects of life, ranging from sleep through to being unable to carry out basic activities of daily living. Many of the women reported considerable support from partners and family. However, there were also reports of serious misunderstandings in the workplace, arising from managers and/or colleagues seeing back pain as a normal part of pregnancy and expecting women to ‘just get on with it’, with resulting lack of support. For some, even attending routine antenatal appointments was difficult to negotiate with their workplace and, consequently, anything that might incur further time away from work was seen as challenging. This is particularly significant because many women reported needing to work as long as possible up to their due date, because of their maternity leave entitlement and for financial reasons. It was clear others in severe pain were unable to work or participate in social activities, with consequences for their mental well-being and relationships, as the following quote illustrates:
My mood at the moment is all over the place anyway [laughs], but it [the pain] affects you, because it does limit me, especially first thing in the morning when I’ve been in one position for a long period of time, it kind of freezes up. So in the morning when I get up, I kind of crawl out of bed rather than spring out of bed.
Individual interview: 56
The women interviewed did not expect to experience immediate pain relief with acupuncture but believed that it would take several treatments to make a difference. The severity of the pain and its impact on activities of daily life meant that they felt that it was unlikely the pain could be completely resolved but rather alleviation was seen as an acceptable outcome:
I know nothing can sort of get rid of my pain completely but perhaps just alleviate, you know, something to alleviate it for a little bit and enable me to sort of get around and move around a little bit more [yeah] you know? I think that would be a pretty good outcome really.
Individual interview: 156
Theme 2: the paucity of treatment options
The responses to the survey indicated that SC varied widely for this patient group. This variation in care and lack of effective treatment options were also reflected in the narratives from women and professionals. It was clear that the emphasis is on self-management strategies, with only the most severely affected women being referred to physiotherapists for individualised advice about posture, movement and gentle exercise. Both midwives and physiotherapists tended to view these women as ‘heart-sink’ patients for whom they could offer very little in the way of effective interventions, as this illustrates:
I think it’s one of the few types of patients that we won’t see more than once because you know that, physio-wise, there’s very little to offer. So it’s a case of give them what they need and leave them on hold for further appointments.
Community physiotherapists: group A, 48
Midwives and physiotherapists reported explaining the causes of back pain during pregnancy as a way of reassuring the women and, although they described offering advice, they felt that this amounted to ‘fobbing off’ their patients, expressing a lack of faith in the effectiveness of their suggestions. Moreover, the advice provided was clearly highly variable, indicating uncertainty among midwives and physiotherapists regarding the most appropriate forms of advice, and there clearly were no consistently used sources of advice in terms of either written leaflets or website resources. Examples of patient information leaflets (PILs) and websites recommended to women were collected from respondents to the national survey, and the 37 different leaflets returned underline the variation in current advice provided to these women. This reflects the uncertainty voiced by the professionals about what constitutes ‘the right advice’ for this group of patients. Most women were advised to try self-management techniques around posture, gentle exercise and pain relief medication. Women’s health physiotherapists reported favouring a ‘hands-off’ approach, with advice on posture, preparation for labour and delivery and feeding positions after delivery. They identified an important part of their role as providing reassurance. The uncertainty about what constituted ‘the right advice’ for this group of patients was reflected in the accounts of the women, who conveyed a sense of being left to ‘get on with it’, as this severely affected individual reported:
No, I refused to take that [co-codamol]. They did prescribe it in the end and I did take it home with me but I haven’t took any because I just don’t agree with that in pregnancy. And after that I was discharged because really there’s nothing you can do. They referred me to the physio back class that I went to, and every time I’ve seen my midwife, she gave me a little tip of how to get in and out of cars, and things like that. But I don’t really think it can be helped. I just think it’s one of them things you’ve got to deal with.
Individual interview: 75
Theme 3: acupuncture as an acceptable intervention for women and midwives, but generating concerns for many physiotherapists
Although some women did express the need for information and reassurance over safety of acupuncture and whether or not the positioning for acupuncture would require them to lie in positions that could exacerbate their pain, in the main women expressed little concern expressed about its use in pregnancy.
I think if people were telling me that it could help my back pain then I would pretty much do anything.
Individual interview: 149
I don’t know where they put the needles in pregnancy. If they were in my tummy I think I’d be a bit like, ‘mmm, not quite sure about that’.
Individual interview: 98
Midwives were generally in favour of the idea that acupuncture could be offered to women with pregnancy-related back pain and that it could offer a useful additional treatment option. They felt that many women would be interested in knowing more about acupuncture for their back pain, particularly those women who are severely affected, and who, they felt, would be willing to try it within the context of a trial. The midwives felt that pregnant women with back pain under their care would have few concerns about acupuncture and these would be most likely linked to the location of and sensations from the needles, as this focus group excerpt indicates:
[They’ll] want to know where you’re going to put the needles.
That’s the first thing I’d ask.
Yeah, and they’d want to know if it hurts.
Community midwives: group B, 373
Physiotherapists were also generally in favour of testing the additional benefit of acupuncture for this patient group in a trial because of the difficulties in treating the pain through other treatment methods.
I mean, it’s [acupuncture] very interesting because drugs do not seem to work for these women. You know, talking about sort of real heavy painkillers . . . We had a lady admitted last week and was immediately put on morphine, it didn’t touch her pain at all. And all that does then is make the baby sleepy, and the mum sleepy. So for some women it is very difficult pain to manage.
Women’s health physiotherapist group
However, the physiotherapists raised concerns about safety of acupuncture in pregnancy, given their previous acupuncture training during which they recalled they had been advised that acupuncture was contraindicated in pregnancy.
And again like the previous two people, I thought acupuncture was contraindicated, that was part of my training. And I wouldn’t have done it to a pregnant lower back pain patient.
Community physiotherapists: group B, 57
Such concerns included the general safety of acupuncture in pregnancy and the specific acupuncture points and techniques to be used, and these concerns were rooted in their lack of confidence and/or experience in caring for pregnant women, as this excerpt indicates:
With them being pregnant, you’re just so aware that they’re pregnant and you feel limited to what you can do because you don’t want to . . .
I think we’re just scared to hurt them, aren’t we?
Community physiotherapists: group A, 81
This fear was related to concerns over a perceived lack of adequate training, specifically in the application of acupuncture in pregnancy:
I don’t think I’ve got the training to do it. There might be other stuff out there, but I don’t feel that I’m well enough equipped to deliver other things.
Is that the same for everybody?
Yeah. I think because we don’t see them often enough, we don’t – there isn’t the training out there. We don’t know exactly . . .
Community physiotherapists: group A, 95
Such fears around possible harm to the mother and/or baby generated a culture of caution, underpinned by a fear of litigation. Although most physiotherapists shared these fears, the three who participated in individual interviews and who practised acupuncture with pregnant women held starkly contrasting views. They worked in NHS musculoskeletal outpatient departments in which acupuncture was available. One had been qualified for 11 years, one for 18 years and one for 28 years. They were confident about the safety and efficacy of acupuncture for this population and indeed considered it safer, in fact, than medication, as illustrated by this quotation:
I would use acupuncture as a first choice of treatment with pregnant ladies over medication because of the safety risks with medication. In fact, I find my pregnant patients respond better [to acupuncture] than perhaps my standard lower back pains.
Physiotherapists’ survey
These interview findings were pivotal in developing the content of the training and support programme offered to physiotherapists participating in the EASE Back pilot trial in phase 2.
In addition, both the midwife and physiotherapist interviews highlighted a number of issues around recruitment, including the importance of detailed patient information and reassurance (about the acupuncture needling, any known side effects on the baby, information about positioning during treatment), flexibility around time and location of treatments and generally minimising the research burden on participants. The fact that the issues emerging through the interviews and focus groups were consistent with some of the survey responses acted as a further form of validation. The qualitative results specifically about physiotherapists’ concerns in using acupuncture during pregnancy also help explain the practice patterns seen in the survey responses. The findings from the qualitative interviews were incorporated into the participant information leaflet, the recruitment methods, the selection of treatment sites, the treatment protocols and the outcomes for the EASE Back pilot trial in phase 2.
Implications for recruitment to the pilot randomised controlled trial
The challenges in recruiting pregnant women to participate in the phase 1 interviews made it clear that we needed to develop and test a range of approaches to identify and recruit eligible women for the pilot trial in phase 2. Originally the plan had been to raise awareness about the pilot trial by inserting a flyer within the booking information pack given when seen by their community midwives and for women with back pain in pregnancy to be given an information pack about the trial by their usual midwife. We tested these approaches in phase 1, and overall these approaches alone were not particularly successful in identifying suitable women who were willing to be involved in the interviews. Recruitment of this population to research in phase 1 was clearly challenging, and therefore we used the results of the interviews with pregnant women, midwives and physiotherapists as well as suggestions for additional recruitment methods from research midwives who had worked on other research studies with pregnant women in order to agree six methods with which to identify and recruit women to the pilot RCT in phase 2. While using six methods was complex for a pilot trial and we had not originally included these costs of some of these methods in the grant application, we were keen to test out the methods in order to identify a smaller set of methods that might work best for a future large trial. The details of the six methods are provided in the next chapter (see Chapter 3, Recruitment methods and procedures), but they included a brief questionnaire that screened for the presence of back pain and willingness to be contacted further among women attending their antenatal 20-week ultrasound scan appointment and a local awareness-raising campaign that included use of a study website, newspaper, radio and other local media in order to take the message about the study directly to local pregnant women who could then opt to self-refer to the research team for eligibility screening.
In addition, we had planned that research midwives would screen all women for eligibility in face-to-face information and consent meetings. Through discussions with the research midwives it was agreed that a much more efficient use of their time would be to conduct brief telephone screening first and invite only those who appeared potentially eligible to face-to-face meetings for full eligibility screening, informed consent and baseline data collection.
Specification of information and interventions for the pilot randomised controlled trial
The development of the participant information leaflet
In order for potential participants to be fully informed about what taking part in the pilot trial in phase 2 would involve, a detailed PIL was developed. The format and content of the PIL was both based on a best practice example provided within the good clinical practice and regulatory requirements for clinical trials and taken from the findings of the qualitative research in phase 1. Information was provided not only on the rationale of the study, why women were being invited to take part, what taking part would involve, issues around anonymity and confidentiality, payment and the funders of the study, but also on the acupuncture treatment. This specific information included the required positioning for treatment, the difference between acupuncture needles and other types of needles (e.g. those used to take blood), whether or not children were able to attend appointments, the ability to drive after treatment and the known risk of specific adverse events from acupuncture during pregnancy. The PIL was reviewed by patient representatives on the Trial Steering Committee (TSC) and amended following feedback. A copy of the PIL is in Appendix 4.
The development of a standard care protocol
Given the variation in SC for pregnancy-related back pain, we sought to use the results of the national survey and the qualitative interviews, along with available research evidence, to specify a SC intervention protocol for the pilot RCT. The protocol included a high-quality and comprehensive self-management booklet and, for those who needed it, an onward pathway to individualised assessment and treatment with an EASE Back study physiotherapist.
Self-management booklet
The national survey resulted in the research team receiving examples of 37 different advice and self-management leaflets currently used by physiotherapists across the UK. These were used to help develop the specific self-management booklet used in the pilot RCT. Other than the professionally produced leaflet Pregnancy-Related Pelvic Girdle Pain, published by the ACPWH, all others were examples of brief and inexpensive leaflets produced by individual NHS trusts or individual clinicians. It was clear that none was clearly fit for purpose for use in the EASE Back pilot RCT and, therefore, we developed the EASE Back: Managing Your Back and Pelvic Girdle Pain in Pregnancy booklet specifically for use in phase 2. The available leaflets were reviewed for common themes and good examples of both content and layout, taking into account the issues raised by pregnant women, midwives and physiotherapists during the phase 1 pre-pilot work. We sought to develop a booklet that would be seen as more comprehensive than those available to date, that was produced in colour, of high quality, with clear photographs of real pregnant women (rather than diagrams only, as was the case in most of the available examples), divided into sections and with clear page numbers and handy hints boxes throughout. We also wanted the booklet to be of a size that women could fit into their handbag so that they could, if they wished, carry it around with them and thus refer to it during the day (most of the available examples were photocopied A4 sheets of paper). Working with the women’s health specialist physiotherapist at the participating hospital [University Hospital of North Staffordshire (UHNS)], who was also a member of the ACPWH, we developed sections for the booklet about the good prognosis of back pain in pregnancy, advice about appropriate self-management of back pain in pregnancy, including pacing between activities and rest, simple exercises to try at home, advice on adaptation in lifting techniques, tips about relieving postures for sitting, standing and sleeping, advice about work and continuing with everyday activities, the use of pelvic supports/belts and supportive pillows, and the use of simple and safe analgesics. We also included some self-management hints and tips, advice for labour and after the birth, a summary and useful websites.
The booklet was reviewed by patient representatives (women with experience of pregnancy-related back pain) on the TSC, physiotherapists and an antenatal and postnatal exercise specialist before we finalised the content, photographs and layout. A copy of the booklet is included in Appendix 5. In the pilot trial, the booklet was posted to all trial participants, who were advised to follow the advice and exercises in the booklet and that, if they felt they needed to see a physiotherapist, they should discuss this with their community midwife (as in usual care) and then book an appointment with an EASE Back study physiotherapist.
One-to-one standard care physiotherapy
We protocolised the number and content of physiotherapy sessions for the pilot RCT using the data from the national survey and qualitative interviews. We knew that women who were severely affected would need help with pain and function, and that onward referral to physiotherapists for assessment, advice and treatment needed to be available within the SC protocol. Therefore, we provided information in the SC information pack on how to access EASE Back study physiotherapy care should both the woman and her midwife feel this was needed and we developed an EASE Back study SC protocol for those women, based on the results of our surveys and interviews from phase 1. This involved an individualised assessment of the problem, individualised advice particularly about posture and a home exercise programme (focusing mainly on stabilising trunk exercise and pelvic floor muscle exercise but which could include stretching, pelvic tilt exercises and gluteal muscle strengthening), with treatment options that included supportive Tubigrip™ (Mölnlycke Health Care Limited, Dunstable, UK), pelvic supports/belts, manual therapy including massage, supervised exercise therapy and use of walking aids for those that might need them. Hydrotherapy, group treatments and acupuncture were not permitted within the protocol for SC alone. If women enquired about or engaged in antenatal aqua classes this was fine, as long as the treatment from the physiotherapist did not involve exercise in water. The episode of care consisted of between two and four treatment sessions over 6 weeks, with the episode of care left open until the end of the pregnancy, in line with our survey findings.
The development of the acupuncture treatment protocol
The results from the national survey and the interviews with physiotherapists who used acupuncture in the management of pregnancy-related low back pain and PGP were used, alongside evidence from previous trials, to specify the content and delivery of the acupuncture treatments in the pilot RCT. We attended to the need for an individualised approach to acupuncture (in terms of selection of initial points to be needled and the flexibility to change the selection of points over the series of treatment sessions) while also needing to be able to describe the range of points that therapists could select from. Thus, following individual patient assessment including examination of tender points, physiotherapists could choose the most appropriate true acupuncture points for the individual patient from a long list of potential points. The agreed list of points was based on our survey findings and previous trials in similar patient populations. We ensured that formal service-level agreements with participating physiotherapy services stipulated between six and eight treatment sessions should be delivered within 6 weeks (based on the survey results and balancing the need to offer sufficient acupuncture sessions to be effective while also providing a treatment course that might be suitable for the NHS in future). Full details of both the true and non-penetrating acupuncture protocols are provided in Chapter 3, Interventions.
Development of training programmes for participating clinicians
Training programme for research midwives and nurses
The research midwives and nurses involved in the EASE Back pilot trial (n = 8) attended a half-day training programme prior to recruitment commencing, which included lectures, practical sessions, role play, group discussion, problem-solving and case studies. During the training programme, the research midwives and nurses were informed about (1) the rationale and design of the EASE Back study, including how the findings from phase 1 had informed the design of the pilot trial and (2) the planned procedures involved in identification of potentially eligible women, screening, gaining written informed consent, audio-recording a sample of the face-to-face screening and consent meeting, baseline data collection and the randomisation and completion of maternity record reviews after trial participants had given birth. Audit procedures were also finalised; these included clinic activities such as informed consent, guiding women in the performance of the two objective tests for PGP, the telephone calls to the randomisation service at the Clinical Trials Unit (CTU) as well as the collection of minimum data over the telephone at follow-up. A summary of the half-day training programme is provided in Appendix 6.
In order to consolidate learning, the initial half-day training programme was followed by a 2-hour refresher session that took place immediately prior to commencing recruitment in the pilot RCT. This included role play of a number of different scenarios from the point of initially identifying potentially eligible women, completing screening and eligibility checking over the telephone and completing the face-to-face screening and consent meeting. Example scenarios included women who were ineligible for various reasons, women who were eligible but who declined participation and women who were eligible and provided informed consent. Throughout all scenarios, study documentation was completed to enable the research midwives and nurses to become familiar with it before starting recruitment, and all research midwives and nurses were observed by a member of the study team to ensure that they were competent in completing all study eligibility screening and recruitment procedures as planned.
Training programme for physiotherapists
All the physiotherapists providing care in the pilot trial were trained in the use of acupuncture for pain conditions, in training programmes that met national standards. The EASE Back pilot trial training programme for participating physiotherapists took place over 3 full days and a copy of the programme content is available in Appendix 7. Day 1 summarised relevant literature, including the changes during pregnancy to women’s bodies, the potential explanations for back pain during pregnancy, assessment of pregnant women with back pain (with or without PGP), and SC for pregnancy-related back pain, including key findings from phase 1. Day 2 focused on acupuncture for pregnancy-related back pain, available data on safety of acupuncture for this patient population and the details of the EASE Back study protocols for both the true and non-penetrating acupuncture treatments. Day 3 combined SC and acupuncture protocols together using patient case studies and included information about the practicalities of the trial, including use of EASE Back trial case report forms (CRFs); how to deliver the trial protocols, stressing the importance of patient blinding; and identification of any adverse events or SAEs. Training included lectures, group discussion and use of patient case examples, as well as practice of assessment and treatment skills. We trained 14 physiotherapists to deliver the treatments in the EASE Back pilot trial, supported by a training team including an expert acupuncturist, a women’s health specialist physiotherapist and a consultant obstetrician. Ongoing support to deliver the treatments in the EASE Back trial was provided by an expert acupuncturist and a women’s health specialist physiotherapist; this support took the form mostly of telephone and e-mail communications as well as some face-to-face visits during which the acupuncturist observed participating physiotherapists’ treatment sessions with patients and provided feedback and support. Physiotherapists completed a brief questionnaire before and immediately after the training programme and at the end of the pilot RCT, in order to describe physiotherapists’ characteristics and explore changes in their intended management of a patient with pregnancy-related low back pain and in their confidence to assess and treat this population. The results from these questionnaires are summarised in Chapter 3, Physiotherapists’ questionnaire results and feedback.
Conclusions
In conclusion, the pre-pilot work in phase 1 provided high-quality data on current UK SC and acupuncture treatment for back pain in pregnancy. The survey and interviews results, particularly those from NHS-based clinicians, were used to help develop the intervention protocols for all the treatment arms in the pilot randomised trial in phase 2 of the EASE Back study. The interview findings from pregnant women, midwives and physiotherapists informed the content of the patient information materials, the recruitment methods and the clinician training programme for the pilot trial in phase 2, reported in Chapter 3.
Chapter 3 Phase 2 pilot randomised controlled trial
Objectives of phase 2 pilot randomised controlled trial
The specific objectives of phase 2 were to:
-
test the trial procedures, training programme for health professionals, interventions and short-term outcomes with pregnant women with back pain, and provide data on recruitment and follow-up rates, treatment fidelity, outcome completion rates and an estimate of between-group difference on key outcomes
-
bring the above findings together, with experts in SC, acupuncture and trial design, in a consensus conference to finalise the design, interventions, sample size, outcome measures and operational aspects of a main EASE Back trial.
Design and setting
We conducted a single-centre pilot three-arm parallel RCT with data collection before randomisation and at 8-week follow-up. The pilot trial included three treatment arms, randomising participants to receive SC, SC plus true acupuncture or SC plus non-penetrating acupuncture. North Staffordshire, including UHNS and associated antenatal clinics including community midwives, and physiotherapy clinics within the North Division of Staffordshire and Stoke-on-Trent Partnership Trust, was the site for the pilot trial.
Ethical approval and research governance
Research ethical approval was sought in December 2012 from West Midlands Staffordshire Research Ethics Committee (REC) and included the usual follow-up reminder procedures for clinical trials overseen by the musculoskeletal CTU at Keele University [a follow-up questionnaire, followed by a postcard reminder if no response, followed by a further full copy of the questionnaire if no response, followed by a minimum data questionnaire if no response, followed by a minimum data collection (MDC) over the telephone if no response]. The REC recommended using a maximum of two reminders, as they were concerned that the planned follow-up processes would be seen as burdensome and one member of the committee felt strongly that this was a vulnerable patient group, some of whom could be suffering with postnatal depression. Despite our formal appeal (25 January 2013, see Appendix 8) in which we provided evidence from the CTU from five previous trials about the importance of all of these follow-up reminders in achieving response rates in excess of 80% and our reassurance to the committee that the follow-up time point of 8 weeks had been chosen so that most women would not yet have given birth, the committee upheld their decision and we had to remove two reminders from our usual follow-up processes. The postcard reminder and minimum data questionnaire were removed and, therefore, the follow-up process in the EASE Back trial comprised an 8-week questionnaire and a further full copy of the questionnaire if no response was obtained in 2 weeks (at 10-week follow-up), followed by a telephone call for MDC if no response was obtained in 2 weeks (at 12-week follow-up). Appendix 8 provides the evidence of the ethics committee appeal (which was conducted with the knowledge of the NIHR HTA programme contact person for the EASE Back study), the evidence from five of our previous trials about the importance of our usual follow-up processes in achieving high response rates and the response from the REC. Following ethics approval on 28 February 2013, we proceeded to apply for research and development approvals for all participating sites. Ethics and research and development approvals were all gained by 22 April 2013 for the pilot trial.
Given the known importance of patients’ expectations in analgesic responses and in particular in acupuncture response, we obtained research ethics approval to explain in the participant information documentation that all trial participants would receive SC and that, in addition, they might or might not receive one of two forms of acupuncture, thus maximising non-specific effects. This approach has previously been successful in acupuncture trials using validated sham Streitberger needles (blunted, non-penetrating needles; Asia-med, Suhl, Germany),33,39 demonstrating both true and non-penetrating acupuncture to be safe and credible to patients.
Amendments
There were no substantial amendments submitted to ethics for the pilot RCT. The following minor amendments were made:
-
5 March 2013: this amendment related to the addition of a number of patient identification centre sites (Stoke-on-Trent Primary Care Trust, North Staffordshire Primary Care Trust, South Staffordshire Primary Care Trust) and a change of named study principal investigator (PI) for the UHNS.
-
9 April 2013: this amendment related to some minor changes to the wording of consent forms, PILs and information relating to the treatment sites.
-
4 June 2013: this amendment related to a minor clarification to the eligibility screening questionnaire.
-
31 July 2013: this amendment related to a minor clarification to the eligibility screening questionnaire and the covering letter for the 8-week follow-up questionnaire.
Participants
Participants were pregnant women with low back pain (with or without PGP) who contacted the research team in response to information about the trial or who were identified from primary care, referrals to the UHNS women’s health physiotherapy service, community midwives and antenatal clinics within UHNS and the North Division of Staffordshire and Stoke-on-Trent Partnership Trust (SSOPT).
Inclusion criteria
Women were eligible to participate in the pilot trial if they were:
-
women with pregnancy-related back pain [defined as self-reported pain in the lumbar area (between the 12th rib and the gluteal fold)] with or without PGP
-
under the care of participating NHS sites and GP practices
-
aged 18 years or over
-
at 13 to 31 weeks’ gestation (chosen in order to ensure that women could receive six to eight treatment sessions within 6 weeks, if they were randomised to SC plus acupuncture, and yet still have their 8-week follow-up questionnaire before they had given birth)
-
naive to acupuncture treatment
-
able to read and communicate in English (to provide full informed consent and to complete the baseline and outcome assessments)
-
willing to participate.
Women who had low back pain episodes before this pregnancy were suitable for inclusion as long as the current episode of low back pain was either attributed to or made worse as a result of this pregnancy.
Exclusion criteria
Women were excluded from participation in the pilot trial if they:
-
had ever had any form of acupuncture previously for any health problem
-
were at high risk of miscarriage (previously had recurrent miscarriage, defined as three or more; abnormalities in the cervix deemed to increase risk of miscarriage; antiphospholipid syndrome; lupus anticoagulant)
-
were at high risk of pre-term labour (previously giving birth before 37 weeks’ gestation), multiple pregnancies, polyhydramnios (an excess of amniotic fluid in the amniotic sac, seen in about 1% of pregnancies), pre-term ruptured membranes (the rupture of membranes prior to the onset of labour in a woman who is at less than 37 weeks’ gestation, seen in 2% of all pregnancies) or had a history to surgery to the uterine cervix (deemed to increase risk of pre-term labour)
-
had diagnosed pre-eclampsia (a rapidly progressive condition characterised by high blood pressure and the presence of protein in the urine, affecting 5–8% of pregnancies)
-
had a history of surgery to the spine or the pelvis
-
had contraindications to any of the treatments (coagulation problems, haemophilia or bleeding disorders, were at increased risk of infection such as skin infections or loss of skin integrity from burns or ulcerations at the site of needling) or had a high needle phobia
-
had pain in the anterior pelvic region only (anterior PGP or pubic symphysis pain only)
-
had a current urinary tract infection.
