Notes
Article history
The research reported in this issue of the journal was funded by the HTA programme as project number 11/95/03. The contractual start date was in November 2012. The draft report began editorial review in August 2014 and was accepted for publication in June 2015. The authors have been wholly responsible for all data collection, analysis and interpretation, and for writing up their work. The HTA editors and publisher have tried to ensure the accuracy of the authors’ report and would like to thank the reviewers for their constructive comments on the draft document. However, they do not accept liability for damages or losses arising from material published in this report.
Declared competing interests of authors
none
Permissions
Copyright statement
© Queen’s Printer and Controller of HMSO 2016. This work was produced by Morrell et al. under the terms of a commissioning contract issued by the Secretary of State for Health. This issue may be freely reproduced for the purposes of private research and study and extracts (or indeed, the full report) may be included in professional journals provided that suitable acknowledgement is made and the reproduction is not associated with any form of advertising. Applications for commercial reproduction should be addressed to: NIHR Journals Library, National Institute for Health Research, Evaluation, Trials and Studies Coordinating Centre, Alpha House, University of Southampton Science Park, Southampton SO16 7NS, UK.
Chapter 1 Background
This chapter details the background to the report and presents an overview of postnatal depression (PND): the size and importance of the problem, the need for prevention, current service provision and the approaches to interventions to prevent the condition.
Description of health problem
Depression is a leading cause of life lived with disability. PND, also termed postpartum depression, is defined using standardised diagnostic criteria as a major depressive disorder in the year following childbirth. 1 PND has a wide range of symptoms measured in clinical practice and in research using symptom self-reports as a proxy for clinical assessment. 1 It is distinguished from the more transient ‘baby blues’ and the rarer and more acute puerperal psychosis. Severe PND is associated with suicide and infanticide, especially when the woman has psychotic symptoms. 2
The Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (DSM-V)3 does not recognise PND as a separate diagnosis, so, to be diagnosed, women must meet the criteria for depression. The specifier is ‘with peripartum onset’ (the most recent episode occurring during pregnancy and in the 4 weeks following delivery). 4 The following symptoms must be present for at least 2 weeks to fulfil the criteria for major depression: a depressed mood or a loss of interest or pleasure in daily activities which represents a change from normal mood; and a clinically significant distress or impairment in social, occupational, educational or other important areas of functioning. Five or more of the symptoms in Box 1 must also be present for a major depressive episode to be determined.
-
Depressed mood most of the day, almost every day, indicated by subjective report or others’ observations.
-
Reduced interest or pleasure in all (or nearly all) activities for most of the day, almost every day.
-
Significant weight loss or weight gain or decrease or increase in appetite almost every day.
-
Insomnia or hypersomnia almost every day.
-
Psychomotor agitation or retardation almost every day.
-
Fatigue or loss of energy almost every day.
-
Feelings of worthlessness or excessive or inappropriate guilt almost every day.
-
Diminished ability to think or concentrate, or indecisiveness, almost every day.
-
Recurrent thoughts of death, recurrent thoughts of suicide without a plan, a plan for committing suicide or a suicide attempt.
In contrast, the World Health Organization’s International Classification of Diseases, Tenth Edition (ICD-10) diagnosis code F53, is for mental disorders associated with the puerperium, that is postnatal or postpartum depression commencing within 6 weeks of delivery, that do not meet the criteria for disorders classified elsewhere. 5 ICD-10 also requires several symptoms to be endorsed for a diagnosis of depression and most cases of PND will meet criteria for disorders classified elsewhere. ICD-10 uses key symptoms of persistent sadness or low mood and/or loss of interest or pleasure, fatigue or low energy; at least one of these symptoms, most days, most of the time for at least 2 weeks. If any of these are present, associated symptoms such as disturbed sleep, poor concentration or indecisiveness, low self-confidence, poor or increased appetite, suicidal thoughts or acts, agitation or slowing of movements and guilt or self-blame define the degree of depression.
Prevalence
Postnatal depression is a public health problem4,6 which occurs in most cultures. 6–8 The prevalence of both major or minor depression during the first postnatal year is 7–13%. 9 Among a sample of more than 8000 women in England, 13% scored 13 or more (the threshold to identify women with probable major depression)2 on the Edinburgh Postnatal Depression Scale (EPDS)10 on at least one postnatal assessment. 11
Some women recover by the time their infant is 6 months old, but in 50% of women depression can last for more than 6 months. 12 Although PND is defined as depression within the 12 months after the birth of an infant, a significant number of women remain depressed for over 1 year,13 and some women remain depressed for 4 years. 12
Although depression postnatally may not be different from depression occurring in non-pregnant women, some women become depressed for the first time postnatally, some experience postnatal recurrence of previous depression13 and, for others, depression begins antenatally and continues postnatally. 14–16 Antenatal depression is the strongest predictor of PND,14 being as common as PND, with 18.4% of women having depressive symptoms throughout pregnancy. 17 Antenatal anxiety is commonly comorbid with antenatal depression and also increases the likelihood of PND. 14,15,18
Additional factors have consistently been associated with PND. Some PND may be biologically mediated and specifically linked to childbirth. 1 Some women with PND may be genetically more reactive to the environmental trigger for depression. 19 In other women, who have a general vulnerability to depression, PND may occur because childbirth is a stressor. 1 The strongest predictors of PND are antenatal anxiety and antenatal depression,14 lack of social support, a history of depression, neuroticism, low self-esteem, stressful life events during pregnancy, poor marital relationship and domestic violence. 1,20,21 Women themselves have reported that the causes of their PND were lack of support, pressure to do things right, their personality (prone to mental health problems), pressure (work or money), hormonal changes and resurfaced memories. 22 As the aetiology is diverse, it is difficult to predict accurately which women will develop PND.
Impact of health problem
The burden of PND can extend, in its most severe form, to suicide and, less frequently, infanticide. 23 The impact of PND on mothers is compounded by impairments to the mother–infant interaction24 and impairments to the infant’s longer-term emotional, cognitive, behavioural and social development. 25,26 The impact of withdrawn behaviour24 and vocally communicated sadness27 appears to be worsened when women live in poorer socioeconomic circumstances, and is worse if the infant is a boy28,29 or if depression becomes a chronic problem. 30,31 Additional later risks for infants are mediated through the effect of chronic depression on the hypothalamic–pituitary–adrenal axis functioning in offspring, into adolescence. 25,32,33
Depressed pregnant women have a greater risk of delivering a low-birthweight infant. 34 Antenatal depression is a risk factor for infant mood33,35 and for depression in offspring at 18 years of age, with higher risk among offspring whose mothers are less educated. 16,36 There is a potential impact on fathers, around 10% of whom are at risk of depression, particularly during the 3–6 months after the infant is born. 37 This depression is moderately positively correlated with maternal depression, but it is unclear if there is an association or a causal influence, and the direction of the influence, if any, is unknown. 37 Furthermore, postnatal paternal depression is associated with depression in offspring. 16
Current service provision
Variation in service and uncertainty about best practice
Free maternity care in the UK, delivered predominantly by midwives and obstetricians, provides opportunities for women to have contact with health-care services. The National Institute for Health and Care Excellence (NICE) provides evidence-based guidelines for antenatal, intrapartum and postnatal care, and for antenatal and postnatal mental health. 38 Among those at low obstetric and medical risk, nine antenatal consultations are recommended for women expecting their first baby and seven consultations for those expecting a subsequent child. 39 Most women give birth in hospital maternity units, or in free-standing or alongside midwifery units and stay in for less than 2 days; fewer than 3% give birth at home. 40
Traditionally in the UK, hospital midwives have provided care in hospital for antenatal, labouring and postnatal women. Community midwifery teams have provided antenatal care in the community, and postnatal care during visits to the woman’s home, community health centres and children’s centres for up to 28 days after birth. Care is usually transferred on postnatal day 10 to the health visiting service and is provided by health visitors; specially trained public health nurses. Most health visitors now offer antenatal visits.
National Institute for Health and Care Excellence guidance38 recommends that primary health-care professionals should routinely enquire about past and current mental illness, and family history of perinatal mental illness, at a woman’s first appointment in early pregnancy, and postnatally (4–6 weeks and 3 or 4 months) to identify predictive risk factors. NICE guidance38 also recommends that midwives enquire within the first 24 hours after birth about a woman’s experience of her labour. In some locations, midwife-provided services have developed to provide an opportunity for women to discuss their birth experiences, but these do not always include access to formal psychological support.
The community midwife’s role includes an increased focus on improving public health and current pre-registration midwifery education covers the identification of potential mental health issues for childbearing women. The Maternal Mental Health Pathway41 guidance focuses on the health visitor’s role in maternal mental health and wellbeing during pregnancy and postnatally, recognising the contribution of midwives, mental health practitioners and general practitioners (GPs).
Other maternity support roles include maternity support workers and volunteers, such as breastfeeding peer supporters, counsellors and doula support (women who provide support to other women), during pregnancy, labour and birth and the early postnatal period.
Infrequently in the UK, and more commonly in the USA and a small number of other countries, CenteringPregnancy® (Centering Healthcare Institute, Boston, MA, USA) is available. 42,43 The CenteringPregnancy44 approach provides group care to women at similar stages of pregnancy by means of a health assessment and provision of education and peer support. Health-care professionals help women to participate in their own care and to learn from each other about pregnancy and care of the new infant.
Identification of postnatal and antenatal depression
There has been a lack of consistency in the routine approach to the identification of PND9,45,46 by primary health-care professionals. 47 NICE advocates a case-finding approach for depressive symptoms,38 based on two questions, the Patient Health Questionnaire (PHQ)-2, from the PHQ-9, as follows:48,49 ‘Over the last 2 weeks, how often have you been bothered by any of the following problems?’ (1) ‘Little interest or pleasure in doing things’ and (2) ‘Feeling, down, depressed, or hopeless’. 49 The EPDS,10 the Hospital Anxiety and Depression Scale (HADS)50 and the full PHQ-9 are to be used as follow-up tools as part of a fuller assessment process. The EPDS is frequently used as it performs well for major and minor depression,45 and is acceptable to women and health-care professionals. 51 The EPDS is not used systematically throughout the UK to identify depressive symptoms during pregnancy or postnatally partly because it ‘does not satisfy the National Screening Committee’s criteria for the adoption of a screening strategy as part of national health policy’. 52
Current service costs
Apart from the distress for women and the potential long-term consequences for infants, there are additional public health, social and economic consequences of maternal depression. 4 The cost of PND to the UK government is estimated as £45M53 to £61M per year. 4 For each exposed child, the estimated cumulative economic costs of adverse child development linked to a mother’s depression is £8190. 54 The health-care costs associated with postnatal paternal depression have been estimated for fathers with depression as £11,041, for fathers at high risk of developing depression as £1075 and for fathers without depression as £945 at 2008 prices. 55 In New Zealand, the potential value for money of implementation of a PND screening programme was assessed and the programme was found to be cost-effective. 56 In contrast, following a cost-effectiveness analysis, a system to identify PND in the UK was reported not to represent value for money based on the assumed cost of false positives. 57 Little is known about the economic consequences of PND or the cost-effectiveness of interventions aiming to prevent or alleviate PND symptoms. 58 Substantial economic returns have been estimated for investment in the prevention of mental health problems, with potential long-term pay-offs continuing into adulthood. 59
Despite the ‘case-finding’ approach to identify women at greater risk of PND, mainly based on earlier experience of mental health problems, little attention is paid to the prevention of PND, and no specific instruments are available to reliably predict PND among asymptomatic women. Some health visitors in the UK use the EPDS, but this practice varies nationally. It is likely that even less attention is paid to identifying depression and anxiety antenatally than postnatally.
Description of technology under assessment
Preventive interventions for postnatal depression
This section provides an overview of the rationale for the prevention of PND and a description of approaches that have been explored to prevent PND. There is evidence of the effectiveness of pharmacological60 and psychological interventions61–63 to treat PND within four main approaches: general counselling, interpersonal psychotherapy (IPT), cognitive–behavioural therapy (CBT) and psychodynamic therapy. 1 Prevention of a major depressive episode implies reducing the intensity, duration and frequency of depressive symptoms. 64
NHS England has provided a £1.8M budget for public health responsibilities, covering screening, immunisation and health-visiting services. 65 Less than 5% of NHS funding in England is spent on prevention, of all conditions. 65 The Marmot et al. 66 review aims to strengthen the role and impact of ill-health prevention, prioritising prevention and early detection of mental health conditions and early intervention. Traditionally primary, secondary and tertiary prevention activities are designed, respectively, to reduce the risk of developing health problems, to identify and manage pre-symptomatic ill health and to reduce the impact of the disease.
Three levels of preventive intervention are relevant to the prevention of PND:67
-
Universal preventive interventions are available to all women in a defined population not identified on the basis of increased risk for PND.
-
Selective preventive interventions are offered to women or subgroups of the population whose risk of developing PND are significantly higher than average, because they have one or more social risk factors.
-
Indicated preventive interventions are offered to women at high risk of developing PND on the basis of psychological risk factors, above-average scores on psychological measures or other indications of a predisposition to PND but who do not meet diagnostic criteria for PND at that time.
Universal preventive approaches may be less stigmatising than selective preventive interventions, but little attention has been paid to universal prevention in pregnant women, partly because the cost of a universal programme is likely to be high63 compared with a selective approach to identify higher-risk women. For example, 81% of women do not have an EPDS score 13 or more during pregnancy. 14 However, there is a rationale for providing a preventive intervention to women with subthreshold symptoms of depression who may otherwise go on to develop depression. 18,64
The outcomes for a selective intervention depend on how the population and risks are identified and defined. 63 Although indicated preventive interventions for PND could be regarded as addressing prodromal symptoms and therefore are not actually preventive, they could be regarded as early intervention. 68
The rationale for antenatal prevention of PND is based on data from the Avon Longitudinal Study of Parents and Children study14 showing that 43.7% of women with an EPDS score 13 or more at 32 weeks of pregnancy experienced elevated symptoms postnatally. Aiming to prevent, identify and treat antenatal depression presupposes that this will lead to a reduction in antenatal maternal morbidity and severity, deleterious effects on the developing infant, postnatal maternal morbidity and severity and other adverse outcomes in the offspring. 16,69 Hence, investment during pregnancy and postnatally may yield future benefits and financial savings in different areas of health and social care.
Evidence of preventive interventions
A wide range of support and treatment approaches have been explored because of the diverse aetiology of PND (physiological, social or psychological) with the aim of changing the mechanisms leading to PND. 68 Several interventions to prevent PND have been developed as modifications of promising interventions to treat PND. These are classified as psychotherapeutic, biological, pharmacological, educational or social support. Cochrane and other systematic reviews have provided some contradictory findings about the potential to prevent PND. Not enough is known about the effectiveness of these preventive interventions.
Psychological approaches to the prevention and treatment of depression
The psychological literature attests to the large effort expended on research into differing psychological approaches to the prevention70 and treatment of depression. 71–75 Although depression has often been the initial target condition for testing psychological approaches, it has equally often proved to be a more challenging condition when attempting to establish mechanisms of change that are specific to particular models of therapeutic interventions. A review of 101 randomised controlled trials (RCTs) on the treatment of major depression concluded that IPT, CBT and behaviour therapy are effective, while brief dynamic therapy and emotion-focused therapy are possibly effective. 72
A different body of literature suggests relatively small differences between the outcomes of different psychological interventions for depression. An earlier review which controlled for researcher allegiance (belief in the superiority of a treatment) found small effect sizes from comparisons between specific therapies. 73 This finding has been broadly supported in a meta-analysis of 58 outcome studies for depression which made direct comparisons between specific therapies, which yielded similarly small effect sizes. 74 However, arguments suggesting that researcher allegiance bias is related to treatment effects have been both supported76 and challenged. 77
A wide-ranging review of the efficacy and effectiveness of psychological therapies in general concluded that they were broadly effective for depression with little difference between theoretically diverse interventions. 78 Estimates of the proportion of outcome variance attributable to components of therapy comprised the following: extra-therapeutic factors, 40% (e.g. delivered individually or in a group or the number of sessions); relationship, 30%; placebo/expectancy effects, 15%; and specific techniques, 15%. 78,79 A subsequent meta-analysis in which common factor control groups were employed supported these estimates. 80
Extensive efforts have been afforded in relation to the development of measures81 and the measurement of outcomes82 in psychotherapeutic interventions, and the role of non-specific (common) factors, such as congruence, positive regard and empathy, has long been recognised. 83,84 The account of broadly similar outcomes despite diverse therapeutic interventions (termed the equivalence paradox)85 has yielded sophisticated accounts to explain this phenomenon, with the existence of common factors persisting as one major explanatory source. 85 However, others have argued that there is no clear evidence supporting a causal link between common factors and therapeutic outcomes. 86 The debate is not so much focused on the validity of the concept but rather on the absence of experimental manipulation as a route to determining which common factors, if any, impact on therapeutic change. The concepts of hope and expectancy, among others, have been posited as common factors, but the main focus for research has been on the concept of the therapeutic relationship or alliance.
Educational interventions
Attention has been paid to developing preventive strategies or interventions that focus on couple communication or parenting skills to ease the transition to parenthood. 87 Antenatal preparation for parenthood has traditionally focused on aspects of the woman’s pregnancy and on preparation for childbirth, with less attention paid to what to expect when the infant arrives or to couple communication or parenting. 88,89 Dyadic relationship quality is adversely affected90 in 67% of new mothers91 and 45% of new fathers92 during the first year of parenthood. Despite the central role of partner support in maternal mood,93 new parent couples have reported being shocked by and unprepared for adverse changes in their relationship, feeling sad and bemused that no one had talked to them about the changes they would experience in their relationships. 94
Some preventive educational interventions have been delivered universally to all expectant parents, making use of the opportunities to access this population through established antenatal care pathways, thereby reaching couples who may not otherwise seek such support. 95 These, and more targeted, approaches cover a variety of levels of intensity and format and timings.
Social support
Social support is a multidimensional concept that incorporates appraisal, companionship, informational, motivational and instrumental support; that is ‘. . . information leading the subject to believe that they are cared for and loved, esteemed and a member of a network of mutual obligations’. 96 Social support involves both social relationships that are embedded, such as relationships with family members or friends, and those that are created. 97
There are several pathways through which social relationships and social support can affect mental health. Social support can operate to promote health directly by enhancing feelings of well-being or by buffering the negative influences of stressful events. Integration in a social network might also directly produce positive psychological states, including sense of purpose, belonging and recognition of self-worth. 98 These positive states, in turn, might benefit mental health because of an increased motivation for self-care, as well as the modulation of the neuroendocrine response to stress. 98 Being part of a social network enhances the likelihood of accessing various forms of social support, which in turn protects against distress. 99 Members of a social network can exert a salutary influence on mental health by role modelling health-relevant behaviours. 100
Several different psychosocial mechanisms link aspects of social relationships to physical and emotional well-being: social influence/social comparison, social control, role-based purpose and meaning (mattering), self-esteem, sense of control, belonging and companionship and perceived support availability. 101 Given the importance of social support on mental health outcomes, enhancing social support has been used as a strategy for both the prevention and treatment of PND.
Pharmacological interventions or supplements
Some of the earliest interventions for the treatment and prevention of PND were hormonal. Uncontrolled studies used progesterone,102–104 but no controlled studies have been conducted of progesterone or oestradiol, as either a treatment or prevention.
Compared with the results of trials supporting antidepressant treatment for major depression, there is relatively little evidence to guide the clinician in treating or preventing PND. The mainstay of treatment has been antidepressant medication but women are reluctant to take antidepressants,60 as they are concerned about their safety when breastfeeding and the potential for side effects to disturb their interaction with their infant. 105
It has been reported that fish consumption and omega-3 status after childbirth are not associated with PND,106 but there is still interest in exploring the role of omega-3 fatty acids in PND, alone or combined with supportive psychotherapy. 107
Complementary and alternative medicine
This review adopts a generic definition of complementary and alternative medicine (CAM): ‘A group of diverse medical and health-care systems, practices and products that are not presently considered to be part of conventional medicine’. 108 Although this definition meets with problems in many areas of medical practice, in that what were once regarded as CAM are now provided as part of conventional medical service, it works reasonably well in perinatal depression, as CAMs are not generally provided in perinatal services.
Complementary and alternative medicine is widely used by pregnant women in the Western world, particularly those who are highly educated and have high incomes,109 often to reduce stress and improve mood; however, their use remains controversial. 110 Controversy extends beyond the definition of CAM, to the nature of the effects of CAM and to the quality of CAM research. CAM is also widely used by the general public, particularly women,111,112 many of whom do not report its use to their doctors. It is often used to promote wellness in the positive holistic sense as well as in the management of symptoms and disease. CAM has been offered to women with the aim of treating both antenatal depression63,113–115 and PND,63,116 alone or in combination.
The CAM interventions most commonly explored in these studies include aromatherapy, massage, hypnosis and other forms of relaxation therapy, herbal medicine, mindfulness and meditation, acupuncture and general traditional Chinese medicine, Ayurvedic medicine and homeopathy. Acupuncture is a popular form of treatment for depression outside the perinatal period, and there is evidence that its effectiveness is equivalent to that of antidepressants117 and that side effects are rare. Acupuncture in the context of antenatal depression was examined by a Cochrane review118 that reported inconclusive evidence.
Mind–body therapies have also been used to treat depression in general and in the perinatal period specifically,116,119 and for many there is some evidence of effectiveness. 120 Mindfulness has received specific attention in the context of perinatal depression121 and is supported by an evidence base showing that it is effective in depression in general. 122
Yoga and tai chi/qi gong are practised both alone and as a component of Ayurvedic and traditional Chinese medicine and are used by pregnant women to improve their health. 110,119 The health effects of these traditional medical approaches are held to extend beyond physical fitness, suppleness and strength, and they overlap with those of simple physical activity, which has also been investigated as an intervention to reduce depressive symptoms in pregnant women. 123
Summary
In summary, the prevention of PND is an important and somewhat neglected area in the UK in terms of the potential impact on women and their infants and families. Within the NHS, effort is currently directed towards treating identified depression in perinatal women, particularly postnatally. A range of psychological, educational, pharmacological social support and CAM interventions have been explored to minimise the development of and the intensity, duration, and frequency of depressive symptoms. The next chapter defines the decision problem.
Chapter 2 Definition of the decision problem
Decision problem
The focus of this report is the prevention of PND and optimisation of the mental health of pregnant and postnatal women, and consequently the health of their infants.
The population comprised all pregnant women (universal), pregnant women or subgroups whose risk of developing PND was significantly higher than average because they had one or more social risk factor (selective), and pregnant women at high risk of developing PND on the basis of psychological risk factors, above-average scores on psychological measures or other indications of a predisposition to PND or diagnosed depression (indicated). The population also included all postnatal women in their first 6 postnatal weeks (universal), postnatal women or subgroups whose risk of developing PND was significantly higher than average because they had one or more social risk factor (selective), and postnatal women at high risk of developing PND on the basis of psychological risk factors, above-average scores on psychological measures or other indications of a predisposition to PND (indicated), but not postnatal women diagnosed with depression.
All interventions suitable for pregnant women and women in the first 6 postnatal weeks were included. All usual care and enhanced usual-care control and active comparisons were considered. In the review of both the quantitative and the qualitative research literature, all outcomes were considered.
Overall aim and objectives of assessment
The overall aim of the report was to evaluate the clinical effectiveness, cost-effectiveness, acceptability and safety of antenatal and postnatal interventions to prevent PND. The purpose of the study was to apply rigorous methods of systematic reviewing of quantitative and qualitative studies, evidence synthesis and decision-analytic modelling to evaluate the preventive impact on women and their infants and families.
The objectives of the review were as follows:
-
to determine the clinical effectiveness of antenatal interventions and postnatal interventions to prevent PND (systematic review of quantitative research)
-
a. to identify moderators and mediators of the effectiveness of preventive interventions
-
b. to undertake a meta-analysis of available evidence [including a network meta-analysis (NMA) as appropriate]
-
-
to provide a detailed service user and service provider perspective on the uptake, acceptability and potential harms of antenatal and postnatal interventions (systematic review of qualitative research)
-
a. to examine the main service models for prevention of PND in relation to the underlying programme theory and mechanisms, with a focus on group- and individual-based approaches (realist synthesis)
-
-
to undertake an economic analysis, including a systematic review of economic evaluations and the identification of other evidence needed to populate an economic model
-
to determine the potential value of collecting further information on all or some of the input parameters (expected value of information analysis).
Service user involvement
The Nottingham Expert Patient (EP) committee is a group of women who have experienced the distressing effects of severe PND. Three of the women in the group were admitted to a mother and baby unit and all received community psychiatric care. The EP committee, established in 2009, has acted as the patients’ ‘voice’, advising the East Midlands Perinatal Mental Health Clinical Network Board on how to develop local services to meet the needs of women who experience mental health problems in pregnancy and after childbirth. The EP committee has joined the newly formed National Perinatal Mental Health Clinical Reference Group to ensure that the experiences and views of patients inform and influence the planning and delivery of the specialised service.
The EP committee were pleased to be invited to contribute to this review, to be involved in the development of the research proposal and to provide patient and public involvement (PPI) advice throughout the research. The EP committee reviewed the draft research proposal and provided detailed feedback to the principal investigator. The EP committee has maintained involvement through contact with the principal investigator (JM), ad-hoc meetings, having an EP committee member sit on the Expert Clinical/Methodological Group and providing input into this report.
Service user feedback on the draft proposal
The EP committee was initially somewhat sceptical that interventions could prevent PND. Early detection and treatment of PND was considered more of a priority than prevention. The importance of educating health professionals in the detection of and impact of PND was also highlighted. Further discussion and consideration led to collective acknowledgement that all members of the EP committee had experienced the most severe PND, which may not have been preventable. It was agreed that prevention, or at least a reduction in severity of moderate or mild PND, may be possible and worth investigating.
Service user feedback on the proposal and ongoing review
The EP committee questioned the meaning of PND, especially with regard to the term ‘depression’, as for many of the women anxiety was the major symptom. The research team decided to include maternal anxiety or stress as a secondary outcome, with depression as the primary outcome.
It was suggested that both infanticide (although rare) and the decision to terminate a pregnancy (if PND had been experienced in a previous pregnancy) should be considered as outcomes. Maternal suicide (no longer the most common cause of maternal death)23 was another potentially preventable outcome. It was agreed to cover these outcomes in the background section of this report. Family outcomes were also emphasised, as the entire EP committee reported the impact of their PND on their children and family members. Of particular note was the impact of their PND on partners, who also may become depressed or anxious.
The group discussed the distinction between prevention and treatment. The question was posed, ‘When is an intervention considered treatment and when is it prevention?’ One EP committee member had been on antidepressant medication before conceiving (although symptom free) because she experienced PND with her first child. This medication was increased at the end of the first trimester when she developed symptoms of anxiety. This also calls into question the term postnatal depression, as many women also become ill in the antenatal period. There was some debate around EPDS scores in the literature and the cut-off point for including studies as prevention studies. It was decided that trials in which included women had a raised EPDS but no diagnosis of PND would be classed as prevention studies.
Service user feedback on acceptability of interventions to prevent postnatal depression
Given their relatively extreme experiences of PND, the EP committee’s view on potential interventions to prevent PND was very open. When faced with a life-changing and potentially life-threatening illness, they felt the choice of intervention was likely to be focused on proven effectiveness.
Medication during pregnancy was perceived to be acceptable to women who have experienced PND in a previous pregnancy, especially severe PND. However, they felt that preventive medication was probably undesirable for those women in their first pregnancy who are asymptomatic but deemed ‘at risk’. Other non-pharmacological interventions, such as those being investigated in this review, were considered more likely to be acceptable to the majority of pregnant women.
Overall, the acceptability of interventions to prevent PND was perceived to be influenced by many factors, not least whether or not a woman has a history of PND. The potential for prevention or lessening the severity of PND was viewed by the EP committee as a very encouraging and exciting prospect.
Chapter 3 Review methods
Overview of review methods
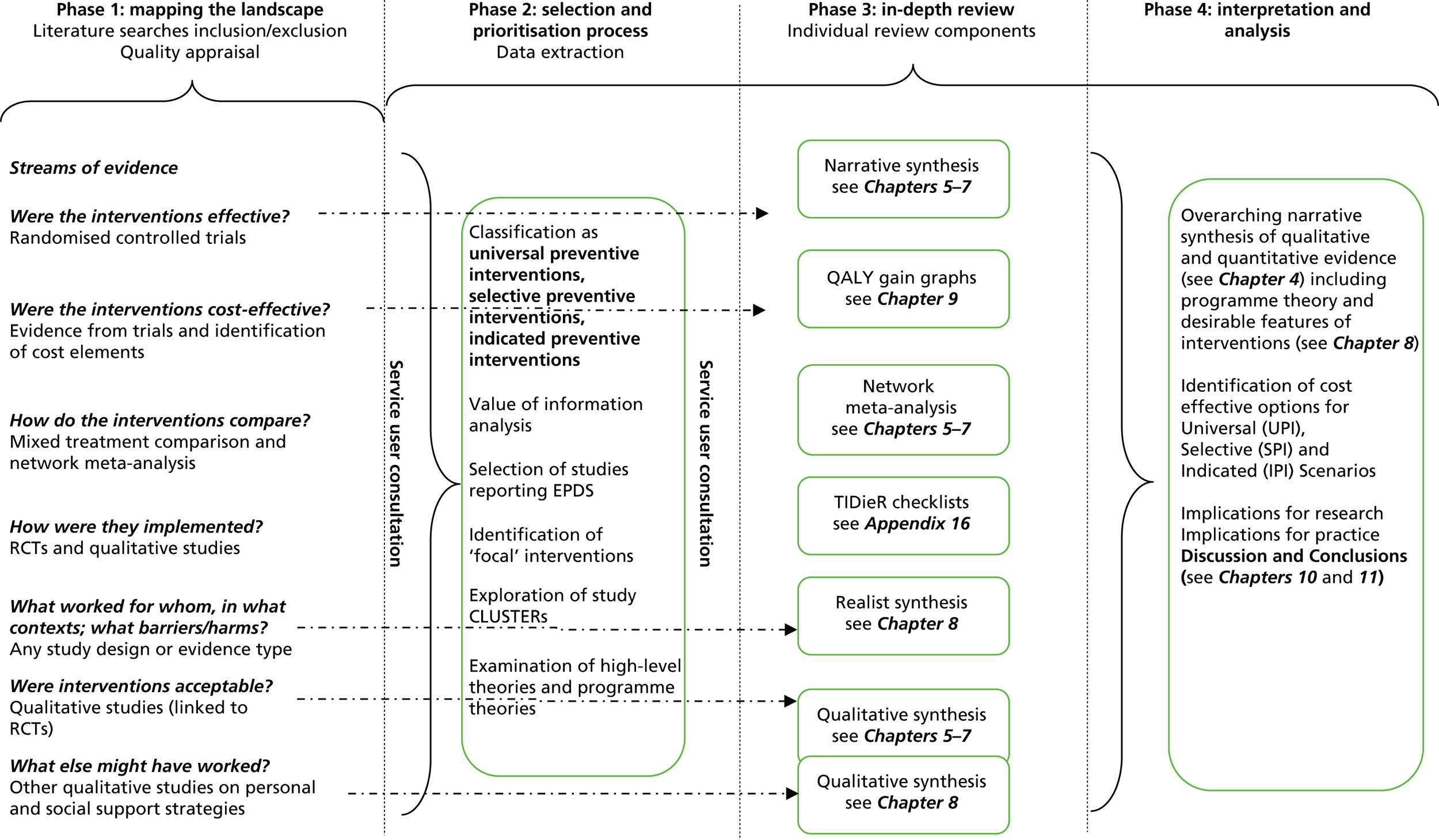
This chapter details the methods used to identify RCTs, systematic and other reviews and qualitative studies suitable for inclusion in the review. Figure 1 illustrates the four phases of the review, including the data extraction, analysis and interpretation phases.
FIGURE 1.
Overview of review methods. Key: IPI, indicated preventive intervention; QALY, quality-adjusted life-year; SPI, selective preventive intervention; TIDieR, template for intervention description and replication; UPI, universal preventive intervention. This is an Open Access article124 distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 3.0) license, which permits others to distribute, remix, adapt, build upon this work non- commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/3.0/.
Methods for reviewing and assessing clinical effectiveness
Search strategies for identification of studies
The review of effectiveness of interventions to prevent PND constituted the central platform for this report. The objectives of the individual RCTs and the data available from them determined what NMAs were feasible. The analysis of effectiveness determined the subsequent qualitative synthesis and economic analyses. The leading candidate interventions, demonstrated in terms of potential effectiveness, became the focus for the realist synthesis. This filtered approach recognised that it would not be feasible to conduct rich interpretive explorations across the wide heterogeneity of possible interventions and, therefore, interpretive resources were focused where they were most likely to yield insights on current and future interventions.
Search strategy for randomised controlled trials and systematic reviews
Search activities were as follows:
-
searches of electronic databases
-
searches of the internet
-
searches of specific websites
-
citation searches
-
reference lists of relevant studies
-
hand searches of relevant journals
-
scrutiny of references listed in reviews of the prevention of PND
-
suggestions from experts and those working in the field.
Searches of electronic databases
A comprehensive search of 12 electronic bibliographic databases was undertaken to identify systematically clinical effectiveness literature comparing different interventions to prevent PND. The literature search strategy is presented in Appendix 1. The list of electronic bibliographic databases searched for published and unpublished clinical effectiveness research evidence is presented here:
-
The Cochrane Library including the Cochrane Systematic Reviews Database, Cochrane Controlled Trials Register, Database of Abstracts of Reviews of Effects (DARE), Health Technology Assessment (HTA) and NHS Economic Evaluation Database (NHS EED) 1991; searched on 28 November 2012
-
MEDLINE (via Ovid) 1946–week 3 November 2012; searched on 30 November 2012
-
PreMEDLINE (via Ovid) 4 December 2012; searched on 5 December 2012
-
EMBASE (via Ovid) 1974–4 December 2012; searched on 5 December 2012
-
Cumulative Index to Nursing and Allied Health Literature (CINAHL; via EBSCOhost) 1982; searched on 11 December 2012
-
PsycINFO (via Ovid) 1806–week 4 November 2012; searched on 5 December 2012
-
Science Citation Index (via ISI Web of Science) 1899; searched on 5 December 2012
-
Social Science Citation Index (via ISI Web of Science) 1956; searched on 5 December 2012
-
Applied Social Sciences Index and Abstracts (ASSIA) (via ProQuest) 1987; searched on 19 December 2012
-
Allied and Complementary Medicine Database (AMED) (via Ovid) 1985–December 2012; searched on 5 December 2012
-
Conference Proceedings Citation Index–Science (CPCI-S) (via ISI Web of Science) 1990; searched on 5 December 2012
-
Midwives Information and Resource Service (MIDIRS) Reference Database 1991; searched on 24 July 2013.
Further searches for grey literature were conducted from January to March 2013 on additional resources. A list of the additional resources is presented in Appendix 1.
Search strategy search terms
The search strategy was developed using an iterative approach. The search used a combination of thesaurus and free-text terms for postnatal and antenatal depression combined with terms for prevention or risk factors or generic terms for interventions. The search comprised four facets:
-
Facet 1 comprised terms for the population (pregnant and postnatal women).
-
Facet 2 comprised terms for prevention.
-
Facet 3 comprised terms for known risk factors for PND.
-
Facet 4 comprised generic terms for interventions.
Facet 1 was combined separately with facets 2, 3 and 4. The major search refinement was to reduce the number of search terms in facet 1, then extra terms were added for facets 2, 3 and 4. In addition, the searches were combined with search filters for specific study designs when appropriate. All searches were performed by an information specialist (AC) from November to December 2012. Copies of The Cochrane Library and all the other search strategies are presented in Appendix 1.
The search strategy was used to search the Cochrane Central Register of Controlled Trials (CENTRAL) and then to search other databases not indexed by Clinical Trials. CENTRAL runs sensitive strategies on MEDLINE and EMBASE to identify relevant published RCTs; therefore, MEDLINE and EMBASE were not searched retrospectively. Records were retrieved through planned manual searching of a journal or conference proceedings to identify all reports of RCTs and controlled clinical trials. 125 The search was run with a systematic reviews filter to find Cochrane and other systematic reviews. The number of RCT and systematic review results obtained for the various databases searched is presented in Appendix 2.
Citation searches, reference lists, relevant journals and clinical experts
Reference tracking of all included and relevant studies was performed and reference lists of relevant reviews and systematic reviews were scrutinised to identify additional, relevant studies not retrieved by the electronic search to identify further potentially eligible RCTs. Searching of key journals, selected following consultation with clinical experts, was conducted using electronic table of contents alerts from January to July 2013 for 33 journals, presented in Appendix 3. Clinical advisors were also contacted about further potentially relevant RCTs.
Search outcome summary for the randomised controlled trials
Search result citations were imported and merged into Reference Manager, version 12126 (Thomson ResearchSoft, San Francisco, CA, USA), and duplicates were removed by Reference Manager or deleted manually (by JM and AC).
Review protocol
The population, intervention, comparators, outcomes, study designs (PICOS) process was used to break down the research question into concepts and search terms. Recognising that systems of care differ internationally, rather than concentrating solely on UK-based RCTs, we were deliberately inclusive in our search to capture RCTs of all interventions, irrespective of their health-care context. The research protocol is registered on PROSPERO (registration number CRD42012003273).
Inclusion and exclusion criteria for quantitative studies
Population
The population included women of all ages who were either pregnant or had given birth in the previous 6 weeks. The population was separated according to level of risk of PND into three levels, universal, selective or indicated, as follows:
-
Universal: all women in a defined population not identified on the basis of increased risk of PND.
-
Selective: women or subgroups of the population whose risk of developing PND was significantly higher than average because they had one or more social risk factors such as general vulnerability, aged less than 18 years, at risk of violence, ethnic minority, human immunodeficiency virus (HIV) positive, living in deprivation or financial hardship or poverty, or single, socially disadvantaged or unsupported.
-
Indicated: women at high risk of developing PND on the basis of psychological risk factors, above-average scores on psychological measures or other indications of a predisposition to PND but who did not meet diagnostic criteria for PND at that time, such as antenatal depression, a raised symptom depression score and a history of PND or history of major depression.
The population dimension for the PICOS framework is presented in Box 2.
Pregnant women (universal).
Postnatal women with a live baby born within the previous 6 weeks (universal).
Vulnerable pregnant or postnatal women who were aged less than 18 years; at risk of violence; an ethnic minority; HIV positive; living in deprivation, financial hardship or poverty; or single, socially disadvantaged or unsupported (selective).
Pregnant or postnatal women with a raised score on the antenatal risk questionnaire, Beck Depression Inventory, Center for Epidemiologic Studies Depression scale, the Cooper predictive index, depression symptom checklist, EPDS, HADS, Hamilton Depression Rating Scale, Health during pregnancy questionnaire; a past history of PND or major depression (indicated).
Pregnant women with a diagnosis of depression using Research Diagnostic Criteria or DSM-IV criteria (indicated).
ExcludedPostnatal women with a diagnosis of PND.
Pregnant women with comorbid psychiatric disorders.
Postnatal women with major medical problems.
DSM-IV, Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition.
Interventions
The preventive interventions were also separated into three levels of preventive intervention according to the population for which the intervention was intended:
-
Universal preventive interventions: interventions available for all women in a defined population not identified on the basis of increased risk of PND.
-
Selective preventive interventions: interventions offered to women or subgroups of the population whose risk of developing PND was significantly higher than average because they had one or more social risk factors.
-
Indicated preventive interventions: interventions offered to women at high risk of developing PND on the basis of psychological risk factors, above-average scores on psychological measures or other indications of a predisposition to PND but who did not meet diagnostic criteria for PND at that time.
Seven main classes of interventions were also categorised as presented in Box 3.
Pharmacological agents or supplements: prescribed antidepressants, calcium, dietary supplements, hormone therapy, thyroid therapy.
Psychological: the breadth of psychological interventions and approaches which comprise components of a psychotherapeutic approach.
Social support: home visits, telephone-based peer support, doula support, social support.
Educational: educational information booklets and classes.
Organisation of maternity care: alternative forms of contact with care providers, primary care strategies.
CAM or other: music, acupuncture, tai chi, yoga, pregnancy massage, aromatherapy, exercise and herbal medicine.
Midwifery-led interventions: different approaches to antenatal care, CenteringPregnancy, team midwife care, caseload midwifery.
ExcludedTreatment trials for women with PND.
Interventions initiated preconceptually.
Interventions initiated more than 6 weeks postnatally.
Comparators
All comparison arms for all eligible studies in all countries were included, whether usual care, enhanced usual care, or an active comparison group.
Outcomes
The main outcome was a validated measure of symptoms of maternal depression or a diagnostic measure of depression from 6 weeks to 12 months postnatally. Other maternal outcomes of anxiety and well-being were included. Binary, categorical or continuous outcomes were included, whether as a single measure or assessed at more than one postbaseline treatment time point. The outcomes dimension is presented in Box 4.
Depression symptoms measured on a validated self-completed instrument.
Depression diagnosis.
Anxiety symptoms.
Diagnostic measure of anxiety.
Birth outcomes.
Infant outcomes.
Family outcomes.
ExcludedNo measure of PND reported in the results.
Outcome measurements more than 12 months postnatally.
Outcome measurements less than 6 weeks postnatally.
Physiological measurement.
Unvalidated measures of depression.
Study designs
The study designs dimension is presented in Box 5.
RCTs.
Economic evaluations alongside RCTs.
Systematic reviews of the prevention of PND.
ExcludedBefore-and-after studies.
Case–control studies.
Cohort studies.
Commentary or clinical overviews.
Cross-sectional surveys.
Description of a study.
Non-randomised control groups.
Non-systematic reviews.
Not a PND prevention trial.
Ongoing RCTs.
Protocols for a RCT.
Reviews not about prevention of PND.
Secondary analysis of data from a RCT.
Studies reported in non-English language.
Systematic reviews not about prevention of PND.
Search strategy and outcome summary for the qualitative studies
Electronic databases
The search for the clinical effectiveness evidence was run with a qualitative filter to identify qualitative studies. The list of electronic bibliographic databases searched is presented in Appendix 1. The search was run again with a mixed-methods filter (devised with AB) to find papers that used quantitative and qualitative methodology. The numbers of qualitative studies and mixed-methods studies retrieved for the various databases searched are presented in Appendix 4.
Study selection
Study selection criteria and procedures for the quantitative review
Two reviewers (JM and PS) independently screened the titles and abstracts to identify papers for possible inclusion. If no abstract was available, the full paper was retrieved for scrutiny. Full papers for RCTs were obtained if the abstract showed that the study fulfilled the inclusion criteria or it was unclear from the abstract whether or not the inclusion criteria were fulfilled. All full papers retrieved were independently reviewed by two reviewers. Papers were not excluded on quality at this selection stage. The full papers had to fulfil the inclusion criteria presented in Tables 2–5. Where there was no consensus following discussion about inclusion at the full-paper stage, a third reviewer or clinical expert (CLD, HS or SS-B) was consulted. The reasons for exclusion are presented in Appendix 5.
Study quality assessment checklists and procedures for the randomised controlled trials
Risk-of-bias assessment
The quality of each paper was assessed independently by two reviewers (JM and PS) using the Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. 126 Any disagreements about risk of bias were resolved by a third reviewer. The risks assessed were:
-
risk of selection bias (random sequence generation and allocation concealment)
-
risk of performance bias (blinding of participants and personnel)
-
risk of detection bias (blinding of outcome assessors)
-
risk of attrition bias (incomplete outcome data)
-
risk of reporting bias (selective reporting of the outcome, subgroups or analysis)
-
risk of other sources of bias (any important concerns about other possible sources of bias such as funding source, adequacy of statistical methods used, type of analysis, baseline between-group imbalance in important prognostic factors).
The risks were assessed as low risk of bias, high risk of bias or unclear risk of bias. For each assessed risk, the reviewers provided a statement, description or direct quotation to support their judgement. A summary assessment of risk was made across all the risks, to inform the interpretation of plausible bias and summary risk of bias is presented in Chapter 4, the overview of results for quantitative and qualitative studies.
Data extraction for randomised controlled trials
Data from the full papers were entered on to a specially designed, pre-piloted and tailored data extraction form, to summarise the intervention. The primary aim of the study was documented (PND prevention, antenatal well-being, birth outcomes, general health, general psychological well-being, infant outcomes or family outcomes). The intervention and comparison arms were described. The data extraction form indicating the main RCT characteristics is presented in Appendix 6.
Outcomes were recorded as maternal, neonatal and family outcomes, using mean [standard deviation (SD)] values when available and numbers and proportions of participants in specific outcome categories. The quality of the extracted data was checked (JM and PS).
Potential moderators
Potential moderators are variables describing population characteristics, for which the intervention may have a different effect for different values of the moderator variable. 127 These were documented when there was some basis for believing that the maternal population characteristics might have a moderating effect on the outcomes, for example maternal age, parity, being a sole parent, history of mental health problems and history of PND. Baseline depression scores were recorded to estimate the population mean depression score for women who entered the studies.
Potential mediators
Potential mediators are variables that could help explain the process by which an intervention was effective. 127 These were documented, such as the timing of the intervention, the provider, the number of sessions offered and whether the intervention was individual based or group based.
Data synthesis of randomised controlled trials
A large number of RCTs and systematic reviews were eligible for inclusion according to our broad inclusion characteristics. We conducted a narrative description of the studies according to the level of preventive intervention (universal, selective or indicated), class of intervention and the context within which the RCTs were undertaken.
Meta-analysis of randomised controlled trials
Methods of evidence synthesis
The extracted data and quality assessment variables were presented, for each study, in structured tables and as a narrative description. Both conventional RCTs, in which individual women were randomised to interventions, and cluster RCTs (CRCTs) were eligible for inclusion. Estimates of treatment effect and standard error of treatment effects from CRCTs were included in the analyses after allowing for the cluster design.
The reference treatment, for comparative purposes and for estimating intervention effects, was defined as usual care. Usual care in the UK, Australia, Canada, France, Norway and the USA was assumed to be sufficiently similar to be interchangeable and was collectively defined as ‘usual care’ for the purpose of the analysis.
The evidence was synthesised using a NMA. 128 A NMA (also known as a mixed-treatment comparison or a multiple treatment comparison) is an extension of a standard (pairwise) meta-analysis. It allows evidence from RCTs comparing different interventions to be combined to provide an internally consistent set of intervention effects while respecting the randomisation used in individual studies. The NMA enables a simultaneous comparison of all evaluated interventions in a single coherent analysis; thus, all interventions can be compared with one another, including comparisons not evaluated within individual studies. The only requirement is that each study must be linked to at least one other study through having at least one intervention in common. The analysis preserves the within-study randomised treatment comparison of each study and assumes that there is consistency across evidence. As with standard pairwise meta-analyses, treatment effects are assumed to be exchangeable across studies. In addition, it is assumed that treatment effects are transitive such that if the effect of intervention 2 relative to intervention 1 is d21 and the effect of intervention 3 relative to intervention 1 is d31, then the effect of intervention 3 relative to intervention 2 is d32 = d31 – d21; this allows a synthesis of direct and indirect evidence about intervention effects and a simultaneous comparison between interventions. Evidence from RCTs presenting data at any assessment time up to 12 months were considered relevant to the decision problem.
Methods for the estimation of efficacy
Statistical model for Edinburgh Postnatal Depression Scale threshold score
The number of women who had an EPDS score greater than a specified threshold was available from several studies at four different postnatal stages depending on the study (i.e. 6 weeks, 3 months, 6 months and 12 months). Most studies used one threshold, although the thresholds varied across studies (i.e. threshold score of 10, 11, 12 and 13). One study129 reported the number of women who had an EPDS score at two thresholds (i.e. 10 and 13).
The EPDS threshold scores were regarded as being ordered categorical data with categories 0–9, 10, 11, 12, 13 and 14 or more. We assumed an underlying proportional odds model such that:
where αj is the cumulative log-odds for the control intervention (x = 0) and β is the log-odds ratio for the experimental intervention (x = 1) relative to the control intervention. The model assumes that the cumulative log-odds ratios are independent of the threshold so that the effect of treatment does not depend on the threshold. Although this may be a strong assumption, it cannot be assessed in studies that use only one threshold, which are all but one study.
Studies were classified as follows:
-
RCTs randomising women to interventions and reporting data using one threshold
-
RCTs randomising women to interventions and reporting data using two thresholds
-
CRCTs.
Randomised controlled trials randomising women to interventions and reporting data using one threshold
For RCTs, randomising women to interventions and reporting data using one threshold, we let rik be the number of women with a response greater than the threshold for each arm out of nik women for arm k in study i. We assumed that the data follow a binomial likelihood such that:
where pik is the probability that a women has a response greater than the threshold in arm k of study i. The pik values are transformed to the real line using a logit link function such that:
where
µi is the study-specific baseline log-odds of having a response greater than the threshold in the control intervention of the study and δi,bk is the study-specific log-odds ratios of having a response greater than the threshold in the intervention group compared with the control intervention, b.
Randomised controlled trials randomising women to interventions and reporting data using two thresholds
For RCTs randomising women to interventions and reporting data using two thresholds, we fitted a proportional odds model using the freely available software package R (The R Foundation for Statistical Computing, Vienna, Austria) using the ‘polr’ function within the MASS package and obtained the sample estimate of the log-odds ratio, yi,bk, and its standard error, Vi,bk, for intervention k relative to intervention b in study i. We assumed that the sample log-odds ratios arose from a normal likelihood such that:
Cluster randomised controlled trials
For two-arm CRCTs (which reported data using one threshold), the sample estimate of the log-odds ratio, yi,bk, and its adjusted standard error, Vi,bk, for intervention k relative to intervention b in study i were extracted and assumed to have arisen from a normal likelihood such that:
For three-arm CRCTs (which reported data using one threshold), the two intervention effects are correlated because they are both estimated relative to the same control. The likelihood function for study i was defined to be bivariate normal such that:
where yi,bk and Vi,bk are as defined before, and se2i,1 is the variance of the control intervention log-odds.
The population standard errors of the log-odds ratios and the population standard error of the control intervention in a three-arm cluster randomised trial were assumed to be known and equal to the sample estimates.
For a random (intervention)-effects model, we assumed that the study-specific log-odds ratios arose from a common population distribution such that:
where d1k is the population log-odds ratios for intervention k relative to the reference intervention (i.e. usual care) and τ is the between-study SD. We assumed a homogenous variance model in which the between-study SD was assumed to be common to all treatment effects. For multiarm trials, these univariate normal distributions are replaced by a multivariate normal distribution to account for correlation between treatment effects within a multiarm study.
Parameters were estimated using Markov chain Monte Carlo simulation conducted using the freely available software package WinBUGS 1.4.3. (MRC Biostatistics Unit, Cambridge, UK). 130
The model was completed by giving the parameters prior distributions:
-
Vague prior distributions for the trial-specific baselines, µi ∼ N(0,1000).
-
Vague prior distributions for the treatment effects relative to reference treatment, d1t ∼ N(0,1000).
Weakly informative prior distribution for the between-study SD of treatment effects, τ ∼ HN(0, 0.322) [in addition, as a sensitivity analysis, the model was also run using the conventional vague prior distribution τ ∼ U(0,2)].
Vague prior distributions were used for trial-specific baseline and treatment effect parameters. However, a weakly informative prior distribution was used for the between-study SD because there were insufficient studies with which to estimate it from the sample data alone; this prior distribution was chosen to ensure that, a priori, 95% of the study-specific odds ratios were within a factor of 2 from the median odds ratio for each treatment comparison.
Convergence of the Markov chains to their stationary distributions was assessed using the Gelman–Rubin statistic. 131 The chains converged within 25,000 iterations; a burn-in of 30,000 iterations was used. We retained a further 10,000 iterations of the Markov chain with which to estimate parameters.
Results are presented as odds ratios [and 95% credible intervals (CrIs)], the between-study SD (and its 95% CrI) and rankograms (i.e. the probability of treatment rankings). CrIs provide an x% interval such that there is a x% probability that the true parameter lies within the interval. Rankograms provide the probabilities of each treatment being ranked as the best, second best, and so on through to the lowest-ranked treatment. The between-study SD provides a measure of heterogeneity in treatment effects between studies; on the log-odds scale, a between-study SD less than 0.5 is indicative of mild heterogeneity, of between 0.5 and 1 is indicative of moderate heterogeneity and of greater than 1 is indicative of extreme heterogeneity.
Statistical model for Edinburgh Postnatal Depression Scale mean scores
The analysis of the EPDS score data was conducted in two stages: (1) a treatment-effects model in which the effect of each intervention was estimated relative to usual care and (2) a baseline (i.e. usual-care) model in which the absolute response to usual care was estimated. The treatment-effects model provides estimates of relative treatment effects which are used to make inferences about the relative effects of interventions. The estimates of treatment effects relative to usual care were combined with the baseline model to provide estimates of absolute responses for each intervention; these estimates were used as inputs to the economic model.
Treatment-effects model
In general, each study provided data for each intervention in each study at baseline and at least one on-treatment assessment time. We excluded the baseline data from the treatment-effects model; the remaining data are longitudinal (i.e. repeated measures) and are correlated between times.
We began by supposing that we have observations, yij = (xij, Sij), for i = 1, 2, . . ., I and j = 1, 2, . . ., J for women in study i receiving intervention j, that is we suppose that the sample mean EPDS scores for women in study i receiving treatment j at times t can be denoted by the vector xij = (xij1, . . ., xijT)T, and that the sample mean variance–covariance matrix, Sij, is:
where the diagonal elements are the variances of the sample means at each time, the off-diagonal elements are the covariances between sample means at different times and the rijSi are the sample estimates of the within-study correlation coefficients, which depend on study si.
Although the woman-specific EPDS scores are discrete in the range 0–30, and the underlying distribution of EPDS scores is unlikely to be normal, we appeal to the central limit theorem which states that as the sample size approaches infinity for any underlying distribution with finite mean and variance, then the distribution of the sample mean is normal. Therefore, we assume that the likelihood for the samples means for women in study i, receiving treatment j is:
where vij = (vij1, . . ., vijT)T represents the study-specific population mean vector of EPDS scores for treatment j in study i.
Published papers provided no information on the correlation between sample means at different times. Therefore, we began by assuming that the rijSi is zero. We also assumed that the population standard errors, σijtnijt were known and equal to the sample standard errors, sijt, where σijt are the population SDs of an individual observation for women in study i, receiving treatment j at time t.
The model for the treatment effects follows that for a NMA of repeated measures as presented by Dakin et al. 132 We estimate the treatment effects separately for each time such that:
where µit is the population mean EPDS score for the baseline treatment (which is allowed to vary between studies) in study i at time t and δijt is the population mean effect of treatment j in study i at time t.
We used an unconstrained baseline model in which the effect of the baseline treatment in each study is fixed at each time, thereby preserving the randomisation within each study. We assumed that the effects of treatment j in study i at time t arose from a normal distribution such that:
where ai,k indicates the treatment used in the kth arm of study i. We assumed a homogeneous variance model in which the between-study SD was assumed to be common to all treatment effects and also across times. For multiarm trials, these univariate normal distributions are replaced by a multivariate normal distribution to account for correlation between treatment effects within a multiarm study.
Parameters were estimated using Markov chain Monte Carlo simulation conduction using WinBUGS 1.4.3. 130
The model was completed by giving the parameters prior distributions:
-
Vague prior distributions for the trial-specific baselines, μi ∼ N(0,1000).
-
Vague prior distributions for the treatment effects relative to reference treatment, d1t ∼ N(0,1000).
-
A weakly informative prior distribution for the between-study SD of treatment effects, τ ∼ HN(0,2).
Vague prior distributions were used for trial-specific baseline and treatment effect parameters. However, a weakly informative prior distribution was used for the between-study SD because there were insufficient studies with which to estimate it from the sample data alone; this prior distribution has median 0.95 (95% CrI 0.04 to 3.17) and was chosen to ensure that, a priori, 95% of the study-specific differences between interventions in mean EPDS scores were within a range ± 3.1 for each treatment comparison.
Convergence of the Markov chains to their stationary distributions was assessed using the Gelman–Rubin statistic. 131 The chains converged within 25,000 iterations; therefore, a burn-in of 30,000 iterations was used. We retained a further 10,000 iterations of the Markov chain to estimate parameters.
Results are presented as differences between intervention in mean EPDS scores and 95% CrIs, the between-study SD (and its 95% CrI) and rankograms (i.e. the probability of treatment rankings) at each time. Crls provide an x% interval such that there is a x% probability that the true parameter lies within the interval. Rankograms provide the probabilities of each treatment being ranked the best, second best, through to the lowest-ranked treatment. The between-study SD provides a measure of heterogeneity in treatment effects between studies; for continuous outcome measures the extent to which the between-study SD indicates mild, moderate or extreme heterogeneity depends on the scale of measurement and the variation within study.
Baseline model
In general, studies in which the control intervention was usual care provided data at baseline and at least one on-treatment assessment time. Therefore, the data are longitudinal (i.e. repeated measures) and are correlated between times.
We began by supposing that we have observations yi = (xi,Si), for i = 1, 2, . . ., I, for women in study i, that is we suppose that the sample mean EPDS scores for women in study i, receiving usual care at times t, can be denoted by the vector xi = (x1i, . . ., xiT)T, and that the sample mean variance–covariance matrix, Si, is:
where the diagonal elements are the variances of the sample means at each time, the off-diagonal elements are the covariances between sample means at different times and the rijSi are the sample estimates of the within-study correlation coefficients, which depend on study si. In practice, not all women provide data at each time and the covariances depend on the number of women who provide data at each time as well as the number of women who provide data at both times. Therefore, the covariance between sample means within a study at times t and t’ is:
Although the woman-specific EPDS scores are discrete in the range 0–30, and the underlying distribution of EPDS scores is unlikely to be normal, we appeal to the central limit theorem which states that as the sample size approaches infinity for any underlying distribution with finite mean and variance, then the distribution of the sample mean is normal. Therefore, we assume that the likelihood for the samples means for women in study i is:
where vi = (vi1, . . ., viT)T represents the study-specific population mean vector of EPDS scores for women in study i, receiving usual care at times t. Studies do not provide data at all times so that the number of times with data, Ti, in study i is such that 1 ≤ Ti ≤ T.
Published papers provided no information on the correlation between sample means at different times. However, using individual woman-level data from the PoNDER (PostNatal Depression Economic evaluation and Randomised controlled trial), we obtained estimates of the correlation coefficients between sample EPDS scores at baseline, 6 months and 12 months to be rb,6m = 0.345, rb,12m = 0.369 and r6m,12m = 0.721. In the absence of any additional external evidence, we made the assumptions as follows:
The model for the baseline effects follows that presented by Wei and Higgins. 133 We let υi∼MVN(Xiµ,XiΩXiT) where Xi is a Ti × T design matrix defining which of the T times are included in the study, µ is a T × 1 vector of underlying mean EPDS scores across studies, and Ω is a T × T matrix representing the between study covariance matrix for all T times. Thus, the studies are linked through the parameters that characterise the distribution of the random effects.
All analyses were conducted in WinBUGS 1.4.3. 130 The model was completed by giving the parameters prior distributions:
-
Vague prior distributions for the treatment effects relative to the reference treatment, d1t ∼ N(0,1000).
-
Weakly informative prior distributions for the between-study SD of treatment effects, τ ∼ HN(0,2).
-
Weakly informative prior distributions for the correlation coefficients U(–1,1).
Vague prior distributions were used for treatment effect parameters. However, a weakly informative prior distribution was used for the between-study SD because there were insufficient studies with which to estimate it from the sample data alone; this prior distribution has a median of 0.95 (95% CrI 0.04 to 3.17) and was chosen to ensure that, a priori, 95% of the study-specific differences in means lie within a range ± 3.1 for each treatment comparison.
Convergence of the Markov chains to their stationary distributions was assessed using the Gelman–Rubin statistic. 131 The chains converged within 10,000 iterations so a burn-in of 10,000 iterations was used. We retained a further 10,000 iterations of the Markov chain to estimate parameters after thinning the chains by retaining every 10th iteration to account for correlation between successive iterations of the Markov chain.
Results are presented as means (and 95% CrIs) and the between-study SD (and its 95% CrI) at each time.
The mean EPDS scores and the covariance matrix were extracted and were coupled with the treatment-effects model to generate absolute EPDS scores for each treatment as inputs to the economic model. Riley134 showed that, in the context of multivariate meta-analyses, ignoring the within-study correlation can have substantial impact on parameter estimates and their correlation expect when the within-study variation is small relative to the between-study variation. Morrell et al. 61 provided information about usual care, cognitive–behavioural approach (CBA)-based intervention and a person-centred approach (PCA)-based intervention at baseline, 6 months and 12 months, and was used to estimate the within-study correlation coefficients.
Methods for reviewing and assessing qualitative studies
Study selection criteria and procedures for the effectiveness review
A two-stage sifting process for inclusion of studies (title and abstract then full paper sift) was undertaken. Titles and abstracts of the qualitative studies were scrutinised by one assessor (AS) using the inclusion and exclusion criteria. No papers were excluded on the basis of quality at this stage. Full papers were obtained for potentially included studies and for where the abstract provided too little information. One-fifth of the total citations identified by electronic database searching (n = 2313) were checked for inclusion or exclusion by AB (n = 427).
Inclusion and exclusion criteria for qualitative studies
The PICOS process was used to clarify the inclusion and exclusion criteria (Box 6).
Population
Studies of populations of antenatal women and postnatal women, at any point postnatally (but with qualitative data concerning the first postnatal year), and health-care practitioners involved in delivering preventive interventions for PND were relevant.
ExcludedStudies of pregnant or postnatal women with diagnosed PND or other comorbid psychiatric disorders or major medical problems.
Comparators
All comparators were considered, whether they were usual care, other controls or specific, alternative comparators.
Outcomes
All outcome measures were considered. All types of data, including case studies, interview data and observations, were considered.
Study designs
No study designs were excluded from the qualitative review (Box 7).
-
Qualitative studies concerning acceptability to pregnant women and service providers, potential harm and adverse effects were extracted.
-
Studies reporting qualitative research, qualitative data elicited via a survey or a mixed-methods study including qualitative data on the perspectives and attitudes of either: (1) those who had received preventive interventions for PND, regardless of modality, in order to examine issues of acceptability; or (2) from women who had not experienced PND, regarding PSSSs that they believed helped them to avoid the condition, in order to identify promising components of any candidate intervention.
-
Qualitative data, embedded in trial reports or in accompanying process evaluations, to inform an understanding of how issues of acceptability were likely to affect the clinical effectiveness of current and potential interventions.
-
Qualitative data, either from separately conceived research or embedded within quantitative study reports, reporting the acceptability of interventions to health-care practitioners.
PSSSs, personal and social support strategies.
Study quality assessment checklists and procedures for qualitative studies
Studies meeting the inclusion criteria were evaluated by two reviewers (AS and AB) using the CERQual (Confidence in the Evidence from Reviews of Qualitative research) approach,135 which aims to assess how much certainty could be placed in the qualitative research evidence, and were rated as ‘very low’, ‘low’, ‘moderate’ or ‘high’. A summary assessment was made for each study, based on the methodological quality of each included study and the coherence of the review findings (the extent to which a clear pattern was identifiable across the individual study data). Coherence was assessed by examining whether or not the review findings were consistent across multiple contexts and incorporated explanations for variation across individual studies. Coherence was strengthened when individual studies contributing to the findings were drawn from a wide range of settings.
The methodological quality of individual studies was appraised using an abbreviated version of the Critical Appraisal Skills Programme (CASP) quality assessment tool for qualitative studies. 136 Two reviewers (AS and AB) independently applied the set of quality criteria to each included study.
Review findings were subsequently graded as ‘high’, ‘moderate’, ‘low’ or ‘very low’ according to the CASP assessment, the number and richness of the data in the studies, the consistency of the data within the studies across study settings and populations and the relevance of the findings to the review question.
Data extraction strategy for qualitative studies
Data extraction from included studies was undertaken by AS using a data extraction tool adapted and tailored for the qualitative review. A 20% sample of data extractions were checked by AB. When data for included studies were missing, reviewers attempted to contact the authors at their last known e-mail address.
Selective extraction of findings137 was undertaken when the data were pertaining to an optimal intervention to be delivered antenatally or postnatally to prevent PND. A framework for extraction was developed to elicit data extraction elements related directly to the review question. The data extraction elements for the data extraction for the studies are presented in Appendix 6. The level of extracted evidence included information on characteristics of the intervention, identified in the results and discussion sections and author comments and interpretation.
Data synthesis for qualitative studies
Qualitative meta-synthesis was undertaken by highlighting women’s and service providers’ issues around the acceptability of interventions, and elucidating evidence around regarding personal and social support strategies (PSSSs) applied by women, using the data extraction framework and thematic synthesis to aggregate the findings. 138 Evidence about interventions from women and service providers and evidence about PSSSs are presented separately (see Appendix 7).
Synthesis drawing upon realist approaches
Identification of key potential CLUSTERs
To exploit the potential of realist synthesis approaches requires rich conceptual and contextual data. Reporting limitations and the varied emphases of published reports make it unlikely that all relevant data are included in a single report of a study. However, the scale and expense of a RCT increases the likelihood that multiple research reports have been produced relating to the study of interest. Such reports may include supplementary qualitative work, process evaluations, student projects, pilot studies, feasibility studies and follow-up studies. All such papers may help us to understand the study context, mechanisms and outcomes. Therefore, a key task is to move from analysis of a single study report to a detailed examination of a cluster of related papers. Such forensic examination looks not only for directly related ‘sibling studies’, but also for tangentially related ‘kinship’ papers (i.e. papers that may represent replication of an existing programme in a different context, thus allowing for comparison and contrast). Finally, syntheses, analyses and theoretical papers may locate the study within a wider context of exemplars or case studies, thereby expanding the potential for comparison. Selection of clusters is necessarily limited by the resources available for analysis. In-depth analysis, as typically performed for realist synthesis, typically precludes the comprehensive and exhaustive approaches prescribed by systematic review methods. In selecting focal study clusters, the team considered both the likely success of the programme and the availability of sibling and/or kinship study reports. At this stage, the Preparing for Parenthood cluster was excluded, as even though it possessed several companion reports the trial did not demonstrate potential effectiveness.
Searching for CLUSTER documents
Searching for documents to populate a study cluster has, until recently, been viewed as essentially an unsystematic and arbitrary procedure. Conceptually it draws upon the long-established retrieval practices outlined in Bates’ seminal paper139 on ‘berry picking’ including ‘backward chaining’ (following up cited references) and ‘forward chaining’ (following up cited articles). Recent years have revealed a prodigious potential yield from supplementary documents. For example, a review by Jagosh et al. 140 revealed several clusters with an average of 12 reports per cluster. We used systematic methods previously developed by one of the authors of our study (AB) for implementing cluster to become CLUSTER searching, for which a full published description of the CLUSTER methods (Citations, Lead authors, Unpublished materials, Scholar searches, Theories, Early examples, Related projects) is openly available. 141 In essence, the research team undertook persistent pursuit of study links, contextual links and theoretical links from the source study or studies to other related reports which then, themselves, initiated a further cause for searching. CLUSTER searching is reliant on relatively rapid judgements on potential links between a referring document and its referent. 141 When papers shared a study identifier or acronym (e.g. PoNDER) or a RCT identifying number, such connections were easy to establish. However, more typically a sibling relationship between papers relies on similarities in authorship, study context and sponsoring institution. However, further checks involve pursuing cross-citation and co-citation so that a network of studies could be constructed.
Synthesis and construction of a theoretical model
For the synthesis stage we developed a rapid realist review approach, provisionally labelled as ‘best-fit realist synthesis’. This involves:
-
identification of a provisional ‘best-fit’ conceptual framework as a starting point for data analysis
-
population of the conceptual framework with ‘if–then’ statements from the identified articles
-
construction of pathways or chains from ‘if–then’ statements to surface potential mechanisms by which outcomes might be achieved
-
identification of existing theory underpinning individual mechanisms
-
development of a programme theory to explain how PND prevention programmes may work
-
testing of the programme theory with contextual data from included studies.
Identification of provisional ‘best fit’ conceptual framework
Given the prominence of group care approaches among the candidate interventions (e.g. CenteringPregnancy or IPT) the research team decided to focus initial analytical attempts on the group-care model and then to seek to highlight similarities and differences with behavioural interventions delivered on an individual basis, either via face to face or via telephone. A search was conducted on Google Scholar (Google Inc., Mountain View, CA, USA), harnessing its extensive full-text searching functionality, using the terms ‘group care’ OR ‘group visits’ AND ‘health education’ AND ‘model’ OR ‘framework’.
Population of the conceptual framework
In examining CLUSTER documents the research team sought to identify mechanisms by which outcomes were achieved in a particular context. Mechanisms were operationalised by construction of a series of ‘if–then’ statements based on causal relationships advanced by the RCT, or hypothesised explanations proposed by either the qualitative research or derived from the ‘Discussion’ sections of the associated study reports.
Construction of pathways or chains from ‘if–then’ statements
‘If–then’ statements were subsequently constructed into complete pathways or partial chains to form an embryonic basis for a theoretical model that attempted to explain how the intervention works for different populations in different contexts from first action through to ultimate outcome. Given the heterogeneity of the interventions present in the initial clusters, it is unsurprising to note the presence of different mechanisms (e.g. between group- and individual-based approaches) and yet common success factors, for example, the establishment of ‘trust’, whether this be between a woman and a health-care provider, between a woman and other members in her group, or between peers. This modelling process provided the facility to explain both generalisable mechanisms and specific areas of variance.
Identification of existing theory underpinning individual mechanisms
Examination of mechanisms by which the interventions sought to meet the various needs of the pregnant women identified several key concepts. In several instances, these concepts were explicitly linked within the study to specific theory or an implicit connection was readily identifiable (e.g. by using terminology associated with a theory).
Development of a programme theory
Based on the conceptual framework, and starting from the premises involved in the group-based model, the research team constructed a programme theory to explain how such a model might work in preventing PND. This overarching programme theory was then examined in more detail to identify where individual-based approaches were unable to meet the same programme requirements and either attempted to substitute for them (e.g. in substituting the resources of the individual peer supporter for the collective resources of facilitator plus group) or offered features not possible within the constraints of the group approach (e.g. in targeting and making application of strategies to the specific needs of the individual).
Data from included studies, quantitative and qualitative, were used to examine the evidence in support of the programme theory. Realist synthesis also accommodates the bringing to bear of a wider evidence base. In this review more proximate evidence was first accessed, identified via a CLUSTER searching approach,141 and then expanded where necessary to a wider set of theoretical and empirical papers. For example, ‘direct’ qualitative data related to the experience of group-based interventions was used to identify the features of such approaches and this was then supplemented by theoretical understandings of the basis underpinning the interventions142 and by middle-range theory examining mechanisms for PND. 143 In this way the explanatory power of the review was broadened beyond the tight focus prescribed by the inclusion criteria.
The supporting data may be limited and may be at a level of abstraction that makes it difficult to identify the exact mechanism by which cause achieves effect. As a consequence, synthesis is to a certain extent an interpretive process which may require the reviewer to identify hypothetical intermediate links in a chain144 by which, for example, training leads to self-efficacy. A further challenge of this method relates to reliance on the detail and quality of reporting; while it is legitimate for the reviewer to generate potential explanations by which a particular outcome is affected, more typically these connections are advanced in the published literature. As a consequence certain explanations may be well rehearsed but poorly substantiated, whereas others may be novel and consequently unsupported. A key stage is therefore the subsequent validation of the ‘if–then’ statements such that they are supported by empirical data or at the very least they are internally consistent with a range of published data sources. To a certain extent the process is analogous with brainstorming processes in which idea generation is deliberately divorced from subsequent validation. In summary, a complete explanation is initially privileged over a high-quality one, with the realisation that a poorly constructed study may perversely yield valuable explanatory insights. Validation of ‘if–then’ statements therefore follows as an important supplemental stage.
Integrating quantitative and qualitative findings
Methodological work to date has been unable to establish the superiority of conducting the qualitative and quantitative synthesis in parallel or of conducting quantitative followed by qualitative, qualitative followed by quantitative or some more iterative approach. Our choice of method of combining data has been determined by the needs of this particular review in which the quantitative data are the main focus and the qualitative data are used for their explanatory potential. Having initially intended to use methods similar to those described by Noyes et al. 145 to explore an effectiveness review in the light of supporting qualitative research data, further examination revealed significant heterogeneity across the types of behavioural intervention used within the included studies. We therefore decided to expand the explanatory potential of our study by drawing upon the methods of realist synthesis.
Typically, realist synthesis explores variation around a single programme type intended to achieve predefined outcomes with much of the variation relating to the population for whom the intervention works). Early examination revealed that most interventions to be included in the review gravitated primarily to either group- or individual-based approaches and we therefore decided to start by examining the programme theory for group-based approaches and then to re-examine this in the light of individual-based approaches. As mentioned previously, realist synthesis embraces the widest possible range of data sources. It therefore becomes a method by which quantitative and qualitative data might potentially be integrated. For example, an hypothesis generated by a qualitative report may be substantiated by a trial that formally establishes the mechanism of cause and effect. Alternatively, the qualitative report may enable the review to help explain how a particular outcome might be achieved. It may also specify aspects of an intervention considered important by women that may map to specific components either present in a current intervention or mooted for inclusion in a future intervention yet to be studied within a trial.
Chapter 4 Overview of results for quantitative and qualitative studies
Literature search for the quantitative review
The electronic searches identified 3072 references; following removal of duplicates, 2064 remained. A total of 180 additional records were identified from other sources. Following removal of duplicates, there were 2244 records to be screened, of which 1910 were excluded at title/abstract level. The full text of the remaining 256 records was examined, following which 122 (representing 86 unique studies) were included in the review and 134 were excluded. The 122 included papers reported 80 conventional RCTs in which individual women were randomised to interventions and six CRCTs. 61,146–150 The 86 RCTs were reported in multiple publications; one study61 included two levels of analysis that were reported in different publications. 151,152 Throughout this review, these 86 RCTs are cited according to the first author of their corresponding original publications.
The search of ongoing trials in Clinical Trials.gov, Current Controlled Trials and UK Clinical Research Network Portfolio databases (carried out in September 2013) retrieved 47 potentially relevant records. However, none of these met the criteria for inclusion in the review.
A flow diagram outlining the process of identifying relevant literature and the 86 included RCTs, along with reasons for exclusion of full-text articles, is provided in Figure 2.
FIGURE 2.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart of studies included in the quantitative review.

Quantitative review study characteristics
An overview of the 86 included RCTs is presented here. 61,121,123,129,146–150,153–229
Yield of systematic reviews
Twenty-three reviews were included (i.e. Austin et al. ,230 Bennett et al. ,231 Cuijpers et al. ,68 Dale et al. ,232 Dennis and Creedy,233 Dennis,234 Dennis,118 Dennis,235 Dennis and Kingston,236 Dennis et al. ,237 Dennis,238 Dodd and Crowther,239 Fontein-Kuipers et al. ,240 Howard et al. ,241 Jans et al. ,242 Lawrie et al. ,243 Leis et al. ,244 Lumley et al. ,245 Marc et al. ,246 Miller et al. ,247 Sado et al. ,248 Shaw et al. 249 and Sockol et al. 250), of which one provided an additional included study not identified in the searches. 191 The included reviews are summarised in Appendix 8.
Quantitative review study characteristics
Some studies are reported in multiple references, for example Armstrong et al. 1999,164,251,252 Brugha et al. 2000,188,253,254 Chabrol et al. 2002,158,255,256 Cooper et al. 2009,153,257 Dennis et al. 2009,205,258 Gamble et al. 2005,221,259,260 Harrison-Hohner et al. 2001,208,261 Ickovics et al. 2011,222,262 Lumley et al. 2006,147,263 MacArthur et al. 2002,146,264 Makrides et al. 2010,211,265 Morrell et al. 2000,199,266 Morrell et al. 2009,61,151,152 Petrou et al. 2006,174,267 Reid et al. 2002,200,268 Richter et al. 2014,203,269 Rotheram-Borus et al. 2011,226,270 Sen 2006,191,271 Stamp et al. 1995,195,272 Wisner et al. 2001,215,273 Wisner et al. 2004216,274 and Wolman et al. 1993. 204,275,276 Henceforth studies are referred to by the first identifying reference only.
Level of preventive intervention
The 86 RCTs, one reporting both a universal preventive intervention level of analysis and an indicated preventive intervention level of analysis,61,151 comprised:
-
37 trials reporting a universal preventive intervention61,123,129,146,147,150,153–157,180–187,197–200,207–212,217–220,225–228
-
20 trials reporting a selective preventive intervention149,158–163,188–192,201–204,213,221–223
-
30 trials reporting an indicated preventive intervention. 61,121,148,164–179,193–196,205,206,214–216,224,229
Study location
In total, 15 of the included RCTs were undertaken in the UK,61,146,149,150,174,177,188,191,199–201,206,213,219,224 31 in the USA,121,160,161,163,166–173,178–181,187,190,192,197,198,202,208,210,212,214–216,222,227,229 18 in Australia,123,147,159,164,165,182,184,185,189,195,196,211,217,218,220,221,223,225 five in South Africa,153,203,204,209,226 three in the China,154,157,162 two in Canada,186,205 two in Hong Kong,156,175 two in the Republic of China (Taiwan)183,193 and one each in France,158 Germany,176 Hungary,155 Japan,228 Mexico,194 the Netherlands,207 Norway129 and Pakistan. 148
Participants
A total of 66,418 participants were randomised across the 86 trials, with the individual trial sample sizes ranging from 25 to 18,555 participants. The mean number of participants was 772.3 (SD 2210). The mean (SD) age of participants was 27.16 years (SD 4.06 years).
Intervention class
Seven intervention types were identified across the 86 RCTs, these were:
Outcome assessment
The studies varied in their duration and assessment times: 6–8 weeks, 10–12 weeks, 3 or 4 months, 5 months, 6 months, 7 months, and 12 months postnatally.
Following the description of the overall study quality, the RCTs are described fully according to the level of preventive intervention in Chapters 5–7.
Quality of quantitative studies
Overall risk of bias of randomised controlled trials
Selection bias
Of all the 86 RCTs, 64 (74.4%) reported an adequate method for random sequence generation (low risk of bias), 16 (19.0%) were unclear about the allocation method (unclear risk of bias) and six (7.0%) had used a non-random process (high risk of bias). The greatest level of risk was associated with allocation concealment. Furthermore, 50 RCTs (58.1%) reported adequate treatment allocation concealment (low risk of bias), 27 (31.4%) were unclear (unclear risk of bias) and nine (10.5%) were at high risk of bias.
Performance bias
The nature of most of the interventions made blinding of participants and caregivers not possible, but it is unlikely that the lack of blinding could not have affected the results. Therefore, 73 RCTs (84.9%) were rated as being at low risk of performance bias for the assessment of blinding for participants and staff, 12 (14.0%) were rated as being at unclear risk of bias and one RCT (1.2%) was rated as at high risk of bias for failing to report blinding status of the women and study personnel. In 61 RCTs (71%), outcome assessors were reported to be blinded (low risk of bias), in 24 (28.0%) it was not clear if the outcome assessors were blinded (unclear risk of bias) and in one RCT the risk of bias was rated as high.
Attrition bias
The risk of attrition bias was assessed as low for 51 (59.3%) RCTs, and unclear for 27 RCTs (31.4%); eight (9.3%) RCTs were assessed as being at high risk for selective outcome and/or analysis bias.
Reporting bias and other bias
The risk of reporting bias was assessed as low in 74 RCTs (86%), unclear in eight RCTs (9.3%) and high in four RCTs (4.7%).
The risk of other bias (e.g. funding source or inappropriate analysis) was judged to be low for 54 RCTs (62.8%), unclear for 28 (32.6%) and high for four (4.7%).
Overall, the risks of bias were rated as higher for universal preventive intervention studies than for the selective and indicated preventive interventions; this was most notable for selection bias and attrition bias. The judgements about each risk of bias domain are presented in Tables 1–3 for each included study according to the level of preventive intervention (universal, selective or indicated) and summarised in Figure 3 for all included studies.
| First author, year, reference number | Selection bias | Performance bias | Detection bias | Attrition bias | Reporting bias | Other bias | |
|---|---|---|---|---|---|---|---|
| Random sequence generation | Allocation concealment | Blinding of participants/personnel | Blinding of outcome assessors | Incomplete outcome data | Selective reporting of the outcome, subgroups, or analysis | Funding source, adequacy of statistical methods used, type of analysis (ITT/PP), baseline imbalance in important characteristics | |
| Christie, 2011150 | Low | Low | Unclear | Low | Low | Low | Low |
| Cooper, 2009153 | Low | Unclear | Unclear | Low | Low | Low | Low |
| Doornbos, 2009207 | Low | Unclear | Low | Low | High | Low | Unclear |
| Feinberg, 2008180 | Unclear | Unclear | Unclear | Low | Low | Low | Low |
| Fujita, 2006228 | Unclear | Unclear | Low | Low | High | Low | Unclear |
| Gao, 2010154 | Low | Low | Low | Low | Low | Low | Low |
| Gjerdingen, 2002181 | Low | Unclear | Unclear | Low | Unclear | High | High |
| Gunn, 1998225 | Low | Low | Low | Low | Low | Low | Low |
| Harrison-Hohner, 2001208 | Low | Low | Unclear | Unclear | High | High | High |
| Hayes, 2001182 | Low | Low | Low | Unclear | Low | Low | Unclear |
| Ho, 2009183 | High | High | Low | Low | Low | Low | Unclear |
| Hodnett, 2002197 | Low | Low | Low | Unclear | Low | Low | Low |
| Kieffer, 2013198 | Low | Low | Low | Low | Low | Low | Low |
| Kozinsky, 2012155 | High | High | Unclear | Unclear | Unclear | High | High |
| Lawrie, 1998209 | Low | Low | Low | Low | Low | Low | Low |
| Leung, 2012156 | Low | Low | Low | Low | Low | Low | Low |
| Llorente, 2003210 | Low | Low | Low | Unclear | Unclear | Low | Unclear |
| Lumley, 2006147 | Low | Unclear | Low | Low | Unclear | Low | Low |
| MacArthur, 2002146 | Low | Low | Low | Low | Low | Low | Low |
| Makrides, 2010211 | Low | Low | Low | Low | Low | Low | Low |
| Mao, 2012157 | Low | Low | Low | Low | Low | Low | Unclear |
| Matthey, 2004184 | Unclear | Unclear | Low | Low | Low | Low | Unclear |
| Milgrom, 2011185 | Low | Low | Low | Unclear | Unclear | Low | Low |
| Mokhber, 2011212 | Unclear | Unclear | Low | Low | Unclear | Low | Unclear |
| Morrell, 2000199 | Low | Low | Low | Low | Low | Low | Low |
| Morrell, 200961 | Low | Low | Low | Low | Low | Low | Low |
| Norman, 2010123 | Low | Low | Low | Low | Unclear | Unclear | Unclear |
| Priest, 2003217 | Low | Unclear | Low | Low | Low | Low | Low |
| Reid, 2002200 | Low | Low | Low | Low | Low | Low | Low |
| Rotheram-Borus, 2011226 | Low | Low | Low | Low | Low | Low | Low |
| Sealy, 2009186 | High | High | Low | Low | Unclear | Low | Unclear |
| Selkirk, 2006218 | High | High | High | Low | High | Low | Low |
| Serwint, 1991227 | High | High | Low | Low | Low | Low | Low |
| Shapiro, 2005187 | Unclear | Unclear | Low | High | High | Low | Unclear |
| Shields, 1997219 | Low | Unclear | Low | Low | Unclear | Unclear | Low |
| Songøygard, 2012129 | Low | Low | Low | Low | Unclear | Unclear | Unclear |
| Waldenstrom, 2000220 | Low | Low | Low | Low | Unclear | Low | Low |
| First author, year, reference number | Selection bias | Performance bias | Detection bias | Attrition bias | Reporting bias | Other bias | |
|---|---|---|---|---|---|---|---|
| Random sequence generation | Allocation concealment | Blinding of participants/personnel | Blinding of outcome assessors | Incomplete outcome data | Selective reporting of the outcome, subgroups, or analysis | Funding source, adequacy of statistical methods used, type of analysis (ITT/PP), baseline imbalance in important characteristics | |
| Barnes, 2009149 | Unclear | Unclear | Low | Low | Unclear | Low | Unclear |
| Brugha, 2000188 | Low | Unclear | Low | Unclear | Low | Low | Low |
| Buist, 1999189 | Unclear | Unclear | Low | Low | Unclear | Unclear | Unclear |
| Chabrol, 2002158 | Unclear | High | Low | Unclear | Unclear | Low | Unclear |
| Cupples, 2011201 | Low | Low | Low | Low | Low | Low | Low |
| Gamble, 2005221 | Low | Low | Low | Low | Low | Low | Low |
| Hagan, 2004159 | Low | Low | Low | Low | Low | Low | Low |
| Harris, 2002213 | Low | Unclear | Low | Low | Unclear | Unclear | Unclear |
| Howell, 2012190 | Low | Low | Low | Low | Low | Low | Low |
| Ickovics, 2011222 | Low | Low | Low | Low | Low | Low | Low |
| Logsdon, 2005202 | Low | Unclear | Unclear | Low | Unclear | Low | Unclear |
| Phipps, 2013160 | Low | Low | Low | Low | Low | Low | Low |
| Richter, 2014203 | Low | Low | Low | Unclear | High | Unclear | Unclear |
| Sen, 2006191 | Low | Low | Low | Low | Low | Low | Low |
| Silverstein, 2011161 | Low | Low | Low | Low | Low | Low | Low |
| Small, 2000223 | Low | Low | Low | Low | Low | Low | Low |
| Tam, 2003162 | Low | Low | Unclear | Unclear | Unclear | Low | Unclear |
| Walkup, 2009192 | Low | Low | Low | Low | Unclear | Low | Low |
| Wolman, 1993204 | Low | Low | Low | Unclear | Unclear | Low | Low |
| Zlotnick, 2011163 | Low | Low | Low | Unclear | Low | Low | Low |
| First author, year, reference number | Selection bias | Performance bias | Detection bias | Attrition bias | Reporting bias | Other bias | |
|---|---|---|---|---|---|---|---|
| Random sequence generation | Allocation concealment | Blinding of participants/personnel | Blinding of outcome assessors | Incomplete outcome data | Selective reporting of the outcome subgroups or analysis | Funding source adequacy of statistical methods used type of analysis (ITT/PP) baseline imbalance in important characteristics | |
| Armstrong, 1999164 | Low | Low | Low | Low | Low | Low | Low |
| Austin, 2008165 | Low | Unclear | Low | Low | Unclear | Unclear | Unclear |
| Crockett, 2008166 | Unclear | Unclear | Low | Unclear | Low | Low | Unclear |
| Dennis, 2009205 | Low | Low | Low | Low | Low | Low | Low |
| El-Mohandes, 2008167 | Low | Low | Low | Low | Low | Low | Low |
| Ginsburg, 2012168 | Unclear | Unclear | Low | Unclear | Unclear | Low | Unclear |
| Gorman, 1997169 | Unclear | Unclear | Unclear | Low | Low | Low | Low |
| Grote, 2009170 | Low | Unclear | Low | Unclear | Low | Low | Low |
| Harris, 2006206 | Low | Low | Low | Unclear | Unclear | Unclear | Unclear |
| Heh, 2003193 | High | High | Low | Low | Low | Low | Unclear |
| Lara, 2010194 | Low | Low | Low | Unclear | High | Low | High |
| Le, 2011171 | Low | Low | Low | Unclear | Low | Low | Low |
| Manber, 2004229 | Unclear | Unclear | Unclear | Unclear | Unclear | Low | Unclear |
| Marks, 2003224 | Low | Low | Unclear | Unclear | Low | Low | Unclear |
| McKee, 2006172 | Unclear | Unclear | Low | Unclear | High | Low | Unclear |
| Morrell, 200961 | Low | Low | Low | Low | Low | Low | Low |
| Mozurkewich, 2013214 | Low | Low | Low | Low | Low | Low | Low |
| Munoz, 1998173 | Low | Low | Low | Unclear | Low | Low | Low |
| Petrou, 2006174 | Low | Low | Low | Low | Low | Low | Low |
| Rahman, 2008148 | Low | Low | Low | Low | Low | Low | Low |
| Stamp, 1995195 | Low | Low | Low | Low | Low | Low | Low |
| Tiwari, 2005175 | Low | Low | Low | Low | Low | Low | Low |
| Vieten, 2008121 | Unclear | Unclear | Low | Low | Unclear | High | Unclear |
| Webster, 2003196 | Low | Low | Low | Low | Unclear | Low | Low |
| Weidner, 2010176 | Low | High | Low | Low | Unclear | Low | Low |
| Wilson, 2013177 | Low | High | Low | Unclear | Unclear | Low | Low |
| Wisner, 2001215 | Low | Low | Low | Low | Low | Low | Low |
| Wisner, 2004216 | Low | Low | Low | Low | Low | Low | Low |
| Zlotnick, 2001178 | Unclear | Unclear | Low | Unclear | Low | Low | Low |
| Zlotnick, 2006179 | Low | Unclear | Low | Unclear | Low | Low | Low |
FIGURE 3.
Risk-of-bias graph for all included RCTs: authors’ judgements about each risk-of-bias item. Key: ITT, intention to treat; NA, not applicable; PP, per protocol.
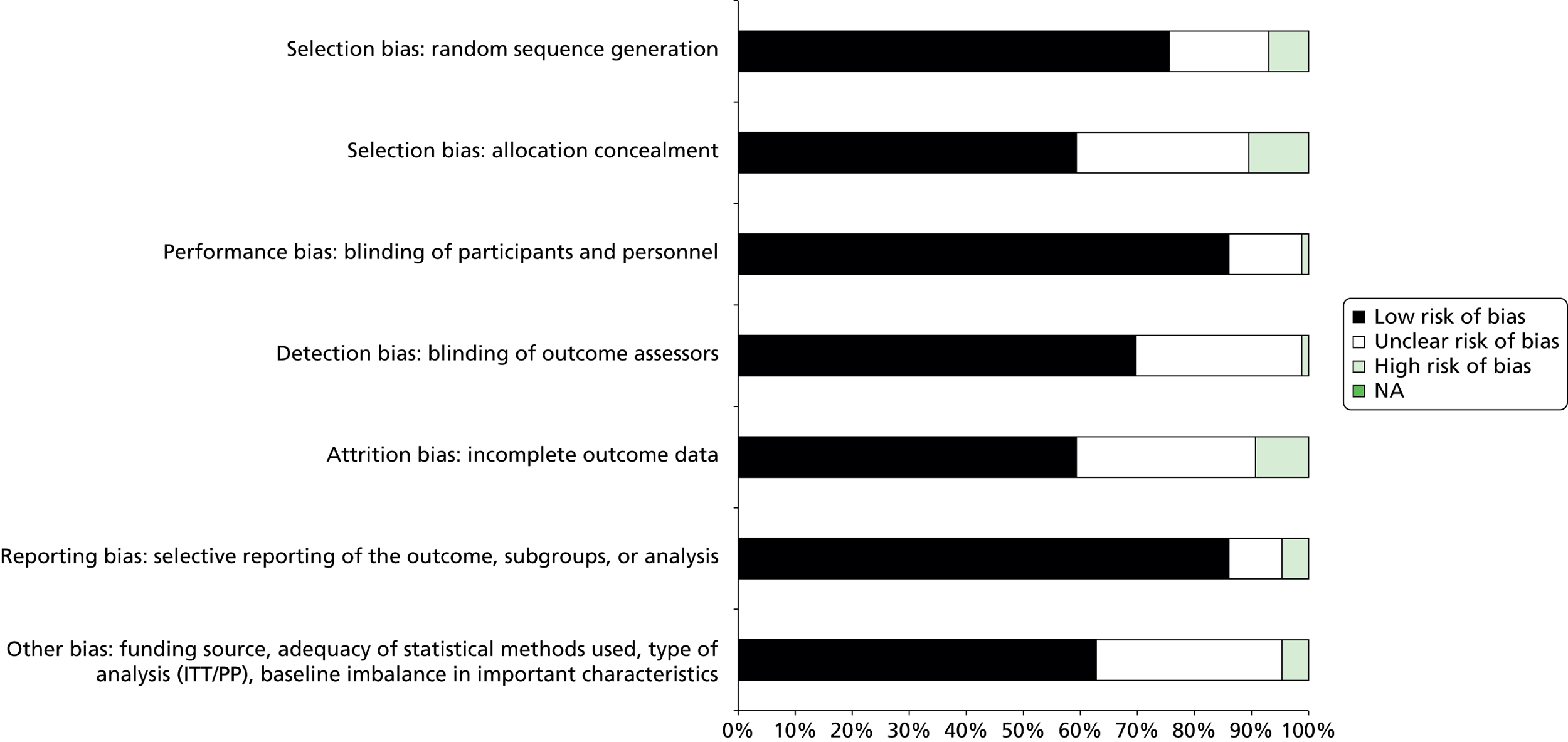
Quality of systematic and other reviews
No quality assessment was undertaken for the systematic reviews.
Literature search for the qualitative review
The electronic searches identified 2131 records after removal of duplicates and a further 20 records that were from other sources. Overall, 2151 records were screened by title and abstract and 1991 were excluded. The remaining 56 records (representing 44 unique studies) were included and the full text examined. A flow diagram outlining the identification of relevant included qualitative studies and reasons for exclusion of full-text articles is provided in Figure 4.
FIGURE 4.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart of studies included in the qualitative review. Key: PTSD, post-traumatic stress disorder.