Recruitment methods and procedures
Building on the findings from phase 1, we tested several ways to identify and recruit women to the EASE Back pilot RCT. Six methods were tested and participant flow through each is summarised in Appendix 9 and explained below.
Method 1: research midwives identified women in antenatal clinics and determined eligibility
Research midwives identified potentially eligible women in usual antenatal clinics, discussed the trial directly with them and provided a PIL. If both the woman and the research midwife had the time to do so on the same day, a face-to-face appointment proceeded at which full eligibility was confirmed and written informed consent gained.
Method 2: brief screen for back pain at the 20-week ultrasound scan appointment
On arrival for their routine 20-week ultrasound scan, all pregnant women were to be given a study flyer and a screening questionnaire to complete either before or after they had their scan, and were asked to return the completed brief questionnaire to a dedicated box within the ultrasound scanning clinic. Questions included the presence of pregnancy-related back pain and a consent form for further contact. Questionnaires were collected on a weekly basis by research staff and screened by a research midwife. The research midwife telephoned potentially eligible women to determine their eligibility and their interest in the trial. If eligible, women were posted the PIL and a face-to-face appointment was booked to confirm full eligibility and to gain informed consent. If no contact could be made, the trial information leaflet and an EASE Back study card were posted to the woman, advising her to telephone the study administrator if she was interested in participating.
Method 3: women identified from the University Hospital of North Staffordshire women’s health physiotherapy service referrals
Research midwives screened referrals from GPs, community midwives and antenatal clinic to the UHNS women’s health physiotherapy service. A research midwife contacted all potentially eligible participants to determine their interest in the study and their eligibility. If eligible and interested, they were sent the PIL by post and a face-to-face appointment was booked to confirm full eligibility and to gain informed consent. If no contact could be made, the trial information leaflet and the EASE Back study card were posted to the woman, advising her to telephone the study administrator if she was interested in participating.
Method 4: research midwives identified women in antenatal clinics
Research midwives identified potentially eligible women in usual antenatal clinics. However, if either the woman or the research midwife did not have time to complete a face-to-face visit there and then, or if the woman wanted further time to think about participation, the research midwife provided the woman with an EASE Back study card, which directed the woman to telephone the study administrator.
Method 5: clinicians gave pregnant women with back pain an EASE Back study card
In the fifth method, we contacted participating GPs, obstetricians and community midwives to identify potentially eligible women and give them an EASE Back study card, which directed women to telephone the study administrator.
Method 6: self-referral from local awareness raising
Pregnant women with back pain who were made aware of the trial through our local media awareness raising could directly telephone the EASE Back study administrator (termed ‘self-referring’ women). We used several approaches to raise awareness about the pilot trial among local pregnant women and clinicians. Study flyers were included in the standard information booking packs that all pregnant women received at their first booking visit with a midwife, and were also to be given to women at their 20-week ultrasound scan appointment. The study flyers included details of how women could find more information (providing both a contact telephone number and a website address). We developed a study-specific website for the EASE Back trial and a YouTube (YouTube, LLC, San Bruno, CA, USA) video clip that was linked to the website; while we sought to include information about the trial on other internet sites including Facebook (Facebook, Inc., Menlo Park, CA, USA), Twitter (Twitter, Inc., San Francisco, CA, USA), Mumsnet and Pelvic Partnership, this was not possible in the end. In addition, study flyers and posters were distributed to, and displayed in, local GP practices, children’s centres and the UHNS maternity centre and women’s health department. We raised awareness of the trial through local radio (including one-off, free interviews about the trial on Radio Stoke and Six Towns Radio as well as professionally produced radio infomercials running frequently on 3 consecutive days on the local commercial radio station, Signal Radio), a free two-page spread in a local newspaper with wide readership (The Sentinel) and paid advertisements about the study on local buses. These awareness-raising methods were tested throughout the recruitment period and were phased in over time. The need for such advertising and payment for advertising had not been originally included in the grant application but the research team felt it was important to test out different methods in order to estimate their likely value for a future large trial.
Eligibility screening and informed consent
Women identified through method 1 were screened for eligibility by research midwives on the same day as their antenatal appointment. Those who appeared eligible were provided with a PIL. If time permitted, and the woman wished to do so, she completed the full eligibility checks, consent process and baseline data collection and was randomised on the same day. If time did not allow this, or if the woman wished to have more time to consider participation, then a further face-to-face research appointment was booked with a research midwife or research nurse or the woman was advised to telephone the study administrator if she was subsequently interested in participating (method 4).
In all other methods there was a brief initial eligibility check over the telephone (confirming intended clinical site of birth as UHNS, presence of back pain related to this pregnancy, age of18 years or over, at gestational weeks 13 to 31 and naive to acupuncture treatment). If women met these initial eligibility criteria, a study letter and PIL were posted out to them and a research midwife or research nurse then contacted them by telephone to complete further eligibility checking. If the woman was eligible and interested in participating, a face-to-face appointment was booked for her with a research midwife or research nurse at a choice of either an EASE Back study research clinic at UHNS or the woman’s own home for confirmation of final eligibility, consent, baseline assessments and randomisation.
If the woman was eligible and willing to participate, written consent to participate was obtained. Full baseline data collection took place, including completion of the baseline questionnaire and completion of two self-administered pain provocation tests (see Baseline data collection). Women had a choice in location and times of EASE Back study eligibility and consent appointments and in treatment location and times. Ineligible women and those who declined to participate were signposted back to normal care pathways. In order to explore generalisability, anonymised data were captured from women who were ineligible or declined participation.
Audio-recordings of eligibility and consent meetings
The purposes of these audio-recordings were to explore how the trial was explained and presented to women by those involved in obtaining informed consent, the potential usefulness and acceptability of the information provided and any concerns on the part of the women, in particular about acupuncture in pregnancy and/or the acceptability of randomisation to the different treatment groups. Previous research has pointed to frequent difficulties in recruitment to randomised trials. 57,62 Such difficulties pose major threats to external validity, increase costs and reduce research staff productivity. 63–65 Such research also highlights the importance of a clear understanding among potentially eligible participants of the concept of clinical equipoise, of threats to recruitment because of patient preferences66,67 and of tensions in the process of informed consent. 68 As part of testing the trial procedures in the light of these challenges, we examined in detail a sample of the face-to-face meetings that took place between the research midwife or research nurse and potentially eligible women.
Details on how to use the recorders, label the audio files to ensure anonymity, upload them to the secure research e-mail address and delete once confirmation of their safe arrival had been received were including in the training session for the research midwives and nurses. These recordings were transcribed in an anonymised format. Data collection stopped after 30 audio recordings, when data saturation was clear. 69 Analysis was carried out based on the constant comparative method60 with transcripts read and text segments coded in order to identify themes which were then discussed within the research team.
Baseline data collection
The baseline data collection included a baseline questionnaire (see Appendix 10) and two objective self-administered tests of pain provocation. The baseline questionnaire included sociodemographic questions about age, education (highest qualification), marital status, social support (living alone), number of children and pregnancies, job title, work status, physical demands of work, time taken off work because of the back pain, performance at work and overall work satisfaction, as well as current body mass index (BMI) and pre-pregnancy BMI. The baseline questionnaire also included questions about symptoms including pain location using a body chart [in which responses were coded into low back pain only, low back pain with anterior PGP, low pain back with pain in other bodily regions (such as the thoracic spine, neck, shoulders and arms) or low back pain with anterior PGP and pain in other bodily regions], pain duration of this episode, pain severity using a pain index [mean score of three Numeric Rating Scales (NRSs) of least, usual and current pain70], pain intensity before going to bed,33 frequency of pain preventing being able to fall asleep, frequency of pain waking the woman up at night, impact of pain on everyday activities [measured using both the Oswestry Disability Index (ODI)71 and the Pelvic Girdle Questionnaire (PGQ), a recently validated tool that captures self-reported symptoms and impact on activities specifically for pregnant and postpartum women72,73], overall quality of life [measured by the European Quality of Life-5 Dimensions (EQ-5D)74 and Short Form questionnaire-12 items (SF-12)75], use of both over-the-counter and prescribed medications, treatments or appliances, treatment preferences and expectations for both SC and SC plus acupuncture. In order to further assess the proportion of participants in the trial with low back pain only or low back pain with PGP, the research midwife or research nurse instructed participants to conduct two self-administered tests for PGP. These were the self-test P4, which is a participant-generated thigh thrust, and the bridging test, where the woman performs a pelvic bridging manoeuvre with extension of one leg (see Appendix 11). Both tests are conducted in a supine position, can be performed by pregnant women and have been shown to have high sensitivity and specificity for posterior PGP compared with reference standard tests. 76 Compared with a reference standard, the sensitivity of the self-test P4 was 90% and for the bridging test 97%, with specificity being reported as 92% and 87% for the self-test P4 and bridging test respectively. Olsen et al. 76 report a positive pain drawing as the most sensitive (96%) and specific (85%) method of identifying anterior PGP (and we included a body chart in the baseline questionnaire on which women were asked to shade the areas of pain). The research midwives instructed the women to undertake the self-test P4 and the bridging test in a standardised way using a pre-prepared script. A positive test was a reproduction of their familiar pain in the sacroiliac region.
Randomisation and allocation concealment
Participants were randomised using the musculoskeletal CTU (registered CTU), a process of third-party remote randomisation. A random allocation sequence was used, based on computer-generated random numbers. The research midwife or research nurse telephoned the CTU administrator on the same day (whenever possible) or on the next working day following the face-to-face meeting at which written consent was taken and a research administrator conducted the concealed randomisation process and directly informed the participants about their treatment allocation, in writing, within 2–3 days of randomisation (in the next available post). This ensured that the person involved in randomisation was unaware of the baseline data of each trial participant. Given that back pain tends to worsen as pregnancy progresses, we stratified randomisation based on gestation weeks (dichotomised into two groups, less than or more than 24 weeks), in order to ensure that equal proportions of women at earlier and later gestation were randomised to each of the three treatment groups. The randomisation was also blocked (using randomly varying blocks of sizes 3 and 6) to ensure that the number of participants was equally distributed among the three treatment arms. All participants continued with their usual care from their midwife and other antenatal carers, and this was recorded in the follow-up questionnaire at 8 weeks. Participants were posted written confirmation of their treatment allocation along with the EASE Back study self-management booklet. Those randomised to SC alone also received information about how to access physiotherapy should both they and their community midwife feel they needed it. Those randomised to receive one of the acupuncture interventions also received, in the same postal package, information about the next steps for them to start their treatment. We developed written service-level agreements with participating physiotherapy services to facilitate the commencement of treatment within 2 weeks of randomisation to one of the acupuncture treatments and agreed the process of communication between trial participants and the physiotherapy service (through administrators in the existing physiotherapy hub who arrange all physiotherapy appointments in the participating trust).
Blinding
The women randomised to SC plus either true or non-penetrating acupuncture were blinded to whether they were receiving true or non-penetrating acupuncture. Physiotherapists providing the treatments were not involved in the baseline data collection or follow-up outcome assessment processes. The NIHR Clinical Research Network West Midlands research midwives and nurses dealing with the baseline and outcome data collection were blinded to the intervention assignments. Selection bias was avoided by the system of remote allocation to treatments described earlier. Data about outcomes were collected using self-completed questionnaires (and telephone follow-up for a minimum data set). These data were collected and entered by staff without knowledge of the allocation of the individual concerned. In addition, analyses of patient-reported outcomes at 8-weeks follow-up were conducted and verified by blinded statisticians.
Training and auditing processes
Research midwives in the Childbirth And REproductive health (CARE) for Comprehensive Local Research Network (CLRN) West Midlands North network and research nurses in the Clinical Research Network West Midlands were key to identifying potentially eligible women for the pilot trial, to providing full information to potentially eligible women, to determining eligibility for the trial and to gaining women’s written consent and full baseline data. Following written consent, research midwives and research nurses were also responsible for telephoning the randomisation service. In addition, our EASE Back study administrator conducted brief initial eligibility screens during a telephone call initiated by interested women. Several training events led by the study team for these key staff ensured the processes for identification, explanation, screening and consent were feasible and clear (see Chapter 2, Training programme for research midwives and nurses, for full details of the research midwife and nurse training programme). This was facilitated by a named lead research midwife and a named lead research nurse, clear flow charts and a pro forma for completion during the eligibility screening and checking meetings (see Appendix 12 for the full eligibility screening pro forma). The research team conducted audits of these eligibility screening and consent meetings.
The processes for identifying potentially eligible women, completing screening and eligibility checks, audio-recording face-to-face meetings, obtaining informed consent, collecting baseline data including guiding women to complete the two objective tests for PGP and contacting the CTU for randomisation were initially assessed as mock scenarios within the training session prior to commencing recruitment (see Chapter 2, Training programme for research midwives and nurses). During the recruitment period, any new members of the research nurse team who joined the study were also trained and assessed by the lead research nurse to ensure they were competent in these processes. The lead research nurse was audited by the trial co-ordinator. The lead research nurse then carried out audits on all other research midwives and nurses. The audit found that all research midwives and nurses were competent in the process of taking informed consent and guiding women to perform the objective tests, and that the pilot trial procedures were being adhered to.
The lead research nurse ran a training session on MDC telephone calls after the 8-week questionnaire with the research nurse team and listened to the telephone follow-up calls until she was happy that the nurses were competent in collecting follow-up data. This was checked again halfway through the MDC period by the lead research nurse, to ensure consistency across all the nurse team, and no problems were identified.
Physiotherapists’ questionnaire results and feedback
Questionnaire results
Fourteen physiotherapists (13 female) who delivered the EASE Back pilot trial interventions completed three questionnaires (before and immediately after the training programme, and at the end of the EASE Back pilot RCT). Their demographic and practice characteristics are summarised in Table 6. All had prior experience (although mostly ‘infrequently’) of treating pregnancy-related back pain. The majority had previously received postgraduate training in back pain, but only one in women’s health. Eleven currently used acupuncture in the management of musculoskeletal pain, including back pain, but none currently used acupuncture for back pain in pregnant women.
| Characteristics (denominatora) | |
|---|---|
| Years of clinical experience, median (IQR) | 8.5 (5.0–17.5) |
| Use acupuncture for musculoskeletal pain, n (%) | 11 (78.6) |
| Work setting (13) | |
| Exclusively NHS, n (%) | 6 (42.9) |
| Combination of NHS and non-NHS, n (%) | 7 (50.0) |
| Frequency of treating pregnant women with back pain (13) | |
| Infrequent – at most one in last 6 months, n (%) | 10 (71.4) |
| Somewhat frequent – between two and five in last 6 months, n (%) | 2 (14.3) |
| Very frequent – at least one per week, n (%) | 1 (7.7) |
| Circumstances under which pregnant women access physiotherapyb (13) | |
| Referred from their midwife, n (%) | 1 (7.7) |
| Referred from their GP, n (%) | 12 (92.3) |
| Referred from their obstetrician, n (%) | 1 (7.7) |
| Self-referred to physiotherapy, n (%) | 1 (7.7) |
| Postgraduate training (14) | |
| In women’s health, n (%) | 1 (7.14) |
| In back pain in general, n (%) | 13 (92.9) |
| In back pain in pregnancy, n (%) | 2 (14.3) |
Physiotherapist questionnaires sought information about their self-confidence in managing pregnant women with back pain and their clinical management of a typical patient with this problem (in a patient case vignette), before and immediately after the training programme, and after delivering the EASE Back study interventions to participants. The results are summarised in Table 7. Self-confidence in diagnosis and management of back pain in pregnancy increased after the training and remained high at the end of the pilot RCT. In terms of SC, the large majority of respondents reported that they would manage the patient case in one-to-one treatment sessions, and the number of times the patient would typically be seen increased after the EASE Back study training, with many preferring to see the patient more than twice.
| Physiotherapists’ questionnaire results | Before training (n = 14) | After training (n = 14) | At trial end (n = 12) |
|---|---|---|---|
| Self-confidence in diagnosis and management of back pain in pregnancy,a median (IQR) | 8.0 (6.0–11.0) | 16.0 (16.0–17.0) | 16.0 (16.0–17.0) |
| Patient would normally be seen in individual, face-to-face sessions, n (%) | 12 (85.7) | 12 (85.7) | 11 (91.7) |
| Patient would normally be seen as part of group, but could access one-to-one sessions, n (%) | 1 (7.1) | 1 (7.1) | 1 (8.3) |
| Patient seen in up to two treatment sessions, n (%) | 9 (64.3) | 5 (35.7) | 4 (33.3) |
| Patient seen in more than two treatment sessions, n (%) | 5 (35.7) | 8 (64.3) | 8 (67.3) |
| Care episode would last 3–4 weeks, n (%) | 10 (71.4) | 4 (28.6) | 6 (50.0) |
| Care episode would last > 4 weeks, n (%) | 4 (28.6) | 9 (71.4) | 6 (50.0) |
| Typical length of session: up to 30 minutes, n (%) | 11 (78.6) | 8 (57.1) | 10 (83.3) |
| Care would finish after treatment, re-referral required for further treatment, n (%) | 3 (21.4) | 0 (0) | 1 (8.3) |
| Care would be left open for duration of the pregnancy, n (%) | 7 (50.0) | 9 (69.2) | 6 (50.0) |
| Care would be left open for a defined period of time after end of treatment, n (%) | 3 (21.3) | 4 (30.8) | 5 (41.7) |
The questionnaire sought information on physiotherapists’ reported advice to, and management of, the patient case before and immediately after the training programme for the EASE Back study and at the end of the pilot RCT. Figure 4 summarises the advice that therapists reported they would offer and Figure 5 the clinical management approaches. We observed increases in the reported use of written advice on self-management, advice to continue with everyday activities, advice about safe pharmacological treatment options and advice about the use of home massage (see Figure 4), following the EASE Back study training programme. We also observed increases in the use of various management approaches after the training programme including exercises supervised by a physiotherapist, strengthening exercise, pelvic floor exercise and acupuncture see Figure 5).
FIGURE 4.
The EASE Back study physiotherapists’ use of advice for the typical patient case.

FIGURE 5.
The EASE Back study physiotherapists’ management of the typical patient case.
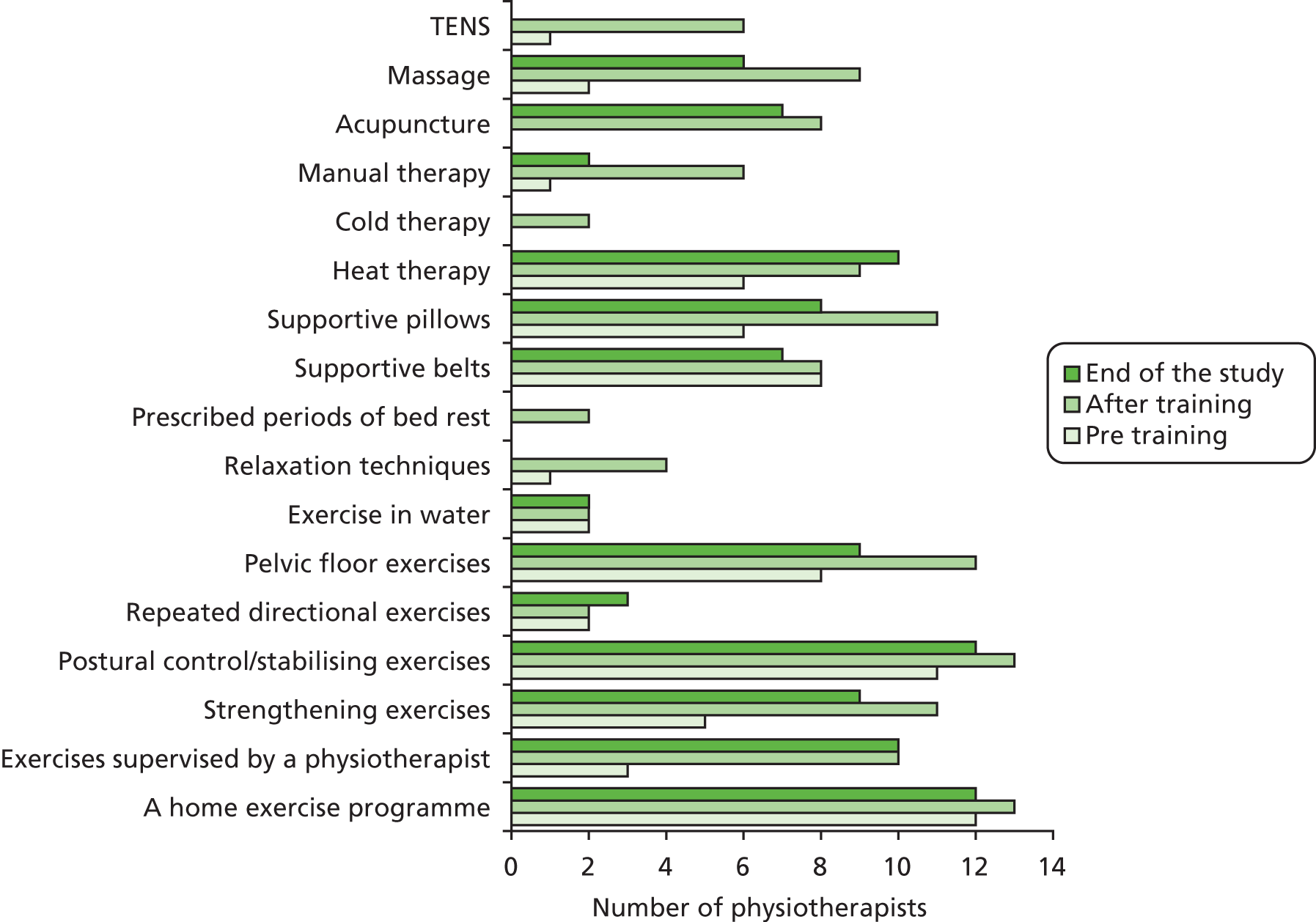
Physiotherapist feedback
Fourteen physiotherapists attended the EASE Back study training programme, 12 of whom provided treatment to the pilot trial participants. Each physiotherapist treated a median [interquartile range (IQR)] of five (two to nine) participants; six physiotherapists treated between two and four participants, three treated between five and eight participants and three treated between 10 and 19 participants. These differences were a result of women choosing some geographical treatment sites more frequently than others. Following the end of all treatment in the pilot trial, we invited the physiotherapists to a half-day feedback workshop (in April 2014) to gain their views of participation in the pilot trial, to explore what worked well and less well from their perspectives, in order to inform the future main RCT and any future training programme. Several key issues were highlighted including the following:
-
Some women had not read the self-management study booklet prior to their first physiotherapy appointment, which meant that much of the first treatment session was taken up with the therapist needing to explain the self-management information before starting acupuncture,
-
Uncontrolled epilepsy, allergy to metal and allergy to Tubigrip should be included in the list of exclusion criteria for a future main RCT.
-
Women should receive a full explanation of what participation in the trial means in terms of commitment to attending treatment sessions.
-
The course of physiotherapy treatment for each participant should be blocked out in physiotherapists’ diaries well in advance.
-
The training programme for physiotherapists’ should include more content on management of pubic symphysis pain (anterior PGP).
Feedback from participating physiotherapists highlighted that the following worked particularly well in the pilot trial and should be continued for a future main RCT:
-
the offer of evening treatment times to participants
-
the block booking of participants’ whole treatment course into physiotherapists’ diaries
-
ensuring flexibility in staff providing EASE Back study treatments to cover annual leave
-
a minimum of two physiotherapists trained in the EASE Back study at each treatment site to provide peer support and sufficient capacity to treat participants
-
the mentoring support and supervision from the acupuncture trainer
-
new patient appointment slots that lasted 1 hour to ensure that there was sufficient time to provide advice, start the exercise programme and deliver acupuncture.
Interventions
The pilot trial included three treatment arms, randomising participants to receive SC, SC plus true acupuncture or SC plus non-penetrating acupuncture.
Standard care
Full details and justification for the SC protocol were provided in Chapter 2, The development of a standard care protocol. SC comprised a high-quality and comprehensive self-management booklet plus onward referral, if necessary, for face-to-face physiotherapy. This was felt to be the most appropriate SC package, as it mostly closely reflected current practice, according to which most pregnant women with back pain are not referred to other health professionals for treatment for their back pain but, rather, are advised to self-manage, with only those who are the most severely affected being referred to physiotherapists. This booklet (see Appendix 5) was posted to women in the SC group along with a letter explaining which group they had been randomised to. They were not instructed to avoid other treatments, but their use of other treatments was monitored through self-report questions in the 8-week follow-up questionnaire. We provided information in the SC information pack about how to access EASE Back study physiotherapy care should both the woman and her midwife feel that this was needed and we developed an EASE Back study SC protocol for these women with participating physiotherapists, based on the results of phase 1 surveys and interviews (see Chapter 2, The development of a standard care protocol, for details). Physiotherapists assessing and managing these women completed EASE Back study CRFs (see Appendix 13) to describe the care provided.