Qualitative studies level of preventive intervention
Among the 21 studies (27 citations):
-
Fourteen were studies of a universal preventive intervention. Twelve studies reported qualitative data on the perspectives and attitudes of those who had received universal preventive interventions for PND277–289 (of these, two also reported perspectives and attitudes of service providers on universal preventive interventions287,288 and two studies reported only on the perspectives and attitudes of service providers to preventive interventions). 290,291
-
Four studies presented data from those who had received a selective preventive intervention292–298 (with one study additionally presenting data relating to an indicated population). 296–298 Of these, one study also reported perspectives and attitudes of service providers on selective preventive interventions. 296–298
-
Three studies presented data from those who had received an indicated preventive intervention. 253,256,299,300 One study, with a separate citation,301 additionally reported on the perspectives of and attitudes of service providers on indicated preventive interventions.
These data are synthesised in Chapters 5–7. The remaining 29 (23 studies) citations about PSSSs that women believed helped prevent PND are synthesised in Chapter 8, the realist synthesis and are presented separately (see Appendix 7).
Qualitative review study characteristics
Study location
Of the included studies, two were undertaken in the UK,253,254,287 seven in the USA,283,284,286,291–298 one in Sweden,277 one in Ireland,278,279 four in Australia,280,288,289,300 three in Canada281,285,290,299,301 and one in China. 282
Participants
The studies contained qualitative data from 940 service users (when reported) and from 29 service providers (when reported). Service provider data came from four clinicians,296–298 three nurses,288 two certified nurse-midwives and two medical assistants,293–295 three physicians,290 four certified nurse midwives, five health centre staff and five administrators,284 from support workers, midwives and health visitors287 and from peer volunteers. 301 The age range of the women was reported in eight studies. Age ranged from 13 to 45 years. Ethnicity was reported in 13 studies. 280,282–286,290,292–298,300 For further details of participant characteristics see Appendix 9.
Qualitative review study characteristics: personal and social support strategy studies
A total of 23 studies (n = 29 citations) reported qualitative data on perspectives and attitudes of women who had not experienced PND, regarding PSSSs that they believe helped them to prevent the condition. 7,302–325 This included five citations from three intervention studies which included PSSS evidence. 286,292,296–298
Study location
Ten studies were conducted in the UK,304,306–315,319,321,322,324 seven studies were conducted in the USA,286,292,296–298,302,303,318,320 one in Switzerland,316 one in Canada,317 one in Norway,323 one in India,325 one in China305 and one in multiple centres. 7
Participants
The total number of reported participants contributing qualitative evidence was 801 (one study did not provide the number of participants who contributed to qualitative findings). 7 Fifteen studies provided data from participants who were part of the general population in the country of study, whereas the remaining studies examined evidence from minority groups within the country of study. The minority groups either were a culturally different group based within the country of study (n = 5)304,306–311,314,318 or were a selective group (n = 3). 292,296–298,315 For details of participant characteristics, see Appendix 9.
Quality of the qualitative intervention studies
All studies met the requirement to report either qualitative research or qualitative data within mixed-methods studies, indicated in Table 4. All included studies also adequately described the context and aims of the study. Few (29%) demonstrated evidence of researcher reflexivity (i.e. awareness of the researcher’s contribution to the construction of meanings throughout the research process and an acknowledgement of the impossibility of remaining ‘outside’ one’s subject matter while conducting research); among those which did, these descriptions were brief. A number of studies illustrated that reflexivity in the research process had been incorporated, such as making changes to the interview guide as necessary and responding to participants’ wishes. All 21 studies provided adequate descriptions of recruitment methods, just over half (n = 13) provided adequate descriptions of data collection methods, although such descriptions tended to be brief. The study methods used involved interview methods in nine studies, supplemented by other methods such as focus groups and observation in three studies. Qualitative data came from open-ended questions as part of a questionnaire in three studies. Two studies used focus groups and one study used online messages. Twelve studies provided an adequate description of data analysis methods, and 13 studies provided sufficiently in-depth, detailed and rich data. The absence of detail in the remaining studies may have been, in part, because of limitations imposed by journal reporting requirements.
| Question | Yes/somewhat, (n = 21 studies) | |
|---|---|---|
| 1 | Is the study qualitative research/or provide qualitative data? | 21/21 |
| 2 | Is the study context and aims clearly described? | 21/21 |
| 3 | Is there evidence of researcher reflexivity? | 6/21 |
| 4 | Are the sampling methods clearly described and appropriate for the research question? | 21/21 |
| 5 | Are the methods of data collection clearly described and appropriate to the research question? | 13/21 |
| 6 | Is the method of analysis clearly described and appropriate to the research question? | 12/21 |
| 7 | Are the claims made supported by sufficient evidence? That is, did the data provide sufficient depth, detail and richness? | 13/21 |
Certainty of the review findings: intervention studies
The CERQual approach137 was used to assess the certainty of the review findings, graded as ‘very low’, ‘low’, ‘moderate’ or ‘high’. A summary assessment was based on the CASP quality assessment finding,136 the number and richness of the study data, the consistency of the data across study settings and populations, and the relevance of the finding to the review question. There were 37 findings in women’s evidence: nine were assessed as of moderate certainty, 25 as low and three as of very low certainty. For service providers’ evidence, there were 25 findings: one finding was assessed as being of moderate certainty, 18 as of low certainty and six as of very low certainty. No findings were assessed as high certainty.
Overview of main findings from qualitative intervention studies (all levels)
Psychological
Women reported that IPT served to promote the development of relationships with other group members, which had a normalising effect. 282–285 It facilitated gaining support from family members. Women also reported that they appreciated the support of the midwife as part of the intervention. Participants reported learning useful and applicable practical strategies. 282 IPT facilitated the gaining of knowledge and the active participation of women in their own health care specifically, in realistic information about motherhood and in the empowerment to ask for help.
Educational
The Preparing for Parenthood intervention was aimed at improving women’s knowledge and active participation in their own health care,253,254 specifically gaining information about sensitive subjects such as PND. Although appearing to want information about PND, women who attended the Preparation of Parentedhood intervention were reluctant to ask for information because of the fear of stigma. Other women appeared to avoid information about PND; authors interpreted this as a belief that lack of knowledge could operate as a protective factor. Although most women reported benefits of the group environment, a few did not want to join because of privacy concerns. Most participants valued the opportunity provided for their partner to join the group and were interested in the partner involvement session.
Social support
The qualitative review demonstrated that both women and service providers felt the support group and support intervention adequately provided emotional and informational support, reassurance and validation. Participants of the support worker intervention287 reported that the intervention would have been more beneficial if it were more intensive. Concerns articulated by service providers included worries about their own ability to deal with unpredictable situations and women’s overdependence on the service. 287,288
Midwifery-led interventions
Peer support, partner support and support from health professionals were particularly helpful aspects of the CenteringPregnancy intervention. 277,283,285,289–294 Specifically, a supportive environment and the opportunity to share experiences were appreciated. However, some women reported a dislike for the group environment and the inclusion of partners because of concerns regarding privacy. 277 Some partners also felt uncomfortable with their own inclusion for similar reasons. 277 Women felt the health professionals were able to pay more attention to their own concerns and offer them more solutions,285 although the skill of the midwife was an important factor in the success of the intervention. 277 Service providers felt the intervention promoted better communication between providers and users and between health providers. They were able to develop better relationships with the intervention recipients and the enhanced communication served to facilitate information exchange. 290 Education and information about pregnancy and the postnatal period were valued. 283,284,293,294 However, the evidence indicated283,289 that some women wanted more, and more intensive, education on issues relating to labour, birth and parenting, particularly about the early weeks of parenting.
Organisation of maternity care
The support women received from the health professionals delivering the service was felt to be helpful,288,300 although a lack of understanding of the role of the maternal and child health nurse created a potential barrier to accessing the service. 288 Women reported that they felt able to rely on the service, particularly if they needed the service urgently. 300 However, concerns included feeling intimidated by the thought of referral to the specialist perinatal and infant mental health service,300 worries about stigma associated with using the service288 and concerns about being ready to be discharged. 300
Complementary and alternative medicine or other intervention
Women reported that the CAM interventions provided peer support, specifically by the sharing of experiences and birth stories, and the facilitation of family support. 278–280,286 They reported the practical use of strategies learned during the intervention. 278,279,286 However, some difficulty in being able to apply learned techniques in practice was expressed,286 together with a concern that the use of the learned strategies could result in unexpected emotional responses. 278,279 The interventions facilitated preparation for birth, both emotionally278–280 and physically. 280
Tables 5–12 provide a synthesis of the qualitative evidence across all types of intervention.
| Meta-theme | Subtheme | Mechanism (with examples) | Evidence source: CASPa | Certainty in CERQual137 |
|---|---|---|---|---|
| Support | Peer support | Peer support, providing reassurance, normalisation of experiences, emotional support, practical advice and informational advice. Achieved through reading about peer experiences,281 sharing experiences277,283 and through the development of friendship and relationships and forming a connection with others280 | Moderate (× 6)/low | Moderate |
| Family support | Practical and emotional support from the family facilitated by educating family members, through provision for men/partners to join the group to be supported283 and partners being encouraged to be actively involved in intervention289 through family joining the group and participants teaching their partner or mother the song learned in the group278,279 | Moderate (× 3)/low | Moderate | |
| Educating the intervention recipients about ‘doing the month’ served to facilitate development of a relationship with the mother-in-law, leading to her providing practical support282 | Moderate | Moderate | ||
| Health professional support | Health professionals leading the intervention were seen as having concern for participants, providing emotional and practical support. Specifically, discussions with nurses,288 support workers287 or social support from the midwife, through telephone follow-up282 were reported as being helpful | Moderate (× 3)/low (× 2) | Moderate | |
| Partner support | Partners’ support in applying techniques learned through the intervention, which went on to facilitate better communication between the partners286,289 | High/low | Low | |
| Empowerment | Education/active participation in own health care | Participants empowered by being allowed to weigh themselves,283 providing education and information280,282,284 | Moderate | Moderate |
| Learning practical strategies/skills/knowledge | Learning practical strategies, such as singing,278,279 problem-solving skills, mind–body exercises and techniques286 to be applied during pregnancy or in the postpartum period . These included the ability to calm the infant,278,279 the gaining of information about sensitive subjects such as PND282 and realistic information about motherhood; thus helping participants accept the reality of early motherhood282 | Moderate/high/moderate | Moderate | |
| Self-esteem | Yoga provided emotional preparation for birth280 | Moderate | Low | |
| Interventions promoted abilities in dealing with offers of support and asking for support, and developing a good relationship with mother-in-law, to be empowered to ask for help282 | Moderate | Low | ||
| Time out/relaxation/socialisation | – | Reduction of stress and anxiety, and countering isolation by the provision of socialisation in a group278,279 or via a one-to-one intervention287 | Moderate/moderate/low | |
| Physical preparation/recovery | – | Yoga practice as part of the group intervention promoted preparation for birth and quicker physical recovery from birth280 | Moderate | Low |
| Reduced waiting times | – | A group, rather than individual, format resulted in reduced waiting times289 | Low | Very low |
| Continuity of care | – | Group intervention promoted continuity of care277 | Moderate | Low |
| Connecting with the baby | – | Yoga aspect of group intervention promoted connection with unborn baby280 | Moderate | Low |
| Safe space | – | Group intervention provided a safe space280 | Moderate | Low |
| An intervention for the prevention of PND was unhelpful when it resulted in a perception of | Evidence source: CASP | Certainty in CERQual137 |
|---|---|---|
| Lack of support, as a result of partners feeling uncomfortable with discussions and thus disengaging283 | Moderate | Moderate |
| Inability to implement learned strategies without the support of the group286 | High | Moderate |
| Difficult to raise questions with partners present at group intervention84,283 | Moderate | Moderate |
| An unexpected emotional response because of the application of the strategies learned in the group (singing) resulting in a ‘profound’ emotional response85,279 | Moderate | Low |
| Feeling rushed by health professionals during the intervention90 | Moderate | Low |
| Lack of privacy during the intervention90 | Moderate | Low |
| Lack of consideration for workload, specific to a service in a military setting90 | Moderate | Low |
| Midwife being too controlling, and not asking about the wishes of the group84 | Moderate | Low |
| Service was not family centred and older children were not welcome at the service90 | Moderate | Low |
| Service providers were scrimping and cost-saving on care (women were asked to deliver their own samples to the laboratory)90 | Moderate | Low |
| Not being able to implement strategies because of forgetfulness3 | High | Low |
| Format of the sessions was not ideal because a 2-hour session was too long96 | Low | Low |
| A long interval between first and second group meetings84 | Moderate | Moderate |
| Group format was disliked84 | Moderate | Low |
| An intervention for prevention of PND should have included | Evidence source: CASP | Certainty in CERQual137 |
|---|---|---|
| Education, specifically about the early weeks of parenting289 | Low | Very low |
| More intensive intervention, more visits and longer visits287 | Low | Very low |
| Something different from the mainstream (CAM)280 | Moderate | Low |
| Structure to the group aspect280 | Moderate | Low |
| More drinks/refreshments283 | Moderate | Low |
| Barriers to participation included | Evidence source: CASPa | Certainty in CERQual137 |
|---|---|---|
| Poor access to the service, including practical difficulties in getting to appointments and physical limitations (bleeding) which hindered attendance283 | Moderate | Low |
| Unhelpful front-desk staff, long waits and ‘brush-offs’283 | Moderate | Low |
| Not understanding role of the service provider288 | Moderate | Low |
| Not associating the depression with pregnancy/postpartum period286,288 | Moderate/high | Moderate |
| Perceived stigma related to the admission of not being able to cope286,288 | Moderate/high | Moderate |
| Being unable to see use of strategies learned during pregnancy for the postpartum period286 | High | Low |
| Being unable to find the time to implement strategies learned286 | High | Low |
| Things helpful for the intervention recipients | Evidence source: CASPa | Certainty in CERQual137 |
|---|---|---|
| Peer support through sharing experiences providing reassurance, normalisation of experiences, emotional support, practical support and informational advice287,290,291 | Moderate/moderate/low | Moderate |
| Education, group environment provided more opportunity for teaching284,291 | Moderate | Low |
| Women’s active participation in their own health care (empowerment); the group environment allowed more time to be allocated to this284,290 | Moderate | Low |
| Better communication between provider and user, facilitating information exchange in the group setting290 | Moderate | Low |
| Health professional developed better relationships with service users in the group setting290 | Moderate | Low |
| Provision of richer care provided in a group setting290,291 | Moderate | Low |
| Women’s enthusiasm about a group setting served to increase participation284 | Moderate | Low |
| Group setting allowed more women to be seen in same amount of time, thereby addressing waiting time issues284 | Moderate | Low |
| Sensitivity to the women and a subtle and non-threatening manner in approach to issues288 | Moderate | Low |
| Things helpful for the health professionals delivering the intervention | ||
| Group setting resulted in more efficient use of time290 | Moderate | Low |
| Health professionals found delivering the group intervention enjoyable, satisfying and a rewarding experience290,291 | Moderate | Low |
| Delivering an innovative (group) intervention brought recognition to the site (health centre)284 | Moderate | Low |
| Things that health professionals thought did not help prevent PND | Evidence source: CASPa | Certainty in CERQual137 |
|---|---|---|
| Restricting service to selective groups, through staff and provider bias, for example only for teens291 | Moderate | Low |
| Difficulties in funding the service284,291 | Moderate | Low |
| Difficulties in facilitating access to the service because of work conflicts for service providers and transportation difficulties for women attending groups, and also for support workers travelling to women’s homes to deliver the one-to-one intervention287,291 | Moderate/low | Low |
| Women’s resistance to the intervention or discontinuation of the intervention because of participants’ resistance to a group format291 or the individual support worker visit was anxiety inducing287 | Moderate/low | Low |
| Group interventions result in provider having less opportunity for one-to-one care284 | Moderate | Low |
| Inability to address deeply personal issues in group setting. Service providers felt that deeper issues were not appropriate to be discussed in a group setting284 | Moderate | Low |
| Scheduling difficulties as while one provider was doing group care the other had to deal with everything else284 | Moderate | Low |
| Potential for participants to become dependent on the intervention287 | Low | Very low |
| Potential conflicts or threats to provider roles287 | Low | Very low |
| Potential for invasion of participant privacy287 | Low | Very low |
| Being unable to deal with unpredictable situations or those for which they were unqualified. Anxieties about their own abilities, skills and helpfulness287 | Low | Very low |
| Health professionals’ thought an intervention for prevention of PND should include: | Evidence source: CASP | Certainty in CERQual |
|---|---|---|
| Closer integration with other service providers (primary care team)287 | Low | Very low |
| Target vulnerable groups287 | Low | Very low |
| Question | Yes/somewhat, (n = 23 studies) | |
|---|---|---|
| 1 | Is the study qualitative research/or does it provide qualitative data? | 23/23 |
| 2 | Is the study context and are the aims clearly described? | 23/23 |
| 3 | Is there evidence of researcher reflexivity? | 16/23 |
| 4 | Are the sampling methods clearly described and appropriate for the research question? | 21/23 |
| 5 | Are the methods of data collection clearly described and appropriate to the research question? | 21/23 |
| 6 | Is the method of analysis clearly described and appropriate to the research question? | 18/23 |
| 7 | Are the claims made supported by sufficient evidence, i.e. did the data provide sufficient depth, detail and richness? | 20/23 |
Quality of the qualitative personal and social support strategy studies
As shown in Table 12, all included studies reported either qualitative research or qualitative data within mixed-methods studies. All included studies adequately described the context and aims of the study. Sixteen of the 23 studies demonstrated evidence of researcher reflexivity. As in the intervention studies, few PSSS studies made explicit reference to researcher reflexivity, and in those which did descriptions were often brief. Most studies adequately described recruitment methods (n = 21) and data collection methods (n = 21), although such descriptions tended to be brief. Eighteen studies used interview methods, four used focus groups and one study used an online survey. Eighteen of 23 of studies provided an adequate description of data analysis methods, and 20 of the 23 studies provided sufficiently in-depth, detailed and rich data.
Certainty of the review findings personal and social support strategy studies
The CERQual approach137 was applied to assess the certainty of the review findings, graded as low, moderate or high. In each case a summary assessment was made of the CASP quality assessment finding, the number of studies contributing to the finding, the consistency of study setting and the population. The PSSS data yielded 19 findings: one assessed as high certainty, 11 assessed as moderate certainty and seven assessed as low certainty.
The findings were used to inform the realist synthesis and are presented in Chapter 8.
Qualitative studies further analysis by level of preventive intervention: universal, selective and indicated
Further quantitative and qualitative results are presented in Chapter 5 (37 universal preventive interventions trials, 14 qualitative studies), Chapter 6 (20 selective preventive interventions trials, four qualitative studies) and Chapter 7 (30 indicated preventive interventions trials, three qualitative studies). One study presented two levels of intervention and analysis. 61
Chapter 5 Results for universal preventive intervention studies
Characteristics of randomised controlled trials of universal preventive interventions
There were 37 RCTs included in the universal preventive interventions group,61,123,129,146,147,150,153–157,180–187,197–200,207–212,217–220,225–228,266,287 in the seven intervention classes defined as:
The results are presented in this order for the RCTs of universal preventive interventions. There was limited replication of interventions across the trials. The 37 universal preventive intervention trials are described first by their intervention context, mechanisms and measured outcomes within the seven classes.
Description of qualitative studies of universal preventive interventions
There were 14 studies relating to 15 citations reporting qualitative data on universal preventive interventions for PND. 277–291 Twelve studies relating to 13 citations reported the perspectives and attitudes of women who had received an intervention. 277–289 Four studies reported perspectives and attitudes of service providers of universal preventive interventions. 286,287,290,291
The qualitative studies related to five of the seven intervention classes:
For ease of reference the universal preventive interventions have been given short-version descriptive labels (Table 13).
| First author, year, reference number | Short-version descriptive label | Fuller description |
|---|---|---|
| Gunn, 1998225 | Early contact with care provider | A postnatal check-up with a GP 1 week after hospital discharge |
| Harrison-Hohner, 2001208,261 | Calcium | 2000 mg of elemental calcium per day during pregnancy |
| Hodnett, 2002197 | Support in labour | Continuous labour support by a specially trained nurse |
| Lumley, 2006147,263 | Primary care- and community-based strategies | Complex multifaceted primary care- and community-based strategies |
| MacArthur, 2002;146 2003264 | Midwifery redesigned postnatal care | Redesigned midwifery-led community postnatal care |
| Makrides, 2010211,265 | DHA | 800 mg of DHA in DHA-rich fish oil capsules in pregnancy |
| Matthey, 2004184 | Baby play | A session focused on the importance of play with a baby, with videotapes and discussion on how parents can play with infants |
| Matthey, 2004184 | Education on preparing for parenting | A session focusing on postpartum psychosocial issues related to becoming first-time parents |
| Mokhber, 2011212 | Selenium | 100 µg of selenium as selenium yeast daily during pregnancy |
| Morrell, 2000;199,266 2002287 | Social support | Up to 10 home visits in the first postnatal month by a community postnatal support worker |
| Morrell, 200961,151,152,326 | CBT-based intervention | HV training in the assessment of postnatal women, with CBA sessions for eligible women |
| Morrell, 200961,151,152,326 | PCA-based intervention | HV training in the assessment of postnatal women, combined with PCA sessions for eligible women |
| Norman, 2010123 | Exercise | An 8-week ‘Mother and Baby’ programme, of specialised exercise provided by a physical therapist combined with parenting education |
| Norman, 2010123 | Educational information | An 8-week ‘Mother and Baby’ programme, with parenting education |
| Sealy, 2009186 | Booklet on PND | An educational pamphlet ‘Why is everyone happy but me?’ mailed at 4-weeks postpartum, that explained the symptoms of PPD and identified local services for PPD |
| Shields, 1997219 | Midwife-managed care | A new programme of midwife-managed care (Midwifery Development Unit) |
| Songøygard, 2012129 | Exercise | A 12-week exercise programme of aerobic and strengthening exercises, during pregnancy; a weekly physiotherapy-led group session and home exercises encouraged twice a week |
| Waldenstrom, 2000220 | Midwifery team care | Team midwife care: eight midwives who provided antenatal and intrapartum care and follow-up visits to the postnatal ward |
Universal preventive interventions: psychological interventions
Characteristics and main outcomes of randomised controlled trials of universal preventive interventions of psychological interventions
Of the 37 universal preventive interventions, six studies evaluated a psychological intervention,61,153–157 including promotion of parent–infant interaction,153 psychoeducation,155 IPT,154,157 CBT-based interventions61,157 and PCA. Comparators included usual care in specific countries61,153,154,156,157 and educational information. 155 Three studies provided the intervention using a group format,154–156 whereas two involved individual sessions61,153 and one combined both group and individual sessions. 157 Two trials provided interventions in the home setting,61,153 whereas in the other four trials the intervention was provided in the antenatal setting. 154–157 Three trials provided the intervention in the antenatal period only,155–157 whereas one trial initiated the intervention postnatally61 and two trials provided the intervention across the perinatal period both during pregnancy and following childbirth. 153,154 The interventions were provided by different health-care providers including community workers,153 midwives,154 health visitors,155 psychologists156 and obstetricians,157 with the number of intervention contacts ranging from two154 to 16153 and with the duration of contact ranging from 1 to 2 hours.
A summary of the characteristics and main outcomes is provided in Table 14. In the psychological intervention trials, PND was assessed using various measures including the EPDS,61,153,154,156,157 General Health Questionnaire,154 Leverton Questionnaire,155 the Short Form questionnaire-36 items (SF-36) mental component summary (MCS),328 the Clinical Outcomes in Routine Evaluation-Outcome Measure (CORE-OM),151 the PHQ-9157 and the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders (SCID). 157 The State–Trait Anxiety Inventory (STAI) was the only anxiety outcome reported151 and the Perceived Stress Scale (PSS) the only stress outcome. 156 Family outcomes included the Dyadic Adjustment Scale,61 the Parenting Stress Index (PSI),151 the Relationship Efficacy Measure,156 the Satisfaction with Interpersonal Relationships Scale154 and mother–infant interaction (maternal sensitivity and intrusiveness). 153 The three infant outcomes reported were the Ainsworth Strange Situation Assessment of Infant Attachment,153 the Behaviour Screening Questionnaire61 and the Checklist for Autism in Toddlers. 61 General health and other outcomes included the Short Form questionnaire-12 items (SF-12), the SF-36 physical component summary (PCS), the Short-Form questionnaire-6 Dimensions (SF-6D)61 and the Subjective Happiness Scale. 156
| Intervention summary | First author, year, reference number | Country | Total number of women randomised | Place | Timing | Type of session | Provider | Comparison group(s) | Number of contacts | Duration of contact (minutes) | Depression outcomes | Other outcomes | Main findings | Overall risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CBT-based intervention | Mao, 2012157 | China | 204 | Antenatal setting | Antenatal | Individually and group | Obstetrician | Usual care in China | 4 | 90 | EPDS mean score (Chinese version), PHQ-9 score (Chinese version), SCID | – | On completion of the program, IG reported significantly lower mean PHQ-9 and EPDS scores than CG157 | Unclear |
| The mean EPDS score at 6 weeks postnatally was lower in the intervention group (mean 6.45, SD 1.09) than in the control group (mean 9.23, SD 2.91) (t = 1.95; p = 0.04) | ||||||||||||||
| Fewer participants from the IG were diagnosed as having PND using the SCID for DSM-IV157 | ||||||||||||||
| CBT-based intervention and PCA-based intervention | Morrell, 200961,151,152,326 | UK | 2241 | Home visits | Postnatal | Individually | Health visitor | Usual care in the UK | 1 | – | EPDS score 12 or more, SF-12 MCS score, CORE-OM score | STAI, DAS, PSI, BSQ, CHAT, SF-12, PCS, SF-6D | At 6 months, among all of the women who had returned both a 6-week and a 6-month questionnaire, 16.4% in CG scored 12 or more on the EPDS versus 11.7% in IG. Absolute difference was 4.7% (95% CI 0.7% to 8.6%) (p = 0.003)61 | Low |
| Mean EPDS score was 6.4 (SD 5.2) in CG and 5.5 (SD 4.7) in IG. Difference was statistically significant (p = 0.001)61 | ||||||||||||||
| IPT-based intervention | Gao, 2010;154 2012327 | China | 194 | Antenatal setting | Antenatal and postnatal | Group | Midwife | Usual care in China | 2 | 90 | EPDS score 13 or more (Chinese version) GHQ score 4 or more | SWIRS (devised by first author) | Women receiving the childbirth psychoeducation programme had significantly better psychological well-being (t = –3.33, p = 0.001), fewer depressive symptoms (t = –3.76, p = 0.000) and better interpersonal relationships (t = 3.25, p = 0.001) at 6 weeks postpartum compared with those who received only routine childbirth education152 | Low |
| IPT-based intervention | Leung, 2012156 | China (Hong Kong) | 156 | Antenatal setting | Antenatal | Group | Psychologist | Usual care in Hong Kong | 2 or more | – | EPDS score 13 or more | PSS (four-items), REM, SHS | Intention-to-treat analysis showed IG had significantly lower perceived stress and greater happiness than CG immediately after the intervention (in pregnancy). Effects not sustained at postnatal follow-up156 | Low |
| Promoting parent–infant interaction | Cooper, 2009153 | South Africa | 449 | Home visits | Antenatal and postnatal | Individually | Community worker (Lay) | Usual care in South Africa | 16 | 60 | EPDS mean score, SCID (DSM-IV) | Mother–infant interaction, maternal sensitivity and intrusiveness, ASSA | At 6 months and 12 months postnatally, the SCID indicated non-statistically significant differences in depression in the intervention and control group (χ2 = 0.85, df = 1, p = 0.36 at 6 months; χ2 = 1.16, df = 1, p = 0.21 at 12 months) | Unclear |
| With regard to maternal depressive symptoms (the continuous EPDS), the mean scores for those in the IG were lower at both assessments than were those for the CG, but the benefit of treatment was significant only at 6 months (z = 2.05, p = 0.041 at 6 months; z = 0.24, p = 0.813 at 12 months)153 | ||||||||||||||
| Psychoeducational intervention | Kozinsky, 2012155 | Hungary | 1762 | Antenatal setting | Antenatal | Group | Hungarian health visitors | Educational information | 4 | 180 | Leverton Questionnaire score | – | Leverton scores appeared to indicate a reduction in the risk of depression in the intervention group (OR = 0.69). The risk was reduced by around 18% among women who were depressed in pregnancy and 0.5% in women not depressed in pregnancy | High |
| At 6 weeks postnatally, the prevalence of depression was 12.7% in the intervention group and 17.5% in the control group (χ2; p < 0.01; OR 0.68). Leverton scores were 9.43 (± 2.168) vs. 10.12 (± 3.632) in the intervention and control groups, respectively |
Description and findings from qualitative studies of universal preventive interventions of psychological interventions
A description of the qualitative study evaluating a psychological intervention is provided in Table 15.
| First author | CASP quality grading | Country | Intervention details | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Name | Setting | Delivered antenatal/postnatal | Group/individual | Numbers in group | Number of sessions | Duration of session (minutes) | Facilitator/service provider | |||
| Gao282 | Moderate | China | IPT-oriented programme | Secondary care – teaching hospital | Antenatal and postnatal | Group and individual | NR | Two classes and a postnatal follow-up telephone call | 90 | Midwife |
Support
The qualitative study of a psychological intervention was IPT based and was conducted in China. 282 Data from participants demonstrated that the intervention promoted the development of relationships and connection with other group members, normalised their experience,282 helped them to harness support from family members282 and educated them about the Chinese cultural ritual known as ‘doing the month’ (which they had felt was unscientific and out of date) and how it could help them to develop a better relationship and elicit support from their mother-in-law. 282 Women appreciated the social support they received from the midwife through a telephone follow-up. 282
Learning practical strategies
Participants learned useful and applicable practical strategies as part of the intervention,282 gaining knowledge and skills to cope with the postpartum period. 282
Education/active participation in own health care
The intervention promoted knowledge gain and active participation in their own health care. 282 Specifically, participants reported that they were able to gain realistic information about motherhood, that it helped them to accept the reality of early motherhood282 and that they felt empowered to ask for help. 282
Universal preventive interventions: educational interventions
Characteristics and main outcomes of randomised controlled trials of universal preventive interventions of educational interventions
Eight included studies evaluated an educational intervention for the universal prevention of PND, none of which were conducted in the UK. 180,182–187 Two main types of educational interventions were identified: education on preparing for parenting180,181,184,185,187 and various advisory booklets on PND. 182,183,186 Comparisons were made with usual care in specific countries180–184,186 and educational information. 185 Four trials provided the educational intervention via group format,180,181,184,187 while the remaining four trials involved individual sessions. 182,183,185,186 Only one trial provided the intervention in the home setting. 186 Four trials provided the intervention in the antenatal period only,181,182,185,187 whereas two trials initiated the intervention postnatally183,186 and two trials provided the intervention across the perinatal period both during pregnancy and following childbirth. 180,184 The interventions were provided by psychologists,180,181,184,185 midwives182 and nurses. 183,186 The number of contacts ranged from two to eight and the duration of contact ranged from 30 minutes to 4 hours.
A summary of the characteristics and main outcomes is provided in Table 16. No qualitative studies were found for educational interventions as a universal preventive intervention.
| Intervention summary | First author, year, reference number | Country | Total number of women randomised | Place | Timing | Type of session | Provider | Comparison group(s) | Number of contacts | Duration of contact (minutes) | Depression outcomes | Other outcomes | Main findings | Risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Booklet on PND | Hayes, 2001;182 2004329 | Australia | 188 | Antenatal setting | Antenatal | Individually | Midwife | Usual care in Australia | 1 | – | POMS | NSSQ | Significant and steady reduction in scores (overall and on the subscales) was observed over time for both groups that showed significant improvement in symptoms of depression. No difference when comparing IG vs. CG182 | Unclear |
| Booklet on PND | Ho, 2009183 | Taiwan | 200 | Primary care | Postnatal | Individually | Postpartum ward nurse | Usual care in Taiwan | 1 | – | EPDS score 10 or more (Chinese version) | – | No significant difference for IG vs CG at 6 weeks (χ2 = 1.90, df = 1, p = 0.17) and 3 months postpartum (χ2 = 1.02, df = 1, p = 0.31)183 | High |
| Booklet on PND and available services | Sealy, 2009186 | Canada | 256 | Home visits | Postnatal | Individually | Nurse | Usual care in Canada | 1 | – | EPDS score 12 or more | The Parkyn tool | Women in IG had EPDS scores significantly lower than women in CG, IG 4.14; CG 5.01; t = 2.180; df = 254; p = 0.030186 | High |
| Education on preparing for parenting | Feinberg, 2008180 | USA | 169 | Antenatal setting | Antenatal and postnatal | Group | Psychologist | Usual care in the USA | 8 | – | CES-D (subset of 7 items) | – | Intent-to-treat analyses indicated significant program effects on coparental support, maternal depression and anxiety, distress in the parent–child relationship, and several indicators of infant regulation180 | Unclear |
| Results indicate a significant intervention effect on maternal depression and anxiety180 | ||||||||||||||
| Education on preparing for parenting | Gjerdingen, 2002181 | USA | 151 | Antenatal setting | Antenatal | Group | Psychologist | Usual care in the USA | 2 | 30 | SF-36 5-item mental health scale | Partner satisfaction and caring, SF-36 5-items | No significant group differences on postpartum health or work outcomes181 | High |
| Education on preparing for parenting | Matthey, 2004184 | Australia | 268 | Antenatal setting | Antenatal and postnatal | Group | Psychologist | Usual care in Australia | 7 | 120 | CES-D, DIS, (DSM-IV), EPDS, POMS | SOS, CSEI | No significant effects were obtained for either measure of caseness at 6 months postpartum184 | Unclear |
| Findings point strongly to differential effects of an intervention dependent upon the woman’s level of self-esteem184 | ||||||||||||||
| Education on preparing for parenting | Milgrom, 2011185 | Australia | 143 | Telephone | Antenatal | Individually | Psychologist | Educational information | 8 | – | BDI, DASS score, EPDS score 13 or more | RAC | Significantly fewer cases scoring above threshold for mild to severe depression/anxiety symptoms postnatally vs. routine care185 | Unclear |
| IG reported significantly lower levels of depression (BDI-II) post-treatment than participants in routine care (F1,86 = 7.82, p < 0.01. Cohen’s d = 0.6)185 | ||||||||||||||
| Education on preparing for parenting | Shapiro, 2005187 | USA | 38 | Antenatal setting | Antenatal | Group | Psychologist | Usual care in the USA | 2 | 420 | SCL score (data extracted using digitising software) | Marital Adjustment Test | In general, intervention was effective compared to CG for wife and husband marital quality, for wife and husband postpartum depression187 | High |
| The major change in postpartum depression was from 3 months to 1 year: CG increased and IG decreased, t(32) = 2.13, p < 0.05187 |
Universal preventive interventions: social support
Characteristics and main outcomes of randomised controlled trials of universal preventive interventions of social support
Of the 37 RCTs of universal preventive interventions, four (11%) evaluated a social support intervention,197–200 two of which were conducted in the UK. 199,200 Several types of social support were identified including support in labour197 and self-help support. 200 Comparisons were made with usual care in specific countries197,199,200 and educational information. 198 One intervention involved a group session,200 two studies involved individual sessions197,199 and one involved both group and individual sessions. 198 One study took place in the home setting. 199 None of the studies were undertaken in the antenatal period only, two were in the postnatal period only,199,200 two were in a combination of both antenatal and postnatal periods198 and one was at the stage of labour. 197 As with other types of included interventions, these were provided by different health-care providers: community workers,198 midwives,200 nurses197 and support workers. 198 The number of contacts ranged from one to 14 but duration of contact (10–378 minutes) was reported in only one study. 199
A summary of the characteristics and main outcomes is provided in Table 17.
| Intervention summary | First author, year, reference number | Country | Total number of women randomised | Place | Timing | Type of session | Provider | Comparison group(s) | Number of contacts | Duration of contact (minutes) | Depression outcomes | Other outcomes | Main findings | Overall risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Self-help support | Reid, 2002200,268 | UK | 1004 | Primary care | Postnatal | Group | Midwife group facilitator | Usual care in the UK | 2 or more | – | EPDS score 12 or more | – | There were no significant differences in EPDS scores between the control and trial arms at 3 and 6 months, nor were there differences in the SF-36 and the SSQ6 scores | Low |
| Social support | Kieffer, 2013198 | USA | 278 | Antenatal setting | Antenatal and postnatal | Individually and group | Community health worker | Educational information | 14 | – | CES-D score 16 or more | – | IG less likely than CG to be at risk for depression at follow-up198 | Low |
| From baseline to postpartum, the mean CES-D score of the MOMs group decreased 1.45 points more than the mean CES-D score of the CG, although this difference in overall change scores was not significant (95% CI –3.26, 0.37; p = 0.12)198 | ||||||||||||||
| Social support | Morrell, 2000199,266,287 | UK | 623 | Home visits | Postnatal | Individually | Postnatal support worker | Usual care in the UK | 10 | Range 10–378 | EPDS score 12 or more | Breastfeeding, SF-36, DUFSS, resource use, costs | At 6 weeks no significant improvement in health status among the women in the IG | Low |
| Support in labour | Hodnett, 2002197 | Canada | 6915 | Labour ward | Labour | Individually | Nurse | Usual care in the USA | 1 | – | EPDS score 13 or more | Caesarean delivery, LAS, LSQ | No significant differences in women’s perceived control during childbirth or in depression, measured at 6–8 weeks postpartum. A total of 245 women in IG (8.7%) had evidence of postpartum depression vs. 277 women (10.1%) in CG (p = 0.08) | Unclear |
Description and findings from qualitative studies of universal preventive interventions of social support
Of the two qualitative studies of social support included in the universal preventive interventions category, one was conducted in the UK287 and one in Canada. 281 One intervention was an online discussion group281 and the other a postnatal support worker intervention. 287 Further details are provided in Table 18.
| First author, year, reference number | CASP Quality Grading | Country | Intervention details | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Name | Setting | Delivered antenatal/postnatal | Group/individual | Number in group | Number of sessions | Duration of session | Facilitator/service providers | |||
| Evans, 2012281 | Moderate | Canada | Online discussion support group | Online forum | Postnatal | Virtual group (online forum) | NA | NA | NA | Peers |
| Morrell, 2000;199,266 2002287 | Low | UK | Postnatal support worker intervention | Home visits | Postnatal | Individual | NA | Up to 10 sessions | Up to 3 hours | Support workers trained to NVQ level 2 for the role |
Findings from qualitative studies of universal preventive interventions of social support
Support
Participants reported that helpful aspects of the intervention were emotional and informational support, the development of relationships with peers,281,287 reassurance and validation (appraisal support), normalisation of their feelings, practical advice281 and practical support. 287
I would just like to say the support worker who came to help me was fantastic. I had twins by caesarean so I couldn’t move around too good. She sent me off to bed and when I’d get up the house would be straight, ironing done, babies bathed and my 3-year-old amused. J was brilliant. I think the support worker is good and hope you can carry it on.
Participant287
Providers of the support worker intervention reported that it provided women with emotional, informational and appraisal support. 287 However, one concern about the interventions was whether or not women would become overdependent on the additional support. 287
Service delivery
Participants287 reported that the intervention would be more beneficial if it were more intensive, for example if visits were longer and/or more frequent. Midwives raised concern about the support worker’s role threatening their own role. Service providers were concerned that the intervention represented an invasion of the women’s privacy287 and were worried that they would be unable to deal with unpredictable situations which they were not qualified to address. In the study, the authors suggested that service providers wanted closer integration with other service providers such as the primary care team and that the intervention should be targeted at vulnerable groups. 287
Universal preventive interventions: pharmacological agents or supplements
Characteristics and main outcomes of randomised controlled trials of universal preventive intervention of pharmacological agents or supplements
Of the six trials that evaluated a specific supplement or drug for the universal prevention of PND, none were conducted in the UK. 207–212 Several types of pharmacological agents or supplements were identified including docosahexaenoic acid (DHA) at different doses,207,210,211 calcium,208 norethisterone ethanate209 and selenium. 212 All six studies compared the interventions with usual care in specific countries. 207–212 All six studies involved individual sessions. 207–212 Three studies took place in the antenatal period208,211,212 and two in the postnatal period;209,210 one combined both antenatal and postnatal periods. 207 Included interventions were all delivered by the provider. A summary of the characteristics and main outcomes is provided in Table 19. No qualitative studies were identified of pharmacological agents or supplements aimed at a universal population.
| Intervention summary | First author, year, reference number | Country | Total number of women randomised | Place | Timing | Type of session | Provider | Comparison group | Number of contacts | Depression outcomes | Other outcomes | Main findings | Overall risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Calcium | Harrison-Hohner, 2001208,261 | USA | 468 | Antenatal setting | Antenatal | Individually | Prescriber | Usual care in the USA | 2 or more | EPDS score 14 or more | Norbeck’s modified Sarason’s Life Events Survey | There was a trend among 293 women who scored 14 on more on the 6-week EPDS towards less depression in the intervention group. At 12 weeks postnatally, the intervention group were less depressed (p = 0.04) | High |
| The authors suggested that calcium supplementation could have had a preventive effect at one centre, but no effect at another and that these outcomes were difficult to explain | |||||||||||||
| DHA | Doornbos, 2009207 | The Netherlands | 119 | Antenatal setting | Antenatal and postnatal | Individually | Prescriber | Usual care in the Netherlands | 2 or more | EPDS score 12 or more (Dutch version) | OOS | IG did not differ in mean EPDS scores or changes in EPDS scores, nor in incidence or severity of postpartum blues | High |
| DHA 200 mg/day | Llorente, 2003210 | USA | 89 | Postnatal setting | Postnatal | Individually | Prescriber | Usual care in the USA | 2 or more | BDI, EPDS mean score, SCID-CV | Plasma phospholipid, DHA acid content | After 4 months, no difference between groups in either self-rating or diagnostic measures of depression | Unclear |
| DHA 800 mg | Makrides, 2010211,265 | Australia | 2399 | Antenatal setting | Antenatal | Individually | Prescriber | Usual care in Australia | 2 or more | EPDS score 13 or more | BSID | The percentage of women with high levels of depressive symptoms during the first 6 months postpartum did not differ for IG vs. CG (9.67% vs. 11.19%; adjusted relative risk, 0.85; 95% CI 0.70 to 1.02; p = 0.09) | Low |
| Norethisterone ethanate 200 mg administered intramuscularly | Lawrie, 1998209 | South Africa | 180 | Postnatal setting | Postnatal | Individually | Prescriber | Usual care in South Africa | 1 | EPDS score 12 or more, MADRS | Breastfeeding, vaginal bleeding, somatic complaints | Mean depression scores significantly higher in IG vs. CG at 6 weeks postpartum (mean MADRS score 8.3 vs. 4.9: p = 0.0111: mean EPDS score 10.6 vs. 7.5: p = 0.0022)209 | Low |
| Selenium | Mokhber, 2011212 | Iran | 166 | Antenatal setting | Antenatal | Individually | Prescriber | Usual care in Iran | 2 or more | EPDS score 13 or more (Iranian version) | – | Mean EPDS score in selenium group significantly lower than in CG (p < 0.05) | Unclear |
Universal preventive interventions: midwifery-led interventions
Characteristics and main outcomes of randomised controlled trials of universal preventive interventions of midwifery-led interventions
Of the five studies146,217–220 evaluating midwifery-led interventions for the universal prevention of PND, two were conducted in the UK. 146,219 Several types of midwifery-led interventions were identified, including midwifery redesigned postnatal care,146 midwife-led debriefing or counselling after childbirth,217,218 midwife-managed care219 and team midwife care. 220 Comparisons were made with usual care in specific countries. 146,217–220 All six trials involved individual sessions. 146,217–220 None of the trials provided the intervention only antenatally; three initiated the intervention postnatally,146,217,264 and two trials initiated the intervention during the pregnancy and continued it postnatally. 219,220 The provision of the midwifery care varied in the number of contacts, with duration ranging from 15 minutes to 1 hour. A summary of the characteristics and main outcomes is provided in Table 20.
| Intervention summary | First author, year, reference number | Country | Total number of women randomised | Place | Timing | Type of session | Provider | Comparison group | Number of contacts | Duration of contact (minutes) | Depression outcomes | Other outcomes | Main findings | Risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Midwife-led debriefing or counselling after childbirth | Priest, 2003;217 Henderson, 1998330 | Australia | 1745 | Postnatal setting | Postnatal | Individually | Midwife | Usual care in Australia | 1 | Range 15–60 | EPDS score 13 or more, SCID, SADs | IoE Scale (revised) (psychological trauma) | No significant differences for CG vs. IG in scores on IoE Scale or EPDS at 2, 6 or 12 months postpartum or in the proportions of women who met diagnostic criteria for a stress disorder (intervention 0.6% vs. control 0.8%; p = 0.58) or major or minor depression [intervention, 17.8% vs. control, 18.2%; relative risk 0.99 (95% CI 0.87 to 1.11)] during the postpartum year. No differences in median time to onset of depression [intervention 6 (interquartile range 4–9) weeks vs. control 43–8 weeks; p = 0.84], or duration of depression (intervention 2412–46 weeks vs. control 2210–52 weeks; p = 0.98) | Unclear |
| Midwife-led debriefing or counselling after childbirth | Selkirk, 2006218 | Australia | 149 | Postnatal setting | Postnatal | Individually | Midwife | Usual care in Australia | 1 | Range 30–60 | EPDS mean score, SCL-90 | STAI, IES, DAS, FAD, PSI, IIS, POBS | No significant differences for IG vs. CG on measures of personal information, depression, anxiety, trauma, perception of the birth, or parenting stress at any assessment points, postpartum218 | High |
| Midwife-managed care | Shields, 1997219 | UK | 1299 | Antenatal setting | Antenatal and postnatal | Individually | Midwife | Usual care in the UK | 2 or more | – | EPDS mean score (question 10 on self-harm was excluded) | Infant feeding | EPDS has not been validated as a 9-item scale. It was not possible to give a ‘true’ measure of point prevalence of PND219 | Unclear |
| The mean scores for women in the MDU were lower than those for the traditional care group (8.1, SD 4.9 vs. 9.0, SD 4.9). 16.7% of women in the MDU vs. 23.2% women in usual care had an EPDS score 13 or more (95% CI –12.1% to –0.9%) | ||||||||||||||
| Midwifery-redesigned postnatal care | MacArthur, 2002;146 2003264 | UK | 2064 | Postnatal setting | Postnatal | Individually | Midwife | Usual care in the UK | 2 or more | – | EPDS score 13 or more, SF-36 MCS | SF-36 PCS | Women’s mental health measures were significantly better in the IG (MCS, 3.03 [95% CI 1.53–4.52]; EPDS –1.92 [–2.55 to –1.29]; EPDS 13 + odds ratio 0.57 [0.43–0.76]) than in controls, but the physical health score did not differ146 | Low |
| Team midwife care | Waldenstrom, 2000220 | Australia | 1000 | Antenatal setting | Antenatal and postnatal | Individually | Midwife | Usual care in Australia | 2 or more | – | EPDS score 13 or more | – | Team midwife care associated with increased satisfaction. Differences between groups most noticeable for intrapartum care and least noticeable for postpartum care. No differences for team midwife care vs. standard care in medical interventions or in women’s emotional well-being 2 months after the birth220 | Unclear |
Description and findings from qualitative studies of universal preventive interventions of midwifery-led interventions
Seven qualitative reports were identified of women’s experiences of midwifery-led interventions. 277,283–285,289–291 All seven reports related to the CenteringPregnancy initiative (Table 21).
| Name | CASP quality grading | First author, year, reference number | Country | Setting | Delivered antenatal/postnatal | Group/individual | Number of women in group | Number of sessions | Duration of session (hours) | Facilitator/service providers |
|---|---|---|---|---|---|---|---|---|---|---|
| CenteringPregnancy | Moderate | Andersson, 2012277 | Sweden | Secondary care – antenatal clinic | Antenatal and postnatal | Group and individual | 6–8 | NR | NR | Midwives |
| CenteringPregnancy | Moderate | Kennedy, 2009283 | USA | Secondary care – air force base/US Navy hospital | Antenatal (one postnatal reunion) from 12–16 weeks of pregnancy | Group and individual | 8–12 | 10 | 2 | Midwives/nurse |
| CenteringPregnancy | Moderate | Klima, 2009284 | USA | Secondary care – antenatal clinic | Antenatal and postnatal | Group and individual | 4–10 | NR | NR | Certified nurse-midwives |
| CenteringPregnancy | Moderate | McNeil, 2012285 | Canada | Secondary care – antenatal clinic | Antenatal and postnatal | Group and individual | 8–12 | 10 | 2 | Family physician and a perinatal educator |
| CenteringPregnancy | Moderate | McNeil, 2013290 | Canada | Secondary care – antenatal clinic | Antenatal and postnatal | Group and individual | 8–12 | 10 | 2 | Family physician and a perinatal educator |
| CenteringPregnancy | Low | Teate, 2011289 | Australia | Secondary care – antenatal clinic/community health centres | Antenatal and postnatal | Group and individual | 8–12 | NR | NR | Midwives, student midwives, social workers |
| CenteringPregnancy | Moderate | Tanner-Smith, 2012291 | USA | Secondary care – antenatal clinic/community health centres – multisite | Antenatal and postnatal | Group and individual | 8–12 | NR | NR | NR |
Findings from the qualitative studies of universal preventive interventions of midwifery-led interventions
Peer support
Several respondents in the seven studies277,283–285,289–291 reported gaining support, particularly in the CenteringPregnancy intervention. Service providers were positive about their experience and thought the intervention facilitated peer support. 290,291 In addition, the women felt that they had benefited from a supportive environment and from sharing experiences:277,283,289
I really enjoyed having others who were at the same stage of pregnancy as me to talk to and compare feelings and symptoms.
Participant289
Women talked about building relationships with peers,283,289 receiving reassurance and normalisation of their experiences during the pregnancy, during birth and postnatally. 289 Women also valued the emotional, informational and appraisal support received from peers. 289 One woman did not find the group environment helpful:
It wasn’t a good idea in the beginning of the pregnancy. I would not want the pregnancy be open to the public.
Participant277
Partners
Respondents felt that their partners needed and appreciated the support from the intervention:283,289
It was good for the husbands. They all came and it was nice [that] they were included . . . my husband liked it because before he had to wait in the waiting room and now he was involved.
Participant283
Some women felt more of the intervention focus should be on partners;277 although one woman was ambivalent:277,283
I think it’s good if they can come, but when they were present, there were things you did not want to ask in front of others. I did not want to raise questions in front of them.
Participant277
Authors’ interpretations277,283 revealed either that partners had difficulty contributing to the group because of shyness277 or that women felt that partners were uncomfortable with intimate discussions. 283
Service providers’ skills
Participants found the midwives’ support and group skills in running the intervention helpful,277,285,289 because they were able to pay attention to women’s concerns and offer women solutions,277,285 although some midwives required more training to lead groups:
I was disappointed that the midwife did not ask about the wishes of the group.
Participant277
Participants felt midwives should focus more on their partners. 277 Others appreciated the midwife’s skills, knowledge, warmth, providing suggestions for group discussion and allowing unstructured discussion. 277 Service providers felt the intervention improved communication between them and participants which promoted a better relationship and facilitated information exchange. 290 Service providers said they enjoyed delivering the intervention, and found it a satisfying and rewarding experience in that it provided richer care to women. 290,291
Active participation/education
Another important theme related to how participants might actively participate in their own health care, including the provision of education and the gaining of information and knowledge. 283–285,289 Several respondents said that they valued receiving education and information about pregnancy and the postnatal period. 283,284 The women felt empowered by being allowed to undertake certain health monitoring tasks, such as weighing themselves and taking their own blood pressure. 283 In two studies,283,289 the women wanted more and more intensive education on issues relating to labour, birth and parenting and the early weeks of parenting:
At the time, we were given ample information. I was very well informed for my birth. More information about coping with a newborn would be helpful.
Participant289
Group setting
Service providers in two studies reported that, compared with individual care, the group environment provided more opportunity for teaching and enhanced education. 284,291 Providers across studies felt that the intervention encouraged women to be active participants in their own health care. 284,290 They reported that women were enthusiastic about the group setting, and this enthusiasm served to increase participation. 284
Service delivery and barriers to participation
Practical aspects relating to how the service is delivered has important implications regarding intervention up-take. Participants reported the format reduced waiting times285,289 and promoted continuity of care. 277 In a study in a US military setting,283 participants found ‘front-desk staff’ unhelpful:
You would have to wait for a really long time on the phone or for them to call back. And then it felt like they just brushed you off.
Participant283
They complained about the lack of child care and consideration for children. 283 Participants reported they felt they had few assessments and that they experienced ‘scrimping and cost saving’ as they were asked to undertake tasks such as taking samples to the laboratory. They felt they would not have had to undertake these activities if their care been delivered in a civilian setting. 283
Suggested improvements
Ways suggested to improve the service were to reduce the period of time between first and second group meetings,277 to reduce the 2-hour session,289 to address the rushed feeling,283 to improve the lack of privacy,277,283 to address the lack of healthy snacks283 and to add individual appointments:
As a first-time mom, you need more reassurance to talk with a caregiver. Or perhaps have an open time where you can go in – perhaps before or after to talk with them.
Participant283
Service providers reported the group intervention helped to address waiting time issues in one study284 and suggested that the intervention was a more efficient use of time:290
I can’t impart everything I’ve learned from 20 years of delivering babies in . . . five 7-minute visits . . . but, I can get more of that across in . . . all their 2-hour groups.
Participant290
The intervention was still restricted to groups, such as teenagers, because of provider bias. 291 There were difficulties gaining funding to keep the intervention running284,291 and attendance difficulties because of transport or work conflict issues. Some women were resistant to the group format,291 which service providers felt did not allow ‘deeper issues’ to be addressed. 284 Service providers reported concerns that the group intervention took a provider away from one-to-one care284 and that they experienced difficulties with scheduling:
There is no system for scheduling. While one provider does the group, the other provider gets dumped on.
Participant284
Universal preventive interventions: organisation of maternity care
Characteristics and main outcomes of randomised controlled trials of universal preventive interventions of organisation of maternity care
Of the five studies147,150,225–227 evaluating the organisation of maternity care for the universal prevention of PND, only one was conducted in the UK. 150 Several types of organisation of maternity care interventions were identified, including planned health visitor visits,150 early contact with care provider,225 primary care and community care strategies,147 programmes for HIV, alcohol and mental health226 and early contact with care provider. 227 Comparisons were made with usual care in specific countries. 147,225–227 All five studies involved individual contacts. 147,150,225–227
None of the studies were undertaken in only the antenatal period, three in only the postnatal period150,225,227 and two used a combination of both antenatal and postnatal periods. 226,227 The interventions were provided by different health-care providers including health visitors,150 GPs,225 primary care nurses, community development workers,147 community health workers, peer mentors,226 paediatric house officer or nurse practitioners. 227 The number of contacts varied greatly. A summary of the characteristics and main outcomes is provided in Table 22.
| Intervention summary | First author, year, reference number | Country | Total number of women randomised | Place | Timing | Type of session | Provider | Comparison group | Number of contacts | Duration of contact | Depression outcomes | Other outcomes | Main findings | Risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Early contact with care provider | Gunn, 1998225 | Australia | 475 | Primary care | Postnatal | Individually | GP | Usual care in Australia | 1 | – | EPDS score 13 or more | Breastfeeding, SF-36 | No significant differences between groups in: EPDS and SF-36 scores; number of problems; breastfeeding rates; or satisfaction with general practitioner care. IG less likely to attend for their check-up (76.4% vs. 88.4%; p = 0.001)225 | Low |
| Early contact with care provider | Serwint, 1991227 | USA | 251 | Postnatal setting | Postnatal | Individually | Paediatric house officer or nurse practitioner | Usual care in the USA | 1 | – | CES-D | Maternal knowledge, use of services | No differences for IG vs. CG for emergency room utilisation, percentage who received immunisations by 90 days of age, maternal knowledge of infant care, maternal anxiety, or postpartum depression | High |
| Primary care and community care strategies | Lumley, 2006147,263 | Australia | 18,555 | Primary care | Antenatal and postnatal | Individually | Primary care nurse and community development worker | Usual care in Australia | 2 or more | – | EPDS score 13 or more, SF-36 MCS | SF-36 PCS | There were no differences in mean scores for the MCS or EPDS. There were no differences in the proportion of women scoring 13 or more on the EPDS. There were also no differences in the mean PCS scores | Unclear |
| The combination of primary care and community based strategies did not reduce the symptoms of depression or improve the physical health of women at 6 months postnatally | ||||||||||||||
| Program for HIV, alcohol, mental health | Rotheram-Borus, 2011;226 le Roux, 2013270 | South Africa | 1144 | Antenatal setting | Antenatal and postnatal | Individually | Community health worker (peer mentors) | Usual care in South Africa | 11 | – | EPDS score 14 or more, GHQ | – | PIP is a model for countries facing significant reductions in HIV funding whose families face multiple health risks. Healthcare, maternal depression, social support, and % of mothers securing the child grant were similar across conditions270 | Low |
| Six planned health visitor visits | Christie, 2011150 | UK | 295 | Home visits | Postnatal | Individually | Health visitor | Health visitor single visit | 6 | – | EPDS | PSI, role restriction attachment self-efficacy, PES, baby nurture, breastfeeding, use of services, satisfaction | There were no differences in outcomes for the intervention group compared with the control group, apart from the EPDS score which was higher (indicating more symptoms of depression) in the intervention group at 8 weeks postnatally. Compared with the control group, women in the intervention group reported higher levels of satisfaction and lower use of emergency services up to 8 weeks postnatally | Unclear |
Description and findings from qualitative studies of universal preventive interventions of organisation of maternity care
One qualitative study288 reported women’s experiences of interventions aimed at a universal population involving the organisation of maternity care (Table 23).
| First author, year, reference number | Country | Intervention details | CASP quality grading | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Name | Setting | Delivered antenatal/postnatal | Group/individual | Number of women in group | Number of sessions | Duration of session | Facilitator/service providers | |||
| Scott, 1987288 | Australia | Maternal and child health nurses | Secondary care – maternal and child health centres | Postnatally | Individual | NA | Multiple contact | NA | Nurses | Moderate |
Findings from qualitative studies of universal preventive interventions of organisation of maternity care
Support
Women found the service provider’s support helpful288 and appreciated the infant welfare sister’s concern expressed for them and the baby. They also talked about the nurse as maternal figure for themselves:
She’s a supplement to my own mother. She’s easy to talk to. I depend on her. She’s not just there to take care of the baby but for the mothers too. She started a group for us new mothers.
Participant288
However, this positive effect may have become a barrier to effective service use in situations in which women reported that they did not understand the role of the maternal and child health nurse. 288 One woman reported:
. . . I never thought I had a right to talk about emotional problems as I was never told what the role of the nurse covers.
Participant288
Service delivery and barriers to participation
Women reported that they did not understand that depression was associated with the baby and, therefore, did not talk to the nurse about their feelings, or they were worried about stigma if they approached the nurse for emotional support. 288
Universal preventive interventions: complementary and alternative medicine or other
Characteristics and main outcomes of randomised controlled trials of universal preventive interventions of complementary and alternative medicine or other
None of the three studies123,129,228 evaluating the CAMs for the universal prevention of PND were conducted in the UK. Several types of CAMs interventions were identified including baby massage228 and exercise. 123,129 Comparisons were made with usual care in specific countries129,228 and educational information. 123 All three studies involved individual sessions. One was undertaken in the antenatal period only129 and two in the postnatal period only. 123,228 The provider of these interventions was a massage instructor228 or physical therapist. 123,129 The number of contacts varied and the length of contact was 1 hour in two studies. 123,129 A summary of the characteristics and main outcomes is provided in Table 24.
| Intervention summary | First author, year, reference number | Country | Total number of women randomised | Place | Timing | Type of session | Provider | Comparison group | Number of contacts | Duration of contact (minutes) | Depression outcomes | Other outcomes | Main findings | Risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baby massage | Fujita, 2006228 | Japan | 57 | Postnatal setting | Postnatal | Individually | Massage instructor | Usual care in Japan | 2 or more | – | POMS, (Japanese version) | Salivary cortisol | Significant differences in the POMS score seen in depression and vigor between two groups at 3 months. No significant differences in the salivary cortisol levels. 3 months after delivery scores had improved more positively in depression and vigor in IG vs. CG (D; t = –2:57, p = .02, V; t = 2:39, p = .02)228 | High |
| Exercise | Norman, 2010123 | Australia | 161 | Postnatal setting | Postnatal | Group | Physical therapist | Educational information | 8 | 60 | EPDS score 13 or more | PABS | There was a reduction in mean EPDS score in the Mother and Baby Program intervention group at 8 weeks, compared with the education-only group, maintained for 4 weeks | Unclear |
| Exercise | Songøygard, 2012129 | Norway | 855 | Antenatal setting | Antenatal | Group | Physiotherapist | Usual care in Norway | 12 | 60 | EPDS score 10 or more, EPDS score 13 or more | – | 14/379 (3.7%) women in IG and 17 of 340 (5.0%) in CG had an EPDS score of 10 or more (p = 0.46), and 4/379 (1.2%) women in IG and 8/340 (2.4%) in CG had an EPDS score of 13 or more (p = 0.25)129 | Unclear |
Description and findings of qualitative studies of universal preventive interventions of complementary and alternative medicine or other
Three qualitative studies278–280,286,288 reported women’s experiences of interventions aimed at a universal population involving the CAMs or other intervention (Table 25).
| Name | CASP quality grading | First author, year, reference number | Country | Setting | Delivered antenatal/postnatal | Group/individual | Number of women in group | Number of sessions | Duration of session (minutes) | Facilitator/service providers |
|---|---|---|---|---|---|---|---|---|---|---|
| Singing lullabies | Moderate | Carolan, 2012278,279 | Ireland | Secondary care – antenatal clinic | Antenatally | Group | 6 | 4 | 45 | Musicians |
| Yoga and discussion group | Moderate | Doran, 2013280 | Australia | Secondary care – community based feminist non-government women’s health centre | Antenatally and postnatally | Group | NR | Ongoing/flexible | NR | Midwife and a yoga teacher |
| Mind–body exercise techniques | High | Migl, 2009286 | USA | Secondary care – prenatal support group | Antenatally | Group | NR | 5 weekly sessions | NR | NR |
Support
Support was an important theme in studies of a group mind–body exercise (MBE) intervention,286 a singing lullabies group intervention278,279 and a yoga and discussion group. 280 In two studies,278–280 the benefit of peer support was reported by participants, especially the sharing of experiences and birth stories and in the development of connections with their fellow group members:
. . . (when I was giving birth) . . . I thought of all the women in the lullaby project having their babies . . . it just connected me and I didn’t feel so nervous . . .
Women who took part in the MBE techniques reported that when partners supported them in applying the MBE techniques this facilitated communication between them and their partners. 286 Participants reported that family support was also facilitated by teaching the songs learned in the lullaby intervention. 278,279 The study author reported that participants found it difficult to apply MBE techniques learned during the intervention without group support. 286
Learning practical strategies
Beneficial aspects of the interventions were reported by participants as the practical use of strategies learned during the intervention. 278,279,286 Participants reported that they served to prevent panic attacks, combat physical symptoms of stress and could be used in combination with existing strategies. 286 Participants in one study286 reported that they valued techniques that were easy to use in any setting and for a short period and being able to take the specific parts of the intervention they needed:
[MBE was] . . . something new and easy to use in almost any setting and for period a short period of time . . .
Participant286
However, in one study278,279 it was reported that the use of the learned strategies could result in unexpected emotional responses:
. . . I was told you’re going to get blue . . . so I was expecting that. I didn’t expect [what happened] . . . At first I’d start crying was when I was singing that song . . . I was crying at the time. It was so strong . . .
In one study286 the authors reported that the women found it difficult to allocate time to use the practical strategies learned, forgot to implement the strategies or were resistant to using techniques because of stigma in that they felt certain MBE techniques were not accepted by wider society. One woman reported that she could not see the value in the use of the techniques during the postpartum period. 286
Results from network meta-analysis for universal preventive interventions for Edinburgh Postnatal Depression Scale threshold score
A NMA is an extension of a standard meta-analysis that enables a simultaneous comparison of all evaluated interventions in a single coherent analysis. In this way, all interventions can be compared with one another, including comparisons not evaluated within individual studies. The only requirement is that each study must be linked to at least one other study through having at least one intervention in common.
Among the trials excluded because they could not be connected to the main network (see Appendix 10, Table of universal preventive intervention studies omitted from network meta-analysis), three were conducted in South Africa,153,209,226 three in China,154,156,157 one in Japan,228 one in the Republic of China (Taiwan)183 and one in Hungary. 155 Three of these trials were at high risk of bias155,183,228 and two were of uncertain risk of bias. 153,157
Among the other excluded trials, three had no usual-care comparator. 150,185,198 Six trials did not report an EPDS score180–182,187,227,329 and in two the EPDS score was unusable. 200,268 Two trials of social support, one conducted in the UK200 and one in the USA,198 were at low risk of bias and found no evidence of an effect. There were five studies at high risk of bias. 181,187,207,218,227 In all of the other studies the risk of bias was unclear. Three of these studies did not have negative results. 150,180,185 A US trial of education on preparing for parenting found ‘a [statistically] significant intervention effect on maternal depression and anxiety’180 using a subset of seven items from the Center for Epidemiologic Studies Depression (CES-D) scale. An Australian trial of education on preparing for parenting found ‘participants in the intervention reported significantly lower levels of depression [Beck Depression Inventory (BDI-II)] post-treatment than participants in routine care’. 185 A UK-based trial of six planned health visitor visits150 found that the ‘intervention had no impact on most outcomes; however, it was associated with an increased EPDS score at eight weeks (before accounting for outliers) but not at seven months’.
Results for universal preventive interventions for Edinburgh Postnatal Depression Scale threshold score at 6 weeks postnatally
Data were available from five studies presenting the EPDS threshold score at 6 weeks postnatally. 197,208,211,219,220 The results for the five universal preventive intervention trials presenting an EPDS threshold score are combined here. A NMA compared the effects of support in labour,197 midwife-managed care,219 DHA,211 calcium208 and team midwife care220 relative to usual care on EPDS threshold. Figure 5 presents the network of evidence. There were five intervention effects (relative to usual care) to estimate from five studies.
FIGURE 5.
Universal preventive interventions EPDS threshold score at 6 weeks postnatally: network of evidence.

Figure 6 presents the odds ratios of each intervention relative to usual care and Figure 7 presents the probabilities of treatment rankings. The total residual deviance was 10.04, which is compared with the total number of data points, 10, included in the analysis. This implies a good fit of the model to the data. The between-study SD was estimated to be 0.26 (95% CrI 0.01 to 0.72), which implies mild heterogeneity of intervention effects between studies.
FIGURE 6.
Universal preventive interventions EPDS threshold score at 6 weeks postnatally: odds ratios for all treatment comparisons. Key: OR, odds ratio.

FIGURE 7.
Universal preventive interventions EPDS threshold score at 6 weeks postnatally: probability of treatment rankings (ranks 1–6).
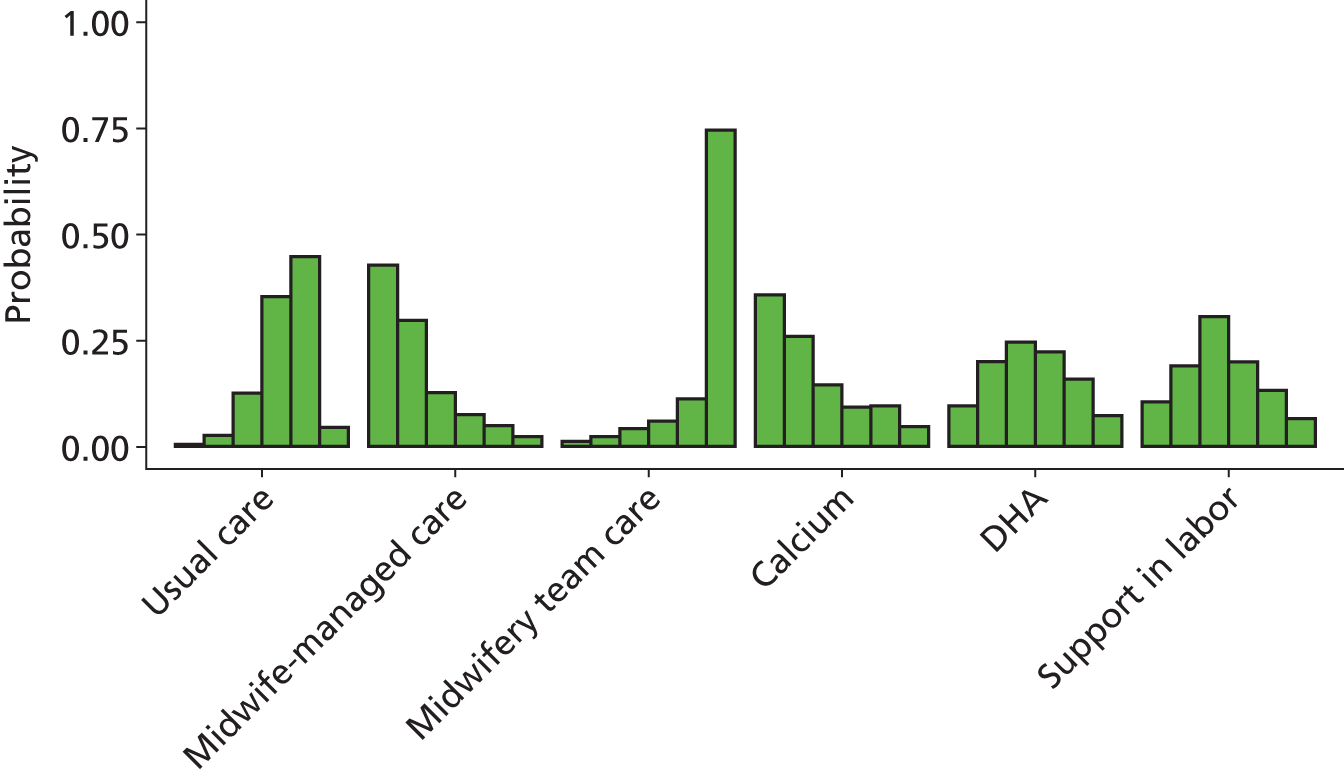
For all interventions except midwifery team care the odds ratio was less than 1, suggesting a beneficial effect compared with usual care. However, none of the comparisons were statistically significant at a conventional 5% level (see Figure 6). The interventions with the highest probabilities of being the best were midwife-managed care and calcium (probability 0.43 and 0.36, respectively).
Midwifery team care was associated with an increased odds ratio compared with usual care (1.39, 95% CrI 0.65 to 3.01) and had a 74% chance of being the least effective among the six interventions (see Figure 7).
Results for universal preventive interventions for Edinburgh Postnatal Depression Scale threshold score at 3 months postnatally
A NMA was used to compare the effects of calcium,208 booklet on PND,186 exercise129 and early contact with care provider225 relative to usual care on EPDS threshold. Data were available from four studies comparing five interventions. Figure 8 presents the network of evidence. There were four intervention effects to estimate from four studies. 129,186,208,225
FIGURE 8.
Universal preventive interventions EPDS threshold score at 3 months postnatally: network of evidence.

Figure 9 presents the odds ratios of each intervention relative to usual care and Figure 10 presents the probabilities of treatment rankings. The total residual deviance was 7.04, which is compared with the total number of data points, seven, included in the analysis. This implies a good fit of the model to the data. The between-study SD was estimated to be 0.23 (95% CrI 0.00 to 0.74), which implies mild heterogeneity between studies in intervention effects.
FIGURE 9.
Universal preventive interventions EPDS threshold score at 3 months postnatally: odds ratios for all treatment comparisons. Key: OR, odds ratio.
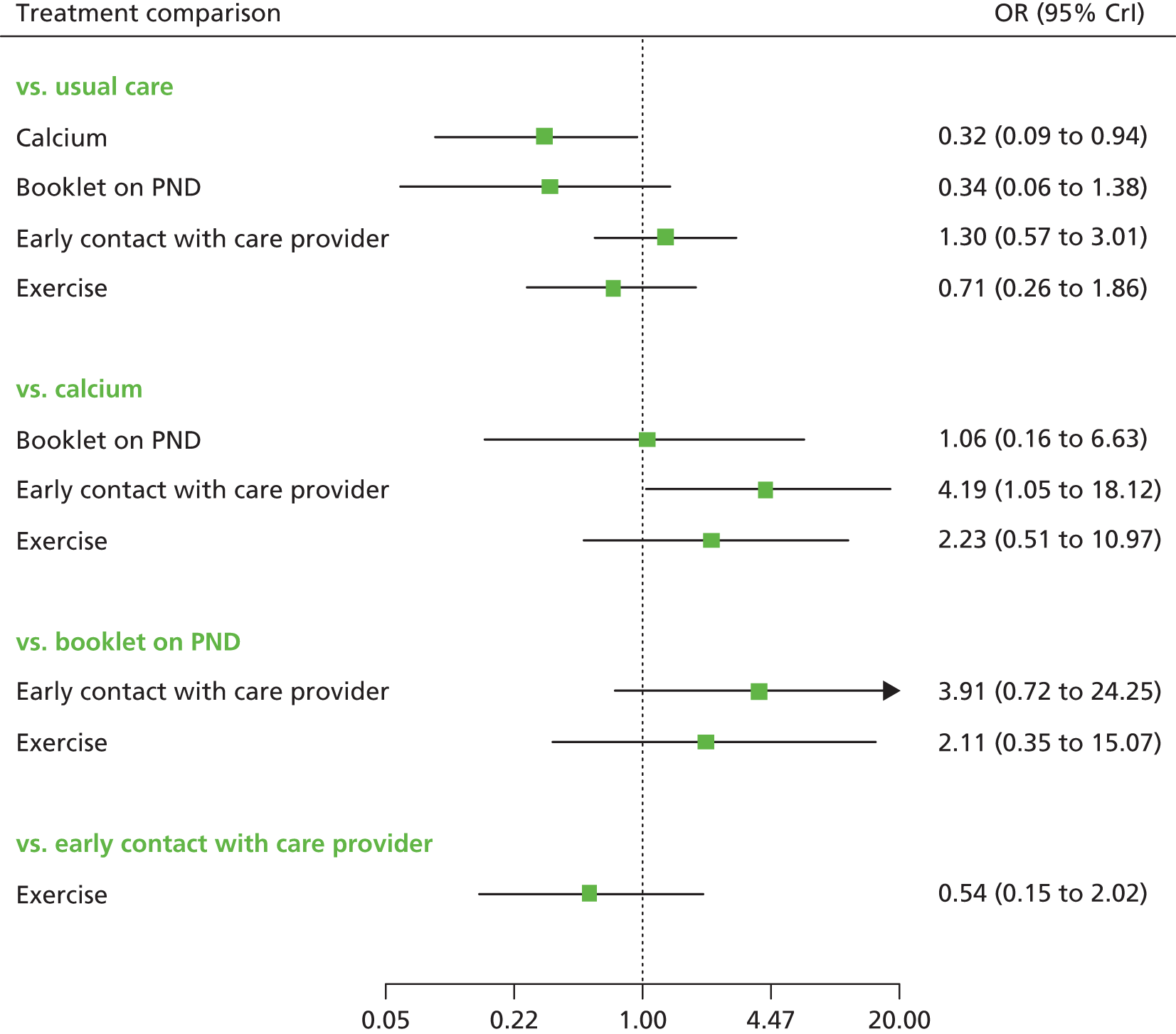
FIGURE 10.
Universal preventive interventions EPDS threshold score at 3 months postnatally: probability of treatment rankings (ranks 1–5).

The odds ratios of calcium, a booklet on PND and exercise were less than 1, suggesting a beneficial effect compared with usual care. Early contact with care provider had an odds ratio greater than 1, suggesting a worsening effect (see Figure 9). However, only the effect of calcium was statistically significant at a conventional 5% level. The interventions with the highest probabilities of being the best were calcium and booklet on PND (probability 0.48 and 0.45, respectively).
Results for universal preventive interventions for Edinburgh Postnatal Depression Scale threshold score at 6 months postnatally
A NMA was used to compare the effects of DHA,211 CBT-based intervention,61 PCA-based intervention,61 primary care and community care strategies147 and early contact with care provider225 relative to usual care on EPDS threshold. Data were available from four studies comparing six interventions. Figure 11 presents the network of evidence. There were five intervention effects to estimate from four studies. 61,147,211,225
FIGURE 11.
Universal preventive interventions EPDS threshold score at 6 months postnatally: network of evidence. Dashed lines represent three-arm trials.

Figure 12 presents the odds ratios of each intervention relative to usual care and Figure 13 presents the probabilities of treatment rankings. The total residual deviance was 7.04, which is compared with the total number of data points, seven, included in the analysis. This implies a good fit of the model to the data. The between-study SD was estimated to be 0.22 (95% CrI 0.00 to 0.71), which implies mild heterogeneity of intervention effects between studies.
FIGURE 12.
Universal preventive interventions EPDS threshold score at 6 months postnatally: odds ratios all treatment comparisons. Key: OR, odds ratio.
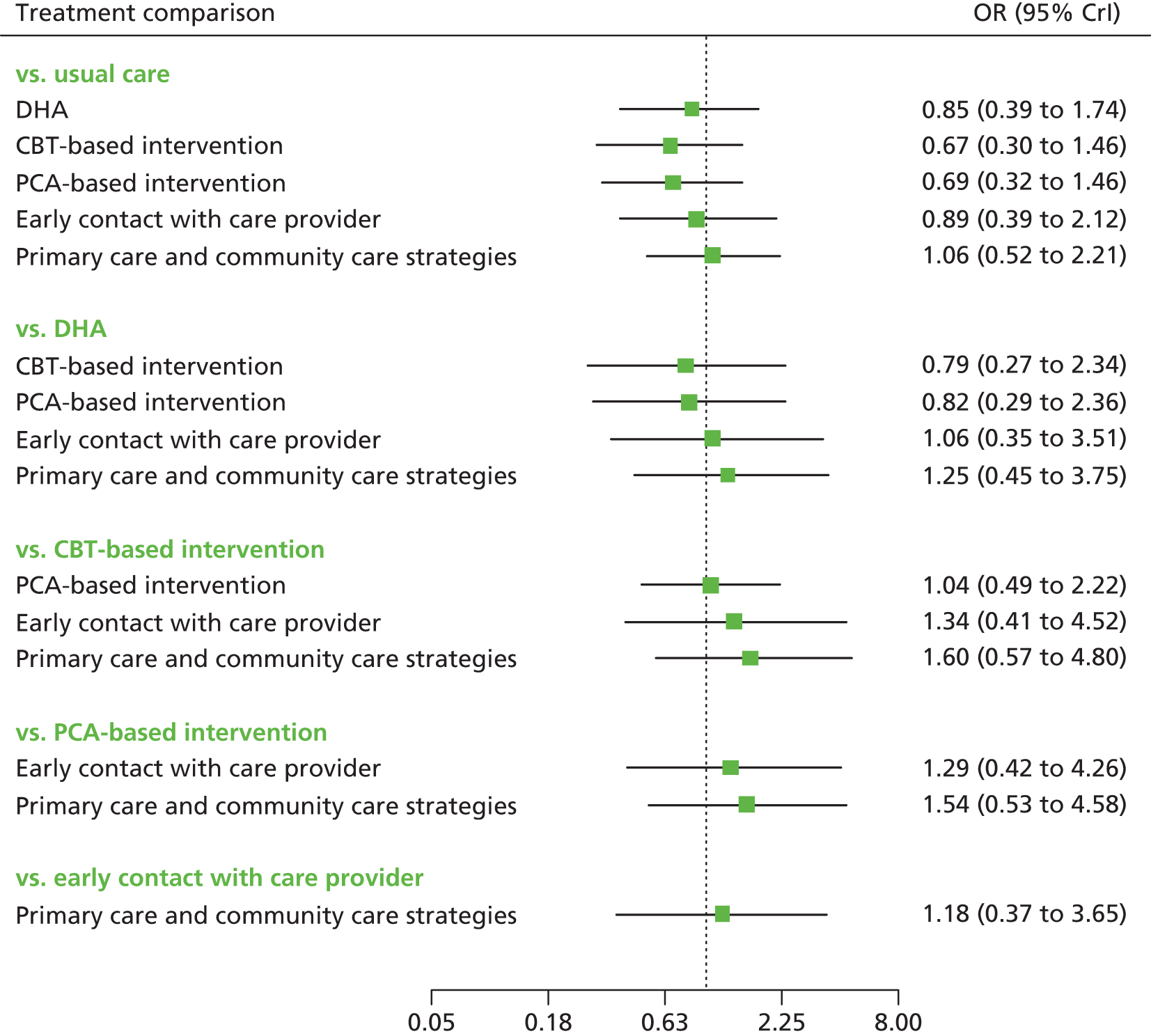
FIGURE 13.
Universal preventive interventions EPDS threshold score at 6 months postnatally: probability of treatment rankings (ranks 1–6).

For all interventions except primary care and community care strategies the odds ratio compared with usual care was less than 1, suggesting a beneficial effect. However, none of the comparisons were statistically significant at a conventional 5% level (see Figure 12). The interventions with the highest probabilities of being the best were CBT-based intervention and PCA-based intervention (probabilities 0.38 and 0.29, respectively) (see Figure 13).
Results for universal preventive interventions for Edinburgh Postnatal Depression Scale threshold score at 12 months postnatally
A NMA was used to compare the effects of CBT-based intervention,61 PCA-based intervention61 and midwifery redesigned postnatal care146 relative to usual care on EPDS threshold. Data were available from two studies comparing four interventions. Figure 14 presents the network of evidence. There were three intervention effects to estimate from two studies. 61,146
FIGURE 14.
Universal preventive interventions EPDS threshold score at 12 months postnatally: network of evidence.
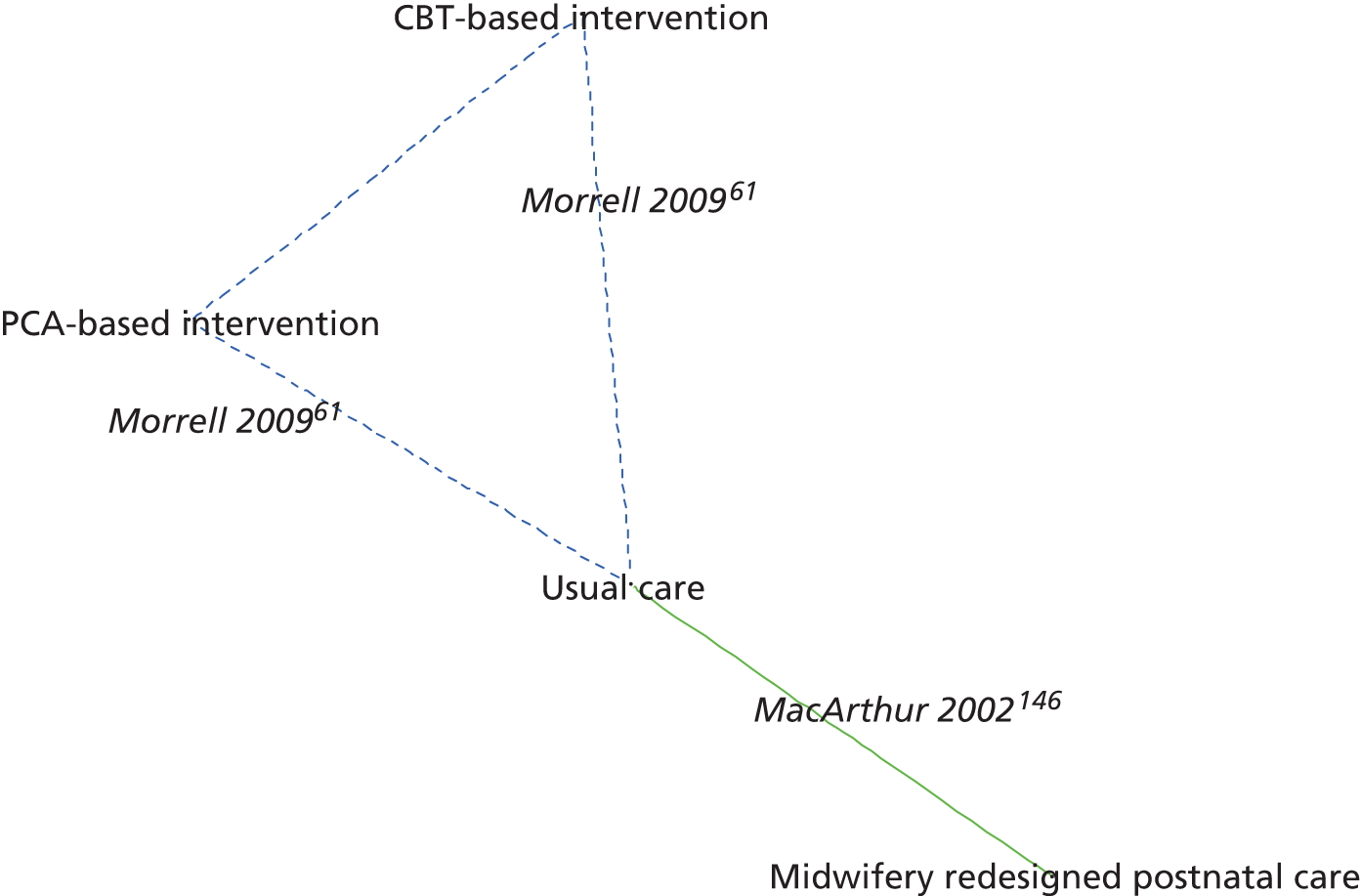
All three interventions were associated with a beneficial effect, although the results were statistically inconclusive (Figure 15). The probability of the intervention being the best was 0.43, 0.32 and 0.25 for midwifery redesigned postnatal care,146 CBT-based intervention61 and PCA-based intervention,61 respectively (Figure 16).
FIGURE 15.
Universal preventive interventions EPDS threshold score at 12 months postnatally: odds ratios for all treatment comparisons. Key: OR, odds ratio.
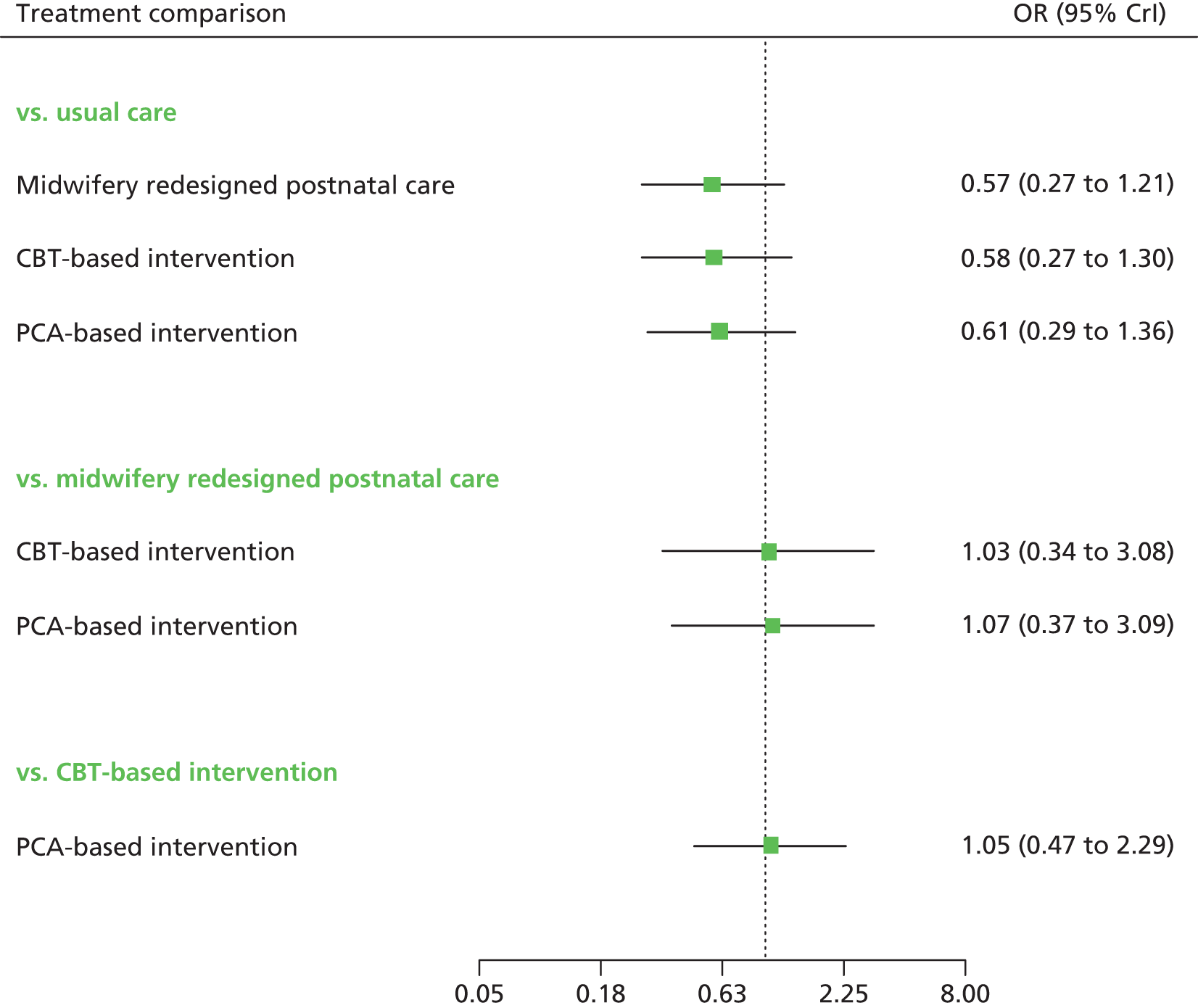
FIGURE 16.
Universal preventive interventions EPDS threshold score at 12 months postnatally: probability of treatment rankings (ranks 1–4).

Summary of results from network meta-analysis for universal preventive interventions for Edinburgh Postnatal Depression Scale threshold score
In general, the intervention effects were inconclusive, although calcium was associated with a statistically significant benefit relative to usual care at 3 months. Intervention effects tended to vary over time. The interventions most likely to be the best among those evaluable at each assessment were:
-
at 6 weeks postnatally, midwife-managed care219 and calcium208 (the included studies were of unclear and high risk of bias, respectively)
-
at 3 months postnatally, booklet on PND186 and calcium208 (the included studies were both at high risk of bias)
-
at 6 months postnatally, CBT-based intervention61 and PCA-based intervention61
-
at 12 months postnatally midwifery redesigned postnatal care,146 CBT-based intervention61 and PCA-based intervention. 61
However, there was considerable uncertainty associated with the results and none of the probabilities of being the best intervention exceeded 0.5.
A weakly informative prior distribution was used for the between-study SD because there were insufficient studies with which to estimate it from the sample data alone. This prior distribution was chosen to ensure that, a priori, 95% of the study-specific odds ratios were within a factor of 2 of the median odds ratio for each treatment comparison. The sensitivity analysis is presented for completeness in Appendix 11.
Results from network meta-analysis for universal preventive interventions for Edinburgh Postnatal Depression Scale mean scores
A NMA was used to compare the effects of baby play,184 booklet on PND,186 calcium,208 CBT-based intervention,61 early contact with care provider,225 education on preparing for parenting,184 educational information,123 exercise,129 midwife-managed care,219 midwifery redesigned postnatal care,146 PCA-based intervention,61 primary care and community care strategies,147 selenium212 and social support,199 relative to usual care on EPDS mean scores. Data were available from 12 studies comparing 15 interventions so that there were 14 intervention effects (relative to usual care) to estimate from 12 studies. 61,123,129,146,147,184,186,199,208,212,219,225 Figure 17 presents the network of evidence.
FIGURE 17.
Universal preventive interventions EPDS mean scores: network of evidence. Dashed lines represent three-arm trials.

Figure 18 presents the differences in EPDS mean scores of each intervention relative to usual care. The between-study SD was estimated to be 0.81 (95% CrI 0.04 to 2.61), which implies moderate heterogeneity of intervention effects between studies.
FIGURE 18.
Universal preventive interventions EPDS mean scores: mean differences of treatment comparisons vs. usual care across all time points.

The interventions associated with the greatest reduction in EPDS mean score were selenium212 (–1.90, 95% CrI –4.83 to 1.38 at 6–8 weeks) and midwifery redesigned postnatal care146 (–1.64, 95% CrI –4.07 to 1.07 at 3–4 months; –1.43, 95% CrI –4.00 to 1.36 at 12 months). None of the comparisons against usual care were statistically significant at a conventional 5% level.
Figures 19–22 present the probabilities of treatment rankings at 6–8 weeks, 3–4 months, 6–7 months and 12 months, respectively.
FIGURE 19.
Universal preventive interventions EPDS mean scores: probability of treatment rankings at 6–8 weeks postnatally (ranks 1–6).

FIGURE 20.
Universal preventive interventions EPDS mean scores: probability of treatment rankings at 3–4 months postnatally (ranks 1–7).
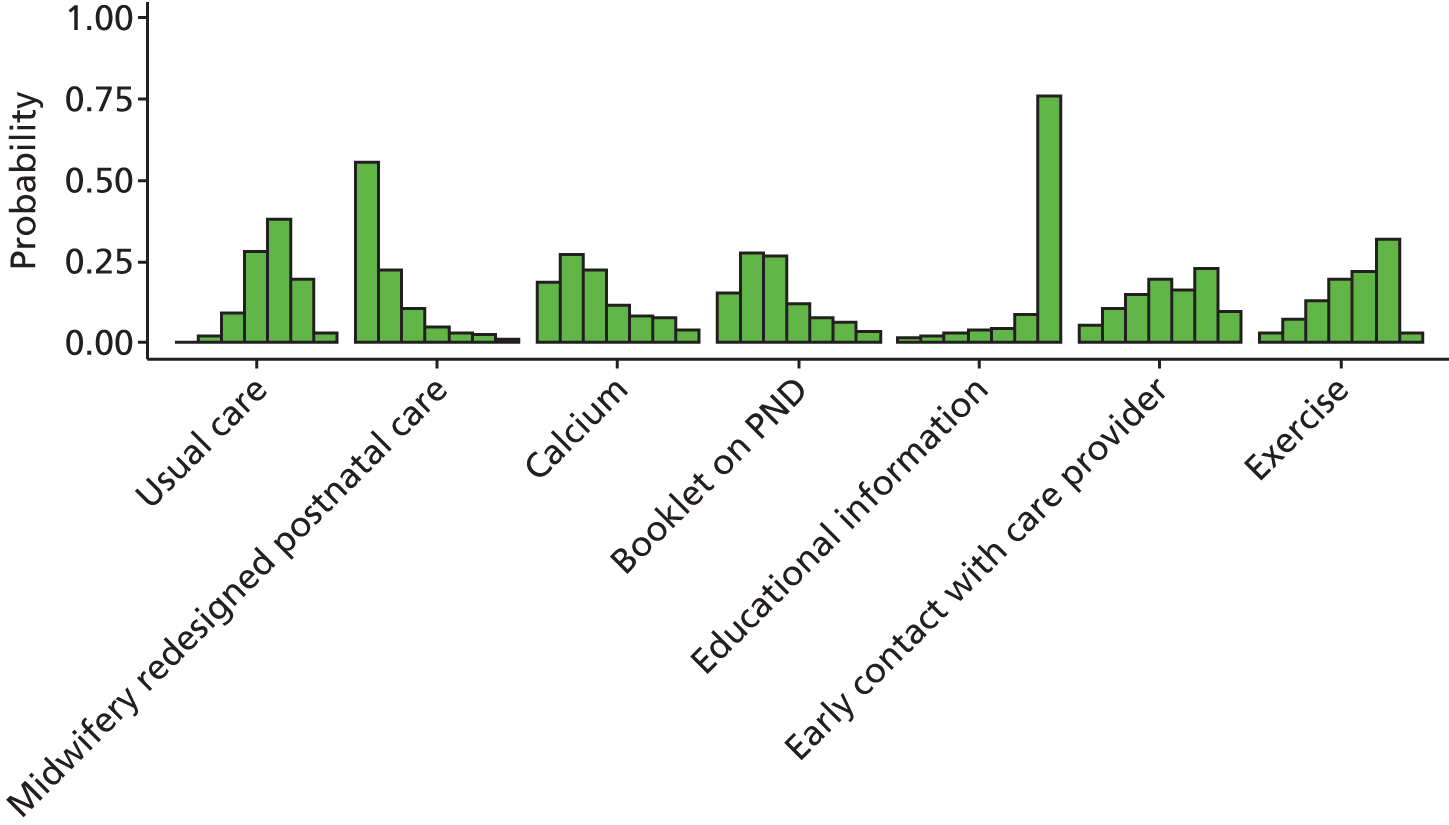
FIGURE 21.
Universal preventive interventions EPDS mean scores: probability of treatment rankings at 6–7 months postnatally (ranks 1–8).
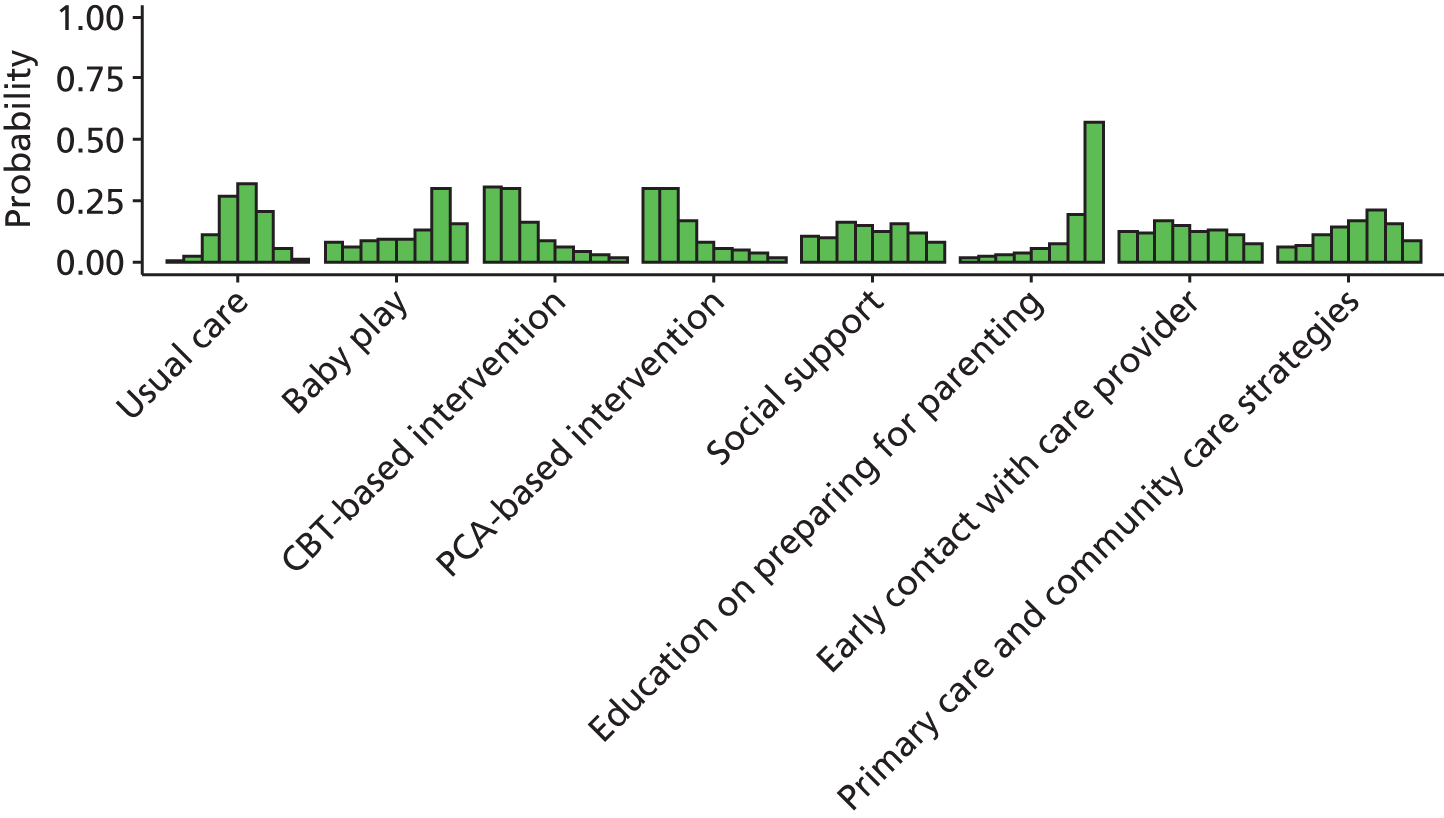
FIGURE 22.
Universal preventive interventions EPDS mean scores: probability of treatment rankings at 12 months postnatally (ranks 1–4).

The intervention with the highest probability of being the best at 6–8 weeks postnatally was selenium212 (probability 0.59); at 3–4 months postnatally the intervention with the highest probability of being the best was midwifery redesigned postnatal care (probability 0.55), while at 6–7 months postnatally CBT-based intervention and PCA-based intervention were equally likely to be the best (probability 0.30 in each case) and at 12 months postnatally the highest probabilities were associated with midwifery redesigned postnatal care146 and PCA-based intervention (probability 0.58 and 0.25, respectively).
Summary of results from network meta-analysis for universal preventive intervention studies for Edinburgh Postnatal Depression Scale mean scores
Not all studies provided information about intervention effects at each time, making it difficult to draw inferences across all interventions at each time. In general, the intervention effects were inconclusive and the CrIs were wide. Intervention effects tended to vary over time. The interventions most likely to be the best among those evaluable at each assessment were:
-
6–8 weeks postnatally: selenium212 (the risk of bias for this study was unclear so the benefit of selenium estimated in this NMA should be treated with some caution)
-
3 months postnatally: midwifery redesigned postnatal care146
-
6 months postnatally: CBT-based intervention61 and PCA-based intervention61
-
12 months postnatally: midwifery redesigned postnatal care,146 CBT-based intervention61 and PCA-based intervention. 61
Summary of results for universal preventive interventions for Edinburgh Postnatal Depression Scale threshold and Edinburgh Postnatal Depression Scale mean scores
Overall summary of results for universal preventive interventions for Edinburgh Postnatal Depression Scale threshold and Edinburgh Postnatal Depression Scale mean scores
Table 26 indicates the results of the NMAs for the EPDS threshold scores and EPDS mean scores at all assessment times. The results indicate that the universal preventive intervention with the best-quality evidence and the most enduring effect were midwifery redesigned postnatal care,146 CBT-based intervention61 and PCA-based intervention. 61
| Time postnatally | EPDS mean score | EPDS threshold score | Overall risk of bias | ||
|---|---|---|---|---|---|
| Difference in mean (95% CrI) | Probability of being the besta | Odds ratio (95% CrI) | Probability of being the besta | ||
| 6 weeks postnatally | |||||
| Midwife-managed care219 | –0.89 (–3.49 to 1.84) | 0.17 | 0.66 (0.30 to 1.40) | 0.43b | Unclear |
| Calcium208 | NE | NE | 0.70 (0.29 to 1.64) | 0.36b | High |
| 3 months postnatally | |||||
| Midwifery redesigned postnatal care146 | –1.64 (–4.07 to 1.07) | 0.55c | NE | NE | Low |
| Calcium208 | –0.90 (–3.56 to 1.85) | 0.19 | 0.32 (0.09 to 0.94) | 0.48d | High |
| Booklet on PND186 | –0.87 (–3.31 to 1.89) | 0.15c | 0.34 (0.06 to 1.38) | 0.45d | High |
| 6 months postnatally | |||||
| CBT-based intervention61 | –0.91 (–3.41 to 1.76) | 0.30e | 0.67 (0.30 to 1.46) | 0.38b | Low |
| PCA-based intervention61 | –0.90 (–3.32 to 1.74) | 0.30e | 0.69 (0.32 to 1.46) | 0.29b | Low |
| 12 months postnatally | |||||
| Midwifery redesigned postnatal care146 | –1.43 (–4.00 to 1.36) | 0.58f | 0.57 (0.27 to 1.21) | 0.43f | Low |
| PCA-based intervention61 | –0.97 (–3.54 to 1.71) | 0.25f | 0.61 (0.29 to 1.36) | 0.25f | Low |
| CBT-based intervention61 | –0.78 (–3.41 to 1.91) | 0.15f | 0.58 (0.27 to 1.30) | 0.32f | Low |
The qualitative data indicated that women appreciated the benefits from IPT, the reassurance and normalisation of social support, and the support received from peers while taking part in midwifery-led interventions and group-based CAM interventions.
Chapter 6 Results for selective preventive intervention studies
Characteristics of randomised controlled trials of selective preventive interventions
There were 20 RCTs in the selective preventive interventions group, in five of the seven intervention classes defined as:
-
pharmacological agents or supplements (n = 1)213
-
organisation of maternity care (n = 0)
-
CAM or other (n = 0).
Results are presented in this order for the RCTs of selective preventive interventions. There was limited replication of interventions across the trials. The 20 selective preventive intervention trials are described by their intervention context, mechanisms and measured outcomes within the seven classes. The results of the NMAs are presented for the EPDS threshold score and EPDS mean scores, followed by the findings of the qualitative data.
Description of qualitative studies of selective preventive interventions
The qualitative synthesis identified four studies in the selected preventive interventions group, within three of the seven intervention classes:
For ease of reference the selective preventive interventions have been given short-version descriptive labels (Table 27).
| First author, year, reference number | Short-version descriptive labels | Fuller description |
|---|---|---|
| Barnes, 2009149 | Peer support | Home-Start UK volunteer visits |
| Brugha, 2000188 | Education on preparing for parenting | Preparing for Parenthood is a series of six structured 2-hour long antenatal classes. These are preceded by an initial introductory meeting with the woman and her partner. The classes are designed to increase social support and problem-solving skills |
| Buist, 1999189 | Education on preparing for parenting | Ten classes in pregnancy and postpartum, focusing on parenting and coping strategies. Sessions covered physical preparing for parenting, but focused on emotional issues and highlighted the reality of parenting. Didactic teaching was combined with interactive group work, films and experiential exercises |
| Chabrol, 2002158 | CBT-based intervention | One cognitive–behavioural prevention session during hospitalisation |
| Gamble, 2005221 | Midwife-led debriefing or counselling after childbirth | Face-to-face counselling within 72 hours of birth and again via telephone at 4–6 weeks postpartum for women who report a distressing birth experience |
| Harris, 2002213 | Thyroxine | 100 µg of thyroxine tablets daily in thyroid antibody-positive women |
| Sen, 2006191 | Education on preparing for parenting | A twin midwife advisor, invitation to attend a series of education sessions, additional home visits and attendance at an antenatal twin clinic for women with twins |
| Small, 2000223 | Midwife-led debriefing or counselling after childbirth | Midwife-led debriefing after operative childbirth, before discharge from hospital |
| Zlotnick, 2011163 | IPT-based intervention | An interpersonally based intervention for low-income pregnant women with intimate partner violence |
Selective preventive interventions: psychological interventions
Characteristics and main outcomes of randomised controlled trials of selective preventive interventions of psychological interventions
Of the six included selective preventive intervention trials evaluating a psychological intervention,158–163 none were conducted in the UK. Three types of psychological interventions were evaluated: psychoeducational therapy,162 IPT160,163 and CBT. 158,159,161 Comparisons were made with usual care in specific countries158,159,161–163 and educational information. 160 One trial provided the intervention in a group format159 and five trials incorporated individual sessions. 158,160–163 None of the interventions were provided in the home setting. One trial provided the intervention in the antenatal period only,160 whereas three trials initiated the intervention postnatally159,161,162 and two trials provided the intervention across the perinatal period from pregnancy to after childbirth. 158,163 Interventions were provided by a variety of service providers. The number of contacts ranged from one to six (mean 4.3) and contact duration ranged from 25 minutes to 2 hours.
A summary of the characteristics and main outcomes is provided in Table 28.
| Intervention summary | First author, year, reference number | Country | Total number of women randomised | Place | Timing | Type of session | Provider | Comparison group | Number of contacts | Duration of contact (minutes) | Depression outcomes | Other outcomes | Main findings | Overall risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CBT-based intervention | Chabrol, 2002158,255,256 | France | 258 | Antenatal setting | Antenatal and postnatal | Individually | Psychologist | Usual care in France | 1 | 60 | BDI, EPDS score 11 or more, HDRS, MINI, SIGH-D | – | Compared with the control group, women in the prevention group had significant reductions in the frequency of probable depression (30 ± 2% vs. 48 ± 2%). Recovery rates based on HDRS scores of < 7 and BDI scores of < 4 were also significantly greater in the treated group than in the control group158 | High |
| The study suggests that this programme for prevention and treatment of post-partum depression is reasonably well-accepted and efficacious158 | ||||||||||||||
| CBT-based intervention | Hagan, 2004159 | Australia | 199 | Postnatal setting | Postnatal | Group | Midwife | Usual care in Australia | 6 | 120 | BDI, DSM-IV, EPDS median (interquartile range), GHQ, SADs | – | Fifty-four mothers (27%) in the trial were diagnosed with minor or major depression in the 12 months following very preterm delivery, 29 (29%) in the intervention group and 25 (26%) in the control group [relative risk 1.1 (95% CI 0.80–1.5)]159 | Low |
| There were no differences in the time of onset or the duration of the episodes of depression between the groups159 | ||||||||||||||
| Our intervention program did not alter the prevalence of depression in these mothers159 | ||||||||||||||
| CBT-based intervention | Silverstein, 2011161 | USA | 50 | Postnatal setting | Postnatal | Individually | Social worker | Usual care in the USA | 4 | 25–60 | QIDS | – | Forty-four per cent of control group mothers experienced an episode of moderately severe depression symptoms over the follow-up period, compared to 24% of PSE mothers. Control mothers experienced an average 1.19 symptomatic episodes over the 6 months of follow-up, compared to 0.52 among PSE mothers161 | Low |
| PSE appears feasible and may be a promising strategy to prevent depression among mothers of preterm infants161 | ||||||||||||||
| IPT-based intervention | Phipps, 2013160 | USA | 106 | Antenatal setting | Antenatal | Individually | Psychologist | Educational information | 6 | 60 | KID-SCID | – | The overall rate of depression in the intervention group (12.5%) was lower than the control group (25%) with a hazard rate ratio of 0.44 (95% confidence interval, 0.17–1.15) at 6 months after delivery160 | Low |
| An intervention that is delivered during the prenatal period has the potential to reduce the risk for postpartum depression in primiparous adolescent mothers160 | ||||||||||||||
| IPT-based intervention | Zlotnick, 2011163 | USA | 54 | Antenatal setting | Antenatal and postnatal | Individually | Interventionist | Usual care in the USA | 5 | 60 | EPDS mean, LIFE, SCID/NP | DTS, Criterion A of PTSD module of SCID-NP, CTS2 | The intervention was not associated with a reduction in major depressive episodes, PTSD, or IPV in pregnant or postnatal women. There was some effect in lowering symptoms of PTSD and depression among pregnant women. For women up to 3 months postnatally, there was a larger effect for PTSD symptomsThis study suggests some initial support for our intervention. Larger randomized trials are needed to further examine the intervention both during and after pregnancy163 | Low |
| Psychoeducational intervention | Tam, 2003162 | China | 516 | Postnatal setting | Postnatal | Individually | Nurse | Usual care in China | 4 | – | CGI, GHQ, HADS | WHO-QOL (Chinese version) | There was no significant difference in psychological morbidity, quality of life or client satisfaction between the counselling group and the control group162 | Unclear |
Description and findings from qualitative studies of selective preventive interventions of psychological interventions
There was one US-based study reporting qualitative data on selective preventive interventions for PND. 296–298 The IPT intervention for teenagers promoted support from peers and clinicians, and participants were able to gain practical skills and felt empowered (Table 29).
| First author, year, reference number | Country | Intervention details | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Name | Setting | Delivered antenatal/postnatal | Group/individual | Number of women in group | Number of sessions | Duration of session | Facilitator/service providers | ||
| Shanok, 2007296–298 Moderate CASP quality | USA | IPT (n = 14 current depressive disorder); n = 28, no inclusion/exclusion criteria | Secondary care: school for pregnant/parenting teenagers | Majority antenatal | Group | 7 | 12 weekly | 75 minutes | Clinical psychologist and co-therapist with training in IPT |
Findings from qualitative studies of selective preventive interventions of psychological interventions: support, learning practical strategies and empowerment
Participants reported that the intervention promoted the development of relationships and connection with other group members, and that it was a normalising experience. 296–298 Service providers said gaining practical skills was an important aspect of the intervention and that the intervention was beneficial when the group was supportive, and when the group members could share experiences and give advice. 296–298 Clinicians raised the importance of supporting the women and the validation of the pregnancy as part of an IPT intervention for teenagers:296–298
That we honored the arrival of motherhood, supported it as valid and no less valid even though they were young and poor.
Helping them to think about what’s next, how to get the child care, how to find a school for the child, how to negotiate with the difficult people in their lives to get what they need.
Being able to self-advocate and establish personal boundaries was interpreted by the authors as two benefits of IPT. 296–298
Selective preventive interventions: educational interventions
Characteristics and main outcomes of randomised controlled trials of selective preventive intervention of educational interventions
Of five included trials of a selective preventive intervention evaluating an educational intervention,188–190,192,271 two were conducted in the UK. 188,191 Two main types of interventions were identified: education on preparing for parenting188,189,192,271 and a booklet on PND and social worker telephone call. 190 Comparisons were made with usual care in specific countries. 188,189,192,271 One study evaluated the effect of group sessions,188 two studies evaluated the effect of individual sessions only190,192 and two studies evaluated a combination of individual and group sessions. 189,191 One trial provided the intervention in a home setting. 192 Three trials provided the intervention in the antenatal period only,188,189,191 whereas one trial initiated the intervention in the postnatal period190 and one trial provided the intervention across the antenatal and postnatal periods. 192 The interventions were provided by a variety of service providers, with the number of contacts ranging from 1 to 25 (mean 9.6 contacts) and the duration varying between 1 and 2 hours. A summary of the characteristics and main outcomes is provided in Table 30.
| Intervention summary | First author, year, reference number | Country | Total number of women randomised | Place | Timing | Type of session | Provider | Comparison group | Number of contacts | Duration of contact (minutes) | Depression outcomes | Other outcomes | Main findings | Risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Booklet on PND and social worker call | Howell, 2012190 | USA | 540 | Postnatal setting | Postnatal | Individually | Social worker | Educational information | 1 | – | EPDS score 10 or more, PHQ-9 | An intention-to-treat repeated measures analysis for up to 6 months of follow-up demonstrated that mothers in the intervention group were less likely to screen positive for depression versus enhanced usual care (odds ratio of 0.67; 95% CI 0.47–0.97 number needed to treat, 16; 95% CI: 9–112)190 | Low | |
| For black and Latina postnatal women, the action oriented behavioural educational intervention was associated with fewer depressive symptoms | ||||||||||||||
| Education on preparing for parenting | Brugha, 2000188,254,331 | UK | 209 | Antenatal setting | Antenatal | Group | Nurse and occupational therapist | Usual care in the UK | 6 | 120 | EPDS score 11 or more, GHQ-D, SCAN | Assignment to the IG did not significantly impact on PND [odds ratio for GHQ-Depression 1.22 (95% CI 0.63 to 2.39), p = 0.55] or on risk factors for depression188 | Unclear | |
| Attenders benefited no more than non-attenders188 | ||||||||||||||
| Education on preparing for parenting | Buist, 1999189 | Australia | 44 | Antenatal setting | Antenatal | Individually and group | Midwife, psychologist, nurse | Usual care in Australia | 10 | – | BDI, EPDS score 13 or more | STAI, DAS, SSS | Postpartum . . . no differences in depression scores, however, anxiety less at 6 weeks in IG189 | Unclear |
| Education on preparing for parenting | Sen, 2006191,271 | UK | 162 | Antenatal setting | Antenatal | Individually and group | Midwife | Usual care in the UK | 6 | 90 | EPDS score 13 or more, HADS | HADS subscale for anxiety, PSI, marital relationship, mother–infant attachment, social support | Non significant differences were noted at 6 weeks (8% vs. 20%; p = 0.52); 12 weeks (11 vs. 22; p = 0.20) and 26 weeks postnatal (9% vs. 19%; p = 0.08) but not at 52 weeks postnatal (18% vs. 20%; p = 0.68)191 | Low |
| Future provision of care for twin pregnancy, birth and parenting requires careful consideration. The intervention resulted in improved psychological benefit other than depression191 | ||||||||||||||
| Education on preparing for parenting | Walkup, 2009192 | USA | 167 | Home visits | Antenatal and postnatal | Individually | Community women | Educational information | 25 | 60 | CES-D | PSI, Parenting knowledge test, HOME, Parent involvement, ITSEA, Social Support self-report measure, substance use | No between-group differences found for maternal involvement, home environment, or mothers’ stress, social support, depression, or substance use192 | Unclear |
| Supports efficacy of paraprofessional-delivered Family Spirit home-visiting intervention for young American Indian mothers on maternal knowledge and infant behavior outcomes192 |
Description and findings from qualitative studies of selective preventive interventions of educational interventions
One qualitative study of an educational intervention was included in the indicated preventive interventions category. 253,254 This study was linked to the trial of education on preparing for parenting. 188 Further details are provided in Table 31.
| First author, year, reference number | Country | Intervention details | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Name | Setting | Delivered antenatal/postnatal | Group/individual | Numbers in group | Number of sessions | Duration of session | Facilitator/service providers | ||
| Wheatley, 1999,253 2003256 | UK | Preparing for parenthood | Secondary care – antenatal clinic | Antenatal | Group | 10–15 | One introductory meeting, six group sessions and one postnatal reunion | 2 hours | NR |
Findings from the qualitative review
Support
Data from participants of the group intervention demonstrated that the intervention promoted the development of relationships and connection with other group members and that it was a normalising experience. 253,256 One participant refused to take part in the intervention and said the idea of being in room full of people who did not know each other was ‘strange’. 253,254
Recipients reported that the intervention helped them to harness support from family members. 253,254 Authors’ interpretations indicated that participants valued the provision for their partner to join the group and that they were most interested in the session that included partner involvement. Participants found it helpful having another person with them to hear information that was provided. 253,254
Learning practical strategies
Participants reported that they had learned useful practical strategies as part of the intervention. 253,254 Specifically, participants learned, and were then able to apply, the SODAS (situation, options, disadvantages, advantages, solution) problem-solving system. 253,254
Education/active participation in own health care
The intervention promoted the gaining of knowledge and active participation in their own health care. 253,254 Specifically, the recipients reported that they were able to gain information about sensitive subjects such as PND. 253,254
Service delivery and barriers to participation
Although the majority of service user perspectives on psychological interventions were positive, a number of suggestions for improvement were provided. Authors of one study253,254 reported participants wanted more time for sharing of experiences. The women reported that they wanted to keep groups intimate:
And then when there were four of us there was more trust, you could be honest, it became like a little family.
Participants also reported that they would have liked written information such as handouts to be able to re-read them at a later point. 253,254
The authors253,254 also raised the point that when women were provided with information about the intervention they were told that only some women would be invited to take part. At the same time they were told the primary aim of the intervention was to reduce the likelihood of PND. The authors concluded that the selected women may have made the assumption that they were considered as of increased vulnerability for PND, but as it was never confirmed it may have left them with unresolved questions and anxieties. This may have implications for how information about interventions is presented to women.
A participant in one study253,254 reported difficulties in accessing the service:
I mean I wish I hadn’t missed the others, you know what I mean, to carry on really but just, what with getting there as well and my bleeding – so like you know I was upset that I missed quite a few sessions.
Other barriers were less visible and concerned how women approached the taboo subject of PND. The authors of one study253,254 reported that women appeared to want information about PND but were resistant to ask for this information in fear that they would be thought of as ‘going mad’. Other women appeared to actively avoid information about PND; when one woman was asked if she had found out about PND from health professionals she replied:
Well no, not really. I just didn’t want to know. I think I thought if I didn’t know about it, it wouldn’t happen!
The authors concluded that some participants avoided information about PND, as they believed a lack of knowledge could operate as a protective factor. When this information about PND was provided to them in the context of the intervention it appeared most were receptive to it.
Selective preventive interventions: social support interventions
Characteristics and main outcomes of randomised controlled trials of selective preventive interventions of social support
Of the five included trials149,201–204 evaluating social support interventions for the selective prevention of PND, only two were conducted in the UK. 149,201 Peer support was the main type of social support intervention identified: booklet on PND,149,201,203 as well as support in labour204 and a booklet plus video. 202 One trial provided the intervention using a group format,203 whereas the remaining four trials provided individual sessions. 149,201,202,204 Two trials provided the intervention in a home setting. 149,201 One trial provided the intervention in the antenatal period only,202 and no trial initiated the intervention postnatally. Three trials provided the intervention in both the antenatal and postnatal time periods. 149,201,203 One trial provided the intervention during labour. 204 As in the other included trials, the interventions were provided by a variety of lay and professional service providers. The number of contacts varied greatly with duration of contact (300 minutes) reported in only one trial. 204
A summary of the characteristics and main outcomes is provided in Table 32.
| Intervention summary | First author, year, reference number | Country | Total number of women randomised | Place | Timing | Type of session | Provider | Comparison group | Number of contacts | Duration of contact (minutes) | Depression outcomes | Other outcomes | Main findings | Risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Booklet plus video | Logsdon, 2005202 | USA | 128 | Antenatal setting | Antenatal | Individually | Nurse | Usual care in the USA | 1 | – | CES-D | PSQ, RSE | No significant differences found in Center for Epidemiological Trials of Depression instrument scores among groups at 6 weeks postpartum202 | Unclear |
| No significant difference | ||||||||||||||
| Peer mentors living with HIV | Richter, 2014;203 Rotheram, 2014269 | South Africa | 262 | Primary care | Antenatal and postnatal | Group | Peer mentors | Usual care in South Africa for women with HIV | 8 | – | EPDS score 13 or more, GHQ | Infant health, weight-for-age z-score, health-care utilisation, social support, HIV transmission-related behaviours | Compared to standard care women living with HIV, Enhanced Intervention women were less likely to report depressed mood (OR = 2.55; p = 0.003) | High |
| Adherence to clinic intervention groups was low, yet, there were benefits for maternal and infant health at 1.5 months post birth203 | ||||||||||||||
| Significant difference | ||||||||||||||
| Peer support | Barnes, 2009149 | UK | 527 | Home visits | Antenatal and postnatal | Individually | Home-Start volunteers | Usual care in the UK | 2 or more | – | EPDS score 13 or more, SCID | PSI, ICQ, MSSI | Volunteer support had no identifiable impact on the emergence of maternal depression from 2 to 12 months or on depression symptoms when infants were 12 months149 | Unclear |
| Informal support initiated following screening for disadvantage in pregnancy did not reduce the likelihood of depression for mothers with infants149 | ||||||||||||||
| No significant difference | ||||||||||||||
| Peer support | Cupples, 2011201 | UK | 343 | Home visits | Antenatal and postnatal | Individually | Peer mentors | Usual care in the UK | 2 or more | – | SF-36 | BSID-II | IG and CG did not differ in BSID-II psychomotor (mean difference 1.64, 95% CI −0.94 to 4.21) or mental (−0.81, −2.78 to 1.16) scores, nor SF-36 physical functioning (−5.4, −11.6 to 0.7) or mental health (−1.8, −6.1 to 2.6)201 scores | Low |
| No benefit for infant development or maternal health at 1 year201 | ||||||||||||||
| No significant difference | ||||||||||||||
| Support in labour | Wolman, 1993;204 Trotter, 1992;276 Nikodem, 1998275 | South Africa | 189 | Labour ward | Labour | Individually | Supportive labour companion doula | Usual care in South Africa | 1 | 300 | EPDS mean score, HDRS, PDI | STAI, CSEI | The mean depression score of control group mothers was 23.27 (SEM 1.28) and of supported mothers 10.4 (SEM 0.77) (p < 0.001)204 | Unclear |
| The group receiving support attained higher self-esteem scores and lower postpartum depression and anxiety ratings 6 weeks after delivery204 | ||||||||||||||
| According to the data analysis the presence of a supportive labour companion resulted in a significant decrease in depression 3 months after birth: t(61) = 2,18; p < 0.05276 | ||||||||||||||
| There were no differences in postpartum depression scores between two groups at 1 year275 | ||||||||||||||
| Mixed results |
No qualitative studies provided data on social support interventions.
Selective preventive interventions: pharmacological agents or supplements
Characteristics and main outcomes of randomised controlled trials of selective preventive interventions of pharmacological agents or supplements
Only one trial was identified that evaluated a pharmacological agent or supplement intervention for the prevention of PND. 213 This trial was conducted in the UK and evaluated the administration of thyroxine during the postnatal period. The number of contacts involved was two or more but duration length of contact was not reported. A summary of the characteristics and main outcomes is provided in Table 33.
| Intervention summary | First author, year, reference number | Country | Total number of women randomised | Place | Timing | Type of session | Provider | Comparison group(s) | Number of contacts | Duration of contact (minutes) | Depression outcomes | Other outcomes | Main findings | Risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Thyroxine | Harris, 2002213 | UK | 341 | Postnatal setting | Postnatal | Individually | Prescriber | Usual care in the UK | 2 or more | – | EPDS score 13 or more, GHQ, MADRS, RDC | – | No evidence that thyroxine had any effect on occurrence of depression213 | Unclear |
No qualitative studies provided data on studies of pharmacological agents or supplement interventions.
Selective preventive interventions: midwifery-led interventions
Characteristics and main outcomes of randomised controlled trials of selective preventive interventions of midwifery-led interventions
Of the three trials221–223 included in the selective preventive interventions evaluating midwifery-led interventions, none were conducted in the UK. The types of midwifery-led interventions that were identified included midwife-led debriefing after childbirth221,223 and CenteringPregnancy Plus. 222 Comparisons were made with usual care in Australia221,223 and the USA. 222 Two studies evaluated individual sessions221,223 and one study was undertaken in the antenatal period only. 222 Midwives provided the interventions. The number of contacts varied and duration of contact ranged from 1 to 2 hours. A summary of the characteristics and main outcomes is provided in Table 34.
| Intervention summary | First author, year, reference number | Country | Total number of women randomised | Place | Timing | Type of session | Provider | Comparison group(s) | Number of contacts | Duration of contact (minutes) | Depression outcomes | Other outcomes | Main findings | Risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CenteringPregnancy Plus | Ickovics, 2011;222 Ickovics 2007262 | USA | 1047 | Antenatal setting | Antenatal | Group | Midwife | Usual care in the USA | 10 | 120 | CES-D | PSS, SRS social support subscale items, seven SRS social conflict subscale items | Using intention-to-treat models, there were no significant differences in psychosocial function; yet, women in the top tertile of psychosocial stress at study entry did benefit from integrated group care222 | Low |
| Scores for high-stress women in the CenteringPregnancy Plus arm were higher for self-esteem and lower for stress and social conflict in the third trimester, and depression was lower at 1 year postnatally | ||||||||||||||
| No significant difference | ||||||||||||||
| Midwife-led debriefing after childbirth | Gamble, 2005221,259,260 | Australia | 103 | Postnatal setting | Postnatal | Individually | Midwife | Usual care in Australia | 2 or more | – | EPDS score 13 or more, DASS-21 | MINI-PTSD, MSSS | At 3-month follow-up, intervention group women reported decreased trauma symptoms, low relative risk of depression, low relative risk of stress, and low feelings of self-blame221 | Low |
| The midwifery-led intervention for women following a distressing birth experience was associated with a reduction in symptoms of stress, trauma, depression, and self-blame | ||||||||||||||
| Four women in the intervention group and 17 women in the control group had an EPDS score 12 or more at 3 months postnatally (RR 0.25, 95% CI 0.09 to 0.69) | ||||||||||||||
| Significant difference | ||||||||||||||
| Midwife-led debriefing after childbirth | Small, 2000223 | Australia | 1041 | Postnatal setting | Postnatal | Individually | Midwife | Usual care in Australia | 1 | 60 | EPDS score 13 or more | SF-36 subscales | More women allocated to IG scored as depressed 6 months after birth than women allocated to usual postpartum care [81 (17%) vs. 65 (14%)], although this difference was not significant (odds ratio 1.24, 95% CI 0.87 to 1.77) | Low |
| No significant difference |
Description and findings from qualitative studies of selective preventive interventions of midwifery-led interventions
Two US-based studies292–295 included in the selective preventive interventions reported on midwifery-led interventions. Details of these CenteringPregnancy interventions are presented in Table 35.
| First author, year, reference number | CASP Quality Grading | Country | Intervention details | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Name | Setting | Delivered antenatal/postnatal | Group/individual | Number of in group | Number of sessions | Duration of session | Facilitator/service providers | |||
| Lehman, 2012292 | Moderate | USA | CenteringPregnancy | Secondary care – faith-based community health centre | Antenatal and postnatal | Group and individual | NR | 10 (the first four monthly, and then the last six fortnightly) | 2 hours | NR |
| Novick, 2012;293 2013294,295 | High | USA | CenteringPregnancy | Secondary care – antenatal clinic | Antenatal and postnatal | Group and individual | 8–12 | One individual, then 8–10 group | 2 hours | Certified nurse-midwife and a medical assistant |
Findings from the qualitative review
Support
Women reported gaining support of various kinds, such as peer support, as a particularly helpful aspect of the CenteringPregnancy intervention. 292–295 Women talked about building relationships with peers,293–295 receiving reassurance and normalising their experiences of pregnancy, birth and the postpartum period. 293–295 Women reported how they valued the emotional support, informational support and practical advice they gained from peers. 293–295
Service providers were positive about their experience in delivering CenteringPregnancy. They echoed service user views suggesting that the intervention facilitated peer support. 293–295
Women in two studies felt the intervention encouraged family and partner support, and increased family awareness of difficulties in pregnancy. 292–295 Participants in one study felt health professionals’ support was helpful. 292 Service providers reported the intervention facilitated improved communication between health providers, such as between community mental health teams and obstetric providers. 293–295
Active participation/education
One study highlighted how participants might actively participate in their own health care including the provision of education, and gaining information and knowledge. 293–295 Several respondents in one study reported that they valued receiving education and information about pregnancy and the postnatal period. 293–295 Providers across several studies felt that the intervention encouraged women to be active participants in their own health care. 293–295
Service delivery and barriers to participation
Service providers said that the group intervention was a more efficient use of their time. 293–295
The review showed that peer support was an important aspect of the intervention. The intervention also appeared to promote and facilitate support from the woman’s family and partner. Women found the support received from health professionals helpful. Service providers felt that the intervention facilitated improved communication between health providers. Women valued receiving education and information about pregnancy and the postnatal period. Providers felt that the intervention encouraged active participation by the women. Service providers also felt that the intervention was an efficient use of time compared with other models.
Selective preventive interventions: organisation of maternity care
No selective preventive intervention for PND was identified concerning the organisation of maternity care. No qualitative studies provided data on selective preventive interventions of organisation of maternity care.
Selective preventive interventions: complementary and alternative medicine or other interventions
No selective preventive intervention for PND was identified concerning CAMs or other interventions. No qualitative studies provided data on selective preventive interventions of CAMs or other interventions.
Results from network meta-analysis for selective preventive interventions for Edinburgh Postnatal Depression Scale threshold score
Of the 20 selective preventive intervention trials, nine were included in the NMA. 150,160,188,190,213,215,221,223,225 Among the 11 trials excluded because they could not be connected to the main network (see Appendix 10, Table of selective preventive intervention studies omitted from network meta-analysis), two were conducted in South Africa203,204,269,270,275,276 and one in China. 162 Three trials were excluded because they could not be connected to the main network of evidence. 160,190,192
Five trials were excluded because of a lack of EPDS data,159,161,201,202,222,262 and three trials because there was no usual-care comparator. 160,190,192
Three of the trials at low risk of bias found no benefit of CenteringPregnancy Plus for young, ethnic minority women of low socioeconomic status,222,262 of CBT-based intervention for mothers following very preterm delivery,159 or of peer mentors for first-time mothers in socioeconomically deprived communities.
Of the other three trials at low risk of bias, one found that a CBT-based intervention was associated with a reduction in depressive symptoms for women living in financial hardship,161 one found that an IPT-based intervention was associated with an overall lower rate of depression among primiparous adolescent mothers160 and one found that a booklet on PND and social worker call was associated with a reduced likelihood of screening positive for depression among black and Latina mothers postpartum. 190
Results from network meta-analysis for selective preventive intervention for Edinburgh Postnatal Depression Scale threshold score at 6 weeks postnatally
A NMA was used to compare the effects of thyroxine,213 a CBT-based intervention158 and midwife-led debriefing following childbirth221 relative to usual care on EPDS threshold data. Data were available from three trials comparing three interventions. 158,213,221 Figure 23 presents the network of evidence. 158,213,221
FIGURE 23.
Selective preventive interventions EPDS threshold score at 6 weeks postnatally: network of evidence.

Figure 24 presents the odds ratios of each intervention relative to usual care and Figure 25 presents the probabilities of treatment rankings. The total residual deviance was 6.00, compared with the total number of data points, six, included in the analysis. This implies a good fit of the model to the data. The between-study SD was estimated to be 0.21 (95% CrI 0.01 to 0.72), which implies mild heterogeneity of intervention effects between trials.
FIGURE 24.
Selective preventive interventions EPDS threshold score at 6 weeks postnatally: odds ratios all treatment comparisons. Key: OR, odds ratio.

FIGURE 25.
Selective preventive interventions EPDS threshold score at 6 weeks postnatally: probability of treatment rankings (ranks 1–4).
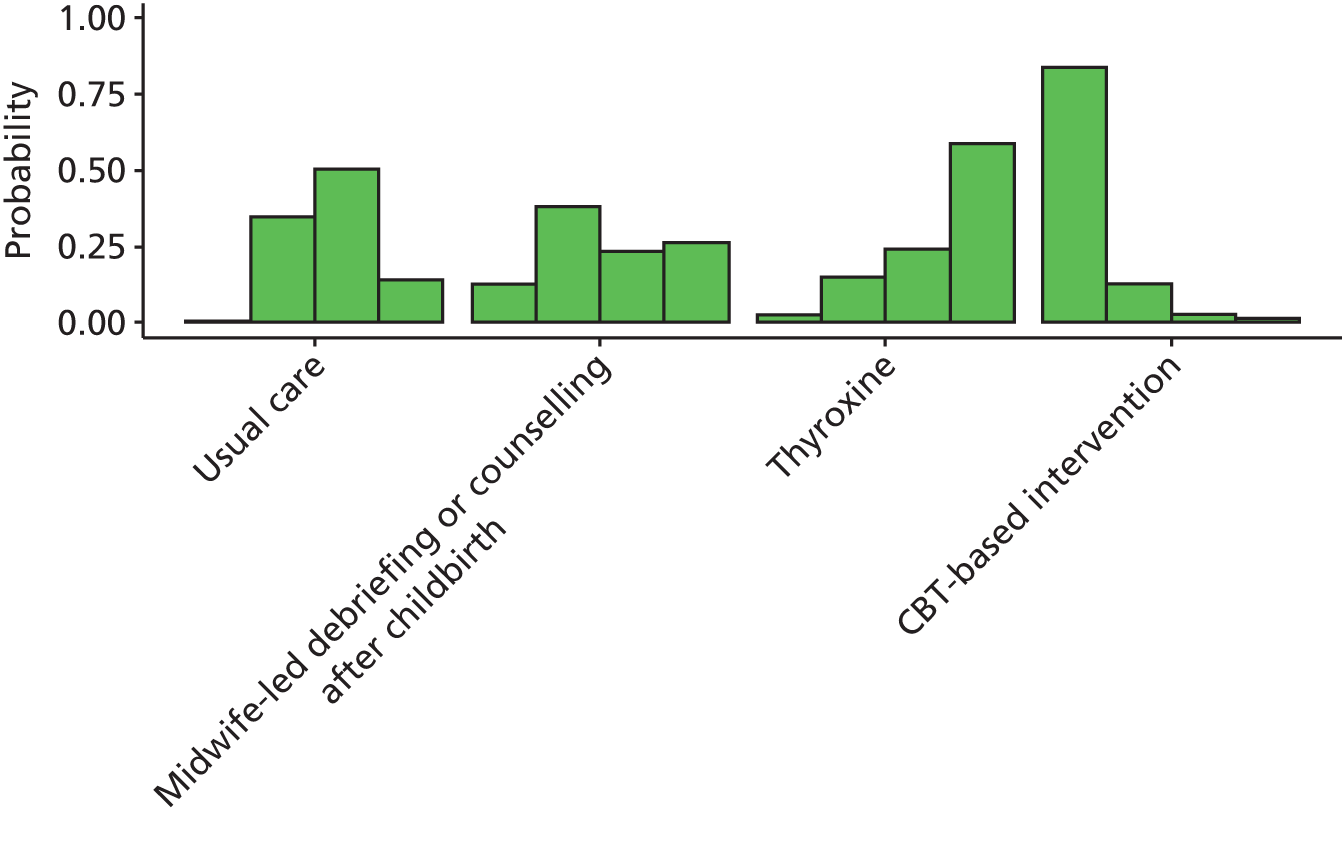
Cognitive–behavioural therapy-based intervention had the biggest effect relative to usual care (odds ratio 0.46, 95% CrI 0.18 to 1.10), although this was not statistically significant at a conventional 5% level (see Figure 24). CBT-based intervention had the highest probability of being the best (probability 0.84) (see Figure 25).
Results from network meta-analysis for selective preventive intervention for Edinburgh Postnatal Depression Scale threshold score at 3 months postnatally
A NMA was used to compare the effects of midwife-led debriefing after childbirth,221 education on preparing for parenting188 and thyroxine213 relative to usual care on EPDS threshold. Data were available from three trials comparing four interventions. 188,213,221 Figure 26 presents the network of evidence. Three treatment effects were estimated from three trials. 188,213,221
FIGURE 26.
Selective preventive interventions EPDS threshold score at 3 months postnatally: network of evidence.
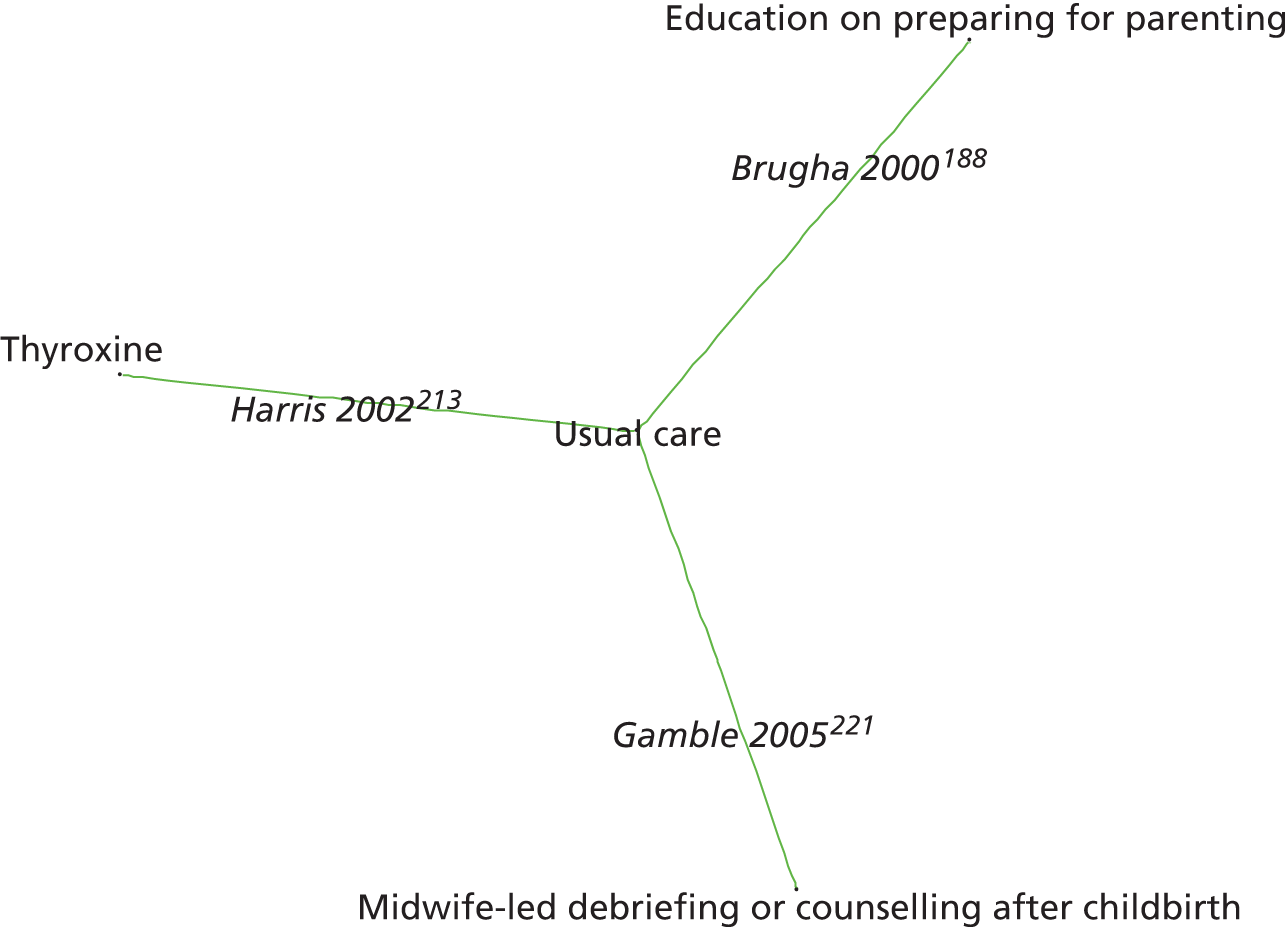
Figure 27 presents the odds ratios of each intervention relative to usual care and Figure 28 presents the probabilities of treatment rankings. The total residual deviance was 6.16, compared with the total number of data points, six, included in the analysis. This implies a good fit of the model to the data. The between-study SD was estimated to be 0.22 (95% CrI 0.01 to 0.73), which implies mild heterogeneity of intervention effects between trials.
FIGURE 27.
Selective preventive interventions EPDS threshold score at 3 months postnatally: odds ratios all treatment comparisons. Key: OR, odds ratio.
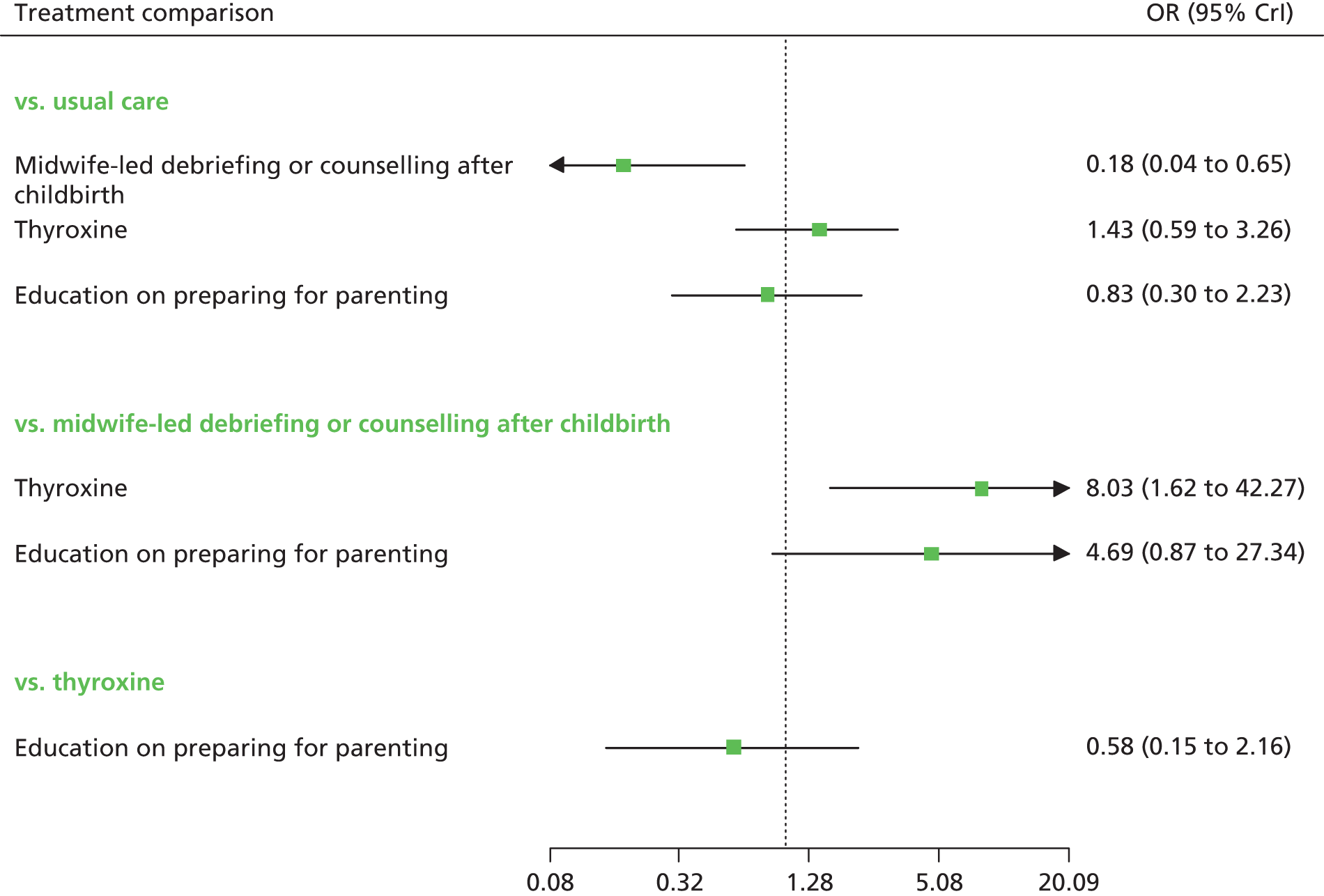
FIGURE 28.
Selective preventive interventions EPDS threshold score at 3 months postnatally: probability of treatment rankings (ranks 1–4).
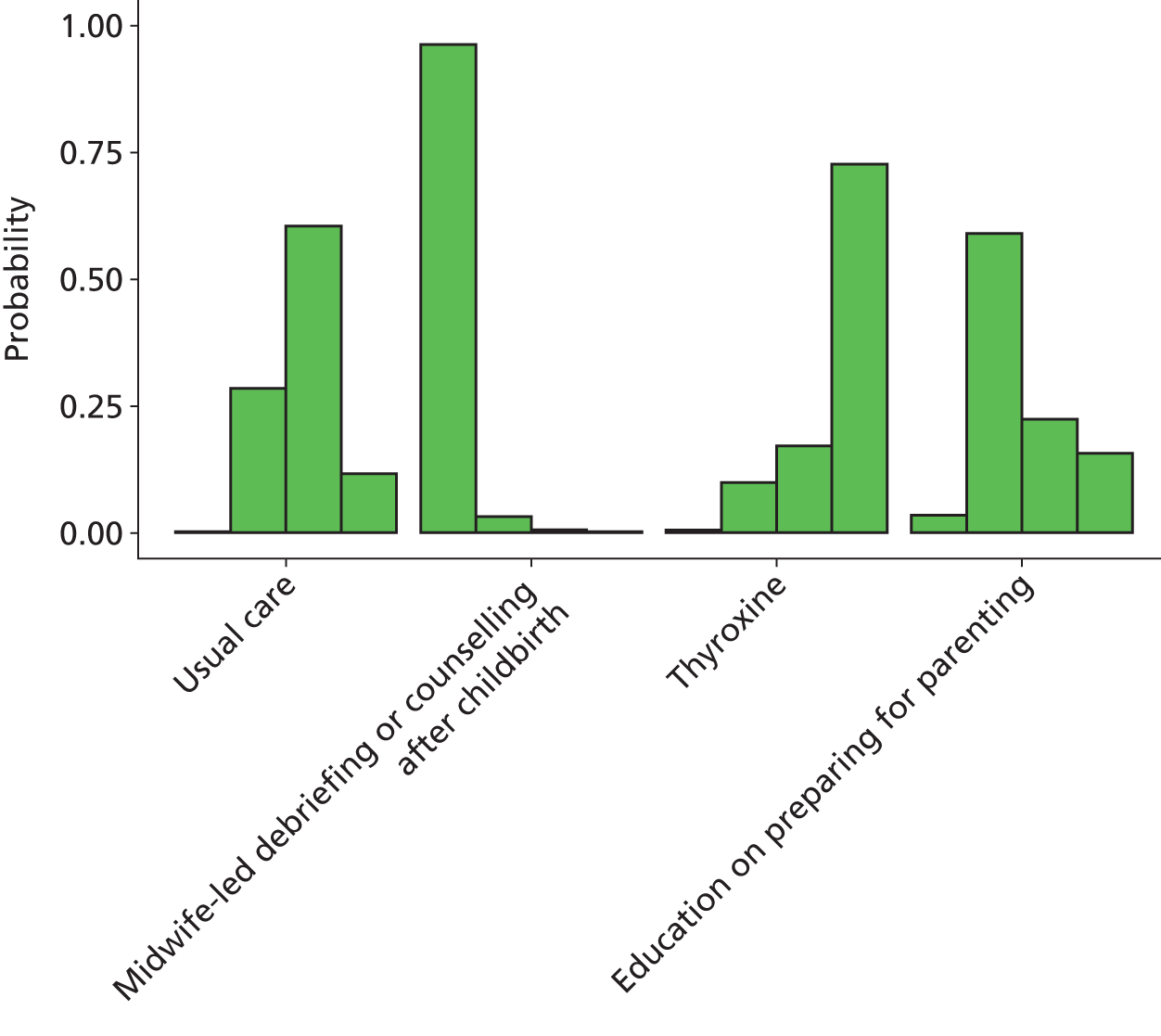
For the selective preventive interventions at 3 months postnatally, midwife-led debriefing or counselling after childbirth had the biggest effect relative to usual care (odds ratio 0.18, 95% CrI 0.04 to 0.65) (see Figure 27). Midwife-led debriefing or counselling after childbirth had the highest probability of being the best (probability 0.96) (see Figure 28).
Results from network meta-analysis for selective preventive intervention for Edinburgh Postnatal Depression Scale threshold score at 6 months postnatally
A NMA was used to compare the effects of thryoxine213 and midwife-led debriefing after childbirth223 relative to usual care on EPDS threshold. Data were available from two trials comparing three interventions. 213,223 Figure 29 presents the network of evidence. There were two treatment effects to estimate from two trials. 213,223
FIGURE 29.
Selective preventive interventions EPDS threshold score at 6 months postnatally: network of evidence.

Figure 30 presents the odds ratios of each intervention relative to usual care and Figure 31 presents the probabilities of treatment rankings. The total residual deviance was 3.99, compared with the total number of data points, four, included in the analysis. This implies a good fit of the model to the data. The between-study SD was estimated to be 0.22 (95% CrI 0.02 to 0.74), which implies mild heterogeneity of intervention effects between trials.
FIGURE 30.
Selective preventive interventions EPDS threshold score at 6 months postnatally: odds ratios all treatment comparisons. Key: OR, odds ratio.
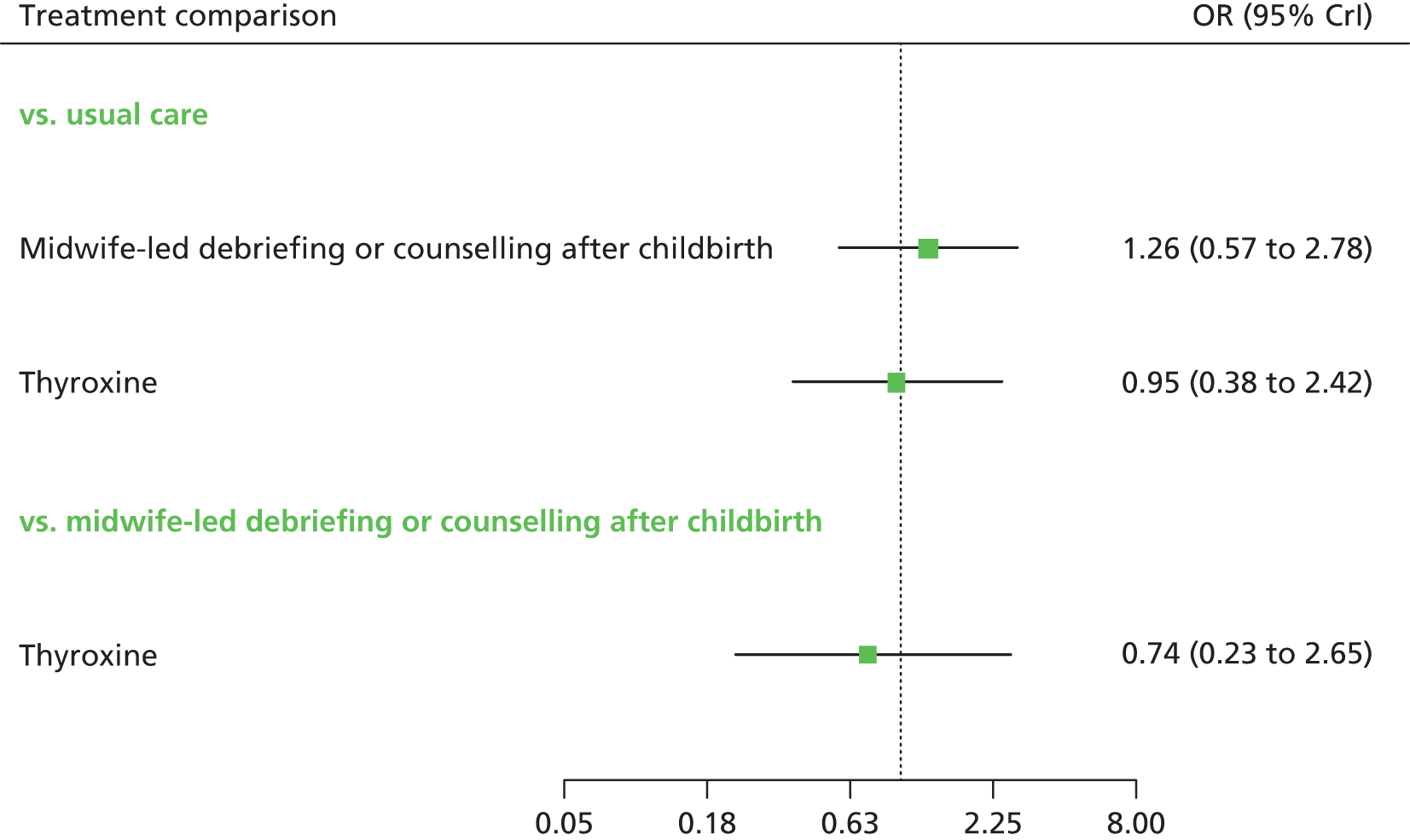
FIGURE 31.
Selective preventive interventions EPDS threshold score at 6 months postnatally: probability of treatment rankings (ranks 1–3).

There was insufficient evidence of a difference in effect between interventions (see Figures 30 and 31).
Summary of results from network meta-analysis for selective preventive interventions Edinburgh Postnatal Depression Scale threshold score
Table 36 indicates the results of the NMAs for the EPDS threshold scores and mean scores at all assessment times. In general, the intervention effects were inconclusive, although midwife-led debriefing after childbirth was associated with a statistically significant benefit at 3 months. When interventions were evaluated at more than one assessment, the effects tended to vary over time.
| Time postnatally | EPDS mean score | EPDS threshold score | Overall risk of bias | ||
|---|---|---|---|---|---|
| Difference in mean (95% CrI) | Probability of being the besta | Odds ratio (95% CrI) | Probability of being the besta | ||
| 6 weeks postnatally | |||||
| CBT-based intervention: Chabrol, 2002158 | –1.75 (–4.25 to 0.71) | 0.75b | 0.46 (0.18 to 1.10) | 0.84c | High |
| Education on preparing for parenting: Sen, 2006;191 Buist, 1999189 | –0.81 (–3.10 to 1.34) | 0.23 3 | NE | NE | Low; uncleard |
| 3 months postnatally | |||||
| Education on preparing for parenting: Sen, 2006;191 Buist, 1999189 | –1.08 (–3.83 to 1.65) | 0.35b | 0.83 (0.30 to 2.23) | 0.03c | Low; uncleard |
| IPT-based intervention: Zlotnick, 2011163 | –1.85 (–5.60 to 2.14) | 0.62b | NE | NE | Unclear |
| 6 months postnatally | |||||
| Education on preparing for parenting: Sen, 2006;191 Buist, 1999189 | –1.32 (–3.54 to 1.10) | 0.83b | NE | NE | Low; uncleard |
Results from network meta-analysis for selective preventive interventions for Edinburgh Postnatal Depression Scale mean scores
A NMA was used to compare the effects of CBT-based intervention,158 education on preparing for parenting,189,191 IPT-based intervention,163 midwife-led debriefing after childbirth223 and peer support149 relative to usual care on EPDS mean scores. Data were available from six trials comparing five interventions. Figure 32 presents the network of evidence. There were five intervention effects to estimate (relative to usual care) from six trials. 149,158,163,189,191,223
FIGURE 32.
Selective preventive interventions EPDS mean scores: network of evidence.

Figure 33 presents the difference in EPDS mean scores of each intervention relative to usual care and Figures 34–37 present the probabilities of treatment rankings at 6–8 weeks, 3–4 months, 6–7 months and 12 months, respectively. The between-study SD was estimated to be 0.68 (95% CrI 0.03 to 2.46), which implies moderate heterogeneity of intervention effects between trials. The interventions associated with the greatest reduction in EPDS mean score were the IPT-based intervention (–1.85, 95% CrI –5.60 to 2.144 at 3–4 months) and CBT-based intervention (–1.75, 95% CrI –4.25 to 0.71 at 6–8 weeks). None of the comparisons against usual care were statistically significant at a conventional 5% level.
FIGURE 33.
Selective preventive interventions EPDS mean scores: mean differences of treatment comparisons vs. usual care across all time points.
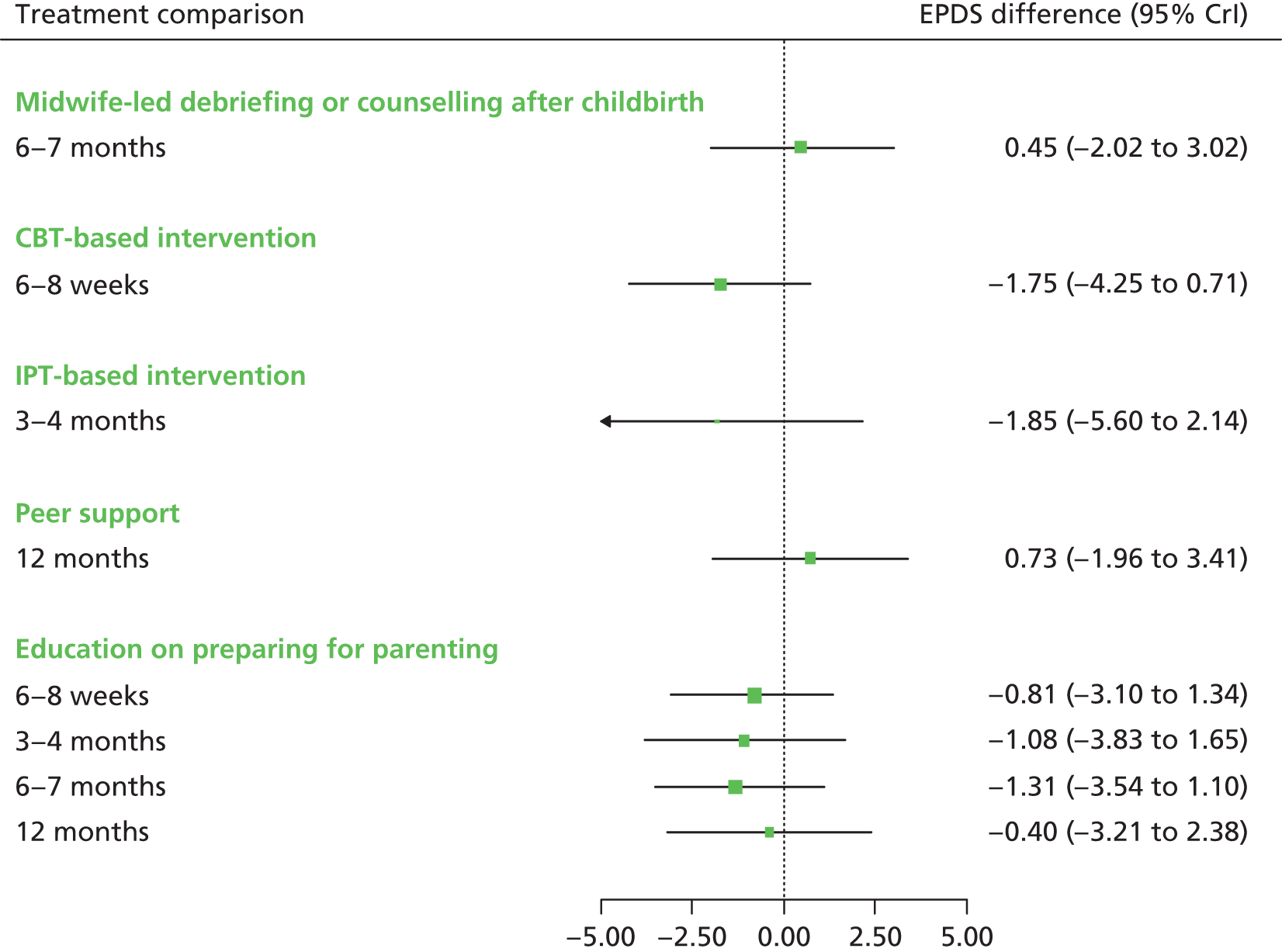
FIGURE 34.
Selective preventive interventions EPDS mean scores: probability of treatment rankings at 6–8 weeks postnatally (ranks 1–3).
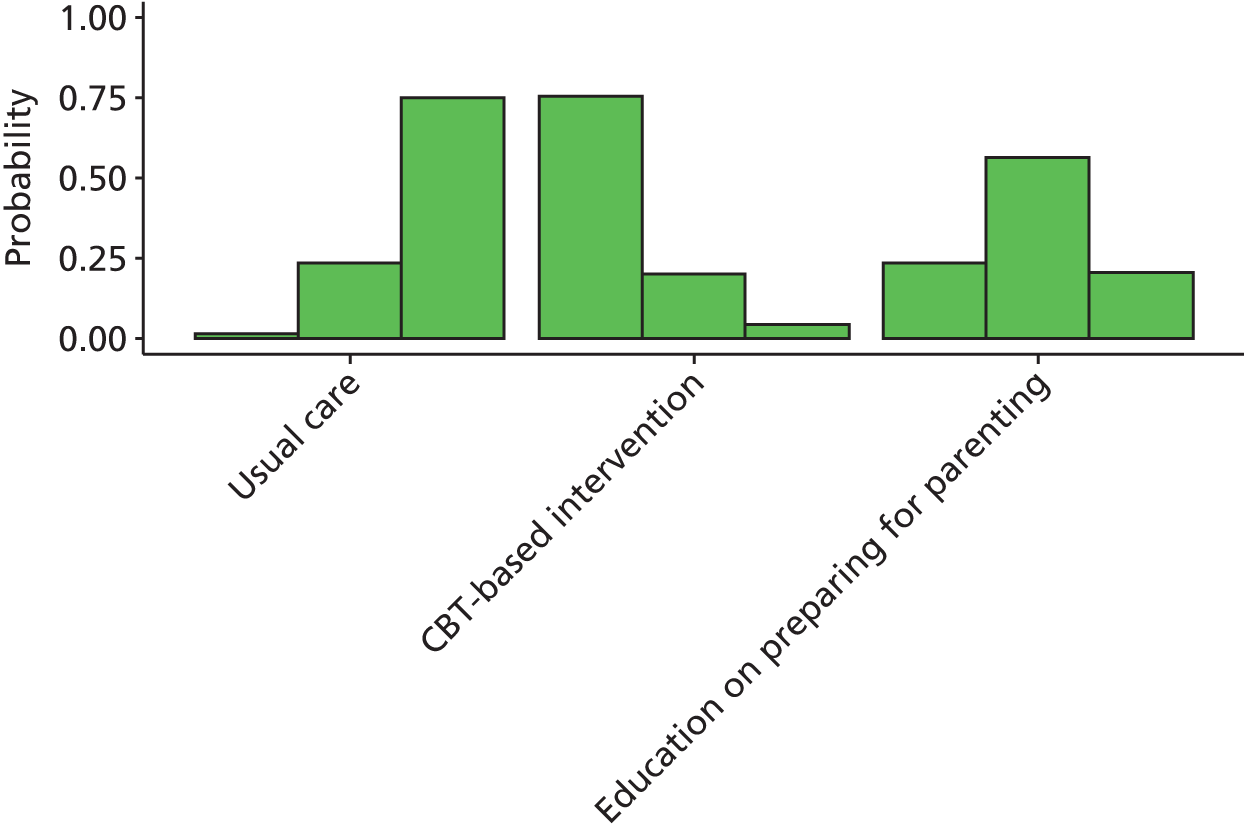
FIGURE 35.
Selective preventive interventions EPDS mean scores: probability of treatment rankings at 3–4 months postnatally (ranks 1–3).
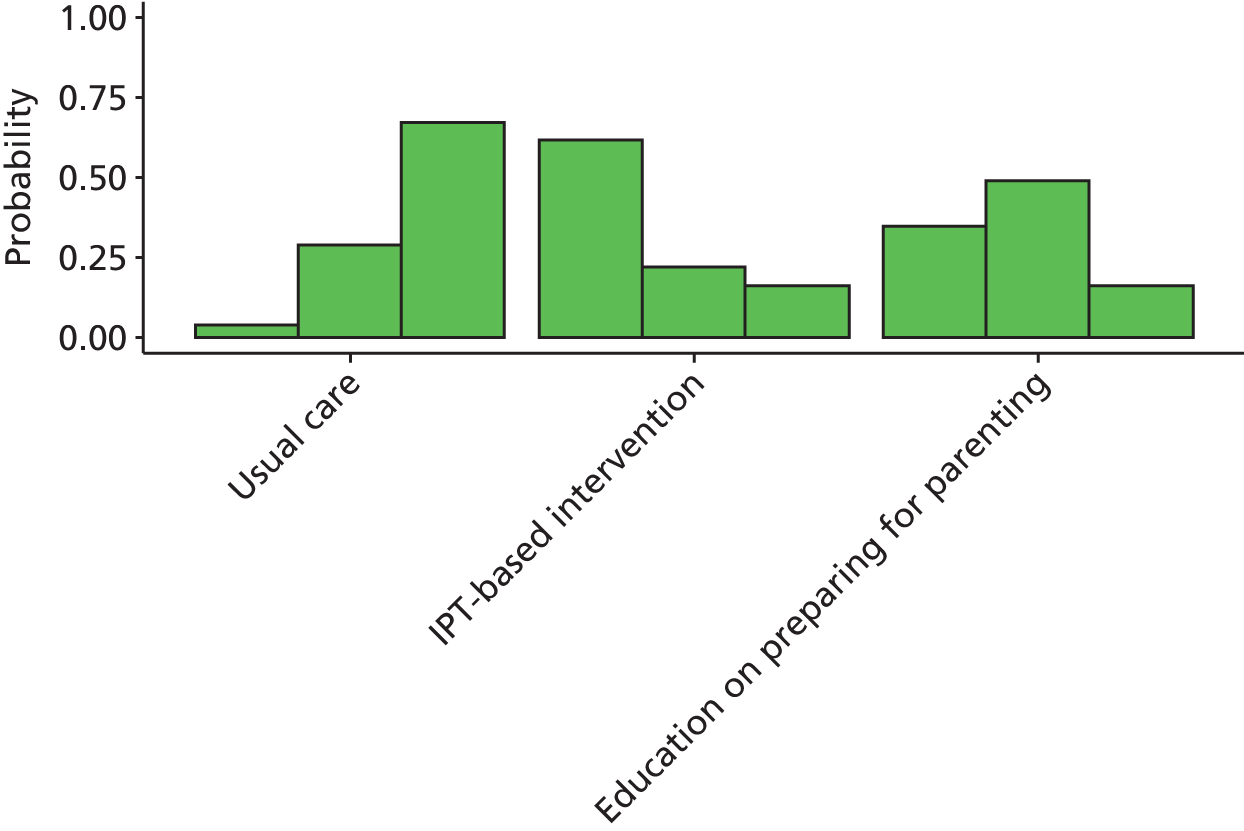
FIGURE 36.
Selective preventive interventions EPDS mean scores: probability of treatment rankings at 6–7 months postnatally (ranks 1–3).

FIGURE 37.
Selective preventive interventions EPDS mean scores: probability of treatment rankings at 12 months (ranks 1–4).

The intervention with the highest probabilities of being the best at 6–8 weeks was the CBT-based intervention (probability 0.75). The intervention with the highest probability of being the best at 3–4 months was the IPT-based intervention (probability 0.62). The intervention with the highest probability of being the best at 6–7 months was education on preparing for parenting (probability 0.83). The intervention with the highest probability of being the best at 12 months was education on preparing for parenting (probability 0.57).
Summary of results from network meta-analysis for selective preventive interventions for Edinburgh Postnatal Depression Scale mean scores
Not all interventions provided information about intervention effects at each time, making it difficult to draw inferences across all interventions at each time. In general, the intervention effects were inconclusive and the CrIs were wide. The most beneficial interventions appeared to be the CBT-based interventions, IPT-based interventions and education on preparing for parenting. However, the evidence for the effect of CBT-based intervention came from the study by Chabrol et al. ,158 which was judged to be at high risk of bias. As such, the benefit of that CBT-based intervention estimated in this NMA should be treated with some caution. In addition, the evidence for the effect of IPT-based interventions at 3–4 months came from a trial which was a small pilot study by Zlotnick et al. 163 and, as such, the results should be treated with caution.
The evidence from the qualitative review demonstrated that the IPT, as a selective intervention, was acceptable to women and they reported benefiting from gaining realistic information about motherhood and from being empowered to ask for help. The educational intervention ‘Preparing for parenthood’ provided participants with an additional opportunity to learn about PND while avoiding the stigma of asking for this information. Benefits of the CenteringPregnancy intervention included facilitation of support, particularly peer support for selective groups.
Chapter 7 Results for indicated preventive intervention studies
Characteristics of randomised controlled trials of indicated preventive interventions
There were 30 RCTs in the indicated preventive interventions group, in six of the seven intervention classes defined as:
-
midwifery-led interventions (n = 1)224
-
organisation of maternity care (n = 0)
-
CAM or other interventions (n = 1). 229
Results are presented in this order for the RCTs of indicated preventive interventions. There was limited replication of interventions across the studies. The 30 indicated preventive intervention studies are described by their intervention context, mechanisms and measured outcomes within the seven classes.
Description and findings from qualitative studies of indicated preventive interventions
There were three qualitative studies in the indicated preventive interventions group, in two of the seven intervention classes:
One study reported on the perspectives and attitudes of service providers to indicated preventive interventions. 298 For ease of reference, indicated preventive interventions were given short-version indicative labels (Table 37).
| First author, year, reference number | Short-version indicative label | Fuller description |
|---|---|---|
| Armstrong, 1999164 | Promoting parent–infant interaction | A structured home-visiting programme of weekly nurse home visiting supported by a social worker and paediatrician when the child was at great risk of poor health and developmental outcomes |
| Austin, 2008165 | CBT-based intervention | An antenatal cognitive–behavioural group intervention in a primary care setting for pregnant women identified with mild to moderate symptoms in pregnancy and/or at risk of developing depression or anxiety in the perinatal period |
| Austin, 2008165 | Educational information | Information booklet for pregnant women identified with mild to moderate symptoms in pregnancy and/or at risk of developing depression or anxiety in the perinatal period |
| Dennis, 2009205 | Peer support | Telephone-based volunteer peer support for women at high risk of PND |
| Ginsburg, 2012168 | CBT-based intervention | An eight-lesson cognitive–behavioural-based programme, Living in Harmony, for reservation-based American Indians |
| Ginsburg, 2012168 | Educational information | An eight-lesson education programme, Education-Support programme, for reservation-based American Indians |
| Gorman, 1997169 | IPT-based intervention | A preventive intervention adapted from IPT for depression, for women at high risk of PND and adjustment problems |
| Grote, 2009170 | Educational information | Written educational materials about depression, and strong encouragement to seek treatment at the behavioural health centre for low-income, pregnant women scoring 13 or more on the EPDS |
| Grote, 2009170 | IPT-based intervention | Culturally relevant, enhanced brief IPT-B consisting of an engagement session, followed by eight acute IPT-B sessions before birth and maintenance IPT up to 6 months postpartum for low-income, pregnant women scoring 13 or more on the EPDS |
| Marks, 2003224 | Midwifery continuous care | Continuous midwifery care of a named midwife who, as far as possible, followed the women through the pregnancy, delivery and postnatally, for women with a history of major depressive disorder |
| Morrell, 200961 | CBT-based intervention | HV training in the assessment of postnatal women combined with cognitive–behavioural approach sessions for eligible women who scored 12 or more on the EPDS |
| Morrell, 200961 | PCA-based intervention | HV training in the assessment of postnatal women combined with Person-Centred Approach sessions for eligible women who scored 12 or more on the EPDS |
| Munoz, 2007173 | CBT-based intervention | Mamás y Bebés/Mothers and Babies Course developed in Spanish and English that uses a cognitive–behavioural mood management framework and incorporates social learning concepts, attachment theory and sociocultural issues, for low-income predominantly Latina women who screened positive for a major depressive episode and/or who scored 16 or more on CES-D |
| Petrou, 2006174 | Promoting parent–infant interaction | Home visits from research health visitors to enhance maternal sensitivity to infant communicative signals and infant responsiveness and to encourage women to express their feelings; for women at raised risk for PND |
| Stamp, 1995195 | Education on preparing for parenting | Two antenatal groups and one postnatal group with a practical and emotional emphasis on planning for and expectations of life changes precipitated by the arrival of a new baby for women vulnerable to developing PND. A non-directive, practical and supportive programme was developed, underpinned by a philosophy that acknowledged the abilities and resourcefulness of the women themselves. Its focus was on access to information, preparation and support, the extension and development of women’s existing networks and goal setting |
| Webster, 2003196 | Booklet on PND | Providing women in the intervention group with a booklet about PND and a list of the phone contacts of PND resources; for pregnant women with risk factors for PND |
Indicated preventive interventions: psychological interventions
Characteristics and main outcomes of randomised controlled trials of indicated preventive interventions of psychological interventions
Of the 19 included studies reporting psychological interventions for the indicated prevention of PND,61,121,148,164–179 only three61,174,177 were conducted in the UK. Six types of psychological interventions were identified: CBT-based interventions,61,148,165,167,168,171–173 empowerment training,175 IPT-based interventions,166,169,170,178,179 mindfulness-based intervention,121 promoting parent–infant interaction164,174,177 and psychoeducational interventions. 176 Comparisons were made with usual care in specific countries61,121,148,164,166,167,169–179 and educational information. 165,168 Seven studies evaluated group sessions,121,165,171,173,177–179 11 evaluated individual sessions61,148,164,167–170,172,174–176 and one evaluated both group and individual sessions. 166 Five studies took place in the home setting. 61,164,168,172,174 Six studies were undertaken in the antenatal period only,121,168,173,175–177 two in the postnatal period only61,164 and 11 in a combination of both antenatal and postnatal periods. 148,165–167,169–172,174,178,179 The interventions were provided by different health-care providers (nurse, social worker, paediatrician, psychologist, counsellor, health visitor, community health workers) and group facilitators. 171,177 The number of contacts varied and length of contact ranged from 30 minutes168 to 2 hours121,165,171,177 A summary of the characteristics and main outcomes is provided in Table 38.
| Intervention summary | First author, year, reference number | Country | Total number of women randomised | Place | Timing | Type of session | Provider | Comparison group(s) | Number of contacts | Duration of contact (minutes) | Depression outcomes | Other outcomes | Main findings | Overall risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CBT-based intervention | Austin, 2008165 | Australia | 277 | Antenatal setting | Antenatal and postnatal | Group | Psychologist | Educational information | 6 | 120 | EPDS mean score (data extracted using digitising software), MINI | STAI (not reported) | Intention-to-treat analyses revealed relatively low mean baseline EPDS scores [range 6.88 (SD 4.43) 8.16 (SD 4.47)], with no reduction in EPDS scores in either group. MINI depression criteria were fulfilled by 19% of all participants at time 1, but there was no reduction in depression in either group; in contrast those with MINI anxiety diagnoses reduced from 28% in late pregnancy to 16% at 4 months postpartum in the CBT group, with similar reductions in the control group | Unclear |
| No significant difference | ||||||||||||||
| CBT-based intervention | El-Mohandes, 2008167 | USA | 1070 | Antenatal setting | Antenatal and postnatal | Individually | Counsellor | Usual care in the USA | 2 or more | 36 | BDI-II, Hopkins symptom checklist | CTS, ETSE | Depression at postpartum interview was 25.5% in the intervention group and 29.0% in the control group; p = 0.303 | Low |
| An integrated multiple risk factor intervention addressing psychosocial and behavioral risks delivered mainly during pregnancy can have beneficial effects in risk reduction postpartum167 | ||||||||||||||
| No significant difference | ||||||||||||||
| CBT-based intervention | Ginsburg, 2012168 | USA | 47 | Home visits | Antenatal | Individually | Paraprofessionals | Educational information | 8 | 30–60 | CES-D, CGAS, DISC, EPDS mean score | SSI | At all post intervention assessments, mothers in both groups showed similar reductions in depressive symptoms and similar rates of MDD. Both groups of participants also showed similar improvements in global functioning. No changes in either group were found on the measure of social support168 | Unclear |
| No significant difference | ||||||||||||||
| CBT-based intervention | Le, 2011171 | USA | 217 | Antenatal setting | Antenatal and postnatal | Group | Group Facilitators | Usual care in the USA | 11 | 120 | BDI-II score 21 or more, Mood Screener | Mood Screener | The cumulative incidence of major depressive episodes was not significantly different between the intervention (7.8%) and UC (9.6%) groups171 | Unclear |
| A CBT intervention for low-income, high-risk Latinas reduced depressive symptoms during pregnancy but not during the postpartum period171 | ||||||||||||||
| No significant difference | ||||||||||||||
| CBT-based intervention | McKee, 2006172 | USA | 90 | Home visits | Antenatal and postnatal | Individually | Psychologist | Usual care in the USA | 8 | – | BDI-II | IRS, NSSQ | The two intervention conditions were equally effective in reducing depression172 | High |
| No significant difference | ||||||||||||||
| CBT-based intervention and PCA-based intervention | Morrell, 200961 | UK | 595 | Home visits | Postnatal | Individually | Health visitors | Usual care in the UK | up to 8 | 60 | CORE-OM, EPDS score 12 or more and mean, SF-36 MCS | PSI, DAS, SF-6D, SF-36 PCS | At 6 months postnatally, 93 of the 271 (34%) women in the IG and 67 of the 147 women in the CG (46%) had an EPDS score 12 or more. The OR for a score 12 or more at 6 months postnatally was 0.62 (95% CI 0.40 to 0.97; p = 0.036) for women in the IG vs. CG | Low |
| Training health visitors to assess women, identify symptoms of PND, and deliver psychologically informed sessions was clinically effective at 6 and 12 months postnatally compared with usual care61 | ||||||||||||||
| Significant difference | ||||||||||||||
| CBT-based intervention | Munoz, 2007173 | USA | 41 | Antenatal setting | Antenatal | Group | Psychologist | Usual care in the USA | 12 | – | CES-D, EPDS mean score; MMS for MDE | – | Differences in terms of depression symptom levels or incidence of MDEs between the two groups did not reach statistical significance in this pilot trial. However, the MDE incidence rates of 14% for the intervention condition versus 25% for the comparison condition represent a small effect size (h = 0.28)173 | Unclear |
| No significant difference | ||||||||||||||
| CBT-based intervention | Rahman, 2008148 | Pakistan | 903 | Antenatal setting | Antenatal and postnatal | Individually | Community health workers | Usual care in Pakistan | 16 | – | HDRS | Weight-for-age Z scores, height-for-age Z scores, MSPSS, BDQ, GAFS | At 6 months, 97 of the 418 (23%) women in the IG and 211 of the 400 women in the CG (53%) had major depression. The OR was 0.22 (95% CI 0.14 to 0.36; p < 0.0001). At 12 months, 27% in the IG (111 out of 412) vs. 59% in the CG (226 out of 386) had major depression. The OR was 0.23 (95% CI 0.15 to 0.36; p < 0.0001) | Low |
| This psychological intervention delivered by community-based primary health workers has the potential to be integrated into health systems in resource-poor settings148 | ||||||||||||||
| Significant difference | ||||||||||||||
| Empowerment training | Tiwari, 2005175 | Hong Kong | 110 | Antenatal setting | Antenatal | Individually | Midwife | Usual care in Hong Kong | 1 | 30 | EPDS score 10 or more | CTS, SF-36 | Twenty-five women from the control group had EPDS scores of 10 or more compared with 9 from the experimental group (relative risk 0.36, 0.15–0.88)175 | Low |
| The experimental group reported less psychological abuse and minor physical violence and their depression symptom scores were lower than the those for the CG | ||||||||||||||
| Significant difference | ||||||||||||||
| IPT-based intervention | Crockett, 2008166 | USA | 36 | Antenatal setting | Antenatal and postnatal | Individually and group | Counsellor | Usual care in the USA | 4 | 90 | DSM-IV, EPDS score 10 or more, SCID | PPAQ, PSI, SAS self-report questionnaire | At 3 months postpartum, the study found no significant differences between the two conditions in degree of depressive symptoms or level of parental stress | Unclear |
| No significant difference | ||||||||||||||
| IPT-based intervention | Gorman, 1997169 | USA | 45 | Antenatal setting | Antenatal and postnatal | Individually | Psychologist | Usual care in the USA | 5 | – | BDI, EPDS score 13 or more, PANAS, SCID, SCL-90-R | DAS, PPAQ | No significant differences between the two groups were found on self-report measures of depressive symptomatology, general psychiatric symptomatology, marital satisfaction or general postpartum adjustment at either 1 or 6 months postpartum169 | Unclear |
| No significant difference | ||||||||||||||
| IPT-based intervention | Grote, 2009170 | USA | 53 | Antenatal setting | Antenatal and postnatal | Individually | Psychologist | Educational information | 8 | – | BDI, DIS, EPDS score 13 or more, SCID (DSM-IV) | BAI, PPAQ new baby subscale (not reported), SAS (Social and Leisure Domain) | At 6 months postnatally, no women in the IPT-B groups had major depression, compared with 16 of 23 (70%) in the UC group. At 6 months postnatally, the EPDS scores indicated a response to treatment in 22 of 25 women in the IPT-B group (88%) vs. 7 of 28 (25%) in the CG with a large effect size (χ2 = 21.16, df = 1, p < .001; Cohen’s h = 1.17)170 | Unclear |
| Findings suggest that enhanced IPT-B ameliorates depression during pregnancy and prevents depressive relapse and improves social functioning up to 6 months postpartum170 | ||||||||||||||
| Significant difference | ||||||||||||||
| IPT-based intervention | Zlotnick, 2001178 | USA | 35 | Antenatal setting | Antenatal and postnatal | Group | Psychologist | Usual care in the USA | 4 | 60 | BDI, SCID | At 3 months postnatally, none of the 17 women in the intervention group, compared with 6 of 18 women in the control group (33%) had major depression. There was a greater reduction in BDI scores in the 17 IG women than in the 18 CG women (t = 3.50, df = 33; p = 0.001). Four antenatal sessions of IPT for financially disadvantaged women appeared to prevent major PND | Unclear | |
| Significant difference | ||||||||||||||
| IPT-based intervention | Zlotnick, 2006179 | USA | 99 | Antenatal setting | Antenatal and postnatal | Group | Nurse | Usual care in the USA | 5 | 60 | BDI | RIFT | At 3 months postnatally, 2 of the 50 women in the intervention group (4%), compared with 8 of 40 women in the control group (20%), had major PND. A brief antenatal IPT-based intervention for financially disadvantaged women appeared to prevent major PND | Unclear |
| Significant difference | ||||||||||||||
| Mindfulness-based intervention | Vieten, 2008121 | USA | 34 | Antenatal setting | Antenatal | Group | Clinical psychologist, yoga instructor | Usual care in the USA | 8 | 120 | CES-D, PANAS-X | STAI, PSS, ARM, MAAS | Differences observed between treatment and wait-list controls at 3-month follow-up were not statistically significant121 | High |
| No significant difference | ||||||||||||||
| Promoting parent–infant interaction | Armstrong, 1999164 | Australia | 181 | Home visits | Postnatal | Individually | Nurse, social worker, paediatrician | Usual care in Australia | 6 | – | EPDS score 13 or more | PSI, breastfeeding, accidental injury, Child Abuse Potential Inventory, HOME, newly-developed measure of preventive infant health care, PSQ-18, use of health services | At 6 weeks, women receiving the home-based programme had significant reduction in PND screening scores as well as improvements in their experience of the parental role and improvement in the ability to maintain their own identity. EPDS in intervention group was 5.67 (SD 4.14) vs. 7.90 (SD 5.89) comparison group; p = 0.004 | Low |
| Significant difference | ||||||||||||||
| Promoting parent–infant interaction | Petrou, 2006;174 Cooper, 2014267 | UK | 151 | Home visits | Antenatal and postnatal | Individually | Health visitor | Usual care in the UK | 2 or more | – | EPDS mean score, SCID for DSM-IV diagnoses | ASSA, BSID II MDI, BSQ | The index intervention had no discernible impact on maternal mood or the quality of maternal parenting behaviours, neither did it benefit the infant outcomes assessed174,267 | Low |
| No significant difference | ||||||||||||||
| Promoting parent–infant interaction | Wilson, 2013177 | UK | 31 | Antenatal setting | Antenatal | Group | Group facilitators | Usual care in the UK | 6 | 120 | EPDS mean score | AWS Salivary cortisol | For a small number of women vulnerable in pregnancy, representing a hard-to-reach population, the Mellow Bumps Group and the Chill-out in Pregnancy group both appeared to have positive effects on the women’s mental health and well-being overall at 8–12 weeks postnatally | High |
| No significant difference | ||||||||||||||
| Psychoeducational intervention | Weidner, 2010176 | Germany | 238 | Antenatal setting | Antenatal | Individually | Psychologist | Usual care in Germany | 22 | – | HADS | Giessen Subjective Complaints list (physical symptoms) | The psychosomatic intervention had a significant effect on anxiety scores (p–0.006), but not on depression scores, physical complaints and characteristics of labour and delivery176 | High |
| No significant difference |
There were no qualitative studies of indicated preventive interventions of psychological interventions.
Indicated preventive interventions: educational intervention
Characteristics and main outcomes of randomised controlled trials of indicated preventive interventions of educational interventions
None of the four included studies193–196 reporting educational interventions for the indicated prevention of PND were conducted in the UK. Two main types of educational interventions were identified: a booklet on PND193,194,196 and education on preparing for parenting. 195 Comparisons were made with usual care in specific countries and educational information. Two studies evaluated group sessions,194,195 and two evaluated individual sessions only. 193,196 No study took place in the home setting. Two studies were undertaken in the antenatal period only,194,196 one in the postnatal period only193 and one in a combination of both antenatal and postnatal periods. 195 The interventions were provided by different health-care providers (nurse, midwife) with the number of contacts ranging from one to eight (mean 3.25) and duration of contact ranging from 1 to 2 hours (mean 1.5 hours). A summary of the characteristics and main outcomes is provided in Table 39.
| Intervention summary | First author, year, reference number | Country | Total number of women randomised | Place | Timing | Type of session | Provider | Comparison group(s) | Number of contacts | Duration of contact (minutes) | Depression outcomes | Other outcomes | Main findings | Overall risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Booklet on PND | Heh, 2003193 | Taiwan | 70 | Postnatal setting | Postnatal | Individually | Nurse | Usual care in Taiwan | 1 | 60 | EPDS score 10 or more (Chinese version) | At 3 months postnatally, Taiwanese women who received information at around 6 weeks postnatally, had lower EPDS scores, (mean 10.8, SD 4.4) than a control group (mean 12.1, SD 3.00) (p = 0.02) | High | |
| Significant difference | ||||||||||||||
| Booklet on PND | Lara, 2010194 | Mexico | 377 | Antenatal setting | Antenatal | Group | Group facilitators | Usual care in Mexico | 8 | 120 | BDI-II, SCID | SCL-90 anxiety subscale | At 6 months postnatally, 6 of 56 women in the intervention group (10.7%) had major depression vs. 15 of 60 women in the control group (25%), but there was no significant effect | High |
| Available data are consistent with the possibility that the incidence of depression may have been reduced by the intervention, but differential attrition makes interpretation of the findings difficult194 | ||||||||||||||
| Mixed results | ||||||||||||||
| Booklet on PND and contact numbers | Webster, 2003196 | Australia | 600 | Antenatal setting | Antenatal | Individually | Leaflet (unclear) | Usual care in Australia | 1 | – | EPDS score 13 or more | The proportion of women who reported an EPDS score of 13 or more was 26%. There were no significant differences between intervention (46/192, 24%) and control groups (50/177, 28.2%) on this primary outcome measure (OR 0.80; 95% CI 0.50–1.28)196 | Unclear | |
| No significant difference | ||||||||||||||
| Education on preparing for parenting | Stamp, 1995195 | Australia | 144 | Antenatal setting | Antenatal and postnatal | Group | Midwife | Usual care in Australia | 3 | – | EPDS score 13 or more | At 6 weeks postnatally, 8 out of 64 women in the intervention group (13%) scored 13 or more on the EPDS compared with 11 out of 64 women in the control group (17%) | Low | |
| At 12 weeks postnatally, 7 out of 63 women in the intervention group (11%) scored 13 or more, compared with 10 out of 65 women in the control group (15%) | ||||||||||||||
| At 6 months postnatally, 9 out of 60 women in the intervention group (15%) scored 13 or more, compared with 6 out of 61 women in the control group (10%) | ||||||||||||||
| No significant difference |
There were no qualitative studies of indicated preventive interventions of educational interventions.
Indicated preventive interventions: social support
Characteristics and main outcomes of randomised controlled trials of indicated preventive interventions of social support
Only one of the included studies206 evaluating social support for the indicated prevention of PND was conducted in the UK. Peer support was the main type of social support intervention identified: a booklet on PND. 205,206 Comparisons were made with usual care in specific countries (i.e. Canada205 and the UK206) Both included studies evaluated individual sessions only. 205,206 One study took place in the home setting206 and one intervention was by telephone. 205 One study was undertaken in the postnatal period only,205 and one in a combination of both antenatal and postnatal periods. 206 Both interventions were provided by different peer volunteers, the number of contacts varied and the length of contact was not specified. A summary of the characteristics and main outcomes is provided in Table 40.
| Intervention summary | First author, year, reference number | Country | Total number of women randomised | Place | Timing | Type of session | Provider | Comparison group(s) | Number of contacts | Duration of contact (minutes) | Depression outcomes | Other outcomes | Main findings | Overall risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Peer support | Dennis, 2009205 | Canada | 701 | Telephone | Postnatal | Individually | Peer volunteers | Usual care in Canada | 8 | – | EPDS score 13 or more, SCID | STAI, UCLA loneliness scale | At 12 weeks postnatally, 40 out of 297 women in the intervention group (14%) scored 13 or more on the EPDS compared with 78 out of 315 women in the control group (25%) (χ2 = 12.5; p < 0.001). The number needed to treat was 8.8 (95% CI 5.9 to 19.6). The relative risk reduction was 0.46 (95% CI 0.24 to 0.62) | Low |
| Significant difference | ||||||||||||||
| Peer support | Harris, 2006206 | UK | 65 | Home visits | Antenatal and postnatal | Individually | Newpin volunteer | Usual care in the UK | 2 or more | – | SCAN, PSE | – | The onset of perinatal major depression was 27% (8/30) for the Newpin befriender group and 54% (19/35) for the control group (χ2 = 4.00, p = 0.045, two-tailed test)206 | Unclear |
| Significant difference |
Description and findings from qualitative studies of indicated preventive interventions of social support
Two qualitative studies of social support interventions were included in the indicated preventive interventions category;299,301 one relating to women’s perceptions and one relating to service provider perceptions of the same intervention. Further details are provided in Table 41.
| First author, year, reference number | Country | Intervention details | ||||||
|---|---|---|---|---|---|---|---|---|
| Name | Setting | Delivered Antenatal/postnatal | Group/individual | Number of sessions | Duration of session | Facilitator/service providers | ||
| Dennis, 2009205 | Canada | Telephone-based peer support | Telephone support | Postnatal | Individual | Mean contacts 8.8 (SD 6 contacts) | Mean length of contact 14.1 minutes (SD 18.5 minutes), range 1–180 minutes | Peer volunteers – mothers from the community with resolved history of PND who participated in a 4-hour training session |
Findings from the qualitative review
Support
Emotional support, informational support and the development of relationships with peers were reported by participants as beneficial aspects of the telephone support intervention. 299
Service delivery
Service providers301 were concerned that the intervention represented an invasion of the recipients’ privacy and also that they would not be able to deal with unpredictable situations for which they were not qualified. One peer volunteer301 reported that providing the service had resulted in the recurrence of her own past emotions and anxieties. Peer volunteers felt uncomfortable discussing emotional issues with the recipients. Some felt they would have benefited from further training, supervision and information to share with the service users. The peer volunteers reported that they would have liked more time to devote to the role. 301
Indicated preventive interventions: pharmacological agents or supplements
Characteristics and main outcomes of randomised controlled trials of indicated preventive interventions of pharmacological agents or supplements
All three included studies214–216 evaluating pharmacological agents or supplements for the indicated prevention of PND were conducted in the USA. Four types of pharmacological agents or supplements were identified: eicosapentaenoic acid (EPA) plus DHA,214 nortriptyline273 and sertraline. 216 One study was undertaken in the antenatal period only214 and two studies were undertaken in the postnatal period only. 215,216 A summary of the characteristics and main outcomes is provided in Table 42.
| Intervention summary | First author, year, reference number | Country | Total number of women randomised | Place | Timing | Type of session | Provider | Comparison group(s) | Number of contacts | Duration of contact (minutes) | Depression outcomes | Other outcomes | Main findings | Overall risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| EPA and DHA | Mozurkewich, 2013214 | USA | 126 | Antenatal setting | Antenatal | Individually | Prescriber | Usual care in the USA | 2 or more | – | BDI, MINI | – | No differences between groups in BDI scores or other depression endpoints at any of the three time points after supplementation214 | Low |
| EPA-rich fish oil and DHA-rich fish oil supplementation did not prevent depressive symptoms during pregnancy or postpartum214 | ||||||||||||||
| No significant difference | ||||||||||||||
| Nortriptyline | Wisner, 2001215 | USA | 51 | Postnatal setting | Postnatal | Individually | Prescriber | Usual care in the USA | 2 or more | – | HDRS (HAM-D) | BRMS | 6 out of the 26 women in the nortriptyline intervention group (23%) compared with 6 out of the 25 women in the control group (24%) had a postnatal recurrence of depression | Low |
| No significant difference | ||||||||||||||
| Sertraline | Wisner, 2004216 | USA | 25 | Postnatal setting | Postnatal | Individually | Prescriber | Usual care in the USA | 2 or more | – | HDRS, SCID | Asberg Side Effects rating | Recurrences in the 17-week preventive treatment period occurred in four of the eight women taking placebo (proportion, 0.50; 95% CI, 0.16–0.84) and in one of the 14 women taking sertraline (proportion, 0.07, 95% CI, 0.00–0.34) (p = 0.04, Fisher’s exact test)216 | Low |
| Significant difference |
There were no qualitative studies of indicated preventive interventions of pharmacological agents or supplements.
Indicated preventive interventions: midwifery-led interventions
Characteristics and main outcomes of randomised controlled trials of indicated preventive interventions of midwifery-led interventions
There was one indicated preventive intervention evaluating midwifery-led interventions, conducted in the UK. 224 A summary of the characteristics and main outcomes is provided in Table 43.
| Intervention summary | First author, year, reference number | Country | Total number of women randomised | Place | Timing | Type of session | Provider | Comparison group(s) | Number of contacts | Duration of contact (minutes) | Depression outcomes | Other outcomes | Main findings | Overall risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Midwifery continuous care | Marks, 2003224 | UK | 98 | Antenatal setting | Antenatal and postnatal | Individually | Midwife | Usual care in the UK | 22 | NR | EPDS mean score, SCID | CAME, MSQ | At 3 months postnatally, the EPDS mean score for the 43 women in the control group was 7.49 (SD 5.33) and for the 42 women in the intervention group was 7.48 (SD 6.54) | Unclear |
| No significant differences |
There were no qualitative studies of indicated preventive interventions of midwifery-led interventions.
Indicated preventive interventions: organisation of maternity care
Characteristics and main outcomes of randomised controlled trials of indicated preventive interventions of organisation of maternity care
No indicated preventive intervention for preventing PND was identified concerning the organisation of maternity care.
Description and findings of qualitative studies of selective preventive interventions of the organisation of maternity care
One qualitative study of an intervention evaluating the organisation of maternity care was included in the indicated preventive intervention category. 300 Further details are provided in Table 44.
| First author, year, reference number | Country | Intervention details | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Name | Setting | Delivered antenatal/postnatal | Group/individual | Numbers in group | Number of sessions | Duration of session | Facilitator/service providers | ||
| Myors, 2014300 | Australia | Specialist perinatal and infant mental health service | Secondary care – location not reported | Antenatal and postnatal | Individual | NA | Multiple contact | NA | Nurse, psychiatrist, psychologist, social workers |
Support
Recipients of the intervention300 reported the support they received from the health professionals delivering the service as helpful and the relationship with the service provider appeared to be of great importance. Women reported that they were able to rely on the service and that if they needed the service urgently it was available to them:
. . . the service was closing and I just rang up and was like ‘I really need some help’, and they called me straight back the next day . . . (M)y clinical nurse . . .immediately started seeing me within a week because they . . . could see how desperate I was for some help . . .
Participant300
They also valued a close relationship they were able to form with their clinician and reported on their kind approach which enabled a feeling of safety. 300
Empowerment (self-esteem)
The authors reported that the women learned to cope without the service, and that it allowed them to gain confidence in themselves. 300
Service delivery and barriers to participation
Women reported feeling intimidated by the thought of referral to the specialist perinatal and infant mental health service. 300 The authors reported that those who did feel able to access the service fully said that they would have liked the service to be extended beyond the infant’s first birthday and felt that they were not ready to be discharged, which caused them stress and anxiety. 300
Indicated preventive interventions: complementary and alternative medicine or other interventions
Characteristics and main outcomes of randomised controlled trials of indicated preventive interventions of complementary and alternative medicine or other interventions
The only included study evaluating CAMs or other interventions for the indicated prevention of PND was conducted in the USA. 229 A summary of the characteristics and main outcomes is provided in Table 45.
| Intervention summary | First author, year, reference number | Country | Total number of women randomised | Place | Timing | Type of session | Provider | Comparison group(s) | Number of contacts | Duration of contact (minutes) | Depression outcomes | Other outcomes | Main findings | Overall risk of bias |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Acupuncture for depression | Manber, 2004229 | USA | 61 | Antenatal setting | Antenatal and postnatal | Individually | Acupuncture specialist | Acupuncture non-specific | 12 | 30 | BDI, HDRS | – | At 10 weeks postnatally, the mean BDI score in the 16 women in the acupuncture group was 6.9 (SD 7.7). In the 19 women in the active control it was 10.8 (SD 9.8) and in the 19 women in the massage group it was 10.2 (SD 6.6). There was no pure control | Unclear |
| Limited by small sample |
There were no qualitative studies of indicated preventive interventions of CAM or other interventions.
Results from network meta-analysis for indicated preventive interventions for Edinburgh Postnatal Depression Scale threshold score
Of the indicated preventive intervention trials, 12 were included in the NMA (see Appendix 10, Table of indicated preventive intervention studies omitted from network meta-analysis). Four trials were excluded because they could not be connected to the main network of evidence148,177,229 and 12 were excluded as a result of lack of available EPDS data. 121,166,167,171,172,176,178,179,206,214–216
The four trials excluded because they could not be connected to the main network were undertaken in China (Hong Kong),175 Mexico,194 Pakistan148 and Taiwan. 193
Of the 14 trials excluded as a result of lack of available EPDS data, four were at high risk of bias and none of these were associated with significant differences in depression. 121,172,176,177 The UK-based trial was small (n = 31) and the results suggested that psychoeducational interventions in pregnancy may benefit women with major psychosocial needs. 177
Of the 14 trials excluded as a result of lack of available EPDS data, six were at unclear risk of bias. 166,171,178,179,206,229 Five of these trials were small, with fewer than 100 participants. 166,178,179,206,229 The largest of these trials, with 217 participants, concluded ‘A CBT intervention for low-income, high-risk Latinas reduced depressive symptoms during pregnancy but not during the postpartum period’. 171 Two of the three trials examining IPT-based intervention found a significant effect using the BDI or DSM-IV [Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition (DSM-IV)] criteria,178,179 but the other did not. 166 In the active acupuncture study there were only 20 participants in each group229 and the UK-based Newpin trial found a significant reduction in the onset of perinatal major depression using the Schedule for Clinical Assessment in Neuropsychiatry (SCAN). 206
One of the four trials at low risk of bias found that EPA- and DHA-rich fish oil supplementation did not prevent depressive symptoms. 214 No difference was found in the rate of recurrence in women treated with nortriptyline compared with those treated with placebo. 215 There were significantly fewer recurrences of depression in women taking sertraline preventive treatment compared with women taking placebo. 216 A CBT-based intervention that integrated multiple risk interventions, delivered mainly during pregnancy, had a non-significant effect in reducing risks for smoking, depression and intimate partner violence, but there was a difference in favour of the intervention group. 167
Results from network meta-analysis for indicated preventive intervention for Edinburgh Postnatal Depression Scale threshold scores at 6 weeks postnatally
A NMA was used to compare the effects of education on preparing for parenting and promoting parent–infant interaction relative to usual care on EPDS threshold. Data were available from two studies comparing three interventions. 166,197 Figure 38 presents the network of evidence. There were two intervention effects to estimate from two studies.
FIGURE 38.
Indicated preventive interventions EPDS threshold score at 6 weeks postnatally: network of evidence.

Figure 39 presents the odds ratios of each intervention relative to usual care and Figure 40 presents the probabilities of treatment rankings. The total residual deviance was 4.12, compared with the total number of data points, four, included in the analysis. This implies a good fit of the model to the data. The between-study SD was estimated to be 0.23 (95% CrI 0.01 to 0.74), which implies mild heterogeneity of intervention effects between studies.
FIGURE 39.
Indicated preventive interventions EPDS threshold score at 6 weeks postnatally: odds ratios all treatment comparisons.

FIGURE 40.
Indicated preventive interventions EPDS threshold score at 6 weeks postnatally: probability of treatment rankings (ranks 1–5).

Promoting parent–infant interaction and education on preparing for parenting reduced the odds of high EPDS scores compared with usual care, although the effect was statistically significant only for promoting parent–infant interaction at a conventional 5% level (see Figure 39).
Promoting parent–infant interaction had the highest probability of being the best (probability 0.84) (see Figure 40).
Results from network meta-analysis for indicated preventive intervention for Edinburgh Postnatal Depression Scale threshold scores at 3 months postnatally
A NMA was used to compare the effects of peer support and education on preparing for parenting relative to usual care on EPDS threshold. Data were available from two studies comparing three interventions. 197,207 Figure 41 presents the network of evidence. There were two intervention effects to estimate from three studies.
FIGURE 41.
Indicated preventive interventions EPDS threshold score at 3 months postnatally: network of evidence.

Figure 42 presents the odds ratios of each intervention relative to usual care and Figure 43 presents the probabilities of treatment rankings. The total residual deviance was 4.05, compared with the total number of data points, four, included in the analysis. This implies a good fit of the model to the data. The between-study SD was estimated to be 0.21 (95% CrI 0.01 to 0.72), which implies mild heterogeneity of intervention effects between studies.
FIGURE 42.
Indicated preventive interventions EPDS threshold score at 3 months postnatally: odds ratios all treatment comparisons.

FIGURE 43.
Indicated preventive interventions EPDS threshold score at 3 months postnatally: probability of treatment rankings.

Both peer support and education on preparing for parenting have reduced odds of high EPDS scores compared with usual care. However, the effects were not statistically significant at a conventional 5% level (see Figure 42). Peer support has the highest probability of being the best (probability 0.69) (see Figure 43).
Results from network meta-analysis for indicated preventive intervention for Edinburgh Postnatal Depression Scale threshold scores at 4 months postnatally
A NMA was used to compare the effects of booklets on PND and promoting parent–infant interaction relative to usual care on EPDS threshold. Data were available from two studies comparing three interventions. 166,198 Figure 44 presents the network of evidence. There were two intervention effects to estimate from two studies.
FIGURE 44.
Indicated preventive interventions EPDS threshold score at 4 months postnatally: network of evidence.
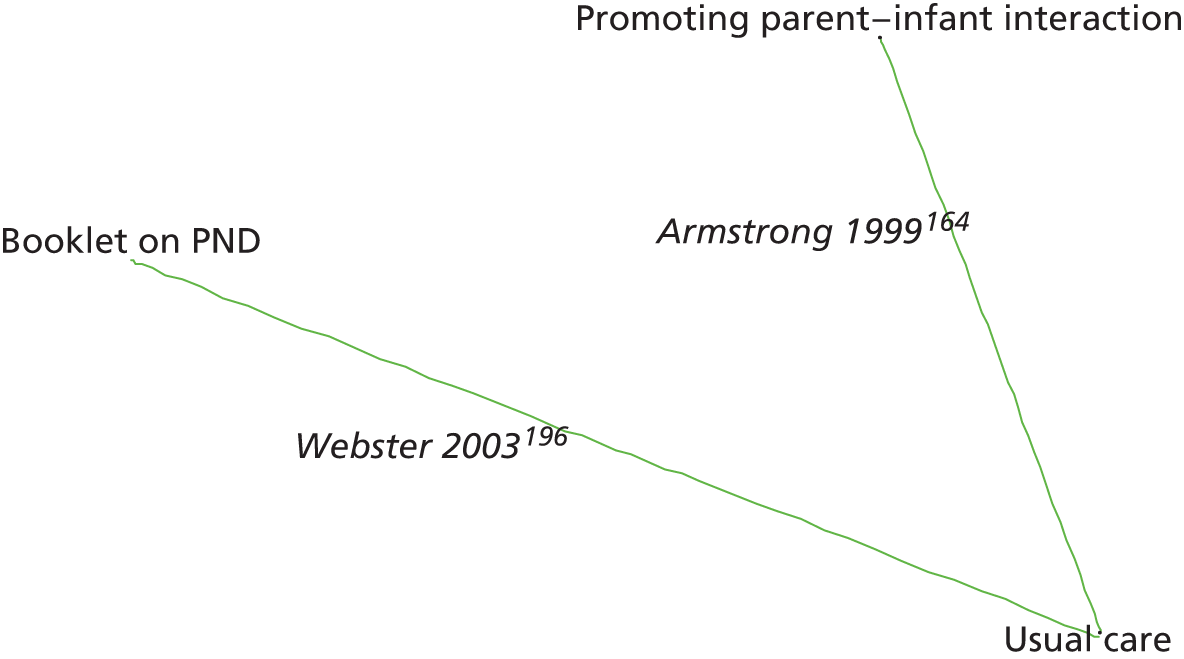
Figure 45 presents the odds ratios of each intervention relative to usual care and Figure 46 presents the probabilities of treatment rankings. The total residual deviance was 3.97, compared with the total number of data points, four, included in the analysis. This implies a good fit of the model to the data. The between-study SD was estimated to be 0.22 (95% CrI 0.01 to 0.70), which implies mild heterogeneity of intervention effects between studies.
FIGURE 45.
Indicated preventive interventions EPDS threshold score at 4 months postnatally: odds ratios all treatment comparisons.
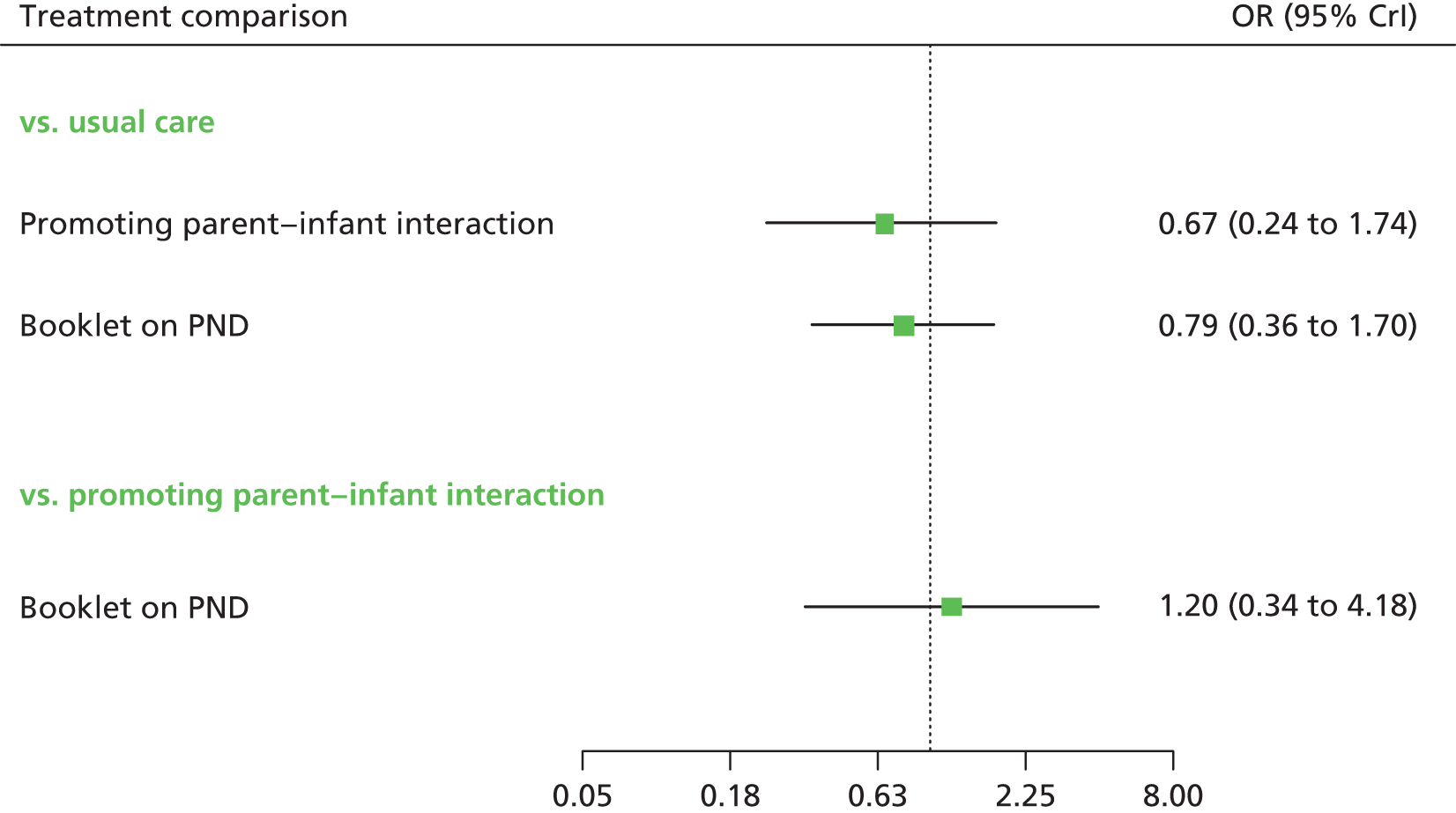
FIGURE 46.
Indicated preventive interventions EPDS threshold score at 4 months postnatally: probability of treatment rankings (ranks 1–3).
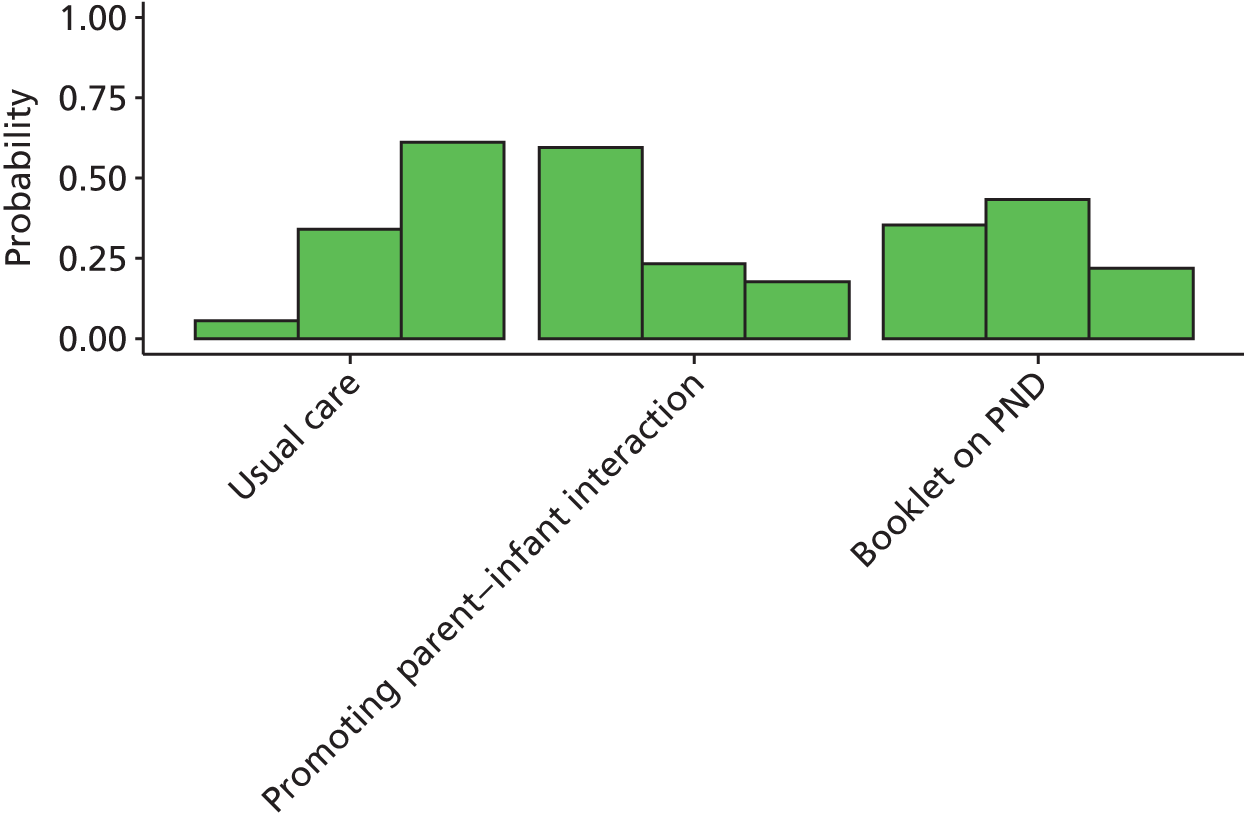
The odds ratio for both promoting parent–infant interaction and booklet on PND was less than 1, suggesting a beneficial effect compared with usual care, although the results were not statistically significant at a conventional 5% level (see Figure 45). Promoting parent–infant interaction has the highest probability of being the best (probability 0.60) (see Figure 46).
Results from network meta-analysis for indicated preventive intervention for Edinburgh Postnatal Depression Scale threshold scores at 6 months postnatally
A NMA was used to compare the effects of CBT-based intervention, PCA-based intervention and education on preparing for parenting relative to usual care on EPDS threshold. Data were available from two studies comparing four interventions. 61,197 Figure 47 presents the network of evidence. There were three intervention effects to estimate from two studies.
FIGURE 47.
Indicated preventive interventions EPDS threshold score at 6 months postnatally: network of evidence.

Figure 48 presents the odds ratios of each intervention relative to usual care and Figure 49 presents the probabilities of treatment rankings. The total residual deviance was 4.12, compared with four data points, included in the analysis. This implies a good fit of the model to the data. The between-study SD was estimated to be 0.22 (95% CrI 0.01 to 0.73), which implies mild heterogeneity of intervention effects between studies.
FIGURE 48.
Indicated preventive interventions EPDS threshold score at 6 months postnatally: odds ratios all treatment comparisons.

FIGURE 49.
Indicated preventive interventions EPDS threshold score at 6 months postnatally: probability of treatment rankings (ranks 1–4).

The CBT- and PCA-based interventions had reduced odds of high EPDS scores compared with usual care. Education on preparing for parenting had an increased odds of a high EPDS score at 6 months compared with usual care. However, none of the odds ratios were statistically significant at a conventional 5% level (see Figure 48). The CBT-based intervention has the highest probability of being the best (probability 0.56) (see Figure 49).
Summary of results from network meta-analysis for indicated preventive intervention for Edinburgh Postnatal Depression Scale threshold scores
In general, the intervention effects were inconclusive, although promoting parent–infant interaction was associated with a statistically significant benefit at 6 weeks. Intervention effects tended to vary over time, with the most beneficial treatments being promoting parent–infant interaction at 6 weeks, peer support at 3 months, promoting parent–infant interaction at 4 months, and CBT- and PCA-based interventions at 6 months.
Results from network meta-analysis for indicated preventive intervention for Edinburgh Postnatal Depression Scale mean scores
A NMA was used to compare the effects CBT-based intervention, educational information, IPT-based intervention, midwifery continuous care, peer support, PCA-based intervention and promoting parent–infant interaction relative to usual care on EPDS mean scores. Data were available from 10 studies comparing eight interventions. 61,166,167,170–172,175,176,207,226 There were seven intervention effects to estimate (relative to usual care) from 10 studies. Figure 50 presents the network of evidence.
FIGURE 50.
Indicated preventive interventions for EPDS mean scores: network of evidence. Dashed lines represent three-arm trials.

Figure 51 presents the differences in EPDS mean scores of each intervention relative to usual care. The between-study SD was estimated to be 1.95 (95% CrI 0.69 to 3.55), which implies moderate heterogeneity of intervention effects between studies. However, there is considerable uncertainty about the between-study SD because of the relatively small number of studies that provided data relative to the number of intervention effects being estimated. The interventions associated with the greatest reduction in EPDS mean score were IPT-based intervention (–4.25, 95% CrI –7.87 to 0.43 at 6–7 months), CBT-based intervention (–2.18, 95% CrI –5.39 to 1.15 at 12 months) and PCA-based intervention (–2.05, 95% CrI –5.90 to 2.12 at 12 months). None of the comparisons with usual care were statistically significant at a conventional 5% level. Figures 52–55 present the probabilities of treatment rankings at 6–8 weeks, 3–4 months, 6–7 months and 12 months, respectively.
FIGURE 51.
Indicated preventive interventions EPDS mean scores: mean differences of treatment comparisons vs. usual care across all time points.
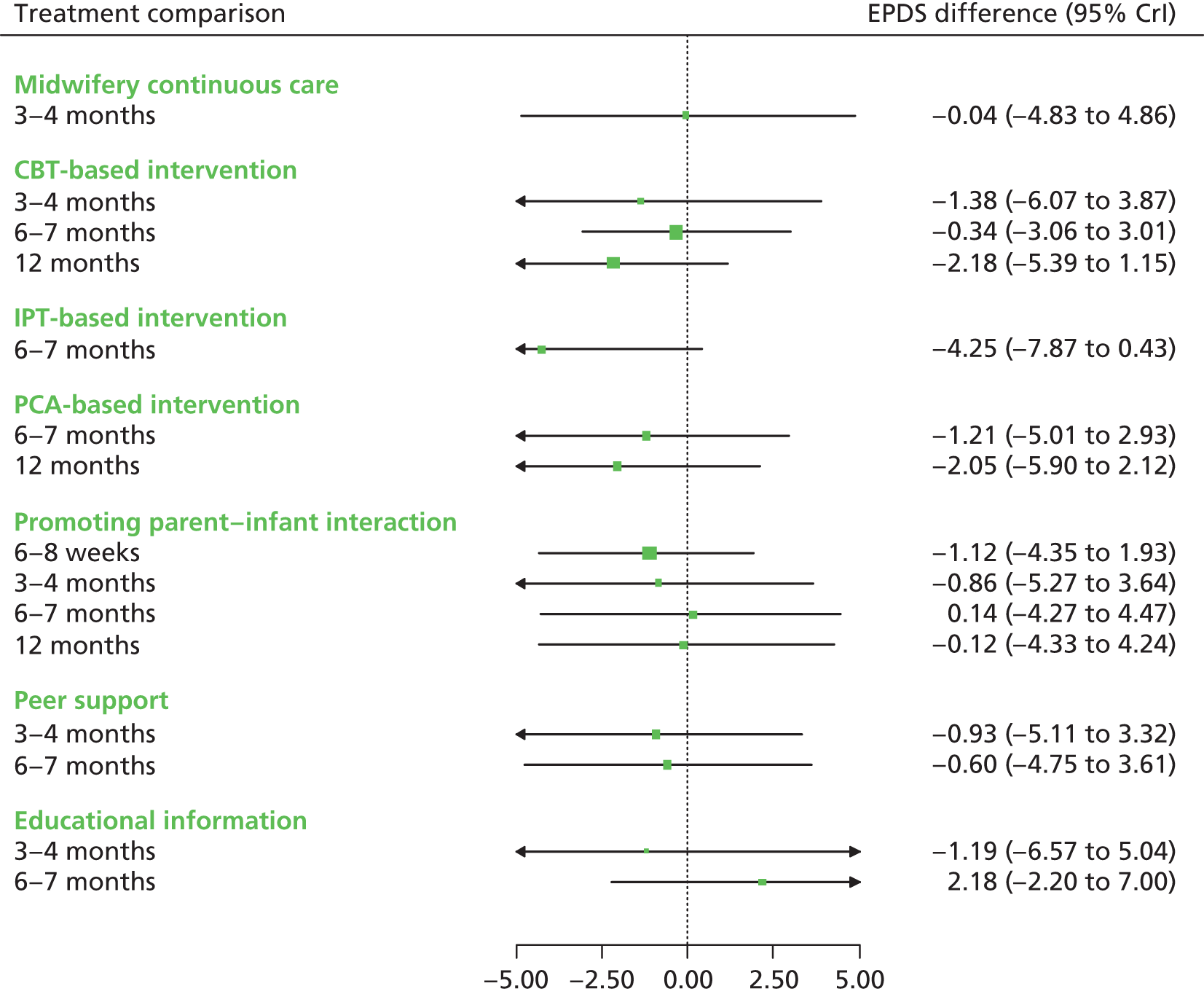
FIGURE 52.
Indicated preventive interventions EPDS mean scores: probability of treatment rankings at 6–8 weeks postnatally (ranks 1–5).
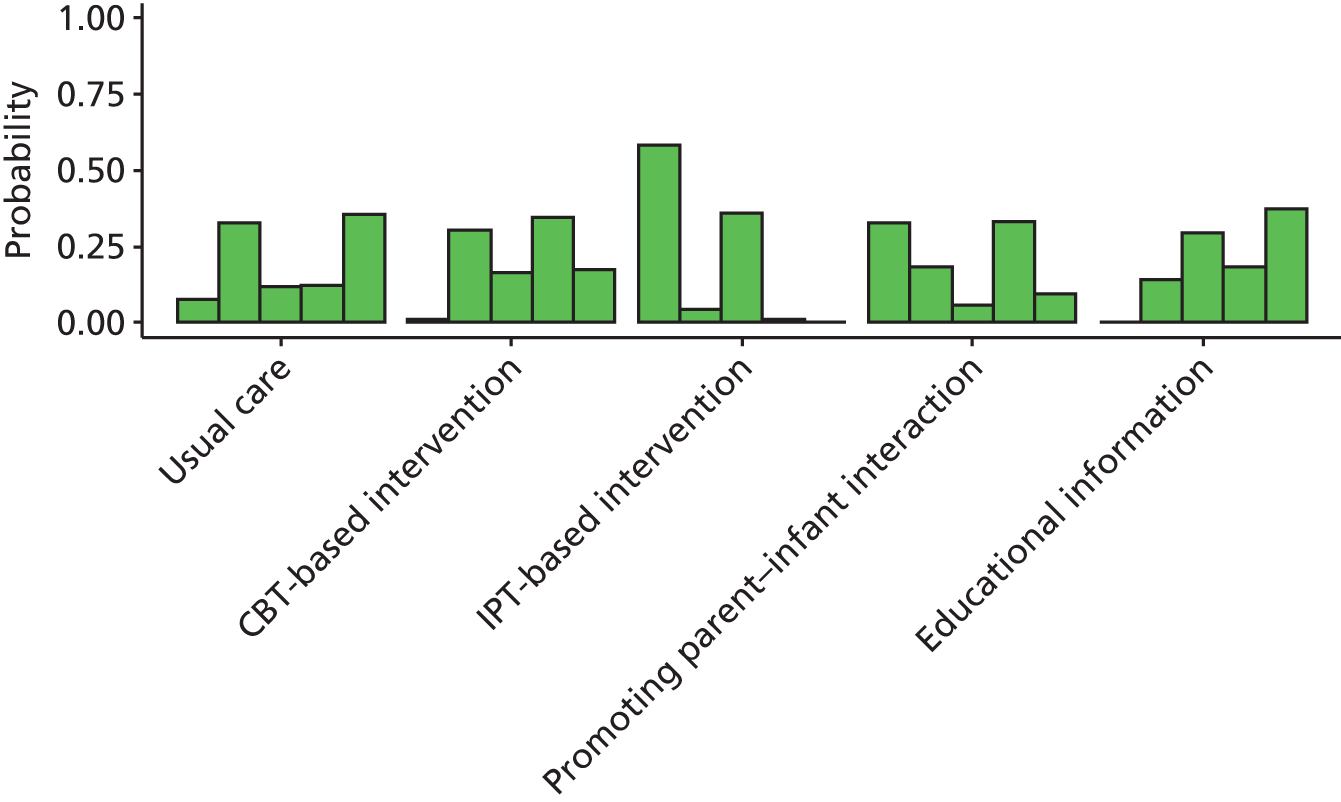
FIGURE 53.
Indicated preventive interventions EPDS mean scores: probability of treatment rankings at 3–4 months postnatally (ranks 1–6).