Standard care plus true acupuncture
The same advice and education package was posted to women randomised to SC plus a course of true acupuncture, along with a letter explaining how to arrange the first physiotherapy appointment and that the first treatment should be within 2 weeks. Physiotherapists provided a course of SC plus true acupuncture informed by findings from the phase 1 surveys and interviews. In addition to SC, participants randomised to also receive true acupuncture were to receive treatment as follows: a patient assessment to ascertain the quality, location and intensity of the presenting back pain (with or without PGP) followed by acupuncture treatment, using acupuncture points from selected from the agreed list of points summarised in Table 8. The list of points was informed by the survey of current practice in phase 1, texts about acupuncture for back pain and PGP in pregnancy and previous RCTs. Point location and depth of insertion were as described in Table 8. The patient was suitably positioned (side-lying wherever possible or prone) and the therapist chose a minimum of six and a maximum of 10 bilateral points in total, thus needling between 12 and 20 acupuncture points. The choice of these points was made using the principles of Western acupuncture and trigger point acupuncture. Acupuncture points were to be in the general location of the patient’s pain (local points) with the addition of distal points. The therapists identified and needled the relevant points at the appropriate depth and rotated the needle to elicit the de-qi sensation. It was intended that all needles be inserted into muscle. Traditional acupuncture needles were used in sizes 50 mm × 30 mm, 40 mm × 30 mm, 70 mm × 30 mm and 30 mm × 30 mm. Therapists could change the points at each treatment session, should they feel this was appropriate, as long as all points used were those from the agreed list in Table 8. All needles were of the disposable, sterile, stainless steel variety. Acupuncture treatment was to last from 20 to 30 minutes, during which time the therapist was to stimulate the needles again, ensuring that the needling sensation (de-qi) was maintained. On completion of the treatment all needles were to be safely removed, any sensations felt by the participant during treatment and any adverse reactions were recorded on the CRF and the patient booked for the next appointment. Between six and eight treatment sessions were to be offered to participants over a period of 6 weeks, and efforts to engage women in treatment after failure to attend were agreed with participating physiotherapy services.
| Local points | ||
|---|---|---|
| Point | Description | Depth of insertion/needle |
| BL23 | 1.5 cun lateral to the spinous process of L2 | 30–40 mm/50 mm |
| BL24 | 1.5 cun lateral to the spinous process of L3 | 30–40 mm/50 mm |
| BL25 | 1.5 cun lateral to the spinous process of L4 | 30–40 mm/50 mm |
| BL26 | 1.5 cun lateral to the spinous process of L5 | 30–40 mm/50 mm |
| BL27 | 1.5 cun lateral to the spinous process of S1 | 30–40 mm/50 mm |
| BL28 | 1.5 cun lateral to the spinous process of S2 | 20–30 mm/40 mm |
| BL54 | 3 cun lateral to the spinous process of S4 | 50–70 mm/75 mm |
| BL31 | Over the first sacral foramen | 20–30 mm/40 mm |
| BL32 | Over the second sacral foramen | 20–30 mm/40 mm |
| BL33 | Over the third sacral foramen | 20–30 mm/40 mm |
| GB30 | Over the piriformis muscle, at junction of lateral third and medial two-thirds of line joining sacral hiatus and greater trochanter of the femur | 50–70 mm/75 mm |
| HJJ L4 | One finger-breadth lateral to the spinous process of L4 | 30–40 mm/50 mm |
| HJJL5 | One finger-breadth lateral to the spinous process of L5 | 30–40 mm/50 mm |
| All of the above points can be needled bilaterally. Tender points over the gluteus minimus and the pelvic rim can also be included. | ||
| Distal points | ||
| GB34 | One finger-breadth anterior and one inferior to the fibular head | 25–30 mm/40 mm |
| ST36 | 3 cun below the joint line of the knee and a finger-breadth lateral to the tibial crest | 25–30 mm/40 mm |
| LR3 | Just distal to the junction of the bases of the first and second metatarsal bones | 25–30 mm/40 mm |
| LI4 | On the highest point of the first dorsal interosseous muscle of the hand | 20–30 mm/30–40 mm |
| BL60 | Midway between the lateral malleolus and the Achilles tendon | 15–25 mm/30 mm |
| BL62 | 1 cun below the tip of the lateral malleolus | 10–20 mm/30 mm |
Standard care plus non-penetrating acupuncture
In order to control for time and attention with physiotherapists, we included a SC plus sham acupuncture arm using non-penetrating needles (the devices look exactly like real needles but the tip is blunted and the shaft of the needle is allowed to slide in the handle, giving an illusion of penetration). This trial arm consisted of the same advice and education booklet posted to women randomised to SC plus a course of non-penetrating acupuncture, along with a letter explaining how to arrange the first physiotherapy treatment session and that the first treatment should be within 2 weeks. The same NHS physiotherapists provided the non-penetrating acupuncture treatment, and the participants’ letters explained that they had been randomised to receive SC plus one of two forms of acupuncture treatment. The non-penetrating Streitberger needle has been validated in several studies and used successfully in two previous trials of acupuncture. 33,39 The device looks exactly like a real needle but has a blunted tip, and is tapped onto the skin, held in place by an O-ring, and gives the illusion of needle insertion. Women were treated in a side-lying or prone position, which permitted both comfortable positioning for the participant and adequate blinding to the non-penetrating acupuncture needles.
In addition to SC, participants randomised to also receive non-penetrating acupuncture received the treatment as follows: the patient was assessed to ascertain the quality, location and intensity of the presenting back pain (with or without PGP), the patient was suitably positioned and the therapist applied the non-penetrating needles bilaterally over the four points detailed in Table 9. After the non-penetrating needles were positioned, no further attempt to stimulate the needles was made. The treatment lasted for 20–30 minutes. On completion of the treatment all needles were safely removed, any sensations felt by participants during treatment and any adverse reactions were recorded on CRFs and the patient was booked for the next appointment. Between six and eight treatment sessions were offered by physiotherapists over a period of 6 weeks.
| Local points | ||
|---|---|---|
| Point | Description | Depth of insertion of the needles |
| BL26 | 1.5 cun lateral to the spinous process of L5 | n/a |
| BL27 | 1.5 cun lateral to the spinous process of S1 | n/a |
| BL54 | 3 cun lateral to the spinous process of S4 | n/a |
| GB30 | Over the piriformis muscle, at junction of lateral third and medial two-thirds of line joining the sacral hiatus and the greater trochanter of the femur | n/a |
Fidelity of treatments
For each participant, physiotherapists recorded full details of the advice and treatments, number and mode of treatment sessions, any non-attendance, acupuncture points used, any sensations during acupuncture treatments and any adverse events on specifically designed CRFs (see Appendix 13). The CRFs also included one NRS to capture pain severity after treatment at each session. These CRFs were audited against the physiotherapists’ clinical notes to ensure accuracy and to determine protocol adherence by participating physiotherapists before collation by the research team in order to fully describe the interventions delivered. Where protocol deviations were noted, these were discussed with the physiotherapists involved in order, whenever possible, to enhance adherence to the agreed intervention protocol. Protocol deviations were mostly related to challenges in getting women to attend for all of their arranged treatment sessions. Where participants did not attend for treatment, physiotherapists attempted to contact them to re-engage them in treatment whenever possible.
Outcome measures and follow-up
Process outcomes
Process outcomes from the pilot trial included recruitment rates (both overall and from each separate recruitment method), follow-up rates at 8 weeks (both overall and in each treatment arm), attendance at treatment sessions, treatment protocol adherence, completion rates on key outcome measures, and floor and ceiling effects of key outcome measures.
Clinical outcomes
Patient-reported outcomes were assessed at the 8-week follow-up (i.e. 8 weeks after randomisation). The decision about the most appropriate follow-up time point for the pilot trial was taken in order to maximise the chances of most participants having received their full course of treatment, but not yet having given birth. We expected that women recruited to the trial at 30 and 31 weeks’ gestation would wait a maximum of 2 weeks for the start of their acupuncture treatment and would have a course of treatment over 6 weeks. Therefore, they should have completed their acupuncture treatment and received their follow-up questionnaire just before the birth of their baby. Studies of low back pain and PGP in pregnant women have previously followed up participants 1 week after the end of treatment33 and at 12 weeks (3 months) post partum. 15,17 We did not plan longer-term follow-ups in this pilot trial but, rather, we provide data on baseline and one follow-up time point only (at 8 weeks), in order to ensure that we delivered the feasibility and pilot study within a period of 24 months.
Outcomes at the 8-week follow-up were collected by postal questionnaire (see Appendix 14) and included the same measures of pain, everyday function and general health as at baseline, overall global rating of change since baseline, whether or not the woman was still pregnant (and, if yes, number of weeks’ gestation), a series of questions about treatment credibility, satisfaction with the treatment package received, satisfaction with the results from treatment and side effects from treatment in the EASE Back study. In addition, we included an open question on the 8-week follow-up questionnaire about the participant’s experience of treatment in the trial. We developed a minimum outcome data set from these wider set of outcomes which was collected over the telephone for those participants who did not respond to the postal reminder.
Cost outcomes
Data collection was undertaken to obtain patient-level cost and outcome data for all women participating in the trial in order to conduct a preliminary economic evaluation and inform the design of a cost–utility analysis alongside a future main trial. The SC plus non-penetrating acupuncture arm of the trial was not included in the economic analysis; therefore, data were analysed for only the SC and SC plus true acupuncture arms.
Resource use associated with SC and acupuncture treatment was based on primary data collected using information from the trial and self-completed questionnaires at 8 weeks. Cost data collection was undertaken on all women and from a broad perspective, taking into account health-care, patient and societal costs. NHS resource use data included GP consultations, visits to health-care professionals, outpatient appointments, investigations or treatments and inpatient stays related to their back pain during pregnancy. Information on costs borne by the patient with regard to over-the-counter medicines and devices was requested in the 8-week questionnaire. In order to assess broader societal economic consequences, productivity costs relating to both absenteeism (absence from work) and presenteeism (working with reduced productivity) were considered. Self-reported data on employment status, occupation and time off work and reduced productivity at work (presenteeism) owing to their back pain over the 8-week study period were collected. As it was assumed that some of the women attending the acupuncture treatment sessions might be in work or have other children, data were also collected regarding the travel costs, time off work and child care costs associated with attending a treatment sessions during the trial. As part of the pilot, the methods of collecting cost data from patient questionnaires and completeness of the data were assessed, in order to inform cost data collection in a future large trial.
Details of the number of treatment sessions attended by each participant were collected as part of the trial. The costs required to deliver the treatments included the acupuncture sessions, other aspects of SC, duration of each session and consumables needed.
For the purpose of costing staff time associated with the treatments, we estimated the average time of a treatment session with a physiotherapist during the study. Both the acupuncture intervention and SC involved, on average, a standard 60-minute initial consultation and follow-up consultations of 40 minutes per session.
In order to enable the calculation of quality-adjusted life-years (QALYs), all patients were asked to complete the five-level version of the EQ-5D questionnaire (i.e. EQ-5D-5L) at baseline and 8 weeks in order to assess quality of life. 77
Maternal/neonatal outcomes
We collected the following additional obstetric birth/neonatal outcomes from maternity records for all participants in order to inform a future main trial: gestation week at time of delivery, live births, length of labour (and second stage of labour), whether or not the woman needed to be induced, mode of delivery, whether or not the woman had an episiotomy or a perineal tear, estimated blood loss at birth, antenatal and postnatal haemoglobin count, pain relief during labour, baby’s sex and weight, Apgar scores at 1 minute and 5 minutes after birth and whether or not the baby was admitted to the neonatal unit.
Adverse events
We collected adverse event data through CRFs completed after each physiotherapy treatment, through self-report of participants in the 8-week follow-up questionnaire and through maternity record reviews. Expected adverse events from the acupuncture interventions include drowsiness/light-headedness, nausea/vomiting, fainting, bruising at needle sites, feeling hot/burning, headaches and transient pain at needle sites. We defined SAEs as death, hospitalisation, significant disability or incapacity, any life-threatening circumstance (to the woman or developing child) or any other medically significant occurrence that were potentially attributable to any of the trial procedures or treatments. Potential SAEs were identified via treating physiotherapists.
Sample size
In line with pilot trial recommendations,45 the EASE Back pilot trial did not have a primary outcome or the usual sort of power calculation that one would expect in a main RCT. The sample size was based on the number of births overseen by the participating maternity centre (UHNS) per year at the time of the funding application and estimates about the proportion of women likely to be eligible and consent to participate. The UNHS maternity service oversaw approximately 6100 births per year and we estimated that between 50% and 66% would self-report back pain at some point in their pregnancy and at least 30% would self-report back pain in gestational weeks 13–31. Thus, we estimated that approximately 1800 women would be potentially eligible over the course of 1 year, equivalent to approximately 600 over a recruitment period of 4–5 months. We estimated that we would need to raise awareness of the EASE Back pilot trial among these 600 pregnant women with back pain and that approximately one in four might agree to participate. To allow for some withdrawal and loss to follow-up, we anticipated needing to approach about 720 women in order to recruit 180 women and provide follow-up data on 150 women.
In reality, we recruited 125 women in 6 months. The research team and the TSC felt that 125 women provided an adequate number to estimate critical parameters in the pilot trial (e.g. recruitment rates, variation in key patient-reported outcome measures, treatment fidelity), using the rule of thumb of 30 patients or greater per group. 78
Analysis
To ensure transparency in analyses, a statistical analysis plan (SAP) was developed by the study statistician (RO), together with the PI (NF), trial co-ordinator (AL), senior CTU statistician (ML), health economists (SJ and JK) and other study team members. The SAP, including all the mock-up tables and figures, was presented to the TSC for review and discussion. All agreed amendments were implemented and the revised SAP was approved and signed off by the TSC.
The analysis of the pilot focused on (1) evaluation of the physiotherapy training programme through analysis of physiotherapy questionnaire data; (2) baseline description of the study population, including pain location and a summary of gestation weeks; (3) assessment of process measures including recruitment rate and methods of recruitment uptake and response to follow-up; (4) exploratory analysis of clinical outcomes; (5) descriptive summaries of treatment received (in relation to adherence with randomised intervention), satisfaction with care and evaluation of the adherence to treatment protocols through analysis of CRF data; (6) extent of missing data and data accuracy; (7) summary of birth and neonatal outcomes; (8) reports of adverse events in any of the treatment arms; and (9) summary of parameters to aid the choice of primary outcome measure and sample size calculation for a full RCT.
In the absence of standard practice regarding the type of economic evaluation to conduct alongside feasibility and pilot studies, a cost–consequence analysis was chosen. This allowed an exploration of the feasibility of conducting an economic evaluation as part of a future RCT testing acupuncture compared with SC in women with pregnancy-related back pain, rather than demonstrating cost-effectiveness at this stage. The SC plus non-penetrating acupuncture arm of the trial was not included in the economic analysis. The main purpose of including a non-penetrating acupuncture treatment was to explore the merits of this for a future main trial, in order to explore the importance of needle penetration in explaining acupuncture effects. The SC plus non-penetrating acupuncture intervention would not be commissioned in actual NHS practice. Therefore, health economic data were analysed for only the SC and SC plus true acupuncture arms. The cost–consequence analysis describes all the important results relating to costs and consequences of the treatments for the management of back pain in pregnant women in the SC and the SC plus true acupuncture arms of the pilot trial. The base case analysis for the evaluation adopted a NHS and Personal Social Services (PSS) perspective, with additional analysis considering a broader societal perspective taking into account patient-incurred costs and productivity losses. Costs are presented for each broad cost category (health-care costs, patient-incurred costs, productivity costs) and in a disaggregated form within each of these cost categories. Unit costs were obtained from various sources including the British National Formulary (BNF),79 NHS reference costs and Unit Costs of Health and Social Care80,81 and multiplied by resource use items from the trial. Unit costs are presented in Table 10. Discounting was not necessary as the follow-up period was 8 weeks. Owing to the lack of nationally representative unit cost estimates for private health-care visits, any private care was costed as the NHS equivalent. Patient-reported costs for over-the-counter treatments and patient-incurred time, travel and child care costs were used to estimate patient-related costs. Productivity losses were assessed using the human capital approach; self-reported days of work absence and reduced productivity at work due to back pain during the 8 weeks were multiplied by the average sex-specific wage estimates identified from annual earnings data and UK Standard Occupational Classification coding. 82,83 Reduced productivity time loss was generated by translating the self-reported scores obtained using a 0–10 scale into work loss based on the actual number of days worked during this period. In addition, time off work and reduced time spent on unpaid activities in order to attend physiotherapy appointments was estimated using a similar approach. Responses to the EQ-5D questionnaire were converted to index scores using the interim crosswalk UK value set. The area-under-the-curve approach that links each patient’s utility scores at different time points was applied to calculate QALYs for each study participant over the 8-week time period. Regression-based adjustment was used to account for baseline differences in EQ-5D score. A complete case analysis was undertaken and all costs and outcomes were summarised using means, SDs and 95% confidence intervals (CIs). Cost and QALY data alongside RCTs are invariably skewed; therefore, bias-corrected accelerated bootstrapping with 1000 replications was used to generate 95% CIs around differences in mean costs and QALYs. All statistical analysis was performed using Stata version 13. The CHEERS (Consolidated Health Economic Evaluation Reporting Standards) statement and checklist were consulted for reporting the economic evaluation. Owing to a cost–consequence analysis being undertaken, some items of the checklist were not appropriate for this study.
| Health-care resource | Unit cost (£) |
|---|---|
| Primary carea | |
| GP consultation (11.7 minutes) | 34 |
| Practice nurse consultation (per hour) | 44 |
| Health visitor (per hour) | 43 |
| Nurse home visit (per hour) | 60 |
| Community physiotherapist (per hour) | 30 |
| Secondary care contactsb | |
| Midwife: first attendance | 96 |
| Midwife: follow-up | 54 |
| Obstetrician: first attendance | 165 |
| Obstetrician: follow-up | 112 |
| Acupuncturist: first attendance | 49 |
| Acupuncturist: follow-up | 44 |
| Physiotherapist: first attendance | 49 |
| Physiotherapist: follow-up | 44 |
| Study treatment sessions | |
| First session: 60 minutes | 30 |
| Follow-up session: 40 minutes | 23 |
| Prescribed medication | Patient specificc |
| Medical investigations/interventions | Patient specificb |
| Day of sickness absence from work | One-fifth of average weekly earning wages |
Patient involvement
Prior to funding application, the study plans were discussed in detail with women attending the antenatal back pain class at the participating hospital (UHNS). The women felt that it was important to be able to offer a number of alternative treatments, as their perspective was that currently few options exist. They considered acupuncture a potentially attractive option but stressed that information had to be clear and particularly needed an explanation of safety issues. They felt that this information had to be given both verbally through health-care professionals, and in a written format which allowed women to reflect on it at home. In addition, two women who had attended the back class and were receiving one-to-one physiotherapy reviewed a draft of the PIL for the pilot RCT and commented on its content, style and readability.
We had two patient representatives on the TSC who:
-
identified the limitations of the Disability Rating Index (included in the original funding application to be used as a second measure of back pain-related disability) for the pregnant population, which led to the inclusion instead of the PGQ, a newly developed outcome assessment tool specifically for those with back and PGP in pregnancy,72 reviewed and fed back on the PIL and the baseline and follow-up questionnaires in the pilot RCT
-
fed back on the visibility of EASE Back study posters and banners when attending antenatal appointments
-
reviewed and fed back on the draft self-management booklet EASE Back: Managing Your Back and Pelvic Girdle Pain in Pregnancy
-
helped with the media advertising by appearing in a newspaper article in The Sentinel about the pilot trial and being the voice of a woman with pregnancy-related low back pain in the Signal Radio infomercials.
Results of the pilot randomised controlled trial
Participant flow
Of 388 women assessed for eligibility in 6 months, 280 were potentially eligible and 125 women (45%) were recruited into the EASE Back pilot trial and randomly allocated to one of the three treatment arms (Figure 6). One participant, in the SC plus non-penetrating acupuncture arm, was randomised in error (she fulfilled criteria for a high-risk pregnancy) and was subsequently withdrawn prior to treatment. Overall, the 8-week follow-up rate was 74% (n = 91).
FIGURE 6.
The CONSORT (Consolidated Standards of Reporting Trials) diagram for the EASE Back pilot trial.
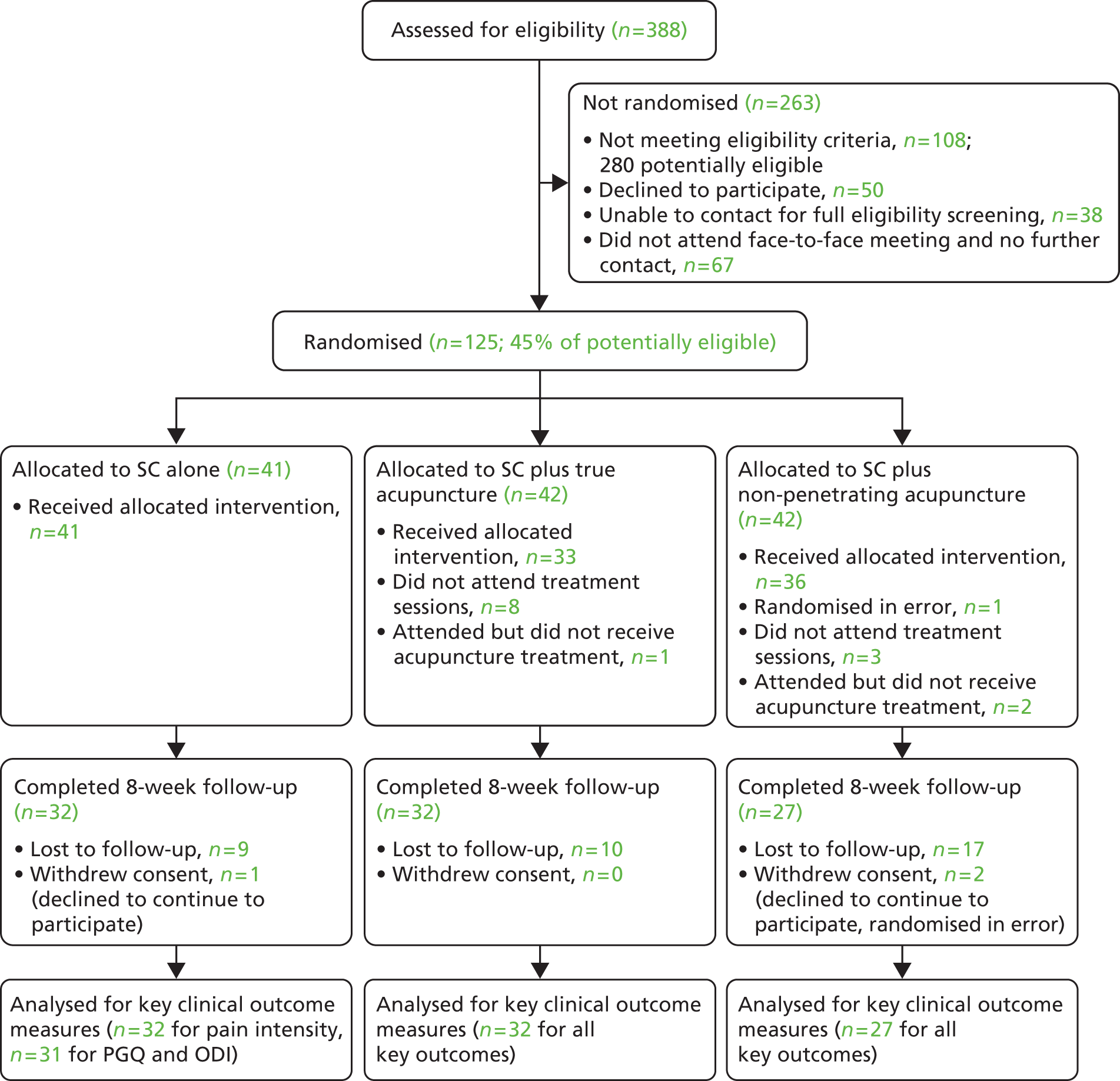
Baseline comparability
Participants’ baseline characteristics (Table 11) were largely similar among the three treatment arms. The mean (SD) age of the 124 participants was 28 (5.3) years; 54 (44%) were married, 87 (70%) were in full/part-time employment and 53 (42%) were ≥ 24 weeks pregnant at the time of inclusion. More than half (68 out of 124) had experienced back pain for more than 6 weeks and the mean (SD) pain severity score (mean score of three Pain NRSs on 0–10 scales) was 4.6 (SD 1.7). About one-third of participants (38 out of 144) had low back pain with anterior PGP and pain in other parts of the body. More than half of the participants (67 out of 124, 54%) had moderate back pain-related disability measured by the ODI.