FIGURE 54.
Indicated preventive interventions EPDS mean scores: probability of treatment rankings at 6–7 months postnatally (ranks 1–7).
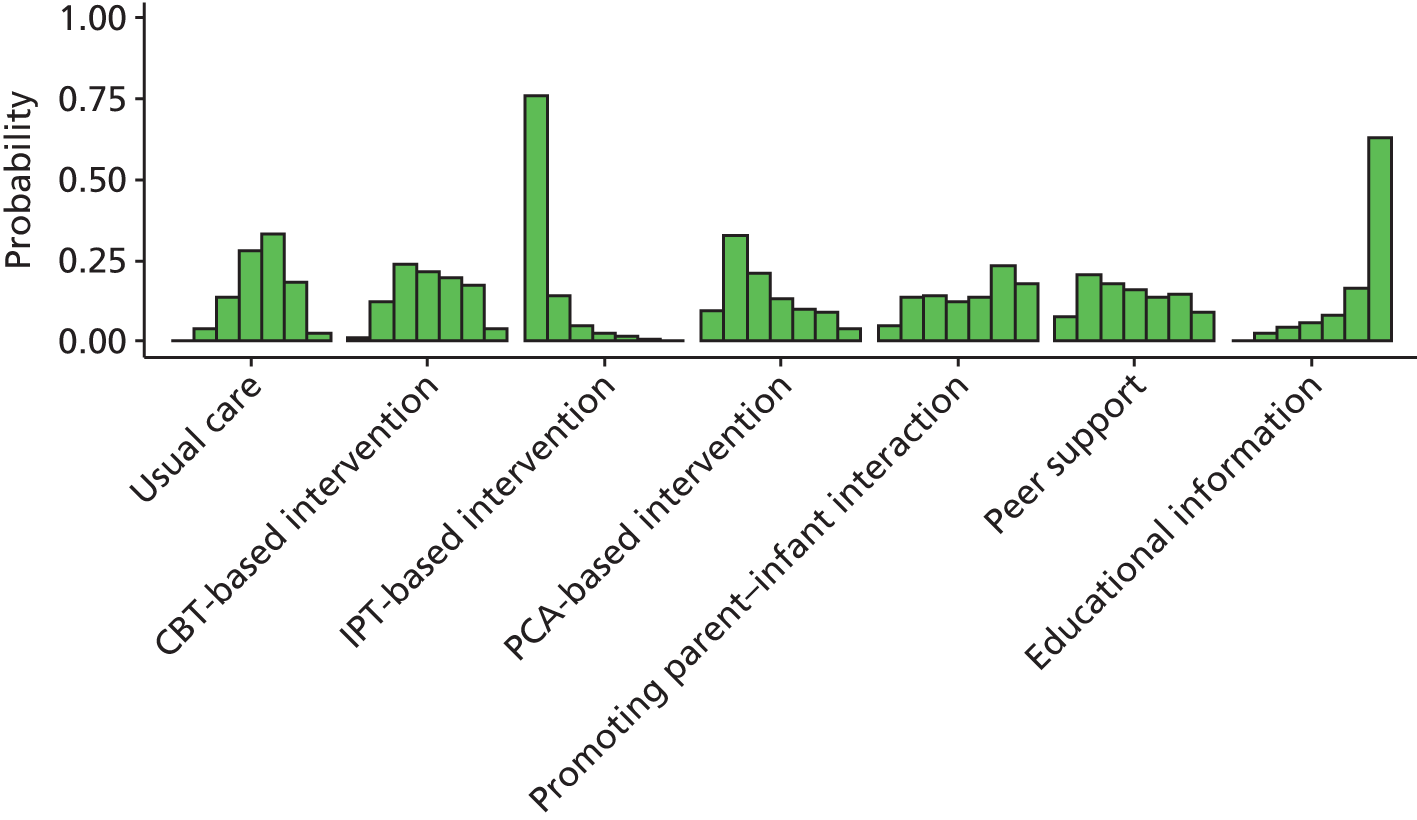
FIGURE 55.
Indicated preventive interventions EPDS mean scores: probability of treatment rankings at 12 months (ranks 1–4).
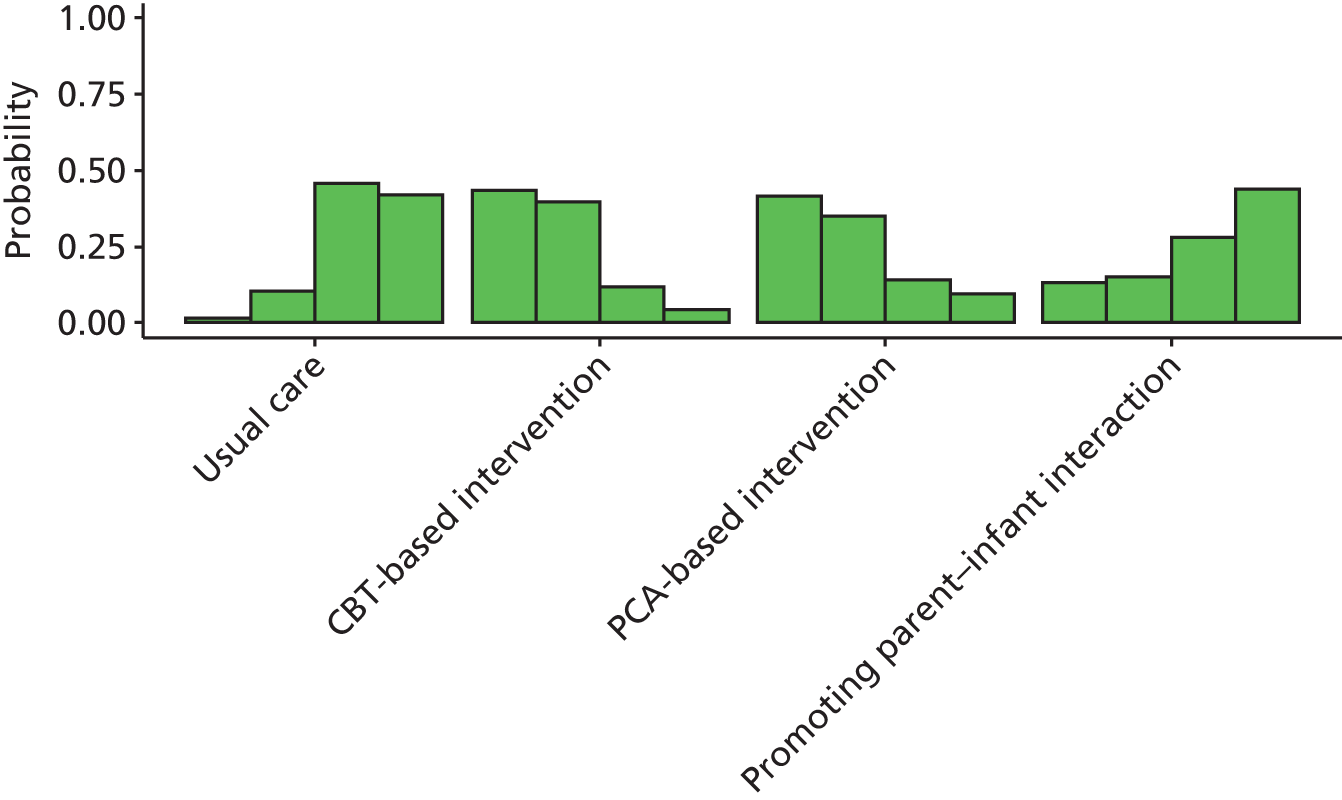
The interventions with the highest probabilities of being the best at 6–8 weeks were the IPT-based intervention and promoting parent–infant interaction (probability 0.60 and 0.32, respectively).
The interventions with the highest probabilities of being the best at 3–4 months were educational information (probability 0.24), CBT-based intervention (probability 0.21), promoting parent–infant interaction (probability 0.20) and peer support (probability 0.20).
The intervention with the highest probability of being the best at 6–7 months was IPT-based intervention (probability 0.77).
The interventions with the highest probabilities of being the best at 12 months were CBT- and PCA-based interventions (probability 0.43 and 0.41, respectively).
Summary of results from network meta-analysis for indicated preventive intervention for Edinburgh Postnatal Depression Scale mean scores
Not all interventions provided information about intervention effects at each time, making inferences across all treatments at each time difficult. In general, the intervention effects were inconclusive and the CrIs were wide. The most beneficial treatments appeared to be IPT-based intervention, educational information, CBT-based intervention and PCA-based intervention. A summary of the results for the threshold and the EPDS mean scores is presented in Table 46.
| Time postnatally | EPDS mean score | EPDS threshold score | Overall risk of bias | ||
|---|---|---|---|---|---|
| Difference in mean (95% CrI) | Probability of being the besta | Odds ratio (95% CrI) | Probability of being the besta | ||
| 6 weeks postnatally | |||||
| Promoting parent–infant interaction164 | –1.12 (–4.35 to 1.93) | 0.60b | 0.21 (0.06 to 0.63) | 0.84c | Low |
| 3 months postnatally | |||||
| CBT-based intervention173 | –1.38 (–6.07 to 3.87) | 0.21d | NE | NE | Unclear |
| Educational information168 | –1.19 (–6.57 to 5.04) | 0.24d | NE | NE | Unclear |
| Peer support205 | –0.93 (–5.11 to 3.32) | 0.20d | 0.47 (0.21 to 1.03) | 0.69c | Low |
| Education on preparing for parenting195 | NE | NE | 0.67 (0.18 to 2.37) | 0.30c | Low |
| Promoting parent–infant interaction164 | –0.86 (–5.27 to 3.64) | 0.20d | NE | NE | Low |
| 4 months postnatally | |||||
| Promoting parent–infant interaction164 | NE | NE | 0.67 (0.24 to 1.74) | 0.60c | Low |
| 6 months postnatally | |||||
| IPT-based intervention169,170 | –4.25 (–7.87 to 0.43) | 0.77e | NE | NE | Unclear |
| PCA-based intervention61 | –1.21 (–5.01 to 2.93) | 0.10e | 0.65 (0.28 to 1.57) | 0.37f | Low |
| CBT-based intervention61 | –0.34 (–3.06 to 3.01) | 0.01e | 0.59 (0.26 to 1.38) | 0.56f | Low |
| 12 months postnatally | |||||
| PCA-based intervention61 | –2.05 (–5.90 to 2.12) | 0.41f | NE | NE | Low |
| CBT-based intervention61,173 | –2.18 (–5.39 to 1.15) | 0.43f | NE | NE | Low; unclearg |
The qualitative evidence suggested that the social support intervention adequately provided emotional and informational support to women. Women reported that they felt able to rely on a perinatal and infant mental health service if they needed to access them urgently and appreciated the support of the health professionals delivering the service. However, barriers to accessing the service included a feeling of intimidation around being referred to such a service, stigma and concerns about being discharged before they felt ready.
Chapter 8 Results of realist synthesis: what works for whom?
Introduction to Best Fit Realist Synthesis
Having characterised the principal seven classes of intervention and having identified focal interventions from among the group- and individual-based approaches, the team sought to examine the main service models for prevention of PND in relation to the underlying programme theory and mechanisms.
Results of the review
The ‘Best Fit Realist Review’ engaged with 96 studies relating to 13 separate intervention programmes. 7,8,42–44,61,146,148,151,152,154,160,163,164,166,170,178,179,184,190,205,206,208,219,221,222,224,236,251,252,262,264,277–340 CenteringPregnancy was the most represented in the literature (with 22 studies). 61,146,148,151,154,164,170,179,190,205,208,219,221,251,252,262,264,327,335–338 Next came telephone peer support and IPT plus telephone (nine studies each), followed by midwifery redesigned postnatal care (eight). Then followed IPT-brief (seven), midwife-managed care (seven), midwife-led brief counselling (six), the Newpin Project (six), Health Visitor PoNDER Training (six), Thinking Healthy Programme (five) and the two-step behavioural educational intervention (five). Finally home-based intervention and IPT plus Reach Out, Stand strong, Essentials for new mothers (ROSE) were both covered by three studies.
Eleven trials were from the effectiveness review, 25 of the studies represented the views of women receiving an intervention and five represented the views of service providers. One study collected the views of both women and service providers. Two represented a cost study or economic evaluation. One study collected measures of women’s satisfaction and costs. 339 Eleven studies were either reviews or evidence syntheses. The remaining 40 studies were study reports but were not RCTs, qualitative studies or economic evaluations. Eight of the qualitative studies were already included in the qualitative synthesis of intervention studies. (See Appendix 9.)
Synthesis drawing upon realist approaches
The realist review began by engaging with the spreadsheet-based matrices of intervention classes and their relative effectiveness and with the qualitative synthesis of intervention study findings. The dearth of qualitative intervention studies further required that the realist synthesis engage with wider qualitative data from beyond the group of intervention studies. These studies are characterised from here onwards as PSSS studies. Such studies identify strategies, used by women who had not experienced PND, that they believe helped to prevent the condition. Although such data must be treated with caution, given that they reflect women’s anticipation of a hypothetical situation, the team believed that this perspective would provide a counterpoint to interventions in which content and delivery had been primarily devised by health professionals. The PSSS studies allow comparison between what women feel is helpful and what is actually being delivered by the interventions themselves.
Description of included personal and social support strategy studies
In total, 23 studies (n = 29 citations) were identified reporting qualitative data on the perspectives and attitudes of women who had not experienced PND regarding PSSSs that they believe helped to prevent the condition (see Appendix 9, Personal and social support strategy studies: population characteristics).
Study respondents in the personal and social support strategy studies
The number of participants contributing qualitative evidence across all studies, where reported, was summed and totalled 801 (one study7 did not provide the number of participants who contributed to the qualitative findings). Fifteen studies provided data from participants from a general population in the country of study,7,286,302,303,305,312,313,316–325 while the remaining studies examined evidence from minority groups within the country of study. The minority groups were either a culturally different group based within the country of study (n = 6)292,306–311,314,315,318 or a selective group (n = 2). 296–298,304 For details of participant characteristics see Appendix 9.
Study setting of the personal and social support strategy studies
Ten studies were conducted in the UK,304,306–315,319,321,322,324 seven studies were conducted in the USA,286,292,296–298,302,303,318,320 one in Switzerland,316 one in Canada,317 one in Norway,323 one in India,325 one in China305 and one in multiple centres. 7
Synthesis of findings across personal and social support strategy studies
Several themes relating to the PSSSs which helped women prevent PND were identified across the included studies. Included studies focused on either general population women, minority groups which were culturally different from the general population of the country of study or, in a small number of cases, selective groups (low-socioeconomic status or vulnerable groups). Two studies305,325 focused on the general population of the country of study, but highlighted findings related to particular cultural practices.
Based on an actual or promising assessment of effectiveness, the review team specified thirteen interventions requiring further in-depth analysis. These 13 interventions became the focus for subsequent investigation of study clusters (Table 47).
| Intervention category | Initiative | Target population | Setting |
|---|---|---|---|
| Psychological | Health Visitor PoNDER Training | Universal and indicated | UK |
| Psychological | Home-based intervention | Indicated | Australia |
| Psychological | IPT plus telephone follow-up | Universal | China |
| Psychological | IPT standard antenatal care plus the ROSE programme | Indicated | USA |
| Psychological | IPT – Brief | Indicated | USA |
| Educational | Two-step behavioural educational intervention | Selective | USA |
| Social Support | Telephone peer support | Indicated | Canada |
| Social Support | The Newpin Project | Indicated | UK |
| Social Support | Thinking Healthy Programme | Indicated | Pakistan and developing world |
| Midwifery-led interventions | CenteringPregnancy | Selective | USA and Australia |
| Midwifery-led interventions | Midwife-led brief counselling | Selective | Australia |
| Midwifery-led interventions | Midwife-managed care332 | Universal | UK |
| Midwifery-led interventions | Midwifery redesigned postnatal care | Universal | UK |
Examination of the RCTs in conjunction with searches for qualitative research revealed 22 published trial reports associated with the 13 interventions (see Table 48). These reports became the ‘index papers’ for our study clusters.
Searching for CLUSTER documents for realist synthesis
Google Scholar citation searches (‘forward chaining’) were conducted for each of the 22 published study reports. 141 A total of 1888 citations were identified (including duplicates). The mean number of citations was 86 (range 0–232). Lists of results for articles citing an index paper were examined carefully for shared authorship, a common study identifier or for other common study-level denominators (e.g. setting or institution). When a directly connected (‘sibling’) report was identified this was used to populate synthesis of the findings from PSSS studies Appendix 7.
In addition, when a similar intervention study (e.g. differing in setting, population, etc.) was identified, this was recorded as a kinship study. Finally, systematic reviews, narrative reviews and qualitative evidence syntheses on the topic were also identified. The reference lists of all 22 original published reports (Table 48), as well as the reference lists of all ‘sibling’ studies, were scrutinised (‘backward chaining’) for earlier sibling studies (e.g. protocols, pilot studies, feasibility studies, etc.) or related ‘kinship studies’ (e.g. studies sharing a common intervention or underpinning theory).
| Study report (first author, year, reference number) | Number of Google Scholar citations |
|---|---|
| Psychological | |
| Health Visitor PoNDER Training | |
| 1. Morrell, 200961 | 44 |
| 2. Morrell, 2009151 | 105 |
| Home-based intervention | |
| 3. Armstrong, 1999164 | 169 |
| 4. Armstrong, 2000251 | 97 |
| 5. Fraser, 2000252 | 93 |
| IPT standard antenatal care plus the ROSE programme | |
| 6. Zlotnick, 2006179 | 117 |
| IPT plus telephone follow-up | |
| 7. Gao, 2010154 | 15 |
| 8. Gao, 2012327 | 10 |
| IPT-brief | |
| 9. Grote, 2009170 | 75 |
| Educational | |
| Two-step behavioural educational intervention | |
| 10. Howell, 2012190 | 9 |
| 11. Howell, 2014335 | 1 |
| 12. Martin, 2013336 | 0 |
| Social support | |
| Telephone peer support | |
| 13. Dennis, 2009205 | 102 |
| The Newpin Project | |
| 14. Harris, 2008206 | 0 |
| Thinking Healthy Programme | |
| 15. Rahman, 2008148 | 209 |
| Midwifery-led interventions | |
| CenteringPregnancy | |
| 16. Ickovics, 2007262 | 199 |
| Midwife-led brief counselling | |
| 17. Gamble, 2005221 | 105 |
| Midwife-managed care | |
| 18. Shields, 1997219 | 37 |
| 19. Shields, 1998337 | 43 |
| 20. Turnbull, 1996338 | 232 |
| Midwifery redesigned postnatal care | |
| 21. MacArthur, 2002146 | 168 |
| 22. MacArthur, 2003264 | 58 |
| Total references | 1888 |
Preliminary synthesis and construction of a theoretical model
A formative stage of the synthesis required becoming familiar with the focal interventions, to sensitise to the study data and to broadly characterise the different programmes against their defining dimensions. Table 49 attempts to locate the included programmes against the following dimensions:
-
whether the programme is delivered at an individual or group level or it has elements of both (‘mixed approach’), or whether it is not directly targeting the women but reaching them indirectly through health professional training
-
whether the programme is delivered face to face, whether it is delivered remotely or whether it uses both methods (‘hybrid delivery’)
-
whether the programme is delivered by health professionals or by lay support, or it is delivered by both (‘joint delivery’).
| Dimension | Individual | Mixed approach | Group | Training |
|---|---|---|---|---|
| Face to face | Midwife-managed care, midwifery redesigned postnatal care | IPT standard antenatal care plus ROSE programme | CenteringPregnancy, Thinking Healthy Programme | Health Visitor PoNDER Training |
| Hybrid delivery | Midwife-led brief counselling plus telephone postpartum, the Newpin Project, two-step behavioural educational intervention | – | IPT plus telephone follow-up | – |
| Remote | Telephone peer support | – | – | – |
This formative analysis helped in looking for similarities and differences across programmes, for example, in characterising the different mechanisms by which lay support might work compared with delivery by health professionals.
Although specific components of one-to-one or group types of approach are determined by the reviews of effectiveness and acceptability, these two types of approach are underpinned by discernibly different assumptions. Consequently, the mechanisms by which such approaches might operate also carry important differences. These are best illustrated by placing the two types of approach in juxtaposition. However, interventions may blend both approaches. For example, CenteringPregnancy, an essentially group-based approach, offers the opportunity for individual consultation with health professionals. IPT is initially conducted in a group environment, but is followed up by one-to-one telephone contact (Table 50).
| Dimension | Individual | Mixed approach | Group | Training |
|---|---|---|---|---|
| Health/care professional | Midwife-managed care, midwifery redesigned postnatal care, midwife-led brief counselling plus telephone postpartum, two-step behavioural educational intervention | IPT standard antenatal care plus the ROSE programme | IPT plus telephone follow-up | Health Visitor PoNDER Training |
| Joint delivery | – | – | CenteringPregnancy | – |
| Lay support | The Newpin Project, telephone peer support | – | Thinking Healthy Programme | – |
Subsequent synthesis involved detailed itemisation of programme components from each cluster of related study reports; use of multiple reports was essential as not all study reports provided a full description of the intervention. The descriptions of the interventions often lacked sufficient detail to allow replication beyond the original programme. 341 The innovative template for intervention description and replication (TIDieR) framework was used as a template for elicitation of relevant programme components. 342 Appendix 16 contains the TIDieR templates for all thirteen focal interventions, with as complete details as cluster reporting allowed.
Identification of provisional ‘best fit’ conceptual framework for realist synthesis
Searches of Google Scholar identified two outputs from a single Veteran Affairs project on group-based approaches. 343,344 In line with the ‘best fit framework’,345,346 these study reports were sufficiently generic to be used as a source of an ‘analytical framework’ (Figure 56) for examining group care approaches during the perinatal period.
FIGURE 56.
Analytical framework to evaluate group visits. Reproduced with permission from Quinones et al. 343 Note: a, Includes gender, race/ethnicity, age, education/health literacy, rurality/geography, chronic conditions/morbidity and other patient demographics. Note: socioeconomic influences such as financial strain (e.g. price of gas) directly affect patient population. Key: CHF/CAD, congestive heart failure/coronary artery disease; COPD, chronic obstructive pulmonary disease; HTN, hypertension; KQ, key question; ED, emergency department; T2DM, type 2 diabetes mellitus.
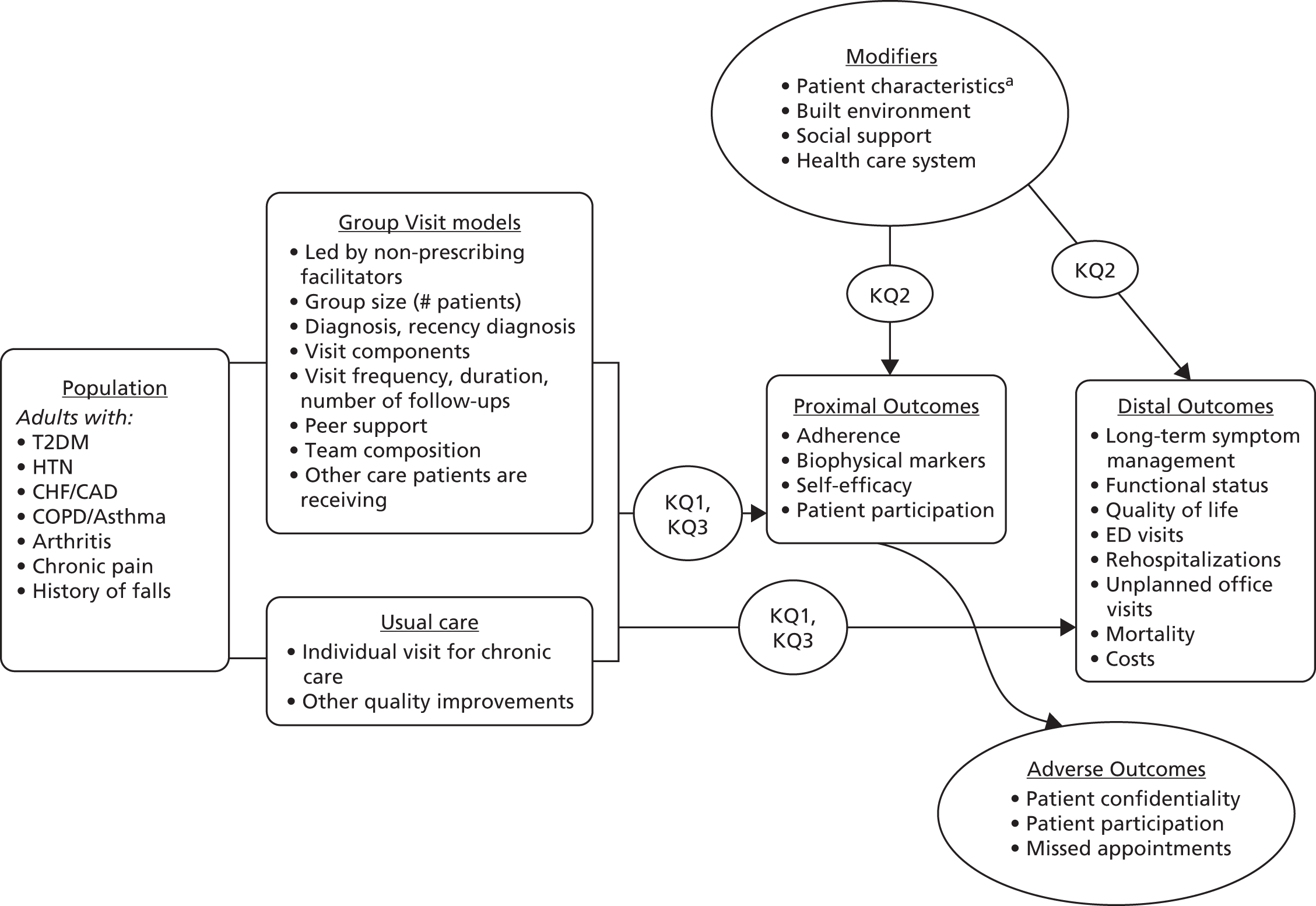
Population of the conceptual framework
Elements of the analytical conceptual framework (see Figure 56) were deconstituted into fields on a data extraction form. Two fields were modified a priori in recognition of the topic: mortality (re-interpreted as suicide ideation) and biophysical markers (re-interpreted as physical signs and symptoms). The Best Fit Framework approach provides for inclusion of additional inductive elements once the deductive stage of the synthesis is completed.
Identification of existing theory underpinning specific mechanisms
Five main bodies of theory seemed to underpin the specific mechanisms of featured interventions:
-
social cognitive/learning theory and self-efficacy
-
social support/social exchange theory (e.g. Brugha et al. 152)
-
locus of control (e.g. Brugha et al. 152)
-
empowerment (e.g. CenteringPregnancy)
-
attachment theory (e.g. home-based intervention and IPT interventions).
The theories underpinning the mechanisms for each study are provided in Table 51. Table 52 indicates the theories relevant for the prevention of PND. Table 53 indicates the mechanism of application of the theories according to the approach used, for example one-to-one or group approach.
| Initiative | Implicit/explicit presence of theory |
|---|---|
| CenteringPregnancy | CenteringPregnancy was developed and piloted by a certified nurse-midwife after experience with successful family-centred approaches to prenatal care and in recognition of repetitiousness [sic] of one-on-one prenatal care for providers. Uses a model of empowerment |
| Health Visitor PoNDER training | Health visitors were trained to deliver psychologically informed sessions based on distinct psychological theories, either cognitive–behavioural principles347 or person-centred principles348 |
| Home-based intervention | Attachment theory349 states that parents’ bonding with their own children and treatment of them is affected by their own earlier attachment history and internal working models. Attachment theory emphasises the importance of consistency in relationships and sensitive understanding of reactions to separation, loss and rejection. The theory of resilience350 recognises personal resilience factors (e.g. positive orientation to problem-solving), and environmental factors (e.g. the help of a supportive adult).351,352 Although some factors are relatively fixed, others can be modified, such as access to support. By exploring individual and family strengths, positive experiences and resources are built upon and enhanced |
| IPT standard antenatal care plus ROSE programme; IPT plus telephone follow-up; IPT-brief | IPT353 is grounded in interpersonal theories354 and attachment theories.355 It is based on the hypothesis that clients who experience social disruption are at increased risk of depression. IPT specifically targets interpersonal relationships and is designed to assist clients in modifying either their relationships or their expectations about relationships. IPT could help new mothers in:
|
| Midwife-led brief counselling | The intervention was based on two theoretical perspectives relating to violence and maternal distress,356,357 focus group discussions with childbearing women and midwives and reviews of the literature |
| Midwife-managed care | The predominant model of shared care – divided among midwives, hospital doctors and GPs (family physicians) – has been called into question. This initiative was designed to address the hypothesis that midwife-managed care would result in fewer interventions, similar (or more favourable) outcomes, similar complications, plus greater satisfaction with care and enhanced continuity of care and carer |
| The Newpin Project340 | A lifespan model of psychosocial origins of depression in women358 pinpoints the role of stressful life events/difficulties (often involving humiliating losses) in bringing on depression/fresh-start events (promising hope of a new beginning) in promoting remission |
| Midwifery redesigned postnatal care | No explicit theory. The intervention was based on UK government reports stating that there was a need for wide-ranging changes to maternity services, emphasising poor assessment and frequently inappropriate delivery of postnatal care. A service led by midwives, with continuity of care and involvement of women, which is supportive and sensitive to individual needs, and preferences is at the centre of the maternity care recommendations |
| Telephone peer support | The intervention was based on research related to maternal dissatisfaction with peer support. Lazarus and Folkman (1984)359 theorised that coping incorporates problem-resolution and emotion-regulation while employing affective, cognitive, and behavioural response systems. Bandura (1977)360 and Bandura (1986)361 social cognitive theory, peer support influences health outcomes by (1) decreasing isolation and feelings of loneliness; (2) swaying health practices and deterring maladaptive behaviours or responses; (3) promoting positive psychological states and individual motivation; (4) providing information regarding access to medical services or the benefits of behaviours that positively influence health and well-being; and (5) preventing risk for, progression of, and promoting recovery from physical illness |
| Thinking Healthy Programme | Holistic approach designed to counter ‘defunct theory of “mind–body” dualism’362 |
| Two-step behavioural educational intervention | Prior research suggests that postpartum physical symptoms, overload from daily demands and poor social support play a major role in generation of depressive symptoms |
| Programme theory | Label | Programme theory – PND will be prevented if . . . | Relevant theory | Elements |
|---|---|---|---|---|
| By activity | ||||
| PT1 | Developing trust | Women develop meaningful relationships with other women in the group and with health-care providers285,363 | Social cognitive theory | Group interaction |
| PT1 | Asking for help | Women are made aware that it is legitimate to ask for help364 and can identify whom to ask365 | Social norms | Modelling within group |
| PT2 | Learning by doing | Women acquire practical366 and communication skills367 that equip them for their new roles366 | Social learning theory, locus of control, self-efficacy | Practical sessions, demonstrations, role play |
| PT3 | Feeling supported | Women feel supported by their partner, health professionals, peer supporters or group members to help them feel comfortable, reduce their anxiety and help them cope with challenges283,285,364,368 | Social support | Group sessions, telephone, individual sessions |
| PT4 | Accessing information | Women are able to access information not before or after but when they need it369 | Social learning theory, locus of control | Group or individual information sessions |
| PT5 | Sharing information | Women are able to harvest resources to support coping184 from their health-care provider370 or from other group members | Social exchange theory | Group or information sessions |
| Symbolic | ||||
| PT6 | Feeling normal | Women come to realise that their experience is not uncommon and that other women come through it364,369 | Social norms | Group sessions or individual interaction with peer or professional |
| PT7 | Dispelling the myth of the ideal mother/birth/baby | Women come to realise that the narratives of the ideal mother,316,371 birth372 and baby are social constructions | Social norms | Group sessions or individual interaction with peer or professional |
| PT8 | Making time for self | Women discover that it is legitimate to make time for themselves320,371 within a baby-centric situation373 | Social norms | Group sessions or individual interaction with peer or professional |
| Mechanism | Underpinning theory (when identified) | Group approaches | One-to-one approaches |
|---|---|---|---|
| Appraisal support (functional support) | Social exchange theory374,375 | Positive: even where facilitator appears unsupportive other group members may compensate | Positive: individuals may develop rapport and trust with their nominated contact |
| Negative: individuals may feel inhibited within a group setting | Negative: individuals may perceive nominated contact as judgemental or unsympathetic | ||
| Emotional support (functional support) | Social exchange theory374,375 | Positive: even where facilitator appears unsupportive other group members may compensate | Positive: individuals may develop rapport, and trust with, and feel able to confide in their nominated contact |
| Negative: individuals may feel inhibited within a group setting | Negative: individuals may not be appropriately matched with nominated contact | ||
| Informational support (functional support) | Social exchange theory374,375 | Positive: facilitator may validate information quality on behalf of the group | Positive: health professional/peer supporter may validate information quality and provide tailored information |
| Positive: other group members may ask a question of relevance to a more reticent member | Positive: individuals may feel comfortable in asking sensitive questions | ||
| Positive: reticent individuals may grow in confidence to ask questions | Negative: health professional/peer supporter may provide inappropriate, unhelpful or factually incorrect information | ||
| Negative: group members may provide unfiltered information leading to incorrect decision or incomplete picture | Negative: individuals may leave personalised concerns unexpressed | ||
| Negative: individuals/partners may feel uncomfortable in asking sensitive questions | |||
| Instrumental support (functional support) | Social exchange theory374,375 | Positive: women may share ideas for sources of practical aid | Positive: facilitator may share ideas for sources of practical aid |
| Negative: individual women may experience increased frustration if sources are not forthcoming | Negative: facilitator may not have full understanding of practical realities | ||
| Support-seeking strategies | Attachment theory355 | Positive: group members access widest range of suggested strategies | Positive: health professional/peer supporter may be able to tailor suggested strategies |
| Negative: others in group may have a limited repertoire of strategies to share | Negative: health professional/peer supporter may have limited repertoire of strategies to share | ||
| Interpersonal relationships | Interpersonal theory354 | Positive: other group members may act as buffer or sounding board for relationship difficulties | Positive: health professional/peer supporter may become confidant for relationship difficulties |
| Negative: group may have limited time to address specific individual relationship difficulties | Negative: individual may feel inhibited from sharing relationship difficulties with health professional/peer supporter | ||
| Negative: individuals may feel inhibited from sharing relationship difficulties with others | |||
| Normalisation | Normalising through connection theory376 | Positive: other group members may affirm validity of individual’s feeling or experience | Positive: health professional/peer supporter may validate individual’s feeling or experience based on previous caseload or professional knowledge |
| Positive: facilitator may validate individual’s feeling or experience based on previous caseload or professional knowledge | Negative: health professional/peer supporter may communicate frequently experienced phenomenon as routine and appear to minimise individual’s personalised experience | ||
| Negative: others in group may not have experienced same feeling or event. Individual may feel strange or isolated | Negative: health professional/peer supporter may perpetuate unrealistic expectations | ||
| Negative: others in group may perpetuate or amplify unrealistic expectations | |||
| Coping | Coping theory359 | Positive: individual is exposed to different models of coping and can select resources appropriately | Positive: health professional/peer supporter may identify most appropriate coping resources to match to individual |
| Negative: individual may compare themselves unfavourably to other group members | Negative: health professional/peer supporter may privilege their own preferred strategies | ||
| Self-efficacy | Self-efficacy theory377 | Positive: group members may help to normalise rationalisations for their symptoms | Positive: care provider may help to normalise rationalisations for their symptoms |
| Negative: group members may affirm belief that PND is unpreventable/untreatable | Negative: care provider may affirm belief that PND is unpreventable/untreatable | ||
| Continuity of care | Not identified | Positive: group facilitation and membership may be relatively stable | Positive: individual receives coherent and cohesive care from a sole provider |
| Negative: group facilitation and membership may be inconsistent | Negative: individual may become overly dependent upon sole provider | ||
| Modelling behaviours | Social learning theory360 | Positive: other group members may be appropriate and realistic role models | Positive: individuals may rehearse appropriate behaviours in a safe environment |
| Negative: group may promote unhelpful norms that counterbalance positive behaviours | Negative: individual may not perceive health professional/peer supporter as appropriate or realistic role model | ||
| Preparing for parenting | Not identified | Positive: facilitator and other group members may contribute to realistic expectations | Positive: health professional/peer supporter may help to actively manage expectations |
| Negative: facilitator and other group members may focus on labour rather than parenthood | Negative: health professional/peer supporter may base advice solely on their own experience | ||
| Negative: health professional/peer supporter may focus on labour rather than parenthood | |||
| Targeting depressive symptoms | Vulnerability-stress theory358 | Positive: even though not every individual experiences every symptom, there is an increased likelihood that at least one member experiences a symptom | Positive: health professional/peer supporter may be able to tailor support/advice to specific needs of individual |
| Targeting anxiety symptoms | Vulnerability-stress theory358 | Positive: not every individual experiences every symptom but there is an increased likelihood that at least one member experiences a symptom | Positive: health professional/peer supporter may be able to tailor support/advice to specific needs of individual |
The social cognitive theory of depression proposes that ‘women for whom motherhood is a highly valued role may be particularly vulnerable to depression if events or difficulties threaten this role’. 378 Interventions that address this theory therefore seek to equip the woman with self-efficacy so that she is better able to manage such events or difficulties or has multiple strategies by which she might attempt to address them. Increased self-efficacy may be seen in the management of her own symptoms or, more generally, in being able to cope with the practical aspects of motherhood that might otherwise be viewed as difficult or problematic. A further aspect to this theory is the modification of the woman’s understanding of the motherhood role so that she is less likely to fall victim to unrealistic expectations of either herself or of others.
The social support theory of depression is underpinned by social exchange theory. Social support has been found to facilitate the adaptation to, and transition to, motherhood and facilitates the flow of emotional concern, instrumental aid, information and appraisal between people, including partners and mothers. Interventions that address this theory therefore seek to reduce the psychological stress of the transition to motherhood. 379 Strategies include the building up of social support networks prior to the birth and being better able to mobilise such support when needed. Group-based interventions may serve to extend social support again in preparation for the birth or as a resource to be accessed after childbirth. Social exchange theory requires a structure through which an interactive process might occur and preventive strategies may help in both the identification of and mobilisation of such structures for interaction. 378
The idea of the locus of control, that is ‘whether a person perceives what happens to her as being within her own control or in the hands of external forces’,380 is believed to be an important aspect of psychological functioning. Clearly this is closely linked with self-efficacy, as discussed above. However, some commentators caution380 that in a childbirth context this may not necessarily translate into greater involvement in decision-making as, for some women, such involvement may actually increase feelings of anxiety. Interventions that engage with the idea of locus of control provide a woman with an opportunity to discuss all aspects of the motherhood experience fully with staff. The woman receives the right amount of information that they personally require. Receiving the right amount of information, both ‘preloaded’ (i.e. prior to the birth) and subsequently ‘on demand’, reduces their anxiety about aspects of the motherhood experience and increases their satisfaction with aspects of the birth experience. Again the mechanism of modifying expectations, to make them more realistic, is present in such interventions.
The empowerment model of prevention of depression is based on the assumption that women are likely to experience negative partner support and therefore need information and coping resources by which to handle this. Interventions that address this theory therefore seek to provide information to help women to identify particular strategies that may be helpful to them. Community resources are identified from which women may draw as appropriate. Empowerment approaches often allow an individualised focus for an intervention so that support can focus on areas of particular need for each woman.
The attachment theory of depression proposes that postpartum depression develops when a mother’s attachment needs are not being satisfied by her partner, whom she feels is irresponsive or inaccessible to her. 381 Although attachment theory originally focused on the importance developing a strong emotional bond between an infant and their mother, more recently this has been extended to include adult relationships, such as the partner and the mother or mother-in-law. Attachment provides a useful resource during times of uncertainty, such as characterise the anxiety-filled birth and postnatal periods. Attachment theory attempts to explain why some women seek to be close to their partner, or significant others, but fear being rejected by them and why others seek to avoid closeness. Interventions that address the attachment theory seek to develop attachment, typically with the partner, so that social support may be readily accessed as and when required. They seek to develop mechanisms by which need for support may be communicated and recognised.
This discussion demonstrates that these theories are not distinct but frequently operate in close proximity. Collectively they explain many intervention components for individual-based and group-centred approaches. Other interventions derive their imperative not from an explicit theoretical basis but from political or social drivers such as the agendas of the UK government264 or of the World Health Organization. 148 For a fuller discussion of principal theories underpinning strategies for treatment and by implication, prevention see the useful summary by Beck. 381
Development of a programme theory
A key issue in developing a programme theory with regard to two different modes of delivery, that is group-based (one-to-many) and individual-based (one-to-one) approaches, relates to whether they offer competing alternatives to meet the same needs or they seek to address different sets of needs. The tables of components (see Appendix 7) assist in identification of important mechanisms that are common to both approaches, those that can substitute for each other, or those that are unique to one of the two approaches.
Group-based interventions
In the case of the group, under a ‘resource-based model’ (i.e. the idea that a group is identifying, sharing and subsequently using its collective emotional and experiential resources) members of a group may provide aspects of information, experience or support beyond the resources of a single facilitator. 302,312,313,321 However, this relies on the existence of mechanisms for releasing the resources for use by the whole group. There is evidence of facilitators being aware of resources or experience within a group that the individuals themselves felt unable or unwilling to share. 293 Consequently, the facilitators felt powerless to offer such experiences without the approval of the individual themselves. Use of group-based mechanisms places additional requirements for group coherence,382 the development of trust with a larger number of individuals and the existence of ground rules that minimise the chance of harmful group behaviours.
Continuity of care
Continuity of care may be present through the ongoing participation of one or more group co-ordinators. The CenteringPregnancy programme identifies ‘stability of group leadership’ as an ‘essential element’ of the approach. 383 Continuity is also sought within team midwifery-based support approaches,224 but that does not necessarily translate into the personalised and tailored care required for the building of confidence, trust and satisfaction with care. If a facilitator does not function well with, or relate well personally to, several or, indeed, all of the group, then this may potentially cause more harm than a problematic one-to-one approach. However, this may be partially compensated for through a form of substitution by good relationships within the group.
Individual-centred interventions
With regard to individual interventions it is perhaps unhelpful to focus on the ‘individual’ part as the intervention (in contrast to the acknowledged effect of the ‘group’). The individual approach offers potential benefits that may or may not be realised. For example, under a resource-based model, a particular supporter, whether professional or lay, may not have experience to draw upon and mobilise for the benefit of the individual. Continuity of care, a claimed advantage of individual-based interventions, may not be realised if staff changes or team processes interfere with this. This may explain why Dennis et al. 384 found a non-significant effect for continuity of care in their systematic review. There may not be a rapport between supporter and woman. If an individual relationship is not built up, then trust and relationships are impaired. Other benefits, such as sharing of confidential, personalised information, are not realised. Dennis et al. 384 refer to this in the specific context of revealing PND to a health professional. However, this may be equally important in prevention when seeking to broach the subject of potential symptoms or causative factors. 385 It is helpful to highlight the personalised, targeted nature of the individual-based approaches, not the fact of the individual relationship per se.
Considerations shared by group-based and individual-centred interventions
The analysis has revealed the shared importance of three preparatory stages in the intervention. Principally, these concern (1) recruitment, whether of health professionals or of lay supporters, (2) training, again irrespective of whether professionals or lay supporters, and (3) the process of targeting or matching the needs of those requiring support to those delivering support. In addition, mechanisms for sustainability within a programme also surface as being important considerations.
Recruitment
Recruitment is a key intervention in relation to lay support. Lay supporters are typically volunteers and are often motivated by a desire to help or to give something back. 301
Training
Clinical staff must make a considerable investment of time to supplement their clinical expertise with facilitation, counselling or support skills. Midwives, to create a favourable impression within a CenteringPregnancy intervention have to be sufficiently skilled, knowledgeable and warm, to provide suggestions for group discussion and to allow unstructured discussion, all of which were appreciated by group members. 277 The intervention by Morrell287 compared training for health visitors in assessment and two different methods of psychological support. Deficiencies in delivery of care sometimes imply a need for further training.
For lay supporters, the potential training burden is substantial. For example, it may include experiential training, such as role-playing and supervision, information on peer support strategies and topic-specific information about PND and medications as well as organisations or further sources to which they could refer. 386 Dennis386 describes the use of a 121-page training manual.
Matching
Behavioural interventions require creation of a rapport between service provider and recipients of care. Those delivering group interventions must be viewed as accessible and welcoming by members of the group. Indeed, effective facilitation requires that the facilitator progressively suppresses his or her own role so that the group becomes functional with minimum and judicious input. In the individual telephone counselling intervention, participants were matched with peer volunteers ‘if the mother desired’. 205 However, this so-called matching was based on residency and ethnicity and was performed by the co-ordinator. The Newpin Intervention saw young befrienders being matched with younger parents. 206,387 However, demographic ‘matching’ may not be sufficient and numerous other variables could be considered when seeking to establish compatibility.
Support to providers
A further ongoing requirement for both approaches is supervision of, or at least support to, those delivering support (whether professionals or lay supporters). This is particularly the case for formal psychological approaches, such as IPT, which often require supervision as a component of intervention delivery. The availability of such support may have a subsequent effect on retention of the facilitators/supporters, the sustainability of the overall programme and, indeed, on further recruitment.
Another consideration for both group and individual approaches that is not determined exclusively by type of intervention delivery relates to the convenience of the intervention sessions. Delivery of sessions at home or over the telephone and integration with routine health-care visits may help to increase the acceptability and feasibility of intervention delivery as well as adherence. 327,388 Hybrid models may seek to optimise the pattern of home visits and regular visits to a health-care provider. Opportunities for improved co-ordination are offered by using such visits to give advice on nutrition, child health, child development programmes, positive parenting programmes, vaccination programmes, routine childbirth education sessions and community health programmes. 389 Group interventions can seek to achieve improved acceptability and feasibility by being offered in conjunction with individual health-care appointments, as in the CenteringPregnancy model.
Components of the interventions
Several features recurred frequently in the qualitative syntheses of interventions and of personal and social strategies, as either actual or suggested components for the intervention, irrespective of the chosen method of delivery. In some cases the feature is implicit within suggestions of what might have helped. For example, the value of family support or of instrumental support translates into a requirement for intervention content that both affirms the validity of help-seeking and provides practical strategies for eliciting such support. A useful intervention, when time and resources permit, includes the following:
-
make provision for continuity of care
-
legitimise help-seeking without framing this as an inability to cope
-
offer strategies for identifying support
-
equip women to delegate tasks without surrendering mother role
-
offer strategies for eliciting emotional, spiritual and instrumental support
-
identify coping strategies to allow self-help
-
help women to access information as and when required
-
feel able to share feelings and experiences without experiencing premature closure
-
facilitate normalisation of feelings
-
create realistic expectations about the birth
-
create realistic expectations about motherhood roles
-
create realistic expectations about health professional support and roles and health services
-
challenge social norms of the ideal birth, the ideal baby or the ideal mother
-
anticipate baby-centric focus of family and health professionals
-
identify strategies for acknowledging and meeting mother’s own needs
-
prepare women for emotional lability
-
anticipate fatigue, pain and slow recovery from labour
-
help women adjust their routines to motherhood
-
widen focus beyond delivery and birth
-
gain strength/joy from baby
-
develop attachment with infant
-
acquire practical skills (breastfeeding, changing nappies, bottle feeding, bathing)
-
understand appropriate use of medication, alternative medicine and counselling services
-
acknowledge and build upon cultural variation
-
adjust to cultural barriers regarding communication or provision of support.
Sustainability
A further key consideration relates to the sustainability of the intervention or programme. Unlike other self-management or peer support programmes, primarily within the domain of chronic diseases, pregnancy is a time-limited condition with definable antenatal and postnatal periods. Sustainability cannot be offered by continuity of group membership. Sustainability may be offered by structural components, for example, a common venue or ongoing facilitators, or by process elements such as training manuals and programmes or a standard curriculum. There is some evidence within the reviewed studies of a cohort approach which seeks to engage a group of mothers to be at a common point and then take them together through the antenatal, birth and postnatal period. Certainly group membership seems less of an issue under a cohort model than with an escalator model, in which mothers can enter or exit at any point in the programme. However, the cohort model is, in turn, predicated upon having sufficient critical mass of women at approximately the same point in their pregnancy for the group to be viable. Here considerations of optimal group size need to be considered against what is feasible and practicable.
Recruitment of the next generation of peer supporters could, in theory, be achieved from within each cohort although timing is an issue as a recent mother, adjusting to such a significant life event, does not correspond to the typical model of one likely to volunteer. Therefore, some mechanism for medium-term follow-up may be needed to keep in touch with potential future peer supporters.
Construction of pathways or chains from ‘if–then’ statements
The subsequent stage to production of ‘if–then’ statements is to seek to integrate these into causal pathways or chains.
Mechanisms for improving appropriateness of strategies
Figures 57 and 58 present schema demonstrating the way in which ‘if–then’ statements might illuminate particular paths or dependencies. 290
FIGURE 57.
The ways in which ‘if-then’ statements might illuminate pathways for individual approaches. Data source: McNeil et al. , 2013. 290
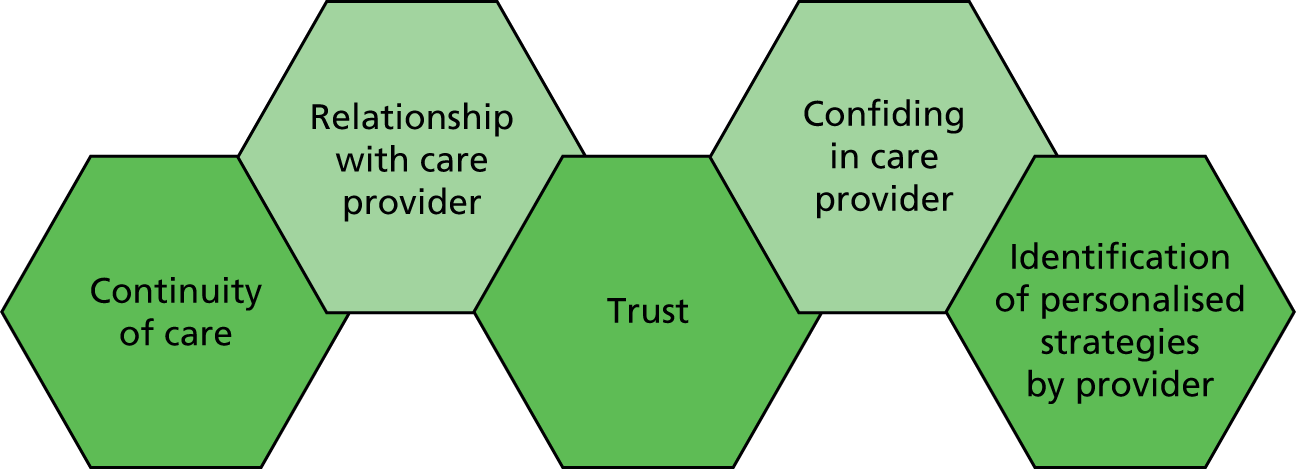
FIGURE 58.
The ways in which ‘if-then’ statements might illuminate pathways for group approaches.

These representations illustrate that a key point in the delivery of interventions, whether group or individual based, is the establishment of a relationship with a care provider, whether professional or a lay helper. Matching of care provider to women, whether individually or collectively, becomes a key factor in the success of such interventions. Building up such a relationship allows the establishment of trust, which then allows open and frank information exchange. 285 When such communication is present it leads, in turn, to a better understanding of the needs of the expectant mother. The establishing of relationships explains, at least in part, why continuity of care283 figures prominently in discussions of the requirements for good-quality antenatal care.
In group-based interventions, the requirement for a successful relationship is further compounded. Relationships need to be built up between mother and care provider and between mother and others in the group. 283,289 However, this element of ‘risk’ to the functioning of the group may potentially be compensated for by the likelihood that support for the group may compensate for inadequacies in the facilitation and also that the group has more resources, in terms of experience to share and a ‘like mind’,390 to offer in support of each individual mother. When support is being provided by care provider and/or by women in a group this may take away some of the pressure on the relationship with fathers or significant others (such as in-laws).
That women need to build up relationships in order for the intervention to work is seen in the experience that groups may initially struggle. 285 Subsequently, they typically weather initial periods of individual anxiety.
On adverse effects
Some women do not welcome the group approach and so, in quantitative terms, are lost to trials prior to randomisation. Similarly, most of the qualitative studies recruited women who had agreed to participate in a group-based approach. This represents an important area of potential methodological bias. Likewise, participation tends to be described in very forgiving terms, for example in the number of women attending one or more sessions. Theoretically, this means that the women are likely to be being delivered a suboptimal ‘dose’ of care. In practical terms, there is the possibility that health provider resources are not used effectively or women may be unable to access groups because available slots are occupied by non-attenders. In addition, there was some evidence that discomfort experienced by partners over the nature of discussions may have caused them to disengage with a subsequent perception of lack of support from the viewpoint of the women themselves. 283 A further complication relates to the potential inclusion of fathers. Fathers may experience difficulty in contributing to the group277 either because of their own shyness or because women felt that men were uncomfortable with intimate discussions. 283 Alternatively, women may feel reticent in bringing up topics when in a mixed group that includes fathers. If women themselves fail to maintain an adequate attendance level, and thus experience a consequent lack of group support, they may perceive an inability to implement strategies that they have learned. 286
Communication with a care provider, and/or with a group, should not be viewed simply in positive terms. Groups or care providers may, albeit unwittingly, create expectations that become difficult or impossible for an individual mother to fulfil. 371 A failure to meet either perceived or actual norms may contribute to a feeling of inadequacy. Social comparison may also be unfavourable if others in the group are handling challenging situations with more ease, even if this reflects individual proficiency rather than the benchmark level for the group as a whole. There was some evidence that established group members would take significant steps to avoid upsetting other group members by creating expectations (e.g. in their support relationships, material circumstances or the pregnancy experience) that they might be unable subsequently to fulfil. 293
Although much is made of the benefits of bringing together women who are facing the common challenges associated with pregnancy, labour and childbirth, it should be recognised that this is not without risk. Given the recognised susceptibility of these women to emotional feelings, it can be seen to be potentially volatile to bring together women when the response of another might well attenuate the emotional effect. A further consideration within a group context is that a lack of privacy during the intervention may result in a mother feeling that her individual care has been sacrificed to the requirements of the group. The very structured CenteringPregnancy protocol also poses specific logistic problems if women perceive that the format of the sessions is not ideal, with a 2-hour session being too long289 or there being too long a period of time between first and second group meetings. 277
A shared concern for both individual- and group-based approaches relates to the fact that any type of service provision raises expectations from the service. If these expectations are subsequently unrealised then this can be an additional source of frustration to women who already feel unsupported. Improved access to a caregiver through a targeted intervention may subsequently raise expectations that might not be met either in individual follow-up care from the provider or by front-desk support staff in their interactions with mothers. 283 Qualitative research revealed specific logistic concerns related to the fact that the choreographed and structured nature of group sessions may induce a feeling of being rushed by a health professional during the intervention. Specifically, within a military setting, CenteringPregnancy was seen to neglect consideration of the associated workload and resource constraints. So, although the CenteringPregnancy Intervention appears to be generally well received, constraint of available resources could have a disproportionate, that is non-symmetrical, effect, if service providers are seen to be scrimping and saving on costs of care. Women may therefore feel that their care is not perceived as a priority.
Other considerations relate to specific facilitation difficulties in which a health professional is perceived as being too controlling or not suitably facilitative in engaging with the wishes of the group. A tension between encouraging women to bring their family, in some cases, when this facilitates their access and attendance but acknowledging the disruption this may pose, in other instances, can lead to the perception that the service is not family centred and that older children are not welcome.
Testing of the programme theory and integrating quantitative and qualitative findings
Having identified hypothesised components for successful inclusion in an intervention or programme enabled us to re-examine their presence or absence in the featured interventions. Although this approach is necessarily limited by the quality of reporting of each intervention this effect was minimised by using all available published reports of each intervention, not solely the primary trial report. It was assumed that the emphasis of the reporting would largely reflect the corresponding emphasis of particular features within an intervention. That is, if a feature is mentioned it is more likely to be considered important to an intervention’s mechanisms of action whereas if a feature is unclear or omitted, particularly given word limit constraints, it is correspondingly unlikely to be considered a key feature, although not necessarily absent. A further limitation relates to the limited ability of an approach based on reporting to establish whether a feature was deliberately planned in the conception of an intervention or was implemented fortuitously or opportunistically. Nevertheless, its presence would indicate that it is feasible both as a feature of the existing intervention and as part of any planned enhancement.
Finally, consideration of desired qualitative features alone is not sufficient for exploration of the candidate interventions. At some point these features must be correlated with data on the effectiveness of each intervention. Table 54 makes an initial link between the presence or absence of reported features and an overall assessment of effectiveness. However, it is important to recognise that this simply represents a correlation and cannot be considered evidence of a cause and effect relationship.
| Element from qualitative findings | Two-step | CenteringPregnancy | Midwife-led brief counselling | Midwife-managed care | Mid-routine primary care | PoNDER | Home based | IPT phone | IPT Rose | IPT-brief | Telephone support | Newpin | Thinking Healthy |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Continuity of care | – | ✓ | – | ✓ | ✓ | – | – | – | – | ✓ | ✓ | – | – |
| Legitimise help-seeking | ✓ | – | – | – | – | – | ✓ | ✓ | – | – | ✓ | ✓ | – |
| Identify support | ✓ | ✓ | – | – | – | – | ✓ | ✓ | – | ✓ | ✓ | ✓ | – |
| Delegate without surrender | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Strategies for eliciting support | ✓ | ✓ | – | ✓ | – | – | – | ✓ | ✓ | – | ✓ | ✓ | – |
| Coping strategies | – | – | – | – | – | ✓ | ✓ | ✓ | ✓ | – | – | – | |
| Access information as required | ✓ | – | ✓ | – | – | ✓ | ✓ | – | ✓ | ✓ | ✓ | ✓ | |
| Able to share feelings without experiencing premature closure | – | – | – | – | – | ✓ | – | – | – | ✓ | ✓ | ✓ | – |
| Normalisation of feelings | ✓ | – | – | – | – | ✓ | – | ✓ | ✓ | ✓ | – | – | |
| Realistic expectations about birth | – | – | – | – | – | – | – | – | – | – | – | – | ✓ |
| Realistic expectations about motherhood roles | – | – | – | – | – | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | ✓ |
| Realistic expectations of professionals and health services | ✓ | – | ✓ | – | – | – | – | – | – | – | ✓ | – | ✓ |
| Challenge ‘ideal’ | – | – | – | – | – | – | – | – | – | – | – | ✓ | ✓ |
| Anticipate baby-centric focus | – | – | – | – | – | – | – | – | – | – | – | – | ✓ |
| Acknowledge mother’s own needs | – | – | – | – | ✓ | – | – | – | – | – | – | – | – |
| Acknowledge emotional lability | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Anticipate fatigue, pain, and recovery from labour | ✓ | – | – | – | – | – | – | – | – | – | – | – | – |
| Adjust routines | ✓ | – | – | – | – | ✓ | – | – | – | – | – | – | – |
| Focus beyond delivery and birth | – | – | – | – | – | – | ✓ | – | – | – | – | – | ✓ |
| Gain strength/joy from baby | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Develop attachment with infant | – | – | – | – | – | – | ✓ | ✓ | ✓ | ✓ | – | – | ✓ |
| Acquire practical skills | – | ✓ | – | – | – | – | – | ✓ | – | – | – | – | ✓ |
| Use of medication, alternative medicine and counselling | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Cultural variation | – | – | – | – | – | – | – | – | ✓ | ✓ | – | – | |
| Cultural barriers regarding communication or support | – | – | – | – | – | – | – | – | ✓ | – | – | – |
Response from the service user group to optimal characteristics identified from the qualitative/realist reviews
Consultation with the PPI group revealed that many characteristics listed resonated with group members’ own experience and feelings. One informant commented that they felt that ‘the list was meaningful and shows good insight into the pregnancy experience and early motherhood’, while another stated that ‘it captures the main concerns’ and a third agreed that it was meaningful. They did identify that the wording of the list would need careful attention if it is to be translated into use with women themselves, as opposed to health professionals.
Modifications to the list
One informant endorsed the need to equip woman to delegate tasks without surrendering the mother role. She made an implicit connection with challenging the concept of the ‘ideal mother’ in stressing to women that ‘help with mothering could be necessary and to avoid making this shameful or neglectful’. Members of the PPI group offered specific observations on the timing of some of the suggested strategies. Practical skills (such as breastfeeding, changing nappies, bottle feeding, bathing) were considered ‘very important skills that need to be acknowledged before the birth’. It was felt that these should be emphasised because, as also revealed by the literature reviews, ‘too much focus is on the birth’. It was also important that women’s own needs be acknowledged before the birth:
I would add also to tell mothers to look after themselves before and after the birth by doing one thing a day they enjoy; five minutes of filing nails, eating something they really enjoy and simple everyday pleasures, which are achievable.
PPI group member
Finally, information on PND needs to be available from the start, for example at antenatal classes.
Additions to the list
In addition, members of the PPI group volunteered observations that triangulated with findings identified elsewhere in the review processes. In particular, the involvement of, and role of, partners was essential with a need to educate partners regarding symptoms and a requirement to ‘keep them involved and to help them understand what is going on’. Comments resonated with the strategies offered by IPT, namely ‘to avoid potential possible relationship difficulties/breakdown which obviously wouldn’t be helpful to the women with PND’. The importance of attachment extends beyond the mother and baby, requiring that partners enjoy ‘some level of involvement to encourage the later bonding process with baby – or it could become very much just the woman’s experience’.
Other findings from the review, reflected by participant responses, included the importance of the need to legitimise help-seeking without framing this as an inability to cope given that women may ‘fear their children may be taken away from them if they open up as to how they are feeling’. The key role of continuity of care was affirmed, particularly in the context of the caregiver being able to identify changes in the woman and therefore offer personalised strategies for eliciting emotional, spiritual and instrumental (i.e. practical) support.
Other important features felt to help avoid PND included:
-
being informed about and prepared for the risks of reccurrence with subsequent pregnancies
-
having a supportive GP
-
not being put under pressure to breast feed if a woman feels uncomfortable doing so
-
providing access to other new mums for example, groups.
An observation, not identified in the literature, related to ‘help with identifying baby’s cries’. A woman described how she ‘felt anxious and found it hard to trust and to connect with [her] baby’. She suggested that help in interpreting baby’s cries might be based on the work of an Australian musician who has ‘observed babies’ cries and discovered how we can interpret them before they become fully fledged; it is called Dunstan’s baby language. 391
Additional nuances emerging from the consultation
One informant, while recognising that the strategies listed were important, highlighted practical difficulties, in implementing the strategies. For example, triggering asking for help may prove problematic because ‘what a woman experiences is “normal” for her and therefore she might not know that she is depressed and therefore not ask for help’. Similarly, equipping a woman with strategies for identifying support is also dependent on a woman herself recognising that she needs support.
Delegation of tasks will not always be possible if a woman has no one to help her or if a partner is of no help and only increases her anxiety. Individual ability to ‘manage everything themselves’ varies from woman to woman and this needs to be recognised by health-care providers. Other comments also highlighted the individualised nature of response to help, advice and support:
Anything that is said to an anxious or depressed woman can have a negative effect but also a positive effect. Her ability to cope must not be doubted. I think professionals need to be very aware.
Summary of findings from realist synthesis review
When planning a group-based intervention, an intervention is:
-
more likely to succeed if a facilitator has been trained in group leadership and facilitation
-
more likely to succeed if a facilitator has personal resources that they can bring to the group
-
more likely to succeed if a facilitator creates a rapport with the group
-
more likely to succeed if the group creates a favourable group dynamic
-
less likely to succeed if the facilitator is seen as controlling or not responding to the wishes of the group.
When planning a one-to-one peer-based intervention, an intervention is more likely to succeed:
-
if a peer has been matched on other than simple demographic variables
-
when peers are recruited based on extroversion and good communication skills.
When planning a one-to-one professional mediated intervention, an intervention is more likely to succeed if:
-
a relationship of trust is built up between the woman and the care provider
-
the health-care provider has significant personal resources on which to draw.
A face-to-face intervention is more likely to be successful if a health-care provider responds to visual, verbal and non-verbal cues that reflect how a woman is feeling.
An intervention delivered at a distance is more likely to be successful if a supporter makes more contacts, has more conversations and leaves messages.
Training interventions for health professionals or peer supporters are more likely to be successful if they:
-
include problem-solving strategies such as role play
-
include demonstrations of practical skills that can subsequently be modelled with individuals and groups of women
-
are relevant to the community as they equip health professionals or peer supporters with appropriate skills to deal with the range of people who receive services within a multicultural society.
Chapter 9 Assessment of cost-effectiveness
Systematic review of existing cost-effectiveness models
Identification of cost-effectiveness studies
A comprehensive search was undertaken to identify systematically cost-effectiveness literature comparing the costs of different interventions to prevent PND. The search used a combination of thesaurus and free-text terms. The search comprised four facets combined together. Facet 1 comprised terms for the population (pregnant and postnatal women). Facet 2 comprised terms for prevention. Facet 3 comprised terms for known risk factors of PND. Facet 4 was generic terms for interventions. To retrieve cost-effectiveness literature, the four facets of the searches were combined with an economic evaluations search filters. The searches were performed by an information specialist (AC) in November and December 2012. The search strategy is reported in Appendix 1. The economic evaluations filter for MEDLINE is provided in Appendix 1, Search strategy used for cost-effectiveness studies with economic evaluations filter for MEDLINE. The list of electronic bibliographic databases searched for cost-effectiveness literature is presented in Appendix 1, Electronic databases searched for the cost-effectiveness literature. All citations were imported into Reference Manager version 12 and duplicates deleted. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart for the studies included in the health economics review is presented in Figure 59.
FIGURE 59.
The PRISMA flow chart of studies included in the health economics review.
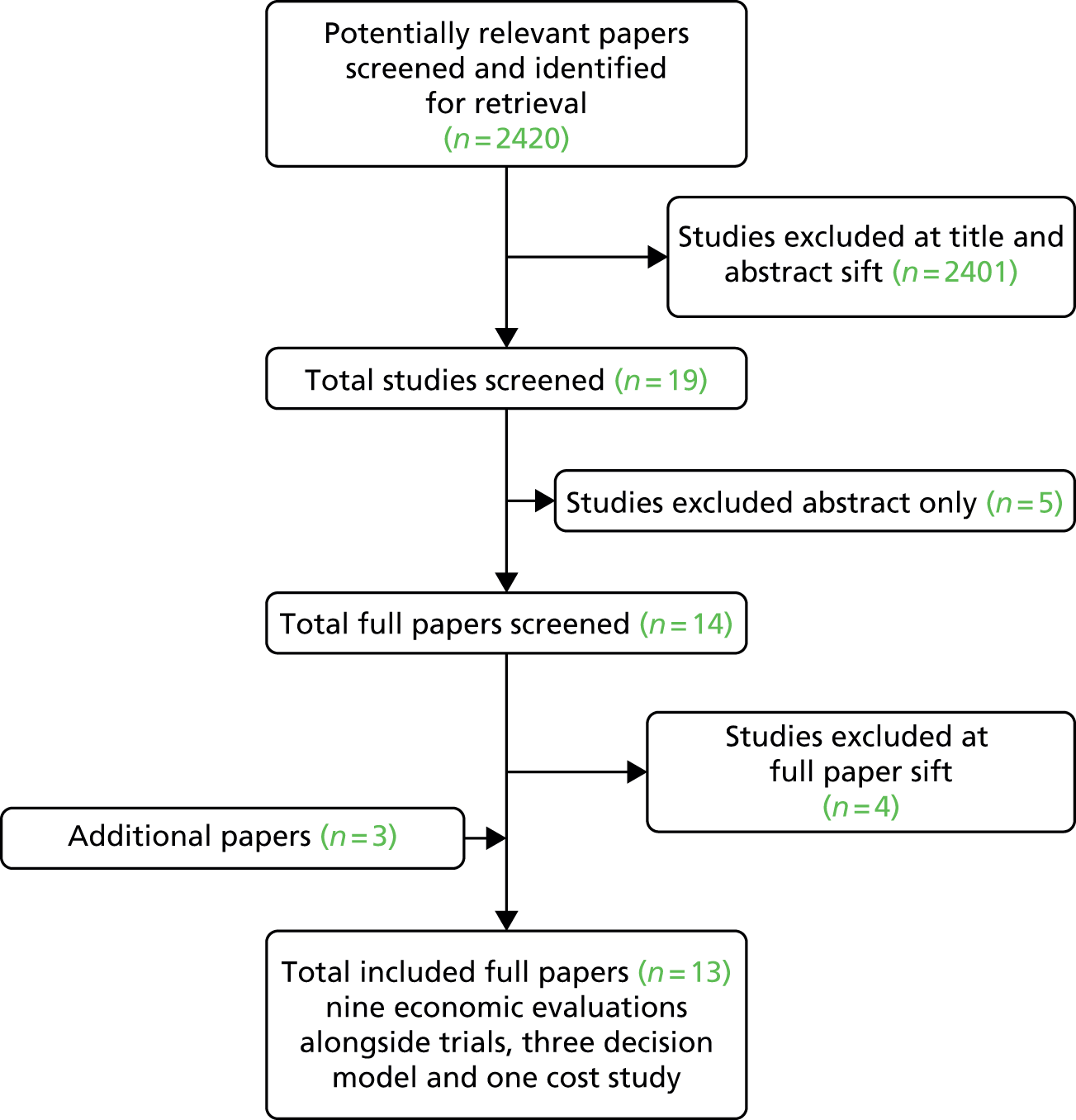
Study selection criteria and procedures for the health economics review
Papers were eligible for inclusion if they included costs or health-related quality-of-life measurements of PND that could be used in an economic decision model. As only a limited number of studies addressing prevention only were found, the inclusion criteria were kept broad to include papers evaluating screening for and treatment of PND, as well as prevention of PND in order to minimise the risk of potentially useful data being excluded. When multiple papers of the same studies were published, the most detailed or most recent (as appropriate) were selected, as recorded in Table 55.
| First author, year, reference number | Reason for exclusion |
|---|---|
| Stevenson, 2010392 | Two papers on same study,392,393 the more detailed paper was selected392 |
| Paulden, 200957 | Two papers on same study,45,57 the more detailed paper was selected45 |
| Buist, 2002394 | Non-economic evaluation, neither costs nor health-related quality of life reported |
| Darcy, 2011395 | Non-economic evaluation, neither costs nor relevant health-related quality of life reported |
There were 2420 papers were identified in the search. The reasons for exclusion at the full paper stage are shown in Table 55. There were two studies for which multiple papers for the same study were found45,57,392,393 and in both cases the more detailed paper was selected. 45,392 An additional paper that was published after the search was completed was identified by a member of the project team who was an author on the paper and the paper was included. 396 It was not identified in a systematic way and other papers that were published after the search was conducted will have been missed. A second paper was identified by a member of the project team during the search for quantitative studies and was included in this health economic review. 56 This paper had been excluded at the title and abstract stage on the basis of the paper title. A further paper was identified during the economic modelling process. 397 It had been excluded at the title and abstract stage as PND or associated terms were not included in the title or abstract. Of the 13 papers identified,61,174,199,264,392–394,398–400 nine described an economic evaluation that was conducted alongside a trial,53,61,174,199,264,299,392,393,400 three papers described an economic decision model45,56,394 and one paper described a cost study. 398
Overview of papers included in the health economics review
Although all included papers described an economic evaluation of a PND intervention, they were heterogeneous in many aspects, including the population, intervention, comparator and outcomes evaluated. The nine economic evaluations53,61,174,199,264,299,392,393,400 and the one cost study398 are described in Table 56 and the three economic decision models45,56,392 are described in Table 57.
| Study (first author, year, reference number) | Country | Intervention | Population | Sample size | Outcomes measured | Main economic outcome reported | Quality-of-life measure | Time horizon | Result |
|---|---|---|---|---|---|---|---|---|---|
| Appleby, 2003398 | England | Health visitors giving cognitive–behavioural counselling | All postnatal women | 97 health visitors | Number of health visitor contacts per depressed woman pre and post training; cost of health visitor time pre and post training | Change in health visitor costs | – | 6 months | A non-significant decrease in mean costs occurred overall |
| Boath, 2003399 | England | PND treatment in a specialised PBDU compared with routine primary care | Women with PND | 60 women (30 in the intervention and 30 in the control group) | Mean costs for women using PBDU and routine primary care; number of women depressed at 6 months | Incremental cost per successfully treated woman | – | 6 months | A move from routine primary care to PBDU would incur an additional cost of £1945 per successfully treated women |
| Dagher, 2012400 | USA | – | Employed postnatal women | 31 depressed, 607 non-depressed | Total health-care resources used at 11 weeks | Difference in health-care resources used | SF-12 | 11 weeks | The mean total cost for health-care resources used was US$681 higher in the depressed group than in the non-depressed group |
| Dukhovny, 2013396 | Canada | Volunteer telephone-based peer support compared with usual care for the prevention of PND | High-risk women (screened postnatally) | 610 women (296 in the intervention and 314 in the control group) | Cases of PND averted at 12 weeks (EPDS), health-service use, cost of intervention, volunteer opportunity cost, hired housework/child care and partner time of work | ICER (per case of PND averted) | – | 12 weeks | An ICER of CA$10,009 per case of PND avoided |
| Gold, 2007397 | Australia | Primary care and community-based interventions to promote the health of new mothers | All postnatal women in study areas | 16 intervention areas: eight in the intervention and eight in the control group | Cost of the intervention and health-care resource use | Cost per woman of the intervention and cost per area | SF-36 (but value not reported in paper) | 24 months | Average cost per woman of AU$129 in rural areas and AU$172 in urban areas. No significant differences in health-care resource use when intervention areas compared with control areas |
| MacArthur, 2003264 | England | Designed to enable midwifery care in community settings to be tailored to women’s individual needs with a focus on the identification and management of physical and psychological health rather than on routine observations | All postnatal women in the selected GP clusters | 1042 (485 in the control group and 557 in the intervention group) | Number and duration of health-service use; EPDS scores | Total health-care resources used. Cost per case of probable depression avoided | – | 12 months | An incremental cost of £700 per case of probable depression prevented |
| Morrell, 2000199 | England | Additional postnatal care by trained community postnatal support workers | Postnatal women | 623 (311 in the intervention group and 312 in the control group) | Number of contacts with health services, SF-36, Duke functional social support scale scores, EPDS scores, other measures of health outcomes | Change in health service costs | SF-36 | 6 week and 6 months | No significant differences in NHS resource use (except for the support worker service) |
| Morrell, 200961 | England | Health visitor psychologically informed training intervention | At-risk women (screened postnatally) and all postnatal women | At-risk women 418; all women 2659 | Cost of health visitor training, health service contacts for interventions and control, EPDS scores | Incremental costs and QALYs | SF-6D | 6 and 12 months | Psychological approaches dominated control group – lower mean cost and higher mean QALY gain |
| Petrou, 2006174 | England | Additional health visitor visits | At-risk women (screened antenatally) | 151 (74 in intervention group and 77 in control group) | Number of contacts with health services, length of PND | Incremental cost per month of PND avoided | – | 18 months | Incremental cost per month of PND avoided of £43.10 |
| Petrou, 200253 | England | – | High-risk women | 206 | Number of contacts with health services | Incremental cost of treating PND | – | 18 months | Mean cost per women with PND £2419; mean cost per women without PND £2027 |
| Study (first author, year, reference number) | Country | Intervention | Population | Costs used | Quality-of-life measure | Outcome measure | Model time horizon | Results |
|---|---|---|---|---|---|---|---|---|
| Hewitt, 200945 | England | Screening for PND (EPDS and BDI) | All postnatal women | Cost of screening; cost of treating PND | Moderate PND | ICER, incremental costs and incremental QALYs | 1 year | EPDS (cut-off score of 6) ICER £41,103 per QALY. The ICER for other strategies ranged from £23,195 to £814,623 |
| Stevenson, 2010392 | England | Group CBT for women with PND | Women with PND | Cost of group CBT | SF-6D (mapped from EPDS) | Mean cost per QALY | 1 year | Mean cost per QALY of £46,462 (£36,062 PSA) |
| Campbell, 200856 | New Zealand | Screening for PND (three-question questionnaire) | All postnatal women | Cost of screening; cost of treating PND | Revicki and Wood general depression values | ICER, incremental costs, incremental QALYs, incremental PND cases detected, incremental PND cases resolved | 1 year | ICER NZ$3461 per QALY, NZ$287 per additional case of PND detected, NZ$400 per additional case of PND resolved |
Population considered in the health economics review
The population under consideration differed between studies. Two of the studies evaluating treatment interventions included only women diagnosed with PND. 392,399 The other two studies that evaluatied the incremental cost of PND included women regarded as having PND400 and women at risk of PND. 51 In the Dagher et al. 400 study, women were regarded as having PND if they scored 13 or more on the EPDS at 5 weeks postpartum. The Petrou et al. 174 study included high-risk women identified antenatally at 26–28 weeks’ gestation using the Cooper predictive index,401 including both psychological and social risk factors. Women were diagnosed with PND using the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders-Third Edition Revised diagnoses at 8 weeks, 18 weeks, 12 months and 18 months postpartum. The population in the screening papers45,56 was all postnatal women. For the papers broadly evaluating the prevention of PND, the population differed with some studies including all postnatal women61,199,264,397 and three studies evaluating women who had been identified as at increased risk of developing PND. 61,174,396
The methods used to identify higher-risk women also varied between studies. The Dukhovny et al. 396 and Morrell et al. 61 studies both used the EPDS but at different cut-off points (score greater than 9 and score greater than 11, respectively) and at different time points (24–48 hours after hospital discharge and at 6 weeks postnatally, respectively). Both the 2002 and the 2006 Petrou et al. papers53,174 identified women antenatally at 26–28 weeks’ gestation using the Cooper predictive index. 401
Interventions in the health economics review
Of the 13 included papers:
-
Six were broadly concerned with the prevention of PND. 61,174,199,264,396,397
-
Four evaluated different strategies for treating PND53,392,399,400 and, of these four, two were concerned with the additional cost of treating PND. 53,400
-
One focused on the impact on health visitors’ time before and after they were given training in cognitive–behavioural counselling. 398
The health impact of the intervention on PND was measured in 10 of the studies;45,56,61,174,199,264,392–394,399 the measure used differed between studies and included the number of cases of, or duration of PND and the EPDS scores. The Appleby et al. 398 study did not report the impact of the intervention on PND, as it was focused on the impact on health visitors and their time spent per depressed woman. The Petrou et al. 53 study and the Dagher et al. 400 study did not contain an intervention, as they were focused on the incremental cost of treating PND in a high-risk population and among employed women, respectively.
Health-related quality-of-life data in the health economics review
Seven of the papers used a measure of health-related quality of life. 45,56,61,199,392,397,400 Five of these papers used a generic measure,61,199,392,397,400 whereas the other two used a patient-generated utility value. 45,56 Of those that used a generic measure, two used the SF-6D,61,392 two used the SF-36199,397 and one used the SF-12. 400 The SF-36 and SF-12 cannot be used in their basic form to estimate quality-adjusted life-year (QALY) values but can be converted into the SF-6D, which provides values that can be used to estimate QALY values for use in an economic decision model. Only the mean and SD were reported for the SF-12 PCS and MCS at 5 postnatal weeks. 400
The remaining two papers45,401 used patient-generated utility values from a study by Revicki and Wood,402 in which patients diagnosed with depression valued hypothetical depression-related states using a standard gamble approach. From this study,402 Hewitt et al. 45 used the value given for moderate depression and applied this to women suffering with PND in their decision model. In contrast, Campbell et al. 56 used values for severe symptoms, mild or moderate symptoms, subthreshold symptoms, drug and psychological treatment response, and response without drug-associated disutility for different health states within their model. There are several issues with using the utility values from the Campbell et al. 56 study. First, the health state valued was a general depression health state and not a specific PND health state. Second, the sample size reported of 70 patients was relatively small and made up of patients suffering with depression and not specifically PND. Third, the health-state values were estimated using a patient population, although the preferred approach is to use a general population sample to value health states. 403
The PoNDER trial61 collected SF-6D data, using the UK tariff, at a baseline of 6 weeks and then at 6, 12 and 18 months postnatally, and these scores were used in the economic evaluation to calculate QALYs. The PoNDER trial61 also collected data on the EPDS at the same time points. The paired data on the change in SF-6D and EPDS scores were used by Stevenson et al. 392 to map change in EPDS to change in SF-6D which was then used in the decision model. 392
Comparison between the QALY estimates used in the three papers is not possible because of the way they were calculated and presented. Hewitt et al. 45 and Campbell et al. 56 used utility values from the Revicki and Wood study. 402 Hewitt et al. 45 used values of 0.63 for women with PND and 0.86 for women without PND and Campbell et al. 56 used values of 0.30 for severe symptoms, 0.63 for mild or moderate symptoms, 0.80 for subthreshold symptoms and response with drug and psychological treatment and 0.86 for response without drug-associated disutility. Whereas Morrell et al. 61 presented the mean difference in QALY values at 6 months for women in the control and intervention groups, Stevenson et al. 392 presented the mean QALY gain.
Costs and health-care resources reported in the health economics review
All included studies reported health-service use for interventions evaluating the prevention or treatment of PND. The nine economic evaluations alongside trials and the one cost study all reported costs associated with the resource use reported during the trials or study, whereas the decision models used estimates from the literature and expert opinion. Costs were inflated using the hospital and community health services index for studies based in England. 404 Canadian costs were inflated using the Canadian Consumer Price Index, health and personal care index,405 US costs were inflated using the medical care Consumer Price Index,406 Australian costs were inflated using the Australian Total Health Price Index407 and the New Zealand costs were inflated using the average of the US and English indexes. The costs used in the economic evaluations identified in the literature review are presented in Table 58.
| First author, year, reference number | Resource use recorded in study | Category of cost | Cost | Base year | Inflated cost (2012/13) | Perspective |
|---|---|---|---|---|---|---|
| Appleby, 2003398 | Health visitor time, pre-training | Per woman | £81 | 1998 | £135 | Health-care system (NHS) perspective – health visitor time |
| Per depressed woman | £116 | £193 | ||||
| Per treated woman | £107 | £178 | ||||
| Health visitor time, post-training | Per woman | £79 | £132 | |||
| Per depressed woman | £108 | £180 | ||||
| Per treated woman | £109 | £182 | ||||
| Boath, 2003399 | Mean cost PBDU patient | PBDU cost | £991 | 1992/3 | £1905 | Health-care system (NHS) and wider societal costs perspective – health-care resource use. Mother and infant costs included |
| GP and health visitor | £203 | £390 | ||||
| Secondary care | £0 | £0 | ||||
| Cost to client | £302 | £581 | ||||
| Medication | £44 | £85 | ||||
| Total | £1540 | £2960 | ||||
| Total excluding cost to client | £1238 | £2380 | ||||
| Mean cost per routine primary care patient | PBDU cost | £0 | 1992/3 | £0 | ||
| GP and health visitor | £266 | £511 | ||||
| Secondary care | £309 | £594 | ||||
| Cost to client | £25 | £48 | ||||
| Medication | £32 | £62 | ||||
| Total | £632 | £1215 | ||||
| Total excluding cost to client | £607 | £1167 | ||||
| Dagher, 2012400 | Mean cost per woman with PND | Emergency department visits | US$84 | 2001 | US$131 | Health-care system perspective (USA) – health-care resource use. Unclear if infant costs included |
| Inpatient hospital stays | US$607 | US$949 | ||||
| Outpatient surgeries | US$93 | US$145 | ||||
| Physician’s office/urgent care centre visits | US$124 | US$194 | ||||
| Mental health counselling | US$138 | US$216 | ||||
| Total | US$1046 | US$1636 | ||||
| £984a | ||||||
| Mean cost per woman without PND | Emergency department visits | US$13 | 2001 | US$20 | ||
| Inpatient hospital stays | US$80 | US$125 | ||||
| Outpatient surgeries | US$138 | US$216 | ||||
| MD office/urgent care centre visits | US$12 | US$189 | ||||
| Mental health counselling | US$13 | US$20 | ||||
| Total | US$365 | US$571 | ||||
| £343a | ||||||
| Dukhovny, 2013396 | Telephone-based peer support group | Public health costs | CA$667 | 2011 | CA$674 | Health-care system and wider societal costs perspective (Canada) – health-care resource use and wider costs included. Mother and infant costs included |
| Volunteer opportunity costs | CA$126 | CA$127 | ||||
| Hired housework | CA$234 | CA$236 | ||||
| Hired child care | CA$194 | CA$196 | ||||
| Family/friend and partner time of work | CA$2374 | CA$2398 | ||||
| Health-care utilisation total | CA$901 | CA$910 | ||||
| Nursing visits | CA$252 | CA$255 | ||||
| Provider visits | CA$371 | CA$375 | ||||
| Mental health visits | CA$43 | CA$43 | ||||
| Inpatient admissions total | CA$227 | CA$229 | ||||
| Mother | CA$42 | CA$42 | ||||
| Infant | CA$185 | CA$187 | ||||
| Ambulance | CA$8 | CA$8 | ||||
| Total | CA$4497 | CA$4543 | ||||
| £2474a | ||||||
| Routine primary care | Public health costs | NA | 2011 | NA | ||
| Volunteer opportunity costs | NA | NA | ||||
| Hired housework | CA$180 | CA$182 | ||||
| Hired child care | CA$137 | CA$138 | ||||
| Family/friend and partner time of work | CA$1983 | CA$2003 | ||||
| Health-care utilisation total | CA$1080 | CA$1091 | ||||
| Nursing visits | CA$256 | CA$259 | ||||
| Provider visits | CA$373 | CA$377 | ||||
| Mental health visits | CA$57 | CA$58 | ||||
| Inpatient admissions total | CA$389 | CA$393 | ||||
| Mother | CA$73 | CA$74 | ||||
| Infant | CA$316 | CA$319 | ||||
| Ambulance | CA$6 | CA$6 | ||||
| Total | CA$3380 | CA$3415 | ||||
| £1860a | ||||||
| Gold, 2007397 | Cost of the intervention | Rural, cost per woman | AU$172 | 2002 | £127a | Cost of the intervention and health-care resource use (Australia) |
| Urban, cost per woman | AU$129 | £95a | ||||
| Rural, cost per area | AU$272,490 | £200,959a | ||||
| Urban, cost per area | AU$313,900 | £231,499a | ||||
| MacArthur, 2003264 | Control group | Total costs | £542 | 1998 | £902 | Health-care system (NHS) perspective – health-care resource use. Infant costs not included |
| Postnatal care cost | £126 | £209 | ||||
| Intervention group | Total costs | £470 | £783 | |||
| Postnatal care costs | £190 | £317 | ||||
| Morrell, 2000199 | Cost of intervention, additional support worker visits | – | £160 | 1996 | £279 | Health-care system (NHS) perspective – cost of the intervention and health-care resource use. Mother and infant costs included |
| Total resources, intervention (6 months) | – | £815 | £1420 | |||
| Total resources, control (6 months) | – | £639 | £1113 | |||
| Morrell, 200961 | Total resources used, all women (6 months) | Control | £272 | 2003/4 | £350 | Health-care system (NHS) perspective – health-care resource use. Mother and infant costs included |
| CBA | £253 | £326 | ||||
| PCA | £250 | £322 | ||||
| Total resources used, at-risk women (12 months) | Control | £374 | £481 | |||
| CBA | £329 | £423 | ||||
| PCA | £353 | £454 | ||||
| Petrou, 2006174 | Cost of additional health visitor visits | – | £121 | 2000 | £185 | Health-care system (NHS) perspective – health-care resource use. Mother and infant costs included |
| Petrou, 200253 | Total resources used, women with PND | – | £2419 | 2000 | £3710 | Health-care system (NHS) perspective – health-care resource use. Mother and infant costs included |
| Total resources used, women without PND | – | £2027 | £3109 | |||
| Hewitt, 200945 | Cost of intervention | EPDS (5 minutes health visitor time) | £8 | 2006/7 | £9 | Health-care system (NHS) perspective – cost of screening and treatment |
| BDI (5 minutes health visitor time and license fee) | £9 | £10 | ||||
| Cost of treatment of PND | Structured psychological therapy | £447 | £517 | |||
| Supportive care | £414 | £479 | ||||
| Stevenson, 2010392 | Group CBT: One session per week for 8 weeks, 2-hour long, groups of four to six women | – | £1500 | 2007/8 | £1687 | Health-care system (NHS) perspective – cost of intervention/treatment |
| Campbell, 200856 | Psychological therapy (IPT- or CBT-based intervention): eight sessions (50 minutes each), provided by a clinical psychologist | – | NZ$268 | 2006/7 | NZ$318 | Health-care system perspective (New Zealand) – cost of screening and treatment |
| £166a | ||||||
| Social support: three group sessions (five women) and three telephone contacts by a qualified counsellor (30 minutes each) | – | NZ$59 | NZ$70 | |||
| £37a | ||||||
| Combination therapy: 16 sessions (50 minutes each) of psychological therapy by a clinical psychologist and 12 weeks’ antidepressant therapy | – | NZ$561 | NZ$666 | |||
| £347a |
In their economic decision model, Hewitt et al. 45 included costs for screening using the EPDS and BDI based on 5 minutes of health visitors’ time plus the licence fee for the BDI screening tool. The costs of treatment of PND were based on NICE clinical guidelines for the treatment of PND and were costed using relevant NHS reference costs. The cost for an undiagnosed woman with depression was estimated as one additional GP visit. Stevenson et al. 392 included costs for an intervention group CBT, which were based on resource use reported in a RCT and from expert opinion. 408 Campbell et al. 56 included the cost of screening and the cost of treatment based on unit costs of health staff and prescriptions. Screening was assumed to take 5 minutes using the EPDS and 3 minutes using the brief three PHQ questions. 49 A further 30-minute appointment with a GP was assumed for all women who screened positive. Half of the women who were severely depressed and did not respond to treatment were assumed to have 1 day of inpatient care in hospital and a further GP appointment. Treatment costs were adjusted for non-compliance, with 10% of the total treatment costs applied to these women.
For their economic evaluations alongside trials, Petrou et al. 53 estimated the health-care resources used from delivery to 18 months by the population of high-risk women and differentiated between those who developed PND and those who did not. Women diagnosed with PND had higher overall resource use, a reported difference of £392, which inflated at 2012/3 prices increased to £601. 404 Part of the Petrou et al. 53 2002 sample included women who were taking part in the Petrou et al. 174 2006 RCT. The report of 2006 trial174 described resource use for the intervention group, additional health visitor visits, and the control group, routine primary care, and not for women who developed PND and those that did not. Mother and infant costs were included in both studies.
A broader perspective was taken in the Dukhovny et al. 396 study, which included both health-care and non-health-care costs. For the intervention, the public health cost and the opportunity cost of the volunteers’ time was included. Costs for the intervention group and the usual-care group were reported at 12 weeks. These included health-care costs as well as costs for hired housework, hired child care and family/friend and partner time off work. Mother and infant costs were included.
The 2009 Morrell et al. 61 paper collected health-care resource use for women in their trial. Total resource use estimates were split into control and intervention groups over periods of 6 and 12 months. The primary analysis was carried out using the 6-month data, which included the costs incurred by the mother. A further analysis on the 12-month data was also carried out, which included the costs incurred by the mother and also the baby. The total resource use was further split into an analysis of at-risk women and an analysis of all women and additionally split between the two intervention approaches of CBA and PCA. The study also collected data on the additional training that would be required for health visitors to be able to provide the psychologically informed intervention sessions and estimated that the additional training would increase the health visitors’ cost per hour of client time by £2, from £77 to £79.
The Morrell et al. 199 paper reported the cost of the intervention under study (additional care by trained community postnatal support workers) and the total health-care resources used by the intervention and control groups. Total health-care resource use was reported at 6 weeks and 6 months. Mother and infant costs were included.
MacArthur et al. 264 collected total health-care resources used for the intervention and control groups in three matrices (presented in Table 59). A subset of the total health-care resources, referred to as postnatal care costs, was also presented. These costs included the standard community services offered to postnatal women including midwife home visits, GP home visits and the postnatal check. For all matrices, total costs were lower in the intervention group than in the control group, while postnatal care costs were higher in the intervention group than in the control group for matrices A and B and lower for matrix C. Costs for matrix A were estimated based on crude data from midwives’ diaries and GPs’ records. A further analysis was conducted that included replacement data from women’s health diaries when estimates from midwives were unavailable (matrix B). Using this approach the total costs for the control group decreased from £542 to £479, whereas the cost of postnatal care increased slightly from £126 to £134. A third analysis using the women’s health diaries to estimate the frequency of midwives’ and GP appointments was undertaken (matrix C). Using this approach the total costs decreased compared with matrix A to £509 and the costs of postnatal care also increased compared with both matrices A and B to £161. The total cost for the intervention group also fell, from £470 to £457, and the costs for postnatal care decreased from £190 to £152 (see Table 66). As the intervention was not intended to impact on health visitors, health visitor costs were not included in the total resource use. Costs incurred by the babies were also not included.
| Matrix | Category of cost | Mean of cluster means | |
|---|---|---|---|
| Control (£) | Intervention (£) | ||
| Matrix A | Total costs | 542 | 470 |
| Postnatal care costs | 126 | 190 | |
| Matrix B | Total costs | 479 | 469 |
| Postnatal care costs | 134 | 190 | |
| Matrix C | Total costs | 509 | 457 |
| Postnatal care costs | 161 | 152 | |
Boath et al. 399 reported the median and mean of total cost for women receiving treatment in a specialised psychiatric parent and baby day unit and for women receiving routine primary care. Costs to the mother and baby were included in the analysis.
Appleby et al. 398 concentrated on what the impact of additional training would be in terms of the amount of time health visitors spent with the women under their care. The amount of time spent with each woman, depressed woman and treated woman before and after the training on cognitive–behavioural counselling, was recorded and costed using the 1998 Unit Costs of Health and Social Care. 409 Further details on the definition of depressed or treated women were not provided.
The Dagher et al. 400 study estimated the extra health-care resources used by women with PND compared with those used by women without PND. Health-care use was estimated using self-reported data from the women themselves. The data on health-care use were then costed using 2001 unit prices of services provided by the Blue Cross Shield of Minnesota. The incremental cost for women with PND compared with women without PND was US$1065. Converted to British pounds using exchange rates correct as of March 2014, this is equivalent to a difference of £641. It is not clear whether or not this included the health-care costs of the infant as well as the mother.
Gold et al. 397 evaluated the economic side of the PRISM (Program of Resources, Information and Support for Mothers) trial. The PRISM trial evaluated primary care and community-based strategies to improve the physical and mental health of new mothers. Costs were collected in relation to the intervention and health-care resource use in the intervention and control areas. No significant differences were found in health-care resource use between the areas. The cost of the intervention was estimated in Australian dollars at AU$272,490 in rural communities and AU$313,900 in urban areas. Inflated from 2002 prices to 2012/13 prices using the Australian Total Health Price Index407 and converted to British pounds using exchanges rates correct as of July 2014, which resulted in costs of £200,959 and £231,499, respectively. The average cost per woman was AU$172.40 for rural areas and AU$128.70 for urban areas which resulted in a cost of £127 and £95, respectively, when inflated and converted.
The differences in the population, intervention, and objective for each study make a comparison of the different costs across the papers difficult. However, as a number of papers report costs of treatment, a speculative comparison could be made. Boath et al. 399 at 6 months reported the highest cost for those undergoing treatment in the parent and baby day unit at £2380 and a lower cost for those undergoing routine primary care at £1167. Stevenson et al. 392 estimated the cost of treating PND with group CBT-based intervention as £1687, but did not include any additional GP appointments or secondary care that a woman with PND may have received. Hewitt et al. 45 estimated the total cost of standard care for women with PND as £996. This is lower than the best comparator for the cost of routine primary care reported by Boath et al. 399 Petrou et al. 53 found a difference of £601 in health-care resources used between high-risk women with PND and high-risk women without PND. This is the lowest of all the estimates of the PND treatment studies, possibly because the control group comprised high-risk women rather than a universal population of all women and, therefore, it estimated the additional cost of treating PND in a high-risk population. The difference between the resource use of women with PND and the resource use of non-high-risk women may have been greater. Based on these figures, £1000 would be a reasonable estimate for the cost of routine care for women with PND.
In the studies not based in England, with costs converted to British pounds, Dagher et al. 400 estimated the incremental cost as £641. This is similar to that found in the Petrou et al. 53 study, but lower than other England-based estimates. This could be because of differences in the health-care systems of the two countries. It could also be as a result of the way health-care resource use was recorded. Dagher et al. 400 relied on self-reported estimates of health-care use from the women in the study and used a recall period of up to 3 months, whereas Boath et al. 399 used women’s case notes, Stevenson et al. 392 used cost estimates from a RCT and Hewitt et al. 45 costed out treatment guidelines.
Main results reported in the health economics review
The outcomes and time horizons evaluated varied between the studies. For the economic evaluations alongside trials, outcomes were evaluated at various time points between 12 weeks and 24 months. Both decision models used a time horizon of 1 year. Four papers reported costs only. 53,397,398,400 Appleby et al. 398 found that giving health visitors training in cognitive–behavioural counselling was associated with a statistically non-significant decrease in mean costs incurred by health visitors. Petrou et al. 53 found a lower mean cost per high-risk woman without PND than per woman with PND in terms of total health-care resources used with a difference of £601 in 2012/3 prices. The Morrell et al. 199 paper found no significant difference between NHS resource used in the intervention and control groups apart from the cost of the intervention itself. The other economic evaluations264,396 alongside trials used incremental costs against a variety of outcome measures including the number of cases of PND prevented, month of PND avoided174 and incremental cost per successfully treated woman. 399 The Morrell et al. 61 paper reported incremental costs and QALYs and found that psychological interventions dominated the control group, with lower mean costs and a higher mean QALY gain. Dagher et al. 400 reported an incremental cost of US$1065 for women with PND compared with women without PND.
All three decision models reported a cost per QALY and included univariate and multivariate sensitivity analyses. Hewitt et al. 45 found that the incremental cost-effectiveness ratio (ICER) for the screening intervention EPDS (cut-off score of 16) to be £41,103 per QALY. This ranged between £23,195 and £814,623 for different screening strategies compared in the sensitivity analyses. The highest ICER values were found when a low EPDS cut-off value was used. Campbell et al. 56 reported an ICER of NZ$3461, a cost per additional case of PND detected of NZ$287, and a cost per additional case of PND resolved of NZ$400. In the sensitivity analyses the ICER ranged from NZ$2959 to NZ$9607 per QALY. Stevenson et al. 392 reported a mean cost per QALY of £46,462 for group cognitive therapy for women with PND. In the sensitivity analyses, this ranged between £19,230 and £61,948, with the lower value representing a set of values favourable to CBT-based intervention and still believed to be plausible. A probabilistic sensitivity analysis (PSA), an expected value of perfect information analysis (EVPI) and an expected value of partial perfect information (EVPPI) on four variables were also conducted. The results of the PSA reported a mean cost per QALY of £36,062, with the results suggesting that some runs had a cost per QALY of under £30,000. The results of the EVPI and EVPPI estimated a maximum value of £64M to remove all uncertainty with large values for removing uncertainty in the cost treatment variable and the relationship between the EPDS and SF-6D variable.
Summary of appropriateness of previously published models
None of the reviewed models were entirely appropriate for answering the decision problem addressed within this review. Thus, a de novo model was constructed.
The de novo model
The conceptual model
The purpose of the de novo model was to estimate the incremental QALYs and incremental costs of each intervention in the NMA of EPDS scores compared with usual care. From these data, fully incremental analyses could be conducted to establish the most cost-effective intervention and the robustness of these conclusions. The conceptual model used an area under the curve approach to calculate the summation of weekly EPDS scores over a year. Data from the NMA of EPDS values identified five time points: baseline (common to all treatments), 6–8 weeks, 3–4 months, 6–7 months and 1 year. For simplicity, the EPDS score between assessments was approximated by a linear relationship. A further simplification was that deaths were not included in the model; it was believed that this would have little impact on the results given the dearth of information on the effect (if any) of interventions on mortality.
A 1-year time horizon was chosen to align with previous modelling work392 and to acknowledge the fact that PND is assumed to be ‘standard’ depression after 12 months postpartum and that different treatment options may become available to the woman. However, it is implausible that any change in utility would immediately be removed after 12 months and therefore a sensitivity analysis assessed the impact of altering the assumption that all effects were assumed to have dissipated at 12 months. This analysis has the limitation that the duration of residual benefit is uncertain and that other events, such as a subsequent pregnancy, could occur that would limit the generalisability of the results in all women. For the base-case discounting was not applied. For the sensitivity analysis a discount rate of 3.5% was applied to utility in the second year as recommended by NICE. 403
Figure 60 illustrates the approach in which data exist for all time points (which is the case only for usual care), whereas Figure 61 provides an illustrative example when only one data point (in addition to the assumed baseline value) is reported. The summation of EPDS scores for other combinations of numbers and position of reported time points are calculated using the same method. Separate analyses were undertaken for the universal, the selective and the indicated preventive intervention groups and the results will be presented in this order.
FIGURE 60.
An illustrative example of calculating the area under the curve when data for an intervention are available for all time points.

FIGURE 61.
An illustrative example of calculating the area under the curve when data for an intervention are available only at time point 3.

For reasons that will be detailed later, the area under the curve is divided into two constituent parts: until time point 1 (0 to 6–8 week data) and from time point 1 to time point 4 (6–8 weeks to 1 year). In the initial time period, the area under the curve is calculated by the addition of rectangle A to triangle B. In the subsequent time period, the area under the curve is the summation of rectangles C, E and G and of triangles D, F and H.
In this example, in order to differentiate between the EPDS values before time points 0 and 1 and between time points 1 and 4, an estimation of the EPDS value at time point 1 must be made. This estimation assumes a linear progression between time points 0 and 3 (for which data were reported in this illustrative example), with the estimated point depicted by the blue star at time point 1 in Figure 61. In the base case it was assumed that at 1 year (time point 4) the EPDS values would be equal for the intervention and usual care. This is depicted as the light-blue star at time point 4 in Figure 61. In order to assess the impact, where it was assumed that any change in EPDS score would persist beyond 1 year, a sensitivity analysis was undertaken which assumes that the value at time point 4 would be the average between the last reported data point and the usual-care value at time point 4.
Model parameters
The parameters required for the model have been divided into four broad categories:
-
the effectiveness data for each intervention
-
the incremental costs associated with each intervention
-
the relationship between utility and EPDS scores
-
the relationship between total health costs and EPDS scores.
The effectiveness data for each intervention
The data used within the mathematical model were taken directly from the Convergence Diagnostic and Output Analysis (CODA) samples generated from the NMA of EPDS values. This approach has the advantage that correlation between parameters is preserved.
The incremental costs associated with each intervention
The incremental cost was estimated for each intervention for each study included in the NMA of EPDS scores. The incremental cost was assumed to be the additional costs associated with the intervention above usual care costs. When more than one study was used to inform the effectiveness of an intervention, for example both Norman et al. 123 and Songøygard et al. 129 were used for the exercise intervention in the universal population, the average cost from the two studies was taken. This simplistic approach was deemed reasonable because of the assumed between-study heterogeneity values used in the NMAs which would provide similar weightings for each study in calculating intervention efficacy.
The size of groups for the group interventions was based on information provided in the studies when available and advice from clinical experts otherwise. The group size was assumed to be 12 for exercise-based intervention groups, eight for CBT group-based interventions and six for antenatal group interventions. The total cost for group interventions was based on the length and number of group sessions multiplied by the staff costs and then divided by the number in the group to give a cost per woman. When the length of appointment or session was not specified in the study, it was assumed to be 2 hours for antenatal group sessions and 1 hour for CBT-based interventions or IPT interventions. For both calcium and selenium, the intervention cost is assumed to be the drug cost only, with no additional tests assumed to be required because of the prescribing of these supplements. For educational information that is given out or posted to recipients, we assumed a cost of £1 per booklet or educational information to cover the costs of postage and printing and accompanying staff costs.
Some studies included an economic evaluation. Although these studies included a difference in total cost of health-care resource use for the intervention compared with the control, the absolute cost of the intervention was used. This was done for consistency with the costing approach applied to the other interventions in which an economic evaluation had not been carried out. In one case, the analysis by Morrell et al. 61 of all women, the only change in total resource use was presented for the costs of CBT and PCA. For this reason, change in total resource use has been used, which results in a negative cost for the intervention. In the case of at-risk women, Morrell et al. 61 presented change in health visitor costs and change in total resource used. As the intervention focused on health visitors, the change in health visitor costs was used to cost the intervention. In the CBT group the intervention resulted in fewer health visitor visits and, therefore, a negative cost for the intervention was applied.
A NHS and personal social services perspective was taken. This meant that only costs that would fall on the NHS or personal social services in full were included in the costing of the interventions. Other costs, such as volunteer opportunity costs and loss of earnings, were excluded.
Staff costs were taken from the 2013 Unit Costs of Health and Social Care404 and are outlined in Table 60. The cost per hour of client contact with qualifications was used when available. A cost per hour was available for all staff roles, apart from GP costs (with or without qualifications). For some staff roles, for example clinical psychologist, health visitor, community nurse and social worker, both a unit cost per hour and a cost per hour of client contact were available. The average difference between the unit cost per hour and the rate per hour of client contact (+182%), was applied to those staff roles for which only a cost per hour was available. However, the rates for social workers were excluded from the calculation of average difference, as the difference value was deemed to be an outlier, being an increase of 383%. When both community and hospital costs were provided for a staff role, the average of the two was used. In addition to those costs presented in Table 60, a mean cost of face-to-face contact was used for health visitors at £47 and for a GP appointment lasting 11.7 minutes at £41.
| Role | Unit cost per hour (£) | Per hour of client contact, including qualification, costs (£) |
|---|---|---|
| Physiotherapist (average community and hospital) | 35.00 | 63.62b |
| Occupational therapist (average community and hospital) | 35.00 | 63.62b |
| Community clinical psychologist | 59.00 | 159.00a |
| Health visitor | 49.00 | 71.00 |
| Midwife (community nurse) | 48.00 | 70.00 |
| Clinical support worker nursing (community)a | 21.00 | 30.00b |
| CBT-based interventiona | 50.00 | 99.00 |
| Hospital dietitian | 35.00 | 63.62b |
| Speech and language therapist (average community and hospital) | 35.00 | 63.62b |
| GP per patient contact lasting 11.7 minutes | – | – |
| GP out of office per hour | – | 267.00 |
| Social worker (children’s services) | 57.00 | 218.00 |
The 2013 Unit Costs of Health and Social Care404 did not include costs for midwives. From the economic evaluations that had included the cost of midwives, two had used local costs61,174 and one had used the cost of a district nurse. 264 The second approach was followed and the cost for a community nurse was used as a substitute for the cost of a midwife.
For CBT-based interventions and IPT-based interventions, when it was not specified in the study who delivered the content or when the content was delivered by psychology students, the reported cost of CBT-based interventions in the 2013 Unit Costs of Health and Social Care404 was used. When it was specified that a clinical psychologist had given the intervention, the cost of a clinical psychologist was used. 404 Any additional costs of training have not been included in the staff costs unless the additional cost was specified in the study. 61
The costs of each intervention are detailed separately for the three populations.
The costs associated with interventions for the universal preventive interventions
For the universal preventive interventions, a number of assumptions were made for specific interventions. A general description of the interventions is given in Table 61.
| Type of intervention | Study | Intervention | Cost (£) | Source reference |
|---|---|---|---|---|
| Educational information | Norman, 2010123 | Education group received written education material every week for 8 weeks through the post | 8.00 | – |
| Exercise | Norman, 2010123 | 8-week programme of 1 hour of group physical therapy exercises given by a physical therapist and a 30-minute education session delivered by health-care professionals each week | 67.86 | PSSRU404 |
| Songøygard, 2012129 | 12-week programme of 1-hour group sessions led by physiotherapists | 63.62 | PSSRU404 | |
| Average cost | 65.74 | – | ||
| Selenium | Mokhber, 2011212 | 100 µg of selenium per day until delivery taken for approximately 6 months | 149.85 | BNF410 |
| Booklet on PND | Sealy, 2009186 | Posted an educational pamphlet at 4 weeks postnatal | 1.00 | – |
| Midwifery redesigned postnatal carea | MacArthur, 2003264 | Changes to postnatal care to systematic identification and management of women’s health problems, led by midwives with GP contact only when required | 107.64 | MacArthur et al.264 |
| Baby play | Matthey, 2004184 | One additional session ‘baby play’ and additional mail-outs (one antenatal and one postnatal); the extra session run by a clinical psychologist (author) and either a female social worker or occupational therapist | 101.94 | PSSRU404 |
| Education on preparing for parenting | Matthey, 2004184 | One additional session which focused on postpartum psychosocial issues and additional mail-outs (one antenatal and one postnatal); the extra session run by a clinical psychologist (author) and either a female social worker or occupational therapist | 101.94 | PSSRU404 |
| PCA-basedb intervention | Morrell, 2009;61 all women | Psychologically informed interventions by health visitors | –28.00 | Morrell et al.61 |
| CBT-basedb intervention | Morrell, 2009;61 all women | Psychologically informed interventions by health visitors | –24.00 | Morrell et al.61 |
| Early contact | Gunn, 1998225 | Changing the 6-week GP appointment to a 1-week appointment (assumes all women still have 6-week appointment in addition) | 41.00 | PSSRU404 |
| Calcium | Harrison-Hohner, 2001208 | Women prescribed 1000 mg of calcium twice a day between 11 and 21 weeks’ gestation until birth | 78.96 | BNF410 |
| Midwife-managed care | Shields, 1997219 | Midwife-managed care – seen by same named midwife (or team) through pregnancy, birth and postnatal period | 0.00 | – |
| Primary care and community care strategies | Lumley, 2006147 | Education and training programmes for GPs and MCHNs. 10 hours of workshops, simulated patients, two clinical practice audits and evidence-based guidelines for GPs. A similar education programme provided for MCHNs with 12 hours training (year 1) and 3 hours (year 2). Information kit for mothers, appointment of full-time community development officer | 94.79 | Gold et al.397 |
| Social supporta | Morrell, 2000199 | Additional support worker visits | 279.00 | Morrell et al.199 |
Norman et al. 123 included an education session for the intervention group as well as the exercise sessions. The education session were given by physiotherapists, dietitians, speech pathologists, health psychologists and midwives. We have assumed that four out of the eight sessions were given by physiotherapists and the other professions gave one session each. For Matthey et al. ,184 the baby play intervention and the education on preparing for parenting were both delivered by a clinical psychologist and either a social worker or occupational therapist. For simplicity, the average cost of a social worker and occupational therapist was used in addition to the clinical psychologist cost. The Gunn et al. 225 study specified that the 6-week GP appointment was changed to a 1-week appointment. However, women could still have the 6-week appointment if required. In costing the intervention, a conservative approach was taken and it was assumed that all women would have an additional GP appointment.
In the case of the two studies looking at the effect of supplements,208,212 the costs of the supplements were taken from the British National Formulary. 410 In the Mokhber et al. 212 study, women took 100 µg of selenium per day for 6 months. A 10-ml bottle contained 500 µg of selenium and, therefore, 37 full bottles were required for the 6-month period. Horrison-Hohner et al. 208 specified that the 2000 mg of calcium per day was started at between 11 and 21 weeks’ gestation. The assumption was made that the midpoint of 16 weeks would be used and therefore the calcium would be taken for 24 weeks assuming a normal pregnancy duration of 40 weeks. A 60-tablet pack of 1000 mg tablets would last 30 days and a woman would therefore require six whole 60-tablet packs over this period.
No incremental cost was applied to the Shields et al. 219 study for the universal preventive interventions which ensured that each woman saw a named midwife or member of the same team throughout the pregnancy and postnatal.
The following approaches were used for the studies that had an economic evaluation component to the trial. To cost the MacArthur et al. 264 study, postnatal care costs were calculated using the matrix A approach to costing, which uses data from midwives’ diaries and GP records. For the Morrell et al. 61 study, the differences between total costs for PCA-based and CBT-based interventions and the cost of usual care were used because no figures related to the cost of the intervention were given for the all-women group. For the earlier Morrell et al. 199 economic evaluation, the additional cost of the support worker visits given in the paper were used as the cost of the intervention. Costs from all economic evaluations were uplifted to 2012/3 prices using the hospital and community health services. 404
Both MacArthur et al. 264 and Morrell et al. 199 included a change in total health-care costs. For MacArthur et al. ,264 the use of the change in total health-care cost would make the intervention of midwifery redesigned care cost saving. The intervention would go from costing £108 to saving £119 per woman compared with usual care. For Morrell et al. ,199 the use of change in total health care would increase the cost of the intervention of social support from £279 to £307 per woman.
The PRISM trial, evaluated by Lumley et al. ,147 also had an economic evaluation, reported in Gold et al. 397 The cost per woman in urban areas was used to cost the intervention, as it was felt that this would better represent the cost of applying the intervention in England (and Wales) than the rural cost. The cost was uplifted using the Australia Total Health Costs Index and converted to British pounds (£) using an exchange rate of AU$0.55 to £1, which was applicable in July 2014. 411
The costs associated with interventions for the selective preventive interventions
For the selective preventive interventions an additional assumption was made for the Barnes et al. 149 study, which evaluated volunteer home visits. Volunteers were given 12 half days of training. The cost of the training was estimated to be £150 per day per six volunteers. This gave a cost of £150 per volunteer for training and it was assumed that the volunteers would see only one family; the impact of this assumption on the overall results will be discussed in the results section. A general description of the other interventions is given in Table 62.
| Type of intervention | Study | Intervention | Cost (£) | Source of cost information |
|---|---|---|---|---|
| Midwife-led debriefing | Zlotnick, 2011163 | 1-hour session with a trained midwife | 70.00 | Small et al.223 |
| IPT-based intervention | Chabrol, 2002158 | Five individual 1-hour sessions – provided by study interventionists | 495.00 | PSSRU404 |
| CBT-based intervention | Barnes, 2009149 | 1-hour prevention session between 2 and 5 days postnatally given by master level psychology students | 99.00 | PSSRU404 |
| Peer support | Buist, 1999189 | Volunteers 12 half-days of training | 150.00 | PSSRU404 |
| Education on preparing for parenting | Sen, 2006191 | Four additional classes, run by midwives, nurse/psychologist, psychologist | 275.67 | PSSRU404 |
| Zlotnick, 2011163 | One individual visit prenatal and postnatal, five antenatal group sessions lasting 2 hours | 256.67 | PSSRU404 | |
| – | Average cost | 266.17 | – |
The costs associated with interventions for the indicated preventive interventions
For indicated preventive interventions a number of assumptions were made for specific interventions. A general description of the interventions is given in Table 63 and, when needed, more detail is provided.
| Type of intervention | Study | Intervention | Cost (£) | Source of cost information |
|---|---|---|---|---|
| Midwifery continuous care | Marks, 2003224 | Named midwife who as far as possible followed the woman through pregnancy, delivery and postnatally | 0.00 | – |
| Promoting parent–infant interaction | Armstrong, 1999;164 Fraser, 2000252 | Average of 22 home nurse visits over 12 months. A weekly case conference held where child health nurses met with team’s social worker and community paediatrician | 1849.47 | PSSRU404 |
| aPetrou, 2006174 | Additional health visitor visits | 185.00 | Petrou et al.174 | |
| Average cost | 1017.23 | – | ||
| Peer support | aDukhovny, 2013394 | Telephone-based peer support | 366.43 | Dukhovny et al.392 |
| IPT-based intervention | Gorman, 1997169 | Five individual sessions on IPT for depression | 495.00 | PSSRU404 |
| Grote, 2009170 | Engagement session followed by eight acute IPT-brief sessions before birth and maintenance IPT in either biweekly or monthly sessions up to 6 months postnatally | 1831.50 | PSSRU404 | |
| Average cost | 1163.25 | – | ||
| Educational information | Grote, 2009170 | Written materials and encouragement to seek care if needed | 1.00 | – |
| Ginsburg, 2012168 | Eight weekly 30–60 minutes in home (or in office) education sessions delivered by Apache paraprofessional family health educators and three booster sessions | 816.75 | PSSRU404 | |
| Austin, 2008165 | Booklet | 1.00 | – | |
| Average cost | 272.92 | – | ||
| CBT-based intervention | Ginsburg, 2012168 | Eight weekly 30–60 minute in home (or in office sessions) of cognitive–behaviourally based programme delivered by Apache paraprofessional family health educators and three booster sessions | 816.75 | PSSRU404 |
| Austin, 2008165 | CBT-group-based intervention comprised six weekly 2-hour sessions (and a later follow-up session) of CBT delivered by a clinical psychologist and specially trained midwife | 400.75 | PSSRU404 | |
| Munoz, 2007173 | CBT-based intervention: 12-week mood management course, and four booster sessions conducted at approximately 1, 3, 6 and 12 months postpartum. Groups of 3–8 pregnant women | 874.50 | PSSRU404 | |
| aMorrell, 200961 at-risk women | Psychologically informed interventions by health visitors | –35.00 | Morrell et al.61 | |
| Average cost | 514.25 | – | ||
| PCA-based intervention | aMorrell, 200961 at-risk women | Psychologically informed interventions by health visitors | 3.00 | Morrell et al.61 |
For the three studies that had an economic evaluation component, we used the additional health visitor costs from Petrou et al. ,174 the public health costs from Dukhovny et al. 396 and the difference from the control arm in terms of the cost of health visitor contacts from Morrell et al. ,61 for both the CBT and PCA arms of the trial for at-risk women.
These three studies also included change in total health-care costs compared with usual care. 61,174,396 The use of total health-care costs would make PCA cost saving, with a reduction in the cost of the intervention from £3 to –£27 per woman compared with usual care. 61 Data from this trial would also increase the cost saving associated with a CBT-based intervention from £35 to £58. However, the effect on the overall cost of CBT-based interventions would be a reduction from £514 to £509 in the average cost for CBT-based interventions. Using change in total health-care costs would reduce the cost of peer support from £366 to £269. 396 The cost of the promoting parent–infant interactions would fall very slightly for the Petrou et al. 174 study, from £185 to £184, with a minimal impact on the overall cost of promoting parent–infant interaction, with this value remaining at £1017 to the nearest pound.
Marks et al. 224 specified that the intervention was to use existing midwifery resources; therefore, no cost was applied to this intervention. Fraser et al. 252 specified that a weekly case conference was held between the home visit nurse and the team social worker and community paediatrician, although the duration of the meeting was not reported. It was stated that 40% of families were referred to a social worker and that the mean number of visits from the nurse per woman was 22. The study did not specify how long each nurse home visit was; therefore, the mean cost of a face-to-face contact with a health visitor was used to cost this part of the intervention. For costing the case conferences, we assumed 22 meetings between the home visit nurse, social worker and the community paediatrician for each family referred to a social worker. We assumed that the costs of the person who would represent the paediatrician should this intervention be made available in England and Wales would equal that of a GP and assumed that a duration of 10 minutes per meeting per family. In the Ginsburg et al. 168 study, which compared a CBT-based intervention with an education-based intervention, Apache paraprofessional health educators were used to deliver both programmes. The cost of CBT-based intervention was used in the analysis for both interventions, as they were delivered by the same professionals in the study. Unlike the grouping of trials in the universal preventive interventions and selective preventive interventions, the trials grouped as certain types of intervention in the indicated group have a much wider range of individual costs. It is unclear what the effect on the results would be if the groupings were made differently.
The relationship between utility and Edinburgh Postnatal Depression Scale scores
In order to allow a meaningful comparison of the cost-effectiveness of interventions for the prevention of PND with other technologies competing for scarce resources it was necessary to transform the depression-specific measure (the EPDS) into a preference-based single index that can be applied to all diseases. Data were obtained from the PoNDER trial,61 which provided absolute values of EPDS and SF-6D for individuals at three different time points: 6 weeks, 6 months and 1 year. These data are depicted as scatterplots in Figures 62–64.
FIGURE 62.
The relationship between EPDS and SF-6D scores at 6 weeks.

FIGURE 63.
The relationship between EPDS and SF-6D scores at 6 months.
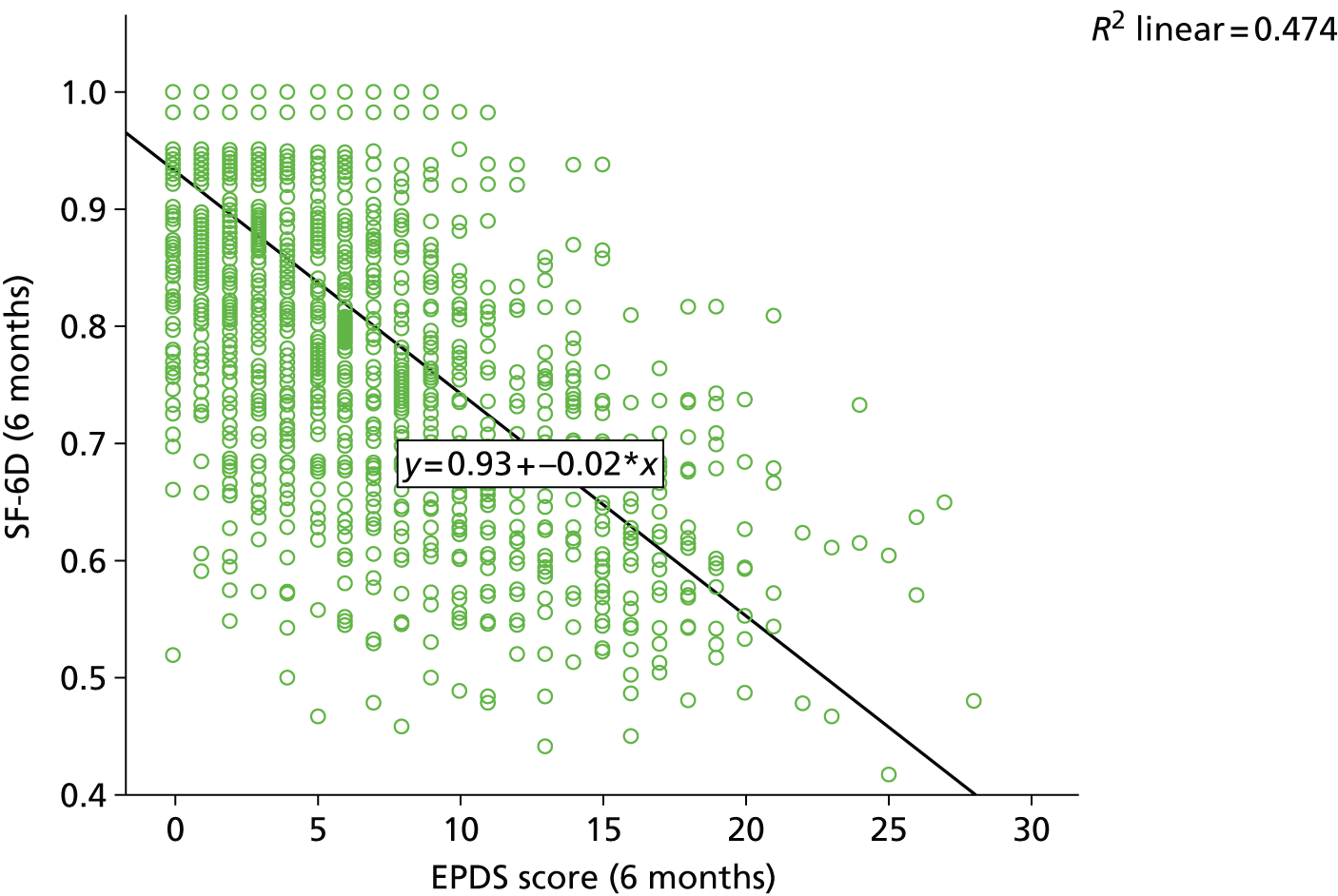
FIGURE 64.
The relationship between EPDS and SF-6D scores at 12 months.
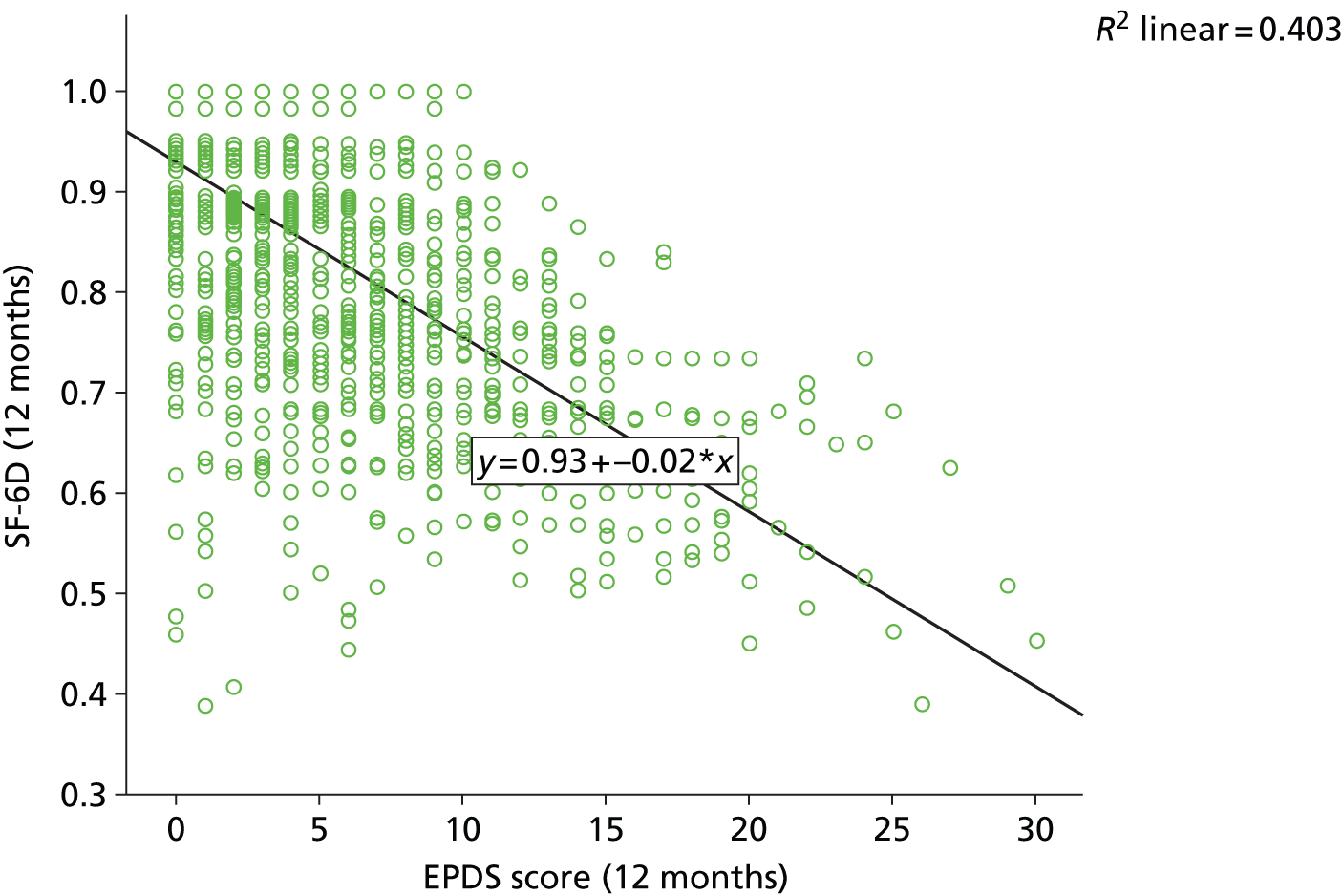
It is seen that there is a moderate relationship between EPDS and SF-6D scores, with an R2 of 0.281, with a prediction that a unit improvement in EPDS score would be associated with a 0.01 improvement in utility.
It is seen that there is a stronger relationship between EPDS and SF-6D scores at 6 months than 6 weeks, with an R2 of 0.474, with a prediction that a unit improvement in EPDS score would be associated with a 0.02 improvement in utility.
It is seen that there is a moderate relationship between EPDS and SF-6D scores at 12 months, with an R2 value of 0.403, with a prediction that a unit improvement in EPDS score would be associated with a 0.02 improvement in utility.
The coefficient of the relationships between EPDS and SF-6D scores appeared to be different for the first 6-week period to that at 6 months and 12 months. Thus, the data for 6 months and 12 months were pooled, with the resulting relationship between EPDS and SF-6D in the combined data set shown in Figure 65.
FIGURE 65.
The relationship between EPDS and SF-6D scores using data at both 6 and 12 months.

When using the combined data for 6 and 12 months, it is seen that there is a moderate relationship between EPDS and SF-6D scores, with an R2 value of 0.448, with a prediction that a 1-point improvement in EPDS scores would be associated with a 0.02-unit improvement in utility. An advantage of combining the data is to reduce the uncertainty in the relationship.
The assumed relationship between EPDS and SF-6D scores used within the model is shown in Table 64. The constant in the regression equation is not considered relevant as this will be applicable to all interventions.
| Time period | Coefficienta | Standard error on the coefficient |
|---|---|---|
| Between baseline and time point 1 | 0.018421 | 0.000312 |
| Between time point 1 and 1 year | 0.009602 | 0.000301 |
The relationship in Table 64 was used to calculate an area under the curve estimate for utility, which was then divided by the number of weeks in a year (52.178) to obtain a QALY value. Subtracting the value of usual care from that of an intervention gave the estimated incremental QALY gain associated with that intervention.
The relationship between total health costs and Edinburgh Postnatal Depression Scale scores
Data were obtained from the PoNDER trial,61 which provided absolute values of EPDS score and total health costs for individuals at three different time points: 6 weeks, 6 months and 1 year. These data are depicted as scatterplots in Figures 66–68.
FIGURE 66.
The relationship between EPDS score and total health costs at 6 weeks.
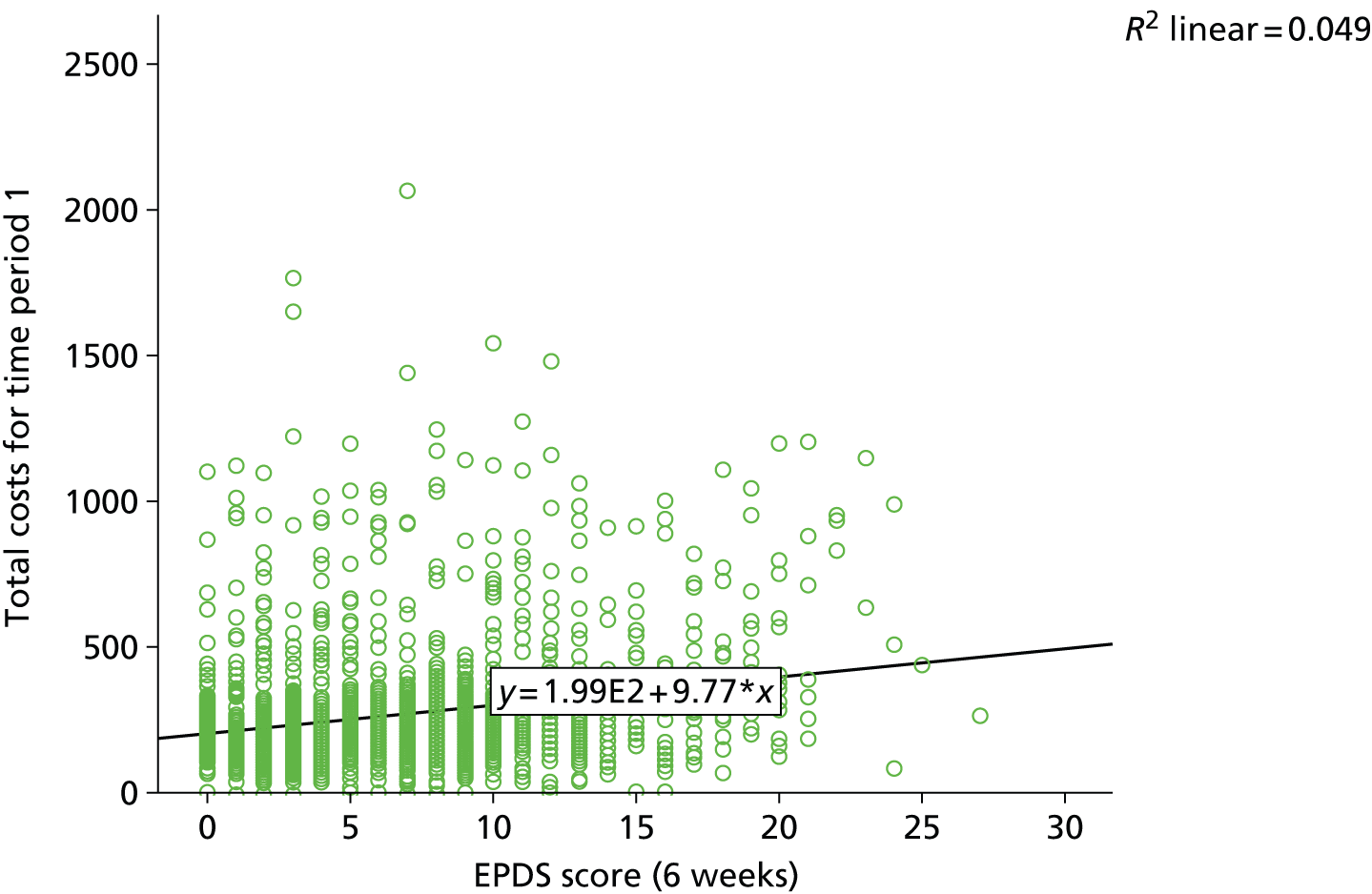
FIGURE 67.
The relationship between EPDS score and total health costs at 6 months.
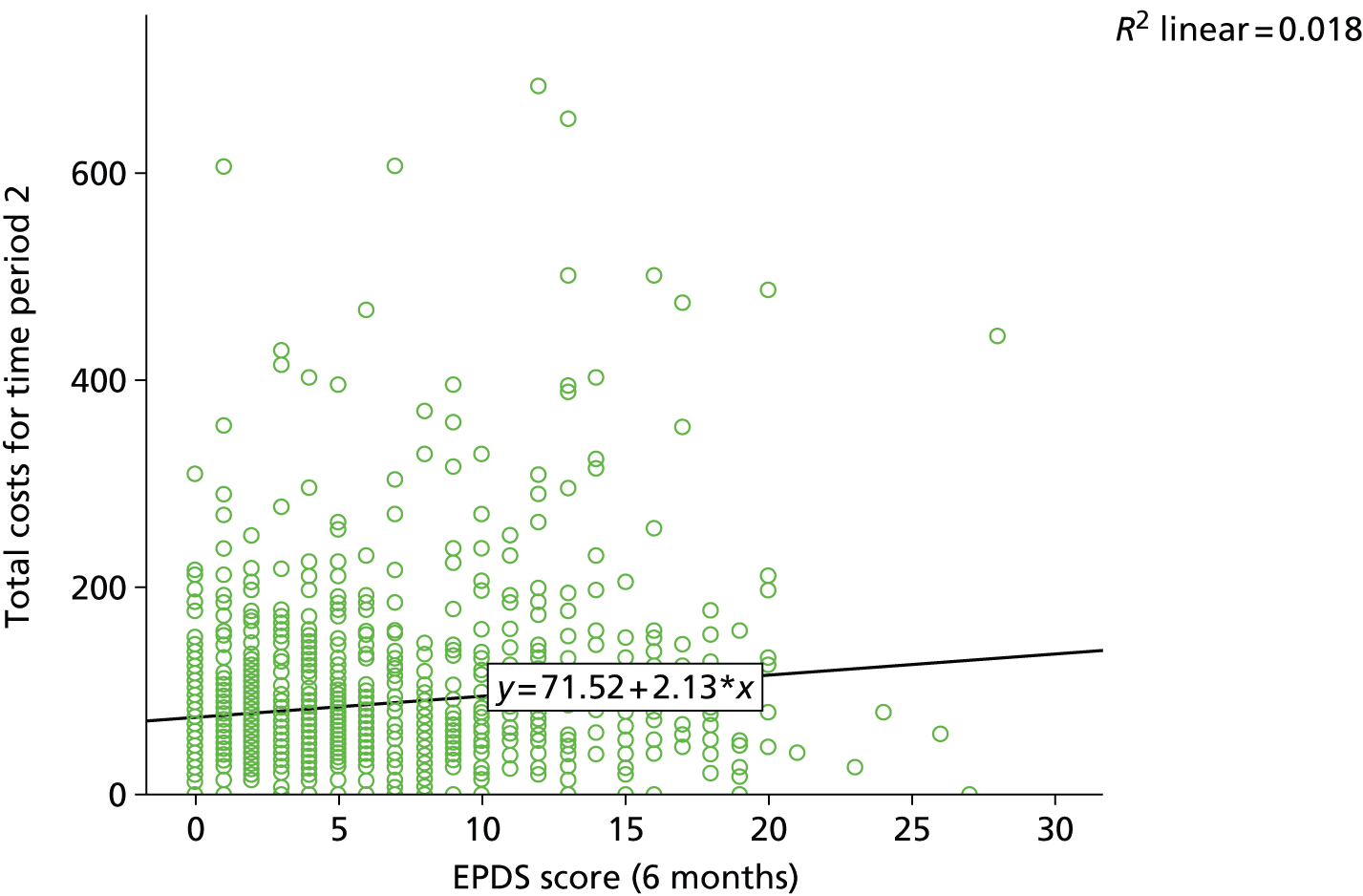
FIGURE 68.
The relationship between EPDS score and total health costs at 12 months.

It is seen that there is a very weak relationship between EPDS score and total health costs at 6 weeks, with an R2 value of 0.049, with a prediction that a 1-unit improvement in EPDS would be associated with a £10 decrease in costs across the 6-week period.
It is seen that there is a very weak relationship between EPDS score and total health costs at 6 months, with an R2 value of 0.018, with a prediction that a 1-unit improvement in EPDS score would be associated with a £2 decrease in costs in the period from 6 weeks to 6 months.
It is seen that there is a very weak relationship between EPDS score and total health costs at 12 months, with an R2 value of 0.020. The regression analysis predicts that a 1-unit improvement in EPDS score would be associated with a £2 decrease in costs across the period from 6 months to 12 months.
Owing to the weak relationship between the EPDS scores and total health-care costs across all time periods and the slight absolute cost impact it was decided not to model a relationship between EPDS scores and total health-care costs.
The analyses undertaken
Probabilistic analyses were undertaken to examine the impact of uncertainty on the results using 1000 probabilistic draws. For effectiveness data, the measures of uncertainty came from the CODA samples provided by the NMA of EPDS values. For the relationship between EPDS and SF-6D, the initial and subsequent time periods coefficients were sampled assuming a normal distribution and using the mean and standard error provided in Table 64. The values between the initial and subsequent period were assumed to be independent.
The probabilistic analyses allowed a graphical display of uncertainty in the form of a cost-effectiveness acceptability curve412 (CEAC), which indicates the probability that an intervention was the most cost-effective. A fully incremental analysis was undertaken to determine the efficiency frontier and the intervention estimated the most cost-effective, assuming a cost per QALY threshold of £20,000, which is a value NICE considers to be appropriate in funding decisions. 401 A further analysis calculated the incremental costs associated with interventions in order that the cost per QALY compared with usual care was £20,000.
In addition, the EVPI413 was estimated. The EVPI provides an indication of the maximum amount a funder would be prepared to pay to remove all uncertainty from the decision. Measures to reduce the uncertainty may take the form of a RCT or may come from other forms of research. The EVPI is calculated directly from the results of the probabilistic analyses by subtracting the net monetary benefit (NMB)414 associated with the strategy perceived to be most cost-effective from the NMB associated with the optimal strategy in each of the PSA configurations, and dividing by the number of PSA runs. The EVPI estimate is then multiplied by the number of women assumed to be affected by the decision over forthcoming years.
The NMB is calculated as incremental QALYs multiplied by the willingness-to-pay threshold (assumed to be £20,000 per QALY in our calculations) minus the incremental costs, and is often compared with a chosen strategy, for example current care. NMB can be compared directly, with the largest value being for the strategy that is most cost-effective.
An example of calculating the EVPI is provided in Table 65, assuming only three PSA iterations and results presented per 100 people. In the example the intervention is more cost-effective, as it has an average NMB of £20,000 [(£50,000 – £30,000 + £40,000)/3] compared with £0 [(£0 + £0 + £0)/3] for current care. However, if the most cost-effective intervention was selected for each PSA run, the average NMB would be £30,000 [(£50,000 +£0 + £40,000)/3] representing an EVPI of £10,000 (£30,000 – £20,000) per 100 people. Should the decision affect 10,000 people the EVPI would be £1,000,000 (10,000 × £10,000/100). If all uncertainty was removed from the model then this would be seen as cost-effective, assuming the £20,000 per QALY threshold, if the cost of removing the uncertainty was less than £1,000,000.
| PSA run | Current care per 100 people (referent), NMB (£) | Intervention per 100 people, NMB (£) | Most cost-effective option per 100 people, NMB (£) |
|---|---|---|---|
| 1 | 0 | 50,000 | 50,000 |
| 2 | 0 | –30,000 | 0 |
| 3 | 0 | 40,000 | 40,000 |
| Average from PSA runs | 0 | 20,000 | 30,000 |
The EVPI can be extended to assess the value of perfect information not for all variables within the model, but for a selected subgroup. This is referred to as the EVPPI. 415
For the analyses conducted within this report two sets of parameters were defined, the first set being the effectiveness parameters (the CODA output from the NMA of EPDS values), and the second set being the relationship between EPDS scores and SF-6D scores. The first group evaluated in the EVPPI analyses assumed that a trial would be commissioned evaluating all interventions for the relevant population. The second group assumed that data were collected for a period of at least 12 months. The EVPPI analyses used the 1000 probabilistic draws for each group, setting each draw to a simulated set of known ‘perfect’ data while maintaining the random variability previously sampled for the remaining EVPPI group. These analyses were performed to assess the relative impact of removing uncertainty in the efficacy of the interventions compared with that of removing uncertainty in the utility mapping.
In order to translate value of information in terms of cost per woman into a societal value, it was assumed that a willingness to pay of £20,000 per QALY was applicable; that the information would be of benefit to women giving birth over a period of 10 years; and that in England and Wales the number of women per year who would benefit from the improved knowledge would be 720,000 in case of the universal preventive interventions, 108,000 in the case of the selective preventive interventions and 72,000 in the case of indicated preventive interventions. The number for the universal preventive interventions was estimated using the average numbers of maternities between 2010 and 2012 reported by the Office for National Statistics416 and rounded to the nearest 10,000. Our clinical experts also estimated that 10% of women would fall in indicated preventive interventions and 15% in the selective preventive interventions. The duration for which the greater knowledge provides benefit to society is uncertain. Although it is arbitrary, 10 years seemed a reasonable period of time to assume that either there were no additional interventions for preventing PND or considerable service reconfiguration would occur. Note that this is different from the duration of benefit assumed for each woman, which remained for a 1-year period.
Results
The estimated quality-adjusted life-year gain compared with usual care for each intervention
The estimated QALY gains per woman for each intervention in the universal preventive interventions, selective preventive interventions and indicated preventive interventions are provided in Figures 69–71. The trials included in each intervention group are fully detailed in Chapter 4. In all analyses the absolute estimated QALY gain in the base case was relatively low and never exceeded 0.026 (equivalent to 10 days of perfect health). In several instances the intervention was shown to be less effective than usual care. In the sensitivity analyses in which it was assumed that the EPDS score associated with an intervention became equal to that of usual care at 2 years, the effect of the intervention was typically larger, as would be expected. However, this was not true for all interventions, as in some time points in some interventions the intervention was estimated to be more effective than usual care, but at other time points usual care was estimated to be more effective.
FIGURE 69.
The estimated incremental QALYs per woman compared with usual care associated with each universal preventive intervention.
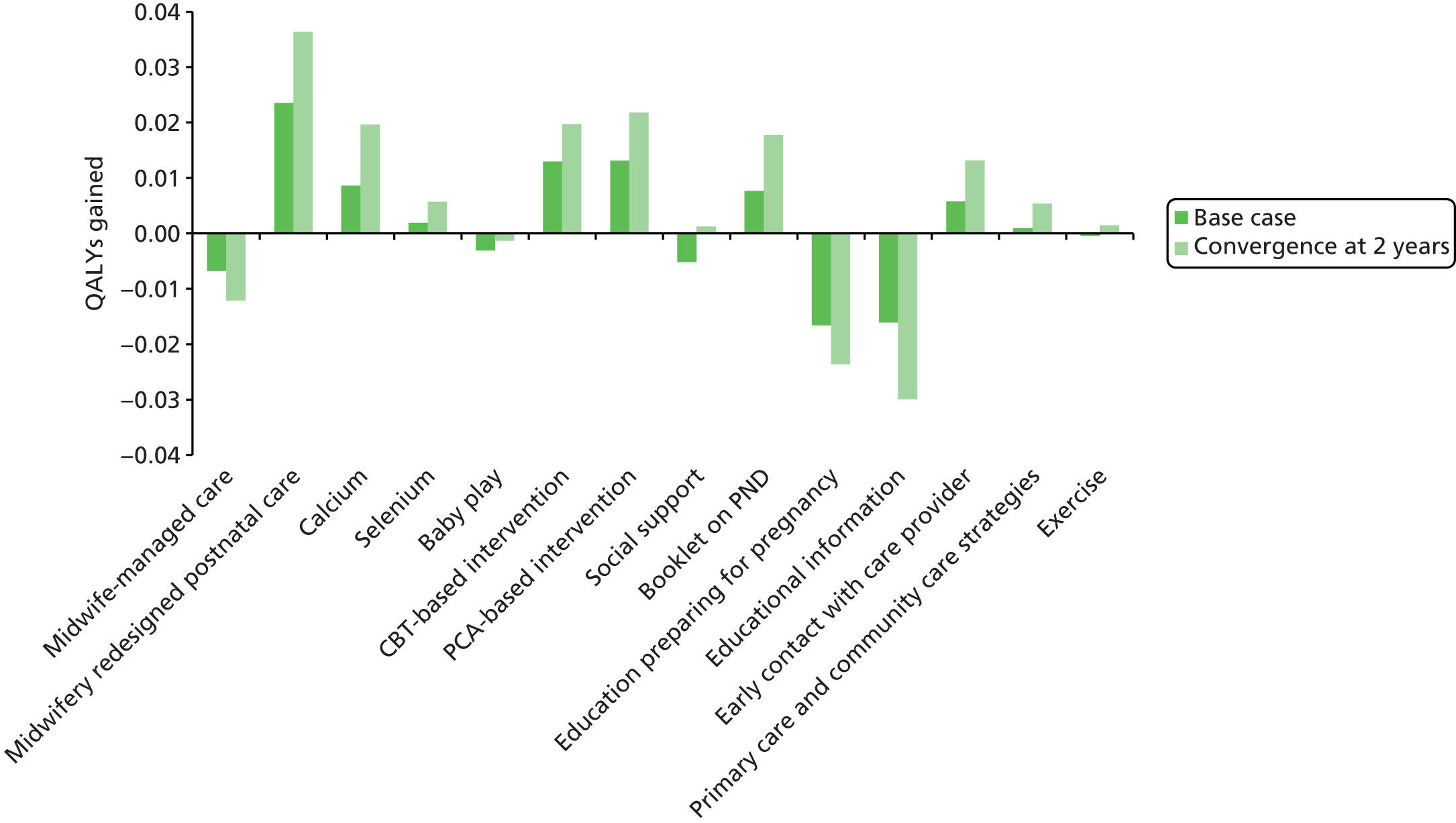
FIGURE 70.
The estimated incremental QALYs per woman compared with usual care associated with each selective preventive intervention.
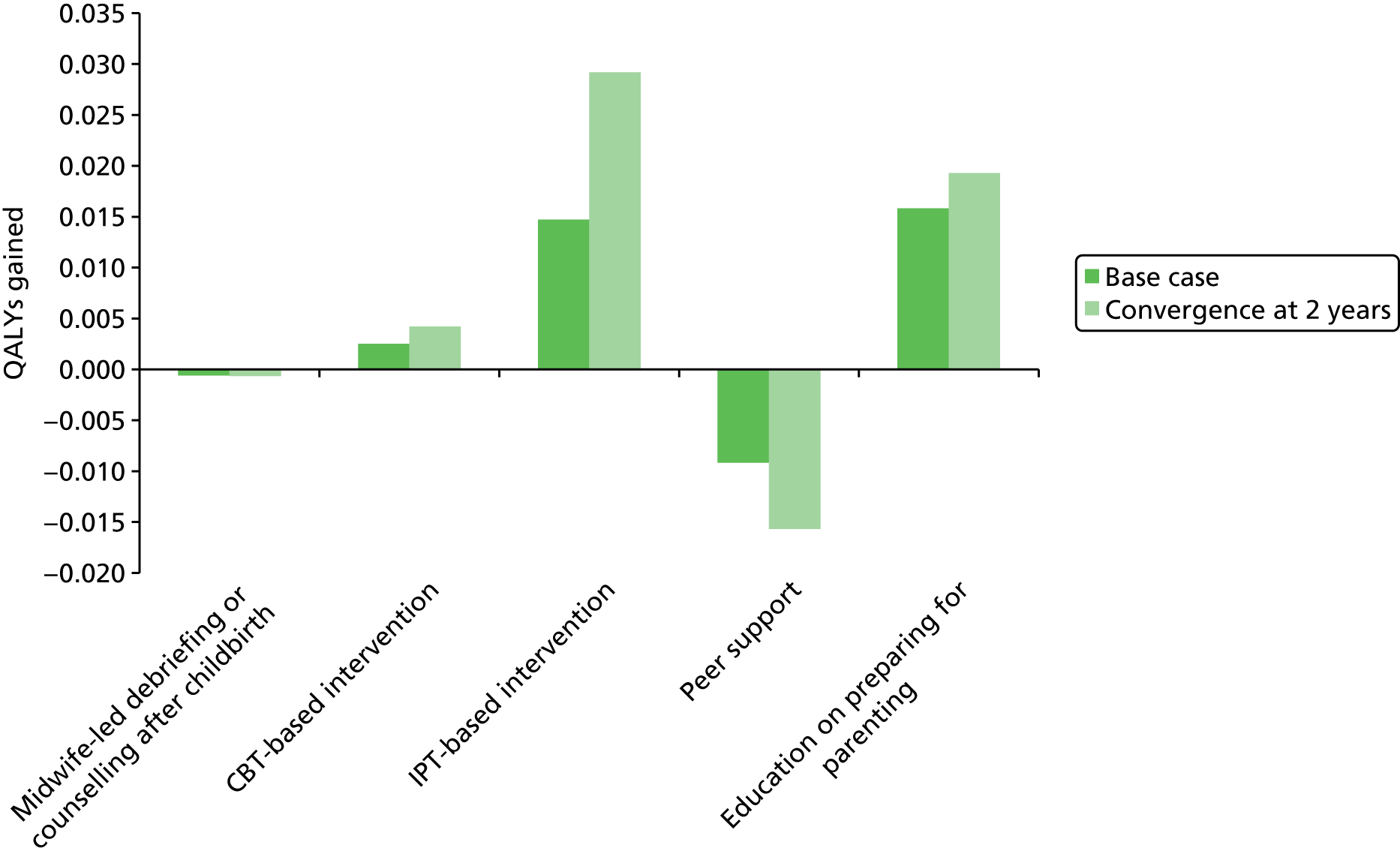
FIGURE 71.
The estimated incremental QALYs per woman compared with usual care associated with each indicated preventive intervention.

Calculating cost per quality-adjusted life-year values
The data presented in Figures 69–71 were combined with the assumed costs of each intervention to estimate a cost per QALY value for each intervention compared with usual care and also to allow a fully incremental analysis to be undertaken. These data are provided in Tables 66–71 for universal preventive interventions, indicated preventive interventions and selective preventive interventions and for the base-case and sensitivity analyses on time of EPDS score convergence. In all tables the intervention estimated to be most cost-effective at a willingness-to-pay threshold of £20,000 per QALY is shaded.
| Intervention | Assumed incremental cost (£)a | Mean incremental QALYsa | Cost per QALY compared with usual care (£) | Percentage of times generating more QALYs than usual care (%) | Incremental cost which results in a cost per QALY of £20,000 (£)b | Fully incremental analyses, cost per QALY (£)c |
|---|---|---|---|---|---|---|
| PCA-based intervention | –28.00 | 0.0131 | Dominating | 84.8 | 262 | – |
| CBT-based intervention | –24.00 | 0.0130 | Dominating | 83.2 | 259 | Dominated |
| Usual care | – | – | – | – | – | Dominated |
| Midwife-managed care | 0.00 | –0.0068 | Dominated | 66.4 | –136 | Dominated |
| Booklet on PND | 1.00 | 0.0076 | 131 | 68.3 | 153 | Dominated |
| Educational information | 8.00 | –0.0161 | Dominated | 20.3 | –322 | Dominated |
| Early contact with care provider | 41.00 | 0.0058 | 7116 | 69.4 | 115 | Dominated |
| Exercise | 65.74 | –0.0004 | Dominated | 49.5 | –9 | Dominated |
| Calcium | 78.96 | 0.0086 | 9189 | 69.7 | 172 | Dominated |
| Primary care and community care strategies | 94.79 | 0.0009 | 101,876 | 51.8 | 19 | Dominated |
| Baby play | 101.94 | –0.0031 | Dominated | 40.2 | –62 | Dominated |
| Education on preparing for parenting | 101.94 | –0.0166 | Dominated | 13.4 | –332 | Dominated |
| Midwifery redesigned postnatal care | 107.64 | 0.0236 | 4570 | 89.2 | 471 | 12,961 |
| Selenium | 149.85 | 0.0019 | 78,422 | 54.2 | 38 | Dominated |
| Social support | 279.00 | –0.0052 | Dominated | 33.3 | –103 | Dominated |
| Intervention | Assumed incremental cost (£)a | Mean incremental QALYsa | Cost per QALY compared with usual care (£) | Percentage of times generating more QALYs than usual care (%) | Incremental cost which results in a cost per QALY of £20,000 (£)b | Fully incremental analyses, cost per QALY (£)c |
|---|---|---|---|---|---|---|
| Usual care | – | – | – | – | – | – |
| Midwife-led debriefing or counselling after childbirth | 70.00 | –0.0006 | Dominated | 46.0 | –12 | Dominated |
| CBT-based intervention | 99.00 | 0.0025 | 39,343 | 56.1 | 50 | Extendedly dominated |
| Peer support | 150.00 | –0.0092 | Dominated | 26.8 | –184 | Dominated |
| Education on preparing for parenting | 266.17 | 0.0158 | 16,811 | 93.3 | 317 | 16,811 |
| IPT-based intervention | 495.00 | 0.0147 | 33,640 | 79.6 | 294 | Dominated |
| Intervention | Assumed incremental cost (£)a | Mean incremental QALYsa | Cost per QALY compared with usual care (£) | Percentage of times generating more QALYs than usual care (%) | Incremental cost which results in a cost per QALY of £20,000 (£)b | Fully incremental analyses, cost per QALY (£)c |
|---|---|---|---|---|---|---|
| Usual care | – | – | – | – | – | – |
| Midwifery continuous care | 0.00 | –0.0032 | Dominated | 45.5 | –63 | Dominated |
| PCA-based intervention | 3.00 | 0.0067 | 447 | 63.5 | 134 | 447 |
| Educational information | 272.92 | –0.0221 | Dominated | 15.6 | –441 | Dominated |
| Peer support | 366.43 | 0.0035 | 103,928 | 58.9 | 71 | Dominated |
| CBT-based intervention | 514.25 | 0.0093 | 55,157 | 73.3 | 186 | Extendedly dominated |
| Promoting parent–infant interaction | 1017.23 | 0.0055 | 183,696 | 61.8 | 111 | Dominated |
| IPT-based intervention | 1163.25 | 0.0254 | 45,884 | 88.9 | 507 | 62,251 |
| Intervention | Assumed incremental cost (£)a | Mean incremental QALYsa | Cost per QALY compared with usual care (£) | Percentage of times generating more QALYs than usual care (%) | Incremental cost which results in a cost per QALY of £20,000 (£)b | Fully incremental analyses, cost per QALY (£)c |
|---|---|---|---|---|---|---|
| PCA-based intervention | –28.00 | 0.0218 | Dominating | 89.0 | 436 | – |
| CBT-based intervention | –24.00 | 0.0197 | Dominating | 86.5 | 394 | Dominated |
| Usual care | – | – | – | – | – | Dominated |
| Midwife-managed care | 0.00 | –0.0121 | Dominated | 36.6 | –243 | Dominated |
| Booklet on PND | 1.00 | 0.0177 | 56 | 69.6 | 355 | Dominated |
| Educational information | 8.00 | –0.0300 | Dominated | 24.0 | –599 | Dominated |
| Early contact with care provider | 41.00 | 0.0131 | 3119 | 70.5 | 263 | Dominated |
| Exercise | 65.74 | 0.0015 | 44,486 | 52.9 | 30 | Dominated |
| Calcium | 78.96 | 0.0196 | 4022 | 71.0 | 393 | Dominated |
| Primary care and community care strategies | 94.79 | 0.0054 | 17,658 | 58.8 | 107 | Dominated |
| Baby play | 101.94 | –0.0013 | Dominated | 46.3 | –27 | Dominated |
| Education on preparing for parenting | 101.94 | –0.0236 | Dominated | 20.7 | –472 | Dominated |
| Midwifery redesigned postnatal care | 107.64 | 0.0363 | 2963 | 92.8 | 727 | 9340 |
| Selenium | 149.85 | 0.0057 | 26,267 | 55.2 | 114 | Dominated |
| Social support | 279.00 | 0.0013 | 221,579 | 52.4 | 25 | Dominated |
| Intervention | Assumed incremental cost (£)a | Mean incremental QALYa | Cost per QALY compared with usual care (£) | Percentage of times generating more QALYs than usual care (%) | Incremental cost which results in a cost per QALY of £20,000 (£)b | Fully incremental analyses, cost per QALY (£)c |
|---|---|---|---|---|---|---|
| Usual care | – | – | – | – | – | – |
| Midwife-led debriefing or counselling after childbirth | 70.00 | –0.0006 | Dominated | 48.8 | –13 | Dominated |
| CBT-based intervention | 99.00 | 0.0042 | 23,429 | 55.4 | 85 | Extendedly dominated |
| Peer support | 150.00 | –0.0157 | Dominated | 26.0 | –313 | Dominated |
| Education on preparing for parenting | 266.17 | 0.0193 | 13,785 | 86.4 | 386 | 13,785 |
| IPT-based intervention | 495.00 | 0.0292 | 16,966 | 79.3 | 584 | 23,191 |
| Intervention | Assumed incremental costa | Mean incremental QALYsa | Cost per QALY compared with usual care | Percentage of times generating more QALYs than usual care (%) | Incremental cost which results in a cost per QALY of £20,000 (£)b | Fully incremental analysesc |
|---|---|---|---|---|---|---|
| Usual care | – | – | – | – | – | – |
| Midwifery continuous care | 0.00 | –0.0036 | Dominated | 47.5 | –72 | Dominated |
| PCA-based intervention | 3.00 | 0.0119 | 251 | 62.9 | 239 | 251 |
| Educational information | 272.92 | –0.0446 | Dominated | 14.6 | –891 | Dominated |
| Peer support | 366.43 | 0.0075 | 49,041 | 57.6 | 149 | Dominated |
| CBT-based intervention | 514.25 | 0.0279 | 18,423 | 84.3 | 558 | Extendedly dominated |
| Promoting parent–infant interaction | 1017.23 | 0.0060 | 168,468 | 56.3 | 121 | Dominated |
| IPT-based intervention | 1163.25 | 0.0604 | 19,259 | 91.5 | 1208 | 23,943 |
The values from each of the individual PSAs run were also used to generate an estimate of the probability that each intervention provided more QALYs than usual care.
Producing cost-effectiveness acceptability curves
Cost-effectiveness acceptability curves have been produced for the base case for each of the three populations. These are reproduced in Figure 72–74.
FIGURE 72.
The CEAC for the universal preventive interventions.

FIGURE 73.
The CEAC for the selective preventive interventions.
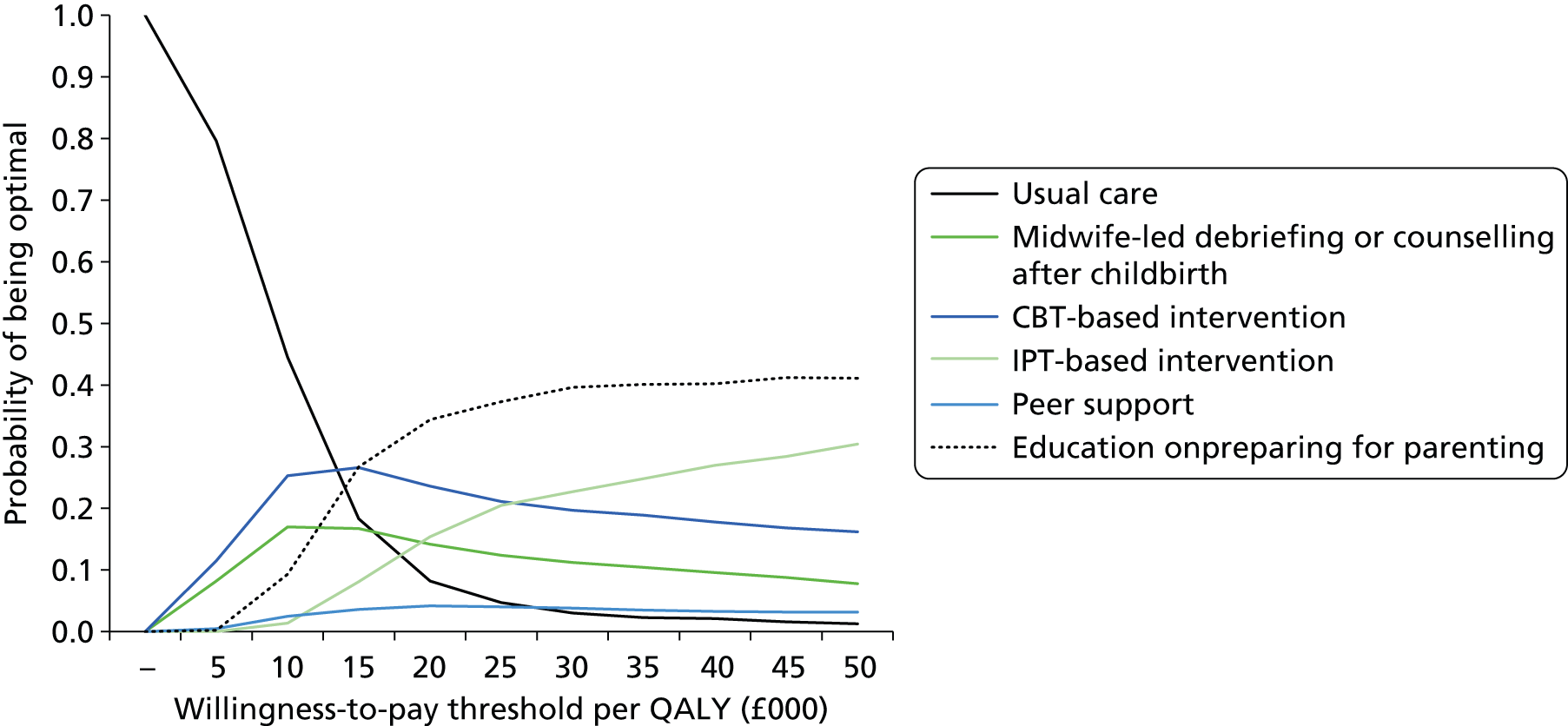
FIGURE 74.
The CEAC for the indicated preventive interventions.

The three universal preventive interventions with a relatively high probability of being optimal are usual care (for low willingness to pay per QALY levels), midwifery redesigned postnatal care and PCA-based intervention.
All-strategies bar peer support have a reasonable probability (> 10%) of being the most cost-effective selective preventive intervention. As the willingness to pay per QALY value increases the probability that IPT-based intervention is optimal increases, indicating it is expected to produce the greatest mean number of QALYs.
The three indicated preventive interventions strategies with a relatively high probability of being optimal are usual care (for low willingness to pay per QALY levels), midwifery continuous care and PCA-based intervention. As the willingness to pay per QALY value increases the probability that IPT-based intervention is optimal increases indicating it is expected to produce the greatest mean QALYs.
At a willingness to pay of £0 per QALY, both usual care and midwifery continuous care were deemed optimal as they shared the lowest cost per intervention. The CEAC has been modified to allocate the optimal strategy to the one with more QALYs in each probabilistic run (51% midwifery continuous care and 49% usual care).
Interpretation of the cost-effectiveness results produced
A brief interpretation of the results for each population is provided. However, a number of factors apply to all populations; these are detailed in advance of the individual sections and serve to highlight the considerable uncertainty in the results.
The analyses undertaken are limited to those interventions that reported EPDS mean values. All other interventions are excluded, adding uncertainty to any conclusion. In all analyses the mean absolute QALY gain estimated was small (less than 0.061 in all analyses) and may not be seen as a worthwhile improvement should services needed to be reconfigured to achieve such benefits. The current results presented assume that capacity of staff is infinite and changes can be achieved without incurring costs, which is an oversimplification.
Uncertainty is large regarding the most cost-effective intervention in all populations. Once a willingness to pay of £20,000 per QALY is reached, no intervention had a probability of being the optimal strategy of greater than 50%.
Furthermore, the costings of each strategy have by necessity been relatively crude. Additional knowledge regarding the costs of any intervention deemed possibly cost-effective will improve the robustness of any decision.
Interventions for the universal preventive interventions
Midwifery redesigned postnatal care was estimated to be the most cost-effective intervention assuming a willingness to pay of £20,000 per QALY. However, in over 10% of simulations midwifery redesigned postnatal care was estimated to produce fewer QALYs than usual care in the base-case analysis. Both PCA-based intervention and CBT-based interventions dominated usual care and would also be candidates for introduction in the NHS. Midwifery redesigned postnatal care remained the intervention estimated to be most cost-effective when a duration of benefit to the woman of 2 years was assumed.
Interventions for the selective preventive interventions
Education on preparing for parenting was estimated to be the most cost-effective of the interventions evaluated with a cost per QALY of approximately £17,000. No other intervention appeared cost-effective compared with usual care alone unless a residual benefit lasting until year 2 was assumed. The mean QALYs produced by the peer support intervention were estimated to be lower than those produced by usual care, meaning that uncertainty in the intervention costs described previously would not affect the conclusions regarding the cost-effectiveness of this strategy. Education on preparing for parenting remained the intervention estimated to be most cost-effective when the duration of benefit to the woman of was assumed to be 2 years. However, the cost per QALY of an IPT-based intervention compared with education on preparing for parenting was reduced to approximately £23,000.
Interventions for indicated preventive interventions
A PCA-based intervention was estimated to be the most cost-effective intervention, although this was estimated to produce more QALYs than usual care on only 64% of simulations. No other intervention appeared cost-effective compared with usual care alone unless a residual benefit lasting until year 2 was assumed. A PCA-based intervention remained the intervention estimated to be most cost-effective when the duration of benefit to the woman was assumed to be 2 years. However, the cost per QALY of an IPT-based intervention compared with a PCT-based intervention was reduced to approximately £24,000 if a benefit of 2 years was assumed.
Assessing the impact of using total health-care costs when these were available rather than intervention costs
In the universal preventive interventions, the changes in assumed costs of the midwifery redesigned postnatal care intervention and the social support intervention did not alter the intervention estimated to be the most cost-effective assuming a willingness to pay of £20,000 per QALY. This remained as midwifery redesigned postnatal care, which now dominated all other interventions using mean values. Social support remained dominated by usual care using mean values.
No studies reported total health-care costs in the selective preventive interventions.
In indicated preventive interventions changes to the assumed costs of a PCA-based intervention, a CBT-based intervention, peer support and promoting parent–infant interaction did not alter the intervention estimated to be the most cost-effective assuming a willingness to pay of £20,000 per QALY, which remained a PCA-based approach. The PCA-based intervention still dominated peer support and promoting parent–infant interaction using mean values, while a CBT-based intervention remained extendedly dominated by a PCA-based approach and an IPT-based approach using mean values.
Value of information results
Expected value of perfect information results
Figure 75–77 present the EVPI per woman for the three defined populations. In all of the figures the value increases as the willingness to pay increases, indicating that there is genuine uncertainty in the most effective intervention. Assuming a willingness to pay of £20,000 per QALY, the population EVPI values are very large, in excess of £150M for all analyses, which would more than cover the costs of studies aimed at reducing the uncertainty in model parameters.
FIGURE 75.
The EVPI associated with the universal preventive interventions.

FIGURE 76.
The EVPI associated with the selective preventive interventions.
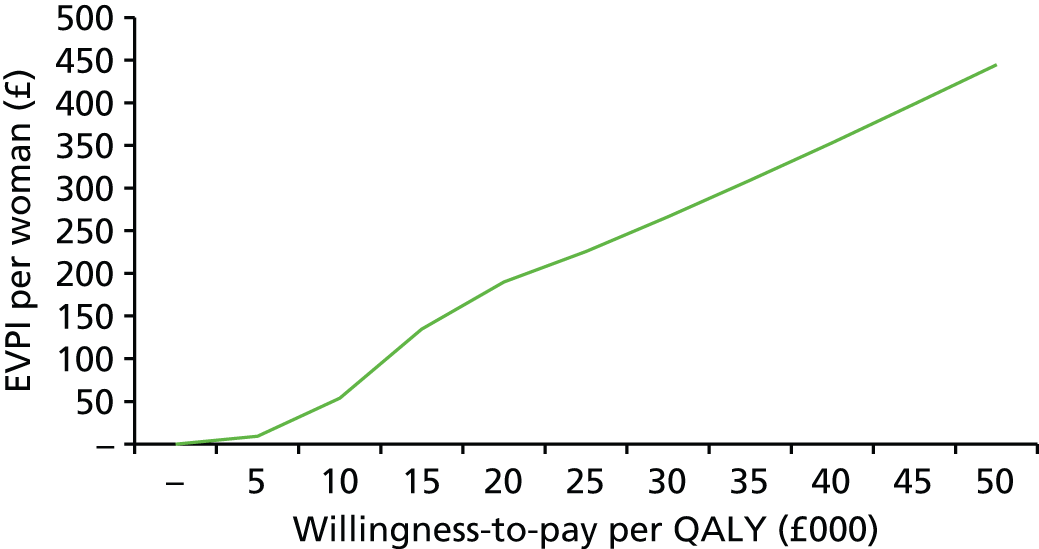
FIGURE 77.
The EVPI associated with the indicated preventive interventions.
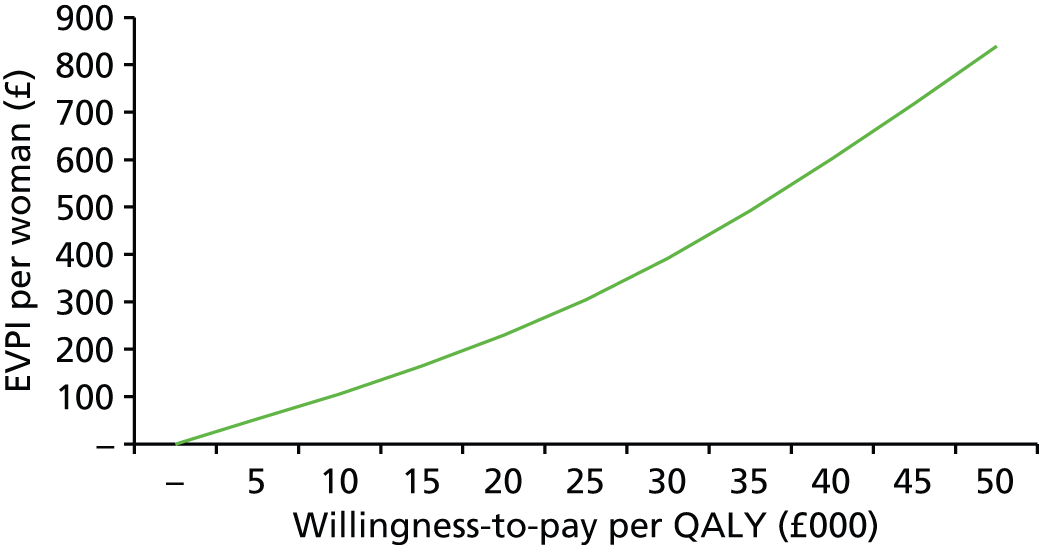
Assuming that 7.20 million women would benefit from improved knowledge in the universal preventive interventions and a willingness to pay of £20,000 per QALY, the population EVPI was estimated to be £1.93B (£267 × 7.20 million).
Assuming that 1.08 million women would benefit from improved knowledge in the selective preventive interventions and a willingness to pay of £20,000 per QALY, the population EVPI was estimated to be £205M (£190 × 1.08 million).
Assuming that 720,000 women would benefit from improved knowledge in indicated preventive interventions and a willingness to pay of £20,000 per QALY, the population EVPI was estimated to be £166M (£230 × 720,000).
Expected value of partial perfect information results
As previously stated the EVPPI analyses were undertaken assuming two broad groups: the efficacy data that represented the correlated CODA output from the NMA and the mapping of EPDS scores to utility values.
The EVPPI for the mapping group was zero, indicating that the value assigned to the relationship between EPDS and utility would not alter the conclusion regarding which intervention was most cost-effective. In stark contrast, having perfect data on the relative efficacies of the interventions could result in a different decision on the most cost-effective intervention and would be valuable. For all populations the EVPPI for the efficacy group equalled the EVPI value. It is seen in Figure 78 that the impact of uncertainty in the efficacy data dwarfs that within the mapping.
FIGURE 78.
Results of the EVPI and EVPPI analyses. The value for the EVPPI for mapping is zero.