| Baseline characteristic | SC (n = 41) | SC + true acupuncture (n = 42) | SC + non-penetrating acupuncture (n = 41) |
|---|---|---|---|
| Age (years), mean (SD) | 27.8 (5.4) | 28.1 (5.1) | 29.0 (5.3) |
| Highest qualification: degree/postgraduate, n (%) | 13 (31.7) | 14 (33.3) | 18 (43.9) |
| Gestation weeks at inclusion: > 24, n (%) | 17 (41.5) | 18 (42.9) | 18 (42.9) |
| Married, n (%) | 16 (39.0) | 19 (45.2) | 19 (46.3) |
| No. of children, n (%) | |||
| 0 | 16 (39.0) | 20 (47.6) | 14 (34.2) |
| 1 | 17 (41.5) | 13 (31.0) | 17 (41.5) |
| 2 or more | 8 (19.5) | 9 (21.4) | 10 (24.4) |
| Working, n (%) | 28 (68.3) | 27 (64.3) | 32 (78.1) |
| Physical demands of current/most recent paid job: heavy/very heavy, n (%) | 12 (29.3) | 13 (32.5) | 11 (26.8) |
| Taken time off during the current pregnancy because of back pain,a n (%) | 8 (28.6) | 9 (33.3) | 15 (46.9) |
| Back pain interference with performance at work (0–10 NRS),a,b mean (SD) | 5.0 (2.5) | 4.9 (2.6) | 5.0 (3.1) |
| Work satisfaction (0–10 NRS),a,c mean (SD) | 6.6 (2.7) | 5.4 (1.9) | 6.6 (2.3) |
| Pain location (manikin), n (%) | |||
| Low back pain only | 7 (17.1) | 9 (21.4) | 7 (17.1) |
| Low back pain with anterior PGP | 8 (19.5) | 6 (14.3) | 4 (9.8) |
| Low back pain with anterior PGP and pain elsewhere | 10 (24.4) | 14 (33.3) | 12 (29.3) |
| Low back pain and pain elsewhere | 16 (39.0) | 13 (31.0) | 18 (43.9) |
| Duration of pain episode: > 6 weeks, n (%) | 23 (56.1) | 20 (47.2) | 25 (61.0) |
| Pain severity (mean score of three NRSs), mean (SD) | 4.5 (1.6) | 4.5 (1.5) | 4.6 (1.8) |
| Pain intensity before going to bed, mean (SD) | 6.8 (1.9) | 6.8 (1.8) | 7.0 (2.2) |
| Woken up most/every night by pain, n (%) | 16 (39.0) | 15 (35.7) | 17 (41.5) |
| ODI score (0–100),d mean (SD) | 34.8 (11.2) | 32.9 (13.7) | 35.7 (13.6) |
| ODI score (categorised), n (%) | |||
| Minimal disability (0–20%) | 5 (12.2) | 8 (19.0) | 4 (9.8) |
| Moderate disability (21–40%) | 24 (58.5) | 20 (47.6) | 23 (56.1) |
| Severe disability (40–60%) | 12 (29.3) | 13 (31.0) | 11 (26.8) |
| Crippled (61–80%) | 0 (0.0) | 1 (2.4) | 3 (7.3) |
| PGQ score (0–100),e mean (SD) | |||
| Total | 56.9 (16.0) | 48.7 (17.2) | 54.2 (17.3) |
| Activity subscale | 54.6 (17.0) | 46.7 (18.1) | 52.7 (18.1) |
| Symptom subscale | 65.4 (17.1) | 56.1 (17.2) | 59.3 (19.9) |
| Pre-pregnancy BMI, n (%) | |||
| Normal/underweight | 16 (40.0) | 19 (47.5) | 12 (31.6) |
| Overweight | 8 (20.0) | 11 (27.5) | 17 (44.7) |
| Obese/morbidly obese | 16 (40.0) | 10 (25.0) | 9 (23.7) |
| Taking prescribed medication, n (%) | 7 (17.1) | 5 (11.9) | 5 (12.2) |
| Treatment preferences: yes, n (%) | 10 (24.4) | 8 (19.1) | 10 (24.4) |
| SF-12 – Physical Component Scale score, mean (SD)f | 36.4 (7.6) | 38.2 (8.0) | 37.0 (9.7) |
| SF-12 – Mental Component Scale score, mean (SD)f | 46.6 (10.1) | 44.7 (12.1) | 48.1 (11.7) |
| Self-assessed P4 test: familiar pain produced or increased in lumbosacroiliac area,g n (%) | 25 (75.8) | 26 (81.3) | 22 (66.7) |
| Bridging with extension of leg: familiar pain produced or increased in lumbosacroiliac area,g n (%) | 25 (89.3) | 24 (80) | 23 (82.1) |
| Positive on both P4 test and bridging test, n (%) | 17 (41.5) | 21 (50.0) | 16 (39.0) |
Process outcomes (recruitment, retention, blinding)
Recruitment
Methods of raising local awareness of the trial
Multiple approaches of raising awareness about the EASE Back pilot trial among potentially eligible women in the local area were pilot tested. Women contacting the research office about the trial were asked how they had come to know about the study. Recruitment lasted for 6 months (27 weeks) from April to October 2013. Flyers and posters were used throughout the entire recruitment period, while the bus advertising campaign ran for 8 weeks (from week 19 to week 25 of the recruitment period). The internet website was available for the entire recruitment period with the addition of a YouTube video about the study from week 9. The radio and newspaper advertising campaign varied; some were one-off short radio advertisements and interviews with the trial PI (NF) and others were in the form of radio infomercials (running many times per day on a local commercial radio station, for 3 consecutive days, in week 25 of recruitment). We also published articles in a local newspaper on two occasions in weeks 7 and 12 of the recruitment period. These articles were linked to the newspaper’s website, where interested women could obtain further information. There was also an advertisement in a local magazine in week 11 of the recruitment period. Table 12 summarises these methods, the number of women identified through them and the number subsequently recruited into the pilot trial. Almost half of the women identified from the local awareness-raising campaign came to know about the study through flyers and posters, and the next most successful method was the advertisements on local radio or in local newspapers.
| Awareness-raising method | Identified, n (%)a | Recruited, n (%)b |
|---|---|---|
| Flyers or posters | 25 (48.1) | 12 (48.0) |
| Advertisements on local radio/newspapers | 18 (34.6) | 5 (27.8) |
| Internet websitec | 2 (3.9) | 1 (50.0) |
| Advertisements on local buses | 3 (5.8) | 3 (100.0) |
| Word of mouth | 4 (7.7) | 3 (75.0) |
| Total | 52 | 24 |
Success of six methods of identification and recruitment
The number and proportion of women identified and recruited through the six methods described in Recruitment methods and procedures are presented in Table 13. The brief screening questionnaire for back pain given to women as they attended their routine 20-week ultrasound scan appointment was the most successful method, followed by community midwives providing women with an EASE Back study card and women self-referring following the local awareness-raising efforts.
| Women identified and recruited | Research midwives identify women through UHNS maternity clinic | Brief questionnaire at 20-week ultrasound scan | Screening of referrals to the women’s health physiotherapy service at UHNS | Research midwives or obstetricians give women EASE Back study card | Community midwives or GP give women EASE Back study card | Self-refer due to local awareness raising | Total |
|---|---|---|---|---|---|---|---|
| Total number of women identified, n (%) | 28 (7.2) | 199 (51.3) | 49 (12.6) | 3 (0.8) | 73 (18.8) | 36 (9.3) | 388 |
| Ineligible at initial screen, n | 4 | 21 | 17 | 0 | 13 | 9 | 64 |
| Ineligible overall (initial screen + full screen), n (% of total) | 9 (32.1) | 42 (21.1) | 20 (40.8) | 1 (33.3) | 21 (28.8) | 15 (41.7) | 108 (27.8) |
| Potentially eligible, n | 19 | 157 | 29 | 2 | 52 | 21 | 280 |
| Declined at initial screen, n | 1 | 22 | 5 | 0 | 0 | 1 | 29 |
| Declined overall, n | 3 | 34 | 7 | 0 | 4 | 2 | 50 |
| Unable to contact for full eligibility screening, n | 0 | 24 | 10 | 0 | 4 | 0 | 38 |
| Did not attend face to face for full screen with no further contact, n | 4 | 51 | 4 | 0 | 5 | 3 | 67 |
| Randomised n (% of potentially eligible) | 12 (63.2) | 48 (30.6) | 8 (27.6) | 2 (100.0) | 39 (75.0) | 16 (76.2) | 125 (44.6) |
Recruitment figures over time
Recruitment is summarised in Table 14. The average weekly recruitment was five women per week (range 0–12). The lowest recruitment (no participants) was in the week of the height of the summer holiday period and highest recruitment (12 participants) was in the week following the radio infomercials on Signal Radio. Estimated (180 women over 5 months) compared with observed recruitment (125 women over 6 months) is presented in Figure 7.
| Week starting | Number recruited | Participant accrual |
|---|---|---|
| 22 April | 1 | 1 |
| 29 April | 2 | 3 |
| 6 May | 6 | 9 |
| 13 May | 2 | 11 |
| 20 May | 3 | 14 |
| 27 May | 4 | 18 |
| 3 June | 3 | 21 |
| 10 June | 4 | 25 |
| 17 June | 7 | 32 |
| 24 June | 6 | 38 |
| 1 July | 7 | 45 |
| 8 July | 3 | 48 |
| 15 July | 6 | 54 |
| 22 July | 5 | 59 |
| 29 July | 5 | 64 |
| 5 August | 6 | 70 |
| 12 August | 4 | 74 |
| 19 August | 3 | 77 |
| 26 August | 0 | 77 |
| 2 September | 6 | 83 |
| 9 September | 6 | 89 |
| 16 September | 5 | 94 |
| 23 September | 5 | 99 |
| 30 September | 5 | 104 |
| 7 October | 6 | 110 |
| 14 October | 12 | 122 |
| 21 October | 3 | 125 |
FIGURE 7.
Expected vs. observed recruitment.
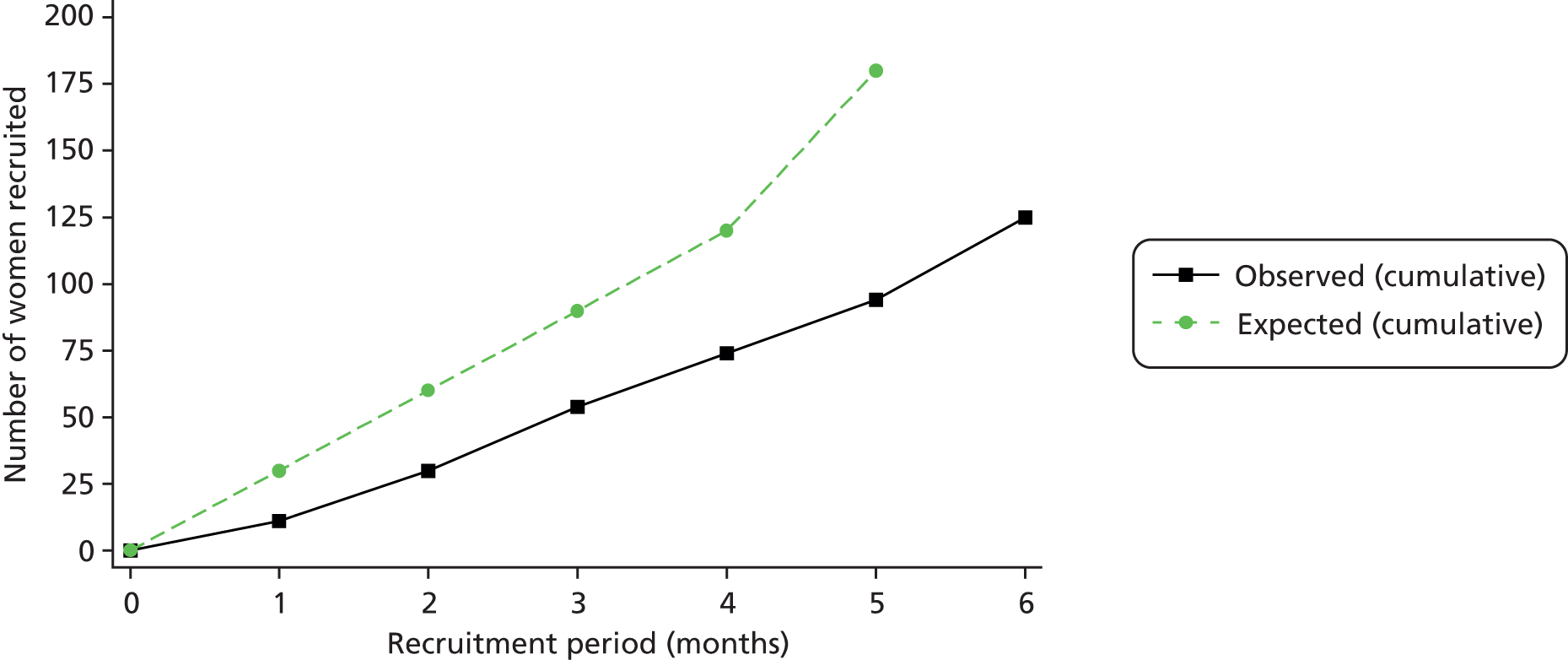
Reasons for ineligibility
From 388 women we contacted, 280 were potentially eligible at initial screens and 108 ineligible. The reasons for ineligibility are presented in Table 15. The most common were previous acupuncture (26 out of 105, 25%), previous pre-term delivery (12%) and the woman being registered at a GP practice outside the included list of practices (11%). The number and proportion of eligible women who declined to participate are presented in Table 13.
| Reason | Frequencya | % of responsesb | % of casesc |
|---|---|---|---|
| Previous acupuncture | 26 | 20.2 | 24.8 |
| Previously given birth before 37 weeks | 13 | 10.1 | 12.4 |
| GP practice not in eligible list for the trial | 11 | 8.5 | 10.5 |
| No current back pain | 9 | 7.0 | 8.6 |
| Recurrent previous miscarriage | 9 | 7.0 | 8.6 |
| Pregnancy classified as high risk | 9 | 7.0 | 8.6 |
| High risk of pre-term delivery | 7 | 5.4 | 6.7 |
| Previous surgery to uterine cervix | 6 | 4.7 | 5.7 |
| Not between 13 and 31 completed weeks of gestation | 5 | 3.9 | 4.8 |
| Unusually high fear or needles | 5 | 3.9 | 4.8 |
| Pregnant with more than one baby | 4 | 3.1 | 3.8 |
| Not planning to give birth at UHNS | 4 | 3.1 | 3.8 |
| Already under care of a physiotherapist | 4 | 3.1 | 3.8 |
| Back pain not caused/worsened by pregnancy | 3 | 2.3 | 2.9 |
| Previous surgery to spine or pelvis | 3 | 2.3 | 2.9 |
| Communication problems | 3 | 2.3 | 2.9 |
| Aged under 18 years | 2 | 1.6 | 1.9 |
| Has ruptured membranes | 2 | 1.6 | 1.9 |
| Not eligible pain location | 1 | 0.8 | 1.0 |
| Abnormalities with uterus | 1 | 0.8 | 1.0 |
| Antiphospholipid syndrome or lupus anticoagulant | 1 | 0.8 | 1.0 |
| Problem with blood clotting | 1 | 0.8 | 1.0 |
| Total | 129 | – | – |
Generalisability of the sample
Table 16 compares key baseline characteristics [age and index of multiple deprivations (from postcodes)] captured from the anonymised data on women who were ineligible or declined participation with the EASE Back trial participants. There was reasonable overall comparability in these key baseline characteristics.
| Key characteristic | Consent (n = 125) | Potentially eligible but did not consent (n = 157) | Non-participantsa (n = 263) |
|---|---|---|---|
| Age (years), mean (SD) | 28.3 (5.3) | 27.1 (6.5) | 27.9 (6.2) |
| Deprivation tertile, n (%) | |||
| Least deprived third | 48 (40.3) | 60 (39.5) | 76 (29.6) |
| Medium | 38 (31.9) | 49 (32.2) | 88 (34.2) |
| Most deprived third | 33 (27.7) | 43 (28.3) | 93 (36.2) |
Retention
The 8-week follow-up rate was 74%. Table 17 presents the details of the follow-up responses (including number of responses after initial mailing, reminder mailing and MDC over the telephone) both overall and for each of the three treatment arms. There was a slight imbalance in the follow-up rates among the treatment arms, with the SC plus non-penetrating acupuncture arm having the lowest response rate at 8 weeks (66%). Only 14% of the women had given birth by the time they returned the 8-week follow-up questionnaire. Three participants withdrew from the trial: one in the SC arm (declined to continue to participate) and two in the SC plus non-penetrating acupuncture arm (one was subsequently ineligible as she had been consented in error; one declined to continue to participate).
| Mailing | Responded, n (%) | |||
|---|---|---|---|---|
| SC (n = 40)a | SC + TA (n = 42) | SC + NPA (n = 41) | Total (n = 123)a | |
| Initial mailing | 14 (35.0) | 9 (21.4) | 12 (29.3) | 35 (28.5) |
| Reminder mailing | 10 (11.5) | 18 (54.5) | 10 (34.5) | 38 (20.5) |
| MDCb | 8 (34.8) | 5 (20.0) | 5 (22.7) | 18 (25.7) |
| Response rate | 32/40 (80.0) | 32/42 (76.2) | 27/41 (65.9) | 91/123 (74.0) |
| Number who had given birth by time of response | 7 (21.9) | 4 (12.5) | 2 (7.4) | 13 (14.3) |
Blinding
During MDC via the telephone, three cases of unblinding out of the 70 MDC calls conducted were recorded between the participant and the research nurse collecting data. All three had been randomised to receive SC plus true acupuncture.
Results from audio-recordings of screening/consent meetings
The face-to-face meeting with a research midwife or nurse comprised a full eligibility screen and informed consent (followed by baseline data collection and randomisation), and we audio-recorded a sample of 30 of these meetings. The section Audio-recordings of eligibility and consent meetings previously described the methods. The average length of the recordings covering the discussion about the trial between the participant and midwife/nurse was 12 minutes. All audio files were transcribed and fully anonymised. Given the brevity of the recordings and early data saturation, it was not possible to apply the same analysis framework as in phase 1 (i.e. an iterative, constructionist grounded theory framework60). Instead, a simplified constant comparative approach within and across cases was undertaken,84 with relevant data for comparison identified as those that were pertinent to the research objectives.
The research midwives and nurses adhered well to the processes of information giving and eligibility screening; they could clearly be heard reading through the PIL and the eligibility criteria in line with the protocol, and from the earliest interviews it was clear that women had very few questions about the trial and those that were asked were consistent with those identified through the qualitative work in phase 1 (i.e. questions around positioning for treatment, whether or not the needles would be painful, the geographical location of treatment centres and the length of time needed for treatment). However, given the brevity of the recordings, it was decided to continue data collection (from the 10 originally foreseen) to 30 to ensure saturation had indeed been reached.
Treatment delivery and adherence
Case report forms were analysed to describe the interventions delivered (Table 18). In total, 4 of the 41 participants (10%) randomised to SC accessed face-to-face physiotherapy. Eight participants randomised to SC plus true acupuncture and four in the SC plus non-penetrating acupuncture arm failed to attend for any treatment and therefore received no acupuncture, and 21 (62%) and 29 (76%) received the number of treatment sessions specified in the protocol (between six and eight treatment sessions) for the arms respectively.
| Treatment delivered | Treatment arm | ||
|---|---|---|---|
| SC (n = 41) | SC + TA (n = 42) | SC + NPA (n = 42) | |
| Participants | |||
| Number of participants who booked appointment to see a physiotherapist | 4 | 37 | 41 |
| Total number of participants who attended at least one treatment session with a physiotherapist | 4 | 34 | 38 |
| Total number of participants who received acupuncture treatment | 0 | 33 | 36 |
| Number of treatment sessions provided (per participant), median (IQR) | 2 (1–4) | 6 (3–7) | 6 (6–7) |
| Number of treatment sessions per participant (categorised), n (% of number of participants seen) | |||
| 1–5 | 4 (100) | 13 (38.2) | 9 (23.7) |
| 6–8 | 0 (0.0) | 17 (50.0) | 27 (71.1) |
| 9–11 | 0 (0.0) | 4 (11.8) | 2 (5.3) |
| Number of treatments per participant in line with protocols,a n (% of number of participants) | 2 (50.0) | 17 (50.4) | 27 (71.1) |
| Treatment sessions: total number planned | 13 | 240 | 273 |
| Total number of treatment sessions provided, n (% of total planned) | 9 (69.2) | 189 (78.8) | 224 (82.1) |
| Total number of sessions that were not attended – DNAs/UTAs, n (% of total planned) | 4 (30.8) | 51 (21.3) | 49 (17.9) |
| Total number of sessions attended where acupuncture was provided, n (% of attended) | 0 (0.0) | 163 (86.2) | 197 (87.9) |
| Treatment content across all sessions, % (SD) | |||
| Assessment/reassessment | 100 (0) | 91.8 (17.7) | 80.6 (25.4) |
| Education and advice | 100 (0) | 81.4 (23.4) | 73.2 (25.7) |
| Tubigrip provided with instruction | 54.2 (41.7) | 15.2 (25.5) | 9.6 (11.6) |
| Pelvic support belt provided with instruction | 50.0 (57.7) | 4.5 (8.1) | 5.4 (17.1) |
| Heat therapy used in clinic | 0 (0.0) | 5.4 (11.6) | 3.9 (8.1) |
| Massage therapy used in clinic | 0 (0.0) | 5.4 (12.0) | 3.9 (8.1) |
| Manual therapy used in clinic | 0 (0.0) | 0 (0.0) | 2.1 (9.2) |
| Supervised exercises in clinic | 6.3 (12.5) | 24.1 (26.1) | 18.1 (24.7) |
| Home exercises given/reviewed | 83.3 (33.3) | 39.7 (29.9) | 35.2 (29.9) |
| Issued walking aids | 31.3 (47.3) | 1.9 (8.8) | 2.4 (6.6) |
| Exercise approaches across all sessions, % (SD) | |||
| Transversus abdominus muscle strengthening | 43.8 (51.5) | 23.4 (28.1) | 19.7 (25.0) |
| Pelvic floor muscle strengthening | 43.8 (51.5) | 23.4 (28.1) | 19.7 (25.0) |
| Pelvic tilt exercise | 52.1 (44.3) | 21.5 (16.9) | 15.8 (17.5) |
| Gluteal muscle strengthening | 27.1 (35.6) | 27.6 (25.1) | 20.9 (21.1) |
| Lower back/pelvic stretching | 12.5 (25.0) | 12.9 (18.2) | 6.0 (11.0) |
| Advice/signposting to general physical activity opportunities | 50 (57.7) | 6.1 (17.9) | 10.3 (20.9) |
| Other exercisesb | 12.5 (25.0) | 13.7 (24.8) | 12.9 (21.4) |
| Pain severity score after treatment (0–10), mean (SD) | 6.0 (0.8) | 1.9 (2.0) | 2.3 (2.3) |
The number of treatments that participants received was lower than expected, mainly as a result of the challenges that prevented women attending for their allocated treatment. The did-not-attend rates ranged from 18% to 31%. While the average number of treatment sessions in both arms receiving acupuncture was six (in line with the specified protocols), 13 (38%) in the SC plus true acupuncture arm and nine (23.7%) in the SC plus non-penetrating acupuncture arm attended fewer than six sessions.
In terms of content of treatment, assessment/re-assessment and advice were provided at the majority of treatment sessions. The very small number of participants accessing face-to-face physiotherapy in the SC arm was expected but makes comparisons across the treatment arms difficult. The use of pelvic supports (belts or Tubigrip) and walking aids appears to have been more frequent in the SC arm. Exercise approaches were commonly used across all treatment arms, mostly a home exercise programme that focused on muscle strengthening of core trunk muscles and pelvic floor muscles as well as pelvic tilting exercises. Overall, the contents of treatment were delivered broadly in line with the specified protocols.
A pain severity NRS score recorded at the end of each treatment session indicated that, on average, those randomised to either of the acupuncture arms reported much lower pain after treatment than those in the SC only arm.