Discussion of the assessment of cost-effectiveness of interventions
Although the cost-effectiveness analyses undertaken allow the most cost-effective intervention in each population to be estimated, these results are far from definitive. Limitations with the analyses include:
-
Interventions that did not report EPDS values have been omitted from the analyses.
-
The incremental costs for each strategy have, by necessity, been estimated in a simplistic manner. Costs of restructuring services, if required, have not been included.
-
The possibility of erroneous grouping of trials as a single intervention within indicated preventive interventions.
-
Simplistic assumptions have been made in estimating the area under the curve when data are not available for all time points.
Limitations with providing a definitive conclusion regarding the most cost-effective intervention include:
-
that absolute QALY gains estimated are small for all interventions
-
that there is considerable uncertainty in the direction of the estimates of QALY change compared with usual care for all interventions, thus usual care could conceivably be the most effective intervention in all three populations.
Value of information analyses were undertaken to estimate the monetary value of removing uncertainty in the efficacy data. These values were shown to be exceedingly high, in the order of hundreds of millions of pounds, which would be sufficient to cover the costs of future research. Although the relationship between EPDS and utility was not shown to influence the decision, given current information, should future research be undertaken it is recommended that utility data be collected. In addition, detailed costing data for each intervention should be recorded in any future research.
Chapter 10 Discussion
Introduction
The purpose of the current review was to evaluate the clinical effectiveness and cost-effectiveness, acceptability and safety of antenatal and postnatal interventions for pregnant and postnatal women to prevent PND. In this chapter, the principal findings of the NMAs and the economic evaluation are interpreted alongside an assessment of the strengths and limitations of the review and the overall strengths and limitations of the individual trials. Uncertainty about intervention effects, implications for further research and implications for practice are highlighted.
Up until 10–15 years ago management of depression in postpartum women was a neglected area59 and even less attention was paid to the prevention of PND in research or practice. 59 However, with increasing knowledge about perinatal mental health59 and particularly its potential long-term impact on the development of infants,33 the need for preventive approaches has become more apparent.
The breadth of approaches aimed at preventing PND evaluated in clinical trials reflects the uncertainty around the aetiology of the condition and which of the many associated factors might be amenable to intervention. Some factors, such as a history of depression (before pregnancy, during pregnancy or postnatally) or a familial or genetic component, are unalterable but levels of risk may be reduced. Other factors, such as lack of social support, are potentially amenable to intervention.
Description of the interventions
As far as we are aware, this is the most comprehensive review of interventions to evaluate the clinical effectiveness and cost-effectiveness, acceptability and safety of antenatal and postnatal interventions for pregnant and postnatal women to prevent PND. In total, 86 RCTs are included. Trials are categorised into one of three levels of preventive intervention (universal, selective and indicated) relevant for particular populations of women; the findings for each of these levels of preventive interventions is reported along with the limitations and implications.
The earlier Cochrane review of psychosocial and psychological interventions to prevent PND417 searched to 30 November 2011 and the current review searched to July 2013. Our review included diverse interventions to prevent PND not just psychosocial and psychological, which is important given the diverse aetiology of PND.
The review includes trials from 16 countries. Trials were classified as psychological (including specific therapeutic approaches), educational, social, pharmacological, organisation of maternity care, midwifery-led interventions and CAM or other approaches to the prevention of PND. All of the universal preventive interventions were considered applicable to selective and indicated populations. Not all selective preventive interventions or indicated preventive interventions were applicable to a universal population. Evidence for some of the interventions was available neither for all populations nor for all follow-up times, meaning an evaluation of some interventions is necessarily incomplete.
The trials which followed up participants until 12 months postnatally provided information about enduring effects. Those trials which had a short-term follow-up of 6 weeks or 3 months did not provide information about whether or not any effect was sustained over the full postnatal year.
Levels of preventive intervention
We defined selective preventive interventions as those provided for maternal populations identified on the basis of social risk (e.g. teenage parenting or poverty) and indicated preventive interventions as those provided for populations with individual risk (e.g. history of depression or a high score on a symptom checklist). Universal preventive interventions were provided for all pregnant and eligible postnatal women.
Categorising the trials into three levels of preventive intervention, relevant for particular populations of women, facilitates decisions on service provision from a service provider or commissioner perspective. The identification of populations of perinatal women for either selective or indicated preventive interventions can follow an assessment of risk of PND only among a population of perinatal women suitable for universal preventive interventions. Risk assessment requires specialised skills. The exceptions are for particular pregnant or postnatal women already known to health services because of a personal history, ongoing depression or anxiety or because of their social circumstances.
Within the trials, definitions of risk were inconsistent. Some trials used clinical criteria such as HIV-positive serostatus, or a screen for trauma symptoms. Other trials applied social criteria, such as being teenage, first-time pregnant, unmarried, from specific ethnic groups (such as Navajo or White Mountain Apache American Indian), or screened positive for domestic violence in the past year. Other trials used a depression diagnostic instrument or a measure of depressive symptoms. Even where a common instrument had been used to identify depressive symptoms, there was inconsistency in the threshold scores used to define level of risk. Some judgement was required for allocating trials to one of the three levels of preventive intervention.
Conceptualisation of postnatal depression and the potential for prevention
Although depression can range on a continuum from mild symptoms to major depressive disorder, it is classified in psychiatry and for research purposes within a dichotomy of diagnosed depression or not depressed. The spectrum of symptoms in one person’s state or mood can vary daily and weekly. We regarded depression in postnatal women as depression which may have begun before pregnancy, during pregnancy or after the baby was born. Trials for which the main focus was treatment of antenatal depression were included if they included a postnatal measure of depressive symptoms or a depression diagnosis, that is the antenatal treatment of depression was regarded as the prevention of PND. The implications of depression for a pregnant mother and her developing baby are different from the implications of depression for a new mother and her newborn and developing infant. There was inconsistency in the definition of antenatal depression as different self-completed measures of depressive symptoms (e.g. EPDS or BDI) or depression diagnostic instruments (e.g. DSM-IV or ICD-10) were used.
Focus of the included interventions
Although all of the trials included a measure of PND, the primary aim of the trials varied from being primarily about PND prevention, antenatal well-being, birth outcomes, general health, general psychological well-being, infant outcomes and family outcomes. The deliberately broad inclusion criteria within our review enabled the capture of all potentially effective interventions whether PND was a primary or secondary outcome, notwithstanding selective reporting and publication bias.
Network meta-analyses
A novel feature of this review was that inferences about intervention effects were made using a NMA. The NMA was used to determine the clinical effectiveness of individual antenatal and postnatal interventions for preventing PND, and to generate the joint distribution of individual antenatal and postnatal interventions which was used to characterise the uncertainty around inputs for the economic model.
A NMA requires trials to form a connected network of interventions, to enable intervention effects to be synthesised and compared. That is, trials included in the review could only be included in the NMA if they shared at least one intervention in common with at least one other study. In addition, trials must have provided information on the outcome measure of interest. The assumption made in the analysis was that any trials that were excluded because they did not provide information on the outcome of interest were missing at random.
Trials were excluded from the NMA if ‘usual care’ was considered to be sufficiently different from that in the UK or if the outcomes reported did not include the EPDS.
Clinical effectiveness of universal preventive interventions
Of the trials included in the NMA, interventions most likely to be the best among those evaluable at each assessment were:
-
at 3 months postnatally, midwifery redesigned postnatal care146
-
at 6 months postnatally, CBT-based intervention61 and PCA-based intervention61
-
at 12 months postnatally, midwifery redesigned postnatal care,146 CBT-based intervention61 and PCA-based intervention. 61
The most promising interventions were selected only from the set of interventions which formed a network.
Psychological interventions
In the PCA-based intervention of health visitor training (the PoNDER trial) health visitors were trained in the assessment of postnatal women, combined with up to eight sessions for eligible women, in one arm a PCA and in the other arm a CBA. 61 The control group and the intervention group health visitors had an ongoing relationship with the women as part of their usual care. This trial had a low risk of bias and had the longest follow-up of 18 months. The trial had an accompanying economic evaluation, which indicated a high probability that the intervention was cost-effective but required what was considered a lengthy training for health visitors, including ongoing clinical supervision and reflective practice, equivalent in total to 8 days. The economic model indicated that, among the universal preventive interventions, the PCA-based intervention61 was a candidate for introduction in the NHS. The trial findings were published in 2009 and were not included in the 2007 NICE guidance on antenatal and postnatal mental health. 38
Pharmacological or supplements
The calcium trial was included within a trial examining the prevention of pre-eclampsia. Outcomes were measured at only 3 months postnatally. The trial was assessed as having a high risk of bias overall. The authors were unable to explain the disparate outcomes in the two centres, Portland and Albuquerque. 208
Midwifery-led interventions
The intervention in the trial of redesigned midwifery-led community postnatal care was designed to enable midwifery care in community settings to be tailored flexibly according to the individual needs of the women. The focus was on the identification and management of women’s physical and psychological health rather than on routine observations. 146 The trial had a low risk of bias. Women in the intervention group had a final check with their midwife at 10–12 weeks, which replaced the GP contact at 6–8-weeks, and overall GP consultation rates during the year were reduced in the intervention group. The economic evaluation indicated that among the universal preventive interventions, this intervention was the most cost-effective given current knowledge.
Despite some evidence of clinical benefit and cost savings, the findings did not substantially change practice or influence guidance. Following the 2004 revision to the GP contract, funding for maternity care was no longer allocated on an ‘item of service’ basis but was included in a global sum paid to GPs. 418 No recent studies have assessed the benefit of the GP role in postnatal care. The National Service Framework419 recommended that all women should be provided with access to a midwife for up to 28 days post birth. NICE guidance420 on routine postnatal care of women and their babies recommended that postnatal contacts should be based on an individual woman’s need. However, many care providers in England continue to discharge some women from midwifery care at around 10–14 days postnatally, to health visitor care, with a routine GP contact offered at 6–8 weeks postnatally. Current NHS resource constraints mean that women are likely to be offered far fewer community contacts than were available in the trial of redesigned midwifery-led community postnatal care. 146 The historical definition of the postnatal period and fragmented organisation of maternity services across health-care sectors have hitherto been major barriers to revising practice in line with evidence, despite policy recognition of the importance of effective maternity care to promote life-long health and to reduce inequalities. 66
In the trial of midwife-managed care within a Midwifery Development Unit (MDU),220 825 women were assessed at only 7 weeks postnatally using an unvalidated nine-item version of the EPDS rather than the usual 10-item EPDS. This model provided a high degree of continuity of care and carer with the aim that women should receive care from no more than four midwives during their hospital and community pregnancy, labour and postnatal care. MDU midwives therefore worked in both community and hospital settings. Birthing rooms used by MDU women were less clinical than those generally available and hospital postnatal care was provided in a dedicated postnatal ward that was designed to provide a more home-like environment. The authors advised at the time that further research should be carried out on the midwife’s training in support, especially emotional support. The benefits of this approach merit consideration, but the various components would require significant changes in midwifery working to those utilised in most of the UK and would also require changes to facilities if the model was replicated.
Universal preventive interventions not included in the network meta-analysis
Some interventions could not be compared in the NMA because trials did not provide the required data. For trials not included in the NMA, there should be caution about relying too heavily on whether or not a test of hypothesis was statistically significant in a particular trial, for example when the trial results showed a p-value less than 0.05 and the investigators concluded that the intervention was effective. One of the universal preventive intervention trials excluded from the NMA was conducted in the UK. 150 This trial, of unclear risk of bias, examining the frequency of health visitors’ visits found no impact on most outcomes.
A US trial of education on preparing for parenting (a psychosocial prevention programme implemented through childbirth education programmes to enhance the co-parental relationship, parental mental health, the parent–child relationship and infant emotional and physiological regulation), with 169 participants, had an unclear risk of bias and found ‘a [statistically] significant intervention effect on maternal depression and anxiety’ using subset of seven items CES-D. 163
An Australian trial of ‘Towards Parenthood’, with 143 women, in the education on preparing for parenting class of interventions was of unclear risk of bias found ‘[statistically] significantly lower levels of depression (BDI-II) post-treatment than participants in routine care’. 185 The different elements of the intervention could not be evaluated separately.
Summary of qualitative findings for universal preventive interventions
Fourteen of the 21 qualitative studies of interventions examined a universal preventive intervention. Included studies provide at least moderate certainty with regard to their findings. Universal approaches must recognise that for a number of women the practical considerations regarding access to the intervention, convenience and challenges of integration with other responsibilities (such as other children or work commitments) may provide significant barriers to attendance at a substantive number of sessions or even attendance at all. Group-based approaches seemed to offer a wide range of resources and strategies, beyond those offered by the facilitator, and, provided that they do not prove too resource intensive or create unrealistic expectations of services, may be a useful supplement to provision. Group-based approaches may compensate for limitations in the formal care provision by providing additional social support, provided the group process is facilitated adequately. However, an important consideration relates to whether or not group approaches are able to offer sufficient individualised attention and continuity of care. Continuity of care was confirmed as an important operator across several interventions, and viewed as important by the EP committee, in that it enabled women to build up a relationship of trust with their health-care provider. This enabled both free communication of problems or concerns and then tailoring of support strategies to the needs of the individual woman. Midwifery redesigned care interventions seek to offer improved continuity. However, such continuity is not an automatic product of a single named provider or a stable team; it requires rapport and skills in facilitation if it is not to become an additional source of stress or anxiety.
The CenteringPregnancy approach is a highly structured, resource-intensive intervention that is being explored in the UK,421 but has not yet been used widely in UK settings and may reveal its limitations within a resource-constrained environment. CenteringPregnancy provides group care to women at similar stages of pregnancy with a health assessment and provision of education and peer support. As a ‘whole-system’ approach it seems to merit wider evaluation, not simply against outcomes of relevance to PND but against a broad range of maternal and infant outcomes, both short and medium term. It may also offer support to partners, considered an important aspect of an intervention by the literature and the expert group of service users. However, such involvement is not unproblematic and may, in fact, exacerbate feelings of lack of support, particularly in comparison to others within the group. Although CenteringPregnancy has been evaluated in a universal context, its greater potential, given the extensive requirement for training and individual follow-up support, seems to lie in it being a more appropriate approach for an indicated population.
Clinical effectiveness of selective preventive interventions
In general, the treatment effects for the selective preventive interventions were inconclusive. Of the studies included in the NMA, the most beneficial treatments appeared to be CBT-based interventions,158 IPT-based interventions163 and education on preparing for parenting. The most promising interventions for a selective population of women are presented within the categories in which the universal preventive interventions were presented.
Psychological interventions
One of the most beneficial selective preventive interventions appeared to be CBT-based intervention158 with IPT-based intervention estimated to provide the most QALYs. IPT is a relatively newly studied specific form of psychological intervention, which focuses on facilitating positive relationships. The studies examining IPT-based interventions were mainly undertaken in the USA, with two in China (one in Hong Kong). IPT has not been as well adopted in the UK as CBT-based approaches. Its use has been supported in a meta-analysis of psychological treatments for PND62,422 and treatment for perinatal depression (including antenatal depression). 250 These studies could be replicated in a selective preventive intervention population.
Educational interventions
Education on preparing for parenting appeared to be one of the more beneficial educational selective preventive interventions. It was estimated to be the most cost-effective of the trials of educational interventions evaluated with a cost of approximately £17,000 per QALY. The individual interventions were dissimilar. One, based in the UK examined the effectiveness of attendance at a twin clinic and provision of additional antenatal education, information, and support by a specialist midwife for women with twins. 191 The other, based in the USA offered 10 classes during pregnancy and postpartum, focusing on parenting and coping strategies, with 44 women, and was of unclear risk of bias. 189
Social support
The trial, conducted in the UK, of 343 young women having their first baby and living in a socioeconomically disadvantaged area examined peer mentor support in pregnancy and postnatally. 201 The failure to demonstrate a difference in the social support peer mentor group was similar to results from the trial of postnatal social support provided for a universal population199 in which there appeared to be a trend for the intervention group scores to reflect poorer health than the scores for women in the control group. The authors recommended further rigorous evaluation of interventions to promote the health of children in socially disadvantaged communities. 392 More attention should be paid to exploring the nature of the support women say they would like, such as peer support, rather than examining the effectiveness of interventions without a particular theoretical basis.
Summary of qualitative findings for selective preventive interventions
Four qualitative studies presented data from those who had received a selective preventive intervention. Included studies provide at least moderate certainty with regard to their findings. CenteringPregnancy was credited as offering support to partners, as well as facilitating support from the wider family and, most importantly, the peer support the intervention offered. IPT appears a well-received approach, although conclusions on the appropriateness of IPT as a selective prevention intervention are based on findings from a single study and constrained by the lack of qualitative evidence on the other types of intervention.
Clinical effectiveness of indicated preventive interventions
The NMA showed that, in general, the treatment effects for the indicated preventive interventions were inconclusive and the CrIs were wide. The most beneficial interventions appeared to be those promoting parent–infant interaction at 6 weeks and 3 months postnatally,164 those providing peer support at 3 months postnatally205 or educational information at 3 months postnatally,168 CBT-based intervention at 3–4 months postnatally,173 IPT-based intervention at 7 months postnatally,169,170 PCA-based intervention at 6 and 12 months postnatally61 and CBT-based intervention at 6 and 12 months postnatally. 61
The economic analysis showed that the indicated preventive interventions strategies with a relatively high probability of being optimal were midwifery continuous care; and PCA-61 and IPT-based interventions.
Indicated preventive interventions not included in the network meta-analysis
Some interventions could not be compared in the NMA because trials did not provide the required data. Apart from one large trial, conducted in Pakistan,148 most of those excluded were small trials or trials without a comparable usual-care control group. Two small trials of women living in poverty178,179 suggested a positive benefit of an IPT-based intervention. However, these results could be a consequence of small study effects and they should be confirmed in a RCT with up to 1 year of follow-up and adequately powered to detect clinically relevant treatment effects.
Social support
Among the trials not included in the NMA, the UK-based trial examined Newpin volunteer peer support in 65 women. 206 The prevalence of perinatal major depression, measured by the SCAN, was 27% (8/30) in the Newpin befriender group and 54% (19/35) in the control group. This diagnostic instrument is more robust than the EPDS and the findings should be taken seriously by replicating the trial with an appropriately large sample size.
Pharmacological or supplements
The findings demonstrating the effectiveness of sertraline216 have been incorporated into clinical practice.
Complementary and alternative medicine or other interventions
The small study of acupuncture, control acupuncture and massage in 61 women at different points in pregnancy (11–28 weeks)229 was of unclear risk of bias and used the BDI at 10 weeks postnatally. All of the trials within CAM or other were at unclear or high risk of bias.
Summary of qualitative findings for indicated preventive interventions
Three qualitative studies presented data from those who had received an indicated preventive intervention and provided at least moderate certainty with regard to their findings. For an indicated population, the specific attention to developing strategies for better management of interpersonal relationships, as offered by IPT approaches, was important. Although the experience of individual women is unique, as affirmed by the expert group of service users, the facility for normalisation and creation of realistic expectations of what to expect and of which strategies might help is key to intervention approaches. However, once again it must be recognised that conclusions on the appropriateness of IPT as an intervention are constrained by the lack of qualitative evidence on the other types of intervention. The good availability of a specialist perinatal and infant mental health service appeared to be an essential part of an indicated preventive intervention although it should be noted that referral and discharge processes could cause anxiety, and how these are dealt with is of key importance.
Economic analysis
This is the most up-to-date review of trials about the prevention or management of PND and provides the first estimate of the cost-effectiveness of preventing PND. The review included economic evaluations alongside trials, decision models and a cost study. In addition to the clinical outcomes, the review was able to combine the effectiveness data with the incremental costs for each intervention. Data from the PoNDER trial61 were used to estimate a relationship between EPDS scores and SF-6D, allowing the QALYs produced by each intervention in the NMA of EPDS scores to be estimated. The incremental costs and QALYs for each intervention compared with standard care were used to estimate the cost-effectiveness of the intervention against standard care. In addition, fully incremental analyses were conducted, as were value of information analyses.
These estimates do not take into account any effects on the infant and the potential for them to benefit from QALY gain throughout their life course.
The universal preventive interventions with a relatively high probability of being optimal, and hence candidates for introduction within the NHS, were redesigned midwifery-led community postnatal care,264 PCA-based interventions61 and CBT-based interventions. 61,173
Education on preparing for parenting was estimated to be the most cost-effective of the selective preventive interventions. 189,191
Of the indicated preventive interventions, a PCA-based intervention was estimated to be the most cost-effective intervention, with the probability of the IPT-based intervention being optimal increasing as the willingness to pay per QALY increased.
There is genuine uncertainty as to the most effective intervention within the three levels of preventive intervention. In addition, the economic analysis has provided an analysis of the value of further research in the area. Assuming a willingness to pay of £20,000 per QALY, the population analysis (EVPI) values are very large, in excess of £150M for all analyses. For the universal preventive interventions, selective preventive interventions and indicated preventive interventions, the EVPI was estimated to be £1930M, £205M and £166M, respectively. These results were limited to those interventions for which an EPDS mean score was available. Overall, there was considerable uncertainty about the most cost-effective intervention in all populations as the cost estimations and estimations of the area under the curve were simple and the absolute QALY gains were small for all interventions. Expected value of information analyses quantify the expected gain from obtaining further information to inform decisions. For further research to be worthwhile, the EVPI must exceed the planned research costs. No definitive answer can be provided regarding the most cost-effective intervention because of the large uncertainty regarding the relative efficacies of the interventions. Given the high EVPPI values which exceed the cost of trials, future trials assessing the relative efficacies of promising interventions appear value for money.
Limitations of the quantitative evidence base
Replication of interventions
One limitation of the evidence base, and therefore the evidence synthesis, was the lack of replication of interventions, other than of usual care as a control intervention. The exceptions were ‘education on preparing for parenting’,189,191 ‘promoting parent–infant interaction’,164,174 ‘CBT-based intervention’61,165,168,173 and ‘IPT-based intervention’. 169,170 Within the interventions there was variation in skills of the care provider and the format, timing and duration of the intervention provided.
It was not possible for the review team to verify any potential benefits suggested by investigators who reported statistically significant effects on small trials of unclear risk of bias. Similarly, when investigators reported statistically non-significant results in trials that were not adequately powered to detect clinically meaningful effects, the results remain uncertain.
Despite the number of interventions assessed for the prevention of PND and the large number of trials conducted, there was generally a lack of replication of trials to confirm intervention effects. The lack of replication meant that there were insufficient sample data (i.e. trials) to estimate the between-trial SD from the data alone. The reasons for the lack of replication concern the complexity of the aetiology of PND and the additional skills required for interventions to be tested in addition to the novelty of the research overall in this generally neglected area of research.
Moderators and mediators
The random (treatment)-effect models assumed that there was heterogeneity of treatment effects between trials. The mean of the random-effects distribution represents the pooled mean across the population and does not relate to women with any specific characteristics. Data were available from trials describing the study-level characteristics of the participants and the intervention provider as continuous or dichotomous outcomes. When there is heterogeneity between trials, it is sometimes possible to use meta-regression to explore whether or not study-level characteristics are treatment effect modifiers. However, it was not possible to perform a meta-regression in this instance because there was insufficient replication of each treatment effect across trials.
Limitations of the included trials
Quality of the trials
The Cochrane risk-of-bias assessment allowed a robust assessment of the risk of bias by two reviewers for the 86 RCTs. The highest level of assessed risk was for allocation concealment, followed by incomplete outcome data, then random sequence generation. Rather than excluding trials on the basis of an assessment of high risk of bias, all of the included trials were incorporated into the NMA irrespective of the assessment of risk of bias. The trials for which there appeared to be the most beneficial treatments were nearly all assessed as being at low risk of bias. Knowledge of the methodological weaknesses of the trials that were assessed as high risk of bias allows recommendations to be made about how to improve the general standard of research in the field.
Heterogeneity of trial participants
The participants’ characteristics reflected the heterogeneity of the individual trials: country, care system, severity of depression, risk factors, age, HIV serostatus, thyroid status, traumatic birth experience and intimate partner violence. The mean age of participants ranged from 16 to 33 years. The trials with young participants were mainly the selective preventive intervention trials.
Intervention provider
More than 30 different health-care professionals (doctors, nurses and midwives), community volunteers and peer workers, and specialists (acupuncture, physiotherapy, counselling, massage, psychology, social work yoga) were involved in providing the interventions. The training ranged from 4 hours for peer support workers to master- and doctoral-level clinicians with supervision and the use of training manuals. It was not possible to determine whether or not a longer length of training was associated with greater effectiveness, although it is likely that the longer the length of training was associated with a greater cost.
Variations in health-care practice are important and may be attributable to components related to practitioners as individuals and women as individuals and the interaction between them. A highly skilled practitioner may be able to develop a trusting relationship with many people; a very much less skilled practitioner with only some people. The skills are trainable but only to some extent. In individual trials with access to individual-level data, with many women and many practitioners it should be possible to carry out multilevel modelling that would enable an estimate of the practitioner effect. When there are few participants and only one or two practitioners providing the intervention, it is not possible to disentangle the practitioner effect.
Usual care in the UK
The reference treatment was usual care but we acknowledge that this varies between countries and within countries. We consulted a number of experts around the world to gain their views on the comparability of usual care in the UK with usual care in the other countries where trials were conducted. Usual perinatal care was defined as routine antenatal or postnatal care for healthy women with uncomplicated pregnancies. The consultation allowed us to conclude that care in Australia, Canada, Europe (France and Norway) and the USA was comparable for the network with usual care in the UK, but that it would not be possible to form a network with usual care provided in China (Hong Kong), Japan, Mexico, Pakistan, South Africa and Taiwan.
Measures of depression
Over 100 different instruments had been used in the included trials, reflecting the lack of focus on particular outcomes or the lack of validated instruments used. Trials using the EPDS were selected as the focus for this review because this was the instrument most frequently used in the trials and because, being a continuous measure, results were presented as mean (SD) values. EPDS data are not normally distributed and methods of analysis should acknowledge the skewness of the data. The EPDS can also be used as a dichotomous measure for use in clinical practice, but a score of below a certain threshold does not confirm the absence of depression. 2 Further research might examine the outcomes of trials which used other primary outcome measures or diagnostic instruments when measuring depression.
Treatment end points
The reason for the measuring outcomes at 6 weeks, 10 weeks, 12 weeks, 16 weeks, 4–5 months, 6 months, 7 months, 9 months and 12 months postnatally is not clear. A reduction in some of the time points to 6 weeks, 12 weeks, 6 months and 12 months postnatally would allow monitoring of any enduring effect to 12 months postnatally and allow a better comparison with the outcomes in other trials.
Infant outcomes
One of the potential effects of PND is the impact on infant development. An infant can be exposed to a ‘cumulative dose of depression’ by either severity or duration and infants may vary in their susceptibility to the effects of PND. Impact of interventions on infants is difficult to determine before the age of 12 months and is often assessed by parental reports or more objective researcher assessments in controlled situations. Few of the trials reported outcomes to 12 months or reported infant outcomes at all. It would be important to use repeated measures analysis to 12 months postnatally or longer, and explore if any effect on infant development varied over time and if infant development scores correlated with maternal depression scores over time. Infants of women who were depressed in pregnancy or postnatally have been followed up to school age and beyond and there is evidence of lifelong effects on infants’ mental health. However, within the context of a RCT, we are only aware of the PoNDER trial which followed up infants to 18 months postnatally. In the included studies which measured infant outcomes,61,149,153,168,174,201,211 using the Ainsworth Strange Situation Assessment of Infant Attachment, Bayley Scales of Infant Development, Behaviour Screening Questionnaire, Children’s Global Assessment Scale, Infant Characteristics Questionnaire and the Infant Toddler Social Emotional Assessment there was no clear benefit for infants in the measures used. It was not possible to perform a NMA. The sample size for trials examining infant outcomes should be appropriately large to determine differences where they exist. The main reason for the expansion of interest in PND in recent years is the recognition of the impact this usually self-limiting maternal condition has on the mental health of the infant across the life course. It is therefore a serious limitation of the review that the effects of intervention on this outcome could not be assessed.
Strengths of the review
We undertook a rigorous systematic review and we believe that we identified all relevant trials evaluating the clinical effectiveness of interventions to prevent PND. Although we appraised and summarised a very large number of trials, much of the evidence was inconclusive because of inconsistency in determining an at-risk population for identifying the level of preventive intervention; outcomes measured; thresholds used in the same outcome measure; follow-up time points; and timing, duration and intensity of individual intervention provided.
The analysis approach differs from that used in previous Cochrane reviews233,417 and other reviews423 which did not distinguish between interventions within trials in terms of the control or comparator interventions. The 2013 Cochrane review417 did not consider specific interventions separately but combined different psychosocial and psychological interventions. In contrast, our objective was to assess the clinical effectiveness and cost-effectiveness of individual interventions and the value of collecting additional information. These reviews were unable to make inferences about the relative effects of specific interventions, beyond class effects for psychological, educational, social and pharmacological interventions. The assumptions that they made were that intervention effects within a class were identical rather than treating them as related and exchangeable.
Previous reviews used standardised effect sizes rather than EPDS scores. Standardised effect sizes have been criticised on the basis that trials with identical results may spuriously appear to give different results. This can lead to estimates that were smaller in magnitude than other trials but appear greater, and vice versa. Working with standardised mean scores would also require a mapping to utility. Previous reviews also tended to ignore the time at which assessments were made, often taking the latest assessment time; this would be reasonable if the treatment effect was constant over time, although little attempt has been made to test this assumption.
A further strength was the development of a de novo model which allowed the cost-effectiveness of each intervention compared with usual care to be estimated. Furthermore, fully incremental analyses and value of information calculations were undertaken.
Limitations of the review
The NMA offers an advance on previous reviews. Nevertheless, there are some limitations with the current analysis:
-
Some trials were omitted because they did not provide EPDS scores and this may have introduced reporting or selection bias. In principle, a multivariate meta-analysis would allow correlation between outcomes to be estimated in trials that provide multiple outcomes. However, this would involve a multivariate NMA of multiarm trials, which is beyond the scope of this review.
-
No adjustment was made for the lack of quality associated with some trials. Evidence was taken at face value and treatment effects may thus be overstated.
-
The analysis of EPDS scores assumes independence of outcomes within trials and independence of population intervention effects between trials. The EPDS scores are longitudinal within trials (i.e. repeated measures) and EPDS mean scores are expected to be more similar within trials than between trials. We would also expect population mean intervention effects to be correlated between trials at different times and for the between study SD to be different at different times. However, the lack of replication of pairs of interventions means that these parameters would be difficult to estimate without external information, which is beyond the scope of this review.
-
A limitation of the economic evaluation was that estimations of incremental costs and the methodology used in the area under the curve model were by necessity, simplistic which may have introduced inaccuracy.
-
Infant outcomes were not examined in detail because of inconsistent published infant outcome data.
-
Family outcomes were not examined in detail because of insufficient outcome data.
Discussion of all qualitative findings
In addition to the 21 qualitative studies of interventions, a further 23 studies reported qualitative data on perspectives and attitudes of women who had not experienced PND, regarding PSSSs that they believe helped them to prevent the condition. Included studies were generally of moderate to high quality and, therefore, taken individually or collectively provide at least moderate certainty with regard to their findings. Although the hypothetical nature of suggested strategies must be acknowledged, this body of evidence clearly provides a useful counterpoint to interventions that are largely hypothesised by service providers. Generally, this wider evidence base confirmed the presence of many features considered important by women within existing interventions. However, the team’s ability to identify these components was constrained by the limited detail of reporting of each intervention. Nevertheless, we believe that each intervention, current or planned, should be evaluated against the list of strategies considered helpful by women who avoided PND. The findings of the qualitative review may therefore make a major contribution to design of future interventions.
The implications of the main findings of this review
Findings associated with the evidence base: methodological implications
Previous reviews have found no evidence to recommend any intervention for preventing PND because of methodological limitations.
Many trials reviewed were pilot studies or had small or non-generalisable samples. Overall, the universal preventive intervention trials were rated to have greater risks of bias than the selective and indicated preventive interventions; this was most notable for selection bias and attrition bias. This may be an inevitable consequence of research with women in this population. Fundamental reporting of quality criteria applicable to all trials, random sequence generation and allocation concealment would, however, improve (when it occurred) the quality assessment of up to 25% of trials.
Implications for future research in the prevention of postnatal depression
The implications of the findings are that a variety of different approaches may be valuable in the prevention of PND. Identifying the single best approach for each level of preventive intervention may be what service commissioners require. Future trials could investigate individual women’s preferences for approaches and the impact on effectiveness of offering women choice. Rather than establish a new practitioner role future trials could examine the effectiveness of the development of additional skills in practitioners who already work with pregnant and postnatal women. Examining the effectiveness of training in a PCA-based intervention, a CBT-based intervention or an IPT-based intervention would require a large enough sample to undertake practitioner-level analysis, to explore practitioner variability.
In future trials, the data generation process for the EPDS should be better considered. EPDS data are ordered categorical data and calculating a sample mean and sample SD for the purpose of statistical inference means appealing to the central limit theorem. In general, the sample sizes were not large enough for the central limit theorem to apply. Future estimates of treatment effect should be based on methods of analysis using ordered categorical techniques. It would still be possible to estimate population EPDS mean scores, rather than sample mean scores, but based on the population proportion of women. Using the current approach of using the sample mean can lead to negative estimates of absolute mean EPDS mean scores when it is assumed that the distribution of EPDS scores is normal.
Edinburgh Postnatal Depression Scale scores may be dichotomised in clinical practice as an assessment of risk and therefore operate as a decision aid for individual women to have further intervention. Within clinical trials, dichotomising EPDS scores according to a threshold for the purpose of making inferences about interventions is less appropriate. It has been recommended that dichotomies should be abandoned so that people are not arbitrarily divided into groups, by using thresholds on an underlying continuous scale. Calculating sample sizes based on dichotomous measures is regarded as inefficient in unnecessarily increasing the size of clinical trials, as well as contributing to overestimates of the extent to which different women respond differently to the same treatment.
Variation in the implementation of these interventions will manifest itself as heterogeneity between trials in treatment effect (i.e. in the estimate of the between-trial SD). When the evidence suggests that interventions are beneficial and cost-effective relative to usual care then it would be necessary to do further research to identify under what circumstances the treatment is beneficial (and not beneficial).
The value of information analyses undertaken produced EVPPI values for the relative efficacy of treatment in excess of £150M for each population. This is more than sufficient to fund research assessing the most effective intervention in each population. Comparing interventions in such a way that feedback loops could be created would create indirect as well as direct evidence (thereby strengthening inference) and would allow an assessment of inconsistency and adjustment for bias.
Implications for individual interventions
There are a number of hypothesised components for successful inclusion in an intervention, presented in full in Chapter 8 and Table 55 specifically. At a minimum, an intervention should allow women to develop trusting relationships with the care provider, feel supported, access information, have continuity of care, have individual-centred care and to have their partner involved. For health-care providers, there should be support with appropriate training, skills and resources, for them to respond to cues about how a woman is feeling.
Different psychological approaches (CBT-based, PCA-based and IPT-based) all were possibly cost-effective within the three levels of preventive interventions. The role of non-specific factors, such as congruence, positive regard and empathy, in psychotherapeutic interventions has been recognised. Skilled therapists may have multiple trainings and select the different approaches to suit clients at particular stages in their intervention. Skills to help women feel that they can trust their care provider and develop a continuing, supportive relationship, for example with a midwife or health visitor, would help address the needs of pregnant and postnatal women.
Chapter 11 Conclusion
Implications from this review for further research
The following recommendations are made for RCTs of preventive interventions for PND:
-
Trials should be designed appropriately powered to address important hypotheses of interest: maternal and infant related.
-
Sample sizes should be based on clear statistical criteria and an understanding of a clinically important difference.
-
Trials should collect and report a battery of a few, consistent outcome measures.
-
Outcomes should be measured at consistent time points – 6 weeks, 12 weeks, 6 months, 12 months postnatally.
-
Outcomes should include anxiety.
-
Trials should be in targeted populations.
-
There should be a clear justification for the interventions being trialled.
-
Women’s perspectives on what they might find helpful should precede a RCT.
-
Attention should be paid to the needs of women for a trusting, supportive, ongoing relationship with a care provider in the intervention development phase.
-
Utility data should be collected for each intervention.
-
Detailed costing data should be collected for each intervention.
-
Women’s and service providers’ perspectives should be gathered alongside an ongoing trial in properly planned qualitative studies.
-
Trials should include multiple interventions.
-
Large data sets resulting from properly populated studies can be combined to allow multilevel modelling to disentangle moderators and mediators and specifically practitioner- and service-level effects.
Implications from this review for service provision
The activity represented by this volume of trials which aimed to prevent PND rather than treat PND emphasises the importance of the condition and the potential benefit for perinatal women, infants and partners. Of the trials included in the NMA, the most beneficial treatments appeared to be midwifery redesigned postnatal care,146 PCA-based intervention61 and CBT-based intervention. 61 The effect of the interventions appeared to be small. Trials of parent–infant interaction including infant outcomes explicitly and replication would be important to confirm these findings. Although one intervention may not prevent the onset of depression, it may reduce the severity of symptoms and extrapolated to a population level that would represent a large benefit.
Suggestions for research priorities
Preventive interventions should be relatively simple and inexpensive, particularly when they are to be applied to a universal population. Small trials are useful in assessing feasibility or generating hypotheses but potential treatment effects need to be confirmed in properly designed and conducted RCTs. Similarly, treatment effects based on small sample sizes from a limited number of trials should also be confirmed in properly designed and conducted RCTs. Specific interventions that are worthy of further evaluation include:
-
As a universal preventive intervention: midwifery redesigned postnatal care, PCA-based interventions, CBT-based interventions and preparing for parenting.
-
As a selective preventive intervention: CenteringPregnancy, IPT-based interventions and education on preparing for parenting.
-
As an indicated preventive intervention: PCA-based interventions, CBT-based interventions, IPT-based interventions, promoting parent–infant interaction, telephone-based peer support and Newpin volunteer peer support.
Acknowledgements
We acknowledge the help from Professor Christine MacArthur, Professor Debra Bick, Professor Jeanette Milgrom, Professor Julie Jomeen, Professor Martin Knapp, Professor Mike O’Hara, Professor Nine Glangeaud, Dr Kari Glavin, Dr Pauline Hall and Michelle Coghlan.
Contributions of authors
All authors were involved in writing draft and final versions of the report.
C Jane Morrell (Associate Professor in Health Research) co-ordinated the review, wrote the background section of the report, and conducted the clinical effectiveness systematic review (screening and retrieving papers, assessing against the inclusion criteria and appraising the quality of papers and abstracting information from papers for synthesis), wrote sections of the results and discussion and assembled the final report.
Paul Sutcliffe (Associate Professor, Deputy Director for Warwick Evidence) co-ordinated the review, wrote the abstract and scientific summary, conducted the clinical effectiveness systematic review (screening and retrieving papers, assessing against the inclusion criteria and appraising the quality of papers and abstracting information from papers for synthesis), and wrote sections of the results and discussion.
Andrew Booth (Reader in Evidence-Based Information Practice) conducted the realist synthesis; and contributed to methodology, data extraction and interpretation of the qualitative synthesis.
John Stevens (Reader in Decision Science, Director, Centre for Bayesian Statistics in Health Economics, Health Economics and Decision Science) led on the quantitative synthesis, co-ordinated the NMA and wrote sections of the results and discussion.
Alison Scope (Research Fellow, Health Economics and Decision Science) led on the qualitative synthesis and completed most of the data extraction and the initial analysis and interpretation.
Matt Stevenson (Professor of HTA, Health Economics and Decision Science) constructed the mathematical model, generated and interpreted the results, and had overall responsibility for the modelling chapter.
Rebecca Harvey (Research Associate in Medical Statistics, Health Economics and Decision Science) carried out the evidence synthesis, assisted with drafting the statistical results and data extraction of the trials included in the NMA.
Alice Bessey (Research Associate Health Economics and Decision Science) undertook the economic evaluation literature review, did the costing of interventions for economic evaluation and contributed to the health economic chapter.
Anna Cantrell (Information Specialist, Information Resources Group, Health Economics and Decision Science) led on the literature searching for the quantitative, qualitative and economic components of the review, managed the reference management database and performed the update procedures.
Cindy-Lee Dennis (Professor in Nursing and Medicine, Department of Psychiatry; Canada Research Chair in Perinatal Community Health) assisted in screening studies and selecting eligible trials for inclusion; contributed to data extraction, assessment of risk of bias, edited chapters; and commented on the final draft
Shijie Ren (Statistician, Health Economics and Decision Science) wrote sections of the background, edited chapters and commented on the final draft.
Margherita Ragonesi (Visiting Clinical Psychology Academic, University of Bologna) developed the data extraction tool and conducted the data extraction.
Michael Barkham (Professor in Clinical Psychology, Department of Psychology) contributed to the original proposal, wrote sections of the background and discussion, edited chapters and commented on final draft.
Dick Churchill (Clinical Associate Professor/Director of Clinical Skills) commented on drafts chapters and wrote sections of the final report.
Carol Henshaw (Psychiatrist, Division of Psychiatry) assisted with the grey literature search, assessing risk of bias of pharmacological interventions and commenting on drafts of the final report.
Jo Newstead (EP Group Co-ordinator) contributed to the research proposal, led the PPI input, co-ordinated the EP group, wrote the sections for the report from a service user perspective, provided comments on all report chapters and drafted the Plain English summary.
Pauline Slade (Professor of Clinical Psychology, Consultant Clinical Psychologist) contributed to the original proposal and commented on drafts of the final report through perinatal clinical psychology expertise.
Helen Spiby (Professor of Midwifery) provided a midwifery perspective; contributed to the design of the research, filtering of the results of the searches and interpretation of the data; wrote sections for the final report; provided critical review of drafts of the report; and commented on the final version.
Sarah Stewart-Brown (Professor of Public Health Statistics and Epidemiology) advised on design of searches and the selection of trials for inclusion with regard to complementary and alternative approaches; advised on classification of preventive interventions and interpretation of findings; and contributed to the final report.
Data sharing statement
Data can be obtained from the corresponding author.
Disclaimers
This report presents independent research funded by the National Institute for Health Research (NIHR). The views and opinions expressed by authors in this publication are those of the authors and do not necessarily reflect those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health. If there are verbatim quotations included in this publication the views and opinions expressed by the interviewees are those of the interviewees and do not necessarily reflect those of the authors, those of the NHS, the NIHR, NETSCC, the HTA programme or the Department of Health.
References
- O’Hara MW, McCabe JE. Postpartum depression: current status and future directions. Annu Rev Clin Psychol 2013;9:379-407. http://dx.doi.org/10.1146/annurev-clinpsy-050212-185612.
- Cox J, Holden J, Henshaw C. Perinatal Mental Health: The Edinburgh Postnatal Depression Scale (EPDS) Manual. Glasgow: RCPsych Publications; 2014.
- Diagnostic and Statistical Manual of Mental Disorders. Arlington, VA: American Psychiatric Association; 2013.
- Maternal Mental Health and Child Health and Development. Improving Maternal Mental Health Millennium Development Goal 5 – Improving Maternal Health. Geneva: WHO; 2010.
- International Statistical Classification of Diseases and Related Health Problems. Geneva: WHO; 2010.
- Almond P. Postnatal depression: a global public health perspective. Perspect Public Health 2009;129:221-7. http://dx.doi.org/10.1177/1757913909343882.
- Oates MR, Cox JL, Neema S, Asten P, Glangeaud-Freudenthal N, Figueiredo B, et al. Postnatal depression across countries and cultures: a qualitative study. Br J Psychiatry 2004;46:s10-16. http://dx.doi.org/10.1192/bjp.184.46.s10.
- Rahman A, Fisher J, Bower P, Luchters S, Tran T, Yasamy MT, et al. Interventions for common perinatal mental disorders in women in low-and middle-income countries: a systematic review and meta-analysis. Bull World Health Organ 2013;91:593-601I. http://dx.doi.org/10.2471/BLT.12.109819.
- Gaynes BN, Gavin N, Meltzer BS, Lohr KN, Swinson T, Gartlehner G, et al. Perinatal Depression: Prevalence, Screening Accuracy, and Screening Outcomes. Rockville, MD: Agency for Healthcare Research and Quality; 2005.
- Cox J, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987;150:782-6. http://dx.doi.org/10.1192/bjp.150.6.782.
- Akman C, Uguz F, Kaya N. Postpartum-onset major depression is associated with personality disorders. Compr Psychiatry 2007;48:343-7. http://dx.doi.org/10.1016/j.comppsych.2007.03.005.
- Kumar R, Robson KM. A prospective study of emotional disorders in childbearing women. Br J Psychiatry 1984;144:35-47. http://dx.doi.org/10.1192/bjp.144.1.35.
- Cooper PJ, Murray L. Postnatal depression. BMJ 1998;316:1884-6. http://dx.doi.org/10.1136/bmj.316.7148.1884.
- Heron J, O’Connor TG, Evans J, Golding J, Glover V. the ALSPAC Study Team . The course of anxiety and depression through pregnancy and the postpartum in a community sample. J Affect Disord 2004;80:65-73. http://dx.doi.org/10.1016/j.jad.2003.08.004.
- Evans J, Heron J, Francomb H, Oke S, Golding J. Cohort study of depressed mood during pregnancy and after childbirth. BMJ 2001;323:257-60. http://dx.doi.org/10.1136/bmj.323.7307.257.
- Pearson RM, Evans J, Kounali D, Lewis G, Heron J, Ramchandani PG, et al. Maternal depression during pregnancy and the postnatal period: risks and possible mechanisms for offspring depression at age 18 years. JAMA Psychiatry 2013;70:1312-19. http://dx.doi.org/10.1001/jamapsychiatry.2013.2163.
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol 2005;106:1071-83. http://dx.doi.org/10.1097/01.AOG.0000183597.31630.db.
- Lee AM, Lam SK, Lau SM, Chong CS, Chui HW, Fong DY. Prevalence, course, and risk factors for antenatal anxiety and depression. Obstet Gynecol 2007;110:1102-12. http://dx.doi.org/10.1097/01.AOG.0000287065.59491.70.
- Engineer N, Darwin L, Nishigandh D, Ngianga-Bakwin K, Smith SC, Grammatopoulos DK. Association of glucocorticoid and type 1 corticotropin-releasing hormone receptors gene variants and risk for depression during pregnancy and post-partum. J Psychiatr Res 2013;47:1166-73. http://dx.doi.org/10.1016/j.jpsychires.2013.05.003.
- Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry 2004;26:289-95. http://dx.doi.org/10.1016/j.genhosppsych.2004.02.006.
- Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM. Risk factors for depressive symptoms during pregnancy: a systematic review. Am J Obstet Gynecol 2010;202:5-14. http://dx.doi.org/10.1016/j.ajog.2009.09.007.
- Russell S, Lang B. Perinatal Mental Health: Experiences of Women and Health Professionals 2013. www.bftalliance.co.uk/wp-content/uploads/2014/02/boots-perinatal-mental-health-09-10-13-web.pdf (accessed July 2014).
- Oates MR. Perinatal psychiatric syndromes: clinical features. Psychiatry 2009;8:1-6. http://dx.doi.org/10.1016/j.mppsy.2008.10.014.
- Murray L, Halligan S, Cooper P, Bremner JG, T. D. Wachs TD. The Wiley-Blackwell Handbook of Infant Development, Volume 2. Hoboken, NJ: Wiley-Blackwell; 2010.
- Murray L, Arteche A, Fearon P, Halligan S, Goodyer I, Cooper P. Maternal postnatal depression and the development of depression in offspring up to 16 years of age. J Am Acad Child Adolesc Psychiatry 2011;50:460-70. http://dx.doi.org/10.1016/j.jaac.2011.02.001.
- Brand SR, Brennan PA. Impact of antenatal and postpartum maternal mental illness: how are the children?. Clin Obstet Gynecol 2009;52:441-55. http://dx.doi.org/10.1097/GRF.0b013e3181b52930.
- Murray L, Marwick H, Arteche A. Sadness in mothers’ ‘baby-talk’ predicts affective disorder in adolescent offspring. Infant Behav Dev 2010;33:361-4. http://dx.doi.org/10.1016/j.infbeh.2010.03.009.
- Hay DF, Pawlby S, Sharp D, Asten P, Mills A, Kumar R. Intellectual problems shown by 11-year-old children whose mothers had postnatal depression. J Child Psychol Psychiatry 2001;42:871-89. http://dx.doi.org/10.1111/1469-7610.00784.
- Murray L, Arteche A, Fearon P, Halligan S, Croudace T, Cooper P. The effects of maternal postnatal depression and child sex on academic performance at age 16 years: a developmental approach. J Child Psychol Psychiatry 2010;51:1150-9. http://dx.doi.org/10.1111/j.1469-7610.2010.02259.x.
- Sinclair D, Murray L. Effects of postnatal depression on children’s adjustment to school. Teacher’s reports. Br J Psychiatry 1998;172:58-63. http://dx.doi.org/10.1192/bjp.172.1.58.
- Morrell J, Murray L. Parenting and the development of conduct disorder and hyperactive symptoms in childhood: a prospective longitudinal study from 2 months to 8 years. J Child Psychol Psychiatry 2003;44:489-508. http://dx.doi.org/10.1111/1469-7610.t01-1-00139.
- Hammen C, Brennan PA. Severity, chronicity, and timing of maternal depression and risk for adolescent offspring diagnoses in a community sample. Arch Gen Psychiatry 2003;60:253-8. http://dx.doi.org/10.1001/archpsyc.60.3.253.
- Hay DF, Pawlby S, Waters CS, Sharp D. Antepartum and postpartum exposure to maternal depression: different effects on different adolescent outcomes. J Child Psychol Psychiatry 2008;49:1079-88. http://dx.doi.org/10.1111/j.1469-7610.2008.01959.x.
- Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry 2010;67:1012-24. http://dx.doi.org/10.1001/archgenpsychiatry.2010.111.
- Huot RL, Brennan PA, Stowe ZN, Plotsky PM, Walker EF. Negative affect in offspring of depressed mothers is predicted by infant cortisol levels at 6 months and maternal depression during pregnancy, but not postpartum. Ann N Y Acad Sci 2004;1032:234-6. http://dx.doi.org/10.1196/annals.1314.028.
- Pawlby S, Hay DF, Sharp D, Waters CS, O’Keane V. Antenatal depression predicts depression in adolescent offspring: prospective longitudinal community-based study. J Affect Disord 2009;113:236-43. http://dx.doi.org/10.1016/j.jad.2008.05.018.
- Paulson JF, Bazemore SD. Prenatal and postpartum depression in fathers and its association with maternal depression: a meta-analysis. JAMA 2010;303:1961-9. http://dx.doi.org/10.1001/jama.2010.605.
- Antenatal and Postnatal Mental Health: The NICE Guideline on Clinical Management and Service Guidance. NICE Clinical Guidelines (CG45). London: NICE; 2007.
- Antenatal Care for Uncomplicated Pregnancies: NICE Clinical Guidelines (CG62). London: NICE; 2008.
- Births in England and Wales by Characteristics of Birth 2, 2012. London: Office for National Statistics; 2013.
- Department of Health . Maternal Mental Health Pathways 2012. www.gov.uk/government/publications/maternal-mental-health-pathway (accessed July 2014).
- Gaudion A, Bick D, Menka Y, Demilew J, Walton C, Yiannouzis K, et al. Adapting the CenteringPregnancy® model for a UK feasibility study. Br J Midwifery 2011;19:433-8. http://dx.doi.org/10.12968/bjom.2011.19.7.433.
- Gaudion A, Menka Y, Demilew J, Walton C, Yiannouzis K, Robbins J, et al. Findings from a UK feasibility study of the CenteringPregnancy® model. Br J Midwifery 2011;19:796-802. http://dx.doi.org/10.12968/bjom.2011.19.12.796.
- Rising SS. Centering pregnancy: an interdisciplinary model of empowerment. J Nurse Midwifery 1998;43:46-54. http://dx.doi.org/10.1016/S0091-2182(97)00117-1.
- Hewitt CE, Gilbody SM, Brealey S, Paulden M, Palmer S, Mann R, et al. Methods to identify postnatal depression in primary care: an integrated evidence synthesis and value of information analysis. Health Technol Assess 2009;13. http://dx.doi.org/10.3310/hta13360.
- Morrell CJ. Review of interventions to prevent or treat postnatal depression. Clin Eff Nurs 2006;9:e135-61. http://dx.doi.org/10.1016/j.cein.2006.11.006.
- Hearn G, Iliff A, Jones I, Kirby A, Ormiston P, Parr P, et al. Postnatal depression in the community. Br J Gen Pract 1998;48:1064-6.
- Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instruments for depression. J Gen Intern Med 1997;12:439-45. http://dx.doi.org/10.1046/j.1525-1497.1997.00076.x.
- Spitzer RL, Kroenke K, Williams JB. The development and validation of a version of PRIME-MD: the PHQ primary care study. JAMA 1999;282:1737-44. http://dx.doi.org/10.1001/jama.282.18.1737.
- Zigmund AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983;67:361-70. http://dx.doi.org/10.1111/j.1600-0447.1983.tb09716.x.
- Brealey SD, Hewitt C, Green JM, Morrell J, Gilbody S. Screening for postnatal depression: is it acceptable to women and healthcare professionals? A systematic review and meta-synthesis. Reprod Infant Psychol 2010;28:328-44. http://dx.doi.org/10.1080/02646838.2010.513045.
- Shakespeare J. An Evaluation of Screening for Postnatal Depression Against the NSC Handbook Criteria. Oxford: National Screening Committee; 2001.
- Petrou S, Cooper P, Murray L, Davidson LL. Economic costs of post-natal depression in a high-risk British cohort. Br J Psychiatry 2002;181:505-12. http://dx.doi.org/10.1192/bjp.181.6.505.
- Bauer A, Pawlby S, Plant D, King D, Pariante C, Knapp M. Perinatal depression and child development: exploring the economic consequences from a South London cohort. Psychol Med 2014;45:51-6. http://dx.doi.org/10.1017/S0033291714001044.
- Edoka IP, Petrou S, Ramchandani PG. Healthcare costs of paternal depression in the postnatal period. J Affect Disord 2011;133:356-60. http://dx.doi.org/10.1016/j.jad.2011.04.005.
- Campbell S, Norris S, Standfield L, Suebwongpat A. Screening for Postnatal Depression Within the Well Child Tamariki Ora Framework. Christchurch: Health Services Assessment Collaboration (HSAC); 2008.
- Paulden M, Palmer S, Hewitt C, Gilbody S. Screening for postnatal depression in primary care: cost effectiveness analysis. BMJ 2009;339. http://dx.doi.org/10.1136/bmj.b5203.
- Petrou S, Morrell CJ, Knapp M, Milgrom J, Gemmill AW. Identifying Perinatal Depression and Anxiety: Evidence-Based Practice in Screening, Psychosocial Assessment and Management. Oxford: Wiley; 2015.
- Knapp M, King D, Healey A, Thomas C. Economic outcomes in adulthood and their associations with antisocial conduct, attention deficit and anxiety problems in childhood. J Ment Health Policy Econ 2011;14:137-47.
- Appleby L, Warner R, Whitton A, Faragher B. A controlled study of fluoxetine and cognitive–behavioural counselling in the treatment of postnatal depression. BMJ 1997;314:932-6. http://dx.doi.org/10.1136/bmj.314.7085.932.
- Morrell CJ, Warner R, Slade P, Dixon S, Walters S, Paley G, et al. Psychological interventions for postnatal depression: cluster randomised trial and economic evaluation. The PoNDER trial. Health Technol Assess 2009;13. http://dx.doi.org/10.3310/hta13300.
- Cuijpers P, Brannmark JG, Straten A. Psychological treatment of postpartum depression: a meta-analysis. J Clin Psychol 2008;64:103-18. http://dx.doi.org/10.1002/jclp.20432.
- Dimidjian S, Goodman S. Nonpharmacologic intervention and prevention strategies for depression during pregnancy and the postpartum. Clin Obstet Gynecol 2009;52:498-515. http://dx.doi.org/10.1097/GRF.0b013e3181b52da6.
- Munoz RF, Beardslee WR, Leykin Y. Major depression can be prevented. Am Psychol 2012;67. http://dx.doi.org/10.1037/a0027666.
- England NHS . A Call to Action: Commissioning for Prevention 2013. www.england.nhs.uk/wp-content/uploads/2013/11/call-to-action-com-prev.pdf (accessed July 2014).
- Marmot MG, Allen J, Goldblatt P, Boyce T, McNeish D, Grady M, et al. Fair Society, Healthy Lives: Strategic Review of Health Inequalities in England Post-2010. London: The Marmot Review; 2010.
- Mrazek PJ, Haggerty RJ. Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research. Washington, DC: National Academies Press; 1994.
- Cuijpers P, Straten A, Smit F. Preventing the incidence of new cases of mental disorders: a meta-analytic review. J Nerv Ment Dis 2005;193:119-25. http://dx.doi.org/10.1097/01.nmd.0000152810.76190.a6.
- Barker ED, Jaffee SR, Uher R, Maughan B. The contribution of prenatal and postnatal maternal anxiety and depression to child maladjustment. Depress Anxiety 2011;28:696-702. http://dx.doi.org/10.1002/da.20856.
- Jane-Llopis EVA, Hosman C, Jenkins R, Anderson P. Predictors of efficacy in depression prevention programmes meta-analysis. Br J Psychiatry 2003;183:384-97. http://dx.doi.org/10.1192/bjp.183.5.384.
- Hollon SD, Thase ME, Markowitz JC. Treatment and prevention of depression. Psychol Sci Public Interest 2002;3:39-77. http://dx.doi.org/10.1111/1529-1006.00008.
- Khan A, Faucett J, Lichtenberg P, Kirsch I, Brown WA. A systematic review of comparative efficacy of treatments and controls for depression. PLOS ONE 2012;7. http://dx.doi.org/10.1371/journal.pone.0041778.
- Hollon SD, Ponniah K. A review of empirically supported psychological therapies for mood disorders in adults. Depress Anxiety 2010;27:891-932. http://dx.doi.org/10.1002/da.20741.
- Robinson LA, Berman JS, Neimeyer RA. Psychotherapy for the treatment of depression: a comprehensive review of controlled outcome research. Psychol Bull 1990;108:30-49. http://dx.doi.org/10.1037/0033-2909.108.1.30.
- Cuijpers P, Van Straten A, Andersson G, van Oppen P. Psychotherapy for depression in adults: a meta-analysis of comparative outcome studies. J Consult Clin Psychol 2008;76. http://dx.doi.org/10.1037/a0013075.
- Munder T, Brutsch O, Leonhart R, Gerger H, Barth J. Researcher allegiance in psychotherapy outcome research: an overview of reviews. Clin Psychol Rev 2013;33:501-11. http://dx.doi.org/10.1016/j.cpr.2013.02.002.
- Leykin Y, DeRubeis RJ. Allegiance in psychotherapy outcome research: Separating association from bias. Clin Psychol (New York) 2009;16:54-65. http://dx.doi.org/10.1111/j.1468-2850.2009.01143.x.
- Lambert MJ, Lambert MJ. Bergin and Garfield’s Handbook of Psychotherapy and Behavior Change. London: John Wiley & Sons; 2013.
- Lambert MJ, Norcoss JC, Goldfried MR. Handbook of Psychotherapy Integration. New York, NY: Basic Books; 1992.
- Cuijpers P, Driessen E, Hollon SD, van Oppen P, Barth J, Andersson G. The efficacy of non-directive supportive therapy for adult depression: a meta-analysis. Clin Psychol Rev 2012;32:280-91. http://dx.doi.org/10.1016/j.cpr.2012.01.003.
- Horvath AO, Greenberg LS. Development and validation of the Working Alliance Inventory. J Couns Psychol 1989;36. http://dx.doi.org/10.1037/0022-0167.36.2.223.
- Martin DJ, Garske JP, Davis MK. Relation of the therapeutic alliance with outcome and other variables: a meta-analytic review. J Consult Clin Psychol 2000;68:438-50. http://dx.doi.org/10.1037/0022-006X.68.3.438.
- Rosenzweig S. Some implicit common factors in diverse methods of psychotherapy. Am J Orthopsychiatry 1936;6. http://dx.doi.org/10.1111/j.1939-0025.1936.tb05248.x.
- Frank JD. Persuasion and Healing: A Comparative Study of Psychotherapy. Baltimore, MD: Johns Hopkins University Press; 1993.
- Stiles WB, Shapiro DA, Elliott R. Are all psychotherapies equivalent?. Am Psychol 1986;41:165-80. http://dx.doi.org/10.1037/0003-066X.41.2.165.
- Kazdin AE. Treatment outcomes, common factors, and continued neglect of mechanisms of change. Clin Psychol (New York) 2005;12:184-8. http://dx.doi.org/10.1093/clipsy.bpi023.
- Petch J, Halford WK. Psycho-education to enhance couples’ transition to parenthood. Clin Psychol Rev 2008;28:1125-37. http://dx.doi.org/10.1016/j.cpr.2008.03.005.
- Billingham K. Preparing for parenthood: the role of antenatal education. Community Pract 2011;84:36-8.
- Nolan ML. Information giving and education in pregnancy: a review of qualitative studies. J Perinat Educ 2009;18:21-30. http://dx.doi.org/10.1624/105812409X474681.
- Mitnick DM, Heyman RE, Smith Slep AM. Changes in relationship satisfaction across the transition to parenthood: a meta-analysis. J Fam Psychol 2009;23:848-52. http://dx.doi.org/10.1037/a0017004.
- Shapiro AF, Gottman JM, Carrere S. The baby and the marriage: identifying factors that buffer against decline in marital satisfaction after the first baby arrives. J Fam Psychol 2000;14:59-70. http://dx.doi.org/10.1037/0893-3200.14.1.59.
- Cowan CP, Cowan PA. Interventions to ease the transition to parenthood: Why they are needed and what they can do. Fam Relat 1995;44:412-23. http://dx.doi.org/10.2307/584997.
- O’Hara MW, Swain AM. Rates and risk of postpartum degression – a meta-analysis. Int Rev Psychiatry 1996;8:37-54. http://dx.doi.org/10.3109/09540269609037816.
- Deave T, Johnson D, Ingram J. Transition to parenthood: the needs of parents in pregnancy and early parenthood. BMC Pregnancy Childbirth 2008;8:30-44. http://dx.doi.org/10.1186/1471-2393-8-30.
- Petch J, Halford WK, Creedy DK, Gamble J. Couple relationship education at the transition to parenthood: a window of opportunity to reach high risk couples. Fam Process 2012;51:498-511. http://dx.doi.org/10.1111/j.1545-5300.2012.01420.x.
- Cobb S. Social support as a moderator of life stress. Psychosom Med 1976;38:300-14. http://dx.doi.org/10.1097/00006842-197609000-00003.
- Dennis CL. Peer support within a health care context: a concept analysis. Int J Nurs Stud 2003;40:321-32. http://dx.doi.org/10.1016/S0020-7489(02)00092-5.
- Cohen S, Underwood L, Gottlieb BH. Social Support Measurement and Intervention: A Guide For Health and Social Scientists. Oxford: Oxford University Press; 2000.
- Lin N, Ye X, Ensel WM. Social support and depressed mood: a structural analysis. J Health Soc Behav 1999;40:344-59. http://dx.doi.org/10.2307/2676330.
- Berkman LF, Glass T, Berkman LF, Kawachi I. Social Epidemiology. New York, NY: Oxford University Press; 2000.
- Thoits PA. Social support as coping assistance. J Consult Clin Psychol 1986;54. http://dx.doi.org/10.1037/0022-006X.54.4.416.
- Dalton K. Progesterone prophylaxis used successfully in postnatal depression. Practitioner 1985;229:507-8.
- Dalton K. Successful prophylactic progesterone for idiopathic postnatal depression. Int J Prenat Perinat Studies 1989;1:323-7.
- Dalton K. Progesterone prophylaxis for postnatal depression. Int J Prenat Perinat Psychol Med 1995;7:447-50.
- Turner KM, Sharp D, Folkes L, Hew-Graham C. Women’s views and experiences of antidepressants as a treatment for postnatal depression: a qualitative study. Fam Pract 2008;25:450-5. http://dx.doi.org/10.1093/fampra/cmn056.
- Browne JC, Scott KM, Silvers KM. Fish consumption in pregnancy and omega-3 status after birth are not associated with postnatal depression. J Affect Disord 2006;90:131-9. http://dx.doi.org/10.1016/j.jad.2005.10.009.
- Freeman MP, Davis M, Sinha P, Wisner KL, Hibbeln JR, Gelenberg AJ. Omega-3 fatty acids and supportive psychotherapy for perinatal depression: a randomized placebo-controlled study. J Affect Disord 2008;110:142-8. http://dx.doi.org/10.1016/j.jad.2007.12.228.
- Barnes PM, Bloom B, Nahin R. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report 2008;10:1-23.
- Pallivalappila AR, Stewart D, Shetty A, Pande B, McLay JS. Complementary and alternative medicines use during pregnancy: a systematic review of pregnant women and healthcare professional views and experiences. Evid Based Complement Alternat Med 2013. http://dx.doi.org/10.1155/2013/205639.
- Beddoe AE, Lee KA. Mind–body interventions during pregnancy. J Obstet Gynecol Neonatal Nurs 2008;37:165-75. http://dx.doi.org/10.1111/j.1552-6909.2008.00218.x.
- Bishop FL, Lewith GT. Who uses CAM? A narrative review of demographic characteristics and health factors associated with CAM use. Evid Based Complement Alternat Med 2010;7:11-28. http://dx.doi.org/10.1093/ecam/nen023.
- Xue CCL, Zhang AL, Lin V, Da Costa C, Story DF. Complementary and alternative medicine use in Australia: a national population-based survey. J Altern Complement Med 2007;13:643-50. http://dx.doi.org/10.1089/acm.2006.6355.
- Field T, Figueiredo B, Hernandez RM, Diego M, Deeds O, Ascencio A. Massage therapy reduces pain in pregnant women, alleviates prenatal depression in both parents and improves their relationships. J Bodyw Mov Ther 2008;12:146-50. http://dx.doi.org/10.1016/j.jbmt.2007.06.003.
- Field T, Deeds O, Diego M, Hernandez RM, Gauler A, Sullivan S, et al. Benefits of combining massage therapy with group interpersonal psychotherapy in prenatally depressed women. J Bodyw Mov Ther 2009;13:297-303. http://dx.doi.org/10.1016/j.jbmt.2008.10.002.
- Field T, Diego MA, Hernandez RM, Schanberg S, Kuhn C. Massage therapy effects on depressed pregnant women. J Psychosom Obstet Gynaecol 2004;25:115-22. http://dx.doi.org/10.1080/01674820412331282231.
- Mantle F. The role of alternative medicine in treating postnatal depression. Complement Ther Nurs Midwifery 2002;8:197-203. http://dx.doi.org/10.1054/ctnm.2002.0647.
- Zhang ZJ, Chen HY, Yip Kc, Ng R, Wong VT. The effectiveness and safety of acupuncture therapy in depressive disorders: systematic review and meta-analysis. J Affect Disord 2010;124:9-21. http://dx.doi.org/10.1016/j.jad.2009.07.005.
- Dennis CL, Allen K. Interventions (other than pharmacological, psychosocial or psychological) for treating antenatal depression. Cochrane Database Syst Rev 2008;4. http://dx.doi.org/10.1002/14651858.cd006795.pub2.
- Field T, Diego M, Hernandez RM, Medina L, Delgado J, Hernandez A. Yoga and massage therapy reduce prenatal depression and prematurity. J Bodyw Mov Ther 2012;16:204-9. http://dx.doi.org/10.1016/j.jbmt.2011.08.002.
- D’Silva S, Poscablo C, Habousha R, Kogan M, Kligler B. Mind–body medicine therapies for a range of depression severity: a systematic review. Psychosomatics 2012;53:407-23. http://dx.doi.org/10.1016/j.psym.2012.04.006.
- Vieten C, Astin J. Effects of a mindfulness-based intervention during pregnancy on prenatal stress and mood: results of a pilot study. Arch Womens Ment Health 2008;11:67-74. http://dx.doi.org/10.1007/s00737-008-0214-3.
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J Consult Clin Psychol 2010;78:169-83. http://dx.doi.org/10.1037/a0018555.
- Norman E, Sherburn M, Osborne RH, Galea MP. An exercise and education program improves well-being of new mothers: a randomized controlled trial. Phys Ther 2010;90:348-55. http://dx.doi.org/10.2522/ptj.20090139.
- Whitaker R, Hendry M, Booth A, Carter B, Charles J, Craine N, et al. Intervention Now To Eliminate Repeat Unintended Pregnancy in Teenagers (INTERUPT): a systematic review of intervention effectiveness and cost-effectiveness, qualitative and realist synthesis of implementation factors and user engagement. BMJ Open 2014;4. http://dx.doi.org/10.1136/bmjopen-2013-004733.
- Cochrane Community . Cochrane Central Register of Controlled Trials (CENTRAL) n.d. http://community.cochrane.org/editorial-and-publishing-policy-resource/cochrane-central-register-controlled-trials-central (accessed July 2014).
- Higgins J, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011;343. http://dx.doi.org/10.1136/bmj.d5928.
- MacKinnon DP. Integrating mediators and moderators in research design. Res Soc Work Pract 2011;21:675-81. http://dx.doi.org/10.1177/1049731511414148.
- Dias S, Sutton AJ, Ades AE, Welton NJ. Evidence synthesis for decision making 2A generalized linear modeling framework for pairwise and network meta-analysis of randomized controlled trials. Med Decis Making 2013;33:607-17. http://dx.doi.org/10.1177/0272989X12458724.
- Songøygard KM, Stafne SN, Evensen KA, Salvesen K, Vik T, Mørkved S. Does exercise during pregnancy prevent postnatal depression? A randomized controlled trial. Acta Obstet Gynecol Scand 2012;91:62-7. http://dx.doi.org/10.1111/j.1600-0412.2011.01262.x.
- Lunn DJ, Thomas A, Best N, Spiegelhalter D. WinBUGS-a Bayesian modelling framework: concepts, structure, and extensibility. Stat Comput 2000;10:325-37. http://dx.doi.org/10.1023/A:1008929526011.
- Brooks SP, Gelman A. Alternative methods for monitoring convergence of iterative simulations. J Comput Graph Stat 1988;7:434-55.
- Dakin HA, Welton NJ, Ades AE, Collins S, Orme M, Kelly S. Mixed treatment comparison of repeated measurements of a continuous endpoint: an example using topical treatments for primary open angle glaucoma and ocular hypertension. Stat Med 2011;30:2511-35. http://dx.doi.org/10.1002/sim.4284.
- Wei Y, Higgins J. Bayesian multivariate meta-analysis with multiple outcomes. Stat Med 2013;32:2911-34. http://dx.doi.org/10.1002/sim.5745.
- Riley RD. Multivariate meta-analysis: the effect of ignoring within-study correlation. J R Stat Soc Ser A 2009;172:789-98. http://dx.doi.org/10.1111/j.1467-985X.2008.00593.x.
- Glenton C, Colvin CJ, Carlsen B, Swartz A, Lewin S, Noyes J, et al. Barriers and facilitators to the implementation of lay health worker programmes to improve access to maternal and child health: qualitative evidence synthesis. Cochrane Database Syst Rev 2013;10. http://dx.doi.org/10.1002/14651858.cd010414.
- 10 Questions to Help you Make Sense of Qualitative Research. Oxford: CASP; 2011.
- Noyes J, Lewin S, Noyes J, Booth A, Hannes K, Harden A, et al. Supplementary Guidance for Inclusion of Qualitative Research in Cochrane Systematic Reviews of Interventions. Version 1. Cochrane Collaboration Qualitative Methods Group; 2011.
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008;8. http://dx.doi.org/10.1186/1471-2288-8-45.
- Bates MJ. The design of browsing and berrypicking techniques for the online search interface. Online Info Rev 1989;13:407-24. http://dx.doi.org/10.1108/eb024320.
- Jagosh J, Macaulay AC, Pluye P, Salsberg J, Bush PL, Henderson J, et al. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. Milbank Q 2012;90:311-46. http://dx.doi.org/10.1111/j.1468-0009.2012.00665.x.
- Booth A, Harris J, Croot E, Springett J, Campbell F, Wilkins E. Towards a methodology for cluster searching to provide conceptual and contextual. BMC Med Res Methodol 2013;13. http://dx.doi.org/10.1186/1471-2288-13-118.
- Beck CT. Postpartum depression: a metasynthesis. Qual Health Res 2002;12:453-72. http://dx.doi.org/10.1177/104973202129120016.
- Marsh J. A middle range theory of postpartum depression: analysis and application. Int J Childbirth Educ 2013;28.
- Guise JM, Chang C, Viswanathan M, Glick S, Treadwell J, Umscheid C, et al. Systematic Reviews of Complex Multicomponent Health Care Interventions. Rockville, MD: Agency for Healthcare Research and Quality; 2014.
- Noyes J, Popay J, Pearson A, Hannes K, Booth A, Higgins JPT, et al. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.0.1. The Cochrane Collaboration; 2008.
- MacArthur C, Winter HR, Bick DE, Knowles H, Lilford R, Henderson C, et al. Effects of redesigned community postnatal care on womens’ health 4 months after birth: a cluster randomised controlled trial. Lancet 2002;359:378-85. http://dx.doi.org/10.1016/S0140-6736(02)07596-7.
- Lumley J, Watson L, Small R, Brown S, Mitchell C, Gunn J. PRISM (Program of Resources, Information and Support for Mothers): a community-randomised trial to reduce depression and improve women’s physical health six months after birth [ISRCTN03464021]. BMC Public Health 2006;6. http://dx.doi.org/10.1186/1471-2458-6-37.
- Rahman A, Malik A, Sikander S, Roberts C, Creed F. Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: a cluster-randomised controlled trial. Lancet 2008;372:902-9. http://dx.doi.org/10.1016/S0140-6736(08)61400-2.
- Barnes J, Senior R, MacPherson K. The utility of volunteer home-visiting support to prevent maternal depression in the first year of life. Child Care Health Dev 2009;35:807-16. http://dx.doi.org/10.1111/j.1365-2214.2009.01007.x.
- Christie J, Bunting B. The effect of health visitors’ postpartum home visit frequency on first-time mothers: cluster randomised trial. Int J Nurs Stud 2011;48:689-702. http://dx.doi.org/10.1016/j.ijnurstu.2010.10.011.
- Morrell CJ, Slade P, Warner R, Paley G, Dixon S, Walters SJ, et al. Clinical effectiveness of health visitor training in psychologically informed approaches for depression in postnatal women: pragmatic cluster randomised trial in primary care. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.a3045.
- Brugha TS, Morrell CJ, Slade P, Walters SJ. Universal prevention of depression in women postnatally: cluster randomized trial evidence in primary care. Psycho Med 2011;41:739-48. http://dx.doi.org/10.1017/S0033291710001467.
- Cooper PJ, Tomlinson M, Swartz L, Landman M, Molteno C, Stein A, et al. Improving quality of mother–infant relationship and infant attachment in socioeconomically deprived community in South Africa: randomised controlled trial. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.b974.
- Gao LL, Chan SW, Li X, Chen S, Hao Y. Evaluation of an interpersonal-psychotherapy-oriented childbirth education programme for Chinese first-time childbearing women: a randomised controlled trial. Int J Nurs Stud 2010;47:1208-16. http://dx.doi.org/10.1016/j.ijnurstu.2010.03.002.
- Kozinszky Z, Dudas RB, Devosa I, Csatordai S, Toth E, Szabo D, et al. Can a brief antepartum preventive group intervention help reduce postpartum depressive symptomatology?. Psychother Psychosom 2012;81:98-107. http://dx.doi.org/10.1159/000330035.
- Leung S, Lam TH. Group antenatal intervention to reduce perinatal stress and depressive symptoms related to intergenerational conflicts: a randomized controlled trial. Int J Nurs Stud 2012;49:1391-402. http://dx.doi.org/10.1016/j.ijnurstu.2012.06.014.
- Mao HJ, Li HJ, Chiu H, Chan WC, Chen SL. Effectiveness of antenatal emotional self-management training program in prevention of postnatal depression in Chinese women. Perspect Psychiatr Care 2012;48:218-24. http://dx.doi.org/10.1111/j.1744-6163.2012.00331.x.
- Chabrol H, Teissedre F, Saint JM, Teisseyre N, Rog B, Mullet E. Prevention and treatment of post-partum depression: a controlled randomized study on women at risk. Psycho Med 2002;32:1039-47. http://dx.doi.org/10.1017/S0033291702006062.
- Hagan R, Evans SF, Pope S. Preventing postnatal depression in mothers of very preterm infants: a randomised controlled trial. BJOG 2004;111:641-7. http://dx.doi.org/10.1111/j.1471-0528.2004.00165.x.
- Phipps MG, Raker CA, Ware CF, Zlotnick C. Randomized controlled trial to prevent postpartum depression in adolescent mothers. Am J Obstet Gynecol 2013;208:192-e1. http://dx.doi.org/10.1016/j.ajog.2012.12.036.
- Silverstein M, Feinberg E, Cabral H, Sauder S, Egbert L, Schainker E, et al. Problem-solving education to prevent depression among low-income mothers of preterm infants: a randomized controlled pilot trial. Arch Womens Ment Health 2011;14:317-24. http://dx.doi.org/10.1007/s00737-011-0222-6.
- Tam WH, Lee DT, Chiu HF, Ma KC, Lee A, Chung TK. A randomised controlled trial of educational counselling on the management of women who have suffered suboptimal outcomes in pregnancy. BJOG 2003;110:853-9. http://dx.doi.org/10.1111/j.1471-0528.2003.02412.x.
- Zlotnick C, Capezza NM, Parker D. An interpersonally based intervention for low-income pregnant women with intimate partner violence: a pilot study. Arch Womens Ment Health 2011;14:55-6. http://dx.doi.org/10.1007/s00737-010-0195-x.
- Armstrong KL, Fraser JA, Dadds MR, Morris J. A randomized, controlled trial of nurse home visiting to vulnerable families with newborns. J Paediatr Child Health 1999;35:237-44. http://dx.doi.org/10.1046/j.1440-1754.1999.00348.x.
- Austin MP, Frilingos M, Lumley J, Hadzi PD, Roncolato W, Acland S, et al. Brief antenatal cognitive behaviour therapy group intervention for the prevention of postnatal depression and anxiety: a randomised controlled trial. J Affect Disord 2008;105:35-44. http://dx.doi.org/10.1016/j.jad.2007.04.001.
- Crockett K, Zlotnick C, Davis M, Payne N, Washington R. A depression preventive intervention for rural low-income African-American pregnant women at risk for postpartum depression. Arch Womens Ment Health 2008;11:319-25. http://dx.doi.org/10.1007/s00737-008-0036-3.
- El-Mohandes AA, Kiely M, Joseph JG, Subramanian S, Johnson AA, Blake SM, et al. An intervention to improve postpartum outcomes in African-American mothers: a randomized controlled trial. Obstet Gynecol 2008;112:611-20. http://dx.doi.org/10.1097/AOG.0b013e3181834b10.
- Ginsburg GS, Barlow A, Goklish N, Hastings R, Baker EV, Mullany B, et al. Postpartum depression prevention for reservation-based American Indians: results from a pilot randomized controlled trial. Child Youth Care Forum 2012;41:229-45. http://dx.doi.org/10.1007/s10566-011-9161-7.
- Gorman L. Prevention of Postpartum Difficulties in a High Risk Sample 1997.
- Grote NK, Swartz HA, Geibel SL, Zuckoff A, Houck PR, Frank E. A randomized controlled trial of culturally relevant, brief interpersonal psychotherapy for perinatal depression. Psychiatr Serv 2009;60:313-21. http://dx.doi.org/10.1176/ps.2009.60.3.313.
- Le HN, Perry DF, Stuart EA. Randomized controlled trial of a preventive intervention for perinatal depression in high-risk Latinas. J Consult Clin Psychol 2011;79:135-41. http://dx.doi.org/10.1037/a0022492.
- McKee MD, Zayas LH, Fletcher J, Boyd RC, Nam SH. Results of an intervention to reduce perinatal depression among low-income minority women in community primary care. J Soc Serv Res 2006;32:63-81. http://dx.doi.org/10.1300/J079v32n04_04.
- Munoz RF, Le HN, Ippen CG, Diaz MA, Urizar GG, Soto J, et al. Prevention of postpartum depression in low-income women: development of the Mamas y Bebes/Mothers and Babies Course. Cogn Behav Pract 2007;14:70-83. http://dx.doi.org/10.1016/j.cbpra.2006.04.021.
- Petrou S, Cooper P, Murray L, Davidson LL. Cost-effectiveness of a preventive counseling and support package for postnatal depression. Int J Technol Assess Health Care 2006;22:443-53. http://dx.doi.org/10.1017/S0266462306051361.
- Tiwari A, Leung WC, Leung TW, Humphreys J, Parker B, Ho PC. A randomised controlled trial of empowerment training for Chinese abused pregnant women in Hong Kong. BJOG 2005;112:1249-56. http://dx.doi.org/10.1111/j.1471-0528.2005.00709.x.
- Weidner K, Bittner A, Junge HJ, Zimmermann K, Siedentopf F, Richter J, et al. A psychosomatic intervention in pregnant in-patient women with prenatal somatic risks. J Psychosom Obstet Gynaecol 2010;31:188-98. http://dx.doi.org/10.3109/0167482X.2010.497233.
- Wilson P, Puckering C, Thompson L, Clarke A, MacBeth A, McAlees S, et al. Antenatal Parenting Support for Women Vulnerable in Pregnancy: An Exploratory Randomised Controlled Trial of Mellow Bumps. Edinburgh: Scottish Collaboration for Public Health Research and Policy; 2013.
- Zlotnick C, Johnson SL, Miller IW, Pearlstein T, Howard M. Postpartum depression in women receiving public assistance: pilot study of an interpersonal-therapy-oriented group intervention. Am J Psychiatry 2001;158:638-40. http://dx.doi.org/10.1176/appi.ajp.158.4.638.
- Zlotnick C, Miller IW, Pearlstein T, Howard M, Sweeney P. A preventive intervention for pregnant women on public assistance at risk for postpartum depression. Am J Psychiatry 2006;163:1443-5. http://dx.doi.org/10.1176/ajp.2006.163.8.1443.
- Feinberg ME, Kan ML. Establishing family foundations: Intervention effects on coparenting, parent/infant well-being, and parent–child relations. J Fam Psychol 2008;22. http://dx.doi.org/10.1037/0893-3200.22.2.253.
- Gjerdingen DK, Center B. A randomized controlled trial testing the impact of a support/work-planning intervention on first-time parents’ health, partner relationship, and work responsibilities. Behav Med 2002;28:84-91. http://dx.doi.org/10.1080/08964280209596045.
- Hayes BA, Muller R, Bradley BS. Perinatal depression: a randomized controlled trial of an antenatal education intervention for primiparas. Birth 2001;28:28-35. http://dx.doi.org/10.1046/j.1523-536x.2001.00028.x.
- Ho SM, Heh SS, Jevitt CM, Huang LH, Fu YY, Wang LL. Effectiveness of a discharge education program in reducing the severity of postpartum depression: a randomized controlled evaluation study. Patient Educ Couns 2009;77:68-71. http://dx.doi.org/10.1016/j.pec.2009.01.009.
- Matthey S, Kavanagh DJ, Howie P, Barnett B, Charles M. Prevention of postnatal distress or depression: an evaluation of an intervention at preparation for parenthood classes. J Affect Disord 2004;79:113-26. http://dx.doi.org/10.1016/S0165-0327(02)00362-2.
- Milgrom J, Schembri C, Ericksen J, Rossb J, Gemmill AW. Towards parenthood: An antenatal intervention to reduce depression, anxiety and parenting difficulties [ACTRN012606000263594]. J Affect Disord 2011;130:385-94. http://dx.doi.org/10.1016/j.jad.2010.10.045.
- Sealy PA, Simpson JP, Evans MK. The effect of a pamphlet on women’s experiences of postpartum depression. Can J Commun Ment Health 2009;28:113-22. http://dx.doi.org/10.7870/cjcmh-2009-0009.
- Shapiro AF, Gottman JM. Effects on marriage of a psycho-communicative-educational intervention with couples undergoing the transition to parenthood, evaluation at 1-year post intervention. J Fam Commun 2005;5:1-24. http://dx.doi.org/10.1207/s15327698jfc0501_1.
- Brugha TS, Wheatley S, Taub NA, Culverwell A, Friedman T, Kirwan P, et al. Pragmatic randomized trial of antenatal intervention to prevent post-natal depression by reducing psychosocial risk factors. Psycho Med 2000;30:1273-81. http://dx.doi.org/10.1017/S0033291799002937.
- Buist A, Westley D, Hill C. Antenatal prevention of postnatal depression. Arch Womens Ment Health 1999;1:167-73. http://dx.doi.org/10.1007/s007370050024.
- Howell EA, Balbierz A, Wang J, Parides M, Zlotnick C, Leventhal H. Reducing postpartum depressive symptoms among black and Latina mothers: a randomized controlled trial. Obstet Gynecol 2012;119:942-9. http://dx.doi.org/10.1097/AOG.0b013e318250ba48.
- Sen DM. A Randomised Controlled Trial of a Midwife-Led Twin Antenatal Programme: The Newcastle Twin Study 2006.
- Walkup JT, Barlow A, Mullany BC, Pan W, Goklish N, Hasting R, et al. Randomized controlled trial of a paraprofessional-delivered in-home intervention for young reservation-based American Indian mothers. J Am Acad Child Adolesc Psychiatry 2009;48:591-60. http://dx.doi.org/10.1097/CHI.0b013e3181a0ab86.
- Heh SS, Fu YY. Effectiveness of informational support in reducing the severity of postnatal depression in Taiwan. J Adv Nurs 2003;42:30-6. http://dx.doi.org/10.1046/j.1365-2648.2003.02576.x.
- Lara MA, Navarro C, Navarrete L. Outcome results of a psycho-educational intervention in pregnancy to prevent PPD: a randomized control trial. J Affect Disord 2010;122:109-17. http://dx.doi.org/10.1016/j.jad.2009.06.024.
- Stamp GE, Williams AS, Crowther CA. Evaluation of antenatal and postnatal support to overcome postnatal depression: a randomized, controlled trial. Birth 1995;22:138-43. http://dx.doi.org/10.1111/j.1523-536X.1995.tb00689.x.
- Webster J, Linnane J, Roberts J, Starrenburg S, Hinson J, Dibley L. IDentify, Educate and Alert (IDEA) trial: an intervention to reduce postnatal depression. BJOG 2003;110:842-6. http://dx.doi.org/10.1111/j.1471-0528.2003.02377.x.
- Hodnett ED, Lowe NK, Hannah ME, Willan AR, Stevens B, Weston JA, et al. Effectiveness of nurses as providers of birth labor support in North American hospitals: a randomized controlled trial. JAMA 2002;288:1373-81. http://dx.doi.org/10.1001/jama.288.11.1373.
- Kieffer EC, Caldwell CH, Welmerink DB, Welch KB, Sinco BR, Guzman JR. Effect of the healthy MOMs lifestyle intervention on reducing depressive symptoms among pregnant latinas. Am J Community Psychol 2013;51:76-89. http://dx.doi.org/10.1007/s10464-012-9523-9.
- Morrell CJ, Spiby H, Stewart P, Walters S, Morgan A. Costs and effectiveness of community postnatal support workers: randomised controlled trial. BMJ 2000;321:593-8. http://dx.doi.org/10.1136/bmj.321.7261.593.
- Reid M, Glazener C, Murray GD, Taylor GS. A two-centred pragmatic randomised controlled trial of two interventions of postnatal support. BJOG 2002;109:1164-70. http://dx.doi.org/10.1111/j.1471-0528.2002.01306.x.
- Cupples ME, Stewart MC, Percy A, Hepper P, Murphy C, Halliday HL. A RCT of peer-mentoring for first-time mothers in socially disadvantaged areas (The MOMENTS Study). Arch Dis Child 2011;96:252-8. http://dx.doi.org/10.1136/adc.2009.167387.
- Logsdon MC, Birkimer JC, Simpson T, Looney S. Postpartum depression and social support in adolescents. J Obstet Gynecol Neonatal Nurs 2005;34:46-54. http://dx.doi.org/10.1177/0884217504272802.
- Richter L, Rotheram-Borus MJ, Heerden AV, Stein A, Tomlinson M, Harwood JM, et al. Pregnant Women Living with HIV (WLH) supported at clinics by peer wlh: a cluster randomized controlled trial. AIDS Behav 2014;18:706-15. http://dx.doi.org/10.1007/s10461-014-0694-2.
- Wolman WL, Chalmers B, Hofmeyr GJ, Nikodem VC. Postpartum depression and companionship in the clinical birth environment: a randomized, controlled study. Am J Obstet Gynecol 1993;168:1388-93. http://dx.doi.org/10.1016/S0002-9378(11)90770-4.
- Dennis CL, Hodnett E, Kenton L, Weston J, Zupancic J, Stewart DE, et al. Effect of peer support on prevention of postnatal depression among high risk women: multisite randomised controlled trial. BMJ 2009;338. http://dx.doi.org/10.1136/bmj.a3064.
- Harris T, Brown GW, Hamilton V, Hodson S, Craig TKJ, Mondy L, et al. Newpin Courage to Change Together 2008. UnitingCare Burnside: North Parramatta, NSW; 2008.
- Doornbos B, Goor SA, Dijck-Brouwer DA, Schaafsma A, Korf J, Muskiet FA. Supplementation of a low dose of DHA or DHA+AA does not prevent peripartum depressive symptoms in a small population based sample. Prog Neuropsychopharmacol Biol Psychiatry 2009;33:49-52. http://dx.doi.org/10.1016/j.pnpbp.2008.10.003.
- Harrison-Hohner J, Coste S, Dorato V, Curet LB, McCarron D, Hatton D. Prenatal calcium supplementation and postpartum depression: an ancillary study to a randomized trial of calcium for prevention of preeclampsia. Arch Womens Ment Health 2001;3:141-6. http://dx.doi.org/10.1007/s007370170011.
- Lawrie TA, Hofmeyr GJ, Jager M, Berk M, Paiker J, Viljoen E. A double-blind randomised placebo controlled trial of postnatal norethisterone enanthate: the effect on postnatal depression and serum hormones. Br J Obstet Gynaecol 1998;105:1082-90. http://dx.doi.org/10.1111/j.1471-0528.1998.tb09940.x.
- Llorente AM, Jensen CL, Voigt RG, Fraley JK, Berretta MC, Heird WC. Effect of maternal docosahexaenoic acid supplementation on postpartum depression and information processing. Am J Obstet Gynecol 2003;188:1348-53. http://dx.doi.org/10.1067/mob.2003.275.
- Makrides M, Gibson RA, McPhee AJ, Yelland L, Quinlivan J, Ryan P. Effect of DHA supplementation during pregnancy on maternal depression and neurodevelopment of young children: a randomized controlled trial. JAMA 2010;304:1675-83. http://dx.doi.org/10.1001/jama.2010.1507.
- Mokhber N, Namjoo M, Tara F, Boskabadi H, Rayman MP, Ghayour MM, et al. Effect of supplementation with selenium on postpartum depression: a randomized double-blind placebo-controlled trial. J Matern Fetal Neonatal Med 2011;24:104-8. http://dx.doi.org/10.3109/14767058.2010.482598.
- Harris B, Oretti R, Lazarus J, Parkes A, John R, Richards C, et al. Randomised trial of thyroxine to prevent postnatal depression in thyroid-antibody-positive women. Br J Psychiatry 2002;180:327-30. http://dx.doi.org/10.1192/bjp.180.4.327.
- Mozurkewich EL, Clinton CM, Chilimigras J, . The Mothers, Omega-3, and Mental Health Study: a double-blind, randomized controlled trial. Am J Obstet Gynecol 2013;208:313-15. http://dx.doi.org/10.1016/j.ajog.2013.01.038.
- Wisner KL, Perel JM, Peindl KS, Hanusa BH, Findling RL, Rapport D. Prevention of recurrent postpartum depression: a randomized clinical trial. J Clin Psychiatry 2001;62:82-6. http://dx.doi.org/10.4088/JCP.v62n0202.
- Wisner KL, Perel JM, Peindl KS, Hanusa BH, Piontek CM, Findling RL. Prevention of postpartum depression: a pilot randomized clinical trial. Am J Psychiatry 2004;161:1290-2. http://dx.doi.org/10.1176/appi.ajp.161.7.1290.
- Priest SR, Henderson J, Evans SF, Hagan R. Stress debriefing after childbirth: a randomised controlled trial. Med J Aust 2003;178:542-5.
- Selkirk R, McLaren S, Ollerenshaw A, McLachlan AJ, Moten J. The longitudinal effects of midwife-led postnatal debriefing on the psychological health of mothers. J Reprod Infant Psychol 2006;24:133-47. http://dx.doi.org/10.1080/02646830600643916.
- Shields N, Reid M, Cheyne H, Holmes A, McGinley M, Turnbull D, et al. Impact of midwife-managed care in the postnatal period: an exploration of psychosocial outcomes. J Reprod Infant Psychol 1997;15:91-108. http://dx.doi.org/10.1080/02646839708404537.
- Waldenstrom U, Brown S, McLachlan H, Forster D, Brennecke S. Does team midwife care increase satisfaction with antenatal, intrapartum, and postpartum care? A randomized controlled trial. Birth 2000;27:156-67. http://dx.doi.org/10.1046/j.1523-536x.2000.00156.x.
- Gamble J, Creedy D, Moyle W, Webster J, McAllister M, Dickson P. Effectiveness of a counseling intervention after a traumatic childbirth: a randomized controlled trial. Birth 2005;32:11-9. http://dx.doi.org/10.1111/j.0730-7659.2005.00340.x.
- Ickovics JR, Reed E, Magriples U, Westdahl C, Schindler RS, Kershaw TS. Effects of group prenatal care on psychosocial risk in pregnancy: results from a randomised controlled trial. Psychol Health 2011;26:235-50. http://dx.doi.org/10.1080/08870446.2011.531577.
- Small R, Lumley J, Donohue L, Potter A, Waldenström U. Randomised controlled trial of midwife led debriefing to reduce maternal depression after operative childbirth. BMJ 2000;321:1043-7. http://dx.doi.org/10.1136/bmj.321.7268.1043.
- Marks MN, Siddle K, Warwick C. Can we prevent postnatal depression? A randomized controlled trial to assess the effect of continuity of midwifery care on rates of postnatal depression in high-risk women. Prog Neuropsychopharmacol Biol Psychiatry 2003;13:119-27. http://dx.doi.org/10.1080/jmf.13.2.119.127.
- Gunn J, Lumley J, Chondros P, Young D. Does an early postnatal check-up improve maternal health: results from a randomised trial in Australian general practice. Br J Obstet Gynaecol 1998;105:991-7. http://dx.doi.org/10.1111/j.1471-0528.1998.tb10263.x.
- Rotheram-Borus MJ, le Roux IM, Tomlinson M, Mbewu N, Comulada WS, le Roux K, et al. Philani Plus (+): a mentor mother community health worker home visiting program to improve maternal and infants’ outcomes. Prev Sci 2011;12:372-88. http://dx.doi.org/10.1007/s11121-011-0238-1.
- Serwint JR, Wilson MH, Duggan AK, Mellits ED, Baumgardner RA, DeAngelis C. Do postpartum nursery visits by the primary care provider make a difference?. Pediatrics 1991;88:444-9.
- Fujita M, Endoh Y, Saimon N, Yamaguchi S. Effect of massaging babies on mothers: pilot study on the changes in mood states and salivary cortisol level. Complement Ther Clin Pract 2006;12:181-5. http://dx.doi.org/10.1016/j.ctcp.2006.01.003.
- Manber R, Schnyer RN, Allen JJ, Rush AJ, Blasey CM. Acupuncture: a promising treatment for depression during pregnancy. J Affect Disord 2004;83:89-95. http://dx.doi.org/10.1016/j.jad.2004.05.009.
- Austin MP, Priest SR, Sullivan EA. Antenatal psychosocial assessment for reducing perinatal mental health morbidity. Cochrane Database Syst Rev 2008;8. http://dx.doi.org/10.1002/14651858.cd005124.pub2.
- Bennett C, Macdonald GM, Dennis J, Coren E, Patterson J, Astin M, et al. Home-based support for disadvantaged adult mothers. Cochrane Database Syst Rev 2007;3. http://dx.doi.org/10.1002/14651858.cd003759.pub2.
- Dale J, Caramlau IO, Lindenmeyer A, Williams SM. Peer support telephone calls for improving health. Cochrane Database Syst Rev 2008;4. http://dx.doi.org/10.1002/14651858.cd006903.pub2.
- Dennis CL, Creedy D. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Syst Rev 2004;4. http://dx.doi.org/10.1002/14651858.cd001134.pub2.
- Dennis CL. Psychosocial and psychological interventions for prevention of postnatal depression: systematic review. BMJ 2005;331:15-21. http://dx.doi.org/10.1136/bmj.331.7507.15.
- Dennis CL. Preventing postpartum depression part I: a review of biological interventions. Can J Psychiatry 2004;49:467-75.
- Dennis CL, Kingston D. A systematic review of telephone support for women during pregnancy and the early postpartum period. J Obstet Gynecol Neonatal Nurs 2008;37:301-14. http://dx.doi.org/10.1111/j.1552-6909.2008.00235.x.
- Dennis CL, Ross LE, Herxheimer A. Oestrogens and progestins for preventing and treating postpartum depression. Cochrane Database Syst Rev 2008;4. http://dx.doi.org/10.1002/14651858.cd001690.pub2.
- Dennis CL. Preventing postpartum depression part II: a critical review of nonbiological interventions. Can J Psychiatry 2004;49:526-38.
- Dodd JM, Crowther CA. Specialised antenatal clinics for women with a multiple pregnancy for improving maternal and infant outcomes. Cochrane Database Syst Rev 2012;8. http://dx.doi.org/10.1002/14651858.cd005300.pub3.
- Fontein-Kuipers YJ, Nieuwenhuijze MJ, Ausems M, Bude L, Vries R. Antenatal interventions to reduce maternal distress: a systematic review and meta-analysis of randomised trials. BJOG 2014;121:389-97. http://dx.doi.org/10.1111/1471-0528.12500.
- Howard LM, Hoffbrand S, Henshaw C, Boath L, Bradley E. Antidepressant prevention of postnatal depression. Cochrane Database Syst Rev 2005;2. http://dx.doi.org/10.1002/14651858.cd004363.pub2.
- Jans LA, Giltay EJ, Does AJ. The efficacy of n-3 fatty acids DHA and EPA (fish oil) for perinatal depression. Br J Nutr 2010;104:1577-85. http://dx.doi.org/10.1017/S0007114510004125.
- Lawrie TA, Herxheimer A, Dalton K. Oestrogens and progestogens for preventing and treating postnatal depression. Cochrane Database Syst Rev 2008;2.
- Leis JA, Mendelson T, Tandon SD, Perry DF. A systematic review of home-based interventions to prevent and treat postpartum depression. Arch Womens Ment Health 2009;12:3-13. http://dx.doi.org/10.1007/s00737-008-0039-0.
- Lumley J, Austin MP, Mitchell C. Intervening to reduce depression after birth: a systematic review of the randomized trials. Int J Technol Assess Health Care 2004;20:128-44. http://dx.doi.org/10.1017/S0266462304000911.
- Marc I, Toureche N, Ernst E, Hodnett ED, Blanchet C, Dodin S, et al. Mind–body interventions during pregnancy for preventing or treating women’s anxiety. Cochrane Database Syst Rev 2011;7. http://dx.doi.org/10.1002/14651858.cd007559.pub2.
- Miller BJ, Murray L, Beckmann MM, Kent T, Macfarlane B. Dietary supplements for preventing postnatal depression. Cochrane Database Syst Rev 2013;10. http://dx.doi.org/10.1002/14651858.cd009104.pub2.
- Sado M, Ota E, Stickley A, Mori R. Hypnosis during pregnancy, childbirth, and the postnatal period for preventing postnatal depression. Cochrane Database Syst Rev 2012;6. http://dx.doi.org/10.1002/14651858.cd009062.pub2.
- Shaw E, Levitt C, Wong S, Kaczorowski J. McMaster University Postpartum Research G . Systematic review of the literature on postpartum care: effectiveness of postpartum support to improve maternal parenting, mental health, quality of life, and physical health. Birth 2006;33:210-20. http://dx.doi.org/10.1111/j.1523-536X.2006.00106.x.
- Sockol LE, Epperson CN, Barber JP. A meta-analysis of treatments for perinatal depression. Clin Psychol Rev 2011;31:839-49. http://dx.doi.org/10.1016/j.cpr.2011.03.009.
- Armstrong KL, Fraser JA, Dadds MR, Morris J. Promoting secure attachment, maternal mood and child health in a vulnerable population: a randomized controlled trial. J Paediatr Child Health 2000;36:555-62. http://dx.doi.org/10.1046/j.1440-1754.2000.00591.x.
- Fraser JA, Armstrong KL, Morris JP, Dadds MR. Home visiting intervention for vulnerable families with newborns: follow-up results of a randomized controlled trial. Child Abuse Negl 2000;24:1399-429. http://dx.doi.org/10.1016/S0145-2134(00)00193-9.
- Wheatley SL, Brugha TS. ‘Just because I like it doesn’t mean it has to work’: personal experiences of an antenatal psychosocial intervention designed to prevent postnatal depression. Int J Ment Health Promot 1999;1:26-31. http://dx.doi.org/10.1108/17465729199900006.
- Wheatley SL, Brugha TS, Shapiro DA. Exploring and enhancing engagement to the psychosocial intervention ‘Preparing for Parenthood’. Arch Womens Ment Health 2003;4:275-85. http://dx.doi.org/10.1007/s00737-003-0025-5.
- Chabrol H, Teissedre F, Saint JM, Teisseyre N, Roge B. Prevention and treatment of post partum depression: A controlled study. Devenir 2003;15:5-25. http://dx.doi.org/10.3917/dev.031.0005.
- Chabrol H, Coroner N, Rusibane S, Séjourné N. Prévention du blues du post-partum : étude pilote (pilot study of prevention of postpartum blues). Gynecol Obstet Fertil 2007;35:1242-4. http://dx.doi.org/10.1016/j.gyobfe.2007.10.014.
- Cooper PJ, Landman M, Tomlinson M, Molteno C, Swartz L, Murray L. Impact of a mother-infant intervention in an indigent peri-urban South African context: pilot study. Br J Psychiatry 2002;180:76-81. http://dx.doi.org/10.1192/bjp.180.1.76.
- Dukhovny D, Dennis CL, Hodnett E, Kenton L, Weston J, Stewart DE, et al. Prospective economic evaluation of a peer support intervention for prevention of postpartum depression amongst high risk women in Ontario, Canada. Am J Perinatol 2013;30:631-42. http://dx.doi.org/10.1055/s-0032-1331029.
- Creedy D. Reducing Postpartum Emotional Distress: A Randomised Controlled Trial n.d.
- Gamble J, Creedy D. Reducing Postpartum Emotional Distress: A Randomised Controlled Trial n.d.
- Levine RJ, Hauth JC, Curet LB, Sibai BM, Catalano PM, Morris CD, et al. Trial of calcium to prevent preeclampsia. N Engl J Med 1997;337:69-77. http://dx.doi.org/10.1056/NEJM199707103370201.
- Ickovics JR, Kershaw TS, Westdahl C, Magriples U, Massey Z, Reynolds H, et al. Group prenatal care and perinatal outcomes: a randomized controlled trial. Obstet Gynecol 2007;110. http://dx.doi.org/10.1097/01.AOG.0000275284.24298.23.
- Lumley J, Small R, Brown S, Watson L, Gunn J, Mitchell C, et al. PRISM (Program of Resources, Information and Support for Mothers) Protocol for a community-randomised trial [ISRCTN03464021]. BMC Public Health 2003;3. http://dx.doi.org/10.1186/1471-2458-3-36.
- MacArthur C, Winter HR, Bick DE, Lilford RJ, Lancashire RJ, Knowles H, et al. Redesigning postnatal care: a randomised controlled trial of protocol-based midwifery-led care focused on individual women’s physical and psychological health needs. Health Technol Assess 2003;7. http://dx.doi.org/10.3310/hta7370.
- Ryan P, Griffith E, McDermott B, Makrides M, Gibson R. Data management tools in the DOMINO trial: DHA in pregnancy to prevent postnatal depressive symptoms and enhance neurodevelopment in children. Clinical Trials 2007;4.
- Morrell C, Spiby H, Stewart P, Walters S, Morgan A. Costs and benefits of community postnatal support workers: a randomised controlled trial. Health Technol Assess 2000;4.
- Cooper P, De Pascalis L, Woolgar M, Romaniuk H, Murray L. Attempting to prevent postnatal depression by targeting the mother–infant relationship: a randomised controlled trial. Prim Health Care Res Dev 2014;16:384-97. http://dx.doi.org/10.1017/S1463423614000401.
- Reid M, Glazener C, Connery L, Mackenzie J, Ismail D, Prigg A, et al. Two interventions for postnatal support. Br J Midwifery 2003;11:294-8. http://dx.doi.org/10.12968/bjom.2003.11.5.11226.
- Rotheram-Borus MJ, Richter L, Rooyen HV, Tomlinson M, Harwood JM, Tang Z, et al. A cluster randomized controlled trial evaluating the efficacy of peer mentors to support South African women living with HIV and their infants. PLOS ONE 2014;9. http://dx.doi.org/10.1371/journal.pone.0084867.
- le Roux IM, Tomlinson M, Harwood JM, O’Connor MJ, Worthman CM, Mbewu N, et al. Outcomes of home visits for pregnant mothers and their infants: a cluster randomized controlled trial. AIDS 2013;27:1461-71. http://dx.doi.org/10.1097/QAD.0b013e3283601b53.
- Sen DM, Robson SC, Bond S. Peripartum depression and anxiety in mothers expecting uncomplicated twin infants-an antenatal model of care in the North East of England. J Reprod Infant Psychol 2004;22.
- Stamp GE, Williams AS, Crowther CA. Predicting postnatal depression among pregnant women. Birth 1996;23:218-23. http://dx.doi.org/10.1111/j.1523-536X.1996.tb00498.x.
- Peindl KS. The Use of Nortriptyline for Prevention of Postpartum Depression in a High-Risk Group of Women n.d.
- Wisner KL, Peindl KS, Perel JM, Hanusa BH, Plontek CM, Findling RL. Sertraline Prevents Postpartum Depression n.d. http://dx.doi.org/10.1016/s0009-9236(03)90455-3.
- Nikodem VC, Nolte AG, Wolman W, Gülmezoglu AM, Hofmeyr GJ. Companionship by a lay labour supporter to modify the clinical birth environment: long-term effects on mother and child. Curationis 1998;21:8-12. http://dx.doi.org/10.4102/curationis.v21i1.596.
- Trotter C, Wolman WL, Hofmeyr J, Nikodem C, Turton R. The effect of social support during labour on postpartum depression. S Afr J Psychol 1992;22:134-9. http://dx.doi.org/10.1177/008124639202200304.
- Andersson E, Christensson K, Hildingsson I. Parents’ experiences and perceptions of group-based antenatal care in four clinics in Sweden. Midwifery 2012;28:502-8. http://dx.doi.org/10.1016/j.midw.2011.07.006.
- Carolan M, Barry M, Gamble M, Turner K, Mascarenas O. Experiences of pregnant women attending a lullaby programme in Limerick, Ireland: a qualitative study. Midwifery 2012;28:321-8. http://dx.doi.org/10.1016/j.midw.2011.04.009.
- Carolan M, Barry M, Gamble M, Turner K, Mascarenas O. The Limerick Lullaby project: an intervention to relieve prenatal stress. Midwifery 2012;28:173-80. http://dx.doi.org/10.1016/j.midw.2010.12.006.
- Doran F, Hornibrook J. Women’s experiences of participation in a pregnancy and postnatal group incorporating yoga and facilitated group discussion: a qualitative evaluation. Women Birth 2013;26:82-6. http://dx.doi.org/10.1016/j.wombi.2012.06.001.
- Evans M, Donelle L, Hume-Loveland L. Social support and online postpartum depression discussion groups: a content analysis. Patient Educ Couns 2012;87:405-10. http://dx.doi.org/10.1016/j.pec.2011.09.011.
- Gao LL, Luo SY, Chan SWC. Interpersonal psychotherapy-oriented program for Chinese pregnant women: delivery, content, and personal impact. Nurs Health Sci 2012;14:318-24. http://dx.doi.org/10.1111/j.1442-2018.2012.00722.x.
- Kennedy HP, Farrell T, Paden R, Hill S, Jolivet R, Willetts J, et al. ‘I wasn’t alone’ – a study of group prenatal care in the military. J Midwifery Womens Health 2009;54:176-83. http://dx.doi.org/10.1016/j.jmwh.2008.11.004.
- Klima C, Norr K, Vonderheid S, Handler A. Introduction of CenteringPregnancy in a public health clinic. J Midwifery Womens Health 2009;54:27-34. http://dx.doi.org/10.1016/j.jmwh.2008.05.008.
- McNeil DA, Vekved M, Dolan SM, Siever J, Horn S, Tough SC. Getting more than they realized they needed: a qualitative study of women’s experience of group prenatal care. BMC Pregnancy Childbirth 2012;12. http://dx.doi.org/10.1186/1471-2393-12-17.
- Migl KS. The Lived Experiences of Prenatal Stress and Mind–body Exercises: Reflections of Post-Partum Women 2009.
- Morrell C. Postnatal Support: Who Wants It, What Is Its Benefit and How Much Does It Cost 2002.
- Scott D. Maternal and child health nurse: role in post-partum depression. Aust J Adv Nurs 1987;5:28-37.
- Teate A, Leap N, Rising SS, Homer CS. Women’s experiences of group antenatal care in Australia – the CenteringPregnancy Pilot Study. Midwifery 2011;27:138-45. http://dx.doi.org/10.1016/j.midw.2009.03.001.
- McNeil DA, Vekved MF, Dolan SM, Siever J, Siever JF, Horn S, et al. A qualitative study of the experience of CenteringPregnancy group prenatal care for physicians. BMC Pregnancy Childbirth 2013;13. http://dx.doi.org/10.1186/1471-2393-13-S1-S6.
- Tanner-Smith EE, Steinka-Fry KT, Lipsey MW. A Multi-site Evaluation of the Centering Pregnancy® Programs in Tennessee. Nashville, TN: Peabody Research Institute, Vanderbilt University; 2012.
- Lehman E. Centering pregnancy: A Combined Quantitative and Qualitative Appraisal of Women’s Experiences of Depression and Anxiety During Group Prenatal Care. Wheaton, IL: Wheaton College; 2012.
- Novick G, Sadler LS, Knafl KA, Groce NE, Kennedy HP. The intersection of everyday life and group prenatal care for women in two urban clinics. J Health Care Poor Underserved 2012;23:589-603. http://dx.doi.org/10.1353/hpu.2012.0060.
- Novick G, Reid A, Lewis J, Kershaw TS, Rising SS, Ickovics J. Group prenatal care: model fidelity and outcomes. Am J Obstet Gynecol 2013;209:112.e1-e6. http://dx.doi.org/10.1016/j.ajog.2013.03.026.
- Novick G, Sadler LS, Knafl KA, Groce NE, Kennedy HP. In a hard spot: providing group prenatal care in two urban clinics. Midwifery 2013;29:690-7. http://dx.doi.org/10.1016/j.midw.2012.06.013.
- Shanok AF, Miller L. Stepping up to motherhood among inner-city teens. Psychol Women Q 2007;31:252-61. http://dx.doi.org/10.1111/j.1471-6402.2007.00368.x.
- Shanok AF, Miller L. Depression and treatment with inner city pregnant and parenting teens. Arch Womens Ment Health 2007;10:199-210. http://dx.doi.org/10.1007/s00737-007-0194-8.
- Shanok AF. Experiences of Pregnancy and Parenting Among Inner City Teens Attending an Alternative Public School 2007.
- Dennis CL. Postpartum depression peer support: maternal perceptions from a randomized controlled trial. Int J Nurs Stud 2010;47:560-8. http://dx.doi.org/10.1016/j.ijnurstu.2009.10.015.
- Myors KA, Schmied V, Johnson M, Cleary M. ‘My special time’: Australian women’s experiences of accessing a specialist perinatal and infant mental health service. Health Soc Care Community 2014;22:268-77. http://dx.doi.org/10.1111/hsc.12079.
- Dennis CL. Peer support for postpartum depression: volunteers’ perceptions, recruitment strategies and training from a randomized controlled trial. Health Promot Int 2013;28:187-96. http://dx.doi.org/10.1093/heapro/das003.
- Corrigan LB. Postpartum Depressive Symptomatology in First-Time Mothers: Relationship to Expectations and Postpartum Perceptions 1997.
- Curtis R, Robertson P, Forst A, Bradford C. Postpartum mood disorders: results of an online survey. Counsel Psychother Res 2007;7:203-10. http://dx.doi.org/10.1080/14733140701706060.
- Hanley J. The emotional wellbeing of Bangladeshi mothers during the postnatal period. Community Pract 2007;80:34-7.
- Leung SSK. Postpartum Depression: Perceived Social Support and Stress Among Hong Kong Chinese Women 2001.
- Edge D. ‘We don’t see black women here’: an exploration of the absence of black Caribbean women from clinical and epidemiological data on perinatal depression in the UK. Midwifery 2008;24:379-89. http://dx.doi.org/10.1016/j.midw.2007.01.007.
- Edge D. Perinatal depression: its absence among black Caribbean women. Br J Midwifery 2006;14. http://dx.doi.org/10.12968/bjom.2006.14.11.22251.
- Edge D, Baker D, Rogers A. Perinatal depression among black Caribbean women. Health Soc Care Community 2004;12:430-8. http://dx.doi.org/10.1111/j.1365-2524.2004.00513.x.
- Edge D, MacKian SC. Ethnicity and mental health encounters in primary care: help-seeking and help-giving for perinatal depression among black Caribbean women in the UK. Ethn Health 2010;15:93-111. http://dx.doi.org/10.1080/13557850903418836.
- Edge D, Rogers A. Dealing with it: black Caribbean women’s response to adversity and psychological distress associated with pregnancy, childbirth, and early motherhood. Soc Sci Med 2005;61:15-2. http://dx.doi.org/10.1016/j.socscimed.2004.11.047.
- Edge D. ‘It’s leaflet, leaflet, leaflet then, ‘see you later’’: black Caribbean women’s perceptions of perinatal mental health care. Br J Gen Pract 2011;61:256-62. http://dx.doi.org/10.3399/bjgp11X567063.
- Lewis SE, Nicolson P. Talking about early motherhood: recognizing loss and reconstructing depression. J Reprod Infant Psychol 1998;16:177-97. http://dx.doi.org/10.1080/02646839808404567.
- Nicolson P. Loss, happiness and postpartum depression: the ultimate paradox. Can Psychol 1999;2:162-78. http://dx.doi.org/10.1037/h0086834.
- Parvin A, Jones CE, Hull SA. Experiences and understandings of social and emotional distress in the postnatal period among Bangladeshi women living in Tower Hamlets. Fam Pract 2004;21:254-60. http://dx.doi.org/10.1093/fampra/cmh307.
- Raymond JE. ‘Creating a safety net’: women’s experiences of antenatal depression and their identification of helpful community support and services during pregnancy. Midwifery 2009;25:39-4. http://dx.doi.org/10.1016/j.midw.2007.01.005.
- Razurel C, Bruchon-Schweitzer M, Dupanloup A, Irion O, Epiney M. Stressful events, social support and coping strategies of primiparous women during the postpartum period: a qualitative study. Midwifery 2011;27:237-42. http://dx.doi.org/10.1016/j.midw.2009.06.005.
- Sword W, Clark AM, Hegadoren K, Brooks S, Kingston D. The complexity of postpartum mental health and illness: a critical realist study. Nurs Inq 2012;19:51-62. http://dx.doi.org/10.1111/j.1440-1800.2011.00560.x.
- Taniguchi H, Baruffi G. Childbirth overseas: the experience of Japanese women in Hawaii. Nurs Health Sci 2007;9:90-5. http://dx.doi.org/10.1111/j.1442-2018.2007.00307.x.
- Thurtle V. First time mothers’ perceptions of motherhood and PND. Community Pract 2003;76:261-5.
- Ugarriza DN, Brown SE, Chang-Martinez C. Anglo-American mothers and the prevention of postpartum depression. Issues Ment Health Nurs 2007;28:781-98. http://dx.doi.org/10.1080/01612840701413624.
- Choi P, Henshaw C, Baker S, Tree J. Supermum, superwife, supereverything: performing femininity in the transition to motherhood. J Reprod Infant Psychol 2005;23:167-80. http://dx.doi.org/10.1080/02646830500129487.
- Furber CM, Garrod D, Maloney E, Lovell K, McGowan L. A qualitative study of mild to moderate psychological distress during pregnancy. Int J Nurs Stud 2009;46:669-77. http://dx.doi.org/10.1016/j.ijnurstu.2008.12.003.
- Haga SM, Lynne A, Slinning K, Kraft P. A qualitative study of depressive symptoms and well-being among first-time mothers. Scand J Caring Sci 2012;26:458-66. http://dx.doi.org/10.1111/j.1471-6712.2011.00950.x.
- Mauthner NS. Re-assessing the importance and role of the marital relationship in postnatal depression: methodological and theoretical implications. J Reprod Infant Psychol 1998;16. http://dx.doi.org/10.1080/02646839808404566.
- Rodrigues M, Patel V, Jaswal S, de SN. Listening to mothers: qualitative studies on motherhood and depression from Goa, India. Soc Sci Med 2003;57:1797-806. http://dx.doi.org/10.1016/S0277-9536(03)00062-5.
- Morrell CJ, Ricketts T, Tudor K, Williams C, Curran J, Barkham M. Training health visitors in cognitive behavioural and person-centred approaches for depression in postnatal women as part of a cluster randomised trial and economic evaluation in primary care: the PoNDER trial. Prim Health Care Res Dev 2011;12:11-20. http://dx.doi.org/10.1017/S1463423610000344.
- Gao Ll, Chan SW-c, Sun K. Effects of an interpersonal-psychotherapy-oriented childbirth education programme for Chinese first-time childbearing women at 3-month follow up: randomised controlled trial. Int J Nurs Stud 2012;3:274-81. http://dx.doi.org/10.1016/j.ijnurstu.2011.09.010.
- Ware JE, Kosinski M, Gandek B. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales. Boston, MA: The Health Institute, New England Medical Centre; 1995.
- Hayes BA, Muller R. Prenatal depression: a randomized controlled trial in the emotional health of primiparous women. Res Theory Nurs Pract 2004;18:165-83. http://dx.doi.org/10.1891/rtnp.18.2.165.61277.
- Henderson J, Sharp J, Priest SR, Hagan R, Evans SF. Postnatal Debriefing: What Do Women Feel about It? 1998;38.
- Wheatley SL, Culverwell A, Brugha TS, Shapiro DA. Preparing for parenthood: background and development of a risk modifying intervention to prevent postnatal depression. Arch Womens Mental Health 2000;3:81-90. http://dx.doi.org/10.1007/s007370070001.
- Lavender T, Walkinshaw SA. Can midwives reduce postpartum psychological morbidity? A randomized trial. Birth 1998;25:215-19. http://dx.doi.org/10.1046/j.1523-536X.1998.00215.x.
- Smith J. An integrated approach to perinatal support by Family Action. J Health Visiting 2013;1:272-6. http://dx.doi.org/10.12968/johv.2013.1.5.272.
- Lara MA, Navarro C, Navarrete L, Le HN. Retention rates and potential predictors in a longitudinal randomized control trial to prevent postpartum depression. Salud Mental 2010;33:429-36.
- Howell EA, Bodnar-Deren S, Balbierz A, Loudon H, Mora PA, Zlotnick C, et al. An intervention to reduce postpartum depressive symptoms: a randomized controlled trial. Arch Womens Ment Health 2014;17:57-63. http://dx.doi.org/10.1007/s00737-013-0381-8.
- Martin A, Negron R, Balbierz A, Bickell N, Howell EA. Recruitment of black and Latina women to a randomized controlled trial. J Health Care Poor Underserved 2013;24:1102-14. http://dx.doi.org/10.1353/hpu.2013.0125.
- Shields N, Turnbull D, Reid M, Holmes A, McGinley M, Smith LN. Satisfaction with midwife-managed care in different time periods: a randomised controlled trial of 1299 women. Midwifery 1998;14:85-93. http://dx.doi.org/10.1016/S0266-6138(98)90003-1.
- Tumbull D, Holmes A, Shields N, Cheyne H, Twaddle S, Gilmour WH, et al. Randomised, controlled trial of efficacy of midwife-managed care. Lancet 1996;348:213-18. http://dx.doi.org/10.1016/S0140-6736(95)11207-3.
- Young D, Shields N, Holmes A, Turnbull D, Twaddle S. A new style of midwife-managed antenatal care: costs and satisfaction. Br J Midwifery 1997;5:540-5. http://dx.doi.org/10.12968/bjom.1997.5.9.540.
- Beynon R, Wafula S. One charity’s approach to perinatal depression and social inclusion. Ment Health Soc Inclusion 2012;16:206-10. http://dx.doi.org/10.1108/20428301211281078.
- Schroter S, Glasziou P, Heneghan C. Quality of descriptions of treatments: a review of published randomised controlled trials. BMJ Open 2012;2. http://dx.doi.org/10.1136/bmjopen-2012-001978.
- Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348. http://dx.doi.org/10.1136/bmj.g1687.
- Quinones AR, Richardson J, Freeman M, Fu R, O’Neil ME, Kansagara D. Group Visits Focusing on Education for the Management of Chronic Conditions in Adults: A Systematic Review 2012.
- Quinones AR, Richardson J, Freeman M, Fu R, O’Neil ME, Motu’apuaka M, et al. Educational group visits for the management of chronic health conditions: a systematic review. Patient Educ Couns 2014;95:3-29. http://dx.doi.org/10.1016/j.pec.2013.12.021.
- Carroll C, Booth A, Cooper K. A worked example of ‘best fit’ framework synthesis: a systematic review of views concerning the taking of some potential chemopreventive agents. BMC Med Res Methodol 2011;11:1-9. http://dx.doi.org/10.1186/1471-2288-11-29.
- Carroll C, Booth A, Leaviss J, Rick J. ‘Best fit’ framework synthesis: refining the method. BMC Med Res Methodol 2013;13. http://dx.doi.org/10.1186/1471-2288-13-37.
- Clark DME, Fairburn CG. Science and Practice of Cognitive Behaviour Therapy. Oxford: Oxford University Press; 1997.
- Sanders P. Mapping person-centred approaches to counselling and psychotherapy. Person-Centred Practice 2000;8:62-74.
- Greenberg MT, Speltz ML, DeKlyen M. The role of attachment in the early development of disruptive behavior problems. Dev Psychopathol 1993;5:191-213. http://dx.doi.org/10.1017/S095457940000434X.
- Fonagy P, Target M. Playing with reality: I. Theory of mind and the normal development of psychic reality. Int J Psychoanal 1996;77:217-33.
- Fonagy P, Steele M, Steele H, Higgitt A, Target M. The Emanuel Miller Memorial Lecture 1992. The Theory and Practice of Resilience. J Child Psychol Psychiatry 1994;35:231-57. http://dx.doi.org/10.1111/j.1469-7610.1994.tb01160.x.
- Gilligan R. Enhancing the resilience of children and young people in public care by mentoring their talents and interests. Child Fam Soc Work 1999;4:187-96. http://dx.doi.org/10.1046/j.1365-2206.1999.00121.x.
- Klerman GL, Weissman MM, Rounsaville B, Chevron ES. Interpersonal Psychotherapy for Depression. New York, NY: University Press; 1996.
- Sullivan HS. The Interpersonal Theory of Psychiatry. New York, NY: Routledge; 2013.
- Bowlby J. Attachment, Vol. 1 of Attachment and Loss. New York, NY: Basic Books; 1969.
- Finkelhor D. The trauma of child sexual abuse two models. J Interpers Violence 1987;2:348-66. http://dx.doi.org/10.1177/088626058700200402.
- Littlewood J, McHugh N. Maternal Distress and Postnatal Depression: The Myth of Madonna. London: Palgrave Macmillan Limited; 1997.
- Brown GW, Harris T. Social Origins of Depression: A Study of Psychiatric Disorder in Women. New York, NY: Routledge; 2012.
- Lazarus RS, Folkman S. Stress, Appraisal and Coping. New York, NY: Springer; 1984.
- Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice-Hall; 1977.
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986.
- Rahman A, Surkan PJ, Cayetano CE, Rwagatare P, Dickson KE. Grand challenges: integrating maternal mental health into maternal and child health programmes. PLOS Med 2013;10. http://dx.doi.org/10.1371/journal.pmed.1001442.
- Novick G, Sadler LS, Kennedy HP, Cohen SS, Groce NE, Knafl KA. Women’s experience of group prenatal care. Qual Health Res 2011;21:97-116. http://dx.doi.org/10.1177/1049732310378655.
- Teng L, Robertson BE, Stewart DE. Healthcare worker’s perceptions of barriers to care by immigrant women with postpartum depression: an exploratory qualitative study. Arch Womens Ment Health 2007;10:93-101. http://dx.doi.org/10.1007/s00737-007-0176-x.
- Holopainen D. The experience of seeking help for postnatal depression. Aust J Adv Nurs 2002;19:39-44.
- Dennis CL, Chung-Lee L. Postpartum depression help-seeking barriers and maternal treatment preferences: a qualitative systematic review. Birth 2006;33:323-31. http://dx.doi.org/10.1111/j.1523-536X.2006.00130.x.
- Heneghan AM, Morton S, DeLeone NL. Paediatricians’ attitudes about discussing maternal depression during a paediatric primary care visit. Child Care Health Dev 2007;33:333-9. http://dx.doi.org/10.1111/j.1365-2214.2006.00648.x.
- Herrman JW, Rogers S, Ehrenthal DB. Women’s perceptions of CenteringPregnancy: a focus group study. MCN Am J Matern Child Nurs 2012;37:19-28. http://dx.doi.org/10.1097/NMC.0b013e3182385204.
- Sword W, Busser D, Ganann R, McMillan T, Swinton M. Women’s care-seeking experiences after referral for postpartum depression. Qual Health Res 2008;18:1161-73. http://dx.doi.org/10.1177/1049732308321736.
- Buultjens M, Liamputtong P. When giving life starts to take the life out of you: women’s experiences of depression after childbirth. Midwifery 2007;23:77-91. http://dx.doi.org/10.1016/j.midw.2006.04.002.
- Williamson VH. A Hermeneutic Phenomenological Study of Women’s Experiences of Postnatal Depression and Health Professional Intervention 2005.
- Everingham CR, Heading G, Connor L. Couples’ experiences of postnatal depression: a framing analysis of cultural identity, gender and communication. Soc Sci Med 2006;62:1745-56. http://dx.doi.org/10.1016/j.socscimed.2005.08.039.
- Barkin JL, Bloch JR, Hawkins KC, Thomas TS. Barriers to optimal social support in the postpartum period. J Obstet Gynecol Neonatal Nurs 2014;43:445-54. http://dx.doi.org/10.1111/1552-6909.12463.
- Blau PM. Exchange and Power in Social Life. Piscataway, NJ: Transaction Publishers; 1964.
- Homans GC. Social Behavior: Its Elementary Forms. New York, NY: Harcourt, Brace & World, Inc.; 1961.
- Scrandis DA. Normalizing postpartum depressive symptoms with social support. J Am Psychiatr Nurses Assoc 2005;11:223-30. http://dx.doi.org/10.1177/1078390305280940.
- Bandura A, Ramachaudran VS. Encyclopedia of Human Behaviour. New York, NY: Academic Press; n.d.
- Champion LA, Power MJ. Social and cognitive approaches to depression: towards a new synthesis. Br J Clin Psychol 1995;34:485-503. http://dx.doi.org/10.1111/j.2044-8260.1995.tb01484.x.
- Leahy-Warren P, McCarthy G, Corcoran P. First-time mothers: social support, maternal parental self-efficacy and postnatal depression. J Clin Nurs 2012;21:388-97. http://dx.doi.org/10.1111/j.1365-2702.2011.03701.x.
- Berg M. Genuine Caring in Caring for the Genuine: Childbearing and High Risk As Experienced by Women and Midwives 2002.
- Beck CT. Postpartum depression: it isn’t just the blues. Am J Nurs 2006;106:40-5. http://dx.doi.org/10.1097/00000446-200605000-00020.
- Novick G, Sadler LS, Knafl KA, Groce NE, Kennedy HP. In a hard spot: providing group prenatal care in two urban clinics. Midwifery 2013;29:690-7. http://dx.doi.org/10.1016/j.midw.2012.06.013.
- Rising SS, Kennedy HP, Klima CS. Redesigning prenatal care through CenteringPregnancy. J Midwifery Womens Health 2004;49:398-404. http://dx.doi.org/10.1111/j.1542-2011.2004.tb04433.x.
- Dennis CL, Ross LE, Grigoriadis S. Psychosocial and psychological interventions for treating antenatal depression. Cochrane Database Syst Rev 2007;3.
- Pennington A. The Student Guide to Counselling and Psycotherapy Approaches 2012.
- Dennis CL. The effect of peer support on postpartum depression: a pilot randomized controlled trial. Can J Psychiatry 2003;48:115-24.
- Harris T, Brown G, Hamilton V, Hodson S, Craig TKJ. The Newpin Antenatal and Postnatal Project: a randomised controlled trial of an intervention for Perinatal Depression. London: Institute of Psychiatry, King’s College London; 2006.
- Rojas G, Fritsch R, Solis J, Jadresic E, Castillo C, Gonzalez M, et al. Treatment of postnatal depression in low-income mothers in primary-care clinics in Santiago, Chile: a randomised controlled trial. Lancet 2007;370:1629-37. http://dx.doi.org/10.1016/S0140-6736(07)61685-7.
- Chowdhary N, Sikander S, Atif N, Singh N, Ahmad I, Fuhr DC, et al. The content and delivery of psychological interventions for perinatal depression by non-specialist health workers in low and middle income countries: a systematic review. Best Pract Res Clin Obstet Gynaecol 2014;28:113-33. http://dx.doi.org/10.1016/j.bpobgyn.2013.08.013.
- Hanley J, Long B. A study of Welsh mothers’ experiences of postnatal depression. Midwifery 2006;22:147-57. http://dx.doi.org/10.1016/j.midw.2005.08.004.
- Dunstan P. Calm the Crying: The Secret Baby Language that Reveals the Hidden Meaning Behind an Infant’s Cry. London: Penguin; 2012.
- Stevenson MD, Scope A, Sutcliffe PA, Booth A, Slade P, Parry G, et al. Group cognitive behavioural therapy for postnatal depression: a systematic review of clinical effectiveness, cost-effectiveness and value of information analyses. Health Technol Assess 2010;14. http://dx.doi.org/10.3310/hta14440.
- Stevenson MD, Scope A, Sutcliffe PA. The cost-effectiveness of group cognitive behavioral therapy compared with routine primary care for women with postnatal depression in the UK. Value Health 2010;13:580-4. http://dx.doi.org/10.1111/j.1524-4733.2010.00720.x.
- Buist AE, Barnett BE, Milgrom J, Pope S, Condon JT, Ellwood DA, et al. To screen or not to screen – that is the question in perinatal depression. Med J Aust 2002;17:S101-S5.
- Darcy JM, Grzywacz JG, Stephens RL, Leng I, Clinch CR, Arcury TA. Maternal depressive symptomatology: 16-month follow-up of infant and maternal health-related quality of life. J Am Board Fam Med 2011;24:249-57. http://dx.doi.org/10.3122/jabfm.2011.03.100201.
- Dukhovny D, Dennis CL, Hodnett E, Weston J, Stewart DE, Mao W, et al. Prospective economic evaluation of a peer support intervention for prevention of postpartum depression among high-risk women in Ontario, Canada. Am J Perinatol 2013;30:631-42. http://dx.doi.org/10.1055/s-0032-1331029.
- Gold L, Shiell A, Hawe P, Riley T, Rankin B, Smithers P. The costs of a community-based intervention to promote maternal health. Health Educ Res 2007;22:648-57. http://dx.doi.org/10.1093/her/cyl127.
- Appleby L, Hirst E, Marshall S, Keeling F, Brind J, Butterworth T, et al. The treatment of postnatal depression by health visitors: impact of brief training on skills and clinical practice. J Affect Disord 2003;77:261-6. http://dx.doi.org/10.1016/S0165-0327(02)00145-3.
- Boath E, Major K, Cox J. When the cradle falls II: the cost-effectiveness of treating postnatal depression in a psychiatric day hospital compared with routine primary care. J Affect Disord 2003;74:159-66. http://dx.doi.org/10.1016/S0165-0327(02)00007-1.
- Dagher RK, McGovern PM, Dowd BE, Gjerdingen DK. Postpartum depression and health services expenditures among employed women. J Occup Environ Med 2012;54:210-15. http://dx.doi.org/10.1097/JOM.0b013e31823fdf85.
- Cooper PJ, Murray L, Hooper R, West A. The development and validation of a predictive index for postpartum depression. Psycho Med 1996;26:627-34. http://dx.doi.org/10.1017/S0033291700035698.
- Revicki DA, Wood M. Patient-assigned health state utilities for depression-related outcomes: differences by depression severity and antidepressant medications. J Affect Disord 1998;48:25-36. http://dx.doi.org/10.1016/S0165-0327(97)00117-1.
- Guide to the Methods of Technology Appraisal. London: NICE; 2013.
- Curtis L. Unit Costs of Health and Social Care 2013. Canterbury: PSSRU, University of Kent; 2013.
- Consumer Price Index, Health and Personal Care, by Province (Canada). Canada: Government of Canada; 2014.
- Trends in Health Care Cost Growth and the Role of the Affordable Care Act. Washington, DC: Executive Office of the President of the United States; 2013.
- Health Expenditure Australia 2011/12. Canberra: Australian Institute of Health and Welfare; 2013.
- Honey KL, Bennett P, Morgan M. A brief psycho-educational group intervention for postnatal depression. British J Clin Psychol 2002;41:405-9. http://dx.doi.org/10.1348/014466502760387515.
- Netten A, Dennet J, Knight J. Unit Costs of Health and Social Care. Canterbury: PSSRU, University of Kent; 1998.
- British National Formulary. London: BMJ Group and Pharmaceutical Press; 2014.
- XE . XE Currency Converter n.d. www.xe.com/currencyconverter/ (accessed August 2014).
- Fenwick E, Claxton K, Sculpher M. Representing uncertainty: the role of cost-effectiveness acceptability curves. Health Econ 2001;10:779-87. http://dx.doi.org/10.1002/hec.635.
- Claxton K, Posnett J. An economic approach to clinical trial design and research priority-setting. Health Econ 1996;5:513-24. http://dx.doi.org/10.1002/(SICI)1099-1050(199611)5:6<513::AID-HEC237>3.0.CO;2-9.
- Stinnett A, Mullahy J. Net health benefits: a new framework for the analysis of uncertainty in cost-effectiveness analyses. Med Decis Making 1998;18:S68-80. http://dx.doi.org/10.1177/0272989X9801800209.
- Felli JC, Hazen GB. Sensitivity analysis and the expected value of perfect information. Medical Decision Making 1998;18:95-109. http://dx.doi.org/10.1177/0272989X9801800117.
- Birth Summary Tables, England and Wales, 2012. London: Office for National Statistics; 2013.
- Dennis CL, Dowswell T. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Syst Rev 2013;2. http://dx.doi.org/10.1002/14651858.CD001134.pub3.
- Smith A, Dixon A, Shakespeare J. The Role of GPS in Maternity Care – What Does The Future Hold? An Inquiry Into the Quality of General Practice in England. London: The King’s Fund; 2010.
- National Service Framework for Children, Young People and Maternity Services (England). London: Department of Health; 2004.
- Routine Postnatal Care of Women and Their Babies. London: NICE; 2006.
- Barnes J, Aistrop D, Allen E, Barlow J, Elbourne D, Macdonald G, et al. First steps: study protocol for a randomized controlled trial of the effectiveness of the Group Family Nurse Partnership (gFNP) program compared to routine care in improving outcomes for high-risk mothers and their children and preventing abuse. Trials 2013;14. http://dx.doi.org/10.1186/1745-6215-14-285.
- Miniati M, Callari A, Calugi S, Rucci P, Savino M, Mauri M, et al. Interpersonal psychotherapy for postpartum depression: a systematic review. Arch Womens Ment Health 2014;17:257-68. http://dx.doi.org/10.1007/s00737-014-0442-7.
- Sockol LE, Epperson CN, Barber JP. Preventing postpartum depression: a meta-analytic review. Clin Psychol Rev 2013;33:1205-17. http://dx.doi.org/10.1016/j.cpr.2013.10.004.
- Hoffenaar PJ, van Balen F, Hermanns J. The impact of having a baby on the level and content of women’s well-being. Soc Indic Res 2010;97:279-95. http://dx.doi.org/10.1007/s11205-009-9503-0.
- Bennett C, Macdonald GM, Dennis J, Coren E, Patterson J, Astin M, et al. Home-based support for disadvantaged adult mothers. Cochrane Database Syst Rev 2008;1. http://dx.doi.org/10.1002/14651858.cd003759.pub3.
- Baldwin KA. Comparison of selected outcomes of CenteringPregnancy versus traditional prenatal care. J Midwifery Womens Health 2006;51:266-72. http://dx.doi.org/10.1016/j.jmwh.2005.11.011.
- Baldwin K, Phillips G. Voices along the journey: midwives’ perceptions of implementing the centering pregnancy model of prenatal care. J Perinat Educ 2011;20. http://dx.doi.org/10.1891/1058-1243.20.4.210.
- Shakespear K, Waite PJ, Gast J. A comparison of health behaviors of women in centering pregnancy and traditional prenatal care. Matern Child Health J 2010;14:202-8. http://dx.doi.org/10.1007/s10995-009-0448-3.
- Shakespear K. Centering Pregnancy and Traditional Prenatal Care: A Comparison of Health Practices 2008.
- Xaverius PK, Grady MA. Centering pregnancy in Missouri: a system level analysis. Sci World J 2014. http://dx.doi.org/10.1155/2014/285386.
- Gaudion A, Menka Y. ‘No decision about me without me’: centering pregnancy. Pract Midwife 2010;13:15-7.
- Teate A, Leap N, Homer CSE. Midwives experiences of becoming CenteringPregnancy facilitators: a pilot study in Sydney, Australia. Women Birth 2013;26:e31-6. http://dx.doi.org/10.1016/j.wombi.2012.08.002.
- Robertson B, Aycock DM, Darnell LA. Comparison of centering pregnancy to traditional care in Hispanic mothers. Matern Child Health J 2009;13:407-14. http://dx.doi.org/10.1007/s10995-008-0353-1.
- Sheeder J, Yorga KW, Kabir-Greher K. A review of prenatal group care literature: the need for a structured theoretical framework and systematic evaluation. Matern Child Health J 2012;16:177-87. http://dx.doi.org/10.1007/s10995-010-0709-1.
- Slade P, Morrell CJ, Rigby A, Ricci K, Spittlehouse J, Brugha TS. Postnatal women’s experiences of management of depressive symptoms: a qualitative study. Br J Gen Pract 2010;60:e440-8. http://dx.doi.org/10.3399/bjgp10X532611.
- Morrell CJ. Nurse-led postpartum discharge education programme including information on postnatal depression reduces risk of high depression scores at 3-month follow-up. Evid Based Nurs 2010;13:48-9. http://dx.doi.org/10.1136/ebn.13.2.48.
- Gao Ll, Sun K, Chan SW-c. Social support and parenting self-efficacy among Chinese women in the perinatal period. Midwifery 2014;30:532-8. http://dx.doi.org/10.1016/j.midw.2013.06.007.
- Ngai FW, Chan S. Psychosocial factors and maternal wellbeing: an exploratory path analysis. Int J Nurs Stud 2011;48:725-31. http://dx.doi.org/10.1016/j.ijnurstu.2010.11.002.
- Grote NK, Zuckoff A, Swartz H, Bledsoe SE, Geibel S. Engaging women who are depressed and economically disadvantaged in mental health treatment. Soc Work 2007;52:295-308. http://dx.doi.org/10.1093/sw/52.4.295.
- Grote NK, Swartz HA, Zuckoff A. Enhancing interpersonal psychotherapy for mothers and expectant mothers on low incomes: adaptations and additions. J Contemp Psychother 2008;38:23-3. http://dx.doi.org/10.1007/s10879-007-9065-x.
- Grote NK, Bledsoe SE, Swartz HA, Frank E. Feasibility of providing culturally relevant, brief interpersonal psychotherapy for antenatal depression in an obstetrics clinic: a pilot study. Res Soc Work Pract 2004;14:397-40. http://dx.doi.org/10.1177/1049731504265835.
- Grote NK, Bledsoe SE, Swartz HA, Frank E. Culturally relevant psychotherapy for perinatal depression in low-income ob/gyn patients. Clin Soc Work J 2004;3:327-47. http://dx.doi.org/10.1023/B:CSOW.0000035111.81205.5b.
- Grote NK, Spieker SJ, Lohr MJ, Geibel SL, Swartz HA, Frank E, et al. Impact of childhood trauma on the outcomes of a perinatal depression trial. Depress Anxiety 2012;29:563-73. http://dx.doi.org/10.1002/da.21929.
- Dennis CL, Ravitz P, Grigoriadis S, Jovellanos M, Hodnett E, Ross L, et al. The effect of telephone-based interpersonal psychotherapy for the treatment of postpartum depression: study protocol for a randomized controlled trial. Trials 2012;13. http://dx.doi.org/10.1186/1745-6215-13-38.
- Fenwick J, Gamble J, Creedy D, Barclay L, Buist A, Ryding EL. Women’s perceptions of emotional support following childbirth: a qualitative investigation. Midwifery 2013;29:217-24. http://dx.doi.org/10.1016/j.midw.2011.12.008.
- Fenwick J, Gamble J, Creedy DK, Buist A, Turkstra E, Sneddon A, et al. Study protocol for reducing childbirth fear: a midwife-led psycho-education intervention. BMC Pregnancy Childbirth 2013;13. http://dx.doi.org/10.1186/1471-2393-13-190.
- Gamble J, Creedy DK. A counselling model for postpartum women after distressing birth experiences. Midwifery 2009;25:e21-30. http://dx.doi.org/10.1016/j.midw.2007.04.004.
- Reed M, Fenwick J, Hauck Y, Gamble J, Creedy DK. Australian midwives’ experience of delivering a counselling intervention for women reporting a traumatic birth. Midwifery 2014;30:269-75. http://dx.doi.org/10.1016/j.midw.2013.07.009.
- Turkstra E, Gamble J, Creedy DK, Fenwick J, Barclay L, Buist A, et al. PRIME: impact of previous mental health problems on health-related quality of life in women with childbirth trauma. Arch Womens Ment Health 2013;16:561-4. http://dx.doi.org/10.1007/s00737-013-0384-5.
- Turnbull D, Shields N, McGinley M, Holmes A, Cheyne H, Reid M, et al. Can midwife-managed units improve continuity of care?. Br J Midwifery 1999;7:499-503. http://dx.doi.org/10.12968/bjom.1999.7.8.8285.
- Shields N, Holmes A, Cheyne H, McGinley M, Young D, Gilmour WH, et al. Knowing your midwife during labour. Br J Midwifery 1999;7:504-10. http://dx.doi.org/10.12968/bjom.1999.7.8.8286.
- Young D, Lees A, Twaddle S. The costs to the NHS of maternity care: midwife-managed vs shared. Br J Midwifery 1997;5:465-72. http://dx.doi.org/10.12968/bjom.1997.5.8.465.
- Ferguson L. Beating the baby blues. Pract Midwife 2012;15:17-9.
- Lederer J. Family Action Southwark Newpin: Prenatal Support Project Evaluation Report. London: Family Action; 2009.
- Barlow J, Coe C. Family Action Perinatal Support Project. Warwick: University of Warwick, Warwick Medical School; 2012.
- Bick D, MacArthur C, Winter H, Fortune H, Henderson C, Lilford R, et al. Redesigning postnatal care: physical and psychological needs. Br J Midwifery 1997;5:621-2. http://dx.doi.org/10.12968/bjom.1997.5.10.621.
- Morrow J, McLachlan H, Forster D, Davey MA, Newton M. Redesigning postnatal care: exploring the views and experiences of midwives. Midwifery 2013;29:159-66. http://dx.doi.org/10.1016/j.midw.2011.11.006.
- MacArthur C, Winter H, Bick D, Henderson C, Knowles H. Re-designed community postnatal care trial. Br J Midwifery 2005;13:319-23. http://dx.doi.org/10.12968/bjom.2005.13.5.18096.
- Glavin K, Smith L, Sorum R, Ellefsen B. Redesigned community postpartum care to prevent and treat postpartum depression in women – a one-year follow-up study. J Clin Nurs 2010;19:3051-62. http://dx.doi.org/10.1111/j.1365-2702.2010.03332.x.
- Furuta M, Sandall J, Bick D. Women’s perceptions and experiences of severe maternal morbidity ‘A synthesis of qualitative studies using a meta-ethnographic approach. Midwifery 2014;30:158-69. http://dx.doi.org/10.1016/j.midw.2013.09.001.
- Bick D, MacArthur C, Winter H. Postnatal Care. London: Elsevier Health Sciences UK; 2008.
- Lavender T, Richens Y, Milan SJ, Smyth R, Dowswell T. Telephone support for women during pregnancy and the first six weeks postpartum. Cochrane Database Syst Rev 2013;7. http://dx.doi.org/10.1002/14651858.cd009338.pub2.
- Rahman A. Challenges and opportunities in developing a psychological intervention for perinatal depression in rural Pakistan – a multi-method study. Arch Womens Ment Health 2007;10:211-19. http://dx.doi.org/10.1007/s00737-007-0193-9.
- Simon GE. CBT improves maternal perinatal depression in rural Pakistan. Evid Based Ment Health 2009;12. http://dx.doi.org/10.1136/ebmh.12.2.45.
- Rahman A, Sikander S, Malik A, Ahmed I, Tomenson B, Creed F. Effective treatment of perinatal depression for women in debt and lacking financial empowerment in a low-income country. Br J Psychiatry 2012;201:451-7. http://dx.doi.org/10.1192/bjp.bp.112.109207.
- Martin A, Horowitz C, Balbierz A, Howell EA. Views of women and clinicians on postpartum preparation and recovery. Matern Child Health J 2013;18:707-13. http://dx.doi.org/10.1007/s10995-013-1297-7.
- Negron R, Martin A, Almog M, Balbierz A, Howell EA. Social support during the postpartum period: mothers’ views on needs, expectations, and mobilization of support. Matern Child Health J 2013;17:616-23. http://dx.doi.org/10.1007/s10995-012-1037-4.
- Novick G. CenteringPregnancy and the current state of prenatal care. J Midwifery Womens Health 2004;49:405-11. http://dx.doi.org/10.1111/j.1542-2011.2004.tb04434.x.
- Fu YY, Heh SS. Effectiveness of informational support in reducing the severity of postnatal depression in Taiwan. J Adv Nurs 2003;42:30-6. http://dx.doi.org/10.1046/j.1365-2648.2003.02576.x.
- Mills EP, Finchilescu G, Lea SJ. Postnatal depression – an examination of psychosocial factors. S Afr Med J 1995;85:99-105.
- Mason WA, Rice MJ, Records K. The lived experience of postpartum depression in a psychiatric population. Perspect Psychiatr Care 2005;41:52-61. http://dx.doi.org/10.1111/j.1744-6163.2005.00011.x.
- Knaak S. ‘Having a tough time:’ towards an understanding of the psycho-social causes of postpartum emotional stress. JMI 2009;11:80-94.
- Guedeney A, Marchand-Martin L, Cote SJ, Larroque B. Perinatal risk factors and social withdrawal behaviour. Eur Child Adolesc Psychiatry 2012;21:185-91. http://dx.doi.org/10.1007/s00787-012-0250-4.
- Saligheh M. Physical Activity in Postpartum Women and its Relationship to Postnatal Depression. Bentley, WA: Curtin University; 2011.
- Frank E, Kupfer DJ, Cornes C, Morris SM, Klerman G, Weissman MM. New Applications of Interpersonal Psychotherapy. Washington, DC: American Psychiatric Press; 1993.
- Zuckoff A, Swartz HA, Grote NK, Arkowitz H, Westra HA, Miller WR, et al. Motivational Interviewing in the Treatment of Psychological Problems. New York, NY: Guilford; 2008.
- Bernal G, Saez-Santiago E. Culturally centered psychosocial interventions. J Community Psychol 2006;34:121-32. http://dx.doi.org/10.1002/jcop.20096.
- Thinking Healthy: Cognitive Behavioural Training for Healthy Mothers and Infants. Training Manual Draft 01-11-2004. Islamabad: Human Development Research Foundation; 2007.
- Ritter C, Gochman DS. Health Behavior. New York, NY: Springer; 1998.
- Collins NL, Dunkel-Schetter C, Lobel M, Scrimshaw SC. Social support in pregnancy: psychosocial correlates of birth outcomes and postpartum depression. J Pers Soc Psychol 1993;65. http://dx.doi.org/10.1037/0022-3514.65.6.1243.
- McGinley M, Turnbull D, Fyvie H, Johnstone I, MacLennan B. Midwifery development unit at Glasgow Royal Maternity Hospital. Br J Midwifery 1995;3:362-71.
- Turnbull D, McGinley M, Fyvie H, Johnstone I, Holmes A, Shields N, et al. Implementation and evaluation of a midwifery development unit. Br J Midwifery 1995;3:465-8.
Appendix 1 Literature search strategies
Electronic bibliographic databases searched for clinical effectiveness evidence
-
The Cochrane Library including the Cochrane Systematic Reviews Database, Cochrane Controlled Trials Register, DARE, HTA and NHS EED databases 1991 (searched on 28 November 2012).
-
MEDLINE (via Ovid) 1946 – November week 3 2012 (searched on 30 November 2012).
-
PreMEDLINE (via Ovid) 4 December 2012 (searched on 5 December 2012).
-
EMBASE (via Ovid) 1974 – 4 December 2012 (searched on 5 December 2012).
-
CINAHL (via EBSCOhost) 1982 (searched on 11 December 2012).
-
PsycINFO (via Ovid) 1806 – November week 4 2012 (searched on 5 December 2012).
-
Science Citation Index (via ISI Web of Science) 1899 – date (searched on 5 December 2012).
-
Social Science Citation Index (via ISI Web of Science) 1956 (searched on 5 December 2012).
-
ASSIA (via ProQuest) 1987 (searched on 19 December 2012).
-
AMED (via Ovid) 1985 – 4 December 2012 (searched on 5 December 2012).
-
CPCI-S (via ISI Web of Science) 1990 (searched on 5 December 2012).
-
MIDIRS reference database 1991 (searched 24 July 2013).
Additional resources used for clinical effectiveness evidence
-
UK Clinical Research Network (searched on 30 January 2013).
-
Current Controlled Trials (searched on 30 January 2013).
-
Clinical Trials.gov (searched on 30 January 2013).
-
PROSPERO (searched on 19 February 2013).
-
Social Care online (searched on 19 February 2013).
-
ProQuest Dissertation and Theses (searched on 26 March 2013).
-
HSRProj (Health Services Research Projects in Progress) (searched on 19 February 2013).
-
Index to Theses (searched on 19 February 2013).
-
OpenGrey (searched on 19 February 2013).
-
relevant websites (searched on 26 March 2013).
-
general internet search using the search engine Google (searched on 19 February 2013).
Search strategy for randomised controlled trials
-
MeSH descriptor: [Depression, Postpartum] explode all trees
-
pnd:ti,ab,kw (Word variations have been searched)
-
MeSH descriptor: [Depression] explode all trees
-
depress*:ti,ab,kw (Word variations have been searched)
-
stress*:ti,ab,kw (Word variations have been searched)
-
anxi*:ti,ab,kw (Word variations have been searched)
-
MeSH descriptor: [Anxiety Disorders] explode all trees
-
MeSH descriptor: [Anxiety] explode all trees
-
MeSH descriptor: [Affective Disorders, Psychotic] explode all trees
-
affective:ti,ab,kw (Word variations have been searched)
-
#3 or #4 or #5 or #6 or #7 or #8 or #9 or #10
-
postpartum or post partum or postpartum:ti,ab,kw (Word variations have been searched)
-
MeSH descriptor: [Postpartum Period] explode all trees
-
postnatal* or post natal* or postnatal*:ti,ab,kw (Word variations have been searched)
-
post-pregnan* or post pregnan* or postpregnan*:ti,ab,kw (Word variations have been searched)
-
ante-natal* or ante natal* or antenatal*:ti,ab,kw (Word variations have been searched)
-
pre-natal* or pre natal* or prenatal*:ti,ab,kw (Word variations have been searched)
-
peri-natal* or peri natal* or perinatal*:ti,ab,kw (Word variations have been searched)
-
#12 or #13 or #14 or #15 or #16 or #17 or #18
-
#11 and #19
-
#1 or #2 or #20
-
MeSH descriptor: [Primary Prevention] explode all trees
-
prevent*:ti,ab,kw (Word variations have been searched)
-
Any MeSH descriptor with qualifier(s): [Prevention & control - PC]
-
prophyla*:ti,ab,kw (Word variations have been searched)
-
decreas* or reduc* or lower* or overcom* or improv* or avoid*:ti,ab,kw (Word variations have been searched)
-
wellbeing or well-being or well being:ti,ab,kw (Word variations have been searched)
-
enhanc* or improv* or increas*:ti,ab,kw (Word variations have been searched)
-
#27 and #28
-
#22 or #23 or #24 or #25 or #26 or #29
-
#21 and #30
-
MeSH descriptor: [Risk Factors] explode all trees
-
MeSH descriptor: [Risk] explode all trees
-
risk* or indicat* or predict* or predispos*:ti,ab,kw (Word variations have been searched)
-
MeSH descriptor: [Social Support] explode all trees
-
social support*:ti,ab,kw (Word variations have been searched)
-
MeSH descriptor: [Socioeconomic Factors] explode all trees
-
MeSH descriptor: [Social Class] explode all trees
-
MeSH descriptor: [Life Change Events] explode all trees
-
history of depression*:ti,ab,kw (Word variations have been searched)
-
MeSH descriptor: [Marriage] explode all trees
-
dyadic adjustment* or parental adjustment*:ti,ab,kw (Word variations have been searched)
-
MeSH descriptor: [Pregnancy Complications] explode all trees
-
MeSH descriptor: [Obstetric Labor Complications] explode all trees
-
complication*:ti,ab,kw (Word variations have been searched)
-
MeSH descriptor: [Parturition] explode all trees
-
#32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43 or #44 or #45 or #46
-
#21 and #47
-
interven* or program* or target* or educat* or strat*:ti,ab,kw (Word variations have been searched)
-
#21 and #49
-
#31 or #48 or #50
Search strategy used on The Cochrane Library
The Cochrane Library including the Cochrane Systematic Reviews Database, Cochrane Controlled Trials Register, DARE, HTA and NHS EED databases, 1991– date (searched on 28 November 2012).
-
MeSH descriptor: [Depression, Postpartum] explode all trees
-
pnd:ti,ab,kw (Word variations have been searched)
-
MeSH descriptor: [Depression] explode all trees
-
depress*:ti,ab,kw (Word variations have been searched)
-
stress*:ti,ab,kw (Word variations have been searched)
-
anxi*:ti,ab,kw (Word variations have been searched)
-
MeSH descriptor: [Anxiety Disorders] explode all trees
-
MeSH descriptor: [Anxiety] explode all trees
-
MeSH descriptor: [Affective Disorders, Psychotic] explode all trees
-
affective:ti,ab,kw (Word variations have been searched)
-
#3 or #4 or #5 or #6 or #7 or #8 or #9 or #10
-
postpartum or post partum or postpartum:ti,ab,kw (Word variations have been searched)
-
postnatal* or post natal* or postnatal*:ti,ab,kw (Word variations have been searched)
-
post-pregnan* or post pregnan* or postpregnan*:ti,ab,kw (Word variations have been searched)
-
ante-natal* or ante natal* or antenatal*:ti,ab,kw (Word variations have been searched)
-
pre-natal* or pre natal* or prenatal*:ti,ab,kw (Word variations have been searched)
-
peri-natal* or peri natal* or perinatal*:ti,ab,kw (Word variations have been searched)
-
#12 or #13 or #14 or #15 or #16 or #17
-
#11 and #18
-
#1 or #2 or #19
Search steps 1–20 are for the population PND.
-
MeSH descriptor: [Primary Prevention] explode all trees
-
prevent*:ti,ab,kw (Word variations have been searched)
-
Any MeSH descriptor with qualifier(s): [Prevention & control - PC]
-
prophyla*:ti,ab,kw (Word variations have been searched)
-
decreas* or reduc* or lower* or overcome* or improve*:ti,ab,kw (Word variations have been searched)
-
#21 or #22 or #23 or #24 or #25
Search steps 21–26 are terms for prevention.
-
#20 and #26
Search step 27 combines the population and prevention terms to find literature on prevention of PND.
-
MeSH descriptor: [Risk Factors] explode all trees
-
MeSH descriptor: [Risk] explode all trees
-
risk* or indicat* or predict* or predispos*:ti,ab,kw (Word variations have been searched)
-
MeSH descriptor: [Social Support] explode all trees
-
social support*:ti,ab,kw (Word variations have been searched)
-
MeSH descriptor: [Socioeconomic Factors] explode all trees
-
MeSH descriptor: [Social Class] explode all trees
-
MeSH descriptor: [Life Change Events] explode all trees
-
history of depression*:ti,ab,kw (Word variations have been searched)
-
MeSH descriptor: [Marriage] explode all trees
-
dyadic adjustment* or parental adjustment*:ti,ab,kw (Word variations have been searched)
-
MeSH descriptor: [Pregnancy Complications] explode all trees
-
MeSH descriptor: [Obstetric Labor Complications] explode all trees
-
#28 or #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 or #37 or #38 or #39 or #40
Search steps 28–30 are terms for risk and 31–40 are terms for known risk factors for PND.
-
#20 and #41
Search step 20 and 41 combines the population and risk terms to find papers about risk factors and PND to find trials that are focused at risk factors.
-
interven* or program* or target* or educat* or strat*:ti,ab,kw (Word variations have been searched)
Search step 43 are different terms around interventions.
-
#20 and #43
Search step 44 combines PND and intervention terms to find trials of PND interventions.
-
#27 or #42 or #44
Search step 45 uses OR to combine the different subsets and try to find all PND trials.
The search retrieved 883 records, 60 systematic reviews, 38 other reviews from DARE, 759 trials, eight technology assessments and nine economic evaluations.
Search strategy used on PreMEDLINE (via Ovid)
MEDLINE (Ovid) 1946 – week 3 November 2012 (searched on 30 November 2012) and PreMEDLINE (Ovid) 4 December 2012 (searched on 5 December 2012).
-
exp Depression, Postpartum /
-
pnd.tw.
-
exp Depression /
-
depress$.tw.
-
stress$.tw.
-
anxi$.tw.
-
exp Anxiety Disorders /
-
exp Anxiety /
-
exp Affective Disorders, Psychotic /
-
affective.tw.
-
3 or 4 or 5 or 6 or 7 or 8 or 9 or 10
-
12.(postpartum or post partum or postpartum).tw.
-
exp Postpartum Period /
-
(postnatal$ or post natal$ or postnatal$).tw.
-
(post-pregnan$ or post pregnan$ or postpregnan$).tw.
-
(ante-natal$ or ante natal$ or antenatal$).tw.
-
(pre-natal$ or pre natal$ or prenatal$).tw.
-
(peri-natal$ or peri natal$ or perinatal$).tw.
-
12 or 13 or 14 or 15 or 16 or 17 or 18
-
11 and 19
-
1 or 2 or 20
Search steps 1–21 are terms for the population PND.
-
exp Primary Prevention /
-
prevent$.tw.
-
pc.fs.
-
prophyla$.tw.
-
(decreas$ or reduc$ or lower$ or overcom$ or improv$ or avoid$).tw.
-
(wellbeing or well-being or well being).tw.
-
(enhanc$ or improv$ or increas$).tw.
-
27 and 28
-
or / 22-26,29
Search steps 22–30 are terms for prevention.
-
21 and 30
Search step 31 combines the population and prevention terms to find literature on prevention of PND.
-
exp Risk Factors /
-
Risk /
-
(risk$ or indicat$ or predict$ or predispos$).tw.
-
exp Social Support /
-
social support$.tw.
-
exp Socioeconomic Factors /
-
exp Social Class /
-
exp Life Change Events /
-
history of depression$.tw.
-
exp Marriage /
-
(dyadic adjustment$ or parental adjustment$).tw.
-
exp Pregnancy Complications /
-
Obstetric Labor Complications /
-
complication$.tw.
-
exp Parturition /
-
or / 32-46
Search steps 22–34 are terms for risk and 35–47 are terms for known risk factors for PND.
-
21 and 47
Search step 48 combines 21 and 47 combining the population and risk terms to find papers about risk factors and PND to find trials that are focused at risk factors.
-
(interven$ or program$ or target$ or educat$ or strat$).tw.
Search step 49 are different terms around interventions.
-
21 and 49
Search step 50 combines PND and intervention terms to find trials of PND interventions.
-
31 or 48 or 50
Search step 51 uses OR to combine the different subsets and try to find all PND trials.
-
Meta-Analysis as Topic /
-
meta analy$.tw.
-
metaanaly$.tw.
-
Meta-Analysis /
-
(systematic adj (review$1 or overview$1)).tw.
-
exp Review Literature as Topic /
-
52 or 53 or 54 or 55 or 56 or 57
-
cochrane.ab.
-
embase.ab.
-
(psychlit or psyclit).ab.
-
(cinahl or cinhal).ab.
-
science citation index.ab.
-
bids.ab.
-
cancerlit.ab.
-
59 or 60 or 61 or 62 or 63 or 64 or 65
-
reference list$.ab.
-
bibliograph$.ab.
-
hand-search$.ab.
-
relevant journals.ab.
-
manual search$.ab.
-
67 or 68 or 69 or 70 or 71
-
selection criteria.ab.
-
data extraction.ab.
-
73 or 74
-
Review /
-
75 and 76
-
Comment /
-
Letter /
-
Editorial /
-
animal /
-
human /
-
81 not (81 and 82)
-
78 or 79 or 80 or 83
-
58 or 66 or 72 or 77
-
85 not 84
Search steps 52–86 are the systematic reviews filter for MEDLINE.
-
51 and 86
Search step 87 combines the search with the systematic reviews filter to retrieve systematic reviews.
-
limit 87 to (English language and humans)
-
exp “costs and cost analysis” /
-
economics /
-
exp economics hospital /
-
exp economics medical /
-
exp economics nursing /
-
economics pharmaceutical /
-
exp “fees and charges” /
-
exp budgets /
-
budget$.tw.
-
cost$.ti.
-
(cost$ adj2 (effective$ or utilit$ or benefit$ or minim$)).ab.
-
(economic$ or pharmacoeconomic$ or pharmaco-economic$).ti.
-
(price or pricing$).tw.
-
(financial or finance or finances or finanaced).tw.
-
(fee or fees).tw.
-
or / 89-103
Search steps 89–104 is the economic evaluations filter for MEDLINE.
-
51 and 104
Search step 105 combines the search with the economic evaluations filter to retrieve economic evaluations.
-
limit 105 to (english language and humans)
-
from 106 keep 1-266
-
mixed method.tw.
-
mixed methods.tw.
-
mixed study.tw.
-
multi method.tw.
-
multiple sources of data.tw.
-
triangulation design.tw.
-
(qualitative adj99 quantitative).tw.
-
108 or 109 or 110 or 111 or 112 or 113 or 114
Search steps 108–115 are terms for mixed-methods research.
-
51 and 115
Search step 116 combines the search with the mixed-methods filter to mixed-methods papers
-
limit 116 to (english language and humans)
-
findings.tw.
-
interview.tw.
-
qualitative.tw.
-
118 or 119 or 120
Search steps 108–115 are the qualitative filter for MEDLINE.
-
51 and 121
Search step 122 combines the search with the qualitative filter to retrieve qualitative studies
-
limit 122 to (english language and humans)
-
*Depression, Postpartum /
-
123 and 124
Search step 125 further refines the search to retrieve qualitative research with *Depression, Postpartum / as a major subject heading.
Search strategy used on EMBASE
EMBASE (Ovid) 1974 – 4 December 2012 (searched on 5 December 2012).
-
puerperal depression /
-
pnd.tw.
-
exp depression /
-
depress$.tw.
-
stress$.tw.
-
anxi$.tw.
-
exp anxiety disorder /
-
exp anxiety /
-
mood disorder /
-
affective.tw.
-
or / 3-10
-
(postpartum or post partum or postpartum).tw.
-
exp puerperium /
-
(postnatal$ or post natal$ or postnatal$).tw.
-
(post-pregnan$ or post pregnan$ or postpregnan$).tw.
-
(ante-natal$ or ante natal$ or antenatal$).tw.
-
(pre-natal$ or pre natal$ or prenatal$).tw.
-
(peri-natal$ or peri natal$ or perinatal$).tw.
-
or / 12-18
-
11 and 19
-
1 or 2 or 20
Search steps 1–21 are terms for the population PND.
-
exp primary prevention /
-
prevent$.tw.
-
pc.fs.
-
prophyla$.tw.
-
(decreas$ or reduc$ or lower$ or overcom$ or improv$ or avoid$).tw.
-
(wellbeing or well-being or well being).tw.
-
(enhanc$ or improv$ or increas$).tw.
-
27 and 28
-
or / 22-26,29
Search steps 22–30 are terms for prevention.
-
21 and 30
Search step 31 combines the population and prevention terms to find literature on prevention of PND.
-
exp risk factor /
-
risk /
-
(risk$ or indicat$ or predict$ or predispos$).tw.
-
exp social support /
-
social support$.tw.
-
exp socioeconomics /
-
exp social class /
-
exp life event /
-
history of depression$.tw.
-
marriage /
-
(dyadic adjustment$ or parental adjustment$).tw.
-
exp pregnancy complication /
-
exp labor complication /
-
complication$.tw.
-
exp birth /
-
or / 32-46
Search steps 32–34 are terms for risk and 35–47 are terms for known risk factors for PND.
-
21 and 47
Search step 48 combines 21 and 47 combining the population and risk terms to find papers about risk factors and PND to find trials that are focused at risk factors.
-
(interven$ or program$ or target$ or educat$ or strat$).tw.
Search step 49 are different terms around interventions.
-
21 and 49
Search step 50 combines PND and intervention terms to find trials of PND interventions.
-
21 or 48 or 50
Search step 51 uses OR to combine the different subsets and try to find all PND trials.
-
Meta Analysis /
-
((meta adj analy$) or metaanalys$).tw.
-
(systematic adj (review$1 or overview$1)).tw.
-
or / 51-53
-
cancerlit.ab.
-
cochrane.ab.
-
embase.ab.
-
(psychlit or psyclit).ab.
-
(psychinfo or psycinfo).ab.
-
(cinal or cinahl).ab.
-
science citation index.ab.
-
bids.ab.
-
or / 55-62
-
reference lists.ab.
-
bibliograph$.ab.
-
hand-search$.ab.
-
manual search$.ab.
-
relevant journals.ab.
-
or / 64-68
-
data extraction.ab.
-
selection criteria.ab.
-
70 or 71
-
review.pt.
-
72 and 73
-
letter.pt.
-
editorial.pt.
-
animal /
-
human /
-
77 not (77 and 78)
-
or / 75-76,79
-
54 or 63 or 69 or 74
-
81 not 80
Search steps 52–83 is the systematic reviews filter for EMBASE.
-
51 and 83
Search step 84 combines the search with the systematic reviews filter to retrieve systematic reviews.
-
exp SOCIOECONOMICS /
-
exp “Cost Benefit Analysis” /
-
exp “Cost Effectiveness Analysis” /
-
exp “Cost of Illness” /
-
exp “Cost Control” /
-
exp Economic Aspect /
-
exp Financial Management /
-
exp “Health Care Cost” /
-
exp Health Care Financing /
-
exp Health Economics /
-
exp “Hospital Cost” /
-
(financial or fiscal or finance or funding).tw.
-
exp “Cost Minimization Analysis” /
-
(cost adj estimate$).mp.
-
(cost adj variable$).mp.
-
(unit adj cost$).mp.
-
or / 83-100
Search steps 85–101 is a economic evaluations filter for EMBASE.
-
51 and 101
Search step 102 combines the search with the economic filter to retrieve economic evaluations.
-
mixed method.tw.
-
mixed methods.tw.
-
mixed study.tw.
-
multi method.tw.
-
multiple sources of data.tw.
-
triangulation design.tw.
-
(qualitative adj99 quantitative).tw.
-
or / 103-109
Search steps 103–110 are terms for mixed methods.
-
51 and 110
Search step 111 combines the search with the terms for mixed-methods to retrieve mixed-methods research.
-
findings.tw.
-
interview.tw.
-
qualitative.tw.
-
or / 112-114
Search steps 112–115 are a qualitative filter for EMBASE.
-
51 and 115
Search step 116 combines the search with the qualitative filter to retrieve qualitative research.
-
*puerperal depression /
-
116 and 117
Search step 118 further refines the search to retrieve qualitative research with *puerperal depression / as a major subject heading.
Search strategy used on Cumulative Index to Nursing and Allied Health Literature
CINAHL (EBSCOhost) 1982 (searched on 11 December 2012).
S53 S51 and S52
S52 (MM “Depression, Postpartum”)
S51 S41 AND S50
S50 TI (findings OR interview OR qualitative) OR AB (findings OR interview OR qualitative)
S49 S41 AND S48
S48 TI (“mixed method” OR “mixed methods” OR “mixed study” OR “multi method” OR “multiple sources of data” OR “triangulation design” OR (qualitative AND quantitative)) OR AB (“mixed method” OR “mixed methods” OR “mixed study” OR “multi method” OR “multiple sources of data” OR “triangulation design” OR (qualitative AND quantitative))
S47 S41 AND S46
S46 TI (economic* OR cost* OR fee* OR charge* OR budget* OR pharmacoeconomic* or price* or pricing*) OR AB (economic* OR cost* OR fee* OR charge* OR budget* OR pharmacoeconomic* or price* or pricing*)
S45 S41 AND S44
S44 TI (meta analy* OR metaanaly* OR meta-analysis OR systematic review OR overview* OR revie) OR AB (meta analy* OR metaanaly* OR meta-analysis OR systematic review OR overview* OR revie)
S43 S41 AND S42
S42 TI (randomised controlled trial* OR randomized controlled trial* OR random* OR blind* OR mask* OR clinical trial* OR placebo*) OR AB (randomised controlled trial* OR randomized controlled trial* OR random* OR blind* OR mask* OR clinical trial* OR placebo*)
S41 S25 OR S38 OR S40
S40 S17 AND S39
S39 TI (interven* or program* or target* or educat* or strat*) OR AB (interven* or program* or target* or educat* or strat*)
S38 S17 AND S37
S37 S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37
S37 (MH “Childbirth+”)
S36 TI complication* OR AB complication*
S35 (MH “Labor Complications+”)
S34 (MH “Pregnancy Complications+”)
S33 TI (dyadic adjustment* or parental adjustment*) OR AB (dyadic adjustment* or parental adjustment*)
S32 (MH “Marriage”)
S31 TI history of depression* OR AB history of depression*
S30 (MH “Life Change Events+”)
S29 (MH “Socioeconomic Factors+”)
S28 TI social support* OR AB social support*
S27 (MH “Support, Psychosocial+”)
S26 TI (risk* or indicat* or predict* or predispos*) OR AB (risk* or indicat* or predict* or predispos*)
S25 S17 AND S24
S24 S18 OR S19 OR S20 OR S23
S23 S21 AND S22
S22 TI (enhanc* or improv* or increas*) OR AB (enhanc* or improv* or increas*)
S21 TI (wellbeing or well-being or well being) OR AU (wellbeing or well-being or well being)
S20 TI (decreas* or reduc* or lower* or overcom* or improv* or avoid*) OR AB (decreas* or reduc* or lower* or overcom* or improv* or avoid*)
S19 TI prophyla* OR AB prophyla*
S18 TI prevent* OR AB prevent*
S17 S1 OR S2 OR S1
S16 (S8 AND S15)
S15 S9 OR S10 OR S11 OR S12 OR S13 OR S14
S14 TI (peri-natal* or peri natal* or perinatal*) OR AB (peri-natal* or peri natal* or perinatal*)
S13 TI (pre-natal* or pre natal* or prenatal*) OR AB (pre-natal* or pre natal* or prenatal*)
S12 TI (ante-natal* or ante natal* or antenatal*) OR AB (ante-natal* or ante natal* or antenatal*)
S11 TI (post-pregnan* or post pregnan* or postpregnan*) OR AB (post-pregnan* or post pregnan* or postpregnan*)
S10 TI (postnatal* or post natal* or postnatal*) OR AB (postnatal* or post natal* or postnatal*)
S9 TI (postpartum or post partum or postpartum) OR AB (postpartum or post partum or postpartum)
S8 S3 OR S4 OR S5 OR S6 OR S7
S7 TI affective OR AB affective
S6 (MH “Anxiety+”)
S5 (MH “Affective Disorders, Psychotic+”)
S4 (MH “Anxiety Disorders+”)
S3 TI (depress* OR stress* OR anxi*) OR AB (depress* OR stress* OR anxi*)
S2 TI pnd OR AB pnd
S1 (MH “Depression, Postpartum”)
Results from search line 43 were saved for RCTs, 45 for systematic reviews, 47 for economic evaluations, 49 for mixed-methods research and 53 for qualitative research.
Search strategy used on PsycINFO
PsycINFO (via Ovid) was searched from 1806 to week 4 November 2012 (searched on 5 December 2012).
-
postpartum depression /
-
pnd.ab,ti.
-
(depress$ or stress$ or anxi*).ab,ti.
-
anxiety /
-
anxiety disorders /
-
or / 3-5
-
postnatal period /
-
(postpartum or post partum or postpartum or postnatal$ or post natal$ or postnatal$ or post-pregnan$ or post pregnan$ or postpregnan$ or ante-natal$ or ante natal$ or antenatal$ or pre-natal$ or pre natal$ or prenatal$ or peri-natal$ or peri natal$ or perinatal$).ab,ti.
-
7 or 8
-
6 and 9
-
1 or 2 or 10
Search steps 1–11 are terms for the population PND.
-
exp Primary Mental Health Prevention /
-
(prevent$ or prophyla$ or decreas$ or reduc$ or lower$ or overcom$ or improv$ or avoid$).ab,ti.
-
(wellbeing or well-being or well being).ab,ti.
-
(enhanc$ or improv$ or increas$).ab,ti.
-
14 and 15
-
12 or 13 or 16
Search steps 12–17 are terms for prevention.
-
11 and 17
Search step 18 combines the population and prevention terms to find literature on prevention of PND.
-
risk factors /
-
(risk$ or indicat$ or predict$ or predispos$).ab,ti.
-
social support /
-
social support$.ab,ti.
-
exp socioeconomic status /
-
life changes /
-
history of depression$.ab,ti.
-
marriage /
-
(dyadic adjustment$ or parental adjustment$).ab,ti.
-
exp obstetrical complications /
-
complication$.ab,ti.
-
birth /
-
19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30
Search steps 19–20 are terms for risk and 21–30 are terms for known risk factors for PND.
-
11 and 31
Search step 32 combines 11 and 31 combining the population and risk terms to find papers about risk factors and PND to find trials that are focused on risk factors.
-
(interven$ or program$ or target$ or educat$ or strat$).ab,ti.
Search step 33 is synonymous for the term intervention.
-
11 and 33
Search step 34 combines PND and intervention terms to find trials of PND interventions.
-
18 or 32 or 34
Search step 35 uses OR to combine the different subsets and try to find all PND trials.
-
limit 35 to (human and english language)
Search steps 36 limits the results of the search to studies about human in English.
-
(double-blind or random: assigned or control).tw.
Search step 37 is a one-line RCT filter for PsycINFO.
-
36 and 37
Search step 38 combines the search with the RCT filter to retrieve RCTs of PND prevention trials.
-
(meta-analysis or search:).tw.
Search step 39 is a one-line systematic reviews filter for PsycINFO.
-
36 and 39
Search strategy used for cost-effectiveness studies with economic evaluations filter for MEDLINE
Search step 38 combines the search with the systematic reviews filter to retrieve systematic reviews on PND prevention.
-
exp “costs and cost analysis”/
-
economics /
-
exp economics hospital /
-
exp economics medical /
-
exp economics nursing /
-
economics pharmaceutical /
-
exp “fees and charges”/
-
exp budgets /
-
budget$.tw.
-
cost$.ti.
-
(cost$ adj2 (effective$ or utilit$ or benefit$ or minim$)).ab.
-
(economic$ or pharmacoeconomic$ or pharmaco-economic$).ti.
-
(price or pricing$).tw.
-
(financial or finance or finances or finanaced).tw.
-
(fee or fees).tw.
-
or / 41-55
Step 56 is an economic evaluation filter for PsycINFO.
-
36 and 56
Step 57 combines the search with the economic evaluation filter to retrieve economic evaluations.
-
mixed method.tw.
-
mixed methods.tw.
-
mixed study.tw.
-
multi method.tw.
-
multiple sources of data.tw.
-
triangulation design.tw.
-
(qualitative adj99 quantitative).tw.
-
or / 58-64
Search step 65 are terms for mixed-methods research.
-
36 and 65
Search step 66 combined the search with the mixed-methods terms to retrieve research that utilises mixed methods.
-
findings.tw.
-
interview.tw.
-
qualitative.tw.
-
or / 67-69
Search step 70 is a qualitative filter for PsycINFO.
-
36 and 70
Search step 71 combines the search with the qualitative filter to retrieve qualitative research.
-
*Depression, Postpartum /
-
71 and 72
Search step 73 further refines the search to retrieve qualitative research with *Depression, Postpartum / as a major subject heading.
Search strategy used on Conference Proceedings Citation Index and Social Science Citation Index Search and Science Citation Index
Science Citation Index (via ISI Web of Science) 1899–date, Social Science Citation Index (via ISI Web of Science) 1956–date and CPCI-S (via ISI Web of Science) 1990–date (searched on 5 December 2012).
# 29 #15 AND #28
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 28 (TS = (randomised controlled trial* OR randomized controlled trial* OR random* OR blind* OR mask* OR clinical trial* OR placebo*)) AND LANGUAGE:(English)
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 27 #15 AND #26
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 26 (TS = (findings OR interview OR qualitative)) AND LANGUAGE: (English)
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 25 #15 AND #34
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 24 #22 OR #23
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 23 (TS = (“mixed method” OR “mixed methods” OR “mixed study” OR “multi method” OR “multiple sources of data” OR “triangulation design”)) AND LANGUAGE: (English)
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 22 (TS = (qualitative AND quantitative)) AND LANGUAGE: (English)
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 21 #15 AND #20
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 20 (TS = (“mixed method” OR “mixed methods” OR “mixed study” OR “multi method” OR “multiple sources of data” OR “triangulation design” OR “qualitative quantitative”)) AND LANGUAGE: (English)
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 19 #15 AND #18
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 18 (TS = (economic* OR cost* OR fee* OR charge* OR budget* OR pharmacoeconomic* or price* or pricing*)) AND LANGUAGE: (English)
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 17 (#16) AND LANGUAGE:(English)
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 16 #12 AND #15
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 15 #13 AND #14
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 14 #10 OR #11
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 13 #3 OR #4
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 12 TI = (meta analy* OR metaanaly* OR meta-analysis OR systematic review OR overview* OR review)
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 11 TI = (interven* OR program* OR target* OR educat* OR strat*)
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 10 #7 OR #8 OR #9
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 9 TI = (prevent* OR prophyla* OR decreas* OR reduc* OR lower* OR overcom* OR improv* OR avoid*)
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 8 TI = (risk* OR indicat* OR predict* OR predispos* OR social support* OR socioeconomic factor* OR social class OR life change event* OR history of depression* OR marriage OR dyadic adjustment* OR parental adjustment* OR complication* OR birth OR parturition)
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 7 #6 AND #5
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 6 TS = (wellbeing OR well-being OR well being)
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 5 TI = (decreas* OR reduc* OR lower* OR overcom* OR improv* or avoid*)
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 4 TS = pnd
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 3 #2 AND #1
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 2 TI = (postpartum OR post partum OR postpartum OR postnatal* OR post natal* OR postnatal* OR post-pregnan* OR post pregnan* OR postpregnan* OR ante-natal* OR ante natal* OR antenatal* OR pre-natal* OR pre natal* OR prenatal* OR peri-natal* OR peri natal* OR perinatal*)
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
# 1 TI = (depress* OR stress* OR anxi* OR affective)
Indexes = SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH Timespan = All years
Results from search line 29 were saved for RCTs, 16 for systematic reviews, 19 for economic evaluations, 25 for mixed-methods research and 27 for qualitative research.
Search strategy used on Applied Social Sciences Index and Abstracts (via ProQuest)
Applied Social Sciences Index and Abstracts (via ProQuest) 1987 – (searched on 19 December 2012)
-
((((SU.EXACT.EXPLODE(“Postnatal depression”) OR pnd) OR ((SU.EXACT(“Depression”) OR (depress* OR stress* OR anxi*) OR SU.EXACT(“Anxiety”) OR SU.EXACT(“Anxiety disorders”) OR SU.EXACT(“Affective disorders”) OR affective) AND (SU.EXACT.EXPLODE(“Postpartum women”) OR all(postpartum OR post partum OR postpartum) OR (postnatal* OR post natal* OR postnatal*) OR (post-pregnan* OR post pregnan* OR postpregnan*) OR (ante-natal* OR ante natal* OR antenatal*) OR all(peri-natal* OR peri natal* OR perinatal*) OR all(pre-natal*) OR all(prenatal*)))) AND (SU.EXACT.EXPLODE(“Primary prevention trials”) OR (prevent* OR prophyla* OR decreas* OR reduc* OR lower* OR overcom* OR improv* OR avoid*) OR ((wellbeing OR well-being OR well being) AND (enhanc* OR improv* OR increas*)))) OR (((SU.EXACT.EXPLODE(“Postnatal depression”) OR pnd) OR ((SU.EXACT(“Depression”) OR (depress* OR stress* OR anxi*) OR SU.EXACT(“Anxiety”) OR SU.EXACT(“Anxiety disorders”) OR SU.EXACT(“Affective disorders”) OR affective) AND (SU.EXACT.EXPLODE(“Postpartum women”) OR all(postpartum OR post partum OR postpartum) OR (postnatal* OR post natal* OR postnatal*) OR (post-pregnan* OR post pregnan* OR postpregnan*) OR (ante-natal* OR ante natal* OR antenatal*) OR all(peri-natal* OR peri natal* OR perinatal*) OR all(pre-natal*) OR all(prenatal*))))
-
(((risk* OR indicat* OR predict* OR predispos*) OR (SU.EXACT. “Risk factors”) OR SU.EXACT(“Risk factors”) OR SU.EXACT.EXPLODE(“Computer based social support” OR “Perceived social support” OR “Social support”) OR (social support*) OR SU.EXACT.EXPLODE(“Aristocracy” OR “Elites” OR “Gentrification” OR “Lumpenproletariat” OR “Middle class people” OR “Peerages” OR “Proletariat” OR “Ruling classes” OR “Social class” OR “Underclasses” OR “Upper class people” OR “Upper class women” OR “Upper middle class people” OR “Working class people”) OR all(history of depress*) OR SU.EXACT.EXPLODE(“Arranged marriages” OR “Brides” OR “Conjugal contracts” OR “Consanguineous marriages” OR “Custody after divorce” OR “Divorce” OR “Endogamy” OR “Engaged couples” OR “Exogamy” OR “Extramarital affairs” OR “Homogamy” OR “Intermarriage” OR “Joint custody” OR “Marital quality” OR “Marital structure” OR “Marriage” OR “Monogamy” OR “Parental divorce” OR “Polyandry” OR “Polygamy” OR “Polygyny” OR “Prenuptial contracts” OR “Racial intermarriage” OR “Remarriages” OR “Serial monogamy” OR “Singleness” OR “Tahlil marriage” OR “Temporary marriages” OR “Transnational divorce” OR “Weddings”) OR (dyadic adjustment* OR parental adjustment* OR complication*) OR SU.EXACT.EXPLODE(“Birth centres” OR “Caesarean section” OR “Childbirth” OR “Dystocia” OR “Home birth” OR “Labour” OR “Natural childbirth” OR “Placenta” OR “Premature labour” OR “Shoulder dystocia” OR “Vacuum extraction” OR “Vaginal birth” OR “Waterbirth”)))
-
(interven* OR program* OR target* OR educat* OR strat*)
-
(random* control* OR blind* OR trial* singl* OR doubl* OR trebl* OR tripl* OR mask* OR placebo*)
Searches 1, 2, 3 and 4 were combined to find RCTs on prevention of PND.
-
(meta-analy* OR meta analy* OR metaanaly* OR review* OR overview*)
Searches 1, 2, 3 and 5 were combined to find systematic reviews on prevention of PND.
-
(economic* OR cost* OR fee* OR charge* OR budget* OR pharmacoeconomic* or price* or pricing*)
Searches 1, 2, 3 and 6 were combined to find economic evaluations.
-
(“mixed method” OR “mixed methods” OR “mixed study” OR “multi method” OR “multiple sources of data” OR “triangulation design” OR “qualitative quantitative”)
Searches 1, 2, 3 and 7 were combined to find mixed-methods research.
-
(findings OR interview OR qualitative)
Searches 1, 2, 3 and 8 were combined to find qualitative research.
Search strategy used on Allied and Complementary Medicine Database (via Ovid)
Allied and Complementary Medicine Database (via Ovid) was searched from 1985 to 4 December 2012 and EconLit (via Ovid) was searched from 1961 to November 2012 (searched on 5 December 2012).
-
pnd.tw.
-
depress$.tw.
-
stress$.tw.
-
anxi$.tw.
-
affective.tw.
-
or / 2-5
-
(postpartum or post partum or postpartum).tw.
-
(postnatal$ or post natal$ or postnatal$).tw.
-
(post-pregnan$ or post pregnan$ or postpregnan$).tw.
-
(ante-natal$ or ante natal$ or antenatal$).tw.
-
(pre-natal$ or pre natal$ or prenatal$).tw.
-
(peri-natal$ or peri natal$ or perinatal$).tw.
-
or / 7-12
-
6 and 13
-
1 or 14
-
prevent$.tw.
-
pc.fs.
-
prophyla$.tw.
-
(decreas$ or reduc$ or lower$ or overcom$ or improv$ or avoid$).tw.
-
(wellbeing or well-being or well being).tw.
-
(enhanc$ or improv$ or increas$).tw.
-
20 and 21
-
or / 16-19,22
-
15 and 23
-
(risk$ or indicat$ or predict$ or predispos$).tw.
-
social support$.tw.
-
social class$.tw.
-
life change event$'.tw.
-
history of depression$.tw.
-
marriage.tw.
-
(dyadic adjustment$ or parental adjustment$).tw.
-
complication$.tw.
-
parturition.tw.
-
or / 25-33
-
15 and 34
-
(interven$ or program$ or target$ or educat$ or strat$).tw.
-
15 and 36
-
24 or 35 or 37
No filters were used for AMED or EconLit due to the small size of the databases.
Search strategy used on Midwives Information and Resource Service
Midwives Information and Resource Service Reference Database 1991 – (searched 24 July 2013)
Owing to the small size of the database, searches were conducted for the population terms only and then reviewed for relevance.
Electronic databases searched for the cost-effectiveness literature
The following electronic databases were searched:
-
MEDLINE (via Ovid) 1946 – November week 3 2012 (searched on 30 November 2012).
-
PreMEDLINE (via Ovid) (searched on 5 December 2012).
-
EMBASE (via Ovid) 1974 – 4 December 2012 (searched on 5 December 2012).
-
CINAHL (via EBSCOhost) 1982 – (searched on 11 December 2012).
-
NHS EED (via Wiley) 1991 – (searched on 28 November 2012).
-
EconLit (via Ovid) 1961 – November 2012 (searched on 5 December 2012).
-
PsycINFO (via Ovid) 1806 – week 4 November 2012 (searched on 5 December 2012).
-
Science Citation Index (via ISI Web of Science) 1899 – (searched on 5 December 2012).
-
Social Science Citation Index (via ISI Web of Science) 1956 – (searched on 5 December 2012).
-
AMED (via Ovid) 1985 – 4 December 2012 (searched on 5 December 2012).
-
ASSIA (via ProQuest) 1987 – (searched on 19 December 2012).
-
MIDIRS reference database 1991 – (searched 24 July 2013).
Appendix 2 Randomised controlled trials and systematic reviews: number retrieved
| Database searched | Number of RCTs | Number of systematic reviews |
|---|---|---|
| Cochrane Systematic Reviews Database | NA | 60 |
| Cochrane Controlled Trials Register | 767 | 0 |
| DARE | NA | 38 |
| HTA | NA | 8 |
| MEDLINE | NA | 268 |
| PreMEDLINE | NA | 27 |
| EMBASE | NA | 393 |
| CINAHL | 408 | 124 |
| PsycINFO | 575 | 126 |
| Citation Indexes (Science and Social Sciences): Science Citation Index expanded (1899 to date); Social Sciences Citation Index (1956 to date); CPCI-S (1990 to date); Conference Proceedings Citation Index – Social Science & Humanities (1990 to date) | 7 | 29 |
| ASSIA | 107 | 132 |
| AMED | 3 | 3 |
| MIDIRS reference database | 2 | 0 |
Appendix 3 Key journals hand-searched via electronic alerts
Acta Psychiatrica Scandinavica.
American Journal of Obstetrics & Gynecology.
American Journal of Psychiatry.
American Journal of Family Therapy.
Archives of General Psychiatry.
Archives of Women’s Mental Health.
Birth.
BJOG: An International Journal of Obstetrics and Gynaecology.
BMC Public Health.
British Journal of General Practice.
British Journal of Clinical Psychology.
British Journal of Psychiatry.
British Medical Journal.
Canadian Journal of Psychiatry.
International Journal of Methods in Psychiatric Research.
International Journal of Nursing Studies.
Journal of Advanced Nursing.
Journal of Affective Disorders.
Journal of Clinical Psychiatry.
Journal of Mental Health.
Journal of Midwifery and Women’s Health.
Journal of Paediatrics and Child Health.
Journal of Psychiatry.
Journal of Psychopharmacology.
Journal of Psychosomatic Research.
Medical Journal of Australia.
Midwifery.
Nursing Research.
Obstetrics and Gynaecology.
Psychological Medicine.
Psychology and Health.
Therapeutic Research.
Therapy.
Appendix 4 Qualitative studies and mixed-methods studies: number retrieved
| Database searched | Number of results | |
|---|---|---|
| Qualitative | Mixed methods | |
| MEDLINE | 581 | 58 |
| PreMEDLINE | 0 | 3 |
| EMBASE | 691 | 78 |
| CINAHL | 304 | 53 |
| PsycINFO | 517 | 69 |
| Citation Indexes (Science and Social Sciences): Science Citation Index expanded (1899 to date); Social Sciences Citation Index (1956 to date); CPCI-S (1990 to date); Conference Proceedings Citation Index – Social Science & Humanities (1990 to date) | 246 | 2 |
| ASSIA | 0 | 21 |
| AMED | 16 | 0 |
| MIDIRS reference database | 0 | 0 |
| Cochrane Systematic Reviews Database; Cochrane Controlled Trials Register; DARE; HTA | NA | NA |
Appendix 5 Reason for exclusion of quantitative studies
| Reference | Reason for exclusion |
|---|---|
| Abel KM. Review: psychosocial and psychological interventions reduce postpartum depressive symptoms. Evid Based Mental Health 2008;11:79 | Commentary or clinical overview |
| Armstrong K, Edwards H. The effectiveness of a pram-walking exercise programme in reducing depressive symptomatology for postnatal women. Int J Nurs practice 2004;10:177–94 | PND treatment trial |
| Armstrong K, Edwards H. The effects of exercise and social support on mothers reporting depressive symptoms: a pilot randomized controlled trial. Int J Ment Health Nursing 2003;12:130–8 | PND treatment trial |
| Austin MP, Lumley J. Antenatal screening for postnatal depression: a systematic review. Acta Psychiatr Scand 2003;107:10–17 | Systematic review not about prevention of PND |
| Austin MP, Priest SR. Clinical issues in perinatal mental health: new developments in the detection and treatment of perinatal mood and anxiety disorders. Acta Psychiatr Scand 2005;112:97–104 | Commentary or clinical overview |
| Austin MP. Targeted group antenatal prevention of postnatal depression: a review. Acta Psychiatr Scand 2003;107:244–50 | Non-systematic review |
| Beddoe AE, Lee KA. Mind–body interventions during pregnancy. JOGNN 2008;37:165–75 | Outcome measurements before 6 weeks postnatally |
| Bennett S, Alpert M, Kubulins V, Hansler RL. Use of modified spectacles and light bulbs to block blue light at night may prevent postpartum depression. Med Hypotheses 2009;73:251–3 | PND treatment trial |
| Bergström M, Kieler H, Waldenström U. Effects of natural childbirth preparation versus standard antenatal education on epidural rates, experience of childbirth and parental stress in mothers and fathers: a randomised controlled multicentre trial. BJOG 2009;116:1167–76 | Not a PND prevention trial |
| Bernard RS, Williams SE, Storfer-Isser A, Rhine W, Horwitz SM, Koopman C, et al. Brief cognitive-behavioral intervention for maternal depression and trauma in the neonatal intensive care unit: a pilot study. J Trauma Stress 2011;24:230–4 | Outcome measurements before 6 weeks postnatally |
| Beucher G, Viaris de LB, Dreyfus M. Maternal outcome of gestational diabetes mellitus. Diabetes Metab 2010;36:522–37 | Review not about prevention of PND |
| Bhutta ZA, Lassi ZS, Blanc A, Donnay F. Linkages among reproductive health, maternal health, and perinatal outcomes. Semin Perinatol 2010;34:434–45 | Not a PND prevention trial |
| Bick DE, Kettle C, Macdonald S, Thomas PW, Hills RK, Ismail KM. Perineal Assessment and Repair Longitudinal Study PEARLS: protocol for a matched pair cluster trial. BMC Pregnancy Childbirth 2010;10:10 | Protocol for or description of a study |
| Bijlenga D, Koopmans CM, Birnie E, Mol BW, Post JA, Bloemenkamp KW, et al. Health-related quality of life after induction of labor versus expectant monitoring in gestational hypertension or preeclampsia at term. Hypertens Pregnancy 2011;30:260–74 | Not a PND prevention trial |
| Bledsoe SE, Grote NK. Treating depression during pregnancy and the postpartum: a preliminary meta-analysis. Res Social Work Prac 2006;16:109–20 | Review not about prevention of PND |
| Boath E, Bradley E, Henshaw C. The prevention of postnatal depression: a narrative systematic review. J Psychosom Obstet Gynecol 2005;26(3):185–92 | Non-systematic review |
| Boulvain M, Perneger TV, Othenin G, V, Petrou S, Berner M, Irion O. Home-based versus hospital-based postnatal care: a randomised trial. BJOG 2004;111:807–13 | Outcome measurements before 6 weeks postnatally |
| Briscoe M. The detection of emotional disorders in the post natal period by health visitors. Health Visitor 1989;62:336–8 | Non-randomised control group |
| Brown S, Small R, Argus B, Davis PG, Krastev A. Early postnatal discharge from hospital for healthy mothers and term infants. Cochrane Database Syst Rev 2002;3:CD002958 | Outcome measurements before 6 weeks postnatally |
| Buist AE, Barnett BE, Milgrom J, Pope S, Condon JT, Ellwood DA, et al. To screen or not to screen – that is the question in perinatal depression. Med J Aust 2002;177(Suppl.):S101–5 | Commentary or clinical overview |
| Burns A, O’Mahen H, Baxter H, Bennert K, Wiles N, Ramchandani P, et al. A pilot randomised controlled trial of cognitive behavioural therapy for antenatal depression. BMC Psychiatry 2013;13:33 | Outcome measurements before 6 weeks postnatally |
| Caramlau I, Barlow J, Sembi S, McKenzie MK, McCabe C. Mums 4 Mums: structured telephone peer-support for women experiencing postnatal depression. Pilot and exploratory RCT of its clinical and cost effectiveness. Trials 2011;12:88 | Protocol for or description of a study |
| Carroll JC, Reid AJ, Biringer A, Midmer D, Glazier RH, Wilson L, et al. Effectiveness of the Antenatal Psychosocial Health Assessment ALPHA form in detecting psychosocial concerns: a randomized controlled trial. CMAJ 2005;173:253–9 | No measure of PND reported |
| Carter FA. Postnatal home visits from healthcare professionals show promise for preventing postnatal depression. Evid Based Mental Health 2005;8:108 | Commentary or clinical overview |
| Carty EM, Bradley CF. A randomized, controlled evaluation of early postpartum hospital discharge. Birth 1990;17:199–204 | Outcome measurements before 6 weeks postnatally |
| Cattell DL, King EA. Estrogen for postnatal depression. J Fam Practice 1996;43:22–3 | Commentary or clinical overview |
| Cerutti R, Sichel MP, Perin M, Grussu P, Zulian O. Psychological distress during puerperium: A novel therapeutic approach using S-adenosylmethionine. Curr Ther Res Clin Exp 1993;53:707–16 | Outcome measurements before 6 weeks postnatally |
| Chang MY, Chen CH, Huang KF. Effects of music therapy on psychological health of women during pregnancy. J Clin Nurs 2008;17:2580–7 | Outcome measurements before 6 weeks postnatally |
| Chen CH, Tseng YF, Chou FH, Wang SY. Effects of support group intervention in postnatally distressed women. A controlled study in Taiwan. J Psychosom Res 2000;49:395–9 | Not a PND prevention trial |
| Cheng S, Kondo N, Aoki Y, Kitamura Y, Takeda Y, Yamagata Z. The effectiveness of early intervention and the factors related to child behavioural problems at age 2: a randomized controlled trial. Early Hum Dev 2007;83:683–91 | Intervention initiated after 6 weeks postnatally |
| Cho HJ, Kwon JH, Lee JJ. Antenatal cognitive-behavioral therapy for prevention of postpartum depression: a pilot study. Yonsei Med J 2008;49:553–62 | Outcome measurements before 6 weeks postnatally |
| Cinciripini PM, Blalock JA, Minnix JA, Robinson JD, Brown VL, Lam C, et al. Effects of an intensive depression-focused intervention for smoking cessation in pregnancy. J Consult Clin Psychol 2010;78:44–54 | Not a PND prevention trial |
| Clark R, Hipke K. Relational group intervention for postpartum depression [NCT00051246]. 2004. URL: http://clinicaltrials.gov/ct2/show/NCT00051246 (accessed May 2013) | PND treatment trial |
| Collado MAO, Saez M, Favrod J, Hatem M. Antenatal psychosomatic programming to reduce postpartum depression risk and improve childbirth outcomes: a randomized controlled trial in Spain and France. BMC Pregnancy Childbirth 2014;14:22 | Outcome measurements before 6 weeks postnatally |
| Conrad P, Adams C. The effects of clinical aromatherapy for anxiety and depression in the high risk postpartum woman – A pilot study. Complement Ther Clin Pract 2012;18:164–8 | Intervention initiated after 6 weeks postnatally |
| Cope CD, Lyons AC, Donovan V, Rylance M, Kilby MD. Providing letters and audiotapes to supplement a prenatal diagnostic consultation: effects on later distress and recall. Prenat Diagn 2003;23:1060–7 | Not a PND prevention trial |
| Costa D, Lowensteyn I, Abrahamowicz M, Ionescu IR, Dritsa M, Rippen N, et al. A randomized clinical trial of exercise to alleviate postpartum depressed mood. J Psychosom Obstetr Gynaecol 2009;30:191–200 | PND treatment trial |
| Craig M, Howard L. Postnatal Depression. BMJ Clinical Evidence. 2009. pii. 1407. URL: http://clinicalevidence.bmj.com/x/systematic-review/1407/overview.html (accessed May 2013) | Review not about prevention of PND |
| Cresci M. Self-help group intervention in post natal depression. National Research Register 1996 [NIHR no longer provide the National Research Register as a searchable online archive following the migration of the NIHR website to a new platform in 2014] | Not a PND prevention trial |
| Crowley SK, Youngstedt SD. Efficacy of light therapy for perinatal depression: a review. J Physiol Anthropol 2012;31:15 | Outcome measurements before 6 weeks postnatally |
| Cuijpers P. Prevention: an achievable goal in personalized medicine. Dialogues Clin Neuroscience 2009;11:2009 | Commentary or clinical overview |
| Curtis K, Weinrib A, Katz J. Systematic review of yoga for pregnant women: current status and future directions. Evid Based Complement Alternat Med 2012;2012:715942 | No measure of PND reported |
| Daley A. Exercise and depression: a review of reviews. J Clin Psychol Med Settings 2008;15:140–7 | PND treatment trial |
| Dennis CL. The effect of peer support on postpartum depression: a pilot randomized controlled trial. Can J Psychiatr 2003;48:115–24 | Intervention initiated after 6 weeks postnatally |
| Di Scalea TL, Wisner KL. Pharmacotherapy of postpartum depression. Expert Opin Pharmacother 2009;10:2009 | Non-systematic review |
| Doucet S, Jones I, Letourneau N, Dennis CL, Blackmore ER. Interventions for the prevention and treatment of postpartum psychosis: a systematic review. Arch Womens Ment Health 2011;14:89–98 | Systematic review not about prevention of PND |
| Dritsa M, Costa D, Dupuis G, Lowensteyn I, Khalifé S. Effects of a home-based exercise intervention on fatigue in postpartum depressed women: results of a randomized controlled trial. Ann Behav Med 2008;35:179–87 | PND treatment trial |
| Elliott SA, Sanjack M, Leverton TJ. Parents Groups in Pregnancy. A Preventive Intervention for Postnatal Depression? In Gottlieb BH, editor. Marshaling Social Support: Formats, Processes and Effects. London: Sage. pp. 87–97 | Non-randomised control group |
| El-Mohandes AA, El-Khorazaty MN, Kiely M, Gantz MG. Smoking cessation and relapse among pregnant African-American smokers in Washington, DC. Matern Child Health J 2011;15(Suppl. 1):96–105 | Secondary analysis of data from a RCT |
| El-Mohandes AA, Kiely M, Gantz MG, El-Khorazaty MN. Very preterm birth is reduced in women receiving an integrated behavioral intervention: a randomized controlled trial. Matern Child Health J 2011;15:19–28 | No measure of PND reported |
| Evans EC, Bullock LF. Optimism and other psychosocial influences on antenatal depression: a systematic review. Nurs Health Sci 2012;14:352–61 | Review not about prevention of PND |
| Feinberg E, Stein R, Diaz LY, Egbert L, Beardslee W, Hegel MT, et al. Adaptation of problem-solving treatment for prevention of depression among low-income, culturally diverse mothers. Fam Commun Health 2012;35:57–67 | No measure of PND reported |
| Field T, Deeds O, Diego M, Hernandez RM, Gauler A, Sullivan S, et al. Benefits of combining massage therapy with group interpersonal psychotherapy in prenatally depressed women. J Bodyw Mov Ther 2009;13:297–303 | Outcome measurements before 6 weeks postnatally |
| Field T, Diego M, Hernandez RM, Medina L, Delgado J, Hernandez A. Yoga and massage therapy reduce prenatal depression and prematurity. J Bodyw Mov Ther 2012;16:204–9 | Outcome measurements before 6 weeks postnatally |
| Field T, Diego MA, Hernandez RM, Schanberg S, Kuhn C. Massage therapy effects on depressed pregnant women. J Psychosom Obstet Gynaecol 2004;25:115–22 | Outcome measurements before 6 weeks postnatally |
| Field T, Figueiredo B, Hernandez RM, Diego M, Deeds O, Ascencio A. Massage therapy reduces pain in pregnant women, alleviates prenatal depression in both parents and improves their relationships. J Bodyw Mov Ther 2008;12:146–50 | Outcome measurements before 6 weeks postnatally |
| Field T, Hernandez RM, Hart S, Theakston H, Schanberg S, Kuhn C. Pregnant women benefit from massage therapy. J Psychosom Obstet Gynaecol 1999;20:31–8 | Outcome measurements before 6 weeks postnatally |
| Field T, Hernandez RM, Taylor S, Quintino O, Burman I. Labor pain is reduced by massage therapy. J Psychosom Obstet Gynaecol 1997;18:286–91 | Outcome measurements before 6 weeks postnatally |
| Fink NS, Urech C, Cavelti M, Alder J. Relaxation during pregnancy: what are the benefits for mother, fetus, and the newborn? A systematic review of the literature. J Perinat Neonat Nurs 2012;26:296–306 | Outcome measurements before 6 weeks postnatally |
| Fisher JRW. Brief behavioural intervention for infant sleep problems reduces depression in mothers. Evid Based Mental Health 2009;12:46 | Commentary or clinical overview |
| Fleming AS, Klein E, Corter C. The effects of a social support group on depression, maternal attitudes and behavior in new mothers. J Child Psychol Psychiatry 1992;33:685–98 | Non-randomised control group |
| Fleming VE, Hagen S, Niven C. Does perineal suturing make a difference? The SUNS trial. BJOG 2003;110:684–9 | Outcome measurements before 6 weeks postnatally |
| Freeman MP, Sinha P. Tolerability of omega-3 fatty acid supplements in perinatal women. PLEFA 2007;77:203–8 | No measure of PND reported |
| Freeman MP. Complementary and alternative medicine for perinatal depression. J Affect Disord 2009;112:1–10 | Non-systematic review |
| Freeman MP. Omega-3 fatty acids and perinatal depression: a review of the literature and recommendations for future research. PLEFA 2006;75:291–7 | Non-systematic review |
| Gagnon AJ, Sandall J. Individual or group antenatal education for childbirth or parenthood, or both. Cochrane Database Sys Rev 2007;3:CD002869 | No measure of PND reported |
| Gamble J, Creedy D. Content and processes of postpartum counseling after a distressing birth experience: a review. Birth ISS Perinat C 2004;31:213–18 | Non-systematic review |
| Gamble JA, Creedy DK, Webster J, Moyle W. A review of the literature on debriefing or non-directive counseling to prevent postpartum emotional distress. Midwifery 2002;18:72–9 | Non-systematic review |
| Gentile S. The role of estrogen therapy in postpartum psychiatric disorders: an update. CNS Spectrums 2005;10:944–52 | Non-systematic review |
| Gjerdingen DK, Yawn BP. Postpartum depression screening: importance, methods, barriers, and recommendations for practice. JABFM 2007;20:280–8 | Non-systematic review |
| Glavin K, Smith L, Sorum R, Ellefsen B. Redesigned community postpartum care to prevent and treat postpartum depression in women – a one-year follow-up study. J Clin Nurs 2010;19:3051–62 | Non-randomised control group |
| Gordon N, Walton D, McAdam E, Derman J, Gallitero G, Garrett L. Effects of providing hospital-based doulas in health maintenance organization hospitals. Obstetr Gynecol 1999;93:422–6 | No measure of PND reported |
| Gordon RE, Gordon KK. Social factors in prevention of postpartum emotional problems. Obstetr Gynecol 1960;15:433–8 | Non-randomised control group |
| Griffiths K, Christensen H, Ellwood D. Online cognitive behaviour therapy MoodGYM for the prevention of postnatal depression in at-risk mothers: a randomised controlled trial [protocol] [ACTRN12609001032246]. Aust NZ Clin Trials Registry 2009. URL: www.anzctr.org.au (accessed May 2013) | Protocol for or description of a study |
| Guse T, Wissing M, Hartman W. The effect of a prenatal hypnotherapeutic programme on postnatal maternal psychological well-being. J Reprod Infant Psychol 2006;24:163–77 | Non-randomised control group |
| Halford WK, Petch J, Creedy DK. Promoting a positive transition to parenthood: a randomized clinical trial of couple relationship education. Prev Sci 2010;11:89–100 | No measure of PND reported |
| Hall W. Mothers were less likely to be depressed after a structured behavioural intervention for infant sleep problems. Evid Based Nursing 2009;12:9 | Commentary or clinical overview |
| Hawkins-Walsh E, Hiscock H, Wake M. A behavioural infant sleep intervention resolved sleep problems. Evid Based Nursing 2003;6:10 | Intervention initiated after 6 weeks postnatally |
| Heh SS, Huang LH, Ho SM, Fu YY, Wang LL. Effectiveness of an exercise support program in reducing the severity of postnatal depression in Taiwanese women. Birth 2008;35:60–5 | Non-randomised control group |
| Hiscock H, Bayer J, Gold L, Hampton A, Ukoumunne OC, Wake M. Improving infant sleep and maternal mental health: a cluster randomised trial. Arch Dis Childhood 2007;92:952–8 | Intervention initiated after 6 weeks postnatally |
| Hiscock H, Bayer JK, Hampton A, Ukoumunne OC, Wake M. Long-term mother and child mental health effects of a population-based infant sleep intervention: cluster-randomized, controlled trial. Pediatrics 2008;122:e621–7 | Outcome measurements after twelve postnatal months |
| Hiscock H, Wake M. Randomised controlled trial of behavioural infant sleep intervention to improve infant sleep and maternal mood. BMJ 2002;324:1062–5 | Intervention initiated after 6 weeks postnatally |
| Hiscock H, Wake M. The impact of an infant sleep intervention on postnatal depression: a randomized controlled trial. J Paediatr Child Health 2001;37:A1 | Intervention initiated after 6 weeks postnatally |
| Horowitz JA, Bell M, Trybulski J, Munro BH, Moser D, Hartz SA, et al. Promoting responsiveness between mothers with depressive symptoms and their infants. J Nurs Scholarsh 2001;33:323–9 | Intervention initiated after 6 weeks postnatally |
| Hoseininasab D, Ahmadianheris S, Taghavi S. The effect of antenatal education on postpartum depression. Int J Gynecol Obstetr 2009;107:S607–8 | Outcome measurements before 6 weeks postnatally |
| Hosli I, Zanetti-Daellenbach R, Holzgreve W, Lapaire O. Role of omega 3-fatty acids and multivitamins in gestation. J Perinatal Medicine 2007;35(Suppl. 1):S19–24 | Non-systematic review |
| Howard LM, Boath E, Henshaw C. Antidepressant prevention of postnatal depression. PLOS Med 2006;3:e389 | Non-systematic review |
| Hubner-Liebermann B, Hausner H, Wittmann M. Recognizing and treating peripartum depression. Dtsches Arztebl Int 2012;109:419–24 | Non-systematic review |
| Ivey LC. Behavioral health matters. Effective nonpharmacological therapies for pregnant women with depression. Evid Based Practice 2006;9(10):9, 1 page. URL: www.fpin.org/wp/wp-content/uploads/2014/10/733-EBP-October-2006.pdf (accessed 4 March 2016) | Commentary or clinical overview |
| Jans LA, Giltay EJ, Van der Does AJ. The efficacy of n-3 fatty acids DHA and EPA (fish oil) for perinatal depression. Br J Nutr 2010;104:1577–85 | Review not about prevention of PND |
| Jesse DE, Blanchard A, Bunch S, Dolbier C, Hodgson J, Swanson MS. A pilot study to reduce risk for antepartum depression among women in a public health prenatal clinic. Issues Ment Health Nurs 2010;31:355–64 | Non-randomised control group |
| Karuppaswamy J, Vlies R. The benefit of oestrogens and progestogens in postnatal depression. J Obstet Gynaecol 2003;23:341–6 | Non-systematic review |
| Kennedy HP, Farrell T, Paden R, Hill S, Jolivet RR, Cooper BA, et al. A randomized clinical trial of group prenatal care in two military settings. Mil Med 2011;176:1169–77 | No measure of PND reported |
| Kenyon S, Jolly K, Hemming K, Ingram L, Gale N, Dann SA, et al. The ELSIPS trial: Evaluation of lay support in pregnant women with social risk: a randomised controlled trial. BMC Pregnancy Childbirth 2012;12:11 | Protocol for or description of a study |
| Kersten-Alvarez LE, Hosman CM, Riksen-Walraven JM, Doesum KT, Hoefnagels C. Which preventive interventions effectively enhance depressed mothers’ sensitivity? A meta-analysis (Provisional abstract). Infant Ment Health J 2011;32:362–76 | Review not about prevention of PND |
| King E. The effectiveness of an internet-based stress management program in the prevention of postpartum stress, anxiety and depression for new mothers. Dissertations Abstracts International: Section B: The Sciences and Engineering 2009;70:2560 | Intervention initiated after 6 weeks postnatally |
| Kitamura T. Midwives’ psychological group and individual support sessions as prevention of postnatal depression: a randomised trial in Japan. J Psychosom Obstet Gynecol 2007;28:14 [Abstract] | No measure of PND reported |
| Kleeb B, Rageth CJ. [Influence of prophylactic information on the frequency of baby blues]. Z Geburtshilfe Neonatol 2005;209:22–8 | Study reported in non-English language (German) |
| Ko YL, Yang CL, Chiang LC. Effects of postpartum exercise program on fatigue and depression during ‘doing-the-month’ period. J Nurs Res 2008;16:177–86 | Non-randomised control group |
| Koh TH, Butow PN, Coory M, Budge D, Collie LA, Whitehall J, et al. Provision of taped conversations with neonatologists to mothers of babies in intensive care: randomised controlled trial. BMJ 2007;334:28 | Not a PND prevention trial |
| Koltyn KF, Schultes SS. Psychological effects of an aerobic exercise session and a rest session following pregnancy. J Sports Med Phys Fitness 1997;37:287–91 | Non-randomised control group |
| Langer A, Farnot U, Garcia C, Barros F, Victora C, Belizan JM, et al. The Latin American trial of psychosocial support during pregnancy: effects on mother’s wellbeing and satisfaction. Latin American Network For Perinatal and Reproductive Research (LANPER). Soc Sci Med 1996;42:1589–97 | No measure of PND reported |
| Lavender T, Walkinshaw SA. Can midwives reduce postpartum psychological morbidity? A randomized trial. Birth 1998;25:215–19 | Outcome measurements before 6 weeks postnatally |
| Lee KO, Kim KR, Ahn SH. Effects of a Qigong prenatal education program on anxiety, depression and physical symptoms in pregnant women. Korean J Womens Health Nurs 2006;12:240–8 | Study reported in non-English language (Korean) |
| Leung SS, Leung C, Lam TH, Hung SF, Chan R, Yeung T, et al. Outcome of a postnatal depression screening programme using the Edinburgh Postnatal Depression Scale: a randomized controlled trial. J Public Health 2011;33:292–301 | Intervention initiated after 6 weeks postnatally |
| Leung, SSK, Lee AM, Chiang VCL, Lam SK, Yung C, Wong DFK. 2013. Culturally sensitive, preventive antenatal group cognitive-behavioural therapy for Chinese women with depression. 2013;19(Suppl. 1):28–37 | Protocol for or description of a study |
| Levitt C, Shaw E, Wong S, Kaczorowski J, Springate R, Sellors J, et al. Systematic review of the literature on postpartum care: methodology and literature search results. Birth 2004;31:196–202 | Systematic review not about prevention of PND |
| Liberto TL. Screening for depression and help-seeking in postpartum women during well-baby pediatric visits: an integrated review. J Pediatr Health Care 2012;26:109–17 | Non-systematic review |
| Manber R, Schnyer RN, Lyell D, Chambers AS, Caughey AB, Druzin M, et al. Acupuncture for depression during pregnancy: a randomised controlled trial. J Obstetr Gynecol 2010;115:511–20 | Outcome measurements before 6 weeks postnatally |
| Matsuoka Y. It’s high time to challenge a collaboration of omega-3s in the prevention. Asia-Pacific Psychiatry Conference: 15th Pacific Rim College of Psychiatrists Scientific Meeting, PRCP 2012. Seoul, South Korea, 25–27 October 2012. Conference Publication: (var. pagings) 2012;4:October | Protocol for or description of a study |
| Matthey S. Telephone based peer support can reduce postnatal depression in women at high risk. Evid Based Mental Health 2009;12:82 | Commentary or clinical overview |
| Medves J. Review: continuous caregiver support during labour has beneficial maternal and infant outcomes. Evid Based Nursing 2002;5:105 | Commentary or clinical overview |
| Mendelson T, Leis JA, Perry DF, Stuart EA, Tandon SD. 2013. Impact of a preventive intervention for perinatal depression on mood regulation, social support, and coping. Arch Womens Mental Health, 1–8 | Secondary analysis of data from a RCT |
| Mercado JM. Changes in depression in pregnant and postpartum adolescents following participation in a comprehensive preventive intervention. Dissertation Abstracts International: Section B: The Sciences and Engineering 2004;65:1046 | Non-randomised control group |
| Middlemiss C, Dawson AJ, Gough N, Jones ME, Coles EC. A randomised study of a domiciliary antenatal care scheme: maternal psychological effects. Midwifery 1989;5:69–74 | Outcome measurements before 6 weeks postnatally |
| Miller BJ, Murray L, Beckmann MM, Kent T, Macfarlane B. Dietary supplements for preventing postnatal depression. Cochrane Database Syst Rev 2011;5:CD009104 | Protocol for or description of a study |
| Moshki M, Beydokhti TB, Cheravi K. The effect of educational intervention on prevention of postpartum depression: an application of health locus of control. J Clin Nurs 2014:23;2256–63. | Outcome measurements before 6 weeks postnatally |
| Mozurkewich E, Chilimigras J, Klemens C, Keeton K, Allbaugh L, Hamilton S, et al. The mothers, Omega-3 and mental health study. BMC Pregnancy Childbirth 2011;11:46 | Protocol for or description of a study |
| Mozurkewich E, Klemens C. Omega-3 fatty acids and pregnancy: current implications for practice. Curr Opin Obstet Gynecol 2012;24:72–7 | Non-systematic review |
| Mulcahy R, Reay RE, Wilkinson RB, Owen C. A randomised control trial for the effectiveness of group Interpersonal Psychotherapy for postnatal depression. Arch Womens Ment Health 2010;13:125–39 | PND treatment trial |
| Murphy KE, Hannah ME, Willan AR, Ohlsson A, Kelly EN, Matthews SG, et al. Maternal side-effects after multiple courses of antenatal corticosteroids MACS: the three-month follow-up of women in the randomized controlled trial of MACS for preterm birth study. JOGC 2011;33:909–21 | Not a PND prevention trial |
| Nanzer N, Rossignol AS, Righetti-Veltema M, Knauer D, Manzano J, Espasa FP. Effects of a brief psychoanalytic intervention for perinatal depression. Arch Womens Ment Health 2012:15;259–68 | Non-randomised control group |
| Nardi B, Laurenzi S, Di NM, Bellantuono C. Is the cognitive-behavioral therapy an effective intervention to prevent the postnatal depression? A critical review. Int J Psychiatry Med 2012;43:211–25 | Non-systematic review |
| Nascimento SL, Surita FG, Cecatti JG. Physical exercise during pregnancy: a systematic review. Curr Opin Obstet Gynecol 2012;24:387–94 | Non-systematic review |
| Ogrodniczuk JS, Piper WE. Preventing postnatal depression: a review of research findings. Harvard Rev Psychiatry 2003;11:291–307 | Non-systematic review |
| Ogrodniczuk JS. Increasing a partner’s understanding of motherhood significantly reduces postnatal distress and depression in first time mothers with low self esteem. Evid Based Mental Health 2004;7:116 | Commentary or clinical overview |
| O’Mahen H, Himle JA, Fedock G, Henshaw E, Flynn H. 2013. A pilot randomized controlled trial of cognitive behavioral therapy for perinatal depression adapted for women with low incomes. Depress Anxiety 2013:30;679–87 | Not a PND prevention trial |
| Ortega RM, Rodriguez-Rodriguez E, Lopez-Sobaler AM. Effects of omega 3 fatty acids supplementation in behavior and non-neurodegenerative neuropsychiatric disorders. Br J Nutr 2012;107(Suppl. 2):S261–70 | Systematic review not about prevention of PND |
| Paul IM. Downs DS, Schaefer EW, Beiler JS, Weisman CS. Postpartum anxiety and maternal-infant health outcomes. Pediatrics 2013;131:1–7 | Secondary analysis of data from a RCT |
| Pearson RM, O’Mahen H, Burns A, Bennert K, Sheppard C, Baxter H, Chauhan D, Evans J. The normalisation of disrupted attentional processing of infant distress in depressed pregnant women following cognitive behavioural therapy. J Affect Disord 2013;145:208–13 | Outcome measurements before 6 weeks postnatally |
| Peindl KS, Wisner KL, Hanusa BH. Identifying depression in the first postpartum year: guidelines for office-based screening and referral. J Affect Disord 2004;80:37–44 | Secondary analysis of data from a RCT |
| Reay R, Matthey S, Ellwood D, Scott M. Long-term outcomes of participants in a perinatal depression early detection program. J Affect Disord 2011;129:94–103 | Outcome measurements after 12 months postnatally |
| Rees AM, Austin MP, Parker GB. Omega-3 fatty acids as a treatment for perinatal depression: randomized double-blind placebo-controlled trial. Aust NZ J Psychiat 2008;42:199–205 | Not a PND prevention trial |
| Robledo-Colonia AF, Sandoval RN, Mosquera-Valderrama YF, Escobar HC, Ramírez VR. Aerobic exercise training during pregnancy reduces depressive symptoms in nulliparous women: a randomised trial. J Physiother 2012;58:9–15 | Outcome measurements before 6 weeks postnatally |
| Roman LA, Gardiner JC, Lindsay JK, Moore JS, Luo Z, Baer LJ, Paneth, N. Alleviating perinatal depressive symptoms and stress: a nurse-community health worker randomized trial. Arch Womens Ment Health 2009;12:379–91 | Outcome measurements after 12 months postnatally |
| Rowan C, Bick D, Silva-Bastos MH. Postnatal debriefing interventions to prevent maternal mental health problems after birth: exploring the gap between the evidence and UK policy and practice (Structured abstract). Worldviews Evid Based Nurs 2007;4:97–105 | Non-systematic review |
| Ryding EL, Wirén E, Johansson G, Ceder B, Dahlström AM. Group counseling for mothers after emergency cesarean section: a randomized controlled trial of intervention. Birth 2004;31:247–53 | Intervention initiated after 6 weeks postnatally |
| Sainz-Bueno JA, Romano MR, Teruel RG, Benjumea AG, Palacín AF, González CA, et al. Early discharge from obstetrics-pediatrics at the Hospital de Valme, with domiciliary follow-up. Am J Obstet Gynecol 2005;193:714–26 | Outcome measurements before 6 weeks postnatally |
| Scott KD, Klaus PH, Klaus MH. The obstetrical and postpartum benefits of continuous support during childbirth. J Womens Health Gend Based Med 1999;8:1257–64 | Non-systematic review |
| Seeman MV. Group oriented interpersonal therapy reduced postpartum depression in women at risk. Evid Based Mental Health 2001;4:118 | Commentary or clinical overview |
| Shivakumar G, Brandon AR, Snell PG, Santiago-Munoz P, Johnson NL, Trivedi MH, et al. Antenatal depression: a rationale for studying exercise. Depress Anxiety 2011;28:234–42 | Systematic review not about prevention of PND |
| Simons J, Reynolds J, Morison L. Randomised controlled trial of training health visitors to identify and help couples with relationship problems following a birth. Br J Gen Practice 2001;51:793–9 | No measure of PND reported |
| Skibniewski-Woods D. A review of postnatal debriefing of mothers following traumatic delivery. Community Pract 2011;84:29–32 | Non-systematic review |
| Spinelli MG, Endicott J. Controlled clinical trial of interpersonal psychotherapy versus parenting education program for depressed pregnant women. Am J Psychiatry 2003;160:555–62 | Outcome measurements before 6 weeks postnatally |
| Stomp-van-den-Berg-SG, Poppel MN, Hendriksen IJ, Bruinvels DJ, Uegaki K, Bruijne MC, et al. Improving return-to-work after childbirth: design of the Mom@Work study, a randomised controlled trial and cohort study. BMC Public Health 2007;7:43 | Protocol for or description of a study |
| Stuart S, O’Hara MW, Gorman LL. The prevention and psychotherapeutic treatment of postpartum depression. Arch Womens Ment Health 2003;6(Suppl. 2):57–69 | Commentary or clinical overview |
| Su KP, Huang SY, Chiu TH, Huang KC, Huang CL, Chang HC, et al. Omega-3 fatty acids for major depressive disorder during pregnancy: results from a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry 2008;69:644–51 | Outcome measurements before 6 weeks postnatally |
| Sunder KR, Wisner KL, Hanusa BH, Perel JM. Postpartum depression recurrence versus discontinuation syndrome: observations from a randomized controlled trial. J Clin Psychiatry 2004;65:1266–8 | Secondary analysis of data from a RCT |
| Surkan PJ, Gottlieb BR, McCormick MC, Hunt A, Peterson KE. Impact of a health promotion intervention on maternal depressive symptoms at 15 months postpartum. Matern Child Health J 2012;16:139–48 | Outcome measurements after 12 months postnatally |
| Svensson J, Barclay L, Cooke M. Randomised controlled trial of two antenatal education programmes. Midwifery 2009;24:114–25 | No measure of PND reported |
| Sword W. Review: some specific preventive psychosocial and psychological interventions reduce risk of postpartum depression. Evid Based Nurs 2005;8:76 | Commentary or clinical overview |
| Taft AJ, Small R, Hegarty KL, Watson LF, Gold L, Lumley JA. Mothers’ advocates in the community mosaic – non-professional mentor support to reduce intimate partner violence and depression in mothers: a cluster randomised trial in primary care. BMC Public Health 2011;11:178 | Intervention initiated after 6 weeks postnatally |
| Tandon SD, Perry DF, Mendelson T, Kemp K, Leis JA. Preventing perinatal depression in low-income home visiting clients: a randomized controlled trial. J Consult Clin Psychol 2011;79:707–12 | Intervention initiated after 6 weeks postnatally |
| Tang YF, Shi SX, Lu W, Chen Y, Wang QQ, Zhu YY, et al. Prenatal psychological prevention trial on postpartum anxiety and depression. Chin Ment Health J 2009;23:83–9 | Study reported in non-English language (Chinese) |
| Teissedre F, Chabrol H. Screening, prevention and postpartum treatment: a randomized comparative study on 450 women. Neuropsychiatr Enfance Adolesc 2004;52:266–73 | Study reported in non-English language (French) |
| Tripathy P, Nair N, Barnett S, Mahapatra R, Borghi J, Rath S, et al. Effect of a participatory intervention with women’s groups on birth outcomes and maternal depression in Jharkhand and Orissa, India: a cluster-randomised controlled trial. Lancet 2010;375:1182–92 | Outcome measurements after 12 months postnatally |
| Ushiroyama T, Sakuma K, Ueki M. Efficacy of the Kampo Medicine Xiong-Gui-Tiao-Xue-Yin Kyuki-Chouketsu-In A. Traditional herbal medicine, in the treatment of maternity blues syndrome in the postpartum period. Am J Chin Med 2005;33:117–26 | Outcome measurements before 6 weeks postnatally |
| Varo I. Impact of a nursing intervention on pregnant women as a preventive tool for postpartum depression. Nure Investigación 2012;1–17 | Study reported in non-English language (Spanish) |
| Vieten C, Astin J. Effects of a mindfulness-based intervention during pregnancy on prenatal stress and mood: results of a pilot study. Arch Womens Ment Health 2008;11:67–74 | No measure of PND reported |
| Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H, et al. Postnatal support for mothers living in disadvantaged inner city areas: a randomised controlled trial. J Epidemiol Commun Health 2005;59:288–95 | Outcome measurements after 12 months postnatally |
| Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H, et al. The Social Support and Family Health Study: a randomised controlled trial and economic evaluation of two alternative forms of postnatal support for mothers living in disadvantaged inner-city areas. Health Technol Assess 2001;8(32) | Outcome measurements after 12 months postnatally |
| Wilton G, Moberg DP, Fleming MF. The effect of brief alcohol intervention on postpartum depression. MCN Am J Matern Child Nurs 2009;34:297–302 | Intervention initiated after 6 weeks postnatally |
| Wirz-Justice A, Bader A, Frisch U, Stieglitz R-D, Aldfer J, Bitzer J, et al. A randomized, double-blind, placebo-controlled study of light therapy for antepartum depression. J Clin Psychiatry 2011;72:986–93 | Outcome measurements before 6 weeks postnatally |
| Wisner KL, Gelenberg AJ, Leonard H, Zarin D, Frank E. Pharmacologic treatment of depression during pregnancy Structured. JAMA 1999;282:1264–9 | Non-systematic review |
| Wisner KL, Wheeler SB. Prevention of recurrent postpartum major depression. Hosp Commun Psych 1994;45:1191–6 | Non-randomised control group |
| Yawn BP, Dietrich AJ, Wollan P, Bertram S, Graham D, Huff J, et al. TRIPPD: A practice-based network effectiveness study of postpartum depression screening and management. Ann Fam Med 2012;10:320–9 | Intervention initiated after 6 weeks postnatally |
| Yonkers KA, Wisner KL, Stewart DE, Oberlander TF, Dell DL, Stotland N, et al. The management of depression during pregnancy: a report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. Gen Hosp Psychiat 2009;31:403–13 | Non-systematic review |
| Zayas LH. Six-month multicomponent intervention improves postnatal depression in low-income settings. Evid Based Mental Health 2008;11:80 [Comment on Rojas G, Fritsch R, Solis J, Jadresic E, Castillo C, Gonzalez, et al. Treatment of postnatal depression in low-income mothers in primary-care clinics in Santiago, Chile: a randomised controlled trial. Lancet 2007;370:1629–37] | Protocol for or description of a study |
Appendix 6 Data extraction
Data extraction for quantitative studies
Data extraction for qualitative studies
| Evidence from women | To inform intervention – elements of the intervention | Service delivery |
|---|---|---|
| Data extraction | Data synthesis | Interpretation |
| What helped? | Which intervention elements helped? | Which intervention elements to include? |
| What did not help? | What not to do | How to counteract unhelpful experiences during pregnancy and postpartum |
| What did you need? | What to do and how to address it | Which intervention elements to include? Will it fit into an intervention? |
| How did you want it? evidence of preferred service delivery | Vehicle? | Delivery types (leaflet, peer group, midwife) |
| What didn’t you want? (service delivery) | Avoid including in interventions; or assess which women were suitable for particular elements | Which elements should be removed from an intervention |
| Barriers to participation | To inform service delivery | Allow for different circumstances (e.g. unable to travel to group/physical limitations |
Appendix 7 Synthesis of findings from personal and social support strategy studies
Themes and subthemes from the synthesis of findings from personal and social support strategy studies
| Themes | Subtheme(s) | Evidence source(s) [CASP] Evidence from studies with general population participants |
Selective group data | Certainty in the evidence (CERQual) | Explanation of certainty in the evidence assessment |
|---|---|---|---|---|---|
| Things that help to prevent feelings of depression from the women’s perspective were . . . | |||||
| Support | Emotional support from family and friends. One respondent illustrated how friends and family provided emotional support:. . . providing extra visits and extra phone calls, checking on me to make sure I’m ok, and if I need anything.Participant320Supporting references286,300,303,312,313,317,323,325 | High/moderate | High/moderate | High certainty | Studies of high to moderate quality; finding seen across several studies, across general populations, and culturally different and selective groups |
| Emotional support from the mothers and grandmothers of the women. Such emotional support appeared to be particularly important for women of selective groups292,296–298 and women who had recently moved to a new country living away from their extended family. A participant reported292 on a relationship with her own grandma:It seems like when I got pregnant we got closer . . . She asks me how my day went and what’s going on with the baby and, you know, I’ll tell her the problems and she’ll be like, oh, well you’ll be okay. Just try to do this and relax.Participant292 | Moderate | High/moderate | |||
| Supporting references296–298,302,305,317,319,323 | High/moderate | Moderate | |||
| Emotional support from midwife/health professionals – this applied to midwives, health visitors and GPs.319 This was particularly important when health professionals had knowledge about PND and related issues.303 Supporting references303,315,319 |
– | Moderate | |||
| Instrumental/practical support from family/friends. Family and friends were providing practical help at home:320I had my mother or mother-in-law who volunteered to stay with me a couple of weeks after the baby was born so I could rest. I have friends from my church who . . . all volunteered to make a dinner and deliver it to my home . . .Participant320Instrumental support took the form of making food, to allow women to sleep and to care for other children.305,317 This was particularly provided by mothers and mother-in-laws.319,320 Supporting references286,292,303,305–310,317,318,320,325 |
High/moderate | High/moderate; moderate | |||
| Instrumental/practical support from partner. Partners were credited for taking on practical tasks to support the women. These tasks included doing the housework and looking after the children. A respondent reported:My husband . . . was running the house, working full time, doing everything with the children. He works nights, he was coming home getting the kids to school, going to sleep for 2 hours, getting up and getting the youngest child from nursery, going back to sleep, he was an absolute legend. Thank God.Participant322Supporting references305,316,317,319,322,323,325 | High/moderate | – | |||
| Instrumental/practical support from midwife/health professionals. However, interactions with health professionals varied:I had a nurse midwife that delivered the baby. She helped me learn how to nurse, but . . . no one told me that it was gonna be that painful . . . I didn’t have that kind of support system from the hospital staff, but . . . I had a wonderful midwife who was great about that.Participant320Supporting references303,304,423 | Moderate/high | Moderate | |||
| Peer support – sharing experiences and normalisation. Benefits for women often appeared to be specific to sharing experiences with peers, who had encountered similar difficulties during pregnancy and the postpartum, which helped to normalise the feelings they were experiencing. Supporting references302,312,313,318,321,322 |
Moderate/high | Moderate | |||
| Adjustment to pregnancy/motherhood | Realistic expectations (because of antenatal education)/being prepared – recognition of the importance of having realistic expectations about pregnancy and the postpartum and being prepared for these. Antenatal education was credited as promoting realistic expectations by a respondent who said:I came into it expecting the worse and it ended up a lot better, you have prepared yourself. . . Basically, I think they told us everything in classesParticipant319 | Moderate/high | – | Moderate certainty | Studies on adjustment to pregnancy and motherhood mainly of moderate quality; finding seen across several studies, although mostly in general populations |
| Awareness of potential PND/learning about emotional lability – For others being prepared meant being aware of potential for PND and learning about emotional lability317,320 Particularly for women with previous depression317 but also in those with no previous history of depression. One respondent reported that she:Talked to all my friends, my family, my husband and said, if you think anything is different with me don’t hesitate to tell me, tell someone immediately because I don’t want the worse that could happen to happenParticipant317 | Moderate/high | – | |||
| Practical experience/having routines/getting to know the baby – Women spoke of importance of having practical experience of looking after the baby320 including having routines322 and getting to know the baby.320 Women reported they needed more practical skills and experience for early postnatal period (e.g. changing nappies, bottle feeding and bathing the baby305,321) | High | – | |||
| Approval of mum at announcement of pregnancy/validation of the pregnancy296–298 | – | Moderate | |||
| Faith/rituals/religion | Praying strategy to help manage emotional distress and to provide emotional and spiritual support317 Supporting references304,306–310,314,318 |
Moderate | Moderate (× 3); high; moderate | Moderate certainty | Studies relating to faith, rituals and religion mainly of moderate quality; finding seen across several studies of culturally different populations |
| Health care | Medication – Respondents had used professional medical and mental health services, such as counselling, consultation with physicians and midwives, and hospitalisation.303 Nearly half of respondents303 reported using medication for emotional distress | Moderate | – | Low certainty | Studies of high to moderate quality; finding seen only in few studies, although in both general population and selective groups |
| Women also reported beneficial effects of alternative treatment modalities such as massage, acupuncture, and hypnotherapy322 | Moderate/High | ||||
| Continuity of care, in the form of one-to-one care from a community midwife, was also particularly helpful in one study315 | Moderate | ||||
| Self-help/coping strategies | Engage in activities (counter isolation)/talking to others/maintaining a sense of being in control/Asking for help/peer support groups/problem-solving/having a cultural identity to be strong. Participants reported that asking for physical help or simply asking for a break was used as a strategy to combat feelings of being down. Asking those around her to give her a break was one important strategy used by a young mother.She said, ‘I’ll just tell them, ‘Look Mom’s got a headache. I need a break. Y’all give me 15 minutes.’ That’s what I’ll tell them. I’ll tell my husband, ‘J. . ., just give me 15 minutes.Participant286Supporting references286,303,306–310,312–314,317,322 | Moderate/High | High/moderate | Moderate certainty | Studies of high to moderate quality; finding seen across several studies, in both general population and cultural groups |
| Baby-related issues | Feelings of wonder and joy/gaining strength from the baby318,319 | High | Moderate | Low certainty | Studies of high to moderate quality; finding seen only in few studies, although in both general population and cultural groups |
| Good infant temperament317 | Moderate | – | |||
| Synthesised finding – things that did not help to prevent depression from the women’s perspective/exacerbated feelings of depression were . . . | |||||
| Lack of support from key people | Lack of support/understanding from partner (Taniguchi318/harassment by baby’s father296–298/fear of abandonment315). Some participants indicated that their distress had a negative impact on their relationship and caused further stress:My partner keeps saying ‘For God’s sake, I wish we’d never got pregnant. I wish you’d have got rid of him’. He doesn’t understand. He’s just ‘What’s up? You in a mood?’ and I find that a bit hardParticipant322 | High/moderate | Moderate/moderate | Moderate certainty | Studies of high to moderate quality; finding seen across several studies, across general populations and across culturally different and selective groups |
| Lack of practical support – a detrimental effect of a lack of practical support was reported.314,318 Respondents reported having to deal with everything by themselves without practical support:You bring the baby home. You need to eat, the family need to eat, have to clean the house, have to wash the children, take them to school, take them to Arabic reading (classes). You have to do all this work in 1 day, how can you get rest?Participant314Contrary to popular beliefs about the nature of the extended Asian family in Britain, help from relatives was not available to many womenParticipant314 | – | Moderate | |||
| Negative interactions with health-care professionals – in some cases care provided by health professionals was seen as inadequate.424 One respondent revealed:The infant cried a lot. I called the midwife and she said ‘what do you want me to do?’ I was very disappointed. I needed someone to give me supportParticipant424 | Moderate | High | |||
| Interference by mother or family members/unreliable mother/rejection by family member/disapproval. In one study a women talked about her mother who she lived with and her sister who lived nearby who were initially very supportive but this support became unhelpful:321I felt quite jealous. He had colic and because he cried from between 6 and 10, and of course my mum’s: ‘Oh give him here. You don’t know what to do with him . . .’ and I remember having a few tears over that because she’d taken him away from me . . .Participant321Teenagers described their own mother as ‘unreliable’, and she could not provide required support305,319,321 | High/moderate | Moderate | |||
| Negative effect of peers – women reported that peers had embellished their own experience to conform to social norms of being a ‘good mother’316 for them only to discover later that their account of their experiences had not been entirely truthful:I asked friends . . . : ‘how is your daughter? . . . They said . . . she never cries. Recently, . . . they then said they could not even take a shower! And I said . . . ‘but I thought that she did not cry?’ And even worse, they had not told me the truth, and I found this extremely distressingParticipant316 | Moderate | – | |||
| – | – | ||||
| Cultural beliefs did not help in accessing support – respondents reported that women were expected to not discuss private matters by other members of their community314 | – | Moderate | – | – | |
| Cultural and community beliefs included that men were not expected to provide support, and therefore women were deprived of the support of their partners314 | – | Moderate | – | – | |
| Unsatisfactory health care | Multiple carers during pregnancy – dissatisfaction with the health-care system was also reported303,311,315,316 including negative perceptions of having multiple carers during pregnancy315 | – | Moderate | Moderate certainty | Studies of high to moderate quality; finding seen across a number of studies, across general populations and across culturally different and selective groups |
| Poor-quality hospital care.311 One respondent reported:. . . the [community] midwife . . . she was very helpful but the midwives in hospital, . . . I would never advise anyone to go and see them . . . You could be crying with pain and [they] will be treating you like a log. I didn’t feel like a human being at allParticipant311 | – | High | |||
| Simply normalising problems – respondents expressed disappointment when seeking health care and felt that health professionals merely focused on normalising problems:323I go there only when I have to . . . I feel I haven’t gotten any help there, they haven’t taken me seriously, and all they say is that ‘this is normal’Participant323 | – | – | |||
| Protocol-driven care – no scope to discuss psychological distress – respondents complained that they found the health-care system to be protocol driven with no room to discuss psychological distress or to deliver interventions to maintain maternal mental health311 | – | High | |||
| Antenatal class did not help – antenatal classes appeared of little use to respondents.316 Women did not want an intervention in the form of a class296–298 | Moderate | – | |||
| Medication did not help – medication made things worse or was ineffective303 | Moderate | – | |||
| Negative effect of self-help/coping strategies/inability to apply self-help/coping strategies | Repetitive cleaning – compulsive behaviours – participants noted that some strategies could become unhelpful, and could in some cases develop into compulsive behaviours, such as repetitive cleaning.322 Respondents complained that they were unable to apply strategies they had relied on in the past because of their inappropriateness in the prenatal and postnatal period, such as drinking alcohol322 | High | – | Low certainty | Finding from one study of high quality; finding cannot be generalised to other populations |
| Too much information – books and internet increased distress322 | High | – | |||
| Inability to apply previously used coping strategies322 | High | – | |||
| Inability to do anything – lack of motivation322 | High | – | |||
| Baby-related difficulties | Baby crying318 | – | Moderate | Low certainty | Finding from one study of moderate quality; finding cannot be generalised to other populations |
| Breast feeding difficulties318 | |||||
| Guilt because of prematurity318 | |||||
| Physical difficulties, physical tiredness ‘limited time for self-care’ | Difficulties included fatigue, pain and the physical recovery from labour and delivery,312,313,317 cognitive difficulties318 and also having limited time for self-care to address such issues312,313 | Moderate/high | Moderate | Moderate certainty | Studies of high to moderate quality; finding seen across a few studies, across general populations and across cultural groups |
| Personal insecurity | Worries about being a good parent, self-doubt, feeling a pressure of responsibility and feelings of inadequacy.286,292,312,313,321 Women reported that they put themselves under a lot pressure to be perfect mothers and experienced feelings of inadequacy when motherhood did not come naturally321 |
High | Moderate | Moderate certainty | Studies of generally high quality; finding seen across several studies, across general populations and across culturally different and selective groups |
| Personal insecurity was associated with a loss of a sense of self. Loss of self included a loss of occupational identity312,313 and a loss of appearance/physical attractiveness312,313 | High | – | |||
| Loss of self included a loss of autonomy in which the focus was on the baby and there was a sense of sacrificing oneself for the baby,312,313,321 and a loss of sexuality312,313 | High | – | |||
| Women reported that having financial concerns was detrimental to their mental health. They believed that they would be better able to counter emotional distress if these concerns were alleviated286,306–310 | High | High | |||
Appendix 8 Included systematic reviews
| First author, year, reference number | Full reference | Review type |
|---|---|---|
| Austin, 2008230 | Austin MP, Priest SR, Sullivan EA. Antenatal psychosocial assessment for reducing perinatal mental health morbidity. Cochrane Database Syst Rev 2008;8:CD005124 | Cochrane review |
| Bennett, 2008425 | Bennett C, Macdonald GM, Dennis J, Coren E, Patterson J, Astin M, et al. Home-based support for disadvantaged adult mothers [Update of Cochrane Database Syst Rev 2007;3:CD003759]. Cochrane Database Syst Rev 2008;1:CD003759 | Cochrane review |
| Cuijpers, 200568 | Cuijpers P, Straten A, Smit F. Preventing the incidence of new cases of mental disorders: a meta-analytic review. J Nerv Ment Dis 2005;193:119–25 | Systematic review and meta-analysis |
| Dale, 2008232 | Dale J, Caramlau IO, Lindenmeyer A, Williams SM. Peer support telephone calls for improving health. Cochrane Database Syst Rev 2008;4:CD006903 | Cochrane review |
| Dennis, 2004233 | Dennis CL, Creedy D. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Syst Rev 2004;4:CD001134 | Cochrane review |
| Dennis, 2005234 | Dennis CL. Psychosocial and psychological interventions for prevention of postnatal depression: systematic review. BMJ 2005;331:15–21 | Systematic review |
| Dennis, 2008118 | Dennis CL, Allen K. Interventions (other than pharmacological, psychosocial or psychological) for treating antenatal depression. Cochrane Database Syst Rev 2008;4:CD006795 | Cochrane review |
| Dennis, 2004235 | Dennis CL. Preventing postpartum depression part I: a review of biological interventions. Can J Psychiatry 2004;49:467–75 | Systematic review |
| Dennis, 2008236 | Dennis CL, Kingston D. A systematic review of telephone support for women during pregnancy and the early postpartum period. J Obstet Gynecol Neonatal Nurs 2008;37:301–14 | Systematic review |
| Dennis, 2008237 | Dennis CL, Ross LE, Herxheimer A. Oestrogens and progestins for preventing and treating postpartum depression. Cochrane Database Syst Rev 2008;4:CD001690 | Cochrane review |
| Dennis, 2004238 | Dennis CL. Preventing postpartum depression part II: A critical review of nonbiological interventions. Can J Psychiatry 2004;49:526–38 | Critical review |
| Dodd, 2012239 | Dodd JM, Crowther CA. Specialised antenatal clinics for women with a multiple pregnancy for improving maternal and infant outcomes. Cochrane Database Syst Rev 2012;8:CD005300 | Cochrane review |
| Fontein-Kuipers, 2014240 | Fontein-Kuipers YJ, Nieuwenhuijze MJ, Ausems M, Bude L, Vries R. Antenatal interventions to reduce maternal distress: a systematic review and meta-analysis of randomised trials. BJOG 2014;121:389–97 | Systematic review |
| Howard, 2005241 | Howard LM, Hoffbrand S, Henshaw C, Boath L, Bradley E. Antidepressant prevention of postnatal depression. Cochrane Database Syst Rev 2005;2:CD004363 | Cochrane review |
| Jans, 2010242 | Jans LA, Giltay EJ, Does AJ. The efficacy of n-3 fatty acids DHA and EPA (fish oil) for perinatal depression. Br J Nutr 2010;104:1577–85 | Review |
| Lawrie, 2008243 | Lawrie TA, Herxheimer A, Dalton K. Oestrogens and progestogens for preventing and treating postnatal depression. Cochrane Database Syst Rev 2008;2:CD001690 | Cochrane review |
| Leis, 2009244 | Leis JA, Mendelson T, Tandon SD, Perry DF. A systematic review of home-based interventions to prevent and treat postpartum depression. Arch Womens Ment Health 2009;12:3–13 | Systematic review |
| Lumley, 2004245 | Lumley J, Austin MP, Mitchell C. Intervening to reduce depression after birth: a systematic review of the randomized trials. Int J Technol Assess Health Care 2004;20:128–44 | Systematic review |
| Marc, 2011246 | Marc I, Toureche N, Ernst E, Hodnett ED, Blanchet C, Dodin S, et al. Mind–body interventions during pregnancy for preventing or treating women’s anxiety. Cochrane Database Syst Rev 2011;7:CD007559 | Cochrane review |
| Miller, 2013247 | Miller BJ, Murray L, Beckmann MM, Kent T, Macfarlane B. Dietary supplements for preventing postnatal depression. Cochrane Database Syst Rev 2013;10:CD009104 | Systematic review and meta-analysis |
| Sado, 2012248 | Sado M, Ota E, Stickley A, Mori R. Hypnosis during pregnancy, childbirth, and the postnatal period for preventing postnatal depression. Cochrane Database Syst Rev 2012;6:CD009062 | Cochrane review |
| Shaw, 2006249 | Shaw E, Levitt C, Wong S, Kaczorowski J, McMaster University Postpartum Research G. Systematic review of the literature on postpartum care: effectiveness of postpartum support to improve maternal parenting, mental health, quality of life, and physical health. Birth 2006;33:210–20 | Systematic review |
| Sockol, 2011250 | Sockol LE, Epperson CN, Barber JP. A meta-analysis of treatments for perinatal depression. Clin Psychol Rev 2011;31:839–49 | Systematic review |
| Sockol, 2013423 | Sockol LE, Epperson CN, Barber JP. Preventing postpartum depression: a meta-analytic review. Clin Psychol Rev 2013;33:1205–17 | Meta-analysis |
Appendix 9 Qualitative review: participant characteristics
Characteristics of participants receiving preventive interventions
Universal preventive interventions: included studies concerned with midwifery models of working (n = 5)
| First author, year, reference number | Country | Intervention name | Sample size (contributing qualitative evidence) | Study methods (yielding qualitative data) | Population details | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General population, minority group | Depression status: none reported/self-reported/mixed/mixed diagnosed | Age (years) | Ethnicity | Socioeconomic status | Parity | Education | Marital status | |||||
| Andersson, 2012277 | Sweden | CenteringPregnancy | 28 (included 8 male partners) | Individual and group interviews | General population | None reported | NR | Swedish, n = 16; non-Swedish, n = 4 | NR | First baby, n = 14; second baby, n = 7 | NR | NR |
| Kennedy, 2009283 | USA | CenteringPregnancy | 234 (both arms) | Semistructured telephone interview | Military population | None reported | Mean 25 (SD 4.9) | African American, 18.4% (n = 29): Latina, 10.8% (n = 17); white, 59.2% (n = 92); Asian/Pacific Islander, 5.7% (n = 9); other 7.0% (n = 11) | WIC eligible (low income), 50.3% (n = 77) | Nulliparous, 59.2% (n = 77) | < High school, 3.5% (n = 5); high school, 35% (n = 50); some college, 47.7% (n = 68); college graduate, 9.8% (n = 14); graduate school 4.2% (n = 6) | Single, 10.8% (n = 17); married, 74.5% (n = 117); partnered, 12.1% (n = 19); divorced/separated, 2.5% (n = 4) |
| Klima, 2009284 | USA | CenteringPregnancy | 5 | Focus group | General population | None reported | NR | All African American | NR | NR | NR | NR |
| McNeil, 2012285 | Canada | CenteringPregnancy | 12 | Interviews and focus groups | General population | None reported | Range 27–39 | 5/12 were born outside Canada and 4/12 were non-Caucasian | 2/12 had less than CA$40,000 annual income and 4/12 had CA$100,000 or more | 10/12 were first-time mothers | Ranged from less than high school to graduate school | 11/12 were married |
| Teate, 2011289 | Australia | CenteringPregnancy | NR | Questionnaire | General population | None reported | NR | NR | NR | NR | NR | NR |
Universal preventive interventions: included studies concerned with CAM (n = 3)
| First author, year, reference number | Country | Intervention name | Sample size (contributing qualitative evidence) | Study methods (yielding qualitative data) | Population details | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General population, minority group | Depression status: none reported/self-reported/mixed/mixed diagnosed | Age (years) | Ethnicity | Socioeconomic status | Parity | Education | Marital status | |||||
| Carolan, 2012278,279 | Ireland | Singing lullabies | 6 | In-depth interview | General population | None reported | 29–35 | NR | 5/6 employed in professional occupations | All primiparous | 5 tertiary, 1 secondary | NR |
| Doran, 2013280 | Australia | Yoga and group discussion | 15 | In-depth interview | General population | None reported | Mean 32 (range 22–45) | 14 women were born in Australia, one of whom identified as Indigenous, and one was born in the Pacific | NR | Mean 1.6 children | All participants had a technical and further education or university qualification | NR |
| Migl, 2009286 | USA | MBE techniques | 10 | Open-ended interview | General population | None reported | 27–38 | 1 Hispanic; 2 African American; 7 Caucasian | 8 in employment | 1–7 pregnancies | High school to graduate degree | 8 married; 2 single |
Universal preventive interventions: included studies concerned with psychological interventions (n = 2)
| First author, year, reference number | Country | Intervention name | Sample size (contributing qualitative evidence) | Study methods (yielding qualitative data) | Population details | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General population, minority group | Depression status: none reported/self-reported/mixed/mixed diagnosed | Age (years) | Ethnicity | Socioeconomic status | Parity | Education | Marital status | |||||
| Gao, 2012282 | China | IPT–oriented programme | 20 | Interview | General population | None reported | Mean 28.8 (SD 2.35), range 25–34 | Chinese | Professional, n = 10; semiprofessional, n = 8; skilled, n = 2 | First-time mothers | High school or below, n = 2; college or above, n = 18 | All married |
Universal preventive interventions: included studies concerned with the organisation of maternity care (n = 1)
| First author, year, reference number | Country | Intervention name | Sample size (contributing qualitative evidence) | Study methods (yielding qualitative data) | Population details | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General population, minority group | Depression status: none reported/self-reported/mixed/mixed diagnosed | Age (years) | Ethnicity | Socioeconomic status | Parity | Education | Marital status | |||||
| Scott, 1987288 | Australia | Maternal and child health nurses | Unclear – 7 (plus 3 nurses) | Interview and observation | General population | Self-reported as depressed | NR | NR | NR | NR | NR | NR |
Universal preventive interventions: included studies concerned with the social support (n = 1)
| First author, year, reference number | Country | Intervention name | Sample size (contributing qualitative evidence) | Study methods (yielding qualitative data) | Population details | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General population, minority group | Depression status: none reported/self-reported/mixed/mixed diagnosed | Age (years) | Ethnicity | Socioeconomic status | Parity | Education | Marital status | |||||
| Evans, 2012281 | Canada | Online discussion support group | 512 postings | Online messages | General population | Self-reported as depressed | NR | NR | NR | NR | NR | NR |
| Morrell, 2002287 | UK | Postnatal support worker | NR | Questionnaire | General population | None reported | NR | NR | NR | NR | NR | NR |
Universal preventive interventions: included studies concerned with usual care (n = 1)
| First author, year, reference number | Country | Intervention name | Sample size (contributing qualitative evidence) | Study methods (yielding qualitative data) | Population details | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General population, minority group | Depression status: none reported/self-reported/mixed/mixed diagnosed | Age (years) | Ethnicity | Socioeconomic status | Parity | Education | Marital status | |||||
| Kennedy, 2009283 | USA | Individual prenatal care | 234 (both arms) | Semistructured telephone interview | Military population | None reported | Mean 25.5 (SD 5.4) | African American, 19.0% (n = 30); Latina, 8.9% (n = 14); white, 60.1% (n = 95); Asian/Pacific Islander, 5.1% (n = 8); other, 7.0% (n = 11) | WIC eligible (low income), 47.8% (n = 69) | Nulliparous 45.9% (n = 61) | < High school, 5.6% (n = 8); high school, 21.1% (n = 30); some college, 50.0% (n = 71); college completed, 12.7% (n = 18) | Single, 9.5% (n = 15); married, 82.9% (n = 131); divorced/separated, 3.8% (n = 6); partnered, 3.8% (n = 6) |
Selective preventive interventions: included studies concerned with midwifery models of working (n = 2)
| First author, year, reference number | Country | Intervention name | Sample size (contributing qualitative evidence) | Study methods (yielding qualitative data) | Population details | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General population, minority group | Depression status: none reported/self-reported/mixed/mixed diagnosed | Age (years) | Ethnicity | Socioeconomic status | Parity | Education | Marital status | |||||
| Lehman, 2011292 | USA | CenteringPregnancy | 10 | Interview | African American/Latina low income | None reported | 20–30 (mean 22) | African American | Low-income | Number of children 1–4 (mean 2.3) | NR | 4 single, 6 unknown |
| Novick, 2011, 294,363 2012,293 2013382 | USA | CenteringPregnancy | 21 pregnant women (18 others attending sessions not interviewed formally) | Interviews and observation | African American/Hispanic low income | None reported | Mean 21.6 | 18 African American; 3 Hispanic | NR | NR | Ranged from grade school to some college | 19 single; 2 married |
Indicated and selective preventive interventions: included studies concerned with psychological interventions (n = 1)
| First author, year, reference number | Country | Intervention name | Sample size (contributing qualitative evidence) | Study methods (yielding qualitative data) | Population details | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General population, minority group | Depression status: none reported/self-reported/mixed/mixed diagnosed | Age (years) | Ethnicity | Socioeconomic status | Parity | Education | Marital status | |||||
| Shanok, 2007296–298 | USA | IPT | 42 (plus 4 clinicians) | Semistructured interviews; clinical interviews; videoed therapy sessions transcribed | Teenagers | 14 participants had a current depressive disorder with no psychotic symptoms. EPDS score 8 or more | 13–19 (mean 5.50, SD 1.47) | 49% Hispanic, 38% black, 10% black and Hispanic | Impoverished urban area | All first child; 93% pregnant; 7% parenting | NR | NR |
Indicated preventive interventions: included studies concerned with social support (n = 1)
| First author, year, reference number | Country | Intervention name | Sample size (contributing qualitative evidence) | Study methods (yielding qualitative data) | Population details | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General population, minority group | Depression status: none reported/self-reported/mixed/mixed diagnosed | Age (years) | Ethnicity | Socioeconomic status | Parity | Education | Marital status | |||||
| Dennis, 2010299 | Canada | Telephone-based peer support | NR | Questionnaire | General population | EPDS score 10 or more | NR | NR | NR | NR | NR | NR |
Indicated preventive interventions: included studies concerned with the organisation of maternity care (n = 1)
| First author, year, reference number | Country | Intervention name | Sample size (contributing qualitative evidence) | Study methods (yielding qualitative data) | Population details | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General population, minority group | Depression status: none reported/self-reported/mixed/mixed diagnosed | Age (years) | Ethnicity | Socioeconomic status | Parity | Education | Marital status | |||||
| Myors, 2013300 | Australia | Specialist perinatal and infant mental health service | 11 | Interview | General population | Identified as having multiple mental health and psychosocial issues | 20–39 | 9 from an English-speaking background | NR | 1–4 children | NR | All women partnered at time of referral |
Selective preventive interventions: included studies concerned with educational interventions (n = 1)
| First author, year, reference number | Country | Intervention name | Sample size (contributing qualitative evidence) | Study methods (yielding qualitative data) | Population details | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General population, minority group | Depression status: none reported/self-reported/mixed/mixed diagnosed | Age (years) | Ethnicity | Socioeconomic status | Parity | Education | Marital status | |||||
| Wheatley, 1999,253 2003,254 | UK | Preparing for parenthood | 9 | Interview | General population | None reported (scoring as high risk on GHQ) | NR | NR | NR | First pregnancy | NR | NR |
Population characteristics for the service providers of preventive interventions
Universal preventive interventions: included studies concerned with midwifery models of working (n = 3)
| First author, year, reference number | Country | Intervention name | Sample size (contributing qualitative evidence) | Study methods (yielding qualitative data) | Population details | |||
|---|---|---|---|---|---|---|---|---|
| Age (years) | Gender | Ethnicity | Parity | |||||
| Klima, 2009284 | USA | CenteringPregnancy | 4 certified nurse midwives; 5 health-centre staff; 5 administrators | Focus groups | NR | NR | NR | NR |
| McNeil, 2013290 | Canada | CenteringPregnancy | 3 physicians | Interview/focus groups | NR | All female | NR | NR |
| Tanner-Smith, 2012291 | USA | CenteringPregnancy | NR | Questionnaire | NR | NR | NR | NR |
Universal preventive interventions: included studies concerned with social support (n = 1)
| First author, year, reference number | Country | Intervention name | Sample size (contributing qualitative evidence) | Study methods (yielding qualitative data) | Population details | |||
|---|---|---|---|---|---|---|---|---|
| Age (years) | Gender | Ethnicity | Parity | |||||
| Morrell, 2002287 | UK | Support workers | NR – SWs, MWs, HVs | Questionnaire | NR | NR | NR | NR |
Universal preventive interventions: included studies concerned with the organisation of maternity care (n = 1)
| First author, year, reference number | Country | Intervention name | Sample size (contributing qualitative evidence) | Study methods (yielding qualitative data) | Population details | |||
|---|---|---|---|---|---|---|---|---|
| Age (years) | Gender | Ethnicity | Parity | |||||
| Scott, 1987288 | Australia | Maternal and child health nurses | 3 nurses | Interview and observation | NR | NR | NR | NR |
Selective preventive interventions: included studies concerned with midwifery models of working (n = 1)
| First author, year, reference number | Country | Intervention name | Sample size (contributing qualitative evidence) | Study methods (yielding qualitative data) | Population details | |||
|---|---|---|---|---|---|---|---|---|
| Age (years) | Gender | Ethnicity | Parity | |||||
| Novick, 2011,363 2012293,294 | USA | CenteringPregnancy | 2 certified nurse-midwife group leaders; 2 medical assistants | Interviews and observation | NR | NR | NR | NR |
Indicated preventive interventions: included studies concerned with social support (n = 1)
| First author, year, reference number | Country | Intervention name | Sample size (contributing qualitative evidence) | Study methods (yielding qualitative data) | Population details | |||
|---|---|---|---|---|---|---|---|---|
| Age (years) | Gender | Ethnicity | Parity | |||||
| Dennis, 2013301 | Canada | Telephone-based peer support | Peer volunteers – mother from the community with resolved history of PND who participated in a 4-hour training session | Questionnaire | NR | NR | NR | NR |
Indicated and selective preventive interventions: included studies concerned with psychological interventions (n = 1)
| First author, year, reference number | Country | Intervention name | Sample size (contributing qualitative evidence) | Study methods (yielding qualitative data) | Population details | |||
|---|---|---|---|---|---|---|---|---|
| Age (years) | Gender | Ethnicity | Parity | |||||
| Shanok, 2007296–298 | USA | IPT | 4 clinicians | Semistructured interviews, clinical interviews, videoed therapy sessions transcribed | 26–35 | All female | 2 Caucasian, 1 Hispanic, 1 Middle Eastern | One pregnant and parenting, others did not have children |
Personal and social support strategy studies: population characteristics
| First author, year, reference number | Country | Sample size (contributing qualitative evidence) | Study methods (yielding qualitative data) | Population details | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| General population, minority group | Specific group if any; cultural, selective | Antenatal/postnatal | Depression status: none reported/self-reported/mixed/mixed diagnosed | Age (years) | Ethnicity | Socioeconomic status | Parity | Education | Marital status | ||||
| Choi, 2005321 | UK | 24 | Interview | General | – | Recruited antenatally | Mixed, some self-reported depression | 27–45 (mean age 35.92, SD 4.43) | Caucasian | Variety of occupations, social classes | 9 first child; 11 had one other and 4 had two others | Variety of educational levels | 22 were married or cohabiting, 1 was single and 1 was divorced |
| Corrigan, 1997302 | USA | 8 | Semistructured interview | General | – | Recruited antenatally | Mixed, half scoring highly on BDI | NR | NR | NR | NR | NR | NR |
| Curtis, 2007303 | USA | 252 | Open-ended online survey | General | – | Recruited postnatally | Self-reported as depressed | 10–62 (mean 37, SD 7.6) | Caucasian, 228; African American, 3; Asian, 1; Latina, 6; Filipino, 1; Native American, 1; mixed ethnicity, 9 | NR | NR | NR | NR |
| Edge, 2005306–310 | UK | 12 | In-depth interviews | Black Caribbean | Cultural | Recruited antenatally | Mixed, sample represented the full range of EPDS scores | 24–42 | Black Caribbean | NR | NR | NR | 6 married, 3 cohabiting, 3 single |
| Edge, 2011311 | UK | 42 | Focus group interviews | Black Caribbean | Cultural | Recruited postnatally | None reported | 18–43 | Black Caribbean | Lived in inner city and suburbs | NR | NR | Married, cohabiting or single |
| Furber, 2009322 | UK | 12 | Interview | General | – | Recruited antenatally | None reported | 24–39 | NR | 12 not working; 4 worked full time; 5 worked part time; 2 studying full time; 1 on maternity leave | 8 primiparous; 16 multiparous | NR | 19 living with partners, 2 not living with partner, 2 single; 1 separated |
| Haga, 2012323 | Norway | 12 | Interview | General | – | Recruited postnatally | Mixed, some self-reported depression | 25–44 (mean 32.8) | NR | NR | All first time mothers | All university or college | All cohabiting with father of baby |
| Hanley, 2007304 | UK | 10 | Focus group interview | Minority | Cultural | Recruited postnatally | Mixed, 2 self-reported as depressed | 16–24 | Bangladeshi | 8 husbands worked in catering industry; 2 professional | 1–4 | 8 educated in Britain | All married |
| aLehman, 2011292 | USA | 10 | Interview | Minority – low income | – | Recruited antenatally | Deprived | 20–30 (mean 22) | African American | Low-income | 1–4 (mean 2.3) | NR | 4 single, 6 unknown |
| Leung, 2001305 | China | 59 | Interviews | General population: Hong Kong Chinese | Cultural: Hong Kong Chinese | Recruited antenatally | Mixed, 32 depressed, 27 non-depressed | NR | Hong Kong Chinese | Working women and housewives | NR | NR | NR |
| Lewis, 1998312,313 | UK | 36 | Interview | General | – | 1 study antenatally; 2 study postnatally | Mixed, some self-reported depression | 22–41 | All city dwellers, 2 were black (in study 1, 1 from Zimbabwe, 1 London with West Indian origin, 1 Irish) remainder British and white | Broad range | 18 already had children with at least 1 under 5 years; 18 expecting first child | NR | 7 single mothers, others in permanent or long-term relationships |
| Maunther, 1998324 | UK | 40 | Interview | General | – | Recruited postnatally | Mixed, some self-reported depression, some diagnosed depression | 20–39 | 39 white; 1 Afro-Caribbean | 5 non-skilled; 7 skilled non-manual; 6 professional | NR | 7 secondary education; 9 vocational training; 2 university | All living with father of children |
| aMigl, 2009286 | USA | 10 | Open-ended interview | General | – | Recruited antenatally | – | 27–38 | 1 Hispanic; 2 African American; 7 Caucasian | 8 in employment | 1 to 7 pregnancies | High school to graduate degree | 8 married, 2 single |
| Oates, 20047 | 15 centres | NR | Interview and focus group | General | – | Recruited postnatally | None reported | NR | NR | NR | NR | NR | NR |
| Parvin, 2004314 | UK | 25 | Focus groups | Minority: cultural/ethnic differences | Cultural | Recruited postnatally | None reported | 21–54 | Bangladeshi and British-Bangladeshi | Head of household skilled 8%, unskilled 50%, unemployed 42% | Mean 3.9 | NR | Living in a nuclear family 73% |
| Raymond, 2009315 | UK | 9 | Semistructured interviews | Minority | Selective | Recruited postnatally | Self-reported as depressed (antenatal depression) | 23–40 | 6 white; 1 black Caribbean; 1 black African; 1 mixed Asian British | Deprived area | 1–3 | NR | 5 living with or had support of partner; 4 not in contact with partner |
| Razurel, 2011316 | Switzerland | 60 | Semistructured interviews | General | – | Recruited postnatally | None reported | Mean 31 | Unclear | 51% – medium category office workers, service workers, skilled manual workers | All primiparous | NR | 97% living as a couple |
| Rodrigues, 2003325 | Goa, India | 39 | Interview | General | – | Recruited antenatally | EPDS score 19 or more | 24.1–29.3 | NR | NR | 10 first-time mothers | 33 literate | NR for participants overall |
| a,bShanok, 2007296–298 | USA | 42 | Semistructured interviews, clinical interviews, videoed therapy sessions transcribed | Minority | Selective (teenagers) | Recruited antenatally | NR | 13–19 (mean 15.50, SD 1.47) | 49% Hispanic, 38% black, 10% black and Hispanic | Impoverished urban area | All first child: 93% pregnant, 7% parenting | NR | NR |
| Sword, 2012317 | Canada | 20 | In-depth interview | General | – | Recruited antenatally | Mixed, some women had previously been depressed | Mean 29.8 (SD 4.5) | White, 18 (90%); other, 2 (10%). 90% born in Canada | Household income CA$10,000–CA$39,999 (10%); CA$40,000–CA$79,999 (20%), CA$80,000 or more (60%) | NR | 1 (5%) high school or less, 9 (45%) some/completed community college or technical school, 10 (50%) university degree | All married or living with partner |
| Taniguchi, 2007318 | USA | 45 | Semistructured interview | Minority: Japanese women in USA | Cultural | Recruited postnatally | Mixed, some self-reported antenatal and PND, some diagnosed | 21–46 | Japanese | NR | 35 primparas, 10 multiparas | > 2 years college | All partnered |
| Thurtle, 2003319 | UK | 14 | Semistructured interview | General | – | Recruited antenatally | Mixed, 1/3 self-reported depressed | 17–38 | NR | All 13 husbands were in employment, socioeconomic groups II/III. Mothers II-IV. Living in self-contained housing | All primiparous | NR | 13 married or living with partner; 1 lone parent |
| Ugarriza, 2007320 | USA | 20 | Open-ended interview | General | – | Postnatal, 1 month to 1 year at time of study | None reported | 23–42 (mean 32) | All Anglo American | NR | 1–4 | Masters n = 3; Bachelors n = 9; some college n = 7; high school n = 1 | 17 married, 3 single |
Qualitative studies of universal preventive interventions
| First author, year, reference number | Full reference |
|---|---|
| Andersson, 2012277 | Andersson E, Christensson K, Hildingsson I. Parents’ experiences and perceptions of group-based antenatal care in four clinics in Sweden. Midwifery 2012;28:502–8 |
| Carolan, 2012278 | Carolan M, Barry M, Gamble M, Turner K, Mascarenas O. Experiences of pregnant women attending a lullaby programme in Limerick, Ireland: a qualitative study. Midwifery 2012;28:321–8 |
| Carolan, 2012279 | Carolan M, Barry M, Gamble M, Turner K, Mascarenas O. The Limerick Lullaby project: an intervention to relieve prenatal stress. Midwifery 2012;28:173–80 |
| Doran, 2012280 | Doran F, Hornibrook J. Women’s experiences of participation in a pregnancy and postnatal group incorporating yoga and facilitated group discussion: a qualitative evaluation. Women Birth 2013;26:82–6 |
| Evans, 2012281 | Evans M, Donelle L, Hume-Loveland L. Social support and online postpartum depression discussion groups: a content analysis. Patient Educ Couns 2012;87:405–10 |
| Gao, 2012282 | Gao LL, Luo SY, Chan SWC. Interpersonal psychotherapy-oriented program for Chinese pregnant women: delivery, content, and personal impact. Nurs Health Sci 2012;14:318–24 |
| Kennedy, 2009283 | Kennedy HP, Farrell T, Paden R, Hill S, Jolivet R, Willetts J, et al. ‘I wasn’t alone’ – a study of group prenatal care in the military. J Midwifery Womens Health 2009;54:176–83 |
| Klima, 2009284 | Klima C, Norr K, Vonderheid S, Handler A. Introduction of CenteringPregnancy in a public health clinic. J Midwifery Womens Health 2009;54:27–34 |
| McNeil, 2012285 | McNeil DA, Vekved M, Dolan SM, Siever J, Horn S, Tough SC. Getting more than they realized they needed: a qualitative study of women’s experience of group prenatal care. BMC Pregnancy Childbirth 2012;12:17 |
| Migl, 2009286 | Migl KS. The Lived Experiences of Prenatal Stress and Mind–body Exercises: Reflections of Post-Partum Women. PhD thesis. Texas: University of Texas Medical Branch Graduate School of Biomedical Sciences; 2009 |
| Morrell, 2002287 | Morrell C. Postnatal Support: Who Wants it, What is its Benefit and How Much Does it Cost. PhD thesis. Sheffield: University of Sheffield; 2002 |
| Scott, 1987288 | Scott D. Maternal and child health nurse: role in post-partum depression. Aust J Adv Nurs 1987;5:28–37 |
| Teate, 2011289 | Teate A, Leap N, Rising SS, Homer CS. Women’s experiences of group antenatal care in Australia – the CenteringPregnancy Pilot Study. Midwifery 2011;27:138–45 |
Qualitative studies (universal) reporting data from service providers
| First author, year, reference number | Full reference |
|---|---|
| McNeil, 2013290 | McNeil DA, Vekved MF, Dolan SM, Siever J, Siever JF, Horn S, et al. A qualitative study of the experience of CenteringPregnancy group prenatal care for physicians. BMC Pregnancy Childbirth 2013;13(Suppl. 1):6 |
| Tanner-Smith, 2012291 | Tanner-Smith EE, Steinka-Fry KT, Lipsey MW. A Multi-site Evaluation of the Centering Pregnancy® Programs in Tennessee. Nashville, TN: Peabody Research Institute, Vanderbilt University. 2012. URL: https://my.vanderbilt.edu/emilytannersmith/files/2012/02/Contract19199-GR1030830-Final-Report.pdf (accessed August 2014) |
Qualitative studies of selective preventive interventions
| First author, year, reference number | Full reference |
|---|---|
| Lehman, 2012292 | Lehman E. Centering pregnancy: A Combined Quantitative and Qualitative Appraisal of Women’s Experiences of Depression and Anxiety During Group Prenatal Care. Wheaton, IL: Wheaton College; 2012 |
| Novick, 2012293 | Novick G, Sadler LS, Knafl KA, Groce NE, Kennedy HP. The intersection of everyday life and group prenatal care for women in two urban clinics. J Health Care Poor Underserved 2012;23:589–603 |
| Novick, 2013295 | Novick G, Sadler LS, Knafl KA, Groce NE, Kennedy HP. In a hard spot: providing group prenatal care in two urban clinics. Midwifery 2013;29:690–7 |
| Novick, 2011363 | Novick G, Sadler LS, Kennedy HP, Cohen SS, Groce NE, Knafl KA. Women’s experience of group prenatal care. Qual Health Res 2011;21:97–116 |
| Shanok, 2007296 | Shanok AF, Miller L. Stepping up to motherhood among inner-city teens. Psychol Women Q 2007;31:252–61 |
| Shanok, 2007297 | Shanok AF, Miller L. Depression and treatment with inner city pregnant and parenting teens. Arch Womens Ment Health 2007;10:199–210 |
| Shanok, 2007298 | Shanok AF. Experiences of Pregnancy and Parenting Among Inner City Teens Attending an Alternative Public School. PhD thesis. New York, NY: Columbia University; 2007 |
| Wheatley, 1999253 | Wheatley SL, Brugha TS. ‘Just because I like it doesn’t mean it has to work’: personal experiences of an antenatal psychosocial intervention designed to prevent postnatal depression. Int J Ment Health Promot 1999;1:26–31 |
| Wheatley, 2003254 | Wheatley SL, Brugha TS, Shapiro DA. Exploring and enhancing engagement to the psychosocial intervention ‘Preparing for Parenthood’. Arch Womens Ment Health 2003;4:275–85 |
Qualitative studies of indicated preventive interventions
| First author, year, reference number | Full reference |
|---|---|
| Dennis, 2010299 | Dennis CL. Postpartum depression peer support: maternal perceptions from a randomized controlled trial. Int J Nurs Stud 2010;47:560–8 |
| Myors, 2014300 | Myors KA, Schmied V, Johnson M, Cleary M. ‘My special time’: Australian women’s experiences of accessing a specialist perinatal and infant mental health service. Health Soc Care Community 2014;22:268–77 |
Qualitative studies (indicated) reporting data from service providers
| First author, year, reference number | Full reference |
|---|---|
| Dennis, 2013301 | Dennis CL. Peer support for postpartum depression: volunteers’ perceptions, recruitment strategies and training from a randomized controlled trial. Health Promot Int 2013;28:187–96 |
Appendix 10 Studies omitted from the network meta-analysis
Universal preventive intervention studies omitted from network meta-analysis
| Intervention summary | First author and reference | Reason not included | Total number of participants | Comparison group(s) | Depression outcomes | Main findings | Overall risk of bias |
|---|---|---|---|---|---|---|---|
| CBT-based intervention | Mao157 | No usual-care comparison | 204 | Usual care in China | EPDS mean score (Chinese version) | In the emotional self-management group-training arm, the EPDS mean score at 6 weeks postnatally was 6.45 (SD 1.09) vs. 9.23 (SD 2.91) in the CG. Using the Structured Clinical Interview for DSM-IV (SCID) 2.7% women (3/113) in the IG had PND vs. 9.3% women (10/108) in the CG | Unclear |
| IPT-based intervention | Gao154,327 | No usual-care comparison | 194 | Usual care in China | EPDS score 13 or more (Chinese version) | In the IG, the EPDS mean score at 6 weeks postnatally was 6.59 (SD 4.10) vs. 8.87 (SD 4.37) in the CG | Low |
| IPT-based intervention | Leung156 | No usual-care comparison | 156 | Usual care in Hong Kong | EPDS score 13 or more | Intention-to-treat analysis showed IG had significantly lower perceived stress and greater happiness than CG immediately after the intervention (in pregnancy). Effects not sustained at postnatal follow-up156 | Low |
| Promoting parent–infant interaction | Cooper153 | No usual-care comparison | 449 | Usual care in South Africa | EPDS mean score | At 6 months postnatally, 12.4% (21/170) women in the IG were depressed according to the SCID, compared with 15.8% (29/184) women in the CG. The EPDS mean score was 2.78 (SD 4.54) in the IG and 3.91 (SD 5.80) in the CG | Unclear |
| Psychoeducational intervention | Kozinszky155 | No EPDS score | 1762 | Usual care in Hungary, educational information | Leverton Questionnaire | Differences 6 weeks postpartum in PPD prevalence ‘(12.7 vs. 17.5%; χ2, p< 0.01; OR: 0.68) and LQ scores (9.43 ± 2.168 vs. 10.12 ± 3.632; Mann-Whitney U probe, p < 0.001) for IG vs. CG, likely reflect the effect of the group intervention155 | High |
| Booklet on PND | Hayes182,329 | No EPDS score | 188 | Usual care in Australia | POMS | Significant and steady reduction in scores (overall and on the subscales) was observed over time for both groups that showed significant improvement in symptoms of depression. No difference when comparing IG vs. CG | Unclear |
| Booklet on PND | Ho183 | No usual-care comparison | 200 | Usual care in Taiwan | EPDS score 10 or more (Chinese version) | No significant difference for IG vs. CG at 6 weeks (χ2 = 1.90, d.f. = 1, p = 0.17) and 3 months postpartum (χ2 = 1.02, d.f. = 1, p = 0.31)183 | High |
| Education on preparing for parenting | Feinberg180 | No EPDS score | 169 | Usual care in the USA | CES-D (subset of seven items) | Intent-to-treat analyses indicated significant program effects on coparental support, maternal depression and anxiety, distress in the parent—child relationship, and several indicators of infant regulation180 | Unclear |
| Education on preparing for parenting | Gjerdingen181 | No EPDS score | 151 | Usual care in the USA | SF-36 | No significant group differences on postpartum health or work outcomes181 | High |
| Education on preparing for parenting | Milgrom185 | No usual-care comparison | 143 | Educational information | BDI, EPDS score 13 or more | IG reported significantly lower levels of depression (BDI-II) post-treatment than participants in routine care (F1, 86 = 7.82, p < 0.01. Cohen’s d = 0.6)185 | Unclear |
| Education on preparing for parenting | Shapiro187 | No EPDS score | 38 | Usual care in the USA | SCL | In general, intervention was effective compared to CG for wife and husband marital quality, for wife and husband postpartum depression. The major change in postpartum depression was from 3 months to 1 year: CG increased and IG decreased, t(32) = 2.13, p < .05187 | High |
| Self-help support | Reid200,268 | No usable EPDS score | 1004 | Usual care in the UK | EPDS score 12 or more | At 3 and 6 months postnatally there were no significant differences in the EPDS scores between the IG and the CG | Low |
| Social support | Kieffer198 | No usual-care comparison | 278 | Educational information | CES-D | From baseline to postpartum, the mean CES-D score of the MOMs group decreased 1.45 points more than the mean CES-D score of the CG, although this difference in overall change scores was not significant (95% CI: –3.26, 0.37; p = 0.12)198 | Low |
| DHA | Doornbos207 | No network | 119 | Usual care in the Netherlands | EPDS score 12 or more (Dutch version) | IG did not differ in mean EPDS scores or changes in EPDS scores or in incidence or severity of postpartum blues | High |
| DHA 200 mg/day | Llorente210 | No network | 89 | Usual care in the USA | BDI, EPDS mean | After 4 months, no difference between groups in either self-rating or diagnostic measures of depression | Unclear |
| Norethisterone ethanate 200 mg administered intramuscular | Lawrie209 | No usual-care comparison | 180 | Usual care in South Africa | EPDS score 12 or more | Mean depression scores significantly higher in IG vs. CG at 6 weeks postpartum (mean MADRS score 8.3 vs. 4.9: p = 0.0111: mean EPDS score 10.6 vs. 7.5: p = 0.0022)209 | Low |
| Midwife-led debriefing or counselling after childbirth | Priest,217 Henderson330 | No network | 1745 | Usual care in Australia | EPDS score 13 or more | No differences in median time to onset of depression (intervention, 6 [interquartile range, 4–9] weeks vs. control, 4 weeks; p = 0.84), or duration of depression (intervention, 24 weeks vs. control, 22 weeks; p = 0.98) | Unclear; unclear |
| Midwife-led Debriefing or Counselling after childbirth | Selkirk218 | No network | 149 | Usual care in Australia | EPDS mean score | No significant differences for IG vs. CG on measures of personal information, depression, anxiety, trauma, perception of the birth, or parenting stress at any assessment points, postpartum218 | High |
| Early contact with care provider | Serwint227 | No EPDS score | 251 | Usual care in the USA | CES-D | No differences for IG vs. CG for emergency room utilisation, % who received immunisations by 90 days of age, maternal knowledge of infant care, maternal anxiety or postpartum depression | High |
| Program for HIV, alcohol, mental health | Rotheram-Borus,226 le Roux270 | No usual-care comparison | 1144 | Usual care in South Africa | EPDS score 14 or more | PIP is a model for countries facing significant reductions in HIV funding whose families face multiple health risks225 | Low |
| Six planned health visitor visits | Christie150 | No usual-care comparison | 295 | Health visitor single visit | EPDS | Intervention had no impact on most outcomes, however, it was associated with an increased EPDS score (after adjustment: 0.16, 2.36 95% CI) at 8 weeks (before accounting for outliers) but not at 7 months (–0.62, 1.65 95% CI) | Unclear |
| Baby massage | Fujita228 | No usual-care comparison. No EPDS score | 57 | Usual care in Japan | POMS Japanese version | 3 months after delivery scores had improved more positively in depression and vigour in IG vs. CG (depression; t = –2:57; p = 0.02, vigour; t = 2:39; p = 0.02) | High |
Selective preventive intervention studies omitted from network meta-analysis
| Intervention summary | First author and reference | Reason not included | Total number of R | Comparison group(s) | Depression outcomes | Main findings | Overall risk of bias |
|---|---|---|---|---|---|---|---|
| CBT-based | Hagan159 | No EPDS score | 199 | Usual care in Australia | BDI | . . . Program did not alter the prevalence of depression in these mothers159 | Low |
| CBT-based | Silverstein161 | No EPDS score | 50 | Usual care in the USA | QIDS | Problem-solving education appears feasible and . . . promising strategy to prevent depression among mothers of preterm infants161 | Low |
| IPT-based | Phipps160 | No usual-care comparison, no EPDS score | 106 | Educational information | KID-SCID | Intervention has potential to reduce risk for postpartum depression in [Hispanic and black] primiparous adolescent mothers160 | Low |
| Psychoeducational | Tam162 | No usual-care comparison, no EPDS score | 516 | Usual care in China | CGI, GHQ, HADS | Educational counselling may have deleterious effect to women’s quality of life in those who had instrumental delivery162 | Unclear |
| Booklet on PND and social worker call | Howell190 | No usual-care comparison | 540 | Educational information | EPDS score 10 or more, PHQ-9 | Intervention reduced positive depression screens among black and Latina postpartum mothers190 | Low |
| Education on preparing for parenting | Walkup192 | No usual-care comparison, no EPDS score | 167 | Educational information | CES-D | Supports efficacy of paraprofessional-delivered Family Spirit home-visiting intervention for young American Indian mothers on maternal knowledge and infant behavior outcomes192 | Unclear |
| Booklet plus video | Logsdon202 | No EPDS score | 128 | Usual care in the USA | CES-D | No significant differences found in CES-D scores among groups at 6 weeks postpartum202 | Unclear |
| Peer mentors living with HIV | Richter,203 Rotheram-Borus269 | No usual-care comparison | 262 | Usual care in South Africa for women with HIV | EPDS score 13 or more, GHQ | Adherence to IGs was low203 | High |
| Significant difference | |||||||
| Peer support | Cupples201 | No EPDS score | 343 | Usual care in the UK | SF-36 | No benefit for infant development or maternal health at 1 year201 | Low |
| Support in labour | Wolman,204 Trotter,276 Nikodem275 | No usual-care comparison | 189 | Usual care in South Africa | EPDS mean score, HDRS, PDI | IG attained higher self-esteem scores and lower postpartum depression and anxiety ratings 6 weeks after delivery204 | Unclear |
| CenteringPregnancy Plus | Ickovics222,262 | No EPDS score | 1047 | Usual care in the USA | CES-D | ‘Bundled’ intervention has promise for improving psychosocial outcomes, especially for young pregnant women222 | Low |
Indicated preventive intervention studies omitted from network meta-analysis
| Intervention summary | First author and reference | Reason not included | Total number of R | Comparison group(s) | Depression outcomes | Main findings | Overall risk of bias |
|---|---|---|---|---|---|---|---|
| CBT-based intervention | El-Mohandes167 | No EPDS score | 1070 | Usual care in the USA | BDI | Depression at postpartum interview was 25.5% in the intervention group and 29.0% in the control group, p = 0.303167 | Low |
| No significant difference | |||||||
| CBT-based intervention | Le171 | No EPDS score | 217 | Usual care in the USA | BDI-II | A CBT intervention for low-income, high-risk Latinas reduced depressive symptoms during pregnancy but not during the postpartum period171 | Unclear |
| No significant difference | |||||||
| CBT-based intervention | McKee172 | No EPDS score | 90 | Usual care in the USA | BDI-II | The two intervention conditions were equally effective in reducing depression172 | High |
| No significant difference | |||||||
| CBT-based intervention | Rahman148 | No usual-care comparison, no EPDS score | 903 | Usual care in Pakistan | HDRS | This psychological intervention delivered by community-based primary health workers has the potential to be integrated into health systems in resource-poor settings148 | Low |
| Significant difference | |||||||
| Empowerment training | Tiwari175 | No usual-care comparison | 110 | Usual care in Hong Kong | EPDS score 10 or more | An empowerment intervention specially designed for Chinese abused pregnant women was effective in reducing IPV and improving the health status of the women175 | Low |
| Significant difference | |||||||
| IPT-based intervention | Crockett166 | No EPDS score | 36 | Usual care in the USA | DSM-IV | At 3 months postpartum, the study found no significant differences between the two conditions in degree of depressive symptoms or level of parental stress | Unclear |
| No significant difference | |||||||
| IPT-based intervention | Zlotnick178 | No EPDS score | 35 | Usual care in the USA | BDI, SCID | A four-session IPT-oriented group intervention was successful in preventing the occurrence of major depression during a postpartum period of 3 months in a group of financially disadvantaged women178 | Unclear |
| Significant difference | |||||||
| IPT-based intervention | Zlotnick179 | No EPDS score | 99 | Usual care in the USA | BDI | This study provides further evidence for the efficacy of a brief intervention to reduce the occurrence of major depressive disorder among financially disadvantaged women during a postpartum period of 3 months179 | Unclear |
| Significant difference | |||||||
| Mindfulness-based intervention | Vieten121 | No EPDS score | 34 | Usual care in the USA | CES-D, PANAS-X | Differences observed between treatment and wait-list controls at 3-month follow-up were not statistically significant121 | High |
| No significant difference | |||||||
| Promoting parent–infant interaction | Wilson177 | No usual-care comparison | 31 | Usual care in the UK | EPDS mean | The results suggest that psychoeducational interventions in pregnancy may benefit women with major psychosocial needs177 | High |
| No significant difference | |||||||
| Psychoeducational intervention | Weidner176 | No EPDS score | 238 | Usual care in Germany | HADS | The psychosomatic intervention had a significant effect on anxiety scores (p – 0.006), but not on depression scores, physical complaints and characteristics of labour and delivery176 | High |
| No significant difference | |||||||
| Booklet on PND | Heh193 | No usual-care comparison | 70 | Usual care in Taiwan | EPDS score 10 or more (Chinese version) | The mean EPDS score was 10.8 SD 4.4, in the intervention group and 12.1 SD 3.0 in the control group (p = 0.02)193 | High |
| Significant difference | |||||||
| Booklet on PND | Lara194,334 | No usual-care comparison | 377 | Usual care in Mexico | BDI-II, SCID | Available data are consistent with the possibility that the incidence of depression may have been reduced by the intervention, but differential attrition makes interpretation of the findings difficult194 | High |
| Mixed results | |||||||
| Peer support | Harris206 | No EPDS score | 65 | Usual care in the UK | SCAN PSE | The onset of perinatal major depression was 27% (8/30) for the Newpin befriender group and 54% (19/35) for the control group (x2 = 4.00, p = .045, two-tailed test)206 | Unclear |
| Significant difference | |||||||
| EPA: 1060 mg EPA plus 274 mg DHA | Mozurkewich214 | No EPDS score | 126 | Usual care in the USA | BDI, MINI | No differences between groups in BDI scores or other depression endpoints at any of the 3 time points after supplementation214 | Low |
| EPA-rich fish oil and DHA-rich fish oil supplementation did not prevent depressive symptoms during pregnancy or postpartum214 | |||||||
| No significant difference | |||||||
| Nortriptyline | Wisner215 | No EPDS score | 51 | Usual care in the USA | HDRS (HAM-D) | Of 26 subjects who took nortriptyline preventively, 6 (0.23, 95% exact confidence interval [CI] = 0.09 to 0.44) suffered recurrences. Of 25 subjects who took placebo, 6 (0.24, 95% exact CI = 0.09 to 0.45) suffered recurrence (Fisher exact p = 1.00)215 | Low |
| No significant difference | |||||||
| Sertraline | Wisner216 | No EPDS score | 25 | Usual care in the USA | HDRS, SCID | Recurrences in the 17-week preventive treatment period occurred in four of the eight women taking placebo (proportion = 0.07, 95% exact CI = 0.00–0.34) (p = 0.04, Fisher’s exact test)216 | Low |
| Significant difference | |||||||
| Acupuncture for depression | Manber229 | No usual-care comparison, no EPDS score | 61 | Acupuncture non-specific | BDI, HDRS | At 10 weeks postnatally, the mean BDI score in the 16 women in the acupuncture group was 6.9 (SD 7.7). In the 19 women in the active control it was 10.8 (SD 9.8) and in the 19 women in the massage group it was 10.2 (SD 6.6). There was no pure control | Unclear |
| Limited by small sample |
Appendix 11 Sensitivity analysis of Edinburgh Postnatal Depression Scale threshold score data using vague prior distribution for the between-study standard deviation
FIGURE 79.
EPDS threshold score for universal preventive interventions at 6 weeks postnatally: odds ratios all treatment comparisons.
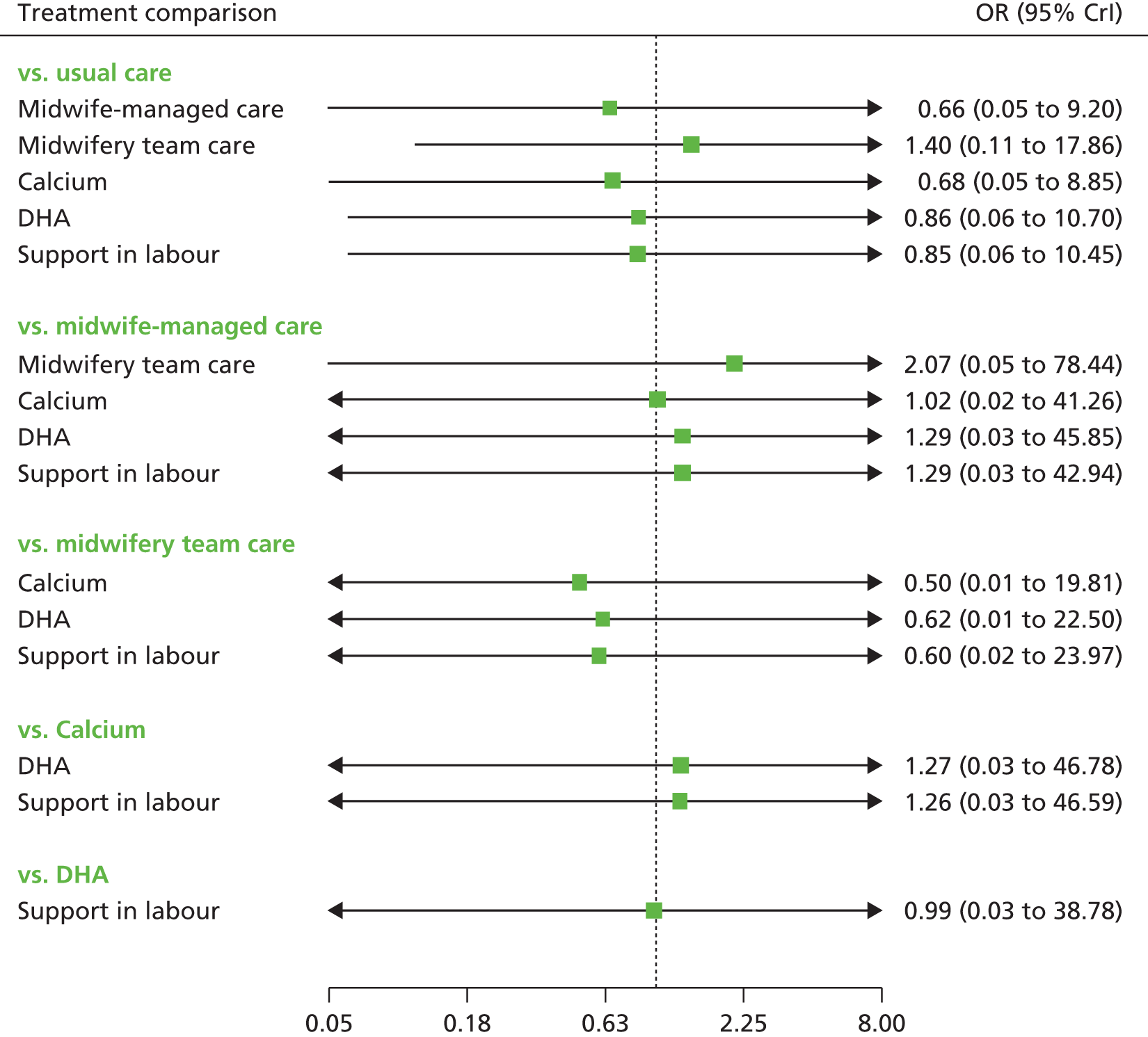
FIGURE 80.
EPDS threshold score for universal preventive interventions at 3 months postnatally: odds ratios all treatment comparisons.