Table 19 shows the acupuncture points used in both the true acupuncture and non-penetrating acupuncture treatment arms. Both of the acupuncture protocols were delivered as intended. In the true acupuncture treatment arm, BL25, BL26, BL31 and BL54 (all points in the area of the lower back) were the most frequently used local points. Distal points were used much less commonly. In the non-penetrating acupuncture arm, the local points specified in the protocol were used in the large majority of sessions.
| Acupuncture point | Treatment sessions | Participantsa | ||||
|---|---|---|---|---|---|---|
| SC + TA (Na,b = 163) | SC + NPA (Na,b = 197) | SC + TA (N = 33)c | SC + NPA (N = 36)c | |||
| Left, n (%)c | Right, n (%) | Left, n (%) | Right, n (%) | n (%) | n (%) | |
| Local points | ||||||
| BL23 | 50 (30.7) | 51 (31.3.0) | – | – | 19 (57.6) | – |
| BL24 | 89 (45.4) | 91 (55.8) | – | – | 23 (69.7) | – |
| BL25 | 155 (95.1) | 155 (95.1) | – | – | 33 (100) | – |
| BL26 | 155 (95.1) | 156 (95.7) | 197 (100) | 196 (99.5) | 33 (100) | 36 (100) |
| BL27 | 93 (42.9) | 92 (56.4) | 196 (99.5) | 195 (99.0) | 22 (66.7) | 36 (100) |
| BL28 | 38 (23.3) | 38 (23.3) | – | – | 9 (27.3) | – |
| BL54 | 128 (78.5) | 134 (82.2) | 195 (99.0) | 196 (99.5) | 28 (84.9) | 36 (100) |
| BL31 | 100 (61.4) | 100 (61.4) | – | – | 25 (75.7) | – |
| BL32 | 46 (28.2) | 46 (28.2) | – | – | 13 (39.4) | – |
| BL33 | 20 (12.3) | 20 (12.3) | – | – | 4 (12.1) | – |
| GB30 | 67 (41.1) | 78 (47.9) | 173 (87.2) | 192 (97.7) | 26 (78.8) | 36 (100) |
| HJJ L4 | 35 (21.5) | 35 (21.5) | – | – | 11 (33.3) | – |
| HJJ L5 | 33 (20.3) | 33 (20.3) | – | – | 10 (30.3) | – |
| Distal points | ||||||
| GB34 | 5 (3.1) | 37 (22.7) | – | – | 8 (24.2) | – |
| ST36 | 0 (0.0) | 7 (4.3) | – | – | 1 (3.0) | – |
| LR3 | 9 (5.5) | 19 (11.7) | – | – | 8 (24.2) | – |
| LI4 | 15 (9.2) | 21 (12.9) | – | – | 8 (24.2) | – |
| BL60 | 42 (25.8) | 43 (26.9) | – | – | 21 (63.6) | – |
| BL62 | 1 (0.6) | 19 (11.7) | – | – | 5 (15.2) | – |
Needle or de-qi sensations
Participants were asked about needling (de-qi) sensations experienced at each treatment session. de-qi sensations such as an ache, a warmth, tingling and pressure were reported in the large majority (94%) of true acupuncture treatment sessions and also in 31% of the non-penetrating acupuncture treatment sessions (Table 20).
| Needling sensation | Treatment arm | |
|---|---|---|
| SC + TA (number of treatment sessions with acupuncture = 163) | SC + NPA (number of treatment sessions with acupuncture = 197) | |
| Number of sessions in which de-qi sensations were reported, n (%) | 153 (93.9) | 61 (31.0) |
| Sensations described during acupuncture n (% of number of sessions in which de-qi sensation was achieved) | ||
| Ache | 66 (43.1) | 14 (23.0) |
| Aching in the back | 35 (22.9) | 7 (11.5) |
| Warmth | 29 (19.0) | 13 (21.3) |
| Tingle | 26 (17.0) | 12 (19.7) |
| Sharpness | 23 (15.0) | 7 (11.5) |
| Tickle | 11 (7.2) | 0 (0.0) |
| Pressure | 11 (7.2) | 0 (0.0) |
| Numbness | 4 (2.6) | 9 (14.8) |
| Heaviness | 4 (2.6) | 3 (4.9) |
| Soreness | 3 (2.0) | 2 (2.8) |
| Sweaty palms | 2 (1.3) | 1 (1.6) |
| An ‘awareness’ | 0 (0.0) | 1 (1.6) |
| Twinge | 0 (0.0) | 0 (0.0) |
| Othera | 35 (22.9) | 10 (16.4) |
Patient-reported outcomes
Exploratory analysis of key clinical outcomes
The descriptive statistics (mean and SD) of the key clinical outcomes (pain and disability outcomes) at baseline and the 8-week follow-up are presented in Table 21. Table 22 shows the differences in the mean scores from baseline. Overall, there was a reduction in pain and disability scores from baseline to the 8-week follow-up. A greater reduction in score was observed in the two arms randomised to receive SC plus acupuncture than in the arm receiving SC alone.
| Key outcome | Baseline (n = 124) | 8-week follow-up (n = 91) | ||||
|---|---|---|---|---|---|---|
| SC | SC + TA | SC + NPA | SC | SC + TA | SC + NPA | |
| ODI score (0–100), mean (SD) | 34.8 (11.2) | 32.9 (13.7) | 35.7 (13.6) | 32.2 (18.8) | 21.3 (17.7) | 26.2 (14.4) |
| PGQ score (0–100), mean (SD) | ||||||
| Total | 56.9 (16.0) | 48.7 (17.2) | 54.2 (17.3) | 52.2 (28.4) | 31.9 (21.8) | 40.3 (21.8) |
| Activity subscale | 54.6 (17.0) | 46.7 (18.1) | 52.7 (18.1) | 51.5 (29.4) | 31.3 (22.1) | 40.0 (23.4) |
| Symptom subscale | 65.4 (17.1) | 56.1 (17.2) | 59.3 (19.9) | 54.4 (26.5) | 33.8 (22.4) | 40.2 (20.2) |
| Pain severity (mean score of three NRSs) | 4.5 (1.6) | 4.5 (1.5) | 4.6 (1.8) | 4.2 (2.2) | 2.4 (2.2) | 2.2 (1.5) |
| Key outcome | SC (n = 32) | SC + TA (n = 32) | SC + NPA (n = 27) |
|---|---|---|---|
| ODI score, mean difference (95% CI) | 1.9 (–5.1 to 8.8) | 7.8 (1.6 to 14.0) | 7.7 (2.9 to 12.5) |
| PGQ score, mean difference (95% CI) | |||
| Total | 5.1 (–5.1 to 15.2) | 14.0 (6.9 to 21.2) | 11.6 (5.2 to 18.0) |
| Activity subscale | 4.1 (–6.4 to 14.6) | 12.8 (5.4 to 20.3) | 10.1 (3.5 to 16.8) |
| Symptom subscale | 8.6 (–1.9 to 19.0) | 18.8 (11.1 to 26.5) | 17.8 (9.7 to 25.8) |
| Pain severity (mean score of three NRSs) | 0.2 (–0.8 to 1.2) | 1.8 (1.1 to 2.5) | 2.1 (1.4 to 2.9) |
Table 23 summarises the differences in mean scores among the treatment arms (with 95% CI) adjusted for baseline scores and other baseline covariates obtained from multiple linear regression. We do not place undue significance on these results since a formal sample size calculation was not carried out; rather we focus on CI estimation. As expected, the CIs are quite imprecise. Several comparisons have been made: SC alone versus SC plus true acupuncture; SC alone versus SC plus non-penetrating acupuncture; and SC plus true acupuncture versus SC plus non-penetrating acupuncture. These comparisons indicated some between-group differences in physical function (mean PGQ) and pain severity between SC alone and SC plus true acupuncture and between SC alone and SC plus non-penetrating acupuncture but not between SC plus true acupuncture and SC plus non-penetrating acupuncture.
| Outcome | Adjusted for baseline scores only | Adjusted for baseline scores and baseline covariatesa | ||
|---|---|---|---|---|
| Marginal mean | Adjusted mean difference (95% CI) | |||
| Marginal mean | Adjusted mean difference (95% CI) | Marginal mean | Adjusted mean difference (95% CI) | |
| SC vs. SC plus acupuncture arms | ||||
| ODI score (0–100) | – | 31.2 | – | – |
| SC (reference) | 23.2 | –8.0 (–16.1 to 0.1) | 31.3 | – |
| SC + TA | 25.2 | –5.9 (–14.2 to 2.4) | 23.3 | –8.0 (–16.2 to 0.2) |
| SC + NPA | – | – | 25.0 | –6.3 (–14.7 to 2.3) |
| PGQ total score (0–100) | – | 48.3 | – | – |
| SC (reference) | 35.8 | –12.6 (–23.8 to –1.3) | 48.3 | – |
| SC + TA | 40.1 | –8.2 (–19.6 to 3.1) | 36.7 | –11.6 (–22.9 to –0.4) |
| SC + NPA | – | – | 39.0 | –9.3 (–20.7 to 2.0) |
| PGQ activity subscale score | – | 47.6 | – | – |
| SC (reference) | 35.3 | –12.3 (–23.9 to –0.8) | 47.7 | – |
| SC + TA | 39.9 | –7.7 (–19.4 to 4.0) | 36.2 | –11.5 (–22.9 to –0.4) |
| SC + NPA | – | – | 38.6 | –9.1 (–20.9 to 2.6) |
| PGQ symptom subscale score | – | 52.0 | – | – |
| SC (reference) | 36.2 | –15.8 (–27.2 to –4.5) | 52.4 | – |
| SC + TA | 40.1 | –11.9 (–23.4 to –0.3) | 36.0 | –16.4 (–27.8 to –5.0) |
| SC + NPA | – | – | 40.0 | –12.4 (–24.1 to –0.7) |
| Pain severity (mean score of three NRSs) | – | – | 4.2 | – |
| SC (reference) | 2.5 | –1.8 (–2.7 to –0.8) | 4.1 | – |
| SC + TA | 2.2 | –2.0 (–3.0 to –1.0) | 2.6 | –1.6 (–2.5 to –0.6) |
| SC + NPA | – | – | 2.2 | –2.0 (–3.0 to –1.0) |
| TA vs. NPA arms | ||||
| ODI score (0–100) | – | 23.2 | – | – |
| SC + TA (reference) | 25.2 | 2.1 (–6.3 to 10.5) | 23.3 | – |
| SC + NPA | – | – | 25.0 | 1.8 (–6.8 to 10.3) |
| PGQ total score (0–100) | – | 35.8 | – | – |
| SC + TA (reference) | 40.1 | 4.3 (–7.0 to 15.6) | 36.7 | – |
| SC + NPA | – | – | 39.0 | 2.6 (–8.9 to 14.2) |
| PGQ activity subscale score | 35.3 | – | – | – |
| SC + TA (reference) | 39.9 | 4.6 (–7.1 to 16.3) | 36.2 | – |
| SC + NPA | – | – | 38.6 | 2.3 (–9.4 to 14.1) |
| PGQ symptom subscale score | – | 36.2 | – | – |
| SC + TA (reference) | 40.1 | 3.9 (–7.5 to 15.5) | 36.0 | – |
| SC + NPA | – | – | 40.0 | 4.0 (–7.6 to 15.6) |
| Pain severity (mean score of three NRSs) | – | – | 2.4 | – |
| SC + TA (reference) | 2.2 | –0.2 (–1.3 to 0.78) | 2.6 | – |
| SC+ NPA | 2.2 | –0.2 (–1.3 to 0.78) | 2.2 | –0.4 (–1.4 to 0.6) |
Estimates of other health outcomes
Table 24 summarises participants’ global assessment of change at follow-up compared with baseline. About half (45 out of 91) reported complete recovery or much improvement. However, this proportion was much lower in the SC arm (6 out of 32, 19%) the SC plus true acupuncture (21 out of 32, 66%) or SC plus non-penetrating acupuncture (18 out of 27, 67%) arm.
| Change since baseline | Overall | SC | SC + TA | SC + NPA | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Completely recovered | 6 | 6.6 | 1 | 3.1 | 4 | 12.5 | 1 | 3.7 |
| Much improved | 39 | 42.9 | 5 | 15.6 | 17 | 53.1 | 17 | 63.0 |
| Somewhat improved | 17 | 18.7 | 8 | 25.0 | 5 | 15.6 | 4 | 14.8 |
| Same | 7 | 7.7 | 2 | 6.3 | 1 | 3.1 | 4 | 14.8 |
| Somewhat worse | 11 | 12.1 | 8 | 25.0 | 2 | 6.3 | 1 | 3.7 |
| Much worse now | 11 | 12.1 | 8 | 25.0 | 3 | 9.4 | 0 | 0.0 |
| Total | 91 | – | 32 | – | 32 | – | 27 | – |
| Completely recovered or much improved | 45 | 49.5 | 6 | 18.8 | 21 | 65.6 | 18 | 66.7 |
Table 25 summarises other participants’ outcomes at the 8-week follow-up. Overall, the majority (78 out of 91, 86%) of women were still pregnant by response to follow-up, with most more than 33 weeks pregnant, and this was fairly balanced across the treatment arms. There was substantial reduction in pain intensity before going to bed and in the proportion of women woken up every/most nights at 8 weeks compared with baseline in those randomised to SC plus acupuncture but not in the SC alone arm. Overall, quality of life did not improve substantially at 8 weeks but there was marked improvement in physical health (measured using the physical component scale of the SF-12) in the SC plus non-penetrating acupuncture arm (–5.7, 95% CI –10.7 to –0.7).
| Key characteristics | SC (n = 32) | SC + TA (n = 32) | SC + NPA (n = 27) |
|---|---|---|---|
| Taken at both baseline and follow-up, n | 24 | 27 | 22 |
| Pain intensity before going to bed, mean (SD) | 6.5 (2.8) | 3.7 (2.8) | 3.5 (2.3) |
| Woken up most/every night by back pain, n (%) | 9 (37.5) | 4 (14.8) | 1 (4.6) |
| SF-12 – Physical Component Scale, mean score(SD)a | 36.5 (10.6) | 41.4 (11.5) | 43.3 (9.5) |
| SF-12 – Mental Component Scale, mean score (SD)a | 49.1 (8.1) | 48.4 (13.8) | 50.2 (12.3) |
| Change from baseline (baseline to 8-week score) | |||
| Pain intensity before going to bed, mean (95% CI) | 0.04 (–1.5 to 1.6) | 2.7 (1.4 to 4.0) | 3.2 (1.8 to 4.5) |
| Woken up most/every night by back pain, percentage difference (95% CI) | 1.5% (–22.9% to 25.9%) | 20.9% (1.2% to 40.6%) | 36.9% (19.5% to 54.3%) |
| SF-12 – Physical Component Scale, mean score difference (95% CI)a | –0.3 (–5.5 to 4.9) | –2.8 (–6.2 to 0.6) | –5.7 (–10.7 to –0.7) |
| SF-12 – Mental Component Scale, mean score difference (95% CI)a | 0.03 (–4.1 to 4.1) | –0.2 (–4.2 to 3.9) | 1.2 (–5.3 to 7.7) |
Health-care use, treatment credibility and satisfaction with care
Table 26 presents use of other health-care services and self-reported satisfaction with care for the 73 participants who completed the full 8-week follow-up questionnaire. Overall, fewer than half of the participants (31 out of 73) had used any over-the-counter medicines, treatments or appliances (e.g. TENS machine, maternity belt), and this number was slightly lower (8 out of 22) among women in the SC plus non-penetrating acupuncture arm. Use of prescribed medicines, treatments or appliances and any other NHS or private health care (e.g. inpatient stays, physiotherapy) was generally low, and was lowest in the SC plus non-penetrating acupuncture treatment arm (see Table 26). No participants had attended either the NHS or private health-care services for investigation or treatments (e.g. radiography, surgery, injection) for back pain within the 8-week follow-up period.
| Treatment arm | |||
|---|---|---|---|
| SC (n = 24) | SC + TA (n = 27) | SC + NPA (n = 22) | |
| Health-care use, n (%) | |||
| Over-the-counter medicines, treatments or appliances for back pain (n = 73) | 12 (50.0) | 11 (40.7) | 8 (36.4) |
| Prescription of medicines or appliances for back pain (n = 72) | 6 (26.1) | 5 (18.5) | 1 (4.6) |
| Attended any other NHS or private health care because of back problem (n = 73) | 7 (29.2) | 7 (25.9) | 2 (9.1) |
| Attended NHS or private health care for investigation or treatments for back pain (n = 72) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Treatment credibility, n (%) | |||
| Confidence with the information/treatment received: very/quite confident (n = 71) | 3 (13.0) | 22 (81.5) | 18 (85.7) |
| Confidence in recommending the information/treatment: very/quite confident (n = 71) | 7 (29.2) | 22 (88.0) | 20 (90.9) |
| How logical the information/treatment seemed: very/quite logical (n = 71) | 13 (54.2) | 21 (84.0) | 20 (90.9) |
| Success of information/treatment in alleviating other complaints: very/quite successful (n = 71) | 3 (12.5) | 19 (76.0) | 16 (72.3) |
| Satisfaction with care, n (%) | |||
| Satisfaction with the treatment package received: very/quite satisfied (n = 72) | 4 (16.7) | 22 (84.6) | 21 (95.5) |
| Satisfaction with results from treatment: very/quite satisfied (n = 72) | 4 (16.7) | 22 (84.6) | 21(95.5) |
In terms of treatment credibility, 60% (43 out of 71) of participants were very or quite confident that the information or treatment they received helped their back problem. In total, 69% (49 out of 71) reported they would be very or quite confident in recommending the information/treatment to a friend who suffered from a similar problem; however, the proportions rating treatment credibility as high were much lower in the SC alone arm (7 out of 24, 29%). Levels of satisfaction with the treatment package received and the results from treatment were high overall (65%) but lower in the SC arm (17%) than in the SC plus true acupuncture (85%) and SC plus non-penetrating acupuncture (96%) arms.
Responses to open question on follow-up questionnaire
In total, 14 women allocated to SC alone, 18 allocated to SC plus true acupuncture and 12 allocated to SC plus non-penetrating acupuncture provided responses to the open question on the follow-up questionnaire about their overall experience. A summary of the responses with examples is given.
Of those in SC alone, eight women expressed negative views of the value of the SC package they received in the trial, while others took the opportunity to explain the impact of back pain on their pregnancy and labour. Examples of comments include:
I don’t feel I benefited at all from the standard care plan and the booklet showed me nothing that I wasn’t already aware of. I do feel the acupuncture would have been better.
The EASE Back study did not help with my back pain at all, and I ended up finishing work sooner than I wanted to.
and
The back pain experienced during labour was unbearable and worse than my contractions, so resulted in me having an epidural for my back pain.
From those receiving SC plus true acupuncture, the comments were overwhelmingly positive (13 of the 18 comments suggested positive experiences). Examples include:
I feel that I have received excellent treatment during this study. I do believe that the acupuncture has really aided my back pain and am certainly in a lot less discomfort at this stage in my pregnancy. The acupuncture has allowed me to carry on with daily activities (especially those at night time) with less pain. I would recommend this treatment to others and would consider it again to treat any other conditions.
I have really benefited from taking part in this study. The treatment and advice given by the physiotherapist have dramatically improved my pain during my pregnancy and I will continue to use some of the techniques afterwards. I really hope this study continues and that more women are offered such treatment. Thank you!
The care received has been excellent despite my initial doubts, it eased my pain an awful lot.
Two comments suggested that participants wanted more acupuncture treatment than they were offered in the study; for example:
I think the course length can be extended to 12 weeks as the more acupuncture done, the pain reduces a lot.
In addition, several participants shared the reasons why they struggled to attend for treatment:
I was unable to attend physiotherapy appointments due to lack of childcare. I proceeded to continue to exercise caution in my daily movements.
I won’t be able to get to any hospitals for acupuncture because of money problems, but the only thing I have for my back pain is paracetamol and my water bottle. Sometimes it works, sometimes it doesn’t, it depends how bad my back pain is.
Finally, the comments made by women allocated to SC plus non-penetrating acupuncture were a little more varied. One felt that the acupuncture had not been helpful:
I didn’t feel that the acupuncture helped at all, but the booklet contained some useful information. Thank you.
Several others particularly emphasised the benefits of the exercise component of treatment, for example:
I found the exercises I was given to do at home helped a lot, when I felt pain starting I would do the exercises and I could keep it under control. I feel the acupuncture also helped but you would need to keep up the exercises.
I have been very pleased with the impact of doing the exercises from the booklet. It was particularly useful having the physio show me exactly how to do the ones I wasn’t sure about. Thank you!
In addition, several women clearly felt they had benefited from the treatment, including:
Fantastic care. I loved the acupuncture and felt more relaxed and comfortable at these sessions than I had in a while. I would often nod off to sleep I felt so relaxed. Although I am now wearing a support belt and walking with elbow crutches I am much more confident dealing with my back pain
The physio was very supportive and provided very good advice and support. The acupuncture was a first time experience and I am very surprised (positively) at the good results. Would recommend this treatment to all pregnant women! Thank you!
Missing data and data accuracy
Missing data levels on key disability outcomes
The Oswestry Disability Index
Missing data on the ODI at baseline were very minimal. Of the 1240 individual ODI items (10 items each for 124 participants), there were only 35 items with missing data (2.8%). The two most frequently missing items were activities reported as ‘not applicable’ by participants with pregnancy-related low back pain (with and without PGP): ‘lifting’ (7.3% missing) and ‘sex life’ (8.9% missing). More than 80% (103 out of 124) of participants completed all the questionnaire items. Missing ODI data at the 8-week follow-up were similarly very low but slightly higher than at baseline. Of the 910 individual ODI items (10 items each for 91 participants), there were 71 items with missing data (7.8%), 62 of which were on questions about lifting and sex life. About half of the participants (43 out of 91) completed all the ODI follow-up questionnaire items.
The Pelvic Girdle Questionnaire
Missing data for the PGQ were very low but slightly higher than for the ODI. Out of 3100 PGQ items at baseline (25 items for each for 124 participants), there were only 191 items with missing data (6.2%). Again missing data on individual items were very minimal except for a few questions frequently reported as not applicable (e.g. running, sporting activities). Forty-six per cent (57 out of 124) completed all the items of the PGQ at baseline. At the 8-week follow-up, the overall rate of missing data was 8.7% [197 out of 2275 items (25 items for each of the 91 participants)]. Forty-one per cent (37 out of 91) completed all the items of the PGQ at 8-week follow-up.
Data accuracy
A random check of 10% of the data entered into the trial database was carried out to verify the data entry accuracy before data cleaning and analysis. Overall, the data entry accuracy was very high, with more than 99.5% accuracy across all the questionnaires.
Health economic evaluation
Baseline and 8-week economic data were available for 73 participants (24 in the SC arm, 27 in the SC plus true acupuncture arm and 22 in the SC plus non-penetrating acupuncture arm); this represented 59% of the sample. The health economic analysis focused on the 51 participants receiving SC versus SC plus true acupuncture that informed the base case analysis. Details of NHS and broader health-care resource use are reported in Table 27. Primary care NHS resource use was similar between the two trial arms (SC vs. SC plus true acupuncture). Participants in the SC plus true acupuncture arm reported more visits to NHS physiotherapists and NHS acupuncturists, although this could be a problem with double-reporting. Despite the question asking for health-care use outside of the EASE Back study, it is possible that participants misunderstood this question.
| Resource use category | SC (n = 24) | SC + TA (n = 27) |
|---|---|---|
| Study back pain visits, mean (SD) | 0.29 (0.9) | 6.03 (2.76) |
| GP visits, mean (SD) | 0.38 (0.9) | 0.52 (1.2) |
| NHS midwife visits, mean (SD) | 0.08 (0.4) | 0.22 (0.6) |
| Private midwife visits, mean (SD) | 0.00 (–) | 0.04 (0.2) |
| ‘NHS acupuncture’ visits, mean (SD) | 0.00 (–) | 0.22 (1.2) |
| NHS physiotherapist visits, mean (SD) | 0.04 (0.2) | 0.37 (1.5) |
| NHS ‘other’ health care professional visits, mean (SD) | 0.25 (1.2) | 0.11 (0.6) |
| ‘Over-the-counter’a treatments, n (%) | 12 (50) | 11 (41) |
| Prescribed medication,a n (%) | 6 (25) | 5 (19) |
| Visited NHS or private practice,a n (%) | 7 (29) | 7 (26) |
Table 28 shows the EQ-5D scores at baseline and at 8 weeks, and the total QALYs in the two arms. At 8 weeks, we observed a lower EQ-5D score in participants in the SC arm and a higher score for the SC plus true acupuncture arm. The mean difference in QALYs was 0.010 (95% CI –0.001 to 0.024). Receiving the acupuncture intervention was, therefore, associated with incremental QALYs over the 8 weeks.
| Complete case analysis | SC | SC + TA |
|---|---|---|
| Baseline | (n = 41) | (n = 42) |
| Mean (SD) | 0.649 (0.12) | 0.651 (0.16) |
| 8 weeks | (n = 24) | (n = 27) |
| Mean (SD) | 0.570 (0.23) | 0.698 (0.22) |
| Total QALYs, mean (SD) | 0.096 (0.02) | 0.106 (0.02) |
| Mean difference (95% CI) | 0.010 (–0.001 to 0.024) | |
| Adjusteda | 0.096 | 0.106 |
| Mean difference (95% CI) | 0.009 (0.000 to 0.019) | |
Table 29 shows the disaggregated mean (SD) costs for each treatment arm. The cost of treatment was reported as part of the total cost of each trial arm. The principal aim of the cost–consequence analysis was to look at all the costs of the two interventions (SC alone vs. SC plus true acupuncture) and compare these with the corresponding outcomes in terms of QALYs gained.
| Complete case analysis | Mean (£) (SD) | |
|---|---|---|
| SC (n = 24) | SC + TA (n = 27) | |
| Intervention cost | 11.52 (43.2) | 149.43 (71.14) |
| GP | 12.75 (29.8) | 17.62 (39.3) |
| NHS midwife | 6.25 (30.6) | 16.66 (48.03) |
| Private midwife | 0.00 (–) | 3.55 (18.4) |
| ‘NHS acupuncture’ | 0.00 (–) | 9.96 (51.76) |
| NHS physiotherapist | 2.04 (10.0) | 16.85 (69.2) |
| ‘Other’ professionals in NHS | 5.83 (28.6) | 3.74 (19.43) |
| Prescriptions | 1.76 (8.6) | 0.54 (2.8) |
| ‘Over-the-counter’ treatments | 8.67 (14.3) | 7.38 (21.7) |
| Back pain-related work absencea | 98.36 (330.3) | 258.86 (517.8) |
| Back pain-related reduced productivity | 806.55 (769.58) | 783.45 (762.7) |
| NHS/PSS cost | 40.15 (90.78) | 214.82 (191.92) |
| Adjusted mean differenceb (95% CI) | 174.67 (102.35 to 271.20) | |
| Incorporation of back pain-related health-care resource use (n = 42) | ||
| Health-care costc | 48.82 (94.18) | 225.77 (205.65) |
| Adjusted mean differenceb (95% CI) | 176.94 (100.73 to 265.50) | |
| Incorporation of back pain-related wider societal resource use (n = 42) | ||
| Societal costd | 953.74 (921.14) | 1268.08 (1207.24) |
| Adjusted mean differenceb (95% CI) | 314.34 (–256.84 to 887.86) | |
The results show that, although the SC plus true acupuncture intervention has a higher total NHS cost and health-care than SC alone, it is the intervention that also achieves higher QALY gains. From a NHS/PSS perspective, the difference in costs between SC plus true acupuncture and SC alone was £174.67 (95% CI £102.35 to £271.20). The differences in cost can be attributed to the additional acupuncture sessions and the relatively small reported increase in utilisation of acupuncture, midwifery and physiotherapy in a few participants in that treatment arm. On the basis of the NHS and health-care perspective, there is no intervention that is dominant (i.e. has lower costs and better outcomes). Acupuncture provided alongside SC, however, appears more effective in treating pregnant women with low back pain, but this increased effectiveness comes at an increased cost.
Work-related outcomes and out-of-pocket costs
Information on time off work and out-of-pocket costs related to treatment is reported in Table 30. Only two (9.5%) participants in the SC alone arm reported taking time off as a result of their back pain, compared with nine (33.3%) women in the SC plus true acupuncture group. The percentage of participants taking time off work as a result of back pain and to attend physiotherapy sessions was slightly higher in the SC plus true acupuncture arm for those in full-time employment and slightly lower for those in part-time employment than SC alone. The associated productivity-related costs showed higher costs among patients in the acupuncture treatment arm attending physiotherapy sessions (£0.81 vs. £16.87). Reduced productivity during paid work was reported by six (22%) women in the SC plus true acupuncture arm. Overall, slightly higher productivity costs were observed in the SC plus true acupuncture intervention arm than in the SC alone arm.
| Work outcome | SC | SC + TA |
|---|---|---|
| Employed at baseline | 28 of 41 | 27 of 42 |
| Employed at 8 weeks | 21 of 24 | 23 of 27 |
| Working full-time in paid job, n (%) | 3 (12.5) | 9 (33.3) |
| Working part-time in paid job, n (%) | 7 (29.2) | 2 (7.4) |
| Employed, but currently off sick as a result of back pain, n (%) | 1 (4.2) | 2 (7.4) |
| Employed, but currently on maternity leave, n (%) | 10 (41.7) | 10 (37.0) |
| Reported taking time off work as a result of back pain, n (%) | 2 (9.5) | 9 (33.3) |
| Mean (SD) number of days lost from work | 1.4 (4.5) | 3.4 (6.9) |
| Mean (SD) cost (£) of days lost from work | 111.48 (352.1) | 284.08 (554.8) |
| Mean (SD) number of days of reduced productivity at work | 15.6 (10.1) | 11.1 (9.0) |
| Mean (SD) cost (£) reduced productivity at work | 921.77 (754.7) | 919.70 (745.9) |
| Reported taking time off work to attend appointments, n (%) | 1 (4.2) | 14 (51.9) |
| Mean (SD) cost (£) of work absence to attend physiotherapy appointments | 0.81 (3.98) | 16.87 (24.34) |
| Reported reduced time in unpaid activities, n (%) | 0 (–) | 6 (22.2) |
| Reported paying someone to look after children, n (%) | 0 (–) | 1 (3.7) |
| Mean (SD) cost (£) of looking after children | 0 (–) | 5 (–) |
| Mode of transport to sessions, n (%) | ||
| Car/van | 2 (8.3) | 18 (66.7) |
| Taxi/train/bus | 0 (–) | 2 (7.4) |
| Foot | 0 (–) | 1 (3.7) |
| Mean (SD) cost (£) of parking | 1 (1.4) | 1.6 (1.1) |
| Mean (SD) cost (£) of bus/taxi/train fare | 0 (–) | 5.5 (0.7) |
Taking a broader societal perspective, the cost of time lost from work during the trial follow-up period of 8 weeks, reduced productivity at work and time taken off work to attend physiotherapy sessions is also reported. From these perspectives, the SC alone treatment arm was the least costly, although it was also associated with higher presenteeism costs.
Maternity record review results
Obstetric birth/neonatal outcomes
Table 31 summarises the birth outcomes obtained from the maternity records of trial participants, overall and by treatment arm. All women who participated in the pilot trial had live births, at a mean gestation week of 40 (SD 1.5 week). Labour duration was similar across all three treatment arms, as were the need to be induced, the mode of delivery, the proportion of women who had either an episiotomy or a perineal tear and the mean estimated blood loss at birth. The majority of women (66.4%) used Entonox® (BOC Ltd, Manchester, UK; gas and air) as pain relief during labour, 32% used pethidine and 21% had an epidural. Pattern of pain relief used during labour was the same across all three treatment arms.
| Birth outcomes | Overall (n = 122) | Treatment arm | ||
|---|---|---|---|---|
| SC (n = 40) | SC + TA (n = 42) | SC + NPA (n = 40) | ||
| Gestation week at delivery, mean (SD) | 39.7 (1.5) | 39.5 (1.6) | 39.6 (1.6) | 40.1 (1.3) |
| Live birth, n (%) | 122 (100) | 40 (100) | 42 (100) | 40 (100) |
| Labour durationa (hours), mean (SD) | 4.1 (4.5) | 3.2 (2.8) | 3.8 (3.7) | 5.2 (6.1) |
| Second-stage labour durationa (minutes), mean (SD) | 45 (57.4) | 41.0 (57.0) | 49.6 (54.1) | 44.3 (62.9) |
| Needed to be induced,a n (%) | 40 (35.7) | 14 (36.8) | 14 (35.9) | 12 (34.3) |
| Mode of delivery, n (%) | ||||
| Spontaneous vaginal delivery | 80 (66.1) | 26 (65.0) | 30 (73.2) | 24 (60.0) |
| Instrumental delivery | 14 (11.6) | 4 (10.0) | 4 (9.8) | 6 (15.0) |
| Elective caesarean section | 18 (14.4) | 9 (22.5) | 4 (9.8) | 5 (12.5) |
| Emergency caesarean section | 9 (7.4) | 1 (2.5) | 3 (7.3) | 5 (12.5) |
| Had an episiotomyb | 17 (18.1) | 5 (16.7) | 6 (17.7) | 6 (20.0) |
| Perineal tear, n (%) | ||||
| No tear | 56 (47.9) | 17 (46.0) | 20 (47.6) | 19 (50.0) |
| First-degree tear | 9 (7.7) | 1 (2.7) | 4 (9.5) | 4 (10.5) |
| Second-degree tear | 35 (29.9) | 13 (35.1) | 10 (23.8) | 12 (31.6) |
| Third-degree tear | 7 (6.0) | 2 (5.4) | 3 (7.1) | 2 (5.3) |
| Information not available | 10 (8.6) | 4 (10.8) | 5 (11.9) | 1 (2.6) |
| Estimated blood loss at birth (ml), median (IQR) | 300 (200–450) | 300 (250–400) | 300 (200–400) | 350 (300–500) |
| Blood loss of 500 ml or more, n (%) | 28 (24.1) | 8 (20.5) | 7 (18.0) | 13 (34.2) |
| Last antenatal haemoglobin count (g/l), n (%) | ||||
| < 115 | 33 (27.3) | 9 (23.1) | 14 (33.3) | 10 (25.0) |
| 115–165 (normal range) | 87 (719.9) | 30 (76.9) | 27 (64.3) | 30 (75.0) |
| > 165 | 1 (0.8) | 0 (0.0) | 1 (2.4) | 0 (0.0) |
| Woman’s postnatal haemoglobin count (g/l),c n (%) | ||||
| < 115 | 19 (70.4) | 7 (77.8) | 7 (77.8) | 5 (55.6) |
| 115–165 | 8 (29.6) | 2 (22.2) | 2 (22.2) | 4 (44.4) |
| Pain relief used during labour,d n (%) | ||||
| TENS machine | 5 (4.1) | 3 (7.5) | 1 (2.4) | 1 (2.5) |
| Water birth | 2 (1.6) | 0 (0.0) | 1 (2.4) | 1 (2.5) |
| Entonox® (gas and air) | 81 (66.4) | 27 (67.5) | 27 (64.3) | 27 (67.5) |
| Pethidine | 40 (32.8) | 14 (35.0) | 17 (40.5) | 9 (22.5) |
| Morphine | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Epidural | 26 (21.3) | 5 (12.5) | 12 (28.6) | 9 (22.5) |
| Spinal | 19 (15.6) | 9 (22.5) | 5 (11.9) | 5 (12.5) |
| General anaesthetic | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Patient-controlled analgesia | 1 (0.8) | 0 (0.0) | 1 (2.4) | 0 (0.0) |
| Information not available | 9 (7.4) | 1 (2.5) | 3 (7.1) | 5 (12.5) |
Neonatal outcomes were also very similar across all three treatment arms (Table 32). Approximately 50% of all babies were male and the majority had a birthweight of 3000–4000 g. In total, only three babies (2.5%) were admitted to the neonatal unit and 95% or more of all babies had an Apgar score of 7–10 at 5 minutes after birth.
| Neonatal outcomes | Overall (n = 122) | Treatment arm | ||
|---|---|---|---|---|
| SC (n = 40) | SC + TA (n = 42) | SC + NPA (n = 40) | ||
| Baby’s sex (female), n (%) | 62 (51.2) | 19 (48.7) | 23 (54.8) | 20 (50.0) |
| Birthweight of baby (g), n (%) | ||||
| < 2500 | 1 (0.8) | 0 (0.0) | 1 (2.4) | 0 (0.0) |
| 2500–3000 | 21 (17.2) | 8 (20.0) | 9 (21.4) | 4 (10.0) |
| 3000–3500 | 41 (33.6) | 12 (30.0) | 16 (38.1) | 13 (32.5) |
| 3500–4000 | 48 (39.3) | 17 (42.5) | 13 (31.0) | 18 (45.0) |
| > 4000 | 11 (9.0) | 3 (7.5) | 3 (7.1) | 5 (12.5) |
| Apgar scorea at 1 minute after birth, n (%) | ||||
| 0–3 | 1 (0.8) | 1 (2.5) | 0 (0.0) | 0 (0.0) |
| 4–6 | 6 (4.9) | 2 (5.0) | 3 (7.1) | 1 (2.5) |
| 7–10 | 115 (94.3) | 37 (92.5) | 39 (92.9) | 39 (97.5) |
| Apgar score at 5 minutes after birth, n (%) | ||||
| 4–6 | 1 (0.8) | 1 (2.5) | 0 (0.0) | 0 (0.0) |
| 7–10 | 121 (99.2) | 39 (95.5) | 42 (100) | 40 (100) |
| Baby admitted to the neonatal unit,b n (%) | 3 (2.5) | 2 (5.0) | 0 (0.0) | 1 (2.5) |
Adverse events
No SAEs attributable to the trial interventions or trial processes were reported. There were four SAEs reported by treating physiotherapists to the trial team (one in SC, two in SC plus true acupuncture and one in SC plus non-penetrating acupuncture), all examples of brief periods of hospitalisation or admission to the maternity assessment unit at UHNS, for reasons other than those related to the trial or treatments. All women were discharged after monitoring and all resumed treatment.
Self-reported side effects
Ten women (five in SC plus true acupuncture and five in SC plus non-penetrating acupuncture) reported some side effects from treatment in response to this question on the 8-week questionnaire, summarised in Table 33.
| Side effect | Number | |
|---|---|---|
| SC + TA | SC + NPA | |
| Nausea | 1 | 1 |
| Vomiting | 1 | 0 |
| Drowsiness/light-headedness | 4 | 4 |
| Fainting | 1 | 0 |
| Headaches | 1 | 0 |
| Pain or soreness | 2 | 3 |
Minor adverse reactions following treatment
Minor adverse reactions reported by physiotherapists on CRFs are summarised in Table 34. All were expected minor adverse effects. The most common was slight bleeding at the needle sites in 35 (21%) treatment sessions in the SC plus true acupuncture arms and in one (0.5%) treatment session in the SC plus non-penetrating acupuncture arm.
| Adverse events | Treatment arm | ||
|---|---|---|---|
| SC (total number of treatment sessions = 9) | SC + TA (number of sessions of acupuncture = 164) | SC + NPA (number of sessions of acupuncture = 197) | |
| Standard care, n (%) | |||
| Pain while exercising | 0 (0.0) | 5 (3.0) | 1 (0.5) |
| Muscle soreness | 0 (0.0) | 1 (0.6) | 0 (0.0) |
| Discomfort as a result of exercise | 0 (0.0) | 0 (0.0) | 1 (0.5) |
| Acupuncture, n (%) | |||
| Slight bleed at needle site | – | 35 (21.3) | 1 (0.5) |
| Pain on needle insertion | – | 6 (3.7) | 0 (0.0) |
| Slight bruising | – | 6 (3.7) | 0 (0.0) |
| Slight soreness | – | 2 (1.2) | 1 (0.5) |
| Muscle spasm | – | 2 (1.2) | 0 (0.0) |
| Numbness | – | 1 (0.6) | 0 (0.0) |
| Feeling slight sharpness | – | 1 (0.6) | 0 (0.0) |
| Feeling uncomfortable | – | 1 (0.6) | 0 (0.0) |
| Slight drowsiness | – | 0 (0.0) | 4 (2.0) |
Primary outcome measure and sample size for a full randomised controlled trial
Choice of primary outcome for future main trial
We included two outcomes measures capturing data on physical function (the ODI and the PGQ) and one measure of pain severity in the pilot trial, in order to help inform the decision about a primary outcome measure for a future main trial. Several factors were taken into consideration in examining the performance of these measures. These included the number of missing data at the item and scale levels; any evidence of floor or ceiling effects; the precision of the outcome measures based on the 95% CI; and their responsiveness to change.
The number of missing data was minimal for both these measures (reported in Missing data and data accuracy). No floor or ceiling effects were shown in the total score of either the ODI (minimum score = 10%, scored by n = 1; maximum score = 66%, scored by n = 1) or the PGQ (minimum score = 13.6, scored by n = 1; maximum score = 85.3, scored by n = 1). The standard errors for the estimated treatment effect were large in both the ODI and the PGQ measures, leading to wider CIs (which could partly be a result of the small sample size). However, the PGQ total score had a slightly larger margin of error than the ODI.
A number of statistical indices were used to assess the relative responsiveness of the key outcome measures. These included standardised effect size (SES), the mean change score divided by the SD of the measure at baseline; standardised response mean (SRM), the mean change score divided by the SD of the change scores; responsiveness statistic (RS), based on the mean change score divided by the SD of change of stable patients; and the paired t-test statistic, overall and in improved patients. The global assessment of improvement used as the anchor was the participant’s self-reported global rating of change in her back pain problem at the 8-week follow-up measured using a 6-point ordinal scale dichotomised into ‘improved’ (combining options ‘completely recovered’, ‘much improved’, ‘somewhat improved’) and ‘not improved’ (combining options ‘same’, ‘somewhat worse’, ‘much worse’). A SES/SRM/RS greater than 0.8 can be considered large, moderate values range from 0.5 to 0.8, and values below 0.5 are small. 85 A higher value of the above indices indicates greater sensitivity to clinical change. For a better comparison of the scores we present standardised pain intensity scores of 0–100 by multiplying each score by 10. All the three outcome measures showed moderate or large SES, SRM and RS; the PGQ symptoms scale particularly outperformed the other outcomes on most of these indices (Table 35).
| Key outcomes | n | Responsiveness measures | Paired t-test statistic (improved) | |||
|---|---|---|---|---|---|---|
| SES | SRM | RS | Paired t-test statistic (overall) | |||
| ODI score (0–100), mean (SD) | 90 | 0.494 | 0.345 | 0.370 | 3.274 | 8.099 |
| PGQ score (0–100), mean (SD) | ||||||
| Total | 90 | 0.598 | 0.461 | 0.474 | 4.378 | 8.893 |
| Activity subscale | 90 | 0.498 | 0.395 | 0.393 | 3.748 | 7.933 |
| Symptom subscale | 90 | 0.829 | 0.625 | 0.712 | 5.930 | 9.794 |
| Pain severity (mean score of three NRSs)a | 91 | 0.814 | 0.549 | 0.656 | 5.236 | 13.088 |
Responsiveness was also quantified through a receiver operating characteristic (ROC) curve analysis by plotting the true positive (sensitivity) versus the false positive (1 - specificity) for multiple cut-off points of the outcome measures against the patient’s global assessment of change. Patients were grouped into improved (‘completely recovered’/’much improved’/’somewhat improved’) or no change and worse (‘same’/’somewhat worse’/’much worse’). The best discrimination occurs with a curve that reaches most to the upper left; a sharp initial rise (high true-positive rate and low false-positive rate), then flattens while the false-positive rate is still small. For each outcome measure (Figure 8) the curve was to the left above the diagonal, showing some discriminative ability, and the areas under the curve were all above 0.85 showing good discrimination.
FIGURE 8.
The ROC curves of key outcomes against self-rated change. AUC, area under the curve.

Based on all of the above parameters, we feel that the PGQ (total score measuring both symptoms and impact of everyday activities) is the best choice of primary outcome measure for a future main RCT.
Sample size estimate for a future main EASE Back trial
A future main trial is likely to be best powered to detect small to moderate differences between SC and SC plus true acupuncture (testing effectiveness) but given the results of this pilot trial we feel it will also be helpful for a future main trial to compare a package of SC plus true acupuncture with SC plus non-penetrating acupuncture (specifically testing the added efficacy of needle penetration and manipulation).
The sample size calculation is therefore based on a three-arm, parallel-group RCT with the PGQ total score as the primary outcome measure and follow-up at 8 weeks as the primary time point. As there are no previous studies reporting a minimum clinically important difference (MCID) for the PGQ in this population, our parameters for the sample size calculation are based on the pilot data. The point estimate for the comparison of true acupuncture with SC was 12.6 (95% CI 1.3 to 23.8) and for true acupuncture with sham acupuncture was 4.3 (95% CI –7.0 to 15.6) with a SD of 17.0 for the PGQ total score at baseline. The best cut-off point that maximises sensitivity and specificity from the ROC curve analysis was found to be approximately a 4-point difference in the total score. At this difference in score, the sensitivity was 0.87 and specificity was 0.79. Since the estimated optimum cut-off sits within the CIs for both the two point estimates, this provides sufficient justification that the MCID would be achievable for testing for superiority in treatment effect in a main trial. We have, therefore, chosen a mean difference of 4 points in the PGQ total score as the minimum important difference for this population of women, and a SD of 18 (one-sided 80% upper limit of the baseline SD) – translating to a small effect size of 0.22. We have adopted a conservative approach of using an 80% upper one-sided confidence limit of the SD rather than the estimate itself, in line with the conservative approach recommended by Browne78 when using pilot data.
Given that the primary analysis will use analysis of covariance to compare the mean score between the two groups 8 weeks after randomisation adjusting for baseline scores, a sample size of 160 participants in each arm will be required to detect a 4-point difference in the mean scores between SC plus true acupuncture and SC plus non-penetrating acupuncture and between SC and SC plus true acupuncture with a power of 80% at a 5% two-sided significance level, assuming an autocorrelation of 0.5. The pilot data showed a correlation of 0.52 between the baseline and 8-week PGQ total scores; thus, an autocorrelation of 0.5 seems reasonable. Therefore, a total of 480 participants will be required. It is expected that no more than 20% of the participants will be lost to follow-up (as we have identified ways to increase the response rate to at least 80% from 74% from pilot data); thus, a future main trial would need to recruit 600 participants in total (200 per arm). Our pilot data have shown that it is possible to recruit an average of five women per week from one maternity centre using six recruitment methods. Therefore, for a main trial we estimate that three maternity centres will need to recruit participants for approximately 12–15 months using the three most successful recruitment methods.
The above suggestions for a primary outcome measure and estimated sample size for a future main EASE Back trial were presented to stakeholders at the EASE Back study dissemination event in May 2014 for discussion (see Chapter 4).
Conclusions
In conclusion, phase 2 of the EASE Back study was a pilot RCT in which participants were recruited over 6 months, randomised to one of three treatment arms (SC alone, SC plus true acupuncture and SC plus non-penetrating acupuncture), and followed up at 8 weeks following randomisation. Through this pilot RCT, we tested six recruitment methods, and randomised 45% of potentially eligible women. Our linked audio-recordings highlighted that women expressed no new concerns about acupuncture treatment that had not been identified in phase 1 interviews. Treatments were delivered in line with intervention protocols, although some women did not attend for treatment. The follow-up rate was 74% at 8 weeks, lower than the usual follow-up rates observed in our previous trials. We believe this resulted from the REC decision to reduce the number of follow-up reminders from our usual procedure. While all analyses of patient-reported clinical outcomes (pain, function, quality of life), health economic outcomes and safety outcomes can be considered only exploratory in this pilot RCT, the results overall tended to favour the addition of acupuncture to SC for pregnancy-related back pain. We used the results from the pilot trial to determine which outcome should be the primary outcome for a future main RCT and to estimate the sample size required for such a trial. All of the findings from the pilot RCT were presented and discussed at an end of study dissemination event in May 2014, summarised in Chapter 4.
Chapter 4 End of study dissemination event
At the end of the pilot trial (May 2014), we hosted a dissemination event to share the key findings of the EASE Back study with a range of stakeholders.
Participants and programme
We shared the results with a wide range of key stakeholders including national experts in the care of pregnant women, international experts from Sweden (Elden and Stener-Victorin) who had conducted the previous high-quality RCTs testing acupuncture for pregnancy-related PGP, representatives from the community and research midwives, physiotherapists, physiotherapy managers and research managers that we had worked with in the study, as well as trial methodologists. Women who had participated in the pilot trial were also invited but were unable to attend because of time and family commitments. In total, 35 people attended the event.
The programme for the day is provided in Appendix 15 and included an overview of the EASE Back study aims and objectives, summaries of the methods and findings of both phase 1 (the pre-pilot work) and phase 2 (the pilot RCT) and a short presentation on the potential aims, design and plans for a future main EASE Back trial. They listened to examples of the radio advertising used to raise local awareness about the pilot trial and reviewed the self-management booklet used in the pilot trial. The key focus of the day was to consider the key findings of the pilot RCT (the process outcomes, and the exploratory safety, clinical and cost outcomes) and their implications, in order to agree whether or not the findings provided sufficient evidence that a future main RCT might be desirable and feasible.
Discussion points
After hearing a summary of all of the results of the EASE Back study, participants worked in three separate multidisciplinary groups to discuss six key questions. The questions and a summary of the feedback from participants are provided:
Is a main trial desirable and feasible? If so, which trial design is best?
All felt that a future main trial was desirable but would benefit from modifications. The rationales for deciding a main trial would be desirable included the need to reduce the negative impact of back pain in pregnancy, the need to improve the quality of life during pregnancy of this group of women, the need for a better evidence base to underpin NHS practice, and the need to test additional treatment options for this population given that referral rates to NHS women’s health specialists were perceived to be rising.
The group felt that a future main trial was also feasible, and that the pilot RCT had provided the evidence needed to inform a larger and multicentre RCT. This group of women were considered to be a challenging group to recruit to RCTs and to commit to a course of treatment. Some modifications were suggested in order to ensure high rates of recruitment, follow-up and treatment attendance in a future main trial (these are described in the following section).
Several options for the design of a future main trial were discussed. These included a two-arm parallel RCT, randomising participants to either SC or a combination of SC and true acupuncture, powered to detect superiority of the addition of acupuncture to SC. Some participants felt that the SC treatment should be further standardised for a future main trial, so that either all women receive the self-management booklet only or all women receive the booklet and at least one session with a physiotherapist who would go through the booklet advice and demonstrate helpful exercises and self-management tips. A second option discussed was a three-arm parallel RCT randomising participants to the same three treatment arms as the pilot RCT, powered to also detect superiority of the SC plus true acupuncture arm in comparison with the SC plus non-penetrating acupuncture arm. Some concerns were raised by acupuncture experts among the stakeholders about the non-penetrating needles still being ‘active’ treatment (and not a true inert or sham treatment). This led to recommendations about using fewer needles and placing them outside the pain area in the sham acupuncture arm of a future main trial. We also discussed the merits of a three-arm parallel RCT with unequal randomisation (1 : 2 : 2 to SC, SC plus true acupuncture and SC plus non-penetrating acupuncture, respectively) and an adaptive trial design that starts with these three arms but is informed by an interim analysis to continue as either a three-arm trial or a two-arm trial (should the interim analysis shown futility in attempting to continue as a three-arm trial that could demonstrate superiority of SC plus true acupuncture over SC plus non-penetrating acupuncture). Some stakeholders felt that the question of most relevance to the NHS would be the one answered by a simple two-arm RCT (thus dropping the idea of a sham acupuncture comparison group altogether) while several others recommended a four-arm design adding in a treatment arm where women all receive one-to-one SC treatment offered by physiotherapists but not acupuncture of any sort. However, the preferred design was the adaptive trial design starting with three arms, as it appeared to offer benefits in terms of greater efficiency for a future large trial; if an interim analysis revealed futility (i.e. even if recruitment to all three arms continued, there would be no differences in patient outcome between the true and non-penetrating acupuncture arms) then recruitment, treatment and follow-up efforts could be directed to two trial arms (SC alone and SC plus true acupuncture). Using the PGQ as the primary outcome measure and an 8-week time point as the primary time point (with longer-term follow-ups at 3 and 6 months) would mean needing to recruit 600 women to a full EASE Back trial. We estimate that this would require three maternity centres with linked community midwifery and physiotherapy services, recruiting for a maximum of 15 months.
How could recruitment be maximised in a future main trial?
Although overall the recruitment rate in the EASE Back pilot trial was high (we recruited 45% of those women who were eligible), it was clear that we did not reach all the pregnant women likely to have back pain in the locality during the 6 months of recruitment (we had contact with 366 women out of the 720 we estimated might be suitable for screening for the pilot trial). The six recruitment methods tested in the pilot RCT had varied success, but the three most successful methods were a brief questionnaire screening for back pain given to women as they attend their routine 20-week ultrasound scan appointment, community midwives giving women under their care the EASE Back study card and self-referral of women in response to local awareness raising, particularly the regular radio infomercials. Overall, the stakeholders at the dissemination event felt that all three of these successful methods should be used in a future main trial but that efforts were needed to ensure, as far as possible, that all women attending their 20-week ultrasound scan appointment were given a screening questionnaire and were also given an EASE Back study flyer to take home with them (in case they currently did not have back pain but developed it later in the pregnancy). Research midwives suggested the use of small voucher incentives for staff within the ultrasound scan clinics to reward those getting most questionnaires completed and returned (based on examples of similar incentives used in other trials with pregnant women). They recommended that there was regular and extensive use of radio advertising to raise awareness of local women about a full trial (and it was ensured that the costs of these were included in any main trial application). Other recommendations included a model in which research midwives dedicate more sessions per week to supporting recruitment in a full trial and a slight change to several exclusion criteria for the trial (to exclude only women with previous acupuncture treatment in the last 2 years, to exclude women who had previously delivered a baby prior to 37 weeks and to include women with anterior pelvic pain only and include acupuncture points in that area such as KI11 and SP12).
How could follow-up rates be improved in a future main trial?