FIGURE 81.
EPDS threshold score for universal preventive interventions at 6 months postnatally: odds ratios all treatment comparisons.

FIGURE 82.
EPDS threshold score for universal preventive interventions at 12 months postnatally: odds ratios all treatment comparisons.
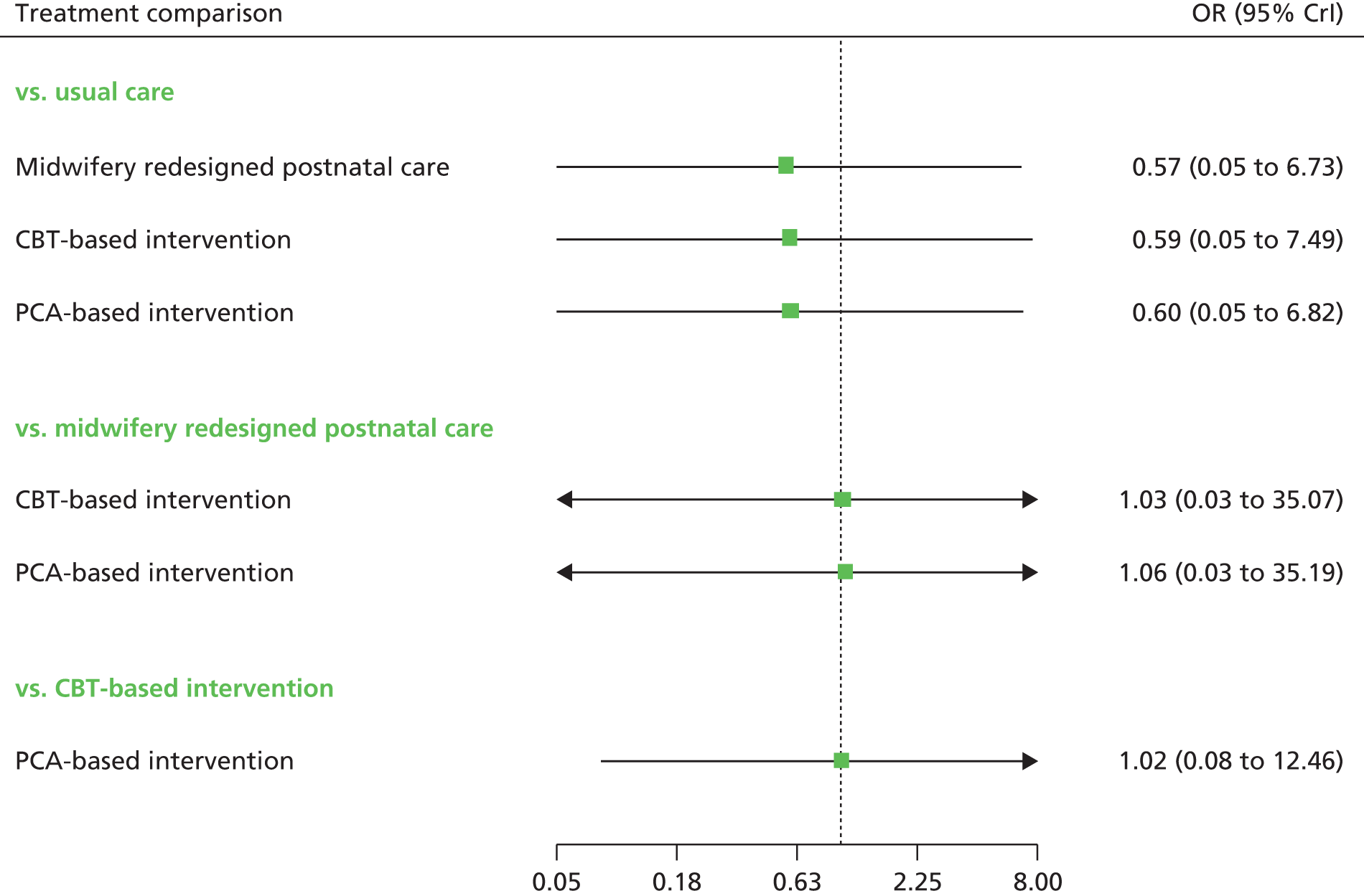
FIGURE 83.
EPDS threshold score for selective preventive interventions at 6 weeks postnatally: odds ratios all treatment comparisons.

FIGURE 84.
EPDS threshold score for selective preventive interventions at 3 months postnatally: odds ratios all treatment comparisons.

FIGURE 85.
EPDS threshold score for selective preventive interventions at 6 months postnatally: odds ratios all treatment comparisons.
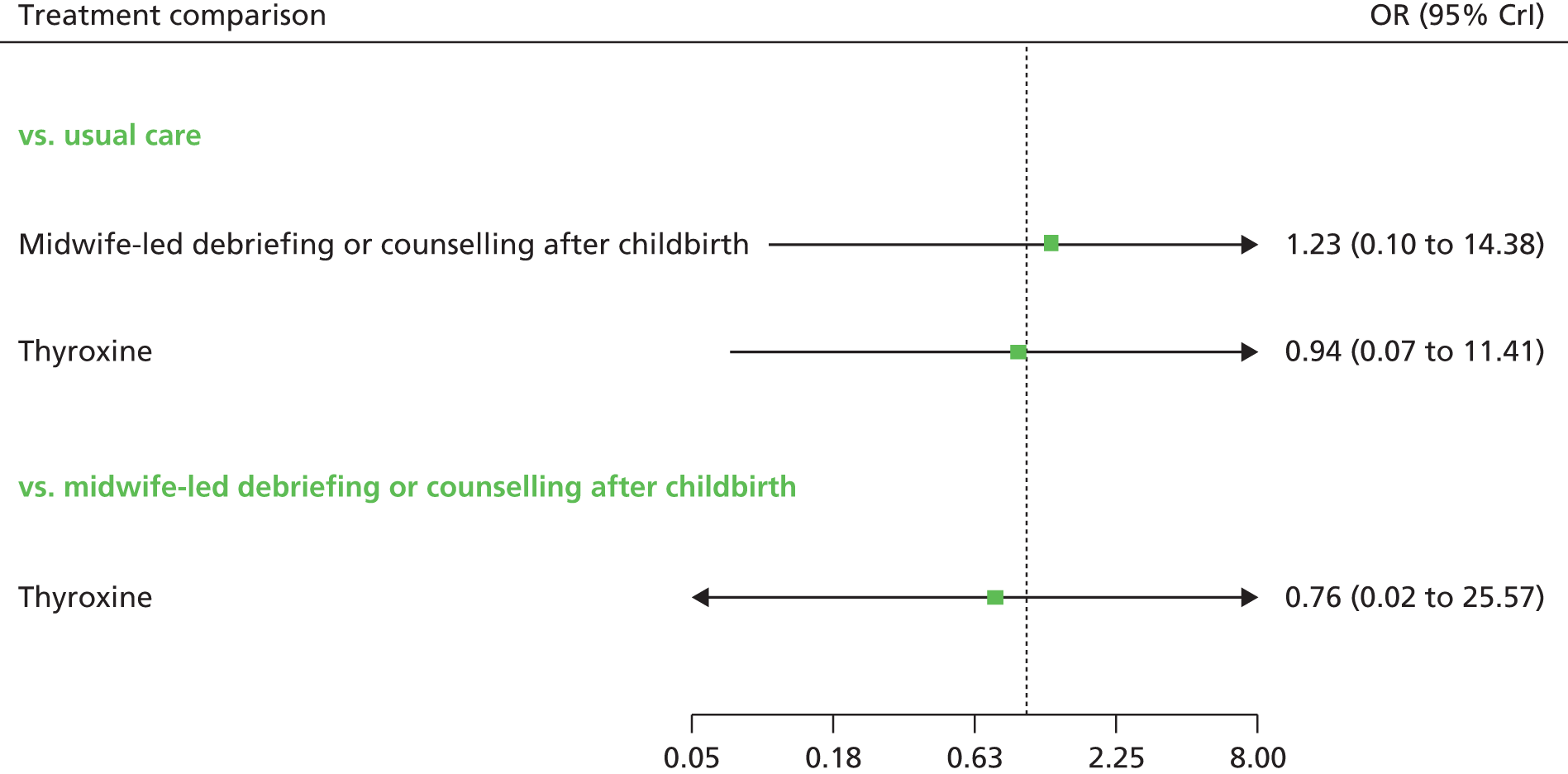
FIGURE 86.
EPDS threshold score for indicated preventive interventions at 6 weeks postnatally: odds ratios all treatment comparisons.
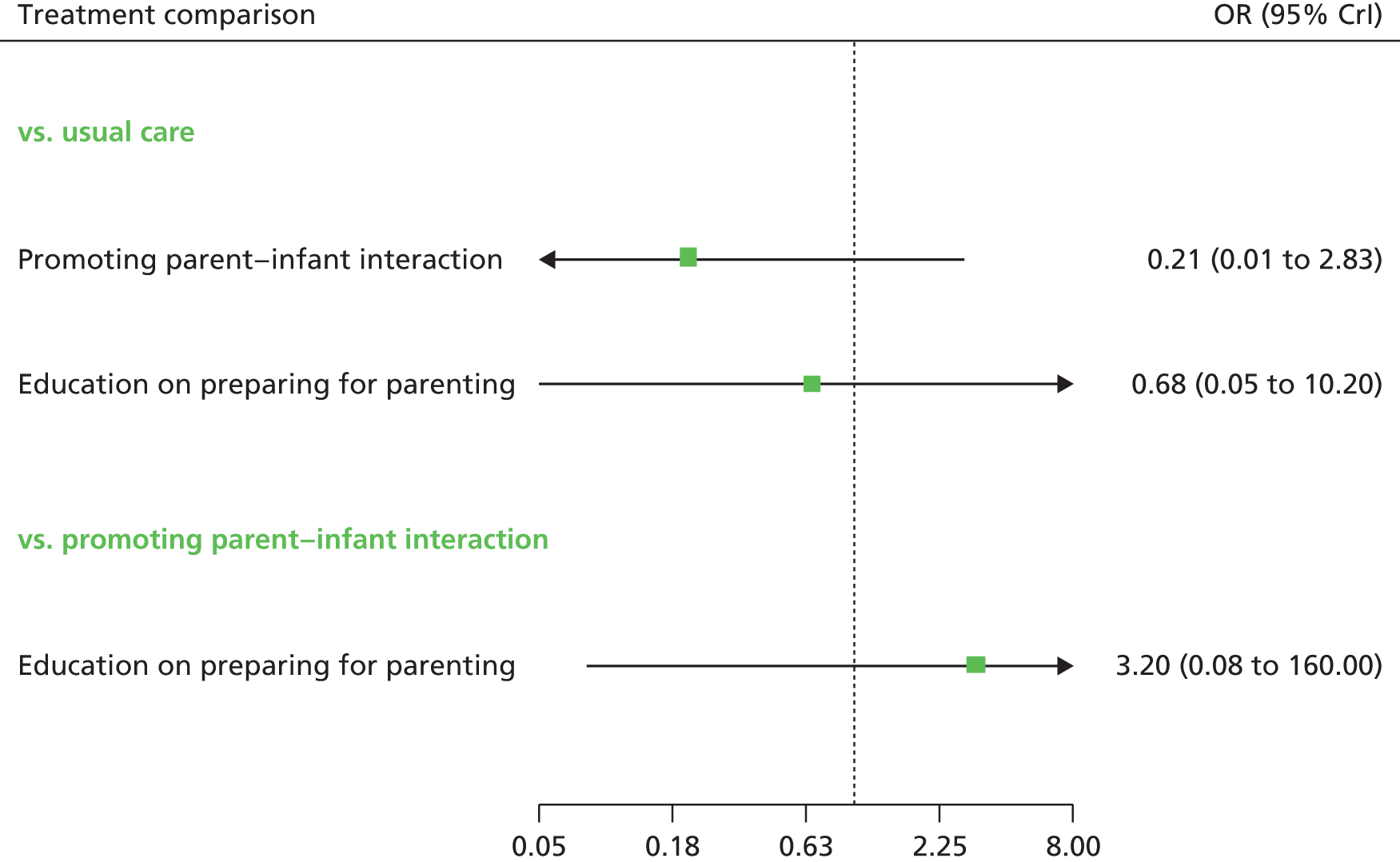
FIGURE 87.
EPDS threshold score for indicated preventive interventions at 3 months postnatally: odds ratios all treatment comparisons.
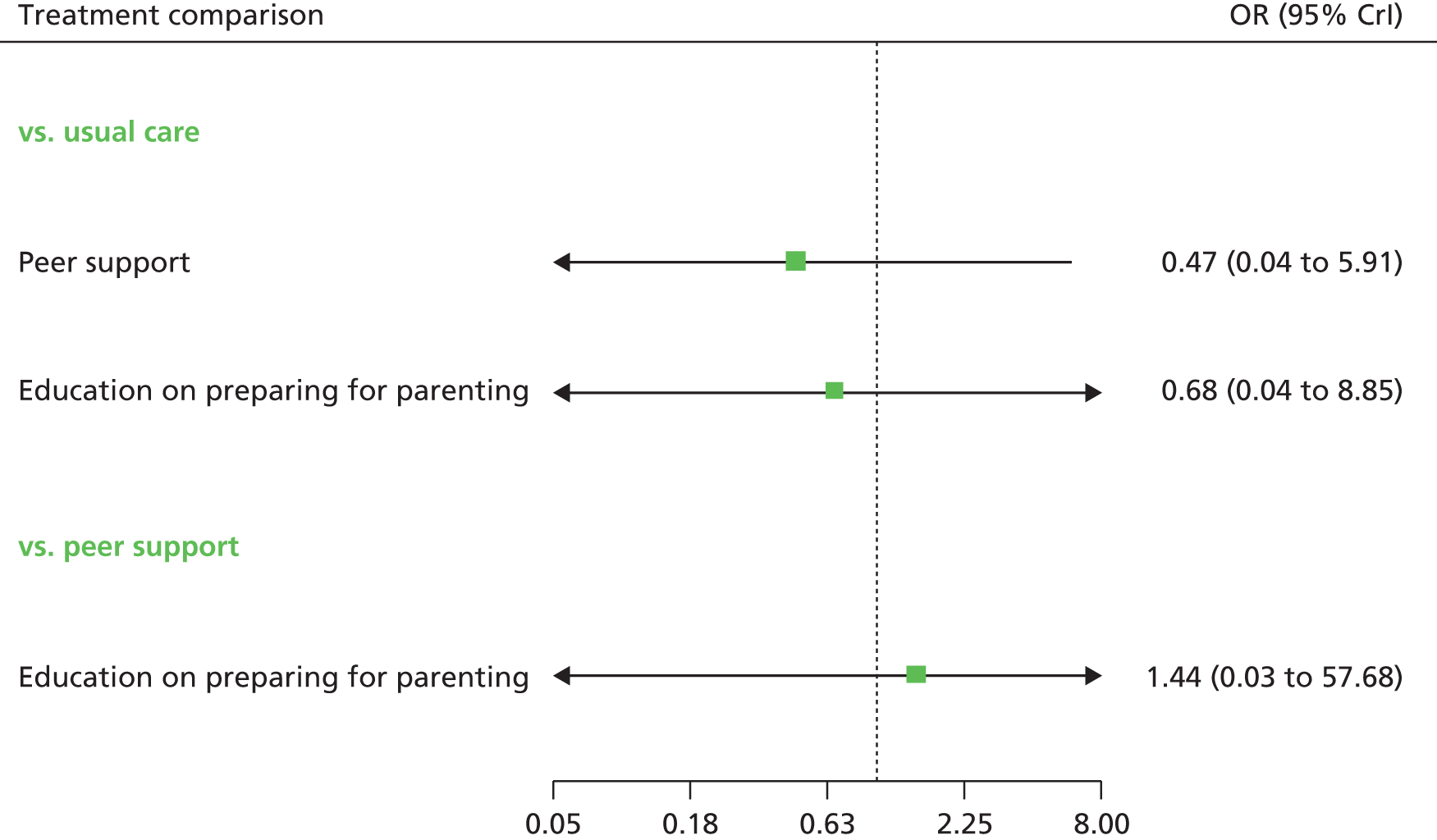
FIGURE 88.
EPDS threshold score for indicated preventive interventions at 4 months postnatally: odds ratios all treatment comparisons.

FIGURE 89.
EPDS threshold score for indicated preventive interventions at 6 months postnatally: odds ratios all treatment comparisons.
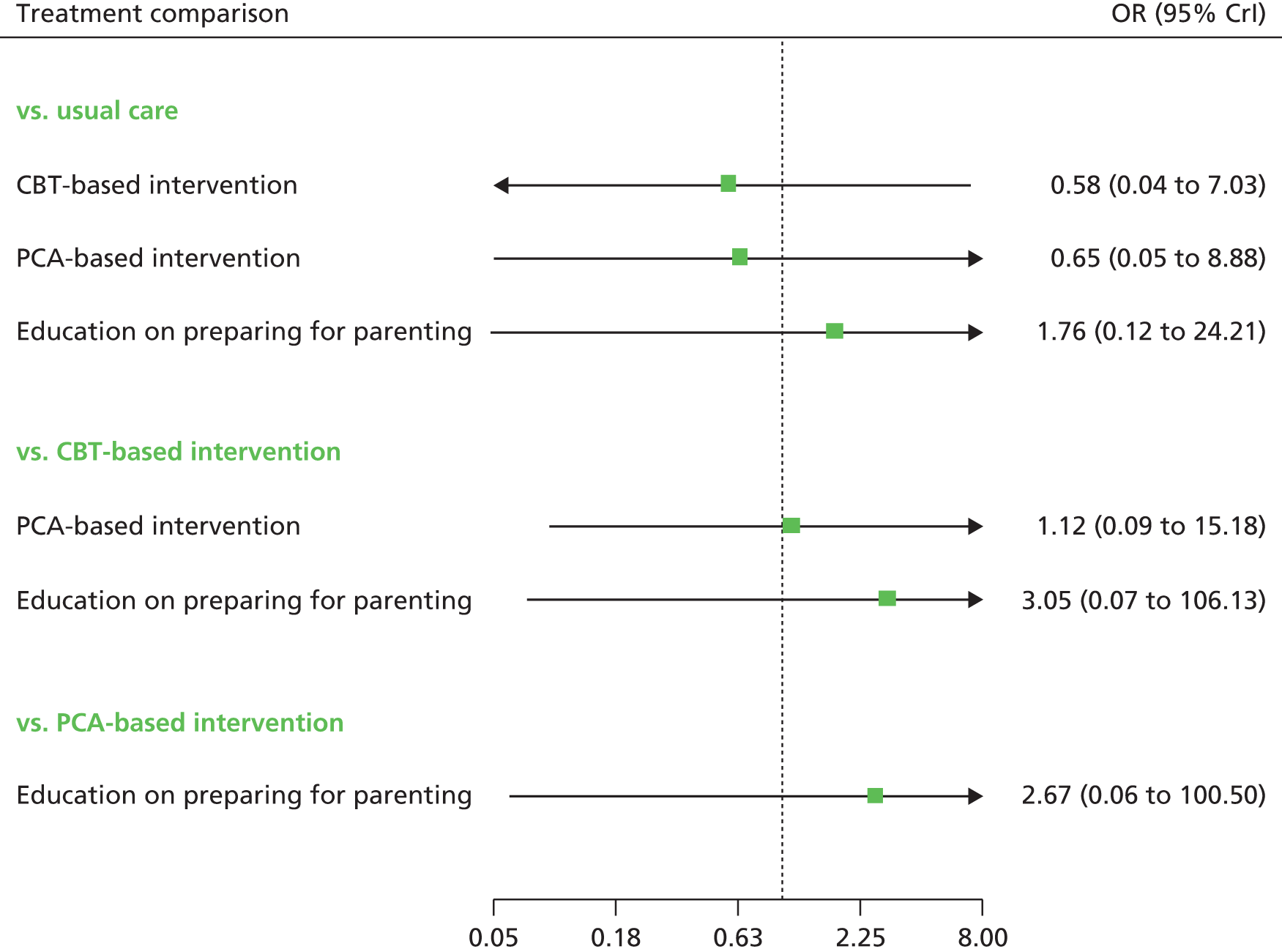
Appendix 12 Similarities and differences between group- and individual-based approaches
Preliminary synthesis and construction of a theoretical model
This formative analysis helped in looking for similarities and differences across programmes, for example, in characterising the different mechanisms by which lay support might work compared with delivery by health professionals.
FIGURE 90.
Theory of change logic model for the prevention of PND.
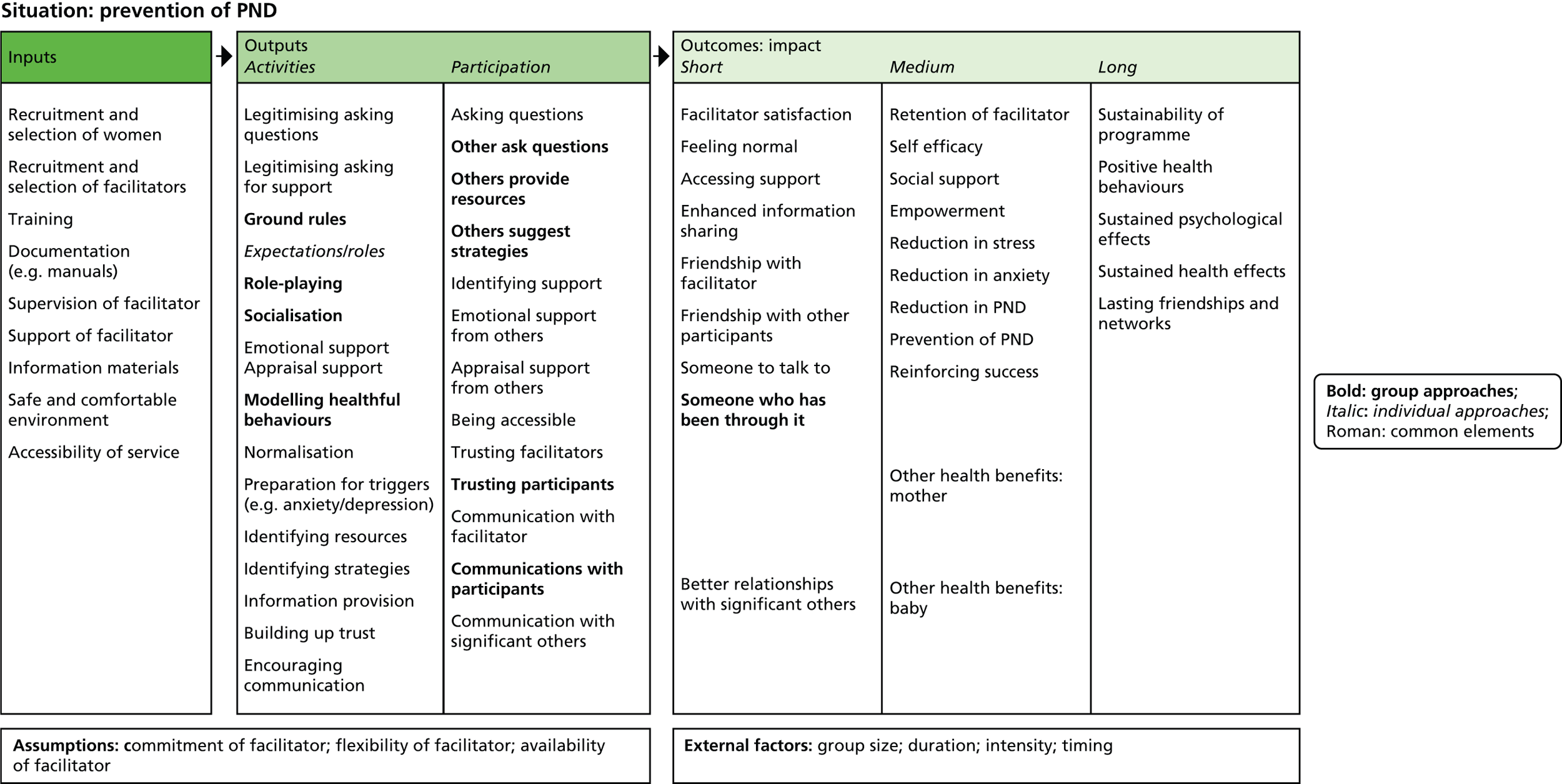
Appendix 13 Findings relating to a potential service/intervention
| Meta-theme | Subtheme(s) | Evidence source(s) (CASP). Evidence from studies with general population participants | Evidence source(s) (CASP) | Certainty in the evidence (CERQual) | Explanation of certainty in the evidence assessment |
|---|---|---|---|---|---|
| Synthesised finding – things that would have been needed to help prevent feelings of depression are . . . [retrospective] | |||||
| Support | Support of midwives was reported as important. Participants felt they needed to be in hospital314 | – | Moderate | Moderate certainty | Studies of generally high quality; finding seen across a small number of studies and in only culturally different and selective groups |
| Deprived women reported that they needed peer support and to share experiences315 | – | High | |||
| Health-care treatment | Mono-ethnic, ‘culturally sensitive’ interventions are favoured less than care and support in mixed ethnic groups311 | – | High | Moderate certainty | Studies of high to moderate quality; finding seen across several studies, across general populations and across culturally different and selective groups |
| Peer support groups315,323 and having somewhere to go (for treatment)315 | – | – | |||
| Counselling306–310 and alternative medicine, such as massage315 | – | High | |||
| The prescription of medication by the GP314 | – | Moderate | |||
| a community-based multiagency women-centred approach – two studies of culturally different women recommended a service to be a community-based multiagency women-centred approach and to address the full spectrum of need311 | – | High | |||
| More open discussion of realities of new motherhood, specifically in relation to breastfeeding323 | High | – | |||
| Practical skills and experience | Knowledge of how to breastfeed and how to bath a baby305,321 | High/moderate | – | Low certainty | Finding seen in only two general population studies of high to moderate quality |
| Barriers to help-seeking | |||||
| Negative perceptions of help seeking | Perceptions of not coping/pressure to be seen as a good mother – fear of being perceived as not able to cope315,319 and thus not being seen as a good mother315,324 | High/moderate | Moderate | Moderate certainty | Studies of high to moderate quality; finding seen across several studies, across general populations and across culturally different and selective groups |
| Stigma/fear of children being removed – women also worried about the stigma attached to help seeking303,315,325 and in some cases a fear of their children being removed if they sought help.303 Women were worried about being labelled as having a mental illness and the effect this may have306–310 | Moderate | Moderate | – | – | |
| Cultural bias towards the unacceptability of help seeking for mental illness for black Caribbean women306–310 – these women felt they were ‘not allowed to get depressed’ and that depression was not recognised in their culture306–310 | – | High | – | – | |
| Barriers to gaining support | Woman’s withdrawal from relationship with their partner and inability to share their feelings with their partner as a result of emotional distress.324,325 Participants felt unable to access partner support | High/moderate | – | Low certainty | Studies of high to moderate quality; finding seen in only a few studies, across general populations and across culturally different groups |
| Cultural beliefs – respondents were advised to perform certain rituals, (e.g. wearing particular items of jewellery or clothing), to ensure protection from harm during pregnancy and the postnatal period.304 A study304 reported a belief in the existence of Jinn (evil spirits). Authors commented that ailments given to women, as a result of being possessed by the Jinn, were indistinguishable from symptoms of PND. Cultural beliefs may create a barrier to seeking help from mainstream routes | – | Moderate | – | – | |
| Barriers to approaching health-care professionals | Not understanding the health visitor’s role (to address mothers’ mental health)/not understanding the GP’s role – respondents reported not feeling that the mothers’ mental health was the role of the health visitor or the GP, and therefore they did not address any symptoms of emotional distress in their interactions with these health professionals304,311,314 | – | Moderate/high | Moderate certainty | Studies of high to moderate quality; finding seen across several studies, across general populations and across culturally different and selective groups |
| Health visitor not appropriate person to discuss with/poor relationship with GP/did not want to discuss with GP – in one study women reported that they did not consider the health visitor or GP an appropriate person with whom to discuss mental health issues.314 Some women felt they had a poor relationship with the GP314 | – | Moderate | |||
| Health professionals’ lack of awareness/uncaring hospital midwives/health-care providers perceived as too busy – women felt that they were a burden. Health professionals, particularly hospital midwives, were considered to have a lack of awareness around emotional distress, they were perceived as uncaring, and too busy, making women feel like they were a burden306–311,315 | High | Moderate | |||
| Respondents reported not knowing how to get help305 | Moderate | – | |||
| Health professional focus on the baby – health visitor focus on baby was a barrier to seeking help for emotional difficulties.315,321 Women reported care givers were concerned only with the well-being of the fetus and never asked about them315 | High | Moderate | – | – | |
| Practical barriers to seeking health care | Long waiting times | – | High | Low certainty | Studies of high to moderate quality; finding seen in only two studies across culturally different and selective groups |
| Lack of black therapists for black women | |||||
| Lack of child-care facilities306–310 | |||||
| Inappropriate (male) interpreter – for some minority group women, a language barrier presented difficulties.314,318 Women reported that they were unable to understand the midwives or gain access to the information they needed | – | Moderate | |||
Appendix 14 CLUSTERs receiving detailed examination
Sibling papers and kinship studies for CLUSTERs examined in detail
| Sibling papers | Kinship studies | Reviews and syntheses |
|---|---|---|
| Definition: papers conducted by same authorial team or describing same phenomenon of interest | Definition: studies that relate to original phenomenon of interest across one or two variables, e.g. use of theory, setting of intervention, main components et cetera | Secondary studies sharing topic or drawing on primary study data from index paper |
| CenteringPregnancy | ||
|
||
| Health Visitor PoNDER Training | ||
| – | – | |
| Home-based intervention | ||
| – | – | |
| IPT standard antenatal care plus the ROSE programme | ||
| – | – | |
| IPT plus telephone follow-up | ||
| IPT– brief | ||
| – |
|
|
| Midwife-led brief counselling | ||
|
– | |
| Midwife-managed care | ||
| – | – | |
| The Newpin Project | ||
| – | – | |
| Midwifery redesigned postnatal care | ||
| – | ||
| Telephone peer support | ||
| – | ||
| Thinking Healthy Programme | ||
| – |
|
|
| Two-step behavioural educational intervention | ||
| – | – | |
Appendix 15 Examples of ‘if–then’ propositions used to refine ‘best fit’ analytic framework
Illustration of ‘if–then’ statements to refine ‘best fit’ analytic framework
| Category number | If . . . | Then | Source reference |
|---|---|---|---|
| Population | First-time mothers attend group care | First-time mothers receive helpful information especially to help prepare for labour | McNeil et al.285 |
| First-time mothers attend group care | First-time mothers know what to expect | McNeil et al.285 | |
| Facilitation | Women feel group leaders extend themselves above and beyond the usual norms of care to help them navigate through complex, even daunting, health systems | Women perceive the programme as successful | Novick et al.293 |
| Providers ensure a favourable group setting and atmosphere | Women realise it is a safe place to ask questions and share | McNeil et al.285 | |
| Group size | Group size falls within range of 8 to 12 women | Group size is efficient for system and effective to promote the process | Rising44 |
| Group size is kept small | Women enjoy the group sessions | Dennis301 | |
| Components | Women gain exposure to different pregnancy experiences and advice derived from diverse perspectives | Women value the group sessions | Novick et al.293 |
| Group leaders spend extended time for discussion in a facilitative format | Group leaders gain a different perspective on women’s lives than they would get from conducting individual visits | Novick et al.293 | |
| Frequency | Group meetings take place weekly | Women look forward to the opportunity to meet with those of like mind | Hanley and Long390 |
| Home visits are more intensive (e.g. longer and more frequent) | Women find intervention more beneficial | Morrell287 | |
| Duration | Women attend 2-hour group appointments (compared with 15-minute individual sessions) | Women have more time to learn about pregnancy-related topics and become ‘active participants in their own health care’ | Novick et al.293 |
| Women are offered inflexibly scheduled 2-hour group appointments | Women do not attend because of limited control over transportation or their daily schedule | Novick et al.293 | |
| Follow-up | Women are offered arrangements for individualised follow-up | Women have opportunity to discuss medical or personal issues requiring more time or privacy | Novick468 |
| Peer support | |||
| Appraisal support | Women are provided with information and appraisal from their peers | Women assimilate knowledge more effectively | Dennis299 |
| Informational support | Women receive informational support about PND within 6 weeks after birth | Women experience PND that is less severe | Fu and Heh469 |
| Peer supporters are recruited for extroversion and communication characteristics | Women perceive that they talk too much | Dennis299 | |
| Emotional support | Women discover that they are not alone in their experiences | Women are ‘delighted and often surprised’ | Kennedy et al.283 |
| Women raise concerns or share frightening stories | Women’s anxieties are heightened, not decreased | Novick et al.293 | |
| Instrumental support | No data | No data | No data |
| Team composition | No data | No data | No data |
| Other contacts | Antenatal support groups are offered separate from antenatal classes | Women do not attend | Stamp et al.195 |
| Women’s characteristics | No data | No data | No data |
| Built environment | Women have comfortable chairs, food and pleasant décor | Women gain a sense of attending a friendly social gathering | Novick et al.293 |
| Dimensions of the group space permit pregnant women to move around comfortably, and an area rug is provided for floor exercises | Women enjoy relaxed, pleasant atmosphere that promotes interaction and development of relationships among women | Novick et al.293 | |
| Social support | Women only receive help if they have to ask for it | Women suffer PND | Brugha et al.152 |
| Women have someone to talk openly with who has shared a similar problem | Women do not suffer PND | Brugha et al.152 | |
| Women lack an intimate confidant or friend to converse with | Women suffer PND | Brugha et al.152 | |
| Women feel socially isolated | Women suffer PND | Mills et al.470 | |
| Partner support | |||
| Appraisal support | No data | No data | No data |
| Informational support | No data | No data | No data |
| Emotional support | Women do not receive support from their partners | Women suffer PND | Mason et al.471 |
| Family support | Women have little or no family support | Women perceive themselves as being under stress | Novick et al.293 |
| Instrumental support | Women have someone to offer practical help | Women are able to get more rest | Ugarriza et al.320 |
| Women feel able to ask for help | Others are likely to provide practical support | Knaak;472 Ugarizza et al.320 | |
| Women ask for help | Others perceive that they are not able to handle things on their own | Knaak472 | |
| Support from health professional | Women experience continuity of care from the health professional | Women develop a relationship with their care provider and trust them with sensitive issues | Novick et al.293 |
| Appraisal support | No data | No data | No data |
| Informational support | Physicians and educators provide information that ‘you can’t get from books’ | Women feel supported | McNeil et al.285 |
| Emotional support | No data | No data | No data |
| Instrumental support | Women are given practical demonstrations of how to bath the baby, change a nappy and put the baby to sleep | Women experience reduction in their perceived stressors | Razurel et al.316 |
| Adherence | Women are members of groups with short duration, high turnover or irregular attendance | Groups are less stable and cohesive and thus less therapeutic | Novick et al.293 |
| Physical signs and symptoms (was biophysical markers) | Women experience high expectations on what they need to purchase for the imminent baby | Women may feel overwhelmed to the point of tears | Migl286 |
| Women learn practical strategies during the group intervention | These strategies prevent panic attacks, combat physical symptoms of stress, and could be combined with existing strategies | Carolan et al.;278,279 Migl286 | |
| Women perceive that depressive symptoms are associated with stigma | Women complain about physical symptoms such as headaches and tiredness | Rodrigues et al.325 | |
| Women hear other women describing and comparing symptoms | Women feel reassured that their own experience is normal | Teate et al.432 | |
| Self-efficacy | |||
| Self-efficacy | Women experience discomfort at the level of responsibility required for self-care | Women do not engage with group care programme | McNeil et al.285 |
| Women experience a loss of control as a result of the feelings engendered by pregnancy | Women feel powerless over their physical responses, emotions and interactions | Mason et al.473 | |
| Women feel able to develop a conscious resistance to dominant cultural norms about good mothering | Women develop ‘realistic’ core beliefs and expectations | Knaak472 | |
| Women’s participation | Women feel that that selection for the intervention is based upon being at increased vulnerability to PND | Women do not participate in programme | Wheatley254 |
| Women find it difficult to access group interventions because of transport constraints | Women do not participate in programme | Wheatley254 | |
| Prevention of PND (was long-term symptom management) | Women learn practical strategies at the group intervention | Women find it difficult to allocate time to use the practical strategies learned | Migl286 |
| Women learn practical strategies at the group intervention | Women report that they forget to implement the strategies | Migl286 | |
| Women learn practical strategies at the group intervention | Women report that they do not use the strategies because of perceptions of stigma | Migl286 | |
| Psychological status (was functional status) | Women do not feel that the mental health of the mother is the role of the health visitor or the GP | Women do not discuss their symptoms of emotional distress in their interactions with these health professionals | Parvin et al.314 |
| Black Caribbean women have a deep-seated fear of mental health services | Women are reluctant to seek help | Edge et al.308 | |
| Quality of life | No data | No data | No data |
| Unplanned utilisation of health services (was emergency department visits, rehospitalisations and unplanned office visits) | No data | No data | No data |
| Suicide ideation (was mortality) | Women isolate themselves from friends, family and providers | Women entertain thoughts of suicide | Beck381 |
| Women put their child’s needs above their own and want to protect their infant | Women resist temptation to attempt suicide | Beck381 | |
| Costs | Classes are run by suitably qualified and experienced staff | Costs may be prohibitive | Saligheh474 |
| Confidentiality | Examinations are conducted in a manner that affords women privacy | Women are more likely to feel comfortable about participation | Novick et al.293 |
| Examination space is located away from other activities, using visual barriers (e.g. screens or large plants), and playing recorded music to create sound privacy | Women feel less anxious about participation | Novick et al.293 | |
| Participation (non-) | First sessions get off to a slow start with reluctance to talk | Women feel sessions are waste of time | McNeil et al.285 |
| Missed appointments | Women do not attend regularly | Other women express disapproval and perceive a lack of commitment | Novick et al.293 |
Appendix 16 TIDieR checklists for focal interventions
TIDier checklist for Health Visitor PoNDER training
| Psychological | |
|---|---|
| Brief name | |
| 1 | Health Visitor PoNDER Training61,151 |
| Why | |
| 2 | Person-centred counselling is based on idea that opportunities to explore difficulties with another, who listens non-judgementally and reflects empathically, allows a person to feel validated as a person and facilitates their abilities to manage their distress and find their own solutions. Cognitive Behavioural Counselling assumes that events, thoughts and feelings are linked in a predictable way and that, by understanding these patterns, particularly where patterns of thinking lead to distress, there is the opportunity to make active change and test out new ways of thinking and behaving |
| What | |
| 3 | Materials: manualised HV training addressed therapy allegiance and prepared HVs to provide appropriate, pragmatic, distinctive, derivative approach, delivering critical elements from CBT or person-centred therapy, not psychotherapy |
| 4 | Procedures: both training approaches sought to enable HVs to acquire further generic skills in developing helpful relationships, for example, positive regard and empathy. CBT-based intervention training emphasised normalising rationale and identification of unhelpful patterns of behaviours, perceptions or thoughts in the woman’s life to help woman to change these herself347 Person-centred training used three principles of the actualising tendency, a non-directive attitude and the necessary and sufficient conditions of change.348 Details of the HV training are provided in the section on training of the intervention group HVs |
| Who provided | |
| 5 | Two main psychotherapist trainers were specialists with experience in practice as trainers and supervisors. They prepared a manual for each HV and a separate trainer’s manual. Manuals included theoretical basis for relevant psychological approach and training plan so that, if necessary, training could be replicated |
| How | |
| 6 | Face-to-face training |
| Where | |
| 7 | No details |
| When and how much | |
| 8 | No details |
| Tailoring | |
| 9 | No details |
| Modifications | |
| 10 | No details |
| How well | |
| 11 | Planned: to enhance rigour and effectiveness of training for both psychotherapeutic approaches, to maximise comparability of programmes and to ensure that trial was a credible and fair test, a training reference group was established before the trial. This comprised experienced academically based psychotherapy trainers from England and Scotland, including representatives of both CBAs and PCAs |
| 12 | Actual: no details |
| Psychological | |
|---|---|
| Brief name | |
| 1 | IPT-brief |
| Why | |
| 2 | Multicomponent model of care derived from IPT.440 It retains essential theory, targets and techniques of IPT by helping women resolve one of four interpersonal problem areas (role transition, role dispute, grief and interpersonal deficits) related to the onset or maintenance of a depressive episode. It differs from IPT in several ways: e.g., to reduce treatment burden and activate change in (participant), format is restructured into eight rather than 16 sessions, a focus on the long-term problem area of interpersonal deficits is avoided, and between-session behavioural activation strategies with interpersonal focus are encouraged |
| What | |
| 3 | Materials: participants given written educational materials about depression |
| 4 | Procedures: participants informed of their diagnoses, given written educational materials and referred for treatment. Interviewer approaches (participant) in culturally sensitive manner consistent with principles of ethnographic interviewing: the interviewer adopts a one-down position as a learner; tries to understand cultural perspectives and values of woman without bias; inquires about the woman’s view of depression, health-related beliefs and coping practices (e.g. the importance of spirituality or familismo in her life); and asks what woman would like in a therapist, including the importance of race-ethnicity |
| Who provided | |
| 5 | One doctoral-level clinician and one master-level clinician, both of whom had supervised training and experience in enhanced IPT-brief, served as therapists, followed detailed treatment manuals and received weekly supervision by an expert |
| How | |
| 6 | Delivered face to face, when participants could not attend treatment, session conducted on phone to maintain continuity |
| Where | |
| 7 | Engagement and IPT-brief sessions delivered in an office in the large obstetrics and gynaecology clinic to make treatment more accessible and less stigmatising. Therapist’s office displayed culturally relevant pictures of racially and ethnically diverse infants |
| When and how much | |
| 8 | Consists of engagement session, followed by eight acute IPT-brief sessions before the birth and maintenance IPT up to 6 months postpartum.475 Engagement session, described elsewhere,439,476 is based on principles of motivational interviewing and ethnographic interviewing and is designed to promote engagement by building trust and addressing the practical, psychological and cultural barriers to care experienced by individuals who are socioeconomically disadvantaged. Biweekly or monthly maintenance IPT sessions help participants deal effectively with social and interpersonal stressors associated with remission.475 As goal of maintenance is to maintain recovery, the woman is encouraged to be watchful for the appearance of early somatic, affective or cognitive symptoms related to prior depressive episodes and to practice skills learned in IPT-brief to prevent relapse. Maintenance IPT differs from IPT-brief in that a woman can focus on more than one interpersonal problem area while in remission |
| Tailoring | |
| 9 | During engagement, interviewer elicits each (participant)’s unique barriers to care and engages in collaborative problem-solving to ameliorate each barrier, for example if (participant) doubts relevance of treatment (e.g. specifically whether enhanced IPT-brief could reduce depression triggered by losing her job) – interviewer would inform her that IPT-brief can assist her in finding a new job or job training, as well as help her manage the interpersonal difficulties resulting from the job loss |
| Modifications | |
| 10 | Augmented with modifications to make it culturally relevant to socioeconomically disadvantaged women.440 Enhanced IPT-brief reflected seven of eight components from culturally centred framework of Bernal and Saez-Santiago477: persons, metaphors, concepts, content, goals, methods and contexts (e.g. addressed component of persons by employing therapists trained in cultural competence with considerable experience working with persons of racial-ethnic minority groups who were living in poverty).477 Components of metaphors and stories from the participants’ cultural background were used to reinforce treatment goals. To address concepts, therapists provided education about depression congruent with (participant)’s culture and used the word ‘stressed’ instead of the word ‘depressed’, if (participant) desired, to minimise perceived stigma of depression. Content addressed by exploring which coping mechanisms and cultural resources, such as spirituality or familismo, had helped participants through adversity in the past and by building on these resources during treatment. Therapists helped clients develop treatment goals personally and culturally relevant to them. Methods addressed by intensive outreach and shortening treatment to reduce (participant) burden. Contexts addressed by pragmatic additions, such as free bus passes, child care and the facilitation of access to needed social services (i.e. food, job training, housing and free baby supplies) |
| How well | |
| 11 | Planned: no details reported |
| 12 | Actual: engagement and IPT-brief sessions were audiotaped, and 77% were reviewed for fidelity to the model |
TIDieR checklist for Thinking Healthy Programme
| Psychological interventions | |
|---|---|
| Brief name | |
| 1 | Thinking Healthy Programme148,463,465 |
| Why | |
| 2 | Intervention: CBT-based intervention especially for developing countries such as Pakistan. Intervention targets mothers who have many psychosocial stresses and may be depressed. However, it can be used as a motivation tool for all mothers living in socioeconomically deprived areas with low literacy rates. It focuses on health of both mother and baby and encourages participation of the whole family. Approach used is simple and pictorial but retains the essential characteristics of CBT |
| What | |
| 3 | Materials: training manual in English and/or Urdu.478 Activity workbooks: Each of five modules had specially designed pictorial activity workbook used by trainer to conduct a session with the mother. Each mother had her own activity workbook where activities carried out in each session were noted. Calendar consists of pictorial and verbal key messages of each session, and serves as a visual cue for whole family to follow programme between sessions. In addition, calendar has monitoring tools to help the mother chart her own progress, and that of infant, throughout the programme |
| 4 | Procedures: Thinking Healthy has five modules covering period from third pregnancy trimester to first year of infant’s life: preparing for the baby, the baby’s arrival and early, mid and late infancy. Each module contains sessions on the mother’s health, her relationship with her baby and the relationships with people around her |
| Who provided | |
| 5 | Designed for delivery by supervised female health workers, following brief 2-day training, strengthened by experiential learning and monthly half-day facilitated group supervision |
| How | |
| 6 | Face-to-face delivery to individual mothers |
| Where | |
| 7 | Delivered in home visits |
| When and how much | |
| 8 | Sixteen-session programme targeted at women with depression and their families, beginning around 30 weeks’ gestation and continuing to 10 months postpartum |
| Tailoring | |
| 9 | No details although has been adapted to Vietnam |
| Modifications | |
| 10 | No details |
| How well | |
| 11 | Planned: no details |
| 12 | Actual: no details |
TIDieR checklist for home-based intervention
| Psychological interventions | |
|---|---|
| Brief name | |
| 1 | Home-based intervention164,251,252 |
| Why | |
| 2 | The focus of the programme was to (1) establish relationship of trust with infant’s family; (2) enhance parenting esteem and confidence through reinforcement of success; (3) provide anticipatory guidance for normal child development; (4) promote preventive child care; and (5) facilitate access to appropriate community services |
| What | |
| 3 | Materials: no details given |
| 4 | Procedures: structured programme of child health nurse visits. Weekly case conference |
| Who provided | |
| 5 | Child health-care nurses; social worker and community paediatrician (for case conferences only) |
| How | |
| 6 | Face to face provided to individuals |
| Where | |
| 7 | In woman’s home |
| When and how much | |
| 8 | Weekly for first 6 weeks, fortnightly until 3 months, then monthly until 6 months postpartum |
| Tailoring | |
| 9 | No details |
| Modifications | |
| 10 | No details |
| How well | |
| 11 | Planned: no details |
| 12 | Actual: no details |
TIDieR checklist for IPT standard antenatal care plus the ROSE programme
| Psychological interventions | |
|---|---|
| Brief name | |
| 1 | IPT standard antenatal care plus the ROSE programme179 |
| Why | |
| 2 | Intervention based on IPT, treatment for depression targeting factors (e.g. poor social support, role transition and life stressors) that may play a crucial role in onset of PND. ROSE programme designed to help mothers-to-be in an ethnically diverse population to improve their close interpersonal relationships and change their expectations about them, build and use their social support networks and master their role transition to motherhood. The emphasis was on social relationships, especially relevant for low-income women who have recently delivered; research suggests that social support can limit the negative effects of chronic stress479 and that social support is inversely associated with perinatal symptoms of depression480 |
| What | |
| 3 | Materials: handouts based on the material presented in each session were given as well as session-related homework assignments. Therapists were nurses who had received intensive training and supervision in delivery of the intervention |
| 4 | Procedures: the intervention, Survival Skills for New Moms, involved four sessions, (1) rationale for the programme and psychoeducation on ‘baby blues’ and postpartum depression; (2) identifying role transitions, changes associated with role transitions and goals for successfully managing role transitions, with emphasis on transition to motherhood; (3) setting goals, developing supports and identifying potential interpersonal conflicts, especially once the baby was born; and (4) skills for resolving interpersonal conflicts and review of main themes of intervention.178 Booster session aims to reinforce skills learned in the group sessions and to address current or expected mood changes associated with interpersonal difficulties on arrival of the newborn infant: ROSE programme |
| Who provided | |
| 5 | Nurses who had received ‘intensive training and supervision’ |
| How | |
| 6 | Face to face, delivered to group |
| Where | |
| 7 | Not specified |
| When and how much | |
| 8 | Four 60-minute group sessions (3–5 women/group) over 4-week period and 50-minute individual booster session after delivery |
| Tailoring | |
| 9 | Not specified |
| Modifications | |
| 10 | Not specified |
| How well | |
| 11 | Planned: no details |
| 12 | Actual: no details |
TIDieR checklist for IPT plus telephone follow-up
| Psychological interventions | |
|---|---|
| Brief name | |
| 1 | IPT plus telephone follow-up154,327 |
| Why | |
| 2 | IPT specifically targets interpersonal relationships and is designed to assist clients in modifying either their relationships or their expectations about those relationships. IPT could help new mothers in three areas:
|
| What | |
| 3 | Materials: written material for programme provided to participants in each session |
| 4 | Procedures: intervention targeted specific concerns and interpersonal problem areas (role transitions and interpersonal conflicts) experienced by women during the postpartum period: Two 2-hour group sessions and one telephone follow-up in postpartum period |
| Each programme consisted of no more than 10 participants. Specific IPT techniques, such as information giving, clarification, communication analysis, role-playing and brainstorming, were applied throughout the programme. During session, participants are encouraged to express emotions attached to each of their new roles in motherhood and to explore any ambivalent feelings. Through role-play and discussion, participants could develop a more balanced view of each role and to modify their expectations and restructure their priorities. Participants were encouraged to share and role-play their experiences. Group could learn from analysing ways of communication through the role-play. Brainstorming session could enable participants to consider different ways to cope with difficulties that they would encounter after delivery | |
| Telephone follow-up provided within 2 weeks after delivery. Aims of follow-up were to reinforce skills learned in sessions to deal with any current or expected mood changes or interpersonal issues during the postpartum period. A brief outline of IPT-oriented childbirth psychoeducation programme is provided154 | |
| Who provided | |
| 5 | Group sessions run by midwife educator, who had received intensive training and supervision in delivery of IPT intervention. Telephone follow-up provided by same midwife educator |
| How | |
| 6 | Two group sessions, telephone follow-up provided individually |
| Where | |
| 7 | Group sessions arranged to follow routine childbirth education sessions to encourage attendance |
| When and how much | |
| 8 | Two group sessions and telephone follow-up within 2 weeks of birth |
| Tailoring | |
| 9 | No details |
| Modifications | |
| 10 | No details |
| How well | |
| 11 | Planned: five experts in postpartum depression and childbirth education confirmed the validity of the intervention |
| 12 | Actual: no details |
TIDieR checklist for two-step behavioural educational intervention
| Education | |
|---|---|
| Brief name | |
| 1 | Two-step behavioural educational intervention190,337,388 |
| Why | |
| 2 | Based on prior research, suggesting that situational factors (i.e. postpartum physical symptoms, overload from daily demands and poor social support) play a major role in generation of depressive symptoms, the team created a behavioural educational intervention aimed at reducing frequency of depressive symptoms in postpartum mothers by preparing women about specific situational triggers of depressive symptoms, bolstering their personal and social resources, suggesting specific actions to enhance self-management skills and buffer postpartum demands. Content of intervention based on prior studies, focus groups with postpartum mothers, obstetricians, psychiatrists, social workers and community advisory board |
| What | |
| 3 | Materials: pamphlet represented each potential trigger of depressive symptoms as a ‘normal’ aspect of the postpartum experience, and provided specific suggestions for management (e.g. prevalence of moderate or heavy vaginal bleeding immediately postpartum was depicted by 8 of 10 female silhouettes coloured red; whereas only 1 of the 10 silhouettes was red 3 months post delivery). Simple ‘to do’ statements (rest; use pads) were listed between the two rows of figures. Postpartum and 3-month rates and intermediate ‘to do’ lists also were provided. A separate page was dedicated to social support and ‘helpful organisations’. A partner summary sheet spelled out the typical pattern of experience for mothers postpartum, that is to ‘normalise’ the feelings and behaviours experienced and enacted by most mothers postpartum and stress the importance of social support for the woman. Content, pictures, wording and length were revised after input from two focus groups and a community advisory board. Materials were translated to Spanish and back, and were translated for accuracy and consistency of meaning |
| 4 | Procedures: 15-minute, in-hospital review of an education pamphlet and partner summary sheet by the mother with social worker. Social worker reviewed the education pamphlet and partner summary sheet with the woman during postpartum hospital stay and answered questions. Two-week post-delivery call when social worker assessed woman’s symptoms, skills in symptom management and other needs. ‘To do’ lists to help alleviate symptoms were reviewed as needed and woman and social worker created action plans to address current needs including accessing community resources |
| Who provided | |
| 5 | 1 and 2: master’s-trained bilingual social worker |
| How | |
| 6 | 1: face-to-face individual interaction. 2: individual telephone call |
| Where | |
| 7 | 1: in hospital. 2: in woman’s home |
| When and how much | |
| 8 | 1: 15-minute session. 2: telephone call – duration unspecified |
| Tailoring | |
| 9 | In the telephone call the social worker assessed the woman’s symptoms, skills in symptom management and other needs |
| Modifications | |
| 10 | Not described |
| How well | |
| 11 | Planned: fidelity of intervention maintained by repeated training and review of scripts for both in person in-hospital and telephone components of intervention |
| 12 | Actual: approximately 5% of in-hospital sessions and 2-week telephone needs assessments were observed by a physician or project manager on the team |
TIDieR checklist for telephone peer support
| Social support | |
|---|---|
| Brief name | |
| 1 | Telephone peer support |
| Why | |
| 2 | Three theoretical mechanisms for behaviour change underpin peer support interventions:
|
| What | |
| 3 | Materials: a Mothers Helping Mothers with Postpartum Depression manual was developed, pilot-tested and distributed to trainees.205 A take-home 121 page training manual developed and piloted by the principal investigator386 was distributed to new peer volunteers to guide the training session and intervention. Manual outlined professional services available for referral and covered: (1) introduction to peer support; (2) potential benefits of peer support; (3) relationship development; (4) techniques for effective telephone support; (5) general postpartum depression information; and (6) the helping process. All peer volunteers participated in a 4-hour training session. Role-playing and strategising were important components of the training session. Focus of training was to develop skills required for effective telephone-based support and to make referrals to health professionals as necessary. Peer volunteers provided with clear guidelines regarding thoughts of self-harm, indicating when to refer mothers to professional health services or crisis care. Training workshop provided opportunity to select applicants best suited for peer support with postpartum mothers |
| 4 | Procedures:
|
| Who provided | |
| 5 | Those whose communication skills were deemed inadequate, who demonstrated difficulties participating in discussions about postpartum depression or who showed evidence of unresolved depression were excluded from the peer support programme. Of those attending training, approximately 86% were accepted as peer volunteers and were matched with at least one new mother in the trial, based on residency and ethnicity if the mother desired |
| How | |
| 6 | By telephone having been matched individually by a volunteer co-ordinator |
| Where | |
| 7 | Based in woman’s own home |
| When and how much | |
| 8 | Each peer volunteer who actively participated in the trial and was matched with a (participant) on average supported two women with a range from one to seven |
| Tailoring | |
| 9 | Only according to ethnicity |
| Modifications | |
| 10 | No details |
| How well | |
| 11 | Planned: during training sessions, peer volunteers were given activity logs to complete for each supported mother. To document initiation of the intervention, the volunteer co-ordinator interacted with the peer volunteer 1 week after matching to confirm that contact was made with the (participant). All peer volunteers were requested to complete an activity log386 for each woman supported to document specific intervention activities and duration to 12 weeks postpartum |
| 12 | Actual: no details |
TIDieR checklist for The Newpin Project
| Social support | |
|---|---|
| Brief name | |
| 1 | The Newpin Project340 |
| Why | |
| 2 | An empowering strengths-based model that helps parents face their responsibilities with support from other parents as well as from trained staff. Lack of marital and extended family support, adverse experiences in the mother’s own childhood and poor material circumstances are implicated not only in the causation and maintenance of maternal depression, but also in child abuse and neglect. Befriending schemes may be accessible to many clients. Volunteers may show more commitment and flexibility in work with the families than is possible by professional health or social services. Such schemes are also cheaper than a professionally staffed service |
| What | |
| 3 | Materials: group uses variety of methods including information handouts, structured group discussion and detailed video feedback on parenting practice |
| 4 | Procedures: key to the model is mutual support, with every member being expected to support other parents by drawing on their own strengths and abilities. The combined support from both trained staff and other parents enables vulnerable families to be held through times of extreme distress |
| Who provided | |
| 5 | Women in the intervention group matched with a Newpin volunteer befriender. Befrienders were recruited through advertising or family centres where service users have already gained some experience of befriending other parents using the centre. Most befrienders were aged 31–45 years and young befrienders were matched with younger parents. Volunteer training consists of two half-days per week over a 6-month period. One session consists of lectures and workshops on topics such as child development, play, marriage and childbirth, problems in parenting and the befriending relationship. The other consists of a self-development group run by a group therapist, in which members are encouraged to explore current and past relationships and to come to terms with earlier trauma and loss. On conclusion of training, volunteers are assigned to support new clients and continue to receive weekly supervision while befriending |
| How | |
| 6 | No details |
| Where | |
| 7 | No details |
| When and how much | |
| 8 | Group ran for one day a week for 12–14 weeks from 10.00 until 14.30 and was open to mothers; it was facilitated by two trainers |
| Tailoring | |
| 9 | The only adaptation is the additional 2 weeks ‘settling in’ period |
| Modifications | |
| 10 | No details |
| How well | |
| 11 | Planned: no details |
| 12 | Actual: no details |
TIDieR checklist for CenteringPregnancy
| Midwifery-led intervention | |
|---|---|
| Brief name | |
| 1 | CenteringPregnancy262 |
| Why | |
| 2 | Founded on set of ‘Essential Elements’ providing structure for effective group prenatal care. Premise of CenteringPregnancy model is that by receiving prenatal care and education through a supportive group process, women gain power and confidence as knowledgeable health consumers, increased personal and maternal self-efficacy and strengthened community networks. Theory of mutual intentionality posits that the giver and recipient of social support make active decisions to give and receive support. Women give support to others as they seek to have their own needs met in the group and less through an active, conscious choice |
| What | |
| 3 | Materials: hand-outs and worksheets facilitate the discussion and are completed during the initial minutes |
| 4 | Procedures: women are invited to join group sessions after initial prenatal assessment and laboratory testing is completed. Sessions comprise prenatal health care and education and within the group space, women learn self-care skills including measuring their own blood pressure and weight, which they record in their medical record and they receive individual physical assessment from prenatal care provider. Women then meet as a group to discuss issues around the content of pregnancy, childbirth and parenting |
| Who provided | |
| 5 | Groups led by a certified nurse midwife /certified midwife or nurse practitioner skilled in group process. An additional person, a nurse or aide, facilitates flow of the group and help with any follow-up necessary. Consistency in leadership is important to provide continuity to the group and ensure comprehensive content presentation. Other professionals who assist as group leaders include social workers, nutritionists, physical therapists, birthing unit nurses and parent educators |
| How | |
| 6 | Face-to-face group sessions supplemented with individual sessions as considered necessary |
| Where | |
| 7 | Hospital clinic, requires space for self-examination activities and possibly private office space for individual consultations |
| When and how much | |
| 8 | Ten 2-hour prenatal group sessions with 8 to 12 women with similar due dates. Sessions begin at 12 to 16 weeks of pregnancy, concluding in the early postpartum |
| Tailoring | |
| 9 | Group discussion, facilitated by prenatal care provider, stimulated by self-assessment sheets geared to the content plan for each session and completed by women at beginning of each session |
| Modifications | |
| 10 | Not identified |
| How well | |
| 11 | Planned: no details |
| 12 | Actual: process fidelity reflected how facilitative leaders were and how involved participants were in each session. Content fidelity reflected whether recommended content was discussed in each session. Fidelity rated at each session by trained researcher294 |
TIDieR checklist for midwife-led brief counselling
| Midwifery-led intervention | |
|---|---|
| Brief name | |
| 1 | Midwife-led brief counselling221 |
| Why | |
| 2 | Counselling intervention based on a theoretical perspective, focus group discussions with childbearing women and midwives, and reviews of the literature |
| What | |
| 3 | Materials: none described |
| 4 | Procedures: counselling processes incorporated elements of critical stress debriefing and issues pertinent to the childbearing context. Content of the intervention specifically reviewed ‘management of labour’. This review of the actions of others, particularly professionals involved in, and possibly contributing to, traumatic aspects of the birth, differs from standardised debriefing or other counselling interventions reported to date |
| Who provided | |
| 5 | A midwife, knowledgeable about childbirth and trained in counselling approach, conducted sessions. Intervention does not require sophisticated psychotherapeutic skills. Model did not require substantial training and were a brief intervention that could be integrated with existing service frameworks |
| How | |
| 6 | Delivered face to face on postnatal ward and then via the telephone |
| Where | |
| 7 | On postnatal ward and then remotely via telephone |
| When and how much | |
| 8 | Intervention group received face-to-face counselling within 72 hours of birth and again via telephone at 4 to 6 weeks postpartum. Counselling duration ranged from 40 to 60 minutes |
| Tailoring | |
| 9 | None described |
| Modifications | |
| 10 | None described |
| How well | |
| 11 | Planned: adherence to a standard time frame enabled the incidence of acute and chronic trauma symptoms in childbearing women to be determined according to DSM-IV criteria |
| 12 | Actual: not described |
TIDieR checklist for midwife-managed care
| Midwifery-led intervention | |
|---|---|
| Brief name | |
| 1 | Midwife-managed care338 |
| Why | |
| 2 | Based on continuity of care and building of relationship of trust with care provider |
| What | |
| 3 | Both intervention and control group women encouraged to access community-based child health services. Provided with written information on service |
| 4 | Procedures: each pregnant woman had named midwife whom she met at first antenatal visit and who aimed to provide the majority of planned episodes of care from booking to discharge to the health visitor |
| Who provided | |
| 5 | Care was provided by group of 20 midwives who volunteered to join the unit from the hospital’s existing complement of midwives. When named midwife was unavailable, the woman was cared for by an associate midwife from the MDU team; women were referred to the obstetric medical team when there was deviation from normal, rather than at routinely specified times. The programme of care in comparison with shared care is care is described elsewhere481,482 |
| How | |
| 6 | Face to face, provided individually |
| Where | |
| 7 | Antenatal and postnatal care provided within existing facilities which included the hospital, home and community health centres. Designated birth rooms provided in hospital so that women could deliver in less clinical surroundings |
| When and how much | |
| 8 | Each mother offered the opportunity of one home visit and unlimited visits to the centre |
| Tailoring | |
| 9 | No details |
| Modifications | |
| 10 | No details |
| How well | |
| 11 | Planned: no details |
| 12 | Actual: no details |
TIDieR checklist for midwifery redesigned postnatal care
| Midwifery-led interventions | |
|---|---|
| Brief name | |
| 1 | Midwifery redesigned postnatal care146,264 |
| Why | |
| 2 | No theory. Government recommendations for wide-ranging changes to maternity, highlighting often inappropriate and fragmented delivery of postnatal care, led to a midwife-led service with continuity of care and involvement of women that is sensitive to the women’s individual needs and preferences at the centre of the reforms |
| What | |
| 3 | Ten evidence-based guidelines for main postpartum disorders identified from literature for subsequent midwife management of physical and psychological disorders, all with clear criteria for referral to GPs. Each guideline peer-reviewed by national experts and summarised in a leaflet. A description of how to use the checklists and guidelines to make visits more flexible also included. A symptom checklist was used alongside usual clinical judgement. An abbreviated version of the checklists was used at the first visit, to assess more immediate symptoms, and then a full list was used at the 10- and 28-day visits and again at the postnatal discharge check. EPDS was also completed at the 28-day visit and at the discharge check to screen for PND |
| 4 | Procedures: particular symptoms or problems included on checklist were main ones shown by literature to occur after birth and those for which guidelines were developed. From this information, care plans were made, after discussing needs with the woman |
| Who provided | |
| 5 | Midwifery-led, with GP contact only if midwife considered necessary, if requested/preferred by woman or GP. Midwife undertook all postnatal home visits and postnatal maternity discharge check. Midwives attached to recruited practices attended an English National Board for Nursing, Midwifery and Health Visiting accredited training day provided by the study team. Midwifery managers were able to claim the cost of bank staff to cover clinical work of attending midwives, although most did not claim. Four training days held and midwives attended in groups of about 15 |
| How | |
| 6 | EPDS used to screen for depression at day 28 and at discharge consultation |
| Where | |
| 7 | In woman’s home |
| When and how much | |
| 8 | To identify specific needs, even if not spontaneously reported by women or observed by midwife, symptom checklist used at first visit (immediate symptoms only), at days 10 and 28 and at discharge consultation at 10–12 weeks |
| Tailoring | |
| 9 | Care plans made/visits scheduled based on EPDS results so care tailored to individual needs rather than based on predetermined schedule |
| Modifications | |
| 10 | No details |
| How well | |
| 11 | Planned: no details |
| 12 | From trial documentation, most midwives in intervention group recorded care plans and visits as part of care, regular use of the guidelines and the completion of symptom checklists, suggesting package was implemented with reasonable fidelity |
Glossary
- Beck Depression Inventory
- A 21-item self-report scale used to determine depression severity. Items are scored on a 0–3 scale, giving a total score range of 0–63. Total scores within the 1–9 range indicate minimal depression, 10–18 indicate mild depression, 19–29 indicate moderate depression and 30–63 indicate severe depression.
- Center for Epidemiological Studies Depression Scale
- A short self-report scale designed to measure depressive symptomology in the general population. The 20-item scale has a possible range of scores from 0 to 60, with higher scores indicating more symptoms, weighted by frequency of occurrence during the past week.
- Cognitive–behavioural therapy
- The pragmatic combination of concepts and techniques from cognitive and behaviour therapies common in clinical practice. Cognitive–behavioural therapy aims to facilitate, through collaboration and guided discovery, recognition and re-evaluation of negative thinking patterns and practising new behaviours.
- Edinburgh Postnatal Depression Scale
- The most widely used self-report scale designed to measure postnatal depression symptomology. The scale consists of a 10-item Likert format relating to depression and anxiety symptomology. Items are scored on a 0–3 scale to give a total range of 0–30. Total scores within the 12–30 range suggest significant depression.
- Indicated preventive interventions
- Interventions offered to women at high risk of developing postnatal depression on the basis of psychological risk factors, above-average scores on psychological measures or other indications of a predisposition to postnatal depression but who did not meet diagnostic criteria for postnatal depression at that time.
- Interpersonal psychotherapy
- A time-limited, structured and psychoeducational therapy which links depression to role transitions, interpersonal disputes, interpersonal sensitivity or losses. It facilitates understanding of recent events in these interpersonal terms and explores alternative ways of handling interpersonal situations.
- Multipara
- A woman who has given birth two or more times.
- Network meta-analysis
- An extension of a standard meta-analysis which enables a simultaneous comparison of all evaluated interventions in a single coherent analysis. Thus, all interventions can be compared with one another, including comparisons not evaluated within individual studies. To perform a network meta-analysis each study must be linked to at least one other study through having at least one intervention in common.
- Postnatal depression (also known as postpartum depression)
- A non-psychotic depressive episode meeting standardised diagnostic criteria for a minor or major depressive disorder, beginning in or extending into the postnatal period.
- Selective preventive interventions
- Interventions offered to women or subgroups of the population whose risk of developing postnatal depression was significantly higher than average, because they had one or more social risk factors.
- Universal preventive interventions
- Interventions available for all women in a defined population not identified on the basis of increased risk for postnatal depression.
List of abbreviations
- AMED
- Allied and Complementary Medicine Database
- ASSIA
- Applied Social Sciences Index and Abstracts
- BDI
- Beck Depression Inventory
- CAM
- complementary and alternative medicine
- CASP
- Critical Appraisal Skills Programme
- CBA
- cognitive–behavioural approach
- CBT
- cognitive–behavioural therapy
- CEAC
- cost-effectiveness acceptability curve
- CENTRAL
- Cochrane Central Register of Controlled Trials
- CERQual
- Confidence in the Evidence from Reviews of Qualitative research
- CES-D
- Center for Epidemiologic Studies Depression scale
- CINAHL
- Cumulative Index to Nursing and Allied Health Literature
- CLUSTER
- Citations, Lead authors, Unpublished materials, Scholar searches, Theories, Early examples, Related projects
- CODA
- Convergence Diagnostic and Output Analysis
- CORE-OM
- Clinical Outcomes in Routine Evaluation-Outcome Measure
- CPCI-S
- Conference Proceedings Citation Index–Science
- CRCT
- cluster randomised controlled trial
- CrI
- credible interval
- DARE
- Database of Abstracts of Reviews of Effects
- DHA
- docosahexaenoic acid
- DSM-IV
- Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition
- DSM-V
- Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition
- EP
- Expert Patient
- EPA
- eicosapentaenoic acid
- EPDS
- Edinburgh Postnatal Depression Scale
- EVPI
- expected value of perfect information
- EVPPI
- expected value of partial perfect information
- GP
- general practitioner
- HADS
- Hospital Anxiety and Depression Scale
- HIV
- human immunodeficiency virus
- HTA
- Health Technology Assessment
- ICD-10
- International Classification of Diseases, Tenth Edition
- ICER
- incremental cost-effectiveness ratio
- IPT
- interpersonal psychotherapy
- MBE
- mind–body exercise
- MCS
- mental component summary
- MDU
- Midwifery Development Unit
- MIDIRS
- Midwives Information and Resource Service
- NHS EED
- NHS Economic Evaluation Database
- NICE
- National Institute for Health and Care Excellence
- NMA
- network meta-analysis
- NMB
- net monetary benefit
- PCA
- person-centred approach
- PCS
- physical component summary
- PHQ
- Patient Health Questionnaire
- PICOS
- population, intervention, comparators, outcomes, study designs
- PND
- postnatal depression
- PoNDER
- PostNatal Depression Economic evaluation and Randomised controlled trial
- PPI
- patient and public involvement
- PRISM
- Program of Resources, Information and Support for Mothers
- PRISMA
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PSA
- probabilistic sensitivity analysis
- PSI
- Parenting Stress Index
- PSS
- Perceived Stress Scale
- PSSS
- personal and social support strategy
- QALY
- quality-adjusted life-year
- RCT
- randomised controlled trial
- ROSE
- Reach Out, Stand strong, Essentials for new mothers
- SCAN
- Schedule for Clinical Assessment in Neuropsychiatry
- SCID
- Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders
- SD
- standard deviation
- SF-12
- Short Form questionnaire-12 items
- SF-36
- Short Form questionnaire-36 items
- SF-6D
- Short-Form 6-Dimensions
- STAI
- State–Trait Anxiety Inventory
- TIDieR
- template for intervention description and replication