The overall follow-up rate in the pilot trial was 74%, and this is lower than previous RCTs led by our team at Keele. We believe that the decision of the REC which reviewed the pilot RCT to allow us to use only two reminders contributed to this low follow-up rate and that a future full RCT using the usual processes of reminders for RCT follow-up in the CTU at Keele would result in approximately 10% higher retention at the 8-week follow-up (see Appendix 8 for evidence from our previous trials). A future main trial would also collect longer-term follow-up data (at 3 and 6 postnatal months) and, therefore, additional efforts were felt to be needed to ensure high longer-term follow-up rates. Therefore, in addition to making a stronger case (with evidence from the pilot RCT) for the need for the usual follow-up reminder process to any future REC reviewing the main RCT, stakeholders at the end of study event also recommended offering women the option of online questionnaire completion prompted through emails and/or reminders by Short Message Service text messaging. Many of those attending also felt that the use of low-value shopping voucher incentives (such as £10 for each returned questionnaire or a total of £20 after return of the last questionnaire) should also be considered, based on the recent systematic review evidence that monetary incentives and offers of monetary incentives increase postal and electronic questionnaire response in randomised trials. 86 Stakeholders felt it important to provide trial participants with the option of declining the vouchers. Home visits to collect outcome data were discussed but felt by the group not to be feasible in a large future trial.
How could participant attendance at treatment be maximised?
Interventions in the EASE Back pilot trial were delivered in line with protocols, in terms of the content of treatment. However, the challenge we observed was in women attending for the full course of treatment (between six and eight treatment sessions in those participants allocated to receive acupuncture). Recommendations from the dissemination event included ensuring that the consent process very clearly describes the commitment needed on the part of included women to engage in the full course of treatment as well as making sure treatment appointments are as flexible as possible (to include evening appointments and to consider the possibility of weekend appointments for those women struggling to attend for treatment owing to work commitments). Additional suggestions included working with a greater number of physiotherapists to deliver EASE Back study interventions (thus offering great flexibility of treatment slots) and using Short Message Service text reminders to participants the day before their appointment to prompt them to attend for treatment.
How should physiotherapists be supported?
All felt that any future main trial should include a similar training and mentoring programme for participating physiotherapists, and that building in plans for peer support and pair-working (with at least two EASE Back-trained physiotherapists per treatment site) would be beneficial. The group of stakeholders recommended regular refresher workshops throughout the recruitment and treatment period of a future main trial, to offer the opportunity to discuss problems, patient case examples and obtain support from those leading the training. They wanted easy telephone contact to community midwives to address questions they might have about normal (and abnormal) features of pregnancy. They suggested that the group of 14 physiotherapists trained in EASE Back study interventions could proceed to support the wider group of therapists who might deliver treatment in a future multicentre trial. Some also suggested using community midwives to offer treatment in a future main trial, where those midwives might already be trained in using acupuncture for pain problems.
Should qualitative research be included in a future main trial?
There was mixed opinion about the value of linked qualitative research within a future main EASE Back trial. Those that felt it would be valuable recommended seeking REC approval to conduct qualitative interviews with those women who are eligible for a main trial but who decline to take part, in order to better understand the reasons for decline, and to interview a sample of women receiving treatment in order to fully understand their experiences of treatment, perceived treatment benefits, challenges faced in committing to a course of treatment and the impact particularly on work, time off work and the start of maternity leave. Such in-depth qualitative data could also help to explain the reasons for the results of a future main trial. A further purpose to qualitative research in the future main trial would be to explore the role of the therapeutic relationship between the women and the physiotherapists. This appeared to be important in the open responses women gave on their 8-week questionnaires.
Key conclusions and recommendations
In summary, a multidisciplinary group attending the end of study dissemination event at which the aims, design, methods and results of the EASE Back feasibility and pilot trial were presented reached the conclusion that a future main RCT testing the additional benefit of acupuncture to SC for women with pregnancy-related back pain (with and without PGP) is desirable and feasible. Recommendations included an adaptive trial design for the main trial with a pre-planned interim futility analysis in order to decide whether to continue with a three-arm full RCT or to stop recruiting to the SC plus non-penetrating acupuncture arm. Other recommendations included ways to maximise recruitment, follow-up rates, attendance at treatment sessions, support of participating physiotherapists and the potential role of linked qualitative research in a future main EASE Back trial.
Chapter 5 Discussion and conclusions
We have shown that that a RCT testing the addition of acupuncture to SC for pregnancy-related back pain is feasible.
Over 24 months, the EASE Back feasibility and pilot trial included (1) a pre-pilot phase comprising a national survey of physiotherapists and qualitative focus group and individual interviews with pregnant women, midwives and physiotherapists; (2) development of SC, true acupuncture and non-penetrating acupuncture treatment protocols; (3) development and delivery of a brief training programme to support physiotherapists to deliver treatment; (4) development of six methods with which to identify and recruit potentially eligible pregnant women; (5) a pilot RCT to assess recruitment rate, treatment fidelity and follow-up rate; (6) several patient-reported outcome measures of pain and function in order to select the most suitable one for use in a future main trial; and (7) a consensus conference with multiple stakeholders to reach agreement on the merits of, and procedures for, a future main trial.
The feasibility and pilot trial specifically:
-
Provided data on current UK SC and acupuncture treatment for low back pain in pregnant women. We described current practice for pregnant women with low back pain and used these data in the development of treatment protocols for SC, SC plus true acupuncture and SC plus non-penetrating acupuncture. Features of the treatment protocols including the number of treatment sessions, the types of advice and exercises, the acupuncture points and the overall course of treatment are, therefore, in line with what the NHS currently provides or would be reasonably expected to provide.
-
Explored the views of pregnant women with back pain about the acceptability of the proposed interventions, the content and delivery of participant information, the outcomes most important to them and the most appropriate timing of outcome measurement. We found that pregnant women and midwives welcome the idea of a trial as they want more treatment options for this clinical problem. Other than minor questions about positioning for treatment, the location of the needles and the time needed to attend for treatment, women expressed very few concerns. The participant information for the pilot trial ensured that these details were explained, including the information about the known risks of minor side effects of acupuncture such as feeling drowsy or light-headed. Women wanted help with the pain but particularly the impact of the pain on their everyday activities, including work. We tested several outcome measures of pain and function in the pilot trial, including a recently developed instrument specifically for this patient population (the PGQ). In order to ensure that most women would not yet have given birth at the time of their follow-up data collection, we selected a follow-up time point of 8 weeks after randomisation. Only 14% of participants had given birth by the time of their follow-up.
-
Optimised trial information, recruitment and consent procedures by learning what works best from the perspectives of pregnant women with low back pain, midwives and physiotherapists. The results of the pre-pilot work highlighted that this patient group are young, busy working women trying to continue to look after other small children and stay in work despite their pain, and these challenges mean they find it difficult to get to NHS appointments and to engage with research. We therefore developed six methods of identifying potentially eligible women for the pilot trial, as we needed to find out which might work best. The methods included a brief screen for back pain when women attend their routine 20-week ultrasound scan appointment, the development of small EASE Back study business cards that midwives could simply give women they look after and a local media awareness-raising campaign to get the message about the pilot trial directly to local women (using YouTube, a website, radio, newspaper and local bus advertisements). We used brief telephone screens to assess initial eligibility before asking women to attend for a full eligibility and information meeting with a research midwife or nurse. We audio-recorded 30 of these meetings and again found that women expressed few concerns other than positioning for treatment and the time commitment required for treatment.
-
Investigated the views of NHS health professionals regarding (1) the acceptability and feasibility of referring women with back pain in pregnancy to physiotherapists for acupuncture, (2) the proposed trial design and interventions and (3) ways in which to maximise recruitment and retention to a trial. The pre-pilot work highlighted that both midwives and physiotherapists felt that there are currently very few effective treatment options for pregnant women with low back pain and that acupuncture has merit and should be researched. Midwives welcomed the trial, felt acupuncture would be very acceptable to women and were keen to ensure that the women they looked after could access care in the trial. Physiotherapists were keen to participate in the trial but had concerns about the safety of acupuncture in pregnancy, mostly related to their original acupuncture training, through which at least some had been told that pregnancy was a contraindication for acupuncture. These concerns informed the development of a training programme for the 14 physiotherapists that took part, led by the research team, including an experienced acupuncturist, a women’s health physiotherapist and a consultant obstetrician. Physiotherapists’ confidence in the diagnosis and management of pregnancy-related back pain increased after the training and remained high to the end of the trial. The findings of the interviews with physiotherapists and midwives highlighted the need to offer women choice about geographical treatment sites, flexibility in the timing of treatment sessions (including evening appointments) and the provision of cover for annual leave periods for participating physiotherapists. Within the constraints of a pilot trial we offered some choice to women in line with these suggestions (of up to four treatment sites, one of which could offer evening appointments) and trained more physiotherapists than needed in order to specifically provide reasonable cover for annual leave and part-time working patterns of physiotherapists.
-
Tested the trial procedures, training programme for health professionals, the interventions and short-term outcomes with pregnant women with back pain, providing data on recruitment and follow-up rates, treatment fidelity, outcome completion rates and an estimate of between-group difference on key outcomes. We recruited 125 women over 6 months (45% of those who were eligible) and randomised them to one of the three treatment arms. Three of the six methods of identifying and recruiting women were more successful. We designed protocols, eligibility criteria, patient information material and CRFs and found that they performed well in the pilot RCT. We trained 14 physiotherapists to deliver the EASE Back study interventions and provided mentoring support during the pilot trial. They delivered the treatments in line with specified protocols, although some women did not attend for their allocated treatments despite efforts to contact them and re-engage them in treatment. Our usual follow-up processes for RCTs were reduced based on the decision of the REC reviewing the pilot trial (despite our appeal and evidence from five previous trials). The follow-up rate at 8 weeks was 74%, lower than we had hoped, but in our view unsurprising given the decision of the REC about using fewer reminders than we have previously used in RCTs. Outcome completion rates on key measures were high, with few missing data. Exploratory analysis of patient-reported clinical outcomes highlighted benefits from acupuncture over SC alone for pain and function and potential benefits of true acupuncture over non-penetrating acupuncture for function. The pilot data allowed us to estimate between-group differences on outcomes of symptoms and impact on activities using the PGQ; we determined the MCID for this measure and concluded that this would be a suitable primary outcome measure for a future main trial. In the pilot trial, the baseline SD for the PGQ total score was 17 (one-sided 80% upper confidence limit = 18) and we determined that the MCID is 4 points; therefore, a future RCT using this measure should be able to demonstrate a SES as low as 0.22. We also tested out ways to collect health economic data and conducted an exploratory health economic analysis. Overall, the preliminary results suggest that adding acupuncture to SC shows potential for providing a cost-effective alternative to SC alone. The results of both the clinical outcomes and health economic analyses presented in this report are exploratory and can inform a future main trial.
-
Brought the above findings together, with experts in SC, acupuncture and trial design, in a consensus conference to finalise the design, interventions, sample size, outcome measures and operational aspects of a main EASE Back trial. We presented all the results at an end of study dissemination event and consensus meeting, and discussed the feasibility and desirability of a future main trial. We estimate that 160 women per arm (480 in total) with pregnancy-related low back pain (with and without PGP) would be required for a full trial to have 80% power, at 5% significance, to detect an effect difference equal to or more than the MCID at the 8-week follow-up between treatment arms. Assuming a 80% follow-up rate (using our CTU standard follow-up processes and adding options for follow-up data collection and the offer of small shopping voucher incentives for response), we estimate a total sample size of 600 women need to be recruited. Being conservative, we estimate this could be achieved from three centres (three maternity centres and linked community services) over 15 months’ recruitment. A full trial would benefit from longer-term follow-up (most likely at 3 and 6 months postpartum) and an adaptive trial design using a pre-specified interim analysis to decide whether the trial should continue with all three treatment arms.
In conclusion, based on the learning from this feasibility and pilot RCT, a future main RCT testing the additional benefit of acupuncture over SC is feasible. The design and structure of the main RCT was developed and tested in this pilot RCT. Recruitment and follow-up were challenging, largely because this patient population comprises young, busy women often with other small children at home and demanding jobs to continue with, despite pain. We have shown that three recruitment methods are successful and these could be made more successful if the changes recommended at the consensus conference are implemented. We also believe that our usual RCT follow-up processes need to be followed in a future trial and we need to work with the REC reviewing the main trial, to help them see the need for all of the reminders. We believe there is a good window of opportunity to proceed to a large, multicentre RCT and have had requests from several sites in the UK interested in working with us on a future large trial.
Acknowledgements
The authors wish to acknowledge funding for this study from the NIHR HTA programme, support from managers and clinicians in the UHNS and SSOPT NHS Trusts, CARE for CLRN West Midlands North network, CLRN and participating clinicians and pregnant women. We would like to thank the women, midwives and physiotherapists who took part in the qualitative work, particularly Hannah Cochrane for helping to organise focus groups with the acupuncture special interest group within SSOPT. Thanks also to the many physiotherapists who responded to the EASE Back study survey in 2012, providing the different examples of information and advice leaflets they give to pregnant women with back and pelvic pain. This information was invaluable in shaping the content of the EASE Back study self-management booklet. We would also like to thank the women with experience of pregnancy-related back pain, physiotherapists and exercise specialist who provided feedback on the draft version of the booklet. We express particular thanks to Kris Wilkinson for acting as deputy study coordinator for phase 1 and for assistance in producing the self-management booklet, and Heather Minors, Helen Myers and Emily Mounsey for their assistance in producing the booklet. We thank Heather Minors for her input into the content and delivery of the physiotherapy training programme for the pilot RCT. We thank Panos Sarigiovannis, Helen Anderson, Noeleen Hellis, Lucy Huckfield and Julie Shufflebotham for their support and engagement of physiotherapy services, Darren Clement and Angela Rooney for the support of the research midwifery team and midwifery services at UHNS, and Sharon Wallis for support from the community midwifery team. Thanks to Professor Shaughn O’Brien and Dr Radha Indusekhar for their support from the obstetrics and gynaecology team at UHNS. Thanks also to Helen Duffy for support in developing service-level agreements and liaison with participating services. We would like to also thank the research midwifery team at UHNS and the research nurse team at Keele University CTU for their help identifying, recruiting and following up women in the EASE Back study. Finally, many thanks to the physiotherapists who were trained and delivered the intervention within the pilot trial and also the physiotherapy administrators who were instrumental in organising EASE Back study appointments. We acknowledge Michelle Robinson, Charlotte Purcell and the administrative team at Keele University for their administrative support, Wendy Clow for database support, Robert Fair for developing the EASE Back study website and Dr Ruth Beardmore for overall support with project management.
Contributions of authors
Professor Nadine E Foster, NIHR Professor of Musculoskeletal Health in Primary Care, led the research as chief investigator. She designed the study, wrote the proposal, supervised the research, facilitated several focus groups and wrote the final report.
Dr Annette Bishop, NIHR Research Fellow, helped plan the study and funding proposal, developed the national physiotherapy survey, facilitated a focus group, contributed to the analyses of the survey and interviews in phase 1 and supported aspects of the training programmes for participating clinicians.
Dr Bernadette Bartlam, Lecturer in Health Services Research, led the qualitative research in phases 1 and 2, conducted and analysed interviews with women, midwives and physiotherapists and contributed to the development of the PIL.
Dr Reuben Ogollah, Research Associate in Biostatistics, performed the quantitative analyses.
Dr Panos Barlas, Lecturer in Physiotherapy and Acupuncture, led the development of the acupuncture treatment protocols, delivered the training in acupuncture, mentored the participating physiotherapists, contributed to the analysis of the qualitative data and was part of the team that considered the adverse effects of treatments.
Dr Melanie Holden, Arthritis Research UK Allied Health Professional Training Fellow, was the study co-ordinator for phase 1, helped develop the survey and interview procedures, developed the participant information, led the development of the research ethics application for the pilot RCT and contributed to the training programmes for participating clinicians.
Professor Khaled Ismail, Professor of Obstetrics and Gynaecology, helped design the study, contributed to the recruitment methods and the training programme for physiotherapists, and was part of the team discussing reported adverse effects.
Dr Sue Jowett, Senior Lecturer in Health Economics, developed the economic data collection and analysis plan and supervised Jesse Kigozi, who conducted the health economic analysis.
Professor Christine Kettle, Professor of Midwifery, helped to design the study and contributed to the recruitment methods and oversight of the delivery of study.
Jesse Kigozi, Research Fellow in Health Economics, conducted health economics analysis.
Dr Martyn Lewis, Reader in Biostatistics and Health Economics, helped to design the study and supervised Dr Reuben Ogollah in developing and delivering the analysis plan.
Alison Lloyd, trial co-ordinator for the pilot RCT, was responsible for the day-to-day running of the trial and supporting the research nurses and midwives working on the trial.
Dr Jackie Waterfield, Senior Lecturer in Physiotherapy, helped to analyse the qualitative data and developed the questionnaire that physiotherapists completed before and after their training programme.
Julie Young, Senior Research Nurse, was the lead research nurse for the study and led the development and delivery of the auditing procedures for recruitment, eligibility screening, consent and MDC.
All authors contributed to the final report and approved the final version.
Publications
Bishop A, Holden MA, Ogollah RO, Foster NE. Current management of pregnancy-related low back pain: a national cross-sectional survey of UK physiotherapists. Physiotherapy 2016;102:78–85.
Waterfield J, Bartlam B, Bishop A, Holden MA, Barlas P, Foster NE. Physical therapists’ views and experiences of pregnancy-related low back pain and the role of acupuncture: qualitative exploration. Phys Ther 2015;95:1234–43.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- Ostgaard HC. Assessment and treatment of low back pain in working pregnant women. Semin Perinatol 1996;20:61-9. http://dx.doi.org/10.1016/S0146-0005(96)80058-9.
- van Tulder M, Becker A, Bekkering T, Breen A, del Real MT, Hutchinson A, et al. Chapter 3: European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J 2006;15:S169-91. http://dx.doi.org/10.1007/s00586-006-1071-2.
- Vleeming A, Albert HB, Ostgaard HC, Sturesson B, Stuge B. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J 2008;17:794-819. http://dx.doi.org/10.1007/s00586-008-0602-4.
- Robinson HS. Pelvic Girdle Pain and Disability during and after Pregnancy: A Cohort Study. Oslo: University of Oslo; 2010.
- Wu WH, Meijer OG, Uegaki K, Mens JM, van Dieën JH, Wuisman PI, et al. Pregnancy related pelvic girdle pain: terminology, clinical presentation and prevalence. Eur Spine J 2004;13:575-89. http://dx.doi.org/10.1007/s00586-003-0615-y.
- Pierce H, Homer C, Dahlen H, King J. Pregnancy Related Low Back and or Pelvic Girdle Pain: Listening to Australian Women n.d.
- Pennick VE, Young G. Interventions for preventing and treating pelvic and back pain in pregnancy. Cochrane Database Syst Rev 2007;2. http://dx.doi.org/10.1002/14651858.cd001139.pub2.
- Robinson HS, Veierød MB, Mengshoel AM, Vøllestad NK. Pelvic girdle pain: associations between risk factors in early pregnancy and disability or pain intensity in late pregnancy – a prospective cohort study. BMC Musculoskelet Disord 2010;11. http://dx.doi.org/10.1186/1471-2474-11-91.
- Sundsbo GV, Faksvag KT, Boldermo NO, Lokas R, Gram MJ, Heiszter ST, et al. Evidence Based Knowledge through an Educational Approach for Pregnant Women With Lumbo Pelvic Pain n.d.
- Olsson C, Nilsson-Wikmar L. Health-related quality of life and physical ability among pregnant women with and without back pain in late pregnancy. Acta Obstet Gynecol Scand 2004;83:351-7. http://dx.doi.org/10.1080/j.0001-6349.2004.00384.x.
- Vermani E, Mittal R, Weeks A. Pelvic girdle pain and low back pain in pregnancy: a review. Pain Pract 2010;10:60-71. http://dx.doi.org/10.1111/j.1533-2500.2009.00327.x.
- Albert H, Godskesen M, Westergaard J. Prognosis in four syndromes of pregnancy-related pelvic pain. Acta Obstet Gynecol Scand 2001;80:505-10. http://dx.doi.org/10.1080/j.1600-0412.2001.080006505.x.
- Röst CC, Jacqueline J, Kaiser A, Verhagen AP, Koes BW. Prognosis of women with pelvic pain during pregnancy: a long-term follow-up study. Acta Obstet Gynecol Scand 2006;85:771-7. http://dx.doi.org/10.1080/00016340600626982.
- Ostgaard HC, Zetherström G, Roos-Hansson E. Back pain in relation to pregnancy: a 6-year follow-up. Spine 1997;22:2945-50. http://dx.doi.org/10.1097/00007632-199712150-00018.
- Gutke A, Ostgaard HC, Oberg B. Predicting persistent pregnancy-related low back pain. Spine 2008;33:E386-93. http://dx.doi.org/10.1097/BRS.0b013e31817331a4.
- Robinson HS, Mengshoel AM, Bjelland EK, Vøllestad NK. Pelvic girdle pain, clinical tests and disability in late pregnancy. Man Ther 2010;15:280-5. http://dx.doi.org/10.1016/j.math.2010.01.006.
- Robinson HS, Mengshoel AM, Veierod MB, Vøllestad N. Pelvic girdle pain: potential risk factors in pregnancy in relation to disability and pain intensity three months postpartum. Man Ther 2010;15:522-8. http://dx.doi.org/10.1016/j.math.2010.05.007.
- Foster NE, Thomas E, Bishop A, Dunn KM, Main CJ. Distinctiveness of psychological obstacles to recovery in low back pain patients in primary care. Pain 2010;148:398-406. http://dx.doi.org/10.1016/j.pain.2009.11.002.
- Grotle M, Foster NE, Dunn KM, Croft P. Are prognostic indicators for poor outcome different for acute and chronic low back pain consulters in primary care?. Pain 2010;151:790-7. http://dx.doi.org/10.1016/j.pain.2010.09.014.
- Vøllestad NK, Stuge B. Prognostic factors for recovery from postpartum pelvic girdle pain. Eur Spine J 2009;18:718-26. http://dx.doi.org/10.1007/s00586-009-0911-2.
- Olsson C, Buer N, Holm K, Nilsson-Wikmar L. Lumbopelvic pain associated with catastrophizing and fear-avoidance beliefs in early pregnancy. Acta Obstet Gynecol Scand 2009;88:378-85. http://dx.doi.org/10.1080/00016340902763210.
- Ammendolia C, Furlan AD, Imamura M, Irvin E, van Tulder M. Evidence-informed management of chronic low back pain with needle acupuncture. Spine J 2008;8:160-72. http://dx.doi.org/10.1016/j.spinee.2007.10.014.
- Fregni F, Imamura M, Chien HF, Lew HL, Boggio P, Kaptchuk TJ, et al. Challenges and recommendations for placebo controls in randomized trials in physical and rehabilitation medicine: a report of the International Placebo Symposium Working Group. Am J Phys Med Rehabil 2010;89:160-72. http://dx.doi.org/10.1097/PHM.0b013e3181bc0bbd.
- Low Back Pain: Early Management of Persistent Non-specific Low Back Pain. London: NICE; 2009.
- Thomas KJ, MacPherson H, Thorpe L, Brazier J, Fitter M, Campbell MJ, et al. Randomised controlled trial of a short course of traditional acupuncture compared with usual care for persistent non-specific low back pain. BMJ 2006;333. http://dx.doi.org/10.1136/bmj.38878.907361.7C.
- Ratcliffe J, Thomas KJ, MacPherson H, Brazier J. A randomised controlled trial of acupuncture care for persistent low back pain: cost-effectiveness analysis. BMJ 2006;333. http://dx.doi.org/10.1136/bmj.38932.806134.7C.
- Furlan AD, van Tulder M, Cherkin D, Tsukayama H, Lao L, Koes B, et al. Acupuncture and dry needling for low back pain: an updated systematic review within the framework of the Cochrane Collaboration. Spine 2005;30:944-63. http://dx.doi.org/10.1097/01.brs.0000158941.21571.01.
- Wedenberg K, Moen B, Norling A. A prospective randomized study comparing acupuncture with physiotherapy for low-back and pelvic pain in pregnancy. Acta Obstet Gynecol Scand 2000;79:331-5. http://dx.doi.org/10.1080/j.1600-0412.2000.079005331.x.
- Ternov NK, Grennert L, Aberg A, Algotsson L, Akeson J. Acupuncture for lower back and pelvic pain in late pregnancy: a retrospective report on 167 consecutive cases. Pain Med 2001;2:204-7. http://dx.doi.org/10.1046/j.1526-4637.2001.01031.x.
- Guerreiro da Silva JB, Nakamura MU, Cordeiro JA, Kulay L. Acupuncture for low back pain in pregnancy: a prospective, quasi-randomised, controlled study. Acupunct Med 2004;22:60-7. http://dx.doi.org/10.1136/aim.22.2.60.
- Kvorning N, Holmberg C, Grennert L, Aberg A, Akeson J. Acupuncture relieves pelvic and low-back pain in late pregnancy. Acta Obstet Gynecol Scand 2004;83:246-50. http://dx.doi.org/10.1111/j.0001-6349.2004.0215.x.
- Elden H, Ladfors L, Olsen MF, Ostgaard HC, Hagberg H. Effects of acupuncture and stabilising exercises as adjunct to standard treatment in pregnant women with pelvic girdle pain: randomised single blind controlled trial. BMJ 2005;330. http://dx.doi.org/10.1136/bmj.38397.507014.E0.
- Elden H, Fagevik-Olsen M, Ostgaard HC, Stener-Victorin E, Hagberg H. Acupuncture as an adjunct to standard treatment for pelvic girdle pain in pregnant women: randomised double-blinded controlled trial comparing acupuncture with non-penetrating sham acupuncture. BJOG 2008;115:1655-68. http://dx.doi.org/10.1111/j.1471-0528.2008.01904.x.
- Ee CC, Manheimer E, Pirotta MV, White AR. Acupuncture for pelvic and back pain in pregnancy: a systematic review. Am J Obstet Gynecol 2008;198:254-9. http://dx.doi.org/10.1016/j.ajog.2007.11.008.
- Wang SM, Dezinno P, Lin EC, Lin H, Yue JJ, Berman MR, et al. Auricular acupuncture as a treatment for pregnant women who have low back and posterior pelvic pain: a pilot study. Am J Obstet Gynecol 2009;201. http://dx.doi.org/10.1016/j.ajog.2009.04.028.
- MacPherson H, Altman DG, Hammerschlag R, Youping L, Taixiang W, White A, et al. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT Statement. PLOS Med 2010;7. http://dx.doi.org/10.1371/journal.pmed.1000261.
- Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P. Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med 2008;148:295-309. http://dx.doi.org/10.7326/0003-4819-148-4-200802190-00008.
- Madsen MV, Gøtzsche PC, Hróbjartsson A. Acupuncture treatment for pain: systematic review of randomised clinical trials with acupuncture, placebo acupuncture, and no acupuncture groups. BMJ n.d.;338. http://dx.doi.org/10.1136/bmj.a3115.
- Foster NE, Thomas E, Barlas P, Hill JC, Young J, Mason E, et al. Acupuncture as an adjunct to exercise based physiotherapy for osteoarthritis of the knee: randomised controlled trial. BMJ 2007;335. http://dx.doi.org/10.1136/bmj.39280.509803.BE.
- Elden H, Ostgaard HC, Fagevik-Olsen M, Ladfors L, Hagberg H. Treatments of pelvic girdle pain in pregnant women: adverse effects of standard treatment, acupuncture and stabilising exercises on the pregnancy, mother, delivery and the fetus/neonate. BMC Complement Altern Med 2008;8. http://dx.doi.org/10.1186/1472-6882-8-34.
- Smith C, Crowther C, Beilby J. Pregnancy outcome following women’s participation in a randomised controlled trial of acupuncture to treat nausea and vomiting in early pregnancy. Complement Ther Med 2002;10:78-83. http://dx.doi.org/10.1054/ctim.2002.0523.
- Melchart D, Weidenhammer W, Streng A, Reitmayr S, Hoppe A, Ernst E, et al. Prospective survey of adverse effects of acupuncture in 97,733 patients. Arch Intern Med 2004;164:104-5. http://dx.doi.org/10.1001/archinte.164.1.104.
- Ernst E, Zhang J. Cardiac tamponade caused by acupuncture: a review of the literature. Int J Cardiol 2011;149:287-9. http://dx.doi.org/10.1016/j.ijcard.2010.10.016.
- Halvorsen TB, Anda SS, Naess AB, Levang OW. Fatal cardiac tamponade after acupuncture through congenital sterna foramen. Lancet 1995;345. http://dx.doi.org/10.1016/S0140-6736(95)91004-2.
- Arain M, Campbell MJ, Cooper CL, Lancaster GA. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med Res Methodol 2010;16. http://dx.doi.org/10.1186/1471-2288-10-67.
- Leech NL, Onwuegbuzie AJ. A typology of mixed methods research designs. Qual Quant 2009;43:265-75. http://dx.doi.org/10.1007/s11135-007-9105-3.
- Konstantinou K, Foster NE, Rushton A, Baxter D. The use and reported effects of mobilization with movement techniques in low back pain management; a cross-sectional descriptive survey of physiotherapists in Britain. Man Ther 2002;7:206-14. http://dx.doi.org/10.1054/math.2002.0469.
- Bishop A, Foster NE, Thomas E, Hay EM. How does the self-reported clinical management of patients with low back pain relate to the attitudes and beliefs of health care practitioners? A survey of UK general practitioners and physiotherapists. Pain 2008;135:187-95. http://dx.doi.org/10.1016/j.pain.2007.11.010.
- Holden MA, Nicholls EE, Hay EM, Foster NE. Physical therapists’ use of therapeutic exercise for patients with clinical knee osteoarthritis in the United Kingdom: in line with current recommendations. Phys Ther 2008;88:1109-21. http://dx.doi.org/10.2522/ptj.20080077.
- Peabody JW, Luck J, Glassman P, Dresselhaus TR, Lee M. Comparison of vignettes, standardized patients, and chart abstraction. JAMA 2000;283:1715-22. http://dx.doi.org/10.1001/jama.283.13.1715.
- Buchbinder R, Jolley D, Wyatt M. Volvo Award winner in clinical studies: effects of a media campaign on back beliefs and its potential influence on management of low back pain in general practice. Spine 2001;26:2535-42. http://dx.doi.org/10.1097/00007632-200112010-00005.
- Evans DW, Breen AC, Pincus T, Sim J, Underwood M, Vogel S, et al. The effectiveness of a posted information package on the beliefs and behaviour of musculoskeletal practitioners: the UK Chiropractors, Osteopaths and Musculoskeletal Physiotherapists Low back pain ManagemENT (COMPLeMENT) randomised trial. Spine 2010;35:858-66. http://dx.doi.org/10.1097/BRS.0b013e3181d4e04b.
- Bishop A, Foster NE. Do physical therapists in the UK recognise psychosocial factors in patients with acute low back pain?. Spine 2005;30:1316-22. http://dx.doi.org/10.1097/01.brs.0000163883.65321.33.
- Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. Thousand Oaks, CA: Sage Publications Inc.; 1994.
- Christ TW. A recursive approach to mixed methods research in a longitudinal study of post-secondary education disability support services. J Mix Methods Res 2007;1:226-41. http://dx.doi.org/10.1177/1558689807301101.
- Davies H, Powell A, Rushmer R. Healthcare Professionals’ Views on Clinician Engagement in Quality Improvement: A Literature Review. London: The Health Foundation; 2007.
- Coakley M, Fadiran EO, Parrish LJ, Griffith RA, Weiss E, Carter C. Dialogues on diversifying clinical trials: successful strategies for engaging women and minorities in clinical trials. J Women’s Health 2012;21:713-16. http://dx.doi.org/10.1089/jwh.2012.3733.
- Morse J, Lewis-Beck M, Bryman AE, Liao TF. The SAGE Encyclopedia of Social Science Research Methods. Thousand Oaks, CA: Sage Publications Inc.; 2004.
- Coyne IT. Sampling in qualitative research: purposeful and theoretical sampling – merging or clear boundaries?. J Adv Nurs 1997;26:623-30. http://dx.doi.org/10.1046/j.1365-2648.1997.t01-25-00999.x.
- Charmaz KC. Constructing Grounded Theory: A Practical Guide through Qualitative Analysis. New York, NY: Sage Publications; 2006.
- Guest G, MacQueen KM, Namey EE. Applied Thematic Analysis. Thousand Oaks, CA: Sage Publications Inc.; 2012.
- Donovan J, Mills N, Smith M, Brindle L, Jacoby A, Peters T, et al. Quality improvement report: improving design and conduct of randomised trials by embedding them in qualitative research – ProtecT (prostate testing for cancer and treatment) study. Commentary: presenting unbiased information to patients can be difficult. BMJ 2002;325:766-70. http://dx.doi.org/10.1136/bmj.325.7367.766.
- Fisher L, Hessler D, Naranjo D, Polonsky W. AASAP: a program to increase recruitment and retention in clinical trials. Patient Educ Couns 2012;86:372-7. http://dx.doi.org/10.1016/j.pec.2011.07.002.
- Glasgow RE, Eakin EG, Toobert DJ. How generalizable are the results of diabetes self-management research? The impact of participation and attrition. Diabetes Educ 1996;22:573-4. http://dx.doi.org/10.1177/014572179602200605.
- Rothwell PM. External validity of randomised controlled trials: ‘to whom do the results of this trial apply?’. Lancet 2005;365:82-93. http://dx.doi.org/10.1016/S0140-6736(04)17670-8.
- Mills N, Donovan JL, Smith M, Jacoby A, Neal DE, Hamdy FC. Perceptions of equipoise are crucial to trial participation: a qualitative study of men in the ProtecT study. Control Clin Trials 2003;24:272-82. http://dx.doi.org/10.1016/S0197-2456(03)00020-5.
- Mills N, Metcalfe C, Ronsmans C, Davis M, Lane JA, Sterne JAC, et al. A comparison of socio-demographic and psychological factors between patients consenting to randomisation and those selecting treatment (the ProtecT study). Control Clin Trials 2006;27:413-19. http://dx.doi.org/10.1016/j.cct.2006.04.008.
- Corrigan O. Empty ethics: the problem with informed consent. Sociol Health Ill 2003;25:768-92. http://dx.doi.org/10.1046/j.1467-9566.2003.00369.x.
- Sim J, Wright C. Research in Health Care: Concepts, Designs and Methods. Cheltenham: Nelson Thomas; 2000.
- Dunn KM, Jordan KP, Croft PR. Recall of medication use, self-care activities and pain intensity: a comparison of daily diaries and self-report questionnaires among low back pain patients. Prim Health Care Res Dev 2010;11:93-102. http://dx.doi.org/10.1017/S1463423609990296.
- Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy 1980;66:271-3.
- Stuge B, Garratt A, Krogstad Jenssen H, Grotle M. The pelvic girdle questionnaire: a condition-specific instrument for assessing activity limitations and symptoms in people with pelvic girdle pain. Phys Ther 2011;91:1096-108. http://dx.doi.org/10.2522/ptj.20100357.
- Grotle M, Garratt AM, Krogstad Jenssen H, Stuge B. Reliability and construct validity of self-report questionnaires for patients with pelvic girdle pain. Phys Ther 2012;92:111-23. http://dx.doi.org/10.2522/ptj.20110076.
- Brooks R. EuroQol Group . EuroQol: the current state of play. Health Policy 1996;37:53-72. http://dx.doi.org/10.1016/0168-8510(96)00822-6.
- Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220-33. http://dx.doi.org/10.1097/00005650-199603000-00003.
- Olsen MF, Gutke A, Elden H, Nordenman C, Fabricus L, Gravesen M, et al. Self-administered tests as a screening procedure for pregnancy-related pelvic girdle pain. Eur Spine J 2009;18:1121-9. http://dx.doi.org/10.1007/s00586-009-0948-2.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727-36. http://dx.doi.org/10.1007/s11136-011-9903-x.
- Browne RH. On the use of a pilot sample for sample size determination. Stat Med 1995;14:1933-40. http://dx.doi.org/10.1002/sim.4780141709.
- British National Formulary. London: BMJ Group and Pharmaceutical Press; 2013.
- Curtis L. Unit Costs of Health and Social Care. Canterbury: PSSRU, University of Kent; 2013.
- Department of Health . NHS Reference Costs 2012 2013 n.d. www.gov.uk/government/publications/nhs-reference-costs-2012-to-2013 (accessed May 2014).
- Office for National Statistics . Standard Occupational Classification 2010. www.ons.gov.uk/ons/guide-method/classifications/current-standard-classifications/soc2010/index.html (accessed May 2014).
- Office for National Statistics . Statistical Bulletin: Annual Survey of Hours and Earnings, 2013 Provisional Results 2013. www.ons.gov.uk/ons/rel/ashe/annual-survey-of-hours-and-earnings/2013-provisional-results/stb-ashe-statistical-bulletin-2013.html (accessed May 2014).
- Morse JM, Field PA. Nursing Research of Qualitative Approaches. Cheltenham: Stanley Thornes; 1998.
- Cohen J. Statistical Power Analysis for the Behavioural Sciences. Hillsdale, NJ: Erlbaum; 1988.
- Brueton VC, Tierney JF, Stenning S, Meredith S, Harding S, Nazareth I, et al. Strategies to improve retention in randomised trials: a Cochrane systematic review and meta-analysis. BMJ Open 2014;4:1-18. http://dx.doi.org/10.1136/bmjopen-2013-003821.
Appendix 1 Survey questionnaire to physiotherapists
Appendix 2 Focus group participant brief questionnaire
Appendix 3 Topic guides for interviews and focus groups
EASE Back study interview topic guide: acupuncturist
-
Introduction.
-
Explain usual arrangements for completion of brief profile, consent, recording, anonymity, focus group rules, etc.
-
NB: signing of consent form to be at termination of discussion as check that consent still in place.
-
-
Experience of back pain among patients.
-
Just to check: what are your qualifications and when did you qualify?
-
Tell me a little about your experience of back pain among your pregnant patients . . .
-
Probe for symptoms, effects on daily life, work, sleep, partner/family relationships, physical activities, mood, etc.
-
Have you received any specific postgraduate training around the area of back pain in pregnancy?
-
-
Views on complementary therapies generally.
-
What are your views on complementary therapies generally other than acupuncture?
-
Have you any experience of using them?
-
If so, which and in what ways?
-
NHS or private?
-
Reasons for use?
-
Outcomes?
-
-
Managing symptoms.
-
Do you feel you can offer any help with managing symptoms other than acupuncture?
-
What would be the usual type of approach you would take with these patients?
-
Probe – how effective, anything else that might be done, does it depend on the severity of the back pain or other symptoms?
-
Are there any ‘standard’ self-management resources that you use?
-
-
Managing patients using acupuncture.
-
Do you provide acupuncture within a private or a NHS setting? Say more . . .
-
Are there particular aspects of a patient’s symptoms that influence your approach?
-
Is acupuncture your first line approach?
-
If yes, are there circumstances in which it might not be?
-
If no, what is? Say more . . .
-
Are there particular points that you would not use? Say more . . .
-
Any particular needles?
-
Any variation on depth?
-
Is there any particular aspect of managing these patients you find difficult? Say more . . .
-
Any adverse effects?
-
What do you feel are patients’ expectations about what you have to offer them?
-
What kinds of explanations about the problem do you use with these women?
-
Do you have any procedures for informed consent?
-
Is there any particular information, and in what format, that you give patients?
-
-
Views on acupuncture in pregnancy – depending on above responses.
-
What sorts of expectations do you think patients have around acupuncture?
-
When do you consider acupuncture most helpful in the course of the pregnancy?
-
What sorts of outcomes are be important to you? To women? Prompts RE: employment, childcare, etc.
-
When would it be most appropriate to assess those outcomes, e.g. directly after a course of treatment, a month of so after the end of treatment but before the birth, after the birth?
-
-
Views on taking part in the trial.
Women:
-
How would you think women might feel about taking part? Reasons and any specific concerns they anticipate women having . . .
-
Any particular groups of women that might/not be willing?
-
What might support/encourage women to take part?
-
What might discourage/inhibit/prevent them?
-
-
Professionals:
-
How would you think professionals might feel about inviting women to take part? Reasons. . .
-
Any particular groups of women that they might/not be willing to invite?
-
What might support/encourage them in inviting women to take part?
-
What might discourage/inhibit/prevent them?
-
-
Close of interview.
-
Any other final remarks/additional views.
-
Signing of consent form as a check that consent is still in place.
-
Reimbursement of travel expenses (where appropriate).
-
EASE Back study interview topic guide: midwives and physiotherapists
-
Introduction.
-
Explain usual arrangements for completion of brief profile, consent, recording, anonymity, focus group rules, etc.
-
NB: signing of consent form to be at termination of discussion as check that consent still in place.
-
-
Experience of back pain among patients.
-
Tell me a little about your experience of back pain among your pregnant patients . . .
-
Probe for symptoms, effects on daily life, work, sleep, partner/family relationships, physical activities, mood, etc.
-
-
Managing symptoms.
-
Do you feel you can offer any help with managing symptoms?
-
What would be the usual type of approach you would take with these patients?
-
Probe – how effective, anything else that might be done, does it depend on the severity of the back pain or other symptoms?
-
Are there any ‘standard’ self-management resources that you use?
-
-
Managing patients.
-
Is there any particular aspect of managing these patients you find difficult? Say more . . .
-
What do you feel are patients’ expectations about what you have to offer them?
-
What kinds of explanations about the problem do you use with these women?
-
How do you usually manage these patients?
-
-
Views on complementary therapies generally and acupuncture specifically.
-
What are your views on complementary therapies generally?
-
Have you any experience of using them?
-
If so, which and in what ways?
-
NHS or private?
-
Reasons for use?
-
Outcomes?
-
Repeat for acupuncture specifically.
-
-
Views on acupuncture in pregnancy – depending on above responses.
-
Have used in pregnancy?
-
Reasons for doing so?
-
If not used, probe for reasons, including specifically any concerns about adverse effects.
-
What sorts of expectations do you think patients have around acupuncture?
-
If acupuncture was to be provided, when would be most helpful in the course of the pregnancy?
-
What sort of outcomes would be important to you?
-
When would it be most appropriate to assess those outcomes, e.g. directly after a course of treatment, a month of so after the end of treatment but before the birth, after the birth?
-
-
Views on taking part in the trial.
Explain the trial.
Women:
-
How would you think women might feel about taking part? Reasons and any specific concerns they anticipate women having . . .
-
Any particular groups of women that might/not be willing?
-
What might support/encourage women to take part?
-
What might discourage/inhibit/prevent them?
-
-
Professionals:
-
How would you think professionals might feel about inviting women to take part? Reasons . . .
-
Any particular groups of women that they might/not be willing to invite?
-
What might support/encourage them in inviting women to take part?
-
What might discourage/inhibit/prevent them?
-
-
Midwives:
-
Which women with back pain do you refer on to physiotherapists? Probe for details.
-
Explain the plan for audio-recording in pilot trial of consent meeting and explore their views of these plans.
-
-
Close of interview.
-
Any other final remarks/additional views.
-
Signing of consent form as a check that consent is still in place.
-
Reimbursement of travel expenses (where appropriate).
-
EASE Back study interview topic guide: women
-
Introduction.
-
Explain usual arrangements for completion of brief profile, consent, recording, anonymity, focus group rules, etc.
-
NB: signing of consent form to be at termination of discussion as check that consent still in place.
-
-
Experience of back pain in pregnancy.
-
Tell me a little about your experience of back pain in your pregnancy . . .
-
Probe for symptoms, effects on daily life, work, sleep, partner/family relationships, physical activities, mood, etc.
-
-
Help received with managing symptoms.
-
Do you feel you have received any help with managing symptoms?
-
If yes, probe who from, what sorts of help, how effective, anything else that might be done?
-
If no, has help been sought?
-
If yes, from whom, what sort of responses received?
-
If no, reasons for not seeking help.
-
Anything else that you have done to help with the pain, including self-help strategies and accessing information, and if so, from where? How effective?
-
-
Expectations after pregnancy.
-
How do you expect the situation to be after the baby is born?
-
Reasons?
-
-
Views on complementary therapies generally and acupuncture specifically.
-
Have you any experience of complementary therapies?
-
If so, which types? (Probes as follows.)
-
NHS or private?
-
Reasons for use?
-
Financial cost?
-
Outcomes?
-
Repeat for acupuncture as appropriate.
-
-
Views on acupuncture in pregnancy – depending on above responses.
-
Willingness to consider acupuncture for back pain in pregnancy – initial ideas about this and any specific concerns.
-
Have you used acupuncture in pregnancy?
-
If used, probe for reasons.
-
How did you decide which acupuncturist to use?
-
NHS or private?
-
Practitioner background?
-
Outcomes?
-
If not used, probe for reasons.
-
If acupuncture was to be provided, when would be most helpful in the course of the pregnancy?
-
What sort of outcomes would be important to you?
-
When would it be most important to you to assess those outcomes, e.g. directly after a course of treatment, a month of so after the end of treatment but before the birth, after the birth?
-
-
Views on taking part in research.
Explain about the trial.
-
How would you feel about taking part? Reasons . . .
-
How do you think women generally might feel? Reasons . . .
-
Any particular concerns about being invited to take part in this type of trial?
-
What might support/encourage women to take part? Specifically what information would they want before deciding to take part?
-
What might discourage/inhibit/prevent them?
-
-
Closing the interview.
-
Any other final remarks/additional views.
-
Signing of consent form as a check that consent is still in place.
-
Reimbursement of travel expenses (where appropriate).
-
Appendix 4 Participant information leaflet
Appendix 5 Self-management booklet
Appendix 6 Training programme for research midwives and nurses
Appendix 7 Training programme for physiotherapists
Appendix 8 Correspondence with Research Ethics Committee
Appendix 9 Participant recruitment methods and flow
Appendix 10 Baseline questionnaire
Appendix 11 Self-tests for pelvic girdle pain
Self-assessed P4 test
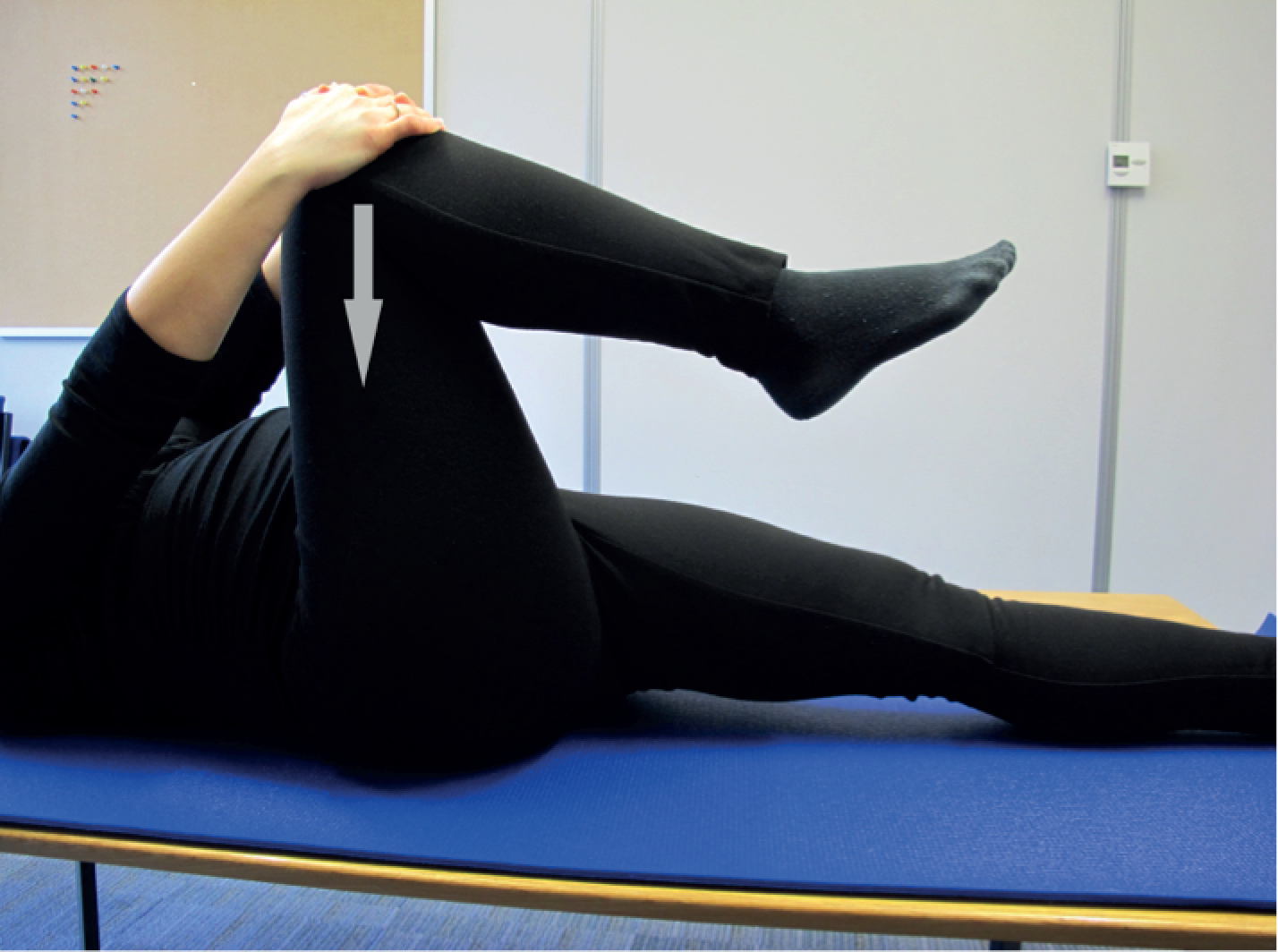
Bridging with extension of the leg

Appendix 12 Eligibility screening proforma
Appendix 13 Physiotherapy case report forms
Appendix 14 Follow-up questionnaire
Appendix 15 Evaluating Acupuncture and Standard carE for pregnant women with Back pain study dissemination event
List of abbreviations
- ACPWH
- Association of Chartered Physiotherapists in Women’s Health
- BMI
- body mass index
- BNF
- British National Formulary
- CARE
- Childbirth And REproductive health
- CI
- confidence interval
- CLRN
- Comprehensive Local Research Network
- CRF
- case report form
- CTU
- Clinical Trials Unit
- EASE Back
- Evaluating Acupuncture and Standard carE for pregnant women with Back pain study
- EQ-5D
- European Quality of Life-5 Dimensions
- GP
- general practitioner
- HTA
- Health Technology Assessment
- IQR
- interquartile range
- MCID
- minimum clinically important difference
- MDC
- minimum data collection
- NIHR
- National Institute of Health Research
- NRS
- Numeric Rating Scale
- ODI
- Oswestry Disability Index
- PGP
- pelvic girdle pain
- PGQ
- Pelvic Girdle Questionnaire
- PI
- principal investigator
- PIL
- patient information leaflet
- PSS
- Personal Social Services
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- REC
- Research Ethics Committee
- ROC
- receiver operating characteristic
- RS
- responsiveness statistic
- SAE
- serious adverse event
- SAP
- statistical analysis plan
- SC
- standard care
- SD
- standard deviation
- SES
- standardised effect size
- SF-12
- Short Form questionnaire-12 items
- SRM
- standardised response mean
- SSOPT
- Staffordshire and Stoke-on-Trent Partnership Trust
- TCM
- traditional Chinese medicine
- TENS
- transcutaneous electrical nerve stimulation
- TSC
- Trial Steering Committee
- UHNS
- University Hospital of North Staffordshire